- Patient Care & Health Information
- Diseases & Conditions
- Childhood obesity
Childhood obesity is a serious medical condition that affects children and adolescents. It's particularly troubling because the extra pounds often start children on the path to health problems that were once considered adult problems — diabetes, high blood pressure and high cholesterol. Childhood obesity can also lead to poor self-esteem and depression.
One of the best strategies to reduce childhood obesity is to improve the eating and exercise habits of your entire family. Treating and preventing childhood obesity helps protect your child's health now and in the future.
Not all children carrying extra pounds are overweight. Some children have larger than average body frames. And children normally carry different amounts of body fat at the various stages of development. So you might not know by how your child looks if weight is a health concern.
The body mass index (BMI), which provides a guideline of weight in relation to height, is the accepted measure of overweight and obesity. Your child's doctor can use growth charts, the BMI and, if necessary, other tests to help you figure out if your child's weight could pose health problems.

When to see a doctor
If you're worried that your child is putting on too much weight, talk to his or her doctor. The doctor will consider your child's history of growth and development, your family's weight-for-height history, and where your child lands on the growth charts. This can help determine if your child's weight is in an unhealthy range.
Lifestyle issues — too little activity and too many calories from food and drinks — are the main contributors to childhood obesity. But genetic and hormonal factors might play a role as well.
More Information
- Mayo Clinic Minute: Out of shape kids and diabetes
Risk factors
Many factors — usually working in combination — increase your child's risk of becoming overweight:
- Diet. Regularly eating high-calorie foods, such as fast foods, baked goods and vending machine snacks, can cause your child to gain weight. Candy and desserts also can cause weight gain, and more and more evidence points to sugary drinks, including fruit juices and sports drinks, as culprits in obesity in some people.
- Lack of exercise. Children who don't exercise much are more likely to gain weight because they don't burn as many calories. Too much time spent in sedentary activities, such as watching television or playing video games, also contributes to the problem. TV shows also often feature ads for unhealthy foods.
- Family factors. If your child comes from a family of overweight people, he or she may be more likely to put on weight. This is especially true in an environment where high-calorie foods are always available and physical activity isn't encouraged.
- Psychological factors. Personal, parental and family stress can increase a child's risk of obesity. Some children overeat to cope with problems or to deal with emotions, such as stress, or to fight boredom. Their parents might have similar tendencies.
- Socioeconomic factors. People in some communities have limited resources and limited access to supermarkets. As a result, they might buy convenience foods that don't spoil quickly, such as frozen meals, crackers and cookies. Also, people who live in lower income neighborhoods might not have access to a safe place to exercise.
- Certain medications. Some prescription drugs can increase the risk of developing obesity. They include prednisone, lithium, amitriptyline, paroxetine (Paxil), gabapentin (Neurontin, Gralise, Horizant) and propranolol (Inderal, Hemangeol).
Complications
Childhood obesity often causes complications in a child's physical, social and emotional well-being.
Physical complications
Physical complications of childhood obesity may include:
- Type 2 diabetes. This chronic condition affects the way your child's body uses sugar (glucose). Obesity and a sedentary lifestyle increase the risk of type 2 diabetes.
- High cholesterol and high blood pressure. A poor diet can cause your child to develop one or both of these conditions. These factors can contribute to the buildup of plaques in the arteries, which can cause arteries to narrow and harden, possibly leading to a heart attack or stroke later in life.
- Joint pain. Extra weight causes extra stress on hips and knees. Childhood obesity can cause pain and sometimes injuries in the hips, knees and back.
- Breathing problems. Asthma is more common in children who are overweight. These children are also more likely to develop obstructive sleep apnea, a potentially serious disorder in which a child's breathing repeatedly stops and starts during sleep.
- Nonalcoholic fatty liver disease (NAFLD). This disorder, which usually causes no symptoms, causes fatty deposits to build up in the liver. NAFLD can lead to scarring and liver damage.
Social and emotional complications
Children who have obesity may experience teasing or bullying by their peers. This can result in a loss of self-esteem and an increased risk of depression and anxiety.
To help prevent excess weight gain in your child, you can:
- Set a good example. Make healthy eating and regular physical activity a family affair. Everyone will benefit and no one will feel singled out.
- Have healthy snacks available. Options include air-popped popcorn without butter, fruits with low-fat yogurt, baby carrots with hummus, or whole-grain cereal with low-fat milk.
- Offer new foods multiple times. Don't be discouraged if your child doesn't immediately like a new food. It usually takes multiple exposures to a food to gain acceptance.
- Choose nonfood rewards. Promising candy for good behavior is a bad idea.
- Be sure your child gets enough sleep. Some studies indicate that too little sleep may increase the risk of obesity. Sleep deprivation can cause hormonal imbalances that lead to increased appetite.
Also, be sure your child sees the doctor for well-child checkups at least once a year. During this visit, the doctor measures your child's height and weight and calculates his or her BMI . A significant increase in your child's BMI percentile rank over one year may be a possible sign that your child is at risk of becoming overweight.
- Helping your child who is overweight. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/weight-management/helping-your-child-who-is-overweight. Oct. 14, 2020.
- Childhood obesity causes and consequences. Centers for Disease Control and Prevention. https://www.cdc.gov/obesity/childhood/causes.html. Accessed Oct. 14, 2020.
- Kliegman RM, et al. Overweight and obesity. In: Nelson Textbook of Pediatrics. 21st ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Oct. 14, 2020.
- Hay WW, et al., eds. Normal childhood nutrition and its disorders. In: Current Diagnosis & Treatment: Pediatrics. 25th ed. McGraw Hill; 2020. https://accessmedicine.mhmedical.com. Accessed Oct. 20, 2020.
- Skelton JA. Management of childhood obesity in the primary care setting. https://www.uptodate.com/contents/search. Accessed Oct. 14, 2020.
- Klish WJ, et al. Definition, epidemiology and etiology of obesity in children and adolescents. https://www.uptodate.com/contents/search. Accessed Oct. 14, 2020.
- Polfuss ML, et al. Childhood obesity: Evidence-based guidelines for clinical practice — Part one. Journal of Pediatric Health Care. 2020; doi:10.1016/j.pedhc.2019.12.003.
- Davis RL, et al. Childhood obesity: Evidence-based guidelines for clinical practice — Part two. Journal of Pediatric Health Care. 2020; doi:10.1016/j.pedhc.2020.07.011.
- Mayo Clinic Children's Center Pediatric Weight Management Clinic
- Mayo Clinic Minute: Weight loss surgery for kids
Associated Procedures
- Bariatric surgery
- Cholesterol test
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 20 October 2015
Biological, environmental, and social influences on childhood obesity
- M. Karen Campbell 1 , 2 , 3 , 4
Pediatric Research volume 79 , pages 205–211 ( 2016 ) Cite this article
49k Accesses
106 Citations
5 Altmetric
Metrics details
- Metabolic disorders
- Risk factors
The prevalence of childhood obesity has increased globally over the past three decades, with evidence of recent leveling off in developed countries. Reduction in the, currently high, prevalence of obesity will require a full understanding of the biological and social pathways to obesity in order to develop appropriately targeted prevention strategies in early life. Determinants of childhood obesity include individual level factors, including biological, social, and behavioral risks, acting within the influence of the child’s family environment, which is, in turn, imbedded in the context of the community environment. These influences act across childhood, with suggestions of early critical periods of biological and behavioral plasticity. There is evidence of sex and gender differences in the responses of boys and girls to their environments. The evidence that determinants of childhood obesity act at many levels and at different stages of childhood is of policy relevance to those planning early health promotion and primary prevention programs as it suggests the need to address the individual, the family, the physical environment, the social environment, and social policy. The purpose of this narrative review is to summarize current, and emerging, literature in a multilevel, life course framework.
Similar content being viewed by others

