- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health

What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
/cdn.vox-cdn.com/uploads/chorus_image/image/72848552/shutterstock_304415033.0.0.0.0.jpg)
What I wish I’d known before I had gender-affirming surgery
The media makes out procedures like the one I had to be cure-alls. They're not.
Share this story
- Share this on Facebook
- Share this on Twitter
- Share this on Reddit
- Share All sharing options
Share All sharing options for: What I wish I’d known before I had gender-affirming surgery
I have nightmares about growing a beard and having a penis. They've occurred more and more frequently the further I've progressed into my transition from male to female.
Last July, New York magazine published a video explaining what nightmares are : our brains' way of taking whatever is bothering or frightening us in life and morphing it into tales that we can process as memories. Thanks to hormone therapy, laser treatments, and vaginoplasty surgery, I no longer grow facial hair or have a penis, but the thought of being a boy still terrifies me and always will. These nightmares are my brain's way of helping me distance myself from that fear.
Much of what you can find about gender-affirming surgeries like vaginoplasty makes you think that after you've had one, all your problems fade away and your life becomes instantaneously better. Take a look at these recent videos by the New York Times and NPR , and this article by NBC : All three leave you with the impression that the surgery is a type of transition denouement. In the video by the Times, for example, Katherine, supported by pleasant and hopeful music, says this about her surgery: "It's, like, the new me. I finally feel like myself, so it kind of, in a sense, is a rebirth day … a renaissance."
NPR similarly ends its video with Jetta'Mae Carlisle, who, having undergone the surgery, says, "I have that white picket fence dream, and that's where my future is." The NBC article quotes Denee Mallon saying, "I feel complete."
These reports obscure the truth: While gender-affirming surgeries can make people more comfortable in their bodies, they're not a fix-it for everything wrong in your life. I know this from my own experience with surgery, and from studying the research on it.
I wish I had better resources to help prepare me for my surgery
People who want to have a vaginoplasty must get referrals from two different therapists. Dr. Molly Parks, a gender therapist in Durham, North Carolina, told me the goal of preoperative therapy is to make sure patients have really thought through their decision, and to determine whether they have any mental health issues that could hamper their decision-making.
"I ultimately think that the client is the only one who can determine whether a procedure is the right decision for them," said Parks.
My pre-op therapy largely went the way Parks described. With my first therapist, I explored how long I'd had gender dysphoria, a medical condition characterized by an extreme discomfort with the primary and secondary sex characteristics of one's body. We talked about how I thought of myself as a girl, therapy history, my relationships with friends and family, what support structures I had in place, and what goals I was pursuing in life. My second therapist and I made sure I was mentally capable of grasping the decision I was making.
Thinking back, though, my pre-op therapy didn't help me realize how extraordinarily hard it would be to recover from the surgery I had: the stress from being unable to eat solid food for a week and a half, and the feeling of helplessness from being so bedridden and unable to walk normally for weeks, to name only two difficulties. I'm also, apparently, not the only one who's had this gap in his or her therapy experience.
"I would think, and hope, that most gender therapists … would talk through the potential difficult side effects of surgery," said Parks. "The therapists I work with do tend to do this, although I have had clients who have come to me from therapists where this was not the case."
Parks said that currently there are "no specific guidelines in place as to what therapy has to look like presurgery." That could change, though — she is a member of the World Professional Association for Transgender Health, and she said she thinks the organization should adopt guidelines for preoperative therapy.
Researching on your own the gender-affirming surgery you need, especially one so enigmatic as vaginoplasty, and without guidance from an informed therapist on the subject, can be excruciating. There was no formal education I could find about vaginoplasty. Even with information provided by my surgeon, I still found myself reading online Q&As, visiting forums, and reading news articles. Trying to form a clear picture of the surgical experience seems impossible when the information you find is so disjointed and often so hateful and frightening.
I've seen several horrible euphemisms used to describe a postoperative vagina: "frankenpussy," "mutilated dickhole," "an open wound," "penis bits." Sometimes the sentiment behind these phrases manifests in very violent ways: Vice published a moving article last year about the 23 trans women killed in 2015.
It's also really easy to come across articles that describe the surgery as mutilation . In her article for Public Discourse , Margaret A. Hagen, a professor at Boston University, described a woman like me as a "mutilated male pumped full of estrogen."
One of the most tiring factors of transitioning is having to be on constant emotional guard everywhere you go. Despite your best efforts, though, you have to wonder how much negativity has been internalized. My vagina is not a mutilation, but I must admit I might not like it as much as I should after reading so much horrible language directed toward it.
What happens when expectations meet reality
Being inadequately prepared for surgery has real consequences.
In an essay published last summer, Don Terry explored the horrible struggles black trans women face. One woman told Terry she knew several people who'd killed themselves after having surgery. "They really thought life was going to be completely different," she said. "Nothing changed. That's a whole lot of money to invest to still have the same life."
If you're in a shit situation before surgery, you'll be in a shit situation after. If your co-workers aren't supportive of your transition, they're not going to change their minds once you have a vagina. The friends you've lost aren't going to come back now that you have female genitalia. If you've made it far enough to get surgery without support from your family, they won't come around in the aftermath of the operation; what they say to you might change, but their true feelings certainly won't.
And you'll still come across news articles that say your vagina is mutilation. You're still going to have people calling you a man. You're still going to see people freak out about you using a certain bathroom. Surgery will not change any of this.
And indeed, people who have gender-affirming surgeries still experience higher suicide and attempted suicide rates than the rest of the population, according to a 2011 study from Sweden. Some cite this research in the hopes of convincing others that the surgeries are ineffective and ultimately harmful , but they do so in error. The researchers go out of their way to explain that the surgeries are not the cause of the high suicide rates: "The results should not be interpreted such as [the surgery] per se increases morbidity and mortality." They say "things might have been even worse" without the surgery.
The latest research shows that it's discrimination and stigma, not surgery itself, that causes the high suicide and attempted suicide rates. A study published in Ontario in 2015 revealed that those who have a supportive social environment (the most important social support being parents) were far less likely to seriously consider suicide. Other factors, like having one official document properly identifying your sex, also correlated with lower suicide attempts and rates.
My major problem, like many others, is employment. According to the National Center for Transgender Equality's 2011 survey , 44 percent of the respondents were experiencing underemployment, the unemployment rate was twice that of the national average, and 90 percent said they had experienced workplace harassment or had to hide who they are to avoid such harassment.
It's been almost two years since I graduated, and I still don't have a full-time job. Though I've been recently accepted to graduate school — a very encouraging development! — I need to find a part-time job soon, because my mom isn't doing so well financially at the moment. I'm terrified, however, of encountering harassment on the job, so I'm forced to be very selective in my search.
Transitioning is a long, challenging road
Transitioning is one of the hardest, most overwhelming experiences someone can go through. It's the kind of gamble you make when your back is against the wall and everything seems at stake. Some people take years to finish if they're lucky enough to finish or start at all; others think they never finish simply because learning what a woman or man is takes a lifetime.
Transitioning is also not a cure. I needed gender-affirming surgery to alleviate gender dysphoria and feel as comfortable in my body as possible, but there is no cure for gender dysphoria — you can only treat the symptoms, and our ability to treat the symptoms is limited. I still experience dysphoria even though my physical results have turned out well. When I'm stressed out, my dysphoria worsens, making it harder to deal with whatever was stressing me out in the first place.
In February 2013, a month into my transition, I admitted myself to a psychiatric ward because I was afraid I was going to hurt myself. Though I've thankfully never had so serious a situation since then, I've had suicidal thoughts every year since I started transitioning. Maybe, hopefully, finally 2016 will be the first where I don't have any at all.
The morning of my surgery, the day of my last big step, I realized that right now in our society, transitioning isn't just some process you go through; it's also something you survive.
I've had vaginoplasty. I've finished transitioning. But I've yet to survive it.
J.L. is a freelance writer.
Will you support Vox today?
We believe that everyone deserves to understand the world that they live in. That kind of knowledge helps create better citizens, neighbors, friends, parents, and stewards of this planet. Producing deeply researched, explanatory journalism takes resources. You can support this mission by making a financial gift to Vox today. Will you join us?
We accept credit card, Apple Pay, and Google Pay. You can also contribute via
Tucker Carlson went after Israel — and his fellow conservatives are furious
Why the case at the center of netflix’s what jennifer did isn’t over yet, alec baldwin’s rust, the on-set shooting, and the ongoing legal cases, explained, sign up for the newsletter today, explained, thanks for signing up.
Check your inbox for a welcome email.
Oops. Something went wrong. Please enter a valid email and try again.
- Patient Care & Health Information
- Tests & Procedures
- Feminizing hormone therapy
Feminizing hormone therapy typically is used by transgender women and nonbinary people to produce physical changes in the body that are caused by female hormones during puberty. Those changes are called secondary sex characteristics. This hormone therapy helps better align the body with a person's gender identity. Feminizing hormone therapy also is called gender-affirming hormone therapy.
Feminizing hormone therapy involves taking medicine to block the action of the hormone testosterone. It also includes taking the hormone estrogen. Estrogen lowers the amount of testosterone the body makes. It also triggers the development of feminine secondary sex characteristics. Feminizing hormone therapy can be done alone or along with feminizing surgery.
Not everybody chooses to have feminizing hormone therapy. It can affect fertility and sexual function, and it might lead to health problems. Talk with your health care provider about the risks and benefits for you.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Feminizing hormone therapy is used to change the body's hormone levels. Those hormone changes trigger physical changes that help better align the body with a person's gender identity.
In some cases, people seeking feminizing hormone therapy experience discomfort or distress because their gender identity differs from their sex assigned at birth or from their sex-related physical characteristics. This condition is called gender dysphoria.
Feminizing hormone therapy can:
- Improve psychological and social well-being.
- Ease psychological and emotional distress related to gender.
- Improve satisfaction with sex.
- Improve quality of life.
Your health care provider might advise against feminizing hormone therapy if you:
- Have a hormone-sensitive cancer, such as prostate cancer.
- Have problems with blood clots, such as when a blood clot forms in a deep vein, a condition called deep vein thrombosis, or a there's a blockage in one of the pulmonary arteries of the lungs, called a pulmonary embolism.
- Have significant medical conditions that haven't been addressed.
