Writing a research proposal
The format of a research proposal varies depending on what or who it is required by. They can vary in length, ie. be very concise or quite long and detailed. Also the headings for the different sections can vary. Therefore, this guide deals with the research proposal in its most generic form, which should be easily modifiable to fit the criteria for any research body.
The ultimate aim of any research proposal is to convince people that your research is important, has not been done before, is worthwhile and is feasible. Hence you have to make a strong argument for your research. The language used should be clear and easy to understand, as often non-experts will assess it. Some funders may, and the Research Ethics Committee application form will, want a ‘lay’ summary in addition to your basic proposal document. It is usually only in the background and methodology sections that writers tend to assume that the intended audience has a particular knowledge of their research area.
Additionally, it is crucial that different sections of your research proposal should link or follow on from each other, eg. the research question should link with the methodology. This may sound obvious, but revisions of one section can lead to mis-matches. Check this before submitting your proposal!

Typical stages in a research proposal
1. The purpose of a research proposal is:
- To help to focus on a relevant and current topic.
- To identify a gap or inadequacy in the research literature.
- To make sure that these are your ideas, and to help you to focus and crystallise your ideas.
- To help you to focus on what the actual stages involved in the research process will be, eg. the exact methodology and data analysis that will be adopted.
- To justify a proposed research project to a particular audience, eg. supervisor, departmental or faculty committee, external funding body etc.
2. Some strategies before you start:
- Search through literature for topic related articles and books, ie. search through databases/catalogues/journals etc.
- Look at what is already being done in the area i.e. existing data and research.
- Read critically, ie. look for interesting and suitable gaps – areas for research.
- Talk to your employer for approval – there is no point in starting research that you will not be allowed to complete.
- Talk to your local research and development teams. They will be able to tell you the specific criteria for any research proposal and may highlight some issues that you have overlooked.
- Talk to experts or supervisors in the field – in person, phone, letters, e-mail.
- If it is helpful, use concept maps to link ideas, and or formulate questions that the literature review should address.
3. Identifying your research question:
Any research proposal needs to have a clear research question for it to succeed. Without a clear question research will become confused and lack direction. Subsequent analysis will be difficult because the research question is key to forming your hypothesis or aims, and later analysis.
Do start by writing a question, not a statement. This will help clarify exactly what the issue is that you are trying to find a solution to. Hypotheses, aims etc can then follow from this.
Your research question should:
- Be as clear and concise as you can make it. Don’t use multi-barrelled questions if you can avoid them.
- Be informative – state your population of interest, locality etc.
- Avoid technical jargon – this is the golden rule in most areas of research proposals. Remember that your research question is what will capture the interest of the reader / assessor.
- Relate to the proposal title – often the research question is quoted as the title of the proposal.
- Relate to the aim of the research – again, the research question is often quoted as the research aim.
It should be obvious from your question alone what the project will aim to do, and on who.
4. Project title:
The title should be brief but informative. It is important that it is clear and easy to understand, and describes what your proposed research is. As previously stated, this is often the research question.
5. Abstract or summary:
This is a very important section which bears a disproportionate share of responsibility for success or failure of a proposal, as it may act as the initial ‘hook’.
It needs to be written for a wider audience, so technical vocabulary has to be limited. The abstract also needs to come quickly to the proposed research. Abstracts for grant proposals usually begin with the objective or purpose of the study, move on to methodology (procedures and design), and close with a modest but precise statement of the projects’ significance.
The significance should:
- Be about one paragraph – if it needs any longer it is advisable to rethink your research or break it down into more manageable chunks.
- Explain to the reader why the study is “significant”, in the sense of advancing general knowledge.
- Explain what the benefits to the patient / health community are.
- Encourage funding.
Although you present this first in the document, write it last so that its content accurately reflects the whole proposal.
6. Introduction:
The introduction is also written so that a more general audience can easily obtain a general idea of what the project is about, and the major concepts involved. It will also typically begin with the purpose of the proposed research. The introduction will typically be quite short, leaving the detail to the background and methodology sections.
7. Background:
It is only in the background and methodology sections that writers tend to assume that their intended audience is a specialist in their research area, and so use more technical language.
This section will include the literature review.
The purpose of a literature review is as follows:
- To become familiar with the research area and keep up to date with the current research in your area of interest.
- Identify an appropriate research question.
- Establish a theoretical framework for the research.
- Justify the need for the research.
Through the actual process of writing the literature review you, the researcher, can explore the relevant literature, formulate a problem, defend the value of the research, and compare the findings and ideas with your own. The literature review establishes a context and orientates the reader to your research topic.
The common structure of the literature review is likened to a “funnel effect”, which goes from general to more specific studies etc directly relating your intended project, ending with your research question, problem or objective.
In summary the stages of a literature review are as follows:
- General statement(s) about the field of research – the setting.
- More specific statements about the previous research.
- Statements that indicate the need for more investigation.
- Very specific statement(s) of the research question, problem or objective.
Your Trust librarians will be able to help with appropriate literature searching techniques if required.
8. Methodology:
The method or methodology section describes the steps you will follow in conducting your research. It is a very important section as assessors will scrutinise it to evaluate the feasibility and likelihood of successful completion of your proposed research.
Examine methodology sections of research articles in your research area. Arrange to discuss your research with a statistical and/or methodological specialist (Trust and other local research clinics / groups). Discuss with other researchers in your discipline the methodologies they have adopted. Consult methodology texts and statistical packages.
Overview of research:
Population/sample to be studied, including:
- How you have arrived at the sample size.
- How they will be recruited.
- Location of the research.
- Restrictions/limiting conditions.
- Sampling technique.
- Procedures.
- Analysis tools and methods.
9. Timescale:
10. Budget:
11. Ethical considerations:
- Benefits vs risks of the involvement in the project.
- Receipt of informed consent.
- Protection of participants (including data protection and storage issues).
- Privacy, minimising discomfort etc.
- Community values.
12. Dissemination strategy:
- The targets of your research eg. staff, patients, service users or carers,
- services locally and/or nationally,
- policies that drive the above services.
13. Bibliography and references:
Good luck with your project!
Useful reading: Bowling A (2002), Research Methods in Health: Investigating Health and Health Services 2Rev Ed edition, Open University Press Polgar S and Thomas SA. (4 th Edition 2004) Introduction to Research in the Health Sciences. Churchill Livingstone. MRC Good Research Practice Guidance
- Technical Support
- Find My Rep
You are here
Writing Research Proposals in the Health Sciences A Step-by-step Guide
- Zevia Schneider
- Jeffrey Fuller
- Description
See what’s new to this edition by selecting the Features tab on this page. Should you need additional information or have questions regarding the HEOA information provided for this title, including what is new to this edition, please email [email protected] . Please include your name, contact information, and the name of the title for which you would like more information. For information on the HEOA, please go to http://ed.gov/policy/highered/leg/hea08/index.html .
For assistance with your order: Please email us at [email protected] or connect with your SAGE representative.
SAGE 2455 Teller Road Thousand Oaks, CA 91320 www.sagepub.com
Well written, comprehensive and easy to use - definitely one I will recommend.
excellent book for healthcare students
Goes through the stages of a research proposal guiding students on the expected content for each section
lovely clear text, concepts clearly set out, an excellent introductory book for health science students
A useful resource to help level 3 students to develop their academic writing. This step by step guide provides clear guidance. Students have found this very useful
Preview this book
For instructors, select a purchasing option, related products.

This title is also available on SAGE Knowledge , the ultimate social sciences online library. If your library doesn’t have access, ask your librarian to start a trial .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 06 May 2021
Co-producing knowledge in health and social care research: reflections on the challenges and ways to enable more equal relationships
- Michelle Farr ORCID: orcid.org/0000-0001-8773-846X 1 , 2 ,
- Philippa Davies ORCID: orcid.org/0000-0002-2678-7126 1 , 2 ,
- Heidi Andrews 1 , 2 ,
- Darren Bagnall 1 , 2 ,
- Emer Brangan ORCID: orcid.org/0000-0002-1288-0960 1 , 2 , 3 &
- Rosemary Davies ORCID: orcid.org/0000-0001-9969-1902 1 , 4
Humanities and Social Sciences Communications volume 8 , Article number: 105 ( 2021 ) Cite this article
5893 Accesses
19 Citations
33 Altmetric
Metrics details
- Health humanities
- Medical humanities
Researchers are increasingly encouraged to co-produce research, involving members of the public, service users, policy makers and practitioners in more equal relationships throughout a research project. The sharing of power is often highlighted as a key principle when co-producing research. However, health and social care research, as with many other academic disciplines, is carried out within embedded hierarchies and structural inequalities in universities, public service institutions, and research funding systems—as well as in society more broadly. This poses significant challenges to ambitions for co-production. This article explores the difficulties that are faced when trying to put ideal co-production principles into practice. A reflective account is provided of an interdisciplinary project that aimed to better understand how to reduce power differentials within co-produced research. The project facilitated five workshops, involving researchers from different disciplines, health, social care and community development staff and public contributors, who all had experience in co-production within research. In the workshops, people discussed how they had attempted to enable more equal relationships and shared ideas that supported more effective and equitable co-produced research. Shared interdisciplinary learning helped the project team to iteratively develop a training course, a map of resources and reflective questions to support co-produced research. The gap between co-production principles and practice is challenging. The article examines the constraints that exist when trying to share power, informed by multidisciplinary theories of power. To bring co-production principles into practice, changes are needed within research practices, cultures and structures; in understandings of what knowledge is and how different forms of knowledge are valued. The article outlines challenges and tensions when co-producing research and describes potential ideas and resources that may help to put co-production principles into practice. We highlight that trying to maintain all principles of co-production within the real-world of structural inequalities and uneven distribution of resources is a constant challenge, often remaining for now in the realm of aspiration.
Introduction
Co-production of research—where researchers, practitioners and members of the public collaborate to develop research together—is promoted as a way to strengthen public involvement, and create and implement more relevant and applicable knowledge, that is used in practice (Staniszewska et al., 2018 ; Hickey et al., 2018 ). Academic disciplines and funding bodies define the concept of co-production differently, using divergent methods and theories (Facer and Enright, 2016 ), with subsequent debate about what co-production is and who may be doing it ‘properly’. We use the INVOLVE definition and principles of co-producing research (Box 1 ) (Hickey et al., 2018 ), which includes the often-agreed principle to share power more equally between partners. However, the extent to which this is achievable within structural inequalities and institutional hierarchies is debatable (Flinders et al., 2016 ).
This commentary article reflects on a project that aimed to:
share interdisciplinary learning about co-produced research
understand how to enable more equal relationships with co-production partners, particularly public contributors—defined as members of the public including patients, potential patients, carers and people who use health and social care services (in contrast to people who have a professional role in health and social care services or research) (NIHR CED, 2020 ).
develop training and resources to support co-produced research.
The project was developed by a team of three applied health researchers, a public involvement lead and three public contributors (with in-depth experiences of co-produced research) undertaken within the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) West, an organisation that develops applied health and social care research. Through facilitating five project workshops, we engaged with eleven researchers from five disciplines; six practitioners; and eleven public contributors with involvement and co-produced research experiences. We shared practical lessons across disciplinary boundaries about how to do co-produced research more equitably (Oliver and Boaz, 2019 ). These workshops helped the project team progressively and iteratively develop a training course, a map of resources (Farr et al., 2020 ) and reflective questions (Davies et al., 2020 ), freely available to support co-produced research.
This article explores the extent to which these multidisciplinary lessons can help us transform knowledge production in more equitable ways, outlining our learning from this project. First, we overview some conceptual issues with the use of the word ‘co-production’. We then discuss key matters raised in our interdisciplinary workshops: ‘Who is involved and when in co-produced research?’; ‘Power dynamics within health and social care research’; and ‘Communication and relationships’. We conclude by highlighting that bringing co-production principles into the real research world is fraught with difficult and messy compromises. Researchers (often lower in the academic hierarchy) may be caught up in battling systems and policies to enable co-production to happen, especially where they attempt to address issues of power and control within the research process.
Box 1: INVOLVE a Definitions and principles of co-produced research (Hickey et al., 2018 )
‘ Co-producing a research project is an approach in which researchers, practitioners and the public work together, sharing power and responsibility from the start to the end of the project, including the generation of knowledge ’ (p. 4).
Principles include:
Sharing power where research is owned by everyone and people are working together in more equal relationships
Including all perspectives and skills to ensure that everyone who wants to make a contribution can do so, with diversity, inclusiveness and accessibility being key
Respecting and valuing the knowledge of everyone , with everyone being of equal importance, and benefitting from the collaboration
Reciprocity and mutuality , building and maintaining relationships and sharing learning
Understanding each other with clarity over people’s roles and responsibilities.
a INVOLVE supported active public involvement in NHS, public health and social care research, with a new NIHR Centre for Engagement and Dissemination (CED) launched in April 2020.
The concept of co-production
The NVOLVE co-production principles (Box 1 ) (Hickey et al., 2018 ) build on public policy co-production literature (Boyle and Harris, 2009 ; Staniszewska et al., 2018 ), which explores how service users can take an active role within the provision of public services (Brudney and England, 1983 ; Ostrom, 1996 ). A key premise is that service users have a fundamental role in producing services and outcomes that are important to them (Brandsen and Honingh, 2016 ). While in our project we particularly wanted to focus on ways of sharing power with service users and public contributors, defining who is involved in co-produced research varies across disciplines. The active involvement of service users/members of the public has sometimes been lost in research that is labelled as co-produced. UK funding councils such as the Economic and Social Research Council (ESRC) talk of co-produced research as developed between academic and non-academic organisations or communities (Campbell and Vanderhoven, 2016 ; ESRC, 2019 ). In health services research, authors have used the non-specific language of ‘stakeholders’ (Oliver et al., 2019 ). Sometimes the main research co-production partner has been practitioners (Heaton et al., 2016 ) and service users have been relegated to ‘context’ (Marshall et al., 2018 ), rather than being active agents and partners. This obfuscation of the role of service users/ members of the public in co-production is detrimental to the drive for inclusivity, democratisation and equity within co-produced research, which addresses the needs of service users/ marginalised citizens (Williams et al., 2020 ), overlooking the long political history of demands from service users to be more democratically involved in health and social care services and research (Beresford, 2019 ).
In our project, we particularly wanted to focus on how to equalise relationships with service users and public contributors (defined above) within co-produced research. The egalitarian and democratic principles of co-production means that service users, who may have been marginalised and are on the receiving end of professional ‘expertise’, now become equal partners in research (Williams et al., 2020 ). Best practice in co-produced research remains contested, with a significant theory-practice gap (Lambert and Carr, 2018 ). We wanted to understand what practices and resources could help bring principles into practice, when we are working within a context of structural inequalities.
Who is involved and when in co-produced research?
INVOLVE states that co-production should ‘occur from the start to the end of the project’ (Hickey et al., 2018 ) (p. 4). The principle to ‘include all perspectives and skills—make sure the research team includes all those who can make a contribution’ (Hickey et al., 2018 ) (p. 4) can be highly aspirational.
In our interdisciplinary workshops we discussed how there is often a lack of funding to pay public contributors to help develop a funding application. Formative ideas about research priorities and design can often be made by researchers before other people are involved. Our workshop discussions noted that involving all stakeholders who potentially have an interest in a project could be a very large and diverse group. It would be difficult to involve everyone, and this could be in tension with the idea that smaller groups can work better together. There are usually practical constraints on team numbers, budgets to pay for public contributors’ time and project scale and size. A tension can exist between the number of people you can viably include, and the diversity of the group you are working with. More generally, workshop participants highlighted problematic issues of claims to representation, where people within a co-production group need to be aware that they don’t speak for everyone—not even everyone in a group they are there to ‘represent’—and there was a need to look for opportunities to draw other perspectives in.
Workshop discussions included that when public contributors join a project there is a need to support people to take on different roles, and for people to also have choice and work from their strengths, rather than assuming that everyone has to do everything. Some group members may feel they lack skills or expertise in particular areas, and so may need training, support and mentoring. There may also be assumptions about who is going to do what work, which may need to be explicitly discussed and agreed. Ensuring proper payment of public contributors is an essential element of co-production. If public contributors are going to collect research data, they need appropriate payment, contracts and to follow all research governance processes. Within UK National Health Service (NHS) research that may mean having Research Passports, Good Clinical Practice training and Disclosure and Barring Service checks, if they are working with vulnerable people or children. Not all these processes are designed for public contributors, they can be potentially problematic to navigate, and researchers may need to support public contributors through this process. Table 1 summarises some of the challenges around who is involved, and when in co-produced research, and potential practices and resources that may help.
Power dynamics within health and social care research
Theoretical perspectives on power.
Critical and interdisciplinary perspectives on power can help us understand how to facilitate more equitable partnerships within research and co-produced work (Farr, 2018 ; Oliver and Boaz, 2019 ). The first principle of co-production is to share power through ‘an equal and reciprocal relationship’ between professionals and people using services (Boyle and Harris, 2009 ) (p. 11). However, several authors highlight how co-production can be a rhetorical device to hide power and social inequities (Flinders et al., 2016 ; Thomas-Hughes, 2018 ). Using Lukes ( 2005 ) dimensions of power, Gaventa ( 2007 ) conceives that power can be visible (institutions, structures, resources, rules), hidden (agenda-setting, some voices more dominant within decision-making), or invisible (embedded in beliefs and language).
Focussing first on visible aspects, structural and resource issues can impinge on people’s ability to co-produce, for example funders’ top-down control of research priorities and funding streams, alongside NHS and government political priorities. University research environments can be competitive, ‘unkind and aggressive’, which can crowd out ‘collegiality and collaboration’ (WellcomeTrust, 2020 ), exactly the kind of principles that academics are being encouraged to adopt through co-production. Traditional research frameworks are ill-fitted to the challenges of transforming power and control that are needed for co-productive practice (Lambert and Carr, 2018 ). Power hierarchies are intrinsic to research processes, with people experiencing competing expectations (from public contributors and communities, co-researchers, colleagues and institutions) when working in this way (Lenette et al., 2019 ). How do researchers create co-production circles of equality, reciprocity and share power with public contributors, when often researchers themselves are on temporary contracts and subject to the pressures of publishing, funding, impact and self-promotion within ‘toxic’ (Wellcome Trust, 2020 ) competitive structures? Understanding who is involved and how in decision-making processes (hidden aspects of power) is essential to understand how power is exercised. However, political scientists have long ago illustrated that ‘even the most internally democratic small collectives cannot in fact achieve equality of power in their decisions’ (Mansbridge, 1996 , p. 54).
Scrutinising invisible aspects of power, power can be seen to operate through knowledge, social relations and the language we use (Foucault, 1977 ). The principle of respecting and valuing the knowledge of all (Hickey et al., 2018 ) can be challenging in a healthcare context where a knowledge hierarchy with traditional positivist epistemological assumptions values an ‘unbiased, objective’ position. Co-productive approaches can be grounded in critical theory (Bell and Pahl, 2018 ; Facer and Enright, 2016 ), as opposed to traditional scientific paradigms. The experiential contextualised and tacit knowledge of people who use services, and related qualitative and participatory action methods, can be valued less than knowledge derived from randomised controlled trials (RCTs). This increases the challenge of co-production, as the values and methods of health and social care research may align less with co-production principles. Indeed the very idea that co-production and the sharing of power can actually happen within mainstream University spaces has been contested, with Rose and Kalathil ( 2019 ) arguing that Eurocentric hierarchical institutions that privilege rationality and reason will never be coming from a place where different knowledges are valued equally.
Understanding power in practice
In our project it was difficult to maintain a focus on power relations in the face of a strong tendency to emphasise practicalities, highlighting the difficulties of bringing these issues into clearer focus. An analysis of power dynamics may be an important aspect of a sociological study, but not one considered of such importance within health and social care research.
Focussing first on visible, structural aspects of power, workshop participants discussed their experience that within research that is formally ‘owned’ by a University (i.e., the Principal Investigator (PI) legally responsible for the project is situated within a University) there are associated issues of accountability and formal responsibility for delivering a funded research project. This creates constraints where projects have to deliver what is described rather than what emerges from the co-production process. How a PI works to develop a collaborative leadership style is an under-researched area. Within our own project we all held some unspoken assumptions about leadership and ensuring progress toward our project objectives. Workshop participants highlighted that organisational systems may not support co-production (e.g., finance, human resources and funding systems) so researchers may have to be tenacious to advocate for system changes in order to achieve things, which can be frustrating and time-consuming. For these myriad reasons, realistic resourcing of researcher time for co-production is needed, and many researchers may still end up putting discretionary time into projects to make co-production a success. There are few tools to help researchers avoid or alleviate risks to themselves and their stakeholders, such risks including practical costs, personal and professional costs to researchers, and costs to stakeholders (Oliver et al., 2019 ).
In relation to decision-making, workshop participants noted that in a pragmatic sense, doing everything by committee and consensus can impede project progress, as no decisions can be made until everyone is present at meetings. Even if decisions are made with everyone present, the power dynamics between people does not necessarily ensure that decisions are shared and agreed by everyone. Within our own project, where we were trying to stick to the principles of co-production, we found that we often had discussions between paid staff members outside of team meetings where thinking was developed and decisions taken. If public contributors are without employment contracts and are not working alongside other staff, there is potential for them to be excluded from informal discussions and decisions in day-to-day tasks. In our workshops there were discussions about whether researchers needed to ‘get out of the way’ and ‘sit on their hands’ in order to make space for others. We discussed how to practically create space for diverse knowledge and skills to be shared and considered whether it is possible to identify shared interests or if there is always a political struggle for power.
Through our project, we reflected as a team how assumptions and practices of how we do healthcare research may be deeply embedded within academic cultures. This links with Foucault’s perspectives on power dynamics (Foucault, 1977 ), every act and assumption we make is imbued with power, which makes power particularly hard to observe, grasp, critique, challenge and transform. We all have subconscious beliefs and work within cultural assumptions, thus continual critical reflective practice, and constant attention to fluctuating power relations is needed (Farr, 2018 ; Bell and Pahl, 2018 ). In workshops, suggested ways to address cultural issues included harnessing the current trends for co-production and using this to start challenging engrained cultures and accepted ways of doing things. Current funder prioritisation of co-production can enable senior researcher support for co-production, as organisational leaders recognise the cultural capital of the word and practices of ‘co-production’. Raising awareness of NIHR and other policy commitments to co-production may be a useful influencing strategy to engage more senior staff, as organisational support can be crucial to facilitate co-production. However, there is always the risk of tokenism and rhetoric (Flinders et al., 2016 ; Thomas-Hughes, 2018 ).
We considered within our project that the relationships between personal experiential knowledge, practice-based knowledge of healthcare staff, and dominant healthcare research need to be better understood if we are to co-produce knowledge together. We reflected on whether the aim of co-production projects is to modify the knowledge hierarchy completely, or to bring in experiential expertise/lived experience to influence the knowledge production process so the knowledge produced is more practical/effective/implementable. This second, more limited aim of making evidence more co-productively, so that it is more useful in practice may be more achievable, whereas modifying the dominant knowledge hierarchy was beyond our scope and influence.
Communication and relationships
The above dimensions of power (Lukes, 2005 ) have been augmented and brought together into a broader theoretical framework (Haugaard, 2012 ), which also incorporates ‘power with’ (Arendt, 1970 ), where emancipatory power can be harnessed through our ‘capacity to act in concert’. Arendt’s work highlights how we can collectively use our power together in more empowering ways. This links with a key principle of co-production, reciprocity, where everyone benefits from working together.
Consideration of what different team members want from working together, and therefore what reciprocity means within a project is needed. We discussed in the interdisciplinary workshops how the kind of benefits wanted by public contributors might include developing skills, confidence and work experience, and meeting such expectations may not usually be considered as research aims. Through our project we saw how co-production is strongly reliant on good communication and relationships. Strong facilitation and chairing skills are needed within meetings, to encourage everyone to contribute and challenge unhelpful behaviours, e.g., using jargon, or one person speaking a lot to the exclusion of others. People in our workshops discussed how some public contributors might need additional support to get more involved, e.g., having pre-meetings to help people get to grips with some information and/or issues, or the provision of materials in different accessible formats. If a co-production project includes people with specific communication needs, the group may need additional time and skills to be able to offer ways of working that are suitable for all. The NIHR is encouraging researchers to involve communities and groups that are often excluded. This means more outreach work to go out and meet with people in the places that they find accessible and comfortable, which can include project meetings in community locations, which may require additional resources.
Developing relationships and trust between team members may take time and requires emotional work. In our workshops we discussed how if the public contributor role includes sharing personal experiences for the benefit of the project, then researchers may also need to drop the ‘professional’ mask and share more personally and expose their own vulnerabilities (Batalden, 2018 ) to support more equal relationships. The challenges of university structural hierarchies were also discussed, including how it was often the responsibility of more ‘junior’ (i.e., lower in the hierarchy) researchers, and often women, to do the relational work (Lenette et al., 2019 ). Senior researchers do not necessarily understand the implications of co-production, for example one person shared how their Principal Investigator assumed that having a public contributor on the team would increase capacity and speed work up, unappreciative of the extra time needed for support, training and communication, including at the weekends, when public contributors could be carrying out work. Meeting the support and learning needs of team members can be challenging, both for researchers and public contributors, as co-produced research may take researchers outside the skills and knowledge usually expected in their professional environment. Even when these needs within a co-production project are recognised, research funders may not understand the resource and capacity implications.
A key element of running a co-production project identified within our work was the ongoing need for time to reflect on group processes to support and maintain different ways of working. Finding time for reflection can be challenging alongside creating an environment where everyone can honestly reflect on what it’s like to be in the group. This requires strong facilitation skills, particularly if there are tensions and conflicts. Addressing communication and relationship challenges are key to developing and sustaining a sense of shared ownership, and we outline some helpful practices in Table 2 .
Reflections on our own attempts at co-production
The conception of our project came initially from conversations between a researcher and public involvement specialist with previous experience as a service user and user-controlled research, wanting to create a space to share interdisciplinary learning between everyone about co-production. It could be argued that as the generation of the idea did not include public members in this first discussion it was not truly co-produced. We acknowledged that there were gaps between the lessons our project produced, and how the project itself had been carried out. It was very challenging to implement all INVOLVE principles (Hickey et al. 2018 ), and we question the extent to which they can ever be fully realised within our current contexts. Practically, we found that we should have allocated more resources to payment of our public contributors to take on additional roles. A focus on relationships and reflection was hard to maintain in the face of a small group trying to deliver an ambitious project to time, alongside other competing commitments. However, in our own reflective discussions we acknowledged that a sense of ongoing commitment to the project from everyone felt key to our group process and successfully getting the project done. In writing this article we met together several times to plan and develop sections, tables and points we wanted to get across. However, the actual writing tended to fall to the academics and public involvement specialist, who had more of the technical knowledge of what was expected. Demands of time, the juggling of commitments, and lack of resources meant that writing the article was not truly ‘co-produced’. Indeed, through the process, a public contributor co-author said they found the reviewers’ comments ‘a bit overwhelming’, with uncertainty of how to approach this. Another public contributor co-author expressed similar experiences with reviewers comments on another paper they had previously co-authored. The publication process can be a challenge to researchers as well, who are more familiar with these traditional academic practices.
Sharing power in the face of embedded hierarchies and inequalities is an obvious challenge for co-production. The gap between co-production principles and practice is a tricky territory. Working with everyone who is interested in an issue, having a focus on meeting the priorities of communities and people we work with, and co-producing all aspects of a project from beginning to end will be difficult to deliver in many projects in health and social care research. Working directly with members of the public is likely to require more adaptation of research project processes and to ‘usual ways of doing things’, alongside additional time and resources. People have different skills and uneven access to resources, and people may need considerable training and support to work together more equally. However, our experience is that funders do not necessarily understand this and doing co-production on a small budget can be particularly challenging. Time investment and the emotional work required to build relationships necessary for successful co-production is both under-appreciated and under-resourced. This reflects disparities in power between those who do this work and those who hold most power in universities. Recognising, recording, documenting and consistently budgeting for this work may help to make it more visible. Timing of funding is also crucial as many research teams do not have access to institutional ‘core’ funding, or seed funding grants, for public contributor involvement at the research development stage. As it is unlikely that most co-production projects will be able to include people with all the relevant perspectives and skills it is important to actively discuss and agree who can be involved and to be open about and discuss restrictions, which can be an act of power in itself.
Oliver and Boaz ( 2019 ) want to ‘open the door’ to more critical multidisciplinary accounts of evidence production and use, highlighting that some people want to direct energies to democratise knowledge for all. Interdisciplinary lessons from this project question the extent to which co-production processes can enable this, given the challenges we have highlighted. We consider that the jury is still out on the viability of co-production in the context of health and social care research. While some (Rose and Kalathil, 2019 ) find the promise of co-production untenable in mental health, we hope we can find a meaningful way forward. However, ‘putting what we already know [about co-production] into practice’ (Oliver and Boaz, 2019 ) can be very challenging. Our own experiences led us to reflect that to be working toward co-production principles means that you have to consistently be challenging ‘business as usual’—we consider a key point here is how to maintain sufficient self and team support to keep trying to do this in practice. Establishing reflective processes that encourage consideration of power issues are likely to be essential. Our approach to help ourselves and others navigate the challenges of co-production has been to identify ways in which groups can start to address power issues as highlighted in Tables 1 and 2 , and to develop practical freely available outputs including a map of resources and reflective questions (Farr et al., 2020 ; Davies et al., 2020 ). We need to understand more about how effective these strategies are, and whether co-production really does make a difference to the use of research. We need to encourage honest reporting of projects, their outcomes and the balance between the benefits and challenges of trying to implement the principles. However, power structures may mitigate against reporting of challenges and problems in research. Other research gaps include understanding what projects will benefit most from a co-production approach. Can co-production deliver more practical and implementable research findings, and if so how? How do we best challenge and change some of the structural inequalities within academia that impede co-production (Williams et al., 2020 )? How do we integrate experiential, practice and research-based knowledge to improve health and social care?
Our experiences on this project highlight the ongoing challenges to truly put the principles of co-production into practice. During this project we used the phrase ‘I am always doing what I can’t do yet in order to learn how to do it’ (van Gogh, 1885 ), to illustrate our limitations, yet continual striving toward an ideal. The quote continues ‘…I’ll end by saying that the work is difficult, and that, instead of quarrelling, the fellows who paint peasants and the common people would do wisely to join hands as much as possible. Union is strength…’ (van Gogh, 1885 ). Forgiving the dated language and connotations of this quote, the principles of joining hands and facilitating union are important co-production ideals that we continually need to remember, relearn and put our hearts into practising.
Arendt H (1970) On violence. Allen Lane, Penguin, London
Google Scholar
Batalden P (2018) Getting more health from healthcare: quality improvement must acknowledge patient coproduction—an essay by Paul Batalden. BMJ 362:k3617. https://doi.org/10.1136/bmj.k3617
Article PubMed Central Google Scholar
Bell DM, Pahl K (2018) Co-production: towards a utopian approach. Int J Soc Res Methodol 21(1):105–117. https://doi.org/10.1080/13645579.2017.1348581
Article Google Scholar
Beresford P (2019) Public participation in health and social care: exploring the co-production of knowledge. Front Sociol 3(41). https://doi.org/10.3389/fsoc.2018.00041
Boyle D, Harris M (2009) The challenge of co-production. New Economics Foundation, London
Brandsen T, Honingh M (2016) Distinguishing different types of coproduction: a conceptual analysis based on the classical definitions. Publ Admin Rev 76(3):427–435. https://doi.org/10.1111/puar.12465
Brudney JL, England RE (1983) Toward a definition of the coproduction concept. Publ Admin Rev 43(1):59–65. https://doi.org/10.2307/975300
Campbell HJ, Vanderhoven D (2016) N8/ESRC research programme. Knowledge that matters: realising the potential of co-production. N8 Research Partnership, Manchester, https://www.n8research.org.uk/media/Final-Report-Co-Production-2016-01-20.pdf . Accessed 23 Mar 2021
Davies R, Andrews H, Farr M, Davies P, Brangan E, Bagnall D (2020) Reflective questions to support co-produced research. National Institute for Health Research (NIHR) ARC West and People in Health West of England, University of Bristol and University of West of England. http://bit.ly/CoProResources . Accessed 23 Mar 2021
ESRC (2019) Guidance for collaboration. Economic and Social Research Council. https://esrc.ukri.org/collaboration/guidance-for-collaboration/ . Accessed 29 Nov 2020
Facer K, Enright B (2016) Creating Living knowledge: the connected communities programme, community-university relationships and the participatory turn in the production of knowledge. University of Bristol/ AHRC Connected Communities, Bristol
Farr M (2018) ‘Power dynamics and collaborative mechanisms in co-production and co-design processes’. Crit Social Policy 38(4):623–644. https://doi.org/10.1177/0261018317747444
Farr M, Davies R, Davies P, Bagnall D, Brangan E, Andrews H (2020) A map of resources for co-producing research in health and social care. University of Bristol and University of West of England, National Institute for Health Research (NIHR) ARC West and People in Health West of England http://bit.ly/CoProResources . Accessed 23 Mar 2021
Flinders M, Wood M, Cunningham M (2016) The politics of co-production: risks, limits and pollution. Evid Policy 12(2):261–279. https://doi.org/10.1332/174426415X14412037949967
Foucault M (1977) Discipline and punish: the birth of the prison. Allen Lane, London
Gaventa J (2007) Levels, spaces and forms of power: analysing opportunities for change. In: Berenskoetter F, Williams MJ (eds) Power in world politics. Routledge, Abingdon, pp. 204–224
Haugaard M (2012) Rethinking the four dimensions of power: domination and empowerment. J Polit Power 5(1):33–54. https://doi.org/10.1080/2158379X.2012.660810
Heaton J, Day J, Britten N (2016) Collaborative research and the co-production of knowledge for practice: an illustrative case study. Implement Sci 11(1):20. https://doi.org/10.1186/s13012-016-0383-9
Article PubMed PubMed Central Google Scholar
Hickey G, Brearley S, Coldham T, Denegri S, Green G, Staniszewska S, Tembo D, Torok K, Turner K (2018) Guidance on co-producing a research project. INVOLVE, Southampton
INVOLVE (2019) Co-production in action: number one. INVOLVE, Southampton
Lambert N, Carr S (2018) ‘Outside the Original Remit’: Co-production in UK mental health research, lessons from the field. Int J Ment Health Nurs. 27(4):1273–1281
Lenette C, Stavropoulou N, Nunn C, Kong ST, Cook T, Coddington K, Banks S (2019) Brushed under the carpet: examining the complexities of participatory research. Res All 3(2):161–179. https://doi.org/10.18546/RFA.03.2.04
Lukes S (2005) Power: a radical view. Macmillan, London
Book Google Scholar
Mansbridge J (1996) Using power/ fighting power: the polity. In: Benhabib S (ed.) Democracy and Difference. Princeton University Press, Princeton, pp. 46–66
Marshall M, Mear L, Ward V, O’Brien B, Davies H, Waring J, Fulop N (2018) Optimising the impact of health services research on the organisation and delivery of health services: a study of embedded models of knowledge co-production in the NHS (Embedded). NIHR. https://www.journalslibrary.nihr.ac.uk/programmes/hsdr/165221/#/ . Accessed 23 Mar 2021
NIHR CED (2020) Centre for engagement and dissemination recognition payments for public contributors. https://www.nihr.ac.uk/documents/centre-for-engagement-and-dissemination-recognition-payments-for-public-contributors/24979#1 . Accessed 23 Mar 2021
Oliver K, Boaz A (2019) Transforming evidence for policy and practice: creating space for new conversations. Pal Commun 5(1):60. https://doi.org/10.1057/s41599-019-0266-1
Oliver K, Kothari A, Mays N (2019) The dark side of coproduction: do the costs outweigh the benefits for health research? J Health Res Policy Syst 17(1):33. https://doi.org/10.1186/s12961-019-0432-3
Ostrom E (1996) Crossing the great divide: coproduction, synergy, and development. World Dev 24(6):1073–1087. https://doi.org/10.1016/0305-750X(96)00023-X
Rose D, Kalathil J (2019) Power, privilege and knowledge: the untenable promise of co-production in mental “health”. Front Sociol 4:57. https://doi.org/10.3389/fsoc.2019.00057
Staniszewska S, Denegri S, Matthews R, Minogue V (2018) Reviewing progress in public involvement in NIHR research: developing and implementing a new vision for the future. BMJ Open 8(7):e017124. https://doi.org/10.1136/bmjopen-2017-017124
Thomas-Hughes H (2018) Ethical ‘mess’ in co-produced research: reflections from a U.K.-based case study. Int J Soc Res Methodol 21(2):231–242. https://doi.org/10.1080/13645579.2017.1364065
van Gogh V (1885) RE: Letter from Vincent van Gogh to Anthon Van Rappard
WellcomeTrust (2020) What researchers think about the culture they work in. Wellcome Trust, London, https://wellcome.org/sites/default/files/what-researchers-think-about-the-culture-they-work-in.pdf . Accessed 23 Mar 2021
Williams O, Sarre S, Papoulias SC, Knowles S, Robert G, Beresford P, Rose D, Carr S, Kaur M, Palmer VJ (2020) Lost in the shadows: reflections on the dark side of co-production. Health Research Policy and Systems 18 (1)
Download references
Acknowledgements
This project was funded by the University of Bristol Public Engagement Seed Funding and Research Staff Development fund. It was supported by the National Institute for Health Research (NIHR) Applied Research Collaboration West (NIHR ARC West). The views expressed in this article are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. Many thanks to everyone who attended our workshops, got involved in and supported the project to help us develop our resources and training. We couldn’t have done this with you!
Author information
Authors and affiliations.
The National Institute for Health Research Applied Research Collaboration West (NIHR ARC West) at University Hospitals Bristol and Weston NHS Foundation Trust, Bristol, UK
Michelle Farr, Philippa Davies, Heidi Andrews, Darren Bagnall, Emer Brangan & Rosemary Davies
Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
Michelle Farr, Philippa Davies, Heidi Andrews, Darren Bagnall & Emer Brangan
School of Health and Social Wellbeing, University of the West of England, Bristol, UK
Emer Brangan
Faculty of Health and Applied Sciences, University of the West of England, Bristol, UK
Rosemary Davies
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Michelle Farr .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Farr, M., Davies, P., Andrews, H. et al. Co-producing knowledge in health and social care research: reflections on the challenges and ways to enable more equal relationships. Humanit Soc Sci Commun 8 , 105 (2021). https://doi.org/10.1057/s41599-021-00782-1
Download citation
Received : 28 February 2020
Accepted : 31 March 2021
Published : 06 May 2021
DOI : https://doi.org/10.1057/s41599-021-00782-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Create to collaborate: using creative activity and participatory performance in online workshops to build collaborative research relationships.
- Alice Malpass
- Astrid Breel
- Michelle Farr
Research Involvement and Engagement (2023)
Coproducing health research with Indigenous peoples
- Chris Cunningham
- Monica Mercury
Nature Medicine (2023)
Patient and public involvement in an international rheumatology translational research project: an evaluation
- Savia de Souza
- Eva C. Johansson
- Ruth Williams
BMC Rheumatology (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Find My Rep
You are here
Your Undergraduate Dissertation in Health and Social Care
- Nicholas Walliman - Oxford Brookes University, UK
- Jane Appleton
- Description
This is a revised edition of Nicholas Walliman's best-selling Your Undergraduate Dissertation , which has been specially tailored to the needs of those studying health, social care and related subjects. All the central topics are covered, with comprehensive information and guidance on crucial issues such as ethics, research governance and appraising the quality of the evidence. Relevant 'real life' examples are also included, drawn from a wide range of settings.
This guide offers a genuinely accessible and supportive source of advice that will be welcomed by undergraduates in working towards their final year dissertation in health and social care. SAGE Study Skills are essential study guides for students of all levels. From how to write great essays and succeeding at university, to writing your undergraduate dissertation and doing postgraduate research, SAGE Study Skills help you get the best from your time at university. Visit the SAGE Study Skills hub for tips, resources and videos on study success!
Supplements
The text is difficult to read and there are far more engaging books on this subject. Really not applicable to widening participation students.
I will be recommending this book for health care degree learners. The book is set out well and has a variety of information that is useful not only when preparing for dissertation in both health care and social work. Some sections go beyond dissertation and thus also can be an invaluable reference book when in professional practice.
this text is recommended for all Undergraduate students about to embark on their major project
very helpful book easy to navigate.
This the perfect text for our public health department's junior year writing course.
This book was sent during the summer when I was unable to review it in enough depth. However I shall be suggesting it as a supplemental text
This book will be recommended to our students. It contains some invaluable chapters that students will find useful.
This is a useful text which contains valuable information for all undergraduate students completing their dissertaion. I have given it a personal recomendation to a number of students who have learning differences as I feel it will benefit them particualrly.
In addition to midwifery students, I will also be recomending this text to nursing, radipgraphy and social work students I am in contact with during Interprofessional learning modules.
A book I have recommended to several students enbarking on writing their dissertation. No feedback as yet as to whether sudents have found it useful.
Presented in a question and answer ‘manual’ style text this book is a must have for undergraduates wishing to get a successful grasp on the complex field of research. It offers a clear introduction to various types, approaches and methods used and accepted within the discipline of Health and Social Care. Te title of the book does not do the text justice - it would be advisable to obtain this user friendly read before approaching any written paper/essay involving research, and can then be referred to during extended projects as a guide to focus and keep on track!! With plenty of suggested further reading this book makes a great companion on an otherwise, LONELY journey.
Preview this book
Sample materials & chapters.
Introduction
Chapter One
For instructors
Please select a format:
Select a Purchasing Option
Order from:.
- VitalSource
- Amazon Kindle
- Google Play
Related Products

