Nursing Case Study for Breast Cancer
Watch More! Unlock the full videos with a FREE trial

Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Natasha is a 32-year-old female African American patient arriving at the surgery oncology unit status post left breast mastectomy and lymph node excision. She arrives from the post-anesthesia unit (PACU) via hospital bed with her spouse, Angelica, at the bedside. They explain that a self-exam revealed a lump, and, after mammography and biopsy, this surgery was the next step in cancer treatment, and they have an oncologist they trust. Natasha says, “I wonder how I will look later since I want reconstruction.”
What assessments and initial check-in activities should the nurse perform for this post-operative patient?
- Airway patency, respiratory rate (RR), peripheral oxygen saturation (SpO2), heart rate (HR), blood pressure (BP), mental status, temperature, and the presence of pain, nausea, or vomiting are assessed upon arrival. Medication allergies, social questioning (i.e. living situation, religious affiliation), as well as education preference are also vital. An admission assessment MUST include an examination of the post-op dressing and any drains in place. This should be documented accordingly.
- The hand-off should be thorough and may be standardized. Some institutions have implemented a formal checklist to provide a structure for the intrahospital transfer of surgical patients. Such instruments help to standardize processes thereby ensuring that clinicians have critical information when patient care is transferred to a new team. The nurse should also prepare to provide education based on surgeon AND oncologist guidance
What orders does the nurse expect to see in the chart?
- Post-op medications, dressing change and/or drain management, strict I&O, no BP/stick on the operative side (rationale is to help prevent lymphedema – Blood pressure (BP) measurement with a cuff on the ipsilateral arm has been posed as a risk factor for the development of LE after-breast cancer therapy for years, regardless of the amount of lymph node excision.)
- Parameters for calling the surgeon are also important. The nurse should also check for an oncology service consult.
After screening and assessing the patient, the nurse finds she is AAOx4 (awake, alert and oriented to date, place, person and situation). The PACU staff gave her ice due to dry mouth which she self-administers and tolerates well. She has a 20G IV in her right hand. She states her pain is 2 on a scale of 1-10 with 10 being the highest. Her wife asks when the patient can eat and about visiting hours. Natasha also asks about a bedside commode for urination and why she does not have a “pain medicine button”. Another call light goes off and the nurse’s clinical communicator (unit issued cell phone) rings.
The nurse heard in report about a Jackson-Pratt drain but there are no dressing change instructions, so she does not further assess the post-op dressing situation in order deal with everything going on at the moment. She then sits down to document this patient.
Medications ordered in electronic health record but not yet administered by PACU: Tramadol 50 mg q 6 hrs. Prn for mild to moderate pain. Oxycodone 5 mg PO q 4 hrs. Prn for moderate to severe pain (5-7 on 1-10 scale) Fentanyl 25 mcg IV q3hrs. Prn For breakthrough pain (no relieve from PO meds or greater than 8 on 1-10 scale) Lactated Ringers 125 mL/hr IV infusion, continuous x 2 liters Naloxone 0.4-2 mg IV/IM/SC; may repeat q2-3min PRN respiratory rate less than 6 bpm; not to exceed 10 mg
BP 110/70 SpO2 98% on Room Air HR 68bpm and regular Ht 157 cm RR 14 bpm Wt 53 kg Temp 36.°5C EBL 130mL CBC -WNL BMP Potassium – 5.4 mEq/L
What education should be conducted regarding post-op medications?
- New post-op pain guidelines rely less on patient-controlled analgesia (aka “pain medicine button”) than in previous years. Most facilities will have an approved standing protocol (i.e., “Multimodal analgesia and Opioid Prescribing recommendation” guideline) or standing orders. The patient must be instructed on how to rate pain using facility-approved tools (aka “pain scales”). She should also report any medication-related side effects and reinforce there is a reversal medication in case of an opioid overdose.
What are some medical and/or non-medical concerns the nurse may have at this point? If there are any, should they be brought up to the surgeon?
- The nurse may request an anti-emetic such as ondansetron 4 mg IV q 6 hrs prn nausea vomiting (N&V) since it is not uncommon post-op for the patient to have N&V. The rate of LR is a little high for such a small patient and could cause electrolyte imbalances. The nurse may also inquire about the oncologist being on the case and ask if the surgeon has discussed reconstruction with the patient yet. She may also want to ask about dressing change orders.
Natasha sleeps through the night with no complaints of pain. Lab comes to draw the ordered labs and the CNA takes vital signs. See below.
CBC HGB 7.2 g/dl HCT 21.6%
BMP Sodium 130 mEq/L Potassium 6.0 mEq/L BUN 5 mg/dL
BP 84/46 SpO2 91% on Room Air HR 109 RR 22 bpm
What should the nurse do FIRST? Is the nurse concerned about the AM labs? AM vital signs? Why or why not?
- Check the dressing and drain for bleeding (assess the patient). The patient should also sit up and allow staff to check the bed for signs of bleeding. Reinforce the dressing as needed. Record output from the drain (or review documentation of all the night’s drain output). Labs and vital signs indicate she may be losing blood.
Check the dressing and drain for BLEEDING (assess the patient). The patient should also sit up and allow staff to check the bed for signs of bleeding. Reinforce the dressing as needed. Record output from the drain (or review documentation of all the night’s drain output). Labs and vital signs indicate she may be losing blood.
What orders does the nurse anticipate from the surgeon?
- The nurse should expect an order to transfuse blood for this patient. Also, dressing reinforcement or change instructions are needed in the case of saturation)
How should the nurse address Natasha’s declaration? What alerts the nurse to a possible complication?
- First, the complication is that “Kingdom Hall” is the site of worship for Jehovah’s Witnesses. They do not accept ANY blood product, not even in emergencies. It is vital the nurse determines the patient’s affiliation and religious exceptions for medical care before moving forward. Next, employ therapeutic communication to elicit more details about Natasha’s concerns. Say things like, “tell me why you think you’re not attractive?” She may discuss reconstruction options or ask the patient to write down specific questions about this option to ask the provider later. Ask about getting family in to provide support. Seek information to give the patient about support groups and other resources available (as appropriate, ie. prosthetics, special undergarments/accessories, etc)
The surgeon orders 1 unit packed red blood cells to be infused. The nurse then goes to the patient to ask about religious affiliation and to discuss the doctor’s order. After verifying that Natasha is not a practicing Jehovah’s Witness, the nurse proceeds to prepare the transfusion.
What is required to administer blood or blood products?
- First, the patient’s CONSENT is required to give blood products. The nurse must also prepare to stay with the patient for at least the first 15 minutes of the transfusion taking a baseline set of V/S prior to infusion. Then, V/S per protocol (frequent). Education is also required. The patient should report feeling flushed, back or flank pain, shortness of breath, chest pain, chills, itching, hives. Normal saline ONLY for infusion setup and flushing: size IV 20g or higher. Always defer infusion time limits to “per policy” because this can differ vastly
How should the nurse respond to this question?
- Planning for post-op cancer treatment should have begun prior to the surgery. Ask the patient if she has discussed plans with her oncologist. Refer to any specialist documentation to see if this is mentioned. Remind the patient of the specialist’s assessment and planning information. Reinforce that testing of the tissue may change the course of treatment as well. Provide education AS PER THE PATIENT’S STATED PREFERENCE and/or resources based on what the plan includes (ie. chemotherapy, radiation, further surgery. Continually assess and reassess patient understanding. Include family and/or support with the patient’s approval.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
References:
View the full transcript, nursing case studies.

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.

NurseStudy.Net
Nursing Education Site

Breast Cancer Nursing Diagnosis and Nursing Care Plan
Last updated on January 28th, 2024 at 08:03 am
Breast Cancer Nursing Care Plans Diagnosis and Interventions
Breast Cancer NCLEX Review and Nursing Care Plans
Breast cancer is a type of cancer that involves the uncontrolled growth and division of breast cancer cells. In the United States, breast cancer is the second most common types of cancer in women, after skin cancer.
Signs and Symptoms of Breast Cancer
- Breast or underarm lump – usually the first symptom of breast cancer; does not go away; can be seen through a mammogram; may be painful or tender
- Swelling – may be seen or felt in the breast or in the lymph nodes located in the armpit or collarbone area
- Indentation or flattened area on a breast
- Changes in breast size, texture, color, contour, or temperature
- Unusual nipple discharge – can be bloody, clear, or any other color
- Other nipple changes such as inward pulling, dimpling, itchiness, soreness, burning sensation
Types of Breast Cancer
- Ductal Carcinoma in Situ (DCIS). The most common breast cancer type, ductal carcinoma occurs in 1 out of 5 new cases of breast cancer. DCIS is a local breast tumor that has not spread in nearby lymph nodes and other tissues. Some cases of DCIS are asymptomatic, while others show bloody nipple discharge or a breast lump.
- Lobular Carcinoma. This type of breast cancer originates in the lobules, the glands where milk is produced. The most common symptoms of lobular carcinoma include swelling, thickening, and/or feeling of fullness in one region of the breast and inverted or flat nipples.
- Infiltrating or Invasive Breast Cancer. When the breast cancer has started spreading from its origin towards the surrounding tissues, it is classified as an invasive breast cancer. The symptoms of infiltrating breast cancer include a rash on the breast skin, dimpling, swelling, pain, and an immovable lump in the breast or armpit.
- Metastatic Breast Cancer. Also known as advanced or secondary breast cancer, metastatic breast cancer is the type when the disease has spread to other organs and parts of the body. The symptoms of metastatic breast cancer depend on where the disease has spread, but may involve bone pain, headache, jaundice , double vision, trouble breathing, belly swelling, weight loss, gastrointestinal problems, muscular weakness, confusion, and changes in brain function.
- Triple Negative Breast Cancer. This type of breast cancer is detected if the tumor produces only low levels of protein called HER-2 and does not contain receptors for estrogen and progesterone hormones. Triple negative breast cancers can be aggressive, thus the treatment protocol is usually different than other types of breast tumors.
- Male Breast Cancer. Breast cancer in males is rare. The symptoms such as lump in the breast or armpit and nipple discharge are the same as that of the females.
- Paget’s Disease of the Breast. This type of breast cancer occurs with ductal carcinoma. The symptoms of this disease include eczema-looking skin, scaly or crusty nipple skin, burning or itching breast skin, inverted or flat nipple, and yellowish or bloody nipple discharge.
Causes and Risk Factors of Breast Cancer
The exact cause of breast cancer is still unknown. However, the risk factors that may increase the chance of getting breast cancer are well-studied.
In general, breast cancer tumors develop from the rapid growth and division of abnormal breast cells (hyperplasia and dysplasia). Eventually, the cells accumulate and form a mass or a lump.
These abnormal breast cells may spread (metastasis) in the other parts of the breast, lymph nodes, or organs of the body.
The risk factors of breast cancer include:
- Gender – being a woman is the biggest risk factor of having breast cancer, although 1% of the cases occur in men.
- Age – 2 of 3 invasive breast cancer cases are seen in women aged 55 years or above
- Family History and Genetics– the risk is doubled if a woman has a first-degree female relative that has been diagnosed with breast cancer (mother, sister, or daughter)
- Past Medical History of Breast Cancer – if the patient has had breast cancer in the past, he/she is 3 to 4 times likely to develop breast cancer in the future; having had benign breast conditions in the past also increase the risk for breast cancer
- Race and Ethnicity – White women have a slightly higher risk for breast cancer than Hispanic, Black, and Asian women
- Exposure to Radiation – if the patient had radiotherapy to the face or chest to treat acne or another cancer type such as lymphoma , the risk for developing breast cancer is higher than average
- Obesity and being overweight
- History of Pregnancy – women who have had their first child after age 30 or have not had any full term pregnancy have a higher risk than women who have had full term pregnancy and/or gave birth before age 30.
- Breastfeeding – studies show that breastfeeding, especially for longer than 1 year, lowers the risk of breast cancer
- Menstrual History – women who had periods younger than age 12 have a higher risk of breast cancer; menopausing older than 55 years old also increases the risk
- Alcohol use and Smoking
- Hormone Replacement Therapy – HRT users have a higher risk of breast cancer
- Sedentary Lifestyle
Complications of Breast Cancer
- Pulmonary insufficiency
- Metastasis to other organs or parts of the body
- Cardiac disease
Diagnosis of Breast Cancer
- Breast Exam. This can be done daily through self-checking. During a breast exam in the clinic, the doctor will observe and feel/palpate the breasts and the lymph nodes in the armpit for any abnormalities such as lumps.
- Mammogram. X-ray of the breast or mammogram is the most common screening test for breast cancer. Women with no history of breast cancer are recommended to have a yearly mammogram once they turn 40 years old.
- Breast Ultrasound. This can determine if a breast lump is a fluid-filled cyst or a solid mass.
- Breast Magnetic Resonance Imaging (MRI). This is used to visualize the breast by creating pictures. MRI involves injection of a dye to see the interior of the breast.
- Breast Biopsy. The definitive way to diagnose breast cancer, biopsy involves taking a sample of breast cells to be studied under the microscope.
- Cancer Staging. After diagnosis, the oncologist will assess the extent or stage of breast cancer, from 0 to IV. Cancer staging depends on the blood test results (complete blood count and tumor markers (i.e., cancer antigen 15-3 or CA 15-3, cancer antigen 27.29 or CA 27.29, and carcinoembryonic antigen or CEA), CT/ PET scan, and other diagnostic results.
Treatment for Breast Cancer
- Breast Surgery. The removal of breast cancer cells through operation can vary depending on the size, grade, and extent of the tumor and disease.
- Lumpectomy – to remove small tumors and a margin of surrounding healthy breast tissues; also known as wide local excision or breast-conserving surgery
- Mastectomy – to remove the entire breast
- Sentinel node biopsy – to remove a limited number of lymph nodes and determine cancer spread in these areas
- Axillary lymph node dissection – to remove additional lymph nodes if the sentinel nodes show signs of cancer
- Medications. Several pharmacologic therapies have been used to treat breast cancer, such as:
- Chemotherapy – uses drugs to kill cancer cells. The most common chemotherapy protocols for breast cancer include combinations of anti-tumor antibiotics and alkylating agents, followed by taxanes.
- Hormone Therapy – used to treat breast cancers that are sensitive to hormones estrogen and/or progesterone
- Targeted Therapy – uses drugs that attack specific abnormalities in the cancer cell, such as human epidermal growth factor receptor 2 (HER2); an example is the use of monoclonal antibodies (MABs)
- Immunotherapy – utilizes the immune system to attack the breast cancer cells; examples include immune system modulators and checkpoint inhibitors
- Radiotherapy. Radiotherapy uses radiation or high-powered energy beams such as protons and X-rays to kill the cancer cells. This can last from 3 days to 6 weeks.
- External beam radiation – aims the energy beams at the affected body area
- Brachytherapy – places radioactive material inside the body in order to perform radiation therapy
Nursing Diagnosis for Breast Cancer
Breast cancer nursing care plan 1.
Nursing Diagnosis: Deficient Knowledge related to new diagnosis of breast cancer as evidenced by patient’s verbalization of “I want to know more about my new diagnosis and care”
Desired Outcome: At the end of the health teaching session, the patient will be able to demonstrate sufficient knowledge of breast cancer and its management.
Breast Cancer Nursing Care Plan 2
Nursing Diagnosis: Imbalanced Nutrition: Less than Body Requirements related to consequences of chemotherapy for breast cancer, as evidenced by abdominal cramping, stomach pain, diarrhea or constipation , bloating, weight loss, nausea and vomiting , and loss of appetite
Desired Outcome: The patient will be able to achieve a weight within his/her normal BMI range, demonstrating healthy eating patterns and choices.
Breast Cancer Nursing Care Plan 3
Nursing Diagnosis: Fatigue related to consequence of chemotherapy for breast cancer (e.g., immunosuppression and malnutrition ) and/or emotional distress due to the diagnosis, as evidenced by overwhelming lack of energy, verbalization of tiredness, generalized weakness, and shortness of breath upon exertion
Desired Outcome: The patient will establish adequate energy levels and will demonstrate active participation in necessary and desired activities.
Breast Cancer Nursing Care Plan 4
Imbalanced Nutrition: Less Than Body Requirements
Nursing Diagnosis: Imbalanced Nutrition: Less Than Body Requirements related to fatigue, emotional distress, and poorly controlled pain due to chemotherapy secondary to breast cancer, as evidenced by expressions of inadequate food intake, loss of interest in food, inability to ingest food, reduced subcutaneous fat, body weight 20 percent below optimum for height and frame, stomach cramps and constipation.
Desired Outcomes:
- The patient will be able to demonstrate a stable weight gain toward the goal with normal laboratory values.
- The patient will not show any indicators of malnutrition.
- The patient will be able to participate in specific interventions to gain appetite and increase dietary intake.
Breast Cancer Nursing Care Plan 5
Risk for Infection
Nursing Diagnosis: Risk for Infection related to insufficient secondary defenses, immunosuppression, and chronic disease process secondary to breast cancer, as evidenced by damaged epidermal tissue, skin irritation on injection site, shortness of breath, presence of mucus in the saliva, nasal drainage, fever of 100.5 °F, sore throat and chills.
- The patent will be able to stay afebrile and achieve timely healing as appropriate.
- The patient will be able to identify and participate in interventions to prevent or minimize the risk of infection.
Breast Cancer Nursing Care Plan 6
Anticipatory Grieving
Nursing Interventions: Anticipatory Grieving related to expected decline in physiological health and perceived risk of dying secondary to breast cancer, as evidenced by alterations in eating habits, changes in sleeping patterns, activity levels, and communication patterns, shortness of breath, acute panic, expressions of fear and crying.
- The patient will be able to recognize their own emotions and convey them effectively.
- The patient will be able to maintain the normal daily routine while planning for the future and looking ahead one day at a time.
- The patient will be able to express awareness of the dying process.
- The patient will demonstrate ways to identify anxiety to prevent going into a panic state.
More Breast Cancer Nursing Diagnosis
- Fear / Anxiety
- Risk for Altered Oral Mucous Membranes
- Risk for Impaired Skin Integrity
- Risk for Disturbed Body Image
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Leave a Comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Breast Cancer: Survivorship Care Case Study, Care Plan, and Commentaries
Affiliation.
- 1 Saint Louis University.
- PMID: 34800110
- DOI: 10.1188/21.CJON.S2.34-42
This case study highlights the patient's status in care plan format and is followed by commentaries from expert nurse clinicians about their approach to manage the patient's long-term or chronic cancer care symptoms. Finally, an additional expert nurse clinician summarizes the care plan and commentaries, emphasizing takeaways about the patient, the commentaries, and additional recommendations to manage the patient. As can happen in clinical practice, the patient's care plan is intentionally incomplete and does not include all pertinent information. Responding to an incomplete care plan, the nurse clinicians offer comprehensive strategies to manage the patient's status and symptoms. For all commentaries, each clinician reviewed the care plan and did not review each other's commentary. The summary commentary speaks to the patient's status, care plan, and nurse commentaries.
Keywords: breast cancer; care plan; case study; survivorship care.
- Breast Neoplasms* / therapy
- Survivorship*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

