PhD Program: Clinical Pharmaceutical Scientist Program
The Clinical Pharmaceutical Scientist Program is a specialty track/program in which students with expertise in pharmacotherapeutics investigate both the clinical and mechanistic elements of drug therapy issues.
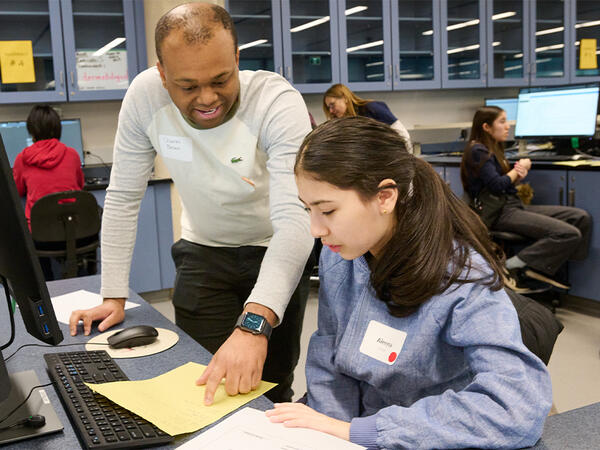
- You will learn experimental design, experimental methods, data analysis, and data interpretation of human-based research projects.
- You will study how research discoveries are translated into practices that promote health and prevent disease.
- You will learn the process required to implement new therapies as standards of care through human-based research projects.
The is a specialized track within the graduate program that educates students to conduct pharmaceutical research at the interface of the bench and bedside. Learn more about the Clinical Pharmaceutical Scientist program »

Pitt is one of the first programs in the country to offer a PhD in clinical and translational research in the pharmaceutical sciences. To date, the program has graduated in excess of forty students who have been recruited to academic, government, and pharmaceutical industry positions. Learn more about why to choose Pitt for Clinical Pharmaceutical Science »

Individuals with a prior advanced degree in the health sciences (PharmD or other degree in the health sciences) will be considered for admission to the Clinical Pharmaceutical Scientist program .

The curriculum is composed of coursework and experiences designed to train students to achieve the core competencies of clinical researchers in the pharmaceutical sciences.

We have identified the core competencies of clinical researchers in the pharmaceutical sciences. Our interactive tool details the skills that all students within the Clinical Pharmaceutical Scientist program achieve through graduate training and can be used to differentiate this training from traditional graduate and fellowship programs

View a list of all students currently in the Clinical Pharmaceutical Scientist program »

View a list of all the Clinical Pharmaceutical Scientist program faculty »

View a list of frequently asked questions »

Primary Contact
Philip E. Empey, PharmD, PhD Associate Professor 205 Salk Pavilion Pittsburgh, PA 15261 Phone: 412-648-7219 Fax: 412-624-1850 E-mail: [email protected]

- Quick Links
Tools & Resources
- Events Calendar
- Strauss Health Sciences Library
- Department A-Z Directory
- Campus Directory
- Faculty & Staff Resources
- Supporter & Alumni Resources
- Student Resources
- Mental Health Resources
- University Policies
CU Campuses
Cu anschutz medical campus.
- CU Colorado Springs
- School of Dental Medicine
- Graduate School
- School of Medicine
- College of Nursing
Skaggs School of Pharmacy and Pharmaceutical Sciences
- Colorado School of Public Health
PhD in Pharmaceutical Outcomes Research
Pharmaceutical Outcomes Research is a PhD program in the graduate program in Clinical Pharmacy. This program is housed in the Center for Pharmaceutical Outcomes Research (CePOR, SEE-por), a school-wide center in the Skaggs School of Pharmacy. Our doctoral curriculum is designed to provide competent and highly skilled researchers in the study of patient, provider, or population-level health care and health system interventions. We most often focus on economic, clinical, and humanistic outcomes such as clinical or cost effectiveness or safety. Areas of focus available to students undertaking this course of study include pharmacoeconomics, pharmacoepidemiology, health services research, and drug policy.
Core faculty are methodological experts and provide collaborative linkage to clinical experts in all pharmacy, medicine, nursing, and public health. Programs of study are tailored to student interests in disease or drug areas, such as cardiology, psychiatry, neurology, and cancer. Opportunities exist to link to more basic science colleagues depending on your topic of interests. For example, students interested in drug safety might link with toxicology faculty, or in gene-environment interactions might link with pharmacogenomics faculty.
Applications for all doctoral programs are submitted electronically through the Graduate School of the University of Colorado Denver. After signing up for an account, select 'PhD' under the 'Academic Interests' menu and scroll down to 'Skaggs School of Pharmacy and Pharmaceutical Sciences' and select "PhD in Pharmaceutical Outcomes Research."
Application requirements are:
- A completed Graduate School application and $50.00 application fee (Domestic) $75.00 application fee (International)
- A baccalaureate degree of arts or science from an accredited college or university with a minimum GPA of 3.0.** One (1) official transcript of all academic work completed to date with awarded baccalaureate degree. University transcripts from other countries must include a transcript evaluation from World Education Services ( WES ). Applicants who complete a transcript evaluation with WES will have their application fee waived automatically.
- All applicants for the program should complete a year of study in the following subjects: general chemistry, organic chemistry, calculus, biology, English and physics. In addition, courses in the following subjects are highly recommended to supplement the student's background: physiology, biochemistry, statistics, cell biology, physical chemistry, and computer science.
- Three (3) letters of recommendation from professors or research supervisors familiar with your aptitude for graduate study
Additionally:
- The GRE (Graduate Record Examination) is not required but is optional.
- The TOEFL is required of applicants for whom English is not their first language, Duolingo and IELTS also accepted (more information on this here )
- Please use 4875 as the Institution Code so that the test results will be sent directly to our institution
- Under special circumstances, deficiencies in important areas may be made up within the first year after entrance into the program. Normally, admission to the program will be based on an undergraduate GPA of 3.0 or better. However, applicants' recommendations, research experience and additional individual accomplishments will also be considered in the admissions process.
Application opens September 1, 2023. Applications will not be reviewed until all required materials have been received. The application deadline for Fall 2024 admission is December 1, 2023 for all students.
Admission to the program may include financial support via a stipend awarded on a 12-month basis.
Although a priority of the School of Pharmacy is to provide financial support to its graduate students, payment of stipend, tuition and any fees by the School of Pharmacy or by grants, contracts or gifts to the School of Pharmacy faculty is contingent upon availability of funding, satisfactory academic progress (as defined by the UCD Graduate School, Graduate Student Handbook) and completion of required teaching duties, core courses, and examinations. The School of Pharmacy also reserves the right to review and adjust its funding policies at any time. All students are expected to work full-time toward program requirements for 12 months of the year.
Generally, the first year of financial support will be in the form of stipend support for working as a teaching assistant. Depending on availability, teaching assistantships may be offered beyond one year to students. Faculty may choose to offer research assistant scholarships to students as well. Other funding opportunities in the form of external student grants and awards also exist. Students are encouraged to talk to the faculty about funding and scholarship opportunities. Funds for travel to one meeting where students are presenting a poster or giving a podium presentation are limited to $500 per fiscal year.
Students who do not remain in good graduate standing (3.0 GPA or above) or maintain satisfactory academic progress are placed on academic probation. Probation and suspension policies are described in the UCD Graduate School, Graduate Student Handbook. Payment of stipend, tuition, insurance and fees for a student while on academic probation is at the discretion of the graduate program committee.
What does "pharmaceutical outcomes research" mean?
What kind of students should pursue a phd degree in pharmaceutical outcomes research why should you apply to this program.
We are looking for students who want to influence healthcare but do not want to be a provider. With the belief that the research done will allow for the application of new knowledge towards health improvement.
What makes the Pharmaceutical Outcomes Research PhD program at the University of Colorado different from other PhD programs?
The benefits of this program are multi-faceted. Housed on a major medical campus, students will be able to collaborate with the schools of pharmacy, medicine, nursing, and public health. Also the University of Colorado Hospital, Children's Hospital, and the Veterans Affairs Medical Center are located on campus.
By having a small group of graduate students, they are allowed more time with the faculty members. With two faculty members from each component, students will be able to have the support necessary to complete their degree.
What are the job prospects for a graduate with a PhD degree in the pharmaceutical sciences? What can you do with this career?
Graduates of the program will have many career options within these areas:
- Pharmaceutical industry
- Government agencies
- Contract research organization (CROs)
- Organized healthcare systems
There is a critical need for individuals who are able to conduct rigorous, credible, and relevant population and patient-based research within stringent ethical and regulatory guidelines; the demand for such researchers is expected to grow given the developing health care reform and the investment in federal development and expansion on comparative effectiveness research.
Past graduates have gone on to be an interim dean at a Regis University and the director of pharmacy at the University of Colorado Hospital
How are current students doing?
Our students often win awards at regional and national symposium (such as Julia Slejko at ISPOR or SMDM). One holds a prestigious pre-doctoral dissertation award in health outcomes from the PhRMA Foundation. Two have completed comprehensive exams are working on defending their dissertation proposals. All these more advanced students have published manuscripts in peer-reviewed journals as first authors with the mentorship of the CePOR faculty.
Faculty comments on the program.
Heather Anderson, PhD What's great about this campus is that we are able to collaborate with other schools such as public health, nursing, and medicine. While many Pharmaceutical Outcomes Research programs have a major focus on economics, we do that and more. Our program has a strong focus on epidemiology and policy too. I actually got my PhD in epidemiology from our School of Public health and can link up students with the best courses and advise on exciting local opportunities for research assistantships.
Kelly Anderson, PhD Training at a world-class medical campus allows PhD students in the Center for Pharmaceutical Outcomes Research to engage with faculty in the center with expertise in outcomes research, drug pricing, economics, epidemiology, and health policy, and also have the opportunity to learn from and collaborate with faculty throughout the Schools of Pharmacy, Public Health, Medicine, Dentistry, and Nursing. For anyone who loves big data, our faculty also work with numerous large data sets: Medicare claims, linked EHR-claims data, and all-payer data just to name a few. As a lot of my work is focused on payment policy, I welcome the opportunity to engage students as they think about the real-world implications of their research for policy makers, health insurers, patients, clinicians, and drug companies and disseminate their findings to these key stakeholders.
R. Brett McQueen, PhD Pharmaceutical outcomes research includes aspects of multiple disciplines including math, economics, and epidemiology. I joined the faculty at CU to contribute to comparative- and cost-effectiveness research and to education both for the PhD and the PharmD programs. Our PhD program emphasizes quality over quantity. We maintain a very favorable student to faculty ratio, we offer competitive student financial support, and we strive to graduate scientific leaders in the field of outcomes research.
Kavita V. Nair, PhD Our expectations for graduate students are high and we have structured the education and training requirements to help you meet these goals. I will require a lot of you as a student but will also be your strongest advocate!
Robert Valuck, PhD, RPh I believe that the strengths of our program are the skills and the diversity of the faculty, and size and connectedness of our program with others on campus and in the state and region. With a smaller number of graduate students in our program, they are able to spend more time with faculty members. Our program is well connected with others on the Anschutz campus, and students have opportunities to collaborate both across campus, and with state agencies, provider groups, and others that have an interest in outcomes research and its applications to patient care and policy.
Advance the science of pharmaceutical outcomes research by training scientists who generate and synthesize evidence to inform practice and policy.
The goal of the PhD n pharmaceutical outcomes research is to develop methodological experts. Graduates will have the knowledge and extensive skills necessary to conduct pharmacoeconomic, pharmacoepidemiologic, health services, and drug policy research. We train individuals who can contribute to T3-T4 clinical translational pharmacy and pharmaceutical sciences, specifically on effective, population health, and policy studies. These contributions should ultimately benefit pharmacists and society with safe, effective, and efficient use of pharmaceutical care.
The Pharmaceutical Outcomes Research PhD program trains graduate students to become proficient and successful investigators who are able to:
- demonstrate an in-depth knowledge of central concepts in Pharmaceutical Outcomes Research, including the areas of pharmacoeconomics, pharmacoepidemiology, and/or drug policy.
- critically appraise existing literature and sources of information.
- formulate hypotheses based on current concepts in the field and accurately and correctly design, conduct, and interpret their own research projects.
- present research results in peer-reviewed publications and in a dissertation.
- perform research that adheres to the principles and guidelines of ethical conduct.
- communicate research results effectively through oral presentations at scientific seminars, conferences, and other venues
The program’s strengths in outcomes research are emphasized in 35 credits of several areas:
- Biostatistics
- Epidemiology
- Health Policy
- Research/Study Design
- Doctoral Thesis
The program has experience in accessing a multitude of data such as MEPS, PHARMetrics, University Health-System, Consortium and MarketScan. Students are encouraged to utilize these datasets as well as primary data collection. Students may enroll in courses not listed (e.g courses in downtown campuses and/or newly developed courses) by consulting with the program director.
Pharmacoepidemiology

Heather Anderson PhD

Robert Valuck PhD, RPh
Pharmacoeconomics.

Mike J. DiStefano PhD, MBE

Kelly Anderson PhD, MPP

R. Brett McQueen PhD
Pharmaceutical and drug related policy.

Kavita Nair PhD

Antal Zemplényi
Antal Zemplényi, PhD, is an Associate Professor at the Center for Health Technology Assessment at the University of Pécs and a senior researcher at the Syreon Research Institute, an international research corporation specializing in health policy, health economic modeling, and technology assessment. He has experience in value assessment, HTA, health economics and outcomes research, and real-world data analysis. He is the past president of the ISPOR Hungary Chapter. Antal is currently a Fulbright Scholar at the University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences working as a visiting research associate in the Pharmaceutical Value (pValue) initiative.

Monica Bianchini
Monica Bianchini is originally from Indianapolis, Indiana. She received a PharmD and MPH from the University of Wisconsin-Madison in 2017. She subsequently completed a hospital pharmacy residency (PGY-1) and Infectious Diseases PGY-2 at Henry Ford Hospital in Detroit, Michigan. Monica joined CePOR in 2019 and currently works as a clinical inpatient pharmacist. Her dissertation will evaluate opportunities to decrease syphilis rates and improve syphilis care in Colorado. Outside of work, she enjoys reading, live music, cooking, and anything outside (running, hiking, backpacking, skiing).
Sue is a fifth year PhD student at CePOR. Her dissertation focuses on characterizing the burden of MS and treatment strategies using real-world claims data. Prior to grad school, she studied Neuroscience in Pomona College. In her free time, Sue enjoys taking her puppies on adventures.

Mahesh Maiyani
Mahesh Maiyani was born and raised in India. He earned his Bachelor of Pharmacy (BPharm) from India in 2006 and then he came to the US to pursue his Master’s in Business administration. He completed his MBA from The University of Findlay in Ohio. He has work experience in clinical trials and heath care research. He joined the Pharmaceutical Outcomes Research PhD program in Fall-2021. His research interests are focused around cost effectiveness in real-world clinical settings. Mahesh enjoys hiking and spending time with family and friends.

Nick Mendola
Nick Mendola was born and raised in Buffalo, New York. He graduated from The University of Akron with a BS in Exercise Science in 2016. He then moved to Washington D.C. to attend The George Washington University Milken Institute School of Public Health, where he obtained his MPH in Epidemiology, in 2018. During this time, he worked researching the impact of the pharmaceutical industry’s marketing to healthcare professionals, and its influence on prescribing practices and population level drug utilization. Nick joined the Pharmaceutical Outcomes Research program in the fall of 2018. Nick’s current work with Dr. Robert Brett McQueen, explores the use of Multi-Criteria Decision Analysis (MCDA) as a novel health technology value assessment tool. His work specifically explores MCDA in evaluating treatments for neuromyelitis optica spectrum disorder (NMOSD), a rare neurological disorder.

Vanessa Paul Patterson
Vanessa Patterson is originally from Kansas City. She graduated from Tulane University School of Public Health and Tropical Medicine with an MPH concentrating in Epidemiology and Maternal and Child Health in 2012. Vanessa went on to work as an applied epidemiologist for government public health agencies for six years. She joined the Pharmaceutical Outcomes Research program at CU in the fall of 2018. Working under the mentorship of Dr. Heather Anderson, Vanessa is currently a PhRMA Foundation Predoctoral Fellow and a PhD candidate. Her dissertation focuses on the utilization of cardioprotective medications among women with a history of breast cancer. In her free time, Vanessa enjoys making pottery and spending time outdoors with family and friends.

Nai-Chia (Sammi) Chen
Sammi is originally from Taiwan. She holds a bachelor’s degree in Pharmacy from Kaohsiung Medical University. After graduation, she had worked in pharmaceutical companies and clinical research organizations for several years before coming to the US. She completed her Master’s training at the University of Pittsburgh, Pharmaceutical Outcomes and Policy Research, in 2022. And then she joined Pharmaceutical Outcomes Research PhD program at CU Anschutz in Fall 2022. Her research interest lies in the intersection of pharmacoeconomics, real-world evidence, and pharmaceutical outcomes. Outside the schoolwork, she enjoys cooking, baking, and snowboarding/skiing in winter.

