
- Practice Areas
- Terminology
- Entrepreneurship
- Medical Billing
- Healthcare Conferences

What is Assignment of Benefits in Medical Billing?

An assignment of benefits is the act of signing documentation authorizing a health insurance company to pay a physician directly. In other words, the insurance company can pay claims without the direct involvement of the patient in the process. There are other situations where AOBs can be helpful, but we’ll focus on their use in relation to medical benefits.
If there isn’t an assignment of benefits agreement in place, the patient would be responsible for paying the other party directly from their own pocket, then filing a claim with their insurance provider to receive reimbursement. This could be time-consuming and costly, especially if the patient has no idea how to file a claim.
The document is typically signed by patients when they undergo medical procedures. The purpose of this form is to assign the responsibility of payment for any future medical bills that may arise after the procedure. It’s important to note that not all procedures require an AOB.
An assignment of benefits agreement might be utilized to pay a medical practitioner the patient didn’t choose, like an anesthesiologist. The patient may have picked a surgeon, but an anesthesiologist assigned on the day of the procedure might issue a separate bill. They’re, in essence, signing that anyone involved in their treatment can receive direct payment from the insurance carrier. It doesn’t have to go through the patient.
This document can also eliminate service fees surrounding processing. As a result, the patient can focus on medical treatment and recovery without being bogged down with the complexities of paying medical bills. The overall intent of an assignment of benefits agreement is to make the process more manageable for the patient, as they don’t need to haggle directly with their insurer.
List of Providers and Services
When the patient signs an AOB agreement, they give a third party right to obtain payment for services the provider performed, and medical billing services are a prime example of where they may sign an AOB agreement.
- Ambulance services
- Medical insurance claims
- Drugs and pharmaceuticals
- Diagnostic and clinical lab services
- Emergency surgical center services
- Dialysis supplies and equipment used in the home
- Physician services for Medicare and Medicaid patients
Services of professionals other than a primary care physician, which includes:
- Physician assistants
- Clinical nurse specialists
- Clinical social workers
- Clinical psychologists
- Certified registered nurse anesthetists

Information Commonly Requested on Assignment of Benefits Form:
- Signature of patient or person legally responsible
- Signature of parent or legal guardian
How AOBs Affect the Medical Practitioner
A medical provider or their administrative staff may feel overwhelmed by the sheer number of forms patients must fill out prior to treatment. Demanding more paperwork from patients may be seen as an added burden on the managerial staff, as well as the patient. However, getting a signed AOB is vital in preserving the interests of everyone involved.
In addition to receiving direct payment from the insurance company without needing to go through the patient, a signed assignment of benefits form will help medical providers appeal denied and underpaid claims. They can ask that payments be made directly to them rather than through the patient. This makes the process more manageable for both the doctors and the patient.
Things to Bear in Mind
The patient gives their rights and benefits to third parties under their current health plan. Depending on the wording in the AOB, their insurer may not be allowed to contact them directly about their claims. In addition, the patient may be unable to negotiate settlements or approve payments on their behalf and enable third parties to endorse checks on behalf of the patient. Finally, when the patient signs an AOB, the insurer may sue the third parties involved in the dispute.
Looking for a qualified medical billing service?
By taking just 1 minute to provide some basic information about your practice, you can get up to 5 pre-screened companies competing for your business.
Related Posts
What Is Cosmetic Dermatology? Your Guide to Treatments, Costs, and More
What is a clia number in medical billing, healthcare revenue cycle management explained, leave a reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- +1 978-683-5115
- +1 978-423-1269
- [email protected]

What Is Assignment Of Benefits In Medical Billing – AOB Complete Guide
The healthcare industry operates with a diverse network of payers and various reimbursement means. From government to private insurance companies, a healthcare practice is simultaneously engaged with multiple payer parties, each linked to a different patient with unique regulations and requirements. This reimbursement workflow and many other factors alone make this already hectic environment business a bit more chaotic if not dealt with properly. With the development and execution of several policies, every healthcare service strives to bring more efficiency and seamlessness to its operations, and the reimbursement system is not an exception in this regard. This is where the assignment of benefits in medical billing comes into play.
What is Assignment of Benefits in Medical Billing?
An assignment of benefits in medical billing is a type of agreement between the healthcare provider, insurance company, and the patient through which a patient authorizes the medical service to collect healthcare policy coverage benefits on their behalf from their insurer for the service they have received from the facility. Once the patient signs this agreement, a direct payment link is made between the facility and the insurance company without communicating every time with the patient, which brings seamlessness and efficiency to the reimbursement process.
Read More: Medical Billing vs Revenue Cycle Management – Key Differences Explained
Medical Services That Use the Assignment of Benefits
Various healthcare providers across different specialties and settings may use Assignment of Benefits (AOB) as part of their billing practices. Some examples of healthcare providers that commonly use AOB include:
- Physicians and Medical Practices
- Hospitals and Medical Centers
- Dentists and Dental Clinics
- Physical Therapy and Rehabilitation Centers
- Ambulatory Surgery Centers
- Imaging Centers
So how does this assignment of benefits in medical billing work? Let’s explore:
What is the Procedure for the Assignment of Benefits in Medical Billing ? – the Methodology
Patient visit.
In the first step, the patient receives medical service from a healthcare facility like a hospital, clinic, etc.
AOB Agreement
Once the services are rendered, the healthcare facility presents an AOB agreement to the patient to transfer their healthcare insurance coverage benefits to the facility directly. The patient is advised to thoroughly review the form before signing for consent as they are establishing a direct form of communication and payment action by authorizing the medical service to collect monetary benefits on their behalf.
Claim Submission
In this stage, the healthcare service document and code all the service encounters with the patient into medical bills and claim, comprising all the details and treatment procedures that are associated with curing the patient. These claims are then sent to the insurance company.
Claim Reviewing
After claim submission, the insurance company meticulously evaluates it on the criteria of its unique requirements, standard policies, and regulations. They also analyze the accuracy of the claim and assess the coverage limit against the payment listed in the claim. If the claim is found to be inaccurate or ineligible for coverage by the insurance company, it reverts back to the facility for denial management.
In the case the claim is approved, the insurance company makes payment directly to the medical service given the AOB policy. This reimbursed amount may cover the full or half of the patient’s medical bills, based on the coverage plan.
Patient Responsibility
Once the insurer pays the billed amount to the medical service, any remaining payment responsibilities come on the shoulder of the patient, like deductibles, co-pays, or services not covered by insurance. The patient may receive an explanation of benefits (EOB) from the insurance company, outlining the details of the claim and any patient responsibility.
Read More: Why Outsourcing Ophthalmology Medical Billing is the Smart
What are the Complications in the Assignment of Benefits in Medical Billing? – the Hindrances
Assignment of benefits does not work well necessarily for all patient encounters. There are some instances where it fails to be applicable or may get denied. So what are those cases? Let’s explore:
Out-of-Network Providers
An insurance policy can deny the assignment of benefits claim if the service acquired by the patient is out of its network of carriers. In this case, the healthcare facility can’t establish any type of reimbursement connection with the insurance policy and must obtain the payments directly from the patient. The patient can then cover their expenditure from their insurance policy.
Non-Covered Services
It is not necessary that a health insurance policy cover all types of patient medical encounters. Every policy has its own limitations and offers reimbursements for medical services according to its regulations. So if a patient seeks a medical facility that is not covered by their healthcare policy, no AOB agreement will be applicable here. In this scenario, a patient is required to pay all the charges from their own pocket.
Preauthorization Requirements
Insurance policies require preauthorization for certain medical treatments, procedures, or medications, and if a patient fails to obtain this preauthorization, the insurance company rejects the assignment of benefits claim, leaving the patient to pay the bills out of their pocket.
Claims Rejection
Even with an AOB in place, insurance companies may reject or deny claims for various reasons, such as incomplete documentation, coding errors, or policy exclusions. In such cases, the provider and the patient may need to work together to resolve the issue and resubmit the claim.
If an AOB gets accepted, it will only cover the services eligible for insurance coverage. Patients are still responsible for any deductibles, co-pays, or non-covered services as per their insurance policy. If the patient fails to pay their portion, it can lead to complications in the billing process.
Billing Disputes
Moreover, billing disputes between healthcare providers and insurance companies are another reason for AOB complications. Occasionally, disputes may arise between the healthcare provider and the insurance company regarding reimbursement rates or claim processing. These disputes can delay or hinder the AOB process, requiring additional efforts to resolve the billing issues. Read More: What Is Down Coding In Medical Billing? – The Complete Guide
Assignment of benefits is an excellent way to increase the efficiency of the reimbursement process in the medical industry. However, for a patient, it is important to thoroughly and meticulously review all the terms and complications associated with the agreement of AOB as it transfers their monetary rights directly to the healthcare service.
Concerning healthcare services, they must ensure a well-communicated, clear, and detailed preparation of this agreement to help patients better understand all the things related to their financial obligations and insurance benefits transfer. Further, the medical facilities should also bring more accuracy and compliance with standards to their billing and overall financial landscape to make the whole process conducive to the acceptance of AOB, effectively navigating the complex web of reimbursements.
Stay in Touch
After hours & weekend physician line
- 978-423-1269
- 978-683-5115
- PRIVACY POLICY
- TERMS AND CONDITIONS

