We will keep fighting for all libraries - stand with us!

Internet Archive Audio

- This Just In
- Grateful Dead
- Old Time Radio
- 78 RPMs and Cylinder Recordings
- Audio Books & Poetry
- Computers, Technology and Science
- Music, Arts & Culture
- News & Public Affairs
- Spirituality & Religion
- Radio News Archive

- Flickr Commons
- Occupy Wall Street Flickr
- NASA Images
- Solar System Collection
- Ames Research Center

- All Software
- Old School Emulation
- MS-DOS Games
- Historical Software
- Classic PC Games
- Software Library
- Kodi Archive and Support File
- Vintage Software
- CD-ROM Software
- CD-ROM Software Library
- Software Sites
- Tucows Software Library
- Shareware CD-ROMs
- Software Capsules Compilation
- CD-ROM Images
- ZX Spectrum
- DOOM Level CD

- Smithsonian Libraries
- FEDLINK (US)
- Lincoln Collection
- American Libraries
- Canadian Libraries
- Universal Library
- Project Gutenberg
- Children's Library
- Biodiversity Heritage Library
- Books by Language
- Additional Collections

- Prelinger Archives
- Democracy Now!
- Occupy Wall Street
- TV NSA Clip Library
- Animation & Cartoons
- Arts & Music
- Computers & Technology
- Cultural & Academic Films
- Ephemeral Films
- Sports Videos
- Videogame Videos
- Youth Media
Search the history of over 866 billion web pages on the Internet.
Mobile Apps
- Wayback Machine (iOS)
- Wayback Machine (Android)
Browser Extensions
Archive-it subscription.
- Explore the Collections
- Build Collections
Save Page Now
Capture a web page as it appears now for use as a trusted citation in the future.
Please enter a valid web address
- Donate Donate icon An illustration of a heart shape
Medical problem solving : an analysis of clinical reasoning
Bookreader item preview, share or embed this item, flag this item for.
- Graphic Violence
- Explicit Sexual Content
- Hate Speech
- Misinformation/Disinformation
- Marketing/Phishing/Advertising
- Misleading/Inaccurate/Missing Metadata
![[WorldCat (this item)] [WorldCat (this item)]](https://archive.org/images/worldcat-small.png)
plus-circle Add Review comment Reviews
4 Favorites
DOWNLOAD OPTIONS
No suitable files to display here.
IN COLLECTIONS
Uploaded by station44.cebu on June 11, 2020
SIMILAR ITEMS (based on metadata)
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Medical problem solving: An analysis of clinical reasoning

Related Papers
Arthur S Elstein
Jan Kiesewetter , Ralf Schmidmaier
Problem-solving in terms of clinical reasoning is regarded as a key competence of medical doctors. Little is known about the general cognitive actions underlying the strategies of problem-solving among medical students. In this study, a theory-based model was used and adapted in order to investigate the cognitive actions in which medical students are engaged when dealing with a case and how patterns of these actions are related to the correct solution. Twenty-three medical students worked on three cases on clinical nephrology using the think-aloud method. The transcribed recordings were coded using a theory-based model consisting of eight different cognitive actions. The coded data was analysed using time sequences in a graphical representation software. Furthermore the relationship between the coded data and accuracy of diagnosis was investigated with inferential statistical methods. The observation of all main actions in a case elaboration, including evaluation, representation and...
Alan Schwartz
Medical Education
ETS Research Report Series
Leonard Baird
International Journal of Psychological Research
Luis Humberto Orozco Pulido
This paper presents a brief analysis of most known problem solving theoretical models realized using epistemological categories such as observer position, object of study, methods and procedures, and descriptive or explicative scope. The review showed linear and cyclical models, the need to recognize method's limitations to generalizing, the relevance of expliciting observer position, and a diffuse delimitation of the object problem solving as a cognitive process. An integrative and molar theoretical model of problem solving as a dependent variable is proposed whose variations go with critical cognitive processes (information processing, comprehension, reasoning, cognitive styles, and attitudes). Its molar feature refers to that it integrates basic and high order processes in a general cognitive activity; this proposal has to be extensively tested.
The Journal of Mathematical Behavior
Thomas Defranco
Journal of Communication Disorders
European Journal of Behavior Analysis
Advances in Health Sciences Education
This paper has five objectives: (a) to review the scientific background of, and major findings reported in, Medical Problem Solving, now widely recognized as a classic in the field; (b) to compare these results with some of the findings in a recent best-selling collection of case studies; (c) to summarize criticisms of the hypothesis-testing model and to show how these led to greater emphasis on the role of clinical experience and prior knowledge in diagnostic reasoning; (d) to review some common errors in diagnostic reasoning; (e) to examine strategies to reduce the rate of diagnostic errors, including evidence-based medicine and systematic reviews to augment personal knowledge, guidelines and clinical algorithms, computer-based diagnostic decision support systems and second opinions to facilitate deliberation, and better feedback.
RELATED PAPERS
Manuel Alcantara
alejandra velasquez
Psicologia em Estudo
Sílvia Zanatta Da Ros
Gustavo Garlet
Genetics and Molecular Biology
Margarida Perecin
Alexey Kavokin
Kevin Anzzolin
Lee Eysturlid
Marianne BERAUD
Endocrine Connections
ALMUDENA VICENTE
International Journal of Science and Management Studies (IJSMS)
Erwin Macua
Jhih-Rong Liao
Archives of gerontology and geriatrics
Lívia Maria Santiago
Journal of pharmacy & pharmaceutical sciences : a publication of the Canadian Society for Pharmaceutical Sciences, Société canadienne des sciences pharmaceutiques
Eduardo Aparecido de Oliveira
International Journal of Advanced Robotic Systems
Mohammed Ouali
Geoambiente On-line
Leonel Macedo
Caroline Moine
El toldo de Astier
Florencia Gietz
Onur Dursun
Canadian Journal of Applied Linguistics Revue Canadienne De Linguistique Appliquee
Marie-Josee Hamel
Gilberto Morales
Medical Problem Solving: An Analysis of Clinical Reasoning.
Elstein AS, ed. Cambridge, MA: Harvard University Press; 1978. ISBN: 9780674561250.
Clinical reasoning lies at the heart of formulating diagnoses and selecting treatments. The results of these medical decisions determine a substantial portion of the dollars spent on health care. Considering the fundamental importance of clinical reasoning, the topic has received surprisingly little systematic study. Even with the widespread interest in medical error and patient safety in recent years, diagnostic errors and other errors in clinical reasoning have received little attention. This classic collection of empiric studies on clinical reasoning in action thus remains highly relevant more than 25 years after its original publication. One finding of particular relevance for those interested in patient safety and quality improvement is that competence may be problem specific; thus, there is no generic approach to clinical problem solving that, when followed, ensures excellent, or even competent, performance in a variety of domains within a field. The authors also provide an excellent overview of theoretic models relevant to the study of clinical reasoning.
Medical Harm: Historical, Conceptual, and Ethical Dimensions of Iatrogenic Illness. March 27, 2005
Human Error. March 27, 2005
Merry and McCall Smith's Errors, Medicine, and the Law. 2nd ed. March 6, 2005
Judgment under Uncertainty: Heuristics and Biases. March 6, 2005
Working Knowledge: How Organizations Manage What They Know. September 14, 2005
First, Do Less Harm: Confronting the Inconvenient Problems of Patient Safety. June 6, 2012
Accountability: Patient Safety and Policy Reform. March 6, 2005
Error and Uncertainty in Diagnostic Radiology. March 20, 2019
Improving Quality and Safety in Healthcare. April 16, 2024
Speaking Up Constructively: Managerial Practices that Elicit Solutions from Front-Line Employees. March 9, 2011
Work Design Drivers of Organizational Learning about Operational Failures: A Laboratory Experiment on Medication Administration. January 9, 2013
A Randomized Field Study of a Leadership WalkRounds-Based Intervention. September 5, 2012
2014 Annual Benchmarking Report: Malpractice Risks in the Diagnostic Process. January 14, 2015
2011 Annual Benchmarking Report: Malpractice Risks in Emergency Medicine. September 26, 2012
Sources of Power: How People Make Decisions. March 6, 2005
Out of the Crisis. March 27, 2005
Unity of Mistakes: A Phenomenological Interpretation of Medical Work. March 6, 2005
The Cognitive Autopsy: A Root Cause Analysis of Medical Decision Making. January 27, 2021
Closing Death’s Door: Legal Innovations to End the Epidemic of Healthcare Harm. July 7, 2021
Oxford Professional Practice: Handbook of Patient Safety. July 27, 2022
Are Workarounds Ethical? Managing Moral Problems in Health Care Systems. February 3, 2016
Listening for What Matters: Avoiding Contextual Errors in Health Care. March 9, 2016
Organizing for Reliability: A Guide for Research and Practice. January 30, 2019
Practical Patient Safety. October 14, 2009
Talking with Patients and Families about Medical Error: A Guide for Education and Practice. February 16, 2011
Improving Patient Safety Through Teamwork and Team Training. January 29, 2014
Patient Safety Ethics: How Vigilance, Mindfulness, Compliance, and Humility can Make Healthcare Safer. July 24, 2019
Quality and Safety in Anesthesia and Perioperative Care. July 17, 2019
Still Not Safe: Patient Safety and the Middle-Managing of American Medicine. December 18, 2019
After Harm: Medical Error and the Ethics of Forgiveness. September 14, 2005
The Challenger Launch Decision: Risky Technology, Culture, and Deviance at NASA. March 27, 2005
The Limits of Safety: Organizations, Accidents and Nuclear Weapons. March 6, 2005
Demanding Medical Excellence. Doctors and Accountability in the Information Age. March 6, 2005
Forgive and Remember: Managing Medical Failure. 2nd ed. March 6, 2005
Failure in Safety-Critical Systems: A Handbook of Accident and Incident Reporting. March 6, 2005
Engaging Patients as Safety Partners: a Guide for Reducing Errors and Improving Satisfaction. June 18, 2008
Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2nd ed. February 13, 2017
Patient Safety: Achieving a New Standard for Care. March 6, 2005
Misadventures in Health Care: Inside Stories. August 24, 2005
Principles of Risk Management and Patient Safety. March 9, 2011
Patient Safety Handbook, Second Edition. August 17, 2013
When We Do Harm: A Doctor Confronts Medical Error. April 22, 2020
A Crisis in Health Care: A Call to Action on Physician Burnout. January 30, 2019
Learning in Action: A Guide to Putting the Learning Organization to Work. March 27, 2005
Maternal and Infant Health Inequality: New Evidence from Linked Administrative Data. February 22, 2023
The Power to Predict: Leveraging Medical Malpractice Data to Reduce Patient Harm and Financial Loss. June 24, 2020
Addressing the Opioid Crisis in the United States. November 2, 2016
IHI Skilled Nursing Facility Trigger Tool for Measuring Adverse Events. January 27, 2016
