- Research article
- Open access
- Published: 06 September 2021

Unhealthy lifestyles, environment, well-being and health capability in rural neighbourhoods: a community-based cross-sectional study
- Anabela Marisa Azul ORCID: orcid.org/0000-0003-3295-1284 1 , 2 , 3 ,
- Ricardo Almendra 4 , 5 ,
- Marta Quatorze 6 ,
- Adriana Loureiro 4 ,
- Flávio Reis 2 , 6 , 7 , 8 ,
- Rui Tavares 1 , 2 , 3 ,
- Anabela Mota-Pinto 6 , 9 ,
- António Cunha 10 , 11 ,
- Luís Rama 12 ,
- João Oliveira Malva 2 , 6 , 7 , 11 ,
- Paula Santana 4 , 5 ,
- João Ramalho-Santos 1 , 2 , 13 &
HeaLIQs4Cities consortium
BMC Public Health volume 21 , Article number: 1628 ( 2021 ) Cite this article
11k Accesses
4 Citations
1 Altmetric
Metrics details
Non-communicable diseases are a leading cause of health loss worldwide, in part due to unhealthy lifestyles. Metabolic-based diseases are rising with an unhealthy body-mass index (BMI) in rural areas as the main risk factor in adults, which may be amplified by wider determinants of health. Changes in rural environments reflect the need of better understanding the factors affecting the self-ability for making balanced decisions. We assessed whether unhealthy lifestyles and environment in rural neighbourhoods are reflected into metabolic risks and health capability.
We conducted a community-based cross-sectional study in 15 Portuguese rural neighbourhoods to describe individuals’ health functioning condition and to characterize the community environment. We followed a qualitatively driven mixed-method design to gather information about evidence-based data, lifestyles and neighbourhood satisfaction (incorporated in eVida technology), within a random sample of 270 individuals, and in-depth interviews to 107 individuals, to uncover whether environment influence the ability for improving or pursuing heath and well-being.
Men showed to have a 75% higher probability of being overweight than women ( p -value = 0.0954); and the reporting of health loss risks was higher in women (RR: 1.48; p -value = 0.122), individuals with larger waist circumference (RR: 2.21; IC: 1.19; 4.27), overweight and obesity (RR: 1.38; p -value = 0.293) and aged over 75 years (RR: 1.78; p -value = 0.235; when compared with participants under 40 years old). Metabolic risks were more associated to BMI and physical activity than diet (or sleeping habits). Overall, metabolic risk linked to BMI was higher in small villages than in municipalities. Seven dimensions, economic development, built (and natural) environment, social network, health care, demography, active lifestyles, and mobility, reflected the self-perceptions in place affecting the individual ability to make healthy choices. Qualitative data exposed asymmetries in surrounding environments among neighbourhoods and uncovered the natural environment and natural resources specifies as the main value of rural well-being.
Conclusions
Metabolic risk factors reflect unhealthy lifestyles and can be associated with environment contextual-dependent circumstances. People-centred approaches highlight wider socioeconomic and (natural) environmental determinants reflecting health needs, health expectations and health capability. Our community-based program and cross-disciplinary research provides insights that may improve health-promoting changes in rural neighbourhoods.
Peer Review reports
Non-communicable diseases (NCD) are the leading causes of health loss globally, accounting for 91% of deaths and almost 87% of disability-adjusted-life-years (DALYs) in Europe [ 1 ], in part due to unhealthy diets and lifestyles [ 2 , 3 ]. A systematic analysis for the Global Burden of Disease [ 4 ], undertaken by the World Health Organisation (WHO) and the Institute for Health, Metrics and Evaluation (IHME) highlight three metabolic risks among the five leading risks of DALYs worldwide: i) high systolic blood pressure (SBP), ii) high fasting plasma glucose and iii) body-mass index (BMI). In parallel, in 2019, a large-scale study including more than 112 million adults across urban and rural neighbourhoods estimated that BMI increased 2.1 kg/m 2 in both women and men in rural neighbourhoods over the past three decades; suggesting that the rising of rural BMI is currently the main health risk factor in adults [ 5 ].
Health loss risks in rural neighbourhoods may be amplified by wider determinants of health and well-being such as the geographic and historical factors across economic and socio-cultural characteristics [ 6 ]. Places are living organisms that produce dynamics, generate environments and create societies [ 7 , 8 ] They are a set of multiple, complex and overlapping environments that support life (e.g., home, social relationships, communities and neighbourhoods) [ 9 ]. The exposure to positive or negative environments, that occur in particular geographic locations, influence human health and well-being throughout the course of life [ 10 , 11 ]. Problems related with built, connective, and relational space present themselves when spatial planning and development models cannot be adjusted in face of a changing landscape, for instance, ageing phenomena [ 12 ]. A growing elderly population accentuates the ability to pursue health in place due to a combination of physical–cognitive and functional–social and psychological fragility [ 10 , 11 , 12 , 13 ].
Communities have a deep understanding of their surrounding environments enabling them to better assess external factors [ 13 , 14 ] impacting health and the ability to make healthy choices. Comprehensive theories of health and social justice [ 15 , 16 , 17 , 18 , 19 ] intersect individual-level data and broader structural and environmental circumstances, for mapping the conditions that reflect health needs, health expectations and health capability gaps at both individual and community levels. In this way, Ruger’ health capability mode of 2010 [ 18 ] includes the capability to reduce/prevent the exposure to metabolic risks factors, to reduce DALYs and early mortality, to pursue healthy lifestyles, or to gain health-related knowledge, which is viewed both as an end for individuals (intrinsic motivation) but also as a driving force for encouraging changes at the community level, e.g., socioeconomic development, built and natural environment, or social cohesion, particularly in rural areas [ 20 ].
Self-management of NCD remains poorly implemented in rural neighbourhoods despite self-adherence to healthy lifestyles evidence reflected in self-ability to make balanced decisions [ 21 , 22 ]. The community-based participatory research (CBPR) is a wide-ranging methodological approach that concedes the possibility of exploring gaps between what is expected and what is afforded and its interconnections and interdependencies [ 23 ], while evidence-based data can be helpful for assessing an individual’s health functionality. Therefore, we propose a qualitatively driven mixed-method design to assess unhealthy lifestyles of people living in rural neighbourhoods, which includes gathering evidence-based data about metabolic risks and health functionality and studying broader contextual determinants of health and well-being associated to place and neighbourhood. We ultimate expect to uncover health and well-being drivers in rural neighbourhoods, and determine whether community circumstances influence health capability at both the individual and community-level.
Study area, design and community setting
The cross-sectional study was conducted in 15 rural neighbourhoods from six municipalities in the Centre region of Portugal (Fig. 1 ), aiming at 1) assessing evidence-based data and describing lifestyles, 2) examining determinants of health and well-being in rural neighbourhoods, and 3) discuss how individuals’ conditions and population’ circumstances can contribute with a better understanding to improve health capability in rural neighbourhoods.
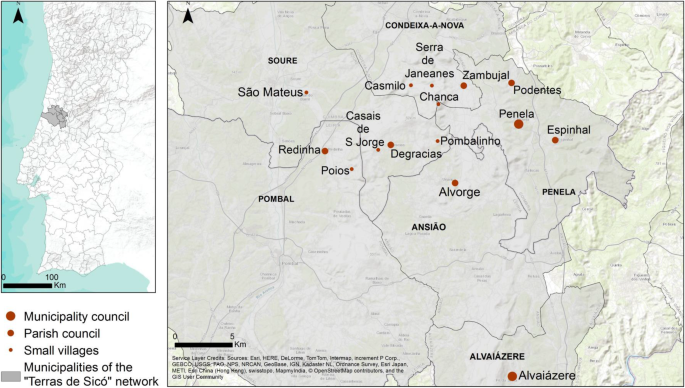
Location of rural neighbourhoods; basemap is provided by ESRI, available as part of the mapping platform ArcGIS Online
The selection of the rural neighbourhoods of the “ Terras de Sicó ” ( Lands of Sicó ) network (Sicó-network) was drawn on a CBPR approach. Given possible differences at the administrative level, which could influence local practices, we considered the three relevant levels of territory administrative structure: small villages, parish councils, and municipalities seats (hereinafter referred as municipality) (Fig. 1 ). According to the Portuguese National Statistics Institute, in 2011, 3879 individuals were living in the 15 rural neighbourhoods (Table 1 ), one third of the population was older than 64 years and with a high rate of limited literacy (e.g., the proportion of individuals that do not know how to read is almost the same as individuals with higher education); which are common characteristics in Portuguese rural areas [ 24 ].
The study encompasses a qualitatively driven mixed-method design, that is, simultaneously, qualitative (QUAL; inductive theoretical drive) and quantitative (quan): QUAL+quan [ 25 ]: quan to describe and examine individuals’ health functioning condition (evidence-based data and lifestyles); QUAL to document how individuals experience their neighbourhood in terms of health and well-being [ 26 ], and to better understand which local circumstances influence the ability to adopt healthier lifestyles and to pursue health [ 18 ].
Our CBPR approach involved the local representatives from the Sicó-network ( n = 20; among policymakers, local community members and stakeholders); advanced training students and young professionals ( n = 13), from biomedical sciences, medicine and sports sciences; a trans-disciplinary research and innovation team ( n = 18) involving researchers from life sciences, medical and health sciences, and social sciences, and developers of advanced technology for health monitoring and e-health services, including two international members of the HeaLIQs consortium and two members of the consortium Ageing@Coimbra. Two local consolidation meetings with local representatives of the Terras de Sicó network and the research and innovation team, held in two municipalities, Penela (May 28, 2019) and Alvaiázere (June 11, 2019), created the bases of the CBPR approach, and a roadmap for local itineraries and local community engagement. Triangulation between local representatives and researchers regarding the CBPR approach contributed to: better characterizing the demography in the 15 neighbourhoods; co-designing the community program adapted to each neighbourhood; co-constructing a health communication strategy and tailored healthy lifestyles-related messages for older adults with limited literacy; discussing the theoretical background [ 14 , 15 , 16 , 17 , 18 , 19 , 20 ] and the QUAL+quan methodology connecting with a questionnaire [ 27 ] incorporated in pre-existing eVida technology [ 28 ]; and training volunteer students and young professionals to operationalize translational research and participatory approaches with community engagement in neighbourhoods. Local representatives collaborated actively in the dissemination of the program via national/regional media (i.e., newspapers, radio, television and flyers), social media (i.e., Facebook) and institutional websites (e.g., Sicó-network, municipalities, local stakeholders and university). Overall, the design took about 9 months, from January to September 2019.
Mobile healthy living room
The community program took place in a mobile Healthy Living Room (mHLR) (Fig. 2 ), designed as a mobile community service, to reach isolated rural neighbourhoods with lower access to health care facilities and awareness about healthy lifestyles. The mHLR was equipped with a healthy lifestyle assessment toolkit, which comprises medical devices and a questionnaire [ 27 ] incorporated in eVida technology. eVida is a tablet-based application centred on the input of the questionnaires (as discussed in detail below), provides a personalized summary of putative health risks associated with individual characteristics and behaviours [ 28 ].

