Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
If your baby is in a breech presentation, their feet or bottom will be closest to your birth canal. The 3 most common types of breech presentation are:
- frank or extended breech — where your baby’s legs are straight up in front of their body, with their feet up near their face
- complete or flexed breech — where your baby is in a sitting position with their legs crossed in front of their body and their feet near their bottom
- footling breech — where one or both of your baby’s feet are hanging below their bottom, so the foot or feet are coming first
Read more on breech presentation .
What are the different positions my baby could be in during pregnancy and birth?
If your baby is headfirst, the 3 main types of presentation are:
- anterior – when the back of your baby’s head is at the front of your belly
- lateral – when the back of your baby’s head is facing your side
- posterior – when the back of your baby’s head is towards your back

How will I know what presentation and position my baby is in?
Your doctor or midwife can usually work out your baby’s presentation by feeling your abdomen. They may also double check it with a portable ultrasound. Your baby’s presentation is usually checked around 36 weeks .
Your doctor or midwife will also confirm your baby’s head position in labour by examining your belly and using an ultrasound , and they may also do a vaginal examination . During the vaginal examination they are feeling for certain ridges on your baby’s head called sutures and fontanelles that help them work out which way your baby is positioned.
What is the ideal presentation and position for baby to be in for a vaginal birth?
For a vaginal birth, your baby will ideally be headfirst with the back of their head at the front of your belly, also known as being in the anterior position. This position is best for labour and birth since it means that the smallest part of your baby’s head goes down the birth canal first.

When does a baby usually get in the ideal presentation and position for birth?
Your baby will usually be in a headfirst position by 37 weeks of pregnancy. Around 3 in every 100 babies will be in breech presentation after 37 weeks.
Your baby’s position can change with your contractions during labour as they move down the birth canal, so their exact position can change during labour.
What are my options if baby isn't in the ideal presentation or position for a vaginal birth?
If your baby is in a breech presentation, your doctor may recommend a technique called an external cephalic version (ECV) to try and move your baby while they are still in the uterus . An ECV involves your doctor using their hands to apply pressure on your belly and help turn your baby to a headfirst position. It has a 1 in 2 chance of success and is a safe option in most pregnancies.
There is no evidence to show that alternative therapies, such as exercises, acupuncture or chiropractic treatments, help your baby change from a breech presentation to headfirst.
If your baby remains breech, your doctor may discuss having a breech vaginal birth. Not all doctors and hospitals offer this option. They may also suggest you birth your baby with a planned caesarean section .
If your baby’s presentation is headfirst but the position of your baby’s head is not ideal for labour, it can lead to a longer labour, and potential complications . The position of your baby’s head will often change as your labour progresses. If it doesn’t, sometimes you can still give birth without assistance, or you may need your doctor to help turn your baby’s head or help your birth with a vacuum or forceps .
Any procedure or decision for a type of birth will only go ahead with your consent . You will be able to discuss all the options with your doctor, and based on your preferences for yourself and your baby’s safety, make a decision together .
Resources and support
The Royal Australian and New Zealand College of Obstetrics and Gynaecology has a factsheet about the options available to you if your baby is in a breech presentation at the end of your pregnancy .
Mercy Perinatal has information on external cephalic version (ECV) safety and benefits if your baby is in a breech presentation at the end of your pregnancy.
The Women’s Hospital has information about the different presentations and positions your baby could be in, and how it can affect your birthing experience.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: October 2023
Related pages
External cephalic version (ecv), malpresentation, breech pregnancy, search our site for.
- Foetal Version
- Breech Presentation
Need more information?
Top results
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
ECV is a procedure to try to move your baby from a breech position to a head-down position. This is performed by a trained doctor.
Having a baby
The articles in this section relate to having a baby – what to consider before becoming pregnant, pregnancy and birth, and after your baby is born.
Anatomy of pregnancy and birth - pelvis
Your pelvis helps to carry your growing baby and is tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Planned or elective caesarean
There are important things to consider if you are having a planned or elective caesarean such as what happens during and after the procedure.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Zink is a board-certified emergency medicine physician with expertise in the wilderness and global medicine.
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

11 templates
20 templates

holy spirit
36 templates
9 templates

25 templates
memorial day
12 templates
Pregnancy Presentation templates
The day you give birth to a child is the best of your entire life. nine months living as one, and then a lifetime of pure parent-child love check out these google slides themes & powerpoint templates about pregnancy, obstetrics and babies. easily customizable for everyone.

It seems that you like this template!
Pregnancy breakthrough infographics.
Medical advances on pregnancy just keep growing! Although we know a lot about obstetrics nowadays, there is always a lot to discover, and there is nothing clearer than an infographic to illustrate medical concepts! If you found our Pregnancy Breakthrough template useful, these infographics that complement that presentation will make...

Premium template
Unlock this template and gain unlimited access
Stages of Development of the Fetus
Nine intense months until a new life is born! If you work in healthcare, you might have seen some informative posters for first-time parents about the development of the fetus. With this template, you can create a full presentation about it! We've used tones of pink to convey love and...
Placental Abnormalities in Pregnancy
Download the Placental Abnormalities in Pregnancy presentation for PowerPoint or Google Slides. Healthcare goes beyond curing patients and combating illnesses. Raising awareness about diseases, informing people about prevention methods, discussing some good practices, or even talking about a balanced diet—there are many topics related to medicine that you could be...

Care Center for Pregnant Mothers
Pregnancy is often referred to as the "miracle of life" because it involves the creation of a brand-new human being. It’s a miracle, yes… Following this, we have a template for promoting a care center for pregnant mothers. The slides are decorated with beautiful flowers, plants, and images of glowing...

Pregnancy Calendar
Are you expecting a baby? Nine months might seem too much time... or maybe not! We have designed a new multi-purpose template whose topic is pregnancy. We wanted to make the slides very visually pleasing, so we've used soft colors and some flowers as decoration. If you want to make...

Pregnancy Medical Center
A soon-to-be-mom? You're probably feeling a mixture of excitement and nervousness, which is completely normal. Medicine and healthcare are pretty much ready to take care of pregnant women, and there's even some medical centers whose specialty is obstetrics. Promote such a center by using the template that we've just released...

Preeclampsia in Pregnancy Case Study
Understanding and managing preeclampsia in pregnancy is a task requiring careful attention and knowledge. With this colorfully illustrated Google Slides and PowerPoint template, you can present a comprehensive case study highlighting the complexities and strategies involved with exceptional clarity. This fully editable slide deck, prepped with additional icons to add...
Social Factors on Teenage Pregnancy Thesis Defense
Download the Social Factors on Teenage Pregnancy Thesis Defense presentation for PowerPoint or Google Slides. Congratulations, you have finally finished your research and made it to the end of your thesis! But now comes the big moment: the thesis defense. You want to make sure you showcase your research in...

Pregnant Mother Minitheme
Congratulations on the new addition to your family! As an expecting mother, it's important to take care of both yourself and your growing baby. Write a minitheme to help other mothers and guide them through a healthy and happy pregnancy. The slides of this template look very cute with a...

Twins Pregnancy Case Study
They say that giving birth to a child is the most beautiful moment for a mother in her entire life. Wait a second, another baby is coming right after the first—they're twins! Use this editable template to prepare a slideshow that shows the case study of pregnancy of twin babies....

Postpartum Ischemic Stroke Case Report
Download the "Postpartum Ischemic Stroke Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals...

Toxoplasmosis Disease
Download the Toxoplasmosis Disease presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical attention....

Download the "Eclampsia" presentation for PowerPoint or Google Slides. Taking care of yourself and of those around you is key! By learning about various illnesses and how they are spread, people can get a better understanding of them and make informed decisions about eating, exercise, and seeking medical attention. This...

World Day for Pregnant, Perinatal and Neonatal Death Awareness
World Day for Pregnant, Perinatal and Neonatal Death Awareness is an important occasion to talk about these tragic subjects. With this template, you can put together a presentation whose look and tone fit the sad nature of the topic being discussed. Its stark design, with white text over a black...

Egg Donation Center
Download the "Egg Donation Center" presentation for PowerPoint or Google Slides. Hospitals, private clinics, specific wards, you know where to go when in need of medical attention. Perhaps there’s a clinic specialized in treating certain issues, or a hospital in your area that is well-known for its state-of-the-art technology. How...

Gestational Diabetes Breakthrough
Download the Gestational Diabetes Breakthrough presentation for PowerPoint or Google Slides.Treating diseases involves a lot of prior research and clinical trials. But whenever there’s a new discovery, a revolutionary finding that opens the door to new treatments, vaccines or ways to prevent illnesses, it’s great news. Should there be a...

Maternity Related Sickness
Bearing a child is a very tough task for a body. Mothers, or soon-to-be, should have time and space to rest, that’s why maternity leaves are so important. In addition, pregnancy can have complications that require medical attention. Speak about them and share the most common ones so that pregnant...


