Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

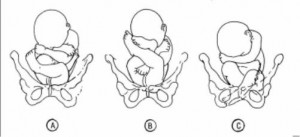
If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Breech presentation.
Caron J. Gray ; Meaghan M. Shanahan .
Affiliations
Last Update: November 6, 2022 .
- Continuing Education Activity
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. This activity reviews the cause and pathophysiology of breech presentation and highlights the role of the interprofessional team in its management.
- Describe the pathophysiology of breech presentation.
- Review the physical exam of a patient with a breech presentation.
- Summarize the treatment options for breech presentation.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by breech presentation.
- Introduction
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of one or both hips extended, also known as footling (one leg extended) breech, or double footling breech (both legs extended). [1] [2] [3]
Clinical conditions associated with breech presentation include those that may increase or decrease fetal motility, or affect the vertical polarity of the uterine cavity. Prematurity, multiple gestations, aneuploidies, congenital anomalies, Mullerian anomalies, uterine leiomyoma, and placental polarity as in placenta previa are most commonly associated with a breech presentation. Also, a previous history of breech presentation at term increases the risk of repeat breech presentation at term in subsequent pregnancies. [4] [5] These are discussed in more detail in the pathophysiology section.
- Epidemiology
Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 28 weeks or less, 25% are breech.
Specifically, following one breech delivery, the recurrence rate for the second pregnancy was nearly 10%, and for a subsequent third pregnancy, it was 27%. Prior cesarean delivery has also been described by some to increase the incidence of breech presentation two-fold.
- Pathophysiology
As mentioned previously, the most common clinical conditions or disease processes that result in the breech presentation are those that affect fetal motility or the vertical polarity of the uterine cavity. [6] [7]
Conditions that change the vertical polarity or the uterine cavity, or affect the ease or ability of the fetus to turn into the vertex presentation in the third trimester include:
- Mullerian anomalies: Septate uterus, bicornuate uterus, and didelphys uterus
- Placentation: Placenta previa as the placenta is occupying the inferior portion of the uterine cavity. Therefore, the presenting part cannot engage
- Uterine leiomyoma: Mainly larger myomas located in the lower uterine segment, often intramural or submucosal, that prevent engagement of the presenting part.
- Prematurity
- Aneuploidies and fetal neuromuscular disorders commonly cause hypotonia of the fetus, inability to move effectively
- Congenital anomalies: Fetal sacrococcygeal teratoma, fetal thyroid goiter
- Polyhydramnios: Fetus is often in unstable lie, unable to engage
- Oligohydramnios: Fetus is unable to turn to vertex due to lack of fluid
- Laxity of the maternal abdominal wall: Uterus falls forward, the fetus is unable to engage in the pelvis.
The risk of cord prolapse varies depending on the type of breech. Incomplete or footling breech carries the highest risk of cord prolapse at 15% to 18%, while complete breech is lower at 4% to 6%, and frank breech is uncommon at 0.5%.
- History and Physical
During the physical exam, using the Leopold maneuvers, palpation of a hard, round, mobile structure at the fundus and the inability to palpate a presenting part in the lower abdomen superior to the pubic bone or the engaged breech in the same area, should raise suspicion of a breech presentation.
During a cervical exam, findings may include the lack of a palpable presenting part, palpation of a lower extremity, usually a foot, or for the engaged breech, palpation of the soft tissue of the fetal buttocks may be noted. If the patient has been laboring, caution is warranted as the soft tissue of the fetal buttocks may be interpreted as caput of the fetal vertex.
Any of these findings should raise suspicion and ultrasound should be performed.
Diagnosis of a breech presentation can be accomplished through abdominal exam using the Leopold maneuvers in combination with the cervical exam. Ultrasound should confirm the diagnosis.
On ultrasound, the fetal lie and presenting part should be visualized and documented. If breech presentation is diagnosed, specific information including the specific type of breech, the degree of flexion of the fetal head, estimated fetal weight, amniotic fluid volume, placental location, and fetal anatomy review (if not already done previously) should be documented.
- Treatment / Management
Expertise in the delivery of the vaginal breech baby is becoming less common due to fewer vaginal breech deliveries being offered throughout the United States and in most industrialized countries. The Term Breech Trial (TBT), a well-designed, multicenter, international, randomized controlled trial published in 2000 compared planned vaginal delivery to planned cesarean delivery for the term breech infant. The investigators reported that delivery by planned cesarean resulted in significantly lower perinatal mortality, neonatal mortality, and serious neonatal morbidity. Also, there was no significant difference in maternal morbidity or mortality between the two groups. Since that time, the rate of term breech infants delivered by planned cesarean has increased dramatically. Follow-up studies to the TBT have been published looking at maternal morbidity and outcomes of the children at two years. Although these reports did not show any significant difference in the risk of death and neurodevelopmental, these studies were felt to be underpowered. [8] [9] [10] [11]
Since the TBT, many authors since have argued that there are still some specific situations that vaginal breech delivery is a potential, safe alternative to planned cesarean. Many smaller retrospective studies have reported no difference in neonatal morbidity or mortality using these specific criteria.
The initial criteria used in these reports were similar: gestational age greater than 37 weeks, frank or complete breech presentation, no fetal anomalies on ultrasound examination, adequate maternal pelvis, and estimated fetal weight between 2500 g and 4000 g. In addition, the protocol presented by one report required documentation of fetal head flexion and adequate amniotic fluid volume, defined as a 3-cm vertical pocket. Oxytocin induction or augmentation was not offered, and strict criteria were established for normal labor progress. CT pelvimetry did determine an adequate maternal pelvis.
Despite debate on both sides, the current recommendation for the breech presentation at term includes offering external cephalic version (ECV) to those patients that meet criteria, and for those whom are not candidates or decline external cephalic version, a planned cesarean section for delivery sometime after 39 weeks.
Regarding the premature breech, gestational age will determine the mode of delivery. Before 26 weeks, there is a lack of quality clinical evidence to guide mode of delivery. One large retrospective cohort study recently concluded that from 28 to 31 6/7 weeks, there is a significant decrease in perinatal morbidity and mortality in a planned cesarean delivery versus intended vaginal delivery, while there is no difference in perinatal morbidity and mortality in gestational age 32 to 36 weeks. Of note, due to lack of recruitment, no prospective clinical trials are examining this issue.
- Differential Diagnosis
- Face and brow presentation
- Fetal anomalies
- Fetal death
- Grand multiparity
- Multiple pregnancies
- Oligohydramnios
- Pelvis Anatomy
- Preterm labor
- Primigravida
- Uterine anomalies
- Pearls and Other Issues
In light of the decrease in planned vaginal breech deliveries, thus the decrease in expertise in managing this clinical scenario, it is prudent that policies requiring simulation and instruction in the delivery technique for vaginal breech birth are established to care for the emergency breech vaginal delivery.
- Enhancing Healthcare Team Outcomes
A breech delivery is usually managed by an obstetrician, labor and delivery nurse, anesthesiologist and a neonatologist. The ultimate decison rests on the obstetrician. To prevent complications, today cesarean sections are performed and experienced with vaginal deliveries of breech presentation is limited. For healthcare workers including the midwife who has no experience with a breech delivery, it is vital to communicate with an obstetrician, otherwise one risks litigation if complications arise during delivery. [12] [13] [14]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Caron Gray declares no relevant financial relationships with ineligible companies.
Disclosure: Meaghan Shanahan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Gray CJ, Shanahan MM. Breech Presentation. [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. [Z Geburtshilfe Neonatol. 1997] [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. Krause M, Fischer T, Feige A. Z Geburtshilfe Neonatol. 1997 Jul-Aug; 201(4):128-35.
- The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. [Early Hum Dev. 1993] The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. Sival DA, Prechtl HF, Sonder GH, Touwen BC. Early Hum Dev. 1993 Mar; 32(2-3):161-76.
- The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. [PLoS One. 2019] The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. Jennewein L, Allert R, Möllmann CJ, Paul B, Kielland-Kaisen U, Raimann FJ, Brüggmann D, Louwen F. PLoS One. 2019; 14(12):e0225546. Epub 2019 Dec 2.
- Review Breech vaginal delivery at or near term. [Semin Perinatol. 2003] Review Breech vaginal delivery at or near term. Tunde-Byass MO, Hannah ME. Semin Perinatol. 2003 Feb; 27(1):34-45.
- Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. [Gynecol Obstet Fertil Senol. 2...] Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. Mattuizzi A. Gynecol Obstet Fertil Senol. 2020 Jan; 48(1):70-80. Epub 2019 Nov 1.
Recent Activity
- Breech Presentation - StatPearls Breech Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Obstetric and Newborn Care I
10.02 key terms related to fetal positions.
a. “Lie” of an Infant.
Lie refers to the position of the spinal column of the fetus in relation to the spinal column of the mother. There are two types of lie, longitudinal and transverse. Longitudinal indicates that the baby is lying lengthwise in the uterus, with its head or buttocks down. Transverse indicates that the baby is lying crosswise in the uterus.
b. Presentation/Presenting Part.
Presentation refers to that part of the fetus that is coming through (or attempting to come through) the pelvis first.
(1) Types of presentations (see figure 10-1). The vertex or cephalic (head), breech, and shoulder are the three types of presentations. In vertex or cephalic, the head comes down first. In breech, the feet or buttocks comes down first, and last–in shoulder, the arm or shoulder comes down first. This is usually referred to as a transverse lie.
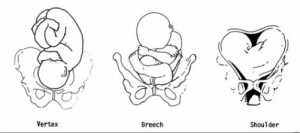
(2) Percentages of presentations.
(a) Head first is the most common-96 percent.
(b) Breech is the next most common-3.5 percent.
(c) Shoulder or arm is the least common-5 percent.
(3) Specific presentation may be evaluated by several ways.
(a) Abdominal palpation-this is not always accurate.
(b) Vaginal exam–this may give a good indication but not infallible.
(c) Ultrasound–this confirms assumptions made by previous methods.
(d) X-ray–this confirms the presentation, but is used only as a last resort due to possible harm to the fetus as a result of exposure to radiation.
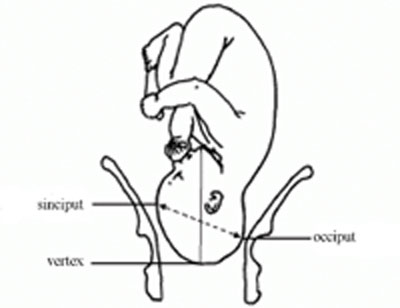
c. Attitude.
This is the degree of flexion of the fetus body parts (body, head, and extremities) to each other. Flexion is resistance to the descent of the fetus down the birth canal, which causes the head to flex or bend so that the chin approaches the chest.
(1) Types of attitude (see figure 10-2).
(a) Complete flexion. This is normal attitude in cephalic presentation. With cephalic, there is complete flexion at the head when the fetus “chin is on his chest.” This allows the smallest cephalic diameter to enter the pelvis, which gives the fewest mechanical problems with descent and delivery.
(b) Moderate flexion or military attitude. In cephalic presentation, the fetus head is only partially flexed or not flexed. It gives the appearance of a military person at attention. A larger diameter of the head would be coming through the passageway.
(c) Poor flexion or marked extension. In reference to the fetus head, it is extended or bent backwards. This would be called a brow presentation. It is difficult to deliver because the widest diameter of the head enters the pelvis first. This type of cephalic presentation may require a C/Section if the attitude cannot be changed.
(d) Hyperextended. In reference to the cephalic position, the fetus head is extended all the way back. This allows a face or chin to present first in the pelvis. If there is adequate room in the pelvis, the fetus may be delivered vaginally.
(2) Areas to look at for flexion.
(a) Head-discussed in previous paragraph, 10-2c(1).
(b) Thighs-flexed on the abdomen.
(c) Knees-flexed at the knee joints.
(d) Arches of the feet-rested on the anterior surface of the legs.
(e) Arms-crossed over the thorax.
(3) Attitude of general flexion. This is when all of the above areas are flexed appropriately as described.
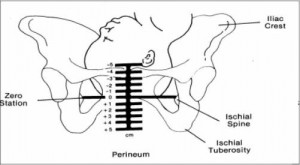
d. Station.
This refers to the depth that the presenting part has descended into the pelvis in relation to the ischial spines of the mother’s pelvis. Measurement of the station is as follows:
(1) The degree of advancement of the presenting part through the pelvis is measured in centimeters.
(2) The ischial spines is the dividing line between plus and minus stations.
(3) Above the ischial spines is referred to as -1 to -5, the numbers going higher as the presenting part gets higher in the pelvis (see figure10-3).
(4) The ischial spines is zero (0) station.
(5) Below the ischial spines is referred to +1 to +5, indicating the lower the presenting part advances.
e. Engagement.
This refers to the entrance of the presenting part of the fetus into the true pelvis or the largest diameter of the presenting part into the true pelvis. In relation to the head, the fetus is said to be engaged when it reaches the midpelvis or at a zero (0) station. Once the fetus is engaged, it (fetus) does not go back up. Prior to engagement occurring, the fetus is said to be “floating” or ballottable.
f. Position.
This is the relationship between a predetermined point of reference or direction on the presenting part of the fetus to the pelvis of the mother.
(1) The maternal pelvis is divided into quadrants.
(a) Right and left side, viewed as the mother would.
(b) Anterior and posterior. This is a line cutting the pelvis in the middle from side to side. The top half is anterior and the bottom half is posterior.
(c) The quadrants never change, but sometimes it is confusing because the student or physician’s viewpoint changes.
NOTE: Remember that when you are describing the quadrants, view them as the mother would.
(2) Specific points on the fetus.
(a) Cephalic or head presentation.
1 Occiput (O). This refers to the Y sutures on the top of the head.
2 Brow or fronto (F). This refers to the diamond sutures or anterior fontanel on the head.
3 Face or chin presentation (M). This refers to the mentum or chin.
(b) Breech or butt presentation.
1 Sacrum or coccyx (S). This is the point of reference.
2 Breech birth is associated with a higher perinatal mortality.
(c) Shoulder presentation.
1 This would be seen with a transverse lie.
2. Scapula (Sc) or its upper tip, the acromion (A) would be used for the point of reference.
(3) Coding of positions.
(a) Coding simplifies explaining the various positions.
1 The first letter of the code tells which side of the pelvis the fetus reference point is on (R for right, L for left).
2 The second letter tells what reference point on the fetus is being used (Occiput-O, Fronto-F, Mentum-M, Breech-S, Shoulder-Sc or A).
3 The last letter tells which half of the pelvis the reference point is in (anterior-A, posterior-P, transverse or in the middle-T).

