- Nurse Spotlight
- Student Resources

The Value of Critical Thinking in Nursing
Gayle Morris
Contributing Writer
Learn about our editorial process .
Updated October 3, 2023

Are you ready to earn your online nursing degree?
Some experts describe a person's ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as "necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation."
"This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice," he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
"Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe."
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
"Nurses are at the patient's bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider," she explains.
Featured Online MSN Programs
Top 5 ways nurses can improve critical thinking skills.
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. "What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?"
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. "Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help." Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It's important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that "critical thinking is a self-driven process. It isn't something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive."
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient's care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient's mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
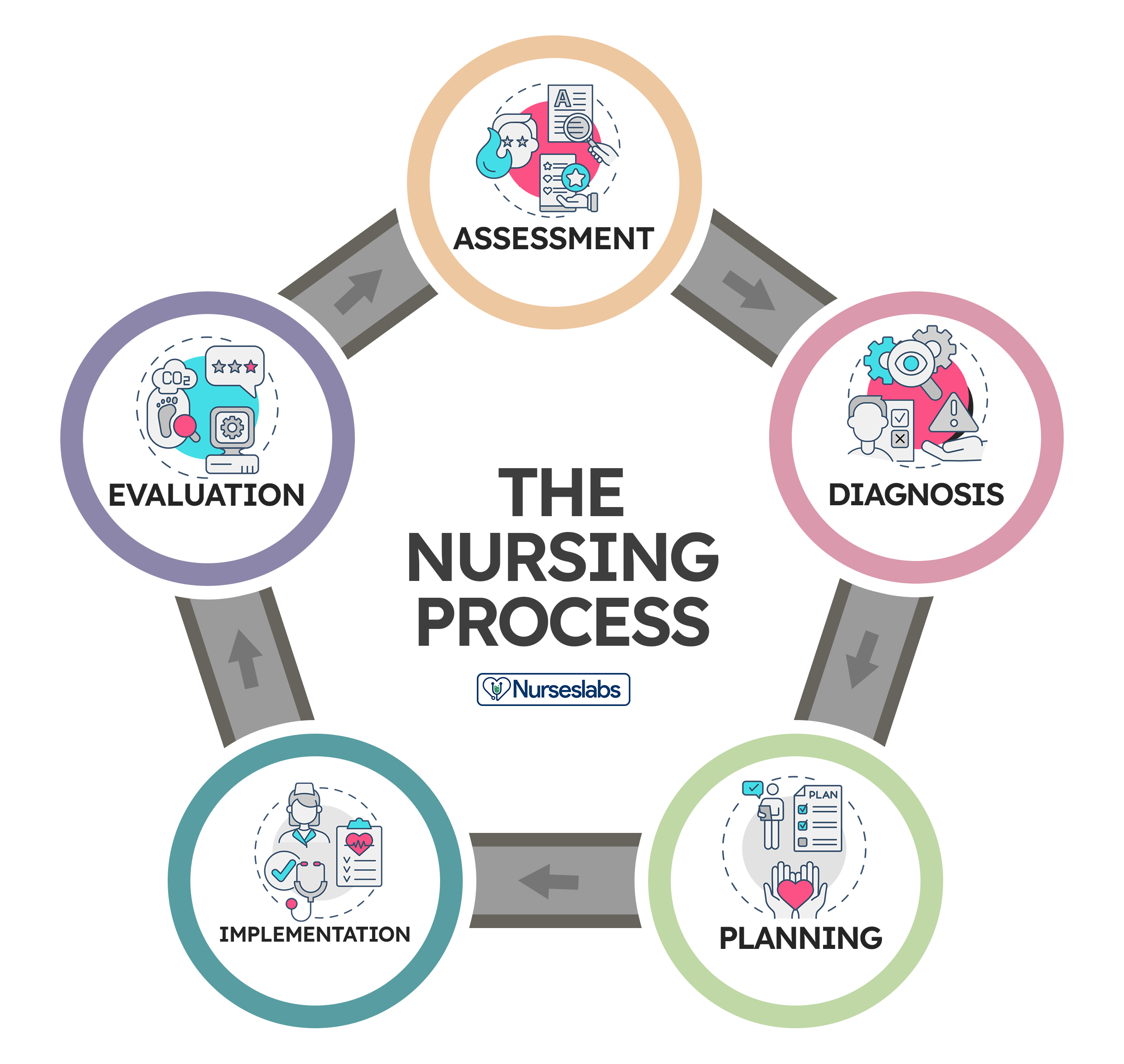
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what's happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
"We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care," he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
"Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient's blood pressure because medication administration is a task that must be completed," Slaughter says. "A nurse employing critical thinking skills would address the low blood pressure, review the patient's blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld."
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient's cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient's overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University's RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter's clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
You might be interested in

HESI vs. TEAS Exam: The Differences Explained
Genevieve Carlton
Published February 14, 2024 · 2 Min Read
Courtnee James
Contributing Editor

10 Nursing Schools That Don’t Require TEAS or HESI Exam

For Chiefs' RB Clyde Edwards-Helaire, Nursing Runs in the Family
Published February 13, 2024 · 2 Min Read
NurseJournal.org is an advertising-supported site. Featured or trusted partner programs and all school search, finder, or match results are for schools that compensate us. This compensation does not influence our school rankings, resource guides, or other editorially-independent information published on this site.
Whether you’re looking to get your pre-licensure degree or taking the next step in your career, the education you need could be more affordable than you think. Find the right nursing program for you.

Brain, Decision Making and Mental Health pp 179–189 Cite as
Critical Thinking in Nursing
- Şefika Dilek Güven 3
- First Online: 02 January 2023
1007 Accesses
Part of the book series: Integrated Science ((IS,volume 12))
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
- Clinical decision-making
- Critical thinking
- Critical thinking skills
- Decision-making
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
Key aspects of critical thinking include:
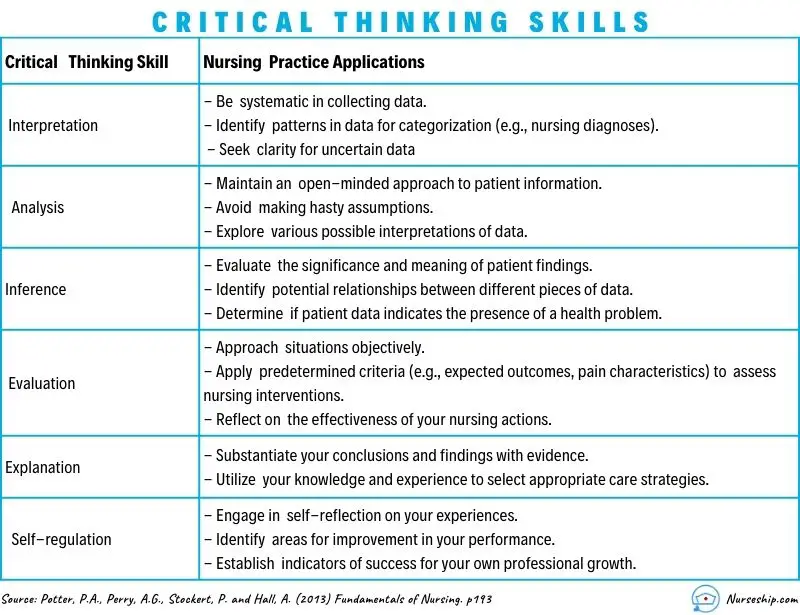
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
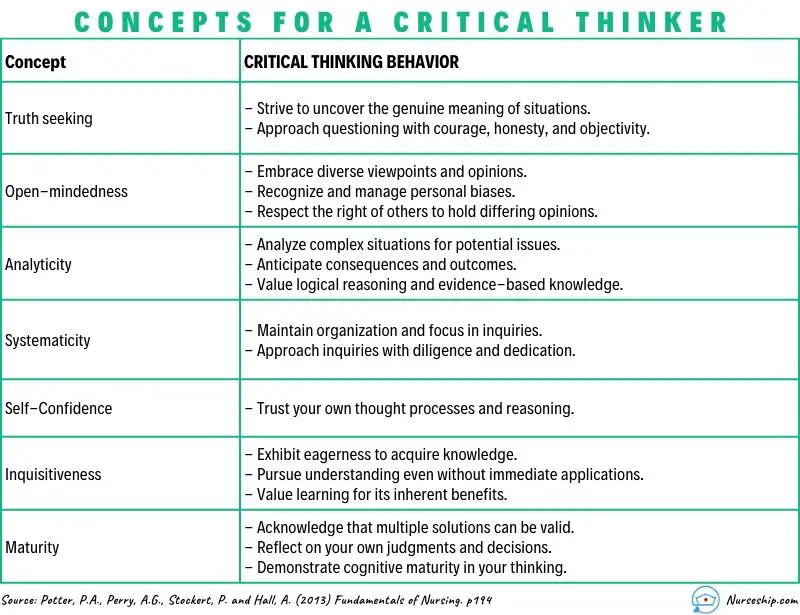
What are the Levels of Critical Thinking in Nursing?
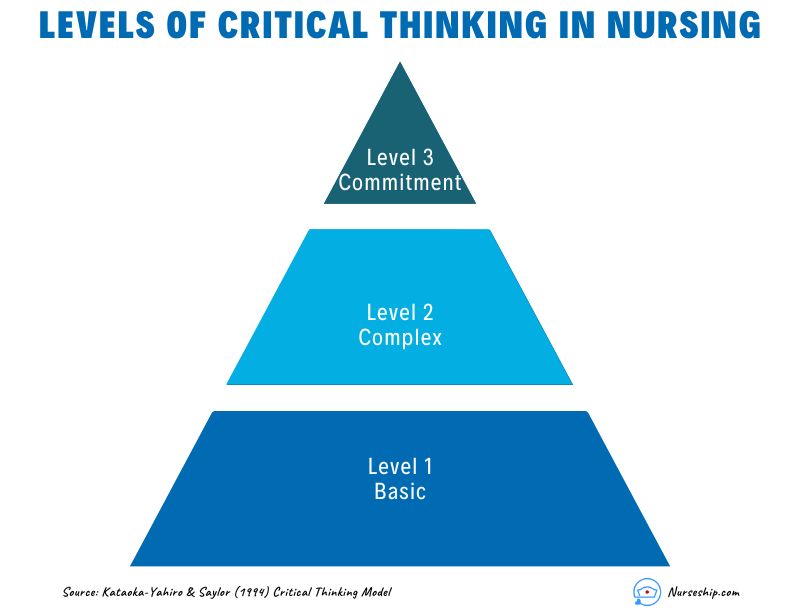
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.
Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.

Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.
What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

The Nursing Process: A Comprehensive Guide

In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse’s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
Application of the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data.
- 2. Diagnosis: “What is the problem?”
Initial Planning
Ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care.
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation. The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch, smell, or hearing, and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure, vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance, facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members, support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history, which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation.
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
2. Diagnosis: “What is the problem?”
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care.
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions. When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement, and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation : “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration , educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking, to reduce the patient’s anxiety, anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing, administering an injection, manipulating equipment, bandaging, moving, lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non-RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory , nursing practice, and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation : “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan, and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan.
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
38 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Leave a Comment Cancel reply
Critical Thinking and the Nursing Process
In today’s health care arena, the nurse is faced with increasingly complex issues and situations resulting from advanced technology, greater acuity of patients in hospital and community settings, an aging population, and complex disease processes, as well as ethical and cultural factors. Traditionally, nurses have used a problem-solving approach in planning and providing nursing care. Today the decision-making part of problem solving has become increasingly complex and requires critical thinking.
Definition of Critical thinking
Critical thinking is a multidimensional skill, a cognitive or mental process or set of procedures. It involves reasoning and purposeful, systematic, reflective, rational, outcome-directed thinking based on a body of knowledge, as well as examination and analysis of all available information and ideas. Critical thinking leads to the formulation of conclusions and the most appropriate, often creative, decisions, options, or alternatives. Critical thinking includes metacognition, the examination of one’s own reasoning or thought processes while thinking, to help strengthen and refine thinking skills. Independent judgments and decisions evolve from a sound knowledge base and the ability to synthesize information within the context in which it is presented. Nursing practice in today’s society mandates the use of high-level critical thinking skills within the nursing process. Critical thinking enhances clinical decision making, helping to identify patient needs and to determine the best nursing actions that will assist the patient in meeting those needs. Critical thinking and critical thinkers have distinctive characteristics. As indicated in the above definition, critical thinking is a conscious, outcome-oriented activity; it is purposeful and intentional. The critical thinker is an inquisitive, fair-minded truth seeker with an open-mindedness to the alternative solutions that might surface.
Critical thinking Process: Rationality and Insight
Critical thinking is systematic and organized. The skills involved in critical thinking are developed over time through effort, practice, and experience. Skills needed in critical thinking include interpretation, analysis, evaluation, inference, explanation, and self-regulation. Critical thinking requires background knowledge and knowledge of key concepts as well as standards of good thinking. The critical thinker uses reality-based deliberation to validate the accuracy of data and the reliability of sources, being mindful of and questioning inconsistencies. Interpretation is used to determine the significance of data that are gathered, and analysis is used to identify patient problems indicated by the data. The nurse uses inference to draw conclusions. Explanation is the justification of actions or interventions used to address patient problems and to help a patient move toward desired outcomes. Evaluation is the process of determining whether outcomes have been or are being met, and self-regulation is the process of examining the care provided and adjusting the interventions as needed. Critical thinking is also reflective, involving metacognition, active evaluation, and refinement of the thinking process. The critical thinker considers the possibility of personal bias when interpreting data and determining appropriate actions. The critical thinker must be insightful and have a sense of fairness and integrity, the courage to question personal ethics, and the perseverance to strive continuously to minimize the effects of egocentricity, ethnocentricity, and other biases on the decision making process.
Components of Critical thinking
Certain cognitive or mental activities can be identified as key components of critical thinking. When thinking critically, a person will do the following:
- Ask questions to determine the reason why certain developments have occurred and to see whether more information is needed to understand the situation accurately.
- Gather as much relevant information as possible to consider as many factors as possible.
- Validate the information presented to make sure that it is accurate (not just supposition or opinion), that it makes sense, and that it is based on fact and evidence.
- Analyze the information to determine what it means and to see whether it forms clusters or patterns that point to certain conclusions.
- Draw on past clinical experience and knowledge to explain what is happening and to anticipate what might happen next, acknowledging personal bias and cultural influences.
- Maintain a flexible attitude that allows the facts to guide thinking and takes into account all possibilities.
- Consider available options and examine each in terms of its advantages and disadvantages.
- Formulate decisions that reflect creativity and independent decision making.
Critical thinking requires going beyond basic problem solving into a realm of inquisitive exploration, looking for all relevant factors that affect the issue, and being an “out-of-the-box” thinker. It includes questioning all findings until a comprehensive picture emerges that explains the phenomenon, possible solutions, and creative methods for proceeding. Critical thinking in nursing practice results in a comprehensive patient plan of care with maximized potential for success.
Critical thinking In Nursing Practice
Using critical thinking to develop a plan of nursing care requires considering the human factors that might influence the plan. The nurse interacts with the patient, family, and other health care providers in the process of providing appropriate, individualized nursing care. The culture, attitude, and thought processes of the nurse, the patient, and others will affect the critical thinking process from the data-gathering stage through the decision-making stage; therefore, aspects of the nurse-patient interaction must be considered. Nurses must use critical thinking skills in all practice settings—acute care, ambulatory care, extended care, and in the home and community. Regardless of the setting, each patient situation is viewed as unique and dynamic. The unique factors that the patient and nurse bring to the health care situation are considered, studied, analyzed, and interpreted. Interpretation of the information presented then allows the nurse to focus on those factors that are most relevant and mostsignificant to the clinical situation. Decisions about what to do and how to do it are then developed into a plan of action.
Fonteyn (1998) identified 12 predominant thinking strategies used by nurses, regardless of their area of clinical practice:
Recognizing a pattern
- Setting priorities
- Searching for information
- Generating hypotheses
- Making predictions
- Forming relationships
- Stating a proposition (“if–then”)
- Asserting a practice rule
- Making choices (alternative actions)
- Judging the value
- Drawing conclusions
- Providing explanations
Fonteyn further identified other, less prominent thinking strategies the nurse might use:
- Posing a question
- Making assumptions (supposing)
- Making generalizations
These thought processes are consistent with the characteristics of critical thinking and cognitive activities discussed earlier. Fonteyn asserted that exploring how these thinking strategies are used in various clinical situations, and practicing using the strategies, might assist the nurse–learner in examining and refining his or her own thinking skills.
Throughout the critical thinking process, a continuous flow of questions evolves in the thinker’s mind. Although the questions will vary according to the particular clinical situation, certain general inquiries can serve as a basis for reaching conclusions and determining a course of action. When faced with a patient situation, it is often helpful to seek answers to some or all of the following questions in an attempt to determine those actions that are most appropriate:
- What relevant assessment information do I need, and how do I interpret this information? What does this information tell me?
- To what problems does this information point? Have I identified the most important ones? Does the information point to any other problems that I should consider?
- Have I gathered all the information I need (signs/symptoms, laboratory values, medication history, emotional factors, mental status)? Is anything missing?
- Is there anything that needs to be reported immediately? Do I need to seek additional assistance?
- Does this patient have any special risk factors? Which ones are most significant? What must I do to minimize these risks?
- What possible complications must I anticipate?
- What are the most important problems in this situation? Do the patient and the patient’s family recognize the same problems?
- What are the desired outcomes for this patient? Which have the highest priority? Does the patient see eye to eye with me on these points?
- What is going to be my first action in this situation? How can I construct a plan of care to achieve the goals?
- Are there any age-related factors involved, and will they require some special approach? Will I need to make some change in the plan of care to take these factors into account?
- How do the family dynamics affect this situation, and will this have an affect on my actions or the plan of care?
- Are there cultural factors that I must address and consider?
- Am I dealing with an ethical problem here? If so, how am I going to resolve it?
- Has any nursing research been conducted on this subject?
Related Posts
Blood glucose monitoring, basal metabolic rate (bmr), hand washing technique.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
4.2 Basic Concepts
Open Resources for Nursing (Open RN)
Before learning how to use the nursing process, it is important to understand some basic concepts related to critical thinking and nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [1] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” [2] To make sound judgments about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [3]
Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, making generalizations, and creating hypotheses. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a patient’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes more clear. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a patient problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a patient, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1. [4] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to take action quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Example: A nurse assesses a patient and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the patient’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.

Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Nurses use standards set by their state’s Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about patient care and solve problems.
Example: Based on research findings, hospital leaders determine patients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2). [5] The nurse further implements this policy by organizing care for patients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all patients regardless if they have difficulty sleeping or not.
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized patient concern, and generate the best possible evidence-based solutions in order to deliver safe patient care.” [6] The NCSBN administers the national licensure exam (NCLEX) that measures nursing clinical judgment and decision-making ability of prospective entry-level nurses to assure safe and competent nursing care by licensed nurses.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.” [7]
Nursing Process
The nursing process is a critical thinking model based on a systematic approach to patient-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing patient care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently. [8] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: A ssessment, D iagnosis, O utcomes Identification, P lanning, I mplementation, and E valuation.
The nursing process is a continuous, cyclic process that is constantly adapting to the patient’s current health status. See Figure 4.3 [9] for an illustration of the nursing process.
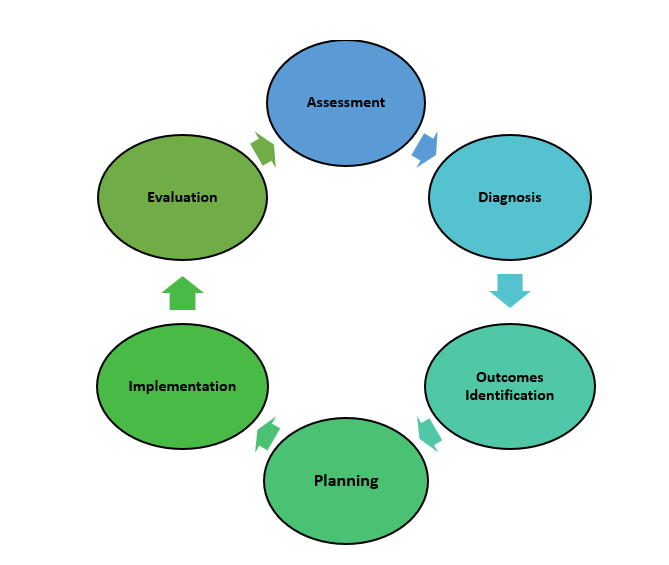
Review Scenario A in the following box for an example of a nurse using the nursing process while providing patient care.
Patient Scenario A : Using the Nursing Process [10]

A hospitalized patient has a prescription to receive Lasix 80mg IV every morning for a medical diagnosis of heart failure. During the morning assessment, the nurse notes that the patient has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F. The nurse reviews the medical record for the patient’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s. The nurse recognizes these cues form a pattern related to fluid imbalance and hypothesizes that the patient may be dehydrated. The nurse gathers additional information and notes the patient’s weight has decreased 4 pounds since yesterday. The nurse talks with the patient and validates the hypothesis when the patient reports that their mouth feels like cotton and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the patient with the nursing diagnosis Fluid Volume Deficit and establishes outcomes for reestablishing fluid balance. The nurse withholds the administration of IV Lasix and contacts the health care provider to discuss the patient’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitor hydration status. By the end of the shift, the nurse evaluates the patient status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the patient, recognizes cues, creates a generalization and hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates the outcome. Additionally, the nurse promotes patient safety by contacting the provider before administering a medication that could cause harm to the patient at this time.
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” [11] A registered nurse uses a systematic method to collect and analyze patient data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized patient in pain includes the patient’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. [12]
The “Assessment” component of the nursing process is further described in the “ Assessment ” section of this chapter.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [13] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses. [14]
The “Diagnosis” component of the nursing process is further described in the “ Diagnosis ” section of this chapter.
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” [15] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the patient based on their assessment data and nursing diagnoses.
The “Outcomes Identification” component of the nursing process is further described in the “ Outcomes Identification ” section of this chapter.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [16] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each patient’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the patient’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care. [17]
The “Planning” component of the nursing process is further described in the “ Planning ” section of this chapter.
Nursing Care Plans
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific patient using the nursing process. Registered nurses (RNs) create nursing care plans so that the care provided to the patient across shifts is consistent among health care personnel. Some interventions can be delegated to Licensed Practical Nurses (LPNs) or trained Unlicensed Assistive Personnel (UAPs) with the RN’s supervision. Developing nursing care plans and implementing appropriate delegation are further discussed under the “ Planning ” and “ Implementing ” sections of this chapter.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” [18] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the patient. Interventions are also documented in the patient’s electronic medical record as they are completed. [19]
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment. [20]
The “Implementation” component of the nursing process is further described in the “ Implementation ” section of this chapter.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [21] During evaluation, nurses assess the patient and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed. [22]
The “Evaluation” component of the nursing process is further described in the “ Evaluation ” section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, patients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality patient care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a patient’s health care problems
- Improves patient safety
- Improves patient satisfaction
- Identifies a patient’s goals and strategies to attain them
- Increases the likelihood of achieving positive patient outcomes
- Saves time, energy, and frustration by creating a care plan or path to follow
By using these components of the nursing process as a critical thinking model, nurses plan interventions customized to the patient’s needs, plan outcomes and interventions, and determine whether those actions are effective in meeting the patient’s needs. In the remaining sections of this chapter, we will take an in-depth look at each of these components of the nursing process. Using the nursing process and implementing evidence-based practices are referred to as the “science of nursing.” Let’s review concepts related to the “art of nursing” while providing holistic care in a caring manner using the nursing process.
Holistic Nursing Care
The American Nurses Association (ANA) recently updated the definition of nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.” [23]
The ANA further describes nursing is a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.” [24]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a patient and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Caring and the Nursing Process
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” [25] Successful use of the nursing process requires the development of a care relationship with the patient. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the patient and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. [26] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, touching, and verbal reassurances while also respecting and being sensitive to the care recipient’s cultural beliefs and meanings associated with caring behaviors. [27] See Figure 4.4 [28] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their patients while creating a healing environment. [29]

Now that we have discussed basic concepts related to the nursing process, let’s look more deeply at each component of the nursing process in the following sections.
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41 (4), 215-221. ↵
- Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15 (7), 37-39. ↵
- “ The Detective ” by paurian is licensed under CC BY 2.0 ↵
- “ In the Quiet Zone… ” by C.O.D. Library is licensed under CC BY-NC-SA 2.0 ↵
- NCSBN. (n.d.). NCSBN clinical judgment model . https://www.ncsbn.org/14798.htm ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “ The Nursing Process ” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Patient Image in LTC.JPG” by ARISE project is licensed under CC BY 4.0 ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (n.d.). The nursing process . https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- Walivaara, B., Savenstedt, S., & Axelsson, K. (2013). Caring relationships in home-based nursing care - registered nurses’ experiences. The Open Journal of Nursing, 7 , 89-95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3722540/pdf/TONURSJ-7-89.pdf ↵
- “ hospice-1793998_1280.jpg ” by truthseeker08 is licensed under CC0 ↵
- Watson Caring Science Institute. (n.d.). Watson Caring Science Institute. Jean Watson, PHD, RN, AHN-BC, FAAN, (LL-AAN) . https://www.watsoncaringscience.org/jean-bio/ ↵
Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.
A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.
A type of reasoning that involves forming generalizations based on specific incidents.
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder.
A judgment formed from a set of facts, cues, and observations.
A proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring.
“Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion.
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies, theories, clinical expertise, health care resources, and patient preferences and values.
An easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.
Individual, family, or group which includes significant others and populations.
Specific documentation of the planning and delivery of nursing care that is required by the Joint Commission.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.
A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the patient and family.
Developing a relationship of mutual trust and understanding.
Nursing Fundamentals Copyright © by Open Resources for Nursing (Open RN) is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
4.1: Nursing Process Introduction
- Last updated
- Save as PDF
- Page ID 52409