- Have behavioral health conditions that haven't been addressed.
- Have a condition that limits your ability to give your informed consent.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Stay Informed with LGBTQ+ health content.
Receive trusted health information and answers to your questions about sexual orientation, gender identity, transition, self-expression, and LGBTQ+ health topics. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing to our LGBTQ+ newsletter.
You will receive the first newsletter in your inbox shortly. This will include exclusive health content about the LGBTQ+ community from Mayo Clinic.
If you don't receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Research has found that feminizing hormone therapy can be safe and effective when delivered by a health care provider with expertise in transgender care. Talk to your health care provider about questions or concerns you have regarding the changes that will happen in your body as a result of feminizing hormone therapy.
Complications can include:
- Blood clots in a deep vein or in the lungs
- Heart problems
- High levels of triglycerides, a type of fat, in the blood
- High levels of potassium in the blood
- High levels of the hormone prolactin in the blood
- Nipple discharge
- Weight gain
- Infertility
- High blood pressure
- Type 2 diabetes
Evidence suggests that people who take feminizing hormone therapy may have an increased risk of breast cancer when compared to cisgender men — men whose gender identity aligns with societal norms related to their sex assigned at birth. But the risk is not greater than that of cisgender women.
To minimize risk, the goal for people taking feminizing hormone therapy is to keep hormone levels in the range that's typical for cisgender women.
Feminizing hormone therapy might limit your fertility. If possible, it's best to make decisions about fertility before starting treatment. The risk of permanent infertility increases with long-term use of hormones. That is particularly true for those who start hormone therapy before puberty begins. Even after stopping hormone therapy, your testicles might not recover enough to ensure conception without infertility treatment.
If you want to have biological children, talk to your health care provider about freezing your sperm before you start feminizing hormone therapy. That procedure is called sperm cryopreservation.
How you prepare
Before you start feminizing hormone therapy, your health care provider assesses your health. This helps address any medical conditions that might affect your treatment. The evaluation may include:
- A review of your personal and family medical history.
- A physical exam.
- A review of your vaccinations.
- Screening tests for some conditions and diseases.
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections.
- Discussion about sperm freezing and fertility.
You also might have a behavioral health evaluation by a provider with expertise in transgender health. The evaluation may assess:
- Gender identity.
- Gender dysphoria.
- Mental health concerns.
- Sexual health concerns.
- The impact of gender identity at work, at school, at home and in social settings.
- Risky behaviors, such as substance use or use of unapproved silicone injections, hormone therapy or supplements.
- Support from family, friends and caregivers.
- Your goals and expectations of treatment.
- Care planning and follow-up care.
People younger than age 18, along with a parent or guardian, should see a medical care provider and a behavioral health provider with expertise in pediatric transgender health to discuss the risks and benefits of hormone therapy and gender transitioning in that age group.
What you can expect
You should start feminizing hormone therapy only after you've had a discussion of the risks and benefits as well as treatment alternatives with a health care provider who has expertise in transgender care. Make sure you understand what will happen and get answers to any questions you may have before you begin hormone therapy.
Feminizing hormone therapy typically begins by taking the medicine spironolactone (Aldactone). It blocks male sex hormone receptors — also called androgen receptors. This lowers the amount of testosterone the body makes.
About 4 to 8 weeks after you start taking spironolactone, you begin taking estrogen. This also lowers the amount of testosterone the body makes. And it triggers physical changes in the body that are caused by female hormones during puberty.
Estrogen can be taken several ways. They include a pill and a shot. There also are several forms of estrogen that are applied to the skin, including a cream, gel, spray and patch.
It is best not to take estrogen as a pill if you have a personal or family history of blood clots in a deep vein or in the lungs, a condition called venous thrombosis.
Another choice for feminizing hormone therapy is to take gonadotropin-releasing hormone (Gn-RH) analogs. They lower the amount of testosterone your body makes and might allow you to take lower doses of estrogen without the use of spironolactone. The disadvantage is that Gn-RH analogs usually are more expensive.
After you begin feminizing hormone therapy, you'll notice the following changes in your body over time:
- Fewer erections and a decrease in ejaculation. This will begin 1 to 3 months after treatment starts. The full effect will happen within 3 to 6 months.
- Less interest in sex. This also is called decreased libido. It will begin 1 to 3 months after you start treatment. You'll see the full effect within 1 to 2 years.
- Slower scalp hair loss. This will begin 1 to 3 months after treatment begins. The full effect will happen within 1 to 2 years.
- Breast development. This begins 3 to 6 months after treatment starts. The full effect happens within 2 to 3 years.
- Softer, less oily skin. This will begin 3 to 6 months after treatment starts. That's also when the full effect will happen.
- Smaller testicles. This also is called testicular atrophy. It begins 3 to 6 months after the start of treatment. You'll see the full effect within 2 to 3 years.
- Less muscle mass. This will begin 3 to 6 months after treatment starts. You'll see the full effect within 1 to 2 years.
- More body fat. This will begin 3 to 6 months after treatment starts. The full effect will happen within 2 to 5 years.
- Less facial and body hair growth. This will begin 6 to 12 months after treatment starts. The full effect happens within three years.
Some of the physical changes caused by feminizing hormone therapy can be reversed if you stop taking it. Others, such as breast development, cannot be reversed.
While on feminizing hormone therapy, you meet regularly with your health care provider to:
- Keep track of your physical changes.
- Monitor your hormone levels. Over time, your hormone dose may need to change to ensure you are taking the lowest dose necessary to get the physical effects that you want.
- Have blood tests to check for changes in your cholesterol, blood sugar, blood count, liver enzymes and electrolytes that could be caused by hormone therapy.
- Monitor your behavioral health.
You also need routine preventive care. Depending on your situation, this may include:
- Breast cancer screening. This should be done according to breast cancer screening recommendations for cisgender women your age.
- Prostate cancer screening. This should be done according to prostate cancer screening recommendations for cisgender men your age.
- Monitoring bone health. You should have bone density assessment according to the recommendations for cisgender women your age. You may need to take calcium and vitamin D supplements for bone health.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing hormone therapy care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/contents/search. Accessed Oct. 10, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Oct. 10, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming hormone therapy (adult). Mayo Clinic; 2022.
- Nippoldt TB (expert opinion). Mayo Clinic. Sept. 29, 2022.
- Gender dysphoria
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
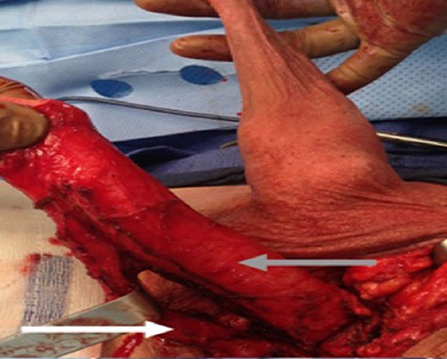
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
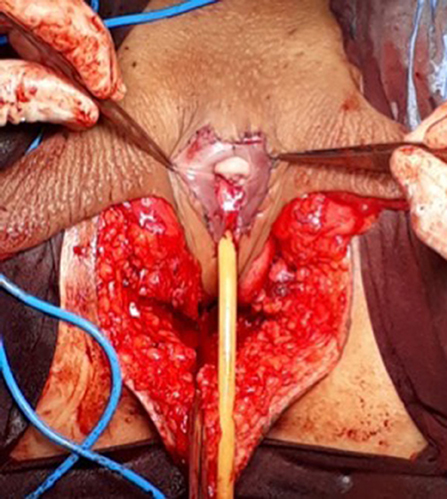
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
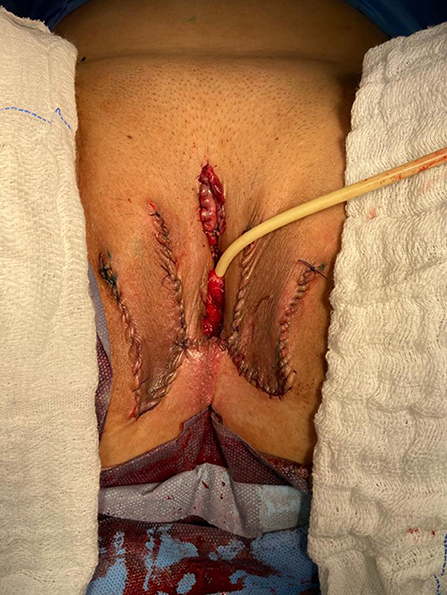
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
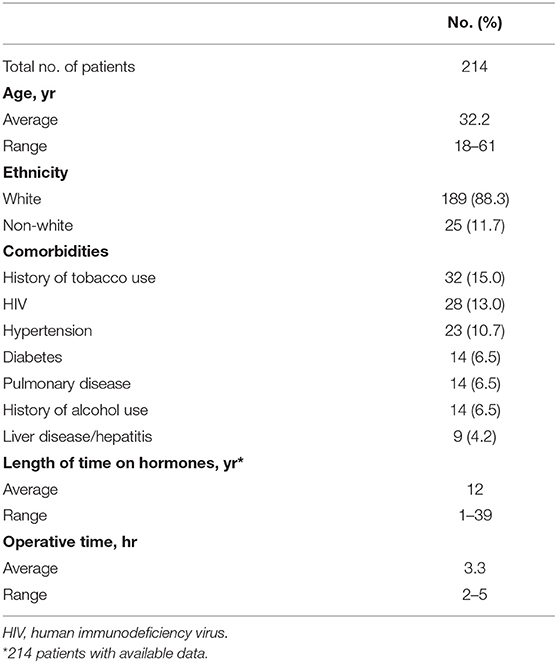
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
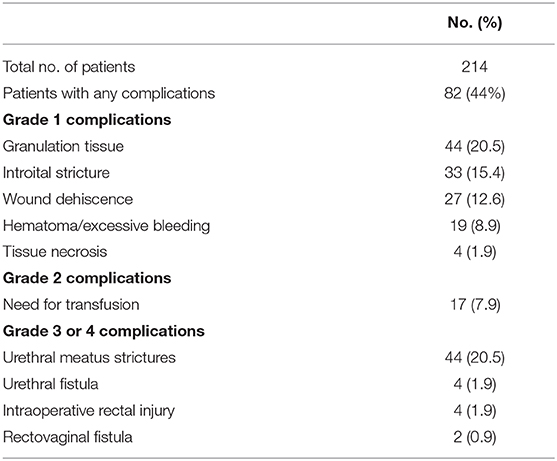
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
Long-term Outcomes After Gender-Affirming Surgery: 40-Year Follow-up Study
Affiliations.