SAGE Knowledge is the premier social sciences platform for SAGE and CQ Press book, reference and video content.
The platform allows researchers to cross-search and seamlessly access a wide breadth of must-have SAGE book and reference content from one source.

- Member Organisations
- Research, Implementation and Impact
- Social Care and Social Work
- Social Care - Kent, Surrey & Sussex Region
- Starting Well: Children's Mental Health
- Primary and Community Health Services
- Living Well with Dementia
- Co-production
- Public Health
- Digital Innovation
- Economics of Health and Social Care
- Implementation
- Public and Community Involvement
- What is PCIE?
- Getting Involved
- Support for researchers
- Introduction
- An overview of ARC KSS
- Who can help you with PCIE?
- Terminology and PCIE
- Why and When to do PCIE
- Why involve members of the public in research?
- Why do members of the public want to get involved in research?
- When to get members of the public involved?
- How to do PCIE
- Communication and Accessibility
- Planning for involvement and engagement
- How to recruit members of the public
- Equality, Diversity and Inclusion (EDI)
- Approaches – different options for undertaking PCIE
- Facilitating meetings and Group dynamics
- Impact and Evaluation
- Examples/Case Studies
- Appendix/Useful tools
- Learning and Development

- Learning and Development Finder
- Researchers Journeys

- Research Week
- Research Week 2023: Poster Competition
- Previous Research Weeks

- Resource Library
Your Health and Social Care Research Quick Guide
This guide is designed for those in practice to navigate the world of research.

In this section
Produced by Dr Diana Ramsey , ARC KSS Darzi Fellow (2021-2022) with insights and support from people working to deliver research in the Health and Social Care region, the Your Health and Social Care Research Quick Guide is a resource to help those working in health or social care to start or develop their research journey.
Packed with information, links and personal stories from people working across Kent, Surrey and Sussex, this guide has been designed to answer any questions you might have in regards to getting involved in research, building networks, research training and resources.
Whatever your research experience, this guide is for you.
View guide here

Subscribe to our newsletter
Sign up here
You can unsubscribe at any time by clicking the link in the footer of our emails. For information about our privacy practices, please visit this page . We use e-shot as our marketing platform. Learn more about e-shot's privacy practices here .
Cookies on Be Part of Research
We use some essential cookies to make this service work.
We would like to use additional cookies to remember your settings, understand how you use Be Part of Research and improve the service.
We also use cookies set by other sites to help us deliver content via their services.
Keep up to date
Sign up for news and information about taking part and shaping research.
I'm looking for research about
- News and features
- Why take part?
- How to take part
- What happens on a study?
- Volunteering without a condition
- UK research registries
- Information for researchers
- Information for health and care professionals
- Web developer resources
What is health and care research?
- How are studies regulated, approved and funded?
- Frequently asked questions
Search for a study
You already conduct research in your day-to-day life. This research informs and broadens your understanding of things before you make a decision. Health and care research is the same. It seeks to find answers to questions about the best options available. It then uses these discoveries to make decisions about improvements or changes. This is so we can:
- diagnose diseases earlier or more accurately
- provide life-changing treatments
- prevent people from developing conditions
- improve health and care for generations to come
- ensure everyone has a better quality of life
Although health professionals already know a great deal, there are still so many questions that need answers. Sometimes, the outcome of research just confirms that what we have at the moment, is the best available to us right now.
How research contributes to our NHS
This short film explains the important role that research plays in the NHS and how important it is for the future that we all consider taking part ( video transcript ).
Good research is:
- Relevant – it answers questions that are important to the health and care of the public
- High quality – it has to follow strict legal standards
- Safe – it puts people’s safety and dignity first
The first clinical trial

The first clinical trial was conducted by James Lind. He was a Scottish doctor and a pioneer of naval hygiene in the Royal Navy. He conducted the first clinical trial in history in 1747.
James wanted to investigate whether citrus fruits cured scurvy. He selected twelve patients with scurvy on a ship, kept them together and gave them all different diets and monitored them. By the end of the week, the sailors whose daily diet included citrus fruits recovered, therefore proving that citrus fruit could cure scurvy.
We still celebrate this milestone each year on International Clinical Trials Day.
Myths about research
Understanding the facts is really important when deciding whether to take part in research. By clicking on the arrow next to each myth you can reveal the facts.
All health and care research is high risk
All health and social care research has to go through very strict ethical and regulatory checks before it can go ahead. There are lots of different ways to get involved with research . Some involve taking a new medicine or having a new form of treatment, others may be as simple as filling out a questionnaire or leaving a sample. People are very closely monitored while they are taking part in research, so although health and care research is not entirely risk-free, the chances of something going wrong are small.
My doctor will tell me about the research available
Not all health and care professionals will be fully informed about all of the research opportunities available to you. They might also not have the time to discuss it with you in your appointment. However, it is important to ask about opportunities to get involved in research as your healthcare professional will know how to find out what might be available. You can search for studies on this website by using the search bar at the very top of each page by typing in your town, postcode, body part, medicine or health condition. You can also find a condition by pressing the “ view conditions ” button.
Research can only take place in hospital
Health and care research can take place in many different places, from schools to care homes depending on the type of research. It is more common than ever before for research to take place in non-clinical settings. Digital technology provides a way of getting people involved from the comfort of their own homes.
Health and care research means taking lots of drugs
Not all health and care research involves taking drugs. The research may involve testing a new device to help monitor or administer a medicine for an illness. It could be about monitoring how certain changes in our diet and lifestyle could help the health of our nation in the future. Research might simply involve talking to someone, completing a short questionnaire or even using an app on a mobile device. There are also many different ways to be involved in research without being a participant in a research study .
People are treated like guinea pigs
Whatever the type of research, anyone who is involved should be treated with respect. The research is not being done to them but with them. People who participate in research often say that they feel well cared for as they have a dedicated contact within the research staff team. Research teams must follow ethical guidance and before the research can take place, they must seek approval for their plan from a Research Ethics Committee. Research that involves new medicines is not tested on people first. It will have gone through a process to ensure it is ready for use with people.
Health and care research is only about finding a cure
Research aims to prevent diseases as well as cure them. There are a range of factors which can contribute to your health, for example: where you live, what you eat and whether you have a good support network of family and friends. Public health research seeks to answer questions about some of these factors.
Research seeks to find ways for people to live well with long-term conditions. It can help to find out the best ways to care for people living with life-limiting illness and pain, which is known as ’palliative care’. Research can lead to improvements in end-of-life care across all diseases and to help patients to live in comfort and die with dignity.
Health and social care research only involves physical diseases, it cannot help with mental health
People’s health is not limited to physical disease, it includes their mental well being. Research therefore seeks to answer questions about mental health such as is medicine, counselling or a combination of both the best treatment for individuals living with depression? Members of the public can have a role in identifying and prioritising where health research is focused . Given increased awareness of the effects our mental health can have on our physical well being, this is likely to be a growing area of health and social care research. Read about all the research happening within the NIHR specialty for mental health .
Children are not allowed to participate in health and care research
Children can take part in health and care research with the permission of their legal guardian. The research team may meet with the child to make sure they understand what the research is about. They may use pictures to explain the study. Research in child health is vital to help find new and better ways to care for children. You can find studies for children by typing "Children" in the search box at the very top of this page.
Research only benefits the drug companies
Health research is funded by drug companies, charities and the government, although when the NHS undertakes research specifically for drug companies, the company pays the full cost. Everyone benefits from the development of new medicines, and without commercial drug companies there would be less research taking place.
Different types of research

Healthcare research
Sometimes health research studies may be referred to as ‘clinical trials’. They usually involve examining and observing people with different conditions and sometimes comparing them with people who don't have the condition. It can also involve research on samples of blood or other tissues, or tests such as scans or X-rays. Researchers can also analyse information in patient records, or the data from health and lifestyle surveys.

Public health research
Tackles some of the bigger health issues that affect society as a whole, for example, the impact of giving up smoking, how many steps a day for good health etc. It also looks at the benefits, costs, acceptability and the wider impact of treatments.

Social care research
Is about improving the lives of people who receive care and support from our social care sector. Research in social care could be about introducing new devices and technologies such as: lifting equipment to help with residents, exploring the impact of technology driven care environments or changing social care policies and practice.
Important research discoveries
.jpg)
Launched in 1961, the contraceptive pill was initially only prescribed to married women, but the law was relaxed in 1967. The pill works by suppressing fertility with either progesterone or oestrogen or, more commonly, a combination of both.

Penicillin was discovered in 1928 and developed into a drug in the early 1940s. Today it’s used to treat a broad range of bacterial infections accounting for around 45% of the antibiotics prescribed in the NHS in England.

Research in the 1980s and 1990s showed that low doses of blood-thinning drugs such as aspirin and warfarin significantly reduced the number of heart attacks and strokes in people at risk.
Before you go
Research is a team effort. We need members of the public, like you, to take part. Without volunteers, it would not be possible for research to happen.
- Reasons why people take part in research
- How to take part in research
- Learn about how studies are made safe
Research Topics & Ideas: Healthcare
100+ Healthcare Research Topic Ideas To Fast-Track Your Project

Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you’ve landed on this post, chances are you’re looking for a healthcare-related research topic , but aren’t sure where to start. Here, we’ll explore a variety of healthcare-related research ideas and topic thought-starters across a range of healthcare fields, including allopathic and alternative medicine, dentistry, physical therapy, optometry, pharmacology and public health.
NB – This is just the start…
The topic ideation and evaluation process has multiple steps . In this post, we’ll kickstart the process by sharing some research topic ideas within the healthcare domain. This is the starting point, but to develop a well-defined research topic, you’ll need to identify a clear and convincing research gap , along with a well-justified plan of action to fill that gap.
If you’re new to the oftentimes perplexing world of research, or if this is your first time undertaking a formal academic research project, be sure to check out our free dissertation mini-course. In it, we cover the process of writing a dissertation or thesis from start to end. Be sure to also sign up for our free webinar that explores how to find a high-quality research topic.
Overview: Healthcare Research Topics
- Allopathic medicine
- Alternative /complementary medicine
- Veterinary medicine
- Physical therapy/ rehab
- Optometry and ophthalmology
- Pharmacy and pharmacology
- Public health
- Examples of healthcare-related dissertations
Allopathic (Conventional) Medicine
- The effectiveness of telemedicine in remote elderly patient care
- The impact of stress on the immune system of cancer patients
- The effects of a plant-based diet on chronic diseases such as diabetes
- The use of AI in early cancer diagnosis and treatment
- The role of the gut microbiome in mental health conditions such as depression and anxiety
- The efficacy of mindfulness meditation in reducing chronic pain: A systematic review
- The benefits and drawbacks of electronic health records in a developing country
- The effects of environmental pollution on breast milk quality
- The use of personalized medicine in treating genetic disorders
- The impact of social determinants of health on chronic diseases in Asia
- The role of high-intensity interval training in improving cardiovascular health
- The efficacy of using probiotics for gut health in pregnant women
- The impact of poor sleep on the treatment of chronic illnesses
- The role of inflammation in the development of chronic diseases such as lupus
- The effectiveness of physiotherapy in pain control post-surgery
Topics & Ideas: Alternative Medicine
- The benefits of herbal medicine in treating young asthma patients
- The use of acupuncture in treating infertility in women over 40 years of age
- The effectiveness of homoeopathy in treating mental health disorders: A systematic review
- The role of aromatherapy in reducing stress and anxiety post-surgery
- The impact of mindfulness meditation on reducing high blood pressure
- The use of chiropractic therapy in treating back pain of pregnant women
- The efficacy of traditional Chinese medicine such as Shun-Qi-Tong-Xie (SQTX) in treating digestive disorders in China
- The impact of yoga on physical and mental health in adolescents
- The benefits of hydrotherapy in treating musculoskeletal disorders such as tendinitis
- The role of Reiki in promoting healing and relaxation post birth
- The effectiveness of naturopathy in treating skin conditions such as eczema
- The use of deep tissue massage therapy in reducing chronic pain in amputees
- The impact of tai chi on the treatment of anxiety and depression
- The benefits of reflexology in treating stress, anxiety and chronic fatigue
- The role of acupuncture in the prophylactic management of headaches and migraines
Topics & Ideas: Dentistry
- The impact of sugar consumption on the oral health of infants
- The use of digital dentistry in improving patient care: A systematic review
- The efficacy of orthodontic treatments in correcting bite problems in adults
- The role of dental hygiene in preventing gum disease in patients with dental bridges
- The impact of smoking on oral health and tobacco cessation support from UK dentists
- The benefits of dental implants in restoring missing teeth in adolescents
- The use of lasers in dental procedures such as root canals
- The efficacy of root canal treatment using high-frequency electric pulses in saving infected teeth
- The role of fluoride in promoting remineralization and slowing down demineralization
- The impact of stress-induced reflux on oral health
- The benefits of dental crowns in restoring damaged teeth in elderly patients
- The use of sedation dentistry in managing dental anxiety in children
- The efficacy of teeth whitening treatments in improving dental aesthetics in patients with braces
- The role of orthodontic appliances in improving well-being
- The impact of periodontal disease on overall health and chronic illnesses
Tops & Ideas: Veterinary Medicine
- The impact of nutrition on broiler chicken production
- The role of vaccines in disease prevention in horses
- The importance of parasite control in animal health in piggeries
- The impact of animal behaviour on welfare in the dairy industry
- The effects of environmental pollution on the health of cattle
- The role of veterinary technology such as MRI in animal care
- The importance of pain management in post-surgery health outcomes
- The impact of genetics on animal health and disease in layer chickens
- The effectiveness of alternative therapies in veterinary medicine: A systematic review
- The role of veterinary medicine in public health: A case study of the COVID-19 pandemic
- The impact of climate change on animal health and infectious diseases in animals
- The importance of animal welfare in veterinary medicine and sustainable agriculture
- The effects of the human-animal bond on canine health
- The role of veterinary medicine in conservation efforts: A case study of Rhinoceros poaching in Africa
- The impact of veterinary research of new vaccines on animal health
Topics & Ideas: Physical Therapy/Rehab
- The efficacy of aquatic therapy in improving joint mobility and strength in polio patients
- The impact of telerehabilitation on patient outcomes in Germany
- The effect of kinesiotaping on reducing knee pain and improving function in individuals with chronic pain
- A comparison of manual therapy and yoga exercise therapy in the management of low back pain
- The use of wearable technology in physical rehabilitation and the impact on patient adherence to a rehabilitation plan
- The impact of mindfulness-based interventions in physical therapy in adolescents
- The effects of resistance training on individuals with Parkinson’s disease
- The role of hydrotherapy in the management of fibromyalgia
- The impact of cognitive-behavioural therapy in physical rehabilitation for individuals with chronic pain
- The use of virtual reality in physical rehabilitation of sports injuries
- The effects of electrical stimulation on muscle function and strength in athletes
- The role of physical therapy in the management of stroke recovery: A systematic review
- The impact of pilates on mental health in individuals with depression
- The use of thermal modalities in physical therapy and its effectiveness in reducing pain and inflammation
- The effect of strength training on balance and gait in elderly patients
Topics & Ideas: Optometry & Opthalmology
- The impact of screen time on the vision and ocular health of children under the age of 5
- The effects of blue light exposure from digital devices on ocular health
- The role of dietary interventions, such as the intake of whole grains, in the management of age-related macular degeneration
- The use of telemedicine in optometry and ophthalmology in the UK
- The impact of myopia control interventions on African American children’s vision
- The use of contact lenses in the management of dry eye syndrome: different treatment options
- The effects of visual rehabilitation in individuals with traumatic brain injury
- The role of low vision rehabilitation in individuals with age-related vision loss: challenges and solutions
- The impact of environmental air pollution on ocular health
- The effectiveness of orthokeratology in myopia control compared to contact lenses
- The role of dietary supplements, such as omega-3 fatty acids, in ocular health
- The effects of ultraviolet radiation exposure from tanning beds on ocular health
- The impact of computer vision syndrome on long-term visual function
- The use of novel diagnostic tools in optometry and ophthalmology in developing countries
- The effects of virtual reality on visual perception and ocular health: an examination of dry eye syndrome and neurologic symptoms
Topics & Ideas: Pharmacy & Pharmacology
- The impact of medication adherence on patient outcomes in cystic fibrosis
- The use of personalized medicine in the management of chronic diseases such as Alzheimer’s disease
- The effects of pharmacogenomics on drug response and toxicity in cancer patients
- The role of pharmacists in the management of chronic pain in primary care
- The impact of drug-drug interactions on patient mental health outcomes
- The use of telepharmacy in healthcare: Present status and future potential
- The effects of herbal and dietary supplements on drug efficacy and toxicity
- The role of pharmacists in the management of type 1 diabetes
- The impact of medication errors on patient outcomes and satisfaction
- The use of technology in medication management in the USA
- The effects of smoking on drug metabolism and pharmacokinetics: A case study of clozapine
- Leveraging the role of pharmacists in preventing and managing opioid use disorder
- The impact of the opioid epidemic on public health in a developing country
- The use of biosimilars in the management of the skin condition psoriasis
- The effects of the Affordable Care Act on medication utilization and patient outcomes in African Americans
Topics & Ideas: Public Health
- The impact of the built environment and urbanisation on physical activity and obesity
- The effects of food insecurity on health outcomes in Zimbabwe
- The role of community-based participatory research in addressing health disparities
- The impact of social determinants of health, such as racism, on population health
- The effects of heat waves on public health
- The role of telehealth in addressing healthcare access and equity in South America
- The impact of gun violence on public health in South Africa
- The effects of chlorofluorocarbons air pollution on respiratory health
- The role of public health interventions in reducing health disparities in the USA
- The impact of the United States Affordable Care Act on access to healthcare and health outcomes
- The effects of water insecurity on health outcomes in the Middle East
- The role of community health workers in addressing healthcare access and equity in low-income countries
- The impact of mass incarceration on public health and behavioural health of a community
- The effects of floods on public health and healthcare systems
- The role of social media in public health communication and behaviour change in adolescents
Examples: Healthcare Dissertation & Theses
While the ideas we’ve presented above are a decent starting point for finding a healthcare-related research topic, they are fairly generic and non-specific. So, it helps to look at actual dissertations and theses to see how this all comes together.
Below, we’ve included a selection of research projects from various healthcare-related degree programs to help refine your thinking. These are actual dissertations and theses, written as part of Master’s and PhD-level programs, so they can provide some useful insight as to what a research topic looks like in practice.
- Improving Follow-Up Care for Homeless Populations in North County San Diego (Sanchez, 2021)
- On the Incentives of Medicare’s Hospital Reimbursement and an Examination of Exchangeability (Elzinga, 2016)
- Managing the healthcare crisis: the career narratives of nurses (Krueger, 2021)
- Methods for preventing central line-associated bloodstream infection in pediatric haematology-oncology patients: A systematic literature review (Balkan, 2020)
- Farms in Healthcare: Enhancing Knowledge, Sharing, and Collaboration (Garramone, 2019)
- When machine learning meets healthcare: towards knowledge incorporation in multimodal healthcare analytics (Yuan, 2020)
- Integrated behavioural healthcare: The future of rural mental health (Fox, 2019)
- Healthcare service use patterns among autistic adults: A systematic review with narrative synthesis (Gilmore, 2021)
- Mindfulness-Based Interventions: Combatting Burnout and Compassionate Fatigue among Mental Health Caregivers (Lundquist, 2022)
- Transgender and gender-diverse people’s perceptions of gender-inclusive healthcare access and associated hope for the future (Wille, 2021)
- Efficient Neural Network Synthesis and Its Application in Smart Healthcare (Hassantabar, 2022)
- The Experience of Female Veterans and Health-Seeking Behaviors (Switzer, 2022)
- Machine learning applications towards risk prediction and cost forecasting in healthcare (Singh, 2022)
- Does Variation in the Nursing Home Inspection Process Explain Disparity in Regulatory Outcomes? (Fox, 2020)
Looking at these titles, you can probably pick up that the research topics here are quite specific and narrowly-focused , compared to the generic ones presented earlier. This is an important thing to keep in mind as you develop your own research topic. That is to say, to create a top-notch research topic, you must be precise and target a specific context with specific variables of interest . In other words, you need to identify a clear, well-justified research gap.
Need more help?
If you’re still feeling a bit unsure about how to find a research topic for your healthcare dissertation or thesis, check out Topic Kickstarter service below.

You Might Also Like:

15 Comments
I need topics that will match the Msc program am running in healthcare research please
Hello Mabel,
I can help you with a good topic, kindly provide your email let’s have a good discussion on this.
Can you provide some research topics and ideas on Immunology?
Thank you to create new knowledge on research problem verse research topic
Help on problem statement on teen pregnancy
This post might be useful: https://gradcoach.com/research-problem-statement/
can you provide me with a research topic on healthcare related topics to a qqi level 5 student
Please can someone help me with research topics in public health ?
Hello I have requirement of Health related latest research issue/topics for my social media speeches. If possible pls share health issues , diagnosis, treatment.
I would like a topic thought around first-line support for Gender-Based Violence for survivors or one related to prevention of Gender-Based Violence
Please can I be helped with a master’s research topic in either chemical pathology or hematology or immunology? thanks
Can u please provide me with a research topic on occupational health and safety at the health sector
Good day kindly help provide me with Ph.D. Public health topics on Reproductive and Maternal Health, interventional studies on Health Education
may you assist me with a good easy healthcare administration study topic
May you assist me in finding a research topic on nutrition,physical activity and obesity. On the impact on children
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
RESEARCH PROPOSAL – “Enhancing Quality in Patient Care”
1. relevant background of the proposed work:.
Patient care has gained immense importance in recent years due to the increased number of medical disorders and increasing awareness amongst people and patients. Increased demand in hospitals and healthcare centres to improve the patient’s health condition has become a formidable factor for all the health care professionals at every hierarchy level. Errors have become a part of the system, due to increase in the number of challenging issues that affect the deteriorating health condition of the patient. Improving the health condition by minimising system and human errors has become a crucial concern in the health industry. Health professionals have identified several causative factors for poor quality and implemented various measures to improve the quality of the situation. Unlike the old paradigm, the person approach, where the percentage of errors recorded was high, the system approach came into existence and is these days reducing the percentage of errors and increasing the complexity of the system (Warburton. 2005). In addition to the improvement of organisation, there are many other improvements underway, which include the public involvement in primary health research (Jonathan et al., 2010). According to the current situation, the health care team is also getting educated to reduce the risk of errors (Colin. 1995). Awareness of errors also created a significant impact on the safety of the patient and hence many resources were created and modified to reduce the risk (Warburton. 2005). These days, usage of health information technologies lead to improvement of the health. In the study by Connie and David (2010), through the innovative technology, the system can be advanced globally to reduce the socioeconomic barriers in various countries. Appropriate use of technology at the right time would cause miracles in the health sector (Connie et al., 2010). Many health care changes initiated in certain categories of patients decreased the risk of errors. Some of the measures included direct, personal supervision and decreased adverse reactions in case of paediatric and geriatric patients (Cambern. 2009). Another main implementation is an introduction of rapid assessment and initial patient treatment team (RAPT) in accident and emergency patients, reducing the risk to life (Cronin et al., 2005).
Summarising all the developments, quality in health care can be achieved by the academic and technical knowledge of the physician along with the communication of the health care assistants and public. In addition, appropriate utilisation of resources and tools is also essential to achieve the improvement of patient’s health condition as a target (Michelle. 1996).
2. HYPOTHESIS: Objective of the current project is to demonstrate new techniques based on studies done in previous years and to improve the quality of patient care, which is a considerable challenge for the health sector.
The tasks to accomplish include:
- To increase safety of patients by relevant initiatives. 12/16/2010 Research Proposal
- Team working within the health care sector and involvement of patients and public in primary research.
- Implementing innovations in patient care.
3. SCOPE: The following tasks would be undertaken as a part of proposed research:
- Task 1: To investigate the past studies on existing and improved health care system.
- Task 2: To appreciate the improvements in the health sector in the recent years.
- Task 3: To design research in order to increase quality in health care system and patient safety by reducing errors and implementing innovations.
4. METHODOLOGY AND APPROACH:
1. Patient Safety Initiatives: Although lots of experiments were done in patient safety in recent decades, it still remains a challenge for health professionals. These days, hospitals are spending enormous resources to reduce errors, which are appreciated. However, implementing all the proposals is not easy (Warburton. 2005). It is cost involving and depends on manpower to a greater extent, which is difficult to control.
The safety improvements cannot be implemented and always be accurate as it changes according to the situation. Improper design and rapid enforcement of safety measures would only cause meagre improvement to patients (Warburton. 2005).
There are several approaches and studies for obtaining maximum benefit out of the available resources. They are:
- Setting up a committee of professionals across the health sector to highlight vital safety measures in the hospital according to the patient conditions (Warburton. 2005). This method is time consuming and complicated. The results obtained were vague and could not improve the quality of patient.
- Another approach, which is my area of research interest, is setting up an Economic Evaluation Loop (EEL), based on the recommendation of Leape and others (1999) which would be based on utilising available evidence to establish priorities. In this approach, priorities would be set according to the analysis of available resources and outcomes of the changes (Warburton. 2005).
Accordingly, evaluation would be based on the benefits and resources available for research. Later, detailed research would be completed according to Warburton (2005), by which alternative assumptions could be identified and compiled. Finally, an additional research network would be framed to fulfil the requirements in the best possible way to reduce critical gaps (Warburton. 2005). This loop is a variant of Technology assessment iterate loop, called TAIL (Tugwell et al., 1986; Tugwell et al., 1995).
By this EEL approach, critical gaps in the research area can be identified by discussions among the health professionals and these gaps, which are usually overlooked, would be considered to provide the best safety measures within the scope of resources.
Increasing research on safety implementation to patients often raises a question of how much safety is essential. Warburton (2005) describes that there is no upper bound for providing safety to patient as demands of improving safety measurements never drop. He explains this fact by the figure depicted in figure 2 of this paper.
The curve depicts total costs of errors to the society against the level of safeguards and clearly reveals that the safety measures are implemented based upon the cost effectiveness. When initial safety methods are employed it is initially cheap, and then with the increase of costs, negligible benefits are obtained due to less reduction of adverse effects when cost measures increases. This continues uphill, further reducing the benefits with increased cost (Warburton. 2005).
The curve depicts total costs of errors to the society against the level of safeguards and clearly reveals that the safety measures are implemented based upon the cost effectiveness. When initial safety methods are employed it is initially cheap, and then with increase of costs, negligible benefits are obtained due to a drop in the reduction of adverse effects when cost measures increases. This continues further reducing the benefits with increased cost (Warburton. 2005).
Figure 2: Cost to the society versus level of safeguards Figure adopted from Warburton (2005).
In my research project, EEL with regards to one of the patient safety will be studied in the clinical environment and conclusions would be compiled accordingly in the thesis work.
2. Patient and Public Involvement in Primary Research: Involvement of potential patients and the public is an import contribution to primary research.
According to Beresford’s argument, the research experiments tend to be more accurate when the distance between the potential patients and the investigator is minimal (Beresford. 2005).
Furthermore the public, the part owners for research as taxpayers, have an equal right to subscribe for the success of research, which would improve their lives directly (Boote et al., 2010).
Additionally, public involvement at all stages of research, especially the primary level, would reduce the initial value of resources by direct focus on potential treatment areas and thus contribute to the quality of care (Boote et al., 2002; Thompson et al., 2009).
One of the approaches by which quality of patient care would be enhanced is performing clinical trials in a particular diseased population. In these clinical trials, design of the study would be based on their relevant experiences. Questionnaires would be prepared accordingly to consider general experiences and needs in that category of patients. These questionnaires are then compiled together to establish a basic structure of description and would form the research theme. Initially consent forms would be taken from the patients, and research would be carried out by contacting them regularly for feedback. All the issues the public need to be addressed would be collected for better supervision and analysis would be carried on to ensure results favouring the potential patients. This attempt ensures that questions of the potential patients would be answered and treatment becomes patient friendly, reducing the stress on the investigator, and the patient.
In this project, clinical trial is closely observed on a class of patients. Later analysis would be done on how the involvement of public and potential patients influences quality of patient care.
3. Team Working Team working is essential for effective health care management, especially in critical conditions like chronic health disorders. To achieve quality team working amongst all the health care professionals, interaction among them in day-to-day service is necessary. To ensure team-working skills in hospitals and health care centres, educating the team would be required.
Education should be a dynamic process that is patient-centred (Coles et al., 1995). Education amongst the health professionals should be multidisciplinary rather than self-centred research.
Patients and their cares should get an education alongside to improve care and hygiene. Thus, quality in health care would be achieved by a patient-centred approach.
In addition, regular team meetings and interaction between the physicians, care takers and patients would improve the quality of patient care. Discussion among patients and physicians during the treatment would be useful to record the treatment procedure, which could be useful in future investigation of the same kind.
In this project, team-working skills within a selected hospital would be improved and quality of patient care would be compared.
4. Innovations in Delivering Patient Care Many advances have been introduced in the health sector in the recent years. Use of modern technology is one that simplified the administration of health sector. Health information technologies (HIT) include mobile phones, computers, self-administration equipment, health decision-making management devices, life style modification devices, monitoring chronic illness and patient education devices (Gustafson et al., 2002). Socioeconomic barriers cause slow penetration of HIT in developing countries (Connie et al., 2010).
Setting up an appropriate HIT within a health sector is a challenge for technologists as many factors would be taken into account while considering it, and to facilitate the system, a framework would be employed. By the use of this framework, approaches could be studied and the best HIT would be employed (Connie et al., 2010). Some factors that would be taken into consideration include situational factors like setting and clinical domain, technological factors and work force (Connie et al., 2010).
Other remarkable innovations include the establishment of RAPT, which is a rapid assessment and initial patient treatment team within accident and emergency, where the patient would be allocated 4 hr of comprehensive treatment in an emergency condition (Cronin et al., 2005).
Personal care within the department of paediatrics and geriatrics is one of the other innovations (Cambern et al., 2009). This would reduce the incidence of risk and errors causing adverse reactions in them.
My intention of study would be to try and implement some of the innovations in a hospital environment and examine the quality in terms of health care. 12/16/2010 Research Proposal.
5. FACILITIES TO BE USED: Many facilities would be used to perform the following objectives in accordance with available resources and these include:
- Discussion with various people across the health sector to set up the economic evaluation loop in order to set up priorities in patient safety.
- Seeking clearance to participate in some clinical trials which would enable to understand the association of public and patients in primary health research.
- Visiting hospitals and health care organisations to examine and record the facilities for a certain group of patients.
- Getting initial training in the system of control within the primary health sector to minimise the occurrence of errors.
- Many paper and poster articles analysing different approaches of patient education.
- Certain use of technology to study the improvement of quality with the use of innovation.
6. PROGRAM SCHEDULE AND DELIVERABLES: (A basic gnat chart without dates, client should set up dates appropriately)
7. FUNDS AVAILABLE: Client has to decide according to available funding
8. REFERENCES: Warburton, R.N. (2005) Patient safety-how much is enough? Health policy,71, pp.223-232.
Perrow, C. (1984) Normal accidents: living with high risk technologies. New York Basic Books.
Leape, L. L., Forward, I.N (1999). Error reduction in health care: a systems approach to improving patient safety. Jossey-Bass.
Tugwell, P.,Bennett, K.,Feeny, D.,Guyatt, G.,Haynes, R.B. (1986) A frame work for the evaluation of technology. Institute in research and public policy, pp.41-56.
Tugwell, P.,Sitthi-Amorn, C.,O’Connor, A.,Hatcher-Roberts ,J.,Bergevin, Y.,Wolfson, M (1995)
Technology assessment. Old, new and needs-based. International Journal of Technology Assesment in Health care, 11(4), 650-662.
Jonathan, B.,Wendy, B.,Claire.,B. (2010) Public involvement at the design stage of primary health research: A narrative review of case examples. Health policy, 95, pp.10-23.
Boote, J.,Telford, R., Cooper, C. (2002) Consumer involvement in health research: a review and research agenda. Health policy, 61(2), pp.213-236.
Beresford, P. (2005) Developing the theoretical basis for service user/survivor-led research and equal involvement in research. Epidemiologia e psichiatria Sociale, 14(1), pp.4-9.
Thompson, J.,Barber, R.,Ward, P.R.,Boote, J.D.,Cooper, C.L.,Armitage, C.J. (2009) Health Researchers’ attitudes towards public involvement in health research. Health expectations, 12(2), pp.209-220.
Coles, C. (1995) Educating the health care team. Patient Education and Counseling, 26, pp.239-244.
Connie, V.C.,David, R.K. (2010) A technology selection frame work for supporting delivery of patient-oriented health interventions in developing countries. Journal of Biomedical Informatics, 43, pp.300-306.
Cambern, K. (1952) A quality improvement program. Pediatrics and child health, pp.5172-5175.
Cronin, J.G.,Wright, J.RN. (2005) Rapid assessment and initial patient treatment team-a way forward for emergency care. Accident and Emergency Nursing, 13, pp.87-92.
Gustafson, D.H.,Hawkins, R.P.,Boberg, E.W.,Mc Tavish, F.,Owens, B.,Wise, M. (2003) 10 years of research and development in consumer health informatics for broad populations, including the underserved. Med inform, 65(3), pp.169-177.
GNATT (1994) Founded by Paul
Cite this page
Similar essay samples.
- Performance Modelling and Evaluation of a Wireless Cellular Network of...
- Essay on Plagiarism
- Essay on How Useful Is the Source in Providing Information About the E...
- Research Paper on Importance of Having a Culture of a Learning Organiz...
- Essay on How Pigeons Became Rats: The Cultural-Spatial Logic of Proble...
- Argument Essay Against Online Censorship by Tech Companies
Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.

Research Programme for Social Care

The NIHR Research Programme for Social Care (RPSC) call is a bi-annual competition specifically for social care proposals.
The aim of RPSC is to fund research that generates evidence to increase the effectiveness of social care services, provides value for money and benefits people who need or use social care services, and carers. Research will cover both adults and children's social care.
RPSC replaced NIHR's Research for Social Care call (RfSC) in September 2023. The final RfSC call was Call 7. For further information about this, please see the relevant call documents .
Latest funding opportunities for Research Programme for Social Care
Research Programme for Social Care - Call 2
All social care funding opportunities
The Research Programme for Social Care encourages applications from researchers from all stages of their careers, and includes a sub stream for early career researchers as well as funding for capacity building.
Proposals should demonstrate appropriate research expertise, and teams should have a track record of relevant published research.
RPSC invites applications from higher education institutions, charities, local authorities/governments and relevant third sector organisations in all four nations of the UK.
What do we fund?
RPSC funds research that generates evidence to improve, expand and strengthen the way social care is provided for users of care services, carers, the social care workforce, and the public across the UK. Please read the full scope for further details.
How long and how much?
The amount awarded and the length of the funding period depends on the nature of the proposed work. Strong justification for the research duration and funding requested is required and will be considered by the reviewing committee.
RPSC also offers opportunities for early career researchers to apply for applications up to £250,000, providing they are supported by an appropriate team which is suitably resourced. These applications will be reviewed by the assessing committee but will not be in direct competition with larger awards or those from non-early career researchers.
As part of NIHR's drive to develop research capacity, RPSC is offering the opportunity to develop and advance social care research capacity building. Applicants to RPSC can include funding for research capacity development, across all stages of the academic career pathway (i.e., from internships to Masters to PhD to post-doctoral), As a general rule, it is anticipated that 10% to 20% of the overall project programme grant budget should be spent on capacity building within the grant, however each request will be reviewed on its merits. More information can be found in the capacity building guidance .
For more information, see the stage 1 finance guidance .
When is funding available?
RPSC has two researcher-led calls per year and also operates commissioned calls on priority highlight topics. See the dates for our funding competitions .
How to apply
All RPSC calls typically use a two stage application process. Please see the applicant guidance for stage 1 to find out more.
Applicants considering submitting a stage 1 application may wish to submit an outline of their proposal for guidance before official submission. This can be done using the pre-submission form . This is not mandatory and purely aimed at helping potential applicants to engage with the requirements of the call (e.g. eligibility and remit).
Research proposals are submitted to RPSC online through the Research Management System. We supply Word document versions of the online application Stage 1 form and Stage 2 form , to help researchers prepare their proposal ahead of submission.
Advice and support is available from the NIHR Research Support Service to develop your research proposal.
If you are applying as a Local Authority, you can find out more information on our Local Authorities page .
If you are applying as a Charity, you can find out more information on our Charities page.
What we fund
Applications through the Research Programme for Social Care should have:
- A clear pathway to social care benefit that could be immediate or over a longer-term
- A strong link with people who need or use social care, carers and organisations which provide social care services or other relevant groups
- An appropriate team, likely consisting of social care researchers, members of the social care workforce, carers, methodologists and people who use social care, reflecting the nature of the application
We are aware that social care is broad. If you are unsure as to whether a topic is within scope for the programme, please see the call specification , contact the team or submit a pre-submission form . We also suggest consulting our logic model, to understand the intended outcomes of the programme, and consider how your topic links to this.
The RPSC team are holding a webinar on 04 April 2024 10am-12 BST, to give more information about the aims of the programme and to provide useful information about the application process. Sign up for the webinar.
Our programme director
Professor Martin Knapp is Director of the Research Programme for Social Care.
Our funding committee
RPSC is a UK-wide programme open to applicants in England, Wales, Scotland and Northern Ireland. Applications are reviewed by a committee comprising social care experts, methodologists, public and practitioner members.
Committee members review all stage 1 and stage 2 applications and make funding recommendations based on the quality of applications, with support from expert peer reviewers.
The committee recommends projects for funding to the Department of Health and Social Care, which approves the projects to be funded.
Members of NIHR committees are required to declare any interests which conflict, or may be considered to conflict, with NIHR business, or may be perceived as influencing decisions made in the course of their work within NIHR programmes. All members are asked to complete the Register of Interest form (annually), which is intended to capture long term predictable interests that could be perceived to lead to conflicts of interest. These and other interests are judged on a case by case basis at individual meetings.
View our current funding committee.
NIHR registry of interests
Interested in joining one of our committees? View our committee vacancies .
We offer a wide variety of assistance during all stages of the research process. If in doubt, please get in touch.
If you would like the team to comment briefly on your research plan please complete the presubmission form . If you have a query not answered in the above documents, please check the FAQs ,
Tel: 020 8843 8057 Email: [email protected] Our operating hours are 9am to 5pm.
For support to develop your research proposal contact the NIHR RSS Specialist Centre for Social Care. The RSS Specialist Centre works nationally to provide free and tailored advice to social care researchers of all levels and experience, offering a broad range of methods expertise and research support, including expert advice on public involvement and developing and delivering inclusive research that incorporates the voice of service users, carers and practitioners.
Latest news about Social Care

Digital training programme improves quality of life for care residents with dementia

NIHR launches £10m funding programme for social care research

New campaign to help develop careers in research

Browse all our research projects by topic We have funded more than 150 external research projects across a range of themes over the last five years
- Share on Twitter
- Share on LinkedIn
- Share on Facebook
- Share on WhatsApp
- Share by email
- Link Copy link
Please click below to see the research projects we've funded on the following topics.
- Analytics and data
- Children and young people
- Commissioning
- Community and voluntary
- Digital technology
- Efficiency and productivity
- Emergency medicine
- End of life care
- Funding and sustainability
- Improvement science
- Inequalities
- Integrated care
- Long-term conditions
- Mental health
- Older people
- Patient experience
- Patient safety
- Person-centred care
- Primary care
- Public health
- Quality improvement
- Quality of care
- Social care
- Social determinants of health
Share this page:
Health Foundation @HealthFdn
- Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
The Q community
Q is an initiative connecting people with improvement expertise across the UK.

Quick links
- News and media
- Events and webinars
Hear from us
Receive the latest news and updates from the Health Foundation
- 020 7257 8000
- [email protected]
- The Health Foundation Twitter account
- The Health Foundation LinkedIn account
- The Health Foundation Facebook account
Copyright The Health Foundation 2024. Registered charity number 286967.
- Accessibility
- Anti-slavery statement
- Terms and conditions
- Privacy policy

We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essays Samples >
- Essay Types >
- Research Proposal Example
Health Care Research Proposals Samples For Students
121 samples of this type
Regardless of how high you rate your writing skills, it's always a worthy idea to check out an expertly written Research Proposal example, especially when you're dealing with a sophisticated Health Care topic. This is exactly the case when WowEssays.com database of sample Research Proposals on Health Care will prove handy. Whether you need to come up with a fresh and meaningful Health Care Research Proposal topic or examine the paper's structure or formatting peculiarities, our samples will provide you with the required material.
Another activity area of our write my paper website is providing practical writing support to students working on Health Care Research Proposals. Research help, editing, proofreading, formatting, plagiarism check, or even crafting fully unique model Health Care papers upon your demand – we can do that all! Place an order and buy a research paper now.
Free Research Proposal On Aims Of The Research
Introduction, example of building health information technology workforce: challenges and strategies research proposal, research proposal on medios electronic health record (ehr) software: the most innovative healthcare technology.
Don't waste your time searching for a sample.
Get your research proposal done by professional writers!
Just from $10/page
Good Research Proposal On Should Businesses Provide Employees Healthcare Insurance
Project overview, good law research proposal example, corruption in health systems research proposal samples, example of health research proposal, free research problem research proposal sample, research outline.
- Abstract - Introduction - Concept - Research problem - Research questions - Research objectives - Research justification - Limitations of the study - Assumptions - Scope of the study - Ethical considerations - Literature review - Research methodology
Free Health Disparities Research Proposal Example
Health disparitiesintroduction, how a bill becomes a law research proposals example, situation: is this something that can be legislated, good example of purpose research proposal.
The aim of this study is to quantify ED-generated follow-up adherence rates amongst white, Black American, and Hispanic patients discharged from the ED of a managed care system.
Problem Statement
Free research proposal on rfp response, proposal overview and requested project, problem, purpose and the question research proposal example, xxxxxxxxxx research proposal, health care.
Introduction Research question, aims and objectives Literature search strategy Appraisal of key study Identification of key themes Literature search strategy
Action plan
Research proposal on master project, master project document one, research proposal on technology in nursing, the legalization of marijuana research proposal, specific aims and hypotheses, future of managed health care delivery system research proposal samples, medical knowledge management: research proposal examples, free research proposal about telemedicine, telemedicine to manage hypertension, diabetes and asthma, grant proposal for health system strengthening in kenya research proposal examples.
Executive Summary
Good Research Proposal On Problem Description
Implementation of information technology in healthcare systems – research proposal, ait case study cover sheet research proposals example.
in Healthcare Systems Past Courses: Please list all course completed and currently taking. Remember that you must complete all prerequisites in order to register for a case study.
Implementation of Information Technology in Healthcare Systems
Non-economic factors that effect on demand for health care research proposal examples, free research proposal about project proposal, introduction to the organization, good example of curbing the risk of infection in healthcare environments research proposal, mission, vision, values, and ethics statements research proposal examples, following the guidelines of the course id guidelinesstudent’s nameuniversity, hand washing: healthcare-acquired infection prevention research proposals examples, data analysis and analytics research utilization project proposal research proposal examples, data analysis and analytics research, good example of cultural diversity at advocate health care research proposal, example of purpose of the study research proposal, good proposed solution research proposal example.
Amongst mentally ill patients at high risk for early readmission, does the utilization of a multi-component transition care plan as compared to usual care help to improve early readmission rates?
Nurse Hand Hygiene Practices Research Proposal
Example of health care reforms research proposal, good the impact of km strategies on hospital performance improvement in saudi arabia research proposal example.
The Saudi Arabian government ensures that it focuses in the implementation of KM strategies to enhance improvements in service provision. The paper looks at the impact of introducing the strategies in the hospitals. It can be seen that KM supports knowledge and information sharing which boosts communication hence facilitating great improvement in hospital sector. Knowledge management helps to solve both existing and emerging issues in healthcare with a goal to improve hospital performance in Saudi Arabia.
Overview & Justification of the Research
Research proposal on target population, ohio state medical center research proposal sample, advocate good samaritan hospital marketing plan research proposal examples, executive summary, good example of slide 1 research proposal, promoting healthy prescription filling behaviors in the elderly to prevent polypharmacy research proposal sample.
The health promotion goal The U.S. health care system’s goal is to maintain health-related quality of life and well-being by evaluating the emotional, physical, mental, and social functioning of an individual. The focus aims at determining the impact of the health status of a person the quality of life in additional to other measures such as causes of death, life expectancy, and population health (Healthy People 2020, 2016). The project aims at improving the health, function, and quality of life by promoting healthy prescription filling behaviors in the elderly adult to prevent Polypharmacy.
Proposed intervention to address the goal
Free wound care education research proposal sample, good research proposal on health, developing a health program in a non-profit family shelter, free critical analysis research proposal sample.
LIMITED UNDERSTANDING OF THE PERCEPTION OF AFRICAN WOMEN IMMIGRANTS IN THE UK AS THE RESULT TO THE CURRENT TREND OF INADEQUATE CLINICAL INTERVENTION FOR POSTNATAL DEPRESSION PATIENTS Limited understanding of the perception of African Women Immigrants in the UK the Cause of the Current trend of inadequate Clinical Intervention
Community Health Proposal Research Proposal Example
Free wound care education for healthcare providers research proposal sample.
There is a growing need for the education of healthcare workers, for them to efficiently cover and treat wounds and prevent contamination. Thus, there should be an evidenced approach in evaluating differences in the approach of treatment that medical practitioners use in various spheres. For this, it is important to examine some evidences on the different treatment of wounds that are being used nowadays in healthcare. This is crucial for medical practitioner training, while providing opportunity for developing proficiencies with regards to proper wound care, which may avert undesired patient outcomes in hospitals.
Evidence Review
Overcoming communication barriers research proposal, free nursing proposal research proposal sample, chapter one: introduction 1.
Background 1 Statement of the Problem 2 Research Objectives 2 Research Questions 3 Significance of the study 3 Chapter Two: Literature Review 4 Introduction 4 Theoretical Literature 4 Empirical Literature 5 System Barriers 5 Healthcare Professional Barrier 7 Social Barriers 7 Patient Barrier 8 Chapter Three: Methodology 8 Introduction 8 Research Design 9 Model Specification 9 Study Area 9 Target Population 10 Data Type and data Source 10 Data collection 10 Data Analysis 10
References 11
Acute myocardial infarction patients are a risk for posttraumatic stress disorder research proposals examples, research design research proposals example, role of the hand washing in the spread of infections in hospital research proposal examples, methodology, research proposal on the spread of infections in hospital, introduction, evaluation of jobs in a surgeon-generals office and the importance each role plays research proposal sample, learn to craft research proposals on scope and challenges of transitional nursing for the elderly population with this example, knowledge, attitude and practice of smoking research proposals example, research proposal on the prevalence of diabetes amongst minority populations, the proposal, diabetes: research proposal research proposal example, diabetes in america: research proposal, exemplar research proposal on problem to write after.
Innovative Change Proposal
It is undeniable that complaints are intrinsic aspects in every working environment in an organization (MetricStream Inc, 2016). In healthcare services, however, complaints are highly critical and always require an immediate resolution. Apparently, the number of patient complaints in our health care quality department continues to rise, and no amicable mechanisms are implemented to resolve this issue. This proposal aims to develop an effective patient resolution policy that will help address this critical concern.
Solution/Benefits: Recommendations
Exemplar research proposal on evaluating emr systems to write after, good example of research proposal on wound care education for health care provider, tittle: wound care education for health care provider.
Introduction The principles of nursing efficiency in respect to wounds care education implies the need for developing nursing programs that adopt and accept effective wound care education. Without efficiency in medical specialization, it becomes imperative that wound care would render the entire spectrum of health care provision challenging (Srivastava & Shainesh, 2015; Islam, et al, 2015). The present status of wound care education informs the need for role socialization, clinical rotation schedule and curriculum objective to enhance the responsibilities of medical specialties.
Aims and Objectives
Example of research proposal on effectiveness of nurse practitioners in health care.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline
This paper is in the following e-collection/theme issue:
Published on 27.3.2024 in Vol 13 (2024)
Assessment of Patient Safety in a Low-Resource Health Care System: Proposal for a Multimethod Study
Authors of this article:

- Ghazal Haque 1 , MBBS, MPH ;
- Fozia Asif 1 , MBBS, MBA, MHQS ;
- Fasih Ali Ahmed 1 , MD ;
- Farwa Ayub 1 , MD ;
- Sabih ul Hassan Syed 1 , MBBS ;
- Nousheen Akber Pradhan 2 , BScN, MSc ;
- Malika Hameed 3 , MBBS ;
- Muhammad Muneeb Ullah Siddiqui 2 , MBBS ;
- Shafaq Mahmood 2 , MBBS ;
- Tahani Zaidi 2 , MBBS ;
- Sameen Siddiqi 2 , MBBS, MSc, PhD ;
- Asad Latif 1, 3 , MD, MPH
1 Center for Patient Safety, Aga Khan University, Karachi, Pakistan
2 Department of Community Health Sciences, Aga Khan University, Karachi, Pakistan
3 Department of Anesthesiology, Aga Khan University Medical College, Karachi, Pakistan
Corresponding Author:
Asad Latif, MD, MPH
Department of Anesthesiology
Aga Khan University Medical College
Stadium Road
Karachi, 74800
Phone: 92 2134864639
Email: [email protected]
Background: The high prevalence of adverse events (AEs) globally in health care delivery has led to the establishment of many guidelines to enhance patient safety. However, patient safety is a relatively nascent concept in low- and middle-income countries (LMICs) where health systems are already overburdened and underresourced. This is why it is imperative to study the nuances of patient safety from a local perspective to advocate for the judicious use of scarce public health resources.
Objective: This study aims to assess the status of patient safety in a health care system within a low-resource setting, using a multipronged, multimethod approach of standardized methodologies adapted to the local setting.
Methods: We propose purposive sampling to include a representative mix of public and private, rural and urban, and tertiary and secondary care hospitals, preferably those ascribed to the same hospital quality standards. Six different approaches will be considered at these hospitals including (1) focus group discussions on the status quo of patient safety, (2) Hospital Survey on Patient Safety Culture, (3) Hospital Consumer Assessment of Healthcare Providers and Systems, (4) estimation of incidence of AEs identified by patients, (5) estimation of incidence of AEs via medical record review, and (6) assessment against the World Health Organization’s Patient Safety Friendly Hospital Framework via thorough reviews of existing hospital protocols and in-person surveys of the facility.
Results: The abovementioned studies collectively are expected to yield significant quantifiable information on patient safety conditions in a wide range of hospitals operating within LMICs.
Conclusions: A multidimensional approach is imperative to holistically assess the patient safety situation, especially in LMICs. Our low-budget, non–resource-intensive research proposal can serve as a benchmark to conduct similar studies in other health care settings within LMICs.
International Registered Report Identifier (IRRID): PRR1-10.2196/50532
Introduction
Adverse events (AEs) are instances of injury or harm to patients as a result of medical care and not their underlying medical condition [ 1 ]. They are ubiquitous, with some estimates saying that up to 1 in 10 hospitalizations involve medical errors [ 2 ]. Underreported and often overlooked, they take a heavy toll on health systems globally. In the United States alone, an estimated 250,000 deaths are attributed to AEs annually, making them the third leading cause of mortality in the country [ 3 ]. Moreover, anywhere from 25% to 80% of these errors—some of which lead to a loss of life or permanent disability—are entirely preventable [ 4 , 5 ]. Due to a myriad of factors including but not limited to, understaffing, resource availability and use, and lack of health literacy, health systems within low- and middle-income countries (LMICs) are estimated to experience far more AEs, with an incidence rate ranging between 2.5% and 18.4% [ 5 ].
Given these facts, it is understandable why the domain of patient safety and harm reduction gained traction around the world. Of note, the publication of the Institute of Medicine’s report “To Err is Human” in 2000 served as a benchmark in establishing the relevance of this aspect of health care delivery [ 6 ]. Since then, it has become increasingly apparent that it is a complex issue requiring a multidimensional approach. This school of thought is also linked to the relatively recent emergence of the “systems thinking” concept. This concept emphasizes recognizing the importance of a systems approach in studying the causes of patient harm and advocates for designing an error-proof system. Such an environment is aimed at preventing human errors and focuses on mitigation rather than the elimination of human factors in health care provision [ 7 ]. Additionally, an open and transparent environment where a culture of patient safety is prevalent is also imperative in fostering safe health care systems, which ultimately reduce the chances of errors and AEs. This safety culture can be nurtured by upholding safety beliefs, values, and attitudes among the majority of the workforce [ 8 ].
Moreover, viewing patient safety through a systems lens is a low-resource exercise since it mainly requires a shift in cultural and systemic perspectives. By considering patient safety problems as a product of the interaction between human and system factors, clinicians can evaluate the factors contributing to patient safety issues without the need for expensive or time-consuming resources [ 7 ]. This is particularly important for LMICs where large groups of the population are catered to using precious scarce resources and more often than not, have fewer human resources available per capita. The low cost of these measures makes the establishment of a patient safety culture a near-ideal step in achieving the provision of safe health care delivery and maximizing the quality and impact of health care services [ 9 ]. The cost-effectiveness of patient safety culture and a systems approach is reflected in the idea that prevention of AEs is much less resource-intensive than treating the complications that arise from them and which impose a heavy burden on already strained health systems [ 1 , 10 ].
Knowledge Gap
Though sparse, the existing literature from LMICs suggests that there are considerable knowledge gaps in the patient safety domain despite a general awareness of its importance [ 11 , 12 ]. However, global awareness of patient safety has also resulted in a shift of focus toward improvement in the quality of care in LMICs [ 13 , 14 ]. The Global Patient Safety Collaborative is one such initiative established by the joint efforts of the World Health Organization (WHO) and the governments of the United Kingdom and Northern Ireland to scale up global efforts to prioritize patient safety and improve the safety of health systems at a country level [ 15 ].
Similarly, the WHO’s Global Patient Safety Action Plan for 2021-2030 [ 16 ] outlines some key points in eliminating preventable harm in health care through their defined goals of completely eliminating avoidable harm and ensuring the delivery of safe clinical processes, building reliable health systems to protect patients’ rights to safe and quality care, empowering both health care providers and patients by engaging in productive dialogue to influence patient safety policies, and ensuring effective information and knowledge sharing among health systems and partners to promote multidisciplinary involvement in patient safety. Therefore, to achieve a holistic understanding of the status of patient safety within a health care system, it is necessary to approach the problem simultaneously from multiple perspectives such as the health care provider’s view of patient safety, the health care consumer’s view of patient safety and AEs, the estimated incidence of AEs happening within a health care setting, and the infrastructure available to cater to these problems. To our knowledge, a unified framework that addresses all such facets of patient safety has not been used at scale, hence our proposal is unique in its approach.
As mentioned above, to establish a proper culture of safety, it is imperative to first assess the existing culture of safety within health systems [ 17 ]. The most commonly used tool for this assessment is the United States Agency for Healthcare Research and Quality’s (AHRQ) Hospital Survey on Patient Safety Culture (HSOPSC), which has been implemented in many countries [ 18 - 21 ], translated into several different languages, and can be adapted to fit the local context of most countries [ 22 ]. Similarly, the AHRQ’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) questionnaire is used globally to assess the patient perspective on health care provision and service delivery. Standards such as the Joint Commission International Accreditation and the WHO’s Patient Safety Friendly Hospital Framework (PSFHF) serve as benchmarks against which health care settings can be measured on their quality indicators.
LMICs can greatly benefit from initiatives like the Global Patient Safety Collaborative and PSFHF and from using tools such as the HSOPSC and HCAHPS, to perform comprehensive risk assessments of their hospitals, deliver patient safety education and training, establish a culture of safety, and expand the capacity for patient safety within their hospitals [ 23 ]. The generalizability of these standardized, validated tools makes them easily adaptable to the local context and can help evaluate patient safety standards across varying health systems. However, there is a considerable dearth of research in this domain in LMICs and to our knowledge, a comprehensive study on patient safety has not been undertaken so far in Pakistan.
With this proposal, our goals are to evaluate, develop, and implement evidence-based patient safety assessment policies and recommend patient safety strategies and plans that can be replicated across low-resource settings. In order to achieve these goals we aim to perform a comprehensive assessment of the patient safety problem at a sample of hospitals in each province in the country. Additionally, we seek to analyze the results of these assessments to establish the status of patient safety problems in local hospitals, in order to recommend practical steps and policy guidelines for improvement.
Patient Safety Assessment Framework
To better comprehend the range of patient safety problems and their contributing factors at a variety of hospitals across the country, we propose a multifaceted, multimethod approach with the goal of developing a holistic understanding of patient safety issues within the local health care system. For this purpose, we have devised a conceptual framework for the holistic assessment of the patient safety status across variable health settings. Our framework for the assessment of patient safety ( Figure 1 ) in a low-resource setting approaches the problem from a systems thinking lens. We aim to evaluate each hospital setting on its safety culture, the incidence of AEs, and existing infrastructural standards against a minimum, preset standard. After the study sites are identified and all necessary approvals are obtained, multiple methodologies will be used to analyze the patient safety situation at these sites within 3 interconnected domains: patient safety culture, AE detection, and patient safety infrastructure. We shall use 6 different approaches that can be variably used in either a multicenter study design or in individual health care settings.