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
Learning Objectives
- Use the nursing process to provide patient care
- Identify nursing diagnoses from evidence-based sources
- Describe the development of a care plan
- Prioritize patient care
- Describe documentation for each step of the nursing process
- Differentiate between the role of the PN and RN
Have you ever wondered how a nurse can receive a quick handoff report from another nurse and immediately begin providing care for a patient they previously knew nothing about? How do they know what to do? How do they prioritize and make a plan?
Nurses do this activity every shift. They know how to find pertinent information and use the nursing process as a critical thinking model to guide patient care. The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients’ well-being and health. This chapter will explain how to use the nursing process as standards of professional nursing practice to provide safe, patient-centered care.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Advanced Search
- Journal List
- Rev Lat Am Enfermagem
Language: English | Portuguese | Spanish
Reflective and critical thinking in nursing curriculum
O pensamento crítico-reflexivo nos currículos de enfermagem, el pensamiento reflexivo y crítico en los currículos de enfermería, maría antonia jiménez-gómez.
1 Universidad Nacional de Colombia, Facultad de Enfermería, Bogotá, Colombia.
Lucila Cárdenas-Becerril
2 Universidad Autónoma del Estado de México, Facultad de Enfermería, Toluca, México.
Margarita Betzabé Velásquez-Oyola
3 Universidad Nacional José Faustino Sánchez Carrión, Facultad de Medicina Humana, Huacho, Lima, Peru.
Marcela Carrillo-Pineda
4 Universidad de Antioquia, Facultad de Enfermería, Medellín, Colombia.
Leyvi Yamile Barón-Díaz
5 Universidad Nacional de Colombia, Facultad de Medicina, Bogotá, Colombia.
to evaluate the teaching of transversal competence of the Reflective and Critical Thinking that is fundamental in the decision-making and solution of nursing problems, in degree programs of public and private institutions in the Andean region.
multi-center, cross-sectional, exploratory-descriptive study, with mixed approach in 5 countries.
76 nursing programs participated in the study. The Reflective and Critical Thinking was found as a subject, subject content and didactic strategies. Of the 562 subjects reviewed, this type of thinking is found in 46% of the humanities area and 42% in the area of research and professional discipline. It is important to train teachers to achieve coherence between the pedagogical model approach, teaching strategies and evaluations.
Conclusion:
nursing programs in the Andean region contemplate the critical thinking as cognitive and personals skills of communication. They also use real situations analysis, supervised practice, simulation labs and specifically learning based in problems to develop the capacity to solve them, decision-making and develop communication skills, including analysis, synthesis and evaluation.
avaliar o ensino da competência transversal do pensamento crítico-reflexivo, fundamental na tomada de decisões e solução de problemas de enfermagem, nos programas de graduação de instituições públicas e privadas da região Andina.
Método:
estudo multicêntrico, transversal, exploratório-descritivo, com abordagem mista em cinco países.
Resultados:
76 programas de Enfermagem participaram do estudo. O pensamento crítico-reflexivo foi constatado como disciplina, conteúdo de disciplina e estratégias didáticas. Das 562 disciplinas revisadas, este tipo de pensamento se encontra em 46% da área de humanidades e 42% na área de pesquisa e profissional-disciplinar. Existe a necessidade de capacitar os docentes para obter coerência entre a proposta do modelo pedagógico, as estratégias didáticas e a avaliação.
Conclusão:
os programas de enfermagem da região Andina contemplam o pensamento crítico como habilidades cognitivas, de comunicação e pessoais. Da mesma forma, utilizam a análise de situações reais, estágio supervisionado, laboratórios de simulação e, principalmente, a aprendizagem baseada em problemas, com a finalidade de desenvolver a capacidade para solucionar problemas, tomar decisões e desenvolver habilidades comunicativas, incluindo análise, síntese e avaliação.
evaluar la enseñanza de la competencia transversal del Pensamiento Reflexivo y Crítico, fundamental en la toma de decisiones y en la solución de problemas de enfermería, en los programas de grado de instituciones públicas y privadas de la región Andina.
estudio multicéntrico, transversal, exploratorio-descriptivo, con abordaje mixto en 5 países.
76 programas de Enfermería participaron en el estudio. El Pensamiento Reflexivo y Crítico se encontró como asignatura, contenido de asignatura y estrategias didácticas. De las 562 asignaturas que han sido revisadas, este tipo de pensamiento se encuentra en el 46% del área de humanidades y el 42% en el área de investigación y profesional disciplinar. Está la necesidad de capacitar a los docentes para lograr coherencia entre el planteamiento del modelo pedagógico, las estrategias didácticas y la evaluación.
Conclusión:
los programas de enfermería de la región Andina contemplan el pensamiento crítico como habilidades cognitivas, de comunicación y personales. Asimismo, utilizan el análisis de situaciones reales, la práctica supervisada, los laboratorios de simulación y, principalmente, el aprendizaje basado en problemas, con la finalidad de desarrollar la capacidad para solucionar los problemas, tomar decisiones y desarrollar habilidades comunicativas, incluyendo el análisis, la síntesis y la evaluación.
Introduction
Globalization brought with it changes in all aspects of life: social, political, economic and cultural. Moreover, the nursing profession is evolving, so that it is increasingly moving away from the biomedical model of care, focused on the instrumental, to focus on people’s health care, with primacy of dialogue and agreements between the professional and the person under care. As part of a multiprofessional team, this requires changes in the curricular proposal and, in turn, a qualifying teacher for a new profile of graduate, whereby reflection, self-criticism and professional responsibility are developed ( 1 ) .
Therefore, it is necessary to work intensely to reduce the dichotomies that are present in nursing programs, namely: between theory-practice; training and the reality of professional practice; and the student as a passive part of the teaching-learning process and the professional who is required, active, proactive, creative, analytical, with contextual perspective, flexible, with logical thinking, able to carry out a permanent and continuous search for information, able to contribute with his profession to the solution of health problems.
The General Conference of the United Nations Educational, Scientific and Cultural Organization (UNESCO), at its 38th session, held in Paris from 3 to 18 November 2015, “Recommendation about Adult Learning and Education” states in one of its objectives the need to develop people’s capacity to think critically and to act with autonomy and a sense of responsibility ( 2 ) .
Critical thinking (CT) is a process and a learning outcome ( 3 - 4 ) and the clinical judgment is the result of this process. The development of the clinical judgment (clinical reasoning skills) is one of the most important and challenging tasks of being a nurse. Clinical reasoning precedes clinical judgment and the decision-making that is important in professional and personal life.
In order to achieve professionals with reflective and critical thinking (RACT), it is necessary to make deep changes in the educational dynamics, in the teaching and student roles, in the use of pedagogy and didactics to transmit knowledge, the curricular structure, the strategies of teaching-learning. These changes are expected to be centered on the student, who must actively participate in the learning process in order to achieve greater development of his or her capacities for reasoning, self-learning, self-evaluation, self-management and self-regulation. Likewise, it is expected that teachers to be critical and creative, attending to individual ways of learning, encouraging the development of good thinking in the student ( 3 ) .
Literature points out that critical thinking is the “essential foundation for education, since it is the basis for adaptation to the individual, social and professional demands of daily life in the 21st century and beyond” ( 4 ) . The world changes fast and new realities arise, so there is a fundamental need of people to develop capabilities that allow them to respond and adapt themselves to these changes.
Critical thinking is “the process of seeking, obtaining, evaluating, analyzing, synthesizing and conceptualizing information as a guide, to develop self-conscious thinking and the ability to use this information by adding creativity and taking risks” ( 4 ) .
Authors pointed out one of the first definitions of critical thinking: “knowledge, skills and attitudes” ( 5 ) and, since the end of 1980, various strategies for its teaching have been discussed at all school levels ( 4 ) . On the other hand, authors point out the importance of generating opportunities to develop RACT in students. Therefore, some authors emphasize the importance of developing it in all health situations in favor of the patient ( 4 , 6 - 7 ) . The nursing professional developing RACT will know where, when and how to use their knowledge, skills, values and attitudes.
The motivation for nurse training in the Andean region became evident in the 1960s. In particular, Colombia generated the first degree program in 1958, which was approved in 1961. In the same period, Venezuela, Ecuador, and Peru initiated undergraduate programs; in the case of Bolivia, it happened only until 1970 ( 8 ) .
The 1980s were marked by the rise of postgraduate programs, increased development of research and the generation of knowledge. The 1990s saw a boom in graduate, specialization, masters, and doctoral programs, the latter especially in education. However, there were also more options for the qualification of nursing professionals for the teaching role. On the other hand, the Higher Education Quality Assurance System ( Sistema de Aseguramiento de la Calidad de la Educación Superior ) was implemented, as well as the Accreditation of the programs and the own regulations or nursing law emerged in each country of the region.
The first decade of the 21st century brought the development of the highest level of nursing education, the doctorate, and, with it, the generation of nursing knowledge in the region and its progress towards consolidation as a discipline ( 8 ) .
Throughout this journey, there was a permanent motivation for balance and congruence between the graduation profiles and the reality of the job, based on the permanent motivation for the adaptation of the curriculum, the teaching-learning strategies, the evaluation processes, and the teacher qualification to respond to this constantly changing context.
The literature ( 9 - 11 ) shows the need to expand the research in the area of education, to achieve greater development of research and to work in education and nursing policies and practices. On the other hand, the latter shows the need to implement and evaluate pedagogical and didactic strategies that help the student to develop a critical judgment, justified decision making, comprehensive memory and communicative competence ( 11 ) .
For its part, the Ibero-American Network for Research in Nursing Education ( Red Iberoamericana de Investigación en Educación en Enfermería - RIIEE), in 2011, identified as a research priority, “The development of RACT in nursing students”, within the tree of the problems detected in its research line Higher Education and Nursing. For the development of this research purpose, the Network suggested a multicenter macroproject with the theme “Strategies to develop the RACT in nursing students: situation in Latin America”. In fact, the conceptual paradigm refers to “critical theory and constructivism, since RACT is an analytical, cyclical, broad and systematic process, but not rigid; its analysis and interpretation allows to have elements for decision-making, as well as to make informed choices” ( 8 - 12 ) .
The project involves five of the six regions that make up the RIIEE: the Andean region (Bolivia, Colombia, Ecuador, Peru and Venezuela), Brazil, the Southern Cone, Europe, and Mexico and the Caribbean. The investigation is planned in three stages: 1. Diagnose; 2. Planning and implementation of interventions; and 3. Evaluation. The diagnostic stage includes: 1. The state of the art on scientific production in RACT and teaching strategies for its development; 2. Characterization of educational strategies for teaching the RACT collected in nursing literature; 3. To determine the development of the RACT competence in the different nursing curriculum; 4. To identify the educational strategies used by teachers to develop the competence of reflective critical thinking in nursing students; 5. To identify levels of critical thinking in nursing students according to the classification of Paul and Elder (unreflective thinker - master thinker). Objectives 4 and 5 are currently being developed.
The analysis of the “Scientific Production in RACT in Nursing in 1990-2012 in Ibero-America” produced among others the following conclusion: the formation of a critical reader and the investigative process are strategies that help university students to be critical and autonomous and to access more critically to the knowledge of the disciplinary area. For this, teachers are required to make of each moment and situation in the teaching-learning relationship an open forum for reflection, debate, questioning and contrasting of the different perspectives around the area of professional training and society’s problems ( 8 ) .
After reviewing the literature on the web of science by using the descriptors critical thinking and nursing, education and curriculum, it was not possible to find studies that analyzed the presence of RACT in the curriculum of nursing degree programs. However, it is very striking the motivation to analyze the importance of its development and studies that demonstrate its value, as well as the use of different and combined teaching-learning strategies to achieve the formation of RACT in nursing students.
This study was done with the purpose of to evaluate the teaching of transversal competence of the Reflective and Critical Thinking that is fundamental in the decision-making and solution of nursing problems, in degree programs of public and private institutions in the Andean region.
The coordinating group of RIIEE developed the research project from which the research groups of each country and region of the Network were made up, integrated by members of the Network and researchers in education and nursing, who are also teachers in Higher Education Institutions (HEI), and mostly with PhD academic level. The HEI in Nursing (HEIN) were identified through the Ministries of Education, the Associations of Schools and Universities of Nursing of each country and the Latin American Association of Schools and Universities of Nursing ( Asociación Latinoamericana de Escuelas y Facultades de Enfermería - ALADEFE).
The project was benefited from the Declaration of Helsinki (Ethical principles for medical research on human subjects) and the current ethics legislation in each country, was approved by the Ethics Committee of the University of Antioquia, Colombia, by Act No. CEI-FE 2015-25 on July 31, 2015. The respect for privacy and confidentiality were ensured to each Program Director, with the informed consent signed by each participant. The project was also sent to them and their understanding was guaranteed. In turn, we conceded the right to choose what information they wanted to share. Confidentiality was maintained by institutional coding. Finally, was given a deadline of 15 days to obtain the response of acceptance to participate.
The target population of this research were 187 undergraduate nursing programs in the Andean region: Bolivia (47), Colombia (47), Ecuador (21), Peru (62) and Venezuela (10). We considered only the nursing curriculum of the HEI, recognized by the Associations of Schools and Colleges of Nursing of each country or its counterpart, regardless of whether they were public or private. Resulting in the nursing curriculum of 76 Institutions that correspond to the 40.64% HEIN that teach undergraduate nursing in the Andean region: Bolivia (7), Colombia (38), Ecuador (11), Peru (14), and Venezuela (6). Due to the difficulty in obtaining the information, we checked web pages, contacted HEIN members, made contacts by telephone, in some cases, we made personal visits and, finally, the complete program was requested in PDF format for the complete the instrument of the research group. In addition, the HEIN did not refused to participate, but some institutions did not respond to the invitation. The result of this process: 30 institutions accepted to participate and provided the complete information, and out of 46 partial results were obtained. An HEIN database of the names, telephone numbers and e-mail addresses of the authorities in charge of managing the programs was created in order to follow up on their responses.
After identifying, during 2011 and 2012, the theoretical and conceptual framework of RACT from different authors and different perspectives (education, pedagogy, psychology and nursing), despite the abundance of literature about the subject, we concluded that the concept is very unclear from a nursing point of view ( 13 - 14 ) .
However, it was necessary to establish a concept that was accepted by the research group of the Network, that allowed to determine a starting point or consensus to carry out this work and, without detriment to seek some level of fidelity to the multiple approaches of the scholars of this research object, that was understandable for the group and reflected what was intended to be done in its research phases and stages.
The Network took as a theoretical framework the approaches made by Paul ( 15 ) and Paul; Elder ( 16 ) , the elements of the CT and the attitudes of the Critical Thinker proposed by these authors. With the material analyzed, RIIEE constructed the following concept: “Reflective and critical thinking is a complex, systematic and deliberate process of reasoning, self-directed and action-oriented. It is primary purpose to choose, based on intellectual and affective processes (cognitive, experiential and intuitive), the best response options that favor the solution of nursing problems, in well-defined contexts and in accordance with the ethical postulates of the profession that allow it to act with rationality and professional autonomy” ( 8 ) .
