Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .

Health economics
- Health care
- Health care sector
- Health insurance
- Pharmacoeconomics
- Get an email alert for Health economics
- Get the RSS feed for Health economics
Showing 1 - 13 of 2,985
View by: Cover Page List Articles
Sort by: Recent Popular
Development of a conceptual framework for defining trial efficiency
Charis Xuan Xie, Anna De Simoni, [ ... ], Clare Relton
Factors associated with the enrollment of commercial medical insurance in China: Results from China General Social Survey
Songyue Xue, Wu Zeng, [ ... ], Guanyang Zou
A cost-benefit analysis of WildFireSat, a wildfire monitoring satellite mission for Canada
Emily S. Hope, Daniel W. McKenney, Lynn M. Johnston, Joshua M. Johnston
The impact of long-term care insurance on family care for older adults: The mediating role of intergenerational financial support
Lianjie Wang, Jing Liu
The effects of digital economy development on social insurance funds revenue: Evidence from China
Xiaoqing Pan, Bo Li, Jing Wu
Inequality of the crowding-out effect of tobacco expenditure in Colombia
Juan Miguel Gallego, Guillermo Paraje, Paul Rodríguez-Lesmes
An assessment of the direct and indirect costs of breast cancer treatment in leading cancer hospitals in Ghana
Patience Gyamenah Okyere Asante, Adobea Yaa Owusu, [ ... ], Edward Nketiah-Amponsah
Impact of aging on acute myeloid leukemia epidemiology and survival outcomes: A real-world, population-based longitudinal cohort study
Hyun Jin Han, Kyungson Choi, Hae Sun Suh
Public attitudes toward medical waste: Experiences from 141 countries
Zhipeng Bai, Xi Liu, Wenbao Ma
Measurement and determinants of multidimensional urban poverty: Evidence from Shandong Province, China
Bo Zhao, Phaik Kin Cheah, Priscilla Moses