A case-case analysis of women with breast cancer: predictors of interval vs screen-detected cancer
Nickolas dreher.
1 University of California San Francisco, San Francisco, CA, USA
2 The Icahn School of Medicine at Mount Sinai, New York, NY, USA
Madeline Matthys
Edward hadeler.
3 University of Miami Miller School of Medicine, Miami, FL, USA
Yiwey Shieh
Irene acerbi, fiona m. mcauley, michelle melisko, martin eklund.
4 Karolinska Institutet, Stockholm, Sweden
Jeffrey A. Tice
Laura j. esserman, laura j. van ‘t veer.
Authors’ contributions: All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Nickolas Dreher, Madeline Matthys, and Edward Hadeler. The first draft of the manuscript was written by Nickolas Dreher and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Associated Data
The Breast Cancer Surveillance Consortium (BCSC) model is a widely-used risk model that predicts five- and ten-year risk of developing invasive breast cancer for healthy women aged 35–74 years. Women with high BCSC risk may also be at elevated risk to develop interval cancers, which present symptomatically in the year following a normal screening mammogram. We examined the association between high BCSC risk (defined as the top 2.5% by age) and breast cancers presenting as interval cancers.
We compared the mode of detection and tumor characteristics of patients in the top 2.5% BCSC risk by age with age-matched (1:2) patients in the lower 97.5% risk. We constructed logistic regression models to estimate the odds ratio (OR) of presenting with interval cancers, and poor-prognosis tumor features, between women from the top 2.5% and bottom 97.5% of BCSC risk.
Our analysis included 113 breast cancer patients in the top 2.5% of risk for their age and 226 breast cancer patients in the lower 97.5% of risk. High-risk patients were more likely to have presented with an interval cancer within one year of a normal screening, OR 6.62 (95% CI 3.28–13.4, p<0.001). These interval cancers were also more likely to be larger, node positive, and higher stage.
Conclusion:
Breast cancer patients in the top 2.5% of BCSC risk for their age were more likely to present with interval cancers. The BCSC model could be used to identify healthy women who may benefit from intensified screening.
Introduction
Interval cancers are invasive breast cancers that present symptomatically within 12 months of a normal screening mammogram. These cancers include both those that develop after a mammogram and those that were not detected (but did exist) at the previous screening mammograms. Interval cancers tend to be more aggressive and faster-growing than screen-detected cancers.[ 1 – 4 ] Identifying women who are at increased risk for interval breast cancers could inform screening strategies, as these women may benefit from supplemental or more frequent screening and risk reduction. However, no consensus regarding how to risk-stratify women for interval breast cancer risk exists. The Breast Cancer Surveillance Consortium (BCSC) model is a validated and widely used risk prediction tool that predicts five- and ten-year risk of developing invasive breast cancer for women age 35–74.[ 5 ] It bases risk prediction on age, race/ethnicity, presence of first degree relative with breast cancer, prior biopsies/benign breast disease, and Breast Imaging-Reporting and Data System (BI-RADS) breast density.[ 5 , 6 ] Past work by Kerlikowske et al. has suggested that the combination of BCSC risk and BI-RADS breast density is one method upon which risk-stratification for interval cancer could be based.[ 7 ]
However, both the BCSC model and breast density itself are correlated with age: as age increases, BCSC score increases and breast density decreases. Providers may be wary of basing recommendations for screening frequency and modality on risk models (such as BCSC) that may enrich for increased screening as age increases. Further, tumor characteristics and morbidity vary by age, with younger women being at increased risk of developing poor prognosis tumors and interval cancers.[ 7 – 9 ] In contrast to using an absolute risk cutoff to identify high risk women, an alternative method is to use age-specific cutoffs. Age-specific BCSC risk distributions are generated directly by the BCSC, and aggregate 5-year age groups have been described in the literature.[ 5 ] The WISDOM study, run by the Athena Breast Health Network, uses these distributions to establish a threshold of the top 2.5% of risk for each age group to initiate counseling on prevention interventions and annual screening. Prior thresholds were not sufficiently high to motivate interest in embarking on risk reduction strategies.[ 10 ] The top 2.5% by age threshold consistently identifies women with lifetime risk of 23–28%, and 20% of these women elect to pursue prevention interventions. This is why it was chosen for the high risk threshold to trigger for annual screening and prevention counseling in WISDOM.[ 10 ]
This study’s primary aim is to validate this top 2.5% by age threshold by determining if these women are more likely to present with interval cancers rather than screen-detected cancers. We also evaluated whether these interval cancers have more aggressive features to confirm the clinical relevance of detecting interval cancers.
Patients and Methods
We conducted a case-case analysis of women treated for invasive breast cancer at the University of California San Francisco Breast Care Center (UCSF BCC). This study included only women with a confirmed diagnosis of invasive breast cancer previously undergoing standard mammography screening. Between 2013 and 2017, 896 patients completed the Athena intake questionnaire (described in Measures ) in the BCC and had available BI-RADS breast density and pathology data. We identified the 180 women in the top 2.5% of BCSC risk for their age. Women were excluded from the study if they deviated from standard screening intervals by having an increased screening frequency (more than 1 mammogram per year) or if they had an “interval” cancer detected more than one year after their prior clear mammogram. Ultimately, information on mode of detection (screen detected versus interval breast cancer) was available for 113 women in the top 2.5% of risk for their age. We then used a random number generator to select age-matched (±1 year) women from the lower 97.5% who also had method of detection available. ( Figure 1 ).

Selection of the study group from women seen at the UCSF Breast Care Center from 2013–2017. Top 2.5% threshold determined from distributions of BCSC 5-year risk estimates.
The UCSF BCC is part of the Athena Breast Health Network, a breast cancer clinical care and research collaborative that includes breast care clinics from five University of California hospitals and Sanford Health in South Dakota.[ 11 ] Athena collects patient characteristics and outcome data across the entire care spectrum from screening and prevention to treatment and survivorship. At the UCSF BCC, questionnaires are distributed to all patients presenting with a new breast problem.
The Athena intake questionnaire at the BCC collects race/ethnicity, family history, personal cancer history, history of prior biopsies, presence of comorbidities, and psychosocial and physical quality of life metrics.[ 12 ] These questionnaires contain all the variables included in the BCSC model ( http://tools.bcsc-scc.org/BC5yearRisk/ ) except for BI-RADS density. Using the electronic medical record, we exported BI-RADS density based on the last negative screening mammogram prior to diagnosis and used it for the BCSC risk assessment. While the BCSC model is intended for women without a history of breast cancer, this allowed for a retrospective estimate of each patient’s 5-year risk of developing cancer at the approximate time of their diagnosis with the assumption that breast density stayed relatively stable between the last negative mammogram and density.[ 13 ] The 97.5 th BCSC risk percentile for each age ( Supplementary Table A ) was estimated by applying the BCSC risk calculator to data collected from more than six million mammograms from eight breast imaging registries across the country.[ 14 ]
The BCSC risk score was calculated for eligible women (those between the ages of 40–74 without a diagnosis of breast cancer prior to the current diagnosis) who completed the online intake questionnaire and whose BI-RADS density was available ( Figure 1 ). These BCSC scores were based on the patient’s age at time of intake. Medical records for all patients in the top 2.5% of risk for their age and two age-matched (±1 year) cases from the bottom 97.5% of risk were reviewed to determine method of cancer detection.
The UCSF Cancer Center registry contains pathology and outcome data linked to state and national registries, and has been described previously.[ 15 , 16 ] We collected information on each patient’s histology, grade, stage, nodal involvement, hormone receptor status, and tumor size from the Registry. If data were not available for a patient, we imported these fields from the UCSF surgical registry. The UCSF BCC maintains an internal surgical registry that is updated weekly with pathology reports from recent surgeries. This dataset, updated in near real-time, was included to capture data that were not yet reported in other registries.
Our primary outcome focused on interval cancers, defined as invasive breast cancers that presented within one year of a normal mammogram, BI-RADS score 1 or 2. Tumor characteristics including hormone receptor status, grade, size, nodal involvement and stage were imported from the registries based on patient medical record number and approximate diagnosis date.
Statistical Analysis
We compared the proportion of interval cancers between the two age-matched groups using conditional logistic regressions in R. We also used logistic regressions to compare tumor characteristics between interval cancers and screen-detected cancers. All tests were two-sided with alpha of 0.05.
In addition to comparing patients in the top 2.5% of risk for their age to patients from the lower 97.5%, we examined two additional risk stratification criteria from the literature: patients with extremely dense breasts (BI-RADS d) or a very high BCSC score irrespective of age (>4.00% 5-year risk of developing breast cancer).[ 7 ] This was an adjunct analysis included to address potential questions from the reader. However, it is important to note that the sample used in this study is not matched based on these two criteria.
Patient Characteristics
Of the 339 patients included in the final analysis, 113 fell in the top 2.5% of risk for their age, and they were compared to 226 from the lower 97.5% of risk ( Figure 1 ). Table 1 summarizes demographic information from the patients included in the analysis. Women in the top 2.5% of risk for their age tended to have higher breast density and more frequently reported a first degree relative with breast cancer and a personal history of breast biopsy (p<0.001 for all comparisons).
Baseline characteristics and demographic data for women in the top 2.5% of risk for their age (n=113) and age-matched women from the lower 97.5% (n=226).
Interval cancer risk by BCSC risk group
Patients from the top 2.5% of risk for their age were more likely to present with an interval cancer within one year of a normal screening mammogram compared to patients in the lower 97.5% of risk, OR 6.62 (95% CI 3.28–13.4, p<0.001) ( Table 2 ). Similar results were seen when we expanded the analysis to include “late-interval” cancers, those discovered within two years of a normal screening mammogram.
Association between three risk stratification criteria and interval cancers. The three risk stratification criteria included the BCSC top 2.5%, BI-RADS d (extremely dense), or BCSC 5-year cancer risk >4.00% (very high).
We also compared the top 2.5% by age threshold to two other common risk stratification criteria: extremely dense breasts (BI-RADS d) or a very high BCSC score irrespective of age (>4.00% 5-year risk of developing breast cancer) ( Table 2 ). The BCSC top 2.5% by age threshold was most strongly associated with interval cancer risk. The mean age for the BCSC top 2.5% threshold was between that of extremely dense breasts and 4% 5-year BCSC risk. Furthermore, a substantial number of women in the top 2.5% of risk for their age would not have been identified by these other risk cutoffs. Specifically, 49 of 113 (43%) women would only be flagged for increased risk using the top 2.5% by age threshold – and these women show a similarly high percentage of interval cancers (32.7%).
Tumor characteristics of interval cancers
Interval cancers had more aggressive features than cancers detected via screening mammogram. Interval cancers were more likely to be lymph node positive (odds ratio, OR 3.24, 95% CI 1.76 – 5.96, p<0.001) and larger than two centimeters (OR 3.49, 95% CI 1.82 – 6.70, p<0.001). Thus, they were more likely to be stage II or higher (OR 4.88, 95% CI 2.34 – 10.2, p<0.001). Likewise, interval cancers tended to be grade 3 and hormone receptor negative, although these trends were not statistically significant ( Table 3 ).
Tumor characteristics of interval cancers compared to screen-detected cancers from 339 breast cancer patients seen at the UCSF Breast Care Center. Certain components of pathology were not available for all patients, most notably tumor size. The ratios represent number of patients with the characteristic per those with data available.
In this study, we compared breast cancer patients in the BCSC top 2.5% of risk for their age to patients from the remaining 97.5%. We found that women in the top 2.5% of risk for their age, who have double the risk of getting breast cancer relative to the average women, had more than six-fold higher odds of presenting with interval cancers. Furthermore, the interval cancers detected in this study were of clinical relevance as they followed trends outlined in the literature and tended to have more aggressive features.
Our study extends the literature by validating an alternative approach to risk stratification, which considers the distribution of risk among similarly aged women, as a predictor of interval cancer risk.[ 17 ] This allows providers to identify women at high risk without selecting certain age groups, as would BCSC score or density alone. A numeric threshold, identical for all ages, also fails to recognize the range of risk in each age group and does not account for lifetime risk. A 1.5% 5-year risk in a 40-year-old, for example, is associated with a much higher lifetime risk than a 1.5% 5-year risk in a 75-year-old. Many patients in the top 2.5% of risk for their age have extremely dense or heterogeneously dense breasts, which may mask tumors and contribute to interval cancer prevalence. However, if density alone drove this effect, we would expect to see the highest interval cancer prevalence in patients with BI-RADS d density. To the contrary, the data presented in this manuscript demonstrate that the top 2.5% by age threshold had the highest proportion of interval cancers when compared to other previously reported risk stratification criteria such as extremely dense breasts (BIRADS d) or a 4% absolute 5-year risk. However, it is important to recognize that this study was not designed to compare these criteria, and in creating the BIRADS d or 4% absolute risk groups age-matching was broken. Further research is necessary to effectively compare risk-stratification criteria; this analysis was included to address common questions from readers but is largely beyond the scope of this work.
We also replicated previous work showing interval cancers to be enriched for aggressive features and linked to poor prognosis.[ 7 , 18 ] In a large case-case study of 431,480 women, Kirsh et al. found interval cancers were more likely to be higher stage, higher grade, estrogen receptor negative, and progesterone receptor negative when compared to screen-detected tumors. We replicated these findings for stage, and while our study may not have been sufficiently powered to detect significant differences in grade and hormone receptor status, it should be noted that trends in our results were aligned with previous findings in the literature.[ 1 , 2 ]
Our work should be interpreted in light of several limitations. First, this was a case-case analysis and our sample size may have limited the precision of our estimates and ability to detect small differences between groups. Larger cohort studies in multiracial/multiethnic populations are needed to validate our main findings. Such studies would also make our work more generalizable, given our study predominately included white patients. Second, we did not review the most recent mammogram to confirm that the tumor represented a “true” interval cancer – rather than merely a missed tumor due to human error in the initial reading. However, missed interval cancers have also been shown to have more aggressive features compared to screen-detected cancers, although to a lesser extent.[ 1 ] Furthermore, these data reflect the limits of what is understood in clinical practice. Ultimately, if this sampling includes tumors that should have been screen-detected, it should only underestimate the unique characteristics of interval cancers. Third, women with higher risk are often offered more intensive screening due to the presence of risk factors such as dense breasts or positive family history. This may also bias these results, but we expect the bias to be toward the null, given that we expect increased screening to decrease interval cancer prevalence in high-risk groups.
Our results have several important clinical implications. Since interval cancers tend to present at later stages and lead to worse prognosis, it follows that a goal of breast cancer screening should be to detect interval cancers at an earlier, more treatable stage. However, increasing screening frequency for all women would likely lead to unsustainable resource usage and unintended effects such as false positives. As such, there is a clear need for risk stratification criteria that can identify women at elevated risk of interval cancers so that they can receive targeted screening and prevention. However, providers may be wary of using existing criteria that tend to select specific age groups for a variety of reasons – such as the prevalence of indolent tumors in older women.[ 19 , 20 ] Our results suggest that a simple top 2.5% by age threshold, based on a widely used risk-assessment tool, may effectively identify women with higher odds of developing interval cancers. This threshold is already being used to target preventative efforts (such as chemoprevention and lifestyle changes) by providers in the Athena Breast Health Network and in the WISDOM (Women Informed to Screen Depending on Measures of risk) Study, a randomized trial of personalized versus annual breast cancer screening that uses the BCSC model as well as genetic predisposition (mutations and polygenic risk).[ 21 , 22 ] Women in the personalized arm who are in the top 2.5% of risk for their age are assigned to annual screening and active outreach for risk reduction counseling; those whose 5-year risk is over 6% get screening every 6 months, alternating annual mammography with annual MRI.
Future work should aim to validate whether the top 2.5% by age threshold is associated with a similar increase in the likelihood of interval cancers in large cohort studies. These studies may also determine that a different sensitivity is optimal, such as top 1% or 5% by age. Cohort studies should ideally be powered to compare alternative risk-stratification criteria and examine the link between BCSC score and other features of aggressiveness, such as HER2 positivity, triple-negative/basal subtype, or high grade or proliferation.
Implications
Breast cancer patients whose BCSC risk, at the time they were diagnosed with breast cancer, was in the top 2.5% of predicted breast cancer risk for their age are significantly more likely to have their cancers detected in the interval between screening mammograms. These interval cancers were more likely to be higher grade and later stage, and thus may be linked to poor prognosis. Women in this elevated-risk category may benefit from tailored screening strategies or preventative interventions such as chemoprevention. A prospective validation is underway in the WISDOM study.
Supplementary Material
Acknowledgments.
We are extremely grateful to Karla Kerlikowske and her team at the San Francisco Mammography Registry (SFMR) for their guidance contextualizing this research and their willingness to collaborate. The SFMR provided access to data that was not ultimately used in this study. We would also like to thank Ann Griffin from the UCSF Cancer Registry and Patrick Wang from the UCSF Breast Care Center Internship Program. Data collection and sharing was supported by the National Cancer Institute-funded Breast Cancer Surveillance Consortium (HHSN261201100031C). You can learn more about the BCSC at: http://www.bcsc-research.org/ . Yiwey Shieh was supported by funding from the National Cancer Institute (1K08CA237829) and the MCL consortium. Dr. Esserman is supported by funding from the NCI MCL consortium (U01CA196406). We would also like to thank the dedicated Athena investigators and advocates for their continued work and support.
Yiwey Shieh was supported by funding from the National Cancer Institute (1K08CA237829) and the MCL consortium. Laura Esserman is supported by funding from the NCI MCL consortium (U01CA196406).
Conflicts of Interest: The authors declare no potential conflicts of interest.
Ethics approval: This work was approved by the UCSF Institutional Review Board and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to participate: All participants consented to have their data used for research that may result in publication.
Consent for publication: All participants consented to have their data used for research that may result in publication.
Availability of data and material: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability: Code used in this analysis will be made available from the corresponding author on reasonable request.