- 1 From the Department of Plastic and Reconstructive Surgery.
- 2 School of Medicine.
- 3 Department of Obstetrics and Gynecology.
- 4 Department of Urology.
- 5 Department of Psychiatry and Neurobehavioral Sciences, University of Virginia, Charlottesville, VA.
- PMID: 36149983
- DOI: 10.1097/SAP.0000000000003233
Background: Gender dysphoria is a condition that often leads to significant patient morbidity and mortality. Although gender-affirming surgery (GAS) has been offered for more than half a century with clear significant short-term improvement in patient well-being, few studies have evaluated the long-term durability of these outcomes.
Methods: Chart review identified 97 patients who were seen for gender dysphoria at a tertiary care center from 1970 to 1990 with comprehensive preoperative evaluations. These evaluations were used to generate a matched follow-up survey regarding their GAS, appearance, and mental/social health for standardized outcome measures. Of 97 patients, 15 agreed to participate in the phone interview and survey. Preoperative and postoperative body congruency score, mental health status, surgical outcomes, and patient satisfaction were compared.
Results: Both transmasculine and transfeminine groups were more satisfied with their body postoperatively with significantly less dysphoria. Body congruency score for chest, body hair, and voice improved significantly in 40 years' postoperative settings, with average scores ranging from 84.2 to 96.2. Body congruency scores for genitals ranged from 67.5 to 79 with free flap phalloplasty showing highest scores. Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria.
Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being. High patient satisfaction, improved dysphoria, and reduced mental health comorbidities persist decades after GAS without any reported patient regret.
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
- Follow-Up Studies
- Gender Dysphoria* / surgery
- Sex Reassignment Surgery*
- Transgender Persons* / psychology
- Transsexualism* / psychology
- FIND A PROVIDER
I'm a Candidate
I'm a Provider
Log In / Sign Up
I'm a candidate
Provider login
I'm a provider
List your practice
FTM Gender Confirmation: Genital Construction
The specifics, the takeaway.
Download the app
As part of a transgender individual’s transition, genital reassignment surgery alters female genitalia into male genitalia.
Written By: Erin Storm, PA-C
Published: October 07, 2021
Last updated: February 18, 2022
- Procedure Overview
- Ideal Candidate
- Side Effects
- Average Cost
thumbs-up Pros
- Can Help Complete A Gender Affirmation Journey
thumbs-down Cons
- Potentially Cost Prohibitive
Invasiveness Score
Invasiveness is graded based on factors such as anesthesia practices, incisions, and recovery notes common to this procedure.
Average Recovery
Application.
Surgical Procedure
$ 50000 - $ 100000
What is a female to male (FTM) gender reassignment surgery?
Female to male (FTM) gender reassignment surgery is also known as sex reassignment surgery (SRS), genital construction, and generally as gender confirmation surgery. These plastic surgery procedures are used by transgender patients to remove and alter female genitalia into traditional male genitalia.
Plastic surgeons will usually perform a hysterectomy and salpingo-oophorectomy to remove the uterus and ovaries. A vaginoplasty or vaginectomy will close the vagina, the erectile tissue of the clitoris is released and with the mons portion of the pubic area a neo-phallus is created (phalloplasty or metoidioplasty). The labia majora then become the scrotum (scrotoplasty), bilateral testicular implants are placed, and finally the urethra is lengthened through the newly created penile tissue.
Typically gender reassignment surgery is performed as a last step in a transgender individuals transition journey. Guidelines on standards of care from The World Professional Association for Transgender Health (WPATH) state candidates must have letters of recommendation from their mental health professional and healthcare provider, have been living full time as a man for one year, and have completed one year of hormonal therapy to be eligible.
Information on facial masculinization surgeries, top surgeries (like a mastectomy), and other female to male gender affirming surgeries as part of a gender transition for transmen can be found in our comprehensive guide to FTM gender affirmation solutions .
What concerns does a FTM gender reassignment surgery treat?
- Transmasculine Bottom Surgery & Genital Construction : Female to male gender reassignment surgery creates male genitalia that are aesthetically authentic and functional.
Who is the ideal candidate for a FTM gender reassignment surgery?
The ideal candidate for FTM gender reassignment surgery is a transgender man seeking to complete his physical embodiment of his gender identity. This reconstructive genital surgery creates functioning male genitalia. FTM gender reassignment surgery is not recommended for those who have not been on hormone therapy for one year, have not been living full time as a man for one year, do not have letters of recommendation from their mental health provider and physician, children under the age of 18, and those with certain chronic medical conditions.
What is the average recovery associated with a FTM gender reassignment surgery?
Most patients experience four to six weeks of recovery time following a FTM gender reassignment surgery. Patients can expect bruising, swelling, and tenderness following the procedure. A urinary catheter is typically used for two to three weeks.
What are the potential side effects of a FTM gender reassignment surgery?
Possible side effects following a FTM gender reassignment surgery include bleeding, swelling, bruising, incision site infection, altered sensation, difficulty urinating due to strictures, difficulty with sexual function, prolonged edema, and complications from anesthesia or the procedure.
What can someone expect from the results of a FTM gender reassignment surgery?
The results of FTM gender reassignment surgery are permanent. This procedure creates functional male genitalia and removes all female genitalia.
What is the average cost of a FTM gender reassignment surgery?
What to expect.
A FTM gender reassignment surgery creates male genitalia. Here is a quick guide for what to expect before, during, and after a FTM gender reassignment surgery:
Before Surgery
- Prophylactic antibiotics or antivirals may be prescribed
- Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol, Aspirin, and prescription anticoagulants
- Stop smoking four weeks prior to the procedure and continue cessation for four weeks post op
- No alcohol two days prior to the procedure
- Do not eat or drink six hours before
During Surgery
- General anesthesia
- A hysterectomy, oophorectomy, and vaginoplasty are performed
- The clitoris is released from suspensory ligaments
- The neo-phallus and scrotum are created with existing tissues
- Testicular implants are placed - The urethra is lengthened

Immediately After Surgery
- Swelling, bruising, and tenderness
1 - 30 Days After Treatment & Beyond
- Resume most activities after a few days
- Swelling typically resolves within a few weeks
- Avoid strenuous activity for two to four weeks
- Remove urinary catheter after two to three weeks
Result Notes
- Results are permanent
- Proper aftercare will ensure optimal results
- Any revisions needed are typically not performed until six months after the initial procedure
Gender confirmation surgeries for transgender individuals are an important component of transgender health and in creating an embodied gender identity. Gender reassignment surgery allows transgender men who feel it is a part of their transition to more fully embrace their gender identity.
To learn more about our content creation practices, visit our Editorial Process page .
Source List
AEDIT uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- American Society of Plastic Surgeons Gender Confirmation Surgeries plasticsurgery.org
- Karel E Y Claes Chest Surgery for Transgender and Gender Nonconforming Individuals PubMed.gov ; 2018-07-02
Related Procedures

FTM Gender Confirmation Solutions

Adam’s Apple Enhancement

FTM Gender Confirmation: Facial Masculinization

FTM Gender Confirmation: Transmasculine Top & Bottom Surgeries
View all procedures
Learn More About FTM Gender Confirmation: Genital Construction in The AEDITION

Gender Transitioning And Skincare: Taking Care Of Your Changing Face
Side effects of hormone therapy often show up on the skin in the form of acne, pigmentation, and uneven skin texture. Here’s what you need to know about the most common skin concerns and treatment options.

Everything You Need To Know About Clavicle Surgery
Clavicle (a.k.a. collarbone) surgery is growing in popularity among patients seeking to change the length and prominence of the bone, enhance their décolleté, and improve the overall proportion of the body.

Finding The Right Plastic Surgeon, Dermatologist, Or Cosmetic Dentist
When considering a cosmetic procedure, it is so important to find the right doctor for you.
Discover more articles

‘Try on’ aesthetic procedures and instantly visualize possible results with AEDIT and our patented 3D aesthetic simulator.
Find Top Aesthetic Providers Near You
Providers by locations.
- Alpharetta, GA Providers
- Chevy Chase, MD Providers
- Fall River, MA Providers
- Glenview, IL Providers
- Lone Tree, CO Providers
- Metairie, LA Providers
- Minneapolis, MN Providers
- More Locations
- New Haven, CT Providers
- San Diego, CA Providers
- Scottsdale, AZ Providers
- Southfield, MI Providers
- Springdale, AR Providers
- Washington, DC Providers
- Winter Park, FL Providers
Providers by Specialties
- Cosmetic Dentistry Providers
- Cosmetic Dermatology Providers
- Cosmetic Surgery Providers
- Dermatologic Surgery Providers
- Dermatology Providers
- Facial Plastic and Reconstructive Surgery Providers
- General Surgery Providers
- Hair Restoration Surgery Providers
- Head and Neck Surgery Providers
- Medspa Providers
- More Procedures
- Oculoplastic Surgery Providers
- Plastic and Reconstructive Surgery Providers
- Vaginal Rejuvenation Providers
Providers by Procedures
- Acne Scar Treatment Providers
- Acne Treatment Providers
- Birthmark Removal Providers
- Blepharoplasty Providers
- Botox Providers
- Brow Lift Providers
- Buccal Fat Removal (Cheek Reduction) Providers
- Cheek Augmentation (Cheek Implants) Providers
- Cheek Surgery Providers
- Chemical Peels Providers
- Chin Surgery (Mentoplasty) Providers
- Dental Treatments Providers
- Dermabrasion Treatment Providers
- Dermal Fillers & Injectables Providers
- More Specialties
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Metabol Open
- v.13; 2022 Mar
The effects of gender-affirming hormone therapy on cardiovascular and skeletal health: A literature review
Nyein chan swe.
