Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article

Presentation
The condition, lessons for the clinician, poster presentations:, section editor’s note, suggested readings, case 5: a 13-year-old boy with abdominal pain and diarrhea.
AUTHOR DISCLOSURE
Drs Sudhanthar, Okeafor, and Garg have disclosed no financial relationships relevant to this article. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Anjali Garg , Sathyan Sudhanthar , Chioma Okeafor; Case 5: A 13-year-old Boy with Abdominal Pain and Diarrhea. Pediatr Rev December 2017; 38 (12): 572. https://doi.org/10.1542/pir.2016-0223
Download citation file:
- Ris (Zotero)
- Reference Manager
A 13-year-old boy presents to his primary care provider with a 5-day history of abdominal pain and a 2-day history of diarrhea and vomiting. He describes the quality of the abdominal pain as sharp, originating in the epigastric region and radiating to his back, and exacerbated by movement. Additionally, he has had several episodes of nonbloody, nonbilious vomiting and watery diarrhea. His mother discloses that several family members at the time also have episodes of vomiting and diarrhea.
He admits to decreased oral intake throughout the duration of his symptoms. He denies any episodes of fever, weight loss, fatigue, night sweats, or chills. He also denies any hematochezia or hematemesis. His medical history is significant for a ventricular septal defect that was repaired at a young age, but otherwise no other remarkable history.
During the physical examination, the adolescent is afebrile and assessed to be well hydrated. Examination of the abdomen reveals tenderness in the epigastric region and the right lower quadrant on light to deep palpation, with radiation to his back on palpation. There are no visible marks or lesions on his abdomen. Physical examination is negative for rebound tenderness, rovsing sign, or psoas sign. The remainder of the examination findings are negative.
Complete blood cell count, liver enzyme levels, pancreatic enzyme levels, and urinalysis results are all within normal limits.
Our patient was asked to observe his hydration status and pain at home and to report any changes. However, he arrived at the emergency department the next day due to increased severity of abdominal pain. The pain had localized into the right lower quadrant. Further imaging revealed the diagnosis.
The differential diagnosis for an adolescent who presents with abdominal pain is broad, including gastrointestinal causes such as gastroenteritis, appendicitis, or constipation and renal causes such as nephrolithiasis or urinary tract infections. With our patient, the more plausible answers were ruled out through laboratory studies and physical examination, and he was assumed to have gastroenteritis based on the history of similar symptoms in his family members. However, with the worsening of his abdominal pain, further diagnostic study became imperative and a computed tomographic (CT) scan of the abdomen was obtained to assess for appendicitis or nephrolithiasis.
The CT scan showed a cecum located midline; the large intestine was on the left side of the abdomen, and the small intestine was on the right ( Figs 1 and 2 ). The appendix was buried deep in the right pelvis, and there was no indication of appendicitis. These findings were consistent with intestinal malrotation. Intestinal malrotation is rare beyond the first year of life. Maintaining a higher index of suspicion in any patient with an acute presentation of severe abdominal pain is imperative because of the severity of potential complications such as bowel obstruction, volvulus, and eventual necrosis. Our patient’s pain is assumed to have been due to compressive effects of the peritoneal bands (Ladd bands), which were irritated by an initial gastroenteritis. He did not have the signs or symptoms of a more severe complication, such as bowel obstruction or volvulus.

Computed tomographic scan of the abdomen showing intestinal malrotation, specifically of the subtype nonrotation. The small bowel is present in the right hemi-abdomen and the large bowel in the left hemi-abdomen. The cecum is midline in the pelvis. Haustra are still present, excluding any sign of obstruction.

Swirling appearance of the mesentery is known as the whirl sign, which is also indicative of malrotation. This computed tomographic scan shows the superior mesenteric vein wrapped around the superior mesenteric artery.
Owing to the severity of the pain, our patient was taken for surgery, specifically, a Ladd procedure and a prophylactic appendectomy. Ladd bands were seen to extend from the cecum to above the duodenum. During the procedure, these bands were lysed, then the mesentery was spread out, and the bowels were rearranged. He tolerated the surgery well and was discharged 3 days after the operation.
His abdominal pain improved after surgery, and he has been doing well at his postoperative checks.
Intestinal malrotation is when the intestines fail to rotate properly in utero. From the fifth to 10th weeks of embryologic development, the small intestine lies in the right aspect of the abdomen, with the ileocecal junction midline, and the large intestine in the left hemi-abdomen. The segments are then pushed out of the abdomen into the umbilical cord. Both segments grow in the first stage of rotation. During the second stage of rotation, the small intestine rotates counterclockwise 270 degrees around the superior mesenteric artery. The remaining intestine is pulled into the abdomen, and the mesentery is fixed to the retroperitoneal space. The large intestine comes in last, with the final segment of the cecum lying anterior to the small intestine in the right lower quadrant.
Nonrotation is the most frequent cause of intestinal malrotation. Nonrotation occurs when the 270-degree rotation does not occur and, thus, the mesentery is not fixed to the retroperitoneal space. Derangements of the second stage of rotation are defined as having the small intestine in the right hemi-abdomen, with the cecum midline in the pelvis, and the large intestine in the left hemi-abdomen.
One percent of the population has intestinal rotation disorders. The incidence decreases with age. Approximately 90% of patients are diagnosed within the first year of their life, with 80% among them within the first month after birth. Due to a delay in diagnosis, the 10% of patients who present beyond that first year after birth can have severe complications.
Symptoms of malrotation are different in infants compared with adolescents. Neonates typically will have bilious emesis. In contrast, children and adults commonly exhibit acute abdominal pain. Some older patients have had chronic abdominal pain that goes unnoticed; others may be asymptomatic before diagnosis. The co-occurrence of intestinal malrotation with congenital cardiac anomalies is a common finding. Twenty-seven percent of intestinal malrotation patients were found to have a concurrent cardiovascular defect such as ventricular septal defect or another minor/major abnormality.
The diagnostic modality of choice is an upper gastrointestinal tract contrast study. This study modality shows any obstruction and depicts the malrotation through contrast media. Sometimes a contrast medium is not needed for diagnosis, as in the case of our patient, where CT scanning was enough to diagnose the malrotation.
Asymptomatic neonates and all symptomatic individuals, regardless of age, go through the Ladd procedure to correct the abnormality. However, the guidelines are not as clear for treatment of children older than 1 year who are asymptomatic. Currently, there is some consensus for performance of the procedure regardless of symptom status because of the severity of the complications or mortality that can occur due to malrotation. The narrow pedicle of the mesentery that forms in malrotation is prone to volvulus and ischemia, leading to complications at any point in an individual’s life. A diagnostic laparoscopy should be performed at the very least and can be therapeutic as well. Removal of the appendix has been suggested to prevent any diagnostic complications on future presentation. Additionally, the Ladd procedure can lyse Ladd bands, which are abnormal fibrous adhesions from the cecum that also arch over the duodenum. Removal of these bands is imperative because they can cause intestinal obstruction and ischemia as well.
Diagnosis of intestinal malrotation should be considered in a patient presenting acutely with severe abdominal pain, especially in a patient with known cardiac anomalies.
Often the symptoms of intestinal malrotation can be vague, and a patient can be asymptomatic for years before presentation.
The diagnostic modality of choice is an upper gastrointestinal tract series, but other imaging, such as computed tomographic scan, can help diagnose the presence of malrotation in emergency situations.
A Ladd procedure should be conducted on a patient even if he/she does not have current symptoms of obstruction due to increased risk of obstruction or complications such as volvulus and gut necrosis with this disease.
This case is based on a presentation by Ms Anjali Garg and Drs Sathyan Sudhanthar and Chioma Okeafor at the 39th Annual Michigan Family Medicine Research Day Conference in Howell, MI, May 26, 2016.
Poster Session: Student and Resident Case Report Poster Presentation
Poster Number: 23
This case is based on a presentation by Ms Anjali Garg and Drs Sathyan Sudhanthar and Chioma Okeafor at the 2016 AAP National Conference and Exhibition in San Francisco, CA, October 22-25, 2016.
Poster Session: Section on Pediatric Trainees Clinical Case Competition
Abdominal Pain in Children: https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Abdominal-Pain-in-Children.aspx
Diarrhea: https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Diarrhea.aspx
For a comprehensive library of AAP parent handouts, please go to the Pediatric Patient Education site at http://patiented.aap.org .
This case was selected for publication from the finalists in the 2016 Clinical Case Presentation program for the Section on Pediatric Trainees of the American Academy of Pediatrics (AAP). Ms Anjali Garg, BS, was a medical student from Michigan State University College of Human Medicine, East Lansing, MI, when she wrote this case report, and she now is a medical resident at Rainbow Babies and Children's Hospital in Cleveland, OH. Choosing which case to publish involved consideration of not only the teaching value and excellence of writing but also the content needs of the journal. Other cases have been chosen from the finalists presented at the 2017 AAP National Conference and Exhibition and will be published in 2018.
Competing Interests
Advertising Disclaimer »
Citing articles via
Email alerts.
Affiliations
- Editorial Board
- ABP Content Spec Map
- Pediatrics On Call
- Online ISSN 1526-3347
- Print ISSN 0191-9601
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
DIARRHEA IN CHILDREN
Sep 04, 2014
4.61k likes | 17.92k Views
DIARRHEA IN CHILDREN. Maria Naval C. Rivas Department of Pediatrics The Medical City. SOURCES. Nelson’s Textbook of Pediatrics 18 th edition World Health Organization: A Manual for Physicians and Other Senior Health Workers, 2005. DEFINITION.
Share Presentation
- watery diarrhea
- acute diarrhea
- dry mucous membranes
- acute diarrhea 2 weeks

Presentation Transcript
DIARRHEA IN CHILDREN Maria Naval C. Rivas Department of Pediatrics The Medical City
SOURCES • Nelson’s Textbook of Pediatrics 18th edition • World Health Organization: A Manual for Physicians and Other Senior Health Workers, 2005
DEFINITION • passage of unusually loose or watery stools • at least 3 times in a 24 hour period • Acute diarrhea: < 2 weeks • Chronic diarrhea: > 2 weeks
EPIDEMIOLOGY • 2nd leading cause of morbidity • 1,135 cases per 100,000 population • 6th leading cause of mortality • 5.3 deaths per 100,000 population • 1000M episodes of diarrhea/year in children <5y • 5M deaths in <5y • 80% deaths in 1st 2y of life (1/3 of all deaths) Sources: Carlos M.D., C. & Saniel M.D., M. Etiology and Epidemiology of Diarrhea. Research Institute for Tropical Medicine : Philippine Health Statistics, 2000
APPROACH TO A CHILD WITH ACUTE DIARRHEA Main Objectives 1. assess degree of dehydration and provide fluid and electrolyte replacement 2. prevent spread of enteropathogen 3. in select episodes, determine etiologic agent and provide specific therapy if indicated
APPROACH TO A CHILD WITH ACUTE DIARRHEA Pertinent Data oral intake frequency of stools volume of stools presence of blood or mucus in stool general appearance & activity of child frequency of urination
APPROACH TO A CHILD WITH ACUTE DIARRHEA others: day care attendance recent travel to a diarrhea endemic area use of antibiotics exposure to contacts with similar symptoms intake of seafood, uncooked meat, unpasteurized milk, unwashed vegetables, contaminated water systemic sx: fever, vomiting, seizure
APPROACH TO A CHILD WITH ACUTE DIARRHEA Degree of Dehydration MILD DEHYDRATION (3-5%) - normal or increased pulse, decreased urine output, thirsty, normal physical examination MODERATE DEHYDRATION (7-10%) - tachycardia, little or no urine output, irritable/ lethargic, dry mucous membranes, mild tenting of skin, delayed capillary refill, cool and pale
APPROACH TO A CHILD WITH ACUTE DIARRHEA Degree of Dehydration SEVERE DEHYDRATION (10-15%) - rapid and weak pulse, decreased blood pressure, no urine output, very sunken eyes and fontanel, no tears, dry mucous membranes tenting of the skin, very delayed capillary refill, cold and mottled
ASSESSMENT OF DIARRHEA PATIENTS FOR DEHYDRATION
APPROACH TO A CHILD WITH ACUTE DIARRHEA Treatment Plan A - home therapy to prevent dehydration and malnutrition • Give the child more fluids than usual • ORS solution • salted drinks (e.g. salted water, salted yoghurt drink) • vegetable or chicken soup with salt • Give supplemental zinc (10-20mg) for 10-14 days • Continue to feed the child