Prenatal Healthcare Center
Before giving birth to a child, there are so many things to be prepared for a smooth labor. Did you know that there are several exercises and movements that can help a woman to be relaxed and release the pain during childbirth? We are sure that you know that better...
- Page 1 of 8
Great presentations, faster
Slidesgo for Google Slides :
The easy way to wow
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Identification of breech presentation
Evidence review L
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation?
Introduction
Breech presentation in late pregnancy may result in prolonged or obstructed labour for the woman. There are interventions that can correct or assist breech presentation which are important for the woman’s and the baby’s health. This review aims to determine the most effective way of identifying a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
One single centre randomised controlled trial (RCT) was included in this review ( McKenna 2003 ). The study was carried out in Northern Ireland, UK. The study compared ultrasound examination at 30-32 and 36-37 weeks with maternal abdomen palpation during the same gestation period. The intervention group in the study had the ultrasound scans in addition to the abdomen palpation, while the control group had only the abdomen palpation. Clinical management options reported in the study based on the ultrasound scan or the abdomen palpation include referral for full biophysical assessment which included umbilical artery Doppler ultrasound, early antenatal review, admission to antenatal ward, and induction of labour.
The included study is summarised in Table 2 .
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D . No meta-analysis was conducted (and so there are no forest plots in appendix E ).
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
One study, a cost utility analysis was included ( Wastlund 2019 ).
See the literature search strategy in appendix B and economic study selection flow chart in appendix G .
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of studies included in the economic evidence review
For full details of the economic evidence, see the economic evidence tables in appendix H and economic evidence profiles in appendix I .
Wastlund (2019) assessed the cost effectiveness of universal ultrasound scanning for breech presentation at 36 weeks’ gestational age in nulliparous woman (N=3879). The comparator was selective ultrasound scanning which was reported as current practice. In this instance, fetal presentation was assessed by palpation of the abdomen by a midwife, obstetrician or general practitioner. The sensitivity of this method ranges between 57%-70% whereas ultrasound scanning is detected with 100% sensitivity and 100% specificity. Women in the selective ultrasound scan arm only received an ultrasound scan after detection of a breech presentation by abdominal palpation. Where a breech was detected, a woman was offered external cephalic version (ECV). The structure of the model undertook a decision tree, with end states being the mode of birth; either vaginal, elective or emergency caesarean section. Long term health outcomes were modelled based on the mortality risk associated with each mode of birth. Average lifetime quality-adjusted life years (QALYs) were estimated from Euroqol general UK population values.
Only the probabilistic results (n=100000 simulations) were reported which showed that on average, universal ultrasound resulted in an absolute decrease in breech deliveries by 0.39% compared with selective ultrasound scanning. The expected cost per person with breech presentation of universal ultrasound was £2957 (95% Credibility Interval [CrI]: £2922 to £2991), compared to £2,949 (95%CrI: £2915 to £2984) from selective ultrasound. The expected QALYs per person was 24.27615 in the universal ultrasound cohort and 24.27582 in the selective ultrasound cohort. The incremental cost effectiveness ratio (ICER) from the probabilistic analysis was £23611 (95%CrI: £8184 to £44851).
A series of one-way sensitivity analysis were conducted which showed that the most important cost parameter was the unit cost of a universal ultrasound scan. This parameter is particularly noteworthy as the study costed this scan at a much lower value than the ‘standard antenatal ultrasound’ scan in NHS reference costs on the basis that such a scan can be performed by a midwife during a routine antenatal care visit in primary care. According to the NICE guideline manual economic evaluation checklist this model was assessed as being directly applicable with potentially severe limitations. The limitations were mostly attributable to the limitations of the clinical inputs.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. routine ultrasound scan versus selective ultrasound scan, critical outcomes, unexpected breech presentation in labour.
No evidence was identified to inform this outcome.
Mode of birth
- Moderate quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of women who had elective caesarean section: RR 1.22 (95% CI 0.91 to 1.63).
- Moderate quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on number of women who had emergency caesarean section: RR 1.20 (95% CI 0.90 to 1.60).
- High quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on number of women who had vaginal birth: RR 0.95 (95% CI 0.89 to 1.01).
Important outcomes
Maternal anxiety, women’s experience and satisfaction of care, gestational age at birth.
- High quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of babies’ born between 39-42 gestational weeks: RR 0.98 (95% CI 0.94 to 1.02).
Admission to neonatal unit
- Low quality evidence from 1 RCT (N=1993) showed that there is no clinically important difference between routine ultrasound scan at 36-37 weeks and selective ultrasound scan on the number of babies admitted into the neonatal unit: RR 0.83 (95% CI 0.51 to 1.35).
Economic evidence statements
One directly applicable cost-utility analysis from the UK with potentially serious limitations compared universal ultrasound scanning for breech presentation at 36 weeks’ gestational age with selective ultrasound scanning, stated as current practice. Universal ultrasound scanning was found to be borderline cost effective; the incremental cost-effectiveness ratio was £23611 per QALY gained. The cost of the scan was seen to be a key driver in the cost effectiveness result.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Unexpected breech presentation in labour and mode of birth were prioritised as critical outcomes by the committee. This reflects the different options available to women with a known breech presentation in pregnancy and the different choices that women make. There are some women and/or clinicians who may feel uncomfortable with the risks of aiming for vaginal breech birth, and for these women and/or clinicians avoiding an unexpected breech presentation in labour would be the preferred option.
As existing evidence suggests that aiming for vaginal breech birth carries greater risk to the fetus than planned caesarean birth, it is important to consider whether earlier detection of the breech presentation would reduce the risk of these outcomes.
The committee agreed that maternal anxiety and women’s experience and satisfaction of care were important outcomes to consider as the introduction of an additional routine scan during pregnancy could have a treatment burden for women. Gestational age at birth and admission to neonatal unit were also chosen as important outcomes as the committee wanted to find out whether earlier detection of breech presentation would have an impact on whether the baby was born preterm, and as a consequence admitted to the neonatal unit. These outcomes were agreed to be important rather than critical as they are indirect outcomes of earlier detection of breech presentation.
The quality of the evidence
The quality of the evidence ranged from low to high. Most of the evidence was rated high or moderate, with only 1 outcome rated as low. The quality of the evidence was downgraded due to imprecision around the effect estimates for emergency caesarean section, elective caesarean section and admissions to neonatal unit.
No evidence was identified for the following outcomes: unexpected breech presentation in labour, maternal anxiety, women’s experiences and satisfaction of care.
The committee had hoped to find evidence that would inform whether early identification of breech presentation had an impact on preterm births, and although the review reported evidence for gestational age as birth, the available evidence was for births 39-42 weeks of gestation.
Benefits and harms
The available evidence compared routine ultrasound scanning with selective ultrasound scanning, and found no clinically important differences for mode of birth, gestational age at birth, or admissions to the neonatal unit. However, the committee discussed that it was important to note that the study did not focus on identifying breech presentation. The committee discussed the differences between the intervention in the study, which was an ultrasound scan to assess placental maturity, liquor volume, and fetal weight, to an ultrasound scan used to detect breech presentation. Whilst the ultrasound scan in the study has the ability to determine breech presentation, there are additional and costlier training required for the assessment of the other criteria. As such, it is important to separate the interventions. The committee also highlighted that the study did not look at whether an identification of breech presentation had an impact on the outcomes which were selected for this review.
In light of this, the committee felt that they were unable to reach a conclusion as to whether routine scanning to identify breech presentation, was associated with any benefits or harms. The committee agreed that while this review suggests routine ultrasound scanning to be no more effective than selective scanning, it does not definitively establish equivalence. Therefore, the committee agreed to recommend a continuation of the current practice with selective scanning and make a research recommendation to compare the clinical and cost effectiveness of routine ultrasound scanning versus selective ultrasound scanning from 36 weeks to identify fetal breech presentation.
Cost effectiveness and resource use
The committee acknowledged that there was included economic evidence on the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
The 1 included study suggested that offering a routine scan for breech is borderline cost effective. A key driver of cost effectiveness was the cost of the scan, which was substantially lower in the economic model than the figure quoted in NHS reference costs for routine ultrasound scanning. The committee noted that a scan for breech presentation only is a simpler technique and uses a cheaper machine. The committee agreed that the other costing assumptions presented in the study seemed appropriate.
However, the committee expressed concerns about the cohort study which underpinned the economic analysis which had a high risk of bias. The committee noted that a number of assumptions in the model which were key drivers of cost effectiveness, including the palpation diagnosis rates and prevalence of breech position, were from this 1 cohort study. This increased the uncertainty around the cost effectiveness of the routine scan. The committee also noted that, whilst the cost of the scan was fairly inexpensive, the resource impact would be substantial if a routine scan for breech presentation was offered to all pregnant women.
Overall, the committee felt that the clinical and cost effectiveness evidence presented was not strong enough to recommend offering a routine ultrasound scan given the potential for a significant resource impact. The recommendation to offer abdominal palpation to all pregnant women, and to offer an ultrasound scan where breech is suspected reflects current practice and so no substantial resource impact is anticipated.
McKenna 2003
Wastlund 2019
Appendix A. Review protocols
Review protocol for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 244K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 370K)
Appendix C. Clinical evidence study selection
Clinical study selection for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 117K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 213K)
Appendix E. Forest plots
Forest plots for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
This section includes forest plots only for outcomes that are meta-analysed. Outcomes from single studies are not presented here, but the quality assessment for these outcomes is provided in the GRADE profiles in appendix F .
Appendix F. GRADE tables
GRADE tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 196K)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
A single economic search was undertaken for all topics included in the scope of this guideline. One economic study was identified which was applicable to this review question. See supplementary material 2 for details.
Appendix H. Economic evidence tables
Economic evidence tables for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 143K)
Appendix I. Economic evidence profiles
Economic evidence profiles for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 129K)
Appendix J. Economic analysis
Economic evidence analysis for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation, clinical studies, table 8 excluded studies and reasons for their exclusion.
View in own window
Economic studies
A single economic search was undertaken for all topics included in the scope of this guideline. No economic studies were identified which were applicable to this review question. See supplementary material 2 for details.
Appendix L. Research recommendations
Research recommendations for review question: What is the effectiveness of routine scanning between 36+0 and 38+6 weeks of pregnancy compared to standard care regarding breech presentation? (PDF, 164K)
Evidence reviews underpinning recommendations 1.2.36 to 1.2.37
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Identification of breech presentation: Antenatal care: Evidence review L. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (518K)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Management of breech presentation: Antenatal care: Evidence review M [ 2021] Review Management of breech presentation: Antenatal care: Evidence review M National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- [The effect of the woman's age on the course of pregnancy and labor in breech presentation]. [Akush Ginekol (Sofiia). 1996] [The effect of the woman's age on the course of pregnancy and labor in breech presentation]. Dimitrov A, Borisov S, Nalbanski B, Kovacheva M, Chintolova G, Dzherov L. Akush Ginekol (Sofiia). 1996; 35(1-2):7-9.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- Review Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). [Cochrane Database Syst Rev. 2005] Review Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior). Hofmeyr GJ, Kulier R. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD001063. Epub 2005 Apr 18.
Recent Activity
- Identification of breech presentation Identification of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