(b) Each presenting part has the possibility of six positions. They are normally recognized for each position–using “occiput” as the reference point.
1 Left occiput anterior (LOA).
2 Left occiput posterior (LOP).
3 Left occiput transverse (LOT).
4 Right occiput anterior (ROA).
5. Right occiput posterior (ROP).
6 Right occiput transverse (ROT).
(c) A transverse position does not use a first letter and is not the same as a transverse lie or presentation.
1 Occiput at sacrum (O.S.) or occiput at posterior (O.P.).
2 Occiput at pubis (O.P.) or occiput at anterior (O.A.).
(4) Types of breech presentations (see figure10-4).
(a) Complete or full breech. This involves flexion of the fetus legs. It looks like the fetus is sitting in a tailor fashion. The buttocks and feet appear at the vaginal opening almost simultaneously.
A–Complete. B–Frank. C–Incomplete.
(b) Frank and single breech. The fetus thighs are flexed on his abdomen. His legs are against his trunk and feet are in his face (foot-in-mouth posture). This is the most common and easiest breech presentation to deliver.
(c) Incomplete breech. The fetus feet or knees will appear first. His feet are labeled single or double footing, depending on whether 1 or 2 feet appear first.
(5) Observations about positions (see figure 10-5).
(a) LOA and ROA positions are the most common and permit relatively easy delivery.
(b) LOP and ROP positions usually indicate labor may be longer and harder, and the mother will experience severe backache.
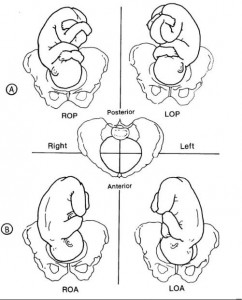
(c) Knowing positions will help you to identify where to look for FHT’s.
1 Breech. This will be upper R or L quad, above the umbilicus.
2 Vertex. This will be lower R or L quad, below the umbilicus.
(d) An occiput in the posterior quadrant means that you will feel lumpy fetal parts, arms and legs (see figure 10-5 A). If delivered in that position, the infant will come out looking up.
(e) An occiput in the anterior quadrant means that you will feel a more smooth back (see figure 10-5 B). If delivered in that position, the infant will come out looking down at the floor.
Distance Learning for Medical and Nursing Professionals
- MSD careers
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Fetal Presentation, Position, and Lie (Including Breech Presentation)
, MD, Children's Hospital of Philadelphia
Variations in Fetal Position and Presentation
- 3D Models (0)
- Calculators (0)
- Lab Test (0)

Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).

The fetus has a birth defect Overview of Birth Defects Birth defects, also called congenital anomalies, are physical abnormalities that occur before a baby is born. They are usually obvious within the first year of life. The cause of many birth... read more .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
Sometimes the doctor can turn the fetus to be head first before labor begins by doing a procedure that involves pressing on the pregnant woman’s abdomen and trying to turn the baby around. Trying to turn the baby is called an external cephalic version and is usually done at 37 or 38 weeks of pregnancy. Sometimes women are given a medication (such as terbutaline ) during the procedure to prevent contractions.
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada)—dedicated to using leading-edge science to save and improve lives around the world. Learn more about the MSD Manuals and our commitment to Global Medical Knowledge .
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Edition
- IN THIS TOPIC
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Christine Zink, MD, is a board-certified emergency medicine with expertise in the wilderness and global medicine. She completed her medical training at Weill Cornell Medical College and residency in emergency medicine at New York-Presbyterian Hospital. She utilizes 15-years of clinical experience in her medical writing.
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Fetal Presentation, Position, and Lie (Including Breech Presentation)
, MD, Children's Hospital of Philadelphia
Variations in Fetal Position and Presentation
- 3D Models (0)
- Calculators (0)
- Lab Test (0)

Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).

The fetus has a birth defect Overview of Birth Defects Birth defects, also called congenital anomalies, are physical abnormalities that occur before a baby is born. They are usually obvious within the first year of life. The cause of many birth... read more .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
Sometimes the doctor can turn the fetus to be head first before labor begins by doing a procedure that involves pressing on the pregnant woman’s abdomen and trying to turn the baby around. Trying to turn the baby is called an external cephalic version and is usually done at 37 or 38 weeks of pregnancy. Sometimes women are given a medication (such as terbutaline ) during the procedure to prevent contractions.
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.
Drugs Mentioned In This Article

Was This Page Helpful?

