How to Prepare a Paper Presentation?
- First Online: 02 February 2019

Cite this chapter

- Timothy Lording 8 , 9 &
- Jacques Menetrey 10 , 11
2309 Accesses
Presenting your paper at a meeting is an important part of sharing your research with the orthopaedic community. Presentations are generally short and sharp, and careful preparation is key to ensure that the premise, findings, and relevance of your work are successfully conveyed. For most conference papers, the structure will mirror that of a scientific manuscript, with an introduction, materials and methods, results, discussion, and conclusions. Anticipation of potential questions will help to clarify your research for the audience.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Elmansori A, Lording T, Dumas R, Elmajri K, Neyret P, Lustig S. Proximal tibial bony and meniscal slopes are higher in ACL injured subjects than controls: a comparative MRI study. Knee Surg Sports Traumatol Arthrosc. 2017;25:1598–605.
Article Google Scholar
Lording T, Corbo G, Bryant D, Burkhart TA, Getgood A. Rotational laxity control by the anterolateral ligament and the lateral meniscus is dependent on knee flexion angle: a cadaveric biomechanical study. Clin Orthop Relat Res. 2017;90:1922–8.
Google Scholar
Shybut TB, Vega CE, Haddad J, Alexander JW, Gold JE, Noble PC, Lowe WR. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43:905–11.
Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43:1702–7.
Article CAS Google Scholar
Sonnery-Cottet B, Mogos S, Thaunat M, Archbold P, Fayard JM, Freychet B, Clechet J, Chambat P. Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:1873–80.
Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? Knee Surg Sports Traumatol Arthrosc. 2007;16:112–7.
Download references
Author information
Authors and affiliations.
Melbourne Orthopaedic Group, Windsor, VIC, Australia
Timothy Lording
The Alfred Hospital, Melbourne, VIC, Australia
Centre de Médecine du Sport et de l’Exercice, Hirslanden Clinique la Colline, Geneva, Switzerland
Jacques Menetrey
Service de Chirurgie Orthopédique et Traumatologie de l’Appareil Moteur, University Hospital of Geneva, Geneva, Switzerland
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Timothy Lording .
Editor information
Editors and affiliations.
UPMC Rooney Sports Complex, University of Pittsburgh, Pittsburgh, PA, USA
Volker Musahl
Department of Orthopaedics, Sahlgrenska Academy, Gothenburg University, Sahlgrenska University Hospital, Gothenburg, Sweden
Jón Karlsson
Department of Orthopaedic Surgery and Traumatology, Kantonsspital Baselland (Bruderholz, Laufen und Liestal), Bruderholz, Switzerland
Michael T. Hirschmann
McMaster University, Hamilton, ON, Canada
Olufemi R. Ayeni
Hospital for Special Surgery, New York, NY, USA
Robert G. Marx
Department of Orthopaedic Surgery, NorthShore University HealthSystem, Evanston, IL, USA
Jason L. Koh
Institute for Medical Science in Sports, Osaka Health Science University, Osaka, Japan
Norimasa Nakamura
Rights and permissions
Reprints and permissions
Copyright information
© 2019 ISAKOS
About this chapter
Lording, T., Menetrey, J. (2019). How to Prepare a Paper Presentation?. In: Musahl, V., et al. Basic Methods Handbook for Clinical Orthopaedic Research. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-58254-1_24
Download citation
DOI : https://doi.org/10.1007/978-3-662-58254-1_24
Published : 02 February 2019
Publisher Name : Springer, Berlin, Heidelberg
Print ISBN : 978-3-662-58253-4
Online ISBN : 978-3-662-58254-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