Experience of healthcare personnel on Co-payment mechanism and the implications on its use in private drug outlets in Uganda
Moses Ocan, Racheal Bakubi, [ ... ], Nsobya Sam
Individual and community level determinants of delayed antenatal care initiation in Ethiopia: A multilevel analysis of the 2019 Ethiopian Mini Demographic Health Survey
Addisu Alehegn Alemu, Liknaw Bewket Zeleke, [ ... ], Marjan Khajehei
Evaluating digital literacy of health professionals in Ethiopian health sectors: A systematic review and meta-analysis
Alex Ayenew Chereka, Agmasie Damtew Walle, [ ... ], Mathias Nega Tadesse
Connect with Us
- PLOS ONE on Twitter
- PLOS on Facebook
- Frontiers in Public Health
- Health Economics
- Research Topics
Insights in Health Economics: 2021
Total Downloads
Total Views and Downloads
About this Research Topic
We are now entering the third decade of the 21st Century, and, especially in the last years, the achievements made by scientists have been exceptional, leading to major advancements in the fast-growing field of Health Economics. Frontiers has organized a series of Research Topics to highlight the latest ...
Keywords : health economics, health financing, health systems
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
- Open access
- Published: 14 May 2024
An overview of the perspectives used in health economic evaluations
- Manit Sittimart 1 ,
- Waranya Rattanavipapong 1 ,
- Andrew J. Mirelman 2 ,
- Trinh Manh Hung 3 ,
- Saudamini Dabak 1 ,
- Laura E. Downey 4 , 5 ,
- Mark Jit 6 , 7 ,
- Yot Teerawattananon 1 , 8 &
- Hugo C. Turner 9
Cost Effectiveness and Resource Allocation volume 22 , Article number: 41 ( 2024 ) Cite this article
459 Accesses
2 Altmetric
Metrics details
The term ‘perspective’ in the context of economic evaluations and costing studies in healthcare refers to the viewpoint that an analyst has adopted to define the types of costs and outcomes to consider in their studies. However, there are currently notable variations in terms of methodological recommendations, definitions, and applications of different perspectives, depending on the objective or intended user of the study. This can make it a complex area for stakeholders when interpreting these studies. Consequently, there is a need for a comprehensive overview regarding the different types of perspectives employed in such analyses, along with the corresponding implications of their use. This is particularly important, in the context of low-and-middle-income countries (LMICs), where practical guidelines may be less well-established and infrastructure for conducting economic evaluations may be more limited. This article addresses this gap by summarising the main types of perspectives commonly found in the literature to a broad audience (namely the patient, payer, health care providers, healthcare sector, health system, and societal perspectives), providing their most established definitions and outlining the corresponding implications of their uses in health economic studies, with examples particularly from LMIC settings. We then discuss important considerations when selecting the perspective and present key arguments to consider when deciding whether the societal perspective should be used. We conclude that there is no one-size-fits-all answer to what perspective should be used and the perspective chosen will be influenced by the context, policymakers'/stakeholders’ viewpoints, resource/data availability, and intended use of the analysis. Moving forward, considering the ongoing issues regarding the variation in terminology and practice in this area, we urge that more standardised definitions of the different perspectives and the boundaries between them are further developed to support future studies and guidelines, as well as to improve the interpretation and comparison of health economic evidence.
What is the perspective in health economic evaluations?
Health economic analyses, particularly economic evaluations and costing studies, have an important role in investigating the value-for-money of health interventions and supporting decision-making surrounding resource allocation within the health sector [ 1 , 2 , 3 ]. Such studies are a key element of Health Technology Assessment (HTA) processes and other priority-setting or decision-making processes [ 1 , 4 , 5 ]. When conducting an economic evaluation of a particular health intervention or technology, understanding the perspective, or the point of view from which the evaluation is conducted is important, as it determines the boundary of the study and which types of costs and consequences/outcomes are included within the analysis [ 6 ]. Note that cost is a general term that refers to the value of resources/inputs used to produce a good or service. As different perspectives include (or exclude) different costs and outcomes, they can substantially influence the results of health economic studies and the subsequent recommendations and policies informed by these studies [ 7 ]. Therefore, it is vital that the perspective is carefully considered when conducting, reviewing, or interpreting health economic analyses.
Different types of perspectives have been adopted in health economic studies. However, there is no universally accepted “right” answer regarding which perspective should be applied, and this decision will depend on the context, type of analysis, decision-maker and question that the evaluation aims to answer [ 7 ]. Due to contextual considerations, the perspective is one of the methodological areas that exhibits the largest variation within the currently available guidelines for health economic studies [ 8 , 9 , 10 ]. Therefore, this is a potentially challenging area for stakeholders when conducting and/or interpreting these studies. Consequently, there is a need for an overview outlining the key types of perspectives, along with the corresponding implications of using different perspectives in health economic analyses. This is particularly important in the context of low-and-middle-income countries (LMICs), where there are less well-established guidelines and infrastructure (including data) for conducting economic evaluations and subsequently the potential for more variation in methodology between studies. To date, the Guide to Economic Analysis and Research (GEAR) resource has only identified 14 national guidelines from LMICs related to conducting health economic evaluations [ 11 ].
This article aims to outline and introduce the main types of perspectives used in economic evaluations, as well as to discuss their implications on cost-effectiveness calculations. We also outline ongoing issues and considerations related to perspectives that are important to be aware of when comparing and interpreting economic evaluations. It is expected that greater awareness of these concepts will lead to better consistency in future health economic studies and improve the interpretation and comparison of health economic evidence.
What are the main types of perspectives?
Here we provide a breakdown of the most commonly used perspectives within health economic evaluations and costing studies. These are derived from a review of key texts [ 8 , 12 , 13 ], and recommendations from multiple international and national economic evaluation guidelines listed in the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) and Guide to Economic Analysis and Research (GEAR) websites [ 11 , 14 , 15 ]. That said, it is important to note that there is variation in terminology used within the field to describe perspectives as well as other terms for perspectives not included here. We have endeavoured to highlight what we consider to be the most established definitions.
The differences between these perspectives relate to what cost (and cost saving) items may be included within an analysis. Figure 1 provides an overview of the different perspectives and the variation of included costs. In the context of cost-effectiveness and cost-utility analysis, the inclusion of non-monetary health outcomes (such as disability-adjusted life year (DALY), quality-adjusted life year (QALY) or cases averted) in the denominator of the cost-effectiveness ratio calculations would not typically be influenced by these perspectives whereas the costs in the numerator would be directly influenced.
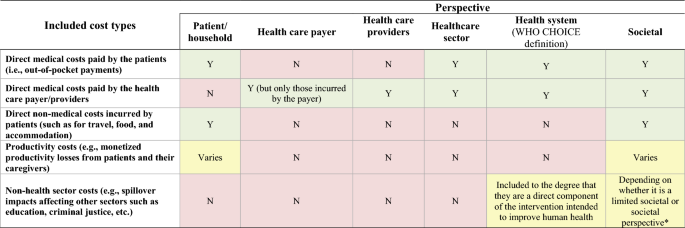
Overview of the different perspectives and the variation of included costs within economic evaluations. Y: Included; N: Not included; * The limited societal perspective excludes spillover impacts affecting sectors other than health care whereas the (non-limited) societal perspective includes the spillover impacts on at least one non-health care sector. Note that there is variation in terminology used within the field to describe these different perspectives as well as others not included here. Therefore, it is possible some studies would apply these perspectives differently to what we have outlined
Patient/household
The patient or household perspectives are used to describe the costs borne by individuals or their households, respectively. The patient perspective may be limited to the costs incurred by the patient whereas the household perspective also includes the costs incurred by other members of the household. This distinction is not always made as the terms are at times used interchangeably. Under the patient/household perspective, all costs that patients incur when facing a health issue could be included, such as direct medical costs that are not covered by the patient's health insurance (i.e., out-of-pocket costs, co-payments, and deductibles), direct non-medical costs (such as those from transport to health facilities), and potentially productivity costs—also known as indirect costs (i.e., monetised productivity losses resulting from lost paid and unpaid work due to an illness or an intervention). The extent to which these cost types are included depends on the type of study being conducted. Within the context of an economic evaluation of a health system intervention, all costs borne by the patient would be included. While the patient/household perspective is more likely to be used within cost-of-illness studies or analysis of patient health expenditure/analyses of financial risk protection [ 16 ], it is rarely applied within full economic evaluations. However, some have advocated for using this perspective in economic evaluations in the context of the increasing focus on patient-centred outcomes in health policy research [ 8 , 12 ].
Health care payer or payer
The health care payer perspective includes costs incurred by specific health care payer(s)—typically a third party, such as a specific health organisation, specific control programme or agency that manages an insurance programme [ 9 ]. This would include the costs incurred by a specific health care payer related to treatment, disease management or other health care services [ 9 , 16 ]. However, the costs that are not borne by this specific payer will not be considered (such as the out-of-pocket payments paid by patients). It is important to note that the payer perspective would only relate to the part of the organisation that the funds have been planned or budgeted for [ 17 ]. Therefore, it would capture the costs incurred by a specific control programme but not the costs incurred by the broader health care provider(s). It is noteworthy that in some settings there can be multiple relevant payers (such as multiple insurance programmes).
Health care provider(s)
The health care provider’s perspective will include all costs incurred by a given provider (or group of providers in the health system) in delivering care services to patients. Depending on the context, this can be the same as the health care payer perspective. However, the health care provider(s) perspective is usually broader in terms of its scope of costs included; as the payer perspective only relates to the specific part of the organisation that the funds have been planned/budgeted for [ 17 ]. The difference between the payer and provider perspectives will depend on the context of the study, but it is plausible that the provider’s perspective will give a more complete picture of total costs and hence is used more often in costing exercise [ 16 ].
Healthcare sector
The healthcare sector perspective is similar to the health care provider(s) perspective but broader and accounts for all the costs directly associated with the healthcare sector, regardless of who will bear such costs. This means that it not only includes the direct medical costs incurred by specific third-party payers (such as national health services), but it also includes the out-of-pocket payments for health care made by patients [ 9 ]. Costs that are not directly related to medical services/the health sector are considered outside of the scope of the healthcare sector perspective—such as costs related to the patients' travel or accommodation and productivity costs (indirect costs) [ 18 ]. The distinction between health care payer/provider and healthcare sector perspectives may be particularly important in LMIC settings where out-of-pocket payments by patients can be a significant source of health care expenditure [ 19 ].
Health system
The definition of the health system perspective is more variable within the literature [ 20 , 21 , 22 , 23 , 24 ]. The latest WHO-CHOICE guidelines [ 20 , 21 ] defined the health system perspective as including an ensemble of actions and actors whose primary intent is to improve human health. This therefore includes all direct, market-valued costs, whether public or private, that are required to deliver the intervention, regardless of payer. This would also cover the out-of-pocket payments for health care made by patients but would not account for the patients’ direct non-medical costs (such as travel-related costs), and productivity costs. This definition is subtly broader than the healthcare sector perspective (Fig. 1 ), as it can potentially include costs from other sectors when they are a direct component of the intervention intended to improve human health (e.g., the costs associated with developing health legislation and costs associated with regulation of health care and products) [ 20 ]. It is debatable how often these are included. Costs outside of the health system that are not primarily health oriented would not be included. It should be noted that in some cases, it is possible that the term health system perspective is being defined differently—such as to refer to the costs incurred by a particular publicly funded national healthcare provider. If this was the case, it could be more equivalent to the use of the health care provider(s) perspective as outlined above.
The societal perspective is the broadest and includes all healthcare-related costs, regardless of who is paying, including the patients'/caregivers’ costs for accessing an intervention (such as for travel and accommodation etc.) and their productivity costs [ 9 ]. This perspective can also potentially include other “relevant” non-health-related impacts in other sectors [ 25 ] such as those on social services, education, legal or criminal justice, environment, etc. In practice, there is variation in how far the societal perspective is taken and whether the impact on other sectors is included [ 13 ]. Kim et al. stratified the societal perspective by whether it is limited or not (Fig. 1 ) [ 9 ]. The limited societal perspective includes all healthcare-related costs (including the patients' costs) but excludes spillover impacts affecting sectors other than health care. In contrast, the (non-limited) societal perspective is broader and also includes the cost impacts on at least one non-healthcare sector [ 9 ]. In macroeconomic models, the societal perspective would also include the sectoral impact on other sectors due to changes in demand and supply in the economy [ 26 , 27 ].
It should be noted that there will be other types of perspectives not captured here that can fall in between these categories. For example, the National Institute for Health and Care Excellence (NICE) in the UK recommends “The perspective adopted on costs should be that of the NHS and personal social services.” [ 28 ]. This would be broader than the health system perspective as defined here as it includes the social care related costs, but not as broad as the societal perspective.
Some guidelines now recommend the use of a disaggregated societal perspective [ 29 , 30 ], where the costs and outcomes are disaggregated, either by sector of the economy or by who incurs them—and therefore it is possible to interest the results from a range of perspectives.
It should be noted that there are types of costs that may be excluded from the societal perspective [ 22 ]. For example, some interventions may result in transfer costs or payments; financial flows from one part of society to another, that do not consume resources but simply transfer the power to use resources from one person or sector to another (such as import tariffs as well as unemployment or sickness benefits) [ 31 ]. Transfer payments can be a cost to the paying government or control programme, but a financial gain to another sector or a patient. Therefore, because they do not use or create resources, transfer payments are typically not considered when estimating economic costs using a societal perspective [ 22 , 32 ], but can be included when using a narrower perspective (such as the health care payer perspective).
Implications on economic evaluations
There are several implications of the study perspective on health economic evaluations. The first is the scope of costs related to the intervention that are included. Generally, in terms of the cost of the intervention, the broader the perspective the higher the potential cost of the intervention (the impact will depend on the context). For example, when looking at the costs of providing a vaccine at a health clinic, the health care provider(s) perspective would only include the costs that are incurred by the government’s health service (such as those associated with the staff’s time, and the purchase of the vaccine etc.). However, under the societal perspective, the costs that are incurred by the patients in order to go to the clinic and get the vaccine would also be included (such as their travel costs and potentially their productivity costs associated with lost paid or unpaid work), increasing the overall cost of the intervention. Similarly, for cost-of-illness studies, the broader the perspective the wider the scope of costs included.
A related implication is that the choice of study perspective can have a significant impact on both the source of cost data and the method used for data collection. For example, this determines whether patient interviews may be needed. Having different sources of cost data and the way they are collected can contribute to the variation of cost values included in studies. For example, the costs for treating a patient at a hospital may be based on 'reimbursement rates’ under the payer perspective whereas the full cost of the resources utilised may be used under the health care provider perspective.
It is also important to note that, theoretically, the chosen perspective of an economic evaluation should not influence whether financial or economic costs should be adopted [ 33 ]. Nonetheless, the chosen perspective can influence how economic costs are valued and whether adjustments to market prices are required [ 33 ]. For example, if adopting the health care provider or payer perspective, it might be appropriate to use the market prices of a drug or vaccine that the provider has procured. However, if using the societal perspective, these prices may need to be adjusted to reflect their social opportunity costs (their value in their next best alternative use—only reflecting their short-run manufacturing and distribution costs), rather than their market price [ 22 , 34 ].
A further implication within economic evaluations is that the perspective will determine the consequences/outcomes that are included. A key example is that it affects if/what “cost savings” or cost offsets are included within the analysis. These “cost savings” are effectively deducted from the intervention cost within the cost-effectiveness ratios. These cost savings could include the costs associated with disease cases that are averted due to the intervention (for example in the case of measles vaccination, they would consider the cost savings associated with the averted measles cases that it prevents—such as the medical costs associated with hospitalised cases). The broader the perspective, the broader the types of costs included within these savings, and with the societal perspective, it can include prevented productivity costs that would have been associated with the morbidity and mortality of the cases and even costs outside the healthcare sector.
A further implication of the perspective is regarding the inclusion of future unrelated costs within these analyses [ 35 , 36 , 37 , 38 , 39 ]. Health interventions can increase the life expectancy of patients and consequently influence the consumption of both unrelated medical and non-medical resources during the additional lifetime they generate. These future unrelated costs are typically grouped into future medical costs (e.g., the costs of treating people with other future unrelated health conditions) and future non-medical costs (the costs related to consumption of non-medical resources, such as food, housing, utilities etc.). Which types of future unrelated costs that could be included within an economic evaluation, would be influenced by the perspective (with the societal perspective potentially including both future unrelated medical and non-medical costs). If these future costs are taken into account, adopting a broader perspective, could lead to a greater increase in the net cost of the intervention when it impacts the patient’s survival. This can therefore subsequently impact the estimated cost-effectiveness of the intervention. There is currently ongoing debate about the inclusion of these future unrelated costs in health economic analyses [ 35 , 36 , 37 , 38 , 39 ]. This debate and variation should be considered when interpreting different studies. The inclusion of future unrelated costs is still uncommon, and further guidance on this area is needed [ 35 ].
A particular area of debate is regarding the inclusion of future unrelated medical costs [ 35 ]. A key issue here is that the costs and outcomes of unrelated events in the future will depend on decisions not yet made and are therefore difficult to predict. This debate and variation should be considered when interpreting different studies.
Ultimately, although in some cases the use of different perspectives may only have a small impact on the cost-effectiveness ratios, it can also have a significant impact and could fundamentally change the conclusions of studies (Table 1 ). In some cases, broadening the perspective will not greatly change the estimated cost of the intervention, but could result in more cost-savings being included, resulting in the estimated cost-effectiveness ratio decreasing (Table 1 ). On the other hand, it is also possible that broadening the perspective would increase the cost of an intervention—potentially making its cost-effectiveness ratio increase (if this increase in the intervention cost outweighs any potential increase in the cost-savings). This relative impact and direction of the change on the cost-effectiveness ratio will depend on the context of the study and the intervention being investigated (Table 1 ). It should be noted that in some cases, health interventions may be estimated to be cost saving (i.e., have negative ICER values) even when using a more restricted perspective. For example, Owen et al. [ 40 ] found that among the cost-effectiveness analysis of public health interventions examined between 2005 to 2018 by the National Institute for Health and Care Excellence (NICE) in the UK, 21% were projected to generate cost savings even without using a societal perspective. In these cases, changing to a societal perspective would be unlikely to influence the results/policy recommendation. However, this will not always be the case and the perspective can have a significant impact (Table 1 ). This is particularly important to consider in countries in which the patients incur higher costs for assessing/receiving health care.
Due to this variation, if studies have used different perspectives, a direct comparison of results may be misleading. Of concern, even when the same perspective is reported to be used, the variation in the specific cost items included (Table 1 ) could still negatively impact the comparability of studies. A key driver in the variation of cost-effectiveness ratios between the use of the societal and other perspectives, is the specific types of costs being considered and if/what types of productivity costs are being included. Notably, there are issues surrounding the inclusion of productivity costs and potential double counting (outlined in Box 1). This highlights the importance of considering the perspective when comparing studies and the need to clearly report methodology regarding productivity costs.
Box 1: Issues surrounding productivity costs within economic evaluations (adapted from [ 46 ])
What is used in practice.
A review of the perspectives used in costing in cost-effectiveness analysis between 1974–2018 has been conducted by Kim et al. [ 9 ]. Interestingly, they found that studies often misspecified or did not clearly state the perspective used. After re-classification by registry reviewers, they found that a healthcare sector or payer perspective was the most common (74%) and that cost-effectiveness analysis rarely included impacts on non-healthcare sectors [ 9 ].
In terms of the available national economic evaluation guidelines (including from high income countries), a cross-country comparison by Sharma et al. [ 13 ] found that of the 31 guidelines they reviewed, 15 (48%) recommended using one of the non-societal perspectives (such as payer, health care provider health sector, health system etc.). However, the corresponding terminology used to describe these perspectives was variable. Three guidelines (10%) stated that any perspective relevant to the research question may be considered. Eight guidelines (26%) recommended using the societal perspective for the primary analysis, and 10 (26%) recommended using the societal perspective for additional analysis if required [ 13 ]. Yet, Sharma et al. also highlighted that even when the societal perspective was recommended, there was variation regarding the specific recommendations on the type of costs that should be included [ 13 ]. For example, the guidelines for Portugal recommended that intangible costs should also be included under the societal perspective [ 58 ], whereas the guidelines for Norway recommended using a societal perspective but the inclusion of productivity costs was optional [ 59 ]. In addition, while several guidelines recommended including all costs and outcomes within and outside the healthcare sector, others recommended for the more limited societal perspective excluding the impacts of the intervention on non-healthcare sectors [ 13 ]. This highlights the notable variation surrounding the societal perspective. A recent review of how the societal perspective is defined within guidelines by Avşar et al. also found substantial variation of the definition, including insufficient guidance on what to include under different perspectives [ 8 ]. Among 46 guidelines included in their review, the societal perspective featured in 30 guidelines, of which 21 (70%) explicitly considered this perspective (at times it was recommended within additional analysis). In several guidelines where productivity costs were allowed in additional analysis, this was usually referred to as a broader perspective (than healthcare), instead of explicitly defining it as a societal perspective. Interestingly, countries with multiple payers in the health systems were more likely to consider the societal perspective.
Table 2 highlights the recommendations regarding what perspective to use within key international/LMIC economic evaluation guidelines. The national economic evaluation guidelines were extracted from GEAR [ 11 ] (please note that some guidelines were not included as their text was not available in English). The focus on LMICs in Table 2 was chosen because literature providing contextual insights/case studies from LMICs are typically limited (despite the need for increased capacity in these settings). In terms of international guidelines, the WHO-CHOICE 2003 guidelines on cost-effectiveness analysis recommended using the societal perspective but excluding productivity costs [ 55 ]. The WHO-CHOICE's latest guidelines have now adopted a health system perspective [ 21 ]. In contrast, the International Decision Support Initiative (iDSI) reference case for economic evaluation recommended using a disaggregated societal perspective (where the costs and outcomes are disaggregated, either by sector of the economy or by who incurs them, making it possible to interpret the results from a range of perspectives) [ 29 , 30 ]. In terms of the available LMIC national economic evaluation guidelines, recommendations for the use of one of the non-societal perspectives were the most common. This could be because adopting these non-societal perspectives is relatively less complex and requires fewer data. That said, the societal perspective was recommended in several cases. In contrast, the perspective recommended for budget impact analysis is generally more consistent within guidelines, with the public payer or service purchaser perspectives typically recommended [ 60 ].
Selecting the perspective
In practice, it is important to note that there is no one-size-fits-all recommendation regarding what perspective should be used. The right perspective will depend on the research question, context, and goals of the decision-makers [ 7 , 34 , 71 ]. For example, if the goal is to understand the affordability of an intervention, the payer perspective may be the most appropriate.
When choosing the perspective, it is important to consider the role of patient out-of-pocket payments. Crucially, the payer and health care providers perspectives will not account for any costs paid by patients (including their out-of-pocket payments). They therefore may not be suitable for interventions that require co-payment by patients—as they will underestimate the cost of the intervention and potentially lead to inefficient policy recommendations. This is particularly important in a global heath context as patient out-of-pocket payments are one of the most critical healthcare funding sources in many LMICs [ 72 ]. In this context, at least the use of a healthcare sector perspective (if not a broader perspective) would be needed to account for these out-of-pocket payments (as outlined in Fig. 1 ).
Key considerations regarding navigating the use of societal perspective
In terms of selecting perspective, it should be noted that there is ongoing debate regarding the role of the societal perspective and when it should be used. The societal perspective is often referred to as the gold standard for economic evaluations [ 73 , 74 , 75 ] and recommended in several guidelines. The reasons for this relate to the fact that it considers a more complete picture of costs and consequences/outcomes. This has important advantages in the context of evaluating health interventions and promoting total welfare and the good of society. For example, since the societal perspective considers a full set of information regarding conceivable costs and outcomes, it has been argued that it offers a higher level of decision-supportive power and will be less dependent on the study commissioners, as well as the political and social character of the society that the study is intended for [ 73 , 74 , 76 , 77 , 78 ]. A focus solely on the health care payer/provider perspective could overlook interventions that demonstrate cost-effectiveness from a broader societal standpoint. Furthermore, excluding important costs and outcomes within an economic evaluation, as seen in more restricted perspectives, could lead to inefficient resource allocation decisions [ 78 ]. The societal perspective can identify cost-shifting between sectors and on to patients/their families [ 78 ] (e.g., if the costs to the health systems are decreased but the costs to patients are increased), which may not be accounted for with more restricted perspectives. Consequently, many have argued that the societal perspective is preferable to others [ 73 , 75 , 78 ].
However, there are important further considerations that need to be made when considering the societal perspective—particularly in a global health context [ 7 , 71 ]. Firstly, having an all-inclusive analysis from a societal perspective, where in theory all conceivable costs and outcomes are considered, may require more costs and effort in order to acquire the additional data and information. As such, there needs to be a balance between the costs of acquiring additional information needed to use the societal perspective and increasing the quality of the decision being made. In the context of having inadequate or inaccessible datasets (such as those related to epidemiology, resource uses, unit costs, baseline distribution of health outcomes and data to inform the cost-effectiveness threshold), there is a greater challenge to the adoption of a broader perspective [ 79 ]. This is the rationale why the proponents of adaptive HTA suggest that a more limited perspective can be used in more nascent systems [ 80 ]. Applying a narrower perspective, especially in the cases of limited data, may be more pragmatic, albeit presenting some degree of omitted variable bias.
Although the societal perspective has often been advocated for, less consideration has been given to what this should include and its practical implementation [ 74 , 81 ]. In practice, it is not always easy to define what the conceivable or relevant costs and outcomes to be captured are. Consequently, there can be uncertainty regarding which costs should be included, and the way the societal perspective is conceptualised and interpreted can vary [ 82 ]. Even studies that state they are using it can omit potentially relevant costs and outcomes, and the societal perspective is often less comprehensive than it could be [ 8 ]. This is notable as the choice of its conceptualisation can seriously affect the result of a health economic analysis and the variation in how it is implemented can make comparisons more challenging. More generally, it could be argued that the societal perspective increases the risk of gaming as methods are less standardised, and there are more prominent data gaps [ 7 ].
A further consideration surrounding the use of the societal perspective and the variation in its implementation relates to the ongoing debate regarding the inclusion of indirect non-health benefits within economic evaluations (i.e., averted productivity costs) [ 52 , 53 , 55 ]. From a broad utilitarian moral standpoint, including these benefits in economic evaluations is important to ensure the maximisation of the collective benefit to society from the allocation of healthcare resources. However, including productivity gains could lead to the prioritization of the treatment of one group of patients over another because one group generates greater non-health benefits, thereby failing to give equal moral concern and weight to each person’s health care needs. Consequently, there is also a potential moral argument for ignoring productivity gains, in line with Kant's moral theory and that the equitable distribution of healthcare resources should be based on individual health needs [ 83 ]. A further factor is that quantifying all relevant non-health outcomes and productivity gains could potentially be double-counting the effectiveness of interventions [ 53 ], and this is an area of debate within the field (outlined previously in Box 1). Due to these factors, even under the societal perspective, the inclusion of productivity costs (as well as types of productivity costs) is variable. It is also important to note that productivity costs are particularly sensitive to the methodology used to calculate them, and the different methods used can generate significantly different results (Box 1) [ 84 ]. It is vital to consider this variation regarding the types of productivity costs being considered and their calculation within economic evaluations when making comparisons between studies.
A further issue relates to what “society” should be considered under the societal perspective: does “society” refer to the entire world or the society of an individual country. This issue becomes more prominent when evaluating interventions with a limited supply or that involve cross-border issues [ 22 ]. Although this can influence to what degree societal costs will be included, it is not always clear what is the scope of the society of interest within studies.
Even if the societal perspective is being used correctly, it can be unclear how the information produced informs choices across different settings and decision-makers—particularly when decision-makers may have different judgements about what outcomes are relevant to their relative values [ 85 ]. This is an important limitation for which progress is being made: for example, Walker et al . [ 74 ] developed a framework for the economic evaluation of policies with the costs and outcomes falling on different sectors (e.g., health, criminal justice, education) and involving different decision makers.
To summarise, while the societal perspective offers some significant advantages, corresponding issues and challenges should also be acknowledged, particularly in LMIC settings. It is worth noting that the societal perspective will not always be required as, ultimately, economic evaluations must align with and serve the stated goals of the decision-maker. In the United Kingdom, the primary focus of the decision-maker is to enhance health outcomes efficiently within a fixed health budget [ 28 , 85 ]. Therefore, in this context, adopting a health care provider perspective is typically considered more justifiable than a societal perspective. In contrast, this perspective could be misleading in settings where co-payments by the patients are notable, when the goal is to enhance the health system’s efficiency as a whole. Consequently, the choice of the perspective will depend on the purpose of the analysis, who needs to know/use the results and policymakers'/stakeholders’ viewpoints. It is also important to consider that the adoption of the societal perspective can involve notable additional data needs and the corresponding resource needs for collecting this data. This is not to discourage adoption of the societal perspective but rather to highlight that it is not a universal gold standard and the aforementioned factors/challenges are a consideration regarding its adoption.
Recommendations for policy and research
The terminology used to describe perspectives is variable within the literature. We have endeavoured to use the most established definitions, but it is possible that studies have interpreted and used them differently as well as potentially referred to terminology not included here. We recommend that the global health economic field set more standard definitions of the different perspectives and boundaries between these terms. This is to prevent confusion and misunderstanding not only among researchers but also policymakers and the public as a whole.
