Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 03 October 2022

How COVID-19 shaped mental health: from infection to pandemic effects
- Brenda W. J. H. Penninx ORCID: orcid.org/0000-0001-7779-9672 1 , 2 ,
- Michael E. Benros ORCID: orcid.org/0000-0003-4939-9465 3 , 4 ,
- Robyn S. Klein 5 &
- Christiaan H. Vinkers ORCID: orcid.org/0000-0003-3698-0744 1 , 2
Nature Medicine volume 28 , pages 2027–2037 ( 2022 ) Cite this article
38k Accesses
115 Citations
492 Altmetric
Metrics details
- Epidemiology
- Infectious diseases
- Neurological manifestations
- Psychiatric disorders
The Coronavirus Disease 2019 (COVID-19) pandemic has threatened global mental health, both indirectly via disruptive societal changes and directly via neuropsychiatric sequelae after SARS-CoV-2 infection. Despite a small increase in self-reported mental health problems, this has (so far) not translated into objectively measurable increased rates of mental disorders, self-harm or suicide rates at the population level. This could suggest effective resilience and adaptation, but there is substantial heterogeneity among subgroups, and time-lag effects may also exist. With regard to COVID-19 itself, both acute and post-acute neuropsychiatric sequelae have become apparent, with high prevalence of fatigue, cognitive impairments and anxiety and depressive symptoms, even months after infection. To understand how COVID-19 continues to shape mental health in the longer term, fine-grained, well-controlled longitudinal data at the (neuro)biological, individual and societal levels remain essential. For future pandemics, policymakers and clinicians should prioritize mental health from the outset to identify and protect those at risk and promote long-term resilience.
Similar content being viewed by others

The serotonin theory of depression: a systematic umbrella review of the evidence
Joanna Moncrieff, Ruth E. Cooper, … Mark A. Horowitz
Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population
Yunhe Wang, Binbin Su, … Daniel Prieto-Alhambra

MDMA-assisted therapy for moderate to severe PTSD: a randomized, placebo-controlled phase 3 trial
Jennifer M. Mitchell, Marcela Ot’alora G., … MAPP2 Study Collaborator Group
In 2019, the COVID-19 outbreak was declared a pandemic by the World Health Organization (WHO), with 590 million confirmed cases and 6.4 million deaths worldwide as of August 2022 (ref. 1 ). To contain the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) across the globe, many national and local governments implemented often drastic restrictions as preventive health measures. Consequently, the pandemic has not only led to potential SARS-CoV-2 exposure, infection and disease but also to a wide range of policies consisting of mask requirements, quarantines, lockdowns, physical distancing and closure of non-essential services, with unprecedented societal and economic consequences.
As the world is slowly gaining control over COVID-19, it is timely and essential to ask how the pandemic has affected global mental health. Indirect effects include stress-evoking and disruptive societal changes, which may detrimentally affect mental health in the general population. Direct effects include SARS-CoV-2-mediated acute and long-lasting neuropsychiatric sequelae in affected individuals that occur during primary infection or as part of post-acute COVID syndrome (PACS) 2 —defined as symptoms lasting beyond 3–4 weeks that can involve multiple organs, including the brain. Several terminologies exist for characterizing the effects of COVID-19. PACS also includes late sequalae that constitute a clinical diagnosis of ‘long COVID’ where persistent symptoms are still present 12 weeks after initial infection and cannot be attributed to other conditions 3 .
Here we review both the direct and indirect effects of COVID-19 on mental health. First, we summarize empirical findings on how the COVID-19 pandemic has impacted population mental health, through mental health symptom reports, mental disorder prevalence and suicide rates. Second, we describe mental health sequalae of SARS-CoV-2 virus infection and COVID-19 disease (for example, cognitive impairment, fatigue and affective symptoms). For this, we use the term PACS for neuropsychiatric consequences beyond the acute period, and will also describe the underlying neurobiological impact on brain structure and function. We conclude with a discussion of the lessons learned and knowledge gaps that need to be further addressed.
Impact of the COVID-19 pandemic on population mental health
Independent of the pandemic, mental disorders are known to be prevalent globally and cause a very high disease burden 4 , 5 , 6 . For most common mental disorders (including major depressive disorder, anxiety disorders and alcohol use disorder), environmental stressors play a major etiological role. Disruptive and unpredictable pandemic circumstances may increase distress levels in many individuals, at least temporarily. However, it should be noted that the pandemic not only resulted in negative stressors but also in positive and potentially buffering changes for some, including a better work–life balance, improved family dynamics and enhanced feelings of closeness 7 .
Awareness of the potential mental health impact of the COVID-19 pandemic is reflected in the more than 35,000 papers published on this topic. However, this rapid research output comes with a cost: conclusions from many papers are limited due to small sample sizes, convenience sampling with unclear generalizability implications and lack of a pre-COVID-19 comparison. More reliable estimates of the pandemic mental health impact come from studies with longitudinal or time-series designs that include a pre-pandemic comparison. In our description of the evidence, we, therefore, explicitly focused on findings from meta-analyses that include longitudinal studies with data before the pandemic, as recently identified through a systematic literature search by the WHO 8 .
Self-reported mental health problems
Most studies examining the pandemic impact on mental health used online data collection methods to measure self-reported common indicators, such as mood, anxiety or general psychological distress. Pooled prevalence estimates of clinically relevant high levels of depression and anxiety symptoms during the COVID-19 pandemic range widely—between 20% and 35% 9 , 10 , 11 , 12 —but are difficult to interpret due to large methodological and sample heterogeneity. It also is important to note that high levels of self-reported mental health problems identify increased vulnerability and signal an increased risk for mental disorders, but they do not equal clinical caseness levels, which are generally much lower.
Three meta-analyses, pooling data from between 11 and 61 studies and involving ~50,000 individuals or more 13 , 14 , 15 , compared levels of self-reported mental health problems during the COVID-19 pandemic with those before the pandemic. Meta-analyses report on pooled effect sizes—that is, weighted averages of study-level effect sizes; these are generally considered small when they are ~0.2, moderate when ~0.5 and large when ~0.8. As shown in Table 1 , meta-analyses on mental health impact of the COVID-19 pandemic reach consistent conclusions and indicate that there has been a heterogeneous, statistically significant but small increase in self-reported mental health problems, with pooled effect sizes ranging from 0.07 to 0.27. The largest symptom increase was found when using specific mental health outcome measures assessing depression or anxiety symptoms. In addition, loneliness—a strong correlate of depression and anxiety—showed a small but significant increase during the pandemic (Table 1 ; effect size = 0.27) 16 . In contrast, self-reported general mental health and well-being indicators did not show significant change, and psychotic symptoms seemed to have decreased slightly 13 . In Europe, alcohol purchase decreased, but high-level drinking patterns solidified among those with pre-pandemic high drinking levels 17 . When compared to pre-COVID levels, no change in self-reported alcohol use (effect size = −0.01) was observed in a recent meta-analysis summarizing 128 studies from 58 (predominantly European and North American) countries 18 .
What is the time trajectory of self-reported mental health problems during the pandemic? Although findings are not uniform, various large-scale studies confirmed that the increase in mental health problems was highest during the first peak months of the pandemic and smaller—but not fully gone—in subsequent months when infection rates declined and social restrictions eased 13 , 19 , 20 . Psychological distress reports in the United Kingdom increased again during the second lockdown period 15 . Direct associations between anxiety and depression symptom levels and the average number of daily COVID-19 cases were confirmed in the US Centers for Disease Control and Prevention (CDC) data 21 . Studies that examined longer-term trajectories of symptoms during the first or even second year of the COVID-19 pandemic are more sparse but revealed stability of symptoms without clear evidence of recovery 15 , 22 . The exception appears to be for loneliness, as some studies confirmed further increasing trends throughout the first COVID-19 pandemic year 22 , 23 . As most published population-based studies were conducted in the early time period in which absolute numbers of SARS-CoV2-infected individuals were still low, the mental health impacts described in such studies are most likely due to indirect rather than direct effects of SARS-CoV-2 infection. However, it is possible that, in longer-term or later studies, these direct and indirect effects may be more intertwined.
The extent to which governmental policies and communication have impacted on population mental health is a relevant question. In cross-country comparisons, the extent of social restrictions showed a dose–response relationship with mental health problems 24 , 25 . In a review of 33 studies worldwide, it was concluded that governments that enacted stringent measures to contain the spread of COVID-19 benefitted not only the physical but also the mental health of their population during the pandemic 26 , even though more stringent policies may lead to more short-term mental distress 25 . It has been suggested that effective communication of risks, choices and policy measures may reduce polarization and conspiracy theories and mitigate the mental health impact of such measures 25 , 27 , 28 .
In sum, the general pattern of results is that of an increase in mental health symptoms in the population, especially during the first pandemic months, that remained elevated throughout 2020 and early 2021. It should be emphasized that this increase has a small effect size. However, even a small upward shift in mental health problems warrants attention as it has not yet shown to be returned to pre-pandemic levels, and it may have meaningful cumulative consequences at the population level. In addition, even a small effect size may mask a substantial heterogeneity in mental health impact, which may have affected vulnerable groups disproportionally (see below).
Mental disorders, self-harm and suicide
Whether the observed increase in mental health problems during the COVID-19 pandemic has translated into more mental disorders or even suicide mortality is not easy to answer. Mental disorders, characterized by more severe, disabling and persistent symptoms than self-reported mental health problems, are usually diagnosed by a clinician based on the International Classification of Diseases, 10th Revision (ICD-10) or the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria or with validated semi-structured clinical interviews. However, during the COVID-19 pandemic, research systematically examining the population prevalence of mental disorders has been sparse. Unfortunately, we can also not strongly rely on healthcare use studies as the pandemic impacted on healthcare provision more broadly, thereby making figures of patient admissions difficult to interpret.
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic has led to a 28% (95% uncertainty interval (UI): 25–30) increase in major depressive disorders and a 26% (95% UI: 23–28) increase in anxiety disorders. It should be noted that these estimations come with high uncertainty as the assumption that transient pandemic-related increases in mental symptoms extrapolate into incident mental disorders remains disputable. So far, only four longitudinal population-based studies have measured and compared current mental (that is, depressive and anxiety) disorder prevalence—defined using psychiatric diagnostic criteria—before and during the pandemic. Of these, two found no change 30 , 31 , one found a decrease 32 and one found an increase in prevalence of these disorders 33 . These studies were local, limited to high-income countries, often small-scale and used different modes of assessment (for example, online versus in-person) before and during the pandemic. This renders these observational results uncertain as well, but their contrast to the GBD calculations 29 is striking.
Time-series analysis of monthly suicide trends in 21 middle-income to high-income countries across the globe yielded no evidence for an increase in suicide rates in the first 4 months of the pandemic, and there was evidence of a fall in rates in 12 countries 34 . Also in the United States, there was a significant decrease in suicide mortality in the first pandemic months but a slight increase in mortality due to drug overdose and homicide 35 . A living systematic review 36 also concluded that, throughout 2020, there was no observed increase in suicide rates in 20 studies conducted in North America, Europe and Asia. Analyses of electronic health record data in the primary care setting showed reduced rates of self-harm during the first COVID-19 pandemic year 37 . In contrast, emergency department visits for self-harm behavior were unchanged 38 or increased 39 . Such inconsistent findings across healthcare settings may reflect a reluctance in healthcare-seeking behavior for mental healthcare issues. In the living systematic review, eight of 11 studies that examined service use data found a significant decrease in reported self-harm/suicide attempts after COVID lockdown, which returned to pre-lockdown levels in some studies with longer follow-up (5 months) 36 .
In sum, although calculations based on survey data predict a global increase of mental disorder prevalence, objective and consistent evidence for an increased mental disorder, self-harm or suicide prevalence or incidence during the first pandemic year remains absent. This observation, coupled with the only small increase in mental health symptom levels in the overall population, may suggest that most of the general population has demonstrated remarkable resilience and adaptation. However, alternative interpretations are possible. First, there is a large degree of heterogeneity in the mental health impact of COVID-19, and increased mental health in one group (for example, due to better work–family balance and work flexibility) may have masked mental health problems in others. Various societal responses seen in many countries, such as community support activities and bolstering mental health and crisis services, may have had mitigating effects on the mental health burden. Also, the relationship between mental health symptom increases during stressful periods and its subsequent effects on the incidence of mental disorders may be non-linear or could be less visible due to resulting alternative outcomes, such as drug overdose or homicide. Finally, we cannot rule out a lag-time effect, where disorders may take more time to develop or be picked up, especially because some of the personal financial or social consequences of the COVID pandemic may only become apparent later. It should be noted that data from low-income countries and longer-term studies beyond the first pandemic year are largely absent.
Which individuals are most affected by the COVID-19 pandemic?
There is substantial heterogeneity across studies that evaluated how the COVID pandemic impacted on mental health 13 , 14 , 15 . Although our society as a whole may have the ability to adequately bounce back from pandemic effects, there are vulnerable people who have been affected more than others.
First, women have consistently reported larger increases in mental health problems in response to the COVID-19 pandemic than men 13 , 15 , 29 , 40 , with meta-analytic effect sizes being 44% 15 to 75% 13 higher. This could reflect both higher stress vulnerability or larger daily life disruptions due to, for example, increased childcare responsibilities, exposure to home violence or greater economic impact due to employment disruptions that all disproportionately fell to women 41 , thereby exacerbating the already existing pre-pandemic gender inequalities in depression and anxiety levels. In addition, adolescents and young adults have been disproportionately affected compared to younger children and older adults 12 , 15 , 29 , 40 . This may be the result of unfavorable behavioral and social changes (for example, school closure periods 42 ) during a crucial development phase where social interactions outside the family context are pivotal. Alarmingly, even though suicide rates did not seem to increase at the population level, studies in China 43 and Japan 44 indicated significant increases in suicide rates in children and adolescents.
Existing socio-cultural disparities in mental health may have further widened during the COVID pandemic. Whether the impact is larger for individuals with low socio-economic status remains unclear, with contrasting meta-analyses pointing toward this group being protected 15 or at increased risk 40 . Earlier meta-analyses did not find that the mental health impact of COVID-19 differed across Europe, North America, Asia and Oceania 13 , 14 , but data are lacking from Africa and South America. Nevertheless, a large-scale within-country comparison in the United States found that the mental health of Black, Hispanic and Asian respondents worsened relatively more during the pandemic compared to White respondents. Moreover, White respondents were more likely to receive professional mental healthcare during the pandemic, and, conversely, Black, Hispanic, and Asian respondents demonstrated higher levels of unmet mental healthcare needs during this time 45 .
People with pre-existing somatic conditions represent another vulnerable group in which the pandemic had a greater impact (pooled effect size of 0.25) 13 . This includes people with conditions such as epilepsy, multiple sclerosis or cardiometabolic disease as well as those with multiple comorbidities. The disproportionate impact may reflect this groupʼs elevated COVID-19 risk and, consequently, more perceived stress and fear of infection, but it could also reflect disruptions of regular healthcare services.
Healthcare workers faced increased workload, rapidly changing and challenging work environments and exposure to infections and death, accompanied by fear of infecting themselves and their families. High prevalences of (subthreshold) depression (13% 46 ), depressive symptoms (31% 47 ), (subthreshold) anxiety (16% 46 ), anxiety symptoms (23% 47 ) and post-traumatic stress disorder (~22% 46 , 47 ) have been reported in healthcare workers. However, a meta-analysis did not find a larger mental health impact of the pandemic as compared to the general population 40 , and another meta-analysis (of 206 studies) found that the mental health status of healthcare workers was similar to or even better than that of the general population during the first COVID year 48 . However, it is important to note that these meta-analyses could not differentiate between frontline and non-frontline healthcare workers.
Finally, individuals with pre-existing mental disorders may be at increased risk for exacerbation of mental ill-health during the pandemic, possibly due to disease history—illustrating a higher genetic and/or environmental vulnerability—but also due to discontinuity of mental healthcare. Already before the pandemic, mental health systems were under-resourced and disorganized in most countries 6 , 49 , but a third of all WHO member states reported disruptions to mental and substance use services during the first 18 months of the pandemic 50 , with reduced, shortened or postponed appointments and limited capacity for acute inpatient admissions 51 , 52 . Despite this, there is no clear evidence that individuals with pre-existing mental disorders are disproportionately affected by pandemic-related societal disruptions; the effect size for pandemic impact on self-reported mental health problems was similar in psychiatric patients and the general population 13 . In the United States, emergency visits for ten different mental disorders were generally stable during the pandemic compared to earlier periods 53 . In a large Dutch study 22 , 54 with multiple pre-pandemic and during-pandemic assessments, there was no difference in symptom increase among patients relative to controls (see Fig. 1 for illustration). In absolute terms, however, it is important to note that psychiatric patients show much higher symptom levels of depression, anxiety, loneliness and COVID-fear than healthy controls. Again, variation in mental health changes during the pandemic is large: next to psychiatric patients who showed symptom decrease due to, for example, experiencing relief from social pressures, there certainly have been many patients with symptom increases and relapses during the pandemic.
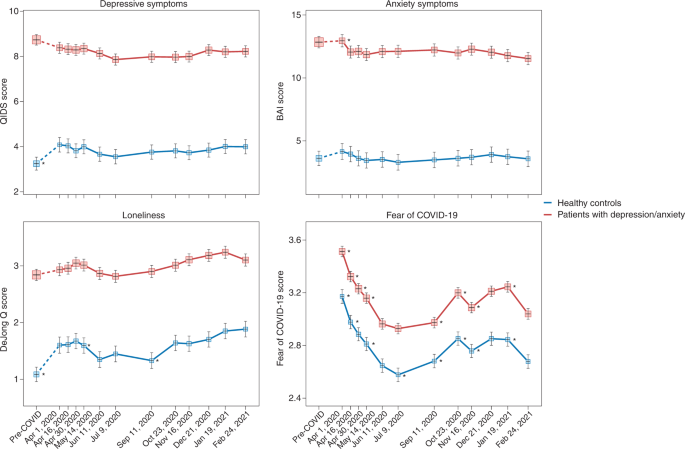
Trajectories of mean depressive symptoms (QIDS score), anxiety symptoms (BAI score), loneliness (De Jong questionnaire score) and Fear of COVID-19 score before and during the first year of the COVID-19 pandemic in healthy controls (blue line, n = 378) and in patients with depressive and/or anxiety disorders (red line, n = 908). The x -axis indicates time with one pre-COVID assessment (averaged over up to five earlier assessments conducted between 2006 and 2019) and 11 online assessments during April 2020 through February 2021. Symbols indicate the mean score during the assessment with 95% CIs. As compared to pre-COVID assessment scores, the figure shows a statistically significant increase of depression and loneliness symptoms during the first pandemic peak (April 2020) in healthy controls but not in patients (for more details, see refs. 22 , 54 ). Asterisks indicate where subsequent wave scores differ from the prior wave scores ( P < 0.05). The figure also illustrates the stability of depressive and anxiety symptoms during the first COVID year, a significant increase in loneliness during this period and fluctuations of Fear of COVID-19 score that positively correlate with infection rates in the Netherlands. Raw data are from the Netherlands Study of Depression and Anxiety (NESDA), which were re-analyzed for the current plots to illustrate differences between two groups (healthy controls versus patients). BAI, Beck Anxiety Inventory; QIDS, Quick Inventory of Depressive Symptoms.
Impact of COVID-19 infection and disease on mental health and the brain
Not only the pandemic but also COVID-19 itself can have severe impact on the mental health of affected individuals and, thus, of the population at large. Below we describe acute and post-acute neuropsychiatric sequelae seen in patients with COVID-19 and link these to neurobiological mechanisms.
Neuropsychiatric sequelae in individuals with COVID-19
Common symptoms associated with acute SARS-CoV-2 infection include headache, anosmia (loss of sense of smell) and dysgeusia (loss of sense of taste). The broader neuropsychiatric impact is dependent on infection severity and is very heterogeneous (Table 2 ). It ranges from no neuropsychiatric symptoms among the large group of asymptomatic COVID-19 cases to milder transient neuropsychiatric symptoms, such as fatigue, sleep disturbance and cognitive impairment, predominantly occurring among symptomatic patients with COVID-19 (ref. 55 ). Cognitive impairment consists of sustained memory impairments and executive dysfunction, including short-term memory loss, concentration problems, word-finding problems and impaired daily problem-solving, colloquially termed ‘brain fog’ by patients and clinicians. A small number of infected individuals become severely ill and require hospitalization. During hospital admission, the predominant neuropsychiatric outcome is delirium 56 . Delirium occurs among one-third of hospitalized patients with COVID-19 and among over half of patients with COVID-19 who require intensive care unit (ICU) treatment. These delirium rates seem similar to those observed among individuals with severe illness hospitalized for other general medical conditions 57 . Delirium is associated with neuropsychiatric sequalae after hospitalization, as part of post-intensive care syndrome 58 , in which sepsis and inflammation are associated with cognitive dysfunction and an increased risk of a broad range of psychiatric symptoms, from anxiety to depression and psychotic symptoms with hallucinations 59 , 60 .
A subset of patients with COVID-19 develop PACS 61 , which can include neuropsychiatric symptoms. A large meta-analysis summarizes 51 studies involving 18,917 patients with a mean follow-up of 77 days (range, 14–182 days) 62 . The most prevalent neuropsychiatric symptom associated with COVID-19 was sleep disturbance, with a pooled prevalence of 27.4%, followed by fatigue (24.4%), cognitive impairment (20.2%), anxiety symptoms (19.1%), post-traumatic stress symptoms (15.7%) and depression symptoms (12.9%) (Table 2 ). Another meta-analysis that assessed patients 12 weeks or more after confirmed COVID-19 diagnosis found that 32% experienced fatigue, and 22% experienced cognitive impairment 63 . To what extent neuropsychiatric symptoms are truly unique for patients with COVID remains unclear from these meta-analyses, as hardly any study included well-matched controls with other types of respiratory infections or inflammatory conditions.
Studies based on electronic health records have examined whether higher levels of neuropsychiatric symptoms truly translate into a higher incidence of clinically overt mental disorders 64 , 65 . In a 1-year follow-up using the US Veterans Affairs database, 153,848 survivors of SARS-CoV-2 infection exhibited an increased incidence of any mental disorder with a relative risk of 1.46 and, specifically, 1.35 for anxiety disorders, 1.39 for depressive disorders and 1.38 for stress and adjustment disorders, compared to a contemporary group and a historical control group ( n = 5,859,251) 65 . In absolute numbers, the incident risk difference attributable to SARS-CoV-2 for mental disorders was 64 per 1,000 individuals. Taquet et al. 64 analyzed electronic health records from the US-based TriNetX network with over 81 million patients and 236,379 COVID-19 survivors followed for 6 months. In absolute numbers, 6-month incidence of hospital contacts related to diagnoses of anxiety, affective disorder or psychotic disorder was 7.0%, 4.5% and 0.4%, respectively. Risks of incident neurological or psychiatric diagnoses were directly correlated with COVID-19 severity and increased by 78% when compared to influenza and by 32% when compared to other respiratory tract infections. In contrast, a medical record study involving 8.3 million adults confirmed that neuropsychiatric disorders were significantly elevated among COVID-19 hospitalized individuals but to a similar extent as in hospitalized patients with other severe respiratory disease 66 . In line with this, a study using language processing of clinical notes in electronic health records did not find an increase in fatigue, mood and anxiety symptoms among COVID-19 hospitalized individuals when compared to hospitalized patients for other indications and adjusted for sociodemographic features and hospital course 67 . It is important to note that research based only on hospital records might be influenced by increased health-seeking behavior that could be differential across care settings or by increased follow-up by hospitals of patients with COVID-19 (compared to patients with other conditions).
Consequently, whether PACS symptoms form a unique pattern due to specific infection with SARS-CoV-2 remains debatable. Prospective case–control studies that do not rely on hospital records but measure the incidence of neuropsychiatric symptoms and diagnoses after COVID-19 are still scarce, but they are critical for distinguishing causation and confounding when characterizing PACS and the uniqueness of neuropsychiatric sequalae after COVID-19 (ref. 68 ). Recent studies with well-matched control groups illustrate that long-term consequences may not be so unique, as they were similar to those observed in patients with other diseases of similar severity, such as after acute myocardial infarction or in ICU patients 56 , 66 . A first prospective follow-up study of COVID-19 survivors and control patients matched on disease severity, age, sex and ICU admission found similar neuropsychiatric outcomes, regarding both new-onset psychiatric diagnosis (19% versus 20%) and neuropsychiatric symptoms (81% versus 93%). However, moderate but significantly worse cognitive outcomes 6 months after symptom onset were found among survivors of COVID-19 (ref. 69 ). In line with this, a longitudinal study of 785 participants from the UK Biobank showed small but significant cognitive impairment among individuals infected with SARS-CoV-2 compared to matched controls 70 .
Numerous psychosocial mechanisms can lead to neuropsychiatric sequalae of COVID-19, including functional impairment; psychological impact due to, for example, fear of dying; stress of being infected with a novel pandemic disease; isolation as part of quarantine and lack of social support; fear/guilt of spreading COVID-19 to family or community; and socioeconomic distress by lost wages 71 . However, there is also ample evidence that neurobiological mechanisms play an important role, which is discussed below.
Neurobiological mechanisms underlying neuropsychiatric sequelae of COVID-19
Acute neuropsychiatric symptoms among patients with severe COVID-19 have been found to correlate with the level of serum inflammatory markers 72 and coincide with neuroimaging findings of immune activation, including leukoencephalopathy, acute disseminated encephalomyelitis, cytotoxic lesions of the corpus callosum or cranial nerve enhancement 73 . Rare presentations, including meningitis, encephalitis, inflammatory demyelination, cerebral infarction and acute hemorrhagic necrotizing encephalopathy, have also been reported 74 . Hospitalized patients with frank encephalopathies display impaired blood-brain barrier (BBB) integrity with leptomeningeal enhancement on brain magnetic resonance images 75 . Studies of postmortem specimens from patients who succumbed to acute COVID-19 reveal significant neuropathology with signs of hypoxic damage and neuroinflammation. These include evidence of BBB permeability with extravasation of fibrinogen, microglial activation, astrogliosis, leukocyte infiltration and microhemorrhages 76 , 77 . However, it is still unclear to what extent these findings differ from patients with similar illness severity due to acute non-COVID illness, as these brain effects might not be virus-specific effects but rather due to cytokine-mediated neuroinflammation and critical illness.
Post-acute neuroimaging studies in SARS-CoV-2-recovered patients, as compared to control patients without COVID-19, reveal numerous alterations in brain structure on a group level, although effect sizes are generally small. These include minor reduction in gray matter thickness in the various regions of the cortex and within the corpus collosum, diffuse edema, increases in markers of tissue damage in regions functionally connected to the olfactory cortex and reductions in overall brain size 70 , 78 . Neuroimaging studies of post-acute COVID-19 patients also report abnormalities consistent with micro-structural and functional alterations, specifically within the hippocampus 79 , 80 , a brain region critical for memory formation and regulating anxiety, mood and stress responses, but also within gray matter areas involving the olfactory system and cingulate cortex 80 . Overall, these findings are in line with ongoing anosmia, tremors, affect problems and cognitive impairment.
Interestingly, despite findings mentioned above, there is little evidence of SARS-CoV-2 neuroinvasion with productive replication, and viral material is rarely found in the central nervous system (CNS) of patients with COVID-19 (refs. 76 , 77 , 81 ). Thus, neurobiological mechanisms of SARS-CoV-2-mediated neuropsychiatric sequelae remain unclear, especially in patients who initially present with milder forms of COVID-19. Symptomatic SARS-CoV-2 infection is associated with hypoxia, cytokine release syndrome (CRS) and dysregulated innate and adaptive immune responses (reviewed in ref. 82 ). All these effects could contribute to neuroinflammation and endothelial cell activation (Fig. 2 ). Examination of cerebrospinal fluid in patients with neuroimaging findings revealed elevated levels of pro-inflammatory, BBB-destabilizing cytokines, including interleukin-6 (IL-6), IL-1, IL-8 and mononuclear cell chemoattractants 83 , 84 . Whether these cytokines arise from the periphery, due to COVID-19-mediated CRS, or from within the CNS, is unclear. As studies generally lack control patients with other severe illnesses, the specificity of such findings to SARS-CoV-2 also remains unclear. Systemic inflammatory processes, including cytokine release, have been linked to glial activation with expression of chemoattractants that recruit immune cells, leading to neuroinflammation and injury 85 . Cerebrospinal fluid concentrations of neurofilament light, a biomarker of neuronal damage, were reportedly elevated in patients hospitalized with COVID-19 regardless of whether they exhibited neurologic diseases 86 . Acute thromboembolic events leading to ischemic infarcts are also common in patients with COVID-19 due to a potentially increased pro-coagulant process secondary to CRS 87 .
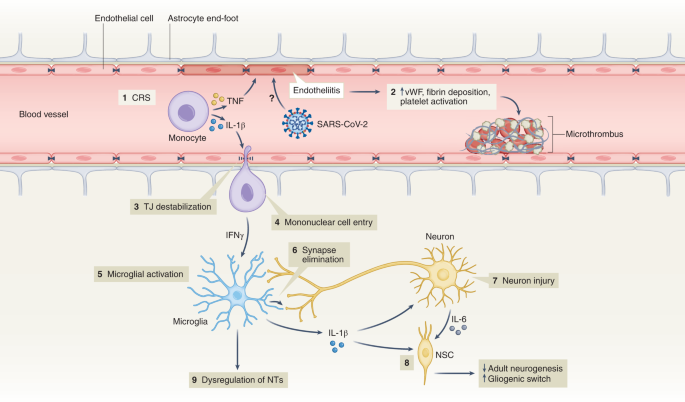
(1) Elevation of BBB-destabilizing cytokines (IL-1β and TNF) within the serum due to CRS or local interactions of mononuclear and endothelial cells. (2) Virus-induced endotheliitis increases susceptibility to microthrombus formation due to platelet activation, elevation of vWF and fibrin deposition. (3) Cytokine, mononuclear and endothelial cell interactions promote disruption of the BBB, which may allow entry of leukocytes expressing IFNg into the CNS (4), leading to microglial activation (5). (6) Activated microglia may eliminate synapses and/or express cytokines that promote neuronal injury. (7) Injured neurons express IL-6 which, together with IL-1β, promote a ‘gliogenic switch’ in NSCs (8), decreasing adult neurogenesis. (9) The combination of microglial (and possibly astrocyte) activation, neuronal injury and synapse loss may lead to dysregulation of NTs and neuronal circuitry. IFNg, interferon-g; NSC, neural stem cell; NT, neurotransmitter; TJ, tight junction; TNF, tumor necrosis factor; vWF, von Willebrand factor.
It is also unclear whether hospitalized patients with COVID-19 may develop brain abnormalities due to hypoxia or CRS rather than as a direct effect of SARS-CoV-2 infection. Hypoxia may cause neuronal dysfunction, cerebral edema, increased BBB permeability, cytokine expression and onset of neurodegenerative diseases 88 , 89 . CRS, with life-threatening levels of serum TNF-α and IL-1 (ref. 90 ) could also impact BBB function, as these cytokines destabilize microvasculature endothelial cell junctional proteins critical for BBB integrity 91 . In mild SARS-CoV-2 infection, circulating immune factors combined with mild hypoxia might impact BBB function and lead to neuroinflammation 92 , as observed during infection with other non-neuroinvasive respiratory pathogens 93 . However, multiple studies suggest that the SARS-CoV-2 spike protein itself may also induce venous and arterial endothelial cell activation and endotheliitis, disrupt BBB integrity or cross the BBB via adoptive transcytosis 94 , 95 , 96 .
Reducing neuropsychiatric sequelae of COVID-19
The increased risk of COVID-19-related neuropsychiatric sequalae was most pronounced during the first pandemic peak but reduced over the subsequent 2 years 64 , 97 . This may be due to reduced impact of newer SARS-CoV-2 strains (that is, Omicron) but also protective effects of vaccination, which limit SARS-CoV-2 spread and may, thus, prevent neuropsychiatric sequalae. Fully vaccinated individuals with breakthrough infections exhibit a 50% reduction in PACS 98 , even though vaccination does not improve PACS-related neuropsychiatric symptoms in patients with a prior history of COVID-19 (ref. 99 ). As patients with pre-existing mental disorders are at increased risk of SARS-CoV-2 infection, they deserve to be among the prioritization groups for vaccination efforts 100 .
Adequate treatment strategies for neuropsychiatric sequelae of COVID-19 are needed. As no specific evidence-based intervention yet exists, the best current treatment approach is that for neuropsychiatric sequelae arising after other severe medical conditions 101 . Stepped care—a staged approach of mental health services comprising a hierarchy of interventions, from least to most intensive, matched to the individual’s need—is efficacious with monitoring of mental health and cognitive problems. Milder symptoms likely benefit from counseling and holistic care, including physiotherapy, psychotherapy and rehabilitation. Individuals with moderate to severe symptoms fulfilling psychiatric diagnoses should receive guideline-concordant care for these disorders 61 . Patients with pre-existing mental disorders also deserve special attention when affected by COVID-19, as they have shown to have an increased risk of COVID-19-related hospitalization, complications and death 102 . This may involve interventions to address their general health, any unfavorable socioenvironmental factors, substance abuse or treatment adherence issues.
Lessons learned, knowledge gaps and future challenges
Ultimately, it is not only the millions of people who have died from COVID-19 worldwide that we remember but also the distress experienced during an unpredictable period with overstretched healthcare systems, lockdowns, school closures and changing work environments. In a world that is more and more globalized, connectivity puts us at risk for future pandemics. What can be learned from the last 2 years of the COVID-19 pandemic about how to handle future and longstanding challenges related to mental health?
Give mental health equal priority to physical health
The COVID-19 pandemic has demonstrated that our population seems quite resilient and adaptive. Nevertheless, even if society as a whole may bounce back, there is a large group of people whose mental health has been and will be disproportionately affected by this and future crises. Although various groups, such as the WHO 8 , the National Health Commission of China 103 , the Asia Pacific Disaster Mental Health Network 104 and a National Taskforce in India 105 , developed mental health policies early on, many countries were late in realizing that a mental health agenda deserves immediate attention in a rapidly evolving pandemic. Implementation of comprehensive and integrated mental health policies was generally inconsistent and suboptimal 106 and often in the shadow of policies directed at containing and reducing the spread of SARS-CoV-2. Leadership is needed to convey the message that mental health is as important as physical health and that we should focus specific attention and early interventions on those at the highest risk. This includes those vulnerable due to factors such as low socioeconomic status, specific developmental life phase (adolescents and young adults), pre-existing risk (poor physical or somatic health and early life trauma) or high exposure to pandemic-related (work) changes—for example, women and healthcare personnel. This means that not only should investment in youth and reducing health inequalities remain at the top of any policy agenda but also that mental health should be explicitly addressed from the start in any future global health crisis situation.
Communication and trust is crucial for mental health
Uncertainty and uncontrollability during the pandemic have challenged rational thinking. Negative news travels fast. Communication that is vague, one-sided and dishonest can negatively impact on mental health and amplify existing distress and anxiety 107 . Media reporting should not overemphasize negative mental health impact—for example, putative suicide rate increases or individual negative experiences—which could make situations worse than they actually are. Instead, communication during crises requires concrete and actionable advice that avoids polarization and strengthens vigilance, to foster resilience and help prevent escalation to severe mental health problems 108 , 109 .
Rapid research should be collaborative and high-quality
Within the scientific community, the topic of mental health during the pandemic led to a multitude of rapid studies that generally had limited methodological quality—for example, cross-sectional designs, small or selective sampling or study designs lacking valid comparison groups. These contributed rather little to our understanding of the mental health impact of the emerging crisis. In future events that have global mental health impact, where possible, collaborative and interdisciplinary efforts with well-powered and well-controlled prospective studies using standardized instruments will be crucial. Only with fine-grained determinants and outcomes can data reliably inform mental health policies and identify who is most at risk.
Do not neglect long-term mental health effects
So far, research has mainly focused on the acute and short-term effects of the pandemic on mental health, usually spanning pandemic effects over several months to 1 year. However, longer follow-up of how a pandemic impacts population mental health is essential. Can societal and economic disruptions after the pandemic increase risk of mental disorders at a later stage when the acute pandemic effects have subsided? Do increased self-reported mental health problems return to pre-pandemic levels, and which groups of individuals remain most affected in the long-term? We need to realize that certain pandemic consequences, particularly those affecting income and school/work careers, may become visible only over the course of several years. Consequently, we should maintain focus and continue to monitor and quantify the effects of the pandemic in the years to come—for example, by monitoring mental healthcare use and suicide. This should include specific at-risk populations (for example, adolescents) and understudied populations in low-income and middle-income countries.
Pay attention to mental health consequences of infectious diseases
Even though our knowledge on PACS is rapidly expanding, there are still many unanswered questions related to who is at risk, the long-term course trajectories and the best ways to intervene early. Consequently, we need to be aware of the neuropsychiatric sequelae of COVID-19 and, for that matter, of any infectious disease. Clinical attention and research should be directed toward alleviating potential neuropsychiatric ramifications of COVID-19. Next to clinical studies, studies using human tissues and appropriate animal models are pivotal to determine the CNS region-specific and neural-cell-specific effects of SARS-CoV-2 infection and the induced immune activation. Indeed, absence of SARS-CoV-2 neuroinvasion is an opportunity to learn and discover how peripheral neuroimmune mechanisms can contribute to neuropsychiatric sequelae in susceptible individuals. This emphasizes the importance of an interdisciplinary approach where somatic and mental health efforts are combined but also the need to integrate clinical parameters after infection with biological parameters (for example, serum, cerebrospinal fluid and/or neuroimaging) to predict who is at risk for PACS and deliver more targeted treatments.
Prepare mental healthcare infrastructure for pandemic times
If we take mental health seriously, we should not only monitor it but also develop the resources and infrastructure necessary for rapid early intervention, particularly for specific vulnerable groups. For adequate mental healthcare to be ready for pandemic times, primary care, community mental health and public mental health should be prepared. In many countries, health services were not able to meet the population’s mental health needs before the pandemic, which substantially worsened during the pandemic. We should ensure rapid access to mental health services but also address the underlying drivers of poor mental health, such as mitigating risks of unemployment, sexual violence and poverty. Collaboration in early stages across disciplines and expertise is essential. Anticipating disruption to face-to-face services, mental healthcare providers should be more prepared for consultations, therapy and follow-up by telephone, video-conferencing platforms and web applications 51 , 52 . The pandemic has shown that an inadequate infrastructure, pre-existing inequalities and low levels of technological literacy hindered the use and uptake of e-health, both in healthcare providers and in patients across different care settings. The necessary investments can ensure rapid upscaling of mental health services during future pandemics for those individuals with a high mental health need due to societal changes, government measures, fear of infection or infection itself.
Even though much attention has been paid to the physical health consequences of COVID-19, mental health has unjustly received less attention. There is an urgent need to prepare our research and healthcare infrastructures not only for adequate monitoring of the long-term mental health effects of the COVID-19 pandemic but also for future crises that will shape mental health. This will require collaboration to ensure interdisciplinary and sound research and to provide attention and care at an early stage for those individuals who are most vulnerable—giving mental health equal priority to physical health from the very start.
WHO Coronavirus (COVID-19) Dashboard (WHO, 2022; https://covid19.who.int/
Rando, H. M. et al. Challenges in defining long COVID: striking differences across literature, electronic health records, and patient-reported information. Preprint at https://www.medrxiv.org/content/10.1101/2021.03.20.21253896v1 (2021).
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27 , 601–615 (2021).
Article CAS PubMed PubMed Central Google Scholar
Abbafati, C. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1204–1222 (2020).
Article Google Scholar
Penninx, B. W., Pine, D. S., Holmes, E. A. & Reif, A. Anxiety disorders. Lancet 397 , 914–927 (2021).
Article PubMed PubMed Central Google Scholar
Herrman, H. et al. Time for united action on depression: a Lancet –World Psychiatric Association Commission. Lancet 399 , 957–1022 (2022).
Article PubMed Google Scholar
Radka, K., Wyeth, E. H. & Derrett, S. A qualitative study of living through the first New Zealand COVID-19 lockdown: affordances, positive outcomes, and reflections. Prev. Med. Rep. 26 , 101725 (2022).
Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact (WHO, 2022).
Dragioti, E. et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 94 , 1935–1949 (2022).
Zhang, S. X. et al. Mental disorder symptoms during the COVID-19 pandemic in Latin America—a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 31 , e23 (2022).
Zhang, S. X. et al. Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. Eur. J. Psychotraumatol . 13 , 2000132 (2022).
Racine, N. et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 175 , 1142–1150 (2021).
Robinson, E., Sutin, A. R., Daly, M. & Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 296 , 567–576 (2022).
Article CAS PubMed Google Scholar
Prati, G. & Mancini, A. D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 51 , 201–211 (2021).
Patel, K. et al. Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Netw. Open 5 , e227629 (2022).
Ernst, M. et al. Loneliness before and during the COVID-19 pandemic: a systematic review with meta-analysis. Am. Psychol . 77 , 660–677 (2022).
Kilian, C. et al. Changes in alcohol use during the COVID-19 pandemic in Europe: a meta-analysis of observational studies. Drug Alcohol Rev . 41 , 918–931 (2022).
Acuff, S. F., Strickland, J. C., Tucker, J. A. & Murphy, J. G. Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: a systematic review and meta-analysis. Psychol. Addict. Behav. 36 , 1–19 (2022).
Varga, T. V. et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health Eur . 2 , 100020 (2021).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8 , 141–149 (2021).
Jia, H. et al. National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic—United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 70 , 1427–1432 (2021).
Kok, A. A. L. et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in Dutch case–control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J. Affect. Disord. 305 , 85–93 (2022).
Su, Y. et al. Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: a systematic review and meta-analysis. Int. Psychogeriatr. https://doi.org/10.1017/S1041610222000199 (2022).
Knox, L., Karantzas, G. C., Romano, D., Feeney, J. A. & Simpson, J. A. One year on: what we have learned about the psychological effects of COVID-19 social restrictions: a meta-analysis. Curr. Opin. Psychol. 46 , 101315 (2022).
Aknin, L. B. et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health 7 , e417–e426 (2022).
Lee, Y. et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 290 , 364–377 (2021).
Wu, J. T. et al. Nowcasting epidemics of novel pathogens: lessons from COVID-19. Nat. Med. 27 , 388–395 (2021).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Santomauro, D. F. et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398 , 1700–1712 (2021).
Knudsen, A. K. S. et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Reg. Health Eur . 4 , 100071 (2021).
Ayuso-Mateos, J. L. et al. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol. Psychiatr. Sci . 30 , e49 (2021).
Vloo, A. et al. Gender differences in the mental health impact of the COVID-19 lockdown: longitudinal evidence from the Netherlands. SSM Popul. Health 15 , 100878 (2021).
Winkler, P. et al. Prevalence of current mental disorders before and during the second wave of COVID-19 pandemic: an analysis of repeated nationwide cross-sectional surveys. J. Psychiatr. Res. 139 , 167–171 (2021).
Pirkis, J. et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 8 , 579–588 (2021).
Faust, J. S. et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, March–August 2020. JAMA 326 , 84–86 (2021).
John, A. et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. F1000Res. 9 , 1097 (2020).
Steeg, S. et al. Temporal trends in primary care-recorded self-harm during and beyond the first year of the COVID-19 pandemic: time series analysis of electronic healthcare records for 2.8 million patients in the Greater Manchester Care Record. EClinicalMedicine 41 , 101175 (2021).
Rømer, T. B. et al. Psychiatric admissions, referrals, and suicidal behavior before and during the COVID-19 pandemic in Denmark: a time-trend study. Acta Psychiatr. Scand. 144 , 553–562 (2021).
Holland, K. M. et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry 78 , 372–379 (2021).
Kunzler, A. M. et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health 17 , 34 (2021).
Flor, L. S. et al. Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: a comprehensive review of data from March, 2020, to September, 2021. Lancet 399 , 2381–2397 (2022).
Viner, R. et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. 176 , 400–409 (2022).
Zheng, X. Y. et al. Trends of injury mortality during the COVID-19 period in Guangdong, China: a population-based retrospective analysis. BMJ Open 11 , e045317 (2021).
Tanaka, T. & Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 5 , 229–238 (2021).
Thomeer, M. B., Moody, M. D. & Yahirun, J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J. Racial Ethn. Health Disparities https://doi.org/10.1007/s40615-021-01006-7 (2022).
Hill, J. E. et al. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. J. Adv. Nurs. 78 , 1551–1573 (2022).
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R. & Guessoum, S. B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126 , 252–264 (2021).
Phiri, P. et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine 34 , 100806 (2021).
Jorm, A. F., Patten, S. B., Brugha, T. S. & Mojtabai, R. Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 16 , 90–99 (2017).
Third Round of the Global Pulse Survey on Continuity of Essential Health Services during the COVID-19 Pandemic (WHO, 2021).
Baumgart, J. G. et al. The early impacts of the COVID-19 pandemic on mental health facilities and psychiatric professionals. Int. J. Environ. Res. Public Health 18 , 8034 (2021).
Raphael, J., Winter, R. & Berry, K. Adapting practice in mental healthcare settings during the COVID-19 pandemic and other contagions: systematic review. BJPsych Open 7 , e62 (2021).
Anderson, K. N. et al. Changes and inequities in adult mental health-related emergency department visits during the COVID-19 pandemic in the US. JAMA Psychiatry 79 , 475–485 (2022).
Pan, K. Y. et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case–control cohorts. Lancet Psychiatry 8 , 121–129 (2021).
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W. & Kelley, K. W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 9 , 46–56 (2008).
Nersesjan, V. et al. Central and peripheral nervous system complications of COVID-19: a prospective tertiary center cohort with 3-month follow-up. J. Neurol. 268 , 3086–3104 (2021).
Wilson, J. E. et al. Delirium. Nat. Rev. Dis. Prim . 6 , 90 (2020).
Rawal, G., Yadav, S. & Kumar, R. Post-intensive care syndrome: an overview. J. Transl. Intern. Med. 5 , 90–92 (2017).
Pandharipande, P. P. et al. Long-term cognitive impairment after critical illness. N. Engl. J. Med. 369 , 1306–1316 (2013).
Girard, T. D. et al. Long-term cognitive impairment after hospitalization for community-acquired pneumonia: a prospective cohort study. J. Gen. Intern. Med. 33 , 929–935 (2018).
Crook, H., Raza, S., Nowell, J., Young, M. & Edison, P. Long covid—mechanisms, risk factors, and management. BMJ 374 , n1648 (2021).
Badenoch, J. B. et al. Persistent neuropsychiatric symptoms after COVID-19: a systematic review and meta-analysis. Brain Commun . 4 , fcab297 (2021).
Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 101 , 93–135 (2022).
Taquet, M., Geddes, J. R., Husain, M., Luciano, S. & Harrison, P. J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8 , 416–427 (2021).
Xie, Y., Xu, E. & Al-Aly, Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ 376 , e068993 (2022).
Kieran Clift, A. et al. Neuropsychiatric ramifications of severe COVID-19 and other severe acute respiratory infections. JAMA Psychiatry 79 , 690–698 (2022).
Castro, V. M., Rosand, J., Giacino, J. T., McCoy, T. H. & Perlis, R. H. Case–control study of neuropsychiatric symptoms following COVID-19 hospitalization in 2 academic health systems. Mol. Psych. (in the press).
Amin-Chowdhury, Z. & Ladhani, S. N. Causation or confounding: why controls are critical for characterizing long COVID. Nat. Med. 27 , 1129–1130 (2021).
Nersesjan, V. et al. Neuropsychiatric and cognitive outcomes in patients 6 months after COVID-19 requiring hospitalization compared with matched control patients hospitalized for non-COVID-19 illness. JAMA Psychiatry 79 , 486–497 (2022).
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604 , 697–707 (2022).
Zhang, H. et al. Psychological experience of COVID-19 patients: a systematic review and qualitative meta-synthesis. Am. J. Infect. Control 50 , 809–819 (2022).
Mazza, M. G. et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 89 , 594–600 (2020).
Moonis, G. et al. The spectrum of neuroimaging findings on CT and MRI in adults With COVID-19. AJR Am. J. Roentgenol. 217 , 959–974 (2021).
Asadi-Pooya, A. A. & Simani, L. Central nervous system manifestations of COVID-19: a systematic review. J. Neurol. Sci . 413 , 116832 (2020).
Lersy, F. et al. Cerebrospinal fluid features in patients with Coronavirus Disease 2019 and neurological manifestations: correlation with brain magnetic resonance imaging findings in 58 patients. J. Infect. Dis. 223 , 600–609 (2021).
Thakur, K. T. et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain 144 , 2696–2708 (2021).
Cosentino, G. et al. Neuropathological findings from COVID-19 patients with neurological symptoms argue against a direct brain invasion of SARS-CoV-2: a critical systematic review. Eur. J. Neurol. 28 , 3856–3865 (2021).
Tian, T. et al. Long-term follow-up of dynamic brain changes in patients recovered from COVID-19 without neurological manifestations. JCI Insight 7 , e155827 (2022).
Lu, Y. et al. Cerebral micro-structural changes in COVID-19 patients—an MRI-based 3-month follow-up study. EClinicalMedicine 25 , 100484 (2020).
Qin, Y. et al . Long-term microstructure and cerebral blood flow changes in patients recovered from COVID-19 without neurological manifestations. J. Clin. Invest . 131 , e147329 (2021).
Matschke, J. et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 19 , 919–929 (2020).
Shivshankar, P. et al. SARS-CoV-2 infection: host response, immunity, and therapeutic targets. Inflammation 45 , 1430–1449 (2022).
Manganotti, P. et al. Cerebrospinal fluid and serum interleukins 6 and 8 during the acute and recovery phase in COVID-19 neuropathy patients. J. Med. Virol. 93 , 5432–5437 (2021).
Farhadian, S. et al. Acute encephalopathy with elevated CSF inflammatory markers as the initial presentation of COVID-19. BMC Neurol . 20 , 248 (2020).
Francistiová, L. et al. Cellular and molecular effects of SARS-CoV-2 linking lung infection to the brain. Front. Immunol . 12 , 730088 (2021).
Paterson, R. W. et al. Serum and cerebrospinal fluid biomarker profiles in acute SARS-CoV-2-associated neurological syndromes. Brain Commun . 3 , fcab099 (2021).
Cryer, M. J. et al. Prothrombotic milieu, thrombotic events and prophylactic anticoagulation in hospitalized COVID-19 positive patients: a review. Clin. Appl. Thromb. Hemost . 28 , 10760296221074353 (2022).
Nalivaeva, N. N. & Rybnikova, E. A. Editorial: Brain hypoxia and ischemia: new insights into neurodegeneration and neuroprotection. Front. Neurosci . 13 , 770 (2019).
Brownlee, N. N. M., Wilson, F. C., Curran, D. B., Lyttle, N. & McCann, J. P. Neurocognitive outcomes in adults following cerebral hypoxia: a systematic literature review. NeuroRehabilitation 47 , 83–97 (2020).
Del Valle, D. M. et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 26 , 1636–1643 (2020).
Daniels, B. P. et al. Viral pathogen-associated molecular patterns regulate blood–brain barrier integrity via competing innate cytokine signals. mBio 5 , e01476-14 (2014).
Reynolds, J. L. & Mahajan, S. D. SARS-COV2 alters blood brain barrier integrity contributing to neuro-inflammation. J. Neuroimmune Pharmacol. 16 , 4–6 (2021).
Bohmwald, K., Gálvez, N. M. S., Ríos, M. & Kalergis, A. M. Neurologic alterations due to respiratory virus infections. Front. Cell. Neurosci . 12 , 386 (2018).
Khaddaj-Mallat, R. et al. SARS-CoV-2 deregulates the vascular and immune functions of brain pericytes via spike protein. Neurobiol. Dis . 161 , 105561 (2021).
Qian, Y. et al. Direct activation of endothelial cells by SARS-CoV-2 nucleocapsid protein is blocked by simvastatin. J Virol. 95 , e0139621 (2021).
Rhea, E. M. et al. The S1 protein of SARS-CoV-2 crosses the blood–brain barrier in mice. Nat. Neurosci. 24 , 368–378 (2021).
Magnúsdóttir, I. et al. Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: an observational study. Lancet Public Health 7 , e406–e416 (2022).
Antonelli, M. et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case–control study. Lancet Infect. Dis. 22 , 43–55 (2022).
Wisnivesky, J. P. et al. Association of vaccination with the persistence of post-COVID symptoms. J. Gen. Intern. Med . 37 , 1748–1753 (2022).
De Picker, L. J. et al. Severe mental illness and European COVID-19 vaccination strategies. Lancet Psychiatry 8 , 356–359 (2021).
Cohen, G. H. et al. Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry 74 , 1251–1258 (2017).
Vai, B. et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry 8 , 797–812 (2021).
Xiang, Y. T. et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7 , 228 (2020).
Newnham, E. A. et al. The Asia Pacific Disaster Mental Health Network: setting a mental health agenda for the region. Int. J. Environ. Res. Public Health 17 , 6144 (2020).
Article CAS PubMed Central Google Scholar
Dandona, R. & Sagar, R. COVID-19 offers an opportunity to reform mental health in India. Lancet Psychiatry 8 , 9–11 (2021).
Qiu, D. et al. Policies to improve the mental health of people influenced by COVID-19 in China: a scoping review. Front. Psychiatry 11 , 588137 (2020).
Su, Z. et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Global Health 17 , 4 (2021).
Petersen, M. B. COVID lesson: trust the public with hard truths. Nature 598 , 237 (2021).
van der Bles, A. M., van der Linden, S., Freeman, A. L. J. & Spiegelhalter, D. J. The effects of communicating uncertainty on public trust in facts and numbers. Proc. Natl Acad. Sci. USA 117 , 7672–7683 (2020).
Titze-de-Almeida, R. et al. Persistent, new-onset symptoms and mental health complaints in Long COVID in a Brazilian cohort of non-hospitalized patients. BMC Infect. Dis. 22 , 133 (2022).
Carfì, A., Bernabei, R. & Landi, F. Persistent symptoms in patients after acute COVID-19. JAMA 324 , 603–605 (2020).
Bliddal, S. et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci. Rep. 11 , 13153 (2021).
Kim, Y. et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect. Dis . 22 , 93 (2022).
Download references
Acknowledgements
The authors thank E. Giltay for assistance on data analyses and production of Fig. 1 . B.W.J.H.P. discloses support for research and publication of this work from the European Union’s Horizon 2020 research and innovation programme-funded RESPOND project (grant no. 101016127).
Author information
Authors and affiliations.
Department of Psychiatry, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands
Brenda W. J. H. Penninx & Christiaan H. Vinkers
Amsterdam Public Health, Mental Health Program and Amsterdam Neuroscience, Mood, Anxiety, Psychosis, Sleep & Stress Program, Amsterdam, The Netherlands
Biological and Precision Psychiatry, Copenhagen Research Center for Mental Health, Mental Health Center Copenhagen, Copenhagen University Hospital, Copenhagen, Denmark
Michael E. Benros
Department of Immunology and Microbiology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
Departments of Medicine, Pathology & Immunology and Neuroscience, Center for Neuroimmunology & Neuroinfectious Diseases, Washington University School of Medicine, St. Louis, MO, USA
Robyn S. Klein
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Brenda W. J. H. Penninx .
Ethics declarations
Competing interests.
The authors declare no conflicts of interest.
Peer review
Peer review information.
Nature Medicine thanks Jane Pirkis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Penninx, B.W.J.H., Benros, M.E., Klein, R.S. et al. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med 28 , 2027–2037 (2022). https://doi.org/10.1038/s41591-022-02028-2
Download citation
Received : 06 June 2022
Accepted : 26 August 2022
Published : 03 October 2022
Issue Date : October 2022
DOI : https://doi.org/10.1038/s41591-022-02028-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Mental health disturbance in preclinical medical students and its association with screen time, sleep quality, and depression during the covid-19 pandemic.
- Tjhin Wiguna
- Valerie Josephine Dirjayanto
- Erik Kinzie
BMC Psychiatry (2024)
Protocol for a pilot cluster randomised controlled trial of a multicomponent sustainable return to work IGLOo intervention
- Oliver Davis
- Jeremy Dawson
- Fehmidah Munir
Pilot and Feasibility Studies (2024)
- Daniel Prieto-Alhambra
Nature Human Behaviour (2024)
Possible temporal relationship between SARS-CoV-2 infection and anti-NMDA receptor encephalitis: a meta-analysis
- Veronika Vasilevska
- Paul C. Guest
- Johann Steiner
Translational Psychiatry (2024)
The end of COVID-19: not with a bang but a whimper
- Fiona McNicholas
Irish Journal of Medical Science (1971 -) (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