Contact our breast care nurses
0808 800 6000
- Information and support
- For healthcare professionals
- Secondary breast cancer nursing toolkit
Secondary breast care case studies
Below are case studies that support the information in the Secondary Breast Cancer Nursing toolkit.
Effective Data Collection, Frimley Park, Surrey
How the trust uses the Somerset Cancer Register and a team approach to accurately record data about patients with secondary breast cancer
Stratified patient follow up, The Christie, Manchester
How the team re-designed their service, using a co-production approach in order to meet the varying needs of a large caseload.
Developing a new service, Western General Hospital, Edinburgh
How the hospital designed a new service for secondary breast cancer patients.
Delivering a multi-disciplinary service, Velindre Cancer Centre, Cardiff
How the hospital established the first dedicated metastatic MDT in Wales and works with non-clinical teams to ensure patients’ holistic needs are addressed.
The case for a new secondary breast cancer specialist nurse, Truro
How the hospital expanded their service from one to two nurses to meet increasing patient demand
Reallocation of work in a CNS team, Lanarkshire
How reorganising the way the team worked enabled them to provide more consistent support to their patients with secondary breast cancer.
Joint Breast CNS & Specialist Pharmacy led clinics for patients with oestrogen receptor positive metastatic breast cancer, Sheffield
How joint Macmillan Nurse and Pharmacist led clinics reduced patient waiting times, freed up consultant time and addressed a wider range of patient needs.
The role of Band 4 Support Worker alongside CNS Secondary Breast Cancer , Northampton
The use of a Band 4 Support worker to maximise CNS time spent with patients.
Connect with us
- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Daily Do Lesson Plans
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning
MyNSTA Community
- My Collections
In Search of a Cure for Breast Cancer
By Jolanta Skalska
Share Start a Discussion

In this directed case study, students analyze data, draw a research-based conclusion, interpret experimental results, and discuss the relevance of research findings for clinical practice. Specifically, students examine the effects of chemotherapeutic drugs on newly generated cell lines and explain research outcomes using their prior knowledge of signal transduction pathways (G-protein coupled receptors), hormones, glycolysis, oxidative phosphorylation, and DNA structure and function as they follow the story of "Emily," an undergraduate student who is accepted into an internship program focusing on the breast cancer cell line MCF-7. Emily learns that MCF-7 cells can survive the treatment of tamoxifen and a hormone deprivation regimen, which leads to the generation of new cell lines (Tam3 and TamR3) that do not activate the mTOR signaling pathway. Emily attempts to predict how the Tam3 and TamR3 cells will respond to the mTOR inhibitor rapamycin, and then incorporates drugs used for chemotherapy into her experiments. Originally written for upper-level undergraduate biology majors, the case study is also appropriate for courses focusing on cell biology, pharmacology, and cancer biology.
Download Case
Date Posted
- List the functions of the steroid hormones, classify receptors, and summarize the mechanism of action and effects of chemotherapeutic drugs.
- Interpret experimental data and explain the outcomes of experiments described in the case study.
- Determine the differences between cell lines based on data, present signaling transduction pathways, and predict research outcomes.
- Explain the phenotypical differences between three cell lines, debate experimental outcomes and present them in the form of a written discussion.
Breast cancer; camptothecin; competitive inhibitor; cisplatin; doxorubicin; fluorouracil; G-protein coupled receptors; MCF-7; ER+; PR+; membrane receptors; mTOR; signaling pathway; oxidative phosphorylation; reactive oxygen species; tamoxifen
Subject Headings
EDUCATIONAL LEVEL
Undergraduate upper division
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials.
The optional PowerPoint presentation below can be used to pace students as they work through the case study in class.
- breast_cancer_direct.pptx (~100 KB)
You may also like
Web Seminar
Join us on Thursday, June 13, 2024, from 7:00 PM to 8:00 PM ET, to learn about the science and technology of firefighting. Wildfires have become an e...
Join us on Thursday, October 10, 2024, from 7:00 to 8:00 PM ET, for a Science Update web seminar presented by NOAA about climate science and marine sa...
Disclosure: This site contains some affiliate links. We might receive a small commission at no additional cost to you.
Breast cancer is a significant health concern that affects millions of individuals worldwide. Nurses play a critical role in the management and treatment of breast cancer, providing essential care that spans the spectrum from early detection to end-of-life support.
Effective nursing interventions for breast cancer are multifaceted, requiring comprehensive knowledge, skills, and empathy. These interventions are aimed at improving the quality of life for patients and may include managing symptoms, offering psychological support, and administering treatments in collaboration with other healthcare professionals.
The expertise of nursing professionals in this field includes creating personalized care plans that address the unique needs of each patient.
As research advances and treatments evolve, nurses must stay informed about the latest developments in breast cancer management. They educate patients and their families on the disease process, treatment options, and self-care strategies.
Moreover, they are responsible for evaluating the effectiveness of nursing interventions and modifying care plans based on patient response and clinical outcomes, ensuring an evidence-based and patient-centered approach.
Key Takeaways
- Nurses are integral in providing patient-centered care and managing symptoms throughout the breast cancer treatment process.
- Ongoing education and adaptation of care are essential as treatments and nursing practices evolve with new research.
- Nurses evaluate and adjust interventions to improve patient outcomes, involving education and support for patients and families.
Breast Cancer Overview

This section offers an in-depth look at breast cancer, focusing on its nature, risk factors , and the signs and symptoms that facilitate early detection and treatment.
Understanding Breast Cancer
Breast cancer arises when cells in the breast grow uncontrollably, often forming a tumor that can be detected via a mammogram or felt as a lump . This malignancy is responsible for a significant mortality rate, yet early detection and advanced treatments have improved survival.
The incidence of breast cancer varies globally but it remains one of the most common cancers affecting individuals, primarily women as they age .
Assessing Risk Factors
Several risk factors contribute to the likelihood of developing breast cancer. They include age , with higher incidence in older women, a genetic predisposition to cancer, evidenced by mutations in genes such as BRCA1 and BRCA2, and exposure to radiation .
Lifestyle factors such as smoking and alcohol use can also elevate risk. Moreover, individuals with dense breast tissue may have a higher risk, underlining the importance of regular mammograms for early diagnosis .
Signs and Symptoms
Recognizing the early signs and symptoms of breast cancer is crucial for prompt diagnosis and treatment.
Common symptoms include lumps or swelling in the breast or underarm, pain in the breast that is not cyclic, changes in the color or feel of the breast skin, like dimpling or puckering, and unusual nipple discharge .
It is vital for individuals to be aware of these symptoms as they do not always indicate cancer but should prompt a medical consultation.
Nursing Interventions

Nursing interventions for breast cancer are multifaceted, focusing on managing symptoms , educating patients, and implementing evidence-based care plans tailored to individual needs.
Developing a Nursing Care Plan
A comprehensive nursing care plan begins with a thorough nursing diagnosis, which helps in identifying patient-specific needs and setting up goals.
This plan outlines the systematic approach nurses follow to address the various symptoms and complications associated with breast cancer. It is critical to ensure that the plan is adaptable to changes in the patient's condition and treatment response.
Pain and Symptom Management
Effective pain and symptom management are central to breast cancer care. Key interventions include:
- Assessment : Regularly evaluating the intensity and characteristics of pain using appropriate scales.
- Management : Utilizing a mix of pharmacological and non-pharmacological strategies to manage pain, fatigue , and nausea and vomiting .
- Nurses monitor for side effects of pain medication and adjust care as necessary to alleviate discomfort and improve quality of life .
Nurse-Led Teaching and Counselling
Nurse-led teaching and counselling are essential components. This includes:
- Education : Providing information on disease process, treatment options, side effects, and self-care techniques.
- Counselling : Addressing emotional concerns, offering support for dealing with anxiety , and depression , and facilitating coping strategies.
A systematic review highlighted the positive impact of nurse-led interventions on the health-related quality of life for breast cancer patient s, exemplifying clinical effectiveness in the nursing role.
Treatment and Management
In the context of breast cancer, a range of medical and surgical options are available, each with distinct goals and potential complications . Treatment efforts strive to remove or destroy cancerous cells while aiming to minimize morbidity associated with the disease and its management.
Surgical Interventions
Surgery remains a cornerstone in treating breast cancer, wherein a mastectomy or lumpectomy is performed to remove cancer tissue.
Post-surgical complications can include infection and lymphedema , a condition characterized by swelling due to lymphatic system disruption. Precise surgical techniques aim to reduce these risks and subsequent morbidity .
Chemotherapy and Radiotherapy
Chemotherapy and radiotherapy serve as adjuncts to surgery, attempting to eradicate microscopic disease and decrease recurrence. They can be administered pre- or post-operatively.
However, these treatments often come with significant side effects such as fatigue, nausea, and an increased risk of infection, which require careful management to maintain the patient's quality of life.
Newer Therapies and Trials
Emerging treatments, including immunotherapy and targeted drugs, offer hope for better outcomes with fewer side effects.
Ongoing clinical trials and randomised controlled trials continue to evaluate the safety and effectiveness of these new interventions, contributing to evidence-based practice and possibly reducing morbidity associated with conventional therapies.
Specialized Nursing Care
Specialized nursing care in the context of breast cancer encompasses a range of targeted interventions designed for optimizing patient outcomes. Nurses play a crucial role in case management, education, and improving the health-related quality of life for patients.
Case Management and Nurse-Led Surveillance
Nurse-led surveillance is a vital aspect of oncology nursing. It includes regular monitoring of a patient's condition, ensuring timely intervention, and tracking progress .
Several studies have shown that nurse-led surveillance can be as effective as physician-led care in terms of safety and effectiveness for breast cancer patients. These interventions involve coordinated care planning and comprehensive case management that can include scheduling follow-up appointments and managing treatment plans.
Self-Management Education
Nurses provide self-management education , equipping patients with the necessary skills to manage their symptoms and treatment side effects.
These educational initiatives often cover a wide range of topics, such as medication management, nutrition guidelines, and exercise recommendations. Empowering patients through education leads to better behavioral outcomes, helping them gain a sense of control over their health .
Health-Related Quality of Life Measures
Oncology nurses assess and implement strategies to improve the quality of life for breast cancer patients. This includes psychosocial support and interventions that aim to address both the physical and emotional challenges associated with breast cancer.
The effectiveness of specialist breast care nurses on psychosocial outcomes has been positively noted, indicating an improvement in general health-related quality of life and satisfaction with care.
Psychosocial Support
Psychosocial support is an integral component of comprehensive breast cancer care, addressing the complex emotional and psychological needs of patients throughout their cancer trajectory. It encompasses various interventions aimed at managing survivorship challenges, including emotional distress, anxiety, and symptom burden.
Emotional and Psychological Support
Nurses play a pivotal role in delivering emotional and psychological support to individuals diagnosed with breast cancer. They are trained to recognize signs of psychological distress and provide emotional support .
This support includes reassuring patients, offering hope, and assisting with grieving processes. Specialist breast care nurses act as a consistent presence, guiding patients through treatment and helping them adapt to changes in body image and self-perception.
Interventions such as counseling services and support groups are part of this support. These interventions aid in the mitigation of anxiety and enhance patients' coping mechanisms.
Resources for Emotional Support:
- Individual counseling
- Support groups
- Educational workshops
- Peer support networks
Coping with Chronic Symptoms
Chronic symptom management is critical in improving quality of life for breast cancer survivors.
Nurses are essential in educating patients about effective strategies for managing chronic pain and other long-term symptoms that may arise from treatment or disease progression.
Nurse-led interventions might include pain management education, prescription of pain relievers, or referral to physical therapy. By addressing the symptom burden , nurses help patients maintain daily activities and improve overall well-being.
Strategies for Symptom Management:
- Pain medication regimens
- Physical therapy
- Stress-reduction techniques (e.g., mindfulness, relaxation exercises)
- Lifestyle adjustments (e.g., dietary changes, exercise plans)
Implementation of Interventions
Proper implementation of interventions in breast cancer care stands as a critical facilitator for improving patient outcomes. Nursing interventions that prioritize evidence-based resources and collaborative practices are leading to enhanced healthcare delivery.
Utilizing Evidence-Based Resources
Nurse-led interventions have demonstrated effectiveness in promoting health-related quality of life for women with breast cancer, but their successful implementation is contingent upon the use of evidence-based resources.
A systematic review reinforced the significance of interventions grounded in solid research. This research is often established through randomized controlled trials (RCTs) and confidence intervals to assess their efficacy.
For instance, nursing interventions are scrutinized through the Cochrane risk-of-bias tool . This ensures that their clinical effectiveness is supported by reliable evidence before being recommended for practice.
Nurse educators and clinicians also rely on registries like PROSPERO for identifying relevant studies that influence breast cancer care guidelines.
The rigorous approach to scrutinizing evidence ensures that the nursing interventions incorporated are not only safe but are optimal for patient-centered care.
Collaboration with Multidisciplinary Teams
Effective consultation between nurses and the broader healthcare team is essential for the successful implementation of breast cancer interventions.
Research underscores that nurse-led care is as safe and effective as physician-led care , particularly when nurses are equipped with proper guidance and resources.
Emphasizing the role of collaboration , it's found that multidisciplinary teamwork in symptom management and patient counseling leads to favorable outcomes.
To enforce a seamless integration of nursing practices, channels for communication and consultation among physicians, nurses, support staff, and even the patients, are established. This ensures that all aspects of patient care are covered and bolsters the confidence of nursing staff to take initiative and apply evidence-based practices more autonomously.
Outcomes and Effectiveness

The assessment of nursing interventions in breast cancer care is crucial, focusing on the patients' quality of life, symptom management, and the clinical effectiveness of treatments. These outcomes are directly linked to behavioral changes and overall health status of survivors, showcasing the importance of precise measurement and consistent reporting protocols.
Measuring Clinical Outcomes
Clinical outcomes in breast cancer treatment are pivotal indicators of progress. They are often characterized by patient-reported improvements in quality of life and symptom management, including reductions in fatigue .
Using the Omaha System Intervention Classification Scheme , healthcare professionals can classify and standardize the interventions applied in breast cancer care.
This categorization assists in evaluating the direct effects of nursing care on clinical and behavioral outcomes.
Reporting and Documentation
Accurate reporting and documentation are fundamental for tracking the progression and responses to nursing interventions.
They provide essential data that feeds into larger compendiums used for case management and further analyses. This systematic approach ensures that all facets of patient care, from the physical to the psychosocial, are meticulously recorded, aiding in the continuous enhancement of cancer care protocols.
Systematic Reviews and Meta-Analysis
Systematic reviews and meta-analyses offer comprehensive perspectives on the effectiveness of nursing interventions for breast cancer patients.
These methods synthesize data from numerous studies and can assert the influence of nursing on symptom management and other outcomes.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines are often employed to ensure high-quality reporting in these types of research, thus contributing to the field's body of knowledge with well-substantiated findings.
Continuing Education and Training

Continuing education and training are pivotal for nurses to stay abreast of the latest nursing interventions and guidelines for breast cancer care. It ensures that nurses are equipped with the knowledge and skills necessary to provide optimal patient outcomes.
Training for Nurses
The foundation of effective breast cancer care lies in robust training programs that focus on current best practices.
Training for nurses often includes understanding the complexities of breast cancer biology and becoming proficient in patient-centered nursing interventions.
Nurses are encouraged to participate in hands-on workshops and simulations, which can be found through programs such as the Miami Breast Cancer Conference .
Nurses also have access to databases such as CINAHL and EMBASE for the latest research, including randomized controlled trials (RCTs), to inform evidence-based practice.
This research is essential for nurses who take part in developing and implementing patient care plans that include current nursing interventions.
Advancing Nurse Knowledge
Continuous education is vital for advancing nurse knowledge as it relates to breast cancer.
Programs like the Mayo Clinic's Medical Breast Training Program offer online courses that tackle risk assessment, management of breast complaints, and care for breast cancer survivors.
Nurses can deepen their understanding and apply these competencies to improve patient care.
Furthermore, education that fosters guidance and teaching roles amongst nurses supports a culture of learning and quality improvement.
Resources such as NCCN Continuing Education and the Medicine Learning Center at Medscape offer specialized modules that enhance critical thinking and clinical decision-making skills related to breast cancer care.
Preventive Strategies