A related issue is that broader perspectives consider a wider range of costs, and therefore are likely to capture greater potential cost savings resulting from health interventions. If the healthcare budget is fixed, then this would imply that the cost-effectiveness threshold should be lower for a broader perspective, i.e. that different perspectives should be accompanied by different thresholds. However, the implications go beyond simply lowering the threshold. Some of these cost savings may extend beyond the designated budget holder (e.g. the health care provider), and the presence of budget constraints and trade-offs with other sectors need to be considered. For example, switching from the health care provider perspective to the societal perspective would mean that the provider (e.g. Department of Health) is effectively subsidising other sectors and without increasing the budget, the change could effectively decrease the amount of health being generated. Hence, we recommend that future studies further explore how to more accurately account for the interaction between the chosen perspective and appropriate cost-effectiveness threshold, considering the corresponding impact of budget constraints and trade-offs with other sectors [ 85 ]. In addition, not accounting for the impact of the use of different perspectives could potentially lead to biases in decision making, with interventions that have been evaluated with the societal perspective (including more cost savings) more likely to be favoured compared to those that have been evaluated with a narrower perspective.
A factor that needs to be further investigated on the implications of the chosen perspectives is the presence and impact of budget constraints as well as the desired time scale of investment returns.
A key issue to consider when evaluating and interpreting health economic studies is the potential inclusion of productivity costs when using the societal perspective. Estimates of productivity costs are highly sensitive to the method used [ 56 ], and it is important to be aware of the potential variation in methodology when comparing studies. In addition, the types of productivity costs included can vary—even when using the societal perspective. We recommend that this is an area that should have more comprehensive and consistent reporting in future studies. Having more standardised productivity cost estimates (potentially within country specific economic evaluation reference cases/guidelines) could be helpful to ensure increased consistency between studies for a particular country setting.
In this paper, we focused on the implications of the perspectives used in economic evaluations such as cost-effectiveness and cost-utility analysis. However, it is also important for future work to consider how the perspective interacts with other health economics methods and frameworks used within public health [ 86 , 87 , 88 , 89 ].
When conducting an economic evaluation of a particular intervention, or health technology, the concept of perspective is paramount. There are different types of perspectives which are used in economic evaluations with corresponding differences in the types of costs that are considered, as well as what outcomes are included (for example it can affect if/what “cost savings” are included). The choice of perspective can have a significant impact on the results of economic evaluations. Its relative impact on the results will depend on the context of the study and the intervention being investigated.
When choosing the perspective, it is important to consider the role of patient out-of-pocket payments. Crucially, the payer and health care provider(s) perspectives will not account for any costs paid by patients (including other out-of-pocket payments). They therefore may not be suitable for interventions that require co-payments by patients, as they could underestimate the cost of interventions and potentially lead to inefficient policy recommendations. This is particularly an important consideration in LMIC settings where out-of-pocket payments can be a significant source of health care expenditure [ 19 ].
Concerningly, the terminology used to describe the different perspectives is variable within the literature. We have endeavoured to highlight what we consider to be the most established definitions. We recommend that the global health economic field set more standard definitions of the different perspectives and boundaries between these terms.
Finally, it is important to note that despite the advantages of the societal perspective, its adoption does involve additional data needs and there is notable variation in how it is implemented, particularly surrounding what types of productivity costs are considered. Ultimately, there is no universal gold standard regarding what perspective should be used as it depends on the context (including policymakers'/stakeholders’ viewpoints and data/resource availability) as well as the question that the evaluation aims to provide an answer to [ 7 ].
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article.
Kristensen FB, Husereau D, Huić M, Drummond M, Berger ML, Bond K, et al. Identifying the need for good practices in health technology assessment: summary of the ISPOR HTA Council Working Group Report on Good Practices in HTA. Value Health. 2019;22(1):13–20.
Article PubMed Google Scholar
Nemzoff C, Ruiz F, Chalkidou K, Mehndiratta A, Guinness L, Cluzeau F, et al. Adaptive health technology assessment to facilitate priority setting in low-and middle-income countries. BMJ Glob Health. 2021;6(4): e004549.
Article PubMed PubMed Central Google Scholar
World Health Organization. SEA/RC66/R4-Health intervention and technology assessment in support of universal health coverage. WHO Regional Office for South-East Asia; 2013.
Oortwijn W, Jansen M, Baltussen R. Evidence-informed deliberative processes for health benefit package design—part II: a practical guide. Int J Health Policy Manage. 2022;11(10):2327–36.
Google Scholar
Baltussen R, Jansen M, Oortwijn W. Evidence-informed deliberative processes for legitimate health benefit package design—part I: conceptual framework. Int J Health Policy Manage. 2022;11(10):2319–26.
York Health Economics Consortium (YHEC). Perspective. 2016. Available from: https://yhec.co.uk/glossary/perspective/ .
Chalkidou K, Culyer AJ, Nemzoff C. Perspective in economic evaluations of health care interventions in low-and middle-income countries—one size does not fit all. CGD Policy Paper. 2018.
Avşar TS, Yang X, Lorgelly P. How is the societal perspective defined in health technology assessment? Guidelines from Around the Globe. Pharmacoeconomics. 2023;41(2):123–38.
Kim DD, Silver MC, Kunst N, Cohen JT, Ollendorf DA, Neumann PJ. Perspective and costing in cost-effectiveness analysis, 1974–2018. Pharmacoeconomics. 2020;38(10):1135–45.
Culyer A, Chalkidou K, Teerawattananon Y, Santatiwongchai B. Rival perspectives in health technology assessment and other economic evaluations for investing in global and national health. Who decides? Who pays? F1000 Res. 2018;7:72.
Article Google Scholar
GEAR. Guidelines Comparison. Available from: http://www.gear4health.com/gear/health-economic-evaluation-guidelines .
Tai BB, Bae YH, Le QA. A systematic review of health economic evaluation studies using the patient’s perspective. Value Health. 2016;19(6):903–8.
Sharma D, Aggarwal AK, Downey LE, Prinja S. National healthcare economic evaluation guidelines: a cross-country comparison. Pharmacoecon Open. 2021;5(3):349–64.
ISPOR. Pharmacoeconomic Guidelines: Russian Federation 2018. Available from: https://www.ispor.org/heor-resources/more-heor-resources/pharmacoeconomic-guidelines/pe-guideline-detail/russian-federation .
ISPOR. Pharmacoeconomic Guidelines: Brazil. 2014. Available from: https://www.ispor.org/heor-resources/more-heor-resources/pharmacoeconomic-guidelines/pe-guideline-detail/brazil .
Özaltın A, Cashin C. Costing of health services for provider payment: a practical manual based on country costing challenges, trade-offs, and solutions. Washington, DC: Joint Learning Network for Universal Health Coverage; 2014.
Vassall A, Sweeney S, Kahn J, Gomez Guillen G, Bollinger L, Marseille E, et al. Reference case for estimating the costs of global health services and interventions. 2017. Available from: https://ghcosting.org/pages/standards/reference_case .
Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG. Cost-effectiveness in health and medicine. Oxford: Oxford University Press; 2016.
Book Google Scholar
World Health Organization. Public spending on health: a closer look at global trends. World Health Organization; 2018. Report No.: 9240040331.
Bertram MY, Stenberg K, Brindley C, Li J, Serje J, Watts R, et al. Disease control programme support costs: an update of WHO-CHOICE methodology, price databases and quantity assumptions. Cost Effect Resour Allocat. 2017;15:21.
Bertram MY, Lauer JA, Stenberg K, Edejer TTT. Methods for the economic evaluation of health care interventions for priority setting in the health system: an update from WHO CHOICE. Int J Health Policy Manag. 2021;10(11):673–7.
PubMed PubMed Central Google Scholar
Garrison LP Jr, Mansley EC, Abbott TA III, Bresnahan BW, Hay JW, Smeeding J. Good research practices for measuring drug costs in cost-effectiveness analyses: a societal perspective: the ispor drug cost task force report—Part II. Value in Health. 2010;13(1):8–13.
Henrikson NB, Skelly AC. Economic studies part I: basics and terms. Evid Based Spine Care. 2012;3(4):7–11.
Abbott JH, Wilson R, Pryymachenko Y, Sharma S, Pathak A, Chua JYY. Economic evaluation: a reader’s guide to studies of cost-effectiveness. Arch Physiother. 2022;12(1):28.
Garrison LP Jr, Pauly MV, Willke RJ, Neumann PJ. An overview of value, perspective, and decision context—a health economics approach: an ISPOR Special Task Force Report [2]. Value Health. 2018;21(2):124–30.
Smith KM, Machalaba CC, Seifman R, Feferholtz Y, Karesh WB. Infectious disease and economics: the case for considering multi-sectoral impacts. One Health. 2019;7: 100080.
Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–93.
National Institute for Health and Care Excellence (NICE). NICE health technology evaluations: the manual. 2022. Available from: https://www.nice.org.uk/process/pmg36/chapter/introduction-to-health-technology-evaluation .
Wilkinson T, Sculpher MJ, Claxton K, Revill P, Briggs A, Cairns JA, et al. The international decision support initiative reference case for economic evaluation: an aid to thought. Value Health. 2016;19(8):921–8.
Claxton KP, Revill P, Sculpher M, Wilkinson T, Cairns J, Briggs A. The gates reference case for economic evaluation: the Bill and Melinda Gates Foundation; 2014.
Hutton G, Baltussen R. Cost valuation in resource-poor settings. Health Policy Plan. 2005;20(4):252–9.
Hay JW, Smeeding J, Carroll NV, Drummond M, Garrison LP, Mansley EC, et al. Good research practices for measuring drug costs in cost effectiveness analyses: issues and recommendations: the ISPOR Drug Cost Task Force Report—Part I. Value Health. 2010;13(1):3–7.
Turner HC, Sandmann FG, Downey LE, Orangi S, Teerawattananon Y, Vassall A, et al. What are economic costs and when should they be used in health economic studies? Cost Effect Resour Allocat. 2023;21(1):31.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th ed. Oxford: Oxford University Press; 2015.
De Vries LM, Van Baal PHM, Brouwer WBF. Future costs in cost-effectiveness analyses: past, present. Future Pharmacoecon. 2019;37(2):119–30.
Garber AM, Phelps CE. Future costs and the future of cost-effectiveness analysis. J Health Econ. 2008;27(4):819–21.
Meltzer D. Accounting for future costs in medical cost-effectiveness analysis. J Health Econ. 1997;16(1):33–64.
Article CAS PubMed Google Scholar
Kellerborg K, Wouterse B, Brouwer W, van Baal P. Estimating the costs of non-medical consumption in life-years gained for economic evaluations. Soc Sci Med. 2021;289: 114414.
Morton A, Adler AI, Bell D, Briggs A, Brouwer W, Claxton K, et al. Unrelated future costs and unrelated future benefits: reflections on NICE guide to the methods of technology appraisal. Health Econ. 2016;25(8):933–8.
Owen L, Fischer A. The cost-effectiveness of public health interventions examined by the National Institute for Health and Care Excellence from 2005 to 2018. Public Health. 2019;169:151–62.
Turner HC, Quyen DL, Dias R, Huong PT, Simmons CP, Anders KL. An economic evaluation of Wolbachia deployments for dengue control in Vietnam. PLoS Negl Trop Dis. 2023;17(5): e0011356.
Kim SY, Goldie SJ, Salomon JA. Cost-effectiveness of rotavirus vaccination in Vietnam. BMC Public Health. 2009;9:29.
Le P, Griffiths UK, Anh DD, Franzini L, Chan W, Swint JM. Cost-effectiveness of Haemophilus influenzae type b vaccine in Vietnam. Vaccine. 2015;33(36):4639–46.
Turner HC, Lauer JA, Tran BX, Teerawattananon Y, Jit M. Adjusting for inflation and currency changes within health economic studies. Value Health. 2019;22(9):1026–32.
World Bank. GDP deflator (base year varies by country). Available from: https://data.worldbank.org/indicator/NY.GDP.DEFL.ZS .
Turner HC, Archer RA, Downey LE, Isaranuwatchai W, Chalkidou K, Jit M, et al. An introduction to the main types of economic evaluations used for informing priority setting and resource allocation in healthcare: key features, uses, and limitations. Front Public Health. 2021;9: 722927.
Brouwer WB, Koopmanschap MA, Rutten FF. Productivity costs measurement through quality of life? A response to the recommendation of the Washington Panel. Health Econ. 1997;6(3):253–9.
Brouwer WB, Koopmanschap MA, Rutten FF. Productivity costs in cost-effectiveness analysis: numerator or denominator: a further discussion. Health Econ. 1997;6(5):511–4.
Sculpher M. The role and estimation of productivity costs in economic evaluation. In: Drummond M, McGuire A, editors. Economic evaluation in health care: merging theory with practice. Oxford University Press: Oxford; 2001. p. 94–112.
Chapter Google Scholar
Olsen JA, Richardson J. Production gains from health care: what should be included in cost-effectiveness analyses? Soc Sci Med. 1999;49(1):17–26.
Liljas B. How to calculate indirect costs in economic evaluations. Pharmacoeconomics. 1998;13(1):1–7.
Pritchard C, Sculpher M. Productivity costs: principles and practice in economic evaluation. Office of Health Economics; 2000.
Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996.
Neumann PJ, Thorat T, Zhong Y, Anderson J, Farquhar M, Salem M, et al. A systematic review of cost-effectiveness studies reporting cost-per-DALY averted. PLoS ONE. 2016;11(12): e0168512.
World Health Organization. Making choice in health: WHO guide to cost effectiveness analysis. Geneva: WHO; 2003.
Krol M, Brouwer W, Rutten F. Productivity costs in economic evaluations: past, present, future. Pharmacoeconomics. 2013;31(7):537–49.
Hung TM, Shepard DS, Bettis AA, Nguyen HA, McBride A, Clapham HE, et al. Productivity costs from a dengue episode in Asia: a systematic literature review. BMC Infect Dis. 2020;20(1):1–18.
Da Silva EA, Pinto CG, Sampaio C, Pereira J, Drummond M, Trindade R. Guidelines for economic drug evaluation studies. Lisbon, Portugal: Infarmed. 1998.
Agency NM. Guidelines for the submission of documentation for single technology assessment (STA) of pharmaceuticals. Norwegian Medicines Agency Oslo (Norway); 2018.
Chugh Y, De Francesco M, Prinja S. Systematic literature review of guidelines on budget impact analysis for health technology assessment. Appl Health Econ Health Policy. 2021;19(6):825–38.
ISPOR. Pharmacoeconomic Guidelines: Thailand 2019: Available from: https://www.ispor.org/heor-resources/more-heor-resources/pharmacoeconomic-guidelines/pe-guideline-detail/thailand .
Department of Health Research, Ministry of Health & Family Welfare, Government of India. Health Technology Assessment in India: A Manual. New Delhi: Department of Health Research; 2018.
Elsisi GH, Kaló Z, Eldessouki R, Elmahdawy MD, Saad A, Ragab S, et al. Recommendations for reporting pharmacoeconomic evaluations in Egypt. Value Health Reg Issues. 2013;2(2):319–27.
Health Technology Assessment Unit, Department of Health—Philippines. P Philippine HTA Methods Guide, Health Technology Assessment Unit Department of Health - Philippines: Department of Health; 2020.
Indonesian Health Technology Assessment Committee (InaHTAC). Health technology assessment (HTA) guideline. Jakarta: Pusat Pembiayaan dan Jaminan Kesehatan Kementerian Kesehatan RI. 2017;143.
Ministry of Health Malaysia. Pharmacoeconomic Guideline for Malaysia (2nd Edition). Pharmaceutical Services Programme; 2020.
Moreno Viscaya M, Mejía Mejía A, Castro Jaramillo HE. Manual para la elaboración de evaluaciones económicas en salud. Bogotá: Instituto de Evaluación Tecnológica en Salud. 2014.
Yue X, Li Y, Wu J, Guo J. Current development and practice of pharmacoeconomic evaluation guidelines for universal health coverage in China. Value Health Reg Issues. 2021;24:1–5.
Consejo de Salubridad General. Guía para la conducción de estudios de evaluación económica para la actualización del cuadro básico y catálogo de insumos del sector salud en México. México, DF: CSG. 2017.
Cuba Ministry of Health. Methodological Guidelines for Health Economic Evaluation. 2003.
Culyer AJ. “Perspectives” in health technology assessment. AMA J Ethics. 2021;23(8):619–23.
World Health Organization. Public spending on health: a closer look at global trends. World Health Organization; 2018.
Johannesson M, Jönsson B, Jönsson L, Kobelt G, Zethreaus N. Why should economic evaluations of medical technologies have a societal perspective. OHE Briefing Paper London: Office of Health Economics. 2009.
Walker S, Griffin S, Asaria M, Tsuchiya A, Sculpher M. Striving for a societal perspective: a framework for economic evaluations when costs and effects fall on multiple sectors and decision makers. Appl Health Econ Health Policy. 2019;17(5):577–90.
Gold M. Panel on cost-effectiveness in health and medicine. Medical Care. 1996:DS197–DS9.
Drost RMWA, Paulus ATG, Evers SMAA. Five pillars for societal perspective. Int J Technol Assess Health Care. 2020;36(2):72–4.
Byford S, Raftery J. Perspectives in economic evaluation. BMJ. 1998;316(7143):1529–30.
Article CAS PubMed PubMed Central Google Scholar
Jöonsson B. Ten arguments for a societal perspective in the economic evaluation of medical innovations. Eur J Health Econ. 2009;10:357–9.
Chalkidou K. A Global Burden of Disease Data Plus Model to Inform Domestic Decision-Making: In Search of Super-local Data. Blog post of the Center for Global Development. 2017. Available from: https://www.cgdev.org/blog/global-burden-disease-data-plus-model-inform-domestic-decision-making-search-super-local-data .
Nemzoff C, Ruiz F, Chalkidou K, Mehndiratta A, Guinness L, Cluzeau F, et al. Adaptive health technology assessment to facilitate priority setting in low- and middle-income countries. BMJ Glob Health. 2021;6(4): e004549.
Evers SM, Hiligsmann M, Adarkwah CC. Risk of bias in trial-based economic evaluations: identification of sources and bias-reducing strategies. Psychol Health Econ Rev. 2015;30(1):52–71.
Drost RM, Van der Putten IM, Ruwaard D, Evers SM, Paulus AT. Conceptualizations of the societal perspective within economic evaluations: a systematic review. Int J Technol Assess Health Care. 2017;33(2):251–60.
Sullivan RJ. Immanuel Kant’s moral theory. Cambridge: Cambridge University Press; 1989.
Van den Hout W. The value of productivity: human-capital versus friction-cost method. Ann Rheum Dis. 2010;69(Suppl 1):i89–91.
Claxton K, Walker S, Palmer S, Sculpher M. Appropriate perspectives for health care decisions. Centre for Health Economics, University of York, Working Papers. 2010.
Fischer AJ, Ghelardi G. The precautionary principle, evidence-based medicine, and decision theory in public health evaluation. Front Public Health. 2016;4:107.
Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2(1):55–64.
PubMed Google Scholar
Baltussen R, Marsh K, Thokala P, Diaby V, Castro H, Cleemput I, et al. Multicriteria decision analysis to support health technology assessment agencies: benefits, limitations, and the way forward. Value Health. 2019;22(11):1283–8.
Coast J, Kinghorn P, Mitchell P. The development of capability measures in health economics: opportunities, challenges and progress. Patient. 2015;8(2):119–26.
Download references
Acknowledgements
The authors alone are responsible for the views expressed, which do not necessarily represent the views, decisions or policies of the institutions with which the authors are affiliated.
HCT acknowledges funding from the MRC Centre for Global Infectious Disease Analysis (reference MR/X020258/1), funded by the UK Medical Research Council (MRC). This UK funded award is carried out in the frame of the Global Health EDCTP3 Joint Undertaking. The Health Intervention and Technology Assessment Program (HITAP) is a semi-autonomous research unit in the Ministry of Public Health, Thailand, and supports evidence-informed priority-setting and decision-making for healthcare. HITAP is funded by national and international public funding agencies. HITAP is also supported by the Health Systems Research Institute (HSRI), the Thai Health Promotion Foundation (ThaiHealth), the World Health Organization (WHO), the Access and Delivery Partnership, which is hosted by the United Nations Development Programme and funded by the Government of Japan, among others. The findings, interpretations and conclusions expressed in this article do not necessarily reflect the views of the funding agencies. MJ was supported by the NIHR Health Protection Research Unit in Modelling and Health Economics (grant code HPRU-2019-NIHR200908). MJ was also supported by the NIHR Health Protection Research Unit in Immunisation (HPRU-2019-NIHR200929). The views expressed are those of the authors and not necessarily those of the United Kingdom (UK) Department of Health and Social Care, the National Health Service, the National Institute for Health Research (NIHR), or the UK Health Security Agency. For the purpose of open access, the author has applied a ‘Creative Commons Attribution’ (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and affiliations.
Health Intervention and Technology Assessment Program (HITAP), Nonthaburi, Thailand
Manit Sittimart, Waranya Rattanavipapong, Saudamini Dabak & Yot Teerawattananon
World Health Organization, Geneva, Switzerland
Andrew J. Mirelman
Oxford University Clinical Research Unit (OUCRU), Ho Chi Minh City, Vietnam
Trinh Manh Hung
The George Institute for Global Health, School of Public Health, Imperial College London, London, UK
Laura E. Downey
The George Institute for Global Health, University of New South Wales, Sydney, Australia
Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, UK
School of Public Health, University of Hong Kong, Hong Kong Special Administrative Region, Hong Kong, China
Saw Swee Hock School of Public Health, National University of Singapore (NUS), Singapore, Singapore
Yot Teerawattananon
MRC Centre for Global Infectious Disease Analysis, School of Public Health, Imperial College London, London, UK
Hugo C. Turner
You can also search for this author in PubMed Google Scholar
Contributions
MS and HCT wrote the original draft. WR, AJM, TMH, SD, LED, MJ and YT contributed to the writing, reviewing and editing of the draft. All authors read and approved the final draft.
Corresponding author
Correspondence to Hugo C. Turner .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sittimart, M., Rattanavipapong, W., Mirelman, A.J. et al. An overview of the perspectives used in health economic evaluations. Cost Eff Resour Alloc 22 , 41 (2024). https://doi.org/10.1186/s12962-024-00552-1
Download citation
Received : 15 January 2024
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12962-024-00552-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Perspective
- Economic evaluation
- Health economics
- Global health
Cost Effectiveness and Resource Allocation
ISSN: 1478-7547
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
Healthcare Expenditure and Economic Performance: Insights From the United States Data
Viju raghupathi.
1 Koppelman School of Business, Brooklyn College of the City University of New York, Brooklyn, NY, United States
Wullianallur Raghupathi
2 Gabelli School of Business, Fordham University, New York, NY, United States
Associated Data
Publicly available datasets were analyzed in this study. These can be found here: CMS; BEA; BLS; https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData ; https://www.bea.gov/iTable/iTable.cfm?reqid=70&step=1&isuri=1&acrdn=2#reqid=70&step=1&isuri=1 ; https://www.bls.gov/lpc/data.htm ; https://www.bls.gov/webapps/legacy/tusa_1tab1.htm .
This research explores the association of public health expenditure with economic performance across the United States. Healthcare expenditure can result in better provision of health opportunities, which can strengthen human capital and improve the productivity, thereby contributing to economic performance. It is therefore important to assess the phenomenon of healthcare spending in a country. Using visual analytics, we collected economic and health data from the Bureau of Economic Analysis and the Bureau of Labor Statistics for the years 2003–2014. The overall results strongly suggest a positive correlation between healthcare expenditure and the economic indicators of income, GDP, and labor productivity. While healthcare expenditure is negatively associated with multi-factor productivity, it is positively associated with the indicators of labor productivity, personal spending, and GDP. The study shows that an increase in healthcare expenditure has a positive relationship with economic performance. There are also variations across states that justify further research. Building on this and prior research, policy implications include that the good health of citizens indeed results in overall better economy. Therefore, investing carefully in various healthcare aspects would boost income, GDP, and productivity, and alleviate poverty. In light of these potential benefits, universal access to healthcare is something that warrants further research. Also, research can be done in countries with single-payer systems to see if a link to productivity exists there. The results support arguments against our current healthcare system's structure in a limited way.
Introduction and Background
Healthcare spending and the impact that it has on economic performance are important considerations in an economy. Some studies have shown that improvements in health can lead to an increase in Gross Domestic Product (GDP) and vice versa ( 1 – 3 ). Healthcare holds a significant place in the quality of human capital. The increased expenditure in healthcare increases the productivity of human capital, thus making a positive contribution to economic growth ( 4 , 5 ). However, there is ongoing debate on what kinds of healthcare spending and what level of optimal spending is beneficial for economic development ( 6 – 8 ).
The theory of welfare economics is relevant to the current research. Welfare economics is a branch that deals with economic and social welfare by analyzing how the resources of the economy are allocated among the social agents ( 9 , 10 ). Here, we analyze the allocation of resources in terms of spending within the healthcare sector and assess its influence on economic welfare. In addition to this, we draw from several related studies in laying a strong foundation for our research. The relationship between health and economic growth has been examined extensively across multiple studies ( 11 – 16 ). Based on a study that examined the impact of health on economic growth in developing countries, it was evident that a decrease in birth rates positively affected economic growth ( 17 ). During the period of study, health expenditures rose threefold, from $83M to $286M, and outpaced growth in GDP. The study showed that health and income mutually affected each other and concluded that problems affecting healthcare delivery caused negative impact on economic growth ( 18 ). Arora ( 19 ) investigated the effects of health on economic growth for industrialized countries and found a strong association. In a study of the impact of health indicators for the period 1965–1990 for developed and developing countries, economic performance in developing countries increased significantly with an improvement in public health ( 20 ). Studies have proposed that an annual improvement of 1 year in life expectancy increases economic growth by 4% ( 1 , 21 ). Similarly, another study in 2001 emphasized that the existence of a healthy population may be more important than education, for human capital in the long term ( 22 ). Examining 21 African countries for the 1961–1995 period and 23 Organization for Economic Cooperation and Development (OECD) countries for the 1975–1994 period with the extended Solow growth model, authors found that 23 OECD health stocks affect growth rate of per capita income ( 23 ). Muysken ( 24 ) also investigated whether health is one of the determinants of economic growth and concluded that an iterative relationship exists between economic growth and health—high economic growth leads to investments in human capital and to health advancement, and good population health leads to more labor productivity and economic growth. Aghion et al. ( 25 ) utilized the Schumpeterian growth theory to analyze channels associated with the influence of national health on economic growth. The theory emphasizes the importance of maternal and child health on the critical dimensions of human capital. Another element that has been shown to be a critical element for sustainable economic growth is high life expectancy ( 26 ). Aghion et al. ( 27 ) applied the endogenous growth theory, which proposes that a better life expectancy enhances growth, to analyze the relationship between health and economic growth. The study examined life expectancy for various ages in OECD countries and concluded that a decline in mortality rates for the age groups below 40 has the effect of increasing economic growth Aghion et al. ( 27 ).
Based on the above-mentioned studies, we surmise that higher income per capita is associated not only with life expectancy, but also with numerous other measures of health status. While health is not the only indicator of economic development—indeed, we need to consider the impact of other factors, such as education, political freedom, gender, and many other social attributes ( 1 , 3 , 28 )—health is definitely an integral non-income component that should be considered in a measure of economic development. People generally give high priority and value to a long and healthy life ( 2 , 25 ). Secondly, the rate of achievement of this goal to aspire for a long and healthy life differs widely across countries ( 11 , 13 , 29 ). The Human Development Index, in addition to suggesting a correlation between income and health, also expresses a strong correlation between an individual's place in the income distribution and his or her health outcomes within a country ( 2 , 30 ). This within-country correlation is particularly strong in developing countries. In comparing the growth of income with improvements in health outcomes, it is common to account for simultaneous causation. As an example, people who are healthy have the ability to be more productive in school and at work, reflecting that good health can be a precursor for better economic development ( 4 ). Additionally, a higher income allows individuals or governments to make investments that yield better health ( 28 ). Finally, differences in the quality of education, government, health, and other institutions across countries, in human capital, or in the level of technology can induce correlated movements in health and income ( 16 ). One also needs to account for the dynamic effects built into many of the potential causal outlets. For example, improvements in health may only result in increased worker productivity after a lag of several decades. Similarly, when life expectancy rises, there can be increases in population growth that may temporarily reduce income per capita ( 31 ).
The per capita health expenditures of countries vary in terms of economic development.
Whereas, high-income countries spend, on average on healthcare, $3,000 on each citizen, low-income countries only spend up to $30 per capita. It is also important to consider healthcare expenditure expressed as a percentage of GDP ( 5 , 14 ). While some countries spend higher than 12% of GDP on healthcare, others spend as little as 3% ( 32 ). There are at least two methods that can explain the association between a country's healthcare expenditure and economic performance. In the first scenario, healthcare expenditure is considered an investment in human capital. Human capital accumulation is then perceived to be a source of economic growth (e.g., via increased productivity). Therefore, an increase in healthcare expenditure is likely to be associated with a higher GDP ( 30 , 33 ). In the second scenario, an increase in healthcare expenditure can lead to regular health interventions (e.g., annual medical-checkups, preventive screening, etc.), which are likely to improve labor and productivity; this, in turn, will increase the GDP ( 34 ). Both these mechanisms reflect an iterative phenomenon between healthcare and GDP. Nevertheless, the relationship needs to be checked for endogeneity—which we aim to study in this research.
An important dimension in the relationship between health expenditure and economic performance is the factor of the productivity of workers. In developed countries, labor is scarce, and capital is abundant as a factor of production ( 2 , 31 , 35 ). But this situation is reversed in developing countries where economic growth and economies are based on labor. Here, an increase in individuals' poor health will likely lead to a loss in labor workforce and productivity ( 4 , 16 ). Therefore, addressing public health and health expenditures, though important for both developed and developing countries, is more critical for the latter ( 3 , 4 , 11 , 13 , 16 , 36 ). It is generally assumed from common knowledge that individuals who are healthier are able to work more effectively, in terms of physical and mental workload. Also, adults who were healthier as children will have acquired more human capital in the form of education, which is explained by the proximate effect of health on the level of income ( 37 ). Simultaneously, the impact of individual income on health is also important ( 38 , 39 ). Higher income can result in better health by facilitating access to better nutrition, preventative treatment, good sanitation, safe water, and affordable quality healthcare. Additionally, health can also be a cause of high income, by allowing individuals to work more, be more productive and earn higher income during the lifetime ( 35 ).
The impact of health on education is an important factor that plays a role in healthcare expenditure and economic performance ( 30 , 33 ). Children who enjoy good health can attend school regularly and have the potential of high learning ability and cognitive development. Also, if good health continues through adulthood, it will enable the population to recover the investments in education ( 30 , 33 , 39 ).
Another significant dimension in the relationship that healthcare spending has with economic development is the impact of health on savings. Good health can increase the life expectancy and encourage an individual's motivation to have savings (such as for retirement) and to make more business investments, both of which are beneficial activities for economic performance ( 1 ). Population health is an important healthcare component whose impact should be considered. A healthy population can reduce the expense on national healthcare and increase the potential for earnings. In this manner, the economic impact of population health can occur at the micro and macro levels ( 1 , 2 , 4 , 5 ). It is no surprise that some countries assign a higher value to gains from health than gains from income ( 36 , 40 – 43 ). Additionally, most countries have witnessed an increase in life expectancy despite a persistent income gap over the last 50 years ( 44 ), reflecting the monetary benefits that can accrue from investing in healthcare ( 2 , 44 ).
In this research, we acknowledge the significance of healthcare expenditure and analyze its association with the economic performance. We conduct the analysis at a national level for the United States using the data from the Bureau of Economic Analysis (BEA) and the Bureau of Labor Statistics (BLS). We incorporate the techniques of visual and descriptive analytics ( 45 – 47 ). Our findings provide insight on the differences in health spending and economic performance across the various states of the U.S. The research offers implications for governments 2008; and national policy makers to identify dimensions of healthcare that contribute to national economic performance. It is especially important for policy that addresses population health issues of a nation.
The rest of the paper is organized as follows: section Research 2 describes the methodology; section 3 presents the analyses and results; section 4 contains a discussion of results with implications; section 5 offers the scope and limitations of the research; and finally, section 6 presents the conclusions.
Research Methodology
Data collection and variables.
We analyze state-level data and ascertain patterns that offer insight into the healthcare spending and economic performance of various states in the United States. Our methodology includes the stages of data collection and variable selection, data preparation, analytics platform and tool selection, and analytics implementation. We collected economic and health data from the Centers for Medicare and Medicaid Services (CMS) ( https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData ), Bureau of Economic Analysis (BEA) ( https://www.bea.gov/iTable/iTable.cfm?reqid=70&step=1&isuri=1&acrdn=2#reqid=70&step=1&isuri=1 ), and the Bureau of Labor Statistics (BLS) ( https://www.bls.gov/lpc/data.htm ; https://www.bls.gov/webapps/legacy/tusa_1tab1.htm ) for a period of 12 years (2003–2014). The variables relate to various economic performance and healthcare spending indicators. Table 1 shows the variables in the research.
List of variables.
The data was analyzed using the business intelligence tool Tableau for visualization, R programming language for regression analysis, and SPSS Modeler for neural network analysis.
Visual Analytics Method
We utilize visual analytics to analyze healthcare spending and economic performance data. With visual analytics, one can discover patterns and relationships that are unexpected, and get timely and rational assessments of the phenomenon that is being analyzed ( 46 , 48 ). Descriptive analytics, as a technique in visual analytics, helps one understand past and current trends and make informed decisions in a domain ( 48 ). By deploying this approach, we take a more data-driven approach to understanding the trends and associations between healthcare expenditure and economic performance scenario.
The technology of analytics is used increasingly in the domain of healthcare. As a business intelligence component, analytics allows statistical and quantitative analyses of large data repositories, enabling evidenced-based decision making ( 49 ). Specifically, in the domain of healthcare, analytics offers timely, relevant and quality information that can help healthcare entities and governments optimize health resource allocation goals effectively ( 50 ).
We deploy visual analytics based on the belief that it offers an effective tool to comprehend healthcare expenditure at a national level and analyze its impact on economic performance. We now discuss the results of our analyses in the following section.
Analyses and Results
We analyzed the data for patterns and relationships between the indicators of healthcare spending and economic performance. Healthcare expenditure refers to aggregate healthcare spending in an economy, including expenditure relating to hospitals, home health agencies, prescription drugs, nursing facilities, and personal healthcare.
Distribution of Hospital Expenditure Per Capita by Hospitals
To get an idea of the state of hospital expenditure we looked at the distribution of expenditure by hospitals in the country ( Figure 1 ). Hospital expenditure includes all service provided to patients, including room, ancillary charges, physician services, in-patient pharmacy services, and nursing home and home care. In Figure 1 , the intensity of color of the bars depicts the number of hospitals such that the darker the color, the higher the number of hospitals with the expenditure. Clearly, the distribution is right-skewed. While the majority of the hospital expenditures per capita rank between $1,600 and $3,500, there are several outliers on the right side. Additionally, even though per capita hospital expenditure on average is within $3,500, there are still some hospitals where the average cost is higher.