(888) 444-6041

What is Assignment of Benefits in Medical Billing
The health care industry has a wide network of health care insurance payers that make payments on behalf of patients having insurance plans. Without insurance plans, many patients would not be able to seek medical services. Whenever a patient visits a doctor for the treatment he/she needs to ensure that the insurance payer makes the payment for all the medical benefits he/she may have received. This is where the assignment of benefits comes in.
Definition of Assignment of Benefits
The term assignment of benefits (AOB) may be referred to as an agreement that transfers the health insurance claims benefits of the policy from the patient to the health care provider. This agreement is signed by the patient as a request to pay the designated amount to the health care provider for the health benefits he/she may have received. On the patient’s request the insurance payer makes the payment to the hospital/doctor.
Understanding of Assignment of Benefits
The assignment of benefits is generally transferred by designing a legal document— for which, the format may vary across medical offices. This document is called the ‘Assignment of Benefits’ form. While signing the form, the patient also authorizes the insurance company to release any and all written information that is required by the hospital for reimbursement purposes. This also means that any medical billing and collection company hired by the hospital is free to use the released information for billing purposes. In addition to this, the patient agrees to appoint anyone from the hospital as a representative on his/her behalf to seek payment from the insurance payer. In other words, once the document has been signed, the patient is no longer required to deal directly with the insurance company or its representative, unless asked to do so.
It is important to note that the assignment of benefits occurs only when a claim has been successfully processed with the insurance company/payer. However, the insurance company may not always honor and accept the request for AOB. The acceptance or rejection of AOB depends on the patient’s or member’s health benefits contract and/or the State Law. Therefore all three parties— patient, health care provider, and the insurance company must stay updated with the State Law and also, review the patient’s health benefit plan thoroughly. This will help in saving time and unnecessary paperwork if the chances of the insurance company rejecting the AOB seem to be high.
Following are some providers or medical services that use AOB:
- Ambulance services.
- Ambulatory surgical center services.
- Clinical diagnostic laboratory services.
- Biological(s) and drugs.
- Home dialysis equipment and supplies.
- Physician services for patients having Medicare and Medicaid plans.
- Services of medical professionals other than a primary physician, including certified registered nurse anesthetists, clinical nurse specialists, clinical psychologists, clinical social workers, nurse midwives, nurse practitioners, and physician assistants.
- Simplified billing roster for vaccines, such as— influenza virus and pneumococcal.
AOB plays an important role in medical billing by establishing direct contact with the patient’s health care insurance payer. The purpose is to increase the chances of reimbursement and accelerate the process without contacting the patient additionally..
Popular Blog
Want to learn more about our solutions?
Connect with us.
- (888) 444 6041
- 3838 N Sam Houston Pkwy E. Suite 430 Houston, TX. 77032

Get in Touch
Medical Billing
Medical Billing and RCM Experts
Aob in medical billing: your 14 questions answered.
Everyone wants to get insured for possible medical treatments in the future. But when it comes to billing, people face huge difficulty in paying expensive hospital bills . Even when you have insurance coverage, there is a small amount that you owe to the hospital, that appears not so small at all. Additionally, you wouldn’t want to stress yourself up when you have finished taking medical treatment. So you might opt for AOB in medical billing.
But if you are confused about whether to go for it or not, today, you’ll know the answers to all questions you might have related to AOB contract.
What Exactly Is AOB In Medical Billing?
AOB stands for “Assignment of Benefits”. AOB in medical billing is a contract between healthcare provider and patient, signed by the patient and sent to the insurance payers.
After signing this document, the patient transfers all claim rights to the healthcare providers and they are out of the process.
Now it is only the healthcare provider and insurance payer in the operation. The hospital communicates directly to the insurance payer and gets the payment.
As the name indicates, it is the allocation of benefits from the patient to the healthcare provider. In this process, patients contract with a reliable person within the healthcare facility where they have received the medical services.
Then, that person on behalf of the patient deals with the insurance payer and gets the reimbursement payment.
How Does It Work?
Let us tell you the process in simple words. Imagine you are getting your house roof repaired.
When the contractor asks for the payment, you sign an AOB document after which the contractor will contact your insurance company and ask for the repair payment to them. You are completely out of the picture.
Similarly, in healthcare, when you sign an AOB in medical billing, you are free to pay your bills, get medical service, go home, and take rest. Your insurance company will pay for your service and you are required to do nothing.
Here is the process we have summed up in 5 points:
- After taking the medical service, you and your healthcare partner or contractor agree to signup AOB in medical billing
- The contract is signed. Paperwork is done
- The contractor then sends the AOB to the insurance company which reviews the document and makes any concerns clear
- The settlement check is made that contains the name of the contractor (or an agreed-upon individual) as specified.
- After all the information is verified, the insurance payer will issue the check and the process is marked as complete.
Faq’s About AOB
Table of Contents
Even after understanding the definition and purpose of AOB in medical billing, there may be more questions running through your head. Like isn’t that similar to a normal insurance agreement? What if I change my mind and cancel the contract? And so on.
Have a look at these questions. I am sure you will find all your answers after reading that.
1. How Does It Differ From The Normal Billing Process?
In contrast to the standard billing procedure , AOB transfers payment responsibility from you to the healthcare provider.
By direct billing and receiving payment from the insurance provider using an AOB, the provider minimizes your involvement in handling medical bills.
2. When Should I Use AOB In Medical Billing?
If you want to give your healthcare provider permission to bill your insurance company directly and receive payments on your behalf, you can use an Assignment of Benefits (AOB).
It is frequently used by patients who want to simplify the billing procedure, lower their financial obligation, and guarantee that insurance benefits are utilized properly.
By using an AOB in medical billing, you give the healthcare provider control over billing and payment arrangements, which is convenient and might reduce out-of-pocket costs.
3. What Services I Can Use AOB For?
- Ambulance services
- Ambulatory surgical centers
- biological(s) and drugs
- Clinical diagnostic lab services
- Dialysis at-home equipment and supplies
- Can be used by those patients that have Medicaid and Medicare plans
- Professionals include clinical nurse specialists, certified nurse anesthetists, clinical social workers, clinical psychologists, nurse practitioners, physician assistants, and nurse midwives to deliver their services.
- Vaccinations like influenza
4. What Information Is Included In The AOB Document?
- Patient Information: The patient’s entire name, address, phone number, and insurance policy number.
- Healthcare Provider Information: Name, address, and phone number of the facility or healthcare provider providing the services.
- Insurance Company Details: The name of the patient’s insurance provider, the policy number, and any other pertinent insurance details.
- Assignment Authorization: The patient’s permission for the healthcare professional to bill the insurance company directly for services rendered will be expressly stated in the paperwork.
- Payment Assignment: Statement that the patient authorizes the insurance company to pay the healthcare facility or provider directly.
- Effective Dates: The start and end dates of the assignment, together with the duration for which the authorization is valid.
- Signatures: The patient’s signature and, in some situations, that of the healthcare professional or another designated representative is required on the document.
- Terms and Conditions: Specific terms and conditions about billing, reimbursement, confidentiality, and any other relevant information may be included in the AOB.
5. What If I Have To Cancel The Contract?
If you need to terminate the Assignment of Benefits (AOB) contract, you must do so by the steps laid out in the contract. The procedures you must follow to revoke or terminate the AOB in medical billing will often be outlined in the contract.
It can entail giving written notice of your desire to terminate the contract to the healthcare provider and the insurance provider, together with the cancellation’s effective date.
It’s crucial to analyze the AOB contract’s terms and conditions regarding cancellation or revocation to comprehend any potential implications or repercussions.
It is essential to abide by any cancellation requirements included in contracts because some may have strict deadlines or requirements.
6. What Are The Pros And Cons Of Signing An AOB?
Every AOB contract has different terms, so the consequences may vary. Here are the common pros and cons of opting for AOB in medical billing:
- After signing the contract you don’t need to pay a single penny upfront.
- Many people love the idea of not getting into a clash during negotiations with the insurance payer.
- If your insurance payer refuses to pay for you or they don’t know about such a contract, it could create huge trouble
- Some healthcare providers make it mandatory to sign up AOB in medical billing. This could restrict your selection of diverse healthcare facilities that don’t require AOB
- There are also some privacy concerns associated with the contract, as it involves the transfer of your insurance and healthcare details. Though all stakeholders are obliged to respect your privacy, there is always some risk.
7. How Does An AOB Affect My Medical Billing?
Your medical billing may be impacted by an Assignment of Benefits (AOB), which permits your healthcare provider to charge your insurance company directly for services delivered.
The requirement for upfront payment and reimbursement is removed. Direct payments to your provider will be made by the insurance company after processing the claims.
Your financial obligation may therefore be limited to coinsurance, deductibles, or copayments.
8. Will Signing An AOB Impact My Out-Of-Pocket Expenses?
Your out-of-pocket costs may change if you sign an AOB in medical billing. Your healthcare provider will submit a direct claim to your insurance carrier via an AOB.
Your financial obligation may therefore be limited to the deductibles, copayments, or coinsurance that your insurance plan specifies.
To ascertain how the AOB will particularly affect your out-of-pocket costs, it is crucial to analyze its provisions and comprehend your insurance coverage.
9. How Does An AOB Impact My Relationship With My Insurance Company?
By transferring the communication and payment process to your healthcare provider, signing an Assignment of Benefits might influence your relationship with your insurance provider.
The insurance company will pay the provider directly as specified in the AOB. They will serve as the primary point of contact for billing and claims.
10. Can I Choose Whether Or Not To Sign An AOB?
Yes, you typically have the option to sign an AOB in medical billing or not. You have the option to permit your healthcare practitioner to contact your insurance company directly; it is not required.
It’s crucial to weigh the potential advantages and disadvantages of signing an AOB and comprehend how it may impact your medical billing procedure and financial obligations.
Dive Deeper into AOB Basics
11. what happens if i don’t sign an aob.
Your healthcare provider won’t be able to bill your insurance carrier directly if you decide not to sign AOB in medical billing.
Instead, you will be in charge of covering the medical costs upfront before submitting a claim for reimbursement to your insurance provider by the terms of your policy.
Without an AOB, you will have more control over the billing procedure but will also be responsible for handling claim submission and insurance company communication.
It’s crucial to speak with your doctor and insurance provider to fully grasp the implications and available options if you choose not to sign an AOB.
12. How Can I Ensure That My Insurance Company Receives My Medical Bills Through The AOB Process?
You should confirm that your healthcare provider accepts AOB in medical billing and has the necessary information to start the process if you want to make sure that your insurance company receives your medical bills through the Assignment of Benefits (AOB) procedure.
Provide proper insurance information, check-up with your physician to make sure the bill was submitted, and maintain copies of all supporting paperwork. If you need advice, speak with your insurance provider directly.
13. What Should I Do If There Are Issues Or Discrepancies With My AOB Or The Billing Process?
Take the following actions if there are problems or anomalies with your Assignment of Benefits (AOB) or the billing procedure:
- Contact your healthcare practitioner to address the issue
- Contact your insurance provider for support
- Record all correspondence
- Request explanation from both sides
- If required, include a third party
14. How Can I Better Understand The AOB Language And Terms In My Insurance Policy?
Read your insurance policy carefully and look for the section on AOB in medical billing to get a better understanding of its terminology and conditions.
If you have any inquiries, speak with the customer service department of your insurance provider or seek advice from an insurance agent or broker.
Legal counsel and online sites can also offer insightful information.
Common Frauds Associated With AOB In Medical Billing
As the contract AOB in medical billing assigns your billing rights to a third party, your essential billing and personal information too are transferred.
But unfortunately, if your data comes into the hands of fraudulent third-party providers, you could get into huge trouble. Misuse of your data may lead to fraudulent activities like:
Identity Theft
Your name, date of birth, and social security number are just a few examples of the personal data thieves might exploit to steal your identity.
They might use your name to open credit accounts, request loans, or make unauthorized transactions, which would hurt your finances and your credit.
Medical Identity Theft
If your medical information is stolen, scammers can use it to buy prescription medicines or medical services in your name. This may result in inaccurate medical records, poor care, and possible health hazards.
Billing Fraud
Fraudsters may use your billing information to create fictitious insurance claims or charge for services that were never rendered.
This may lead to increased medical costs, financial damage, and possible legal repercussions for both you and the participating healthcare practitioner.
Insurance Fraud
Your information may be used fraudulently to obtain insurance benefits by inventing illnesses or injuries, for example. This kind of deception may result in higher insurance costs, a loss of coverage, and negative legal consequences.
Unauthorized Access to Financial Accounts
Fraudsters may attempt to acquire unauthorized access to your financial accounts, including bank accounts, credit cards, and online payment systems, using your personal information.
They have the ability to withdraw money, carry out deceptive activities, and steal private financial data.
Phishing Scams
Fraudsters may target you with phishing scams, such as false emails or phone calls impersonating reputable businesses, using the information they have about you.
They might try to con you into giving them more financial or personal information, putting you in danger of identity theft or other financial losses.
Medical Equipment or Prescription Fraud
Your information could be used by fraudsters to get pricey medical supplies or prescription pharmaceuticals that they can then resell for a profit.
This kind of scam can damage your medical care and general health in addition to having an adverse effect on your financial situation.
False Medical Services
Your information could be used by scammers to bill for medical treatments that were never delivered. This could lead to incorrect insurance costs, which would raise your premiums and raise the possibility of coverage problems.
Subscribe our newsletter to see latest published content.
Preventing billing frauds by all possible means.
Preventing fraud during AOB in medical billing is a huge concern for many patients as they don’t want their info to be exposed over a non-reliable third party but still want to benefit from this agreement.
If you are one of them, what should you do? Follow these precautionary measures before signing a contract:
1. Research Reputable Healthcare Providers
Researching and selecting credible healthcare providers is an essential first step.
Look for service suppliers who have a good track record of moral behavior. You can make a wise choice by reading patient testimonials, examining credentials, and confirming licenses.
2. Thoroughly Review the AOB Agreement
Examine and comprehend each of the agreement’s terms and conditions of AOB in medical billing in detail before you sign. Pay special attention to any warning signs or provisions that can suggest possible fraud.
If necessary, get advice from an impartial third party, such as a lawyer or trusted advisor, to make sure you know the agreement completely.
3. Understand the Scope of Services Covered
Make sure you comprehend the services that are covered by the AOB agreement and that they meet your medical requirements.
If the contract specifies extraneous or unrelated services, proceed with caution as this may point to possible fraud.
4. Question and Validate Billing Practices
Spend some time finding out how the healthcare provider bills. Make sure their charging practices are honest and ethical. Find out how they handle billing disputes and problems.
You can judge someone’s credibility by asking about their billing practices in clear terms and with transparency.
5. Maintain Copies of All Relevant Documents
Keep copies of the signed agreement, bills, and any correspondence that pertains to AOB in medical billing. It will be essential to have these data on hand in case there are any later disagreements or disputes.
It gives you supporting information and records that you can use later on if necessary.
6. Regularly Review Explanation of Benefits (EOB) Statements
Examine the Explanation of Benefits (EOB) documents that your insurance provider has sent you carefully.
Make sure everything is accurate and that the services being charged correspond to the care given. Report any anomalies or questionable invoicing to your insurance provider right away.
7. Report Suspected Fraud
Report any suspected fraudulent actions or billing procedures to your insurance provider, the appropriate authorities, and regulatory organizations.
In order to prevent fraud and to guarantee that providers who commit fraud are dealt with appropriately, reporting is crucial.
AOB vs Self-Payment: What Should I Choose?
Now after eliminating most of your concerns and exploring potential frauds related to the process, you might still be confused should I opt for AOB in medical billing or self-payment would work just fine?
To remove your doubts, we have come up with a comparison you should have a look at:
Based on this comparison, you can now make a final determination about whether to go for AOB or not. The decision is totally up to you, but if you go for it make sure to follow our guide and strategies to protect your billing data.
Making An Informed Decision
We hope our guide has helped you better understand what is AOB in medical billing. Overall, it is a good idea to sign this contract as it saves you from a lot of complications.
In fact, to further streamline the claims process, experts predict that by 2025, the use of AI and machine learning for AOB identification and resolution will double.
But before signing the contract, it is crucial to read all terms and conditions and act accordingly.
1 thought on “AOB In Medical Billing: Your 14 Questions Answered”
Pingback: How Does Assignment Of Benefits (AOB) Work? Ins & Outs
Comments are closed.
Automated page speed optimizations for fast site performance
+1 (888) 655- 3729 | [email protected]

