Ontario.ca needs JavaScript to function properly and provide you with a fast, stable experience.
To have a better experience, you need to:
- Go to your browser's settings
- Enable JavaScript

Gender confirming surgery
How to apply for gender confirming surgery (also known as sex reassignment surgery) in Ontario. If you are eligible, this service is covered under OHIP .
As of March 1, you can seek an assessment for surgery from qualified health care providers across the province.
On this page Skip this page navigation
Affirming gender identity.
Gender confirming surgery (also known as sex reassignment or gender affirming surgery) does more than change a person’s body. It affirms how they think and feel about their own gender and what it means to who they are.
Ontario is funding surgery as an option for people who experience discomfort or distress with their sex or gender at birth.
How to qualify
Ontario funds two types of gender-confirming surgery: genital and chest.
To qualify for funding, you must:
- be assessed and recommended for surgery by either one or two healthcare providers (e.g. a qualified doctor, nurse practitioner, registered nurse, psychologist or registered social worker)
- have a referral for surgery completed and submitted to the Ministry of Health and Long-Term Care by a physician or nurse practitioner; and
- have the surgery approved by the Ministry of Health and Long-Term Care before the surgery takes place
Approval for genital surgery
To be approved for genital surgery, you’ll need:
- one of the assessments must be from a doctor or nurse practitioner
- you have a diagnosis of persistent gender dysphoria
- have completed 12 continuous months of hormone therapy (unless hormones are not recommended)
- you have lived 12 continuous months in the gender role you identify with (for genital surgery only)
If you have surgery before getting approval from the ministry, the cost of the surgery will not be covered.
Approval for chest surgery
To be approved for chest surgery you’ll need:
- have a diagnosis of persistent gender dysphoria
- have completed 12 months of continuous hormone therapy with no breast enlargement (unless hormones are not recommended) if you’re seeking breast augmentation
After being approved for chest surgery, your family doctor or nurse practitioner can refer you to a specialist who can perform the surgery.
Apply for surgery
To apply for gender confirming surgery, your doctor or nurse practitioner needs to fill out and submit the application along with the assessments and recommendations for surgery, to the Ministry of Health and Long-Term Care. The application is for patients seeking services in Ontario, out of province but within Canada or outside of the country.
Your doctor or nurse practitioner will let you know if your application is approved.
Once you receive approval from the ministry, talk with your health care provider to get ready for the surgery
Additional resources
You can find useful information from organizations, such as:
- find out about their ongoing project, Trans Health Connection
- consult their service directory
- find out about the Gender Identity Clinic (Adult)
Information for healthcare providers
Find out more about your role in providing gender-confirming surgery funded by Ontario.
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
Home » Surgeon News
Canada Finally Has Nation-Wide Funding For Gender-Affirming Surgeries

With last week’s announcement from the Government of Nunavut confirming that the territory will pay for mental health services and transition treatments for transgender and non-binary residents, Canada will now have nation-wide funding available for gender-affirming surgeries. Nunavut’s Health Department is partnering with GrS Montréal to provide the surgeries.
Health care in Canada is delivered by the provinces and territories and funding for gender-affirming surgeries varies depending on where a person lives. This patchwork of coverage has resulted in barriers to accessing care that have disproportionately affected people living in Canada’s territories in the North, which includes Yukon, Northwest Territories and Nunavut. While expansion of surgery funding in Canadian provinces has continually progressed over the last decade, comprehensive coverage has only been established in the territories over the past three years.
Nation-wide coverage is obviously a very positive development but advocacy is still needed to continue the work of dismantling barriers for Canadians to access surgical care. Current challenges include:
Getting coverage across the country for Facial Feminization , Breast Augmentation and Male Chest Contouring , procedures that are excluded from funding policies in some jurisdictions.
Surgeons who practice gender-affirming genital surgery are only located in Montreal, Toronto and Vancouver. This means that many transgender and non-binary Canadians need to travel great distances to access surgeons for primary surgeries, follow-ups and specialized care for complications, incurring significant expenses that aren’t universally covered or subsidized.
Wait times are a problem that is not unique to gender-affirming surgical care in Canada but with few experts performing these surgeries patients can wait up to three years just for a consultation with a surgeon.
With the Government of Nunavut’s funding commitment, the goal of nation-wide coverage for gender-affirming surgery in Canada has been achieved. Improvements to provincial and territorial funding policies are still needed but this is a milestone to be celebrated.
Review Funding Policies by Province and Territory:
- British Columbia
- New Brunswick
- Newfoundland and Labrador
- Nova Scotia
- Ontario – PDF
- Prince Edward Island
- Saskatchewan – PDF
- Northwest Territories – PDF
- Nunavut – News article: GN transgender, non-binary health services a positive step
- Yukon – News article: Yukon’s new gender-affirming care policy is most comprehensive in Canada
Search The Canadian Encyclopedia
Enter your search term
Why sign up?
Signing up enhances your TCE experience with the ability to save items to your personal reading list, and access the interactive map.
- MLA 8TH EDITION
- James-Abra, Erin. "The Road to Inclusion: Transgender Health Care in Canada". The Canadian Encyclopedia , 29 July 2014, Historica Canada . www.thecanadianencyclopedia.ca/en/article/the-road-to-inclusion-transgender-health-care-in-canada. Accessed 26 April 2024.
- The Canadian Encyclopedia , 29 July 2014, Historica Canada . www.thecanadianencyclopedia.ca/en/article/the-road-to-inclusion-transgender-health-care-in-canada. Accessed 26 April 2024." href="#" class="js-copy-clipboard b b-md b-invert b-modal-copy">Copy
- APA 6TH EDITION
- James-Abra, E. (2014). The Road to Inclusion: Transgender Health Care in Canada. In The Canadian Encyclopedia . Retrieved from https://www.thecanadianencyclopedia.ca/en/article/the-road-to-inclusion-transgender-health-care-in-canada
- The Canadian Encyclopedia . Retrieved from https://www.thecanadianencyclopedia.ca/en/article/the-road-to-inclusion-transgender-health-care-in-canada" href="#" class="js-copy-clipboard b b-md b-invert b-modal-copy">Copy
- CHICAGO 17TH EDITION
- James-Abra, Erin. "The Road to Inclusion: Transgender Health Care in Canada." The Canadian Encyclopedia . Historica Canada. Article published June 16, 2014; Last Edited July 29, 2014.
- The Canadian Encyclopedia . Historica Canada. Article published June 16, 2014; Last Edited July 29, 2014." href="#" class="js-copy-clipboard b b-md b-invert b-modal-copy">Copy
- TURABIAN 8TH EDITION
- The Canadian Encyclopedia , s.v. "The Road to Inclusion: Transgender Health Care in Canada," by Erin James-Abra, Accessed April 26, 2024, https://www.thecanadianencyclopedia.ca/en/article/the-road-to-inclusion-transgender-health-care-in-canada
- The Canadian Encyclopedia , s.v. "The Road to Inclusion: Transgender Health Care in Canada," by Erin James-Abra, Accessed April 26, 2024, https://www.thecanadianencyclopedia.ca/en/article/the-road-to-inclusion-transgender-health-care-in-canada" href="#" class="js-copy-clipboard b b-md b-invert b-modal-copy">Copy
Thank you for your submission
Our team will be reviewing your submission and get back to you with any further questions.
Thanks for contributing to The Canadian Encyclopedia.
The Road to Inclusion: Transgender Health Care in Canada
Article by Erin James-Abra
Published Online July 29, 2014
Last Edited July 29, 2014

As a child growing up in Trail , British Columbia , she remembers wanting to play dolls with the other girls. Instead she was given a toy truck. Playtime proved good practice when, as an adult, Natasha spent three years as a long-haul truck driver. During this time she drove a trailer from Calgary to Los Angeles and back again. The week-long trips would often begin in Taber , Alberta, where Natasha would fill her 75-foot rig with McCain french fries. After each driving day she would sleep in the six-by-seven bunk behind the driver’s seat. Once in L.A., it would take a full day to switch loads, exchanging french fries for Ikea furniture in Kern County, wicker chairs in Tijuana, or organic bananas in San Diego. And then it was back north, taking her new load to Saskatoon or Prince Albert , Grand Prairie or Fort Nelson , before returning to Calgary.
“It took its toll,” Natasha says of the job. “I ended up with all these ailments because of the road, living on it 16 hours a day.” First it was gallstones, then chronic bladder infections, and finally, an enlarged prostate. After an operation on her prostate, Natasha was impotent. “That became my turning point,” she says. “I said to hell with it, I’m going to go this route.”
In Alberta, Natasha’s route to becoming a woman will necessarily lead to the office of Dr. Lorne Warneke. In fact, the letter she so desperately needed from any one of the six doctors she visited, was to allow her to see Alberta’s “gender specialist” at his psychiatry practice at Grey Nuns Hospital in Edmonton. Warneke is one of only two psychiatrists in Alberta who diagnoses, assesses and provides patients with the referrals they need to access hormone therapy and sex reassignment surgery.
“Transgenderism was once thought to be very rare, and in fact it’s much, much more common than once previously thought,” he says. “Certainly, I’m so backlogged that there could be two or three or four transgender psychiatrists, maybe not full time but at least seeing transgender patients.”
Over the years, the continued existence of Warneke’s practice has depended on his enthusiasm and commitment. Warneke has worked at Catholic hospitals in Edmonton for 34 years. In 1996, he started seeing enough trans patients to make it a specialized service at his clinic, and after some lobbying, the Alberta Health Services Capital Region provided him with an additional staff member.
In April 2009, when SRS was removed from the list of provincially funded services in Alberta, multiple news outlets asked Warneke to comment on the policy change, making the Edmonton diocese more aware of his work. Warneke was told he was to stop seeing transgender patients. Assisting them in “changing their body” went against Catholic dogma. In an effort to deflect the administration’s anger, Warneke sought support from the Alberta Medical Association, the Alberta Psychiatric Association, the College of Physicians and Surgeons of Alberta, the Canadian Medical Protective Association and members of his own department. All of them turned their backs. As a result of the dust-up, Warneke now carries out all clinic correspondence on his own letterhead, but for the most part has proceeded as usual. After a three-year hiatus, SRS was relisted in June 2012.
Warneke’s persistence stems in part from his own experience. As a gay man who didn’t come out until his early 40s, he has a sense of the stigma many trans people still experience today. “I love to fight for their rights,” he says. “It’s just my passion.”
The word transsexual was first coined in 1923 when German sexologist Dr. Magnus Hirschfeld used the expression “seelischer transsexualismus” (psychic transsexualism) in a journal paper. Since Hirschfeld wrote about a wide range of topics in sexuality, it wasn’t until another German born sexologist, Dr. Harry Benjamin, published The Transsexual Phenomenon in 1966 that transsexuality truly entered the medical literature.
Benjamin was one of the first physicians in North America to work with trans patients and became influential in the development of trans care. He wrote The Transsexual Phenomenon at the age of 81.
The book isn’t an average piece of medical literature. Benjamin’s writing is often poetic, especially as he describes the moral and political notions surrounding trans care. “I have seen too many transsexual patients to let their picture and their suffering be obscured by uninformed albeit honest opposition,” he wrote. “Furthermore, I felt that after fifty years in the practice of medicine, and in the evening of life, I need not be too concerned with a disapproval that touches much more on morals than on science.”
Founded in 1979, the World Professional Association for Transgender Health—an international group that provides standards of care for trans patients—was originally named after Benjamin. The WPATH standards guide the better part of the work of trans health care providers across Canada, such as the Sherbourne Health Centre, a community-based clinic in downtown Toronto . They state, for example, how many letters of referral a patient needs for chest surgery (one) or genital surgery (two).
Despite the time that has passed since Benjamin published The Transsexual Phenomenon, certain observations remain true. “The difficulty in procuring surgical help is not the only plight of the TS patient,” Benjamin wrote. “Any medical help, including hormone treatment, may be denied him by overcautious and over-conservative physicians.” Benjamin also included his vision for the future: “It is my hope that this volume may induce doctors as well as laymen who may come across the transsexual phenomenon to assume a tolerant and rational attitude and let the light of facts replace the ever-present twilight of prejudices.”
Forty-eight years later, Benjamin’s words seem naively hopeful. With the exception of heavily populated regions like Ontario and British Columbia, most provinces have only a handful of primary health care providers familiar and comfortable with trans issues. As the number of trans patients grows, the future care of trans Canadians can no longer rest in the hands of just a few physicians.
Sex reassignment surgery is often used as a catch-all term for multiple procedures. For male-to-female patients the list may include facial feminization, breast augmentation, and vaginoplasty (the creation of a vagina), and for female-to-male patients, mastectomy, hysterectomy, or phalloplasty (the creation of a penis). While not every trans person opts for hormonal or surgical treatment, research suggests an overwhelming majority do: In Ontario, over 75 per cent of trans people have either completed a medical transition, are in the process, or plan to begin in the near future.
Opponents of sex reassignment surgery, particularly opponents of government funding, often put the procedure in the same category as cosmetic surgery. It’s a dangerous misunderstanding. “There is mortality associated with untreated gender dysphoria and it’s usually in the form of suicide,” says Dr. Ian Whetter, a physician at Trans Health Klinic in Winnipeg . Numbers from the Ontario Trans Pulse survey back up Whetter’s conviction: Of the respondents still waiting to begin a medical transition, 46 per cent were considering suicide. That number dropped to 23 per cent for those who had completed the process. “There are known treatments that reduce the mortality associated with [transgenderism],” Whetter continues, “which are crossgender hormone therapy and sexual reassignment surgery.”
Satisfaction rates among those who undergo sex reassignment surgery are increasing steadily, according to the WPATH Standards of Care.
Anna Travers is director of Rainbow Health Ontario, a province-wide initiative designed to promote access to health services in the LGBT community. “I don’t exactly know,” she says, “but I think there’s something about people crossing gender lines that really freaks people out.”
Transphobia, whether it manifests itself in violence or stubborn ignorance, is, without question, one of the reasons trans health care in Canada is inconsistent and inadequate. Through education and training, Rainbow Health is doing its part to remedy the situation. It runs a service called Trans Health Connection, which partners with health care organizations in communities across Ontario. Launched in April 2011, the program offers training sessions to health care teams working with trans people. The topics discussed in the four day-long sessions range from respectful language to pre- and post-surgical care, and are open to all primary health care providers, be they doctors, nurses, counsellors, or social workers. No similar training model exists elsewhere in Canada.
“It’s important because no one else is doing work like this,” says Jordan Zaitzow, Trans Health Connection coordinator. “I get calls from trans people across the province every single week looking for [support],” he says. “And I get even more calls from providers [who say] I would love to do this work, but I don’t have the resources. I need more training.”
Now in its fourth year, the program is a success. Training sessions held across Ontario communities are attended by as many as 80 health care and social service workers per day. While pleased with the program, Zaitzow is conscious of the magnitude of the problem he’s trying to fix. The popularity of the sessions is in large part due to the lack of LGBT education in medical, nursing and social work schools. “I think for trans health in particular it’s been seen up until very recently as a very specialized area,” Travers says. “It’s only recently that it’s being seen as something that’s within the scope of a family doctor.”
Both Travers and Zaitzow would prefer LGBT health to be a part of the curriculum at the professional school level, rather than having organizations like Rainbow Health deliver training as a part of continuing education. Others agree. “I think that there should be standard medical education,” Whetter says. “It’s trickier to diagnose depression than it is to diagnose gender dysphoria.”
While policy makers debate who should shoulder the burden of trans health training, patients are often the ones educating their doctors — if they’re brave enough to visit the doctor in the first place. “Trans people don’t see themselves in any health studies, health information and health literature,” Zaitzow says. “So then if trans people don’t see themselves reflected in [the medical world], the message is that primary health care services are not for them.” Because so many trans people have had bad experiences accessing health care, many choose not to go at all, adding to their list of health concerns.
After 10 months on the waiting list, and three and a half hours driving from Calgary to Edmonton, Natasha was happy to spend a mere five minutes in the waiting room at Grey Nuns Hospital before her name was called. First, an intern interviewed her, taking note of her history and her experience living as a woman. When finally Natasha met Dr. Warneke, the meeting was short.
Going into the appointment, Natasha hoped Warneke would provide her with one of the referral letters she needs for genital surgery. Instead, she discovered she must spend nearly a year before surgery on spironolactone, an androgen inhibitor, as well estrogen, which she will be on for the rest of her life. Adding to her frustration is the fact Warneke remains the only gender specialist in the province. “It seems like I’m going to be doing a lot of commuting between here and Edmonton to maintain my program,” she says dispiritedly.
Despite feeling weary, in a way, Natasha’s experience as a truck driver was preparation for the process she’s going through now. Years ago, the long stretches of highway between Calgary and Los Angeles would put her in an almost meditative state, helping to pass the time between the two cities. It’s this kind of patience Natasha continues to draw on to this day. She uses the word transgender to describe the stage she’s at, as though it were just a pit stop on the way to place she’s going. “It doesn’t fit my mind,” she says of being transgender. “To me it’s just a journey you go through.”
Like the long distances she used to travel, Natasha’s transgender journey is also coming to a close — or at least moving on to the next pit stop. About two years after her first appointment with Dr. Warneke, Natasha is scheduled for genital surgery in September 2014. Given all she’s been through she’s hesitant to celebrate just yet. “I’m still beside myself,” she says. “It’s still a fantasy. I won’t believe it until it’s here.” Occasionally, however, Natasha allows herself to imagine what life might be like after her operation. “I’m looking to re-establish myself as a human being,” she says.
Recommended
Lesbian, gay, bisexual and transgender rights in canada, queer culture.