a Department of Cardiology, Cardiovascular Prevention, Lenox Hill Hospital, 110 East 59th Street, Suite 8A, New York, NY, 10022, USA
Samihah Ahmed
b Division of Endocrinology, Lenox Hill Hospital, 110 East 59th Street, Suite 8B, New York, NY, 10022, USA
Leonid Poretsky
c Department of Medicine, Lenox Hill Hospital, 110 East 59th Street, Suite 8B, New York, NY, 10022, USA
d Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, 110 East 59th Street, Suite 8B, New York, NY, 10022, USA
e Feinstein Institutes for Medical Research, 110 East 59th Street, Suite 8B, New York, NY, 10022, USA
Eugenia Gianos
f Zucker School and Medicine, 110 East 59th Street, Suite 8A, New York, NY, 10022, USA
g Cardiovascular Prevention, Northwell Health, 110 East 59th Street, Suite 8A, New York, NY, 10022, USA
h Western Region, Katz Institute Women's Heart Program, 110 East 59th Street, Suite 8A, New York, NY, 10022, USA
i Women's Heart Program, Lenox Hill Hospital, 110 East 59th Street, Suite 8A, New York, NY, 10022, USA
Natalie E. Cusano
j Zucker School of Medicine at Hofstra/Northwell, 110 East 59th Street, Suite 8B, New York, NY, 10022, USA
k Bone Metabolism Program, Lenox Hill Hospital, 110 East 59th Street, Suite 8B, New York, NY, 10022, USA
Approximately 1.5 million people in the United States currently identify as transgender. The use of gender affirming hormone therapy is integral to routine clinical care of transgender individuals, yet our understanding of the effects of this therapy is limited. There are reasons to believe that gender affirming hormone therapy may have important effects on cardiovascular risk and bone health in transgender individuals. The purpose of this review article is to summarize the evidence for the cardiovascular effects (including coronary artery disease, hypertension and stroke) as well as the effects on bone metabolism associated with gender affirming hormone therapy in both transgender men and transgender women.
1. Introduction
Approximately 1.5 million adults in the United States (0.6% of the population in 2016) identify as transgender, with 99.5% of these individuals younger than 65 years [ 1 ]. Transgender persons are a diverse group whose gender identity differs from the sex assigned at birth [ 2 ]. Some transgender persons undergo medical treatment which includes gender-affirming hormone therapy (GAHT) and/or surgery to align their physical characteristics with their gender identity and to alleviate gender dysphoria. GAHT is provided in order to induce feminizing or masculinizing changes [ 2 ].
The prevalence of transgender population in the United States has been increasing. This is likely due to the fact that transgender individuals are now more likely to identify as such in demographics surveys [ 3 ]. Understanding the terminology used to describe transgender individuals ( Table 1 ) and the commonly used hormone therapies ( Table 2 ) is essential to improve care for this population. Awareness of the potential side effects of GAHT is needed to make informed decisions and to individualize GAHT. This article reviews the available evidence regarding the effects of GAHT on the cardiovascular and skeletal health in the transgender population.
Definitions of terms [ 2 , 53 ].
Gender-affirming hormone therapy (GAHT) used in transgender persons [ 32 , 42 ].
Abbreviations: GnRH, Gonadotropin releasing hormone, IM, intramuscularly; SC, subcutaneously; TD, transdermal.
*Not available in the US, Cyproterone acetate is also an anti-androgen.
In transgender women, estrogen is often used together with either anti-androgen or GnRH analog.
1.1. Research methodology
We searched online electronic databases (Embase, Medline Cochrane Library, Google Scholar and Pubmed) to identify all relevant studies from 1990 until 2022. We used keywords such as “transgender”, “gender”, “gender dysphoria”, “cisgender”, “sex assigned at birth”, “natal sex”, “gender affirming therapy”, “gender affirming surgery”, “cardiovascular”, “cardiovascular disease”, “myocardial infarction”, “stroke”, “cerebrovascular disease”, “cardiometabolic”, “diabetes”, “lipid”, “cholesterol”, “dyslipidemia”, “body fat”, “visceral fat”, “pulmonary embolism”, “venous thromboembolism”, “bone mineral density”, “bone health” in order to screen studies that included gender affirming therapy effects on our desired outcome.
Retrospective studies, prospective studies, observational studies, systematic reviews, meta-analyses and randomized trials were all included when applicable.
A total of 150 articles were screened. 53 articles were retained based on the outcomes related to our review.
2. Cardiovascular health
2.1. transgender women, 2.1.1. ischemic heart disease.
Two early observational studies reported that the crude incidence of myocardial infarction and mortality related to myocardial infarction in transgender women receiving GAHT were not different from sex assigned at birth men [ 4 , 5 ]. Nokoff et al. analyzed the data from a 2015 behavioral risk factor surveillance survey (BRFSS) and found that transgender women on GAHT had a higher risk of myocardial infarction than sex assigned at birth women (OR 2.9; 95% CI 1.6–5.3) but this risk was not higher than in sex assigned at birth men (OR 1.09; 95% CI 0.59–2.03) [ 6 ]. Similar results were found by Getahun et al. in a retrospective cohort study of 2842 transgender women (mean study duration: 4 years): transgender women receiving GAHT had higher risk of ischemic heart disease than sex assigned at birth women (HR 1.9; 95% CI 1.3–2.6) but the risk was not different from that of sex assigned at birth men [ 7 ].
A case control study showed a higher prevalence of myocardial infarction in transgender women who had received GAHT for an average of 7.7 years compared with sex assigned at birth women (18.7/1000 cases vs. 0; P = 0.001), with the prevalence of myocardial infarction similar to sex assigned at birth men [ 8 ]. The incidence of myocardial infarction in transgender women on GAHT was similarly higher than in sex assigned at birth women (SIR 2.64 [95% CI 1.81–3.72]) and similar to sex assigned at birth men in a retrospective cohort [ 9 ].
Transgender women were found to have higher mortality rate due to ischemic heart disease than adjusted expected mortality of the general population (SMR 1.64; 95% CI: 1.43–1.87) in a retrospective cohort study. Transgender women treated with ethinyl estradiol had a particularly high event rate with a 3-fold increased risk of cardiovascular mortality compared with former users or never-users (HR 3.12; 95% CI 1.28–7.63) [ 10 ].
Overall, the available data indicate that transgender women on GAHT are at a higher risk of ischemic heart disease (including myocardial infarction) compared with sex assigned at birth women, however transgender women appear to have similar cardiovascular risk when compared to sex assigned at birth men.
2.1.2. Cerebrovascular disease
The incidence of cerebrovascular disease in transgender women receiving GAHT was found to be similar to sex assigned at birth men [ 4 ] and to the general population [ 5 ] in two early retrospective observational studies. In a retrospective cohort study of 966 transgender women receiving GAHT, the mortality related to cerebrovascular disease in transgender women was not statistically different from the general population [ 10 ].
In a case-control study of 214 transgender women on GAHT, the prevalence of ischemic stroke in transgender women was however higher than that in sex assigned at birth men (23.4/1000 cases vs. 9.4/1000 cases; P = 0.03), but similar to sex assigned at birth women [ 8 ].
In contrast, a subsequent retrospective cohort study (n = 2842) found that the risk of ischemic stroke in transgender women receiving GAHT was higher than that in sex assigned at birth women (HR 1.9; 95% CI 1.4–2.7) but similar to that of sex assigned at birth men (median follow up: 4 years) [ 7 ]. In the subgroup analysis, transgender women who had received GAHT for longer than 6 years (n = 853) had higher risk of ischemic stroke than both sex assigned at birth men (HR 9.9; 95% CI 3.0–33.1) and sex assigned at birth women (HR 4.1; 95% CI 1.5–11.4) indicating increased risk of stroke with prolonged exposure to hormone therapy [ 7 ]. A similar higher risk of ischemic stroke in transgender women on GAHT compared with both sex assigned at birth men (SIR 1.80 [95% CI 1.23–2.56]) and sex assigned at birth women (SIR 2.42 [95% 1.65–3.42]) was shown in another retrospective cohort of 2517 patients [ 9 ].
Overall, the available data for cerebrovascular disease are equivocal. However there seems to be an increased long-term risk of ischemic stroke in transgender women on GAHT compared to both sex assigned at birth men and women.
2.1.3. Cardiometabolic risk factors
A meta-analysis of 29 studies, which included 3231 transgender women, showed no significant differences in total cholesterol (TC), LDL-C, HDL-C or triglyceride levels (TG) in transgender women receiving GAHT at 3–6 months, 12 months or ≥ 24 months compared to baseline [ 11 ]. Serum TG level was higher than baseline after 24 months of GAHT [ 11 ]. A prospective cohort study of 30 transgender women found no significant changes in lipid profiles after 6 months of estrogen therapy compared with baseline [ 12 ].
In contrast, a prospective observational study showed that GAHT in transgender women was associated with deleterious alteration in lipid prolife: TC, TG, LDL-C increased and HDL-C decreased after 1 year and 2 years of GAHT compared with baseline [ 13 ]. The study also demonstrated alteration in glyco-insulinemic profile in transgender women with homeostatic model assessment-insulin resistance index (HOMA-IR index) of 6.57 (SD 2.69) after 2 years of GAHT compared with baseline HOMA-IR index of 3.63 (SD 0.77) [ 13 ]. A higher prevalence of diabetes was observed in transgender women receiving estrogen compared with both sex assigned at birth men and sex assigned at birth women in a case-control study [ 8 ]. While data regarding insulin resistance in transgender patients are limited, a recent systematic review of 26 studies showed that in transgender women feminizing hormone therapy (estradiol, with or without anti-androgen agents) decreases lean mass, increases fat mass, and may worsen insulin resistance. However, the data on insulin resistance are not as consistent due to paucity of randomized prospective research, small cohorts and short follow up periods. More data are needed for better and more consistent results [ 14 ]. In a recent prospective study, the cardiometabolic profile of 179 transgender women on GAHT was evaluated at 1 year. The authors found that total body fat had increased without a change in visceral fat. These changes were not associated with a change in the lipid profile or HOMA-IR index [ 15 ].
Conflicting effects of GAHT on the lipid profile of transgender women were observed in some studies. LDL-C decreased (−12%), HDL-C increased (+24%) while TG increased (+86%) and TC remained unchanged after one year of GAHT compared with baseline in an observational study of 20 transgender women (mean age 26 ± 6) 16 . Reductions in TC, LDL-C, TG, HDL-C were observed after one year of GAHT compared with baseline in a prospective cohort study of 53 transgender women [ 17 ]. A similar pattern compared to baseline was seen in another cohort study of 242 transgender women after one year of GAHT [ 18 ].