Study Site Selection
In our proposal, a cross-section of public and private hospitals providing varying levels of care to urban or rural populations will be considered for these assessments. Since there is not a single electronic health record network or a unique quality standard implemented across all hospitals in Pakistan, our aim would be to include hospitals participating in the World Health Organization’s Patient Safety Friendly Hospital Initiative. The Patient Safety Friendly Hospital Initiative involves a basic, easily implemented framework for hospital quality standards developed by the WHO Regional Office for the Eastern Mediterranean and has been successfully piloted in 7 countries including Pakistan [ 24 ]. Attempts will be made to include 1 secondary or tertiary hospital from each province to accommodate for regional variations in a decentralized health system. Following this, key personnel will be identified from the selected centers and stakeholder meetings will be conducted to get the appropriate permissions from all relevant parties on board for subsequent hospital assessments.
Ethical Considerations
Prior to data collection, separate approvals will be obtained from the institutional research review board or an equivalent body of each participating institute. An overarching approval will also be obtained from the institution conducting the research. For study components requiring individual responses, an informed consent form in either English or a certified Urdu translation will be obtained per the respondent’s preference. Each respondent will also be offered a blank copy of the consent form.
For study components requiring medical record access, a review of the participating health center’s policy on data governance and sharing will be conducted before any medical records are requested for the study. Consent will be obtained from all relevant institutional authorities prior to medical record reviews. All identifying information will be coded to ensure strict patient confidentiality and anonymity. The collected data will be stored on secure servers with limited access provided only to authorized research personnel. All information generated will be used exclusively for research purposes in accordance with local regulations.
Safety Culture
Focus group discussions.
To assess the existing infrastructure and culture of patient safety and quality improvement at the study sites, focus groups will be conducted with teams comprising each hospital’s leadership, unit-level management, and frontline health care workers. Administrative staff, physicians, nurses, and technicians will be targeted for responses in representative proportions. During these discussions, in-depth interviews will be conducted to try to capture informal methods of health care delivery that might be in practice at each institute, to get an idea of the local understanding of patient safety, and to identify the problems associated with it. A qualitative analysis will be performed following these interviews to identify the relevant codes and themes pertaining to the patient safety situation in these hospitals. Textbox 1 shows a sample of the prompts that will be used for these interviews.
- What is your understanding of quality and patient safety?
- What processes/activities/mechanism currently exist at your hospital for quality improvement and patient safety?
- Please share the last unexpected/adverse event that you have encountered/observed at your hospital
- What activities (if any) are planned for initiating/strengthening the existing quality and patient safety culture at the hospital?
- What are your suggestions to improve/strengthen patient safety at your hospital?
Evaluation of Existing Patient Safety Culture
To evaluate the existing safety culture in the participating hospitals, a survey will be conducted using the Agency for Healthcare Research and Quality’s HSOPSC [ 25 ]. HSOPSC is a standardized, validated tool consisting of 42 items that assess patient safety culture across 12 basic dimensions ( Textbox 2 ). For this survey, a minimum of 2 available personnel belonging to five categories—doctors, nurses, technicians, hospital management, and hospital aides—will be included via quota sampling from the participating hospitals, with a minimum of 10 personnel per hospital. Responses to most items in this survey will be based on a Likert scale, some of which will be dichotomized during analysis to be measured against the predefined composites listed in Textbox 2 .
- Staffing and work pace
- Organizational learning—continuous improvement
- Response to error
- Supervisor, manager, or clinical leader support for patient safety
- Communication about error
- Communication openness
- Reporting patient safety events
- Hospital management support for patient safety
- Hands-off and information exchange
- Number of events reported
- Patient safety rating
Note: Survey items included in the HSOPSC are grouped by safety culture composite measures [ 25 ].
Inpatient Hospital Experience Survey
To measure the quality of the inpatient hospital experience from the patients’ perspective, a modified version of the AHRQ’s Hospital Consumer Assessment of Healthcare Providers and Systems questionnaire will be used to conduct an interview-based survey. The HCAHPS is a widely used standardized survey used to measure patient satisfaction with in-hospital care [ 26 ]. The standard HCAHPS survey contains 29 questions split into 7 discrete categories, which measure the patient’s experience during their hospital stay in specific areas of inpatient health care delivery. As a standard practice, it should be administered randomly to adult patients between 48 hours and 6 weeks after discharge from the hospital and a minimum of 300 patients should be surveyed per hospital, from 1 calendar year.
Our modified HCAHPS questionnaire adds one more category with additional questions on pain management, adapted from the Qatar Ministry of Public Health’s Patient Experience Survey for Hospitals ( Textbox 3 ). Using quota sampling for this survey, we aim to target a minimum of 20 patients being discharged from each participating hospital. Most responses in the HCAHPS are measured with a 4-point Likert scale, which during analysis, will be dichotomized into binary values to elicit the highest positive responses to the items—the so-called “top box percentages.”
- Nurse communication
- Doctor communication
- Hospital environment
- In-hospital care experience
- Pain management
- Discharge or transfer information
- Overall hospital rating
- Understanding your care transition upon discharge
Note: Survey categories are based on a standard HCAHPS survey form modified to include questions on pain management [ 26 ].
Adverse Event Detection
Patient–reported incidence of ae.
To understand the patients’ perspective of AEs during health care delivery, we propose a questionnaire-based survey to assess patient safety–related issues including patients’ understanding and experiences of AEs, preventable harm, and local reporting. This survey is adapted from a tool implemented by Southwick et al [ 27 ] to suit the local health care setting. The original study design surveyed almost 700 patients in nearly a 4-year period through a web-based form.
To account for low digital literacy within LMICs we propose using quota sampling to screen patients within the outpatient departments at the study sites to survey those who have availed health care services. Participants will be requested to recall potential AEs experienced during health care delivery using the standardized questionnaire, and the responses will be recorded by a member of the investigating team. The results will be analyzed descriptively to determine the nature and severity of AEs, and their effects as perceived by patients who have received medical care. At least 50 respondents will be interviewed at each study site.
Medical Record–Based Incidence of AEs
To calculate the incidence of AEs during hospitalization, a review of medical records will be performed at each hospital. The sample size for this study will be calculated based on the annual inpatient volume at each hospital with a 5% significance, a precision of 3%, and an estimated 10% dropout rate due to unavailability or poor quality of medical records. A range of prevalence of 10%-18% will be assumed as representative of the population. A team of investigators will also perform a data quality check of the existing medical records against a standardized checklist prior to the review [ 28 ].
Following this, a retrospective chart review of the medical records will be conducted in a 2-step process. In the first step, all charts will be screened using a standardized AE screening form, “Review Form 1” (RF1) to identify any potential AEs. All AEs identified using RF1 will then be evaluated using “Review Form 2” (RF2) to establish the nature, causality, and the factors contributing to these AEs. Both review forms have been adapted from the WHO patient safety research tools for data-poor hospitals and contain extensive screening and investigative questions to assess and analyze “harmful incidents” or “adverse events” [ 29 ]. The incidence of AEs will be calculated using the following formula:
Additionally, a descriptive analysis will be performed on the types of AEs, their potential causes, and the likely systemic and human factors contributing to the event.
Patient Safety Infrastructure Assessment Against the WHO’s Patient Safety Friendly Hospital Framework
The PSFHF is based primarily on 5 domains and 22 standards [ 30 ], which together comprise 134 criteria that are prioritized into critical, core, and developmental categories ( Table 1 ).
The 25 critical criteria are the basic minimum requirements that hospitals are encouraged to achieve in terms of quality improvement. To assess each hospital’s standing against the PSFHF criteria, members of the investigating team will conduct in-person surveys of the facilities to observe the implementation of standards. They will also review standard operating procedures and existing hospital protocol documents, and check for the existence of an AE reporting system. Interviews with staff members and patients will also be conducted. All these observations will be recorded against the existing standard criteria set within the PSFHF and after a comprehensive review, a list of recommendations will be provided by the investigators in light of their findings.
Project Execution
In order to conduct all the above study components in an organized and timely manner, the investigating team will comprise health care professionals recruited from the core team and regional partners, who will be trained in conducting each survey. All survey instruments will be developed and recorded in English, whereas the written consent forms for participant recruitment will be translated into the local language as well. The interviewers will be fluent in both languages. The proposed timeline of events for conducting each component of the assessment is given in Figure 2 .
It should be noted that as part of a theoretical framework, this proposed timeline includes a timeframe for the completion of each part of this multimodal approach, carried out simultaneously by multiple teams at each site. However, the authors understand that various levels of care within various health care systems require different facets of evaluation. Thus, it is recommended that the approach within this framework be modified according to the local organizational and operational structures and the given limitations of the health care setting being assessed. Subsequently, the project timeline can vary depending on the number of assessments being conducted.

A thorough quantitative and qualitative analysis will be conducted which will be aimed for publication in the form of a technical report.
Patient safety culture is an essential component of health care provision and can significantly impact patient outcomes. The beliefs, attitudes, and behaviors of health care providers can significantly affect their understanding of and commitment to ensuring patient safety [ 10 ]. Research has consistently shown that a positive patient safety culture leads to improved patient outcomes, increased staff satisfaction, and reduced health care costs [ 31 ]. Conversely, a lack of an open, transparent culture focused on patient safety can result in medical errors, AEs, and poor patient outcomes [ 17 ]. LMICs in particular fall behind in prioritizing patient safety due to a lack of practical policies and procedures, inadequate education and training, and lacking a culture of transparency and open communication to ensure the best possible patient outcomes [ 5 ]. These are largely attributed to the chronically depleted health resources in the region, however, establishing a culture of safety does not necessarily require high-cost interventions. Additionally, in order to establish a sustainable culture of safety, it is essential to first identify the gaps that lie within this system.
Studying the incidence and prevalence of AEs within a health system is an effective way to gauge the status of patient safety. Historically, this has been achieved using incident reporting systems and retrospective chart reviews to record error prevalence [ 32 , 33 ], health consumer and provider surveys [ 19 , 23 , 34 ], and by studying medical litigation cases [ 35 ]. There is a considerable amount of literature from high-income countries that highlights the incidence and impact of AEs in health care [ 2 , 27 , 36 ], however, the same is not true for LMICs [ 5 ]. Moreover, patient safety problems are multifactorial and therefore require a diverse yet intertwined approach to obtain a comprehensive understanding of the problems involved, such as system-based issues, which tend to be locally unique at the unit, hospital, or even regional level. For example, an inpatient hospital setup might have patient safety concerns due to culture issues, while the emergency room at the same hospital might have patient safety concerns due to inadequate resources for their volumes. Similarly, the same type of work area in variably resourced settings, such as the intensive care unit in a public versus a private hospital might have vastly different reasons for gaps in patient safety. Therefore, a comprehensive risk assessment of factors contributing to patient safety concerns is the first step in identifying these issues and subsequently addressing them.
Therefore, our proposed multimodal methodology for assessing patient safety issues in the Pakistani health care system is a pragmatic approach to the problem. With the participation of local and federal stakeholders, the application of our research proposal is easily achievable at a very low cost to the health system. Estimating the incidence of AEs from retrospective chart reviews and patient interviews, assessing the presence of a safety culture within hospitals by interviewing health care providers, learning from patient experiences within the hospital through surveys, and examining hospital compliance to quality improvement measures are all technically sound methods to ascertain the dynamics and challenges within patient safety culture.
Challenges and Solutions
However, even with a less resource-intensive approach such as ours, the local health system still poses many challenges. Implementation of patient safety protocols for quality health care provision in LMICs is limited, mainly due to the unavailability of resources and proper infrastructure. A significant number of health care facilities in Pakistan lack essential equipment, life-saving medications, and adequately trained staff to provide safe and effective care to patients [ 37 ]. Additionally, given the diversity in the local population in terms of language and regional lifestyle differences, health care providers can encounter cultural and linguistic barriers that hinder their ability to communicate effectively with patients, which can subsequently compromise patient safety.
Furthermore, the lack of access to continuing medical and nursing education and training opportunities results in poor understanding and implementation of patient safety protocols among health care providers. Additionally, a decentralized health care system paired with political instability and poor governance frequently results in inadequate funding [ 37 ] and a dearth of regulations for implementing patient safety protocols effectively. Consequently, health care providers in Pakistan continually navigate these multifaceted challenges while striving for the provision of safe, effective, and quality care for their patients [ 38 ].
We anticipate all these issues to surface during our research project as well. To begin with, a significant challenge in collaborative risk assessments in a decentralized health system is to have all the various stakeholders agree on a singular model. Additionally, the lack of a common understanding of the concept of patient safety risk assessment results in discrepancies in the identification and management of risks by the health care providers at different institutions. Moreover, limited channels of communication among the local health care systems also mean that effective collaboration and information sharing among health care providers is almost nonexistent.
Another significant challenge in our research will likely be the absence or inadequacy of medical records within the local hospitals. Poor medical records result in incomplete or incorrect information about medical histories, leading to inaccurate diagnoses, inappropriate treatment, and consequently, AEs. Predictably, poor medical records might limit our ability to track patient progress and treatment outcomes, which can hinder the identification and management of AEs in a retrospective analysis of medical errors and near-misses.
In order to mitigate these problems head-on, we shall aim to diligently communicate with all federal and provincial stakeholders, listen to their concerns, and with the help of our subject matter experts, express our research ideas, intentions, and expected outcomes as transparently as possible. Additionally, the investigating team will include regional partners who can provide valuable cultural and linguistic context to the data collection process. To streamline the project focus, we shall invite all the major stakeholders to a brainstorming session where their perceptions and practices regarding patient safety will be discussed and incorporated within the data analysis. To combat the problem of poor quality of medical records, all reviewed charts will undergo a quality assessment [ 28 ] before they are included in the data set and a wider margin for dropouts will be adjusted in the sample size calculation if needed. Finally, given the law-and-order situation in the country, all efforts will be made to ensure the physical security of the investigating team and the project data.
Our patient- and provider-centered approach to patient safety assessment incorporates the Global Patient Safety Action Plan goals [ 16 ] of empowering patients, encouraging health care workers to participate in fostering a culture of safety, sharing valuable information across health systems, promoting transparency in incidence event reporting and making health care delivery safer to produce better outcomes. Building on this knowledge of the patient safety status in Pakistan, we hope to inform and inspire policy making and strive to align local patient safety standards with global recommendations.
Strengths and Limitations
Our research proposal has many strengths. Given the proposed diversity of health care facilities in our study sample, and their varying capacities for health care provision, no single assessment tool can provide an exhaustive description of the patient safety situation in these hospitals. Hence, our diverse multimethod approach is not only unique within patient safety research in LMICs, but it will also provide a comprehensive assessment of the situation. The inclusion of patient safety and quality experts within the research group is also a unique feature for a survey of this magnitude. The relatively low cost of our proposed methodology and short execution time will encourage stakeholder interest in the project. Moreover, our final analysis is expected to provide a first-of-its-kind perspective on the patient safety situation, particularly within the public health care system.
Some of the limitations of our study include the significant disparity in the perception of health economics and literacy in the study population. This can result in a wide shift in the perception of quality indicators in health care between high and low-income countries. This requires adjusting the existing global standards in quality health care delivery against the local perception of it. Moreover, the reliance on retrospective chart reviews limits information availability, while patient interviews introduce the possibility of respondent recall bias in assessing the incidence of AEs. Additionally, some geographical areas of interest for our study might not be logistically or politically feasible for inclusion. There might also be concerns among the participating hospitals regarding data sharing with other institutions. However, all efforts will be made to ensure compliance with confidentiality standards.
Conclusions
Our multidimensional, multimethod research proposal to assess and analyze the patient safety situation on a large scale within the Pakistani health care system is a unique approach to broaching the domain of patient safety in the country. We are confident that our methodology will produce good quality data so that we can use our study results in writing situation analyses, offering policy recommendations, and hopefully, instigating some real change in prioritizing and implementing a safety culture in Pakistani hospitals. Moreover, our research proposal can be easily implemented in other LMICs with a few minor adjustments in the local context.
Acknowledgments
All authors declared that they had insufficient or no funding to support open access publication of this manuscript, including from affiliated organizations or institutions, funding agencies, or other organizations. JMIR Publications provided article processing fee (APF) support for the publication of this article.
Data Availability
Data sharing is not applicable to this article as no data sets were generated or analyzed during this study.
Authors' Contributions
AL, F Asif, and SS contributed to the conceptualization and design of the study. GH drafted the manuscript. AL, F Asif, FAA, F Ayub, SHS, NAP, MH, MMUS, SM, and TZ reviewed and edited the manuscript.
Conflicts of Interest
None declared.
- Rodziewicz TL, Houseman B, Hipskind JE. Medical error reduction and prevention. In: StatPearls. Treasure Island (FL). StatPearls Publishing; 2023. [ Medline ]
- de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. Jun 2008;17(3):216-223. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. May 03, 2016;353:i2139. [ CrossRef ] [ Medline ]
- Schwendimann R, Blatter C, Dhaini S, Simon M, Ausserhofer D. The occurrence, types, consequences and preventability of in-hospital adverse events - a scoping review. BMC Health Serv Res. Jul 04, 2018;18(1):521. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wilson RM, Michel P, Olsen S, Gibberd RW, Vincent C, El-Assady R, et al. Patient safety in developing countries: retrospective estimation of scale and nature of harm to patients in hospital. BMJ. Mar 13, 2012;344:e832. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Institute of Medicine Committee on Quality of Health Care in America. In: Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington (DC). National Academies Press (US); 2000. [ CrossRef ]
- Carayon P, Wooldridge A, Hoonakker P, Hundt AS, Kelly MM. SEIPS 3.0: Human-centered design of the patient journey for patient safety. Appl Ergon. Apr 2020;84:103033. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Guldenmund FW. (Mis)understanding safety culture and its relationship to safety management. Risk Anal. Oct 2010;30(10):1466-1480. [ CrossRef ] [ Medline ]
- Kaur G, Prinja S, Lakshmi PVM, Downey L, Sharma D, Teerawattananon Y. Criteria used for priority-setting for public health resource allocation in low- and middle-income countries: a systematic review. Int J Technol Assess Health Care. 2019;35(6):474-483. [ CrossRef ] [ Medline ]
- Bates DW, Singh H. Two decades since to err is human: an assessment of progress and emerging priorities in patient safety. Health Aff (Millwood). Nov 2018;37(11):1736-1743. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nabilou B, Feizi A, Seyedin H. Patient safety in medical education: students' perceptions, knowledge and attitudes. PLoS One. 2015;10(8):e0135610. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shah N, Jawaid M, Shah N, Ali SM. Patient safety: perceptions of medical students of Dow Medical College, Karachi. J Pak Med Assoc. Dec 2015;65(12):1261-1265. [ Medline ]
- Patient Safety: Making Health Care Safer. World Health Organization. 2017. URL: https://www.who.int/publications/i/item/WHO-HIS-SDS-2017.11 [accessed 2022-12-10]
- The Lancet. The struggle for universal health coverage. Lancet. Sep 08, 2012;380(9845):859. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Global patient safety collaborative. World Health Organization. 2019. URL: https://www.who.int/initiatives/global-patient-safety-collaborative [accessed 2022-12-06]
- Global Patient Safety Action Plan 2021-2030: Towards Eliminating Avoidable Harm in Health Care. World Health Organization. 2021. URL: https://www.who.int/teams/integrated-health-services/patient-safety/policy/global-patient-safety-action-plan [accessed 2023-01-20]
- Hellings J, Schrooten W, Klazinga N, Vleugels A. Challenging patient safety culture: survey results. Int J Health Care Qual Assur. 2007;20(7):620-632. [ CrossRef ] [ Medline ]
- El-Jardali F, Jaafar M, Dimassi H, Jamal D, Hamdan R. The current state of patient safety culture in Lebanese hospitals: a study at baseline. Int J Qual Health Care. Oct 2010;22(5):386-395. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chen IC, Li HH. Measuring patient safety culture in Taiwan using the Hospital Survey on Patient Safety Culture (HSOPSC). BMC Health Serv Res. Jun 07, 2010;10:152. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Waterson P, Griffiths P, Stride C, Murphy J, Hignett S. Psychometric properties of the hospital survey on patient safety culture: findings from the UK. Qual Saf Health Care. Oct 2010;19(5):e2. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bodur S, Filiz E. Validity and reliability of Turkish version of "Hospital Survey on Patient Safety Culture" and perception of patient safety in public hospitals in Turkey. BMC Health Serv Res. Jan 28, 2010;10:28. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Palmieri PA, Leyva-Moral JM, Camacho-Rodriguez DE, Granel-Gimenez N, Ford EW, Mathieson KM, et al. Hospital survey on patient safety culture (HSOPSC): a multi-method approach for target-language instrument translation, adaptation, and validation to improve the equivalence of meaning for cross-cultural research. BMC Nurs. 2020;19:23. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ahmed FA, Asif F, Munir T, Halim MS, Feroze Ali Z, Belgaumi A, et al. Measuring the patient safety culture at a tertiary care hospital in Pakistan using the Hospital Survey on Patient Safety Culture (HSOPSC). BMJ Open Qual. Mar 2023;12(1):e002029. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Siddiqi S, Elasady R, Khorshid I, Fortune T, Leotsakos A, Letaief M, et al. Patient safety friendly hospital initiative: from evidence to action in seven developing country hospitals. Int J Qual Health Care. Apr 2012;24(2):144-151. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yount N, Sorra J, Famolaro T, Gray L, Rockville W. Hospital Survey on Patient Safety Culture Version 2.0: User's Guide. Rockville, MD. Agency for Healthcare Research and Quality; 2021. URL: https://www.ahrq.gov/sops/surveys/hospital/index.html [accessed 2024-02-07]
- Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). Baltimore, MD. Centers for Medicare & Medicaid Services URL: https://hcahpsonline.org/ [accessed 2023-05-11]
- Southwick FS, Cranley NM, Hallisy JA. A patient-initiated voluntary online survey of adverse medical events: the perspective of 696 injured patients and families. BMJ Qual Saf. Oct 2015;24(10):620-629. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Joint Commission International Accreditation Standards for Hospitals: Including Standards for Academic Medical Center Hospitals. Joint Commission International. 2020. URL: https://www.jointcommissioninternational.org/-/media/jci/jci-documents/accreditation/hospital-and-amc/jci-errata-standards-only_7th-ed-hospital.pdf [accessed 2023-01-17]
- Assessing and Tackling Patient Harm: A Methodological Guide for Data-Poor Hospitals. World Health Organization. 2010. URL: https://iris.who.int/bitstream/handle/10665/77100/9789241500388_eng.pdf?sequence=1 [accessed 2023-06-11]
- Patient Safety Assessment Manual: Third Edition. World Health Organization Regional Office for the Eastern Mediterranean. 2020. URL: https://applications.emro.who.int/docs/9789290223221-eng.pdf [accessed 0000-00-00]
- Meterko M, Mohr DC, Young GJ. Teamwork culture and patient satisfaction in hospitals. Med Care. May 2004;42(5):492-498. [ CrossRef ] [ Medline ]
- de Feijter JM, de Grave WS, Muijtjens AM, Scherpbier AJJA, Koopmans RP. A comprehensive overview of medical error in hospitals using incident-reporting systems, patient complaints and chart review of inpatient deaths. PLoS One. 2012;7(2):e31125. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zanetti ACB, Gabriel CS, Dias BM, Bernardes A, Moura AA, Gabriel AB, et al. Assessment of the incidence and preventability of adverse events in hospitals: an integrative review. Rev Gaucha Enferm. 2020;41:e20190364. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kiaei MZ, Ziaee A, Mohebbifar R, Khoshtarkib H, Ghanati E, Ahmadzadeh A, et al. Patient safety culture in teaching hospitals in Iran: assessment by the Hospital Survey on Patient Safety Culture (HSOPSC). Health Manag Inf Sci. 2016;3(2):51-56. [ FREE Full text ]
- Oyebode F. Clinical errors and medical negligence. Med Princ Pract. 2013;22(4):323-333. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rafter N, Hickey A, Conroy RM, Condell S, O'Connor P, Vaughan D, et al. The Irish National Adverse Events Study (INAES): the frequency and nature of adverse events in Irish hospitals-a retrospective record review study. BMJ Qual Saf. Feb 2017;26(2):111-119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kurji Z, Premani ZS, Mithani Y. Analysis of the health care system of Pakistan: lessons learnt and way forward. J Ayub Med Coll Abbottabad. 2016;28(3):601-604. [ FREE Full text ] [ Medline ]
- Bashir S, Nasir M, Grasic K, Moulin M, Ali S. Association between efficiency and quality of care of public healthcare facilities: evidence from Pakistan. Int J Health Plann Manage. Jul 2022;37(4):2240-2255. [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 15.08.23; peer-reviewed by F Al Dhabbari, M Letaief; comments to author 02.12.23; revised version received 09.01.24; accepted 19.01.24; published 27.03.24.
©Ghazal Haque, Fozia Asif, Fasih Ali Ahmed, Farwa Ayub, Sabih ul Hassan Syed, Nousheen Akber Pradhan, Malika Hameed, Muhammad Muneeb Ullah Siddiqui, Shafaq Mahmood, Tahani Zaidi, Sameen Siddiqi, Asad Latif. Originally published in JMIR Research Protocols (https://www.researchprotocols.org), 27.03.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Research Protocols, is properly cited. The complete bibliographic information, a link to the original publication on https://www.researchprotocols.org, as well as this copyright and license information must be included.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
How Health Care Organizations Should Support Social Services
- 1 The Brookings Institution, Washington, DC
In a recent JAMA Health Forum article, Glied and D’Aunno ask whether health sector investment in social services is “a bridge too far” and raise concerns about differing priorities, skills, finances, and functions of the 2 sectors that question whether this is a good match for collaboration. 1
As health care organizations ponder their role, if any, in supporting social services, there is growing evidence of health benefits from certain investments in social services (including housing and nutrition). But it is hard to make a traditional return-on-investment (ROI) case for many instances of health systems funding social service programs. For instance, to the extent that this “upstream” social funding helps improve household and community health, it means reduced revenues to hospitals and fee-for-service medical practices—so, not good for business. Managed care organizations do have a stronger business incentive to address their enrollees’ health-influencing social conditions. Still, although there is evidence that certain investments in housing, nutrition, etc do yield health care savings , the direct ROI to the health sector is often questionable. 2
The ROI Conundrum
This does not actually mean such investments have a poor return; it’s just that the principal returns often do not accrue to the investor. Health organization investments typically have positive spillover effects in areas beyond immediate health savings, such as economic improvement, better school graduation rates, and better long-term community health. But this form of value-added is not captured as revenue or savings by the health sector investor—a classic “ wrong pockets ” problem. In the same way, improvements in housing conditions financed by a housing authority, or a reduction in violence-caused injuries from new policing programs, can generate large spillover health care savings, yet the financial value of those health benefits do not accrue to the budget bottom line of housing authorities or police departments. The result in each case is usually suboptimal levels of investment in the general well-being of a community.
The key to achieving an optimal level of health system funding of social services, in which public funding is supplemented with health sector funding aimed at improving health, is to organize these investments through multisector partnerships in a community, with each partner strategically investing in community needs that generate spillover benefits to all partners. If designed and implemented well, this partnership approach encourages investments by all community partners to create a strong social return on investment ( SROI ), with benefits and savings shared by each partner as it advances its goal. Of course, reaching that result requires the investing partners to agree on their shares. That can easily lead to difficult negotiations and heightened distrust. Nichols and Taylor are among those testing procedures in communities to create a positive climate, in their case through an innovative bidding process run by a neutral broker and designed to align each partner’s investment commitment with the benefits it will receive from joint action.
Government Encouragement
There are several ways to encourage appropriate health sector investments in social services.
Government initiatives can help in several ways. At the state and local level, the government can act as an honest broker to foster joint investments within communities; states can use Medicaid contracts to require managed care plans to include community engagement, with community partners involved from the beginning. Tweaking community benefit requirements is another way. As a condition of their tax exemption, nonprofit hospitals are already required by law to invest in their communities to improve general health. The Internal Revenue Service (IRS) establishes the rules and over many years has broadened the types of community investments that qualify, including “community building activities.” The IRS could and should encourage nonprofit hospitals to be more creative in supporting innovative social service investments that appear to improve the long-term health and vitality of their communities.
The federal government can provide much clearer guidance on how programs can be used to foster local partnerships with braided funds . It can also help the development of community-level referral systems between health and social services through pilots and more grants to states and communities. More sophisticated referral infrastructure would help facilitate better coordination of social and medical care for households. It would also create important data to help improve our ability to quantify the multisector impacts of investments. In addition, analyzing the impact of recent Medicaid 1115 waivers allowing states, such as Arkansas and New Jersey , more flexibility to mix medical and social services to improve health outcomes will also generate valuable insights on how to best structure health sector investments in social services that will improve community health.
Taking a Back Seat in Partnerships
Effective partnerships require trust, understanding, and the effective use of complementary skills. Indeed, a review of health-human services partnerships suggests that the quality of the relationship is key. This is not easy to achieve between health and social service organizations when communities often doubt the motives and commitment of large health institutions that, in turn, can be skeptical of the expertise of community organizations.
Health systems need to adapt to this reality for their investments to be most beneficial. In 2017, Kaiser Permanente considered supporting a public health and economic development project in Baltimore, Maryland; however, the organization was not then well known in the mid-Atlantic area. So it first partnered with Bon Secours hospital , a very small but highly respected institution in the community; essentially, Bon Secours “credentialled” Kaiser within the community.
CommonSpirit Health has been a pioneer in developing trusted partnerships with social service organizations in communities. CommonSpirit recognizes that there is a critically important difference between functioning as a catalyst for action and being in the driver’s seat. It has partnered with the Pathways Community HUB Institute (PCHI) in 6 communities. In the PCHI model, a neutral hub operated by a local entity links a network of community organizations, health systems, and community health workers to help coordinate care and address health-related social needs. CommonSpirit, along with competing health systems in each area, funds a “community bank” that helps fund the hub’s operating costs and covers otherwise nonreimbursable service costs. It is an intriguing example of how a community partnership can function and how competing health systems can collaborate in a “co-opetition” model for their common benefit. 3
We have come to appreciate that achieving healthier communities requires a larger focus on social factors contributing to ill health. For that to happen, we need to design better SROI techniques and ways in which community savings are distributed. Health systems need to deploy investment resources in ways that prevent illness as well as treat it. Their levels and type of investment should also reflect the broad economic value of prevention and better health. And they must appreciate the importance of sharing control of decision-making over the use of their own investments.
That is not an easy equation to get right. But we have been making steady progress and should be encouraging health systems to explore more partnerships.
Published: November 9, 2023. doi:10.1001/jamahealthforum.2023.4569
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Butler SM. JAMA Health Forum .
Corresponding Author: Stuart M. Butler, PhD, The Brookings Institution, Economic Studies, 1775 Massachusetts Ave NW, Washington, DC, 20036 ( [email protected] ).
Conflict of Interest Disclosures: None reported.
See More About
Butler SM. How Health Care Organizations Should Support Social Services. JAMA Health Forum. 2023;4(11):e234569. doi:10.1001/jamahealthforum.2023.4569
Manage citations:
© 2024
Artificial Intelligence Resource Center
Best of JAMA Network 2022
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Open access
- Published: 21 March 2024
A rapid review to inform the policy and practice for the implementation of chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people in primary care
- Uday Narayan Yadav ORCID: orcid.org/0000-0002-6626-1604 1 , 2 na1 ,
- Jasmine Meredith Davis 3 ,
- Keziah Bennett-Brook 4 ,
- Julieann Coombes 4 ,
- Rosemary Wyber 1 , 5 na1 &
- Odette Pearson 6 , 7
Health Research Policy and Systems volume 22 , Article number: 34 ( 2024 ) Cite this article
383 Accesses
14 Altmetric
Metrics details
More than 35% of Aboriginal and Torres Strait Islander adults live with cardiovascular disease, diabetes, or chronic kidney disease. There is a pressing need for chronic disease prevention and management among Aboriginal and Torres Strait Islander people in Australia. Therefore, this review aimed to synthesise a decade of contemporary evidence to understand the barriers and enablers of chronic disease prevention and management for Aboriginal and Torres Strait Islander People with a view to developing policy and practice recommendations.
We systematically searched for peer-reviewed published articles between January 2014 to March 2023 where the search was performed using subject headings and keywords related to “Aboriginal and Torres Strait Islander peoples,” “Chronic Disease,” and “Primary Health Care”. Quality assessment for all included studies was conducted using the Aboriginal and Torres Strait Islander Quality Appraisal Tool. The data were extracted and summarised using a conventional content analysis approach and applying strength-based approaches.
Database searches identified 1653 articles where 26 met inclusion criteria. Studies varied in quality, primarily reporting on 14 criteria of the Aboriginal and Torres Strait Islander Quality Appraisal Tool. We identified six key domains of enablers and barriers of chronic disease prevention and management programs and implied a range of policy and practice options for improvement. These include culturally acceptable and safe services, patient-provider partnerships, chronic disease workforce, primary health care service attributes, clinical care pathways, and accessibility to primary health care services. This review also identified the need to address social and cultural determinants of health, develop the Aboriginal and Torres Strait Islander and non-Indigenous chronic disease workforce, support multidisciplinary teams through strengthening clinical care pathways, and engage Aboriginal and Torres Strait Islander communities in chronic disease prevention and management program design and delivery.
Enabling place-based partnerships to develop contextual evidence-guided strategies that align with community priorities and aspirations, with the provision of funding mechanisms and models of care through policy and practice reforms will strengthen the chronic disease prevention and management program for Aboriginal and Torres Strait Islander people.
Peer Review reports
Introduction
Aboriginal and Torres Strait Islander people have continuously demonstrated strength, tenacity, and resilience in the face of a high burden of chronic disease associated with profound health, social, economic and cultural and wellbeing impacts. The disproportionate burden of chronic disease—particularly cardiovascular disease (CVD), type II diabetes and chronic kidney disease (CKD)—is driven by the effects of colonisation. These effects include intergenerational trauma, racism and commercial determinants such as the introduction of ultra-processed foods, tobacco, sugar-sweetened beverages, and alcohol [ 1 , 2 ].
More than 35% of Aboriginal and Torres Strait Islander adults report having CVD, diabetes or CKD, 38% have two of these conditions and 11% have all three [ 3 ]. Nearly 70% of Australia’s burden of disease from CVD is attributable to modifiable risk factors including high blood pressure, dietary risks, high body weight, high cholesterol and smoking [ 4 ]. These risk factors, and subsequent disease, can be prevented. This prevention can be primordial (by addressing the structural drivers at a population level, such as food supply and recreation facilities) or primary (through identifying people at risk and taking individual steps to reduce that risk).
Primary prevention and management of chronic disease among Aboriginal and Torres Strait Islander people in Australia predominantly occurs in primary care settings. Universal primary care in Australia is largely funded through a fee-for-service model via the Medicare Benefits Scheme (MBS), with some augmentation for Aboriginal and Torres Strait Islander people through the Indigenous Australian’ Health Programme [ 5 ]. Primary care is delivered by a range of providers, including Aboriginal Community Controlled Health Organisations (ACCHOs) which are governed by a local board, Aboriginal Medical Services run by State and Territory governments, and private primary care services (sometimes referred to as ‘mainstream’ providers). Chronic disease services in primary care include risk assessment, support for healthy behaviours, referrals to allied health and pharmacology for risk reduction. High quality, culturally safe primary care can prevent the development of disease, and manage complications, for individuals and communities [ 6 , 7 , 8 ]. Strengthening primary care is a key strategic priority of the Australian government, [ 9 , 10 ] peak bodies and other stakeholders working to improve the health and well-being of Aboriginal and Torres Strait Islander communities [ 11 , 12 ].
Understanding how primary care services, prevention and management programs can best meet the needs of Aboriginal and Torres Strait Islander people, who are living with or at risk of chronic disease, is critical to addressing disparity in outcomes. A review conducted by Gibson et al. in 2015 explored chronic disease care for Indigenous communities globally, but there has been no comprehensive contextual evidence available focusing on Aboriginal and Torres Strait Islander people [ 13 ]. Therefore, there is a need for local evidence disease on chronic prevention and management for Aboriginal and Torres Strait Islander people in Australia. The Aboriginal and Torres Strait Islander People’s Health Assessment (MBS item number 715) is an annual health check funded for Aboriginal and Torres Strait Islander people and a cornerstone of early detection for chronic disease [ 14 ]. The number of Health Assessments fell for the first time in 2020 and 2021 after years of sustained growth [ 15 ]. The reduction in Health Assessments is likely to reflect disruption to routine primary care services during the COVID-19 pandemic [ 16 ].
Our team were contracted by the Australian Commonwealth Department of Health and Aged Care to understand best practice delivery of chronic disease care for Aboriginal and Torres Strait Islander people in 2020. The effects of the COVID-19 pandemic accelerated the need for this research and necessitated a pivot to rapid review strategy. The Oxford Centre for Evidence-Based Medicine highlights [ 17 ] that rapid review methodology can be used to meet the needs of commissioning bodies in policy-relevant timeframes. Therefore, this rapid review aims to synthesise contemporary and contextually relevant barriers and enablers for chronic disease care in primary care settings for Aboriginal and Torres Strait Islander people with a view to developing near term policy and practice recommendations.
This review applied the SelecTing Approaches for Rapid Reviews (STARR) decision tool that includes interaction with commissioners, scoping the literature, selecting approaches to literature search, methods for data extraction and evidence synthesis [ 18 ]. It was conducted based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guideline [ 19 ]. We searched two databases (Medline and Web of Science) to identify relevant studies from January 2014 to March 2023. These two databases were chosen because of following reasons: (i) Medline database provides access to articles from 5,200 journals in about 40 languages covering the biomedical and life sciences including Aboriginal and Torres Strait Islander peoples as a MeSH Headings and (ii) Web of Science is the world’s oldest interdisciplinary and widely used database of research publications that covers over 34,000 journals today.
This timeframe follows on from a systematic review conducted by Gibson et al. [ 13 ] which included data up to December 2013. This rapid review mirrors the Gibson methodology with two main changes: i) narrowing focus from Indigenous communities globally to Aboriginal and Torres Strait Islander contexts in Australia, ii) narrowing focus from all chronic diseases to focus on the three major contributors to chronic disease burden (cardiovascular disease, diabetes and chronic kidney disease). The review was performed between January to August 2023.
In this review, Aboriginal and Torres Strait Islander researchers and Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members rather than Thiitu Tharrmay Aboriginal Reference Group members were actively engaged and consulted in all steps, from the inception of the research questions to the completion of this review. Throughout the process, the research team met monthly with the Australian Commonwealth Department of Health and Aged Care during the period of this review to inform the scope of evidence synthesis.
Positionality: The senior author of this review Pearson (nee Gibson, first author of the 2015 review), is Kuku Yalnji/Torres Strait Islander health systems researcher. KB-B ( Torres Strait Islander ) and JC ( Gumbaynggir ) are experienced researchers with particular expertise in quality assessment of Aboriginal and Torres Strait Islander research studies. UNY ( Madhesi, Nepal ) is an implementation scientist, JD is a non-Indigenous medical student and RW is a non-Indigenous practising general practitioner and researcher.
Operational definition of key terminology used in this review:
Holistic care or support: The care process that involved strategies to support mental, physical, cultural and spiritual health which is beyond the individual level that values family and community capacity and governance [ 20 ].
Systems thinking: Systems thinking is c onceptual orientation concerned with inter-relationships between different levels, institutions, systems, and people nested within social, cultural, economic, political contexts to deliver a holistic care [ 21 ].
Place-based partnerships: Place-based partnerships involve collaborative arrangements the unique needs and circumstances of both the community and service provider. In this context, place-based partnerships involve a formal partnership among government, service providers and First Nations representatives. These partnerships are specific to geographical locations and population groups and are aimed at designing or delivering services that directly respond to community needs, aspirations and local priorities, while valuing local cultural values [ 22 , 23 ].
Scoping the literature:
The search was performed using a combination of subject headings and keywords related to “Aboriginal and Torres Islander peoples,” “Chronic Disease,” and “Primary Health Care” using “OR” and “AND” iterated from the search strategy described in a study by Gibson et al. [ 13 ] The search strategy has been provided in Box 1. The search results obtained from two databases were imported to Endnote and uploaded on the Covidence platform for title and abstract and full-text screening [ 24 ]. Three reviewers (UNY, JMD and RW) independently screened the titles and abstracts of potential studies for eligibility based on inclusion and exclusion criteria (Table 1 ). Full-text articles were assessed by two reviewers and any disagreement that appeared during the screening process was resolved through discussion with the third reviewer (RW). The details of the screening process are documented as a PRISMA flow diagram (Fig. 1 ).
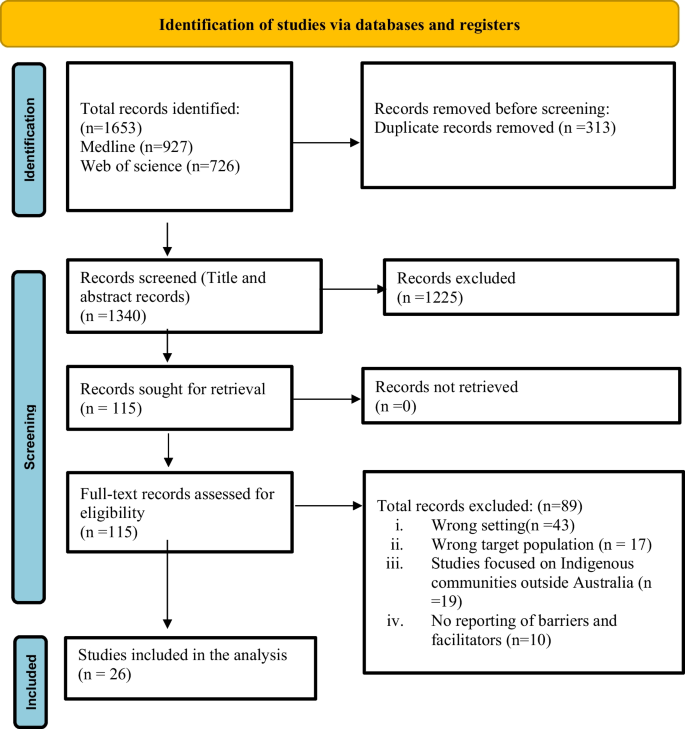
PRISMA 2020 flow diagram that included searches of databases and included studies
Box 1: Search strategy
Data extraction.
An iterative process was used to define data extraction domains. A total of fourteen potential domains were identified from the systematic review conducted by Gibson et al., alongside the He Pikinga Waiora Implementation Framework [ 25 ] and an access framework for Aboriginal and Torres Strait Islander people [ 26 ]. Further, three discussions were held within the team and with other Aboriginal and Torres Strait Islander researchers that identified eight domains of interest for both barriers and enablers (design attributes, chronic disease workforce, patient/provider partnership, clinical care pathways, access-accessibility, access-acceptability, system thinking and knowledge translation). A data extraction tool was prepared to extract information about the study characteristics (title, author, publication year, study setting, study objective, study design, types of services) and eight domains decided from the discussions mentioned above. A data extraction tool was shared with the Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members rather than Thiitu Tharrmay Aboriginal Reference Group members at the National Centre for Aboriginal and Torres Strait Islander Wellbeing Research at the Australian National University for their input. Based on inputs from Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members rather than Thiitu Tharrmay Aboriginal Reference Group members and team discussion, some domains were consolidated and made an agreement of extracting data focusing six domains (culturally acceptable and safe services, patient provider partnerships, chronic disease workforce, primary health care service attributes, clinical care pathways and accessibility to primary health care services) the final data extraction tool included study characteristics and six domains (Fig. 2 )focusing both barriers and enablers. The data extraction tool was piloted on five included studies that facilitated shared understanding of approach to data extraction between team members. The data were extracted by UNY and JMD between May to June 2023.