APPROACH TO A CHILD WITH ACUTE DIARRHEA • Take child back to health worker if there are signs of dehydration or other problems • starts to pass many stools • repeated vomiting • becomes very thirsty • eating or drinking poorly • develops a fever • has blood in the stool • child does not get better in 3 days
APPROACH TO A CHILD WITH ACUTE DIARRHEA Treatment Plan B • oral rehydration therapy with ORS in a health facility • monitoring progress of oral rehydration • supplemental zinc (10-20mg) for 10-14 days • food should not be given during initial 4-hour rehydration period • breastmilk may be given continuously
Treatment Plan B: Approximate amount of ORS to give in the initial 4 hours
APPROACH TO A CHILD WITH ACUTE DIARRHEA Reduced osmalarity ORS mmol/liter Sodium 75 Chloride 65 Glucose 75 Potassium 20 Citrate 10 TOTAL OSMOLARITY 245
APPROACH TO A CHILD WITH ACUTE DIARRHEA Treatment Plan C • rapid intravenous rehydration • may give oral ORS if child can already drink - usually after 1-4 hours • monitoring progress of IV hydration • if IV therapy not available, give ORS by NGT at 20cc/kg/hr x 6 hrs. • manage electrolyte disturbance
IV Treatment of Children & Adults with Severe Dehydration
IV Treatment of Children & Adults with Severe Dehydration 1. Restore intravascular volume • normal saline: 20ml/kg over 20 mins • repeat until intravascular volume is restored 2. Calculate 24-hr water needs • calculate maintenance water • 0-10kg 100ml/kg • 11-20kg 1000ml + 50ml/kg for each kg > 10kg • > 20kg 1500ml + 20ml/kg for each kg > 20kg • calculate deficit water • Percent dehydration x weight
IV Treatment of Children & Adults with Severe Dehydration 3. Calculate 24-hour electrolyte needs • calculate maintenance sodium and potassium • calculate deficit sodium and potassium • Na deficit = water deficit x 80 mEq/L • K deficit = water deficit x 30 mEq/L 4. Select an appropriate fluid • nornal saline or Ringer lactate 5. Replace any ongoing losses as they occur
APPROACH TO A CHILD WITH ACUTE DIARRHEA Electrolyte Disturbances • Hypernatremic Dehydration (serum Na > 150 mmol/L) - due to drinks with excessive sugar or salt - e.g. soft drinks, commercial fruit drinks, concentrated infant formula - s/sx: extreme thirst convulsions
APPROACH TO A CHILD WITH ACUTE DIARRHEA Electrolyte Disturbances • Hyponatremic Dehydration (serum Na < 130 mmol/L) - due to drinking mostly water or drinks with little salt - common in Shigellosis and in severe malnutrition with edema - s/sx: lethargy
APPROACH TO A CHILD WITH ACUTE DIARRHEA Electrolyte Disturbances • Hypokalemia (serum K+ < 3 mmol/L) - s/sx: muscle weakness, paralytic ileus, cardiac arrhythmia, impaired kidney function
CLINICAL TYPES OF DIARRHEA • Acute Watery Diarrhea • Acute Bloody Diarrhea • Persistent Diarrhea
ACUTE WATERY DIARRHEA Viruses Rotavirus Astrovirus Adenovirus Calcivirus ( e.g. Norwalk agent )
ACUTE WATERY DIARRHEA Pathogenesis - destroy villus tip cells in the SI • imbalance in ratio of intestinal absorption and secretion • malabsorption of complex carbohydrates, sp. lactose - gastric mucosa is not affected - greatly enhances intestinal permeability to macromolecules increase risk of food allergies
ACUTE WATERY DIARRHEA Pathogenesis - increased vulnerability of infants • decreased intestinal reserve function • lack of specific immunity • decreased non-specific host defense mechanisms (e.g. gastric acid, mucus)
ACUTE WATERY DIARRHEA Rotavirus - most common viral cause; RNA virus - > 125 M of cases / yr in < 5 y/o - 600,000 deaths per year - most severe in ages 3mos – 24mos - transmission: fecal-oral route days before and after the clinical illness
Rotavirus in the Philippines - based on 2005 data of PPS - most common viral cause - 3,700 deaths from total of 14,500 deaths related to childhood diarrhea - most severe in ages 3mos – 24mos - 65% of diarrhea-related hospital admissions
Clinical Manifestations incubation: < 48 hours mild to moderate vomiting & fever onset of frequent, watery diarrhea Complications: dehydration, severe and prolonged symptoms in malnourished and immunocompromised children
Diagnosis - clinical and epidemiological features - enzyme immunoassays : 90% specificity/ sensitivity - stool exam : free of blood and leukocytes Treatment - rehydration - probiotics (Lactobacillus species) , zinc - no role for antiviral nor antibacterial drugs - no role for antiemetics nor antidiarrheal drugs
Prognosis - after initial infection, 38% protection against subsequent infection 77% against diarrhea 87% against severe diarrhea Prevention - good hygiene and isolation - breastfeeding - vaccine: > 80% protection against severe disease
Differential Diagnosis 1. Astrovirus – RNA virus - milder with less significant dehydration 2. Norwalk virus – RNA virus - short incubation period (<12 hrs) - vomiting and nausea tend to predominate - clinical picture resembles “food poisoning” by S. aureus
Differential Diagnosis 3. Adenovirus – DNA virus - 5-9% of diarrhea in children - mainly a respiratory virus that grows well in the epithelium of SI - diarrhea is watery but of longer duration ( 10-14 days )
Differential Diagnosis 3. Adenovirus - may be assoc with conjunctivitis, myocarditis, hemorrhagic cystitis, intussusception, encephalomyelitis - transmission: respiratory fecal-oral routes - diagnosis: virus detection by culture or PCR increase in antibody titers
ACUTE WATERY DIARRHEA Enterotoxigenic Escherichia coli (ETEC) - major cause of infantile diarrhea - important etiologic agent of traveler’s diarrhea - 20-30% of diarrhea worldwide and in the Philippines
Pathogenesis - colonization of SI and subsequent elaboration of enterotoxins - enterotoxins: heat-labile (LT) heat- stable (ST) - require a large inoculum of organisms to induce disease - mode of transmission: food or water-borne
ACUTE WATERY DIARRHEA Enteropathogenic Escherichia coli (EPEC) - major cause of infant diarrhea and mortality in < 2 years - pathogenesis: “attaching and effacing lesion” • intimate attachment of bacteria to epithelial surface and effacement of host cell microvilli
Clinical Manifestations - explosive, watery, non-bloody, non-mucoid - abdominal pain - nausea and vomiting - +/- fever - self-limited: 3-5 days but occassionally > 1week
Diagnosis - clinical features seldom distinctive - laboratory studies not readily available: • isolation of bacteria from stool cultures • biochemical criteria (fermentation patterns) • tissue culture • identification of specific virulence factors • detection of antibodies
Treatment - rehydration - early refeeding - history of travel from developing country - DOC: Trimethoprim-Sulfamethoxazole Prevention - prolonged breastfeeding - personal hygiene - proper food and water handling - public health measures
ACUTE WATERY DIARRHEA CHOLERA (Vibrio cholerae) - 5-7M cases and > 100,000 deaths/yr. - an EMERGENCY!! - latest epidemic in 1990s in Americas death rate = 12,000 deaths/70,000 cases -V. cholerae is a gram-negative rod with a polar, flagellum - 2 strains: O1 and O139
Pathogenesis colonization of SI by > 10 viable vibrios production of cholera toxin (CT) entry of toxin into intestinal epithelial cells high cAMP level decrease absorption of Na and Cl by villous cells active secretion of Cl by crypt cells 8
Clinical Manifestations - most are asymptomatic - ¼ with mild to moderate disease - 2-5% with severe disease - hallmark: massive loss of fluids and electrolytes - incubation: 6 hours – 5 days - watery diarrhea, vomiting, low-grade fever - severe: profuse, painless, watery diarrhea with rice-water consistency and fishy odor
Diagnosis - primarily clinical - laboratory confirmation during epidemics • culture by thiosulfate-citrate-bile-sucrose(GOLD STANDARD) • appear as large, yellow colonies against bluish-green medium • culture by tellurite-taurocholate-gelatin agar • small, opaque colonies with zone of cloudiness around them
Treatment - fluid and electrolyte replacement - refeeding does not affect purging rates or duration of illness - success of ORT shown in Peru epidemic in 1991 with <1% mortality - antibiotics for moderate or severe disease DOC: tetracycline and doxycycline resistant strains: TMP-SMZ, Erythromycin, Furazolidone
Complications - dehydration: hypoglycemia acute tubular necrosis - hypokalemia: cardiac arrhythmia paralytic ileus - sodium disturbance: lethargy seizures coma
Prevention - prolonged breastfeeding - safe food and water handling - improved vaccine is priority - Cholera vaccine • 50% efficacy, highly reactogenic, does not protect against O139 vibrios • used only for very high-risk persons (e.g. achlorhydria) with high probability of exposure • not recommended for < 6 mos old
ACUTE WATERY DIARRHEA Staphylococcus aureus - most common cause of food poisoning - ingestion of pre-formed enterotoxins sudden, severe vomiting watery diarrhea - treatment: supportive - prevention: • eat/refrigerate prepared food immediately • exclude those with Staphylococcal skin infections from food handling or preparations 2-7 hours
ACUTE WATERY DIARRHEA GIARDIASIS (Giardia lamblia) - frequently identified during outbreaks assoc with drinking water - high prevalence during childhood - role of child-care centers - transmission: water and food borne low infectious dose extended periods of cyst shedding resistant to chlorination and UV light irradiation
- More by User
Diarrhea. Definition. Increased liquidity, frequency or decreased consistency of stools. Mechanisms. Osmotic Diarrhea Secretory Diarrhea Deranged Motility Exudation. Osmotic Diarrhea. results from poorly absorbable osmotically active solutes in the gut lumen
1.86k views • 41 slides
DIARRHEA. MODULE FOR TEACHERS. OBJECTIVES. Define diarrhea Present major causes and symptoms associated with diarrhea Provide guidance as to when to seek medical attention for diarrhea Students should know: When diarrhea requires medical attention
959 views • 23 slides
CHRONIC DIARRHEA IN CHILDREN
CHRONIC DIARRHEA IN CHILDREN. Asaad M. A. Abdullah Assiri Professor of Pediatrics & Consultant Pediatric Gastroenterologist Department of Pediatrics King Khalid University Hospital. OBJECTIVES.
2.81k views • 113 slides
Evidence based Medicine on Acute Diarrhea in Children
Evidence based Medicine on Acute Diarrhea in Children. Dr.H.K.Takvani, MD Ped., FIAP
1.09k views • 39 slides

diarrhea. intro. Generally > 3 stools per day daily stool weight exceeding 200 grams Up to 5% of ER visits Four mechanisms: increased intestinal secretion decreased intestinal absorption increased osmotic load abnormal intestinal motility . Clinical features. History Camping Travel
478 views • 16 slides
Diarrhea . Brian Rempe MD. Goals. Define Diarrhea Statistics Approach to the Patient Who to work up How to work them up Who to treat and with what. Definitions. Any increase in daily stool weight above normal –roughly 200g per day (in men)
1.26k views • 73 slides
DIARRHEA. Dr. Therese C. Macatula Section of Gastroenterology Department of Medicine The Medical City. What is diarrhea ?. Diarrhea is caused by an imbalance in the physiologic mechanisms of the GI tract, resulting in impaired absorption and excessive secretion
1.6k views • 53 slides
Diarrhea. A messy subject. Case. A 1 year old girl is brought to clinic with 3 days of watery brown diarrhea, vomiting, and irritability. On exam the child is lethargic, afebrile, with sunken eyes and a weak pulse of 140/minute. Which of the following is the best management plan?
783 views • 26 slides
Nutrition For Children With Diarrhea
Nutrition For Children With Diarrhea. Why is diarrhea a concern for parents?. Dehydration, poor nutrition, and poor health 200,000 hospitalizations per year in U.S. 300 deaths per year in U.S. How can I tell if my child has diarrhea?.
491 views • 16 slides
Diarrhea in ICU setting
Diarrhea in ICU setting. B89401129 楊展輝. Patient. 蘇 xx 娥 4226891 72 y/o Female ER 10/16 4:46pm acute onset chest pain radiating to back + cold sweating since that afternoon 4pm T/P/R 35.9/96/24 BP 194/80mmHg Rectal CA s/p OP, C/T and cholecystectomy at 和信 H. 10+ yrs ago
525 views • 23 slides
Rehydration in acute diarrhea
Rehydration in acute diarrhea. Jorge Amil Dias Porto, Portugal [email protected]. Water and electrolyte movement across the intestinal mucosa. K Hodges and R Gill, Gut Microbes, 2010. K Hodges and R Gill, Gut Microbes, 2010. K Hodges and R Gill, Gut Microbes, 2010.
607 views • 33 slides
Prebiotics for acute diarrhea in adults and children
Prebiotics for acute diarrhea in adults and children. Rüdiger Schultz, MD, PhD Pediatrician Ilembula Hospital. Probiotics. The definition of Probiotics: -Living micro-organisms that, upon ingestion in certain numbers, exert health benefiting effects beyond inherent general nutrition
328 views • 11 slides
Antibiotics associated Diarrhea ( Nosocromial Diarrhea)
Antibiotics associated Diarrhea ( Nosocromial Diarrhea). Thananont Krittayawiwat MD. Donchedi Hospital. เชื้อสาเหตุ. Clostridium difficile Gram Positive, Normal commensal organism in Human Gut Major Source : Nosocromial Diarrhea Pseudomembranous Colitis
796 views • 12 slides
DIARRHEA. A pathophysiological Approach to Diagnosis and Treatment Prof. J. Zimmerman Gastroenterology Hadassah-Hebrew University Medical Center. Diarrhea = Increased loss of water from the GI tract. Diarrhea is a common complaint.
690 views • 44 slides
DIARRHEA. WHAT TO ORDER. Criteria for Conducting Stool Studies:. Perform a complete history which includes the following: Travel history Sexual practices Antibiotics in the past 2 months or usage any other medications
1.16k views • 29 slides
DIARRHEA. What is DIARRHEA ?. MOST CAUSATIVE AGENT. Pathophysiology: OSMOTIC DIARRHEA. SECRETORY DIARRHEA. Agents inducing SECRETORY DIARRHEA. INFLAMMATORY & INFECTIOUS DIARRHEA. PATHOGENS ASSOCIATED W/ INFECTIOUS DIARRHEA. DIARRHEA W/ DERANGED MOTILITY. EPIDEMIOLOGY.