Understanding childhood obesity in the US: the NIH environmental influences on child health outcomes (ECHO) program
Frances A. Tylavsky, Assiamira Ferrara, … Leonardo Trasande
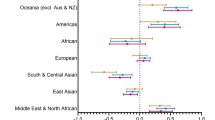
Mediators of differences by parental education in weight-related outcomes in childhood and adolescence in Norway
Teferi Mekonnen, Anne-Lise Brantsæter, … Eleni Papadopoulou
Differences in weight status among Australian children and adolescents from priority populations: a longitudinal study
Thomas Lung, Anagha Killedar, … Alison Hayes
Introduction
The prevalence of childhood obesity has increased globally over the past three decades, with more rapid increases recently occurring in low-income countries ( 1 ). In the United States, more than 30% of children are now overweight or obese ( 1 ), with evidence that the prevalence has leveled off ( 2 ). Children and adolescents are exhibiting obesity-related conditions such as type 2 diabetes, elevated blood pressure, low-density lipoprotein cholesterol, and higher fasting insulin levels ( 3 , 4 , 5 , 6 ). In addition, childhood obesity predicts adulthood obesity and its known health consequences ( 7 , 8 ). Treatment of obesity is notoriously difficult, with weight loss rarely sustained in adults ( 9 ). Therapeutic interventions in childhood are somewhat more successful, particularly if the intervention occurs prior to onset of puberty ( 10 ). However, real and sustained progress in combating the obesity epidemic will require a full understanding of the biological and social pathways to obesity in order to develop appropriately targeted prevention strategies in early life.
Pathways to childhood obesity are complex. It is therefore helpful to discuss determinants of obesity within a conceptual framework. A multilevel conceptual model, Bronfenbrenner’s Bioecological Systems Theory ( 11 ), has previously been applied to the conceptualization of childhood obesity by Davison and Birch ( 12 ). This framework depicts individual-level factors, including biological, social, and behavioral risks, as acting within the influence of the child’s family environment, which is, in turn imbedded in the context of the community environment. It is also helpful to consider critical periods for obesity risk and, as will be further illustrated in a later section, there are likely critical periods of biological and behavioral plasticity beginning as early as fetal life ( 13 ) with risk factors accumulating, and interacting with each other, across the life course. This is consistent with a life course model of chronic disease epidemiology ( 14 ). Specific determinants of obesity will be discussed below within this multilevel framework and life course perspective.
This narrative review will discuss both biological and social determinants of childhood obesity at three levels (individual, family, and community) and across early childhood. The relationship between childhood stress and obesity will be explored in greater detail as this is an important pathway of active interest in current literature. In addition, the review will address recent attention to sex- and gender-based differences in obesity risk. A key purpose in undertaking this review was to summarize evidence regarding pathways to obesity in boys and girls by integrating established plus emerging perspectives in the literature. These include an overview of important factors at each level. Given the breadth of the literature, it was not the intention to cover all literature on each determinant but rather to provide these as key examples of the many dimensions of obesity risk.
Individual-, Family-, and Community-Level Determinants of Obesity
At the individual level, the most direct determinant of children’s obesity is the energy balance between nutritional intake and activity, the latter being influenced by both physical activity and sedentary behaviors ( 15 , 16 , 17 ). These behavioral factors are therefore frequent targets for both preventive and therapeutic interventions. However, nutrition and activity are “downstream” factors that can be influenced by many “upstream” causes. The energy balance required to maintain an appropriate fat mass varies among individuals due to differences in metabolism and in lipostatic set point, which will influence appetite and activity preferences ( 18 ). Metabolism and lipostatic set point, while to some degree influenced by genetic predisposition ( 18 ), can be altered by gene–environment interactions ( 19 , 20 , 21 ).
The family, physical, and social environment influence children’s obesity risk in two ways: through a direct influence on children’s nutrition and activity behaviors and through indirect influences via stress as will be discussed later in this paper. Higher parental education, parental nurturing, and higher self-esteem reduce obesity risk in girls ( 22 ). There is an abundance of evidence that the home food environment ( 23 , 24 , 25 ), shared family meals ( 26 , 27 ), and electronic media use influence children’s obesity ( 28 ) largely through behavioral pathways. Mothers primarily establish the home food environment and are role models for eating behaviors ( 29 ) with evidence of strong correlation between the eating patterns of mothers and children ( 25 , 29 ). Appetite control and food preferences are established early in life ( 30 ), and there is a high correlation between parental obesity and their children’s obesity ( 20 , 22 ).
The community environment is increasingly obesogenic, with increased use of convenience foods, automobiles, and electronic and televised forms of entertainment ( 31 , 32 , 33 ) leading to higher consumption of calorie-dense foods and more sedentary lifestyles. Food choices have been shown to be influenced by proximity to fast food outlets, supermarkets, and farmers markets ( 34 , 35 , 36 , 37 , 38 ). Physical activity levels are influenced by public recreation opportunities, transit availability, and neighborhood walkability ( 35 , 37 , 39 , 40 , 41 , 42 ). In addition, lower obesity levels are observed in areas where the natural environment has high recreational value ( 43 ). While evidence suggests that the above environmental factors affect risk behaviors and obesity, there is still a gap in understanding how children interface with the obesogenic environment ( 44 ).
Prenatal and Postnatal Influences
There is emerging interest in prenatal factors, postnatal factors, and their interactions. These are critical time periods of metabolic and endocrine plasticity and may condition later physiologic responses to environmental influences ( 13 ). This field of research has been labeled as the developmental origins of health and disease and is the subject of much attention in the biomedical and epidemiologic sciences.
For the past two decades, there has been intense interest in the possible effect of fetal undernutrition on later obesity. The interest in this proposed association was precipitated by seminal work by Barker ( 45 ). In humans, fetal undernutrition may be a consequence of maternal undernutrition, maternal smoking, or placental dysfunction from preeclampsia. Markers of fetal undernutrition, which include fetal growth restriction and its proxy indicator small birth weight for gestational age, have been shown to be associated with a modestly elevated risk of obesity. It has been suggested that this effect is due to an in utero adaptation that becomes a mismatch to a postnatal environment in which nutrition is abundant ( 46 , 47 ). Animal studies, often based on maternal dietary restriction, confirm evidence for such fetal metabolic adaptations to undernutrition ( 48 ). In both animal and human studies, there is evidence of the permanence of these adaptations. The greatest elevation in obesity risk is for those who were born small, but experienced rapid “catch up growth” postnatally ( 48 , 49 , 50 , 51 , 52 ).
Emerging literature is challenging the relationship of fetal undernutrition as a determinant of obesity. First, if the association does exist, is a genetic component partially responsible? Specific adult obesity gene loci have been implicated as associated both with fetal growth ( 53 ) and with growth velocity in infancy ( 54 ). In this genomic era, this will be an aspect of the literature to watch, although to date the predictive value of individual gene loci for obesity risk has been modest. There is emerging speculation as to whether this association indeed exists at all, despite the abundance of literature on the topic. Part of this speculation is based on a statistical argument that, in the zealous effort to control for the myriad of potential confounders, most studies looking at the relationship between fetal growth restriction or small birth weight for gestational age and later chronic conditions have controlled for variables along the causal pathway and thus introduced bias ( 55 , 56 ). Moreover, recent carefully analyzed studies have suggested the inverse; that small birth weight for gestational age is associated with a lower risk of obesity ( 57 ). This question remains an active topic of interest in the literature, despite the recognition that the association, if real, is a small magnitude association with no clear implications for prevention ( 58 ).
Fetal overnutrition, evidenced by large infant birth weight for gestational age, is a strong predictor of obesity in childhood and later life ( 59 , 60 , 61 ). A caveat is that, while large infant birth weight for gestational age is generally an indicator of excess fat mass, it may also reflect other growth parameters such that a subset of large infant birth weight for gestational age infants may have increased lean mass ( 62 , 63 ). Risk factors for large infant birth weight for gestational age include maternal obesity and maternal gestational diabetes ( 64 , 65 ) with African-American women exhibiting risk at lower maternal BMI thresholds ( 66 ). It is suggested that fetal hyperglycemia triggers fetal insulin production which in turn triggers fetal growth and adiposity ( 67 ). Animal studies demonstrate that fetal hyperinsulinemia may invoke permanent changes in the CNS mechanisms for regulating metabolism and body weight ( 67 ). Thus, fetal overnutrition may be a mechanism of intergenerational transmission of obesity and diabetes ( 67 , 68 ).
Early postnatal experiences are also important contributors to obesity risk. Breastfed infants are at lower risk for later obesity ( 69 , 70 , 71 , 72 , 73 ) for hypothesized reasons including that formula-fed infants develop greater reliance on external hunger cues ( 74 ) and have higher intake of protein ( 75 ), which may contribute to obesity risk through behavioral and physiologic mechanisms, respectively. The benefits of breastfeeding appear to be confined to exclusive breastfeeding; mixed infant feeding of breastmilk and formula do not reduce obesity risks associated with formula feeding ( 76 ). In addition, the timing and choice of complementary foods introduced into an infant’s diet may influence their food preferences in the long term ( 77 ). In general, obesity risk is elevated for those who experienced rapid early weight gain in infancy ( 78 , 79 , 80 ). Based on this knowledge, strategies for primary prevention in high-income countries may include support for long-term breastfeeding ( 81 ).
Psychosocial Vulnerabilities
There is evidence that psychosocial stress is associated with obesity in children. Measures of stress vary from study to study ( 82 ), but the findings are consistent. Whether this association is causal is not known, but there are theoretical frameworks that suggest causality. For example, the life course–stress process perspective introduced by Pearlin et al . ( 83 ) has been discussed by Wickrama et al . ( 84 ) in the context of body mass. A pathway from stress to obesity could include inflammatory mechanisms ( 85 ) including arousal of the hypothalamic–pituitary–adrenal axis leading to increased cortisol levels and subsequent metabolic disruption and increased hunger ( 84 , 86 , 87 , 88 ). If so, nutrition may mediate the relationship between stress and obesity, or lifestyle factors may be coexisting with environmental stressors ( 89 , 90 ). Some of the reported associations of environmental stressors with childhood overweight and obesity include negative life events ( 82 ), maltreatment ( 91 ), how well the family communicates ( 90 ), and parental stress ( 92 ).
Depression and obesity are often comorbid in both children and adults. This comorbidity may be due to common genetic and environmental etiologies ( 93 , 94 , 95 , 96 ) or common pathways via dysregulation of the hypothalamic–pituitary–adrenal system ( 93 , 95 , 96 ). Increased food intake and reduced physical activity are characteristic of both conditions ( 94 ). Bidirectional causation is also plausible, with suggestions that obesity may be a determinant of later depression in children ( 97 , 98 , 99 ) and conversely hypothesized mechanisms for depression causing obesity ( 93 , 95 , 98 , 99 , 100 ). Indeed, it has more recently been suggested that these two comorbid conditions may mutually reinforce a progressive downward spiral in each other ( 101 ) and that additional insight into their longitudinal interaction may be important for intervention strategies ( 102 ).
Mothers’ mental and emotional well-being has been shown to be associated with childhood obesity. Children of mothers with depressive symptoms are more likely to be obese or overweight in infancy ( 103 , 104 ), childhood ( 105 , 106 ), and adolescence ( 107 ). Prenatal exposure to maternal stress and distress has been shown to be associated with both children’s obesity and rapid postnatal growth ( 108 , 109 ). Proposed mechanisms for the association include infant feeding practices ( 110 ), mother–infant interaction ( 111 ), mother–infant feeding interactions ( 112 ), parenting style ( 113 ), and a direct effect of stressors leading to central adiposity via arousal of the child’s hypothalamic–pituitary–adrenal axis ( 86 ). It has also been suggested that, due to the comorbidity between maternal overweight and emotion regulation, these pathways may also play into the intergenerational transfer of overweight and obesity ( 112 ), as well as the roles of shared genes and environment ( 86 ). A recent systematic review noted the need for more prospective studies to confirm and explain these associations ( 114 ).
Consistently, in high-income countries, socioeconomic disadvantage has been shown to be associated with obesity risk in childhood and persistently throughout life ( 115 , 116 , 117 ). Socioeconomic disadvantage may exert its influence as early as the prenatal and postnatal period, through its association with maternal depression ( 106 , 118 ) and its consequences. Moreover, poverty may be associated with poorer individual diet ( 119 ), poorer retail food and recreational environment ( 34 , 120 , 121 ), suboptimal family food routines ( 118 , 122 ), and environmental stressors such as living in a higher crime neighborhood ( 121 ). The risks associated with socioeconomic disadvantage may accumulate and compound throughout childhood ( 123 ). Miller and Chen ( 124 ) present a theoretical model, with corresponding research evidence, linking poverty to the development of a proinflammatory phenotype and subsequent elevated risk for chronic conditions in childhood and beyond. Overall, it appears that poverty is associated with later obesity through its association with other obesity risk factors and through the stress process.
There is an increasing attention in the literature to the differences in vulnerabilities in boys and girls, suggesting different pathways to obesity. Much of the literature, to date, has looked at determinants of childhood obesity while statistically controlling for children’s sex. However, to truly understand the developmental processes leading to obesity, researchers may need to look at boys and girls separately in order to recognize both sex-specific (biological) and gender-specific (social and cultural) differences in the ways in which boys and girls interact with their physical and social environments. Some biological differences include body composition and growth patterns, with clear sex differences in the distribution of adiposity beginning as early as the neonatal period and continuing through adulthood ( 125 ). Energy requirements and the aptitude for specific physical activities exhibit sex differences, while specific gender differences include how boys and girls interact with their family and their food environment as well as their overall physical activity levels ( 126 ). There are also gender differences in metabolic responses to stress ( 87 ) and family disruption or conflict ( 127 ). Responses to the physical and social environment will influence, and be influenced by, pubertal development ( 47 , 48 , 125 ). Pubertal timing itself has significant influence on insulin resistance and metabolic syndrome, particularly in girls ( 128 , 129 ). The pubertal transition is also well established as a time when depression rates rise dramatically, particularly for females; indeed, this developmental stage is when the gender difference in depression emerges ( 130 , 131 ). Finally, pubertal timing and growth influence later adult cardiovascular risk in both males and females ( 128 ). Additional research focusing on the gendered dimensions of childhood obesity is needed.
Summary and Implications
In undertaking a review of this broad area of significant health promotion interest, I have used the narrative review method. It has been argued that narrative reviews have advantages when the scope and literature coverage is broad and covers a range of issues within a given topic ( 132 ). This broader coverage comes at the expense of the more explicit methods, reporting and reproducibility, that are associated with systematic reviews, which tend to focus on narrower topics using prescribed search methods ( 132 ). Given the methodological limitations of the narrative method, and the acknowledged potential for selection biases in study selection when a nonsystematic review is undertaken, the reader should turn to determinant-specific systematic reviews for exhaustive discussion of the specific determinants covered in this review. The main objective of this review was to summarize key early determinants of childhood obesity within the important framework of individual-, family-, and community-level biological and social influences acting across early life.
Consideration of determinants of obesity within this broader multilevel framework may imply that strategies for health promotion and primary prevention should include attention to determinants at all levels. The upstream influences on childhood obesity occur at many levels, including the family and the community, and begin very early in the life course. Health promotion activities typically target individual lifestyle factors, despite emerging evidence of the importance of broader environmental prevention targets ( 133 ). Family-based interventions to improve the home food environment ( 90 ) and parenting style ( 134 ) and policies to reduce the costs of healthy food choices ( 135 ) are needed. Prevention efforts should also include programs to reduce financial stress in families and programs aimed at teaching children on how to cope with stressors in their environment ( 86 ). It has been suggested that overweight and obesity reductions may accrue if the prevention focus is shifted, more broadly, to promoting healthy lifestyles and healthy environments and beyond the focus on individual children’s body weight as the outcome ( 136 ). The opportunities for early health promotion require attention simultaneously to many levels ( 30 ), suggesting the need to address the individual, family, and physical environment, the social environment, and social policy.
Statement of Financial Support
none; there are no conflicts of interest.
Lobstein T, Jackson-Leach R, Moodie ML, et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015; 385 :2510–20.
Article PubMed PubMed Central Google Scholar
Rokholm B, Baker JL, Sørensen TI. The levelling off of the obesity epidemic since the year 1999–a review of evidence and perspectives. Obes Rev 2010; 11 :835–46.
Article CAS PubMed Google Scholar
Daniels SR. The consequences of childhood overweight and obesity. Future Child 2006; 16 :47–67.
Article PubMed Google Scholar
Amed S, Dean HJ, Panagiotopoulos C, et al. Type 2 diabetes, medication-induced diabetes, and monogenic diabetes in Canadian children: a prospective national surveillance study. Diabetes Care 2010; 33 :786–91.
Clarson CL, Mahmud FH, Baker JE, et al. Metformin in combination with structured lifestyle intervention improved body mass index in obese adolescents, but did not improve insulin resistance. Endocrine 2009; 36 :141–6.
Thompson DR, Obarzanek E, Franko DL, et al. Childhood overweight and cardiovascular disease risk factors: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr 2007; 150 :18–25.
Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr 2002; 76 :653–8.
Steinberger J, Moran A, Hong CP, Jacobs DR Jr, Sinaiko AR. Adiposity in childhood predicts obesity and insulin resistance in young adulthood. J Pediatr 2001; 138 :469–73.
Stelmach-Mardas M, Mardas M, Walkowiak J, Boeing H. Long-term weight status in regainers after weight loss by lifestyle intervention: status and challenges. Proc Nutr Soc 2014; 73 :509–18.
Wiegand S, Keller KM, Lob-Corzilius T, et al. Predicting weight loss and maintenance in overweight/obese pediatric patients. Horm Res Paediatr 2014; 82 :380–7.
Bronfenbrenner U, Ceci SJ. Nature-nurture reconceptualized in developmental perspective: a bioecological model. Psychol Rev 1994; 101 :568–86.
Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev 2001; 2 :159–71.
Article CAS PubMed PubMed Central Google Scholar
Hanson MA, Gluckman PD. Early developmental conditioning of later health and disease: physiology or pathophysiology? Physiol Rev 2014; 94 :1027–76.
Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol 2002; 31 :285–93.