Test your knowledge
Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada)—dedicated to using leading-edge science to save and improve lives around the world. Learn more about the Merck Manuals and our commitment to Global Medical Knowledge .
- Permissions
- Cookie Settings
- Terms of use
- Veterinary Edition

- IN THIS TOPIC
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Malpresentation
8-minute read
If you feel your waters break and you have been told that your baby is not in a head-first position, seek medical help immediately .
- Malpresentation is when your baby is not facing head-first down the birth canal as birth approaches.
- The most common type of malpresentation is breech — when your baby’s bottom or feet are facing downwards.
- A procedure called external cephalic version can sometimes turn a breech baby into a head-first position at 36 weeks.
- Most babies with malpresentation are born by caesarean, but you may be able to have a vaginal birth if your baby is breech.
- There is a serious risk of cord prolapse if your waters break and your baby is not head-first.
What are presentation and malpresentation?
‘Presentation’ describes how your baby is facing down the birth canal. The ‘presenting part’ is the part of your baby’s body that is against the cervix .
The ideal presentation is head-first, with the crown (top) of the baby’s head against the cervix, with the chin tucked into the baby’s chest. This is called ‘vertex presentation’.
If your baby is in any other position, it’s called ‘malpresentation’. Malpresentation can mean your baby’s face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix.
It’s safest for your baby’s head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you will have a more complex vaginal birth or a caesarean.
If my baby is not head-first, what position could they be in?
Malpresentation is caused by your baby’s position (‘lie’). There are different types of malpresentation.
Breech presentation
This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a ‘footling presentation’).
Breech presentation is the most common type of malpresentation.
Face presentation
This is when your baby is head-first but stretching their neck, with their face against the cervix.
Transverse lie
This is when your baby is lying sideways. Their back, shoulders, arms or legs may be the first to enter the birth canal.
Oblique lie
This is when your baby is lying diagonally. No particular part of their body is against the cervix.
Unstable lie
This is when your baby continually changes their position after 36 weeks of pregnancy.
Cord presentation
This is when the umbilical cord is against the cervix, between your baby and the birth canal. It can happen in any situation where your baby’s presenting part is not sitting snugly in your pelvis. It can become an emergency if it leads to cord prolapse (when the cord is born before your baby, potentially reducing placental blood flow to your baby).
What is malposition?
If your baby is lying head-first, the best position for labour is when their face is towards your back.
If your baby is facing the front of your body (posterior position) or facing your side (transverse position) this is called malposition. Transverse position is not the same as transverse lie. A transverse position means your labour may take a bit longer and you might feel more pain in your back. Often your baby will move into a better position before or during labour.
Why might my baby be in the wrong position?
Malpresentation may be caused by:
- a low-lying placenta
- too much or too little amniotic fluid
- many previous pregnancies, making the muscles of the uterus less stable
- carrying twins or more
Often no cause is found.

Is it likely that my baby will be in the wrong position?
Many babies are in a breech position during pregnancy. They usually turn head-first as pregnancy progresses, and more than 9 in 10 babies in Australia have a vertex presentation (ideal presentation, head-first) at birth.
You are more likely to have a malpresentation if:
- this is your first baby
- you are over 40 years old
- you've had a previous breech baby
- you go into labour prematurely
How is malpresentation diagnosed?
Malpresentation is normally diagnosed when your doctor or midwife examines you, from 36 weeks of pregnancy. If it’s not clear, it can be confirmed with an ultrasound.
Can my baby’s position be changed?
If you are 36 weeks pregnant , it may be possible to gently turn your baby into a head-first position. This is done by an obstetrician using a technique called external cephalic version (ECV).
Some people try different postures or acupuncture to correct malpresentation, but there isn’t reliable evidence that either of these work.
Will I need a caesarean if my baby has a malpresentation?
Most babies with a malpresentation close to birth are born by caesarean . You may be able to have a vaginal birth with a breech baby, but you will need to go to a hospital that can offer you and your baby specialised care.
If your baby is breech, an elective (planned) caesarean is safer for your baby than a vaginal birth in the short term. However, in the longer term their health will be similar, on average, regardless of how they were born.
A vaginal birth is safer for you than an elective caesarean. However, about 4 in 10 people planning a vaginal breech birth end up needing an emergency caesarean . If this happens to you, the risk of complications will be higher.
Your doctor can talk to you about your options. Whether it’s safe for you to try a vaginal birth will depend on many factors. These include how big your baby is, the position of your baby, the structure of your pelvis and whether you’ve had a caesarean in the past.
What are the risks if I have my baby when it’s not head-first?
If your waters break when your baby is not head-first, there is a risk of cord prolapse. This is an emergency.
Vaginal breech birth
Risks to your baby can include:
- Erb’s palsy
- fractures, dislocations or other injuries
- bleeding in your baby’s brain
- low Apgar scores
- their head getting stuck – this is an emergency
Risks to you include:
- blood loss or blood clots
- infection in the wound
- problems with the anaesthetic
- damage to other organs nearby, such as your bladder
- a higher chance of problems in future pregnancies
- a longer recovery time than after a vaginal birth
Risks to your baby include:
- trouble with breathing — this is temporary
- getting a small cut during the surgery
Will I have a malpresentation in my future pregnancies?
If you had a malpresentation in one pregnancy, you have a higher chance of it happening again, but it won’t necessarily happen in future pregnancies. If you’re worried, it may help to talk to your doctor or midwife so they can explain what happened.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: July 2022
Related pages
Labour complications.
- Interventions during labour
- Giving birth - stages of labour
Breech pregnancy
Search our site for.
- Caesarean Section
- Foetal Version
Need more information?
Top results
When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

Presentation and position of baby through pregnancy and at birth
Presentation and position refer to where your baby’s head and body is in relation to your birth canal. Learn why it’s important for labour and birth.
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Labour and Delivery Care Module: 8. Abnormal Presentations and Multiple Pregnancies
Study session 8 abnormal presentations and multiple pregnancies, introduction.
In previous study sessions of this module, you have been introduced to the definitions, signs, symptoms and stages of normal labour, and about the ‘normal’ vertex presentation of the fetus during delivery. In this study session, you will learn about the most common abnormal presentations (breech, shoulder, face or brow), their diagnostic criteria and the required actions you need to take to prevent complications developing during labour. Taking prompt action may save the life of the mother and her baby if the delivery becomes obstructed because the baby is in an abnormal presentation. We will also tell you about twin births and the complications that may result if the two babies become ‘locked’ together, preventing either of them from being born.
Learning Outcomes for Study Session 8
After studying this session, you should be able to:
8.1 Define and use correctly all of the key words printed in bold . (SAQs 8.1 and 8.2)
8.2 Describe how you would identify a fetus in the vertex presentation and distinguish this from common malpresentations and malpositions. (SAQs 8.1 and 8.2)
8.3 Describe the causes and complications for the fetus and the mother of fetal malpresentation during full term labour. (SAQ 8.3)
8.4 Describe how you would identify a multiple pregnancy and the complications that may arise. (SAQ 8.4)
8.5 Explain when and how you would refer a woman in labour due to abnormal fetal presentation or multiple pregnancy. (SAQ 8.4)
8.1 Normal and abnormal presentations
8.1.1 vertex presentation.
In about 95% of deliveries, the part of the fetus which arrives first at the mother’s pelvic brim is the highest part of the fetal head, which is called the vertex (Figure 8.1). This presentation is called the vertex presentation . Notice that the baby’s chin is tucked down towards its chest, so that the vertex is the leading part entering the mother’s pelvis. The baby’s head is said to be ‘well-flexed’ in this position.
During early pregnancy, the baby is the other way up — with its bottom pointing down towards the mother’s cervix — which is called the breech presentation . This is because during its early development, the head of the fetus is bigger than its buttocks; so in the majority of cases, the head occupies the widest cavity, i.e. the fundus (rounded top) of the uterus. As the fetus grows larger, the buttocks become bigger than the head and the baby spontaneously reverses its position, so its buttocks occupy the fundus. In short, in early pregnancy, the majority of fetuses are in the breech presentation and later in pregnancy most of them make a spontaneous transition to the vertex presentation.
8.1.2 Malpresentations
You will learn about obstructed labour in Study Session 9.
When the baby presents itself in the mother’s pelvis in any position other than the vertex presentation, this is termed an abnormal presentation, or m alpresentation . The reason for referring to this as ‘abnormal’ is because it is associated with a much higher risk of obstruction and other birth complications than the vertex presentation. The most common types of malpresentation are termed breech, shoulder, face or brow. We will discuss each of these in turn later. Notice that the baby can be ‘head-down’ but in an abnormal presentation, as in face or brow presentations, when the baby’s face or forehead (brow) is the presenting part.
8.1.3 Malposition
Although it may not be so easy for you to identify this, the baby can also be in an abnormal position even when it is in the vertex presentation. In a normal delivery, when the baby’s head has engaged in the mother’s pelvis, the back of the baby’s skull (the occiput ) points towards the front of the mother’s pelvis (the pubic symphysis ), where the two pubic bones are fused together. This orientation of the fetal skull is called the occipito-anterior position (Figure 8.2a). If the occiput (back) of the fetal skull is towards the mother’s back, this occipito-posterior position (Figure 8.2b) is a vertex malposition , because it is more difficult for the baby to be born in this orientation. The good thing is that more than 90% of babies in vertex malpositions undergo rotation to the occipito-anterior position and are delivered normally.
You learned the directional positions: anterior/in front of and posterior/behind or in the back of, in the Antenatal Care Module, Part 1, Study Session 3.
Note that the fetal skull can also be tilted to the left or to the right in either the occipito-anterior or occipito-posterior positions.