Malpractice Risks in Communication Failures: 2015 Annual Benchmarking Report. February 10, 2016
Respectful Management of Serious Clinical Adverse Events. Second Edition. October 27, 2010
How-to Guide: Multidisciplinary Rounds. March 10, 2010
Annual Benchmarking Report: Malpractice Risks in Surgery. June 9, 2010
Thinking Outside the Pillbox: A System-wide Approach to Improving Patient Medication Adherence for Chronic Disease. September 9, 2009
Achieving an Exceptional Patient and Family Experience of Inpatient Hospital Care. March 23, 2011
How-to Guides: Improving Transitions from the Hospital to Reduce Avoidable Rehospitalizations. August 8, 2012
How-to Guide: Prevent Obstetrical Adverse Events. October 24, 2012
Optimizing a Business Case for Safe Health Care: An Integrated Approach to Safety and Finance. July 12, 2017
A Framework for Safe, Reliable, and Effective Care. February 15, 2017
Closing the Loop: A Guide to Safer Ambulatory Referrals in the EHR Era. December 13, 2017
Addressing the Opioid Epidemic: Is There a Role for Physician Education? August 23, 2017
IHI Framework for Improving Joy in Work. August 9, 2017
Patient Safety in the Home: Assessment of Issues, Challenges, and Opportunities. September 6, 2017
Safer Together Survey: Advancing Patient and Workforce Safety January 18, 2023
IHI Global Trigger Tool for Measuring Adverse Events. 2nd Edition. May 9, 2009
Leadership Guide to Patient Safety: Resources and Tools for Establishing and Maintaining Patient Safety. September 28, 2005
Seven Leadership Leverage Points for Organization-Level Improvement in Health Care. Second edition. June 1, 2005
Organizational Learning from Experience in High-Hazard Industries: Problem Investigations as Off-line Reflective Practice. March 6, 2005
The Public's Views on Medical Error in Massachusetts. December 17, 2014
Safety Quality and Informatics Leadership Program. January 7, 2015
When safety event reporting is seen as punitive: "I've been PSN-ed!" September 9, 2020
Organizational readiness to change as a leverage point for improving safety: a national nursing home survey. September 8, 2021
Adverse events present on arrival to the emergency department: the ED as a dual safety net. March 11, 2020
The Emperor’s New Clothes: Or Whatever Happened To “Human Error”? January 1, 2001
Resident Projects for Improvement. June 19, 2013
Normal Accidents: Living with High-Risk Technologies. March 6, 2005
Patient Safety: Research into Practice. September 13, 2006
Medication errors reported in a pediatric intensive care unit for oncologic patients. September 14, 2011
The Patient Safety Leadership WalkRounds Guide. November 19, 2008
Hospitalists as emerging leaders in patient safety: targeting a few to affect many. August 31, 2005
Drug, Healthcare and Patient Safety. November 7, 2012
Mistaking error. March 27, 2005
Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. August 2, 2017
Organisational Failure: An Exploratory Study in the Steel Industry and Medical Domain. March 6, 2005
Implementing Patient Safety: Addressing Culture, Conditions and Values to Help People Work Safely. October 23, 2019
SHOT Annual Report. July 19, 2023
Patient Safety Culture: Theory, Methods and Application. January 21, 2015
Patient Safety: Perspectives on Evidence, Information and Knowledge Transfer. June 4, 2014
The Role of Hospitalists in Patient Safety. December 2, 2009
Pediatric Patient Safety in the Emergency Department. April 28, 2010
The Value of Close Calls in Improving Patient Safety. February 2, 2011
Error Reduction in Health Care: A Systems Approach to Improving Patient Safety, Second edition. June 1, 2011
Impact of Medical Errors and Malpractice on Health Economics, Quality, and Patient Safety. April 26, 2017
Surgical Patient Safety: A Case-Based Approach. October 18, 2017
Getting Results: Reliably Communicating and Acting on Critical Test Results. July 12, 2006
Improving Healthcare Team Communication: Building on Lessons from Aviation and Aerospace. June 25, 2008
Clinical Risk Management. Enhancing Patient Safety. 2nd ed. March 27, 2005
Human Error in Medicine. March 27, 2005
Saving Mothers' Lives: Reviewing Maternal Deaths to Make Motherhood Safer—2003–2005. January 2, 2008
The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. May 19, 2021
Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. January 30, 2003
All in Her Head. The Truth and Lies Early Medicine Taught Us About Women's Bodies and Why It Matters Today. March 20, 2024
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Annual Perspective
Formalizing the hidden curriculum of performance enhancing errors. March 22, 2023
Impact of medical education on patient safety: finding the signal through the noise. February 8, 2023
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. September 21, 2022
Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. April 27, 2022
NCICLE Pathways to Excellence: Expectations for an Optimal Clinical Learning Environment to Achieve Safe and High-Quality Patient Care, 2021. November 24, 2021
Developing critical thinking skills for delivering optimal care July 28, 2021
Resident-faculty overnight discrepancy rates as a function of number of consecutive nights during a week of night float. January 13, 2021
ACGME Summary Report: The Pursuing Excellence Pathway Leaders Patient Safety Collaborative. November 18, 2020
Misdiagnosis, mistreatment, and harm - when medical care ignores social forces. April 8, 2020
Assessing clinical reasoning: targeting the higher levels of the pyramid. September 18, 2019
Professionalism lapses and adverse childhood experiences: reflections from the island of last resort. August 14, 2019
Association of residency work hour reform with long term quality and costs of care of US physicians: observational study. July 24, 2019
Effects on resident work hours, sleep duration and work experience in a Randomized Order Safety Trial Evaluating Resident-physician Schedules (ROSTERS). June 26, 2019
Pediatric faculty knowledge and comfort discussing diagnostic errors: a pilot survey to understand barriers to an educational program. June 12, 2019
Health Professions Education. June 12, 2019
Associations between in-hospital mortality, health care utilization, and inpatient costs with the 2011 resident duty hour revision. May 15, 2019
Perception of the usability and implementation of a metacognitive mnemonic to check cognitive errors in clinical setting. April 10, 2019
Patient safety outcomes under flexible and standard resident duty-hour rules. March 13, 2019
Sleep and alertness in a duty-hour flexibility trial in internal medicine. March 13, 2019
"Does your knee make more of a click or a clack?"; teaching "Car Talk" to new docs. March 13, 2019
Teaching about diagnostic errors through virtual patient cases: a pilot exploration. February 27, 2019
Adjusting to duty hour reforms: residents' perception of the safety climate in interdisciplinary night-float rotations. February 20, 2019
Data omission by physician trainees on ICU rounds. February 6, 2019
Utilizing a Systems and Design Thinking Approach for Improving Well-Being Within Health Professional Education and Health Care. January 16, 2019

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- Architecture and Design
- Asian and Pacific Studies
- Business and Economics
- Classical and Ancient Near Eastern Studies
- Computer Sciences
- Cultural Studies
- Engineering
- General Interest
- Geosciences
- Industrial Chemistry
- Islamic and Middle Eastern Studies
- Jewish Studies
- Library and Information Science, Book Studies
- Life Sciences
- Linguistics and Semiotics
- Literary Studies
- Materials Sciences
- Mathematics
- Social Sciences
- Sports and Recreation
- Theology and Religion
- Publish your article
- The role of authors
- Promoting your article
- Abstracting & indexing
- Publishing Ethics
- Why publish with De Gruyter
- How to publish with De Gruyter
- Our book series
- Our subject areas
- Your digital product at De Gruyter
- Contribute to our reference works
- Product information
- Tools & resources
- Product Information
- Promotional Materials
- Orders and Inquiries
- FAQ for Library Suppliers and Book Sellers
- Repository Policy
- Free access policy
- Open Access agreements
- Database portals
- For Authors
- Customer service
- People + Culture
- Journal Management
- How to join us
- Working at De Gruyter
- Mission & Vision
- De Gruyter Foundation
- De Gruyter Ebound
- Our Responsibility
- Partner publishers

Your purchase has been completed. Your documents are now available to view.
Medical Problem Solving
An analysis of clinical reasoning.
- Arthur S. Elstein , Lee S. Shulman and Sarah A. Sprafka
- In collaboration with: Linda Allal , Michael Gordon , Jason Hilliard , Norman Kagan , Michael J. Loupe and Ronald D. Jordan
The publication that you have attempted to download requires a license.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Clinical problem...
Clinical problem solving and diagnostic decision making: selective review of the cognitive literature
- Related content
- Peer review
This article has a correction. Please see:
- Clinical problem solving and diagnostic decision making: selective review of the cognitive literature - November 02, 2006
- Arthur S Elstein , professor ( aelstein{at}uic.edu ) ,
- Alan Schwarz , assistant professor of clinical decision making.
- Department of Medical Education, University of Illinois College of Medicine, Chicago, IL 60612-7309, USA
- Correspondence to: A S Elstein
This is the fourth in a series of five articles
This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential approaches: problem solving 1 , 2 , 3 and decision making. 4 , 5 , 6 , 7 , 8 Problem solving research was initially aimed at describing reasoning by expert physicians, to improve instruction of medical students and house officers. Psychological decision research has been influenced from the start by statistical models of reasoning under uncertainty, and has concentrated on identifying departures from these standards.
Summary points
Problem solving and decision making are two paradigms for psychological research on clinical reasoning, each with its own assumptions and methods
The choice of strategy for diagnostic problem solving depends on the perceived difficulty of the case and on knowledge of content as well as strategy
Final conclusions should depend both on prior belief and strength of the evidence
Conclusions reached by Bayes's theorem and clinical intuition may conflict
Because of cognitive limitations, systematic biases and errors result from employing simpler rather than more complex cognitive strategies
Evidence based medicine applies decision theory to clinical diagnosis
Problem solving
Diagnosis as selecting a hypothesis.
The earliest psychological formulation viewed diagnostic reasoning as a process of testing hypotheses. Solutions to difficult diagnostic problems were found by generating a limited number of hypotheses early in the diagnostic process and using them to guide subsequent collection of data. 1 Each hypothesis can be used to predict what additional findings ought to be present if it were true, and the diagnostic process is a guided search for these findings. Experienced physicians form hypotheses and their diagnostic plan rapidly, and the quality of their hypotheses is higher than that of novices. Novices struggle to develop a plan and some have difficulty moving beyond collection of data to considering possibilities.
