An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

A systematic review of substance use and substance use disorder research in Kenya

Florence Jaguga
1 Department of Mental Health, Moi Teaching & Referral Hospital, Eldoret, Kenya
Sarah Kanana Kiburi
2 Department of Mental Health, Mbagathi Hospital, Nairobi, Kenya
Eunice Temet
3 Department of Mental Health & Behavioral Sciences, Moi University School of Medicine, Eldoret, Kenya
Julius Barasa
4 Population Health, Academic Model Providing Access to Healthcare, Eldoret, Kenya
Serah Karanja
5 Department of Mental Health, Gilgil Sub-County Hospital, Gilgil, Kenya
Lizz Kinyua
6 Intensive Care Unit, Aga Khan University Hospital, Nairobi, Kenya
Edith Kamaru Kwobah
Associated data.
All relevant data are within the paper and its Supporting information files.
The burden of substance use in Kenya is significant. The objective of this study was to systematically summarize existing literature on substance use in Kenya, identify research gaps, and provide directions for future research.
This systematic review was conducted in line with the PRISMA guidelines. We conducted a search of 5 bibliographic databases (PubMed, PsychINFO, Web of Science, Cumulative Index of Nursing and Allied Professionals (CINAHL) and Cochrane Library) from inception until 20 August 2020. In addition, we searched all the volumes of the official journal of the National Authority for the Campaign Against Alcohol & Drug Abuse (the African Journal of Alcohol and Drug Abuse). The results of eligible studies have been summarized descriptively and organized by three broad categories including: studies evaluating the epidemiology of substance use, studies evaluating interventions and programs, and qualitative studies exploring various themes on substance use other than interventions. The quality of the included studies was assessed with the Quality Assessment Tool for Studies with Diverse Designs.
Of the 185 studies that were eligible for inclusion, 144 investigated the epidemiology of substance use, 23 qualitatively explored various substance use related themes, and 18 evaluated substance use interventions and programs. Key evidence gaps emerged. Few studies had explored the epidemiology of hallucinogen, prescription medication, ecstasy, injecting drug use, and emerging substance use. Vulnerable populations such as pregnant women, and persons with physical disability had been under-represented within the epidemiological and qualitative work. No intervention study had been conducted among children and adolescents. Most interventions had focused on alcohol to the exclusion of other prevalent substances such as tobacco and cannabis. Little had been done to evaluate digital and population-level interventions.
The results of this systematic review provide important directions for future substance use research in Kenya.
Systematic review registration
PROSPERO: CRD42020203717.
Introduction
Globally, substance use is associated with significant morbidity and mortality. In the 2017 Global Burden of Disease (GBD) study, substance use disorders (SUDs) were the second leading cause of disability among the mental disorders with 31,052,000 (25%) Years Lived with Disability (YLD) attributed to them [ 1 ]. In 2016, harmful alcohol use resulted in 3 million deaths (5.3% of all deaths) worldwide and 132.6 (5.1%) million disability-adjusted life years (DALYs) [ 2 ]. Tobacco use, the leading cause of preventable death, kills more than 8 million people worldwide annually [ 3 ]. Alcohol and tobacco use are leading risk factors for non-communicable diseases for example cardiovascular disease, cancer, and liver disease [ 3 , 4 ]. Even though the prevalence rate of opioid use is small compared to that of tobacco and alcohol use, opioid use disorder contributes to 76% of all deaths from SUDs [ 4 ]. Other psychoactive substances such as cannabis and amphetamines are associated with mental health consequences including increased risk of suicidality, depression, anxiety and psychosis [ 5 , 6 ]. In addition to the effect on health, substance use is associated with significant socio-economic costs arising from its impact on health and criminal justice systems [ 7 ].
Low- and middle-income countries (LMICs) bear the burden of substance use. Over 80% of the 1.3 billion tobacco users worldwide live in LMICs [ 3 ]. In 2016, the alcohol-attributable disease burden was highest in LMICs compared to upper-middle-income and high-income countries (HICs) [ 2 ]. In Kenya, a nationwide survey conducted in 2017 reported that over 10% of Kenyans between the ages of 15 to 65 years had a SUD [ 8 ]. In another survey, 20% of primary school children had ever used at least one substance in their lifetime [ 9 ]. Moreover, Kenya has the third highest total DALYs (54,000) from alcohol use disorders (AUD) in Africa [ 4 ] Unfortunately, empirical work on substance use in LMICs is limited [ 10 , 11 ]. In a global mapping of SUD research, majority of the work had been conducted in upper-middle income and HICs (HICs) [ 11 ]. In a study whose aim was to document the existing work on mental health in Botswana, only 7 studies had focused on substance use [ 10 ]. Information upon which policy and interventions could be developed is therefore lacking in low-and-middle income settings.
Since the early 1980s, scholars in Kenya began engaging in research to document the burden and patterns of substance use [ 12 ]. In 2001 the National Authority for the Campaign Against Alcohol and Drug Abuse (NACADA) was established in response to the rising cases of harmful substance use in the country particularly among the youth. The mandate of the Authority was to educate the public on the harms associated with substance use [ 13 ]. In addition to prevention work, NACADA contributes to research by conducting general population prevalence surveys every 5 years and recently launched its journal, the African Journal of Alcohol and Drug Abuse (AJADA) [ 14 ]. The amount of empirical work done on substance use in Kenya has expanded since these early years but has not been systematically summarized. The evidence gaps therefore remain unclear.
In order to guide future research efforts and adequately address the substance use scourge in Kenya, there is need to document the scope and breadth of available scientific literature. The aim of this systematic review is therefore: (i) to describe the characteristics of research studies conducted on substance use and SUD in Kenya; (ii) to assess the methodological quality of the studies; (iii) to identify areas where there is limited research evidence and; (iv) to make recommendations for future research. This paper is in line the Vision 2030 [ 15 ], Kenya’s national development policy framework, which directs that the government implements substance use treatment and prevention projects and programs, and target 3.5 of the Sustainable Development Goals (SDGs) which requires that countries strengthen the treatment and prevention for SUDs [ 16 ].
Materials and methods
Protocol and registration.
In conducting this systematic review we adhered to the recommendations from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [ 17 ]. A 27-item PRISMA checklist is available as an additional file to this protocol ( S1 Checklist ). Our protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO): CRD42020203717.
Search strategy
A search was carried out in five electronic databases on 20 th August 2020: PubMed, PsychINFO, Web of Science, Cumulative Index of Nursing and Allied Professionals (CINAHL) and Cochrane Library. The full search strategy can be found in S1 File and takes the following form: (terms for substance use) and (terms for substance use outcomes of interest) and (terms for region) . The searches spanned the period from inception to date. No filter was applied. A manual search was done in Volumes 1, 2 and 3 (all published volumes by the time of the search) of the recently launched AJADA journal by NACADA, and additional articles identified.
[ 14 , 18 , 19 ].
Study selection
Following the initial search, all articles were loaded onto Mendeley reference manager where initial duplicate screening and removal was done. After duplicate removal, the articles were loaded onto Rayyan, a soft-ware for screening and selecting studies during the conduct of systematic reviews [ 20 ]. The abstract and titles of retrieved articles were independently screened by two authors based on a set of pre-determined eligibility criteria. A second screening of full text articles was also done independently by two authors and resulted in an 88.7% agreement. Disagreements during each stage of the screening were resolved through discussion and consensus.
Inclusion criteria
Since we sought to map existing literature on the subject, our inclusion criteria were broad. We included articles on substance use if (i) the sample or part of the sample was from Kenya, (ii) they were original research articles, (iii) they had a substance use or SUD exposure, (iv) they had a substance use or SUD related outcome such as prevalence, pattern of use, prevention and treatment, and (iv) they were published in English or had an English translation available. We included studies conducted among all age groups and studies that used all designs including quantitative, qualitative and mixed methods.
Exclusion criteria
Studies were excluded if: (i) they were cross-national and did not report country specific results (ii) they did not report substance use or SUD as an exposure, and did not have substance use or SUD related outcomes or as part of the outcomes, (iii) they were review articles, dissertations, conference presentations or abstracts, commentaries or editorials, (iv) and the full text articles were not available.
Data extraction
We prepared 3 data extraction forms based on three emerging categories of studies i.e.:
- Studies reporting on the epidemiology of substance use or SUD
- Studies evaluating substance use or SUD interventions and programs
- Studies qualitatively exploring various themes on substance use or SUD (but not evaluating interventions or programs)
The forms were piloted by F.J. and S.K. and adjustments made to the content. Data extraction was then done using the final form by all authors and double checked by F.J. for completeness and accuracy. Discrepancies were resolved by discussion with S.K. and E.T. until consensus was achieved. The following data was extracted for each study category:
- Studies reporting on the epidemiology of substance use or SUD: study design, study population characteristics, study setting, sample size, age and gender distribution, substance(s) assessed, standardized tool or criteria used, main findings (prevalence, risk factors, other key findings).
- Studies evaluating substance use or SUD interventions and programs: study design, study objective, sample size, name of the intervention or program, person delivering intervention, outcomes and measures, and main findings.
- Studies qualitatively exploring various aspects of substance use or SUD other than programs and interventions: study objective, methods of data collection, study setting, study population, age and gender distribution, theoretical framework used, and main findings.
Data synthesis
The results have been summarized descriptively and organized by the three categories above. Within each category, a general description of the study characteristics has been provided followed by a narrative synthesis of findings organized by sub-themes inductively derived from the data. The sub-themes within each category are as follows:
- Studies reporting on the epidemiology of substance use or SUD : Epidemiology of alcohol use, epidemiology of tobacco use, epidemiology of khat use, epidemiology of cannabis use, epidemiology of opioid and cocaine use, epidemiology of other substance use (sedatives, inhalants, hallucinogens, prescription medication, emerging drugs, ecstasy).
- Studies evaluating substance use or SUD interventions and programs: Individual level interventions (Individual-level interventions for harmful alcohol use, individual-level interventions for khat use, individual level intervention for substance use in general); Programs (Methadone programs, needle-syringe programs, tobacco cessation programs, out-patient SUD treatment programs); Population-level interventions : Population-level tobacco interventions, population-level alcohol interventions.
- Studies qualitatively exploring various aspects of substance use or SUD other than programs and interventions : Injecting drug use and heroin use, alcohol use, substance use among youth and adolescents, other topics.
Quality assessment of the studies
Quality assessment was conducted by S.K. using the Quality Assessment Tool for Studies with Diverse Designs (QATSDD) [ 21 ]. F.J. & J.B. double checked the scores for completeness and accuracy. Any disagreements were discussed and resolved by consensus. We had initially planned to use the National Institute of Health (NIH) set of quality assessment tools but due to the diverse nature of study designs, the authors agreed to use the QATSDD tool. The QATSDD is a 16-item tool for both qualitative and quantitative studies. Each item is scored on a 4-point scale (0–3), with a total of 14 criteria for each study design and 16 for studies with mixed methods. Scoring relies on guidance notes provided as well as judgment and expertise from the reviewers. The criteria used are: (i) theoretical framework; (ii) statement of aims or objectives; (iii) description of research setting; (iv) sample size consideration; (v) representative sample of target group (vi) data collection procedure description; (vii) rationale for choice of data collection tool(s); (viii) detailed recruitment data; (ix) statistical assessment of reliability and validity of measurement tools (quantitative only); (x) fit between research question and method of data collection (quantitative only); (xi) fit between research question and format and content data collection (qualitative only); (xii) fit between research question and method of analysis; (xiii) justification of analytical method; (xiv) assessment of reliability of analytical process (qualitative only); (xv) user involvement in design and (xvi) discussion on strengths and limitations[ 21 ]. Scores are awarded for each criterion as follows: 0 = no mention at all; 1 = very brief description; 2 = moderate description; and 3 = complete description. The scores of each criterion are then summed up with a maximum score of 48 for mixed methods studies and 42 for studies using either qualitative only or quantitative only designs. For ease of interpretation, the scores were converted to percentages and classified as low (<50%), medium (50%–80%) or high (>80%) quality of evidence [ 22 ].
Search results
The search from the five electronic databases yielded 1535 results: 950 from PubMed, 173 from PsychINFO, 210 from web of science, 123 from CINAHL and 79 from Cochrane library. Thirteen additional studies were identified through a manual search of the AJADA journals (Volumes 1, 2 and 3). Studies were assessed for duplicates and 1154 articles remained after removal of duplicates. The 1154 studies underwent an initial screening based on abstracts and titles, and 946 articles were excluded. A second screen of full text articles was done for the 208 studies that were potentially eligible for the review. Twenty three studies were excluded as follows: 21 did not meet the eligibility criteria and 2 had duplicated results. A total of 185 studies were found to meet the inclusion criteria and were included in the review ( Fig 1 ).

General characteristics of the studies
Of the 185 studies included in this review, 144 (77.8%) investigated the epidemiology of substance use or SUD, 18 (9.7%) evaluated substance use or SUD interventions and programs, and 23 (12.4%) were qualitative studies exploring perceptions on various substance use or SUD topics other than interventions and programs (Table 4). The studies were published between 1982 and 2020. The number of studies published has gradually increased in number over the years, particularly in the past decade. Fig 2 shows the publication trends for substance use research in Kenya.

Quality assessment
The QATSDD scores ranged from 28.6% [ 23 ] to 92.9% [ 24 ]. Only 14 studies [ 12 , 23 , 25 – 36 ] (all quantitative) had scores of less than 50%. Of these, the main items driving low quality were: no mention of user involvement in study design (n = 14) [ 12 , 23 , 25 – 36 ], no explicit mention of a theoretical framework (n = 10) [ 12 , 23 , 25 – 28 , 30 , 33 , 35 , 36 ] and a lack of a statistical assessment of reliability and validity of measurement tools (n = 10) [ 12 , 23 , 25 , 28 , 30 – 33 , 35 , 36 ] Table 1 .
Studies examining the epidemiology of substance use or SUD
General description of epidemiological studies.
One hundred and forty-four studies examined the prevalence and or risk factors for various substances. The studies were published between 1982 and 2020. The four main study designs used were cross-sectional (n = 126), cohort (n = 5), case-control (n = 10), and mixed methods (n = 2). One study used a combination of the multiplier method, Wisdom of the Crowds (WOTC) method, and a published literature review to document the size of key populations [ 164 ]. The sample size for this category of studies ranged from 42 [ 130 ] to 72292 [ 128 ].
The studies were conducted in diverse settings including the community (n = 72), hospitals (n = 40), institutions of learning (n = 24), streets (n = 5), prisons and courts (n = 3), charitable institutions (n = 1), methadone maintenance therapy (MMT) clinics (n = 1), and in needle-syringe program (NSP) sites (n = 1). Of the studies conducted within the community, 12 were conducted in informal settlements. The study populations were similarly diverse as follows: general population adults & adolescents (n = 39), persons with NCDs (n = 11), primary and secondary school students (n = 15), people who inject drugs (PWID) (n = 11), general patients (n = 5), men who have sex with men (MSM) (n = 8), university and college students (n = 9), commercial sex workers (n = 7), psychiatric patients (n = 6), orphans and street connected children and youth (n = 6), people living with HIV (PLHIV) (n = 6), healthcare workers (n = 3), law offenders (n = 3), military (n = 1), and teachers (n = 1). Only one study was conducted among pregnant women [ 131 ].
Sixty-nine studies (47.6%) used a standardized diagnostic tool to assess for substance use. The Alcohol Use Disorder Identification Test (AUDIT) (n = 21) and the Alcohol, Smoking & Substance Use Involvement Screening Test (ASSIST) questionnaire (n = 10) were the most frequently used tools. Most papers assessed for alcohol ( n = 109) and tobacco use ( n = 80). Other substances assessed included khat (n = 34), opioids (n = 21), sedatives (n = 19), cocaine (n = 19), inhalants (n = 16), cannabis (n = 14), hallucinogens (n = 7), prescription medication (n = 4), emerging drugs (n = 1) and ecstasy (n = 1). Most studies (n = 93) assessed for more than one substance.
Epidemiology of alcohol use
One hundred and nine papers assessed for the prevalence and or risk factors for alcohol use. Using the AUDIT, the 12-month prevalence rate for hazardous alcohol use ranged from 2.9% among adults drawn from the community [ 97 ] to 64.6% among female sex workers (FSW) [ 77 ]. Based on the same tool, the lowest and highest 12-month prevalence rates for harmful alcohol use were both reported among FSWs i.e. 9.3% [ 80 ] and 64.0% [ 174 ] respectively, while the prevalence of alcohol dependence ranged from 8% among FSWs living with HIV [ 203 ] to 33% among MSM who were commercial sex workers [ 144 ]. The highest lifetime prevalence rate for alcohol use was reported by Ndegwa & Waiyaki [ 151 ]. The authors found that 95.7% of undergraduate students had ever used alcohol.
Alcohol use, was associated with several socio-demographic factors including being male [ 50 , 112 , 114 , 140 , 158 , 168 , 182 , 191 ], being unemployed [ 114 ], being self-employed [ 97 ], having a lower socio-economic status (SES) [ 128 ], being single or separated, living in larger households [ 97 ], having a family member struggling with alcohol use, and alcohol being brewed in the home [ 143 ]. Alcohol use was linked to various health factors including glucose intolerance [ 81 ], poor cardiovascular risk factor control [ 111 ], having a diagnosis of diabetes mellitus [ 134 ], hypertension [ 112 , 139 ], default from tuberculosis (TB) treatment [ 148 ], depression [ 113 ], psychological Intimate Partner Violence (IPV) [ 205 ], tobacco use [ 182 , 205 ], and increased risk of esophageal cancer [ 137 , 179 ]. Finally, alcohol use was associated with involvement in Road Traffic Accidents (RTAs) [ 88 ], and having injuries [ 88 , 171 ] and suicidal behavior [ 109 ].
Epidemiology of tobacco use
Eighty papers assessed for the prevalence and risk factors for tobacco use. The lifetime prevalence of tobacco use ranged from 23.5% among healthcare workers (HCWs) [ 140 ] to 84.3% among psychiatric patients [ 110 ]. The highest lifetime prevalence rate for tobacco use was reported by Ndegwa & Waiyaki [ 151 ]. The authors found that 95.7% of undergraduate students had ever used tobacco.
Tobacco use was associated with socio-demographic factors such as being male [ 112 , 140 , 168 ] and living in urban areas [ 163 ]. Several health factors were linked to tobacco use including hypertension [ 112 ], development of oral leukoplakia [ 32 ], pneumonia [ 146 ], increased odds of laryngeal cancer [ 136 ], ischemic stroke [ 100 ] and diabetes mellitus [ 134 ]. In addition, tobacco use was associated with having had an injury in the last 12 months [ 171 ], emotional abuse [ 110 ], and psychological IPV [ 205 ]. Longer duration of smoking was associated with a diagnosis of diabetes mellitus [ 73 ], lower SES [ 128 ], and hypertension [ 98 , 142 ]. Peltzer et al. [ 181 ] reported that early smoking initiation among boys was associated with ever drunk from alcohol use, ever used substances, and ever had sex. Among girls, the authors found that early smoking initiation was associated with higher education, ever drunk from alcohol use, parental or guardian tobacco use, and suicide ideation.
Epidemiology of khat use
The epidemiology of khat use was investigated by 34 studies. The lifetime prevalence rate for khat use ranged from 10.7% among general hospital patients [ 168 ] to 88% among a community sample [ 23 ]. Khat use was associated with being male [ 114 , 168 ]; unemployment [ 114 ]; being employed [ 25 ]; younger age (less than 35 years), higher level of income, comorbid alcohol and tobacco use [ 166 ] and age at first paid sex of less than 20 years among FSWs [ 195 ]. Further, khat use was associated with increased odds of negative health outcomes [ 130 , 146 , 166 , 201 ].
Higher odds of reporting psychotic [ 166 , 201 ], and PTSD (Post-Traumatic Stress Disorder) symptoms [ 201 ], having thicker oral epithelium [ 130 ], and pneumonia [ 146 ], were reported among khat users compared to non-users.
Epidemiology of cannabis use
Fourteen studies evaluated the prevalence of cannabis use. The lifetime prevalence rate of cannabis use ranged from 21.3% among persons with AUD [ 120 ] to 64.2% among psychiatric patients [ 110 ]. Cannabis use was associated with being male [ 140 , 168 ], and with childhood exposure to physical abuse [ 110 ].
Epidemiology of opioid and cocaine use
Twenty-one studies investigated the prevalence of opioid use. The lifetime prevalence rate of opioid use ranged from 1.1% among PLHIV [ 132 ] to 8.2% among psychiatric patients [ 110 ].
Nineteen studies assessed for the prevalence of cocaine use. The highest reported prevalence rates were 76.2% among PWID use (current use) [ 190 ]; 8.8% among healthcare workers (lifetime use) [ 140 ]; and 6.7% among PLHIV (lifetime use) [ 132 ].
Epidemiology of IDU
One study assessed the prevalence for IDU. Key population size estimates for PWID use was reported as 6107 for Nairobi [ 164 ]. IDU was associated with depression, risky sexual behavior [ 149 ], Hepatitis-C Virus (HCV) infection [ 173 ], and HIV-HCV co-infection [ 68 ].
Epidemiology of other substance use (sedatives, inhalants, hallucinogens and prescription medication, emerging drugs, ecstasy)
The epidemiology of sedative use was investigated by 19 studies, inhalant use by 16 studies, hallucinogen use by 7 studies, prescription medication by 4 studies, and emerging drugs and ecstasy by one study each. The highest lifetime prevalence rate for sedative use was reported as 71.4% among a sample of psychiatric patients [ 28 ], while the highest prevalence rate for inhalant use was 67% among children living in the streets [ 86 ]. The lifetime prevalence rates for hallucinogen use ranged from 1.4% among university students [ 160 ] to 3.7% among psychiatric patients [ 110 ]. The highest prevalence rate for the use of prescription medication was reported as 21.2% among PWID [ 190 ]. One study each reported on the prevalence of emerging drugs [ 122 ] and ecstasy [ 153 ]. The studies were both conducted among adolescents and youth. The authors found the lifetime prevalence rates for the two substances to be 11.8% [ 122 ] and 4.0% [ 153 ] respectively.
Other topics explored by the epidemiology studies
In addition to prevalence and associated factors, the epidemiological studies explored other topics.
Papas et al. [ 176 ] explored the agreement between self-reported alcohol use and the biomarker phosphatidyl ethanol and reported a lack of agreement between self-reported alcohol use and the biomarker phosphatidyl ethanol among PLHIV with AUD.
One study investigated the self-efficacy of primary HCWs for SUD management and reported that self-efficacy for SUD management was lower in those practicing in public facilities and among those perceiving a need for AUD training. Higher self-efficacy was associated with attending to a higher proportion of patients with AUD, and the belief that AUD is manageable in outpatient settings [ 196 ].
Five studies investigated the reasons for substance use. Common reasons for substance use included leisure, stress and peer pressure among psychiatric patients[ 28 ], curiosity, fun, and peer influence among college students [ 123 ], peer influence, idleness, easy access, and curiosity among adults in the community [ 25 ], and peer pressure, to get drunk, to feel better and to feel warm among street children [ 74 ]. Atwoli et al. 2011 [ 72 ] reported that most students were introduced to substances by friends.
Kaai et al. [ 99 ] conducted a study regarding quit intentions for tobacco use and reported that 28% had tried to quit in the past 12 months, 60.9% had never tried to quit, and only 13.8% had ever heard of smoking cessation medication. Intention to quit smoking was associated with being younger, having tried to quit previously, perceiving that quitting smoking was beneficial to health, worrying about future health consequences of smoking, and being low in nicotine dependence. A complete description of the prevalence studies has been provided in Table 2 .
a khat (catha edulis) is a plant with stimulant properties and is listed by WHO as a psychoactive substance. Its use is common in East Africa
b kuber is a type of smokeless tobacco product.
Studies evaluating substance use or SUD programs and interventions
General description of studies evaluating programs and interventions.
A total of eighteen studies evaluated specific interventions or programs for the treatment and prevention of substance use. These were carried out between 2009 and 2020. Eleven studies focused on individual-level interventions, 5 studies evaluated programs, and 2 studies evaluated population-level interventions. The studies used various approaches including randomized control trials (RCT) (n = 7), mixed methods (n = 3), non-concurrent multiple baseline design (n = 1), quasi experimental (n = 1), cross-sectional (n = 2), and qualitative (n = 3). One study employed a combination of qualitative methods and mathematical modeling.
Individual-level interventions
Individual-level interventions for harmful alcohol use . Nine studies evaluated either feasibility, acceptability, and or efficacy for individual-level interventions for harmful alcohol use [ 38 , 40 , 90 , 94 , 127 , 141 , 175 , 178 , 193 ]. All the interventions were tested among adult populations including persons attending a Voluntary Counseling & Testing (VCT) center (38), PLHIV [ 40 , 175 ], and adult males and females drawn from the community [ 94 , 141 ] and FSWs [ 127 , 178 ].
Two studies evaluated a six session CBT intervention for harmful alcohol use among PLHIV. The intervention was reported as feasible, acceptable [ 40 ] and efficacious [ 175 ] in reducing alcohol consumption among PLHIV. The intervention was delivered by trained lay providers.
Giusto et al [ 90 ] evaluated the preliminary efficacy of an intervention aimed at reducing men’s alcohol use and improving family outcomes. The intervention was delivered in 5 sessions by trained lay-providers, and utilized a combination of behavioral activation, motivational interviewing (MI) and gender norm transformative strategies. The intervention showed preliminary efficacy for addressing alcohol use and family related problems.
Five studies evaluated brief interventions that ranged from 1 to 6 sessions and were delivered by primary HCWs, lay providers and specialist mental health professionals [ 38 , 94 , 127 , 178 , 193 ]. The brief interventions were reported as feasible, acceptable [ 38 ], and efficacious in reducing alcohol consumption [ 94 , 127 , 178 , 193 ]. The brief interventions additionally resulted in reductions to IPV, participation in sex work [ 178 ], and risky sexual behavior [ 127 ].
One study evaluated the efficacy of a mobile delivered MI intervention and found that at 1 month, AUDIT-C scores were significantly higher for waiting-list controls compared to those who received the mobile MI [ 94 ].
Moscoe at al. [ 141 ] found no effect of a prize-linked savings account on alcohol, gambling and transactional sex expenditures among men.
Individual-level interventions for khat use . One study utilized a randomized control trial (RCT) approach to evaluate the effect of a three-session brief intervention for khat use on comorbid psychopathology (depression, PTSD, khat induced psychotic symptoms) and everyday functioning. The intervention was delivered by trained college graduates and was found to result in reduced khat use and increased functioning levels, but had no benefit for comorbidity symptoms (compared to assessments only) [ 202 ].
Individual level intervention for any substance use . One study evaluated the efficacy of a four-session psychoeducation intervention using an RCT approach. The study found that the intervention was effective in reducing the severity of symptoms of any substance abuse at 6 months compared to no intervention. The intervention was additionally effective in reducing symptoms for depression, hopelessness, suicidality, and anxiety [ 145 ].
Methadone programs . Two studies utilized qualitative methods to evaluate the perceptions of persons receiving methadone on the benefits of the programs [ 61 , 62 ]. The methadone programs were perceived as having potential to aid in recovery from opioid use and to reduce HIV transmission among PWID [ 61 , 62 ].
Needle-syringe programs (NSPs) . One paper explored the impact of NSPs programs on needle and syringe sharing among PWID. The study reported that the introduction of NSPs led to significant reductions in needle and syringe sharing [ 56 ].
Tobacco cessation programs . One study evaluated HCWs knowledge and practices on tobacco cessation and found that the knowledge and practice on tobacco cessation was inadequate [ 89 ].
Out-patient SUD treatment programs . One paper investigated the impact of community based outpatient SUD treatment services and reported a 42% substance use abstinence rate 0–36 months following treatment termination [ 84 ].
Population-level interventions
Population-level tobacco interventions . One study evaluated the appropriateness and effectiveness of HIC anti-tobacco adverts in the African context and found the adverts to be effective and appropriate [ 183 ].
Population-level alcohol interventions . One paper examined community members’ perspectives on the impact of the government’s public education messages on alcohol abuse and reported that the messages were ineffective and unpersuasive [ 55 ].
A complete description of studies investigating programs and interventions is in Table 3 .
Studies qualitatively exploring various substance use or SUD topics (other than interventions)
General description of qualitative studies.
There were 23 qualitative studies included in our review. The studies were conducted between 2004 and 2020. Data was collected using several approaches including in-depth interviews (IDIs) only (n = 6), focus group discussions (FGDs) only (n = 2), a combination of FGDs and IDIs (n = 10), a combination of observation and individual IDIs (n = 2), a combination of observation, IDIs and FGDs (n = 1), a combination of literature review, observation, IDIs and FGDs (n = 1). One study utilized the participatory research and action approach [ 60 ]. The target populations for the qualitative studies included persons using heroin (n = 3), males and females with IDU (n = 11) adolescents and youth (n = 3), FSWs (n = 2), refugees and Internally Displaced Persons (IDPs) (n = 1), and PLHIV (n = 2).
Injecting drug use and heroin use
Thirteen studies explored various themes related to IDU and heroin use with most of them (n = 8) focusing on issues related to women. Three studies explored the drivers of IDU among women and found them to include influence of intimate partners [ 48 , 49 ], stress of unexpected pregnancies [ 49 ], gender inequality, and social suffering [ 67 ]. One study found that IDU among women interfered with utilization of antenatal and maternal and child health services [ 57 ], while another reported that women who inject drugs linked IDU to amenorrhea hence did not perceive the need for contraception [ 51 ].
Mburu et al [ 47 ] explored the social contexts of women who inject drugs and found that these women experienced internal and external stigma of being injecting drug users, and external gender-related stigma of being female injecting drug users. Using a socio-ecological approach, Mburu et al [ 50 ] reported that IDU during sex work was an important HIV risk behavior. In another study, FSWs reported that they used heroin to boost courage to engage in sex work [ 65 ].
Other than IDU and heroin use among women, five studies investigated other themes. One study explored the experiences of injecting heroin users and found that the participants perceived heroin injection as cool [ 42 ]. Guise et al. 2015 [ 44 ] conducted a study to explore transitions from smoking to injecting and reported that transitions from smoking to IDU were experienced as a process of managing resource constraints, or of curiosity, or search for pleasure. One study explored the experiences of persons on MMT as regards integration of MMT with HIV treatment. The study was guided by the material perspective in sociology theory and Annmarie’s Mol’s analysis of logic of care. Persons on MMT preferred that they have choice over whether to seek care for HIV and MMT in a single, or in separate settings.
Alcohol use
Six studies focused on alcohol use. Three studies explored perceptions of service providers and communities on the effects of alcohol use. Alcohol use was perceived as having a negative impact on sexual and reproductive health [ 53 , 54 ] and on socio-economic status [ 43 , 46 ]. One study explored the reasons for alcohol use among PLHIV and found that reasons for alcohol use included stigma and psychological problems, perceived medicinal value, and poverty [ 60 ].
Youth and adolescent substance use
Three studies focused on substance use among youth and adolescents. In one study, the adolescents perceived that substance use contributed to risky sexual behavior including unprotected sex, transactional sex, and multiple partner sex [ 58 ]. The youth identified porn video shows and local brew dens as places where risky sexual encounters between adolescents occurred [ 59 ]. Ssewanyana et al. [ 63 ] utilized the socio-ecological model to explore perceptions of adolescents and stakeholders on the factors predisposing and contributing to substance use. Substance use among adolescents was perceived to be common and to be due to several socio-cultural factors e.g. access to disposable income, idleness, academic pressure, low self-esteem etc.
Other topics
Utilizing the syndemic theory, one study explored how substance use, violence and HIV risk affect PrEP (Pre-exposure prophylaxis) acceptability, access and intervention needs among male and female sex workers. The study found that co-occurring substance use, and violence experienced by sex workers posed important barriers to PrEP access [ 41 ].
A complete description of included qualitative studies is in Table 4 .
This is to our knowledge, the first study to summarize empirical work done on substance use and SUDs in Kenya. More than half (77.8%) of the reviewed studies investigated the area of prevalence and risk factors for substance use. Less common were qualitative studies exploring various themes (12.4%) and studies evaluating interventions and programs (9.7%). The first study was conducted in 1982 and since then the number of publications has gradually risen. Most of the research papers (92.4%) were of moderate to high quality. In comparison to two recent scoping reviews conducted in South Africa and Botswana, more research work has been done on substance use in Kenya. Our study found that 185 papers on substance use among Kenyans had been published by the time of the search while Opondo et al. [ 11 ] and Tran et al. [ 10 ] reported that only 53 and 7 papers focusing on substance use had been published in South Africa (between 1971 and 2017) and in Botswana (between 1983 and 2020) respectively.
Epidemiology of substance use or SUD
Studies investigating the prevalence, and risk factors for substance use dominated the literature. The studies, which were conducted across a broad range of settings and populations, focused on various substances including alcohol, tobacco, cannabis, opioids, cocaine, sedatives, inhalants, hallucinogens, prescription medication, and ecstasy. In addition, a wide range of important health and socio-demographic factors were examined for their association with substance use. Most studies had robust sample sizes and were conducted using diverse designs including cross-sectional, case-control and cohort. The studies showed a significant burden of substance use among both adults and children and adolescents. In addition, substance use increased the odds of negative mental and physical health outcomes consistent with findings documented in global reports [ 2 , 3 ]. These findings highlight the importance of making the treatment and prevention for substance use and SUDs of high priority in Kenya.
- Two main evidence gaps were identified within this category: The prevalence and risk factors for substance use among certain vulnerable populations for whom substance use can have severe negative consequences, had not been investigated. For example, no study had included police officers or persons with physical disability, only one study had its participants as pregnant women [ 113 ], and only 2 studies had been conducted among HCWs [ 140 , 196 ].
- Few studies had explored the epidemiology of hallucinogens, prescription medication, ecstasy, IDU, and emerging substances e.g. synthetic cannabinoids. These substances are a public health threat globally [ 207 , 208 ] yet their use remains poorly documented in Kenya.
Interventions and programs
Given the significant documented burden of substance use and SUDs in Kenya, it was surprising that few studies had focused on developing and testing treatment and prevention interventions for SUDs. A possible reason for this is limited expertise in the area of intervention development and testing. For example, research capacity in implementation science has been shown to be limited in resource-poor settings such as ours [ 209 ].
Of note is that most of the tested interventions had been delivered by lay providers [ 40 , 90 , 175 ] and primary HCWs [ 38 , 127 , 178 ] indicating a recognition of task-shifting as a strategy for filling the mental health human resource gap in Kenya.
Several research gaps were identified within this category.
- Out of the 11 individual-level interventions tested, nine had targeted harmful alcohol use except one which focused on khat [ 202 ] and another that targeted several substances [ 145 ]. No studies had evaluated individual-level interventions targeting tobacco and cannabis use, despite the two being the second and third most commonly used substances in Kenya [ 8 ]. Further, no individual-level interventions had focused on other important SUDs like opioid, sedative and cocaine use disorders.
- Few studies had evaluated the impact of substance use population-level interventions [ 55 , 183 ]. Several cost-effective population-level interventions have been recommended by WHO e.g. mass media education and national toll free quit line services for tobacco use, and brief interventions integrated into all levels of primary care for harmful alcohol use [ 210 ]. Such strategies need to be tested for scaling up in Kenya.
- None of the interventions had been tested among important vulnerable populations for whom local research already shows a significant burden e.g. children and adolescents, the Lesbian Gay Bisexual Transgender & Queer (LGBTQ) community, HCWs, prisoners, refugees, and IDPs. In addition, no interventions had been tested for police officers and pregnant women, and no studies had evaluated interventions to curb workplace substance use.
- Only one study evaluated digital strategies for delivering substance use interventions [ 94 ] yet the feasibility of such strategies has been demonstrated for other mental health disorders in Kenya [ 211 ]. Moreover, the time is ripe for adopting such an approach to substance use treatment given the fact that the country currently has a mobile subscriptions penetration of greater than 90% [ 212 ].
- No studies had evaluated the impact of other interventions such as mindfulness and physical exercise. Meta-analytic evidence suggests that such strategies hold promise for reducing the frequency and severity of substance use and craving [ 213 , 214 ].
Qualitative studies
The qualitative studies focused on a broad range of themes including drivers and impact of substance use, drug markets, patterns of substance use, stigma, and access to treatment. Most of the work however focused on PWID and heroin users. Future qualitative work should explore issues relating to other populations for example persons with other mental disorders, persons with physical disabilities, police officers, and persons using other commonly used substances such as tobacco, khat, and cannabis.
Limitations
The aim of this systematic review was to provide an overview of the existing literature on substance use and SUD research in Kenya. We therefore did not undertake a meta-analysis and detailed synthesis of the findings of studies included in this review. In addition, variability in measurements of substance use outcomes precluded our ability to more comprehensively summarize the study findings. For quality assessment, detailed assessments using design specific tools were not possible given the diverse methodological approaches utilized in the studies. We therefore used a single tool for the quality assessment of all studies. The results of the quality assessment are therefore to be interpreted with caution. Nonetheless this review describes for the first time the breadth of existing literature on substance use and SUDs in Kenya, identifies research gaps, and provides important directions for future research.
The purpose of this systematic review was to map the research that has been undertaken on substance use and SUDs in Kenya. Epidemiological studies dominated the literature and indicated a significant burden of substance use among both adults and adolescents. Our findings indicate that there is a dearth of literature regarding interventions for substance use and we are calling for further research in this area. Specifically, interventions ought to be tested not just for alcohol but for other substances as well, and among important at risk populations. In addition, future research ought to explore the feasibility of delivering substance use interventions using digital means, and the benefit of other interventions such as mindfulness and physical exercise. Future qualitative work should aim at providing in-depth perspectives on substance use among populations excluded from existing literature e.g. police officers, persons using other substances such as tobacco, cannabis and khat, and persons with physical disability.
Supporting information
S1 checklist, abbreviations, funding statement.
The author(s) received no specific funding for this work.
Data Availability
- PLoS One. 2022; 17(6): e0269340.
Decision Letter 0
28 Mar 2022
PONE-D-22-00681A systematic review of substance use and substance use disorder research in KenyaPLOS ONE
Dear Dr. JAGUGA,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
Please submit your revised manuscript by May 12 2022 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: https://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
We look forward to receiving your revised manuscript.
Kind regards,
Judith I Tsui
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. We noticed you have some minor occurrence of overlapping text with the following previous publication(s), which needs to be addressed:
- Tsuei, S.HT., Clair, V., Mutiso, V. et al. Factors Influencing Lay and Professional Health Workers’ Self-efficacy in Identification and Intervention for Alcohol, Tobacco, and Other Substance Use Disorders in Kenya. Int J Ment Health Addiction 15, 766–781 (2017). https://doi.org/10.1007/s11469-017-9775-6
The text that needs to be addressed involves lines 279-283 in your submission.
In your revision ensure you cite all your sources (including your own works), and quote or rephrase any duplicated text outside the methods section. Further consideration is dependent on these concerns being addressed
3. In your Data Availability statement, you have not specified where the minimal data set underlying the results described in your manuscript can be found. PLOS defines a study's minimal data set as the underlying data used to reach the conclusions drawn in the manuscript and any additional data required to replicate the reported study findings in their entirety. All PLOS journals require that the minimal data set be made fully available. For more information about our data policy, please see http://journals.plos.org/plosone/s/data-availability .
Upon re-submitting your revised manuscript, please upload your study’s minimal underlying data set as either Supporting Information files or to a stable, public repository and include the relevant URLs, DOIs, or accession numbers within your revised cover letter. For a list of acceptable repositories, please see http://journals.plos.org/plosone/s/data-availability#loc-recommended-repositories . Any potentially identifying patient information must be fully anonymized.
Important: If there are ethical or legal restrictions to sharing your data publicly, please explain these restrictions in detail. Please see our guidelines for more information on what we consider unacceptable restrictions to publicly sharing data: http://journals.plos.org/plosone/s/data-availability#loc-unacceptable-data-access-restrictions . Note that it is not acceptable for the authors to be the sole named individuals responsible for ensuring data access.
We will update your Data Availability statement to reflect the information you provide in your cover letter.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Partly
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: N/A
Reviewer #2: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #2: Yes
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
Reviewer #1: No
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: This manuscript adds value in an under-research area by summarizing main learnings from substance use and substance use disorder research in Kenya. Major revisions are needed though for the article to be presented as a scientifically- acceptable piece. These revision include punctuation, grammar errors (eg: inappropriate use of upper case letter on line 84- 86), and overall flow of some sentences such as line 31, line 39, line 50, line 58, line 69, line 83, line 87- 91, line 104, line 172, line 175 to list a few.
In addition to these revision, below are proposed consideration:
- In the abstract, please specify the start date used in the search strategy.
- Line 53- tobacco kills 8million people where? Worldwide? On a specific continent? Please specify
-Line 57- you mentioned one consequence so far ie death which others are you referring to here?
- Line 104- inception of what?
-Line 111 who checked the duplicates? Was the software used for this or did the authors do it? It's a bit unclear
-Line 124-125: Were mixed methods studies included as well? The way this is phrased it sounds like "all designs" refers more to qualitative and quantitative studies
-Avoid over using "/" in sentences. If need be list item a "or" b throughout the manuscript. Eg: substance use or SUDs
-Line 182- 183- did you mean that 13 additional studies were identified? Please consider reviewing and rephrasing your sentences to improve clarity
-Line 185- Is "These" referring to the studies? If yes, can you be a bit more explicit?
-Line 238- are you referring to MSM who are commercial sex workers? Please use appropriate languages throughout the manuscript
- For the result presentation, it might be helpful to have as part of the main manuscript (not supplemental information) a summary table of the final literature reviewed including information on the title of the article, authors, methods, findings and gap from the articles that were included in the review instead of having long references throughout the result section.
- Line 313 Lay healthcare providers might be more appropriate same for line 314 for primary healthcare workers not primary care workers
-Line 331-332 that last sentence seems incomplete, please consider reviewing it
-Line 371- 372- What are estimates then on what has been done elsewhere in SSA? Is this conclusion based mainly on the 2 scoping work from SA and Bostwana? How about other SSA countries including countries neighboring Kenya like Uganda, Tanzania, etc?
How do you define a lot?
-Line 392- Emerging substances like which ones?
- Line 404- Was the study specifically assessing feasibility? If that was not the case, making such claim is misleading
Reviewer #2: This systematic review highlights several gaps in licit and illicit substance use (SU) and substance use disorder (SUD) literature within Kenya, with the goal of summarizing research within three broad domains: (1) epidemiologic studies, (2) intervention and/or programs and (3) qualitative studies. The authors apply sound methods, with attention to details around decision-making processes when including articles in their review. The attention to target study populations (e.g., community, hospitals, prisons, etc.) is extremely valuable and calls for additional studies within specific populations. In addition, the authors make the case that their review is needed in order to address Kenya’s Vision 2030 and moves towards accomplishing SDG’s. I commend the authors for completing this large undertaking and offer feedback to strengthen and improve their paper.
Major Edits
• There is an absolute need for SU and SUD systematic review; however, this paper may have limited applications in its current state. In the introduction, the authors state this paper will “guide future research efforts”; however, most SUD researchers work with one substance or one category of substances. It would be helpful within the key findings sections to expand on SU categories, which are discussed briefly in the introduction (e.g., tobacco, alcohol, opioids, cannabis, and stimulants.) Another option may be to reformat the paragraphs according to SU categories and discuss the current epidemiologic, interventions/programs, and qualitative studies.
• In your criteria, you do not mention whether you included studies conducted out of methadone clinics or harm reduction sites (i.e., drop-in centres, NSPs), specifically. However, when I look over the publications, several were conducted within these sites. Please clarify whether these terms were part of your search categories and include them on Page 11, lines 215-217.
• Throughout the descriptions and key findings sections, there should be more syntheses of the data instead of frequencies, which are already conveyed in your tables. For example, under the epidemiology section of SU/SUD, you say that 47% of the studies used evidence-based diagnostic tools, but this should be followed by the key findings of those studies (i.e., X-X% of participants indicated hazardous or harmful alcohol consumption, and X-X% of participants indicated alcohol dependence.) This is just one example, but all of the key finding’s sections should provide more data syntheses.
• As it stands, the key findings and other findings sections are a little difficult to follow and are heavily focused on alcohol and tobacco use. For example, in the epidemiologic key findings section the paragraphs are organized as follows: (1) youth and substance use, (2) adults and tobacco use, (3) adults and alcohol use, and (4) two case control studies. Again, this may have a better flow if the authors organized the key findings by SU categories (e.g., tobacco, alcohol, opioids, cannabis, and stimulants.) By structuring the paragraphs by SU categories, the reader is able to quickly decipher where there are gaps in the literature. Alternatively, the authors may want to consider narrowing the scope of their paper by solely focusing on alcohol and tobacco use, which seem to be the main focus throughout the paper.
• In the qualitative study key findings section, most of the studies apply frameworks and/or theories to their analysis (e.g., stages of change, risk environment framework), which should be synthesized and included as a column in Additional File 5/Qualitative Studies.
Minor Edits
• Please review the PLOS ONE Guidelines on formatting references and edit references.
• Page 11 (line 220) “People with injecting drug use” should be “people (or persons) who inject drugs.”
• Page 11 (line 221) “Men who have Sex with Men” should not contain capital letters.
• Page 11 (lines 218-225) This section does not sum up to the total studies in the epidemiology section n=144.
• Page 11 (line 210-213) Please be consistent in how you mention the study designs with corresponding references. This was completed in the interventions and programs section, but not for the epidemiological studies.
• Page 15 (lines 299-303) Conversely, please indicate in the programs and intervention section, how may studies were included in each of the study designs.
• Page 12 (line 229) typo, please change to “opioids (n=21)”
• In the findings section, please define “hospital,” and whether this includes methadone clinics.
• Page 20 (line 398) “Substance use” should be “substance use disorder.”
• Page 21 (line 423-424) “Mental disorders” should be “mental health disorders.”
• Additional File 3/Epidemiological Studies: The SU category should not include how people consume their drugs (“injection drugs”), which is only seen a few times, but what drugs categories were examined. Please be more specific than “illicit drugs.”
• Additional File 4/Interventions and Program: Please review the sample sizes for each study, particularly for those with “not reported.”
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #2: No
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Submitted filename: PONE-D-22-00681.pdf
Author response to Decision Letter 0
12 May 2022
Reviewer #1: This manuscript adds value in an under-research area by summarizing main learnings from substance use and substance use disorder research in Kenya. Major revisions are needed though for the article to be presented as a scientifically- acceptable piece. These revision include punctuation, grammar errors (eg: inappropriate use of upper case letter on line 84- 86), and overall flow of some sentences such as line 31, line 39, line 50, line 58, line 69, line 83, line 87- 91, line 104, line 172, line 175 to list a few.
We thank the reviewer for this comment. We have thoroughly proof read the paper and made corrections to grammar and punctuation.
We have specified that the search was conducted from inception (line 27).
We have clarified that it is worldwide (line 58)
The paragraph has been revised to include health consequences of alcohol, tobacco and other substances (line 58-63)
Inception means from the earliest available study. This term is commonly used in systematic review searches when no date limits have been set
The Mendeley Reference manager was used to identify and remove duplicates. This has been clarified on line 116-117.
Yes, we included studies with qualitative, quantitative and mixed methods designs. This has now been clarified (line 133).
This has been corrected throughout the manuscript
The sentence has been reviewed to improve clarity (line 208)
We have reworded the sentence to make it more explicit (line 210)
The authors are referring to MSM who were commercial sex workers. We have corrected this (line 273).
We have included the tables within the main manuscript (line 367, 439, 504)
This has been corrected line 388, 391, 395, 551, 552
This sentence has been revised (line 428-430)
We have reworded the paragraph to show that we are comparing our findings with available scoping reviews (line 513-520)
How do you define a lot? We have revised this sentence and used the word “more…” (line 515)
An example has been given (line 541)
This line has been deleted (line 554).
Reviewer #2: This systematic review highlights several gaps in licit and illicit substance use (SU) and substance use disorder (SUD) literature within Kenya, with the goal of summarizing research within three broad domains: (1) epidemiologic studies, (2) intervention and/or programs and (3) qualitative studies. The authors apply sound methods, with attention to details around decision-making processes when including articles in their review. The attention to target study populations (e.g., community, hospitals, prisons, etc.) is extremely valuable and calls for additional studies within specific populations. In addition, the authors make the case that their review is needed in order to address Kenya’s Vision 2030 and moves towards accomplishing SDG’s. I commend the authors for completing this large undertaking and offer feedback to strengthen and improve their paper.
We thank the reviewer for their comments.
We acknowledge this comment. We have organized the key findings sections by substance use categories and expanded on the findings (line 162, 266-366, 373-439, 446-503).
NSP sites has been included in the general characteristics of epidemiological studies (line 248)
• We have now provided more synthesis of data in the results section
(line 266-366, 373-439, 446-503).
We have incorporated the theoretical frameworks into the results section (line 468,478, 492, 499), and added a column presenting information on theoretical frameworks to the table 4 (line 505).
The references have been edited in line with PLOS one guidelines
This has been corrected (line 251)
This has been corrected (line 252)
Yes. This is true because some populations overlapped e.g. some studies were conducted among general population adults with NCDs.
We have now deleted references in the general description section for the intervention studies (line 375-378) and qualitative studies (448-457) to ensure uniformity
This has been indicated. Line 386-389
This has been corrected. Line 261
We have separated out studies done within hospitals and those done within methadone clinics (line 247; Kisilu et al. 2019 on table 2 line 367)
This has been corrected. Line 551
This has been corrected. Line 578
The studies described the substances as just IDU and illicit substances, and did not provide descriptions of the specific substances assessed for. We have included the phrase ‘not specified’ next to the term illicit drugs and IDU for clarity. (Table 2 line 367)
These were reviewed and appropriate sample sizes reported (table 3 line 443)
Editors’ comments
We have addressed this (line 349-354)
About data availability. All analyzed data has been included in the main manuscript and in the supporting information files 1 and 2. (line 1264)
Decision Letter 1
19 May 2022
PONE-D-22-00681R1
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
Acceptance letter
26 May 2022
Dear Dr. Jaguga:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Judith I Tsui
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
A systematic review of substance use and substance use disorder research in Kenya
Roles Conceptualization, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Mental Health, Moi Teaching & Referral Hospital, Eldoret, Kenya
Roles Conceptualization, Methodology, Supervision, Writing – review & editing
Affiliation Department of Mental Health, Mbagathi Hospital, Nairobi, Kenya
Roles Formal analysis, Validation, Writing – review & editing
Affiliation Department of Mental Health & Behavioral Sciences, Moi University School of Medicine, Eldoret, Kenya
Affiliation Population Health, Academic Model Providing Access to Healthcare, Eldoret, Kenya
Roles Formal analysis, Writing – review & editing
Affiliation Department of Mental Health, Gilgil Sub-County Hospital, Gilgil, Kenya
Affiliation Intensive Care Unit, Aga Khan University Hospital, Nairobi, Kenya
Roles Formal analysis, Supervision, Writing – review & editing
- Florence Jaguga,
- Sarah Kanana Kiburi,
- Eunice Temet,
- Julius Barasa,
- Serah Karanja,
- Lizz Kinyua,
- Edith Kamaru Kwobah

- Published: June 9, 2022
- https://doi.org/10.1371/journal.pone.0269340
- Peer Review
- Reader Comments
The burden of substance use in Kenya is significant. The objective of this study was to systematically summarize existing literature on substance use in Kenya, identify research gaps, and provide directions for future research.
This systematic review was conducted in line with the PRISMA guidelines. We conducted a search of 5 bibliographic databases (PubMed, PsychINFO, Web of Science, Cumulative Index of Nursing and Allied Professionals (CINAHL) and Cochrane Library) from inception until 20 August 2020. In addition, we searched all the volumes of the official journal of the National Authority for the Campaign Against Alcohol & Drug Abuse (the African Journal of Alcohol and Drug Abuse). The results of eligible studies have been summarized descriptively and organized by three broad categories including: studies evaluating the epidemiology of substance use, studies evaluating interventions and programs, and qualitative studies exploring various themes on substance use other than interventions. The quality of the included studies was assessed with the Quality Assessment Tool for Studies with Diverse Designs.
Of the 185 studies that were eligible for inclusion, 144 investigated the epidemiology of substance use, 23 qualitatively explored various substance use related themes, and 18 evaluated substance use interventions and programs. Key evidence gaps emerged. Few studies had explored the epidemiology of hallucinogen, prescription medication, ecstasy, injecting drug use, and emerging substance use. Vulnerable populations such as pregnant women, and persons with physical disability had been under-represented within the epidemiological and qualitative work. No intervention study had been conducted among children and adolescents. Most interventions had focused on alcohol to the exclusion of other prevalent substances such as tobacco and cannabis. Little had been done to evaluate digital and population-level interventions.
The results of this systematic review provide important directions for future substance use research in Kenya.
Systematic review registration
PROSPERO: CRD42020203717.
Citation: Jaguga F, Kiburi SK, Temet E, Barasa J, Karanja S, Kinyua L, et al. (2022) A systematic review of substance use and substance use disorder research in Kenya. PLoS ONE 17(6): e0269340. https://doi.org/10.1371/journal.pone.0269340
Editor: Judith I. Tsui, University of Washington, UNITED STATES
Received: January 8, 2022; Accepted: May 18, 2022; Published: June 9, 2022
Copyright: © 2022 Jaguga et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: ASI, Addiction Severity Index; ASSIST, Alcohol Smoking and Substance Involvement Screening Test; AUD, Alcohol Use Disorder; AUDIT, Alcohol Use Identification Test; AUDIT-C, Alcohol Use Identification Test–Concise; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; BHS, Behavioral Health Screen; BMI, Body Mass index; BSIS, Beck Suicidal Intent Scale; CAD, Coronary Artery Disease; CAGE, Cut, Annoyed, Guilty, Eye-opener; CIDI, Composite International Diagnostic Interview; CINAHL, Cumulative Index of Nursing and Allied Professionals; CRAFFT, Car, Relax, Alone, Forget, Friends, Trouble; DAST, Drug Abuse Screening Test; DSM-III, Diagnostic & Statistical Manual Third Edition; DSM-III R, Diagnostic & Statistical Manual Third Edition Revised; DSM-IV, Diagnostic & Statistical Manual Fourth Edition; DSM-V, Diagnostic & Statistical Manual Fifth Edition; DUSI-R, Drug Use Screening Inventory—Revised; FGD, Focus Group Discussion; FSW, Female Sex Workers; GSHS, Global School-based Health Survey; HCV, Hepatitis C Virus; HCW, Healthcare worker; HIC, High Income Country; HIV, Human Immunodeficiency Virus; ICD, International Classification of Disease; IDI, In-depth Interviews; IDP, Internally Displaced Persons; IPV, Intimate Partner Violence; KIIs, Key Informant Interviews; K-SADS, Kiddie-Schedule for Affective Disorders; LGBTQ, Lesbian, Gay, Bisexual, Transgender, Queer; LMIC, Low and Middle Income Country; MAST, Michigan Alcohol Screening Test; MI, Motivational Interviewing; MINI, Mini International Neuropsychiatric Interview; MMT, Methadone Maintenance Therapy; MPBI, Multiple Problem Behavior Inventory; MSM, Men who have Sex with Men; MSME, Men who have Sex with Men Exclusively; MSMW, Men who have Sex with Men & Women; NIH, National Institute of Health; NSP, Needle Syringe Program; OST, Opioid Substitution Therapy; PLHIV, People Living with HIV; PrEP, Pre-exposure Prophylaxis; PTSD, Post-Traumatic Stress Disorder; PWID, People Who Inject Drugs; QATSDD, Quality Assessment Tool for Studies with Diverse Designs; RCT, Randomized controlled trial; RTAs, Road Traffic Accidents; SCID, Structured Clinical interview for DSM; SES, Socio-economic Status; SSA, Sub-Saharan Africa; TB, Tuberculosis; UNODC, United Nations Office on Drugs and Crime; VCT, Voluntary Counseling & Testing; WOTC, Wisdom of the Crowds
Introduction
Globally, substance use is associated with significant morbidity and mortality. In the 2017 Global Burden of Disease (GBD) study, substance use disorders (SUDs) were the second leading cause of disability among the mental disorders with 31,052,000 (25%) Years Lived with Disability (YLD) attributed to them [ 1 ]. In 2016, harmful alcohol use resulted in 3 million deaths (5.3% of all deaths) worldwide and 132.6 (5.1%) million disability-adjusted life years (DALYs) [ 2 ]. Tobacco use, the leading cause of preventable death, kills more than 8 million people worldwide annually [ 3 ]. Alcohol and tobacco use are leading risk factors for non-communicable diseases for example cardiovascular disease, cancer, and liver disease [ 3 , 4 ]. Even though the prevalence rate of opioid use is small compared to that of tobacco and alcohol use, opioid use disorder contributes to 76% of all deaths from SUDs [ 4 ]. Other psychoactive substances such as cannabis and amphetamines are associated with mental health consequences including increased risk of suicidality, depression, anxiety and psychosis [ 5 , 6 ]. In addition to the effect on health, substance use is associated with significant socio-economic costs arising from its impact on health and criminal justice systems [ 7 ].
Low- and middle-income countries (LMICs) bear the burden of substance use. Over 80% of the 1.3 billion tobacco users worldwide live in LMICs [ 3 ]. In 2016, the alcohol-attributable disease burden was highest in LMICs compared to upper-middle-income and high-income countries (HICs) [ 2 ]. In Kenya, a nationwide survey conducted in 2017 reported that over 10% of Kenyans between the ages of 15 to 65 years had a SUD [ 8 ]. In another survey, 20% of primary school children had ever used at least one substance in their lifetime [ 9 ]. Moreover, Kenya has the third highest total DALYs (54,000) from alcohol use disorders (AUD) in Africa [ 4 ] Unfortunately, empirical work on substance use in LMICs is limited [ 10 , 11 ]. In a global mapping of SUD research, majority of the work had been conducted in upper-middle income and HICs (HICs) [ 11 ]. In a study whose aim was to document the existing work on mental health in Botswana, only 7 studies had focused on substance use [ 10 ]. Information upon which policy and interventions could be developed is therefore lacking in low-and-middle income settings.
Since the early 1980s, scholars in Kenya began engaging in research to document the burden and patterns of substance use [ 12 ]. In 2001 the National Authority for the Campaign Against Alcohol and Drug Abuse (NACADA) was established in response to the rising cases of harmful substance use in the country particularly among the youth. The mandate of the Authority was to educate the public on the harms associated with substance use [ 13 ]. In addition to prevention work, NACADA contributes to research by conducting general population prevalence surveys every 5 years and recently launched its journal, the African Journal of Alcohol and Drug Abuse (AJADA) [ 14 ]. The amount of empirical work done on substance use in Kenya has expanded since these early years but has not been systematically summarized. The evidence gaps therefore remain unclear.
In order to guide future research efforts and adequately address the substance use scourge in Kenya, there is need to document the scope and breadth of available scientific literature. The aim of this systematic review is therefore: (i) to describe the characteristics of research studies conducted on substance use and SUD in Kenya; (ii) to assess the methodological quality of the studies; (iii) to identify areas where there is limited research evidence and; (iv) to make recommendations for future research. This paper is in line the Vision 2030 [ 15 ], Kenya’s national development policy framework, which directs that the government implements substance use treatment and prevention projects and programs, and target 3.5 of the Sustainable Development Goals (SDGs) which requires that countries strengthen the treatment and prevention for SUDs [ 16 ].
Materials and methods
Protocol and registration.
In conducting this systematic review we adhered to the recommendations from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [ 17 ]. A 27-item PRISMA checklist is available as an additional file to this protocol ( S1 Checklist ). Our protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO): CRD42020203717.
Search strategy
A search was carried out in five electronic databases on 20 th August 2020: PubMed, PsychINFO, Web of Science, Cumulative Index of Nursing and Allied Professionals (CINAHL) and Cochrane Library. The full search strategy can be found in S1 File and takes the following form: (terms for substance use) and (terms for substance use outcomes of interest) and (terms for region) . The searches spanned the period from inception to date. No filter was applied. A manual search was done in Volumes 1, 2 and 3 (all published volumes by the time of the search) of the recently launched AJADA journal by NACADA, and additional articles identified.
[ 14 , 18 , 19 ].
Study selection
Following the initial search, all articles were loaded onto Mendeley reference manager where initial duplicate screening and removal was done. After duplicate removal, the articles were loaded onto Rayyan, a soft-ware for screening and selecting studies during the conduct of systematic reviews [ 20 ]. The abstract and titles of retrieved articles were independently screened by two authors based on a set of pre-determined eligibility criteria. A second screening of full text articles was also done independently by two authors and resulted in an 88.7% agreement. Disagreements during each stage of the screening were resolved through discussion and consensus.
Inclusion criteria
Since we sought to map existing literature on the subject, our inclusion criteria were broad. We included articles on substance use if (i) the sample or part of the sample was from Kenya, (ii) they were original research articles, (iii) they had a substance use or SUD exposure, (iv) they had a substance use or SUD related outcome such as prevalence, pattern of use, prevention and treatment, and (iv) they were published in English or had an English translation available. We included studies conducted among all age groups and studies that used all designs including quantitative, qualitative and mixed methods.
Exclusion criteria
Studies were excluded if: (i) they were cross-national and did not report country specific results (ii) they did not report substance use or SUD as an exposure, and did not have substance use or SUD related outcomes or as part of the outcomes, (iii) they were review articles, dissertations, conference presentations or abstracts, commentaries or editorials, (iv) and the full text articles were not available.
Data extraction
We prepared 3 data extraction forms based on three emerging categories of studies i.e.:
- Studies reporting on the epidemiology of substance use or SUD
- Studies evaluating substance use or SUD interventions and programs
- Studies qualitatively exploring various themes on substance use or SUD (but not evaluating interventions or programs)
The forms were piloted by F.J. and S.K. and adjustments made to the content. Data extraction was then done using the final form by all authors and double checked by F.J. for completeness and accuracy. Discrepancies were resolved by discussion with S.K. and E.T. until consensus was achieved. The following data was extracted for each study category:
- Studies reporting on the epidemiology of substance use or SUD: study design, study population characteristics, study setting, sample size, age and gender distribution, substance(s) assessed, standardized tool or criteria used, main findings (prevalence, risk factors, other key findings).
- Studies evaluating substance use or SUD interventions and programs: study design, study objective, sample size, name of the intervention or program, person delivering intervention, outcomes and measures, and main findings.
- Studies qualitatively exploring various aspects of substance use or SUD other than programs and interventions: study objective, methods of data collection, study setting, study population, age and gender distribution, theoretical framework used, and main findings.
Data synthesis
The results have been summarized descriptively and organized by the three categories above. Within each category, a general description of the study characteristics has been provided followed by a narrative synthesis of findings organized by sub-themes inductively derived from the data. The sub-themes within each category are as follows:
- Studies reporting on the epidemiology of substance use or SUD : Epidemiology of alcohol use, epidemiology of tobacco use, epidemiology of khat use, epidemiology of cannabis use, epidemiology of opioid and cocaine use, epidemiology of other substance use (sedatives, inhalants, hallucinogens, prescription medication, emerging drugs, ecstasy).
- Studies evaluating substance use or SUD interventions and programs: Individual level interventions (Individual-level interventions for harmful alcohol use, individual-level interventions for khat use, individual level intervention for substance use in general); Programs (Methadone programs, needle-syringe programs, tobacco cessation programs, out-patient SUD treatment programs); Population-level interventions : Population-level tobacco interventions, population-level alcohol interventions.
- Studies qualitatively exploring various aspects of substance use or SUD other than programs and interventions : Injecting drug use and heroin use, alcohol use, substance use among youth and adolescents, other topics.