- Coronavirus Disease 2019
The Psychological Impact of COVID-19
New research provides insight into the psychological impact of covid-19..
Posted September 30, 2020 | Reviewed by Jessica Schrader

As the COVID-19 pandemic sweeps the globe bringing uncertainty, fear , loss, isolation, and hardship, individuals find themselves in a time of collective trauma. Situations like COVID-19 that can elicit collective trauma may lead to a number of psychological, relational, physiological, and spiritual consequences for those impacted (Aydin, 2017; Saul, 2014; for more information on collective trauma and its effects see " What is Collective Trauma? "). As the COVID-19 pandemic continues to uproot the lives of millions, current research seeks to understand the impact of the pandemic and how to mitigate the negative consequences that may be surfacing in response.
Since the onset of the COVID-19 pandemic in 2019, research has noted a variety of mental health consequences that have been experienced in response. Some of these consequences have included: stress , depression , anxiety , feelings of panic, feelings of hopelessness, frustration, feelings of desperation, and struggles with suicidal ideation and behavior, insomnia , irritability, emotional exhaustion, grief , and traumatic stress symptoms. Although the impact of COVID-19 is individual-specific and based on a number of factors (e.g. the length of quarantine, risk factors, trauma history, mental health history, etc.), some trends in mental health consequences have begun to emerge among the general population (Serafini et al., 2020).