What is Assignment of Benefits (AOB) in Medical Billing
The healthcare sector has an extensive network of payers for health insurance who make payments on behalf of clients with insurance policies. The assignment of benefits is used in this situation. Insurance programs allow many patients to receive medical care. Patients must ensure that their insurance provider covers all medical benefits when they visit the doctor.
Keep reading as we go through everything related to the assignment of benefits in medical billing , including what it comprises and what components it should contain.
What is Assignment of Benefits (AOB)?
The assignment of benefits (AOB) is undoubtedly one of the most significant legal documents that make up the healthcare system. It is an agreement conveying the medical professional’s right to claim medical services and obtain benefits from the patient’s insurance plan. The medical professional receives payment for patient services under this agreement.
Therefore, the insurance payer must pay the doctor when the patient signs this paper allowing payment. Without the AOB, the patient’s sole obligation is to pay the cost of any medical services obtained from the physician before filing a claim with the insurance provider for prompt payment.
Various components of the assignment of benefits (AOB)
Different formats.
AOB must be written considering its complexity because it is an important document. Although it is a legal document, it can be created in various ways because each medical officer or team may use a different structure or style.
Exchange of information
Patients must sign a letter allowing the insurance company to supply the medical practitioner with information to get reimbursed. Thus, by signing this contract, the patient implicitly permits the insurance provider to provide essential information and data to medical providers.
In addition, the signatures attest that the patient has authorized a medical practitioner’s staff member to approach the insurance provider on the patient’s behalf to request the necessary payments as outlined in the contract.
Establishes a line of communication
Thanks to this paperwork, the patients are also released from the obligation to contact the insurance provider or the doctor directly for payment-related issues. He can leave it after allowing both parties to interact with one another and carry out the subsequent actions without being held responsible for making the connection himself.
Transfer of the financial obligation
The benefits assignment occurs once the insurance company/payer’s claim process has been successfully completed. This is the precise moment when the patient shifts payment responsibility to the insurance provider.
Outsourced billing services might be engaged by medical professionals who need help keeping up with the billing. AOB requests might not be approved by the insurance company involved in the specific process; it is necessary to note this.
Rejection may occur for several reasons, including the patient’s health benefits contract clauses or State Law.
Relational to state laws
The doctor, patient, and insurance company must stay abreast of state legislation changes because of this. A single clause modification can generate significant problems with insurance benefits. It is essential to keep up with the evolving state laws and regulations because doing so saves time and reduces paperwork.
The doctor or hospital must analyze each patient’s health benefit program to ensure the claim is accepted. Several things influence the operation of AOB and its success.
These include state legislation, the type of medical services the healthcare provider offers, and the insurance plan the consumer has chosen. The patient gives up his right to bargain with the insurance provider over the provider’s services by signing the AOB.
What should be included in an AOB?
It is crucial to carefully craft the AOB because only one signature establishes a binding legal relationship between the three parties. The elements listed below make up a proper assignment of benefits:
Business’s full name
Even a tiny error in the company’s name that needs compensation can prevent progress and cause unneeded delays. In addition, while preparing the medical billing papers, the business organization’s name must be added with the utmost level of precision in the assignment of benefits.
Even if a provider of outsourced medical billing services is involved in the procedure, it is still required to ensure that the name listed in the contract is correct.
The concept of Irrevocability
The term “irrevocable” is crucial and significant for contracts that establish legal responsibilities. Using this phrase, the patient signifies that they cannot reverse the benefit assignment later.
Demonstration of Rights
The court is instructed by the rights demonstrated in this contract to investigate the advantages paid by the patient to the doctor. These rights are granted to the insurance carrier, which will compensate the healthcare practitioner.
Benefits of Not Paying for Treatment
A provider forfeits their right to demand payment at the time of service in return for the ability to sue the insurance provider if they are not paid in full. The patient will forfeit their right to sue, but payment is unnecessary.
Genuine signature provided by the patients
This is the crucial clause in the contract. The patient must accurately sign this document to be legally binding and establish rights and obligations. Finding the best medical billing service that guarantees prompt payment reimbursement can be challenging.
RCM Matter is the only place to go if you’re looking for a business that can provide adequate medical billing services.
What channel is opened between the patient, doctor, and insurance company thanks to the assignment of benefits?
The benefits assignment permits communication between the insurance company and the doctor for financial matters. By doing this, the patient is released from having direct contact with both parties on payment-related issues.
What happens when the insurance company has processed your claim successfully?
After completing a claim, the insurance provider takes over the patient’s financial responsibilities. This allows the insurance company to pay the doctor directly.
What should a document containing an assignment of benefits have?
The precise name of the medical professional or firm, the word “irrevocable” to indicate that the patient cannot revoke the assignment, a clear display of the rights assigned to the insurance company for payment, and an actual signature by the patient to verify the agreement all need to be required in an assignment of benefits document.
AOB establishes a direct line of communication with the patient’s health insurance payer, playing a significant role in medical billing. The goal is to speed up the process without further contacting the patient while increasing the likelihood that the claim will be reimbursed.
Similar Posts
Things to remember regarding cms2022 final rule.
The Centers for Medicare and Medicaid Services (CMS) has issued a range of information for healthcare providers to know about invoicing Medicare in the New Year as we prepare for 2022. We’ve compiled a list of the few things suppliers should be aware of.
Guide to Provider Enrollment and Credentialing Services
Although provider enrollment and credentialing are frequently used interchangeably, they both have significant functions in the healthcare industry.
Myopia Disease: it’s an environmental, rather than a genetic issue
Myopia is a condition that causes blurred vision and may result in significant sight-threatening eye conditions. Myopia is often diagnosed in childhood due to the eye developing abnormally long from the front to the rear of the head (axial length). To view distant things, such as a school board, a television across the room, or a wall clock, is problematic in Myopia. In childhood and adolescence, nearsightedness symptoms generally worsen. Nearsightedness is a hereditary disorder.
5 Practice Management Trends to follow in 2022!
this year demands more attention to the revenue management system and overall practice management. RCM Matter brings you the top 5 trends that you need to look up to for Practice Management:
Key Factors to help Modernize Patient Scheduling
Patient scheduling is one of the most important parts of a healthcare system. It is important to make this method efficient for the patients to ensure future appointments and services. RCM MATTER is a leading company that provides the right services for modernizing your scheduling system.
Advantages of Mobile Apps in Healthcare
To provide superior services across borders, healthcare institutions are contemplating mobile apps. Over the last several years, health apps have gai…