The objective of preventive strategies in breast cancer is twofold: to identify the disease at the earliest stage through effective screening and to reduce the overall likelihood of its development by modifying certain lifestyle factors.
Early Detection and Screening
Early detection and screening are paramount in the battle against breast cancer.
Nurses play a crucial role in educating patients on the importance of regular mammograms , the standard method for breast cancer screening.
It's recommended that women start mammography at an age based upon individual risk factors.
Nursing care plans often emphasize the need for routine checks, as they are associated with earlier diagnosis and better treatment options.
Execution of such plans is vital to mitigate the risk of bias in delayed diagnosis due to lack of awareness.
Lifestyle Changes and Risk Reduction
Healthcare professionals, including nurses, advocate for several lifestyle changes to aid in the primary prevention of breast cancer:
- Nutrition : Encourage a diet high in vegetables, fruits, and whole grains.
- Exercise : Suggest regular physical activity to maintain a healthy weight, which can be a protective factor against breast cancer.
- Smoking Cessation : Guide patients on strategies for quitting smoking, a known risk factor for many cancers.
Implementing these changes can significantly curtail the risk and contribute positively to both physical and psychological health. Nurses develop and administer educational programs that provide patients with tools to make these changes, supporting a comprehensive approach to prevention.
Patient and Family Education
Educating on treatment options.
Patients and their families are provided with detailed information on various breast cancer treatments. These may include surgery, chemotherapy, radiation therapy, hormone therapy, and targeted therapy.
Nurses play a pivotal role by explaining how each treatment works, discussing the potential side effects of medications, and outlining the individualized nursing care plan.
- Surgery : Nurses clarify the differences between lumpectomy and mastectomy, and the expected post-operative care.
- Chemotherapy : The regimen's specifics, scheduling, medication names, and management of side effects are thoroughly discussed.
- Radiation Therapy : Instruction on the treatment's duration, frequency, and side effect management is provided.
- Hormone Therapy and Targeted Therapy : Information about how these treatments can prevent cancer recurrence is shared, along with their potential side effects.
Guiding Through Cancer Care Journey
Nurses offer guidance through the different stages of the cancer care journey, from diagnosis to survivorship. A critical aspect is establishing a robust follow-up care schedule, which includes regular medical check-ups and monitoring for signs of recurrence.
- Family Support : Emphasizing the need for family involvement and support throughout treatment and recovery.
- Nursing Care Plan : Outlining a plan that addresses the patient's unique health needs and promotes recovery.
- Survivorship Checklist : Introducing a checklist to help patients manage their long-term health post-treatment, including nutritional advice, exercise recommendations, and strategies to cope with the emotional impact of cancer.
Nurses are responsible for empowering patients and their families with education and guidance, ensuring they are prepared to manage their health effectively during and after breast cancer treatment.
Nursing Research and Future Trends
In the ever-evolving field of healthcare, nursing research plays a crucial role in enhancing breast cancer treatment and care. This section delves into the specific areas of nursing research, the incorporation of innovation in patient care, and analyzes both global trends and statistics that are shaping the future of nursing interventions for breast cancer patients.

Exploring Research Areas
Recent studies have focused on evaluating the effectiveness of nursing interventions in breast cancer care. Randomized controlled trials (RCTs) have revealed that nurse-led surveillance is just as safe and effective as physician-led care.
These interventions, as mentioned in the BMJ Supportive & Palliative Care , include guidance, teaching, counseling, and case management for symptom management.
The growth in the Cochrane Controlled Register of Trials and databases like MEDLINE help to advance these research initiatives by compiling a vast array of clinical studies crucial for evidence-based practice.
Integrating Innovation in Care
Innovation in nursing care plan development has had a significant impact on quality of life for patients. Advanced technologies and methodologies are being integrated into patient care, translating research findings into practical interventions.
For instance, the introduction of telemedicine and mobile health has allowed for continued patient support beyond the clinical setting.
Nursing care is becoming more personalized, adapting to patients' unique needs, which is particularly important for diseases with high incidence rates such as breast and lung cancer.
Global Trends and Statistics
Global trends and statistics indicate a varied prevalence of cancer. Countries like Iran have been conducting research to establish the local incidence of breast cancer and determine the best approaches for nursing interventions tailored to their population.
It's critical for nursing research to consider these various influences, as the disease burden differs around the world. By understanding these trends, nursing care can adapt to meet global health challenges effectively and improve patient outcomes on an international scale.
Regulatory and Ethical Considerations
In the landscape of oncology nursing, regulatory compliance and ethical considerations form the cornerstone of patient care. Nurses must navigate the complexities of maintaining patient rights and confidentiality while adhering to informed consent protocols.
Ethical Issues in Oncology Nursing
Oncology nursing involves critical ethical issues that must be handled with care and professionalism. The Omaha System Intervention Classification Scheme provides a structured approach to address these issues, ensuring that interventions are appropriate and ethical.
Ethical concerns such as maintaining patient confidentiality and providing thorough guidance on treatment options require a deep understanding of both ethical frameworks and the legal aspects of patient care.
- Confidentiality : Nurses are duty-bound to protect patient information, only sharing details with relevant healthcare professionals involved in the patient's care.
- Informed Consent : Patients have the right to be informed about their care. Nurses play a key role in explaining treatment plans and ensuring that patients understand the implications before consenting.
Complying with Health Care Standards
Regulatory compliance is essential for oncology nursing practice, impacting patient safety and quality of care. The Omaha System Intervention Classification Scheme is often employed as a tool to standardize nursing care and maintain adherence to healthcare standards.
- Regulatory Compliance : Nurses must stay current with regulations governing oncology care, and any changes to these regulations must be integrated into practice in a timely manner.
- Patient Rights : Upholding patient rights is a regulatory requirement that incorporates ethical obligations to protect patients' autonomy and dignity.
This appendix provides a structured overview of the tools and databases relevant to nursing interventions for breast cancer, highlighting their applications and value in research and clinical practice.
Databases :
- PubMed/MEDLINE : A comprehensive database for medical literature that includes nursing interventions for breast cancer.
- CINAHL : Catering specifically to nursing and allied health professionals, this database is crucial for identifying nursing-focused studies.
- EMBASE : Valuable for its extensive coverage of pharmacological and biomedical literature, crucial for interventions research.
- Cochrane Controlled Register of Trials : Essential for locating randomized and quasi-randomized controlled trials in breast cancer nursing.
- PROSPERO : An international database for systematic review protocols, which helps in identifying research before completion to minimize duplication.
Tools and Schemes :
- The Omaha System Intervention Classification Scheme : Employed to standardize the terminology and categorization of nursing interventions.
- Cochrane Risk-of-Bias Tool : Applied in systematic reviews to assess the risk of bias within studies, ensuring the integrity of research findings.
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) : An evidence-based minimum set of items for reporting systematic reviews, aiding in the synthesis of nursing intervention data.
Frequently Asked Questions
The following FAQs cover the specifics of nursing interventions tailored to meet the unique needs of patients with breast cancer through various stages of their treatment and recovery.
What are the components of an effective nursing care plan for patients diagnosed with breast cancer?
An effective nursing care plan for breast cancer includes assessment of the patient's physical and emotional needs, formulation of nursing diagnoses related to breast cancer, planning and implementation of interventions, and evaluation of patient outcomes. It addresses symptoms management, education on treatment options, and psychosocial support.
How does preoperative nursing management contribute to positive outcomes for breast cancer surgeries?
Preoperative nursing management plays a crucial role in preparing patients for surgery, which involves ensuring patients understand the procedure, managing expectations, and providing guidance on post-operative care. Comprehensive assessments and patient education are instrumental in reducing anxiety and promoting recovery.
Can you describe the role of nurses in providing post-mastectomy care and support?
Nurses provide critical post-mastectomy care by managing drainage tubes, monitoring for signs of infection, assisting with pain management, and supporting emotional and physical recovery. They also educate patients on arm exercises to prevent lymphedema and instruct on how to recognize potential complications.
What are the commonly used NANDA nursing diagnoses for breast cancer?
Commonly used NANDA nursing diagnoses for breast cancer may include acute pain, disturbed body image, risk for infection, and impaired skin integrity. These diagnoses focus on the most frequent challenges faced by patients undergoing treatment for breast cancer.
In what ways can nurses assist patients in managing the side effects of breast cancer treatment?
Nurses assist patients in managing the side effects of treatment by providing medication for symptom relief, offering nutritional support, guidance on lifestyle modifications, and interventions to manage fatigue and nausea. They also educate patients on self-care techniques valuable throughout the treatment process.
How do nursing interventions support patient education and coping strategies for breast cancer?
Nursing interventions support patient education by delivering accurate information about the disease process, treatment options, and self-care after procedures.
Nurses also teach coping strategies, provide resources for support groups, and ensure patients have access to mental health professionals when needed.
Related posts:
- Breast Cancer Lawyers: Finding Legal Assistance for Your Case
- Spironolactone and Breast Cancer: Unveiling the Connection
- TNBC Skin Manifestations: Identifying Cutaneous Symptoms Linked to Triple-Negative Breast Cancer
- Coffee and Triple-Negative Breast Cancer: What You Need to Know
Leave a Comment
Your email address will not be published. Required fields are marked
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Pathophysiology
Normal physiology of the human breast.
Prior to sexual maturity, male and female breasts are structurally and functionally similar; they are both comprised of small immature nipples, fatty and fibrous tissue and several duct-like arrangements beneath the areola.
When puberty is underway in males and females, this is where the major structural development occurs. Male breasts remain unchanged due to the lack of high levels of estrogen and progesterone. Females, on the other hand, have significant changes occur due to an assortment of hormones (estrogen, growth hormone, insulin-like growth factor-1, progesterone, and prolactin) (p.739) that cause the female breast to develop into a lactating system.
The mature female breast’s foundational unit is the lobe (each breast contains 15-20) a system of ducts which is comprised of and supported by Cooper ligaments. Each lobe is made up of 20-40 lobules (glands that produce milk). The lobules contain alveolar cells, which are complicated spaces lined with epithelial cells that secrete milk and sub-epithelial cells that contract, passing milk into the arrangement of ducts that leads to the nipple (p. 739).
The lobes and lobules are enclosed and separated by muscle strands and adipose connective tissue which varies in amount depending on weight, genetics, endocrine factors and contributes to the diversity of breast size and shape.
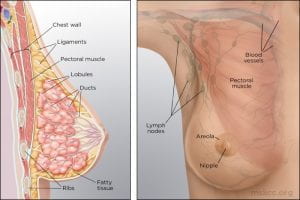
(Memorial Sloan Kettering Cancer Center)
During the reproductive years, breast tissue undergoes cyclic changes in response to hormonal changes of the menstrual cycle. After menopause, adipose deposits and connective tissue increases, glandular breast tissue becomes involuted, and breasts are reduced in size and form. Due to elevated aromatase (decreases circulating estrogen) there can be an increase in white adipose tissue inflammation (p.740).
The function of the female breast is primarily to provide a source of nourishment for the newborn; however, breasts are also a source of pleasurable sexual sensation and in Western cultures have become a sexual symbol (p.741).
(McCance, K. L., & Heuther, S. E. (2019). Pathophysiology: The biological basis for disease in adults and children (8th ed., pp.739-741). St. Louis, MO: Mosby.)
Pathophysiology of Breast Cancer
Except for skin cancer, breast cancer is the most common cancer in American women. Most breast cancer occurs in women older than 50 years. The major risk factors for breast cancer are classified as reproductive, such as nulliparity and pregnancy-associated breast cancer; familial, such as inherited gene syndromes; and environmental and lifestyle, such as hormonal factors and radiation exposure. Some examples of known carcinogenic agents with sufficient evidence in humans that contribute to the development of breast cancer are alcoholic beverages, diethylstilbestrol, estrogen-progestogen contraceptives, estrogen-progestogen menopausal therapy, X-radiation and γ-radiation (Rote, 2019). Other important factors are delayed involution of the mammary gland and increased breast density.
Overall, lifetime risk of breast cancer is reduced in parous women compared to nulliparous women, but pregnancy must occur at a young age. The influence of pregnancy on the risk of cancer also depends on family history, lactation postpartum, and overall parity. Breast gland involution after pregnancy and lactation uses some of the same tissue remodeling pathways activated during wound healing. The presence of macrophages in the involuting mammary gland contributes to carcinogenesis.
Most breast cancers are adenocarcinomas and first arise from the ductal/lobular epithelium as carcinoma in situ. Carcinoma in situ is an early-stage, noninvasive, proliferation of epithelial cells that is confined to the ducts and lobules, by the basement membrane. About 84% of all in situ disease is ductal carcinoma in situ (DCIS); the remainder is mostly lobular carcinoma in situ (LCIS) disease. Ductal carcinoma in situ (DCIS) refers to a heterogenous group of proliferative lesions limited to ducts and lobules without invasion to the basement membrane. DCIS occurs predominantly in women but can also occur in men. DCIS has a wide spectrum of risk for invasive cancers. Preinvasive lesions do not invariably progress to invasive malignancy. Lobular carcinoma in situ (LCIS) originates from the terminal duct-lobular unit. Unlike DCIS, LCIS has a uniform appearance; thus, the lobular structure is preserved. The cells grow in non-cohesive clusters, typically because of a loss of the tumor-suppressive adhesion protein E-cadherin . Also, unlike DCIS, LCIS is found as an incidental lesion from a biopsy and not mammography, is more likely to be present bilaterally.
(Winslow, 2012)
Breast cancer is a heterogeneous disease with diverse, molecular, genetic, phenotypic, and pathologic changes. Tumor heterogeneity results from the genetic, epigenetic, and microenvironmental influences (selective pressure) that tumor cells undergo during cancer progression. Cellular subpopulations from different sections of the same tumor vary in many ways including growth rate, immunogenicity, ability to metastasize, and drug response, demonstrating significant heterogeneity. The biological attributes of a tumor as a whole are strongly influenced by its subpopulation of cells with cellular populations communicating through paracrine or contact-dependent signaling (juxtacrine) from ligands and mediated from components of the microenvironment such as blood vessels, immune cells, and fibroblasts.
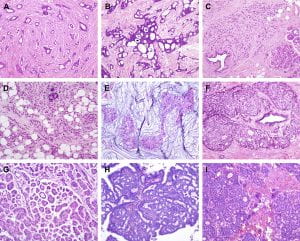
Figure 1. Histological special types of breast cancer preferentially oestrogen receptor positive. (A) Tubular carcinoma, (B) cribriform carcinoma, (C) classic invasive lobular carcinoma, (D) pleomorphic invasive lobular carcinoma, (E) mucinous carcinoma, (F) neuroendocrine carcinoma, (G) micropapillary carcinoma, (H) papillary carcinoma, (I) low grade invasive ductal carcinoma with osteoclast-like giant cells. (Weigelt, Geyer, & Reis-Filho, 2010)
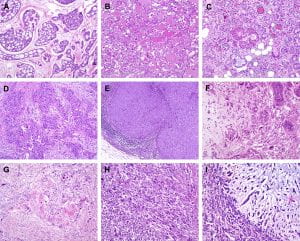
Figure 2. Histological special types of breast cancer preferentially oestrogen receptor negative. (A) Adenoid cystic carcinoma, (B) secretory carcinoma, (C) acinic-cell carcinoma, (D) apocrine carcinoma, (E) medullary carcinoma, (F) metaplastic carcinoma with heterologous elements, (G) metaplastic carcinoma with squamous metaplasia, (H) metaplastic spindle cell carcinoma, (I) metaplastic matrix-producing carcinoma. (Weigelt, Geyer, & Reis-Filho, 2010)
Gene expression profiling studies have identified major subtypes classified as luminal A, luminal B, HER2+, basal-like, Claudin-low, and normal breast. These subtypes have different prognoses and responses to therapy. Tumors can be stratified with gene expression profiles such as Oncotype Dx, Prosigna, and MammaPrint on the basis of genetic profiles. This information helps personalize breast cancer treatment and determine which women need aggressive systemic treatment for high-risk cancers versus close surveillance for indolent tumors.
Many models of breast carcinogenesis have been suggested and the expanding themes include (1) gene addiction, (2) phenotype plasticity, (3) cancer stem cells, (4) hormonal outcomes affecting cell turnover of mammary epithelium, stem cells, extracellular matrix, and immune function.
Cancer gene addiction includes oncogene addiction, whereby these driver genes play key roles in breast cancer development and progression. In non-oncogene addiction, these genes may not initiate cancer but play roles in cancer development and progression. Examples of key driver genes include HER2 and MYC, and examples of tumor-suppressor genes include TP53, BRCA1, and BRCA2. Once a founding tumor clone is established, genomic instability may assist through the establishment of other subclones and contribute to both tumor progression and therapy resistance.
Phenotypic plasticity is exemplified by a distinctive phenotype called epithelial-to-mesenchymal transition (EMT) . EMT is involved in the generation of tissues and organs during embryogenesis, is essential for driving tissue plasticity during development, and is hijacked during cancer progression. The EMT-associated programming is involved in many cancer cell characteristics, including suppression of cell death or apoptosis and senescence. It is reactivated during wound healing and is resistant to chemotherapy and radiation therapy. Remodeling or reprogramming of the breast during post-pregnancy involution is important because it involves inflammatory and “wound healing-like” tissue reactions known as reactive stroma or inflammatory stroma . The reactive stroma releases various signals and interleukins that affect nearby carcinoma cells, inducing these cells to activate their previously silent EMT programs. The activation is typically reversible (i.e., plasticity), and those EMT programs may revert through mesenchymal-epithelial (MET) to the previous phenotypic state before the induction of the EMT program. Reactive stroma increases the risk for tumor invasion and may facilitate the transition of carcinoma in situ to invasive carcinoma. Activation of an EMT program during cancer development often requires signaling between cancer cells and neighboring stromal cells. In advanced primary carcinomas, cancer cells recruit a variety of cell types into the surrounding stroma. Overall, increasing evidence suggests that interactions of cancer cells with adjacent tumor-associated stromal cells induce malignant phenotypes.
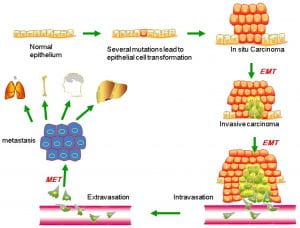
Figure 3. Putative EMT and MET in breast cancer progression. Normal epithelial cells undergo a series of transformational changes to become malignant tumor cells. Clonal proliferation of malignant cells gives rise to invasive carcinoma. Some of these cells undergo EMT and enter into the neighboring blood vessels or lymphatic vessels. These cells may remain in the circulation as circulating tumor cells or may extravasate at a distant site. The extravasated tumor cells form macrometastasis by a reverse mechanism known as MET. EMT, epithelial-mesenchymal transition; MET, mesenchymal-epithelial transition. (Liu, Gu, Shan, Geng, & Sang, 2016)
Using a mouse model of tumor heterogeneity, investigators demonstrated different clones within the heterogeneous population had distinct properties, such as the ability to dominate the primary tumor, or to contribute to metastatic populations, or to enter the lymphatic or vascular systems via vascular mimicry.
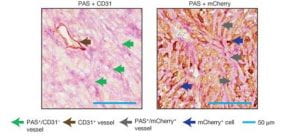
(Wagenblast et al., 2015)
Figure 4. Two adjacent sections of a mouse breast tumor. Tissue at left is stained so that normal blood vessels can be seen (brown arrow). Extending from these vessels are blood filled channels (green arrows). On the right, the tissue is stained for a fluorescent protein expressed by the tumor cells. Here it is seen that blood-filled channels are actually formed by tumor cells in a process known as vascular mimicry. The team demonstrate that the tumor cells lining these channels help drive metastasis, the process by which tumors spread. (Ravindran, 2019)
Invasion by primary tumor cells typically involves the collective migration of large cohesive groups into adjacent tissue rather than the scattering of individual carcinoma cells. However, still unknown are the precise events occurring at the invasive stage. Dormant carcinoma cells called minimal residual disease (MRD) appear to perpetuate carcinogenesis and form the precursors of eventual metastatic relapse and, sometimes, rapid cancer recurrence. Dormant cells have exited the cell cycle and are not proliferating. Thus current treatments that preferentially kill proliferating cells render dormant cells intrinsically more resistant and may remain after initial chemotherapy, radiotherapy, and surgery.
Emerging evidence supports three main prerequisites that must be met for metastatic colonization to succeed: the capacity to seed and maintain a population of tumor-initiating stem cells; the ability to create adaptive, organ-specific colonization programs; and the development of a supportive microenvironmental niche. Metastases may also occur early in the process of neoplastic transformation.
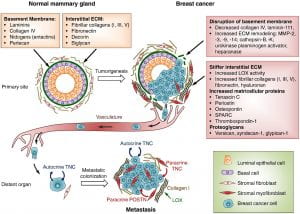
Figure 5 . Extracellular matrix (ECM) changes in breast cancer progression and metastasis. The primary components of the ECM in normal mammary gland are significantly changed in breast cancer. A desmoplastic reaction is associated with breast cancer development, due to the increased production of fibrous ECM by activated fibroblasts and cancer cells. The increased collagen deposition and crosslinking by lysyl oxidase (LOX) enzymes, together with the increased production of fibronectin and other ECM components, stiffens the ECM, which in turn promotes tumor aggressiveness. The basement membrane surrounding the mammary gland epithelium is broken down by ECM remodeling enzymes like MMPs, heparanase and others. Matricellular proteins that promote cancer cell fitness such as tenascin C, periostin, osteopontin, SPARC and thrombospondin-1 are also upregulated. Breast cancer cells from the primary tumor, that include cells with the ability to establish metastatic colonies, enter the blood circulation, disseminate and can reach distant sites. While the vast majority of disseminated cancer cells are eliminated or undergo dormancy due to the adverse environment, few cancer cells are able to resist the selective pressure and establish a metastatic colony. These cells may rely on signals from the ECM such as type I collagen (collagen I), crosslinked by LOX. Tenascin C (TNC) and periostin (POSTN), which are crucial ECM proteins of the metastatic niche, promote stem/progenitor pathways and metastatic fitness in disseminated breast cancer cells. (Insua-Rodríguez & Oskarsson, 2016)
The first clinical manifestation of breast cancer is usually a small, painless lump in the breast. Other manifestations include palpable lymph nodes in the axillae, dimpling of the skin, nipple and skin retraction, nipple discharge, ulcerations, reddened skin, and bone pain associated with bony metastases.
Treatment is based on the extent or stage of the cancer and includes surgery, radiation, chemotherapy, hormone therapy, and biologic therapy.
(Unless otherwise cited, all pathophysiology information was gathered from Danhausen, Phillippi, & McCance, 2019)
- Around the Practice
- Between the Lines
- Contemporary Concepts
- Readout 360
- Insights from Experts at Mayo Clinic on Translating Evidence to Clinical Practice
- Optimizing Outcomes in Patients with HER2+ Metastatic Breast Cancer