According to a recent article by Serafini et al. (2020), although there may be varied responses to the COVID-19 pandemic, there are several common psychological reactions to COVID-19 that are surfacing amongst the general population. These reactions include intense and uncontrolled fear related to infection, pervasive anxiety, frustration, boredom , and disabling loneliness . Understandably, psychological consequences included in these findings may impair an individual’s well-being and quality of life. Although this is the case, Serafini et al. (2020) note that an individual’s resilience and social support may be factors that can aid them in adapting to this crisis.
The recent findings of Serafini et al. (2020) provide further insight into the ways in which the COVID-19 pandemic may be impacting many. Although these findings may be challenging to acknowledge, these findings provide important information as we continue to battle the COVID-19 crisis. These findings may provide a source of important validation to many about their experiences and increase awareness about what steps may need to be taken on individual and societal levels to minimize the psychological consequences of the COVID-19 pandemic. As discussed by Serafini et al. (2020) the recognition of these findings or the “the psychological impact of fear and anxiety induced by the rapid spread of pandemic needs to be clearly recognized as a public health priority for both authorities and policymakers” to reduce the mental health consequences of this pandemic.
Aydin, C. (2017). How to Forget the Unforgettable? On Collective Trauma, Cultural Identity, and Mnemotechnologies, Identity, 17:3, 125-137, DOI: 10.1080/15283488.2017.1340160
Saul, J. (2014). Collective trauma, collective healing: Promoting resilience in the aftermath of disaster. New York, NY: Routledge.
Serafini, G., Parmigian, B., Amerio, A., Aguglia, A., Sher, L., & Amore, M. (2020). The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine, 529-535, doi: 10.1093/qjmed/hcaa201 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7337855/pdf/hcaa201.pdf

Danielle Render Turmaud, Ph.D., NCC , is a Counseling Professional who specializes in working with survivors of trauma and complex trauma; specifically, sexual trauma, childhood trauma, and interpersonal violence.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Affective Forecasting
- Neuroscience
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to take your pulse
- How to measure your respiratory rate
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
PERSPECTIVE article
The psychological and social impact of covid-19: new perspectives of well-being.
A commentary has been posted on this article:
Commentary: The psychological and social impact of COVID-19: New perspectives of well-being
- Read general commentary

- 1 Department of Human Sciences, Society and Health, University of Cassino and Southern Lazio of Cassino, Cassino, Italy
- 2 Independent Researcher, Milan, Italy
- 3 Department of Political and Social Studies, Sociology, University of Salerno, Fisciano, Italy
The recent Covid-19 pandemic has had significant psychological and social effects on the population. Research has highlighted the impact on psychological well-being of the most exposed groups, including children, college students, and health workers, who are more likely to develop post-traumatic stress disorder, anxiety, depression, and other symptoms of distress. The social distance and the security measures have affected the relationship among people and their perception of empathy toward others. From this perspective, telepsychology and technological devices assume important roles to decrease the negative effects of the pandemic. These tools present benefits that could improve psychological treatment of patients online, such as the possibility to meet from home or from the workplace, saving money and time and maintaining the relationship between therapists and patients. The aim of this paper is to show empirical data from recent studies on the effect of the pandemic and reflect on possible interventions based on technological tools.
Introduction
The Covid-19 pandemic led to a prolonged exposure to stress. As a consequence, researchers showed an increased interest in measuring social and community uneasiness in order to psychologically support the population. This increased attention might help in managing the current situation and other possible epidemics and pandemics. The security measures adopted in managing the pandemic had different consequences on individuals, according to the social role invested. Some segments of the population seem to be more exposed to the risk of anxious, depressive, and post-traumatic symptoms because they are more sensitive to stress.
The following article has two focuses of interest: (1) the evaluation of the psychological and social effects of the pandemic on the population, mostly children, college students, and health professionals; and (2) the identification of new perspectives of intervention based on digital devices and in line with the social security measures and mental health promotion. Telepsychology, for instance, is a valid tool, effective in taking charge of the psychological suffering caused by the pandemic and in preventing the chronicity of the disease. The prolonged stress could involve anxiety, depression, and the inability to manage traumatic and negative emotions. Furthermore, the constant fear of contagion affects daily life and leads to social isolation, modifying human relations.
COVID-19 and At-Risk Populations: Psychological and Social Impact of the Quarantine
Studies of pandemics faced over time, such as SARS, Ebola, H1N1, Equine Flu, and the current COVID-19, show that the psychological effects of contagion and quarantine is not limited on the fear of contracting the virus ( Barbisch et al., 2015 ). There are some elements related to the pandemic that affect more the population, such as separation from loved ones, loss of freedom, uncertainty about the advancement of the disease, and the feeling of helplessness ( Li and Wang, 2020 ; Cao et al., 2020 ). These aspects might lead to dramatic consequences ( Weir, 2020 ), such as the rise of suicides ( Kawohl and Nordt, 2020 ). Suicidal behaviors are often related to the feeling of anger associated with the stressful condition widely spread among people who lived/live in the most affected areas ( Miles, 2014 ; Suicide Awareness Voices of Education, 2020 ; Mamun and Griffiths, 2020 ). In light of these consequences, a carefully evaluation of the potential benefits of the quarantine is needed, taking into account the high psychological costs ( Day et al., 2006 ; Mazza et al., 2020 ).
As reported in a recent survey administered during the Covid-19 pandemic, children and young adults are particularly at risk of developing anxious symptoms ( Orgilés et al., 2020 ). The research involved a sample of 1,143 parents of Italian and Spanish children (range 3–18). In general, parents observed emotional and behavioral changes in their children during the quarantine: symptoms related to difficulty concentrating (76.6%), boredom (52%), irritability (39%), restlessness (38.8%), nervousness (38%), sense of loneliness (31.3%), uneasiness (30.4%), and worries (30.1%). From the comparison between the two groups—Spanish and Italian parents—it emerged that the Italian parents reported more symptoms in their children than the Spanish parents. Further data collected on a sample of college students at the time of the spread of the epidemic in China showed how anxiety levels in young adults are mediated by certain protective factors, such as living in urban areas, the economic stability of the family, and cohabitation with parents ( Cao et al., 2020 ). On the contrary, having infected relatives or acquaintances leads to a worsening in anxiety symptoms. Furthermore, the economic problems and the slowdown in academic activities are related with anxious symptoms ( Alvarez et al., 2020 ). In addition, an online survey conducted on the general population in China found that college students are more likely to experiencing stress, anxiety, and depression than others during the pandemic ( Li et al., 2020 ). These results suggest monitoring and promoting mental health of youths in order to reduce the negative impact of the quarantine ( CSTS, 2020 ; Fessell and Goleman, 2020 ; Li et al., 2020 ).
Health-care workers (HCWs) are another segment of population particularly affected by stress ( Garcia-Castrillo et al., 2020 ; Lai et al., 2020 ). HCWs are at risk to develop symptoms common in catastrophic situations, such as post-traumatic stress disorder, burnout syndrome, physical and emotional exhaustion, depersonalization, and dissociation ( Grassi and Magnani, 2000 ; Mache et al., 2012 ; Øyane et al., 2013 ). However, an epidemic presents different peculiarities compared to a catastrophic event, for instance, the stigmatizing attitudes in particular toward health professionals, who are in daily contact with the risk of infection ( Brooks et al., 2020 ). During SARS, up to 50% of health-care professionals suffered from acute psychological stress, exhaustion, and post-traumatic stress, caused by the fear of contagion of their family members and the prolonged social isolation ( Tam et al., 2004 ; Maunder et al., 2006 ).
As a consequence of the pandemic, the health professionals who were overworked suffered high level of psychophysical stress ( Mohindra et al., 2020 ). Health professionals also lived/live in daily life a traumatic condition called secondary traumatic stress disorder ( Zaffina et al., 2014 ), which describes the feeling of discomfort experienced in the helping relationship when treatments are not available for all patients and the professional must select who can access them and who cannot ( Roden-Foreman et al., 2017 ; Rana et al., 2020 ). Data from a survey on 1,257 HCWs who assisted patients in Covid-19 wards and in second- and third-line wards showed high percentages of depression (50%), anxiety (44.6%), insomnia (34%), and distress (71.5%) ( Lai et al., 2020 ). Also, the constant fear of contagion leads to obsessive thoughts ( Brooks et al., 2020 ), increasing the progressive closure of the person and reducing social relationships. In line with these results, Rossi et al. (2020) evaluated mental health outcomes among HCWs in Italy during the pandemic, confirming a high score of mental health issues, particularly among young women and front-line workers. Furthermore, Spoorthy et al. (2020) conducted a review on the gendered impact of Covid-19 and found that 68.7–85.5% of medical staff is composed of women, and the mean age ranged between 26 and 40 years. Also, women are more likely to be affect by anxiety, depression, and distress ( Lai et al., 2020 ; Zanardo et al., 2020 ). Liang et al. (2020) also found a relation between age and depressive symptoms associated with the pandemic. Indeed, the medical staff at younger ages (<30 years) reports higher self-rated depression scores and more concern about infecting their families than those of older age. Staff > 50 years of age reported increased stress due to patient’s death, the prolonged work hours, and the lack of personal protective equipment. Cai et al. (2020) also found that nurses felt more nervous compared to doctors.
As emerged by the recent literature, the promotion of psychological interventions on the specific population who is more likely to develop pathologies and suffering is needed. The Lancet Global Mental Health Commission’s observation ( Patel, 2018 ) reported that the use of digital technologies can provide mental health interventions in order to reduce anxiety and stress levels and increase self-efficacy ( Kang et al., 2020 ; Xiao et al., 2020 ).
Telepsychology: Training and Promotion of Psychological Well-Being
In order to reduce anxiety and depression symptoms widespread among the population, the World Health Organization (2019) and the Centers for Disease Control and Prevention (2020) proposed specific guidelines on the correct use of health protection with the aim to minimize the distress associated with health-care professions.
At the same time, as a consequence of the emerging issues, psychotherapists provided psychological support online, addressing the technological challenge ( Greenberg et al., 2020 ); Liu et al., 2020 ). In line with the technological progress, professional organizations promoted specific guidelines and policies related to customer protection, privacy, screening, evaluation, and development of self-help products ( Duan and Zhu, 2020 ; Zhou et al., 2020 ). Technological development in mental health foreshadows future trends that include “smart” mobile devices, cloud computing, virtual worlds, virtual reality, and electronic games in addition to the traditional psychotherapy tools. In this perspective, it is important to help future generations of psychologists and patients to collaborate in the potential growth areas, through education and training on the benefits and effectiveness of telepsychology ( Maheu et al., 2012 ).
Indeed, more awareness of the potentials of the online services is needed, exploring the main differences between the devices (chat, video-audio consultation, etc.) in order to use them in relation to the specific purposes identified by the professional. For example, the Italian Service of Online Psychology conducted a study based on a service of helpdesk on Facebook. This service guided people in asking for psychological help, working on their personal motivation. At the same time, another helpdesk on Skype provided some psychological sessions via webcam ( Gabri et al., 2015 ). In this line, telecounseling is a diffuse online method used by counselors and psychologists during the recent pandemic ( De Luca and Calabrò, 2020 ).
One of the future goals of public and private psychological organizations should be the promotion of specific training for psychologists and psychotherapists, with the following aims: (1) developing the basic skills in managing the effects of a pandemic and of emergency situations; and (2) sensitizing patients to online therapeutic relationship, providing the main rules and benefits of the process ( Stoll et al., 2020 ; Joint Task Force for the Development of Telepsychology Guidelines for Psychologists, 2013 ). On this line, a significant example is the Virginia Commonwealth University (VCU) which proposed PhDs in telepsychology, with the aim of training future psychologists in managing the psychological effects of the pandemic through an online psychology service ( Baylor et al., 2019 ). The service provided by the VCU had been effective in reducing anxiety, depression ( Sadock et al., 2017 ), and hospital recoveries ( Lanoye et al., 2017 ). As shown, telepsychology assumes a key role in the improvement of health care. Online psychological services avoid geographical barriers and are suitable to become a useful integrated tool in addition to traditional psychotherapy ( APS, 2020 ; Perrin et al., 2020 ).
Advantages of Psychological Support and Online Psychotherapy
Online psychological services provide several advantages, especially in the current situation of pandemic. First of all, online services help people in a short period of time, reducing the risk of contagion and the strong feeling of anxiety in both psychotherapists and patients, who feel uncomfortable in doing traditional psychotherapy due to the pandemic ( Békés and Aafjes-van Doorn, 2020 ). Furthermore, Pietrabissa et al. (2015) identified some of the main advantages of telepsychology, such as the decrease in waiting for the consultation, because it takes place from home or from the workplace, saving time and expense, less travel and rental costs for the office, for those who provide the service and for those who use it. As reported by the authors, online psychological services facilitate access to people who struggle to find support close to their social environment, avoiding difficulties related to mobility. Also, online services help people who have less confidence in psychotherapy. Indeed, mostly online psychotherapy takes place in one’s comfort zone, facilitating the expression of problems and feelings.
According to the situations, online services could provide a different medium. For instance, the chat is a useful tool to establish a first assessment of a person who feels uncomfortable in using video. Indeed, the online psychotherapy is perceived as more “acceptable.” Suler (2004) defined the term online disinhibition effect demonstrating how the web, unlike the real life, leads to the failure of the hierarchical relationship based on dominant-dominated among individuals; this aspect, according to the author, allows a greater sense of freedom in expressing oneself and less concern related to judgment ( ibid .). Other researchers ( Mantovani, 1995 ; Tosoni, 2004 ) have integrated to the construct of online disinhibition effect the concept of social space, emphasizing the role of the “situation,” of the “social norms” ( Brivio et al., 2010 , p. 811), of the tools (“artifacts”), and of the cyberplace, which allow different levels of interaction. Each person has a different experience of the network and several levels of disinhibition. For instance, a mild disinhibition could be a person who chooses to ask for help talking with a psychologist about their problems; while a high disinhibition could be represented by flaming, an expression of online bullying or cyberstalking.
Online psychological services should be integrated with the various territorial services in order to provide the patients local references in relation to the specific health and economic needs. Finally, the possibility for the therapist and for the patient to record the sessions via chat and in audio/video mode—with the informed consent of the participants ( Wells et al., 2015 )—provides another useful tool to compare the sessions and to underline the positive outcomes and the effectiveness of the therapeutic process. According to this perspective, online psychological support and psychotherapy become a resource for psychotherapists and patients in a co-build relationship ( Algeri et al., 2019 ).
Psychological and Social Suffering and the Empathic Process
In analyzing the psychological impact of the quarantine, the importance for individuals to feel integral part of the society emerged, an aspect often undervalued in psychological well-being. Experts of public health believe that social distancing is the better solution to prevent the spread of the virus. However, although it is not possible to predict the duration of the pandemic, we know very well the serious impact of these measures on the society, on relationships and interactions, in particular on the empathic process. In the early 90s, empathy was described as a form of identification in the psychological and physiological states of others. This definition led to a debate between the disciplines of philosophy of psychology and philosophy of the mind ( Franks, 2010 ). Willard Van Orman Quine (1908–2000) renewed attention to the debate on empathy with a thesis on the development of language and mind in the analytical philosophy. According to Quine, the attribution of the so-called intentional states, through which the psychology commonly explains human behavior, is based on empathy ( Treccani, 2020 ) and leads people to attribute beliefs, desires, and perceptions ( Quine, 1990 , 1992 , Pursuit of Truth: Revised Edition, 1992). Analyzing this aspect within the recent situation of the pandemic, an increment of antithetical positions and attitudes could be noticed. On the one hand, people identify themselves with those who suffer (neighbors, friends, relatives who are living stressful events), promoting activities such as the so-called “suspended expenses.” For instance, solidarity and humanitarian activities, food, and medicine delivery for people who are unable to go to the supermarket. On the other hand, there is a part of the population who experiences a feeling of “forced empathy.” This aspect could be also emphasized by the use of technological devices that might lead to a depersonalization of relationships, forcing the sense of closeness, at least virtually. The hyperconnection of feelings becomes a way to reduce the self-isolation and its consequences, representing the contrary of the idea of Durkheim (1858–1917), who considered society as a specific entity, built on social facts ( Durkheim, 1922 ). The sensation “to be forced to feel” could lead people to distance themselves from others after the emergency situation, incrementing social phobias.
Also, human communication is changing. The formal question “how are you?” at the beginning of a conversation is no longer just a formality, as before the pandemic. For example, the relationship between employee and the manager is different, leading to more responsibilities in listening and understanding feelings expressed during the video call, generating a forced reciprocity. Hence, the aforementioned “forced empathy” may be common in this period because the social distance and the emergency situation make people want to be heard and appreciated, and the simple question “how are you?” becomes an anchor to express fears and emotions ( Pasetti, 2020 ).
The Covid-19 pandemic has affected the way people live interpersonal relationships. The lockdown was characterized of a different organization of daily life, with an incrementation of time at home and a reduction of distance through digital devices. This period was also seen as an evolution in the concept of empathy, producing new perspectives in the study of the phenomenon according to a sociological and neurological points of view. Indeed, empathy—defined as the ability to understand and share the feelings of another—involves several elements, such as: (a) social context and historical period of the individual, (b) neurological mechanisms, and (c) psychological and behavioral responses to feelings of others. The neuro-sociological perspective analyzes the mechanisms involved in the empathic process, focusing on human communication and interpersonal relationships ( Singer and Lamm, 2009 ; Decety and Ickes, 2009 ). Specifically, in this historical period characterized by an increment in the man–machine relationship, neurosociology could become one of the principal sciences for the study of human relations and technology. “We live increasingly in a human–machine world. Anyone who doesn’t understand this, and who is not struggling to adapt to the new environment—whether they like that environment or not—is already being left behind. Adapting to the new, fast-changing, technologically enhanced context is one of the major challenges of our times. And that certainly goes for education” ( Prensky, 2012 , p. 64).
According to the abovementioned considerations, our suggestion consists in:
Primary prevention. Studying the impact of the pandemic toward an at-risk population to reduce symptoms related to stress and providing specific online psychological counseling based on the target (students, medical staff, parents, and teachers).
Secondary prevention. Overcoming the limitations of the human interaction based on digital devices: (1) developing new spaces of inter- and intrasocial communication and new tools of support and psychological treatment, reproducing the multisensory experienced during the face-to-face interaction (Virtual Reality, holograms, serious game etc.); (2) training the next generation of psychotherapists in managing online devices and in implementing their adaptive and personal skills; and (3) sensitizing the general population on telepsychology and its advantages.
Research according to the neurosociological perspective . Studying human interaction mediated by new technologies and the role of empathy, associating neuroscience, sociology, and psychology.
Author Contributions
VS, DA, and VA conceptualized the contribution. VS wrote the paper, reviewed the manuscript, and provided the critical revision processes as PI. All authors approved the submission of the manuscript.
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Algeri, D., Gabri, S., and Mazzucchelli, L. (2019). Consulenza psicologica online. Esperienze pratiche, linee guida e ambiti di intervento. Firenze: Giunti Editore.
Google Scholar
Alvarez, F., Argente, D., and Lippi, F. (2020). A simple planning problem for Covid-19 lockdown. Covid Econ. 14, 1–33. doi: 10.3386/w26981
CrossRef Full Text | Google Scholar
APS (2020). Psychologists welcome health fund telehealth support of Australians’ mental health during COVID-19 outbreak. Australia: Tratto da Australian Psuchology Society.
Barbisch, D., Koenig, K., and Shih, F. (2015). Is there a case for quarantine? Perspectives from SARS to Ebola . Dis. Med. Pub. Health Prepar. 9, 547–553. doi: 10.1017/dmp.2015.38
PubMed Abstract | CrossRef Full Text | Google Scholar
Baylor, C., Burns, M., McDonough, K., Mach, H., and Yorkstona, K. (2019). Teaching Medical Students Skills for Effective Communication With Patients Who Have Communication Disorders. Am. J. Spe. Lang. Pathol. 28, 155–164. doi: 10.1044/2018_ajslp-18-0130
Békés, V., and Aafjes-van Doorn, K. (2020). Psychotherapists’ attitudes toward online therapy during the COVID-19 pandemic. J. Psychother. Integr. 30, 238–247. doi: 10.1037/int0000214
Brivio, E., Ibarra, F., Galimberti, C., and Cilento. (2010). “An Integrated Approach to Interactions in Cyberplaces: The Presentation of Self in Blogs,” in Handbook of Research on Discourse Behavior and Digital Communication: Language Structures and Social Interaction , eds E. Brivio, F. Ibarra, and C. Galimberti (Pennsylvania: Information Science Reference/IGI Global), 810–829. doi: 10.4018/978-1-61520-773-2.ch052
Brooks, S., Webster, R. S., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395:10227. doi: 10.1016/S0140-6736(20)30460-8
Cai, H., Tu, B., Ma, J., Chen, L., Fu, L., Jiang, Y., et al. (2020). Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID19) in Hubei. China. Med. Sci. Monit. 2020:26. doi: 10.12659/MSM.924171
Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., et al. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psych. Res. 287:112934. doi: 10.1016/j.psychres.2020.112934
Centers for Disease Control and Prevention (2020). Preparedness Tools for Healthcare Professionals and Facilities Responding to Coronavirus (COVID-19) . Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/preparedness-checklists.html
CSTS (2020). Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Pub Health 17:1729. doi: 10.3390/ijerph17051729
Day, T., Park, A., Madras, N., Gumel, A., and Wu, J. (2006). When Is Quarantine a Useful Control Strategy for Emerging Infectious Diseases? Am. J. Epidemiol. 163, 479–485. doi: 10.1093/aje/kwj056
De Luca, R., and Calabrò, R. S. (2020). How the COVID-19 Pandemic is Changing Mental Health Disease Management: The Growing Need of Telecounseling in Italy. Innov. Clin. Neurosci. 17, 16–17.
Decety, J., and Ickes, W. (eds) (2009). The Social Neuroscience of Empathy. Cambridge, MA: MIT Press.
Duan, L., and Zhu, G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. Lancet. Psych. 7, 300–302. doi: 10.1016/s2215-0366(20)30073-0
Durkheim, E. (1922). Education et Sociologie. Milano: Ledizioni.
Fessell, D., and Goleman, D. (2020). How Healthcare Personnel Can Take Care of Themselves. US: HBR.
Franks, D. (2010). Neurosociology the nexus between neuroscience and social psychology. Londra. Springer.
Gabri, S., Mazzucchelli, S., and Algeri, D. (2015). The request for psychological help in the digital age: offering counseling through chat and video counseling. E J. Psychother. 2015, 2–10.
Garcia-Castrillo, L., Petrino, R., and Leach, R. (2020). European Society For Emergency Medicine position paper on emergency medical systems’ response to COVID-19. Eur. J. Emerg. Med. 27, 174–1777. doi: 10.1097/mej.0000000000000701
Grassi, L., and Magnani, K. (2000). Psychiatric Morbidity and Burnout in the Medical Profession: An Italian Study of General Practitioners and Hospital Physicians. Psychother. Psychosom. 69, 329–334. doi: 10.1159/000012416
Greenberg, N., Docherty, M., Gnanapragasam, S., and Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 368:m1211. doi: 10.1136/bmj.m1211
Joint Task Force for the Development of Telepsychology Guidelines for Psychologists (2013). Guidelines for the practice of telepsychology. Am. Psychol. 68, 791–800. doi: 10.1037/a0035001
Kang, L., Ma, S., and Chen, M. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 87, 11–17. doi: 10.1016/j.bbi.2020.03.028
Kawohl, W., and Nordt, C. (2020). COVID-19, unemployment, and suicide. Lancet Psych. 7, 389–390. doi: 10.1016/s2215-0366(20)30141-3
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., et al. (2020). Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
Lanoye, A., Stewart, K., Rybarczyk, B., Auerbach, S., Sadock, E., Aggarwal, A., et al. (2017). The impact of integrated psychological services in a safety net primary care clinic on medical utilization. J. Clin. Psychol. 73, 681–692. doi: 10.1002/jclp.22367
Li, L. Z., and Wang, S. (2020). Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psych. Res. 291, 0165–1781. doi: 10.1016/j.psychres.2020.113267
Li, S., Wang, Y., Yang, Y., Lei, X., and Yang, Y. (2020). Analysis of influencing factors of anxiety and emotional disorders in children and adolescents during home isolation during the epidemic of novel coronavirus pneumonia. Chin. J. Child Heal 2020, 1–9.
Liang, Y., Chen, M., Zheng, X., and Liu, J. (2020). Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 133, 1101–1102. doi: 10.1016/j.jpsychores.2020.110102
Liu, S., Yang, L., Zhang, C., Xiang, Y. T., Liu, Z., Hu, S., et al. (2020). Online mental health services in China during the COVID-19 outbreak. Lancet. Psych. 7, E17–E18. doi: 10.1016/S2215-0366(20)30077-8
Mache, S., Vitzthum, K., and Klapp, B. (2012). Stress, health and satisfaction of Australian and German doctors-a comparative study. World Hosp Health 48, 21–27.
Maheu, M. P., McMenamin, J., and Posen, L. (2012). Future of telepsychology, telehealth, and various technologies in psychological research and practice. Profess. Psychol. Res. Prac. 43, 613–621. doi: 10.1037/a0029458
Mamun, M. A., and Griffiths, M. D. (2020). First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian J. Psych. 51:102073. doi: 10.1016/j.ajp.2020.102073
Mantovani, G. (1995). Comunicazione e Identità: dalle situazioni quotidiane agli ambienti virtuali. Bologna: il Mulino.
Maunder, R. G., Lancee, W. J., Balderson, K. E., Bennett, J. P., and Borgundvaag, B. (2006). Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 12, 1924–1932. doi: 10.3201/eid1212.060584
Mazza, C., Ricci, E., Biondi, S., Colasanti, M., Ferracuti, S., Napoli, C., et al. (2020). Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Publ. Health 17:3165. doi: 10.3390/ijerph17093165
Miles, S. (2014). Kaci Hickox: Public Health and the Politics of Fear. Tratto da Bioethics . Available online at: http://www.bioethics.net/2014/11/kaci-hickox-public-health-and-the-politics-of-fear/ (accessed June 2, 2020).
Mohindra, R. R. R., Suri, V., Bhalla, A., and Singh, S. M. (2020). Issues relevant to mental health promotion in frontline health care providers managing quarantined/isolated COVID19 patients. Asian J. Psych. 51:102084. doi: 10.1016/j.ajp.2020.102084
Orgilés, M., Morales, A., Delvecchio, E., Mazzeschi, C., and Espada, J. (2020). Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. PsyArXiv 2020, 1–13. doi: 10.1017/s0033291720001841
Øyane, N. P. S., Elisabeth, M., Torbjörn, A., and Bjørn, B. (2013). Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One 2013:e70228. doi: 10.1371/journal.pone.0070228
Pasetti, J. (2020). Smart-working, costretti all’empatia da convenevoli forzati. Tratto da Sole24Ore . Available online at: https://alleyoop.ilsole24ore.com/2020/03/20/covid-19-empatia/?refresh_ce=1 (accessed June 3, 2020).
Patel, V. (2018). The Lancet Commission on global mental health and sustainable development. Lancet 392, 1553–1598. doi: 10.1016/S0140-6736(18)31612-X
Perrin, P., Rybarczyk, B., Pierce, B., Jones, H., Shaffer, C., and Islam, L. (2020). Rapid telepsychology deployment during the COVID-19 pandemic: A special issue commentary and lessons from primary care psychology training. Clin. Psychol. 76, 1173–1185. doi: 10.1002/jclp.22969
Pietrabissa, G., Manzoni, A., Algeri, D., Mazzucchelli, L., Carella, A., Pagnini, F., et al. (2015). Facebook Use as Access Facilitator for Consulting Psychology. Austr. Psychol. 50, 299–303. doi: 10.1111/ap.12139
Prensky, M. (2012). What ISN’T Technology Good At? Empathy for One Thing!. Educat. Technol. 52:64.
Quine, W. (1990). Pursuit of Truth. New York: Harvard University Press.
Quine, W. (1992). Pursuit of Truth: Revised Edition. New York: Harvard University Press.
Rana, W., Mukhtar, S., and Mukhtar, S. (2020). Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J. Psych. 51:102080. doi: 10.1016/j.ajp.2020.102080
Roden-Foreman, K., Solis, J., Jones, A., Bennett, M., Roden-Foreman, J., Rainey, E., et al. (2017). Prospective Evaluation of Posttraumatic Stress Disorder and Depression in Orthopaedic Injury Patients With and Without Concomitant Traumatic Brain Injury. J. Orthop. Trauma 31, e275–e280. doi: 10.1097/BOT.0000000000000884
Rossi, R., Socci, V., and Pacitti, F. (2020). Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw Open. 3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185
Sadock, E., Perrin, P., Grinnell, R., Rybarczyk, B., and Auerbach, S. (2017). Initial and follow-up evaluations of integrated psychological services for anxiety and depression in a safety net primary care clinic. Am. Psycol. Assoc. 73, 1462–1481. doi: 10.1002/jclp.22459
Singer, T., and Lamm, C. (2009). The Social Neuroscience of Empathy. Ann. N. Y. Acad. Sci. 2009, 81–96. doi: 10.1111/j.1749-6632.2009.04418.x
Spoorthy, M. S., Pratapa, S. K., and Mahant, S. (2020). Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psych. 51:1876. doi: 10.1016/j.ajp.2020.102119
Stoll, J., Müller, J., and Trachsel, M. (2020). Ethical Issues in Online Psychotherapy: A Narrative Review. Front. Psych. 10:993. doi: 10.3389/fpsyt.2019.00993
Suicide Awareness Voices of Education (2020). Preventing Suicide During and After the COVID-19 Pandemic . Available online at: https://save.org/blog/preventing-suicide-covid-19-pandemic (accessed June 5, 2020).
Suler, J. (2004). The Online Disinhibition Effect. Cyb. Psychol. Behav. 7, 321–326. doi: 10.1089/1094931041291295
Tam, C., Pang, E., Lam, L., and Chiu, H. (2004). Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 34, 1197–1204. doi: 10.1017/s0033291704002247
Tosoni, S. (2004). Identità virtuali: comunicazione mediata da computer e processi di costruzione dell’identità personale. Milano: FrancoAngeli.
Treccani (2020). Einfuhlung. Tratto da Treccani . Available online at: http://www.treccani.it/enciclopedia/einfuhlung/ (accessed June 10, 2020).
Weir, K. (2020). Grief and COVID-19: Mourning our bygonelives. Washington: American Psychological Association.
Wells, S. W., Moreno, L., Butler, E., and Glassman, L. (2015). “The informed consent process for therapeutic communication in clinical videoconferencing,” in Clinical videoconferencing in telehealth: Program development and practice , eds P. W. Tuerk and P. Shore (Berlin: Springer Inernational Publishing), 133–166. doi: 10.1007/978-3-319-08765-8_7
World Health Organization (2019). Emergency Global Supply Chain System (COVID-19) Catalogue . Available online at: https://www.who.int/publications/i/item/emergency-global-supply-chain-system-(covid-19)-catalogue (accessed June 10, 2020).
Xiao, H., Zhang, Y., Kong, D., Li, S., and Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 26:e923549. doi: 10.12659/MSM.923549
Zaffina, S., Camisa, V., Monducci, E., Vinci, M., Vicari, S., and Bergamaschi, A. (2014). Disturbo post traumatico da stress in operatori sanitari coinvolti in un incidente rilevante avvenuto in ambito ospedaliero. La Med. Del Lav. 105:2014.
Zanardo, V., Manghina, V., Giliberti, L., Vettore, M., Severino, L., and Straface, G. (2020). Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Gynechol. Obst. 150, 184–188. doi: 10.1002/ijgo.13249
Zhou, X., Snoswell, C. L., and Harding, L. E. (2020). The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemed. E Health. 26, 377–379. doi: 10.1089/tmj.2020.0068
Keywords : COVID-19, empathy, psychological disease, psychotherapy, social distancing, telepsychology
Citation: Saladino V, Algeri D and Auriemma V (2020) The Psychological and Social Impact of Covid-19: New Perspectives of Well-Being. Front. Psychol. 11:577684. doi: 10.3389/fpsyg.2020.577684
Received: 29 June 2020; Accepted: 03 September 2020; Published: 02 October 2020.
Reviewed by:
Copyright © 2020 Saladino, Algeri and Auriemma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Valeria Saladino, [email protected] ; [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 12
- Impact of the COVID-19 pandemic on mental health and well-being of communities: an exploratory qualitative study protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-0180-0213 Anam Shahil Feroz 1 , 2 ,
- Naureen Akber Ali 3 ,
- Noshaba Akber Ali 1 ,
- Ridah Feroz 4 ,
- Salima Nazim Meghani 1 ,
- Sarah Saleem 1
- 1 Community Health Sciences , Aga Khan University , Karachi , Pakistan
- 2 Institute of Health Policy, Management and Evaluation , University of Toronto , Toronto , Ontario , Canada
- 3 School of Nursing and Midwifery , Aga Khan University , Karachi , Pakistan
- 4 Aga Khan University Institute for Educational Development , Karachi , Pakistan
- Correspondence to Ms Anam Shahil Feroz; anam.sahyl{at}gmail.com
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours, myths and inaccurate information about the virus are spreading rapidly, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes of community members towards COVID-19 and its impact on their daily lives and mental well-being.
Methods and analysis This formative research will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews with community members. The study will be conducted in the Karimabad Federal B Area and in the Garden (East and West) community settings in Karachi, Pakistan. The community members of these areas have been selected purposively for the interview. Study data will be analysed thematically using NVivo V.12 Plus software.
Ethics and dissemination Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The results of the study will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
- mental health
- public health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-041641
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The mental health impact of the COVID-19 pandemic is likely to last much longer than the physical health impact, and this study is positioned well to explore the perceptions and attitudes of community members towards the pandemic and its impact on their daily lives and mental well-being.
This study will guide the development of context-specific innovative mental health programmes to support communities in the future.
One limitation is that to minimise the risk of infection all study respondents will be interviewed online over Zoom and hence the authors will not have the opportunity to build rapport with the respondents or obtain non-verbal cues during interviews.
The COVID-19 pandemic has affected almost 180 countries since it was first detected in Wuhan, China in December 2019. 1 2 The COVID-19 outbreak has been declared a public health emergency of international concern by the WHO. 3 The WHO estimates the global mortality to be about 3.4% 4 ; however, death rates vary between countries and across age groups. 5 In Pakistan, a total of 10 880 cases and 228 deaths due to COVID-19 infection have been reported to date. 6
The worldwide COVID-19 pandemic has not only incurred massive challenges to the global supply chains and healthcare systems but also has a detrimental effect on the overall health of individuals. 7 The pandemic has led to lockdowns and has created destructive impact on the societies at large. Most company employees, including daily wage workers, have been prohibited from going to their workplaces or have been asked to work from home, which has caused job-related insecurities and financial crises in the communities. 8 Educational institutions and training centres have also been closed, which resulted in children losing their routine of going to schools, studying and socialising with their peers. Delay in examinations is likewise a huge stressor for students. 8 Alongside this, parents have been struggling with creating a structured milieu for their children. 9 COVID-19 has hindered the normal routine life of every individual, be it children, teenagers, adults or the elderly. The crisis is engendering burden throughout populations and communities, particularly in developing countries such as Pakistan which face major challenges due to fragile healthcare systems and poor economic structures. 10
The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. 8 Further, the highly contagious nature of COVID-19 has also escalated confusion, fear and panic among community residents. Moreover, social distancing is often an unpleasant experience for community members and for patients as it adds to mental suffering, particularly in the local setting where get-togethers with friends and families are a major source of entertainment. 9 Recent studies also showed that individuals who are following social distancing rules experience loneliness, causing a substantial level of distress in the form of anxiety, stress, anger, misperception and post-traumatic stress symptoms. 8 11 Separation from family members, loss of autonomy, insecurity over disease status, inadequate supplies, inadequate information, financial loss, frustration, stigma and boredom are all major stressors that can create drastic impact on an individual’s life. 11 Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. 12 With the widespread use of social media, 13 rumours, myths and inaccurate information about COVID-19 are also spreading rapidly, not only among adults but are also carried on to children, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. 9 The psychological symptoms associated with COVID-19 at the community level are also manifested as anxiety-driven panic buying, resulting in exhaustion of resources from the market. 14 Some level of panic also dwells in the community due to the unavailability of essential protective equipment, particularly masks and sanitisers. 15 Similarly, mental health issues, including depression, anxiety, panic attacks, psychotic symptoms and even suicide, were reported during the early severe acute respiratory syndrome outbreak. 16 17 COVID-19 is likely posing a similar risk throughout the world. 12
The fear of transmitting the disease or a family member falling ill is a probable mental function of human nature, but at some point the psychological fear of the disease generates more anxiety than the disease itself. Therefore, mental health problems are likely to increase among community residents during an epidemic situation. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes towards COVID-19 among community residents and the impact of these perceptions and attitude on their daily lives and mental well-being.
Methods and analysis
Study design.
This study will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews (IDIs) with community members. The IDIs aim to explore perceptions of community members towards COVID-19 and its impact on their mental well-being.
Study setting and study participants
The study will be conducted in two communities in Karachi City: Karimabad Federal B Area Block 3 Gulberg Town, and Garden East and Garden West. Karimabad is a neighbourhood in the Karachi Central District of Karachi, Pakistan, situated in the south of Gulberg Town bordering Liaquatabad, Gharibabad and Federal B Area. The population of this neighbourhood is predominantly Ismailis. People living here belong mostly to the middle class to the lower middle class. It is also known for its wholesale market of sports goods and stationery. Garden is an upmarket neighbourhood in the Karachi South District of Karachi, Pakistan, subdivided into two neighbourhoods: Garden East and Garden West. It is the residential area around the Karachi Zoological Gardens; hence, it is popularly known as the ‘Garden’ area. The population of Garden used to be primarily Ismailis and Goan Catholics but has seen an increasing number of Memons, Pashtuns and Baloch. These areas have been selected purposively because the few members of these communities are already known to one of the coinvestigators. The coinvestigator will serve as a gatekeeper for providing entrance to the community for the purpose of this study. Adult community members of different ages and both genders will be interviewed from both sites, as mentioned in table 1 . Interview participants will be selected following the eligibility criteria.
- View inline
Study participants for indepth interviews
IDIs with community members
We will conduct IDIs with community members to explore the perceptions and attitudes of community members towards COVID-19 and its effects on their daily lives and mental well-being. IDI participants will be identified via the community WhatsApp group, and will be invited for an interview via a WhatsApp message or email. Consent will be taken over email or WhatsApp before the interview begins, where they will agree that the interview can be audio-recorded and that written notes can be taken. The interviews will be conducted either in Urdu or in English language, and each interview will last around 40–50 min. Study participants will be assured that their information will remain confidential and that no identifying features will be mentioned on the transcript. The major themes will include a general discussion about participants’ knowledge and perceptions about the COVID-19 pandemic, perceptions on safety measures, and perceived challenges in the current situation and its impact on their mental well-being. We anticipate that 24–30 interviews will be conducted, but we will cease interviews once data saturation has been achieved. Data saturation is the point when no new themes emerge from the additional interviews. Data collection will occur concurrently with data analysis to determine data saturation point. The audio recordings will be transcribed by a transcriptionist within 24 hours of the interviews.
An interview guide for IDIs is shown in online supplemental annex 1 .
Supplemental material
Eligibility criteria.
The following are the criteria for inclusion and exclusion of study participants:
Inclusion criteria
Residents of Garden (East and West) and Karimabad Federal B Area of Karachi who have not contracted the disease.
Exclusion criteria
Those who refuse to participate in the study.
Those who have experienced COVID-19 and are undergoing treatment.
Those who are suspected for COVID-19 and have been isolated/quarantined.
Family members of COVID-19-positive cases.
Data collection procedure
A semistructured interview guide has been developed for community members. The initial questions on the guide will help to explore participants’ perceptions and attitudes towards COVID-19. Additional questions on the guide will assess the impact of these perceptions and attitude on the daily lives and mental health and well-being of community residents. All semistructured interviews will be conducted online via Zoom or WhatsApp. Interviews will be scheduled at the participant’s convenient day and time. Interviews are anticipated to begin on 1 December 2020.
Patient and public involvement
No patients were involved.
Data analysis
We will transcribe and translate collected data into English language by listening to the audio recordings in order to conduct a thematic analysis. NVivo V.12 Plus software will be used to import, organise and explore data for analysis. Two independent researchers will read the transcripts at various times to develop familiarity and clarification with the data. We will employ an iterative process which will help us to label data and generate new categories to identify emergent themes. The recorded text will be divided into shortened units and labelled as a ‘code’ without losing the main essence of the research study. Subsequently, codes will be analysed and merged into comparable categories. Lastly, the same categories will be grouped into subthemes and final themes. To ensure inter-rater reliability, two independent investigators will perform the coding, category creation and thematic analyses. Discrepancies between the two investigators will be resolved through consensus meetings to reduce researcher bias.
Ethics and dissemination
Study participants will be asked to provide informed, written consent prior to participation in the study. The informed consent form can be submitted by the participant via WhatsApp or email. Participants who are unable to write their names will be asked to provide a thumbprint to symbolise their consent to participate. Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The study results will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
The findings of this study will help us to explore the perceptions and attitudes towards the COVID-19 pandemic and its impact on the daily lives and mental well-being of individuals in the community. Besides, an indepth understanding of the needs of the community will be identified, which will help us develop context-specific innovative mental health programmes to support communities in the future. The study will provide insights into how communities are managing their lives under such a difficult situation.
- World Health Organization
- Nielsen-Saines K , et al
- Worldometer
- Ebrahim SH ,
- Gozzer E , et al
- Snoswell CL ,
- Harding LE , et al
- Nargis Asad
- van Weel C ,
- Qidwai W , et al
- Brooks SK ,
- Webster RK ,
- Smith LE , et al
- Tripathy S ,
- Kar SK , et al
- Schwartz J ,
- Maunder R ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
ASF and NAA are joint first authors.
Contributors ASF and NAA conceived the study. ASF, NAA, RF, NA, SNM and SS contributed to the development of the study design and final protocols for sample selection and interviews. ASF and NAA contributed to writing the manuscript. All authors reviewed and approved the final version of the paper.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Virtual Reality & Nature Lab, Department of Parks, Recreation and Tourism Management, Clemson University, Clemson, SC, United States of America
Roles Conceptualization, Data curation, Investigation, Methodology, Visualization, Writing – review & editing
Affiliation Department of Parks, Recreation and Tourism Management, North Carolina State University, Raleigh, NC, United States of America
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Writing – review & editing
Affiliation Department of Parks, Recreation and Tourism Management, Clemson University, Clemson, SC, United States of America
Roles Conceptualization, Data curation, Methodology, Writing – review & editing
Affiliation Department of City and Metropolitan Planning, The University of Utah, Salt Lake City, UT, United States of America
Roles Data curation, Writing – review & editing
Affiliation Sustainability and Happiness Research Lab, School of Sustainability, Arizona State University, Tempe, AZ, United States of America
Roles Formal analysis, Methodology, Visualization, Writing – review & editing
Affiliation Advanced Computing & Data Science, Clemson Computing & Information Technology, Clemson University, Clemson, SC, United States of America
Affiliation Department of Society and Conservation, W.A. Franke College of Forestry and Conservation, University of Montana, Missoula, MT, United States of America
Roles Data curation, Methodology, Visualization, Writing – review & editing
Affiliation Recreation, Park, and Tourism Management Department, College of Health and Human Development, Pennsylvania State University, PA, United States of America
Affiliation Forest Ecosystems and Society, College of Forestry, Oregon State University, Corvallis, OR, United States of America
Roles Methodology, Software, Writing – review & editing
Affiliation Department of Human Geography and Spatial Planning, Faculty of Geosciences, Utrecht University, Utrecht, The Netherlands
Roles Methodology, Writing – review & editing
Affiliation Environment & Well-Being Lab, School of Environmental and Forest Sciences, University of Washington, Seattle, WA, United States of America
Affiliation School of Nursing, Oregon Health & Science University, Portland, OR, United States of America
- Matthew H. E. M. Browning,
- Lincoln R. Larson,
- Iryna Sharaievska,
- Alessandro Rigolon,
- Olivia McAnirlin,
- Lauren Mullenbach,
- Scott Cloutier,
- Tue M. Vu,
- Jennifer Thomsen,