Quality assessment of the studies
Quality assessment was conducted by S.K. using the Quality Assessment Tool for Studies with Diverse Designs (QATSDD) [ 21 ]. F.J. & J.B. double checked the scores for completeness and accuracy. Any disagreements were discussed and resolved by consensus. We had initially planned to use the National Institute of Health (NIH) set of quality assessment tools but due to the diverse nature of study designs, the authors agreed to use the QATSDD tool. The QATSDD is a 16-item tool for both qualitative and quantitative studies. Each item is scored on a 4-point scale (0–3), with a total of 14 criteria for each study design and 16 for studies with mixed methods. Scoring relies on guidance notes provided as well as judgment and expertise from the reviewers. The criteria used are: (i) theoretical framework; (ii) statement of aims or objectives; (iii) description of research setting; (iv) sample size consideration; (v) representative sample of target group (vi) data collection procedure description; (vii) rationale for choice of data collection tool(s); (viii) detailed recruitment data; (ix) statistical assessment of reliability and validity of measurement tools (quantitative only); (x) fit between research question and method of data collection (quantitative only); (xi) fit between research question and format and content data collection (qualitative only); (xii) fit between research question and method of analysis; (xiii) justification of analytical method; (xiv) assessment of reliability of analytical process (qualitative only); (xv) user involvement in design and (xvi) discussion on strengths and limitations[ 21 ]. Scores are awarded for each criterion as follows: 0 = no mention at all; 1 = very brief description; 2 = moderate description; and 3 = complete description. The scores of each criterion are then summed up with a maximum score of 48 for mixed methods studies and 42 for studies using either qualitative only or quantitative only designs. For ease of interpretation, the scores were converted to percentages and classified as low (<50%), medium (50%–80%) or high (>80%) quality of evidence [ 22 ].
Search results
The search from the five electronic databases yielded 1535 results: 950 from PubMed, 173 from PsychINFO, 210 from web of science, 123 from CINAHL and 79 from Cochrane library. Thirteen additional studies were identified through a manual search of the AJADA journals (Volumes 1, 2 and 3). Studies were assessed for duplicates and 1154 articles remained after removal of duplicates. The 1154 studies underwent an initial screening based on abstracts and titles, and 946 articles were excluded. A second screen of full text articles was done for the 208 studies that were potentially eligible for the review. Twenty three studies were excluded as follows: 21 did not meet the eligibility criteria and 2 had duplicated results. A total of 185 studies were found to meet the inclusion criteria and were included in the review ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0269340.g001
General characteristics of the studies
Of the 185 studies included in this review, 144 (77.8%) investigated the epidemiology of substance use or SUD, 18 (9.7%) evaluated substance use or SUD interventions and programs, and 23 (12.4%) were qualitative studies exploring perceptions on various substance use or SUD topics other than interventions and programs (Table 4). The studies were published between 1982 and 2020. The number of studies published has gradually increased in number over the years, particularly in the past decade. Fig 2 shows the publication trends for substance use research in Kenya.
https://doi.org/10.1371/journal.pone.0269340.g002
Quality assessment
The QATSDD scores ranged from 28.6% [ 23 ] to 92.9% [ 24 ]. Only 14 studies [ 12 , 23 , 25 – 36 ] (all quantitative) had scores of less than 50%. Of these, the main items driving low quality were: no mention of user involvement in study design (n = 14) [ 12 , 23 , 25 – 36 ], no explicit mention of a theoretical framework (n = 10) [ 12 , 23 , 25 – 28 , 30 , 33 , 35 , 36 ] and a lack of a statistical assessment of reliability and validity of measurement tools (n = 10) [ 12 , 23 , 25 , 28 , 30 – 33 , 35 , 36 ] Table 1 .
https://doi.org/10.1371/journal.pone.0269340.t001
Studies examining the epidemiology of substance use or SUD
General description of epidemiological studies..
One hundred and forty-four studies examined the prevalence and or risk factors for various substances. The studies were published between 1982 and 2020. The four main study designs used were cross-sectional (n = 126), cohort (n = 5), case-control (n = 10), and mixed methods (n = 2). One study used a combination of the multiplier method, Wisdom of the Crowds (WOTC) method, and a published literature review to document the size of key populations [ 164 ]. The sample size for this category of studies ranged from 42 [ 130 ] to 72292 [ 128 ].
The studies were conducted in diverse settings including the community (n = 72), hospitals (n = 40), institutions of learning (n = 24), streets (n = 5), prisons and courts (n = 3), charitable institutions (n = 1), methadone maintenance therapy (MMT) clinics (n = 1), and in needle-syringe program (NSP) sites (n = 1). Of the studies conducted within the community, 12 were conducted in informal settlements. The study populations were similarly diverse as follows: general population adults & adolescents (n = 39), persons with NCDs (n = 11), primary and secondary school students (n = 15), people who inject drugs (PWID) (n = 11), general patients (n = 5), men who have sex with men (MSM) (n = 8), university and college students (n = 9), commercial sex workers (n = 7), psychiatric patients (n = 6), orphans and street connected children and youth (n = 6), people living with HIV (PLHIV) (n = 6), healthcare workers (n = 3), law offenders (n = 3), military (n = 1), and teachers (n = 1). Only one study was conducted among pregnant women [ 131 ].
Sixty-nine studies (47.6%) used a standardized diagnostic tool to assess for substance use. The Alcohol Use Disorder Identification Test (AUDIT) (n = 21) and the Alcohol, Smoking & Substance Use Involvement Screening Test (ASSIST) questionnaire (n = 10) were the most frequently used tools. Most papers assessed for alcohol ( n = 109) and tobacco use ( n = 80). Other substances assessed included khat (n = 34), opioids (n = 21), sedatives (n = 19), cocaine (n = 19), inhalants (n = 16), cannabis (n = 14), hallucinogens (n = 7), prescription medication (n = 4), emerging drugs (n = 1) and ecstasy (n = 1). Most studies (n = 93) assessed for more than one substance.
Epidemiology of alcohol use.
One hundred and nine papers assessed for the prevalence and or risk factors for alcohol use. Using the AUDIT, the 12-month prevalence rate for hazardous alcohol use ranged from 2.9% among adults drawn from the community [ 97 ] to 64.6% among female sex workers (FSW) [ 77 ]. Based on the same tool, the lowest and highest 12-month prevalence rates for harmful alcohol use were both reported among FSWs i.e. 9.3% [ 80 ] and 64.0% [ 174 ] respectively, while the prevalence of alcohol dependence ranged from 8% among FSWs living with HIV [ 203 ] to 33% among MSM who were commercial sex workers [ 144 ]. The highest lifetime prevalence rate for alcohol use was reported by Ndegwa & Waiyaki [ 151 ]. The authors found that 95.7% of undergraduate students had ever used alcohol.
Alcohol use, was associated with several socio-demographic factors including being male [ 50 , 112 , 114 , 140 , 158 , 168 , 182 , 191 ], being unemployed [ 114 ], being self-employed [ 97 ], having a lower socio-economic status (SES) [ 128 ], being single or separated, living in larger households [ 97 ], having a family member struggling with alcohol use, and alcohol being brewed in the home [ 143 ]. Alcohol use was linked to various health factors including glucose intolerance [ 81 ], poor cardiovascular risk factor control [ 111 ], having a diagnosis of diabetes mellitus [ 134 ], hypertension [ 112 , 139 ], default from tuberculosis (TB) treatment [ 148 ], depression [ 113 ], psychological Intimate Partner Violence (IPV) [ 205 ], tobacco use [ 182 , 205 ], and increased risk of esophageal cancer [ 137 , 179 ]. Finally, alcohol use was associated with involvement in Road Traffic Accidents (RTAs) [ 88 ], and having injuries [ 88 , 171 ] and suicidal behavior [ 109 ].
Epidemiology of tobacco use.
Eighty papers assessed for the prevalence and risk factors for tobacco use. The lifetime prevalence of tobacco use ranged from 23.5% among healthcare workers (HCWs) [ 140 ] to 84.3% among psychiatric patients [ 110 ]. The highest lifetime prevalence rate for tobacco use was reported by Ndegwa & Waiyaki [ 151 ]. The authors found that 95.7% of undergraduate students had ever used tobacco.
Tobacco use was associated with socio-demographic factors such as being male [ 112 , 140 , 168 ] and living in urban areas [ 163 ]. Several health factors were linked to tobacco use including hypertension [ 112 ], development of oral leukoplakia [ 32 ], pneumonia [ 146 ], increased odds of laryngeal cancer [ 136 ], ischemic stroke [ 100 ] and diabetes mellitus [ 134 ]. In addition, tobacco use was associated with having had an injury in the last 12 months [ 171 ], emotional abuse [ 110 ], and psychological IPV [ 205 ]. Longer duration of smoking was associated with a diagnosis of diabetes mellitus [ 73 ], lower SES [ 128 ], and hypertension [ 98 , 142 ]. Peltzer et al. [ 181 ] reported that early smoking initiation among boys was associated with ever drunk from alcohol use, ever used substances, and ever had sex. Among girls, the authors found that early smoking initiation was associated with higher education, ever drunk from alcohol use, parental or guardian tobacco use, and suicide ideation.
Epidemiology of khat use.
The epidemiology of khat use was investigated by 34 studies. The lifetime prevalence rate for khat use ranged from 10.7% among general hospital patients [ 168 ] to 88% among a community sample [ 23 ]. Khat use was associated with being male [ 114 , 168 ]; unemployment [ 114 ]; being employed [ 25 ]; younger age (less than 35 years), higher level of income, comorbid alcohol and tobacco use [ 166 ] and age at first paid sex of less than 20 years among FSWs [ 195 ]. Further, khat use was associated with increased odds of negative health outcomes [ 130 , 146 , 166 , 201 ].
Higher odds of reporting psychotic [ 166 , 201 ], and PTSD (Post-Traumatic Stress Disorder) symptoms [ 201 ], having thicker oral epithelium [ 130 ], and pneumonia [ 146 ], were reported among khat users compared to non-users.
Epidemiology of cannabis use.
Fourteen studies evaluated the prevalence of cannabis use. The lifetime prevalence rate of cannabis use ranged from 21.3% among persons with AUD [ 120 ] to 64.2% among psychiatric patients [ 110 ]. Cannabis use was associated with being male [ 140 , 168 ], and with childhood exposure to physical abuse [ 110 ].
Epidemiology of opioid and cocaine use.
Twenty-one studies investigated the prevalence of opioid use. The lifetime prevalence rate of opioid use ranged from 1.1% among PLHIV [ 132 ] to 8.2% among psychiatric patients [ 110 ].
Nineteen studies assessed for the prevalence of cocaine use. The highest reported prevalence rates were 76.2% among PWID use (current use) [ 190 ]; 8.8% among healthcare workers (lifetime use) [ 140 ]; and 6.7% among PLHIV (lifetime use) [ 132 ].
Epidemiology of IDU.
One study assessed the prevalence for IDU. Key population size estimates for PWID use was reported as 6107 for Nairobi [ 164 ]. IDU was associated with depression, risky sexual behavior [ 149 ], Hepatitis-C Virus (HCV) infection [ 173 ], and HIV-HCV co-infection [ 68 ].
Epidemiology of other substance use (sedatives, inhalants, hallucinogens and prescription medication, emerging drugs, ecstasy).
The epidemiology of sedative use was investigated by 19 studies, inhalant use by 16 studies, hallucinogen use by 7 studies, prescription medication by 4 studies, and emerging drugs and ecstasy by one study each. The highest lifetime prevalence rate for sedative use was reported as 71.4% among a sample of psychiatric patients [ 28 ], while the highest prevalence rate for inhalant use was 67% among children living in the streets [ 86 ]. The lifetime prevalence rates for hallucinogen use ranged from 1.4% among university students [ 160 ] to 3.7% among psychiatric patients [ 110 ]. The highest prevalence rate for the use of prescription medication was reported as 21.2% among PWID [ 190 ]. One study each reported on the prevalence of emerging drugs [ 122 ] and ecstasy [ 153 ]. The studies were both conducted among adolescents and youth. The authors found the lifetime prevalence rates for the two substances to be 11.8% [ 122 ] and 4.0% [ 153 ] respectively.
Other topics explored by the epidemiology studies.
In addition to prevalence and associated factors, the epidemiological studies explored other topics.
Papas et al. [ 176 ] explored the agreement between self-reported alcohol use and the biomarker phosphatidyl ethanol and reported a lack of agreement between self-reported alcohol use and the biomarker phosphatidyl ethanol among PLHIV with AUD.
One study investigated the self-efficacy of primary HCWs for SUD management and reported that self-efficacy for SUD management was lower in those practicing in public facilities and among those perceiving a need for AUD training. Higher self-efficacy was associated with attending to a higher proportion of patients with AUD, and the belief that AUD is manageable in outpatient settings [ 196 ].
Five studies investigated the reasons for substance use. Common reasons for substance use included leisure, stress and peer pressure among psychiatric patients[ 28 ], curiosity, fun, and peer influence among college students [ 123 ], peer influence, idleness, easy access, and curiosity among adults in the community [ 25 ], and peer pressure, to get drunk, to feel better and to feel warm among street children [ 74 ]. Atwoli et al. 2011 [ 72 ] reported that most students were introduced to substances by friends.
Kaai et al. [ 99 ] conducted a study regarding quit intentions for tobacco use and reported that 28% had tried to quit in the past 12 months, 60.9% had never tried to quit, and only 13.8% had ever heard of smoking cessation medication. Intention to quit smoking was associated with being younger, having tried to quit previously, perceiving that quitting smoking was beneficial to health, worrying about future health consequences of smoking, and being low in nicotine dependence. A complete description of the prevalence studies has been provided in Table 2 .
https://doi.org/10.1371/journal.pone.0269340.t002
Studies evaluating substance use or SUD programs and interventions
General description of studies evaluating programs and interventions..
A total of eighteen studies evaluated specific interventions or programs for the treatment and prevention of substance use. These were carried out between 2009 and 2020. Eleven studies focused on individual-level interventions, 5 studies evaluated programs, and 2 studies evaluated population-level interventions. The studies used various approaches including randomized control trials (RCT) (n = 7), mixed methods (n = 3), non-concurrent multiple baseline design (n = 1), quasi experimental (n = 1), cross-sectional (n = 2), and qualitative (n = 3). One study employed a combination of qualitative methods and mathematical modeling.
Individual-level interventions.
Individual-level interventions for harmful alcohol use . Nine studies evaluated either feasibility, acceptability, and or efficacy for individual-level interventions for harmful alcohol use [ 38 , 40 , 90 , 94 , 127 , 141 , 175 , 178 , 193 ]. All the interventions were tested among adult populations including persons attending a Voluntary Counseling & Testing (VCT) center (38), PLHIV [ 40 , 175 ], and adult males and females drawn from the community [ 94 , 141 ] and FSWs [ 127 , 178 ].
Two studies evaluated a six session CBT intervention for harmful alcohol use among PLHIV. The intervention was reported as feasible, acceptable [ 40 ] and efficacious [ 175 ] in reducing alcohol consumption among PLHIV. The intervention was delivered by trained lay providers.
Giusto et al [ 90 ] evaluated the preliminary efficacy of an intervention aimed at reducing men’s alcohol use and improving family outcomes. The intervention was delivered in 5 sessions by trained lay-providers, and utilized a combination of behavioral activation, motivational interviewing (MI) and gender norm transformative strategies. The intervention showed preliminary efficacy for addressing alcohol use and family related problems.
Five studies evaluated brief interventions that ranged from 1 to 6 sessions and were delivered by primary HCWs, lay providers and specialist mental health professionals [ 38 , 94 , 127 , 178 , 193 ]. The brief interventions were reported as feasible, acceptable [ 38 ], and efficacious in reducing alcohol consumption [ 94 , 127 , 178 , 193 ]. The brief interventions additionally resulted in reductions to IPV, participation in sex work [ 178 ], and risky sexual behavior [ 127 ].
One study evaluated the efficacy of a mobile delivered MI intervention and found that at 1 month, AUDIT-C scores were significantly higher for waiting-list controls compared to those who received the mobile MI [ 94 ].
Moscoe at al. [ 141 ] found no effect of a prize-linked savings account on alcohol, gambling and transactional sex expenditures among men.
Individual-level interventions for khat use . One study utilized a randomized control trial (RCT) approach to evaluate the effect of a three-session brief intervention for khat use on comorbid psychopathology (depression, PTSD, khat induced psychotic symptoms) and everyday functioning. The intervention was delivered by trained college graduates and was found to result in reduced khat use and increased functioning levels, but had no benefit for comorbidity symptoms (compared to assessments only) [ 202 ].
Individual level intervention for any substance use . One study evaluated the efficacy of a four-session psychoeducation intervention using an RCT approach. The study found that the intervention was effective in reducing the severity of symptoms of any substance abuse at 6 months compared to no intervention. The intervention was additionally effective in reducing symptoms for depression, hopelessness, suicidality, and anxiety [ 145 ].
Methadone programs . Two studies utilized qualitative methods to evaluate the perceptions of persons receiving methadone on the benefits of the programs [ 61 , 62 ]. The methadone programs were perceived as having potential to aid in recovery from opioid use and to reduce HIV transmission among PWID [ 61 , 62 ].
Needle-syringe programs (NSPs) . One paper explored the impact of NSPs programs on needle and syringe sharing among PWID. The study reported that the introduction of NSPs led to significant reductions in needle and syringe sharing [ 56 ].
Tobacco cessation programs . One study evaluated HCWs knowledge and practices on tobacco cessation and found that the knowledge and practice on tobacco cessation was inadequate [ 89 ].
Out-patient SUD treatment programs . One paper investigated the impact of community based outpatient SUD treatment services and reported a 42% substance use abstinence rate 0–36 months following treatment termination [ 84 ].
Population-level interventions.
Population-level tobacco interventions . One study evaluated the appropriateness and effectiveness of HIC anti-tobacco adverts in the African context and found the adverts to be effective and appropriate [ 183 ].
Population-level alcohol interventions . One paper examined community members’ perspectives on the impact of the government’s public education messages on alcohol abuse and reported that the messages were ineffective and unpersuasive [ 55 ].
A complete description of studies investigating programs and interventions is in Table 3 .
https://doi.org/10.1371/journal.pone.0269340.t003
Studies qualitatively exploring various substance use or SUD topics (other than interventions)
General description of qualitative studies..
There were 23 qualitative studies included in our review. The studies were conducted between 2004 and 2020. Data was collected using several approaches including in-depth interviews (IDIs) only (n = 6), focus group discussions (FGDs) only (n = 2), a combination of FGDs and IDIs (n = 10), a combination of observation and individual IDIs (n = 2), a combination of observation, IDIs and FGDs (n = 1), a combination of literature review, observation, IDIs and FGDs (n = 1). One study utilized the participatory research and action approach [ 60 ]. The target populations for the qualitative studies included persons using heroin (n = 3), males and females with IDU (n = 11) adolescents and youth (n = 3), FSWs (n = 2), refugees and Internally Displaced Persons (IDPs) (n = 1), and PLHIV (n = 2).
Injecting drug use and heroin use.
Thirteen studies explored various themes related to IDU and heroin use with most of them (n = 8) focusing on issues related to women. Three studies explored the drivers of IDU among women and found them to include influence of intimate partners [ 48 , 49 ], stress of unexpected pregnancies [ 49 ], gender inequality, and social suffering [ 67 ]. One study found that IDU among women interfered with utilization of antenatal and maternal and child health services [ 57 ], while another reported that women who inject drugs linked IDU to amenorrhea hence did not perceive the need for contraception [ 51 ].
Mburu et al [ 47 ] explored the social contexts of women who inject drugs and found that these women experienced internal and external stigma of being injecting drug users, and external gender-related stigma of being female injecting drug users. Using a socio-ecological approach, Mburu et al [ 50 ] reported that IDU during sex work was an important HIV risk behavior. In another study, FSWs reported that they used heroin to boost courage to engage in sex work [ 65 ].
Other than IDU and heroin use among women, five studies investigated other themes. One study explored the experiences of injecting heroin users and found that the participants perceived heroin injection as cool [ 42 ]. Guise et al. 2015 [ 44 ] conducted a study to explore transitions from smoking to injecting and reported that transitions from smoking to IDU were experienced as a process of managing resource constraints, or of curiosity, or search for pleasure. One study explored the experiences of persons on MMT as regards integration of MMT with HIV treatment. The study was guided by the material perspective in sociology theory and Annmarie’s Mol’s analysis of logic of care. Persons on MMT preferred that they have choice over whether to seek care for HIV and MMT in a single, or in separate settings.
Alcohol use.
Six studies focused on alcohol use. Three studies explored perceptions of service providers and communities on the effects of alcohol use. Alcohol use was perceived as having a negative impact on sexual and reproductive health [ 53 , 54 ] and on socio-economic status [ 43 , 46 ]. One study explored the reasons for alcohol use among PLHIV and found that reasons for alcohol use included stigma and psychological problems, perceived medicinal value, and poverty [ 60 ].
Youth and adolescent substance use.
Three studies focused on substance use among youth and adolescents. In one study, the adolescents perceived that substance use contributed to risky sexual behavior including unprotected sex, transactional sex, and multiple partner sex [ 58 ]. The youth identified porn video shows and local brew dens as places where risky sexual encounters between adolescents occurred [ 59 ]. Ssewanyana et al. [ 63 ] utilized the socio-ecological model to explore perceptions of adolescents and stakeholders on the factors predisposing and contributing to substance use. Substance use among adolescents was perceived to be common and to be due to several socio-cultural factors e.g. access to disposable income, idleness, academic pressure, low self-esteem etc.
Other topics.
Utilizing the syndemic theory, one study explored how substance use, violence and HIV risk affect PrEP (Pre-exposure prophylaxis) acceptability, access and intervention needs among male and female sex workers. The study found that co-occurring substance use, and violence experienced by sex workers posed important barriers to PrEP access [ 41 ].
A complete description of included qualitative studies is in Table 4 .
https://doi.org/10.1371/journal.pone.0269340.t004
This is to our knowledge, the first study to summarize empirical work done on substance use and SUDs in Kenya. More than half (77.8%) of the reviewed studies investigated the area of prevalence and risk factors for substance use. Less common were qualitative studies exploring various themes (12.4%) and studies evaluating interventions and programs (9.7%). The first study was conducted in 1982 and since then the number of publications has gradually risen. Most of the research papers (92.4%) were of moderate to high quality. In comparison to two recent scoping reviews conducted in South Africa and Botswana, more research work has been done on substance use in Kenya. Our study found that 185 papers on substance use among Kenyans had been published by the time of the search while Opondo et al. [ 11 ] and Tran et al. [ 10 ] reported that only 53 and 7 papers focusing on substance use had been published in South Africa (between 1971 and 2017) and in Botswana (between 1983 and 2020) respectively.
Epidemiology of substance use or SUD
Studies investigating the prevalence, and risk factors for substance use dominated the literature. The studies, which were conducted across a broad range of settings and populations, focused on various substances including alcohol, tobacco, cannabis, opioids, cocaine, sedatives, inhalants, hallucinogens, prescription medication, and ecstasy. In addition, a wide range of important health and socio-demographic factors were examined for their association with substance use. Most studies had robust sample sizes and were conducted using diverse designs including cross-sectional, case-control and cohort. The studies showed a significant burden of substance use among both adults and children and adolescents. In addition, substance use increased the odds of negative mental and physical health outcomes consistent with findings documented in global reports [ 2 , 3 ]. These findings highlight the importance of making the treatment and prevention for substance use and SUDs of high priority in Kenya.
- Two main evidence gaps were identified within this category: The prevalence and risk factors for substance use among certain vulnerable populations for whom substance use can have severe negative consequences, had not been investigated. For example, no study had included police officers or persons with physical disability, only one study had its participants as pregnant women [ 113 ], and only 2 studies had been conducted among HCWs [ 140 , 196 ].
- Few studies had explored the epidemiology of hallucinogens, prescription medication, ecstasy, IDU, and emerging substances e.g. synthetic cannabinoids. These substances are a public health threat globally [ 207 , 208 ] yet their use remains poorly documented in Kenya.
Interventions and programs
Given the significant documented burden of substance use and SUDs in Kenya, it was surprising that few studies had focused on developing and testing treatment and prevention interventions for SUDs. A possible reason for this is limited expertise in the area of intervention development and testing. For example, research capacity in implementation science has been shown to be limited in resource-poor settings such as ours [ 209 ].
Of note is that most of the tested interventions had been delivered by lay providers [ 40 , 90 , 175 ] and primary HCWs [ 38 , 127 , 178 ] indicating a recognition of task-shifting as a strategy for filling the mental health human resource gap in Kenya.
Several research gaps were identified within this category.
- Out of the 11 individual-level interventions tested, nine had targeted harmful alcohol use except one which focused on khat [ 202 ] and another that targeted several substances [ 145 ]. No studies had evaluated individual-level interventions targeting tobacco and cannabis use, despite the two being the second and third most commonly used substances in Kenya [ 8 ]. Further, no individual-level interventions had focused on other important SUDs like opioid, sedative and cocaine use disorders.
- Few studies had evaluated the impact of substance use population-level interventions [ 55 , 183 ]. Several cost-effective population-level interventions have been recommended by WHO e.g. mass media education and national toll free quit line services for tobacco use, and brief interventions integrated into all levels of primary care for harmful alcohol use [ 210 ]. Such strategies need to be tested for scaling up in Kenya.
- None of the interventions had been tested among important vulnerable populations for whom local research already shows a significant burden e.g. children and adolescents, the Lesbian Gay Bisexual Transgender & Queer (LGBTQ) community, HCWs, prisoners, refugees, and IDPs. In addition, no interventions had been tested for police officers and pregnant women, and no studies had evaluated interventions to curb workplace substance use.
- Only one study evaluated digital strategies for delivering substance use interventions [ 94 ] yet the feasibility of such strategies has been demonstrated for other mental health disorders in Kenya [ 211 ]. Moreover, the time is ripe for adopting such an approach to substance use treatment given the fact that the country currently has a mobile subscriptions penetration of greater than 90% [ 212 ].
- No studies had evaluated the impact of other interventions such as mindfulness and physical exercise. Meta-analytic evidence suggests that such strategies hold promise for reducing the frequency and severity of substance use and craving [ 213 , 214 ].
Qualitative studies
The qualitative studies focused on a broad range of themes including drivers and impact of substance use, drug markets, patterns of substance use, stigma, and access to treatment. Most of the work however focused on PWID and heroin users. Future qualitative work should explore issues relating to other populations for example persons with other mental disorders, persons with physical disabilities, police officers, and persons using other commonly used substances such as tobacco, khat, and cannabis.
Limitations
The aim of this systematic review was to provide an overview of the existing literature on substance use and SUD research in Kenya. We therefore did not undertake a meta-analysis and detailed synthesis of the findings of studies included in this review. In addition, variability in measurements of substance use outcomes precluded our ability to more comprehensively summarize the study findings. For quality assessment, detailed assessments using design specific tools were not possible given the diverse methodological approaches utilized in the studies. We therefore used a single tool for the quality assessment of all studies. The results of the quality assessment are therefore to be interpreted with caution. Nonetheless this review describes for the first time the breadth of existing literature on substance use and SUDs in Kenya, identifies research gaps, and provides important directions for future research.
The purpose of this systematic review was to map the research that has been undertaken on substance use and SUDs in Kenya. Epidemiological studies dominated the literature and indicated a significant burden of substance use among both adults and adolescents. Our findings indicate that there is a dearth of literature regarding interventions for substance use and we are calling for further research in this area. Specifically, interventions ought to be tested not just for alcohol but for other substances as well, and among important at risk populations. In addition, future research ought to explore the feasibility of delivering substance use interventions using digital means, and the benefit of other interventions such as mindfulness and physical exercise. Future qualitative work should aim at providing in-depth perspectives on substance use among populations excluded from existing literature e.g. police officers, persons using other substances such as tobacco, cannabis and khat, and persons with physical disability.
Supporting information
S1 checklist. prisma checklist..
https://doi.org/10.1371/journal.pone.0269340.s001
S1 File. Search terms for PsychINFO.
https://doi.org/10.1371/journal.pone.0269340.s002
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Hammer JH, Parent MC, Spiker DA, World Health Organization. Global status report on alcohol and health 2018. https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1 . Accessed 12 June 2021
- 3. World Health Organisation. Tobacco [Internet]. 2020. https://www.who.int/news-room/fact-sheets/detail/tobacco . Accessed 12 June 2021
- 4. World Health Organization. Alcohol and drug use disorders: Global health estimates. 2017. http://www.who.int/substance_abuse/activities/fadab/msb_adab_2017_GHE_23June2017.pdf . Accessed 12 June 2021
- 7. International Narcotics Control Board. Chapter 1: Economic consequences of drug abuse. 2013. https://www.incb.org/documents/Publications/AnnualReports/AR2013/English/AR_2013_E_Chapter_I.pdf . Accessed 12 June 2021
- 8. National Authority for the Campaign Against alcohol and Drug Abuse. Rapid Situation Assessment of Drugs abd Substance Abuse in Kenya. 2017. https://nacada.go.ke/sites/default/files/2019-10/National%20ADA%20Survey%20Report%202017_2_2.pdf . Accessed 12 June 2021
- 9. National Authority for the Campaign Against alcohol and Drug Abuse, Kenya Institute for Public Policy Research and Analysis. Status of Drugs and Substance Abuse among Primary School Pupils in Kenya. 2019. https://nacada.go.ke/sites/default/files/2019-10/Report%20on%20the%20Status%20of%20Drugs%20and%20Substance%20Abuse%20among%20Primary%20School%20Pupils%20in%20Kenya.pdf . Accessed 12 June 2021
- 13. The National Authority for the Campaign aganist Alcohol and Drug Abuse [Internet]. http://www.nacada.go.ke . Accessed 12 June 2021
- 14. The National Authority for the Campaign Aganist Alcohol and Drug Abuse. African Journal of Alcohol & Drug Abuse (Volume 2). https://nacada.go.ke/sites/default/files/AJADA/AJADA%202%20ammended/AJADA%20Volume%20II%20(Full%20Booklet).pdf . Accessed 12 june 2021
- 15. Republic of Kenya. The National Treasury and Planning. Third Medium Term Plan 2018–2022. Kenya Vision 2030. https://planning.go.ke/wp-content/uploads/2018/12/THIRD-MEDIUM-TERM-PLAN-2018-2022.pdf . Accessed 20 June 2020
- 16. United Nations Development Programme. The 2030 Agenda for Sustainable Development, A/RES/70/1. Undp. 2015.
- 18. The National Authority for the Campaign Aganist Alcohol and Drug Abuse. African Journal of Alcohol & Drug Abuse (Volume 3). https://nacada.go.ke/sites/default/files/AJADA/AJADA%203/NACADA%20AJADA%20Vol%203-%20Full%20Booket.pdf . Accessed 12 june 2021
- 19. The National Authority for the Campaign Aganist Alcohol and Drug Abuse. African Journal of Alcohol & Drug Abuse (Volume 1). https://nacada.go.ke/sites/default/files/AJADA/AJADA%201%20ammended/AJADA%20Volume%20I%20(Full%20Booklet).pdf . Accessed 12 june 2021
- 207. United Nations Office on Drugs and Crime. New psychoactive substances.2020. https://www.unodc.org/documents/scientific/NPS-Leaflet_WEB_2020.pdf . Accessed 12 June 2021
- 208. UNODC World Drug Report 2020: Global drug use rising; while COVID-19 has far reaching impact on global drug markets. 2020. https://www.unodc.org/unodc/press/releases/2020/June/media-advisory—global-launch-of-the-2020-world-drug-report.html
- 210. World Health Organisation 2017. ‘ Best Buys ‘ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases; “the updated Appendix 3 of the WHO Global NCD Action Plan 2013–2020. https://www.who.int/ncds/management/WHO_Appendix_BestBuys.pdf . Accessed 12 June 2021
- 212. Business Today. Kenya leads Africa in smartphone usage [Internet]. 2020. https://businesstoday.co.ke/kenya-leads-africa-smartphone-usage/ . Accessed 12 June 2021.
- Open access
- Published: 21 June 2021
A review of research-supported group treatments for drug use disorders
- Gabriela López 1 ,
- Lindsay M. Orchowski ORCID: orcid.org/0000-0001-9048-3576 2 ,
- Madhavi K. Reddy 3 ,
- Jessica Nargiso 4 &
- Jennifer E. Johnson 5
Substance Abuse Treatment, Prevention, and Policy volume 16 , Article number: 51 ( 2021 ) Cite this article
26k Accesses
7 Citations
3 Altmetric
Metrics details
This paper reviews methodologically rigorous studies examining group treatments for interview-diagnosed drug use disorders. A total of 50 studies reporting on the efficacy of group drug use disorder treatments for adults met inclusion criteria. Studies examining group treatment for cocaine, methamphetamine, marijuana, opioid, mixed substance, and substance use disorder with co-occurring psychiatric conditions are discussed. The current review showed that cognitive behavioral therapy (CBT) group therapy and contingency management (CM) groups appear to be more effective at reducing cocaine use than treatment as usual (TAU) groups. CM also appeared to be effective at reducing methamphetamine use relative to standard group treatment. Relapse prevention support groups, motivational interviewing, and social support groups were all effective at reducing marijuana use relative to a delayed treatment control. Group therapy or group CBT plus pharmacotherapy are more effective at decreasing opioid use than pharmacotherapy alone. An HIV harm reduction program has also been shown to be effective for reducing illicit opioid use. Effective treatments for mixed substance use disorder include group CBT, CM, and women’s recovery group. Behavioral skills group, group behavioral therapy plus CM, Seeking Safety, Dialectical behavior therapy groups, and CM were more effective at decreasing substance use and psychiatric symptoms relative to TAU, but group psychoeducation and group CBT were not. Given how often group formats are utilized to treat drug use disorders, the present review underscores the need to understand the extent to which evidence-based group therapies for drug use disorders are applied in treatment settings.
Drug use disorders are a significant public health concern in the United States. According to the National Epidemiologic Survey of Alcohol and Related Conditions-III, the lifetime prevalence rate of DSM-5 drug use disorders is 9.9%, which includes amphetamine, cannabis, club drug, cocaine, hallucinogen, heroin, opioid, sedative/tranquilizer, and solvent/inhalant use disorders [ 1 ]. Drug use disorders are defined in terms of eleven criteria including physiological, behavioral and cognitive symptoms, as well as consequences of criteria, any two of which qualify for a diagnosis [ 2 , 3 ]. The individual and community costs of drug use are estimated at over $193 billion [ 4 , 5 ] and approximately $78.5 billion [ 6 ] for opioids alone. Consequences include overdose [ 7 ], mental health problems [ 8 ], and a range of medical consequences such as human immunodeficiency virus [ 9 , 10 ], hepatitis C virus [ 9 ], and other viral and bacterial infections [ 11 ].
Evidence-based practice was formally defined by Sackett et al. [ 12 ] in 1996 to refer to the “conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients” (p. 71). In 2006, the American Psychological Association [ 13 ] developed a policy on evidence-based practice (EBP) of psychotherapy, which emphasized the integration of best research evidence (i.e., data from meta-analyses, randomized controlled trials, effectiveness trials, and other forms of systematic case studies and reviews) with clinical expertise and judgment to deliver treatment in the context of a patient’s individual needs, preferences and culture. The shift towards EBP for substance use disorders has multiple benefits for practitioners and patients, including an increased focus on the implementation of treatments that are safe and cost-effective [ 14 ]. A recent survey of clinicians’ practices with substance use treatment found that clinicians often conducted therapy in groups [ 15 ]. While most clinicians who completed the survey reported use of evidence-based treatment practices (EBT) some also reported the use of non-EBT practices [ 15 ]. Ensuring that clinicians can readily access information regarding the current state of evidence regarding group-based therapies for substance use disorders is critical for fostering increased use of EBTs.
Although any effort to summarize a literature as large and complex as the psychological treatment literature is useful, there are several limitations. With few exceptions, research-supported treatment lists categorize treatments by formal change theory (e.g., cognitive-behavioral, interpersonal) and describe little about the context, format, or setting in which treatments were conducted and tested [ 16 ]. As a result, it is often difficult to ascertain from existing resources whether research supported treatments were conducted in group or individual format. A group format is often used in substance use treatment [ 17 ] and aftercare programs [ 18 , 19 , 20 , 21 , 22 ] . The discrepancy between the wide-spread use of group therapy in clinical practice and the relative paucity of research on the efficacy of group treatments has been noted by treatment researchers [ 23 ] and clinicians [ 24 ]. According to Lundahl’s [ 25 ] 2010 meta-analysis of studies evaluating the efficacy of motivational interviewing (MI), a commonly used treatment for substance use disorders, examination of the 119 studies concluded that studies of MI in a group format were too rare to draw solid conclusions about the efficacy of group MI. Also, it is possible that efficacy of treatments developed for individual delivery will be altered when delivered in a group format and vice versa. Given the limited empirical inquiry on group treatments for substance use, a framework organizing the literature on the efficacy of group therapy to treat substance use disorders would be useful. There is also a need for a more recent rigorous review of the empirical evidence to support group-based treatments for substance use disorders. Over 15 years ago, Weiss and colleagues conducted a review of 24 treatment outcome studies within the substance use disorder intervention literature comparing group therapy to other treatments conditions (i.e., no group therapy, individual therapy, group therapy plus individual therapy), and found no differences between group and individual therapy [ 26 ].
Given the importance of understanding the current evidence base for group-delivered treatments for substance use disorders, the present review sought to provide a summary of the literature on the benefits of group treatments for drug use disorders. Group treatments are potentially cost-effective, widely disseminable, and adaptable to a variety of populations but are lagging individual treatments in terms of research attention. Thus, highlighting characteristics of group treatments that are potentially efficacious is of import to stimulate further empirical inquiry. The review is organized by drug type (cocaine, methamphetamine, marijuana, opiate, mixed substance use disorders; SUD) and co-occurring SUD and psychiatric problems. We excluded studies focused on alcohol use disorder alone as this literature is summarized elsewhere (see Orchowski & Johnson, 2012). Given research suggesting that several factors impact outcomes of group treatments, including formal change theory driving the treatment approach (i.e., cognitive-behavioral, motivational interviewing), as well as patient factors [ 27 ], the review begins by first reviewing each theory of change (i.e., type of treatment), and then concludes by summarizing the research examining the extent to which patient factors influence the efficacy of group treatments for SUD.
To locate studies that evaluated a group treatment for SUD that met review inclusion criteria, the authors conducted a comprehensive literature search of PsycINFO and MedLine through 2020. Three individuals then examined abstracts of the articles for relevance. In addition, the authors utilized the reference lists of review studies and meta-analyses of SUD- treatments to locate additional studies that might meet the review inclusion criteria. The authors and a research assistant then reviewed full articles with relevance to the current study and excluded any studies that did not meet the review inclusion criteria (see Fig. 1 ).
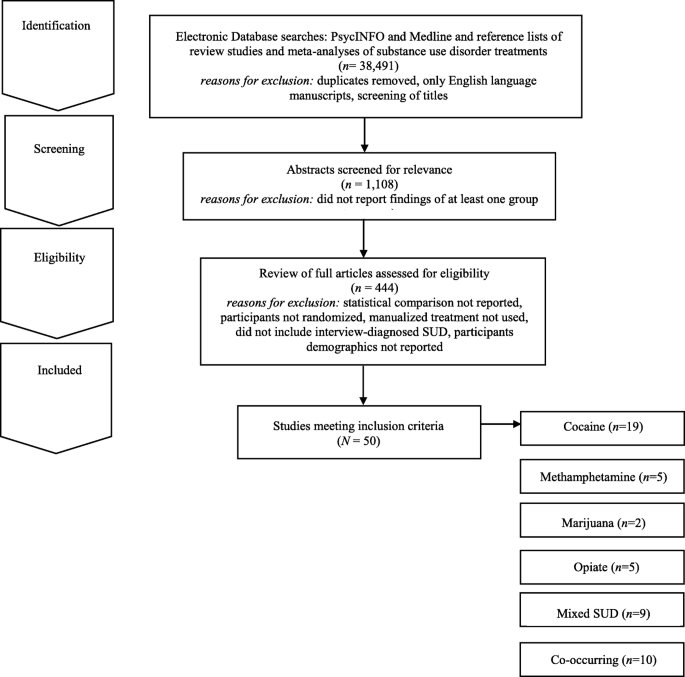
Electronic Search Strategy Flowchart
For inclusion in the review, studies needed to meet the following criteria: 1) report the findings of at least one group treatment; 2) provide at least one statistical comparison between the group treatment and a control condition; 3) randomize participants between the group treatment and control condition; 4) utilize a manualized treatment; 5) include patients with an interview-diagnosed SUD; and 6) provide information regarding the demographic characteristics of the participants in the study. Studies’ methods and results were used for data extraction. Studies which maintained a primary focus on the treatment of SUD, but also included treatment of a co-occurring psychiatric condition, were included in the review. Studies which included alcohol use as a comorbid diagnosis along another substance use were included. Studies examining the efficacy of group treatment for only alcohol use were excluded. The final set of articles included were 50 research studies that utilized a group treatment modality for the treatment of SUD, including separately examining cocaine, methamphetamine, marijuana, opioid, mixed substance, or SUD with comorbid psychiatric problems in adults.
It should be noted that several studies that met inclusion criteria were not reported in the present review because they did not report the use of a specific screening instrument for SUD as a part of the study inclusion/exclusion criteria. These studies are as follows and include these comparisons: group-based relational therapy [ 28 ] two studies by Guydish et al. [ 29 , 30 ] comparing a day treatment program to residential treatment (RT) program, a day treatment program to a coping skills group [ 31 ], standard care to a harm reduction group [ 32 ], 12 step group to a CBT group [ 33 ], medical management treatment (MMT) with CBT group to an MMT plus treatment reinforcement plan [ 34 ], treatment as usual to contingency management (CM) [ 35 ], professionally led recovery training group to treatment as usual (TAU) [ 36 ], two 4 month residential treatment programs [ 37 ], varying lengths of therapeutic community program (TPC) with and without relapse prevention [ 38 ], and Information and Referral plus peer advocacy to a Motivational group with CBT group [ 39 ].
Review of evidence-based theories of change
The 50 research studies meeting inclusion criteria tested the following group treatment modalities: contingency management (CM), motivational interviewing (MI), relapse prevention (RP), social support (SS), cognitive-behavioral (CBT), coping skills (CS), harm reduction (HR), cognitive therapy (CT), drug counseling (DC), recovery training (RT), standard group therapy (SGT), family therapy (FT), intensive group therapy (IGT), 12 step facilitation group therapy (12SG), relational psychotherapy mothers’ group (RPMG), psychoeducational therapy group (PET), behavioral skills (BS), and seeking safety (SS). Below, we briefly review the theory of change that drives each of these treatments.
Several treatment approaches are grounded in behavioral therapies and/or cognitive therapies. Broadly, cognitive therapy is an approach that focuses exclusively on targeting thoughts that are identified as part of a diagnosis or behavioral problem [ 28 ]. Cognitive-behavioral (CBT) therapy is an approach that targets specific symptoms, thoughts, and behaviors that are identified as part of a diagnosis or presenting problem [ 28 ]. Under the umbrella of CBT several other treatment modalities exist. For example, relapse prevention is a CBT treatment that hypothesizes that there are cognitive, behavioral, and affective mechanism that underlie the process of relapse [ 40 ]. Recovery training is a more specific form of relapse prevention, including education on addiction and recovery and reinforcing relapse prevention skills (e.g., understanding triggers, coping with cravings etc.) [ 41 , 42 ]. Other treatments focus on coping skills more broadly. For example, coping skills treatments include a focus on components of adaptability in interpersonal relationships, thinking and feeling, as well as approaches to self and life [ 28 ]. Some treatment approaches also recognize that individuals may not be ready to change their substance use. For example, motivational interviewing is often described as a therapy guiding technique in which the therapist is a helper in the behavior change process and expressed acceptance of the patient [ 43 ]. Standard group therapy includes 90 min sessions approximately twice a week in a group setting, [ 44 ] whereas intensive group therapy is a heavier dose of standard group therapy that includes 120-min sessions up to five times a week [ 44 ]. Psychoeducational therapy group focused on providing information on the immediate and delayed problems of substance use disorders to patients [ 45 ]. Lastly, dialectical behavior therapy (DBT) is a type of CBT therapy that focuses on helping regulate intense emotional states and provides skills to reduce arousal levels, and increase mindfulness, emotional regulation, and interpersonal skills [ 46 ].
Grounded within behavioral therapies, are behavioral skills training which focused on developing behaviors that are adaptive [ 28 ]. Contingency management is a type of behavioral therapy in which patients are reinforced or rewarded for positive behavioral change [ 47 ]. Harm reduction is a term for interventions aiming to reduce the problematic effects of behaviors [ 48 ]. Several treatment approaches also focus on interpersonal networks and building interpersonal skills. For example, social support is any psychological resources provided by a social network to help patients cope with stress [ 49 ]. Twelve-step facilitation group therapy is a more specific form of social support, which focuses on introducing patients to the 12 steps of alcoholics anonymous or related groups (i.e., cocaine or narcotics anonymous) to encourage 12-step meeting attendance in their community [ 33 , 50 ]. Seeking Safety is a present-focused and empowerment-based intervention focused on coping skills that emphasizes the importance of safety within interpersonal relationships [ 51 ]. Drug counseling describes treatment that aims to facilitate abstinence, encourage mutual support, and provide coping skills [ 52 ]. Finally, family therapy is a family-based intervention that aims to change, parenting behaviors and family interactions [ 53 ]. Overall, there are many overlapping components and skill sets in the models discussed above (See Table 1 ).
Group-based cocaine use treatments for adults
Nineteen studies were identified that targeted cocaine use and utilized some form of group therapy, the most of any drug in this review (see Table 2 ). Overall, the studies showed that all of the group therapy modalities included in this review generally reduced cocaine use when compared to treatment as usual (TAU), including day hospital groups [ 54 ]. Two studies, Magura et al. (1994) and Magura et al. (2002) did not find group differences between 8 months CBT and 8 months of TAU that consisted of methadone maintenance therapy among 141 patients with cocaine disorder [ 60 , 69 ]. When compared directly, individuals in CBT groups achieved longer abstinence than individuals in 12 step facilitation groups [ 33 ] or low intensity groups [ 64 , 65 ]. However, in another study, individuals with cocaine dependence receiving 12-step based Group Drug Counseling (GDC; similar to 12-step facilitation) had similar cocaine abstinence outcomes with or without additional individual CBT [ 41 ]. This may suggest that group 12-step facilitation is an effective intervention for cocaine dependence. Two studies demonstrated the superiority of CM groups for reducing cocaine use as compared to CBT [ 62 ] or TAU groups [ 61 , 62 ] at 12 weeks [ 54 ], 17 weeks [ 53 ], 26 weeks [ 53 ] and 52 weeks follow up [ 51 ]. Therefore, CBT group therapy and contingency management groups appear to be more effective at reducing cocaine use than TAU groups.
Group-based methamphetamine use treatments for adults
Only five treatment studies were identified that examined group treatments for methamphetamine use (see Table 3 ). Three studies found longer periods of abstinence for the group treatment (CM or drug+CM) than for TAU or non-CM conditions. The first study conducted by Rawson and colleagues compared matrix model (MM) with TAU in eight community outpatient settings [ 71 ]. The MM consisted of CBT groups, family education groups, social support groups, and individual counseling sessions along with weekly urine screens for 16 weeks. Participants in the MM condition attended more sessions, stayed in treatment longer, had more than twice as many contacts, evidence longer abstinence and greater self-reported psychosocial functioning relative to the TAU group. However, these significant differences did not persist 6 months later at follow-up.
Shoptaw et al. (2006) [ 73 ] compared four groups for treating methamphetamine dependence sertraline + CM, sertraline only, placebo + CM, and placebo [ 73 ]. Additionally, all participants attended a relapse prevention group conducted three times a week over a 14-week period. Findings provided support for the efficacy of CM for amphetamine use disorders. Group treatment (CM or drug + CM) was more effective for sustaining longer periods of abstinence relative to TAU or non-CM conditions. Roll et al. [ 72 ] found that effects of CM relative to TAU became larger as the duration of CM increased. Jaffe et al. [ 70 ] evaluated a culturally tailored intervention for 145 methamphetamine dependent gay and bisexual males. Participants in the Gay Specific CBT condition reported the most rapid decline in levels of methamphetamine use relative to standard CBT, CBT + CM, suggesting benefits for culturally appropriate group methamphetamine interventions.
Group-based marijuana use treatments for adults
Two studies examining group treatments for adults with marijuana use disorders were identified (see Table 4 ). Both studies were conducted by the same research group, utilizing the same inclusion criteria for marijuana use (50 times in 90 days). The studies examined group relapse prevention (RP) [ 76 ], specifically designed for adult marijuana users. The first trial [ 75 ] ( n = 212) comparing relapse prevention to a social support group found participants in both group treatment conditions did well overall, with two-thirds (65%) reporting abstinence of marijuana use for 2 weeks after session 4 or the quit date and 63% reporting abstinence during the last 2 weeks of treatment. Gender differences emerged; no differences between group treatments were found for women, but men in the relapse prevention group reported reduced marijuana use at the 3-month follow-up compared to men in the social support group.
A second trial [ 74 ] randomized participants to 14 sessions of group RP enhanced with cognitive behavioral skills training, two sessions of motivational interviewing (MI) with feedback and advice on cognitive behavioral skills (modeled after the Drinkers Check-up) [ 77 ], or a 4-month delayed treatment control (DTC) group which consisted of the RP group or individual MI treatment of the participants choosing. Compared to individuals randomly assigned to the DTC condition, participants in the group RP and individual MI conditions evidenced a significantly greater reduction in marijuana use and related problems over 16-month follow-up. However, examination of participants’ reactions to DTC assignment indicated that participants who felt that changing their marijuana use was their own responsibility were more likely than those who did not to change their use patterns without treatment engagement.
Group-based opiate use treatments for adults
Five group treatment studies for opioid use were identified (see Table 5 ). Two studies compared the effectiveness of pharmacotherapy plus group therapies [ 79 , 80 , 81 ] to pharmacotherapy alone in samples of opioid dependent persons, and both found that adding group treatment improved outcomes. The first study compared Naltrexone with monthly medical monitoring visits to an enhanced group condition (EN) consisting of Naltrexone plus a Matrix Method (MM) [ 79 ]. MM consisted of hourly individual sessions, 90-min CBT group, and 60 min of cue-exposure weekly for weeks 1–12; hourly individual sessions and CBT group sessions for weeks 13–26; and 90-min social support group sessions for weeks 27–52. Results found that EN participants took more study medication, were retained in treatment longer, used less opioids while in treatment, and showed greater improvement on psychological and affective dimensions than Naltrexone only participants. No difference by treatment condition was found at 6- and 12-month follow-ups. Similarly, Scherbaum et al. [ 80 ] compared routine Methadone Maintenance Therapy (MMT) with routine MMT plus group CBT psychotherapy (20 90-min sessions for 20 weeks). MMT plus group CBT participants showed less drug use than participants in the MMT group (i.e., control group). In contrast, a higher dose of group therapy provided without methadone maintenance was less effective for heroin use than was a lower dose of group therapy with methadone maintenance (Sees et al. [ 81 ]. This suggests that the combination of pharmacotherapy and group therapy for opioid use is optimal.
Shaffer et al. [ 22 ] compared psychodynamic group therapy with a hatha yoga group. All participants received methadone maintenance and individual therapy. No differences between two treatment conditions were found. For all participants, longer participation in treatment was associated with reduction in drug use and criminal activity. Lastly, Des Jarlais et al. [ 78 ] compared a group social learning AIDS/drug injection treatment program (4 sessions, 60–90 min, over 2 weeks) to a control condition. All participants received information about AIDS and HIV antibody test counseling. Compared to control participants, intervention participants reported lower rates of drug injection over time.
Group treatments for mixed SUD for adults
Nine treatment studies were identified that targeted mixed substance use with group treatments (see Table 6 ). Three involved CBT. Downey et al. [ 82 ] compared group CBT plus individual CBT to group CBT plus vouchers in a sample of 14 polysubstance users (cocaine and heroin) maintained on buprenorphine. The study was significantly underpowered and they found no significant differences on treatment outcomes. Marques and Formiogioni [ 84 ] compared individual CBT to group CBT in a sample of 155 participants with alcohol and/or drug dependence. They found that both formats resulted in similar outcomes, with higher compliance in the group CBT participants (66.7% compliance with treatment). Rawson et al. [ 87 ] compared three 16-week treatments: CM, group CBT, and CM plus group CBT, among 171 participants with cocaine disorder or methamphetamine abuse. They found that CM produced better retention and lower rates of stimulant use than CBT during treatment, but CBT produced comparable longer-term outcomes.
Two studies involved Group Drug Counseling (GDC). Greenfield et al. [ 52 ] compared a group drug counseling (GDC) (mixed gender) to a women’s recovery group (WRG) that both met weekly, for 12 weeks, for 90-min sessions among 44 participants that had a substance use disorder other than nicotine. WRG evidenced significantly greater reductions in drug and alcohol use over the follow up compared with GDC. Schottenfeld et al. [ 88 ] compared GDC (weekly, 1-h group sessions) to a community reinforcement approach (CRA; twice weekly sessions for the first 12 weeks and then weekly the following 12 weeks) among 117 patients with an opioid and cocaine use disorder. There were no differences in retention or drug use.
Remaining studies examined other interventions. Margolin et al. [ 83 ] compared an HIV Harm reduction program (HHRP) that met twice weekly for 2 h to an active control group that met six times in a sample of 90 HIV-seropositive methadone-maintained injection drug users with opioid dependence, and abuse or dependence on cocaine. At follow up, they had lower addiction severity scores and were less likely to have engaged in high risk behaviors compared to control. McKay et al. [ 85 ] compared weekly phone monitoring and counseling plus a support group in the first 4 weeks (TEL), twice-weekly individualized relapse prevention, and twice-weekly standard group counseling (STND) among 259 referred participants with alcohol use disorder or cocaine disorder. STND resulted in more days abstinent than TEL. Nemes et al. [ 86 ] compared a 12-month group program (10 months inpatient and 2 months outpatient) to an abbreviated group program (6 months inpatient, 6 months outpatient) among 412 patients with multiple drug/alcohol use disorders. Results indicated that both groups had reduction in arrests and drug use. There were no significant difference between groups. Lastly, Smith et al. [ 89 ] compared a standard treatment program (STP, daily group counseling, family outreach, 12-step program introduction, four 2 h sessions for family) to an enhanced treatment program (ETP; twice weekly group on relapse prevention and interpersonal violence in additional to all STP components) among 383 inpatient veterans meeting for an alcohol, cocaine, or amphetamine use disorder. Results indicated that ETP had enhanced abstinence rates at 3-month and 12-month follow up compared to STP, regardless of type of drug use.
Group Treatments for SUD and Co-Occurring Psychiatric Problems
Individuals with psychiatric distress are at high risk for comorbid SUD [ 90 ]. Ten randomized controlled studies meeting our inclusion criteria examined the efficacy of group therapy for SUD and co-occurring psychiatric problems (see Table 7 ). Three studies described group treatment of SUD and co-occurring DSM-IV Axis II disorders [ 18 , 91 , 96 ], three studies examined group treatment of drug abuse and co-occurring DSM-IV classified Axis I disorders [ 92 , 93 , 99 ], one study explored group drug abuse treatment and co-occurring psychiatric problems among homeless individuals without limiting to DSM-IV Axis I or Axis II diagnoses [ 97 ], and one study focused on group drug treatment among individuals testing positive for HIV [ 98 ]. Within this diverse set of RCTs, participants generally included individuals diagnosed with any form of SUD; however, some studies focused specifically on individuals using cocaine [ 91 , 97 ] or cocaine/opioids [ 98 ].
A range of group treatment approaches are represented, including group psychoeducational therapy, group CBT approaches, group DBT, Seeking Safety and CM. DiNitto and colleagues [ 92 ] evaluated the efficacy of adding a group-based psychoeducational program entitled “Good Chemistry Groups” to standard inpatient SUD treatment services among 97 individuals with a dual diagnosis of SUD and a DSM-IV Axis I psychological disorder. The nine 60-min Good Chemistry Group sessions were offered 3 times per week for 3 weeks. When compared to standard inpatient treatment, the addition of the psychoeducational group was not associated with any changes in medical, legal, alcohol, drug, psychiatric or family/social problems among participants.
The efficacy of adding a psychoeducational group treatment to standard individual therapy to address HIV risk among cocaine users has also been examined [ 91 ]. Participants were randomly assigned to complete the following: 1) individually-administered Standard Intervention developed by the NIDA Cooperative Agreement Final Cohort sites [ 100 ] including HIV testing, and pre- and post-HIV testing counseling on risks relating to cocaine use, transmission of STDs/HIV, condom use, cleaning injection equipment, and the benefits of treatment; or) Standard Intervention plus four 2-h peer-delivered psychoeducational groups addressing stress management, drug awareness, risk reduction strategies, HIV education and AIDS. Among the sample of 966 individuals completing the 3-month follow-up, the group psychoeducational treatment was not differentially effective in reducing drug use and HIV risk behavior in comparison to standard treatment alone at 3-months post-baseline, regardless of treatment type, individuals with antisocial personality disorder (ASPD) demonstrated less improvement in crack cocaine use compared to individuals without ASPD or depression.
The following types of group CBT have sustained research evaluation meeting our inclusion criteria to address co-occurring SUD and Axis I or Axis II disorders: 1) group behavioral skills training; 2) group cognitive behavioral therapy; 3) group-based Seeking Safety [ 51 ], and 4) group dialectical behavioral therapy. Specifically, Jerrell and Ridgely [ 93 ] examined the efficacy of group behavioral skills (BS) training, group-based 12-step facilitation (TS) treatment, and intensive case management among 132 individuals with a dual diagnosis of SUD and another Axis I psychiatric problem over the course of 24-months. Based on the Social and Independent Living Skills program [ 101 ], the BS group included one group per week addressing self-management skills designed to enhance abstinence, including medication management, relapse prevention, social skills, leisure activities and symptom monitoring. Relative to participants in TS groups, participants in the BS groups evidenced increased psychosocial functioning and decreased psychiatric symptoms (i.e., schizophrenia, depressive symptoms, mania, drug use and alcohol use) across the 6-, 12- and 18-month follow-up assessments after treatment entry.
Lehman and colleagues’ [ 95 ] examination of the efficacy of group CBT for substance abuse compared to TAU among 54 individuals with SUD and either schizophrenia or a major affective disorder revealed no differences between treatment groups over the course of a 1-year follow-up period. More promising findings were reported in Fisher and Bentley’s [ 18 ] evaluation of a group CBT and group therapy based in the disease and recovery model (DRM) among 38 individuals with dual diagnosis of SUD and a personality disorder. Groups met three times per week for 12 weeks and were compared to TAU. Individuals in group CBT and group DRM indicated improved social and family functioning compared to TAU, and among those who completed the group in an outpatient setting, CBT was more effective in reducing alcohol use, enhancing psychological functioning and improving social and family functioning compared to DRM and TAU.
Group behavioral therapy plus abstinence contingent housing and work administered in the context of a day treatment program was compared to behavioral group treatment alone among individuals with cocaine abuse/dependence, non-psychotic psychiatric conditions, and homelessness [ 97 , 102 ]. The group behavioral therapy included 8 weeks of daily treatment (4 h and 50 min per day) of groups addressing relapse prevention training, assertiveness training, AIDS education, 12-step facilitation, relaxation, recreation development, goal setting, and goal planning. Participants also engaged in a process-oriented group as well as individual counseling and urine monitoring and engaged in a weekly 90 min psychoeducational group therapy during months 3–6 following treatment enrollment. Individuals who received contingency-based work and housing were provided with rent-free housing and employment in construction or food service industries after 2 consecutive weeks of abstinence [ 103 ]. Relative to BS groups alone, group behavioral day treatment plus contingency management was associated with greater abstinence at 2- and 6-month follow-ups [ 102 ] and were less likely to relapse [ 97 ], although gains were not maintained at 12-months [ 104 ]. Both groups evidenced positive changes in drug use overtime compared to baseline [ 104 ].
Zlotnick, Johnston and Najavits [ 99 ] evaluated the efficacy of Seeking Safety (SS), in comparison to treatment as usual (TAU) among 49 incarcerated women with substance use disorder (SUD) and full or subthreshold posttraumatic stress disorder (PTSD). SS aims to decrease PTSD and SUD through psychoeducational and present-focused and empowerment-based instruction on coping skills that emphasize abstinence and safety [ 51 ]. The SS group treatment included 90-min group sessions held three times per week, that were completed in addition to the 180 to 240 h of group and individual therapy provided in TAU. All participants showed similar improvement on assessments of PSTD, SUD, legal problems and other psychiatric concerns at 12-week, 3- and 6-month follow-ups following prison release. Nonetheless, there was a trend for improved PTSD and continued improvements in psychiatric symptoms at follow-up among participants completing SS compared to TAU. Greater completion of SS sessions was associated with increased improvement in PTSD as well as drug use among women [ 99 ].
Dialectical behavioral group therapy (DBT), a CBT-focused treatment for individuals with borderline personality disorder (BPD), has also been evaluated in comparison to TAU among individuals with BPD and co-occurring SUD [ 96 ]. Core elements of DBT are manualized [ 105 ], and have been evaluated in prior research [ 106 , 107 , 108 ]. Techniques center on providing the participant with acceptance and validation while maintaining a continual focus on behavior change, and include the following: mindfulness skills training, behavioral analysis of dysfunctional behavior, cognitive restructuring, coping skills training, exposure-based strategies addressing maladaptive emotions, and behavioral management skills training. DBT was administered through 2 ¼ hour weekly group sessions administered in combination with 60 min of weekly individual therapy and the opportunity for skills-coaching phone calls. Relative to TAU, participants randomly assigned to DBT demonstrated greater reductions in drug use during the 12-month treatment and at the 16-month follow-up assessment, as well as greater gains in adjustment at the 16-month follow-up assessment.
Although contingency management is commonly administered individually, Petry and colleagues [ 98 ] examined the efficacy of weekly 60-min group-based contingency management (CM) for reinforcing health behaviors and HIV-positive individuals with cocaine or opioid disorders ( N = 170) in comparison to 12-step facilitation (TS) over the course of a 24-week period. Overall, participants in CM were more likely than those in TS to submit consecutive drug-free urine specimens, although the overall proportion of drug-free specimens did not vary between groups during treatment or over the follow-up period. Notably, during treatment, group CM was associated with greater reductions in HIV-risk behaviors as well as overall viral load compared to TS; although effects were not maintained over the follow-up period.
Across these studies, many trials showed positive gains for both group treatments examined [ 18 , 97 , 98 ], or no difference between groups when examining the benefit of adding group treatment to existing TAU [ 91 , 92 , 95 , 99 ]. However, one study demonstrated greater reductions in drug use among individuals with BPD and SUD who completed group DBT in comparison to TAU [ 96 ]. Further, BS groups were more effective than TS groups in improving psychosocial functioning and decreasing substance use [ 93 ]. Finally, CBT was more effective than DRM in reducing alcohol use, enhancing psychological functioning and improving social and family functioning compared to DRM and TAU among individuals dually diagnosed with SUD and a personality disorder [ 18 ].
Factors associated with treatment efficacy
Gender and treatment efficacy.
Five of the studies included in the present review examined whether treatment was differentially effective for men and women. Although Jarrell and Ridgely’s [ 93 ] evaluation of group BS, group TS and individual case management for individuals with SUD and co-occurring Axis I disorders did not examine whether group treatment types were differentially effective for men and women, data indicated that women—regardless of treatment group—reported higher role functioning (i.e.., independent living, work productivity, as well as immediate and extended social relationships), increased psychiatric symptomatology (depression, mania, drug use, alcohol use) across the follow-up periods compared to men.
Race and ethnicity and treatment efficacy
Among the studies included in the present review, only three examined whether treatment efficacy varied as a function of race and ethnicity. A secondary examination of the efficacy of group BS in comparison to group TS and individual case management [ 93 ] suggested that outcomes in each group treatment among ethnic and racial minority clients were equivalent to White participants during the 6-month follow [ 94 ]. The initial evaluation indicated that—regardless of group treatment type—racial/ethnic minority participants reported lower scores in personal well-being, lower life satisfaction (i.e., satisfaction with living), worse role functioning (i.e., independent living, work productivity, immediate and extended social relationships) over the follow-up periods compared to White participants [ 93 ].