Community program intervention design; credits: the research team
The community intervention involved 1) the assessment of evidence-based data (e.g., BMI, waist circumference, and self-assessment of illnesses or chronic diseases, medication and sleep habits), 2) lifestyle characterization (e.g., diet, active lifestyles, quality of life and self-assessment of health and well-being), 3) demographic information (i.e., sex, age, employment status and level of education), complemented with 4) the self-assessment of neighbourhood satisfaction, all incorporated in eVida technology, and 5) the individual in-depth interview about the contexts in place to pursue good health in the neighbourhood. Each participant was accompanied by a trained team member and community intervention included two to four team members and four to six students/young professionals, depending on the neighbourhoods’ population.
At the end, participants received the results of the eVida questionnaire and prevention recommendations in an individualised report as well as short cartoon-like active healthy lifestyles messages, about diet, physical activity, social cohesion, and mental health and well-being.
This research was part of a collaborative European research project, Healthy Lifestyle Innovation Quarters for Cities and Citizens (HeaLIQs4Cities), funded by the European Institute of Innovation and Technology for Health (EIT Health), that unite researchers and neighbourhoods from Coimbra (Portugal), Groningen (The Netherlands) and Copenhagen (Denmark), around the concept of health capability and drivers of health and well-being. Among the stakeholders, the consortium Ageing@Coimbra represents a reference site in Centro region of Portugal within the European Innovation Partnership (EIP) on Active and Healthy Ageing (AHA), that is founded on a quadruple helix-based innovation model for improving active and healthy ageing in Europe [ 28 ].
Data collection
One dimension of the data aimed at collecting evidence-based data, lifestyles and self-assessment of neighbourhood satisfaction incorporated in eVida, as mentioned above, while another dimension of the data aspired at documenting the contexts in place influencing the ability to pursue health and well-being in the neighbourhood. The weight and waist circumference were measured and BMI assessed; the factors associated with illnesses or chronic diseases, medication, and sleep habits were self-reported. The quality of life followed EQ-5D-5L questionnaire: mobility, self-care, usual activities, pain/discomfort and anxiety/depression (each dimension is rated on scale with 5 levels: no problems, slight problems, moderate problems, severe problems and extreme problems). We also considered two additional dimensions of self-assessment of health and well-being of ‘quality of life’ (with 5 levels, strongly disagree, disagree, neither agree nor disagree, agree, strongly agree) and ‘health condition’ (with 5 levels, very good, good, reasonable, bad, very bad). Regarding the description of lifestyles, diet was categorized per food groups per day and per week (following 5 levels in the Likert scale).
Qualitative research advances the possibilities of a deeper understanding of people’s perceptions and expectations and exploring unique topics within the research aims. For that purpose, we conducted the open-ended question in an in-depth interview: “ What would you change in your neighbourhood to have a healthier life? ”. To reduce eventual desirability bias, participants were ensured prior the eVida questionnaire that were no right or wrong responses and a privacy environment was ensured during the interview; the eVida and interview took in between 45 to 60 min.
Through eVida, information was collected on a random sample of 270 individuals living in rural neighbourhoods from the Sicó-network, considering the dimension and location of the neighbourhood (small villages, parish council and municipalities), constituting a sample with a margin of error of 5.75% and confidence level of 95%. The sample size for the interviews was determined by applying the saturation point criteria, and was stopped after 107 testimonials were collected. This study design was considered the most appropriate way to describe individuals’ lifestyles and communities’ environments. The collection of QUAL+quan data was performed by researchers with background on life sciences, medical and health sciences, and social sciences; the CBPR approach from the very early stages revealed to be determinant for the research methodology and outcomes. Furthermore, the first day of intervention was followed by a preliminary assessment and discussion by the advanced training students (and young professionals) and the team, in order to identify personal bias, optimize the use of eVida and the interview, and minimize any other form of unintended coercion with participants. Data collection was conducted between September 4 and 23, 2019.
Ethical considerations
This study was approved by the Ethics Committee of the Centre Regional Health Administration of Portugal: Reference 91/2019. Participants were required to be 18 years or older and were asked to sign a written informed consent before initiating the community intervention. At the end, participants received a bag with the individualised report and the short cartoon-like active healthy lifestyles messages, about diet, physical activity, social cohesion, and mental health and well-being.
Data analysis
Testimonies were documented in writing, and then transcribed and translated to English. Each participant was linked the age, sex and municipality council in order to present direct quotations (e.g., Female, 68, Small Village, Pombalinho 610). The first four authors performed an independent analysis in all testimonies developing a parallel codification on drivers of health and well-being at community level in the rural neighbourhoods. After several collective discussions rounds (over a period of 3 months), seven consensual dimensions were identified a priori: economic development, built environment, social network, health care, demography, active lifestyles and mobility. The a priori themes were used to code the qualitative data in which subtopics were built upon [ 29 ].
All testimonies were imported to MAXQDA Analytics Pro 2020 version 20.0.0 (Berlin, Germany: VERBI Software GmbH) for coding and analysis. The coding was done in three stages. In the first stage, the testimonies were coded based on the selected dimensions. In a second stage of coding, the resulting identification of sub-topics for each of the 7 dimensions based on mention frequency, and the identification of predominant topics, in both individual accounts and different neighbourhoods, was carried out independently across researchers. Any new codes were consensually debated during regular team meetings. In the third stage, all testimonies were coded once more by applying the final coding scheme. All coded testimonies were evaluated for emerging topics. We used several strategies to ensure quality in data coding. The composition of coding pairs was changed after 10 to 15 testimonies to reduce possible systematic bias. Using this approach, we were able to examine the in situ community needs in the 15 rural neighbourhoods. We also documented the clear individual positive perceptions of living in rural neighbourhoods: i) in terms of healthy living and well-being; ii) the different ways of describing and explaining lifestyles and daily habits; iii) the multiples ways of living and be engaged with community environment; iv) access to health care and health services.
Authors involved in the analyses maintained the explanatory map of the CBPR process from the research goals to data collection and analysis. The number and the frequency of subjects mentioned by participants in different topics support the reliability and credibility of our findings. We also used the lexical search on the MAXQDA program for key codes, to identify the frequency and number of mentions for consistency in participants’ responses.
To supplement the qualitative analysis, binomial logistic regression models were applied: BMI (classified in two categories: 1. overweight and obesity and 2. normal and low weight), waist circumference (classified in two categories: 1. and 2.), self-assessed health status (classified in two categories: 1. good and very good and 2. less than good), were assessed as dependent variables and sex, age (continuous), place of residence (classified in the three classes: 1. small villages, 2. parish councils and 3. municipalities), as independent.
Demographic characteristics
Two hundred seventy people participated (84 in small villages, 112 in parish councils and 74 in municipalities). Women made up a larger proportion of the participants (63%) in the three levels (Table 1 ). The median age was 69 years (1st quartile: 58 years; 3rd quartile: 77 years), with 78% of the participants above 55 years of age. Most of the participants were retired (64%), with a higher proportion (77%) in small villages. The level of education varied along the neighbourhoods, with a small proportion (9%) having receiving higher education (4 and 3% in small villages and parish councils, and 24% in municipalities); the largest share of participants completed the first two grades of basic education (69%), and 14% did not receiving primary education (29, 9 and 7% in small villages, parish councils and municipalities, respectively).
Individual health functionality
The proportion of participants with normal BMI was substantially lower above 55 years of age, with a higher proportion of women presenting normal BMI than men for the participants aged 55 to 74 years (Additional file 1 : Table S1). The proportion of participants with obesity was slightly higher in women aged 55 to 74 years and lower in the other range of ages (< 54 years, > 75 years). In terms of obesity data by rural neighbourhood, the proportion of participants with obesity was lower in municipalities (32%) than in small villages (38%) and parish councils (45%). For the participants aged 55 to 74 years (Fig. 3 a), excess weight was lower in women in all types of neighbourhoods (48 and 54% in small village; 27 and 55% in parish councils; 29 and 50% in municipalities; respectively); obesity was higher in men in municipalities (43 and 38%, respectively). Overall, men had a 75% higher probability of being overweight than women ( p -value: 0.0954), while waist circumference measurements reflected obesity over age, being consistently higher in participants > 75 years of age; the risk of having high waist circumference was 2.45 (IC: 1.1; 5.7) times higher in individuals living in small villages than in municipalities.
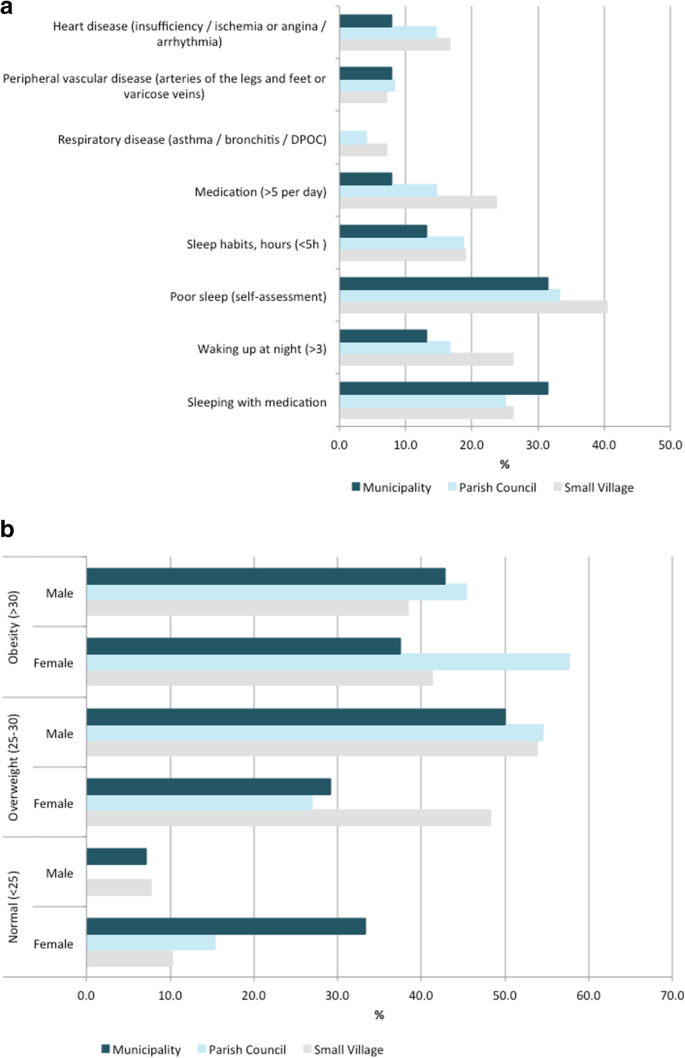
Evidence-based data by rural neighbourhood for participants aged 55 to 74 years
NCD risks associated to chronic diseases were reported by 25% of the participants aged 55 to 74 years (Fig. 3 b) including: (i) heart disease (heart failure, ischemia or angina, arrhythmia) was declared by 13% (17% in small villages, 15% in parish councils and 8% in municipalities); (ii) peripheral vascular disease (problems in arteries of the legs and feet, or varicose veins) was mentioned by 8% (7% in small villages, 8% in parish councils and 8% in municipalities); and (iii) respiratory disease (asthma, bronchitis, chronic obstructive pulmonary disease) was declared by 4% (7% in small villages and 4% in parish councils) (the information for all participants is presented in supplementary Table S1 ). The lowest prevalence of medication was documented in parish councils (33%) and municipalities (32%) (Additional file 1 : Table S1); overall, a substantial proportion of the participants (59%) reported were taking 2–5 medications a day, and a lower proportion (16%) reported taking > 5 medications a day.
Sleeping habits ranged from ≥7 h for 38% of the individuals and less than 5 hours for 17% of the individuals, with a clear trend of more sleeping hours in individuals living in municipalities (Additional file 1 : Table S1). Sleep without interruption was reported by 48% of the individuals, with higher prevalence (55%) in individuals living in municipalities. Consistently with sleeping hours, 35% of the individuals considered having poor sleep quality (41, 33 and 32%, in small villages, parish councils and municipalities, respectively; supplementary Table S1 ).
Self-rated health condition ranged from good (47%) to reasonable (42%), with little differences in neighbourhoods. About 5% of participants referred having very good health, consistently in all neighbourhoods, contrasting with the 5% of participants that mentioned having bad health, with lower incidence in municipalities (3%). Severe or extreme pain was reported by 6 and 1% of the individuals, respectively, with higher incidence from participants living in small villages. In terms of self-rated well-being, a large proportion of participants (74%) reported having a good quality of life, with 25% of the individuals attributing the highest score (18% living in small villages, 30% in parish council and 26% in municipalities). Across data, participants with higher waist circumference had a 2.21 (IC: 1.19; 4.27) higher probability of presenting a poor self-evaluation of their health status.
Unhealthy lifestyles according to rural neighbourhood type
The description of lifestyles in the 15 rural neighbourhoods is shown in Table 2 . A large proportion of participants (81%) reported eating fruit and vegetables 0–1 times per day. Only 1% of the participants mentioned eating fruit and vegetables fewer than once. A substantial proportion of individuals reported eating fish, meat and eggs (87%) 0–1 times per week in all neighbourhoods; also, a considerable share of individuals reported eating bread, pasta or cereal (82%) 0–1 per day, ranging from 78% in parish councils to 89% in small villages. Many participants reported drinking milk (66%) 0–1 per day, ranging from 50% of individuals living in municipalities to 60% of respondents from small villages; 6 and 9% mentioned drinking milk once a week or never, respectively, with little differences in all neighbourhood types. The majority of the population (69%) referred eating fried and salty foods once a week or less, in all neighbourhoods. Some participants (59%) mentioned eating sweets once a week or never, and 7% reported eating more than once a day (2% in small villages, 11% in parish council and 8% in municipalities). Regarding active lifestyles, a large proportion of participants (67%) reported having daily active routines. A lower proportion of participants (21%) reported regular vigorous physical activity, ranging from 11% doing gymnastics (e.g., fitness, Pilates, yoga), 4% water-based exercise (e.g., swimming or water aerobics), 2% bicycling, 1% running and 3% other sports. In general, those living in the municipalities assess better quality of life (following EQ-5D-5L questionnaire); regarding the self-assessment of health and well-being, the inferior levels were observed in small villages.
Characterization of community environment
Individual reflections pinpointed seven dimensions as the main drivers to pursue health and well-being in rural neighbourhoods. These include: economic development, built (and natural) environment, social network, health care, demography, active lifestyles and mobility (Fig. 4 ; supplementary Table S 2 ). Such reflections envision people-centred expectations and a deeper understanding of valuable surrounding environments connected to well-being, which contribute to unforeseen wider ‘needs’ and ‘benefits’ of rural areas.
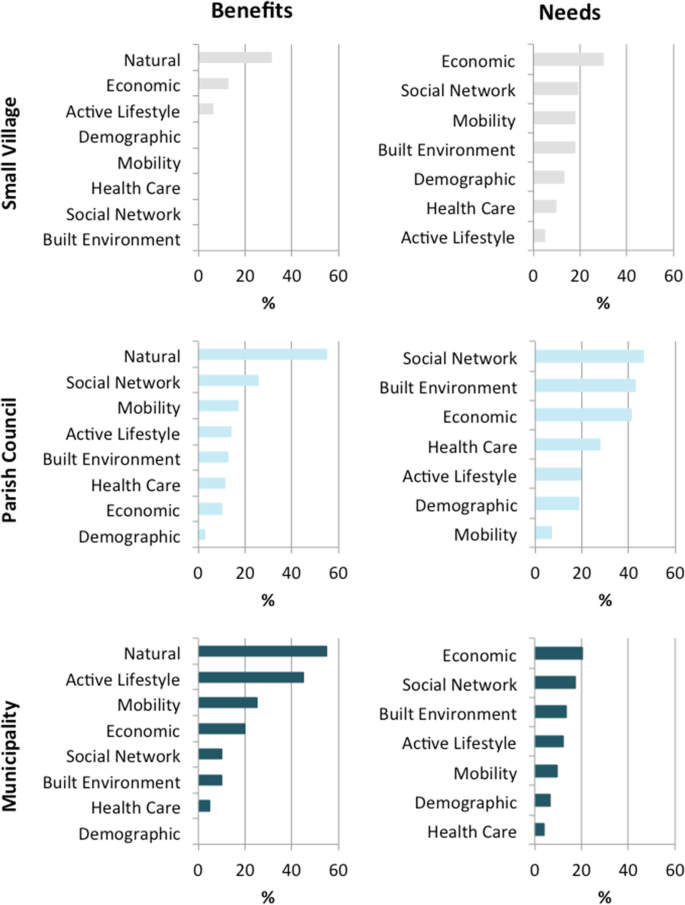
Individual’s reflections about community circumstances influencing health and well-being in their rural neighbourhood
One third of the participants (86) stressed economic development as the main community need –financial, technological and digitalisation investment, high-value-added industry, industrial infrastructures, digitalisation for remote working–, with particular focus on economic innovation and diversification to encourage the establishment of young people in rural areas. Regional policies to improve investment and attractiveness of high-skilled young workers were mentioned by 12 participants.
Built environment, goods and services, underlined by 73 participants, emphasize the need for maintenance and conservation of (i) infrastructures for social interaction, ranging from cultural activities (24), green-blue areas for practicing physical activity and exercise, e.g., green public spaces, camping areas, river beaches, playing areas for children (18), to connected green-blue infrastructures for enjoying nature (14); (ii) infrastructures for promoting the inclusive walkability, namely for youth and elderly people with morbidities, such as smooth and safe walking paths and resting places (10) or sound barriers (2); and (iii) the patrimonial rehabilitation for tourism and habitation (3). Among the services needed, cafes, grocery stores or restaurants, bank, book stores and shopping facilities were mentioned. However, built environment reflected asymmetries in the neighbourhoods; some participants (7) underlined the accessibility to cafes, supermarkets and restaurants in their respective neighbourhoods as an additional benefit of living in rural areas, while others (11) mentioned safe streets, infrastructures for practicing exercise, e.g., gymnasium, swimming pool, tennis court and walking routes, and cultural activities, e.g., folk activities, folk music, cinema and theatre.
Social relationships and networks in neighbourhoods, mentioned by 81 participants, included local community-based initiatives and means of communication to reinforce social connections and dynamics. Asymmetrically, other participants (20) reinforcing local networks and dynamics as a benefit of living in their neighbourhoods, exemplifying with the active participation in collective grape/olive picking, or cultural and recreation activities.
Health care, mentioned by 42 participants, was mostly associated to elderly dependency and included the need for better and long-term health care services (39), support in transport to health care services (1) and pharmacies (2). Asymmetrically, the suitable health care support and services, primary health care services and pharmacies, emphasized by 9 participants, reflected the beneficial aspects mentioned in some neighbourhoods. Adult social care support, particularly day centres and nursing homes, underlined by 21 participants, including childcare and family care were also among the needs reported in rural neighbourhoods.
Demographic factors, mentioned by 37 participants, focused particularly on population ageing and the need of (young) people (30) as social pressure to improve education and (re)open schools (3) and kindergartens (3). The local education, stressed by 2 participants, was reported as a main benefit in their own neighbourhood, to promote well-being.
Active lifestyles, emphasized by 35 participants, include the need for (i) lifelong learning opportunities and digital inclusion, e.g., internet, information and communication technologies (ICTs) (17 participants); (ii) access to places for practicing physical activity and exercise, e.g., soccer, yoga, Pilates, fitness, pool, and walking (10 participants); and (iii) cultural activities, e.g., dance, music, cinema (8 participants). Mobility, mentioned by 30 participants, included the need of accessible public transport (25) and safe accessible walking routes (5). Asymetrycally, several participants (16) underlined the functionality in mobility –public transports systems– and accessibility and linkages (highways) to villages and cities nearby as a main benefit of their neighbourhood.
Natural resources and natural environment were in the centre of health and well-being in rural neighbourhoods. The majority of the individuals (237) mentioned to like living in their neighbourhood and 55 participants featured the natural environment was as the main community benefit to improve quality of life, describing their neighbourhood as calm, beautiful, healthy and safe. The prioritisation on quality of life include (i) daily routines linked to land use, e.g., gardening, agriculture, silvo-pastoral practices; (ii) biodiversity; (iii) connectivity with nature, e.g., swimming and fishing in rivers, walking in green spaces, woodlands and mountains; and (iv) environmental quality, e.g., lower exposure to air / noise pollution. More than two thirds of the participants (192) mentioned they would not live elsewhere if they could and one third (92) revealed they would not change anything in their neighbourhood. Overall, 216 participants underlined that their own neighbourhood is a good place to live. Specific testimonies on these issues are sampled below (Table 3 ).
To the best of our knowledge, this is the first qualitatively driven mixed-method approach to assess whether unhealthy lifestyles and surrounding environments are reflected into metabolic risks and health capability at individual and community-level in rural neighbourhoods.
In terms of the main findings, excess weight and obesity are more prevalent in men between 55 to 74 years and in individuals younger than 54 years, respectively, while in women obesity predominates between 55 to 74 years while excess weight is more predominant in individuals younger than 54. Considering the overall population, NCD risk linked to BMI was superior in small villages than in municipalities. NCD risk associated to unhealthy lifestyles was less evident for diet and sleep habits than for (lack of) physical activity. Diet habits reported by the participants strongly evidenced the adherence to a Mediterranean dietary pattern, which is linked to healthy lifestyles due to its protective effect against several metabolic risks and NCD, namely type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), obesity, cancers and total mortality [ 30 ]. Diet and metabolic risks were described as the second and third leading risks factors of early mortality in a recent survey for Portugal [ 31 ]; but it did not address rural and urban neighbourhoods separately. In Europe, DALYs and risks evidences from NCD also often expose dietary and metabolic risk factors [ 12 ], but again little is known about the relationship between NCD burden and community environment. Healthy diet habits reported in our study suggest that the accessibility to healthy food in own gardens and farms as well as in local markets enable the ability to make healthy choices. Indeed, several participants from small villages mentioned they produce their own food (e.g., vegetables and legumes, fruits and nuts, cereals, meat, eggs, cheese, olive oil), whereas participants from parish councils and municipalities mentioned obtaining local products in grocery stores or the local weekly markets.
Low level of regular physical activity and exercise was admitted by most of the participants in all neighbourhoods. Physical inactivity has been recognized as the fourth leading risk factor for global mortality [ 32 ] and the most pressing public health burden of the current century [ 33 ]. Portugal is the second country in the euro-area with higher physical inactivity in people over 60 years of age and among the countries with higher prevalence of multi-morbidity in people between 60 and 65 years [ 34 ]. Two previous reviews have highlighted that physical inactivity may be explained by pursuing health focused on individual-level determinants, such as self-motivation or literacy, whereas surrounding environment also determines the ability to prevent metabolic risks and choose healthy lifestyles [ 35 , 36 ].
The qualitative research revealed people-centred health and well-being expectations, allowing us to identify seven main dimensions in community circumstances: economic development, built and natural environment, social network, health care, demography, active lifestyles, and mobility, affecting the options to improve or pursue healthier lifestyles, with asymmetries among the neighbourhoods. In fact, participants reframed the narratives, “ I like where I am! ”, underlining the benefits of living in their own neighbourhood; while two thirds of the participants revealed they wouldn’t live elsewhere if they could. Several studies have previously researched the effect of place of residence in terms of availability and accessibility in order to improve health [ 37 , 38 , 39 , 40 ].
Economic development and built environment emerged as the main community needs, namely via financial, technological, and digitalisation investment to attract high-skilled young workers to rural areas, and social interaction and lifelong learning activities, respectively, given that built and natural environment are the setting for the development of human activities [ 41 ]. Natural resources and natural environment were stressed as the main value of rural well-being. However some participants mentioned missing planned and oriented structures to connect with nature, such as functional green-blue areas to exercise / be physically active, or socialize, which can be also an opportunity to come with co-benefits for biodiversity and nature protection and conservation [ 42 ]. Some rural neighbourhoods have been associated with less vigorous physical activity due to socio-economic disadvantages, including less availability to, and use of, facilities for sports and recreational activities [ 43 , 44 ]. By contrast rural neighbourhoods with available green spaces and higher accessibility or walkability tend to contribute to metabolic risk prevention, namely for T2DM [ 36 ]. However the (perceived) accessibility of walkability in rural and urban neighbourhoods may vary in different parts of the world. The low use of the bicycle as a mode of transportation reported in our study can be associated with the absence of specific infrastructures for cycling safety (e.g. on-road bike routes, on-road marked bike lanes), mentioned by some participants, but could also be due to the (high) average participant age. Notably, previous qualitative studies have stressed the positive association between adapted designing interventions in the environment for promoting active lifestyles and PA in rural adults, with gains to social cohesion and individual health conditions [ 43 , 44 , 45 , 46 , 47 ].
Rural neighbourhoods in Portugal are characterized by a higher ageing index, lower geographical access to health care, lower average income and declining population [ 48 , 49 ], but there still is an underestimation of health capability versus disease burden and environment. DALYs have been relevant in terms of the costs to direct health care, namely to the public sector [ 50 ]; however, the translation of such knowledge rarely results into positive contributions and policies to rural neighbourhoods [ 20 ]. Some key subjects need to be considered in further research, including whether the 1) prevalence of women is associated with the demographic uneven structure of the elderly populations, or with women involvement in community, such as agriculture and social activities; 2) increase in evidence-based health and well-being is accompanied by an improvement in community environment, and whether common causes of choosing to live in rural neighbourhoods, such as greater food security, safety, connection with nature, quality of environment, improve metabolic risks and NCD over time [ 8 ] and thus health capability. The ambition of creating accessibility of ‘health-promoting environments’ in green and public areas, to reduce the NCD is well reflected on goal 11.7 of the World Health Organization’s sustainable development goals (2016) [ 51 ]. Populations in rural areas have access to, among other things, healthy food and healthy environmental resources; however rural structural capacities are often under-represented in developing and implementing socioeconomic policies.
In fact, rural marginalization affects health and social justice [ 52 ] and impacts metabolic risks and co-morbidities in populations [ 5 ]. BMI and waist measures observed in this study combined with the participatory approach about lifestyles and community environment, configure an opportunity to act differently in terms of improving health capability in Portuguese rural neighbourhoods, and these findings could thus serve as a driving force for encouraging healthy changes at both individual and community levels [ 18 ].
There are some limitations to this study. The approach was conducted in a single region of the country; thus, results cannot be generalized to other rural neighbourhoods or remote regions. Moreover, data was collected during standard working hours of the week, which might have influenced the sample, including ageing index and the prevalence of women participating. However, we did cover a representative sample of rural populations in Portugal. The eVida has been designed to be user friendly and of almost immediate understanding to participants (10 to 20 min to complete) [ 27 ]. Although the eVida has been re-designed to record information about external environment factors, testimonies were mostly documented in writing and then transcribed. Future research in health innovation devices should also focus on developing programs that can incorporate context-based information, and with it, a better understanding of how ability to pursue health come as a whole from internal and external factors. The use of technology-based devices is increasingly modifying resources and support of health care services and health monitoring, traditionally carried out by health providers in medical facilities. Such innovative devices and adapted strategies have been suggested to encourage active self-management and to ‘empower’ behaviours, and as a way to acquire reliable health-related knowledge to make self-balance decisions [ 28 ].
The qualitative driven mixed-method design allowed us to gather data concerning unhealthy lifestyles of individuals but also to collect in-depth information about community environments that facilitate / weaken individual health and well-being, and their ability to make healthy choices (data saturation was achieved by characterizing broader determinants of health and well-being in neighbourhoods). We believe that the mixed-method described is one way to combine multiple components acting independently and inter-dependently, in order to better understand health capability at both the individual and community levels. The main strengths of the study include the co-designing community program involving the local representatives of the Sicó-network and advanced training students (and young professionals), working together with a trans-disciplinary research team. With the advantages of CBPR, the involvement of community in the early stage of the study provided the opportunity for discussing and adapting the health-related messages for a population with a high ageing index and limited literacy living in the Sicó-network (Portuguese National Statistics, 2019). Such involvement of community and its degrees of negotiation, and flexibility, enabled researchers to uncover gaps regarding (natural) environment contextual-dependent circumstances influencing the ability of individuals to pursue health in their own neighbourhoods.
Our findings are relevant for raising healthy lifestyles awareness and health seeking-skills to improve the self-ability to make balanced decisions, for implementing technology-based devices combined with participatory dynamics, as well as for encouraging the active engagement of local representative planners (governments and other stakeholders) in research to enhance the capacity building and thus the capability for improving heath in rural areas. There are specific contexts of marginalized rural areas for whom the (itinerant) health promotion services and support seem to be an important component of cohesion and equity [ 53 , 54 , 55 ]. The impact of design and intervention with community representatives is planned and further reflexion on follow-up of the healthy lifestyle assessment in rural (and urban) neighbourhoods is required, which is feasible using the tools in a reference site of the collaborative network European innovation partnership on active and healthy ageing (EIP on AHA) [ 28 , 56 , 57 , 58 ].
Revisiting our initial research aim to assess whether unhealthy lifestyles and environment in rural neighbourhoods are reflected into metabolic risks and health capability, we observed that NCD risk in overweight individuals (aged 55 to 74 years) was higher in men in all neighbourhoods; and metabolic risks were more associated to BMI and physical activity than diet (or sleeping habits). The qualitative research allowed us to uncovering seven environmental circumstances reflecting health needs, health expectations and health capability at community-level: economic development, built (and natural) environment, social network, health care, demography, active lifestyles, and mobility, which also underline the asymmetries among neighbourhoods. Notably, participants often reframed their narratives to express the benefits of living in rural areas. Natural resources and environment were pinpointed as the main value of rural well-being, with a particular focus on land use, biodiversity and connectivity with nature, as well as environmental quality. Our CBPR approach contributed for the active involvement of the local representatives and to adapt the health-related messages for older adults with limited literacy. The co-benefits from this co-designing community program and cross-disciplinary research provide further evidence to support people-centred approaches for pushing health and well-being at a broader social, health care and natural environment agenda in rural neighbourhoods.
Availability of data and materials
Datasets used in the study are available from the corresponding author upon request.
Abbreviations
Active and Healthy Ageing
Body Mass Index
Cardiovascular Disease
Community-Based Participatory Research
Disability-Adjusted-Life-Years
European Innovation Partnership
European Institute of Innovation and Technology for Health
Healthy Lifestyle Innovation Quarters for Cities and Citizens
Information and Communication Technologies
Institute for Health, Metrics and Evaluation
mobile Healthy Living Room
Non-Communicable Diseases
Systolic blood pressure
Type 2 diabetes mellitus
World Health Organisation
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 Diseases and Injuries for 195 countries and territories, 1990-2017: A systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789–858.
Article Google Scholar
Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, et al. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005;81(2):341–54. https://doi.org/10.1093/ajcn.81.2.341 .
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and National Burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. https://doi.org/10.1016/j.jacc.2017.04.052 .
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Non-Communicable Diseases Risk Factor Collaboration (NCD-RisC). Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569:260–4.
Reid S. The rural determinants of health: using critical realism as a theoretical framework. Rural Remote Health. 2019;19:5184.
PubMed Google Scholar
Barton H, Tsourou C. Healthy urban planning in practice: experience of European cities. Report of the WHO City Action Group on Healthy Urban Planning. In: A WHO guide to planning for people: WHO Regional Office for Europe. Copenhagen, Denmark; 2000.
Samoggia A, Bertazzoli A, Ruggeri A. European rural development policy approaching health issues: an exploration of programming schemes. Int J Environ Res Public Health. 2019;16(16):2973. https://doi.org/10.3390/ijerph16162973 .
Article PubMed Central Google Scholar
Santana P. Urbanização e saúde. Janus. 2009;2009:1–7.
Google Scholar
Santana P, Nogueira H, Costa C, Santos R. Identificação das vulnerabilidades do ambiente físico e social na construção da Cidade Saudável. Coimbra: A Cidade e a Saúde; 2007. p. 165–81.
Corburn J. Urban place and health equity: critical issues and practices. Int J Environ Res Public Health. 2017;14(2):117. https://doi.org/10.3390/ijerph14020117 .
WHO. Action Plan for the Prevention and Control of Noncommunicable Diseases in the WHO European Region 2016-2025. 2016.
Creswell JW, Hirose M. Mixed methods and survey research in family medicine and community health. Fam Med Community Health. 2019;7:86.
Hilger-Kolb J, Ganter C, Albrecht M, Bosle C, Fischer JE, Schilling L, et al. Identification of starting points to promote health and wellbeing at the community level - a qualitative study. BMC Public Health. 2019;19(1):75. https://doi.org/10.1186/s12889-019-6425-x .
Nussbaum M. Nature, function, and capability: aristotle on political distribution. In: Oxford studies in ancient philosophy: Supplementary volume: Oxford University Press. Oxford, United Kingdom; 1988. p. 145–84.
Nussbaum M. Creating capabilities: the human development approach. Cambridge: Harvard University Press; 2011. https://doi.org/10.4159/harvard.9780674061200 .
Book Google Scholar
Ruger JP. Health, capability, and justice: toward a new paradigm of health ethics, policy and law. Cornell J Law Public Policy. 2006;15(2):403–82.
Ruger JP. Health capability: conceptualization and operationalization. Am J Public Health. 2010;100(1):41–9. https://doi.org/10.2105/AJPH.2008.143651 .
Article PubMed Google Scholar
Ruger JP. Ethics of the social determinants of health. Lancet. 2004;364(9439):1092–7. https://doi.org/10.1016/S0140-6736(04)17067-0 .
Article PubMed PubMed Central Google Scholar
OECD/European Union. Health at a Glance: Europe 2018: State of Health in the EU Cycle. Brussels: OECD Publishing; 2018.
WHO. Global Status Report on Noncommunicable Diseases 2014. 2014.
WHO. Noncommunicable Diseases Progress Monitor 2020. 2020.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173–202. https://doi.org/10.1146/annurev.publhealth.19.1.173 .
Article CAS PubMed Google Scholar
Mota-Pinto A, Rodrigues V, Botelho A, Veríssimo MT, Morais A, Alves C, et al. A socio-demographic study of aging in the Portuguese population: the EPEPP study. Arch Gerontol Geriatr. 2011;52(3):304–8. https://doi.org/10.1016/j.archger.2010.04.019 .
Morse JM, Niehaus L. Mixed method design: principles and procedures. New York: Routledge; 2009.
Barton H, Grant M. A health map for the local human habitat. J R Soc Promot Heal. 2006;126(6):252–3. https://doi.org/10.1177/1466424006070466 .
Reis F, Sá-Moura B, Guardado D, Couceiro P, Catarino L, Mota-Pinto A, et al. Development of a healthy lifestyle assessment toolkit for the general public. Front Med. 2019;6:134.
Malva JO, Amado A, Rodrigues A, Mota-Pinto A, Cardoso AF, Teixeira AM, et al. The quadruple Helix-based innovation model of reference sites for active and healthy ageing in Europe: the ageing@Coimbra case study. Front Med. 2018;5. https://doi.org/10.3389/fmed.2018.00132 .
Carroll C, Booth A, Cooper K. A worked example of “best fit” framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11(1). https://doi.org/10.1186/1471-2288-11-29 .
Miller V, Webb P, Micha R, Mozaffarian D. Defining diet quality: a synthesis of dietary quality metrics and their validity for the double burden of malnutrition. Lancet Planetary Health. 2020;4(8):e352–70. https://doi.org/10.1016/S2542-5196(20)30162-5 .
General Directorate of Health and Institute for Health Metrics and Evaluation. Portugal: The Nation’s Health 1990–2016: An overview of the Global Burden of Disease Study 2016 Results. Direção-Geral da Saúde, Lisboa, Portugal. Institute for Health Metrics and Evaluation, Seattle, USA; 2018.
WHO. Global Recommendations on Physical Activity for Health. Geneva: WHO; 2010.
Al Tunaiji H, Davis JC, Mansournia MA, Khan KM. Population attributable fraction of leading non-communicable cardiovascular diseases due to leisure-time physical inactivity: a systematic review. BMJ Open Sport Exerc Med. 2019;5(1):e000512. https://doi.org/10.1136/bmjsem-2019-000512 .
WHO. World Report on Ageing and Health. 2015.
Van Holle V, Deforche B, Van Cauwenberg J, Goubert L, Maes L, Van de Weghe N, et al. Relationship between the physical environment and different domains of physical activity in European adults: a systematic review. BMC Public Health. 2012;12(1):807. https://doi.org/10.1186/1471-2458-12-807 .
DenBraver NR, Lakerveld J, Rutters F, Schoonmade LJ, Brug J, Beulens JWJ. Built environmental characteristics and diabetes: a systematic review and meta-analysis. BMC Med. 2018;16(1):12. https://doi.org/10.1186/s12916-017-0997-z .
Article CAS Google Scholar
Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–9. https://doi.org/10.2105/AJPH.91.11.1783 .
Article CAS PubMed PubMed Central Google Scholar
Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55(1):125–39. https://doi.org/10.1016/S0277-9536(01)00214-3 .
Cummins S, Stafford M, Macintyre S, Marmot M, Ellaway A. Neighbourhood environment and its association with self rated health: evidence from Scotland and England. J Epidemiol Community Health. 2005;59(3):207–13. https://doi.org/10.1136/jech.2003.016147 .
Barton H, Thompson S, Burgess S, Grant M. The Routledge handbook of planning for health and well-being. Shaping a sustainable and healthy future. Devon: Routledge; 2015.
Bird EL, Ige JO, Pilkington P, Pinto A, Petrokofsky C, Burgess-Allen J. Built and natural environment planning principles for promoting health: an umbrella review. BMC Public Health. 2018;18(1):930. https://doi.org/10.1186/s12889-018-5870-2 .
Ten Brink P, Mutafoglu K, Schweitzer J-P, Kettunen M, Twigger-Ross C, Kuipers Y, et al. The health and social benefits of Nature and biodiversity protection-executive summary. London/Brussels: Institute for European Environmental Policy; 2016.
Kegler MC, Swan DW, Alcantara I, Feldman L, Glanz K. The influence of rural home and neighborhood environments on healthy eating, physical activity, and weight. Prev Sci. 2014;15(1):1–11. https://doi.org/10.1007/s11121-012-0349-3 .
Chrisman M, Nothwehr F, Yang G, Oleson J. Environmental influences on physical activity in rural Midwestern adults: a qualitative approach. Health Promot Pract. 2015;16(1):142–8. https://doi.org/10.1177/1524839914524958 .
Barnidge EK, Baker EA, Estlund A, Motton F, Hipp PR, Brownson RC. A participatory regional partnership approach to promote nutrition and physical activity through environmental and policy change in rural Missouri. Prev Chronic Dis. 2015;12:140593. https://doi.org/10.5888/pcd12.140593 .
Hege A, Christiana RW, Battista R, Parkhurst H. Active living in rural Appalachia: using the rural active living assessment (RALA) tools to explore environmental barriers. Prev Med Rep. 2017;8:261–6. https://doi.org/10.1016/j.pmedr.2017.11.007 .
Luo Y, Zhang L, Pan X. Neighborhood environments and cognitive decline among middle-aged and older people in China. J Gerontol B Psychol Sci Soc Sci. 2019;74(7):e60–71. https://doi.org/10.1093/geronb/gbz016 .
de Almeida SJ, Augusto GF, Fronteira I, Hernandez-Quevedo C. Portugal: health system review. Health Syst Transit. 2017;19:1–184.
Soares da Silva D, Figueiredo E, Eusébio C, Carneiro MJ. The countryside is worth a thousand words – Portuguese representations on rural areas. J Rural Stud. 2016;44:77–88.
European Commission and Economic Policy Committee (Ageing Working Group). The 2018 Ageing report: economic and budgetary projections for the EU member states (2016-2070). European Commission, Brussels; 2018.
WHO. Sustainable Development Goal 11. 2016.
Braveman PA, Kumanyika S, Fielding J, LaVeist T, Borrell LN, Manderscheid R, et al. Health disparities and health equity: The issue is justice. Am J Public Health. 2011;101(SUPPL. 1):S149.
Article PubMed Central PubMed Google Scholar
Walsh K, O’Shea E. Responding to rural social care needs: older people empowering themselves, others and their community. Health Place. 2008;14(4):795–805. https://doi.org/10.1016/j.healthplace.2007.12.006 .
Nimegeer A, Farmer J. Prioritising rural authenticity: community members’ use of discourse in rural healthcare participation and why it matters. J Rural Stud. 2016;43:94–103. https://doi.org/10.1016/j.jrurstud.2015.11.006 .
Winterton R, Warburton J, Keating N, Petersen M, Berg T, Wilson J. Understanding the influence of community characteristics on wellness for rural older adults: a meta-synthesis. J Rural Stud. 2016;45:320–7. https://doi.org/10.1016/j.jrurstud.2015.12.010 .
Sá-Moura B, Couceiro P, Catarino L, Guardado D, Brito M, Gomes B, et al. Bridging health and social care with the citizens – the case of EIT health project “Healiqs4cities” and “Praça Vida+”, in Portugal. Care Wkly. 2018;2:21–4.
Bousquet J, Malva J, Nogues M, Mañas LR, Vellas B, Farrell J, et al. Operational definition of active and healthy aging (AHA): the European innovation partnership (EIP) on AHA reference site questionnaire: Montpellier October 20–21, 2014, Lisbon July 2, 2015. J Am Med Dir Assoc. 2015;16(12):1020–6. https://doi.org/10.1016/j.jamda.2015.09.004 .
Bousquet J, Illario M, Farrell J, Batey N, Carriazo AM, Malva J, et al. The reference site collaborative network of the European innovation partnership on active and healthy ageing. Transl Med. 2019;19:66–81 http://www.ncbi.nlm.nih.gov/pubmed/31360670 . Accessed 28 May 2021.
Download references
Acknowledgements
Advanced training students and young professionals that helped in the implementation of the community program in the 15 neighbourhoods of the Sicó-network: Adriana Caldo, Ana Pedrosa, André Caseiro, Beatriz Vaz, Carlos Farinha, Catarina Santos, Fernanda Silva, Inês Cipriano, Larissa Theil, Lilian Merini, Márcio Cascante, Rafael Rodrigues and Rafael Neves; the members of the Association Terras de Sicó (Lands of Sicó) and all the local stakeholders that helped implementing and disseminating our activities. HeaLIQs4Cities Consortium involved, which is composed by António Cunha, André Pardal, Eugénia Peixoto, Diana Guardado from the Instituto Pedro Nunes (IPN, Coimbra, Portugal); Marieke Zwaving from Rijksuniversiteit Groningen (The Netherlands); Eduardo Briones Pérez De La Blanca from Servicio Andaluz de Salud (SAS, Seville, Spain); Roel A. van der Heijden, Ruth Koops van ‘t Jagt and Daan Bultje from University Medical Center Groningen (UMCG, The Netherlands); João Malva, Flávio Reis, Luís Rama, Manuel Veríssimo, Ana Teixeira, Margarida Lima, Lèlita Santos, Filipe Palavra, Pedro Ferreira, Anabela Mota Pinto, Paula Santana, Ricardo Almendra, Adriana Loureiro, Inês Viana, Marta Quatorze, Anabela Marisa Azul, João Ramalho-Santos from the University of Coimbra (Portugal); Catharina Thiel Sandholdt and Maria Kristiansen from University of Copenhagen (UCPH, Denmark). We thank to the Reviewers the comments, which contributed for improving the manuscript. This research work was also developed under the European Regional Development Fund (ERDF), through the COMPETE 2020 – Operational Programme for Competitiveness and Internationalisation and Portuguese national funds via FCT – Fundação para a Ciência e a Tecnologia, the project UID/NEU/04539/2019, the Centro 2020 Regional Operational Programme: project CENTRO-01-0145-FEDER-000012-HealthyAging2020, the FOIE GRAS project, funded by the European Union’s Horizon 2020, Research and Innovation programme under the Marie Skłodowska-Curie Grant Agreement No. 722619, and the Decree Law 57/2016 (amended by Law 57/2017).
This research was developed in the scope of the European project Healthy Lifestyle Innovation Quarters for Cities and Citizens (HeaLIQs4Cities), funded by the European Institute of Innovation and Technology for Health (EIT Health) [Project Number 18036]. The funder had no role in the study design, data collection, analysing or interpreting data, or in writing the manuscript.
Author information
Authors and affiliations.
Center for Neuroscience and Cell Biology (CNC), University of Coimbra, 3004-504, Coimbra, Portugal
Anabela Marisa Azul, Rui Tavares & João Ramalho-Santos
Center for Innovative Biomedicine and Biotechnology (CIBB), University of Coimbra, 3030-789, Coimbra, Portugal
Anabela Marisa Azul, Flávio Reis, Rui Tavares, João Oliveira Malva & João Ramalho-Santos
University of Coimbra, Institute for Interdisciplinary Research (IIIUC), 3030-789, Coimbra, Portugal
Anabela Marisa Azul & Rui Tavares
Centre of Studies in Geography and Spatial Planning (CEGOT), Faculty of Arts and Humanities, Colégio de São Jerónimo, University of Coimbra, 3004-530, Coimbra, Portugal
Ricardo Almendra, Adriana Loureiro & Paula Santana
Department of Geography and Tourism, Faculty of Arts and Humanities, Colégio de São Jerónimo, University of Coimbra, 3004-530, Coimbra, Portugal
Ricardo Almendra & Paula Santana
Coimbra Institute for Clinical and Biomedical Research (iCBR), Faculty of Medicine, University of Coimbra, 3030-789, Coimbra, Portugal
Marta Quatorze, Flávio Reis, Anabela Mota-Pinto & João Oliveira Malva
Institute of Pharmacology & Experimental Therapeutics, Faculty of Medicine, University of Coimbra, 3030-370, Coimbra, Portugal
Flávio Reis & João Oliveira Malva
Clinical Academic Center of Coimbra (CACC), 3030-370, Coimbra, Portugal
Flávio Reis
CIMAGO-Center for Research in the Environment, Genetics and Oncobiology, Faculty of Medicine, University of Coimbra, Coimbra, Portugal
Anabela Mota-Pinto
IPN-Laboratory of Automatics and Systems, Pedro Nunes Institute, 3030-199, Coimbra, Portugal
- António Cunha
Ageing@Coimbra, EIP on AHA Reference Site, Coimbra, Portugal
António Cunha & João Oliveira Malva
Faculty of Sport Sciences and Physical Education, University of Coimbra, 3040-256, Coimbra, Portugal
Department of Life Sciences (DCV), Faculty of Sciences and Technology, University of Coimbra, 3000-456, Coimbra, Portugal
João Ramalho-Santos
You can also search for this author in PubMed Google Scholar
- , André Pardal
- , Eugénia Peixoto
- , Diana Guardado
- , Marieke Zwaving
- , Eduardo Briones Pérez De La Blanca
- , Roel A. van der Heijden
- , Ruth Koops Van’t Jagt
- , Daan Bultje
- , João Malva
- , Flávio Reis
- , Luís Rama
- , Manuel Veríssimo
- , Ana Teixeira
- , Margarida Lima
- , Lèlita Santos
- , Filipe Palavra
- , Pedro Ferreira
- , Anabela Mota Pinto
- , Paula Santana
- , Ricardo Almendra
- , Adriana Loureiro
- , Inês Viana
- , Marta Quatorze
- , Anabela Marisa Azul
- , João Ramalho-Santos
- , Catharina Thiel Sandholdt
- & Maria Kristiansen
Contributions
AMA was involved in the conceptualization and design of the study, all stages of data collection, curation, and analysis and led on writing the paper: original draft. RA, MQ, AL, PS and JRS were involved in the conceptualization and design of the study, all stages of data collection, curation, and analysis and writing the paper. FR, AMP, AC, LR, JOM, were involved in the conceptualization and design, data collection and writing the paper. RT was involved in the visual content. AC, JOM and HeaLIQs4Cities Consortium were involved in the funding acquisition. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Anabela Marisa Azul or João Ramalho-Santos .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table s1..
Evidence-based data by neighbourhoods’ type.
Additional file 2: Table S2.
Characterization of the community environment needs by neighbourhoods’ type and self-assessment of neighbourhood’ satisfaction.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Azul, A.M., Almendra, R., Quatorze, M. et al. Unhealthy lifestyles, environment, well-being and health capability in rural neighbourhoods: a community-based cross-sectional study. BMC Public Health 21 , 1628 (2021). https://doi.org/10.1186/s12889-021-11661-4
Download citation
Received : 11 November 2020
Accepted : 25 August 2021
Published : 06 September 2021
DOI : https://doi.org/10.1186/s12889-021-11661-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Non-communicable diseases
- Healthy lifestyles
- Health loss
- Health capability
- Qualitative driven mixed-methods
- Participatory community-based research
- Built environment
- Natural environment
- Rural areas
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Food and mood: how do...
Food and mood: how do diet and nutrition affect mental wellbeing?
Read our food for thought 2020 collection.
- Related content
- Peer review
This article has a correction. Please see:
- Food and mood: how do diet and nutrition affect mental wellbeing? - November 09, 2020
- Joseph Firth , research fellow 1 2 ,
- James E Gangwisch , assistant professor 3 4 ,
- Alessandra Borsini , researcher 5 ,
- Robyn E Wootton , researcher 6 7 8 ,
- Emeran A Mayer , professor 9 10
- 1 Division of Psychology and Mental Health, Faculty of Biology, Medicine and Health, Oxford Road, University of Manchester, Manchester M13 9PL, UK
- 2 NICM Health Research Institute, Western Sydney University, Westmead, Australia
- 3 Department of Psychiatry, Columbia University Vagelos College of Physicians and Surgeons, New York, USA
- 4 New York State Psychiatric Institute, New York, NY, USA
- 5 Section of Stress, Psychiatry and Immunology Laboratory, Institute of Psychiatry, Psychology and Neuroscience, Department of Psychological Medicine, King’s College London, London, UK
- 6 School of Psychological Science, University of Bristol, Bristol, UK
- 7 MRC Integrative Epidemiology Unit, Oakfield House, Bristol, UK
- 8 NIHR Biomedical Research Centre, University Hospitals Bristol NHS Foundation Trust and University of Bristol, Bristol, UK
- 9 G Oppenheimer Center for Neurobiology of Stress and Resilience, UCLA Vatche and Tamar Manoukian Division of Digestive Diseases, UCLA, Los Angeles, CA, USA
- 10 UCLA Microbiome Center, David Geffen School of Medicine, UCLA, Los Angeles, CA, USA
- Correspondence to: J Firth joseph.firth{at}manchester.ac.uk
Poor nutrition may be a causal factor in the experience of low mood, and improving diet may help to protect not only the physical health but also the mental health of the population, say Joseph Firth and colleagues
Key messages
Healthy eating patterns, such as the Mediterranean diet, are associated with better mental health than “unhealthy” eating patterns, such as the Western diet
The effects of certain foods or dietary patterns on glycaemia, immune activation, and the gut microbiome may play a role in the relationships between food and mood
More research is needed to understand the mechanisms that link food and mental wellbeing and determine how and when nutrition can be used to improve mental health
Depression and anxiety are the most common mental health conditions worldwide, making them a leading cause of disability. 1 Even beyond diagnosed conditions, subclinical symptoms of depression and anxiety affect the wellbeing and functioning of a large proportion of the population. 2 Therefore, new approaches to managing both clinically diagnosed and subclinical depression and anxiety are needed.
In recent years, the relationships between nutrition and mental health have gained considerable interest. Indeed, epidemiological research has observed that adherence to healthy or Mediterranean dietary patterns—high consumption of fruits, vegetables, nuts, and legumes; moderate consumption of poultry, eggs, and dairy products; and only occasional consumption of red meat—is associated with a reduced risk of depression. 3 However, the nature of these relations is complicated by the clear potential for reverse causality between diet and mental health ( fig 1 ). For example, alterations in food choices or preferences in response to our temporary psychological state—such as “comfort foods” in times of low mood, or changes in appetite from stress—are common human experiences. In addition, relationships between nutrition and longstanding mental illness are compounded by barriers to maintaining a healthy diet. These barriers disproportionality affect people with mental illness and include the financial and environmental determinants of health, and even the appetite inducing effects of psychiatric medications. 4