Boone-Heinonen J, Gordon-Larsen P, Adair LS. Obesogenic clusters: multidimensional adolescent obesity-related behaviors in the U.S. Ann Behav Med 2008; 36 :217–30.
Nelson MC, Gordon-Larsen P, Adair LS, Popkin BM. Adolescent physical activity and sedentary behavior: patterning and long-term maintenance. Am J Prev Med 2005; 28 :259–66.
Owen N, Leslie E, Salmon J, Fotheringham MJ. Environmental determinants of physical activity and sedentary behavior. Exerc Sport Sci Rev 2000; 28 :153–8.
CAS PubMed Google Scholar
Speakman JR. Obesity: the integrated roles of environment and genetics. J Nutr 2004; 134 :Suppl 8:2090S–105S.
Bouchard C. Gene-environment interactions in the etiology of obesity: defining the fundamentals. Obesity (Silver Spring) 2008; 16 :Suppl 3:S5–S10.
Article CAS Google Scholar
Kosti RI, Panagiotakos DB, Tountas Y, et al. Parental body mass index in association with the prevalence of overweight/obesity among adolescents in Greece; dietary and lifestyle habits in the context of the family environment: the Vyronas study. Appetite 2008; 51 :218–22.
Qi L, Cho YA. Gene-environment interaction and obesity. Nutr Rev 2008; 66 :684–94.
Crossman A, Anne Sullivan D, Benin M. The family environment and American adolescents’ risk of obesity as young adults. Soc Sci Med 2006; 63 :2255–67.
Rosenkranz RR, Dzewaltowski DA. Model of the home food environment pertaining to childhood obesity. Nutr Rev 2008; 66 :123–40.
Haines J, Neumark-Sztainer D, Wall M, Story M. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity (Silver Spring) 2007; 15 :2748–60.
Article Google Scholar
Arcan C, Neumark-Sztainer D, Hannan P, van den Berg P, Story M, Larson N. Parental eating behaviours, home food environment and adolescent intakes of fruits, vegetables and dairy foods: longitudinal findings from Project EAT. Public Health Nutr 2007; 10 :1257–65.
Pinard CA, Yaroch AL, Hart MH, Serrano EL, McFerren MM, Estabrooks PA. Measures of the home environment related to childhood obesity: a systematic review. Public Health Nutr 2012; 15 :97–109.
Haines J, Kleinman KP, Rifas-Shiman SL, Field AE, Austin SB. Examination of shared risk and protective factors for overweight and disordered eating among adolescents. Arch Pediatr Adolesc Med 2010; 164 :336–43.
Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res 2006; 21 :770–82.
Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, Baur LA. Associations between the home food environment and obesity-promoting eating behaviors in adolescence. Obesity (Silver Spring) 2007; 15 :719–30.
Gluckman P, Nishtar S, Armstrong T. Ending childhood obesity: a multidimensional challenge. Lancet 2015; 385 :1048–50.
Jeffery RW, Utter J. The changing environment and population obesity in the United States. Obes Res 2003; 11 :Suppl:12S–22S.
Gilliland J . The built environment and obesity: trimming waistlines through neighbourhood design. In: Bunting E, Filion P, Walker R, eds. Canadian Cities in Transition . Don Mills, ON: Oxford University Press, 2010:391–410.
Google Scholar
Gilliland JA, Rangel CY, Healy MA, et al. Linking childhood obesity to the built environment: a multi-level analysis of home and school neighbourhood factors associated with body mass index. Can J Public Health 2012; 103 :Suppl 3:eS15–21.
Ford PB, Dzewaltowski DA. Disparities in obesity prevalence due to variation in the retail food environment: three testable hypotheses. Nutr Rev 2008; 66 :216–28.
Rahman T, Cushing RA, Jackson RJ. Contributions of built environment to childhood obesity. Mt Sinai J Med 2011; 78 :49–57.
Zhang X, van der Lans I, Dagevos H. Impacts of fast food and the food retail environment on overweight and obesity in China: a multilevel latent class cluster approach. Public Health Nutr 2012; 15 :88–96.
Epstein LH, Raja S, Daniel TO, et al. The built environment moderates effects of family-based childhood obesity treatment over 2 years. Ann Behav Med 2012; 44 :248–58.
He M, Tucker P, Gilliland J, Irwin JD, Larsen K, Hess P. The influence of local food environments on adolescents’ food purchasing behaviors. Int J Environ Res Public Health 2012; 9 :1458–71.
Lopez RP, Hynes HP. Obesity, physical activity, and the urban environment: public health research needs. Environ Health 2006; 5 :25.
Oreskovic NM, Winickoff JP, Kuhlthau KA, Romm D, Perrin JM. Obesity and the built environment among Massachusetts children. Clin Pediatr (Phila) 2009; 48 :904–12.
Tucker P, Irwin JD, Gilliland J, He M, Larsen K, Hess P. Environmental influences on physical activity levels in youth. Health Place 2009; 15 :357–63.
Larsen K, Gilliland J, Hess PM. Route-based analysis to capture the environmental influences on a child’s mode of travel between home and school. Ann Assoc Am Geogr 2012; 102 :1348–65.
Björk J, Albin M, Grahn P, et al. Recreational values of the natural environment in relation to neighbourhood satisfaction, physical activity, obesity and wellbeing. J Epidemiol Community Health 2008; 62 :e2.
Penney TL, Almiron-Roig E, Shearer C, McIsaac JL, Kirk SF. Modifying the food environment for childhood obesity prevention: challenges and opportunities. Proc Nutr Soc 2014; 73 :226–36.
Barker DJ. The fetal and infant origins of adult disease. BMJ 1990; 301 :1111.
Zafon C. Oscillations in total body fat content through life: an evolutionary perspective. Obes Rev 2007; 8 :525–30.
Gluckman PD, Hanson MA, Beedle AS, Raubenheimer D. Fetal and neonatal pathways to obesity. Front Horm Res 2008; 36 :61–72.
Gluckman PD, Hanson MA. Developmental and epigenetic pathways to obesity: an evolutionary-developmental perspective. Int J Obes (Lond) 2008; 32 :Suppl 7:S62–71.
Eriksson JG, Forsén T, Tuomilehto J, Winter PD, Osmond C, Barker DJ. Catch-up growth in childhood and death from coronary heart disease: longitudinal study. BMJ 1999; 318 :427–31.
Eriksson JG, Forsén T, Tuomilehto J, Osmond C, Barker DJ. Early growth and coronary heart disease in later life: longitudinal study. BMJ 2001; 322 :949–53.
Soto N, Bazaes RA, Peña V, et al. Insulin sensitivity and secretion are related to catch-up growth in small-for-gestational-age infants at age 1 year: results from a prospective cohort. J Clin Endocrinol Metab 2003; 88 :3645–50.
Nobili V, Alisi A, Panera N, Agostoni C. Low birth weight and catch-up-growth associated with metabolic syndrome: a ten year systematic review. Pediatr Endocrinol Rev 2008; 6 :241–7.
PubMed Google Scholar
Morgan AR, Thompson JM, Murphy R, et al. Obesity and diabetes genes are associated with being born small for gestational age: results from the Auckland Birthweight Collaborative study. BMC Med Genet 2010; 11 :125.
Article PubMed PubMed Central CAS Google Scholar
Elks CE, Loos RJ, Sharp SJ, et al. Genetic markers of adult obesity risk are associated with greater early infancy weight gain and growth. PLoS Med 2010; 7 :e1000284.
Kramer MS. Invited commentary: association between restricted fetal growth and adult chronic disease: is it causal? Is it important? Am J Epidemiol 2000; 152 :605–8.
Tu YK, West R, Ellison GT, Gilthorpe MS. Why evidence for the fetal origins of adult disease might be a statistical artifact: the “reversal paradox” for the relation between birth weight and blood pressure in later life. Am J Epidemiol 2005; 161 :27–32.
Kramer MS, Martin RM, Bogdanovich N, Vilchuk K, Dahhou M, Oken E. Is restricted fetal growth associated with later adiposity? Observational analysis of a randomized trial. Am J Clin Nutr 2014; 100 :176–81.
Joseph KS. Should we intervene to improve fetal and infant growth? In: Kuh D, Ben-Shlomo Y, eds. A Life Course Approach to Chronic Disease Epidemiology . New York: Oxford University Press, 2004:399–414.
Adair LS. Child and adolescent obesity: epidemiology and developmental perspectives. Physiol Behav 2008; 94 :8–16.
Huang JS, Lee TA, Lu MC. Prenatal programming of childhood overweight and obesity. Matern Child Health J 2007; 11 :461–73.
Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 2005; 115 :e290–6.
Murphy MJ, Metcalf BS, Jeffery AN, Voss LD, Wilkin TJ. Does lean rather than fat mass provide the link between birth weight, BMI, and metabolic risk? EarlyBird 23. Pediatr Diabetes 2006; 7 :211–4.
Singhal A, Wells J, Cole TJ, Fewtrell M, Lucas A. Programming of lean body mass: a link between birth weight, obesity, and cardiovascular disease? Am J Clin Nutr 2003; 77 :726–30.
Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA. Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics 2003; 111 :e221–6.
Kim SY, Sharma AJ, Sappenfield W, Wilson HG, Salihu HM. Association of maternal body mass index, excessive weight gain, and gestational diabetes mellitus with large-for-gestational-age births. Obstet Gynecol 2014; 123 :737–44.
Sridhar SB, Ferrara A, Ehrlich SF, Brown SD, Hedderson MM. Risk of large-for-gestational-age newborns in women with gestational diabetes by race and ethnicity and body mass index categories. Obstet Gynecol 2013; 121 :1255–62.
Dabelea D, Crume T. Maternal environment and the transgenerational cycle of obesity and diabetes. Diabetes 2011; 60 :1849–55.
Ma RC, Tutino GE, Lillycrop KA, Hanson MA, Tam WH. Maternal diabetes, gestational diabetes and the role of epigenetics in their long term effects on offspring. Prog Biophys Mol Biol 2015; 118 :55–68.
Gillman MW, Rifas-Shiman SL, Camargo CA Jr, et al. Risk of overweight among adolescents who were breastfed as infants. JAMA 2001; 285 :2461–7.
Hediger ML, Overpeck MD, Kuczmarski RJ, Ruan WJ. Association between infant breastfeeding and overweight in young children. JAMA 2001; 285 :2453–60.
Hawkins SS, Cole TJ, Law C ; Millennium Cohort Study Child Health Group. An ecological systems approach to examining risk factors for early childhood overweight: findings from the UK Millennium Cohort Study. J Epidemiol Community Health 2009; 63 :147–55.
Arenz S, Rückerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity–a systematic review. Int J Obes Relat Metab Disord 2004; 28 :1247–56.
Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics 2005; 115 :1367–77.
Fisher JO, Birch LL, Smiciklas-Wright H, Picciano MF. Breast-feeding through the first year predicts maternal control in feeding and subsequent toddler energy intakes. J Am Diet Assoc 2000; 100 :641–6.
Kirchberg FF, Harder U, Weber M, et al.; European Childhood Obesity Trial Study Group. Dietary protein intake affects amino acid and acylcarnitine metabolism in infants aged 6 months. J Clin Endocrinol Metab 2015; 100 :149–58.
Rossiter MD, Colapinto CK, Khan MK, et al. Breast, formula and combination feeding in relation to childhood obesity in Nova Scotia, Canada. Matern Child Health J 2015; 19 :2048–56.
Mennella JA, Trabulsi JC. Complementary foods and flavor experiences: setting the foundation. Ann Nutr Metab 2012; 60 :Suppl 2:40–50.
Stettler N, Zemel BS, Kumanyika S, Stallings VA. Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics 2002; 109 :194–9.
Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ 2005; 331 :929.
Dubois L, Girard M. Early determinants of overweight at 4.5 years in a population-based longitudinal study. Int J Obes (Lond) 2006; 30 :610–7.
Çamurdan MO, Çamurdan AD, Polat S, Beyazova U. Growth patterns of large, small, and appropriate for gestational age infants: impacts of long-term breastfeeding: a retrospective cohort study. J Pediatr Endocrinol Metab 2011; 24 :463–8.
Lumeng JC, Wendorf K, Pesch MH, et al. Overweight adolescents and life events in childhood. Pediatrics 2013; 132 :e1506–12.
Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: some conceptual perspectives. J Health Soc Behav 2005; 46 :205–19.
Wickrama KK, O’Neal CW, Oshri A. Are stressful developmental processes of youths leading to health problems amplified by genetic polymorphisms? The case of body mass index. J Youth Adolesc 2014; 43 :1096–109.
Magrone T, Jirillo E. Childhood obesity: immune response and nutritional approaches. Front Immunol 2015; 6 :76.
Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev 2011; 12 :e54–63.
Huybrechts I, De Vriendt T, Breidenassel C, et al.; HELENA Study Group. Mechanisms of stress, energy homeostasis and insulin resistance in European adolescents–the HELENA study. Nutr Metab Cardiovasc Dis 2014; 24 :1082–9.
Pasquali R. The hypothalamic-pituitary-adrenal axis and sex hormones in chronic stress and obesity: pathophysiological and clinical aspects. Ann NY Acad Sci 2012; 1264 :20–35.
Vanaelst B, Michels N, Clays E, et al. The association between childhood stress and body composition, and the role of stress-related lifestyle factors–cross-sectional findings from the baseline ChiBSD survey. Int J Behav Med 2014; 21 :292–301.
Renzaho AM, Dau A, Cyril S, Ayala GX. The influence of family functioning on the consumption of unhealthy foods and beverages among 1- to 12-y-old children in Victoria, Australia. Nutrition 2014; 30 :1028–33.
Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry 2014; 19 :544–54.
Shankardass K, McConnell R, Jerrett M, et al. Parental stress increases body mass index trajectory in pre-adolescents. Pediatr Obes 2014; 9 :435–42.
Bornstein SR, Schuppenies A, Wong ML, Licinio J. Approaching the shared biology of obesity and depression: the stress axis as the locus of gene-environment interactions. Mol Psychiatry 2006; 11 :892–902.
de Wit L, Luppino F, van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res 2010; 178 :230–5.
McElroy SL, Kotwal R, Malhotra S, Nelson EB, Keck PE, Nemeroff CB. Are mood disorders and obesity related? A review for the mental health professional. J Clin Psychiatry 2004; 65 :634–51, quiz 730.
Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biol Psychiatry 2003; 54 :330–7.
Erickson SJ, Robinson TN, Haydel KF, Killen JD. Are overweight children unhappy?: Body mass index, depressive symptoms, and overweight concerns in elementary school children. Arch Pediatr Adolesc Med 2000; 154 :931–5.
Needham BL, Crosnoe R. Overweight status and depressive symptoms during adolescence. J Adolesc Health 2005; 36 :48–55.
Ross CE. Overweight and depression. J Health Soc Behav 1994; 35 :63–79.
Duclos M, Gatta B, Corcuff JB, Rashedi M, Pehourcq F, Roger P. Fat distribution in obese women is associated with subtle alterations of the hypothalamic-pituitary-adrenal axis activity and sensitivity to glucocorticoids. Clin Endocrinol (Oxf) 2001; 55 :447–54.
Penninx BW, Milaneschi Y, Lamers F, Vogelzangs N. Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Med 2013; 11 :129.
Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010; 67 :220–9.
Surkan PJ, Kawachi I, Peterson KE. Childhood overweight and maternal depressive symptoms. J Epidemiol Community Health 2008; 62 :e11.
Wang L, Anderson JL, Dalton Iii WT, et al. Maternal depressive symptoms and the risk of overweight in their children. Matern Child Health J 2013; 17 :940–8.
Ramasubramanian L, Lane S, Rahman A. The association between maternal serious psychological distress and child obesity at 3 years: a cross-sectional analysis of the UK Millennium Cohort Data. Child Care Health Dev 2013; 39 :134–40.
Gross RS, Velazco NK, Briggs RD, Racine AD. Maternal depressive symptoms and child obesity in low-income urban families. Acad Pediatr 2013; 13 :356–63.
Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, Davies WH. Controlled study of critical parent and family factors in the obesigenic environment. Obesity (Silver Spring) 2007; 15 :126–36.
Stout SA, Espel EV, Sandman CA, Glynn LM, Davis EP. Fetal programming of children’s obesity risk. Psychoneuroendocrinology 2015; 53 :29–39.
Hohwü L, Henriksen TB, Grønborg TK, Hedegaard M, Sørensen TI, Obel C. Maternal salivary cortisol levels during pregnancy are positively associated with overweight children. Psychoneuroendocrinology 2015; 52 :143–52.
Article PubMed CAS Google Scholar
Farrow CV, Blissett JM. Is maternal psychopathology related to obesigenic feeding practices at 1 year? Obes Res 2005; 13 :1999–2005.
Wachs TD. Multiple influences on children’s nutritional deficiencies: a systems perspective. Physiol Behav 2008; 94 :48–60.
de Campora G, Giromini L, Larciprete G, Li Volsi V, Zavattini GC. The impact of maternal overweight and emotion regulation on early eating behaviors. Eat Behav 2014; 15 :403–9.
McConley RL, Mrug S, Gilliland MJ, et al. Mediators of maternal depression and family structure on child BMI: parenting quality and risk factors for child overweight. Obesity (Silver Spring) 2011; 19 :345–52.
Milgrom J, Skouteris H, Worotniuk T, Henwood A, Bruce L. The association between ante- and postnatal depressive symptoms and obesity in both mother and child: a systematic review of the literature. Womens Health Issues 2012; 22 :e319–28.
O’Dea JA, Chiang H, Peralta LR. Socioeconomic patterns of overweight, obesity but not thinness persist from childhood to adolescence in a 6-year longitudinal cohort of Australian schoolchildren from 2007 to 2012. BMC Public Health 2014; 14 :222.
Kakinami L, Séguin L, Lambert M, Gauvin L, Nikiema B, Paradis G. Poverty’s latent effect on adiposity during childhood: evidence from a Québec birth cohort. J Epidemiol Community Health 2014; 68 :239–45.
Lee H, Andrew M, Gebremariam A, Lumeng JC, Lee JM. Longitudinal associations between poverty and obesity from birth through adolescence. Am J Public Health 2014; 104 :e70–6.
McCurdy K, Gorman KS, Kisler T, Metallinos-Katsaras E. Associations between family food behaviors, maternal depression, and child weight among low-income children. Appetite 2014; 79 :97–105.
de Jong E, Visscher TL, HiraSing RA, Seidell JC, Renders CM. Home environmental determinants of children’s fruit and vegetable consumption across different SES backgrounds. Pediatr Obes 2015; 10 :134–40.
Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med 2013; 95 :106–14.
Lovasi GS, Schwartz-Soicher O, Quinn JW, et al. Neighborhood safety and green space as predictors of obesity among preschool children from low-income families in New York City. Prev Med 2013; 57 :189–93.
Malhotra K, Herman AN, Wright G, Bruton Y, Fisher JO, Whitaker RC. Perceived benefits and challenges for low-income mothers of having family meals with preschool-aged children: childhood memories matter. J Acad Nutr Diet 2013; 113 :1484–93.
Hernandez DC, Pressler E. Accumulation of childhood poverty on young adult overweight or obese status: race/ethnicity and gender disparities. J Epidemiol Community Health 2014; 68 :478–84.
Miller GE, Chen E. The biological residue of childhood poverty. Child Dev Perspect 2013; 7 :67–73.
Wisniewski AB, Chernausek SD. Gender in childhood obesity: family environment, hormones, and genes. Gend Med 2009; 6 :Suppl 1:76–85.
Sweeting HN. Gendered dimensions of obesity in childhood and adolescence. Nutr J 2008; 7 :1.
Hernandez DC, Pressler E. Gender disparities among the association between cumulative family-level stress & adolescent weight status. Prev Med 2015; 73 :60–6.
Widén E, Silventoinen K, Sovio U, et al. Pubertal timing and growth influences cardiometabolic risk factors in adult males and females. Diabetes Care 2012; 35 :850–6.
Goran MI, Gower BA. Longitudinal study on pubertal insulin resistance. Diabetes 2001; 50 :2444–50.
Hankin BL, Abramson LY. Development of gender differences in depression: an elaborated cognitive vulnerability-transactional stress theory. Psychol Bull 2001; 127 :773–96.
Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol 1998; 107 :128–40.
Collins JA, Fauser BC. Balancing the strengths of systematic and narrative reviews. Hum Reprod Update 2005; 11 :103–4.
Alvaro C, Jackson LA, Kirk S, et al. Moving Canadian governmental policies beyond a focus on individual lifestyle: some insights from complexity and critical theories. Health Promot Int 2011; 26 :91–9.
Kakinami L, Barnett TA, Séguin L, Paradis G. Parenting style and obesity risk in children. Prev Med 2015; 75 :18–22.
Morrissey TW, Jacknowitz A, Vinopal K. Local food prices and their associations with children’s weight and food security. Pediatrics 2014; 133 :422–30.
Penney TL, Kirk SF. The health at every size paradigm and obesity: missing empirical evidence may help push the reframing obesity debate forward. Am J Public Health 2015; 105 :e38–42.
Download references
Author information
Authors and affiliations.
Department of Epidemiology and Biostatistics, The University of Western Ontario, London, Ontario, Canada
M. Karen Campbell
Department of Pediatrics, The University of Western Ontario, London, Ontario, Canada
Department of Obstetrics & Gynecology, The University of Western Ontario, London, Ontario, Canada
Children’s Health Research Institute, Lawson Health Research Institute, London, Ontario, Canada
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to M. Karen Campbell .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Campbell, M. Biological, environmental, and social influences on childhood obesity. Pediatr Res 79 , 205–211 (2016). https://doi.org/10.1038/pr.2015.208
Download citation
Received : 17 April 2015
Accepted : 30 September 2015
Published : 20 October 2015
Issue Date : January 2016
DOI : https://doi.org/10.1038/pr.2015.208
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Bayesian spatial modeling of childhood overweight and obesity prevalence in costa rica.
- Mario J. Gómez
- Luis A. Barboza
- Paula Moraga
BMC Public Health (2023)
Likelihood of obesity in early and late childhood based on growth trajectory during infancy
- George Moschonis
- Anela Halilagic
- Yannis Manios
International Journal of Obesity (2023)
Rare genetic forms of obesity in childhood and adolescence, a comprehensive review of their molecular mechanisms and diagnostic approach
- Francesca Mainieri
- Saverio La Bella
- Francesco Chiarelli
European Journal of Pediatrics (2023)
Neighborhood Walkability, Historical Redlining, and Childhood Obesity in Denver, Colorado
- Katharina Kowalski
- Jeremy Auerbach
- Sheryl Magzamen
Journal of Urban Health (2023)
Mothers as advocates for healthier lifestyle behaviour environments for their children: results from INFANT 3.5-year follow-up
- Christine Delisle Nyström
- Karen J Campbell
- Kylie D Hesketh
BMC Public Health (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Home — Essay Samples — Nursing & Health — Childhood Obesity — The Main Causes Of Childhood Obesity: Child’s Environment
The Main Causes of Childhood Obesity: Child's Environment
- Categories: Child Obesity Childhood Obesity Obesity
About this sample