Conclusions
In general, participants in group treatment for drug use disorders exhibit more improvement on typical measures of outcome (e.g., abstinence & use rates, objective measures, urinalysis) when compared to standard care without group [ 18 , 109 ] and those who refuse or drop out of treatment [ 110 ]. Specifically, CBT and CM appear to be more effective at reducing cocaine use than TAU groups. CM is effective in increasing periods of abstinence among users of methamphetamine. Both relapse prevention and social support group therapy were effective for marijuana use although relapse prevention was more helpful for men than for women. Brief MI and relapse prevention were both effective at reducing marijuana use. CBT and CBT-related treatments (including the matrix model) when added to pharmacotherapy were more effective for opioid use disorder than pharmacotherapy alone. Effective treatments for Mixed SUD include group CBT, CM, and women’s recovery group. Longer relapse prevention periods appear to be more helpful in reducing mixed SUD. Behavioral skills and behavioral skills plus contingency management helped decreased psychiatric symptoms and drug use behaviors. Psychoeducation groups alone, a commonly used intervention, were not effective at addressing SUD and co-occurring psychiatric problems. Additionally, it is important to note that there is potential for risk of bias in the studies included across four domains: participants, predictors, outcome, and analysis [ 111 ]. The current study did not comprehensively assess for risk of bias and this is a study limitation. Future research could assess for risk of bias by following the guidelines suggested by the Cochrane Handbook [ 112 ].
The current literature offers a wide variety of group treatments with varying goals and based on varying formal change theories. Overall, studies that reported between-group effect size ( n = 7) reported small to medium effect sizes potentially suggesting differences were moderate but of potential theoretical interest. Of those seven studies, only two studies reported large effect sizes (both comparing an active treatment to a delayed treatment/untreated condition). In order to better characterize magnitude of intervention effects, future studies should report effect sizes and their confidence intervals [ 113 , 114 ]. Moreover, groups based on cognitive-behavioral theory [ 35 ], motivational enhancement theory [ 43 ], stages of change theory [ 115 ], 12-step theory [ 41 ] and psychoeducational group models [ 116 ] have all been the subject of recent studies. Steps of treatment have also been used to classify groups for acutely ill individuals with SUD versus middle stage (recovering) or after care groups, with the latter mainly focusing on relapse prevention. Group therapy is provided – at least as an augment to multimodal interventions – in most of the outpatient and inpatient programs in English speaking and European countries [ 17 , 117 ]. Therefore, continued efforts to implement and scale up group-based treatments for SUD known to be effective are needed. CM appears to be effective at addressing various drug use problems and further research should evaluate whether it would also be useful for marijuana use.
Future Research Questions
Studies of other group treatments for SUD that use rigorous, interview-based diagnosis, use control groups, randomly assign participants to condition, report the ethnic and racial composition of the sample, are adequately powered, implement a treatment manual, and compare outcomes to individual treatment as well are necessary.
Little is known regarding the possible mediators and moderators of treatment outcome in group interventions for SUD
Key Learning Objectives
Group treatment approaches are widely utilized and are often less costly to implement than individual treatments, currently we know very little whether one group approach is superior to another in the treatment of SUD.
Group treatment approaches seem to be more effective at improving positive outcomes (e.g., abstinence, use rates, objective measures, urinalysis) when compared to standard care without group [ 18 , 109 ], and those who refuse and drop out of treatment
More thorough randomized controlled trials of group SUD treatments are needed [ 110 ].
Availability of data and materials
Not applicable. The present study does not include original data. However, the authors of the study have listed all articles reviewed in this study in the reference section.
Abbreviations
Twelve Step Facilitation Group Therapy
Alcohol Dependence
Acquired Immunodeficiency Syndrome
Addiction Severity Index
Antisocial Personality Disorder
Abbreviated Program
Behavioral Skills
Borderline Personality Disorder
Cognitive Behavioral Therapy
Cocaine Dependence
Composite Diagnostic Interview Schedule
Contingency Management
Community Reinforcement Approach
Coping Skills
Cognitive Therapy
Dialectical Behavioral Therapy
Day Treatment
Drug Counseling
Diagnostic Interview Schedule
Diagnostic and Statistical Manual
Disease and Recovery Model
Delayed to Control
Evidence-Based Practice
Evidence-Based Treatment Practice
Enhanced Group Condition
Enhanced Treatment Program
Family Therapy
Group Drug Counseling
Human Immunodeficiency Virus
HIV Harm Reduction
Harm Reduction
Intensive Group Therapy
Individual Therapy
Motivational Interviewing
Matrix Model
Methadone Maintenance Therapy
National Institute of Drug Abuse
Psychoeducational Therapy Group
Pre-Post with Comparison Group (matched or otherwise)
Post Traumatic Stress Disorder
Random Assignment with Control
Relapse Prevention
Recovery Training
Random Assignment to Active Treatment
Relational Psychotherapy Mothers’ Group
Structured Clinical Interview for Diagnosis
Social Support
Standard Group Therapy
Substance Use Disorder
Seeking Safety
Standard Group Counseling
Standard Treatment Program
Treatment as Usual
Phone Monitoring and Counseling, with Support Group
Therapeutic Community Program
Twelve Step
Women’s Recovery Group
Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on alcohol and related conditions-III. JAMA Psychiatry. 2016;73(1):39–47.
Article PubMed PubMed Central Google Scholar
Edition F. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed; 2013.
Google Scholar
Rehm J, Marmet S, Anderson P, Gual A, Kraus L, Nutt DJ, et al. Defining substance use disorders: do we really need more than heavy use? Alcohol Alcohol. 2013;48(6):633–40.
Article CAS PubMed Google Scholar
Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–67.
Article PubMed Google Scholar
Center NDI. National Drug Threat Assessment. Washington: United States Department of Justice; 2011.
Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–6.
Kamal R, Cox C, Rousseau D, Foundation ftKF. Costs and outcomes of mental health and substance use disorders in the US. JAMA. 2017;318(5):415.
Hall WD, Patton G, Stockings E, Weier M, Lynskey M, Morley KI, et al. Why young people's substance use matters for global health. Lancet Psychiatry. 2016;3(3):265–79.
Khalsa JH, Treisman G, McCance-Katz E, Tedaldi E. Medical consequences of drug abuse and co-occurring infections: research at the National Institute on Drug Abuse. Subst Abus. 2008;29(3):5–16.
McCoy CB, Lai S, Metsch LR, Messiah SE, Zhao W. Injection drug use and crack cocaine smoking: independent and dual risk behaviors for HIV infection. Ann Epidemiol. 2004;14(8):535–42.
Contoreggi, md C, Rexroad, rph VE, Lange, md, et al. Current Management of Infectious Complications in the injecting drug user. J Subst Abus Treat. 1998;15(2):95–106.
Article Google Scholar
Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71–2.
Article CAS PubMed PubMed Central Google Scholar
American Psychological Association PTFoE-BP. Evidence-based practice in psychology. Am Psychol. 2006;61:271–85.
Pope C. Resisting evidence: the study of evidence-based medicine as a contemporary social movement. Health. 2003;7(3):267–82.
Wendt D. Group therapy for substance use disorders: a survey of clinician practices. J Groups Addict Recover. 2017;12(4):243 EOA.
Johnson J. Using research-supported group treatments. J Clin Psychol In Session. 2008;64(11):1206–24.
Stinchfield RD, Owen P, Winters K. Group therapy for substance abuse: A review of the empirical research. In: Burlingame AFG, editor. Handbook of group psychotherapy. New York: Wiley; 1994. p. 458–88.
Fisher MS Sr, Bentley KJ. Two group therapy models for clients with a dual diagnosis of substance abuse and personality disorder. Psychiatr Serv. 1996;47(11):1244–50.
Kaminer Y, Burleson JA, Blitz C, Sussman J, Rounsaville BJ. Psychotherapies for adolescent substance abusers: a pilot study. J Nerv Ment Dis. 1998;186(11):684–90.
McKay JR, Alterman AI, Cacciola JS, O'Brien CP, Koppenhaver JM, Shepard DS. Continuing care for cocaine dependence: comprehensive 2-year outcomes. J Consult Clin Psychol. 1999;67(3):420–7.
McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O'Brien CP, Koppenhaver J. Group counseling versus individualized relapse prevention aftercare following intensive outpatient treatment for cocaine dependence: initial results. J Consult Clin Psychol. 1997;65(5):778–88.
Shaffer HJ, LaSalvia TA, Stein JP. Comparing hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: a randomized clinical trial. Altern Ther Health Med. 1997;3(4):57–66.
CAS PubMed Google Scholar
Morgan-Lopez AA, Fals-Stewart W. Analytic methods for modeling longitudinal data from rolling therapy groups with membership turnover. J Consult Clin Psychol. 2007;75(4):580–93.
Weiss RD. Treating patients with bipolar disorder and substance dependence: lessons learned. J Subst Abus Treat. 2004;27(4):307–12.
Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res Soc Work Pract. 2010;20(2):137–60.
Weiss RD, Jaffee WB, de Menil VP, Cogley CB. Group therapy for substance use disorders: what do we know? Harvard Rev Psychiatry. 2004;12(6):339–50.
Burlingame GM, MacKenzie KR, Strauss B. Bergin & Garfields Handbook Of Psychotherapy And Behavior Change. Small group treatment: Evidence for effectiveness and mechanisms of change. In: Lambert M, editor. Handbook of psychotherapy and behavior change. 5th ed. New York: Wiley; 2003. p. 647–96.
Beck AT. Cognitive therapy: nature and relation to behavior therapy. Behav Ther. 1970;1(2):184–200.
Guydish J, Sorensen JL, Chan M, Werdegar D, Bostrom A, Acampora A. A randomized trial comparing day and residential drug abuse treatment: 18-month outcomes. J Consult Clin Psychol. 1999;67(3):428–34.
Guydish J, Werdegar D, Sorensen JL, Clark W, Acampora A. Drug abuse day treatment: a randomized clinical trial comparing day and residential treatment programs. J Consult Clin Psychol. 1998;66(2):280–9.
Avants SK, Margolin A, Sindelar JL, Rounsaville BJ, Schottenfeld R, Stine S, et al. Day treatment versus enhanced standard methadone services for opioid-dependent patients: a comparison of clinical efficacy and cost. Am J Psychiatry. 1999;156(1):27–33.
Avants SK, Margolin A, Usubiaga MH, Doebrick C. Targeting HIV-related outcomes with intravenous drug users maintained on methadone: a randomized clinical trial of a harm reduction group therapy. J Subst Abus Treat. 2004;26(2):67–78.
Maude-Griffin PM, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, Hall SM. Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. J Consult Clin Psychol. 1998;66(5):832–7.
Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. J Consult Clin Psychol. 2000;68(3):515–20.
Beck ATW, F. D.; Newman, C. F.; Liese, B. S. Cognitive therapy of substance abuse. New York: Guilford; 1993.
McAuliffe WE. A randomized controlled trial of recovery training and self-help for opioid addicts in New England and Hong Kong. J Psychoactive Drugs. 1990;22(2):197–209.
Czuchry M, Dansereau DF. Node-link mapping and psychological problems. Perceptions of a residential drug abuse treatment program for probationers. J Subst Abus Treat. 1999;17(4):321–9.
Article CAS Google Scholar
McCusker J, Bigelow C, Frost R, Garfield F, Hindin R, Vickers-Lahti M, et al. The effects of planned duration of residential drug abuse treatment on recovery and HIV risk behavior. Am J Public Health. 1997;87(10):1637–44.
Rosenblum A, Magura S, Kayman DJ, Fong C. Motivationally enhanced group counseling for substance users in a soup kitchen: a randomized clinical trial. Drug Alcohol Depend. 2005;80(1):91–103.
Marlatt GA, Donovan DM. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. 2nd ed. New York: The Guilford Press; 2005. p. xiv, 416-xiv
Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse collaborative cocaine treatment study. Arch Gen Psychiatry. 1999;56(6):493–502.
Luthar SSS, N.E.; Altomare, M. Relational psychotherapy Mother’s group: A randomized clinical trial for substance abusing mothers. Dev Psychopathol. 2007;19:243–61.
Miller WRR, S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991.
Hoffman JA, Caudill BD, Koman JJ 3rd, Luckey JW, Flynn PM, Mayo DW. Psychosocial treatments for cocaine abuse. 12-month treatment outcomes. J Subst Abus Treat. 1996;13(1):3–11.
Kaminer Y, Burleson JA, Goldberger R. Cognitive-behavioral coping skills and psychoeducation therapies for adolescent substance abuse. J Nerv Ment Dis. 2002;190(11):737–45.
Linehan M. DBT skills training manual. 2nd ed. London: The Guilford Press; 2015.
Petry NM. Contingency management: what it is and why psychiatrists should want to use it. Psychiatrist. 2011;35(5):161–3.
Logan DE, Marlatt GA. Harm reduction therapy: a practice-friendly review of research. J Clin Psychol. 2010;66(2):201–14.
PubMed PubMed Central Google Scholar
Ellis B, Bernichon T, Yu P, Roberts T, Herrell JM. Effect of social support on substance abuse relapse in a residential treatment setting for women. Eval Program Plan. 2004;27(2):213–21.
Nowinski J, Baker S. The twelve-step facilitation handbook: A systematic approach to early recovery from alcoholism and addiction. San Francisco: Jossey-Bass; 1992. p. xxii. 215-xxii
Najavits LM. Seeking safety: a treatment manual for PTSD and substance abuse. New York: Guilford; 2002.
Greenfield SF, Trucco EM, McHugh RK, Lincoln M, Gallop RJ. The Women's recovery group study: a stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug Alcohol Depend. 2007;90(1):39–47.
Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: results of a randomized clinical trial. Am J Drug Alcohol Abuse. 2001;27(4):651–88.
Coviello DM, Alterman AI, Rutherford MJ, Cacciola JS, McKay JR, Zanis DA. The effectiveness of two intensities of psychosocial treatment for cocaine dependence. Drug Alcohol Depend. 2001;61(2):145–54.
Crits-Christoph P, Siqueland L, McCalmont E, Weiss RD, Gastfriend DR, Frank A, et al. Impact of psychosocial treatments on associated problems of cocaine-dependent patients. J Consult Clin Psychol. 2001;69(5):825–30.
Siqueland L, Crits-Christoph P, Gallop R, Barber JP, Griffin ML, Thase ME, et al. Retention in psychosocial treatment of cocaine dependence: predictors and impact on outcome. Am J Addict. 2002;11(1):24–40.
Mercer D, Carpenter G, Daley D. The adherence and competence scale for group addiction counseling for TCACS: Center for Psychotherapy Research, Department of Psychiatry, University of Pennsylvania Medical School; 1994.
Luborsky L. Principles of psychoanalytic psychotherapy a manual for supportive-expressive treatment; 1984.
Epstein DH, Hawkins WE, Covi L, Umbricht A, Preston KL. Cognitive-behavioral therapy plus contingency management for cocaine use: findings during treatment and across 12-month follow-up. Psychol Addict Behav. 2003;17(1):73–82.
Magura S, Rosenblum A, Lovejoy M, Handelsman L, Foote J, Stimmel B. Neurobehavioral treatment for cocaine-using methadone patients: a preliminary report. J Addict Dis. 1994;13(4):143–60.
Petry NM, Alessi SM, Hanson T. Contingency management improves abstinence and quality of life in cocaine abusers. J Consult Clin Psychol. 2007;75(2):307–15.
Rawson RA, Huber A, McCann M, Shoptaw S, Farabee D, Reiber C, et al. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance treatment for cocaine dependence. Arch Gen Psychiatry. 2002;59(9):817–24.
Rohsenow DJ, Monti PM, Rubonis AV, Gulliver SB, Colby SM, Binkoff JA, et al. Cue exposure with coping skills training and communication skills training for alcohol dependence: 6- and 12-month outcomes. Addiction. 2001;96(8):1161–74.
Rosenblum A, Magura S, Foote J, Palij M, Handelsman L, Lovejoy M, et al. Treatment intensity and reduction in drug use for cocaine-dependent methadone patients: a dose-response relationship. J Psychoactive Drugs. 1995;27(2):151–9.
Rosenblum A, Magura S, Palij M, Foote J, Handelsman L, Stimmel B. Enhanced treatment outcomes for cocaine-using methadone patients. Drug Alcohol Depend. 1999;54(3):207–18.
Volpicelli JR, Markman I, Monterosso J, Filing J, O'Brien CP. Psychosocially enhanced treatment for cocaine-dependent mothers: evidence of efficacy. J Subst Abus Treat. 2000;18(1):41–9.
Weinstein SP, Gottheil E, Sterling RC. Randomized comparison of intensive outpatient vs. individual therapy for cocaine abusers. J Addict Dis. 1997;16(2):41–56.
Gottheil E, Weinstein SP, Sterling RC, Lundy A, Serota RD. A randomized controlled study of the effectiveness of intensive outpatient treatment for cocaine dependence. Psychiatr Serv. 1998;49(6):782–7.
Magura S, Rosenblum A, Fong C, Villano C, Richman B. Treating cocaine-using methadone patients: predictors of outcomes in a psychosocial clinical trial. Subst Use Misuse. 2002;37(14):1927–55.
Jaffe A, Shoptaw S, Stein J, Reback CJ, Rotheram-Fuller E. Depression ratings, reported sexual risk behaviors, and methamphetamine use: latent growth curve models of positive change among gay and bisexual men in an outpatient treatment program. Exp Clin Psychopharmacol. 2007;15(3):301–7.
Rawson RA, Marinelli-Casey P, Anglin MD, Dickow A, Frazier Y, Gallagher C, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99(6):708–17.
Roll JM, Chudzynski J, Cameron JM, Howell DN, McPherson S. Duration effects in contingency management treatment of methamphetamine disorders. Addict Behav. 2013;38(9):2455–62.
Shoptaw S, Huber A, Peck J, Yang X, Liu J, Jeff D, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2006;85(1):12–8.
Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68(5):898–908.
Stephens RS, Roffman RA, Simpson EE. Treating adult marijuana dependence: a test of the relapse prevention model. J Consult Clin Psychol. 1994;62(1):92–9.
Marlatt GAG, J.R. Relapse prevention (unpublished manuscript). In: Luther SSS, Boltas D, editors. Relational parenting Mother’s group: A therapist’s manual. New York: Guilford Press; 1985.
Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol. 1993;61(3):455–61.
Des Jarlais DC, Casriel C, Friedman SR, Rosenblum A. AIDS and the transition to illicit drug injection--results of a randomized trial prevention program. Br J Addict. 1992;87(3):493–8.
Rawson RA, McCann MJ, Shoptaw SJ, Miotto KA, Frosch DL, Obert JL, et al. Naltrexone for opioid dependence: evaluation of a manualized psychosocial protocol to enhance treatment response. Drug Alcohol Rev. 2001;20(1):67–78.
Scherbaum N, Kluwig J, Specka M, Krause D, Merget B, Finkbeiner T, et al. Group psychotherapy for opiate addicts in methadone maintenance treatment--a controlled trial. Eur Addict Res. 2005;11(4):163–71.
Sees KL, Delucchi KL, Masson C, Rosen A, Clark HW, Robillard H, et al. Methadone maintenance vs 180-day psychosocially enriched detoxification for treatment of opioid dependence: a randomized controlled trial. JAMA. 2000;283(10):1303–10.
Downey KK, Helmus TC, Schuster CR. Treatment of heroin-dependent poly-drug abusers with contingency management and buprenorphine maintenance. Exp Clin Psychopharmacol. 2000;8(2):176–84.
Margolin A, Avants SK, Warburton LA, Hawkins KA, Shi J. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health Psychol. 2003;22(2):223–8.
Marques AC, Formigoni ML. Comparison of individual and group cognitive-behavioral therapy for alcohol and/or drug-dependent patients. Addiction. 2001;96(6):835–46.
McKay JR, Lynch KG, Shepard DS, Morgenstern J, Forman RF, Pettinati HM. Do patient characteristics and initial progress in treatment moderate the effectiveness of telephone-based continuing care for substance use disorders? Addiction. 2005;100(2):216–26.
Nemes S, Wish ED, Messina N. Comparing the impact of standard and abbreviated treatment in a therapeutic community. Findings from the district of Columbia treatment initiative experiment. J Subst Abus Treat. 1999;17(4):339–47.
Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, et al. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–74.
Schottenfeld RS, Pantalon MV, Chawarski MC, Pakes J. Community reinforcement approach for combined opioid and cocaine dependence. Patterns of engagement in alternate activities. J Subst Abus Treat. 2000;18(3):255–61.
Smith TL, Volpe FR, Hashima JN, Schuckit MA. Impact of a stimulant-focused enhanced program on the outcome of alcohol- and/or stimulant-dependent men. Alcohol Clin Exp Res. 1999;23(11):1772–9.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA. 1990;264(19):2511–8.
Compton WM, Cottler LB, Ben-Abdallah A, Cunningham-Williams R, Spitznagel EL. The effects of psychiatric comorbidity on response to an HIV prevention intervention. Drug Alcohol Depend. 2000;58(3):247–57.
DiNitto DM, Webb DK, Rubin A. Gender differences in dually-diagnosed clients receiving chemical dependency treatment. J Psychoactive Drugs. 2002;34(1):105–17.
Jerrell JM, Ridgely MS. Comparative effectiveness of three approaches to serving people with severe mental illness and substance abuse disorders. J Nerv Ment Dis. 1995;183(9):566–76.
Jerrell JM, Wilson JL. Ethnic differences in the treatment of dual mental and substance disorders. A preliminary analysis. J Subst Abus Treat. 1997;14(2):133–40.
Lehman AF, Herron JD, Schwartz RP, Myers CP. Rehabilitation for adults with severe mental illness and substance use disorders. A clinical trial. J Nerv Ment Dis. 1993;181(2):86–90.
Linehan MM, Schmidt H 3rd, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8(4):279–92.
Milby JB, Schumacher JE, Vuchinich RE, Wallace D, Plant MA, Freedman MJ, et al. Transitions during effective treatment for cocaine-abusing homeless persons: establishing abstinence, lapse, and relapse, and reestablishing abstinence. Psychol Addict Behav. 2004;18(3):250–6.
Petry NM, Weinstock J, Alessi SM, Lewis MW, Dieckhaus K. Group-based randomized trial of contingencies for health and abstinence in HIV patients. J Consult Clin Psychol. 2010;78(1):89–97.
Zlotnick C, Johnson J, Najavits LM. Randomized controlled pilot study of cognitive-behavioral therapy in a sample of incarcerated women with substance use disorder and PTSD. Behav Ther. 2009;40(4):325–36.
Wechsberg WM, MacDonald BR, Dennis ML, Inciardi JA, Surratt HL, Leukefeld CG, et al. The standard intervention for reduction in HIV risk behavior; protocol changes suggested by the continuing HIV/AIDS epidemic. Bloomington: Lighthouse Institute; 1997.
Liberman RP, Massel HK, Mosk MD, Wong SE. Social skills training for chronic mental patients. Hosp Community Psychiatry. 1985;36(4):396–403.
Milby JB, Schumacher JE, McNamara C, Wallace D, Usdan S, McGill T, et al. Initiating abstinence in cocaine abusing dually diagnosed homeless persons. Drug Alcohol Depend. 2000;60(1):55–67.
Milby JB, Schumacher JE, Raczynski JM, Caldwell E, Engle M, Michael M, et al. Sufficient conditions for effective treatment of substance abusing homeless persons. Drug Alcohol Depend. 1996;43(1–2):39–47.
Milby JB, Schumacher JE, Wallace D, Frison S, McNamara C, Usdan S, et al. Day treatment with contingency management for cocaine abuse in homeless persons: 12-month follow-up. J Consult Clin Psychol. 2003;71(3):619–21.
Linehan MMD, L.A. Dialectical behavior therapy manual of treatment interventions for drug abusers with borderline personality disorder. Seattle: University of Washington; 1997.
Linehan MM, Heard HL, Armstrong HE. Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1993;50(12):971–4.
Linehan MM, Tutek DA, Heard HL, Armstrong HE. Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. Am J Psychiatry. 1994;151(12):1771–6.
Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060–4.
Burtscheidt W, Schwarz R, Redner C, Gaebel W. Behavioral therapeutic methods in ambulatory treatment of alcoholism. Early results of an experimental study. Fortschr Neurol Psychiatr. 1999;67(6):274–80.
Sandahl C, Herlitz K, Ahlin G, Rönnberg S. Time-limited group psychotherapy for moderately alcohol dependent patients: A randomized controlled clinical trial. Psychother Res. 1998;8(4):361–78.
Wolff RF, Moons KG, Riley RD, Whiting PF, Westwood M, Collins GS, et al. PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med. 2019;170(1):51–8.
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. In: Cochrane handbook for systematic reviews of interventions; 2019. p. 205–28.
Chapter Google Scholar
Diener MJ. The Corsini Encyclopedia of Psychology; 2010. p. 1.
Book Google Scholar
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11(1):1–8.
Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Prog Behav Modif. 1992;28:183–218.
Drake RE, McLaughlin P, Pepper B, Minkoff K. Dual diagnosis of major mental illness and substance disorder: an overview. New Dir Ment Health Serv. 1991;1991(50):3–12.
Kunzke D, Strauss B, Burtscheidt W. The effectiveness of psychodynamic group therapy in the treatment of alcohol abuse. A review. Gruppenpsychotherapie und Gruppendynamik. 2002;38:53–70.
Download references
Acknowledgements
The authors have no acknowledgements.
The study is not supported through funding.
Author information
Authors and affiliations.
Center for Alcohol and Addiction Studies, Brown University, Providence, RI, 02912, USA
Gabriela López
Alpert Medical School of Brown University, Department of Psychiatry and Human Behavior, Providence, RI, 02904, USA
Lindsay M. Orchowski
Walter Reed Army Institute of Research, Silver Spring, MD, 20910, USA
Madhavi K. Reddy
Massachusetts General Hospital, Harvard Medical School, Boston, MA, 02115, USA
Jessica Nargiso
Division of Public Health, Michigan State University, Flint, MI, 48502, USA
Jennifer E. Johnson
You can also search for this author in PubMed Google Scholar
Contributions
All authors participated in the review of manuscripts included in the study, writing of sections of the manuscript, as well as final editing of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Lindsay M. Orchowski .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
López, G., Orchowski, L.M., Reddy, M.K. et al. A review of research-supported group treatments for drug use disorders. Subst Abuse Treat Prev Policy 16 , 51 (2021). https://doi.org/10.1186/s13011-021-00371-0
Download citation
Accepted : 03 April 2021
Published : 21 June 2021
DOI : https://doi.org/10.1186/s13011-021-00371-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Substance use disorders
- Group therapy
Substance Abuse Treatment, Prevention, and Policy
ISSN: 1747-597X
- General enquiries: [email protected]
A Systematic Literature Review of Substance-Use Prevention Programs Amongst Refugee Youth
- Original Paper
- Open access
- Published: 09 April 2024
Cite this article
You have full access to this open access article
- Elijah Aleer 1 ,
- Khorshed Alam ORCID: orcid.org/0000-0003-2232-0745 2 &
- Afzalur Rashid ORCID: orcid.org/0000-0003-3413-1757 1
This paper aims at exploring existing literature on substance use prevention programs, focusing on refugee youth. A comprehensive search for relevant articles was conducted on Scopus, PubMed, and EBSCOhost Megafile databases including Academic Search Ultimate, APA PsycArticles, APA PsycInfo, CINAHL with Full Text, E-Journals, Humanities Source Ultimate, Psychology and Behavioural Sciences Collection, and Sociology Source Ultimate. Initially, a total of 485 studies were retrieved; nine papers were retained for quality assessment after removing duplicates. Of the nine studies that met the inclusion criteria, only three are found to partially addressed substance use prevention programs. The two substance use prevention programs that emerge from the study are Adelante Social and Marketing Campaign (ASMC), and Screening and Brief Intervention (SBI). Six others explored protective factors and strategies for preventing substance use. The study findings show that refugee youth held negative attitudes toward institutions that provide substance use prevention programs. This review concluded that refugee youth often experience persistent substance use as they are not aware of prevention programs that may reduce the prevalence and/or severity of such misuse.
Avoid common mistakes on your manuscript.
Introduction
Increasingly, literature suggests that refugee youth face a heightened vulnerability to substance use, coupled with a limited awareness of substance use prevention programs. Refugees’ susceptibility to substance use is linked to adverse living conditions and maladaptive coping mechanisms (Posselt et al., 2015 ; Ramachandran et al., 2019 ; Roberts et al., 2011 ). As a result, research suggests that the prevalence of substance use amongst refugees ranges from 17 to 37% in camps and 4% to7% in the community setting (Horyniak et al., 2016a ). Another study revealed that 14.9% of men and 0.7% of women from refugee background exhibited substance use (Ramachandran et al., 2019 ). The concerning aspect of this situation lies in the fact that substance use and its associated risks are well-documented within refugee setting (Gire et al., 2019 ; Luitel et al., 2013 ), with a growing call to integrate substance use prevention programs into refugee services due to the prevalence of the phenomenon (Horyniak et al., 2016a ). Such recommendation emphasises the importance of addressing the knowledge gap on substance use prevention programs amongst the refugee youth. Research indicates that if the substance use prevention programs are not made known to those at risk individuals, it could have detrimental effects on such individuals (Bauman and Phongsavan, 1999 ). Failure to address the knowledge gap of substance use prevention programs could place, refugee youth at an increasing risk of various negative outcomes such as disorder, higher mortality, accidental injury, liver diseases, violence, dysfunctional work, and school dropout due to substance use (Ji et al., 2021 ; Kuntsche et al., 2017 ; Li et al., 2017 ; Momeñe et al., 2021 ). Hence, it is important to document the knowledge of substance use prevention programs amongst refugee youth in the literature to ensure that the groups are informed about the negative consequences.
As per this study, substance use prevention programs refer to a myriad of substance-free and medication treatments administered to assist individuals to reduce substance use (Alayan et al., 2021 ). While substance use refers to as a prolonged harmful use of any substance, which can result in problems such as non-fulfilling social roles, withdrawal and tolerance symptoms, substance use disorders and attributable to burden of disease and mortality (American Psychiatric Association, 2013 ; Rehm et al., 2013 ). In this case, substances can include alcohol, cannabis, methamphetamine and other stimulants drugs, non-medical use of pharmaceutical drugs, illicit opioids including heroin, tobacco and other emerging psychoactive substances (AIHW, 2020 ). In Australia, youth refers to a person aged between 12 and 24 years (AIHW, 2021 ). Accordingly, refugee youth in this study are those between the ages of 12 and 24.
Substance Use Prevention Programs
There are several substance use prevention programs in the literature, the aim of which are to reduce harms of substance use. The last two decades have witnessed a surge in studies conducted on substance use prevention programs for different socio-demographic groups that produced information about the initiation, prevalence and associated behavioural, social, and educational outcomes (Fishbein et al., 2006 ; Gau et al., 2012 ; Gruenewald et al., 2009 ; Springer et al., 2004 ). The surge in research reaffirms that substance use prevention programs play an important role in reducing the consequences of substance use. Notably, there are several factors which permit individuals to engage in use substance. These include peer pressure, poor neighbourhood, inability to cope with difficulties, cultural norms, family history of drug use and lower level of education. Family structure and mental disorder play a vital role in initiation and maintenance of substance use (Gattamorta et al., 2017 ; Peloso et al., 2021 ). The knowledge of various factors, that induce individuals to use substances is vital as they play a significant role when designing substance use prevention programs.
Some of the known substance use prevention programs include individual and group counselling, alternative programs, and family and community interventions (Barrett et al., 1988 ; Foss-Kelly et al., 2021 ; Radoi, 2014 ). These programs are designed to influence social and psychological factors associated with the initiation and maintenance of substance use (Barrett et al., 1988 ). The social factors include peer pressure, a deviation from conventional values. Including those of one’s family, school, and religion, while the psychological characteristics include low self-esteem and an attitude of tolerance towards deviancy (Barrett et al., 1988 ; Hater et al., 1984 ; Radoi, 2014 ). Substance use prevention programs aim to approach social and psychological factors in a unique way depending on their goal and outcome. Each of the factors requires a different approach when designing a substance use prevention program. For example, the primary objective of providing counselling to young individuals who engage in substance use is to assist them in overcoming their low self-esteem and embracing the positive societal norms that are linked to such behaviour (Barrett et al., 1988 ). The effectiveness of an individual program depends on the participants’ attitude toward intervention and their outcomes (Espada et al., 2015 ). For instance, participants sometimes refuse to join the prevention program due to fear of being reported to authorities (Kvillemo et al., 2021 ).
Peer pressure is widely acknowledged as a significant source of the initiation and maintenance of substance use amongst youth. According to social learning theory, youth substance use is a consequence of peer pressures originating from their reference groups (Watkins, 2016 ). To address the substance use where such pressure is deemed to be the initiation and maintenance factor, group counselling is believed to be a key prevention program (Barrett et al., 1988 ). This is because peer relations play a powerful influence, and therefore, researchers often use group counselling rather than individual counselling to promote healthy and acceptable relationships, foster social skills, and thus to develop healthy forms of recreational activities amongst peers.
Apart from counselling, adopting alternative programs such as substance-free strategies reduce the initiation and maintenance factors of substance use. Behavioural economic theory suggests that an increase in rewarding substance-free activities can lead to a reduction in substance use (Murphy et al., 2019 ). The structured substance-free activities approach is based on the relationship between the reinforcement derived from substance-related activities to the reinforcement derived from substance-free activities (Correia et al., 2005 ). Research shows that substance use programs that are supplemented with either relaxation training or a behavioural economic session focused on increasing substance-free activities are associated with reductions in substance use (Murphy et al., 2019 ). Notably, increasing substance-free activities is suggested to be useful in substance use prevention in vulnerable youth (Andrabi et al., 2017 ).
Community, family, academic engagements, work, and religious activities play a significant role in reducing the initiation and maintenance of substance use and its related consequences. Similarly, individual and group counselling, alternative programs, and family and community interventions have also led to a reduction in the initiation and maintenance of substance use amongst youth. Research demonstrated a negative relationship between commitment to conventional values such as family, religion, and education, and substance use amongst the youth (Sussman et al., 2006 ). This evidence is supported by social bond theory, which postulates that commitment to conventional values of one’s family, religion, and school act to prevent deviant responses (Nijdam-Jones et al., 2015 ). Similarly, the Family Interaction Theory suggests that social learning, parent attachment, and intrapersonal characteristics equally discourage youth risk-taking behaviours (Ismayilova et al., 2019 ). The evidence appeared in several substance use prevention programs (Huang et al., 2014 ; Ishaak et al., 2015 ; Liddle et al., 2006 ). For instance, the Adolescent Day Treatment Program (ADTP) in Canada implements a social learning approach stressing positive support for appropriate substance, anti-social coping behaviour, and social skills (Liddle et al., 2006 ).
Some substance use prevention programs are designed to assist individuals with the development of skills and attitudes through a community approach. The approach has seen youth cessation of substance use and helped them make changes leading to substance-free lifestyles (Wade-Mdivanian et al., 2016 ). One of the substance use prevention programs, which adopts a community approach is Multidimensional Family Treatment (DFT). DFT targets the initiation and maintenance of youth substance use by addressing coping strategies, parenting practices, other family members, and interactional patterns that contribute to the continuation of substance use and related consequences (Liddle et al., 2006 ). DFT also addresses the functioning of youth and family using the social systems influencing the youth’s life such as school, work, peer networks, and the juvenile justice system (Liddle et al., 2006 ; Valente et al., 2007 ). In support of the community approach, researchers argue for the inclusion of the perspectives of community members in substance use prevention programs because they understand the unique needs of the people with whom they share a bond (Bermea et al., 2019 ). Researchers also focus the interconnected nature of their socio-environmental relationships that can facilitate advocacy for change at the community level (Bermea et al., 2019 ).
Research Gap
Despite the vast knowledge of substance use prevention programs in the literature, research on the refugee youth remains scarce. The lack of research on substance use prevention programs for refugee youth may be due to many factors. First, scholars might have ignored the severity of the issues amongst the groups. Secondly, the socio-economic benefits of the prevention programs might have been underestimated in the literature. Thirdly, the political aspect of substance use prevention programs for refugee youth might have not been thoroughly evaluated in the policy frameworks. The socio-economic benefit of substance use prevention programs underscores a pressing need to begin synthesizing evidence given the deleterious nature of substance use if it is left unmitigated. The knowledge of substance use prevention programs is significant to vulnerable groups like refugee youth because they seek assistance whenever they succumb to substance use. As a result, they will avoid the negative consequences of substance use and subsequently exploit the social benefit. Furthermore, the knowledge of substance use prevention programs can assist organisations and advocacy groups assisting refugee youth to provide them with better services.
This study aims at contributing to substance use prevention programs literature by conducting a systematic literature review to synthesize evidence on such programs, their attitudes towards the program, and amongst refugee youth to fill the gaps in knowledge and provide directions for future research.
Research Questions
The following questions are designed to achieve the aims and objectives of the systematic literature review:
What different substance use prevention programs are used to assist refugee youth with substance use?
What is the refugee youth’s attitude toward substance use prevention programs?
What are the outcomes of a substance use prevention program?
To ensure the validity and reliability of this study, systematic review guidelines are followed (Toews, 2017 ). This is because the systematic review is useful in mapping out areas of uncertainty, identifying the lack of research on a particular topic, and pointing out an area where research is needed (Rethlefsen et al., 2021 ). The systematic review method provides complete and accurate reporting, which facilitates assessment of how well reviews have been conducted (Toews, 2017 ).
Unlike a traditional review, a systematic review uses a transparent, replicable, and scientific steps purposely to mitigate the risk of bias by conducting a comprehensive literature search and providing an audit trail of procedures, decisions, and conclusions (Caldwell and Bennett, 2020 ). The systematic review reports a reproducible search strategy that increases the reliability and validity of the study.
By following systematic review guidelines, this study will mitigate bias and increase its validity and reliability. The following steps are adopted to conduct the systematic review:
Step 1: Identifying Keywords
To synthesize the evidence of substance use prevention programs available in the literature amongst refugee youth, a database search began with a simple string of “substance use AND Prevention AND Refugee AND youth” in the library. Then other search terms were obtained using a permutation of the keywords in EBSCOhost Megafile Ultimate (Table 1 ).

Step 2: Search Strategy
In the next step, a comprehensive search for relevant articles was conducted on 12th of October 2021 on three major databases: Scopus, PubMed, and EBSCOhost Megafile databases including Academic Search Ultimate, APA PsycArticles, APA PsycInfo, CINAHL with Full Text, E-Journals, Humanities Source Ultimate, Psychology and Behavioural Sciences Collection, and Sociology Source Ultimate. A total of 485 studies were retrieved following the comprehensive search of the databases (Table 2 ).
Study Selection
All the retrieved studies were exported to Endnote X9, and 199 duplicates were removed. The titles and abstracts of the remaining 286 studies were reviewed and 253 studies were excluded for not focusing on substance use prevention programs. A total of 33 studies were further screened using inclusion and exclusion criteria. As a result of the exercise, 24 studies were excluded and nine were included for quality assessment. The PRISMA workflow diagram below shows the process of identifying and selecting eligible studies for this systematic review (Fig. 1 ). The data visualisation displays identified, included, and excluded papers and their explanations.
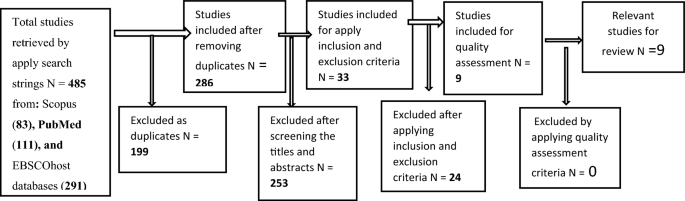
PRISMA of workflow
Exclusion and Inclusion Criteria
This systematic literature review on substance use prevention programs amongst refugee youth was conducted after adopting exclusion and inclusion criteria. To assist in the process of selecting relevant studies in this systematic literature review, studies were limited to peer-reviewed articles published in the English language. Unpublished articles were excluded, and no restriction was placed on the date of publication of the studies.
Furthermore, the selection of articles was restricted to the following eligibility criteria:
Inclusion Criteria
Studies that explored substance use and prevention/reduction/treatment/intervention programs amongst refugee youth.
Studies that explored substance use amongst refugee youth included another perspective of substance use prevention programs.
Studies that investigated and reported motivation for substance use refugee youth.
Exclusion Criteria
Studies that addressed substance use but did not include any intervention.
Studies that addressed substance use prevention and never mentioned refugee youth.
Studies that addressed substance use prevention programs amongst refugees in general.
Studies that addressed immigrant youth but did not mention refugees.
Quality Assessment
The quality of studies included in the systematic literature review was evaluated using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement checklist (von Elm et al., 2007 ). This quality assessment tool is chosen for this study because to its usefulness and applicability to all studies (Vandenbroucke et al., 2014 ; von Elm et al., 2007 ). The explanation and elaboration of the different components of the STROBE provide readers with a clear understanding of the study (Vandenbroucke et al., 2014 ).
A total of twenty STROBE items from the checklist were used to assess the quality of the studies. These include 1 A. title, 1B. abstract, 2. background/rationale, 3. objective, 4. design, 5. setting, 6. eligibility of the participants, 7. variables, 8. data source/measurement, 10. study size, 13a. participant number, 14a. descriptive data, 15. outcome data, 16a. main result, 16b. Category of Continuous variable, 19. limitation, 20. interpretation, 21. generalisation, and 22. funding (items 1 A, 1B, 2, 3, 4, 5, 6, 7, 8, 10, 13a, 14a, 15, 16a, 18, 19, 20, 21, 22). Each item was coded as: Y = present, N = not present, P = partially present, N/A = not applicable, and finally, the percentage of the positive judgement’s total calculation (Table 3 ). If an article’s total percentage of positive judgement is less than 50%, then it is deemed poor quality and excluded from the study.
Table 3 : Quality Assessment .
Data Extraction
Systematic reviews conduct data extraction to minimise human error and bias (Tranfield et al., 2003 ). The purpose of the data extraction is to directly link to the formulated review question and the planned assessment of the incorporated studies, providing as a visual representation and historical record of decisions made during the process, and as the data-repository for the analysis (Tranfield et al., 2003 ). Below is the data extraction table developed for this systematic literature review (Table 4 ). Data extractions contain valuable information such as title, author, findings, concepts, journal, study design, setting, population, and emerging themes.
Study Characteristics
Study objectives and designs.
The study designs include four qualitative, one ethnographic, two mixed methods, one random controlled trial, and one two-cluster sample. The studies were published in nine different journals (Table 5 ).
Study Setting and Participants
Nine peer-reviewed articles met the inclusion criteria for this systematic literature review. They were published from 2009 to 2020. Four studies were conducted in the USA, two in Australia, two in the Middle East, and one in Kenya. Participants in these studies are refugees youth from these host countries.
The findings revealed a gap in the literature about substance use prevention programs amongst refugee youth. In the nine articles that met the inclusion criteria for this study, only two substance use prevention programs emerged. The substance use prevention programs identified in the study included Adelante Social and Marketing Campaign (ASMC) and Screening and Brief Intervention (SBI).
ASMC is a community-based intervention program offered by the Advance Centre for the Advancement of Immigrant/Refugee Health in Washington, DC, USA. This is a well-known primary prevention program, which addresses risk factors for substance use and other co-occurrences amongst Latino adolescents aged 12 to 19 years in a suburb of Washington, DC (Andrade et al., 2018 ; Edberg et al., 2015 ). The study employed the 4-year Adelante primary prevention program to address risk factors for substance use and other issues amongst Latino adolescents, aged 12 to 19 years (Andrade et al., 2018 ). In the two studies, ASMC was used to investigate two distinct scenarios. Firstly, it was used to identify post contents and features that resulted in greater user engagement (Andrade et al., 2018 ). Secondly, Edberg et al. ( 2015 ) used ASMC to provide a brief description of the background for community-level health disparities intervention that aims to help close the gap. The intervention is organised in a group of one to five short psychotherapeutic sessions for substance users (Karno et al., 2021 ; Widmann et al., 2017 ). Participants engage in a standardized screening for substance use problems, receive systematic feedback on substance-related risks, and participate in a motivational intervention to reduce substance use (Saitz, 2014 ).
On the other hand, SBI is used by non-psychiatric healthcare providers for substance use prevention. The approach relies on motivational interviewing focusing on empowering patients during the intervention (Karno et al., 2021 ; Widmann et al., 2017 ). SBI was successfully used to assist refugee youth in addressing substance use issues.
Six studies explore the strategies and protective factors for substance use prevention. Giuliani et al. ( 2010 ) and McCann et al. ( 2016 ) identified protective factors that influence the cessation of substance use amongst refugee youth, including strong community support systems, family, and friends. Protective factors such as trustworthiness, confidentiality of help sources, perceived expertise of formal help sources, and increasing young people’s and parents’ substance use literacy play a vital role in reducing the initiation and maintenance of substance use. Research has shown that providing refugee youth woth counselling, ongoing case management coordination, residential detoxification programmes, and individual strategies such as self-imposed physical isolation can mitigate substance use amongst them (Horyniak et al., 2016a ; McCleary et al., 2016 ). Moreover, researchers identified protective factors including academic success, and participation in voluntary activities can assist in reducing substance use (Massad et al., 2016 ).
The findings highlight protective factors that shield refugee youth from substance-use. These protective factors included religion, positive peer pressure, health, relief, and social services (Giuliani et al., 2010 ; Khader et al., 2009 ; McCann et al., 2016 ). More importantly, connecting with substance use treatment is suggested to be one way refugee youth can reduce substance use (McCann et al., 2016 ; McCleary et al., 2016 ).
Participants’ Attitudes toward Substance use Prevention Programs
The studies that attempt to investigate the attitude of refugee youth towards substance use prevention programs have revealed mixed results. First and foremost, refugee youth demonstrated a lack of confidence in the institution that provides substance use prevention programs (Massad et al., 2016 ; McCann et al., 2016 ). For instance, refugee youth in substance use treatment expressed a sense of scepticism towards the institution that provides counselling and rehabilitation (McCann et al., 2016 ; McCleary et al., 2016 ). Other researchers found out that refugee youth’s participation in substance use treatments is not motivated and therefore they are too reluctant to seek treatment (McCann et al., 2016 ; McCleary et al., 2016 ). While other research shows that refugee youth are unaware of any local institutions to support youth with substance use problems (Massad et al., 2016 ). The refugee youth who participated in the Adelante intervention and utilise social media demonstrated a positive propensity towards engaging in more passive forms of social media usage (Andrade et al., 2018 ).
Outcomes of Substance Use Prevention Programs
ASMC showed that prevention topics were significantly associated with post-engagement behaviour, such as substance use (Andrade et al., 2018 ). ASMC also identified the inequalities that promote substance use amongst the refugee youth such as a lack of community attachment, social support and social space, isolation rather than connection, and a racialized identity (Andrade et al., 2018 ; Edberg et al., 2015 ). The study indicated lack of social space leading to refugee youth finding sanctuary in gang activities (Edberg et al., 2015 ). ASMC also indicated that the most engaging topic discussed in social media posts was substance use prevention, which accounted for 8.4% of the posts with the p-value < 0.001 (Andrade et al., 2018 ).
The outcome for SBI was significant. The findings indicate that there was a decline in the amount of time that refugee youth spent using substances as their functional time increased among refugee youth (Widmann et al., 2017 ). As a result, SBIs appear to reduce substance use to some extent.
Overview of the Findings
The study aimed to explore different substance use prevention programs, summarise refugee youth’s attitudes towards these programs and outline the outcomes of the prevention programs. This systematic literature review appeared to be the first of its kind to systematically synthesis substance use prevention programs amongst refugee youth. The findings from this study supported the hypothesis that research on substance use prevention programs amongst refugee youth is scarce. Only two substance use prevention programs were identified in the study: SBI and ASMC. Although ASMC was included in only one study on substance use prevention programs, its main objectives were to identify the activities in which refugee youth participate and to outline potential areas for intervention. ASMC did not employ strategies to reduce substance use. Moreover, most studies included in this context outlined strategies and protective factors that assist in reducing substance use and related consequences amongst refugee youth. If refugee youth adhere to protective factors such as family attachment, religion, and commitment to social norms, then there is a likelihood that they can avoid the initiation and maintenance factors of substance use. Another important strategy that emerges from this study is the need to increase refugee youth and parents’ substance use literacy. Increasing literacy can help refugee youth to understand the risk substance use can have on their health, social interactions, and economic wellbeing.
Previous studies asserted that the efficacy of substance use prevention program depends on the participants’ attitude towards intervention and its outcomes (Espada et al., 2015 ). However, what is alarming is refugee youth have a negative attitude about institutions providing substance reduction services. Although the ASMC and SBI demonstrated positive outcome, such an approach can be associated with high dropout rates and subsequently, poor outcomes in substance use prevention programs. Individuals who have confidence in professional services are more likely to seek assistance and therefore, reduce substance use.
Implication
The dearth of research on substance use prevention programs programmes may have significant ramifications, considering the substantial body of literature indicating the widespread occurrence of substance use amongst refugee youth. There exists convincing evidence that the refugee youth cohort could be at risk of substance use disorders but are not seeking help. Substance use has a debilitating impact on an individual’s health, social and economic well-being. For refugee youth not seeking assistance to reduce substance use may indicate they are suffering significant consequences on top of their challenges before and after migration.
Previous studies conducted on youth in general has identified many substance use prevention programs in the literature that can mitigate the prevalence of substance use and related consequences (Barrett et al., 1988 ). However, little is known in the literature about the extent and effectiveness of substance use prevention programs including individual and group counselling, alternative programs, and family and community interventions, applicable for refugee youth (Barrett et al., 1988 ; Foss-Kelly et al., 2021 ; Radoi, 2014 ). Researchers only indicated that refugees are aware of some substance use treatment services. There are substantial differences between being aware of a service and actively interacting and engaging with it. Therefore, it is significant for refugee youth to be aware of substance use prevention programs and seek assistance to reduce substance dependence.
Refugee youth’s lack understanding of substance use prevention programs might be compounded by their inability to seek professional help. Scholarly literature suggest that refugee youth do not seek professional help because of barriers including lack of understanding of the new health system, poor mental literacy, language problem, limited transportation and cultural differences (Posselt et al., 2014 ; Shaw et al., 2019 ). Additionally, young refugees, particularly those who are forced to flee their countries due to persecution or violence, frequently encounter substantial trauma and stress without adequate access to mental health services. The pressures encompass a dearth of livelihood opportunities, familial separation, risky journeys, and vulnerability to assault and abuse. Despite managing to escape life-threatening situations in their native countries, these youth individuals often face further prejudice and become targets of in their host countries. They frequently encounter challenges accessing appropriate services, especially when it comes to disparities in mental healthcare services caused by socio-cultural factors. While additional resources and support are necessary, it is crucial to provide culturally sensitive and customised interventions to refugee youth.
Conclusion and Future Research
In conclusion, prevention programs for substance use remain obscure despite the prevalence of substance use amongst refugee youth. The prominent finding of this review is that the majority of the investigations failed to address substance use prevention programs, as their focus was primarily on protective factors and strategies to reduce substance-use. While the study does make an attempt to address substance use prevention programs, it also incorporates other risk behaviours as well. In such investigations, it is difficult to deduce the outcome and attitudes of the participants. Future research is warranted regarding the implementation of substance use prevention programs amongst refugee youth. The findings are an indication of the need to conduct a robust substance use prevention program such as individual and group counselling, alternative programs, and family and community interventions tailored specifically to refugee youth. Furthermore, research should demonstrate the efficacy of each substance use prevention program by exploring participants’ attitudes towards intervention and measuring the outcome of the study. This can fill the gap in the literature with empirical evidence on how refugee youth participate in substance use prevention programs and maximise the benefits by reducing substance use.
It is essential to acknowledge the limitations of this study. The primary constraint lies in the study’s narrow focus on refugee youth, restricting the search to this specific keyword. Consequently, fewer articles satisfied the inclusion criteria. The study may have overlooked relevant articles that employ alternative terms such as ‘immigrant’, ‘migrant’, or ‘cultural linguistic diverse individuals’. Using broader and more inclusive terms can improve the quality of future research by redesigning the search strategy. .
AIHW (2020). Australian Institute Of Health And Welfare Retrieved from https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/summary .
AIHW (2021). Australian’s Youth Retrieved from June 2022. https://www.aihw.gov.au/reports/cws/81/australias-youth .
Alayan, N., Naal, H., Makhoul, M., Avedissian, T., Assaf, G., Talih, F., et al. (2021). Primary care screening, brief intervention, and referral to treatment for adolescent substance use in lebanon: A National Cross-Sectional Study. Substance Abuse: Research & Treatment, 1. https://doi.org/10.1177/1178221821994608
Article Google Scholar
American Psychiatric Association (2013). American psychiatric association, arlington, Va: diagnostic and statistical manual of mental disorders (Dsm–5) Retrieved from https://www.psychiatry.org/psychiatrists/practice/dsm .
Andrade, L., Evans, D., Barrett, N., Edberg, C., & Cleary, D. (2018). Strategies to increase latino immigrant youth engagement in health promotion using social media: Mixed-methods study. Jmir Public Health Surveill, 4 (4), E71. https://doi.org/10.2196/Publichealth.9332
Article PubMed PubMed Central Google Scholar
Andrabi, N., Khoddam, R., & Leventhal, A. M. (2017). Socioeconomic disparities in adolescent substance use: Role of enjoyable alternative substance-free activities. Social Science & Medicine (1982) , 176 , 175–182. https://doi.org/10.1016/J.Socscimed.2016.12.032 .
Barrett, E., Simpson, D., & Lehman, K. (1988). Behavioral changes of adolescents in drug abuse intervention programs. Journal of Clinical Psychology , 44 (3), 461–473.
Article CAS PubMed Google Scholar
Bauman, A., & Phongsavan, P. (1999). Epidemiology of substance use in adolescence: Prevalence, trends and policy implications. Drug and Alcohol Dependence, 55 (3), 187–207. https://doi.org/10.1016/S0376-8716(99)00016-2
Bermea, M., Lardier, T., Forenza, B., Garcia-Reid, P., & Reid, J. (2019). Communitarianism and youth empowerment: Motivation for participation in A Community‐based substance abuse Prevention Coalition. Journal of Community Psychology , 47 (1), 49–62. https://doi.org/10.1002/Jcop.22098 .
Article PubMed Google Scholar
Caldwell, Y., & Bennett, T. (2020). Easy Guide to conducting a systematic review. Journal of Paediatrics and Child Health , 56 (6), 853–856. https://doi.org/10.1111/Jpc.14853 .
Correia, J., Benson, T. A., & Carey, B. (2005). Decreased substance use following increases in alternative behaviors: A preliminary investigation. Addictive Behaviors, 30 (1), 19–27. https://doi.org/10.1016/J.Addbeh.2004.04.006
Edberg, M., Cleary, S., Simmons, B., Cubilla-Batista, I., Andrade, L., & Gudger, G. (2015). Defining the ‘Community’: Applying ethnographic methods for a latino immigrant health intervention. Human Organization, 74 (1), 27–41. https://doi.org/10.17730/Humo.74.1.6561p4u727582850
Espada, P., Gonzálvez, T., Lloret, D., Guillén-Riquelme, A., & Orgilés, M. (2015). Meta-analysis of the effectiveness of school substance abuse prevention programs in Spain. Meta-Análisis De La Eficacia De Los Programas De Prevención Escolares Del Abuso De Sustancias En España, 27 (1), 5–12. https://doi.org/10.7334/Psicothema2014.106
Fishbein, H., Hyde, C., Eldreth, D., Paschall, J., Hubal, R., & Das, A. (2006). Neurocognitive skills moderate urban male adolescents’ responses to preventive intervention materials. Drug & Alcohol Dependence , 82 (1), 47–60. https://doi.org/10.1016/J.Drugalcdep.2005.08.008 .
Foss-Kelly, L., Generali, M., & Crowley, M. J. (2021). Making choices and reducing risk (Mcarr): School counseling primary prevention of substance use. Professional Counselor, 11 (3), 352–369. https://doi.org/10.15241/Llfk.11.3.352
Gattamorta, A., Varela, A., Mccabe, E., Mena, P., & Santisteban, D. A. (2017). Psychiatric symptoms, parental attachment, and reasons for Use as correlates of heavy substance use among treatment-seeking hispanic adolescents. Substance Use & Misuse, 52 (3), 392–400. https://doi.org/10.1080/10826084.2016.1229338
Gau, J., Stice, E., Rohde, P., & Seeley, J. (2012). Negative life events and substance use moderate cognitive behavioral adolescent depression prevention intervention. Cognitive Behaviour Therapy, 41 (3), 241–250. https://doi.org/10.1080/16506073.2011.649781
Gire, T., & Ibaishwa, R. L. (2019). Patterns of substance Use among internally displaced persons in Borno State, Nigeria. African Journal of Drug and Alcohol Studies, 18 (1), 17–30.
Google Scholar
Giuliani, W., Mire, O., Ehrlich, C., Stigler, H., & Dubois, K. (2010). Characteristics and prevalence of Tobacco use among Somali Youth in Minnesota. American Journal of Preventive Medicine, 39 (6, Suppl 1), S48–S55. https://doi.org/10.1016/J.Amepre.2010.09.009
Gruenewald, J., Johnson, K., Shamblen, R., Ogilvie, A., & Collins, D. (2009). Reducing adolescent use of harmful legal products: Intermediate effects of a community prevention intervention. Substance Use & Misuse, 44 (14), 2080–2098. https://doi.org/10.3109/10826080902855223
Hater, J., Singh, K., & Simpson, D. (1984). Influence of family and religion on long-term outcomes among opioid addicts. Advances in Alcohol & Substance Abuse, 4 (1), 29–40. https://doi.org/10.1300/J251v04n01_04
Article CAS Google Scholar
Horyniak, D., Melo, S., Farrell, M., Ojeda, D., & Strathdee, A. (2016a). Epidemiology of substance use among forced migrants: A global systematic review. Plos One, 11 (7), E0159134–E0159134. https://doi.org/10.1371/Journal.Pone.0159134
Horyniak, D., Higgs, P., Cogger, S., Dietze, P., & Bofu, T. (2016b). Heavy alcohol consumption among marginalised African Refugee Young people in Melbourne, Australia: Motivations for drinking, experiences of alcohol-related problems and strategies for managing drinking. Ethnicity & Health, 21 (3), 284–299. https://doi.org/10.1080/13557858.2015.1061105
Huang, S., Cordova, D., Estrada, Y., Brincks, M., Asfour, S., & Prado, G. (2014). An application of the complier average causal effect analysis to examine the effects of a family intervention in reducing illicit drug use among high-risk hispanic adolescents. Family Process, 53 (2), 336–347. https://doi.org/10.1111/Famp.12068
Ishaak, F., De Vries, K., & Van Der Wolf, K. (2015). Design of study without drugs–A surinamese school-based drug-prevention program for adolescents. Bmc Public Health, 15 (1), 1046–1057. https://doi.org/10.1186/S12889-015-2374-1
Ismayilova, L., Terlikbayeva, A., & Rozental, Y. (2019). Computerized intervention to prevent drug use among at-risk adolescents in Central Asia: Preliminary family-level findings from a pilot mixed methods trial. International Journal of Drug Policy, 68 , 75–85. https://doi.org/10.1016/J.Drugpo.2019.03.022
Ji, X., Cummings, R., Mertens, C., Wen, H., & Effinger, E. (2021). Substance use, substance use disorders, and treatment in adolescent and young adult cancer survivors—results from a national survey. Cancer (0008543x), 127 (17), 3223–3231. https://doi.org/10.1002/Cncr.33634
Karno, P., Rawson, R., Rogers, B., Spear, S., Grella, C., & Mooney, J. (2021). Effect of screening, brief intervention and referral to treatment for unhealthy alcohol and other drug use in mental health treatment settings: A randomized controlled trial. Addiction (Abingdon England), 116 (1), 159–169. https://doi.org/10.1111/Add.15114
Khader, A., Shaheen, Y., Turki, Y., El Awa, F., Fouad, H., & Warren, W. (2009). Tobacco use among palestine refugee students (Unrwa) aged 13–15. Preventive Medicine, 49 (1), 224–228. https://doi.org/10.1016/J.Ypmed.2009.06.001
Kuntsche, E., Kuntsche, S., Thrul, J., & Gmel, G. (2017). Binge drinking: Health impact, prevalence, correlates and interventions. Psychology & Health, 32 (8), 976–1017. https://doi.org/10.1080/08870446.2017.1325889
Kvillemo, P., Hiltunen, L., Demetry, Y., Carlander, K., Hansson, T., & Gripenberg, J. (2021). How to prevent alcohol and illicit drug use among students in affluent areas: A qualitative study on motivation and attitudes towards prevention. Substance Abuse Treatment Prevention & Policy, 16 (1), 1–13. https://doi.org/10.1186/S13011-021-00420-8
Li, J., Cho, B., Salvatore, E., Edenberg, J., Agrawal, A., & Chorlian, B. (2017). The impact of peer substance use and polygenic risk on trajectories of Heavy Episodic drinking across adolescence and emerging adulthood. Alcoholism Clinical and Experimental Research, 41 (1), 65–75. https://doi.org/10.1111/Acer.13282
Liddle, A., Rowe, L., Gonzalez, A., Henderson, E., Dakof, A., & Greenbaum, E. (2006). ChangiNg provider practices, program environment, and improving outcomes by transporting multidimensional family therapy to an adolescent drug treatment setting. American Journal on Addictions, 15 , 102-S112. https://doi.org/10.1080/10550490601003698
Luitel, P., Jordans, M., Murphy, A., Roberts, B., & Mccambridge, J. (2013). Prevalence and patterns of hazardous and harmful alcohol consumption assessed using the audit among Bhutanese refugees in Nepal. Alcohol and Alcoholism , 48 (3), 349–355. https://doi.org/10.1093/Alcalc/Agt009 .
Massad, S. G., Shaheen, M., Karam, R., Brown, R., Glick, P., & Linnemay, S. (2016). Substance use among palestinian youth in the West Bank, Palestine: A qualitative investigation. Bmc Public Health, 16 (1), 1–9. https://doi.org/10.1186/S12889-016-3472-4
Mccann, V., Mugavin, J., Renzaho, A., & Lubman, I. (2016). Sub-Saharan African Migrant Youths’ help-seeking barriers and facilitators for mental health and substance use problems: A qualitative study. Bmc Psychiatry . https://doi.org/10.1186/S12888-016-0984-5
Mccleary, S., Shannon, J., & Cook, L. (2016). Connecting refugees to substance use treatment: A qualitative study. Social Work in Public Health, 31 (1), 1–8. https://doi.org/10.1080/19371918.2015.1087906
Momeñe, J., Estévez, A., Pérez-García, A. M., Jiménez, J., Dolores Chávez-Vera, M., Olave, L., & Iruarrizaga, I. (2021). Substance abuse and its relationship to emotional dependence, attachment and emotional regulation in adolescents. El Consumo De Sustancias Y Su Relación Con La Dependencia Emocional El Apego Y La Regulación Emocional En Adolescentes, 37 (1), 121–132. https://doi.org/10.6018/Analesps.404671
Murphy, G., Dennhardt, A., Martens, P., Borsari, B., Witkiewitz, K., & Meshesha, Z. (2019). A randomized clinical trial evaluating the efficacy of a brief alcohol intervention supplemented with a substance-free activity session or relaxation training. Journal of Consulting and Clinical Psychology, 87 (7), 657–669. https://doi.org/10.1037/Ccp0000412
Nijdam-Jones, A., Livingston, D., Verdun-Jones, S., & Brink, J. (2015). Using social bonding theory to examine ‘recovery’ in a forensic mental health hospital: A qualitative study. Criminal Behaviour and Mental Health, 25 (3), 157–168. https://doi.org/10.1002/Cbm.1918
Peloso, M., De Freitas, C., Henriques, D., De Souza Magalhães, B., Marques, S., & Lima, M. (2021). Factors associated with drug use among adolescents. Revista Ciência E Natura, 43 , 1–15. https://doi.org/10.5902/2179460x43556
Posselt, M., Galletly, C., De Crespigny, C., & Procter, N. (2014). Mental health and drug and alcohol comorbidity in young people of refugee background: A review of the literature. Mental Health & Substance Use: Dual Diagnosis, 7 (1), 19–30. https://doi.org/10.1080/17523281.2013.772914
Posselt, M., Procter, N., Galletly, C., & De Crespigny, C. (2015). Aetiology of coexisting mental health and alcohol and other drug disorders: Perspectives of refugee youth and service providers. Australian Psychologist, 50 (2), 130–140. https://doi.org/10.1111/Ap.12096
Radoi, M. (2014). Preventing drug abuse - from explanatory theories to intervention models. Scientific Annals of the ‘Al I Cuza’ University Iasi Sociology & Social Work / Analele Stiintifice Ale Universitatii ‘Al I Cuza’ Iasi Sociologie Si Asistenta Sociala , 7 (1), 116–128.