Hypothesised relationship between diet, physical health, and mental health. The dashed line is the focus of this article.
- Download figure
- Open in new tab
- Download powerpoint
While acknowledging the complex, multidirectional nature of the relationships between diet and mental health ( fig 1 ), in this article we focus on the ways in which certain foods and dietary patterns could affect mental health.
Mood and carbohydrates
Consumption of highly refined carbohydrates can increase the risk of obesity and diabetes. 5 Glycaemic index is a relative ranking of carbohydrate in foods according to the speed at which they are digested, absorbed, metabolised, and ultimately affect blood glucose and insulin levels. As well as the physical health risks, diets with a high glycaemic index and load (eg, diets containing high amounts of refined carbohydrates and sugars) may also have a detrimental effect on psychological wellbeing; data from longitudinal research show an association between progressively higher dietary glycaemic index and the incidence of depressive symptoms. 6 Clinical studies have also shown potential causal effects of refined carbohydrates on mood; experimental exposure to diets with a high glycaemic load in controlled settings increases depressive symptoms in healthy volunteers, with a moderately large effect. 7
Although mood itself can affect our food choices, plausible mechanisms exist by which high consumption of processed carbohydrates could increase the risk of depression and anxiety—for example, through repeated and rapid increases and decreases in blood glucose. Measures of glycaemic index and glycaemic load can be used to estimate glycaemia and insulin demand in healthy individuals after eating. 8 Thus, high dietary glycaemic load, and the resultant compensatory responses, could lower plasma glucose to concentrations that trigger the secretion of autonomic counter-regulatory hormones such as cortisol, adrenaline, growth hormone, and glucagon. 5 9 The potential effects of this response on mood have been examined in experimental human research of stepped reductions in plasma glucose concentrations conducted under laboratory conditions through glucose perfusion. These findings showed that such counter-regulatory hormones may cause changes in anxiety, irritability, and hunger. 10 In addition, observational research has found that recurrent hypoglycaemia (low blood sugar) is associated with mood disorders. 9
The hypothesis that repeated and rapid increases and decreases in blood glucose explain how consumption of refined carbohydrate could affect psychological state appears to be a good fit given the relatively fast effect of diets with a high glycaemic index or load on depressive symptoms observed in human studies. 7 However, other processes may explain the observed relationships. For instance, diets with a high glycaemic index are a risk factor for diabetes, 5 which is often a comorbid condition with depression. 4 11 While the main models of disease pathophysiology in diabetes and mental illness are separate, common abnormalities in insulin resistance, brain volume, and neurocognitive performance in both conditions support the hypothesis that these conditions have overlapping pathophysiology. 12 Furthermore, the inflammatory response to foods with a high glycaemic index 13 raises the possibility that diets with a high glycaemic index are associated with symptoms of depression through the broader connections between mental health and immune activation.
Diet, immune activation, and depression
Studies have found that sustained adherence to Mediterranean dietary patterns can reduce markers of inflammation in humans. 14 On the other hand, high calorie meals rich in saturated fat appear to stimulate immune activation. 13 15 Indeed, the inflammatory effects of a diet high in calories and saturated fat have been proposed as one mechanism through which the Western diet may have detrimental effects on brain health, including cognitive decline, hippocampal dysfunction, and damage to the blood-brain barrier. 15 Since various mental health conditions, including mood disorders, have been linked to heightened inflammation, 16 this mechanism also presents a pathway through which poor diet could increase the risk of depression. This hypothesis is supported by observational studies which have shown that people with depression score significantly higher on measures of “dietary inflammation,” 3 17 characterised by a greater consumption of foods that are associated with inflammation (eg, trans fats and refined carbohydrates) and lower intakes of nutritional foods, which are thought to have anti-inflammatory properties (eg, omega-3 fats). However, the causal roles of dietary inflammation in mental health have not yet been established.
Nonetheless, randomised controlled trials of anti-inflammatory agents (eg, cytokine inhibitors and non-steroidal anti-inflammatory drugs) have found that these agents can significantly reduce depressive symptoms. 18 Specific nutritional components (eg, polyphenols and polyunsaturated fats) and general dietary patterns (eg, consumption of a Mediterranean diet) may also have anti-inflammatory effects, 14 19 20 which raises the possibility that certain foods could relieve or prevent depressive symptoms associated with heightened inflammatory status. 21 A recent study provides preliminary support for this possibility. 20 The study shows that medications that stimulate inflammation typically induce depressive states in people treated, and that giving omega-3 fatty acids, which have anti-inflammatory properties, before the medication seems to prevent the onset of cytokine induced depression. 20
However, the complexity of the hypothesised three way relation between diet, inflammation, and depression is compounded by several important modifiers. For example, recent clinical research has observed that stressors experienced the previous day, or a personal history of major depressive disorders, may cancel out the beneficial effects of healthy food choices on inflammation and mood. 22 Furthermore, as heightened inflammation occurs in only some clinically depressed individuals, anti-inflammatory interventions may only benefit certain people characterised by an “inflammatory phenotype,” or those with comorbid inflammatory conditions. 18 Further interventional research is needed to establish if improvements in immune regulation, induced by diet, can reduce depressive symptoms in those affected by inflammatory conditions.
Brain, gut microbiome, and mood
A more recent explanation for the way in which our food may affect our mental wellbeing is the effect of dietary patterns on the gut microbiome—a broad term that refers to the trillions of microbial organisms, including bacteria, viruses, and archaea, living in the human gut. The gut microbiome interacts with the brain in bidirectional ways using neural, inflammatory, and hormonal signalling pathways. 23 The role of altered interactions between the brain and gut microbiome on mental health has been proposed on the basis of the following evidence: emotion-like behaviour in rodents changes with changes in the gut microbiome, 24 major depressive disorder in humans is associated with alterations of the gut microbiome, 25 and transfer of faecal gut microbiota from humans with depression into rodents appears to induce animal behaviours that are hypothesised to indicate depression-like states. 25 26 Such findings suggest a role of altered neuroactive microbial metabolites in depressive symptoms.
In addition to genetic factors and exposure to antibiotics, diet is a potentially modifiable determinant of the diversity, relative abundance, and functionality of the gut microbiome throughout life. For instance, the neurocognitive effects of the Western diet, and the possible mediating role of low grade systemic immune activation (as discussed above) may result from a compromised mucus layer with or without increased epithelial permeability. Such a decrease in the function of the gut barrier is sometimes referred to as a “leaky gut” and has been linked to an “unhealthy” gut microbiome resulting from a diet low in fibre and high in saturated fats, refined sugars, and artificial sweeteners. 15 23 27 Conversely, the consumption of a diet high in fibres, polyphenols, and unsaturated fatty acids (as found in a Mediterranean diet) can promote gut microbial taxa which can metabolise these food sources into anti-inflammatory metabolites, 15 28 such as short chain fatty acids, while lowering the production of secondary bile acids and p-cresol. Moreover, a recent study found that the ingestion of probiotics by healthy individuals, which theoretically target the gut microbiome, can alter the brain’s response to a task that requires emotional attention 29 and may even reduce symptoms of depression. 30 When viewed together, these studies provide promising evidence supporting a role of the gut microbiome in modulating processes that regulate emotion in the human brain. However, no causal relationship between specific microbes, or their metabolites, and complex human emotions has been established so far. Furthermore, whether changes to the gut microbiome induced by diet can affect depressive symptoms or clinical depressive disorders, and the time in which this could feasibly occur, remains to be shown.
Priorities and next steps
In moving forward within this active field of research, it is firstly important not to lose sight of the wood for the trees—that is, become too focused on the details and not pay attention to the bigger questions. Whereas discovering the anti-inflammatory properties of a single nutrient or uncovering the subtleties of interactions between the gut and the brain may shed new light on how food may influence mood, it is important not to neglect the existing knowledge on other ways diet may affect mental health. For example, the later consequences of a poor diet include obesity and diabetes, which have already been shown to be associated with poorer mental health. 11 31 32 33 A full discussion of the effect of these comorbidities is beyond the scope of our article (see fig 1 ), but it is important to acknowledge that developing public health initiatives that effectively tackle the established risk factors of physical and mental comorbidities is a priority for improving population health.
Further work is needed to improve our understanding of the complex pathways through which diet and nutrition can influence the brain. Such knowledge could lead to investigations of targeted, even personalised, interventions to improve mood, anxiety, or other symptoms through nutritional approaches. However, these possibilities are speculative at the moment, and more interventional research is needed to establish if, how, and when dietary interventions can be used to prevent mental illness or reduce symptoms in those living with such conditions. Of note, a recent large clinical trial found no significant benefits of a behavioural intervention promoting a Mediterranean diet for adults with subclinical depressive symptoms. 34 On the other hand, several recent smaller trials in individuals with current depression observed moderately large improvements from interventions based on the Mediterranean diet. 35 36 37 Such results, however, must be considered within the context of the effect of people’s expectations, particularly given that individuals’ beliefs about the quality of their food or diet may also have a marked effect on their sense of overall health and wellbeing. 38 Nonetheless, even aside from psychological effects, consideration of dietary factors within mental healthcare may help improve physical health outcomes, given the higher rates of cardiometabolic diseases observed in people with mental illness. 33
At the same time, it is important to be remember that the causes of mental illness are many and varied, and they will often present and persist independently of nutrition and diet. Thus, the increased understanding of potential connections between food and mental wellbeing should never be used to support automatic assumptions, or stigmatisation, about an individual’s dietary choices and their mental health. Indeed, such stigmatisation could be itself be a casual pathway to increasing the risk of poorer mental health. Nonetheless, a promising message for public health and clinical settings is emerging from the ongoing research. This message supports the idea that creating environments and developing measures that promote healthy, nutritious diets, while decreasing the consumption of highly processed and refined “junk” foods may provide benefits even beyond the well known effects on physical health, including improved psychological wellbeing.
Contributors and sources: JF has expertise in the interaction between physical and mental health, particularly the role of lifestyle and behavioural health factors in mental health promotion. JEG’s area of expertise is the study of the relationship between sleep duration, nutrition, psychiatric disorders, and cardiometabolic diseases. AB leads research investigating the molecular mechanisms underlying the effect of stress and inflammation on human hippocampal neurogenesis, and how nutritional components and their metabolites can prevent changes induced by those conditions. REW has expertise in genetic epidemiology approaches to examining casual relations between health behaviours and mental illness. EAM has expertise in brain and gut interactions and microbiome interactions. All authors contributed to, read, and approved the paper, and all the information was sourced from articles published in peer reviewed research journals. JF is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare the following: JF is supported by a University of Manchester Presidential Fellowship and a UK Research and Innovation Future Leaders Fellowship and has received support from a NICM-Blackmores Institute Fellowship. JEG served on the medical advisory board on insomnia in the cardiovascular patient population for the drug company Eisai. AB has received research funding from Johnson & Johnson for research on depression and inflammation, the UK Medical Research Council, the European Commission Horizon 2020, the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust, and King’s College London. REW receives funding from the National Institute for Health Research Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. EAM has served on the external advisory boards of Danone, Viome, Amare, Axial Biotherapeutics, Pendulum, Ubiome, Bloom Science, Mahana Therapeutics, and APC Microbiome Ireland, and he receives royalties from Harper & Collins for his book The Mind Gut Connection. He is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and the US Department of Defense. The views expressed are those of the authors and not necessarily those of the organisations above.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of series commissioned by The BMJ. Open access fees are paid by Swiss Re, which had no input into the commissioning or peer review of the articles. T he BMJ thanks the series advisers, Nita Forouhi, Dariush Mozaffarian, and Anna Lartey for valuable advice and guiding selection of topics in the series.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Friedrich MJ
- Johnson J ,
- Weissman MM ,
- Lassale C ,
- Baghdadli A ,
- Siddiqi N ,
- Koyanagi A ,
- Gangwisch JE ,
- Salari-Moghaddam A ,
- Larijani B ,
- Esmaillzadeh A
- de Jong V ,
- Atkinson F ,
- Brand-Miller JC
- Seaquist ER ,
- Anderson J ,
- American Diabetes Association ,
- Endocrine Society
- Towler DA ,
- Havlin CE ,
- McIntyre RS ,
- Nguyen HT ,
- O’Keefe JH ,
- Gheewala NM ,
- Kastorini C-M ,
- Milionis HJ ,
- Esposito K ,
- Giugliano D ,
- Goudevenos JA ,
- Panagiotakos DB
- Teasdale SB ,
- Köhler-Forsberg O ,
- N Lydholm C ,
- Hjorthøj C ,
- Nordentoft M ,
- Yahfoufi N ,
- Borsini A ,
- Horowitz MA ,
- Kiecolt-Glaser JK ,
- Fagundes CP ,
- Andridge R ,
- Osadchiy V ,
- Martin CR ,
- O’Brien C ,
- Sonnenburg ED ,
- Sonnenburg JL
- Rampelli S ,
- Jeffery IB ,
- Tillisch K ,
- Kilpatrick L ,
- Walsh RFL ,
- Wootton RE ,
- Millard LAC ,
- Jebeile H ,
- Garnett SP ,
- Paxton SJ ,
- Brouwer IA ,
- MooDFOOD Prevention Trial Investigators
- Francis HM ,
- Stevenson RJ ,
- Chambers JR ,
- Parletta N ,
- Zarnowiecki D ,
- Fischler C ,
- Sarubin A ,
- Wrzesniewski A
- Harrington D ,
The Different Lifestyle Issues that Affect People’s Health Essay
Introduction, works cited.
This essay discusses the different life style issues that affect people’s health. Many diseases and disorders result from lifestyle choices. Through life style changes, individuals can afford a life free from diseases. Physical exercise and proper relaxation have been identified as critical to avoiding stress, obesity and even other complicated conditions like cancer.
By avoiding smoking, alcohol and drug abuse, individuals avoid associated diseases and social problems. This essay covers issues to do with stress, tobacco use, alcohol consumption, drug abuse, diabetes and cancer. For each of the mentioned issues, I consider the causes and best ways of stopping or limiting related destructive behavior.
Stress happens when we are stretched or straining. Straining can happen in the psychological, physical, emotional or mental self. When one thinks a lot, it will translate into stress. The same happens when one does too much physical activity. Stress can largely be associated with unhealthy lifestyles. Unhealthy lifestyles are characterized by overdoing of some things and neglect of given aspects of self. For example, people who over eat are likely to suffer from stress induced by effects of overweight.
Stress often registers both as a feeling and a physical condition (Ratcliff 69). Some people realize they are stressed when they start to behave in certain awkward ways e.g. making simple mistakes at work.
Stress induces sleeplessness, headaches, stomachaches, general tension in the body, general fatigue, bouts of anger, nervousness, lack of appetite, overeating, mood swings, loss of enthusiasm for life and unexplained anxiety (Ratcliff 52). The signs and symptoms vary from individual to individual. In extreme cases, individuals turn to drug abuse or alcoholic tendencies when stressed.
To avoid stress, individuals have to learn to balance work and relaxation. Life is neither about work nor leisure. Everything has to be done in the right dose i.e. work hard but also relax enough. For students, stress management would require budgeting well for time. The timetables should allow for study time, physical exercise time and some time of pure relaxation.
Tobacco smoking has been practiced for a very long time. Many people smoke tobacco for pleasure. Smoking is an addiction that people take to out of influence especially from company. Tobacco has chemical properties so that when inhaled they activate the body and make the body alert (Connolly 22).
Smoking tobacco has been scientifically proved to be the cause of many breathes system related complications and cancer. Smoke particle perforate the lungs in the long run leading to lung failure or lung cancers (Connolly 37). It is also known that tobacco smoke contains carcinogens which affect body cells making them cancerous.
Widespread smoking is associated with advertisement or marketing campaigns by tobacco companies. In the advertisement, thought currently, highly restricted, smokers were depicted as the cool guys (Connolly 75). Smoking was associated with achievement or being super.
Currently, despite antismoking campaigns, smoking continues. As an individual, I can not imagine myself smoking because there is no recorded benefit that one gains from smoking. More sensitization and legislation against tobacco smoking is a sure way of stopping and limiting smoking.
Alcohol is used almost world wide. Continued use of alcoholic drinks results in addiction and development of health problems. Individuals who are addicted to alcohol have a compulsion to be drunk always. Stress, socio-economic problems or frustration is the key reason why people become alcoholics. Those who start taking alcohol at a young age are more likely to become alcohol dependent (Goodwin 18).
Alcoholism has many negative effects in the life of an individual. Continued dependence on alcohol translates into an individual draining his or her finances. Alcohol is one of the greatest expenditure for alcoholics. Alcoholics develop ill health due to the effect of alcohol on the liver (Goodwin 10).
There are also a number of cognitive problems associated with excessive consumption of alcohol. Alcoholics also develop negative social behavior e.g. withdrawing from social activity, becoming abusive and intolerant. In the extreme conditions, alcoholism makes individuals to develop suicidal behavior; when drunk, the fear of doing the unthinkable is found. Furthermore, alcoholics tend towards violence and such deviance as rape or other crimes.
Alcoholism is managed through use of medicines and therapy (Goodwin 133). It is considered that given the effects of alcohol on the body, detoxification or purification is necessary. Group therapy or counseling is necessary to help people confront and acknowledge that alcoholism is a problem they have. Group therapy is encouraging as it helps one realize there are others suffering from the same but breaking from it is possible. The best way of dealing with alcoholism is avoiding alcohol completely.
Drug abuse is use of generally associated with use of certain drugs that make an individual psychoactive or enhances performance (Abadinsky 2). There are a number of drugs that produce unhealthy reactions in the human body. They suppress the nervous system, induce over secretion of fight or flight hormones, or generally lead to over-excitement.
In the long run, such drugs either impair ones mental capacity or physical performance. Examples of such drugs include opium, cocaine, heroine etc. although the drugs, on the short term, induce a happy feeling in the user; in the long run they are addictive and affect the individual adversely.
Drug abuse often causes individuals a lot of problems. When found out, drug abuse often carries some form of criminal penalty. People who abuse drugs also have high propensity towards violence, unprotected sex, lawlessness, crime, and suicide. Drug abuse also leads to addiction or dependence that makes individuals virtually unproductive. It has been proved that some drugs when used cause physiological damage to the brain and the nervous system (Abadinsky 18). Many psychiatric problems result from drug abuse e.g. smoking of bhang.
Generally, efforts to limit or control abuse of drugs are effected through legislation and harmful effect sensitization. It is criminal to handle or use certain substances such as heroine or cocaine (Abadinsky 37). Government, non governmental organizations and even religions do a lot to sensitize community against drug abuse. As an individual, being principled and avoiding peer pressure comes in handy in avoiding the drug abuse traps.
Diabetes is a condition that results in the body not being able to regulate blood sugar. This is caused by the pancreas producing less or too much insulin (Moran and Merriman 3). Due to the insulin available being in abnormal amount, it does not work properly producing an abnormal condition in the body. This happens when one eats too many sugary food stuffs, due to bacteria attack or exposure to chemical toxins.
Although diabetes is sometimes inherited, many cases of the disease are acquired due to lifestyle related issues. Eating of sugary things contributes in a big way to occurrence of diabetes cases (Moran and Merriman 41). From very early ages, parents often find themselves trapped in appeasing their children with sweet things as cakes and sweets.
However, these sweet foods only increase blood sugar to the level where the pancreas becomes overworked or the insulin produced is not enough to facilitate breakdown of sugar. Lack of physical exercise also contributes in a big way to sugar levels going high (Moran and Merriman 73). Physical exercise uses energy which is obtained from breakdown of sugar thus leading to reduction of blood sugar levels.
To avoid diabetes, one has to regulate the amount of sugary foods he or she takes. Physical exercise is critical for proper metabolism and catabolism in the body. This helps towards breakdown or use of much blood sugar, reducing risk of overworking pancreas.
Cancer refers to a condition when body cells grow uncontrollably forming a lump called a tumor. There are different kinds of tumor that register in the body in different ways. Some cancerous cells (cells that are growing abnormally and replicating out of control) spread around the body while others are often localized. When cancerous lumps or tumors form, they affect the normal flow in the body. They normal destroy the body system within which they grow.
Cancer is believed to be hereditary i.e. it inherited through the genetic disposition in families. Old age is the second uncontrollable factor that disposes people to cancer.
In old age the immune system becomes weaker and possibility of cell mutations I higher. However, it also largely depends on exposure to certain risks in life. Carcinogens are known to increase likelihood of getting cancer as they damage DNA thus leading to cells growing uncontrollably (Anderson 29). Smoking is widely believed to be the number one contributor to carcinogens presence in the human body.
Carcinogen is also accessed through inhaling exhaust fumes. Many sexually transmitted disease causing viruses are also closely associated with cancer and they lower body immunity. Eating a poor diet puts an individual at the risk of cancer because body immunity and proper cell formation is depended on diet. Lack of exercising and obesity are associated with cancer because proper functioning of body is affected.
Cancer can be prevented through avoiding of certain destructive behaviors. Smoking and drinking alcohol only raise the risks of getting cancer. Individuals have to avoid expressing themselves to the chemicals and radiation that is also associated with cell mutation (Anderson 123). Individuals have to eat right because health largely depends on what individuals eat.
This essay considers the different destructive behaviors that people engage in. From the different issues discussed, it is clear that lifestyle choices play a critical role in ensuring health living. It is advisable that individuals eat well, avoid smoking, resist any form of drug abuse, do physical exercises and avoid exposure to harmful chemicals or radiation to avoid risk of disease or other social defects.
Abadinsky Howard. Drug Abuse: An Introduction. 3 rd Ed. Chicago: Nelson-Hall Publishers, 1997
Anderson, Greg. Cancer: 50 Essential Things to Do. 3 rd Ed. New York: Plume, 2009.
Connolly, Sean. Tobacco . Mankato: Black Rabbit Books, 2006.
Goodwin, Donald W. Alcoholism, the Facts. 3 rd Ed. Oxford: Oxford University Press, 2000
Moran, Katherine, and Merriman Lisa. Diabetes: The Ultimate Teen Guide. New York:Scarecrow Press, 2004
Ratcliffe, Gail. Take Control Of Your Life: The Five Step Stress Management Plan. London: Simon & Schuster, 1995
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, January 20). The Different Lifestyle Issues that Affect People’s Health. https://ivypanda.com/essays/destructive-behavior/
"The Different Lifestyle Issues that Affect People’s Health." IvyPanda , 20 Jan. 2020, ivypanda.com/essays/destructive-behavior/.
IvyPanda . (2020) 'The Different Lifestyle Issues that Affect People’s Health'. 20 January.
IvyPanda . 2020. "The Different Lifestyle Issues that Affect People’s Health." January 20, 2020. https://ivypanda.com/essays/destructive-behavior/.
1. IvyPanda . "The Different Lifestyle Issues that Affect People’s Health." January 20, 2020. https://ivypanda.com/essays/destructive-behavior/.
Bibliography
IvyPanda . "The Different Lifestyle Issues that Affect People’s Health." January 20, 2020. https://ivypanda.com/essays/destructive-behavior/.
- The Facts About Alcoholism
- Alcoholism Causes and Curing
- Do Alcoholic People Interact Differently?
- Alcoholism Disease or Self Will
- Alcoholism: The Disease Is Often Progressive and Fatal
- Teenage Depression and Alcoholism
- Alcoholism, Domestic Violence and Drug Abuse
- Alcoholism as a Social Problem
- Genetic Predisposition to Alcohol: The Appreciation and Therapy for Alcoholism
- Alcoholism as a Social Issue and Its Effect on Families
- Fundamental Causality and Race
- Life Expectancy in the Developing World
- Stress at the Workplace for Correctional Officers
- National Health Care System for Insurance Program in America
- Detrimental Effects of Unemployment on People’s Health
Talk to our experts
1800-120-456-456
- Healthy Lifestyle Essay