It is possible to collect data thoroughly but nevertheless to ignore, to misunderstand, or to misinterpret some findings, but also possible for a clinician to be too economical in collecting data and yet to interpret accurately what is available. Accuracy and thoroughness are analytically separable.
Pattern recognition or categorisation
Expertise in problem solving varies greatly between individual clinicians and is highly dependent on the clinician's mastery of the particular domain. 9 This finding challenges the hypothetico-deductive model of clinical reasoning, since both successful and unsuccessful diagnosticians use hypothesis testing. It appears that diagnostic accuracy does not depend as much on strategy as on mastery of content. Further, the clinical reasoning of experts in familiar situations frequently does not involve explicit testing of hypotheses. 3 10 , 11 , 12 Their speed, efficiency, and accuracy suggest that they may not even use the same reasoning processes as novices. 11 It is likely that experienced physicians use a hypothetico-deductive strategy only with difficult cases and that clinical reasoning is more a matter of pattern recognition or direct automatic retrieval. What are the patterns? What is retrieved? These questions signal a shift from the study of judgment to the study of the organisation and retrieval of memories.
Problem solving strategies
Hypothesis testing
Pattern recognition (categorisation)
By specific instances
By general prototypes
Viewing the process of diagnosis assigning a case to a category brings some other issues into clearer view. How is a new case categorised? Two competing answers to this question have been put forward and research evidence supports both. Category assignment can be based on matching the case to a specific instance (“instance based” or “exemplar based” recognition) or to a more abstract prototype. In the former, a new case is categorised by its resemblance to memories of instances previously seen. 3 11 This model is supported by the fact that clinical diagnosis is strongly affected by context—for example, the location of a skin rash on the body—even when the context ought to be irrelevant. 12
The prototype model holds that clinical experience facilitates the construction of mental models, abstractions, or prototypes. 2 13 Several characteristics of experts support this view—for instance, they can better identify the additional findings needed to complete a clinical picture and relate the findings to an overall concept of the case. These features suggest that better diagnosticians have constructed more diversified and abstract sets of semantic relations, a network of links between clinical features and diagnostic categories. 14
The controversy about the methods used in diagnostic reasoning can be resolved by recognising that clinicians approach problems flexibly; the method they select depends upon the perceived characteristics of the problem. Easy cases can be solved by pattern recognition: difficult cases need systematic generation and testing of hypotheses. Whether a diagnostic problem is easy or difficult is a function of the knowledge and experience of the clinician.
The strategies reviewed are neither proof against error nor always consistent with statistical rules of inference. Errors that can occur in difficult cases in internal medicine include failure to generate the correct hypothesis; misperception or misreading the evidence, especially visual cues; and misinterpretations of the evidence. 15 16 Many diagnostic problems are so complex that the correct solution is not contained in the initial set of hypotheses. Restructuring and reformulating should occur as data are obtained and the clinical picture evolves. However, a clinician may quickly become psychologically committed to a particular hypothesis, making it more difficult to restructure the problem.
Decision making
Diagnosis as opinion revision.
From the point of view of decision theory, reaching a diagnosis means updating opinion with imperfect information (the clinical evidence). 8 17 The standard rule for this task is Bayes's theorem. The pretest probability is either the known prevalence of the disease or the clinician's subjective impression of the probability of disease before new information is acquired. The post-test probability, the probability of disease given new information, is a function of two variables, pretest probability and the strength of the evidence, measured by a “likelihood ratio.”
Bayes's theorem tells us how we should reason, but it does not claim to describe how opinions are revised. In our experience, clinicians trained in methods of evidence based medicine are more likely than untrained clinicians to use a Bayesian approach to interpreting findings. 18 Nevertheless, probably only a minority of clinicians use it in daily practice and informal methods of opinion revision still predominate. Bayes's theorem directs attention to two major classes of errors in clinical reasoning: in the assessment of either pretest probability or the strength of the evidence. The psychological study of diagnostic reasoning from this viewpoint has focused on errors in both components, and on the simplifying rules or heuristics that replace more complex procedures. Consequently, this approach has become widely known as “heuristics and biases.” 4 19
Errors in estimation of probability
Availability —People are apt to overestimate the frequency of vivid or easily recalled events and to underestimate the frequency of events that are either very ordinary or difficult to recall. Diseases or injuries that receive considerable media attention are often thought of as occurring more commonly than they actually do. This psychological principle is exemplified clinically in the overemphasis of rare conditions, because unusual cases are more memorable than routine problems.
Representativeness —Representativeness refers to estimating the probability of disease by judging how similar a case is to a diagnostic category or prototype. It can lead to overestimation of probability either by causing confusion of post-test probability with test sensitivity or by leading to neglect of base rates and implicitly considering all hypotheses equally likely. This is an error, because if a case resembles disease A and disease B equally, and A is much more common than B, then the case is more likely to be an instance of A. Representativeness is associated with the “conjunction fallacy”—incorrectly concluding that the probability of a joint event (such as the combination of findings to form a typical clinical picture) is greater than the probability of any one of these events alone.
Heuristics and biases
Availability
Representativeness
Probability transformations
Effect of description detail
Conservatism
Anchoring and adjustment
Order effects
Decision theory assumes that in psychological processing of probabilities, they are not transformed from the ordinary probability scale. Prospect theory was formulated as a descriptive account of choices involving gambling on two outcomes, 20 and cumulative prospect theory extends the theory to cases with multiple outcomes. 21 Both prospect theory and cumulative prospect theory propose that, in decision making, small probabilities are overweighted and large probabilities underweighted, contrary to the assumption of standard decision theory. This “compression” of the probability scale explains why the difference between 99% and 100% is psychologically much greater than the difference between, say, 60% and 61%. 22
Support theory
Support theory proposes that the subjective probability of an event is inappropriately influenced by how detailed the description is. More explicit descriptions yield higher probability estimates than compact, condensed descriptions, even when the two refer to exactly the same events. Clinically, support theory predicts that a longer, more detailed case description will be assigned a higher subjective probability of the index disease than a brief abstract of the same case, even if they contain the same information about that disease. Thus, subjective assessments of events, while often necessary in clinical practice, can be affected by factors unrelated to true prevalence. 23
Errors in revision of probability
In clinical case discussions, data are presented sequentially, and diagnostic probabilities are not revised as much as is implied by Bayes's theorem 8 ; this phenomenon is called conservatism. One explanation is that diagnostic opinions are revised up or down from an initial anchor, which is either given in the problem or subjectively formed. Final opinions are sensitive to the starting point (the “anchor”), and the shift (“adjustment”) from it is typically insufficient. 4 Both biases will lead to collecting more information than is necessary to reach a desired level of diagnostic certainty.
It is difficult for everyday judgment to keep separate accounts of the probability of a disease and the benefits that accrue from detecting it. Probability revision errors that are systematically linked to the perceived cost of mistakes show the difficulties experienced in separating assessments of probability from values, as required by standard decision theory. There is a tendency to overestimate the probability of more serious but treatable diseases, because a clinician would hate to miss one. 24
Bayes's theorem implies that clinicians given identical information should reach the same diagnostic opinion, regardless of the order in which information is presented. However, final opinions are also affected by the order of presentation of information. Information presented later in a case is given more weight than information presented earlier. 25
Other errors identified in data interpretation include simplifying a diagnostic problem by interpreting findings as consistent with a single hypothesis, forgetting facts inconsistent with a favoured hypothesis, overemphasising positive findings, and discounting negative findings. From a Bayesian standpoint, these are all errors in assessing the diagnostic value of clinical evidence—that is, errors in implicit likelihood ratios.
Educational implications
Two recent innovations in medical education, problem based learning and evidence based medicine, are consistent with the educational implications of this research. Problem based learning can be understood as an effort to introduce the formulation and testing of clinical hypotheses into the preclinical curriculum. 26 The theory of cognition and instruction underlying this reform is that since experienced physicians use this strategy with difficult problems, and since practically any clinical situation selected for instructional purposes will be difficult for students, it makes sense to provide opportunities for students to practise problem solving with cases graded in difficulty. The finding of case specificity showed the limits of teaching a general problem solving strategy. Expertise in problem solving can be separated from content analytically, but not in practice. This realisation shifted the emphasis towards helping students acquire a functional organisation of content with clinically usable schemas. This goal became the new rationale for problem based learning. 27
Evidence based medicine is the most recent, and by most standards the most successful, effort to date to apply statistical decision theory in clinical medicine. 18 It teaches Bayes's theorem, and residents and medical students quickly learn how to interpret diagnostic studies and how to use a computer based nomogram to compute post-test probabilities and to understand the output. 28
We have selectively reviewed 30 years of psychological research on clinical diagnostic reasoning. The problem solving approach has focused on diagnosis as hypothesis testing, pattern matching, or categorisation. The errors in reasoning identified from this perspective include failure to generate the correct hypothesis; misperceiving or misreading the evidence, especially visual cues; and misinterpreting the evidence. The decision making approach views diagnosis as opinion revision with imperfect information. Heuristics and biases in estimation and revision of probability have been the subject of intense scrutiny within this research tradition. Both research paradigms understand judgment errors as a natural consequence of limitations in our cognitive capacities and of the human tendency to adopt short cuts in reasoning.
Both approaches have focused more on the mistakes made by both experts and novices than on what they get right, possibly leading to overestimation of the frequency of the mistakes catalogued in this article. The reason for this focus seems clear enough: from the standpoint of basic research, errors tell us a great deal about fundamental cognitive processes, just as optical illusions teach us about the functioning of the visual system. From the educational standpoint, clinical instruction and training should focus more on what needs improvement than on what learners do correctly; to improve performance requires identifying errors. But, in conclusion, we emphasise, firstly, that the prevalence of these errors has not been established; secondly, we believe that expert clinical reasoning is very likely to be right in the majority of cases; and, thirdly, despite the expansion of statistically grounded decision supports, expert judgment will still be needed to apply general principles to specific cases.
Series editor J A Knottnerus
Preparation of this review was supported in part by grant RO1 LM5630 from the National Library of Medicine.
Competing interests None declared.
“The Evidence Base of Clinical Diagnosis,” edited by J A Knottnerus, can be purchased through the BMJ Bookshop ( http://www.bmjbookshop.com/ )
- Elstein AS ,
- Shulman LS ,
- Bordage G ,
- Schmidt HG ,
- Norman GR ,
- Boshuizen HPA
- Kahneman D ,
- Sox HC Jr . ,
- Higgins MC ,
- Mellers BA ,
- Schwartz A ,
- Chapman GB ,
- Sonnenberg F
- Glasziou P ,
- Pliskin J ,
- Brooks LR ,
- Coblentz CL ,
- Lemieux M ,
- Kassirer JP ,
- Kopelman RI
- Sackett DL ,
- Haynes RB ,
- Guyatt GH ,
- Richardson WS ,
- Rosenberg W ,
- Tversky A ,
- Fischhoff B ,
- Bostrom A ,
- Quadrell M J
- Redelmeier DA ,
- Koehler DJ ,
- Liberman V ,
- Wallsten TS
- Bergus GR ,
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Med (Lausanne)
Rethinking clinical decision-making to improve clinical reasoning
Salvatore corrao.