- Published: January 7, 2021
- https://doi.org/10.1371/journal.pone.0245327
- Peer Review
- Reader Comments
26 Aug 2022: Browning MHEM, Larson LR, Sharaievska I, Rigolon A, McAnirlin O, et al. (2022) Correction: Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLOS ONE 17(8): e0273938. https://doi.org/10.1371/journal.pone.0273938 View correction
University students are increasingly recognized as a vulnerable population, suffering from higher levels of anxiety, depression, substance abuse, and disordered eating compared to the general population. Therefore, when the nature of their educational experience radically changes—such as sheltering in place during the COVID-19 pandemic—the burden on the mental health of this vulnerable population is amplified. The objectives of this study are to 1) identify the array of psychological impacts COVID-19 has on students, 2) develop profiles to characterize students' anticipated levels of psychological impact during the pandemic, and 3) evaluate potential sociodemographic, lifestyle-related, and awareness of people infected with COVID-19 risk factors that could make students more likely to experience these impacts.
Cross-sectional data were collected through web-based questionnaires from seven U.S. universities. Representative and convenience sampling was used to invite students to complete the questionnaires in mid-March to early-May 2020, when most coronavirus-related sheltering in place orders were in effect. We received 2,534 completed responses, of which 61% were from women, 79% from non-Hispanic Whites, and 20% from graduate students.
Exploratory factor analysis on close-ended responses resulted in two latent constructs, which we used to identify profiles of students with latent profile analysis, including high (45% of sample), moderate (40%), and low (14%) levels of psychological impact. Bivariate associations showed students who were women, were non-Hispanic Asian, in fair/poor health, of below-average relative family income, or who knew someone infected with COVID-19 experienced higher levels of psychological impact. Students who were non-Hispanic White, above-average social class, spent at least two hours outside, or less than eight hours on electronic screens were likely to experience lower levels of psychological impact. Multivariate modeling (mixed-effects logistic regression) showed that being a woman, having fair/poor general health status, being 18 to 24 years old, spending 8 or more hours on screens daily, and knowing someone infected predicted higher levels of psychological impact when risk factors were considered simultaneously.
Inadequate efforts to recognize and address college students’ mental health challenges, especially during a pandemic, could have long-term consequences on their health and education.
Citation: Browning MHEM, Larson LR, Sharaievska I, Rigolon A, McAnirlin O, Mullenbach L, et al. (2021) Psychological impacts from COVID-19 among university students: Risk factors across seven states in the United States. PLoS ONE 16(1): e0245327. https://doi.org/10.1371/journal.pone.0245327
Editor: Chung-Ying Lin, Hong Kong Polytechnic University, HONG KONG
Received: August 4, 2020; Accepted: December 28, 2020; Published: January 7, 2021
Copyright: © 2021 Browning et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
1 Introduction
A large number of studies support that the conclusion that the novel coronavirus (SARS-CoV-2) and its corresponding disease (COVID-19) have dramatically impacted people's mental health and behavior [ 1 – 5 ], with very few studies suggesting otherwise [ 6 ]. Mental health hotlines in the United States experienced 1,000% increases during the month of April, when most people were under lockdown because of the pandemic [ 7 ]. Some medical facilities have seen more deaths from suicide, presumably because of exceedingly poor mental health, than from COVID-19 infections [ 8 ]. Substance disorders in many people who were previously abstinent are expected to relapse during COVID-19, which will cause long-term economic and health impacts [ 9 ].
Although impacts are felt across populations—and especially in socially-disadvantaged communities and individuals employed as essential workers—college students are among the most strongly affected by COVID-19 because of uncertainty regarding academic success, future careers, and social life during college, amongst other concerns [ 10 ]. Even before the pandemic, students across the globe experienced increasing levels of anxiety, depressive moods, lack of self-esteem, psychosomatic problems, substance abuse, and suicidality [ 11 ]. Therefore, students may need additional resources and services to deal with the physical and mental health repercussions of the disease.
University administrators could best serve students if they better understood the impacts of COVID-19 and the risk factors of its psychological impacts. These impacts are of critical importance to warrant immediate mental health interventions focused on prevention and treatment [ 12 ]. Psychiatric and counseling services have historically been underutilized by college students [ 13 , 14 ]. Understanding what subpopulations may suffer from unique combinations of psychological impacts may facilitate targeted interventions and successful treatment and coping strategies for individuals at greatest risk.
A recent review highlights some of the documented psychological impacts of COVID-19 on college students [ 15 ]. Many feel increased stress levels and anxiety and depressive symptoms as a result of changed delivery and uncertainty of university education, technological concerns of online courses, being far from home, social isolation, decreased family income, and future employment. These impacts have been observed in universities across the world [ 10 ].
Studies of the psychological impacts of COVID-19 on college studies in the United States, however, have been limited in their generalizability [ 10 ] due to examination of single institutions only [ 10 , 16 , 17 ]. We are aware of no studies that have been conducted with college students at multiple institutions across the United States during the pandemic. These schools collectively represent a somewhat unique context within higher education. The United States educates large numbers of students from around the world [ 18 , 19 ]. Diverse student bodies may show different risk factors from more culturally-homogenous student bodies because of the diversity of value orientations [ 20 ] and sources of media consumption [ 16 , 21 – 23 ]. Further, colleges in the United States cost more than higher education institutions nearly anywhere else in the world [ 24 ]; therefore, financial concerns may be particularly apparent in the United States. The United States also experienced the lowest global recovery rate from infection–in other words, the highest mortality rate post-infection–in the weeks leading up to the timing of the current study (April and May, 2020) [ 25 ]. This country continues to witness the highest incidence and mortality rates among Global North countries [ 26 ]. Such high rates aggravate the psychological impacts of the disease on infected and non-infected individuals [ 1 ].
In the current study, we investigate the psychological impacts of COVID-19 and associated risk factors on college students at seven universities across the United States. Our objectives are three-fold: 1) identify the array of psychological impacts COVID-19 has on students, 2) develop profiles to characterize students' anticipated levels of psychological impact during the pandemic, and 3) evaluate potential sociodemographic, lifestyle-related, and awareness of people infected with COVID-19 risk factors that could make students more likely to experience these impacts.
2.1 Study population
In spring 2020, 14,174 participants were recruited cross-sectionally from representative and targeted samples at seven large, state universities, which in sum enroll more than 238,000 students. Universities included Arizona State University in Tempe, AZ (approximately 52,000 undergraduate/graduate students enrolled in 2019); Clemson University in Clemson, SC (approx. 25,000); North Carolina State University in Raleigh, NC (approx. 34,000); Oregon State University in Corvallis, OR (approx. 29,000); Pennsylvania State University in State College, PA (approx. 54,000); University of Montana in Missoula, MT (approx. 11,000); and The University of Utah in Salt Lake City, UT (approx. 33,000). One institution (North Carolina State University) was able to utilize a university-wide representative sample. Other institutions used targeted samples in the home college(s) or department(s) of the corresponding author. Selection of sampling scheme (i.e., representative or targeted) was determined by human subject review board allowances and listserv availability. (Recruitment occurred over email listservs and course website announcements.)
This research was deemed exempt from the Clemson University Institutional Review Board. Also, all subjects provided written consent when they completed the online survey.
Recruitment started as soon as human subject approval was awarded and occurred over a two-to-three-week window at each institution. Because approval took longer at some institutions, nationwide recruitment was staggered. No compensation for participation was provided. Sampling frames and recruitment windows are detailed in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0245327.t001
Of the 14,174 students invited to participate in the survey, we received 2,534 responses with data on most of the relevant variables; thus, this sample size was available for most of the descriptive statistics and bivariate associations. Missing/not reported data on race/ethnicity and gender occurred in approximately 11% of respondents. Therefore, complete data for multivariate analyses with all risk factors entered simultaneously—including race/ethnicity and gender—were available for 2,140 students. Table 2 provides the sample characteristics.
https://doi.org/10.1371/journal.pone.0245327.t002
2.2 Measures
2.2.1 psychological impacts..
2 . 2 . 1 . 1 Qualitative assessment . We expected that it would be difficult to parsimoniously and comprehensively capture the broad array of impacts from COVID-19 on students with quantitative measures. Therefore, we utilized an open-ended questionnaire item that asked respondents, "We are interested in the ways that the coronavirus (COVID-19) pandemic has changed how you feel and behave. What are the first three ways that come to mind?" Three responses were required, and a fourth response was optional. This question was placed at the beginning of the questionnaire to avoid priming and order effects [ 27 , 28 ].
2 . 2 . 1 . 2 Quantitative assessment . Regarding our selection of quantitative impacts to measure, we chose nine survey items based on information gathered from a review of previous research and new interview data. These nine survey items measured the following concepts: negative emotion states, preoccupation with COVID-19, feeling stressed, worry, and time demands.
Regarding the review of previous research, we examined studies of other large-scale disasters (i.e., the World Trade Center terrorist attacks on September 11, 2001; previous epidemics requiring quarantine), which are almost always associated with psychological impacts on the general population [ 29 ]. These studies provided some guidance on what impacts to measure for the impacts of COVID-19 on college students.
Regarding new interview data, the corresponding author of the current study conducted unstructured interviews with adults on their experiences in the early stages of the COVID-19 pandemic. These interviews consisted of recruiting ten participants aged 18 years or older in February 2020. Recruitment occurred in both low-risk and high-risk regions of the United States, including urban areas in Washington and rural areas in Tennessee, Iowa, and South Carolina. The interviews captured the feelings that interviewees experienced during the pandemic.
Negative emotion states comprised four of the survey items. Each item explained one of the basic negative emotions (i.e., being afraid, irritable, guilty, and sad) identified during the development of the positive and negative affect schedule (PANAS) [ 30 ]. Items were measured using the visual analogue scale (VAS) to provide data across a wide range of responses (1–100) with minimal participant burden [ 31 ]. Prompts asked respondents to indicate the extent to which they felt these things when they thought about the pandemic.
Preoccupation and feeling stressed comprised two more survey items. These were also measured with the VAS. Prompts once again asked respondents to indicate the extent to which they felt these things when they thought about the pandemic.
One more survey item measured worry—specifically anxious arousal. It was measured with a single item ("I worry a lot") from the Penn State Worry Questionnaire (PSWQ) that is strongly associated with the entire 16-item PSWQ, r = 0.80 [ 32 ]. Therefore, this single item succinctly captures the concept of worry/anxious arousal. A 5-point Likert-type agree-disagree response scale was used.
Two more survey items measured time demands. These were developed from survey prompts in the eating disorder literature [ 33 ]. Specifically, we asked to what extent respondents believed they spent a lot of time/thought on the pandemic, and to what extent they believed they spent too much time/thought on the pandemic. Once again, a 5-point Likert-type agree-disagree response scale was used.
The prompts for all nine of these survey items were delivered as reactions to the coronavirus rather than measures of general psychological states. Example include: "how stressed do you feel when you think about coronavirus," and "to what extent do you agree/disagree with the following: I worry about coronavirus all of the time."
2.2.2 Risk factors.
Sociodemographic factors were self-reported and allowed identification of potential differences in impact levels by gender, age, race/ethnicity, socioeconomic status (SES), and academic status (undergraduate vs. graduate-seeking). SES was measured with perceived social class, which has been shown to accurately represent SES in student populations, using a battery of seven questions on class, parental education, and relative family income [ 34 , 35 ]. To measure academic status, we asked respondents whether they were in pursuit of an undergraduate or graduate degree.
To account for possible lifestyle-related risk factors, we first considered general health factors such as general health status and body mass index (BMI). Health status was measured with a single item on respondents' "health in general" and a 5-point response scale (poor to excellent) [ 36 ]. BMI was calculated from self-reported height and weight. BMI has been implicated as a risk factor or confounder of the psychological impacts of COVID-19 [ 37 , 38 ].
Another set of plausible lifestyle-related risk factors was time use. We utilized a recent recall question structure from the American Time Use Survey that strongly predicts objective time use and activity measures [ 39 ]. Three items were used to ask respondents to indicate how many hours they spent outdoors (at a park, on a greenway/trail, in a neighborhood/yard, etc.), in front of a screen (on a smartphone/computer, watching television, online gaming, etc.), and engaged in moderate or vigorous physical activity that caused an increase in breathing or heart rate (fast walking, running, etc.) in the past 24 hours [ 40 , 41 ].
Regarding awareness of COVID-19 victims as a potential risk factor, we included two measures of knowing people who were diagnosed with the virus: someone in their family and someone in their community [ 42 ].
2.3 Analyses
To accomplish Objective 1, qualitative data from the open-ended responses were analyzed using content analysis with an inductive approach [ 43 , 44 ]. Two independent researchers examined the data systematically to identify patterns and codes [ 43 ]. Each response was coded separately and reviewed for agreement [ 45 , 46 ]. Interrater/intercoder agreement (kappa) score was 94.94% [ 47 ].
Objective 2 was accomplished in three steps. These included data imputations, data reduction, and profile identification.
We imputed missing values by bag imputation, which fits a machine learning regression tree model for each predictor as a function of all others [ 48 ]. In our dataset, 5.2% of the quantitative data were missing and imputed.
Next, we reduced the survey items related to levels of psychological impact into latent constructs using exploratory factor analysis (EFA) with oblimin rotation [ 49 ]. Scree plots and Very Simple Structure (VSS) criterion were used to identify the number of factors [ 50 ]. The VSS criterion evaluates the magnitude of the changes in goodness of fit with each increase in the number of extracted factors.
Last, using the composite scores from the EFA, we used the identified latent constructs from the psychological impact survey items as input variables in a latent profile analysis (LPA) [ 51 ]. Criteria for determining the number of profiles in the LPA included statistical adequacy of the solution and interpretability of each profile [ 52 ]. Indices used to determine statistical adequacy included the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC) and sample-size adjusted Bayesian Information Criterion [ 53 ]. For each of these indices, lower values represented better model fit. Also, the entropy criterion was calculated as a measure of classification precision [ 54 ]. We favored a parsimonious solution with fewer profiles over a more complex solution if this improved the interpretability of the LPA [ 53 ]. Z-scores of the input variables were used to interpret the profiles. The criteria to assign low and high values is not established and so we adopted previous studies' thresholds [ 53 ]. These included standardized scores between +0.5 and -0.5 being labelled as moderate, scores above 0.5 being labelled as high, and scores below -0.5 being labelled as low levels of psychological impact from COVID-19.
Objective 3 was achieved by modeling unadjusted (bivariate) and adjusted (multivariate) relationships between risk factors and profiles from the LPA. Unadjusted results are presented because multivariate models used a dichotomous outcome variable to distinguish students in the highest profile of psychological impact from those in the moderate or low profiles of impact (see Results for profile development and sample sizes within each profile). Determining risk factors for being in the high impact profile was deemed more important and actionable by university administrators than determining risk factors for each of the lower impact profiles, as would have been accomplished with a multinomial model. Thus, this modeling approach served a practical function; results could inform university administrators with tight budgets on how to prioritize funding for mental health interventions amongst students at greatest risk of high levels of psychological impact. Unadjusted results remained relevant, however, since they served the function of comparing risk factors between each level of impact profile in a simpler format than the output of a multinomial regression model.
For the unadjusted results, risk factors were evaluated with chi-squared contingency tables. Residuals from observed versus expected count comparisons determined the direction of the effect of the risk factors (i.e., more or less likely that a group was classified to a higher impact profile than another profile). Statistical significance of risk factors was calculated with Bonferroni adjustments to reduce Type I Error [ 55 ]. Continuous measures were reduced to dichotomous or categorical factors based on clinically meaningful levels, past research, and data distributions. BMI was classified into four categories (less than 18 = underweight; 18 to 24.99 = normal; 25 to 29.99 = overweight; 30.0 and over = obese) [ 56 ]. General health was separated into two groups: poor/fair health and good/very good/excellent health [ 53 ]. Screen time was separated into less than eight hours on a device and eight or more hours on a device [ 57 ]. Time outdoors was split into three groups: Less than 1.00 hour, 1.00 to 1.99 hours, and 2.00 hours or more [ 58 , 59 ]. Time spent exercising was also split into three groups: 30.00 minutes or less, 30.01 to 59.99 minutes, and 1.00 hour or more [ 60 ]. In addition, social class and relative income were split into three levels: below average, average, or above average. Levels of education were split into two levels: less than a 4-year college degree and a 4-year college degree or more [ 61 ].
For the adjusted results, we conducted generalized mixed-effects logistic regression to examine risk factors simultaneously and control for random (grouping) effects by institutional affiliation. To avoid collinearity in SES measures, whichever item correlated most strongly with psychological impacts was entered in the model. We used Variance Inflation Factor (VIF) values to test for multicollinearity. The proportion of variance explained was measured with conditional and marginal R 2 coefficients of determination [ 62 – 64 ]. Marginal R 2 represents the contribution of the predictors, which are modelled as fixed effects, whereas conditional R 2 accounts for the additional contribution of institutional affiliation (random effect) in addition to the fixed effects.
As a sensitivity analysis, we ran a logistic regression model with a subsample of respondents from the university that obtained a representative sample (North Carolina State University). This allowed us to evaluate the robustness of our nationwide sample, which otherwise utilized a convenience sampling approach.
Analyses were conducted in Excel for Mac Version 16.38 and R Version 3.6.2.
3.1 Array of impacts
Qualitative data from the open-ended responses demonstrated a broad array of impacts from COVID-19 on college students’ feelings ( Table 3 ) and behaviors ( Table 4 ). The most common changes in how students felt compared to before the pandemic were increased lack of motivation, anxiety, stress, and isolation. For example, one of the students reflected, “I'm normally extremely motivated, and I've never struggled with depression, but have recently felt very sluggish and melancholy.” Another student described their feelings related to isolation as “I feel trapped. I don't have anywhere I need to go since I can't socialize, and I have schoolwork. But yet I still feel trapped due to actual restrictions and suggestions.” The most frequent changes in student behavior compared to before the pandemic included more social distancing, more education changes, and less going out. Other concerning changes ranged from entrapment, boredom, fatigue, hopelessness, guilt, and inconvenience to hygiene, sleep, housing, employment, personal finances, and caretaking. For example, some students expressed their frustration with the financial situation, including one statement indicating: “I am BROKE. I lost my job because of this pandemic and now I can’t pay for groceries.” Other students were concerned about online learning. For example, one student commented: “I am constantly on edge about coursework: Did the computer register I submitted my exam? Did I see everything my teacher posted in Moodle? What happens if my internet goes out and I miss an assignment?”
https://doi.org/10.1371/journal.pone.0245327.t003
https://doi.org/10.1371/journal.pone.0245327.t004
Smaller numbers of students reported positive changes from the COVID-19 pandemic as well. These included optimism, productivity, adaptation, and empathy, as highlighted in the following quotes: “I've affirmed that people are capable of adapting in any circumstances” and “[I felt a] higher degree of empathy toward my community”.
3.2 Psychological impact profiles
Mean values of the psychological impact survey items are shown in Table 5 . Eight of these were included in the EFA. (Feeling guilty demonstrated low communality ( h 2 = .21) and was removed from further analyses.) All eight items displayed relatively normal distributions ( S1 Fig ). Criteria of the resulting model were acceptable: Tucker Lewis Index = 0.95; Kaiser-Meyer-Olkin (KMO) factor adequacy measure of sampling adequacy (MSA) = .89 [ 65 ]; significant Bartlett's test of sphericity, χ 2 (28) = 10503, p < .001. The VSS Criterion [ 50 ] achieved a maximum of .93 with a two-factor solution, compared to .89 for a one-factor solution or .94 for a three-factor solution ( S1 Table , S2 and S3 Figs). We labelled the first factor as "Emotional Distress" since it was composed largely of negative affect items (afraid, irritable, sad, preoccupied and stressed). The second factor was composed of three items dealing with how time was spent presumably in worry during the pandemic (worry, too much time and a lot of time), and so we labelled it "Worry Time." This is a term from clinical psychology that describes time spent reflecting on all the possible impacts of a health concern, including those worries that an individual cannot do anything about [ 66 ]. The internal reliability of the factors was high, Cronbach's ⍺ = .87 for Worry Time and .83 for Emotional Distress.
https://doi.org/10.1371/journal.pone.0245327.t005
A three-profile solution fit the data best for the LPA. Information criteria decreased with additional profiles up to a five-profile solution, indicating a better model fit ( S2 Table , S4 Fig ). The elbow plot suggested minor improvements in model fit after a three-profile solution. Adding a fourth or fifth profile provided less interpretable results. Based on the combined information from the statistical criteria and interpretability, we retained a three-profile solution as our final model.
The three levels of psychological impact from COVID-19 resulting from the LPA are depicted in Fig 1 . Positive z-scores indicate higher levels of impact and negative z-scores indicate lower levels of impact, compared to the average. Profile 1 ("high") represented students with higher than average levels of the two factors measuring psychological impacts (Emotional Distress, Worry Time) stemming from COVID-19. Profile 2 ("moderate") represented students with moderate levels of the two factors, and profile 3 ("low") represented students with low levels of the two factors. Regarding profile membership, 45.2% of students (n = 1,146) were within the high impact profile, whereas 40.4% (n = 1,025) were in the moderate profile and 14.3% (n = 363) were in the low profile.
Means and standard errors shown.
https://doi.org/10.1371/journal.pone.0245327.g001
3.3 Risk factors
A summary of the risk factors with significant differences between impact profiles based on bivariate Chi-square tests is depicted in Fig 2 . With respect to sociodemographic factors, women were more likely to be at risk than men ( χ 2 (2) = 88, p < .001). Specifically, women were more likely to be in the high profile (residuals (RES) = 8.02, p < .001) and less likely to be in the moderate (RES = -2.75, p = .036) or low (RES = -7.54, p < .001) profile. Men demonstrated the opposite pattern. We did not observe differences by academic status ( χ 2 (2) = .3, p = .9), although we did observe differences by age ( χ 2 (4) = 15, p = .005). Students who were 18 to 24 years old were more likely to be in the moderate profile (RES = 3.81, p = .0013), and students who were 25 to 32 years old were less likely to be in the moderate profile (RES = -3.03, p = .022) than other profiles. No other significant differences between age groups by profile were found, p > .05.
Sociodemographic (a), lifestyle (b), and COVID-19 victim awareness (c) risk factors associated with high, moderate, and low psychological impact profiles for students across the United States. Residuals from Pearson's chi-squared tests depict likelihood of profile membership based on risk factor. Only significant factors ( p < .05) are reported. Reference groups include men; over 32 age; other race/ethnicity; average/above average SES (social class and relative family income); good/very good/excellent general health; less than 2 hours of time outdoors; less than 8 hours of screen time; and not knowing someone infected (COVID-19).
https://doi.org/10.1371/journal.pone.0245327.g002
We also observed racial/ethnic and SES differences in psychological impact levels. Specifically, we found differences by race/ethnicity ( χ 2 (6) = 18, p = .007) with non-Hispanic Whites being more likely to be in the low profile (RES = 2.98, p = .035) and Non-Hispanic Asians being less likely to be in the low impact profile (RES = -3.42, p = .0076). No differences in impact profiles were observed for non-Hispanic Black students or Hispanic students, although sample sizes were small ( n = 95 and 98, respectively). Parental educational achievement measures further showed no differences in profiles, p = .5 for maternal and .9 for paternal. No differences were observed for parental social class either, p = .1 for maternal and .2 for paternal. In contrast, student social class ( χ 2 (4) = 14, p = .008), and relative family income ( χ 2 (4) = 14, p = .008) differed by impact profile. Students who reported above-average social class were more likely to be in the low profile (RES = 3.07, p = .019), and students who reported below-average relative family income were more likely to be in the high profile (RES = 3.38, p = .0065). No other significant differences between ethnoracial groups or SES measures by profile were found, p > .05.
Lifestyle-related factors predicted differences in impact profiles. For instance, general health predicted assignment to different impact profiles ( χ 2 (2) = 41, p < .001). Students with fair/poor health were more likely to be in the high profile (RES = 5.90, p < .001) and less likely to be in the moderate (RES = -2.67, p = .045) or low profile (RES = -4.58, p < .001). Students with good/very good/excellent health displayed the opposite pattern. No difference in impact profiles was observed for BMI ( χ 2 (6) = 9, p = .2). We observed differences in impact profiles by time outdoors ( χ 2 (4) = 13, p = .01) and screen time ( χ 2 (2) = 14, p = .001) but not by exercise time ( χ 2 (4) = 6, p = .2). Students who reported spending two or more hours outdoors were less likely to be in the high profile (RES = -3.17, p = .014), and students who reported spending more than eight hours on a device were more likely to be in the high profile (RES = 3.06, p = .013) and less likely to be in the moderate profile (RES = -3.67, p = .0014). Students spending less than eight hours on a device displayed the exact opposite trend. No other pair-wise comparisons in lifestyle-related factors were significant, p > .05.
Lastly, knowing someone who was infected with COVID-19 increased the likelihood of being at risk of psychological impacts ( χ 2 (2) = 14, p < .001). Students who knew someone in their family or community who was infected were more likely to be in the high profile (RES = 3.06, p = .013) and less likely to be in the moderate profile (RES = -3.67, p = .0014). Students who did not know an infected person displayed the opposite pattern.
Five variables remained significant predictors of impact profiles in models adjusting for all risk factors simultaneously while controlling for institutional affiliation ( Table 6 ). The SES measure entered in these models was social class of student, because it correlated more highly with psychological impact levels than other measures ( S5 Fig ). Students who were women, fair/poor general health, 18 to 24 years old, reporting 8 or more hours of screen time, and who knew someone infected with COVID-19 were more likely to be in the high profile. Non-Hispanic Asian students were marginally more likely to be in the high impact profile, p = .091. Effect sizes varied; women were approximately twice as likely to be assigned to the high impact profile as the moderate/low profile. Other predictors increased (or decreased) the likelihood of being in the high impact profile by approximately 20% to 40%. No institutions emerged as significant random effects ( S6 Fig ). VIF values < 2.0 indicated no multicollinearity. Approximately 7% of the variance was explained by the predictors and institutional affiliations.
https://doi.org/10.1371/journal.pone.0245327.t006
Sensitivity analyses with a subsample of respondents from the representative sample at North Carolina State University identified a similar set of predictors of psychological impact levels ( S3 Table ). Gender, age, general health, and knowing someone infected remained significant predictors. In contrast, screen time was no longer significant. Being Non-Hispanic Asian as marginally significant, p = .070, and social class was significant, p = .0038. Students of above average social class were 23.0% less likely to be assigned to the high impact profile.
4 Discussion
4.1 key findings and interpretation of results.
To evaluate the psychological impacts of COVID-19 on students in the United States, we collected over 2,500 survey responses from students at seven universities in late-February to mid-May 2020. Qualitative data from open-ended responses showed students experienced largely negative impacts of COVID-19 on psychological health and lifestyle behaviors. Among the most commonly reported changes were lack of motivation, anxiety, stress, and isolation, as well as social distancing, education changes, and going out less. Similar findings were reported by another study exploring the impact of COVID-19 on students at a single college in the United States, revealing increases in sedentary lifestyle, anxiety, and depressive symptoms [ 16 ]. A global study examining experiences of students in 62 countries, including one university in the United States, found that students’ expressed concerns about their academic and professional careers, as well as feelings of boredom, anxiety and frustration [ 10 ]. Increased anger, sadness, anxiety and fear were also reported by students in China [ 67 ]. Students in Switzerland reported a decrease in social interaction and higher levels of stress, anxiety, and loneliness [ 68 ]. More generally, adults have reported decreases in physical activity and food consumption increases during the COVID-19 pandemic quarantine compared to beforehand, as well as increases in binge drinking on average [ 69 ], which was identified in a small portion of our student respondents as well. Slight differences between our studies' results and results from studies conducted elsewhere may be due to the differences in student experience by geographical location. The United States is providing relatively little financial relief to college students during the pandemic compared to other Global North countries [ 70 ].
Quantitative survey measures captured the majority of the content that students entered in the open-ended responses (i.e., worry, stress, and fear) and informed the development of impact profiles. Students were assigned to one of three profiles—low (14% of the sample), moderate (40%) and high (45%)—based on the psychological impacts they reported experiencing in response to COVID-19.
In unadjusted models, students who were women, non-Hispanic Asian, in fair/poor health, of below-average relative family income, or someone who knew a family/community member infected with COVID-19 were at risk of higher levels of psychological impact. Students who were non-Hispanic White, above-average social class, spent at least two hours outside in the past day, or spent less than eight hours on screens in the past day were at less risk.
In multivariate models controlling, being a woman, being younger (18 to 24 years old), having poor/fair general health, reporting more screen time, and knowing someone infected were statistically significant risk factors. SES and identifying as non-Hispanic Asian were additional significant risk factors in the subsample of respondents obtained from representative sampling, whereas screen time was not significant in this sensitivity analysis.
These risk factor findings generally match those found in other studies that employed a case study approach within single United States universities/colleges. One longitudinal study of students at a public university in Nevada (n = 205) found that anxiety and depressive symptoms were greater in April 2020 than in prior months [ 17 ]. Women reported greater disruption to daily activities, mental and physical health, and personal finances than men. Contrary to our unadjusted findings, Asian or Asian-American students in the Nevada study reported lower levels of anxiety and depression than other races. A second longitudinal study with undergraduate students (n = 217) at a small liberal arts college in New Hampshire also found increases in anxiety, depression, and sedentary time during April 2020 relative to prior months [ 16 ]. COVID-19 risk factors for college students at other countries have been strikingly similar, as explained below.
Over ten studies, including several with college student populations, identify women as being at greater risk of psychological distress during the COVID-19 pandemic [ 1 , 10 , 21 , 71 – 77 ]. Women are generally prone to depression and anxiety disorders [ 14 ], and although initial evidence indicated men were more susceptible to infection [ 77 ], our study supports the assertion that women appear to be more strongly impacted by the long-term psychological impacts of the pandemic. This observation may be attributable to higher levels of pre-existing psychopathology in women as well as gender differences in fear processing, which could translate to exacerbations of symptoms [ 78 ]. Also, male students tend to have higher confidence in the computer skills necessary for the transition to online course delivery [ 10 ]. Meanwhile, women are more concerned about impacts on their professional career and ability to study than men, on average [ 10 ]. One study attributed these gender differences to greater emotional expression, less tolerance for uncertainty, and less-effective coping strategies amongst students who are women [ 75 ]. Women have also reported being more susceptible to "emotional hunger" and subsequent increased food intake than men during COVID-19 quarantine; these behaviors can lead to weight gain and poor mental health [ 73 ].
Our findings that fair/poor general health is a risk factor has been documented in numerous other populations during COVID-19 [ 79 , 80 ]. In addition to comorbidity between mental and physical health status, people with pre-existing health problems and those with poor mental health show lower preparedness for disasters and suffer disproportionately more from disaster-related outcomes [ 81 ].
Several reasons explain our findings that younger students may be at greater risk than older students. Younger students (i.e., 18 to 24 years old, regardless of academic status) tend to be more worried about their future education and ability to pay for college education than older students [ 10 ]. Younger people also engage in social media more than older people during the pandemic [ 12 , 82 ]. Given the dominance of the COVID-19 pandemic in the news, younger "always-on" students may be exposed to greater amounts of risk-elevating messages, which can lead to anxiety and poor mental health [ 16 , 75 ].
Regarding our findings that non-Hispanic Asian students may be at greater risk than other races/ethnicities, several studies show higher psychological distress from COVID-19 in this population [ 10 ]. Asians and Asian Americans have reported being discriminated against by other students on social media during the pandemic [ 83 ]. Further, this population has experienced long-standing barriers to receiving and participating in mental health services [ 84 ].
The current study provides some support toward the mounting evidence that excessive screen time, including during the pandemic, may negatively impact mental health [ 85 ]. People who manage COVID-19 anxiety with excessive use of smartphones and other screen-based technology inadvertently learn more about the virus from the news, which fuels anxiety and ongoing coping through screens, thus causing a downward spiral [ 82 ]. Excessive use of digital media also detracts from time that could be spent on other health-promoting activities such as outdoor recreation [ 86 ]. Our study supports these relationships, suggesting negative impacts of screen time and positive impacts of "green time" on students' psychological health. The unadjusted analyses suggested that outdoor time predicted psychological impacts of COVID-19, although this variable was not significant in multivariate models. Other studies justify its consideration as a risk factor by university administrators. Both outdoor recreation [ 87 ] and nature exposure [ 88 , 89 ] can improve psychosocial and eudaimonic well-being [ 90 , 91 ]. Recent studies of people across the world show protective psychological effects of park and green space access during the pandemic [ 92 ] as well as lower rates of infection and mortality [ 93 ].
The finding that knowing someone infected is a risk factor for psychological impacts of COVID-19 is intuitive. Familiarity can increase the salience and perceived risk of becoming infected and dealing with subsequent health concerns, like COVID-19-related death [ 79 ]. Also, the threat of death from COVID has been associated with students' mental health and explainable by unhealthy levels of smartphone use [ 82 ].
As suggested in our unadjusted analyses and the multivariate model with the representative sample, SES may influence students' mental health during the pandemic. This might be a result of financial concerns affecting college students and their families [ 10 ]. SES has been documented as a predictor of COVID-19 fear and mental health concerns in other populations [ 10 , 74 , 79 , 94 – 98 ]. Students coming from low-SES families may be more concerned about basic needs, like food and shelter, caused by loss of their or their parent's income [ 99 ]. Furthermore, since low-SES families are more susceptible to COVID-19 infection [ 98 ], students may be more concerned for their own and their families' safety.
4.2 Recommendations for universities
Given the large percentage of students assigned to the high psychological impact profile, universities would be well-served to address the mental health needs of their entire student body. Select programs that have promoted mental health—such as those at the University of Connecticut, University of Kentucky, and Northeastern—include virtual group exercise and meditation/mindfulness sessions, accountability buddies and exercise challenges and tele-medicine/counseling visits [ 99 ]. These group meetings may be helpful not only in lowering anxiety but also in decreasing the sense of isolation reported by the students in this study. Digital interventions for students with clinical levels of anxiety or depression as well as potential for self-harm or suicide can involve automated and blended therapeutic interventions (such as apps and online programs), calls/text messages to reach those with less digital resources, suicide risk assessments, chatlines and forums, and other technologies to monitor risk either passively or actively [ 80 ]. Recently, Chen et al. [ 100 ] recommended a six-step intervention for the reduction in psychological impact risk amongst Chinese college students. These steps included the delivery of positive pandemic-related information, reduction in negative behavior, learning about stress management techniques, improvements in family relationships, increases in positive behavior, and adjustments in academic expectations.
Given the likelihood of ongoing psychological distress from COVID-19, universities may also consider helping students maintain healthy mindsets rather than avoiding stress [ 101 ]. In support of this proposition are recent findings that cognitive and behavioral avoidance (i.e., avoiding situations where exposure is possible and difficult thoughts about the pandemic) was the most consistent predictor of increased anxiety and depressive symptoms during the pandemic [ 17 ]. Cognitive reappraisal of stressful situations can alter their negative impacts [ 102 , 103 ]. Training students to shift their educational experience mind-set to one that focuses on the "silver linings" and emerging opportunities may lead to "stress-related growth" and "toughening" [ 104 , 105 ]. Adaptive mindsets can also help reorganize priorities to develop deeper relationships and greater appreciation of life [ 106 ], as well as help students to adjust to new ways of learning. Since a portion of the students in this study reported feeling less motivated, productive, and able to focus, switching to an adaptive mindset may help students persevere in their education and later in life. Finally, mindset reappraisals can increase well-being, decrease negative health symptoms, and boost physiological functioning under acute stress when a family member becomes infected or the pandemic creates rapid shifts in policies and procedures that affect students [ 107 , 108 ].
Universities can further develop platforms that facilitate safe student social interaction. Many students seek out social interaction during their university experience [ 109 – 111 ]. However, as the findings of this study revealed, students’ opportunities for socializing significantly decreased in the early stages of COVID-19. Missing "going out" and important milestone events (e.g., graduation, last sporting event) was a frequent response from our student participants. Other studies found that in order to maintain students' mental health during the first wave of the COVID-19 pandemic, they communicated online with close family members or roommates at least daily [ 10 ]. With college students, physical distancing does not and should not require "social distancing" [ 101 ]. Both synchronous (i.e., Zoom) and asynchronous (i.e., Facebook group) online interactions can foster bonding and bridging social connection [ 112 – 115 ], which can extend beyond social media posts and email listservs. Normal venues where people congregate such as places of worship, gyms, cafeterias, yoga studios and classes can be replicated online or even held outdoors in temperate weather on a schedule similar to what was in place prior to the pandemic [ 116 ]. Other recently-successful interventions include the facilitated online sharing of recipes, books, and podcasts as well as virtual movie, game, trivia, or happy hour nights [ 99 ]. Providing support to student organizations to coordinate these virtual social activities could accelerate the availability of these resources.
Colleges and universities also have a moral obligation to boost their outreach to particularly vulnerable groups–that is, populations at risk of high levels of psychological impact from COVID-19 [ 14 ]. As documented in the impact profiles of our study, people at increased risk include women, younger students, students with pre-existing health concerns, students spending at least one-third of their day (including time spent sleeping) on screens, and students with family or community members who are infected with COVID-19. Monitoring and reporting rates of anxiety, depression, self-harm, suicide and other mental health issues within these groups is necessary to allocate counseling services and intervene pre-emptively and at times of acute symptomology [ 80 ]. Further, universities can provide accommodations for assignments and exams using a more personalized approach to learning and create enhanced opportunities for virtual social interactions with peers. These efforts may help at-risk groups succeed academically, build stronger relationships, and enhance their sense of belonging during distant learning [ 117 ].
Students in this study also expressed stress and anxiety associated with changes in education mode during the pandemics. As previous research has found, academic success may be supported with virtual town halls, regular email check-ins, virtual office hours, and peer mentoring [ 104 ]. Globally, students' satisfaction with university response to COVID-19 is predicted by students' satisfaction with pre-recorded videos during online course delivery, sufficient information on exams, satisfaction with teaching staff, satisfaction with websites and social media information with regular updates from the university, hopefulness, (lack of) boredom, (lack of) study issues, being on scholarship, being able to pay for school, and study discipline (social sciences tend to be less impacted than hard sciences or engineering) [ 10 ]. Universities may be encouraged by findings from another study on the switch to online courses; this study found many students were not challenged by the transition because of their aptitude toward digital learning and new technologies [ 118 ]. However, another study found new software platforms can be a challenge for some students [ 10 ].