Assignment of benefits
Assignment of benefits is a legal agreement where a patient authorizes their healthcare provider to receive direct payment from the insurance company for services rendered.
Boost patient experience and your bottom line by automating patient cost estimates, payer underpayment detection, and contract optimization in one place.
What is Assignment of Benefits?
Assignment of benefits (AOB) is a crucial concept in the healthcare revenue cycle management (RCM) process. It refers to the legal transfer of the patient's rights to receive insurance benefits directly to the healthcare provider. In simpler terms, it allows healthcare providers to receive payment directly from the insurance company, rather than the patient being responsible for paying the provider and then seeking reimbursement from their insurance company.
Understanding Assignment of Benefits
When a patient seeks medical services, they typically have health insurance coverage that helps them pay for the cost of their healthcare. In most cases, the patient is responsible for paying a portion of the bill, known as the copayment or deductible, while the insurance company covers the remaining amount. However, in situations where the patient has assigned their benefits to the healthcare provider, the provider can directly bill the insurance company for the services rendered.
The assignment of benefits is a legal agreement between the patient and the healthcare provider. By signing this agreement, the patient authorizes the healthcare provider to receive payment directly from the insurance company on their behalf. This ensures that the provider receives timely payment for the services provided, reducing the financial burden on the patient.
Difference between Assignment of Benefits and Power of Attorney
While the assignment of benefits may seem similar to a power of attorney (POA) in some respects, they are distinct legal concepts. A power of attorney grants someone the authority to make decisions and act on behalf of another person, including financial matters. On the other hand, an assignment of benefits only transfers the right to receive insurance benefits directly to the healthcare provider.
In healthcare, a power of attorney is typically used in situations where a patient is unable to make decisions about their medical care. It allows a designated individual, known as the healthcare proxy, to make decisions on behalf of the patient. In contrast, an assignment of benefits is used to streamline the payment process between the healthcare provider and the insurance company.
Examples of Assignment of Benefits
To better understand how assignment of benefits works, let's consider a few examples:
Sarah visits her primary care physician for a routine check-up. She has health insurance coverage through her employer. Before the appointment, Sarah signs an assignment of benefits form, authorizing her physician to receive payment directly from her insurance company. After the visit, the physician submits the claim to the insurance company, and they reimburse the physician directly for the covered services.
John undergoes a surgical procedure at a hospital. He has health insurance coverage through a private insurer. Prior to the surgery, John signs an assignment of benefits form, allowing the hospital to receive payment directly from his insurance company. The hospital submits the claim to the insurance company, and they reimburse the hospital for the covered services. John is responsible for paying any copayments or deductibles directly to the hospital.
Mary visits a specialist for a specific medical condition. She has health insurance coverage through a government program. Mary signs an assignment of benefits form, granting the specialist the right to receive payment directly from the government program. The specialist submits the claim to the program, and they reimburse the specialist for the covered services. Mary is responsible for any applicable copayments or deductibles.
In each of these examples, the assignment of benefits allows the healthcare provider to receive payment directly from the insurance company, simplifying the billing and reimbursement process for both the provider and the patient.
Assignment of benefits is a fundamental concept in healthcare revenue cycle management. It enables healthcare providers to receive payment directly from the insurance company, reducing the financial burden on patients and streamlining the billing process. By understanding the assignment of benefits, patients can make informed decisions about their healthcare and ensure that their providers receive timely payment for the services rendered.
Improve your financial performance while providing a more transparent patient experience
Related terms, base payment rate.
Base payment rate is the predetermined amount established by payers for specific healthcare services, serving as the starting point for reimbursement calculations.
National coverage determination (NCD)
National coverage determination (NCD) is a Medicare policy that specifies whether a particular medical service or item is covered and reimbursed by the program.

Subscribe to the

Healthcare Clarified newsletter
Get the latest insights on RCM and healthcare policy in your inbox

- Construction Accidents
Practice Areas

Assignment of Benefits: What You Need to Know
- August 17, 2022
- Steven Schwartzapfel