1 Department of Internal Medicine, National Relevance and High Specialization Hospital Trust ARNAS Civico, Palermo, Italy
2 Dipartimento di Promozione della Salute Materno Infantile, Medicina Interna e Specialistica di Eccellenza “G. D’Alessandro” (PROMISE), University of Palermo, Palermo, Italy

Christiano Argano
Associated data.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid cognitive errors through correct educational training. This article examines clinical approaches and educational gaps in training medical students and young doctors. The authors explore the core elements of clinical reasoning, including metacognition, reasoning errors and cognitive biases, reasoning strategies, and ways to improve decision-making. The article addresses the dual-process theory of thought and the new Default Mode Network (DMN) theory. The reader may consider the article a first-level guide to deepen how to think and not what to think, knowing that this synthesis results from years of study and reasoning in clinical practice and educational settings.
Introduction
Clinical reasoning is based on complex and multifaceted cognitive processes, and the level of cognition is perhaps the most relevant factor that impacts the physician’s clinical reasoning. These topics have inspired considerable interest in the last years ( 1 , 2 ). According to Croskerry ( 3 ) and Croskerry and Norman ( 4 ), over 40 affective and cognitive biases may impact clinical reasoning. In addition, it should not be forgotten that both the processes and the subject matter are complex.
In medicine, there are thousands of known diagnoses, each with different complexity. Moreover, in line with Hammond’s view, a fundamental uncertainty will inevitably fail ( 5 ). Any mistake or failure in the diagnostic process leads to a delayed diagnosis, a misdiagnosis, or a missed diagnosis. The particular context in which a medical decision is made is highly relevant to the reasoning process and outcome ( 6 ).
More recently, there has been renewed interest in diagnostic reasoning, primarily diagnostic errors. Many researchers deepen inside the processes underpinning cognition, developing new universal reasoning and decision-making model: The Dual Process Theory.
This theory has a prompt implementation in medical decision-making and provides a comprehensive framework for understanding the gamma of theoretical approaches taken into consideration previously. This model has critical practical applications for medical decision-making and may be used as a model for teaching decision reasoning. Given this background, this manuscript must be considered a first-level guide to understanding how to think and not what to think, deepening clinical decision-making and providing tools for improving clinical reasoning.
Too much attention to the tip of the iceberg
The New England Journal of Medicine has recently published a fascinating article ( 7 ) in the “Perspective” section, whereon we must all reflect on it. The title is “At baseline” (the basic condition). Dr. Bergl, from the Department of Medicine of the Medical College of Wisconsin (Milwaukee), raised that his trainees no longer wonder about the underlying pathology but are focused solely on solving the acute problem. He wrote that, for many internal medicine teams, the question is not whether but to what extent we should juggle the treatment of critical health problems of patients with care for their coexisting chronic conditions. Doctors are under high pressure to discharge, and then they move patients to the next stage of treatment without questioning the reason that decompensated the clinical condition. Suppose the chronic condition or baseline was not the fundamental goal of our performance. In that case, our juggling is highly inconsistent because we are working on an intermediate outcome curing only the decompensation phase of a disease. Dr. Bergl raises another essential matter. Perhaps equally disturbing, by adopting a collective “base” mentality, we unintentionally create a group of doctors who prioritize productivity rather than developing critical skills and curiosity. We agree that empathy and patience are two other crucial elements in the training process of future internists. Nevertheless, how much do we stimulate all these qualities? Perhaps are not all part of cultural backgrounds necessary for a correct patient approach, the proper clinical reasoning, and balanced communication skills?
On the other hand, a chronic baseline condition is not always the real reason that justifies acute hospitalization. The lack of a careful approach to the baseline and clinical reasoning focused on the patient leads to this superficiality. We are focusing too much on our students’ practical skills and the amount of knowledge to learn. On the other hand, we do not teach how to think and the cognitive mechanisms of clinical reasoning.
Time to rethink the way of thinking and teaching courses
Back in 1910, John Dewey wrote in his book “How We Think” ( 8 ), “The aim of education should be to teach us rather how to think than what to think—rather improve our minds to enable us to think for ourselves than to load the memory with the thoughts of other men.”
Clinical reasoning concerns how to think and make the best decision-making process associated with the clinical practice ( 9 ). The core elements of clinical reasoning ( 10 ) can be summarized in:
- 1. Evidence-based skills,
- 2. Interpretation and use of diagnostic tests,
- 3. Understanding cognitive biases,
- 4. Human factors,
- 5. Metacognition (thinking about thinking), and
- 6. Patient-centered evidence-based medicine.
All these core elements are crucial for the best way of clinical reasoning. Each of them needs a correct learning path to be used in combination with developing the best thinking strategies ( Table 1 ). Reasoning strategies allow us to combine and synthesize diverse data into one or more diagnostic hypotheses, make the complex trade-off between the benefits and risks of tests and treatments, and formulate plans for patient management ( 10 ).
Set of some reasoning strategies (view the text for explanations).
However, among the abovementioned core element of clinical reasoning, two are often missing in the learning paths of students and trainees: metacognition and understanding cognitive biases.
Metacognition
We have to recall cognitive psychology, which investigates human thinking and describes how the human brain has two distinct mental processes that influence reasoning and decision-making. The first form of cognition is an ancient mechanism of thought shared with other animals where speed is more important than accuracy. In this case, thinking is characterized by a fast, intuitive way that uses pattern recognition and automated processes. The second one is a product of evolution, particularly in human beings, indicated by an analytical and hypothetical-deductive slow, controlled, but highly consuming way of thinking. Today, the psychology of thinking calls this idea “the dual-process theory of thought” ( 11 – 14 ). The Nobel Prize in Economic Sciences awardee Daniel Kahneman has extensively studied the dichotomy between the two modes of thought, calling them fast and slow thinking. “System 1” is fast, instinctive, and emotional; “System 2” is slower, more deliberative, and more logical ( 15 ). Different cerebral zones are involved: “System 1” includes the dorsomedial prefrontal cortex, the pregenual medial prefrontal cortex, and the ventromedial prefrontal cortex; “System 2” encompasses the dorsolateral prefrontal cortex. Glucose utilization is massive when System 2 is performing ( 16 ). System 1 is the leading way of thought used. None could live permanently in a deliberate, slow, effortful way. Driving a car, eating, and performing many activities over time become automatic and subconscious.
A recent brilliant review of Gronchi and Giovannelli ( 17 ) explores those things. Typically, when a mental effort is required for tasks requiring attention, every individual is subject to a phenomenon called “ego-depletion.” When forced to do something, each one has fewer cognitive resources available to activate slow thinking and thus is less able to exert self-control ( 18 , 19 ). In the same way, much clinical decision-making becomes intuitive rather than analytical, a phenomenon strongly affected by individual differences ( 20 , 21 ). Experimental evidence by functional magnetic resonance imaging and positron emission tomography studies supports that the “resting state” is spontaneously active during periods of “passivity” ( 22 – 25 ). The brain regions involved include the medial prefrontal cortex, the posterior cingulate cortex, the inferior parietal lobule, the lateral temporal cortex, the dorsal medial prefrontal cortex, and the hippocampal formation ( 26 ). Findings reporting high-metabolic activity in these regions at rest ( 27 ) constituted the first clear evidence of a cohesive default mode in the brain ( 28 ), leading to the widely acknowledged introduction of the Default Mode Network (DMN) concept. The DMN contains the medial prefrontal cortex, the posterior cingulate cortex, the inferior parietal lobule, the lateral temporal cortex, the dorsal medial prefrontal cortex, and the hippocampal formation. Lower activity levels characterize the DMN during goal-directed cognition and higher activity levels when an individual is awake and involved in the mental processes requiring low externally directed attention. All that is the neural basis of spontaneous cognition ( 26 ) that is responsible for thinking using internal representations. This paradigm is growing the idea of stimulus-independent thoughts (SITs), defined by Buckner et al. ( 26 ) as “thoughts about something other than events originating from the environment” that is covert and not directed toward the performance of a specific task. Very recently, the role of the DMN was highlighted in automatic behavior (the rapid selection of a response to a particular and predictable context) ( 29 ), as opposed to controlled decision making, suggesting that the DMN plays a role in the autopilot mode of brain functioning.
In light of these premises, everyone can pause to analyze what he is doing, improving self-control to avoid “ego-depletion.” Thus, one can actively switch between one type of thinking and the other. The ability to make this switch makes the physician more performing. In addition, a physician can be trained to understand the ways of thinking and which type of thinking is engaged in various situations. This way, experience and methodology knowledge can energize Systems 1 and 2 and how they interact, avoiding cognitive errors. Figure 1 summarizes all the concepts abovementioned about the Dual Mode Network and its relationship with the DMN.

Graphical representation of the characteristics of Dual Mode Network, including the relationship between the two systems by Default Mode Network (view the text for explanations).
Emotional intelligence is another crucial factor in boosting clinical reasoning for the best decision-making applied to a single patient. Emotional intelligence recognizes one’s emotions. Those others label different feelings appropriately and use emotional information to guide thinking and behavior, adjust emotions, and create empathy, adapt to environments, and achieve goals ( 30 ). According to the phenomenological account of Fuchs, bodily perception (proprioception) has a crucial role in understanding others ( 31 ). In this sense, the proprioceptive skills of a physician can help his empathic understanding become elementary for empathy and communication with the patient. In line with Fuchs’ view, empathic understanding encompasses a bodily resonance and mediates contextual knowledge about the patient. For medical education, empathy should help to relativize the singular experience, helping to prevent that own position becomes exclusive, bringing oneself out of the center of one’s own perspective.