much more than surgery
The quality and safety in our care and services; Your peace of mind. Excellence is a core value that drives the decisions and actions of every member of our staff.
EXPERIENCED SURGEONS
Our surgeons have performed more than 10 000 gender-affirming surgeries over the past 12 years.
PERSONALIZED FOLLOW-UP
Care is provided in the spirit of patient support and in consideration of the uniqueness of your own experience. From the preoperative period to your postoperative follow-ups, we will be right beside you.
QUALITY FACILITIES
Surgeries are performed at the Centre Métropolitain de Chirurgie, our private hospital centre accredited with exemplary standing. For some surgeries, a stay at the Asclépiade convalescent home is necessary.
A WORRY-FREE STAY
No matter where you come from, we will help you plan your stay.

Dr Pierre Brassard, FRCSC

Dre Maud Bélanger, FRCSC

Dre Valérie J. Brousseau, FRCSC

Dr Alex Laungani, FRCSC

Dr Chen Lee, FRCSC

Dr Dru Perkins
Dr Mar Aristeo Poncio
Male to Female / MTF / MTX
Vaginoplasty, Vaginoplasty without vaginal cavity, Breast Augmentation, Adam's Apple Reduction, Voice Surgery, Facial and Body Feminization, Corrective surgeries: Secondary Vaginoplasty, Genital Scar Revision, Vulvar Reconstruction, Labioplasty, Correction of the Clitoris
Female to Male / FTM / FTX
Masculinization of the Torso or Mastectomy, Metoidioplasty, Phalloplasty, Insertion of Testicular Implant(s), Insertion of Penile Implants , Masculinization of the Face and Body surgeries, Corrective surgeries: Torso Scar Removal, Nipple Correction, Secondary Phalloplasty, Phallus Revision

Transition-Related Surgery
Transition-related surgery (TRS) refers to a range of surgical options that can help people feel that their physical characteristics more closely reflect their gender identity or expression. These options can support one in feeling more comfortable in their body and may help to improve your mental wellness.
In order to receive provincially-funded transition-related surgeries, you will need a surgery assessment from one or two health providers, depending on the surgery, one of which being a qualified primary care provider like a Physician or Nurse Practitioner.
If you have a primary care provider and would like to start a discussion with them about transition-related surgery, you can click here for tips on how to start that conversation.
If you do not have a primary care provider and would like to access transition-related surgery, you can reach out to Centretown Community Health Centre’s Trans Health Program to get connected with surgery referral support.
Provincially Funded Transition-Related Surgeries
Disclaimer: this section uses medical terminology.
Upper Surgery (Chest or Breast Augmentation) needs one assessment by a qualified Physician or Nurse Practitioner. Lower Surgery (Genital Surgery) needs an additional assessment from any qualified Physician, Nurse Practitioner, Psychologist, or Registered Social Worker (Master’s Degree).
Under the Ministry of Health and Long-Term Care (MOHLTC), the following surgical procedures are provincially-funded:
For “Assigned Male at Birth” individuals:
- Vaginoplasty
- Orchiectomy
- Augmentation Mammoplasty a (breast enlargement)*
*Patient must have completed twelve continuous months of hormone therapy with no breast enlargement unless hormones are contraindicated
For “Assigned Female at Birth” individuals:
- Hysterectomy
- Clitoral release with vaginectomy
- Metoidioplasty
- Phalloplasty
- Testicular implants with scrotoplasty
- Penile implant
Eligibility
Prior to beginning the referral process for transition-related surgeries, the following eligibility criteria must be met:
- Has a diagnosis of persistent gender dysphoria
- For breast augmentation surgery: Has completed 12 continuous months of hormone therapy with no breast enlargement (unless hormones are not appropriate for the person)
- For External Genital Surgery Only: Has completed 12 continuous months living as gender(s)
Not Covered
As of right now, OHIP does not cover the following procedures identified as medically necessary by the World Professional Association for Transgender Health:
- Liposuction
- Electrolysis
- Chest contouring/masculinization
- LASER hair removal
- Hair transplants
- Tracheal shave
- Voice modification surgery
- Chin, nose, cheek or buttock implants
- Facial feminization/masculinization
*OHIP does not cover travel costs involved in obtaining surgery. If you are in financial need and must travel to obtain an OHIP approved procedure, Hope Air can provide free air travel and accommodation. You can learn more about this option here.
For an overview of transition-related surgeries, risks, benefits and additional information, review Rainbow Health Ontario’s TRS Summary Sheets here .
The Referral Process
Step 1: Connect with Qualified Providers.
The MOHLTC requires 2 qualified providers submit a “Request for Prior Approval for Funding of Sex Reassignment Surgery” form (can be found on the “Clinical Resources” section of our resource library ).
Who is a qualified provider?
The MOHLTC criteria for a qualified provider includes Physicians, Nurse Practitioners, Registered Nurses, Psychologists and Registered Social Workers. Eligible providers are expected to self-assess if providing transition-related surgical referrals is within the scope of their practice. There is no single training course that “qualifies” a provider, but providers are encouraged to undertake professional development and training activities to build their capacity on trans health services.
If your primary care provider is not able to submit a Prior Approval form on your behalf, Centretown Community Health Centre can help.
Step 2: Participate in a Transition-Related Surgery (TRS) Planning Visit
A TRS planning visit is a collaborative visit between a patient and a qualified provider to discuss TRS and how to optimize the patient’s experience and outcome. Topics discussed include reviewing World Professional Association for Transgender Health (WPATH) and MOHLTC criteria, confirming the diagnosis of gender dysphoria, reviewing the stability of medical and mental health conditions, confirming surgery-specific informed consent and planning aftercare.
Step 3: Complete the Prior Approval Form
Following your Transition-Related Surgery Planning Visit, your provider can complete, sign, and submit the “Request for Prior Approval for Funding of Sex-Reassignment Surgery” (also known as the “Prior Approval” form) to the MOHLTC.
The number of qualified providers who must complete independent TRS surgery planning visits and sign a Prior Approval form is based on the type of surgery requested.
Upper body surgery requires a TRS planning visit(s) by one qualified provider (either a P hysician or Nurse Practitioner).
Gonadal or external genital surgery requires independent TRS planning visits with two qualified providers, one of whom must be a Physician or Nurse Practitioner, while the second can be a Physician, Nurse Practitioner, Registered Nurse, Psychologist, or a Registered Social Worker with a Masters of Social Work.
Once the application is submitted, the MOHLTC will then send a response letter with the outcome of the funding application.
If approval is not received, your qualified provider can contact the MOHLTC to provide additional information, the application can be resubmitted, and/or an internal review of the initial application can be requested by your provider.
Step 4: TRS Referral Letter Sent to TRS Surgeon
Once an approval letter is received from the MOHLTC, your provider can send a referral letter to the transition-related surgery surgeon. TRS referral letters are often more in-depth than typical referral notes and often include details about your TRS planning visits. Surgeons will often request additional documentation, including medication lists, lab results and other information.
Step 5: Complete TRS and After Care
Once referred to a TRS surgeon, you will be contacted by the surgeon or clinic to sort out additional details, and will receive more information as your surgery date nears.
In partnership with:

Hundreds of trans teens under 18 have had breasts removed in Canada, new data show
Concerns have been raised about mastectomies in teens when uncertainties exist about long-term health effects and the possibility of regret
You can save this article by registering for free here . Or sign-in if you have an account.
Article content
As tensions rise over the medical care of trans children, a new analysis shows hundreds of adolescents in Canada have undergone female-to-male “top surgery” — double mastectomies — over the past five years.
Hospitalizations and day surgery visits for bilateral mastectomies for gender reassignment surgery have risen sharply, from 536 in 2018-19, to 985 in fiscal 2022-23, according to data compiled for National Post by the Canadian Institute for Health Information.
Enjoy the latest local, national and international news.
- Exclusive articles by Conrad Black, Barbara Kay, Rex Murphy and others. Plus, special edition NP Platformed and First Reading newsletters and virtual events.
- Unlimited online access to National Post and 15 news sites with one account.
- National Post ePaper, an electronic replica of the print edition to view on any device, share and comment on.
- Daily puzzles including the New York Times Crossword.
- Support local journalism.
Create an account or sign in to continue with your reading experience.
- Access articles from across Canada with one account.
- Share your thoughts and join the conversation in the comments.
- Enjoy additional articles per month.
- Get email updates from your favourite authors.
Don't have an account? Create Account
Of the 4,071 visits in total involving gender-affirming mastectomies or breast reductions reported since 2018, 602 involved youth 18 and under.
Of those, 303 involved teens 17 and younger. The youngest age was 14.
The numbers tell only part of the story. The CIHI data exclude Quebec hospitals as well as surgeries performed in private clinics like the McLean Clinic in Mississauga, which describes its surgeons as “industry pioneers” for top surgery — mastectomies and breast reductions in those assigned female at birth, and breast augmentation for those born male transitioning to female.
One specialist in transgender health issues said that, when applying for OHIP funding for people seeking top surgery, “50 to 70 per cent will go to McLean.”
Female-to-male chest surgery involves removing the breasts to achieve a flatter, more masculinized torso, to better align the person’s physical body with their gender identity and reduce gender dysphoria, defined as the persistent distress that can accompany the incongruence between the gender one identifies with and one’s gender at birth.
Get a dash of perspective along with the trending news of the day in a very readable format.
- There was an error, please provide a valid email address.
By signing up you consent to receive the above newsletter from Postmedia Network Inc.
A welcome email is on its way. If you don't see it, please check your junk folder.
The next issue of NP Posted will soon be in your inbox.
We encountered an issue signing you up. Please try again
If this was just about ... kids being allowed to wear what they want and say what they want and be called whatever name they want and it stopped there, who would care?
But concerns have been raised about intervening with permanent, body-altering surgeries in adolescents when uncertainties exist about the long-term health effects, the possibility of regret and whether their trans identity will be lifelong.
Last week thousands gathered in cities across the country for duelling protests over gender policies in schools. Earlier this month delegates to the federal Conservative party’s policy convention voted 69 per cent in favour of prohibiting “life altering medicinal or surgical interventions” on minors under 18 to treat gender confusion or dysphoria.
Sweden, the world’s first country to authorize legal gender transitions in 1972, last year began limiting mastectomies for teenage girls to research settings. “The uncertain state of knowledge calls for caution,” the head of Sweden’s National Board of Health and Welfare said in a statement reported by AFP.
Public coverage for the surgeries varies from province to province. Most cover the cost of the mastectomy itself, but not several thousand dollars or more in extra add on fees for “chest contouring,” liposuction procedures to give the body a more sculpted, masculine look.
The rise in surgeries reflects a dramatic shift in the sex ratio of children and teens being referred to specialized gender identity clinics across the country, from once predominantly young boys to children born female.
One study involving 174 trans and non-binary children and teens referred to 10 gender identity clinics in Canada found 34 per cent of those assigned female at birth were referred for top surgery. Most were 15 or 16 at the time of referral.
Ontario’s Health Ministry declined to respond when asked the number of OHIP approvals for gender-affirming mastectomies in the most recent year available, including the proportion in youth. The McLean Clinic said its surgeons were unable to accommodate a request for an interview.
According to CIHI, of the 536 hospital visits for transgender reassignment mastectomies in 2018-19, 76, or 14 per cent, involved 18-year-olds and younger.
That age group accounted for 18 per cent of visits for mastectomies (174 out of 991) reported in fiscal 2021-22, and 14 per cent of visits (135 out of 985) in 2022-23.
The percentage dipped last year as hospitals grappled with pandemic-driven surgical backlogs. “But the private clinics just kept churning them through,” said one doctor familiar with trans medicine who requested anonymity fearing professional repercussions.
“The fact that you can’t get the numbers from private clinics…. It’s very cloak-and-dagger,” the doctor said. “They’re still billing OHIP. That’s tax dollars. That should be publicly accessible information. We need to see these numbers and ask questions,” the doctor said.
“If this was just about the schools, and just about kids being allowed to wear what they want and say what they want and be called whatever name they want and it stopped there, who would care? But medicine got involved.”
For a double mastectomy, typically two incisions are made on the bottom border of the pectoral muscle or chest area, according to the McLean Clinic’s website. “The skin is then lifted to surgically remove the breast tissue underneath.” The nipples are removed, re-sized and repositioned by grafting “to suit the new masculine appearance of the chest.”
It’s a day-surgery procedure performed under general anesthesia that takes approximately two hours. Complications can include bruising, wound infections and scarring. People lose nipple sensation as well as the ability to breastfeed should they become pregnant.
The uncertain state of knowledge calls for caution
Major medical groups like the American Academy of Pediatrics have strongly endorsed a gender-affirming approach to care to promote “optimal physical, mental and social wellbeing.” Eligibility for gender-affirmative surgeries in teens should be determined on a case-by-case basis, the AAP said in a 2018 policy statement the organization recently reaffirmed, while at the same time calling for a review of the evidence to develop an “expanded set of guidance.”
The growth in referrals to specialized clinics could be due to greater awareness and social acceptance, and the teaching of gender identity in school, experts said. But it’s not clear why it’s concentrated in children and teens born female.
Denying or holding back access to gender-affirming care “can have negative consequences for some youth,” SickKids in Toronto said in a statement. “Decisions for care should be made by youth, their families and their health-care providers, who are best-positioned to support them.”
Trans teens are known to be at higher risk of harassment and cyberbullying, wrote the authors of a recent review on the surgical and ethical considerations of gender affirming surgery in teens. Early access to surgery may reduce the bullying, they said, or help facilitate “age-appropriate romantic and sexual development in adolescents who may otherwise be prevented from engaging in these activities due to gender dysphoria.”
But the evidence is largely anecdotal, they said. The handful of published studies on surgery in minors involved relatively short follow-up periods.
“What we do know is that regret does take place, and it does take place later on in life,” said one trans medicine specialist, who also agreed to speak on the condition of anonymity for fear of being labelled “transphobic.”
“If we know that people can come to this realization that maybe this may have not been the best decision for them, if that takes place after five years or 10 years, we don’t have all the information to allow patients to make an informed decision.”
For such a permanent decision as the removal of healthy breasts, “I’m always looking at the why, and because that hasn’t been answered yet, that’s what leads to my ambivalence,” the specialist said.
“What all this says to me is that we need to be much more thoughtful in our approach and in our assessments.”
National Post
Our website is the place for the latest breaking news, exclusive scoops, longreads and provocative commentary. Please bookmark nationalpost.com and sign up for our daily newsletter, Posted, here .
Postmedia is committed to maintaining a lively but civil forum for discussion. Please keep comments relevant and respectful. Comments may take up to an hour to appear on the site. You will receive an email if there is a reply to your comment, an update to a thread you follow or if a user you follow comments. Visit our Community Guidelines for more information.
'Nessie' photo at Scotland's Loch Ness puts Canadians in media spotlight
Cupe president silences members who call her out for wearing keffiyeh at union meeting, subscriber only. john ivison: how canada’s military-industrial complex made sure ottawa bought its preferred fighter jet, rex murphy: hatred of israel is the great moral disorder of our time, jewish student sues tmu over 'poisoned' antisemitic environment, breathe easy with our favourite air purifiers.
A reliable air purifier can effectively remove airborne particles and improve air quality
The best online deals in the Canadian retail space right now
Good American, Brooklinen and Our Place, to name a few
Advertisement 2 Story continues below This advertisement has not loaded yet, but your article continues below.
Makeup tutorial: Blue and green are great eyeliner alternatives
Here’s a high-low comparison of luxury brand Make Up For Ever Aqua Resist Color Pencil Eyeliner versus drugstore brand Annabelle Smoothliner
Supermodel, L'Oréal ambassador Soo Joo Park shares her approach to beauty, aging
The longtime L'Oréal Paris ambassador admits her approach to skin care and makeup has shifted.
New Star Wars LEGO sets released for 2024
Celebrating 25 years of Star Wars LEGO
This website uses cookies to personalize your content (including ads), and allows us to analyze our traffic. Read more about cookies here . By continuing to use our site, you agree to our Terms of Service and Privacy Policy .
You've reached the 20 article limit.
You can manage saved articles in your account.
and save up to 100 articles!
Looks like you've reached your saved article limit!
You can manage your saved articles in your account and clicking the X located at the bottom right of the article.
The road to gender-affirming care is complex and expensive: ‘Even if something is big-C covered, it’s not little-C covered’
This article was published more than 6 months ago. Some information may no longer be current.
Magan Carty spoke to the Globe and Mail about gender-affirming healthcare and their personal experience with the financial side of top surgery on Sept. 13 in Ottawa. Ashley Fraser/The Globe and Mail
When Magan Carty got their date for top surgery in August, 2022, they had roughly four months to pull together about $4,000.
Mx. Carty, a 31-year-old radio producer in Toronto , had been seeking top surgery since March, 2020. It took a year and a half to get a referral letter from a qualified doctor. Then came the nine-month wait for approval from the Ontario Health Insurance Plan. Even though there was no reason to think they wouldn’t be approved for coverage, Mx. Carty was nervous. “Because without it, it’s about $10,000.”
The approval came through in June. But while OHIP covers the surgery to remove breast tissue, costing $6,500, it doesn’t cover the $3,500 chest masculinization procedure. Mx. Carty, who also paid $300 for a chest compression vest and $500 in taxes on the surgery, had to pay the full amount before the procedure.
At the suggestion of their roommate, they started a GoFundMe campaign, setting the goal at $2,000 and paying a little more than $2,000 from their own savings. Though they knew there would be expenses, Mx. Carty said they were “adamant” the surgery had to be done “for my well-being.”
And the crowdfunding campaign was a success: “I was overwhelmed with people who wanted to help me. ”
Trans and non-binary Canadians seeking gender-affirming care often need to not only navigate a complex path to approval and wait times for provincially covered surgeries but also potentially plan for out-of-pocket health care costs, which can run from hundreds to tens of thousands of dollars, prompting them to dig into their own savings, launch crowdfunding campaigns or take out medical loans – or to put off care indefinitely.
“It can get very expensive very quickly,” said Laura Whiteland, a certified financial planner and founder of Inclusive Financial Planning in Truro, N.S. “With provincial health insurance, it’s a very specific category of things that they’ll cover.”
Accessing publicly funded gender-affirming health care depends largely on where a person lives. All provinces and territories cover transition-related surgeries, but most require approval and referral from one or two medical professionals.
There are also exceptions: While all provinces cover surgeries to remove breast tissue, many do not cover the contouring procedures that make a chest look more masculine. Most public plans don’t fund breast augmentation or only cover it under certain conditions.
But there can be more to someone’s transition than just those surgeries, including facial feminization surgeries, vocal surgeries or voice training, liposuction and other body contouring, or hair transplants or removal.
Facial feminization procedures run from between $10,000 to more than $15,000. Laser hair removal or electrolysis can costs hundreds of dollars. Voice training specialists typically charge $60 to $150 an hour. According to 2021 figures from the Aesthetic Society, a California-based association of plastic surgery and cosmetic medicine professionals from the United States and Canada, body contouring procedures such as liposuction cost more than US$2,000 each. Yukon pays for all of these (its coverage is considered the best in North America) but most public plans cover only some or none.
Riley Nielson-Baker, executive director of Gender Affirming Care Nova Scotia, an advocacy and policy organization, said a transition is often highly dependent on “who you can afford to see and the quality of care you can afford.”
OHIP reverses course, will fund gender-affirming surgery for Ottawa public servant
The Canada Health Act entitles Canadians to medically necessary health care . Procedures seen as cosmetic are excluded, though provinces have leeway to decide what medically necessary means. Advocates argue that gender-affirming care that isn’t currently publicly funded should fall under medicare, as research has demonstrated an ability to access to such care improves mental health and reduces suicide risk.
Mx. Nielson-Baker said better provincial coverage would also contribute to trans and non-binary Canadians’ economic security “because people are no longer trying to privately fund their own procedures” and could instead focus on other financial goals.
Even for surgeries covered by the public system, other expenses crop up, Ms. Whiteland said. There are only three clinics that perform surgeries such as vaginoplasties and phalloplasties – in Montreal, Toronto and British Columbia – and travel and accommodation costs are rarely covered. Most surgeries require days or weeks off work to recover.
As well, not all provinces fund the cost of mental-health professionals or hormone therapy, despite some requiring an assessment from a psychiatrist or a certain amount of months on hormone therapy to be approved for surgeries.
“Even if something is big-C covered, it’s not little-C covered,” Ms. Whiteland said. “I travel an hour to see a specialist for hormones, and it’s not uncommon to travel 100 to 300 kilometres to get to a doctor who will even prescribe those.”
Canadian employers have started adding financial support for gender-affirming care as part of organizational diversity, equity and inclusion initiatives and to attract top talent. Twenty-one per cent of Canadian employers cover gender-affirmation benefits and a further 33 per cent are interested in covering them, according to a 2022 survey of more than 500 employers and other benefits-plan sponsors by trade publication Benefits Canada.
In the past few years employers including most of the big five banks, the University of Toronto, KPMG Canada, Molson Coors and Toyota Motor Manufacturing Canada have added coverage to their plans. Toronto Dominion Bank and Accenture were among the first to offer such coverage, dating back more than a decade ago.
The public service health care plan, which covers federal employees, has one of the most generous plans, covering gender-affirming procedures up to a lifetime maximum of $75,000.
The benefits generally fill in the gaps of provincial or territorial health plans, said Stephanie Lue-Kim, principal of total health management at employee benefits consulting firm Mercer Canada.
Ms. Lue-Kim has seen more companies show interest in such benefits. “Employers understand they need to match benefits to the current population’s needs, one of which is gender affirming care,” she said.
Mx. Carty said they have known they wanted top surgery since they were 19. But if they had actually tried to pursue it at that time, the cost would have been an insurmountable barrier.
“If you don’t have the money or a way to pay for it, it stops you before you can even start.”
Are you a young Canadian with money on your mind? To set yourself up for success and steer clear of costly mistakes, listen to our award-winning Stress Test podcast .
Report an editorial error
Report a technical issue
Editorial code of conduct
Follow related authors and topics
- Health Follow You must be logged in to follow. Log In Create free account
Authors and topics you follow will be added to your personal news feed in Following .
Interact with The Globe
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Gender Confirmation Surgery (GCS)
What is Gender Confirmation Surgery?
- Transfeminine Tr
Transmasculine Transition
- Traveling Abroad
Choosing a Surgeon
Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures. These are both respectful terms.
Gender dysphoria , an experience of misalignment between gender and sex, is becoming more widely diagnosed. People diagnosed with gender dysphoria are often referred to as "transgender," though one does not necessarily need to experience gender dysphoria to be a member of the transgender community. It is important to note there is controversy around the gender dysphoria diagnosis. Many disapprove of it, noting that the diagnosis suggests that being transgender is an illness.
Ellen Lindner / Verywell
Transfeminine Transition
Transfeminine is a term inclusive of trans women and non-binary trans people assigned male at birth.
Gender confirmation procedures that a transfeminine person may undergo include:
- Penectomy is the surgical removal of external male genitalia.
- Orchiectomy is the surgical removal of the testes.
- Vaginoplasty is the surgical creation of a vagina.
- Feminizing genitoplasty creates internal female genitalia.
- Breast implants create breasts.
- Gluteoplasty increases buttock volume.
- Chondrolaryngoplasty is a procedure on the throat that can minimize the appearance of Adam's apple .
Feminizing hormones are commonly used for at least 12 months prior to breast augmentation to maximize breast growth and achieve a better surgical outcome. They are also often used for approximately 12 months prior to feminizing genital surgeries.
Facial feminization surgery (FFS) is often done to soften the lines of the face. FFS can include softening the brow line, rhinoplasty (nose job), smoothing the jaw and forehead, and altering the cheekbones. Each person is unique and the procedures that are done are based on the individual's need and budget,
Transmasculine is a term inclusive of trans men and non-binary trans people assigned female at birth.
Gender confirmation procedures that a transmasculine person may undergo include:
- Masculinizing genitoplasty is the surgical creation of external genitalia. This procedure uses the tissue of the labia to create a penis.
- Phalloplasty is the surgical construction of a penis using a skin graft from the forearm, thigh, or upper back.
- Metoidioplasty is the creation of a penis from the hormonally enlarged clitoris.
- Scrotoplasty is the creation of a scrotum.
Procedures that change the genitalia are performed with other procedures, which may be extensive.
The change to a masculine appearance may also include hormone therapy with testosterone, a mastectomy (surgical removal of the breasts), hysterectomy (surgical removal of the uterus), and perhaps additional cosmetic procedures intended to masculinize the appearance.
Paying For Gender Confirmation Surgery
Medicare and some health insurance providers in the United States may cover a portion of the cost of gender confirmation surgery.
It is unlawful to discriminate or withhold healthcare based on sex or gender. However, many plans do have exclusions.
For most transgender individuals, the burden of financing the procedure(s) is the main difficulty in obtaining treatment. The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed.
A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019.
Traveling Abroad for GCS
Some patients seek gender confirmation surgery overseas, as the procedures can be less expensive in some other countries. It is important to remember that traveling to a foreign country for surgery, also known as surgery tourism, can be very risky.
Regardless of where the surgery will be performed, it is essential that your surgeon is skilled in the procedure being performed and that your surgery will be performed in a reputable facility that offers high-quality care.
When choosing a surgeon , it is important to do your research, whether the surgery is performed in the U.S. or elsewhere. Talk to people who have already had the procedure and ask about their experience and their surgeon.
Before and after photos don't tell the whole story, and can easily be altered, so consider asking for a patient reference with whom you can speak.
It is important to remember that surgeons have specialties and to stick with your surgeon's specialty. For example, you may choose to have one surgeon perform a genitoplasty, but another to perform facial surgeries. This may result in more expenses, but it can result in a better outcome.
A Word From Verywell
Gender confirmation surgery is very complex, and the procedures that one person needs to achieve their desired result can be very different from what another person wants.
Each individual's goals for their appearance will be different. For example, one individual may feel strongly that breast implants are essential to having a desirable and feminine appearance, while a different person may not feel that breast size is a concern. A personalized approach is essential to satisfaction because personal appearance is so highly individualized.
Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review . Transgend Health . 2018;3(1):159-169. doi:10.1089/trgh.2018.0014
Morrison SD, Vyas KS, Motakef S, et al. Facial Feminization: Systematic Review of the Literature . Plast Reconstr Surg. 2016;137(6):1759-70. doi:10.1097/PRS.0000000000002171
Hadj-moussa M, Agarwal S, Ohl DA, Kuzon WM. Masculinizing Genital Gender Confirmation Surgery . Sex Med Rev . 2019;7(1):141-155. doi:10.1016/j.sxmr.2018.06.004
Dowshen NL, Christensen J, Gruschow SM. Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information . Transgend Health . 2019;4(1):131-135. doi:10.1089/trgh.2018.0055
American Society of Plastic Surgeons. Rhinoplasty nose surgery .
Rights Group: More U.S. Companies Covering Cost of Gender Reassignment Surgery. CNS News. http://cnsnews.com/news/article/rights-group-more-us-companies-covering-cost-gender-reassignment-surgery
The Sex Change Capital of the US. CBS News. http://www.cbsnews.com/2100-3445_162-4423154.html
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
The Financial Cost of Being Transgender in Canada
Part 2: we focus on some of the financial challenges faced by the transgender community, both hidden and open.