Barriers and enablers to chronic disease prevention and management for Aboriginal and Torres Strait Islander people
Evidence synthesis and quality appraisal
Quality assessment for all included studies was conducted using the Aboriginal and Torres Strait Islander Quality Appraisal Tool that privileges Aboriginal and Torres Strait Islander people’s (knowing) epistemology, (being) ontology, (doing) axiology and ethical research governance [ 27 ]. The extracted data were analysed and summarised using a conventional content analysis approach [ 28 ] that allows the categories and the name of the categories to flow from the data and applying strength-based approaches [ 29 ].
Study selection and its characteristics
For the period 2013- 2023, a total of 1653 articles were retrieved from Medline ( n = 927) and Web of Science ( n = 726) databases. Of the total, 313 were duplicates which left 1340 articles for screening. Following the screening, 115 studies were selected for the full-text review. Upon full-text review, 89 articles were excluded, leaving 26 articles to be included for extraction and evidence synthesis. Service delivery models of the included studies were ACCHOs, government-run Aboriginal Medical Services and private general practice. The majority of the studies applied qualitative or mixed-method evaluation approaches (see Additional file 1 ).
Quality appraisal results
All studies met two criteria from the Aboriginal and Torres Strait Islander Quality Appraisal Tool: priority determined by community (criterion 1) and use of an Indigenous research paradigm (criterion 9). Over 92% studies met criteria for community protocols (criterion 5), 80% of studies met criteria addressing community consultation and engagement (criterion 2), Aboriginal and Torres Strait Islander leadership (criterion 3) and 76% studies had demonstrated Aboriginal and Torres Strait Islander governance in research (criterion 4). While 30% or less of the studies addressed existing intellectual and cultural property (criterion 6 and 7), 70% studies met the following criteria: Aboriginal and Torres Strait Islander people control over collection and management of research materials (criteria 8), use of strength based approach and acknowledging practices that have harmed Aboriginal and Torres Strait Islander communities (criterion 10) translation of findings into sustainable changes (criterion 11), benefit the participants and Aboriginal and Torres Strait Islander communities (criterion 12), demonstrate capacity strengthening for Aboriginal and Torres Strait Islander people (criterion 13), and researchers have opportunities to learn from each other (criterion 14). Details are provided in Table 2 .
Enablers and barriers to the implementation of chronic disease initiatives
Enablers and barriers (see Additional file 2 ) are presented under six thematic domains and relevant sub-themes presented below:
Primary health care service attributes
Aboriginal and Torres Strait Islander engagement and Aboriginal leadership in system design: Aboriginal and Torres Strait Islander project leadership and community engagement were overwhelmingly identified as key determinants for system design [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Engagement through outreach cultural community events and stakeholder partnerships appear to amplify these effects [ 48 ]. Six studies investigated how information was exchanged between knowledge-users and researchers throughout the studies [ 30 , 38 , 44 , 45 , 46 , 47 ]. Knowledge users included Aboriginal and Torres Strait Islander communities, primary health care providers (ACCHOs and mainstream providers), Aboriginal and/ or Torres Strait Islander health workers and practitioners, other service providers, and policymakers. Alongside this, one study acknowledged the utilisation of cultural and scientific evidence to provide best-practice healthcare [ 37 ]. Aboriginal and Torres Strait Islander project leadership consistently facilitated trust and satisfaction. Use of evidence-based clinical care guideline in project implementation within community and services were other key benefits of knowledge translation.
Primary health car responsive to local community needs: Prospective analysis of potential barriers for program development were essential to program success, in order to actively address these in the program design and implementation. Many studies clearly demonstrated how barriers were overcome through tailored solutions including: outreach services to save patient time and cost [ 30 , 31 , 45 , 49 ]; free of charge services [ 31 , 49 , 50 , 51 ]; 24-h culturally safe service [ 32 , 37 , 50 ]; and telehealth specialist services [ 51 , 52 ]. Outreach services (delivered outside of the clinic facility) included home medication delivery, general visits by health workers to build trust and screening for conditions at community-based events. Services which were free at point of care included medications, nicotine patches, hospital specialist clinics, supplementary services (e.g. cooking class, aged care services), and preventive initiatives (e.g. blood pressure measurement, glucose monitor and health promotion activities). Innovative primary care models for Aboriginal and Torres Strait Islander patients included flexible appointment systems [ 32 , 37 , 50 ], multidisciplinary teams for providing holistic care [ 37 , 38 , 51 ], and clinical audits for quality improvement were also effective [ 31 , 34 , 39 , 45 , 46 ]. Incorporating chronic disease prevention into primary care occurred through health promotion initiatives [ 30 , 35 , 37 , 50 , 51 ], and patient-led prevention initiatives and management plans [ 30 , 46 , 50 ] were also found to be invaluable in addressing community needs. Six studies explicitly emphasised the importance of adequate resources and flexible funding for primary care services to meet local Aboriginal and Torres Strait Islander community priorities and needs [ 30 , 32 , 36 , 37 , 38 , 39 ].
A holistic approach to care: Aligned with Aboriginal and Torres Strait Islander peoples’ perception of health , holistic support [ 30 , 38 , 44 ] and care coordination was critical, necessitating flexible funding, and systems thinking and innovative, locally-adapted reforms [ 30 , 31 , 46 ]. Social referral approaches that connected people to non-clinical services were an important component in Aboriginal community controlled primary care settings, for example: connecting patients to exercise groups, providing access to housing, opportunities for hobbies, or home care services such as ‘Meals on Wheels’ [ 38 , 40 , 41 , 53 ].
Primary care access: Several barriers were identified, including: a lack of support specific to Aboriginal and Torres Strait Islander leadership [ 34 , 39 , 51 , 53 , 54 ]; competing priorities of healthcare service delivery [ 30 , 34 , 39 ]; and a lack of funding specifically address social determinants of health [ 31 , 55 ]. These were more pronounced in Aboriginal PHC. There were also insufficient resources to engage stakeholders in the co-development of primary care programs. This contributed to poor connections and relationships between multidisciplinary teams in health centres and other actors, including clinical information management systems [ 34 , 48 , 51 , 54 ], and high turnover of trained staff [ 34 , 50 , 54 ]. Some studies highlighted challenges in creating culturally appropriate services, due to the heterogeneity of Aboriginal and Torres Strait Islander populations [ 32 , 39 , 55 ]. Moreover, accessing primary care services was particularly challenging for people with the greatest health needs [ 31 ], including those with limited health literacy which made it difficult for people to engage with chronic disease care [ 48 , 49 ].
Chronic disease workforce
Creating supportive environment and building capacity of primary healthcare workforce: Enabling safe and good work environments for Aboriginal and Torres Strait Islander Health Workers and Practitioners [ 30 , 35 , 54 ], and a shared sense of purpose amongst staff to address the complex needs of patients [ 30 , 47 ] were consistently identified as enablers. Eight studies highlighted the importance of dedicated staff for chronic disease management, with clear delegation of responsibilities and a positive team culture created through an engaging and collaborative work environment [ 30 , 36 , 37 , 39 , 43 , 46 , 51 , 54 ]. Establishing the health care workforce with chronic disease ‘portfolios’ were considered more able to provide recurrent, culturally safe, preventative, and responsive healthcare for Aboriginal and Torres Strait Islander people because they had a greater chance of forming trusting relationships [ 32 , 41 , 48 , 50 ]. Included studies highlighted the need for training and development of the primary healthcare workforce [ 30 , 31 , 33 , 55 ]. Four studies had a particular focus on local Aboriginal and Torres Strait Islander Health Workers and Practitioners including the importance of recruitment and retention strategies [ 31 , 34 , 39 , 46 ], alongside a need to clarify their roles, provide Aboriginal and Torres Strait Islander role models [ 40 , 41 , 50 , 52 ], and ensure they are involved in clinical decision making [ 30 , 33 , 35 , 37 , 39 , 43 , 44 , 52 , 54 ]. The importance of intensive cultural safety training for staff to deliver safe care was emphasised in five studies [ 37 , 47 , 49 , 54 , 55 ].
Barriers to sustainable chronic disease workforce at primary health care services: Nine studies noted staff shortages and high staff turnover as adversely impacting continuity of care [ 32 , 33 , 34 , 39 , 43 , 46 , 50 , 51 , 53 ], and three studies noted inadequate clinical training for non-Indigenous staff [ 32 , 46 , 53 ]. Workforce limitations contributed to lack of time and resources to reach the patients that needed healthcare the most [ 31 , 45 , 46 ]. Nine studies specifically emphasised the substantial shortages, high turnover, and high rates of burnout of Aboriginal and Torres Strait Islander staff [ 33 , 34 , 39 , 43 , 46 , 51 , 53 , 54 , 55 ]. Work overload, inadequate support and a sense of being undervalued contributed to these issues [ 32 , 33 , 43 ]. Four studies noted shortages of specialists as a key barrier to integrated chronic disease management pathway [ 34 , 43 , 46 , 47 ].
Patient-provider partnerships
Optimal care achieved by effective trustful patient-provider partnerships: Eight studies found that enablers of trusting patient-provider relationships included strengthening patient knowledge through interactive learning, culturally appropriate conversation, and strengths-focused clinical engagement [ 30 , 32 , 33 , 35 , 38 , 50 , 53 , 55 ]. Numerous studies highlighted that holistic care required mechanisms for communities, families/carers and community leaders to be engaged with service providers [ 30 , 45 , 52 , 53 , 54 ]. ACCHOs were generally identified as meeting these needs by offering culturally safe care, longer consultation times to facilitate patient/provider partnerships [ 32 , 37 ], and communicating with the community when there were changes in services, or the implementation of new programs [ 31 ].
Contextual barriers to patient-provider partnership: Barriers to partnership included competing priorities for patients [ 53 ], patient experiences of racism and discrimination [ 32 ], patient discomfort with non-Indigenous services [ 32 ], and patients sensing that their holistic needs were unmet [ 42 ]. Two studies reported that limited health literacy with little shared provider-consumer understanding of chronic conditions were barriers to forming positive relationships [ 31 , 46 ]. Three studies noted a general lack of connection between the clinician and patient but did not interrogate the contributors to this [ 32 , 49 , 55 ].
Clinical care pathways
Enablers to effective clinical information systems: Nine studies found in-house information technology support within primary healthcare services was crucial for effective patient referral, coordination, and follow-up care [ 30 , 31 , 32 , 34 , 38 , 39 , 43 , 46 , 55 ]. Of these, two highlighted the importance of partnership-enabled integration across health service organisations using a shared electronic health record system, disease registration multidisciplinary care plans, and a patient recall system [ 30 , 36 ]. While translation of evidence-based care guidelines were not mentioned, five studies explained the importance of capacity building of staff and investment in systems development for the effective use of clinical information systems [ 30 , 34 , 39 , 43 , 51 ].
Barriers to efficient clinical information systems: Information technology barriers were profound, including poor integration information technology systems, mixed paper and electronic records [ 43 , 46 , 51 , 53 ], and poor infrastructure – most notably internet access [ 34 , 52 , 54 ]. Four studies noted shortages of trained and regular staff to implement new pathways, as a key barrier to integrated chronic disease management pathways [ 34 , 43 , 46 , 47 ]. Inconsistent models of care [ 44 ], and poor communication between different hospital and primary care systems [ 50 ] were also barriers.
Access to primary health care services
Many of the recognised domains of healthcare access (accessibility, accommodation, availability, accessibility and affordability) were identified [ 56 ].
People and family-centred reforms improve access to adequate primary care: Enablers of access to primary health care services were identified in ten studies [ 30 , 31 , 32 , 38 , 39 , 40 , 41 , 43 , 45 , 49 , 53 ]. Transportation support was a determining and/or motivating factor for clients to access health services [ 31 , 38 , 39 ] Other studies [ 45 , 49 ] [ 43 ] identified accommodation factors, particularly flexible appointment systems, reduced waiting times and co-location with allied health services as key enablers. In this review, a number of motivational factors were identified for people to attend services, including support or referral from family members, higher motivation to look after oneself following the death of a family member, and motivation texts or invitational messages for health check from service providers [ 32 , 41 , 53 ]. In addition, one study identified providing financial incentives as an enabler for health checks [ 32 ].
Unaddressed social determinants prevent access to primary care services: Barriers to accessing primary health care services related to socio-economic factors, health system factors and lack of health promotion factors. Socio-economic factors included accessibility and affordability considerations; lack of transport [ 30 , 31 , 32 , 44 , 46 , 49 , 50 , 53 , 54 , 55 ], inability to afford health and social services, and medication costs [ 31 , 32 , 44 , 47 , 49 ]. Some studies alluded to socioeconomic factors being prioritised over primary care attendance, including household crowding and food insecurity. Ensuring that services account for competing priorities, including family and cultural responsibilities, was an important enabler [ 45 , 55 ].
System related access barriers: Health system factors included high staff turnover, lack of availability of appointments, long waiting periods, physically inaccessible clinics [ 43 , 44 , 46 ], poor leadership of primary care services [ 32 , 45 , 47 , 48 , 49 ], and limited internet and computer access [ 47 ]. Inadequate awareness of available services was also problematic [ 31 , 33 , 49 ]; initiatives run by primary care services had limited uptake when the community was not made aware of these programs [ 46 ]. Health systems need to be able to deliver services and information multimodally. For example, not all patients have phones or phone credit all the time, so several forms of communication may be required.
Culturally acceptable and safe services
Enablers to deliver culturally safe and acceptable services: Cultural safety is essential to the development of a mutually respectful relationship between providers and Aboriginal and Torres Strait Islander people. A systems level approach is needed to address racism experienced by Aboriginal and Torres Strait Islander people in primary care settings [ 30 , 44 ]. Strategies for addressing or achieving cultural safety varied by context, but the role of Aboriginal and Torres Strait Islander healthcare workers including cultural brokerage was emphasised in two studies [ 31 , 52 ]. The need for gender-specific services and gender sensitivity was emphasised by five papers as an important part of providing culturally safe care. This included delivery of programs such as gender-based exercise groups, private consultation areas for males and females, gender specific health assessment days, and employing male and female Aboriginal and Torres Strait Islander healthcare workers [ 31 , 41 , 45 , 46 , 52 ]. The provision of culturally safe services also included a need for culturally appropriate education materials, artwork, and Aboriginal and Torres Strait Islander people’s voices and images as signifiers of belonging [ 30 , 44 , 45 , 46 , 53 ]. Three studies recognised the importance of enabling Aboriginal and Torres Strait Islander patients and staff access to flexibly attend to family, community, cultural and spiritual responsibilities, and obligations to provide a culturally safe service [ 37 , 42 , 44 ]. One study identified the need for robust anonymous feedback systems for staff and patients to improve culturally safe care delivery [ 47 ].
Barriers to deliver culturally safe and acceptable services: Barriers to delivering culturally safe and acceptable services related to systems, structures and lived experiences. Systems issues to providing culturally safe services included language barriers [ 32 ], poor health literacy among patients [ 54 ], long wait times due to staff shortages [ 32 , 50 , 54 ], a sense that services were superficial/rushed [ 31 , 42 ], and lack of physical space to provide holistic care or gender-based services [ 43 , 44 , 46 ]. Lived experiences of treatment of Aboriginal and Torres Strait Islander people within Western systems, including health and social services, elicits feelings of harm rather than help: a fear of discrimination and racism was a key barrier to Aboriginal and Torres Strait Islander patients accessing healthcare services in five studies [ 31 , 32 , 44 , 49 , 53 ] alongside fear of diagnosis due to historical trauma [ 53 ]. These barriers were amplified where there was limited access to Indigenous-specific services [ 32 , 44 , 46 ]. One study mentioned a tokenistic approach where very limited community input to governance, planning, and program design was sought to develop culturally safe initiatives [ 46 ].
This is the first review since 2014 [ 13 ] to present the barriers and enablers of implementing chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people. The enablers and barriers found in this study have several policy and practice implications that should be considered in design, implementation, and funding targets for future chronic disease prevention and management programs.
The most striking addition to our findings, relative to the 2014 [ 13 ] review, is the acknowledgment of Aboriginal and Torres Strait Islander culture (including staff, protocols, leadership, practices and ways of doing business) as a key enabler to engagement and care delivery. Partly, this is attributable to this review’s narrower focus on the Australian context. It also likely reflects increasingly detailed academic descriptions of the ways in which leadership and governance tangibly affect care delivery as part of contemporary Closing the Gap reform. All studies included in this review made some acknowledgement of culture, albeit with variations in how deeply culture was considered as an enabler of care. Our review team grappled with how best to reflect this focus on culture, given that it is both a distinct concept and intimately embedded in all thematic domains. Ultimately, we have chosen to keep Aboriginal and Torres Strait Islander culture as a separate domain to ensure that culture is given independent consideration, in addition to attention within other thematic domains. It is evident that access to culturally appropriate, affordable and comprehensive services are vital for preventing and managing chronic conditions [ 37 ]. There is no one-size-fits-all approach for models of care for Aboriginal and Torres Strait Islander communities, and programs must be tailored to local context. Recent studies have identified numerous opportunities for improving access to primary care services: creating welcoming spaces, improving the cultural safety of healthcare services, building strong trustworthy relationships between patients and providers, and building primary healthcare workforce capacity [ 37 , 57 , 58 ]. The span of this theme is necessarily broad, encompassing Aboriginal and Torres Strait Islander leadership, physically welcoming spaces, training for non-Indigenous staff, time to build trusting relationships. Ensuring that culture is prospectively and proactively considered in funding and delivery of primary care of chronic disease should be a priority for practitioners and policy makers.
There is clear evidence that addressing holistic needs of Aboriginal and Torres Strait Islander people enables greater engagement, rather than a narrow clinical focus on physical aspects of health. This requires primary care services to acknowledge and address the broader social and cultural determinants of health for Aboriginal and Torres Strait Islander people. Many of these have a direct impact on both chronic disease risk factors and capacity to access care (chronic disease management), including poor access to healthy and nutritious food, inadequate housing, rurality, lack of transportation, and financial barriers [ 59 , 60 ].Some of these disparities more pronounced in remote and rural Australia, where Aboriginal and Torres Strait Islander communities are further marginalised by distance and poverty [ 61 , 62 ]. Enablers of chronic disease care, such as outreach services, transportation, and referrals networks to other allied health and community groups are more likely to be effective where holistic approaches are adopted. This is consistent with data from the Australian Institute of Health and Welfare highlighting the experiences of social inequity in Aboriginal and Torres Strait Islander communities and the positive impact on health outcomes when inequities are reduced [ 63 ]. Previous studies [ 13 , 64 ] have identified various obstacles to accessing primary health care services which include inadequate infrastructure, inflexible and inadequate funding to care for people holistically. Evidence also suggests that for Aboriginal and Torres Strait Islander people, travel to access health care means being separated from their country, family and social network that directly impacts their health and wellbeing as described by Milroy’s Dance of Life [ 65 ]. While government subsidies are in place, travel and accommodation costs incurred by Aboriginal and Torres Strait Islander people to access healthcare, may require upfront payment or indirect costs, perpetuating financial barriers for Aboriginal and Torres Strait Islander people living in rural and remote areas [ 66 ]. Therefore, it is crucial that primary health care initiatives take a holistic and system thinking approach to program design, considering the impact of social and cultural determinants on the health of individual, family members and their communities, with every attempt to reduce systemic barriers to access to healthcare where possible.This is only possible when funding mechanisms and models of care are flexible enough to account for local and individual contexts.
The profound impact of workforce was clear throughout this review. Recruiting, and retaining staff and effective training, were found to be key barriers to implementing and maintaining holistic patient-centred chronic disease prevention and management programs [ 13 , 67 ]. Evidence has shown that Aboriginal and Torres Strait Islander people prefer support delivered by Aboriginal and/or Torres Strait Islander staff and clinicians who have a better understanding of Indigenous wellbeing [ 64 , 68 ]. Despite the growth of the Aboriginal and/or Torres Strait Islander health workforce over time, this expansion has not matched the Aboriginal and Torres Strait Islander population growth [ 69 ] and increasing incidence of chronic disease. Unsurprisingly, being members of the community, they serve, Aboriginal and/or Torres Strait Islander Health Workers play an essential and unique role in delivering culturally safe and holistic care. However, a demanding work environment, low salary, inadequate support, [ 70 ] and demanding cultural brokerage with non-Indigenous colleagues [ 70 , 71 ] contribute to burnout that contributes to poor retention rates of Aboriginal and Torres Strait Islander primary care staff. This requires urgent attention, by individual primary care providers and through the National Aboriginal and Torres Strait Islander Health Workforce Strategic Framework and Implementation Plan 2021 – 2031 [ 72 ]. Given the ongoing need for the non-Indigenous workforce in fulfilling workforce gaps required to deliver services for Aboriginal and Torres Strait Islander people, building cultural competence, continuing appropriate training and education pathways and strategies, providing job security and adequate remuneration are also crucial to address primary care workforce issues including the overburdening of the Aboriginal and Torres Strait Islander workforce [ 58 , 71 , 73 ]. Our findings highlight the need to develop the overall chronic disease workforce, with a specific focus for recruitment and retention of Aboriginal and Torres Strait Islander Health Workers and Practitioners and providing cultural safety training for all non-Indigenous staff. Alongside this, mechanisms for recognising the value and load of cultural mentorship/education should be developed. This reflects a recent research findings that showed 39% of Aboriginal and/or Torres Strait Islander workers ( n = 1033) across Australia experienced high cultural load in terms of extra work demands and their engagement in educating others [ 74 ].
Chronic disease management requires multidisciplinary team input for effective care delivery [ 75 ]. When optimally resourced, primary care can serve a coordinating role in patient care, and effectively ensure patients have access to all allied health and specialist care they need [ 76 ]. Therefore, in order to engage Aboriginal and Torres Strait Islander people with chronic disease care and maintain continuity of care, there needs to be established, streamlined, and practitioner and patient friendly systems in place [ 76 , 77 ]. Existing evidence also documented inadequate number of general practitioners and lack of specialists in rural and remote settings of Australia compared to urban or city areas which hinders individuals, particularly Aboriginal and Torres Strait Islander people, to receive timely treatment for their co-occurring conditions in an integrated care approach [ 78 , 79 ]. A lack of integrated IT systems, poor infrastructure, and poor communication between primary care team members were found in this review to impede provision of such care. It is evident that strategies like GP care plans and tertiary care follow up are important sources of information for primary care providers, hospitals and patients which are supported by IT infrastructure [ 80 ]. Previous research highlighted the feasibility of system integration through utilising continuous quality improvement processes and community co-design [ 81 ]. Infrastructure investment such as internet access, in-house IT support and automated systems for follow-up care, is urgently required to ensure that patients who do present or engage with primary care in regional or remote settings, are retained in the system to enable coordinated access to the multidisciplinary care required for chronic disease management. Moreover, rapidly evolving technology such as tele-health, videoconferencing and Point-of-Care Testing may can facilitate access to the Aboriginal and Torres Strait Islander people in remote and rural areas. However, implementing these tools should be part of broader strategy rather than a substitute for solving problems faced by PHC such as workforce retention, undersupply or maldistribution issues [ 82 ]. Therefore, when implementing an integrated team care program [ 83 ] or any other integrated model of care, both barriers and facilitators identified herein should be applied to improve the continuity of care with considering the context.
Effective engagement of Aboriginal and Torres Strait Islander communities and their leadership in program design, delivery and evaluation of chronic disease programs is integral to improving Aboriginal and Torres Strait Islander health and increasing access to primary care services [ 84 , 85 ]. Previous studies have identified the following factors that enable engagement with Aboriginal and Torres Strait Islander communities: employment of local Aboriginal health workforce; trust and relationships; Aboriginal and Torres Strait Islander leadership; availability of flexible services to address holistic needs of local communities; benefits of engagement in service design and delivery; cost of participation and recognition of local Aboriginal knowledge and cultural traditions on study design implementation and dissemination [ 84 , 86 , 87 , 88 ]. These enablers align with those reported in health service research that engaged with Indigenous and marginalised communities in an international context [ 89 ]. Similarly, this review identified a range of impeding factors to engagement of Aboriginal and Torres Strait Islander people with primary health care. Key factors included: a fear or lack of trust on mainstream health facilities, lack of respect from health care providers, experiences of interpersonal and structural racism, lack of understanding of cultural differences to initiate an open discussion and a narrow concept of health that fails to consider the Aboriginal definition of health which is more comprehensive than the Western biomedical perspective of health that focuses on treating health conditions [ 90 , 91 , 92 ]. Evidence also shows that Aboriginal and Torres Strait Islander people in rural and remote communities do not have equitable access to PHC services, including lack of local available services to meet their holistic needs, inadequate infrastructure, high costs, long travel distance and insufficient workforce [ 59 , 93 ]. Therefore, trustful, and culturally safe engagement of Aboriginal and Torres Strait Islander communities through all aspects of the program design, implementation and evaluation is essential to program success, and where possible, the Aboriginal Health Workforce and ACCHOs should be utilised.
Policy and practice recommendations: This study identified several policy and practice recommendations (Table 3 ) that need to be considered for the implementation of chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people in primary care. Our recommendations align with Australia’s Primary Health Care 10 Year Plan 2022–2032 ($632.8 million new investment) that has identified three streams of work: future focused health care; person-centred primary health care supported by funding reform; and integrated care, locally delivered [ 94 ].
Strengths and limitations
Strengths of the present study include (i) the generation of an evidence summary required to guide policy and practice is a short time frame, (ii) the application of iterative process from the design to completion of review with engagement of Aboriginal and Torres Strait Islander researchers and Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members rather than Thiitu Tharrmay Aboriginal Reference Group members , (iii) a quality appraisal of the included studies using Aboriginal and Torres Strait Islander Quality Appraisal Tool that privileges Aboriginal and Torres Strait Islander people’s ways of knowing, being, doing and (iv) interpretation of findings validated by Aboriginal and Torres Strait Islander knowledge champions.
One limitation of this review was that search was restricted to only two databases as the decision makers seek the evidence is a short period of time and were based on peer reviewed articles published in English language. We also acknowledge that the findings might not be comprehensive as the review was conducted in short timeframe, limitations in key words used and subjected to publication bias, as we omitted published program reports, grey literature, and policy guidelines from our inclusion criteria. Moreover, our search was limited to specific databases and terms, which could result in overlooking articles present in other databases or identified through alternate search terms. Despite these limitations, this review is Aboriginal and Torres Strait Islander researchers led that allowed Indigenous perspectives and knowledge to be integrated in the evidence synthesis; ensuring findings are meaningful for the broader sector.
This rapid review synthesises the barriers and enablers to designing and implementing chronic disease prevention and management programs for Aboriginal and Torres Strait Islander communities. While there is no one-size-fits-all approach to the heterogeneous Aboriginal and Torres Strait Islander communities, several policy and practice recommendations are broadly applicable to service providers. These include addressing social and cultural determinants of health, developing the Aboriginal and Torres Strait Islander and non-Indigenous chronic disease workforce, supporting multidisciplinary teams through strengthening clinical care pathways, and engaging Aboriginal and Torres Strait Islander communities in design and delivery of chronic disease prevention and management programs. This requires funding mechanisms and models of care that are flexible enough to account for local and individual context through policy and practice reforms. Moreover, enabling place-based partnerships to develop local and population-based strategies that align with community priories and aspiration is crucial for tackling increasing burden of chronic disease.
Availability of data and materials
All available materials are available as Additional material.
Abbreviations
Aboriginal Community Controlled Health Organisations
Medicare Benefits Schedule
Cardiovascular Disease
Chronic Kidney Disease
Preferred Reporting Items for Systematic Review and Meta-analysis Protocols
SelecTing Approaches for Rapid Reviews
Kairuz CA, Casanelia LM, Bennett-Brook K, Coombes J, Yadav UN. Impact of racism and discrimination on physical and mental health among Aboriginal and Torres Strait islander peoples living in Australia: a systematic scoping review. BMC Public Health. 2021;21(1):1302.
Article PubMed PubMed Central Google Scholar
Penm, E., Cardiovascular disease and its associated risk factors in Aboriginal and Torres Strait Islander peoples 2004–05, 2008, Australian Institute of Health and Welfare: Canberra.
Cardiovascular disease, diabetes and chronic kidney disease-Australian facts: Aboriginal and Torres Strait Islander people 2015 [ https://www.aihw.gov.au/reports/heart-stroke-vascular-disease/cardiovascular-diabetes-chronic-kidney-indigenous/summary ]
Australian Burden of Disease Study 2018-Key findings [ https://www.aihw.gov.au/reports/burden-of-disease/burden-of-disease-study-2018-key-findings ]
Swerissen H, Duckett S, Moran G. Mapping primary care in Australia. 2018. Grattan Institute. Available from: https://grattan.edu.au/wp-content/uploads/2018/07/906-Mapping-primary-care.pdf .
Shi L, Macinko J, Starfield B, Politzer R, Xu J. Primary care, race, and mortality in US states. Soc Sci Med. 2005;61(1):65–75.
Article PubMed Google Scholar
Lavoie JG, Forget EL, Prakash T, Dahl M, Martens P, O’Neil JD. Have investments in on-reserve health services and initiatives promoting community control improved First Nations’ health in Manitoba? Soc Sci Med. 2010;71(4):717–24.
Thomas SL, Zhao Y, Guthridge SL, Wakerman J. The cost-effectiveness of primary care for Indigenous Australians with diabetes living in remote Northern Territory communities. Med J Aust. 2014;200(11):658–62.
Commonwealth of Australia, Department of the Prime Minister and Cabinet. Closing the Gap Prime Minister’s report 2017. Canberra: Department of the Prime Minister and Cabinet, 2017. Available at www.niaa.gov.au/sites/default/files/publications/ctg-report-2017.pdf .
Australian Institute of Health and Welfare 2023. Aboriginal and Torres Strait Islander Health Performance Framework: summary report July 2023. Canberra: AIHW. Viewed:17/07/2023.
The Royal Australian College of General Practitioners. Vision for general practice and a sustainable healthcare system. East Melbourne, Vic: RACGP, 2019. Available at www.racgp.org.au/advocacy/advocacy-resources/the-vision-for-general-practice/the-vision .
TOWARDS A NATIONAL PRIMARY HEALTH CARE STRATEGY: FULFILLING ABORIGINAL PEOPLES ASPIRATIONS TO CLOSE THE GAP.National Aboriginal Community Controlled Health Organisation, February 2009. https://www.naccho.org.au/publications-resources/ .
Gibson O, Lisy K, Davy C, Aromataris E, Kite E, Lockwood C, Riitano D, McBride K, Brown A. Enablers and barriers to the implementation of primary health care interventions for Indigenous people with chronic diseases: a systematic review. Implement Sci. 2015;10:71.
Yadav UN, Smith M, Agostino J, Sinka V, Williamson L, Wyber R, Butler DC, Belfrage M, Freeman K, Passey M, et al. Understanding the implementation of health checks in the prevention and early detection of chronic diseases among Aboriginal and Torres Strait Islander people in Australia: a realist review protocol. BMJ Open. 2023;13(6): e071234.
Australian Institute of Health and Welfare. Indigenous-specific health checks during the COVID-19 pandemic. https://www.aihw.gov.au/reports/indigenous-australians/indigenous-health-checks-during-the-covid-pandemic/contents/about
Follent D, Paulson C, Orcher P, O’Neill B, Lee D, Briscoe K, Dimopoulos-Bick TL. The indirect impacts of COVID-19 on Aboriginal communities across New South Wales. Med J Aust. 2021;214(5):199-200.e191.
Plüddemann A, Aronson JK, Onakpoya I, Heneghan C, Mahtani KR. Redefining rapid reviews: a flexible framework for restricted systematic reviews. BMJ Evid Based Med. 2018;23(6):201–3.
Pandor A, Kaltenthaler E, Martyn-St James M, Wong R, Cooper K, Dimairo M, O’Cathain A, Campbell F, Booth A. Delphi consensus reached to produce a decision tool for SelecTing approaches for rapid reviews (STARR). J Clin Epidemiol. 2019;114:22–9.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Lutschini M. Engaging with holism in Australian Aboriginal health policy–a review. Aust New Zealand Health Policy. 2005;2:15.
Oetzel J, Scott N, Hudson M, Masters-Awatere B, Rarere M, Foote J, Beaton A, Ehau T. Implementation framework for chronic disease intervention effectiveness in Māori and other indigenous communities. Glob Health. 2017;13(1):69.
Article Google Scholar
National Indigenous Australians agency. Priority Reform One: Formal partnerships and shared decision-making. 2023 Commonwealth Closing the Gap Implementation Plan. [ https://www.niaa.gov.au/2023-commonwealth-closing-gap-implementation-plan ].
Naylor C, Charles A. Place-based partnerships explained. The King's Fund. 2022 [ https://www.kingsfund.org.uk/publications/place-based-partnerships-explained ].
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. www.covidence.org .
Oetzel J, Scott N, Hudson M, Masters-Awatere B, Rarere M, Foote J, Beaton A, Ehau T. Implementation framework for chronic disease intervention effectiveness in Māori and other indigenous communities. Global Health. 2017;13(1):69.
Davy C, Harfield S, McArthur A, Munn Z, Brown A. Access to primary health care services for Indigenous peoples: a framework synthesis. Int J Equity Health. 2016;15(1):163.
Harfield S, Pearson O, Morey K, Kite E, Canuto K, Glover K, Gomersall JS, Carter D, Davy C, Aromataris E, et al. Assessing the quality of health research from an Indigenous perspective: the Aboriginal and Torres Strait Islander quality appraisal tool. BMC Med Res Methodol. 2020;20(1):79.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Martin K, Mirraboopa B. Ways of knowing, being and doing: A theoretical framework and methods for indigenous and indigenist re‐search. J Aus Stud. 2003;27(76):203–214.
Askew DA, Togni SJ, Schluter PJ, Rogers L, Egert S, Potter N, Hayman NE, Cass A, Brown ADH. Investigating the feasibility, acceptability and appropriateness of outreach case management in an urban Aboriginal and Torres strait Islander primary health care service: a mixed methods exploratory study. BMC Health Serv Res. 2016;16:178.
Bailie J, Schierhout G, Laycock A, Kelaher M, Percival N, O’Donoghue L, McNeair T, Bailie R. Determinants of access to chronic illness care: a mixed-methods evaluation of a national multifaceted chronic disease package for Indigenous Australians. BMJ Open. 2015;5(11): e008103.
Canuto K, Wittert G, Harfield S, Brown A. “I feel more comfortable speaking to a male”: Aboriginal and Torres Strait Islander men’s discourse on utilizing primary health care services. Int J Equity Health. 2018;17(1):185.
Deshmukh T, Abbott P, Reath J. 'It’s got to be another approach’: an Aboriginal health worker perspective on cardiovascular risk screening and education. Aust Fam Physician. 2014;43(7):475–8.
PubMed Google Scholar
Bailie J, Laycock A, Matthews V, Bailie R. System-level action required for wide-scale improvement in quality of primary health care: synthesis of feedback from an interactive process to promote dissemination and use of aggregated quality of care data. Front Public Health. 2016;4:86.
Barrett E, Salem L, Wilson S, O’Neill C, Davis K, Bagnulo S. Chronic kidney disease in an Aboriginal population: a nurse practitioner-led approach to management. Aust J Rural Health. 2015;23(6):318–21.
Reeve C, Humphreys J, Wakerman J, Carroll V, Carter M, O’Brien T, Erlank C, Mansour R, Smith B. Community participation in health service reform: the development of an innovative remote Aboriginal primary health-care service. Aust J Prim Health. 2015;21(4):409–16.
Davy C, Kite E, Sivak L, Brown A, Ahmat T, Brahim G, Dowling A, Jacobson S, Kelly T, Kemp K, et al. Towards the development of a wellbeing model for aboriginal and Torres Strait islander peoples living with chronic disease. BMC Health Serv Res. 2017;17(1):659.
Blignault I, Norsa L, Blackburn R, Bloomfield G, Beetson K, Jalaludin B, Jones N. “You Can’t Work with My People If You Don’t Know How to”: Enhancing Transfer of Care from Hospital to Primary Care for Aboriginal Australians with Chronic Disease. Int J Environ Res Public Health. 2021;18(14):7233.
Bailie J, Matthews V, Laycock A, Schultz R, Burgess CP, Peiris D, Larkins S, Bailie R. Improving preventive health care in Aboriginal and Torres Strait Islander primary care settings. Global Health. 2017;13(1):48.
Seear KH, Atkinson DN, Henderson-Yates LM, Lelievre MP, Marley JV. Maboo wirriya, be healthy: community-directed development of an evidence-based diabetes prevention program for young Aboriginal people in a remote Australian town. Eval Program Plann. 2020;81: 101818.
Seear KH, Atkinson DN, Lelievre MP, Henderson-Yates LM, Marley JV. Piloting a culturally appropriate, localised diabetes prevention program for young Aboriginal people in a remote town. Aust J Prim Health. 2019;25(5):495–500.
Spurling GK, Bond CJ, Schluter PJ, Kirk CI, Askew DA. 'I’m not sure it paints an honest picture of where my health’s at’—identifying community health and research priorities based on health assessments within an Aboriginal and Torres Strait Islander community: a qualitative study. Aust J Prim Health. 2017;23(6):549–53.
Stoneman A, Atkinson D, Davey M, Marley JV. Quality improvement in practice: improving diabetes care and patient outcomes in Aboriginal community controlled health services. BMC Health Serv Res. 2014;14:481.
Webster E, Johnson C, Kemp B, Smith V, Johnson M, Townsend B. Theory that explains an Aboriginal perspective of learning to understand and manage diabetes. Aust N Z J Public Health. 2017;41(1):27–31.
Wood AJ, Graham S, Boyle JA, Marcusson-Rababi B, Anderson S, Connors C, McIntyre HD, Maple-Brown L, Kirkham R. Incorporating Aboriginal women’s voices in improving care and reducing risk for women with diabetes in pregnancy—a phenomenological study. BMC Pregnancy Childbirth. 2021;21(1):624.
Woods C, Carlisle K, Larkins S, Thompson SC, Tsey K, Matthews V, Bailie R. Exploring systems that support good clinical care in indigenous primary health-care services: a retrospective analysis of longitudinal systems assessment tool data from high-improving services. Front Public Health. 2017;5:45.
Sebastian S, Thomas DP, Brimblecombe J, Arley B, Cunningham FC. Perceived impact of the characteristics of the Indigenous Queensland B.strong brief intervention training program on uptake and implementation. Health Promot J Austr. 2022;33(1):245–56.
Kirkham R, Trap-Jensen N, Boyle JA, Barzi F, Barr ELM, Whitbread C, Van Dokkum P, Kirkwood M, Connors C, Moore E, et al. Diabetes care in remote Australia: the antenatal, postpartum and inter-pregnancy period. BMC Pregnancy Childbirth. 2019;19(1):389.
Article CAS PubMed PubMed Central Google Scholar
Cuesta-Briand B, Saggers S, McManus A. “It still leaves me sixty dollars out of pocket”: experiences of diabetes medical care among low-income earners in Perth. Aust J Prim Health. 2014;20(2):143–50.
Govil D, Lin I, Dodd T, Cox R, Moss P, Thompson S, Maiorana A. Identifying culturally appropriate strategies for coronary heart disease secondary prevention in a regional Aboriginal Medical Service. Aust J Prim Health. 2014;20(3):266–72.
Kirkham R, Boyle JA, Whitbread C, Dowden M, Connors C, Corpus S, McCarthy L, Oats J, McIntyre HD, Moore E, et al. Health service changes to address diabetes in pregnancy in a complex setting: perspectives of health professionals. BMC Health Serv Res. 2017;17(1):524.
Macniven R, Gwynn J, Fujimoto H, Hamilton S, Thompson SC, Taylor K, Lawrence M, Finlayson H, Bolton G, Dulvari N, et al. Feasibility and acceptability of opportunistic screening to detect atrial fibrillation in Aboriginal adults. Aust N Z J Public Health. 2019;43(4):313–8.
Conway J, Tsourtos G, Lawn S. The barriers and facilitators that indigenous health workers experience in their workplace and communities in providing self-management support: a multiple case study. BMC Health Serv Res. 2017;17(1):319.
Schmidt B, Campbell S, McDermott R. Community health workers as chronic care coordinators: evaluation of an Australian Indigenous primary health care program. Aust N Z J Public Health. 2016;40(Suppl 1):S107-114.
Campbell S, Roux N, Preece C, Rafter E, Davis B, Mein J, Boyle J, Fredericks B, Chamberlain C. Paths to improving care of Australian Aboriginal and Torres Strait Islander women following gestational diabetes. Prim Health Care Res Dev. 2017;18(6):549–62.
Saurman E. Improving access: modifying Penchansky and Thomas’s theory of access. J Health Serv Res Policy. 2016;21(1):36–9.
Davy C, Cass A, Brady J, DeVries J, Fewquandie B, Ingram S, Mentha R, Simon P, Rickards B, Togni S, et al. Facilitating engagement through strong relationships between primary healthcare and Aboriginal and Torres Strait Islander peoples. Aust N Z J Public Health. 2016;40(6):535–41.
Jongen C, McCalman J, Campbell S, Fagan R. Working well: strategies to strengthen the workforce of the Indigenous primary healthcare sector. BMC Health Serv Res. 2019;19(1):910.
Nolan-Isles D, Macniven R, Hunter K, Gwynn J, Lincoln M, Moir R, Dimitropoulos Y, Taylor D, Agius T, Finlayson H, et al. Enablers and Barriers to Accessing Healthcare Services for Aboriginal People in New South Wales, Australia. Int J Environ Res Public Health. 2021;18(6):3014.
Christidis R, Lock M, Walker T, Egan M, Browne J. Concerns and priorities of Aboriginal and Torres Strait Islander peoples regarding food and nutrition: a systematic review of qualitative evidence. Int J Equity Health. 2021;20(1):220.
Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016;188(17–18):E474-e483.
Markwick A, Ansari Z, Sullivan M, Parsons L, McNeil J. Inequalities in the social determinants of health of Aboriginal and Torres Strait Islander People: a cross-sectional population-based study in the Australian state of Victoria. Int J Equity Health. 2014;13(1):91.
Australian Institute of Health and Welfare (2022). Australia’s health 2022: in brief, catalogue number AUS 241. Australia’s health series number 18, AIHW, Australian Government. https://www.aihw.gov.au/reports/australias-health/australias-health-2022-in-brief/summary .
Hayman N. Strategies to improve indigenous access for urban and regional populations to health services. Heart Lung Circ. 2010;19(5–6):367–71.
Purdie P., Dudgeon P., Walker R. Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice. 2nd ed. Australian Government Department of the Prime Minister and Cabinet. ACT; Canberra, Australia: 2014.
Kelly J, Dwyer J, Willis E, Pekarsky B. Travelling to the city for hospital care: access factors in country Aboriginal patient journeys. Aust J Rural Health. 2014;22(3):109–13.
Moore L, Britten N, Lydahl D, Naldemirci Ö, Elam M, Wolf A. Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scand J Caring Sci. 2017;31(4):662–73.
McGrath PD, Patton MA, Ogilvie KF, Rayner RD, McGrath ZM, Holewa HA. The case for Aboriginal health workers in palliative care. Aust Health Rev. 2007;31(3):430–9.
Lahn J., Puszka S., Lawton P., Dinku Y., Nichols N. and Markham F. (2020) Beyond Parity in Aboriginal and Torres Strait Islander Health Workforce Planning: Achieving Equity through Needs-Based and Strengths-Based Approaches, Commissioned Report No. 6, Centre for Aboriginal Economic Policy Research, Australian National University. https://doi.org/10.25911/5f88175975c5b
Lai GC, Taylor EV, Haigh MM, Thompson SC. Factors Affecting the retention of indigenous Australians in the health workforce: a systematic review. Int J Environ Res Public Health. 2018;15(5):914.
Gwynne K, Lincoln M. Developing the rural health workforce to improve Australian Aboriginal and Torres Strait Islander health outcomes: a systematic review. Aust Health Rev. 2017;41(2):234–8.
Australian Government Department of Health . National Aboriginal and Torres Strait Islander Health Workforce Strategic Framework and Implementation Plan 2021–2031. Available from: https://www.health.gov.au/sites/default/files/documents/2022/03/national-aboriginal-and-torres-strait-islander-health-workforce-strategic-framework-and-implementation-plan-2021-2031.pdf . In .
McCalman J, Campbell S, Jongen C, Langham E, Pearson K, Fagan R, Martin-Sardesai A, Bainbridge R. Working well: a systematic scoping review of the Indigenous primary healthcare workforce development literature. BMC Health Serv Res. 2019;19(1):767.
Diversity Council Australia/Jumbunna Institute (Brown, C., D’Almada-Remedios, R., Gilbert, J. O’Leary, J. and Young, N.) Gari Yala (Speak the Truth): Centreing the Work Experiences of Aboriginal and/or Torres Strait Islander Australians, Sydney, Diversity Council Australia/Jumbunna Institute, 2020.
Harris MF, Jayasinghe UW, Taggart JR, Christl B, Proudfoot JG, Crookes PA, Beilby JJ, Davies GP. Multidisciplinary team care arrangements in the management of patients with chronic disease in Australian general practice. Med J Aust. 2011;194(5):236–9.
Digital technologies and chronic disease management. Australian Journal for General Practitioners 2014, 43:842-846.
Michielsen L, Bischoff EWMA, Schermer T, Laurant M. Primary healthcare competencies needed in the management of person-centred integrated care for chronic illness and multimorbidity: results of a scoping review. BMC Primary Care. 2023;24(1):98.
Street TD, Somoray K, Richards GC, Lacey SJ. Continuity of care for patients with chronic conditions from rural or remote Australia: a systematic review. Aust J Rural Health. 2019;27(3):196–202.
Comorbidity Guidelines. Rural and remote populations [ https://comorbidityguidelines.org.au/part-c-specific-population-groups/rural-and-remote-populations#:~:text=The%20lack%20of%20specialists%20in%20rural%20and%20remote,of%20employed%20medical%20practitioners%20decreasing%20according%20to%20remoteness .]
Trankle SA, Usherwood T, Abbott P, Roberts M, Crampton M, Girgis CM, Riskallah J, Chang Y, Saini J, Reath J. Integrating health care in Australia: a qualitative evaluation. BMC Health Serv Res. 2019;19(1):954.
McCalman J, Bainbridge R, James YC, Bailie R, Tsey K, Matthews V, Ungar M, Askew D, Fagan R, Visser H, et al. Systems integration to promote the mental health of Aboriginal and Torres Strait Islander children: protocol for a community-driven continuous quality improvement approach. BMC Public Health. 2020;20(1):1810.
Thomas SL, Wakerman J, Humphreys JS. Ensuring equity of access to primary health care in rural and remote Australia—what core services should be locally available? Int J Equity Health. 2015;14(1):111.
Australian Government Department of Health and Aged Care. Integrated Team Care Program.
Durey A, McEvoy S, Swift-Otero V, Taylor K, Katzenellenbogen J, Bessarab D. Improving healthcare for Aboriginal Australians through effective engagement between community and health services. BMC Health Serv Res. 2016;16(1):224.
Banks E, Haynes A, Lovett R, Yadav UN, Agostino J. Output-orientated policy engagement: a model for advancing the use of epidemiological evidence in health policy. Health Res Policy Syst. 2023;21(1):6.
O’Brien P, Prehn R, Rind N, Lin I, Choong PFM, Bessarab D, Coffin J, Mason T, Dowsey MM, Bunzli S. Laying the foundations of community engagement in Aboriginal health research: establishing a community reference group and terms of reference in a novel research field. Res Involve Engage. 2022;8(1):40.
Barnett L, Kendall E. Culturally appropriate methods for enhancing the participation of Aboriginal Australians in health-promoting programs. Health Promot J Austr. 2011;22(1):27–32.
Bessarab D, Durey A, Christou A, Katzenellenbogen JM, Taylor K, Brankovich J. Evaluation of the South Metropolitan Health Service Community Engagement Process Perth: Curtin University. 2014.
Yadav UN, Lloyd J, Baral KP, Bhatta N, Mehata S, Harris M. Evaluating the feasibility and acceptability of a co-design approach to developing an integrated model of care for people with multi-morbid COPD in rural Nepal: a qualitative study. BMJ Open. 2021;11(1): e045175.
Kaihlanen A-M, Hietapakka L, Heponiemi T. Increasing cultural awareness: qualitative study of nurses’ perceptions about cultural competence training. BMC Nurs. 2019;18(1):38.
Askew DA, Foley W, Kirk C, Williamson D. “I’m outta here!”: a qualitative investigation into why Aboriginal and non-Aboriginal people self-discharge from hospital. BMC Health Serv Res. 2021;21(1):907.
Gee G, Dudgeon P, Schultz C, Hart A, Kelly K. Aboriginal and Torres Strait Islander Social and Emotional Wellbeing. In: Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. 2014.
Bywood P, Katterl R, Lunnay B. Disparities in primary health care utilisation: Who are the disadvantaged groups? How are they disadvantaged? What interventions work? Adelaide: Primary Health Care Research and Information Service (PHCRIS), Policy Issue Review; 2011.
Australian Government Department of Health. Future focused primary health care: Australia’s Primary Health Care 10 Year Plan 2022–2032. 2022.Canberra ACT 2601.
Download references
Acknowledgements
We are grateful for the support of Chelsea Liu assisted with the use of the Quality Appraisal Tool and the support of Dr. Deborah Wong (Research Coordinator- Chronic Disease | Cervical Cancer) in designing Fig. 2 . We would also like to acknowledge Thiitu Tharrmay Aboriginal and Torres Strait Islander Reference Group members rather than Thiitu Tharrmay Aboriginal Reference Group members at the National Centre for Aboriginal and Torres Strait Islander Wellbeing Research at the Australian National University for their continuous feedback without which this research piece wouldn’t have been completed.
The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions or policies of their affiliated institutions.
This work was supported by funding from the Australian Government Department of Health-—First Nations Health Division. The funding body had no role in the writing of this article.
Author information
Uday Narayan Yadav and Rosemary Wyber have contributed equally to this work.
Authors and Affiliations
National Centre for Aboriginal and Torres Strait Islander Wellbeing Research, Australian National University, Canberra, ACT, Australia
Uday Narayan Yadav & Rosemary Wyber
Centre for Primary Health Care and Equity, University of New South Wales, Sydney, Australia
Uday Narayan Yadav
Melbourne Medical School, The University of Melbourne, Melbourne, Australia
Jasmine Meredith Davis
The George Institute for Global Health, Sydney, Australia
Keziah Bennett-Brook & Julieann Coombes
Telethon Kids Institute, Perth, WA, Australia
Rosemary Wyber
South Australian Health and Medical Research Institute, Adelaide, SA, Australia
Odette Pearson
Faculty of Health and Medical Science, University of Adelaide, Adelaide, SA, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization & original draft: Uday Narayan Yadav and Rosemary Wyber. Data curation: Uday Narayan Yadav, Jasmine Meredith Davis and Rosemary Wyber. Review, edits and revision: Uday Narayan Yadav, Jasmine Meredith Davis, Keziah Bennett-Brook, Julieann Coombes, Rosemary Wyber and Odette Pearson.
Corresponding author
Correspondence to Uday Narayan Yadav .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for Publication
Competing interests.
The authors have no competing interests to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Study characteristics.
Additional file 2.
Meta aggregated study findings.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yadav, U.N., Davis, J.M., Bennett-Brook, K. et al. A rapid review to inform the policy and practice for the implementation of chronic disease prevention and management programs for Aboriginal and Torres Strait Islander people in primary care. Health Res Policy Sys 22 , 34 (2024). https://doi.org/10.1186/s12961-024-01121-x
Download citation
Received : 26 October 2023
Accepted : 10 February 2024
Published : 21 March 2024
DOI : https://doi.org/10.1186/s12961-024-01121-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Aboriginal and Torres Strait Islander people
- Barriers and enablers Chronic disease prevention and management
- Primary health care
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Australian Government Department of Health and Aged Care
Final report of the Aged Care Taskforce
This report examines the recommendations proposed by the Aged Care Taskforce to support an aged care system that is sustainable, fair and facilitates greater innovation in the sector.
Scroll down to access downloads and media.
Download [Publication] Final report of the Aged Care Taskforce (PDF) as PDF - 1.36 MB - 64 pages
Download [Publication] Final report of the Aged Care Taskforce (Word) as Word - 1.89 MB - 64 pages
We aim to provide documents in an accessible format. If you're having problems using a document with your accessibility tools, please contact us for help .
We held a presentation on the Aged Care Taskforce report on Tuesday 12 March 2024. A recording of this presentation will be available soon. You can still submit questions by email .
Is there anything wrong with this page?
Help us improve health.gov.au
If you would like a response please use the enquiries form instead.
Mobile Menu Overlay
The White House 1600 Pennsylvania Ave NW Washington, DC 20500
FACT SHEET: President Biden Issues Executive Order and Announces New Actions to Advance Women’s Health Research and Innovation
In his State of the Union address, President Biden laid out his vision for transforming women’s health research and improving women’s lives all across America. The President called on Congress to make a bold, transformative investment of $12 billion in new funding for women’s health research. This investment would be used to create a Fund for Women’s Health Research at the National Institutes of Health (NIH) to advance a cutting-edge, interdisciplinary research agenda and to establish a new nationwide network of research centers of excellence and innovation in women’s health—which would serve as a national gold standard for women’s health research across the lifespan.
It is long past time to ensure women get the answers they need when it comes to their health—from cardiovascular disease to autoimmune diseases to menopause-related conditions. To pioneer the next generation of discoveries, the President and the First Lady launched the first-ever White House Initiative on Women’s Health Research , which aims to fundamentally change how we approach and fund women’s health research in the United States.
Today, President Biden is signing a new Executive Order that will direct the most comprehensive set of executive actions ever taken to expand and improve research on women’s health. These directives will ensure women’s health is integrated and prioritized across the federal research portfolio and budget, and will galvanize new research on a wide range of topics, including women’s midlife health.
The President and First Lady are also announcing more than twenty new actions and commitments by federal agencies, including through the U.S. Department of Health and Human Services (HHS), the Department of Defense (DoD), the Department of Veterans Affairs (VA), and the National Science Foundation (NSF). This includes the launch of a new NIH-wide effort that will direct key investments of $200 million in Fiscal Year 2025 to fund new, interdisciplinary women’s health research—a first step towards the transformative central Fund on Women’s Health that the President has called on Congress to invest in. These actions also build on the First Lady’s announcement last month of the Advanced Research Projects Agency for Health (ARPA-H) Sprint for Women’s Health , which committed $100 million towards transformative research and development in women’s health.
Today, the President is issuing an Executive Order that will:
- Integrate Women’s Health Across the Federal Research Portfolio . The Executive Order directs the Initiative’s constituent agencies to develop and strengthen research and data standards on women’s health across all relevant research and funding opportunities, with the goal of helping ensure that the Administration is better leveraging every dollar of federal funding for health research to improve women’s health. These actions will build on the NIH’s current policy to ensure that research it funds considers women’s health in the development of study design and in data collection and analysis. Agencies will take action to ensure women’s health is being considered at every step in the research process—from the applications that prospective grantees submit to the way that they report on grant implementation.
- Prioritize Investments in Women’s Health Research . The Executive Order directs the Initiative’s constituent agencies to prioritize funding for women’s health research and encourage innovation in women’s health, including through ARPA-H and multi-agency initiatives such as the Small Business Innovation Research Program and the Small Business Technology Transfer Program. These entities are dedicated to high-impact research and innovation, including through the support of early-stage small businesses and entrepreneurs engaged in research and innovation. The Executive Order further directs HHS and NSF to study ways to leverage artificial intelligence to advance women’s health research. These additional investments—across a wide range of agencies—will support innovation and open new doors to breakthroughs in women’s health.
- Galvanize New Research on Women’s Midlife Health . To narrow research gaps on diseases and conditions associated with women’s midlife health or that are more likely to occur after menopause, such as rheumatoid arthritis, heart attack, and osteoporosis, the President is directing HHS to: expand data collection efforts related to women’s midlife health; launch a comprehensive research agenda that will guide future investments in menopause-related research; identify ways to improve management of menopause-related issues and the clinical care that women receive; and develop new resources to help women better understand their options for menopause-related symptoms prevention and treatment. The Executive Order also directs the DoD and VA to study and take steps to improve the treatment of, and research related to, menopause for Service women and women veterans.
- Assess Unmet Needs to Support Women’s Health Research . The Executive Order directs the Office of Management and Budget and the Gender Policy Council to lead a robust effort to assess gaps in federal funding for women’s health research and identify changes—whether statutory, regulatory, or budgetary—that are needed to maximally support the broad scope of women’s health research across the federal government. Agencies will also be required to report annually on their investments in women’s health research, as well as progress towards their efforts to improve women’s health.
Today, agencies are also announcing new actions they are taking to promote women’s health research , as part of their ongoing efforts through the White House Initiative on Women’s Health Research. Agencies are announcing actions to:
Prioritize and Increase Investments in Women’s Health Research
- Launch an NIH-Cross Cutting Effort to Transform Women’s Health Throughout the Lifespan. NIH is launching an NIH-wide effort to close gaps in women’s health research across the lifespan. This effort—which will initially be supported by $200 million from NIH beginning in FY 2025—will allow NIH to catalyze interdisciplinary research, particularly on issues that cut across the traditional mandates of the institutes and centers at NIH. It will also allow NIH to launch ambitious, multi-faceted research projects such as research on the impact of perimenopause and menopause on heart health, brain health and bone health. In addition, the President’s FY25 Budget Request would double current funding for the NIH Office of Research on Women’s Health to support new and existing initiatives that emphasize women’s health research.
This coordinated, NIH-wide effort will be co-chaired by the NIH Office of the Director, the Office of Research on Women’s Health, and the institute directors from the National Institute on Aging; the National Heart, Lung, and Blood Institute; the National Institute on Drug Abuse; the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Institute on Arthritis, Musculoskeletal and Skin Diseases.
- Invest in Research on a Wide Range of Women’s Health Issues. The bipartisan Congressionally Directed Medical Research Program (CDMRP), led out of DoD, funds research on women’s health encompassing a range of diseases and conditions that affect women uniquely, disproportionately, or differently from men. While the programs and topic areas directed by Congress differ each year, CDMRP has consistently funded research to advance women’s health since its creation in 1993. In Fiscal Year 2022, DoD implemented nearly $490 million in CDMRP investments towards women’s health research projects ranging from breast and ovarian cancer to lupus to orthotics and prosthetics in women. In Fiscal Year 2023, DoD anticipates implementing approximately $500 million in CDMRP funding for women’s health research, including in endometriosis, rheumatoid arthritis, and chronic fatigue.
- Call for New Proposals on Emerging Women’s Health Issues . Today, NSF is calling for new research and education proposals to advance discoveries and innovations related to women’s health. To promote multidisciplinary solutions to women’s health disparities, NSF invites applications that would improve women’s health through a wide range of disciplines—from computational research to engineering biomechanics. This is the first time that NSF has broadly called for novel and transformative research that is focused entirely on women’s health topics, and proposals will be considered on an ongoing basis.
- Increase Research on How Environmental Factors Affect Women’s Health. The Environmental Protection Agency (EPA) is updating its grant solicitations and contracts to ensure that applicants prioritize, as appropriate, the consideration of women’s exposures and health outcomes. These changes will help ensure that women’s health is better accounted for across EPA’s research portfolio and increase our knowledge of women’s environmental health—from endocrine disruption to toxic exposure.
- Create a Dedicated, One-Stop Shop for NIH Funding Opportunities on Women’s Health. Researchers are often unaware of existing opportunities to apply for federal funding. To help close this gap, NIH is issuing a new Notice of Special Interest that identifies current, open funding opportunities related to women’s health research across a wide range of health conditions and all Institutes, Centers, and Offices. The NIH Office of Research on Women’s Health will build on this new Notice by creating a dedicated one-stop shop on open funding opportunities related to women’s health research. This will make it easier for researchers and institutions to find and apply for funding—instead of having to search across each of NIH’s 27 institutes for funding opportunities.
Foster Innovation and Discovery in Women’s Health
- Accelerate Transformative Research and Development in Women’s Health. ARPA-H’s Sprint for Women’s Health launched in February 2024 commits $100 million to transformative research and development in women’s health. ARPA-H is soliciting ideas for novel groundbreaking research and development to address women’s health, as well as opportunities to accelerate and scale tools, products, and platforms with the potential for commercialization to improve women’s health outcomes.
- Support Private Sector Innovation Through Additional Federal Investments in Women’s Health Research. The NIH’s competitive Small Business Innovation Research Program and the Small Business Technology Transfer Program is committing to further increasing—by 50 percent—its investments in supporting innovators and early-stage small businesses engaged in research and development on women’s health. These programs will solicit new proposals on promising women’s health innovation and make evidence-based investments that bridge the gap between performance of basic science and commercialization of resulting innovations. This commitment for additional funds builds on the investments the Administration has already made to increase innovation in women’s health through small businesses, including by increasing investments by sevenfold between Fiscal Year 2021 and Fiscal Year 2023.
- Advance Initiatives to Protect and Promote the Health of Women. The Food and Drug Administration (FDA) seeks to advance efforts to help address gaps in research and availability of products for diseases and conditions that primarily impact women, or for which scientific considerations may be different for women, and is committed to research and regulatory initiatives that facilitate the development of safe and effective medical products for women. FDA also plans to issue guidance for industry that relates to the inclusion of women in clinical trials and conduct outreach to stakeholders to discuss opportunities to advance women’s health across the lifespan. And FDA’s Office of Women’s Health will update FDA’s framework for women’s health research and seek to fund research with an emphasis on bridging gaps in knowledge on important women’s health topics, including sex differences and conditions that uniquely or disproportionately impact women.
- Use Biomarkers to Improve the Health of Women Through Early Detection and Treatment of Conditions, such as Endometriosis. NIH will launch a new initiative dedicated to research on biomarker discovery and validation to help improve our ability to prevent, diagnose, and treat conditions that affect women uniquely, including endometriosis. This NIH initiative will accelerate our ability to identify new pathways for diagnosis and treatment by encouraging multi-sector collaboration and synergistic research that will speed the transfer of knowledge from bench to bedside.
- Leverage Engineering Research to Improve Women’s Health . The NSF Engineering Research Visioning Alliance (ERVA) is convening national experts to identify high-impact research opportunities in engineering that can improve women’s health. ERVA’s Transforming Women’s Health Outcomes Through Engineering visioning event will be held in June 2024, and will bring together experts from across engineering—including those in microfluidics, computational modeling, artificial intelligence/imaging, and diagnostic technologies and devices—to evaluate the landscape for new applications in women’s health. Following this event, ERVA will issue a report and roadmap on critical areas where engineering research can impact women’s health across the lifespan.
- Drive Engineering Innovations in Women’s Health Discovery . NSF awardees at Texas A&M University will hold a conference in summer 2024 to collectively identify challenges and opportunities in improving women’s health through engineering. Biomedical engineers and scientists will explore and identify how various types of engineering tools, including biomechanics and immuno-engineering, can be applied to women’s health and spark promising new research directions.
Expand and Leverage Data Collection and Analysis Related to Women’s Health
- Help Standardize Data to Support Research on Women’s Health. NIH is launching an effort to identify and develop new common data elements related to women’s health that will help researchers share and combine datasets, promote interoperability, and improve the accuracy of datasets when it comes to women’s health. NIH will initiate this process by convening data and scientific experts across the federal government to solicit feedback on the need to develop new NIH-endorsed common data elements—which are widely used in both research and clinical settings. By advancing new tools to capture more data about women’s health, NIH will give researchers and clinicians the tools they need to enable more meaningful data collection, analysis, and reporting and comprehensively improve our knowledge of women’s health.
- Reflect Women’s Health Needs in National Coverage Determinations. The Centers for Medicare & Medicaid Services (CMS) will strengthen its review process, including through Coverage with Evidence Development guidance, to ensure that new medical services and technologies work well in women, as applicable, before being covered nationally through the Medicare program. This will help ensure that Medicare funds are used for treatments with a sufficient evidence base to show that they actually work in women, who make up more than half of the Medicare population.
- Leverage Data and Quality Measures to Advance Women’s Health Research. The Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration (HRSA) are building on existing datasets to improve the collection, analysis, and reporting of information on women’s health. The CDC is expanding the collection of key quality measures across a woman’s lifespan, including to understand the link between pregnancy and post-partum hypertension and heart disease, and plans to release the Million Hearts Hypertension in Pregnancy Change Package. This resource will feature a menu of evidence-informed strategies by which clinicians can change care processes. Each strategy includes tested tools and resources to support related clinical quality improvement. HRSA is modernizing its Uniform Data System in ways that will improve the ability to assess how women are being served through HRSA-funded health centers. By improving the ability to analyze data on key clinical quality measures, CDC and HRSA can help close gaps in women’s health care access and identify new opportunities for high-impact research.
Strengthen Coordination, Infrastructure, and Training to Support Women’s Health Research
- Launch New Joint Collaborative to Improve Women’s Health Research for Service Members and Veterans. DoD and VA are launching a new Women’s Health Research collaborative to explore opportunities that further promote joint efforts to advance women’s health research and improve evidence-based care for Service members and veterans. The collaborative will increase coordination with the goal of helping improve care across the lifespan for women in the military and women veterans. The Departments will further advance research on key women’s health issues and develop a roadmap to close pressing research gaps, including those specifically affecting Service women and women veterans.
- Coordinate Research to Advance the Health of Women in the Military. DoD will invest $10 million, contingent on available funds, in the Military Women’s Health Research Partnership. This Partnership is led by the Uniformed Services University and advances and coordinates women’s health research across the Department. The Partnership is supporting research in a wide range of health issues affecting women in the military, including cancers, mental and behavioral health, and the unique health care needs of Active Duty Service Women. In addition, the Uniformed Services University established a dedicated Director of Military Women’s Health Research Program, a role that is responsible for identifying research gaps, fostering collaboration, and coordinating and aligning a unified approach to address the evolving needs of Active Duty Service Women.
- Support EPA-Wide Research and Dissemination of Data on Women’s Health. EPA is establishing a Women’s Health Community of Practice to coordinate research and data dissemination. EPA also plans to direct the Board of Scientific Counselors to identify ways to advance EPA’s research with specific consideration of the intersection of environmental factors and women’s health, including maternal health.
- Expand Fellowship Training in Women’s Health Research. CDC, in collaboration with the CDC Foundation and American Board of Obstetrics and Gynecology, is expanding training in women’s health research and public health surveillance to OBGYNs, nurses and advanced practice nurses. Through fellowships and public health experiences with CDC, these clinicians will gain public health research skills to improve the health of women and children exposed to or affected by infectious diseases, mental health and substance use disorders. CDC will invite early career clinicians to train in public health and policy to become future leaders in women’s health research.
Improve Women’s Health Across the Lifespan
- Create a Comprehensive Research Agenda on Menopause. To help women get the answers they need about menopause, NIH will launch its first-ever Pathways to Prevention series on menopause and the treatment of menopausal symptoms. Pathways to Prevention is an independent, evidence-based process to synthesize the current state of the evidence, identify gaps in existing research, and develop a roadmap that can be used to help guide the field forward. The report, once completed, will help guide innovation and investments in menopause-related research and care across the federal government and research community.
- Improve Primary Care and Preventive Services for Women . The Agency for Healthcare Research and Quality (AHRQ) will issue a Notice of Intent to publish a funding opportunity announcement for research to advance the science of primary care, which will include a focus on women’s health. Through this funding opportunity, AHRQ will build evidence about key elements of primary care that influence patient outcomes and advance health equity—focusing on women of color—such as care coordination, continuity of care, comprehensiveness of care, person-centered care, and trust. The results from the funding opportunity will shed light on vital targets for improvements in the delivery of primary healthcare across a woman’s lifespan, including women’s health preventive services, prevention and management of multiple chronic diseases, perinatal care, transition from pediatric to adult care, sexual and reproductive health, and care of older adults.
- Promote the Health of American Indian and Alaska Native Women. The Indian Health Service is launching a series of engagements, including focus groups, to better understand tribal beliefs related to menopause in American Indian and Alaska Native Women. This series will inform new opportunities to expand culturally informed patient care and research as well as the development of new resources and educational materials.
- Connect Research to Real-World Outcomes to Improve Women’s Mental and Behavioral Health. The Substance Abuse and Mental Health Services Administration (SAMHSA) is supporting a range of health care providers to address the unique needs of women with or at risk for mental health and substance use disorders. Building on its current efforts to provide technical assistance through various initiatives , SAMHSA intends, contingent on available funds, to launch a new comprehensive Women’s Behavioral Health Technical Assistance Center. This center will identify and improve the implementation of best practices in women’s behavioral health across the life span; identify and fill critical gaps in knowledge of and resources for women’s behavioral health; and provide learning opportunities, training, and technical assistance for healthcare providers.
- Support Research on Maternal Health Outcomes. USDA will fund research to help recognize early warning signs of maternal morbidity and mortality in recipients of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and anticipates awarding up to $5 million in Fiscal Year 2023 to support maternal health research through WIC. In addition, research being conducted through the Agricultural Research Service’s Human Nutrition Research Centers is focusing on women’s health across the lifespan, including the nutritional needs of pregnant and breastfeeding women and older adults.
Stay Connected
We'll be in touch with the latest information on how President Biden and his administration are working for the American people, as well as ways you can get involved and help our country build back better.
Opt in to send and receive text messages from President Biden.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Rev Saude Publica