- Conferences
- Publications
Case 1: 48-Year-Old Patient With HER2+ Metastatic Breast Cancer

EP: 1 . Best Practices: HER2+ MBC With Brain Mets

EP: 2 . Frontline Standards of Care for HER2+ MBC

EP: 3 . Case 1: 48-Year-Old Patient With HER2+ Metastatic Breast Cancer

EP: 4 . Treatment Strategies for Relapsed/Refractory HER2+ MBC

EP: 5 . Case 2: 61-Year-Old Patient With R/R HER2+ MBC
EP: 6 . Cancer Network Around the Practice: Relapsed/Refractory HER2+ Metastatic Breast Cancer
Adam M. Brufsky, MD, PhD: Let’s talk about this case. This is a 48-year-old woman who presented to her primary care physician a number of years ago with a lump in her breast. She had a 4.4-cm left breast mass and 3 palpable axillary lymph nodes. Her ultrasound and mammogram confirmed these physical findings.
She was referred to a medical oncologist and had a core needle biopsy that showed ER- [estrogen receptor-negative]/PR- [progesterone receptor-negative], HER2 [human epidermal growth factor receptor 2]-positive by IHC [immunohistochemistry score] that was 3+. A CT scan of the chest, abdomen, and pelvis showed 3 liver lesions, the largest being 3.1 cm. This is the de novo patient we always talk about. She had an MRI of the brain and it was negative for metastasis. She received 6 cycles of THP [docetaxel, trastuzumab, pertuzumab], followed by HP [trastuzumab, pertuzumab] for another 12 months. That’s 18 months of therapy.
She had a partial response in her breast mass, and her liver lesions fully responded. Later, she suddenly began to have rapid unexplained weight loss. The CT scan only showed 2 new liver lesions, so not quite the symptom I would imagine. She then got a brain MRI that showed about 30 widely scattered lesions, the largest being about 0.5 or 0.6 [cm]. They have all these little punctate ones; you’ve all seen those.
The question is: what treatment would you give this person? Let’s say the brain MRI shows 3 lesions, all in the frontal cortex, with the largest being 1.5 cm. That makes it a little bit of a different question because if there are widely scattered lesions, we’re not going to want to do SRS [stereotactic radiosurgery]. We are probably going to want to do whole brain radiation. Let’s say she’s asymptomatic with no edema. The polling question is: what treatment would you recommend? T-DM1 [trastuzumab emtansine], tucatinib/trastuzumab/capecitabine, SRS to the brain metastases, clinical trial, or other.
You guys could answer that question. Let me start with Sara. How would you approach this?
Sara A. Hurvitz, MD, FACP: They’re not totally mutually exclusive, right? You could do SRS and switch systemic therapy. She is progressing systemically in the liver, so I think switching systemic therapy makes sense. I like tucatinib because it does penetrate the blood-brain barrier, but I would still be tempted and would probably talk to my radiation oncology and neurosurgery colleagues. We’d probably end up doing both the SRS and tucatinib-based therapy.
Adam M. Brufsky, MD, PhD: That’s reasonable. VK, do you have any other comments on this?
VK Gadi, MD, PhD: Yes, I agree. The tolerability of the regimen is good. You might even give this lady an opportunity to fly without SRS and have that in your back pocket. If you’re not seeing control, you can go to SRS at a later time. I don’t think there’s a wrong answer here. You could probably do it both ways.
Adam M. Brufsky, MD, PhD: Neil, do you have something to add?
Neil M. Iyengar, MD: No. She fits perfectly into the HER2CLIMB population, so I agree with everything that has been said because there is demonstrated activity of the tucatinib-based regimen in terms of CNS [central nervous system] response. Coupling that with SRS is reasonable. This is the patient we were talking about earlier with whom we would discuss foregoing local therapy to the brain. That’s a reasonable discussion here. It’s a tricky poll question because my kneejerk response would be to put her on a clinical trial. We should all be trying to prioritize clinical trials, but in the absence of that clinical availability, tucatinib plus or minus radiation is a reasonable option.
Adam M. Brufsky, MD, PhD: There’s a clinical trial that’s great; it’s not scientifically spectacular, but clinically, it’s fabulous. I believe it’s called DESTINY. In fact, I put a patient on it today with trastuzumab deruxtecan and tucatinib together. That’s a great trial that’s going to accrue quickly. If we could put as many people as we can on that, we can answer the clinical question quickly. I would agree.
I have 1 last question before we go on to the last 25 minutes and the last segment. What do you tell people about [adverse] effects? Are you seeing a lot of [adverse] effects with tucatinib? Do you have to dose reduce it at all when you give it? These are questions people who haven’t had a lot of experience with it usually ask. I’ll start with Neil. Do you see a lot of diarrhea? Do you have to dose reduce with tucatinib?
Neil M. Iyengar, MD: In my experience, this regimen is quite tolerable. We all, as oncologists, have unfortunately become very comfortable with managing diarrhea, along with oncology nursing and so forth. What I have found with the tucatinib-based regimen is that with the initiation of antidiarrheal agents, the diarrhea usually resolves or improves pretty quickly. People have to know about it and be prepared to deal with it immediately. It does come on early, usually within the first cycle.
The other consideration to keep in mind with tucatinib is that many of the [adverse] effects are likely related to capecitabine. We’re all very comfortable with managing capecitabine-related toxicity and dose modifying capecitabine as needed. We see in the HER2CLIMB data that patients in the tucatinib arm stayed on study longer and were therefore exposed to capecitabine for longer than those in the placebo arm. I think a lot of the toxicities are familiar ones that are related to capecitabine and are quite manageable.
Adam M. Brufsky, MD, PhD: Great. VK and Sara, do you have any other comments about this toxicity? Do you see any toxicity at all with this, more than you’d expect?
Sara A. Hurvitz, MD, FACP: It’s well tolerated. About 13% had grade 3/4 diarrhea. Before getting on this call, I had to dose reduce a patient on this therapy. It’s hard to tell. On the clinical trial we enrolled patients, and I had a patient on who had severe colitis, hospitalization, etc, and I was sure she was getting tucatinib. When she was unblinded after the data came out, it turned out that she wasn’t on tucatinib. She was on placebo. I completely agree that these are [adverse] effects we’re used to with capecitabine. There’s not a whole lot of difference. Tucatinib is pretty well tolerated.
VK Gadi, MD, PhD: I agree. I think the capecitabine is the real culprit. The people on the trial were actually on it for so much longer that the toxicities from capecitabine emerged ongoing on the study. That has been my experience. Something important we don’t yet have is the PRO [patient-reported outcomes] data from these studies. A lot of my colleagues, especially those in communities where patients come in from a long way away, know that this is a tremendous pill burden with this regimen. Sometimes a parenteral regimen that you’re giving every 3 weeks is better for patients. I’m curious to see what those data look like when they come out. From our perspective as physicians, this is a slam dunk and it’s easy to give, but that’s not always the perspective that matters.
Adam M. Brufsky, MD, PhD: I agree.
Sara A. Hurvitz, MD, FACP: Yes, I think the quality of life PRO data were presented at the San Antonio [Breast Cancer Symposium]. I’m trying to pull it up. I don’t have it right at my fingertips, but my recollection was that it looked fairly good, that the quality of life was maintained.
Adam M. Brufsky, MD, PhD: Right, but they’re not going to tell you that they’re struggling to take all those pills. It’s a lot.
Sara A. Hurvitz, MD, FACP: That’s true.
Adam M. Brufsky, MD, PhD: It’s about 9 pills a day, which is a lot.
Neil M. Iyengar, MD: The quality of life data are always interesting because the end point of choice is time to deterioration and whether we are avoiding that. I think that’s a fairly low bar.
Adam M. Brufsky, MD, PhD: Exactly. Women are going to do anything they can.
Transcript edited for clarity.
- Open access
- Published: 24 April 2024
Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review
- Virginia Dickson-Swift 1 ,
- Joanne Adams 1 ,
- Evelien Spelten 1 ,
- Irene Blackberry 2 ,
- Carlene Wilson 3 , 4 , 5 &
- Eva Yuen 3 , 6 , 7 , 8
BMC Women's Health volume 24 , Article number: 256 ( 2024 ) Cite this article
27 Accesses
Metrics details
This scoping review aimed to identify and present the evidence describing key motivations for breast cancer screening among women aged ≥ 75 years. Few of the internationally available guidelines recommend continued biennial screening for this age group. Some suggest ongoing screening is unnecessary or should be determined on individual health status and life expectancy. Recent research has shown that despite recommendations regarding screening, older women continue to hold positive attitudes to breast screening and participate when the opportunity is available.
All original research articles that address motivation, intention and/or participation in screening for breast cancer among women aged ≥ 75 years were considered for inclusion. These included articles reporting on women who use public and private breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The Joanna Briggs Institute (JBI) methodology for scoping reviews was used to guide this review. A comprehensive search strategy was developed with the assistance of a specialist librarian to access selected databases including: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Web of Science and PsychInfo. The review was restricted to original research studies published since 2009, available in English and focusing on high-income countries (as defined by the World Bank). Title and abstract screening, followed by an assessment of full-text studies against the inclusion criteria was completed by at least two reviewers. Data relating to key motivations, screening intention and behaviour were extracted, and a thematic analysis of study findings undertaken.
A total of fourteen (14) studies were included in the review. Thematic analysis resulted in identification of three themes from included studies highlighting that decisions about screening were influenced by: knowledge of the benefits and harms of screening and their relationship to age; underlying attitudes to the importance of cancer screening in women's lives; and use of decision aids to improve knowledge and guide decision-making.
The results of this review provide a comprehensive overview of current knowledge regarding the motivations and screening behaviour of older women about breast cancer screening which may inform policy development.
Peer Review reports
Introduction
Breast cancer is now the most commonly diagnosed cancer in the world overtaking lung cancer in 2021 [ 1 ]. Across the globe, breast cancer contributed to 25.8% of the total number of new cases of cancer diagnosed in 2020 [ 2 ] and accounts for a high disease burden for women [ 3 ]. Screening for breast cancer is an effective means of detecting early-stage cancer and has been shown to significantly improve survival rates [ 4 ]. A recent systematic review of international screening guidelines found that most countries recommend that women have biennial mammograms between the ages of 40–70 years [ 5 ] with some recommending that there should be no upper age limit [ 6 , 7 , 8 , 9 , 10 , 11 , 12 ] and others suggesting that benefits of continued screening for women over 75 are not clear [ 13 , 14 , 15 ].
Some guidelines suggest that the decision to end screening should be determined based on the individual health status of the woman, their life expectancy and current health issues [ 5 , 16 , 17 ]. This is because the benefits of mammography screening may be limited after 7 years due to existing comorbidities and limited life expectancy [ 18 , 19 , 20 , 21 ], with some jurisdictions recommending breast cancer screening for women ≥ 75 years only when life expectancy is estimated as at least 7–10 years [ 22 ]. Others have argued that decisions about continuing with screening mammography should depend on individual patient risk and health management preferences [ 23 ]. This decision is likely facilitated by a discussion between a health care provider and patient about the harms and benefits of screening outside the recommended ages [ 24 , 25 ]. While mammography may enable early detection of breast cancer, it is clear that false-positive results and overdiagnosis Footnote 1 may occur. Studies have estimated that up to 25% of breast cancer cases in the general population may be over diagnosed [ 26 , 27 , 28 ].
The risk of being diagnosed with breast cancer increases with age and approximately 80% of new cases of breast cancer in high-income countries are in women over the age of 50 [ 29 ]. The average age of first diagnosis of breast cancer in high income countries is comparable to that of Australian women which is now 61 years [ 2 , 4 , 29 ]. Studies show that women aged ≥ 75 years generally have positive attitudes to mammography screening and report high levels of perceived benefits including early detection of breast cancer and a desire to stay healthy as they age [ 21 , 30 , 31 , 32 ]. Some women aged over 74 participate, or plan to participate, in screening despite recommendations from health professionals and government guidelines advising against it [ 33 ]. Results of a recent review found that knowledge of the recommended guidelines and the potential harms of screening are limited and many older women believed that the benefits of continued screening outweighed the risks [ 30 ].
Very few studies have been undertaken to understand the motivations of women to screen or to establish screening participation rates among women aged ≥ 75 and older. This is surprising given that increasing age is recognised as a key risk factor for the development of breast cancer, and that screening is offered in many locations around the world every two years up until 74 years. The importance of this topic is high given the ambiguity around best practice for participation beyond 74 years. A preliminary search of Open Science Framework, PROSPERO, Cochrane Database of Systematic Reviews and JBI Evidence Synthesis in May 2022 did not locate any reviews on this topic.
This scoping review has allowed for the mapping of a broad range of research to explore the breadth and depth of the literature, summarize the evidence and identify knowledge gaps [ 34 , 35 ]. This information has supported the development of a comprehensive overview of current knowledge of motivations of women to screen and screening participation rates among women outside the targeted age of many international screening programs.
Materials and methods
Research question.
The research question for this scoping review was developed by applying the Population—Concept—Context (PCC) framework [ 36 ]. The current review addresses the research question “What research has been undertaken in high-income countries (context) exploring the key motivations to screen for breast cancer and screening participation (concepts) among women ≥ 75 years of age (population)?
Eligibility criteria
Participants.
Women aged ≥ 75 years were the key population. Specifically, motivations to screen and screening intention and behaviour and the variables that discriminate those who screen from those who do not (non-screeners) were utilised as the key predictors and outcomes respectively.
From a conceptual perspective it was considered that motivation led to behaviour, therefore articles that described motivation and corresponding behaviour were considered. These included articles reporting on women who use public (government funded) and private (fee for service) breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The scope included high-income countries using the World Bank definition [ 37 ]. These countries have broadly similar health systems and opportunities for breast cancer screening in both public and private settings.
Types of sources
All studies reporting original research in peer-reviewed journals from January 2009 were eligible for inclusion, regardless of design. This date was selected due to an evaluation undertaken for BreastScreen Australia recommending expansion of the age group to include 70–74-year-old women [ 38 ]. This date was also indicative of international debate regarding breast cancer screening effectiveness at this time [ 39 , 40 ]. Reviews were also included, regardless of type—scoping, systematic, or narrative. Only sources published in English and available through the University’s extensive research holdings were eligible for inclusion. Ineligible materials were conference abstracts, letters to the editor, editorials, opinion pieces, commentaries, newspaper articles, dissertations and theses.
This scoping review was registered with the Open Science Framework database ( https://osf.io/fd3eh ) and followed Joanna Briggs Institute (JBI) methodology for scoping reviews [ 35 , 36 ]. Although ethics approval is not required for scoping reviews the broader study was approved by the University Ethics Committee (approval number HEC 21249).
Search strategy
A pilot search strategy was developed in consultation with an expert health librarian and tested in MEDLINE (OVID) and conducted on 3 June 2022. Articles from this pilot search were compared with seminal articles previously identified by the members of the team and used to refine the search terms. The search terms were then searched as both keywords and subject headings (e.g., MeSH) in the titles and abstracts and Boolean operators employed. A full MEDLINE search was then carried out by the librarian (see Table 1 ). This search strategy was adapted for use in each of the following databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medical Literature Analysis and Retrieval System Online (MEDLINE), Web of Science and PsychInfo databases. The references of included studies have been hand-searched to identify any additional evidence sources.
Study/source of evidence selection
Following the search, all identified citations were collated and uploaded into EndNote v.X20 (Clarivate Analytics, PA, USA) and duplicates removed. The resulting articles were then imported into Covidence – Cochrane’s systematic review management software [ 41 ]. Duplicates were removed once importation was complete, and title and abstract screening was undertaken against the eligibility criteria. A sample of 25 articles were assessed by all reviewers to ensure reliability in the application of the inclusion and exclusion criteria. Team discussion was used to ensure consistent application. The Covidence software supports blind reviewing with two reviewers required at each screening phase. Potentially relevant sources were retrieved in full text and were assessed against the inclusion criteria by two independent reviewers. Conflicts were flagged within the software which allows the team to discuss those that have disagreements until a consensus was reached. Reasons for exclusion of studies at full text were recorded and reported in the scoping review. The Preferred Reporting Items of Systematic Reviews extension for scoping reviews (PRISMA-ScR) checklist was used to guide the reporting of the review [ 42 ] and all stages were documented using the PRISMA-ScR flow chart [ 42 ].
Data extraction
A data extraction form was created in Covidence and used to extract study characteristics and to confirm the study’s relevance. This included specific details such as article author/s, title, year of publication, country, aim, population, setting, data collection methods and key findings relevant to the review question. The draft extraction form was modified as needed during the data extraction process.
Data analysis and presentation
Extracted data were summarised in tabular format (see Table 2 ). Consistent with the guidelines for the effective reporting of scoping reviews [ 43 ] and the JBI framework [ 35 ] the final stage of the review included thematic analysis of the key findings of the included studies. Study findings were imported into QSR NVivo with coding of each line of text. Descriptive codes reflected key aspects of the included studies related to the motivations and behaviours of women > 75 years about breast cancer screening.
In line with the reporting requirements for scoping reviews the search results for this review are presented in Fig. 1 [ 44 ].
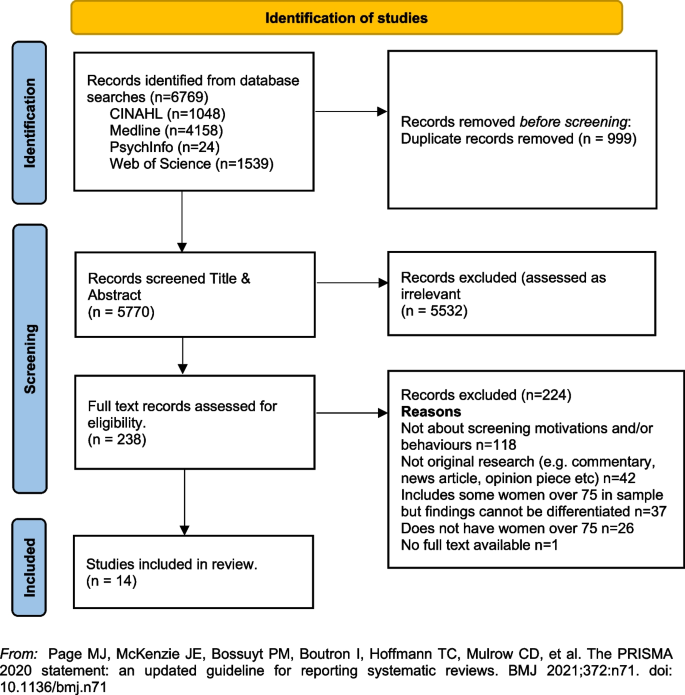
PRISMA Flowchart. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
A total of fourteen [ 14 ] studies were included in the review with studies from the following countries, US n = 12 [ 33 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ], UK n = 1 [ 23 ] and France n = 1 [ 56 ]. Sample sizes varied, with most containing fewer than 50 women ( n = 8) [ 33 , 45 , 46 , 48 , 51 , 52 , 55 ]. Two had larger samples including a French study with 136 women (a sub-set of a larger sample) [ 56 ], and one mixed method study in the UK with a sample of 26 women undertaking interviews and 479 women completing surveys [ 23 ]. One study did not report exact numbers [ 50 ]. Three studies [ 47 , 53 , 54 ] were undertaken by a group of researchers based in the US utilising the same sample of women, however each of the papers focused on different primary outcomes. The samples in the included studies were recruited from a range of locations including primary medical care clinics, specialist medical clinics, University affiliated medical clinics, community-based health centres and community outreach clinics [ 47 , 53 , 54 ].
Data collection methods varied and included: quantitative ( n = 8), qualitative ( n = 5) and mixed methods ( n = 1). A range of data collection tools and research designs were utilised; pre/post, pilot and cross-sectional surveys, interviews, and secondary analysis of existing data sets. Seven studies focused on the use of a Decision Aids (DAs), either in original or modified form, developed by Schonberg et al. [ 55 ] as a tool to increase knowledge about the harms and benefits of screening for older women [ 45 , 47 , 48 , 49 , 52 , 54 , 55 ]. Three studies focused on intention to screen [ 33 , 53 , 56 ], two on knowledge of, and attitudes to, screening [ 23 , 46 ], one on information needs relating to risks and benefits of screening discontinuation [ 51 ], and one on perceptions about discontinuation of screening and impact of social interactions on screening [ 50 ].
The three themes developed from the analysis of the included studies highlighted that decisions about screening were primarily influenced by: (1) knowledge of the benefits and harms of screening and their relationship to age; (2) underlying attitudes to the importance of cancer screening in women's lives; and (3) exposure to decision aids designed to facilitate informed decision-making. Each of these themes will be presented below drawing on the key findings of the appropriate studies. The full dataset of extracted data can be found in Table 2 .
Knowledge of the benefits and harms of screening ≥ 75 years
The decision to participate in routine mammography is influenced by individual differences in cognition and affect, interpersonal relationships, provider characteristics, and healthcare system variables. Women typically perceive mammograms as a positive, beneficial and routine component of care [ 46 ] and an important aspect of taking care of themselves [ 23 , 46 , 49 ]. One qualitative study undertaken in the US showed that few women had discussed mammography cessation or the potential harms of screening with their health care providers and some women reported they would insist on receiving mammography even without a provider recommendation to continue screening [ 46 ].
Studies suggested that ageing itself, and even poor health, were not seen as reasonable reasons for screening cessation. For many women, guidance from a health care provider was deemed the most important influence on decision-making [ 46 ]. Preferences for communication about risk and benefits were varied with one study reporting women would like to learn more about harms and risks and recommended that this information be communicated via physicians or other healthcare providers, included in brochures/pamphlets, and presented outside of clinical settings (e.g., in community-based seniors groups) [ 51 ]. Others reported that women were sometimes sceptical of expert and government recommendations [ 33 ] although some were happy to participate in discussions with health educators or care providers about breast cancer screening harms and benefits and potential cessation [ 52 ].
Underlying attitudes to the importance of cancer screening at and beyond 75 years
Included studies varied in describing the importance of screening, with some attitudes based on past attendance and some based on future intentions to screen. Three studies reported findings indicating that some women intended to continue screening after 75 years of age [ 23 , 45 , 46 ], with one study in the UK reporting that women supported an extension of the automatic recall indefinitely, regardless of age or health status. In this study, failure to invite older women to screen was interpreted as age discrimination [ 23 ]. The desire to continue screening beyond 75 was also highlighted in a study from France that found that 60% of the women ( n = 136 aged ≥ 75) intended to pursue screening in the future, and 27 women aged ≥ 75, who had never undergone mammography previously (36%), intended to do so in the future [ 56 ]. In this same study, intentions to screen varied significantly [ 56 ]. There were no sociodemographic differences observed between screened and unscreened women with regard to level of education, income, health risk behaviour (smoking, alcohol consumption), knowledge about the importance and the process of screening, or psychological features (fear of the test, fear of the results, fear of the disease, trust in screening impact) [ 56 ]. Further analysis showed that three items were statistically correlated with a higher rate of attendance at screening: (1) screening was initiated by a physician; (2) the women had a consultation with a gynaecologist during the past 12 months; and (3) the women had already undergone at least five screening mammograms. Analysis highlighted that although average income, level of education, psychological features or other types of health risk behaviours did not impact screening intention, having a mammogram previously impacted likelihood of ongoing screening. There was no information provided that explained why women who had not previously undergone screening might do so in the future.