8.2 Causes and consequences of malpresentations and malpositions
In the majority of individual cases it may not be possible to identify what caused the baby to be in an abnormal presentation or position during delivery. However, the general conditions that are thought to increase the risk of malpresentation or malposition are listed below:
Multiple pregnancy is the subject of Section 8.7 of this study session. You learned about placenta previa in the Antenatal Care Module, Study Session 21.
- Abnormally increased or decreased amount of amniotic fluid
- A tumour (abnormal tissue growth) in the uterus preventing the spontaneous inversion of the fetus from breech to vertex presentation during late pregnancy
- Abnormal shape of the pelvis
- Laxity (slackness) of muscular layer in the walls of the uterus
- Multiple pregnancy (more than one baby in the uterus)
- Placenta previa (placenta partly or completely covering the cervical opening).
If the baby presents at the dilating cervix in an abnormal presentation or malposition, it will more difficult (and may be impossible) for it to complete the seven cardinal movements that you learned about in Study Sessions 3 and 5. As a result, birth is more difficult and there is an increased risk of complications, including:
You learned about PROM in Study Session 17 of the Antenatal Care Module, Part 2.
- Premature rupture of the fetal membranes (PROM)
- Premature labour
- Slow, erratic, short-lived contractions
- Uncoordinated and extremely painful contractions, with slow or no progress of labour
- Prolonged and obstructed labour, leading to a ruptured uterus (see Study Sessions 9 and 10 of this Module)
- Postpartum haemorrhage (see Study Session 11)
- Fetal and maternal distress, which may lead to the death of the baby and/or the mother.
With these complications in mind, we now turn your attention to the commonest types of malpresentation and how to recognise them.
8.3 Breech presentation
In a b reech presentation , the fetus lies with its buttocks in the lower part of the uterus, and its buttocks and/or the feet are the presenting parts during delivery. Breech presentation occurs on average in 3–4% of deliveries after 34 weeks of pregnancy.
When is the breech position the normal position for the fetus?
During early pregnancy the baby’s bottom points down towards the mother’s cervix, and its head (the largest part of the fetus at this stage of development) occupies the fundus (rounded top) of the uterus, which is the widest part of the uterine cavity.
8.3.1 Causes of breech presentation
You can see a transverse lie in Figure 8.7 later in this study session.
In the majority of cases there is no obvious reason why the fetus should present by the breech at full term. In practice, what is commonly observed is the association of breech presentation at delivery with a transverse lie earlier in the pregnancy, i.e. the fetus lies sideways across the mother’s abdomen, facing a sideways implanted placenta. It is thought that when the placenta is in front of the baby’s face, it may obstruct the normal process of inversion, when the baby turns head-down as it gets bigger during the pregnancy. As a result, the fetus turns in the other direction and ends in the breech presentation. Some other circumstances that are thought to favour a breech presentation during labour include:
- Premature labour, beginning before the baby undergoes spontanous inversion from breech to vertex presentation
- Multiple pregnancy, preventing the normal inversion of one or both babies
- Polyhydramnios: excessive amount of amniotic fluid, which makes it more difficult for the fetal head to ‘engage’ with the mother’s cervix (polyhydramnios is pronounced ‘poll-ee-hy-dram-nee-oss’. Hydrocephaly is pronounced ‘hy-droh-keff-all-ee’)
- Hydrocephaly (‘water on the brain’) i.e. an abnormally large fetal head due to excessive accumulation of fluid around the brain
- Placenta praevia
- Breech delivery in the previous pregnancy
- Abnormal formation of the uterus.
8.3.2 Diagnosis of breech presentation
On abdominal palpation the fetal head is found above the mother’s umbilicus as a hard, smooth, rounded mass, which gently ‘ballots’ (can be rocked) between your hands.
Why do you think a mass that ‘ballots’ high up in the abdomen is a sign of breech presentation? (You learned about this in Study Session 11 of the Antenatal Care Module.)
The baby’s head can ‘rock’ a little bit because of the flexibility of the baby’s neck, so if there is a rounded, ballotable mass above the mother’s umbilicus it is very likely to be the baby’s head. If the baby was ‘bottom-up’ (vertex presentation) the whole of its back will move of you try to rock the fetal parts at the fundus (Figure 8.3).
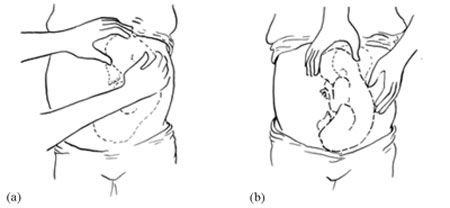
Once the fetus has engaged and labour has begun, the breech baby’s buttocks can be felt as soft and irregular on vaginal examination. They feel very different to the relatively hard rounded mass of the fetal skull in a vertex presentation. When the fetal membranes rupture, the buttocks and/or feet can be felt more clearly. The baby’s anus may be felt and fresh thick, dark meconium may be seen on your examining finger. If the baby’s legs are extended, you may be able to feel the external genitalia and even tell the sex of the baby before it is born.
8.3.3 Types of breech presentation
There are three types of breech presentation, as illustrated in Figure 8.4. They are:
- Complete breech is characterised by flexion of the legs at both hips and knee joints, so the legs are bent underneath the baby.
- Frank breech is the commonest type of breech presentation, and is characterised by flexion at the hip joints and extension at the knee joints, so both the baby’s legs point straight upwards.
- Footling breech is when one or both legs are extended at the hip and knee joint and the baby presents ‘foot first’.
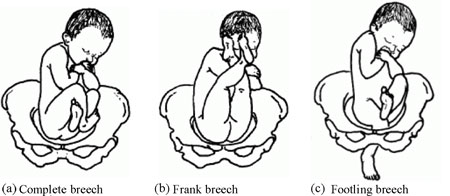
8.3.4 Risks of breech presentation
Regardless of the type of breech presentation, there are significant associated risks to the baby. They include:
- The fetal head gets stuck (arrested) before delivery
- Labour becomes obstructed when the fetus is disproportionately large for the size of the maternal pelvis
- Cord prolapse may occur, i.e. the umbilical cord is pushed out ahead of the baby and may get compressed against the wall of the cervix or vagina
- Premature separation of the placenta (placental abruption)
- Birth injury to the baby, e.g. fracture of the arms or legs, nerve damage, trauma to the internal organs, spinal cord damage, etc.
A breech birth may also result in trauma to the mother’s birth canal or external genitalia through being overstretched by the poorly fitting fetal parts.
Cord prolapse in a normal (vertex) presentation was illustrated in Study Session 17 of the Antenatal Care Module, and placental abruption was covered in Study Session 21.
What will be the effect on the baby if it gets stuck, the labour is obstructed, the cord prolapses, or placental abruption occurs?
The result will be hypoxia , i.e. it will be deprived of oxygen, and may suffer permanent brain damage or die.
You learned about the causes and consequences of hypoxia in the Antenatal Care Module.
8.4 Face presentation
Face presentation occurs when the baby’s neck is so completely extended (bent backwards) that the occiput at the back of the fetal skull touches the baby’s own spine (see Figure 8.5). In this position, the baby’s face will present to you during delivery.
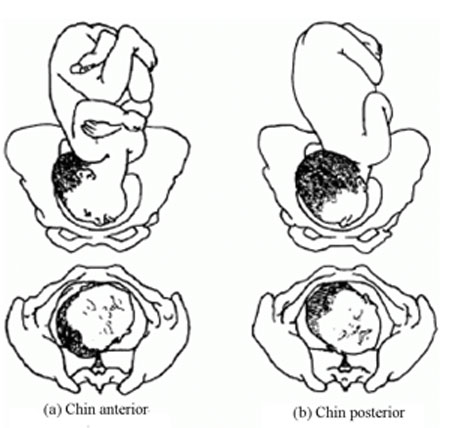
Refer the mother if a baby in the chin posterior face presentation does not rotate and the labour is prolonged.
The incidence of face presentation is about 1 in 500 pregnancies in full term labours. In Figure 8.5, you can see how flexed the head is at the neck. Babies who present in the ‘chin posterior’ position (on the right in Figure 8.5) usually rotate spontaneously during labour, and assume the ‘chin anterior’ position, which makes it easier for them to be born. However, they are unlikely to be delivered vaginally if they fail to undergo spontaneous rotation to the chin anterior position, because the baby’s chin usually gets stuck against the mother’s sacrum (the bony prominence at the back of her pelvis). A baby in this position will have to be delivered by caesarean surgery.
8.4.1 Causes of face presentation
The causes of face presentation are similar to those already described for breech births:
- Laxity (slackness) of the uterus after many previous full-term pregnancies
- Multiple pregnancy
- Polyhydramnios (excessive amniotic fluid)
- Congenital abnormality of the fetus (e.g. anencephaly, which means no or incomplete skull bones)
- Abnormal shape of the mother’s pelvis.
8.4.2 Diagnosis of face presentation
Face presentation may not be easily detected by abdominal palpation, especially if the chin is in the posterior position. On abdominal examination, you may feel irregular shapes, formed because the fetal spine is curved in an ‘S’ shape. However, on vaginal examination, you can detect face presentation because:
- The presenting part will be high, soft and irregular.
- When the cervix is sufficiently dilated, you may be able to feel parts of the face, such as the orbital ridges above the eyes, the nose or mouth, gums, or bony chin.
- If the membranes are ruptured, the baby may suck your examining finger!
But as labour progresses, the baby’s face becomes o edematous (swollen with fluid), making it more difficult to distinguish from the soft shape you will feel in a breech presentation.
8.4.3 Complications of face presentation
Complications for the fetus include:
- Obstructed labour and ruptured uterus
- Cord prolapse
- Facial bruising
- Cerebral haemorrhage (bleeding inside the fetal skull).
8.5 Brow presentation

In brow presentation , the baby’s head is only partially extended at the neck (compare this with face presentation), so its brow (forehead) is the presenting part (Figure 8.6). This presentation is rare, with an incidence of 1 in 1000 deliveries at full term.
8.5.1 Possible causes of brow presentation
You have seen all of these factors before, as causes of other malpresentations:
- Lax uterus due to repeated full term pregnancy
- Polyhydramnios
8.5.2 Diagnosis of brow presentation
Brow presentation is not usually detected before the onset of labour, except by very experienced birth attendants. On abdominal examination, the head is high in the mother’s abdomen, appears unduly large and does not descend into the pelvis, despite good uterine contractions. On vaginal examination, the presenting part is high and may be difficult to reach. You may be able to feel the root of the nose, eyes, but not the mouth, tip of the nose or chin. You may also feel the anterior fontanel, but a large caput (swelling) towards the front of the fetal skull may mask this landmark if the woman has been in labour for some hours.
Recall the appearance of a normal caput over the posterior fontanel shown in Figure 4.4 earlier in this Module.
8.5.3 Complications of brow presentation
The complications of brow presentation are much the same as for other malpresentations:
- Cerebral haemorrhage.
Which are you more likely to encounter — face or brow presentations?
Face presentation, which occurs in 1 in 500 full term labours. Brow presentation is more rare, at 1 in 1,000 full term labours.
8.6 Shoulder presentation
Shoulder presentation is rare at full term, but may occur when the fetus lies transversely across the uterus (Figure 8.7), if it stopped part-way through spontaneous inversion from breech to vertex, or it may lie transversely from early pregnancy. If the baby lies facing upwards, its back may be the presenting part; if facing downwards its hand may emerge through the cervix. A baby in the transverse position cannot be born through the vagina and the labour will be obstructed. Refer babies in shoulder presentation urgently.
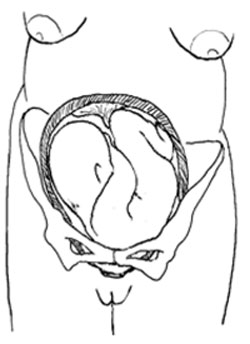
8.6.1 Causes of shoulder presentation
Causes of shoulder presentation could be maternal or fetal factors.
Maternal factors include:
- Lax abdominal and uterine muscles: most often after several previous pregnancies
- Uterine abnormality
- Contracted (abnormally narrow) pelvis.
Fetal factors include:
- Preterm labour
- Placenta previa.
What do ‘placenta previa’ and ‘polyhydramnios’ indicate?
Placenta previa is when the placenta is partly or completely covering the cervical opening. Polyhydramnios is an excess of amniotic fluid. They are both potential causes of malpresentation.
8.6.2 Diagnosis of shoulder presentation
On abdominal palpation, the uterus appears broader and the height of the fundus is less than expected for the period of gestation, because the fundus is not occupied by either the baby’s head or buttocks. You can usually feel the head on one side of the mother’s abdomen. On vaginal examination, in early labour, the presenting part may not be felt, but when the labour is well progressed, you may feel the baby’s ribs. When the shoulder enters the pelvic brim, the baby’s arm may prolapse and become visible outside the vagina.
8.6.3 Complications of shoulder presentation
Complications include:
- Trauma to a prolapsed arm
- Fetal hypoxia and death.
Remember that a shoulder presentation means the baby cannot be born through the vagina; if you detect it in a woman who is already in labour, refer her urgently to a higher health facility.
8.7 Multiple pregnancy
In this section, we turn to the subject of multiple pregnancy , when there is more than one fetus in the uterus. More than 95% of multiple pregnancies are twins (two fetuses), but there can also be triplets (three fetuses), quadruplets (four fetuses), quintuplets (five fetuses), and other higher order multiples with a declining chance of occurrence. The spontaneous occurrence of twins varies by country : it is lowest in East Asia n countries like Japan and China (1 out of 1000 pregnancies are fraternal or non-identical twins), and highest in black Africans , particularly in Nigeria , where 1 in 20 pr egnancies are fraternal twins. In general, compared to single babies, multiple pregnancies are highly associated with early pregnancy loss and high perinatal mortality, mainly due to prematurity.
8.7.1 Types of twin pregnancy
Twins may be identical (monozygotic) or non-identical and fraternal (dizigotic). Monozygotic twins develop from a single fertilised ovum (the zygote), so they are always the same sex and they share the same placenta . By contrast, dizygotic twins develop from two different zygotes, so they can have the same or different sex, and they have separate placenta s . Figure 8.8 shows the types of twin pregnancy and the processes by which they are formed.