Per capita hospital expenditure distribution.
Hospital Expenditure Per Capita and GDP Per Capita by State
We now looked to see if there was any association between the hospital expenditure per capita and the GDP rank of the state ( Figure 2 ). The figure depicts the per capita hospital expenditures by the intensity of the color (the darker the color, the higher the expenditures), and the state rank in terms of GDP per capita as a label in the state. We see that progressive states such as California with a high GDP rank have lower per person hospital expenditure; Nevada has a higher GDP rank than South Dakota but has a lower per capita hospital expenditure. In fact, the hospital expenditure in South Dakota is almost double that of Nevada. This suggests that the states that have higher economic performance (GDP) have legislative and innovative measures that support healthcare research, thereby resulting in lowered costs to the patients.

Per capita hospital expenditures and per capita GDP rank by state.
Population and Per Capita Healthcare Expenditure
Having compared the healthcare expenditure of a state with its GDP, we now wanted to see if there was any association with the population of a state ( Figure 3 ). In the bubble chart the size depicts the population of the state and the color depicts the healthcare expenditure (darker colors represent higher expenditures). Interestingly, we see that sparsely populated states such as District of Columbia (DC) have higher healthcare spending than densely populated states like Texas. On the other hand, states like New York have high population and high expenditure. Therefore, there appears to be no correlation between population size and total average per capita expenditure, proving that population qualifies as a control variable in our dataset.