A mixed methods study in the UK reported similar findings [ 23 ]. Utilising interviews ( n = 26) and questionnaires ( n = 479) with women ≥ 70 years (median age 75 years) the overwhelming result (90.1%) was that breast screening should be offered to all women indefinitely regardless of age, health status or fitness [ 23 ], and that many older women were keen to continue screening. Both the interview and survey data confirmed women were uncertain about eligibility for breast screening. The survey data showed that just over half the women (52.9%) were unaware that they could request mammography or knew how to access it. Key reasons for screening discontinuation were not being invited for screening (52.1%) and not knowing about self-referral (35.1%).
Women reported that not being invited to continue screening sent messages that screening was no longer important or required for this age group [ 23 ]. Almost two thirds of the women completing the survey (61.6%) said they would forget to attend screening without an invitation. Other reasons for screening discontinuation included transport difficulties (25%) and not wishing to burden family members (24.7%). By contrast, other studies have reported that women do not endorse discontinuation of screening mammography due to advancing age or poor health, but some may be receptive to reducing screening frequency on recommendation from their health care provider [ 46 , 51 ].
Use of Decision Aids (DAs) to improve knowledge and guide screening decision-making
Many women reported poor knowledge about the harms and benefits of screening with studies identifying an important role for DAs. These aids have been shown to be effective in improving knowledge of the harms and benefits of screening [ 45 , 54 , 55 ] including for women with low educational attainment; as compared to women with high educational attainment [ 47 ]. DAs can increase knowledge about screening [ 47 , 49 ] and may decrease the intention to continue screening after the recommended age [ 45 , 52 , 54 ]. They can be used by primary care providers to support a conversation about breast screening intention and reasons for discontinuing screening. In one pilot study undertaken in the US using a DA, 5 of the 8 women (62.5%) indicated they intended to continue to receive mammography; however, 3 participants planned to get them less often [ 45 ]. When asked whether they thought their physician would want them to get a mammogram, 80% said “yes” on pre-test; this figure decreased to 62.5% after exposure to the DA. This pilot study suggests that the use of a decision-aid may result in fewer women ≥ 75 years old continuing to screen for breast cancer [ 45 ].
Similar findings were evident in two studies drawing on the same data undertaken in the US [ 48 , 53 ]. Using a larger sample ( n = 283), women’s intentions to screen prior to a visit with their primary care provider and then again after exposure to the DA were compared. Results showed that 21.7% of women reduced their intention to be screened, 7.9% increased their intentions to be screened, and 70.4% did not change. Compared to those who had no change or increased their screening intentions, women who had a decrease in screening intention were significantly less likely to receive screening after 18 months. Generally, studies have shown that women aged 75 and older find DAs acceptable and helpful [ 47 , 48 , 49 , 55 ] and using them had the potential to impact on a women’s intention to screen [ 55 ].
Cadet and colleagues [ 49 ] explored the impact of educational attainment on the use of DAs. Results highlight that education moderates the utility of these aids; women with lower educational attainment were less likely to understand all the DA’s content (46.3% vs 67.5%; P < 0.001); had less knowledge of the benefits and harms of mammography (adjusted mean ± standard error knowledge score, 7.1 ± 0.3 vs 8.1 ± 0.3; p < 0.001); and were less likely to have their screening intentions impacted (adjusted percentage, 11.4% vs 19.4%; p = 0.01).
This scoping review summarises current knowledge regarding motivations and screening behaviours of women over 75 years. The findings suggest that awareness of the importance of breast cancer screening among women aged ≥ 75 years is high [ 23 , 46 , 49 ] and that many women wish to continue screening regardless of perceived health status or age. This highlights the importance of focusing on motivation and screening behaviours and the multiple factors that influence ongoing participation in breast screening programs.
The generally high regard attributed to screening among women aged ≥ 75 years presents a complex challenge for health professionals who are focused on potential harm (from available national and international guidelines) in ongoing screening for women beyond age 75 [ 18 , 20 , 57 ]. Included studies highlight that many women relied on the advice of health care providers regarding the benefits and harms when making the decision to continue breast screening [ 46 , 51 , 52 ], however there were some that did not [ 33 ]. Having a previous pattern of screening was noted as being more significant to ongoing intention than any other identified socio-demographic feature [ 56 ]. This is perhaps because women will not readily forgo health care practices that they have always considered important and that retain ongoing importance for the broader population.
For those women who had discontinued screening after the age of 74 it was apparent that the rationale for doing so was not often based on choice or receipt of information, but rather on factors that impact decision-making in relation to screening. These included no longer receiving an invitation to attend, transport difficulties and not wanting to be a burden on relatives or friends [ 23 , 46 , 51 ]. Ongoing receipt of invitations to screen was an important aspect of maintaining a capacity to choose [ 23 ]. This was particularly important for those women who had been regular screeners.
Women over 75 require more information to make decisions regarding screening [ 23 , 52 , 54 , 55 ], however health care providers must also be aware that the element of choice is important for older women. Having a capacity to choose avoids any notion of discrimination based on age, health status, gender or sociodemographic difference and acknowledges the importance of women retaining control over their health [ 23 ]. It was apparent that some women would choose to continue screening at a reduced frequency if this option was available and that women should have access to information facilitating self-referral [ 23 , 45 , 46 , 51 , 56 ].
Decision-making regarding ongoing breast cancer screening has been facilitated via the use of Decision Aids (DAs) within clinical settings [ 54 , 55 ]. While some studies suggest that women will make a decision regardless of health status, the use of DAs has impacted women’s decision to screen. While this may have limited benefit for those of lower educational attainment [ 48 ] they have been effective in improving knowledge relating to harms and benefits of screening particularly where they have been used to support a conversation with women about the value of screening [ 54 , 55 , 56 ].
Women have identified challenges in engaging in conversations with health care providers regarding ongoing screening, because providers frequently draw on projections of life expectancy and over-diagnosis [ 17 , 51 ]. As a result, these conversations about screening after age 75 years often do not occur [ 46 ]. It is likely that health providers may need more support and guidance in leading these conversations. This may be through the use of DAs or standardised checklists. It may be possible to incorporate these within existing health preventive measures for this age group. The potential for advice regarding ongoing breast cancer screening to be available outside of clinical settings may provide important pathways for conversations with women regarding health choices. Provision of information and advice in settings such as community based seniors groups [ 51 ] offers a potential platform to broaden conversations and align sources of information, not only with health professionals but amongst women themselves. This may help to address any misconception regarding eligibility and access to services [ 23 ]. It may also be aligned with other health promotion and lifestyle messages provided to this age group.
Limitations of the review
The searches that formed the basis of this review were carried in June 2022. Although the search was comprehensive, we have only captured those studies that were published in the included databases from 2009. There may have been other studies published outside of these periods. We also limited the search to studies published in English with full-text availability.
The emphasis of a scoping review is on comprehensive coverage and synthesis of the key findings, rather than on a particular standard of evidence and, consequently a quality assessment of the included studies was not undertaken. This has resulted in the inclusion of a wide range of study designs and data collection methods. It is important to note that three studies included in the review drew on the same sample of women (283 over > 75)[ 49 , 53 , 54 ]. The results of this review provide valuable insights into motivations and behaviours for breast cancer screening for older women, however they should be interpreted with caution given the specific methodological and geographical limitations.
Conclusion and recommendations
This scoping review highlighted a range of key motivations and behaviours in relation to breast cancer screening for women ≥ 75 years of age. The results provide some insight into how decisions about screening continuation after 74 are made and how informed decision-making can be supported. Specifically, this review supports the following suggestions for further research and policy direction:
Further research regarding breast cancer screening motivations and behaviours for women over 75 would provide valuable insight for health providers delivering services to women in this age group.
Health providers may benefit from the broader use of decision aids or structured checklists to guide conversations with women over 75 regarding ongoing health promotion/preventive measures.
Providing health-based information in non-clinical settings frequented by women in this age group may provide a broader reach of information and facilitate choices. This may help to reduce any perception of discrimination based on age, health status or socio-demographic factors.
Availability of data and materials
All data generated or analysed during this study is included in this published article (see Table 2 above).
Cancer Australia, in their 2014 position statement, define “overdiagnosis” in the following way. ‘’Overdiagnosis’ from breast screening does not refer to error or misdiagnosis, but rather refers to breast cancer diagnosed by screening that would not otherwise have been diagnosed during a woman’s lifetime. “Overdiagnosis” includes all instances where cancers detected through screening (ductal carcinoma in situ or invasive breast cancer) might never have progressed to become symptomatic during a woman’s life, i.e., cancer that would not have been detected in the absence of screening. It is not possible to precisely predict at diagnosis, to which cancers overdiagnosis would apply.” (accessed 22. nd August 2022; https://www.canceraustralia.gov.au/resources/position-statements/overdiagnosis-mammographic-screening ).
World Health Organization. Breast Cancer Geneva: WHO; 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=Reducing%20global%20breast%20cancer%20mortality,and%20comprehensive%20breast%20cancer%20management .
International Agency for Research on Cancer (IARC). IARC Handbooks on Cancer Screening: Volume 15 Breast Cancer Geneva: IARC; 2016 [Available from: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Handbooks-Of-Cancer-Prevention/Breast-Cancer-Screening-2016 .
Australian Institute of Health and Welfare. Cancer in Australia 2021 [Available from: https://www.canceraustralia.gov.au/cancer-types/breast-cancer/statistics .
Breast Cancer Network Australia. Current breast cancer statistics in Australia 2020 [Available from: https://www.bcna.org.au/media/7111/bcna-2019-current-breast-cancer-statistics-in-australia-11jan2019.pdf .
Ren W, Chen M, Qiao Y, Zhao F. Global guidelines for breast cancer screening: A systematic review. The Breast. 2022;64:85–99.
Article PubMed PubMed Central Google Scholar
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(8):1194–220.
Article CAS PubMed Google Scholar
Hamashima C, Hattori M, Honjo S, Kasahara Y, Katayama T, Nakai M, et al. The Japanese guidelines for breast cancer screening. Jpn J Clin Oncol. 2016;46(5):482–92.
Article PubMed Google Scholar
Bevers TB, Helvie M, Bonaccio E, Calhoun KE, Daly MB, Farrar WB, et al. Breast cancer screening and diagnosis, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Net. 2018;16(11):1362–89.
Article Google Scholar
He J, Chen W, Li N, Shen H, Li J, Wang Y, et al. China guideline for the screening and early detection of female breast cancer (2021, Beijing). Zhonghua Zhong liu za zhi [Chinese Journal of Oncology]. 2021;43(4):357–82.
CAS PubMed Google Scholar
Cancer Australia. Early detection of breast cancer 2021 [cited 2022 25 July]. Available from: https://www.canceraustralia.gov.au/resources/position-statements/early-detection-breast-cancer .
Schünemann HJ, Lerda D, Quinn C, Follmann M, Alonso-Coello P, Rossi PG, et al. Breast Cancer Screening and Diagnosis: A Synopsis of the European Breast Guidelines. Ann Intern Med. 2019;172(1):46–56.
World Health Organization. WHO Position Paper on Mammography Screening Geneva WHO. 2016.
Google Scholar
Lansdorp-Vogelaar I, Gulati R, Mariotto AB. Personalizing age of cancer screening cessation based on comorbid conditions: model estimates of harms and benefits. Ann Intern Med. 2014;161:104.
Lee CS, Moy L, Joe BN, Sickles EA, Niell BL. Screening for Breast Cancer in Women Age 75 Years and Older. Am J Roentgenol. 2017;210(2):256–63.
Broeders M, Moss S, Nystrom L. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(suppl 1):14.
Oeffinger KC, Fontham ETH, Etzioni R, Herzig A, Michaelson JS, Shih YCT, et al. Breast cancer screening for women at average risk: 2015 Guideline update from the American cancer society. JAMA - Journal of the American Medical Association. 2015;314(15):1599–614.
Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311:1336.
Article CAS PubMed PubMed Central Google Scholar
Braithwaite D, Walter LC, Izano M, Kerlikowske K. Benefits and harms of screening mammography by comorbidity and age: a qualitative synthesis of observational studies and decision analyses. J Gen Intern Med. 2016;31:561.
Braithwaite D, Mandelblatt JS, Kerlikowske K. To screen or not to screen older women for breast cancer: a conundrum. Future Oncol. 2013;9(6):763–6.
Demb J, Abraham L, Miglioretti DL, Sprague BL, O’Meara ES, Advani S, et al. Screening Mammography Outcomes: Risk of Breast Cancer and Mortality by Comorbidity Score and Age. Jnci-Journal of the National Cancer Institute. 2020;112(6):599–606.
Demb J, Akinyemiju T, Allen I, Onega T, Hiatt RA, Braithwaite D. Screening mammography use in older women according to health status: a systematic review and meta-analysis. Clin Interv Aging. 2018;13:1987–97.
Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ. Screening for Breast Cancer in Average-Risk Women: A Guidance Statement From the American College of Physicians. Ann Intern Med. 2019;170(8):547–60.
Collins K, Winslow M, Reed MW, Walters SJ, Robinson T, Madan J, et al. The views of older women towards mammographic screening: a qualitative and quantitative study. Br J Cancer. 2010;102(10):1461–7.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–13.
Hersch J, Jansen J, Barratt A, Irwig L, Houssami N, Howard K, et al. Women’s views on overdiagnosis in breast cancer screening: a qualitative study. BMJ : British Medical Journal. 2013;346:f158.
De Gelder R, Heijnsdijk EAM, Van Ravesteyn NT, Fracheboud J, Draisma G, De Koning HJ. Interpreting overdiagnosis estimates in population-based mammography screening. Epidemiol Rev. 2011;33(1):111–21.
Monticciolo DL, Helvie MA, Edward HR. Current issues in the overdiagnosis and overtreatment of breast cancer. Am J Roentgenol. 2018;210(2):285–91.
Shepardson LB, Dean L. Current controversies in breast cancer screening. Semin Oncol. 2020;47(4):177–81.
National Cancer Control Centre. Cancer incidence in Australia 2022 [Available from: https://ncci.canceraustralia.gov.au/diagnosis/cancer-incidence/cancer-incidence .
Austin JD, Shelton RC, Lee Argov EJ, Tehranifar P. Older Women’s Perspectives Driving Mammography Screening Use and Overuse: a Narrative Review of Mixed-Methods Studies. Current Epidemiology Reports. 2020;7(4):274–89.
Austin JD, Tehranifar P, Rodriguez CB, Brotzman L, Agovino M, Ziazadeh D, et al. A mixed-methods study of multi-level factors influencing mammography overuse among an older ethnically diverse screening population: implications for de-implementation. Implementation Science Communications. 2021;2(1):110.
Demb J, Allen I, Braithwaite D. Utilization of screening mammography in older women according to comorbidity and age: protocol for a systematic review. Syst Rev. 2016;5(1):168.
Housten AJ, Pappadis MR, Krishnan S, Weller SC, Giordano SH, Bevers TB, et al. Resistance to discontinuing breast cancer screening in older women: A qualitative study. Psychooncology. 2018;27(6):1635–41.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil HAE, et al. Chapter 11: Scoping reviews. JBI Manual for Evidence Synthesis 2020 [Available from: https://jbi-global-wiki.refined.site/space/MANUAL .
Peters MD, Godfrey C, McInerney P, Khalil H, Larsen P, Marnie C, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI evidence synthesis. 2022;20(4):953–68.
Fantom NJ, Serajuddin U. The World Bank’s classification of countries by income. World Bank Policy Research Working Paper; 2016.
Book Google Scholar
BreastScreen Australia Evaluation Taskforce. BreastScreen Australia Evaluation. Evaluation final report: Screening Monograph No 1/2009. Canberra; Australia Australian Government Department of Health and Ageing; 2009.
Nelson HD, Cantor A, Humphrey L. Screening for breast cancer: a systematic review to update the 2009 U.S. Preventive Services Task Force recommendation2016.
Woolf SH. The 2009 breast cancer screening recommendations of the US Preventive Services Task Force. JAMA. 2010;303(2):162–3.
Covidence systematic review software. [Internet]. Veritas-Health-Innovation 2020. Available from: https://www.covidence.org/ .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Beckmeyer A, Smith RM, Miles L, Schonberg MA, Toland AE, Hirsch H. Pilot Evaluation of Patient-centered Survey Tools for Breast Cancer Screening Decision-making in Women 75 and Older. Health Behavior and Policy Review. 2020;7(1):13–8.
Brotzman LE, Shelton RC, Austin JD, Rodriguez CB, Agovino M, Moise N, et al. “It’s something I’ll do until I die”: A qualitative examination into why older women in the U.S. continue screening mammography. Canc Med. 2022;11(20):3854–62.
Article CAS Google Scholar
Cadet T, Pinheiro A, Karamourtopoulos M, Jacobson AR, Aliberti GM, Kistler CE, et al. Effects by educational attainment of a mammography screening patient decision aid for women aged 75 years and older. Cancer. 2021;127(23):4455–63.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Gilliam EA, Primeau S, et al. Evaluation of a mammography decision aid for women 75 and older at risk for lower health literacy in a pretest-posttest trial. Patient Educ Couns. 2021;104(9):2344–50.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Siska M, Schonberg MA. Modifying a mammography decision aid for older adult women with risk factors for low health literacy. Health Lit Res Prac. 2021;5(2):e78–90.
Gray N, Picone G. Evidence of Large-Scale Social Interactions in Mammography in the United States. Atl Econ J. 2018;46(4):441–57.
Hoover DS, Pappadis MR, Housten AJ, Krishnan S, Weller SC, Giordano SH, et al. Preferences for Communicating about Breast Cancer Screening Among Racially/Ethnically Diverse Older Women. Health Commun. 2019;34(7):702–6.
Salzman B, Bistline A, Cunningham A, Silverio A, Sifri R. Breast Cancer Screening Shared Decision-Making in Older African-American Women. J Natl Med Assoc. 2020;112(5):556–60.
PubMed Google Scholar
Schoenborn NL, Pinheiro A, Kistler CE, Schonberg MA. Association between Breast Cancer Screening Intention and Behavior in the Context of Screening Cessation in Older Women. Med Decis Making. 2021;41(2):240–4.
Schonberg MA, Kistler CE, Pinheiro A, Jacobson AR, Aliberti GM, Karamourtopoulos M, et al. Effect of a Mammography Screening Decision Aid for Women 75 Years and Older: A Cluster Randomized Clinical Trial. JAMA Intern Med. 2020;180(6):831–42.
Schonberg MA, Hamel MB, Davis RB. Development and evaluation of a decision aid on mammography screening for women 75 years and older. JAMA Intern Med. 2014;174:417.
Eisinger F, Viguier J, Blay J-Y, Morère J-F, Coscas Y, Roussel C, et al. Uptake of breast cancer screening in women aged over 75years: a controversy to come? Eur J Cancer Prev. 2011;20(Suppl 1):S13-5.
Schonberg MA, Breslau ES, McCarthy EP. Targeting of Mammography Screening According to Life Expectancy in Women Aged 75 and Older. J Am Geriatr Soc. 2013;61(3):388–95.
Download references
Acknowledgements
We would like to acknowledge Ange Hayden-Johns (expert librarian) who assisted with the development of the search criteria and undertook the relevant searches and Tejashree Kangutkar who assisted with some of the Covidence work.
This work was supported by funding from the Australian Government Department of Health and Aged Care (ID: Health/20–21/E21-10463).
Author information
Authors and affiliations.
Violet Vines Centre for Rural Health Research, La Trobe Rural Health School, La Trobe University, P.O. Box 199, Bendigo, VIC, 3552, Australia
Virginia Dickson-Swift, Joanne Adams & Evelien Spelten
Care Economy Research Institute, La Trobe University, Wodonga, Australia
Irene Blackberry
Olivia Newton-John Cancer Wellness and Research Centre, Austin Health, Melbourne, Australia
Carlene Wilson & Eva Yuen
Melbourne School of Population and Global Health, Melbourne University, Melbourne, Australia
Carlene Wilson
School of Psychology and Public Health, La Trobe University, Bundoora, Australia
Institute for Health Transformation, Deakin University, Burwood, Australia
Centre for Quality and Patient Safety, Monash Health Partnership, Monash Health, Clayton, Australia
You can also search for this author in PubMed Google Scholar
Contributions
VDS conceived and designed the scoping review. VDS & JA developed the search strategy with librarian support, and all authors (VDS, JA, ES, IB, CW, EY) participated in the screening and data extraction stages and assisted with writing the review. All authors provided editorial support and read and approved the final manuscript prior to submission.
Corresponding author
Correspondence to Joanne Adams .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval and consent to participate was not required for this study.
Consent for publication
Consent for publication was not required for this study.
Competing interest
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dickson-Swift, V., Adams, J., Spelten, E. et al. Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review. BMC Women's Health 24 , 256 (2024). https://doi.org/10.1186/s12905-024-03094-z
Download citation
Received : 06 September 2023
Accepted : 15 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12905-024-03094-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Mammography
- Older women
- Scoping review
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- Grand Rounds
Breast Conference Tumor Board
Case studies and presentations for breast cancer, friday, april 12, 2024 at 7:30 am.
This grand round has already taken place.
Description
At our weekly Breast Conference, we discuss Breast Cancer planning and treatment options with our multidisciplinary team. These case presentations and discussions rely on national Breast Cancer standards (as defined by the NCCN) in this way, we afford best clinical practice for our patients, as well as provide continued medical education at the same time. Both of these essential components of our Breast Conference aim to bridge the gap between historical clinical practices and newer cutting-edge treatments. Through our case presentations and many lectures series, we aim to maximize the chances that our clinical faculty follow national cancer treatment standards, as well as understand and offer newer cutting-edge treatments.
- Additional Info
Accreditation
Dates and times.
Start: 4/12/2024 7:30 AM End: 4/12/2024 8:30 AM
Upon completion of the case presentations at this meeting, participants should be able to: Recognize suspicious findings on mammograms Discuss factors that influence decision about breast Conservation vs. mastectomy Utilize NCCN guidelines to help guide treatment Understand the implication of positive BRCA testing
- left breast malignancy, poss metaplastic. Surgery first vs NAC.
- Review of HER2, adjuvant therapy options.
HSC Level 2, Pathology Conference Room 750 Stony Brook University Medical Center 101 Nicols Rd Stony Brook, NY 11794
The School of Medicine, State University of New York at Stony Brook, is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
The School of Medicine, State University of New York at Stony Brook designates this live activity for a maximum of 1.00 AMA PRA Category 1 Credit(s) ™ . Physicians should only claim the credit commensurate with the extent of their participation in the activity.
Need help with this Grand Round Session?
Please contact the Grand Round coordinator listed below:
Nicole Vella Department: Surgery Phone: (631) 444-5976 Email: [email protected]
Relationship With Partner Affects Outcomes for Breast Cancer Survivors
By Dennis Thompson HealthDay Reporter