Mouna Dardouri
Mouna was born and raised in Tunisia. She graduated with a PharmD from the University of Pharmacy of Monastir in 2016. She then worked for two years at a consulting company focusing on pharmaceuticals’ Pricing, Reimbursement and Market Access (PRMA) in Europe. After that, she was awarded with the Fulbright Foreign student scholarship and moved to Colorado, where she obtained her MPH in Global Health Systems, management, and Policy in 2022. Mouna joined the Pharmaceutical Outcomes Research program in the fall of 2022. Her research interests include evaluating the use of Health Technology Assessment in the context of low- and middle- income countries and developing tools that permit equitable patients’ access to cost-effective technologies. In her free time, Mouna enjoys learning new languages, improv theatre and cooking.
Why CU's Pharmaceutical Outcomes Research PhD Program?
“One key reason I chose to join CePOR at CU was the tight-knit group of faculty and students. Given the program is smaller, the faculty has a better opportunity to stay in touch with all the students and provide support for everyone's research, regardless if they're on the student's committee or not. The student group is also very close as we are together for weekly seminars and enjoy out-of-school gatherings when possible. Another draw of CU's POR program is the diverse expertise of our faculty and alumni. Our current faculty have a range of expertise including: pharmacoepidemiology using big data sources, pharmacoeconomics and drug pricing, rare diseases, opioid use disorder and treatment, and Medicare payment models. Recent alumni have found work in a variety of different fields from consulting to academia to the pharmaceutical industry and the public health department. The wide range of backgrounds and areas of expertise covered by our faculty and alumni provide so many resources for mentorship and future career planning. Finally, there are so many unique opportunities within CePOR to work with different data sources (e.g. electronic health records, national claims data, Medicaid claims data) and different methodology experts, so I am confident that our program could be a great fit for prospective PhD students of all backgrounds.” – Monica Bianchini, PharmD, MPH
“CU's Pharmaceutical Outcomes Research Program produces robust interdisciplinary research that spans from pharmacoepidemiology to pharmaceutical economics with a variety of collaborators, such as Institute for Clinical and Economic Review (ICER) and Colorado Department of Public Health & Environment (CDPHE).” – Sue Kwon, BA
“I joined the POR program because my previous research was focused on population drug utilization and the pharmaceutical industry’s impact on prescribing practices, and the POR program seemed like a natural fit for me to be able to keep learning about the areas of pharmacoepidemiology and drug related policy. What I like most about the program so far has been the core faculty in our program. They seem to truly care about student success and how we progress both academically and professionally. ” – Nick Mendola, MPH
PhD Student Research Projects
- Comparative Effectiveness of Rare Disease Therapies Using Multi-Criteria Decision Analysis: Case Example in Neuromyelitis Optica Spectrum Disorder, a Rare Neurological Disorder
- Characterizing Real-world Burden of Multiple Sclerosis and Treatment Strategies in a Colorado-representative Population
- Utilization of Cardioprotective Medication Strategies Among Women with a History of Breast Cancer
- Opportunities to Improve Syphilis Care in Colorado
Mission: To educate, increase awareness and promote growth within the 'Pharmacoeconomics and Outcomes Research' field in general and to increase the CU Denver presence among the international society ISPOR. To collaborate across different sciences on campus and different departments worldwide.
Description: Promote pharmacoeconomics and outcomes research education by holding regular seminars on current issues in the field and presenting research at least once a year at the annual meeting in the US-Canada region.
Membership requirements: We expect members to be passionate about the kind of research that is involved related to public health, epidemiology, pharmacoeconomics, and policy. Also, attending our regular educational seminars/webinars is highly encouraged.
Activities: Details will be emailed to members soon!
Benefits: The opportunity to present research, network and collaborate with faculty from different universities around the world, professionals from industry and research organizations at a global level.
Julia Slejko, PhD ('12) Associate Professor Practice, Sciences, and Health Outcomes Research University of Maryland School of Pharmacy
R. Brett McQueen, PhD ('13) Associate Professor Department of Clinical Pharmacy, Skaggs School of Pharmacy and Pharmaceutical Sciences University of Colorado Anschutz Medical Campus
William Padula, PhD ('13) Assistant Professor of Pharmaceutical and Health Economics, School of Pharmacy Fellow, Leonard D. Schaeffer Center for Health Policy & Economics University of Southern California
David Tabano, PhD ('18) Principal Health Economist Evidence for Access (E4A) | Public Affairs & Access Genentech, Inc.
Katie Sullivan, PhD ('18) Prescription Drug Epidemiologist Colorado Department of Public Health and Environment
Angela Czaja, MD, PhD ('19) Associate Professor Pediatrics-Critical Care Medicine Children’s Hospital Colorado Anschutz Medical Campus
Chong Kim, PhD ('20) Associate Director Global Value & Access | HEOR Gilead Sciences
Katia Hannah, PhD ('21) Lead HEOR Specialist Dexcom
Kimberly Deininger, PhD ('22) HEOR Manager Amgen
For questions regarding graduate school programs contact:
Isabella Jaramillo Email: [email protected] Phone: 303.724.7263

Kelly Anderson, PHD, MPP
Assistant Professor; Director, Pharmaceutical Outcomes Research PhD Program Email: [email protected] Phone: 434-466-1990
CU Anschutz
Pharmacy and Pharmaceutical Sciences Building
12850 East Montview Boulevard
Aurora, CO 80045
303-724-2882
- Pharmacy Directory
- Continuing Education
- Academic Calendar
- Request information
- Virtual Advising
- Scholarships & Financial Aid
- Career Services
- Experiential Program
- CORE for Students
- UCD-Access Portal
- Zoom Web Conferencing
- Payroll and Benefits
- Campuswide Directory
- University Laws and Policies
- CORE for Preceptors, Faculty, and Staff
Pharmacology, PhD
School of medicine.
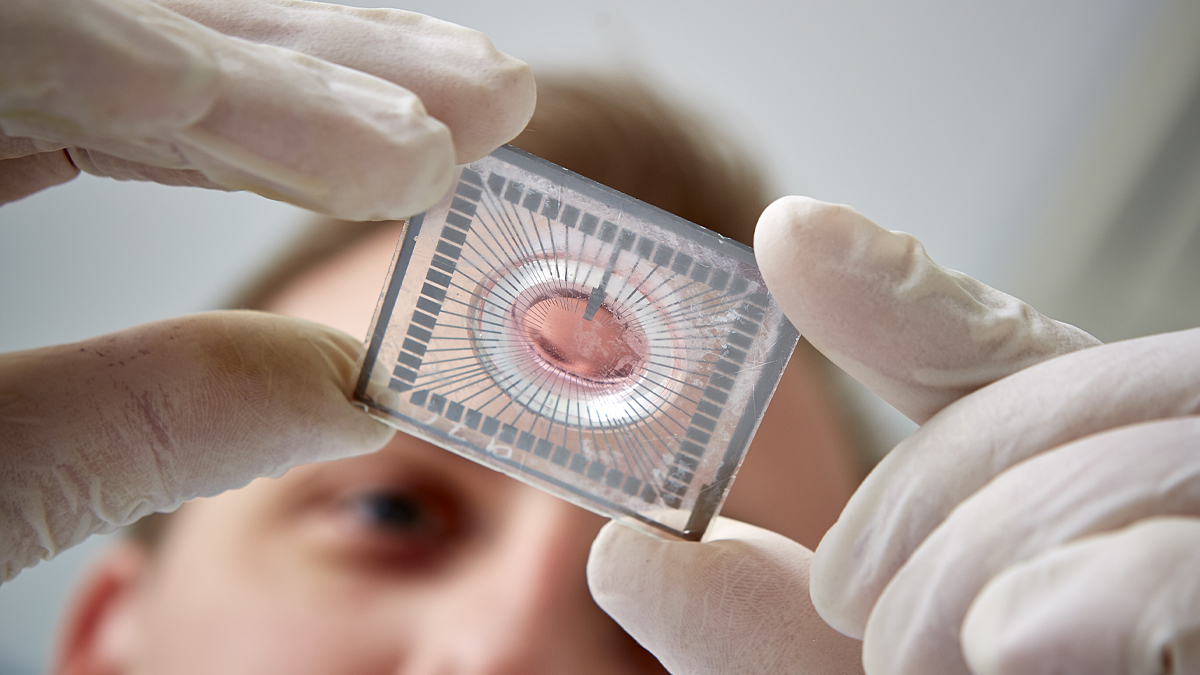
The Department of Pharmacology and Molecular Sciences hosts the Pharmacology Graduate Program, which offers a program of study and research leading to the Ph.D. degree. Research training opportunities within the program cover a broad spectrum of biomedical sciences including chemical biology, immunology, virology, cancer, and neuroscience. The mission of departmental research is to understand the molecular processes underlying physiology and pathology, and to apply this knowledge to discovering new drug targets and developing novel therapeutics. Within the program, students may choose to focus their efforts in any of a large number of specific research areas including signal transduction, structural biology and drug design, NMR spectroscopy, molecular genetics, cancer chemoprevention, viral immunosuppression, cancer immunology, cell-mediated immunity, mechanisms of HIV infection, vaccine development, glycobiology, biomedical mass spectrometry, clinical pharmacology, drug delivery, anti-parasite drug development, histone acetylation and gene regulation, melatonin and circadian rhythm, drug metabolism, Vitamin D pharmacology, natural product biosynthesis, telomerase and chromosome stability, T cell activation and tolerance, DNA repair, DNA topoisomerases, molecular imaging, and the clinical pharmacology of cardiovascular agents. The department is also pleased to host students and award doctoral degrees to M.D./Ph.D. degree candidates and students in other Ph.D. graduate programs in which Pharmacology faculty participate (Biochemistry, Cellular and Molecular Biology, Cellular and Molecular Medicine, Immunology, Neuroscience, and Pathobiology).
Financial Support
Financial support covering normal living costs, individual medical insurance, and tuition is provided.
Admission Requirements
Applicants should have a B.A. or B.S. degree with a major in any of the biological or physical sciences. Entering students are expected to have completed college-level courses in chemistry (inorganic, organic, and physical), calculus, and physics; a strong background in biochemistry is particularly desirable. A completed application form, at least three letters of recommendation, undergraduate transcripts, and a statement of interest must be received by December 8th.
Program Requirements
Students in the Pharmacology program must successfully complete the following courses:
Students must also take two advanced elective courses selected from those offered by this or other departments. Students are able to select a course of studies uniquely suited to their own career goals.
During their first year of study, students will complete ~10-week research rotations in addition to their coursework. They will initiate dissertation research by the end of their first year and complete elective courses relevant to their developing interests in subsequent years of training.
During the second year of study, students will be required to pass a qualifying examination conducted as prescribed by the Doctor of Philosophy Board of the University. This examination will probe the depth and breadth of the student’s knowledge of the biomedical subjects taught in the core courses.
The candidate is required to present a written dissertation based on original research undertaken while in residence as a graduate student and to present a departmental seminar describing the thesis research.
Combined M.D.-Ph.D. Degrees
Students seeking admission to or who are already participating in the M.D. program in the School of Medicine may participate in a program leading to both the M.D. and the Ph.D. degrees.
- Research Areas
- Centres & Initiatives
- Graduate Students
- Postdoctoral Fellows & Research Staff
- Research Seminars
- Undergraduate Research
- Funding Opportunities
header pattern
Clinical Pharmacy Research
The goal of researchers in this area is to improve the prevention and management of disease and injury in individuals.
Our research explores hypotheses and answers questions that arise in clinical practice. The focus is on enhancing the health and quality of life of individuals by optimizing the safety and effectiveness of medications. Specific areas of expertise of our researchers include clinical trials, clinical pharmacology, clinical pharmacokinetics, clinical pharmacodynamics, clinical pharmacogenomics, medication therapy management, and medication stewardship.
Investigators
- Marisa Battistella
- Heather Boon
- Carlo DeAngelis
- Lisa Dolovich
- Sara Guilcher
- Brian Hardy
- Shoshana Hahn-Goldberg
- Murray Krahn
- Lisa McCarthy
- Peter Pennefather
- Lalitha Ramen-Wilms
- Winnie Seto
- Beth Sproule
- Anna Taddio
- Sandra Walker
- Scott Walker
Research News

Celebrating excellence with U of T-wide student services award
Celebrating our community: spotlight on pharmacy education
High school students explore pharmacy practice at PharmPath event
- Pharmacy's Pandemic Response
- Leverage Our Expertise
- Student Spotlight
- By the Numbers
- Our Research
- Our Education
- Our Community
- Message from the Dean
- Champion Equity, Diversity, and Inclusion
- Educate Pharmacy for Tomorrow
- Deliver Impact through Cutting-Edge Discovery
- Build Leadership, Wellness and Community
- Advance Use of Digital Technology
- Support Sustainability in Health Care
- What pharmaceutical sciences research areas can I explore?
- What pharmaceutical sciences graduate degrees are offered?
- What courses can I take as a pharmaceutical sciences graduate student?
- What are the application requirements for a pharmaceutical sciences graduate student?
- How do I find a supervisor?
- How much does graduate school cost?
- What is the application deadline for the graduate department of pharmaceutical sciences?
- Sign up to learn more
- How to become a pharmacist
- Why should I become a pharmacist?
- What are the Leslie Dan Faculty of Pharmacy Admission Requirements
- What high school courses are required to become a pharmacist in Canada?
- What university program should I take before applying to pharmacy school?
- How much is pharmacy school tuition?
- Why should I choose to earn my PharmD at the Leslie Dan Faculty of Pharmacy
- What can pharmacists do other than fill prescriptions?
- Upcoming Events
- News Stories
- Pharmacy Leadership and Education
- Graduate Programs
- Prospective Students
- Current Students
- Faculty & Staff
- Degree Programs >
PHD, Clinical & Administrative Pharmacy
This interdisciplinary program prepares students to address complex socio-political problems relating to ethical drug consumption, manufacturing, distribution, and payment mechanisms. Elective concentrations are business, psychology, statistics, political science, and more.
Degree Type: Doctoral
Degree Program Code: PHD_PHRM
Degree Program Summary:
The department includes the general areas of pharmacy administration, pharmacy practice, and experimental therapeutics. The synergy of these areas provides the means for pharmacy professionals to integrate and apply all prior course material to the identification and assessment of patient problems, collecting and utilizing patient information, developing solutions to patients’ drug related problems, selecting and recommending therapies and appropriate follow up to assess outcomes. The program in experimental therapeutics provides opportunities for basic clinical and pharmacological research. Integral to these areas the department also teaches and explores the economic, social, behavioral and political aspects of developing and providing pharmacy care services. These areas of study prepare the student to address the complex socio-political and therapeutic challenges associated with ethical drug use in our society. Mission Statement The department seeks to provide students with the knowledge and problem solving skills needed to deliver pharmaceutical care. The department is committed to improving the quality and relevance of its program to the contemporary practice of pharmacy. These efforts are aimed at advancing the profession of pharmacy and the provision of health care services to improve patient health outcomes.
Clinical and administrative pharmacy includes the general areas of pharmaceutical health services, outcomes, and policy, as well as clinical and experimental therapeutics. Pharmaceutical health services, outcomes, and policy is the study of the economic, social, behavioral, and political aspects of pharmaceutical services. It is an interdisciplinary program which may contain elective concentration of courses in business, psychology, statistics, political science, and other disciplines which impact on ethical drug issues. The program prepares the student to address the complex socio-political problems relating to ethical drug consumption, manufacturing, distribution, and payment mechanisms.
Clinical and experimental therapeutics is a multi-disciplinary program which involves the investigation of disease processes and the therapeutic regimens in their treatment. Current areas of interest include diseases of the cardiovascular system, learning and memory, immunology, and renal diseases. Additionally, the efficacy of therapeutic regimens in special populations (e.g. geriatric, women, minority) are also of interest. The graduate program is designed to develop competencies in clinical and experimental therapeutics which is translational between the basic, applied and clinical settings.
Locations Offered:
Athens (Main Campus)
College / School:
College of Pharmacy
250 W. Green Street Athens, GA 30602
706-542-1911
Department:
Clinical and Administrative Pharmacy
Graduate Coordinator(s):
Dr. Somanth Shenoy
Phone Number:
706-542-5415
Search for another degree
Find your graduate program.
Offering 200+ degrees, certificates and programs of study, we’ll help you get started on your graduate journey.
or
Search by keyword, program of study, department or area of interest
Interested in earning both a bachelor’s & master’s degree in five years or less?
Learn more about Double Dawgs .
Unlocking potential. Building futures.
Apply Today
The Graduate School Brooks Hall 310 Herty Drive Athens, GA 30602 706.542.1739
- Administration
- Graduate Bulletin
- Strategic Plan
- Virtual Tour
- Request Information
- Requirements
- Application Fee
- Check Status
- UGA Main Campus
- UGA Gwinnett
- UGA Griffin
- UGA Atlanta-Buckhead

We use cookies on reading.ac.uk to improve your experience, monitor site performance and tailor content to you
Read our cookie policy to find out how to manage your cookie settings
This site may not work correctly on Internet Explorer. We recommend switching to a different browser for a better experience.
Pharmacy practice PhD research supervision areas