Overview of population size and total per capita healthcare expenditure.
Association of Hospital Expenditure With GDP Per Capita and Changes in Multifactor Productivity Over Time
We wanted to study the pattern of growth of hospital expenditure with GDP and with changes in multifactor productivity, from 2003 to 2014 ( Figure 4 ). Both associations are shown side by side in Figure 4 .

Relationship of hospital expenditures with per capita GDP, and changes in multifactor productivity.
In Figure 4 , the circles represent the performance for a year, with the intensity of the color indicating the recency of the year. In terms of the graph showing average per capita GDP and average per capita hospital expenditure, we see that since 2003, as the average per capita GDP increases, so does the per capita hospital expenditure. The positive correlation between the average per capita GDP and average per capita hospital expenditure implies that, by proxy, healthcare has a positive effect on GDP (economic performance).
The other graph in Figure 4 shows the relationship of Multifactor Productivity (MFP) with hospital expenditure. MFP is a measure of economic performance that reflects the overall efficiency with which inputs are used to produce outputs. Figure 4 shows that since 2003, the average per capita hospital expenditure has been increasing, but there is no obvious pattern in association with the changes in multifactor productivity. Also, it is worth noting that the trend line shows that there is a slight negative correlation between the changes in multifactor productivity and average per capita hospital expenditure.
Association of Personal Healthcare Costs With Average Hours Per Day Spent on Purchasing Goods and Services, and With Changes in Multifactor Productivity (MFP)
Personal healthcare expenditure determines the out-of-pocket costs incurred by the population. Figure 5 represents two associations of hospital expenditure side by side—with general purchases of the population, and with changes in MFP. In the association of hospital expenditure with general purchases of the population, we estimated the purchasing power of the population using the average hours spent per day on purchasing goods and services. The figure shows a negative relationship such that as personal healthcare costs increase, the average time spent on purchases declines. This is because as personal healthcare costs increase, the amount of available money for spending decreases, affecting the time spent on buying goods and services. Figure 5 also shows the association between hospital expenditure and changes in MFP. The line chart/trend line in the figure indicates that there is no obvious correlation between personal healthcare costs and percent change in MFP. This is consistent with the analysis of hospital expenditure which also had no association with MFP. One can infer that that a change in healthcare costs does not affect the economic cycle.

Relationship of personal healthcare costs with average hours per day spent on purchasing goods and services, and changes in multifactor productivity.
Association of Healthcare Expenditure With Per Capita Personal Income
In looking for associations between healthcare expenditure and personal income ( Figure 6 ) we see that between 2003 and 2014, personal income mostly increased while total healthcare spending has increased as a percentage of income. This confirms two trends—Americans spend more on healthcare over time; and personal income increases faster than that of healthcare expenditure in terms of dollar amount.

Association between per capita healthcare spending and personal income.
Association of Hospital and Physician Expenditures With Labor Productivity
Physician expenditure and hospital expenditure are components of overall healthcare costs of a state. We wanted to analyze if there was any association of labor productivity with physician expenditure and hospital expenditure ( Figure 7 ). The scatterplot in the figure shows that spending in physician or hospital costs is positively correlated with an increase in labor productivity. It appears that healthcare spending has a positive relationship with labor productivity in the United States.

Correlation between labor productivity and hospital and physician expenditures.
Association of Per Capita Healthcare Expenditure With Labor Productivity and With GDP
In terms of healthcare expenditure, the above analysis revealed that physician and hospital expenditure were positively associated with labor productivity. We next explored if total healthcare expenditure which is an aggregate of all components is also associated with labor productivity, and with per capita GDP, both shown side by side ( Figure 8 ). The figure shows that as the total healthcare expenditure increases, labor productivity also increases. There is a positive correlation between total per capita healthcare expenditure and labor productivity. Thus, by increasing healthcare expenditure, the health status of Americans will improve, increasing labor productivity. Figure 8 also shows the association of total healthcare expenditure with an alternate measure of economic performance, namely the GDP. The figure depicts a chart with a trend line that shows that as total healthcare expenditures increase, GDP also increases. Healthcare expenditure of a state has a positive relationship with the GDP of the state.

Relationship between total per capita healthcare expenditures and labor productivity.
Associations Between Personal Healthcare Expenditure, Hospital Expenditure, Nursing Expenditure, and Average Weekly Hours Worked
It is important to see the relationship between average hours worked (weekly) as a measure of economic performance and healthcare expenditure comprising personal healthcare, nursing, and hospital costs ( Figure 9 ). From the figure we can see that as each of the health costs increases, there is no obvious change for average weekly hours. There appears to be no correlation between health costs and average weekly hours, which indicates there is no effect on productivity.

Relationship between personal health, hospital, nursing costs, and average weekly hours.

Association of Personal Healthcare Expenditure With Per Capita GDP
Figure 10 shows the association between personal healthcare expenditure and GDP per capita.

Correlation between per capita personal healthcare expenditure and per capita GDP.
In the figure the bar graph depicts the GDP and the trend line represents the personal healthcare expenditure. The last 2 years, which have a lighter color, represent the forecasted result. The chart shows that personal expenditure costs have steadily risen over the years, while the GDP does not show large fluctuations. A correlation is hard to establish between personal healthcare costs and GDP; it is possible that there may be extraneous types of healthcare expenditure that have an influence on the GDP.
Distribution of Various Types of Healthcare Expenditures Across Years
It is important to explore the different types of healthcare expenditure and their distribution over the years ( Figure 11 ). Personal healthcare expenditure (includes private and public insurance) has the highest average of the types of spending in the years 2003 to 2014. This is followed by hospital and physician expenditure. The rise in personal healthcare expenditure has led to a high demand for reasonably priced private health insurance across the United States. The government needs to increase the affordability of public insurance to increase the reach and benefit more people.

Distribution of various types of healthcare expenditures across years.
Association Between Personal Healthcare Expenditure Per Capita and Total Hours Worked
Figure 12 shows the relationship between personal healthcare expenditure and total hours worked for the years 2003 to 2014. The growth of expenditure costs is not proportional to the rate of change in working hours. There appears to be no correlation between expenditure and working hours; however, from the other analyses, we know that healthcare expenditure has a positive correlation with income.

Relationship between hours worked and per capita personal healthcare expenditure.
Association Between Personal Healthcare Expenditure and Other Personal Expenditure
The relationship between personal healthcare expenditure and other personal expenditure is shown in Figure 13 . The scatterplot shows the personal health expenditure having a positive correlation with the other personal expenditure. The ratio between them basically stays the same, which shows that an increase in personal health care expenditure does not impose a burden, significant enough to cause a reduction in other personal spending.