8.7.2 Diagnosis of twin pregnancy
On abdominal examination you may notice that:
- The size of the uterus is larger than the expected for the period for gestation.
- The uterus looks round and broad, and fetal movement may be seen over a large area. (The shape of the uterus at term in a singleton pregnancy in the vertex presentation appears heart-shaped rounder at the top and narrower at the bottom.)
- Two heads can be felt.
- Two fetal heart beats may be heard if two people listen at the same time, and they can detect at least 10 beats different (Figure 8.6).
- Ultrasound examination can make an absolute diagnosis of twin pregnancy.

8.7.3 Consequences of twin pregnancy
Women who are pregnant with twins are more prone to suffer with the minor disorders of pregnancy, like morning sickness, nausea and heartburn. Twin pregnancy is one cause of hyperemesis gravidarum (persistent, severe nausea and vomiting). Mothers of twins are also more at risk of developing iron and folate-deficiency anaemia during pregnancy.
Can you suggest why anaemia is a greater risk in multiple pregnancies?
The mother has to supply the nutrients to feed two (or more) babies; if she is not getting enough iron and folate in her diet, or through supplements, she will become anaemic.
Other complications include the following:
- Pregnancy-related hypertensive disorders like pre-eclampsia and eclampsia are more common in twin pregnancies.
- Pressure symptoms may occur in late pregnancy due to the increased weight and size of the uterus.
- Labour often occurs spontaneously before term, with p remature delivery or premature rupture of membranes (PROM) .
- Respiratory deficit ( shortness of breath, because of fast growing uterus) is another common problem.
Twin babies may be small in comparison to their gestational age and more prone to the complications associated with low birth weight (increased vulnerability to infection, losing heat, difficulty breastfeeding).
You will learn about low birth weight babies in detail in the Postnatal Care Module.
- Malpresentation is more common in twin pregnancies, and they may also be ‘locked’ at the neck with one twin in the vertex presentation and the other in breech. The risks associated with malpresentations already described also apply: prolapsed cord, poor uterine contraction, prolonged or obstructed labour, postpartum haemorrhage, and fetal hypoxia and death.
- Conjoined twins (fused twins, joined at the head, chest, or abdomen, or through the back) may also rarely occur.
8.8 Management of women with malpresentation or multiple pregnancy
As you have seen in this study session, any presentation other than vertex has its own dangers for the mother and baby. For this reason, all women who develop abnormal presentation or multiple pregnancy should ideally have skilled care by senior health professionals in a health facility where there is a comprehensive emergency obstetric service. Early detection and referral of a woman in any of these situations can save her life and that of her baby.
What can you do to reduce the risks arising from malpresentation or multiple pregnancy in women in your care?
During focused antenatal care of the pregnant women in your community, at every visit after 36 weeks of gestation you should check for the presence of abnormal fetal presentation. If you detect abnormal presentation or multiple pregnancy, you should refer the woman before the onset of labour.
Summary of Study Session 8
In Study Session 8, you learned that:
- During early pregnancy, babies are naturally in the breech position, but in 95% of cases they spontaneously reverse into the vertex presentation before labour begins.
- Malpresentation or malposition of the fetus at full term increases the risk of obstructed labour and other birth complications.
- Common causes of malpresentations/malpositions include: excess amniotic fluid, abnormal shape and size of the pelvis; uterine tumour; placenta praevia; slackness of uterine muscles (after many previous pregnancies); or multiple pregnancy.
- Common complications include: premature rupture of membranes, premature labour, prolonged/obstructed labour; ruptured uterus; postpartum haemorrhage; fetal and maternal distress which may lead to death.
- Vertex malposition is when the fetal head is in the occipito-posterior position — i.e. the back of the fetal skull is towards the mother’s back instead of pointing towards the front of the mother’s pelvis. 90% of vertex malpositions rotate and deliver normally.
- Breech presentation (complete, frank or footling) is when the baby’s buttocks present during labour. It occurs in 3–4% of labours after 34 weeks of pregnancy and may lead to obstructed labour, cord prolapse, hypoxia, premature separation of the placenta, birth injury to the baby or to the birth canal.
- Face presentation is when the fetal head is bent so far backwards that the face presents during labour. It occurs in about 1 in 500 full term labours. ‘Chin posterior’ face presentations usually rotate spontaneously to the ‘chin anterior’ position and deliver normally. If rotation does not occur, a caesarean delivery is likely to be necessary.
- Brow presentation is when the baby’s forehead is the presenting part. It occurs in about 1 in 1000 full term labours and is difficult to detect before the onset of labour. Caesarean delivery is likely to be necessary.
- Shoulder presentation occurs when the fetal lie during labour is transverse. Once labour is well progressed, vaginal examination may feel the baby’s ribs, and an arm may sometimes prolapse. Caesarean delivery is always required unless a doctor or midwife can turn the baby head-down.
- Multiple pregnancies are always at high risk of malpresentation. Mothers need greater antenatal care, and twins are more prone to complications associated with low birth weight and prematurity.
- Any presentation other than vertex after 34 weeks of gestation is considered as high risk to the mother and to her baby. Do not attempt to turn a malpresenting or malpositioned baby! Refer the mother for emergency obstetric care.
Self-Assessment Questions (SAQs) for Study Session 8
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 8.1 (tests Learning Outcomes 8.1, 8.2 and 8.4)
Which of the following definitions are true and which are false? Write down the correct definition for any which you think are false.
A Fundus — the ‘rounded top’ and widest cavity of the uterus.
B Complete breech — where the legs are bent at both hips and knee joints and are folded underneath the baby.
C Frank breech — where the breech is so difficult to treat that you have to be very frank and open with the mother about the difficulties she will face in the birth.
D Footling breech — when one or both legs are extended so that the baby presents ‘foot first’.
E Hypoxia — the baby gets too much oxygen.
F Multiple pregnancy — when a mother has had many babies previously.
G Monozygotic twins — develop from a single fertilised ovum (the zygote). They can be different sexes but they share the same placenta.
H Dizygotic twins — develop from two zygotes. They have separate placentas, and can be of the same sex or different sexes.
A is true. The fundus is the ‘rounded top’ and widest cavity of the uterus.
B is true. Complete breech is where the legs are bent at both hips and knee joints and are folded underneath the baby.
C is false . A frank breech is the most common type of breech presentation and is when the baby’s legs point straight upwards (see Figure 8.4).
D is true. A footling breech is when one or both legs are extended so that the baby presents ‘foot first’.
E is false . Hypoxia is when the baby is deprived of oxygen and risks permanent brain damage or death.
F is false. Multiple pregnancy is when there is more than one fetus in the uterus.
G is false. Monozygotic twins develop from a single fertilised ovum (the zygote), and they are always the same sex , as well as sharing the same placenta.
H is true. Dizygotic twins develop from two zygotes, have separate placentas, and can be of the same or different sexes.
SAQ 8.2 (tests Learning Outcomes 8.1 and 8.2)
What are the main differences between normal and abnormal fetal presentations? Use the correct medical terms in bold in your explanation.
In a normal presentation, the vertex (the highest part of the fetal head) arrives first at the mother’s pelvic brim, with the occiput (the back of the baby’s skull) pointing towards the front of the mother’s pelvis (the pubic symphysis ).
Abnormal presentations are when there is either a vertex malposition (the occiput of the fetal skull points towards the mother’s back instead towards of the pubic symphysis), or a malpresentation (when anything other than the vertex is presenting): e.g. breech presentation (buttocks first); face presentation (face first); brow presentation (forehead first); and shoulder presentation (transverse fetal).
SAQ 8.3 (tests Learning Outcomes 8.3 and 8.5)
- a. List the common complications of malpresentations or malposition of the fetus at full term.
- b. What action should you take if you identify that the fetus is presenting abnormally and labour has not yet begun?
- c. What should you not attempt to do?
- a. The common complications of malpresentation or malposition of the fetus at full term include: premature rupture of membranes, premature labour, prolonged/obstructed labour; ruptured uterus; postpartum haemorrhage; fetal and maternal distress which may lead to death.
- b. You should refer the mother to a higher health facility – she may need emergency obstetric care.
- c. You should not attempt to turn the baby by hand. This should only be attempted by a specially trained doctor or midwife and should only be done at a health facility.
SAQ 8.4 (tests Learning Outcomes 8.4 and 8.5)
A pregnant woman moves into your village who is already at 37 weeks gestation. You haven’t seen her before. She tells you that she gave birth to twins three years ago and wants to know if she is having twins again this time.
- a. How would you check this?
- b. If you diagnose twins, what would you do to reduce the risks during labour and delivery?
- Is the uterus larger than expected for the period of gestation?
- What is its shape – is it round (indicative of twins) or heart-shaped (as in a singleton pregnancy)?
- Can you feel more than one head?
- Can you hear two fetal heartbeats (two people listening at the same time) with at least 10 beats difference?
- If there is access to a higher health facility, and you are still not sure, try and get the woman to it for an ultrasound scan.
- Be extra careful to check that the mother is not anaemic.
- Encourage her to rest and put her feet up to reduce the risk of increased blood pressure or swelling in her legs and feet.
- Be alert to the increased risk of pre-eclampsia.
- Expect her to go into labour before term, and be ready to get her to the health facility before she goes into labour, going with her if at all possible.
- Get in early touch with that health facility to warn them to expect a referral from you.
- Make sure that transport is ready to take her to a health facility when needed.