Grow your potential in pharmacy practice research, by joining one of the PhD projects we have available at the University of Reading. If you're looking for a career in pharmacy practice, this is the perfect place to start.
This is a taster of some of the PhD projects you can be involved in at the University of Reading. To discuss the different projects available, please contact Dr Graeme Cottrell by emailing [email protected] .
Perceptions and ethical considerations of experiments with animals and animal tissues in the development of pharmaceuticals and cosmetics
With dr amelia hollywood (pharmacy practice) and prof vitaliy khutoryanskiy (pharmaceutics).
This interdisciplinary project will explore perceptions and ethical considerations of experiments with animals and animal tissues in the development of pharmaceuticals and cosmetics. Qualitative and quantitative research methods will be used. Data will be collected globally to ensure the findings have international significance and impact.
Pain and health behaviours
With dr amelia hollywood.
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage. The experience, treatment and management of pain is multifactorial, including biological, psychological and social factors. Various projects can be devised from this theme and will focus on the patient perspective. Both qualitative and quantitative research methodologies are likely to be employed, with potential methodologies including questionnaires, interviews and developing behaviour change interventions. The aim of this project is to improve care for those experiencing pain.
Sport and health
This project is a multidisciplinary approach to sports health focussing on the care of the competitive or recreational athlete. Various projects can be devised from this theme, including medicine use in athletes, pain management in sport and the impact of chronic conditions on performance. Both qualitative and quantitative research methodologies are likely to be employed, with potential methodologies including questionnaires, interviews and developing behaviour change interventions. An interest in working as part of a multi-disciplinary team and strong communication skills are essential.
Development of an interprofessional intervention for prescriber management of respiratory tract infections
With dr rosemary lim, resilience in the use of iv insulin infusions in hospital in-patients with diabetes, supporting people with dementia and their informal carers with their medicines, clinical pharmaceutics, with dr nilesh patel, medicines use and health services evaluation, cultural competence in pharmacy, with dr atta naqvi.
UK hosts a large multicultural population and changes in the immigration, business and work regulations have also resulted in increased migration and settlement from different parts of the world. This influx has enriched the culturally diverse society. This is also reflected in figures for pharmacists registered in the UK. Healthcare service delivery may be affected by the level of cultural competence among pharmacists in communication with other healthcare professionals when working in diverse team-based settings. Besides, having patients from different cultures and backgrounds would also require cross-cultural competency to deliver effective healthcare. This theme will explore cultural competence in academic as well as practice areas, develop strategies to improve cultural competence, and assess their effectiveness. The aim is to create reliable resources that can assist in assessing and improving cultural competence.
Pharmacists’ role in chronic pain management and opioid stewardship
Chronic pain affects roughly a third to one-half of UK's population. The UK has a large burden of chronic pain with a prevalence of 43%. Opioid prescription have increased in last few years leading to an opioid epidemic. Pharmacists are one of the most trusted healthcare professionals in the UK's healthcare system and are viewed as reliable source of information for addressing healthcare needs such as opioid therapy optimization for chronic non-cancer pain. This theme will explore pharmacists' role in managing chronic non-cancer pain and opioid medication therapy, from the perspective of pharmacists, patients, and other stakeholders. The studies can be designed both as qualitative and quantitative. In addition, a mix methods approach can be selected. The aim is to provide recommendations to the concerned departments, societies, and the NHS, with a focus on improving service delivery for the patients.
Adherence issues in practice
Non-adherence to medication and treatment among patients with chronic conditions remains a challenge for clinicians in practice. Patients may exhibit non-adherence to medications as well treatment such as physical therapy, etc. Adherence could be intentional or un-intentional. It may also be affected due to multi-morbidity, logistics and financial issues that the patients face. The aim of this project is to develop new and/or improve existing measures, create new resources to facilitate adherence to medications and treatments in this population. Such resources could help in identifying and signposting patients for further evaluation as well as improve adherence to treatment.

CPD from CIPPET
Our research

Find out more from our students and staff about what it's like to study and work in the University of Reading School of Pharmacy.
Take the next step
- How to Apply
- Get a prospectus
- Ask us a question
- Learn about the Doctoral and Researcher College

Alternatively, use our A–Z index

Attend an open day
PhD/MPhil Pharmacy Practice / Programme details
Year of entry: 2024
- View full page
Programme description
Our PhD/MPhil Pharmacy Practice programme enables you to undertake a research project that will improve the practise of pharmacy, the prescribing of medicines to optimise therapy and how patients take their medicines. There are 3 working centres in Pharmacy Practice which include the Centre for Pharmacy Workforce Studies chaired by Dr Ellen Schafheutle , Pharmacoepidemiology and Drug Safety chaired by Prof Darren Aschroft , and Prescribing and Patient Safety chaired by Dr Penny Lewis. There is a lot of interplay between the centres so there is maximum impact to the patient and to the research. We work with patient groups, prescribers, and pharmacists to gather the necessary information to conduct research, but also healthcare databases to maximise the study population size for robust results. We have a diverse skill base including clinical and community pharmacists, biostatisticians, epidemiologist, qualitative specialist researchers and health economists.
A research project is usually supervised by 2 co-supervisors that could be from different types of research backgrounds, but with this combination a unique and blended research experience is gained by the student. Research projects include pharmacoepidemiology studies, drug utilisation research, regulations, patient and medicines safety, organisational systems, transfer of care and disease specific research.
Our PhD research projects in Pharmacy Practice for international students primarily involve evaluation of practice and drug policy, pharmacoepidemiology using anonymous data, evaluating practice from already collected data or data collected by a third party or quantitative and qualitative analysis of national clinical data sets. These projects involve clinical knowledge and judgement and gaining skills in database management, analysis of large dataset and thematic analysis. All of these projects do not involve the international professional student having direct contact with NHS patients. Unfortunately, the NHS regulations on clinical contact with patients (including medical notes) is very strict and reserved for UK registered pharmacists and practitioners. Therefore a PhD in Clinical Pharmacy is not available to students wanting to attend the University of Manchester for this programme of study.
Special features
Training and development
All of our postgraduate researchers attend the Doctoral Academy Training Programme delivered by the Researcher Development team . The programme provides key transferable skills and equips our postgraduate researchers with the tools to progress beyond their research degree into influential positions within academia, industry and consultancy. The emphasis is on enhancing skills critical to developing early-stage researchers and professionals, whether they relate to effective communication, disseminating research findings and project management skills.