Words: 746 |
Published: Feb 9, 2022
Words: 746 | Pages: 2 | 4 min read
Works Cited
- Berall, G. (2002). Walking to school: a step to healthy children. Canadian Medical Association Journal, 166(3), 322-323.
- Ogden, C. L. (2011). Genetics of childhood obesity. Pediatrics, 128(Supplement 2), S152-S155.
- Rosenfield, S. (2007). Perspectives on the prevention and treatment of childhood obesity. Journal of School Health, 77(3), 124-128.
- Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., & Bhadoria, A. S. (2015). Childhood obesity: causes and consequences. Journal of Family Medicine and Primary Care, 4(2), 187-192.
- Singh, A. S., Mulder, C., Twisk, J. W., van Mechelen, W., & Chinapaw, M. J. (2008). Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity Reviews, 9(5), 474-488.
- Swinburn, B. A., Sacks, G., Hall, K. D., McPherson, K., Finegood, D. T., Moodie, M. L., & Gortmaker, S. L. (2011). The global obesity pandemic: shaped by global drivers and local environments. The Lancet, 378(9793), 804-814.
- U.S. Department of Health and Human Services. (2018). Physical Activity Guidelines for Americans, 2nd Edition. U.S. Department of Health and Human Services. https://health.gov/our-work/physical-activity/current-guidelines
- Vogels, N., Posthumus, D. L., Marang-van de Mheen, P. J., & Renders, C. M. (2018). Behavioral factors related to the development of healthy and unhealthy habits in overweight preschool children: a cross-sectional study. International Journal of Behavioral Nutrition and Physical Activity, 15(1), 1-9.
- Ward, D. S., Welker, E., Choate, A., Henderson, K. E., Lott, M., Tovar, A., & Wilson, A. (2015). Strength of obesity prevention interventions in early care and education settings: A systematic review. Preventive Medicine, 78, 23-33.
- Whitaker, R. C., Wright, J. A., Pepe, M. S., Seidel, K. D., & Dietz, W. H. (1997). Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine, 337(13), 869-873.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 649 words
2 pages / 955 words
5 pages / 2799 words
3 pages / 1486 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Childhood Obesity
Centers for Disease Control and Prevention. (2021). Childhood Obesity Facts. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK436791/pdf/Bookshelf_NBK436791.pdf
In today's modern society, the issue of childhood obesity has become an alarming concern. As the rates continue to rise at an unprecedented pace, it is imperative that we address this issue with urgency and determination. One [...]
Buzzell, L. (2019, August 13). Benefits of a Healthy Lifestyle. Johns Hopkins Medicine. https://www.healthline.com/health/healthy-eating-on-a-budget#1.-Plan-meals-and-shop-for-groceries-in-advance
In conclusion, while Zinczenko's analysis in "Don't Blame the Eater" offers valuable insights into the rise of childhood obesity and the role of the fast-food industry, it is necessary to critically examine his claims. While [...]
It is, indeed disheartening that a large proportion of people the world over is becoming obese. This is a serious socio-economic problem, and it is largely attributed to the modern lifestyle. Although, the majority of parents [...]
It is well known today that the obesity epidemic is claiming more and more victims each day. The Centers for Disease Control and Prevention writes “that nearly 1 in 5 school age children and young people (6 to 19 years) in the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
StarsInsider
Childhood obesity: what are the causes and how you can fight it
Posted: December 20, 2023 | Last updated: December 20, 2023