Work and Money Under Canada’s Federal Employment Act , employers “shall implement employment equity by identifying and eliminating employment barriers against persons in designated groups”. The four designated groups are women, aboriginal peoples, persons with disabilities, and members of visible minorities. Neither sexual orientation nor gender identity are protected classes. However, transgender Canadians are not without anti-discrimination protections. Gender and sexual minority people are named in and protected by Section 3(1) of the Canadian Human Rights Act . Still, there’s a gap between theory and practice. Egale , a Canadian advocacy group and a leader in research on the nation’s LGBTIQ2S issues, has perhaps the most up-to-date and comprehensive data on this matter. In their 2020 report on workplace discrimination , Egale notes that LGBTIQ2S Canadians continue to face widespread inequity, particularly in terms of access to safe work, and inequity is more pronounced for transgender, Two Spirit, and gender non-conforming people. This is borne out by the Trans PULSE 2011 report on workplace discrimination , which found that just 37% of transgender Ontarians were working full-time, while 20% were unemployed or on disability. The higher rates of un- or under-employment in these populations “are despite having an overall higher rate of qualifications.” A reported 71% have some college or university but approximately half earn $15,000 or less per year. As with the broader community, the effects of workplace discrimination go far beyond wage loss. Employment can provide access to good housing and educational opportunities, as well as benefits like medical, mental health care, and dental coverage, bonuses, paid leave and vacations, and investment power in the form of RRSP contribution room and matching employer contributions. Health Care Canadians enjoy universal healthcare—but just how universal is it? Among the services not covered are prescription drugs, dentistry, and mental health care. For those without employer plans, these expenses can be out of reach, particularly for low income Canadians. The Standing Committee on Health released a report in 2019 on the health of LGBTIQ2S Canadians and found that between 20% and 30% of transgender people who needed emergency services did not go to the ER, and of those who did, 52% had negative experiences. Refusal of service, inappropriate or invasive questions, misgendering, and other forms of discrimination all contribute to a health care system that can be hostile to transgender people. In this context, it’s not surprising that transgender Canadians underuse available health care services. For a more comprehensive discussion of the costs of health care refer to part one of this series. Specific to the transgender community, there are two aspects of health care worth a closer look: fertility and adoption, and gender affirmation. Fertility and Adoption In addition to adoption and reproductive technologies like intra-uterine insemination (IUI), surrogacy, or in vitro fertilization (IVF), there are fertility preservation strategies for transgender people who have eggs or sperm. For those who have eggs , in addition to IUI or IVF, embryo or egg freezing and storage, prior to hormone therapy (if applicable) may be an option. The costs of this procedure varies by clinic but are estimated to be about $10,000 to extract and $300 per year to store. If and when the time comes to transfer, there is an addition fee of around $2,000. For those who have sperm , banking for future use may a good option. As always, costs vary but the sperm extraction is usually in the neighbourhood of $2,000 with an additional $450 to freeze and around $400 per year to store. There may also be extra handling fees. Gender Affirmation Although medical interventions are only one aspect of the transition process, and not necessary to claim a transgender identity, many trans folks opt for one or all of the following: counselling, hormone therapy, or surgery. Visits with psychologists or clinical counsellors are not covered by basic health care but may be within some employer or extended plans. That said, there some programs across the country, such as Gender Journeys through Sherbourne Health Centre in Toronto, that offer free group sessions for transgender or questioning Canadians. For those without local resources or who want to go the private route, fees for psychologists or counsellors run anywhere between $100 and $300 per hour. Hormone therapies include the administration of testosterone, estrogen, and hormone blockers, all of which are designed to alter secondary sex characteristics such as body hair, voice, and fat distribution. Some Canadians with employer benefits or extended health care plans, or those on disability or social assistance, may be eligible for funding towards their hormone therapies but these are generally an out-of-pocket expense. Gender affirming surgeries include “top surgeries” such as a mastectomy or breast implants and “bottom surgeries” like a hysterectomy, vaginectomy, vulvoplasty, orchiectomy, metoidioplasty, scrotoplasty, and phalloplasty. Coverage for these procedures varies but many are available under provincial health care plans. Extended insurance might broaden the coverage. Other costs to consider that are not typically covered are facial feminization or masculinization procedures, vocal coaching, prosthetics, hair removal, and body contouring. Identity Documentation Should a transgender person want to change their name, it will cost between $100 and $137, depending on province of residence. Afterwards, or in the case of changing a gender marker, they’ll need to update their identification. Again, the fees differ according to location but in Ontario, the cost for a replacement birth certificate is $35. A replacement driver’s license is $35.75. Note: *LGBTIQ2S is an acronym for lesbian, gay, bisexual, transgender, intersex, queer, and Two Spirit. It is uniquely Canadian, and may be understood in place of LGBT+. **In this piece, transgender is used to identify people within the “trans umbrella”. That is, people who identify as transgender, transsexual, genderqueer, non-binary, agender, bigender, and Two Spirit, among other identities of transgender experience. Importantly, a person may claim these identities independent of medical interventions like surgery or hormones, or of legal documentation such as name or sex designation markers.
To view this article, become a Morningstar Basic member.
Do you want to take control of your finances.
Find The Tools Here

These companies have come out with actions that speak louder than words

Now it's only the small investors who fall prey

The pandemic has amplified systemic injustices facing minority groups, women, immigrants, and ...

Activate your money for sustainability and impact

Investors need to step up in Nova Scotia lobster fishing rights issue
- ...Search the Article Archive

Does the dominance of aggressive growth stocks in your portfolio make you nervous?

Make it less painful and go in prepared.

Solid first quarter of revenue growth at Facebook and Instagram owner but shares fall on higher s...
:quality(80)/cloudfront-us-east-1.images.arcpublishing.com/morningstar/Q3KIND5VXRCNHHH6JQHCCYBSSA.png)
The stock of this narrow-moat company is undervalued by a remarkable 50%.

Value investor Dave Jiles is holding these ‘under-followed and under-appreciated’ Canadian names ...
About Author

Keph Senett Keph Senett is a Canadian freelance writer specializing in sport and community development, travel and culture, human rights, and personal finance--and the intersections between these interests.
- Company Website
- Our Signature Methodologies
Connect With Us
- Global Contacts
- Advertising Opportunities
Terms of Use Privacy Policy Disclosures Accessibility
The Morningstar Star Rating for Stocks is assigned based on an analyst's estimate of a stocks fair value. It is projection/opinion and not a statement of fact. Morningstar assigns star ratings based on an analyst’s estimate of a stock's fair value. Four components drive the Star Rating: (1) our assessment of the firm’s economic moat, (2) our estimate of the stock’s fair value, (3) our uncertainty around that fair value estimate and (4) the current market price. This process culminates in a single-point star rating that is updated daily. A 5-star represents a belief that the stock is a good value at its current price; a 1-star stock isn't. If our base-case assumptions are true the market price will converge on our fair value estimate over time, generally within three years. Investments in securities are subject to market and other risks. Past performance of a security may or may not be sustained in future and is no indication of future performance. For detail information about the Morningstar Star Rating for Stocks, please visit here
The Morningstar Medalist Rating is the summary expression of Morningstar’s forward-looking analysis of investment strategies as offered via specific vehicles using a rating scale of Gold, Silver, Bronze, Neutral, and Negative. The Medalist Ratings indicate which investments Morningstar believes are likely to outperform a relevant index or peer group average on a risk-adjusted basis over time. Investment products are evaluated on three key pillars (People, Parent, and Process) which, when coupled with a fee assessment, forms the basis for Morningstar’s conviction in those products’ investment merits and determines the Medalist Rating they’re assigned. Pillar ratings take the form of Low, Below Average, Average, Above Average, and High. Pillars may be evaluated via an analyst’s qualitative assessment (either directly to a vehicle the analyst covers or indirectly when the pillar ratings of a covered vehicle are mapped to a related uncovered vehicle) or using algorithmic techniques. Vehicles are sorted by their expected performance into rating groups defined by their Morningstar Category and their active or passive status. When analysts directly cover a vehicle, they assign the three pillar ratings based on their qualitative assessment, subject to the oversight of the Analyst Rating Committee, and monitor and reevaluate them at least every 14 months. When the vehicles are covered either indirectly by analysts or by algorithm, the ratings are assigned monthly. For more detailed information about these ratings, including their methodology, please go to here
- CSPS Executive
- Why Choose a Plastic Surgeon?
- Testimonials
- Locate a Surgeon
- Choosing a Plastic Surgeon
- Birth Conditions
- Breast Reconstruction
- Breast Reduction
- Burn Reconstruction
- Hand Surgery
- Skin Cancer
- Body & Wound
- Blepharoplasty (Eyelid Lift)
- Body Contouring
- Breast Augmentation
- Breast Lift
- Liposuction
- Rhinoplasty (Nose Job)
- Soft Tissue Fillers
- Skin Resurfacing
- Laser Hair and Tattoo Removal
- Moles, Cysts and Skin Blemishes
- Apply to be a Member
- Registration
- Scientific Program
- Scientific Award Winners
- Call for Abstracts
- Abstract Reviewer Login
- Code of Ethics
- Training Programs
- Young Surgeons
- Fellowships
- International Meetings
- Canadian Wait Times Alliance
- Plastic Surgery Education Network
- Lifetime Achievement Award
- Clinical or Outcomes Research Grant
- Philanthropic donations
- Global Surgery Map
- Global Surgery Map Submissions
Gender-Affirming Surgery
- Members only
- Past Scientific Programs
- Practice Opportunities
- Women Plastic Surgeons of Canada
- President’s Medal
- Board of Directors
- Visiting Professor Funding
- Humanitarian Missions
Plastic surgeons provide gender-affirming surgeries for the treatment of gender dysphoria with the aim of helping a person physically actualize their internal sense of self. The goals of these procedures are therefore patient specific and can vary beyond the gender binary.
Gender-affirming surgeries can be grouped into four main domains: facial, chest, body and genital procedures. Talking to your plastic surgeon about your individual transition will help direct which surgery options are best for you. Below are some commonly performed procedures, however, all patients should discuss both variations and the spectrum of options with their surgeon individually to make sure their chosen procedures match their individual needs and goals.
Please click here ( https://www.wpath.org/publications/soc ) for information from the World Professional Association of Transgender Health (WPATH) on information on preparing for Gender-affirming surgery.
Facial Gender-Affirming Surgery
Facial procedures can either masculinize or feminize the appearance of the face.
To enhance a feminine appearance, both bony anatomy and soft tissue augmentation can be done. Hairline lowering, forehead shortening and forehead contouring are typically done in a combination to achieve an overall feminine appearance of the upper face. Alterations to the middle face include rhinoplasty and upper lip lifts. Fat grafting can also be used to create fuller and softer cheeks. For the lower face, the jawline can be softened and reduced with mandible contouring. Finally, the thyroid cartilage can be reduced to feminize the appearance of the “Adam’s apple” and voice procedures can be used to increased vocal pitch.
Due to the effects of gender-affirming hormones therapy (testosterone) on the skin and facial hair growth, facial masculinization surgery is much less common. Some examples of surgical procedures include facial implants for augmentation of the jawline or chin.
Gender-Affirming Chest Surgery
Gender-affirming mastectomy is the most commonly performed gender-affirming surgical procedure, often referred to as “top surgery”. The most frequently performed technique is the “double incision with free nipple graft” where the breast tissue and excess skin is removed in addition to removing, re-sizing, re-shaping and replacing the nipples as free grafts. Some patients choose not to keep their nipples. Alternative techniques exist when minimal skin removal is needed. Additionally, chest reduction surgery is an option for patients who wish to keep some of their breast tissue.
Breast augmentation is available for patients who aim to increase their breast size. A minimum of 12 months of gender-affirming hormone therapy with estrogen should take place prior to considering or evaluating an individual for breast augmentation. Usually, silicone implants are used. Your surgeon will discuss variation in scar placement techniques.
Genital Gender-Affirming Surgery
For individuals assigned male at birth, options for orchiectomy (testicle removal) in isolation or in combination with vulvar procedures can be done for gender affirmation. Vulvar procedures include either a vulvoplasty or a vaginoplasty. Vulvoplasty refers to creation of an external vulva without a vaginal canal while vaginoplasty similarly creates the external genitalia in addition to a vaginal canal capable of receptive penetrative intercourse. The preoperative preparation for these surgeries varies and may influence your choice of treatment. Vaginoplasty typically requires extensive pre-operative hair removal and a post-operative dilation regimen.
Genital gender-affirming surgery for individual’s with assigned female at birth anatomy falls into two main categories: metoidioplasty and phalloplasty. In both categories the main differentiating factor between the various surgical options is the desire to stand to urinate. While metoidioplasty is done using only pre-existing genital tissue, phalloplasty requires tissue to be transferred from somewhere else on the body to construct the penis. Phalloplasty surgery is often done over multiple stages meaning more than one surgery is required to obtain a functioning phallus capable of standing urination. Many variations of phalloplasty exist. The traditional phalloplasty includes urethral lengthening with the goal of standing urination. Other variations of phalloplasty, referred to as “shaft-only” phalloplasty are increasingly performed. Shaft-only phalloplasty refers to the creation of a phallus without lengthening the uretha. Options in addition to a shaft only phalloplasty include vaginectomy, perineal urostomy, clitoral burial and scrotoplasty, depending on patient goals and individual preference.
Gender-Affirming Body Contouring
Gender-affirming body contouring includes liposuction or fat grating to change the distribution of adipose tissue in the body. Liposuction is done to help narrow the hips and alter the shape of the body. Conversely fat grafting can help augment the buttock and hips to accentuate curves.

Breast Reconstruction Awareness Day - BRA-Day
BRA Day is an initiative designed to promote education, awareness and access for women who may wish to consider post-mastectomy breast reconstruction.
Only physicians who are certified in Plastic Surgery are Plastic Surgeons. There is no foolproof way to choose a Plastic Surgeon or to guarantee your results. However, there are a few basics, which can help you to decide.
Medical Professionals
The Canadian Society of Plastic Surgeons comprises nearly 500 Plastic Surgeons and is focused on sharing knowledge and expertise, improving quality of care, and advancing the practice of plastic surgery in Canada.
- 2021 CSPS Conference Archives
- Global Outreach
- History of the CSPS
- Reconstructive Procedures
- Aesthetic Procedures
- President’s Medal
- Membership Application
- Pay Member Dues
- Annual Meeting
- Information for Plastic Surgeons
- Continuing Professional Development
- Dr. Kimit Rai Family Scholarship
- Privacy Policy
Mailing Address
Street address.
- Contactez-nous
- Politique de confidentialité
Ontario boosts access for trans people seeking gender confirmation surgery
People left waiting 2 years to get surgical referral from camh gender identity clinic.