In summary, the existing literature related to dyslipidemia and cardiometabolic profiles in transgender women is mixed and it is difficult to draw conclusions about any consistent effects of estrogen therapy on lipid profile in transgender women. While data on total cholesterol, LDL-C and insulin resistance are equivocal, there seems to be consistent evidence for the increase in TG levels and total body fat.
2.1.4. Blood pressure
The incidence of hypertension (defined then as BP > 160/90 mmHg) in transgender women receiving GAHT was shown to be similar to sex assigned at birth men (crude incidence 14 [95% CI 7.8–23.1] vs. 18.708) in a study reported in 1989 [ 4 ]. A small prospective observational study in 1993 found significantly decreased level of endothelin in transgender women after 4 months of GAHT [ 19 ]. The effect of lower endothelin level on blood pressure, however, remains unclear. Modest reduction of blood pressure was seen in transgender women receiving GAHT in multiple observational studies lasting 6 months to one year [ 17 , 18 , 20 ]. The subjects in these studies were taking various formulations of GAHT including oral estradiol valerate and transdermal estradiol.
In contrast, an observational study of 79 transgender women showed an increase in blood pressure (both systolic and diastolic) after 1 year and 2 years of GAHT compared with baseline [ 13 ]. A similar increase in blood pressure was seen in another prospective observational study of 20 transgender women [ 16 ].
In summary, evidence for the effects of GAHT on BP in transgender women remains scarce and equivocal making it difficult to draw definite conclusions.
2.1.5. Venous thromboembolism
Two early observational studies showed increased risk of VTE and pulmonary embolism in transgender women: one study showed a 45-fold increase in risk compared to sex assigned at birth men (crude incidence 19 [95% CI 11.7–29.4] vs. 0.42) [ 4 ] while another showed a 20-fold increase in risk compared to general population (SIR 19.56 [95% CI 12.27–26.18]) 5 ; all cases of VTE occurred in patients using oral ethinyl estradiol except for one patient using transdermal 17 β-estradiol in the latter study.
Similarly, a retrospective cohort study of 2842 transgender women found higher risk of VTE in transgender women receiving GAHT compared to sex assigned at birth men (HR 1.9 [95% CI 1.4–2.7]) and sex assigned at birth women (HR 2.0; 95% CI 1.4–2.8) with the highest risk seen with longer exposure to hormone therapy [ 7 ]. In a recently published retrospective observational study of 6793 transgender persons, higher incidence of VTE was seen in transgender women receiving GAHT compared with both sex assigned at birth men (SIR 4.55 [95% CI 3.59–5.69]) and sex assigned at birth women (SIR 5.52 [95% CI 4.36–6.90]) [ 9 ].
In contrast to the studies described above, no cases of VTE were detected in a retrospective cohort study of 162 transgender women who received GAHT for a mean duration of 4.4 years. Of note, all the subjects in this study received transdermal 17β-estradiol along with cyproterone acetate and finasteride rather than oral estrogen, suggesting that the increased risk of VTE with estrogen therapy applies to oral formulations [ 21 ].
In regards to progesterone in transfeminine care, it is not currently recommended by clinical guidelines for routine GAHT. This is mostly due to lack of efficacy and safety data. However, there are increasing data in favor of the use of progesterone and its derivatives in transgender women for feminization, bone health and mood disorders. Data regarding cardiovascular safety remain scarce [ 22 , 23 ].
In summary, the data for VTE in transgender women are consistent and show an increased risk of VTE and pulmonary embolism in transgender women compared to both sex assigned at birth men and women.
2.2. Transgender men
2.2.1. ischemic heart disease and cerebrovascular disease.
A retrospective observational study of 293 transgender men taking GAHT in the Netherlands found a similar incidence of myocardial infarction between transgender men and the general Dutch population over 2418 patient-years (SIR 0.34 [0.01–1.92]) [ 5 ]. Multiple observational studies have not found an increased risk of myocardial infarction or increased mortality related to myocardial infarction in transgender men receiving GAHT compared with sex assigned at birth men or sex assigned at birth women [ [6] , [7] , [8] , 10 ]. Similarly, a cohort study that followed 50 transgender men receiving testosterone (mean age 37 ± 8.2 years) for an average of 10 years (range 2–35 years) did not report any cases of myocardial infarction [ 24 ].
One cross-sectional study using population-based data (BRFSS data from 2014 to 2017) found that transgender men had a >4-fold and 2-fold increased risk of myocardial infarction compared with sex assigned at birth women (OR 4.90 [95% CI 2.21–10.90], P < 0.01) and sex assigned at birth men (OR 2.53 [95% CI 1.14–5.63], P 0.02) [ 25 ]. Information regarding specific hormone therapy was not provided in this study making it difficult to assess the factors related to this increased risk [ 25 ]. The risk and prevalence of ischemic stroke in transgender men on GAHT were also shown to be similar to those of sex assigned at birth men and sex assigned at birth women [ 7 , 8 , 10 ].
In summary, while data are scarce and not consistent, there seems to be no increased risk of cardiovascular disease, myocardial infarction or stroke in transgender men on hormone therapy.
2.2.2. Cardiometabolic risk factors
Deleterious changes in lipid profile were observed in two prospective cohorts: TC, LDL-C and TG increased and HDL-C decreased in transgender men after one year of GAHT compared with baseline values [ 17 , 18 ]. A similar pattern of changes in lipid profile was seen in transgender men in another prospective cohort study after two years of GAHT compared with baseline [ 13 ].
This unfavorable trend in lipid profile in transgender men was supported by a meta-analysis of 29 studies, which included 1500 transgender men. The authors concluded that LDL-C and TG increased and HDL-C decreased significantly while TC remained unchanged after 2 years of GAHT compared with baseline, with mixed results seen before 2 years of GAHT, indicating that longer duration of GAHT is associated with undesirable effects on lipid profile [ 11 ].
Unfavorable changes in lipid profile in transgender men receiving GAHT were fairly consistent in multiple studies despite some mixed results: a cross-sectional study of 111 transgender men showed that transgender men treated with testosterone had higher TC, TG and lower HDL-C compared with transgender men not treated with testosterone [ 26 ]; two additional prospective observational studies showed that TG increased and HDL-C decreased in transgender men after one year [ 16 ] and two years [ 27 ] of GAHT compared to baseline while TC and LDL-C remained unchanged. Another prospective study reported decreased HDL-C in transgender men after one year of GAHT with other lipid parameters unchanged [ 28 ].
The data on the risk for diabetes mellitus in transgender men are mixed. A case-control study showed increased prevalence of diabetes in transgender men receiving GAHT compared with sex assigned at birth women but it was not different from sex assigned at birth men [ 8 ]. Conversely, HOMA-IR in transgender men was not different from baseline after one year and two years of GAHT in a prospective observational study [ 13 ]. HbA1c was similar in transgender men treated with GAHT and those not treated with GAHT in a cross-sectional study [ 26 ]. In a recent prospective study, the cardiometabolic factors of 162 transgender men was evaluated before and after 1 year of GAHT. The authors found that total body fat decreased without changes in visceral fat. Those changes were not related to changes in blood lipids or HOMA-IR index [ 15 ]. The investigators concluded that cardiometabolic effects of GAHT are not related to changes in visceral fat and total body fat.
In summary, GAHT seems to increase LDL-C, TGL and decease HDL-C in transgender men. Some studies indicate that these changes are more pronounced after 2 years of therapy.
2.2.3. Blood pressure
Two observational studies published in 1989 and 1997 did not find an increased incidence of hypertension (defined then as blood pressure >160/95 mmHg and >160/90 mmHg) respectively in transgender men receiving GAHT compared with the general population [ 4 , 5 ]. Chandra et al. also found no changes in mean arterial blood pressure in a prospective cohort study of 12 transgender men after one year of GAHT [ 28 ]. Giltay et al. demonstrated a slightly decreased blood pressure in transgender men after 3–4 months of GAHT in an observational study [ 29 ].
In contrast, a cross-sectional study of 111 transgender men (48 on IM testosterone esters and 63 not on any hormone therapy) showed that transgender men treated with androgens had significantly higher blood pressure (systolic, diastolic, and mean arterial pressure) than those who were not treated over mean study duration of 45 ± 38.1 months [ 26 ]. A variable increase in systolic blood pressure (+4.1–13.4 mmHg) was seen in transgender men after receiving GAHT for 1–2 years compared with baseline across observational studies ranging in sample size from 43 to 50 individuals [ 13 , 17 , 27 ].
In summary, data on blood pressure in changes in transgender men on GAHT remain controversial and it is thus difficult to draw definite conclusions without better data. Table 3 summarizes the effect of GAHT on the cardiovascular risk and different cardiometabolic parameters in transgender men and women.
The effect of GAHT on the cardiovascular health in transgender women and men.
Abbreviation: LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
↑ denotes a significant increase.
↓ denotes a significant decrease.
↔︎ denotes no significant change.
∴ denotes inconclusive results.
Table format adapted from Connelly PJ et al. Hypertension.2019 [ 53 ].
3. Skeletal health
Bone strength, which determines fracture risk, reflects the integration of bone density and bone quality. Dual energy X-ray absorptiometry (DXA), a noninvasive measurement of bone density, is the current standard of care to diagnose osteoporosis and to assess fracture risk [ 30 ]. Bone quality assessment involves macro- and microarchitectural characteristics of bone tissue and can be conducted invasively (using a bone biopsy), or noninvasively (using a program to measure the trabecular bone score, a marker of variation obtained from the lumbar spine bone density image).
Sex steroids are major determinants of bone homeostasis. Estrogen plays a significant role in bone remodeling [ 31 ]. A deficiency in estrogen is associated with increased bone resorption, increased bone loss, and increased fracture risk in the general population. Testosterone plays an important role in bone gain and maintenance in sex assigned at birth men, and testosterone deficiency is associated with increased bone resorption, bone loss, and fracture risk.