Childhood obesity rates are rising and global figures don't make for easy reading. The World Health Organization (WHO) estimates that over 124 million children and teenagers around the world are obese, resulting in a host of health concerns for the next generation.
Click on to learn about the causes of childhood obesity and get some tips to combat it.
You may also like: 10 countries with exceptionally beautiful women

You may also like: Celebrities who died in mysterious circumstances

You may also like: The foods Americans miss the most when abroad

Methodology

You may also like: Random everyday things you'll be shocked to learn have names

Most effected
The study showed that white American and Asian-American children had significantly lower obesity rates than other groups, such as African Americans and Hispanic Americans.

You may also like: High IQ: these are the world's smartest countries

You may also like: Wildlife photos captured at the perfect moment

Omnipresent
You may also like: Environmentally destructive foods we all consume

Advertising
You may also like: The weirdest and most shocking cults of all time


Urgent appeal

Consumption
You may also like: American foods that are banned around the world

Recommendation

You may also like: Stars who took method acting to extremes

You may also like: Stars who have come out as LGBT in 2019

You may also like: The most unbelievably expensive weddings in history

Other factors
The CDC (Centers for Disease Control and Prevention) added that use of medication and sleep patterns should be taken into account.

You may also like: Why you're washing your hair wrong (and what to do about it)

Immediate risks
Childhood obesity can effect the body in many ways. The CDC warns that overweight children are more vulnerable to high blood pressure and high cholesterol, which can lead to cardiovascular disease.
You may also like: Must-try street food for travelers

The CDC also warns that obese kids may display breathing problems like asthma or sleep apnea.
Kids can develop problems later on such as muscular discomfort as well as liver problems, gallstones, and heartburn.

The CDC also notes the psychological side. Overweight children are more vulnerable to anxiety and depression.
They are also more vulnerable to low self-esteem as well as bullying and other problems.
You may also like: Amber Tamblyn, David Cross share how couples therapy helped both on- and off-screen

Future risks
Adulthood obesity is linked to numerous serious illnesses, such as heart disease, type 2 diabetes and cancer, according to the CDC.
Sources: (WHO) (PBS)
See also: How to strengthen your immune system
More for You
18 Of Our Best Cold Sandwich Recipes
Ice Cream Recall in 16 States As Dire Warning Issued
Dustin by Steve Kelley and Jeff Parker
10 Things You Should Never Clean with a Mr. Clean Magic Eraser
The worst Western movie released every year since 1930
The Advantages Of Having Red Hair
5 Subs To Order At Subway And 5 You Might Want To Skip
Are eggs bad for cholesterol? New study reveals how many you can eat
7 Things To Know If You Withdraw More Than $10,000 From Your Checking Account
For Better Or For Worse by Lynn Johnston
The Best Beach in Every State
The Plastic Wrap Hack Every Handyman Will Want To Know When Working With Tools
31 '80s Icons You've Forgotten (But Shouldn't Have)
7 High-Protein Snacks to Lower High Cholesterol, Recommended by a Dietitian
Major storm to sweep United States with severe weather, snow, flooding
Harvard psychologist shares 5 toxic things 'highly narcissistic' people always do in relationships
What's The Difference Between A Chicken And A Cornish Hen?
Rose Is Rose by Don Wimmer and Pat Brady
Remove A Tree Stump With One Common Household Ingredient
The best lake towns in America to live in year-round, based on data
Advertisement
Environment
Wildfire smoke may be deadliest effect of climate change in us.
Smoke from wildfires made worse by climate change is set to cause thousands of additional deaths each year in the US
By James Dinneen
25 March 2024

Increased exposure to wildfire smoke is one of the most damaging effects of climate change
Nasa's Earth Observatory
Exposure to rising levels of wildfire smoke could lead to more than 10,000 additional deaths each year in the US by 2050. This could make deaths due to wildfire smoke the costliest consequence of climate change for the country, accounting for nearly as much economic damage as all other climate-related impacts combined.
“It completely reshapes how we think about the climate impact in the US,” says Minghao Qiu at Stanford University in California. Exposure…
Sign up to our weekly newsletter
Receive a weekly dose of discovery in your inbox! We'll also keep you up to date with New Scientist events and special offers.
To continue reading, subscribe today with our introductory offers
No commitment, cancel anytime*
Offer ends 2nd of July 2024.
*Cancel anytime within 14 days of payment to receive a refund on unserved issues.
Inclusive of applicable taxes (VAT)
Existing subscribers
More from New Scientist
Explore the latest news, articles and features
Dust clouds from the Sahara are reaching Europe more frequently
Subscriber-only
The war in Gaza is creating a health crisis that will span decades
Eerie green sunsets after 1883 krakatoa eruption finally explained, 1 in 8 people worldwide has obesity, popular articles.
Trending New Scientist articles
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Obesity in children and adolescents: epidemiology, causes, assessment, and management
Hiba jebeile.
a Sydney Medical School, The University of Sydney, Sydney, NSW, Australia
b Institute of Endocrinology and Diabetes, The Children's Hospital at Westmead, Westmead, NSW, Australia
Aaron S Kelly
d Department of Pediatrics and Center for Pediatric Obesity Medicine, University of Minnesota Medical School, Minneapolis, MN, USA
Grace O'Malley
e School of Physiotherapy, RCSI University of Medicine and Health Sciences, Dublin, Ireland
f Child and Adolescent Obesity Service, Children's Health Ireland at Temple Street, Dublin, Ireland
Louise A Baur
c Weight Management Services, The Children's Hospital at Westmead, Westmead, NSW, Australia
This Review describes current knowledge on the epidemiology and causes of child and adolescent obesity, considerations for assessment, and current management approaches. Before the COVID-19 pandemic, obesity prevalence in children and adolescents had plateaued in many high-income countries despite levels of severe obesity having increased. However, in low-income and middle-income countries, obesity prevalence had risen. During the pandemic, weight gain among children and adolescents has increased in several jurisdictions. Obesity is associated with cardiometabolic and psychosocial comorbidity as well as premature adult mortality. The development and perpetuation of obesity is largely explained by a bio-socioecological framework, whereby biological predisposition, socioeconomic, and environmental factors interact together to promote deposition and proliferation of adipose tissue. First-line treatment approaches include family-based behavioural obesity interventions addressing diet, physical activity, sedentary behaviours, and sleep quality, underpinned by behaviour change strategies. Evidence for intensive dietary approaches, pharmacotherapy, and metabolic and bariatric surgery as supplemental therapies are emerging; however, access to these therapies is scarce in most jurisdictions. Research is still needed to inform the personalisation of treatment approaches of obesity in children and adolescents and their translation to clinical practice.
Introduction
Obesity in children and adolescents is a global health issue with increasing prevalence in low-income and middle-income countries (LMICs) as well as a high prevalence in many high-income countries. 1 Obesity during childhood is likely to continue into adulthood and is associated with cardiometabolic and psychosocial comorbidity as well as premature mortality. 2 , 3 , 4 The provision of effective and compassionate care, tailored to the child and family, is vital. In this Review, we describe current knowledge on the epidemiology and causes of child and adolescent obesity, considerations for assessment, and current management approaches.
Epidemiology
Definitions of overweight and obesity in children and adolescents.
WHO defines overweight and obesity as an abnormal or excessive fat accumulation that presents a risk to health. For epidemiological purposes and routine clinical practice, simple anthropometric measures are generally used as screening tools. BMI (weight/height 2 ; kg/m 2 ) is used as an indirect measure of body fatness in children and adolescents 5 and should be compared with population growth references adjusted for sex and age. The WHO 2006 Growth Standard is recommended in many countries for children aged 0–5 years, and for children aged 0–2 years in the USA. 6 For older children and adolescents, other growth references are used, including the WHO 2007 Growth Reference, recommended for those aged 5–19 years (overweight defined as BMI ≥1SD and obesity as BMI ≥2SD of the median for age and sex), and the United States Centers for Disease Control and Prevention (CDC) Growth Reference for those aged 2 to 20 years (overweight is >85th to <95th percentile and obesity is ≥95th percentile based on CDC growth charts). 6 , 7 The International Obesity Task Force tables for children aged 2 to 18 years are used for epidemiological studies. 8
Abdominal or central obesity is associated with increased cardiometabolic risk in children and adolescents. 9 For waist circumference there are regional and international growth references allowing adjustment for age and sex. 10 , 11 , 12 A waist-to-height ratio of more than 0·5 is increasingly used as an indicator of abdominal adiposity in clinical and research studies, with no need for a comparison reference. 13
Various definitions have been suggested to identify more extreme values of BMI in children and adolescents. The International Obesity Task Force defined morbid obesity as equivalent to age-adjusted and sex-adjusted BMI of 35kg/m 2 or more at age 18 years, a definition specifically for epidemiological use. 14 The American Heart Association characterises severe obesity as a BMI of 120% or more of the 95th percentile of BMI for age and sex (based on CDC2000 growth charts), a definition that can be used in both clinical practice and research. 15 There are marked limitations in transforming very high BMI values to z-scores, particularly when using CDC2000 growth charts because reductions in BMI can be underestimated. 15
The prevalence of paediatric obesity 16 has increased worldwide over the past five decades. From 1975 to 2016, the global age-standardised prevalence of obesity in children and adolescents aged 5–19 years increased from 0·7% (95% credible interval [CrI] 0·4–1·2) to 5·6% (4·8–6·5) for girls and from 0·9% (0·5–1·3) to 7·8% (6·7–9·1) for boys. 17 Since 2000, the mean BMI has plateaued, usually at high levels, in many high-income countries but has continued to rise in LMICs. In 2016, obesity prevalence in this age group was highest (>30%) in many Pacific Island nations and was high (>20%) in several countries in the Middle East, north Africa, Micronesia (region of the western Pacific), Polynesia (subregion of Oceania), the Caribbean, as well as in the USA. 17
In 2019, the World Obesity Federation estimated there would be 206 million children and adolescents aged 5–19 years living with obesity in 2025, and 254 million in 2030. 1 Of the 42 countries each estimated to have more than 1 million children with obesity in 2030, the top ranked are China, followed by India, the USA, Indonesia, and Brazil, with only seven of the top 42 countries being high-income countries.
The prevalence of severe obesity in the paediatric population has grown in many high-income countries, even though overall prevalence of obesity has been stable. 18 , 19 , 20 , 21 In a survey of European countries, approximately a quarter of children with obesity were classified with severe obesity, a finding that has implications for delivery of obesity clinical services, because such children will need more specialised and intensive therapy. 19
There are socioeconomic disparities in paediatric obesity prevalence within countries. In lower-income to middle-income countries, children of higher socioeconomic status are at greater risk of being affected by overweight or obesity than children of a lower socioeconomic status, whereas in high-income countries, it is children living in socioeconomic disadvantage who are at higher risk. 22 , 23 , 24
Reports from China, Europe, and the USA have documented increased weight gain among children and adolescents during the COVID-19 pandemic compared with the rate before the pandemic, 25 , 26 , 27 , 28 , 29 an apparent consequence of decreases in physical activity, increased screen time, changes in dietary intake, food insecurity, and increased family and individual stress. 30
Development and perpetuation of obesity: a bio-socioecological framework
The development and perpetuation of obesity in modern society can largely be explained by a bio-socioecological framework that has created the conditions for a scenario in which biological predisposition, socioeconomic forces, and environmental factors together promote deposition and proliferation of adipose tissue and resistance to efforts of obesity management. A high degree of biological heterogeneity exists in bodyweight regulation and energy dynamics such that some individuals can maintain healthy levels of adipose tissue with little effort while others face a lifelong struggle with regulating levels. Further, adipose tissue is heterogeneous such that white, brown, and beige forms exist with a variety of physiological functions. 31 The anatomical sites where adipose tissue is stored can translate into varying health risks (eg, central accumulation of adipose tissue is associated with cardiometabolic disease compared to peripheral stores). 32 At a fundamental level, the relative function of the energy regulatory system (the complex interplay of central and peripheral pathways driving appetite, satiety, pleasure-seeking behaviours, and metabolic efficiency) strongly influences body composition. More specifically, the bodyweight set point theory posits the existence of a tightly regulated and complex biological control system, which drives a dynamic feedback loop aimed at defending a predetermined relative or absolute amount of adiposity. 33 Support for this theory comes from evidence in adults demonstrating immediate and sustained alterations in levels of hormones driving appetite and satiety, perceptions of food palatability, and resting energy expenditure following attempts at weight loss. 34 , 35 Other biobehavioural factors such as poor sleep quality, adversity, stress, and medications (causing iatrogenic weight gain) can also serve to exacerbate dysfunction of the energy regulatory system favouring weight gain.
Environmental and behavioural associations of obesity
Over the past few decades the rise in obesity prevalence has been profoundly influenced by changes in the broader obesogenic environment. 36 These changes operate at the level of the family (eg, family modelling of physical activity, food habits, sleep, screen use), local community (eg, child care and schools, parks, green space, public transport and food outlets), or the broader sociopolitical environment (eg, government policies, food industry, food marketing, transport systems, agricultural policies and subsidies). Such influences have been described as having the ability to exploit people's biological, psychological, social, and economic vulnerabilities. 37 Figure 1 depicts a socioecological model incorporating some of the personal and environmental factors influencing paediatric obesity. 38