Social Sharing
There are potentially more than 800 health-care professionals across the province who can now assess patients for sex-reassignment surgery, a change Ontario adopted March 1 to trim the more than two-year wait list for referral.
- Ontario expands referrals for sex-reassignment surgery
- Why transgender people can't get surgery approval in Thunder Bay
Until last week, transgender people hoping to undergo sex-reassignment — also known as gender confirmation surgery — could only get a referral through the adult Gender Identity Clinic at Toronto's Centre for Addiction and Mental Health.
And that wait list for referral has stretched to more than 1,500, the psychiatrist who heads up the clinic said.
"The model of having only one clinic for all of Ontario might have worked when only a small number of seeking these services, but now there are far more," Dr. Chris McIntosh said. "We really feel like this is a great step forward in terms of increasing access."
The province announced the change to the referral process in November, which will see a wide range of health-care practitioners able to refer patients once they are trained in the assessment criteria created by World Professional Association for Transgender Health.
No surgical options in Ontario
Rainbow Health Ontario has already taken more than 800 health professionals through the training, which includes information about surgical and hormone options, how to help someone prepare for a procedure and the necessary support a patient will need after an operation. The majority of those trained so far have been mental health professionals, according to a spokesperson for Rainbow Health.
Donna Turner said the group is still waiting to learn exactly how clinicians who have taken that training can ensure their patients are included in the pipeline for insured candidates receiving gender confirmation surgery in Montreal.
Right now there are no surgical options in Ontario, although Health Minister Eric Hoskins said the expansion of the referral program includes a promise of $2 million, some of which will go toward supporting a program for chest surgery that could run out of Women's College Hospital. A spokesman for the ministry could not say when such a program might begin.
Dr. McIntosh acknowledged that the expansion of the referral service could mean "the bottleneck stops being at CAMH and starts happening in Montreal," but both he and Turner said the Quebec clinic has indicated it can take on more patients.

Rainbow Health and CAMH both expect to help with continued training for surgical referral, McIntosh and Turner said. Some of the provincial funding has already been earmarked to hire more staff at CAMH to clear the backlog of those waiting — and so practitioners there can begin training others, according to a statement from the health ministry.
In an announcing plans to expand the referral system, the health minister said last fall that an increasing number of Ontarians are experiencing gender dysphoria, defined as the distress caused by a conflict between a person's gender identity and their assigned sex at birth.
"One of the most vulnerable times for trans people is when they are ready for surgery, but face a prolonged wait," Hoskins said in November. "This change would reduce wait times by allowing many trans clients to get surgical approvals from their own local primary care teams.
Getting family doctors involved
McIntosh said that's a huge advantage to the expansion. A patient's own doctor — who understands their history — can now be part of a critical medical decision, the psychiatrist said.
Those on the waiting list, however, should not cancel their appointments at CAMH, McIntosh said, until they are certain they can see another physician or nurse practitioner who has the appropriate training to make a referral.
Two referrals are still needed for people seeking genital surgery, while only one is necessary for chest surgery.
If two referrals are needed, one can be performed by a nurse, a social worker with a masters degree or a psychologist. But a physician or a nurse practitioner must be always involved in at least one referral for surgery, according to the guidelines.
"This provides flexibility that the person's own care provider — that's known the person for a long time … can contribute to the decision of assessing someone's readiness for surgery," McIntosh said.
Clarifications
- A previous version of the story indicated that nurses, social workers, and psychologists could provide a referral for chest surgery. In fact, only a physician or a nurse practitioner can, while qualified mental health professionals can provide a second referral for genital surgery. Mar 07, 2016 12:24 AM ET
Related Stories
- Ontario expands referrals for gender reassignment surgery
- Audio Why transgender people can't get surgery approval in Thunder Bay

- Before & After Aesthetics
- Out of Town Patients
You must be at least 19 years old to view this site.
Are you at least 19 years old?
Sorry, you are not old enough to view this site.
Book a Consultation
Don’t hesitate to contact McLean Clinic today to learn more about double incision top surgery and other types of FTM top surgery. A member of our staff will be more than happy to assist you.
How Long It Takes to Get Gender-Affirming Surgery Across Canada
Share article.

In the recent years, transgender health care in Canada has seen dramatic improvements. More provinces have expanded their public healthcare packages to accommodate gender-affirming surgeries, including FTM/N top surgery or genital reconstruction procedures, for gender dysphoria treatment. However, access and availability of transition-related treatments are still far from reach for most members of the LGBTQ+ community because of the long wait times.
What's the average waiting time to get a gender-affirming surgery in Canada? The country's first study on transgender patients' experiences published in 2017 by researchers from the University of British Columbia revealed it's anywhere from one month to nine years. The results of the study showed frustrating inconsistencies in trans patients' experience across the country.
In this article, we break down the study's key findings to pinpoint where the bottleneck is coming from and what's causing the delay in delivering life-saving surgical procedures for the Canadian LGBTQ+ population .
1. Surgery Readiness Assessment
The application process towards a gender-affirming surgery in Canada is divided into several steps. The first one is a surgery readiness assessment. Whether you are getting a transition-related operation done from a publicly funded or private clinic , a surgical readiness assessment is required by most surgeons to ensure that a potential patient is prepared and will get the best results post-surgery.
According to Trans Care BC , the primary criteria for most types of gender-affirming surgery in British Columbia are:
- Persistent gender dysphoria
- Capacity to consent to the procedure
- Medical and mental health conditions are reasonably well-controlled
- Being of the age of majority (In BC, the age of majority is 19. If you're under 19, your surgeon may recommend additional surgery readiness assessment steps).
The Assessment Process
Before even receiving a readiness assessment, the individual needs to follow several processes to qualify for one. This can range from:
Getting referred to an assessor through your primary care provider:
- They can send a referral for a surgical readiness assessment directly to a qualified assessor, or
- Can send a request to your province's health care office who can refer you to a qualified assessor in your community, or
- They are a qualified assessor who can carry out the assessment themselves.
Depending on the type of gender-reaffirming surgery, one or two assessments carried out by different assessors may be required. Surgical readiness assessments can be covered if they are qualified assessors working in the publicly-funded health care system. You can also have them conducted by qualified private assessors, such as psychologists or clinical counsellors.
Getting assessed:
Once you've been referred, you have to wait for a schedule for your surgical readiness assessment. The actual appointment lasts between one to two hours, where you'll discuss your gender identity , medical history, and surgical aftercare plan . In some cases, you may be asked to come back to provide additional information.
Get a recommendation:
The qualified assessor may or may not recommend you for surgery or recommend you return for further assessment. They would send their recommendation directly to your primary care physician, who will send you a referral for surgery.

Waiting Time for Surgery Readiness Assessment
In British Columbia, most people (60%) easily or very easily got referred to an assessor, and half of these trans people (50%) did not have to spend any money on their assessment appointment(s).
Half (50%) of the respondents in BC waited 150 days or less between the referral and their most recent surgery readiness assessment appointment. This is in contrast to the average of 180 days other patients in the country reported. However, BC's wait time also had unusual fluctuations, with some people waiting for a single day to as long as 1,825 days or more than five years.
On the other hand, the average wait time between referral and assessment in BC also differed according to the types of gender-affirming surgery planned.
- Vaginoplasty - 212 days
- Labiaplasty - 255 days
- Chest surgery - 318 days
- Orchiectomy - 322 days
- Hysterectomy-336 days
- Tracheal shave* - 364 days
- Phalloplasty- 383 days
- Breast augmentation -572 days
- Facial feminization - 607 days
2. Funding Approval
Data suggests that for all types of gender-affirming surgery in Canada, 71% had their surgery paid for, at least partially, through a government health care plan . The vast majority (93%) only had one source of funding. Almost seven out of 10 Canadians had their transition-related surgery funded with a public health plan, and one in three people said they used their own money as their sole source for surgery funding.
Unfortunately, not everyone receives approval for the life-changing surgery they had in mind. Aside from having an existing medical condition that increases the risk of being on general anesthesia, many hopefuls are deemed ineligible due to two primary reasons:
- Breast augmentation criteria MSP criteria specifies that the patient should have been on hormone replacement therapy for at least 18 months (unless not clinically indicated) and that there's been less than an AA cup of breast growth or significant asymmetric breast growth greater than one and a half cup size difference. Most respondents feel that these are not enough to make them feel good or feminine enough about their bodies
- BMI (body mass index) Many gender-affirming surgeons have BMI eligibility criteria of 35 and below. They say they will not operate on an individual above this BMI due to hospital or clinical restrictions, clinical safety, and patient results.
3. Waiting for Surgery
After getting approved for funding, the vast majority of participants (84%) said they did not have any problem getting a referral to a surgeon for gender-affirming surgery. More than half (57%) also said they were able to choose the surgeon they wanted.
The average wait time between getting an approval and surgery date was less than 12 months or less for half of the surgeries in BC. In other parts of Canada, the wait time was eight months or less for half the surgeries.
The researchers said each patient's experiences were so diverse, with waiting times ranging from a month up to 108 months or nine years. The longest wait times were reported in the following gender-reaffirming surgeries in Canada:
- Orchiectomy
- Breast augmentation
- Phalloplasty
- Chest surgery
Interestingly, the researchers also noted that 50% of the people taking the survey were currently waiting for their surgery and/or had a scheduled surgery date, and had already been waiting for at least 17 months. Half of the people who were now waiting for surgery but did not have a scheduled surgery date had been waiting 11 months or more when they took the survey.

What's Taking So Long?
Elizabeth Saewyc, one of the lead authors on the study, gave VICE a few valid points regarding what her thoughts were on the potential causes of the long waiting process for accessing gender-affirming surgery in Canada .
- Different training in general physicians and frontline medical staff
- Saewyc says the wait time during the pre-approval stage could be due to doctors who are clueless about where to begin, contributing to the "lack of clarity in the pathway" and impeding the transition process for trans patients.
- Capacity issue
- There's a lack of surgeons and specialists in the field, which is why it takes time before one can get an appointment with, say, a top surgeon.
- Lack of specialty clinics
- For "bottom" surgeries, like vaginoplasty and phalloplasty, Canadians are limited in choice to only one clinic located in Montreal.
Wait Times Worsened by the COVID-19 Pandemic
The long wait times for gender-affirming surgery in Canada have been exacerbated exponentially by the unexpected arrival of the COVID-19 pandemic. Both public and private hospitals and clinics had to cancel scheduled surgeries and other transition-related procedures to adhere to stringent lockdown restrictions placed in different countries worldwide. Currently, we see many health care providers tackling their backlogs with surgeries booked up to 2022.
The Negative Impact of Long Wait Times
One of the biggest concerns caused by the long wait times in gender-affirming surgery in Canada would be its detrimental effects on the mental health of the LGBTQ+ population , who are already at an increased risk for:
- Depression
- Obsessive-compulsive and phobic disorders
- Substance use
- Post-traumatic stress disorder
- Suicide and self-harm
This is cemented in a quote by N. Nicole Nussbaum, former president of Canadian Professional Association for Transgender Health and staff lawyer at Legal Aid Ontario, "Trans people are at the highest risk of suicide and self-harm between the period that they've mentally decided to transition and when they complete their medical transition ."
For inquiries about gender-affirming surgery in Canada or to learn more about what an FTM top surgery at McLean Clinic is like , don’t hesitate to reach out to us. A member of our team will be more than happy to answer your questions.
Contact McLean Clinic today!
Related Articles