Except for third party materials and/or otherwise stated (see terms and conditions ) the content in OpenLearn is released for use under the terms of the Creative Commons Attribution-NonCommercial-Sharealike 2.0 licence . In short this allows you to use the content throughout the world without payment for non-commercial purposes in accordance with the Creative Commons non commercial sharealike licence. Please read this licence in full along with OpenLearn terms and conditions before making use of the content.
When using the content you must attribute us (The Open University) (the OU) and any identified author in accordance with the terms of the Creative Commons Licence.
The Acknowledgements section is used to list, amongst other things, third party (Proprietary), licensed content which is not subject to Creative Commons licensing. Proprietary content must be used (retained) intact and in context to the content at all times. The Acknowledgements section is also used to bring to your attention any other Special Restrictions which may apply to the content. For example there may be times when the Creative Commons Non-Commercial Sharealike licence does not apply to any of the content even if owned by us (the OU). In these stances, unless stated otherwise, the content may be used for personal and non-commercial use. We have also identified as Proprietary other material included in the content which is not subject to Creative Commons Licence. These are: OU logos, trading names and may extend to certain photographic and video images and sound recordings and any other material as may be brought to your attention.
Unauthorised use of any of the content may constitute a breach of the terms and conditions and/or intellectual property laws.
We reserve the right to alter, amend or bring to an end any terms and conditions provided here without notice.
All rights falling outside the terms of the Creative Commons licence are retained or controlled by The Open University.
Head of Intellectual Property, The Open University
- Open access
- Published: 20 March 2024
A new classification allowing assessment of instrumental vaginal-birth practices
- Marine Schaeffer 1 ,
- Marie-Caroline Faisant 1 ,
- Alexandre Buisson 1 ,
- Manon Vanneaux 2 ,
- Pascale Hoffmann 1 &
- Didier Riethmuller 1
BMC Pregnancy and Childbirth volume 24 , Article number: 210 ( 2024 ) Cite this article
69 Accesses
Metrics details
Instrumental vaginal birth, a very common intervention in obstetrics, concerns nearly one in eight women in France. Instrumentally assisted vaginal childbirth can be for maternal and/or fetal indications. Although it reduces recourse to caesarean section, it is subject to risks. Practices concerning instrumental birth are disparate, varying among different practitioners, maternity units and countries, and it is essential to be able to evaluate them. Our objective was to create a classification tool of women requiring instrumental birth to facilitate the analysis of practices within our maternity unit as well as to enable temporal and geographical comparisons.
Materials and methods
We propose a simple and robust classification based on the same principles as Robson's classification. It is made up of seven totally inclusive and mutually exclusive groups. Our classification was refined and validated using the Delphi method by a panel of 14 experts from throughout France, and tested in our maternity unit using data from throughout 2021.
The seven clinically relevant groups are based on five obstetric criteria (multiplicity, presentation, gestational age, previous type of birth, induction of labor). To classify each woman in a group, five successive questions are posed in a predefined order. The classification has been validated by the experts with highly satisfactory overall agreement.
In order to improve the quality of care, we propose a tool to standardize the evaluation of instrumental vaginal birth practice (called the “Isère classification”, after the county where we work in south-eastern France). It will also facilitate the comparison the practices among different maternity units in a network, a country or even among different countries.
Peer Review reports
Instruments such as the ventouse, forceps, or spatulas are often used to assist vaginal birth. The medical indications for instrumental vaginal birth (IVB) can be maternal, such as no progress of cervical dilatation and fetal descent or ineffective maternal efforts, and/or fetal such as an abnormal fetal heart rate. Even if IVB often seems to be preferable to caesarean birth for indications in the second stage of labor [ 1 ], in order to preserve the subsequent obstetric prognosis of parturients [ 2 , 3 ]. However, like caesarean section, it is not devoid of risks and complications [ 4 , 5 ], in order to provide high quality care it is necessary to be able to analyze this common obstetric practice since it concerns nearly one parturient in eight in France (12%) and like caesarean birth is considered as an operative birth.
To date and to our knowledge, however, there are few recognized tools for the evaluation of practices concerning IVB. Our objective was to create a tool for evaluating IVB practices based on the same principles as Robson's classification of caesarean birth delivery [ 6 ]. This new tool would classify parturients according to their obstetric profile in terms of only five parameters, facilitating analysis of IVB practices in each maternity unit, as well as geographical and temporal comparisons.
Our classification, which we have called “the Isère classification” (after the county where we work in south-eastern France) is based on predefined obstetric criteria. Our initial criteria were that must be simple to use, robust and require only data that are readily available to the obstetrician in the birthing room. It must be reproducible with a very low rate of inter-observer variation. The number of groups must be sufficient to differentiate the situations encountered in routine practice but sufficiently limited so as not to lose sight of the whole. The order in which the questions are presented and the relationships between the groups are also important allowing an intuitive use and a quick classification of each case. Groups must be fully inclusive, meaning that each woman can be included in one of the groups; and mutually exclusive, which means that each woman can belong to only one group. The different groups in the classification should reflect, as far as possible, the situations most relevant to routine clinical practice.
To meet these requirements, we proposed a series of questions to be posed to the attending obstetrician or midwife, in a predefined order. Only simple yes/no answers were needed before moving to the next question. The groups and questions we initially proposed concerned the multiplicity of the pregnancy, the presentation of the fetus(es), gestational age (GA), type of any previous childbirth (vaginal or cesarian), whether labor was induced or not, and scarred uterus. We aimed for the minimum number of questions that would allow us to form a reasonable number of well-defined groups in the new classification.
We refined and validated our classification using the Delphi method [ 7 ]. This is an interactive technique that makes it possible to highlight differences and convergences in opinions and obtain a consensus from a group of experts about the proposed classification. A Delphi study is conducted with a group of people considered to have expertise (both professional and based on experience) in the field, in our case obstetrics. For our classification, an email invitation was sent to 14 national experts. They were all active practitioners in the field and represented the whole of France. Those who responded to the invitation and agreed to participate in all phases of the Delphi process provided written and informed consent to participate and were included in the expert panel. Panel members were blinded to the identities of the other experts. The experts filled out all questionnaires anonymously and then received feedback including answers from all the other experts in the panel. At each round, experts could add comments or suggestions. This process was repeated until the range of expert responses narrowed enough to build a consensus or near-consensus on some or all points.
In the first round, we asked the experts to fill a questionnaire on clinical relevance of each proposed group of our draft classification using a Likert scale with five response options ("not at all relevant", "not very relevant", “no opinion”, “fairly relevant” and “very relevant”). They were also asked to explain their choice when their answer was “not at all relevant” or “not very relevant”. Then, modifications were made to the proposed groups according to the answers. In the second round the revised classification and questionnaire was submitted to the panel along with explanations. Each group of our classification was validated if more than half of the experts considered it to be "fairly relevant" or "very relevant".
Lastly, we conducted a retrospective study to describe the IVB practices in our French level III maternity unit in 2021 (over the whole year), using the new classification.
All 14 experts we had contacted agreed to participate in the expert panel. Consensus was quickly obtained for each of the seven groups after only two rounds. After the 1st round, on the recommendation of the experts we modified the title of groups 1 to 3 by removing the mention “scarred uterus included” because the characteristics (multiplicity, presentation and gestational age) are sufficient to classify them. We also changed the numbering of the groups to make our classification easier to use. These modifications were validated during the second round, accompanied by explanations.
The overall consensus regarding the proposed classification was good. Of the seven proposed groups two were deemed relevant by all 14 experts, two by 13 experts, and three by 12 experts. Thus, all groups could be validated as more than half of the experts judged each one to be "fairly relevant" or "very relevant". No group was deemed to be “not at all relevant”.
Our final classification is based on five obstetric criteria present in all medical records: 1) number of fetuses (singleton or multiple pregnancy), 2) fetal presentation (cephalic or breech), 3) gestational age in weeks of amenorrhea (< or ≥ at 37 GA), 4) any previous history or not of vaginal birth, and 5) the mode of entry into labor. It is made up of seven groups deemed clinically relevant (Fig. 1 ).
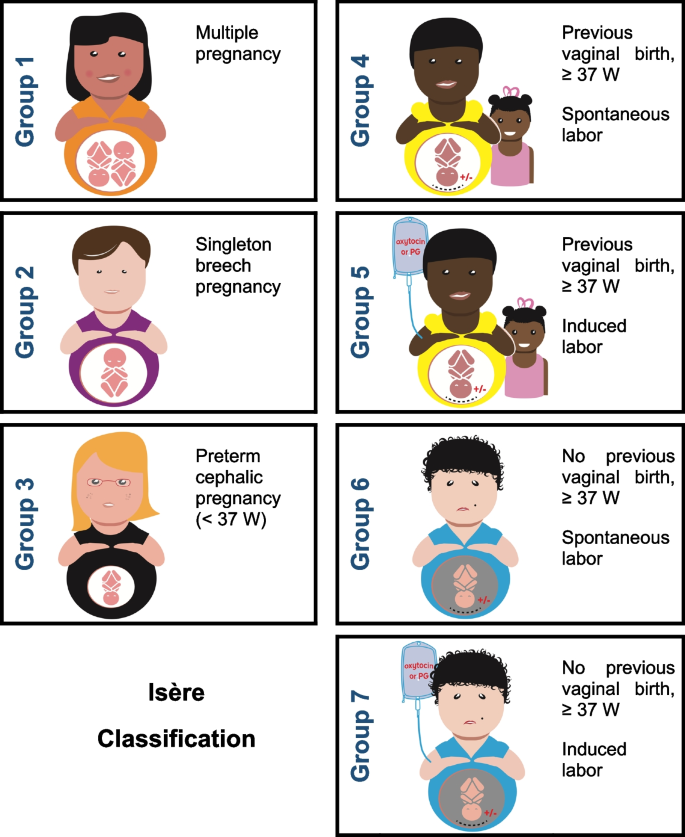
The 7 groups of the “Isère classification” for instrumental vaginal births. Groups 4 and 5 are women with full-term pregnancies who have already given birth vaginally (scarred uterus included); groups 6 and 7 are women who have never given birth vaginally (scarred uterus included). Among groups 4 to 7, groups 4 and 6 are women with spontaneous labor and groups 5 and 7 had undergone induction of labor