4.3 Strengths and limitations
The primary strength of this study is the development of psychological impact profiles using data from universities across the United States. This sampling approach is also a limitation, however. Whereas all the included universities were teaching exclusively online during the study, their respective states and localities may have experienced differing levels of social distancing policy and enforcement. Another limitation related to the sample is the high percentage of non-Hispanic Whites. This occurrence was likely the result of the demographic composition of the colleges and departments targeted for recruitment [ 119 ]. Selection bias related to which students participated in the study questionnaire based on interest and access/availability is also possible [ 3 ].
Another limitation is the quantitative assessment of the psychological impacts of COVID-19, which could have limited the utility of our impact profiles. We did not measure substance abuse, which is expected to be a ramification of the virus [ 116 ] and which anxious individuals are prone to under-report [ 120 ]. Such counterproductive coping behaviors could be particularly problematic for college students [ 121 ]. Further, because our predictors explained a small amount of variance of the profiles, other unmeasured (or better measured) factors might predict students’ psychological risk. For example, our single-item measures of leisure time activities could be improved with a more comprehensive assessment of time budgets such as those employed in episodic time use surveys [ 122 ].
We were primarily interested in reactions to the pandemic rather than how people were feeling/behaving during the pandemic. Therefore, we did not employ standardized measures of stress, anxiety, depression, or well-being. This limits our findings from being directly compared to other studies and pooled in meta-analyses.
Lastly, our measures were retrospective rather than longitudinal, which decreases our ability to say with confidence that the reported impacts were caused by COVID-19. However, we are fairly confident that the findings are attributable to the pandemic given our survey prompts. They specified students' responses to COVID-19 rather than asked generalized psychological states, and the findings strongly aligned with those of longitudinal studies of college students during the pandemic [ 16 , 17 , 37 , 123 – 125 ].
5 Conclusion
Our cross-sectional study found that being a woman, being of younger age, experiencing poor/fair general health, spending extensive time on screens, and knowing someone infected with COVID-19 were risk factors for higher levels of psychological impact during the pandemic among college students in the United States. Unadjusted analyses also suggested that students who were non-Hispanic White, were not non-Hispanic Asian, were of higher-SES, or spent at least two hours outside experienced lower levels of psychological impact. That said, all students surveyed reported being negatively affected by the pandemic in some way, and 59% of respondents experienced high levels of psychological impact.
At the time that these data were collected, the education of over 1.5 billion students across the world were affected by COVID-19 [ 126 ]. Rates of student psychological distress were as high as 90% [ 17 , 127 ]. Students must "Maslow before they can Bloom; " in other words, their basic physiological, psychological, and safety needs must be met prior to them focusing on–much less excelling–in academic life [ 99 ]. We recommend that university administrators take aggressive, proactive steps to support the mental health and educational success of their students at all times, but particularly during times of uncertainty and crisis–notably, the COVID-19 pandemic.
Supporting information
S1 fig. distributions and relationships between covid-19 psychological impact survey items, including histograms, pearson correlation coefficients, and scatter plots..
https://doi.org/10.1371/journal.pone.0245327.s001
S2 Fig. Diagram of EFA on COVID-19 psychological impact survey items.
https://doi.org/10.1371/journal.pone.0245327.s002
S3 Fig. Scree plot of EFA on COVID-19 psychological impact survey items.
https://doi.org/10.1371/journal.pone.0245327.s003
S4 Fig. Elbow plot of the information criteria for the latent profile analysis.
https://doi.org/10.1371/journal.pone.0245327.s004
S5 Fig. Correlations between socio-economic measures and the two psychological impact profiles.
https://doi.org/10.1371/journal.pone.0245327.s005
S6 Fig. Conditional mean values ("condval") and standard deviations of institutional affiliation (university) random effects from mixed-effects logistic regression predicting high versus medium/low psychological impact profile from COVID-19.
https://doi.org/10.1371/journal.pone.0245327.s006
S1 Table. Item loadings and fit statistics of EFA on COVID-19 psychological impact survey items.
https://doi.org/10.1371/journal.pone.0245327.s007
S2 Table. Fit indices, entropy and model comparisons for estimated latent profile analyses models.
https://doi.org/10.1371/journal.pone.0245327.s008
S3 Table. Results of binomial logistic regression modelling likelihood of risk factors predicting high versus low/moderate levels of COVID-19 psychological impact for students at North Carolina State University, where a representative sample was collected ( N = 1,312).
https://doi.org/10.1371/journal.pone.0245327.s009
https://doi.org/10.1371/journal.pone.0245327.s010
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. Academic Press; 2020. https://doi.org/10.1016/j.bbi.2020.05.048 pmid:32485289
- 4. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. American Academy of Child & Adolescent Psychiatry; 2020; 1–46. https://doi.org/10.1016/j.jaac.2020.05.009 pmid:32504808
- 5. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Research. Elsevier Ireland Ltd; 2020;291: 113190. https://doi.org/10.1016/j.psychres.2020.113190 pmid:32563745
- 7. Cunningham PW, Firozi P. The Health 202: Texts to federal government mental health hotline up roughly 1,000 percent. In: washingtonpost.com [Internet]. 4 May 2020 [cited 23 Jun 2020] pp. 1–15. Available: https://www.washingtonpost.com/news/powerpost/paloma/the-health-202/2020/05/04/the-health-202-texts-to-federal-government-mental-health-hotline-up-roughly-1-000-percent/5eaae16c602ff15fb0021568/
- 8. Hollyfield A. Coronavirus impact: Suicides on the rise amid shelter-in-place order, Bay Area medical professionals say. In: abcnews.com [Internet]. 21 May 2020 [cited 23 Jun 2020] pp. 1–4. Available: https://abc7news.com/suicide-covid-19-coronavirus-rates-during-pandemic-death-by/6201962/
- 10. Aristovnik A, Keržič D, Ravšelj D, Tomaževič N, Umek L. Impacts of the COVID-19 pandemic on life of higher education students: A global perspective. preprints.org . 2020. https://doi.org/10.20944/preprints202008.0246.v2
- 12. Stieger S, Lewetz D, Swami V. Psychological well-being under conditions of lockdown: An experience sampling study in Austria during the COVID-19 pandemic. psyarxiv.com . 2020. https://doi.org/10.31234/osf.io/qjhfp
- 13. Gruttadaro D, Crudo D. College students speak: A survey on mental health [Internet]. National Alliance on Mental Health. Fairfax, VA; 2012 Nov pp. 1–24. Available: https://www.nami.org/Support-Education/Publications-Reports/Survey-Reports/College-Students-Speak_A-Survey-Report-on-Mental-H
- 15. Sankhi S, Marasine NR. Impact of COVID-19 Impact of COVID-19 pandemic on mental health of the general population, students, and health care workers: A review. preprints.org . 2020. https://doi.org/10.20944/preprints202007.0616.v1
- 17. Zimmermann M, Bledsoe C, Papa A. The impact of the COVID-19 pandemic on college student mental health: A longitudinal examination of risk and protective factors. psyarxiv.com . 2020. https://doi.org/10.31234/osf.io/2y7hu
- 24. Marmolejo F. America spends more on college than virtually any other country. In: Forbes.com [Internet]. 10 Sep 2020 [cited 10 Sep 2020] pp. 1–9. Available: https://www.forbes.com/sites/prestoncooper2/2019/09/22/america-spends-more-on-college-than-virtually-any-other-country/#2fe46f483348
- 25. Bhagavathula AS, Rahmani J, Aldhaleei WA, Kumar P, Rovetta A. Global, regional and national incidence and case-fatality rates of novel coronavirus (COVID-19) across 154 countries and territories: A systematic assessment of cases reported from January to March 16, 2020. medRxiv.org . 2020. https://doi.org/10.1101/2020.03.26.20044743
- 30. Watson D, Clark LA. The PANAS-X: Manual for the positive and negative affect schedule-expanded form. University of Iowa; 1994.
- 36. Centers for Disease Control and Prevention. Healthy Days Core Module: HRQOL-14 Measure. In: cdc.gov . 31 Oct 2018 pp. 1–10.
- 37. Xiao J, Jiang Y, Zhang Y, Gu X, Ma W, Zhuang B. The impact of psychology interventions on changing mental health status and sleep quality in university students during the COVID-19 pandemic. medRxiv.org . 2020. https://doi.org/10.1101/2020.09.01.20186411
- 43. Lune H, Berg BL. Qualitative Research Methods for the Social Sciences. Pearson; 2016.
- 44. Maxwell JA. Qualitative Research Design: An Interactive Approach. SAGE; 2013.
- 48. Kuhn M. caret: Classification and Regression Training. In: cran.r-project.org [Internet]. 20 Mar 2020 [cited 24 Jun 2020] pp. 1–2. Available: https://cran.r-project.org/web/packages/caret/index.html
- 51. Hennig C, Meila M, Murtagh F, Rocci R. Handbook of Cluster Analysis. Chapman and Hall/CRC; 2015.
- 65. Tabachnick BG, Fidell LS. Using multivariate statistics. 5 ed. Boston, MA: Allyn & Bacon; 2007.
- 69. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of COVID-19 home confinement on physical activity and eating behaviour Preliminary results of the ECLB-COVID19 international online-survey. medRxiv.org . 2020. pp. 1–24. https://doi.org/10.1101/2020.05.04.20072447
- 70. Holzer HJ. The COVID-19 crisis: How do U.S. employment and health outcomes compare to other OECD countries? In: Brookings Institute [Internet]. Jun 2020 [cited 17 Sep 2020] pp. 1–12. Available: https://www.brookings.edu/research/the-covid-19-crisis-how-do-u-s-economic-and-health-outcomes-compare-to-other-oecd-countries/
- 83. Duong V, Pham P, Yang T, Wang Y, Luo J. The Ivory Tower lost: How college students respond differently than the general public to the COVID-19 pandemic. arxiv.org . 2020.
- 93. Klompmaker JO, Hart JE, Holland I, Sabath MB, Wu X, Laden F, et al. County-level exposures to greenness and associations with COVID-19 incidence and mortality in the United States. medRxiv.org . 2020. pp. 1–14. https://doi.org/10.1101/2020.08.26.20181644 pmid:32908990
- 126. UNESCO. School closures caused by Coronavirus (Covid-19). In: en.unesco.org . 11 Sep 2020 pp. 1–4.
- 127. Krakauer Hubner von C, Bruscatto ML, Lima RD. Distress among Brazilian university students due to the Covid-19 pandemic: survey results and reflections. medRxiv.org . 2020. https://doi.org/10.1101/2020.06.19.20135251
How Psychology Has Changed Our Minds