15 Chapter 15 – Conception, Pregnancy, and Birth
Ericka Goerling, PhD and Emerson Wolfe, MS
Learning Outcomes
- Analyze psychosocial and cultural factors impacting abortion, pregnancy and the birthing process and discuss best practices to promote equity within healthcare systems.
- how to enhance the possibility of conception
- infertility problems and how they might be dealt with
- spontaneous and elective abortion
- aspects of a healthy pregnancy
- sexual interaction during pregnancy
- stages of childbirth
- psychological and sexual adjustments postpartum
Introduction
This week’s reading is all about conception, pregnancy and birth. Much of the content we’ll be covering will be physiological, in nature. However, as you go through the material, please keep your intersectional lens on. For example, when we’re discussing the biology of fertilization, how might environmental conditions influence the process (conception through intercourse versus IVF). Or perhaps when we consider pregnancy, how might socio-economic status and/or race impact folks’ access to prenatal care? And when we address issues of birth, note the disparity in how everything from pain care to maternal and infant mortality impact BIPOC. As with many of these topics in human sexuality, we can marvel at the complexities and wonder of our bodies and their many responses. At the same time, we can challenge the areas in which culture, race, poverty, ethnicity, abilities, and marginalization can impede some people’s opportunities.
One more note
This chapter is very much a work-in-progress. One of the challenges we’ve had authoring this chapter is finding the balance of maintaining the respectful and safe space that pregnancy and birthing has afforded generations of women. This is especially true for BIPOC communities that push back against dominant, white, medical establishments. At the same time, we seek to broaden the language, awareness, and understanding of pregnancy and birth, since so much of the traditional, western approaches have excluded gender-diverse people and families. In that vein, we are embracing the and ; that is- we’re striving to consistently honor our foremothers and visionaries of birth who’ve held safe space for women, as well as respectfully embrace our non-binary, trans, and gender-diverse families in the amazing process of pregnancy and birth.
Fertilization occurs when a sperm and an oocyte (egg) combine and their nuclei fuse. Because each of these reproductive cells is a haploid cell containing half of the genetic material needed to form a human being, their combination forms a diploid cell. This new single cell, called a zygote, contains all of the genetic material needed to form a human—half from the egg and half from the sperm.
Transit of Sperm
Fertilization is a numbers game. During ejaculation, hundreds of millions of sperm (spermatozoa) are released into the vagina. Almost immediately, millions of these sperm are overcome by the acidity of the vagina, and millions more may be blocked from entering the uterus by thick cervical mucus. Of those that do enter, thousands are destroyed by phagocytic uterine leukocytes. Thus, the race into the uterine tubes, which is the most typical site for sperm to encounter the oocyte, is reduced to a few thousand contenders. Their journey—thought to be facilitated by uterine contractions—usually takes from 30 minutes to 2 hours. If the sperm do not encounter an oocyte immediately, they can survive in the uterine tubes for another 3–5 days. Thus, fertilization can still occur if intercourse takes place a few days before ovulation. In comparison, an oocyte can survive independently for only approximately 24 hours following ovulation. Intercourse more than a day after ovulation will therefore usually not result in fertilization.
During the journey, fluids in the female reproductive tract prepare the sperm for fertilization through a process called capacitation, or priming. The fluids improve the motility of the spermatozoa. They also deplete cholesterol molecules embedded in the membrane of the head of the sperm, thinning the membrane in such a way that will help facilitate the release of the lysosomal (digestive) enzymes needed for the sperm to penetrate the oocyte’s exterior once contact is made. Sperm must undergo the process of capacitation in order to have the “capacity” to fertilize an oocyte. If they reach the oocyte before capacitation is complete, they will be unable to penetrate the oocyte’s thick outer layer of cells.
Contact Between Sperm and Oocyte
Upon ovulation, the oocyte released by the ovary is swept into—and along—the uterine tube. Fertilization must occur in the distal uterine tube because an unfertilized oocyte cannot survive the 72-hour journey to the uterus.
As it is swept along the distal uterine tube, the oocyte encounters the surviving capacitated sperm, which stream toward it in response to chemical attractants released by the cells of the corona radiata. To reach the oocyte itself, the sperm must penetrate the two protective layers. Eventually, a single sperm makes contact with sperm-binding receptors on the oocyte’s plasma membrane. The plasma membrane of that sperm then fuses with the oocyte’s plasma membrane, and the head and mid-piece of the “winning” sperm enter the oocyte interior.
How do sperm penetrate the corona radiata? As you can see, the first sperm to reach the oocyte is never the one to fertilize it. Rather, hundreds of sperm cells must undergo the acrosomal reaction, each helping to degrade the corona radiata and zona pellucida until a path is created to allow one sperm to contact and fuse with the plasma membrane of the oocyte. If you consider the loss of millions of sperm between entry into the vagina and degradation of the zona pellucida, you can understand why a low sperm count can cause infertility.
Most of the time, a single egg is released during an ovulation cycle. However, in approximately 1 percent of ovulation cycles, two eggs are released and both are fertilized. Two zygotes form, implant, and develop, resulting in the birth of dizygotic (or fraternal) twins. Because dizygotic twins develop from two eggs fertilized by two sperm, they are no more identical than siblings born at different times.
Much less commonly, a zygote can divide into two separate offspring during early development. This results in the birth of monozygotic (or identical) twins. Although the zygote can split as early as the two-cell stage, splitting occurs most commonly during the early blastocyst stage, with roughly 70–100 cells present. These two scenarios are distinct from each other, in that the twin embryos that separated at the two-cell stage will have individual placentas, whereas twin embryos that form from separation at the blastocyst stage will share a placenta and a chorionic cavity.
In Vitro Fertilization
IVF, which stands for in vitro fertilization, is an assisted reproductive technology. In vitro, which in Latin translates to “in glass,” refers to a procedure that takes place outside of the body. There are many different indications for IVF. For example, someone may produce normal eggs, but the eggs cannot reach the uterus because the uterine tubes are blocked or otherwise compromised. There are also challenges with low sperm count, low sperm motility, sperm with an unusually high percentage of morphological abnormalities, or sperm that are incapable of penetrating the zona pellucida of an egg.
A typical IVF procedure begins with egg collection. A normal ovulation cycle produces only one oocyte, but the number can be boosted significantly (to 10–20 oocytes) by administering a short course of gonadotropins. The course begins with follicle-stimulating hormone (FSH) analogs, which support the development of multiple follicles, and ends with a luteinizing hormone (LH) analog that triggers ovulation. Right before the ova would be released from the ovary, they are harvested using ultrasound-guided oocyte retrieval. In this procedure, ultrasound allows a physician to visualize mature follicles. The ova are aspirated (sucked out) using a syringe.
In parallel, sperm are obtained from a partner or from a donor/sperm bank. The sperm are prepared by washing to remove seminal fluid because seminal fluid contains a peptide, FPP (or, fertilization promoting peptide), that—in high concentrations—prevents capacitation of the sperm. The sperm sample is also concentrated, to increase the sperm count per milliliter.
Next, the eggs and sperm are mixed in a petri dish. The ideal ratio is 75,000 sperm to one egg. If there are severe problems with the sperm—for example, the count is exceedingly low, or the sperm are completely nonmotile, or incapable of binding to or penetrating the zona pellucida—a sperm can be injected into an egg. This is called intracytoplasmic sperm injection (ICSI).

The embryos are then incubated until they either reach the eight-cell stage or the blastocyst stage. In the United States, fertilized eggs are typically cultured to the blastocyst stage because this results in a higher pregnancy rate. Finally, the embryos are transferred to the uterus using a plastic catheter (tube).
IVF is a relatively new and still evolving technology, and until recently it was necessary to transfer multiple embryos to achieve a good chance of a pregnancy. Today, however, transferred embryos are much more likely to implant successfully, so countries that regulate the IVF industry cap the number of embryos that can be transferred per cycle at two. This reduces the risk of multiple-birth pregnancies.
Pregnancy begins with the fertilization of an egg and continues through to the birth of the individual. The length of time of gestation varies among animals, but is very similar among the great apes: human gestation is 266 days, while chimpanzee gestation is 237 days, a gorilla’s is 257 days, and orangutan gestation is 260 days long. The fox has a 57-day gestation. Dogs and cats have similar gestations averaging 60 days. The longest gestation for a land mammal is an African elephant at 640 days. The longest gestations among marine mammals are the beluga and sperm whales at 460 days.
Twenty-four hours before fertilization, the egg has finished meiosis and becomes a mature oocyte. When fertilized (at conception) the egg becomes known as a zygote. The zygote travels through the oviduct to the uterus. The developing embryo must implant into the wall of the uterus within seven days, or it will deteriorate and die. The outer layers of the zygote (blastocyst) grow into the endometrium by digesting the endometrial cells, and wound healing of the endometrium closes up the blastocyst into the tissue. Another layer of the blastocyst, the chorion, begins releasing a hormone called human beta chorionic gonadotropin (β-HCG) which makes its way to the corpus luteum and keeps that structure active. This ensures adequate levels of progesterone that will maintain the endometrium of the uterus for the support of the developing embryo. Pregnancy tests determine the level of β-HCG in urine or serum. If the hormone is present, the test is positive.
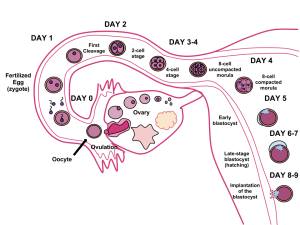
The gestation period is divided into three equal periods or trimesters. During the first two to four weeks of the first trimester, nutrition and waste are handled by the endometrial lining through diffusion. As the trimester progresses, the outer layer of the embryo begins to merge with the endometrium, and the placenta forms. This organ takes over the nutrient and waste requirements of the embryo and fetus, with the parent’s blood passing nutrients to the placenta and removing waste from it.
First Trimester
Internal organs and body structures begin to develop during the first trimester. By five weeks, limb buds, eyes, the heart, and liver have been basically formed. By eight weeks, the term fetus applies, and the body is essentially formed, as shown in Figure 15.4. The individual is about five centimeters (two inches) in length and many of the organs, such as the lungs and liver, are not yet functioning. Exposure to any toxins is especially dangerous during the first trimester, as all of the body’s organs and structures are going through initial development. Anything that affects that development can have a severe effect on the fetus’ survival.

Figure 15.4 Fetal development is shown at nine weeks gestation. (Credit: Ed Uthman)
Second Trimester
During the second trimester, the fetus grows to about 30 cm (12 inches), as shown in Figure 15.5. It becomes active and the mother usually feels the first movements. All organs and structures continue to develop. The placenta has taken over the functions of nutrition and waste and the production of estrogen and progesterone from the corpus luteum, which has degenerated. The placenta will continue functioning up through the delivery of the baby.
Third Trimester
During the third trimester, the fetus grows to 3 to 4 kg (6 ½ -8 ½ lbs.) and about 50 cm (19-20 inches) long. This is the period of the most rapid growth during the pregnancy. Organ development continues to birth (and some systems, such as the nervous system and liver, continue to develop after birth).
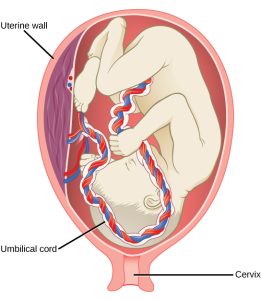
Changes During Pregnancy
A full-term pregnancy lasts approximately 270 days (approximately 38.5 weeks) from conception to birth. Because it is easier to remember the first day of the last menstrual period (LMP) than to estimate the date of conception, obstetricians set the due date as 284 days (approximately 40.5 weeks) from the LMP. This assumes that conception occurred on day 14 of the woman’s cycle, which is usually a good approximation. The 40 weeks of an average pregnancy are usually discussed in terms of three trimesters, each approximately 13 weeks. During the second and third trimesters, the pre-pregnancy uterus—about the size of a fist—grows dramatically to contain the fetus, causing a number of anatomical changes in the pregnant person.
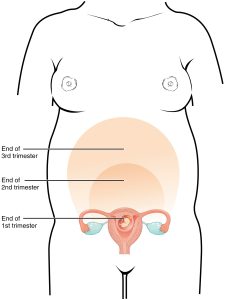
Weight Gain
The second and third trimesters of pregnancy are associated with dramatic changes in anatomy and physiology. The most obvious anatomical sign of pregnancy is the dramatic enlargement of the abdominal region, coupled with weight gain. This weight results from the growing fetus as well as the enlarged uterus, amniotic fluid, and placenta. Additional breast tissue and dramatically increased blood volume also contribute to weight gain (Table 15.1). Surprisingly, fat storage accounts for only approximately 2.3 kg (5 lbs) in a normal pregnancy and serves as a reserve for the increased metabolic demand of breastfeeding.
During the first trimester, the parent does not need to consume additional calories to maintain a healthy pregnancy. However, a weight gain of approximately 0.45 kg (1 lb) per month is common. During the second and third trimesters, the pregnant person’s appetite increases, but it is only necessary for them to consume an additional 300 calories per day to support the growing fetus. Contributors to Weight Gain During Pregnancy
Changes in Organ Systems During Pregnancy
As the body adapts to pregnancy, characteristic physiologic changes occur. These changes can sometimes prompt symptoms often referred to collectively as the common discomforts of pregnancy.
Digestive and Urinary System Changes
Nausea and vomiting, sometimes triggered by an increased sensitivity to odors, are common during the first few weeks to months of pregnancy. This phenomenon is often referred to as “morning sickness,” although the nausea may persist all day. The source of pregnancy nausea is thought to be the increased circulation of pregnancy-related hormones, specifically circulating estrogen, progesterone, and hCG. Decreased intestinal peristalsis may also contribute to nausea. By about week 12 of pregnancy, nausea typically subsides.
A common gastrointestinal complaint during the later stages of pregnancy is gastric reflux, or heartburn, which results from the upward, constrictive pressure of the growing uterus on the stomach. The same decreased peristalsis that may contribute to nausea in early pregnancy is also thought to be responsible for pregnancy-related constipation as pregnancy progresses.
The downward pressure of the uterus also compresses the urinary bladder, leading to frequent urination. The problem is exacerbated by increased urine production. In addition, the maternal urinary system processes both maternal and fetal wastes, further increasing the total volume of urine.
Integumentary System Changes
The dermis (skin) stretches extensively to accommodate the growing uterus, breast tissue, and fat deposits on the thighs and hips. Torn connective tissue beneath the dermis can cause striae (stretch marks) on the abdomen, which appear as red or purple marks during pregnancy that fade to a silvery white color in the months after childbirth.
An increase in melanocyte-stimulating hormone, in conjunction with estrogens, darkens the areolae and creates a line of pigment from the umbilicus to the pubis called the linea nigra (Figure 15.8). Melanin production during pregnancy may also darken or discolor skin on the face to create a chloasma, or “mask of pregnancy.”