Reasoning errors and cognitive biases
Errors in reasoning play a significant role in diagnostic errors and may compromise patient safety and quality of care. A recently published review by Norman et al. ( 32 ) examined clinical reasoning errors and how to avoid them. To simplify this complex issue, almost five types of diagnostic errors can be recognized: no-fault errors, system errors, errors due to the knowledge gap, errors due to misinterpretation, and cognitive biases ( 9 ). Apart from the first type of error, which is due to unavoidable errors due to various factors, we want to mention cognitive biases. They may occur at any stage of the reasoning process and may be linked to intuition and analytical systems. The most frequent cognitive biases in medicine are anchoring, confirmation bias, premature closure, search satisficing, posterior probability error, outcome bias, and commission bias ( 33 ). Anchoring is characterized by latching onto a particular aspect at the initial consultation, and then one refuses to change one’s mind about the importance of the later stages of reasoning. Confirmation bias ignores the evidence against an initial diagnosis. Premature closure leads to a misleading diagnosis by stopping the diagnostic process before all the information has been gathered or verified. Search satisficing blinds other additional diagnoses once the first diagnosis is made posterior probability error shortcuts to the usual patient diagnosis for previously recognized clinical presentations. Outcome bias impinges on our desire for a particular outcome that alters our judgment (e.g., a surgeon blaming sepsis on pneumonia rather than an anastomotic leak). Finally, commission bias is the tendency toward action rather than inaction, assuming that only good can come from doing something (rather than “watching and waiting”). These biases are only representative of the other types, and biases often work together. For example, in overconfidence bias (the tendency to believe we know more than we do), too much faith is placed in opinion instead of gathered evidence. This bias can be augmented by the anchoring effect or availability bias (when things are at the forefront of your mind because you have seen several cases recently or have been studying that condition in particular), and finally by commission bias—with disastrous results.
Novice vs. expert approaches
The reasoning strategies used by novices are different from those used by experts ( 34 ). Experts can usually gather beneficial information with highly effective problem-solving strategies. Heuristics are commonly, and most often successfully, used. The expert has a saved bank of illness scripts to compare and contrast the current case using more often type 1 thinking with much better results than the novice. Novices have little experience with their problems, do not have time to build a bank of illness scripts, and have no memories of previous similar cases and actions in such cases. Therefore, their mind search strategies will be weak, slow, and ponderous. Heuristics are poor and more often unsuccessful. They will consider a more comprehensive range of diagnostic possibilities and take longer to select approaches to discriminate among them. A novice needs specific knowledge and specific experience to become an expert. In our opinion, he also needs special training in the different ways of thinking. It is possible to study patterns, per se as well. It is, therefore, likely to guide the growth of knowledge for both fast thinking and slow one.
Moreover, learning by osmosis has traditionally been the method to move the novice toward expert capabilities by gradually gaining experience while observing experts’ reasoning. However, it seems likely that explicit teaching of clinical reasoning could make this process quicker and more effective. In this sense, an increased need for training and clinical knowledge along with the skill to apply the acquired knowledge is necessary. Students should learn disease pathophysiology, treatment concepts, and interdisciplinary team communication developing clinical decision-making through case-series-derived knowledge combining associative and procedural learning processes such as “Vienna Summer School on Oncology” ( 35 ).
Moreover, a refinement of the training of communicative skills is needed. Improving communication skills training for medical students and physicians should be the university’s primary goal. In fact, adequate communication leads to a correct diagnosis with 76% accuracy ( 36 ). The main challenge for students and physicians is the ability to respond to patients’ individual needs in an empathic and appreciated way. In this regard, it should be helpful to apply qualitative studies through the adoption of a semi-structured or structured interview using face-to-face in-depth interviews and e-learning platforms which can foster interdisciplinary learning by developing expertise for the clinical reasoning and decision-making in each area and integrating them. They could be effective tools to develop clinical reasoning and decision-making competencies and acquire effective communication skills to manage the relationship with patient ( 37 – 40 ).
Clinical reasoning ways
Clinical reasoning is complex: it often requires different mental processes operating simultaneously during the same clinical encounter and other procedures for different situations. The dual-process theory describes how humans have two distinct approaches to decision-making ( 41 ). When one uses heuristics, fast-thinking (system 1) is used ( 42 ). However, complex cases need slow analytical thinking or both systems involved ( 15 , 43 , 44 ). Slow thinking can use different ways of reasoning: deductive, hypothetic-deductive, inductive, abductive, probabilistic, rule-based/categorical/deterministic, and causal reasoning ( 9 ). We think that abductive and causal reasoning need further explanation. Abductive reasoning is necessary when no deductive argument (from general assumption to particular conclusion) nor inductive (the opposite of deduction) may be claimed.
In the real world, we often face a situation where we have information and move backward to the likely cause. We ask ourselves, what is the most plausible answer? What theory best explains this information? Abduction is just a process of choosing the hypothesis that would best explain the available evidence. On the other hand, causal reasoning uses knowledge of medical sciences to provide additional diagnostic information. For example, in a patient with dyspnea, if considering heart failure as a casual diagnosis, a raised BNP would be expected, and a dilated vena cava yet. Other diagnostic possibilities must be considered in the absence of these confirmatory findings (e.g., pneumonia). Causal reasoning does not produce hypotheses but is typically used to confirm or refute theories generated using other reasoning strategies.
Hypothesis generation and modification using deduction, induction/abduction, rule-based, causal reasoning, or mental shortcuts (heuristics and rule of thumbs) is the cognitive process for making a diagnosis ( 9 ). Clinicians develop a hypothesis, which may be specific or general, relating a particular situation to knowledge and experience. This process is referred to as generating a differential diagnosis. The process we use to produce a differential diagnosis from memory is unclear. The hypotheses chosen may be based on likelihood but might also reflect the need to rule out the worst-case scenario, even if the probability should always be considered.
Given the complexity of the involved process, there are numerous causes for failure in clinical reasoning. These can occur in any reasoning and at any stage in the process ( 33 ). We must be aware of subconscious errors in our thinking processes. Cognitive biases are subconscious deviations in judgment leading to perceptual distortion, inaccurate assessment, and misleading interpretation. From an evolutionary point of view, they have developed because, often, speed is more important than accuracy. Biases occur due to information processing heuristics, the brain’s limited capacity to process information, social influence, and emotional and moral motivations.
Heuristics are mind shortcuts and are not all bad. They refer to experience-based techniques for decision-making. Sometimes they may lead to cognitive biases (see above). They are also essential for mental processes, expressed by expert intuition that plays a vital role in clinical practice. Intuition is a heuristic that derives from a natural and direct outgrowth of experiences that are unconsciously linked to form patterns. Pattern recognition is just a quick shortcut commonly used by experts. Alternatively, we can create patterns by studying differently and adequately in a notional way that accumulates information. The heuristic that rules out the worst-case scenario is a forcing mind function that commits the clinician to consider the worst possible illness that might explain a particular clinical presentation and take steps to ensure it has been effectively excluded. The heuristic that considers the least probable diagnoses is a helpful approach to uncommon clinical pictures and thinking about and searching for a rare unrecognized condition. Clinical guidelines, scores, and decision rules function as externally constructed heuristics, usually to ensure the best evidence for the diagnosis and treatment of patients.
Hence, heuristics are helpful mind shortcuts, but the exact mechanisms may lead to errors. Fast-and-frugal tree and take-the-best heuristic are two formal models for deciding on the uncertainty domain ( 45 ).
In the recent times, clinicians have faced dramatic changes in the pattern of patients acutely admitted to hospital wards. Patients become older and older with comorbidities, rare diseases are frequent as a whole ( 46 ), new technologies are growing in a logarithmic way, and sustainability of the healthcare system is an increasingly important problem. In addition, uncommon clinical pictures represent a challenge for clinicians ( 47 – 50 ). In our opinion, it is time to claim clinical reasoning as a crucial way to deal with all complex matters. At first, we must ask ourselves if we have lost the teachings of ancient masters. Second, we have to rethink medical school courses and training ones. In this way, cognitive debiasing is needed to become a well-calibrated clinician. Fundamental tools are the comprehensive knowledge of nature and the extent of biases other than studying cognitive processes, including the interaction between fast and slow thinking. Cognitive debiasing requires the development of good mindware and the awareness that one debiasing strategy will not work for all biases. Finally, debiasing is generally a complicated process and requires lifelong maintenance.
We must remember that medicine is an art that operates in the field of science and must be able to cope with uncertainty. Managing uncertainty is the skill we have to develop against an excess of confidence that can lead to error. Sound clinical reasoning is directly linked to patient safety and quality of care.
Data availability statement
Author contributions.
SC and CA drafted the work and revised it critically. Both authors have approved the submission of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
- Open access
- Published: 24 May 2024
Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial
- Jian Zhao 1 na1 ,
- Xin Gong 1 na1 ,
- Jian Ding 1 ,
- Kepin Xiong 2 ,
- Kangle Zhuang 3 ,
- Rui Huang 1 ,
- Shu Li 4 &
- Huachun Miao 1
BMC Medical Education volume 24 , Article number: 571 ( 2024 ) Cite this article
Metrics details
Case-based learning (CBL) methods have gained prominence in medical education, proving especially effective for preclinical training in undergraduate medical education. Tetralogy of Fallot (TOF) is a congenital heart disease characterized by four malformations, presenting a challenge in medical education due to the complexity of its anatomical pathology. Three-dimensional printing (3DP), generating physical replicas from data, offers a valuable tool for illustrating intricate anatomical structures and spatial relationships in the classroom. This study explores the integration of 3DP with CBL teaching for clinical medical undergraduates.
Sixty senior clinical medical undergraduates were randomly assigned to the CBL group and the CBL-3DP group. Computed tomography imaging data from a typical TOF case were exported, processed, and utilized to create four TOF models with a color 3D printer. The CBL group employed CBL teaching methods, while the CBL-3DP group combined CBL with 3D-printed models. Post-class exams and questionnaires assessed the teaching effectiveness of both groups.
The CBL-3DP group exhibited improved performance in post-class examinations, particularly in pathological anatomy and TOF imaging data analysis ( P < 0.05). Questionnaire responses from the CBL-3DP group indicated enhanced satisfaction with teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities ( P < 0.05). These findings underscore the potential of 3D printed models to augment the effectiveness of CBL, aiding students in mastering instructional content and bolstering their interest and self-confidence in learning.
The fusion of CBL with 3D printing models is feasible and effective in TOF instruction to clinical medical undergraduates, and worthy of popularization and application in medical education, especially for courses involving intricate anatomical components.
Peer Review reports
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease(CHD) [ 1 ]. Characterized by four structural anomalies: ventricular septal defect (VSD), pulmonary stenosis (PS), right ventricular hypertrophy (RVH), and overriding aorta (OA), TOF is a focal point and challenge in medical education. Understanding anatomical spatial structures is pivotal for learning and mastering TOF [ 2 ]. Given the constraints of course duration, medical school educators aim to provide students with a comprehensive and intuitive understanding of the disease within a limited timeframe [ 3 ].