H ow does the mind work? How can we explain consciousness, development, memory, language, rationality, emotions, racism, kindness, and hatred—the most important and intimate aspects of ourselves?
Solving these mysteries is the business of experimental psychology, the field I’ve devoted my life to. But not everyone is satisfied with how we’re doing our job. Some feel that psychology isn’t scientific enough in its approach and believe that the real answers are going to come from studies of the brain. Out with psychology; in with neuroscience! Others reject a scientific approach altogether and seek answers from mystics, self-help celebrities, and internet gurus.
This skepticism is understandable. Our field is going through a replication crisis , as many of our best-known findings have failed to hold up. And, like any field, progress in psychology can be slow, and the answers we give are often tentative and qualified.
But I am bullish about psychology. The field has come up with some striking findings that shatter common-sense conceptions about how the mind works. I’ll tell you about four of them.
More From TIME
1. babies know more than we could have imagined.
The idea that we start off with empty heads was an accepted view by many scholars. In 1890, William James described the mental life of a baby as “a blooming, buzzing confusion.” A century earlier, Jean-Jacques Rousseau made this point in harsher terms, saying that if a child were born in an adult body, “such a child-man would be a perfect idiot”
Maybe you believe this too—babies sure don’t seem very smart. But psychologists have employed clever methods to capitalize on the few things babies are good at, such as sucking on a pacifier and moving their eyes. This might not sound like much, but in the hands of clever researchers, these behaviours can reveal the secrets of the infant soul.
We have discovered an inborn system for reasoning about objects, one present in babies as young as researchers are able to test (and also present in species other than humans, such as newborn baby chicks). Babies know, for instance, that objects that go out of sight continue to exist.
We know that, early on, babies also have some understanding of people. Imagine a table with two different objects on it, and a hand reaching for one of them. Then the objects switch places. Adults know that hands are attached to people, and people have goals, and a reasonable goal for a person is to reach for a particular object, not to go to a specific location. Six-month-olds have the same expectation. They are even capable of rudimentary moral judgments. If you show them a character who helps someone and another character who gets in that person’s way, six-month-olds prefer the helper. When you look into the big eyes of a baby, there’s someone smart looking back.
2. Memory is not to be trusted
Some people believe that we make perfect recordings of the world. Any memory can be recovered if we work hard enough at it, whether through self-reflection, hypnotic regression, or probing by a patient psychiatrist.
None of this is true. Memory is fuzzy and vague; much of what we experience never gets stored in our brains, and much of what is stored gets distorted over time. When we try to remember something, it’s not like a computer retrieving information; it’s more of a storytelling process—an on-the-fly reconstruction.
One way we know this is through studies where psychologists implant false memories in their subjects. Sometimes this is subtle—showing people a scene and later asking them “did you see children getting on the school bus?” makes them more likely, later, to remember a school bus, even if it wasn’t there. Sometimes it’s more heavy-duty. In one study, psychologists asked college students’ family members for information about events from their childhoods and interviewed students about their memories. The twist is that for each interview, one event—being lost in a shopping mall, nearly drowning, spilling punch on a bride’s parents during a wedding, being attacked by a vicious animal—was entirely fabricated by the researchers. Despite this, many of the subjects came to remember these false events as actually occurring.
This research has led to a revolution in the law. Memory research has helped us appreciate that police interrogations that are intended to retrieve memories can instead shape and create them. On a more personal level, it’s worth knowing—maybe when you’re arguing with your partner!—that you can be perfectly confident in a memory and yet entirely mistaken about it.
3. Consciousness is surprisingly limited
When you close your eyes and open them again, would you notice if everything changed?
One of the great discoveries of cognitive psychology finds that only a small fraction of sensory experience makes its way in; everything else is ignored and lost forever. In one famous study, reported in a paper titled “Gorillas in Our Midst,” subjects are shown a video in which people in white shirts and black shirts are standing in a hallway passing basketballs back and forth. The subjects’ task is to focus on the white shirts and count the passes they make. People don’t find this hard, but it does take all their attention. Here’s the twist: In the middle of the video someone dressed as a gorilla walks onto the scene, stops in the middle and pounds his chest, then walks off. About half of the subjects don’t see this at all, though the presence of the gorilla is screamingly obvious for anyone who is not told to focus on the passing of the basketballs.
We tend to be ignorant of these limitations. It feels like we are conscious of the world, not just a small sliver of it. It feels like we can attend to multiple things at the same time, rather than being forced to move our attention back and forth. Our limitations are harmless enough if we are listening to a podcast while mowing the lawn. But they can be fatal in cases where something needs our full attention, such as driving. Talking on the phone, even using a hands-free device, slows our reaction time on the road to an extent that is roughly the same as being legally intoxicated.
4. Insights from the new science of happiness
A few decades ago, a group of psychologists worried that there has been too much focus on the negative. We haven’t done enough research into what goes into a pleasant and meaningful and satisfying life. A new movement, known as positive psychology, emerged to change all this. And now we have a lot of data, some from studies of millions of people, that help us appreciate the conditions for human flourishing.
Some of the findings are common sense. Money does lead to happiness, both at the level of individuals (richer people are happier) and countries (citizens of richer countries are happier)—though there are diminishing returns once the numbers get high enough. Social connections are even more important; one study, published in the journal Science , found that being lonely has a worse effect on health than obesity and smoking.
Other findings are more surprising. Research into aging and happiness find that for many people, the 50s are the saddest period of their lives, and then happiness starts to rise—for many, the eighties are the happiest times of their lives. Who would have thought?
Happiness researchers have also discovered a paradox. There is a strong relationship between thinking a lot about happiness and … being sad. The moral here is: don’t spend too much time pouring over the happiness research!
There are so many other findings that could have made the list, and there will be more in the future. I’m most excited by debates over how well deep learning (how ChatGPT and other AIs work) can work as a model for human thinking, as well in recent developments in clinical psychology, including trials of mind-altering drugs such as ketamine and psylocibin, as treatments for depression and anxiety. These are exciting times to be a psychologist.
More Must-Reads From TIME
- Jane Fonda Champions Climate Action for Every Generation
- Passengers Are Flying up to 30 Hours to See Four Minutes of the Eclipse
- Biden’s Campaign Is In Trouble. Will the Turnaround Plan Work?
- Essay: The Complicated Dread of Early Spring
- Why Walking Isn’t Enough When It Comes to Exercise
- The Financial Influencers Women Actually Want to Listen To
- The Best TV Shows to Watch on Peacock
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
You May Also Like
- Open access
- Published: 06 July 2023
Pros & cons: impacts of social media on mental health
- Ágnes Zsila 1 , 2 &
- Marc Eric S. Reyes ORCID: orcid.org/0000-0002-5280-1315 3
BMC Psychology volume 11 , Article number: 201 ( 2023 ) Cite this article
363k Accesses
13 Citations
89 Altmetric
Metrics details
The use of social media significantly impacts mental health. It can enhance connection, increase self-esteem, and improve a sense of belonging. But it can also lead to tremendous stress, pressure to compare oneself to others, and increased sadness and isolation. Mindful use is essential to social media consumption.
Social media has become integral to our daily routines: we interact with family members and friends, accept invitations to public events, and join online communities to meet people who share similar preferences using these platforms. Social media has opened a new avenue for social experiences since the early 2000s, extending the possibilities for communication. According to recent research [ 1 ], people spend 2.3 h daily on social media. YouTube, TikTok, Instagram, and Snapchat have become increasingly popular among youth in 2022, and one-third think they spend too much time on these platforms [ 2 ]. The considerable time people spend on social media worldwide has directed researchers’ attention toward the potential benefits and risks. Research shows excessive use is mainly associated with lower psychological well-being [ 3 ]. However, findings also suggest that the quality rather than the quantity of social media use can determine whether the experience will enhance or deteriorate the user’s mental health [ 4 ]. In this collection, we will explore the impact of social media use on mental health by providing comprehensive research perspectives on positive and negative effects.
Social media can provide opportunities to enhance the mental health of users by facilitating social connections and peer support [ 5 ]. Indeed, online communities can provide a space for discussions regarding health conditions, adverse life events, or everyday challenges, which may decrease the sense of stigmatization and increase belongingness and perceived emotional support. Mutual friendships, rewarding social interactions, and humor on social media also reduced stress during the COVID-19 pandemic [ 4 ].
On the other hand, several studies have pointed out the potentially detrimental effects of social media use on mental health. Concerns have been raised that social media may lead to body image dissatisfaction [ 6 ], increase the risk of addiction and cyberbullying involvement [ 5 ], contribute to phubbing behaviors [ 7 ], and negatively affects mood [ 8 ]. Excessive use has increased loneliness, fear of missing out, and decreased subjective well-being and life satisfaction [ 8 ]. Users at risk of social media addiction often report depressive symptoms and lower self-esteem [ 9 ].
Overall, findings regarding the impact of social media on mental health pointed out some essential resources for psychological well-being through rewarding online social interactions. However, there is a need to raise awareness about the possible risks associated with excessive use, which can negatively affect mental health and everyday functioning [ 9 ]. There is neither a negative nor positive consensus regarding the effects of social media on people. However, by teaching people social media literacy, we can maximize their chances of having balanced, safe, and meaningful experiences on these platforms [ 10 ].
We encourage researchers to submit their research articles and contribute to a more differentiated overview of the impact of social media on mental health. BMC Psychology welcomes submissions to its new collection, which promises to present the latest findings in the emerging field of social media research. We seek research papers using qualitative and quantitative methods, focusing on social media users’ positive and negative aspects. We believe this collection will provide a more comprehensive picture of social media’s positive and negative effects on users’ mental health.
Data Availability
Not applicable.
Statista. (2022). Time spent on social media [Chart]. Accessed June 14, 2023, from https://www.statista.com/chart/18983/time-spent-on-social-media/ .
Pew Research Center. (2023). Teens and social media: Key findings from Pew Research Center surveys. Retrieved June 14, 2023, from https://www.pewresearch.org/short-reads/2023/04/24/teens-and-social-media-key-findings-from-pew-research-center-surveys/ .
Boer, M., Van Den Eijnden, R. J., Boniel-Nissim, M., Wong, S. L., Inchley, J. C.,Badura, P.,… Stevens, G. W. (2020). Adolescents’ intense and problematic social media use and their well-being in 29 countries. Journal of Adolescent Health , 66(6), S89-S99. https://doi.org/10.1016/j.jadohealth.2020.02.011.
Marciano L, Ostroumova M, Schulz PJ, Camerini AL. Digital media use and adolescents’ mental health during the COVID-19 pandemic: a systematic review and meta-analysis. Front Public Health. 2022;9:2208. https://doi.org/10.3389/fpubh.2021.641831 .
Article Google Scholar
Naslund JA, Bondre A, Torous J, Aschbrenner KA. Social media and mental health: benefits, risks, and opportunities for research and practice. J Technol Behav Sci. 2020;5:245–57. https://doi.org/10.1007/s41347-020-00094-8 .
Article PubMed PubMed Central Google Scholar
Harriger JA, Thompson JK, Tiggemann M. TikTok, TikTok, the time is now: future directions in social media and body image. Body Image. 2023;44:222–6. https://doi.org/10.1016/j.bodyim.2021.12.005 .
Article PubMed Google Scholar
Chi LC, Tang TC, Tang E. The phubbing phenomenon: a cross-sectional study on the relationships among social media addiction, fear of missing out, personality traits, and phubbing behavior. Curr Psychol. 2022;41(2):1112–23. https://doi.org/10.1007/s12144-022-0135-4 .
Valkenburg PM. Social media use and well-being: what we know and what we need to know. Curr Opin Psychol. 2022;45:101294. https://doi.org/10.1016/j.copsyc.2020.101294 .
Bányai F, Zsila Á, Király O, Maraz A, Elekes Z, Griffiths MD, Urbán R, Farkas J, Rigó P Jr, Demetrovics Z. Problematic social media use: results from a large-scale nationally representative adolescent sample. PLoS ONE. 2017;12(1):e0169839. https://doi.org/10.1371/journal.pone.0169839 .
American Psychological Association. (2023). APA panel issues recommendations for adolescent social media use. Retrieved from https://apa-panel-issues-recommendations-for-adolescent-social-media-use-774560.html .
Download references
Acknowledgements
Ágnes Zsila was supported by the ÚNKP-22-4 New National Excellence Program of the Ministry for Culture and Innovation from the source of the National Research, Development and Innovation Fund.
Author information
Authors and affiliations.
Institute of Psychology, Pázmány Péter Catholic University, Budapest, Hungary
Ágnes Zsila
Institute of Psychology, ELTE Eötvös Loránd University, Budapest, Hungary
Department of Psychology, College of Science, University of Santo Tomas, Manila, 1008, Philippines
Marc Eric S. Reyes
You can also search for this author in PubMed Google Scholar
Contributions
AZ conceived and drafted the Editorial. MESR wrote the abstract and revised the Editorial. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Marc Eric S. Reyes .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors have no competing interests to declare relevant to the content of this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zsila, Á., Reyes, M.E.S. Pros & cons: impacts of social media on mental health. BMC Psychol 11 , 201 (2023). https://doi.org/10.1186/s40359-023-01243-x
Download citation
Received : 15 June 2023
Accepted : 03 July 2023
Published : 06 July 2023
DOI : https://doi.org/10.1186/s40359-023-01243-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social media
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- UTHealth Houston
The impact of bullying on mental health
There has been a lot of conversation in the media lately about bullying and the damaging impact it can have on mental health. Bullying is defined as the unwanted, aggressive behavior that presents in an engagement with another individual or individuals that involves a real or perceived power imbalance. Thinking back, most people can probably identify a time when they experienced bullying and how it made them feel. Bullying happens everywhere: schools, workplace, friend groups, online, and it’s important to remember it does not just happen to children.
With the technological world that we have moved in to, access to bullying has grown significantly. Cyberbullying, which refers to being bullied online or through digital devices and can happen through text messages, social media apps, gaming chats and platforms, and pretty much anywhere people view and share content. According to the Center for Disease Control and Prevention’s 2019 Youth Risk Behavior Surveillance System , data shows that an estimated 15.7% of high school students were electronically bullied in the 12 months prior to the survey.
Just because many of us are going to school or working from home doesn’t mean the bullying has stopped. The pandemic has led to youth being connected significantly more than before to their digital devices. For some, digital contact has been the only way they have communicated within the past year. L1ght , an organization that tracks online harassment, is reporting that cyberbullying has increased 70% in just the past few months.
The effects of bullying have serious and lasting negative impacts on our mental health and overall wellbeing. Bullying can cause feelings of rejection, exclusion, isolation, low self-esteem, and some individuals can develop depression and anxiety as a result. In some cases it can even develop into Acute Stress Disorder or Post Traumatic Stress Disorder. Research has shown that being a victim of bullying can lead to longer term impacts including interpersonal violence, substance use, sexual violence, poor social functioning, and poor performance. Even witnessing bullying can impact one’s wellbeing.
Being bullied at a young age can affect someone well past childhood and can cause lifelong psychological damage. During these young years, children are identifying roles, developing personalities, and figuring out who they are. When a young person is bullied, it can lead to problems with trust in others, self-esteem, and anger. It can be hard to develop relationships with others at an older age when you may not have had any at a younger age. When we’re repeatedly presented with blows about who we are or what we are doing, we create a poor self-image and expect that others see us in the same light.
Bullying often leaves us with lingering feelings, turning into anger towards others or ourselves. When one goes through bullying over a long period of time, they may begin to blame themselves for being bullied. Thinking thoughts such as “If I wasn’t so ugly, people would leave me alone,” or “If I tried harder, people wouldn’t make fun of me.” The types of thoughts can change how we see and feel about ourselves and leave long-term impacts.
If you are a parent to a digital teen and you are working from home, you are spending more time than ever with your children. We have a great opportunity to be mindful of what our youth are doing online and how these interactions with others may be affecting them. Create rules on internet use that limits screen time. This can be challenging, since those of us working from home are stuck to screens all day, but these rules can help create a balance around positive, healthy social time and engaging in other activities that make them less likely to engage in cyberbullying. Allow youth to stay connected with others through positive engagement, such as Facetime or weekly Zoom chats that can help balance connectivity. It is very difficult for children and teens to not be connected to others, as these connections are necessary for growth and development. Have open communication and ensure your children know they can talk to you about what is going on in their lives.
If you are concerned that you or your child are experiencing lingering feelings from the results of bullying, it may be helpful to connect with a mental health professional to identify concerns and negative thinking patterns that may still be present. The STOMP Out Bullying HelpChat Line is a free confidential online chat that helps youth ages 13-24 with issues around bullying and cyberbullying. If you are interested in reading about bullying statistics here is a great resource: Pacer’s National Bullying Prevention Center
Written by: Meaghan Warner, LCSW-S
- McGovern Medical School Facebook Page
- McGovern Medical School X Page
- McGovern Medical School Instagram Page
- McGovern Medical School YouTube Page
- McGovern Medical School LinkedIn Page
- Medical School IT (MSIT)
- Campus Carry
- Emergency Info
- How to report sexual misconduct
- University Website Policies
Home — Essay Samples — Social Issues — Gun Violence — The psychological impact of gun violence on communities
The Psychological Impact of Gun Violence on Communities
- Categories: Gun Violence
About this sample

Words: 673 |
Published: Mar 25, 2024
Words: 673 | Page: 1 | 4 min read
Table of contents
Introduction:, impact on survivors:, witnesses and bystanders:, community-level impact:, intergenerational effects:, addressing the psychological impact:, conclusion:.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Social Issues