The Average Cost of Top Surgery Across Canada

10 Reasons Why Toronto is the Most LGBTQ+ Friendly City

A Brief History of Toronto’s Gay Village


Frequently Asked Questions Regarding Change of Sex Designation For Trans Persons
Home » GET INFORMED » Talk Rights » Frequently Asked Questions Regarding Change of Sex Designation For Trans Persons
May 19, 2015
Like all content on this website, this document is not legal advice and is provided solely for the purpose of public information and education. If you are facing a legal issue or have a question about your specific situation, you should consider seeking independent legal advice. You can find a list of legal clinics and other resources to help you here.
The CCLA is a national organization that works to protect and promote fundamental human rights and civil liberties. To fulfill this mandate, the CCLA focuses on litigation, law reform, advocacy and public education. Our organization is not a legal clinic. As such, we are typically not in a position to provide members of the public with legal advice or direct legal representation. However, we do try to provide general legal information and appropriate referrals where possible. For questions about this document, email publicenquiries [at] ccla [dot] org.
How can Trans Persons Change the Sex Designation on their Birth Certificate?
This guide is focused on issues relating to how trans persons can change the sex designation on their birth certificates. For information on how trans persons can legally change the name used on their identification documents, see this guide .
This page is intended to help trans persons with issues related to changing the sex designation on their birth certificates. As such, some of this information may not be helpful to those seeking to change their birth certificates for another reason.
Note: Every effort has been made to ensure comprehensiveness and accuracy (as of May 2015). However, this FAQ may not fully reflect the current state of the law.
We use the term “trans” to include anyone who does not identify with the sex designation they were assigned at birth.
Questions addressed in this FAQ:
Why might I want to change the sex designation on my birth certificate?
Should i have to have surgery in order to change the sex designation on my birth certificate, are sex designations on birth certificates even necessary, how can i change the sex designation on my birth certificate, where do i apply to change the sex designation on my birth certificate, what proof do i need to show in order to change the sex designation on my birth certificate do i need to show proof of surgery, can i apply if i am younger than 18 or 19, can i apply even if i was born outside of my current province/territory.
You can download a PDF of this document here: CCLA Change of Sex Designation FAQ .
Many trans persons consider the sex they were assigned at birth to be inaccurate. If this is you, changing the sex designation on your birth certificate may be important for your well-being. It is also important for legal reasons as well.
In order to enjoy a greater degree of safety and freedom from discrimination, you may want to have identification documents that match the gender with which you identify and present yourself. The information on most identification documents is drawn from birth certificates, so changing your birth certificate is often a necessary first step. “Sex” is a category on most driver’s licenses, passports and health cards, and so you may find yourself being forced to discuss your gender identity – sometimes even your genitals – with a stranger. This is even worse when that stranger is empowered to make decisions that greatly affect you, such as whether to write you a traffic ticket, offer you a job, refer you for medical treatment, or let you enter the country.
Trans persons face widespread discrimination and high rates of violence. Of trans Ontarians surveyed by the Trans PULSE Project, 26% reported being hit or beaten up because they were trans, 73% reported being made fun of, and 39% reported being turned down for a job. In 2010, Trans PULSE estimated that 50% of trans Ontarians had seriously considered suicide at some point in their lives because of the discrimination they faced. Involuntary outing on a regular basis, such as by having an inaccurate gender specified on your identification documents, eliminates one of the few mechanisms you may have to protect yourself from transphobia.
In 2014, a judge in Alberta considered the constitutionality of the provincial law that regulated gender markers on birth certificates. The judge struck down that law, because it was contrary to the Canadian Charter of Rights and Freedoms . In doing so, the judge cited a prior decision of the Ontario Human Rights Tribunal. That decision detailed some of the discrimination faced by trans persons (referred to here as “transgendered” [sic]):
“[T]ransgendered persons as a group tend to face very high rates of verbal harassment and physical assault and are sometimes even murdered because of their transgendered status. […] [I]t is very difficult for a transgendered person to find employment, […] there are very high rates of unemployment among transgendered people generally, and […] many transgendered people are fired once they are exposed in the workplace as being transgendered.”
These concerns also extend to young trans persons, who may be forced to endure bullying by their peers if the sex designation on school records does not match their gender identity.
Many trans persons want the benefits of official documents that correspond to their identity but may not want to undergo surgery. They may be content with the use of hormones or simply by presenting themselves consistently with their gender identity.
Gender reassignment surgery can be expensive, difficult to access, and carries the risks associated with any surgery. In addition, it has been reported to typically cause sterility . Gabrielle Bouchard of the Montreal-based Centre for Gender Advocacy has said the surgical requirement in order for official documents to be changed amounts to mandatory sterilization. The surgery requirement also emphasizes biological sex characteristics rather than gender identity. Even after surgery has been performed, a second doctor must sometimes “confirm” the surgery. C.F., the plaintiff in the Alberta court case mentioned earlier, told the Edmonton Journal :
“What this legislation requires is that you not only submit to dangerous, risky surgery, but then actually attend for a humiliating genital inspection before two separate physicians, both of whom will make a value judgment about whether your genitals are sufficiently female[.] It’s like something from ages gone by. It’s very disturbing stuff.”
Due to these types of concerns, there have been and continue to be legal challenges to the various provincial legislation that require reassignment surgery in order to change sex designation. In the Ontario and Alberta decisions discussed earlier, the requirement for gender reassignment surgery was found to be discriminatory. As a result of these rulings, several provinces, including Alberta, British Columbia, Manitoba, Ontario, and Quebec, have taken steps to amend their laws to remove reassignment surgery from the requirements necessary in order for you to change your sex designation. Nova Scotia has also indicated that it plans to amend its legislation to remove the surgery requirement.
Some activists have argued for the removal of sex designations from identification documents altogether, on the basis that gender identity is not a binary classification. The binary does not accommodate people who do not identify with a binary gender classification.
Ongoing cases challenging legislation in British Columbia , Saskatchewan and Quebec are seeking the removal of sex designations from birth certificates. So far, although several provinces have removed the surgery requirement, no province has taken the step of removing sex designations altogether or providing for a third non-binary option.
In contrast, several countries, including Australia and Germany , now allow persons to designate their sex on their passport with an “X”. However, some trans rights advocates argue that the “X” continues to out trans persons, and is used as an excuse for not eliminating the surgery requirement. An Australian court has ordered the government to register a third category of sex designations on birth certificates and name change certificates.
For more on the possibility of non-binary gender designations, see the BC Law Institute’s report , where the Institute highlights the implications and consequences of different solutions to providing a non-binary sex designation in Canada.
All provinces and territories except Nunavut have procedures for changing sex designations when a person has undergone gender reassignment surgery.
The rules for changing the sex designation on a birth certificate vary from province to province. They are also changing rapidly. In all provinces except Quebec, where the Civil Code governs these issues, the law concerning birth registration is found in the provincial Vital Statistics Act and associated regulations. These laws and regulations can be consulted for free on http://canlii.org . Note that a province may have policies that are not in the legislation. For more information about requirements, check with the government agency responsible for birth certificates in your province or territory (listed below), or with a trans advocacy organization, such as Egale Canada .
Many provinces require letters from a mental health professional in order to change a person’s gender marker or name. Such a letter may also be required to access sex reassignment surgery.
Online government information is limited outside British Columbia, Manitoba and Ontario. Where specific information regarding change of sex designation is unavailable on a province’s website, the links below provide contact information for the appropriate agency.
Until recently, all provinces and territories required you to have gender reassignment surgery if you wanted to change the sex designation on your birth certificate. Ontario became the first province to drop this requirement in 2012 when, as mentioned previously, its human rights tribunal ruled the requirement was discriminatory. The Alberta Court of Queen’s Bench handed down a similar ruling in April 2014. Ontario has not officially amended their legislation, but are now registering changes without proof of surgery as a matter of policy. British Columbia, Alberta and Manitoba are the only provinces that have formally amended their legislation to eliminate the surgery requirement. In Alberta, the new requirements are set out in regulations .
New Brunswick, Newfoundland and Labrador, PEI and Saskatchewan all require applicants to document that they have undergone gender reassignment surgery, usually by having at least two physicians – the surgeon who performed the surgery and another who did not – certify that fact. Quebec and Nova Scotia also currently require proof of surgery, but changes to the law are on their way (see below). In Quebec, the second physician must practice medicine in Quebec. In New Brunswick and the Northwest Territories, the second physician must be licensed in any Canadian jurisdiction.
The law in this area is changing rapidly as legislation is amended and court challenges are brought regarding surgery requirements. Consulting the relevant statutes will not always give a full picture of the current requirements or upcoming amendments. For current information, contact a trans advocacy organization, such as Egale Canada .
You must provide:
A declaration, which provides your date of birth, and states that you identify with and maintain the gender identity that corresponds with your desired sex designation; and
Confirmation from a licensed doctor or psychologist licensed in Alberta or another jurisdiction that the sex designation on your birth certificate does not correspond with your gender identityBritish ColumbiaNo proof of surgery required;
A declaration, which states you have assumed, identify with and intend to maintain the gender identity that corresponds with your desired sex designation; and
Confirmation from a doctor or psychologist licensed in BC or the province or territory where you live that the sex designation on your birth certificate does not correspond with your gender identityManitobaNo proof of surgery required;
A declaration, which states you identify with the requested sex designation, you are currently living full-time in a manner consistent with the requested sex designation and you intend to continue doing so; and
A supporting letter from a health care professional licensed in Canada or where you live that your gender identity corresponds with the requested sex designationNew BrunswickProof of surgery requiredNewfoundland and LabradorProof of surgery requiredNova ScotiaProof of surgery still required, but a bill to eliminate the requirement has received royal assent. Under the new law, which is not yet in force, you will written statements from themselves and a member of a profession to be prescribed in the regulations that confirm your gender identity.OntarioNo proof of surgery required;
A declaration, which states your gender identity); and
A note from a doctor or psychologist licensed to practice in Canada that confirms your gender identityPrince Edward IslandProof of surgery requiredQuebecProof of surgery required, but change is pending;
The requirements under the new law have not been set yet.SaskatchewanProof of surgery requiredNorthwest TerritoriesProof of surgery requiredYukonProof of surgery requiredNunavutThere is no provision in the Vital Statistics Act for changing sex designation, even with surgery
Sex reassignment surgery is generally not performed on those under the provincial age of majority, as all clinics in Canada that currently perform reassignment surgery conform to the recognized Standards of Care . These Standards, which are regarding health care for trans persons, forbid irreversible interventions (such as surgery) on patients before they reach the age of majority. As a result, if you are a minor in Canada, you generally cannot change your sex designation in provinces or territories where proof of surgery is required.
In provinces that do not require surgery, the age requirements vary:
Note that legal challenges to the minimum age requirements are currently proceeding in several provinces, including Quebec and Saskatchewan . Click here to listen to an interesting radio interview with a 10 year old who would like to change the sex designation on her birth certificate.
Under new law (not yet in force) : No age minimum, but if you are under 16, you must have parental/guardian permission or apply to the Supreme Court of Nova Scotia for an order dispensing with the requirement of parental consent.OntarioNo age minimum, but if you are under 16, you must have parental/guardian permissionPrince Edward IslandNo age minimum, but surgery is required and will not be performed if you are under 18; in addition, if you are under the age of majority (18), you must have parental/guardian permissionQuebecAge minimum is 18.SaskatchewanNo age minimum, but surgery is required and will not be performed if you are under 18; in addition, if you are under the age of majority (18), you must have parental/guardian permissionNorthwest TerritoriesNo age minimum, but surgery is required and will not be performed if you are under 18; in addition, if you are under the age of majority (19), you must have parental/guardian permissionNunavutThere is no provision in the Vital Statistics Act for changing sex designationYukonNo age minimum, but surgery is required and will not be performed if you are under 18; in addition, if you are under the age of majority (19), you must have parental/guardian permission
British Columbia, Ontario and Northwest Territories will change sex designations only for births registered in their respective provinces. Some provinces will register a change of sex and then transmit it to the jurisdiction where the birth was registered.
Under new law (not yet in force) : Legislation requires that the applicant was born in Nova Scotia.OntarioLegislation requires that the applicant was born in OntarioPrince Edward IslandApplicants born outside of Prince Edward Island may apply, and the province will transmit their request to the jurisdiction where their birth was registered.SaskatchewanNo explicit requirement that the applicant was born in SaskatchewanQuebec Under the new law (not yet in force) : Legislation requires that the applicant was born in Canada and resides in Quebec, or that the applicant was born in Quebec and resides in a place where change of sex designation is unavailable or impossibleNorthwest TerritoriesLegislation requires that the applicant was born in Northwest TerritoriesNunavutThere is no provision in the Vital Statistics Act for changing sex designationYukonApplicants born outside of Yukon may apply, and the province will transmit their request to the jurisdiction where their birth was registered
For more information:
The Trans PULSE Project prepared a report for the Canadian Human Rights Commission on sex designation in federal and provincial IDs in 2012. The report was prepared for hearings on Bill C-279, a proposal to add gender identity and expression to the Canadian Human Rights Act and to hate crime provisions of the Criminal Code . The report can be found here .
In 2014, the British Columbia Law Institute prepared a report for the Uniform Law Conference of Canada on the state of the Canadian law regarding change of sex designation, and regarding options for reform in 2014. The report can be found here .
About the Canadian Civil Liberties Association
The CCLA is an independent, non-profit organization with supporters from across the country. Founded in 1964, the CCLA is a national human rights organization committed to defending the rights, dignity, safety, and freedoms of all people in Canada.
For the Media
For further comments, please contact us at [email protected] .
For Live Updates
Please keep referring to this page and to our social media platforms. We are on Instagram , Facebook , and Twitter .
Guest Author
Recommended for you.
Explainer: Alberta’s Controversial Critical Infrastructure Defence Act
Comments are closed.
400-124 Merton Street Toronto, ON M4S 2Z2 (416) 363-0321
STAY INFORMED
- Join Our Mailing List
- Get Involved
- Privacy Policy
- Social Media Policy
Charitable Registration Number: 754802288 RR0001
© 2024 CCLA.
- Race Religion & Ethnicity
- Indigenous Peoples
- Freedom of Expression
- Freedom of Religion
- Freedom of Association
- Right to Protest
- Democratic Rights
- Police Powers, Use of Force & Police Accountability
- Fair Trial, Due Process & Sentencing
- Prisons, Jails and Community Supervision
- Privacy Law Reform
- Surveillance & Technology
- Search & Seizure
- National Security
- Visit CCLET.org
- Bill 28 & Notwithstanding Clause
- Emergencies Act
- Federal Strip Searches
- Fighting Solitary Confinement
- Free Speech
- Racial Profiling
- Reproductive Rights
- Strip Searches in Ontario Prisons
- Toronto’s Smart City
- Vaccine Passports
- Press Releases
- In the News
- Our Mission
- How We Work
- Our History
- CCLA & The Charter of Rights and Freedoms
- The National Council
- Job Opportunities
- Financials and Annual Reports
- Clayton Ruby Fund
- Donation FAQs
- Make a Bequest in Your Will
- Law Students
- General Volunteering
- Run a Fundraiser
- Walk for Freedom
- Talk Rights
- Know Your Rights Guides & Other Resources
- Français du Canada
Wait times for bottom surgery in Canada can be as long as eight years. The impact on individuals can be deadly
The story of a 30-something Albertan shows how broken the Canadian system is. It may also be a gross violation of their human rights