Teaching and learning
Applicants are specifically matched with a Primary Supervisor and individual project based on their research interests and background.
International applicants interested in this research area can also consider our PhD programme with integrated teaching certificate .
This unique programme will enable you to gain a Postgraduate Certificate in Teaching and Learning, whilst also carrying out independent research on your chosen project.
Attendance Requirement for Distance Learning Programme
Students must maintain expected virtual presence and communication with their Supervisor in order to remain registered on the programme and follow all online progression milestones as for any PGR student.
Students must attend, in person, the Welcome and Induction activities organised by the Doctoral Academy in September. As a result, a September start date is preferable. Students should also attend, in person, the compulsory `Life as a PhD Student' training.
Students are encouraged to consider undertaking additional training offered via the Doctoral Academy Training Programme.
It is expected that students will spend a minimum of one working week (5 days) in attendance at the University (in addition to welcome/induction days). This may coincide with formal study weeks (ie in NMSW) and will present the opportunity for the student to spend time with their Supervisory team, visit the Library or local research facilities.
Students must participate in the formal Annual Review meeting, ideally in person, but attendance via Skype etc can be considered.
The final oral examination will be held at the University of Manchester. Only in very exceptional circumstances will a student be allowed to undertake the viva remotely.
Scholarships and bursaries
Funded programmes and projects are promoted throughout the year. Funding is available through UK Research Councils, charities and industry. We also have other internal awards and scholarships for the most outstanding applicants from within the UK and overseas.
For more information on available the types of funding we have available, please visit the funded programmes and funding opportunities pages.
What our students say
Disability support.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Pharm J (Ott)
- v.149(4); 2016 Jul
Pharmacy Practice Research Abstracts
Table of contents.
This year, the Canadian Pharmacists Association (CPhA) and the Alberta Pharmacists’ Association (RxA) partnered to deliver four days of exciting educational sessions, exceptional keynote speakers, social events and networking opportunities at the annual Canadian Pharmacists Conference.
The Canadian Pharmacists Conference is an excellent opportunity for pharmacists from across Canada to network with colleagues and to share new and exciting ideas, research and innovation. Our oral and poster pharmacy practice research presentations provide an opportunity for members of the pharmacy community to engage in sessions that promote evidence-based practice and decision-making.
To help promote and disseminate pharmacy practice research, CPhA publishes the abstracts of the research presented at the conference in this special supplement of the Canadian Pharmacists Journal .
PHARMACY PRACTICE AND CARDIOVASCULAR HEALTH
S1 ECG screening in community pharmacy: An innovative pilot program to improve detection of cardiac arrhythmias in high-risk patients
S2 Impact of the Community Pharmacists Assisting Total Cardiovascular Health (CPATCH) strategy for improving medication adherence from community pharmacies – A cluster-randomized trial
S3 The Alberta Vascular Risk Reduction Community Pharmacy Project: RxEACH
SUCCESSFUL PHARMACISTS: POINT OF CARE AND MORE
S4 Implementation of a standardized HbA1c clinic worksheet to improve detection of drug therapy problems: Results from a multi-pharmacy pilot program
S5 Community pharmacist bone density point-of-care screening with osteoporosis and fracture risk estimation
S6 Defining characteristics of successful pharmacists
THE ELDERLY IN PHARMACY
S7 Development and implementation of a pharmacist intervention for frail elderly patients in an interdisciplinary primary care team: A qualitative analysis
S8 Identifying drug-related problems in retirement home residents following community pharmacist administered flu vaccinations
S9 Deprescribing guidelines for the elderly: Overview of findings from a 3-year program of research
MEDICATION ASSESSMENT AND MODELS OF CARE
S10 Community pharmacist standardized home medication consultation program by referral: Structured approach to identifying drug-related problems in the home-bound population
S11 The Medication Assessment Centre: A novel student training and patient care program
S12 Collaborative care model involving eHealth to improve treatment adherence and health outcomes of patients with gout
HOT TOPICS IN PHARMACY PRACTICE RESEARCH
S13 Effectiveness of community-based pharmacist interventions in chronic non-cancer pain: A systematic review
S14 The consideration of sex/gender and vulnerable populations in pharmacy practice research
POSTER ABSTRACTS
S15 Introducing a unit-based clinical pharmacist: A pilot study
S16 Patient-centered renovations
S17 Medication reconciliation practices on discharge into primary care homes in Prince George, British Columbia
S18 Stakeholder perspectives on economic analyses of billable pharmacy services in Ontario
S19 Opportunity and cost: Self-monitoring of blood glucose in Manitoba, 2000-2013
S20 Ibuprofen provides superior antipyretic efficacy vs. acetaminophen in childhood fever: Pooled analysis of 2 randomized trials
S21 Development of a hormonal contraception decision support tool for pharmacists
S22 The pharmacy services framework: Communicating the shift to clinical pharmacy services in Alberta
S23 Provider and patient perspectives regarding a community pharmacist-based case finding and intervention program — Alberta Vascular Risk Reduction Community Pharmacy project: RxEACH
S24 An audit of 8 centres’ use of anticoagulant therapies when discharging patients from hospital with acute venous thromboembolism
S25 An audit of 8 centres’ use of anticoagulant therapies when discharging patients from the emergency department
S26 Enhancing depression outcomes with better use of antidepressants: Evaluation of a pharmacy benefit manager–sponsored depression disease state management program
S27 Pharmacist intervention for a frail elderly population in primary care
S28 Impact of pharmacist assessment on classes of high-risk medications in a geriatric outpatient clinic
S29 Description of medication management problems and supports used in community-dwelling seniors
S30 Effectiveness of the peer-to-peer mentoring model for transitioning from classroom to professional practice
S31 Community pharmacy reports of potential QTc-prolonging drug interactions involving fluoroquinolones or macrolides: A multi-incident analysis
S32 Medication incidents involving insulin: A multi-incident analysis
S33 Potentially inappropriate medication use in older adults: A multi-incident analysis
S34 Patient counseling: An overarching method to mitigate medication errors and ensure continuity of care
S35 Older people’s attitudes towards deprescribing: A community study in Quebec
S36 The effect of health media reporting on self-medication use
S37 Documentation of functional medication management in older adults within an acute care hospital
S38 Global citizenship framework — Application to pharmacy student experience
S39 How does pharmacist prescribing fit with family physicians’ practice in Alberta? Developing a knowledge translation strategy
S40 Medication incidents involving smoking cessation therapies
S41 Medication incidents involving immunosuppressive agents
S42 Medication incidents that could have been prevented at the prescribing stage
S43 Direct oral anticoagulant medication incidents
S44 Drug allergy incidents in community pharmacies
S45 Medication incidents associated with hospital discharge
S46 Successful pharmacists: A qualitative study to understand pharmacists’ definitions of successful pharmacy practices
ECG screening in community pharmacy: An innovative pilot program to improve detection of cardiac arrhythmias in high-risk patients
John Papastergiou, BScPhm; Larissa Boychuk, BSc, PharmD candidate
Objectives:
Undiagnosed arrhythmias such as atrial fibrillation and torsades de pointes can have serious health consequences. Atrial fibrillation causes 1/3 of strokes and 1.4% of these patients are undiagnosed. Over 150 medications are known to prolong QT intervals. The purpose of this study is to assess point-of-care ECG screening in identifying undiagnosed abnormalities in high-risk patients in a community pharmacy setting.
High-risk patients were invited to participate in ECG screening at two community pharmacies in Toronto, Ontario. Patients met eligibility requirements if they were at risk of QT prolongation or atrial fibrillation secondary to medication therapy or a CHADS2 score of >2, respectively. Using the HeartCheckPenTM handheld device, a 30 second lead II screening test was performed. Data was uploaded to an ECG reading service where results were interpreted by a qualified professional. Results were forwarded to the pharmacy for follow-up. Pharmacists referred all patients with abnormal readings to their primary care physician for further investigation.
Thirty-five patients participated in the program. Eleven were identified at risk for atrial fibrillation and 18 for QT prolongation — 5 patients met both criteria. Screening identified 10 (28.6%) patients with one or more abnormal rhythms. These included premature atrial contraction (n=3), wide QRS (n=4), sinus arrhythmia (n=1), sinus tachycardia (n=3) and QT prolongation (n=1). Pharmacists referred all patients and, in the case of QT prolongation, intervened to alter therapy.
Conclusions:
Our experience demonstrates that point-of-care ECG testing can be successfully integrated into pharmacy workflow. The results illustrate the prevalence of abnormal rhythms in high-risk patients. They highlight a significant opportunity for pharmacists to use point-of-care screening as a tool to detect abnormal rhythms, intervene when warranted, and improve medication safety.
Impact of the Community Pharmacists Assisting Total Cardiovascular Health (CPATCH) strategy for improving medication adherence from community pharmacies – A cluster-randomized trial
David Blackburn, PharmD; Charity Evans, PhD; Jeff Taylor, PhD; Kerry Mansell, PharmD; Derek Jorgenson, PharmD; Yvonne Shevchuk, PharmD; Alfred Rémillard, PharmD; Dean Eurich, PhD; Bill Semchuk, PharmD; Anne Champagne, BSP
The highest risk for non-adherence occurs during the first year after starting a new chronic medication. Community pharmacists are well positioned to identify problems and provide support during this critical time.
Thirty community pharmacies in Saskatchewan, Canada, were randomized to deliver a brief adherence intervention or usual care to new users of HMG-CoA reductase inhibitors (statins). The intervention consisted of screening for new statin users, assessment for adherence barriers, and individualized follow-up when appropriate. The primary endpoint was mean statin adherence measured by the proportion of days covered (PDC). During follow-up, intervention pharmacies performed monthly assessments to estimate compliance with the study protocol.
A total of 1,906 new statin users were followed for six to twelve months following their first statin dispensation. No significant differences between intervention and control pharmacies were observed for mean adherence (72% (SD 33) vs 71% (SD 33); p=0.64), median adherence (89% versus 88%; p=0.84), or the percentage of subjects achieving optimal adherence (i.e., PDC ≥80%: 57.3% (520/907) versus 55.8% (558/999); p=0.51). However, several intervention stores reported poor compliance to the study protocol. In post-hoc analyses, mean adherence among pharmacies reporting good compliance with the study protocol was substantially higher than stores with poor compliance (76% versus 66%; p<0.01), and the percentage of patients achieving optimal adherence was 63% vs 52% (p<0.01) respectively.
The CPATCH strategy was not effective for improving statin adherence compared to usual care in community pharmacies. However, post-hoc analyses suggested that successful implementation might be the key to achieving important benefits.
The Alberta Vascular Risk Reduction Community Pharmacy Project: RxEACH
Yazid Al-Hamarneh, BS(Pharm), PhD; Ross T. Tsuyuki, BSc(Pharm), PharmD, MSc; Charlotte A. Jones, MD, PhD; Brenda R. Hemmelgarn MD, PhD
Despite the risk associated with hypertension, diabetes, dyslipidemia, and smoking, these cardiovascular disease (CVD) risk factors remain poorly identified and controlled. To evaluate the effect of a community pharmacy-based case finding and intervention program on estimated cardiovascular risk.
Design: Randomized controlled trial. Setting: 56 community pharmacies across Alberta. Population: Adults at high risk for CVD events, including those with diabetes, chronic kidney disease, vascular disease and/or Framingham score > 20% who have at least one uncontrolled risk factor (hypertension, LDL-cholesterol (LDL-c), HbA1c, or current smoking). Randomization: Participants were randomized (1:1 basis) into advanced or usual care groups. Advanced care: Pharmacists provided participants with: Physical and laboratory assessments; Individualized CVD risk assessment and education; Pharmacists prescribed where appropriate to achieve treatment targets; Regular monthly follow-ups for 3 months. Usual care: Usual pharmacist care with no specific intervention for 3 months. Primary outcome: The difference in change in estimated CVD risk between advanced and usual care groups, calculated using a relevant risk calculator based on participants’ co- morbidities (Framingham, International, or UKPDS).
We enrolled 723 patients. Median age was 62 years (interquartile range 54-69), 57% were male and 27% were smokers. After adjusting for baseline values, the difference in change in CVD risk was 21% (p<0.001): a change of 0.2 mmol/L in LDL-c (p<0.001), 9.4 mmHg in systolic blood pressure (p<0.001), 0.92% in HbA1c (p<0.001), and 20.2% in smoking cessation (p=0.002) between advanced and usual care groupsaccess (96% and 91%).
This is the first large randomized trial of CVD risk reduction in community pharmacy settings. Patients in the advanced care group were 21% less likely to have a heart attack, stroke, or peripheral artery disease when compared to those in the usual care group. RxEACH provides evidence for the benefit of pharmacist care on both global CVD risk and individual risk factors
Implementation of a standardized HbA1c clinic worksheet to improve detection of drug therapy problems: Results from a multi-pharmacy pilot program
John Papastergiou, BScPhm; Bryan Gray, BScPharm, RPh, CDE
Point-of-care HbA1c screening devices are a valuable tool that community pharmacists can use to monitor patients with diabetes and improve their overall management. Here, we report data from a multi-pharmacy pilot program where a standardized worksheet was used by pharmacists offering HbA1c clinics in order to standardize the structure of the patient interviews and improve detection of drug therapy problems.
Thirteen community pharmacies from across Ontario interested in offering HbA1c screening as part of their professional programmes participated in the pilot program. Pharmacists received training on the use of the standardized worksheet and were provided with all the tools required to hold a clinic. HbA1c analysis was performed using the Roxon A1c Now®. Data collection took place over a period of 4 months beginning August 2015.
Eighty-eight patient attended the clinics. The mean HbA1c of the population was 7.76. Overall, 36% of patients had optimal glycaemic control (A1c <7.0%), 45% were hyperglycaemic (A1c >7 and <9%) and 19% of patients had marked hyperglycaemia (A1c >9.0). A total of 204 interventions were performed by pharmacists. An average of 2.32 interventions were performed per patient, and we observed a trend towards increased numbers of interventions in patients with poorer glycemic control. Interestingly, 23% and 15% of patients met the CDA guideline requirements for therapy with a statin and an ACE/ARB, respectively, but were identified by pharmacists as not receiving the appropriate therapy.
These results illustrate the prevalence of suboptimal glycaemic control among patients with diabetes in the community. They highlight a significant opportunity for pharmacists to use point-of-care screening in combination with a standardized worksheet to more readily detect drug therapy problems and intervene to improve disease management when warranted.
Community pharmacist bone density point-of-care screening with osteoporosis and fracture risk estimation
Bryan Gray, BScPharm, RPh, CDE
Point-of-care bone density screening is a valuable tool that community pharmacists can use to identify and educate patients at risk for osteoporosis and fractures. Here, we report data from screening 66 patients (12 male) at structured bone density clinics held at a community pharmacy in Thunder Bay, ON.
Bone density analysis was performed using the Omnisense 8000. Fracture risk factors and the point of care T-scores were interpreted with both the Canadian CAROC estimator and the WHO FRAX risk estimator to provide a 10-year fracture risk assessment. Recruitment involved in-pharmacy promotion to all patients. Data collection took place over a period of 3 months.
Testing successfully identified patients potentially at risk for osteoporosis and fracture. The CAROC found 5, 7, and 54 patients at high, moderate, low risk, respectively, for developing fracture over a 10-year period. The WHO FRAX calculator found a similar distribution with ten patients receiving a major fracture risk estimate 10% or greater, and five patients with a hip fracture risk estimate 5% or greater. The average patient age was 61, and the average BMI was overweight at 29. A total of 273 recommendations were provided by the pharmacist — average 4.13 per patient.
These results illustrate the prevalence of potentially undiagnosed osteoporosis for patients in the community. Our intervention data suggests that a structured bone density consultation by a community pharmacist can identify patients at risk for fractures. Patients at low risk were given evidence based and practical recommendations to maintain their bone health and reduce the risk of developing osteoporosis. Continued expansion in scope of pharmacy practice may contribute to increased osteoporosis identification and reduction in fracture risk.
Defining characteristics of successful pharmacists
Jay Mutch, BScPharm (student); Lydia Cheung, BScPharm (student); Theresa Charrois, BScPharm, ACPR, MSc; Jill Hall, BScPharm, ACPR, PharmD; Meagen Rosenthal, PhD; Ken Cor, PhD
Our primary objective was to identify the self-described characteristics of pharmacists that contribute to their success. Our working definition of success in pharmacy is based on the premise that successful pharmacists practice to the full extent of their knowledge and skills. The definition was derived from a literature review as well as the Blueprint for Pharmacy.
Semi-structured individual interviews were conducted with selected pharmacists. The interview tool was developed using previous research on success in health care professions and was modified based on trial interviews with faculty and practitioners. Potential candidates were nominated by prominent pharmacists in the field, using our definition of success. Lists from the nominators were compared and 10 pharmacists who appeared on more than one list were invited to participate.
A total of 8 out of 10 interviews have been analyzed to date. All 8 pharmacists had additional prescribing authorization (APA), with 4 of those pharmacists being early adopters (receiving APA prior to remuneration model implementation). In terms of factors contributing to success, participants noted strong communication skills and developing relationships as important. When asked what success meant to them, participants believed that self-development played a large role. Participants also felt a focus on emotional intelligence would help ensure the success of pharmacist practice in the future.
A clearly delineated definition of success was developed and used to frame interviews with practitioners viewed as successful by their peers. Communication skills were the most prominent factor that contributed to success. This data will help individual pharmacists become aware of what characteristics they may want to foster in themselves in order to have success in practice.
Development and implementation of a pharmacist intervention for frail elderly patients in an interdisciplinary primary care team: A qualitative analysis
Tejal Patel, PharmD; Lindsay Donaldson, BA; Linda Lee, MD; Jillian Bauer, BScPharm; Cathy Schill, BScPharm
There is a paucity of published literature describing activities involved in the implementation of an intervention in an interdisciplinary primary care environment. The objective of this research is to describe the development and implementation of the pharmacist intervention (PI) for frail elderly patients in an interdisciplinary primary care team.
This study is a deductive qualitative analysis of emails and meeting minutes pertaining to the PI for frail patients. Classical content analysis was conducted to quantify previously established codes and themes pertaining to: 1. Goal of the PI (e.g. codes: literature review, objectives of PI, etc); 2. Delivery of the PI (e.g. codes: care provision, follow-up, tracking outcomes, etc); 3. Work Environment (e.g. codes: roles and responsibilities, availability of staff, workflow processes, etc) and 4. Sustainability of PI (e.g. codes: scheduling, etc).
Of the 2,830 email items and minutes of 4 meetings between pharmacists, physicians, nurses, receptionists and administrators that were reviewed, 172 emails and 4 meeting minutes were eligible for classical content analysis. Of the resulting 718 coded items, 40% were related to Work Environment, 36% to the Delivery of the PI, 12%, each, to the Goal and Sustainability of the PI. The number of items coded for Goal of PI decreased from a high of 50 items in the period of 6 months pre-initiation to 2 items at the end of 24 months post initiation of PI. The number of items pertaining to the codes, “tracking” and “follow-up” of patients increased from 4 and 0 at 6 months pre-initiation to 19 and 39 at 24 months post-initiation of PI, respectively.
The impact and importance of the different aspects, such as the goal, delivery of the program, working environment and relationships changed with time. This analysis may be used to improve planning of other interventions in primary care in the future.
Identifying drug-related problems in retirement home residents following community pharmacist administered flu vaccinations
Community pharmacist administered flu vaccinations serve as an opportunity to screen patient’s medication profiles for drug-related problems. Here, we report data from medication consultations of 58 patients (16 male) from three retirement homes in Thunder Bay, ON.
Consenting retirement home residents were scheduled for a flu vaccination and a subsequent medication consultation. Following intramuscular vaccine administration, resident’s medication regimens and health status were screened for potential drug-related problems. Following consultation, the community pharmacist communicated potential drug-related problems to the resident’s primary care provider. Data collection took place over a period of 1 month.
Following vaccination, standardized medication consultations identified a total of 579 potential drug-related problems — an average of 9.98 interventions per patient. Very few of the patients were aware of their overall vaccination status (291 recommendations). Many patients were receiving inappropriate cardiovascular disease medications (over treating hypertension or lipids (76 recommendations). Consolidation of the medication regimen was very well received by residents (46 recommendations). The average patient age was 87 years old, with 9.5 medications per patient (average), with an average number of dosing intervals of 3.6 per day. Recommendations to improve adherence could reduce dosing intervals to 1.9 per day. Patients were appreciative to have their medication regimen and health status reviewed by the pharmacist instead of waiting independently for the 15 minutes post vaccination time period to pass.
In addition to the benefits provided by vaccination, subsequent medication consultations successfully identified potential drug-related problems.This data suggests that retirement home residents may be at risk for drug-related problems which may be mitigated by pharmacist intervention.
Deprescribing guidelines for the elderly: Overview of findings from a 3-year program of research
Barbara Farrell, BScPhm, PharmD, FCSHP; Lalitha Raman-Wilms, BScPhm, PharmD, FCSHP; James Conklin, PhD; Lisa McCarthy, BScPhm, PharmD, MSc; Kevin Pottie; MD MCISc; Carlos Rojas-Fernandez, BSc(Pharm), PharmD; Lise Bjerre, MD, PhD, MCFP; Hannah Irving, MA
Class-specific deprescribing guidelines are a potential solution to address the problem of polypharmacy. Optimal approaches to developing and implementing such guidelines with practitioners have yet to be identified. The purpose of the study was to understand factors associated with successful deprescribing guideline development, implementation and uptake and whether self-efficacy for deprescribing was affected.
Deprescribing guidelines were developed using AGREE-II (Appraisal of Guidelines for Research and Evaluation), and GRADE (Grading of Recommendations Assessment, Development, and Evaluation) to rate certainty of evidence and strength of recommendations. Developmental evaluation was performed using ethnographic methods: observations and interviews with guideline development and site implementation teams, and facilitated feedback sessions to discuss and agree on process improvements. Self-efficacy surveys were completed. Setting and participants included guideline development team members; members of three Family Health Teams and three Long-Term Care sites in Ottawa, Canada; and study team members.
Three evidence-based deprescribing guidelines were developed (proton pump inhibitors, benzodiazepine receptor agonists and antipsychotics). Process components and resulting decision-aid algorithms will be presented. Factors that facilitate successful development include team members’ expertise in content/ methods, access to additional expertise/resources through professional networks, and staff support. Development processes were modified for the 2nd and 3rd guidelines to ensure clarity in scope and responsibilities. Site implementation experience suggests practitioners are more interested in how to implement deprescribing approaches versus existing evidence to support stopping medications, that practice site priorities and processes shape ability to incorporate recommendations and that aligning guidelines with existing processes is critical to implementation success. Self-efficacy increased among 9 consistent respondents across all guidelines. Examples of how site experiences influence development of deprescribing guidelines will be provided.
Optimizing a deprescribing guideline development and implementation process aims to facilitate clinicians’ ability to address polypharmacy. Developmental evaluation contributes to the improvement of processes used to develop and implement such guidelines.
Community pharmacist standardized home medication consultation program by referral: Structured approach to identifying drug-related problems in the home-bound population
Bryan Gray, BScPharm, RPh, CDE; Laura Bron, BScPharm, RPh, CDE
Perform home medication consultation to identify drug-related problems and communicate concerns to the primary prescriber. Secondary objectives: Identify trends across the different intervention categories, identify drug-related problem trends by disease states and project the anticipated cost savings from avoided hospital admissions.
A referring agency in Thunder Bay, ON, sent requests for Home Medication Consultations for 33 patients (11 male) over a 3 month period. Pharmacists screened the patient’s medication regimen and health status for potential drug-related problems. Following consultation, the community pharmacist communicated potential drug-related problems to the resident’s primary care provider.
A total of 223 interventions (average of 6.76 per patient) were provided to 23 different prescribers. Average age was 76 years. Twelve were immediately accepted, 8 were immediately declined, and the remaining 203 would be discussed at the patient’s next visit Secondary outcome: Pharmaceutical Opinion Classification Trends — The majority of recommendations were related to: requiring additional drug therapy, adherence, and sub-optimal response to current therapy. Secondary outcome: Disease State DRP Trends — Based upon disease state and medical conditions, immunization/vaccination status was the most common DRP, followed by adherence (opportunity to reduce dosing frequency, merge drugs to combination therapy, and adherence packaging), and mental health (8 DRPs related to sleep/insomnia, 14 DRPs related to depression/mood/anxiety, and 2 DRPs related to smoking). Secondary outcome: Projected Case Cost Forecasted Savings — This totals $12,062.19 cost savings for avoided hospital admissions with 2 avoided hospital admissions.
A standardized and structured approach to performing home medication consultations successfully identified potential drug-related problems.
The Medication Assessment Centre: A novel student training and patient care program
Derek Jorgenson, BSP, PharmD, FCSHP; Eric Landry, BSP, ACPR; Katherine Lysak, BSP, MSc candidate
The Medication Assessment Centre (MAC) was launched in 2011 by the College of Pharmacy and Nutrition (University of Saskatchewan), with the dual purposes of: (1) providing access to pharmacist-led comprehensive medication assessments for highly complex patients who cannot access the service elsewhere; and, (2) creating a novel faculty supervised experiential training program for pharmacy students, located on campus. The objective of this project was perform an evaluation of this program from the perspective of patients and physicians.
A retrospective chart review was performed on all patients who attended at least one MAC appointment between March 2014 and July 2015 to measure: number/ description of patients; referral sources; and numbers/severity of drug therapy problems (DTPs). An experience/satisfaction survey was mailed to patients and their physicians who utilized MAC between April and October 2015.
A total of 173 patients were included in the chart review. Patients were referred from both health professionals (65.9%) and self-referrals (34.1%). Patient mean age was 64.8, with a mean of 6.5 diagnoses and 13.8 different chronic medications each. Pharmacists identified 6.2 DTPs per patient (31.1% moderate severity using Schneider criteria). Surveys were mailed to 121 patients and 81 physicians (response rates 66.9% and 43.2%, respectively). Almost 95% of both groups described their experience as very satisfied/satisfied and reported that they would refer MAC to their friends/family/colleagues; 59.2% of patients and 88.6% of physicians felt MAC improved patient outcomes; 98.8% of patients felt they were treated with dignity/ respect and that the pharmacist listened to their concerns; and 97.5% of patients felt they were involved in decisions about their health.
MAC is meeting its objective of providing access to medication assessments for highly complex patients. Physician and patient experience has been very positive and highly supportive of the program.
Collaborative care model involving eHealth to improve treatment adherence and health outcomes of patients with gout
Nicole Tsao, BSc, BScPharm, MScPharm; Kam Shojania, MD; Alison Kydd, MD, PhD; Jessica Galo, BSc; Alyssa Howren, BSc; Carlo Marra, BScPharm, PharmD, PhD; Mary De Vera, PhD
The prevalence of gout is increasing and despite availability of efficacious therapies, sub-optimal clinical outcomes persist due largely to medication non adherence. Pharmacists may have a role in supporting patients to improve their gout management. The objective of this study is to pilot the feasibility of an interdisciplinary care model involving rheumatology, pharmacy, and dietetics using shared electronic medical records (EMRs) to provide gout care.
This is a proof-of-concept study that employs a pharmacist-driven protocol whereby they are responsible for providing medication management, adherence counselling, interpretation of lab tests, and corresponding titration of urate-lowering therapies. Eligible patients are adults age ≥19 who have been diagnosed with gout by a rheumatologist for ≥1 year, ≥1 flare in the past year, and serum uric acid (SUA) >360 µmol/L within past 2 months. Remotely located health team members use shared EMRs to exchange patient information and communicate on care plans. Study outcomes include the impact of the care model on patients’: SUA levels (target <360 µmol/L); medication adherence (Compliance Questionnaire for Rheumatology 5-items); functional status (HAQ); and quality of life (EQ-5D); assessed at 0, 3, 6, and 12 months. Target enrollment is 50 patients.
Preliminary results on 21 patients enrolled from 3 rheumatology clinics since Feb. 2015 include 85% males, mean age 56 years (SD 15). All patients were prescribed allopurinol. At 6 months, adherence rate was 50%, and average SUA was 350 µmol/L versus 445 µmol/L at baseline. To date, pharmacy has provided 71 consultations and dietetics 12 consults. Anecdotal pharmacist interventions also included drug dose increases, discontinuation of unnecessary medications, and prescription continuations.
A virtual interdisciplinary clinic for gout management with expanded pharmacists’ role appears feasible with preliminary data showing improvement in SUA.
Effectiveness of community-based pharmacist interventions in chronic non-cancer pain: A systematic review
Feng Chang, BScPhm, PharmD; Mo Chen, BSc, MSc candidate; Tejal Patel, BScPhm, PharmD
Chronic pain is a common condition that has significant impact on patients’ physical and psychological well-being. Pharmacists have a key role in providing patient-centred care to optimize drug therapy used in the management of chronic pain. To evaluate the effectiveness of interventions by pharmacists providing care in community settings for ambulatory patients with chronic non-cancer pain.
Six electronic databases (PubMed, Cumulative Index to Nursing and Allied Health Literature, COCHRANE, PsychInfo, EMBASE and International Pharmaceutical Abstract) were searched for randomized controlled trials (RCT) and non-randomized studies (NRS) published in the English language involving pharmacists providing direct care in the management of chronic non-cancer pain. Team based approaches were included if a pharmacist was involved. Manual bibliography searches with retrieved articles were conducted. Risk of bias was assessed for all included studies.
The search strategy identified 17 full-text articles from 14 studies. Six of the studies were based on pharmacist-only interventions and the other 8 involved pharmacists working as part of an interprofessional team. The most frequently used pharmacist intervention was consultation involving medication review, recommendations, follow-up, and patient education. There was variation across pain measures and other self-reported measures in the included studies, but most studies showed positive results. Pharmacist interventions significantly decreased pain scores, improved quality of life and patient satisfaction, and reduced medication-related side effects and cost. Pain intensity reduction achieved ranged 8%-21%.