The case-based learning (CBL) teaching model incorporates a case-based instructional approach that emphasizes typical clinical cases as a guide in student-centered and teacher-facilitated group discussions [ 4 ]. The CBL instructional methods have garnered widespread attention in medical education as they are particularly appropriate for preclinical training in undergraduate medical education [ 5 , 6 ]. The collection of case data, including medical records and examination results, is essential for case construction [ 7 ]. The anatomical and hemodynamic consequences of TOF can be determined using ultrasonography, computed tomography (CT), and magnetic resonance imaging techniques. However, understanding the anatomical structures from imaging data is a slow and challenging psychological reconstruction process for undergraduate medical students [ 8 ]. Three-dimensional (3D) visualization is valuable for depicting anatomical structures [ 9 ]. 3D printing (3DP), which creates physical replicas based on data, facilitates the demonstration of complex anatomical structures and spatial relationships in the classroom [ 10 ].
During the classroom session, 3D-printed models offer a convenient means for hands-on demonstration and communication, similar to facing a patient, enhancing the efficiency and specificity of intra-team communication and discussion [ 11 ]. In this study, we printed TOF models based on case imaging data, integrated them into CBL teaching, and assessed the effectiveness of classroom instruction.
Research participants
The study employed a prospective, randomized controlled design which received approval from the institutional ethics committee. Senior undergraduate students majoring in clinical medicine at Wannan Medical College were recruited for participation based on predefined inclusion criteria. The researchers implemented recruitment according to the recruitment criteria by contacting the class leaders of the target classes they had previously taught. Notably, these students were in their third year of medical education, with anticipation of progressing to clinical courses in the fourth year, encompassing Internal Medicine, Surgery, Obstetrics, Gynecology, and Pediatrics. Inclusion criteria for participants encompassed the following: (1) proficient communication and comprehension abilities, (2) consistent attendance without absenteeism or truancy, (3) absence of failing grades in prior examinations, and (4) capability to conscientiously fulfill assigned learning tasks. Exclusion criteria were (1) absence from lectures, (2) failure to complete pre-and post-tests, and (3) inadequate completion of questionnaires. For their participation in the study, Students were provided access to the e-book “Localized Anatomy,” authored by the investigators, as an incentive for their participation. Voluntary and anonymous participation was emphasized, with participants retaining the right to withdraw from the study at any time without providing a reason.
The study was conducted between May 1st, 2023, and June 30, 2023, from recruitment to completion of data collection. Drawing upon insights gained from a previous analogous investigation which yielded an effect size of 0.95 [ 10 ]. Sample size was computed, guided by a statistical consultant, with the aim of 0.85 power value, predicated on an effect size of 0.8 and a margin of error set at 0.05. A minimum of 30 participants per group was calculated using G*Power software (latest ver. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), resulting in the recruitment of a total of 60 undergraduate students. Each participant was assigned an identification number, with codes placed in boxes. Codes drawn from the boxes determined allocation to either the CBL group or the CBL-3DP group. Subsequently, participants were randomly assigned to either the CBL group, receiving instruction utilizing the CBL methodology, or the CBL-3DP group, which received instruction integrating both CBL and 3D Printed models.
Printing of TOF models
Figure 1 A shows the printing flowchart of the TOF models. A typical TOF case was collected from the Yijishan Hospital of Wannan Medical College. The CT angiography imaging data of the case was exported. Mimics Research 20.0 software (Mimics Innovation Suite version 20, Materialize, Belgium) was used for data processing. The cardiovascular module of the CT-Heart tool was employed to adjust the threshold range, independently obtain the cardiac chambers and vessels, post-process the chambers and vessels to generate a hollow blood pool, and merge it with the myocardial volume to construct a complete heart model. The file was imported into Magics 24.0 software (version 24.0; Materialize, Belgium) for correction using the Shell tool page. After repairs, the model entered the smoothing page, where tools such as triangular surface simplification, local smoothing, refinement and smoothing, subdivision of components, and mesh painting were utilized to achieve varying degrees of smoothness. Finally, optimized data were obtained and exported as stereolithography (STL) files. An experienced cardiothoracic surgeon validated the anatomical accuracy of the digital model.
The STL files were imported into a 3D printer (J401Pro; Sailner 3D Technology, China) for model printing. This printer can produce full-color medical models using different materials. The models were fabricated using two distinct materials: rigid and flexible. Both materials are suitable for the observational discussion of the teaching objectives outlined in our study. From the perspective of observing pathological changes in the TOF, there is no significant difference between the two materials.
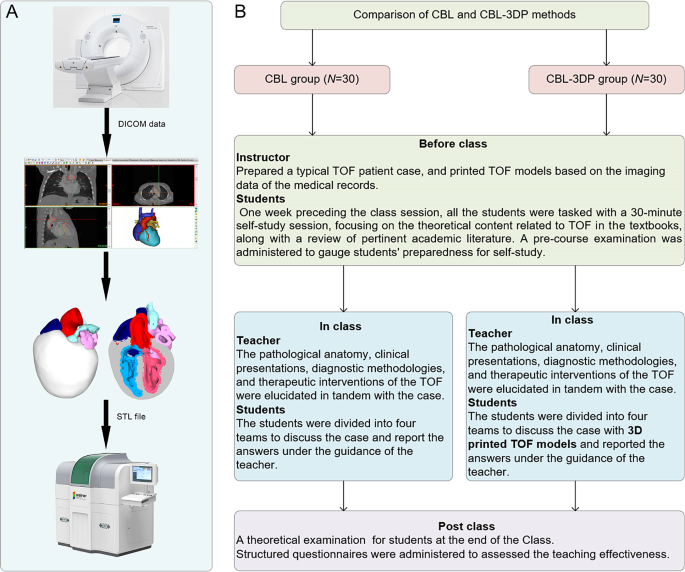
Experimental flow chart of this study. A TOF model printing flow chart. B The instructional framework
Teaching implementation
Figure 1 B illustrates the instructional framework employed in this study. One week preceding the class session, all the students were tasked with a 30-minute self-study session, focusing on the theoretical content related to TOF as outlined in the Pediatrics and Surgery textbooks, along with a review of pertinent academic literature. Both groups received co-supervision from two basic medicine lecturers boasting over a decade of teaching experience, alongside a senior cardiothoracic surgeon. Teaching conditions remained consistent across groups, encompassing uniform assessment criteria and adherence to predefined teaching time frames, all conducted in a Project-Based Learning (PBL) classroom at Wannan Medical College. Additionally, a pre-course examination was administered to gauge students’ preparedness for self-study.
In adherence to the curriculum guidelines, the teaching objectives aimed to empower students to master TOF’s clinical manifestations, diagnostic modalities, and differential diagnoses, while acquainting them with treatment principles and surgical methodologies. Additionally, the objectives sought to cultivate students’ clinical reasoning abilities and problem-solving skills. the duration of instruction for the TOF theory session was standardized to 25 min. The didactic content was integrated with the TOF case study to construct a coherent pedagogical structure.
During the instructional session, both groups underwent teaching utilizing the CBL methodology. Clinical manifestations and case details of TOF cases were presented to stimulate students’ interest and curiosity. Subsequently, the theory of TOF, including its etiology, pathogenesis, pathologic anatomy, clinical manifestations, diagnostic methods, and therapeutic interventions, was briefly elucidated. Emphasis was then placed on the case, wherein selected typical TOF cases were explained, guiding students in analysis and discussion. Students were organized into four teams under the instructors’ supervision, fostering cooperative learning and communication, thereby deepening their understanding of the disease through continuous inquiry and exploration (Fig. 2 L). In the routinely equipped PBL classroom with standard heart models (Fig. 2 J, K), all students had prior exposure to human anatomy and were familiar with these models. Both groups were provided with four standard heart models for reference, while the CBL-3DP group received additional four 3D-printed models depicting TOF anomalies, enriching their learning experience (Fig. 2 D, G). After the lesson, summarization, and feedback sessions were conducted to consolidate group discussions’ outcomes, evaluate teaching effectiveness, and assess learning outcomes.
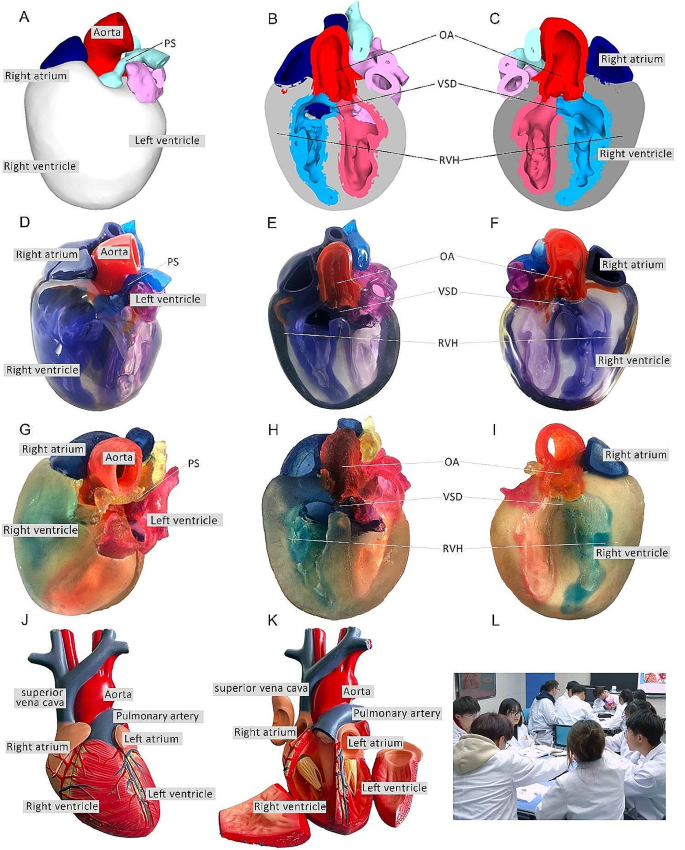
Heart models utilized in instructional sessions. A External perspective of 3D digital models. B, C Cross-sectional views following trans-septal sagittal dissection of the 3D digital model (PS: Pulmonary Stenosis; OA: Overriding Aorta; VSD: Ventricular Septal Defect; RVH: Right Ventricular Hypertrophy). D External depiction of rigid 3D printed model. E, F Sagittal sections of the rigid 3D printed model. G External portrayal of flexible 3D printed model. H, I Sagittal sections of the flexible 3D printed model. J, K The normal heart model employed in the instruction of the CBL group. L Ongoing classroom session
Teaching effectiveness assessment
Following the instructional session, participants from the two groups underwent a theoretical examination to assess their comprehension of the taught material. This assessment covered domains such as pathological anatomy, clinical manifestations, imaging data interpretation, diagnosis, and treatment relevant to TOF. Additionally, structured questionnaires were administered to evaluate the efficacy of the pedagogical approach employed. The questionnaire consisted of six questions designed to gauge participants’ understanding of the teaching content, enhancement of diagnostic skills, cultivation of critical thinking and clinical reasoning abilities, bolstering of confidence in managing TOF cases, satisfaction with the teaching mode, and satisfaction with the CBL methodology.