Figure 15.8 Linea Nigra The linea nigra, a dark medial line running from the umbilicus to the pubis, forms during pregnancy and persists for a few weeks following childbirth.
Labor is the physical efforts of expulsion of the fetus and the placenta from the uterus during birth (parturition). Toward the end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin. At this time, the baby reorients, facing forward and down with the back or crown of the head engaging the cervix (uterine opening). This causes the cervix to stretch and nerve impulses are sent to the hypothalamus, which signals for the release of oxytocin from the posterior pituitary. The oxytocin causes the smooth muscle in the uterine wall to contract. At the same time, the placenta releases prostaglandins into the uterus, increasing the contractions. A positive feedback relay occurs between the uterus, hypothalamus, and the posterior pituitary to assure an adequate supply of oxytocin. As more smooth muscle cells are recruited, the contractions increase in intensity and force.
Stages of Childbirth
The process of childbirth can be divided into three stages: cervical dilation, expulsion of the newborn, and afterbirth ( Figure 15.9).
Cervical Dilation
For vaginal birth to occur, the cervix must dilate fully to 10 cm in diameter—wide enough to deliver the newborn’s head. The dilation stage is the longest stage of labor and typically takes 6–12 hours. However, it varies widely and may take minutes, hours, or days, depending in part on whether the mother has given birth before; in each subsequent labor, this stage tends to be shorter.

Figure 15.9 Stages of Childbirth The stages of childbirth include Stage 1, early cervical dilation; Stage 2, full dilation and expulsion of the newborn; and Stage 3, delivery of the placenta and associated fetal membranes. (The position of the newborn’s shoulder is described relative to the mother.)
True labor progresses in a positive feedback loop in which uterine contractions stretch the cervix, causing it to dilate and efface, or become thinner. Cervical stretching induces reflexive uterine contractions that dilate and efface the cervix further. In addition, cervical dilation boosts oxytocin secretion from the pituitary, which in turn triggers more powerful uterine contractions. When labor begins, uterine contractions may occur only every 3–30 minutes and last only 20–40 seconds; however, by the end of this stage, contractions may occur as frequently as every 1.5–2 minutes and last for a full minute.
Each contraction sharply reduces oxygenated blood flow to the fetus. For this reason, it is critical that a period of relaxation occur after each contraction. Fetal distress, measured as a sustained decrease or increase in the fetal heart rate, can result from severe contractions that are too powerful or lengthy for oxygenated blood to be restored to the fetus. Such a situation can be cause for an emergency birth with vacuum, forceps, or surgically by Caesarian section.
The amniotic membranes rupture before the onset of labor in about 12 percent of women; they typically rupture at the end of the dilation stage in response to excessive pressure from the fetal head entering the birth canal.
Expulsion Stage
The expulsion stage begins when the fetal head enters the birth canal and ends with birth of the newborn. It typically takes up to 2 hours, but it can last longer or be completed in minutes, depending in part on the orientation of the fetus. The vertex presentation known as the occiput anterior vertex is the most common presentation and is associated with the greatest ease of vaginal birth. The fetus faces the maternal spinal cord and the smallest part of the head (the posterior aspect called the occiput) exits the birth canal first.
In fewer than 5 percent of births, the infant is oriented in the breech presentation, or buttocks down. In a complete breech, both legs are crossed and oriented downward. In a frank breech presentation, the legs are oriented upward. Before the 1960s, it was common for breech presentations to be delivered vaginally. Today, most breech births are accomplished by Caesarian section.
Vaginal birth is associated with significant stretching of the vaginal canal, the cervix, and the perineum. Until recent decades, it was routine procedure for an obstetrician to numb the perineum and perform an episiotomy, an incision in the posterior vaginal wall and perineum. The perineum is now more commonly allowed to tear on its own during birth. Both an episiotomy and a perineal tear need to be sutured shortly after birth to ensure optimal healing. Although suturing the jagged edges of a perineal tear may be more difficult than suturing an episiotomy, tears heal more quickly, are less painful, and are associated with less damage to the muscles around the vagina and rectum.
Upon birth of the newborn’s head, an obstetrician will aspirate mucus from the mouth and nose before the newborn’s first breath. Once the head is birthed, the rest of the body usually follows quickly. The umbilical cord is then double-clamped, and a cut is made between the clamps. This completes the second stage of childbirth.
The delivery of the placenta and associated membranes, commonly referred to as the afterbirth, marks the final stage of childbirth (Figure 15.10). After expulsion of the newborn, the myometrium continues to contract. This movement shears the placenta from the back of the uterine wall. It is then easily delivered through the vagina. Continued uterine contractions then reduce blood loss from the site of the placenta. Delivery of the placenta marks the beginning of the postpartum period—the period of approximately 6 weeks immediately following childbirth during which the pregnant person’s body gradually returns to a non-pregnant state. If the placenta does not birth spontaneously within approximately 30 minutes, it is considered retained, and the obstetrician may attempt manual removal. If this is not successful, surgery may be required.
It is important that the obstetrician examines the expelled placenta and fetal membranes to ensure that they are intact. If fragments of the placenta remain in the uterus, they can cause postpartum hemorrhage. Uterine contractions continue for several hours after birth to return the uterus to its pre-pregnancy size in a process called involution, which also allows the abdominal organs to return to their pre-pregnancy locations. Breastfeeding facilitates this process.
Miscarriages
Unfortunately, some instances of pregnancy do not end in a healthy birth. Miscarriage, or spontaneous pregnancy loss before 28 weeks of gestation, occurs in up to 20-25 percent of pregnancies (Sohr-Preston, Morain, Chapman, Pardue, & Ford, 2018; Bellhouse, Temple-Smith, & Bilardi, 2018). The majority of these miscarriages tend to occur before 12 weeks of gestation (often before women realize they’re pregnant). Nearly half of all miscarriages have no known cause, leading to widespread misperceptions about frequency. In cases where there is a known cause, half are attributed to chromosomal abnormalities. Consequently, most miscarriages are largely out of the control of the expectant parent. Additionally, most miscarriages do not inform the parent’s past or future success in bringing a baby to full-term (Sohr-Preston, et al, 2018).
In addition to some confusion regarding prevalence and frequency of miscarriage rates, there are often mixed responses to families impacted by miscarriage from the medical community, the general public, family members and friends. In so many ways, pregnancy loss is a time when many people need emotional support from those around them. There are a number of grass-roots agencies and hospital facilitated programs now in place to support families who’ve experienced loss. Partners are often a huge source of support, but research also identifies the need for more public discourse and education around pregnancy loss generally, which boosts well-being for all members of the families involved (Bellhouse, Temple-Smith, & Bilardi, 2018).
The issues surrounding abortion, the deliberate termination of a pregnancy, remain highly charged throughout the United States and around the globe. In the US, there were over 600,000 abortions in 2018 reported to the Centers for Disease Control (CDC); a rate of 11.3 abortions per 1,000 women aged 15-44 years (Kortsmit, Jatlaoui, Mandel, Reeves, Oduyebo, Petersen, & Whiteman, 2020). Over half of the abortions (57.7%) in 2018 occurred among women in their 20s. Interestingly, 2018 was the first year in almost a decade where there was a slight increase in the rate of abortions (1-2% across measure). Overall, the total number of reported abortions, abortion rate, and abortion ratio decreased 22% from 2009-2018 (Kortsmit, et al, 2020). For more details on the CDC data, which outlines age of parent, gestational periods, race/ethnicity, and more can be found here and below.
On June 24, 2022, the US Supreme Court overturned Roe v. Wade, the 1973 Supreme Court decision protecting a pregnant person’s liberty to choose to have an abortion without government prohibition. Over decades, research has demonstrated that abortion bans most severely impact people in marginalized groups who already struggle to access health care, including abortion.
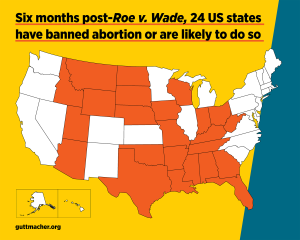
Interestingly, states with the most limitations in access to abortion care also tend to have the most conservative (or absence) of sex education, the highest rates of unintended pregnancies and the lowest indicators of infant/child well-being (Dreweke, 2016; Medoff, 2018).
Caesarean Section
Cesarean section (c-sections), the surgical operation to remove an infant out of their pregnant parent’s body, has been part of human culture since ancient times (Sewel, 1998). Since 1996, c-sections have been on an almost steady rise in the United States. In 2018, approximately one-third (31.9%) of all births occurred through cesarean delivery (Martin, Hamilton, Osterman, & Driscoll, 2019). There is no question that c-sections can save lives; both of parents and children. However, there is a rising concern that many of these procedures are unnecessary, causing needless risk of complications to both mother and baby, as well as potential long-term implications (e.g. following the first c-section, there is a low probability, 10%, of later vaginal delivery; Osterman & Martin, 2014).
One of the ongoing criticisms about the high rate of c-sections is that it is primarily financially driven in terms of payout to physicians/hospitals, rather than due to patient care. Considering that a c-section costs twice as much as a vaginal delivery, the economic boon for attending medical staff/facilities can be high. On the public side of things, almost half of US births are compensated through Medicaid (with double the payout for c-sections; Kozhimannil, Graves, Ecklund, Shah, Aggarwal, & Snowden, 2018). Added to that, one meta-analysis found that c-sections are more likely to be performed on privately insured women as compared with women using public health insurance coverage (Hoxha, Syrogiannouli, Braha, Goodman, da Costa, & Jüni, 2017). Thankfully, more efforts are being examined and implemented to reduce unnecessary births via cesarean section (Kozhimannil, et al, 2018).