Insurance can be useful, but dealing with the back-and-forth between insurance companies and contractors, medical specialists, and others can be a time-consuming and ultimately unpleasant experience. You want your medical bills to be paid without having to act as a middleman between your healthcare provider and your insurer.
However, there’s a way you can streamline this process. With an assignment of benefits, you can designate your healthcare provider or any other insurance payout recipient as the go-to party for insurance claims. While this can be convenient, there are certain risks to keep in mind as well.
Below, we’ll explore what an assignment of insurance benefits is (as well as other forms of remediation), how it works, and when you should employ it. For more information, or to learn whether you may have a claim against an insurer, contact Schwartzapfel Lawyers now at 1-516-342-2200 .
What Is an Assignment of Benefits?
An assignment of benefits (AOB) is a legal process through which an insured individual or party signs paperwork that designates another party like a contractor, company, or healthcare provider as their insurance claimant .
Suppose you’re injured in a car accident and need to file a claim with your health insurance company for medical bills and related costs. However, you also need plenty of time to recover. The thought of constantly negotiating between your insurance company, your healthcare provider, and anyone else seems draining and unwelcome.
With an assignment of benefits, you can designate your healthcare provider as your insurance claimant. Then, your healthcare provider can request insurance payouts from your healthcare insurance provider directly.
Through this system, the health insurance provider directly pays your physician or hospital rather than paying you. This means you don’t have to pay your healthcare provider. It’s a streamlined, straightforward way to make sure insurance money gets where it needs to go. It also saves you time and prevents you from having to think about insurance payments unless absolutely necessary.
What Does an Assignment of Benefits Mean?
An AOB means that you designate another party as your insurance claimant. In the above example, that’s your healthcare provider, which could be a physician, hospital, or other organization.
With the assignment of insurance coverage, that healthcare provider can then make a claim for insurance payments directly to your insurance company. The insurance company then pays your healthcare provider directly, and you’re removed as the middleman.
As a bonus, this system sometimes cuts down on your overall costs by eliminating certain service fees. Since there’s only one transaction — the transaction between your healthcare provider and your health insurer — there’s only one set of service fees to contend with. You don’t have to deal with two sets of service fees from first receiving money from your insurance provider, then sending that money to your healthcare provider.
Ultimately, the point of an assignment of benefits is to make things easier for you, your insurer, and anyone else involved in the process.
What Types of Insurance Qualify for an Assignment of Benefits?
Most types of commonly held insurance can work with an assignment of benefits. These insurance types include car insurance, healthcare insurance, homeowners insurance, property insurance, and more.
Note that not all insurance companies allow you to use an assignment of benefits. For an assignment of benefits to work, the potential insurance claimant and the insurance company in question must each sign the paperwork and agree to the arrangement. This prevents fraud (to some extent) and ensures that every party goes into the arrangement with clear expectations.
If your insurance company does not accept assignments of benefits, you’ll have to take care of insurance payments the traditional way. There are many reasons why an insurance company may not accept an assignment of benefits.
To speak with a Schwartzapfel Lawyers expert about this directly, call 1-516-342-2200 for a free consultation today. It will be our privilege to assist you with all your legal questions, needs, and recovery efforts.
Who Uses Assignments of Benefits?
Many providers, services, and contractors use assignments of benefits. It’s often in their interests to accept an assignment of benefits since they can get paid for their work more quickly and make critical decisions without having to consult the insurance policyholder first.
Imagine a circumstance in which a homeowner wants a contractor to add a new room to their property. The contractor knows that the scale of the project could increase or shrink depending on the specifics of the job, the weather, and other factors.
If the homeowner uses an assignment of benefits to give the contractor rights to make insurance claims for the project, that contractor can then:
- Bill the insurer directly for their work. This is beneficial since it ensures that the contractor’s employees get paid promptly and they can purchase the supplies they need.
- Make important decisions to ensure that the project completes on time. For example, a contract can authorize another insurance claim for extra supplies without consulting with the homeowner beforehand, saving time and potentially money in the process.
Practically any company or organization that receives payments from insurance companies may choose to take advantage of an assignment of benefits with you. Example companies and providers include:
- Ambulance services
- Drug and biological companies
- Lab diagnostic services
- Hospitals and medical centers like clinics
- Certified medical professionals such as nurse anesthetists, nurse midwives, clinical psychologists, and others
- Ambulatory surgical center services
- Permanent repair and improvement contractors like carpenters, plumbers, roofers, restoration companies, and others
- Auto repair shops and mechanic organizations
Advantages of Using an Assignment of Benefits
An assignment of benefits can be an advantageous contract to employ, especially if you believe that you’ll need to pay a contractor, healthcare provider, and/or other organization via insurance payouts regularly for the near future.
These benefits include but are not limited to:
- Save time for yourself. Again, imagine a circumstance in which you are hospitalized and have to pay your healthcare provider through your health insurance payouts. If you use an assignment of benefits, you don’t have to make the payments personally or oversee the insurance payouts. Instead, you can focus on resting and recovering.
- Possibly save yourself money in the long run. As noted above, an assignment of benefits can help you circumvent some service fees by limiting the number of transactions or money transfers required to ensure everyone is paid on time.
- Increased peace of mind. Many people don’t like having to constantly think about insurance payouts, contacting their insurance company, or negotiating between insurers and contractors/providers. With an assignment of benefits, you can let your insurance company and a contractor or provider work things out between them, though this can lead to applications later down the road.
Because of these benefits, many recovering individuals, car accident victims, homeowners, and others utilize AOB agreements from time to time.
Risks of Using an Assignment of Benefits
Worth mentioning, too, is that an assignment of benefits does carry certain risks you should be aware of before presenting this contract to your insurance company or a contractor or provider. Remember, an assignment of benefits is a legally binding contract unless it is otherwise dissolved (which is technically possible).
The risks of using an assignment of benefits include:
- You give billing control to your healthcare provider, contractor, or another party. This allows them to bill your insurance company for charges that you might not find necessary. For example, a home improvement contractor might bill a homeowner’s insurance company for an unnecessary material or improvement. The homeowner only finds out after the fact and after all the money has been paid, resulting in a higher premium for their insurance policy or more fees than they expected.
- You allow a contractor or service provider to sue your insurance company if the insurer does not want to pay for a certain service or bill. This can happen if the insurance company and contractor or service provider disagree on one or another billable item. Then, you may be dragged into litigation or arbitration you did not agree to in the first place.
- You may lose track of what your insurance company pays for various services . As such, you could be surprised if your health insurance or other insurance premiums and deductibles increase suddenly.
Given these disadvantages, it’s still wise to keep track of insurance payments even if you choose to use an assignment of benefits. For example, you might request that your insurance company keep you up to date on all billable items a contractor or service provider charges for the duration of your treatment or project.
For more on this and related topic, call Schwartzapfel Lawyers now at 1-516-342-2200 .
How To Make Sure an Assignment of Benefits Is Safe
Even though AOBs do carry potential disadvantages, there are ways to make sure that your chosen contract is safe and legally airtight. First, it’s generally a wise idea to contact knowledgeable legal representatives so they can look over your paperwork and ensure that any given assignment of benefits doesn’t contain any loopholes that could be exploited by a service provider or contractor.
The right lawyer can also make sure that an assignment of benefits is legally binding for your insurance provider. To make sure an assignment of benefits is safe, you should perform the following steps:
- Always check for reviews and references before hiring a contractor or service provider, especially if you plan to use an AOB ahead of time. For example, you should stay away if a contractor has a reputation for abusing insurance claims.
- Always get several estimates for work, repairs, or bills. Then, you can compare the estimated bills and see whether one contractor or service provider is likely to be honest about their charges.
- Get all estimates, payment schedules, and project schedules in writing so you can refer back to them later on.
- Don’t let a service provider or contractor pressure you into hiring them for any reason . If they seem overly excited about getting started, they could be trying to rush things along or get you to sign an AOB so that they can start issuing charges to your insurance company.
- Read your assignment of benefits contract fully. Make sure that there aren’t any legal loopholes that a contractor or service provider can take advantage of. An experienced lawyer can help you draft and sign a beneficial AOB contract.
Can You Sue a Party for Abusing an Assignment of Benefits?
Sometimes. If you believe your assignment of benefits is being abused by a contractor or service provider, you may be able to sue them for breaching your contract or even AOB fraud. However, successfully suing for insurance fraud of any kind is often difficult.
Also, you should remember that a contractor or service provider can sue your insurance company if the insurance carrier decides not to pay them. For example, if your insurer decides that a service provider is engaging in billing scams and no longer wishes to make payouts, this could put you in legal hot water.
If you’re not sure whether you have grounds for a lawsuit, contact Schwartzapfel Lawyers today at 1-516-342-2200 . At no charge, we’ll examine the details of your case and provide you with a consultation. Don’t wait. Call now!
Assignment of Benefits FAQs
Which states allow assignments of benefits.
Every state allows you to offer an assignment of benefits to a contractor and/or insurance company. That means, whether you live in New York, Florida, Arizona, California, or some other state, you can rest assured that AOBs are viable tools to streamline the insurance payout process.
Can You Revoke an Assignment of Benefits?
Yes. There may come a time when you need to revoke an assignment of benefits. This may be because you no longer want the provider or contractor to have control over your insurance claims, or because you want to switch providers/contractors.
To revoke an assignment of benefits agreement, you must notify the assignee (i.e., the new insurance claimant). A legally solid assignment of benefits contract should also include terms and rules for this decision. Once more, it’s usually a wise idea to have an experienced lawyer look over an assignment of benefits contract to make sure you don’t miss these by accident.
Contact Schwartzapfel Lawyers Today
An assignment of benefits is an invaluable tool when you need to streamline the insurance claims process. For example, you can designate your healthcare provider as your primary claimant with an assignment of benefits, allowing them to charge your insurance company directly for healthcare costs.
However, there are also risks associated with an assignment of benefits. If you believe a contractor or healthcare provider is charging your insurance company unfairly, you may need legal representatives. Schwartzapfel Lawyers can help.
As knowledgeable New York attorneys who are well-versed in New York insurance law, we’re ready to assist with any and all litigation needs. For a free case evaluation and consultation, contact Schwartzapfel Lawyers today at 1-516-342-2200 !
Schwartzapfel Lawyers, P.C. | Fighting For You™™
What Is an Insurance Claim? | Experian
What is assignment of benefits, and how does it impact insurers? | Insurance Business Mag
Florida Insurance Ruling Sets Precedent for Assignment of Benefits | Law.com
Related Posts

What Can Cause You To Lose Your Social Security Disability Benefits?
Social Security disability benefits are intended to financially support people who are too disabled to work for a living. These

What Does Workers’ Compensation Cover?
Workplace injuries happen, even when workplace safety protocols are in place and diligently followed. That’s why workers’ compensation insurance exists.