Pharmacist interventions were positive in several domains studied. However, the clinical significance remains debatable due to heterogeneity in relation to intervention, outcome measures, clinical setting, sample size, and study duration.
The consideration of sex/gender and vulnerable populations in pharmacy practice research
Nancy Waite, PharmD; Martin Cooke, PhD; Katie Cook, MA; Emily Milne, PhD; Feng Chang, PhD; Lisa McCarthy, PharmD; Beth Sproule, PharmD
Funders often now require that sex and gender are main considerations in research programs, but provide little guidance about how this can be accomplished. The Ontario Pharmacy Research Collaboration (OPEN), a multi-institutional and multidisciplinary research program, adopted a sex/gender and vulnerable population (GVP) model within the collaboration to promote incorporation of sex, gender and other dimensions of vulnerability across OPEN’s research projects. This presentation (1) addresses why the consideration of GVPs matter to pharmacy practice and (2) describes the GVP model’s mandate, activities and experiences.
This mixed method study incorporates: (1) literature search of published work on this topic; (2) critical reflection of co-leads of the GVP team with regards to the creation and implementation of the model; and (3) surveys (n=37) and interviews (n=23) conducted with OPEN members about their knowledge of GVP issues and engagement with GVP services.
The consideration of sex/gender and vulnerable populations within pharmacy practice research is necessary, but lacking. Within OPEN, a GVP team was established to support research projects in their incorporation of sex/gender and various dimensions of vulnerability into research design, analysis and interpretation. According to OPEN members, knowledge pertaining to GVP issues in research increased through OPEN involvement. The GVP model “surfaced” domains traditionally neglected in the field but important to ensuring quality pharmacist practice. OPEN members have been receptive and engaged with the GVP model and mandate. However, more work needs to be done in order to fully translate this awareness into research practices.
There is a need for increased awareness and consideration of sex/gender and vulnerable populations in pharmacy practice research. The experience of OPEN suggests that a cross-project structure can help integrate these considerations into a large and complex research project. We encourage practitioners to consider GVP focused initiatives, tools, and models within their work.
Introducing a unit-based clinical pharmacist: A pilot study
Vinita Arora, RPh, BScPhm, ACPR, MEd, PharmD; Heather Parker, RPh, BScPhm; Alexandra Hernandez, PhD; Karyn Li, BSc candidate; Mehrdad Alizadeh, RPh, PharmD
A pharmacist was stationed on a forensic mental health unit to more fully participate in the interprofessional team. Since clinical pharmacy services were previously centralized, we evaluated the impact of this change on staff and patients of a forensic wing.
We administered anonymous surveys at three time periods, post 1, post 2, and post 3, at 1, 5, and 12 months, respectively (72 beds; nstaff 25, 27, 28; npatients 21, 21, 18) to examine themes of accessibility, education, and medication therapy management (MTM). Non-parametric chi-square analyses were used to examine differences in overall satisfaction (Strongly Agree and Agree responses combined) scores over the time periods. We also compared percentages of satisfaction in these themes and qualitative changes over time.
The average change in staff satisfaction from post 1 to post 3 was 8% for the Accessibility theme, 9.5% for the Education theme (2 to 17%) and 11% for the MTM theme (1 to 30%), with the increase in MTM satisfaction approaching significance (x2=5.911, p=0.052). The average change in patient satisfaction from post 1 to post 3 for questions in the Education theme was -12.5% (-5 to -24%) and -28% for questions in the Accessibility theme, however the decreases were not statistically significant. Qualitatively, there were positive changes stated by staff in all themes, most notably, accessibility; while patients expressed desire for increased services in all themes.
Being situated on a forensic mental health unit enhances involvement of the clinical pharmacist in the interprofessional team. Accessibility may be a precursor to provision of increased MTM and education. Limitations surrounding patient satisfaction need further consideration.
Patient-centered renovations
Joan Cochrane, BSP
My object was to renovate my pharmacy to make it easy for my pharmacists to provide better patient care.
We have designed our pharmacy so that the pharmacist is the first point of contact for the patient. The pharmacist is situated in a semi-private area at the front of the store. Our design has 2 of these “pharmacist interaction stations” to decrease wait time. The patient comes to the pharmacy, gives their prescription, refill or new, to the pharmacist and sits down across from the pharmacist. The pharmacist station has a computer with Internet access, a phone, a scanner and a computerized blood pressure monitoring system. This allows the pharmacist to handle the prescription in a single efficient interaction with the patient. If there are no problems to solve, the pharmacist can fill the prescription, the label prints at the island in the main dispensary area, if in the robot, it is automatically counted, if not, the technician assembles the medication and then brings it over to the pharmacist, who can hand it out. The pharmacist has been talking to the patient about the prescription and giving the appropriate information. Then the prescription is handed to the patient who is directed to the cash station. If there are problems, drug interactions, 3rd party coverage issues, etc., they can be taken care of right away.
Our staff and patients are very happy with the layout. We are doing more prescriptions every month and yet have found that we have more time than we used to. Our patients feel that when it is their turn with the pharmacist they have their undivided attention. They like that both they and the pharmacist are sitting down.
It is much easier to provide meaningful patient care if you have a pharmacy that is designed primarily with this function in mind. This new design with pharmacist stations and a work island for the techs replacing the long counter has proven to be very effective.
Medication reconciliation practices on discharge into primary care homes in Prince George, British Columbia
Robert Pammett, BSc, BSP, MSc
Medication reconciliation is an integral part of safe medication practices, and should occur at all stages of hospital transition, including discharge to the primary care home (PCH). Ensuring that the PCH has an up to date list of patient medications after discharge can help avoid medication misadventures. The objectives of this study were: (1) to determine the proportion of patients who had a discharge medication list communicated to the primary care home which contained discrepancies from the hospital medication list, and (2) to categorize discrepancies as prescription medication, non-prescription medication, or medication dose.
Two PCHs were recruited to participate in the retrospective chart review. Records of 50 patients who received a hospital discharge from June 1 2014 to May 31 2015 were identified at each PCH. The list of hospital medications at discharge was compared to the medication list that was communicated to the PCH at discharge. Discrepancies between these lists were identified and categorized, as was the medium in which the medication list was communicated to the PCH.
Seventy-eight cases were included in the final data analysis. Mean age of patients was 46.7 years, 59% being female. The mean number of medications taken was 6.3 per case. Four cases had no medication use. All discharge medication information was communicated via a dictated discharge summary. The total number of discrepancies identified was 280, a mean of 3.6 per case. The majority of discrepancies were prescription medication omissions or errors (69%). The remaining discrepancies were non-prescription medication omissions or errors (18%) and medication dose discrepancies (13%).
A large number of discrepancies were present between the hospital chart and the discharge summary that was sent to the PCH. Improving communication of the medication list at discharge should be encouraged to reduce potential medication errors.
Stakeholder perspectives on economic analyses of billable pharmacy services in Ontario
Sherilyn Houle, BSP, PhD; Jilan Yang, MD, MSc, PhD
A number of pharmacy services in Ontario are government-funded; however, little is known about the costs and benefits of these services. This study solicited stakeholder perspectives on the most valuable economic analysis designs, the priority services, and concerns related to the conduct of the research or dissemination of results.
Semi-structured telephone interviews were conducted with 16 stakeholders from government, academia, pharmacy industry/associations/regulators, and insurers in March and April 2015. Interviews were audiotaped, transcribed verbatim, and coded both manually and using NVivo. Data analysis employed the constant comparison approach to identify emerging themes and patterns.
There was consensus among stakeholders that high-quality economic evaluations of pharmacy services are needed. While evaluation of MedsCheck reviews was considered highest priority, influenza vaccination was widely identified as a suitable starting point given data availability and clear patient outcome measurement. A broad perspective including those of government/payers, the pharmacy profession, and patients is encouraged, with patient outcomes identified as more valuable than financial outcomes. However, accurate and complete patient outcome data collection was identified as a key challenge. Stakeholders reported a desire to be actively involved in economic evaluations and knowledge dissemination.
Researchers considering economic evaluations of pharmacy services are encouraged by stakeholders to incorporate broad perspectives beyond solely the interests of the profession. While patient health outcomes are valued above financial outcomes, care should be taken to ensure this outcome data is accurate and complete to minimize the impact of assumptions on the validity of the results. Stakeholder engagement at all stages of the research can help ensure the relevance and uptake of economic analyses conducted.
Opportunity and cost: Self-monitoring of blood glucose in Manitoba, 2000-2013
Olena Serwylo, BSc(Pharm), PharmD candidate; Kevin Friesen, BSc(Pharm), MSc candidate; Jamie Falk, BSc(Pharm), PharmD; Shawn Bugden, BSc(Pharm), MSc, PharmD
Given the limited evidence of benefit of frequent self-monitoring of blood glucose (SMBG) by non-insulin using patients with diabetes, new guidelines and test strip limit policies have been suggested and implemented in various Canadian jurisdictions. The objective of this study was to assess the overall utilization and cost associated with blood glucose test strips (BGTS) and lancets for SMBG in Manitoba from 2000 to 2013 and to assess potential implications of such a policy.
A cohort of all patients with diabetes in Manitoba from 2000-2013 was established. Test strip and lancet utilization and cost were assessed for the overall cohort and for subgroups based on the type of diabetes treatment. The potential opportunity for a more selective practice of SMBG was assessed.
In the year 2000, 8 million BGTS were dispensed in Manitoba, and this increased by 270% to 21.7 million by 2013. Insulin users accounted for the majority of test strip use. However, it was estimated that test strip use could be reduced by 16 million test strips over 5 years by taking a guideline based approach to monitoring, with 95% of the potential reduction occurring in groups not using insulin. Over the next 5 years, a guideline based approach is projected to save $12.35 million, including $7.3 million in government spending.
Some provinces have placed therapy-linked limits on BGTS use. Whether or not a test strip limit policy is in place there is an important opportunity for pharmacists to help guide patients with diabetes to determine optimal frequency of SMBG. Expenditures above guideline recommendations represent an opportunity cost, money which could be redirected to programs and more useful interventions for the growing population of patients with diabetes in Manitoba.
Ibuprofen provides superior antipyretic efficacy vs. acetaminophen in childhood fever: Pooled analysis of 2 randomized trials
David Kellstein, PhD; Shyamalie Jayawardena, PhD
Compare antipyretic efficacy and safety of ibuprofen (IBU) vs acetaminophen (APAP) in children with fever from a pooled analysis of 2 studies.
Two IRB-approved, randomized, double-blind studies enrolled children 0.5 - 11 y, 13 - 95 lb with fever (101.5 - 104.9°F, rectally, ages 0.5 - 3 y; 101.0 - 103.9°F, orally, ages 4 - 11 y) for ≥2-h duration to single-dose IBU suspension (Children’s Advil® Suspension 7.5 mg/kg) or APAP suspension (Children’s Tylenol® Suspension 10 – 15 mg/kg) based on labelled dose/age. Temperatures (temperature; average of 2 readings) were assessed at baseline (predose) and after single dose of study medication at 15, 30 and 45 min and hourly from 1 - 8 h thereafter. Primary efficacy: time-weighted sum of temp difference from baseline over 8 h evaluated via analysis of variance. Secondary efficacy endpoints included time to onset and duration of temp control (temp: <100°F orally or <101°F rectally) via Cox proportional hazards; percentage with temperature control (Cochran-Mantel-Haenszel); safety was monitored throughout.
In total, 319 children (144 male, 175 female; 94% white; mean age 4.6 y; mean weight 42 lb) were evaluable for efficacy; 333 comprised the safety set. On primary efficacy, IBU 7.5 mg/kg was significantly better in terms of time-weighted sum of temperature differences vs APAP 10 – 15 mg/kg: mean (SD) -11.1 (8.5) vs -7.6 (8.0); p<0.001. Onset of temperature control occurred significantly earlier (median: 94.5 vs 111.6 min; p<0.001), lasted significantly longer (median: 191.3 vs 122.7 min; p=0.042) and occurred in a significantly higher percentage of children (89.6 vs 66.7%; p<0.001) with IBU suspension vs APAP suspension. Fifteen AEs occurred in each group; none severe. Most common AE was vomiting (4.6%: IBU; 6.3%: APAP; p>0.05).
IBU paediatric suspension (7.5mg/kg) is superior to APAP suspension (10 - 15mg/ kg) in treating paediatric fever, with better temperature reduction that was faster and of longer duration compared with APAP. Both products were well tolerated.
Development of a hormonal contraception decision support tool for pharmacists
Nese Yuksel, BScPharm, PharmD, FCSHP, NCMP; Humirah Sultani; Tasneem Siyam, BScPharm, MSc
Hormonal contraception continues to be a popular and effective method of contraception among women. With the expanded scope of practice in Alberta, pharmacists are perfectly positioned to manage the hormonal contraceptive needs of women, including initiating and adjusting hormonal contraceptives. The objective of this project is to develop a decision support tool to help pharmacists manage hormonal contraceptives in the community.
Development of the decision support tool involved a panel of local pharmacists with expertise in women’s health. Content of the tool was informed by current contraception guidelines, published literature and research team experience. The developed prototype was then reviewed by experts in the field including a pharmacist and nurse specialized in contraception, an obstetrician-gynecologist and a family physician with interest in women’s health. The modified prototype was alpha tested in a small cohort of community pharmacists (n=10) for acceptability and usability.
The tool includes 4 sections: (1) Patient Assessment — includes screening for indications, contraindications and risk factors, (2) Initiating Hormonal Contraceptives — includes guidance in choosing among different products, (3) Patient Education — provides an educational overview for shared decision making, and (4) Managing Ongoing Therapy — includes monitoring recommendations, approaches to dealing with side effects and adjusting therapy. An appendix with available Canadian Hormonal Contraceptives is also provided.
An evidence based clinical decision support tool may be a useful tool for pharmacists managing hormonal contraception in the community. Future plans are to evaluate the feasibility and applicability of the tool in the community setting.
The pharmacy services framework: Communicating the shift to clinical pharmacy services in Alberta
Theresa J. Schindel, BSP, MCE; Christine A. Hughes, BScPharm, PharmD; René Breault, BScPharm, PharmD; Deborah Hicks, MA, MLIS
To gain insight into communication of the Compensation Plan for Pharmacy Services, known as the Pharmacy Services Framework (PSF), by interpreting information described in news media articles, policies, government reports, and communications about the PSF.
Publicly available documents published 2012 - 2015 were obtained from websites such as the Government of Alberta, Alberta Blue Cross, the Alberta College of Pharmacists, the Alberta Pharmacists’ Association, and the Blueprint for Pharmacy. Searches using the Canadian Newsstand database and Google identified additional documents. Search terms included “Pharmacy Services Framework,” “Compensation Plan for Pharmacy Services,” pharm*, compensat*, reimburse*, and Alberta. One research team member completed initial analysis of documents using a grounded theory approach and the entire team reviewed emerging thematic categories. During the analysis, attention was paid to how the PSF was presented to pharmacists and other audiences.
Preliminary analysis of documents written for practicing pharmacists consisting of government policies, newsletters, and other communications identified four main themes: reimbursing patient care services, legitimizing pharmacists’ professionalism, shifting focus to patient care role, and collaborating with health care team members. The PSF was framed as payment for professional services and as offering external validation and legitimization for pharmacists’ changing professional service roles. Further analysis of news media and communications directed to other audiences is underway.
Preliminary findings provide insight into how the PSF was communicated to pharmacists and other audiences. Researchers need to consider political and societal contexts that influence provision and reimbursement of clinical services. The results of this study will provide a foundation for future research on how clinical services reimbursed by the PSF are implemented.
Provider and patient perspectives regarding a community pharmacist-based case finding and intervention program — Alberta Vascular Risk Reduction Community Pharmacy project: RxEACH
Maoliosa Donald, BSc, MSc; Kathryn King-Shier, PhD; Ross T. Tsuyuki, BSc(Pharm), PharmD, MSc; Yazid Al Hamarneh, PhD; Charlotte Jones, MD; Braden Manns, MSc, MD; Marcello Tonelli, SM, MD; Brenda Hemmelgarn, PhD, MD
To gain firsthand knowledge of pharmacists’ and patients’ experiences with pharmacist-based management of adults at risk for cardiovascular events.
Design: Qualitative descriptive — one on one telephone interviews. Setting: Community — Alberta. Population: Community pharmacists and patients. Data analysis: Multi-step process using conventional qualitative content analysis.
We completed 35 telephone interviews — 21 pharmacists and 14 patients, where we had 14 dyads (pharmacist and patient relationship). The majority of pharmacists were female (57%) between the ages of 36-45, and worked in an urban setting (57%) with 10 or less years of practice. Pharmacists reported a variety of factors that affected their ability to manage patients’ cardiovascular risk. These included features of their workplace (i.e., work autonomy, resources and physical space); their personal outlook and perspective (i.e., expanded professional role and professional development); collaborative physician/pharmacist relationship; and patient uptake. Common themes identified by patients included their trust of the pharmacist, ease of access to pharmacist services and presumed health care cost.
Understanding the provider and patient perspectives are key to maximizing the impact and sustainability of a pharmacy-based program to manage patients at high cardiovascular risk. Generally, patients were pleased with the clinical services provided by the pharmacist and pharmacists embraced the expanded clinical role.
An audit of 8 centres’ use of anticoagulant therapies when discharging patients from hospital with acute venous thromboembolism
Tammy Bungard, BSP, PharmD; Bruce Ritchie, MD; Cindy Jones, BScPharm; Jennifer Bolt, BScPharm, ACPR, PharmD; William Semchuk, MSc, PharmD, FCSHP
To report anticoagulant (AC) therapies patients receive for acute venous thromboembolism (VTE) upon hospital discharge.
This retrospective chart review from April 2014 to March 2015 included 4 urban Edmonton hospitals, 2 urban Regina hospitals and 3 rural Alberta hospitals. Patients > 18 years of age who were discharged with a diagnosis of VTE (DVT or PE) that lacked another indication for anticoagulant therapy and had an anticipated lifespan > 3 months were included. We primarily sought to assess the anticoagulant regimen prescribed for patients at hospital discharge and with whom follow-up care was to occur. Moreover, we sought to compare differences among the urban and rural centres.
After screening 1,047 patients, 692 (66.1%) were included. The majority of patients discharged from hospital had a PE (Edmonton 84.4%, Regina 81.2%, rural Alberta 63.3%). Novel oral anticoagulants (NOACS) were the most common discharge therapy in rural Alberta (50.0%), followed by warfarin (+/- a parenteral AC) (30.0%). In rural Alberta follow-up most commonly occurred with the GP (66.7%). In Regina, the most common therapy at discharge was warfarin (+/- a parenteral AC (59.0%) followed by a NOAC (23.9%), and a parenteral AC alone (16.2%). In Regina, the majority of follow-up was with the GP (52.1%) or specialist (52.1%). In Edmonton, 40.5% were discharged on warfarin (+/- a parenteral AC), 29.2% a parenteral agent alone, and 28.4% on a NOAC. Follow-up most commonly was with the general practitioner [GP] (29.9%) or VTE clinic (29.1%) in Edmonton.
The majority discharged after VTE-related hospitalizations have PEs, and NOACs are used more commonly in rural Alberta (50%) compared to urban centres (~25%). Depending on the centre, follow-up is either done via the family doctor or through specialists / VTE clinic.
An audit of 8 centres’ use of anticoagulant therapies when discharging patients from the emergency department
To report anticoagulant (AC) therapies patients receive for acute venous thromboembolism (VTE) upon discharge from the emergency department (ED).
This retrospective chart review included patients discharged from the ED with a diagnosis of VTE (DVT or PE) between April 2014 and March 2015. Two urban Edmonton hospitals having VTE clinics (Edm-VTE), 2 without VTE clinics (Edm), 2 urban Regina hospitals and 3 rural Alberta hospitals were included. We primarily sought to assess the AC regimen at ED discharge to the community and with whom follow-up care was to occur. Moreover, we compared differences among the urban and rural centres.
After screening 1,734 patients, 418 (24.1%) were included. The majority were discharged with DVT as compared to PE/PE plus DVT (Edm-VTE 54.5%, Edm 59.0%, Regina 91.7%, rural Alberta 80.0%). For Edm-VTE, discharge therapy with a parenteral AC alone (60.1%) or novel oral anticoagulant (NOAC) (20.0%) with follow up in the VTE clinic (80.6%) was most common. The majority for Edm were prescribed a parenteral AC (41.0%) or NOAC (40.3%) with either general practitioner [GP] (28.1%) or VTE clinic (33.8%) follow-up. In Regina, the majority (75.0%) were discharged on a parenteral AC with warfarin, with 11.9% each on a parenteral AC or NOAC, with GP follow-up (56.0%). Rural Alberta sites most commonly used NOACs (43.3%) or a parenteral AC with warfarin (26.7%), with GP follow up (53.3%).
Urban Alberta sites discharge more patients with PE (43.4%) from ED compared with Regina or rural Alberta sites. Traditional therapy with a parenteral AC (+/- warfarin) is still most commonly used at discharge, with anywhere from 12-43%receiving a NOAC across the sites assessed. NOAC use was most common (~40%) in rural Alberta and at the Edmonton site not having a VTE clinic. Variation in practice is evident.
Enhancing depression outcomes with better use of antidepressants: Evaluation of a pharmacy benefit manager– sponsored depression disease state management program
Katherine Giannoulis, BScPharm, CGP; Leanne McFarlane, BScPharm; Heather Creighton, BScPharm; Moira Reiley, BScPharm, CGP
Non-adherence to antidepressants is associated with poor health outcomes and is common in people with depression. Studies using medication possession ratio (MPR) or proportion of days covered (PDC) to calculate adherence found 34-56% of patients were adherent to therapy. Persistence to antidepressants at 1, 3 and 6 months is estimated to be 70-75%, 56-60% and 40-43% respectively. To improve adherence and patient depression outcomes MHCSI developed and funded a two-year pharmacist Depression Disease State Management (DSM) pilot program for plan members.
Pharmacists within MHCSI’s Preferred Provider Network were encouraged to have multiple consultations with each patient in-program over a one-two year period. Pharmacists received equal compensation for each consultation. Adherence was calculated at program completion based on drug claims data using the PDC method. Patients were considered adherent if the PDC was >80%. Persistence was calculated for patients new to antidepressant therapy. Pharmacists completed a Patient Outcome Survey for each patient.
There were 59 patients in the Depression DSM program. Patients had an average of three consults. The percentage of patients considered adherent to antidepressant therapy was 70%. The average proportion of days covered for participants was 81%. Persistence to 1, 3 and 6 months was 100%, 89% and 61%. Patient Outcome Surveys were completed for 57 of the 59 patients with 81% of respondents reporting that the patient had a better understanding of condition/treatment, 65% of the patients reported “feeling better” and 54% reported productivity gains.
This suggests a pharmacist longitudinal follow-up model may improve adherence to antidepressant medication with the goal of improving patient health outcomes.
Pharmacist intervention for a frail elderly population in primary care
Tejal Patel, PharmD; Jillian Bauer, BScPharm; Linda Lee, MD; Cathy Schill, BScPharm
In 2013, the Centre for Family Medicine Family Health Team initiated a new program called the “Case-Finding for Complex Chronic Conditions in seniors 75+ (C5-75)” to systematically screen for frailty among all persons aged 75 years and older to address medical conditions appropriately and to avert crises. As a component of this program, a pharmacist intervention was developed to address medication-related problems (MRPs). The objectives of this study are to describe the medication use in the population referred and activities performed by pharmacists in this program.
This was a retrospective medical records review of frail elderly patients seen by pharmacists in the C5-75 program from April 2013 to August 2015. Data pertaining to patient demographics, medical conditions, and medication history as well as activities performed and recommendations made by pharmacists were abstracted.
Of 142 patients (54 males and 88 females, mean age 85 years [range: 75-98]) identified as frail, 54 patients accepted the offer of a medication review with a pharmacist in the C5-75 program. At initial visit with the pharmacist, the means for number of total medications was 11.60 (range: 5-23), for prescribed medications, 7.67 (range: 3-20), and for over-the-counter medications, 3.93 (0-15). Polypharmacy and high-risk medication use was highly prevalent (83% and 93%, respectively). A total of 218 MRPs were identified among the 41 patients with at least one follow-up visit with the pharmacist. Pharmacists made a total of 222 recommendations. Of the 138 that were measurable, physicians had accepted 70% and 50% were implemented at most recent follow-up.
Polypharmacy, high-risk medication use and MRPs are highly prevalent in the frail elderly in primary care. Pharmacists were able to address these problems with recommendations, many of which were accepted and implemented.
Impact of pharmacist assessment on classes of high-risk medications in a geriatric outpatient clinic
Sharon Ong, BPharm, PharmD; Alexandra Marin, MD, CCFP, Dip. COR; Imran Hassan, MSc; Ross T. Tsuyuki, BSc(Pharm), PharmD, MSc, FCSHP, FACC; Cheryl Sadowski, BSc(Pharm), PharmD, FCSHP
Seniors often take multiple medications because of a high burden of chronic diseases. This complex population is vulnerable to medication-related problems. Pharmacists can improve suboptimal prescribing in older adults, however, the evidence base for this is weak. Our objective was to determine if pharmacist assessment is effective in reducing classes of high-risk medications in seniors at a geriatric clinic.
We reviewed the medical charts of 245 patients aged 65 and over who were referred to our outpatient geriatric clinic and assessed using comprehensive geriatric assessment (CGA). The CGA team consisted of a geriatrician, medical trainee (student, resident or fellow), pharmacist (available part-time), and nurse. Since the pharmacist was only in the clinic on certain days, we conducted a non-randomized comparison of medication use in those seen by a pharmacist versus those who were not. Number of medications was compared using t-test and exact McNemar’s test was performed to assess medication changes.
The mean number of medications of patients assessed by pharmacist (n=99) vs not assessed by pharmacist (n=89) was 10.5 (SD 5.5) vs 9.4 (SD 4.7) with a mean difference of 1.07 (95% CI, -0.41 to 2.55), p=0.157. The proportions of patients taking acetylcholinesterase inhibitor in both pharmacist and non-pharmacist groups increased, respectively, from 20% to 37%, p<0.001 and 14% to 28%, p=0.001. Other classes of medication with statistical significant changes were exclusively in the pharmacist group, such as selective serotonin reuptake inhibitor from 20% to 27%, p=0.007; over-the-counter analgesic e.g. acetaminophen from 30% to 41%, p=0.002; non-steroidal anti-inflammatory drug from 22% to 16%, p=0.013; and antihistamine or other anticholinergic (not for overactive bladder) from 7% to 2%, p=0.016.
Pharmacist assessment as part of an interprofessional geriatric clinic team led to an improvement in medication use.
Description of medication management problems and supports used in community-dwelling seniors
Objective(s).
Seniors commonly have problems managing their medications due to extensive medication use, medication regimen complexity, and functional or cognitive limitations. With an aging population, it is important to identify these problems so that resources can be directed to meet their health care needs. The purpose of our study was to describe the medication management problems of seniors living in the community.
A retrospective chart review of patients aged 65 years and over who were referred to our geriatric clinic and assessed using comprehensive geriatric assessment (CGA). The CGA team consisted of a geriatrician, medical trainee (student, resident or fellow), pharmacist and nurse. Data were analyzed descriptively and McNemar’s test was used for changes in calendar packaging.
The mean age was 80.6 (SD 7.2) years, 41% lived alone and 46% lived with spouse/ partner. On admission, the mean number of medications (n=236) per patient was 9.8 (SD 4.8), and 46% had medications administered via a non-oral route. Medication-related problems were non-adherence (43%), difficulty managing medication (40%) and dependence with medication use (49%). The dependent patients obtained assistance from spouse or partner (37%), family member/living separately (25%), family member/living with (18%), formal home care cueing/ administration (11%) or monitoring (8%), and caregiver (9%). Calendar packaging from 55% to 70%, p<0.001, and community care services from 27% to 42%, following assessment.
Conclusion(s)
About half the seniors seen at the geriatric outpatient clinic had complex medication regimens, were non-adherent, had difficulty managing medications and were dependent with medication use. There appeared to be a high dependency on their spouse and family members in medication management. As such, assessing seniors for medication management and inquiring about supports for medication assistance are important roles for pharmacists in a geriatric practice.
Effectiveness of the peer-to-peer mentoring model for transitioning from classroom to professional practice
Thomas Huang, PharmD (student); Annie Lee, MSc(T), ACPR; Certina Ho, RPh, BScPhm, MISt, MEd; Edric Paw Cho Sing, PharmD; Michael Vinh, PharmD
To better prepare pharmacy students for practice by implementing a peer-to-peer mentoring model of student-led pharmacotherapy sessions (SLPS) in the PharmD program. The learning impact and the utility of the model for student preparedness for Advanced Pharmacy Practice Experiences and the licensing exam were examined.
Fourth-year students delivered SLPS on Cardiology, Infectious Diseases, and Patient Self-Care online and live to both third- and fourth-year students. Retrospective self-assessment surveys were administered after each SLPS. Five knowledge domains (etiology, clinical presentation, pharmacotherapy, monitoring/follow-up, and overall knowledge) were assessed. A paired t-test was utilized to evaluate the survey data. Thematic analysis was applied to the qualitative comments on the survey.
Eighty-one students (59% third-years; 41% fourth-years) responded to the survey. Prior to the SLPS, 46.8% of students rated their knowledge “Average” (3 of 5), while 33.1% rated their knowledge “Above Average” (4 of 5) in all knowledge domains. After the SLPS, 53.6% of students rated their knowledge to be “Above Average” (4 of 5), while 27.5% rated their knowledge “Excellent” (5 of 5) in all knowledge domains. Statistically significant increase (p<0.001) was shown in all five knowledge domains post-SLPS for both third- and fourth-year students. Students stated that cases, drug charts and therapeutic overview were the most useful. Suggestions for improvement included increased interactions, counselling points, and providing practice examples.
The peer-to-peer mentoring model was an effective model for student learning. Students perceived a therapeutic knowledge increase after attending the SLPS. Student presenters developed public speaking skills and built confidence while consolidating knowledge. This model has proven to be effective in developing skills and knowledge for students transitioning into professional practice.
Community pharmacy reports of potential QTc-prolonging drug interactions involving fluoroquinolones or macrolides: A multi-incident analysis
Roshan Tahavori, RPh, BScPhm, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Significantly prolonged QTc may lead to torsades de pointes (TdP) in at-risk patients. Fluoroquinolones (FQs) and macrolides have the potential to prolong the QTc, and given their widespread use, are implicated in relatively high number of significant QTc-prolongation events. The purpose of this project was to analyze incidents of potential QTc-prolonging drug interactions involving FQs and macrolides, in order to fill in patient-safety gaps.
We searched the Community Pharmacy Incident Reporting program for QTc-related incidents involving FQs and macrolides between April 2010 and January 2015. Using a qualitative, multi-incident analysis approach, we analyzed 56 incidents, identified themes, potential contributing factors, and provided recommendations.