Essay on Healthy Lifestyle
The top secret of being physically fit is adopting a healthy lifestyle. A healthy lifestyle includes regular exercise, a healthy diet, taking good care of self, healthy sleep habits, and having a physically active daily routine. Lifestyle is the most prevailing factor that affects one’s fitness level. A person leading a sedentary lifestyle has a low fitness level whereas living a healthier life not only makes a person fit but also extends life. Good health has a direct impact on our personality. A person with a good and healthy lifestyle is generally more confident, self-assured, sociable, and energetic.
A good and healthy lifestyle allows one to relish and savor all the pleasures in life without any complications. Even all the wealth is less valuable when compared to sound health. Having all the luxuries in the world does not fulfill its purpose when one is continuously ill, depressed, or suffering from a significant health complication. A healthy person has a clear and calm perception of everything without prejudice. His actions and decisions are more practical and logical and are hence more successful in life.
A good habit is a key factor for a healthy lifestyle. To maintain a stable body and mind, one needs to inculcate good habits. Waking up early in the morning, regularly exercising or a good morning walk helps to keep our body energetic and refresh our mind. Maintaining a balanced and nutritious diet throughout the day is vital for maintaining a good lifestyle. Too much indulgence in alcohol or smoking excessively is not at all appropriate for a healthy lifestyle.
Self-Discipline
Self-discipline is important for maintaining a good lifestyle. When we are self-disciplined then we are more organized and regular in maintaining good health. A disciplined life is a regulated life. A man without discipline is a ship without a rudder. Discipline needs self-control. One who cannot control himself can seldom control others. The level of discipline and perseverance largely determines a person’s success. Self-discipline is the act of disciplining one’s own feelings, desires, etc. especially with the intention of improving oneself. It strengthens our willpower. The stronger our will power the positive will be our decision. It enables us to conquer our own self.
Punctuality
Punctuality is the habit of doing things on time. It is the characteristic of every successful person and everyone must observe punctuality in order to win success in life. Punctuality is necessary for maintaining a healthy lifestyle. It should become a habit with us. A punctual person is able to fulfill all his responsibilities and hence is treated with respect in society. It is needed in every walk of life.
Diet is an important component for overall fitness and works best in combination with exercise. A balanced diet and exercise regularly help to maintain good health. It is necessary to reduce weight if one is overweight or obese, failing which one cannot be physically fit for long. For people with obesity, more exercise and a strict regime are necessary, preferably under guidance. There are many ways of making the diet healthier.
Use less sugar and salt while cooking food.
Use less oil while cooking. Avoid deep-frying as much as possible.
Eat more fruits daily. They provide more vitamins and minerals to our bodies.
Add sprouts of gram and moong dal to at least one meal in a day. Add fiber to your diet. Use whole grains instead of polished cereals. Eat lots of salad and yogurt.
Eat fermented food regularly. Fermented food contains many useful bacteria that help in the process of digestion.
Prevention of Lifestyle Diseases
By adopting a healthy lifestyle one can avoid lifestyle diseases. The following are some ways in which we can prevent lifestyle diseases.
Eat a balanced diet that contains important nutrients. One must include more fresh fruits and green vegetables in the diet. Refrain from eating junk food. Stay away from foods that contain large amounts of salt or sugar.
Exercise regularly. Spend more time outdoors and do activities such as walking, running, swimming, and cycling.
One must avoid overindulgence in alcohol, junk food, smoking, and addiction to drugs and medicines.
Avoid spending too much on modern gadgets like mobile phones, laptops, televisions, etc. Spend time on these gadgets for short intervals of time only.
Set a healthy sleeping routine for every day. Waking early in the morning and going to bed early at night should be a daily habit. Lead an active life.
Unhealthy Lifestyle
Bad food habits and an unhealthy lifestyle such as less or no physical activity may lead to several diseases like obesity, high blood pressure or hypertension, diabetes, anemia, and various heart diseases. An unhealthy lifestyle reduces productivity and creativity in a person. It also adversely affects moods and relationships. It leads to depression and anxiety in human beings.
Maintaining a healthy lifestyle not only makes a person confident and productive but also drives him to success. A person with a healthy lifestyle will enjoy both personal and social life.