Credit: Getty Images; Elham Numan/Xtra
“It’s harrowing.”
That’s how Ash describes the process of trying to access gender-confirming bottom surgery in their home province of Alberta. (Ash is not their real name. In order to protect them from possible retaliation by Alberta Health, Xtra has agreed to use a pseudonym.)
Almost three years after Ash, who is now in their 30s, got a referral from their family doctor to one of the province’s gender clinics, they still haven’t received provincial approval for this medically necessary operation—and it will likely be another nine months before they hear from the province. Even then, they’re not guaranteed to get approved at all. All it takes is one bureaucrat at Alberta Health to say no and they’re back to square one.
If Ash is approved for surgery, they’re still facing a wait of up to four years at the one clinic in all of Canada that performs bottom surgeries for trans Albertans. All told, even if Ash is approved soon, they’ll be facing a wait of about eight years total to receive care.
“It’s awful waking up every day and just feeling this weight, this misfortune of … having the wrong body parts that could be fixed,” Ash says. “Some days you wake up, and the only way to continue moving forward with your day is just to completely dissociate from yourself, which, of course, impacts how you go about interacting with other people. People do notice.”
Get free Xtra newsletters
Xtra is being blocked on Facebook and Instagram for Canadians as part of Meta’s response to Bill C18. Stay connected, and tell a friend.
Often, dissociating is the only way they can keep functioning. “The dissociation isn’t something that can be helped; it’s either that, or I let in the full emotion, discomfort, tangible pain of my existence.”
Ash received no mental health supports from Alberta Health Services during the years they were waiting for the gender clinic to process their referral. The waiting game they are currently playing with Alberta Health has caused them major depression, which they have had to hide for fear that their application for bottom surgery funding will be denied—a legitimate concern given that Alberta Health criteria prevents people with symptomatic depression from receiving funding.
The relational cost of that depression has been severe. “The depression, dysphoria and the dissociation I use as a defence mechanism have completely destroyed my marriage,” they say. “A relationship in which one individual is physically in limbo for such a long period of time simply can’t be maintained in a healthy way.”
All the while, they feel they’ve been “watching their life go by,” and worry constantly about whether they will receive bottom surgery at all.
“Is one person along the way with more power than me going to decide that, actually no, this person doesn’t deserve this surgery?” they ask.
Ash’s story is one told many times over across the country. The story of trans healthcare in Canada is one of lack of access, gatekeeping and provincial inaction. Many argue that these systemic problems may also be a gross violation of human rights.
A bureaucratic nightmare just to start access
Getting vaginoplasty and phalloplasty—more commonly known as “bottom surgery” or gender confirmation surgery—is an intensively bureaucratic process in Canada, one that involves a complicated interplay between public and private health agencies. A recent improvement in the bureaucratic tangle in Alberta reveals just how complicated it is to navigate the system in Canada.
In 2022, Alberta Health quietly revised its criteria for approving trans patients for gender confirmation surgery. Previously, approval required a psychiatrist’s diagnosis and referral, a slow process given the few qualified psychiatrists in the province. Now, any physician can make the required diagnosis of gender dysphoria, and any “ practitioner with extensive training or clinical experience in assessing and managing the needs of the transgender population ” may make a valid referral.
It would be difficult to overstate the sea change in trans health policy this revision represents.
Alberta Health Services operates a gender clinic in each of Alberta’s major cities: The Gender Program in Edmonton and the Adult Gender Clinic in Calgary . Both offer comprehensive medical, psychological and social support for people experiencing gender dysphoria. Until this year, both were also the only places in the province where trans people could reliably obtain referrals for gender-affirming bottom surgery.
The problem with the gender clinic model is, of course, facilitating access to the gender clinics themselves. At Edmonton’s Gender Program, the wait time for adults was between four and eight months in September 2022. At Calgary’s Adult Gender Clinic, wait times are currently closer to two years. And those are just the wait times to begin the process of securing the necessary documentation and referral for bottom surgery approval.
Xtra reached out to Alberta minister of health Adriana LaGrange to ask what the province was doing to reduce wait times at the gender clinics and received no response from the minister’s office as of press time.
However, by allowing any qualified physician to refer trans patients for bottom surgery—not just those psychiatrists who work at a gender clinic—Alberta is allowing patients to bypass the backlogged gender clinics, throwing open the door to vaginoplasty and phalloplasty access. Not a small thing in what is arguably Canada’s most conservative province. Indeed, this puts Alberta ahead of neighbouring Saskatchewan , which only accepts funding applications that include a referral from one of four provincially recognized physicians; and, in this respect, even British Columbia , which still requires trans people seeking bottom surgery to obtain a surgical recommendation from a pre-approved list of clinicians.
This doesn’t mean, however, that the fight for trans healthcare in Alberta has been easy, or that it’s over. By removing one bottleneck, the policy change in Alberta smacks hard against an even bigger bottleneck: there are only three clinics in the whole country that offer bottom surgery and two of them are off-limits to out-of-province residents. That means most Canadians, including those from Alberta, are funnelled into one clinic in Montreal where wait times can be up to four years long.
Accessing funding is one thing, accessing surgery is something very different
Like most provinces, Alberta outsources gender confirmation surgeries to a private hospital in Montreal: the Centre Métropolitain de Chirurgie (CMC).
Founded in 1973 , the CMC is the only private hospital in Quebec and one of only a handful of such hospitals in Canada. (Though privately run, the hospital accepts provincial health coverage, meaning patients access surgery for free.) Currently owned by Dr. Pierre Brassard, the CMC performs upward of 1,000 gender confirmation surgeries every year. It has been the exclusive provider of bottom surgery for Albertans since 1990, as well as, until recently, for most trans Canadians. The latest available data , published in 2019, indicates that in the three previous years, 90 percent of the patients who came to the CMC for gender-affirming surgery hailed from Canada with: 26 percent coming from Quebec, 35 percent from Ontario, 26 percent from the Western provinces and six percent from the Maritimes.
The CMC offers patients everything from a preoperative stay at the hospital’s partner hotel in Laval, Quebec, to a postoperative stay at the Asclépiade , the only hospital-affiliated convalescent home in the world dedicated specifically to the care of trans patients who have received bottom surgery, to the care of five surgeons specializing in some or all aspects of gender confirmation surgery.
But the wait-list to access gender confirmation surgery at the CMC is notoriously long. The hospital did not respond to a request from Xtra to confirm current average wait times for the operation. However, reporting by the CBC in March 2023 found that the current wait time to access surgery is currently more than four years from the time the CMC receives a referral from a provincial funding body, regardless of which province is submitting the referral.
And as Alberta increases the accessibility of public funding for bottom surgery, that wait time is likely to increase. That’s exactly what happened when Ontario similarly opened up the funding gates in 2016. In that province, the loosened referral rules caused a nearly threefold jump in the number of gender confirmation surgeries funded each year, from 158 in 2015 to 414 three years later.
Long wait times have been an issue for trans Albertans since the province began funding bottom surgery on an ad hoc basis in 1984 . That year, at the urging of trans healthcare advocate Dr. Lorne Warneke , the province sent three trans patients to Belgium for their surgeries.
In April 2022, the University of Calgary’s Public Interest Law Clinic (PILC) authored a report on the history and state of trans healthcare in Alberta. That report, which is not public, but has been provided to Xtra by the PILC, drew on internal government records obtained from Alberta Health through a 2018 Freedom of Information and Protection of Privacy request. It shows that, from the beginning, gender-confirmation surgery has been underfunded and inaccessible.
For the first decade that funding was available, from 1984 to 1994, there was no official policy or system for facilitating access to this medically necessary procedure. “It is most likely,” the report concludes, “that Dr. Warneke was pushing each application through the system [himself].”
It was only in 1996 , when Warneke founded the Edmonton Gender Program , that the Alberta government launched an official program to fund bottom surgeries out of the CMC. For the first 12 years that the program was in operation, however, funding was strictly limited to 16 surgeries per year—far short of the demand from trans Albertans. Just five months into the province’s 2008–2009 budgetary year, that quota had already been filled and trans patients were being wait-listed for surgeries in the following year.
Then, in order to save $700,000 a year—or roughly $0.18 per Albertan based on the population at the time—Alberta Health announced in April 2009 that it would be discontinuing funding for gender confirmation surgeries as an austerity measure. As Ron Liepert, minister of health and wellness at the time, put it in a speech to the provincial legislature, the decision to defund the program “was not based on medical decisions.”
The province never truly followed through on its plan to eliminate funding for bottom surgery; funding kept flowing in a limited capacity, and in 2012, Alberta officially reinstated the program with an annual budget of $1.1 million. That would be enough to cover approximately 25 bottom surgeries per year. In 2016 and 2017, that number grew to 38 surgeries; and in 2018 and 2019, the province funded 83 surgeries, a more than fivefold increase from the original 16 surgery cap.
As the number of surgeries increased, so, too, did wait times. While Edmonton’s Gender Program saw 580 patients in 2019 (the most recent year for which data is available), more than 650 other patients were on the wait-list for an initial consultation.
In September 2019, the clinic’s director, Dr. Michael Marshall, publicly resigned, citing the clinic’s financial precarity as his reason for leaving. With one exception, he and his entire staff were dependent on University of Alberta grants—not provincial healthcare dollars—for their funding. “Securing grants as a means of providing care is not sustainable,” Dr. Marshall told Global News at the time.
The two other clinics in Canada don’t accept out-of-province patients
The CMC does not have a monopoly on the provision of bottom surgery in Canada.
In 2019 , the Women’s College Hospital in Toronto —a public healthcare institution—began offering vaginoplasty to trans Ontarians. That came two years after the hospital launched the Trans Health Expansion Partnership, an undertaking in partnership with Sherbourne Health Centre, the Centre for Addiction and Mental Health and community consultants meant to increase the availability of transition-related healthcare across Ontario.
Also in 2019 , British Columbia began offering its trans residents access to bottom surgeries at the Vancouver General Hospital. This made it the first province in Western Canada to offer gender-confirmation surgeries for both transmasculine and transfeminine people.
Ontario’s gender-affirming surgical clinic “has the capacity to perform 40 vaginoplasty surgeries in an average year,” according to Emery Potter, nurse practitioner and clinical lead of the Women’s College Hospital’s Transition-Related Surgery program. Last year, the program received 75 referrals for vaginoplasty—almost twice as many as the hospital had the capacity to perform, evidencing the high demand for the health services the program offers.
In B.C., patients move toward bottom surgery in stages. “The first phase includes an intake and consult,” Vancouver Coastal Health told Xtra via email. At this stage, “the wait time is typically 12 to 18 months.” Patients then have the choice to pursue pre-surgery hair removal, which takes about 12 to 18 months by itself; or “intra-operative hair removal” (permanent hair removal during bottom surgery), which can reduce their wait time considerably. Either way, “Once patients are deemed ready, the provincial objective is to ensure that patients wait no longer than six months for surgery.” In the most recent fiscal year, 2022–2023, Vancouver Coastal Health performed 44 vaginoplasties under this program.
Perhaps accounting for their shorter wait times, neither clinic accepts out-of-province patients. (British Columbia’s program does accept referrals from patients in the Yukon, however.) This means that trans people in Canada’s other provinces and territories must still brave the much lengthier wait-list at the CMC, or pay out-of-pocket costs of upward of CAD 13,000 to 20,000 to receive their bottom surgery in another country, like Thailand, for example.
The latter speaks to a deeper problem with the state of healthcare for trans people in Canada. The country has, with two major exceptions, effectively privatized vaginoplasty and phalloplasty. Those with the money to do so can access these procedures fast by going elsewhere. Those without must go to the back of a very long line.
For many trans people, delayed access to gender-affirming bottom surgery is more than an inconvenience. It’s a matter of life or death.
The suicide rate among Canada’s trans population is notoriously high. Compared to the cis lesbian, gay and bisexual population as a whole, trans Canadians are twice as likely to consider or attempt suicide. In 2019 alone, 31 percent of trans Canadians considered suicide and six percent attempted it.
Adequate access to gender-affirming care can help to reduce that risk. Gender-affirming surgeries demonstrably reduce psychological distress and suicidal ideation, according to research undertaken by Harvard University’s T.H. Chan School of Public Health. And a 2020 Dutch study found that, among trans youth, accessing gender-affirming medical care reduced rates of suicidal thoughts compared to those seen in the cis population.
One Alberta trans woman, Donna Battaglia, told CBC News in March that the wait time to access vaginoplasty in Montreal drove her close to suicide twice. She ended up receiving the operation from a local surgeon who agreed to provide it in tandem with cancer-correction surgery. But there is currently no official mechanism for trans people to obtain any gender-affirming bottom surgery at an in-province clinic because neither gender-affirming vaginoplasty nor phalloplasty are listed on Alberta’s Schedule of Medical Benefits —the list of services that Alberta’s public healthcare program will fund with public money. So while there are surgeons in the province capable of performing bottom surgeries, they don’t usually do so.
All of which raises a pointed legal question.
Might it be a violation of trans Canadians’ human rights to deny them ready access to life-saving genital surgeries like vaginoplasty and phalloplasty?
Are the provinces violating trans Canadians’ human rights?
There’s no free-standing right to healthcare in Canada . But there is a right to be free from healthcare discrimination on the basis of one’s gender identity .
Calgary psychiatrist Joe Raiche thinks Alberta Health has violated that right. He helped develop the city’s Adult Gender Clinic and, in February 2017, filed a human rights complaint against Alberta Health alleging discrimination against the province’s trans population.
The quota in place at the time—which limited funding to 25 bottom surgeries per budgetary year—created a “funding bottleneck,” Raiche argued in his complaint, “since there are always more than 25 Albertans perpetually applying for surgery in a given year.”
“By virtue of being transgender, certain Albertans will be discriminated against as they not only need to wait for medical care/surgery (uniformly seen in healthcare), but also need to wait an additional time specifically for funding (not seen in other areas of healthcare). A medical diagnosis of gender dysphoria is the only condition where an additional barrier exists based solely on waiting for funding. This amounts to discrimination based on gender identity, as only transgender patients will experience this additional burden.”
Government records provided to Xtra by the Calgary lawyer who worked with Raiche, Drew Yewchuk , indicate that Alberta Health chose to eliminate the cap on bottom surgery funding rather than fight Raiche in front of the Alberta Human Rights Commission Tribunal. Indeed, an internal government memo submitted in November 2017 to the assistant deputy minister of health indicated that “in response to public calls to reduce the wait time for [bottom surgery] funding approval from transgender Albertans, the media and some of Alberta’s referring psychiatrists, including [Raiche’s] Human Rights challenge, decreasing and eliminating the wait time for [Final Stage Gender Reassignment Surgery] FSGRS funding approval is a program priority.”
In other words, the combination of public outcry and human rights litigation was enough to force the province to dramatically restructure its program for providing trans healthcare. That should offer some hope to trans activists and their allies: change is possible.
And change is needed. Alberta Health may have lifted the formal quota on the number of surgeries it will fund each year, but it still only allocates $1.1 million toward bottom surgeries annually. That would be enough to cover approximately 40 vaginoplasties, Raiche tells Xtra . But the money also has to cover phalloplasties, which can cost four to five times as much. In practice, this means funding for bottom surgery continues to be strictly limited in a province whose population is now estimated to be over 4.5 million residents.
That $1.1 million funding cap needs to go, Raiche says, and vaginoplasty and phalloplasty need to be listed in the provincial Schedule of Medical Benefits . Doing so would place both surgeries on par with other publicly funded operations like gallbladder removal or urethral repair and “allow [Albertans] to have a funding system in place that’s scalable and expands or contracts depending on the needs of the population … at the time.”
Xtra asked Adriana LaGrange why gender-confirming vaginoplasty and phalloplasty are not in the Schedule, as well as when they would be added to it. Spokesperson Andrew Livingstone declined to say when that would happen.
Ideally, there needs to be surgeons in the province performing bottom surgeries under the Alberta Health Services umbrella.
Alberta is moving in the right direction by increasing the availability of public funding for gender-confirmation surgeries. But its progress will remain minimal so long as the province continues to send trans patients out of province. It, along with every other province and territory without its own bottom surgery clinic, needs to follow the lead of Ontario and British Columbia and open up a local clinic for the provision of this surgery.
“There are no legal barriers to Alberta providing such a service in the province,” according to University of Calgary law professor and health law expert Lorian Hardcastle . As far as funding goes, “it is extremely easy for the government to make changes and add new insured services to the Schedule of Medical Benefits.”
The absence of a bottom surgery clinic in the province “seems to be the product of policy choices either by government” or Alberta Health Services (AHS). “These policy choices may be deliberate decisions that the government or AHS has consciously made to send patients out of province, or it may be policy inaction.”
Indeed, “it would be interesting to know,” Hardcastle says, “what AHS has done to try to encourage or facilitate the opening of such a clinic.”
The answer, it seems, is nothing.
According to Raiche, in 2019 a multidisciplinary group of Alberta physicians—including psychiatrists, surgeons, endocrinologists and primary care providers—put together a proposal for an in-province centre for gender-confirmation surgery. Alberta Health Services rejected that proposal due to “budgetary constraints.”
“It’s not that Alberta doesn’t have the providers or the clinicians necessary,” Raiche says. “I think we have a really strong network of particular surgeons who are very passionate and committed to trans care. It is just a financial funding decision that, right now, Alberta Health would rather choose to pay for people to go to Montreal as opposed to working together with AHS to create a surgical program here.”
Indeed, when Xtra asked LaGrange what Alberta Health is doing to facilitate the opening of a bottom surgery clinic in the province, the minister’s office declined to say.
Inaction from provincial governments ultimately means that trans Canadians will face more suffering.
Canada’s provinces are, with two exceptions, failing their trans residents. By relying on a backlogged clinic in Montreal to provide a medically necessary and life-saving operation, the provinces are putting trans people’s health, safety and well-being at risk.
- “ Alberta Healthcare Insurance Bulletin ,” Aug. 20, 2012
- “ Funding for Transition Surgeries ,” Alberta Health Services, 2023
- “ The Gender Program ,” Alberta Health Services, 2023
- “ Adult Gender Clinic ,” Alberta Health Services, 2023
- “ Saskatchewan Medical Transition Guide ,” Saskatchewan Trans Health Coalition, Jan. 2019
- “ Surgical Care Planning ,” Trans Care B.C., 2023
- “ CENTRE MÉTROPOLITAIN DE CHIRURGIE—CMC ,” TransAvenue, Nov. 8, 2019
- “ D'où viennent les patients du Centre Métropolitain de Chirurgie? ” TransAvenue, Dec. 16, 2019
- “ La maison de convalescence Asclepiade fête ses 15 ans! ” TransAvenue, Sept. 22, 2022
- “ Advocates push for gender surgery funding within Alberta amid years-long backlog in Montreal ,” Katarina Szulc, CBC, March 16, 2023
- “ Toronto’s Women’s College Hospital launches new program for gender-reassignment surgery ,” Kelly Grant, Globe and Mail, June 17, 2019
- “ Dr. Lorne Warneke remembered as pivotal LGBTQ pioneer in Alberta ,” CBC News, Sept. 3, 2020
- “ Trans rights trailblazer reflects on 50 years of social change ,” Kristen Bauer, University of Alberta, Sept. 25, 2017
- “ Province of Alberta 27th legislative Session ,” April 14, 2009
- “ Head of program’s resignation raises questions about accessibility to transgender care in Alberta ,” Jill Croteau, Global News, Sept. 16, 2019
- “ The Gender Surgery Program B.C. ” Vancouver Coastal Health, 2023
- “‘ It’s wonderful’: Community reacts to news B.C. will offer gender-affirming lower surgeries ,” Micki Cowan, CBC, Nov. 16, 2018
- “ Price List ,” Transgender Thailand, 2023
- “ Transgender people and suicide fact sheet ,” Mental Health Commission of Canada, May 10, 2019
- “ Mental health benefits associated with gender-affirming surgery ,” Harvard, 2021
- “ Psychological Functioning in Transgender Adolescents Before and After Gender-Affirmative Care Compared With Cisgender General Population Peers ,” Journal of Adolescent Health, June 2020
- “ Alberta Health Care Insurance Plan: schedule of medical benefits as of 01 April 2023 ,” Alberta government, April 1, 2021
- “ Alberta’s population expected to hit 5 million later this decade, possibly as early as 2025 ,” Robson Fletcher, CBC, July 7, 2023
Sources And Methodology

Charlotte Dalwood is an English-speaking freelance journalist and JD student based in Calgary, AB. Her other publications include a monthly column on 2SLGBTQ+ and legal issues for rabble.ca.
Read More About:
Corrections or feedback.