Most incidents were pharmacy-intercepted drug interactions (i.e., near misses) involving moxifloxacin, ciprofloxacin, clarithromycin, and azithromycin. Commonly reported classes of interacting drugs were antidepressants, antiarrhythmics, and antipsychotics. The following themes and possible contributing factors were captured: 1) Prescriber-triggered potential for QTc-prolongation due to absence of drug-interaction assessment, 2) Potentially inappropriate pharmacist-intervention due to absence of patient risk-assessment, and 3) Patient-potentiated risk for harm due to polydoctoring and polypharmacy practices while failing to disclose complete medication lists to the providers.
Prescribers should seek patients’ complete medication list and medical history, and make TdP risk-assessment when prescribing drugs with QTc-liability. Pharmacists should assess patients’ risk factors for QTc-prolongation before intervening on drug-interactions. We developed a QTc-Prolongation Risk Factors Checklist to facilitate these assessments. Patients should regularly be provided with a comprehensive medication list and educated on safe medication use by pharmacists.
Medication incidents involving insulin: A multi-incident analysis
Carolyn Kasprzak, RPh, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Insulin is a life-saving pharmacological therapy for many diabetic patients. However, insulin has been identified as a high alert medication as it has the potential to cause detrimental patient harm when used in error; particularly, an excessive dose can lead to life-threatening hypoglycemia. The objective of this multi-incident analysis was to examine insulin-related medication incidents and determine potential system-based improvements that may be customized in pharmacy practice to enhance medication safety.
Reports of medication incidents involving insulin were extracted from a national incident reporting database between January and December 2014. After a review of 226 incidents, 81 were included in this qualitative, multi-incident analysis. The incidents were then analyzed and categorized into main themes and subthemes.
The four main themes identified were: (1) product selection (related to unique insulin properties), with prescribing, order entry and dispensing as subthemes; (2) therapeutic regimen change; (3) dosage calculations; and (4) storage requirements. Potential solutions for prevention of insulin-related incidents included the use of standardized pre-printed order forms, integrating warning flags into pharmacy software, incorporation of independent double checks throughout the entire pharmacy workflow, and conducting comprehensive diabetes-focused medication reviews with patients.
Medication incidents involving insulin in pharmacy practice are common and have the potential to cause serious patient harm. Findings from this analysis are intended to educate health care professionals on the vulnerabilities in the medication-use process that may contribute to insulin-specific medication incidents and offer recommendations to prevent such events from recurring.
Potentially inappropriate medication use in older adults: A multi-incident analysis
Kelly Ng, BSc, PharmD candidate; Certina Ho, RPh, BScPhm, MISt, MEd; Roger Cheng, RPh, BScPhm, PharmD
Potentially inappropriate medication use in older adults can lead to preventable adverse events, which may account for a significant portion of emergency room visits and hospitalization. This multi-incident analysis identifies points of intervention in the community setting in order to prevent medication incidents that may compromise patient safety.
A qualitative, multi-incident analysis was conducted on medication incidents reported to the Community Pharmacy Incident Reporting (CPhIR) program. Reports of medication incidents involving drug therapy problems, contraindications, and duplications in patients over 65 years of age were extracted between 2010 and 2015. In total, 184 incidents met the inclusion criteria of this multi-incident analysis.
Two main themes were identified: (1) patient-specific factors and (2) drug interactions. Patient specific factors include incidents where the medication was not best suited for the patient due to their intolerances or allergies, medical conditions, and inappropriate dosing/prescribing for older adults over 65 years old. Medication incidents involving drug interactions include antibiotic and chronic medication interactions, interactions between different therapeutic classes, and drug duplications of the same therapeutic class. Comprehensive medication reviews (such as MedsChecks in Ontario) help to ensure patients are safely and appropriately using medication therapies and reduce potential adverse drug events when transitioning between points of care.
Although the use of multiple medications may be appropriate in older adults, the complexity of these medication regimens increases the risk of errors and adverse effects. Implementing system-based strategies in the pharmacy workflow can help pharmacists improve patient safety and mitigate the risks of potentially inappropriate medication use in older adults.
Patient counseling: An overarching method to mitigate medication errors and ensure continuity of care
Tracy He, PharmD candidate; Certina Ho, RPh, BScPhm, MISt, MEd
To explore the methods and behavioural tools in which community pharmacists utilize patient counselling to prevent medication incidents. The findings of this qualitative, multi-incident analysis will substantiate the strongholds in which pharmacists mitigate errors and the role of patient education in encouraging health literacy and continuity of care.
A multi-incident analysis was performed on medication incidents reported to the Community Pharmacy Incident Reporting Program (CPhIR) developed by the Institute for Safe Medication Practices Canada. The keywords in the incident description included patient-counselling terminology, such as “identified,” “counsel,” “explain,” and “teach.” The incidents included in this analysis spanned from September 2014 to August 2015. They were then stratified thematically based on their modes of identification.
Of the 115 incidents that met the inclusion criteria, two emergent themes were identified: pharmacist-led and patient-led identification of medication incidents. The themes gave rise to further subthemes respectively, focussing on prescription reconciliation, therapy evaluation and clarification, storage education, patient identifier verification, and product demonstration. Reinforcement of safe medication use at the stage of patient counselling can also gear pharmacists towards patient-focused care and effective medication therapy management.
Community pharmacy practitioners can effectively identify near misses and medication incidents at the stage of patient counselling. Having a dialogue with patients at the point of care will not solely be helpful for the mitigation of errors, but also serve as a quality assurance of continuity of care.
Older people’s attitudes towards deprescribing: A community study in Quebec
Caroline Sirois, BPharm, PhD; Nicole Ouellet, PhD; Marie-Eve Gagnon, BInf; Joanie Renaud; Lyndia Huard
Polypharmacy is very common among older individuals and has been associated with adverse outcomes. Reducing the number of medications (deprescribing) might be a valuable option to reduce the risks. However, little is known about older individuals’ attitudes towards deprescribing.
We ran a pilot study to evaluate the feasibility of using a self-administered questionnaire among community-dwelling older individuals to address their perceptions towards deprescribing. We used a French version of the Australian Patient’s Attitudes Towards Deprescribing Questionnaire. The questionnaires were distributed in ten community pharmacies and two community centers in the province of Quebec. The participants (n=129) completed the questionnaire containing 10 Likert type questions about polypharmacy/deprescribing and 5 multiple-choice questions. We used descriptive statistics to summarize the participants’ characteristics. We performed chi-square tests to compare the proportions of agreement, and evaluated correlations with Spearman’s Rho (alpha=0.05).
The participants were mostly women (63%) with a median age of 76 years (IQR:7180). The median number of daily medication was 6 (IQR: 3-8). Half of the participants considered they were taking a lot of medications, but 80% judged these medications were necessary and felt comfortable with the number they were taking. More than 80% would agree to take more medications for their health condition if required. Nonetheless, 50% of the participants mentioned they would like to reduce the number of medications they were taking. If their doctor said it would be possible, 71% would be willing to reduce the number of medications used. Those who thought they were taking a lot of medications were more willing to have their number reduced (p<0.001).
The results show that older individuals in the community are eager to undertake deprescribing, conditional on their doctor’s approval.
The effect of health media reporting on self-medication use
I fan Kuo, BSc (Pharm), ACPR, MSc, PharmD; Amanda Church, BSc (Pharm) candidate; Christopher Louizos, BSc (Pharm), PharmD; Brenna Shearer, PhD
The news media serves the crucial role of conveying complex scientific findings and health issues to the general public. The main objectives of this study are (1) to describe the public’s perception of health-related content in the news media and their dependence on the media in decision-making surrounding self-medication use, and (2) to examine potential factors, both individual and media-related, that influence self-medication behaviour.
Twenty-Nine adult volunteers participated in five focus group interviews that were conducted at the College of Pharmacy, University of Manitoba in Winnipeg. Each 90 minute interview was moderated by a study coordinator, audio-recorded, and transcribed. Two study team members independently analyzed the transcripts.
The general public expressed varying degrees of uncertainty towards the reliability of health reporting in news media. Most felt overwhelmed and frustrated by the excess sources of information, and the often mixed and transient messages in health news reports. A trusting relationship with a pharmacist or physician was identified as the most important factor in self-medication decision, but not all individuals had access to health care providers, due to a variety of reasons. Other influences on over-the-counter product use include education background, previous experience, upbringing, credentials of the sources, and the individual’s social circle.
Decision-making surrounding the use of over-the-counter products is a complex process, often implicitly influenced by health news reporting in the media. Trusting interaction with health care providers, especially pharmacists is an important component in choosing non-prescription product use, but one that is not always readily accessible. Pharmacists are yet to maximize the opportunity in filling this health care gap.
Documentation of functional medication management in older adults within an acute care hospital
Monika Bolina, BScPharm, ACPR; Allyson Jones, PhD; Sheri Koshman, BScPharm, PharmD, ACPR; Erin Heintz, BScPharm, ACPR; Ronald Lehmann, BScPharm, ACPR; Cheryl Sadowski, BSc(Pharm), PharmD, FCSHP
To describe the documentation of functional medication management (FMM) in adults, age 65 years and older, on medicine wards, during their hospital stay. The secondary objective was to describe the characteristics of the health care providers (HCP) documenting on FMM.
This study was a retrospective chart review of a random selection of 140 patients admitted at the University of Alberta Hospital from January 2013 to October 2014. FMM was defined as the process of taking medications (including ordering, picking up, organizing, preparing, monitoring, and administering medications). This ability requires assessing factors such as physical function (including vision, dexterity, and swallowing ability) related to medications and cognitive function.
A total of 140 patient charts were reviewed. The average age was 78.9 (SD 8.4) years, 68 (48%) male, and mean 8 (SD 3.1) scheduled oral medications taken. Commonly documented components of FMM included administration of medications (52%), organizing of medication (33%), assessments of physical function including vision (25%), swallowing ability of medications (18%), and cognitive function (21%). Documention of these activities was most frequently done by physicians (39%), occupational therapists (34%), and pharmacists (17%).
Clinicians occasionally document FMM. Given the complexity of medication regimens and the functional demands of handling these, there is a need to incorporate these assessments when evaluating patients.
Global citizenship framework — Application to pharmacy student experience
Cheryl Sadowski, BSc(Pharm), PharmD, FCSHP; Lynette Shultz, PhD, Marlene Gukert, BScPharm, ACPR; Cheryl Cox, BSP, MBA
The role of pharmacists as citizens is important in terms of community engagement, public health, and advocacy. Student exposure to global citizenship is important in order to develop a view of citizenship in their future role as pharmacists. The purpose of our research was to apply a framework for global citizenship to student experiences in an international course taught in Italy.
This was an exploratory qualitative study. Students at the University of Alberta enrolled in Pharm 453 (Intercultural Exploration of Pharmacy & Health) between 2011 and 2013 were invited to participate after completing the course. Students who consented individually participated in a semi-structured interview regarding their experience. We applied a published framework and the data was transcribed and analyzed by content analysis methods.
The framework included 4 main components, with examples of application in practice. The components were politics/ideology, social/collective, self/ subjectivity, and praxis/engagement. Examples of each component include: (1) politics — awareness of food insecurity, injustices; (2) social — appreciation of interconnectedness, inclusion of those with different values; (3) self — being aware of one’s own perspectives, concern for social justice; (4) praxis — ethical action and active participation in society.
Applying a framework in describing student experiences with global citizenship through an international course was valuable, and demonstrated that students can be engaged with important citizenship issues.
How does pharmacist prescribing fit with family physicians’ practice in Alberta? Developing a knowledge translation strategy
Chowdhury Faruquee, BPharm, MPharm, MBA; Amandeep Khera, MD, CCFP, MPH; Lisa Guirguis, BSc Pharm, PhD
Alberta family physicians are seeing patients with an increasing number of chronic diseases and complex medication regimens. Pharmacists are medication experts with prescribing authority who can help both physicians and patients to manage medications. However, literature and anecdotes suggest physicians have low level of understanding and speculative beliefs about pharmacist prescribing. Our objective is to develop a knowledge translation strategy to address family physicians’ gap in understanding of pharmacist prescribing.
Qualitative interviews were used to explore Alberta family physicians’ understanding and experience with pharmacist prescribing. We used purposeful sampling method with semi structured face to face or telephone interviews. We planned to interview 12 to 15 Alberta family physicians having experience of pharmacist prescribing in their practice as well as pharmacists who are working with these physicians. Gaps in physicians’ understanding were identified and will be used to develop infographics to communicate pharmacists’ roles in prescribing medications
To date we have interviewed 11 physicians and one pharmacist. Often, family physicians first learned of pharmacist prescribing after receiving notification that a patient received this service or from the pharmacists they work with on teams. Preliminary themes include interprofessional hierarchy, assorted acceptability, building trust, and shared goals. Gaps include knowledge about pharmacist expertise and pharmacist prescribing authority, and communication strategies to foster collaboration. We will create infographics as educational tools, addressing the gaps. We will develop a usability testing survey to test its usability and will refine the educational tools using feedback. We will disseminate our infographics to both physicians and pharmacists through Alberta PCN leads, professional associations, and encourage pharmacists to use it with individual physicians.
We confirmed that some Alberta family physicians have limited understanding of pharmacist prescribing, resulting in lack of trust. Future research should evaluate the effectiveness of this knowledge translation strategy in the Alberta context.
Medication incidents involving smoking cessation therapies
Phillip Yang, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Ontario pharmacists have been granted the authority to prescribe medications for smoking cessation in their expanded scope of practice. To help pharmacists minimize errors when prescribing for smoking cessation, medication incidents involving varenicline and bupropion must be examined. The objective of this project was to identify areas of vulnerability when prescribing and dispensing smoking cessation therapies.
A qualitative, multi-incident analysis was conducted using anonymous incident reports submitted to the Institute for Safe Medication Practices Canada Community Pharmacy Incident Reporting Program. Medication incidents involving varenicline and bupropion were included in the analysis.
A total of 360 incidents were analyzed. Our findings were divided into two main themes according to the medication therapies: (1) varenicline and (2) bupropion. The main themes were then further divided into subthemes, comprising prescription instructions, quantity of tablets, and drug formulation. Safety interventions include separation of instructions for starter pack and continuation packs, implementation of preprinted order forms and independent double checks in the pharmacy workflow, and verification of the medication with patients during patient counselling.
As more patients access smoking cessation therapies, there are more opportunities for pharmacist-patient interactions. With pharmacists’ expanded scope of practice, there is also a new potential for near misses and incidents involving prescribing errors in the pharmacy. Through shared learning of existing smoking cessation medication incidents from this project, pharmacists will be more prepared and aware of safe medication use when executing their expanded scopes.
Medication incidents involving immunosuppressive agents
Melody Truong, RPh, BScPhm, PharmD; Amanda Chen, RPh, BSc, BScPhm, ACPR, PharmD; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Immunosuppressants are potent, immune-modulating medications that can cause significant harm to patients if used incorrectly. The objective of this multi-incident analysis is to assess the challenges of managing immunosuppressive therapy in the community setting and identifying system-based vulnerabilities.
Oral immunosuppressive agents of interest, such as azathioprine and cyclosporine, were retrieved from the American Hospital Formulary Service classification system. Intravenous agents were excluded due to a lack of presence in the community setting. Relevant medication incidents were gathered from ISMP Canada’s Community Pharmacy Incident Reporting (CPhIR) Program between January 2010 and May 2015. From an initial collection of 61 cases, a total of 47 medication incidents met inclusion criteria and were analyzed and reviewed by two analysts independently.
Quantitative analysis found that of the initial 61 medication incidents, 59% (36) were near-misses, 18% (11) resulted in no harm, and 3% (2) resulted in mild harm to the patient. The remaining 20% (12) were excluded due to insufficient narrative information provided by the reporter. Qualitative analysis uncovered three major themes that ran prevalent throughout all 47 incidents: (1) indication, (2) effectiveness, and (3) safety. Indication referred to incidents where an incorrect drug was being prescribed or dispensed due to look-alike/sound-alike names and/ or formulation oversight. Effectiveness primarily focused on medication errors arising from sub-therapeutic dosing that resulted in therapy failure, while safety referred to incidents that resulted in toxicity due to either supra-therapeutic dosing or drug interactions. System-based vulnerabilities included factors such as confirmation bias, practitioner’s knowledge gap, and lack of independent double checks in pharmacy workflow.
Immunosuppressive agents are commonly used by all patient populations within the community. Analysis of medication incidents provides an opportunity for health care practitioners to learn from errors and advance safe medication practices for quality patient care.
Medication incidents that could have been prevented at the prescribing stage
Kacy Park, BSc, PharmD candidate; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
As the initial step in the medication-use process, prescribing errors can lead to a cascade effect that ultimately places the patient at risk for harm. The goal of this multi-incident analysis was to identify and prevent the occurrence of these systematic errors to mitigate patient harm.
Data were gathered from the Community Pharmacy Incident Reporting (CPhIR) Program between January 2010 and April 2015. Search criteria excluded incidents that did not occur during the “Prescribing” stage and/or resulted in “No Error.” A total of 111 incidents met the initial search criteria with 50 incidents being excluded due to insufficient narrative descriptions. The remaining 61 incidents were then analyzed.
Of the 61 medication incidents analyzed, quantitative analysis showed that 84% (51) resulted in mild harm and 16% (10) resulted in moderate harm. No incidents resulted in patient death. Qualitatively, two main themes were extrapolated from these incidents: (1) Therapeutic Plan Error and (2) Therapeutic Plan Execution Error. Therapeutic Plan Error consisted of incidents that occurred due to incorrect dose, medication discrepancy, drug allergies or drug-drug interactions. Underlying contributing factors included a lack of reliable Computerized Decision Support Systems to help capture potential drug therapy problems, and limited communication networks between health care professionals within the patient’s circle of care. Therapeutic Plan Execution Error included incidents that occurred due to incomplete prescriptions, illegible writing, or wrong patients. Potential contributing factors included a lack of system-based or forcing functions to support prescribers when prescribing and documenting medication therapies.
The prescribing stage represents a key step in the patient’s encounter with the medication-use process. Both physicians and pharmacists can improve patient safety by developing system-based strategies to prevent medication incidents at this crucial stage of patient care.
Direct oral anticoagulant medication incidents
Nusrat Amin, PharmD; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Direct oral anticoagulation utilizing apixaban, dabigatran and rivaroxaban has become highly prevalent due to their ease of use and convenient monitoring parameters. Though their unique pharmacologic properties make them a popular choice among health care professionals, increasing use has also led to an increase in medication incidents involving these medications. This multi-incident analysis serves to explore themes that contribute to incidents involving direct oral anticoagulation medications in the community setting.
Incidents were extracted from the Community Pharmacy Incident Reporting (CPhIR) Program between January 2010 and April 2015. A total of 145 incidents met the initial search criteria with 36 being excluded due to insufficient narrative descriptions. The remaining 109 incidents were then analyzed.
Qualitative, multi-incident analysis found a total of five major themes underlying all medication incidents involving direct oral anticoagulants. These included look-alike/ sound-alike medications, drug-drug interactions, transition of care, intricacies of anticoagulant dosing/frequency, and pharmacy operation. Although the primary focus of the analysis was on medication incidents in the community, transition of care presented a unique challenge as it referred to medication incidents that occurred when patients were transitioning from a different health care setting into the community setting. Numerous contributing factors such as confirmation bias, a lack of reliable Computerized Decision Support Systems, and knowledge deficit of health care practitioners all played a role in facilitating these medication incidents.
The expanding role of direct oral anticoagulants in conventional chronic drug therapy requires increased vigilance from health care professionals. In the community setting, long-term use of direct oral anticoagulants can place the patient at risk of harm if not managed and monitored appropriately. By developing safe medication practices, pharmacists can help educate patients and prevent anticoagulant medication incidents.
Drug allergy incidents in community pharmacies
Leo Kim, RPh, PharmD; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Drug-induced allergic reactions are frequent, unpredictable events of medication usage in the community setting. The lack of homogeneity in their presentation and severity can range from mild, localized discomfort to systemic, life-threatening anaphylaxis, which presents a challenge for community pharmacists to manage. The objective of this multi-incident analysis was to identify common themes underlying drug allergy medication incidents, involving patients with documented allergies, and offer recommendations to help prevent future incidents in the community setting.
Incidents were extracted from the Community Pharmacy Incident Reporting (CPhIR) Program utilizing the inclusion criteria of “Drug Therapy Problem Documented allergy” for the type of medication incident, and generalized signs and symptoms of anaphylaxis as key words in the narrative description. A total of 273 medication incidents were captured and reviewed in this multi-incident analysis.
The three major themes identified were: (1) missing documentation, (2) computer detection incapacity, and (3) alert bypass. Missing documentation involved medication incidents that stemmed from both prescriber and pharmacy-related databases, while computer detection incapacity and alert bypass incidents only involved pharmacy-related dispensing systems. Recommendations primarily focused on the proper usage/maintenance of computer databases and communication strategies with patients. System-based strategies such as various enhancements to existing pharmacy databases, along with other continuous quality improvement programs, provide further solutions to prevent patient harm.
Drug-induced allergies can be easily screened and documented given the right tools and appropriate resources. Although unpredictable in nature, the presence of an existing drug allergy should prompt health care professionals to be mindful and cautious when prescribing and/or dispensing medications.
Medication incidents associated with hospital discharge
John Cao, PharmD; Kelly Ng, BSc, PharmD candidate; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Hospital discharge is a form of transitional patient care that involves multistep processes with multiple health care professionals at different levels of care. Due to its innate complexity, this process places patients at high risk for medication errors and potential subsequent hospital readmissions. This project examines common themes that are prevalent in medication incidents associated with hospital discharge, and provides insight into system-based recommendations for advancing safe medication practices.
Incidents were extracted from ISMP Canada’s Community Pharmacy Incident Reporting (CPhIR) Program between April 2010 and December 2014. A total of 83 incidents met the inclusion criteria. These incidents were analyzed and reviewed by two analysts independently.
A qualitative, multi-incident analysis revealed three main themes underlying these medication incidents: (1) error on the discharge prescription, (2) communication issues, and (3) community integration. Error on the discharge prescription involved preparation errors in the hospital such as inappropriate medications being ordered, inadvertent omission of medications, dosing errors, and wrong patient name on discharge prescriptions. Communication issues referred to miscommunication incidents between the hospital and community that involved illegible writing/ print on faxed and written discharge prescriptions, as well as complex medication orders. Finally, community integration explored the lack of continuity between hospital and community care that facilitated medication errors. This included issues such as duplication in medication therapy, different preparations used in the hospital compared to community, and interruptions/additions to multi-medication compliance aids. Medication reconciliation is an effective strategy that can empower community pharmacists to mitigate patient harm and enhance transitional care during hospital discharge.
Patients discharged from hospitals will continue to experience harm from medication incidents if system-based vulnerabilities are not addressed properly. The results of this multi-incident analysis, along with further investigations, will help develop or improve seamless and comprehensive transitional care practices.
Successful pharmacists: A qualitative study to understand pharmacists’ definitions of successful pharmacy practices
Meagen Rosenthal, PhD; Joseph A Dikun, PharmD; Ashley S Crumby, PharmD AAHIVP; Jill Hall, BScPharm, ACPR, PharmD; Theresa L. Charrois; BScPharm, ACPR, MSc
Efforts to improve uptake of advanced pharmacy practice services by various pharmacy professional organizations have included the development of definitions of pharmacists’ role in patient care, meant to transmit what is a successful pharmacy practice. However, there is little evidence of how these messages are reaching practicing pharmacists. The objective of this study is to understand success in pharmacy practice from the perspective of pharmacy practitioners in various settings.
In-depth semi-structured interviews were undertaken. Pharmacist participants were identified through reviews of national professional organization awardee lists and contact with state professional organizations in Mississippi, USA. The interview guide was developed from a scoping review by the authors. Interviews continued until saturation had been achieved. Qualitative content analysis was completed on all transcribed interviews.
A total of 14 interviews were conducted. There was an even split between participants practicing in community and hospital/ambulatory care settings. Two major themes emerged in the analysis. First, success was the development of meaningful relationships with patients, which led to the perceived improved uptake by patients of pharmacists’ recommendations. Second, success was achieving job satisfaction. Job satisfaction was often described as knowing they were making a difference in lives of patients. Participants also identified factors contributing to success, which included communication skills, self-confidence, and a supportive work environment.
The number, or kind, of advanced pharmacy services being provided to patients was not part of the definition of practice success offered. This implies a gap between the objectives of pharmacy professional organizations and practicing pharmacists. This study provides insight into the definition of success by practitioners, and direction for how professional organizations can improve communications with practitioners.
- UB Directory
- School of Pharmacy and Pharmaceutical Sciences >
- Departments >
- Pharmacy Practice >
Refugee education sessions improve pharmacy education and public health
By Samantha Nebelecky
Published March 29, 2024
The UB School of Pharmacy and Pharmaceutical Sciences (SPPS) recently hosted two refugee education sessions to help educate newly arrived refugees on medical health literacy in the United States.
Related Links
- View photos from the Medication Literacy Clinic on 2-29-24
- View photos from the Medication Literacy Clinic on 3-14-24
Our Refugee Medication Health Literacy Program is one of the only programs in the country that assists displaced refugees with medication management education through culturally sensitive materials. This community-driven outreach initiative helps newly arrived refugees entering the Western New York area learn how to navigate the U.S. healthcare system.
Small group teaching sessions work to improve medication literacy for newly arrived refugees from across the globe and gives them a better understanding of the U.S. healthcare system, including how, when, and why medications have been provided to them. The sessions also provide them with the opportunity to ask questions and feel more comfortable working with a pharmacist.
Gina Prescott, PharmD, director, global and community outreach and clinical professor, Department of Pharmacy Practice, leads the sessions and says they help educate our students just as much as they help educate newly arrived refugees. “The program teaches our students how to work with patients who have limited health literacy, how to recognize their different needs, as well as how to work with an interpreter to understand different cultural perspectives on health.”
The first education session was held on February 29 at the International Institute of Buffalo, an organization dedicated to improving the future of Western New York for immigrants and refugees. At the session SPPS faculty, students and alumni helped educate 14 newly arrived refugees speaking Farci, Arabic, Burmese, Spanish and Swahili.
The second education session on March 14 was held at the Buffalo Public Schools Adult Education Division, English Language School, an educational and workforce skills training provider in Western New York that helps non-native speakers develop English language skills. During this session, 30 newly arrived refugees speaking Farci, Arabic, Bengali, Vietnamese, Ukrainian, Portuguese, French, Somali, Spanish and Swahili were assisted.
Both education sessions taught newly arrived refugees essential aspects of medication use including how to navigate the U.S. pharmacy and healthcare system, understand medication side effects, interpret medication labels, determine pediatric dosing and use dosing tools.
Some commentary from former refugee workshop participants included, “It was very important to learn the proper way to measure,” “I learned how to remove the childproof lids from the bottles, which I didn't know how to do,” and “I found it useful particularly information pertaining to reading actual labels, showing the medication bottles, and medication safety.”
Prescott has future plans to expand and enhance the Refugee Medication Health Literacy Program. She looks forward to continuing to work with the International Institute of Buffalo and English language schools to provide additional programming on topics such as preventative health and non-communicable diseases.
For over 135 years, the University at Buffalo School of Pharmacy and Pharmaceutical Sciences has continually been a leader in the education of pharmacists and pharmaceutical scientists, renowned for innovation in clinical practice and research. The school is accredited by the American Council of Pharmaceutical Education and is the No. 1 ranked school of pharmacy in New York State and No. 14 in the United States by U.S. News & World Report.
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
- Search Results
- Study Record Detail