FAQs on Healthy Lifestyle Essay
What Do You Understand about a Healthy Lifestyle?
A healthy lifestyle is a lifestyle that includes regular exercise, a healthy diet, taking good care of self, healthy sleep habits and having a physically active daily routine.
How is Punctuality Important for Maintaining a Healthy Lifestyle?
Punctuality is the habit of doing things on time. It is the characteristic of every successful person and everyone must observe punctuality in order to win success in life. It should become a habit with us. A punctual person is able to fulfil all his responsibilities and hence is treated with respect in society. It is needed in every walk of life.
What Happens When One Does Not Maintain a Healthy Lifestyle?
When one does not maintain a healthy lifestyle then several diseases like obesity, high blood pressure or hypertension, diabetes, anaemia and various heart diseases can occur. An unhealthy lifestyle reduces productivity and creativity in a person. It also adversely affects moods and relationships. It leads to depression and anxiety in human beings.
What are the Main Factors that Determine a Good and Healthy Lifestyle?
In order to maintain a good and healthy lifestyle, one must be self-disciplined, self-motivated, maintain punctuality and have good habits like waking early in the morning and maintain a regular fitness regime and a balanced and nutritious diet.
Is writing an essay hard?
Essay writing is a difficult task that needs a great deal of study, time, and focus. It's also an assignment that you can divide down into manageable chunks such as introduction, main content, and conclusion. Breaking down and focusing on each individually makes essay writing more pleasant. It's natural for students to be concerned about writing an essay. It's one of the most difficult tasks to do, especially for people who aren't confident in their writing abilities. While writing a decent essay is difficult, the secret to being proficient at it is reading a lot of books, conducting extensive research on essential topics, and practicing essay writing diligently.
Why is it important for one to aspire to have a healthy lifestyle?
A healthy lifestyle is an important way for reducing the occurrence and impact of health problems, as well as for recovery, coping with life stressors, and improving the overall quality of life. An increasing collection of scientific data suggests that our habits have a significant impact on our health. Everything we eat and drink, as well as how much exercise we get and whether we smoke or use drugs, has an impact on our health, not just in terms of life expectancy but also in terms of how long we may expect to live without developing chronic illness. A large proportion of fatalities are caused by conditions such as heart attacks, stroke, diabetes, joint disease, and mental illness. A healthy lifestyle can help to avoid or at least delay the onset of many health issues.
How to download the Essay on Healthy Lifestyle from the Vedantu website?
The Essay on Healthy Lifestyle, which is accurate and well-structured, is available for download on the Vedantu website. The Essay is accessible in PDF format on Vedantu's official website and may be downloaded for free. Students should download the Essay on Healthy Lifestyle from the Vedantu website to obtain a sense of the word limit, sentence structure, and fundamental grasp of what makes a successful essay. Vedantu essay is brief and appropriate for youngsters in school. It is written in basic English, which is ideal for kids who have a restricted vocabulary. Following the Vedantu essay ensures that students are adequately prepared for any essay subject and that they will receive high grades. Click here to read the essay about a healthy lifestyle.
Who prepares the Essay for Vedantu?
The Essay on Healthy Lifestyle designed for the Vedantu is created by a group of experts and experienced teachers. The panel of experts has created the essay after analyzing important essay topics that have been repeatedly asked in various examinations. The Essays that are provided by Vedantu are not only well-structured but also accurate and concise. They are aptly suited for young students with limited vocabulary. For best results, the students are advised to go through multiple essays and practice the topics on their own to inculcate the habits of time management and speed.
What constitutes a healthy lifestyle?
Healthy life is built on the pillars of a good diet, frequent exercise, and appropriate sleep. A healthy lifestyle keeps people in excellent shape, it also gives you more energy throughout the day, and lowers your chance of developing many diet-related chronic diseases. Healthy living is considered a lifestyle choice that allows you to enjoy more elements of your life. Taking care of one's physical, emotional, and spiritual well-being is part of living a healthy lifestyle.
Good Nutrition, Eating Right and proper diet.
Getting Physically Fit, Beneficial Exercise and working out often.
Adequate rest and uninterrupted sleep.
Proper Stress Management.
Self-Supportive Attitudes.
Positive Thoughts are encouraged.
Positive Self-Image and body image.
Inner Calmness and peace.
Openness to Your Creativity and Self-care.
Trust in Your Inner Knowing and your gut feeling.
English that goes straight to the heart
Essay on Unhealthy Lifestyle
An essay is a piece of writing that revolves around a particular theme and contains the academic opinions of the person writing it. A basic essay mainly consists of three parts: Introduction, Body, and Conclusion.
In this post, you will find a brilliant essay on Unhealthy Lifestyles.
Daily Test - Attempt Now

Essay on Unhealthy Lifestyle (600+ Words)
In today’s busy world, it is very common for people to fall victim to the dangers of an unhealthy lifestyle. Sedentary habits, poor dietary choices, and neglecting self-care have become the norm for many, leading to detrimental consequences. However, it is crucial to acknowledge the profound impact of such a lifestyle and take the necessary steps to reclaim our well-being.
One of the primary contributors to an unhealthy lifestyle is the lack of physical activity. Many people find themselves leading sedentary lives, spending long hours sitting at desks or engrossed in digital screens. This dearth of movement not only paves the way for weight gain and obesity but also heightens the risk of chronic conditions such as cardiovascular disease, diabetes, and certain cancers. Our bodies are designed to be active, and the absence of regular exercise deprives us of vitality and robust health.
In conjunction with physical inactivity, poor dietary choices compound the perils of an unhealthy lifestyle. Fast food, processed snacks, sugary beverages, and excessive consumption of refined carbohydrates dominate many individuals’ diets. These choices often pack a caloric punch and contain unhealthy fats, sodium, and sugar, while lacking essential nutrients. Consequently, weight gain becomes an inevitable outcome, and the likelihood of developing metabolic disorders, cardiovascular problems, and other chronic diseases skyrockets. Furthermore, a diet devoid of fruits, vegetables, whole grains, and lean proteins deprives our bodies of vital nourishment, weakening our immune system and compromising our overall well-being.
An unhealthy lifestyle doesn’t merely take a toll on physical health; it also wreaks havoc on mental well-being. Chronic stress, irregular sleep patterns, and neglecting self-care routines contribute to heightened levels of anxiety, depression, and overall mental distress. The demands of modern life often lead individuals to sacrifice their own well-being in pursuit of success, leaving them emotionally drained and vulnerable to mental health challenges. Neglecting self-care activities, such as relaxation, leisure, and engaging in hobbies, further perpetuates this cycle of stress and burnout.
Escaping the clutches of an unhealthy lifestyle necessitates a deliberate commitment to change. It commences with making small yet significant adjustments to our daily routines. Incorporating regular physical activity, even in the form of brisk walks or short workouts, can yield profound benefits for our health. Prioritizing a balanced diet that encompasses abundant fruits, vegetables, whole grains, and lean proteins furnishes our bodies with the essential nutrients required for optimal functioning. Adequate hydration is also vital, as consuming a sufficient amount of water facilitates digestion, bolsters energy levels, and supports overall well-being.
Equally vital is nurturing our mental and emotional health. Engaging in stress-reducing activities like meditation, mindfulness, or practicing relaxation techniques can help restore equilibrium and enhance our resilience in the face of life’s challenges. Establishing boundaries and carving out time for self-care activities, be it pursuing a hobby, immersing oneself in nature, or simply indulging in moments of self-reflection, plays a pivotal role in maintaining emotional well-being.
It is essential to recognize that an unhealthy lifestyle not only jeopardizes our personal well-being but also places a burden on society as a whole. The healthcare system bears the brunt of preventable chronic diseases, while the economic impact of reduced productivity and heightened healthcare costs is significant. By embracing a healthier lifestyle, we not only enhance our own quality of life but also contribute to the construction of a healthier and more sustainable society.
In conclusion, an unhealthy lifestyle carries substantial risks for our physical and mental well-being. It is imperative that we break free from sedentary habits, poor dietary choices, and neglect of self-care that have become ingrained in our lives.
You Asked, We Listened – Get Free Access to All Writing Lists 😍😍

Top 10 Biography Examples
Read More »

What is the Problem Solution Paragraph?

Top 10 Short Stories for Kids
Daily reading comprehension test - attempt now, discover more from english luv.
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Health Risks of an Inactive Lifestyle
What is an inactive lifestyle.
Being a couch potato. Not exercising. A sedentary or inactive lifestyle. You have probably heard of all of these phrases, and they mean the same thing: a lifestyle with a lot of sitting and lying down, with very little to no exercise.
In the United States and around the world, people are spending more and more time doing sedentary activities. During our leisure time, we are often sitting: while using a computer or other device, watching TV, or playing video games. Many of our jobs have become more sedentary, with long days sitting at a desk. And the way most of us get around involves sitting - in cars, on buses, and on trains.
How does an inactive lifestyle affect your body?
When you have an inactive lifestyle,:
- You burn fewer calories. This makes you more likely to gain weight.
- You may lose muscle strength and endurance, because you are not using your muscles as much
- Your bones may get weaker and lose some mineral content
- Your metabolism may be affected, and your body may have more trouble breaking down fats and sugars
- Your immune system may not work as well
- You may have poorer blood circulation
- Your body may have more inflammation
- You may develop a hormonal imbalance
What are the health risks of an inactive lifestyle?
Having an inactive lifestyle can be one of the causes of many chronic diseases. By not getting regular exercise, you raise your risk of:
- Heart diseases , including coronary artery disease and heart attack
- High blood pressure
- High cholesterol
- Metabolic syndrome
- Type 2 diabetes
- Certain cancers, including colon , breast , and uterine cancers
- Osteoporosis and falls
- Increased feelings of depression and anxiety
Having a sedentary lifestyle can also raise your risk of premature death. And the more sedentary you are, the higher your health risks are.
How can I get started with exercise?
If you have been inactive, you may need to start slowly. You can keep adding more exercise gradually. The more you can do, the better. But try not to feel overwhelmed, and do what you can. Getting some exercise is always better than getting none. Eventually, your goal can be to get the recommended amount of exercise for your age and health.
There are many different ways to get exercise; it is important to find the types that are best for you . You can also try to add activity to your life in smaller ways, such as at home and at work.
How can I be more active around the house?
There are some ways you can be active around your house:
- Housework, gardening, and yard work are all physical work. To increase the intensity, you could try doing them at a more vigorous pace.
- Keep moving while you watch TV. Lift hand weights, do some gentle yoga stretches, or pedal an exercise bike. Instead of using the TV remote, get up and change the channels yourself.
- Work out at home with a workout video (on your TV or on the internet)
- Go for a walk in your neighborhood. It can be more fun if you walk your dog, walk your kids to school, or walk with a friend.
- Stand up when talking on the phone
- Get some exercise equipment for your home. Treadmills and elliptical trainers are great, but not everyone has the money or space for one. Less expensive equipment such as yoga balls, exercise mats, stretch bands, and hand weights can help you get a workout at home too.
How can I be more active at work?
Most of us sit when we are working, often in front of a computer. In fact, less than 20% of Americans have physically active jobs. It can be challenging to fit physical activity into your busy workday, but here are some tips to help you get moving:
- Get up from your chair and move around at least once an hour
- Stand when you are talking on the phone
- Find out whether your company can get you a stand-up or treadmill desk
- Take the stairs instead of the elevator
- Use your break or part of your lunch hour to walk around the building
- Stand up and walk to a colleague's office instead of sending an email
- Have "walking" or standing meetings with co-workers instead of sitting in a conference room
- Get Real about Getting Active (American Heart Association)
- Overcoming Barriers to Physical Activity (Centers for Disease Control and Prevention) Also in Spanish
- Screen time and children (Medical Encyclopedia) Also in Spanish
- Standing or Walking Versus Sitting on the Job in 2016 (Department of Labor)
- What Are the Risks of Sitting Too Much? (Mayo Foundation for Medical Education and Research) Also in Spanish
Clinical Trials
Journal articles references and abstracts from medline/pubmed (national library of medicine).
- Article: Secular trends in the prevalence of meeting 24-hour movement guidelines among...
- Article: Measurement of Sedentary Behavior-The Outcomes of the Angle for Posture Estimation...
- Article: The sedentary behavior reduction in pregnancy intervention (SPRING) pilot and feasibility...
- Health Risks of an Inactive Lifestyle -- see more articles
The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health.
Poor Nutrition

Measure Breastfeeding Practices and Eating Patterns
Support breastfeeding in the hospital and community, offer healthier food options in early care and education facilities and schools, offer healthier food options in the workplace, improve access to healthy foods in states and communities, support lifestyle change programs to reduce obesity and type 2 diabetes risk.
Good nutrition is essential to keeping current and future generations healthy across the lifespan. A healthy diet helps children grow and develop properly and reduces their risk of chronic diseases. Adults who eat a healthy diet live longer and have a lower risk of obesity, heart disease, type 2 diabetes, and certain cancers. Healthy eating can help people with chronic diseases manage these conditions and avoid complications.
However, when healthy options are not available, people may settle for foods that are higher in calories and lower in nutritional value. People in low-income communities and some racial and ethnic groups often lack access to convenient places that offer affordable, healthier foods.
Most people in the United States don’t eat a healthy diet and consume too much sodium, saturated fat, and sugar, increasing their risk of chronic diseases. For example, fewer than 1 in 10 adolescents and adults eat enough fruits or vegetables. In addition, 6 in 10 young people aged 2 to 19 years and 5 in 10 adults consume at least one sugary drink on any given day.
CDC supports breastfeeding and works to improve access to healthier food and drink choices in settings such as early care and education facilities, schools, worksites, and communities.
In the United States:

3 IN 4 INFANTS
are not exclusively breastfed for 6 months.

9 IN 10 AMERICANS
consume too much sodium.

1 in 6 PREGNANT WOMEN
have iron levels that are too low.

NEARLY $173 BILLION
a year is spent on health care for obesity.
The Harmful Effects of Poor Nutrition
Overweight and obesity.
Eating a healthy diet, along with getting enough physical activity and sleep, can help children grow up healthy and prevent overweight and obesity. In the United States, 20% of young people aged 2 to 19 years and 42% of adults have obesity, which can put them at risk of heart disease, type 2 diabetes, and some cancers.
Heart Disease and Stroke

Two of the leading causes of heart disease and stroke are high blood pressure and high blood cholesterol. Consuming too much sodium can increase blood pressure and the risk for heart disease and stroke . Current guidelines recommend getting less than 2,300 mg a day, but Americans consume more than 3,400 mg a day on average.
Over 70% of the sodium that Americans eat comes from packaged, processed, store-bought, and restaurant foods. Eating foods low in saturated fats and high in fiber and increasing access to low-sodium foods, along with regular physical activity, can help prevent high blood cholesterol and high blood pressure.
Type 2 Diabetes
People who are overweight or have obesity are at increased risk of type 2 diabetes compared to those at a healthybecause, over time, their bodies become less able to use the insulin they make. Of US adults, 96 million—more than 1 in 3—have prediabetes , and more than 8 in 10 of them don’t know they have it. Although the rate of new cases has decreased in recent years, the number of adults with diagnosed diabetes has nearly doubled in the last 2 decades as the US population has increased, aged, and become more overweight.
An unhealthy diet can increase the risk of some cancers. Consuming unhealthy food and beverages, such as sugar-sweetened beverages and highly processed food, can lead to weight gain, obesity and other chronic conditions that put people at higher risk of at least 13 types of cancer, including endometrial (uterine) cancer, breast cancer in postmenopausal women, and colorectal cancer. The risk of colorectal cancer is also associated with eating red and processed meat.
CDC’s Work to Promote Good Nutrition
CDC’s Division of Nutrition, Physical Activity, and Obesity uses national and state surveys to track breastfeeding rates and eating patterns across the country, including fruit, vegetable, and added sugar consumption. The division also reports data on nutrition policies and practices for each state. Data from these surveys are used to understand trends in nutrition and differences between population groups.
CDC partners use this information to help support breastfeeding and encourage healthy eating where people live, learn, work, and play, especially for populations at highest risk of chronic disease.

Breastfeeding is the best source of nutrition for most infants. It can reduce the risk of some short-term health conditions for infants and long-term health conditions for infants and mothers. Maternity care practices in the first hours and days after birth can influence whether and how long infants are breastfed.
CDC funds programs that help hospitals use maternity care practices that support breastfeeding . These programs have helped increase the percentage of infants born in hospitals that implement recommended practices 1. CDC also works with partners to support programs designed to improve continuity of care and community support for breastfeeding mothers.

Nearly 56 million US children spend time in early care and education (ECE) facilities or public schools. These settings can directly influence what children eat and drink and how active they are—and build a foundation for healthy habits.
CDC is helping our nation’s children grow up healthy and strong by:
- Creating resources to help partners improve obesity prevention programs and use nutrition standards.
- Investing in training and learning networks that help child care providers and state and local child care leaders meet standards and use and share best practices .
- Providing technical assistance, such as training school staff how to buy, prepare, and serve fruits and vegetables or teach children how to grow and prepare fruits and vegetables.
The CDC Healthy Schools program works with states, school systems, communities, and national partners to promote good nutrition . These efforts include publishing guidelines and tips on how schools and parents can model healthy behaviors and offer healthier school meals, smart snacks , and water access.
CDC also works with national groups to increase the number of salad bars in schools. As of 2021, the Salad Bars to School program has delivered almost 6,000 salad bars to schools across the nation, giving over 2.9 million children and school staff better access to fruits and vegetables.
Millions of US adults buy foods and drinks while at work. CDC develops and promotes food service guidelines that encourage employers and vendors to increase healthy food options for employees. CDC-funded programs are working to make healthy foods and drinks (including water) more available in cafeterias, snack shops, and vending machines. CDC also partners with states to help employers comply with the federal lactation accommodation law and provide breastfeeding mothers with places to pump and store breast milk, flexible work hours, and maternity leave benefits.

People living in low-income urban neighborhoods, rural areas, and tribal communities often have little access to affordable, healthy foods such as fruits and vegetables. CDC’s State Physical Activity and Nutrition Program , High Obesity Program , and Racial and Ethnic Approaches to Community Health program fund states and communities to improve food systems in these areas through food hubs, local stores, farmers’ markets, and bodegas.
These programs, which also involve food vendors and distributors, help increase the variety and number of healthier foods and drinks available and help promote and market these items to customers.
CDC’s National Diabetes Prevention Program (National DPP) is a partnership of public and private organizations working to build a nationwide delivery system for a lifestyle change program proven to prevent or delay type 2 diabetes in adults with prediabetes. Participants in the National DPP lifestyle change program learn to make healthy food choices, be more physically active, and find ways to cope with stress. These changes can cut their risk of developing type 2 diabetes by as much as 58% (71% for those over 60).
Social_govd
Get Email Updates
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Home — Essay Samples — Life — Healthy Lifestyle — The Effect Of Choosing A Healthy Lifestyle

Healthy Lifestyle: The Key Factors Impacting a Person's Health and The Ways to Address Them
- Categories: Healthy Lifestyle
About this sample

Words: 1193 |
Published: Nov 26, 2019
Words: 1193 | Page: 1 | 6 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Life

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 613 words
2 pages / 1006 words
2 pages / 1044 words
1 pages / 483 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Healthy Lifestyle
Living a healthy and balanced lifestyle is crucial for maintaining physical, mental, and emotional well-being. As a young adult, I am constantly seeking ways to improve my lifestyle and make sustainable choices that benefit not [...]
Living a healthy lifestyle is a fundamental aspect of maintaining one's physical and mental well-being. In this essay about healthy lifestyle, we will delve into the various components that constitute a healthy way of life and [...]
Exercise is an essential component of a healthy lifestyle, and its benefits are well-documented. Engaging in regular physical activity has been shown to improve both physical and mental health, reduce the risk of chronic [...]
Virginian luxuries refer to the extravagant lifestyle and possessions of the wealthy elite in the colonial state of Virginia. During the 17th and 18th centuries, Virginia was a hub for the cultivation of tobacco, which brought [...]
As the saying goes, “laugh and the world will laugh with you.” Laughing really is undeniably contagious and this has been proven in multiple situations, including public service announcements and social experiments. According to [...]
Currently, the world is facing an epidemic rise in Non-Communicable diseases like diabetes and high blood pressure. These diseases are caused in a part by the trend of rising in obesity which corresponds to the declining rate of [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