1.28k views • 23 slides
541 views • 41 slides
405 views • 33 slides
Diarrhea in Cancer Patients
Diarrhea in Cancer Patients. By. Abdallah H. Elsheref. Diarrhea. WHO Definition: The passage of more than 3 unformed stools in 24 hours. Or Frequent passage of loose stools with urgency. NCI Grading of Diarrhea. Causes of diarrhea in cancer paients. Chemotherapy induced diarrhea
566 views • 23 slides
136 views • 11 slides
A Person is considered to have diarrhea if a person has loose bowel movement three or more times a day. Diarrhea is a condition in which loose, watery stools (bowel movement) appear. www.vaidjagjitsingh.com
480 views • 1 slides

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
Chapter 5 Diarrhoea Case I
Published by Savanna Passon Modified over 9 years ago
Similar presentations
Presentation on theme: "Chapter 5 Diarrhoea Case I"— Presentation transcript:
Diarrhoea and Vomiting in Children Under 5yrs
Diarrhoea and Dehydration Paediatric Palliative Care For Home Based Carers Funded by British High Commission, Pretoria Small Grant Scheme.
Danger Signs in Children Paediatric Palliative Care For Home Based Carers Funded by British High Commission, Pretoria Small Grant Scheme.
Chapter 6 Fever Case I.
Nutrition For Children With Diarrhea
Nurul Sazwani. Definition : a state of negative fluid balance decreased intake increased output fluid shift.
Chapter3 Problems of the neonate and young infant - Neonatal resuscitation.
Chapter 9 Common surgical problems Burns. Case study: Alisher Alisher, a 10 months old girl was brought to the district hospital by her mother. At presentation.
Control of Diarrheal Diseases (CDD) BASIC TRAINING FOR BARANGAY HEALTH WORKERS Calasiao, Pangasinan.
Diarrhea Dr. Adnan Hamawandi Professor of Pediatrics.
DIARRHEA and DEHYDRATION
HAFIZ USMAN WARRAICH Roll#17-C Diarrhea and Dehydration Dr Shreedhar Paudel 25/03/2009.
Doug Simkiss Associate Professor of Child Health Warwick Medical School Management of sick neonates.
Chapter 5 Diarrhoea Case II
Chapter 4 Cough or difficult breathing Case I. Case study: Faizullo Faizullo is a 3-year old boy presented in the hospital with a 3 day history of cough.
Chapter 6 Fever (and joint pain). Case study: Mere Mere is an 11 year old girl brought to hospital after 4 days of fever. She has pain in her right knee.
Chapter 7 Severe Malnutrition
Chapter 4 Cough or Difficult Breathing Case II. Case study: Ratu 11 month old boy with 5 days of cough and fever, yesterday he became short of breath.
IMCI Dr. Bulemela Janeth (Mmed. Pead) 1IMCI for athens.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
- Open access
- Published: 30 November 2021
Determinants of diarrheal diseases among under five children in Jimma Geneti District, Oromia region, Ethiopia, 2020: a case-control study
- Dejene Mosisa 1 ,
- Mecha Aboma 1 ,
- Teka Girma 1 &
- Abera Shibru 1
BMC Pediatrics volume 21 , Article number: 532 ( 2021 ) Cite this article
10k Accesses
10 Citations
1 Altmetric
Metrics details
Globally, in 2017, there were nearly 1.7 billion cases of childhood diarrheal diseases, and it is the second most important cause of morbidity and mortality among under-five children in low-income countries, including Ethiopia. Sanitary conditions, poor housing, an unsanitary environment, insufficient safe water supply, cohabitation with domestic animals that may carry human pathogens, and a lack of food storage facilities, in combination with socioeconomic and behavioral factors, are common causes of diarrhea disease and have had a significant impact on diarrhea incidence in the majority of developing countries.
A community-based unmatched case-control study was conducted on 407 systematically sampled under-five children of Jimma Geneti District (135 with diarrhea and 272 without diarrhea) from May 01 to 30, 2020. Data was collected using an interview administered questionnaire and observational checklist adapted from the WHO/UNICEF core questionnaire and other related literature. Descriptive, bivariate, and multivariate binary logistic regression analyses were done by using SPSS version 20.0.
Sociodemographic determinants such as being a child of 12–23 months of age (AOR 3.3, 95% CI 1.68–6.46; P < 0.05) and mothers’/caregivers’ history of diarrheal diseases (AOR 7.38, 95% CI 3.12–17.44; P < 0.05) were significantly associated with diarrheal diseases among under-five children. Environmental and behavioral factors such as lack of a hand-washing facility near a latrine (AOR 5.22, 95% CI 3.94–26.49; P < 0.05), a lack of hand-washing practice at critical times (AOR 10.6, 95% CI 3.74–29.81; P < 0.05), improper domestic solid waste disposal (AOR 2.68, 95% CI 1.39–5.18; P < 0.05), and not being vaccinated against rotavirus (AOR 2.45, 95% CI 1.25–4.81; P < 0,05) were found important determinants of diarrheal diseases among under-five children.
The unavailability of a hand-washing facility nearby latrine, mothers’/caregivers’ history of the last 2 weeks’ diarrheal diseases, improper latrine utilization, lack of hand-washing practice at critical times, improper solid waste disposal practices, and rotavirus vaccination status were the determinants of diarrheal diseases among under-five children identified in this study. Thus, promoting the provision of continuous and modified health information programs for households on the importance of sanitation, personal hygiene, and vaccination against rotavirus is fundamental to decreasing the burden of diarrheal disease among under-five children.
Peer Review reports
Introduction
The World Health Organization (WHO) defines diarrhea as the passage of three or more loose or liquid stools per day due to an abnormally high fluid content of stool or an abnormal increase in daily stool fluidity, frequency, and volume from what is considered normal for an individual and is caused by bacterial, viral, protozoa, and parasitic organisms [ 1 ]. In low-income countries, the two most common etiological agents of moderate-to-severe diarrhea are rotavirus and Escherichia coli [ 2 ]. Diarrhea is more common when there is a lack of adequate sanitation and hygiene, safe water supply for drinking, cooking, and cleaning, improper feeding practices, and a poor housing situation [ 3 ].
Globally, in 2017, a large number of deaths and more than 1.7 billion cases of childhood diarrheal disease occur every year. Sub-Saharan African and South Asian countries account for roughly 80% of morbidity and mortality. According to 2018 WHO reports, in each year, diarrhea kills more than 525, 000 under-5 years’ children. Five countries accounted for 50 % of the deaths, one of which was Ethiopia [ 4 , 5 ]. Despite the global achievement in the reduction of all-cause of diarrheal diseases, particularly mortality, in the past 30 years, worldwide diarrhea remains the second most important cause of death due to infections among children under 5 years of age [ 6 ]. Likewise, in developing countries, childhood mortality is almost 10 times higher than in developed nations. In Africa, it is estimated that children below 5 years old experience a minimum of five episodes of diarrhea a year and about 800,000 children succumb to diarrhea annually [ 7 ]. Similarly, diarrheal disease is the most important community health problem in Sub-Saharan African countries and is accountable for greater than 50% of childhood illnesses and 50–80% of childhood deaths in the countries [ 1 , 8 ]. Ethiopia is one of the emerging sub-Saharan-African countries contributing to the tall burden of diarrheal illness and death [ 9 ]. In the year of 2016 alone, generally, 1 in every 15 children dies before reaching their fifth birthday. Among these deaths, diarrhea kills almost fifteen thousand under-five children in Ethiopia [ 10 ]. In Ethiopia in particular, diarrheal diseases alone accounted for 23% of the causes of child mortality, which is greater than the annual deaths due to malaria, HIV/AIDS and measles all together [ 11 , 12 ]. These were due to living conditions, high incidence of illness, lack of safe drinking water supply, sanitation and, hygiene, as well as poorer overall health and nutritional status [ 1 ]. In spite of all advances in health technology, improved management, and increased use of oral rehydration therapy in the past decades, diarrheal diseases still continue to be a major cause of morbidity and mortality. Moreover, there is no dramatic change in evidence about whether the health extension program has had an effect on the risk factors of childhood diarrhea [ 13 , 14 ].
According to the Ethiopia Demographic and Health Surveys (EDHS), under-five mortality declined from 166 deaths per 1000 live births in 2000 to 67 deaths per 1000 live births in 2016. This indicates a 60% decrease in under-five mortality over a period of 16 years. However, the under-five mortality rate in the Oromia regional state was 79 per 1000, which is higher than the national mortality rate. According to this survey, there was no significant change in the prevalence of diarrheal disease among under-five children, which has dropped only from 13% in 2011 to 12% in 2016 [ 10 ].
According to the 2019/2020 Jimma Geneti District Health Office performance report, the prevalence of diarrheal diseases among under-five children is 13.5%. Despite the emphasis given by the Ethiopian Federal Ministry of Health, respective regional health offices, Zonal department, and district health offices to improve child health, there is still higher morbidity and mortality among under-five children due to diarrheal disease, specifically in Jimma Geneti District [ 15 ]. Generally, the burden of diarrheal diseases in developing countries is associated with different factors. Evidences revealed that, there is a significant variation in the determinants of diarrhea in Ethiopia, i.e., the determinants of diarrhea identified so far by different scholars was not uniform across the districts. Most of the research conducted in Ethiopia was cross-sectional, institutional-based, and used EDHS data to determine its prevalence. While there are insufficient reports on determinants of under-five diarrheal disease in the studied region, and there is no similar study in Jimma Ganti District, where the prevalence of diarrhea is high and higher child mortality and morbidity due to diarrhea were registered. Thus, to achieve the Sustainable Development Goal (SDG) targeting childhood mortality reduction, operational research designed to identify determinants of diarrhea across different geographical settings is required. Therefore, in this study, we aimed to identify determinants of diarrheal disease among under-five children in the Jimma Geneti District, Oromia Region, Ethiopia, which has important public health implications for planning suitable interventions and appropriate strategies to decrease the impact of diarrheal disease [Fig. 1 ].
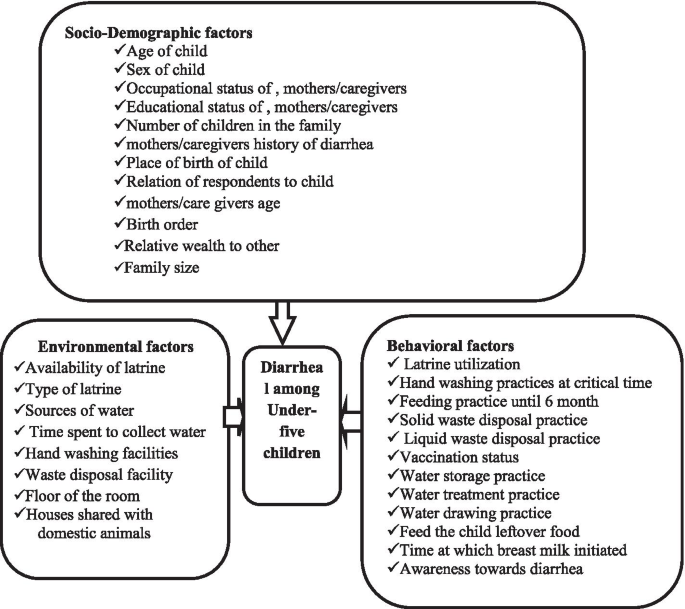
Conceptual framework on Determinants of Diarrheal Diseases among under-five children in Jimma Geneti District, Oromia regional state, Western Ethiopia, May, 2020 [ 16 , 17 ]
Study area and period
The study was conducted in Jimma Geneti District, from May 01 to 30, 2020. Jimma Geneti District is located in Horo Guduru Wollega Zone, Oromia Regional state, the western part of Ethiopia, 273 km from the Capital City, Addis Ababa. In the district there were 44,278 males and 46,086 females, among whom 5755 (6.4%) were urban and 84,609 (93.6%) were rural, and 18,826 total households. There are 19,998 women of reproductive age and 14,848 under-five children [ 15 ] [Fig. 2 ].
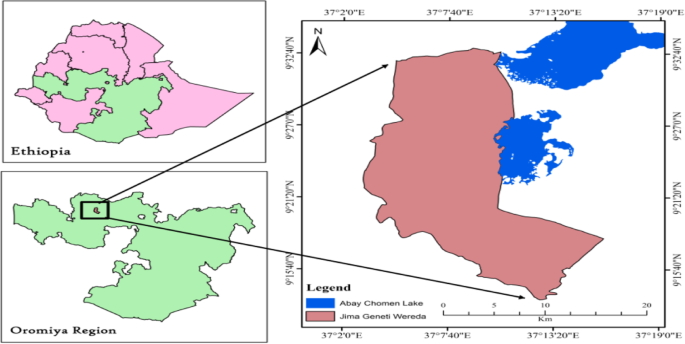
Location map of Jimma Geneti District: Nation, Region and, District, Oromia Regional state, Western Ethiopia, May, 2020 [ 15 ]. Source: - Ethiopian Map Agency 2007 [Using GIS Arc map 10.3.1 version 15]
Study design sample size and sampling procedures
A community-based unmatched case-control study design was conducted to assess determinants of diarrheal diseases among under-five children. The district had 14 kebeles (the district’s smallest administrative unit), four of which were chosen by lottery. The households who had under-five children and residents of the study area in randomly selected kebeles were a sampling unit of this study. While randomly selected under-five children in the households in the preceding 2 weeks before the survey, with a report of diarrhea disease, for cases and without a report of diarrhea disease for controls, were the study units included in this study.