Missing data has led some users of the Robson classification to create a category ‘‘99’’ for these women. We believe this suggestion is very relevant and is why we propose the addition of this “99” group to the Isère classification to make it completely ‘‘totally inclusive’’. The size of the group ‘‘99’’ can be useful to audit the quality of the data. This additional group includes, apart from unclassifiable women, also women with fetal deaths in-utero and medical terminations of pregnancy (therapeutic abortion).
Group 1: Multiple pregnancy
Group 2: Singleton in breech presentation
Group 3: Singleton in cephalic presentation at GA < 37 weeks
Group 4: Singleton in cephalic presentation at GA ≥ 37 weeks, with a history of at least one vaginal birth, spontaneous labor (scarred uterus included)
Group 5: Singleton in cephalic presentation at GA ≥ 37 weeks, with a history of at least one vaginal birth, induced labor (scarred uterus included)
Group 6: Singleton in cephalic presentation at GA ≥ 37 weeks, without previous vaginal birth, spontaneous labor (scarred uterus included)
Group 7: Singleton in cephalic presentation at GA ≥ 37 weeks, without previous vaginal birth, induced labor (scarred uterus included)
Group 99: In-utero fetal death , medical termination of pregnancy (therapeutic abortion), unclassifiable women (missing data)
In order to classify each woman into the appropriate group, only five consecutive questions are needed (Fig. 2 ). The numbering of the groups was defined according to the order of the questions. For each question, if the answer is positive, the woman is placed in the corresponding group. Conversely, if the answer is negative, the process is continued until a positive answer is given. For groups 4 to 7, the final question concerns the mode of entry into labor, spontaneous or induced.
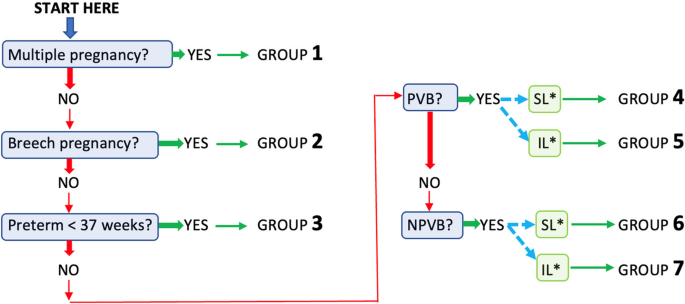
Sequence of the 5 questions allowing each woman to be classified into one of the classification groups (PVB = prior vaginal birth; NPVB = no prior vaginal birth; SL = spontaneous labor; IL = induced labor)
While a multiple pregnancy (group 1) represents only a small proportion of women giving birth, medicalized childbirth, whether by cesarean or by vaginal birth, is very frequent in France for this group.
Breech presentation of a singleton (group 2) represents a small part of IVBs, but because of its particularity it cannot be included in another group (forceps or spatulas are usually used for the after-coming head).
The specificities of singleton birth in cephalic presentation at < 37 weeks GA (group 3) justifies the creation of a group of its own.
The birth of a singleton in cephalic presentation at GA ≥ 37 weeks (groups 4 to 7) account for the majority of IVBs. We considered it useful to classify these women according to whether or not they had previously given birth by vaginal delivery and not according to their parity, and then to subdivide them according to their mode of entry into labor.
The different groups in our classification reflect the most frequent situations seen in clinical practice with regard to IVBs and account for a significant proportion of IVBs in most maternity units. However, this first classification does not address the problems particular to each group. For this, intra-group analyzes need to be made according to obstetrical criteria such as a history of scarred uterus, the sequential use of instruments, the indication for IVB, the fetal position (rearward or forward), whether analgesia is used during labor, fetal macrosomia, etc.
Our retrospective study of IVB practices over a one-year period (year 2021) in our level III French maternity unit (competent for the management of high-risk pregnancies) found a IVB rate of 17.5% ( n = 441) for a caesarean section rate of 19.7%. Groups 6 and 7 were predominant in this year of IVB practice, accounting for 70% of IVBs (54% and 16% respectively), and groups 4 and 5 included almost 19% of parturients. No patients were included in the "99" group.
Instrumental vaginal birth is frequent in France and in many other European countries [ 8 , 9 , 10 ]. It is often preferred to cesarean delivery for indications in the 2nd stage of labor, but it is not devoid of risks and complications depending on the obstetric prognosis of parturients. A large-scale European study [ 8 ] showed that IVB rates varied greatly from country to country and were not always correlated with caesarean section rates within the same country. In metropolitan France, the IVB rate has been stable since 1998 at around 12% [ 9 ]. A survey of practices in Europe in 2019 [ 10 ] showed large disparities with the lowest IVB rate at 1.4% in Croatia and the highest rate in Spain at 14.4%. This ratio of 1 to 10 is incomprehensible in itself and a more detailed evaluation of practices with dedicated tools seems necessary to improve maternity care of mothers and newborns. To our knowledge, there was no recognized and widely used evaluation tool for this practice described in the literature. Some authors have analyzed the rate of IVBs compared with caesarean section rates, attempting to explain this rate but without using a tool to classify IVBs [ 11 , 12 ]. They suggested that calculating the ratio in different institutions could help with the analysis of obstetric practices and might lead to a reduction in unnecessary major surgery.
In France, the high rate of operative vaginal birth, involving nearly one in eight parturients justifies the creation of a classification system to monitor and compare IVB practices within and among institutions and among different populations, to analyze trends over time, as well as to compare maternal and perinatal outcomes. While the overall IVB rate in France is acceptable compared to international standards, it is imperative that health systems and facilities are aware of some specific subgroups that could benefit from improvements in the quality and appropriateness of care.
Another interest of our classification is to facilitate evaluations of practices over short periods of time. It could be used in the analysis of the impact of measures implemented to improve the quality of care or of new recommendations for clinical practice. O'Leary et al. [ 13 ] suggested that the Robson classification of caesarean section should be used to classify parturients who received instrumental assistance. However, some of Robson’s groups are not applicable to vaginal delivery (such as groups 2b and 4b that are patients whose caesarean section is performed before labor begins, and group 9 (transverse fetal presentation) where vaginal delivery is not possible. Nevertheless, we were influenced by Robson's classification [ 14 ].
We propose a classification for women requiring IVB made up of seven mutually exclusive and totally inclusive groups based on five readily available and reliably collected variables. These groups are easy to use, clinically relevant and easy to implement at local, regional, national or even international level. All groups can be further subdivided in order to determine common denominators during the analysis of the results and thus better target the populations at risk of IVB.
Using the same approach as for the recently published Grenoble classification of induced labor [ 15 ], our IVB classification was submitted to 14 national experts using a Delphi method. This qualitative method reflects the subjective and consensual opinions of a group of experts [ 16 ]. It makes it possible to generate a reasoned consensus opinion that can be used to legitimize the choices made when creating the classification. In the first-round we immediately proposed a classification with the groups defined in advance. An alternative approach would have been to question the experts about their proposals for the initial obstetrical criteria io be used; gradually creating the different groups.
While the randomized controlled study by Grobman et al. (2018) [ 17 ] found no statistically significant differences in resort to IVB whether or not labor was induced (7.3% if induced vs. 8.5% if spontaneous, p = 0.07), it should be remembered that induction practices in certain European countries are very different from those in France (with a rate of at least 15% in nulliparous women). In addition, this study only concerned low-risk nulliparous women, whereas multiparous women represent a significant proportion of births in France (58.6% according to the 2021 National Perinatal Survey [ 8 ]).
After searching the literature, we found no convincing tool to assess the impact of induction of labor on the use of IVB. This is why it seemed judicious to decern between the types of labor in parturients with or without previous vaginal delivery. In the study by O'Leary et al. [ 13 ], a higher rate of IVB in their population of nulliparous women with induced labor was observed as compared to spontaneous labor. This increased risk could be related to the reason for induction of labor. However, it seemed important to be able to objectify it in order to best advise patients, particularly as the onset of labor plays a key part in the management of childbirth.
We chose not to reason in terms of the overall parity of the woman but according to a precedent of at least one vaginal birth. This made it possible to group together nulliparous women with multiparous women who had never given birth vaginally (history of 1 or 2 caesarean sections in their previous births); and to group-together women who already had a history of vaginal birth, whether or not they had a scarred uterus. The latter represented 19% of the women included in our retrospective study of practices in 2021.
In order to limit interpretation bias the experts recommended no to take into account the medical indication for IVB, although this could be included in more detailed studies.
The failure of an attempt at instrumental vaginal birth was not included in our classification since it generally results in caesarean section. Nevertheless, every establishment should be aware of the failure rate of the instrumental vaginal route. An evaluation of IVB practices using our classification could lead to actions aimed at improving practices, for some if not all groups. The widespread use of this classification might make it easier to analyze IVB practices at local, regional, national or even international level. It should assist in improving our ability to compare relatively obstetrically homogeneous populations of women and thus contribute to improving the quality of maternity care.
The retrospective study of practices in our maternity unit enabled us to highlight groups with a relatively high proportion of IVBs. These were mainly women with a singleton pregnancy in cephalic presentation at ≥ 37 weeks GA, without previous vaginal birth, with spontaneous labor (scarred uterus included) (group 6).
In the future, we plan to continue more detailed analysis of our own practices in order to provide high quality maternity care and to monitor its evolution over time. The comparison of our practices with those of other maternity units using the Isère classification would be of great interest.