Ramachandran, A., Makhashvili, N., Javakhishvili, J., Karachevskyy, A., Kharchenko, N., Shpiker, M., Ezard, M., Fuhr, N., & Roberts, B. (2019). Alcohol use among conflict-affected persons in Ukraine: Risk factors, coping and access to mental health services. European Journal of Public Health, 29 (6), 1141–1146. https://doi.org/10.1093/Eurpub/Ckz117
Rehm, J., Marmet, S., Anderson, P., Gual, A., Kraus, L., & Nutt, J. (2013). Defining substance use disorders: Do we really need more than heavy use? Alcohol and Alcoholism, 48 (6), 633–640. https://doi.org/10.1093/Alcalc/Agt127
Rethlefsen, L., Kirtley, S., Waffenschmidt, S., Ayala, P., Moher, D., & Page, J. (2021). Prisma-S: An extension to the prisma statement for reporting literature searches in systematic reviews. Systematic Reviews, 10 (1), 39–39. https://doi.org/10.1186/S13643-020-01542-Z
Roberts, B., Felix Ocaka, K., Browne, J., Oyok, T., & Sondorp, E. (2011). Alcohol disorder amongst forcibly displaced persons in Northern Uganda. Addictive Behaviors , 36 (8), 870–873. https://doi.org/10.1016/J.Addbeh.2011.03.006 .
Saitz, R. (2014). Screening and brief intervention for unhealthy drug use: Little or no efficacy. Frontiers in Psychiatry, 5 , 121–121. https://doi.org/10.3389/Fpsyt.2014.00121
Shaw, A., Ward, P., & Pillai, V. (2019). Assessing mental health and service needs among refugees in Malaysia. International Journal of Social Welfare, 28 (1), 44–52. https://doi.org/10.1111/Ijsw.12313
Springer, F., Sale, E., Hermann, J., Sambrano, S., Kasim, R., & Nistler, M. (2004). Characteristics of effective substance abuse prevention programs for high-risk youth. The Journal of Primary Prevention, 25 (2), 171–194. https://doi.org/10.1023/B:Jopp.0000042388.63695.3f
Sussman, S., Skara, S., Rodriguez, Y., & Pokhrel, P. (2006). Non drug use- and drug use-specific spirituality as one-year predictors of drug use among high-risk youth. Substance Use & Misuse, 41 (13), 1801–1816. https://doi.org/10.1080/10826080601006508
Toews, C. (2017). Compliance of systematic reviews in Veterinary journals with preferred reporting items for systematic reviews and meta-analysis (prisma) literature search reporting guidelines. Journal of the Medical Library Association, 105 (3), 233–239. https://doi.org/10.5195/Jmla.2017.246
Tranfield, D., Denyer, D., & Smart, P. (2003). Towards a methodology for developing evidence-informed management knowledge by means of systematic review. British Journal of Management , 14 (3), 207–222. https://doi.org/10.1111/1467-8551.00375 .
Valente, W., Ritt-Olson, A., Stacy, A., Unger, B., Okamoto, J., & Sussman, S. (2007). Peer acceleration: Effects of a social network tailored substance abuse prevention program among high-risk adolescents. Addiction (Abingdon England), 102 (11), 1804–1815. https://doi.org/10.1111/J.1360-0443.2007.01992.X
Vandenbroucke, P., Von Elm, E., Altman, G., Gøtzsche, C., Mulrow, D., & Pocock, S. J. (2014). Strengthening the reporting of observational studies in epidemiology (Strobe): Explanation and elaboration. International Journal of Surgery (London England), 12 (12), 1500–1524. https://doi.org/10.1016/J.Ijsu.2014.07.014
Von Elm, D., Altman, P., Egger, P., Pocock, P., Gøtzsche, D., & Vandenbroucke, P. (2007). The strengthening the reporting of observational studies in epidemiology (Strobe) statement: Guidelines for reporting observational studies. The Lancet (British Edition), 370 (9596), 1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Wade-Mdivanian, R., Anderson-Butcher, D., Newman, J., Ruderman, E., Smock, J., & Christie, S. (2016). Exploring the long-term impact of a positive youth development-based alcohol, tobacco and other drug prevention program. Journal of Alcohol & Drug Education, 60 (3), 67–90.
Watkins, C. (2016). A social learning approach to prescription drug misuse among college students. Deviant Behavior, 37 (6), 601–614. https://doi.org/10.1080/01639625.2015.1060799
Widmann, M., Apondi, B., Musau, A., Warsame, A. H., Isse, M., Mutiso, V., Veltrup, V., Ndetei, D., & Odenwald, M. (2017). Comorbid psychopathology and everyday functioning in a brief intervention study to reduce Khat use among somalis living in Kenya: Description of baseline multimorbidity, its effects of intervention and its moderation effects on substance use. Social Psychiatry and Psychiatric Epidemiology: The International Journal for Research in Social and Genetic Epidemiology and Mental Health Services, 52 (11), 1425–1434. https://doi.org/10.1007/S00127-017-1368-Y
Download references
Open Access funding enabled and organized by CAUL and its Member Institutions. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and affiliations.
Faculty of Business, Education, Law and Arts, School of Business, University of Southern Queensland, Toowoomba, QLD, 4350, Australia
Elijah Aleer & Afzalur Rashid
Faculty of Business, Education, Law and Arts, School of Business, Centre for Health Research, University of Southern Queensland, Toowoomba, QLD, 4350, Australia
Khorshed Alam
You can also search for this author in PubMed Google Scholar
Contributions
Elijah Aleer: study concept, developed review protocol and conceptual framework for study classification, data acquisition, extraction, analysis and interpretation of data, initial draft and critical revision of manuscript, and characteristics of studies tables. Khorshed Alam: review supervision, study concept, review protocol and conceptual framework for study classification, data acquisition, extraction, analysis and interpretation of data, draft and critical revision of manuscript. Afzalur Rashid: review supervision, peer reviewed of search strategies, data acquisition, extraction and interpretation, critical revision of protocol and manuscript.
Corresponding author
Correspondence to Afzalur Rashid .
Ethics declarations
Conflict of interest.
The authors report no conflict of interest.
Ethical Approval
Ethical standards were followed with this research and a formal human ethics approval were not required as the data were collected from the secondary available sources.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Aleer, E., Alam, K. & Rashid, A. A Systematic Literature Review of Substance-Use Prevention Programs Amongst Refugee Youth. Community Ment Health J (2024). https://doi.org/10.1007/s10597-024-01267-6
Download citation
Received : 18 September 2023
Accepted : 09 March 2024
Published : 09 April 2024
DOI : https://doi.org/10.1007/s10597-024-01267-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Refugee youth
- Systematic literature review
- Substance use prevention programs
- Find a journal
- Publish with us
- Track your research
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
A Review of CBT Treatments for Substance Use Disorders
Jean-François Morin, Department of Psychology, Univesité de Montreal
Maggie Harris, CHU-Ste-Justine
Patricia J. Conrod, Department of Psychiatry, Université de Montreal
- Published: 05 October 2017
- Cite Icon Cite
- Permissions Icon Permissions
This review article presents a summary of the existing literature on well-established CBT treatments for substance use disorder. It provides an overview of the origins, procedure, and evidence for six CBT treatment models: relapse prevention (RP) and mindful-based relapse prevention (MBRP), guided self-change (GSC), community reinforcement approach (CRA), behavioral couples therapy (BCT), and personality-targeted brief interventions. Common intervention components include orienting clients towards a meaningful goal, teaching necessary skills to reduce substance use and successfully achieve the goal, and establishing plans to face potential relapses, which generally appear to produce moderate to large effects across contexts and substance-related outcomes.
Introduction
Substance use disorders (SUD) can be defined as “a cluster of cognitive, behavioral and physiological symptoms indicating that the individual continues using the substance despite significant substance-related problems” ( APA, 2013 ). It can emerge from a dysfunctional pattern of behaviors and emotions related to the consumption of psychoactive substances, like alcohol, cannabis, cocaine, and opioids. Substance misuse typically manifests in early adulthood, with some individuals already struggling with substance misuse in adolescence. According to an epidemiological study, about 17–19% of the population suffers from substance misuse ( Kessler et al., 1996 ), which makes it the second most prevalent class of disorders within the Diagnostic and Statistical Manual of Mental Disorders–5 (DSM-5; APA, 2013 ). In a recent report, the World Health Organization (WHO) stated that problematic substance use was on the rise, afflicting more than 5% of the world population, and representing about 3.3 million deaths worldwide ( WHO, 2014 ). Western countries, including Canada, the United Kingdom, and the United States, are experiencing a rapid increase in growth of substance misuse compared to other countries ( WHO, 2014 ). Though rates of substance misuse in adolescents within these countries have been decreasing over the last 15 years, rates of substance abuse and dependence have remained stable over that time period ( CASA, 2010 ).
SUDs are highly prevalent conditions ( Kessler et al., 1996 ; Peer et al., 2013 ) and probably the most prevalent disorder to co-occur with other mental health conditions ( Kessler, 2004 ; Lai et al., 2015 ). Alcohol use disorders (AUD) have been linked to a variety of other psychiatric conditions, including major depressive disorder, generalized anxiety disorder, conduct disorder, antisocial personality disorder, schizophrenia, and bipolar disorder ( APA, 2013 ; Kessler et al., 1996 ). Alcohol abuse has also been linked to gastrointestinal, cardiovascular, and nervous systems damage ( APA, 2013 ). In addition to its impact on health, alcohol inflicts significant economic and social harms ( Goetzel et al., 2003 ; Sanderson & Andrews, 2002 ) that are bound to increase with world’s population growth, making it a healthcare priority ( WHO, 2014 ).
This review focuses on five cognitive-behavioral therapy (CBT) models of intervention for SUDs. The relapse prevention (RP) model is the most commonly described CBT intervention for SUDs and was developed to assist clients who had achieved abstinence through detoxification in order to maintain abstinence over the long term. The RP is based on the understanding of a “relapse” as a process by which internal and external triggers for substance use are managed using problematic coping skills and expectancies that increase the likelihood than an individual will believe that substance use is the only way to manage that high-risk situation. In brief, the intervention approach helps clients identify internal and external high-risk situations and triggers, and then offers behavioral and cognitive interventions to promote the use of new skills and effective coping strategies to increase self-efficacy in managing high-risk situations without using substances ( Marlatt & Donovan, 2005 ).
Other interventions have been developed based on the CBT framework, but designed to target clients in different psychosocial contexts and stages in the course of SUD. These less utilized approaches include guided self-change (GSC), behavioral couples therapy (BCT), and community reinforcement approach (CRA). More recently, these interventions have been adapted to address specific features of SUD that might not have been addressed in earlier treatment models, such as managing cravings in alcohol dependence, addressing psychiatric comorbidity, and offering solutions for prevention. The RP model was recently adapted to include a mindfulness component with mindfulness-based relapse prevention (MBRP), a short-term treatment that helps clients identify and learn to effectively cope with situations that trigger the urge to consume, using mindfulness techniques. The GSC model is a very brief, motivationally based treatment that helps clients formulate a goal for change, which will serve as the focus of treatment. BCT focuses on substance-misuse treatment in the context of intimate relationships. CRA is a multimodal treatment, which leads the client to perceive sobriety as a desirable goal, by effecting change through social mechanisms. Finally, personality-targeted CBT intervention represents a more personalized version of the CBT model to address heterogeneity and comorbidity within SUDs by targeting common personality risk factors for behavioral and mental health problems that co-occur with SUDs. These cognitive-behavioral interventions for SUD are reviewed in more detail later.
Relapse Prevention: Framework for Cognitive Behavior Therapy in SUDs
For any mental health professional working with substance-misusing clients, addressing the risk for relapse following abstinence or drug detoxification is essential for the maintenance of long-term positive outcomes. The cognitive behavioral model that first addressed the importance of relapse within the context of substance use was the RP model, first described by Marlatt and Gordon (1985) .
This well-established model within CBT states that, when trying to maintain sobriety or reduced substance use, recovering individuals are likely to experience a “lapse,” defined as a momentary failure to uphold their goal. The initial lapse occurs when clients encounter “high-risk situations.” High-risk situations can be external (e.g., walking near a bar) or internal (e.g., feeling depressed). From an initial lapse, two outcomes are possible: either one returns to the initial substance-use behavior (a “relapse”; Marlatt & Gordon, 1985 ), or one gets back on track with one’s abstinence goals (a “prolapse”; Marlatt & Gordon, 1985 ). Accordingly, relapses have both affective and cognitive components: the feelings of guilt, shame, and hopelessness associated with relapse constitute the affective component, while attribution of the lapse to internal and uncontrollable factors constitutes the cognitive component ( Marlatt & Donovan, 2005 ). The latter contributes to the “abstinence violation effect” whereby such cognitive processes can lead to giving up on abstinence goals, and strongly contributes to heavy and uncontrolled substance use in the context of a relapse. Figure 1 is a reprint from Marlatt and Gordon (1985) demonstrating the RP model of substance misuse.
Relapse Prevention Model.
According to this model, there are numerous potential targets for psychological intervention. Therapists and clients must identify internal and external high-risk situations. Then behavioral and cognitive interventions can be delivered to develop new skills, teach effective coping strategies, increase self-efficacy and augment feelings of mastery in high-risk situations ( Marlatt & Donovan, 2005 ).
There are several manualized versions of RP interventions ( Carroll, 1998 ; Kadden et al., 1992 ; Monti et al., 1989 ). Treatment typically consists of about 20 sessions. The main objective is to teach different behaviors and coping strategies to manage internal and external high-risk situations that trigger consumption. All models seem to include five CBT strategies: (1) functional analysis of substance use, (2) identification of intrapersonal and interpersonal triggers for relapse, (3) coping-skills training, (4) behavioral skills training for drug-refusal, and (5) increased activities unrelated to substance use.
Magill and Ray (2009) conducted a meta-analysis gathering data from 52 studies for a total of 9,308 participants. Using Hedges’s g , an indicator of standardized mean difference comparable to Cohen’s d , they found that CBT treatments, including RP treatments, have a small positive effect ( g = 0.15) over post-treatment alcohol use, cannabis use, cocaine use, etc., when compared to various control conditions (mostly treatment as usual and medication). The effects slightly diminished over time. Hedges’s g decreased to 0.11 in the short term (6–9-month follow-up), and further diminished to 0.09 at the 12-month follow-up. Another meta-analysis by Dutra et al. (2008) , compiling data from 34 studies ( n = 2,340), reported a low to moderate effect of CBT programs, including RP interventions, on substance use outcomes ( d = 0.32). Though both meta-analyses suggest an effect of RP interventions, it is important to note that these meta-analyses reviewed other kinds of CBT treatments as well (e.g., coping-skills training). The great majority of the treatment reviewed, however, integrate components of the RP model. Though RP models’ efficacy cannot be determined with certainty on the basis of these reviews, their results suggest a certain efficacy of treatments based on the RP model.
Other investigations explored the possibility of certain client attributes’ being associated with a more favorable response to RP interventions. The RP model revised by Monti et al. (1989) , a 27-session group CBT intervention, was compared to interactional group therapy ( Kadden et al. 1989 ). Survival analyses conducted two years after the trial ( Cooney et al., 1991 ) suggested that clients high on psychopathology and sociopathy scales responded more favorably to relapse prevention than to interactional group therapy. They remained abstinent longer after receiving a CBT intervention, compared to interactional group therapy.
The model was later adapted to individual therapy in the context of Project MATCH ( Kadden et al., 2003 ). Project MATCH was a multi-site clinical trial investigating the differential effect of CBT, motivational interviewing, and Twelve-Step Facilitation Therapy. The study also aimed to identify client attributes that might predict differential treatment response. The final CBT model consisted of 14 sessions (eight core sessions and six elective sessions) addressing different topics. The topics were: coping skills teaching, cognitive restructuring, problem solving, and behavioral skills training.
Project MATCH reported that all three intervention conditions resulted in equivalent and very positive substance use outcomes: ratios of days without drinking were about 70–80% at 12 months post-treatment for all three intervention conditions. The study only modestly validated the client–treatment matching hypothesis ( Longabaugh. Wirtz, Mattson, & Myers, 2001 ): psychiatrically more severe clients were shown to have a slightly beneficial outcome on RP intervention than the motivational enhancement intervention. Considering the small differences between treatments, the study later concluded that all treatments evaluated, including the CBT relapse prevention model, were well-supported treatments for SUDs.
The RP model is now integrated into other CBT interventions targeting non-addictive psychopathologies that are now understood as having a more chronic and relapsing nature, such as depression ( Bockting et al., 2005 ), bipolar disorder ( Scott, Colom, & Vieta, 2007 ), and schizophrenia ( Garety et al., 2008 ). This expansion of the RP model to other areas of psychopathology led to mutual enhancements and adaptations, whereby the RP treatment model integrated newer psychological principles coming from these other fields, such as mindfulness, as a helpful strategy for managing emotional distress and cravings.
Mindfulness-Based Relapse Prevention: An Extension of the RP Treatment Model
The mindfulness-based relapse prevention program was developed by Bowen, Chawla, and Marlatt (2010) . This eight-session, group-based program was designed to assist clients with substance-use problems to identify and effectively cope with situations that may trigger relapse after their treatment has ended. MBRP sessions address topics such as recognizing triggers for substance use, identifying automatic reactions to those triggers, behaving differently when confronted with triggers, and using mindfulness as a way of redirecting attention and suppressing the urge to consume ( Bowen, Chawla, & Marlatt, 2010 ).
Origins of MBRP
In the 1990s, cognitive psychologists adopted the concept of mindfulness from Eastern philosophy to address ruminative thinking in mental disorders ( Segal, Teasdale, & Williams, 2004 ). “Mindfulness” can be defined as a state of consciousness that emerges from purposefully redirecting one’s attention to the present moment, and living the experience without judgment ( Kabat-Zinn, 2003 ). This creates new ways for the client to interact with his or her subjective experience, understanding him- or herself, and developing new ways to act in a given situation. Mindfulness has been shown to reduce the severity of symptoms in many different domains, including anxiety and depression ( Amir, Weber, Beard, Bomyea, & Taylor, 2008 ; Heeren, Lievens, & Philippot, 2011 ). In the context of SUD, mindfulness gives individuals the opportunity to develop many skills, such as coping skills, tolerating and reframing cravings, self-motivation, meta-cognitive awareness, self-compassion, and self-efficacy ( Witkiewitz, Martlatt, & Walker, 2005 ).
MBRP is a group intervention delivered in eight sessions of 120 minutes ( Bowen, Chawla, & Marlatt, 2010 ). This is a structured program, with a detailed schedule for each meeting. MBRP also offers worksheets, practice exercises, DVDs borrowed from traditional CBT interventions, and mindfulness homework to continue skill building between the sessions. Despite the firm structure of the treatment, “creativity and shared curiosity” are encouraged as part of the group dynamic, and they aid the success of MBRP ( Bowen, Chawla, & Marlatt, 2010 ). The process of MBRP also differs from other group treatments of SUD, due to its commitment to the present moment. Despite clients’ natural tendencies to tell stories about their experiences, or share judgments and impressions about treatment, the goal is to connect and cope with emotions and thoughts that naturally arise in the context of the sessions. Facilitators of the groups must foster a safe and familiar environment, where mindful contemplation and open communication can be shared.
MBRP sessions follow a specific routine, which usually begins with a review of the material that was prepared or worked on since the previous meeting. A mindfulness exercise is presented, followed by a present-focused “inquiry” phase, which involves clients’ sharing their thoughts and feelings about the present moment. At the end of the meetings, the facilitator explains the homework and readings for the next session.
The first session addresses the issue of automatic response and relapse. After an introduction of the technical aspects of the treatment (e.g., rules, confidentiality, format of group), the facilitator leads a mindfulness exercise for the group, called the raisin exercise . The raisin exercise involves clients’ contemplating, smelling, touching and finally eating a raisin in order fully appreciate and connect with each moment of the experience ( Bowen, Chawla, & Marlatt, 2010 ). The group then discusses the exercise, and the facilitator highlights how most reactions tend to be automatic and mindless compared to the raisin exercise.
The second session focuses on dissecting reactions in high-risk situations, by exposing patients to triggers, cravings, and thoughts related to consumption, while encouraging them to resist reacting in an automatic way. Time is devoted to identifying sensations, emotions, and thoughts of consumption-related triggers and cravings. Mindfulness is introduced as a way of expanding the patients’ possible choices and actions when faced with those difficulties.
The SOBER method (Stop, Observe, Breathe, Expand, and Respond) is presented in the third session as a way to adapt mindfulness to everyday contexts, which diminishes the risk of reacting in an impulsive manner ( Bowen, Chawla, & Marlatt, 2010 ). This session also marks the beginning of official meditation practices.
The mindfulness strategies are further refined in session four, when the group learns coping skills to use when faced with high-risk situations. Coping with and tolerating intense emotional reactions with mindfulness is key for success. For example, a client might take a moment to consider his or her thoughts when confronted with a high-risk situation and choose self-control, as opposed to reacting automatically and consuming substances.
The fifth session concentrates on the acceptance of unwanted thoughts, emotions, and sensations, as a way to move forward and take care of oneself. The concept of “breathing spaces” ( Bowen, Chawla, & Marlatt, 2010 ) is introduced, which consists of disengaging their attention from the external environment and focusing on breathing. Then, clients can progressively re-engage their attention towards their surroundings. This exercise is meant to help clients act in a mindful way, rather than a mindless and automatic way. Meditation techniques are encouraged for daily use, as well.
The sixth session consists of reframing clients’ experiences of their thoughts to accent the element of choice and opportunity, rather than believing their thoughts must be reality. Thoughts are presented merely as thoughts, disassociated from any obligation to act on them ( Bowen, Chawla, & Marlatt, 2010 ).
The seventh meeting underscores the importance of self-care and balance in recovery from SUD. Self-compassion, lifestyle choices, healthy activities, and warning signs of relapse are addressed as important aspects of maintaining positive change.
The last session serves as a brief review of the skills developed over the course of therapy. The group discusses the significance of a support system and the integration of mindfulness practices to preserve the gains that have been achieved ( Bowen, Chawla, & Marlatt, 2010 ).
Summary of Evidence
Overall, MBRP is a relatively novel treatment attempting to integrate mindful meditation as an adjunct to classical RP intervention. Investigations conducted so far by Bowen, Marlatt, and Witkiewitz established that mindful meditation was associated with reduced use of many different substances and reduced intensity of psychiatric symptoms. These reductions seem mediated by client’s reduced tendency for thought-avoidance and reduced self-reported intensity of cravings. A systematic review of mindfulness-based programs for substance misuse corroborated the findings of Bowen, Marlatt, and Witkiewitz. Table 1 presents the sources reviewed in this section.
Detailed Review
The very first study to evaluate MBRP on substance use outcomes was reported by Bowen and colleagues (2006) , who offered a Vipassana course, teaching a form of Buddhist mindfulness meditation practices to a group of incarcerated individuals (79.2% male), who were abusing substances ( n = 173). Participants were randomized to either a ten-day course of silent meditation for periods of 8–10 hours per day, or treatment as usual (TAU), which consisted of chemical dependency treatment and substance use education. The findings revealed that participants enrolled in the mindful meditation class showed a significant reduction in their alcohol, cocaine, or marijuana consumption after three months when compared to the TAU group, but no effects were found for tobacco ( Bowen et al., 2006 ). In addition to reduced consumption rates, participants in the mindfulness meditation class also experienced a decrease in their psychiatric symptoms. Positive psychosocial outcomes, such as locus of control over substance use and level of optimism, also significantly improved by the three-month follow up. Using the same data, a secondary analysis established that levels of thought-suppression mediated the relationship between participation in the Vipassana workshops and alcohol use at follow-up: participation in the mindfulness training was associated with lower levels of thought avoidance, which was then related to less alcohol intake ( Bowen, Witkiewitz, Dillworth, & Marlatt, 2007 ). The mechanisms responsible for this relationship might been due to the new perspective clients developed towards intrusive thoughts, like urges to consume. If clients are taught to neither avoid nor react to substance use urges, this would be likely to lead to reduced substance use.
The effects of mindfulness training on more severe cases of SUD were explored in another study by Bowen et al. (2009) . Individuals suffering from substance abuse ( n = 168) were randomly assigned to either MBRP or treatment as usual, which consisted of a 12-step program, process-oriented groups, and psychoeducation. These patients had previously been in inpatient or outpatient units for about two weeks. Data were collected at pre-treatment, and at two- and four-month follow-ups. Analyses revealed a significant difference in substance use at four months post-intervention for the MBRP compared to controls. Participants enrolled in the MBRP program also reported fewer cravings, and more acceptance and mindful acting than controls. Bowen et al. (2009) also concluded that the MBRP treatment was feasible for patients, since they observed high compliance rates with homework, high attendance, and positive feedback.
The most rigorous evaluation of MBRP was reported recently by Bowen et al. (2014) , who compared the efficacy of MBRP to regular relapse prevention treatment, and to treatment as usual (12-step program and psychoeducation) over a 12-month period. A total of 286 individuals who had recently received treatment for substance use were assigned to either MBRP ( n = 103), regular relapse prevention ( n = 84), or treatment as usual ( n = 95) as part of an aftercare program. The frequency of consumption and relapse were measured at baseline, 3-, 6-, and 12-month follow-ups. Results indicated that both MBRP and traditional relapse prevention were more successful than treatment as usual in reducing relapse and decreasing substances consumed at the 6-month follow-up. After 12 months, the MBRP group had fewer consumption days and heavy drinking episodes, relative to both standard relapse program and treatment as usual recipients ( Bowen et al., 2014 ). This illustrates that MBRP can supplement the other two conditions by reducing heavy drinking and the number of consumption days. Targeted mindfulness training may support long-term recovery by teaching individuals how to tolerate discomfort associated with cravings or negative affect, and behaving in a healthier way.
Additional studies by this same research team indicate that MBRP is also effective in helping college students reduce smoking behavior ( Bowen & Marlatt, 2009 ), ethnic minority groups reduce their substance use ( Witkiewitz, Greenfield, & Bowen, 2013 ), and clients with concurrent depressive symptoms reduce their elevated cravings and substance use that were linked to their depressive symptoms ( Witkiewitz & Bowen, 2010 ).
Additionally, many different adaptations of mindfulness-based therapy for substance use have been conducted by other research teams. A systematic review conducted by Chiesa and Serretti (2014) gathered results from a total of 24 studies investigating mindfulness-based programs, such as Vipassana meditation, acceptance and commitment therapy (ACT), spiritual self-schema therapy (3S-T), mindfulness-based stress reduction (MBSR), dialectical-behavioral therapy (DBT), mindfulness-based cognitive therapy (MBCT) and MBRP. They concluded that mindfulness-based models such as MBRP outperformed waitlist control, non-specific support groups, and treatment as usual conditions on outcomes such as alcohol, cocaine, tobacco, marijuana, and opiates misuse. The review’s finding gave some support for the hypothesis that MBRP is particularly effective in reducing cravings and increasing self-reported mindfulness.
The MBRP model is an excellent post-treatment program, designed to maintain the gains made in therapy for SUD sufferers. Evidence suggests potentially lasting effects for clients in a variety of settings (e.g., forensic, clinical, community) with diverse substance addictions (e.g., alcohol, cocaine), and for members of different cultural backgrounds, with minority women in particular. Beyond interest in their intervention model, the research team behind MBRP is also assessing the relationship between brain changes and mindfulness practices, as well as the development of reliable measures to understand and assess dimensions of mindfulness. For more information, the team’s website is http://www.mindfulrp.com/ .
Community Reinforcement Approach (CRA)
Another cognitive-behavioral approach to aftercare treatment is the community reinforcement approach, which focuses more on the environmental and behavioral factors that maintain substance use, such as social, recreational, familial, and/or vocational reinforcers. The approach is also based on basic principles of behavioral reinforcement applied to the context of addiction and aims to reduce factors that maintain consumption behaviors and increase activities that reinforce non-addictive behaviors.
Origins of CRA
It is common knowledge in psychology that punishment is not the most effective means to modify human behavior. CRA, a behavioral intervention for substance abuse, proposes a model for rewarding sober behavior, rather than punishing substance use through confrontational means ( Hunt & Azrin, 1973 ). CRA was first tested in the early 1970s, developed as an alternative treatment to 12-step programs. Its novel modular construction, dispensed in a time-limited, goal-oriented format, distinguished itself from the treatment available at that time. The intention behind this program was to reinforce activities and decision making that promoted the maintenance of abstinence and to teach skills to help clients to achieve these activities.
CRA is a multi-modal treatment of substance abuse, meaning it offers a variety of interventions targeting key domains of social functioning that are likely to promote a sober lifestyle. The entire set of components is rarely offered systematically, except for functional analysis and treatment planning modules, which serve as starting points for all clients. Depending on clients’ needs, they can navigate through the modules in any way they see fit. What follows is a list of modules that can be used under the umbrella of the CRA intervention.
Functional analysis: In line with the CBT evaluation method, functional analysis is an essential part of assessment. Information collected here focuses on the context of substance use, both external (e.g., situation, time, social setting, presence of key members of social group) and internal (e.g., thoughts, feelings, sensations, emotions). Details of the consumption behavior, like the nature, quantity, and consumption method, are gathered. The consequences of the behavior, both negative and positive, are also part of the evaluation. A well-conducted functional analysis will set the stage for a successful treatment ( Meyers & Smith, 1995 ).
Treatment plan: The CRA treatment plan entails the completion of two questionnaires, the Happiness Scale and the Goals of Counselling form. The Happiness Scale measures self-reported degree of satisfaction in ten areas of social life (e.g., work, relationships, personal habits). Based on the Happiness Scale, domains are selected for a targeted intervention. Once the domains of intervention are established, the client uses the Goals of Counselling form to specify goals to attain in each of the ten identified domains. Strategies to reach said goals, with the projected timeframes, are also included on the form ( Meyers & Smith, 1995 ).
Sobriety sampling: Instead of beginning treatment by stating that clients should achieve complete abstinence, which can be an overwhelming goal for the client, CRA proposes to negotiate a period of soberness. During this period, clients are taught some behavioral skills to stay sober, and the therapist highlights the advantages of sobriety. After the prescribed time period ends, the client and therapist renegotiate the benefits of another sobriety period ( Meyers & Smith, 1995 ).
Behavioral skills training: Therapists and clients may rapidly identify that some behavioral skills are lacking. This module offers clients the opportunity to work on three behaviors: problem solving, assertive communication, and substance refusal. The short behavioral training topics comprise segments on psychoeducation, suggested behaviors, and role-playing exercises to consolidate acquired skills ( Meyers & Smith, 1995 ).
Job skills: For many individuals, work is a key component of social life. Beyond simply obtaining and keeping a job, CRA also promotes the belief that a job should be intellectually, socially, and financially satisfying. The first phase of job-seeking relies heavily upon the Job Club Counselor’s manual, and previously described behavioral skills are taught as job-maintenance strategies ( Meyers & Smith, 1995 ).
Social and recreational counselling: Many intervention models believe that by lowering consumption, clients will immediately find new activities from which to seek enjoyment and satisfaction. Yet, some clients seem to struggle when reorienting their lives after terminating their substance abuse. In this CRA module, clients are encouraged to identify and try different social activities. The clients’ concerns about socializing when sober, and the challenges of having a social circle mostly built around substance use are also discussed. Beyond counseling, attending a CRA social club is another possibility, to help clients learn that sober socializing can be enjoyable in a non-threatening setting ( Meyers & Smith, 1995 ).
Relationship counseling: CRA’s community approach also applies to intimate relationships. In some cases, clients wish to address their relationship with their significant other. Couples start by setting objectives for themselves, using the Happiness Scale and the Perfect Relationship form (an adaptation of the Goals of Counselling form), at the beginning of meetings. For example, to reintroduce pleasant activities in the relationship, couples can set a daily reminder to be nice and to appreciate one another ( Meyers & Smith, 1995 ).
Relapse prevention: This module gathers most of its material for intervention in the functional analysis and behavioral skills module. Clients and therapists investigate each of the triggers for substance use, and use behavioral skills (e.g., problem solving, assertive communication, substance refusal) to avoid future relapse ( Meyers & Smith, 1995 ).
CRA has been adapted to treat clients using a variety of substances (e.g., alcohol, cocaine, heroin, marijuana) and from different sociocultural contexts (e.g., homeless individuals, adolescents), and has been used in conjunction with other treatment approaches. Interestingly, CRA has even been adapted for relatives of substance users, as a means of offering support to the families and encouraging potential substance users to seek treatment (Community Reinforcement Approach: Family Training; Smith, Meyers, & Austin, 2008 ). Table 2 presents the sources reviewed in this section.
CRA was initially tested for alcohol-abusing inpatients ( Hunt & Azrin, 1973 ). The trial comprised 16 participants suffering from alcohol addiction, assigned to either CRA ( n = 8) or a 12-step intervention ( n = 8). Six months after treatment, individuals who followed CRA protocol were favored when compared to 12-step controls; the CRA group only reported drinking on 14% of days, while the other group reported drinking on 79% of days ( Hunt & Azrin, 1973 ). The CRA group also used mental health services less frequently, and had higher employment rates compared to people in a 12-step program. A second CRA trial also showed similar results, with even higher drinking abstinence rates in the CRA group relative to controls (90% non-drinking over two years; Azrin, 1976 ). The treatment was modified to include a disulfiram observance program ( Azrin, 1976 ).
In the early 1980s, the treatment was expanded to outpatient alcoholics ( Azrin et al., 1982 ). Participants ( n = 43) were randomly assigned to one of three conditions: 12-step + disulfiram prescription ( n = 14), 12-step + disulfiram compliance training ( n = 15), or CRA + disulfiram compliance training. At a six-month follow-up, results showed that members of the CRA + disulfiram compliance training program performed better than the other two groups in percentage of days abstained (97% CRA + disulfiram training, 74% 12-step + disulfiram training, and 45% 12-step + disulfiram prescription; Azrin et al., 1982 ).
A replication of this study by Miller, Meyers, Tonigan, and Grant (2001) further refined the experimental design. A sample of 237 participants was recruited, including individuals who were eligible and ineligible for a disulfiram prescription. Disulfiram-eligible participants were randomized in the same three conditions as the original study by Azrin et al. (1982) . For disulfiram-eligible participants, a fourth condition of CRA without disulfiram was added to assess the specific contribution of CRA and establish whether disulfiram was necessary for CRA to be effective. For disulfiram-ineligible cases, CRA or treatment as usual were offered as the two random conditions. CRA conditions seemed to outperform other conditions between one and six-month follow-ups, but the effects decreased by the 12- and 18-month follow-ups. For the disulfiram-ineligible participants, CRA had significantly fewer dropouts than treatment as usual (9% CRA vs. 41% control), but no effects of intervention were observed on drinking outcomes ( Miller et al., 2001 ).
The treatment was also adapted to help homeless adults struggling with alcoholism. Smith, Meyers, and Delaney (1998) compared the outcomes of 106 clients in a group adaptation of CRA to the standard treatment offered by a large shelter in the community (12-steps + job program). The changes in CRA included case management and independent living skills. Follow-ups were conducted at two, four, six, nine, and 12-months post-admission. Follow-up response rates were very high among participants of the CRA program (76–93% across time points), with better outcomes for their substance use at the end of the program than the start ( Smith et al., 1998 ). Comparisons between the two groups showed that clients who followed CRA had consumed significantly fewer standard units of alcohol in between follow-ups, had significantly fewer drinking days, and presented significantly lower blood alcohol levels than controls.
New evidence has examined how homeless youth can benefit from CRA as well ( Slesnick et al., 2007 ). Youth between the ages 14 and 22 who lived on the streets and met criteria for substance abuse ( n = 180) were recruited from a community center. They were assigned to either CRA ( n = 96) or treatment as usual ( n = 84), which consisted of case management and referral to different services at the youth’s request. The results favored CRA: youth in CRA reported a larger decrease in their substance use and depression, and a greater increase in their social stability than controls at the six-month follow up ( Slesnick et al., 2007 ).
The CRA approach was also expanded to users of other substances, notably cocaine, opiates, and marijuana. In the early 1990s, Higgins and colleagues (1993) investigated the effect of combined CRA and contingency management (CM). The CM approach for substance use treatment consists of offering tangible rewards to immediately rival the rewarding aspect of substance use. When clients provide drug-negative urine samples, they are given vouchers exchangeable for goods. Thirty-eight cocaine users were randomized into CRA + CM or standard counseling conditions. In the CRA + CM group, 58% of participants completed the 24-week program, while only 11% of the control group did. Regarding abstinence rates, the percentage of CRA + CM participants who remained continuously abstinent after eight and 16 weeks was 68% and 42%, respectively, while the control group only managed 11% and 5% abstinence at the same time points. In a different study, CRA plus CM seemed to be better than CM alone in reducing cocaine use, improving treatment adherence and employment outcomes during the treatment phase ( Higgins et al., 2003 ). Opiate and marijuana addicts were also investigated as potential targets for CRA intervention with a combined CRA and CM model. People with both substance problems seemed to respond favorably to CRA + CM ( Bickel et al., 1997 ; Budney et al., 2006 ).
As substance use problems generally start in adolescence, a youth adaptation of the program was developed. Godley and colleagues (2001) investigated a modified version of CRA, the Adolescent Community Reinforcement Approach (A-CRA), which featured components relating to school functioning, friendship, and anger management. A-CRA was also altered to include caregivers in the therapy, and was shown to be as effective as motivational enhancement therapy plus CBT and multidimensional family therapy for adolescent substance abusers ( Dennis et al., 2004 ).
The last addition to the CRA model was the development of an intervention targeting significant others of the abusers. The CRA Family Training (CRAFT) has been shown to improve the well-being of substance abusers’ relatives, while also assisting sufferers seeking help for their substance problem. The treatment attempts to teach family members to reward their relative’s sobriety, and withhold rewards when said relative is using substances. It also seeks to enhance the overall happiness of family members. There is strong supportive evidence for CRAFT; it has been shown to successfully engage about two out of three treatment-refusing individuals in treatment ( Kirby et al., 1999 ; Meyers, Miller, Hill, & Tonigan, 1999 ; Meyers, Smith, & Waldorf, 1999 ; Meyers, Miller, Smith, & Tonigan, 2002 ; Miller, Meyers, & Tonigan, 1999 ; Smith, Meyers, & Austin, 2008 ; Roozen et al., 2010 ).
In conclusion, CRA is a multifaceted cognitive behavioral program adapted to many different potential needs. It has been extensively researched and continues to expand to different cultures. The manuals have been translated into Dutch, Finnish, German, and Korean. The research findings are now being disseminated in communities worldwide ( Godley, Garner, Smith, Meyers, & Godley, 2011 ).
Brief Interventions and Guided Self-Change
These interventions consist of a small number of therapy sessions, usually four, with the possibility of adding additional appointments at the client’s request. This motivationally based treatment orients the client towards a goal of his or her choice regarding substance use. These goals typically include substance use reduction or abstinence. The intervention is focused on highlighting and resolving the client’s ambivalence towards change, and to foster the client’s ability to identify and cope with situations or emotions that may trigger substance abuse.
Origins of Brief Interventions
The foundation for brief interventions dates back to the late 1970s. In their investigation of the effect of a short intervention on problematic alcohol consumption, Edwards et al. (1977) observed no significant differences in recovery status between alcohol-abusing men who followed a prolonged treatment program, and alcohol-abusing men who received supportive advice about their alcohol consumption. This effect was observable beyond advice-seeking outside the experiment and level of adherence to treatment. Many participants who received supportive advice sought services outside the context of the study in a similar proportion to clients following the experimental treatment program. In fact, men with a moderate alcohol problem who received single advice sessions reported high satisfaction for the help they received, and seemed to perform better than their peers at a second follow-up. This observation led to the hypothesis that, for individuals with moderate alcohol problems, very brief counselling sessions might be a time- and cost-efficient alternative to formal inpatient or outpatient treatment ( Edwards et al., 1977 ).
In the late 1970s and early 1980s, these observations were followed by two seminal reviews on brief interventions for “problem drinkers,” or people suffering from non-severe alcohol misuse ( Babor, Ritson, & Hodson, 1986 ; Bien, Miller, & Tonigan, 1993 ). Researchers started shifting from the original assumption that individuals struggling with substance use problems lacked the skills to regulate their consumption, and moved towards a motivation-based model in which motivation is understood as a “multi-determined state of readiness” that permits a person to achieve meaningful change; if the individual wants to change, he or she already has the resources to do so (Miller 1985 , 1987 ; Miller & Hester, 1986 ; Miller & Rollnick, 1991 ). In this view, the aim of a brief or early intervention for substance misuse is to assist motivated clients to find the tools they need to address their substance-related concerns. These original studies set the stage for the development of motivational interviewing and motivational enhancement therapy. Another example of a brief, early intervention for problem substance use is the guided self-change method (GSC), developed by Sobell & Sobell (1993) .
A key component of GSC is the motivational interviewing (MI) style. According to Miller and Rollnick (1991) , MI aims to identify and work with the client’s objectives and personal goals. This technique facilitates the client’s exploration and resolution of ambivalence to change. MI is a way to interact with the client, rather than a set of specific techniques; it is an unstructured interview that favors the client’s autonomy. In order to achieve this, (1) the client’s personal motivation is what leads the interview, rather than the counselor’s; (2) the client is responsible for investigating and solving his or her own uncertainty and difficulties; and (3) the counselor and client develop a partnership rather than a hierarchical therapist–patient relationship ( Miller & Rollnick, 1991 ).
In this treatment, the client is able to select his or her own goal regarding substance misuse. Many treatment programs, most notably the 12-step, Alcoholics Anonymous inspired programs, often advocate abstinence as the only realistic goal to pursue when striving for sobriety. In the case of the GSC model, adherence to MI’s style means the client is encouraged to formulate his or her own personal goal, as long as it is compatible with a healthy lifestyle (e.g., less than three drinks on any occasion; avoid drinking all days of the week). Giving the client autonomy to select a goal has the added bonus of solidifying the therapeutic alliance and providing the client with a meaningful personal goal to pursue ( Sobell & Sobell, 1993 ).
The first session of GSC therapy consists of a two-hour, thorough assessment of the client’s substance use. It aims to determine the nature of the substance(s) used by the client, the frequency and intensity of consumption episodes, the contextual elements of substance use, and the level of motivation and self-efficacy regarding change for these behaviors. To achieve this goal, therapists often employ open-ended interviewing and formal assessment tools. A list of these questionnaires includes: Alcohol Use Disorder Identification Test, Drug Abuse Screening Test–10 items, Drug Use History Questionnaire, Brief Situational Competence Questionnaire (BSCQ), Where Are You Now Scale, and Timeline Followback ( Sobell & Sobell, 1993 ). In between the evaluation and the first intervention session, the client is asked to complete some homework, including a self-observation of his or her substance use between the two sessions, and a goal evaluation form, in which the client sets his or her abstinence or reduction goal for the treatment ( Sobell & Sobell, 1993 ).
The next session starts with a review of the material completed since the initial assessment, and the clinician provides personalized feedback, creating a portrait of the client’s substance use. The client and counsellor first review the client’s goal. Then the therapist reviews the self-observation homework and puts it in context with the information gathered from the first session. The therapist also provides feedback, comparing the client’s consumption to normative drinking patterns, and illustrating the client’s consumption-risk profile. They then address and explore the client’s ambivalence towards change. The next sessions aim to further explore high-risk situations for the client, and help him or her identify steps that can be taken to reduce the risk of consumption ( Sobell & Sobell, 1993 ).
The final session prepares the client for the conclusion of therapy and addresses the issue of relapse. Great effort is invested in framing relapse as a normal experience from which the client can learn and grow. The client is taught to identify and limit the impact of relapse when it occurs, and is also taught to consider it a learning opportunity for refining the initial plan of persistent change. This is discussed in an effort to avoid the client’s potential devaluation of his or her ability to maintain change ( Sobell & Sobell, 1993 ).
GSC has been the subject of investigations for over 20 years and has demonstrated that a very brief treatment can still help some substance-misusing clients to reduce their consumption. GSC’s efficiency seems not to be improved by adding more sessions, or different components, suggesting that this very simple model is quite well optimized in its current form. The treatment has also been tested successfully in different sociocultural settings, a great asset for teams interested in testing the model internationally. Table 3 presents the sources reviewed in this section.
The GSC model for the treatment of SUDs has been extensively researched. In the first GSC clinical trial, conducted by Sobell and Sobell (1993) , 100 participants with an alcohol problem were randomized to receive either a GSC intervention alone ( n = 50) or a GSC intervention and two RP module sessions at the end of the intervention ( n = 50). The investigators found that both interventions were successful in reducing the amount of alcohol consumed from last year self-reported drinking levels to 12-months post-treatment drinking levels by 54%, but the two conditions were not significantly different from one another, raising questions about the empirical strength of the RP module. Though the RP module was deemed potentially inefficient, it remained in the intervention because it made little clinical sense to exclude the topic of relapse within an SUD treatment ( Sobell & Sobell, 1993 ). The study also revealed the treatment was well received by clients, 97% of whom rated the treatment highly ( Sobell & Sobell, 1993 ).
The second randomized controlled trial of GSC examined the potential benefits of involving significant others in the treatment ( Sobell, Sobell, & Leo, 2000 ). Fifty-six problem-drinking males received the GSC intervention. Their spouses were randomly assigned to two sessions of “natural social support” ( n = 28), which consisted of information sessions and readings about alcohol problems, or two sessions of “directed social support” ( n = 28), which consisted of training sessions and readings to help the partners be proactive and supportive of the abusers’ treatment. Results suggested that, though all participants improved over the course of treatment, no between-group effects were observable ( Sobell, Sobell, & Leo, 2000 ). This could suggest that the GSC intervention model is a sufficient, self-contained treatment for alcohol problems, and it does not need the added couple component to be efficient. The lack of significant results could also indicate that the control condition was already sufficient to generate effects comparable to the directed condition. Most participants responded favorably to the length of treatment: two-thirds reported the number of sessions as being sufficient, while one-third would have liked more sessions ( Sobell, Sobell, & Leo, 2000 ).
Another trial was conducted to assess the need for a supplementary session for clients who were still problem drinkers after receiving the full intervention ( Breslin et al., 1999 ). Here, 69 males who still drank heavily after the third session were randomized to one of two conditions. A first group received a supplemental or “stepped” session ( n = 33), including a re-evaluation of the client’s obstacles to change, and received personalized flash card reminders to use outside the therapist’s office. The other group received no additional session ( n = 36). The results were not significant for the additional session. The authors mentioned that, since the additional session was very similar to what clients received in regular GSC sessions, participants might have obtained full benefits from the previous GSC sessions, explaining the non-significant effect ( Breslin et al., 1999 ; Sobell & Sobell, 2005 ). A new approach altogether might be warranted for GSC-resistant cases.
The format of therapy was also investigated in the development of the GSC model. Sobell, Sobell, Brown and Cleland (1995) created an intervention targeting problematic drug consumption, and a second group-based format for both alcohol and drug abusers. Both treatments comprised four sessions presenting GSC topics and material. The individual sessions were about 60 minutes long, while the group sessions were between 90 and 120 minutes long. A total of 287 participants (232 drinkers and 55 non-injecting, non-heroin drug users) were randomized. The group format was not deemed significantly different from the individual format, meaning it helped participants reduce their alcohol and drug consumption at a similar level to the already validated individual GSC treatment ( Sobell, Sobell, Brown & Cleland, 1995 ). It is also important to note that the authors observed a considerable cost efficiency (41% less therapist time required by participant for group intervention) and logistic advantage (8 times fewer appointments missed) with the group format. A replication of these findings was recently obtained by Sobell, Sobell, & Agrawal (2009) , confirming the efficacy of group GSC treatment.
Another contemporary adaptation of GSC concerns the treatment of young women at risk for alcohol-exposed pregnancies ( Floyd et al., 2007 ). A group of 830 women, aged 18–44 years, were recruited from Florida, Texas, and Virginia in the United States. These women were randomized to either receive informational sessions ( n = 414), or information with GSC plus a contraception consultation ( n = 416). Women who received the GSC program plus a contraception consultation were twice as likely as the controls to reduce their drinking and/or use efficient contraception at three months, six months, and nine months after the end of the intervention ( Floyd et al., 2007 ).
The efficiency of the GSC model has also been validated in diverse cultural contexts. A series of studies by Ayala et al. (1998 ; Lozano-Blanco, Sobell, & Ayala, 2002 ) adapted the intervention model by translating all the relevant material to Spanish for its delivery to problem drinkers in Mexico. The treatment was also modified to be delivered in Stockholm, Sweden ( Andréasson, Hansagi, & Österlund, 2002 ). Both studies reported significantly reduced alcohol consumption for clients in their respective settings.
The GSC model of intervention has been shown to be an effective brief treatment for individuals in the United States, Mexico, and Sweden who suffer from problematic alcohol or drug use. GSC appears to be well suited for an individual or a group-based intervention, which can be useful as a community approach that is also cost-effective. Though the program is proficient with people who misuse various substances, it seems to be best suited to non-severe alcohol users, since treatment-resistant cases do not seem to respond to more GSC sessions, as was seen in Breslin et al. (1999) . Evidence suggests that severe alcohol abusers could benefit from brief motivational interventions ( Edwards & Taylor, 1994 ; Match Research Group, 1998 ), but no research has investigated the specific effect of GSC on this population. The community responsible for the development of this treatment is still looking for better ways to disseminate this program. For example, they are expanding their alcohol-exposed pregnancy program to college students using a mail-based administration of the program, and they are developing an app- and email-supported version of GSC (iSelf-Change TM ). The GSC webpage ( Healthy Lifestyles Guided Self-Change Program, 2014 , http://www.nova.edu/gsc/ ) provides a variety of assessment tools and exercises that can help practitioners intervene with substance abusing clients. The dissemination of this very brief and flexible intervention as a first line of substance use problem treatment would be highly beneficial for clients and clinicians alike.
Behavioral Couples Therapy
Another CBT option for substance users is behavioral couples therapy (BCT), which is far less utilized in the field, despite promising outcomes. Substance abuse can be detrimental to one’s physical and mental health, but it can also be harmful to the people closest to the abuser. BCT is a therapy targeting couples with one substance abusing partner. This model of treatment has been shown to reduce the addicted partner’s substance use and improve the quality of the couple’s relationship. BCT also addresses the non-abusing partner’s relationship satisfaction and the overall discord within the family environment, which could potentially improve children’s well-being.
In the 1970s, research on social dynamics revealed that family relationships and processes might inadvertently maintain substance use behavior, and interventions were developed tailored to the needs of families struggling with substance addiction. A number of family intervention models exist that address family dynamics in SUD (e.g., multisystemic family therapy), but only a few family-based treatments are strictly based on CBT principles. Using many of the concepts from behavioral interventions, Keller (1974) developed BCT as a response to the needs of struggling families. BCT has since become one of the most empirically supported treatments for alcohol abuse ( Epstein & McCrady, 1998 ), and it has been expanded to clients suffering from various substance use problems, including cocaine and heroin dependence.
BCT aims to maintain the couple’s drug and alcohol abstinence by teaching partners how to reward sobriety, which diminishes the occurrence of substance use, and favors supportive communication to prevent relapses. The treatment consists of 10–20 weekly couple sessions.
The sessions follow a structured format, starting with a presentation of the schedule. The clinician also inquires about the clients’ consumption behavior since the previous session. They then revise assignments and exercises, addressing previously encountered difficulties. If any problems have arisen since the last session, time is devoted to discussing and solving those issues. The session proceeds with new material, which can be delivered by psychoeducation, skills training, or role-play exercises. The session ends with new homework assignments for both the client and partner to work on until the next session ( McCrady & Epstein, 2009 ).
The “sobriety contract” was one of the first concepts established in BCT ( Keller, 1974 ). It describes the daily ritual where the person suffering from SUD formulates his/her intention to stay sober that day, and the partner verbally expresses support for those efforts. Clients who are receiving pharmacotherapy for their substance problem can take their medication at this time, as part of the routine. Adherence to the “sobriety contract” can be logged into a calendar for the therapist and client to monitor. Explicit instructions are given for the couple to refrain from talking about the addict’s past substance use outside the therapist’s office, in order to minimize the risk of substance-related conflicts. This type of situation can be periodically rehearsed in session for the therapist to provide feedback, if necessary ( McCrady & Epstein, 2009 ).
In sessions and through various assignments, BCT attempts to enhance the client and partner’s relationship by promoting positive and gratifying paired activities. These include the “Catch Your Partner Doing Something Nice” assignment, or the “Caring Day” assignment. Shared rewarding activities is paramount for reintroducing positive feelings in the relationship. Effective and supportive communication skills are also taught. These skills include paraphrasing, empathizing, and validating one another’s experiences ( McCrady & Epstein, 2009 ). These techniques are designed to increase relationship satisfaction and positive feelings, while diminishing the negative effects of stressors.
Another goal in BCT is relapse management. At the end of each session, therapists and clients discuss how to avoid relapses and what to do if they occur. Strategies commonly employed to avoid relapses are adherence to the “sobriety contract” and continued attendance at self-help group meetings. If relapses occur, clients are instructed to contact the therapist and resume with the skills they have learned in treatment. Great care is also invested in reframing what relapses signify: they should not be indicative of failure, but rather seen as opportunities to learn and adapt on the road to recovery ( McCrady & Epstein, 2009 ).
Clients and therapists also negotiate pharmacological treatment for SUD. For example, alcohol-dependent clients can discuss their disulfiram prescription and negotiate a gradual reduction in dosage. They first discuss this topic in session, and it can later be integrated into the “sobriety contract” ( McCrady & Epstein, 2009 ).
BCT has been validated as an evidence-based treatment for alcohol misusing clients. It has been evaluated as equivalent or superior to other existing group interventions and couples therapy. Though most research applies to heterosexual couples whose male partner struggle with alcohol misuse, some evidence suggests benefits for couples whose female partner struggles with alcohol misuse. BCT’s findings remain limited to alcohol misuse, and further efforts should expand the investigation on other substance and polysubstance misuse. Table 4 presents the sources reviewed in this section.
BCT has been compared to individual treatment, group interventions, and other couple therapies. When compared to individual therapy, BCT seems to offer delayed effects ( Bowers & al-Redha, 1990 ): levels of alcohol consumption were not significantly different across the different conditions immediately after treatment, but six months later, clients who received BCT maintained lower consumption compared to individual therapy recipients. Relationship ratings were also increased in the BCT condition at both six-month and one-year follow-ups.
In O’Farrell and colleagues’ study (1992) comparing BCT to interactional couples’ group therapy, BCT showed an initial advantage over group therapy, with lower levels of alcohol consumed during treatment, but the effects faded as treatment terminated. Marital outcomes (e.g., days spent separated, wife’s reported relationship satisfaction) were improved in the BCT condition, but the effect sizes diminished over time ( O’Farrell et al., 1992 ). When BCT was compared to other couple therapies for alcohol abuse treatment, BCT was the only couples treatment to show continually decreasing alcohol intake outcomes as time went on, while other treatments showed weaker effects past the nine-month follow-up ( McCrady et al., 1991 ).
In addition to the effectiveness of BCT, it has been shown to have positive cost–benefit outcomes. In O’Farrell and colleagues’ (1996) study, the cost–benefit ratio of BCT was compared to that of individual therapy and interactional couples’ groups. Findings indicated that the BCT group showed decreased judicial and medical costs in the two years following the intervention, relative to the other treatment types. Medical centers saved resources by offering BCT, since the therapy cost the centers less time and money than the standard procedures. The intervention was also shown to be more helpful than the other two treatments with respect to increasing abstinence for women reporting poor couple-adjustment at baseline ( O’Farrell et al., 1996 ).
Although most evidence for BCT has come from analyses of couples where men are struggling with alcoholism, recent findings ( McCrady, Epstein, Cook, Jensen, & Hildebrandt, 2009 ) show that alcohol-abusing women similarly benefit from BCT. They reported more days abstinent and a reduced number of days of heavy alcohol use, compared to individual therapy controls. These differences were maintained at follow-ups (6 and 12 months).
Unfortunately, there is a paucity of research exploring the efficacy of BCT for individuals misusing substances other than alcohol. Considering that this intervention model has great potential for reducing substance use problems and their secondary effects on significant others, we encourage further investigations by new research teams examining the evidence for BCT.
This model of treatment has been widely described in the literature, and empirical studies provide support for the approach, particularly for alcohol abusing clients. New research should investigate the effects of BCT on clients using non-alcohol substances or on clients suffering from polysubstance misuse to confirm the efficacy of this program for a wider range of clients.
Personality-Targeted Brief Interventions for Substance Misuse and Comorbid Psychopathology: A New Treatment Approach
SUDs have a high rate of co-occurrence with other psychiatric conditions, and as highlighted previously, comorbid psychopathology has been identified as a moderator of treatment response, even for traditional CBT interventions. Conrod and Stewart (2005) proposed an adaptation to the RP model for SUDs to incorporate findings from a large literature on common and specific risk factors across substance use and other psychiatric symptoms.
This literature indicates that risk for SUDs and concurrent psychiatric problems exist along a number of continua, often based on personality traits and underlying cognitive/motivational profiles ( Castellanos-Ryan et al., 2013 ; Rioux et al., 2016 ). These profiles can explain risk for future substance misuse, reasons for substance use/misuse, types of substances that are likely to be abused, and other important cognitive and behavioral tendencies, such as proneness towards disinhibited and antisocial behavior, depressive symptoms, or panic/anxiety ( Conrod & Nikolaou, 2016 ). As illustrated in Figure 2 , risk for psychopathology and SUD can be represented along five trait dimensions, each with its own specific cognitive, motivational profile and pattern of substance misuse and comorbid psychiatric problems. These risk trajectories have been shown to be associated with very different reasons for substance use. For example, an anxiety-sensitivity profile is consistently associated with substance use motives for anxiety and emotion regulation, whereas a sensation-seeking profile tends to be associated with substance use for enhancement reasons (e.g., Woicik et al., 2009 ). Beyond simple risk factors, these personality dimensions can also contribute to maintenance of substance related problems once they occur, making the personality profiles relevant as a target for treatment. For example, anxiety sensitivity is associated with intolerance of nicotine withdrawal symptoms and risk for early relapse during a smoking cessation attempt ( Zvolensky et al., 2008 ).
Figure 3 is a reprint from Stewart and Conrod (2008) demonstrating how the RP model can be modified to differentially address these underlying risk trajectories in order to address vulnerability to substance misuse and psychiatric symptoms in a more personalized manner.
Personality risk factors for SUDs and other mental health problems.
Integrating personality risk factors in the Relapse Prevention Model.
Personality-targeted interventions can be offered in group or individual-based interventions, which tend to be brief (one to four sessions), due to the targeted nature of the intervention. As interventions target risk factors rather than problem symptoms, they can be offered as brief interventions for substance misuse or as a selective preventative intervention. In either format, four different intervention manuals have been developed to specifically target four personality risks: anxiety sensitivity, hopelessness, impulsivity, and sensation seeking. These traits are reliably measured using the Substance Use Risk Profile Scale (SURPS), a 23-item scale measuring these four traits ( Woicik et al., 2009 ). This scale has been translated into several different languages and evaluated for use with individuals 12 years old and older. When SURPS is used as a screening tool, it is recommended to use the procedure described and validated by Castellanos-Ryan et al., (2011) , by which individuals are identified as high-risk based on a standard deviation from the population from which they were screened. In other settings, this is not possible, so it is recommended to either use deviation from published standard norms, or the highest mean score of all four scales when deciding which personality-targeted intervention is most appropriate for an individual. In both scenarios, when an individual scores high (screens positive) on more than one personality risk factor, it is recommended to start intervening on the most deviant personality trait. Individuals with similar personality profiles are guided through the intervention when the scale is administered in group format.
The school-based intervention program is a very brief treatment offered over two to three sessions of 90 minutes over a two- to three-week period, for a total of three hours of therapy. The targeted nature of this intervention is conducive to brief therapy, given that the discussion topics and exercises are tailored to the needs of each specific personality profile. The treatment follows a structured format, using manuals to guide discussions and present exercises for each sessions. Manuals also feature vignettes to facilitate exchanges, normalize experiences related to the targeted trait, and encourage participant disclosure. The intervention manuals have been tailored to youth as young as 12 years of age (Preventure; Conrod et al., 2008 ; 2010) and for college students ( Watt et al., 2006 ).
The first session aims to build a positive and engaging group dynamic, while building a common understanding of the problem. Clients start by setting long-term personal goals for themselves. After a brief discussion about obstacles to goal pursuit, the group is introduced to the personality trait, a frequent obstacle when pursuing personal goals. This component sets the personality trait as the center of therapy, and begins to focus attention on tackling obstacles and diminishing the consequences associated with the trait. To assist clients in managing their personality trait, the therapist presents a decision-making exercise that the group applies to a vignette. Clients then learn to deconstruct their experiences in sensation, thoughts, and behaviors, and to identify automatic thoughts as the catalyst for problematic behaviors and ineffective coping strategies. As homework, clients are asked to describe and deconstruct a situation in which they had difficulty managing their personality trait.
In the second session, clients learn to identify their cognitive distortions and challenge them. Cognitive distortions most relevant to each personality profile (e.g., jumping to conclusion for Impulsivity, catastrophizing for Anxiety Sensitivity, or internalization for Hopelessness) are presented, and members of the group share opinions about the distortions. The group moves on to identifying and confronting the distortion illustrated in a vignette. As a final exercise, clients retrospectively identify and challenge their own cognitive distortions. The treatment ends with a review of the material covered across the two workshops and a discussion about the importance of maintaining a healthy lifestyle and social relations in the pursuit of personal goals.
Personality-targeted interventions have also been evaluated when delivered in an individual format to adults living in the community who suffer from SUDs ( Conrod et al., 2000 ) or anxiety disorders ( Olthuis et al., 2015 ). The adult, individual format is very similar to the group-based format described heretofore and can even be distance-delivered through telephone or email coaching ( Olthuis et al., 2015 ).
A recent review of personality-based model of intervention for substance misuse has been conducted by Conrod and Nikolaou (2016) . Table 5 is a reformatted version of the table presented in Conrod and Nikolaou (2016) . A description of individual studies follows.
The personality-targeted CBT approach has been evaluated in a number of randomized trials. One trial used a treatment-matching design in which substance misusing participants were randomized to participate in brief personality-targeted interventions or identical brief CBT interventions that did not target their primary personality profile, and both interventions were compared to a brief supportive counselling session ( Conrod et al., 2000 ). This trial showed that substance using women reporting a range of substance use behaviours and problems responded more favorably to a brief intervention if that intervention targeted their most prominent personality trait. These findings were subsequently replicated in samples of early-onset adolescent drinkers ( Conrod et al., 2006 ) and anxiety-sensitive college students ( Watt et al., 2006 ). Since the personality-targeted approach mainly addresses the management of personality risk, rather than specifically managing substance misuse, many of these trials also showed that concurrent mental health symptoms were reduced by the intervention, in addition to problematic substance use behaviours ( Castellanos-Ryan & Conrod, 2006 ; O’Leary-Barrett et al., 2013 ; Olthuis et al., 2015 ; Watt et al., 2006 ). Furthermore, as these traits have been shown to be highly predictive of adolescent-onset substance use, misuse, and problems (see Castellanos-Ryan et al., 2013 ), the personality-targeted approach has also been shown to be a highly effective strategy for preventing substance misuse and concurrent emotional and behavioral problems among high-risk youth (Conrod et al., 2008 , 2010 , 2011 , 2013 ; Mahu et al., 2015 ; O’Leary-Barrett et al., 2010 ; 2013 ). This approach has proven to be effective when delivered in different cultural and educational contexts as well (e.g., Lammers et al., 2011 and Newton et al., 2016 ).
This novel treatment model shows great promise as both an effective model for detection and prevention of substance related problems in youth, as well as an effective model to personalize interventions, while maintaining their brevity for active substance misusers. The interventions also have the advantage of addressing concurrent mental health and personality factors that are known to maintain many substance use problems, and complicate their treatment. Furthermore, because the intervention approach does not directly target substance use behaviors, but rather risk factors for such behaviors, the approach can be easily adapted to the context of early intervention or prevention as well as the relapse prevention stage, and can address all forms of substance misuse associated with a particular personality trait, rather than having to focus on one target behavior.
Concluding Remarks
It is clear that there are many readily available, effective CBT treatments for substance abusing clients. This chapter reviewed several CBT interventions targeting substance misuse, including RP, MBRP, CRA, GSC, BCT, and personality-targeted interventions. The relapse prevention model applies cognitive behavioral strategies to help substance users achieve and maintain sobriety.