MONDAY, April 22, 2024 (HealthDay News) -- A strong relationship can help a breast cancer survivor thrive in the aftermath of their terrible ordeal, a new study finds.
Diagnosis and treatment of breast cancer places tremendous stress on the women and their partners, researchers said.
Those women in a solid relationship with their partner tend to have less depression and fatigue following their treatment, as well as better physical functioning, the study results show.
For example, they were better able to carry groceries, walk around the block and perform other typical day-to-day tasks, researchers found.
U.S. Cities With the Most Homelessness

On the other hand, weaker relationships were associated with poor emotional and physical outcomes for breast cancer survivors.
“How the breast cancer survivor and partner communicated and handled stressful events, particularly those related to breast cancer, were linked to emotional and physical health for the survivor, with better agreement related to better outcomes,” said lead study author Eric Vachon . He's a research scientist with the Regenstrief Institute and Indiana University School of Nursing.
However, part of the strength of a relationship rests on a shared understanding between the partners, the study also found.
Couples where one person rated the relationship more highly than their partner tended to reap worse outcomes, results show.
“Interestingly, breast cancer survivors who rated their relationship satisfaction as high did not necessarily have better agreement with their partner or better well-being than those survivors who viewed their relationship less positively,” Vachon said. “It’s the communication and relationship between the survivor and partner that are determinant.”
For the study, researchers analyzed survey data from 387 couples, including 220 couples with a breast cancer survivor and 167 with no breast cancer. The average age of study participants was mid-40s.
“We knew from the literature that breast cancer survivors’ rating of their relationship satisfaction is linked with some poor physical and emotional outcomes,” Vachon said in an institute news release.
“We took that knowledge to the next level and combined the breast cancer survivors’ and partners’ views of relationship satisfaction and relationship agreement and determined impact on survivors’ health,” he added.
The satisfaction that breast cancer survivors had with their relationship was significantly associated with better physical function, ability to focus and sleep quality.
The findings were published recently in a special issue of the journal Healthcare .
“This work points to the critical importance of both members of the couple focusing on strengthening the relationship,” Vachon said. “Difficulties among couples can have devastating effects for your physical and emotional health.”
More information
Susan G. Komen has more on social support during breast cancer treatment .
SOURCE: Regenstrief Institute, news release, April 18, 2024
Copyright © 2024 HealthDay . All rights reserved.
Join the Conversation
Tags: breast cancer , marriage
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