An Open Comparative Study of the Effectiveness and Incomparable Study of the Immunogenicity and Safety of the Vaccine (CoviVac) for Adults Aged 60 Years and Older
- Study Details
- Tabular View
- No Results Posted

Inclusion Criteria:
Volunteers must meet the following inclusion criteria:
Type of participants
• Healthy volunteers or volunteers with a history of stable diseases that do not meet any of the criteria for non-inclusion in the study.
Other inclusion criteria
- Written informed consent of volunteers to participate in a clinical trial
- Volunteers who are able to fulfill the Protocol requirements (i.e., fill out a self-observation Diary, come to control visits).
Exclusion Criteria:
SARS-CoV-2 infection • A case of established COVID-19 disease confirmed by PCR and/or ELISA in the last 6 months.
Diseases or medical conditions
- Serious post-vaccination reaction (temperature above 40 C, hyperemia or edema more than 8 cm in diameter) or complication (collapse or shock-like condition that developed within 48 hours after vaccination; convulsions, accompanied or not accompanied by a feverish state) to any previous vaccination.
- Burdened allergic history (anaphylactic shock, Quincke's edema, polymorphic exudative eczema, serum sickness in the anamnesis, hypersensitivity or allergic reactions to the introduction of any vaccines in the anamnesis, known allergic reactions to vaccine components, etc.).
- Guillain-Barre syndrome (acute polyradiculitis) in the anamnesis.
- The axillary temperature at the time of vaccination is more than 37.0 ° C.
- Acute infectious diseases (recovery earlier than 4 weeks before vaccination) according to anamnesis.
- Donation of blood or plasma (in the amount of 450 ml or more) less than 2 months before inclusion in the study.
- Severe and/or uncontrolled diseases of the cardiovascular, bronchopulmonary, neuroendocrine systems, gastrointestinal tract, liver, kidneys, hematopoietic, immune systems.
- Is registered at the dispensary for tuberculosis, leukemia, oncological diseases, autoimmune diseases.
- Any confirmed or suspected immunosuppressive or immunodeficiency condition in the anamnesis.
- Splenectomy in the anamnesis.
- Neutropenia (decrease in the absolute number of neutrophils less than 1000/mm3), agranulocytosis, significant blood loss, severe anemia (hemoglobin less than 80 g/l) according to anamnesis.
- Anorexia according to anamnesis.
Prior or concomitant therapy
- Vaccination with any vaccine carried out within 30 days before vaccination / the first dose of the studied vaccine or planned administration within 30 days after vaccination / the last dose of the studied vaccine.
- Prior vaccination with an experimental or registered vaccine that may affect the interpretation of the study data (any coronavirus or SARS vaccines).
- Long-term use (more than 14 days) of immunosuppressants or other immunomodulatory drugs (immunoregulatory peptides, cytokines, interferons, immune system effector proteins (immunoglobulins), interferon inducers (cycloferon) during the six months preceding the study, according to anamnesis.
- Treatment with systemic glucocorticosteroids (≥ 20 mg of prednisone, or an analog, for more than 15 days during the last month).
- Volunteers who received immunoglobulin preparations or blood transfusion during the last 3 months prior to the start of the study according to anamnesis.
Other non-inclusion criteria
• Participation in any other clinical trial within the last 3 months.
Exclusion criteria:
- Withdrawal of Informed consent by a volunteer;
- The volunteer was included in violation of the inclusion/non-inclusion criteria of the Protocol;
- Any condition of a volunteer that requires, in the reasoned opinion of a medical researcher, the withdrawal of a volunteer from the study;
- Taking unauthorized medications (see section 6.2);
- The volunteer refuses to cooperate or is undisciplined (for example, failure to attend a scheduled visit without warning the researcher and/or loss of communication with the volunteer), or dropped out of observation;
- For administrative reasons (termination of the study by the Sponsor or regulatory authorities), as well as in case of gross violations of the Protocol that may affect the results of the study.
- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services