Do Pre-Existing Injuries Affect Claims?
If you’re currently living with an injury or chronic condition, you’re already living with pain. If an accident, a car
We'll Fight For You
Schwartzapfel® lawyers has a 99% client satisfaction rate.
Quick Links
- News & Events
- Verdicts & Settlements
- Video Gallery
- Wrongful Death
- Vehicle Accidents
- Slip & Fall
- Medical Malpractice
- Workers' Compensation
- Personal Injuries
- Product Liability
- Garden City
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How the UB-04 Form Is Used to Bill Insurance Companies
- Institutions Using the Form
- Tips for Preparing the Form
- UB-04 Fields
The UB-04 uniform medical billing form is the standard claim form that institutional providers use, such as hospitals and community mental health care centers. It is used to bill Medicare, Medicaid, and other health insurance companies for inpatient or outpatient services.
Although developed by the Centers for Medicare and Medicaid Services (CMS), the paper form has become the standard claim form used by all insurance carriers. The National United Billing Committee, the governing body for medical claims billing forms, is responsible for the design and printing of the UB-04 form.
This article explains who can fill out the form and what the form's various sections mean.
Who Can Bill Claims Using the UB-04?
Any institutional provider can use the UB-04 for billing medical claims . Non-institutional providers or suppliers, such as physicians or providers of durable medical equipment, use the CMS-1500 form.
Institutional providers that can use the UB-04 form include:
- Community mental health centers
- Comprehensive outpatient rehabilitation facilities
- Critical access hospitals
- End-stage renal disease facilities
- Federally qualified health centers
- Histocompatibility laboratories
- Home health agencies
- Indian Health Services facilities
- Organ procurement organizations
- Outpatient physical therapy services
- Occupational therapy services
- Speech pathology services
- Religious non-medical healthcare institutions
- Rural health clinics
- Skilled nursing facilities
How Is the UB-04 Form Different Than an Itemized Bill?
An itemized medical bill lists in detail all the services that were provided during a visit or stay—such as a blood test or physical therapy—and may be sent to the patient directly. The UB-O4 form is used by institutions to bill insurance companies.
Tips for Preparing the UB-04
To fill out the form accurately and completely:
- Check with each insurance payer to determine what data is required.
- Ensure that all data is entered accurately and in the correct fields.
- Enter insurance information, including the patient's name exactly as it appears on the insurance card.
- Use correct diagnosis codes (ICD-10 or ICD-11) and procedure codes (CPT/HCPCS) using modifiers when required.
- Use only the physical address for the service facility location field.
- Include National Provider Identifier (NPI) information where indicated.
More detailed instructions can be found at www.cms.gov or www.nubc.org .
Fields of the UB-04
There are 81 fields or lines on a UB-04. They're referred to as form locators or "FL." Each form locator has a unique purpose:
- 1 : Billing provider name, street address, city, state, zip, telephone, fax, and country code
- 2 : Billing provider's pay-to name, address, city, state, zip, and ID if it's different from field 1
- 3 : Patient control number and the medical record number for your facility
- 4 : Type of bill (TOB). This is a four-digit code beginning with zero, according to the National Uniform Billing Committee guidelines.
- 5 : Federal tax number for your facility
- 6 : Statement from and through dates for the service covered on the claim, in MMDDYY (month, date, year) format
- 7 : Number of Administratively Necessary Days
- 8 : Patient name in Last, First, MI format
- 9 : Patient street address, city, state, zip, and country code
- 10 : Patient birthdate in MMDDCCYY (month, day, century, year) format
- 11 : Patient sex (M, F, or U)
- 12 : Admission date in MMDDCCYY format
- 13 : Admission hour using a two-digit code from 00 for midnight to 23 for 11 p.m.
- 14 : Type of visit: 1 for emergency, 2 for urgent, 3 for elective, 4 for newborn, 5 for trauma, 9 for information not available
- 15 : Point of origin (source of admission)
- 16 : Discharge hour in the same format as line 13
- 17 : Discharge status using the two-digit codes from the NUBC manual
- 18-28 : Condition codes using the two-digit codes from the NUBC manual for up to 11 occurrences
- 29 : Accident state (if applicable) using a two-digit state code
- 30 : Accident date
- 31-34 : Occurrence codes and dates using the NUBC manual for codes
- 35-36 : Occurrence span codes and dates in MMDDYY format
- 37 : Not in use
- 38 : Responsible party name and address
- 39-41 : Value codes and amounts for special circumstances from the NUBC manual
- 42 : Revenue codes from the NUBC manual
- 43 : Revenue code description, investigational device exemption (IDE) number, or Medicaid drug rebate NDC (national drug code)
- 44 : HCPCS Healthcare Common Procedure Coding System), accommodation rates, HIPPS (health insurance prospective payment system) rate codes
- 45 : Service dates
- 46 : Service units
- 47 : Total charges
- 48 : Non-covered charges
- 49 : Page_of_ and Creation date
- 50 : Payer Identification (a) Primary (b) Secondary and (c) Tertiary
- 51 : Health plan ID (a) Primary (b) Secondary and (c) Tertiary
- 52 : Release of information (a) Primary (b) Secondary and (c) Tertiary
- 53 : Assignment of benefits (a) Primary (b) Secondary and (c) Tertiary
- 54 : Prior payments (a) Primary (b) Secondary and (c) Tertiary
- 55 : Estimated amount due (a) Primary (b) Secondary and (c) Tertiary
- 56 : Billing provider national provider identifier (NPI)
- 57 : Other provider ID (a) Primary (b) Secondary and (c) Tertiary
- 58 : Insured's name (a) Primary (b) Secondary and (c) Tertiary
- 59 : Patient's relationship (a) Primary (b) Secondary and (c) Tertiary
- 60 : Insured's unique ID (a) Primary (b) Secondary and (c) Tertiary
- 61 : Insurance group name (a) Primary (b) Secondary and (c) Tertiary
- 62 : Insurance group number (a) Primary (b) Secondary and (c) Tertiary
- 63 : Treatment authorization code (a) Primary (b) Secondary and (c) Tertiary
- 64 : Document control number also referred to as Internal control number (a) Primary (b) Secondary and (c) Tertiary
- 65 : Insured's employer name (a) Primary (b) Secondary and (c) Tertiary
- 66 : Diagnosis codes (ICD)
- 67 : Principle diagnosis code, other diagnosis, and present on admission (POA) indicators
- 68 : Not in use
- 69 : Admitting diagnosis codes
- 70 : Patient reason for visit codes
- 71 : Prospective payment system (PPS) code
- 72 : External cause of injury code and POA indicator
- 73 : Not in use
- 74 : Other procedure code and date
- 75 : Not in use
- 76 : Attending provider NPI, ID, qualifiers, and last and first name
- 77 : Operating physician NPI, ID, qualifiers, and last and first name
- 78 : Other provider NPI, ID, qualifiers, and last and first name
- 79 : Other provider NPI, ID, qualifiers, and last and first name
- 80 : Remarks
- 81 : Taxonomy code and qualifier
Institutions use the UB-04 form to bill insurance for inpatient or outpatient medical and mental health claims. Examples include hospitals, hospices, rural health clinics, and comprehensive outpatient rehabilitation facilities. When filling out the form, be sure to understand the meaning of each of the 81 fields and to make sure that the information is accurate.
National Uniform Billing Committee. National Uniform Billing Committee Official Data Specifications Manual .
National Uniform Billing Committee. National Uniform Billing Committee Official Data Specifications Manual .
Centers for Medicare and Medicaid Services. Professional paper claim form (CMS-1500) .
CMS.gov. Medicare Claims Processing Manual .
By Joy Hicks Joy B. Hicks, PhD, MBA, is an expert on the health insurance industry with over 15 years of experience in patient financial services.
- 888-666-0604
- [email protected]
What is the assignment of benefits in medical billing?
What is the revenue code in medical billing, all about cdt d4346 dental procedure code billing questions.
- Billing & Collection
Assignment of benefit, widely known as AOB, is a contractual agreement signed by a policyholder which enables a third party to file a claim, asking them to pay the designated amount directly to your provider for the rendered service. As AOB authorizes a third party to file a claim, make a decision, repair, and collect the payment from the insurer does not require your involvement and takes up to one month to receive the reimbursement.
Purpose of Assignment of Benefit
An assignment of benefits is efficient or customer-friendly to leave that claim to the contractor without the policyholder losing too much sleep.
Understanding Assignment of Benefit
- By signing the assignment of benefits document, a patient authorizes a third party to make payments directly to the treating provider. That benefits the providers tremendously by having insurance reimbursements directly instead of the patient for further appeals, denials, or underpayments from the carrier.
- For instance, if a patient is getting treatment from a non-participating provider or out-of-network provider, in that case, there is no legal contract between the provider and the third party for the negotiated rates for the rendered service. By having signed Assignments of Benefits, the out-of-network provider may submit the document with the claim in the expectation of receiving the payment at the actual billed charges directly to the provider. That is convenient for both the patient as well as for the provider.
- Also, if the out-of-network provider files the claim and the insurance company does not agree or pays less than the actual billed charges, then the provider can appeal the denial or underpayment. Although, it does not guarantee to recover the underpaid reimbursement from the insurer.
Services that use Assignment of Benefits
- Ambulatory services
- Ambulatory surgical center services
- Biological(s) and drugs
- Clinical diagnostic laboratory services
- Home dialysis equipment and supplies
- Medical services for patients that have Medicaid and Medicare plans
- Services of professionals like clinical nurse specialists, certified nurse anesthetics, clinical social workers, clinical psychologists, nurse practitioners, physician assistants, and nurse midwives use AOB.
- Vaccinations such as pneumococcal and influenza virus
Protecting your patients from the Assignment of Benefits fraud
- Before hiring a contractor, get an estimate for the claim cost.
- Check for reviews and references before hiring them.
- Read the contract and get everything in writing, such as time schedules for the work, payment schedules, cost of the work, what will be the work, and check documents that are sent to the insurer to avoid any abuse by inflating claim cost and charging unnecessary.
Impact of Assignment of Benefits on the Insurance Industry
Inflated claims and massive legal actions can dwarf the benefits to the patients by increasing the cost of the insurance premiums and more restrictive terms and conditions. The legal handling cost of the insurers will rise, eventually resulting in deductions leaving the policyholders out of pocket for potentially significant loss.
Related posts
Insurance credentialing tips for dentists, how to conduct a competitive analysis for your dental practice, how can i increase my dental practice revenue, get started.
+1 (224) 999-6997

What is Assignment of Benefits (AOB) in Medical Billing and What Should An AOB Form Include?

There are three major components/members of the healthcare industry, including the healthcare provider, the patient getting the medical treatments done and the insurance taking care of the payments. For the entire system to run smoothly, there is a need for each of these parties to be systematic and coherent in their activities. If even a single party showcases incompetency, it may end up affecting the entire system negatively. A major role played in the working of this network and turning it into a great success is the AOB, also known as the Assignment of Benefits in medical billing.
This article will walk you through everything associated with the assignment of benefits in medical billing, what it entails, and what elements should be a part of it.
Assignment of Benefits
It won’t be wrong to say that assignment of benefits is one of the most crucial documents that are a part of the healthcare system. In simple words, the assignment of benefits refers to an agreement that transfers the insurance claim related to healthcare and the benefits associated with the policy chosen by the patient to the medical practitioner or healthcare provider. This document leads to the transfer of payment to the healthcare provider against all the benefits offered to the patient. Hence, once this document is signed by the patient, the insurance payer is bound to reimburse the medical practitioner.
In the absence of the AOB, it would be the sole responsibility of the patient to pay the cost of medical services taken from the medical practitioner and then file the claim to the insurance company to make timely reimbursement.
Elements of The Assignment of Benefits
Varied formats.
Being a crucial document, AOB has to be created keeping in mind the intricacy associated with it. Though it’s a legal document, it comes in various formats as each medical officer or his team may be following a different pattern or format while creating this document.
Information Sharing
Patients sign the form allowing the insurance company to let out the relevant information required by the medical caregiver for reimbursement purposes. Hence, once this document is signed by the patient, he indirectly gives the authority to the insurance company to give away the required information and data to the medical practitioners.
At the same time, the signatures also confirm that the patient has concurred to nominate someone from the medical practitioner’s staff to seek the required payments from the insurance company in the agreement.
Creates A Communication Channel