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 955 words
3 pages / 1355 words
1 pages / 499 words
2 pages / 858 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Gun Violence
Why are guns dangerous? Guns, often considered tools for personal protection, pose significant dangers that extend far beyond their intended purposes. This essay delves into the inherent dangers of firearms by analyzing the [...]
Public health plays a vital role in addressing gun violence by employing a comprehensive, evidence-based approach. Surveillance and data collection enable the identification of patterns and high-risk populations, contributing to [...]
"Gun violence is a pervasive and complex issue that has far-reaching effects on individuals, communities, and society as a whole. From mass shootings to daily incidents of violence, the impact of gun violence is profound and [...]
Trebuchets and catapults are two of the most iconic and widely recognized. Both of these machines were used in warfare for centuries, and they played a crucial role in the outcome of many battles and sieges. Despite their [...]
The language of gun control legislation plays a crucial role in shaping public opinion and influencing policy decisions. By analyzing the rhetorical strategies employed, the implications of specific terminology, and the [...]
The end of the 2010 decade is soon to come, over 1.2 million American lives have been either lost to gun violence or have been severely injured. Approximately 329 people are shot daily in America. Gun violence is a [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Open access
- Published: 12 December 2023
Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review
- C. E. Hall 1 , 2 ,
- H. Wehling 1 ,
- J. Stansfield 3 ,
- J. South 3 ,
- S. K. Brooks 2 ,
- N. Greenberg 2 , 4 ,
- R. Amlôt 1 &
- D. Weston 1
BMC Public Health volume 23 , Article number: 2482 ( 2023 ) Cite this article
1772 Accesses
21 Altmetric
Metrics details
The ability of the public to remain psychologically resilient in the face of public health emergencies and disasters (such as the COVID-19 pandemic) is a key factor in the effectiveness of a national response to such events. Community resilience and social capital are often perceived as beneficial and ensuring that a community is socially and psychologically resilient may aid emergency response and recovery. This review presents a synthesis of literature which answers the following research questions: How are community resilience and social capital quantified in research?; What is the impact of community resilience on mental wellbeing?; What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, What types of interventions enhance community resilience and social capital?
A scoping review procedure was followed. Searches were run across Medline, PsycInfo, and EMBASE, with search terms covering both community resilience and social capital, public health emergencies, and mental health. 26 papers met the inclusion criteria.
The majority of retained papers originated in the USA, used a survey methodology to collect data, and involved a natural disaster. There was no common method for measuring community resilience or social capital. The association between community resilience and social capital with mental health was regarded as positive in most cases. However, we found that community resilience, and social capital, were initially negatively impacted by public health emergencies and enhanced by social group activities.
Several key recommendations are proposed based on the outcomes from the review, which include: the need for a standardised and validated approach to measuring both community resilience and social capital; that there should be enhanced effort to improve preparedness to public health emergencies in communities by gauging current levels of community resilience and social capital; that community resilience and social capital should be bolstered if areas are at risk of disasters or public health emergencies; the need to ensure that suitable short-term support is provided to communities with high resilience in the immediate aftermath of a public health emergency or disaster; the importance of conducting robust evaluation of community resilience initiatives deployed during the COVID-19 pandemic.
Peer Review reports
For the general population, public health emergencies and disasters (e.g., natural disasters; infectious disease outbreaks; Chemical, Biological, Radiological or Nuclear incidents) can give rise to a plethora of negative outcomes relating to both health (e.g. increased mental health problems [ 1 , 2 , 3 , 4 ]) and the economy (e.g., increased unemployment and decreased levels of tourism [ 4 , 5 , 6 ]). COVID-19 is a current, and ongoing, example of a public health emergency which has affected over 421 million individuals worldwide [ 7 ]. The long term implications of COVID-19 are not yet known, but there are likely to be repercussions for physical health, mental health, and other non-health related outcomes for a substantial time to come [ 8 , 9 ]. As a result, it is critical to establish methods which may inform approaches to alleviate the longer-term negative consequences that are likely to emerge in the aftermath of both COVID-19 and any future public health emergency.
The definition of resilience often differs within the literature, but ultimately resilience is considered a dynamic process of adaptation. It is related to processes and capabilities at the individual, community and system level that result in good health and social outcomes, in spite of negative events, serious threats and hazards [ 10 ]. Furthermore, Ziglio [ 10 ] refers to four key types of resilience capacity: adaptive, the ability to withstand and adjust to unfavourable conditions and shocks; absorptive, the ability to withstand but also to recover and manage using available assets and skills; anticipatory, the ability to predict and minimize vulnerability; and transformative, transformative change so that systems better cope with new conditions.
There is no one settled definition of community resilience (CR). However, it generally relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ]. Social capital (SC) is considered a major determinant of CR [ 12 , 13 ], and reflects strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats. SC is often broken down into further categories [ 15 ], for example: cognitive SC (i.e. perceptions of community relations, such as trust, mutual help and attachment) and structural SC (i.e. what actually happens within the community, such as participation, socialising) [ 16 ]; or, bonding SC (i.e. connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ]) and bridging SC (i.e. acquaintances or individuals loosely connected that span different social groups [ 18 ]). Generally, CR is perceived to be primarily beneficial for multiple reasons (e.g. increased social support [ 18 , 19 ], protection of mental health [ 20 , 21 ]), and strengthening community resilience is a stated health goal of the World Health Organisation [ 22 ] when aiming to alleviate health inequalities and protect wellbeing. This is also reflected by organisations such as Public Health England (now split into the UK Health Security Agency and the Office for Health Improvement and Disparities) [ 23 ] and more recently, CR has been targeted through the endorsement of Community Champions (who are volunteers trained to support and to help improve health and wellbeing. Community Champions also reflect their local communities in terms of population demographics for example age, ethnicity and gender) as part of the COVID-19 response in the UK (e.g. [ 24 , 25 ]).
Despite the vested interest in bolstering communities, the research base establishing: how to understand and measure CR and SC; the effect of CR and SC, both during and following a public health emergency (such as the COVID-19 pandemic); and which types of CR or SC are the most effective to engage, is relatively small. Given the importance of ensuring resilience against, and swift recovery from, public health emergencies, it is critically important to establish and understand the evidence base for these approaches. As a result, the current review sought to answer the following research questions: (1) How are CR and SC quantified in research?; (2) What is the impact of community resilience on mental wellbeing?; (3) What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?
By collating research in order to answer these research questions, the authors have been able to propose several key recommendations that could be used to both enhance and evaluate CR and SC effectively to facilitate the long-term recovery from COVID-19, and also to inform the use of CR and SC in any future public health disasters and emergencies.
A scoping review methodology was followed due to the ease of summarising literature on a given topic for policy makers and practitioners [ 26 ], and is detailed in the following sections.
Identification of relevant studies
An initial search strategy was developed by authors CH and DW and included terms which related to: CR and SC, given the absence of a consistent definition of CR, and the link between CR and SC, the review focuses on both CR and SC to identify as much relevant literature as possible (adapted for purpose from Annex 1: [ 27 ], as well as through consultation with review commissioners); public health emergencies and disasters [ 28 , 29 , 30 , 31 ], and psychological wellbeing and recovery (derived a priori from literature). To ensure a focus on both public health and psychological research, the final search was carried across Medline, PsycInfo, and EMBASE using OVID. The final search took place on the 18th of May 2020, the search strategy used for all three databases can be found in Supplementary file 1 .
Selection criteria
The inclusion and exclusion criteria were developed alongside the search strategy. Initially the criteria were relatively inclusive and were subject to iterative development to reflect the authors’ familiarisation with the literature. For example, the decision was taken to exclude research which focused exclusively on social support and did not mention communities as an initial title/abstract search suggested that the majority of this literature did not meet the requirements of our research question.
The full and final inclusion and exclusion criteria used can be found in Supplementary file 2 . In summary, authors decided to focus on the general population (i.e., non-specialist, e.g. non-healthcare worker or government official) to allow the review to remain community focused. The research must also have assessed the impact of CR and/or SC on mental health and wellbeing, resilience, and recovery during and following public health emergencies and infectious disease outbreaks which affect communities (to ensure the research is relevant to the review aims), have conducted primary research, and have a full text available or provided by the first author when contacted.
Charting the data
All papers were first title and abstract screened by CH or DW. Papers then were full text reviewed by CH to ensure each paper met the required eligibility criteria, if unsure about a paper it was also full text reviewed by DW. All papers that were retained post full-text review were subjected to a standardised data extraction procedure. A table was made for the purpose of extracting the following data: title, authors, origin, year of publication, study design, aim, disaster type, sample size and characteristics, variables examined, results, restrictions/limitations, and recommendations. Supplementary file 3 details the charting the data process.
Analytical method
Data was synthesised using a Framework approach [ 32 ], a common method for analysing qualitative research. This method was chosen as it was originally used for large-scale social policy research [ 33 ] as it seeks to identify: what works, for whom, in what conditions, and why [ 34 ]. This approach is also useful for identifying commonalities and differences in qualitative data and potential relationships between different parts of the data [ 33 ]. An a priori framework was established by CH and DW. Extracted data was synthesised in relation to each research question, and the process was iterative to ensure maximum saturation using the available data.
Study selection
The final search strategy yielded 3584 records. Following the removal of duplicates, 2191 records remained and were included in title and abstract screening. A PRISMA flow diagram is presented in Fig. 1 .
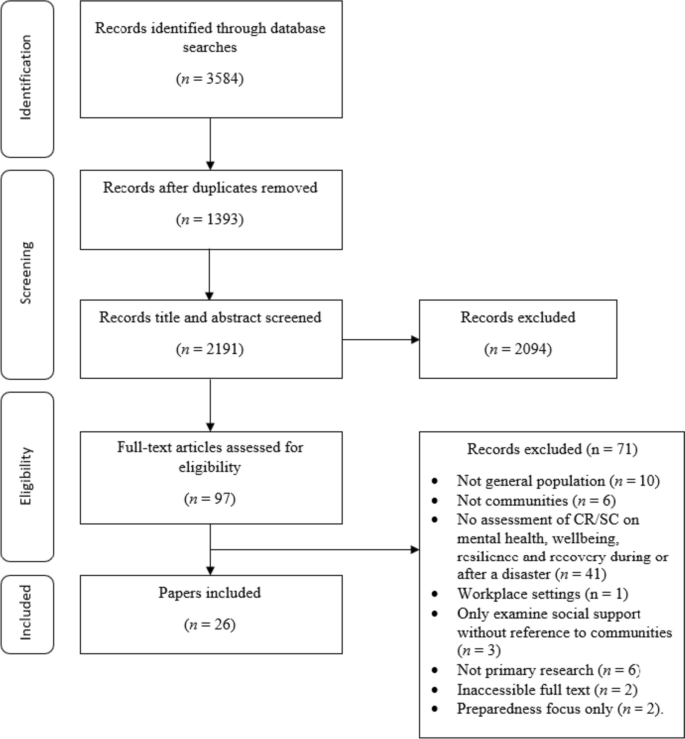
PRISMA flow diagram
At the title and abstract screening stage, the process became more iterative as the inclusion criteria were developed and refined. For the first iteration of screening, CH or DW sorted all records into ‘include,’ ‘exclude,’ and ‘unsure’. All ‘unsure’ papers were re-assessed by CH, and a random selection of ~ 20% of these were also assessed by DW. Where there was disagreement between authors the records were retained, and full text screened. The remaining papers were reviewed by CH, and all records were categorised into ‘include’ and ‘exclude’. Following full-text screening, 26 papers were retained for use in the review.
Study characteristics
This section of the review addresses study characteristics of those which met the inclusion criteria, which comprises: date of publication, country of origin, study design, study location, disaster, and variables examined.
Date of publication
Publication dates across the 26 papers spanned from 2008 to 2020 (see Fig. 2 ). The number of papers published was relatively low and consistent across this timescale (i.e. 1–2 per year, except 2010 and 2013 when none were published) up until 2017 where the number of papers peaked at 5. From 2017 to 2020 there were 15 papers published in total. The amount of papers published in recent years suggests a shift in research and interest towards CR and SC in a disaster/ public health emergency context.
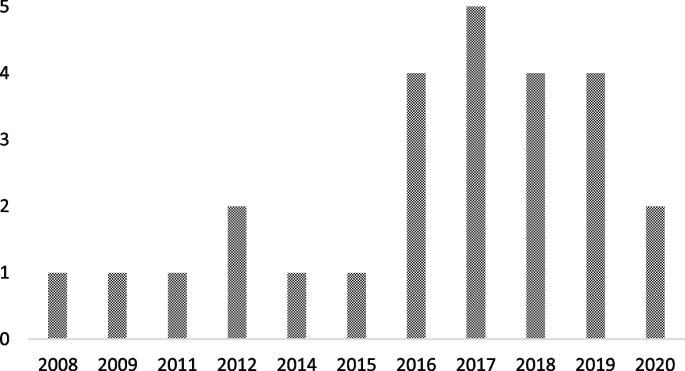
Graph to show retained papers date of publication
Country of origin
The locations of the first authors’ institutes at the time of publication were extracted to provide a geographical spread of the retained papers. The majority originated from the USA [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ], followed by China [ 42 , 43 , 44 , 45 , 46 ], Japan [ 47 , 48 , 49 , 50 ], Australia [ 51 , 52 , 53 ], The Netherlands [ 54 , 55 ], New Zealand [ 56 ], Peru [ 57 ], Iran [ 58 ], Austria [ 59 ], and Croatia [ 60 ].
There were multiple methodological approaches carried out across retained papers. The most common formats included surveys or questionnaires [ 36 , 37 , 38 , 42 , 46 , 47 , 48 , 49 , 50 , 53 , 54 , 55 , 57 , 59 ], followed by interviews [ 39 , 40 , 43 , 51 , 52 , 60 ]. Four papers used both surveys and interviews [ 35 , 41 , 45 , 58 ], and two papers conducted data analysis (one using open access data from a Social Survey [ 44 ] and one using a Primary Health Organisations Register [ 56 ]).
Study location
The majority of the studies were carried out in Japan [ 36 , 42 , 44 , 47 , 48 , 49 , 50 ], followed by the USA [ 35 , 37 , 38 , 39 , 40 , 41 ], China [ 43 , 45 , 46 , 53 ], Australia [ 51 , 52 ], and the UK [ 54 , 55 ]. The remaining studies were carried out in Croatia [ 60 ], Peru [ 57 ], Austria [ 59 ], New Zealand [ 56 ] and Iran [ 58 ].
Multiple different types of disaster were researched across the retained papers. Earthquakes were the most common type of disaster examined [ 45 , 47 , 49 , 50 , 53 , 56 , 57 , 58 ], followed by research which assessed the impact of two disastrous events which had happened in the same area (e.g. Hurricane Katrina and the Deepwater Horizon oil spill in Mississippi, and the Great East Japan earthquake and Tsunami; [ 36 , 37 , 38 , 42 , 44 , 48 ]). Other disaster types included: flooding [ 51 , 54 , 55 , 59 , 60 ], hurricanes [ 35 , 39 , 41 ], infectious disease outbreaks [ 43 , 46 ], oil spillage [ 40 ], and drought [ 52 ].
Variables of interest examined
Across the 26 retained papers: eight referred to examining the impact of SC [ 35 , 37 , 39 , 41 , 46 , 49 , 55 , 60 ]; eight examined the impact of cognitive and structural SC as separate entities [ 40 , 42 , 45 , 48 , 50 , 54 , 57 , 59 ]; one examined bridging and bonding SC as separate entities [ 58 ]; two examined the impact of CR [ 38 , 56 ]; and two employed a qualitative methodology but drew findings in relation to bonding and bridging SC, and SC generally [ 51 , 52 ]. Additionally, five papers examined the impact of the following variables: ‘community social cohesion’ [ 36 ], ‘neighbourhood connectedness’ [ 44 ], ‘social support at the community level’ [ 47 ], ‘community connectedness’ [ 43 ] and ‘sense of community’ [ 53 ]. Table 1 provides additional details on this.
How is CR and SC measured or quantified in research?
The measures used to examine CR and SC are presented Table 1 . It is apparent that there is no uniformity in how SC or CR is measured across the research. Multiple measures are used throughout the retained studies, and nearly all are unique. Additionally, SC was examined at multiple different levels (e.g. cognitive and structural, bonding and bridging), and in multiple different forms (e.g. community connectedness, community cohesion).
What is the association between CR and SC on mental wellbeing?
To best compare research, the following section reports on CR, and facets of SC separately. Please see Supplementary file 4 for additional information on retained papers methods of measuring mental wellbeing.
- Community resilience
CR relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ].
The impact of CR on mental wellbeing was consistently positive. For example, research indicated that there was a positive association between CR and number of common mental health (i.e. anxiety and mood) treatments post-disaster [ 56 ]. Similarly, other research suggests that CR is positively related to psychological resilience, which is inversely related to depressive symptoms) [ 37 ]. The same research also concluded that CR is protective of psychological resilience and is therefore protective of depressive symptoms [ 37 ].
- Social capital
SC reflects the strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats.
There were inconsistencies across research which examined the impact of abstract SC (i.e. not refined into bonding/bridging or structural/cognitive) on mental wellbeing. However, for the majority of cases, research deems SC to be beneficial. For example, research has concluded that, SC is protective against post-traumatic stress disorder [ 55 ], anxiety [ 46 ], psychological distress [ 50 ], and stress [ 46 ]. Additionally, SC has been found to facilitate post-traumatic growth [ 38 ], and also to be useful to be drawn upon in times of stress [ 52 ], both of which could be protective of mental health. Similarly, research has also found that emotional recovery following a disaster is more difficult for those who report to have low levels of SC [ 51 ].
Conversely, however, research has also concluded that when other situational factors (e.g. personal resources) were controlled for, a positive relationship between community resources and life satisfaction was no longer significant [ 60 ]. Furthermore, some research has concluded that a high level of SC can result in a community facing greater stress immediately post disaster. Indeed, one retained paper found that high levels of SC correlate with higher levels of post-traumatic stress immediately following a disaster [ 39 ]. However, in the later stages following a disaster, this relationship can reverse, with SC subsequently providing an aid to recovery [ 41 ]. By way of explanation, some researchers have suggested that communities with stronger SC carry the greatest load in terms of helping others (i.e. family, friends and neighbours) as well as themselves immediately following the disaster, but then as time passes the communities recover at a faster rate as they are able to rely on their social networks for support [ 41 ].
Cognitive and structural social capital
Cognitive SC refers to perceptions of community relations, such as trust, mutual help and attachment, and structural SC refers to what actually happens within the community, such as participation, socialising [ 16 ].
Cognitive SC has been found to be protective [ 49 ] against PTSD [ 54 , 57 ], depression [ 40 , 54 ]) mild mood disorder; [ 48 ]), anxiety [ 48 , 54 ] and increase self-efficacy [ 59 ].
For structural SC, research is again inconsistent. On the one hand, structural SC has been found to: increase perceived self-efficacy, be protective of depression [ 40 ], buffer the impact of housing damage on cognitive decline [ 42 ] and provide support during disasters and over the recovery period [ 59 ]. However, on the other hand, it has been found to have no association with PTSD [ 54 , 57 ] or depression, and is also associated with a higher prevalence of anxiety [ 54 ]. Similarly, it is also suggested by additional research that structural SC can harm women’s mental health, either due to the pressure of expectations to help and support others or feelings of isolation [ 49 ].
Bonding and bridging social capital
Bonding SC refers to connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ], and bridging SC refers to acquaintances or individuals loosely connected that span different social groups [ 18 ].
One research study concluded that both bonding and bridging SC were protective against post-traumatic stress disorder symptoms [ 58 ]. Bridging capital was deemed to be around twice as effective in buffering against post-traumatic stress disorder than bonding SC [ 58 ].
Other community variables
Community social cohesion was significantly associated with a lower risk of post-traumatic stress disorder symptom development [ 35 ], and this was apparent even whilst controlling for depressive symptoms at baseline and disaster impact variables (e.g. loss of family member or housing damage) [ 36 ]. Similarly, sense of community, community connectedness, social support at the community level and neighbourhood connectedness all provided protective benefits for a range of mental health, wellbeing and recovery variables, including: depression [ 53 ], subjective wellbeing (in older adults only) [ 43 ], psychological distress [ 47 ], happiness [ 44 ] and life satisfaction [ 53 ].
Research has also concluded that community level social support is protective against mild mood and anxiety disorder, but only for individuals who have had no previous disaster experience [ 48 ]. Additionally, a study which separated SC into social cohesion and social participation concluded that at a community level, social cohesion is protective against depression [ 49 ] whereas social participation at community level is associated with an increased risk of depression amongst women [ 49 ].
What is the impact of Infectious disease outbreaks / disasters and emergencies on community resilience?
From a cross-sectional perspective, research has indicated that disasters and emergencies can have a negative effect on certain types of SC. Specifically, cognitive SC has been found to be impacted by disaster impact, whereas structural SC has gone unaffected [ 45 ]. Disaster impact has also been shown to have a negative effect on community relationships more generally [ 52 ].
Additionally, of the eight studies which collected data at multiple time points [ 35 , 36 , 41 , 42 , 47 , 49 , 56 , 60 ], three reported the effect of a disaster on the level of SC within a community [ 40 , 42 , 49 ]. All three of these studies concluded that disasters may have a negative impact on the levels of SC within a community. The first study found that the Deepwater Horizon oil spill had a negative effect on SC and social support, and this in turn explained an overall increase in the levels of depression within the community [ 40 ]. A possible explanation for the negative effect lays in ‘corrosive communities’, known for increased social conflict and reduced social support, that are sometimes created following oil spills [ 40 ]. It is proposed that corrosive communities often emerge due to a loss of natural resources that bring social groups together (e.g., for recreational activities), as well as social disparity (e.g., due to unequal distribution of economic impact) becoming apparent in the community following disaster [ 40 ]. The second study found that SC (in the form of social cohesion, informal socialising and social participation) decreased after the 2011 earthquake and tsunami in Japan; it was suggested that this change correlated with incidence of cognitive decline [ 42 ]. However, the third study reported more mixed effects based on physical circumstances of the communities’ natural environment: Following an earthquake, those who lived in mountainous areas with an initial high level of pre-community SC saw a decrease in SC post disaster [ 49 ]. However, communities in flat areas (which were home to younger residents and had a higher population density) saw an increase in SC [ 49 ]. It was proposed that this difference could be due to the need for those who lived in mountainous areas to seek prolonged refuge due to subsequent landslides [ 49 ].
What types of intervention enhance CR and SC and protect survivors?
There were mixed effects across the 26 retained papers when examining the effect of CR and SC on mental wellbeing. However, there is evidence that an increase in SC [ 56 , 57 ], with a focus on cognitive SC [ 57 ], namely by: building social networks [ 45 , 51 , 53 ], enhancing feelings of social cohesion [ 35 , 36 ] and promoting a sense of community [ 53 ], can result in an increase in CR and potentially protect survivors’ wellbeing and mental health following a disaster. An increase in SC may also aid in decreasing the need for individual psychological interventions in the aftermath of a disaster [ 55 ]. As a result, recommendations and suggested methods to bolster CR and SC from the retained papers have been extracted and separated into general methods, preparedness and policy level implementation.
General methods
Suggested methods to build SC included organising recreational activity-based groups [ 44 ] to broaden [ 51 , 53 ] and preserve current social networks [ 42 ], introducing initiatives to increase social cohesion and trust [ 51 ], and volunteering to increase the number of social ties between residents [ 59 ]. Research also notes that it is important to take a ‘no one left behind approach’ when organising recreational and social community events, as failure to do so could induce feelings of isolation for some members of the community [ 49 ]. Furthermore, gender differences should also be considered as research indicates that males and females may react differently to community level SC (as evidence suggests males are instead more impacted by individual level SC; in comparison to women who have larger and more diverse social networks [ 49 ]). Therefore, interventions which aim to raise community level social participation, with the aim of expanding social connections and gaining support, may be beneficial [ 42 , 47 ].
Preparedness
In order to prepare for disasters, it may be beneficial to introduce community-targeted methods or interventions to increase levels of SC and CR as these may aid in ameliorating the consequences of a public health emergency or disaster [ 57 ]. To indicate which communities have low levels of SC, one study suggests implementing a 3-item scale of social cohesion to map areas and target interventions [ 42 ].
It is important to consider that communities with a high level of SC may have a lower level of risk perception, due to the established connections and supportive network they have with those around them [ 61 ]. However, for the purpose of preparedness, this is not ideal as perception of risk is a key factor when seeking to encourage behavioural adherence. This could be overcome by introducing communication strategies which emphasise the necessity of social support, but also highlights the need for additional measures to reduce residual risk [ 59 ]. Furthermore, support in the form of financial assistance to foster current community initiatives may prove beneficial to rural areas, for example through the use of an asset-based community development framework [ 52 ].
Policy level
At a policy level, the included papers suggest a range of ways that CR and SC could be bolstered and used. These include: providing financial support for community initiatives and collective coping strategies, (e.g. using asset-based community development [ 52 ]); ensuring policies for long-term recovery focus on community sustainable development (e.g. community festival and community centre activities) [ 44 ]; and development of a network amongst cooperative corporations formed for reconstruction and to organise self-help recovery sessions among residents of adjacent areas [ 58 ].
This scoping review sought to synthesise literature concerning the role of SC and CR during public health emergencies and disasters. Specifically, in this review we have examined: the methods used to measure CR and SC; the impact of CR and SC on mental wellbeing during disasters and emergencies; the impact of disasters and emergencies on CR and SC; and the types of interventions which can be used to enhance CR. To do this, data was extracted from 26 peer-reviewed journal articles. From this synthesis, several key themes have been identified, which can be used to develop guidelines and recommendations for deploying CR and SC in a public health emergency or disaster context. These key themes and resulting recommendations are summarised below.
Firstly, this review established that there is no consistent or standardised approach to measuring CR or SC within the general population. This finding is consistent with a review conducted by the World Health Organization which concludes that despite there being a number of frameworks that contain indicators across different determinants of health, there is a lack of consensus on priority areas for measurement and no widely accepted indicator [ 27 ]. As a result, there are many measures of CR and SC apparent within the literature (e.g., [ 62 , 63 ]), an example of a developed and validated measure is provided by Sherrieb, Norris and Galea [ 64 ]. Similarly, the definitions of CR and SC differ widely between researchers, which created a barrier to comparing and summarising information. Therefore, future research could seek to compare various interpretations of CR and to identify any overlapping concepts. However, a previous systemic review conducted by Patel et al. (2017) concludes that there are nine core elements of CR (local knowledge, community networks and relationships, communication, health, governance and leadership, resources, economic investment, preparedness, and mental outlook), with 19 further sub-elements therein [ 30 ]. Therefore, as CR is a multi-dimensional construct, the implications from the findings are that multiple aspects of social infrastructure may need to be considered.
Secondly, our synthesis of research concerning the role of CR and SC for ensuring mental health and wellbeing during, or following, a public health emergency or disaster revealed mixed effects. Much of the research indicates either a generally protective effect on mental health and wellbeing, or no effect; however, the literature demonstrates some potential for a high level of CR/SC to backfire and result in a negative effect for populations during, or following, a public health emergency or disaster. Considered together, our synthesis indicates that cognitive SC is the only facet of SC which was perceived as universally protective across all retained papers. This is consistent with a systematic review which also concludes that: (a) community level cognitive SC is associated with a lower risk of common mental disorders, while; (b) community level structural SC had inconsistent effects [ 65 ].
Further examination of additional data extracted from studies which found that CR/SC had a negative effect on mental health and wellbeing revealed no commonalities that might explain these effects (Please see Supplementary file 5 for additional information)
One potential explanation may come from a retained paper which found that high levels of SC result in an increase in stress level immediately post disaster [ 41 ]. This was suggested to be due to individuals having greater burdens due to wishing to help and support their wide networks as well as themselves. However, as time passes the levels of SC allow the community to come together and recover at a faster rate [ 41 ]. As this was the only retained paper which produced this finding, it would be beneficial for future research to examine boundary conditions for the positive effects of CR/SC; that is, to explore circumstances under which CR/SC may be more likely to put communities at greater risk. This further research should also include additional longitudinal research to validate the conclusions drawn by [ 41 ] as resilience is a dynamic process of adaption.
Thirdly, disasters and emergencies were generally found to have a negative effect on levels of SC. One retained paper found a mixed effect of SC in relation to an earthquake, however this paper separated participants by area in which they lived (i.e., mountainous vs. flat), which explains this inconsistent effect [ 49 ]. Dangerous areas (i.e. mountainous) saw a decrease in community SC in comparison to safer areas following the earthquake (an effect the authors attributed to the need to seek prolonged refuge), whereas participants from the safer areas (which are home to younger residents with a higher population density) saw an increase in SC [ 49 ]. This is consistent with the idea that being able to participate socially is a key element of SC [ 12 ]. Overall, however, this was the only retained paper which produced a variable finding in relation to the effect of disaster on levels of CR/SC.
Finally, research identified through our synthesis promotes the idea of bolstering SC (particularly cognitive SC) and cohesion in communities likely to be affected by disaster to improve levels of CR. This finding provides further understanding of the relationship between CR and SC; an association that has been reported in various articles seeking to provide conceptual frameworks (e.g., [ 66 , 67 ]) as well as indicator/measurement frameworks [ 27 ]. Therefore, this could be done by creating and promoting initiatives which foster SC and create bonds within the community. Papers included in the current review suggest that recreational-based activity groups and volunteering are potential methods for fostering SC and creating community bonds [ 44 , 51 , 59 ]. Similarly, further research demonstrates that feelings of social cohesion are enhanced by general social activities (e.g. fairs and parades [ 18 ]). Also, actively encouraging activities, programs and interventions which enhance connectedness and SC have been reported to be desirable to increase CR [ 68 ]. This suggestion is supported by a recent scoping review of literature [ 67 ] examined community champion approaches for the COVID-19 pandemic response and recovery and established that creating and promoting SC focused initiatives within the community during pandemic response is highly beneficial [ 67 ]. In terms of preparedness, research states that it may be beneficial for levels of SC and CR in communities at risk to be assessed, to allow targeted interventions where the population may be at most risk following an incident [ 42 , 44 ]. Additionally, from a more critical perspective, we acknowledge that ‘resilience’ can often be perceived as a focus on individual capacity to adapt to adversity rather than changing or mitigating the causes of adverse conditions [ 69 , 70 ]. Therefore, CR requires an integrated system approach across individual, community and structural levels [ 17 ]. Also, it is important that community members are engaged in defining and agreeing how community resilience is measured [ 27 ] rather than it being imposed by system leads or decision-makers.
In the aftermath of the pandemic, is it expected that there will be long-term repercussions both from an economic [ 8 ] and a mental health perspective [ 71 ]. Furthermore, the findings from this review suggest that although those in areas with high levels of SC may be negatively affected in the acute stage, as time passes, they have potential to rebound at a faster rate than those with lower levels of SC. Ongoing evaluation of the effectiveness of current initiatives as the COVID-19 pandemic progresses into a recovery phase will be invaluable for supplementing the evidence base identified through this review.
- Recommendations
As a result of this review, a number of recommendations are suggested for policy and practice during public health emergencies and recovery.
Future research should seek to establish a standardised and validated approach to measuring and defining CR and SC within communities. There are ongoing efforts in this area, for example [ 72 ]. Additionally, community members should be involved in the process of defining how CR is measured.
There should be an enhanced effort to improve preparedness for public health emergencies and disasters in local communities by gauging current levels of SC and CR within communities using a standardised measure. This approach could support specific targeting of populations with low levels of CR/SC in case of a disaster or public health emergency, whilst also allowing for consideration of support for those with high levels of CR (as these populations can be heavily impacted initially following a disaster). By distinguishing levels of SC and CR, tailored community-centred approaches could be implemented, such as those listed in a guide released by PHE in 2015 [ 73 ].
CR and SC (specifically cognitive SC) should be bolstered if communities are at risk of experiencing a disaster or public health emergency. This can be achieved by using interventions which aim to increase a sense of community and create new social ties (e.g., recreational group activities, volunteering). Additionally, when aiming to achieve this, it is important to be mindful of the risk of increased levels of CR/SC to backfire, as well as seeking to advocate an integrated system approach across individual, community and structural levels.
It is necessary to be aware that although communities with high existing levels of resilience / SC may experience short-term negative consequences following a disaster, over time these communities might be able to recover at a faster rate. It is therefore important to ensure that suitable short-term support is provided to these communities in the immediate aftermath of a public health emergency or disaster.
Robust evaluation of the community resilience initiatives deployed during the COVID-19 pandemic response is essential to inform the evidence base concerning the effectiveness of CR/ SC. These evaluations should continue through the response phase and into the recovery phase to help develop our understanding of the long-term consequences of such interventions.
Limitations
Despite this review being the first in this specific topic area, there are limitations that must be considered. Firstly, it is necessary to note that communities are generally highly diverse and the term ‘community’ in academic literature is a subject of much debate (see: [ 74 ]), therefore this must be considered when comparing and collating research involving communities. Additionally, the measures of CR and SC differ substantially across research, including across the 26 retained papers used in the current review. This makes the act of comparing and collating research findings very difficult. This issue is highlighted as a key outcome from this review, and suggestions for how to overcome this in future research are provided. Additionally, we acknowledge that there will be a relationship between CR & SC even where studies measure only at individual or community level. A review [ 75 ] on articulating a hypothesis of the link to health inequalities suggests that wider structural determinants of health need to be accounted for. Secondly, despite the final search strategy encompassing terms for both CR and SC, only one retained paper directly measured CR; thus, making the research findings more relevant to SC. Future research could seek to focus on CR to allow for a comparison of findings. Thirdly, the review was conducted early in the COVID-19 pandemic and so does not include more recent publications focusing on resilience specifically in the context of COVID-19. Regardless of this fact, the synthesis of, and recommendations drawn from, the reviewed studies are agnostic to time and specific incident and contain critical elements necessary to address as the pandemic moves from response to recovery. Further research should review the effectiveness of specific interventions during the COVID-19 pandemic for collation in a subsequent update to this current paper. Fourthly, the current review synthesises findings from countries with individualistic and collectivistic cultures, which may account for some variation in the findings. Lastly, despite choosing a scoping review method for ease of synthesising a wide literature base for use by public health emergency researchers in a relatively tight timeframe, there are disadvantages of a scoping review approach to consider: (1) quality appraisal of retained studies was not carried out; (2) due to the broad nature of a scoping review, more refined and targeted reviews of literature (e.g., systematic reviews) may be able to provide more detailed research outcomes. Therefore, future research should seek to use alternative methods (e.g., empirical research, systematic reviews of literature) to add to the evidence base on CR and SC impact and use in public health practice.
This review sought to establish: (1) How CR and SC are quantified in research?; (2) The impact of community resilience on mental wellbeing?; (3) The impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?. The chosen search strategy yielded 26 relevant papers from which we were able extract information relating to the aims of this review.
Results from the review revealed that CR and SC are not measured consistently across research. The impact of CR / SC on mental health and wellbeing during emergencies and disasters is mixed (with some potential for backlash), however the literature does identify cognitive SC as particularly protective. Although only a small number of papers compared CR or SC before and after a disaster, the findings were relatively consistent: SC or CR is negatively impacted by a disaster. Methods suggested to bolster SC in communities were centred around social activities, such as recreational group activities and volunteering. Recommendations for both research and practice (with a particular focus on the ongoing COVID-19 pandemic) are also presented.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Social Capital
Zortea TC, Brenna CT, Joyce M, McClelland H, Tippett M, Tran MM, et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts. Crisis. 2020;42(6):474–87.
Article PubMed PubMed Central Google Scholar
Davis JR, Wilson S, Brock-Martin A, Glover S, Svendsen ER. The impact of disasters on populations with health and health care disparities. Disaster Med Pub Health Prep. 2010;4(1):30.
Article Google Scholar
Francescutti LH, Sauve M, Prasad AS. Natural disasters and healthcare: lessons to be learned. Healthc Manage Forum. 2017;30(1):53–5.
Article PubMed Google Scholar
Jones L, Palumbo D, Brown D. Coronavirus: How the pandemic has changed the world economy. BBC News; 2021. Accessible at: https://www.bbc.co.uk/news/business-51706225 .
Below R, Wallemacq P. Annual disaster statistical review 2017. Brussels: CRED, Centre for Research on the Epidemiology of Disasters; 2018.
Google Scholar
Qiu W, Chu C, Mao A, Wu J. The impacts on health, society, and economy of SARS and H7N9 outbreaks in China: a case comparison study. J Environ Public Health. 2018;2018:2710185.
Worldometer. COVID-19 coronavirus pandemic. 2021.
Harari D, Keep M. Coronavirus: economic impact house of commons library. Briefing Paper (Number 8866); 2021. Accessible at: https://commonslibrary.parliament.uk/research-briefings/cbp-8866/ .
Nabavi N. Covid-19: pandemic will cast a long shadow on mental health, warns England’s CMO. BMJ. 2021;373:n1655.
Ziglio E. Strengthening resilience: a priority shared by health 2020 and the sustainable development goals. No. WHO/EURO: 2017-6509-46275-66939. World Health Organization; Regional Office for Europe; 2017.
Asadzadeh A, Kotter T, Salehi P, Birkmann J. Operationalizing a concept: the systematic review of composite indicator building for measuring community disaster resilience. Int J Disaster Risk Reduct. 2017;25:147.
Sherrieb K, Norris F, Galea S. Measuring capacities for community resilience. Soc Indicators Res. 2010;99(2):227.
Poortinga W. Community resilience and health: the role of bonding, bridging, and linking aspects of social capital. Health Place. 2011;18(2):286–95.
Ferlander S. The importance of different forms of social capital for health. Acta Sociol. 2007;50(2):115–28.
Nakagawa Y, Shaw R. Social capital: a missing link to disaster recovery. Int J Mass Emerge Disasters. 2004;22(1):5–34.
Grootaert C, Narayan D, Jones VN, Woolcock M. Measuring social capital: an integrated questionnaire. Washington, DC: World Bank Working Paper, No. 18; 2004.
Adler PS, Kwon SW. Social capital: prospects for a new concept. Acad Manage Rev. 2002;27(1):17–40.
Aldrich DP, Meyer MA. Social capital and community resilience. Am Behav Sci. 2015;59(2):254–69.
Rodriguez-Llanes JM, Vos F, Guha-Sapir D. Measuring psychological resilience to disasters: are evidence-based indicators an achievable goal? Environ Health. 2013;12(1):115.
De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental Illness: a systematic review. J Epidemiol Community Health. 2005;59(8):619–27.
Bonanno GA, Galea S, Bucciarelli A, Vlahov D. Psychological resilience after disaster: New York City in the aftermath of the september 11th terrorist attack. Psychol Sci. 2006;17(3):181.
World Health Organization. Health 2020: a European policy framework and strategy for the 21st century. World Health Organization. Regional Office for Europe; 2013.
Public Health England. Community-Centred Public Health: Taking a Whole System Approach. 2020.
SPI-B. The role of Community Champion networks to increase engagement in the context of COVID19: Evidence and best practice. 2021.
Public Health England. Community champions: A rapid scoping review of community champion approaches for the pandemic response and recovery. 2021.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
World Health Organisation. WHO health evidence network synthesis report: what quantitative and qualitative methods have been developed to measure health-related community resilience at a national and local level. 2018.
Hall C, Williams N, Gauntlett L, Carter H, Amlôt R, Peterson L et al. Findings from systematic review of public perceptions and responses. PROACTIVE EU. Deliverable 1.1. 2019. Accessible at: https://proactive-h2020.eu/wp-content/uploads/2021/04/PROACTIVE_20210312_D1.1_V5_PHE_Systematic-Review-of-Public-Perceptions-and-Responses_revised.pdf .
Weston D, Ip A, Amlôt R. Examining the application of behaviour change theories in the context of Infectious disease outbreaks and emergency response: a review of reviews. BMC Public Health. 2020;20(1):1483.
Article PubMed PubMed Central CAS Google Scholar
Patel SS, Rogers MB, Amlôt R, Rubin GJ. What do we mean by ‘community resilience’? A systematic literature review of how it is defined in the literature. PLoS Curr. 2017;9:ecurrents.dis.db775aff25efc5ac4f0660ad9c9f7db2.
PubMed PubMed Central Google Scholar
Brooks SK, Weston D, Wessely S, Greenberg N. Effectiveness and acceptability of brief psychoeducational interventions after potentially traumatic events: a systematic review. Eur J Psychotraumatology. 2021;12(1):1923110.
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review-a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(1_suppl):21–34.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:1–8.
Bearman M, Dawson P. Qualitative synthesis and systematic review in health professions education. Med Educ. 2013;47(3):252–60.
Heid AR, Pruchno R, Cartwright FP, Wilson-Genderson M. Exposure to Hurricane Sandy, neighborhood collective efficacy, and post-traumatic stress symptoms in older adults. Aging Ment Health. 2017;21(7):742–50.
Hikichi H, Aida J, Tsuboya T, Kondo K, Kawachi I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku Earthquake and tsunami. Am J Epidemiol. 2016;183(10):902–10.
Lee J, Blackmon BJ, Cochran DM, Kar B, Rehner TA, Gunnell MS. Community resilience, psychological resilience, and depressive symptoms: an examination of the Mississippi Gulf Coast 10 years after Hurricane Katrina and 5 years after the Deepwater Horizon oil spill. Disaster med. 2018;12(2):241–8.
Lee J, Blackmon BJ, Lee JY, Cochran DM Jr, Rehner TA. An exploration of posttraumatic growth, loneliness, depression, resilience, and social capital among survivors of Hurricane Katrina and the deepwater Horizon oil spill. J Community Psychol. 2019;47(2):356–70.
Lowe SR, Sampson L, Gruebner O, Galea S. Psychological resilience after Hurricane Sandy: the influence of individual- and community-level factors on mental health after a large-scale natural disaster. PLoS One. 2015;10(5):e0125761.
Rung AL, Gaston S, Robinson WT, Trapido EJ, Peters ES. Untangling the disaster-depression knot: the role of social ties after deepwater Horizon. Soc Sci Med. 2017;177:19–26.
Weil F, Lee MR, Shihadeh ES. The burdens of social capital: how socially-involved people dealt with stress after Hurricane Katrina. Soc Sci Res. 2012;41(1):110–9.
Hikichi H, Aida J, Matsuyama Y, Tsuboya T, Kondo K, Kawachi I. Community-level social capital and cognitive decline after a Natural Disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Soc Sci Med. 2018;257:111981.
Lau AL, Chi I, Cummins RA, Lee TM, Chou KL, Chung LW. The SARS (severe acute respiratory syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment Health. 2008;12(6):746–60.
Sun Y, Yan T. The use of public health indicators to assess individual happiness in post-disaster recovery. Int J Environ Res Public Health. 2019;16(21):4101.
Wong H, Huang Y, Fu Y, Zhang Y. Impacts of structural social capital and cognitive social capital on the psychological status of survivors of the yaan Earthquake. Appl Res Qual Life. 2018;14:1411–33.
Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921.
PubMed PubMed Central CAS Google Scholar
Matsuyama Y, Aida J, Hase A, Sato Y, Koyama S, Tsuboya T, et al. Do community- and individual-level social relationships contribute to the mental health of disaster survivors? A multilevel prospective study after the great East Japan earthquake. Soc Sci Med. 2016;151:187–95.
Ozaki A, Horiuchi S, Kobayashi Y, Inoue M, Aida J, Leppold C, Yamaoka K. Beneficial roles of social support for mental health vary in the Japanese population depending on disaster experience: a nationwide cross-sectional study. Tohoku J Exp Med. 2018;246(4):213–23.
Sato K, Amemiya A, Haseda M, Takagi D, Kanamori M, Kondo K, et al. Post-disaster changes in Social Capital and Mental Health: a natural experiment from the 2016 Kumamoto Earthquake. Am J Epidemiol. 2020;189(9):910–21.
Tsuchiya N, Nakaya N, Nakamura T, Narita A, Kogure M, Aida J, Tsuji I, Hozawa A, Tomita H. Impact of social capital on psychological distress and interaction with house destruction and displacement after the great East Japan earthquake of 2011. J Neuropsychiatry Clin Neurosci. 2017;71(1):52–60.
Brockie L, Miller E. Understanding older adults’ resilience during the Brisbane floods: social capital, life experience, and optimism. Disaster Med Pub Health Prep. 2017;11(1):72–9.
Caldwell K, Boyd CP. Coping and resilience in farming families affected by drought. Rural Remote Health. 2009;9(2):1088.
PubMed Google Scholar
Huang Y, Tan NT, Liu J. Support, sense of community, and psychological status in the survivors of the Yaan earthquake. J Community Psychol. 2016;44(7):919–36.
Wind T, Fordham M, Komproe H. Social capital and post-disaster mental health. Glob Health Action. 2011;4(1):6351.
Wind T, Komproe IH. The mechanisms that associate community social capital with post-disaster mental health: a multilevel model. Soc Sci Med. 2012;75(9):1715–20.
Hogg D, Kingham S, Wilson TM, Ardagh M. The effects of spatially varying earthquake impacts on mood and anxiety symptom treatments among long-term Christchurch residents following the 2010/11 Canterbury Earthquakes, New Zealand. Health Place. 2016;41:78–88.
Flores EC, Carnero AM, Bayer AM. Social capital and chronic post-traumatic stress disorder among survivors of the 2007 earthquake in Pisco, Peru. Soc Sci Med. 2014;101:9–17.
Rafiey H, Alipour F, LeBeau R, Salimi Y, Ahmadi S. Exploring the buffering role of social capital in the development of posttraumatic stress symptoms among Iranian earthquake survivors. Psychol Trauma. 2019;14(6):1040–6.
Babcicky P, Seebauer S. The two faces of social capital in private Flood mitigation: opposing effects on risk perception, self-efficacy and coping capacity. J Risk Res. 2017;20(8):1017–37.
Bakic H, Ajdukovic D. Stability and change post-disaster: dynamic relations between individual, interpersonal and community resources and psychosocial functioning. Eur J Psychotraumatol. 2019;10(1):1614821.
Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91(1):93–114.
Lindberg K, Swearingen T. A reflective thrive-oriented community resilience scale. Am J Community Psychol. 2020;65(3–4):467–78.
Leykin D, Lahad M, Cohen O, Goldberg A, Aharonson-Daniel L. Conjoint community resiliency assessment measure-28/10 items (CCRAM28 and CCRAM10): a self-report tool for assessing community resilience. Am J Community Psychol. 2013;52:313–23.
Sherrieb K, Norris FH, Galea S. Measuring capacities for community resilience. Soc Indic Res. 2010;99:227–47.
Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. 2015;69(10):1021–8.
Pfefferbaum B, Van Horn RL, Pfefferbaum RL. A conceptual framework to enhance community resilience using social capital. Clin Soc Work J. 2017;45(2):102–10.
Carmen E, Fazey I, Ross H, Bedinger M, Smith FM, Prager K, et al. Building community resilience in a context of climate change: the role of social capital. Ambio. 2022;51(6):1371–87.
Humbert C, Joseph J. Introduction: the politics of resilience: problematising current approaches. Resilience. 2019;7(3):215–23.
Tanner T, Bahadur A, Moench M. Challenges for resilience policy and practice. Working paper: 519. 2017.
Vadivel R, Shoib S, El Halabi S, El Hayek S, Essam L, Bytyçi DG. Mental health in the post-COVID-19 era: challenges and the way forward. Gen Psychiatry. 2021;34(1):e100424.
Article CAS Google Scholar
Pryor M. Social Capital Harmonised Standard. London: Government Statistical Service. 2021. Accessible at: https://gss.civilservice.gov.uk/policystore/social-capital/ .
Public Health England NE. A guide to community-centred approaches for health and wellbeing. 2015.
Hawe P. Capturing the meaning of ‘community’ in community intervention evaluation: some contributions from community psychology. Health Promot Int. 1994;9(3):199–210.
Uphoff EP, Pickett KE, Cabieses B, Small N, Wright J. A systematic review of the relationships between social capital and socioeconomic inequalities in health: a contribution to understanding the psychosocial pathway of health inequalities. Int J Equity Health. 2013;12:1–12.
Download references
Acknowledgements
Not applicable.
This study was supported by the National Institute for Health Research Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between Public Health England, King’s College London and the University of East Anglia. The views expressed are those of the author(s) and not necessarily those of the NIHR, Public Health England, the UK Health Security Agency or the Department of Health and Social Care [Grant number: NIHR20008900]. Part of this work has been funded by the Office for Health Improvement and Disparities, Department of Health and Social Care, as part of a Collaborative Agreement with Leeds Beckett University.
Author information
Authors and affiliations.
Behavioural Science and Insights Unit, Evaluation & Translation Directorate, Science Group, UK Health Security Agency, Porton Down, Salisbury, SP4 0JG, UK
C. E. Hall, H. Wehling, R. Amlôt & D. Weston
Health Protection Research Unit, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
C. E. Hall, S. K. Brooks & N. Greenberg
School of Health and Community Studies, Leeds Beckett University, Portland Building, PD519, Portland Place, Leeds, LS1 3HE, UK
J. Stansfield & J. South
King’s Centre for Military Health Research, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
N. Greenberg
You can also search for this author in PubMed Google Scholar
Contributions
DW, JSo and JSt had the main idea for the review. The search strategy and eligibility criteria were devised by CH, DW, JSo and JSt. CH conducted the database searches. CH and DW conducted duplicate, title and abstract and full text screening in accordance with inclusion criteria. CH conducted data extraction, CH and DW carried out the analysis and drafted the initial manuscript. All authors provided critical revision of intellectual content. All authors approved the final manuscript.
Authors’ information
Corresponding author.
Correspondence to D. Weston .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., additional file 4., additional file 5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hall, C.E., Wehling, H., Stansfield, J. et al. Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review. BMC Public Health 23 , 2482 (2023). https://doi.org/10.1186/s12889-023-17242-x
Download citation
Received : 04 April 2022
Accepted : 16 November 2023
Published : 12 December 2023
DOI : https://doi.org/10.1186/s12889-023-17242-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Community cohesion
- Public health emergency
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
The Impact of Psychological Problems on a Person Essay
Introduction, the psychological issues, the aspects of children’s psychological problems, references list.
Psychological problems are those problems that affect an individual mental stability leading to various other problems. These problems can occur when one loses a beloved one, experiences a tragic event or is a survivor from a tragic event. These kinds of problems are very common today and the right measures should be taken to help cope with them. It is important for those going through any sort of psychological problems to undergo the required therapy to help them lead a normal life. (Gazzaniga, & Heatherton, 2006)
These people are likely to suffer from mental problems and poor physical health after being exposed to such traumatizing conditions. These conditions lead to depression and anxiety because of the associated symptoms of mental problems. Individuals feel anxious all the time with mood swings changing very often for no apparent reason. This causes one to be completely depressed all the time and unable to perform their duties. Many of the activities one was participating in no longer seem enjoyable with the result of one withdrawing from any social gatherings. This leads to severe problems in concentration and one feels uncomfortable all the time. (WebMD, 2005)
The other psychological problem these individuals are likely to suffer is emotional instability with one always feeling sad and withdrawn all the time. Psychologically one is distressed and always nervous on what may happen next. Some of these psychological problems lead to people involving in violence behavior. There is behavioral problems and exposing oneself to danger without caring at all. Others get into drug abuse in order to try and forget the ordeal by all means even if that is not possible. The real issues are not dealt with in many cases causing such individuals to be always angry for no apparent reason. (Gazzaniga, & Heatherton, 2006)
The other psychological issue that occurs after being exposed to such a disaster is Posttraumatic Stress Disorder (PTSD) that is a form of mental condition. This causes one to be mentally unstable hallucinating and disengaged. The individual in most cases is not aware of what is happening around him anymore and does not care at all. There are also those individuals who have problems in sleeping during the night or any other time. This causes prolonged depression and distress for such a person as they are not getting enough sleep. Others stay away from any situations that may act as a reminder of what happened. They get nervous whenever the tragedy is mentioned thus they keep away from any social gatherings. (Post Traumatic Stress, n.d.)
Children are also affected by this ordeal in many ways that keeps them afraid all the time that something bad is going to happen. They are always alert and startled easily by any little disturbance. They always harbor flashbacks of what happened and they constantly have fear of what will happen in the future. There is loss of memory among children in most cases and they have problems trusting people. Others engage in anti-social activities and refuse to apologize even when they have been caught red-handed. (Post Traumatic Stress, n.d.)There also cases where they have serious resentment and always afraid that they may lose their parents or guardian. They also experience problems in concentrating and are always participating in criminal activities.
Psychological problems are very common when people are exposed to very tragic situations. It is common to have mental problems and other psychological disorders once one goes through such an ordeal. It is important for the society to provide the necessary help before things go out of hand. Government and other organizations should ensure that the required healthcare is given in the right way in order to help this victims cope with life. It is also necessary to give them counseling so that they are able to understand what is happening to them.
Gazzaniga, M.S., & Heatherton, T.F. (2006). Psychological Science . New York: W.W. Norton & Company, Inc.
Post Traumatic Stress. (n.d.). The causes of PTSD . Web.
WebMD, Inc. (2005). Mental Health: Types of Mental Illness . Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, December 22). The Impact of Psychological Problems on a Person. https://ivypanda.com/essays/the-impact-of-psychological-problems-on-a-person/
"The Impact of Psychological Problems on a Person." IvyPanda , 22 Dec. 2021, ivypanda.com/essays/the-impact-of-psychological-problems-on-a-person/.
IvyPanda . (2021) 'The Impact of Psychological Problems on a Person'. 22 December.
IvyPanda . 2021. "The Impact of Psychological Problems on a Person." December 22, 2021. https://ivypanda.com/essays/the-impact-of-psychological-problems-on-a-person/.
1. IvyPanda . "The Impact of Psychological Problems on a Person." December 22, 2021. https://ivypanda.com/essays/the-impact-of-psychological-problems-on-a-person/.
Bibliography
IvyPanda . "The Impact of Psychological Problems on a Person." December 22, 2021. https://ivypanda.com/essays/the-impact-of-psychological-problems-on-a-person/.
- The Ordeal of Being a Woman: When Feminist Ideas Dissipate
- The Ordeal of Elizabeth Marsh: A Woman in World History Book
- Community Gatherings and Collective Memory
- Criminal Justice System: “Lucky” by Alice Sebold
- “Vietnam: An American Ordeal” by George Moss
- Experience With Death in Personal Life
- The Effects of Tragic Tales on Audience
- Child Sexual Abuse: Impact and Consequences
- Researching of Kumbh Mela in India
- Anxiety, Somatoform, and Dissociative Disorders
- The Life of My Teacher’s Handbag
- Clinical Psychology, Its Issues and Purposes
- Media Attention to Psychology
- Realistic Encounters Emphasizing Recovery
- Depression, Hallucination, and Suicide: Mental Cases
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.12(6); 2020 Jun