A socioecological model for understanding the dynamic interrelationships between various personal and environmental factors influencing child and adolescent obesity.
Adapted from the Centers for Disease Control and Prevention social-ecological model framework for prevention. 38 *Defined as being traversable on foot, compact, physically enticing, and safe.
Dietary factors contributing to obesity risk in children and adolescents include excessive consumption of energy-dense, micronutrient-poor foods; a high intake of sugar-sweetened beverages; and the ubiquitous marketing of these and fast foods. 39 , 40 The relative effect of other factors such as specific eating patterns (eg, frequent snacking, skipping breakfast, not eating together as a family, the window of time from first to last daily meal), portion sizes, the speed of eating, macronutrient intake, and glycaemic load on obesity development remain unclear, although all might be important. 41 , 42
The link between screen time and obesity in childhood and adolescence was initially documented through cross-sectional and longitudinal studies of television viewing. 43 , 44 The past two decades have seen the increase of mobile and gaming devices. Screen exposure influences risk of obesity in children and adolescents via increased exposure to food marketing, increased mindless eating while watching screens, displacement of time spent in more physical activities, reinforcement of sedentary behaviours, and reduced sleep time. 44 , 45
Children's physical activity levels decline around the age of 6 years and again at age 13 years, with girls usually exhibiting more marked declines than boys. Overall, children with obesity tend to engage in lower levels of moderate-vigorous activity than leaner peers. 46 , 47 , 48 Sedentary time increases from the age of 6 years in general, although accelerometery studies report no differences between children with obesity compared with leaner peers. 48 Lower levels of physical activity and increasing sedentary behaviours throughout childhood in all children contribute to obesity development. 49 In most countries, children and adolescents are not sufficiently active due to the loss of public recreation space, the increase in motorised transport and decrease in active transport (eg, cycling, walking, public transport), perceptions of lack of safety in local neighbourhoods leading to less active behaviour, as well as an increase in passive entertainment. 39 , 49
There is growing evidence that short sleep duration, poor sleep quality and a late bedtime are associated with a higher obesity risk, sedentary behaviours, poor dietary patterns, and insulin resistance. In addition, there is a possible link with increased screen time, decreased physical activity, and changes in ghrelin and leptin levels. 50 Many of these obesity-conducive behaviours co-occur. For example, increased screen time is associated with delayed sleep onset and shortened sleep duration, and insufficient sleep is associated with increased food intake and lower levels of physical activity. 50
Early life factors
Several factors in early life put children at increased risk of developing obesity. These factors include maternal obesity before pregnancy, excessive gestational weight gain, and gestational diabetes, all associated with increased birth weight. 51 , 52 Infant and young child feeding practices have variable influences on childhood obesity. Meta-analyses from systematic reviews suggest that breastfeeding has a modest but protective effect against later child obesity. 53 , 54 There is some evidence suggesting that the very early introduction of complementary foods and beverages, before the age of 4 months, especially in formula-fed babies, is associated with higher odds of overweight and obesity. 55 Parental approaches to feeding, especially in the preschool age group (aged 1–4 years), might influence obesity risk, with a systematic review showing a small but significant association between controlling child feed practices (eg, restriction of specific foods or the overall amount of food) and higher child weight. 56 Studies of the role of responsive feeding, whereby the caregiver attends to the baby's cues of hunger and satiety, show that non-responsive feeding is associated with increased child BMI or overweight or obesity. 57 , 58 By contrast, a responsive feeding style that recognises the child's cues of hunger and satiety appears to support healthy weight gain trajectories. 58 , 59 However, in all such studies of infant and young child feeding, the effect of residual confounding on child weight status cannot be discounted.
Other environmental exposures in early life that influence child obesity risk include maternal smoking during pregnancy, 60 second-hand exposure to smoke, and air pollution. 61 Antibiotic exposure in infancy is associated with a slight increase in childhood overweight and obesity, especially if there are repeated treatments, an association that might be mediated by alterations in the gut microbiome. 62 Importantly, there is increased recognition that adverse childhood experiences, such as abuse, family dysfunction and neglect are associated with the development of childhood obesity. This association appears to be especially the case for sexual abuse and for co-occurrence of multiple adverse experiences. 63
Medical conditions associated with obesity
Obesity might occur secondary to a range of medical conditions including several endocrine disorders (eg, hypothyroidism, hypercortisolism, growth hormone deficiency), central nervous system damage (ie, hypothalamic-pituitary damage because of surgery or trauma) and post-malignancy (eg, acute leukaemia). Several pharmacological agents are associated with excess weight gain, including glucocorticoids, some anti-epileptics (eg, sodium valproate), insulin, and several atypical antipsychotics (eg, risperidone, olanzapine, clozapine). 64 The rapid and large weight gain associated with the latter class of drugs suggests that anticipatory weight management strategies should be formally used when commencing such therapy, although evidence is largely from adult studies. 65
Weight stigma
Weight stigma refers to the societal devaluation of a person because they have overweight or obesity, and includes negative stereotypes that individuals are lazy and lack motivation and willpower to improve health. 66 , 67 Higher body mass is associated with a greater degree of weight stigma, although longitudinal studies have shown associations between weight stigma and BMI to be bidirectional. 68 Stereotypes manifest in different ways, leading to discrimination and social rejection, often expressed as teasing, bullying and weight-based victimisation in children and adolescents. 66 , 67 Bodyweight is consistently reported to be the most frequent reason for teasing and bullying in children and adolescents, with a quarter to half of youth reporting being bullied based on their bodyweight. 69 Parents and health-care providers can also be sources of weight stigma. 69 , 70 Weight stigma is associated with poor mental health, impaired social development and education, and engagement in disordered eating behaviours including binge eating. 69 Of concern, youth who have experienced weight related teasing or bullying have higher rates of self-harm behaviours and suicidality compared with peers of the same weight who have not felt stigmatised. 67
Experience of weight stigma is a barrier to accessing health care. 67 Health professionals have a responsibility to help reduce weight stigma experienced by children, adolescents, and families through the use of supportive, compassionate, and non-stigmatising language while providing care. 69 In 2020, an international consensus statement was endorsed by more than 100 organisations pledging to reduce weight stigma. 66 Additionally, the American Academy of Paediatrics recommends paediatricians help mitigate weight stigma within clinical practice by role-modelling professional behaviours, using non-stigmatising language, using patient-centred behaviour change counselling, creating a safe and welcoming clinical environment accommodating of all body sizes, and conducting behavioural health screening for signs of weight-based bullying including emotional comorbidities. 67
Health complications
All body systems can be affected by obesity in the short, medium, or longer term, depending upon age and obesity severity. Figure 2 depicts the possible complications of obesity that can occur anywhere from childhood and adolescence to adulthood. It is important that complications are assessed in childhood and treated alongside obesity to prevent progression of both. Recent reviews provide additional detail regarding complications. 2 , 3 , 4 , 48 , 72 , 73 , 74 , 76 , 77 , 78 , 79 , 84 , 85 , 86 , 87 , 88 , 91 , 92 , 94 , 95