Each maternity unit, network, region or country may have different expectations regarding IVB practices depending on the extent of use. For maternities whose IVB rate is higher than the national rate, the objective could be to reduce it by increasing the rate of spontaneous vaginal births. One of the avenues for improvement to promote spontaneous birth would be to consider a longer duration of the 2nd stage of labor, and to allow an extension of the duration of expulsive efforts in certain groups. Appropriate use of a classification for IVBs could help improve practices of instrumental vaginal birth and coupled with the Robson classification, it would clearly be useful in describing the practices of all operative births in each maternity unit and beyond.
We have created a tool for classifying women in childbirth according to their obstetric circumstances to facilitate the evaluation of instrumental vaginal birth practices. This will make it easier not only to analyze practices within each maternity unit but also to be able to make geographical and temporal comparisons. The tool is a simple, robust classification, comprising seven groups based on five obstetric criteria easily available in each woman's medical file.
Availability of data and materials
The de-identified datasets used and analyzed during the study are available from the corresponding author on reasonable request.
Abbreviations
Gestational age
Instrumental vaginal birth
Induced labor
Prior vaginal birth
No prior vaginal birth
Spontaneous labor
Hendler I, Kirshenbaum M, Barg M, et al. Choosing between bad, worse and worst: what is the preferred mode of delivery for failure of the second stage of labor? J Matern Fetal Neonatal Med. 2017;30(15):1861–4.
Article CAS PubMed Google Scholar
Silver RM. Implications of the first cesarean: perinatal and future reproductive health and subsequent cesareans, placentation issues, uterine rupture risk, morbidity, and mortality. Semin Perinatol. 2012;36(5):315–23.
Article PubMed Google Scholar
Paré E, Quiñones JN, Macones GA. Vaginal birth after caesarean section versus elective repeat caesarean section: assessment of maternal downstream health outcomes. BJOG. 2006;113:75–85.
Lowder JL, Burrows LJ, Krohn MA, Weber AM. Risk factors for primary and subsequent anal sphincter lacerations: a comparison of cohorts by parity and prior mode of delivery. Am J Obstet Gynecol. 2007;196(4):344.e1-344.e5.
Demissie K, Rhoads GG, Smulian JC, et al. Operative vaginal delivery and neonatal and infant adverse outcomes: population based retrospective analysis. BMJ. 2004;329(7456):24–9.
Article PubMed PubMed Central Google Scholar
Robson MS. Can we reduce the caesarean section rate ? Best Pract Res Clin Obstet Gynaecol. 2001;15(1):179–94.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15.
MacFarlane A, Blondel B, Mohangoo A, et al. Wide differences in mode of delivery within Europe: risk-stratified analyses of aggregated routine data from the Euro-Peristat study. BJOG. 2016;123(4):559–68.
Enquête nationale périnatale Rapport. 2021. On line: https://enp.inserm.fr/wp-content/uploads/2022/10/rapport-2022-v5.pdf .
Europeristat. 2022. On line: https://www.europeristat.com/images/Euro-Peristat_Fact_sheets_2022_for_upload.pdf .
Bakke E, Hammer Øseth E, Fofanah T, Sesay I, et al. Vacuum births and barriers to its use: an observational study in governmental hospitals in Sierra Leone. BMJ Open. 2022;12(11):e060773.
van Roosmalenl J, Mbaruku G, Cotiro M, Hoestermann C, Verkuyl DAA, Meguid T. Ratio of instrumental vaginal delivery and caesarean section: a new indicator of the quality of obstetric care. Int J Gynecol Obstet. 2000;70:A21.
Google Scholar
O’Leary BD, Kane DT, Kruseman Aretz N, Geary MP, Malone FD, Hehir MP. Use of the Robson Ten Group classification system to categorise operative vaginal delivery. Aust N Z J Obstet Gynaecol. 2020;60:858–64.
Robson MS. Classification of caesarean sections. Fetal Matern Med Rev. 2001;12(1):23–39.
Article Google Scholar
Vanneaux M, Forey PL, Equy V, Hoffmann P, Riethmuller D. Induction of labour: creation of a classification of Grenoble allowing an assessment of the evaluation of practices. BMC Pregnancy Childbirth. 2022;22:143.
McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38(3):655–62.
PubMed PubMed Central Google Scholar
Grobman WA, Rice MM, Reddy UM, et al. Labor Induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513–23.
Download references
Acknowledgements
We would like to thank the 14 experts for participating in in the Delphi method. We also thank Mr. Jouan for having created the illustrations of the classification. Finally, we thank Alison Foote PhD (an independent medical writer based in Grenoble, France) for critically reading, translating and structuring the manuscript.
There was no specific funding for this article.
Author information
Authors and affiliations.
Department of Gynecology-Obstetrics and Reproductive Medicine, Grenoble Alpes University Hospital, Grenoble, 38043, France
Marine Schaeffer, Marie-Caroline Faisant, Alexandre Buisson, Pascale Hoffmann & Didier Riethmuller
Gynecology-Obstetrics Department, Annecy Genevois Hospital, Epagny Metz-Tessy, 74370, France
Manon Vanneaux
You can also search for this author in PubMed Google Scholar
Contributions
M.S and D.R created the new classification for instrumental-vaginal birth practices, designed the classification illustration (Fig. 1) and wrote the manuscript with M.V. They carried out the Delphi method by communicating with the 14 experts. M-C.F, A.B and P.H analyzed the retrospective study of practices in our maternity unit, reviewed, and corrected the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Didier Riethmuller .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations in France. The approval for the study was waived by the Ethics Committee (CECIC—Comité d’Ethique des Centres d’Investigation Clinique) of the Rhône‐Alpes‐Auvergne région, according to French regulations. All of the experts who participated in the Delphi method were clearly informed of its purpose, risks and benefits. They knew how the Delphi method worked and the implications of their participation. Each one gave their informed written consent to participate.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schaeffer, M., Faisant, MC., Buisson, A. et al. A new classification allowing assessment of instrumental vaginal-birth practices. BMC Pregnancy Childbirth 24 , 210 (2024). https://doi.org/10.1186/s12884-024-06410-5
Download citation
Received : 27 May 2023
Accepted : 11 March 2024
Published : 20 March 2024
DOI : https://doi.org/10.1186/s12884-024-06410-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Instrumental delivery
- Classification
- Practice assessment
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
Possible fetal positions can include: Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section.
During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex presentation before labor, usually at 37 or 38 weeks.
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one ...
Presentation of twins in Der Rosengarten ("The Rose Garden"), a standard medical text for midwives published in 1513. In obstetrics, the presentation of a fetus about to be born specifies which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation.
Is vertex presentation the same as cephalic position? Yes, they essentially mean the same thing. Cephalic presentation means a fetus is in a head-down position. Vertex refers to the fetus's neck being tucked in. There are other types of cephalic presentations like brow and face. These mainly describe how the fetus's neck is flexed.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant patient's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the position of a fetus is facing rearward (toward the woman's back) with the face and body angled to one side and the neck flexed, and presentation is head first. An abnormal position is facing forward, and abnormal presentations include face, brow, breech ...
Introduction. Cephalic presentation is the most physiologic and frequent fetal presentation and is associated with the highest rate of successful vaginal delivery as well as with the lowest frequency of complications 1.Studies on the frequency of breech presentation by gestational age (GA) were published more than 20 years ago 2, 3, and it has been known that the prevalence of breech ...
Presentation refers to that part of the fetus that is coming through (or attempting to come through) the pelvis first. (1) Types of presentations (see figure 10-1). The vertex or cephalic (head), breech, and shoulder are the three types of presentations.
If your baby is headfirst, the 3 main types of presentation are: anterior - when the back of your baby's head is at the front of your belly. lateral - when the back of your baby's head is facing your side. posterior - when the back of your baby's head is towards your back. Top row: 'right anterior — left anterior'.
Fetal presentation is the body part of the baby that leads the way out of the birth canal. ... 5 Types of Fetal Positions and Presentations. During pregnancy and when preparing for childbirth, there are exercises moms can do when the baby is active to get it in the optimal fetal position, which is known as baby spinning. Starting at the 35th ...
When a fetus faces up, the neck is often straightened rather than bent, and the head requires more space to pass through the birth canal. Delivery by a vacuum extractor or forceps Operative Vaginal Delivery Operative vaginal delivery is delivery using a vacuum extractor or forceps. A vacuum extractor consists of a small cup made of a rubberlike material that is connected to a vacuum.
Compound presentation means that a fetal hand is coming out with the fetal head. This is a problem because: The amount of baby that must come through the birth canal at one time is increased. There is increased risk of mechanical injury to the arm and shoulder, including fractures, nerve injuries and soft tissue injury.
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one ...
There are different types of malpresentation. Breech presentation. This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a 'footling presentation'). Breech presentation is the most common type of malpresentation. Face presentation
8.1 Normal and abnormal presentations 8.1.1 Vertex presentation. In about 95% of deliveries, the part of the fetus which arrives first at the mother's pelvic brim is the highest part of the fetal head, which is called the vertex (Figure 8.1).This presentation is called the vertex presentation.Notice that the baby's chin is tucked down towards its chest, so that the vertex is the leading ...
Only simple yes/no answers were needed before moving to the next question. The groups and questions we initially proposed concerned the multiplicity of the pregnancy, the presentation of the fetus(es), gestational age (GA), type of any previous childbirth (vaginal or cesarian), whether labor was induced or not, and scarred uterus.