Relationship between personal health expenditure and other personal expenditure.
Important Healthcare Expenditure Predictors of Per Capita GDP
We wanted to explore which type of healthcare expenditure has the most significant influence on GDP. Figure 14 shows a machine learning based neural network model to analyze which type of healthcare spending affects the per capita GDP the most. The bars indicate to what extent the associated variable is determined by the target variable, namely per capita GDP. Among the different types of healthcare spending, hospital expenditure affects the per capita GDP the most, followed by personal healthcare. It confirms the fact that the effect of healthcare spending in the different care areas will have differential effects on the economy.

Importance of healthcare expenditure predictors for per capita GDP.
Our research offers several important findings that have implications for policy. While healthcare expenditure is negatively associated with multi-factor productivity, it is positively associated with labor productivity, personal spending, and GDP. However, this is not a causal relationship, and our inference is limited. Nevertheless, the research establishes, within the scope of the study, that an increase in healthcare expenditure has a positive relationship with economic performance. There are also variations across states that justify further research. Building on this and prior research, policy implications include that the good health of citizens indeed results in overall better economy. Therefore, investing carefully in various healthcare aspects would boost income, GDP, and productivity, and alleviate poverty. In light of these potential benefits, universal access to healthcare is something that warrants further research. Also, research can be done in countries with single-payer systems to see if a link to productivity exists there. Our results support arguments against our current healthcare system's structure in a limited way.
Scope And Limitations
Our research has a few limitations. First, economic events such as recession may affect the validity of our results. Also, this research uses several proxies for productivity. Ideally, we should also track the hours of time spent being sick, which will affect both attendance and productivity; however due to unavailability of data this was not feasible. This research studies the data at a state level while other studies may drill down further to county and city level. Our research uses secondary data and is therefore subject to the limitations posed by the secondary source in terms of availability and veracity. Finally, the effects of healthcare spending on a different group (such as varying age groups) within a state were not studied. Nevertheless, the study offers a window into the relevance of healthcare expenditure in overall economic performance at a national level.
Conclusions
Our findings suggest that, in general, there is a positive association between healthcare spending and the economic indicators of labor productivity, personal income, per capita GDP, and other spending. Also, personal healthcare spending adversely impacts time spent on purchases of goods and services. There is no association between healthcare spending and change in multi-factor productivity (MFP) or working hours. Different states require varied investment in personal health expenditure, even if they have the same level of labor productivity. Overall, the study contributes to the growing literature on healthcare expenditure and economic performance. It outlines how the government can allocate healthcare expenditure in key dimensions that can stimulate economic growth while also improving the well-being of the population. It is also critical that policy makers implement appropriate policies at the macroeconomic level—targeted at public health expenditure and economic development. Overall, in light of the potential benefits of healthcare to the economy, universal access to healthcare is an area that warrants further research.
Data Availability Statement
Ethics statement.
Since this study uses aggregated national data, both ethical approval and written informed consent from the participants were not required for this study in accordance with the local legislation and institutional requirements.
Author Contributions
VR and WR contributed equally to all parts of manuscript preparation and submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- HEOR Resources
Interest in the field of health economics and outcomes research (HEOR) has grown exponentially.
Top 10 heor trends, the future of he+or, about real-world evidence.
- Clinical Outcomes
- Digital Health, Devices, and Diagnostics
- Economic Evaluation
- Epidemiology
- Healthcare Delivery
- Health Policy
- Health Technology Assessment
- Methodology
- Patient-Centered Research
- Real-World Data
- Specialized Treatment Areas
- CHEERS Related Videos
- Health Technology Assessment Central
- ISPOR Presentations Database
- Media Center
- HEOR News Desk
- Company Listings
- Sponsored Webinars
- Assessing the Evidence
- US Healthcare System Overview-Background
- US Healthcare System Overview-Decision Makers and Influencers
- US Healthcare System Overview-Pharmaceuticals
- US Healthcare System Overview-Medical Devices and In Vitro Diagnostics
- US Healthcare System Overview-Documentation Requirements
- US Healthcare System Overview-Acknowledgements
- US Healthcare System Overview-References
- Pharmacoeconomic Guidelines Around the World
- COVID-19 Resources
What Is HEOR?
Interest in the field of health economics and outcomes research (HEOR) has grown exponentially as governments and other payers grapple with how to provide the best possible health outcomes at affordable costs. At ISPOR, we believe that every healthcare decision should be informed by the best scientific research derived from rigorous, proven methodologies. Toward that goal, the Society’s mission is to promote HEOR excellence to improve decision making for health globally.
In today's world, healthcare decision makers across the globe are often faced with the need to select therapeutic "interventions" from multiple treatment options, including biopharmaceuticals, medical devices, and healthcare services. However, the benefits and costs of these interventions can range dramatically and the benefits can be economic, clinical, both, or may include hard to measure costs or benefits the patient experiences directly. Health economics and outcomes research (HEOR) can help healthcare decision makers—including clinicians, governments, payers, health ministries, patients, and more—to adequately compare and choose among the available options.
HEOR Defined
What is health economics and outcomes research (heor).
Outcomes research comprises a set of scientific disciplines that evaluate the effect of healthcare interventions on patients.
Health economics and outcomes research (HEOR) is the confluence of 2 fields that work together to provide powerful data and insights for healthcare decision makers.
ISPOR—The Professional Society for Health Economics and Outcomes Research (HEOR) continues to monitor healthcare trends and conduct horizon scanning around the world.
The “ISPOR 2024-2025 Top 10 HEOR Trends” marks the fifth publication of the Society’s biennial report, which is based on input from its members and strategic curation from its Health Science Policy Council .
View the Top 10 Trends
HEOR and ISPOR
During ISPOR’s 25+ year history, the Society has become the leading source for scientific conferences, peer-reviewed and MEDLINE ® -indexed publications, good practices guidance, education, collaboration, and tools/resources in the field of health economics and outcomes research. Learn more about how ISPOR contributes to the global HEOR community:
Related Resources
- ISPOR Science Strategy
- ISPOR Strategic Plan
- Real-World Evidence Strategic Initiative
- Payer Engagement in HEOR
- Patient Engagement in HEOR
- Value Assessment Strategic Initiative
- Dialogue With Decision Makers
HEOR Topics
ISPOR has defined the following HEOR topics in its taxonomy that are the key areas of focus for the organization and its membership:
- Epidemiology and Public Health
- Health Policy and Regulatory
- Health Service Delivery and Process of Care
- Medical Technologies
- Real-World Data and Information Systems
- Specific Diseases and Conditions
- Study Approaches
- Methodological and Statistical Research
- Organizational Practices
Subscribe to HEOR News and Events
Connect with the global community of healthcare stakeholders and stay informed on the latest and greatest happenings in the world of HEOR.
Your browser is out-of-date
ISPOR recommends that you update your browser for more security, speed and the best experience on ispor.org. Update my browser now
Aims and scope
Benefits of publishing with bmc, high visibility.
Health Economics Review 's open access policy allows maximum visibility of articles published in the journal as they are available to a wide, global audience.
Speed of publication
Health Economics Review offers a fast publication schedule whilst maintaining rigorous peer review; all articles must be submitted online, and peer review is managed fully electronically (articles are distributed in PDF form, which is automatically generated from the submitted files). Articles will be published with their final citation after acceptance, in both fully browsable web form, and as a formatted PDF.
Flexibility
Online publication in Health Economics Review gives you the opportunity to publish large datasets, large numbers of color illustrations and moving pictures, to display data in a form that can be read directly by other software packages so as to allow readers to manipulate the data for themselves, and to create all relevant links (for example, to PubMed , to sequence and other databases, and to other articles).
Promotion and press coverage
Articles published in Health Economics Review are included in article alerts and regular email updates. Some may be highlighted on Health Economics Review ’s pages and on the BMC homepage.
In addition, articles published in Health Economics Review may be promoted by press releases to the general or scientific press. These activities increase the exposure and number of accesses for articles published in Health Economics Review . A list of articles recently press-released by journals published by BMC is available here .
As an author of an article published in Health Economics Review you retain the copyright of your article and you are free to reproduce and disseminate your work (for further details, see the BMC license agreement ).
For further information about the advantages of publishing in a journal from BMC, please click here .
Open access
All articles published by Health Economics Review are made freely and permanently accessible online immediately upon publication, without subscription charges or registration barriers. Further information about open access can be found here .
As authors of articles published in Health Economics Review you are the copyright holders of your article and have granted to any third party, in advance and in perpetuity, the right to use, reproduce or disseminate your article, according to the BMC license agreement .
For those of you who are US government employees or are prevented from being copyright holders for similar reasons, BMC can accommodate non-standard copyright lines. Please contact us if further information is needed.
Article processing charges (APC)
Authors who publish open access in Health Economics Review are required to pay an article processing charge (APC). The APC price will be determined from the date on which the article is accepted for publication.
The current APC, subject to VAT or local taxes where applicable, is: £2090.00/$2790.00/€2390.00
Visit our open access support portal and our Journal Pricing FAQs for further information.
Open access funding
Visit Springer Nature’s open access funding & support services for information about research funders and institutions that provide funding for APCs.
Springer Nature offers agreements that enable institutions to cover open access publishing costs. Learn more about our open access agreements to check your eligibility and discover whether this journal is included.
Springer Nature offers APC waivers and discounts for articles published in our fully open access journals whose corresponding authors are based in the world’s lowest income countries (see our APC waivers and discounts policy for further information). Requests for APC waivers and discounts from other authors will be considered on a case-by-case basis, and may be granted in cases of financial need (see our open access policies for journals for more information). All applications for discretionary APC waivers and discounts should be made at the point of manuscript submission; requests made during the review process or after acceptance are unable to be considered.
Indexing services
All articles published in Health Economics Review are included in:
- Current Contents - Social & Behavioral Sciences
- Emerging Sources Citation Index
- PubMed Central
- Research Papers in Economics
- Social Sciences Citation Index
- Summon by Serial Solutions
The full text of all articles is deposited in digital archives around the world to guarantee long-term digital preservation. You can also access all articles published by BMC on SpringerLink . Health Economics Review has an Impact Factor of 2.306.
Peer-review policy
Peer-review is the system used to assess the quality of a manuscript before it is published. Independent researchers in the relevant research area assess submitted manuscripts for originality, validity and significance to help editors determine whether the manuscript should be published in their journal. You can read more about the peer-review process here .
Health Economics Review operates a double-blind peer-review system, where the reviewers do not know the names or affiliations of the authors and the reviewer reports provided to the authors are anonymous. Submitted manuscripts will generally be reviewed by two to three experts who will be asked to evaluate whether the manuscript is scientifically sound and coherent, whether it duplicates already published work, and whether or not the manuscript is sufficiently clear for publication. Reviewers will also be asked to indicate how interesting and significant the research is. The Editors will reach a decision based on these reports and, where necessary, they will consult with members of the Editorial Board.
Editorial policies
All manuscripts submitted to Health Economics Review should adhere to BMC's editorial policies .
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Citing articles in Health Economics Review
Articles in Health Economics Review should be cited in the same way as articles in a traditional journal. Because articles are not printed, they do not have page numbers; instead, they are given a unique article number.
Article citations follow this format:
Authors: Title. Health Econ Rev [year], [volume number]:[article number].
e.g. Roberts LD, Hassall DG, Winegar DA, Haselden JN, Nicholls AW, Griffin JL: Increased hepatic oxidative metabolism distinguishes the action of Peroxisome Proliferator-Activated Receptor delta from Peroxisome Proliferator-Activated Receptor gamma in the Ob/Ob mouse. Health Econ Rev 2009, 1 :115.
refers to article 115 from Volume 1 of the journal.
Appeals and complaints
Authors who wish to appeal a rejection or make a complaint should follow the procedure outlined in the BMC Editorial Policies .
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2022 Citation Impact 2.4 - 2-year Impact Factor 2.8 - 5-year Impact Factor 1.204 - SNIP (Source Normalized Impact per Paper) 0.836 - SJR (SCImago Journal Rank)
2023 Speed 11 days submission to first editorial decision for all manuscripts (Median) 220 days submission to accept (Median)
2023 Usage 566,888 downloads 483 Altmetric mentions
- More about our metrics
- ISSN: 2191-1991 (electronic)
Health Economics Review
ISSN: 2191-1991
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Preventing Chronic Diseases: What You Can Do Now
- Living with a Chronic Condition
- Chronic Disease Data
- Community Health Workers
- Workgroup on Translation Tools
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP)
Fast Facts: Health and Economic Costs of Chronic Conditions
At a glance.
Chronic diseases account for most illness, disability, and deaths in the United States and are the leading drivers of health care costs.