There are currently no estimates on the prevalence of osteoporosis or low bone mass in transgender persons. Screening for osteoporosis in transgender individuals should be performed with DXA similar to the general population according to the Endocrine Society Clinical Practice Guidelines [ 32 ]. Risk factors to be assessed to determine the need for DXA screening include age, medical conditions and or medications that increase the risk of osteoporosis [ 33 ]. The T-score represents the number of standard deviations above or below the average bone density of a young healthy Caucasian sex assigned at birth woman. The T-score establishes fracture risk and the need for further treatment and lifestyle modifications.
A recent study evaluating BMD in pre-pubertal transgender youth showed decreased BMD in the transgender group compared to their sex assigned at birth counterparts, suggesting the need for BMD surveillance at an even earlier stage [ 34 ].
There are limited data on the long-term risks of GAHT on skeletal health. Most of the studies in transgender individuals have been cross-sectional or retrospective, with very few prospective or longitudinal studies and data prior to 2019 were summarized in 2 large meta-analyses. Below we provide a review of those two meta-analyses.
A systematic review and meta-analysis 35,36 of the effects of gender affirming hormone therapy on bone mass in transgender individuals were performed in 2017 [ 35 ] and later updated in 2019 [ 36 ]. A single study has been performed using trabecular bone score in transgender individuals [ 37 ]. The 2017 systematic review and meta-analysis examined 13 studies published from 1980 to 2015. 35 The outcomes of interest were bone mineral density and the incidence of fractures. 392 transgender women and 247 transgender men were identified. The updated 2019 systematic review and meta-analysis selected 19 studies published before August 2018. The quality of the studies was assessed by the National Institutes of Health scale to be fair and/or good. 812 transgender women and 487 transgender men were identified. A list of individual studies is shown in Table 4 .
Studies included in the 2017 and 2019 Meta-analyses of Studies Examining Skeletal Health in Transgender Individuals.
Abbreviations: mos, months; yrs, years.
Adapted and expanded from Singh-Ospina N et al. J Clin Endocrinol Metab. 2017 [ 35 ].
The study on trabecular bone score reviewed patient data from the American University Medical Center in the Netherlands from 1972 to 2016. DXA scan results along with additional clinical data corresponding to bone health were retrieved. The trabecular bone score was calculated based on lumbar spine DXA imaging. 535 transgender women and 473 transgender men were included.
3.1. Transgender women
In both meta-analyses, transgender women showed an increase in bone mineral density in the lumbar region at 12 and 24 months. Fracture rates were only evaluated in a single cohort study with no reported events in either gender. The trabecular bone scores (TBS) in transgender women regardless of age, were found to be higher compared to baseline (+0.04, 95%CI + 0.00; +0.08). TBS, calculated from the lumbar region of the DXA scan, in both meta-analyses had an associated increase in bone mineral density.
3.2. Transgender men
In both meta-analyses transgender men showed no statistically significant changes in bone mineral density in the lumbar spine, femoral neck, or total hip at 12 or 24 months. Most transgender men received IM preparations of testosterone, and some received transdermal or oral androgens. All patients had a baseline DXA scan prior to initiation of GAHT. Among the transgender men less than 40 years of age, TBS tended to be lower in those who used GAHT compared to the baseline groups. For transgender men greater than 40 years of age, TBS was lower in those using 5 years GAHT versus baseline (−0.05, 95%CI −0.08; −0.01) [ 37 ]. Although there was evidence of a decrease, the score remained above 1.3, which is in normal architectural range. There was no obvious increase in fracture risk.
In summary, the available data show that in transgender women, GAHT increases bone mineral density and TBS. In transgender men, there was a decrease in TBS which nevertheless remained above 1.3, still in normal architectural range. There was no increase in fracture risk in both populations. Those results are also summarized in Table 5 .
The effects of GAHT on Skeletal health in transgender women and men.
Abbreviation: GAHT, gender affirming hormone therapy; BMD, bone mineral density; TBS, trabecular bone score.
^ TBS decreases but is still within normal range.
4. Discussion
GAHT is a collective term that encompasses androgen and estrogen therapy in different formulations and routes of administration along with other endocrine therapies. The inconsistent and conflicting results found in the current literature can be explained by the highly heterogenous GAHT used in different studies as well as lack of information on lifestyle and psychosocial aspects of the included transgender individuals.
Transgender women appear to have higher risk of myocardial infarction than sex assigned at birth women but not sex assigned at birth men and higher risk of ischemic stroke than both sex assigned at birth men and sex assigned at birth women. It is unclear if the increase in cardiovascular morbidity and mortality in transgender women is due to alterations in cardiovascular risk factors or a direct effect of GAHT. The current literature, however, has not shown a consistent undesirable alteration in conventional cardiovascular risk factors (i.e., hypertension, hyperlipidemia, and diabetes) in transgender women receiving GAHT.
Administration of GAHT to transgender women suppresses the natal androgens resulting in reduced testosterone levels in transgender women compared with sex assigned at birth men. Sex assigned at birth men with low testosterone levels have a high prevalence of cardiovascular disease [ 38 , 39 ] and low baseline testosterone levels are inversely related to cardiovascular mortality in sex assigned at birth men [ 40 ]. Suppressed testosterone levels in transgender women along with the greater plaque burden of the natal gender [ 41 ] might be one of the mechanisms responsible for the increased cardiovascular morbidity and mortality in this population.
GAHT is associated with increased risk of VTE in transgender women. Oral ethinyl estradiol is now less commonly prescribed due to this recognized higher risk, with micronized estradiol and estradiol valerate now the preferred forms of oral estrogen [ 42 ]. To the best of our knowledge, no study had demonstrated increased risk of VTE in transgender men receiving GAHT.
Alteration in the lipid profile, particularly an increase in TG and a decrease in HDL-C, was found to be fairly consistent in transgender men receiving GAHT along with mixed results for TC and LDL-C. Blood pressure was also found to be elevated in some studies although there are conflicting results. The evidence of elevated cardiovascular risk in transgender men is limited. .
It is important to note that transgender men initiate GAHT at ages younger than transgender women. The individuals in the current studies are relatively young and reported study durations are too short to detect cardiovascular events in the primary prevention setting. A prospective study of longer duration or a registry that collects data on lifestyle and psychosocial history would be ideal to assess the cardiovascular effects of GAHT in transgender individuals. Addition of “gender identity” variable to the national health registry may also help assess long-term cardiovascular and metabolic risk in this population [ 43 ].
Transgender individuals experience stress due to minority identity, self-stigma, and discrimination [ 44 ] and may be more likely to smoke tobacco, drink alcohol and be less physically active compared with cisgender population [ 43 ]. A study has also shown that transgender patients are more likely to suffer from drug use disorder, with the highest risk seen with amphetamine (aOR 2.22, 95% CI 1.82–2.70), but also cocaine (aOR 1.59, 95% CI 1.29–1.95), and cannabis (aOR 1.82, 95% CI 1.62–2.05) [ 45 ]. Transgender individuals are also more likely to have poor mental health [ 46 ]. There is evidence that mental health improves in both transgender men and transgender women after gender affirming therapy, including surgery although not necessarily with GAHT [ 47 ].
Additional evidence documents a link between discrimination and cardiovascular health indexes (e.g., tobacco use, hypertension, and obesity) in this stigmatized population [ 48 , 49 ].
Fracture risk in transgender individuals remains uncertain. Estrogen therapy has a positive correlation with TBS and bone mineral density in the lumbar region of transgender women but not elsewhere. Testosterone therapy produces no significant changes in bone mineral density in transgender men. The decrease in the trabecular bone score in transgender men had no significant association with fracture risk since TBS remained in the normal range. The studies conducted so far have been mainly retrospective and of short duration. The average age of the patients was young (20–30 years), and they were followed for about 12–24 months ( Table 4 ). The analysis of additional factors that affect bone health such as smoking, physical activity and vitamin D status was limited. There are limited fracture data.
Further prospective and longitudinal studies are necessary to obtain useful data to assess risk of osteoporosis in the transgender population. Additional factors that can affect bone mineral density need to be assessed. Bone mineral density as considered in the studies and practice is compared to natal reference ranges. With further research, guidelines with reference values for bone mineral density should be established for transgender individuals.
5. Conclusion
Current limited evidence from non-randomized studies suggests that transgender women taking GAHT have increased risks of myocardial infarction, ischemic stroke and VTE. The current evidence does not indicate increased cardiovascular risk in transgender men receiving GAHT. Estrogen therapy has a positive correlation with trabecular bone score and bone mineral density in the lumbar region of transgender women but not elsewhere. The literature should be interpreted with caution due to the risk of bias in these studies.
The evidence shows that GAHT decreases or resolves gender dysphoria in transgender individuals and improves their quality of life [ 50 , 51 ]. Awareness of the potential risk of GAHT by clinicians can help transgender individuals make better informed decisions and can guide clinicians towards early intervention to prevent adverse cardiovascular outcomes. Transgender individuals receiving GAHT should be monitored for conventional cardiovascular risk factors and managed according to current guidelines with lifestyle programs and optimal preventive medical therapy [ 52 ]. The psychological well-being of transgender individuals should also be addressed with referral to mental health professionals as needed. Prospective randomized controlled studies are needed to elucidate the mechanisms and effects on GAHT on cardiovascular and skeletal health.
Declaration of competing interest
The authors disclose no conflict of interest related to this manuscript. This work was supported by the Empire Clinical Research Investigator Program (ECRIP) from the New York State Department of Health.
Treatment - Gender dysphoria
Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary.
What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
Treatment for children and young people
If your child may have gender dysphoria, they'll usually be referred to one of the NHS Children and Young People's Gender Services .
Your child or teenager will be seen by a multidisciplinary team including a:
- clinical psychologist
- child psychotherapist
- child and adolescent psychiatrist
- family therapist
- social worker
The team will carry out a detailed assessment, usually over 3 to 6 appointments over a period of several months.
Depending on the results of the assessment, options for children and teenagers include:
- family therapy
- individual child psychotherapy
- parental support or counselling
- group work for young people and their parents
- regular reviews to monitor gender identity development
- referral to a local Children and Young People's Mental Health Service (CYPMHS) for more serious emotional issues
Most treatments offered at this stage are psychological rather than medical. This is because in many cases gender variant behaviour or feelings disappear as children reach puberty.
Hormone therapy in children and young people
Some young people with lasting signs of gender dysphoria who meet strict criteria may be referred to a hormone specialist (consultant endocrinologist). This is in addition to psychological support.