The research process included the conceptual and theoretical analysis of the curriculum, the updating of the context of research development in nursing education in each country of the region, the characterization of the HEIN and, finally, the results of the state of the art on teaching strategies for the development of the RACT 1990-2012, Andean region.
Once the exhaustive bibliographic review was carried out, the instrument was designed based on the concept of Stenhouse ( 17 ) , the curriculum as a macro concept that encompasses the socializing function of the school is at the same time pedagogical ideas, structure of contents in a particular form, precision of them, reflection of educational aspirations more difficult to translate in concrete terms and skills to promote in the students ( 16 ) . In Posner ( 18 ) , who raised the great number of phenomena involved in the curriculum; Gimeno-Sacristán; Pérez-Gómez ( 19 ) , there is five categories in which the definitions of curriculum can be articulated: as an organized knowledge structure, production technology system, instructional plan, set of learning experiences and problems solution.
Based on the aforementioned, the specific instrument for this investigation was constructed with three parts. The first with 10 items, with general information from the HEI or University. Each University is subdivided into Centers that are parted into Colleges and these are divided into programs: name, geographic location, type of institution, accreditation data, mission, vision, objectives, curricular guidelines for degree programs, web page, and data about who completed the instrument. The second, 28 items, for the College, School, Department or Nursing Program (typology to identify HEIN in the region), with the following subsections: general aspects of the nursing program, character within the institution, number of sites where the program is offered, accreditation data (date, resolution, and time of accreditation), program justification, mission, vision and objectives of the program, evaluation process, graduation profile, pedagogical model, number of hours and credits, curricular structure (nursing program subjects that correspond to each area or component). Finally, the general characteristics of the teachers: kind of affiliation with the institution, time worked, and maximum educational level achieved. The third, 9 items, for specific information about each of the subjects: name, component or area to which it belongs, number of hours and credits, type of subject (theoretical, practical and theoretical-practical), contents, teaching-learning methodologies and evaluation process.
The members of the research group carried out an analysis of the validity of the content of the instrument. Afterwards, the pilot test was conducted, starting with its implementation in each of the HEI in which the researchers worked; the results were analyzed and the corresponding adjustments were made in its structure. Subsequently, the adjusted instrument was tested with five members from the region, one from each country, but different from the research group. Because of this test, we decided to design a guide to facilitate the completion of the instrument and ensure objectivity in the collection of information, because of the language differences. It is possible to obtain the final version of the instrument from the authors of the project.
Each participant received the letter of invitation, the project, the informed consent, the instrument to collect the information and the corresponding guide for its completion in hands and by e-mail.
The information obtained was reviewed and, in some cases, it was necessary to request the complementation of some aspects of the instrument. Then we proceeded to codify the HEI or Universities and the HEIN. The information was included in Excel tables designed with the predetermined categories and subcategories, which were later incorporated into the SPSS statistical analysis program, version 19. The information was processed using descriptive statistics, with frequency distributions and average analysis, and analyzed by institution, by country and as an Andean region, according to the categories and subcategories determined, allowing comparisons between countries and conclusions to be drawn as a region.
The analysis of the information was carried out using the deductive-inductive method, considering the objectives of the project and the revised conceptual theoretical framework, with the aim of determining the presence of the RACT, explicit and implicit, in each categories, the coherence of the approaches between University-College-Program, the coherence between the objectives, contents, teaching-learning strategies and the evaluation process in each subject. In this sense, we analyzed the linearity or coherence with respect to what was proposed, developed and evaluated in relation to the RACT and, finally, the contradictions and inconsistencies found in the aforementioned approaches were pointed out. We considered national and international studies about the subject for the analysis and discussion of the results obtained, in addition to the documents mentioned above.
According to the information obtained by the research group, the Andean region has 2,552 HEI; 410 with character of universities and 160 are public, 220 are private and 14 are in special regime. There are 167 universities with nursing programs, 146 affiliated and recognized by the respective Associations of Schools and Colleges of Nursing in each country. The number of accredited nursing programs in the Andean region is 43: Colombia (20), Peru (20) and Bolivia (3). Precisely, of the 20 accredited institutions in Colombia, 11 already have their certifications renewed, which are of 8, 6 and 4 years; 5 and 6 years for Ecuador and 3 years for Peru. Bolivia is just beginning the process and Venezuela has no information about it.
The total population of HEIN by country was Bolivia 47, Colombia 42, Ecuador 21, Peru 62 and Venezuela 10. A total of 76 HEIN answered: Bolivia 7; Colombia 38; Ecuador 11; Peru 14 and Venezuela, 6. These institutions constituted the sample of the study.
Twenty-one of these institutions are certified: in Colombia 20 and in Bolivia 1; 12 did not include this information and 41 were not yet certificated. Of the total number of institutions that provided the information, 47 are public, 26 private and three do not know the information. Administratively, 36 are programs; 22 Colleges; 21 Schools and one Department.
The number of hours and credits of the programs showed considerable heterogeneity: the average number of hours was 5,552.3, corresponding on average to 232.11 credits. Regarding the number of hours per credit, the lowest is in Peru, which has 13 hours per credit, and the highest is in Colombia, with 48 hours corresponding to one credit. There are institutions that do not work with credits, especially in Bolivia; others did not included this information, among them Ecuador and Venezuela.
The main characteristics of the 912 teachers developing nursing programs in the Andean region are: 501 (54.9%) with a Specialist degree; 634 (69.51%) with a Master’s degree and 58 (6.35%) with a PhD; 249 (27.3%) with a postgraduate degree in Education.
From a general perspective, it should be noted that of the five countries in the region only Venezuela and Peru explicitly present the RACT in their Organic Law (OL) or Higher Education Law in terms of integral and permanent formation of reflective critical citizens (LOE, 2009, or Organic Law of Education, in Venezuela) ( 20 ) and (Law 30220, 2014, or University Law, in Peru) ( 21 ) .
The results of RACT’s presence are presented below: Universities or HEI; in Colleges, Programs, Schools and Departments, that is, in HEIN; and in the subjects.
When analyzing the information of the Universities or HEI, we found the RACT as direct mention, indirect mention and evidence of traditional positions was found. Directly, it was found as a training purpose in Bolivia, Colombia and Peru: receptor and analytical constructor, with critical conscience; as methodology to achieve it, in Colombia and Peru: “ promoting reasoning, the CT and creative”; as a result of learning in Ecuador and Venezuela: capable of solving problems, CT promoter.
The indirect mention was found as result in the five countries of the Region, as a strategy in Bolivia, Ecuador, Peru and Venezuela: integral formation, relation practical theory; and as objective in Colombia: future graduates with ethical conscience, autonomy, democratic spirit and highly qualified.
There are still traditional postures: teaching, evaluation as a final product, training in instrumental action, the educational process as providing knowledge.
By going a little deeper into the HEI, we found that 88% (38) consider the RACT: 63% (27) in the mission; 7% (3) in the vision; 51% (22) in the objectives and 30% (13) in the curricular guidelines. Among these, three defining categories were identified. The first, as a training purpose: prepare professionals and leaders with CT and social conscience . The second, as a methodological strategy to achieve its development: to develop and implement pedagogical methods that encourage reasoning, CT and creativity, and that encourage habits of discipline and productive work . And the third, as a result of the formation process that includes the subject: Training of critical, self-managed, creative and proactive men and women; and, moreover, refers to the projection and utility: with the promotion of CT and the generation of knowledge, thanks to the strengthening of critical analysis, anticipation and vision of the future and development of viable alternatives to the problems.
At HEIN, RACT is expressed in the graduation profile, objectives, curricular guidelines and mission. Table 1 shows the data summarized in relation to the number and percentage in which the RACT is presented in the subcategories and with regard to the total. The information recovered allows us to identify that the RACT ranks first with 38.3% in the graduation profile, followed by 35% both in the curricular guidelines and in the objectives; thirdly, is in the mission, 26.7%, and finally, with 11.7% it is in the vision. Bolivia has the highest percentage of presence in its curricular guidelines, followed by Colombia in its graduation profile, objectives, and mission, while Venezuela is in one before the last place with a 28% of presence in its mission and is not present in the profile or in the curricular guidelines. Peru has the last place and presents it only in the objectives of the programs.
In a cross-sectional view of what is proposed by curricular programs, three categories were identified to be highlighted. The first, the development of cognitive and personal skills, expressed as the training of professionals with scientific, technical, critical, analytical and reflective knowledge, as well as communication, oral and written expression skills; and referred to a critical, creative, participative, supportive, innovative and sensitive attitude towards social change.
The second, the way in which its development could be achieved, among which the research stands out: promote and develop research, generating knowledge in the different areas of nursing that contribute to universal science and the solution of health problems; and the use of technologies: learns permanently developing the capacity of abstraction, analysis, synthesis and using information technologies . The third, its finality, related to the ability of individuals, families and community groups to interfere and make decisions in the solution of health problems, to provide comprehensive care with the capacity to solve health problems in changing and emerging environments.
Concerning the pedagogical models expressed in the HEIN, a variety was found in the denomination. First of all, the constructivist approaches are highlighted in eight (8) Institutions, with some connotations as the model social-critical-constructivist and second, the cognitive - humanistic in four (4). Other models or approaches were also identified, among them: dialectic, technological, psychological, the problematic schools, the Active, Reflective, Dialectic, Innovative and Critical . Finally one institution works with the model based on the pillars of education , in which learning to know, learning to do, learning to be and learning to live together, which includes, educating for life, educating for life, educating for work, educating in society and for society ( 22 ) .
The RACT in the subjects of the programs of Nursing in the Andean region
Only 29 of the 76 HEIN participants in the study were able to obtain information on subjects (38.15%), and 22 (75.86%) of these in nursing programs, RACT was present in different elements of the subjects. 562 subjects were reviewed, 159 (29%) of which have no information about teaching strategies or evaluation. Moreover, some programs record the same teaching and assessment strategies for all subjects in the program, 45 (8%).
Table 2 presents the results by subcategory and the total presence of RACT in the different groups of subjects, basic area or foundation subjects (which introduce and contextualize the student in the field of knowledge), Research, Humanities (the study of the behavior, conditions and performance of the human being), disciplinary professional area (gives the basic grammar of the profession and discipline) and those of the flexible area (the student chooses them according to personal interests, allow to the learner to approach, contextualize and study in depth aspects of the profession and discipline, allowing to learn tools and other kinds of knowledge, leading to develop interdisciplinarity, flexibility and diversity).
The information provided makes it possible to indicate RACT as a subject: Workshop of Critical Thinking and Introduction to CT ; second, as a subject content: CT in Nursing, and, third, RACT is evidenced in teaching-learning strategies.
The highest percentage of subjects in which RACT is evident correspond to the area of humanities, with 46% (55), in which analysis of real situations, group work, concept maps, role playing and seminars are predominant.
In second place, it is in the professional-disciplinary area with 42% (307) subjects with the predominance of the following strategies: supervised clinical practice, clinical case, problem-based learning, simulation laboratories, and the nursing process. The research is in the same place, 42% (41) subjects. The most commonly used strategies are: critical discussions of research reports and articles, project development, workshops, and problem-based learning.
In the last place, subjects from the basic or foundation area 144 (24%). Including discussion workshops, concept maps and case studies.
A great variety of strategies have been identified, among them are: presentation and discussion of clinical case, group work, clinical practice, flipchart, observation guides, debates, discussion about specific topics, resolution of case studies, support of the nursing care plan, investigative reports , workshop development.
What is evaluated: the development of competencies, the acquisition of skills, the development of superior cognitive processes, the professional spirit and the development of processes and independence.
Finally, in some of the subjects, the intentionality of the evaluation of the RACT is explicitly presented: written works about the topics of each seminar in which the proper handling of the bibliography is evidenced, the capacity for criticism, analysis and synthesis, evidence of problem solving, case analysis and Nursing Based in Evidences , didactic relationship analysis and fundamental elements of the RACT, conceptual knowledge, written and oral reflections, group work, practical reflections and group discussions.
It is evident that traditional evaluation techniques still exist: evaluating procedural aspects, dexterity, motivation and initiative in the procedures, memory evaluation, participation in class, oral and written interventions and, finally, the replication of the topics studied in classes.
Therefore, the analyzed programs show interest in including as an important element in their future graduates the development of the RACT. This aspect is vanishing in the development of the subjects. It is evident in the pedagogical strategies, but it is lost until disappearing in most of the evaluative processes.
The analysis results of the plans and programs of the HEI and HEIN allow to conclude that the proposes of the Law of Higher Education to develop the RACT in the students does not guarantee that it is included in the subjects and evaluations.
What is stated in HEI and HEIN allows us to infer that epistemological and theoretical contradictions are present in the Institutions and among them. It makes necessary an epistemological, theoretical and methodological consideration in order to achieve alignment and coherence between the purposes in the curricular guidelines and what is programmed in the curricular plans for the concrete work with the students. This matter goes against comprehensive training, since it is demonstrated that critical and reflective skills contribute to train professionals with greater ability to care for patients ( 23 ) .
It should be noted that it is the University or HEI that determines the philosophical bases that will guide the academic units that compose it, so that they, in turn, incorporate these principles into their academic programs. The results show that there is no linearity between the proposals of the university with respect to its mission, vision, objectives, graduation profile, curricular guidelines, and what is proposed in the nursing degree programs. There is more linearity in Institutions with a longer trajectory and development, private and public ones.
The analysis of the areas in which the subjects are grouped made it possible to identify that the subjects of the humanities area have the highest percentage of presence of the RACT. This result can be explained by the strategies used, but even more by the subjects under study, since it has been demonstrated that the teaching-learning strategies based on the humanities have a significant impact on the development of skills such as clinical reasoning ( 24 ) . The subjects in the professional area use strategies such as case study, supervised clinical practice and other relatively new ones as problem-based learning and simulation laboratories. Strategies that, by involving simulation or potential practical actions, contribute to enhance critical skills and make decisions that lead to the future professional committing fewer errors during the care of patients ( 25 - 26 ) .