Disparities in Prenatal and Perinatal Care
Racial and ethnic disparities in maternal care have been an issue in the United States for generations. Just as we discussed in last week’s reading, abuse against black and brown bodies has been excessive and consequential. In terms of prenatal and perinatal care, there have been ongoing discrepancies in care, resulting in inexcusable outcomes. Nearly a quarter of black women experience delays in their prenatal healthcare and they are almost twice as likely to experience pregnancy complications (Slaughter-Acey, Sneed, Parker, Keith, Lee, & Misra, 2019).
Among industrialized nations, the US has the highest level of maternal deaths (Declercq & Zephyrin, 2020). Wang and her colleagues (2021) reported that black women are three to four times more likely to die of pregnancy-related causes compared to non-Hispanic White women. A black or indigenous person is up to 5 times more likely to die in pregnancy or up to a year after pregnancy than their white peer (Maykin & Tsai, 2020). This disparity is akin to what we saw in the 1940s (Declercq & Zephyrin, 2020).
Importantly, when controlling for other variables, such as education, socio-economic status, accessibility, findings consistently suggest that lived experiences, in the form of racial microaggressions, influence Black women’s use of health care, particularly perinatal services (Slaughter-Acey, et al, 2019). Despite advances in healthcare, antibiotics, surgical processes, and accessibility, the data provides a stark reality of rampant, systemic inequity. As Declercq and Zephyrin (2020) note, “The US has to intentionally focus on disparities between Black and white women, in particular by naming and seeking to reduce the impacts of structural racism” (p. 12). Please see the Commonwealth Fund’s recent briefing here.
There is a great deal of work to do to rectify the massive inequities facing this country. There are a variety of initiatives at both state-wide and the national level to address the disparities in perinatal care. To see a state by state comparison, go here . The Centers for Disease Control also has launched the “ Hear Her Campaign .”
To be clear, the disparities in maternal health are not the result of any one, single factor. It’s at the intersection of sexism and racism, that many women of color are not being heard or seen. The initiatives noted above are a very small part in rectifying this. Continued efforts to name and eliminate structural racism, as well as provide comprehensive health care for pregnant bodies, are essential.
This week’s reading covers a wide range of concepts related to conception, pregnancy, and birth. Additionally, we highlighted some of the major disparities of perinatal care for BIPOC. There are other marginalized populations that need further examination; individuals with disabilities and gender nonconforming folks. There are also other stakeholders that were omitted from this section; partners, surrogates, midwives, and doulas. Finally, some considerations about lactation and postpartum adjustments can be explored further. Still, hopefully you got a solid introduction into the brilliance of conception, the marvel of pregnancy and birth, as well as the pressing issue of our time; building equity into the wrap-around healthcare of all people.
Licenses & Attributions
OpenStax College. (2019). Anatomy & physiology. OpenStax. http://cnx.org/content/col11496/latest/ Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License 4.0 license.
OpenStax College. (2018). Biology, 2e. OpenStax. https://www.oercommons.org/courseware/lesson/15163/student/244841 . Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License 4.0 license.
Adaptations: Reformatted. Added learning objectives. Modified content for language, application to subject and cohesion. Updated sources. All Rights Reserved
Assefi, N. & Levine, B. A. (2015, May). How in vitro fertilization (IVF) works [Video]. https://www.ted.com/talks/nassim_assefi_and_brian_a_levine_how_in_vitro_fertilization_ivf_works?language=en . Creative Commons BY–NC–ND 4.0 International.
BabyCenter (2019, July 31). 8 positions to ease labor pain [Video]. https://www.youtube.com/watch?v=rpzBPqKgvGk&t=24s . License: All Rights Reserved. License Terms: Standard YouTube license.
Centers for Disease Control and Prevention. HearHer Campaign [Video]. https://www.youtube.com/watch?v=nxGz3naF_JQ Creative Commons Attribution 3.0 License.
Howell, E. (2019). How we can improve maternal healthcare – before, during, and after pregnancy. TEDMed. https://www.youtube.com/watch?v=XOySX6sE_8s. Creative Commons BY–NC–ND 4.0 International.
Jemyao. (2016, November 18). Miracle of life – 9 months in 4 minutes [Video]. https://www.youtube.com/watch?v=GE_lI86boUU&t=3s License: All Rights Reserved. License Terms: Standard YouTube license.
Nucleus Medical Media (2013, January 31). Fertilization [Video]. https://youtu.be/_5OvgQW6FG4 License: All Rights Reserved. License Terms: Standard YouTube license.
TEDEd (2020, October 10). The surprising effects of pregnancy [Video]. https://www.youtube.com/watch?v=F_ssj7-8rYg . Creative Commons BY–NC–ND 4.0 International.
Aina, A. D., Asiodu, I. V., Castillo, P., Denson, J., Drayton, C., Aka-James, R., … & Wolfe, T. (2019). Black Maternal Health Research Re-Envisioned: Best Practices for the Conduct of Research with, for, and by Black Mamas. Harv. L. & Pol’y Rev., 14, 393.
Bellhouse, C., Temple-Smith, M. J., & Bilardi, J. E. (2018). “It’s just one of those things people don’t seem to talk about…” women’s experiences of social support following miscarriage: a qualitative study. BMC women’s health, 18(1), 1-9.
Betts, J. G., Young, K. A., Wise, J. A. Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M. & DeSaix, P. (2019). Anatomy and physiology. OpenStax. http://cnx.org/content/col11496/latest/
Byrnes, L., & Hickey, M. (2016). Perinatal care for women with disabilities: clinical considerations. The Journal for Nurse Practitioners, 12(8), 503-509.
Centers for Disease Control & Prevention. (2020). Hear her campaign. https://www.cdc.gov/hearher/ . National Center for Chronic Disease Prevention and Health Promotion, Division of Reproductive Health.
Clark, M. A., Douglas, M. & Choi, J. (2018). Biology, 2nd Edition. OpenStax https://www.oercommons.org/courseware/lesson/15163/student/244841
Creanga, A. A., Syverson, C., Seed, K., & Callaghan, W. M. (2017). Pregnancy-related mortality in the United States, 2011–2013. Obstetrics and Gynecology, 130(2), 366. https://journals.lww.com/greenjournal/Fulltext/2017/08000/Pregnancy_Related_Mortality_in_the_United_States ,.15.aspx
Declercq, E. & Zephyrin, L. (2020). Maternal mortality in the United States: A primer. The Commonwealth Fund. https://www.commonwealthfund.org/publications/issue-brief-report/2020/dec/maternal-mortality-united-states-primer
Goode, K., & Katz Rothman, B. (2017). African‐American midwifery, a history and a lament. American Journal of Economics and Sociology, 76(1), 65-94.
Guttmacher Institute. (2020). State policies on abortion. https://www.guttmacher.org/united-states/abortion/state-policies-abortion
Hoxha, I., Syrogiannouli, L., Braha, M., Goodman, D. C., da Costa, B. R., & Jüni, P. (2017). Caesarean sections and private insurance: systematic review and meta-analysis. BMJ open, 7(8).
Kortsmit, K., Jatlaoui, T. C., Mandel, M. G., Reeves, J. A., Oduyebo, T., Petersen, E., & Whiteman, M. K. (2020). Abortion surveillance—United States, 2018. MMWR Surveillance Summaries, 69(7), 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7713711/
Kozhimannil, K. B., Graves, A. J., Ecklund, A. M., Shah, N., Aggarwal, R., & Snowden, J. M. (2018). Cesarean Delivery Rates and Costs of Childbirth in a State Medicaid Program After Implementation of a Blended Payment Policy. Medical care, 56(8), 658–664. https://doi.org/10.1097/MLR.0000000000000937
Light, A. D., Obedin-Maliver, J., Sevelius, J. M., & Kerns, J. L. (2014). Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstetrics & Gynecology, 124(6), 1120-1127.
Martin, J. A., Hamilton, B. E., Osterman, M., & Driscoll, A. K. (2019). Births: Final Data for 2018. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 68(13), 1–47. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_13-508.pdf
Maykin, M., & Tsai, S. P. J. (2020). Our mothers are dying: The current state of maternal mortality in Hawai ‘i and the United States. Hawai’i Journal of Health & Social Welfare, 79(10), 302.
Medoff M. (2016). Pro-choice versus pro-life: The relationship between state abortion policy and child well-being in the United States. Health Care for Women International, 37(2), 158–169. https://doi.org/10.1080/07399332.2013.841699
Obedin-Maliver, J., & Makadon, H. J. (2016). Transgender men and pregnancy. Obstetric Medicine, 9(1), 4-8.
Osterman, M. J., & Martin, J. A. (2014). Trends in low-risk cesarean delivery in the United States, 1990-2013. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 63(6), 1–16. https://pubmed.ncbi.nlm.nih.gov/25383560/
Sewel, J. E. (1998). Cesarean section: A brief history. https://www.nlm.nih.gov/exhibition/cesarean/index.html
Shorter, J. M., Koelper, N., Sonalkar, S., Oquendo, M. A., Sammel, M. D., & Schreiber, C. A. (2020). Racial Disparities in mental health outcomes among women with early pregnancy loss. Obstetrics and Gynecology, 137(1), 156. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7737857/
Slaughter-Acey, J. C., Sneed, D., Parker, L., Keith, V. M., Lee, N. L., & Misra, D. P. (2019). Skin tone matters: Racial microaggressions and delayed prenatal care. American Journal of Preventive Medicine, 57(3), 321-329.
Sohr-Preston, S. L., Morain, S., Chapman, A., Pardue, S., & Ford, S. (2018). Examining misperceptions about miscarriage in US adults. Journal of Prenatal & Perinatal Psychology & Health, 32(4), 285-305.
Wang, E., Glazer, K. B., Sofaer, S., Balbierz, A., & Howell, E. A. (2020). Racial and ethnic disparities in severe maternal morbidity: A qualitative study of women’s experiences of peripartum care. Women’s Health Issues. https://www.sciencedirect.com/science/article/pii/S1049386720301006?casa_token=_cuyMu_v-BQAAAAA:0wixvLium4n7tUwzlW6oYwqcAIXxzX-xbJjgODfzFMTxXIP_39BrKuvOYKhM06_NUIEuQ_crlg
Introduction to Human Sexuality Copyright © 2022 by Ericka Goerling, PhD and Emerson Wolfe, MS is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Signs and Symptoms
- How It Spreads
- Areas with Risk
- Dengue in the United States
- Dengue Print Resources
- Dengue Vaccine
- Clinical Features
- Clinical Testing and Diagnosis
- Dengue Clinical Care
- Dengue Course
Dengue During Pregnancy
At a glance.
- Data are limited on health outcomes of dengue in pregnancy and effects of maternal infection on the developing fetus.
- Pregnant people can transmit dengue virus to the fetus during pregnancy or around the time of birth.
- Dengue can have harmful effects, including death of the fetus, low birth weight, and premature birth.