Short-term and long-term health complications and comorbidities associated with child and adolescent obesity
Health complications and comorbidities include neurological, 71 dental, 72 cardiovascular, 2 , 73 , 74 , 75 psychosocial, 2 , 4 , 76 , 77 , 78 respiratory, 79 , 80 , 81 , 82 , 83 endocrine, 73 , 84 , 85 musculoskeletal, 80 , 86 , 87 , 88 renal, 89 , 90 gastrointestinal, 90 , 91 skin, 92 function, and participation. 48 , 93
Clinical assessment
A detailed clinical examination screens for underlying causes of obesity, and assesses for possible obesity-related complications, risk of future disease, and whether potentially modifiable behavioural factors exist. Adapted from various national or regional level clinical practice guidelines, 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 summaries of the main aspects to be explored in history taking and physical examination are included in the panel and table . Laboratory tests can complement clinical assessment, looking for cardio-metabolic complications and some underlying causes of obesity. These tests are appropriate in most adolescents with obesity, and in all patients with severe obesity, with clinical signs or history suggestive of complications (eg, acanthosis nigricans), or with a family history of cardio-metabolic disease. Investigations would generally include liver function tests, lipid profile, fasting glucose, and glycated haemoglobin, and might include an oral glucose tolerance test and additional endocrine or genetic studies. 96 , 97 , 98 , 99 , 100 , 101 , 102
Elements of history taking
General history
- • Prenatal and birth history, including gestational obesity, gestational diabetes, maternal smoking, gestational age, birth weight, and neonatal concerns
- • General medical history, including psychiatric or behavioural diagnoses and previous malignancy
- • Developmental history, including any delays in motor, speech, or cognitive developmental, and therapy received
- • Infant feeding, including breastfeeding and duration and timing of introduction of complementary foods
- • Current medications, including glucocorticoids, anti-epileptics (eg, sodium valproate), and antipsychotics (eg, clozapine, risperidone, and olanzapine)
Growth history
- • Height and weight growth trajectories
- • Onset of obesity and timing of weight concerns of child or adolescent and family
- • Previous obesity management, whether supervised or self-initiated
- • Previous and current dieting and exercise behaviours or use of supplements
Complications history
- • Psychological impacts of obesity, including bullying, poor self-esteem, anxiety, depression, and disordered eating
- • Sleep routines, presence of snoring or possible sleep apnoea (eg, poor refreshment after sleep, daytime somnolence, and witnessed apnoea)
- • Exercise tolerance, exercise-induced bronchoconstriction, dyspnoea, hypertension, and fatigue levels
- • Specific symptoms including acne and hirsutism (girls), morning headache and visual disturbance, nocturnal enuresis, daytime dribbling, constipation, hip and knee joint pain, and gastrointestinal complaints (vomiting, abdominal pain, constipation, and gastrointestinal reflux)
- • Menstrual history (girls)
Family history
- • Ethnicity (high risk groups for cardiometabolic complications include First Nations peoples, Latin American, south Asian, east Asian, Mediterranean, and Middle Eastern)
- • Family members with a history of obesity; type 2 diabetes and gestational diabetes; hypertension, dyslipidaemia, and cardiovascular disease; obstructive sleep apnoea; polycystic ovary disease; bariatric surgery; eating disorders; and mental health disorders
- • Home environment including household members, parental relationship, parental employment, hours, and home supervision
Social history, including welfare, and safety
- • Housing or accommodation situation (stable or homeless) and residential care
- • Family income (or proxy) and food insecurity
- • Previous social services involvement
- • School attendance, additional educational assistance, learning difficulties, and behavioural difficulties
- • Hobbies and interests
- • Friends in school or neighbourhood
- • Use of tobacco, alcohol, or recreational drugs
- • Parenting style and child–parent interactions
Behavioural risk factors
- • Nutrition and eating behaviours: breakfast consumption; eating patterns including snacking, grazing, sneaking or hiding food, fast-food intake, binge-eating; beverage consumption (sodas, juices, other sugary drinks); family routines around food and eating; and active dieting
- • Physical activity: transport to and from school; participation in physical education class; participation in organised sport, dance, or martial arts; gym membership; after-school and weekend recreation; and family activities
- • Sedentary behaviours: time spent sitting each day; screen-time per day (television, video game, mobile phone, tablet, computer use); number of devices in the household and bedrooms; patterns of screen viewing (eg, during meals, at night); and use of social media
- • Sleep behaviours: bedtime routines; sleep and wake times on weekdays and weekends; and daytime napping
Clinical findings on examination by organ system
Obesity treatment in children and adolescents aims to reduce adiposity, improve related physical and psychosocial complications, and prevent the development of chronic diseases. The degree of BMI reduction needed to improve obesity related complications is currently unknown. However, some evidence suggests that BMI z-score reductions greater than 0·25 and 0·5 might represent clinically important thresholds. 104 Several high-quality clinical practice guidelines are in use internationally. 96 , 97 , 98 , 99 , 100 , 101 , 102 Treatment type and intensity depends upon obesity severity, the age and developmental stage of the child, needs and preferences of the patient and family, clinical competency and training of the clinician(s), and the health-care system in which treatment is offered. 105 Treatment integrates multiple components including nutrition, exercise and psychological therapy, pharmacotherapy, and surgical procedures. It should be delivered by suitably qualified paediatric health professionals who incorporate behavioural support and non-stigmatising child-focused and youth-focused communication into their practice. 69
Multicomponent behavioural interventions
Behavioural support strategies in obesity management include a combination of addressing dietary intake, physical activity, sedentary behaviours, sleep hygiene, and behavioural components within the context of a family-based and developmentally appropriate approach aiming for long-term behaviour modification. 106 , 107 , 108 Tailoring of interventions to various subgroups based on age, gender, and culture might be needed. For example, with young children the therapy might be largely parent-focussed 109 and for adolescents a greater degree of autonomy might be required. 107
Dietary intervention
Dietary interventions might include dietary education alone or combined with a moderate energy restriction, 110 with structured dietary plans or advice preferred over broad dietary principles, particularly for adolescents. 111 Principles of dietary education focus on adoption of dietary intake patterns consistent with local dietary guidelines—eg, increased intake of vegetables and fruit, reductions in energy-dense nutrient-poor foods and sugar sweetened beverages, and improvement in dietary behaviours such as encouraging mealtime routines and family meals. 110 , 112 One common approach, the traffic light diet, categorises foods by energy density, with green low-energy foods that can be eaten freely, yellow foods eaten moderately, and red foods eaten occasionally due to a higher energy-density. 107 Dietary approaches aim to be nutritionally complete and to address and prevent nutritional deficiencies. 113 , 114 However, children and adolescents might present for obesity treatment with relatively poor diet quality; 115 therefore, an initial goal of improving the baseline diet might be appropriate. Selection of dietary strategies should be informed by individual preference and circumstances, family environment, and available support.
Physical activity
Physical activity components might include provision of education or a structured exercise programme, or both, in line with local guidelines. The goals of exercise interventions should be to offer a safe, supportive, fun, and non-judgemental environment for children with obesity to engage in active play. It can also enable socialisation with peers and facilitate motor competence, confidence, and optimisation of fundamental motor skills. The aims of exercise itself are to increase physical fitness, reduce or attenuate obesity-related complications, improve quality of life, and support the child to reach age-appropriate physical activity levels. 116 , 117 Studies have found that the most effective exercise interventions consist of sessions lasting 60 min or more on at least 3 days per week for at least 12 weeks duration. 118 Training programmes should be tailored to the child's physical abilities and fitness level evaluated at baseline using standardised and age-appropriate outcome measures. Intervention should be fun, leverage the preferences of the child while following frequency, intensity, duration, type, volume, and progression principles. 119
Children with obesity often experience personal barriers to movement and exercise. Therefore tailoring and adapting paediatric exercise interventions will often be necessary, particularly for those that report musculoskeletal pain, high rates of fatigue, urinary incontinence, skin chafing, or have impaired motor skills. Additionally, the presence of intellectual or physical disabilities should be considered. As such, the type of exercise intervention offered will vary according to the child's clinical presentation and the desired outcome (eg, improvements in aerobic fitness, increased enjoyment, or reduction of fat-mass). The health professional might need to consider whether the intervention incorporates weight-bearing or non-weight bearing games, aerobic, proprioceptive and resistance exercises, individual or group-based work, or whether specific physiotherapy approaches might also need to be integrated to address underlying impairments. Appropriate monitoring and evaluation of the exercise intervention is recommended and should include the perspective of the child in addition to psychometrically robust outcome measurement. Additional guidance is available elsewhere. 120 , 121 , 122
Screen time and sedentary behaviours
Sedentary behaviours, including screen time, are distinct from physical activity and need to be addressed as part of a comprehensive behavioural change programme. Interventions that are successful in decreasing screen time in the short term include strong parental engagement, structural changes in the home environment (eg, removing or replacing home or bedroom electronic games access), and e-monitoring of time on digital devices. 123 These interventions tend to be more effective in young children.
There are few trials targeting sleep in the treatment of paediatric obesity, especially in older children and adolescents. Sleep interventions in preschool-aged children are associated with reduced weight gain. 124 Improvements in sleep hygiene, such as a consistent bedtime routine, regular sleep-wake times, and reduced screen times in the evening, are likely to have many co-benefits and positive effects on other weight-related behaviours.
Behavioural support strategies
Changes in dietary intake, physical activity, sedentary behaviours, and sleep are underpinned by strategies supporting behaviour change with the vast majority of interventions using a form of behavioural therapy. Common behaviour change techniques include goal setting, stimulus control (modifying the environment), and self-monitoring. 107 , 125 Motivational interviewing techniques such as reflective listening and shared decision making might also be used by healthcare workers to improve motivation for behaviour change. 126 , 127
The effectiveness of behaviour change interventions are well described, with modest reductions in weight-related outcomes 128 , 129 and improvements in cardiometabolic health. 130 The 2017 Cochrane reviews 128 , 129 found that behaviour changing interventions were more successful than no treatment or usual care comparators in reducing BMI (–0·53 kg/m 2 [95% CI –0·82 to –0·24], low-quality evidence in children; –1·18 kg/m 2 [–1·67 to –0·69], low-quality evidence in adolescents), and BMI z score (–0·06 units [–0·10 to –0·02], low-quality evidence in children; –0·13 [–0·21 to –0·05], low quality evidence in adolescents). 128 , 129 Effects were maintained at 18 to 24 months' follow-up for both BMI and BMI z-score in adolescents. 128 In children and adolescents aged 5–18 years, behavioural interventions are also associated with reductions in total cholesterol, triglycerides, fasting insulin, and HOMA-insulin resistance 130 as well as increased sleep duration and a reduced prevalence of obstructive sleep apnea. 131
A systematic review of 109 randomised controlled trials (RCTs) found that dietary interventions achieve a modest reduction in energy intake, reduced intake of sugar sweetened beverages, and increased intake of fruit and vegetables in children and adolescents aged 2–20 years. 132 The beneficial effects of supervised exercise in children and adolescents with obesity on measures of anthropometry and adiposity include reductions in BMI, bodyweight, waist circumference, and percent body fat. 133 Improvements in obesity-related complications are also observed, independent of changes in anthropometry including increased cardiorespiratory fitness, 134 improved muscle performance 80 and fundamental motor skills, 135 reductions in insulin resistance, reductions in fasting glucose and insulin levels, 136 improved lipid profile, 137 and reductions in blood pressure. 138 , 139 Exercise might also yield additional benefits related to appetite and response to food cues.
Behavioural obesity treatment is also associated with improved psychosocial health, including improved quality of life, 128 , 140 and body image 141 compared with no treatment or usual care comparators post-intervention and improvements in self-esteem at latest follow-up in those aged 4–19 years at baseline. 141 In assessing mental health, no difference between intervention and no-treatment comparator groups have been seen for the changes in symptoms of depression, 142 anxiety, 142 and eating disorders, 143 during the intervention period. However, symptoms of depression, anxiety, and eating disorders are reduced post-intervention or at follow-up in intervention arms, with no worsening of symptoms within groups. 142 , 143 , 144 , 145 Adverse effects of lifestyle interventions are poorly reported. 128 , 129 Where reported, no significant differences in adverse events between intervention and control groups are seen. 146
Psychological interventions
Psychological interventions, incorporated alongside traditional behavioural obesity treatment strategies, or as stand-alone interventions, target psychological factors that might contribute to eating behaviours and obesity, including distorted body image, negative mood, and stimulus control. 125 , 147 A core objective of psychological interventions is to reduce barriers for behaviour change. 147 Cognitive behavioural therapy (CBT) is the most frequently used approach, and addresses the relationship between cognitions, feelings, and behaviours using behavioural therapy techniques to modify behaviours and cognitive techniques to modify dysfunctional cognitions. 125 CBT-based interventions have been shown to result in healthier food habits, improved psychosocial health, quality of life, self-esteem, and anthropometric variables including BMI and waist circumference in children and adolescents. 125 Acceptance and commitment therapy (ACT), which encourage acceptance rather than avoidance of internal experiences (eg, food cravings), have shown to be effective in the management of obesity in adults and are an emerging area of research in adolescence. Pilot studies have found ACT-based interventions to be feasible and acceptable in adolescents with obesity, 148 , 149 with further research underway. Weight-neutral interventions, aiming to promote healthy behaviours and improve physical and psychosocial health without promoting weight loss, are an emerging area of practice in adults. There is currently insufficient evidence to guide the use of weight-neutral approaches in paediatrics.
Mode of intervention delivery
Evidence for behavioural change programmes encompass a variety of modes of delivery including group programmes, one-on-one therapist sessions, and various forms of e-health support. 128 , 129 , 150 , 151 No one form is necessarily superior to another, although a combination of such approaches might be used in a comprehensive integrated programme. Availability of resources; time constraints for health professionals, patients, and families; and appropriate health professional training will influence treatment provided alongside the child's developmental stage and patient or parent preferences. The COVID-19 pandemic has highlighted the need for effective interventions that can be delivered remotely without exacerbating existing social and technological disparities. 152 A 2021 review describes the considerations for successful implementation for such telemedicine approaches. 153
Eating disorders risk management
Children and adolescents with obesity are vulnerable to the development of eating disorders because obesity and eating disorders have several shared risk factors. 76 , 154 Disordered eating attitudes and behaviours, as precursors to eating disorders, are also elevated in children and adolescents with obesity. 155 Although obesity treatment helps improve eating disorder symptoms, including binge eating and loss of control in most youth with obesity, 143 , 144 a small number undergoing obesity treatment might develop an eating disorder during or after an intervention. 143 Although whether this low risk of developing eating disorders differs in youth who do not present for clinical treatment remains unclear, it is an important consideration for clinicians providing obesity care. For over a decade, it has been recommended that there be screening of disordered eating attitudes and behaviours before obesity treatment, 76 , 154 particularly with the use of dietary interventions, 112 to identify undiagnosed eating disorders. However, guidance on how this should occur in practice is scarce. Screening tools that assess for binge eating disorder specifically in children 156 and adolescents 157 with obesity are available but a self-report screening tool to assess for the broad spectrum of eating disorders for those with obesity and with adequate diagnostic accuracy is lacking. Eating disorder symptoms should not prevent the provision of obesity care; 158 rather, a combination of self-report questionnaires and clinical assessment might be needed to assess and monitor eating disorder risk in practice. 76
Intensive dietary interventions
Use of intensive dietary interventions is an emerging area of research and practice, particularly in post-pubertal adolescents with obesity related comorbidity or severe obesity. 110 , 159 Prescriptive dietary approaches may be delivered within the context of a multicomponent behavioural intervention, by experienced paediatric dietitians with medical supervision. 159 Very Low Energy Diets (VLEDs), consisting of an energy prescription of approximately 800 kcal/day or less than 50% of estimated energy requirements, often involving the use of nutritionally complete meal replacement products, are one such option. A meta-analysis of 20 studies found VLEDs to be effective at inducing rapid short term weight loss in children and adolescents with obesity (–10·1kg [95% CI 8·7 to 11·4] over 3 to 20 weeks), though follow-up beyond 12-months is scarce. 160 Data on VLEDs in the treatment of youth with early onset type 2 diabetes are limited to a small pilot study 161 and a medical chart review, 162 however, they have shown early short-term success and the possibility of reducing the requirement for medication, including insulin, and inducing remission of diabetes. 163 However, there is need for further research. 163 Variations in macronutrient distribution have been widely studied due to hypothesised effects on satiety, particularly higher protein (20–30% of energy intake from protein) approaches and very low carbohydrate diets (<50g per day or <10% energy from carbohydrate) aiming to induce ketosis. Although lower carbohydrate approaches show a significantly greater reduction in weight-related outcomes in the short-term (<6 months), dietary patterns with varied macronutrient distribution do not show superior effects in the longer term in children and adolescents. 164 Pilot studies on the use of various regimens of intermittent energy restriction in adolescents with obesity have shown these to be feasible and acceptable. 165 , 166 Larger trials are underway.
Anti-obesity medications
Anti-obesity medications are an important part of comprehensive obesity treatment. Pharmacotherapy, when combined with behavioural change interventions, can be particularly useful in patients for whom behavioural approaches alone have proven suboptimal or unsuccessful in reducing BMI and improving obesity-related complications. Although regulatory approval and availability varies by country and region, there is one anti-obesity medication that is approved by most regulatory agencies (including the United States Food and Drug Administration and the European Medicines Agency) for chronic obesity treatment in adolescents aged 12–18 years, which is liraglutide at 3 mg daily. Liraglutide, delivered via subcutaneous injection, belongs to the glucagon-like peptide-1 receptor agonist class, which acts on its receptors in the hypothalamus to reduce appetite, slow gastric motility, and act centrally on the hind brain to enhance satiety. 167 In the largest RCT of liraglutide 3 mg among adolescents (12 to <18 years old) with obesity, whereby all participants also received lifestyle therapy, the mean placebo-subtracted BMI reduction was approximately 5% with one year of treatment. 168 More participants in the liraglutide versus placebo group had a decline in BMI by 5% (43·3% liraglutide vs 18·7% placebo) and 10% (26·1% liraglutide vs 8·1% placebo). Importantly, no new safety signals were observed in the adolescent trial in relation to previous adult trials. The most reported adverse events were gastrointestinal and were more frequent in the liraglutide group (64·8% liraglutide vs 36·5% placebo). No statistically significant improvements in cardiometabolic risks factors or quality of life were observed between groups.
Other medications have been evaluated for the treatment of paediatric obesity yet are not approved in the EU and many other countries. These medications include orlistat (mean placebo-subtracted BMI reduction <3%), phentermine (no randomised, controlled trials conducted in children or adolescents), topiramate (mean placebo-subtracted BMI reduction <3%), and metformin (mean placebo-subtracted BMI reduction of around 3%). 169 , 170 , 171 , 172 Two anti-obesity medications are currently under evaluation for the treatment of adolescent obesity: semaglutide 2·4 mg weekly ( {"type":"clinical-trial","attrs":{"text":"NCT04102189","term_id":"NCT04102189"}} NCT04102189 ) and the combination of phentermine and topiramate ( {"type":"clinical-trial","attrs":{"text":"NCT03922945","term_id":"NCT03922945"}} NCT03922945 ). Results from these clinical trials are expected in 2022 with regulatory review and perhaps approval in 2022–23. Additional therapies are available for monogenic forms of obesity, 173 details of which are beyond the scope of the current Review.
Metabolic and bariatric surgery
Metabolic and bariatric surgery is the most effective and durable treatment for inducing weight loss in adolescents with obesity, with average BMI reductions in various longitudinal studies of the Roux-en-Y gastric bypass and vertical sleeve gastrectomy ranging from approximately 25–40% at 1–9 years post-surgery. 174 , 175 , 176 , 177 , 178 Beyond weight loss, metabolic and bariatric surgery leads to clinically meaningful improvements in obesity-related complications, cardiometabolic risk factors, musculoskeletal pain, and functional mobility. 174 , 178 , 179 , 180 Importantly, although the relative degree of weight loss with metabolic and bariatric surgery is similar between adults and adolescents, emerging data suggest that serious complications like type 2 diabetes and hypertension might be more likely to remit in adolescents than in adults. 177 Improved quality of life and reduced symptoms of depression are also seen following metabolic and bariatric surgery in the short term. 181 , 182 However, incidence and remission of mental health problems are highly variable following metabolic and bariatric surgery; a proportion of youth will continue to experience mental health concerns post-surgery that can persist long-term, with a subset experiencing suicidal ideations and behaviours. 183 , 184 , 185 , 186 Pre-surgical and post-surgical psychological support is recommended 187 and is associated with improved psychosocial health and weight loss maintenance. 188 Mortality rates 5 years following metabolic and bariatric surgery in adolescents (1·9%) appear to be similar to that of adults (1·8%) but adolescents tend to require abdominal reoperations more frequently than adults and have a higher incidence of low levels of ferritin, 177 requiring monitoring of nutritional status. 189 Until approximately 5 years ago, clinical practice guidelines for metabolic and bariatric surgery restricted eligibility to older adolescents having reached skeletal maturity. However, contemporary guidelines have now suggested that there need not be any lower age limit for consideration of metabolic and bariatric surgery as long as other medical eligibility requirements are met (detailed rationale and other considerations such as pubertal progression, linear growth, and pregnancy). 190 , 191 The uptake of metabolic and bariatric surgery has been extremely limited as surgery is typically reserved for the most severe forms of obesity and for patients with significant obesity-associated complications. 192 Other factors probably contributing to the low use of metabolic and bariatric surgery among adolescents include the perceived invasiveness and irreversibility of the procedures, lingering concerns regarding long-term safety, lack of access to surgical centres, poor insurance coverage, and referral bias.
Treatment selection
Treatment outcomes for paediatric obesity are highly variable 193 , 194 , 195 and a thorough baseline assessment guides the health professional on the appropriate treatment at a given time for a given patient. Baseline factors known to negatively predict weight-related outcomes with treatment include high levels of picky eating in preschool age children, 196 poor family functioning, or low self-concept 193 in the child and maternal psychological distress. 197 Positive predictors of treatment effect on weight include younger age, lower baseline BMI, higher global self-esteem, and adherence 198 to follow up. Predictors of treatment response represents a critically important area of future research as the ultimate goal is to match the appropriate patient to the treatment most likely to provide benefit and minimise potential risks from a non-suitable treatment plan.
Barriers to obesity treatment
Despite its growing evidence base, there remain many barriers to delivery of effective obesity treatment. For example, most RCTs have not been undertaken in culturally diverse populations, in people with complex health needs or disabilities, nor in those living with social disadvantage, all of which might make adherence to standard therapies more challenging. 199 Further, there are failures in implementing the known evidence into routine service delivery. An audit of adult and paediatric obesity services in 68 countries revealed poor resourcing and staffing of clinical services; a lack of integration of services across primary, secondary and tertiary level care; inadequate health professional training; widespread health system stigma towards people with obesity; and frequent unaffordability and inaccessibility of services. 200 Future research is needed to both develop the evidence base for obesity treatment in priority populations and in LMICs, as well as bring an implementation science perspective to obesity service delivery.
Conclusions
Structured, supported and life-long care for children and adolescents with obesity and their families is essential. The provision of care will change over time based on growth, development, life stage, and available support. More research is needed on management of obesity in disadvantaged communities and in those from LMICs, and on the real-world implementation of management approaches. Importantly, clinical care needs to be underscored by modifications to the social, commercial, and built environments which currently promote, rather than protect against, obesity, together with associated policy changes.
Search strategy and selection criteria
References for this Review were identified through searches of Medline (PubMed) and the Cochrane Database of Systematic Reviews for articles published up to Nov 1, 2021, using combinations of terms such as “child”, “adolescent”, “obesity”, “epidemiology”, “aetiology”, “complications”, “co-morbidity”, “treatment”, “behaviour change”, “prevention”, “bariatric surgery”, “metabolic surgery”, “pharmacotherapy”, and “BMI”. Articles published in English were included. We also reviewed reference lists of published manuscripts, clinical guidelines, and other relevant reviews and meta-analyses.
Declaration of interests
ASK serves as an unpaid consultant for Novo Nordisk, Vivus, Eli Lilly, and Boehringer Ingelheim; and receives donated drug and placebo from Vivus for a National Institutes of Health funded clinical trial. LAB serves on the Advisory Committee of the ACTION Teens study, sponsored by Novo Nordisk, for which an honorarium is paid to her hospital research cost centre. All other authors declare no competing interests.
Acknowledgements
HJ was supported by the Sydney University Medical Foundation. GO was supported by funding from the Royal College of Surgeons in Ireland StAR programme (grant number 2151).
Contributors
All authors contributed to the literature search, writing, reviewing, and editing of the manuscript.