By contrast, it is not the same with the subjects of the foundation or basic area in which it is necessary to return to some knowledge aspects that already exists, such as anatomy, physiology, anthropology, psychology, statistics, among many others. For some students these topics are very difficult and involve, on several occasions, an excellent dose of memory. However, the teaching strategies that develop the RACT are not so frequent. It is important doing more research on this point to sustain if it is true.
On the other hand, for the majority of HEIN, training is conceived as qualification and progress achieved by people and as a principle of theories, concepts, methods, models, strategies and courses of pedagogical action that aim to understand and qualify the teaching. In some cases, the transfer of knowledge is approached, but it still underlies the concept of learning as acquisition of knowledge built and finished; the teacher is the one who has the knowledge and the student is who learns what teacher knows.
The curricula of the Andean region include explicit elements that contribute to the development of the RACT, such as reading, writing and reasoning, allowing to the future professional to know how to learn, reason, think creatively, generate and evaluate ideas, make decisions and solve problems ( 24 ) . It includes as proposals the development of social skills, with emphasis on oral and written communication, cognitive skills including problem solving, establish different alternatives, understand the consequences of actions, make decisions and critical thinking ( 16 ) . Also, intend to achieve in the student some characteristics of the critical thinker like to be creative, innovative, proactive, analytical, participatory, entrepreneurial, self-critical, supportive, humanistic, ethical and scientific ( 27 ) .
Regarding the pedagogical models proposed by the HEIN, inconsistencies between the approach of constructivist approach and meaningful learning are evident. The axis is the student and the repetitive approach in the subjects with master class methodology, reading guides and analysis made by teacher, but not by the student. It shows a traditional model centered on the teacher, with an emphasis on memory, comprehension and the application of concepts. Some subjects focus learning on the acquisition of concepts, despite using the integrating project as a teaching-learning strategy, workshops and practice as evaluation. The pretense for the development of the RACT is not in line with the evaluation, with the examination, in the application of contents, since it is centralized in aspects of memory and knowledge, in an asymmetric theory-practice relationship.
Although significant learning is intended and the importance of integrating it into the formation of learning approaches with the intention of promoting critical thinking, added with successful learning experiences ( 28 ) , it is not really concrete how it could be achieved. Strategies such as simple repetition and teaching for the acquisition of concepts show the persistence of the traditional educational models.
This study found there is no a clear structure to operationalize the theories of the proposed pedagogical models, even though there are expressions that point to RACT. Thus, the elements important for its development are presented in the teaching and learning strategies in a more remarkable way.
The curricular guidelines express the intention to transcend technical rationality and behavioral objectives ( 29 ) , from the positivist, rationalist or empirical analyst paradigm, to the humanist and critical curriculum ( 30 ) to the socio-critical paradigm and critical thinking based on hermeneutic processes ( 31 ) . The social and contextual (political, economic and cultural) aspects that influence and determine the health behaviors of the people are still incipient in the curricula ( 32 ) .
According to what has been demonstrated, it is possible to state that there is no predominance of a pedagogical model, but a mixture of several models in the same program with varied influences. The presence of the following models was identified: Traditional Pedagogical, Behavioral, Cognitive, and Social Pedagogical, the latter being very tenuous ( 33 ) .
There are four fundamental elements to forming critical thinkers: first, the question; second, the creation of continuous opportunities to participate in dialogue, debate, research, and critique; third, self-evaluation and hetero-evaluation; and fourth, teachers as models of critical thinkers ( 32 ) . Considering these elements, we can assure that the creation of opportunities is present with more intensity in some curricula, and self-evaluation and hetero-evaluation have begun to be implemented especially in public institutions.
Mentioning the subjects, it is not evident that the thought is motivated by complex kind of questions that encourage exploration, generate evaluation, create concepts and knowledge ( 33 ) .
The literature points out that the Socratic questions stimulate the student to use existing knowledge, since they promote a greater understanding and integration of new knowledge, they foment the habit of thinking critically ( 8 , 34 ) . Other authors suggest, for the reports, questions about the purpose, information, concepts, assumptions, implications, points of view and the questions, as elements that favor analysis, the evaluation of ideas and reasoning ( 24 , 35 ) .
Like other researches, this study found that the most used strategies in the progress of the professional area that promote the development of RACT are the case study ( 24 , 36 ) , problem-based learning ( 24 ) , supervised clinical practice ( 37 ) , the nursing process ( 4 , 38 ) and simulation laboratories ( 34 , 37 - 38 ) . In this article, we only refer to two of these strategies, which were selected because of the great advance of information and communications technologies. The growing need to access this kind of infrastructure as a fundamental part in the training of future professionals and as an example of a single teaching and learning strategy is not sufficient to achieve the RACT, rather, the use of different techniques enhance its development, as we will see below.
We agree with the conclusion of authors who suggest that Problem-Based Learning and simulation labs are active strategies that develop RACT in nursing students ( 37 ) .
The case study, moreover, promotes active learning, helps to solve clinical problems, promotes the development of critical thinking skills ( 34 - 35 ) , in addition, it allows to integrate knowledge, to think as a professional, to analyze individual situations in specific contexts from different angles, to use theoretical concepts in the delimitation of a concrete problem ( 36 ) . It also stimulates collaborative and team work, the work with different points of view. The question-problem is the motivator in the search for alternative solutions, is useful in simple and complex situations, allows to apply theory in practice, promotes the exchange of ideas, teaches students to learn to control their own thinking and promote the exchange of ideas and intellect ( 37 ) . In addition, it helps to incorporate time management and take responsibility. It also facilitates the integration of the four elements of the Nursing metaparadigm: the person receiving the care, health as purpose, the nature of the nursing and the context or environment.
The case study allows the simultaneous implementation of other strategies that further enhance the development of RACT, such as concept maps, the analysis and selection of scientific evidence, the nursing process, nursing history, role-playing, argued discussion and debate.
In contradiction to all the positive aspects of the case study in the development of RACT, the dichotomy between theory and practice in a large number of the curricula reviewed is an obstacle to achieving all the benefits pointed out. Since some teachers are in charge of the development of the theoretical subject in the classroom, others are in charge of their practical part in other spaces that require this care.
Regarding the practice based on simulation models, a study ( 38 ) shows how the promotion of RACT is relevant. In this connection, it highlights the importance of including simulation as a key element in curricula, because it ensures skills in this kind of thinking ( 38 ) and gives students the opportunity to show their ability in decision-making, critical thinking and other skills ( 39 ) . Other authors emphasize its importance when students reflect it on their thinking process and show how it guided their actions ( 34 ) .
There is efficiency of simulation laboratories when accompanied by active strategies, such as the conceptual map before each laboratory session, a visual aid that allows the concepts, objectives, justification, expected results and possible complications to be described in a logical manner if the procedure is not carried out in the appropriate manner ( 34 ) . The same author suggests the use of high-level questions to stimulate reason more than memory. He also suggests assigning an observer, who will ensure analysis and reflection on patient safety, communication, teamwork and leadership, among others ( 34 ) . The reflection of the group around the whole process carried out will be the end of the laboratory ( 15 , 34 ) .
Another study concluded that simulation as a pedagogical method allows students to recognize, interpret and integrate new information with previous knowledge in order to make decisions about the best direction to follow. The authors state that simulation, as an educational method, provides an opportunity to systematically structure learning to help students acquire deep content knowledge and to facilitate the development of thought processes; that simulation experiences stimulate students’ RACT skills and help them become more competent in caring for patients in complex conditions ( 37 ) .
We agree with what has been found in other studies emphasizing that simulation laboratories by themselves do not guarantee the development of RACT skills, but if combined with other strategies and implemented with adequate pedagogy, the results will be much more effective in terms of CT skills ( 34 , 37 - 38 ) .
It is also possible to find correspondence with that was discovered in the State of the Art of scientific production in RACT in the Andean region. The students perceive that “Clinical simulation is a valuable strategy for the acquisition, complementation and integration of the theoretical part with the practical part, because it seeks to make decisions according to the CT” ( 38 ) .
The evaluation of the subjects is cumulative and formative. In some cases, a diagnosis of the level of the student’s participation in the subject is made; it is evaluated in the intermediate and at the end with the objective of promotion to another level. In other cases, a teaching-learning balance is done to verify the fulfillment of the objectives and competences. Self-evaluation and heteroevaluation are increasingly used, implying a process of reflection, analysis and self-criticism.
Precisely, evaluation appears as one of the weakest points when analyzing the presence of RACT in curricula. Therefore, we agree that the “best teaching practice begins by establishing learning outcomes and continues with a focus on helping the student to achieve satisfactory results”. If the proposal is to achieve a higher order thinking, the evaluation will be oriented towards the synthesis, analysis and evaluation of knowledge ( 40 ) .
Overall, the strong approaches to RACT training formulated at HEI, HEIN, as evidenced by some of the teaching and learning strategies presented in the subjects, become much weaker in the evaluation process, with predominance of traditional evaluation models, and in some cases, the intention to evaluate RACT is outlined.
The curricula of Colleges and Schools of Nursing in the Andean region explicitly contemplate reflective and critical thinking in their mission, vision, objectives, graduation profile and didactic strategies, and implicitly as integral formation. However, there is a tension between what is proposed by the HEI and HEIN and what is implemented and evaluated in the subjects. The presence of RACT in the proposed didactic strategies is much more evident, but it is not sufficiently objective or explicit in the evaluation processes.
Despite the great diversity of pedagogical models, there is a clear intention to facilitate the development of RACT. In addition, although a constructivist model is proposed centered on the student, dialogical, active, reflexive, innovative and critical, this model is more centered on the teacher than on the student; on knowledge over a relationship between equals; more on results than on the learning process. Likewise, knowledge is considered as something finished, fixed and the ultimate truth.
In order to be able to teach the RACT to the nursing student it is necessary to include it in the nursing curriculum, teachers who are professionals in the areas of Education and Nursing and with RACT in their training. Teachers should create spaces for the development of RACT, know and implement the different and complementary didactic strategies that facilitate its learning and that analyze the students in relation to the level of RACT achieved.
The authors of this article suggest that the projects currently developed with teachers and students in Ibero-America should be finalized and retaken with the implementation and evaluation of strategies that value the development of RACT.
RACT is considered an indispensable element in personal and professional development, in order to have autonomy, confidence, the ability to make decisions, reach clinical judgment and, the most important, provide individualized, comprehensive and human nursing care. In summary, graduates should be able to work as members of the health team with sufficient clarity of the role and identity they should have, because they have to integrate and experience the four paradigms of the Nursing.
The limitations of the study are
The complexity of the project due to the number of participating countries and the different research groups;
The large number of public and private nursing schools and colleges in the Andean region;
The limitation in accessibility to the complete information of the curricula of each institution;
The minimal presence of information on the official web pages of each institution, school or nursing college;
No response and lack of interest from different schools and nursing colleges, public and private, to participate of this project;
Limited access of current and recent updates of the curricula of nursing colleges to develop this project.
The research group made efforts to reduce these limitations and devised multiple options that were proposed to the institutions, in order to facilitate the provision of information and its complementation when necessary.
Applications for practice
The innovation and contributions expected with this research are based fundamentally on documenting and analyzing of the diverse existing evidences about if RACT is contemplated in the nursing curricula or not, the strategies used by teachers to create and promote it in nursing students and the evaluation processes employed. It provides insights about how RACT’s competence in nursing is addressed in the context of the Andean region and other regions of Ibero-America, its weaknesses and strengths, as well as the improvements that can be made. The final intention of the research is to offer, as a network and collegial body, proposals for teaching, learning and evaluation that will enable the empowerment of new generations of nurses, using RACT as a center of innovation and development.
Clinical decision-making processes among graduate nurses, specialist nurses and nurse practitioners A collaborative international study
Affiliations.
- 1 University of South-Eastern Norway, Kongsberg, Norway.
- 2 Novia University of Applied Sciences, Vaasa, Finland.
- 3 Åland University of Applied Sciences, Mariehamn, Finland.
- 4 Dublin City University, School of Nursing, Psychotherapy & Community Health, Dublin, Ireland.
- 5 Åbo Akademi University, Vaasa, Finland.
- 6 University College Cork, School of Nursing and Midwifery, Cork, Ireland.
- PMID: 38450783
- DOI: 10.1111/inr.12951
Aim: To explore clinical decision-making by comparing the processes used by three groups of nurses in the emergency departments of three hospitals: in Norway, Finland and Ireland.
Background: Clinical decision-making in an emergency department environment is a complex process often occurring in times of crisis. It is an important aspect contributing to the quality of care. However, empirical research is limited regarding the decision-making process in different nursing roles.
Methods: In accordance with the consolidated criteria for reporting qualitative research, a qualitative and observational study was conducted to explore clinical decision-making by comparing the processes used by three groups of nurses in the emergency departments of three hospitals: in Norway, Finland and Ireland. Six Registered Nurses, six Nurse Specialists and six Nurse Practitioners were observed. A total of 40 hours of observation was made at each setting according to a structured observation guideline, followed by clarifying questions. The data material was analysed by means of a qualitative manifest and latent content analysis.
Results: Three themes arose: acting in accordance with routines, previous experience and intuition; considering patient experience; and facilitating new alternatives based on critical thinking. The Registered Nurses mainly used the first approach, the Nurse Specialists used the first and the second approaches, and the Nurse Practitioners used all three approaches.
Conclusions: The results highlight the differences in decision-making processes between these groups. Nurse Practitioners were the only group that facilitated and evaluated new alternatives using their clinical autonomy, such as stepping up and making independent and collaborative decision-making.
Implication: The results can be used in countries developing advanced practice nursing education and defining their scope of practice to inform stakeholders.
Keywords: Clinical decision-making; content analysis; nurse practitioner; nurse specialist; observational study; registered nurse.
© 2024 The Authors. International Nursing Review published by John Wiley & Sons Ltd on behalf of International Council of Nurses.
Grants and funding
- Norwegian Research Council
Critical thinking definition