Essay on Lifestyle
Students are often asked to write an essay on Lifestyle in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Lifestyle
What is lifestyle.
Lifestyle is the way in which a person lives. It includes the choices we make about how we spend our time, what we eat, how active we are, and our attitudes. Our lifestyle can be influenced by our family, friends, and the society we live in.
Types of Lifestyles
There are many types of lifestyles. Some people lead a healthy lifestyle, eating nutritious food and exercising regularly. Others might have a busy lifestyle, filled with work and social activities. Some might prefer a quiet lifestyle, enjoying peaceful activities like reading or gardening.
Importance of Lifestyle
Our lifestyle plays a big role in our health and happiness. A healthy lifestyle can help us feel good, stay strong, and live longer. On the other hand, a lifestyle with bad habits, like eating junk food or not getting enough sleep, can lead to health problems.
Lifestyle Choices
We all have the power to make choices about our lifestyle. We can choose to eat healthy food, get regular exercise, and get enough sleep. We can also choose to spend our time doing things we love, like playing sports, making art, or spending time with friends and family.
Changing Your Lifestyle
Changing your lifestyle can be hard, but it’s possible. Start by making small changes, like eating more fruits and vegetables, or walking more. Over time, these small changes can add up to big improvements in your health and happiness.
250 Words Essay on Lifestyle
Lifestyle means the way we live. It includes our habits, attitudes, tastes, moral standards, and how we spend our time. It’s about what we eat, how we dress, how we work, and how we relax. It also includes our beliefs, values, and goals.
There are many types of lifestyles. Some people lead a simple life, while others live in luxury. Some people are very active and do lots of sports, while others prefer quiet activities like reading or painting. Some people are very social and love to be around others, while some prefer to spend time alone.
Healthy Lifestyle
A healthy lifestyle is very important. It means eating a balanced diet, getting regular exercise, and getting enough sleep. It also means avoiding harmful habits like smoking or drinking too much alcohol. A healthy lifestyle can help us stay fit, feel good, and live longer.
Effects of Lifestyle
Our lifestyle can have a big impact on our health and happiness. A healthy lifestyle can help prevent diseases like heart disease and diabetes. It can also help us feel more positive and less stressed. On the other hand, an unhealthy lifestyle can lead to health problems and stress.
In conclusion, our lifestyle is a big part of who we are. It affects our health, our happiness, and even our future. That’s why it’s important to choose a lifestyle that is healthy and makes us feel good. Remember, it’s never too late to make positive changes in our lifestyle.
500 Words Essay on Lifestyle
Lifestyle is the way we live. It includes our daily habits, attitudes, moral standards, and economic level. It’s about how we spend our time, what we eat, how much physical activity we do, and our behavior with others. Lifestyle can be healthy or unhealthy based on our choices. It’s important to choose a healthy lifestyle for a long, happy, and healthy life.
There are many types of lifestyles. Some people have a simple lifestyle. They live in a simple way, eat simple food, and enjoy simple pleasures. They don’t need a lot of money or fancy things to be happy.
On the other hand, some people have a luxurious lifestyle. They live in big houses, eat expensive food, and enjoy high-end pleasures. They need a lot of money to maintain this kind of lifestyle.
Then, there are people who live an active lifestyle. They do a lot of physical activities like sports, exercise, and outdoor adventures. They eat healthy food and avoid unhealthy habits. This lifestyle is good for physical and mental health.
Choosing a Lifestyle
Choosing a lifestyle is a personal decision. It depends on our values, interests, and goals. We should choose a lifestyle that makes us happy and healthy. It’s not about what others are doing or what society expects from us. It’s about what feels right for us.
To choose a lifestyle, we need to think about our likes and dislikes. We need to consider our physical and mental health. We need to think about our future. And most importantly, we need to listen to our heart.
Impact of Lifestyle
Our lifestyle has a big impact on our life. It affects our health, happiness, and success. A healthy lifestyle can make us feel good, look good, and live longer. It can reduce the risk of many diseases like heart disease, diabetes, and cancer.
A healthy lifestyle can also make us happier. It can boost our mood, reduce stress, and improve our self-esteem. It can make us more productive and successful in life.
On the contrary, an unhealthy lifestyle can harm our health and happiness. It can make us feel bad, look bad, and live shorter. It can increase the risk of many diseases and mental health problems.
In conclusion, lifestyle is a key part of our life. It’s about how we live, what we do, and who we are. It’s about our choices and actions. It’s about our health and happiness. So, let’s choose a healthy lifestyle. Let’s eat healthy, stay active, avoid bad habits, and live happily. Remember, our lifestyle is our life. Let’s make it the best it can be.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Lifelong Learning
- Essay on Life’s Greatest Miracle
- Essay on Life Worst Experience
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Poor Health Related Quality of Life and Unhealthy Lifestyle Habits in Weight-Loss Treatment-Seeking Youth
Enza mozzillo.
1 Department of Translational Medical Science, Section of Pediatrics, Regional Center of Pediatric Diabetes, University of Naples Federico II, 80131 Naples, Italy; moc.liamg@azneollizzom (E.M.); ti.aninu@eseznarf (A.F.)
Eugenio Zito
2 Department of Social Sciences, University of Naples Federico II, 80138 Naples, Italy; [email protected]
Valeria Calcaterra
3 Pediatrics and Adolescentology Unit, Department of Internal Medicine, University of Pavia, 27100 Pavia, Italy; [email protected]
4 Department of Pediatrics, “Vittore Buzzi” Children’s Hospital, 20154 Milan, Italy
Nicola Corciulo
5 Unit of Auxology and Pediatric Endocrinology, Sacred Heart of Jesus Hospital, Gallipoli, 73014 Lecce, Italy; [email protected]
Mario Di Pietro
6 Pediatrics Unit, Hospital of Atri, 64032 Atri, Italy; moc.liamg@61orteipidoiram
Anna Di Sessa
7 Department of Woman, Child, and General and Specialized Surgery, University of Campania “Luigi Vanvitelli”, 80138 Naples, Italy; [email protected]
Roberto Franceschi
8 Pediatric Unit, S. Chiara Hospital, 38122 Trento, Italy; [email protected]
Maria Rosaria Licenziati
9 Obesity and Endocrine Disease Unit, Department of Neurosciences, Santobono-Pausilipon Children’s Hospital, 80129 Naples, Italy; moc.liamg@itaiznecilrm
Giulio Maltoni
10 Pediatric Unit, IRCCS Azienda Ospedaliero-Universitaria di Bologna, 40138 Bologna, Italy; [email protected]
Giuseppe Morino
11 Research Unit for Multifactorial Diseases, Bambino Gesù Children’s Hospital, 00165 Rome, Italy; [email protected]
Barbara Predieri
12 Department of Medical and Surgical Sciences of the Mother, Children and Adults—Pediatric Unit University of Modena and Reggio Emilia, 41124 Modena, Italy; [email protected]
Maria Elisabeth Street
13 Department of Mother and Child, Azienda USL-IRCCS di Reggio Emilia, 42123 Reggio Emilia, Italy; [email protected]
Giuliana Trifirò
14 Endocrinology and Metabolism Division, IRCCS Policlinico San Donato, 20097 Milan, Italy; ti.orebil@ifirtg
Francesca Gallè
15 Department of Movement Sciences and Wellbeing, Parthenope University of Naples, 80133 Naples, Italy; [email protected]
Adriana Franzese
Giuliana valerio, associated data.
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy reasons.
Obesity is associated with unhealthy lifestyle behaviors and poor Health Related Quality of Life (HRQOL). The cumulative effect of lifestyle behaviors on HRQOL has been demonstrated in chronically ill adolescents, but not in adolescents with obesity. The present study aimed to assess the association between HRQOL and adherence to the Mediterranean Diet (MD) and/or low levels of physical activity (PA) in a large sample of outpatient adolescents with overweight or obesity seeking weight loss treatment. Four-hundred-twenty participants were enrolled from 10 Italian outpatient clinics. The demographics and anthropometric features, KIDMED scores, and exercise levels of the participants were collected, together with parental features. The HRQOL was assessed by the Pediatric Quality of Life Inventory (PedsQL™), Adolescents Version 4.0. PedsQL total score and functioning subscales were lower in adolescents who reported one or two unhealthy habits. Compared with the high/intermediate groups, the risk of low HRQOL was twice as high for each unit increase in BMI SDS, while the percentage was reduced by 12.2% for every unit increase in the KIDMED score and by 32.3% for each hour increase of exercise. The clustering of these two unhealthy behaviors conferred a 120% higher risk of low HRQOL. Similarly, adolescents displaying better diet quality and/or a physically more active lifestyle have better physical and psychological functioning. Further studies are needed to disclose whether these characteristics may be predictive of better adherence to weight loss treatment.
1. Introduction
Pediatric obesity, a multifactorial condition resulting from a complex interaction between individual, social, and environmental factors, represents a global public health problem [ 1 ]. Energy balance related behaviors leading to increased weight gain, such as inactivity and unbalanced diet, typically initiate in childhood, are reinforced during adolescence, a period of substantial physical, social and psychological changes, and are maintained throughout adulthood [ 2 ]. The literature has shown that these unhealthy behaviors are likely to cluster in the same individual [ 3 ] and exert their additive effect on the risk of pediatric obesity [ 4 ]. Parental characteristics (i.e., weight status, education, and socioeconomic level) are also important risk factors for children’s overweight and obesity [ 5 , 6 , 7 ].
The prevalence of severe obesity is increased in pediatric age [ 8 , 9 , 10 ] and it is associated with various complications, which undermine not only physical health but also psychological and social wellbeing [ 11 ]. Specifically, youth who are obese may experience peer victimization/bullying, poor self-esteem, dissatisfaction with body image, difficulties in interpersonal relationships or social isolation, behavioral problems, depression or anxiety [ 12 ]. These psychosocial consequences may significantly impact school achievement, attendance, behavior in school, and limit sports participation [ 13 , 14 ].
According to the WHO definition, health is not simply the absence of disease but rather a condition of complete bio-psycho-social wellbeing [ 15 ]. The Health Related Quality of Life (HRQOL) [ 16 ] is a global measure of perceived health and burden of a disease. The HRQOL, a multidimensional and subjective measure of an individual’s health, encompasses physical, emotional, and social wellbeing and is used to assess the individual’s perceptions of the impact of their disease [ 17 ].
A significant and negative impact of obesity on HRQOL has been demonstrated in adults [ 18 ] as well as in children [ 19 ]. Indeed, systematic reviews and meta-analyses have shown that children and adolescents with obesity have lower HRQOL scores compared to youths with healthy weight [ 19 ]. This is particularly evident in the industrial societies [ 19 , 20 , 21 , 22 , 23 , 24 , 25 ].
Few studies have focused on the link between HRQOL in adolescents and health related behaviors, such as an adherence to the Mediterranean diet (MD) or the levels of physical activity (PA) [ 26 , 27 ]. A positive relationship between healthy diet or high PA levels and physical health or psychosocial wellbeing has been reported in adolescents [ 28 , 29 ]. Adolescents spending more time in PA and less time in screen viewing showed higher HRQOL scores, particularly in physical and social domains [ 30 ].
However, few studies have analyzed the influence of the cumulative effect of obesogenic lifestyle behaviors in adolescents with a chronic disease [ 31 ]. In particular, the association between individual or clustered unhealthy lifestyle habits and HRQOL has been little investigated in adolescents with obesity. Therefore, our aim was to evaluate the variables associated with the self-reported and parent-proxy reported HRQOL, such as gender, body mass index (BMI), dietary behaviors, PA levels, and parental BMI and education level in a large sample of Italian adolescents seeking weight loss treatment in outpatient clinics of the Italian Society of Pediatric Endocrinology and Diabetology (ISPED). The combined effect of unhealthy behaviors on the HRQOL was also assessed.
2. Materials and Methods
This cross-sectional multicenter study was carried out by the Childhood Obesity study Group of the Italian Society for Pediatric Endocrinology and Diabetology (ISPED). Participants were represented by youths seeking for weight loss treatment; they were recruited in 10 outpatient clinics for the care of Pediatric Obesity at community or university hospitals throughout the Italian country. The inclusion criteria were age 13.0–17.0 years; Caucasian ethnicity; overweight or obesity; first visit at the outpatient clinic. The exclusion criteria were secondary causes of obesity (genetic, endocrine or iatrogenic forms); presence of other chronic diseases or mental illness. Four-hundred-twenty adolescents (187 boys, 233 girls; mean age 14.2 ± 1.1 years; range 13–17) were consecutively enrolled over a 12-month period (January–December 2017). Demographic data (age and gender) were collected from medical records. The height and weight of the adolescents were measured by the same investigator in each center. Height was measured to the nearest 0.1 cm with a wall-mounted stadiometer, while weight was determined to the nearest 0.1 kg on a medical scale. The BMI was calculated (weight/height 2 ) for both parents and adolescents. Furthermore, the BMI standard deviation score (BMI-SDS) was computed in adolescents as measure of relative BMI adjusted for age and sex. Adolescents were asked to answer on their lifestyle habits (adherence to the MD, PA levels). Parents were asked to report their own weight and height and the highest grade and year of education attained according to the Italian education system [elementary (five years), middle school (three years), high school (five years), degree (over three years)]. Adolescents’ self-reported and parent-proxy reported data about HRQOL were collected by an ad hoc questionnaire.
The research protocol was approved by the Ethics Committee of the University of Naples Federico II, coordinating center of the study (protocol number 88/16), and subsequently by the Ethics Committee of the other participating centers. Written informed consent was obtained from both the adolescents and their parents in accordance with the new version of the Helsinki Declaration. The data of participants and their parents were anonymously registered in a database using an alphanumeric and progressive identification code.
2.1. Dietary Behaviors
Dietary behaviors were assessed through the KIDMED questionnaire, which allows assessing a variety, or combination of different foods and beverage and the frequency with which they are habitually consumed, providing an estimate of an individual’s adherence to the MD pattern [ 32 ]. The KIDMED questionnaire is composed by the following 16 questions: (1) Takes a fruit or a fruit juice every day; (2) Has a second fruit every day; (3) Has fresh or cooked vegetables regularly once a day; (4) Has fresh or cooked vegetables more than once a day; (5) Consumes fish regularly (at least 2–3 times per week); (6) Goes more than once a week to a fast-food (hamburger) restaurant; (7) Likes pulses and eats them more than once a week; (8) Consumes pasta or rice almost every day (5 or more times per week); (9) Has cereals or grains (bread, crackers, etc.) for breakfast; (10) Consumes nuts regularly (at least 2–3 times per week); (11) Uses olive oil at home; (12) Skips breakfast; (13) Has a dairy product for breakfast (yoghurt, milk, etc.); (14) Has commercially baked goods or pastries for breakfast; (15) Takes two yoghurts and/or some cheese (40 g) daily; (16) Takes sweets and candy several times every day. These questions were posed by the same pediatrician to each participant through an interview. For each “yes” response, one point was given to answers representing positive food habits (items 1–5, 7–11, 13, 15), and one point was subtracted for those representing negative food habits (items 6, 12, 14, 16). Two categories of adherence were defined according to a score ≤3 (poor adherence) and ≥4 (average/good adherence) [ 32 ].
2.2. Physical Activity
PA habits were examined by asking the weekly average amount of hours spent for sports (except for physical education at school) or other structured types of PA (dancing, formal exercise programs or use of fitness centers). Adolescents who exercised <3 h/week were classified as less active, while adolescents engaged in ≥3 h of exercise per week were classified as “active” [ 33 ].
2.3. Clustering of Unhealthy Lifestyle Habits
The clustering of unhealthy lifestyle habits was calculated by adding for each participant the number of unhealthy behaviors adopted, namely low MD adherence indicated by a KIDMED score ≤3 [ 32 ] and low PA expressed by less than 3 h of regular exercise per week [ 33 ].
2.4. Health Related Quality of Life
HRQOL was measured by using the Pediatric Quality of Life Inventory (PedsQL™), Italian Version 4.0 for adolescents (13–18 years old) [ 16 , 34 ]. This is a generic tool and allows a parallel adolescent self-report and a parent proxy-report. The multidimensional instrument PedsQL is a validated 23-item scale comprising four subscales—Physical Functioning (8 items) (e.g., problems with running, lifting something heavy), Emotional Functioning (5 items) (e.g., feeling afraid, trouble sleeping), Social Functioning (5 items) (e.g., getting along with other children), and School Functioning (5 items) (e.g., paying attention in class). Answers were scored along a 5-point Likert-type scale: never (0), almost never (1), sometimes (2), often (3), or almost always (4). Items were reversely scored and transformed to a 0–100 (0 = 100, 1 = 75, 2 = 50, 3 = 25, 4 = 0) scale so that higher scores reflected better HRQOL, as per scoring guidelines. Subscale scores were computed from sum and average of the total items within each subscale. The Total Functioning Score is the sum and average of all items across the four subscales. We created three levels of total functioning score based on tertiles of the total score obtained in our population of adolescents: high functioning ≥73.3, intermediate functioning between 73.2 and 68.4 and low functioning ≤68.5.
2.5. Statistical Analyses
Statistical analyses were performed using SPSS for Windows, version 25.0 (SPSS Inc., Chicago, IL, USA). A two-sided p value of ≤0.05 was considered statistically significant in all analyses. All the variables were not normally distributed and were expressed as medians (25th–75th percentile); categorical data were presented as absolute frequencies and percent values.
The Mann–Whitney U test was used to compare variables between two groups (i.e., males vs. females), while the Wilcoxon Rank-Sum Test was used to compare children and parent scores on the PedsQL 4.0 Generic Core Scales. The Kruskal–Wallis H test was used to compare groups stratified according to tertiles of HRQOL scores or the clustering of unhealthy lifestyle habits; a Mann–Whitney U test with a Bonferroni correction was performed to ascertain which pairs of groups differed significantly from one another. Chi-squared test was used to compare proportions. Intra-class correlation coefficients (ICCs) were utilized to evaluate agreement between patient self-report and parent proxy-report on the PedsQL scales (ICCs ≤ 0.40 poor to fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 good agreement, and 0.81–1.00 excellent agreement). The Eta squared (small effect 0.01, medium 0.06, large 0.14) or the Cramer’s V (no or little effect <0.1, low 0.1–0.3, moderate 0.3–0.5, high >0.5) were calculated as measures of effect size for these comparisons [ 35 ].
Two models of multiple logistic regression analysis were applied to calculate the Odds Ratios (ORs) and 95% Confidence Intervals (CIs). In both models the low functioning total score of PedsQL was the dependent variable and the intermediate/high functioning was the reference category. In the first model the independent variables were represented by BMI-SDS, parents’ education level, KIDMED score and PA levels; in the second model variables related with diet and PA were replaced with clustering of unhealthy lifestyle habits in order to assess their possible cumulative role in determining HRQOL.
The demographic and anthropometric features, lifestyle habits, parental characteristics, and PedsQL scores of the total sample and stratified by gender are presented in Table 1 .
Participants’ demographic and anthropometric features, lifestyle habits, parental characteristics, and PedsQL scores of adolescents and parents of the total sample and stratified by gender.
Parent-proxy PedsQl was available in 413 parents. η2 Eta squared; d Cohen’s d ; V Cramer’s V. Mann–Whitney U test was used to compare gender groups; Chi-squared test was used to compare proportions between genders. Significant differences between genders are shown in the column. Wilcoxon Rank-Sum Test was used to compare adolescents’ self-reported scores and parent-proxy reported scores in the whole group and by gender: asterisks denote significant differences between adolescents’ and parents’ scores. *** p <0.001; ** p < 0.01; * p < 0.05.
Self-report forms of the PedsQL were completed by 420 adolescents and proxy-reports forms were completed by 413 parents. Girls were slightly older than boys. No differences were found between genders in the total PedsQL score and subscales, except for emotional functioning, which was lower in girls. Similar data were registered for the emotional functioning reported by parents ( Table 1 ). However, the effect size of these differences was small. Across all PedsQL scales, adolescents self-reported significantly higher scores than their parents, with the most significant differences ( p < 0.001) related with total functioning, physical functioning and social functioning both in the whole sample and by gender ( Table 1 ).
ICCs between adolescent self-report and parent proxy report across the PedsQL 4.0 Generic Core Scales are presented in Table 2 . The ICCs were in the good agreement range; the greatest agreement was found for the total score, whereas the lowest on emotional functioning.
Intra-class correlation coefficients (ICC) between adolescent self-report and parent proxy-report.
CI: Confidence intervals; ICCs are designated as 0.40 poor to fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 good agreement, and 0.81–1.00 excellent agreement.
Adolescents within the low total functioning HRQOL showed higher BMI-SDS, and lower KIDMED score, weekly hours of exercise, father’s and mother’s education level compared with youths with intermediate and/or high functioning HRQOL ( Table 3 ). The effect size was small for all these differences but for weekly hours of exercise.
Demographic, anthropometric features and lifestyle habits, and parental characteristics among adolescents stratified by total HRQOL functioning.
V Cramer’s V; η2 Eta squared. Chi-squared test was used to compare proportions. Kruskal–Wallis H test was used to compare the overall p among the three groups of total HRQOL functioning. Overall significant differences among groups are shown in the p column. Mann-Whitney test with a Bonferroni correction was performed to ascertain the difference between each pair of groups of low, intermediate and high HRQOL: a significant differences between intermediate and low, b significant differences between high and low ( p < 0.05).
Considering the cluster of unhealthy lifestyle habits, 79 adolescents (18.8%) reported no unhealthy lifestyle component, 236 (56.2%) one unhealthy habit and 105 (25.0%) two unhealthy habits. No differences were found regarding gender distribution, age, BMI, and BMI-SDS among these groups, while adolescents reporting two unhealthy lifestyle habits presented significantly lower father’s and mothers’ education level than those with no unhealthy component ( Table 4 ). All the PedsQL scores (total and subscales) significantly decreased with the increase of one or two unhealthy habits. The effect size was medium for total scores and physical functioning in both adolescents and parents, medium for social functioning in the youths and small for the other domains.
Demographic and anthropometric features of participants and adolescents’ self-reported and parent-proxy reported PedsQL scores by clusters of unhealthy lifestyle habits.
V Cramer’s V; η2 Eta squared. Chi-squared test was used to compare proportions. Kruskal–Wallis H test was used to compare the overall p among the three groups with and without unhealthy habits. Overall significant differences among groups are shown in the p column. Mann-Whitney test with a Bonferroni correction was performed to ascertain the difference between each pair of groups with none, one or two unhealthy habits: a significant differences between intermediate and low, b significant differences between high and intermediate, c significant differences between high and low ( p < 0.05).
Multiple logistic regression analyses showed that, when the unhealthy behaviors were considered separately, low total functioning was positively associated with BMI-SDS and negatively associated with KIDMED score and weekly hours of exercise, while the association with parents’ education level was not confirmed. When the clustering of unhealthy habits was included in the model in place of the single components, adolescents within the low functioning scores showed a twofold risk of having low HRQOL total score compared with their respective counterpart with high/intermediate functioning ( Table 5 ).
Multiple logistic regression analyses of the associations between low total functioning and parents’ or adolescents’ characteristics (high/intermediate functioning was used as reference category).
NI not included. ** p < 0.001; * p = 0.004.
4. Discussion
The present study demonstrated that severity of obesity, adherence to the MD, and levels of exercise were independently associated with worse HRQOL in a population of outpatient adolescents seeking weight loss. HRQOL total score decreased as the number of unhealthy components increased. Clustering of unhealthy habits conferred a twofold risk of low functioning compared with adolescents with high/intermediate functioning.
The adverse consequences of pediatric obesity on physical and psychosocial health and their effects on the HRQOL are widely acknowledged [ 19 , 36 , 37 ]. Most dimensions of HRQOL are consistently affected in overweight and obese children and adolescents compared to normal-weight youths [ 19 ]. Among the different dimensions of the PedsQL, the emotional functioning appeared to be more affected in obese youths recruited from clinical setting than from general population [ 19 ] both in the self-reported and the parent-proxy reported studies. Previous studies [ 19 ] showed gender-related differences in HRQOL for social functioning, physical appearance, self-esteem, and total scores, with girls being generally more affected than boys [ 26 ]. In our sample of youths with obesity we found no gender-related differences in the HRQOL total score and in the other sub-domains, with the exception of emotional functioning that scored worse in girls than boys. Numerous studies have demonstrated that weight stigma is highly prevalent in individuals with obesity [ 38 ]. Adolescents with obesity experience higher rates of weight teasing or bullying [ 39 ] and may suffer of several psychosocial complaints [ 12 ]. Although adolescents of both genders are exposed to pressures to conform to an ideal body image, the lower score found in the emotional functioning in girls may reflect the fact that perception of body weight may be generally more strongly associated with low life satisfaction among girls compared to boys [ 40 ]. A relationship between body dissatisfaction and its effects on HRQOL may start very early in life, since it has been reported that girls as early as 6 years are already exposed to peers and media influence on body image and dieting awareness [ 41 , 42 ].
Despite the restricted range of BMI status (BMI-SDS between 1.9–2.7) in our sample, adolescents with lower functioning of the total HRQOL score showed a more severe degree of obesity compared with youths with intermediate and/or high functioning. This finding is in agreement with other studies performed in clinical samples [ 43 , 44 ], suggesting that the weight related differences, usually reported in the general population, may also occur among the very severely youths with obesity.
Combinations of unhealthy lifestyle behaviors are key elements for unfavorable weight gain in children and adolescents [ 45 , 46 , 47 , 48 ]. Several cross-sectional and longitudinal studies have reported a positive association between individual lifestyle behaviors and physical or mental health in adolescents [ 26 , 49 , 50 ]. We found that adolescents within the lower total functioning of HRQOL showed lower KIDMED scores and more time spent in weekly exercise compared with youths with intermediate and/or high functioning. MD is one of the healthiest dietary models that shows benefits regarding life expectancy and cardiovascular diseases that are frequently related to obesity [ 51 ]. A great consumption of fruits and vegetables has been shown to have a beneficial impact on physical health through several pathways associated to numerous biologically active components [ 52 ]. Moreover, diet quality has a beneficial effect on self-perception and is associated with fewer externalizing problems that are usually linked to negative behaviors as being bullied [ 53 , 54 ]. Regarding lifestyle, the association between PA, sedentary behavior, and HRQOL in the general healthy population of children and adolescents has been systematically reviewed by Wu et al. [ 29 ]. Higher levels of PA and less sedentary behavior were associated with better HRQOL with a dose-response relationship. Of note, Gopinath et al. demonstrated that regular PA was prospectively associated with a higher perceived HRQOL in a cohort of Australian adolescents [ 30 ]. Unhealthy behaviors tend to be associated each other and may significantly predict global health. MD adherence and PA engagement were associated with better perception of physical and psychological wellbeing, and improved family relationships, autonomy support and perceptions of the school environment in Spanish adolescents [ 55 ]. A combination of unhealthy lifestyle behaviors and poor HRQOL was also reported by Gopinath et al. in Australian school children [ 56 ]. The combination of high levels of physical fitness and optimal adherence to Mediterranean diet was positively associated with better HRQOL scores in Portuguese adolescents [ 57 ].
As far as we are aware, no study has previously analyzed the association of unhealthy behaviors in adolescents with obesity and self-reported HRQOL. As it was reported in the general population, lower functioning of the total HRQOL score was independently associated with lower KIDMED score or weekly hours of exercise in our sample of obese adolescents. The risk of low HRQOL was twice as high for each unit increase in BMI SDS while the percentage was reduced by 12.2% for every unit increase in the KIDMED score and by 32.3% for each hour increase of exercise. The clustering of these two unhealthy behaviors conferred a 120% higher risk of low HRQOL.
Treating obese adolescents implies good adherence to lifestyle changes. Of note, among the determinants of weight loss, the participation in exercise groups before the beginning of weight loss treatment was a strong predictor of success [ 58 , 59 ]. Furthermore, several studies reported the beneficial effect of weight loss on the improved HRQOL [ 60 , 61 ], but the quality of life at baseline may also impact adherence and treatment outcomes in obese adolescents [ 62 ]. Therefore, a virtuous circle between healthy lifestyle and better HRQOL may have an impact on success of obesity treatment.
The median BMI of both parents in our study was in the overweight range. The strong association between parental weight status and childhood obesity [ 63 ] may imply that parents have a role in the development of child overweight and obesity through both genetics and shared environmental factors. At the same time, parents are also significant agents for change in the treatment of adolescent obesity [ 64 , 65 ] and their point of view on the physical and psychosocial implications related to obesity may provide complementary information to their child’s report. Therefore, we decided to assess both adolescent self-reports and a parent proxy-report of PedsQL. Adolescent-parent concordance was quite good in all the domains (ICC = 0.654–0.737), with the highest agreement on the total score and the lowest on the emotional functioning. Across all PedsQL scales, parents reported significantly lower scores than their children, predominantly on the total score and social health. Our findings are consistent with previous studies that showed that HRQOL scores were significantly lower on the parent reports than on the self-reports of obese youths for some or all of the dimensions studied [ 19 ]. Levels of agreement between adolescent self-report and parent proxy-reports on the PedsQLs can be affected by parents’ education levels or their own quality of life [ 66 , 67 ]. While we did not find any association between low total functioning and parents’ education level, we cannot exclude that parents with obesity themselves experienced negative influences on psychological aspects, such as self-esteem, body image, and emotional state, and projected these bad experiences onto their child’s experiences. Our findings suggest that parents’ distress and worry over the physical and psychosocial implications of overweight may account for overestimation of the effects of obesity on child’s physical functioning and other domains as the social and psychosocial ones [ 68 , 69 , 70 ]. Over the past 10 years, public health organizations from several European countries have been involved in policies to contrast obesity [ 71 ]. Thus, awareness about the causes and consequences of obesity in children is increased not only among health professionals, but also in the general public, including families and teachers. Discrepancies in the perceived HRQOL between parents of children have been also reported in several chronic diseases, such as type 1 diabetes or cystic fibrosis [ 31 , 72 , 73 ].
This study presents some limitations, such as the cross-sectional design and the lack of normal-weight control group, therefore the analyses of the total PedsQL score were done using tertiles calculated on our own population. Only participation to structured PA was considered, while other forms of incidental PA, such as daily activities at school, at home, or during transport were not assessed. This decision was driven by the evidence that estimate of PA levels is challenging in youths, specifically in those affected by obesity, who tend to overestimate PA [ 74 ]. We supposed that focusing the item only on programmed and regular physical activities could have reduced the bias. Lastly, no information was available on the quality of life of parents, which could have allowed to assess its possible modulation effect on the quality of life of their children. Instead, the strength of our study is the multi-centric design and the use of validated questionnaires to analyze diet quality and HRQOL. Moreover, the interpretation of the different levels of agreement between self-reported and parent proxy-reported HRQOL was based on a very high percentage of parents who participated (more than 98%).
5. Conclusions
The main objective of the treatment of pediatric obesity is a permanent change in the child’s eating habits and lifestyle, leading to a negative caloric balance and a progressive weight loss. Another important goal is improving mental health and HRQOL [ 2 ].
Our findings highlight for the first time the influence of the cumulative effect of two unhealthy behaviors, such as unhealthy diet pattern and low PA, on lower general health and physical functioning domains in adolescents with obesity.
The assessment of the HRQOL is crucial in the care of youth seeking weight-loss treatment. Promoting healthy eating behaviors and an active lifestyle in obese adolescents may positively impact their quality of life and establish a virtuous circle of successful treatment.
Further studies are needed to disclose whether the baseline lifestyle characteristics and the HRQOL score may be predictive of better adherence to weight loss treatment in adolescents. These data will be helpful to optimize the management and to apply personalized medicine paths in obesity treatment.
Author Contributions
Conceptualization, E.M., E.Z., A.F., G.V.; methodology, E.M., E.Z., F.G., A.F., G.V.; formal analysis, G.V.; investigation, E.M., V.C., N.C., M.D.P., A.D.S., R.F., M.R.L., G.M. (Giulio Maltoni), G.M. (Giuseppe Morino), B.P., M.E.S., G.T.; resources, E.M., V.C., N.C., M.D.P., A.D.S., R.F., M.R.L., G.M. (Giulio Maltoni), G.M. (Giuseppe Morino), B.P., M.E.S., G.T., A.F.; data curation, E.Z., G.V.; writing—original draft preparation, E.M., G.V.; writing—review and editing, E.M., E.Z., B.P., M.E.S., F.G., G.V.; supervision, G.V. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the University of Naples Federico II, coordinating center of the study (protocol code 88/16, date of approval 27 May 2016), and subsequently by the Ethics Committee of the other participating centers.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Essay on Healthy Lifestyle for Students and Children