The GSC model seems to be best suited for non-severe substance users, and its four-session model makes it an excellent choice for time-efficient first-line care for SUD. Although GSC is efficient, this model cannot serve as the sole line of treatment for substance use problems, given that non-responders do not benefit from additional sessions of GSC.
For clients and partners struggling with substance use, BCT is a worthwhile treatment to consider. It has been recognized as an evidence-based treatment by the American Psychological Association’s 12th Division. Considering the empirical support for BCT in the domain of alcoholism, it is now more urgent than ever to verify its effectiveness for individuals misusing other substances.
For clients facing professional, intimate, and social difficulties associated with substance misuse, the multimodal approach proposed by the CRA model is also very promising. Due to the variety of possible approaches, this treatment can be tailored to best fit clients’ immediate needs. The CRAFT module is an innovative way of reaching and providing support for substance using clients through their significant others, especially for treatment refusing clients who would probably be inaccessible to clinicians with conventional treatment recruitment methods.
MBRP is an innovative treatment in the domain of SUD and the field of addiction in general. Integrating mindfulness meditation with cognitive therapy gives a novel approach to relapse prevention, which usually promotes the avoidance of situations likely to trigger relapses. MBRP does this as well, but through the lens of mindfulness, which can help substance users develop strategies to manage cravings and distress and might provide alternatives to avoiding triggers. Despite the encouraging evidence for MBRP, we would like to point out that the mindfulness exercises may not be suited to certain clients who are unable to engage in meta-cognition or exert control in high-risk situations.
Personality-targeted CBT is a newer adaptation of the CBT model, and it might be particularly helpful when attempting to prevent onset of substance abuse with young adolescents or when addressing concurrent psychiatric problems with adult substance abusing clients.
Each program tackles SUDs in a different way, but, despite obvious differences in their approaches, these models all seem to share the same logic: orienting clients towards a meaningful goal, teaching necessary skills to successfully achieve the goal, and establishing plans to face potential relapses. Given the coherence in these concepts, it is possible that these treatment models can be integrated, which could hopefully lead to a unified program based on the best components each model has to offer.
In terms of treatment efficacy, it is difficult to state whether one intervention is definitively better than another. Considering the conclusions drawn from project MATCH, it is unlikely that CBT treatments differ in any measurable way. Perhaps there is truth is Imel and colleagues’ (2008) remark that most psychotherapies, if conducted in good faith, generate similar outcomes for most alcohol misusing clients. The choice for an appropriate treatment model boils down to the client’s specific needs and the availability of qualified psychotherapists ready to implement these treatments.
Although CBT interventions have demonstrated utility in treating SUDs, for the most part, they have yet to be tested on clients suffering from comorbid disorders. In fact, none of the treatment models described here have developed specific methods tailored to dual diagnosis (i.e., patients with both SUDs and other psychiatric conditions). However, there is some evidence from the MBRP and personality-targeted approaches that concurrent mental health symptoms are affected by these interventions ( Witkiewitz & Bowen, 2010 ; O’Leary-Barrett et al., 2013 ; Olthuis et al., 2015 ). Conrod and Stewart (2005) also observed that few programs seemed to effectively treat dual-diagnosis clients, and those that did show effectiveness targeted depression, which reasserts the hypothesis that CBT for depression and substance use have a conceptual overlap. Moreover, O’Leary-Barrett et al. (2013) showed in an evaluation of the specificity of different personality-targeted interventions that reduction of depression symptoms resulted from brief CBT interventions, regardless of the focus of the interventions, whereas the reduction of conduct problems was only observed in individuals who received interventions targeting impulsivity.
Other well-established treatment models exist to address mental health problems and substance use comorbidity. For example, the Seeking Safety Program, which addresses PTSD and substance use problems, has been shown to be effective in reducing both PTSD symptoms and substance use outcomes. This evidence-based program emphasizes the need for clients to develop a safer lifestyle than the one they were leading before seeking treatment.
Considering the high prevalence of people with substance use problems and mental health difficulties, future research in CBT for SUDs should focus on the development of models that can address the needs of clients with comorbid disorders, and strive to integrate intervention components from various models to provide clients with the best care possible.
Finally, the CBT model does appear to be moderately effective in helping substance using clients reduce their substance use, when tested under rigorous experimental conditions. What is also needed are larger implementation trials to investigate the environmental, social, and clinical conditions that most facilitate the effective implementation of these interventions to patients living in the community in the most cost-effective way. Newer studies are demonstrating that brief interventions for alcohol problems can be delivered over the Web and on average produce small effects on drinking behavior and problems. Higher intensity interventions based on the RP model (e.g., CBT4CBT) have been adapted for Web-based self-guided administration and have been shown to be effective compared to standard care in reducing substance use problems. However, this research is in its infancy and will require larger and more rigorous trials to determine if, and for whom, such Web-based interventions can achieve the same effectiveness as face-to-face therapies (see review by Carroll, 2014 ).
American Psychiatric Association. ( 2013 ). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: APA.
Google Scholar
Google Preview
Amir, N. , Weber, G. , Beard, C. Bomyea, J. , & Taylor, C. T. ( 2008 ). The effect of a single-session attention modification program on response to a public-speaking challenge in socially anxious individuals. Journal of Abnormal Psychology , 117 (4), 860–868.
Andréasson, S. , Hansagi, H. , & Österlund, B. ( 2002 ). Short-term treatment for alcohol-related problems: Four-session guided self-change versus one session of advice—a randomized, controlled trial. Alcohol , 28 , 57–62.
Ayala, H. E. , Echeverria, L. , Sobell, M. B. , & Sobell, L. C. ( 1998 ). Una alternativa de intervencin breve y temprana parabebedores problema en Mexico [An early and brief intervention alternative for problem drinkers in Mexico]. Acta Comportamentalia , 6 , 71–93.
Azrin, N. H. ( 1976 ). Improvements in the community-reinforcement approach to alcoholism. Behavior Research and Therapy , 14 (5), 339–348.
Azrin, N. H. , Sisson, R. W. , Meyers, R. J. , & Godley, M. D. ( 1982 ). Outpatient alcoholism treatment by community reinforcement and disulfiram therapy. Journal of Behavior Therapy and Experimental Psychiatry , 13 , 105–112.
Babor, T. F. , Ritson, E. B. & Hodgson, R. J. ( 1986 ). Alcohol-related problems in the primary health care setting: a review of early intervention strategies. British Journal of Addiction , 81 (1), 23–46.
Bien, T. H. , Miller, W. R. & Tonigan, J. S. ( 1993 ). Brief interventions for alcohol problems: a review. Addiction , 88 , 315–336.
Bickel, W. K. , Amass, L. , Higgins, S. T. , Badger, G. J. , & Esch, R. A. ( 1997 ). Effects of adding behavioral treatment to opioid detoxification with buprenorphine. Journal of Consulting and Clinical Psychology , 65 , 803–810.
Bockting, C. L. H. , Schene, A. H. , Spinhoven, P. , Koeter, M. W. J. , Wouters, L. F. , Huyser, J. , & Kamphuis, J. H. ( 2005 ). Preventing relapse/recurrence in recurrent depression with cognitive therapy: A randomized controlled trial. Journal of Consulting and Clinical Psychology , 73 (4), 647–657.
Bowen, S. , & Marlatt, G. A. ( 2009 ). Surfing the urge: Brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors , 666–671.
Bowen, S. Witkiewitz, K. , Dillworth, T. M. , & Marlatt, G. A. ( 2007 ). The role of thought suppression in the relationship between mindfulness meditation and substance use. Addictive Behaviors , 32 , 2324–2328.
Bowen, S. , Chawla, N. , & Marlatt, G. A. ( 2010 ). Mindfulness-Based Relapse Prevention for the Treatment of Substance Use Disorders: A Clinician’s Guide . New York: Guilford Press.
Bowen, S. , Chawla, N. , Collins, S. , Witkiewitz, K. , Hsu, S. , Grow, J. , … Marlatt, A. ( 2009 ). Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse , 30 , 205–305.
Bowen, S. , Witkiewitz, K. , Clifasefi, S. L. , Grow, G. , Chawla, N. , Hsu, S. H. , … Larimer, M. E. ( 2014 ). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry , 71 (5), 547–556.
Bowen, S. , Witkiewitz, K. , Dillworth, T. M. , Chawla, N. , Simpson, T. L. , Ostafin, B. , … Marlatt, G. A. ( 2006 ). Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors , 20 , 343–347.
Bowers, T. G. , & al-Redha, M. R. ( 1990 ). A comparison of outcome with group/marital and standard/individual therapies with alcoholics. Journal of Studies in Alcohol , 51 (4), 301–309.
Breslin, F. C. , Sobell, M. B. , Sobell, L. C. , Cunningham, J. A. , Sdao-Jarvie, K. , & Borsoi, D. ( 1999 ). Problem drinkers: Evaluation of a stepped care approach. Journal of Substance Abuse , 10 , 217–232.
Budney, A. J. , Moore, B. A. , Rocha, H. L. , & Higgins, S. T. ( 2006 ). Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. Journal of Consulting and Clinical Psychology , 74 , 307–316.
Carroll, K. M. ( 1998 ). A Cognitive-Behavioral Approach: Treating Cocaine Addiction . Rockville, MD: NIDA.
Carroll, K. M. ( 2014 ). Computerized cognitive-behavioral therapy. Alcohol Research Current Reviews , 36 (1), 12–130.
Castellanos-Ryan, N. , & Conrod, P. J. ( 2006 ). Brief interventions targeting personality risk factors for adolescent substance misuse reduce depression, panic and risk-taking behaviors. Journal of Mental Health , 15 (6), 645–658.
Castellanos-Ryan, N. , O’Leary-Barrett, M. , Sully, L. , & Conrod, P. ( 2013 ). Sensitivity and specificity of a brief personality screening instrument in predicting future substance use, emotional, and behavioral problems: 18-month predictive validity of the Substance Use Risk Profile Scale. Alcoholism, Clinical and Experimental Research , 37 (Suppl 1), E281–E290.
Castellanos-Ryan, N. , Rubia, K. , Conrod. P. J. ( 2011 ). Response inhibition and reward response bias mediate the predictive relationships between impulsivity and sensation seeking and common and unique variance in conduct disorder and substance misuse. Alcoholism, Clinical and Experimental Research , 35 (1), 140–155.
Chiesa, A. , Serretti, A. ( 2014 ). Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use and Misuse , 49 (1), 492–512.
Conrod, P. J. , & Stewart, S. H. ( 2005 ). A critical look at dual-focused cognitive-behavioral treatments for comorbid substance use and psychiatric disorders: Strengths, limitations and future directions. Journal of Cognitive Psychotherapy , 19 (3), 261–284.
Conrod, P. J. , & Nikolaou, K. ( 2016 ). Annual Research review: On the developmental neuropsychology of substance use disorders. Journal of Child Psychology and Psychiatry , 57 (3), 371–394.
Conrod, P. J. , Castellanos, N. , & Mackie, C. ( 2008 ). Personality-targeted interventions delay the growth of adolescent drinking and binge drinking. Journal of Child Psychology and Psychiatry , 49 (2), 181–190.
Conrod, P. J. , Castellanos, N. , & Mackie, C. ( 2011 ). Long-term effects of a personality-targeted intervention to reduce alcohol use in adolescents. Journal of Consulting and Clinical Psychology , 79 (3), 296–306.
Conrod, P. J. , Castellanos-Ryan, N. , & Strang, J. ( 2010 ). Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Archives of General Psychiatry , 67 (1), 85–93.
Conrod, P. J. , O’Leary-Barrett, M. , Newton, N. , Topper, L. , Castellanos-Ryan, N. , Mackie, C. , & Girard, A. ( 2013 ). Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA Psychiatry , 70 (3), 334–342.
Conrod, P. J. , Stewart, S. H. , Comeau, N. , & Maclean, A. M. ( 2006 ). Efficacy of cognitive-behavioral interventions targeting personality risk factors for youth alcohol misuse. Journal of Clinical Child & Adolescent Psychology , 35 (4), 550–563.
Conrod, P. J. , Stewart, S. H. , Pihl, R. O. , Côté, S. , Fontaine, V. , & Dongier, M. ( 2000 ). Efficacy of brief coping skills interventions that match different personality profiles of female substance abusers. Psychology of Addictive Behaviors , 14 (3), 231–242.
Cooney, N. L. , Kadden, R. M. , Litt, M. D. , & Getter, H. ( 1991 ). Matching alcoholics to coping skills or interactional therapies: Two-year followup results. Journal of Consulting and Clinical Psychology , 59 , 598–601.
Dennis, M. L. , Godley, S. H. , Diamond, G. , Tims, F. M. , Babor, T. , Donaldson, J. , … Funk, R. ( 2004 ). The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment , 27 , 197–213.
Dutra, L. , Stathopoulou, G. , Basden, S. L. , Leyro, T. M. , Powers, M. B. , & Otto, M. W. ( 2008 ). A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry , 165 , 179–187.
Edwards, G. , & Taylor, C. ( 1994 ). A test of the matching hypothesis: Alcohol dependence, intensity of treatment, and 12-month outcome. Addiction , 89 (5), 553–561.
Edwards, G. , Orford, J. , Egert, S. , Guthrie, S. , Hawker, A. , Hensman, C. , … Taylor, C. ( 1977 ). Alcoholism: A controlled trial of “treatment” and “advice. ” Journal of Studies on Alcohol , 38 (5), 1004–1031.
Epstein, E. E. , & McCrady, B. S. ( 1998 ). Behavioral couples treatment of alcohol and drug use disorders: Current status and innovations. Clinical Psychology Review , 18 , 689–711.
Floyd, R. L. , Sobell, M. , Velasquez, M. M. , Ingersoll, K. , Nettleman, M , Sobell, L. , … on behalf of the Project CHOICES Efficacy Study Group ( 2007 ). Preventing alcohol-exposed pregnancies: A randomized controlled trial. American Journal of Preventive Medicine , 32 (1), 1–10.
Garety, P. A. , Fowler, D. G. , Freeman, D. , Bebbington, P. , Dunn, G. , & Kuipers, E. ( 2008 ). Cognitive-–behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: Randomised controlled trial. The British Journal of Psychiatry , 192 (6), 412–423.
Godley, S. H. , Garner, B. R. , Smith, J. E. , Meyers, R. J. , & Godley, M. D. ( 2011 ). A large-scale dissemination and implementation model for evidence-based treatment and continuing care. Clinical Psychology: Science and Practice , 18 , 67–83.
Godley, S. H. , Meyers, R. J. , Smith, J. E. , Karniven, T. , Titus, J. C. , Godley, M. D. , … Kelberg, P. ( 2001 ). The Adolescent Community Reinforcement Approach for Adolescent Cannabis Users: Cannabis Youth Treatment (CYT) Series, Vol. 4 (DHHS Publication No. 01-3489). Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration.
Goetzel, R. Z. , Hawkins, K. , & Ozminkowski, R. J. ( 2003 ). The health and productivity cost burden of the “top 10” physical and mental conditions affecting six large U.S. employers in 1999. Journal of Occupational Environmental Medicine , 45 , 5–14.
Healthy Lifestyles Guided Self-Change Program. (2014, July 8). Retrieved from http://www.nova.edu/gsc/ .
Heeren, A. , Lievens, L. , & Philippot, P. ( 2011 ). How does attention training work in social phobia: Disengagement from threat or re-engagement to non-threat? Journal of Anxiety Disorders , 25 (8), 1108–1115.
Higgins, S. T. , Budney, A. J. , Bickel, W. K. , Hughes, J. R. , Foerg, F. , & Badger, G. ( 1993 ). Achieving cocaine abstinence with a behavioral approach. American Journal of Psychiatry , 150 , 763–769.
Higgins, S. T. , Sigmon, S. C. , Wong, C. J. , Heil, S. H. , Badger, G. J. , Donham, R. , … Anthony, S. ( 2003 ). Community reinforcement therapy for cocaine-dependent outpatients. Archives of General Psychiatry , 60 , 1043–1052.
Hunt, G. M. , & Azrin, N. H. ( 1973 ). A community-reinforcement approach to alcoholism. Behavior Research and Therapy , 11 (1), 91–104.
Imel, Z. E. , Wampold, B. E. , Miller, S. D. , & Reg, R. ( 2008 ). Distinctions without a difference: Direct comparisons of psychotherapies for alcohol use disorders. Psychology of Addictive Behaviors , 22 (4), 533–543.
Kabat-Zinn, J. ( 2003 ). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science & Practice 10 (2), 144–156.
Kadden, R. M. , Cooney, N. L. , Getter, H. , & Litt, M. D. ( 1989 ). Matching alcoholics to coping skills or interactional therapies: Posttreatment results. Journal of Consulting and Clinical Psychology , 57 , 698–704.
Kadden, R. , Carroll, K. , Donovan, D. , Cooney, N. , Monti, P. , Abrams, D. , … Hester, R. ( 1992 ). Cognitive-Behavioral Coping Skills Therapy Manual: A Clinical Research Guide for Therapists Treatment Individuals with Alcohol Abuse and Dependence . Washington, D.C.: NIAAA Project MATCH Monigraph Series.
Kadden, R. , Carroll, K. , Donovan, D. , Cooney, N. , Monti, P. , Abrams, D. , … Mattson, M. E. ( 2003 ). Volume 3: Cognitive-Behavioral Coping Skills Therapy Manual, a Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence . Rockville, MD: National Institute on Alcohol Abuse and Alcoholism Project MATCH Monograph Series.
Keller, M. (Ed.). ( 1974 ). Trends in treatment of alcoholism. In Second Special Report to the U.S. Congress on Alcohol and Health (pp. 111–128). Washington, DC: Department of Health, Education, and Welfare.
Kessler, R. C. ( 2004 ). The epidemiology of dual diagnosis. Biological Psychiatry , 56 (10), 730–737.
Kessler, R. C. , Nelson, C. B. , McGonagle, K. A. , Lui, J. , Swartz, M. , & Blazer, D. G. ( 1996 ). Comorbidity of DSM-III-R major depressive disorder in the general population: Results from the National Comorbidity Survey. British Journal of Psychiatry , 168 , 17–30.
Kirby, K. C. , Marlowe, D. B. , Festinger, D. S. , Garvey, K. A. , & LaMonaca, V. ( 1999 ). Community reinforcement training for family and significant others of drug abusers: A unilateral intervention to increase treatment entry of drug users. Drug and Alcohol Dependence , 56 (1), 85–96.
Lai, H. M. X. , Cleary, M. , Sitharthan, T. , Hunt, G. E. ( 2015 ). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence , 154 , 1–13.
Lammers, J. , Goossens, F. , Lokman, S. , Monshouwer, K. , Lemmers, L. , Conrod, P. J. , … Kleinjan, M. ( 2011 ). Evaluating a selective prevention programme for binge drinking among young adolescents: Study protocol of a randomised controlled trial. BMC Public Health , 11 , 126–134.
Longabaugh, R. , Wirtz, P. W. , Mattson, M. E. , & Myers, J. K. ( 2001 ). Volume 8: Project MATCH Hypotheses: Results and Causal Chain Analyses . Rockville, MD: National Institute on Alcohol Abuse and Alcoholism Project MATCH Monograph Series.
Lozano-Blanco, C. , Sobell, L. C. , & Ayala, H. V. ( 2002 ). Diseminación del modelo de tratamiento autocambio dirigido para bebedores excesivos del alcohol en instituciones de salud de México [Dissemination of the guided self-change model of treatment in medical settings in Mexico]. Revisita Mexicana Latinoamericana de Psicologia , 34 (3), 259–273.
Magill, M. , & Ray, L. A. ( 2009 ). Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs , 70 , 516–527.
Mahu, I. T. , Doucet, C. , O'Leary-Barrett, M. , & Conrod, P. J. ( 2015 ). Can cannabis use be prevented by targeting personality risk in schools? Twenty-four-month outcome of the adventure trial on cannabis use: A cluster-randomized controlled trial. Addiction , 110 (10), 1625–1633.
Marlatt, G. A. , & Donovan, D. M. ( 2005 ). Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors (2nd ed.). New York: Guilford Press.
Marlatt, G. A. , & Gordon, J. R. (Eds.). ( 1985 ). Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York: Guilford Press.
McCrady, B. S. , & Epstein, E. E. ( 2009 ). Overcoming Alcohol Problems: A Couples-Focused Program . New York: Oxford University Press.
McCrady, B. S. , Epstein, E. E. , Cook, S. , Jensen, N. & Hildebrandt, T. ( 2009 ). A randomized trial of individual and couple behavioral alcohol treatment for women. Journal of Consulting and Clinical Psychology , 77 (2): 243–256.
McCrady, B. S. , Noel, N. E. , Stout, R. L. , Abrams, D. B. , & Nelson, H. F. ( 1991 ). Effectiveness of three types of spouse involved behavioural alcoholism treatment: Outcome 18 months after treatment. British Journal of Addictions , 86 , 1415–1424.
Meyers, R. J. & Smith, J. E. ( 1995 ). Clinical Guide to Alcohol Treatment: The Community Reinforcement Approach. New York, NY: Guilford Press.
Meyers, R. J. , Miller, W. R. , Hill, D. E. , & Tonigan, J. S. ( 1999 ). Community reinforcement and family training (CRAFT): Engaging unmotivated drug users in treatment. Journal of Substance Abuse , 10 (3), 291–308.
Meyers, R. J. , Miller, W. R. , Smith, J. E. , & Tonigan, J. S. ( 2002 ). A randomized trial of two methods for engaging treatment-refusing drug users through concerned significant others. Journal of Consulting and Clinical Psychology , 70 , 1182–1185.
Meyers, R. J. , Smith, J. E. , & Waldorf, V. A. ( 1999 ). Application of the Community Reinforcement Approach. In E. Dowd & L. Rugle (Eds.), Comparative Treatments of Substance Abuse (pp. 210–233). New York: Springer Publishing Company.
Miller, W. R. , & Rollnick, S. ( 1991 ). Motivational Interviewing: Preparing People to Change Addictive Behavior . New York: Guilford Press.
Miller, W. R. ( 1985 ). Motivation for treatment: A review with special emphasis on alcoholism. Psychological Bulletin , 98 , 84–107.
Miller, W. R. ( 1987 ). Techniques to modify hazardous drinking patterns. Recent Development in Alcohol , 5 , 425–438.
Miller, W. R. , & Hester, R. K. ( 1986 ). Inpatient alcoholism treatment: Who benefits? American Psychologist , 41 (7), 794–805.
Miller, W. R. , Meyers, R. J. & Tonigan, S. ( 1999 ). Engaging the Unmotivated in Treatment for Alcohol Problems: A Comparison of Three Strategies for Intervention Through Family Members. Journal of Consulting and Clinical Psychology , 67 (5), 688–697.
Miller, W. R. , Meyers, R. J. , Tonigan, J. S. , & Grant, K. A. ( 2001 ). Community reinforcement and traditional approaches: Findings of a controlled trial. In R. Meyers & W. Miller (Eds.), A Community Reinforcement Approach to Addiction Treatment (pp. 79–103). Cambridge, UK: University Press.
Mindfulness-Based Relapse Prevention (MBRP). Retrieved from http://www.mindfulrp.com/ .
Monti, P. M. , Abrams, D. B. , Kadden, R. M. , & Cooney, N. L. ( 1989 ). Treating Alcohol Dependence: A Coping Skills Training Guide . New York: Guilford Press.
Newton, N. C. , Barrett, E. L. , Castellanos-Ryan, N. , Kelly, E. , Champion, K. E. , Stapinski, L. , … Teesson, M. ( 2016 ). The validity of the Substance Use Risk Profile Scale (SURPS) among Australian adolescents. Addictive Behaviors , 53 , 23–30.
O’Farrell, T. J. , Choquette, K. A. , Cutter, H. S. G. , Floyd, F. J. , Bayog, R. D. , Brown, E. D. , … Deneault, P. ( 1996 ). Cost–benefit and cost-effectiveness analyses of behavioral marital therapy as an addition to outpatient alcoholism treatment. Journal of Substance Abuse , 8 , 145–166.
O’Farrell, T. J. , Cutter, H. S. G. , Choquette, K. A. , Floyd, F. J. , & Bayog, R. D. ( 1992 ). Behavioral marital therapy for male alcoholics: Marital and drinking adjustment during the two years after treatment. Behavior Therapy , 23 , 529–549.
O'Leary-Barrett, M. , Mackie, C. J. , Castellanos-Ryan, N. , Al-Khudhairy, N. , & Conrod, P. J. ( 2010 ). Personality-targeted interventions delay uptake of drinking and decrease risk of alcohol-related problems when delivered by teachers. Journal of the American Academy of Child and Adolescent Psychiatry , 49 (9), 954–963.
O'Leary-Barrett, M. , Topper, L. , Al-Khudhairy, N. , Pihl, R. O. , Castellanos-Ryan, N. , Mackie, C. J. , & Conrod, P. J. ( 2013 ). Two-year impact of personality-targeted, teacher-delivered interventions on youth internalizing and externalizing problems: A cluster-randomized trial. Academy of Child and Adolescent Psychiatry , 52 (9), 911–920.
Olthuis, J. V. , Watt, M. C. , Mackinnon, S. P. , & Stewart, S. H. ( 2015 ). CBT for high anxiety sensitivity: Alcohol outcomes. Addictive Behaviors , 46 , 19–24.
Peer, K. , Rennert, L. , Lynch, K. G. , Farrer, L. , Gelernter, J. , & Kranzler, H. R. ( 2013 ). Prevalence of DSM-IV and DSM-5 alcohol, cocaine, opioid and cannabis use disorders in a largely substance dependent sample. Drug and Alcohol Dependence , 127 (1–3), 215–219.
Project MATCH Research Group. ( 1998 ). Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism: Clinical and Experimental Research , 22 , 1300–1311.
Rioux, C. , Castellanos-Ryan, N. , Parent, S. , & Séguin, J. R. ( 2016 ). The interaction between temperament and the family environment in adolescent substance use and externalizing behaviors: Support for diathesis-stress or differential susceptibility? Developmental Review , 40 , 117–150.
Roozen, H. G. , de Waart, R. , & van der Kroft, P. ( 2010 ). Community reinforcement and family training: An effective option to engage treatment-resistant substance-abusing individuals in treatment. Addiction , 105 (10), 1729–1738.
Sanderson, K. , & Andrews, G. ( 2002 ). Prevalence and severity of mental health-related disability and relationship to diagnosis. Psychiatric Services , 53 (1), 80–86.
Scott, J. , Colom, F. , & Vieta, E. ( 2007 ). A meta-analysis of relapse rates with adjunctive psychological therapies compared to usual psychiatric treatment for bipolar disorders. The International Journal of Neuropsychopharmacology , 10 (1), 123–129.
Segal, Z. V. , Teasdale, J. D. , & Williams, J. M. ( 2004 ). Mindfulness-based cognitive therapy: Theoretical rationale and empirical status. In S. C. Hayes , V. M. Follette , & M. M. Linehan (Eds.), Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition (pp. 45–65). New York: Guilford Press.
Slesnick, N. , Prestopnik, J. L. , Meyers, R. J. , & Glassman, M. ( 2007 ). Treatment outcome for street-living, homeless youth. Addictive Behavior , 32 (6), 1237–1251.
Smith, J. E. , Meyers, R. J. , & Austin, J. L. ( 2008 ). Working with family members to engage treatment-refusing drinkers: The CRAFT program. Alcoholism Treatment Quarterly , 26 , 169–193.
Smith, J. E. , Meyers, R. J. , & Delaney, H. D. ( 1998 ). Community reinforcement approach with homeless alcohol-dependent individuals. Journal of Consulting and Clinical Psychology , 66 , 541–548.
Sobell, L. C. , Sobell, M. B. , & Agrawal, S. ( 2009 ). Randomized controlled trial of a cognitive-behavioral motivational intervention in a group versus individual format for substance use disorders. Psychology of Addictive Behaviors , 23 (4), 672–683.
Sobell, L. C. , Sobell, M. B. , Brown, J. , & Cleland, P. A. (1995). A randomized trial comparing group versus individual guided self-change treatment for alcohol and drug abusers. Poster presented at the 29th Annual Meeting of the Association for Advancement of Behavior Therapy, Washington, DC.
Sobell, M. B. , & Sobell, L. C. ( 1993 ). Problem Drinkers: Guided Self-Change Treatment . New York: Guilford Press.
Sobell, M. B. & Sobell, L. C. ( 2005 ). Guided Self-Change Treatment for Substance Abusers. Journal of Cognitive Psychotherapy , 19 (3), 199–210.
Sobell, M. B. , Sobell, L. C. , & Leo, G. I. ( 2000 ). Does enhanced social support improve outcomes for problem drinkers in guided self-change treatment? Journal of Behavior Therapy & Experimental Psychiatry , 31 (1), 41–54.
Stewart, S. H. , & Conrod, P. J. ( 2008 ). Anxiety disorder and substance use disorder co-morbidity: Common themes and future directions. In M. M. Antony (Ed.), Series in Anxiety and Related Disorders (pp. 239–257). New York: Springer.
The National Center on Addiction and Substance Abuse at Columbia University (CASA). ( 2010 ). National Survey of American Attitudes on Substance Abuse XV: Teens and Parents. New York, NY: CASA.
Watt, M. , Stewart, S. , Birch, C. , & Berner, D. ( 2006 ). Brief CBT for high anxiety sensitivity decreases drinking problems, relief alcohol outcome expectancies, and conformity drinking motives: Evidence from a randomized controlled trial. Journal of Mental Health , 15 , 683–695.
WHO. ( 2014 ). Global Status Report on Alcohol and Health . Geneva: World Health Organization.
Witkiewitz, K. , & Bowen, S. ( 2010 ). Depression, craving and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology , 78 , 362–374.
Witkiewitz, K. , Greenfield, B. L. , & Bowen, S. ( 2013 ). Mindfulness-based relapse prevention with racial and ethnic minority women. Addictive Behaviors , 38 (12), 2821–2824.
Witkiewitz, K. , Marlatt, G. A. & Walker, D. ( 2005 ). Mindfulness based relapse prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy , 19 , 211–228.
Woicik, P. A. , Stewart, S. H. , Pihl, R. O. , & Conrod, P. J. ( 2009 ). The substance use risk profile scale: A scale measuring traits linked to reinforcement-specific substance use profiles. Addictive Behaviors , 34 (12), 1042–1055.
Zvolensky, M. J. , Stewart, S. H. , Vujanovic, A. A. , Gavric, D. , & Steeves, D. ( 2008 ). Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine and Tobacco Research , 11 (3), 323–331.
For Further Reading
Epstein, E. E. , & McCrady, B. S. ( 2002 ). Couple therapy in the treatment of alcoholism. In A. S. Gurman & N. Jacobson (Eds.), Clinical Handbook of Marital Therapy (3rd ed., pp. 597–628). New York: Guilford Publications.
McCrady, B. S. , & Epstein, E. E. ( 2009 ). Overcoming Alcohol Problems: Workbook for Couples . New York: Oxford University Press.
Pattison, E. M. , Sobell, M. B. , & Sobell, L. C. ( 1977 ). Emerging Concepts of Alcohol Dependence . New York: Springer.
Powers, M. B. , Vedel, E. , & Emmelkamp, P. M. G. ( 2008 ). Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical Psychology Review , 28 (6), 952–962.
Witkiewitz, K. , & Villarroel, N. A. ( 2009 ). Dynamic association between negative affect and alcohol lapses following alcohol treatment. Journal of Consulting and Clinical Psychology , 77 (4), 633–644.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 05 April 2024
Substance use patterns, sociodemographics, and health profiles of harm reduction service recipients in Burlington, Vermont
- Tyler G. Erath 1 , 2 ,
- Rosalie LaCroix 3 ,
- Erin O’Keefe 3 ,
- Stephen T. Higgins 1 , 2 , 4 &
- Richard A. Rawson 1 , 2 , 4
Harm Reduction Journal volume 21 , Article number: 76 ( 2024 ) Cite this article
162 Accesses
Metrics details
Understanding current substance use practices is critical to reduce and prevent overdose deaths among individuals at increased risk including persons who use and inject drugs. Because individuals participating in harm reduction and syringe service programs are actively using drugs and vary in treatment participation, information on their current drug use and preferred drugs provides a unique window into the drug use ecology of communities that can inform future intervention services and treatment provision.
Between March and June 2023, 150 participants in a harm reduction program in Burlington, Vermont completed a survey examining sociodemographics; treatment and medication for opioid use disorder (MOUD) status; substance use; injection information; overdose information; and mental health, medical, and health information. Descriptive analyses assessed overall findings. Comparisons between primary drug subgroups (stimulants, opioids, stimulants-opioids) of past-three-month drug use and treatment participation were analyzed using chi-square and Fisher’s exact test.
Most participants reported being unhoused or unstable housing (80.7%) and unemployed (64.0%) or on disability (21.3%). The drug with the greatest proportion of participants reporting past three-month use was crack cocaine (83.3%). Fentanyl use was reported by 69.3% of participants and xylazine by 38.0% of participants. High rates of stimulant use were reported across all participants independent of whether stimulants were a participant’s primary drug. Fentanyl, heroin, and xylazine use was less common in the stimulants subgroup compared to opioid-containing subgroups ( p < .001). Current- and past-year MOUD treatment was reported by 58.0% and 77.3% of participants. Emergency rooms were the most common past-year medical treatment location (48.7%; M = 2.72 visits).
Conclusions
Findings indicate high rates of polysubstance use and the underrecognized effects of stimulant use among people who use drugs—including its notable and increasing role in drug-overdose deaths. Crack cocaine was the most used stimulant, a geographical difference from much of the US where methamphetamine is most common. With the increasing prevalence of fentanyl-adulterated stimulants and differences in opioid use observed between subgroups, these findings highlight the importance and necessity of harm reduction interventions (e.g., drug checking services, fentanyl test strips) and effective treatment for individuals using stimulants alongside MOUD treatment.
In 2021, an estimated 106,699 drug-involved overdose deaths occurred in the United States (US), a record-high and astonishing twofold increase from 52,404 deaths in 2015 [ 1 , 2 ]. Much of the current overdose epidemic is driven by a rise in synthetic opioids such as illicitly manufactured fentanyl, a contributor to approximately 71,000 deaths in 2021 [ 2 , 3 ]. However, psychomotor stimulants including cocaine and methamphetamine are also contributing to record numbers of unintentional poisonings and overdose deaths, both alone and in combination with fentanyl, dramatically rising from approximately 12,000 deaths in 2015 to over 53,000 deaths in 2021 [ 2 , 3 , 4 ].
These recent data indicate a “fourth wave” of the overdose crisis wherein co-occurring use of fentanyl and stimulants is a primary contributor to overdose deaths [ 5 , 6 ]. Indeed, underpinning this public health crisis are differences in the most used polysubstance combinations, which vary by geographic location and rurality. For example, whereas national data indicate that co-use of methamphetamine and fentanyl is the most common drug combination found in overdose deaths in much of the US, cocaine and fentanyl is the most common combination in the northeastern US [ 5 , 7 ].
The provision of harm reduction services is a primary component of addressing the ongoing overdose epidemic, as indicated by its inclusion in the Biden-Harris Administration’s approach to substance use and the U.S. Department of Health and Human Services Overdose Prevention Strategy [ 8 ]. Syringe service programs (SSPs) are community-based programs that provide a range of harm reduction services [ 9 ]. Since their initial creation to help reduce and prevent the transmission of blood-borne infectious diseases (e.g., human immunodeficiency virus [HIV], hepatitis C virus [HCV]), SSPs have expanded to offer many harm reduction services and evidence-based interventions now commonly alongside providing sterile syringes for people who use drugs (PWUD). These additional services often include overdose education and naloxone distribution, case management and counseling, adulterant test strips (e.g., fentanyl, xylazine), safer smoking supplies, and referrals and linkage to substance use treatment, medical care, and mental health treatment among others [ 10 , 11 , 12 , 13 , 14 ]. The provision of medication for opioid use disorder (MOUD) is another emerging service with 32% of SSPs from the National SSP Evaluation Survey ( n = 158 SSPs) offering on-site treatment in 2021 [ 15 ].
Amidst an everchanging drug landscape, understanding of current substance use practices is important to reduce and prevent overdose deaths—both in general and among individuals who are at an increased risk for overdose and other drug-related harms, such as persons who inject drugs (PWID) in particular [ 16 , 17 ]. SSPs are an ideal setting to inquire about current substance use practices, as their “low barrier” approach is well-liked, offering non-judgmental services and supports for individuals who often face stigma in other healthcare settings [ 16 , 18 ]. Because most individuals who receive services at SSPs are actively using drugs and vary in treatment and recovery service participation, collecting information on their current drug use provides a unique window into the drug use ecology of communities. The goal of this observational study was to inform future intervention services and treatment provision by assessing drug use practices, sociodemographics, and health profiles of individuals participating in a low-barrier, community-based SSP in Burlington, Vermont that also provides a range of other harm reduction services and on-site MOUD treatment. A primary focus was to examine how one’s primary (i.e., preferred) drug affected drug-use practices, treatment participation, and other related findings.
Study participants and setting
The study population consisted of 150 individuals participating in harm reduction services in Burlington, Vermont. Howard Center Safe Recovery is primarily a SSP that provides sterile syringe services and other harm reduction services including free fentanyl and xylazine test strips, Narcan overdose reversal kits, and safer smoking supplies. Other treatment and service programs are also available on-site including low-barrier buprenorphine access, case management, HIV and HCV counseling, drug treatment counseling, and free legal clinics, among others. Safe Recovery is an anonymous program, thus, no identifiable information is collected or stored about participants.
All study procedures were conducted on-site at the SSP. This study was approved by the University of Vermont Institutional Review Board. All data were collected between March and June 2023 by a trained SSP staff member. Individuals participating in services were informed by a SSP staff member about an opportunity to participate in the study. If interested, prospective participants were provided with an information sheet. To protect anonymity, verbal informed consent was obtained from each participant and a consent process documentation form was completed. Individuals who consented to participate in the study were asked to answer a series of questions, described in detail below; all procedures were conducted in a private room. Completion of this study was one-time and accomplished in one visit. To be eligible, participants had to meet the following criteria: (a) be 18 years or older, (b) report past 30-day drug use, and (c) participation in harm reduction services at Safe Recovery. For their time and participation, participants were compensated with a $25 gift card.
The primary data collection instrument was the University of Washington Alcohol and Drug Abuse Institute’s Washington State SSP Health Survey [ 19 , 20 , 21 ]. Areas queried on this structured survey included questions on (a) sociodemographics, housing, and employment status; (b) treatment and MOUD status; (c) substance use; (d) injection information; (e) overdose information; and (f) mental health, medical care, and other health information.
Sociodemographic questions asked about age, race/ethnicity, gender, monthly legal income, and being in jail or prison in the last year. Housing questions included current living situation and housing status. Current employment status was recorded. MOUD status was assessed via questions on current and past-year treatment.
Regarding drug use, participants reported which drug(s) was their primary (i.e., preferred) drug via an open-ended question. Additionally, participants were asked to indicate which drugs they had used in the past three months from the following list: (1) heroin, (2) methamphetamine, (3) methamphetamine and heroin mixed together (i.e., goofball), (4) crack cocaine, (5) powder cocaine, (6) cocaine and heroin mixed together (i.e., speedball), (7) fentanyl (and was it purposeful use?), (8) xylazine, and (9) alcohol. For each drug used, participants reported the route(s) of administration (injected, smoked, snorted) and the number of days used in the past seven days. If the drug was injected, participants also reported the number of days injected in the past week. Percentages for the use of each drug were calculated as the proportion of participants endorsing past-three month use among all participants and the sample size for each subgroup. Percentages for each route of administration were calculated as the proportion of participants endorsing route use among those who reported use of the drug. The average number of days used and injected in the past week was calculated across participants who reported use of the drug.
For participants reporting injection, a series of follow-up questions included the number of people they were picking up syringes for, number of days they picked up syringes from SSP in the past month, age of first injection, number of injections on an average day, number of times a syringe is used before discarded, frequency of being alone when injecting, frequency of injecting in a public place, and any abscesses or skin infections, blood clots, or endocarditis.
Overdose information included the number of past year personal overdoses, past year number of overdoses observed, and use of naloxone/Narcan kit in the past three months. Two mental health questions assessed a participant’s concern for depression and anxiety. Regarding medical information, participants reported their type of health insurance, time of last HIV and HCV test, if they ever had HCV, and if ever treated for HCV. For medical care, participants reported treatment places where services had been received within the past year.
Descriptive statistics and frequency distributions were generated to assess sociodemographics, injection and overdose information, and mental health, health and service utilization. Comparisons between primary drug subgroups of past-three-month use of each drug and treatment participation were analyzed using chi-square and Fisher’s exact test. All analyses were performed using GraphPad Prism 10 (Boston, MA).
Results for all tables and topics are reported for all participants ( n = 150), followed by columns for the subgroups categorized by primary drug. Three subgroups were created based on participant reported primary drug(s); the subgroups include stimulants ( n = 72), opioids ( n = 56), and both stimulants and opioids ( n = 17; hereafter referred to as stimulants-opioids). Five participants who reported alcohol as their primary drug are included in the overall but not the subgroup analyses.
Sociodemographics, housing, employment, and incarceration status
Table 1 contains detailed information on sociodemographics, housing, employment, and incarceration status. The mean age across all participants was approximately 39 years old; 51.3% were male and most were white (90.0%), aligning with state demographics. Most participants were either unhoused (46.0%) or in temporary or unstable housing (34.7%), with 18.7% of participants reporting permanent housing. The most common living situations were alone (38.7%) or with a significant other (34%). For employment, 64.0% of participants were unemployed, 21.3% on disability, and 4.7% indicated full-time work. Forty participants (26.7%) reported being in jail or prison in the last year.
Table 2 contains information on current and past year treatment for all participants and each of the three subgroups with results organized by type of treatment. Regarding MOUD, 87 participants (58.0%) reported current treatment, with 33.3% and 24.7% of participants receiving methadone or buprenorphine/suboxone, respectively. Past-year MOUD treatment was reported by 116 participants (77.3%). There was a statistically significant difference in current buprenorphine/suboxone treatment between the primary drug subgroups ( p = 0.016).
Substance use
Table 3 contains detailed information on drug use for all participants and each subgroup with results organized by drug. The term Used refers to reported use in the past three months.
Stimulants main drug subgroup
Seventy-two participants identified stimulants as their primary drug. Crack cocaine was the primary drug for 45 participants (62.5%), methamphetamine for 19 participants (26.4%), powder cocaine for 6 participants (8.3%), and crack cocaine and powder cocaine for 2 participants (2.8%). Crack cocaine was the stimulant and drug overall with the highest proportion of participants reporting use in the past three months ( n = 61; 84.7%). Smoking was the most endorsed route of administration (100%) although approximately 10% of participants also reported injecting. Use of methamphetamine and powder cocaine in the past three months was reported by 37 participants (51.4%) and 21 participants (29.2%). Cumulatively, 46 participants (63.9%) reported use of opioids in the past three months, with 33 participants (45.8%) reporting fentanyl use and 37 participants (51.4%) reporting heroin use.
Opioids main drug subgroup
Fifty-six participants identified opioids as their primary drug. Heroin was the primary drug for 42 participants (75%), fentanyl for 7 participants (12.5%), heroin and fentanyl for 3 participants (5.4%), heroin, fentanyl, and xylazine for 3 participants (5.4%) and methadone for 1 participant (1.8%). The drugs with the highest proportion of participants reporting use in the past three months were heroin ( n = 51; 91.1%) and fentanyl ( n = 50; 89.3%). The most endorsed route of administration was injection for heroin (76.5%) and fentanyl (74.0%). Cumulatively, 49 participants (87.5%) reported use of stimulants in the past three months, with 43 participants (76.8%), 26 participants (46.4%), and 18 participants (32.1%) reporting use of crack cocaine, methamphetamine, and powder cocaine, respectively.
Stimulants and opioids main drug subgroup
Seventeen participants identified both stimulants and opioids as their primary drug. Crack cocaine and heroin were the primary drugs for 12 participants (70.6%), methamphetamine and heroin for 2 participants (11.8%), and powder cocaine and fentanyl for 1 participant (5.9%); 2 participants (11.8%) reported preference for any available drug. Crack cocaine, heroin and fentanyl were the drugs with the highest proportion reporting use in the past three months with use reported by 17 participants (100.0%), 16 participants (94.1%), and 16 participants (94.1%). The most endorsed route of administration was injection for heroin (75.0%) and fentanyl (68.8%) and smoking for crack cocaine (94.1%).
Subgroup differences
Differences in drugs used, frequency of use, and routes of administration were observed across the subgroups. Regarding opioid use, there was a statistically significant difference between the subgroups for past-three-month use of fentanyl ( p < 0.001) and heroin ( p < 0.001), as well as xylazine ( p < 0.001). Use of fentanyl was more prevalent in the stimulants-opioids (94.1%) and opioids (89.3%) subgroups compared to the stimulants subgroup (51.4%). Purposeful use of fentanyl was different between subgroups ( p = 0.002) with greater proportional use in the opioids (56.0%) and stimulants-opioids (50.0%) subgroups than the stimulants subgroup (18.9%). Injection was the most common route of administration among users in the opioids (74.0%), stimulants-opioids (68.8%), and stimulants subgroup (48.6%) although smoking was almost equally endorsed by users in the stimulants subgroup (45.9%). Use and subgroup differences for heroin were similar to fentanyl. Heroin use was proportionally much higher in the stimulants-opioids (94.1%) and opioids (91.1%) subgroups than the stimulants subgroup (45.8%) and injection the most common route of administration. Xylazine use was greater in the stimulants-opioids (70.6%) and opioids (55.4%) subgroups than the stimulants subgroup (19.4%).
Regarding stimulant use, there was no significant difference between the subgroups for past-three-month use of any stimulant. Crack cocaine use was proportionally highest in the stimulants-opioids subgroup (100.0%), followed by the stimulants (84.7%) and opioids (76.8%) subgroups. Methamphetamine use was highest for the stimulants-opioids subgroup (76.5%) and comparatively lower in the stimulants (51.4%) and opioids (46.4%) subgroups. Whereas users in the stimulants subgroup were most likely to smoke methamphetamine (59.5%), users in the opioids and stimulants-opioids subgroups were most likely to inject (73.1% and 69.2%). However, those in the stimulants subgroup who did inject did so more frequently (i.e., 5.4 days in the past week) than participants in the opioid-containing subgroups. Powder cocaine use was proportionally highest for the stimulants-opioids subgroup (47.1%) followed by the opioids (32.1%) and stimulants (29.2%) subgroups. Like methamphetamine, injection was the most common route of administration among users in the opioids (77.8%) and stimulants-opioids subgroups (75.0%) compared to snorting in the stimulants subgroup (61.9%).
Substance use among participants in current MOUD treatment
Examination of drug use among the 87 participants (58.0%) in current MOUD treatment was undertaken to better understand this subpopulation of the overall sample (see Additional file 1 : Table S1). High rates of stimulant use were reported by participants currently on MOUD. The stimulant used by the most participants in the past three months was crack cocaine ( n = 77; 88.5%) followed by methamphetamine ( n = 36; 41.4%) and powder cocaine ( n = 31; 35.6%). For both these latter drugs, injection was the most common route of administration. Opioid use was also prevalent among participants on MOUD. Fentanyl had the highest proportional use in the past three months ( n = 60; 69.0%) and injection the most common route of administration (60.0%). Among other drugs, 29 participants (33.3%) reported use of xylazine with injection the most endorsed route of administration (62.1%).
Injection information
Ninety participants (60.0%) reported injecting a drug (Table 4 ). The average age of first injection of any drug was 23 years old. The average number of past-week days injected and injections per day was 5.34 and 5.43, respectively. Most participants reported either never injecting alone (42.2%) or only sometimes alone (30.0%). The percentage reporting any abscesses or skin infections was 43.3%. Blood clots or blood infections and endocarditis were reported by 12.2% and 5.6%. Skin infections were more commonly reported in the opioids (56.8%) and stimulants-opioids (41.7%) subgroups than the stimulants (28.1%) subgroup.
Overdose information
Table 5 contains detailed information on overdoses. The average number of personally experienced overdoses in the past year was 0.7, with the stimulants subgroup reporting the fewest personal overdoses among the subgroups ( M = 0.32). The average number of overdoses a participant witnessed in the past year was 3.3. 113 participants (76.9%) reported having naloxone or a Narcan kit on them in the past three months.
Mental health, health, and medical information
Table 6 contains detailed mental health, health, and medical information. Concern about depression and anxiety was high among all participants. Approximately 81% and 88% of participants were concerned about depression and anxiety, respectively. Most participants reported an HIV and HCV test within the past year (64.4% and 60.4%). Medicaid was the primary type of health insurance (93.3%). Regarding medical care, the most common place participants reported past-year treatment was from the emergency room (ER)/urgent care (48.7%) with an average of 2.7 visits per person. The next most used medical care services were the doctor’s office (30.7%), SSP (5.3%), and jail/prison (5.3%).
In this observational study, sociodemographics, drug use practices, treatment participation, and health profiles of individuals participating in harm reduction services in Burlington, Vermont were explored overall and by primary drug subgroups. High rates of stimulant use were reported by all participants whether stimulants, opioids, or both were identified as their “primary drug”. Considering the notable and growing prevalence of stimulants in overdose deaths [ 4 , 5 ], these findings highlight a critical need for evidence-based interventions for stimulant use (e.g., Contingency Management) [ 7 , 22 ] including providing such interventions in SSPs and other harm reduction settings for individuals who may be interested.
These findings illustrate an illicit drug supply that now more than ever includes both stimulants and fentanyl [ 23 , 24 ]. We sought to better understand nuance of drug use practices and other related outcomes by categorizing participants by their primary (i.e., preferred) drug resulting in three subgroups—users of stimulants, opioids, and a combination of stimulants and opioids. Crack cocaine was the drug with the greatest proportion of individuals reporting use in the past three months across all participants, aligning with epidemiological data indicating cocaine as the most used stimulant in the Northeast US [ 5 , 6 ]. However, subgroup evaluations revealed crack cocaine was the drug with the highest proportion reporting use for the stimulants and stimulants-opioids subgroups only. In the opioids subgroup, fentanyl and heroin had the highest proportion reporting use. These results suggest that most service recipients whose primary drug is an opioid also regularly used stimulants. Comparatively, service recipients who primarily use stimulants used opioids to a lesser extent. Examining drug use by routes of administration also provided insight into subgroup differences. For example, injection of methamphetamine and powder cocaine was the most endorsed route for the opioid subgroups. However, injection was less common in the stimulant subgroup for these drugs, with smoking methamphetamine and snorting powder cocaine preferred. Such findings have implications for drug-involved overdoses and other health-related harms [ 25 , 26 ].
Approximately 70% of participants reported using fentanyl; however, purposeful use was much lower (41.3%). Purposeful fentanyl use was significantly higher in the opioid subgroups than the stimulant subgroup. The increasing prevalence of fentanyl-adulterated stimulants may be exacerbating overdoses if used unknowingly or inadvertently by individuals who report that they primarily use stimulants [ 27 , 28 ]. As such, this finding highlights the critical importance and necessity of harm reduction interventions such as drug checking services [ 29 ], naloxone distribution [ 10 ], and fentanyl test strips [ 12 ] (the latter two services are offered at this SSP) for people who primarily use stimulants as well as those who primarily use opioids. Commonly, participants whose primary drug was an opioid reported assuming fentanyl was in their drug supply and referred to heroin and fentanyl interchangeably.
Current participation in MOUD treatment was reported by 58.0% of participants. When asked about MOUD treatment in the past year, this number increased to 77.3%. These data suggest that among this sample of harm reduction service recipients, many individuals on MOUD continue to use illicit drugs in general and stimulants in particular. Thus, these data suggest that additional services may be needed to help service recipients reduce or stop their drug use.
Collecting information from individuals participating in harm reduction programs provides insight into the drug use ecology that is not currently being captured by other epidemiological sources. The people who make use of syringe exchange and other harm reduction services provide an important source of real-time information on the drugs currently being used, how they are being used, the effects of the current supply, and information on new drugs and drug use patterns. For example, xylazine was first reported by SSP service recipients in Burlington, Vermont at least twelve months before it was reported by treatment providers. Data from SSP service recipients is a valuable source of information that can provide health care providers, community providers, and health departments with an early warning system about emerging drug problems.
This study has several limitations that should be considered when interpreting these findings. One limitation is this study was conducted in one harm reduction program in a very small Northeastern city. As such, these findings should be considered in their environmental (e.g., geographic, sociodemographic) context and may not be generalizable to other regions, both within and outside of the state of Vermont. Compared to the Burlington metropolitan area with approximately 225,000 residents, much of the rest of the state is rural with 64.9% of residents living in rural areas [ 30 ]. Future research should be conducted to evaluate the generalizability of these findings to other areas of Vermont and the Northeast US.
A second limitation is that all data were collected via participant self-report which could have impacted the results in several different ways. Because drug use was based on self-report, its correspondence with objective measures is unknown and it is possible that participants may have used or not used other drugs (e.g., xylazine) unknowingly. Additionally, findings on current and past-year MOUD treatment should be interpreted while also considering that access to low-barrier MOUD is offered in the same building as this SSP. Finally, findings on routes of administration may have been impacted by the study population (i.e., SSP service recipients) and the availability of safer smoking supplies as another service [ 31 ].
This study expands what is known about important sociodemographic, substance use, and health-related variables among individuals participating in a SSP in Vermont that also provides other harm reduction services. Specifically, these findings add to the literature by assessing differences in the types of drugs used and treatment participation—including MOUD—based on one’s primary (i.e., preferred) drug. Findings among this sample of service recipients indicate that polysubstance substance use was common [ 32 ], an important risk factor for experiencing a drug overdose [ 33 , 34 ] that also has direct implications for the types of evidence-based interventions and services offered in this setting. Taken together, these findings highlight the important role of SSPs in providing community-based services [ 35 ] and provide knowledge that can inform future intervention services and treatment provision in this setting to help address the ongoing overdose epidemic.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to institutionally approved protocols but are available from the corresponding author on reasonable request.
Abbreviations
United States
Syringe Service Program
Human Immunodeficiency Virus
Hepatitis C Virus
People who use drugs
People who inject drugs
Medication for opioid use disorder
Spencer MR, Miniño AM, Warner M. Drug overdose deaths in the United States, 2001–2021. NCHS Data Brief. 2022;457:1–8.
Google Scholar
Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National center for health statistics. 2023 [cited 2023 Oct 1]. Available from: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
National Center for Health Statistics. U.S. Overdose Deaths in 2021 increased half as much as in 2020—but are still up 15% [Internet]. Centers for Disease Control and Prevention; 2022 May [cited 2023 Sep 12]. Available from: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm#:~:text=Provisional%20data%20from%20CDC's%20National,93%2C655%20deaths%20estimated%20in%202020
National Institute on Drug Abuse. Drug overdose death rates. 2023 [cited 2023 Sept 12]. Available from: https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
Friedman J, Shover C. Charting the fourth wave: geographic, temporal, race/ethnicity, and demographic trends in polysubstance fentanyl overdose deaths in the United States, 2010–2021. MedRxiv. 2022:2022–11.
Jenkins RA. The fourth wave of the US opioid epidemic and its implications for the rural US: a federal perspective. Prev Med. 2021;152: 106541.
Article PubMed Google Scholar
Korthuis PT, Cook RR, Foot CA, Leichtling G, Tsui JI, Stopka TJ, Leahy J, Jenkins WD, Baker R, Chan B, Crane HM. Association of methamphetamine and opioid use with nonfatal overdose in rural communities. JAMA Netw Open. 2022;5(8): e2226544.
Article PubMed PubMed Central Google Scholar
Knopf A. HHS moves toward harm reduction for the first time. Alcohol Drug Abuse Wkl. 2021;33(42):6.
Article Google Scholar
Centers for Disease Control and Prevention. Syringe service programs fact sheet. Syringe Service Programs. 2019 [cited 2023 Oct 1]. Accessed from: https://www.cdc.gov/ssp/syringe-services-programs-factsheet.html
Lambdin BH, Wenger L, Bluthenthal R, Bartholomew TS, Tookes HE, LaKosky P, O’Neill S, Kral AH. How do contextual factors influence naloxone distribution from syringe service programs in the USA: a cross-sectional study. Harm Reduct J. 2023;20(1):26.
Krawczyk N, Allen ST, Schneider KE, Solomon K, Shah H, Morris M, Harris SJ, Sherman SG, Saloner B. Intersecting substance use treatment and harm reduction services: exploring the characteristics and service needs of a community-based sample of people who use drugs. Harm Reduct J. 2022;19(1):1.
Peiper NC, Clarke SD, Vincent LB, Ciccarone D, Kral AH, Zibbell JE. Fentanyl test strips as an opioid overdose prevention strategy: findings from a syringe services program in the Southeastern United States. Int J Drug Policy. 2019;63:122–8.
Des Jarlais DC, McKnight C, Goldblatt C, Purchase D. Doing harm reduction better: syringe exchange in the United States. Addiction. 2009;104(9):1441–6.
Jakubowski A, Fowler S, Fox AD. Three decades of research in substance use disorder treatment for syringe services program participants: a scoping review of the literature. Addict Sci Clin Pract. 2023;18(1):1–22.
Glick S, Kong T, Fang C, Pindyck T, Adams M, Furukawa N, Burnett J, Baugher A, Emerson B, Chavez PR. Program and operational characteristics of syringe services programs in the United States, 2020 and 2021.
Frost MC, Austin EJ, Corcorran MA, Briggs ES, Behrends CN, Juarez AM, Frank ND, Healy E, Prohaska SM, LaKosky PA, Kapadia SN. Responding to a surge in overdose deaths: perspectives from US syringe services programs. Harm Reduct J. 2022;19(1):1–1.
Blanco C, Ali MM, Beswick A, Drexler K, Hoffman C, Jones CM, Wiley TR, Coukell A, Recovery Working Group. The American opioid epidemic in special populations: five examples. NAM Perspectives. 2020;2020.
Muncan B, Walters SM, Ezell J, Ompad DC. “They look at us like junkies”: influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduct J. 2020;17:1–9.
Banta-Green CJ, Kingston S, Ohta J, Taylor M, Sylla L, Tinsley J, Smith R, Couper F, Harruff R, Freng S, Von Derau K. 2016 Drug Use Trends in King County, Washington. University of Washington, Alcohol & Drug Abuse Institute; 2017.
Frost MC, Williams EC, Kingston S, Banta-Green CJ. Interest in getting help to reduce or stop substance use among syringe exchange clients who use opioids. J Addict Med. 2018;12(6):428–34.
McMahan VM, Kingston S, Newman A, Stekler JD, Glick SN, Banta-Green CJ. Interest in reducing methamphetamine and opioid use among syringe services program participants in Washington State. Drug Alcohol Depend. 2020;216: 108243.
Article CAS PubMed PubMed Central Google Scholar
Rawson RA, Erath TG, Chalk M, Clark HW, McDaid C, Wattenberg SA, Roll JM, McDonell MG, Parent S, Freese TE. Contingency management for stimulant use disorder: progress, challenges, and recommendations. J Ambul Care Manag. 2023;46(2):152–9.
Ciccarone D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry. 2021;34(4):344.
Ahmed S, Sarfraz Z, Sarfraz A. A changing epidemic and the rise of opioid-stimulant co-use. Front Psychol. 2022;13: 918197.
Fitzpatrick T, McMahan VM, Frank ND, Glick SN, Violette LR, Davis S, Jama S. Heroin pipe distribution to reduce high-risk drug consumption behaviors among people who use heroin: a pilot quasi-experimental study. Harm Reduct J. 2022;19(1):103.
Islam S, Piggott DA, Moriggia A, Astemborski J, Mehta SH, Thomas DL, Kirk GD. Reducing injection intensity is associated with decreased risk for invasive bacterial infection among high-frequency injection drug users. Harm Reduct J. 2019;16:1–8.
Coffin PO, McMahan VM, Murphy C. Evidence of pre-mortem opioid use among fentanyl overdose decedents in a safety net healthcare system. J Urban Health. 2022;99(5):865–72.
Hedegaard H, Miniño AM, Warner M. Co-involvement of opioids in drug overdose deaths involving cocaine and psychostimulants.
Carroll JJ, Mackin S, Schmidt C, McKenzie M, Green TC. The Bronze Age of drug checking: barriers and facilitators to implementing advanced drug checking amidst police violence and COVID-19. Harm Reduct J. 2022;19(1):1–3.
United States Census Bureau. Nations urban and rural populations shift following 2020 census. 2022 [cited 2023 Sept 15]. Available from: https://www.census.gov/newsroom/press-releases/2022/urban-rural-populations.html
Applewhite D, Regan S, Mackin S, Schmidt C, Duffy J, Washington K, Micklos N, Casey S, Sawyer S, Kehoe L, Howard S. Individuals reporting past 3-month smoked stimulant use are placed at risk for infection and injury amid COVID-19. J Addict Med. 2023;17(2):e129–31.
Beckham SW, Glick JL, Schneider KE, Allen ST, Shipp L, White RH, Park JN, Sherman SG. Latent classes of polysubstance use and associations with HIV risk and structural vulnerabilities among cisgender women who engage in street-based transactional sex in Baltimore City. Int J Environ Res Public Health. 2022;19(7):3783.
Mahoney JJ III, Winstanley EL, Lander LR, Berry JH, Marshalek PJ, Haut MW, Marton JL, Kimble WD, Armistead M, Wen S, Cai Y. High prevalence of co-occurring substance use in individuals with opioid use disorder. Addict Behav. 2021;114: 106752.
Schneider KE, Nestadt PS, Shaw BR, Park JN. Trends in substances involved in polysubstance overdose fatalities in Maryland, USA 2003–2019. Drug Alcohol Depend. 2021;223: 108700.
Thakarar K, Sankar N, Murray K, Lucas FL, Burris D, Smith RP. Injections and infections: understanding syringe service program utilization in a rural state. Harm Reduct J. 2021;18:1–8.
Download references
Acknowledgements
Not applicable.
This research was supported by the National Institute of General Medical Sciences (NIGMS) Center of Biomedical Research Excellence award P20GM103644 (STH, RAR, TGE).
Author information
Authors and affiliations.
Vermont Center on Behavior and Health, Burlington, VT, USA
Tyler G. Erath, Stephen T. Higgins & Richard A. Rawson
Department of Psychiatry, University of Vermont, University Health Center, 1 S. Prospect St., Burlington, VT, 05401, USA
Howard Center Safe Recovery, Burlington, VT, USA
Rosalie LaCroix & Erin O’Keefe
Center on Rural Addictions, University of Vermont, Burlington, VT, USA
Stephen T. Higgins & Richard A. Rawson
You can also search for this author in PubMed Google Scholar
Contributions
TE and RR conceptualized the study; RL led the data collection; TE and RR were involved in writing the initial draft; TE and RR led the data analysis; TE, RR, EO, and SH provided feedback and revisions to the manuscript; TE, RL, EO, RR, and SH agreed to the final version submitted for publication.
Corresponding author
Correspondence to Tyler G. Erath .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by University of Vermont’s Institutional Review Board (study #00002041). Verbal informed consent was obtained from each participant and a consent process documentation form was completed prior to study participation.
Consent for publication
Competing interests.
The authors declare they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. Table S1 . Drug Use Among Participants Currently in MOUD Treatment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Erath, T.G., LaCroix, R., O’Keefe, E. et al. Substance use patterns, sociodemographics, and health profiles of harm reduction service recipients in Burlington, Vermont. Harm Reduct J 21 , 76 (2024). https://doi.org/10.1186/s12954-024-00995-y
Download citation
Received : 23 October 2023
Accepted : 31 March 2024
Published : 05 April 2024
DOI : https://doi.org/10.1186/s12954-024-00995-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Harm reduction
- Syringe service program
- Substance use treatment
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]
- Research Article
- Open access
- Published: 15 December 2022
Prevalence and factors associated with substance use among university students in South Africa: implications for prevention
- Stacey Blows ORCID: orcid.org/0000-0002-7276-9404 1 &
- Serena Isaacs ORCID: orcid.org/0000-0002-5952-8614 1
BMC Psychology volume 10 , Article number: 309 ( 2022 ) Cite this article
11k Accesses
8 Citations
Metrics details
Substance use is an important public health concern in many countries across the globe. Among the general public, institutions of higher learning have developed a reputation for inducing new substance use among students. In addition to socio-demographic factors, substance use and abuse among university students often appear to be related to psychological stressors typically related to the demand to adapt to the new environment and the pressures associated with academia. The purpose of this study was to identify the prevalence of, and factors associated with substance use among university students.