Critical thinking, as described by Oxford Languages, is the objective analysis and evaluation of an issue in order to form a judgement.
Active and skillful approach, evaluation, assessment, synthesis, and/or evaluation of information obtained from, or made by, observation, knowledge, reflection, acumen or conversation, as a guide to belief and action, requires the critical thinking process, which is why it's often used in education and academics.
Some even may view it as a backbone of modern thought.
However, it's a skill, and skills must be trained and encouraged to be used at its full potential.
People turn up to various approaches in improving their critical thinking, like:
- Developing technical and problem-solving skills
- Engaging in more active listening
- Actively questioning their assumptions and beliefs
- Seeking out more diversity of thought
- Opening up their curiosity in an intellectual way etc.
Is critical thinking useful in writing?
Critical thinking can help in planning your paper and making it more concise, but it's not obvious at first. We carefully pinpointed some the questions you should ask yourself when boosting critical thinking in writing:
- What information should be included?
- Which information resources should the author look to?
- What degree of technical knowledge should the report assume its audience has?
- What is the most effective way to show information?
- How should the report be organized?
- How should it be designed?
- What tone and level of language difficulty should the document have?
Usage of critical thinking comes down not only to the outline of your paper, it also begs the question: How can we use critical thinking solving problems in our writing's topic?
Let's say, you have a Powerpoint on how critical thinking can reduce poverty in the United States. You'll primarily have to define critical thinking for the viewers, as well as use a lot of critical thinking questions and synonyms to get them to be familiar with your methods and start the thinking process behind it.
Are there any services that can help me use more critical thinking?
We understand that it's difficult to learn how to use critical thinking more effectively in just one article, but our service is here to help.
We are a team specializing in writing essays and other assignments for college students and all other types of customers who need a helping hand in its making. We cover a great range of topics, offer perfect quality work, always deliver on time and aim to leave our customers completely satisfied with what they ordered.
The ordering process is fully online, and it goes as follows:
- Select the topic and the deadline of your essay.
- Provide us with any details, requirements, statements that should be emphasized or particular parts of the essay writing process you struggle with.
- Leave the email address, where your completed order will be sent to.
- Select your prefered payment type, sit back and relax!
With lots of experience on the market, professionally degreed essay writers , online 24/7 customer support and incredibly low prices, you won't find a service offering a better deal than ours.