500+ Words Essay on Healthy Lifestyle
It is said that it is easy to learn and maintain bad habits but it is very difficult to switch them back. The issue of a healthy lifestyle is very serious but the people take it very lightly. Often, it is seen that the people take steps to improve their lifestyle but due to lack of determination quits in the midway.
Moreover, for a healthy lifestyle is it important that you take small and one-step at a time. Also, do not go overboard with it. Besides, this healthy lifestyle will help you in life in a lot of ways.

Habits That Keeps You Healthy
For keeping your body and mind healthy you have to follow certain rules that will help you achieve your goal. Besides, there are certain measures that will help you to stay healthy.
First of all, for being healthy you have to plan and follow a strict diet. This diet should contain all the essential minerals and vitamins required by the body. Also, eat only healthy food and avoid junk and heavily carbohydrate and fatty food.
In addition, wake up early in the morning because first of all, it’s a healthy habit. Secondly, waking up early means you can get ready for your work early, spend some quality time with your family. Besides, this decides time for your sleep and sleep early because it de-stresses body.
Doing exercise regularly makes your body more active and it also releases the pent-up stress from the muscles.
Avoid the mobile- the biggest drawback of this generation is that they are obsessed with their mobile phones. Moreover, these phones cause many physical and mental problem for them. So, to avoid the negative effects of mobile the usage volume of them should be reduced.
Connecting with positive minds because the more you indulge with these people then less you will go to the negative side.
Get the huge list of more than 500 Essay Topics and Ideas
The things that should be avoided for a healthy lifestyle
We knew that there are several bad habits that affect our healthy lifestyle. These habits can cause much harm to not only to the body but to the society too. In addition, these habits are also the cause of many evils of society. The major healthy lifestyle destroying habits are smoking, drinking, junk food, addiction , meal skipping, and overuse of pills.
All these activities severely damage body parts and organs which cannot be replaced easily. Besides, they not only cause physical damage but mental damage too.
Benefits of a Healthy Lifestyle
A healthy lifestyle has many benefits not only for the body but for the mind too. Also, if you follow a healthy lifestyle then you can reduce the risk of having cancer, heart disease, diabetes, obesity, and osteoporosis.
To sum it up, we can say that there are various benefits of living a healthy lifestyle. Also, a healthy lifestyle has many benefits to your social as well as personal life. Besides, it improves the relationships in the family. Most importantly, the person who lives a healthy lifestyle lives longer as compared to those who do not.
FAQs on Healthy Lifestyle
Q.1 Give some tips to live a healthy lifestyle. A.1 Some tips for staying healthy are eating a balanced diet, maintain weight, having enough sleep, sleep early and wake up early, use mobile lesser, etc.
Q.2 What is good health? A.2 Good health means freedom from sickness and diseases. It is a costly gift of nature to us for living a purposeful life. Also, good health means that we can do more work than our capacity without getting tired.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Subscribe Now! Get features like

- Latest News
- Entertainment
- Real Estate
- KKR vs RCB Live Score
- UP Board Result
- Election Schedule 2024
- Win iPhone 15
- IPL 2024 Schedule
- IPL Points Table
- IPL Purple Cap
- IPL Orange Cap
- AP Board Results 2024
- The Interview
- Web Stories
- Virat Kohli
- Mumbai News
- Bengaluru News
- Daily Digest

How to avoid unhealthy comparison - the thief of joy
Mental health experts share some pointers that can help address unhealthy comparison inflicted by self or others.
Unhealthy comparisons can be the bane of our existence, therefore it is not unsurprising that Theodore Roosevelt called comparison the “thief of joy ”! While the argument for it is that social comparison has the ability to motivate people to improve, unfortunately for young teenage minds, it mostly ends up promoting judgmental and biased attitudes and overly competitive behaviour.

In an interview with HT Lifestyle, Nandini Ghatak, Principal of Modern High School International, shared, “It is inherently human to measure ourselves “up” with people who are apparently doing “better” or are seemingly “smarter”. However, this kind of comparison makes young teens feel a sense of self-deprecation and in the long term it is highly likely that they will end up as adults who lack self-worth. Constant comparisons to other “better performers” contribute significantly to making adolescents feel incapable, frustrated and thereby unhappy about who they are and what they have accomplished. This is because they are constantly being taught to look up towards standards that we as parents believe that they should be achieving.”
She revealed, “Social media makes this even worse as they are constantly exposed to exaggerated content exacerbating the situation. Young adolescents wanting “glass skin”, “eight-pack” or “zero sizes” are often pushed into making uninformed and risky decisions detrimental to their physical and mental wellbeing. Parents and teachers ideally should be encouraging young children to focus on self-improvement instead of engaging in unnecessary comparisons. We should help them to understand how to control their impulses so that they learn to take better decisions rather than being spurred on by envy, jealousy and resentment.”
According to Deanna Fugle, Licensed Counsellor working as "Senior counsellor" at JAIN International Residential School (JIRS), family is the first place where we receive messages from significant others and it provides us with the feeling of adequacy and inadequacy, acceptance and rejection. She said, “Even before children can speak, people make evaluations of them. The earliest months of life are full of messages that shape the self-concept. The amount of time parents allow their children to cry before attending to their needs communicates, nonverbally to the children over a period of time, just how important they are to their parents.”
Highlighting that the parents' method of handling infants speaks volumes, she elaborated -
- Children learn what they live: If a child lives with criticism he learns to condemn, listening is the first step in tackling any situation and getting a solution to that.
- Offering unrequested advice: Sometimes parents believe that when students bring problems they are seeking for advice which isn't true but they are actually wanting a listening ear. Advising is an appropriate response but not when it's unrequested.
- Passing judgment: It's usually isn't encouraging to hear. “You know”. It's your own fault. You really shouldn't have done that. This type of response suggests that the listener is playing judge rather than walking in your shoes.
- An important aspect of authority versus submission: Problems is when and how parents exercise discipline and administer punishment. Scolding appears to be the most frequent form of punishment, and comparing their children with others or with their peers is harassment and damage to the growth of children both physically as well as mentally.
To avoid unhealthy comparisons, Deanna Fugle advised:
- Parents must distinguish carefully between what is firm but fair and what is harsh and perhaps unfair.
- Some degree of strictness strengthens the growing child's personality. when strictness approaches rigidity, the boundaries and standards become so sharply defined as to confine rather than guide.
- The child's resultant feelings of hostility, resentment, and fear may generalize toward all authority.
- The adolescent’s attitude towards authority is based upon the reaction he had learned towards his parents in this childhood, whether passively accepting under stress, conditionally accepting, overtly rebellious, or resentful will have their overtones in subsequent stages throughout an individual's life.
- Parents are also important as comrades to adolescent children. Another role is that of the mother or guide. When the parents do not fulfill their rolls, the adolescents may feel let down and fall prey to unhealthy influences outside home.
- Each child purses his parent's roll according to his own needs. The parents who may be viewed by the dependent child as a loving protector, may be seen by the more independent one as a prohibitor.
- Parents need to modify the roles according to the children's needs.
- The overt expressions of conflicts serve as catharsis which, if repressed takes the form of anxiety.
- Parents should treat teenagers not as children but as adults in the making but at the same time should guard them from traumatic experiences however at the same time avoiding too much of guidance.
- Prescriptions for a specific parent-child relationship cannot be laid down. Parents who lack insight or are deeply involved in their difficulties may meet troubles.
- Healthy acceptance of their children without comparisons is warm support to the child without being overly possessive. Children whose attachment to their parents is moderate are actually happier than those whose relations is a very intimate.
- Adolescents do need complete confidence in the love of their parents. They should know that their parents will support them always, no matter what his/her situation is.
Talking about the impact of unhealthy comparison on student well-being, Smitha Rahul, Rehabilitation Psychologist, Student Counsellor Academic Co-ordinator and Psychology lecturer at St. Claret P.U. College in Bengaluru, said, “Unhealthy comparison can have a significant negative effect on a young person's development, particularly on their mental well-being, sense of self-worth, level of confidence, social skills, and general personality.”
Let's examine a few consequences of these harmful comparisons -
- Mental Health: Feelings of inadequacy, anxiety, and sadness can result from continuously comparing oneself to others. This never-ending loop of comparison can erode general mental health and lead to unfavourable thought patterns.
- Confidence and Self-esteem : Unhealthy comparison frequently leaves one feeling less confident and worthless. People who constantly compare themselves to the unattainable standards that other people set for them may internalise emotions of inadequacy and failure, which can lower their self-esteem.
- Behaviour: Harmful comparisons may lead to display of behaviours like perfectionism, avoiding difficult situations, or looking to other people for approval. These behaviours may impede a child's ability to grow and develop personally and may be maladaptive.
- Social Skills: By encouraging rivalry, resentment, and jealousy, comparison can have a detrimental effect on interpersonal relationships. Students who are always comparing themselves to others or who are jealous of the accomplishments of their peers may find it difficult to connect with people on a real level.
- Personality: Unhealthy comparing habits have the potential to negatively alter a child's personality over time. It could result in a persistent need for approval, a fear of failing, or a propensity to gauge one's value more by extraneous characteristics than by fundamental ones. This may impede the growth of a robust and genuine personality.
How to combat the effects of unhealthy comparison?
Smitha Rahul said, “In general, unhealthy comparison can have a substantial negative impact on conduct, social skills, personality, behaviour, self-esteem, and confidence. It is critical to proactively address these problems by developing self-awareness, self-compassion, and a positive mindset that celebrates each person's unique abilities and accomplishments.” Here are some pointers that can help address unhealthy comparison inflicted by self or others -
- Self-Awareness: Encourage students to recognize when they are comparing themselves to others excessively. Awareness is the first step towards change.
- Focus on Strengths: Help students identify and appreciate their own unique strengths and talents. Remind them that everyone has different abilities and it's okay not to excel in every area.
- Set Personal Goals : Encourage students to set goals based on their own aspirations and values, rather than trying to measure up to others' standards. This promotes a sense of autonomy and self-direction.
- Encourage Collaboration : Foster an environment where students support and celebrate each other's successes rather than viewing them as threats. Emphasise the value of teamwork and cooperation.
- Challenge Negative Thoughts : Teach students to challenge negative thoughts and beliefs about themselves. Help them reframe comparisons in a more positive and realistic light.
- Limit exposure to Social Media : Social media can exacerbate feelings of inadequacy by showcasing curated and often unrealistic portrayals of others' lives. Educate them about these facts related to social media and it can help them view it more objectively. Encourage students to limit their time on such platforms and focus on real-life connections.
- Promote Gratitude: Encourage students to practise gratitude for their own accomplishments and blessings. This helps shift the focus away from what they lack compared to others.
- Open communication : Create a safe space for students to express their feelings of inadequacy or insecurity without fear of judgement. Offer guidance and support to help them navigate these emotions constructively.
Addressing the Role of Parents, Teachers, and peers:
- Model healthy behaviour: Adults should lead by example by avoiding comparisons and promoting a culture of acceptance and appreciation for individual differences.
- Provide constructive feedback: Offer feedback that focuses on improvement rather than comparison to others. Encourage students to strive for personal growth rather than outperforming their peers.
- Promote inclusivity: Create inclusive environments where all students feel valued and respected regardless of their abilities or achievements. Encourage collaborative, cooperative endeavours rather than competition.
- Educate about the dangers of comparison: Teach students about the negative effects of comparison on mental health and self-esteem. Empower them to resist societal pressures and embrace their own uniqueness.
- Cultivate Empathy and Compassion: Teach students to empathise with their peers and recognize that everyone faces their own challenges and insecurities. Encourage acts of kindness and compassion within peer groups.
By implementing these strategies, we can help students develop a healthier mindset and foster a supportive and nurturing educational environment.
Sakshi Maheshwari, Clinical Psychologist at Niyama Digital Healthcare, said, “As humans, we have this inherent habit of comparing ourselves with others. Comparison is a double-edged sword; the way it will impact you depends on your perception of it. Sadly, most of us fail to use comparison to boost ourselves or grow our strengths. We rather end up demeaning ourselves, feeling miserable, and lowering our self-esteem, confidence, and whatnot. And this comparison starts from the day one is born. Parents start looking at other children and comparing how pretty their kid is, or how quickly other’s kids are achieving their milestones. As children grow a little older, they also start having these desires to own identical toys or backpacks as their buddies. As children become older and reach school almost every time their grades and performances are compared by the teachers and we never get to see when that comparison starts choking them every day.”
With the advent of social media, easy access to surmount information and ever-changing trends, this generation of teenagers especially has become more susceptible to being hit by comparison to the point that some of them fall into a trap of anxiety, depression and even have thoughts of suicide. Sakshi Maheshwari concluded, “I have come across so my teenagers during my therapy who come with issues of low self-esteem, deteriorating self-confidence, and no one to confide in. They feel so pressured by their caregivers’ expectations of doing good that they forget to explore, feel happy, and excited. It's understandable that as long as we are humans’ comparisons will persist, but to turn it into a healthy norm is in our hands, especially the caregivers. Parents want the best for their children, so sit down and ask them what they want for themselves too. This will help them gain autonomy and also give them a relief that there is someone they can lean back on, and let them explore and navigate this world. You and I did it, they can do it too.”
- Mental Health
Join Hindustan Times
Create free account and unlock exciting features like.

- Terms of use
- Privacy policy
- Weather Today
- HT Newsletters
- Subscription
- Print Ad Rates
- Code of Ethics
- Elections 2024
- DC vs SRH Live Score
- India vs England
- T20 World Cup 2024 Schedule
- IPL 2024 Auctions
- T20 World Cup 2024
- Cricket Teams
- Cricket Players
- ICC Rankings
- Cricket Schedule
- Other Cities
- Income Tax Calculator
- Budget 2024
- Petrol Prices
- Diesel Prices
- Silver Rate
- Relationships
- Art and Culture
- Taylor Swift: A Primer
- Telugu Cinema
- Tamil Cinema
- Exam Results
- Competitive Exams
- Board Exams
- BBA Colleges
- Engineering Colleges
- Medical Colleges
- BCA Colleges
- Medical Exams
- Engineering Exams
- Horoscope 2024
- Festive Calendar 2024
- Compatibility Calculator
- The Economist Articles
- Explainer Video
- On The Record
- Vikram Chandra Daily Wrap
- PBKS vs DC Live Score
- KKR vs SRH Live Score
- EPL 2023-24
- ISL 2023-24
- Asian Games 2023
- Public Health
- Economic Policy
- International Affairs
- Climate Change
- Gender Equality
- future tech
- Daily Sudoku
- Daily Crossword
- Daily Word Jumble
- HT Friday Finance
- Explore Hindustan Times
- Privacy Policy
- Terms of Use
- Subscription - Terms of Use
- Share full article