Social Media Use and Its Connection to Mental Health: A Systematic Review
Fazida karim.
1 Psychology, California Institute of Behavioral Neurosciences and Psychology, Fairfield, USA
2 Business & Management, University Sultan Zainal Abidin, Terengganu, MYS
Azeezat A Oyewande
3 Family Medicine, California Institute of Behavioral Neurosciences and Psychology, Fairfield, USA
4 Family Medicine, Lagos State Health Service Commission/Alimosho General Hospital, Lagos, NGA
Lamis F Abdalla
5 Internal Medicine, California Institute of Behavioral Neurosciences and Psychology, Fairfield, USA
Reem Chaudhry Ehsanullah
Safeera khan.
Social media are responsible for aggravating mental health problems. This systematic study summarizes the effects of social network usage on mental health. Fifty papers were shortlisted from google scholar databases, and after the application of various inclusion and exclusion criteria, 16 papers were chosen and all papers were evaluated for quality. Eight papers were cross-sectional studies, three were longitudinal studies, two were qualitative studies, and others were systematic reviews. Findings were classified into two outcomes of mental health: anxiety and depression. Social media activity such as time spent to have a positive effect on the mental health domain. However, due to the cross-sectional design and methodological limitations of sampling, there are considerable differences. The structure of social media influences on mental health needs to be further analyzed through qualitative research and vertical cohort studies.
Introduction and background
Human beings are social creatures that require the companionship of others to make progress in life. Thus, being socially connected with other people can relieve stress, anxiety, and sadness, but lack of social connection can pose serious risks to mental health [ 1 ].
Social media
Social media has recently become part of people's daily activities; many of them spend hours each day on Messenger, Instagram, Facebook, and other popular social media. Thus, many researchers and scholars study the impact of social media and applications on various aspects of people’s lives [ 2 ]. Moreover, the number of social media users worldwide in 2019 is 3.484 billion, up 9% year-on-year [ 3 - 5 ]. A statistic in Figure 1 shows the gender distribution of social media audiences worldwide as of January 2020, sorted by platform. It was found that only 38% of Twitter users were male but 61% were using Snapchat. In contrast, females were more likely to use LinkedIn and Facebook. There is no denying that social media has now become an important part of many people's lives. Social media has many positive and enjoyable benefits, but it can also lead to mental health problems. Previous research found that age did not have an effect but gender did; females were much more likely to experience mental health than males [ 6 , 7 ].

Impact on mental health
Mental health is defined as a state of well-being in which people understand their abilities, solve everyday life problems, work well, and make a significant contribution to the lives of their communities [ 8 ]. There is debated presently going on regarding the benefits and negative impacts of social media on mental health [ 9 , 10 ]. Social networking is a crucial element in protecting our mental health. Both the quantity and quality of social relationships affect mental health, health behavior, physical health, and mortality risk [ 9 ]. The Displaced Behavior Theory may help explain why social media shows a connection with mental health. According to the theory, people who spend more time in sedentary behaviors such as social media use have less time for face-to-face social interaction, both of which have been proven to be protective against mental disorders [ 11 , 12 ]. On the other hand, social theories found how social media use affects mental health by influencing how people view, maintain, and interact with their social network [ 13 ]. A number of studies have been conducted on the impacts of social media, and it has been indicated that the prolonged use of social media platforms such as Facebook may be related to negative signs and symptoms of depression, anxiety, and stress [ 10 - 15 ]. Furthermore, social media can create a lot of pressure to create the stereotype that others want to see and also being as popular as others.
The need for a systematic review
Systematic studies can quantitatively and qualitatively identify, aggregate, and evaluate all accessible data to generate a warm and accurate response to the research questions involved [ 4 ]. In addition, many existing systematic studies related to mental health studies have been conducted worldwide. However, only a limited number of studies are integrated with social media and conducted in the context of social science because the available literature heavily focused on medical science [ 6 ]. Because social media is a relatively new phenomenon, the potential links between their use and mental health have not been widely investigated.
This paper attempt to systematically review all the relevant literature with the aim of filling the gap by examining social media impact on mental health, which is sedentary behavior, which, if in excess, raises the risk of health problems [ 7 , 9 , 12 ]. This study is important because it provides information on the extent of the focus of peer review literature, which can assist the researchers in delivering a prospect with the aim of understanding the future attention related to climate change strategies that require scholarly attention. This study is very useful because it provides information on the extent to which peer review literature can assist researchers in presenting prospects with a view to understanding future concerns related to mental health strategies that require scientific attention. The development of the current systematic review is based on the main research question: how does social media affect mental health?
Research strategy
The research was conducted to identify studies analyzing the role of social media on mental health. Google Scholar was used as our main database to find the relevant articles. Keywords that were used for the search were: (1) “social media”, (2) “mental health”, (3) “social media” AND “mental health”, (4) “social networking” AND “mental health”, and (5) “social networking” OR “social media” AND “mental health” (Table 1 ).
Out of the results in Table 1 , a total of 50 articles relevant to the research question were selected. After applying the inclusion and exclusion criteria, duplicate papers were removed, and, finally, a total of 28 articles were selected for review (Figure 2 ).

PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Inclusion and exclusion criteria
Peer-reviewed, full-text research papers from the past five years were included in the review. All selected articles were in English language and any non-peer-reviewed and duplicate papers were excluded from finally selected articles.
Of the 16 selected research papers, there were a research focus on adults, gender, and preadolescents [ 10 - 19 ]. In the design, there were qualitative and quantitative studies [ 15 , 16 ]. There were three systematic reviews and one thematic analysis that explored the better or worse of using social media among adolescents [ 20 - 23 ]. In addition, eight were cross-sectional studies and only three were longitudinal studies [ 24 - 29 ].The meta-analyses included studies published beyond the last five years in this population. Table 2 presents a selection of studies from the review.
IGU, internet gaming disorder; PSMU, problematic social media use
This study has attempted to systematically analyze the existing literature on the effect of social media use on mental health. Although the results of the study were not completely consistent, this review found a general association between social media use and mental health issues. Although there is positive evidence for a link between social media and mental health, the opposite has been reported.
For example, a previous study found no relationship between the amount of time spent on social media and depression or between social media-related activities, such as the number of online friends and the number of “selfies”, and depression [ 29 ]. Similarly, Neira and Barber found that while higher investment in social media (e.g. active social media use) predicted adolescents’ depressive symptoms, no relationship was found between the frequency of social media use and depressed mood [ 28 ].
In the 16 studies, anxiety and depression were the most commonly measured outcome. The prominent risk factors for anxiety and depression emerging from this study comprised time spent, activity, and addiction to social media. In today's world, anxiety is one of the basic mental health problems. People liked and commented on their uploaded photos and videos. In today's age, everyone is immune to the social media context. Some teens experience anxiety from social media related to fear of loss, which causes teens to try to respond and check all their friends' messages and messages on a regular basis.
On the contrary, depression is one of the unintended significances of unnecessary use of social media. In detail, depression is limited not only to Facebooks but also to other social networking sites, which causes psychological problems. A new study found that individuals who are involved in social media, games, texts, mobile phones, etc. are more likely to experience depression.
The previous study found a 70% increase in self-reported depressive symptoms among the group using social media. The other social media influence that causes depression is sexual fun [ 12 ]. The intimacy fun happens when social media promotes putting on a facade that highlights the fun and excitement but does not tell us much about where we are struggling in our daily lives at a deeper level [ 28 ]. Another study revealed that depression and time spent on Facebook by adolescents are positively correlated [ 22 ]. More importantly, symptoms of major depression have been found among the individuals who spent most of their time in online activities and performing image management on social networking sites [ 14 ].
Another study assessed gender differences in associations between social media use and mental health. Females were found to be more addicted to social media as compared with males [ 26 ]. Passive activity in social media use such as reading posts is more strongly associated with depression than doing active use like making posts [ 23 ]. Other important findings of this review suggest that other factors such as interpersonal trust and family functioning may have a greater influence on the symptoms of depression than the frequency of social media use [ 28 , 29 ].
Limitation and suggestion
The limitations and suggestions were identified by the evidence involved in the study and review process. Previously, 7 of the 16 studies were cross-sectional and slightly failed to determine the causal relationship between the variables of interest. Given the evidence from cross-sectional studies, it is not possible to conclude that the use of social networks causes mental health problems. Only three longitudinal studies examined the causal relationship between social media and mental health, which is hard to examine if the mental health problem appeared more pronounced in those who use social media more compared with those who use it less or do not use at all [ 19 , 20 , 24 ]. Next, despite the fact that the proposed relationship between social media and mental health is complex, a few studies investigated mediating factors that may contribute or exacerbate this relationship. Further investigations are required to clarify the underlying factors that help examine why social media has a negative impact on some peoples’ mental health, whereas it has no or positive effect on others’ mental health.
Conclusions
Social media is a new study that is rapidly growing and gaining popularity. Thus, there are many unexplored and unexpected constructive answers associated with it. Lately, studies have found that using social media platforms can have a detrimental effect on the psychological health of its users. However, the extent to which the use of social media impacts the public is yet to be determined. This systematic review has found that social media envy can affect the level of anxiety and depression in individuals. In addition, other potential causes of anxiety and depression have been identified, which require further exploration.
The importance of such findings is to facilitate further research on social media and mental health. In addition, the information obtained from this study can be helpful not only to medical professionals but also to social science research. The findings of this study suggest that potential causal factors from social media can be considered when cooperating with patients who have been diagnosed with anxiety or depression. Also, if the results from this study were used to explore more relationships with another construct, this could potentially enhance the findings to reduce anxiety and depression rates and prevent suicide rates from occurring.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.

IMAGES
VIDEO
COMMENTS
Physical distancing due to the COVID‐19 outbreak can have drastic negative effects on the mental health of the elderly and disabled individuals. Physical isolation at home among family members can put the elderly and disabled person at serious mental health risk. It can cause anxiety, distress, and induce a traumatic situation for them.
Awareness of the potential mental health impact of the COVID-19 pandemic is reflected in the more than 35,000 papers published on this topic. ... S. K. et al. The psychological impact of ...
Purpose of the present study. In the present study, we took advantage of a growing evidence base using more sophisticated methodologies. When experimental randomized trials are neither feasible nor ethical, both longitudinal within-person designs (with at least one data collection point before and one during the lockdown) and natural experiments involving a control group provide a ...
Although the impact of COVID-19 is individual-specific and based on a number of factors (e.g. the length of quarantine, risk factors, trauma history, mental health history, etc.), some trends in ...
The recent Covid-19 pandemic has had significant psychological and social effects on the population. Research has highlighted the impact on psychological well-being of the most exposed groups, including children, college students, and health workers, who are more likely to develop post-traumatic stress disorder, anxiety, depression, and other symptoms of distress.
Impact of COVID-19 Pandemic on Utilization of Healthcare Services and Spending Patterns in Dubai, United Arab Emirates: A Cross-Sectional Study, Healthcare, 12, 4, (473), (2024). https://doi.org ...
Talking about dying or harming oneself. Recent loss through death, divorce, separation, even loss of interest in friends, hobbies and activities previously enjoyed. Changes in personality like sadness, withdrawal, irritability or anxiety. Changes in behavior, sleep patterns and eating habits. Erratic behavior, harming self or others.
Background The declaration of COVID-19 as a global pandemic by the World Health Organisation (WHO) in 2020 catapulted institutions of higher education into an emergency transition from face-to-face to online teaching. Given the nature of the COVID-19 pandemic and the continuing after-effects thereof, the study explored the psychological impact of the COVID-19 pandemic on academics. Methods A ...
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
Furthermore, Spoorthy et al. (2020) conducted a review on the gendered impact of Covid-19 and found that 68.7-85.5% of medical staff is composed of women, and the mean age ranged between 26 and 40 years. Also, women are more likely to be affect by anxiety, depression, and distress ( Lai et al., 2020; Zanardo et al., 2020 ).
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours ...
The objectives of this study are to 1) identify the array of psychological impacts COVID-19 has on students, 2) develop profiles to characterize students' anticipated levels of psychological impact during the pandemic, and 3) evaluate potential sociodemographic, lifestyle-related, and awareness of people infected with COVID-19 risk factors that ...
Insights from the new science of happiness. A few decades ago, a group of psychologists worried that there has been too much focus on the negative. We haven't done enough research into what goes ...
Introduction. The impact of the coronavirus disease 2019 (COVID-19) pandemic was diverse and had impacted physical, psychological, economic, and social contexts globally (Álvarez-Iglesias et al., Reference Álvarez-Iglesias, Garman and Lund 2021; Zheng et al., Reference Zheng, Feng, Liu, Targher, Byrne and Zheng 2021).Some populations were at higher risk of facing those impacts.
As people grapple with these health, social and economic impacts, mental health has been widely affected. Plenty of us became more anxious; but for some COVID-19 has sparked or amplified much more serious mental health problems. A great number of people have reported psychological distress and symptoms of depression, anxiety or post-traumatic ...
Overall, findings regarding the impact of social media on mental health pointed out some essential resources for psychological well-being through rewarding online social interactions. However, there is a need to raise awareness about the possible risks associated with excessive use, which can negatively affect mental health and everyday ...
Physical Effects. Stress is associated with various physical health impacts on an individual. In an online cross-sectional survey by Keech et al. (2020) to determine the association between stress and the physical and psychological health of police officers, the findings illustrate that stress negatively impacts physical and psychological well-being.
Along with its high infectivity and fatality rates, the 2019 Corona Virus Disease (COVID-19) has caused universal psychosocial impact by causing mass hysteria, economic burden and financial losses. Mass fear of COVID-19, termed as "coronaphobia", has generated a plethora of psychiatric manifestations across the different strata of the society.
The effects of bullying have serious and lasting negative impacts on our mental health and overall wellbeing. Bullying can cause feelings of rejection, exclusion, isolation, low self-esteem, and some individuals can develop depression and anxiety as a result. In some cases it can even develop into Acute Stress Disorder or Post Traumatic Stress ...
Background. In a short time, the COVID-19 pandemic turned into a global emergency. The fear of becoming infected and the lockdown measures have drastically changed people's daily routine. The aim of this study is to establish the psychological impact that the COVID-19 pandemic is entailing, particularly with regards to levels of stress, anxiety ...
Conclusion. In summary, research has extensively documented the diverse physiological and psychological impacts of stress. From increased risk of cardiovascular disease, cognitive decline, and mental illness, chronic stress exposure induces cumulative wear and tear on the body and brain.Understanding these harmful effects highlights the need for careful stress management using evidence-based ...
This essay aims to explore the multifaceted psychological ramifications of gun violence, analyzing its effects on survivors, witnesses, and the community as a whole. By examining the psychological toll of gun violence, we can better understand its long-term consequences and develop effective interventions to promote healing and resilience.
There were mixed effects across the 26 retained papers when examining the effect of CR and SC on mental wellbeing. ... Nakamura T, Narita A, Kogure M, Aida J, Tsuji I, Hozawa A, Tomita H. Impact of social capital on psychological distress and interaction with house destruction and displacement after the great East Japan earthquake of 2011. J ...
Psychological problems are those problems that affect an individual mental stability leading to various other problems. These problems can occur when one loses a beloved one, experiences a tragic event or is a survivor from a tragic event. These kinds of problems are very common today and the right measures should be taken to help cope with ...
Abstract. Social media are responsible for aggravating mental health problems. This systematic study summarizes the effects of social network usage on mental health. Fifty papers were shortlisted from google scholar databases, and after the application of various inclusion and exclusion criteria, 16 papers were chosen and all papers were ...
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
The impact of climate change on student psychological distress. Indonesia is now experiencing abnormal severe hot weather, where El-Nino causes the increasing temperature to be above the average. Although El Nino is a common phenomenon that occurs naturally, climate change factors exacerbate the adverse impact of El Nino on human life.