- The potential for vertical transmission should be considered for mothers with dengue who are symptomatic late in pregnancy or at delivery.
- Newborns usually develop symptoms within 14 days of birth (commonly within the first week), but most babies are asymptomatic.
- Clinical presentation in babies varies from mild common symptoms of dengue to severe dengue with shock and hemorrhagic manifestations.
Learn about dengue viruses, how dengue spreads, how to prevent dengue, and the areas with risk of dengue.
For Everyone
Health care providers.

Pregnancy and Birth
Jul 29, 2014
100 likes | 293 Views
Pregnancy and Birth. Pregnancy and Birth. A new Beginning Fertilization- when the sperm from a man and the ovum from a woman join together, the genes of the mother and the father combine Implantation- the attachment of the developing cells to the uterus
Share Presentation
- month periods
- second trimester
- emotional changes
- major organs

Presentation Transcript
Pregnancy and Birth • A new Beginning • Fertilization- when the sperm from a man and the ovum from a woman join together, the genes of the mother and the father combine • Implantation- the attachment of the developing cells to the uterus • Pregnancy- the time when the new cell formed during fertilization grows and develops into a baby in the women’s uterus. • Embryo- the developing human for the 1st 8 weeks • Fetus- the developing human from week 8 until birth.
Pregnancy and Birth • Changes in the Mother’s Body • Once pregnant, woman’s uterus produces certain hormone • Pregnancy test • Some hormones make the women nausea (morning sickness) • These hormones produce milk • Enlarged abdomen • Swelling legs • Difficulty sleeping • Become clumsy • Emotional changes
Pregnancy and Birth • Nourishing the fetus • Placenta- an organ that grows in the woman’s uterus during pregnancy and allows nutrients, gases, and wastes to be exchanged between the mother and the fetus. • Mother’s blood on one side, fetus’s blood on the other. • Fetus gets nutrients from mother, and anything else.
Pregnancy and Birth • Pregnancy lasts about 40 weeks, or 9 months • Doctors divide the 9 months into 3 month periods called Trimesters • If a baby goes until the end of the ninth month it is full term, before this it is premature
The First Trimester • The first 12 weeks or 3 months of the pregnancy • Begins as single cell, but continuously divides • The heart is formed and begins to beat in the 4th week, along with the brain and the limbs. • 10,000 times bigger than 1st • Brain waves are detected • All major organs are formed by week 8 • Week 9 it is a fetus
The second trimester • 4th-6th month, 13th -27th week • Fetus is 3 inches long • By end of trimester it will be 3 times this size • Mother feels movement • Week 14-18 the sex of the fetus is determined • Fingers and toes grow nails • Calcium in bones • Hair is formed
The third trimester • 7th-9th month, 28th-40th week • Fetus is 10 inches long, 2 pounds • Develops more muscles and begins to move more • Fat deposited under skin • Eyes open, lungs function • Fetus can hear voices • By end of this trimester the fetus is fully developed and ready to live in the outside world
Pregnancy and Birth • Birth • The passage of a baby from its mother’s uterus to outside her body • Uterus contracts many times • Labor- the process that lasts from the time contractions start until the delivery of the child and placenta. • 3 stages of labor • Caesarean Section- a procedure when the doctor surgically removes the baby and the placenta • After birth the umbilical cord is cut for some women pregnancy, labor and delivery involve problems that range from mild to life threatening
- More by User
The Wonder of Pregnancy & Birth
The Wonder of Pregnancy & Birth. By: Amanda Davis. National Geographic, The Human Body. 2002 Educational film This movie followed the stories of 3 different people. Each situation was different in showing how amazing the human body is in adapting and healing.
278 views • 14 slides
Judicial Intervention in Pregnancy & Birth
Judicial Intervention in Pregnancy & Birth. Rels 300 / Nurs 330 19 March 2014. What does “judicial intervention” mean?. Using laws and court decisions to control the behaviour and choices of a pregnant woman.
387 views • 27 slides
Pregnancy, Birth, and Childhood
Pregnancy, Birth, and Childhood. Development Before Birth. The Beginning of the Life Cycle. During sexual intercourse sperm are deposited into the vagina. If a egg is on its way to the uterus, a sperm may fertilize it. This moment of fertilization is called conception.
431 views • 28 slides
Pregnancy and Birth. The Beginning of the life cycle. Fertilization / Conception. When the males sperm enters the females egg 1 sperm / 1 egg Within seconds of fertilization, the surface of the egg changes so that no more sperm may enter the egg. Zygote. The united egg and sperm
578 views • 42 slides
Pregnancy and child birth
Pregnancy and child birth. 1. To look at health issues surrounding pregnancy 2. To look at stages of development of the foetus 3. To look at the stages of birth 4. To look at care for the mother during pregnancy 5. To look at care of mother and baby at birth 6. Health and infancy
476 views • 30 slides
Pregnancy and Birth. EQ . Why do parents decide to have children? DE Health Standard 2- Students will analyze the influence of family, peers, culture, media on health behaviors. Journal. Why do you think the teen pregnancy rate in the United States is so high?
749 views • 61 slides
3.14 Pregnancy: Fertilization to Birth
3.14 Pregnancy: Fertilization to Birth . (Sec 4.3 pg 117) . The ‘simplest’ part of reproduction is bringing the sperm and the egg together. After that event, many very complex events must take place before a healthy baby is born . . Fertilization:
323 views • 10 slides
Menstrual Cycle, Pregnancy, & Birth
Anatomy & Physiology Mrs. Halkuff. Menstrual Cycle, Pregnancy, & Birth. Menstrual Cycle. A series of hormonal changes that help to prepare a woman’s body for pregnancy. Menarche : First female period that usually occurs around age 12.
518 views • 20 slides
Pregnancy, Injury, and Birth Outcomes: Linking birth/fetal death certificates to hospital data
Pregnancy, Injury, and Birth Outcomes: Linking birth/fetal death certificates to hospital data. Melissa Schiff, MD, MPH Victoria Holt, PhD Janet Daling, PhD. Injury during Pregnancy. A leading cause of morbidity and mortality during pregnancy Occurs in 1 out of 12 pregnancies
364 views • 18 slides
Unit 2: Pregnancy & Birth
Unit 2: Pregnancy & Birth. Chapter 3: Prenatal Development Chapter 4: Preparing for Birth Chapter 5: The Baby’s Arrival. Chapter 3: Prenatal Development. Objectives: To help you: Name the 3 stages of pregnancy and describe the prenatal development in each
401 views • 21 slides
Chapter 15: The Female Reproductive System; Pregnancy and Birth
Chapter 15: The Female Reproductive System; Pregnancy and Birth. Chapter Objectives. Female reproductive tract and describe the function of each part. Structure and function of the mammary glands. Menstrual cycle. Main disorders of the female reproductive system.
1.63k views • 105 slides
Herbal Medicine in Pregnancy, Birth, and Lactation
Herbal Medicine in Pregnancy, Birth, and Lactation. Mary Bove ND Brattleboro Naturopathic Clinic www.bncvt.com. Issues Arising for Herbal Medicines in Pregnancy. Source of information: literature review, clinical trials, survey, clinical observation, empirical data
1.73k views • 130 slides
Pregnancy, Birth, and the Newborn Chapter 5 Unit 2
Pregnancy, Birth, and the Newborn Chapter 5 Unit 2. Michelle Fischer, ACSW, LSW, MSW. Nice job on the discussion board last week! Keep up the good work! Don’t forget to review the seminar archive if you missed our seminar last week. This week you will be reading about pregnancy.
534 views • 36 slides
Birth Control & Teen Pregnancy
Birth Control & Teen Pregnancy. Mark Peters 9 th -12 th Grade. Birth Control Pill. The pill is most popular type of birth control. It usually comes in packs of 21 or 28. The pill is 92 to 99.7 percent effective if used correctly.
345 views • 20 slides
Normal pregnancy and birth defects
HuWenSheng Women’s Hospital School of Medicine Zhejiang University. Normal pregnancy and birth defects. Normal Pregnancy-- Terminology. Pregnancy The course that the embryo and the fetus grow in the maternal body Stages of pregnancy Early pregnancy: ≤12 weeks
1.52k views • 109 slides
Quitting Smoking During Pregnancy and Birth Outcomes:
RESULTS. BACKGROUND. OBJECTIVE. METHODS. CONCLUSIONS. Quitting Smoking During Pregnancy and Birth Outcomes: Evidence of Gains Following Cessation by Third Trimester. Beth A. Bailey, PhD; Judy G. McCook, PhD, RNC; Andrea D. Clements, PhD; Lana U. McGrady, MS.
209 views • 1 slides
Section 3: Pregnancy, Development, and Birth
Section 3: Pregnancy, Development, and Birth. What are the changes that occur to the zygote, embryo, and fetus during development? How is the developing embryo protected and nourished? What happens during childbirth? What changes occur as a person develops from infancy to adulthood?.
224 views • 8 slides
Birth Spacing and Pregnancy Planning/Prevention in Home Visiting
Birth Spacing and Pregnancy Planning/Prevention in Home Visiting. Webinar hosted by The National Campaign to Prevent Teen and Unplanned Pregnancy June 17, 2014 3:00PM – 4:30PM (EDT). What we will hear. Welcome/Introductions
1.16k views • 74 slides
KIC-Guaranteed Pregnancy and Live Birth
About Kiran Infertility Center: Guaranteed pregnancy and live birth package is an option which is feasible and beneficial for the couple as well as for us.
171 views • 5 slides
Guaranteed Pregnancy and Live Birth
Guaranteed pregnancy and live birth package is an option which is feasible and beneficial for the couple as well as for us. We work hard to make sure the maximum achievement for our patients so that we can take our name to a new level of success.
160 views • 5 slides
Judicial Intervention in Pregnancy & Birth. Rels 300 / Nurs 330 Febr uary 2016. What does “judicial intervention” mean?. Using laws and court decisions to control the behaviour and choices of a pregnant woman.
341 views • 27 slides
1.12k views • 109 slides
Baby Your Baby- Maternal Mental Health: Mood Disorders During and After Birth
by Intermountain Health
New Moms May Be at Risk for Peripartum Mood Disorders During pregnancy and during the year after birth
The month of May means a lot of focus on mental health as May is Mental health Month. There is also a focus on moms and the issues that affect them, and it’s also Maternal Mental Health Awareness Month worldwide.
“Being pregnant or being a new mom means a woman and those around her (whether her partner, other kids, family, etc) will be making a lot of changes. Even planned, sought-after changes bring stress. By nature, moms have another person’s needs to care for and think about, besides managing their own personal needs,” said Kim Myers, Behavioral Health Clinical Program Manager at Intermountain Health. “Not to mention the physiological changes such as hormonal changes and significant changes to sleep patterns.
Factors that may contribute to being at risk for peripartum mood disorders
During pregnancy and after delivery women’s hormone levels are changing. On top of that, many new mothers are unable to get the rest they need to fully recover from giving birth. Constant sleep deprivation can lead to physical discomfort and exhaustion.
For all of these reasons, pregnancy and the postpartum period are a time when women are susceptible to mood disorders like depression and anxiety.
“In addition, being a new parent, may increase anxiety about the baby’s well-being and social isolation, and also lead to life stressors like a job change or moving. That’s a lot of things that can factor into a woman’s mental health. A happy time can become an isolated one.
Many women may wonder if their feelings are “normal”, or if they are just the baby blues, or if they may be experiencing true depression or anxiety.
Postpartum depression is common
A better term is actually peripartum mood disorders, because they can occur during pregnancy or after birth. Mood disorders can manifest not only as depression, but in other ways like anxiety or obsessive-compulsive disorder, even psychosis.
Up to 1 in 8 women in Utah experience postpartum depression.
Risk factors for postpartum depression
- Previous mental illness or family history of such
- A stressful life event during pregnancy or soon after birth (job change, moving, divorce, death of a loved one)
- Traumatic labor and delivery or medical complications of mother or baby
- Mixed feelings about the pregnancy
- Isolation or lack of emotional support from family or friends
- Alcohol or drug abuse problems
- Unplanned pregnancy
Medical complications, including contracting COVID-19 while pregnant, add a level of stress. Stress can build on itself to the point of a diagnosable mental health disorder, especially in vulnerable populations.
How is postpartum depression different from the “baby blues”?
- The “baby blues” is used to describe feelings of worry, unhappiness, and fatigue many women experience after having a baby. This occurs in 80% of women.
- Babies require a lot of care, so it’s normal for mothers to be worried about or tired from providing that care.
- Baby blues includes feelings that are somewhat mild, last a week or two, and go away on their own. Doing things like taking a break or a nap and eating well usually help.
It’s ok to talk about mental health concerns with your primary care provider
“Parenting is often romanticized and therefore struggling with parenthood and/or a new baby can make a parent reluctant to ask for help. This is a major life adjustment and some struggle is normal,” said Lash. Don’t be embarrassed to talk to your provider about anxiety or depression. At Intermountain, mental health screenings are part of primary care. It’s ok to ask questions. The world has gone through significant changes in the last year. Help is everywhere. Just open your mouth and ask.
Anxiety is like a virus and runs around and attaches to whatever it wants. Under normal conditions, women are somewhat socially isolated when they have a baby. They’ve taken time off work or quit their job and are spending more time at home. Isolation is different right now, because everyone has felt some isolation during the pandemic.
“While this is maternal mental health month, let’s not forget that adjustment can be hard for the partners, too,” said Lash.
How to know when to see a behavioral health provider
If you are experiencing any symptoms of depression or anxiety and it is significantly interferes with your ability to function in your life for more than a couple of days then it is worth a conversation with your doctor or pediatrician. There is such a continuum of mental health from illness to full health and anytime of suboptimal functioning it is worth exploring what supports and strategies are available for you.
In terms of peripartum mood disorders, here are some things to look for:
Symptoms of postpartum depression that need urgent treatment
- Having trouble bonding or forming an emotional attachment with her baby
- Persistently doubting her ability to care for her baby
- Never feeling good
- Thinking about harming herself or her baby.
- Experiencing anger or rage
- Fear of taking medications
- Psychosis – thoughts that are irrational
Signs of postpartum anxiety
- Worry more than normal about the newborn
- Terrified of hurting the baby.
- Panic attacks
Signs of obsessive-compulsive disorders postpartum
- Obsessed with checking things over and over
- Irrationally concerned about baby’s safety or wellness
- Intrusive thoughts become prevalent and occur often.
- Taking action to avoid intrusive thoughts.
Where to get help
- Talk to your OB or primary care physician about your mental health and ask for a referral. Intermountain has integrated mental health screening into primary care. There are resources available even if you don’t have insurance.
- Call the Intermountain Behavioral Health Services Navigation Line at 833-442-2211 . It’s free and can be reached seven days a week from 8 am to 8 pm. It connects callers with a trained care coordinator who can provide appropriate self-care tools, peer support, treatment options, crisis resources, and more.
- Go to an Intermountain Behavioral Health Access Center
Intermountain LDS Hospital in Salt Lake, McKay Dee Hospital in Ogden and St George Regional Medical Center in St. George offer walk in behavioral health access centers that are open extended hours. Check with other Intermountain behavioral health locations to see if they have urgent appointments available.
For more information about these locations go to intermountainhealthcare.org .
For other community resources, visit the Utah webpage for Postpartum Support International.