Let Them Eat … Everything
In the age of Ozempic, the “fat activist” Virginia Sole-Smith is inspiring and infuriating her followers.
Virginia Sole-Smith at her home in Cold Spring, N.Y. Credit... Marisa Langley for The New York Times
Supported by
By Lisa Miller
- April 21, 2024
The sheet-pan chicken and roasted broccoli are out of the oven, and white rice is steaming on the stove. Virginia Sole-Smith, who has spent a decade writing about how women think and feel about their bodies — and how they pass along those feelings to their children through food — is about to serve dinner to her daughters, Violet, 10, and Beatrix, 6.
Sole-Smith tries not to be a short-order cook. “Respect the labor,” is how she puts it, reminding her children that if they don’t like what she has prepared, there’s other stuff to eat in the house. A pullout shelf in the pantry holds Tate’s chocolate chip cookies, Goldfish crackers, pea snaps, and chocolate kisses. There are raspberries and grape tomatoes in the fridge.
What Sole-Smith hopes to model, she said in a five-hour interview at her home in Cold Spring, N.Y., is “that you can be a mom who doesn’t live solely in service of other people.” That “you deserve time to yourself and that you’re a person with needs, that those needs matter.”
She ferries the girls’ plastic plates to the front-porch table, evading the miniature Bernedoodle, Penelope. A year ago, Sole-Smith published “Fat Talk: Parenting in the Age of Diet Culture,” a guide to helping parents grapple with their discomfort and anxiety about weight and food. At the moment when Ozempic-like drugs are enabling people to become thin, Sole-Smith has become one of the country’s most visible fat activists, calling out the bias and discrimination faced by people in bigger bodies, especially from doctors and research scientists.
She asserts her own right to be “fat,” the preferred adjective in her corner of the internet. In Sole-Smith’s house there are neither “good” or “bad” foods nor “healthy” or “unhealthy” ones; doughnuts and kale hold equivalent moral value and no one polices portion size. By relieving herself and her family of rules about eating, Sole-Smith believes she will have a better chance of raising children who are proud of their bodies, trust themselves to enjoy their food and leave the table when they’re full. She serves dessert and snacks, like Cheez-Its, along with the dinner entree; her kids can eat their meal in any order.
“Fat Talk” is, in a way, Sole-Smith’s manifesto of liberation from what nutritionists call “diet culture”: the enormous pressure American women, in particular, feel to be thin and to raise thin children. For many years, she covered health (including for The New York Times), and her reporting on the pursuit of thinness prompted her rejection of it.
For Sole-Smith, “diet culture” has come to symbolize all the crushing expectations under which American women live. In her Substack newsletter and podcast, Burnt Toast, she muses on whether hewing to a household budget , gardening only with native plants , or limiting kids’ screen time can be regarded as diets.
Sole-Smith separated from her husband Dan Upham last June, and in that upheaval has had to reconsider many family rituals, including dinner. Sole-Smith and Upham attempted a regular dinner hour — Upham said he considered it “sacrosanct” — but when they split, neither child wanted to come to the table at all. And then Sole-Smith hit on a fix: She released her kids from the pressure to politely converse by allowing them to read at the table.
At dinner on this cool night, each girl grabs a brownie and then, after a few bites of broccoli or chicken, wanders off to play on the large rocks that line the front lawn. As she eats, Sole-Smith wonders aloud whether heterosexual marriage itself might be a diet.
“There’s a thing with marriage where you’re like, ‘But he’s a good guy. But it’s pretty good. Like, this is fine. Like, I shouldn’t blow up our lives,” she said. At the same time, she continued, “Shouldn’t I want more freedom than this?” Just as Sole-Smith progressed from trying to wrestle her body into thinness in her 20s to accepting herself at 42, she is also trying to relinquish the notion that marriage — “especially to this thin, attractive man who finds me sexy” — is a marker of success.
“We would all do a lot better to be less afraid of divorce, just as we would do a lot better to be less afraid of being fat,” she said. “What if you just let go?”
No Pro-Weight-Loss Comments Allowed
Sole-Smith has emerged as an inspirational, infuriating voice on the subject of bodies at a moment when there is no neutral zone. Since “Fat Talk” became a New York Times best seller last May, Burnt Toast has grown to nearly 50,000 subscribers — mostly white, straight, millennial mothers who have struggled with eating, body image, and weight. In Sole-Smith’s reader survey, about half of her audience identified as “fat.” On Burnt Toast no pro-weight-loss comments are allowed.
The most fervent 10 percent of Burnt Toast adherents pay $50 or more per year for extra content, which provides Sole-Smith an annual salary of about $200,000, twice as much as she ever made as a freelance writer. Her fans love her for giving them permission to stay off the scale at the doctor’s office and for teaching them how to talk to their kids about bodies and food. Amy Nemirow, a subscriber from suburban Philadelphia, said the community at Burnt Toast helps her “look in the mirror and appreciate how I look and what my body is capable of.”
Sole-Smith relies on scientific research to bolster her message. Data shows that being shamed about weight is linked to depression, anxiety and social isolation , as well as poor physical health . Significant weight loss through dieting is extremely hard to sustain . Bias from doctors can lead to avoidance of medical care and worse health outcomes. Eating disorders — including bingeing and anorexia — are common in people in larger bodies .
“The consequences are clearly demonstrated,” said Kelly Brownell, a professor emeritus of public policy at Duke University who has spent five decades studying obesity and its prevention. “They’re social in nature, psychological, and medical, too. When you add all that up, it clearly means that weight stigma is having an impact on health.”
The relationship between weight and health is extremely complex, and longitudinal studies can’t predict any individual’s vulnerability to disease. Still, decades of research demonstrates a strong association between excess fat and increased risk of five of the top 10 leading causes of death in the United States: cardiovascular disease , cancer , stroke , diabetes and liver disease . Doctors who focus on obesity are alarmed by the growing percentages of Americans who have it — 42 percent by the latest count .
“I think it’s possible to simultaneously hold in your mind that the condition of obesity is concerning, while at the same time protecting the rights of the people who have it,” Brownell said. “You can think of many other parallels, like depression or alcoholism, where you don’t want the people who have these things to be stigmatized — there are clearly negative effects of that — but it doesn’t mean you discount the ravages of those diseases.”
Like most internet personalities, Sole-Smith deploys her persona — a self-confident suburban mother with enviable hair and an obsession with gardening — in service of her battle cry: a body is not anyone else’s problem to solve. Sole-Smith does not dispute that in some cases, excess fat may contribute to disease, but she believes that weight stigma is “the foundation of everything about weight and health that nobody has been looking at for so long.” She is part of a fractious, vocal band of activists and advocates who argue that the real epidemic is bias, not obesity. Some reject even the word “obesity,” which is a medical diagnosis, as derogatory, too tangled with a long history of sexism and racism from doctors, advertisers, and health editors to be neutral.
What most riles readers who encounter Sole-Smith is the calm assurance with which she lays down arguments that seem to defy common sense. This is especially true when she talks about Oreos, as she has done many times, and did again when I asked her about them in Cold Spring. Her position is, in a way, the wedge that divides her fans from her haters and draws attention online. Sole-Smith says that parents need not be concerned about how many Oreos their children eat (the same goes for Halloween candy and ice cream), and when I asked her whether a boundary — say, three Oreos at a time — might be sensible, she pushed back.
“What happens when your kid goes on a play date to my house? I can tell you. Your kid eats nine Oreos,” she said. If parents put restrictions on foods, then children will never figure out how to eat according to their bodies’ own needs, she explained.
When she said such things publicizing her book, readers went mad. A short, positive review in the Washington Post garnered more than 1,700 comments, with an overwhelming number calling Sole-Smith silly, immoderate, and anti-science. “Just letting kids be fat is a form of abuse,” one reader wrote. In The Cut , one commenter, of more than 340, wrote, “It’s like saying kids will intuitively choose math lessons over cartoons and video games.”
But Sole-Smith is committed to her stance. At her last checkup, her blood work showed high cholesterol for the first time, and her doctor suggested she limit saturated fats and start baking cookies with margarine. She’s waiting to see her results “in a year when I’m not launching a book and getting divorced,” she said, with a small laugh. If her cholesterol warrants medication at her next visit, “then great. Medication,” she said. “But no. I will not pursue intentional weight loss to manage a cholesterol level.” As she sees it, the risks to her mental health by restricting her diet outweigh whatever other benefit she might gain.
‘What Your Body Is Meant to Be’
Sole-Smith was raised by divorced parents in Guilford, Connecticut, an affluent suburb of New Haven. Her mother, who is English, was an insurance executive. Her father was a political science professor at Yale, and later at the University of Pennsylvania. Marian Sole preferred a restaurant meal after a long day at work. Rogers Smith, an avid exerciser, would pat his belly when offered dessert and say, “TFA,” which meant, “too fat already.”
Through her father, Sole-Smith belongs to the family that founded H.D. Smith, a national pharmaceutical wholesaler acquired in 2018 by AmerisourceBergen. “It was the back story of my life, and it does shape my life,” Sole-Smith said. “It provides a lot of financial security for my family,” she added. “It is not a privilege I earned, and it is an enormous privilege.”
Sole-Smith started out in women’s magazines in the early 2000s, when “thin” equaled “healthy” and master cleanses were de rigueur. She didn’t consider herself a dieter, but she scheduled her workday around her trips to the gym, which in turn were timed around reruns of “The West Wing,” because, she said, “I could only stand to be on the treadmill if I was watching ‘The West Wing.’” She ran half marathons. “They were the ‘can you have it all’ years,” she said. “You’re going for the big job. You’re going for the perfect body. You’re going for the great marriage. You’re going for motherhood. You’re going for the perfect home.”
She did not begin to reconsider her relationship to food and fat until 2013, when Violet, then four weeks old, was diagnosed with a severe congenital heart defect. Violet required a dozen surgeries, and for most of the first two years of her life was fed through tubes. One consequence was that when she was physically strong enough, she did not know how to eat . Having been passively nourished for so much of her life, her brain did not recognize her appetite.
“The Eating Instinct: Food Culture, Body Image, and Guilt in America,” Sole-Smith’s first book, published in 2018, described how she learned to relinquish her fantasies about motherhood and nourishing her child so that Violet might survive. “The Eating Instinct” offered up “ intuitive eating ,” a feeding method established in the 1990s that was gaining traction among millennial parents. It suggested that all the old rules — “clean your plate” and “no dessert until after dinner” — might not apply. When Violet was 2, Sole-Smith and Upham had to overcome their acculturated anxieties about the sugar and fat in chocolate milk. Violet started drinking half a gallon each week.
In Cold Spring, Sole-Smith said she would write the book very differently today. For one thing, she was still using the words “obese” and “obesity” without qualification. And some part of her was blaming people in bigger bodies for a lack of discipline. “I was still thinking at that point that a fat body was a problem to solve,” she said, “versus this is what your body is meant to be.” “The Eating Instinct,” a quiet book, sold about 2,000 copies in print. “I do think being more clear on a provocative argument, versus asking careful questions about it, is just more marketable,” she said, in retrospect.
A Job Becomes a Calling
Sole-Smith didn’t have a moment of radicalization. It was more like a gradual shift in perspective. After “The Eating Instinct,” she began to encounter ideas she hadn’t previously grappled with, she said. She was already familiar with the work of the nutritionist Lindo Bacon , whose 2010 book, “Health at Every Size: The Surprising Truth About Your Weight,” challenged doctors to treat patients without recommending weight loss. Sole-Smith also knew Lisa DuBreuil, a clinical social worker in Boston who sees people with eating disorders. When introducing someone to fat activism, DuBreuil often starts by saying that “it’s normal for there to be a wide range of body sizes. That fat people have always existed,” she said in an interview. The relief and recognition can be very strong. Educating Sole-Smith was like watching a person “stepping out of the matrix,” she added.
In 2019, Sole-Smith read “Fearing the Black Body: The Racial Origins of Fat Phobia” by Sabrina Strings, a sociologist at the University of California, Santa Barbara, which reframes the cultural and medical concern about obesity as “a way to craft and legitimate race, sex, and class hierarchies.” Sole-Smith started to absorb the larger capitalist critique: Even fat activism had been co-opted by women’s magazines, advertisers, and fitness companies and turned into “body positivity,” a defanged version that “really centers, you know, ‘small fat’ white women like me,” Sole-Smith said, using the identifier she learned around then. Sole-Smith started to spell the word “ob*sity” wherever she could.

Sole-Smith began to feel that her freelance specialty, analyzing obesity research studies for editors at mainstream publications , was “just exhausting and not moving the needle.” She increasingly felt that discrimination was the problem, not proving or disproving that excess fat made people sick. “It doesn’t matter what people’s health status is. Right? Drug addicts are worthy of dignity and respect in medical care. Like, it doesn’t matter whether you caused it, doctors are supposed to meet you where you are,” Sole-Smith said in Cold Spring. Upham saw a change come over her. “When she was in magazines, that was a job. This felt more like a calling,” he said.
In September 2020, Sole-Smith wrote “ What If Doctors Stopped Prescribing Weight Loss ?” an article that evoked the analogy between weight stigma and racism. By then, she had given up trying to dress to de-emphasize her shape. She had moved, definitively, into plus sizes, and found freedom in finally accepting herself. She embraced horizontal stripes, conventionally proscribed for women in bigger bodies. It felt “a little subversive,” she said.
An Argument About Butter
Life in the Cold Spring house grew stressful as the pandemic wore on. The dog wouldn’t stop barking. Violet was attending second grade at her private school in a mask and mostly outdoors. Beatrix was 3. Sole-Smith was working on “Fat Talk” and building Burnt Toast. The extroverted Upham, who worked in communications, was going stir crazy in isolation. He had always been outdoorsy, hiking in the White Mountains or trail running in the Shawangunks. But now, cut off from his friends and two years into sobriety, he began running with urgency on the trails by their house. “I ran hundreds of miles,” he said. Child care was on the list of topics they argued about, Upham said.
For her part, Sole-Smith was newly aware of “the value of comfort eating,” she said. “We demonize it so much.” She began to think about all the ways that she and her friends had punished themselves by abstaining from food. “I deserve softness. I deserve a little tenderness,” she said. “Everything is chaos. It’s nice I can make brownies.”
In almost every respect, Upham had “an easy time” with Sole-Smith’s radicalization, he said. But he did find the notion of “de-prioritizing exercise” to be “challenging” — and not because he regards physical activity as a virtue. Hardcore exercise is his way of life. “It’s hard for me to see past that sometimes,” he said.
In the spring of 2021, with Americans exhausted and edgy and many only recently vaccinated, Sole-Smith emerged as a voice of reassurance. In April, she published a piece in Good Housekeeping saying she had no intention of getting her prepandemic body back. “When it’s safe to re-enter the world, my sweatpants are coming with me,” she wrote. When new studies reported trends of pandemic weight gain , Sole-Smith went on Brian Lehrer, the WNYC call-in show. “Anything you had to do for your mental health in the last year, whether that was more comfort eating, more sleep, more anything, that was a good choice for your health,” she told a listener who felt terrible about regaining the 50 pounds he lost before the pandemic.
It was around this time that she and Upham had an argument about butter. Beatrix had eaten a whole stick, “jammed it in her mouth,” Sole-Smith said in Cold Spring, because she thought it was cheese. Upham — whom Sole-Smith describes as more of a “rules guy” — wanted to intervene, but Sole-Smith disagreed. “If I put butter on the table and a kid wants to eat the butter, that’s fine with me,” Sole-Smith said. (Upham said he now regrets his response. He probably thought eating a whole stick of butter was “just disgusting,” he said, “but I really am on team calories.”)
Answering Critics By Eating Brownies
Ozempic became a national obsession in the winter of 2023, just as Sole-Smith was heading out to promote “Fat Talk,” giving her a foothold in the news cycle that she could not have anticipated. The more she became known for dismantling anti-fatness, the more editors and bookers invited her to give her opinion.
That January, Sole-Smith wrote an opinion piece for The New York Times responding to new guidelines issued by the American Academy of Pediatrics that recommended Ozempic-like drugs for a subset of obese children as young as 12. The first chapter of “Fat Talk” is titled “The Myth of the Childhood Obesity Epidemic,” and in her article, she wrote, “We cannot solve anti-fat bias by making fat kids thin.”
This view prompted an outcry. Dr. Barry Reiner, a pediatric endocrinologist in Baltimore, was “personally infuriated,” he said, and stayed up past midnight one night writing a letter to the editor . Historically, Type 2 diabetes has been an adult-onset disease, but “for the past several years, I’ve been seeing a lot more of it,” Dr. Reiner said. “These children are not going to have a healthy life, or a normal life span.” While it’s theoretically possible for a person to carry a lot of excess weight into maturity and remain healthy, “I think that’s a vast minority, maybe approaching a myth,” Dr. Reiner added.
In his newsletter ConscienHealth, Ted Kyle, who formerly worked in obesity policy for GlaxoSmithKline, called out Sole-Smith for ignoring facts, “which don’t melt away because our feelings are strong.” He linked to a study from Yale University that showed a rising prevalence of fatty liver disease during the pandemic among children with obesity — a condition that can lead to “liver cancer, cirrhosis, and death,” Kyle wrote.
Then, in April, Sole-Smith went on “Fresh Air” and offered a political analysis. “Celebrating a thin white body as the ideal body is a way to other and demonize Black and brown bodies, bigger bodies, anyone who doesn’t fit into that norm,” she said. Social media predictably exploded at this. On Fox, Greg Gutfeld mocked Sole-Smith’s “horrible, stupid” remarks. On the Reddit channel “ fatlogic ,” one person queried whether it wasn’t racist for “middle class white women to be casting themselves as the victims of racist violence and chattel slavery,” while another wondered, “Has she not seen black people that already are skinny/slim/fit? We’re not all ‘thick’ or obese.”
In May, after “Fat Talk” hit the best-seller list, Sole-Smith took a victory lap on Instagram . Wearing a bright pink dress, she posted some of the hate messages she had received. “I can see why you’re single. No one wants to spend time with a fat slob shoving pizza in her fat mouth,” read one. As these notes flashed across the screen, she ostentatiously ate a brownie.
Earlier in our conversation in Cold Spring, Sole-Smith talked about all the ways in which every person undermines their own health, by drinking alcohol, say, or opting out of the gym; even people who refuse to wear motorcycle helmets are freer from judgment than fat people, she said. During dinner, with the girls playing in the yard, this question of autonomy came up again, in a more philosophical way. I asked Sole-Smith what it meant to make less-than-optimal choices about personal health in the name of autonomy when others — children, family members, friends, a community — are dependent on you.
“Health is a resource and a privilege so many people don’t have access to,” Sole-Smith began. There are mothers who are substance users, older mothers, and mothers with congenital health conditions. No parent has an obligation to pursue good health, and to believe so “is fundamentally a very ableist perspective,” she said.
She continued, “Is health that I eat this broccoli for dinner? Or is health that I managed to have a few minutes of connection with my daughter today?”
Sole-Smith announced her separation in September in the most viral issue of Burnt Toast to date, but neither she nor Upham will say why they split. They had been together since high school, and Upham has been a character in Sole-Smith’s work at least since Violet was born. What Sole-Smith does say is that she’s become “deeply critical of the institution of marriage and what it asks from straight women.” In her writing and talking about marriage (and divorce) on Burnt Toast, she denounces the unequal division of emotional labor that so many women in her cohort complain of: the hours spent planning meals and communicating with teachers and arranging play dates in addition to their full-time jobs.
“Deciding to get divorced is terrible. Being divorced is amazing,” she said.
As Sole-Smith considers all the ways she is enjoying her release from what she calls “the hyper-competent oldest daughter in me,” she notices that Beatrix is beginning to shiver in her thin T-shirt. Another rule to which Sole-Smith fails to adhere is appropriate outerwear, she said, with a laugh. Her girls are always either overdressed or underdressed. She yells toward Beatrix. “Are you done with your chicken?” But Beatrix, wearing headphones, doesn’t hear. Sole-Smith leans down and gives Beatrix’s dinner to the dog.
Advertisement

IMAGES
VIDEO
COMMENTS
What are 5 effects of unhealthy lifestyle? 1. Unhealthy lifestyle can lead to an increased risk of developing chronic diseases such as heart disease, diabetes, and cancer.2. Unhealthy lifestyle can lead to poor mental health, such as depression and anxiety.3. Unhealthy lifestyle can lead to an increased risk of obesity and weight gain.4.
Lifestyle may effect on sleep and sleep has a clear influence on mental and physical health. Sexual behavior: Normal sex relation is necessary in healthy life. Dysfunction of sex relation is the problem of most of societies and it has a significant effect on mental and physical health. It can be said that dysfunctional sex relation may result ...
An unhealthy lifestyle is one of the principal causes of many diseases and conditions that afflict humanity today. It is a global problem, transcending geographical boundaries, age, and socioeconomic classes. This essay aims to explore the concept of an unhealthy lifestyle, its causes, consequences, and possible solutions.
Lifestyle may effect on sleep and sleep has a clear influence on mental and physical health ( 9 ). Sexual behavior: Normal sex relation is necessary in healthy life. Dysfunction of sex relation is the problem of most of societies and it has a significant effect on mental and physical health.
1. Introduction. Quality of life (QoL) is a broad multidimensional concept that is significant as a desired health outcome. It represents the expectation and concern for one's own health and life, including both positive and negative aspects of QoL in the context of the culture and value systems [].The 36-item Short-Form Health Survey (SF-36) is a widely used health-related QoL tool that is ...
The effects of an unhealthy lifestyle foster the dysregulation of macrophages that then remain in an M1 phenotype. Transforming growth factor-β (TGF-β) released by lymphocytes and macrophages appears to be one of the primary factors that leads to dysregulation in fibroblasts ( Wynn, 2008 ; Meng et al., 2016 ).
The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK Biobank cohort. Lancet Public Health 2018; 3: e576-85. doi: 10.1016/S2468-2667(18)30200-7. pmid: 30467019
Background Non-communicable diseases are a leading cause of health loss worldwide, in part due to unhealthy lifestyles. Metabolic-based diseases are rising with an unhealthy body-mass index (BMI) in rural areas as the main risk factor in adults, which may be amplified by wider determinants of health. Changes in rural environments reflect the need of better understanding the factors affecting ...
250 Words Essay on Effects Of Modern Lifestyle On Health Introduction. ... Unhealthy Eating Habits. One of the major effects of modern lifestyle on health is seen in eating habits. People tend to eat more fast food and processed foods because they are easy to prepare and consume. These foods are often high in sugar, salt, and unhealthy fats ...
A more recent explanation for the way in which our food may affect our mental wellbeing is the effect of dietary patterns on the gut microbiome—a broad term that refers to the trillions of microbial organisms, including bacteria, viruses, and archaea, living in the human gut. The gut microbiome interacts with the brain in bidirectional ways ...
The same happens when one does too much physical activity. Stress can largely be associated with unhealthy lifestyles. Unhealthy lifestyles are characterized by overdoing of some things and neglect of given aspects of self. For example, people who over eat are likely to suffer from stress induced by effects of overweight.
With increasing access to unhealthy foods and a shift towards a sedentary lifestyle across all ages, maintaining healthy dietary patterns and physical activity levels needs to be emphasized.
Essay on Healthy Lifestyle. The top secret of being physically fit is adopting a healthy lifestyle. A healthy lifestyle includes regular exercise, a healthy diet, taking good care of self, healthy sleep habits, and having a physically active daily routine. Lifestyle is the most prevailing factor that affects one's fitness level.
Essay on Unhealthy Lifestyle (600+ Words) In today's busy world, it is very common for people to fall victim to the dangers of an unhealthy lifestyle. Sedentary habits, poor dietary choices, and neglecting self-care have become the norm for many, leading to detrimental consequences. However, it is crucial to acknowledge the profound impact of ...
Having an inactive lifestyle can be one of the causes of many chronic diseases. By not getting regular exercise, you raise your risk of: Obesity. Heart diseases, including coronary artery disease and heart attack. High blood pressure. High cholesterol. Stroke. Metabolic syndrome. Type 2 diabetes.
An unhealthy diet can increase the risk of some cancers. Consuming unhealthy food and beverages, such as sugar-sweetened beverages and highly processed food, can lead to weight gain, obesity and other chronic conditions that put people at higher risk of at least 13 types of cancer, including endometrial (uterine) cancer, breast cancer in ...
In early childhood the ability to develop and thrive closely relates to a wide range of outcomes throughout a child's life. Having good communication and language skills are linked with higher level qualifications and success in education, resulting in higher incomes and better overall health (IHE, 2020).
A healthy lifestyle can make us feel good, look good, and live longer. It can reduce the risk of many diseases like heart disease, diabetes, and cancer. A healthy lifestyle can also make us happier. It can boost our mood, reduce stress, and improve our self-esteem. It can make us more productive and successful in life.
The Change Of Unhealthy Lifestyle. The Change in Unhealthy Lifestyle Many children and adults these days live unhealthy lifestyles. They are eating more processed food and fast food. Lack of sleep and alcohol are also common in unhealthy lifestyles. Some people are even born into families that have unhealthy habits such as smoking.
1. Introduction. According to the World Health Organization (WHO), the behavioral factors associated with an unhealthy lifestyle include the consumption of a diet with inadequate fruit and vegetables, tobacco smoking, physical inactivity, a sedentary lifestyle, and alcohol consumption [].The literature identifies the fact that people who exercise and eat healthy food have a higher chance of ...
2.3. Clustering of Unhealthy Lifestyle Habits. The clustering of unhealthy lifestyle habits was calculated by adding for each participant the number of unhealthy behaviors adopted, namely low MD adherence indicated by a KIDMED score ≤3 and low PA expressed by less than 3 h of regular exercise per week .
The worst lifestyle habits that can affect students' academic life (Survey item No. 4) The main effect of bad habits on students'academic performance (Survey item No. 8) Responses for some ...
500+ Words Essay on Healthy Lifestyle. It is said that it is easy to learn and maintain bad habits but it is very difficult to switch them back. The issue of a healthy lifestyle is very serious but the people take it very lightly. Often, it is seen that the people take steps to improve their lifestyle but due to lack of determination quits in ...
The deleterious effects of an unhealthy lifestyle are being widely recognized by the public. Fortunately, lifestyle behaviors are modifiable, for instance, through maintaining a healthy mental state, sleeping enough and regularly, ceasing smoking, limiting alcohol consumption, keeping a healthy diet pattern, and engaging in physical exercise.
Talking about the impact of unhealthy comparison on student well-being, Smitha Rahul, Rehabilitation Psychologist, Student Counsellor Academic Co-ordinator and Psychology lecturer at St. Claret P ...
In Sole-Smith's house there are neither "good" or "bad" foods nor "healthy" or "unhealthy" ones; doughnuts and kale hold equivalent moral value and no one polices portion size ...