The sample size was determined using OpenEpi’s unmatched case-control model with the assumptions of power = 80%; confidence level = 95%; case to control ratio = 1:2; P1 = proportion of diarrheic children who had not used latrine for disposal of child feces, P2 = proportion of non-diarrheic children who had not used latrine for disposal of child feces as the main predictors of the outcome, which was 33.0 and 19.1% among cases and controls respectively [ 13 ]. And an adjusted odds’ ratio (AOR = 2.09) and 10% of none response rates were considered. Finally, a 407 (135 for cases and 272 for controls) sample size was generated.
A total of 3745 households with under-five children in the selected kebeles were obtained from the family folders of health extension workers (HEWs). Cases and controls were identified by the census through a house-to-house survey, and then 156 under-five children with diarrhea and 3589 under-five children without diarrhea in the selected kebeles were registered and coded with the guidance of HEWs. The case was confirmed from reports of mother’s/caregiver’s history of last 2 weeks period of diarrhea. Afterward, the calculated sample size for control was proportionally allocated to the size of household with under-five children for each selected kebeles. Finally, a total of 272 controls were selected by using the systematic random sampling technique, and all the registered 135 cases who fulfilled the inclusion criteria were included in the study [Fig. 3 ]. Both cases and controls were recruited from different households, and when there were more than one under-five child in the same household, the youngest child was included in the study since they are more vulnerable to the outcome variable [ 1 ].
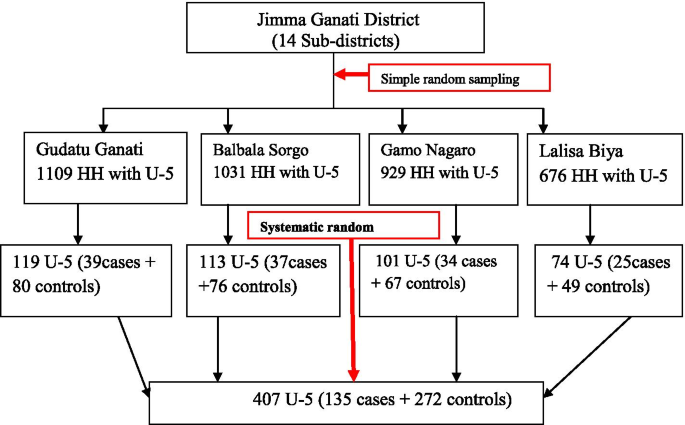
Diagrammatic presentation of sampling technique of under-five children in Jimma Geneti district, Oromia Regional state, Western Ethiopia, May, 2020
Data collection tool and personnel
Data was collected by eight trained B.Sc. nurses under the supervision of four health officers and with guidance of HEWs using a pretested structured questionnaire adapted from the WHO/UNICEF core questionnaire and other related literature [ 16 , 17 , 18 ]. In addition, an observational checklist was used to observe water storage containers, the presence or absence of feces around the latrine and compound, availability, and types of the latrine, and the presence or absence of hand-washing facilities nearby the latrine.
Data quality control and analysis
Data quality was assured through pre-test on 5% of the total sample size in different sub-districts of the study area. Data collectors and supervisors were trained for 1 day by the principal investigator on the study instruments and consent form, how to interview and data collection procedures. The data collection processes were closely supervised by supervisors and investigators. Before data entry, the questionnaires were checked for completeness, consistency, and correction measures made by supervisors and investigators. Then, the data was coded and entered into Epi Info and was exported to SPSS for data processing, cleaning, and analysis. Descriptive analysis like frequency and percentage was carried out to describe sociodemographic characteristics of the respondents and environmental and behavioral determinants of diarrhea among under-five children and results were presented in texts and tables. Bivariate and multivariate analyses were done using a binary logistic regression model to identify determinants of diarrheal diseases among under-five children. Candidate variables for the final model (multivariate logistic regression) were identified using a bivariate logistic regression model with P < 0.25. Multivariate logistic regression was used to determine the independent effect of each explanatory variable on the study variable, with significance set to P < 0.05.
The Hosmer and Lemeshow goodness-of-fit ( P -value = 0.348) was checked to test for model fitness. The independent variables were tested for multi-co-linearity using the Variance Inflation Factor (VIF) and the Tolerance tests, and no variables were found to have a VIF greater than 2 to be omitted from the analysis.
Terms and operational definition
Is defined as having three or more loose or watery stools in a 24-h period in the household within the two-week period before the survey is administered, as reported by the mothers/caregivers of the child [ 10 ].
Mothers/caregivers
Parried-child mother/caregivers, a person who is responsible for taking care of a child; the person can be a relative of the child or a non-relative.
Relative wealth to others
Households are categorized based on the number and kinds of domestic animals they own, ranging from a hen to a cow or ox, in addition to farmland ownership, with the amount of productivity per year and housing characteristics such as consumer goods, toilet facilities, and flooring materials. Each household was ranked by their living standard, and then the distribution was divided into three categories: model, middle, and poor [ 19 ].
Improved water sources
It includes piped water into the dwelling, piped water to the yard, tube well, or borehole, public standpipes, protected dug wells, protected springs, and rainwater. An improved source is one that is likely to provide “safe” water [ 6 ].
Improper waste disposal
Is the disposal of waste in a way that has an impact on the environment. Examples include littering, hazardous waste that is dumped into the ground, and not recycling and disposing of refuse in open fields [ 6 ].
Hand-washing during the critical time
Refers to mothers’/caregivers’ hand-washing practice after the utilization of the latrine, after helping their child defecate, before food preparation, and before self-feeding and child-feeding. If yes, for all critical times of hand-washing, it is concluded as good, otherwise poor practice.
Proper latrine utilization
Households with functional latrines and at least no observable feces in the compound, observable fresh feces through the squat hole, and the footpath to the latrine were uncovered with grasses.
Good awareness towards diarrhea
mothers/caregivers who mentioned at least three causes of diarrhea such as microorganisms, flies, contaminated food/water, three ways of transmission such as by eating contaminated food, by flies, and by physical contact with the diseased person and its prevention such as vaccination of rotavirus vaccine, early initiation, and exclusive breastfeeding, use safe water for drinking and food preparation, proper waste disposal.
Sociodemographic characteristics of study participants
Totally, 407 under five-children (135 cases and 272 controls) were sampled for this study. However, data gathered from 399 under-five children of study participants (127 among cases and 272 among controls) showed a response rate of 94% for cases and 100% for controls. Among those studied children, 76 (59.8%) of cases and 156 (57.4%) of controls were male children and 44 (34.6%) cases and 128 (47.1%) controls were found in the age group of 24–59 months. The mean (+SD) of the age of cases and controls was 18.79 (+ 5.2) and 21.09 (+ 5.9) months respectively. Among these children, 107 (84.3%) of cases and 231 (84.9%) of controls were born at the health facility.
Of all the mothers/caregivers, 118 (92.9%) among cases and 266 (97.8%) among controls were biological mothers. Out of the total mothers/caregivers, 106 (81.9%) cases and 247 (87.9%) controls were found in the age group of 25–35 years.
The majority of mothers/caregivers, 108 (85%) cases, and 201 (73.9%) controls were housewives by occupation. Most of the mothers/caregivers, 115 (90.6%) cases, and 255 (93.8%) controls were married. More than half of the mothers/caregivers in both study groups; 69 (54.3%) cases and 151 (55.5%) controls, had no formal education.
Out of the total, 90 (70.9%) of the mothers/caregivers of the cases and 196 (72.1%) of the controls were protestant religious followers. By ethnicity, approximately 126 (99.2%) of cases and 267 (98.2%) of controls were Oromo.
Regarding the family size of the households in both groups, 62 (48.8%) of cases and 139 (51.1%) of controls were had > = 5 members and the number of under-five children in the households in both groups was one among more than half of the households, 65 (51.2%) of cases and 153 (56.2%) of controls.
Among all households, 34 (26.8%) mothers/caregivers of cases and 14 (5.1%) mothers/caregivers of controls had last two-week history of diarrhea (Table 1 ).
Environmental related characteristics of study participants respondents
The majority of households, 117 (92.1%) among cases and 258 (94.9%) among controls, had latrine facilities in their compound. From these households that had latrines, more than half, 66 (56.4%) among cases and 160 (62.0%) among controls, used pit latrines without a slab.
About 92 (72.4%) of cases and 201 (73.9%) of controls of households were used improved sources of water supply, and 36 (28.3%) of cases and 87 (32.0%) of controls of households traveled more than 30 min to collect water from the sources.
More than half of households with latrines, 73 (57.5%) of cases and 163 (59.9%) of controls, had a hand-washing facility, and 70 (55.1%) of cases and 163 (59.9%) of controls had a waste disposal facility in their compound.
The majority of the floors of the households, 94 (74.0%) of cases, and 214 (78.7%) of controls, were made of soil. About 112 (88.2%) of cases and 258 (84.9%) of controls of households had separated kitchens from their houses. From the total households, 104 (81.9%) of the cases and 251 (92.3%) of the controls were not shared houses with domestic animals (Table 2 ).
Behavioral characteristics of study participants
Regarding behavioral characteristics’ majority of households, 75 (59.1%) among cases, and 220 (80.9%) among controls were properly practiced latrine utilization. Greater than three fourth, 102 (80.3%) among cases and 265 (97.4%) among controls of respondents have washed their hands at critical times. Sixty-four (50.4%) of households from cases and 176 (64.7%) of households from controls were disposed domestic solid refuse properly, while 65 (51.2%) from cases and 113 (41.5%) from controls were disposed of liquid waste improperly.
More than half of under-five children, 73 (62.9%) from cases and 198 (77.6%) from controls, were vaccinated for the measles vaccine. And 73 (57.5%) of cases and 208 (76.5%) of controls were received rotavirus vaccine. From all mother/caregivers, 78 (61.4%) among cases and 171 (62.9%) among controls had good awareness towards diarrheal morbidity (Table 3 ).
Determinants of diarrheal disease among under-five children
The result of backward likelihood multivariate logistic regression analysis revealed that age of child, availability of hand-washing facility, nearby latrine, mothers’/caregivers’ history of the last 2 weeks’ diarrheal disease, latrine utilization, hand-washing practice during a critical time, domestic solid waste refusal practice, and rotavirus vaccination status showed that they were statistically significantly associated with diarrheal diseases among under-five children, after controlling for potential confounders.
Thus, the odds of developing diarrheal disease among under-five children were 2.5 and 3 times higher among children of age 6–11 and 12–23 months, respectively, as compared to children of age 24–59 months (AOR 2.46; 95%CI: 1.09–5.57 and AOR 3.3; 95%CI: 1.68–6.46; P 0.05).
When compared to counterparts, the odds of developing diarrheal disease among under-five children from households with no hand-washing facility near their latrine were five times higher (AOR 5.2; 95% CI: 3.94–26.49; P 0.05). Under-five children whose mothers’/caregivers’ had a history of diarrheal disease in the last 2 weeks had 7 times more likely to develop the disease as compared with their counterparts (AOR 7.38; 95%CI: 3.12–17.44; P < 0.05).
The odds of developing diarrheal disease among under-five children was about 2 times higher among households who had not utilized latrines properly when compared to households who had properly utilized them (AOR 2.34; 95%CI: 1.16, 4.75; P < 0.05). The odds of developing diarrheal disease were 10.6 times higher among under-five children whose mothers’/caregivers’ did not wash their hands during critical time compared with under-five children whose mothers’/caregivers’ did wash their hands during critical times (AOR 10.6; 95%CI: 3.7–29.8; P < 0.05).
Odds of developing diarrheal disease among under-five children whose mothers/caregivers practiced improper domestic solid waste disposal were about 2.7 times higher than under-five children whose mothers’/caregivers’ practiced proper domestic solid waste disposal (AOR 2.68; 95%CI: 1.39–5.18; P < 0.05).
Unvaccinated under-five children were 2.5 times more likely to develop diarrhea disease compared to rotavirus vaccinated children, (AOR 2.45; 95%CI: 1.25–4.81 mothers’/caregivers’) (Table 4 ).
Case = under-five children with diarrhea, Control = under-five children without diarrhea, Crude odds’ ratio (COR), adjusted odds’ ratio (AOR), Confidence interval (CI), P -value derived from multivariate logistic regression based on likelihood ratio test, significant CI of the models are indicated in the bold letter, * p < 0.05; ** p < 0.001.
The result of this study showed that children’s age groups 6–11 and 12–23 months were 2.5 and 3 times more likely to develop diarrhoea disease as compared to children in the age group 24–59 months, respectively. This result was consistent with the results of other case-control studies conducted in Medebay Zane District, Gobi District, and Rural Ethiopia [ 20 , 21 , 22 ].
Similarly, this result was consistent with the study reported from Indonesia and Guatemala [ 23 , 24 ]. In general, children older than 24 months had a lower risk of having diarrheal diseases than children whose ages were between 6 and 23 months. The likely explanation for this risk might be that children between the ages of 6–23 months are undergoing complementary feeding, which may make them vulnerable to diarrheal disease-causing infectious agents due to their undeveloped immunity. Moreover, children at these ages are starting to crawl and walk, thus they may pick dirty or other contaminated objects and take them to their mouth. Likewise, the 2016 EDHS report revealed that diarrhoea prevalence remains high (18%) at the age of 12–23 months, for the reason that weaning and walking often occur during these ages, which contribute to the increased risk of contamination from the environment [ 10 ].
The unavailability of a hand-washing facility near the latrine was positively associated with childhood diarrheal disease. In this study, under five-year-old children from households that had no hand-washing facilities adjacent to the latrines were about five times more likely to have diarrheal diseases than under-five-year-old children from households that had hand-washing facilities adjacent to the latrines. The result of this study was consistent with the study conducted in Jimma District and Yama Gulale [ 25 , 26 ]. This might be expressed as where the hand-washing facilities were unavailable near the toilet; the mothers/caregivers may not frequently practice hand-washing after using the toilet and unintentionally feed their children with contaminated hands, which could be contributing to the high prevalence of under-five diarrheal diseases in the district.