IMAGES
VIDEO
COMMENTS
PhD Program: Clinical Pharmaceutical Scientist Program. The Clinical Pharmaceutical Scientist Program is a specialty track/program in which students with expertise in pharmacotherapeutics investigate both the clinical and mechanistic elements of drug therapy issues. You will learn experimental design, experimental methods, data analysis, and ...
Pharmaceutical Outcomes Research is a PhD program in the graduate program in Clinical Pharmacy. This program is housed in the Center for Pharmaceutical Outcomes Research (CePOR, SEE-por), a school-wide center in the Skaggs School of Pharmacy. Our doctoral curriculum is designed to provide competent and highly skilled researchers in the study of ...
Faculty of Pharmacy, Charles University, Department of Pharmacology and Toxicology . Drug resistance represents a critical obstacle to successful anticancer pharmacotherapy. Read more. Supervisor: Assoc Prof J Hofman. 30 April 2024 PhD Research Project Funded PhD Project (Students Worldwide) More Details.
Research Areas. The UCSF Pharmaceutical Sciences and Pharmacogenomics Graduate Program offers six areas of research emphasis: 1. Pharmacogenomics and functional genomics. Pharmacogenomics and functional genomics are increasingly recognized scientific areas that are critical to precision medicine.
Research Group: Institute of Cancer Therapeutics. We invite applications for a fully-funded, full-time 3-year PhD studentship to develop novel inhibitors for the treatment of advanced prostate cancer, one of the leading causes of male cancer deaths. Read more. Supervisors: Dr J Muller, Dr H Sheldrake, Dr M Sutherland, Dr S Shnyder.
The Department of Pharmacology and Molecular Sciences hosts the Pharmacology Graduate Program, which offers a program of study and research leading to the Ph.D. degree. Research training opportunities within the program cover a broad spectrum of biomedical sciences including chemical biology, immunology, virology, cancer, and neuroscience.
The goal of researchers in this area is to improve the prevention and management of disease and injury in individuals. Our research explores hypotheses and answers questions that arise in clinical practice. The focus is on enhancing the health and quality of life of individuals by optimizing the safety and effectiveness of medications.
PHD, Clinical & Administrative Pharmacy. This interdisciplinary program prepares students to address complex socio-political problems relating to ethical drug consumption, manufacturing, distribution, and payment mechanisms. Elective concentrations are business, psychology, statistics, political science, and more. Degree Type: Doctoral.
These may include new drug discovery, clinical pharmacy, pharmaceutics, pharmacology and microbiology (to name a few examples). How long does it take to get a PhD in Pharmacy? As a full-time doctoral student in the UK, it should take you 3 years to earn a PhD Pharmacy. If you're studying for a part-time PhD, expect to need about 6 years to ...
Pharmacy practice PhD research supervision areas. Browse our PhD project areas. Grow your potential in pharmacy practice research, by joining one of the PhD projects we have available at the University of Reading. If you're looking for a career in pharmacy practice, this is the perfect place to start. This is a taster of some of the PhD ...
Our PhD/MPhil Pharmacy Practice programme enables you to undertake a research project that will improve the practise of pharmacy, the prescribing of medicines to optimise therapy and how patients take their medicines. There are 3 working centres in Pharmacy Practice which include the Centre for Pharmacy Workforce Studies chaired by Dr Ellen Schafheutle, Pharmacoepidemiology and Drug Safety ...
In parallel, clinical pharmacy and practice research is evolving. Research evidence should be used to identify new areas for improved health service delivery and rigorously evaluate new services in pharmacy. ... Topic guides: Topic guides guide the discussions in focus groups and individual interviews, and contain open-ended questions and ...
Some typical research topics in Pharmacy include: Typical Pharmacy PhD research projects take between three and four years to complete. During a standard PhD day, you will either be in the laboratory performing, preparing, or planning experiments, (if your project is laboratory based), researching pharmacy practice and policy, writing up ...
Hot Topics in Pharmaceutical Research. In this virtual issue, we highlight some of the most impactful recent articles in the journal as reflected by citations in 2022. Highly cited articles provide insight into which research topics are attracting the most attention and reflect innovative new discoveries, or timely reviews and perspectives on ...
HOT TOPICS IN PHARMACY PRACTICE RESEARCH. S13 Effectiveness of community-based pharmacist interventions in chronic non-cancer pain: A systematic review. S14 The consideration of sex/gender and vulnerable populations in pharmacy practice research. POSTER ABSTRACTS. S15 Introducing a unit-based clinical pharmacist: A pilot study
Research Methodology Workshop Series Topic -... 27 January, 2024 | K K Birla Goa. ... Clinical Research and Clinical Pharmacy; Pharmaceutical Biotechnology ... Full-time PhD students admitted into the PhD program are eligible to be considered for an Institute fellowship of Rs. 28,000 or Rs. 31,000 per month in the first year based on their ...
Doctor of Pharmacy (PharmD) MS in Clinical and Translational Therapeutics; ... to work with the International Institute of Buffalo and English language schools to provide additional programming on topics such as preventative health and non-communicable diseases. ... 10/12/23 Pharmaceutical Sciences (BS, BS/MS, MS and PhD) 12/2/22 Dual Degree ...
This cross-disciplinary PhD project is between the School of Biomedical Science at UWL and the School of Pharmacy at UCL, and Pharmaceutical company to investigate the feasibility of developing an inhalation form of biotherapeutics for severe chronic inflammatory diseases. Read more. Supervisors: Dr H Khalili, Dr J Lam.
Randomized, double-blind, placebo controlled, multi-center clinical trials of the tolerability, safety and immunogenicity of the inactivated whole-virion concentrated purified vaccine against COVID-19, manufactured by FSBSI "Chumakov FSC R&D IBP RAS", of childrens aged 12-17" (Clinical trials, phase III).
This cross-disciplinary PhD project is between the School of Biomedical Science at UWL and the School of Pharmacy at UCL, and Pharmaceutical company to investigate the feasibility of developing an inhalation form of biotherapeutics for severe chronic inflammatory diseases. Read more. Supervisors: Dr H Khalili, Dr J Lam.
Written informed consent of volunteers to participate in a clinical trial; Volunteers who are able to fulfill the Protocol requirements (i.e., fill out a self-observation Diary, come to control visits). Exclusion Criteria: SARS-CoV-2 infection • A case of established COVID-19 disease confirmed by PCR and/or ELISA in the last 6 months.
Diagnostics and psychological assistance in modern clinical psychology: The problem of scientific and ethical foundations" (November 18—19, 2020, Moscow) and summarize its outcomes.
Advancement of clinical pharmacy practice and optimisation of antimicrobials prescribing. Ulster University - Coleraine Campus Faculty of Life and Health Sciences. Research Group: Biomedical Sciences. Clinical pharmacy services (CPS) is where pharmacists work collaboratively with other healthcare providers to ensure safe, effective, and ...
Catalysis Conference is a networking event covering all topics in catalysis, chemistry, chemical engineering and technology during October 19-21, 2017 in Las Vegas, USA. Well noted as well attended meeting among all other annual catalysis conferences 2018, chemical engineering conferences 2018 and chemistry webinars.