IMAGES
VIDEO
COMMENTS
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills. ... Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize ...
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
In 1958, Ida Jean Orlando started the nursing process that still guides nursing care today. Defined as a systematic approach to care using the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EDP) recommendations, and nursing intuition. Holistic and scientific postulates are integrated to provide the basis for ...
Critical thinking in nursing is the process of applying skills to solve problems related to patient care. It is essential for efficient, safe, and skillful nursing care. Learn what critical thinking is, why it is important, how to improve it, and see 18 examples of poor and excellent critical thinking in nursing.
Critical thinking is a process where nurses use logic and evidence to gather information and make decisions. It is vital for excellent patient outcomes and safety. Learn how nurses use critical thinking skills, improve them, and avoid common mistakes.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
The nursing process is a systematic, rational, and continuous method of planning, providing, and evaluating individualized nursing care. This chapter introduces the basic concepts of the nursing process, such as assessment, diagnosis, planning, implementation, and evaluation. It also explains the relationship between the nursing process and critical thinking, clinical reasoning, and clinical ...
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Therefore, critical thinking in nursing is the process of making clinical decisions through thinking by using knowledge, experience, evidence, and intuition to define patient problems and choose among alternatives. It involves inquiry, collection, analysis, synthesis, and interpretation of data, reasoning inductively and deductively, using ...
Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student ...
Critical Thinking in Nursing. Critical thinking in nursing profession has been defined as "the process of reflective and reasonable thinking about nursing problems without a single solution and is focused on deciding what to believe and do" (Yildrim and Ozkahraman, 2011, p.257). From: Nurse Education Today, 2018.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed. It's a dynamic process that enhances clinical reasoning, problem-solving, and overall patient outcomes.
Excerpt. In 1958, Ida Jean Orlando started the nursing process that still guides nursing care today. Defined as a systematic approach to care using the fundamental principles of critical thinking, client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EDP) recommendations, and nursing intuition.
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
Critical Thinking. Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years. There are several key definitions for critical thinking to consider. ... The process of critical thinking is stimulated by integrating the essential ...
The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes. Nursing Process Steps. The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation.
Critical thinking is a multidimensional skill, a cognitive or mental process or set of procedures. It involves reasoning and purposeful, systematic, reflective, rational, outcome-directed thinking based on a body of knowledge, as well as examination and analysis of all available information and ideas. Critical thinking leads to the formulation ...
The nursing process is a critical thinking model based on a systematic approach to patient-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing patient care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses ...
For courses in Success in Nursing, Critical Thinking, Fundamentals of Nursing, and Nursing Concepts. This innovative text uses concrete examples and hands-on exercises to help students clearly understand and apply the steps of the nursing process to today's rapidly changing healthcare environment. Moving beyond step-by-step instructions, the book encourages students to think about each part of ...
The National League for Nursing Accreditation Commission (NLNAC) defines critical thinking in nursing this way: "the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief-based. This is demonstrated in nursing by clinical ...
Nurses do this activity every shift. They know how to find pertinent information and use the nursing process as a critical thinking model to guide patient care. The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients' well-being and health.
Critical thinking (CT) is a process and a learning outcome (3-4) and the clinical judgment is the result of this process. The development of the clinical judgment (clinical reasoning skills) is one of the most important and challenging tasks of being a nurse. ... To identify levels of critical thinking in nursing students according to the ...
However, empirical research is limited regarding the decision-making process in different nursing roles. ... and facilitating new alternatives based on critical thinking. The Registered Nurses mainly used the first approach, the Nurse Specialists used the first and the second approaches, and the Nurse Practitioners used all three approaches. ...
AORN Journal is a perioperative nursing journal providing evidence-based practice information to help meet the physiological, behavioral, and safety needs of patients. It is time to move from the nursing process to critical thinking - Koch - 1997 - AORN Journal - Wiley Online Library
Critical thinking, as described by Oxford Languages, is the objective analysis and evaluation of an issue in order to form a judgement. Active and skillful approach, evaluation, assessment, synthesis, and/or evaluation of information obtained from, or made by, observation, knowledge, reflection, acumen or conversation, as a guide to belief and action, requires the critical thinking process ...