Additionally, the findings of this study showed that mothers’/caregivers’ history of diarrheal diseases was significantly associated with diarrhea diseases among under-five children. Children whose mothers/caregivers had diarrheal diseases in the last 2 weeks prior to this study were 7 times more likely to develop diarrheal diseases than children whose mothers/caregivers had no history of diarrheal diseases in the last 2 weeks. The result of this study was similar to the study findings conducted in Ethiopia Harar Town, Medebay Zana District, and Pawi Hospital, Northwest Ethiopia [ 14 , 20 , 27 ]. The fact is that mothers/caregivers are the main food handlers in the family and the main childcare providers; hence, the possibility of diarrheal diseases among children with mothers/caregivers who have had diarrheal diseases is a common event. It also indicates poor hygienic practice in the household results in the occurrence of diarrheal diseases among under-five children. This might be due to mothers/caregivers with diarrheal diseases being considered as a source of infection for diarrheal diseases among under-five children. Moreover, the mother/caregivers might not be providing appropriate and comprehensive care for the child, which could be a contributing factor to the overall burden of under-five diarrhea and its consequences in the study area. The result of this study also revealed that households who improperly utilized latrines were 2 times more likely to develop diarrheal diseases among under-five children compared to households that utilized latrines properly. The result of this study was comparable with the study findings reported from West Gojjam, Ethiopia [ 13 ] and the Kawangware Slum in Nairobi County, Kenya [ 28 ]. This showed that the presence of a latrine alone does not ensure the prevention of diarrheal diseases among under-five children unless properly utilized. Many microorganisms that cause diarrheal diseases may be controlled when latrines are used properly.
This study found that children whose mothers/caregivers did not practice hand-washing during the critical period were 10.6 times more likely to be affected by diarrheal disease than children whose mothers/caregivers did practice hand-washing during the critical times. This finding was in line with the studies conducted in Adama Rural and Harena Buluk woreda in Ethiopia [ 29 , 30 ] and in Zambia [ 31 ]. This might indicate that diarrheal diseases are largely spread through contaminated hands, water and food supplies. This contamination occurs mainly from inadequate hygiene and sanitation. Contaminated hand is the main source of infection thus; mothers/caregivers should wash their hands at a critical time to prevent diarrheal diseases.
The findings of this study revealed that improper domestic solid waste disposal practices were 2.7 times more likely to be at risk of developing diarrhea diseases compared to their counterparts. The results of this study were consistent with the studies conducted in the Medebay Zana District and Jamma District in Ethiopia [ 20 , 26 ] and in Kenya [ 28 ]. This might be due to improper disposal of domestic solid waste, which serves as a source of infectious agents and reproduction sites for insects. As well, improper domestic solid waste disposal practices create a favorable environment for flies that carry pathogens and could be sources of contamination for water, food, and food utensils. These might cause children to be exposed to contaminated environments and are a leading risk factor for diarrheal diseases among under-five children.
The result of our study finding indicated that children who were not received the rotavirus vaccine were 2.5 times more likely to develop diarrheal diseases as compared to those children who were received the rotavirus vaccine. This finding was in line with the studies conducted at Harena Buluk Woreda, Bahir Dar, and Debre Berhan in Ethiopia [ 29 , 32 , 33 ] and in sub-Saharan Africa countries, Cameroon, and Madagascar [ 34 , 35 ]. These findings were reported that the rotavirus vaccine showed a significant association with the occurrence of diarrheal diseases among under-five children. This confirmed that the rotavirus vaccination is one of the best ways to prevent diarrheal morbidity and its consequences, together with improvements of sanitation and hygienic practices. Thus, two-dose rotavirus vaccines should be given for children as part of a comprehensive approach to control diarrhea. Evidence from experts review on vaccines suggests that rotavirus vaccines effectiveness provide sufficient prevention against rotavirus episodes among under-five children thus reducing the morbidity of diarrhea among this age group [ 36 , 37 ].

Strength and limitation of the study
One of the strengths of this study was that it was conducted community-based using a case-control study design and using the WHO/UNICEF core-based standard questionnaire for data collection. Some behavioral practices, including hand-washing practices at a critical time, reports of mother’s/caregiver’s history of the last 2 weeks of diarrhea, and treatment of drinking water at home used in the analysis were self-reported by the mothers/caregivers, which might introduce imprecision and information bias. Not including data on breastfeeding status, HIV sero-status and social factors could be considered as an additional limitation of this study.
The unavailability of a hand-washing facility nearby latrine, mother’s/caregiver’s history of the last 2 weeks’ diarrheal diseases, improper latrine utilization, lack of hand-washing practice at a critical time, improper solid waste disposal practices, and rotavirus vaccination status were the determinants of diarrheal diseases among under-five children identified in this study. Most of the identified determinants of diarrheal disease among under-five children in the study area are preventable. Thus, promoting the provision of continuous and modified health information programs for households on the importance of sanitation (proper domestic solid waste disposal and latrine utilization), personal hygiene (hand-washing facilities and proper hand-washing practices at critical times), and vaccination against rotavirus are fundamental to decreasing the burden of diarrheal disease among under-five children.
Recommendations
The District Health Office and Zonal Health Department should encourage the community to install a hand-washing facility nearby the latrine, motivate the community to utilize the latrine properly and practice hand-washing during a critical time, and strengthen rotavirus vaccination for all under-five children.
Health Extension Workers should facilitate and give health information to mothers/caregivers on the importance of the availability of hand-washing facilities near the latrine, personal hygiene, and proper latrine utilization, hand-washing practices during a critical time, proper solid waste disposal practices, vaccination of rotavirus, and homemade drinking water treatment practices. Local NGOs should collaborate with the District Health Office and other stakeholders on the construction of nearby hand-washing facilities, personal hygiene to prevent the transmission of diarrhea disease from mother to child, the introduction of hand-washing practices at a critical time, and the preparation of areas for proper solid waste disposal practices.
Availability of data and materials
The dataset used and analyzed throughout the present study accessible from the corresponding author based on reasonable request.
Abbreviations
Acquired immunodeficiency syndrome
Adjusted odds ratio
Confidence interval
Crude odds ratio
Ethiopian demographic and health survey
Health officer
Principal investigators
Standard deviation
Sustainable development goal
Statistical package for social science
Sub Saharan Africa
Under five years old children
United Nations Children’s Fund
UNICEF, WHO. Diarrhoea: Why children are still dying and what can be done, Unicef-WHO. New York: UNICEF/WHO 2009. doi, 10, pp.S0140–6736.
Peterson KM, Diedrich E, Lavigne J. Strategies for Combating Waterborne Diarrheal Diseases in the Developing World. 2008.
Chopra M, Binkin NJ, Mason E, Wolfheim C. Integrated management of childhood illness: what have we learned and how can it be improved? Arch Dis Child. 2012;97(4):350–4.
Article Google Scholar
WHO, Diarrhoeal disease. 2017.
Google Scholar
UNICEF, Diarrhoeal disease. 2018.
World Health Organization. Progress on drinking water, sanitation and hygiene: 2017 update and SDG baselines. 2017.
Dairo MD, Ibrahim TF, Salawu AT. Prevalence and determinants of diarrhoea among infants in selected primary health centres in kaduna north local government area, nigeria. Pan Afr Med J. 2017;28:109 PubMed| Google Scholar.
Azage M, Haile D. Factors associated with safe child feces disposal practices in Ethiopia: evidence from demographic and health survey. Arch Public Health. 2015;73(1):40.
Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405–16.
Csa I. Central statistical agency (CSA)[Ethiopia] and ICF. Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA. 2016.
Fenta AA. Kassahun Angaw, Dessie Abebaw, prevalence and associated factors of acute diarrhea among under-five children in Kamashi district, western Ethiopia: community-based study. BMC Pediatr. 2020;20(1):236.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, E., and Rockville, Maryland, USA: CSA and ICF; 2016.
Girma M, Gobena T, Medhin G, Gasana J, Roba KT. Determinants of childhood diarrhea in West Gojjam, Northwest Ethiopia: a case control study. Pan Afr Med J. 2018;30:234. https://doi.org/10.11604/pamj.2018.30.234.14109 . PMID: 30574253; PMCID: PMC6295292.
Brhanu H, Negese D, Gebrehiwot M. Determinants of acute diarrheal disease among under-five children in pawi hospital, Northwest Ethiopia. Am J Pediatr. 2017;2(2):29–36.
Jimma Geneti district health office first-quarter performance work report. 2019/2020.
Tarekegn M, Enquselassie F. A case control study on determinants of diarrheal morbidity among under-five children in Wolaita Soddo town, southern Ethiopia. Ethiop J Health Dev. 2012;26(2):78–85.
Ayalew AM, Mekonnen WT, Abaya SW, Mekonnen ZA. Assessment of diarrhea and its associated factors in under-five children among open defecation and open defecation-free rural settings of Dangla District, Northwest Ethiopia. J Environ Public Health. 2018;2018.
WHO/UNICEF. Core questions on drinking water and sanitation for household surveys. 2006.
Jimma Geneti agricultural and natural resource office annual work report. report. 2019.
Asfaha KF, Tesfamichael FA, Fisseha GK, Misgina KH, Weldu MG, Welehaweria NB, et al. Determinants of childhood diarrhea in Medebay Zana District, Northwest Tigray, and Ethiopia: a community based unmatched case–control study. BMC Pediatr. 2018;18(1):120.
Megersa S, Benti T, Sahiledengle B. Prevalence of diarrhea and its associated factors among under-five children in open defecation free and non-open defecation free households in Goba District Southeast Ethiopia: a comparative cross-sectional study. Clin Mother Child Health. 2019;16:324.
Ferede MM. Socio-demographic, environmental and behavioural risk factors of diarrhoea among under-five children in rural Ethiopia: further analysis of the 2016 Ethiopian demographic and health survey. BMC Pediatr. 2020;20(1):1–9.
Rohmawati N, Panza A, Lertmaharit S. Factors associated with diarrhea among children under five years of age in Banten Province, Indonesia. J Health Res. 2012;26(1):31–4.
Edward A, Jung Y, Chhorvann C, Ghee AE, Chege J. Association of mother's handwashing practices and pediatric diarrhea: evidence from a multi-country study on community oriented interventions. BMC Public Health. 2019;60(2):E93–e102.
CAS Google Scholar
Degebasa MZ, Weldemichael DZ, Marama MT. Diarrheal status and associated factors in under five years old children in relation to implemented and unimplemented community-led total sanitation and hygiene in Yaya Gulele in 2017. Pediatric Health Med Ther. 2018;9:109.
Workie GY, Akalu TY, Baraki AG. Environmental factors affecting childhood diarrheal disease among under-five children in Jamma district, south Wello zone, Northeast Ethiopia. BMC Infect Dis. 2019;19(1):804.
Getachew B, Mengistie B, Mesfin F, Argaw R. Factors associated with acute diarrhea among children aged 0-59 months in Harar town, eastern Ethiopia. East Afr J Health Biomed Sci. 2018;2(1):26–35.
Reuben Mutama DM, Wakibia J. Risk factors associated with diarrhea disease among children under-five years of age in Kawangware slum in Nairobi County, Kenya. Food and Public Health. 2019;9(1):1–6.
Beyene SG, Melku AT. Prevalence of diarrhea and associated factors among under five years children in Harena Buluk Woreda Oromia region, south East Ethiopia, 2018. J Public Health Int. 2018;1(2):9.
Regassa W, Lemma S. Assessment of diarrheal disease prevalence and associated risk factors in children of 6-59 months old at Adama District rural Kebeles, eastern Ethiopia, and January/2015. Ethiop J Health Sci. 2016;26(6):581–8.
Musonda C, Siziya S, Kwangu M, Mulenga D. Factors associated with diarrheal diseases in under-five children: a case control study at arthur davison children’s hospital in Ndola. Zambia Asian Pac J Health Sci. 2017;4(3):228–34.
Shine S, Muhamud S, Adanew S, Demelash A, Abate M. Prevalence and associated factors of diarrhea among under-five children in Debre Berhan town, Ethiopia 2018: a cross sectional study. BMC Infect Dis. 2020;20(1):1–6.
Shumetie G, Gedefaw M, Kebede A, Derso T. Exclusive breastfeeding and rotavirus vaccination are associated with decreased diarrheal morbidity among under-five children in Bahir Dar, Northwest Ethiopia. Public Health Rev. 2018;39:28.
Ayuk TB, Carine NE, Ashu NJ, et al. Prevalence of diarrhoea and associated risk factors among children under-five years of age in Efoulan health district- Cameroon, sub-Saharan Africa. MOJ Public Health. 2018;7(6):259–64. https://doi.org/10.15406/mojph.2018.07.00248 .
Randremanana RV, Razafindratsimandresy R, Andriatahina T, Randriamanantena A, Ravelomanana L, Randrianirina F, et al. Etiologies, risk factors and impact of severe diarrhea in the under-fives in Moramanga and Antananarivo, Madagascar. PLoS One. 2016;11(7):e0158862.
O’Ryan M, Giaquinto C, Benninghoff B. Human rotavirus vaccine (Rotarix): focus on effectiveness and impact 6 years after first introduction in Africa. Expert Rev Vaccines. 2015;14(8):1099–112.
Parashar UD, Tate JE. The control of diarrhea, the case of a rotavirus vaccine. Salud Pública De México. 2020;62(1):1–5.