This quantitative study employed convenience sampling to recruit university students who were 18 years and older from a university in the Western Cape. The study made use of self-administered online questionnaires, which participants completed via SurveyMonkey. The sample consisted of 2915 students. Descriptive statistics were used to describe and provide the prevalence and overview of the demographic characteristics of the respondents. Associations between variables were explored using Chi-square and Mann–Whitney U tests.
The main findings revealed a substance use prevalence rate of 62.7%. The most prominent substances used by students were alcohol (80.6%), cannabis (46%), and ecstasy (5.3%). The study further revealed clear associations between students’ substance use and mental health. Students who reported substance use at university reported higher depression and anxiety scores than those who did not. However, findings reveal no significant association ( p = 0.233) between being a substance user and a nonsubstance user and students' respective self-perceived stress scores.
Results show the majority of sampled students had started using substances (both alcohol and other substances) only after entering university. The results call into question seminal findings relating to substance use and the university environment. The novel findings of this study could serve as a baseline input to inform policymakers, programme developers, service providers, parents, and other stakeholders who are involved in the design and implementation of more effective awareness, prevention and, needs-based intervention services.
Peer Review reports
Substance use is an important public health concern in many countries across the globe. Among the general public, institutions of higher learning have developed a reputation for inducing new substance use among students [ 1 , 2 , 3 ]. In addition to reporting novice use, studies have also found that students who had prior exposure to substance use increased their frequency once exposed to the university environment [ 4 , 5 ]. A growing body of research has also shown that university students reported using a number of substances at a greater rate than their non-student peers [ 1 , 6 , 7 , 8 , 9 ]. Findings of such studies show that the use of alcohol, particularly getting drunk and binge drinking [ 1 , 6 ], marijuana [ 1 ] and non-prescription amphetamine, were considerably higher among university students when compared with their non-university attending peers [ 1 , 7 , 8 , 9 ].
Research suggests that there could exist some conditions within the environment of higher education settings that makes students more susceptible to the use and/or abuse substances [ 4 , 10 , 11 , 12 ]. The term "substance use" refers to the use of alcohol, tobacco, illicit drugs, prescription and over-the-counter medications [ 13 ]. “Substance abuse” refers to the continued misuse of drugs, alcohol, tobacco and other psychoactive drugs even though the individual has knowledge that their usage of these substances may cause several debilitating problems and may eventually lead to some form of addiction [ 14 ].
Although much is known about students’ substance use rates on a global scale, very few representative studies have been conducted in South Africa (see e.g., [ 15 , 16 , 17 , 18 , 19 ]). Among the few studies carried out in South Africa, very high rates of student alcohol use have been reported [ 16 , 17 , 19 ]. For example, Young and De Klerk [ 17 ] found alcohol prevalence rates of almost 50% at Rhodes University. At the same South African university, 2 years later, Young and Mayson [ 19 ] found that 57.9% of the sample reported hazardous alcohol consumption, i.e., four or more drinks at a time on at least three separate days in the previous three months.
Similarly, another South African study carried out by Kyei and Ramagona [ 15 ], at the University of Venda, found that while over 65% of the students surveyed use alcohol, 49% of those students abuse it. A more recent study conducted by Du Preez and colleagues [ 2 ], which focused on the drinking behaviour of students at Stellenbosch University reported that 71% of males and 54% of females reported hazardous drinking patterns. In addition, the study also found that 13% of the sample indicated harmful drinking behaviour.
The concern of such findings lies in the potential short- and long-term adverse effects associated with the use of substances on students’ overall health and well-being. As substance use has been associated with an increased risk of contracting communicable diseases such as HIV/AIDS and TB [ 20 ]; non-communicable diseases such as mental illnesses; maternal and child maternal and child morbidity and mortality [ 21 ]; as well as injury and trauma. The previously noted consequences of substance use and abuse notwithstanding, it has also been recognised to contribute to epidemics of crime and violence, high university dropout rates, unemployment, and high levels of poverty and crime [ 22 ].
Research has shown that to intervene effectively and prevent the negative consequences of substance use, it is important to identify socio-demographic [ 18 , 23 , 24 ], environmental and psychological factors [ 25 , 26 , 27 ] contributing to the use and misuse of substances. According to Becker et al. [ 25 ] and NIDA [ 27 ], mental conditions such as stress, anxiety, and depression are important factors predisposing students to use and subsequently abuse substances [ 25 , 26 ]. The present study, therefore, aimed to establish the prevalence and associated factors of substance use among students at a historically disadvantaged university in the Western Cape, South Africa.
The study attempted to answer the following questions: (1) What is the prevalence rate of substance use amongst students at the University? (2) What types of substances do the students commonly use? (3) What are the factors associated with substance use among university students?
Design and context
This quantitative study employed convenience sampling to recruit university students who were 18 years and older from one of 26 public universities situated in South Africa. The university consists of seven faculties and four schools. Faculties are made up of Arts, Community and Health Sciences, Dentistry, Economic and Management Sciences, Education, Law and Natural Science. The schools include Pharmacy, Government, Nursing and Science and Mathematics. The study was primarily borne out of the realisation that very little was known about the current prevalence and factors associated with substance use and abuse at universities in the Western Cape, even though it is situated in the region where alcohol and drug use is reported to be four times higher than the national average in South Africa [ 28 ].
Procedure and ethics
The study was approved by the university and its ethics committee (BM18/9/1). After receiving a list of all registered students (N = 25,226) from the Registrar of the university, we sent out emails (as well as reminders) to all the student email addresses. The email included the description of the study and the link to the questionnaire. The questionnaire was administered online using SurveyMonkey for a period of two months (31 July to 30 September 2019). A link to the questionnaire was sent to students' university email addresses. Upon accessing the questionnaire, participants were provided with an information sheet and consent form which outlined the purpose, aims and, objectives of this study, the rights and responsibilities of the participants, as well as what it is that would be expected from them should they agree to take part in the research. Through the information sheet and consent forms, participants were also assured that their identity would remain confidential, and their responses used for research purposes only. This was ensured by not requiring any identifiable information from participants, thus maintaining their anonymity. The participants in this study were provided with referral pathways, should the need for counselling services or emergency intervention arise as a result of their participation in this study. Should students have required any additional referrals for social or mental health support, they were provided with telephone and email contact details of possible referrals. The researcher’s contact information was also available should they not have been successful on their own.
Participants
After excluding incomplete and missing data, 2915 questionnaires were deemed valid for analysis (11.6% response rate). Participants with two missing values on either the AUDIT or the DUDIT as well as corresponding missing values for their demographic information, which would have resulted in biased calculations, were removed. See Table 1 for the demographic characteristics of the population under study.
The final sample consisted of 34% men, 64% women and 1.7% who presented as “other” in terms of ‘gender’. Participants’ ages were captured categorically, ranging from 18–24 years to 75 years and older. The majority of the sample fell into the two youngest categories, i.e. [18–24 years (n = 2164 (63.9%)] and 25–34-year-old category (17%) respectively. With reference to the sample’s level of study, a large proportion of the participants were 1st year (28.8%), 2nd year (25.7%) and 3rd year (22.9%), undergraduate students. Most of the sample (34.8%) was from the faculty of Economic and Management Sciences. This statistic was succeeded by the second largest grouping 22% of students in the faculty of Arts and Humanities.
The substance use questionnaire consisted of five different instruments namely, the demographic section (please see Additional file 1 for a copy of the demographic section of this questionnaire), the Alcohol Use Disorders Identification Test [ 29 ], The Drug Use Disorders Identification Test [ 30 ], The Perceived Stress Scale [ 31 ] and The Self-Reporting Questionnaire [ 32 ].
Demographic section
A demographic section was developed in order to ascertain demographic information relevant to the current study’s aims and objectives. Questions regarding the students’ substance use, age, gender, education level, year level, marital status and onset of substance.
The Alcohol Use Disorders Identification Test (AUDIT)
The Alcohol Use Disorders Identification Test (AUDIT) was employed to help screen, categorise and diagnose the incidence of safe, hazardous, harmful and dependent drinking among students. The AUDIT is a brief 10-item, 5-point Linkert scale, self-administered questionnaire, with responses ranging from 0 (never) to 4 (4 + times per week) [ 33 ]. The AUDIT has demonstrated a high degree of internal consistency, yielding a Cronbach’s Alpha score of 0.83, with a range of 0.75–0.97 [ 34 ]. For the current sample, Cronbach’s alpha was 0.82.
The Drug Use Disorders Identification Test (DUDIT)
The DUDIT was employed in order to determine the extent of drug use among students. The DUDIT was developed to assist in the screening, diagnosing and categorising the severity of use of substances other than alcohol [ 30 ]. This self-report questionnaire uses a 5-point Likert scale which categorises individuals into three broad categories of drug use, namely, “no drug related problems”, “harmful use or dependence” and “heavily dependent on drugs”. The DUDIT was found to be a psychometrically sound instrument with high convergent validity (r = 0.85) when compared to 44 similar measures such as the DAST-10 and has a Cronbach's alpha of 0.94 [ 35 ]. For the current sample, the Cronbach’s alpha was 0.88.
The Perceived Stress Scale (PSS-10)
The PSS-10 is one of the most extensively used instruments for measuring self-perceived stress on a scale from 0 (never) to 4 (very often) [ 36 ]. Tallied PSS scores are used to detect three categories of stress. An individual is considered to be experiencing low stress is their respective scores ranges from 0 to 13. Scores ranging from 14–26 suggests moderate stress while scores ranging from 27 to 40 would suggest high perceived stress [ 31 ]. The PSS-10 has shown to have good internal and test–retest reliability (α = 0.84–0.86) and it has demonstrated convergent validity with measures of anxiety, depression, and health, and divergent validity with measures of sensations-seeking, religious faith, and aggression among university students [ 37 , 38 ]. For the current sample, Cronbach’s alpha was 0.58.
The Self-Reporting Questionnaire (SRQ-20)
Developed by the World Health Organization (WHO), this questionnaire is a self-rating scale specifically designed to screen for psychological discomfort among individuals, particularly in developing countries. The SRQ-20 was therefore employed to assess the frequency and severity of 20 symptoms related to depression and anxiety among students. The SRQ has proven to be a valid (Cronbach’s α = 0.85) [ 39 ] and reasonably stable instrument in a several studies in different cultural contexts [ 40 , 41 ]. Both the PSS-10 and SRQ-20 are two of the most widely used instrument to measure perceived stress [ 36 , 37 , 38 ] and psychological distress among populations in several different cultural contexts in and around South Africa [ 40 , 41 ]. For the current sample, Cronbach’s alpha was 0.89.
Data analysis
Data were entered into an Excel spreadsheet, and analysis was conducted using the IBM Statistical Package for Social Sciences Version SPSS 26.0 software. Percentages and frequencies were used to report categorical variables. Descriptive statistics was used to summarise the participants’ socio-demographic characteristics and bivariate analysis to examine the associations between background characteristics and alcohol and drug use. The Chi-square test for independence (using α = 0.05) was used to determine whether there were significant differences between student’s substance use before and after their university enrolment. A chi-square test is commonly used when analysing two categorical variables from a single population [ 42 ]. Because scores were not normally distributed, Mann–Whitney U-tests were used to determine the association between students’ self-reported mental health and their use of substances. A p value of less than 0.05 was determined to be statistically significant.
Prevalence of substance use amongst students
The prevalence rates of substance use among the sampled students are presented in the table below (Table 2 ). The prevalence results presented were based on the results obtained questions in the demographic questionnaire. For students to have been labelled as a “substance user” students had to have responded ‘yes’ to the question, which read, “Are you still using any of the substances mentioned above?”. In order to be considered a “non-substance user”, students had to have indicated ‘no’ substance use with respect to this question. Respondents were labelled “unsure” if they indicated ‘yes’ to this question but had not selected any of the substances listed in the question which followed on the survey.
The findings presented in Table 2 show that the majority of respondents reported using substances after they enrolled at the university (62.7%). In this dataset, chi-square analysis indicated a narrow interval span of 60.89–64.43% can be observed among students with an odds ratio of 0.5, and a 95% confidence level. This is indicative of the chances of using substances after being exposed to the university environment is 50%.
Types of substances used
Table 3 (below) displays a list of the substances reported to have been used by the participants after their enrolment at university. Alcohol was the most used substance among students (80.6%) ( n = 1472). The second-most used substance reported by respondents is cannabis, which is commonly known in the Western Cape as ‘dagga’ or weed. The percentage of students reporting cannabis use amounts to 46% ( n = 841) of the sampled respondents. The third largest proportion of students (96 students) indicated that they used ecstasy.
Table 3 further reveals that 8% of the students reported using substances that were not explicitly listed in the questionnaire. These substances were listed by participants as: Ritalin ( n = 33), Poppers ( n = 32), Ketamine ( n = 31), Mescaline ( n = 30), other over-the-counter-medicine ( n = 28), Dimethyltryptamine (DMT or N) ( n = 27), Xanax ( n = 26), Vape ( n = 25) Traditional beer ( n = 24), Pethidine ( n = 21) Tramadol ( n = 20), Rock ( n = 19), Hookah ( n = 18), Flakka ( n = 17), CAT ( n = 16) MD (n = 15), MDMA ( n = 14), Acid ( n = 10) LSD ( n = 12) Mushrooms ( n = 13) and Cocaine ( n = 11).
Level of Alcohol and Drug Use among University Students (AUDIT and DUDIT)
The AUDIT and DUDIT were used to determine the amount of alcohol and drug use among the sample of students who stated that they were current substance users in order to supplement the results from the prevalence findings presented above. The results of the Alcohol Use Disorder Identification Test (AUDIT) and the Drug Use Disorder Identification Test (DUDIT) are presented in Table 4 below. In order to determine the extent of substance use by those who identified as using substances, the analysis was conducted on the 1827 participants who reported using substances after enrolling at university.
A total of 1164 (63.7%) of the 1827 students labelled as ‘substance users’ completed the AUDIT. Although the majority of that cohort indicated ‘low-risk drinking’, a total of 349 students indicated ‘hazardous’, ‘harmful’ drinking patterns and ‘alcohol dependence’.
Most respondents (87.2%) who completed the DUDIT reported, what the DUDIT defines as, ‘no drug-related problems’ while 184 students reported ‘harmful/dependence’ and ‘heavily dependent’ use.
Factors associated with substance use
Self-report questionnaire-20.
A cut off score of 7/8 is used to indicate the presence of depression and anxiety [ 41 ] or as Harpham et al. [ 43 ] reports, ‘mental ill health’. Thomas [ 44 ] used a cut-off score of 7/8’s in a study in Durban, South Africa. The table below (Table 5 ) indicates that 32.5% of the total sample, or 45.1% who completed the SRQ-20 presented with a possible case of mental ill health. This indicates the prevalence of mental health distress as reported within this sample.
A Mann–Whitney U Test was conducted in order to test the significance of the association between those who used substances, those who did not and their associated SRQ score. The results are presented in Table 6 below.
The results found in Table 6 and Figs. 1 and 2 reveals a significant association ( p < 0.01) between being a substance user and non-substance user and students’ respective SRQ scores. The results indicated that students who scored higher in the SRQ-20 (possibly indicating depression and anxiety symptoms) were students who reported substance use at university.

SRQ-25 × Substance Use Histogram
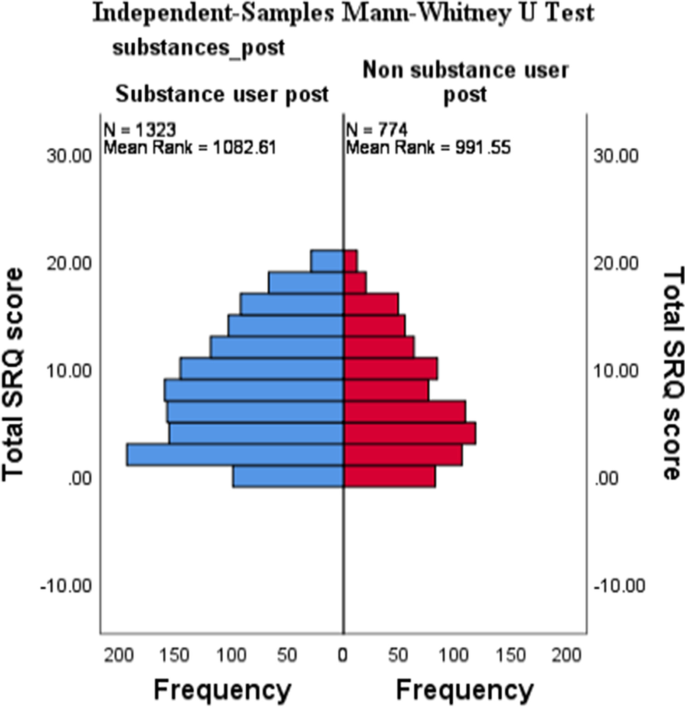
SRQ-25 ×Substance Use Independent-Samples Mann-Whitney U test
A further cross tabulation presented in Table 7 above highlights that those students who reported hazardous, harmful drinking and alcohol dependence also report higher levels of mental health concerns (SRQ-20). Table 8 , below, also indicates that those who report hazardous, harmful drinking and alcohol dependence also report higher levels of perceived stress as compared to those with lower levels of stress. It is interesting to note that all everyone who reported moderate to high perceived stress participated in hazardous or harmful drinking. This speaks to other protective factors which might buffer alcohol use.
Perceived stress scale-10 results
To ascertain the levels of stress students’ experience during their time at university, the PSS-10 was administered and analysed. The PSS-10 measures the level at which respondents appraise life events as being unpredictable, overwhelming, or challenging. Individual scores on the PSS range from 0 to 40, with higher scores indicating higher perceived stress between 0 and 13 are perceived to have low stress. Scores ranging from 14 to 26 would indicate those whose scores are considered as having moderate stress. The final category of scores, i.e. ranging from 27 to 40 would be indicative of individuals having high perceived stress. It is within this context that respondents were scored, and findings were analysed.
Table 9 indicates that substance users have a higher level of perceived stress versus those who do not use substances. The table below indicates whether this difference was significant using a Mann–Whitney U Test (Table 10 ).
The results in Table 8 above and Figs. 3 and 4 below show that there is no significant association ( p > 0.05) between being a substance user and nonsubstance user post university enrolment and students respective PSS-10 scores. The levels of perceived stress appear to be similar for both cohorts.
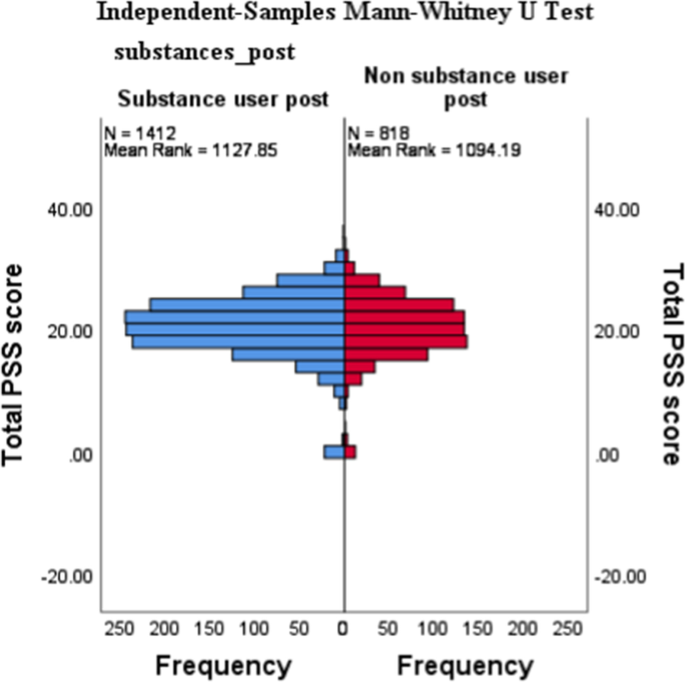
PSS-10 × Substance Use Independent-Samples Mann-Whitney U test

PSS-10 × Substance Use Histogram
Table 11 above, is a cross tabulation of the drug use categories according to the DUDIT and the SRQ. According to the table, those who displayed harmful use or are heavily dependent on substances also report the presence of more mental ill health symptoms. Interestingly, 749 of the 1744 students who reported mental ill health challenges did not indicate drug-related problems.
A similar cross tabulation (Table 12 ) was conducted on the DUDIT categories and students’ perceived levels of stress. Although many students indicated a moderate to high level of perceived stress (n = 1608 and 125 respectively), these students did not report problems with drug use. However, a larger number of students reported moderate to high perceived stress who were also using substances in a harmful or dependent manner.
Prevalence of substance use
The aim of this study was to determine the prevalence of, or patterns, of substance abuse among university students as well as mental health factors that may be influencing this use. The term substances refer to both alcohol and drug use. Results from the study show that 62.7% of sampled students indicated, not only that they used substances but that this use (both alcohol and other substances) started after enrolling at the university. The prevalence rates found in this study appear to align with key findings which, similarly, found high substance use rates after students had enrolled at their respective university/college [ 1 , 4 , 10 , 11 , 12 ].
The extent of alcohol and drug use was evaluated using the AUDIT and DUDIT. These results are particularly interesting as it revealed that the majority of students in the sample reported ‘low-risk drinking' (70.4%) and ‘no drug-related problems’ (87.2%). These results are in direct contrast with similar studies in the field which report relatively high prevalence of substance abuse among university students, particularly in South Africa [ 2 , 15 , 19 ]. The substance use rates reported could be due to a variety of reasons, one of which concerns social desirability bias, which refers to the tendency respondents have to present and align themselves and their reality with what they believe to be socially acceptable. However, each questionnaire was self-report and could be completed alone, without the presence of an interviewer or someone known to the student. The majority use notwithstanding, both the AUDIT and DUDIT revealed a number of students who should be considered for either brief or intensive interventions for substance use.
Types of substances used by students
The three most commonly used substances reported were alcohol (80.6%), cannabis (46%) and ecstasy (5.3%) amongst those who used substances after university enrolment. Interestingly, ecstasy use was found to be higher than methamphetamine use among students in the Western Cape, an area well-known for its increased methamphetamine use [ 45 ]. “Other” substances accounted for 8% of the sample, important to note here is that the number of “other” substances evidently surpasses commonly well-known and well-documented substances such as ecstasy (n = 96), methamphetamine (n = 14), buttons (n = 6) and unga (n = 1). This noteworthy and rather unanticipated finding could be indicative of a shift in the types of substances commonly reported/used by university students at this point in time. Although the sample is not representative, this finding is important as it provides an opportunity for researchers and healthcare practitioners to be mindful of the types of substances being used by individuals of a certain age range in the Western Cape.
Mental health of students
The results of this study revealed a significant association ( p < 0.01) between students’ substance use and their respective SRQ scores. These results appear to be in consensus with much of the available literature which interchangeably associates some aspect of mental health with substance among university students [ 25 , 27 , 46 ]. However, although valuable, the results presented are likewise unable to support or refute the three main hypotheses offered in the literature review which varied from conclusions relating to whether substance use leads to mental health problems [ 47 ]; whether mental health problems cause substance [ 48 ] or whether these concepts are so closely related that it could not be studied in isolation [ 49 ]. It is likewise unfortunate that results were unable to answer the question as to whether students who already present mental health problems prior to attending universities are at an even higher risk of experimenting with substances, as the new environment could exacerbate their already existing symptoms [ 50 ]. What it does however show, is that there appears to be a significant difference between the two groups in terms of their mental health and use of substances, i.e., students who identified as non-users reported fewer symptoms of anxiety and depression (according to the SRQ-20) than students who indicated that they were substances users. Which is indicative of there being some validity to the claims concerning the complex relationship between substance use and mental health, particularly among university students.
This study used the PSS-10 to measure psychological stress among students mainly because it defines stress as an interaction between environmental demands and the individual’s capacity to cope [ 31 ]. Results demonstrate that there is no significant association ( p > 0.05) between being a substance user and a nonsubstance user post university enrolment and students' respective PSS-10 scores. Figures 1 and 2 furthermore support and expand on the results found in Table 9 by showing how scores cluster around the 19/20 mark in both groups. In terms of students’ level of stress, the results from Figs. 1 and 2 furthermore indicate that the majority of students in both groups fall within the moderate stress levels as per PSS-10. These results found above are in contrast with a body of literature that found significant associations between respondents who suffered from psychological distress and their use of substance use. Substance use was commonly reported as being used by distressed respondents to cope with academic pressures and demands [ 50 , 51 ]. Interestingly, even though we did not account for risk and protective factors, based on the results of the AUDIT/DUDIT category cross tabulation with the SRQ and PSS, protective factors could be moderating or mediating the relationship between stress/mental ill health and students’ either using substances or not. Such factors could account for those with high stress and mental health challenges and not having a substance use problem per se. Considering the scarcity of knowledge about the risk and protective factors of substance abuse among university students, a follow-up study to investigate such factors should be prioritised.
Implications of the study
The insights to be gained from this study could serve several purposes and contribute towards the prevention and reduction of substance use and/or abuse among university students in several ways. In its entirety, the study contributes to the overall scarcity of existing knowledge on substance use and abuse among university students in South Africa. The study sheds light on the current prevalence and the extent to which students’ use and/or abuse substances in a previously underexplored population in the Western Cape. Although it does show that the large majority do not necessarily have harmful or hazardous substance use patterns, it is noteworthy that a minimum of 184 to a maximum of 359 students reported harmful/hazardous/dependent use. Therefore, awareness campaigns and varying degrees of referrals and interventions should be made available to students.
In addition to reporting on the “conventionally” well-documented substances, such as alcohol, marijuana, methamphetamine and heroin in South Africa, this study also provided a platform where students could disclose their use and/or abuse of other types of substance use. This information could prove useful for any future attempts to tailor, inform and/or contextualise research endeavours of a similar nature. The unanticipated findings relating to the assortment of substances could be indicative of a gradual paradigm shift in the types of substances commonly reported/used by students. The novel findings of this study could serve as a baseline input to inform policy makers, programme developers, service providers, parents, and other stakeholders who are involved in the design and implementation of more effective awareness, prevention and needs-based intervention services; and the findings of this study could also serve as a feature map for future research relating to substance use in and around South Africa.
Conclusions
Limitations.
The results produced in this research study, although valuable, reflects a single, purposefully selected university in the Western Cape. Since the prevalence and nature of substance abuse among university students in the Western Cape may vary depending on the environments where the universities are found, the generalisation of the current study’s findings should be done with caution. A general limitation of a correlational study is that it can determine the association between variables but cannot predict causation. Another limitation of inherent is such studies is the ability of respondents to accurately recall past events. In this case, the time intervals for which respondents were asked to report their substance use were not specific, i.e., no reference periods were used to restrict and specify the time intervals for which respondents reported their use of substances. This oversight may have produced unclear assumptions regarding the prevalence of substances among students. In addition, tobacco use was not classified as a problematic substance in this study. This is perhaps something to consider in future studies of this nature.
It is also essential to mention here that the questionnaire was disseminated in only one of the three official languages within the Western Cape, i.e., English. This was done in order to align with the University’s primary medium of teaching and of examination, which is, English. This being said, the official language policy of the Western Cape Government (Western Cape Government 2019) encourages the promotion and use of all of the three official languages of the Western Cape, namely Afrikaans, isiXhosa and English where possible. It is thus recommended that future research carried out in different provinces and or countries consider the official languages of the population under study and strive to provide the respondent with an equal opportunity to interpret and answer questions in their mother tongues.
The social desirability bias, inherent in the self-report measures on substance use, may have resulted in students providing socially acceptable rather than honest answers. Apart from the social desirability bias, it is important to bear in mind that students received the online link via their university student email addresses within a specific timeframe, from 29 July to 27 September 2019. The implications here are that students who were absent, or who did not have access to the necessary resource to complete the questionnaire could have been excluded. Although useful, the cross-sectional design has been criticised for only examining aspects of individual’s beliefs and behaviours without paying concerted consideration to the context in which these beliefs and behaviours occur, which could account for misinterpretation of meanings of the beliefs and/or behaviour recorded. As such, it is necessary to exercise caution when interpreting the results of this study.
Recommendations of the study
Taking the aforesaid findings into consideration, it is hoped that the current study’s results would call upon researchers to further investigate the association of factors in relation to an array of substances other than alcohol. This might be essential in the identification of an increase and/or decrease of many substances, and the identification of newly introduced substances, which is vital for the creatiion of awareness-, and prevention- campaigns as well as intervention strategies aimed at the population under study.
A conclusion of the limitations and recommendations of this study cannot be complete without calling for more comprehensive efforts (multidisciplinary) when investigating the use and abuse amongst individuals in our society. Since this research is observational, experimental research is recommended to identify effective intervention options for mitigating the burden of substance abuse among university students.
Discovering these influencing factors (both risk- and protective) would decrease the probability of an individual using drugs, and would once again pinpoint areas one could focus on with interventions, which would empower those in need of intervention, as opposed to educating only. A determination should also be done on evidence-based “best practices” for primary prevention, as well as the treatment of substance abuse among adolescents in South Africa.
In attempts to promote and adhere to the ethicical principles of avoiding harm, giving respect and protecting participants’ integrity, the author's advocacy plea is to cultivate more inclusivity in future research endeavours, especially in the social sciences. Such efforts could begin by exploring social constructs such as gender on a non-binary spectrum. In addition to this, more culturally sensitive, multi-wave longitudinal research needs to be carried out in order to improve on and expand the understanding of substance use and abuse among young people in South Africa, particularly those transitioning from childhood to adolescence to young adulthood, during which pervasive individual and contextual change is the bedrock of these developmental transitions.
The overall aim of the study was to explore the prevalence and factors associated with substance among university students in South Africa in order to provide baseline information that could inform the development and/or tailoring of any awareness and or prevention campaigns designed to reduce substance use and abuse among students in South Africa. Perhaps more importantly, it is hoped that the results, implications, limitation, and recommendation of the present study invokes increased focus and ignites novel or innovative thinking when undertaking research of similar nature.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Alpha (level of significance)
Equals the size of the population
Equals the sample size
Schulenberg JE, Johnston LD, O'Malley PM, Bachman JG, Miech RA, Patrick ME. Monitoring the Future national survey results on drug use, 1975–2016: Volume II, college students and adults ages; 2017. p. 19–55.
Du Preez R, Pentz CD, Lategan BW. Why students drink: a study of South African university students’ drinking behaviour. S Af J High Educ. 2016;30(2):73–93.
Google Scholar
Yi S, Peltzer K, Pengpid S, Susilowati IH. Prevalence and associated factors of illicit drug use among university students in the association of southeast Asian nations (ASEAN). Subst Abuse Treat Prev Policy. 2017;12(1):1–7.
Article Google Scholar
Arria AM, Caldeira KM, Bugbee BA, Vincent KB, O’Grady KE. The academic opportunity costs of substance use during college. College Park: Center on Young Adult Health and Development; 2013.
Jafari F, Zamani AH, Alizadeh K. Reviewing the prevalence of (cigarette) smoking and its related factors in students of Tehran University, Iran. Addict Health. 2011;3(3–4):105.
Dawson DA, Grant BF, Stinson FS, Chou PS. Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. J Stud Alcohol. 2004;65(4):477–88.
Schulenberg JE, Patrick ME. Historical and developmental patterns of alcohol and drug use among college students: framing the problem. In: White HR, Rabiner D, editors. College drinking and drug use. New York: Guilford; 2012. p. 13–35.
National Institute on Drug Abuse, [Internet]. College-Age & Young Adults. 2017 [cited 2019 Nov 5]. https://www.drugabuse.gov/related-topics/college-age-young-adults .
Center for Behavioral Health Statistics and Quality [Internet]). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16-4984, NSDUH Series H-51). 2016 [cited 2019 Nov 5]. http://www.samhsa.gov/data/ .
Bennett TH, Holloway KR. Drug misuse among university students in the UK: implications for prevention. Subst Use Misuse. 2014;49(4):448–55.
Jaouahir I, Azzaoui FZ, Lotfi S, Ahami A, Faid M, Rusinek S. Listening withdrawal psychotherapy from psychoactive substances addiction among young Moroccan trainees. Int J Multidiscip Approach Stud. 2015;2(6):158–65.
O’Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. J Stud Alcohol Suppl. 2002;14:23–39.
Edmonds L, Wilcocks L. Teen drug scene-South Africa: a guide for parents and schools. Wendywood: Little Oak; 1995.
World Health Organization [Internet]. Substance abuse. 2018 [cited 2019 Nov 5]. https://www.who.int/topics/substance_abuse/en/ .
Kyei KA, Ramagoma M. Alcohol consumption in South African universities: prevalence and factors at the University of Venda. Limpopo province. J Soc Sci. 2013;36(1):77–86.
Pengpid S, Peltzer K, Van Der Heever H. Problem alcohol use and associated factors in a sample of university students in South Africa. J Psychol Afr. 2013;23(2):243–9.
Young C, de Klerk V. Patterns of alcohol use on a South African university campus: the findings of two annual drinking surveys. Afr J Drug Alcohol Stud. 2008. https://doi.org/10.4314/ajdas.v7i2.46367 .
Young C, de Klerk V. Correlates of heavy alcohol consumption at Rhodes University. J Child Adolesc Ment Health. 2012;24(1):37–44.
Young C, Mayson T. The Alcohol Use Disorders Identification Scale (AUDIT) normative scores for a multiracial sample of Rhodes University residence students. J Child Adolesc Ment Health. 2010;22(1):15–23.
Puljević C, Learmonth D. Substance abuse prevention in Cape Town’s peri-urban settlements: local health trainers’ perspectives. Health Psychol Behav Med Open Access J. 2014;2(1):183–97.
Wolfe EL, Davis T, Guydish J, Delucchi KL. Mortality risk associated with perinatal drug and alcohol use in California. J Perinatol. 2005;25(2):93–100.
Griffin KW, Lowe SR, Acevedo BP, Botvin GJ. Affective self-regulation trajectories during secondary school predict substance use among urban minority young adults. J Child Adolesc Subst Abuse. 2015;24(4):228–34.
Beck F, Legleye S, Chomynova P, Miller P. A quantitative exploration of attitudes out of line with the prevailing norms toward alcohol, tobacco, and cannabis use among European students. Subst Use Misuse. 2014;49(7):877–90.
White HR, Labouvie EW, Papadaratsakis V. Changes in substance use during the transition to adulthood: a comparison of college students and their noncollege age peers. J Drug Issues. 2005;35(2):281–306.
Becker JB, Perry AN, Westenbroek C. Sex differences in the neural mechanisms mediating addiction: a new synthesis and hypothesis. Biol Sex Differ. 2012;3(1):1–35.
Fernander AF, Flisher AJ, King G, Noubary F, Lombard C, Price M, Chalton D. Gender differences in depression and smoking among youth in Cape Town, South Africa. Ethn Dis. 2006;16(1):41.
National Institute on Drug Abuse (NIDA). Principles of adolescent substance use disorder treatment: a research-based guide. Washington DC: NIDA Publication; 2014.
City of Cape Town. Crime in Cape Town: drug related 2003–2012. Cape Town: Strategic Development Information and Government Communication and Information System (GCIS); 2013.
Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804.
Berman AH, Bergman H, Palmstierna T, Schlyter F. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res. 2005;11(1):22–31.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;1:385–96.
Harding TW, De Arango V, Baltazar J, Climent CE, Ibrahim HH, Ladrido-Ignacio L, Wig NN. Mental disorders in primary health care: a study of their frequency and diagnosis in four developing countries. Psychol Med. 1980;10(2):231–41.
Leedy PD, Ormrod JE. Practical research. Saddle River: Pearson Custom; 2005.
Reinert DF, Allen JP. The alcohol use disorders identification test: an update of research findings. Alcohol Clin Exp Res. 2007;31(2):185–99.
Voluse AC, Gioia CJ, Sobell LC, Dum M, Sobell MB, Simco ER. Psychometric properties of the Drug Use Disorders Identification Test (DUDIT) with substance abusers in outpatient and residential treatment. Addict Behav. 2012;37(1):36–41.
Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. Meas Stress Guide Health Soc Sci. 1994;10(2):1–2.
Peltzer K, Malaka DW, Phaswana N. Sociodemographic factors, religiosity, academic performance, and substance use among first-year university students in South Africa. Psychol Rep. 2002;91(1):105–13.
Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. J Coll Couns. 2006;9(2):135–47.
Stewart RC, Kauye F, Umar E, Vokhiwa M, Bunn J, Fitzgerald M, Tomenson B, Rahman A, Creed F. Validation of a Chichewa version of the self-reporting questionnaire (SRQ) as a brief screening measure for maternal depressive disorder in Malawi, Africa. J Affect Disord. 2009;112(1–3):126–34.
Giang KB, Allebeck P, Kullgren G, Van Tuan N. The Vietnamese version of the Self Reporting Questionnaire 20 (SRQ-20) in detecting mental disorders in rural Vietnam: a validation study. Int J Soc Psychiatry. 2006;52(2):175–84.
Stratton KJ, Aggen SH, Richardson LK, Berenz EC, Tran TL, Trung LT, Tam NT, Tuan T, Buoi LT, Ha TT, Thach TD. Using the SRQ–20 factor structure to examine changes in mental distress following typhoon exposure. Psychol Assess. 2014;26(2):528.
Field A. Discovering statistics using IBM SPSS statistics. London: Sage; 2013.
Harpham T, Reichenheim M, Oser R, Thomas E, Hamid N, Jaswal S, Ludermir A, Aidoo M. Measuring mental health in a cost-effective manner. Health Policy Plan. 2003;18(3):344–9.
Thomas C. Assessment of mental distress in undergraduate medical students. J Educ Res Med Teach. 2014;2(1):14–7.
Dada S, Burnhams NH, Laubscher R, Parry C, Myers B. Alcohol and other drug use among women seeking substance abuse treatment in the Western Cape, South Africa. S Afr J Sci. 2018;114(9–10):1–7.
Shafer AB, Koenig JA, Becker EA. Relation of mental health to alcohol and substance use among Texas college students. Tex Med. 2017;113(4):e1–e1.
Deykin EY, Levy JC, Wells V. Adolescent depression, alcohol and drug abuse. Am J Public Health. 1987;77(2):178–82.
Kushner MG, Sher KJ. Comorbidity of alcohol and anxiety disorders among college students: effects of gender and family history of alcoholism. Addict Behav. 1993;18(5):543–52.
Brook JS, Cohen P, Brook DW. Longitudinal study of co-occurring psychiatric disorders and substance use. J Am Acad Child Adolesc Psychiatry. 1998;37(3):322–30.
Demery R, Thirlaway K, Mercer J. The experiences of university students with a mood disorder. Disabil Soc. 2012;27(4):519–33.
Lin HJ, Yusoff MS. Psychological distress, sources of stress and coping strategy in high school students. Int Med J. 2013;20(6):672–6.
Download references
Acknowledgements
Not applicable.
Authors did not receive any funding to carry out this research.
Author information
Authors and affiliations.
Department of Psychology, Faculty of Community and Health Sciences, University of the Western Cape, Western Cape, South Africa
Stacey Blows & Serena Isaacs
You can also search for this author in PubMed Google Scholar
Contributions
The concept was drafted by SB and SI. Both authors contributed to the comprehensive writing of the article. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Stacey Blows .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for the study was obtained from all the relevant committees at the university. These include the Community and Health Sciences Higher Degrees Committee; Biomedical Research Ethics Committee (BMREC Registration Number: BM18/9/1) as well as the Registrar of the university in the Western Cape, South Africa. The study followed and adhered to all the required ethics procedures set out by the Biomedical Research Ethics Committee (BMREC Registration Number: BM18/9/1). All participants provided written informed consent to partake in the study.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. Demographic Section. A demographic section was developed in order to ascertain demographic information relevant to the current study’s aims and objectives. Questions regarding the students’ substance use, age, gender, education level, year level, marital status and onset of substance.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Blows, S., Isaacs, S. Prevalence and factors associated with substance use among university students in South Africa: implications for prevention. BMC Psychol 10 , 309 (2022). https://doi.org/10.1186/s40359-022-00987-2
Download citation
Received : 03 January 2022
Accepted : 13 November 2022
Published : 15 December 2022
DOI : https://doi.org/10.1186/s40359-022-00987-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Substance use
- Young adults
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders in Patients With Posttraumatic Stress Disorder: A Review of the Literature
- Leslie K. Jacobsen , M.D. ,
- Steven M. Southwick , M.D. , and
- Thomas R. Kosten , M.D.
Search for more papers by this author
OBJECTIVE: Alcohol use disorders and other substance use disorders are extremely common among patients with posttraumatic stress disorder (PTSD). This article reviews studies pertaining to the epidemiology, clinical phenomenology, and pathophysiology of comorbid PTSD and substance use disorders. METHOD: Studies were identified by means of computerized and manual searches. The review of research on the pathophysiology of PTSD and substance use disorders was focused on studies of the hypothalamic-pituitary-adrenal axis and the noradrenergic system. RESULTS: High rates of comorbidity suggest that PTSD and substance use disorders are functionally related to one another. Most published data support a pathway whereby PTSD precedes substance abuse or dependence. Substances are initially used to modify PTSD symptoms. With the development of dependence, physiologic arousal resulting from substance withdrawal may exacerbate PTSD symptoms, thereby contributing to a relapse of substance use. Preclinical work has led to the proposal that in PTSD, corticotropin-releasing hormone and noradrenergic systems may interact such that the stress response is progressively augmented. Patients may use sedatives, hypnotics, or alcohol in an effort to interrupt this progressive augmentation. CONCLUSIONS: Vigorous control of withdrawal and PTSD-related arousal symptoms should be sought during detoxification of patients with comorbid PTSD and substance use disorders. Inclusion of patients with comorbid PTSD and substance use disorders in neurobiologic research and in clinical trials will be critical for development of effective treatments for this severely symptomatic patient population.
Substance use disorders, particularly abuse of and dependence on central nervous system (CNS) depressants, are common in patients with posttraumatic stress disorder (PTSD). This article reviews clinical, epidemiologic, and neurobiologic studies relevant to the problem of comorbid PTSD and substance use disorders and discusses the clinical implications of these findings.
Clinical Phenomenology and Epidemiology
PTSD develops in some people after exposure to a severe traumatic event. The DSM-IV diagnosis of PTSD consists of symptoms in three clusters: 1) reexperiencing symptoms, including intrusive recollections of the trauma that are triggered by exposure to cues symbolizing the trauma; 2) avoidance symptoms, which involve diminished participation in activities and avoidance of thoughts, people, places, and memories associated with the trauma; and 3) arousal symptoms, which include difficulty sleeping, irritability, difficulty concentrating, hypervigilance, and exaggerated startle response.
Although intoxication and withdrawal symptoms vary across abused substances, all substance use disorders share key features. They include a maladaptive pattern of substance use leading to failure to fulfill work, school, or home obligations; legal problems; and substance-related interpersonal problems. Substance dependence further includes tolerance, withdrawal symptoms upon cessation of use, unsuccessful efforts to control use, and continued use despite persistent substance-related physical or psychological problems.
Persons with PTSD have elevated rates of comorbid psychiatric disorders. Studies of both combat veterans and civilians with PTSD have demonstrated that, among men with PTSD, alcohol abuse or dependence is the most common co-occurring disorder, followed by depression, other anxiety disorders, conduct disorder, and nonalcohol substance abuse or dependence (1 , 2) . Among women with PTSD, rates of comorbid depression and other anxiety disorders are highest, followed by alcohol abuse and dependence (1 , 2) . High rates of comorbidity of PTSD and substance use disorders were first reported in war-related studies, in which as many as 75% of combat veterans with lifetime PTSD also met criteria for alcohol abuse or dependence (2) . Among civilian populations, estimates of the prevalence of lifetime substance use disorders have ranged from 21.6% to 43.0% in persons with PTSD, compared with 8.1% to 24.7% in persons without PTSD (1 , 3 , 4) . Similarly, among substance abusers in the general population, the reported rate of PTSD is 8.3% (5) . Rates of PTSD appear to be higher among patients in inpatient substance abuse treatment (up to 42.5%) (6) and among pregnant women in residential treatment for substance abuse (62%) (7) . Surveys of substance-dependent adolescents have also found rates of PTSD ranging up to 19.2% (8) .
Patients with both PTSD and a substance use disorder have significantly higher rates of comorbid axis I and II disorders, psychosocial and medical problems, substance- or alcohol-related inpatient admissions, and relapse to substance use, compared with patients whose substance use is not complicated by PTSD (4 , 9) . Furthermore, patients with PTSD and substance use disorders tend to suffer from more severe PTSD symptoms, particularly those in the avoidance and arousal symptom clusters, than do patients with PTSD alone (10) . Conversely, one longitudinal study of patients with PTSD and a comorbid substance use disorder found at 6-month posttreatment follow-up that patients whose PTSD symptoms had remitted reported significantly less substance use than did patients with unremitted PTSD (11) .
Relationship of Substance Use to PTSD Symptoms
Elevated rates of comorbid depressive and anxiety disorders in patients with PTSD greatly complicate any effort to develop a model of the relationship between PTSD and substance use. High rates of comorbidity suggest that PTSD and substance use disorders are functionally related to one another. Two primary pathways have been described to explain these high rates of comorbidity. In the first, substance abuse precedes PTSD. To sustain their habit, some substance abusers repetitively place themselves in dangerous situations and, as a result, experience high levels of physical and psychological trauma (5) . For example, in a study of patients with PTSD and comorbid cocaine abuse, patients whose cocaine abuse developed first later developed PTSD as a result of trauma sustained in the context of procurement and use of cocaine (12) . Given that chronic substance use can lead to higher levels of arousal and anxiety as well as to sensitization of neurobiologic stress systems (13) , substance abuse may result in a higher level of vulnerability to development of PTSD after exposure to trauma.
In the second pathway, PTSD precedes development of substance use disorders. In this model, the use of substances is a form of self-medication. Patients report that CNS depressants, such as alcohol, cannabis, opioids, and benzodiazepines acutely improve PTSD symptoms (14) . Consistent with this, patients with PTSD report that onset and severity of substance abuse parallel the onset and escalation of PTSD symptoms (14) . In addition, clinical evidence suggests that the choice of substances of abuse (CNS depressants versus CNS stimulants) may stem from the particular constellation of PTSD symptoms that patients experience. For example, PTSD patients with alcohol dependence exhibit significantly more arousal symptoms that do PTSD patients with cocaine dependence (10) .
In the second model, withdrawal from substances, particularly CNS depressants, may initiate a cycle that perpetuates relapse and continued substance use. The withdrawal syndromes associated with many CNS depressants overlap extensively with the arousal symptoms of PTSD (15) ( Figure 1 ). Substances may be taken initially to ameliorate PTSD symptoms. As noted earlier, patients with PTSD have reported that CNS depressants acutely provide symptom relief (14) . Furthermore, objectively measured startle responses are reduced by alcohol (16) . However, the physiologic arousal resulting from substance withdrawal may have an additive effect with arousal symptoms stemming from PTSD. The resulting hyperaroused state may serve as a conditioned reminder of traumatic events and thus precipitate an increase in reexperiencing symptoms. Exacerbation of PTSD symptoms may then prompt relapse to substance use in an attempt to self-medicate. Thus, for the PTSD patient who already has symptoms of arousal, the additional arousal that accompanies withdrawal from substances may be intolerable. Alternatively, substances may be used to cope with the traumatic event itself (17) . This pattern may particularly apply when trauma that leads to PTSD occurs during adulthood. The initial calming effects from substance use may cue patients to resume substance use when PTSD symptoms reemerge.
Most published data support the second model, in which substance use follows or parallels traumatic exposure and the development of PTSD (18) . In a longitudinal study conducted by Chilcoat and Breslau (19) , 1,007 adults were reevaluated 3 and 5 years after an initial assessment. The researchers found that preexisting substance abuse did not increase subjects’ risk of subsequent exposure to trauma or their risk of developing PTSD after exposure to trauma. The relationship between exposure to trauma and increased risk for development of a substance use disorder was found to be specific to PTSD, as exposure to trauma without subsequent development of PTSD did not increase risk for development of a substance use disorder (19) . Of note, one study of patients with cocaine dependence and PTSD found that patients in whom PTSD preceded the onset of cocaine use were significantly more likely to suffer from comorbid major depression and to use benzodiazepines and opiates than were patients in whom PTSD developed after the onset of cocaine use (12) .
Pathophysiology
Our review of the literature on the pathophysiologic basis of comorbid PTSD and addiction selectively focuses on studies of the hypothalamic-pituitary-adrenal (HPA) axis and the noradrenergic system, as these have been most extensively studied in PTSD. It must be emphasized that many other neurobiological systems are involved in both the acute and chronic adaptation to stress and to substance use. These systems include the dopaminergic, γ-aminobutyric acid, benzodiazepine, and serotonergic systems, as well as the thyroid axis. Interactions among these systems in patients with comorbid PTSD and substance dependence are enormously complex. Thus, the potential relationships we discuss between the HPA axis, the noradrenergic system, and symptoms in patients with comorbid PTSD and substance use disorders should be viewed as one part of a far more complex whole.
HPA Axis in PTSD and Addiction
In humans and animals, acute stress elicits a cascade of neurohormonal events, including increased turnover of norepinephrine in terminal projection regions of the locus ceruleus and liberation of hypothalamic corticotropin-releasing hormone (CRH) into the pituitary portal system, which stimulates release of ACTH from the pituitary, which in turn triggers release of cortisol (human) or corticosterone (rat) from the adrenals (20) . Animal and human research has implicated this cascade in the pathophysiology of both substance use disorders and PTSD.
Humans with substance dependence most frequently identify stress and negative mood states as reasons for relapse and ongoing substance abuse (21) . Recently, a personalized stress imagery task was shown to reliably increase cocaine craving and salivary cortisol in cocaine-dependent patients (22) . Animal studies have shown that stress induces relapse to heroin and to cocaine self-administration in rats trained to self-administer these substances and then subjected to a prolonged drug-free period (23 , 24) . Similarly, in animals naive to illicit substances, a large range of stressors increases the proclivity toward drug self-administration (25) . Initial work on the pathophysiology of this phenomenon indicated that stress-induced or stress-enhanced drug self-administration is mediated by corticosterone (26) .
Evidence has accumulated to support a role for CRH in mediating the effects of stress on drug self-administration. Central, but not peripheral, administration of CRH has been shown to induce a long-lasting enhancement (sensitization) of the locomotor response to d-amphetamine (27) , and pretreatment with a CRH antagonist has been shown to block the development of stress-induced sensitization to d-amphetamine (28) . Indeed, central administration of anti-CRH antibody or the CRH receptor antagonist α-helical CRH has been found to block the locomotor hyperactivity induced by cocaine (29) .
Withdrawal from chronic cocaine or alcohol administration in rats produces anxiety-like behavior and decreased exploration that is associated with selective increases in CRH in the hypothalamus, amygdala, and basal forebrain (30 , 31) . Pretreatment with anti-CRH immunoserum or α-helical CRH, blocking the effects of CRH, completely prevents the development of these withdrawal-associated behaviors (30) . Consistent with these observations, CSF CRH is elevated in humans in acute alcohol withdrawal and then normalizes or decreases below normal levels with extended abstinence and resolution of withdrawal symptoms (32) . Shaham and colleagues (33) found that intracerebroventricular injection of CRH reinstated heroin seeking after extinction in rats trained to self-administer the drug. In addition, α-helical CRH attenuated the reinstatement effect of footshock stress (33) . Neither adrenalectomy nor chronic or acute exposure to the corticosterone synthesis inhibitor metyrapone interfered with the reinstatement effects of priming injections of heroin or of footshock stress. A potent, selective CRF1 receptor antagonist, CP-154,526, has been found to attenuate reinstatement of drug seeking induced by footshock stress after up to 14 days of extinction in rats trained to self-administer heroin or cocaine (34) .
Findings from both animal and human studies of the effects of chronic stress or of PTSD on HPA axis function vary depending on the experimental paradigm used or the population studied. In patients with PTSD, elevated (35) , reduced (36) , and normal (37) levels of cortisol secretion have been reported. A series of studies performed by Yehuda and colleagues demonstrated that patients with PTSD have an elevated number of lymphocyte glucocorticoid receptors (38) , enhanced suppression of cortisol after administration of dexamethasone (39) , a greater than normal decrease in the number of lymphocyte glucocorticoid receptors after administration of dexamethasone (39) , and higher than normal increases in ACTH after metyrapone blockade of cortisol synthesis (40) . All of these findings suggest that glucocorticoid negative feedback is enhanced in PTSD.
Animal studies examining the effects of uncontrollable stress on HPA axis function have reported initial increases of corticosterone secretion, followed by normalization of corticosterone secretion with ongoing chronic stress (41) . However, some investigators have failed to demonstrate normalization of corticosterone secretion with chronic uncontrollable stress (42) , particularly in animals that have been reared under stressful conditions (43) or when levels of chronic stress are high (44) . In a pattern similar to that found in humans with PTSD, animals subjected to a single episode of prolonged stress and then briefly restressed after a stress-free period showed enhancement of glucocorticoid negative feedback (45) .
Although both animal and human studies have suggested that glucocorticoid negative feedback may be enhanced in PTSD, the implications of these observations for CRH secretion in this disorder are unclear. As noted earlier, CRH-producing cells and CRH receptors exist both in the hypothalamus and in extrahypothalamic sites. Findings from some studies have suggested that hypothalamic and extrahypothalamic CRH-producing cells may respond differently to corticosterone. Specifically, corticosterone appears to restrain hypothalamic CRH-producing cells while stimulating extrahypothalamic CRH-producing cells, particularly those in the amygdala (46) . Replacement of corticosterone in adrenalectomized rats decreases CRH production in the parvocellular nucleus of the hypothalamus while increasing CRH production in the central nucleus of the amygdala (47) . This region-specific pattern of regulation is also seen in adrenally intact rats treated with high-stress levels of corticosterone for extended periods of time (48) . Thus, while glucocorticoid feedback may decrease CRH production and release in the hypothalamus, it may stimulate CRH production and release in other brain regions, including the amygdala. This possibility has been addressed in two studies of patients with PTSD, one that examined CSF concentrations of CRH at a single time point (49) and one that examined CSF concentrations of CRH at serial time points over a 6-hour period (37) . Both found significantly higher levels of CSF CRH in patients with PTSD than in normal comparison subjects. However, although elevated CSF CRH suggests that brain CRH may be elevated, the specific brain tissues producing CRH elevations cannot be determined from CSF data alone.
The possibility that brain CRH levels are elevated in PTSD is of great interest because of a rich preclinical literature indicating that elevated levels of CRH in the brain, particularly in the amygdala, potentiate fear-related behavioral responses, including the startle response (50) . These anxiogenic effects of CRH are reversed by administration of CRH antagonists (50) . As noted earlier, findings from animal and human studies have supported a role for CRH in mediating some effects of drugs of abuse, including stress- or priming-induced relapse to drug self-administration and symptoms of withdrawal (27 , 28 , 32 – 34) . Thus, elevated levels of CRH in the brain in PTSD may mediate both the symptoms of hyperarousal as well as the increased risk for substance abuse and dependence seen in this disorder. More specifically, elevated levels of CRH in the brain in PTSD may enhance the euphorigenic properties of certain drugs, such as stimulants, and may worsen the severity of withdrawal symptoms, thereby prompting patients to relapse to drug use. Conversely, brain CRH elevations induced by withdrawal from substance use may exacerbate symptoms of hyperarousal, which could trigger other symptoms of PTSD, prompting relapse to substance use.
Noradrenergic System in PTSD and Addiction
During chronic uncontrollable stress, norepinephrine turnover increases in specific brain regions, including the locus ceruleus, hypothalamus, hippocampus, amygdala, and cerebral cortex (51) . Evidence for noradrenergic dysregulation in patients with PTSD has included elevated 24-hour urinary epinephrine and norepinephrine excretion, a lower than normal number of platelet α 2 -adrenergic receptors, elevated 24-hour plasma norepinephrine, and exaggerated cardiovascular and 3-methoxy-4-hydroxyphenylglycol (MHPG) (a norepinephrine metabolite) responses to intravenous yohimbine (52) . Noradrenergic dysregulation has also been reported during states of withdrawal from chronic self-administration of alcohol and other abused substances. The levels of noradrenaline, norepinephrine, and MHPG in both plasma and CSF have been found to be increased and the number of platelet α 2 -adrenergic receptors decreased in alcoholics during acute withdrawal (53 , 54) . The severity of alcoholic withdrawal symptoms has been positively correlated with the concentration of MHPG in CSF (54) . Evidence for noradrenergic dysregulation in opiate withdrawal has included findings of elevated plasma MHPG in humans and elevated plasma and brain MHPG in animals (55 , 56) . In animals, the level of noradrenergic activity was significantly correlated with the severity of withdrawal symptoms (56) . These findings have prompted the use of the α 2 -adrenergic receptor agonist clonidine in the treatment of both opiate withdrawal symptoms and PTSD (57 , 58) .
Noradrenergic System/HPA Axis Interactions
Evidence that brain CRH and noradrenergic systems modulate each other has been reported. Stress has been shown to increase CRH levels in the locus ceruleus (59) , a primary source of noradrenergic projections to all cortices as well as to the thalamus and hypothalamus, while intraventricular administration of CRH has been found to increase the discharge rates of locus ceruleus neurons and to increase norepinephrine turnover in hippocampus, hypothalamus, and prefrontal cortex (60 – 62) . Conversely, stress-induced activation of the locus ceruleus has been blocked by administration of CRH antagonists (63) . Similar evidence exists for the interaction of the CRH and noradrenergic systems in the hypothalamus (64) and the amygdala, where stress induces increases in both CRH and norepinephrine (65) . Furthermore, norepinephrine in the amygdala appears to stimulate release of CRH (66) .
These observations have prompted the proposal by Koob (20) that interactions of the CRH and noradrenergic systems in the brain may, under some conditions, function as a feed-forward system, leading to the progressive augmentation of the stress response with repeated stress exposure that is characteristic of PTSD. This progressive augmentation of response with repeated stress has previously been conceptualized as kindling (67) . A feed-forward interaction between the CRH and noradrenergic systems may represent one neurobiologic underpinning of both PTSD and substance use disorders. More specifically, stress, including stress related to self-administration of or withdrawal from substances, may stimulate CRH release in the locus ceruleus, leading to activation of the locus ceruleus and release of norepinephrine in the cortex, which in turn may stimulate the release of CRH in the hypothalamus and amygdala (20) . Such an interaction between the brain noradrenergic and CRH systems may mediate the symptoms of hyperarousal seen in PTSD, including exaggerated startle response. The proclivity toward misuse of CNS depressants by patients with PTSD may reflect an attempt to interrupt this feed-forward interaction by suppressing activity of the locus ceruleus with these agents (68) .
Conclusions
Clinical and epidemiologic studies confirm that comorbidity of PTSD with substance use disorders is common and that the symptoms of patients with this comorbidity tend to be more severe and more refractory to treatment than those of patients suffering from either disorder alone. Despite the frequency with which patients with both diagnoses present for treatment, no systematic treatment approach of proven efficacy has been developed for this population. Furthermore, little is known about the impact on substance use disorder outcomes of the medications and psychosocial interventions commonly used to treat PTSD, or vice versa.
These limitations notwithstanding, the research conducted to date can inform both clinical practice and future clinical and preclinical research. For example, clinical research suggests that PTSD patients with substance dependence, particularly those who are addicted to CNS depressants, may find the physiologic arousal resulting from substance withdrawal intolerable due to additive effects with preexisting arousal symptoms related to PTSD. Successful detoxification of these patients may thus require inpatient admission to permit vigorous control of withdrawal and PTSD-related arousal symptoms.
Neurobiologic research indicates that high levels of CRH in the brain, particularly in the amygdala, may be common to both PTSD and to substance withdrawal states. Further, CRH antagonists reduce both the anxiety and the enhanced response to illicit substances (sensitization) that are induced by higher levels of brain CRH. These observations suggest that CRH antagonists could potentially have a role in the treatment of patients with PTSD and comorbid substance dependence. Although at present no CRH antagonist has been approved for human use, a series of CRH antagonists that can be administered peripherally have been developed and have been shown to cross the blood brain barrier (34 , 69) . These agents will be important tools for further defining the potential role of CRH antagonism in the treatment of patients with PTSD and substance dependence and will hopefully lead to development of orally active preparations.
Evidence of noradrenergic dysregulation in both PTSD and in withdrawal from CNS depressants has prompted the use of the α 2 -adrenoceptor agonist clonidine in both disorders (57 , 58) . Data from both preclinical and clinical research suggest that this agent, as well as the selective α 2 -adrenoceptor agonist guanfacine, would be effective in reducing noradrenergic hyperactivity in patients with PTSD and comorbid substance dependence. Guanfacine, given its greater selectivity, may offer a more favorable side effect profile. Given the dearth of established treatments for this patient population, controlled clinical trials to establish the efficacy of these agents are clearly indicated.
Finally, although preclinical work has resulted in considerable progress toward delineating the contributions of the HPA axis and noradrenergic systems to the pathophysiologic underpinnings of PTSD with comorbid substance dependence, few neurobiologic studies have been conducted in this patient population. The inclusion of subjects with this comorbidity may render such studies more complicated, but the data emerging from this work would better inform the clinical management of the difficult-to-treat symptoms of these frequently encountered patients. At the minimum, patients who participate in studies of PTSD or of substance dependence must be thoroughly evaluated for the presence of this comorbidity to permit adequate control of the effects of the comorbid condition on the neurobiologic processes under study.
Received May 11, 2000; revision received Aug. 22, 2000; accepted Nov. 17, 2000. From the Department of Psychiatry, Yale University School of Medicine, New Haven, Conn., and the VA Connecticut Healthcare System. Address correspondence to Dr. Jacobsen, Department of Psychiatry (116A), VA Connecticut Healthcare System, Yale University–West Haven Campus, 950 Campbell Ave., West Haven, CT 06516; [email protected] (e-mail). Supported in part by grants DA-00167, DA-04060, and DA-09250 from the National Institute on Drug Abuse.
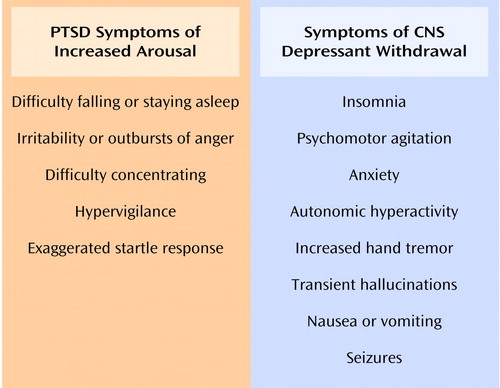
Figure 1. Symptoms of Increased Arousal in PTSD and Symptoms Associated With Withdrawal From CNS Depressants a
a From the DSM-IV criteria for PTSD, alcohol withdrawal, and sedative, hypnotic, or anxiolytic withdrawal.
1. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048- 1060 Google Scholar
2. Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, Brunner/Mazel, 1990 Google Scholar
3. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991 ; 48:216-222 Crossref , Medline , Google Scholar
4. Breslau N, Davis GC, Peterson EL, Schultz L: Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry 1997 ; 54:81-87 Crossref , Medline , Google Scholar
5. Cottler LB, Compton WM III, Mager D, Spitznagel EL, Janca A: Posttraumatic stress disorder among substance users from the general population. Am J Psychiatry 1992 ; 149:664-670 Link , Google Scholar
6. Dansky BS, Saladin ME, Brady KT, Kilpatrick DG, Resnick HS: Prevalence of victimization and posttraumatic stress disorder among women with substance use disorders: comparison of telephone and in-person assessment samples. Int J Addict 1995; 30:1079- 1099 Google Scholar
7. Thompson MP, Kingree JB: The frequency and impact of violent trauma among pregnant substance abusers. Addict Behav 1998 ; 23:257-262 Crossref , Medline , Google Scholar
8. Deykin EY, Buka SL: Prevalence and risk factors for posttraumatic stress disorder among chemically dependent adolescents. Am J Psychiatry 1997 ; 154:752-757 Link , Google Scholar
9. Najavits LM, Gastfriend DR, Barber JP, Reif S, Muenz LR, Blaine J, Frank A, Crits-Christoph P, Thase M, Weiss RD: Cocaine dependence with and without PTSD among subjects in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Am J Psychiatry 1998 ; 155:214-219 Abstract , Google Scholar
10. Saladin ME, Brady KT, Dansky BS, Kilpatrick DG: Understanding comorbidity between PTSD and substance use disorders: two preliminary investigations. Addict Behav 1995 ; 20:643-655 Crossref , Medline , Google Scholar
11. Ouimette PC, Brown PJ, Najavits LM: Course and treatment of patients with both substance use and posttraumatic stress disorders. Addict Behav 1998 ; 23:785-795 Crossref , Medline , Google Scholar
12. Brady KT, Dansky BS, Sonne SC, Saladin ME: Posttraumatic stress disorder and cocaine dependence. Am J Addict 1998 ; 7:128-135 Crossref , Medline , Google Scholar
13. Aouizerate B, Schluger JH, Perret G, McClary K, Ho A, Piazza PV, Kreek MJ: Enhanced sensitivity to negative glucocorticoid feedback in methadone patients with ongoing cocaine dependence, in Proceedings of the College on Problems of Drug Dependence Annual Meeting. Bethesda, Md, National Institute on Drug Abuse, CPDD, 1998, p 3 Google Scholar
14. Bremner JD, Southwick SM, Darnell A, Charney DS: Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry 1996 ; 153:369-375 Link , Google Scholar
15. van der Kolk B, Greenberg M, Boyd H, Krystal J: Inescapable shock, neurotransmitters, and addiction to trauma: toward a psychobiology of post traumatic stress. Biol Psychiatry 1985 ; 20:314-325 Crossref , Medline , Google Scholar
16. Hutchison KE, Rohsenow D, Monti P, Palfai T, Swift R: Prepulse inhibition of the startle reflex: preliminary study of the effects of a low dose of alcohol in humans. Alcohol Clin Exp Res 1997; 21:1312- 1319 Google Scholar
17. Mirin SM, McKenna GJ: Combat zone adjustment: the role of marihuana use. Mil Med 1975 ; 140:482-485 Crossref , Medline , Google Scholar
18. Keane TM, Gerardi RJ, Lyons JA, Wolfe J: The interrelationship of substance abuse and posttraumatic stress disorder: epidemiological and clinical considerations. Recent Dev Alcohol 1988 ; 6:27-48 Medline , Google Scholar
19. Chilcoat HD, Breslau N: Posttraumatic stress disorder and drug disorders: testing causal pathways. Arch Gen Psychiatry 1998 ; 55:913-917 Crossref , Medline , Google Scholar
20. Koob GF: Corticotropin-releasing factor, norepinephrine, and stress. Biol Psychiatry 1999; 46:1167- 1180 Google Scholar
21. Brewer DD, Catalano RF, Haggerty K, Gainey RR, Fleming CB: A meta-analysis of predictors of continued drug use during and after treatment for opiate addiction. Addiction 1998 ; 93:73-92 Crossref , Medline , Google Scholar
22. Sinha R, Catapano D, O’Malley S: Stress-induced craving and stress response in cocaine dependent individuals. Psychopharmacology (Berl) 1999 ; 142:343-351 Crossref , Medline , Google Scholar
23. Shaham Y, Stewart J: Stress reinstates heroin-seeking in drug-free animals: an effect mimicking heroin, not withdrawal. Psychopharmacology (Berl) 1995 ; 119:334-341 Crossref , Medline , Google Scholar
24. Erb S, Shaham Y, Stewart J: Stress reinstates cocaine-seeking behavior after prolonged extinction and a drug-free period. Psychopharmacology (Berl) 1996 ; 128:408-412 Crossref , Medline , Google Scholar
25. Piazza PV, Deminiere JM, Le Moal M, Simon H: Stress- and pharmacologically-induced behavioral sensitization increases vulnerability to acquisition of amphetamine self-administration. Brain Res 1990 ; 514:22-26 Crossref , Medline , Google Scholar
26. Deroche V, Marinelli M, LeMoal M, Piazza PV: Glucocorticoids and behavioral effects of psychostimulants, II: cocaine intravenous self-administration and reinstatement depend on glucocorticoid levels. J Pharmacol Exp Ther 1997; 281:1401- 1407 Google Scholar
27. Cador M, Cole BJ, Koob GF, Stinus L, Le Moal M: Central administration of corticotropin releasing factor induces long-term sensitization to d-amphetamine. Brain Res 1993 ; 606:181-186 Crossref , Medline , Google Scholar
28. Cole BJ, Cador M, Stinus L, Rivier J, Vale W, Koob GF, Le Moal M: Central administration of a CRF antagonist blocks the development of stress-induced behavioral sensitization. Brain Res 1990 ; 512:343-346 Crossref , Medline , Google Scholar
29. Sarnyai Z, Hohn J, Szabo G, Penke B: Critical role of endogenous corticotropin-releasing factor (CRF) in the mediation of the behavioral action of cocaine in rats. Life Sci 1992; 51:2019- 2024 Google Scholar
30. Sarnyai Z, Biro E, Gardi J, Vecsernyes M, Julesz J, Telegdy G: Brain corticotropin-releasing factor mediates “anxiety-like” behavior induced by cocaine withdrawal in rats. Brain Res 1995 ; 675:89-97 Crossref , Medline , Google Scholar
31. Merlo-Pich E, Koob GF, Heilig M, Menzaghi F, Vale W, Weiss F: Corticotropin-releasing factor release from mediobasal hypothalamus of the rat as measured by microdialysis. Neuroscience 1993 ; 55:695-707 Crossref , Medline , Google Scholar
32. Adinoff B, Anton R, Linnoila M, Guidotti A, Nemeroff CB, Bissette G: Cerebrospinal fluid concentrations of corticotropin-releasing hormone (CRH) and diazepam-binding inhibitor (DBI) during alcohol withdrawal and abstinence. Neuropsychopharmacology 1996 ; 15:288-295 Crossref , Medline , Google Scholar
33. Shaham Y, Funk D, Erb S, Brown TJ, Walker C-D, Stewart J: Corticotropin-releasing factor, but not corticosterone, is involved in stress-induced relapse to heroin-seeking in rats. J Neurosci 1997; 17:2605- 2614 Google Scholar
34. Shaham Y, Erb S, Leung S, Buczek Y, Stewart J: CP-154,526, a selective, non-peptide antagonist of the corticotropin-releasing factor 1 receptor attenuates stress-induced relapse to drug seeking in cocaine- and heroin-trained rats. Psychopharmacology (Berl) 1998 ; 137:184-190 Crossref , Medline , Google Scholar
35. Maes M, Lin A, Bonaccorso S, van Hunsel F, Van Gastel A, Delmeire L, Biondi M, Bosmans E, Kenis G, Scharpe S: Increased 24-hour urinary cortisol excretion in patients with post-traumatic stress disorder and patients with major depression, but not in patients with fibromyalgia. Acta Psychiatr Scand 1998 ; 98:328-335 Crossref , Medline , Google Scholar
36. Mason JW, Giller EL, Kosten TR, Ostroff RB, Podd L: Urinary free-cortisol levels in posttraumatic stress disorder patients. J Nerv Ment Dis 1986 ; 174:145-149 Crossref , Medline , Google Scholar
37. Baker DG, West SA, Nicholson WE, Ekhator NN, Kasckow JW, Hill KK, Bruce AB, Orth DN, Geracioti TD Jr: Serial CSF corticotropin-releasing hormone levels and adrenocortical activity in combat veterans with posttraumatic stress disorder. Am J Psychiatry 1999 ; 156:585-588 Abstract , Google Scholar
38. Yehuda R, Lowy MT, Southwick SM, Shaffer D, Giller EL Jr: Lymphocyte glucocorticoid receptor number in posttraumatic stress disorder. Am J Psychiatry 1991 ; 148:499-504 Link , Google Scholar
39. Yehuda R, Boisoneau D, Lowy MT, Giller EL: Dose-response changes in plasma cortisol and lymphocyte glucocorticoid receptors following dexamethasone administration in combat veterans with and without posttraumatic stress disorder. Arch Gen Psychiatry 1995 ; 52:583-593 Crossref , Medline , Google Scholar
40. Yehuda R, Levengood RA, Schmeilder J, Wilson S, Guo LS, Gerber D: Increased pituitary activation following metyrapone administration in post-traumatic stress disorder. Psychoneuroendocrinology 1996 ; 21:1-16 Crossref , Medline , Google Scholar
41. Kant GJ, Bauman RA, Anderson SM, Mougey EH: Effects of controllable vs uncontrollable chronic stress on stress-responsive plasma hormones. Physiol Behav 1992; 51:1285- 1288 Google Scholar
42. Irwin J, Ahluwalia P, Zacharko RM, Anisman H: Central norepinephrine and plasma corticosterone following acute and chronic stressors: influence of social isolation and handling. Pharmacol Biochem Behav 1986; 24:1151- 1154 Google Scholar
43. Gamallo A, Villanua A, Trancho G, Fraile A: Stress adaptation and adrenal activity in isolated and crowded rats. Physiol Behav 1986 ; 36:217-221 Crossref , Medline , Google Scholar
44. Young EA, Akana S, Dallman MF: Decreased sensitivity to glucocorticoid fast feedback in chronically stressed rats. Neuroendocrinology 1990 ; 51:536-542 Crossref , Medline , Google Scholar
45. Liberzon I, Krstov M, Young EA: Stress-restress: effects on ACTH and fast feedback. Psychoneuroendocrinology 1997 ; 22:443-453 Crossref , Medline , Google Scholar
46. Schulkin J, Gold PW, McEwen BS: Induction of corticotropin-releasing hormone gene expression by glucocorticoids; implication for understanding the states of fear and anxiety and allostatic load. Psychoneuroendocrinology 1998 ; 23:219-243 Crossref , Medline , Google Scholar
47. Makino S, Gold PW, Schulkin J: Corticosterone effects on corticotropin-releasing hormone mRNA in the central nucleus of the amygdala and the parvocellular region of the paraventricular nucleus of the hypothalamus. Brain Res 1994 ; 640:105-112 Crossref , Medline , Google Scholar
48. Makino S, Gold PW, Schulkin J: Effects of corticosterone on CRH mRNA and content in the bed nucleus of the stria terminalis; comparison with the effects in the central nucleus of the amygdala and the paraventricular nucleus of the hypothalamus. Brain Res 1994 ; 657:141-149 Crossref , Medline , Google Scholar
49. Bremner JD, Licinio J, Darnell A, Krystal JH, Owens MJ, Southwick SM, Nemeroff CB, Charney DS: Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. Am J Psychiatry 1997 ; 154:624-629 Link , Google Scholar
50. Swerdlow NR, Britton KT, Koob GF: Potentiation of acoustic startle by corticotropin-releasing factor (CRF) and by fear are both reversed by alpha-helical CRF (9-41). Neuropsychopharmacology 1989 ; 2:285-292 Crossref , Medline , Google Scholar
51. Tanaka T, Yokoo H, Mizoguchi K, Yoshida M, Tsuda A, Tanaka M: Noradrenaline release in the rat amygdala is increased by stress: studies with intracerebral microdialysis. Brain Res 1991 ; 544:174-176 Crossref , Medline , Google Scholar
52. Southwick SM, Bremner JD, Rasmusson A, Morgan CA, Arnsten A, Charney DS: Role of norepinephrine in the pathophysiology and treatment of posttraumatic stress disorder. Biol Psychiatry 1999; 46:1192- 1204 Google Scholar
53. Smith AJ, Brent PJ, Henry DA, Foy A: Plasma noradrenaline, platelet alpha 2-adrenoceptors, and functional scores during ethanol withdrawal. Alcohol Clin Exp Res 1990 ; 14:497-502 Crossref , Medline , Google Scholar
54. Hawley RJ, Major LF, Schulman EA, Linnoila M: Cerebrospinal fluid 3-methoxy-4-hydroxyphenylglycol and norepinephrine levels in alcohol withdrawal: correlations with clinical signs. Arch Gen Psychiatry 1985; 42:1056- 1062 Google Scholar
55. Charney DS, Redmond DE, Galloway MP, Kleber HD, Heninger GR, Murberg M, Roth RH: Naltrexone precipitated opiate withdrawal in methadone addicted human subjects: evidence for noradrenergic hyperactivity. Life Sci 1984; 35:1263- 1272 Google Scholar
56. Swann AC, Elsworth JD, Charney DS, Jablons DM, Roth RH, Redmond DE, Maas JW: Brain catecholamine metabolites and behavior in morphine withdrawal. Eur J Pharmacol 1982 ; 86:167-175 Crossref , Medline , Google Scholar
57. Agren H: Clonidine treatment of the opiate withdrawal syndrome: a review of clinical trials of a theory. Acta Psychiatr Scand Suppl 1986 ; 327:91-113 Medline , Google Scholar
58. Harmon RJ, Riggs PD: Clonidine for posttraumatic stress disorder in preschool children. J Am Acad Child Adolesc Psychiatry 1996; 35:1247- 1249 Google Scholar
59. Chappell PB, Smith MA, Hilts CD, Bissette G, Ritchie J, Andersen C, Nemeroff CB: Alterations in corticotropin-releasing factor-like immunoreactivity in discrete rat brain regions after acute and chronic stress. J Neurosci 1986; 10:2908- 2916 Google Scholar
60. Valentino RJ, Foote SL, Aston-Jones G: Corticotropin-releasing factor activates noradrenergic neurons of the locus coeruleus. Brain Res 1983 ; 270:363-367 Crossref , Medline , Google Scholar
61. Zhang JJ, Swiergiel AH, Palamarchouk VS, Dunn AJ: Intracerebroventricular infusion of CRF increases extracellular concentrations of norepinephrine in the hippocampus and cortex as determined by in vivo voltametry. Brain Res Bull 1998 ; 47:277-284 Crossref , Medline , Google Scholar
62. Lavicky J, Dunn AJ: Corticotropin-releasing factor stimulates catecholamine release in hypothalamus and prefrontal cortex in freely moving rats as assessed by microdialysis. J Neurochem 1993 ; 60:602-612 Crossref , Medline , Google Scholar
63. Valentino RJ, Page ME, Curtis AL: Activation of noradrenergic locus coeruleus neurons by hemodynamic stress is due to local release of corticotropin-releasing factor. Brain Res 1991 ; 555:25-34 Crossref , Medline , Google Scholar
64. Pacak K, Palkovits M, Kopin IJ, Goldstein DS: Stress-induced norepinephrine release in the hypothalamic paraventricular nucleus and pituitary-adrenocortical and sympathoadrenal activity: in vivo microdialysis studies. Front Neuroendocrinol 1995 ; 16:89-150 Crossref , Medline , Google Scholar
65. Pich EM, Lorang M, Yeganeh M, Rodriquez de Fonseca F, Raber J, Koob GF, Weiss F: Increase of extracellular corticotropin-releasing factor-like immunoreactivity levels in the amygdala of awake rats during restraint stress and ethanol withdrawal as measured by microdialysis. J Neurosci 1995; 15:5439- 5447 Google Scholar
66. Raber J, Koob GF, Bloom FE: Interleukin-2 (IL-2) induces corticotropin-releasing factor (CRF) release from the amygdala and involves a nitric oxide-mediated signaling: comparison with the hypothalamic response. J Pharmacol Exp Ther 1995 ; 272:815-824 Medline , Google Scholar
67. Post RM, Weiss SRB, Smith M, Li H, McCann U: Kindling versus quenching; implications for the evolution and treatment of posttraumatic stress disorder. Ann NY Acad Sci 1997 ; 821:285-295 Crossref , Medline , Google Scholar
68. Kosten TR, Krystal J: Biological mechanisms in posttraumatic stress disorder: relevance for substance abuse. Recent Dev Alcohol 1988 ; 6:49-68 Medline , Google Scholar
69. Arai K, Ohata H, Shibasaki T: Non-peptidic corticotropin-releasing hormone receptor type 1 antagonist reverses restraint stress-induced shortening of sodium pentobarbital-induced sleeping time of rats: evidence that an increase in arousal induced by stress is mediated through CRH receptor type 1. Neurosci Lett 1998 ; 255:103-106 Crossref , Medline , Google Scholar
- The Relationship Between Workplace Drug Policies, Opioid Misuse, and Psychological Distress: Evidence From the 2020 National Survey on Drug Use and Health 8 February 2024 | NEW SOLUTIONS: A Journal of Environmental and Occupational Health Policy, Vol. 34, No. 1
- Predictors of Suicidal Ideation and Continued Substance Use Problems Among Patients Receiving Methadone Maintenance Treatment Who Have Co-Occurring Cocaine Use Disorder 15 January 2024 | Substance Use & Misuse, Vol. 59, No. 5
- Health Consequences of Violence Directed at Children in Iran: Need for Global Health Action 19 January 2024 | Journal of Loss and Trauma, Vol. 29, No. 3
- The relationship between discrimination, alcohol use severity, and PTSD symptoms among Latinx heavy drinkers Journal of Substance Use and Addiction Treatment, Vol. 159
- Written exposure therapy for veterans with co-occurring substance use disorders and PTSD: Study design of a randomized clinical trial Contemporary Clinical Trials, Vol. 139
- The impact of substance use on posttraumatic stress disorder symptoms and treatment discontinuation 12 December 2023 | Journal of Traumatic Stress, Vol. 37, No. 2
- Mapping the Pathways Between Posttraumatic Stress Disorder, Depression, and Alcohol and Cannabis Use: A Network Analysis 31 March 2024 | Journal of Dual Diagnosis
- Individual Differences in Substance Use Motives, Trauma, and Stress Among College-Based Polysubstance Users 27 March 2024 | Substance Use & Misuse, Vol. 3
- Post-traumatic stress and future substance use outcomes: leveraging antecedent factors to stratify risk 8 March 2024 | Frontiers in Psychiatry, Vol. 15
- Virtual Reality and Transcranial Direct Current Stimulation for Posttraumatic Stress Disorder 6 March 2024 | JAMA Psychiatry, Vol. 376
- Combat events and negative emotions associated with postdeployment illicit drug use among Army National Guard soldiers 22 November 2022 | Journal of Substance Use, Vol. 29, No. 2
- Do we really need two sessions?: The use of a structured interview as a trauma cue reactivity paradigm 10 July 2023 | International Journal of Methods in Psychiatric Research, Vol. 33, No. 1
- The substance use behaviors change of first-year college students before and during COVID-19 pandemic 16 January 2024 | Journal of American College Health, Vol. 3
- Young People’s Support Needs During the Military–Civilian Transition: “I Would Have Been a Very Different Person if There was More Support Available” 17 July 2022 | Australian Social Work, Vol. 77, No. 1
- Psychodrama group psychotherapy as an effective treatment for PTSD and depression in inpatient substance use treatment: a mixed methods study 17 December 2023 | Social Work With Groups, Vol. 14
- Identifying drivers of increasing opioid overdose deaths among black individuals: a qualitative model drawing on experience of peers and community health workers 13 January 2023 | Harm Reduction Journal, Vol. 20, No. 1
- The impact of PTSD on risk of cardiometabolic diseases: a national patient cohort study in Norway 20 May 2023 | BMC Psychiatry, Vol. 23, No. 1
- Behavioral and neurocognitive factors distinguishing post-traumatic stress comorbidity in substance use disorders 14 September 2023 | Translational Psychiatry, Vol. 13, No. 1
- Resilience and Low Substance Use Among Indigenous College Students from a Sexual Assault Prevention Study 3 November 2023 | Adversity and Resilience Science, Vol. 4, No. 4
- Sex and Gender Differences in Co-Occurring Alcohol Use Disorder and PTSD 22 September 2023 | Current Addiction Reports, Vol. 10, No. 4
- Post-traumatic stress disorder and drug use disorder: examination of aetiological models in a Swedish population-based cohort 6 October 2023 | European Journal of Psychotraumatology, Vol. 14, No. 2
- Examining Differences in Substance Use Outcomes and Related Correlates among Transfeminine and Transmasculine Adults Using the 2017 New York State Patient Characteristics Survey 24 July 2023 | Substance Use & Misuse, Vol. 58, No. 13
- Exposure to smoking and general health problems among university students: mediating role of positive affect and moderating role of parenting 22 July 2022 | Journal of Substance Use, Vol. 28, No. 6
- Correlates of posttraumatic stress in cancer patients and their family caregivers across two years following diagnosis 3 October 2023 | Psycho-Oncology, Vol. 32, No. 11
- Dissociation and Temporality in Substance Abuse: A Clinical Phenomenological Overview 30 October 2023 | Psychopathology
- The Impact of Severe Trauma Exposure in Late Childhood on Longitudinal Treatment Outcomes in Adolescents and Young Adults in Treatment for Drug Use Disorders: A Record-Linkage Study 17 October 2023 | International Journal of Mental Health and Addiction, Vol. 9
- Type of Victimization Exposure, Perpetrator Type, and Timing of Victimization: The Impact on Behavioral Health Outcomes 7 October 2023 | Journal of Interpersonal Violence, Vol. 2
- Monotonic Association of Increasing Past-Year Substance Use Disorder across a Four-Level Trauma Post-Traumatic Stress Disorder (PTSD) Hierarchy in a Nationwide Sample 5 October 2023 | Journal of Dual Diagnosis, Vol. 19, No. 4
- Housing Instability Associated with Return to Stimulant Use among Previously Abstaining Women 26 September 2023 | International Journal of Environmental Research and Public Health, Vol. 20, No. 19
- Treatment of PTSD and SUD for the incarcerated population with EMDR: A pilot study 8 October 2023 | Journal of Addictions & Offender Counseling, Vol. 44, No. 2
- Study protocol: implementing and evaluating a trauma-informed model of care in residential youth treatment for substance use disorders 27 September 2023 | Frontiers in Psychiatry, Vol. 14
- Oxytocin Reduces Sensitized Stress–Induced Alcohol Relapse in a Model of Posttraumatic Stress Disorder and Alcohol Use Disorder Comorbidity Biological Psychiatry, Vol. 94, No. 3
- Examining Interactive Effects of PTSD and Deviant Peer Association for Predicting Violent Offending Risk 2 August 2022 | Crime & Delinquency, Vol. 69, No. 8
- Climate Change and Substance-Use Behaviors: A Risk-Pathways Framework 28 November 2022 | Perspectives on Psychological Science, Vol. 18, No. 4
- Benjamin R. Lewis , M.D. , and
- Kevin Byrne , M.D.
- Are migrants diagnosed with a trauma-related disorder at risk of premature mortality? A register-based cohort study in Denmark Journal of Migration and Health, Vol. 392
- Famine Exposure during Early Life and Risk of Cancer in Adulthood: A Systematic Review and Meta-Analysis 10 July 2023 | The journal of nutrition, health & aging, Vol. 27, No. 7
- The acute effects of psychoactive drugs on emotional episodic memory encoding, consolidation, and retrieval: A comprehensive review Neuroscience & Biobehavioral Reviews, Vol. 150
- The Intersectionality of Sex and Race in the Relationship Between Posttraumatic Stress Disorder and Cardiovascular Disease: A Scoping Review 27 June 2023 | Public Health Reviews, Vol. 44
- PTSD, rumination, and psychological health: examination of multi-group models among military veterans and college students 19 January 2022 | Current Psychology, Vol. 42, No. 16
- Substance use and related disorders among persons exposed to the 9/11 terrorist attacks: Essentials for screening and intervention 27 February 2023 | Archives of Environmental & Occupational Health, Vol. 78, No. 5
- Investigating gender differences in the Co-occurrence of PTSD and food addiction Appetite, Vol. 117
- The Association between Potentially Traumatic Events and Cocaine, Cannabis, and Alcohol Use Differs by Race 21 April 2023 | Substance Use & Misuse, Vol. 10
- Primary Care Considerations for Elderly U.S. Veterans of World War II and the Korean War: A Narrative Review Cureus, Vol. 36
- Affective scaffolding in addiction 28 March 2023 | Inquiry, Vol. 117
- The Role of Pre-Treatment Traumatic Stress Symptoms in Adolescent Substance Use Treatment Outcomes 10 February 2023 | Substance Use & Misuse, Vol. 58, No. 4
- Associations between positive memory count and hazardous substance use in a trauma‐exposed sample: Examining the moderating role of emotion dysregulation 2 March 2023 | Journal of Clinical Psychology, Vol. 10
- Adverse Childhood Experiences and Binge Drinking in Adolescence: the Role of Impulsivity and PTSD Symptoms 16 December 2022 | Journal of Pediatric Neuropsychology, Vol. 9, No. 1
- Neurobiology of Aggression—Review of Recent Findings and Relationship with Alcohol and Trauma 20 March 2023 | Biology, Vol. 12, No. 3
- L’imputabilité d’une addiction à un trouble post-traumatique est-elle envisageable dans le cadre d’une expertise du dommage corporel ? Annales Médico-psychologiques, revue psychiatrique, Vol. 181, No. 3
- Traumatic experiences and PTSD symptoms in substance use disorder: A comparison of recovered versus current users 4 November 2022 | Nordic Studies on Alcohol and Drugs, Vol. 40, No. 1
- Sexual Victimization and Mental Health Among LGBQ + College Students: Examining Social Support and Trauma-Related Drinking as Mediators 23 January 2023 | International Journal of Mental Health and Addiction, Vol. 55
- Improving care for SUD patients with complex trauma–relationships between childhood trauma, dissociation, and suicidal behavior in female patients with PTSD and SUD 12 January 2023 | Frontiers in Psychiatry, Vol. 13
- Overdose Experiences among People Who Inject Drugs in West Virginia: Personal Loss, Psychological Distress, Naloxone, and Fentanyl 13 November 2022 | Substance Use & Misuse, Vol. 58, No. 1
- The Integration of Behavioral Health and Primary Care for Hispanic/Latino Patients with Depression and Comorbid PTSD 9 November 2022 | The Journal of Behavioral Health Services & Research, Vol. 50, No. 1
- Comorbid posttraumatic stress disorder and alcohol use disorder in low- and middle-income countries: A narrative review 12 December 2022 | Cambridge Prisms: Global Mental Health, Vol. 10
- The Role of Adverse Childhood Experiences on People in Opiate Agonist Treatment: The Importance of Feeling Unloved 5 September 2023 | European Addiction Research, Vol. 29, No. 5
- Addictions et groupes spécifiques : les adolescents, les personnes âgées et les femmes
- Violence – suicide and suicidal ideation as sequelae of trauma in substance use disorder inpatients 25 December 2022 | Scandinavian Journal of Psychology, Vol. 34
- Relations Between Posttraumatic Stress Disorder Symptoms and Positive Memory Characteristics Among Women Reporting Intimate Partner Violence: A Micro-Longitudinal Study 21 December 2022 | Journal of Interpersonal Violence, Vol. 142
- Chronic ethanol consumption exacerbates future stress‐enhanced fear learning, an effect mediated by dorsal hippocampal astrocytes 9 November 2022 | Alcoholism: Clinical and Experimental Research, Vol. 46, No. 12
- A Scoping Review of the Literature on Trauma Cue-Induced Drug Craving in Substance Users with Trauma Histories or PTSD 16 November 2022
- The Intertwining of Posttraumatic Stress Symptoms, Alcohol, Tobacco or Nicotine Use, and the COVID-19 Pandemic: A Systematic Review 5 November 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 21
- A mixed-methods study on psychodrama treatment for PTSD and depression in inpatient substance use treatment: A comparison of outcomes pre-pandemic and during Covid-19 The Arts in Psychotherapy, Vol. 81
- Stress- and drug-induced neuroimmune signaling as a therapeutic target for comorbid anxiety and substance use disorders Pharmacology & Therapeutics, Vol. 239
- Clinical Predictors of Engagement in Teleintegrated Care and Telereferral Care for Complex Psychiatric Disorders in Primary Care: a Randomized Trial 2 February 2022 | Journal of General Internal Medicine, Vol. 37, No. 13
- Is Chronic Pain a Disease? The Journal of Pain, Vol. 23, No. 10
- Stress-related disorders and subsequent cancer risk and mortality: a population-based and sibling-controlled cohort study in Sweden 13 August 2022 | European Journal of Epidemiology, Vol. 37, No. 9
- Practical Considerations for Treating Comorbid Posttraumatic Stress Disorder in the Addictions Clinic Psychiatric Clinics of North America, Vol. 45, No. 3
- Posttraumatic stress and risky sex in trauma-exposed college students: the role of personality dispositions toward impulsive behavior 13 October 2020 | Journal of American College Health, Vol. 70, No. 6
- Disordered eating as a repercussion of sexual assault: a consequence to consider 11 January 2022 | Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity, Vol. 27, No. 6
- Quantitative changes in mental health measures with 3MDR treatment for Canadian military members and veterans 18 July 2022 | Brain and Behavior, Vol. 12, No. 8
- Military family dynamics in transition: The experiences of young people when their families leave the Australian Defence Force 30 December 2021 | Child & Family Social Work, Vol. 27, No. 3
- What’s in a name? A data-driven method to identify optimal psychotherapy classifications to advance treatment research on co-occurring PTSD and substance use disorders 22 December 2021 | European Journal of Psychotraumatology, Vol. 13, No. 1
- Fatigue sensitivity and mental health among trauma-exposed firefighters 30 June 2022 | Fatigue: Biomedicine, Health & Behavior, Vol. 10, No. 3
- Post-traumatic stress disorder: a psychiatric disorder requiring urgent attention 2 August 2022 | Medical Review, Vol. 2, No. 3
- Adolescence alcohol exposure impairs fear extinction and alters medial prefrontal cortex plasticity Neuropharmacology, Vol. 211
- The Relationship between Positive Memory Phenomenology and Alcohol Use among Trauma-Exposed Individuals 28 March 2022 | Substance Use & Misuse, Vol. 57, No. 6
- “I Felt It and I Let It Go”: Perspectives on Meditation and Emotional Regulation among Female Survivors of Interpersonal Trauma with Co-occurring Disorders 11 October 2021 | Journal of Family Violence, Vol. 37, No. 4
- Traumatic Stress-Induced Vulnerability to Addiction: Critical Role of the Dynorphin/Kappa Opioid Receptor System 27 April 2022 | Frontiers in Pharmacology, Vol. 13
- Measurement Error-Corrected Estimation of Clinically Significant Change Trajectories for Interventions Targeting Comorbid PTSD and SUDs in OEF/OIF Veterans Behavior Therapy, Vol. 43
- Comorbid alcohol use and post-traumatic stress disorders: Pharmacotherapy with aldehyde dehydrogenase 2 inhibitors versus current agents Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 115
- Effect of patient characteristics on posttraumatic stress disorder treatment retention among veterans: A systematic review 20 November 2021 | Journal of Traumatic Stress, Vol. 35, No. 2
- Long-Term Post-traumatic Stress Disorder After Orthopaedic Injury: Prevalence and Risk Factors Journal of Orthopaedic Trauma, Vol. 36, No. 4
- Bright Light Treatment of Combat-related PTSD: A Randomized Controlled Trial 29 January 2021 | Military Medicine, Vol. 187, No. 3-4
- Case Report: the Comorbidity of Pregabalin-Use Disorder and Post-Traumatic Stress Disorder: Clinical and Pharmacological Issues 30 June 2020 | International Journal of Mental Health and Addiction, Vol. 20, No. 1
- Developing a trauma-informed workforce for the opioid crisis in a rural community in the United States: a case study 3 September 2021 | The Journal of Mental Health Training, Education and Practice, Vol. 17, No. 1
- Correlates of COVID-19 pandemic-related increases in sleep aid and anti-anxiety medication use 9 March 2021 | Journal of Substance Use, Vol. 27, No. 1
- Associations Between Lifetime Panic Attacks, Posttraumatic Stress Disorder, and Substance Use Disorders in a Nationally Representative Sample 29 December 2021 | Journal of Dual Diagnosis, Vol. 18, No. 1
- Sex Differences across Retrospective Transitions in Posttraumatic Stress and Substance Use Disorders 29 December 2021 | Journal of Dual Diagnosis, Vol. 18, No. 1
- Symptoms of PTSD 14 August 2022
- The Role(s) of Psychopharmacology in the Treatment of PTSD
- Posttraumatic Stress Disorder, Suicidal Behavior, Substance Use, and Sexual Victimization Among Adolescent Girls Aged 10-19 Years Living Under Ethnic-Based Civil War in Ethiopia 1 October 2022 | Neuropsychiatric Disease and Treatment, Vol. Volume 18
- New Metabolic, Digestive, and Oxidative Stress-Related Manifestations Associated with Posttraumatic Stress Disorder Oxidative Medicine and Cellular Longevity, Vol. 2021
- Rates and predictors of psychotherapy receipt among U.S. veterans with comorbid posttraumatic stress disorder and substance use disorders Drug and Alcohol Dependence Reports, Vol. 1
- Long-Term Mental Health Effects of a Devastating Wildfire Are Amplified by Sociodemographic and Clinical Antecedents in College Students 15 June 2020 | Disaster Medicine and Public Health Preparedness, Vol. 15, No. 6
- Optogenetic manipulation of the prelimbic cortex during fear memory reconsolidation alters fear extinction in a preclinical model of comorbid PTSD/AUD 4 August 2021 | Psychopharmacology, Vol. 238, No. 11
- Treatment outcomes in individuals diagnosed with comorbid opioid use disorder and Posttraumatic stress disorder: A review Addictive Behaviors, Vol. 122
- Cumulative Violence and PTSD Symptom Severity Among Urban Street-Based Female Sex Workers 2 November 2019 | Journal of Interpersonal Violence, Vol. 36, No. 21-22
- Associations among betrayal trauma, dissociative posttraumatic stress symptoms, and substance use among women involved in the criminal legal system in three US cities Drug and Alcohol Dependence, Vol. 227
- “Stories of starting”: Understanding the complex contexts of opioid misuse initiation 17 May 2023 | Substance Abuse, Vol. 42, No. 4
- Profiles of U.S. Law Enforcement Officers’ Physical, Psychological, and Behavioral Health: Results From a Nationally Representative Survey of Officers 17 February 2021 | Police Quarterly, Vol. 24, No. 3
- The prevalence of hazardous and harmful alcohol use across trauma-exposed occupations: A meta-analysis and meta-regression Drug and Alcohol Dependence, Vol. 226
- An Integrated Model of Nature and Nurture Factors that Contribute to Addiction and Recovery 19 April 2021 | Substance Use & Misuse, Vol. 56, No. 8
- Longitudinal assessment of PTSD and illicit drug use among male and female OEF-OIF veterans Addictive Behaviors, Vol. 118
- A Comparison of Cognitive Processing Therapy and Seeking Safety for the Treatment of Posttraumatic Stress Disorder in Veterans 22 September 2020 | Psychiatric Quarterly, Vol. 92, No. 2
- Prevalence Rates and Correlates of Likely Post-Traumatic Stress Disorder in Residents of Fort McMurray 6 Months After a Wildfire 13 May 2019 | International Journal of Mental Health and Addiction, Vol. 19, No. 3
- Effect of trauma-related stress after alcohol consumption on perceived likelihood of negative consequences and willingness to drive Addictive Behaviors, Vol. 117
- Intersections of food insecurity, violence, poor mental health and substance use among US women living with and at risk for HIV: Evidence of a syndemic in need of attention 26 May 2021 | PLOS ONE, Vol. 16, No. 5
- The administration of sertraline plus naltrexone reduces ethanol consumption and motivation in a long-lasting animal model of post-traumatic stress disorder Neuropharmacology, Vol. 189
- Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta‐analysis 6 October 2020 | Addiction, Vol. 116, No. 5
- Problematic Use of the Internet in Subjects With Bipolar Disorder: Relationship With Posttraumatic Stress Symptoms 26 April 2021 | Frontiers in Psychiatry, Vol. 12
- Diffusion Tensor Imaging Reveals White Matter Differences in Military Personnel Exposed to Trauma with and without Post-traumatic Stress Disorder Psychiatry Research, Vol. 298
- Questioning Precedent in Unprecedented Times: Psychosocial Interventions Supporting Medications for Opioid Use Disorder Journal of Psychosocial Nursing and Mental Health Services, Vol. 59, No. 4
- Associations Between Childhood Trauma and the Age of First-Time Drug Use in Methamphetamine-Dependent Patients 26 March 2021 | Frontiers in Psychiatry, Vol. 12
- Posttraumatic stress or posttraumatic growth? Using network analysis to explore the relationships between coping styles and trauma outcomes Journal of Anxiety Disorders, Vol. 78
- Childhood Maltreatment and Risky Substance Use Behaviors: The Mediating Roles of Posttraumatic Stress Symptoms & Callous Unemotional Traits 10 January 2021 | Substance Use & Misuse, Vol. 56, No. 3
- Post-traumatic stress disorder and risky opioid use among persons living with HIV and chronic pain 4 February 2021 | AIDS Care, Vol. 48
- Childhood trauma and post-trauma environment affect fear memory and alcohol use differently in male and female mice Drug and Alcohol Dependence, Vol. 219
- Internalizing and externalizing subtypes in female patients with co-occurring post-traumatic stress disorder and substance use disorders Journal of Substance Abuse Treatment, Vol. 121
- Factors associated with post-traumatic stress disorder among bereaved family members and surviving students two and half years after the Sewol ferry accident in South Korea Psychiatry Research, Vol. 296
- A psychometric investigation on the diagnostic utility of the posttrauma risky behaviors questionnaire Psychiatry Research, Vol. 296
- Can the migration process influence the clinical expression of heroin use disorder in migrants to Italy? 23 January 2020 | CNS Spectrums, Vol. 26, No. 1
- Early Adolescent Binge Drinking Increases Risk of Psychopathology in Post-9/11 Veterans and Mild Traumatic Brain Injury Exacerbates Symptom Severity 10 August 2020 | Alcohol and Alcoholism, Vol. 56, No. 1
- The Comorbidity of Post-traumatic Stress Disorder (PTSD) and Substance Use Disorders 4 November 2020
- Psychological Trauma: Biological and Psychosocial Aspects of Substance Use Disorders 1 May 2021
- The synthetically produced predator odor 2,5-dihydro-2,4,5-trimethylthiazoline increases alcohol self-administration and alters basolateral amygdala response to alcohol in rats 25 September 2020 | Psychopharmacology, Vol. 238, No. 1
- Prevalence of comorbid substance use disorders with anxiety disorders or post-traumatic stress disorder in people seeking treatment for substance abuse: a systematic review protocol 1 August 2021 | JBI Evidence Synthesis, Vol. 19, No. 8
- The Relationship Between Khat Use Disorder and Post-Traumatic Stress Disorder Among Prisoners with Life Time Trauma Exposure in Ethiopia: A Cross-Sectional Study 1 December 2021 | Neuropsychiatric Disease and Treatment, Vol. Volume 17
- Traumatic brain injury and the misuse of alcohol, opioids, and cannabis
- Acute and Post-Traumatic Stress Disorders: A biased nervous system Revue Neurologique, Vol. 177, No. 1-2
- Twenty seven years of treating survivors of torture and organized violence – associations between torture, gender and ethnic minority status among refugees referred for treatment of PTSD 19 April 2021 | European Journal of Psychotraumatology, Vol. 12, No. 1
- Dorsal hippocampal interleukin-1 signaling mediates heroin withdrawal-enhanced fear learning 28 August 2020 | Psychopharmacology, Vol. 237, No. 12
- Dimensions of childhood trauma and their direct and indirect links to PTSD, impaired control over drinking, and alcohol-related-problems Addictive Behaviors Reports, Vol. 12
- Evaluation of the effect of doxasozin and zonisamide on voluntary ethanol intake in mice that experienced chronic intermittent ethanol exposure and stress Alcohol, Vol. 89
- Chemogenetic Manipulation of Dopamine Neurons Dictates Cocaine Potency at Distal Dopamine Transporters 12 October 2020 | The Journal of Neuroscience, Vol. 40, No. 45
- Impact of cannabis on non-medical opioid use and symptoms of posttraumatic stress disorder: a nationwide longitudinal VA study 9 October 2020 | The American Journal of Drug and Alcohol Abuse, Vol. 46, No. 6
- Zonisamide as an Adjunctive Treatment to Cognitive Processing Therapy for Veterans With Posttraumatic Stress Disorder and Comorbid Alcohol Use Disorder: A Pilot Study 27 May 2020 | The American Journal on Addictions, Vol. 29, No. 6
- The Impact of Indigenous Identity and Treatment Seeking Intention on the Stigmatization of Substance Use 15 November 2019 | International Journal of Mental Health and Addiction, Vol. 18, No. 5
- The Prevalence of Mild Cognitive Impairment in a Convenience Sample of 202 Gulf War Veterans 30 September 2020 | International Journal of Environmental Research and Public Health, Vol. 17, No. 19
- Situating the Continuum of Overdose Risk in the Social Determinants of Health: A New Conceptual Framework 18 August 2020 | The Milbank Quarterly, Vol. 98, No. 3
- COVID-19 stress and substance use: Current issues and future preparations Journal of Anxiety Disorders, Vol. 74
- The Intentional Self-Medication of 9/11-Related PTSD Symptoms with Alcohol: 15 Years after the Disaster 24 July 2020 | International Journal of Environmental Research and Public Health, Vol. 17, No. 15
- Traumatic Events in Dual Disorders: Prevalence and Clinical Characteristics 6 August 2020 | Journal of Clinical Medicine, Vol. 9, No. 8
- Adverse childhood experiences (ACEs), cell-mediated immunity, and survival in the context of cancer Brain, Behavior, and Immunity, Vol. 88
- Chapitre 15. Les troubles addictifs
- The role of catecholamines in modulating responses to stress: Sex‐specific patterns, implications, and therapeutic potential for post‐traumatic stress disorder and opiate withdrawal 20 April 2020 | European Journal of Neuroscience, Vol. 52, No. 1
- Equine-Assisted Therapy for Veterans with PTSD: Manual Development and Preliminary Findings 8 February 2020 | Military Medicine, Vol. 185, No. 5-6
- Post-traumatic stress disorder attributed to traumatic brain injury in children – a systematic review 5 June 2020 | Brain Injury, Vol. 34, No. 7
- The impact of trauma characteristics on post-traumatic stress disorder and substance use disorder outcomes across integrated and substance use treatments Journal of Substance Abuse Treatment, Vol. 113
- The Personality Assessment Inventory Alcohol Scale in Veterans With PTSD: Convergent and Discriminant Relations With the Alcohol Use Disorders Identification Test 23 January 2019 | Assessment, Vol. 27, No. 4
- Long-Term Mental Health Effects of a Devastating Wildfire Are Amplified by Socio-Demographic and Clinical Antecedents in Elementary and High School Staff 26 May 2020 | Frontiers in Psychiatry, Vol. 11
- Mindfulness as a predictor of cognitive-behavioral therapy outcomes in inner-city adults with posttraumatic stress and substance dependence Addictive Behaviors, Vol. 104
- The Utility of College Student Samples in Research on Trauma and Posttraumatic Stress Disorder: A Critical Review Journal of Anxiety Disorders
- Pre‐ and postnatal alcohol exposure delays, in female but not in male rats, the extinction of an auditory fear conditioned memory and increases alcohol consumption 28 September 2019 | Developmental Psychobiology, Vol. 62, No. 4
- Psychosocial factors associated with psychological distress and functional difficulties in recently transitioned and current serving regular Australian Defence Force members Psychiatry Research, Vol. 286
- A Systematic Review of Treatments for Problematic Khat Use 25 November 2019 | Substance Use & Misuse, Vol. 55, No. 4
- Gambling disorder and comorbid behavioral addictions: Demographic, clinical, and personality correlates Psychiatry Research, Vol. 284
- Improving the awareness and care of veterans in healthcare services Nursing Standard, Vol. 35, No. 1
- The Need to Numb: Substance Use and Therapeutic Management 4 August 2020
- Intolerance of uncertainty and addiction
- Cannabinoids as an Emerging Therapy for Posttraumatic Stress Disorder and Substance Use Disorders Journal of Clinical Neurophysiology, Vol. 37, No. 1
- A multisite randomized controlled trial of Seeking Safety vs. Relapse Prevention Training for women with co-occurring posttraumatic stress disorder and substance use disorders 19 February 2019 | European Journal of Psychotraumatology, Vol. 10, No. 1
- Posttraumatic stress disorder symptom clusters and substance use among patients with upper limb amputations due to traumatic injury 5 September 2018 | Disability and Rehabilitation, Vol. 41, No. 26
- Psychiatric comorbidities in alcohol use disorder The Lancet Psychiatry, Vol. 6, No. 12
- Chemogenetic stimulation of the infralimbic cortex reverses alcohol-induced fear memory overgeneralization 30 April 2019 | Scientific Reports, Vol. 9, No. 1
- Trauma exposure and alcohol use disorder among prisoners in Jimma Zone correctional institution, Southwest Ethiopia: a cross-sectional study 19 November 2019 | BMC Research Notes, Vol. 12, No. 1
- The role of stigma and trauma in hepatitis C virus treatment in veterans: Applying the common‐sense model 3 October 2019 | Public Health Nursing, Vol. 36, No. 6
- Baseline resting heart rate variability predicts post‐traumatic stress disorder treatment outcomes in adults with co‐occurring substance use disorders and post‐traumatic stress 10 April 2019 | Psychophysiology, Vol. 56, No. 8
- 40. EMDR et addiction
- Dealing with Complexity and Comorbidity: Opportunity for Transdiagnostic Treatment for PTSD 9 May 2019 | Current Treatment Options in Psychiatry, Vol. 6, No. 2
- Post‐Ebola psychosocial experiences and coping mechanisms among Ebola survivors: a systematic review 20 March 2019 | Tropical Medicine & International Health, Vol. 24, No. 6
- Does trauma-focused exposure therapy exacerbate symptoms among patients with comorbid PTSD and substance use disorders? 23 April 2019 | Behavioural and Cognitive Psychotherapy, Vol. 3
- A systematic review of the psychosocial impact of emotional numbing in US combat veterans 31 December 2018 | Journal of Clinical Psychology, Vol. 75, No. 4
- Attitudes among young adults in Palestine about peers with substance use problems: Challenges and opportunities for community intervention design 19 December 2017 | International Social Work, Vol. 62, No. 2
- Informal Control by Family and Risk Markers for Alcohol Abuse/Dependence in Seoul 8 May 2016 | Journal of Interpersonal Violence, Vol. 34, No. 5
- Why do trauma survivors become depressed? Testing the behavioral model of depression in a nationally representative sample Psychiatry Research, Vol. 272
- International Journal of Mental Health and Addiction, Vol. 17, No. 2
- Journal of Child & Adolescent Trauma, Vol. 12, No. 3
- Role of Stress-Associated Signaling in Addiction
- Addictive Behaviors, Vol. 98
- Behavioural Brain Research, Vol. 368
- Current Opinion in Psychology, Vol. 30
- Journal of Substance Abuse Treatment, Vol. 96
- Sexual trauma history is associated with reduced orbitofrontal network strength in substance-dependent women NeuroImage: Clinical, Vol. 24
- Physiology & Behavior, Vol. 203
- Neurobiology of Stress, Vol. 10
- Substance Use & Misuse, Vol. 54, No. 8
- Journal of Dual Diagnosis, Vol. 15, No. 2
- Journal of Dual Diagnosis, Vol. 15, No. 3
- Military Behavioral Health, Vol. 7, No. 3
- Psychiatry and Clinical Psychopharmacology, Vol. 29, No. 1
- Pain Research and Management, Vol. 2019
- PLOS Medicine, Vol. 16, No. 11
- PLOS ONE, Vol. 14, No. 2
- Cannabis, Vol. 2, No. 1
- Frontiers in Behavioral Neuroscience, Vol. 13
- Frontiers in Psychology, Vol. 10
- Frontiers in Psychiatry, Vol. 10
- Management of Chronic Mental Illnesses and Substance Use Disorders
- Drug use and hazardous drinking are associated with PTSD symptoms and symptom clusters in US Army Reserve/National Guard Soldiers 12 December 2018 | The American Journal on Addictions, Vol. 28, No. 1
- Substance use disorder and posttraumatic stress disorder symptomology on behavioral outcomes among juvenile justice youth 21 December 2018 | The American Journal on Addictions, Vol. 28, No. 1
- Alcohol expectancies and distress tolerance: Potential mechanisms in the relationship between posttraumatic stress and alcohol use Personality and Individual Differences, Vol. 137
- Is Integrated CBT Effective in Reducing PTSD Symptoms and Substance Use in Iraq and Afghanistan Veterans? Results from a Randomized Clinical Trial 23 June 2018 | Cognitive Therapy and Research, Vol. 42, No. 6
- Epilogue to the special issue on the use of mobile technology for real-time assessment and treatment of substance use disorders 25 July 2018 | The American Journal of Drug and Alcohol Abuse, Vol. 44, No. 5
- Does experiential avoidance explain the relationships between shame, PTSD symptoms, and compulsive sexual behaviour among women in substance use treatment? 5 June 2018 | Clinical Psychology & Psychotherapy, Vol. 25, No. 5
- Distress tolerance as a mechanism of PTSD symptom change: Evidence for mediation in a treatment-seeking sample Psychiatry Research, Vol. 267
- After the Escape: Physical Abuse of Offspring, Posttraumatic Stress Disorder, and the Legacy of Political Violence in the DPRK 30 October 2017 | Violence Against Women, Vol. 24, No. 9
- The buffering effect of belonging on the negative association of childhood trauma with adult mental health and risky alcohol use Journal of Substance Abuse Treatment, Vol. 88
- Treating addiction with schema therapy and EMDR in women with co-occurring SUD and PTSD: A pilot study 9 October 2017 | Journal of Substance Use, Vol. 23, No. 2
- CB1 and ethanol effects on glutamatergic transmission in the central amygdala of male and female msP and Wistar rats 28 June 2017 | Addiction Biology, Vol. 23, No. 2
- Trial of Prazosin for Post-Traumatic Stress Disorder in Military Veterans New England Journal of Medicine, Vol. 378, No. 6
- (±)-MDMA and its enantiomers: potential therapeutic advantages of R(−)-MDMA 16 December 2017 | Psychopharmacology, Vol. 235, No. 2
- Journal of Contemporary Psychotherapy, Vol. 48, No. 1
- PTSD symptom presentation among people with alcohol and drug use disorders: Comparisons by substance of abuse Addictive Behaviors, Vol. 76
- Alcohol, Vol. 72
- Contemporary Clinical Trials, Vol. 65
- Comprehensive Psychiatry, Vol. 80
- Clinical Psychology Review, Vol. 62
- Journal of Anxiety Disorders, Vol. 53
- Journal of Substance Abuse Treatment, Vol. 85
- Personality and Individual Differences, Vol. 120
- Psychological Medicine, Vol. 48, No. 16
- Military Psychology, Vol. 30, No. 4
- Journal of Child & Adolescent Substance Abuse, Vol. 27, No. 3
- Journal of Human Behavior in the Social Environment, Vol. 28, No. 3
- Journal of Dual Diagnosis, Vol. 14, No. 1
- Journal of Dual Diagnosis, Vol. 14, No. 2
- Alcoholism: Clinical and Experimental Research, Vol. 42, No. 1
- Epidemiology of allergic rhinitis and associated risk factors in Asia World Allergy Organization Journal, Vol. 11
- Journal of Korean Academy of Psychiatric and Mental Health Nursing, Vol. 27, No. 2
- Revista Brasileira de Psiquiatria, Vol. 40, No. 4
- JMIR Mental Health, Vol. 5, No. 2
- THE KOREAN JOURNAL OF PSYCHOLOGY : GENERAL, Vol. 37, No. 4
- Frontiers in Psychiatry, Vol. 9
- Journal of Clinical Medicine, Vol. 7, No. 2
- Al-Qanṭara, Vol. 39, No. 1
- Dissociation and under-regulation of affect in patients with posttraumatic stress disorder with and without a co-morbid substance use disorder European Journal of Trauma & Dissociation, Vol. 1, No. 4
- Madrid Study (Spain) on the Prevalence and Characteristics of Outpatients With Dual Disorders Addictive Disorders & Their Treatment, Vol. 16, No. 4
- Discovery of endogenous opioid systems: what it has meant for the clinician's understanding of pain and its treatment 21 August 2017 | Pain, Vol. 158, No. 12
- Perceptions of Neighborhood Mediate the Relationship Between PTSD Symptoms and Coping in a Neighborhood-Matched Substance-Using Sample Journal of Addiction Medicine, Vol. 11, No. 6
- Psychotropic Medication Prescribing in Iraq/Afghanistan Veterans and Vietnam Era Veterans With Posttraumatic Stress Disorder Journal of Nervous & Mental Disease, Vol. 205, No. 11
- The effect of post-traumatic stress disorder on the risk of developing prescription opioid use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III Drug and Alcohol Dependence, Vol. 179
- Cancer risk among Holocaust survivors in Israel—A nationwide study 10 July 2017 | Cancer, Vol. 123, No. 17
- Altered metabotropic glutamate receptor 5 markers in PTSD: In vivo and postmortem evidence 17 July 2017 | Proceedings of the National Academy of Sciences, Vol. 114, No. 31
- Treatment of alcohol use disorder and co-occurring PTSD 23 December 2016 | The American Journal of Drug and Alcohol Abuse, Vol. 43, No. 4
- Anna Kim , M.D.
- Impact of Meditation on Mental Health Outcomes of Female Trauma Survivors of Interpersonal Violence With Co-Occurring Disorders: A Randomized Controlled Trial 5 July 2015 | Journal of Interpersonal Violence, Vol. 32, No. 14
- Posttraumatic Stress Symptoms and their Relationship to Drug and Alcohol use in an International Sample of Latino Immigrants 5 May 2016 | Journal of Immigrant and Minority Health, Vol. 19, No. 3
- Assessing PTSD in the military: Validation of a scale distributed to Danish soldiers after deployment since 1998 18 April 2017 | Scandinavian Journal of Psychology, Vol. 58, No. 3
- Trauma in Veterans With Substance Use Disorder: Similar Treatment Need Among Urban and Rural Residents 9 August 2016 | The Journal of Rural Health, Vol. 33, No. 3
- Crime victims’ self-medication 23 January 2017 | International Review of Victimology, Vol. 23, No. 2
- Epigenetic alterations of the BDNF gene in combat‐related post‐traumatic stress disorder 25 November 2016 | Acta Psychiatrica Scandinavica, Vol. 135, No. 2
- Posttraumatic Stress Disorder and Alcohol Use Disorder: A Critical Review of Pharmacologic Treatments 19 January 2017 | Alcoholism: Clinical and Experimental Research, Vol. 41, No. 2
- Social Support and Relationship Satisfaction as Moderators of the Stress-Mood-Alcohol Link Association in US Navy Members Journal of Nervous & Mental Disease, Vol. 205, No. 2
- Social Psychiatry and Psychiatric Epidemiology, Vol. 52, No. 3
- Journal of Psychopathology and Behavioral Assessment, Vol. 39, No. 4
- Psychological Injury and Law, Vol. 10, No. 3
- Very Long-Term Effects of Chronic Cocaine on Anxiety and Stress
- Addictive Behaviors, Vol. 64
- Addictive Behaviors, Vol. 73
- Addictive Behaviors, Vol. 74
- Behavior Therapy, Vol. 48, No. 2
- Drug and Alcohol Dependence, Vol. 180
- European Journal of Trauma & Dissociation, Vol. 1, No. 4
- Journal of Anxiety Disorders, Vol. 51
- Neuropharmacology, Vol. 125
- Psychiatry Research, Vol. 257
- Therapies, Vol. 72, No. 3
- Alcoholism Treatment Quarterly, Vol. 35, No. 3
- Anxiety, Stress, & Coping, Vol. 30, No. 6
- Clinical Psychology: Science and Practice, Vol. 24, No. 1
- Concurrent Treatment with Prolonged Exposure for Co-Occurring Full or Subthreshold Posttraumatic Stress Disorder and Substance Use Disorders: A Randomized Clinical Trial 11 May 2017 | Psychotherapy and Psychosomatics, Vol. 86, No. 3
- Mental Health Help Seeking Among Traumatized Individuals 8 July 2016 | Trauma, Violence, & Abuse, Vol. 18, No. 1
- BMC Psychiatry, Vol. 17, No. 1
- PLOS ONE, Vol. 12, No. 7
- Frontiers in Pharmacology, Vol. 8
- Brain Sciences, Vol. 7, No. 12
- Psychiatry Investigation, Vol. 14, No. 6
- Neurobiology of comorbid post‐traumatic stress disorder and alcohol‐use disorder 18 November 2016 | Genes, Brain and Behavior, Vol. 16, No. 1
- Changes in posttraumatic stress disorders symptoms during and after therapeutic community drug and alcohol treatment Therapeutic Communities: The International Journal of Therapeutic Communities, Vol. 37, No. 4
- Cancer incidence in Holocaust male survivors—An Israeli cohort study 25 August 2016 | International Journal of Cancer, Vol. 139, No. 11
- Exposure to Childhood Abuse and Later Substance Use: Indirect Effects of Emotion Dysregulation and Exposure to Trauma 13 September 2016 | Journal of Traumatic Stress, Vol. 29, No. 5
- Trauma‐ and Stress‐Induced Response in Veterans with Alcohol Dependence and Comorbid Post‐Traumatic Stress Disorder 1 July 2016 | Alcoholism: Clinical and Experimental Research, Vol. 40, No. 8
- Psychological therapies for post-traumatic stress disorder and comorbid substance use disorder 4 April 2016 | Cochrane Database of Systematic Reviews, Vol. 2016, No. 4
- Effects of oxytocin on methamphetamine-seeking exacerbated by predator odor pre-exposure in rats 23 December 2015 | Psychopharmacology, Vol. 233, No. 6
- Alcohol Use Disorders and Comorbid Post-Traumatic Stress Disorder in US Military Veterans: Etiology and Current Treatment Approaches 2 June 2016
- Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz, Vol. 59, No. 1
- Social Psychiatry and Psychiatric Epidemiology, Vol. 51, No. 3
- Social Psychiatry and Psychiatric Epidemiology, Vol. 51, No. 8
- Brain Imaging and Behavior, Vol. 10, No. 4
- Current Treatment Options in Psychiatry, Vol. 3, No. 1
- Behavioural Brain Research, Vol. 306
- Brain Research Bulletin, Vol. 120
- Behaviour Research and Therapy, Vol. 79
- Cognitive and Behavioral Practice, Vol. 23, No. 2
- Drug and Alcohol Dependence, Vol. 161
- Drug and Alcohol Dependence, Vol. 163
- Experimental Neurology, Vol. 284
- Journal of Affective Disorders, Vol. 196
- Journal of Anxiety Disorders, Vol. 38
- Journal of Contextual Behavioral Science, Vol. 5, No. 4
- Psychiatry Research, Vol. 239
- Psychiatry Research, Vol. 243
- Journal of Addictive Diseases, Vol. 35, No. 3
- Journal of Dual Diagnosis, Vol. 12, No. 1
- Journal of Dual Diagnosis, Vol. 12, No. 3-4
- Social Work in Public Health, Vol. 31, No. 1
- Journal of Neurotrauma, Vol. 33, No. 9
- Addiction Biology, Vol. 21, No. 3
- Journal of EMDR Practice and Research, Vol. 10, No. 1
- Frontiers in Psychology, Vol. 7
- Mindfulness and Meditation in the Conceptualization and Treatment of Posttraumatic Stress Disorder
- A systematic review of the methodologies used in research related to adult drug and alcohol rehabilitation in therapeutic communities published 2000-2013 Therapeutic Communities: The International Journal of Therapeutic Communities, Vol. 36, No. 4
- Trauma-related mental health problems among national humanitarian staff: a systematic review of the literature 19 November 2015 | European Journal of Psychotraumatology, Vol. 6, No. 1
- Adolescent social isolation increases anxiety-like behavior and ethanol intake and impairs fear extinction in adulthood: Possible role of disrupted noradrenergic signaling Neuropharmacology, Vol. 97
- To reduce or abstain? Substance use goals in the treatment of veterans with substance use disorders and comorbid PTSD 24 August 2015 | The American Journal on Addictions, Vol. 24, No. 7
- Benzodiazepines for PTSD Journal of Psychiatric Practice, Vol. 21, No. 4
- A randomized controlled trial of treatments for co‐occurring substance use disorders and post‐traumatic stress disorder 12 June 2015 | Addiction, Vol. 110, No. 7
- Les interactions entre les différentes composantes du traumatisme psychique et les conduites d’assuétudes Psychotropes, Vol. Vol. 20, No. 4
- Pathways to change: Use trajectories following trauma-informed treatment of women with co-occurring post-traumatic stress disorder and substance use disorders 4 March 2015 | Drug and Alcohol Review, Vol. 34, No. 3
- A Pilot Trial of Prazosin, an Alpha-1 Adrenergic Antagonist, for Comorbid Alcohol Dependence and Posttraumatic Stress Disorder 1 April 2015 | Alcoholism: Clinical and Experimental Research, Vol. 39, No. 5
- Trauma‐ and Stressor‐Related Disorders: Posttraumatic Stress Disorder, Acute Stress Disorder, and Adjustment Disorder 20 February 2015
- Post‐traumatic Stress Disorder Symptoms Mediate the Relationship Between Trauma Exposure and Smoking Status in College Students 14 January 2014 | Stress and Health, Vol. 31, No. 1
- Human Brain Mapping, Vol. 36, No. 8
- Alcohol Use Disorders and Comorbid Posttraumatic Stress Disorder in US Military Veterans: Etiology and Current Treatment Approaches 23 May 2015
- Maternal and Child Health Journal, Vol. 19, No. 10
- Brain Imaging and Behavior, Vol. 9, No. 3
- Journal of Child & Adolescent Trauma, Vol. 8, No. 3
- Biological Psychiatry, Vol. 77, No. 10
- Biological Psychiatry, Vol. 78, No. 5
- Cognitive and Behavioral Practice, Vol. 22, No. 3
- Clinical Psychology Review, Vol. 38
- Drug and Alcohol Dependence, Vol. 147
- Drug and Alcohol Dependence, Vol. 152
- Journal of Anxiety Disorders, Vol. 29
- Associations between lifetime PTSD symptoms and current substance use disorders using a five-factor model of PTSD Journal of Anxiety Disorders, Vol. 29
- Journal of Anxiety Disorders, Vol. 30
- Neurobiology of Stress, Vol. 1
- Perspectives Psy, Vol. 54, No. 1
- Journal of Psychoactive Drugs, Vol. 47, No. 5
- Journal of Trauma & Dissociation, Vol. 16, No. 2
- Journal of Dual Diagnosis, Vol. 11, No. 3-4
- The American Journal on Addictions, Vol. 24, No. 8
- Screening of Current Post-Traumatic Stress Disorder in Patients with Substance Use Disorder Using the Depression, Anxiety and Stress Scale (DASS-21): A Reliable and Convenient Measure 19 November 2014 | European Addiction Research, Vol. 21, No. 2
- Psychodynamic Psychiatry, Vol. 43, No. 2
- Journal of EMDR Practice and Research, Vol. 9, No. 3
- The American Journal of Drug and Alcohol Abuse, Vol. 41, No. 1
- Klinik Psikofarmakoloji Bülteni-Bulletin of Clinical Psychopharmacology, Vol. 25, No. 4
- Posttraumatic Stress Disorders and Addiction 17 October 2014
- The Comorbidity of Post-Traumatic-Stress Disorder (PTSD) and Substance Use Disorders 30 November 2014
- Posttraumatic Stress Disorder and Impulsive and Risky Behavior: Overview and Discussion of Potential Mechanisms 3 July 2015
- Vulnerability to PTSD: Psychosocial and Demographic Risk and Resilience Factors
- Psychopathology and the Ability to Do Otherwise 8 April 2013 | Philosophy and Phenomenological Research, Vol. 90, No. 1
- Epigenetics and memory: causes, consequences and treatments for post‐traumatic stress disorder and addiction 28 January 2015 | Genes, Brain and Behavior, Vol. 14, No. 1
- Personality Assessment Inventory internalizing and externalizing structure in veterans with posttraumatic stress disorder: Associations with aggression 16 August 2014 | Aggressive Behavior, Vol. 40, No. 6
- Recent Violence in a Community-Based Sample of Homeless and Unstably Housed Women With High Levels of Psychiatric Comorbidity American Journal of Public Health, Vol. 104, No. 9
- Trauma-Related Symptoms in Sri Lankan Adult Survivors After the Tsunami 4 October 2013 | Asia Pacific Journal of Public Health, Vol. 26, No. 4
- Co-occurring prescription opioid use problems and posttraumatic stress disorder symptom severity 8 May 2014 | The American Journal of Drug and Alcohol Abuse, Vol. 40, No. 4
- Psychometric Properties of the Posttraumatic Diagnostic Scale (PDS) in Alcohol-Dependent Patients 10 May 2023 | Substance Abuse, Vol. 35, No. 3
- The Role of Alcohol Expectancies in Drinking Behavior among Women with Alcohol Use Disorder and Comorbid Posttraumatic Stress Disorder 14 July 2014 | Journal of Psychoactive Drugs, Vol. 46, No. 3
- Interactions between disordered sleep, post-traumatic stress disorder, and substance use disorders 3 June 2014 | International Review of Psychiatry, Vol. 26, No. 2
- Constraint theory: A cognitive, motivational theory of dependence 9 April 2013 | Addiction Research & Theory, Vol. 22, No. 1
- Chapitre 6. Psychotraumatisme et pathologies addictives
- Evidence-Based Treatment of Post-Traumatic Stress Disorder Annual Review of Medicine, Vol. 65, No. 1
- European Child & Adolescent Psychiatry, Vol. 23, No. 5
- Cognitive Therapy and Research, Vol. 38, No. 3
- Psychological Injury and Law, Vol. 7, No. 4
- Addictive Behaviors, Vol. 39, No. 2
- Addictive Behaviors, Vol. 39, No. 10
- Comprehensive Psychiatry, Vol. 55, No. 5
- Journal of Anxiety Disorders, Vol. 28, No. 1
- Journal of Anxiety Disorders, Vol. 28, No. 8
- Journal of Psychosomatic Research, Vol. 77, No. 3
- Neuroscience, Vol. 277
- Neurobiology of Learning and Memory, Vol. 112
- Pharmacology Biochemistry and Behavior, Vol. 117
- Evidenzbasierte Psychotherapie bei Patienten mit Substanzabhängigkeit und psychischer Komorbidität 9 January 2014 | PSYCH up2date, Vol. 8, No. 01
- Mental Health and Substance Use, Vol. 7, No. 2
- Mental Health and Substance Use, Vol. 7, No. 3
- Mental Health and Substance Use, Vol. 7, No. 4
- PLoS ONE, Vol. 9, No. 11
- Psychodynamic Psychiatry, Vol. 42, No. 3
- Frontiers in Integrative Neuroscience, Vol. 8
- Associations between Post‐Traumatic Stress Symptoms, Stimulant Use, and Treatment Outcomes: A Secondary Analysis of NIDA's Women and Trauma Study 27 December 2013 | The American Journal on Addictions, Vol. 23, No. 1
- Moving toward Trauma-Informed Practice in Addiction Treatment: A Collaborative Model of Agency Assessment 18 November 2013 | Journal of Psychoactive Drugs, Vol. 45, No. 5
- Poly-victimization among juvenile justice-involved youths Child Abuse & Neglect, Vol. 37, No. 10
- Comparative Safety of Benzodiazepines and Opioids Among Veterans Affairs Patients With Posttraumatic Stress Disorder Journal of Addiction Medicine, Vol. 7, No. 5
- Functional neuroanatomy of the central noradrenergic system 12 June 2013 | Journal of Psychopharmacology, Vol. 27, No. 8
- Traumatic stress reactivity promotes excessive alcohol drinking and alters the balance of prefrontal cortex-amygdala activity 27 August 2013 | Translational Psychiatry, Vol. 3, No. 8
- Abstracts 1 July 2013 | British Journal of Occupational Therapy, Vol. 76, No. 7_suppl
- Trauma‐Related Correlates of Alcohol Use in Recently Deployed OEF/OIF Veterans 20 May 2013 | Journal of Traumatic Stress, Vol. 26, No. 3
- Hvordan kan oppmerksomt nærvær hjelpe ved rusproblemer? 1 March 2013 | Tidsskrift for Norsk psykologforening, Vol. 50, No. 3
- Sub‐clinical trauma in the treatment of partner violent offenders with substance dependence Advances in Dual Diagnosis, Vol. 6, No. 1
- Differential roles of thought suppression and dispositional mindfulness in posttraumatic stress symptoms and craving Addictive Behaviors, Vol. 38, No. 2
- Depression and Anxiety, Vol. 30, No. 12
- Journal of Behavioral Medicine, Vol. 36, No. 2
- Comprehensive Psychiatry, Vol. 54, No. 7
- Cytokine, Vol. 63, No. 2
- Drug and Alcohol Dependence, Vol. 127, No. 1-3
- Drug and Alcohol Dependence, Vol. 128, No. 1-2
- Drug and Alcohol Dependence, Vol. 133, No. 2
- Journal of Substance Abuse Treatment, Vol. 45, No. 2
- Journal of Substance Abuse Treatment, Vol. 45, No. 5
- Journal of Addictive Diseases, Vol. 32, No. 2
- Social Work in Public Health, Vol. 28, No. 3-4
- Addiction, Vol. 108, No. 8
- A randomized, controlled pilot study of MDMA (±3,4-Methylenedioxymethamphetamine)-assisted psychotherapy for treatment of resistant, chronic Post-Traumatic Stress Disorder (PTSD) 31 October 2012 | Journal of Psychopharmacology, Vol. 27, No. 1
- BMC Public Health, Vol. 13, No. 1
- Substance Abuse Treatment, Prevention, and Policy, Vol. 8, No. 1
- Chest, Vol. 144, No. 1
- Korea Journal of Counseling, Vol. 14, No. 3
- Disability and Rehabilitation, Vol. 35, No. 14
- Addiction Research & Theory, Vol. 21, No. 5
- Domestic Violence Courts: The Case of Lady Justice Meets the Serpents of the Caduceus 11 July 2013
- Major Depression and PTSD in Pregnant Smokers Enrolled in Nicotine Gum Treatment Trial 7 February 2013 | The American Journal on Addictions, Vol. 22, No. 1
- Prevalence of post-traumatic stress disorder among patients with substance use disorder: it is higher than clinicians think it is 8 August 2012 | European Journal of Psychotraumatology, Vol. 3, No. 1
- Traumatic Stress in Special Populations 21 November 2012
- Using incentives to reduce substance use and other health risk behaviors among people with serious mental illness Preventive Medicine, Vol. 55
- Written Disclosure Treatment for Posttraumatic Stress Disorder in Substance Use Disorder Inpatients 22 July 2012 | Behavior Modification, Vol. 36, No. 6
- Genotype‐dependent consequences of traumatic stress in four inbred mouse strains 8 November 2012 | Genes, Brain and Behavior, Vol. 11, No. 8
- Association between Adverse Life Events and Addictive Behaviors among Male and Female Adolescents 27 September 2012 | The American Journal on Addictions, Vol. 21, No. 6
- Trauma und Sucht: Implikationen für die Psychotherapie SUCHT, Vol. 58, No. 4
- What is resilience?