‘A Rule for the Ages’
Lauren Camera April 25, 2024

Sale? Ban? What’s Next for TikTok?
Laura Mannweiler April 25, 2024

The Status of the Cases Against Trump
Lauren Camera and Kaia Hubbard April 25, 2024

Economy Slows in First Quarter
Tim Smart April 25, 2024

A ‘Fork in the Road’ for Democracy
Lauren Camera April 24, 2024

Johnson at Columbia: ’Stop the Nonsense’
Aneeta Mathur-Ashton April 24, 2024


Study at Cambridge
About the university, research at cambridge.
- For Cambridge students
- For our researchers
- Business and enterprise
- Colleges and Departments
- Email and phone search
- Give to Cambridge
- Museums and collections
- Events and open days
- Fees and finance
- Postgraduate courses
- How to apply
- Fees and funding
- Postgraduate events
- International students
- Continuing education
- Executive and professional education
- Courses in education
- How the University and Colleges work
- Visiting the University
- Annual reports
- Equality and diversity
- A global university
- Public engagement
Study highlights increased risk of second cancers among breast cancer survivors
- Research home
- About research overview
- Animal research overview
- Overseeing animal research overview
- The Animal Welfare and Ethical Review Body
- Animal welfare and ethics
- Report on the allegations and matters raised in the BUAV report
- What types of animal do we use? overview
- Guinea pigs
- Naked mole-rats
- Non-human primates (marmosets)
- Other birds
- Non-technical summaries
- Animal Welfare Policy
- Alternatives to animal use
- Further information
- Funding Agency Committee Members
- Research integrity
- Horizons magazine
- Strategic Initiatives & Networks
- Nobel Prize
- Interdisciplinary Research Centres
- Open access
- Energy sector partnerships
- Podcasts overview
- S2 ep1: What is the future?
- S2 ep2: What did the future look like in the past?
- S2 ep3: What is the future of wellbeing?
- S2 ep4 What would a more just future look like?
- Research impact

Survivors of breast cancer are at significantly higher risk of developing second cancers, including endometrial and ovarian cancer for women and prostate cancer for men, according to new research studying data from almost 600,000 patients in England.
It’s important for us to understand to what extent having one type of cancer puts you at risk of a second cancer at a different site. Knowing this can help inform conversations with their care teams to look out for signs of potential new cancers Isaac Allen
For the first time, the research has shown that this risk is higher in people living in areas of greater socioeconomic deprivation.
Breast cancer is the most commonly diagnosed cancer in the UK. Around 56,000 people in the UK are diagnosed each year, the vast majority (over 99%) of whom are women. Improvements in earlier diagnosis and in treatments mean that five year survival rates have been increasing over time, reaching 87% by 2017 in England.
People who survive breast cancer are at risk of second primary cancer, but until now the exact risk has been unclear. Previously published research suggested that women and men who survive breast cancer are at a 24% and 27% greater risk of a non-breast second primary cancer than the wider population respectively. There have been also suggestions that second primary cancer risks differ by the age at breast cancer diagnosis.
To provide more accurate estimates, a team led by researchers at the University of Cambridge analysed data from over 580,000 female and over 3,500 male breast cancer survivors diagnosed between 1995 and 2019 using the National Cancer Registration Dataset. The results of their analysis are published today in Lancet Regional Health – Europe .
First author Isaac Allen from the Department of Public Health and Primary Care at the University of Cambridge said: “It’s important for us to understand to what extent having one type of cancer puts you at risk of a second cancer at a different site. The female and male breast cancer survivors whose data we studied were at increased risk of a number of second cancers. Knowing this can help inform conversations with their care teams to look out for signs of potential new cancers.”
The researchers found significantly increased risks of cancer in the contralateral (that is, unaffected) breast and for endometrium and prostate cancer in females and males, respectively. Females who survived breast cancer were at double the risk of contralateral breast cancer compared to the general population and at 87% greater risk of endometrial cancer, 58% greater risk of myeloid leukaemia and 25% greater risk of ovarian cancer.
Age of diagnosis was important, too – females diagnosed with breast cancer under the age of 50 were 86% more likely to develop a second primary cancer compared to the general population of the same age, whereas women diagnosed after age 50 were at a 17% increased risk. One potential explanation is that a larger number of younger breast cancer survivors may have inherited genetic alterations that increase risk for multiple cancers. For example, women with inherited changes to the BRCA1 and BRCA2 genes are at increased risk of contralateral breast cancer, ovarian and pancreatic cancer.
Females from the most socioeconomically deprived backgrounds were at 35% greater risk of a second primary cancer compared to females from the least deprived backgrounds. These differences were primarily driven by non-breast cancer risks, particularly for lung, kidney, head and neck, bladder, oesophageal and stomach cancers. This may be because smoking, obesity, and alcohol consumption – established risk factors for these cancers – are more common among more deprived groups.
Allen, a PhD student at Clare Hall, added: “This is further evidence of the health inequalities that people from more deprived backgrounds experience. We need to fully understand why they are at greater risk of second cancers so that we can intervene and reduce this risk.”
Male breast cancer survivors were 55 times more likely than the general male population to develop contralateral breast cancer – though the researchers stress that an individual’s risk was still very low. For example, for every 100 men diagnosed with breast cancer at age 50 or over, about three developed contralateral breast cancer during a 25 year period. Male breast cancer survivors were also 58% more likely than the general male population to develop prostate cancer.
Professor Antonis Antoniou from the Department of Public Health and Primary Care at the University of Cambridge, the study’s senior author, said: “This is the largest study to date to look at the risk in breast cancer survivors of developing a second cancer. We were able to carry this out and calculate more accurate estimates because of the outstanding data sets available to researchers through the NHS.”
The research was funded by Cancer Research UK with support from the National Institute for Health and Care Research Cambridge Biomedical Research Centre.
Cancer Research UK’s senior cancer intelligence manager, Katrina Brown, said: “This study shows us that the risk of second primary cancers is higher in people who have had breast cancer, and this can differ depending on someone’s socioeconomic background. But more research is needed to understand what is driving this difference and how to tackle these health inequalities.”
People who are concerned about their cancer risk should contact their GP for advice. If you or someone close to you have been affected by cancer and you’ve got questions, you can call Cancer Research UK nurses on freephone 0808 800 4040, Monday to Friday.
Reference Allen, I, et al. Risks of second primary cancers among 584,965 female and male breast cancer survivors in England: a 25-year retrospective cohort study. Lancet Regional Health – Europe; 24 April 2024: DOI: 10.1016/j.lanepe.2024.100903

Read this next

Report highlights inequalities and hidden suffering among people living with breast cancer

£9.2m boost for next generation of Cambridge cancer experts

Cancer's climate innovation

UK's only research institute dedicated to understanding early cancer receives £11 million donation
Media enquiries.
Doctor standing near woman patient doing breast cancer scan
Credit: National Cancer Institute
Search research
Sign up to receive our weekly research email.
Our selection of the week's biggest Cambridge research news sent directly to your inbox. Enter your email address, confirm you're happy to receive our emails and then select 'Subscribe'.
I wish to receive a weekly Cambridge research news summary by email.
The University of Cambridge will use your email address to send you our weekly research news email. We are committed to protecting your personal information and being transparent about what information we hold. Please read our email privacy notice for details.
- breast cancer
- Antonis Antoniou
- Isaac Allen
- School of Clinical Medicine
- Department of Public Health and Primary Care
- Cambridge Cancer Centre
Related organisations
- Cancer Research UK (CRUK)
Connect with us

© 2024 University of Cambridge
- Contact the University
- Accessibility statement
- Freedom of information
- Privacy policy and cookies
- Statement on Modern Slavery
- Terms and conditions
- University A-Z
- Undergraduate
- Postgraduate
- Cambridge University Press & Assessment
- Research news
- About research at Cambridge
- Spotlight on...
CAROLYN CROSS IHUMAN CASE STUDY 41-YEAR-OLD FEMALE CONCER... - $22.45 Add to Cart
CAROLYN CROSS IHUMAN CASE STUDY 41-YEAR-OLD FEMALE CONCERNED ABOUT HER RISK FOR BREAST CANCER GRADED A+ 2024 (NEW!!)
Preview 2 out of 18 pages

Generating Your Document
Purchase the document to get the full access instantly
- 3 Million+ Study Documents
- 100% Money Back Guarantee
- Immediate Download Access

Report Copyright Violation
Case Details
Add To Cart
Add To Wishlist
- Trusted by 800,000+ Students
- 24/7 Money Back Guarantee
- Download is directly available
Specifications
Institution Chamberlain College of Nursing
Study Nursing
Course CAROLYN CROSS IHUMAN CASE STUDY 41-YEAR-OLD FEMALE CONCERNED ABOUT HER RISK FOR BREAST CANCER (SOLV
Language English
Subject Health Care
Updated On Apr 23,2024
Number of Pages 18
Written 2023-2024
Seller Details

Grandnotesplug96
81 documents uploaded
0 documents sold
Member since 1 year
Recommended documents

CAROLYN CROSS iHuman 2024...

CAROLYN CROSS IHUMAN CASE...

what students are saying about us
DocMerit is a great platform to get and share study resources, especially the resource contributed by past students.

Northwestern University Karen
I find DocMerit to be authentic, easy to use and a community with quality notes and study tips. Now is my chance to help others.

University Of Arizona Anna Maria
One of the most useful resource available is 24/7 access to study guides and notes. It helped me a lot to clear my final semester exams.

Devry University David Smith
DocMerit is super useful, because you study and make money at the same time! You even benefit from summaries made a couple of years ago.

Liberty University Mike T
- Follow us on
- Copyright © 2024 | All rights reserved
Register a free account


IMAGES
VIDEO
COMMENTS
Hi guys. My name is Abby, and we're going to go through a case study about breast cancer together. Let's get started. In this scenario, our patient is Natasha. She's 32 years old and an African American patient that arrives at the surgical oncology unit after a left breast mastectomy and lymph node excision.
Iwata H, Masuda N, Yamamoto Y, et al. Validation of the 21-gene test as a predictor of clinical response to neoadjuvant hormonal therapy for ER+, HER2-negative breast cancer: the TransNEOS study ...
When delivering survivorship care, a nurse may start with incomplete information about the cancer survivor's treatment and follow-up. Therefore, this breast cancer package includes an incomplete case study and care plan, and then follows with commentaries from expert nurses about their approach to comprehensive survivorship care.
sity School of Nursing Baltimore, Maryland Case 6. Metastatic Breast Cancer Anne Zobec, MS, AOCNP®, BC Oncology Nurse Practitioner Rocky Mountain Cancer Centers Colorado Springs, Colorado Case 19. The Post-Treatment Phase Disclosure Editors and authors of books and guidelines provided by the Oncology Nursing Society are
Nursing Interventions for Breast Cancer: Rationales: Assess the patient's readiness to learn, misconceptions, and blocks to learning (e.g. denial of diagnosis or poor lifestyle habits)To address the patient's cognition and mental status towards the new diagnosis and to help the patient overcome blocks to learning. Explain what breast cancer is and its symptoms.
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3, 4 ].
This case study highlights the patient's status in care plan format and is followed by commentaries from expert nurse clinicians about their approach to manage the patient's long-term or chronic cancer care symptoms. Finally, an additional expert nurse clinician summarizes the care plan and commentaries, emphasizing takeaways about the patient ...
We conducted a case-case analysis of women treated for invasive breast cancer at the University of California San Francisco Breast Care Center (UCSF BCC). This study included only women with a confirmed diagnosis of invasive breast cancer previously undergoing standard mammography screening.
Below are case studies that support the information in the Secondary Breast Cancer Nursing toolkit. How the team re-designed their service, using a co-production approach in order to meet the varying needs of a large caseload. How the hospital designed a new service for secondary breast cancer patients. How the hospital established the first ...
Materials & Methods: This was a care case study performed on a patient with stage three breast cancer using Watson's model of human care and the Caritas care process in three stages.
The goal of this activity is for learners to be better able to select the most optimal anti-HER2 treatments for patients with HER2-positive breast cancer at every stage of care. Upon completion of this activity, participants will: Have increased knowledge regarding the. Clinical data associated with emerging anti-HER2 regimens for patients with ...
Abstract. In this directed case study, students analyze data, draw a research-based conclusion, interpret experimental results, and discuss the relevance of research findings for clinical practice. Specifically, students examine the effects of chemotherapeutic drugs on newly generated cell lines and explain research outcomes using their prior ...
This section offers an in-depth look at breast cancer, focusing on its nature, risk factors, and the signs and symptoms that facilitate early detection and treatment. Understanding Breast Cancer. Breast cancer arises when cells in the breast grow uncontrollably, often forming a tumor that can be detected via a mammogram or felt as a lump.This malignancy is responsible for a significant ...
Keith RN Case Study breast of chemotherapy jan leisner, 50 years old primary concept perfusion interrelated concepts (in order of emphasis) infection pain fluid ... but childcare considerations will factor into care History of cancer can help determine inheritance for children and disease progression Smoking can compromise lung health and ...
Pathophysiology of Breast Cancer. Except for skin cancer, breast cancer is the most common cancer in American women. Most breast cancer occurs in women older than 50 years. The major risk factors for breast cancer are classified as reproductive, such as nulliparity and pregnancy-associated breast cancer; familial, such as inherited gene ...
Mrs. Whitney's oldest sister died of breast cancer. Mrs. Whitney has a diagnostic mammogram and a fine-needle aspiration biopsy. It is determined that she has stage II breast cancer. Case study Mrs. Whitney will have a lumpectomy with lymph node dissection (partial mastectomy). A Jackson- Pratt (JP) drain will be in place postoperatively.
Breast cancer is the second most common cancer in women, surpassed only by skin cancer (National Institute of Health, 2019). In 2019, approximately 268,000 women were diagnosed with breast cancer (National Cancer Institute, 2020). Approximately seven out of a hundred women will develop breast cancer before the age of seventy (Centers for Disease
Carol Edwards, a 39 year-old premenopausal woman, had a screening mammogram which revealed an abnormality in the right breast. She had no palpable masses on breast exam. A mammographically localized surgical biopsy was done and revealed a small (0.9 cm) grade III infiltrating ductal carcinoma with some associated ductal carcinoma-in-situ (DCIS ...
Adam M. Brufsky, MD, PhD: Let's talk about this case. This is a 48-year-old woman who presented to her primary care physician a number of years ago with a lump in her breast. She had a 4.4-cm left breast mass and 3 palpable axillary lymph nodes. Her ultrasound and mammogram confirmed these physical findings.
However, there are limitations in the current CM approaches, which vary in supporting care for breast cancer patients. Some studies have small sample sizes, limited quality, and lack research support from evidence-based medicine, so there is a need to assess the impact of CM on breast cancer patients through systematic evaluation and meta-analysis.
HESI Breast Cancer Learn with flashcards, games, and more — for free. ... Management of a Skilled Care Unit Case Study. 30 terms. zymaji. Preview. Unit 4 (NP-1) 10 terms. Jm211983. Preview. Chapter 18 - Neurologic Emergencies. 30 terms. Anthony_Booker4. Preview. NCCAOM Formulas. 162 terms. gabriela_alexandra. Preview.
Breast Cancer Case Study Group one. Patient Profile R M. is a 68-year-old white female who went to her healthcare provider with a complaint of "feeling tightness" around a lump in her right breast. She has a history of hypertension and smoking (25 pack- year history). Subjective Data Has a family history of breast cancer-one sister recently had lumpectomy and radiation therapy.
Risks of second primary cancers among 584,965 female and male breast cancer survivors in England: a 25-year retrospective cohort study ... Tamoxifen treatment for breast cancer and risk of endometrial cancer: a case-control study. J Natl Cancer Inst ... This work uses data that has been provided by patients and collected by the NHS as part of ...
Breast cancer is now the most commonly diagnosed cancer in the world overtaking lung cancer in 2021 [].Across the globe, breast cancer contributed to 25.8% of the total number of new cases of cancer diagnosed in 2020 [] and accounts for a high disease burden for women [].Screening for breast cancer is an effective means of detecting early-stage cancer and has been shown to significantly ...
Treatment for breast cancer can be followed by fatigue, sleepless nights, brain fog and other quality-of-life issues. Coping with these matters can be a critical part of the healing process. In fact, some patients report that dealing with these symptoms can be as difficult as dealing with the cancer itself.
Description. At our weekly Breast Conference, we discuss Breast Cancer planning and treatment options with our multidisciplinary team. These case presentations and discussions rely on national Breast Cancer standards (as defined by the NCCN) in this way, we afford best clinical practice for our patients, as well as provide continued medical education at the same time.
For the study, researchers analyzed survey data from 387 couples, including 220 couples with a breast cancer survivor and 167 with no breast cancer. The average age of study participants was mid-40s.
Breast cancer is the most. For the first time, the research has shown that this risk is higher in people living in areas of greater socioeconomic deprivation. ... Professor Antonis Antoniou from the Department of Public Health and Primary Care at the University of Cambridge, the study's senior author, said: "This is the largest study to ...
carolyn cross ihuman case study 41-year-old female concerned about her risk for breast cancer (solved by expert) all sections 100% correctly solved (cc, hpi, pmh, objective, lab tests, special tests, diagnosis, plan and references) graded a+ 2024 (new!!)