The impact of chronic diseases in America
Ninety percent of the nation's $4.5 trillion in annual health care expenditures are for people with chronic and mental health conditions. 1 2 Interventions to prevent and manage these diseases have significant health and economic benefits .
Heart disease and stroke
Nothing kills more Americans than heart disease and stroke . More than 934,500 Americans die of heart disease or stroke every year—that's more than 1 in 4 deaths. 3 These diseases take an economic toll, as well, costing our health care system $251 billion per year and causing $156 billion in lost productivity on the job. Costs from cardiovascular diseases are projected to top $1 trillion by 2035. 3
See the health and economic benefits of high blood pressure interventions .
Each year in the United States, 1.7 million people are diagnosed with cancer , and more than 600,000 die from it, making it the second leading cause of death. The cost of cancer care continues to rise and is expected to reach more than $240 billion by 2030. 4
See the health and economic benefits of interventions for breast cancer , cervical cancer , colorectal cancer , and skin cancer .
More than 38 million Americans have diabetes , and another 98 million adults in the United States have prediabetes, which puts them at risk for type 2 diabetes. Diabetes can cause serious complications, including heart disease, kidney failure, and blindness. In 2022, the total estimated cost of diagnosed diabetes was $413 billion in medical costs and lost productivity. 5
See the health and economic benefits of diabetes interventions .
Obesity affects 20% of children and 42% of adults, putting them at risk of chronic diseases such as type 2 diabetes, heart disease, and some cancers. Over 25% of young people aged 17 to 24 are too heavy to join the U.S. military. Obesity costs the U.S. health care system nearly $173 billion a year. 6
Arthritis affects 53.2 million adults in the United States, which is about 1 in 5 adults. 7 It is a leading cause of work disability in the United States, one of the most common chronic conditions, and a leading cause of chronic pain. Arthritis costs appear to be increasing and were estimated at over $600 billion in 2019. 8 9
Alzheimer's disease
Alzheimer's disease , a type of dementia, is an irreversible, progressive brain disease that affects nearly 7 million Americans, including 1 in 9 adults aged 65 and older. Two-thirds of these older adults (4.1 million) are women. Deaths due to Alzheimer's disease more than doubled between 2000 and 2019, increasing 145%. The cost of caring for people with Alzheimer's and other dementias was an estimated $345 billion in 2023, with projected increases to nearly $1 trillion (in today's dollars) by 2050. 10
In the United States, about 3 million adults and about half a million children and teens younger than 18 have active epilepsy —meaning that they have been diagnosed by a doctor, had a recent seizure, or both. Adults with epilepsy report worse mental health, more cognitive impairment, and barriers in social participation compared to adults without epilepsy. In 2019, total health care costs (epilepsy-attributable and other health-related costs) for noninstitutionalized people with epilepsy was $13.4 billion, of which $5.4 billion were directly attributable to epilepsy. 11
Tooth decay
Cavities (also called tooth decay) are one of the most common chronic diseases in the United States. One in six children aged 6 to 11 years and 1 in 4 adults have untreated cavities. Untreated cavities can cause pain and infections that may lead to problems eating, speaking, and learning. On average, 34 million school hours are lost each year because of unplanned (emergency) dental care, and almost $46 billion is lost in productivity due to dental disease. 12 13
See the health and economic benefits of oral disease interventions .
Risk Factors
Cigarette smoking.
Cigarette smoking is the leading cause of preventable death and disease in the United States. More than 16 million Americans have at least one disease caused by smoking. This amounts to more than $240 billion in health care spending that could be reduced every year if we could prevent young people from starting to smoke and help every person who smokes quit. 14
See the health and economic benefits of tobacco use interventions .
Physical inactivity
Not getting enough physical activity comes with high health and financial costs. It can lead to heart disease, type 2 diabetes, some cancers, and obesity. 15 Physical inactivity also costs the nation $117 billion a year for related health care. 16
Excessive alcohol use
Excessive alcohol use is responsible for 140,000 deaths in the United States each year, including 1 in 5 deaths among adults aged 20 to 49 years. 17 18 Binge drinking is responsible for over 40% these deaths. 17 In 2010, excessive alcohol use cost the U.S. economy $249 billion, or $2.05 a drink, and $2 of every $5 of these costs were paid by the public. 19 Three-quarters of these costs were due to binge drinking.
- Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States . Rand Corp.; 2017.
- National health expenditure data: historical. Center for Medicare & Medicaid Services. Updated December 13, 2023. Accessed February 6, 2024. https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/historical
- Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple Cause of Death 1999–2019 on CDC WONDER Online Database website. http://wonder.cdc.gov/mcd-icd10.html . Accessed February 1, 2023.
- Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29:1304–1312.
- Parker ED, Lin J, Mahoney T, et al. Economic costs of diabetes in the U.S. in 2022. Diabetes Care. 2023. doi: 10.2337/dci23-0085
- Ward ZJ, Bleich SN, Long MW, Gortmaker SL. Association of body mass index with health care expenditures in the United States by age and sex. PLoS One . 2021;16(3):e0247307.
- Fallon EA, Boring MA, Foster AL, et al. Prevalence of diagnosed arthritis—United States, 2019–2021. MMWR Morb Mortal Wkly Rep . 2023;72:1101–1107.
- Murphy LB, Cisternas MG, Pasta DJ, Helmick CG, Yelin EH. Medical expenditures and earnings losses among US adults with arthritis in 2013. Arthritis Care Res (Hoboken) . 2018;70(6):869–876.
- Lo J, Chan L, Flynn S. A systematic review of the incidence, prevalence, costs, and activity and work limitations of amputation, osteoarthritis, rheumatoid arthritis, back pain, multiple sclerosis, spinal cord injury, stroke, and traumatic brain injury in the United States: a 2019 Update. Arch Phys Med Rehabil . 2021;102(1):115–131.
- Alzheimer's Association. 2023 Alzheimer's disease facts and figures. Alzheimers Dement . 2023;19(4).
- Moura LMVR, Karakis I, Zack MM, Tian N, Kobau R, Howard D. Drivers of US health care spending for persons with seizures and/or epilepsies, 2010-2018. Epilepsia . 2022;63(8):2144–2154.
- Righolt AJ, Jevdjevic M, Marcenes W Listl S. Global-, regional-, and country-level economic impacts of dental diseases. J Dent Res. 2018;97(5):501–507.
- Naavaal S, Kelekar U. Hours lost due to planned and unplanned dental visits among US adults. Health Behav Policy Rev. 2018;5(2):66–73.
- Xu X, Shrestha SS, Trivers KF, Neff L, Armour BS, King BA. U.S. healthcare spending attributable to cigarette smoking in 2014. Prev Med . 2021;150:106529.
- U.S. Department of Health and Human Services. Step It Up! The Surgeon General's Call to Action to Promote Walking and Walkable Communities . Office of the Surgeon General; 2015.
- Carlson SA, Fulton JE, Pratt M, Yang Z, Adams EK. Inadequate physical activity and health care expenditures in the United States . Prog Cardiovasc Dis . 2015;57:315–323.
- Centers for Disease Control and Prevention (CDC). Alcohol-Related Disease Impact (ARDI).
- Esser MB, Leung G, Sherk A, et al. Estimated deaths attributable to excessive alcohol use among US adults aged 20 to 64 years, 2015 to 2019. JAMA Netw Open . 2022;5(11):e2239485. doi: 10.1001/jamanetworkopen.2022.39485
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. Am J Prev Med 2015;49(5):e73–e79.
Chronic Disease
Prevalence, costs, risks, prevention, and management of chronic diseases in the United States
For Everyone
Public health.
Economics of Health
Researchers affiliated with the Economics of Health Program study the economic determinants of health, the operation of health care markets, and the financing of health care with particular emphasis on public and private insurance. Core topics of interest include the determinants of "health capital" and the consequences of unhealthy behaviors such as substance abuse, the role of market failure in health care and health insurance markets, and the impact of public policies on health care delivery, expenditures, financing, and innovation. The program is the successor to the Health Care and Health Economics Programs, which merged in July 2023.
Codirectors

Christopher "Kitt" Carpenter is the E. Bronson Ingram Chair and Professor of Economics at Vanderbilt University, where he also holds courtesy appointments in the schools of law and medicine. His research focuses on the effects of public policies on health and family outcomes. He has been an NBER affiliate since 2005.

Amy Finkelstein is the John and Jennie S. MacDonald Professor of Economics at the Massachusetts Institute of Technology and the co-founder and Co-Scientific Director of the Jameel Poverty Action Lab-North America. Her research interests focus on public finance and health economics, particularly market failures and government intervention in insurance and health care markets. She has been an NBER affiliate since 2001.
Featured Program Content
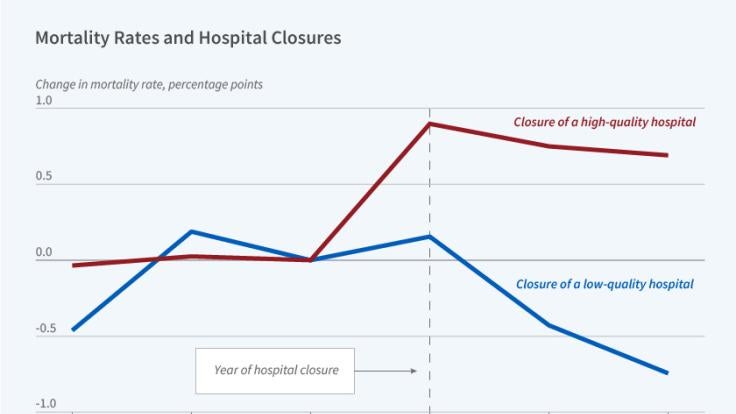
- Authors: Amitabh Chandra , Maurice Dalton & Douglas O. Staiger
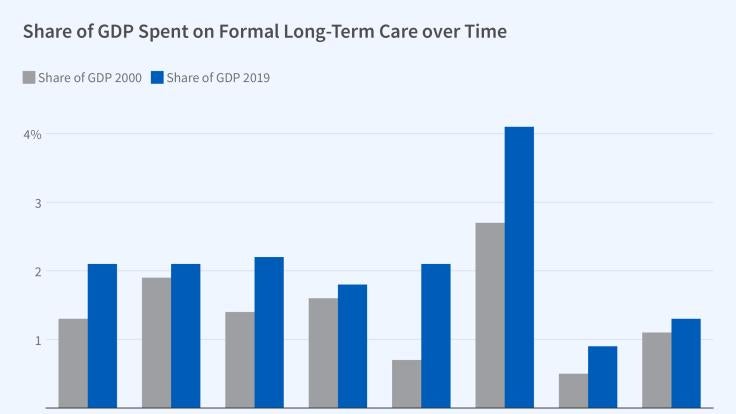
- Authors: Jonathan Gruber , Kathleen M. McGarry & Charles Hanzel
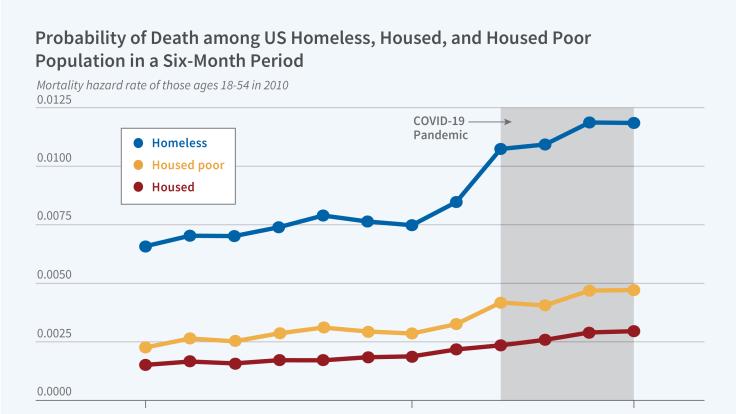
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- New editors
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Active workplace design: current gaps and future pathways
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-9384-5456 Mohammad Javad Koohsari 1 , 2 , 3 ,
- Andrew T Kaczynski 4 ,
- Akitomo Yasunaga 5 ,
- Tomoya Hanibuchi 6 ,
- Tomoki Nakaya 7 ,
- Gavin R McCormack 8 ,
- Koichiro Oka 2
- 1 School of Advanced Science and Technology , Japan Advanced Institute of Science and Technology , Nomi , Japan
- 2 Faculty of Sport Sciences , Waseda University , Tokorozawa , Japan
- 3 School of Exercise and Nutrition Sciences , Deakin University , Geelong , Victoria , Australia
- 4 Arnold School of Public Health , University of South Carolina , Columbia , South Carolina , USA
- 5 Faculty of Health Sciences , Aomori University of Health and Welfare , Aomori , Japan
- 6 Graduate School of Letters , Kyoto University , Kyoto , Japan
- 7 Graduate School of Environmental Studies , Tohoku University , Sendai , Japan
- 8 Department of Community Health Sciences , University of Calgary , Calgary , Alberta , Canada
- Correspondence to Dr Mohammad Javad Koohsari, Japan Advanced Institute of Science and Technology, Nomi, Japan; koohsari{at}jaist.ac.jp
https://doi.org/10.1136/bjsports-2024-108146
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- Public health
- Sedentary Behavior
- Health promotion
Introduction
Insufficient physical activity and excessive sitting time among office-based workers have been linked to various health risks and economic consequences. While health promotion interventions are important, the role of workplace design in encouraging active behaviours is increasingly recognised. However, significant gaps exist in knowledge about how workplace design influences these behaviours. This paper identifies the need to investigate the interactive effects of workplace norms and culture and the role of building layouts on workers’ behaviours, as well as the need for more accurate behavioural measures. Bridging these gaps is crucial for designing workplace interventions and promoting active, healthy and productive work environments.
Workplace design: encouraging movement in workplace settings
Existing gaps and future directions, interactive effects of workplace social environments.
Workplace social environments such as norms and culture can significantly influence sedentary behaviours among office-based workers 4 and can affect how workplace design influences workers’ behaviour. Most previous studies have tested the effects of workplace design on employees’ active and sedentary behaviours within Western contexts, 5 leaving a gap in how these relationships vary in other geographical settings with unique workplace norms and cultures. For instance, in a workplace where extended sitting is a cultural norm, employees may still predominantly engage in sedentary behaviour, regardless of having activity-promoting features in their workplace. Conversely, an activity-promoting environment might help mitigate norms towards sitting or even produce multiplicative positive effects in contexts where activity in the workplace is already customary. Conducting studies across varied geographical settings is necessary to identify similarities and differences in the impact of workplace norms and design on workers’ active and sedentary behaviours. Cross-cultural studies can shed light on the generalisability of findings and help develop customised interventions that address specific norms and cultural challenges. Future research can also employ mixed methods to gain a more thorough understanding of the complex interplay between workplace design, norms and culture, and employees’ behaviour. Additionally, the rise of home and hybrid working arrangements indicates that office social norms could extend to home work environments. For example, a culture of regular stretch breaks in the office might encourage similar practices at home, influencing physical activity behaviours remotely. Understanding the detailed relationship between workplace design, norms and employee behaviour is critical for developing targeted contextually relevant interventions that promote active workplace environments.
Precision in tracking workplace behaviours
Accurately measuring employees’ active and sitting behaviours and identifying the ‘locations’ where these behaviours occur is essential to understand their relationships with workplace design attributes. Global positioning systems (GPS) have been commonly used in combination with accelerometer devices to measure and spatially track people’s active and sedentary behaviour in outdoor environments, such as neighbourhoods and cities. 6 Nevertheless, GPS signals have limited accuracy or can be disrupted within indoor environments, resulting in less precise location data.
An indoor positioning system (IPS) can address the limitations of GPS in indoor environments. 7 IPS is a wayfinding technology that uses existing low-cost WiFi and Bluetooth to provide precise locations of individuals inside buildings. The IPS can be integrated with activity-tracking wearable devices, such as accelerometers, pedometers and heart rate monitors, as well as traditional methods like behavioural mapping. This integration allows for the collection of employees’ location data, movement patterns, activity intensities and other biometric data within workplaces. Additionally, the synergy between IPS and wearable devices effectively differentiates between occupational and leisure physical activities in workplaces. This distinction is key to better understanding the health paradox of the different health effects of these two types of physical activities. 8 Furthermore, with the growth of artificial intelligence (AI), there has been a unique opportunity to employ geospatial AI (GeoAI) in workplace environments and health research. GeoAI techniques aim to integrate innovations in spatial sciences with AI, particularly deep learning. 9 The joint application of IPS and GeoAI would enable precise location data of individuals within the workplace while using the power of spatial analysis. GeoAI can analyse workers’ movement patterns derived from IPS in combination with geospatial layers such as spatial layouts, access to common places, and light conditions. For instance, a GeoAI trained by tracking data on people’s movements in various indoor environments would predict people’s movements and derive estimates of the amount of sedentary behaviour of employed people only from planned indoor layout. This analysis allows for identifying hotspots or areas within the workplace where active and sedentary behaviour is prevalent.
Beyond individual design elements: exploring the influence of building layout on workplace behaviour
Most previous studies have primarily examined individual design elements but fail to consider how the overall spatial layout influences movement and behaviour. Building layout encompasses the spatial arrangement of building elements such as walls, doors, windows, and access ways, and plays a fundamental role in defining the functionality of interior spaces. Once a building layout has been established, making substantial alterations to it becomes challenging or, in some cases, impossible. Therefore, designing (and, if feasible, retrofitting) building interiors to promote health is imperative, but it is still unclear which workplace layouts are most supportive of workers’ active behaviours.
The urban design theory of space syntax has the potential to partially address this gap in knowledge. Space syntax uses a set of graph-based estimators to quantify spatial layouts. 10 It offers a framework to investigate the impact of building layout factors, such as workstation arrangement, common area location, and space accessibility, on workers’ movement patterns and behaviours. It goes beyond isolated design elements and considers the spatial configuration as a whole ( figure 1 ). Additionally, more research on ‘how’ people use and perceive their workspaces could complement the space syntax evaluations of building design.
- Download figure
- Open in new tab
- Download powerpoint
Space syntax examines building layouts as a whole, using the graph theory: (A)a schematic workplace layout, (B)space syntax axial lines (i.e., longest and fewest lines traversing all spaces) of the layout, and (C)the connectivity of all spaces based on the graph theory.
Conclusions
Future research should investigate the interactive effects of workplace norms and culture on behaviour and conduct cross-cultural studies to identify similarities and differences. Innovative measurement methods can also be employed to accurately measure behaviours and locations where those behaviours occur within workplaces. Additionally, exploring the influence of spatial layout, and using the urban design theory of space syntax, can offer valuable insights into the design of work environments that facilitate workers’ engagement in active behaviours.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Sugiyama T ,
- Eakin EE , et al
- Yoshikawa A ,
- Qiu L , et al
- Koohsari MJ ,
- Liao Y , et al
- Waters CN ,
- Chu AHY , et al
- Hadgraft N ,
- Clark BK , et al
- Katapally TR ,
- Pollard B ,
- Engelen L ,
- Held F , et al
- Holtermann A ,
- Hansen JV ,
- Burr H , et al
- Laden F , et al
- Hillier B ,
Contributors MJK conceived the idea and wrote the initial draft of the manuscript. All authors contributed to the writing and assisted with the analysis and interpretation. All authors have read and approved the final manuscript and agree with the order of the presentation of authors.
Funding MJK is supported by the JSPS KAKENHI (grant 23K09701). KO is supported by the JSPS Grants-in-Aid for Scientific Research program (grant 20H04113).
Competing interests None declared. In particular, none of the authors has a financial interest in the Space Syntax Limited company.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