Attitudes of health professionals towards suicidal behavior: an intervention study
Jesiele spindler faria.
I Universidade Federal de Mato Grosso, Faculdade de Enfermagem., Cuiabá MT , Brasil, Universidade Federal de Mato Grosso. Faculdade de Enfermagem. Cuiabá, MT, Brasil
Samira Reschetti Marcon
Alice milani nespollo.
II Universidade Federal de Mato Grosso, Faculdade de Enfermagem, Sinop MT , Brasil, Universidade Federal de Mato Grosso. Faculdade de Enfermagem - Campus Sinop. Sinop, MT, Brasil
Hugo Gedeon Barros dos Santos
III Hospital Universitário Júlio Muller, Unidade de Atenção Psicossocial, Cuiabá MT , Brasil, Hospital Universitário Júlio Muller. Unidade de Atenção Psicossocial. Cuiabá, MT, Brasil
Mariano Martínez Espinosa
IV Universidade Federal de Mato Grosso, Instituto de Ciências Exatas e da Terra, Departamento de Estatística, Cuiabá Mato Grosso , Brasil, Universidade Federal de Mato Grosso. Instituto de Ciências Exatas e da Terra. Departamento de Estatística. Cuiabá, Mato Grosso, Brasil
Kleici Kleslly Brito de Oliveira
Josemara gomes da silva lima.
V Universidade Federal de Mato Grosso, Programa de Pós-Graduação em Saúde Coletiva, Cuiabá MT , Brasil, Universidade Federal de Mato Grosso. Programa de Pós-Graduação em Saúde Coletiva. Cuiabá, MT, Brasil
Authors’ Contribution: Study design and planning: JFS, SRM, AMN, MME. Data collection, analysis, and interpretation: JFS, HGBS, MME, AMN. Manuscript development and review: JFS, SRM, JGSL, KKBO. Final draft approval: JGSL, KKBO, SRM, HGBS. Public responsibility for the content of the article: JFS, HGBS, MME, AMN, JGSL, KKBO, SRM.
To evaluate the effect of an educational intervention on the attitudes of primary healthcare providers regarding patients with suicidal behavior.
Clinical trial randomized by clusters, with a sample of 261 healthcare professionals, from 22 health units selected by stratified sampling, were chosen and randomly allocated, by drawing, into two groups: intervention (n = 87) and control (n = 174). The participants of the intervention group were exposed to a 20-hour training on suicidal behavior. All 261 participants were evaluated before and after the intervention; the groups were compared to evaluate their attitude towards suicidal behavior using the Suicide Behavior Attitude Questionnaire (SBAQ), an evaluation made by comparison of the means via t-Student test, for independent samples, and paired t-test, for dependent samples.
The intervention group, in comparison to their evaluation before and after training, as well as in the comparison with the evaluation of the control group, showed statistically significant differences in attitudes towards suicidal behavior, according to the differences presented in the scores for the domains: “perception of professional capacity,” in all four items; “negative feeling,” in six of the seven items; and in the “right to commit suicide” domain, in three of the five items.
The brief training developed in primary health care was effective to improve the attitudes of the participants who were part of the intervention group regarding patients with suicidal behavior.
INTRODUCTION
Approximately 800,000 people commit suicide annually, which corresponds to a rate of 11.4 deaths per 100,000 inhabitants worldwide, being among the top ten death causes in all age groups 1 . Although the suicide mortality rate in some Western European countries has decreased in recent decades, other countries, such as Mexico, the United States, and Brazil, experienced an increase in cases during the same period 2 . According to national data, more than 10,000 Brazilians committed suicide, meaning 5.5 occurrences per 100,000 inhabitants, in 2015, and 6.5 deaths per 100,000 inhabitants, in 2016, proving an increase over the years 3 . Considering the magnitude of the problem, the World Health Organization – WHO recommends that the prioritization of suicide, both in the care offered and in the development of public health policies 1 .
In this context, the mobilization of the health services is inevitable, since the primary care environment often provides the initial actions for mental health care 4 . This is directly related to the insufficient number of professionals in the psychosocial care network to meet this demand, especially in middle-income countries, such as Brazil, where the coverage of these services encompass only 10% of the individuals who need it 4 .
A systematic review analyzed the contact individuals had with primary healthcare providers before committing suicide and the results showed that, on average, 80% sought the health service in the year prior to suicide and 44%, in the same month of death 5 . Similar findings were described in a Norwegian study that investigated the use of primary healthcare services in 4,926 suicide cases (subjects aged > 15 years) from 2007 to 2015. The results showed that approximately 90% of the individuals consulted a generalist professional in primary care in the year prior to suicide and up to 46.4% in their last month of life 6 .
This suggests that professionals of this level of care are in a unique position to identify and intervene in subjects at suicidal risk, since primary health care is the first contact with the health network 1 . Most professionals, however, manifest negative attitudes when dealing with people with suicidal behavior 7 , commonly due to factors such as unpreparedness or difficulties in dealing with this demand, providing limited initial care, and often referring patients to other services 9 , 10 , compromising the quality of care provided.
An attitude can be defined as a set of cognitive, affective, and behavioral attributes. Therefore, attitude is an inclination of the individual – acquired socially, from personal experiences, and from personality factors – to act in a specific way in relation to certain people, objects, and situations 11 .
In a meta-analysis that reviewed studies developed until 2018, negative attitudes, limited empathy, and some levels of hostility were observed from healthcare providers when attending to people with suicidal behavior. The data also indicated that training and professional qualification on how to deal with these cases promote more positive attitudes 12 . Corroborating these findings, subsequent studies observed a resistance in attending this clientele; care based on beliefs and stigmas; technical and routine activities prioritized over psychological support; deficient knowledge and skills; in addition to the need for training to facilitate therapeutic relationships 13 .
Studies that propose to analyze the effects of educational strategies on the modification of attitudes, although scarce in the Brazilian and international literature, show a predominance in interventions that have the hospital environment as the targeted audience 16 .
Thus, this study questions: can the attitudes of primary healthcare providers be modified after professional training on dealing with suicidal behavior? To answer this question, our study aims to evaluate the effect of an educational intervention on the attitudes of primary healthcare providers regarding suicidal behavior.
This is a two-arm parallel randomized controlled trial inscribed in the Brazilian Registry of Clinical Trials (ReBEC) under the code RBR-9pmjf5w.
Developed in the city of Cuiabá, from May to August 2017, in Family Health Strategy (FHS) units, structured by multidisciplinary teams, composed of at least one nurse, a general practitioner or family doctor, a nursing technician, and community health agents, and can also have an expanded team, including oral health professionals. The city of Cuiabá, in the state of Mato Grosso, has 70 FHS teams, 3 in the rural area of the municipality and 67 in the urban area, distributed in four regions: 24 units in the northern region, 21 in the southern, 11 in the eastern, and 11 in the western. Totaling 298 healthcare providers, including physicians, nurses, and nursing technicians; 697 community health agents; and 86 oral health professionals 23 .
The study population consisted of healthcare providers who functioned as physician, nurses, and nursing technicians; excluding from the study professionals from teams located in the rural area (since they composed the pilot test sample of this study), as well as health agents and oral health professionals (since the instrument used does not target these categories).
A probabilistic sampling was obtained by clustering and stratification; the sampling unit was the health team, composed of a group of professionals, which was stratified by regional health units.
To determine the number of subjects, a formula was used for paired data 24 , in which the mean of the changes in attitude (pre- and post-intervention) and the standard deviations, obtained from a reference study, were determined 25 . A standard deviation of 2.92 was estimated, considering a minimum difference to be detected of 1.0, 95% confidence, and power of 0.80. Thus, the initial sample size adjusted for population (n = 298) was 56 individuals. Since it is a cluster sampling design, a design effect factor was established at 1.22 and an estimated non-response rate was estimated at 22%, which resulted in a final sample of 87 individuals for the intervention group. For the control group, 1 for 2 was considered, i.e., 174 individuals.
The random selection of participants for the intervention and control groups was performed by cluster sampling and stratification proportional to the size of the population, considering the regions (north, south, east, west) as strata and the FHS teams as randomization units, in order to obtain adequate control and reduce methodological bias. The number of professionals selected in each region was defined by multiplying the fraction of professionals by the sample size (87). Subsequently, to define the number of teams to be drawn, the number of healthcare providers per stratum was divided by the number of teams (four), totaling 22 teams randomly drawn by statistical program ( Table 1 ).
FHS: family health strategy.
The Suicide Behavior Attitude Questionnaire (SBAQ), composed of clinical situations frequently experienced by healthcare providers, was used to identify the professional’s attitude towards suicidal behavior 26 . This instrument is divided into factors relating to the feelings professionals have in relation to the patient with suicidal behavior, their self-perception on capacity for care, and the right to suicide. Investigating these factors allows for the positive or negative attitudes to be measured. According to the mean obtained by adding the values of each question and diving by the total number of questions in each domain, we can verify a more positive attitudes by the higher scores for the domain “Perception of professional capacity” and by the lower scores for the domains “Feelings towards the patient” and “Right to suicide 26 .” To verify other variables, such as sociodemographic (age, gender, color, education), professional background (occupation, specializations, training in mental health), and professional practice (previous care to patients with suicidal behavior); a closed instrument was constructed, applied with the SBAQ.
At first, all participating units were visited in order to inform about the study and apply the instruments. The professionals selected for the intervention group, were invited to participate in the intervention (training) in addition to answering the instruments (pre-test). The questionnaires were previously coded and allowed pairing, it did not allow, however, for the personal identification of the participants. The participants who were absent from the health unit at the first attempt were sought two more times, at different moments. Whenever possible and necessary, visits were scheduled.
Subsequently, the intervention group was offered a 20-hour training, aiming to improve the ability to recognize the degree of risk of an individual with suicidal behavior and to intervene; to learn strategies to care for and/or to refer individuals with suicidal behavior; and to recognize and improve one’s own attitude towards a patient with suicidal behavior. The content was defined according to the manual of suicide prevention aimed at primary healthcare teams of the World Health Organization. The training was conducted by psychologists and researchers in Suicidology, with extensive clinical and pedagogical experience in this topic. Immediately after the end of the training, the SBAQ was reapplied to the intervention group (post-test). For the control group, no type of intervention was offered, and the post-test was reapplied later in the health units.
The expected primary outcome was a difference in the level of attitudes towards suicidal behavior between the beginning and end of the intervention, verified through the SBAQ, based on the increase of scores equal to or greater than 3%; the analysis was performed on the principle of intention to treat.
Figure shows the flowchart of participation of individuals involved in the clinical trial, from recruitment to the last evaluation. Of the 87 professionals who were initially exposed to the intervention, 69 (79.3%) participated in the last evaluation, and in the control group 88 (50.6%) remained for analysis. The losses in the study occurred due to refusal to remain in the study (n of the intervention group = 7, n of the control group = 11), incomplete filling of the instruments (n of the intervention group = 11, n of the control group = 37), change of workplace or were not found (n of the control group = 38).