The questionnaire employed a 5-point Likert scale to gauge responses, with 5 indicating “strongly satisfied/agree,” 4 for “satisfied/agree,” 3 denoting “neutral,” 2 reflecting “dissatisfied/disagree,” and 1 indicating “strongly dissatisfied/disagree.” It comprised six questions, with the initial two probing participants’ knowledge acquisition, questions 3 and 4 exploring satisfaction regarding enhanced competence, and the final two assessing satisfaction with teaching methods and modes. Additionally, participants were encouraged to provide suggestions at the end of the questionnaire. To ensure the questionnaire’s validity, five esteemed lecturers in basic medical sciences with more than 10 years of experience verified its content and assessed its Content Validity Ratio and Content Validity Index to ensure alignment with the study’s objectives.
Statistical analysis
Statistical analyses were conducted utilizing GraphPad Prism 9.0 software. Aggregate score data for both groups were presented as mean ± standard deviation (x ± s). The gender comparisons were analyzed with the chi-square (χ2) test, while the other variables were compared using the Mann-Whitney U test. The threshold for determining statistical significance was set at P < 0.05.
Three-dimensional printing models
After configuring the structural colors of each component (Fig. 2 A, B, C), we printed four color TOF models using both rigid and flexible materials, resulting in four life-sized TOF models. Two color TOF models were created using rigid materials (Fig. 2 D, E, F). These models, exhibiting resistance to deformation, and with a firm texture, smooth and glossy surface, and good transparency, allowing visibility of the internal structures, were deemed conducive to teaching and observation. We also fabricated two color TOF models using flexible materials (Fig. 2 G, H, I), characterized by soft texture, opacity, and deformability, allowing for easy manipulation and cutting. It has potential utility beyond observational purposes. It can serve as a valuable tool for simulating surgical interventions and may be employed to create tomographic anatomical specimens. In this study, both material models were suitable for observation in the classroom. The participants were able to discern the four pathological changes characteristic of TOF from surface examination or cross-sectional analysis.
Baseline characteristics of the students
In total, 60 students were included in this study. The CBL group comprised 30 students (14 males and 16 females), with an average age of (21.20 ± 0.76) years. The CBL-3DP group consisted of 30 students (17 males and 13 females) with an average age of 20.96 years. All the students completed the study procedures. There were no significant differences in age, sex ratio, or pre-class exam scores between the two groups ( P > 0.05), indicating that the baseline scores between the two groups were comparable (Table 1 ).
Theoretical examination results
All students completed the research procedures as planned. The post-class theoretical examination encompassed assessment of pathological anatomy, clinical presentations, imaging data interpretation, diagnosis, and treatment pertinent to TOF. Notably, no statistically significant disparities were observed in the scores on clinical manifestations, diagnosis and treatment components between the cohorts, as delineated in Table 2 . Conversely, discernible distinctions were evident whereby the CBL-3DP group outperformed the CBL group notably in pathological anatomy, imaging data interpretation, and overall aggregate scores ( P < 0.05).
Results of the questionnaires
All the 60 participants submitted the questionnaire. Comparing the CBL and CBL-3DP groups, the scores from the CBL-3DP group showed significant improvements in many areas. This included satisfaction with the teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities (Fig. 3 B, C, D, E). All of which improved significantly ( P < 0.05 for the first aspects and P < 0.01 for the rest). However, the two groups were not comparable ( P > 0.05) in terms of understanding of the teaching content and Satisfaction with the CBL methodology (Fig. 3 A, F).
Upon completion of the questionnaires, participants were invited to proffer recommendations. Notably, in the CBL group, seven students expressed challenges in comprehending TOF and indicated a need for additional time for consolidation to enhance understanding. Conversely, within the CBL-3DP group, twelve students advocated for the augmentation of model repertoire and the expansion of disease-related data collection to bolster pedagogical efficacy across other didactic domains.
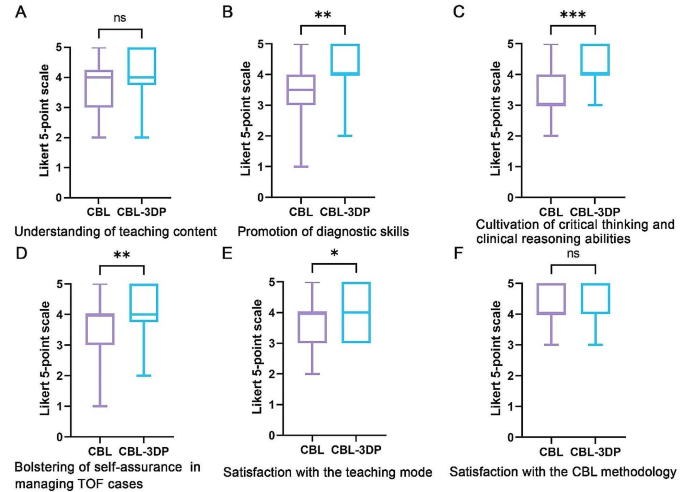
Five-point Likert scores of students’ attitudes in CBL ( n = 30) and CBL-3DP ( n = 30) groups. A Understanding of teaching content. B Promotion of diagnostic skills. C Cultivation of critical thinking and clinical reasoning abilities. D Bolstering of self-assurance in managing TOF cases. E Satisfaction with the teaching mode. F Satisfaction with the CBL methodology. ns No significant difference, * p < 0.05, ** p < 0.01, *** p < 0.001
TOF presents a significant challenge in clinical practice, necessitating a comprehensive understanding for effective diagnosis and treatment [ 12 ]. Traditional teaching methods in medical schools have relied on conventional resources such as textbooks, 2D illustrations, cadaver dissections, and radiographic materials to impart knowledge about complex conditions like TOF [ 13 ]. However, the limitations of these methods in fully engaging students and bridging the gap between theoretical knowledge and practical application have prompted a need for innovative instructional approaches.
CBL has emerged as a valuable tool in medical education, offering students opportunities to engage with authentic clinical cases through group discussions and inquiry-based learning [ 14 ]. By actively involving students in problem-solving and decision-making processes, CBL facilitates the application of theoretical knowledge to real-world scenarios, thus better-preparing students for future clinical practice [ 15 ]. Our investigation revealed that both groups of students exhibited comparable levels of satisfaction with the CBL methodology, devoid of discernible disparities.
CHD presents a formidable challenge due to the intricate nature of anatomical anomalies, the diverse spectrum of conditions, and individual variations [ 16 ]. Utilizing 3D-printed physical models, derived from patient imaging data, can significantly enhance comprehension of complex anatomical structures [ 17 ]. These models have proven invaluable in guiding surgical planning, providing training for junior or inexperienced pediatric residents, and educating healthcare professionals and parents of patients [ 18 ]. Studies indicate that as much as 50% of pediatric surgical decisions can be influenced by the insights gained from 3D printed models [ 19 ]. By providing tangible, anatomically accurate models, 3D printing offers a unique opportunity for people to visualize complex structures and enhance their understanding of anatomical intricacies. Our study utilized full-color, to-scale 3D printed models to illustrate the structural abnormalities associated with TOF, thereby enriching classroom sessions and facilitating a deeper comprehension of the condition.
Comparative analysis between the CBL-3DP group and the CBL group revealed significant improvements in post-test performance, particularly in pathological anatomy and imaging data interpretation. Additionally, questionnaire responses indicated higher levels of satisfaction and confidence among students in the CBL-3DP group, highlighting the positive impact of incorporating 3D printed models into the learning environment, improving the effectiveness of CBL classroom instruction. Despite the merits, our study has limitations. Primarily, participants were exclusively drawn from the same grade level within a single college, possibly engendering bias owing to shared learning backgrounds. Future research could further strengthen these findings by expanding the sample size and including long-term follow-up to assess the retention of knowledge and skills. Additionally, the influence of the 3D models depicting a normal heart on the learning process and its potential to introduce bias into the results warrants consideration, highlighting a need for scrutiny in subsequent studies.
As medical science continues to advance, the need for effective teaching methods becomes increasingly paramount. Our study underscores the potential of combining active learning approaches like CBL with innovative technologies such as 3D printing to enhance teaching effectiveness, improve knowledge acquisition, and foster students’ confidence and enthusiasm in pursuing clinical careers. Moving forward, further research and integration of such methodologies are essential for meeting the evolving demands of medical education, especially in areas involving complex anatomical understanding.
Conclusions
Integrating 3D-printed models with the CBL method is feasible and effective in TOF instruction. The demonstrated success of this method warrants broad implementation in medical education, particularly for complex anatomical topics.
Data availability
All data supporting the conclusions of this research are available upon reasonable request from the corresponding author.
Apitz C, Webb GD, Redington AN. Tetralogy of Fallot. Lancet. 2009;374:1462–71.
Article Google Scholar
Ghosh RM, Jolley MA, Mascio CE, Chen JM, Fuller S, Rome JJ, et al. Clinical 3D modeling to guide pediatric cardiothoracic surgery and intervention using 3D printed anatomic models, computer aided design and virtual reality. 3D Print Med. 2022;8:11.
Chakrabarti R, Wardle K, Wright T, Bennie T, Gishen F. Approaching an undergraduate medical curriculum map: challenges and expectations. BMC Med Educ. 2021;21:341.
Donkin R, Yule H, Fyfe T. Online case-based learning in medical education: a scoping review. BMC Med Educ. 2023;23:564.
Novack JP. Designing cases for case-based immunology teaching in large medical school classes. Front Immunol. 2020;11:995.
Chen HC, Van Den Broek WES, Ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90:431–6.
Wang M, Sun Z, Jia M, Wang Y, Wang H, Zhu X, et al. Intelligent virtual case learning system based on real medical records and natural language processing. BMC Med Inf Decis Mak. 2022;22:60.
Yoo S-J, Thabit O, Kim EK, Ide H, Yim D, Dragulescu A, et al. 3D printing in medicine of congenital heart diseases. 3D Print Med. 2015;2:3.
Yammine K, Violato C. A meta-analysis of the educational effectiveness of three-dimensional visualization technologies in teaching anatomy. Anat Sci Educ. 2015;8:525–38.