- The Role of Posttraumatic Stress and Problem Alcohol Involvement in University Academic Performance 15 May 2012 | Journal of Clinical Psychology, Vol. 68, No. 7
- Post‐traumatic stress disorder, depression and suicidality in inpatients with substance use disorders 26 April 2011 | Drug and Alcohol Review, Vol. 31, No. 3
- Young people's beliefs about the harmfulness of alcohol, cannabis and tobacco for mental disorders: findings from two Australian national youth surveys 21 February 2012 | Addiction, Vol. 107, No. 4
- Psychopharmacology, Vol. 220, No. 4
- Psychopharmacology, Vol. 224, No. 2
- Cognitive Therapy and Research, Vol. 36, No. 3
- Journal of Behavioral Medicine, Vol. 35, No. 1
- Journal of Religion and Health, Vol. 51, No. 4
- Addictive Behaviors, Vol. 37, No. 1
- Annales Médico-psychologiques, revue psychiatrique, Vol. 170, No. 5
- Aggression and Violent Behavior, Vol. 17, No. 1
- Biological Psychiatry, Vol. 71, No. 1
- Drug and Alcohol Dependence, Vol. 124, No. 1-2
- Journal of Psychiatric Research, Vol. 46, No. 8
- Medical Hypotheses, Vol. 79, No. 5
- Neuropharmacology, Vol. 62, No. 2
- Journal of Aggression, Maltreatment & Trauma, Vol. 21, No. 6
- Clinical Psychology: Science and Practice, Vol. 19, No. 3
- European Addiction Research, Vol. 18, No. 2
- Journal of War & Culture Studies, Vol. 5, No. 1
- Jornal Brasileiro de Psiquiatria, Vol. 61, No. 4
- Journal of EMDR Practice and Research, Vol. 6, No. 2
- Comorbid Anxiety and Substance Use Disorders 31 May 2012
- Alcohol and Drug Abuse in Men Who Sustain Intimate Partner Violence 25 October 2011 | Aggressive Behavior, Vol. 38, No. 1
- A Multisite Study of the Association Between Emotion Dysregulation and Deliberate Self-harm Among Substance Use Disorder Inpatients Addictive Disorders & Their Treatment, Vol. 10, No. 4
- Neural Mechanisms of Stress and Addiction 2 November 2011
- Psychotherapie bei Abhängigkeits- erkrankungen und Posttraumatischer Belastungsstörung SUCHT, Vol. 57, No. 5
- Young People's Recognition of Mental Disorders and Beliefs about Treatment and Outcome: Findings from an Australian National Survey 1 October 2011 | Australian & New Zealand Journal of Psychiatry, Vol. 45, No. 10
- Posttraumatic stress hyperarousal symptoms mediate the relationship between childhood exposure to violence and subsequent alcohol misuse in Mi'kmaq youth 6 September 2011 | Journal of Traumatic Stress, Vol. 24, No. 5
- Cocaine-related attentional bias following trauma cue exposure among cocaine dependent in-patients with and without post-traumatic stress disorder 27 July 2011 | Addiction, Vol. 106, No. 10
- Suicidal or Self‐Harming Ideation in Military Personnel Transitioning to Civilian Life 20 May 2011 | Suicide and Life-Threatening Behavior, Vol. 41, No. 4
- Depression and Anxiety, Vol. 28, No. 8
- Social Psychiatry and Psychiatric Epidemiology, Vol. 46, No. 2
- Psychopharmacology, Vol. 214, No. 1
- Psychopharmacology, Vol. 215, No. 1
- Journal of Psychopathology and Behavioral Assessment, Vol. 33, No. 4
- Journal of Family Violence, Vol. 26, No. 6
- International Journal of Mental Health and Addiction, Vol. 9, No. 5
- Clinical Psychology Review, Vol. 31, No. 6
- Drug and Alcohol Dependence, Vol. 118, No. 2-3
- Evaluation and Program Planning, Vol. 34, No. 4
- Journal of Affective Disorders, Vol. 130, No. 1-2
- Journal of Anxiety Disorders, Vol. 25, No. 7
- Neuropharmacology, Vol. 60, No. 2-3
- Psychiatry Research, Vol. 186, No. 1
- Behavioral and Brain Sciences, Vol. 34, No. 6
- Journal of Aggression, Maltreatment & Trauma, Vol. 20, No. 5
- American Journal of Epidemiology, Vol. 174, No. 5
- European Heart Journal, Vol. 32, No. 6
- The American Journal on Addictions, Vol. 20, No. 3
- BMC Psychiatry, Vol. 11, No. 1
- Journal of Cognitive Psychotherapy, Vol. 25, No. 2
- Journal of EMDR Practice and Research, Vol. 5, No. 3
- Trauma, PTSD, and Partner Violence in Military Families 12 October 2010
- Measuring Endocrine (Cortisol) Responses of Zebrafish to Stress 11 October 2010
- Clinical Factors Associated With Prescription Drug Use Disorder in Urban Primary Care Patients with Chronic Pain The Journal of Pain, Vol. 11, No. 11
- Psychological Trauma and Substance Abuse: The Need for an Integrated Approach 7 September 2010 | Trauma, Violence, & Abuse, Vol. 11, No. 4
- Intimate relationships among returning soldiers: The mediating and moderating roles of negative emotionality, PTSD symptoms, and alcohol problems 16 September 2010 | Journal of Traumatic Stress, Vol. 23, No. 5
- Integrated and Holistic Treatment Approach to PTSD and SUD: A Synergy 23 December 2011 | Journal of Addictions & Offender Counseling, Vol. 31, No. 1
- Interactive Effects of Cumulative Stress and Impulsivity on Alcohol Consumption 21 July 2010 | Alcoholism: Clinical and Experimental Research, Vol. 34, No. 8
- Association Between Posttraumatic Stress Disorder and Primary Care Provider-Diagnosed Disease Among Iraq and Afghanistan Veterans Psychosomatic Medicine, Vol. 72, No. 5
- Relationship of alexithymia and temperament and character dimensions with lifetime post‐traumatic stress disorder in male alcohol‐dependent inpatients 24 March 2010 | Psychiatry and Clinical Neurosciences, Vol. 64, No. 2
- PTSD symptoms, hazardous drinking, and health functioning among U.S.OEF and OIF veterans presenting to primary care 26 January 2010 | Journal of Traumatic Stress, Vol. 23, No. 1
- Sudie E. Back , Ph.D.
- Depression and Anxiety, Vol. 27, No. 8
- Cognitive Therapy and Research, Vol. 34, No. 6
- Revista Colombiana de Psiquiatría, Vol. 39
- Addictive Behaviors, Vol. 35, No. 1
- Addictive Behaviors, Vol. 35, No. 6
- Journal of Anxiety Disorders, Vol. 24, No. 1
- Journal of Psychiatric Research, Vol. 44, No. 1
- CNS Spectrums, Vol. 15, No. 8
- Journal of Dual Diagnosis, Vol. 6, No. 2
- JNCI Journal of the National Cancer Institute, Vol. 102, No. 13
- CNS Drugs, Vol. 24, No. 12
- Combat Posttraumatic Stress Disorder, Substance Use Disorders, and Traumatic Brain Injury Journal of Addiction Medicine, Vol. 3, No. 4
- Relationship between Child Abuse and Adult Smoking 5 February 2010 | The International Journal of Psychiatry in Medicine, Vol. 39, No. 4
- A Qualitative Investigation of Long-Term Zopiclone Use and Sleep Quality Among Vietnam War Veterans with PTSD 25 August 2009 | Annals of Pharmacotherapy, Vol. 43, No. 10
- Thoughts on the Interaction of Trauma, Addiction, and Spirituality 23 December 2011 | Journal of Addictions & Offender Counseling, Vol. 30, No. 1
- Evidence-Based Long-Term Treatment of Mental Health Consequences of Disasters among Adults
- Psychotherapies for Trauma and Substance Abuse in Women 27 May 2009 | Trauma, Violence, & Abuse, Vol. 10, No. 3
- Treatment Challenges Associated with Comorbid Substance Use and Posttraumatic Stress Disorder: Clinicians' Perspectives 18 February 2010 | The American Journal on Addictions, Vol. 18, No. 1
- Depression and Anxiety, Vol. 26, No. 12
- The Journal of Behavioral Health Services & Research, Vol. 36, No. 2
- Addictive Behaviors, Vol. 34, No. 10
- Clinical Psychology Review, Vol. 29, No. 6
- Journal of Affective Disorders, Vol. 118, No. 1-3
- Journal of Anxiety Disorders, Vol. 23, No. 4
- Journal of Anxiety Disorders, Vol. 23, No. 5
- Social Science & Medicine, Vol. 69, No. 7
- Journal of Public Health Policy, Vol. 30, No. 3
- Journal of Dual Diagnosis, Vol. 5, No. 1
- Addiction Research & Theory, Vol. 17, No. 4
- JNCI Journal of the National Cancer Institute, Vol. 101, No. 21
- Expert Review of Clinical Pharmacology, Vol. 2, No. 1
- International Review of Psychiatry, Vol. 21, No. 6
- Stress, alcohol and drug interaction: an update of human research 4 December 2008 | Addiction Biology, Vol. 14, No. 1
- Clinical Implications of Epidemiologic Data for Diagnosis and Treatment of Psychiatric Comorbidity Psychiatric Annals, Vol. 38, No. 11
- S 9 January 2012
- Alcohol consumption patterns and risk factors among childhood cancer survivors compared to siblings and general population peers 28 June 2008 | Addiction, Vol. 103, No. 7
- Survey of Alcohol Use in the U.S. Army 11 October 2008 | Journal of Addictive Diseases, Vol. 27, No. 3
- Baseline Subjective Stress Predicts 1-Year Outcomes Among Drug Court Clients 17 July 2007 | International Journal of Offender Therapy and Comparative Criminology, Vol. 52, No. 3
- Oxcarbazepine for Treatment of Posttraumatic Stress Disorder and Alcohol Dependence: A Case Series 1 May 2008 | Journal of Pharmacy Technology, Vol. 24, No. 3
- Predictors of Trauma and PTSD among Heroin Users: A Prospective Longitudinal Investigation 1 April 2008 | Journal of Drug Issues, Vol. 38, No. 2
- EEG Biofeedback as a Treatment for Substance Use Disorders: Review, Rating of Efficacy, and Recommendations for Further Research 24 January 2008 | Applied Psychophysiology and Biofeedback, Vol. 33, No. 1
- Treatment of co-occurring psychiatric and substance use disorders
- Administration and Policy in Mental Health and Mental Health Services Research, Vol. 35, No. 3
- Drug Discovery Today: Disease Models, Vol. 5, No. 4
- Evaluation and Program Planning, Vol. 31, No. 1
- Journal of Psychiatric Research, Vol. 42, No. 10
- Journal de Thérapie Comportementale et Cognitive, Vol. 18, No. 3
- Neuroscience & Biobehavioral Reviews, Vol. 32, No. 3
- Psychoneuroendocrinology, Vol. 33, No. 3
- Journal of Neurotherapy, Vol. 12, No. 1
- Journal of Neurotherapy, Vol. 12, No. 4
- Journal of Groups in Addiction & Recovery, Vol. 3, No. 3-4
- Addiction Research & Theory, Vol. 16, No. 2
- Psychological Outcomes and Measurement of Maternal Posttraumatic Stress Disorder During the Perinatal Period Journal of Perinatal & Neonatal Nursing, Vol. 22, No. 1
- Substance Abuse Treatment, Prevention, and Policy, Vol. 3, No. 1
- Psychiatric Annals, Vol. 38, No. 11
- A Randomized, Double-Blind, Placebo-Controlled Trial of Augmentation Topiramate for Chronic Combat-Related Posttraumatic Stress Disorder Journal of Clinical Psychopharmacology, Vol. 27, No. 6
- Differences in Early Onset Alcohol Use and Heavy Drinking among Persons with Childhood and Adulthood Trauma 19 April 2010 | The American Journal on Addictions, Vol. 16, No. 6
- Epidemiology of disaster mental health
- Clinical challenges in the treatment of patients with posttraumatic stress disorder and substance abuse Current Opinion in Psychiatry, Vol. 20, No. 6
- Karen M. Abram, Ph.D.
- Jason J. Washburn, Ph.D., A.B.P.P.
- Linda A. Teplin, Ph.D.
- Kristin M. Emanuel, M.S.T.
- Erin G. Romero, B.S.
- Gary M. McClelland, Ph.D.
- Long‐term, high‐dose benzodiazepine prescriptions in veteran patients with PTSD: Influence of preexisting alcoholism and drug‐abuse diagnoses 22 October 2007 | Journal of Traumatic Stress, Vol. 20, No. 5
- Integrating Treatment of Posttraumatic Stress Disorder and Substance Use Disorder 23 December 2011 | Journal of Counseling & Development, Vol. 85, No. 4
- Asylum Seekers Seeking Mental Health Services in the United States Journal of Nervous & Mental Disease, Vol. 195, No. 9
- Cognitive-Behavioral Stress Management for Individuals With Substance Use Disorders Journal of Nervous & Mental Disease, Vol. 195, No. 8
- Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event‐exposed marijuana users 22 August 2007 | Journal of Traumatic Stress, Vol. 20, No. 4
- Social defeat stress, sensitization, and intravenous cocaine self-administration in mice 13 February 2007 | Psychopharmacology, Vol. 192, No. 2
- Introductory and Basic Aspects 5 February 2008
- Gender differences in traumatic events and rates of post‐traumatic stress disorder among homeless youth 9 March 2006 | Journal of Adolescence, Vol. 30, No. 1
- Psychopharmacology, Vol. 191, No. 4
- Journal of General Internal Medicine, Vol. 22, No. 6
- Addictive Behaviors, Vol. 32, No. 6
- Best Practice & Research Clinical Rheumatology, Vol. 21, No. 3
- Brain Research, Vol. 1131
- Behaviour Research and Therapy, Vol. 45, No. 10
- Comprehensive Psychiatry, Vol. 48, No. 2
- Drug and Alcohol Dependence, Vol. 90, No. 1
- Journal of Affective Disorders, Vol. 101, No. 1-3
- International Journal of Neuroscience, Vol. 117, No. 9
- Drugs and Alcohol Today, Vol. 7, No. 4
- Advances in Psychiatric Treatment, Vol. 13, No. 5
- Journal of Neurotherapy, Vol. 11, No. 2
- Oral health status in war veterans with post‐traumatic stress disorder 21 December 2006 | Journal of Oral Rehabilitation, Vol. 34, No. 1
- University of Rhode Island Change Assessment–Trauma: Preliminary psychometric properties in an alcohol‐dependent PTSD sample 29 December 2006 | Journal of Traumatic Stress, Vol. 19, No. 6
- Maximizing follow‐up in longitudinal studies of traumatized populations 29 December 2006 | Journal of Traumatic Stress, Vol. 19, No. 6
- Naltrexone and Disulfiram in Patients with Alcohol Dependence and Comorbid Post-Traumatic Stress Disorder Biological Psychiatry, Vol. 60, No. 7
- Symptom Improvement in Co-Occurring PTSD and Alcohol Dependence Journal of Nervous & Mental Disease, Vol. 194, No. 9
- Tobacco use after experiencing a major natural disaster: analysis of a longitudinal study of 2063 young adults 2 June 2006 | Addiction, Vol. 101, No. 7
- Addictive Behaviors, Vol. 31, No. 2
- General Hospital Psychiatry, Vol. 28, No. 1
- Progress in Neurobiology, Vol. 79, No. 5-6
- Psychoneuroendocrinology, Vol. 31, No. 4
- Alcohol Drinking Problems Among New York City Residents after the September 11 Terrorist Attacks 3 July 2009 | Substance Use & Misuse, Vol. 41, No. 9
- Alcoholism: Clinical and Experimental Research, Vol. 30, No. 6
- Journal of Dual Diagnosis, Vol. 2, No. 4
- Jorge L. Armony , Ph.D. ,
- Vincent Corbo , B.Sc. ,
- Marie-Hélène Clément , M.A. , and
- Alain Brunet , Ph.D.
- Work-Based Critical Incidents and Problem Drinking 19 August 2016 | Work and Occupations, Vol. 32, No. 3
- Applying a Public Health Approach to Drug Abuse Research 3 August 2016 | Journal of Drug Issues, Vol. 35, No. 3
- Acceptance and Commitment Therapy in the Treatment of Comorbid Substance Abuse and Post-Traumatic Stress Disorder 24 July 2016 | Clinical Case Studies, Vol. 4, No. 3
- Journal of Traumatic Stress, Vol. 18, No. 5
- Psychopharmacology, Vol. 180, No. 1
- Community Mental Health Journal, Vol. 41, No. 2
- General Hospital Psychiatry, Vol. 27, No. 3
- Psychiatry Research, Vol. 135, No. 3
- Psychoanalytic Psychology, Vol. 22, No. 4
- Theoretical perspective on posttraumatic stress disorder and substance use disorder 3 February 2007 | Australian Psychologist, Vol. 40, No. 2
- Risk factors for alcohol and other drug disorders: A review 2 February 2007 | Australian Psychologist, Vol. 40, No. 2
- Substance Use & Misuse, Vol. 40, No. 13-14
- The American Journal of Drug and Alcohol Abuse, Vol. 31, No. 2
- Substance Use & Misuse, Vol. 40, No. 4
- Journal of Clinical Psychopharmacology, Vol. 25, No. 6
- The Journal of Nervous and Mental Disease, Vol. 193, No. 12
- Journal of Dual Diagnosis, Vol. 1, No. 2
- Expert Review of Neurotherapeutics, Vol. 5, No. 2
- The Effects of PTSD on Treatment Adherence, Drug Relapse, and Criminal Recidivism in a Sample of Incarcerated Men and Women 18 August 2016 | Research on Social Work Practice, Vol. 14, No. 6
- Time-Dependent Alterations in mRNA Expression of Brain Neuropeptides Regulating Energy Balance and Hypothalamo-Pituitary-Adrenal Activity after Withdrawal from Intermittent Morphine Treatment 20 October 2004 | The Journal of Neuroscience, Vol. 24, No. 42
- Substance Abuse and Posttraumatic Stress Disorder 23 June 2016 | Current Directions in Psychological Science, Vol. 13, No. 5
- Anxiety disorders and schizophrenia Current Psychiatry Reports, Vol. 6, No. 4
- Relationship of Alcohol Craving to Symptoms of Posttraumatic Stress Disorder in Combat Veterans Journal of Nervous & Mental Disease, Vol. 192, No. 5
- Social Psychiatry and Psychiatric Epidemiology, Vol. 39, No. 11
- Biological Psychiatry, Vol. 55, No. 6
- Biological Psychiatry, Vol. 55, No. 9
- Biological Psychiatry, Vol. 55, No. 11
- Journal of Anxiety Disorders, Vol. 18, No. 1
- Journal of Psychiatric Research, Vol. 38, No. 6
- Neuroscience & Biobehavioral Reviews, Vol. 28, No. 1
- Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, Vol. 97, No. 1
- Drugs: Education, Prevention and Policy, Vol. 11, No. 1
- American Journal of Psychiatric Rehabilitation, Vol. 7, No. 2
- Psychosomatic Medicine, Vol. 66, No. 1
- Benign Neglect or Neglected Abuse: Drug and Alcohol Withdrawal in U.S. Jails 1 January 2021 | Journal of Law, Medicine & Ethics, Vol. 32, No. 1
- Linking Posttraumatic Stress Disorder and Psychosis Journal of Nervous & Mental Disease, Vol. 191, No. 10
- Substance Use Disorder Comorbidity Among Inpatient Youths With Psychiatric Disorder 17 November 2016 | Australian & New Zealand Journal of Psychiatry, Vol. 37, No. 3
- Posttraumatic Stress Disorder: Do Electrical Startle Responses and Thyroid Function Usefully Supplement Self-Report? A Study of Vietnam War Veterans 17 November 2016 | Australian & New Zealand Journal of Psychiatry, Vol. 37, No. 3
- Current review of the comorbidity of affective, anxiety, and substance use disorders Current Opinion in Psychiatry, Vol. 16, No. 3
- Relationships of Alcohol Use, Stress, Avoidance Coping, and other Factors with Mental Health in a Highly Educated Workforce 25 August 2016 | American Journal of Health Promotion, Vol. 17, No. 4
- Biological Psychiatry, Vol. 54, No. 10
- Neuroscience & Biobehavioral Reviews, Vol. 27, No. 5
- Obstetrics and Gynecology Clinics of North America, Vol. 30, No. 3
- Psychiatry Research: Neuroimaging, Vol. 123, No. 2
- Addictive Behaviors, Vol. 28, No. 9
- Journal of Consulting and Clinical Psychology, Vol. 71, No. 2
- Current Opinion in Psychiatry, Vol. 16, No. 3
- Addictive Disorders & Their Treatment, Vol. 2, No. 2
- Treatment of Drug Addiction in Traumatised Refugees 9 July 2003 | European Addiction Research, Vol. 9, No. 3
- Benzodiazepines 26 October 2007
- Methadone, Morphine and PTSD 17 November 2016 | Australian & New Zealand Journal of Psychiatry, Vol. 36, No. 6
- Drug and Alcohol Dependence, Vol. 66, No. 2
- Sleep And Breathing, Vol. 06, No. 4
- ALCOHOL USE AMONG OUT-OF-TREATMENT CRACK USING AFRICAN–AMERICAN WOMEN 5 August 2002 | The American Journal of Drug and Alcohol Abuse, Vol. 28, No. 3
- Current Opinion in Psychiatry, Vol. 15, No. 2
- Current Opinion in Psychiatry, Vol. 15, No. 3

- Study Guides
- Homework Questions
Literature Review RPN

- Homelessness
- Homelessness and LGBT
- Homelessness and Veterans
- Homeless and Older Men
- Homeless and Women
- Social Media
Literature Review
The Dangers of Substance Use Among the Homeless
Addiction is a multi-faceted dependency on a certain drug or substance. Homelessness is a global issue with colossal implications. Within the current Gerontology literature, numerous articles and studies have attempted to show exactly what the causes of homelessness are. This issue is compounded by the poverty of being homeless. Along with this, homeless people tend to have mental disorders that further aggravate the issue. However, this issue should not be stigmatized but rather met with solutions for housing, social security, and intervention. It is especially dangerous for the homeless who, without support from anyone, become addicted. According to the lancet, cognitive impairment was found to be common among homeless adults and maybe a trans-diagnostic problem that impedes rehabilitative efforts in this population. Individual factors include poverty, family problems, and mental health and substance misuse problems. The availability of low-cost housing is thought to be the most important structural determinant for homelessness. Homeless people have higher rates of premature mortality than the rest of the population, especially from suicide and unintentional injuries, and an increased prevalence of a range of infectious diseases, mental disorders, and substance misuse. High rates of non-communicable diseases have also been described with evidence of accelerated aging. Within the current Gerontology literature, numerous articles and studies have attempted to show exactly what the causes of homelessness are.
Homelessness and Women
In the day and age we live in now there are so many women who end up in the streets, because of substance abuse. I know you might be thinking, “why get addicted to something that’s harmful?”, or “why not get help?”. Well, guess what, majority of the time it is not the fault of the person, for getting hooked on something. Nearly all addicts believe in the beginning that they can stop using drugs on their own, but most try to stop without treatment. Although some people are successful, many attempts result in failure to achieve long term abstinence/sobriety. Research has shown that long term drug abuse results in changes in the brain that persist long after a person stops using drugs. These drug-induced changes in brain function can have many behavioral consequences, including an inability to exert control over the impulse to use drugs despite adverse consequences, which are the defining characteristics of addiction. Drug abuse is the recurrent use of illegal drugs, or the misuse of prescription or over the counter drugs with negative consequences. The two terms, drug abuse or substance abuse can be defined as the use of chemical substances that lead to an increased risk of problems and an inability to control the use of the substance. Although drug and substance abuse do differ from addiction it sometimes can be mistaken for one another. Addiction is a chronic, often relapsing brain disease that causes compulsive drug seeking and use, despite harmful consequences to the addicted individual and to those around him or her. Although the initial decision to take drugs is voluntary for most people, the brain changes that occur over time challenge an addicted person’s self-control and hamper his or her ability to resist intense impulses to take drugs. Most often, an individual who regularly abuses drugs, even if they do not meet the criteria for a diagnosis of drug addiction, has already lost control over their drug use. Drug and substance abuse can result in broken families, destroyed careers, death due to negligence or accident, domestic violence and physical abuse, and child abuse. Drugs contain chemicals that tap into the brain’s communication system and disrupt the way nerve cells normally send, receive, and process information. There are at least two ways that drugs cause this disruption: by imitating the brain’s natural chemical messengers and by overstimulating the “reward circuit” in the brain. Homelessness developed as a national issue in the 1870s. Many homeless people lived in rising urban communities, such as New York City. Into the twentieth century, the Great Depression of the 1930s caused an overwhelming pandemic of neediness, yearning, and homelessness. There were 2,000,000 relocating over the United States. During the 1960s, the deinstitutionalization of patients from state mental emergency clinics, as indicated by the doctor’s medicinal libraries on the utilization of pharmaceuticals, was a hastening factor that seeded the number of inhabitants in individuals that are destitute. The first study, that I came across on google scholar is called, “Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: mediating roles of self-esteem and abuse in adulthood”. The objective of this study is to use the dormant variable methodology, which would investigate but at the same time studies the relative effects of childhood abuse and early parental substance abuse on later chronic homelessness, depression, and substance abuse problems in a sample of homeless women. This study also would explore how self-esteem and recent violence can affect the difference between childhood predictors and dysfunctional outcomes. The example comprises of 581 vagrants dwelling in covers or calm living focuses in Los Angeles (54% African-American, 23% Latina, 22% White, mean age=33.5 years). Different pointer inert factors filled in as indicators and results in auxiliary models. Youth misuse was shown by the sexual, physical, and obnoxious attack. The results were that the youth misuse straightforwardly anticipated later physical maltreatment, interminable vagrancy, gloom, and less confidence. Parent substance utilize legitimately anticipated later substance use issues among the ladies. Later physical maltreatment anticipated ceaseless vagrancy, sadness, and substance use issues. More prominent confidence anticipated less discouragement and less substance use issues. Youth misuse additionally had critical backhanded consequences for melancholy, constant vagrancy, and medication and liquor issues intervened through later physical maltreatment and confidence. In spite of the fact that there was a solid connection between youth misuse and parent medicate use, youth misuse was the more unavoidable and pulverizing indicator of useless results. Youth misuse anticipated a more extensive scope of issues including lower confidence, more exploitation, more misery, and ceaseless vagrancy, and in a roundabout way anticipated medication and liquor issues. The intervening jobs of later physical maltreatment and confidence propose remarkable influence that focuses on change through strengthening preparing and confidence improvement in vagrants. The second study that I came across is called, “Traumatic Transitions: Homeless Women’s Narratives of Abuse, Loss, and Fear”. In this study awful encounters among 21 ladies dwelling in spending lodgings in the wake of lodging relocation. Surrounded in women’s activist and combined injury hypotheses, the motivation behind this examination was to investigate kinds of injury and difficulty preceding and during lodging at spending inns. In this subjective examination, account and all-out substance investigation approaches were led to distinguish basic topics over ladies’ stories. Discoveries uncovered injury accounts of physical and psychological mistreatment, youth abuse, misfortune, budgetary misuse, sexual terrorizing, expulsion nervousness, natural pressure, wrongdoing presentation, and methodical oppression. Injury educated intercession approaches for social work practice are laid out to advance ladies’ strengthening. Endorsement for this subjective, exploratory examination was acquired through Georgia State University and the University of Georgia Institutional Review Boards. Members were occupied with 60-to 90-min private meetings utilizing a semistructured talk with direct. Wide addresses urged ladies to share their anecdotes about close to home encounters previously and during spending lodging stays, for example, “Inform me concerning conditions that made the need to live at an inn,” “What do you like about living here?” “What difficulties have you encountered since living here?” All meetings were directed nearby at different inns where members lived. Every respondent was paid US$25 compensation after an educated assent was given. Sound recorded meetings were translated verbatim and put away in secret key ensured electronic documents. Respondents in this examination ran in age from 19 to 64, with a normal age of 42. African American ladies (76%) dwarfed Caucasian American (19%) and Latin American ladies (5%) in the example. Six ladies were either hitched or drawn in and lived with their accomplices at the inn. Six ladies were separated, isolated, or bereaved. Nine ladies depicted themselves as single and never wedded. Forty-eight percent of ladies went with youngsters at the lodging, kids’ ages ranged from 1 to 18. The normal room rental charge was US$220 every week. The normal lodging remain was 32 weeks. Be that as it may, most ladies (67%) lived at the lodging for about four months or less. All ladies in the example portrayed agitated or fierce home situations before inn living. In their accounts, physical and psychological mistreatment, kid abuse, misfortune, monetary misuse, and sexual terrorizing were basic injury topics before cycling all through vagrancy. The third study I came across is called, “How Can We Stay Sober?” Homeless Women’s Experience in a Substance Abuse Treatment Center”. In this study presents discoveries from an exploratory, subjective assessment of a concentrated outpatient treatment program for vagrants recouping from substance reliance issue. Organized meetings of seven current program customers and three alumni of the program were directed to learn how customers keep up their temperance notwithstanding meeting the exceptional difficulties of being destitute. In view of these meetings, there are four fundamental concerns talked about: absence of correspondence between specialist organizations, irregularity in work force during recuperation, irregularity in backslide approaches, and customers feeling not well arranged to live in “this present reality” after program consummation. Overall, the clients in this study said they profited by the program and announced they are as of now still in recuperation. Our meetings with present and previous customers did anyway distinguish four customer concerns exhibited here: absence of correspondence between specialist organizations, irregularity in faculty during recuperation, irregularity in the utilization of office approaches identified with customer backslide, and saw the viability of the IOT program to get ready customers to re-coordinate into the network after program fulfillment. The arrangement of compelling IOT administrations for vagrants is a significant connection in the substance misuse recuperation administrations continuum of care. The consequences of our customer interviews educate a concise survey regarding the First Steps for Women IOT program and recommendations for program upgrade. Hypothetical systems concerning substance maltreatment among vagrants, including the pressure and adapting worldview of Lazarus and Folkman (1984), just as the wellbeing looking for worldview of Schlotfeldt (1981), demonstrate the basic significance of engaging ladies. Confidence is all around saw as one of the more basic components of getting vagrants to take part in and complete a recuperation program. Setting up confidence inside the setting of a positive and unsurprising social condition is upheld in treatment writing as a methods for enabling the ladies inside an IOT program to never again take part in evasion adapting conduct, for example, medication and liquor misuse (SAMSHA 2006). The treatment writing proposes proficient staff assume a significant job in advancing strengthening by connecting with ladies in their recuperation and making a steady remedial milieu (Hser et al. 2001; Martin et al. 2000). This recommends expanding consistency in staffing may have a huge positive effect on customer achievement. Substance reliance among homeless women presents both treatment and specialist co-ops with numerous difficulties. For treatment suppliers, challenges incorporate how to address essential issues for nourishment and asylum before tending to the plenty of physical and mental indications related with substance reliance. One solution for solving or decreasing the amount of homeless women on the streets can be Federal housing programs are one of the best housing based answers to decrease homelessness. The two biggest government housing programs are open housing and bureaucratic housing vouchers, known as Housing Choice Vouchers or Section 8 vouchers. Housing vouchers permit low-salary families to lease humble market-rate housing of their decision and furnish an adaptable housing vouchers are exceptionally fruitful at decreasing family homelessness and in guaranteeing that these families remain steadily housed out of the asylum framework.
Homeless Men
The first study, Factors associated with substance use in older homeless adults: Results from the HOPE HOME Study, is a non-experimental, qualitative study which shows trends among the homeless, elderly population of Oakland, California. Trends such as substance use, and early morality are present. They begin, “Approximately 1% of the [American] population experiences homelessness…with an estimated 600,000 Americans homeless nightly. Homelessness is defined by the Federal Homeless Emergency Assistance and Rapid Transition to Housing Act of 2009, which defines as homeless: people who lack a fixed, regular residence (i.e. sleeping outdoors, in an emergency shelter, or in a place not meant for habitation), and those who are at imminent risk of losing their housing in the next 14 days”, and “With the aging of the homeless population and the changes in substance use in older adults, little is known about the prevalence of substance use disorders in older homeless adults. There are few community-based samples of substance use in homeless adults since NSHAPC [National Survey of Homeless Assistance Providers and Clients, 1999 survey], and none specifically examining older homeless adults.” This study was conducted by a population-based sampling of homeless individuals aged 50 and older in Oakland, CA. It was approved by the University of California in San Francisco. Some Eligibility criteria included: English speaking, age 50 or over, and homeless based on the HEARTH criteria [lacked a fixed residence, resided in a place not typically used for sleeping, or at risk of losing housing within fourteen days.] This work was funded by the National Institute on Aging at the National Institutes of Health. The funding sources had no role in the preparation, review, or approval of the manuscript. The authors declare that they have no conflicts of interests. The interviews included questions on demographics (age, gender, and race/ethnicity). Whether the interviewee had completed high school or received a GED certificate. If they had served in active duty military, if they had used homeless services in the last 6 months (shelters and free and low-cost meal programs). Interviewees were asked when they first became homeless, if their current episode of homelessness lasted for a year or more, and if they had a history of sexual abuse or physical abuse. Questions from the National Survey of Homeless Assistance Providers and Clients (NSHAPC) were used to gauge the severity of substance abuse. Interviewees were asked what substances they used, when, and for how long. It states, ”Based on the National Health and Nutrition Examination Survey (NHANES), we asked participants to report whether a health care provider had told them that they had diabetes, emphysema or chronic obstructive pulmonary disease (COPD), asthma, stroke, coronary artery disease or a heart attack, congestive heart failure, cirrhosis, or cancer. We asked participants whether they had tested positive for HIV infection or had ever been told they had AIDS.” Interviewees were also evaluated for PTSD and depression. Drug usage was assessed using the questions from the World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test. The time frame was of the previous six months. We categorized AUDIT scores as: low severity (0-7), moderate severity (8–15), and high severity (16+). The results were as follows: the HOPE HOME participants had a median age of 58 years. They continue, “Over three-quarters, (77.1%) were male, and (79.1%) African American; (21.7%) were veterans. Approximately a third (32.6%) had PTSD symptoms and 38.3% had major depressive symptoms; (22.3%) had both depressive and PTSD symptoms. Approximately two-thirds (67.1%) were homeless for at least a year. Almost a third (31.2%) had ever been suspended or expelled from school. Almost all participants (98.4%) used homeless services in the last 6 months. About a third (33.3%) experienced physical abuse as a child, while (13.2%) experienced sexual abuse as a child.” Almost two-thirds of the sample, (63.1%) had used an illicit substance in the last 6 months, and (64.6%) had moderate or greater severity symptoms for at least one illicit drug, with (14.5%) reporting severe symptoms. For illicit drugs, the drugs most commonly used in the last 6 months included cannabis with (48.0%), cocaine with (37.7%), opioids with (7.4%), and amphetamines with (7.1%). The three most commonly reported drugs with moderate or greater severity symptoms were cocaine (43.1%), cannabis (39.1%), and opioids (12.9%). For participants with ASSIST-defined moderate or higher severity illicit drug symptoms, 91.6% had used an illicit substance in the last six months. Some issues with this survey was that the sample was mainly African American, and a narrow age. The second article was titled The Causes of Death Among an Urban Homeless Population Considered by the Medical Examiner , highlights how exactly substance abuse has a detrimental effect on the elderly homeless. This report is based on data from the Office of the Chief Medical Examiner (OCME) for a small homeless population in Alberta, Canana. The time interval was analyzed from January 1, 2007 to December 31, 2009. They state, “One hundred and thirty-two deaths were reported. Most deaths that could be classified were attributed to drug and alcohol use/abuse and to natural causes.” This was a non-experimental, qualitative study. Although people who are homeless in Canada are entitled to equal health care, there are numerous of implicit barriers to that. They list “Problems with access and treatment compliance have been associated with a lack of contact points [telephone, mailing/email addresses] for follow-up, inadequate transportation to ambulatory care settings, financial barriers, mental health/substance abuse problems, and difficulty in storing medications…” Lack of shelter and health care, along with mental/drug issues, make homeless people die at faster rates than the average population. Because of lack of shelter and health care, compounded with mental/drug problems, “Deaths among homeless people occur at rates significantly higher than the general population.” The main cause of this paper was to analyze the cause of the deaths of homeless, “In order to be able to design programs to address the needs of chronically ill and seriously ill people who are homeless… ”Because of the various conflicts between homeless and medical institution, treatment is not always an option. “Existing health care and hospice facilities may be reluctant to accept homeless patients due to behavior and lifestyle concerns (e.g., alcohol and substance abuse), and for their part, people who are homeless may not trust the health care system and its institutions…as a consequence, homeless people die in environments that may not have appropriately met their care needs or their preferences.” The OCME investigated one hundred and thirty-two deaths. The age of the deceased ranged between 18 and 89 years, with a mean age of 46. Drug and alcohol-related illnesses caused the highest number of deaths. Eighty-three percent of the deaths were among men. These deaths were not only the result of overdoses, but were also the consequences of long-term substance use/abuse leading to more chronic, substance-related comorbid conditions.” These small number of studies have shown us that the homeless hold unique fears about death and dying. “These include fears of dying alone and undiscovered, having their remains disposed of without ceremony, receiving inadequate health care or being treated disrespectfully by health care professionals, and not having their wishes respected.” Some issues with this study are the inherent limitations as it is only based on a single urban setting. It is limited in size and scope. Moreover, it did not consider causes of death for those people who were able to find a residence shortly before their deaths, or those who were hospitalized at the time of their death. Potential future research could seek to close the gap of trust between the homeless and medical institutions, and to gather the unique perspectives of the homeless. “In the absence of specialized palliative care and hospice services for people who are homeless…a significant number of homeless people face death without the benefit of a stable home-like environment. Care from mainstream health care institutions may not be suitable or acceptable to this population overall.” Compassion is needed for the homeless and elderly that receive none.
Examining mortality among formerly homeless adults enrolled in Housing First: An observational study
In the third study we can see lack of healthcare is one factor that contributes to a higher mortality rate in the homeless, it is also an overview of the Housing First program. It starts, “Adults who experience prolonged homelessness have mortality rates 3 to 4 times that of the general population…communities including New York City and Philadelphia have enacted surveillance systems to monitor and address mortality in this population…Injuries, substance abuse, heart disease, liver disease, and ill-defined conditions have been reported as accounting for the vast majority of deaths among individuals experiencing homelessness.” Housing First seeks to correct homelessness by providing immediate access to permanent housing, and community-based opportunities. They continue.
To date, however, there has been no research on premature mortality among formerly homeless adults who have enrolled in HF. In the United States, this gap in the literature exists despite research that suggests chronically homeless adults constitute an aging cohort; nearly half are aged 50 years old or older the present study explored mortality among formerly homeless adults who moved into housing as part of an HF program in Philadelphia, PA. We examined death rates and causes of death among HF participants. We then compared HF participant mortality to two groups: members of the general population and the homeless population. We also compared the causes of death and characteristics of decedents in the HF program to a sample of adults identified as homeless at the time of death through formal review We conducted analyses to examine mortality among HF participants from several perspectives. First, we calculated all-cause and cause-specific mortality rates, expressed as deaths per 100,000 person-years of observation, for the entire study cohort. Second, we used survival analysis methods to assess the risk and predictors of death following HF participants’ move to housing. We estimated hazard functions and Kaplan-Meier survival curves to conduct descriptive analyses of the timing and occurrence of death following move to housing and fitted a Cox proportional hazards regression model to assess the relationship between HF participants’ demographic characteristics (gender, race and age) and risk of death following move to housing. We used administrative records from the HF program to identify a cohort of 292 formerly homeless individuals who moved into a housing unit between September 2008, when the HF program first began operations, and October 2013. These values were adjusted for race using direct standardization, with the Philadelphia general population serving as the standard population. We calculated 95 % confidence intervals for these rate ratios using established methods. We obtained mortality data for the Philadelphia general population (2008–2013) from the CDC Wide-ranging Online Data for Epidemiologic Research compressed mortality files regarding underlying cause of death.
To date, however, there has been no research on premature mortality among formerly homeless adults who have enrolled in HF. In the United States, this gap in the literature exists despite research that suggests chronically homeless adults constitute an aging cohort; nearly half are aged 50 years old or older. To begin to address this gap, the present study explored
mortality among formerly homeless adults who moved into housing as part of an HF program in Philadelphia, PA. We examined death rates and causes of death among HF participants. We then compared HF participant mortality to two groups: members of the general population and the homeless population. We also compared the causes of death and characteristics of decedents in the HF program to a sample of adults identified as homeless at the time of death through formal review process in Philadelphia. Fourth, we compared mortality rates in our sample of HF participants to mortality rates of individuals experiencing homelessness as reported in prior studies. To achieve this, we identified published studies that provided mortality rates or information from which such rates could be calculated. We only included studies that
were conducted in North America Finally, we compared the causes of death and characteristics of decedents in the HF program with information on individuals identified as homeless at their time of death in Philadelphia using data from a report by the City of Philadelphia’s Homeless Death Review Team.
Finally, we compared the causes of death and characteristics of decedents in the HF program with information on individuals identified as homeless at their time of death in Philadelphia using data from a report by the City of Philadelphia’s Homeless Death Review Team. Homeless status in the report is determined using the U.S. Department of Housing and Urban Development’s definition of homelessness, which considers individuals to be homeless if they are residing in an emergency shelter or in a place not meant for human habitation
Table 1 presents the characteristics of the 292 individuals in the overall HF participant cohort and decedents. The mean age at move to housing was 51.3, and roughly 80 % of the study cohort was between the ages of 45 and 74 at move to housing. The study cohort was predominantly male (70 %) and African American (68 %). The median duration of follow-up was 3.2 years, resulting in 1045 person-years of observation. Forty-one deaths occurred during the study period, with a mean age at death of 57.2 years. The majority of decedents were male (78 %) and African American (59 %). As shown in Table 2, the crude mortality rate for the study cohort was 3916.1 deaths per 100,000 person- years. Disease of the circulatory system was the leading cause of death, accounting for 29.3 % of deaths in the study cohort. Cancer accounted for 22 % of deaths, whereas drugs or alcohol caused approximately 10 % of deaths. Kidney and respiratory disease caused about 5 % of deaths each, with diabetes, HIV, injury, and liver disease each accounting for about 2 % of deaths. Figure 1 presents the estimated hazard function for death following HF participants’ move to housing.
Table 4 presents the comparison between the 41 HF participants who died during the first 6 years of the program’s operation and the homeless decedents identified by the City of Philadelphia’s Homeless Death Review Team during an overlapping 2-year time period. The majority of decedents in both the HF and homeless groups were between the ages of 45 and 64 at their time of death, although there were proportionally more decedents younger than 45 in the homeless group. Among those in the HF group, 78 % died from natural causes, compared to 49 % in the homeless group. This included 22 % of HF participants as opposed to 7 % in the homeless group who died from cancer. Among homeless adults, 40 % died from an accident, which was significantly more than the 12 % of HF participants who died from an accident. An infectious disease other than HIV caused more than 1 in 10 homeless deaths and hypothermia caused an additional 6 % of deaths; neither of these factors contributed to the death of HF participants. This study is the first to our knowledge to examine mortality among formerly homeless participants in an HF program. Overall, the results from this study are consistent with prior research on early mortality among populations that have experienced long-term homelessness [1, 20, 22] and suggest that adverse health outcomes associated with homelessness persist even after individuals obtain housing. Importantly, we found that risk of death among HF participants residing in housing was highest during the period immediately following their initial entry into housing. On one hand, this may reflect particularly heightened vulnerability and poor health in a certain segment of individuals who die shortly after entering housing. On the other hand, this finding may indicate that the period of transition into housing is one of elevated risk, during which it is of great importance to help individuals access needed health care and other services that may help prevent potentially avoidable deaths. Drug or alcohol usage accounted related deaths accounted for nearly twenty six percent of the deaths from the homeless in Philadelphia.
Homeless Veterans
Addiction to drugs should not be stigmatized and shamed upon but rather should be viewed as a mental illness as it is one. This issue should be taken seriously and offered counseling, support and any other form of help. Many who live on the streets struggle with this problem, and they unfortunately cannot get the help they need due to healthcare problems. “Changes in the American workforce and a general economic recession have resulted in the loss of employment opportunities, especially among low-wage workers. As a result, more individuals and families are living in poverty and at risk of losing their housing,” stated the American Addiction Center. This is a problem considering as people lose jobs, they will also lose housing along with healthcare. The result leads to homelessness which can then lead to drug use.
The homeless veteran population has been increasing throughout the years due to many reasons; some of which can be lack of support, a traumatic event that leads to mental health problems, adjusting back to society. These reasons can lead to drug use among these individuals which puts their health at risk. Opioid use is common among the U.S veterans as they are trying to cope with either a physical pain or in some cases psychological pain. Using addictive opioids can lead to overdose which results in death; and withdrawal sequence is even harder. Why is it that the people who served to protect our country suffer like this on the streets, yet no one does anything about it? To overcome drug abuse and to avoid overdosing the homeless need counseling and proper help rather than to be pushed aside and ignored.
The homeless population continues to grow as the time passes. “Almost 50,000 Veterans were homeless on one night in January 2014” (Ditchter, 2016). 50,000 homeless veterans were on the streets due to unsafe shelters. Homeless shelters may seem like a better alternative than the street but they’re not. In many cases people get abused or mistreated in these shelters, there are many who will steal while some on is asleep. Therefore, many chose to stay on the streets rather than the shelters as they feel safer on the streets. This however becomes a problem especially over the cold season as one might die from hypothermia. Furthermore, once homeless and on the street many resorts to drugs use to ease the pain. In the case of homeless veterans, the need to use drugs could also be psychological. The risk of biopsychosocial challenges is common among the homeless veterans. These challenges are linked with behavior that can put a person at elevated risk of overdose (OD). “U.S. military veterans face many biopsychosocial (BPS) challenges post-service that may elevate risk for opioid-related overdose including physical pain, mental health concerns and social stressors” (Bennett, 2019). The result of mental health challenges and stress can lead to overuse of opioids which can lead to OD.
There were 218 participators who were enlisted via sampling. They finished a baseline assessment in twenty-two opioid-related overdose risk behaviors which measured their past thirty-day opioid engagement this was measured on the Opioid Risk Behavior Scale (ORBS). “Analyses examined associations between ORBS scores and hypothesized demographic, biological/physical, psychological and social predictors. Incident rate ratios estimated the expected relative difference in ORBS score associated with each predictor” (Bennett, 2019). The results from the past thirty-days showed an estimate of 4.72 OD risk behaviors in participants. This was due to many reasons such as: bad living conditions in the homeless shelter, mental health problems, physical pain, painful and stressful life and surviving on the streets.
A study compared comorbidities and nursing home measures of homeless veterans, veterans at risk of being homeless, or veterans who had stable housing in the prior year. Before the community nursing home admissions, the younger homeless veterans were at n = 3355; 62.5 years [SD = 10.3 years]. The stably housed veterans came at n = 64 884; 75.3 years [SD = 11.9 years]. To make the study accurate the study adjusted for demographic differences, homeless veterans showed that they were more likely to be diagnosed with alcohol abuse ARR = 2.18; 95% confidence interval [CI] = 2.05-2.31; and drug abuse at (Adjusted relative risks ARRs) ARR = 3.03; 95% CI = 2.74-3.33. the data for mental health condition was at ARR = 1.49; 95% CI = 1.45-1.54, dementia at ARR = 1.14; 95% CI = 1.04-1.25. Trimorbidy was at ARR = 2.57; 95% CI = 2.40-2.74, in comparison to veterans who were stably housed nursing home users. “Homeless veterans were more likely to be admitted to a nursing home from a hospital (ARR = 1.13; 95% CI = 1.08-1.17) and remain in the nursing home 90 days after admission (ARR = 1.10; 95% CI = 1.04-1.16), but were less likely to die in the facility (ARR = 0.72; 95% CI = 0.67-0.78) compared to stably housed veterans.” (Halladay, 2019). This study illustrates that homeless veterans are safer in the community nursing homes and they were more likely to live if overdosed rather than the stabile housed individuals. We can conclude that with proper care and people around to take care of homeless veterans with substance problems can be safer and more likely to live and survive of risks.
Another study was conducted to research 27,403 Veterans who were screened for homelessness or being at risk of homelessness from November1, of 2012 and January 31, 2013. “During 2013, AORs were calculated using a mixed-effects logistic regression to estimate the likelihood of patients’ receipt of VHA homeless or social work services based on demographic and clinical characteristics” (Ditchter, 2016). Within six months most of the patients received services post-screening, the prediction was diversified by gender. It was found that for women, a diagnosis of drug abuse and psychosis predicted receipt of service. If they were unmarried, they had an increased probability of using services that screened positive for homelessness. Furthermore, if they were diagnosed with PTSD (post-traumatic stress disorder) their probability of receiving services for at-risk women was increased. For men, it was found that being unmarried, younger, having a medical or behavioral health condition, not being service-connect/Medicaid-eligible predicted receipt of services. The major goal of the U.S Department of Veterans Affairs’(VA’s) is to prevent homelessness among the Veterans, like rehouse those who have lost their homes or to identify at-risk Veterans and connect them with homeless prevention services. “Consistent with the Housing First approach, the HSCR is intended to link Veterans with services of their choosing that directly support housing stability” (Ditchter, 2016).
The solution to help the homeless is Housing First, their main priority is to house the homeless. They have created a platform where they not only provide housing but also to help the individuals with their personal goals and improve their quality of life. Housing is a necessity just like food and water, without a place to live it’s hard to find jobs as most employers don’t hire the homeless. Housing First focuses and helps to resolve this issue; furthermore, Housing First gives clients the choice to select a house that they prefer therefore exercising this choice will increase the likelihood of the client’s success and improve their lives. To dive in deeper on this solution we focused on the elements of the housing first program. Housing First will help assist the at-risk of being homeless individuals with rentals depending on the household income and needs. Clients sign a lease that will grant them access to their new homes, and they are also provided with necessary support to help them assist with any issues they might have with the housing. The two common program they offer is Permanent Supportive Housing (PSH) and the second program is rapid re-housing to provide those who have recently lost homes. The purpose of the first program is to target families and individuals with chronic homelessness, mental health problems, disability, illness, and substance use and to help them provide a long-term rental or housing assistance with support service. The second program model’s focus it to help house or rent a place for those families or individuals who have recently lost their homes. This option provides with short-term services and rental assistance. The goal here is to provide and help the families gain quick housing, employment, remain housed and increased self-sufficiency.
Overall, addiction should be recognized as a mental illness and should be treated with proper care. The veterans on the streets have served our country with strength, we as a society should help get them off the streets and into homes and help them get proper professional help to overcome PTSD, and substance use. Once the homeless are provided with proper housing and support to overcome addiction they can get employed and have a fresh start in life. Doing so will prevent OD deaths, help with prevention of diseases, street deaths from hypothermia etc.… Housing First is one step closer to achieving that goal and fixing this issue.
Bennett, A., Watford, A., Elliott, L., Stokfo, B., & Guarino, H. (2019, June 17). Military veterans’ overdose risk behavior: Demographic and biopsychosocial influences. Retrieved from https://www-clinicalkey-com.ccny-proxy1.libr.ccny.cuny.edu/#!/content/journal/1-s2.0-S030646031930156X .
Montgomery, A. E., Dichter, M. E., Thomasson, A. M., & Roberts, C. B. (2016, March 1). Services Receipt Following Veteran Outpatients’ Positive Screen for Homelessness. Retrieved from https://www-clinicalkey-com.ccny-proxy1.libr.ccny.cuny.edu/#!/content/playContent/1-s2.0-S074937971500416X?returnurl=null&referrer=null
E, J., C, H., J, M. G., T, O. T., & L, R. (2019, August 1). Homeless Veterans in Nursing Homes: Care for Complex Medical, Substance Use, and Social Needs. Retrieved from https://www-clinicalkey-com.ccny-proxy1.libr.ccny.cuny.edu/#!/content/medline/2-s2.0-31206592 .
Spinelli MA, Ponath C, Tieu L, Hurstak EE, Guzman D, Kushel M. (Jan 1 2018). Factors associated with substance use in older homeless adults: Results from the HOPE HOME study. Subst Abus. 2017. PMC. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5472372/
Stacey A. Page, Wilfreda E. Thurston & Connie E. Mahoney (2012): Causes of
Death Among an Urban Homeless Population Considered by the Medical Examiner, Journal of Social
Work in End-Of-Life & Palliative Care, 8:3, 265-271

This entry is licensed under a Creative Commons CC0 1.0 Universal Public Domain Dedication license.
Recent Posts
Recent comments.
Powered by WordPress | Designed by Elegant Themes
Need help with the Commons?
Email us at [email protected] so we can respond to your questions and requests. Please email from your CUNY email address if possible. Or visit our help site for more information:

- Terms of Service
- Accessibility
- Creative Commons (CC) license unless otherwise noted


IMAGES
VIDEO
COMMENTS
Studies evaluating substance use or SUD interventions and programs: ... Wisdom of the Crowds (WOTC) method, and a published literature review to document the size of key populations . The sample size for this category of studies ranged from 42 to 72292 . The studies were conducted in diverse settings including the community (n = 72), hospitals ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
A literature review of behavioral health services for youths of racial and ethnic minority groups found that, compared with non-Latino white adolescents with a substance use disorder, Black adolescents with a substance use disorder reported receiving less specialty and informal care, while Latinos with a substance use disorder reported ...
Objectives The burden of substance use in Kenya is significant. The objective of this study was to systematically summarize existing literature on substance use in Kenya, identify research gaps, and provide directions for future research. Methods This systematic review was conducted in line with the PRISMA guidelines. We conducted a search of 5 bibliographic databases (PubMed, PsychINFO, Web ...
Group-based cocaine use treatments for adults. Nineteen studies were identified that targeted cocaine use and utilized some form of group therapy, the most of any drug in this review (see Table 2).Overall, the studies showed that all of the group therapy modalities included in this review generally reduced cocaine use when compared to treatment as usual (TAU), including day hospital groups [].
This systematic literature review on substance use prevention programs amongst refugee youth was conducted after adopting exclusion and inclusion criteria. To assist in the process of selecting relevant studies in this systematic literature review, studies were limited to peer-reviewed articles published in the English language. ...
Abstract. This review article presents a summary of the existing literature on well-established CBT treatments for substance use disorder. It provides an overview of the origins, procedure, and evidence for six CBT treatment models: relapse prevention (RP) and mindful-based relapse prevention (MBRP), guided self-change (GSC), community reinforcement approach (CRA), behavioral couples therapy ...
Introduction. Substance use disorders (SUDs) are defined in the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) as the presence of pathological behaviors associated with the use of any substance falling into one of the nine recognized classes. Citation 1 These behaviors include impaired control over use (eg, using the substance more frequently or in a higher ...
This literature review focuses on initiation of substance use among children and youth. The review describes the scope of substance use among youth, risk factors that can lead to substance use, protective factors that can buffer against initiation, various types of prevention programs and outcome evidence, and limitations to the research ...
Understanding current substance use practices is critical to reduce and prevent overdose deaths among individuals at increased risk including persons who use and inject drugs. ... Three decades of research in substance use disorder treatment for syringe services program participants: a scoping review of the literature. Addict Sci Clin Pract ...
Substance use is an important public health concern in many countries across the globe. Among the general public, institutions of higher learning have developed a reputation for inducing new substance use among students. In addition to socio-demographic factors, substance use and abuse among university students often appear to be related to psychological stressors typically related to the ...
Substance or Drug abuse is a serious public health problem affecting usually adolescents and young adults. It affects both males and females and it is. the major source of crimes in youth and ...
OBJECTIVE: Alcohol use disorders and other substance use disorders are extremely common among patients with posttraumatic stress disorder (PTSD). This article reviews studies pertaining to the epidemiology, clinical phenomenology, and pathophysiology of comorbid PTSD and substance use disorders. METHOD: Studies were identified by means of computerized and manual searches. The review of ...
This document presents a review of literature on youth substance use treatment programs, aimed to reduce alcohol and illicit drug use, and the misuse of licit drugs, in youths who have been clinically diagnosed with a substance use program; it focuses on substance use disorder among youths under 18 years and on the utilization of substance use treatment programs.
In this narrative review, we examine extant literature (PubMed, Google scholar, Medline) for information on the prevalence, trends, and influencers of substance use and the development of ...
Alcohol and Drug Program Literature Review: A Review of the Research on the Treatment of Substance Use Disorders 2014 PREPARED BY MARK STANFORD, PH.D. SYNERGIA CONSULTING . Alcohol and Drug Treatment and Intervention Services 2 Table of Contents
This literature review focuses on initiation of substance use among children and youth. The review describes the scope of substance use among youth, risk factors that can lead to substance use, protective factors that can buffer against initiation, various types of prevention programs and outcome evidence, and limitations to the research currently available.
This protocol outlines a proposed scoping review to characterize evidence on implementation and quality improvement (QI) strategies that aim to improve equitable, evidence-informed care delivery for pregnant and birthing people with substance use disorder (SUD) in acute care. Untreated SUD during pregnancy is associated with an increased risk of overdose and severe maternal morbidity.
3 and goals (Dindo et al., 2017). ACT has been used to treat various mental illnesses including substance use disorders. Common Themes in Literature The majority, if not all research on this topic is quantitative. The main type of instrument used in the studies I will discuss are Likert scales where participants can report their progress throughout treatment.
Literature Review. The Dangers of Substance Use Among the Homeless. Addiction is a multi-faceted dependency on a certain drug or substance. Homelessness is a global issue with colossal implications. Within the current Gerontology literature, numerous articles and studies have attempted to show exactly what the causes of homelessness are.