The distribution of the data was verified by the Shapiro-Wilk test. To compare the two groups, Pearson’s chi-square homogeneity test, t-student test for two independent samples, and U-Mann Whitney test were used. Comparison within the pre- and post-intervention group were performed by the paired t-test for dependent samples and by the Wilcoxon signed-rank test. The level of significance adopted was 5% for all tests. The research project was approved by the research ethics committee in accordance with Resolution 466/2012.
The analysis of sociodemographic data, of previous training, and of attending to suicidal behavior ( Table 2 ) showed no statistically significant difference between the groups.
Table 3 describes the attitudes of healthcare providers in the intervention group and the control group, pre- and post-test. The results did not reveal significant difference for most items of the SBAQ, between the groups in the pre-test, except for item Q17, which presented statistical significance with ranks mean (intervention group = 1.40; control group = 2.70; p-value < 0.001). However, in the evaluation performed after training, there were statistically significant differences between the two groups in all items of the factors “negative feelings towards the patient” and “perception of professional capacity.” In “right to suicide” of the five items that make up the factor, items Q4, Q6, and Q16 underwent statistically significant changes (p-value < 0.05), however, questions Q3 and Q18 did not present significant changes (p-value = 0.131 and p-value = 0.597, respectively).
a Intervention Group evaluation prior to the intervention.
b Control Group evaluation prior to the intervention.
c significant p-value less than 0.05 obtained by student’s t-test.
d Intervention group post-evaluation.
e Control group post-evaluation.
f significant p-value less than 0.05 obtained by the U-Mann Whitney test.
Table 4 describes the attitudes of healthcare providers in the intervention group and the control group, pre- and post-test. In the factor “negative feelings in relation to the patient,” we observed statistically significant gains in six of the seven items that make up the domain (Q2, Q5, Q9, Q13, Q15, and Q19). In question 17, the means of the pre-test, 2.71, and post-test, 2.02 (p-value = 0.070), showed differences, but without statistical significance. Regarding the “perception of professional capacity” there were statistically significant changes for all four items of this factor, with p-value < 0.001. In “right to suicide,” of the five items that make up the factor, items Q4, Q6, and Q16 underwent statistically significant changes (p-value < 0.005), however, questions Q3 and Q18 did not present significant changes (p-value = 0.086 and p-value = 0.234, respectively).
a Intervention Group evaluation before the training.
b Intervention group evaluation after the training.
c Wilcoxon test for paired samples.
d p-value considered significant less than 0.05.
The literature shows that the care given to patients with suicidal behavior can be influenced by several factors, among which are the attitudes of healthcare providers 9 , 10 , 12 .
Attending to patients with suicidal behavior can lead to feelings of frustration, impotence, guilt, contempt, and anger 18 , 27 . Additionally, suicide behavior is surrounded by myths and beliefs, such as those that classify suicide attempts and threats as forms of seeking attention and not as actual intention, or even that people with this behavior are considered cowards 9 , 30 , 31 . An attitude is subject to change, which can be evidenced in our study; regarding the “feeling in relation to the patient,” the post-intervention evaluation showed changes for all items in this domain. These findings demonstrated changes in the understanding of suicidal attempts and threats as potential risk factors and that people in these conditions are in intense suffering, providing a more empathic postures in relation to these patients.
The fact that the professional reacts negatively when attending to a patient with suicidal behavior may, among other aspects, be related to the training process that often does not provide tools for coping with situations of death, especially when associated with the subject’s choice 31 . The lack of desire to live can be conflicting for professionals, since they are instructed to save lives. Thus, aspects such as overcoming the dilemmas of omnipotence and omniscience, which usually cause distress in these situations, were widely discussed in training.
Another aspect that was raised is that the feeling of anxiety, due to a possible error of conduct or evaluation, and the idea of responsibility over the patient’s life can be expressed by the difficulty in establishing a bond or in the fear of talking about suicide for fear of inducing the patient to commit it 32 . However, the discussions generated during the training showed that the professionals were less elusive in getting involved and establishing bonds with patients who attempted suicide and presented a reduction in the feeling of impotence. This may explain the significant changes in the questionnaire responses in this factor.
Perceiving one’s own negative feelings as defense mechanisms, considering death as part of human existence, and identifying the feelings involved in the process of death and dying were a part of the methodology employed and favored the understanding and modification of feelings among professionals. These findings corroborate the study developed with healthcare providers in which, after training, a significant reduction in negative feelings and better accuracy in risk assessment were found 19 .
On the “perception of professional capacity,” the findings showed self-perception of greater capacity for care, better professional preparation, and confidence to deal with patients at risk of suicide. Similar results are found in a Japanese multicenter study that performed a two-hour intervention with 74 healthcare providers. There were significant increases in perceived skills, confidence, and attitude, as well as a greater competence in the assessment of suicidal risk, and more confidence in attending to patients in these conditions 33 .
A study conducted in Australia, in which 248 health professionals participated in a training on suicidal behavior, resulted in improved knowledge, more appropriate attitudes regarding expansion of communication capacity, and increased confidence in providing appropriate care 21 . The literature has emphasized that negative attitudes towards suicidal patients among healthcare providers may be more related to lack of knowledge and uncertainties in how to care for than to a specific hostility 20 . Thus, misinformation about suicide can perpetuate a mistaken approach.
Continuously updated knowledge, especially regarding the assessment of suicidal risk and treatment options, can decrease anxiety about failures and increase the perception of professional capacity. As professionals understand and fulfill their responsibilities in identifying, evaluating, and intervening therapeutically, performing professionally according to evidence, and planning the follow-up of a person at suicidal risk, they become aware that the factors related to professional skills and competences have been contemplated 17 .
Healthcare providers live alongside suffering, pain, fear, hopelessness, losses in various ways and often face the processes of death and dying. Feeling helpless and powerless is common in these situations. The belief that only cure or recovery characterizes as good care, emphasized during academic training and reiterated daily by the culture of therapeutic obstinacy, may contribute to professional insecurity when faced with situations that signal a possible self-inflicted death 34 .
Several authors also highlight the influence of organizational issues of the service, as well as the scarcity of physical structure and especially trained personnel, demonstrating the difficulties and fears of not having resources in the face of the unexpected. During the training, several factors such as those reported above were described as limiting an effective care, accompanied by feelings of insecurity, helplessness, and incompetence. It was emphasized, however, that the fear of error can be gradually replaced by the confidence to intervene when limits and potentials are recognized 17 , 21 , 35 .
The third component investigated in our study refers to the “right to suicide,” in which we observed changes in three of its five items, in the evaluation after intervention. However, one of the items in which no significant changes were observed was the statement: “despite everything, I think a person has the right to suicide.” An Australian study described similar result after a one-day training: in which only 30% agreed with the right to commit suicide. According to the authors, these findings reflect the nature of the items that make up this factor (moral and religious beliefs) are deeply ingrained, with less expectation of modifications, even after an educational intervention 21 .
A healthcare providers should not prioritize their individual principles and convictions when attending a person with suicidal behavior, with the risk of inducing them to adapt to social standards, based on their personal values and beliefs that may not be relevant to the patient, endangering the therapeutic bond necessary for care. Thus, the care provided cannot, in any way, intensify the feeling of guilt in the person with suicidal ideation or tendency and in their families 34 .
When asked about the possibility of changing a suicide intention by means of a conversation, significant positive effects were perceived after training. However, in the statement “when a person talks about ending their life, I try to get it out of their head,” which assumes that the professional themselves are actively involved in the event, the results were not statistically significant. A possible explanation for this refers to the fact that, although the professional believes in the possibility of prevention using therapeutic communication, they do not recognize themselves as an essential element in this process.
Dealing with death triggers countless reactions in humans, among them the perception of finitude itself. Focusing on exclusively technical, bureaucratic, and routine issues when it comes to this theme is part of a posture of denying death, to the extent that it provides power to the healthcare provider and softens the feeling of impotence 35 . Focusing exclusively on the biological aspects and investing in technological resources as alternatives for prolonging life avoid, to some extent, not only contact with death but also a therapeutic communication that could give access to the patient’s feelings. Thus, indirectly, healthcare providers avoid contact with their own death and with their own emotions 34 .
Refusing to speak or think about death is, in a way, comforting since it feeds a fantasy that death can be driven away by not manifesting it with either words or thoughts. The death of the other is characterized as an announcement and anticipation of one’s own death – a threat – and suicide also translates into a mutilation within society by breaking its natural course, stirring the moral bases 35 .
Suicide, since it involves biological, cultural, and social aspects, demands that educational interventions comprise, in addition to clinical management, an understanding of the psychological distress factors that are involved, which are key elements for the therapeutic approach of the multidisciplinary team. Moreover, it is necessary to rethink suicide prevention strategies to provide knowledge that leads to a gaze less regulated by judgments and moral rules, so that the person who experiences this suffering can be welcomed in any context, allowing better conditions for recovery and social rehabilitation 31 .
This study presents as limitation the difficulty of comparative analyses with other interventions, both because they are scarce in the literature and because they differ substantially in relation to the target audience, content taught, teaching-learning methodologies, or forms of result analysis. However, our contributions lie in the type of experimental design that, by raising awareness to the role of the health professional and to the improvement of knowledge about suicidal behavior, has promoted positive change in attitudes and allowed the perception of capacity and confidence to increase regarding the care for these patients, as suggested by the results.
More positive attitudes were observed among professionals towards suicidal behavior after the intervention. This finding contributes to the quality of care in primary care and reinforces the feasibility of training to prevent this condition in the population. Thus, the data evidenced are relevant both for scientific production and for the reality of the services within in the Brazilian Unified Health System.
The results found in this study are in line with the existing literature and collaborate with the current scientific panorama, as they provide support for the development of strategies that contribute to the reduction of the high rates of attempts and suicides in the country.
We suggest for new studies to conduct sequential evaluation or follow-up, observing whether such changes are sustained along the timeline; in addition to verifying the duration of educational intervention programs, aiming to optimize the time spent in such programs, as well as the contents addressed for validation of standardized educational material in order to test and replicate such results in other populations.
- Rev Saude Publica. 2022; 56: 54.
Atitudes dos profissionais de saúde frente a comportamento suicida: estudo de intervenção
I Brasil, Universidade Federal de Mato Grosso. Faculdade de Enfermagem. Cuiabá, MT, Brasil
II Brasil, Universidade Federal de Mato Grosso. Faculdade de Enfermagem - Campus Sinop. Sinop, MT, Brasil
III Brasil, Hospital Universitário Júlio Muller. Unidade de Atenção Psicossocial. Cuiabá, MT, Brasil
IV Brasil, Universidade Federal de Mato Grosso. Instituto de Ciências Exatas e da Terra. Departamento de Estatística. Cuiabá, Mato Grosso, Brasil
V Brasil, Universidade Federal de Mato Grosso. Programa de Pós-Graduação em Saúde Coletiva. Cuiabá, MT, Brasil
Contribuição dos Autores: Concepção e planejamento do estudo: JFS, SRM, AMN, MME. Coleta, análise e interpretação dos dados: JFS, HGBS, MME, AMN. Elaboração ou revisão do manuscrito: JFS, SRM, JGSL, KKBO. Aprovação da versão final: JGSL, KKBO, SRM, HGBS. Responsabilidade pública pelo conteúdo do artigo: JFS, HGBS, MME, AMN, JGSL, KKBO, SRM.
Avaliar o efeito de uma intervenção educativa sobre comportamento suicida nas atitudes dos profissionais de saúde da atenção primária.
MÉTODO
Ensaio clínico randomizado por conglomerados, com amostra de 261 profissionais de saúde, provenientes de 22 unidades de saúde selecionados por amostragem estratificada, elegidos e alocados aleatoriamente, mediante sorteio, em dois grupos: intervenção (n = 87) e controle (n = 174). Os participantes do grupo intervenção foram expostos a uma capacitação sobre comportamento suicida com duração de 20 horas. Todos os 261 participantes foram avaliados, antes e após a intervenção, e os grupos foram comparados para avaliar a atitude frente ao comportamento suicida utilizando o Suicide Behavior Attitude Questionnaire (SBAQ), avaliação feita por comparação das médias via teste t-Student para amostras independentes e Teste t pareado para amostras dependentes.
O grupo intervenção, na comparação intragrupos antes e depois da capacitação, bem como na comparação com o grupo controle, demonstrou diferenças estatisticamente significativas nas atitudes frente ao comportamento suicida, avaliadas a partir das diferenças de scores nos domínios: “percepção da capacidade profissional”, em todos os quatro itens; “sentimento negativo”, em seis dos sete itens; e no domínio “direito ao suicídio”, três dos cinco itens.
CONCLUSÃO
A capacitação breve desenvolvida na atenção primária à saúde foi efetiva para a melhora das atitudes dos participantes que integravam o grupo intervenção frente ao comportamento suicida.
INTRODUÇÃO
Aproximadamente 800 mil pessoas cometem suicídio anualmente, o que corresponde a uma taxa de 11,4 mortes a cada 100 mil habitantes em todo o mundo, figurando entre as dez principais causas de morte em todas as faixas etárias 1 . Embora a taxa de mortalidade por suicídio em alguns países da Europa Ocidental tenha diminuído nas últimas décadas, outros países, como México, Estados Unidos e Brasil, experimentaram um aumento dos casos durante o mesmo período 2 . De acordo com dados nacionais, mais de 10 mil brasileiros se suicidaram, ou seja, 5,5 ocorrências a cada 100 mil habitantes em 2015 e em 2016, 6,5 óbitos para 100 mil habitantes, comprovando um crescimento ao longo dos anos 3 . Considerando a magnitude do problema, a OMS recomenda que o suicídio seja priorizado tanto no atendimento oferecido quanto no desenvolvimento de políticas de saúde pública 1 .
Frente a esse contexto, é inevitável que os serviços de saúde sejam acionados, sendo as ações iniciais de cuidados em saúde mental, frequentemente prestadas em ambiente da atenção básica 4 . Tal fato relaciona-se diretamente ao número insuficiente de profissionais na rede de atenção psicossocial para atender a essa demanda, sobretudo em países de média renda, como o Brasil, em que a cobertura de serviços dessa natureza atende somente a 10% dos indivíduos que necessitam 4 .
Uma revisão sistemática analisou o contato dos indivíduos com profissionais de saúde da atenção primária antes de cometer suicídio e os resultados evidenciaram que, em média, 80% procuraram o serviço de saúde no ano anterior ao suicídio, e 44% no mesmo mês do óbito 5 . Achados semelhantes foram descritos em um estudo norueguês, que investigou a utilização dos serviços de saúde da atenção primária em 4.926 casos de suicídio (sujeitos com idade > 15 anos) durante o período de 2007 a 2015. Os resultados comprovaram que aproximadamente 90% dos indivíduos consultaram um profissional generalista na atenção primária no ano anterior ao suicídio e até 46,4% no último mês de vida 6 .
Isso sugere que os profissionais desse nível de atenção estão em uma posição única para identificar sujeitos em risco suicida e intervir, uma vez que a atenção primária à saúde configura-se porta de entrada na rede de saúde 1 . Entretanto, grande parte dos profissionais, frente a pessoas com comportamento suicida, manifestam atitudes negativas 7 , comumente em decorrência de fatores como despreparo ou dificuldades em lidar com essa demanda, proporcionando um atendimento inicial limitado e frequentemente revertido em encaminhamentos protocolares a outros serviços 9 , 10 , comprometendo a qualidade do cuidado prestado.
Uma atitude pode ser definida como um conjunto de atributos cognitivos, afetivos e comportamentais. Portanto, a atitude é uma inclinação do indivíduo a agir de modo específico em relação a determinadas pessoas, objetos e situações, adquirida socialmente, a partir de experiências pessoais e de fatores de personalidade 11 .
Uma metanálise realizada com pesquisas desenvolvidas até o ano de 2018 apontou atitudes negativas, empatia limitada e algum nível de hostilidade dos profissionais de saúde no atendimento às pessoas com comportamento suicida. Os dados indicaram ainda que treinamento e capacitação sobre como lidar com esses casos promovem atitudes mais positivas 12 . Outros estudos, realizados posteriormente, corroboram esses achados, também em relação à resistência em atender essa clientela; ao cuidado pautado por crenças e estigmas; às atividades técnicas e rotineiras priorizadas em detrimento de suporte psicológico, conhecimento e habilidades deficientes, além da necessidade de treinamento visando facilitar as relações terapêuticas 13 .
Dos estudos que se propõem a analisar os efeitos de estratégias educativas na modificação das atitudes, ainda que escassos na literatura brasileira, mesmo internacionalmente observa-se predomínio de intervenções tendo o ambiente hospitalar como público-alvo 16 .
Diante do exposto, este estudo questiona: as atitudes dos profissionais de saúde da atenção primária poderão ser modificadas após uma capacitação profissional para o atendimento ao comportamento suicida? No intuito de alcançar a resposta para tal indagação, este artigo tem como objetivo avaliar o efeito de uma intervenção educativa sobre comportamento suicida nas atitudes dos profissionais de saúde da atenção primária.
Este é um ensaio clínico randomizado controlado, de alocação paralela, com dois braços, inscrito no Registro Brasileiro de Ensaios Clínicos (ReBEC) sob o código RBR-9pmjf5w.
Desenvolvido no município de Cuiabá, no período de maio a agosto de 2017, nas unidades de estratégia de saúde da família (ESF), que se estruturam equipes multiprofissionais, composta por no mínimo um enfermeiro, um médico generalista ou de família, um técnico de enfermagem e agentes comunitários de saúde (ACS), podendo contar ainda com equipe ampliada, comportando profissionais de saúde bucal. O município de Cuiabá-MT possui 70 equipes de ESF, sendo três na zona rural do município e 67 da zona urbana, distribuídas em quatro regionais: 24 unidades na regional norte, 21 na sul, 11 na leste e 11 na regional oeste. Totalizando 298 profissionais de saúde, entre médicos, enfermeiros e técnicos de enfermagem, 697 agentes comunitários de saúde e 86 profissionais de saúde bucal 23 .
A população do estudo consistiu em profissionais de saúde que exerciam a função de médico, enfermeiro e técnico de enfermagem, excluindo do estudo profissionais de equipes localizadas na zona rural, pois compuseram a amostra de teste piloto no presente estudo, além de agentes de saúde e profissionais de saúde bucal (uma vez que o instrumento utilizado não se direciona para tais categorias).
Adotou-se amostragem probabilística por conglomerados e estratificada, sendo a unidade amostral de sorteio a equipe de saúde que é composta por um grupo de profissionais e estratificada por regionais de saúde.
Para a determinação do número de sujeitos, utilizou-se fórmula para dados pareados 24 , onde foram determinadas as médias de mudança de atitude pré e pós-intervenção e desvios padrão amostrais, obtidos a partir de estudo de referência 25 . Foi estimado um desvio padrão de 2,92, considerada uma mínima diferença a ser detectada de 1,0, confiança de 95% e poder de 0,80. Assim, o tamanho inicial da amostra ajustada para população (n = 298) foi de 56 indivíduos. Por se tratar de delineamento amostral por conglomerado, foi estabelecido fator de efeito de desenho em 1,22 e estimada taxa de não resposta em 22%, o que resultou em uma amostra final 87 indivíduos para o grupo intervenção. Para o grupo controle foi considerado 1 para 2, isto é, 174 indivíduos.
Para seleção aleatória dos participantes dos grupos intervenção e controle foi utilizada amostragem por conglomerados e estratificada proporcional ao tamanho da população, considerando como estratos as regiões (norte, sul, leste, oeste) e como unidade de randomização, a equipe de ESF, a fim de obter controle adequado e reduzir viés metodológico. Definiu-se o número de profissionais selecionados em cada região por multiplicação da fração de profissionais pelo tamanho da amostra (87). Posteriormente, para definir o número de equipes a serem sorteadas dividiu-se o número de profissionais de saúde por estrato pelo número de equipes (quatro), totalizando 22 equipes sorteadas aleatoriamente por programa estatístico, conforme ilustra a Tabela 1 .
ESF: estratégia saúde da família.
Para a identificação da atitude do profissional frente ao comportamento suicida foi utilizado o Suicide Behavior Attitude Questionnaire (SBAQ). Composto por situações clínicas frequentemente vivenciadas por profissionais de saúde 26 . Tal instrumento se divide em fatores que são distribuídos em sentimentos que o profissional tem em relação ao paciente com comportamento suicida, a percepção de sua capacidade para o atendimento e o direito ao suicídio; investigando esses fatores é possível medir uma atitude positiva ou negativa. Espera-se então que, de acordo com a média obtida pela soma dos valores em cada questão divididos pelo número total de questões em cada domínio, possamos verificar atitudes mais positivas por meio de pontuações mais elevadas no domínio “Percepção da capacidade profissional” e mais baixas nos domínios “Sentimentos em relação ao paciente” e “Direito ao suicídio” 26 . Para verificar outras variáveis, sociodemográficas (idade, sexo, cor, escolaridade), relacionadas à formação (profissão, especializações, capacitações e/ou formação em saúde mental) e prática profissional (atendimento anterior a pacientes com comportamento suicida), construiu-se instrumento fechado, aplicado com o SBAQ.
No primeiro momento, todas as unidades participantes foram visitadas, a fim de informar sobre o estudo e aplicar os instrumentos. Os profissionais das equipes sorteadas para o grupo intervenção, além de responder os instrumentos (pré-teste), foram convidados a participar da intervenção (capacitação). Os questionários foram previamente codificados e permitiram o pareamento, mas não a identificação pessoal dos participantes. Os participantes ausentes na unidade de saúde na primeira tentativa, foram procurados, mais duas vezes em horários diferentes. Quando foi possível e necessário, as visitas foram agendadas.
Posteriormente, foi oferecida ao grupo intervenção uma capacitação com duração de 20 horas, visando aprimorar a capacidade de reconhecer o grau de risco de um indivíduo com comportamento suicida e intervir; conhecer estratégias de atendimento e/ou encaminhamento de indivíduos com comportamento suicida; reconhecer a própria atitude perante um paciente com comportamento suicida e aperfeiçoá-la. A definição dos conteúdos abordados teve como direcionador o manual de prevenção ao suicídio voltado para equipes de atenção primária da Organização Mundial da Saúde. A capacitação foi conduzida por psicólogas e pesquisadoras em suicidologia, com ampla experiência clínica e pedagógica nessa temática. Imediatamente após o término da capacitação foi reaplicado o SBAQ para o grupo intervenção (pós-teste). Para o grupo controle não foi oferecido nenhum tipo de intervenção e o pós-teste foi reaplicado posteriormente nas unidades de saúde.
O desfecho primário esperado foi diferença no nível de atitudes frente ao comportamento suicida entre o início e fim da intervenção, verificado por meio do SBAQ, a partir da constatação de aumentos de escores igual ou superior a 3%, avaliado antes e depois da intervenção, a análise foi realizada sobre o princípio de intenção de tratar.
A Figura apresenta o fluxograma de participação dos indivíduos envolvidos no ensaio clínico desde o recrutamento até a última avaliação. Dos 87 profissionais iniciais que foram expostos à intervenção, 69 (79,3%) participaram da última avaliação, e no grupo controle permaneceram para análise 88 (50,6%). As perdas do estudo ocorreram por recusa em permanecer no estudo (n do grupo intervenção = 7, n do grupo controle = 11), preenchimento incompleto dos instrumentos (n do grupo intervenção = 11, n do grupo controle = 37), mudança de local de trabalho ou não foram encontrados ( n do grupo controle = 38).