AI poised to usher in new level of concierge services to the public
Researchers explore how intelligent systems can upgrade hospitality sector.
Concierge services built on artificial intelligence have the potential to improve how hotels and other service businesses interact with customers, a new paper suggests.
In the first work to introduce the concept, researchers have outlined the role an AI concierge, a technologically advanced assistant, may play in various areas of the service sector as well as the different forms such a helper might embody.
Their paper envisions a virtual caretaker that, by combining natural language processing, behavioral data and predictive analytics, would anticipate a customer’s needs, suggest certain actions, and automate routine tasks without having to be explicitly commanded to do so.

“The traditional service industry uses concierges for high-end clients, meaning that only a few people have access to them,” Liu said. “Now with the assistance of AI technology, everybody can have access to a concierge providing superior experiences.”
On that premise, the benefits of incorporating AI into customer service are twofold: It would allow companies to offer around-the-clock availability and consistency in their operations as well as improve how individuals engage with professional service organizations, she said.
Moreover, as the younger workforce gravitates to more tech-oriented jobs and global travel becomes more common, generative AI could be an apt solution to deal with the escalating demands of evolving hospitality trends, said Liu.
“The development of AI technology for hotels, restaurants, health care, retail and tourism has a lot of potential,” she said.
The paper was published recently in the Journal of Service Management .
Despite the social and economic benefits associated with implementing such machines, how effective AI concierges may be at completing a task is dependent on both the specific situation and the type of interface consumers use, said Liu.
There are four primary forms a smart aide might take, each with distinctive attributes that would provide consumers with different levels of convenience, according to Liu.
The first type is a dialogue interface that uses only text or speech to communicate, such as ChatGPT, a conversational agent often used to make inquiries and garner real-time assistance. Many of these interactive devices are already used in hotels and medical buildings for contactless booking or to connect consumers with other services and resources.
The second is a virtual avatar that employs a vivid digital appearance and a fully formed persona to foster a deeper emotional connection with the consumer. This method is often utilized for telehealth consultations and online learning programs.
The third iteration is a holographic projection wherein a simulated 3D image is brought into the physical world. According to the paper, this is ideally suited for scenarios where the visual impact is desired, but physical assistance itself is not necessary.
The paper rounds out the list by suggesting an AI concierge that would present as a tangible, or touchable robot. This form would offer the most human-like sensory experiences and would likely be able to execute multiple physical tasks, like transporting heavy luggage.
Some international companies have already developed these cutting-edge tools for use in a limited capacity. One robotic concierge, known as Sam , was designed to aid those in senior living communities by helping them check in, make fall risk assessments and support staff with non-medical tasks. Another deployed at South Korea’s Incheon International Airport helped consumers navigate paths to their destination and offered premier shopping and dining recommendations.
Yet as advanced computing algorithms become more intertwined in our daily lives, industry experts will likely have to consider consumer privacy concerns when deciding when and where to implement these AI systems. One way to deal with these issues would be to create the AI concierge with limited memory or other safewalls to protect stored personal data, such as identity and financial information, said Liu.
“Different companies are at different stages with this technology,” said Liu. “Some have robots that can detect customers’ emotions or take biometric inputs and others have really basic ones. It opens up a totally different level of service that we have to think critically about.”
What’s more, the paper notes that having a diversity of concierge options available for consumers to choose from is also advantageous from a mental health standpoint.
Because AI is viewed as having less agency than their human counterparts, it might help mitigate psychologically uncomfortable service situations that could arise because of how consumers feel they might be perceived by a human concierge. This reduced apprehension regarding the opinion of a machine may encourage heightened comfort levels and result in more favorable responses about the success of the AI concierge, said Liu.
Ultimately, there’s still much multidisciplinary testing to be done to ensure these technologies can be applied in a widespread and equitable manner. Liu adds that future research should seek to determine how certain design elements, such as the perceived gender, ethnicity or voice of these robotic assistants, would impact overall consumer satisfaction.
More Ohio State News
Nimh director discusses progress, opportunities for research during visit at ohio state.
Earlier this month, the director of the National Institute of Mental Health (NIMH) spent a day at The Ohio State University Wexner Medical Center to help kick off May’s Mental Health Awareness month.
Ohio State appoints new dean and director of Ohio State Newark
The Ohio State University has selected Matthew J. Smith as its next dean and director of The Ohio State University at Newark , effective Aug. 1. Smith currently serves as dean of the College of Humanities and Behavioral Sciences at Radford University , a comprehensive public university in Radford, Virginia, where he is also a professor of communication.
How family economic insecurity can hurt child mental health
Economic difficulty caused by the COVID-19 pandemic led to a cascade of connected problems for some parents – resulting in mental health problems for their children, a new study suggests.

Contact: Admissions | Webmaster | Page maintained by University Communications
Request an alternate format of this page | Web Services Status | Nondiscrimination notice

IMAGES
VIDEO
COMMENTS
This journal seeks articles related to the economics of health and medical care. Its scope will include the following topics: Production and supply of health services; Demand and utilization of health services; Financing of health services; Determinants of health, including investments in health …. View full aims & scope.
Health economics is a thriving sub-discipline of economics. Applied health economics research is considered essential in the health care sector and is used extensively by public policy makers. ... 1.204 - SNIP (Source Normalized Impact per Paper) 0.836 - SJR (SCImago Journal Rank) 2023 Speed 11 days submission to first editorial decision for ...
Health Economics has published a new Virtual Issue The Demand for Health Turns Fifty, and an new retrospective editorial by Dr. Michael Grossman "The demand for health turns 50: Reflections", looking back on the history and development of the demand for health model and its impacts on the field of health economics. The Virtual Issue contains twenty-eight papers from Health Economics ...
Health Economics Review is an open-access journal covering all aspects of health economics, from a micro- to macro-scale. ... health services research and health policy analysis. Further research topics are the individual and institutional aspects of health care management and the growing importance of health economics and health systems in low ...
Health science is evolving extremely rapidly at worldwide level. There is a large volume of articles about health economics that are published each year. The main purpose of this research is to explore health economics in the world's scholarly literature based on a scient metric analysis to outline the evolution of research in the field. The Web of Science repository was used to get the data ...
Given space constraints — and the fact that since the last program report nearly 1,300 NBER Health Economics working papers have been released — this report can only describe a small fraction of the interesting research in these key areas. ... Research by Health Economics Program members has also advanced understanding of the effects of ...
Impact of aging on acute myeloid leukemia epidemiology and survival outcomes: A real-world, population-based longitudinal cohort study. Hyun Jin Han, Kyungson Choi, Hae Sun Suh.
Abstract. Health economics, as an interdisciplinary science, has experienced exceptionally bold evolution through the past eight decades. Generations of committed scholars have built up huge body of knowledge and developed a set of methodological tools to assist health-care authorities with resource allocation process.
1 HEALTH AND HEALTH ECONOMICS. Health economics research will have greater impact on health and health care the more thoughtfully it conceptualizes and measures health (Mullahy, 2018a ). Opportunities to undertake rigorous and relevant measurement of health—in order to understand it, its production, and its consequences—are expanding ...
We are now entering the third decade of the 21st Century, and, especially in the last years, the achievements made by scientists have been exceptional, leading to major advancements in the fast-growing field of Health Economics. Frontiers has organized a series of Research Topics to highlight the latest advancements in science in order to be at the forefront of science in different fields of ...
Dissertation Advisor: Thomas McGuire. Monica Farid. Essays in Health Economics Abstract This dissertation consists of three chapters that relate to the following broad areas in health. economics: care provision for vulnerable populations, challenges in efficient insurance market.
Health Economics resides at the intersection of economics and health-related issues, examining how scarce resources are allocated to improve health and acquire care. The Health Economics Research Network on SSRN is an open access preprint server that provides a venue for authors to showcase their research papers in our digital library, speeding ...
Founded in 1920, the NBER is a private, non-profit, non-partisan organization dedicated to conducting economic research and to disseminating research findings among academics, public policy makers, ... Center for Aging and Health Research; Conference on Research in Income and Wealth; Early Indicators of Later Work Levels, Disease and Death ...
In response to the COVID-19 pandemic, in April 2020 the AJHE began a fast track review for time-sensitive, COVID-19-related health economics research papers. Given the large number of COVID-19 papers submitted and the ongoing challenges facing referees, we have found it increasingly difficult to maintain the goal of a 2-week turnaround on ...
Short Research Articles (Health Economics Letters) (3,000 word limit) - concise reports of new research findings that make a significant contribution to knowledge. Editorials (1,500 word limit) - Summaries of pertinent issues, commentaries on recently published papers, or freestanding pieces expressing an opinion—are typically invited.
Here we provide a breakdown of the most commonly used perspectives within health economic evaluations and costing studies. These are derived from a review of key texts [8, 12, 13], and recommendations from multiple international and national economic evaluation guidelines listed in the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) and Guide to Economic Analysis and ...
Introduction Health economics is a thriving sub-discipline of economics. Applied health economics research is considered essential in the health care sector and is used extensively by public policy makers. For scholars, it is important to understand the history and status of health economics—when it emerged, the rate of research output, trending topics, and its temporal evolution—to ensure ...
The theory of welfare economics is relevant to the current research. Welfare economics is a branch that deals with economic and social welfare ... Based on a study that examined the impact of health on economic growth in ... Canning D. Health as human capital and its impact on economic performance. Geneva Papers Risk Insur. (2003) 28:304 ...
The aim of this study was to assess the cost-effectiveness of extracorporeal photopheresis compared with standard-of-care therapies for the treatment of chronic graft-vs-host disease in Australia. The Journal of HEOR is an open access journal covering all fields and methodologies related to health economics and outcomes research.
nomics can help us avert the situation that arose in the wake of the recent COVID-19 pandemic. Applying the core principles of Health Economics to a situation like that would help avert bad outcomes. In this article, the authors begin by defining and establishing the concepts of Health Economics and then building on them. We further explain the concepts in light of the Indian Economy and ...
the citations in the Journal of Health Economics were to economics journals (excluding health economics), while the papers in Health Economicsdrew less heavily on economics with only 24 percent of citations coming from that field. By contrast, Health Economics papers drew more heavily on health policy, health services research, and medical ...
Health economics and outcomes research (HEOR) is the confluence of 2 fields that work together to provide powerful data and insights for healthcare decision makers. Top 10 HEOR Trends. ... This ISPOR White Paper examines the future of health economics and outcomes research (HEOR), exploring the impact that HEOR and ISPOR will have on healthcare ...
PDF | Top articles in health economics | Find, read and cite all the research you need on ResearchGate. ... Oxford Economic Papers 1971; 23: 189-211.
Health Economics Review is an international high-quality journal covering all fields of Health Economics. A broad range of theoretical contributions, empirical studies and analyses of health policy with a health economic focus will be considered for publication. Its scope includes health economic evaluations, macro- and microeconomics of health ...
More than 934,500 Americans die of heart disease or stroke every year—that's more than 1 in 4 deaths. 3 These diseases take an economic toll, as well, costing our health care system $251 billion per year and causing $156 billion in lost productivity on the job. Costs from cardiovascular diseases are projected to top $1 trillion by 2035. 3.
Amy Finkelstein is the John and Jennie S. MacDonald Professor of Economics at the Massachusetts Institute of Technology and the co-founder and Co-Scientific Director of the Jameel Poverty Action Lab-North America. Her research interests focus on public finance and health economics, particularly market failures and government intervention in insurance and health care markets.
International Economic Review is an economics journal publishing papers in topics across the field, from economic theory to econometrics and applied economics. Abstract This article evaluates the insurance value of the Social Security Disability Insurance (SSDI) program among married households when wives face a trade-off between market hours ...
Insufficient physical activity and excessive sitting time among office-based workers have been linked to various health risks and economic consequences. While health promotion interventions are important, the role of workplace design in encouraging active behaviours is increasingly recognised. However, significant gaps exist in knowledge about how workplace design influences these behaviours ...
[email protected]. Concierge services built on artificial intelligence have the potential to improve how hotels and other service businesses interact with customers, a new paper suggests. In the first work to introduce the concept, researchers have outlined the role an AI concierge, a technologically advanced assistant, may play in various ...
Download the 2024 Gen Z and Millennial Report. 5 MB PDF. To learn more about the mental health findings, read the Mental Health Deep Dive. The 13th edition of Deloitte's Gen Z and Millennial Survey connected with nearly 23,000 respondents across 44 countries to track their experiences and expectations at work and in the world more broadly.