Download references
Acknowledgments
We would like to thank the study participants and all other peoples who had formally or informally involved in the accomplishment of this research.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Public Health, Medicine and Health Sciences College, Ambo University, P.O.BOX:19, Ambo, Oromia, Ethiopia
Dejene Mosisa, Mecha Aboma, Teka Girma & Abera Shibru
You can also search for this author in PubMed Google Scholar
Contributions
DM, MA, TG, ASH carried out all the conception and designing of the study, data collection, performed statistical analysis, wrote final report, reviewing and editing the final draft of the manuscript. All of the authors read and approved the final manuscript.
Corresponding author
Correspondence to Mecha Aboma .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from the Ethical Review Board of Ambo University College of Medicine and Health Sciences, with the Ref. No of PGC/18/2020. Hierarchically, all administrative bodies were communicated and permission was secured. Written informed consent was obtained from the parent/legal guardian for study subjects after explaining the objectives and procedures of the study and their right to participate or to withdraw at any time of the interview. The Research and Ethical Review Committee also approved its ethical issues as there was no procedure that affects the study subject and the data is used only for research purposes. For this purpose, a one-page consent letter was attached to the cover page of each questionnaire stating the general purpose of the study and issues of confidentiality, which were discussed by data collectors before proceeding to the interview. Parent/legal guardian who was found that their children are sick during the study time; they were consulted about the causes of the disease and refer her/him to a health facility nearby. Lastly, we confirm that this study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors declare that no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mosisa, D., Aboma, M., Girma, T. et al. Determinants of diarrheal diseases among under five children in Jimma Geneti District, Oromia region, Ethiopia, 2020: a case-control study. BMC Pediatr 21 , 532 (2021). https://doi.org/10.1186/s12887-021-03022-2
Download citation
Received : 22 February 2021
Accepted : 18 November 2021
Published : 30 November 2021
DOI : https://doi.org/10.1186/s12887-021-03022-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Case-control
- Determinants
- Jimma Geneti
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 09 May 2024
Contextual factors associated with diarrhea among under-five children in the Gambia: a multi-level analysis of population-based data
- Amadou Barrow 1 , 2 ,
- Solomon P.S. Jatta 3 , 4 ,
- Oluwarotimi Samuel Oladele 5 ,
- Osaretin Godspower Okungbowa 6 , 7 &
- Michael Ekholuenetale 8
BMC Infectious Diseases volume 24 , Article number: 453 ( 2024 ) Cite this article
Metrics details
Diarrhea poses a significant threat to the lives of children in The Gambia, accounting for approximately 9% of all deaths among children under the age of five. Addressing and reducing child mortality from diarrhea diseases is crucial for achieving the Sustainable Development Goal (SDG) 3, specifically target 3.2, which aims to eliminate preventable deaths in newborns and children under the age of five by 2030. Thus, this research aims to assess the prevalence and contextual factors associated with diarrhea among under-five children in The Gambia.
This research employed secondary data from the 2019/20 Gambia Demographic Health Survey (GDHS). The study initially involved 8,362 women aged between 15 and 49 years. Of these, 6,929 women with children under five were included in this analysis. Data were analyzed using STATA with cross-tabulation and model fitting. Multilevel logistic regression was applied to accommodate the hierarchical structure of the demographic health survey data. The model comparison parameters were BIC, AIC, deviance, and LLR. Variables with a p -value less than 0.05 were selected for multivariable analysis. The statistical significance of the factors was determined using an adjusted odds ratio with a 95% confidence interval (CI) and a p -value of less than 0.05.
The prevalence of diarrhea in under-five children was 53.2% in males and 46.8% in females. In the final model, Kerewan (aOR = 0.58; 95% CI = 0.33–0.98) and Basse (aOR = 0.59; 95% CI = 0.35–0.98) have significantly lower odds of childhood diarrhea compared to Banjul, female children show slightly lower, yet significant, odds of diarrhea compared to males (aOR = 0.96; 95% CI = 0.86–0.98), deliveries at government health centers are associated with higher odds of childhood diarrhea compared to home births (aOR = 1.24; 95% CI = 1.01–1.52). Mothers with post-secondary education had significantly lower odds of having children with diarrhea than those without any education (aOR = 0.50; 95% CI = 0.26–0.99) after controlling for confounders.
The study findings indicate that several factors significantly impact the risk of childhood diarrhea in The Gambia. These factors include region of residence, sex of the child, place of delivery, and education level of the mother. The study suggests that existing interventions aimed at improving child health outcomes in the country should take into consideration these influential factors. Addressing these modifiable factors can enhance the effectiveness of interventions and promote better health outcomes for children in Gambia.
Peer Review reports
Diarrhea is the passage of three or more watery or loose stools within 24 hours [ 1 ]. It is the second most common cause of death in children under the age of five years, behind pneumonia, and it kills at least one in nine children or in excess of 525 000 children each year [ 1 ]. It is estimated that by 2030, 4.4 million children under the age of five years would die each year from complications associated with infectious illnesses, with Sub-Saharan Africa accounting for 60% of these deaths [ 2 ]. Diarrhea accounts for approximately 3.6% of the global disease burden, as measured by disability-adjusted life years (DALYs) [ 3 ]. Despite a significant reduction in global mortality caused by diarrhea in the past 25 years, its morbidity has not experienced a similar decline. This can be attributed to persistently high levels of risk factors, including inadequate access to clean water, sanitation, and hygiene (WASH), insufficient promotion of breastfeeding, and prevalent malnutrition. These challenges are particularly pronounced in low- and middle-income countries [ 4 ]. In order to mitigate the occurrence of diarrhea, the World Health Organization (WHO) has emphasized the importance of ensuring access to safe drinking water, adequate sanitation facilities, and practice of hand hygiene through the use of soap [ 5 ].
The integrated Global Action Plan for Pneumonia and Diarrhea advocated a holistic approach to ending unnecessary deaths from pneumonia and diarrhea, including WASH interventions [ 6 , 7 ]. As a result of these efforts, the WHO/UNICEF Joint Monitoring Program (JMP) was established to evaluate the status of WASH in families, schools, and healthcare institutions on a global scale [ 8 ]. Most deaths from diarrhea are caused by severe dehydration and fluid loss. Children who are malnourished or have a weakened immune system are at the greatest risk of developing life-threatening diarrhea [ 9 , 10 ]. Diarrheal diseases account for (82%) more than four-fifths of all deaths in children under the age of five in Africa and the Southern countries of Asia [ 11 ]. Approximately half of all deaths caused by pneumonia and diarrhea occur in just five of the world’s poorest countries: India, Nigeria, Democratic Republic of Congo, Pakistan, and Ethiopia [ 12 , 13 ]. Reducing child mortality from diarrhea diseases is critical for achieving the Sustainable Development Goal (SDG) 3 (target 3.2), which aims to eliminate preventable deaths in newborns and children under the age of five by 2030 [ 14 ]. As a result, data on illness predictors and household health-seeking behaviors are critical for developing strategies targeted at reducing disease burden.
Diarrhea is a significant contributor to mortality among children in The Gambia, constituting approximately 9% of total deaths in children below the age of five [ 15 ]. Rotavirus is identified as the predominant etiological agent responsible for severe and fatal cases of diarrhea among young children globally. In The Gambia, this viral infection is responsible for a significant number of deaths and hospitalizations, specifically affecting approximately one-third of all cases of diarrhea disease among children under the age of five. It has been estimated that nearly 300 children in this age group succumb to rotavirus-related complications annually in The Gambia [ 15 ]. The Global Enteric Multicenter Study (GEMS) has confirmed the public health significance of rotavirus in The Gambia as it is identified as the primary cause of moderate-to-severe diarrhea in children below the age of two [ 16 ] and has revealed a significant association between Cryptosporidium infection and a heightened occurrence of moderate to severe infectious diarrhea among children within the age range of 0 to 24 months. According to the GEMS study [ 16 ], Cryptosporidium was identified as a significant cause of gastrointestinal illness in eastern Gambia, responsible for 12% and 8% of cases in children aged 0–11 months and 12–23 months, respectively. The GEMS study was a comprehensive investigation conducted over several years, employing standardized diagnostic protocols to assess the prevalence, distribution, and determinants of various infectious agents associated with diarrhea diseases [ 17 , 18 , 19 ].
In another study that aimed to assess the understanding of rural Gambians on diarrhea disease, it was observed that there was a high prevalence of diarrhea in children under the age of five in a defined group under demographic surveillance. It was concluded that inadequate healthcare facilities and practitioners as well as a lack of awareness in recognizing early indicators of dehydration are major issues amenable to public health interventions [ 20 ]. Thus, this research aims to assess the prevalence and contextual factors associated with diarrhea among under-five children: a multi-level analysis of population-based data in The Gambia.
Data source and study design
The present study employed a cross-sectional analysis methods to examine population-based data derived from the 2020 Gambia Demographic and Health Survey (GDHS). GDHS is a comprehensive survey conducted at the national level. It aims to gather data on various sociodemographic and health-related indicators, including but not limited to childhood diarrhea. Data was collected from the entire administration of Gambia using a sampling procedure consisting of three stages. The primary sampling unit of the survey comprised randomly selected samples from clusters. The study conducted in 2019 involved the participation of 8,362 women between the ages of 15 and 49. This study included a total of 6,929 women who had children under the age of five. The data was obtained from mothers or caregivers of infants who were born alive within the five years prior to the interview date.
Study variables
Dependent variables.
The dependent variable in this study was the occurrence of childhood diarrhea.
Explanatory variable
The possible variables associated with childhood diarrhea were categorized into three levels: child level, mother level, and household level. These variables were selected based on a review of the literature and their theoretical justification. (Table 1 )
Data analysis
The analysis of the secondary data was conducted using Stata version 17 software. The sample data was summarized using descriptive statistics, specifically frequencies and percentages. The data for the 2020 GDHS were obtained through the utilization of a stratified multi-stage cluster sampling technique. This indicates that the data exhibit a hierarchical structure, wherein children are nested within clusters. The survey (‘svy’) module was used to adjust for stratification, clustering and sampling weights to compute the estimates of diarrhea among under-five children in The Gambia. In addition, the interdependence among individual children has significant implications for the analysis. Children who belong to the same cluster exhibit a higher degree of similarity among themselves compared to children who belong to different clusters. This phenomenon can result in the generation of artificially significant findings due to the presence of underestimated standard errors.
To account for the clustering effect of the sample, a multivariable multilevel logistic regression model was used. This type of model can account for a lack of independence across levels of nested data. The model was written as follows:
Where \(i\) and \(j\) are the level 1 (child) and level 2 (mother) and level 3 (household) units, respectively. \(X\) , \(Y\) and \(Z\) refer to child-level, mother-level, and household-level variables, respectively. \({\pi }_{ij}\) is the probability of a child developing diarrhea in the \({t}^{t/t}\) household. The \(\beta\) are the fixed coefficients. \({\beta }_{0}\) is the intercept, or the effect on the probability of developing diarrhea in the absence of predictors. \({u}_{j}\) is the random effect, or the effect of the household on childhood diarrhea for the \({j}^{\text{th }}\) household. \({e}_{ij}\) is the random error at the individual levels.
By assuming each household had different intercepts \(\left({\beta }_{0}\right)\) and fixed coefficients \(\left(\beta \right)\) , the hierarchical (clustered) data nature and the within- and between-household variations were taken into account. Four sequential models were tested:
The null model, which did not include any explanatory variables (empty model) and only divided the total variance into child, mother, and household components.
The second model included only child-level variables.
The third model included only mother-level variables.
The fourth included only household-level variables.
Then the final model included all child-level, mother-level, and household-level variables.
The adjusted odds ratios (AORs) along with their corresponding 95% confidence intervals (CIs) were utilized to present the outcomes of the fixed effects. A P -value equal to or less than 0.05 was deemed to be statistically significant.
The statistical indicators of variability (random effects) encompassed variance, intracluster correlation Coefficient (ICC), a variance partition coefficient (VPC), Akaike information criteria (AIC), and Bayesian information criteria (BIC). The ICC was computed in order to assess whether the variability in childhood diarrhea is predominantly attributable to differences within households or between households. The ICC was calculated using the linear threshold method, as specified by Snijders and Bosker’s formula.: \(C=\frac{{V}_{A}}{{V}_{A}+{\pi }^{2}/{/}_{3}}=\frac{{V}_{A}}{{V}_{A}+3.29}\) , where \({V}_{A}\) is the estimated variance in each model [ 28 ]. VPC wass used to measure the total variation childhood diarrhea attributed to individual and cluster level factors in the multilevel model. It was computed using the formula: \(VPC=\frac{{V}_{A}-{V}_{A}}{{V}_{A}}\) , where \({V}_{A}=\) variance of the initial model, and \({V}_{B}=\) variance of the model with more terms.
The existence of multicollinearity was tested using the variance inflation factor (VIF). A VIF of > 5 is generally considered to be indicative of multicollinearity. However, in this study, the mean VIF was 1.28, the maximum VIF was 1.00, and the minimum VIF was 2.47. These values suggest that there is no evidence of multicollinearity between the independent variables.
Variable selection and measurement
The variables for this study are presented in Table 1 .
Ethical approval
The data in this manuscript was not collected by the authors themselves. Subsequently, authorization was acquired from the MEASURE DHS website to gain access to the data. Upon evaluation and approval in June 2022, the authors’ request for access to the data was granted. Ethics Committee, as well as the Ethics Boards of various partner organizations in different countries, including the Ministry of Health. The methodologies utilized in the surveys were implemented in adherence to relevant guidelines and regulations. During the course of the surveys, the female participants duly granted their informed consent.