Keep Reading

What you need need to know about gender-affirming care for youth

Could this week’s Supreme Court abortion pill case affect gender-affirming care?

Raising the bar: How an Edmonton gym is making exercise accessible

Ohio’s trans healthcare ban sets dangerous precedent ahead of 2024 election
Connect with the writer.
Communication not private: Your email will be forwarded to the writer by an Xtra editor.
This story is over 5 years old.
How long it takes to get gender-affirming surgery across canada.

ONE EMAIL. ONE STORY. EVERY WEEK. SIGN UP FOR THE VICE NEWSLETTER.
By signing up, you agree to the Terms of Use and Privacy Policy & to receive electronic communications from Vice Media Group, which may include marketing promotions, advertisements and sponsored content.
ANALYSIS: What Canada’s Gender-Transition Industry Is Worth in Dollars and Cents
Friends Read Free

Gender-transition surgeries can cost tens of thousands of dollars, depending on the procedure. Puberty blockers can cost about $4,800 annually, and feminizing hormone treatments combined can cost more than $3,000 annually per person.
“A rise in awareness and acceptance of gender-affirming health-care services among younger generations is projected to spur product demand,” Polaris said in its report published January this year. It estimates a compound annual growth rate of 12 percent in the market from now until 2032.
“Pharmaceutical companies have so much vested interest in promoting the sale of their treatments, they also get into the promotion of the ‘disease,’” he said, describing a general phenomenon he has observed in the pharmaceutical industry throughout his decades of research. Often, conditions that don’t require medication are nonetheless treated heavily with drugs—each of which has side effects and may be detrimental to the patient in the long run, Mr. Cassels said.
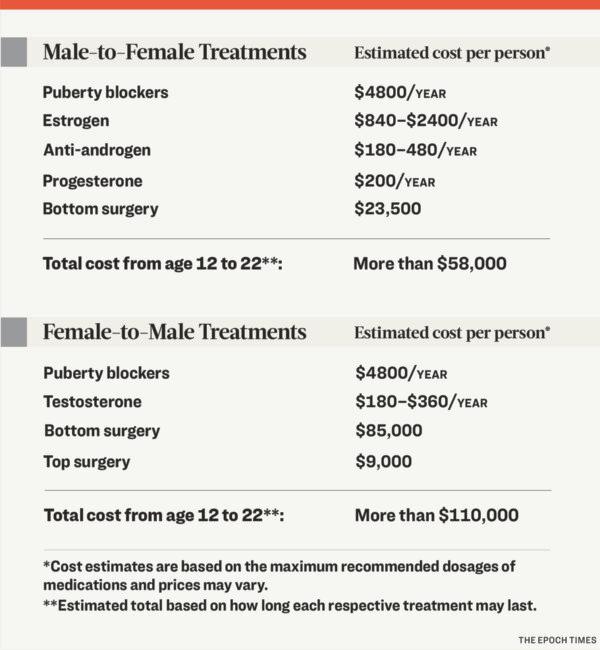
“I’ve studied rational drug policy, and the purpose of providing coverage for drugs always has to be done for appropriate conditions,” Mr. Cassels said. “You don’t give an anti-depressant to someone that doesn’t have diagnosed depression. You shouldn’t be giving drugs that are for high cholesterol to someone who has normal cholesterol.”
When it comes to medical treatment of gender dysphoria, he said, the main question is whether such treatment is appropriate for the patients, especially young patients. “Any dollar spent on a treatment that isn’t needed is a dollar wasted,” he said.
It is difficult to put a precise dollar figure on the market in Canada. The Epoch Times contacted multiple gender clinics to inquire about precise costs of treatments but did not receive replies as of publication. Most provinces and territories, which cover some of the costs of gender-transitioning, also did not respond with requested information about spending.
Puberty Blockers: About $400 Per Month
The company did not respond as of publication time to Epoch Times inquiries about its Lupron product and concerns about puberty blockers, including those raised by Mr. Paxton. Mr. Paxton did not respond to an inquiry regarding the current status of his investigation.
Hormone Treatments: Up to $3,000 Per Year
Estradiol is a commonly prescribed estrogen product. It can cost up to $200 monthly, or $2,400 annually.
A commonly prescribed anti-androgen called Spironolactone costs about $15 monthly, although ACT lists the cost up to $40. At $40 monthly, that would amount to $480 annually. A common progesterone called Medroxyprogesterone acetate costs about $200 annually. Estimates are based on the maximum dosage given by the Canadian Pharmacists Association and cross-referenced with BC PharmaCare coverage prices.
When you combine the costs, a male taking estrogen ($2,400) and an anti-androgen ($480) together could spend $2,880 annually. If you add on progesterone ($200), that’s more than $3,000 on hormonal treatments.
Surgeries: Up to $85,000
Basic top and bottom surgery costs are generally covered by provincial health plans, but a slew of other surgeries generally aren’t. They include facial feminization, vocal surgeries, deduction of the Adam’s apple, and laser hair removal.
A boy starting puberty blockers at the age of 12 and continuing with hormone treatments and bottom surgery through to the age of 22 could spend a total of nearly $59,000 according to these estimated figures.
A girl starting puberty blockers at 12, taking hormones, and getting top and bottom surgery by age 22 could spend more than $110,000.
In addition, various supplies are sold to transgender youth, including devices for women to be able to stand to urinate, for example.
“For the pharmaceutical industry, it’s financial,” Mr. Cassels said. While many doctors feel they are helping youth, he said, it’s also a profitable industry. “People can make significant parts of their livelihood by doing this kind of work, right? So it’s obviously profitable to do it.”
Alberta’s Ongoing COVID-19 Review Looks at Whether Data Justified Lockdowns

From Homelessness to Triathlons: An Alberta Woman’s Fight to Overcome Addictions

Budget 2024’s Tax on the ‘Rich’ Will Backfire, Say Economists

Medindia » News » Research News » A Global Comparison: Best Countries for Gender Reassignment Surgery
A Global Comparison: Best Countries for Gender Reassignment Surgery

Purpose and Procedures
Chest surgery (top surgery) for ftm transitions:, phalloplasty for ftm transitions:, breast augmentation for mtf transitions:, facial feminization surgery (ffs) for mtf transitions:, vaginoplasty for mtf transitions:.
Turkey Emerges as a Budget-Friendly Destination
Latin america offers competitive prices.

Belgium: Affordable and Progressive in Europe
The u.s.: highest costs and legal challenges.
- Expert Q&A: Gender Dysphoria - (https://www.psychiatry.org/patients-families/gender-dysphoria/expert-q-and-a)

- Consult Online Doctor
- Take Telemedicine course
- Health Centers
- Health Tools
- Health info by Speciality
- Know Your Body
- Health and Wellness
- Web Stories
- Health Tips
- Nutrition Facts
- Lifestyle & Wellness
- Beauty Tips
- Diet & Nutrition
- Home Remedies
- Obesity & Weight Loss
- Complementary Medicine
- Special Reports
- Press Releases
- Health Guide
- Health articles
- Health Quiz
- Health Facts
- Travel Health
- Medicine and Movies
- Symptom Articles
- Diabetes Tools
- Pediatric Calculators
- Men's Health
- Women's Health
- Height Weight Tools
- Cardiac Tools
- Pharma Tools
- Wellness Interactive Tools
- Drug Information
- Drugs by Condition
- Drug Price List - Brand Names
- Drug Interaction with Food
- Drug Price List - Generic Names
- Drugs - Side Effects
- Drug Videos
- Drug Database
- Doctor Directory
- Diagnostic Lab Directory
- Hospital Directory
- Pharmacy or Chemist
- Medical Equipment Suppliers
- Pharma Directory
- Emergency Services
- PG Education
- Family Medicine
- Other Resources
- Medical Aphorism
- Health Acts in India
- Health Quotations
- Medical Conference
- Amazing Body Facts
- Health poll

- Editorial Team
- Exclusive Interviews
- In the News
- Partners & Affiliates
- Advertise With Us
- हिन्दी
- français
- Español
- 中文

IMAGES
VIDEO
COMMENTS
Gender confirming surgery (also known as sex reassignment or gender affirming surgery) does more than change a person's body. It affirms how they think and feel about their own gender and what it means to who they are. Ontario is funding surgery as an option for people who experience discomfort or distress with their sex or gender at birth.
Transgender Pride Flag map of Canada by Devin Kira Murphy. Licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license.. With last week's announcement from the Government of Nunavut confirming that the territory will pay for mental health services and transition treatments for transgender and non-binary residents, Canada will now have nation-wide funding available for ...
Nova Scotia. Gender-affirmation surgery (sex-reassignment surgery) is an insured benefit in Nova Scotia. An assessment by a physician, specialist, nurse practitioner, or healthcare professional ...
Most Canadian provinces cover the cost of gender reassignment surgery. However, feminizing surgeries considered cosmetic, such as breast augmentation, voice surgery, ... (Canada) to be allowed to undergo gender reassignment surgery. Therefore, the required age for genital reconstructive surgery is 18 years of age and 16 for masculinization of ...
Everything you need to know about getting top surgery in Canada. It can cost thousands of dollars more out of pocket to get top surgery in Ontario compared to B.C. By Mel Woods • October 14, 2021 1:13 pm EDT ... While it's not necessarily important for everyone's gender journey, ...
Since 17-year-old Seelie Romard of Sydney, N.S., first started seeking gender-affirming treatment in 2021, he says he's visited a pediatrician, a physician who specializes in gender care, and a ...
Gender Surgery Clinic at Gordon and Leslie Diamond Health Care Centre. 2775 Laurel Street, 7th floor, Station 4A. Vancouver, BC V5Z 1M9. See directions on Google Maps. (604) 875-5060. See more details.
Sex reassignment surgery is often used as a catch-all term for multiple procedures. For male-to-female patients the list may include facial feminization, breast augmentation, and vaginoplasty (the creation of a vagina), and for female-to-male patients, mastectomy, hysterectomy, or phalloplasty (the creation of a penis).
Our surgeons are considered to be the most experienced in the field of gender reassignment surgery and perform more than 500 surgical procedures per year. ... Our surgeons have performed more than 10 000 gender-affirming surgeries over the past 12 years. ... Vaginoplasty without vaginal cavity, Breast Augmentation, Adam's Apple Reduction, Voice ...
Step #3. Step 3: Complete the Prior Approval Form. Following your Transition-Related Surgery Planning Visit, your provider can complete, sign, and submit the "Request for Prior Approval for Funding of Sex-Reassignment Surgery" (also known as the "Prior Approval" form) to the MOHLTC. The number of qualified providers who must complete ...
According to CIHI, of the 536 hospital visits for transgender reassignment mastectomies in 2018-19, 76, or 14 per cent, involved 18-year-olds and younger. That age group accounted for 18 per cent ...
When Magan Carty got their date for top surgery in August, 2022, they had roughly four months to pull together about $4,000. Mx. Carty, a 31-year-old radio producer in Toronto, had been seeking ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
The costs of this procedure varies by clinic but are estimated to be about $10,000 to extract and $300 per year to store. If and when the time comes to transfer, there is an addition fee of around $2,000. For those who have sperm, banking for future use may a good option.
The goals of these procedures are therefore patient specific and can vary beyond the gender binary. Gender-affirming surgeries can be grouped into four main domains: facial, chest, body and genital procedures. Talking to your plastic surgeon about your individual transition will help direct which surgery options are best for you.
Gender-affirming surgeries change primary or secondary sex characteristics so that they correspond with one's gender identity. Many trans and gender diverse people are happy with their bodies, or find comfort with their bodies through non-surgical means. Only you can decide whether surgery is right for you . Research shows that gender ...
On July 1, the country's largest health-care plan switched providers to Canada Life Assurance Company, bringing more than 1.7 million federal public servants, retirees and their dependents with ...
The cost of transgender surgery can vary by provider and the type of surgery you choose to get. For a female-to-male transition, masculinization chest surgery (also known as top surgery) might ...
There are potentially more than 800 health-care professionals across the province who can now assess patients for sex-reassignment surgery, a change Ontario adopted March 1 to trim the more than ...
Tracheal shave* - 364 days. Phalloplasty- 383 days. Breast augmentation -572 days. Facial feminization - 607 days. 2. Funding Approval. Data suggests that for all types of gender-affirming surgery in Canada, 71% had their surgery paid for, at least partially, through a government health care plan.
Sex reassignment surgery is generally not performed on those under the provincial age of majority, as all clinics in Canada that currently perform reassignment surgery conform to the recognized Standards of Care. These Standards, which are regarding health care for trans persons, forbid irreversible interventions (such as surgery) on patients ...
The relational cost of that depression has been severe. ... indicates that in the three previous years, 90 percent of the patients who came to the CMC for gender-affirming surgery hailed from Canada with: 26 percent coming from ... "Toronto's Women's College Hospital launches new program for gender-reassignment surgery," Kelly Grant, ...
In BC, the median wait time for a surgery assessment was 150 days, compared to 180 days in the rest of Canada. Some waited as little as one day for an assessment, while others in the same province ...
The gender-reassignment surgery market was worth about US$701 million (C$970 million) globally in 2023, ... The cost varies across Canada based on FTM top surgery methods, the clinic's website ...
Notably, Belgium's healthcare system has recognized transsexualism since 1985, endorsing sex reassignment surgery as a standard treatment. The U.S.: Highest Costs and Legal Challenges