Miao H, Ding J, Gong X, Zhao J, Li H, Xiong K, et al. Application of 3D-printed pulmonary segment specimens in experimental teaching of sectional anatomy. BMC Surg. 2023;23:109.
Sun Z, Wong YH, Yeong CH. Patient-specific 3D-printed low-cost models in medical education and clinical practice. Micromachines (Basel). 2023;14:464.
Downing TE, Kim YY. Tetralogy of Fallot: general principles of management. Cardiol Clin. 2015;33:531–41. vii–viii.
Jia X, Zeng W, Zhang Q. Combined administration of problem- and lecture-based learning teaching models in medical education in China: a meta-analysis of randomized controlled trials. Med (Baltim). 2018;97:e11366.
McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD.S20377.
Zeng N, Lu H, Li S, Yang Q, Liu F, Pan H, et al. Application of the combination of CBL teaching method and SEGUE framework to improve the doctor-patient communication skills of resident physicians in otolaryngology department. Bmc Med Educ. 2024;24:201.
Sun Z. Patient-specific 3D-printed models in pediatric congenital heart disease. Children. 2023;10:319.
Meyer-Szary J, Luis MS, Mikulski S, Patel A, Schulz F, Tretiakow D, et al. The role of 3D printing in planning complex medical procedures and training of medical professionals—cross-sectional multispecialty review. IJERPH. 2022;19:3331.
Sun Z, Wee C. 3D printed models in cardiovascular disease: an exciting future to deliver personalized medicine. Micromachines-basel. 2022;13:1575.
Valverde I, Gomez-Ciriza G, Hussain T, Suarez-Mejias C, Velasco-Forte MN, Byrne N, et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicentre study. Eur J Cardio-thorac. 2017;52:1139–48.
Download references
Acknowledgements
We extend our sincere appreciation to the instructors and students whose invaluable participated in this study.
This paper received support from the Education Department of Anhui Province, China (Grant Numbers 2022jyxm1693, 2022jyxm1694, 2022xskc103, 2018jyxm1280).
Author information
Jian Zhao and Xin Gong are joint first authors.
Authors and Affiliations
Department of Human Anatomy, Wannan Medical College, No.22 West Wenchang Road, Wuhu, 241002, China
Jian Zhao, Xin Gong, Jian Ding, Rui Huang & Huachun Miao
Department of Cardio-Thoracic Surgery, Yijishan Hospital of Wannan Medical College, Wuhu, China
Kepin Xiong
Zhuhai Sailner 3D Technology Co., Ltd., Zhuhai, China
Kangle Zhuang
School of Basic Medical Sciences, Wannan Medical College, Wuhu, China
You can also search for this author in PubMed Google Scholar
Contributions
Jian Zhao and Huachun Miao designed the research. Jian Zhao, Xin Gong, Jian Ding, Kepin Xiong designed the tests and questionnaires. Kangle Zhuang processed the imaging data and printed the models. Xing Gong and Kepin Xiong implemented the teaching. Jian Zhao and Rui Huang collected the data and performed the statistical analysis. Jian Zhao and Huachun Miao prepared the manuscript. Shu Li and Huachun Miao revised the manuscript. Shu Li provided the Funding acquisition. All authors reviewed and approved the final manuscript.
Corresponding authors
Correspondence to Shu Li or Huachun Miao .
Ethics declarations
Ethics approval and consent to participate.
This investigation received ethical approval from the Ethical Committee of School of Basic Medical Sciences, Wannan Medical College (ECBMSWMC2022-1-12). All methodologies adhered strictly to established protocols and guidelines. Written informed consent was obtained from the study participants to take part in the study.
Consent for publication
Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhao, J., Gong, X., Ding, J. et al. Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial. BMC Med Educ 24 , 571 (2024). https://doi.org/10.1186/s12909-024-05583-z
Download citation
Received : 03 March 2024
Accepted : 21 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s12909-024-05583-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Case-based learning
- 3D printing
- Tetralogy of fallot
- Medical undergraduates
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Medical problem solving : an analysis of clinical reasoning ... Medical problem solving : an analysis of clinical reasoning by Elstein, Arthur S. (Arthur Shirle), 1935-Publication date 1978 Topics Diagnostics, Résolution de problème, 44.51 medical diagnostic, Geneeskunde, Diagnose, Probleemoplossing, ...
Medical Problem Solving An Analysis of Clinical Reasoning Arthur S. Elstein Lee S. Shulman Sarah A. Sprafka with Linda Allal Michael Gordon Hilliard Jason Norman Kagan Michael J Loup. e Ronald D. Jordan Harvard Universit Presy s Cambridge, Massachusetts and London, England 1978
Medical Problem Solving, An Analysis of Clinical Reasoning, by Arthur S. Elstein, Lee S. Shulman, and Sarah A. Sprafka. Cambridge, Mass.: Harvard University Press, 1978. 330 pages. $22.50. Reviewed by Wellesley R. Foshay Of the various learning tasks for which instructional developers design instruction, problem solving is perhaps the least ...
Medical Problem Solving: An Analysis of Clinical Reasoning, Cambridge, MA and London, England: Harvard University Press, ... Medical Problem Solving: An Analysis of Clinical Reasoning. Cambridge, MA and London, England: Harvard University Press, 1978. ... Licensed Download PDF: 1: 2. Research in Problem Solving, Judgment, and Decision Making ...
Elstein, Arthur S., Lee S. Shulman, and Sarah A. Sprafka, et al. Medical Problem Solving: An Analysis of Clinical Reasoning. Cambridge, Massachusetts: Harvard ...
Medical Problem Solving studies from the perspective of cognitive psychol-ogy the processes by which physicians make clinical diagnosis decisions. The book reports on a series of studies begun in the early 1970s. It finds little support for the notion that clinical knowledge represents a systematic
PDF (169K) Actions. Cite; Collections. ... an NLM database does not imply endorsement of, or agreement with, the contents by NLM or the National Institutes of Health. Learn more: PMC ... Bull N Y Acad Med. 1979 Oct; 55(9): 886-887. PMCID: PMC1807707. Medical Problem Solving: An Analysis of Clinical Reasoning. Reviewed by David L. Post.
The first comprises narratives or reports of interesting or puzzling cases, clinical mysteries that are somehow explicated by the clever reasoning of an expert. The narrative includes both the solution of the mystery and the problem solver's account of how the puzzle was unraveled.
This paper has five objectives: (a) to review the scientific background of, and major findings reported in, Medical Problem Solving, now widely recognized as a classic in the field; (b) to compare these results with some of the findings in a recent best-selling collection of case studies; (c) to summarize criticisms of the hypothesis-testing model and to show how these led to greater emphasis ...
Medical Problem Solving: An Analysis of Clinical Reasoning. Arthur S. Elstein , Lee S. Shulman , Sarah A. Sprafka
PDF | On Jan 1, 1980, Wellesley R. Foshay published Medical Problem Solving, an Analysis of Clinical Reasoning by Arthur S. Elstein; Lee S. Shulman; Sarah A. Sprafka | Find, read and cite all the ...
This essay reviews the origins, findings and influence of the monograph Medical Problem Solving: An Analysis of Clinical Reasoning. Majorfindings of the monograph are reviewed in the light of subsequent work and the results of selected studies of clinical cognition are related to the book's conclusions, thus sketching the growth of this field of research in the decade since publication.
Medical Problem Solving: An Analysis of Clinical Reasoning Arthur Shirle Elstein , Lee S. Shulman , Sarah A. Sprafka Harvard University Press , 1978 - Medical - 330 pages
The authors describe how scripts are used in diagnostic tasks, how the script concept fits within the clinical reasoning literature, how it contrasts with competing theories of clinical reasoning, how educators can help students build and refine scripts, and how scripts can be used to assess clinical competence. Expand
Medical Problem Solving: An Analysis of Clinical Reasoning. Elstein AS, ed. Cambridge, MA: Harvard University Press; 1978. ISBN: 9780674561250. Elstein AS, ed. Cambridge, MA: Harvard University Press; 1978. ISBN: 9780674561250. View more articles from the same authors. Clinical reasoning lies at the heart of formulating diagnoses and selecting ...
This chapter introduces the concept of clinical reasoning. It attempts to define what clinical reasoning is and what its features are. Solving clinical problems involves the ability to reason about causality of pathological processes, requiring knowledge of anatomy and the working and pathology of organ systems, and it requires the ability to compare patient problems as patterns with instances ...
Medical Problem Solving An Analysis of Clinical Reasoning. Arthur S. Elstein, Lee S. Shulman and Sarah A. Sprafka; In collaboration with: Linda Allal, Michael Gordon, Jason Hilliard, Norman Kagan, Michael J. Loupe and Ronald D. Jordan
Clinical Problem Solving and Decision Psychology: Comment on "The Epistemology of Clinical Reasoning" Elstein, Arthur S. (2000-10) Related Items in Google Scholar ©2009—2024 Bioethics Research Library ... Medical Problem Solving: An Analysis of Clinical Reasoning. Creator. Elstein, Arthur S. Shulman, Lee S. and Sprafka, Sarah A.
Rather than a historical overview as in Chap. 2, this chapter provides the reader with insight into the various approaches that have been used to understand clinical reasoning. We review concepts and major scholars who have been involved in such investigations. Cognitive psychologists Newel and Simon theorized about problem-solving skills and artificial intelligence and initiated the use of ...
This is the fourth in a series of five articles This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential ...
This is the book that many people in the world waiting for to publish, medical problem solving an analysis of clinical reasoning, and the book lovers are really curious to see how this book is actually. Now welcome, the most inspiring book today from a very professional writer in the world, medical problem solving an analysis of clinical reasoning. This is the book that many people in the ...
Background. Clinical reasoning refers to 'the cognitive process that is necessary to evaluate and manage a patient's medical problem' Citation 1.It allows physicians to make diagnoses and decisions (e.g. laboratory tests and drug prescriptions), and is considered as one of the major determining factors of clinical competence Citation 2.Many researchers - including health professionals ...
Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid cognitive ...
DOI: 10.1016/j.teln.2024.04.010 Corpus ID: 269581511; Questioning Training and Critical Thinking of Undergraduate Students of Health and Social Sciences: A Scoping Review @article{Ishtiaq2024QuestioningTA, title={Questioning Training and Critical Thinking of Undergraduate Students of Health and Social Sciences: A Scoping Review}, author={Muhammad Ishtiaq and Raisa Gul and Janet Holt and ...
Additionally, the objectives sought to cultivate students' clinical reasoning abilities and problem-solving skills. the duration of instruction for the TOF theory session was standardized to 25 min. The didactic content was integrated with the TOF case study to construct a coherent pedagogical structure.