At child-level variables, child sex, place of delivery/birth, preceeding birth interval and birth type were not significantly different in the prevalence of diarrhea as shown in Table 2 . Child sex did not significantly affect the incidence of diarrhea (χ 2 = 0.884, p = .347), with comparable rates among males (53.2%) and females (46.8%). Birthplace had a notable impact, albeit not statistically significant, with children born in government health centers displaying slightly higher diarrhea rates (76.6%) than those born at home (18.3%) or in private hospitals (3.4%; χ 2 = 7.188, p = .066). The birth interval did not reveal a clear pattern, but children born after less than a two-year interval had slightly higher diarrhea percentages (14.2%) than those with longer intervals (χ 2 = 7.619, p = .055). The type of birth (single or multiple) showed negligible differences in diarrhea rates (χ 2 = 0.225, p = .635).
At mother-level variables, significant differences were found in the mother’s age at birth and incidence of diarrhea (χ2 = 22.937, p < .001). More specifically, mothers under 20 years of age had higher rates of children with diarrhea (12.7%) than those without diarrhea (9.9%). Other age groups showed varying incidences, but the pattern suggests a decrease in the occurrence of diarrhea with increasing maternal age. Other factors, such as religion, place of residence, and maternal education, were not statistically significant, as shown in Table 3 .
At household-level variables, a significant association was observed between household wealth quintile and diarrhea occurrence ( p -value = 0.001, χ 2 =17.695), with the poor showing a higher incidence of diarrhea compared to other wealth classes. No significant association was found between diarrhea occurrence and water sources ( p -value = 0.539, χ2 = 0.378), toilet facilities ( p -value = 0.067, χ2 = 3.352), health insurance coverage ( p -value = 0.661, χ2 = 0.1927), sex of the household head ( p -value = 0.120, χ2 = 2.415), and family structure ( p -value = 0.824, χ2 = 0.049) as shown in Table 4 .
Multi-level fixed effects of contextual factors associated with childhood diarrhea
The analysis of factors at the child-level variables that relate to childhood diarrhea shows significant differences across regions and places of delivery as shown in Table 5 . When compared to Banjul, which is used as a reference region, children in Kerewan exhibit statistically lower odds of experiencing childhood diarrhea (aOR = 0.61; 95% CI = 0.38–0.98). In relation to places of delivery, children born in government health centers, as compared to those born at home, have a significantly higher likelihood of diarrhea (aOR = 1.29; 95% CI = 1.05–1.58). The effects of different mother-level variables shows that regions such as Kanifing (aOR = 0.63 (95%; CI = 0.41–0.97), Kerewan (aOR = 0.49; 95% CI 0.30–0.79), Janjanbureh (aOR = 0.60; 95% CI = 0.37–0.97), and Basse (aOR = 0.53; 95% CI 0.33–0.83) has reduce odds of childhood diarrhea compared to those from Banjul. Mothers with post-secondary education compared to those with no education were associated with a significantly lower odds of childhood diarrhea, (aOR = 0.58; 95% CI 0.35–0.94). Among household-level variables, several regions such as Kanifing (aOR = 0.64, 95% CI 0.41–0.98), Kerewan (aOR = 0.50, 95% CI 0.32–0.58), Janjanbureh (aOR = 0.62, 95% CI 0.39–0.99), and Basse (aOR = 0.55, 95% CI 0.35–0.86) showed statistically lower odds of childhood diarrhea than Banjul, indicating a decreased risk in these regions.
In the final (full) model, Kerewan (aOR = 0.58; 95% CI = 0.33–0.98) and Basse (aOR = 0.59; 95% CI = 0.35–0.98) had significantly lower odds of childhood diarrhea compared to Banjul, signifying reduced risk in these areas. Regarding the child’s sex, female children show slightly lower, yet significant, odds of diarrhea compared to males (aOR = 0.96; 95% CI = 0.86–0.98). For birthplace, deliveries at government health centers are associated with higher odds of childhood diarrhea compared to home births (aOR = 1.24; 95% CI = 1.01–1.52). Mothers with post-secondary education have significantly lower odds of having children with diarrhea, as compared to those without any education (aOR = 0.50; 95% CI = 0.26–0.99).
Random effects for measures of associations
The analysis began with an empty model (Model 0), which exhibited a variance of 0.34 (SE = 0.06, significant at p < .05). The random effects variance decreased as child-level variables (Model 1), mother-level variables (Model 2), and household-level variables (Model 3) were sequentially added to the models. This drop in variance indicated that these variables contributed to the occurrence of childhood diarrhea. However, the variance remained stable from Model 2 to Model 4 (full model) at 0.24, showing that the addition of household-level variables did not significantly change the model’s explanatory power. The VPC increased from 4.9% in the empty model to 6.6% in the full model, indicating a slight increase in the proportion of total variance attributed to the cluster level. The ICC increased from 0.171 in the empty model to 0.177 in the full model, suggesting a minor increase in the proportion of total variance due to between-cluster differences. In terms of model fit, AIC and BIC both decreased from the empty model to the full model, suggesting that the full model with all variables included provided the best fit to the data. In particular, the full model had an AIC of 5041.9 and a BIC of 5312.1, which were lower than those of any other model. In conclusion, the full model incorporating child, mother, and household-level variables provided the best explanation for the occurrence of childhood diarrhea in The Gambia, highlighting the multifactorial nature of this health issue.
The occurrence of diarrhea at the child level was found to be significantly associated with the region and place of birth. The educational attainment of mothers and the geographical region in which they reside were found to be significant factors at the individual level, specifically in relation to the mothers themselves. However, at the household level, only the geographical region was found to have a significant impact. The findings of this study revealed that the intra-class correlation (ICC) values exceeded 10% for all models pertaining to childhood diarrhea. This observation underscores the necessity of employing a multilevel study design [ 21 ].
The likelihood of diarrhea in female children was found to be less than that in male children. This result is consistent with a cross-sectional study conducted in Ethiopia, which found that boys had 2.52 times greater odds of experiencing acute diarrhea than girls [ 22 ]. Similar findings have been reported in recent studies from SSA including Nigeria [ 23 , 24 ]. The reason for this gender disparity in the incidence of diarrhea illness remains unclear, despite numerous studies highlighting its prevalence in many developing countries [ 25 ]. The disparity is hypothesized to stem from factors tied to gender, such as biological differences, environmental exposure, and cultural influences. One environmental hypothesis proposes that boys, particularly older ones, might have different exposure levels due to activities such as spending more time away from home or accompanying their fathers to work, which may expose them to infectious pathogens more frequently [ 22 , 26 ]. On the biological front, the hypothesis suggests that there may be physiological differences between girls and boys in relation to acute diarrhea, making boys more susceptible [ 27 , 28 ].
The educational attainment of a mother appears to significantly influence the likelihood of childhood diarrhea. The results of this study show that children of mothers who have received post-secondary education are less likely to have diarrhea than children of mothers without education. This aligns with prior research indicating that children of less-educated mothers in East Africa [ 29 ], Ethiopia [ 30 ], Nigeria [ 31 ], and Ghana [ 32 ] had higher odds of experiencing childhood diarrhea. This could be attributed to the fact that mothers with more education are likely to have better knowledge, attitudes, and access to the crucial health information needed to effectively prevent diarrhea. Another likely explanation is that education is anticipated to enhance healthcare and hygiene practices within households. It can equip parents with the necessary knowledge about the prevention and transmission of diarrhea.
Mothers residing in the Kerewan and Basse regions demonstrated lower instances of diarrhea in children under five years, which could be attributed to cultural differences and health-seeking behaviors, compared to mothers from Banjul. These findings are similar to those of a previous study in Gambia, where rural regions reported reduced odds of under-five diarrhea cases compared to urban areas, such as Banjul [ 33 ]. Although the underlying factors specific to these regions have not been extensively studied, the authors suggest that this finding warrants further investigation. Possible explanations for these regional variations could include disparities in sociocultural norms, healthcare accessibility and quality, community participation, stakeholder commitment, and implementation of maternal and child healthcare services.
In this study, place of delivery was significantly associated with under-five diarrhea, as those born at government health centers had increased odds of diarrhea cases compared to those born at home. This implies that children born at government health centers have a higher probability of experiencing diarrhea than those born at home. This information is essential for identifying high-risk groups and creating targeted interventions to reduce childhood diarrhea. It also underlines the importance of focusing not only on individual-level factors but also on regional and health infrastructure-related factors when studying and addressing childhood diarrhea. Further investigations are needed to understand the underlying mechanisms of these associations and develop targeted interventions. There are several possible reasons why diarrhea might be more likely among children delivered in hospitals compared to those delivered at home. Firstly, could be due to hospital-acquired infections. Hospitals are environments where infectious agents are more prevalent, increasing the risk of exposure to pathogens that can cause diarrhea. In hospitals, there is a higher likelihood of antibiotic use, which can disrupt the natural balance of gut bacteria and lead to diarrhea. Hospitals may not always have the same level of sanitation as homes, increasing the risk of exposure to contaminated water or food, which can cause diarrhea. Children who are hospitalized may already have underlying health conditions that make them more susceptible to diarrhea. Moreover, it is important to note that these are potential factors, and the actual reasons can vary depending on the specific hospital practices and circumstances.
Strength and limitation
One advantage of this study is that it utilizes a large, representative dataset from Gambia, which lends credibility to the findings and allows them to be generalized across the country. Another strength of this research is the application of multilevel modeling, a statistical model that accommodates the hierarchical structure of the data and provides more reliable estimates. However, this study had certain limitations. First, the data on childhood diarrhea were self-reported, introducing the potential for recall bias, even though the recall period for illnesses was limited to two weeks prior to the survey. Second, the analyses were based on cross-sectional survey data from the GDHS, which did not allow causal inferences. Third, this study could not capture the impact of seasonal changes on diarrhea morbidity because of the nature of the cross-sectional GDHS data used. Fourth, data from different time frames were combined, assuming minimal changes in demographic characteristics over a 5-year period. Finally, the results could have been influenced by confounders that weren’t measured due to the derivative nature of the data. However, despite these limitations, the utilization of a multilevel model provided an account for the clustered nature of the GDHS data, thereby enhancing the precision of the estimates. Furthermore, the application of nationally representative GDHS data can amplify the generalizability of the results.
The research underscores the fact that factors influencing childhood diarrhea are multi-layered, encompassing not just the geographical region, but also characteristics related to both the child and mother. On the child’s side, aspects like birthplace and gender play a role, while on the mother’s side, education level is statistically significant in relation to childhood diarrhea in Gambia. The study suggests that it’s essential to take into account these changeable factors when enhancing existing health interventions to improve child health outcomes in the country.
Data availability
Data for this study were sourced and available here: http://dhsprogram.com/data/available-datasets.cfm .
Diarrhoea. https://www.who.int/westernpacific/health-topics/diarrhoea . Accessed 22 Oct 2021.
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388:3027–35.
Article PubMed PubMed Central Google Scholar
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392:1859–922.
Article Google Scholar
Okeke IN. Diarrheagenic Escherichia coli in sub-saharan Africa: Status, uncertainties and necessities. J Infect Dev Ctries. 2009;3:817–42.
Article PubMed Google Scholar
World Health Organization. Preventing diarrhoea through better water, sanitaiton and hygiene: exposures and impacts in low- and middle-income countries. 2014.
Qazi S, Aboubaker S, MacLean R, Fontaine O, Mantel C, Goodman T, et al. Ending preventable child deaths from pneumonia and diarrhoea by 2025. Development of the integrated global action plan for the Prevention and Control of Pneumonia and Diarrhoea. Arch Dis Child. 2015;100(Suppl 1):S23–8.
UNICEF, World Health Organization. Ending preventable child deaths from pneumonia and diarrhoea by 2025: the integrated global action plan for pneumonia and diarrhoea (GAPPD). 2013.
World Health Organization. Fund (UNICEF) UNC. Progress on household drinking water, sanitation and hygiene 2000–2017: special focus on inequalities. World Health Organization; 2019.
Carvajal-Vélez L, Amouzou A, Perin J, Maïga A, Tarekegn H, Akinyemi A, et al. Diarrhea management in children under five in sub-saharan Africa: does the source of care matter? A countdown analysis. BMC Public Health. 2016;16:830.
Diarrhoeal disease. https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease . Accessed 22 Oct 2021.
UNICEF. Pneumonia and diarrhoea: tackling the deadliest diseases for the world’s poorest children. New York: UNICEF; 2012.
Google Scholar
Melese B, Paulos W, Astawesegn FH, Gelgelu TB. Prevalence of diarrheal diseases and associated factors among under-five children in Dale District, Sidama Zone, Southern Ethiopia: a cross-sectional study. BMC Public Health. 2019;19:1235.
UNICEF. Organización Mundial De La Salud. Diarrhoea: why children are still dying and what can be done. New York: United Nations Children’s Fund; 2009.
Loewe M, Rippin N. The Sustainable Development Goals of the Post-2015 agenda: comments on the OWG and SDSN proposals. SSRN Electron J. 2015. https://doi.org/10.2139/ssrn.2567302 .
PATH. Rotavirus Disease and Vaccines in The Gambia. PATH Vaccine Access and Delivery Global Program. https://www.path.org/resources/rotavirus-disease-and-vaccines-in-the-gambia/ ; 2013.
Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382:209–22.
World Development Indicators | DataBank. https://databank.worldbank.org/reports.aspx?source=2&country=GMB . Accessed 23 Oct 2021.