How to Use Self Injectable Birth Control Shots Delivered in Ksh 57M UK Initiative
T he United Nations Populations Fund (UNFPA) has donated 450,000 doses of sub-cutaneous Depot Medroxy-Progesterone-Acetate (DMPA), a self-injectable contraceptive consignment valued at Ksh56.4 million.
According to the Ministry of Health Director General Patrick Amoth, the contraceptives will be used to avert over 122 maternal deaths, 12,310 unsafe abortions and 42,750 unintended pregnancies.
Further, the Ministry of Health indicated that the move was a significant step in overcoming barriers to commodity security and addressing the unmet need for family planning services.
Also, Health Cabinet Secretary Susan Nakhumicha said that the consignment will enhance health outcomes for women and families across Kenya.
The consignment has come at a time when there is a growing demand for accessible and convenient contraceptive options, especially after self-injectable contraceptives were approved for use in the county.
Also Read: Family Planning Methods, Benefits and How to Make Your Choice
Details of the Contraceptives and How to Use
Depo-Medroxyprogesterone Acetate (DMPA-SC) is commonly known as the “birth control shot.” When administered correctly and consistently, DMPA-SC is over 99% effective at preventing pregnancy.
It contains the hormone progestin, which prevents pregnancies by preventing ovulation and thickening cervical mucus to prevent sperm from reaching the egg. Also, production of the hormones leads to thinning of the lining of the uterus to prevent implantation of a fertilized egg.
It has gained popularity among users, even in Kenya, because of its long-lasting protection against pregnancy because one requires four injections to last the whole year.
Furthermore, unlike many other forms of contraceptives like implants and intrauterine devices (IUDs), the effects of the birth control shot are reversible after the injections are stopped.
However, some of its common side effects include breast tenderness, and mood changes, irregular menstrual bleeding, weight gain, headaches, and in some instances temporary delay in fertility after discontinuation.
Also, because of its ease of use, the contraceptive can be administered by community health workers, pharmacists, and even women can inject it themselves.
The Reproductive Health Network Kenya (RHNK), notes that DMPA-SC only requires minimal training to be used properly.
“It is reversible and combines the contraceptive drug and needle into a single device that is small, light, and easy to use. It is also 99 per cent effective at preventing unintended pregnancies when administered correctly and on time every three months,” notes the network.
Also Read: No Condoms for Kenyan Teenagers – CS Nakhumicha
Govt Approves Use of the Contraceptive
The Kenya Pharmacy and Poisons Board approved on May 11, 2018, to Pfizer Laboratories Ltd for a label modification enabling self-administration of the contraceptive extending its shelf life to 36 months. Also, the move facilitated the introduction of a 200-pack presentation, that included options for self-injection labeling.
Earlier, the board had demanded a clinical study within the local population to clarify clinical efficacy, safety, and satisfaction outcomes including error rates and confidence in self-administration.
However, to offer women more options for family planning, Jhpiego in collaboration with the Ministry of Health (MOH) and supported by the Bill and Melinda Gates Foundation carried out a study on self-injection of DMPA-SC.
The findings of the study were distributed MOH and presented to stakeholders during the February 2017 Advocates, Researchers, and Development Partners Meeting, where the Kenyan delegation formulated an action plan to outline a roadmap for the implementation and expansion of DMPA-SC.
Follow our WhatsApp Channel for real-time news updates.
https://whatsapp.com/channel/0029VaB3k54HltYFiQ1f2i2C
![The United Nations Populations Fund (UNFPA) has donated 450,000 doses of sub-cutaneous Depot Medroxy-Progesterone-Acetate (DMPA), a self-injectable contraceptive consignment valued at Ksh56.4 million. According to the Ministry of Health Director General Patrick Amoth, the contraceptives will be used to avert over 122 maternal deaths, 12,310 unsafe abortions and 42,750 unintended pregnancies. Further, the Ministry of Health indicated that the move was a significant step in overcoming barriers to commodity security and addressing the unmet need for family planning services. Also, Health Cabinet Secretary Susan Nakhumicha said that the consignment will enhance health outcomes for women and families across Kenya. The […] The United Nations Populations Fund (UNFPA) has donated 450,000 doses of sub-cutaneous Depot Medroxy-Progesterone-Acetate (DMPA), a self-injectable contraceptive consignment valued at Ksh56.4 million. According to the Ministry of Health Director General Patrick Amoth, the contraceptives will be used to avert over 122 maternal deaths, 12,310 unsafe abortions and 42,750 unintended pregnancies. Further, the Ministry of Health indicated that the move was a significant step in overcoming barriers to commodity security and addressing the unmet need for family planning services. Also, Health Cabinet Secretary Susan Nakhumicha said that the consignment will enhance health outcomes for women and families across Kenya. The […]](https://img-s-msn-com.akamaized.net/tenant/amp/entityid/BB1mvFQT.img?w=700&h=350&m=6)

Engineering mini human hearts to study pregnancy complications and birth defects
Ph.D. Candidate in Biomedical Engineering, Michigan State University
Associate Professor of Biomedical Engineering, Michigan State University
Postdoctoral Researcher in Quantitative Health Sciences and Engineering, Michigan State University
Disclosure statement
Aitor Aguirre receives funding from the NIH, AHA, Corewell-MSU Alliance Foundation and HVI.
Aleksandra Kostina and Brett Volmert do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Michigan State University provides funding as a founding partner of The Conversation US.
View all partners
How did your heart form? What triggered your first heartbeat? To this day, the mechanisms of human heart development remain elusive.
Researchers know the heart is the first organ to fully function in the growing human embryo. It begins as a simple tube that starts to pump blood by the fourth week of gestation. By the ninth week, the heart is fully formed. The heart is critical to early development because it provides essential nutrients throughout the developing fetus.
But due to its early formation, the heart is exposed for a long duration to substances a pregnant person might come into contact with, such as medications or pollutants . This may be a main reason why congenital heart disease is the most common type of birth defect in people, occurring in over 1 in 100 births worldwide .
Traditionally, scientists have used animal and cell models to study heart development and disease. However, researchers haven’t been able to produce a cure for congenital heart disease in part because these models are unable to capture the complexity of the human heart . Due to ethical limitations, using human embryos for these studies is out of the question.
To help researchers study heart development and complications in pregnancy, our team of biomedical engineers and cardiovascular scientists have spent the past several years trying to create the next best thing: mini human hearts in the lab .
Human heart organoids
Organoids are complex 3D cellular structures that replicate significant aspects of the structure and function of a specific organ in your body. While organoids are not completely synthetic, functioning organs (yet), they still possess immense power to mimic key aspects of physiology and disease in the lab.
We created our heart organoids using a type of cell called a pluripotent stem cell . Although using these cells in research used to be controversial because they were originally derived from human embryos, this is no longer a concern, as they can be produced from any adult. Pluripotent stem cells have the potential to become any type of cell in the body. This means that cells from nearly any part of your body – typically blood or skin cells – can be turned into your own stem cells to grow your own mini heart.
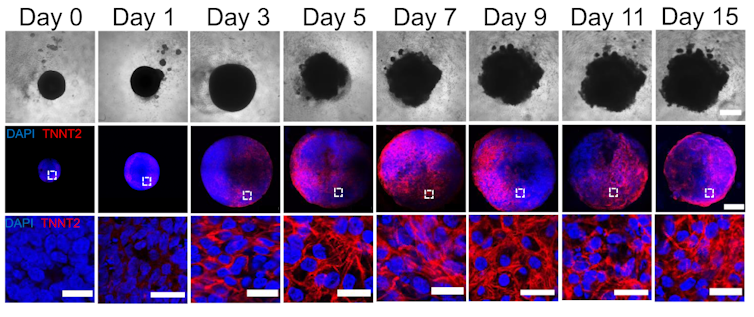
By manipulating the ability of pluripotent stem cells to become any type of cell in the body, we guided these cells to become heart cells . The cells were able to self-assemble, replicating the main stages of human heart development during pregnancy. Our heart organoids have blood vessels and all the cell types found in the human heart, such as cardiomyocytes and pacemaker cells, which give them an edge over 2D cellular models. Furthermore, the electrophysiology and bioenergetics of these heart organoids are very similar to human embryonic hearts in ways that animal models aren’t.
Our heart organoids beat like a tiny baby’s heart, all while smaller than a grain of rice.
Pregnancy and the fetal heart
One area we’re exploring with our heart organoids is maternal and fetal cardiac health. Maternal factors such as diabetes , hypertension or even depression can increase the risk of heart disease in newborns. Studying conditions that increase the risk of congenital heart disease can prevent and reduce the incidence of cardiovascular diseases worldwide.
We can mimic these maternal environments and simulate how they influence fetal heart development with heart organoids. For example, we used heart organoids to show that diabetes, a very common condition, increases the risk of heart disease in embryos . Compared to heart organoids created in healthy conditions, mini hearts exposed to diabetic conditions developed heart abnormalities like those of human fetuses and newborns with diabetic cardiomyopathy.
Our study found that diabetes-related developmental abnormalities of the heart are likely caused by an imbalance of omega-3 fatty acids, the building blocks of cell membranes and signaling molecules. However, dietary supplementation of omega-3 fatty acids could partially restore this imbalance and prevent diabetes-induced congenital heart defects.
Drug safety during pregnancy
The drugs pregnant people take can have significant health effects on both the parent and the fetus. Medications approved for use during pregnancy are not always safe, since adequate testing is complicated . Ethical concerns limit working with biological material from people, so researchers are left with animal models that aren’t able to replicate human physiology closely enough.
Testing medications on human heart organoids allows researchers to better explore and predict potential harmful effects during pregnancy. One example is ondansetron (Zofran), a drug commonly prescribed to prevent nausea and vomiting during pregnancy. Although it has been linked with an increased risk of congenital heart disease , whether it causes the disease hasn’t been confirmed.
We showed that heart organoids exposed to ondansetron had disturbed development of ventricular cells and impaired function, similar to what’s seen in newborns exposed to ondansetron. Our findings provide data that may help update clinical guidelines on the use of the drug.

Another example concerns the use of antidepressants during pregnancy, which is associated with an increased risk of congenital heart defects . Selective serotonin reuptake inhibitors, or SSRIs, the most prescribed antidepressants in pregnant people, work by increasing the availability of serotonin in the body. Serotonin is an important molecule in cardiac development. Maternal serotonin, along with antidepressants, readily pass to the embryo and alter serotonin levels in the developing heart.
In the future, we plan to expose heart organoids to antidepressants and study their effects on the incidence of congenital heart defects. The results of such research on human heart organoids may also inform recommendations for drug replacement or repurposing.
Heart organoids have the potential to help scientists more precisely study how the human heart forms and how it develops disease. In the realm of medical innovation, we believe human heart organoids grown from stem cells are the beating promise of a healthier future.
- Cardiovascular disease
- Biomedical engineering
- Congenital heart defect
- Bioengineering
- Congenital heart disease
- New research
- Disease modeling
- STEEHM new research

Compliance Lead

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

Lecturer/Senior Lecturer, Earth System Science (School of Science)
- International edition
- Australia edition
- Europe edition

Women in the UK: share your experience of maternity care, birth trauma, and postnatal care
We’re keen to hear from women in the UK who experienced birth trauma, and about their experience of care in pregnancy and after giving birth
A health minister has apologised to women affected by birth trauma after a parliamentary inquiry that heard “harrowing” testimonies from more than 1,300 women about giving birth found a “postcode lottery” for maternity care.
The birth trauma inquiry, led by the Conservative MP Theo Clarke and Labour MP Rosie Duffield, will call for an overhaul of the UK’s maternity and postnatal care .
We’d like to hear from women in the UK who have experienced birth trauma, or inadequate care during pregnancy, birth or in their post-natal period.
How has this experience affected you? Did you experience long-term problems affecting your health after giving birth? What might have improved your experience and outcome?
Tell us if you've experienced birth trauma in the UK, or felt that you received problematic care during your pregnancy, delivery or after giving birth.
Please include as much detail as possible
Please note, the maximum file size is 5.7 MB.
Please do leave a phone number if you are happy to be interviewed. Your contact details are helpful so we can contact you for more information. They will only be seen by the Guardian.
Your contact details are helpful so we can contact you for more information. They will only be seen by the Guardian.
If you include other people's names please ask them first.
Contact us on WhatsApp at +447766780300.
For more information, please see our guidance on contacting us via WhatsApp . For true anonymity please use our SecureDrop service instead.
Most viewed
- MSD careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Their first baby came with medical debt. These Illinois parents won't have another.