Puberty blockers and gender-affirming hormones
Puberty blockers (gonadotrophin-releasing hormone analogues) are not available to children and young people for gender incongruence or gender dysphoria because there is not enough evidence of safety and clinical effectiveness.
From around the age of 16, young people with a diagnosis of gender incongruence or gender dysphoria who meet various clinical criteria may be given gender-affirming hormones alongside psychosocial and psychological support.
These hormones cause some irreversible changes, such as:
- breast development (caused by taking oestrogen)
- breaking or deepening of the voice (caused by taking testosterone)
Long-term gender-affirming hormone treatment may cause temporary or even permanent infertility.
However, as gender-affirming hormones affect people differently, they should not be considered a reliable form of contraception.
There is some uncertainty about the risks of long-term gender-affirming hormone treatment.
Children, young people and their families are strongly discouraged from getting puberty blockers or gender-affirming hormones from unregulated sources or online providers that are not regulated by UK regulatory bodies.
Transition to adult gender identity services
Young people aged 17 or older may be seen in an adult gender identity clinic or be referred to one from a children and young people's gender service.
By this age, a teenager and the clinic team may be more confident about confirming a diagnosis of gender dysphoria. If desired, steps can be taken to more permanent treatments that fit with the chosen gender identity or as non-binary.
Treatment for adults
Adults who think they may have gender dysphoria should be referred to a gender dysphoria clinic (GDC).
Find an NHS gender dysphoria clinic in England .
GDCs have a multidisciplinary team of healthcare professionals, who offer ongoing assessments, treatments, support and advice, including:
- psychological support, such as counselling
- cross-sex hormone therapy
- speech and language therapy (voice therapy) to help you sound more typical of your gender identity
For some people, support and advice from the clinic are all they need to feel comfortable with their gender identity. Others will need more extensive treatment.
Hormone therapy for adults
The aim of hormone therapy is to make you more comfortable with yourself, both in terms of physical appearance and how you feel. The hormones usually need to be taken for the rest of your life, even if you have gender surgery.
It's important to remember that hormone therapy is only one of the treatments for gender dysphoria. Others include voice therapy and psychological support. The decision to have hormone therapy will be taken after a discussion between you and your clinic team.
In general, people wanting masculinisation usually take testosterone and people after feminisation usually take oestrogen.
Both usually have the additional effect of suppressing the release of "unwanted" hormones from the testes or ovaries.
Whatever hormone therapy is used, it can take several months for hormone therapy to be effective, which can be frustrating.
It's also important to remember what it cannot change, such as your height or how wide or narrow your shoulders are.
The effectiveness of hormone therapy is also limited by factors unique to the individual (such as genetic factors) that cannot be overcome simply by adjusting the dose.
Find out how to save money on prescriptions for hormone therapy medicines with a prescription prepayment certificate .
Risks of hormone therapy
There is some uncertainty about the risks of long-term cross-sex hormone treatment. The clinic will discuss these with you and the importance of regular monitoring blood tests with your GP.
The most common risks or side effects include:
- blood clots
- weight gain
- dyslipidaemia (abnormal levels of fat in the blood)
- elevated liver enzymes
- polycythaemia (high concentration of red blood cells)
- hair loss or balding (androgenic alopecia)
There are other risks if you're taking hormones bought over the internet or from unregulated sources. It's strongly recommended you avoid these.
Long-term cross-sex hormone treatment may also lead, eventually, to infertility, even if treatment is stopped.
The GP can help you with advice about gamete storage. This is the harvesting and storing of eggs or sperm for your future use.
Gamete storage is sometimes available on the NHS. It cannot be provided by the gender dysphoria clinic.
Read more about fertility preservation on the HFEA website.
Surgery for adults
Some people may decide to have surgery to permanently alter body parts associated with their biological sex.
Based on the recommendations of doctors at the gender dysphoria clinic, you will be referred to a surgeon outside the clinic who is an expert in this type of surgery.
In addition to you having socially transitioned to your preferred gender identity for at least a year before a referral is made for gender surgery, it is also advisable to:
- lose weight if you are overweight (BMI of 25 or over)
- have taken cross-sex hormones for some surgical procedures
It's also important that any long-term conditions, such as diabetes or high blood pressure, are well controlled.
Surgery for trans men
Common chest procedures for trans men (trans-masculine people) include:
- removal of both breasts (bilateral mastectomy) and associated chest reconstruction
- nipple repositioning
- dermal implant and tattoo
Gender surgery for trans men includes:
- construction of a penis (phalloplasty or metoidioplasty)
- construction of a scrotum (scrotoplasty) and testicular implants
- a penile implant
Removal of the womb (hysterectomy) and the ovaries and fallopian tubes (salpingo-oophorectomy) may also be considered.
Surgery for trans women
Gender surgery for trans women includes:
- removal of the testes (orchidectomy)
- removal of the penis (penectomy)
- construction of a vagina (vaginoplasty)
- construction of a vulva (vulvoplasty)
- construction of a clitoris (clitoroplasty)
Breast implants for trans women (trans-feminine people) are not routinely available on the NHS.
Facial feminisation surgery and hair transplants are not routinely available on the NHS.
As with all surgical procedures there can be complications. Your surgeon should discuss the risks and limitations of surgery with you before you consent to the procedure.
Life after transition
Whether you've had hormone therapy alone or combined with surgery, the aim is that you no longer have gender dysphoria and feel at ease with your identity.
Your health needs are the same as anyone else's with a few exceptions:
- you'll need lifelong monitoring of your hormone levels by your GP
- you'll still need contraception if you are sexually active and have not yet had any gender surgery
- you'll need to let your optician and dentist know if you're on hormone therapy as this may affect your treatment
- you may not be called for screening tests as you've changed your name on medical records – ask your GP to notify you for cervical and breast screening if you're a trans man with a cervix or breast tissue
- trans-feminine people with breast tissue (and registered with a GP as female) are routinely invited for breast screening from the ages of 50 up to 71
Find out more about screening for trans and non-binary people on GOV.UK.
NHS guidelines for gender dysphoria
NHS England has published what are known as service specifications that describe how clinical and medical care is offered to people with gender dysphoria:
- Non-surgical interventions for adults
- Surgical interventions for adults
- Interim service specification for specialist gender incongruence services for children and young people
Review of gender identity services
NHS England has commissioned an independent review of gender identity services for children and young people. The review will advise on any changes needed to the service specifications for children and young people.
Page last reviewed: 28 May 2020 Next review due: 28 May 2023
- Find in topic
INTRODUCTION
This topic will discuss the procedures and resultant anatomy for patients transitioning from female to male. Related topics on the care of transgender patients is presented separately.
● (See "Primary care of transgender individuals" .)
● (See "Transgender women: Evaluation and management" .)
● (See "Gender-affirming surgery: Male to female" .)
To continue reading this article, you must sign in . For more information or to purchase a personal subscription, click below on the option that best describes you:
- Medical Professional
- Resident, Fellow or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
Print Options
Advertisement
Hormone therapy in female-to-male transgender patients: searching for a lifelong balance
- Original Article
- Published: 07 October 2020
- Volume 20 , pages 151–159, ( 2021 )
Cite this article

- Luca Maria Schönauer 1 ,
- Miriam Dellino ORCID: orcid.org/0000-0003-3522-4648 2 ,
- Matteo Loverro 3 ,
- Carmine Carriero 1 ,
- Teresa Capursi 1 ,
- Claudia Leoni 4 ,
- Giuseppe Loverro 1 &
- Edoardo Di Naro 1
821 Accesses
4 Citations
2 Altmetric
Explore all metrics
Reassignment of a female-to-male (FtM) person requires gender-affirming, androgenic hormonal treatment that is planned to induce appropriate structural changes. This therapy must be prolonged long term, even after the sex reassignment surgery (SRS). The purpose of this study is to evaluate the effects of hormone therapy with testosterone in FtM subjects during a 24-month follow-up in order to highlight the occasional need for early decompensation and to make adequate hormone therapy modulations.
Fifteen out of 23 FtM persons had been previously treated with SRS, while eight were still awaiting surgery. During hormone therapy, both groups were followed for 24 months, with evaluation of desired changes, adverse effects, and functional or metabolic indicators.
In the group of operated FtM subjects (15/23), a significant increase of total testosterone (total T) and free testosterone (free T) was found after 24 months. Luteinizing hormone (LH) maintained a low level, decreasing after ovariectomy, while FSH increased. Voice deepening, facial and body hair variation, male-pattern balding, and body mass index (BMI) increase are all physical changes due to androgenization. In both groups of patients who have been closely monitored, the side effects and thromboembolic, metabolic, and cardiovascular risks of androgen therapy, even in the long term, appear to be irrelevant.
Total T, free T, and LH dosages are shown to be reliable markers of correct androgenization. Strict monitoring of lipid profile, evaluation of BMI and hematocrit, avoidance of self-initiated therapeutic modifications, adherence to a healthy lifestyle, and avoidance of excessive daily calorie intake can limit risks linked to long-term testosterone administration.