A distribuição dos dados foi verificada pelo teste de Shapiro-Wilk, para a comparação entre os dois grupos foi utilizado o teste de homogeneidade qui-quadrado de Pearson, teste t-Student para duas amostras independentes e teste U-Mann Whitney. As comparações pré e pós-intervenção intragrupos foram realizadas a partir do teste t pareado para amostras dependentes e teste de postos com sinais de Wilcoxon. O nível de significância adotado foi de 5% em todos os testes. O projeto de pesquisa foi aprovado pelo comitê de ética em pesquisa de acordo com a Resolução 466/2012.
A análise dos dados sociodemográficos, de capacitação anterior e de atendimento ao comportamento suicida ( Tabela 2 ) não evidenciou diferença estatisticamente significante entre os grupos.
A Tabela 3 descreve as atitudes dos profissionais de saúde do grupo intervenção e do grupo controle, antes e após a intervenção. Os resultados não revelaram diferença significativa, na maioria dos itens do SBAQ, entre os grupos, na medida do pré-teste, exceto pelo item Q17 que apresentou significância estatística com média dos ranks (grupo intervenção = 1,40; grupo controle = 2,70; p-valor < 0,001). No entanto, na avaliação realizada após a capacitação, verificaram-se diferenças estatisticamente significativas entre os dois grupos em todos os itens dos fatores “sentimentos negativos em relação ao paciente” e “percepção da capacidade profissional”. Em “direito ao suicídio” dos cinco itens que compõem o fator, os itens Q4, Q6 e Q16 sofreram modificações estatisticamente significativas (p-valor < 0,05), todavia, as questões Q3 e Q18 não apresentaram modificações significativas (p-valor = 0,131 e p-valor = 0,597 respectivamente).
a Grupo intervenção avaliação anterior à intervenção.
b Grupo controle avaliação anterior à intervenção.
c p-valor significativo menor que 0,05 obtido por meio do teste t de Student.
d Grupo intervenção avaliação posterior à intervenção.
e Grupo controle avaliação posterior à intervenção.
f p-valor significativo menor que 0,05 obtido por meio do teste U-Mann Whitney.
Na Tabela 4 observam-se as atitudes dos profissionais de saúde do grupo intervenção, antes e após a capacitação. No fator “sentimentos negativos em relação ao paciente”, observam-se ganhos estatisticamente significativos em seis dos sete itens que compõem o domínio (Q2, Q5, Q9, Q13, Q15 e Q19). Na questão 17, as médias pré-teste, 2,71, e pós-teste, 2,02, (p-valor = 0,070) demonstram diferenças, mas sem significância estatística. No que se refere à “percepção da capacidade profissional” houve modificações estatisticamente significativas em todos os quatro itens desse fator, com p-valor < 0,001. Em “direito ao suicídio”, dos cinco itens que compõem o fator, sofreram modificações estatisticamente significativas os itens Q4, Q6 e Q16 (p-valor < 0,005), as questões Q3 e Q18 não apresentaram significância estatística (p-valor = 0,086 e p-valor = 0,234, respectivamente).
a Grupo intervenção avaliação anterior à capacitação.
b Grupo intervenção avaliação posterior à capacitação.
c Teste de Wilcoxon para amostras pareadas.
d p-valor considerado significativo menor que 0,05.
DISCUSSÃO
A literatura demonstra que o atendimento ao paciente com comportamento suicida pode ser influenciado por diversos fatores, dentre os quais estão as atitudes dos profissionais de saúde 9 , 10 , 12 .
O atendimento ao paciente com comportamento suicida pode acarretar sentimentos de frustração, impotência, culpa, desprezo e raiva 18 , 27 , além de ser envolto por mitos e crenças, como as que classificam as tentativas de suicídio como formas e ameaças para chamar a atenção e que não irão se concretizar, ou ainda que pessoas com esse comportamento são covardes 9 , 30 , 31 . A atitude é passível de modificação, o que pode ser evidenciado no presente estudo; quanto ao “sentimento em relação ao paciente”, após a capacitação, foram observadas mudanças em todos os itens desse domínio. Os achados demonstraram mudanças na compreensão das tentativas e ameaças como potenciais fatores de risco e de que pessoas nessas condições estão em intenso sofrimento, propiciando posturas mais empáticas em relação a esses pacientes.
O fato de o profissional reagir de forma negativa ao atender um paciente com comportamento suicida pode, dentre outros aspectos, relacionar-se com o processo de formação que frequentemente não proporciona ferramentas para o enfrentamento de situações de morte, sobretudo quando associada à escolha do sujeito 31 . O desejo de não viver pode ser conflituoso para os profissionais, uma vez que se subentende que devem salvar vidas. Assim, aspectos como superação dos dilemas de onipotência e onisciência, que costumam causar angústia nessas situações, foram amplamente discutidos na capacitação.
Outro aspecto a ser aventado é o de que o sentimento de ansiedade, por um eventual erro de conduta ou de avaliação, e a ideia de responsabilidade sobre a vida do paciente podem ser expressas pela dificuldade em estabelecer vínculo ou no receio de conversar sobre suicídio com medo de induzir o paciente a cometê-lo 32 . No entanto, as discussões geradas durante a capacitação evidenciaram que os profissionais esquivavam-se menos em se envolver e estabelecer vínculo com pacientes que tentaram suicídio e apresentaram redução do sentimento de impotência. Tal fato pode explicar as mudanças significativas das respostas do questionário nesse fator.
Perceber os próprios sentimentos negativos como mecanismos de defesa, considerar a morte com parte da existência humana e identificar os sentimentos envolvidos no processo de morte e morrer fez parte da metodologia empregada e favoreceu a compreensão e modificação dos sentimentos entre os profissionais. Tais achados corroboram o estudo desenvolvido com profissionais de saúde em que se verificou, após uma capacitação, redução significativa dos sentimentos negativos e melhor precisão na avaliação de risco 19 .
Sobre a “percepção da capacidade profissional”, os achados evidenciaram autopercepção de maior capacidade para o atendimento, melhor preparo profissional e segurança para lidar com pacientes em risco de suicídio. Resultados similares são encontrados em uma intervenção com duração de duas horas, oferecida a partir de um estudo multicêntrico japonês a 74 profissionais de saúde. Observou-se ganhos significativos nas habilidades percebidas, confiança, atitude, maior competência na avaliação do risco suicida e mais confiança ao cuidar de pacientes nessas condições 33 .
Um estudo conduzido na Austrália, com 248 profissionais de saúde participantes de um treinamento sobre comportamento suicida, resultou em aprimoramento do conhecimento, atitudes mais adequadas com consequente ampliação da capacidade de comunicação e confiança em fornecer assistência apropriada 21 . A literatura tem enfatizado que as atitudes negativas com pacientes suicidas entre os profissionais de saúde podem estar mais relacionadas à falta de conhecimento e às incertezas em como cuidar do que com a hostilidade especificamente 20 . Desse modo, a desinformação sobre o suicídio pode perpetuar uma abordagem equivocada.
O conhecimento continuamente atualizado, especialmente no que se refere à avaliação do risco suicida e das opções de tratamento, pode diminuir a ansiedade por falhas e aumentar a percepção da capacidade profissional. À medida que os profissionais compreendem e cumprem suas responsabilidades relacionadas à identificação, avaliação e intervenção terapêutica, na atuação profissional baseada em evidências e no planejamento do monitoramento da pessoa com risco suicida, conscientizam-se de que os fatores relacionados a habilidades e competências profissionais foram contemplados 17 .
Os profissionais de saúde convivem com sofrimento, dor, medo, desesperança, perdas de diversos modos e enfrentam frequentemente processos de morte e morrer. Não é raro o sentimento de impotência e incapacidade diante dessas situações. A crença de que apenas a cura ou a recuperação caracterizam o bom cuidado, enfatizado durante a formação acadêmica e reiterada diariamente pela cultura da obstinação terapêutica, pode vir a contribuir para a insegurança profissional ao se deparar com situações que sinalizem uma possível morte autoprovocada 34 .
Diversos autores destacam ainda a influência de questões de ordem organizacional do serviço, bem como a escassez de estrutura física e principalmente pessoal capacitado, demonstrando as dificuldades e o receio de não ter recursos frente ao inesperado. Durante a capacitação, diversos fatores como os relatados acima foram descritos como limitantes de um atendimento efetivo, acompanhados por sentimentos de insegurança, incapacidade e incompetência. No entanto, foi ressaltado que, ao se reconhecerem os limites e potencialidades, o medo de errar pode ser substituído, gradativamente, pela confiança em intervir 17 , 21 , 35 .
O terceiro componente investigado no presente estudo refere-se ao “direito ao suicídio”, em que se verificaram modificações, após a capacitação, em três dos cinco itens que o compõem. No entanto, um dos itens em que não foram observadas mudanças significativas foi a afirmativa: “apesar de tudo, penso que uma pessoa tem o direito de se matar”. Resultado similar foi descrito em pesquisa australiana, após capacitação com duração de um dia: na ocasião apenas 30% concordavam com o direito de cometer suicídio. Segundo os autores, tais achados refletem a natureza dos itens que compõem esse fator (crenças morais e religiosas) profundamente arraigados, com menor expectativa de modificações, mesmo após uma intervenção educativa 21 .
Não cabe aos profissionais de saúde priorizar seus princípios e convicções individuais no atendimento à pessoa com comportamento suicida, com o risco de induzi-lo à adaptação aos padrões sociais, baseados em seus valores e crenças pessoais que podem não ser relevantes para o paciente, pondo em risco o vínculo terapêutico necessário para o atendimento. Assim, o cuidado prestado não pode de forma alguma intensificar o sentimento de culpa na pessoa com ideação ou tentativa de suicídio e em seus familiares 34 .
Quando se questionou sobre a possibilidade de modificar uma decisão de suicídio por meio de uma conversa, perceberam-se efeitos positivos significativos após a capacitação. Porém, na afirmativa “quando uma pessoa fala de pôr fim à vida, tento tirar aquilo da cabeça dela”, que presume o próprio profissional envolvido ativamente no evento, os resultados não foram significativos estatisticamente. Uma possível explicação para o achado refere-se ao fato de que, embora o profissional acredite na possibilidade de prevenção utilizando-se da comunicação terapêutica, ele não se reconhece como um elemento essencial nesse processo.
Lidar com a morte desencadeia inúmeras reações no ser humano, dentre elas a percepção da própria finitude. Atentar para questões exclusivamente técnicas, burocráticas e rotineiras, quando se trata desse tema, faz parte de uma postura de negação da morte, na medida em que fornece poder ao profissional de saúde e ameniza o sentimento de impotência 35 . O foco em cuidar apenas dos aspectos biológicos e o investimento em recursos tecnológicos como alternativas de prolongamento da vida evitam, até certo ponto, não só o contato com a morte, mas também a comunicação terapêutica que poderia dar acesso aos sentimentos do paciente. Assim, indiretamente, os profissionais de saúde evitam o contato com a própria morte e com as próprias emoções 34 .
Deixar de falar ou de pensar na morte conforta, de certo modo, pois alimenta a fantasia de que não concretizá-la em palavras e pensamentos pode, assim, afastá-la. A morte do outro se caracteriza como o anúncio e a antecipação da própria morte, uma ameaça a nós, e o suicídio propriamente dito traduz-se ainda em uma mutilação na sociedade pela quebra do seu curso natural, mexendo em suas bases morais 35 .
O suicídio, por envolver aspectos biológicos, culturais e sociais, demanda que as intervenções educativas compreendam, além do manejo clínico, fatores do sofrimento psíquico envolvido, elementos importantes para a abordagem terapêutica da equipe multidisciplinar. Assim, faz-se necessário repensar estratégias de prevenção ao suicídio que consigam, ao mesmo tempo, fornecer conhecimentos que levem a um olhar menos regulado por julgamentos e regras morais, para que a pessoa que vivencia esse sofrimento seja acolhida em qualquer contexto, possibilitando melhores condições de recuperação e reabilitação social 31 .
Este artigo apresenta como limitação a dificuldade de análises comparativas com outras intervenções, tanto por serem escassas na literatura quanto por diferir substancialmente em relação ao público-alvo, conteúdo ministrado, metodologias de ensino-aprendizagem ou formas de análise dos resultados. Porém, as suas contribuições residem no tipo de delineamento experimental que, por intermédio da conscientização do papel do profissional de saúde e aprimoramento do conhecimento sobre o comportamento suicida, promoveu mudança positiva nas atitudes e possibilitou o aumento da percepção da capacidade e confiança para o atendimento a esses pacientes, conforme sugerem os resultados.
Observaram-se atitudes mais positivas entre os profissionais frente ao comportamento suicida após a intervenção. Tal achado contribui para a qualidade da assistência na atenção primária e reforça a viabilidade de capacitações com vistas a prevenir esse agravo na população. Nesse sentido, os dados evidenciados são relevantes tanto para a produção científica quanto para a realidade dos serviços inseridos no Sistema Único de Saúde.
Os resultados encontrados neste estudo vão ao encontro da literatura existente e colaboram com o panorama científico atual, na medida em que fornecem subsídio para o desenvolvimento de estratégias que contribuam para a redução dos altos índices de tentativas e suicídios no país.
Sugere-se em novos estudos, de avaliação sequencial ou de seguimento, observando se tais mudanças são sustentadas ao longo da linha do tempo; além de verificar a duração dos programas de intervenções educativas, visando otimizar o tempo empregado em tais programações, bem como os conteúdos abordados para validação de material educativo padronizado na intenção de testar e replicar tais resultados em outras populações.
- Skip to content
- Accessibility help
Health and social care robots showcased for NHS Scotland Chief Executive
Published: 27 Mar 2024

Researchers in Robotics and Artificial Intelligence (AI) from Heriot-Watt University and The University of Edinburgh hosted a visit from Caroline Lamb, NHS Scotland Chief Executive and Director - General Health and Social Care, at the National Robotarium on 18 March. The purpose of the visit was to showcase the latest innovations in robotics for healthcare being developed by scientists.
Led by Professor Lynne Baillie, Heriot-Watt’s world-leading expert in Human-Robot Interaction (HRI), the visit included an introduction from Chief Executive of the Robotarium, Stewart Miller, followed by a tour of the high-spec HRI labs and selection of demonstrations from researchers developing cutting-edge robotics and AI solutions to support people’s health, wellbeing and social care, and reduce pressure on clinical and healthcare staff.
“Scotland’s population is ageing more rapidly than ever before. That, alongside the pandemic and other public health crises, is putting strain on existing health services, leading to longer waiting lists and staff burnout. We believe that the safe and responsible application of robotics, AI and data could provide solutions to current challenges facing the sector, facilitating independent-living for longer and improving patient wellbeing overall.” Professor of Human-Robot Interaction, Lynne Baillie
Examples of research included the FEATHER project , a ground-breaking study that is utilising AI and smart home sensors to monitor living habits and enable the early detection of urinary tract infections (UTIs). The project team, a partnership with the Robotarium and School of Informatics at Edinburgh University, is working with social care and residential homes to develop the smart data systems and help improve patient care for the condition, which affects 150 million people worldwide.
The Horizon Europe project SPRING , led by academic co-lead at the National Robotarium Professor Oliver Lemon, was also featured during the tour, with a demonstration of the socially-assistive ARI robots, which have been providing advice and comfort to elderly patients and those with cognitive decline in a hospital in Paris. Recent news of the study has captured the public’s imagination and garnered significant media interest worldwide.
The varied and comprehensive programme also included talks and visual presentations from Research Assistants and doctoral students from Edinburgh Centre for Robotics covering topics such as robotics-assisted surgery and assessment, automated upper-limb protheses and rehabilitation, robotic exoskeletons, wearable devices to combat drug overdoses, healthcare sensors, long-term monitoring resources for an ageing population, and legged robots.
Caroline was accompanied by Professor Soumen Sengupta, Chief Officer of South Lanarkshire Health and Social Care Partnership, throughout the visit. Following the tour, they joined scientists and business figures from the Robotarium in a roundtable discussion on the future of applications of robotics in the NHS and beyond.
Professor Lynne Baillie said: “On behalf of the research teams at Heriot-Watt and The University of Edinburgh, I’d like to express my gratitude to Caroline and Soumen for taking the time to visit the National Robotarium and learn about the wide-ranging robotic applications and solutions we’re developing with input from the health and social care industry.
“As Chief Executive of NHS Scotland and lead of the Digital Health and Care Directorate, Caroline was interested in learning about new innovations that can complement the existing care and support being given to patients across the country.
“Scotland’s population is ageing more rapidly than ever before. That, alongside the pandemic and other public health crises, is putting strain on existing health services, leading to longer waiting lists and staff burnout. We believe that the safe and responsible application of robotics, AI and data could provide solutions to current challenges facing the sector, facilitating independent-living for longer and improving patient wellbeing overall.”
Professor Soumen Sengupta, Chief Officer of South Lanarkshire University Health and Social Care Partnership, said: “Innovation and collaboration with partners across the nation is crucial to how increasingly sophisticated care is being delivered, compassionately, in and with communities. “Indeed, this is something we are actively committed to in South Lanarkshire and across Lanarkshire as a whole.
“These are challenging times for health and social care services – which further reinforces the importance of innovation and collaboration with strategic partners such as our universities.
“From the stimulating presentations and lively discussions with colleagues from Heriot-Watt University and The University of Edinburgh, it is clear that there is huge scope to build upon the exciting developments that are already being progressed with the NHS in Scotland, and to expand the opportunities for collaboration in relation to social care and housing.
“We all clearly share a common, resolute commitment to the ongoing exchange of learning and experience with a view to harnessing all the potential of technology to enhance the vital work of our health and care staff and to improve the quality of lives across our diverse communities.
“I very much look forward to our harnessing the expertise and enthusiasm that is evident within the National Robotarium to contribute to the transformation of health and social care right across Scotland.”
Advertisement
Health care coverage: What is Biden's plan in his 2025 budget proposal?
Copy the code below to embed the wbur audio player on your site.
<iframe width="100%" height="124" scrolling="no" frameborder="no" src="https://player.wbur.org/hereandnow/2024/03/19/health-care-2025-budget"></iframe>
We break down President Biden's plan for health coverage — including his efforts to cement his legacy on drug costs, cancer research and broad health care coverage — in his 2025 budget proposal with STAT reporter Sarah Owermohle .
This segment aired on March 19, 2024.
More from Here & Now

IMAGES
COMMENTS
Typical stages in a research proposal. 1. The purpose of a research proposal is: To help to focus on a relevant and current topic. To identify a gap or inadequacy in the research literature. To make sure that these are your ideas, and to help you to focus and crystallise your ideas.
A long-time priority of health services research has been a focus on issues affecting access to care, including community factors, the availability of social services, and the social determinants of health. Social determinants of health have been defined by Healthy People 2020 as "conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a ...
Reviews. Preview. This is your step-by-step guide on how to write successful research proposals in the health sciences, whether it is for a thesis or dissertation review committee, an ethical review committee or a grant funding committee. Using quantitative, qualitative, and mixed research approaches, follow the journey of Liang and Natasha ...
However, health and social care research, as with many other academic disciplines, is carried out within embedded hierarchies and structural inequalities in universities, public service ...
Health research methodology: A guide for training in research methods FOREWORD Scientific research plays a very important role in our efforts to maintain health and combating diseases. Research helps us create new knowledge and develop proper tools for the use of existing knowledge. Not only does it enable health care providers to diagnose
The Health and Social Care Delivery Research (HSDR) Programme aims to produce rigorous and relevant evidence to improve the quality, accessibility and organisation of health and social care services. ... submit a written summary of your proposal (usually about one side of A4) in a PICO format if appropriate and describe the study briefly in ...
Research proposals to funding bodies also typically include a literature review. Here the purpose is to justify the proposal in terms of a gap in existing ... The systematic review of the literature in health and social care has a differ-ent focus. It aims to contribute to clinical practice through an assessment of the
Significance of Qualitative Research. The qualitative method of inquiry examines the 'how' and 'why' of decision making, rather than the 'when,' 'what,' and 'where.'[] Unlike quantitative methods, the objective of qualitative inquiry is to explore, narrate, and explain the phenomena and make sense of the complex reality.Health interventions, explanatory health models, and medical-social ...
Your Undergraduate Dissertation in Health and Social Care provides a practical step-by-step guide to both the theoretical and practical aspects of the process of doing an undergraduate dissertation, equipping the reader with all the skills necessary to plan, conduct and write up a research project successfully.. This is a revised edition of Nicholas Walliman's best-selling Your Undergraduate ...
Produced by Dr Diana Ramsey, ARC KSS Darzi Fellow (2021-2022) with insights and support from people working to deliver research in the Health and Social Care region, the Your Health and Social Care Research Quick Guide is a resource to help those working in health or social care to start or develop their research journey.. Packed with information, links and personal stories from people working ...
Health and care research is the same. It seeks to find answers to questions about the best options available. It then uses these discoveries to make decisions about improvements or changes. This is so we can: diagnose diseases earlier or more accurately. provide life-changing treatments.
Sample Research Proposals. You will find here two examples of proposals for postgraduate research from the Department of Social Policy and Criminology. They both give good indication of the sorts of things that need to be included. The first, on fathering after divorce or separation, represents first thoughts on the proposed topic, but sets out ...
Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you've landed on this post, chances are you're looking for a healthcare-related research topic, but aren't sure where to start. Here, we'll explore a variety of healthcare-related research ideas and topic thought-starters across a ...
12/16/2010 Research Proposal; Team working within the health care sector and involvement of patients and public in primary research. Implementing innovations in patient care. 3. SCOPE: The following tasks would be undertaken as a part of proposed research: Task 1: To investigate the past studies on existing and improved health care system.
Email: [email protected]. Our operating hours are 9am to 5pm. For support to develop your research proposal contact the NIHR RSS Specialist Centre for Social Care. The RSS Specialist Centre works nationally to provide free and tailored advice to social care researchers of all levels and experience, offering a broad range of methods expertise and ...
Introduction and background. According to the World Health Organization (WHO), social determinants of health (SDH) are defined as the circumstances in which humans are born, develop, live, earn, and age. At the international, regional, and state or local levels, the distribution of money, power, and resources shapes these circumstances [ 1 ].
Recent years have witnessed significant progress in the delivery of integrated health and social care. 1 The move towards integrated care has been motivated by an ageing population with multiple chronic conditions, fragmented and costly care systems, a focus on patient-centred care and empowerment and recognition by service providers of the need for a more joined-up approach to care. 2 ...
Q-Z. Quality improvement. Quality of care. Regulation. Social care. Social determinants of health. Workforce. We have funded more than 150 external research projects across a range of themes over the last five years.
121 samples of this type. Regardless of how high you rate your writing skills, it's always a worthy idea to check out an expertly written Research Proposal example, especially when you're dealing with a sophisticated Health Care topic. This is exactly the case when WowEssays.com database of sample Research Proposals on Health Care will prove handy.
We propose an integrated approach to health care management and leadership education at undergraduate level, to enable doctors to be effective leaders and manage resources appropriately and to ...
Health communication advocacy is an individual and collective approach that we health professionals can use to turn these ideas into generalised realities and to create positive health and social change. A Definition of Health Communication Advocacy Blending science, ethics and politics, health communication advocacy is self-initiated,
Our low-budget, non-resource-intensive research proposal can serve as a benchmark to conduct similar studies in other health care settings within LMICs. However, patient safety is a relatively nascent concept in low- and middle-income countries (LMICs) where health systems are already overburdened and underresourced.
In a recent JAMA Health Forum article, Glied and D'Aunno ask whether health sector investment in social services is "a bridge too far" and raise concerns about differing priorities, skills, finances, and functions of the 2 sectors that question whether this is a good match for collaboration. 1. As health care organizations ponder their role, if any, in supporting social services, there ...
Background More than 35% of Aboriginal and Torres Strait Islander adults live with cardiovascular disease, diabetes, or chronic kidney disease. There is a pressing need for chronic disease prevention and management among Aboriginal and Torres Strait Islander people in Australia. Therefore, this review aimed to synthesise a decade of contemporary evidence to understand the barriers and enablers ...
School of Health Professions Associate Dean for Research Timothy Reistetter, PhD, OTR, FAOTA, a professor in the Department of Occupational Therapy, has secured more than $1.5 million in RO1 grant funding from the Agency for Healthcare Research and Quality to support his research on the effect of social determinants of health on access to post-acute care rehabilitation and quality-of-care ...
The Department of Health and Aged Care acknowledges the traditional owners of country throughout Australia, and their continuing connection to land, sea and community. We pay our respects to them and their cultures, and to elders both past and present.
To narrow research gaps on diseases and conditions associated with women's midlife health or that are more likely to occur after menopause, such as rheumatoid arthritis, heart attack, and ...
DISCUSSION. The literature shows that the care given to patients with suicidal behavior can be influenced by several factors, among which are the attitudes of healthcare providers 9, 10, 12. Attending to patients with suicidal behavior can lead to feelings of frustration, impotence, guilt, contempt, and anger 18, 27.
Examples of research included the FEATHER project, a ground-breaking study that is utilising AI and smart home sensors to monitor living habits and enable the early detection of urinary tract infections (UTIs). The project team, a partnership with the Robotarium and School of Informatics at Edinburgh University, is working with social care and ...
We break down President Biden's plan for health coverage — including his efforts to cement his legacy on drug costs, cancer research and broad health care coverage — in his 2025 budget ...