Kotloff KL, Blackwelder WC, Nasrin D, Nataro JP, Farag TH, van Eijk A, et al. The global enteric Multicenter Study (GEMS) of Diarrheal Disease in infants and Young children in developing countries: epidemiologic and clinical methods of the Case/Control study. Clin Infect Dis. 2012;55 suppl4:S232–45.
The treatment of Diarrhoea. A manual for physicians and other senior health workers | Ministry of Health Knowledge Management Portal. http://library.health.go.ug/publications/communicable-diseases/treatment-diarrhoea-manual-physicians-and-other-senior-health . Accessed 23 Oct 2021.
Saha D, Akinsola A, Sharples K, Adeyemi MO, Antonio M, Imran S, et al. Health Care utilization and attitudes Survey: understanding Diarrheal Disease in Rural Gambia. Am J Trop Med Hyg. 2013;89 1Suppl:13–20.
Theall KP, Scribner R, Broyles S, Yu Q, Chotalia J, Simonsen N, et al. Impact of small group size on neighbourhood influences in multilevel models. J Epidemiol Community Health. 2011;65:688–95.
Anteneh ZA, Andargie K, Tarekegn M. Prevalence and determinants of acute diarrhea among children younger than five years old in Jabithennan District, Northwest Ethiopia, 2014. BMC Public Health. 2017;17:99.
Demissie GD, Yeshaw Y, Aleminew W, Akalu Y. Diarrhea and associated factors among under five children in sub-saharan Africa: evidence from demographic and health surveys of 34 sub-saharan countries. PLoS ONE. 2021;16:e0257522.
Article CAS PubMed PubMed Central Google Scholar
Yaya S, Hudani A, Udenigwe O, Shah V, Ekholuenetale M, Bishwajit G. Improving Water, Sanitation and Hygiene Practices, and Housing Quality to Prevent Diarrhea among under-five children in Nigeria. Trop Med Infect Dis. 2018;3:41.
Sahiledengle B, Teferu Z, Tekalegn Y, Zenbaba D, Seyoum K, Atlaw D, et al. A Multilevel Analysis of Factors Associated with Childhood Diarrhea in Ethiopia. Environ Health Insights. 2021;15:11786302211009894.
Abuzerr S, Nasseri S, Yunesian M, Hadi M, Mahvi AH, Nabizadeh R, et al. Prevalence of diarrheal illness and healthcare-seeking behavior by age-group and sex among the population of Gaza strip: a community-based cross-sectional study. BMC Public Health. 2019;19:704.
Jarman AF, Long SE, Robertson SE, Nasrin S, Alam NH, McGregor AJ, et al. Sex and Gender Differences in Acute Pediatric Diarrhea: a secondary analysis of the DHAKA Study. J Epidemiol Glob Health. 2018;8:42–7.
Siziya S, Muula AS, Rudatsikira E. Correlates of diarrhoea among children below the age of 5 years in Sudan. Afr Health Sci. 2013;13:376–83.
CAS PubMed PubMed Central Google Scholar
Tareke AA, Enyew EB, Takele BA. Pooled prevalence and associated factors of diarrhea among under-five years children in East Africa: a multilevel logistic regression analysis. PLoS ONE. 2022;17:e0264559.
Alebel A, Tesema C, Temesgen B, Gebrie A, Petrucka P, Kibret GD. Prevalence and determinants of diarrhea among under-five children in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2018;13:e0199684.
Desmennu AT, Oluwasanu MM, John-Akinola YO, Opeyemi O, Ayo AS. Maternal Education and Diarrhea among children aged 0–24 months in Nigeria. Afr J Reprod Health. 2017;21.
Apanga PA, Kumbeni MT. Factors associated with diarrhoea and acute respiratory infection in children under-5 years old in Ghana: an analysis of a national cross-sectional survey. BMC Pediatr. 2021;21:78.
Terefe B, Mulat B, Shitu K, Assimamaw NT. Individual and community level factors associated with medical treatment-seeking behavior for childhood diarrhea among the Gambian mothers: evidence from the Gambian demographic and health survey data, 2019/2020. BMC Public Health. 2023;23:579.
Download references
Acknowledgements
The authors express their gratitude to the Demographic and Health Survey (DHS) for granting approval and providing access to the primary data.
The present study did not receive financial support from any public, commercial, or not-for-profit funding agencies.
Author information
Authors and affiliations.
Department of Public & Environmental Health, School of Medicine & Allied Health Sciences, University of The Gambia, Kanifing, The Gambia
Amadou Barrow
Department of Epidemiology, College of Public Health & Health Professions, University of Florida, Gainesville, FL, USA
Amrita School of Sustainable Development, Amrita Vishwa Vidyapeetha University, Kollam, Kerela, India
Solomon P.S. Jatta
School of Public Health, Gambia College, Brikama, The Gambia
Department of Demography and Social Statistics, Faculty of Social Sciences, Federal University Oye-Ekiti, Oye-Ekiti, Ekiti State, Nigeria
Oluwarotimi Samuel Oladele
Department of Economic and Social Research, National Institute for Legislative and Democratic Studies, National Assembly, Abuja, Nigeria
Osaretin Godspower Okungbowa
Department of Economics, Faculty of Social Sciences, University of Benin, Benin City, Nigeria
Department of Epidemiology and Medical Statistics, Faculty of Public Health, College of Medicine, University of Ibadan, Ibadan, Nigeria
Michael Ekholuenetale
You can also search for this author in PubMed Google Scholar
Contributions
AB & ME made significant contributions to the conceptualization and initial preparation of the manuscript. The data analysis was conducted by AB, OSO & ME, who subsequently documented the findings. AB, SPSJ, OSO, OGO & ME made significant contributions to various aspects of the manuscript, including its preparation, study design, literature review, discussion of findings, and critical evaluation of the manuscript’s intellectual content. The final manuscript was read and approved by all of the authors.
Corresponding author
Correspondence to Amadou Barrow .
Ethics declarations
Ethics approval and consent to participate.
This study is a secondary data analysis of the DHS which is publicly available, and approval was granted for its use. Written consent was obtained from mothers/caregivers and data were recorded anonymously at the time of data collection during the DHS.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Barrow, A., Jatta, S.P., Oladele, O.S. et al. Contextual factors associated with diarrhea among under-five children in the Gambia: a multi-level analysis of population-based data. BMC Infect Dis 24 , 453 (2024). https://doi.org/10.1186/s12879-024-09350-9
Download citation
Received : 12 July 2023
Accepted : 24 April 2024
Published : 09 May 2024
DOI : https://doi.org/10.1186/s12879-024-09350-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Contextual factors
- Multi-level
- Under-five children
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
A Simple case diarrhoeA presented at under 5 clinic at SKIMS. Health & Medicine. 1 of 28. Download now. 1. 2. Name: Tabindah Age : 3 ½ years Birth order : Ist R/o : Manigam, Ganderbal Religion: muslim Habitation; Rural Belonging to : Joint family of 5 members Informant: father. 3. Income : Rs 5000 per month Education (HOF): 8th class ...
Imran Iqbal. This document provides an overview of acute diarrhea in children including classification, epidemiology, etiology, clinical features, complications, management, prognosis, and prevention. It discusses the major causes of diarrhea including rotavirus, E. coli, vibrio cholera, and shigella. It covers the pathophysiology of osmotic ...
A 13-year-old boy presents to his primary care provider with a 5-day history of abdominal pain and a 2-day history of diarrhea and vomiting. He describes the quality of the abdominal pain as sharp, originating in the epigastric region and radiating to his back, and exacerbated by movement. Additionally, he has had several episodes of nonbloody, nonbilious vomiting and watery diarrhea. His ...
Case study: Sarah Sarah, a 9 months old girl was brought to the hospital with diarrhoea for 5 days. ... "Chapter 5 Diarrhoea Case I"— Presentation transcript: 1 Chapter 5 Diarrhoea Case I. 2 ... reassess Check the signs of dehydration Check that the child has drank the ORS Check that she has not vomited Select the appropriate plan to continue ...
Older infants, toddlers, and children normally have one to two bowel movements per day. • Diarrhea can usually be defined as an increase in stool frequency to twice the usual number per day in infants, or three or more loose or watery stools per day in older children. 4. • Consistency and color — The consistency and color of a child's ...
DIARRHEA IN CHILDREN Maria Naval C. Rivas Department of Pediatrics The Medical City. SOURCES • Nelson's Textbook of Pediatrics 18th edition • World Health Organization: A Manual for Physicians and Other Senior Health Workers, 2005. DEFINITION • passage of unusually loose or watery stools • at least 3 times in a 24 hour period ...
Presentation on theme: "Chapter 5 Diarrhoea Case I"— Presentation transcript: 1 Chapter 5 Diarrhoea Case I 2 Case study: Sarah Sarah, 9 months old, was brought to the hospital with 5 day history of watery stools.
The author presents a case of gastroenteritis caused by rotavirus in an otherwise healthy but slightly underweight infant presenting with a 2-day history of severe diarrhea and dehydration. 2. Case Presentation. A 4.5-month-old female presented to hospital with a 2-day history of watery diarrhea and fever developed in the 12 hours before ...
The evaluation of the patient with diarrhea can be complex and the treatment challenging. In this article, the definition of diarrhea and the pathophysiologic mechanisms that lead to diarrhea are reviewed. A simplified 5-step approach to the patient with diarrhea is provided and applied in a case-oriented manner applicable to everyday clinical practice. On completion of this article, you ...
Journal of Maternal and Child Health (2021), 06(06): 733-738 Masters Program in Public Health, Universitas Sebelas Maret Case Study e-ISSN: 2549-1172 733 Nursing Intervention in Children with Diarrhea: A Case Study Elly Marce Titihalawa, Dwi Kurniasih, Florida Listavia Panggus Nursing Academy of Dharma Insan, Pontianak, Indonesia ABSTRACT
Prevention and control of childhood diarrhea is a global priority. We conducted a case-control study of childhood diarrhea in Shanghai. Methods: We prospectively recruited diarrheal children in an outpatient setting. Nondiarrheal controls were individually matched to cases. Rotavirus, norovirus and bacterial pathogens were examined.
THE WHITE ARMYClinical case presentation of diarrhoea in a child under preventive and social medicine.Presented by Ms.Nisarga K, 3rd year MBBS, BGSGIMS, Beng...
FINAL-PRESENTATION-ACUTE-GASTROENTERITIS-edited - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Case study of Acute Gastroenteritis
2.1. Severity and trend of diarrhoea among children. The four major infectious diseases that cause death in children under the age of 5 are pneumonia, diarrhoeal diseases, malaria and measles (Figure 1).However, 25% and 31% of the overall diarrhoeal burden has been attributed to diarrhoea among children below the age of 5 in Africa and Asia respectively (Walker et al., 2012), especially Sub ...
Clinical approach. The clinical approach involves, firstly, segregating the cases into acute and chronic diarrhoea. Most childhood diarrhoeal diseases form a continuum, with the majority resolving within the first week of illness.() Chronic diarrhoea refers to persistence of loose stools for at least 14 days() and would entail a more complex approach that involves an age-specific ...
The incidence of diarrhoea obtained (2.6 episodes per child per year) was virtually the same as that estimated by Snyder & Merson in 1982, while the global mortality estimate was lower (3.3 ...
Aug 29, 2020 • Download as PPTX, PDF •. 15 likes • 3,768 views. Arifa T N. PEDIATRIC NURSING. Healthcare. 1 of 60. Download now. DIARRHEAL DISEASE IN CHILDREN - Download as a PDF or view online for free.
We enrolled 9439 children with moderate-to-severe diarrhoea and 13 129 control children without diarrhoea. By analysing adjusted population attributable fractions, most attributable cases of moderate-to-severe diarrhoea were due to four pathogens: rotavirus, Cryptosporidium, enterotoxigenic Escherichia coli producing heat-stable toxin (ST-ETEC; with or without co-expression of heat-labile ...
A community-based unmatched case-control study was conducted on 407 systematically sampled under-five children of Jimma Geneti District (135 with diarrhea and 272 without diarrhea) from May 01 to 30, 2020. ... and there is no similar study in Jimma Ganti District, where the prevalence of diarrhea is high and higher child mortality and morbidity ...
Diarrhoea is defined as the passage of three or more loose stools in 24 hours, or defecation more frequent than what is normal for an individual [1] . Diarrhoea can be classified as: Acute — symptoms lasting less than 14 days; Persistent — symptoms lasting more than 14 days; or. Chronic — symptoms of more than 4 weeks duration [1] .
Diarrhea can be defined by increased stool frequency, liquidity, or volume. Health care professionals typically think of diarrhea as an increase in stool frequency 1; however, for most individuals, the essential characteristic of diarrhea is the passage of loose stools. 2 Diarrhea is objectively defined as passing a stool weight or volume greater than 200 g or 200 mL per 24 hours. 3 Diarrhea ...
Presentation of Case Dr. John A. Weems (Medicine): A 29-year-old woman was evaluated at a primary care clinic affiliated with this hospital because of nausea, vomiting, and diarrhea.
Diarrhea poses a significant threat to the lives of children in The Gambia, accounting for approximately 9% of all deaths among children under the age of five. Addressing and reducing child mortality from diarrhea diseases is crucial for achieving the Sustainable Development Goal (SDG) 3, specifically target 3.2, which aims to eliminate preventable deaths in newborns and children under the age ...
Conclusion: Results of study reveal that Escherichia coli is a predominant bacterial enteropathogen causing diarrhoea and Salmonella is a major contributor to the diarrhoea causing severe dehydration and to the clinical features like fever, vomiting and more than 10 times of frequency of stools.