Trial registration
Retrospectively registered
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Sex Reassignment: Endocrinological Interventions in Adults with Gender Dysphoria
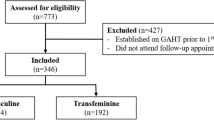
Effects of gender affirming hormone treatment in transgender individuals – a retrospective cohort study

Overview of Gender-Affirming Therapy
Irwig MS (2017) Testosterone therapy for transgender men. Lancet Diabetes Endocrinol 5:301–311
Article CAS Google Scholar
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, fifth edition DSM-5, Washington DC
Coleman E, Bockting W, Botzer M et al (2012) Standards of care for the health of transsexual, transgender, and gender-nonconforming people. Int J Transgenderism 13:165–232
Article Google Scholar
Basson R (2001) Towards optimal hormonal treatment of male to female gender identity disorder. J Sex Reprod Med 1:45–51
Google Scholar
Meriggiola MC, Gava G (2015) Endocrine care of trans-people part I. A review of cross-sex hormonal treatments, outcomes and adverse effects in transmen. Clin Endocrinol 83:597–606
Gooren LJ, Giltay EJ, Bunck MC (2008) Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience. J Clin Endocrinol Metab 93:19–25
Mueller A, Gooren L (2008) Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol 159:197–202
Wierckx K, Elaut E, Delercq E et al (2013) Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans person: a case-control study. Eur J Endocinol Eur Fed Endocr Soc 169:471–478
Wierckx K, Mueller S, Weyers S et al (2012) Long-term evaluation of cross-sex hormone treatment in transsexual persons. J Sex Med 9:2641–2651
Grynberg M, Dubost G, Colau J-C et al (2010) Histology of genital tract and breast tissue after long- term testosterone administration in a female-to-male transsexual population. Reprod BioMed Online 20(4):553–558
Perrone AM, Cerpolini S, Marria Salfi NC et al (2009) Effect of long-term testosterone administration on the endometrium of female-to-male transsexuals. J Sex Med 6:3193–3200
Deutsch MD Guidelines for the primary and Gender-Affirming Care of Transgender and Gender Non binary People. 2th Edition. Available at http://transcare.ucsf.edu/guideline . Accessed 17 June 2016
Getahun D, Nash R, Flanders WD et al (2018) Cross sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann Intern Med 169:205–213
Glueck CJ, Wang P (2014) Testosterone therapy, thrombosis, thrombophilia, cardiovascular events. Metabolism 63:989–994
Gibson DA, Simitsidellis I, Collins F et al (2014) Evidence of androgen action in endometrial and ovarian cancers. Endocr Relat Cancer 21:203–218
Bulun SE, Takayama K, Suzuki T et al (2004) Organization of the human aromatase p 450 (CYP19) gene. Semin Reprod Med 22:5–9
Bruno RD, Njar VC (2007) Targeting cytochrome P450 enzymes: a new approach in anti-cancer drug development. Bioorg Med Chem 15:5047–5060
Berra M, Armillotta F (2006) D’Emidio Let al. Testosterone decreases adiponectin levels in female to male transsexuals. Asian J Androl 8:725–729
Gooren LJ, Wierckx K, Giltay EJ (2014) Cardiovascular disease in transsexual persons treated with cross-sex hormones: reversal of the traditional sex difference in cardiovascular disease pattern. Eur J Endocrinol 170:809–819
Dheine C, Oberg K, Aver S et al (2014) An analysis of all applications for sex reassignment surgery in Sweden, 1960-2010: prevalence, incidence, and regrets. Arch Sex Behav 43:1535–1545
Streed CG, Harfouch O, Marvel F et al (2017) Cardiovascular disease among transgender adults receiving hormone therapy: a narrative review. Ann Intern Med 167:256–267
Giltay EJ, Toorians AWFT, Sarabdjitsingh AR et al (2004) Established risk factors for coronary heart disease are unrelated to androgen-induced baldness in female-to-male transsexuals. J Endocrinol 180:107–112
Asscheman H, T'Sjoen G, Lemaire A et al (2014) Venous thrombo-embolism as a complication of cross-sex hormone treatment of male-to-female transsexual subjects: a review. Andrologia 46:791–795
Gagliano-Jucá T, Basaria S (2019) Testosterone replacement therapy and cardiovascular risk. Nat Rev Cardiol 16:555–574
Liu PY, Death AK, Handelsman DJ (2003) Androgens and cardiovascular disease. Endocr Rev 24:313–340
Wu FCW, Von Eckardstein A (2003) Androgens and coronary artery disease. Endocr Rev 24:183–217
Corona G, Maseroli E, Rastrelli G et al (2014) Cardiovascular risk associated with testosterone boosting medications: a systematic review and meta-analysis. Expert Opin Drug Saf 13:1327–1351
Vigen R, O’Donnell CI, Barón AE et al (2013) Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA 310:1829–1836
Finkle WD, Greenland S, Ridgeway GK et al (2014) Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One 66:175–176
Elamin MB, Garcia MZ, Murad MH et al (2010) Effect of sex steroid use on cardiovascular risk in transsexual individuals: a systematic review and meta-analyses. Clin Endocrinol 72:1–10
Download references
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
This research project was supported in part by the Unit of Obstetrics and Gynecology—University of Bari Aldo Moro, Bari, Italy.
Author information
Authors and affiliations.
Department Interdisciplinary Medicine, Unit of Obstetrics and Gynecology, University of Bari “Aldo Moro”, Bari, Italy
Luca Maria Schönauer, Carmine Carriero, Teresa Capursi, Giuseppe Loverro & Edoardo Di Naro
Interdisciplinary Department of Medicine, Gynecology and Ostetrics Clinic, University of Bary, Bari, Italy
Miriam Dellino
Department of Obstetrics and Gynaecology, ASTT Lecco, Ospedale Leopoldo Mandic, Merate, Italy
Matteo Loverro
Institute of Biomembranes, Bioenergetics and Molecular Biotechnologies, CNR, Bari, Italy
Claudia Leoni
You can also search for this author in PubMed Google Scholar
Contributions
LMS made substantial contributions to drafting the work and substantively revising it, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which he was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
MD (corresponding author) made substantial contributions to the conception of the work, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which she was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
ML made substantial contributions to the design of the work, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which he was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
CC made substantial contributions to the design of the work, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which he was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
TC made substantial contributions to drafting the work and substantively revising it, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which he was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
CL made substantial contributions to revising the work, especially for the statistical reformulation required by the reviewers.
GL made substantial contributions to drafting the work and substantively revising it, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which he was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
ED made substantial contributions to the acquisition and analysis of the data, approved the submitted version, and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even those in which he was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
Corresponding author
Correspondence to Miriam Dellino .
Ethics declarations
Competing interests.
The authors declare that they have no competing interests.
Ethical approval and consent to participate
There was no formal approval of the Ethics Committee, but the procedures were carried out in accordance with the Declaration of Helsinki, as revised in 2013. Informed consent was obtained from the patients through distribution of a dedicated form explaining the study design.
Consent for publication
Written informed consent for the anonymous publication of information relating to the disease is regularly obtained from all individual participants included in the study during the medical interview with the patient prior to the surgical or chemotherapy treatment.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Schönauer, L.M., Dellino, M., Loverro, M. et al. Hormone therapy in female-to-male transgender patients: searching for a lifelong balance. Hormones 20 , 151–159 (2021). https://doi.org/10.1007/s42000-020-00238-2
Download citation
Received : 12 March 2020
Accepted : 17 August 2020
Published : 07 October 2020
Issue Date : March 2021
DOI : https://doi.org/10.1007/s42000-020-00238-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Long-term therapy
- Testosterone
- Transgender
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
In primary male to female (MTF) sex reassignment surgery (SRS), the most frequent postoperative functional complications using the penoscrotal skin technique remain neovaginal stenosis, urinary meatal stenosis and secondary revision surgery. We aimed to retrospectively analyze postoperative functional and anatomical complications, as well as ...
Sex and sexual health tips for transgender women after gender-affirming surgery. Sex after surgery. Achieving orgasm. Libido. Vaginal depth and lubrication. Aftercare. Contraceptions and STIs ...
It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a feminine-appearing outer genital area with a shallow vaginal canal.
Bottom surgery generally refers to one of three surgeries. The first, vaginoplasty, is typically pursued by transgender women and AMAB (assigned male at birth) nonbinary people. Phalloplasty or ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Risks and complications. There are always risks associated with surgery, but vaginoplasty complications are rare. Infections can usually be cleared up with antibiotics. Some immediate postsurgical ...
Abstract. Transsexual issues and sexual reassignment surgery (SRS) are receiving a great deal of attention and support in the media, schools, and government. Given the early age at which youth seek treatment for transsexual attractions (TSA) and gender dysphoria and given the serious risks associated with such treatment, it is essential that ...
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person ...
Commonly performed surgeries include facial feminization (craniomaxillofacial procedures), chest ("top") surgery (eg, breast augmentation), and genital ("bottom") surgery (eg, orchiectomy and vaginoplasty). Knowledge of these commonly performed procedures and the surgical techniques used will aid medical care providers in caring for transgender ...
The NBC article quotes Denee Mallon saying, "I feel complete." These reports obscure the truth: While gender-affirming surgeries can make people more comfortable in their bodies, they're not a fix ...
Feminizing hormone therapy typically is used by transgender women and nonbinary people to produce physical changes in the body that are caused by female hormones during puberty. Those changes are called secondary sex characteristics. This hormone therapy helps better align the body with a person's gender identity.
Medical treatment often includes hormones to expose sex steroid-responsive target tissues to more estrogen and block androgen action. Commonly performed surgeries include facial feminization (craniomaxillofacial procedures), chest ("top") surgery (eg, breast augmentation), and genital ("bottom") surgery (eg, orchiectomy and vaginoplasty).
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current ...
Transwomen (921 men to female) were more frequent than transmen (719 female to male). Transwomen's treatments were based in antiandrogens, estrogens, new drugs, and sex reassignment surgery, meanwhile transmen's surgeries were based in the administration of several forms of testosterone and sex reassignment.
With the onset of puberty, transgender persons typically experience significant psychological distress (gender dysphoria) and consequently seek gender-affirming—or gender reassignment—treatment ( e4 ). With 9% to 11% and 1.5% to 2%, the rates of suicide attempts ( 3) and committed suicides ( 4 ), respectively, are increased among people ...
Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria. Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being ...
A FTM gender reassignment surgery creates male genitalia. Here is a quick guide for what to expect before, during, and after a FTM gender reassignment surgery: Before Surgery. Prophylactic antibiotics or antivirals may be prescribed. Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol ...
Awareness of the potential side effects of GAHT is needed to make informed decisions and to individualize GAHT. ... Definition; Sex: Sex is assigned at birth as male or female, usually based on the appearance of the external genitalia: Gender identity: A person's intrinsic sense of being male, female or an alternative gender (e.g., boygirl ...
Treatment Gender dysphoria. Treatment. Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary. What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
For individuals transitioning from female to male (transgender men), medical treatment includes hormonal therapy with testosterone. Gender-affirming surgery includes "chest" surgery, such as mastectomy, and "genital" or "bottom" surgery, such as hysterectomy, oophorectomy, vaginectomy, metoidioplasty, and phalloplasty.
Reassignment of a female-to-male (FtM) person requires gender-affirming, androgenic hormonal treatment that is planned to induce appropriate structural changes. This therapy must be prolonged long term, even after the sex reassignment surgery (SRS). The purpose of this study is to evaluate the effects of hormone therapy with testosterone in FtM ...