IMAGES
VIDEO
COMMENTS
Firstly, a child can be subject to obesity for a number of reasons, including parents' obesity, exposure to antibiotics, maternal smoking, and diabetes (Deal et al., 2020). This information demonstrates that children's health is formed until they have come into being.
Childhood obesity is a complex chronic (long-term) condition that happens when your child is above a healthy weight for their age, height and sex assigned at birth. The medical definition of childhood obesity is having a body mass index (BMI) at or above the 95th percentile for age and sex in children aged 2 years and older.
Diet. Regularly eating high-calorie foods, such as fast foods, baked goods and vending machine snacks, can cause your child to gain weight. Candy and desserts also can cause weight gain, and more and more evidence points to sugary drinks, including fruit juices and sports drinks, as culprits in obesity in some people. Lack of exercise.
Introduction. Childhood and adolescent obesity have reached epidemic levels in the United States, affecting the lives of millions of people. In the past 3 decades, the prevalence of childhood obesity has more than doubled in children and tripled in adolescents. 1 The latest data from the National Health and Nutrition Examination Survey show that the prevalence of obesity among US children and ...
Obesity in childhood is the most challenging public health issue in the twenty-first century. It has emerged as a pandemic health problem worldwide. The children who are obese tend to stay obese in adulthood and prone to increased risk for diabetes and cardiac problems at a younger age. Childhood obesity is associated with increased morbidity and premature death.[1] Prevention of obesity in ...
Childhood obesity can profoundly affect children's physical health, social, and emotional well-being, and self esteem. It is also associated with poor academic performance and a lower quality of life experienced by the child. These potential consequences are further examined in the following sections.
Introduction. Obesity in children and adolescents is a global health issue with increasing prevalence in low-income and middle-income countries (LMICs) as well as a high prevalence in many high-income countries.1 Obesity during childhood is likely to continue into adulthood and is associated with cardiometabolic and psychosocial comorbidity as ...
Obesity implies a series of associated effects. Some of the effects might reside in such health disorders as high blood pressure, strokes, heart diseases and even diabetes 2 (Haerens, 2012). These diseases reduce the children's life span to five years. In most cases, children with obesity turn into obese adults in future.
Figure 1 shows the share of the U.S. population, by age group, that is obese based on the BMI cutoffs described above.7 During 1971-74 about 5 percent of children aged two to nineteen years were obese. By 1976-80 the share obese was slightly higher, but between 1980 and 1988-94 the share obese nearly doubled.
This Review describes current knowledge on the epidemiology and causes of child and adolescent obesity, considerations for assessment, and current management approaches. Before the COVID-19 pandemic, obesity prevalence in children and adolescents had plateaued in many high-income countries despite levels of severe obesity having increased. However, in low-income and middle-income countries ...
️ 9 Tips for Writing a Childhood Obesity Essay. In many countries, obesity is becoming the leading cause of death. From an overabundance of unhealthy food to a tendency to be less active, the habits of parents often transfer to their children, resulting in the acuteness of a childhood obesity essay.
Childhood obesity can profoundly affect children's physical health, social, and emotional well‑being, and self esteem. It is also associated with poor academic performance and a lower quality ...
The prevalence of childhood obesity continues to rise despite decades of clinical and public health efforts. Early identification of children at risk of developing obesity is essential using newer electronic health systems, which move beyond traditional growth charts to provide a wealth of information about body mass index and other relevant parameters such as social determinants of health and ...
Essay Sample: The epidemic of obesity is a significant, chronic health problem and it is proving to be a major challenge to the adolescents in our society to face. ... The purpose of this paper is to examine childhood obesity causes and effects. According to the Center for Disease Control (CDC), obesity is defined as having ¬¬excess body fat ...
Obesity in childhood can have significant long-term effects on a child's physical health, increasing the risk of developing chronic conditions such as type 2 diabetes, heart disease, and hypertension. Furthermore, obesity can have a profound impact on a child's psychological well-being, leading to low self-esteem, depression, and social isolation.
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression, emanating from negative self-esteem and societal rejection. In some cases, people who become obese lose their friends and may get disapproval from teachers and other personalities ...
The prevalence of childhood obesity has increased globally over the past three decades, with more rapid increases recently occurring in low-income countries ().In the United States, more than 30% ...
The most common causes are genetic factors, lack of physical activity, unhealthy eating patterns, or a combination of these factors. Moreover, socio-economic factors have influence on children, which may cause a child to become obese. In addition, there are certain effects resulted from childhood obesity such as physical, mental, emotional, and ...
There are many different elements which can contribute to the causes of childhood obesity. Children become overweight and obese for a variety of reasons. The main factors which cause childhood obesity are, genetic factors, lack of physical activity, unhealthy eating patterns and lifestyles.
The effect of obesity in children is vital. Self-esteem and confidence of the yout are usually affected. Overweight children have experienced being bullied by other kids. Consequently, depression ...
While the exact cause of MS remains elusive, recent research suggests a potential link between childhood obesity and the development of MS later in life. This article explores the findings of a ...
Childhood obesity can effect the body in many ways. The CDC warns that overweight children are more vulnerable to high blood pressure and high cholesterol, which can lead to cardiovascular disease.
Exposure to rising levels of wildfire smoke could lead to more than 10,000 additional deaths each year in the US by 2050. This could make deaths due to wildfire smoke the costliest consequence of ...
Introduction. Obesity in children and adolescents is a global health issue with increasing prevalence in low-income and middle-income countries (LMICs) as well as a high prevalence in many high-income countries. 1 Obesity during childhood is likely to continue into adulthood and is associated with cardiometabolic and psychosocial comorbidity as well as premature mortality.2, 3, 4 The provision ...