This document also relieves the patients from the requirement to connect with the insurance company or the medical practitioner directly for payment reasons. Once he authorizes both parties to communicate with each other and continue with the following activities, he can come out of it and doesn’t have the liability to connect with them himself.
Transfer Of The Liability To Pay
Upon successful completion of the claim process with the insurance company/payer, the assignment of benefits occurs. This is the exact time when the patient transfers the liability of payment making to the insurance company. For medical practitioners finding it tough to manage the billings, outsourced billing services can be hired.
However, at the same time, there is a need to mention that the insurance company, connected with the particular process, may not accept the AOB request. There may be a rejection for various reasons, and most include the patient’s health benefits contract clauses or the State Law.
Connected To The State Laws
This is why all three parties to the process, the medical practitioner, the patient, and the insurance company must stay updated with the changing state laws. Even a modification of a single clause can lead to extensive problems when it comes to the reimbursement of insurance amounts.
Staying updated with the changing state laws and rules is necessary as it doesn’t only aid in saving time but also helps in reducing the paperwork. A review of the health benefit plan of each patient is a must for the medical care provider to ensure the claim is not rejected later on.
Various factors play their role in the working of AOB and turning it into a success. These include the insurance policy taken up by the patient, laws of the state, and the kind of medical procedures offered by the health care provider. By signing the AOB, the patient surrenders his right to negotiate with the insurance company regarding the provider’s services.
What Should Be In An AOB?
As a single signature creates a legal relationship between the three parties, there is a need to compose the AOB with great precision. An appropriate assignment of benefits includes the following elements:
Exact Name Of The Business
Even a minor mistake in the name of the business that requires reimbursement can lead to blocking the entire process and creating unnecessary delays. For that matter, there is a need to showcase the highest level of perfection while adding the name of the business entity in the assignment of benefits while creating the medical billing documents. Even if an Outsourced medical billing services company is involved in the process, it has to make sure that the name used in the contract is accurate.
The Term ‘Irrevocable’
The term irrevocable is really important and holds great significance in contracts that create legal obligations. This term means that the patient can’t revoke the assignment of benefits later on.
Showcase Of Rights
Showing rights in this contract tells the court to check out the payments, used as benefits, on behalf of the patient to the medical practitioner. These rights are assigned to the insurance company which will then pay the medical health provider .
Benefits Of Non-Payment While Getting Treated

In exchange for the right to sue the insurance company if they are not paid in full, a provider gives up the right to collect payments at the time of service. The patient will give up their right to sue, but will not be required to pay.
Authentic Signature By The Patients
This is probably the most important part of the contract. The patient has to put up his accurate signatures to make this piece of paper a legal entity creating rights and duties.
Looking for the best medical billing compan y that will ensure timely reimbursmsnt of the payments is indeed tough. If you are searching for a company that would offer you efficient services, there is no place better to go than Zee Medical Billing .
Learn more about our Specialities
Mental health billing, urgent care billing, acupuncture billing services, hospitalist billing services, internal medicine billing, see our all specialties, frequently asked questions.
The assignment of benefits refers to an agreement that transfers the insurance claim and associated benefits from the patient to the medical practitioner or healthcare provider. It allows the medical practitioner to receive reimbursement directly from the insurance payer.
The assignment of benefits simplifies the payment process by shifting the responsibility of payment from the patient to the healthcare provider. It ensures that the medical practitioner receives timely reimbursement from the insurance company.
An assignment of benefits document should include the exact name of the healthcare provider or business entity, the term “irrevocable” to indicate the patient cannot revoke the assignment, a clear showcase of rights assigned to the insurance company for payment, and an authentic signature by the patient to validate the contract.
The assignment of benefits allows authorized communication between the medical practitioner and the insurance company for payment reasons. This relieves the patient from the direct responsibility of connecting with both parties regarding payment matters.
Upon successful claim processing, the assignment of benefits takes effect, transferring the liability of payment from the patient to the insurance company. This allows the medical practitioner to receive payment directly from the insurance company.
Get in Touch
More from the category.

ZMB Proactive Approach: Discovering Root Causes of Fraud, Abuse in Healthcare

Zee Medical Billing’s Crucial 6 Steps for Reducing Lag Days

The Impact of Health Information Technology on Patient Safety
The Significance of HIPAA Compliance in Medical Billing
Schedule a meeting.
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CMS Newsroom
Search cms.gov.
- Physician Fee Schedule
- Local Coverage Determination
- Medically Unlikely Edits
- I'm using insurance
- I'm not using insurance
- Contact us for help
- Find an action plan
- Guides and resources
- Cambiar a Español
How to read an explanation of benefits (EOB)
See what an explanation of benefits looks like (PDF)
What’s an explanation of benefits?
An explanation of benefits (eob) shows you the total charges for your visit..
An explanation of benefits isn’t a bill.
It helps you understand how much your health plan covers, and what you'll pay when you get a bill from your provider.
What’s on an explanation of benefits?
General information about you and your health plan.
The explanation of benefits includes information about:
- You (the patient)
- Your health plan
- Who provided your care, and when it was provided
- A reference number called the claim number
- The person who gets reimbursed for any overpayments, called the payee
It will also list your health plan’s phone number . Call your health plan if you have questions about finding a provider or what services they cover.
Details about your claim(s)
The explanation of benefits gives you details about your care, like:
- The date of service
- A service description. This explains what service you had, like a medical visit, lab test, or screening.
Information about your bill
The explanation of benefits lists the cost of your care, and how much your health insurance company will pay.
- “Provider Charges” is the amount your provider bills for your visit.
- “Allowed Charges” is the amount your provider will be paid. This may not be the same as the Provider Charges.
- “Paid by Insurer” is the amount your health plan will pay to your provider.
What you owe
What You Owe , or Patient Balance , is the amount you owe after your insurer has paid everything else.
You may have already paid for part of the Patient Balance. The Explanation of Benefits only shows what you owe, not if you’ve already paid for it.
Your bill should not be higher than the Patient Balance. If it is, talk to your provider.
Remark code
A remark code is a note from the health plan that explains more about the costs, charges, and paid amounts for your visit.
The code is usually 2 or 3 letters and numbers. Check the bottom of the explanation of benefits for a description of each code.
What is Medicare assignment and how does it work?
Kimberly Lankford,
Because Medicare decides how much to pay providers for covered services, if the provider agrees to the Medicare-approved amount, even if it is less than they usually charge, they’re accepting assignment.
A doctor who accepts assignment agrees to charge you no more than the amount Medicare has approved for that service. By comparison, a doctor who participates in Medicare but doesn’t accept assignment can potentially charge you up to 15 percent more than the Medicare-approved amount.
That’s why it’s important to ask if a provider accepts assignment before you receive care, even if they accept Medicare patients. If a doctor doesn’t accept assignment, you will pay more for that physician’s services compared with one who does.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
How much do I pay if my doctor accepts assignment?
If your doctor accepts assignment, you will usually pay 20 percent of the Medicare-approved amount for the service, called coinsurance, after you’ve paid the annual deductible. Because Medicare Part B covers doctor and outpatient services, your $240 deductible for Part B in 2024 applies before most coverage begins.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies , without paying a deductible or coinsurance if the provider accepts assignment.
What if my doctor doesn’t accept assignment?
A doctor who takes Medicare but doesn’t accept assignment can still treat Medicare patients but won’t always accept the Medicare-approved amount as payment in full.
This means they can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive, called “balance billing.” In this case, you’re responsible for the additional charge, plus the regular 20 percent coinsurance, as your share of the cost.
How to cover the extra cost? If you have a Medicare supplement policy , better known as Medigap, it may cover the extra 15 percent, called Medicare Part B excess charges.
All Medigap policies cover Part B’s 20 percent coinsurance in full or in part. The F and G policies cover the 15 percent excess charges from doctors who don’t accept assignment, but Plan F is no longer available to new enrollees, only those eligible for Medicare before Jan. 1, 2020, even if they haven’t enrolled in Medicare yet. However, anyone who is enrolled in original Medicare can apply for Plan G.
Remember that Medigap policies only cover excess charges for doctors who accept Medicare but don’t accept assignment, and they won’t cover costs for doctors who opt out of Medicare entirely.
Good to know. A few states limit the amount of excess fees a doctor can charge Medicare patients. For example, Massachusetts and Ohio prohibit balance billing, requiring doctors who accept Medicare to take the Medicare-approved amount. New York limits excess charges to 5 percent over the Medicare-approved amount for most services, rather than 15 percent.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
How do I find doctors who accept assignment?
Before you start working with a new doctor, ask whether he or she accepts assignment. About 98 percent of providers billing Medicare are participating providers, which means they accept assignment on all Medicare claims, according to KFF.
You can get help finding doctors and other providers in your area who accept assignment by zip code using Medicare’s Physician Compare tool .
Those who accept assignment have this note under the name: “Charges the Medicare-approved amount (so you pay less out of pocket).” However, not all doctors who accept assignment are accepting new Medicare patients.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
What does it mean if a doctor opts out of Medicare?
Doctors who opt out of Medicare can’t bill Medicare for services you receive. They also aren’t bound by Medicare’s limitations on charges.
In this case, you enter into a private contract with the provider and agree to pay the full bill. Be aware that neither Medicare nor your Medigap plan will reimburse you for these charges.
In 2023, only 1 percent of physicians who aren’t pediatricians opted out of the Medicare program, according to KFF. The percentage is larger for some specialties — 7.7 percent of psychiatrists and 4.2 percent of plastic and reconstructive surgeons have opted out of Medicare.
Keep in mind
These rules apply to original Medicare. Other factors determine costs if you choose to get coverage through a private Medicare Advantage plan . Most Medicare Advantage plans have provider networks, and they may charge more or not cover services from out-of-network providers.
Before choosing a Medicare Advantage plan, find out whether your chosen doctor or provider is covered and identify how much you’ll pay. You can use the Medicare Plan Finder to compare the Medicare Advantage plans and their out-of-pocket costs in your area.
Return to Medicare Q&A main page
Kimberly Lankford is a contributing writer who covers Medicare and personal finance. She wrote about insurance, Medicare, retirement and taxes for more than 20 years at Kiplinger’s Personal Finance and has written for The Washington Post and Boston Globe . She received the personal finance Best in Business award from the Society of American Business Editors and Writers and the New York State Society of CPAs’ excellence in financial journalism award for her guide to Medicare.
Discover AARP Members Only Access
Already a Member? Login

More on Medicare

How Do I Create a Personal Online Medicare Account?
You can do a lot when you decide to look electronically

I Got a Medicare Summary Notice in the Mail. What Is It?
This statement shows what was billed, paid in past 3 months
Understanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choices
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS

An official website of the United States government
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Report Fraud
- Get Consumer Alerts
- Search the Legal Library
- Submit Public Comments
Take action
- Report an antitrust violation
- File adjudicative documents
- Find banned debt collectors
- View competition guidance
- Competition Matters Blog
New HSR thresholds and filing fees for 2024
View all Competition Matters Blog posts
We work to advance government policies that protect consumers and promote competition.
View Policy
Search or browse the Legal Library
Find legal resources and guidance to understand your business responsibilities and comply with the law.
Browse legal resources
- Find policy statements
- Submit a public comment
Vision and Priorities
Memo from Chair Lina M. Khan to commission staff and commissioners regarding the vision and priorities for the FTC.
Technology Blog
Consumer facing applications: a quote book from the tech summit on ai.
View all Technology Blog posts
Advice and Guidance
Learn more about your rights as a consumer and how to spot and avoid scams. Find the resources you need to understand how consumer protection law impacts your business.
- Report fraud
- Report identity theft
- Register for Do Not Call
- Sign up for consumer alerts
- Get Business Blog updates
- Get your free credit report
- Find refund cases
- Order bulk publications
- Consumer Advice
- Shopping and Donating
- Credit, Loans, and Debt
- Jobs and Making Money
- Unwanted Calls, Emails, and Texts
- Identity Theft and Online Security
- Business Guidance
- Advertising and Marketing
- Credit and Finance
- Privacy and Security
- By Industry
- For Small Businesses
- Browse Business Guidance Resources
- Business Blog
Servicemembers: Your tool for financial readiness
Visit militaryconsumer.gov
Get consumer protection basics, plain and simple
Visit consumer.gov
Learn how the FTC protects free enterprise and consumers
Visit Competition Counts
Looking for competition guidance?
- Competition Guidance
News and Events
Latest news, ftc finalizes changes to the health breach notification rule.
View News and Events
Upcoming Event
Older adults and fraud: what you need to know.
View more Events
Sign up for the latest news
Follow us on social media
--> --> --> --> -->

Playing it Safe: Explore the FTC's Top Video Game Cases
Learn about the FTC's notable video game cases and what our agency is doing to keep the public safe.
Latest Data Visualization
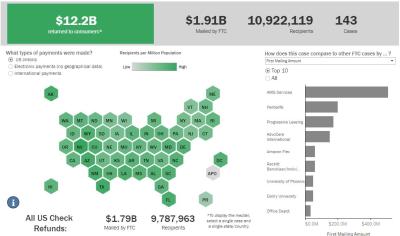
FTC Refunds to Consumers
Explore refund statistics including where refunds were sent and the dollar amounts refunded with this visualization.
About the FTC
Our mission is protecting the public from deceptive or unfair business practices and from unfair methods of competition through law enforcement, advocacy, research, and education.
Learn more about the FTC

Meet the Chair
Lina M. Khan was sworn in as Chair of the Federal Trade Commission on June 15, 2021.
Chair Lina M. Khan
Looking for legal documents or records? Search the Legal Library instead.
- Cases and Proceedings
- Premerger Notification Program
- Merger Review
- Anticompetitive Practices
- Competition and Consumer Protection Guidance Documents
- Warning Letters
- Consumer Sentinel Network
- Criminal Liaison Unit
- FTC Refund Programs
- Notices of Penalty Offenses
- Advocacy and Research
- Advisory Opinions
- Cooperation Agreements
- Federal Register Notices
- Public Comments
- Policy Statements
- International
- Office of Technology Blog
- Military Consumer
- Consumer.gov
- Bulk Publications
- Data and Visualizations
- Stay Connected
- Commissioners and Staff
- Bureaus and Offices
- Budget and Strategy
- Office of Inspector General
- Careers at the FTC
Fact Sheet on FTC’s Proposed Final Noncompete Rule
- Competition
- Office of Policy Planning
- Bureau of Competition
The following outline provides a high-level overview of the FTC’s proposed final rule :
- Specifically, the final rule provides that it is an unfair method of competition—and therefore a violation of Section 5 of the FTC Act—for employers to enter into noncompetes with workers after the effective date.
- Fewer than 1% of workers are estimated to be senior executives under the final rule.
- Specifically, the final rule defines the term “senior executive” to refer to workers earning more than $151,164 annually who are in a “policy-making position.”
- Reduced health care costs: $74-$194 billion in reduced spending on physician services over the next decade.
- New business formation: 2.7% increase in the rate of new firm formation, resulting in over 8,500 additional new businesses created each year.
- This reflects an estimated increase of about 3,000 to 5,000 new patents in the first year noncompetes are banned, rising to about 30,000-53,000 in the tenth year.
- This represents an estimated increase of 11-19% annually over a ten-year period.
- The average worker’s earnings will rise an estimated extra $524 per year.
The Federal Trade Commission develops policy initiatives on issues that affect competition, consumers, and the U.S. economy. The FTC will never demand money, make threats, tell you to transfer money, or promise you a prize. Follow the FTC on social media , read consumer alerts and the business blog , and sign up to get the latest FTC news and alerts .
Press Release Reference
Contact information, media contact.
Victoria Graham Office of Public Affairs 415-848-5121

IMAGES
VIDEO
COMMENTS
An assignment of benefits is the act of signing documentation authorizing a health insurance company to pay a physician directly. In other words, the insurance company can pay claims without the direct involvement of the patient in the process. There are other situations where AOBs can be helpful, but we'll focus on their use in relation to ...
Assignment of benefits occurs after a claim has been successfully processed with an insurance company. As Assignment of Benefits (often abbreviated to AOB) simply means that the patient is asking for their payment of their health benefits to be transferred to the doctor to used as payment. In some medical offices, there is a form known as an ...
An assignment of benefits in medical billing is a type of agreement between the healthcare provider, insurance company, and the patient through which a patient authorizes the medical service to collect healthcare policy coverage benefits on their behalf from their insurer for the service they have received from the facility. Once the patient ...
Definition of Assignment of Benefits. The term assignment of benefits (AOB) may be referred to as an agreement that transfers the health insurance claims benefits of the policy from the patient to the health care provider. ... This also means that any medical billing and collection company hired by the hospital is free to use the released ...
AOB stands for "Assignment of Benefits". AOB in medical billing is a contract between healthcare provider and patient, signed by the patient and sent to the insurance payers. After signing this document, the patient transfers all claim rights to the healthcare providers and they are out of the process.
When you sign an assignment of benefits agreement, you bypass dealing with an insurance company's claims department and allow the benefits to be paid directly to the provider. For example, the assignment of benefits medical definition is when you sign a form that requires your health insurance provider to pay the hospital or physician directly.
The assignment of benefits (AOB) is undoubtedly one of the most significant legal documents that make up the healthcare system. It is an agreement conveying the medical professional's right to claim medical services and obtain benefits from the patient's insurance plan. The medical professional receives payment for patient services under ...
Assignment of benefits is a fundamental concept in healthcare revenue cycle management. It enables healthcare providers to receive payment directly from the insurance company, reducing the financial burden on patients and streamlining the billing process. By understanding the assignment of benefits, patients can make informed decisions about ...
Mar 06, 2020 Share. Assignment of benefits, widely referred to as AOB, is a contractual agreement signed by a policyholder, which enables a third party to file an insurance claim, make repair ...
There are many reasons why an insurance company may not accept an assignment of benefits. To speak with a Schwartzapfel Lawyers expert about this directly, call 1-516-342-2200 for a free consultation today. It will be our privilege to assist you with all your legal questions, needs, and recovery efforts.
The second reimbursement method a physician/supplier has is choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly to the beneficiary.
Non-assignment of Benefits. Non-assigned is the method of reimbursement a physician/supplier has when choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly ...
For Medicare beneficiaries, assignment of benefits means that the person receiving care agrees to allow a nonparticipating provider to bill Medicare directly (as opposed to having the person receiving care pay the bill up front and seek reimbursement from Medicare). Assignment of benefits is authorized by the person receiving care in Box 13 of ...
The UB-04 uniform medical billing form is the standard claim form that institutional providers use, such as hospitals and community mental health care centers. It is used to bill Medicare, Medicaid, and other health insurance companies for inpatient or outpatient services. Although developed by the Centers for Medicare and Medicaid Services ...
Assignment of Benefits. Definition. A procedure whereby a beneficiary/patient authorizes the administrator of the program to forward payment for a covered procedure directly to the treating dentist. How to submit claims for assignment of benefits using the ADA claim form. This is done using box #37 on the ADA claim form.
Assignment of benefit, widely known as AOB, is a contractual agreement signed by a policyholder which enables a third party to file a claim, asking them to pay the designated amount directly to your provider for the rendered service. As AOB authorizes a third party to file a claim, make a decision, repair, and collect the payment from the ...
This document leads to the transfer of payment to the healthcare provider against all the benefits offered to the patient. Hence, once this document is signed by the patient, the insurance payer is bound to reimburse the medical practitioner. In the absence of the AOB, it would be the sole responsibility of the patient to pay the cost of ...
An assignment of benefits is an arrangement where you, the beneficiary, request that your insurance company pay the health benefit payment(s) directly to your health care providers. When you sign the assignment of benefits form, you are essentially entering into a contract with your health care provider to transfer your right of reimbursement ...
Assignment of Benefits (AOB) is an agreement that transfers the insurance claims rights or benefits of the policy to a third party. An AOB gives the third party authority to file a claim, make repair decisions, and collect insurance payments without the involvement of the homeowner. AOBs are commonly used in homeowners' insurance claims by ...
The explanation of benefits lists the cost of your care, and how much your health insurance company will pay. "Provider Charges" is the amount your provider bills for your visit. "Allowed Charges" is the amount your provider will be paid. This may not be the same as the Provider Charges. "Paid by Insurer" is the amount your health ...
Essentially, 'assignment' means that a doctor, (also known as provider or supplier) agrees (or is required by law) to accept a Medicare-approved amount as full payment for covered services. This amount may be lower or higher than an individual's insurance amount, but will be on par with Medicare fees for the services. If a doctor ...
Assignment of benefits is not authorization to submit claims. It is important to note that the beneficiary signature requirements for submission of claims are separate and distinct from assignment of benefits requirements except where the beneficiary died before signing the request for payment for a service furnished by a supplier and the supplier accepts assignment for that service.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies, without paying a deductible or coinsurance if the provider accepts assignment.
Specifically, the final rule defines the term "senior executive" to refer to workers earning more than $151,164 annually who are in a "policy-making position.". The FTC estimates that banning noncompetes will result in: Reduced health care costs: $74-$194 billion in reduced spending on physician services over the next decade.