Medical debt is as much a hallmark of having children as long nights and dirty diapers. The Crivilare family, Andrew, Heather and Rita, 2, are pictured at their kitchen table in Jacksonville, Ill. Neeta Satam for KFF Health News hide caption
Medical debt is as much a hallmark of having children as long nights and dirty diapers. The Crivilare family, Andrew, Heather and Rita, 2, are pictured at their kitchen table in Jacksonville, Ill.
JACKSONVILLE, Ill. — Heather Crivilare was a month from her due date when she was rushed to an operating room for an emergency cesarean section.
The first-time mother, a high school teacher in rural Illinois, had developed high blood pressure, a sometimes life-threatening condition in pregnancy that prompted doctors to hospitalize her. Then Crivilare's blood pressure spiked, and the baby's heart rate dropped. "It was terrifying," Crivilare said.
She gave birth to a healthy daughter. What followed, though, was another ordeal: thousands of dollars in medical debt that sent Crivilare and her husband scrambling for nearly a year to keep collectors at bay.
The Crivilares would eventually get on nine payment plans as they juggled close to $5,000 in bills.
"It really felt like a full-time job some days," Crivilare recalled. "Getting the baby down to sleep and then getting on the phone. I'd set up one payment plan, and then a new bill would come that afternoon. And I'd have to set up another one."
Crivilare's pregnancy may have been more dramatic than most. But for millions of new parents, medical debt is now as much a hallmark of having children as long nights and dirty diapers.
About 12% of the 100 million U.S. adults with health care debt attribute at least some of it to pregnancy or childbirth, according to a KFF poll .
These people are more likely to report they've had to take on extra work, change their living situation, or make other sacrifices.

Heather Crivilare says she wishes there were a grace period for medical debt after the birth of a child, as there is for student loan debt after graduation. Neeta Satam for KFF Health News hide caption
Heather Crivilare says she wishes there were a grace period for medical debt after the birth of a child, as there is for student loan debt after graduation.
Overall, women between 18 and 35 who have had a baby in the past year and a half are twice as likely to have medical debt as women of the same age who haven't given birth recently, other KFF research conducted for this project found.
"You feel bad for the patient because you know that they want the best for their pregnancy," said Eilean Attwood, a Rhode Island OB-GYN who said she routinely sees pregnant women anxious about going into debt.
"So often, they may be coming to the office or the hospital with preexisting debt from school, from other financial pressures of starting adult life," Attwood said. "They are having to make real choices, and what those real choices may entail can include the choice to not get certain services or medications or what may be needed for the care of themselves or their fetus."
Best-laid plans
Crivilare and her husband, Andrew, also a teacher, anticipated some of the costs.
The young couple settled in Jacksonville, in part because the farming community less than two hours north of St. Louis was the kind of place two public school teachers could afford a house. They saved aggressively. They bought life insurance.
And before Crivilare got pregnant in 2021, they enrolled in the most robust health insurance plan they could, paying higher premiums to minimize their deductible and out-of-pocket costs.
Then, two months before their baby was due, Crivilare learned she had developed preeclampsia. Her pregnancy would no longer be routine. Crivilare was put on blood pressure medication, and doctors at the local hospital recommended bed rest at a larger medical center in Springfield, about 35 miles away.
"I remember thinking when they insisted that I ride an ambulance from Jacksonville to Springfield ... 'I'm never going to financially recover from this,'" she said. "'But I want my baby to be OK.'"
For weeks, Crivilare remained in the hospital alone as covid protocols limited visitors. Meanwhile, doctors steadily upped her medications while monitoring the fetus. It was, she said, "the scariest month of my life."
Fear turned to relief after her daughter, Rita, was born. The baby was small and had to spend nearly two weeks in the neonatal intensive care unit. But there were no complications. "We were incredibly lucky," Crivilare said.
When she and Rita finally came home, a stack of medical bills awaited. One was already past due.
Crivilare rushed to set up payment plans with the hospitals in Jacksonville and Springfield, as well as the anesthesiologist, the surgeon, and the labs. Some providers demanded hundreds of dollars a month. Some settled for monthly payments of $20 or $25. Some pushed Crivilare to apply for new credit cards to pay the bills.
"It was a blur of just being on the phone constantly with all the different people collecting money," she recalled. "That was a nightmare."
Big bills, big consequences
The Crivilares' bills weren't unusual. Parents with private health coverage now face on average more than $3,000 in medical bills related to a pregnancy and childbirth that aren't covered by insurance, researchers at the University of Michigan found.
Out-of-pocket costs are even higher for families with a newborn who needs to stay in a neonatal ICU, averaging $5,000. And for 1 in 11 of these families, medical bills related to pregnancy and childbirth exceed $10,000, the researchers found.
"This forces very difficult trade-offs for families," said Michelle Moniz, a University of Michigan OB-GYN who worked on the study. "Even though they have insurance, they still have these very high bills."
Nationwide polls suggest millions of these families end up in debt, with sometimes devastating consequences.
About three-quarters of U.S. adults with debt related to pregnancy or childbirth have cut spending on food, clothing, or other essentials, KFF polling found.
About half have put off buying a home or delayed their own or their children's education.
These burdens have spurred calls to limit what families must pay out-of-pocket for medical care related to pregnancy and childbirth.
In Massachusetts, state Sen. Cindy Friedman has proposed legislation to exempt all these bills from copays, deductibles, and other cost sharing. This would parallel federal rules that require health plans to cover recommended preventive services like annual physicals without cost sharing for patients. "We want ... healthy children, and that starts with healthy mothers," Friedman said. Massachusetts health insurers have warned the proposal will raise costs, but an independent state analysis estimated the bill would add only $1.24 to monthly insurance premiums.
Tough lessons
For her part, Crivilare said she wishes new parents could catch their breath before paying down medical debt.
"No one is in the right frame of mind to deal with that when they have a new baby," she said, noting that college graduates get such a break. "When I graduated with my college degree, it was like: 'Hey, new adult, it's going to take you six months to kind of figure out your life, so we'll give you this six-month grace period before your student loans kick in and you can get a job.'"
Rita is now 2. The family scraped by on their payment plans, retiring the medical debt within a year, with help from Crivilare's side job selling resources for teachers online.

The Crivilares paid off the medical debt for Rita's birth, but they are shouldering some more since Rita needed surgery for recurrent ear infections. Neeta Satam for KFF Health News hide caption
The Crivilares paid off the medical debt for Rita's birth, but they are shouldering some more since Rita needed surgery for recurrent ear infections.
But they are now back in debt, after Rita's recurrent ear infections required surgery last year, leaving the family with thousands of dollars in new medical bills.
Crivilare said the stress has made her think twice about seeing a doctor, even for Rita. And, she added, she and her husband have decided their family is complete.
"It's not for us to have another child," she said. "I just hope that we can put some of these big bills behind us and give [Rita] the life that we want to give her."
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.
- medical debt

VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's ...
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant patient's spine) with the face and body angled to one side and the neck flexed. Abnormal presentations include face, brow, breech, and shoulder.
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Breech presentation happens when your little one's feet or buttocks are in position to be delivered first, and make up just under 5 percent of all pregnancies. Your provider will likely order an ultrasound toward the end of your pregnancy if they suspect your baby is in a breech position.
The vertex presentation describes the orientation a fetus should be in for a safe vaginal delivery. It becomes important as you near your due date because it tells your pregnancy care provider how they may need to deliver your baby. Vertex means "crown of the head.". This means that the crown of the fetus's head is presenting towards the ...
In the last weeks of pregnancy, a fetus usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation.A breech presentation occurs when the fetus's buttocks, feet, or both are in place to come out first during birth. This happens in 3-4% of full-term births.
Presentation of twins in Der Rosengarten ("The Rose Garden"), a standard medical text for midwives published in 1513. In obstetrics, the presentation of a fetus about to be born specifies which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation.
Compound presentation is a fetal presentation in which an extremity presents alongside the part of the fetus closest to the birth canal. The majority of compound presentations consist of a fetal hand or arm presenting with the head [ 1 ]. This topic will review the pathogenesis, clinical manifestations, diagnosis, and management of this ...
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or ...
Presentation refers to which part of your baby's body is facing towards your birth canal. Position refers to the direction your baby's head or back is facing. Your baby's presentation will be checked at around 36 weeks of pregnancy. Your baby's position is most important during labour and birth.
The Trusted Provider of Medical Information since 1899
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
Pregnancy Presentation templates The day you give birth to a child is the best of your entire life. Nine months living as one, and then a lifetime of pure parent-child love! Check out these Google Slides themes & PowerPoint templates about pregnancy, obstetrics and babies. Easily customizable for everyone!
Unexpected breech presentation in labour and mode of birth were prioritised as critical outcomes by the committee. This reflects the different options available to women with a known breech presentation in pregnancy and the different choices that women make. There are some women and/or clinicians who may feel uncomfortable with the risks of ...
A full-term pregnancy lasts approximately 270 days (approximately 38.5 weeks) from conception to birth. Because it is easier to remember the first day of the last menstrual period (LMP) than to estimate the date of conception, obstetricians set the due date as 284 days (approximately 40.5 weeks) from the LMP.
Details. With engaging 3-D animation of the labor and birth process, this PowerPoint delivered on a USB flash drive comprehensively covers all the current teaching points from pregnancy through postpartum. Using gender-neutral and inclusive language, the presentation features a diverse group of families and experts to engage learners.
Dengue During Pregnancy. The potential for vertical transmission should be considered for mothers with dengue who are symptomatic late in pregnancy or at delivery. Newborns usually develop symptoms within 14 days of birth (commonly within the first week), but most babies are asymptomatic.
Pregnancy and Birth. Pregnancy and Birth. A new Beginning Fertilization- when the sperm from a man and the ovum from a woman join together, the genes of the mother and the father combine Implantation- the attachment of the developing cells to the uterus Slideshow 2600683 by kirima ... During download, if you can't get a presentation, the file ...
New Moms May Be at Risk for Peripartum Mood Disorders During pregnancy and during the year after birth. The month of May means a lot of focus on mental health as May is Mental health Month.
Mother's Day is Sunday, May 12. If you're thinking about getting pregnant or if you've just given birth, Life Kit is here to help. Our archive of episodes on maternal and reproductive health can ...
Depo-Medroxyprogesterone Acetate (DMPA-SC) is commonly known as the "birth control shot." When administered correctly and consistently, DMPA-SC is over 99% effective at preventing pregnancy.
The drugs pregnant people take can have significant health effects on both the parent and the fetus. Medications approved for use during pregnancy are not always safe, since adequate testing is ...
We're keen to hear from women in the UK who experienced birth trauma, and about their experience of care in pregnancy and after giving birth Guardian community team Mon 13 May 2024 05.52 EDT ...
Access to dignified healthcare and supportive community conditions during pregnancy and birth should be a basic right. This means having safe housing, nutritious food, and social services that support the health of the child and parent. The stark reality, however, is that structural racism continues to drive disparities in care for people of ...
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed.
Millions of new parents in the U.S. are swamped by medical debt during and after pregnancy, forcing many to cut back on food, clothing, and other essentials.