iss-sic.com
issmembership.com
Abstract Volume
Abstract volume for download now available..
.png)
Abstract information
Go to submission: https://b-com.mci-group.com/abstractsubmission/isw2022.aspx guidelines: go to, please note, that the submission is provided by the congress organizer mci group. topics:.
General Topics (incl. Burns by ISBI, Military Surgery by APIMSF, Pediatric Surgery) organized by ISS/SIC
Digestive Surgery organized by ISDS
Endocrine Surgery organized by IAES
Trauma & Intensive Care organized by IATSIC
Breast Surgery organized by BSI
Anesthesia & Rural Surgery organized by ASAP
Nutrition & Metabolism organized by IASMEN
Abstract prizes
Iss/sic lloyd m. nyhus prize session, the 6 best abstracts intended for a free paper presentation in the program of the international society of surgery iss/sic are presented in the "lloyd m. nyhus prize session" and are awarded a certificate. a jury of internationally renowned experts will choose the best presentation in this prize session. a prize money of usd 1'000.00 for the best presentation will be awarded to the presenting author. the prize will be given at the iss/sic general assembly on wednesday., iss/sic poster prize, a jury of internationally renowned experts will nominate the best poster (regardless of category "poster discussion" or "poster exhibition only") in the program of iss/sic. the presenting author will be awarded a certificate and prize money of usd 500.00. the prize will be given at the iss/sic general assembly on wednesday., iaes abstract guidelines, presenting authors of an accepted free paper (oral) presentation from the iaes in the field of endocrine surgery must submit a full manuscript to world journal of surgery (wjs) by june 1, 2022 (noon gmt) at https://mc.manuscriptcentral.com/wjs . failure to do so may void the opportunity for a podium presentation. the authors must comply with all the rules and regulation of the wjs and note in their cover letter to the journal that this article is part of the iaes meeting in vienna. final revisions are to be submitted to wjs by august 24, 2022., final decision of the manuscripts including editorials will be october 9, 2022., iaes free paper awards for trainees only (residents/registrars, fellows, and medical students), the international association of endocrine surgeons (iaes) awards the presenting author of the best clinical free paper (the dr charles proye award) and the best basic science free paper (the dr selwyn taylor award) each prize money of usd 1'000.00. only presenting authors who are trainees are eligible for these awards. to be considered for the award, the presenting author will need to check the appropriate box the work was done primarily by a trainee in the abstract submission form at the time of submission. note: medical students who present an abstract must register within the category of "trainee"., iaes poster prize for trainees (residents/registrars, fellows, and medical students), the international association of endocrine surgeons (iaes) awards the presenting authors of the best clinical poster (the dr john farndon award) and the best basic science poster (the dr michael brauckhoff award) each prize money of usd 500.00. only presenting authors who are trainees are eligible for these poster awards. to be considered for the award, the presenting author will need to check the appropriate box indicating the work was done primarily by a trainee in the abstract submission form. note: medical students who present an abstract must register within the category of "trainee"., iatsic free paper prize, the international association for trauma surgery and intensive care (iatsic) will evaluate the best free paper presentation in one of the regular iatsic free paper sessions. the presenting author of the best presentation in this field will be awarded a prize money of usd 1'000.00 and a certificate., iatsic poster prize, iatsic will evaluate the best poster on trauma surgery and will award the presenting author a prize money of usd 500.00 with a certificate (regardless of category "poster discussion" or "poster exhibition only")., iasmen free paper prize, the international association for surgical metabolism and nutrition (iasmen) will include the best graded free papers submitted amongst this specific field to be presented within the iasmen prize session. the presenting author of the best presentation in this session will be awarded a prize money of usd 1'000.00 and a certificate., bsi free paper prize, abstracts in the field of breast surgery based on unpublished original work will be selected for presentation in the bsi best paper award session. individuals interested for their abstracts to be considered for the award will need to check the appropriate box in the abstract submission form. the selected presenters will be informed of the decision by march 31, 2022. they will be asked to fully register for the congress and submit a full length manuscript of the paper to be presented, conforming to the format of original articles in world journal of surgery wjs through its online submission platform https://mc.manuscriptcentral.com/wjs the latest by april 30, 2022. these manuscripts may be published in the bsi issue of wjs after undergoing the usual peer-review process. failure to register and submit the full length manuscript in time may preclude the selected abstract from being presented in the congress. all selected papers will be presented in the "best paper competition session". the presenting author of the best bsi paper in the award session as judged by a panel of eminent breast surgeons will be awarded a usd 500.00 prize. the runner-up will be awarded a usd 250.00 prize., bsi poster prize, all posters displayed in the bsi program at isw 2022 will be evaluated by a panel of eminent experts during the poster viewing session. prizes consisting of usd 400.00 and usd 200.00 respectively will be awarded to those judged as the best and second best posters. the presenting author will be asked to fully register for the congress latest by april 30, 2022. failure to register in time may preclude the selected abstract from being presented at the congress. the presenting authors, on their discretion may consider submitting a full length manuscript of the paper to be presented, conforming to the format of original articles in world journal of surgery through its online submission platform https://mc.manuscriptcentral.com/wjs . these manuscripts may be published in the bsi issue of wjs after undergoing the usual peer-review process., isds grassi prize session, the grassi prize will be awarded to a young surgeon (less than 40 years of age) who presents the best paper focusing on benign and/or open surgery of the gastrointestinal tract. this is in keeping with the expertise and talents of prof. grassi in whose honor this award was established. one of the authors of the abstract must be current member of isds (confirm qualification for the prize by checking the appropriate box in the abstract submission form). the presenting author of the best presentation within the grassi prize session will be awarded a prize of usd 1'000.00. the selected presenters within the grassi prize sessions will be informed by march 31, 2022. they will be asked to fully register for the congress and submit a full length manuscript of the paper to be presented, conforming to the format of original articles in world journal of surgery wjs through its online submission platform https://mc.manuscriptcentral.com/wjs the latest by april 30, 2022. failure to register or submit the full length manuscript in time may preclude the selected abstract from being presented at the congress., isds kitajima prize session, the kitajima prize will be awarded to two young surgeons (less than 40 years of age) who present the best papers on malignant and/or laparoscopic surgery of the gastrointestinal tract. this is to honor the generous gift of prof. kitajima who established this prize to encourage the research talents of young surgeons. one of the authors of the abstract must be current member of isds (confirm qualification for the prize by checking the appropriate box in the abstract submission form). the presenting authors of the best two presentations in the kitajima prize session will each be awarded a prize of usd 1'000.00. the selected presenters within the kitajima prize sessions will be informed by march 31, 2022. they will be asked to fully register for the congress and submit a full length manuscript of the paper to be presented, conforming to the format of original articles in world journal of surgery wjs through its online submission platform https://mc.manuscriptcentral.com/wjs the latest by april 30, 2022. failure to register or submit the full length manuscript in time may preclude the selected abstract from being presented at the congress., ambroise paré and rajasinha the second memorial prize for oral free papers, the best abstract for a free paper presentation in the program of apimsf (military surgery) are presented in the apimsf prize session and are awarded a certificate. the selection will then usually be made at the congress by the apimsf jury. a prize money of usd 500.00 for the best presentation will be awarded to the presenting author., ambroise paré and rajasinha the second memorial poster prize, apimsf jury will nominate the best poster in the program of apimsf (military surgery). the presenting author will be awarded a certificate and prize money of usd 400.00. .
Jump to content
American College of Surgeons | Online Learning
Bookmark/search this post.

You are here
Ten hot topics in general surgery.

Accreditation
- Register/Take course
Session Description
This rapid-fire/quick-shot session will cover ten currently popular issues in general surgery.
Moderator: Kenneth W. Sharp, MD, FACS, Nashville, TN
Co-Moderator: E. Christopher Ellison, MD, FACS, Powell, OH
Presentations
Bullet Removal: Pros and Cons John A. Weigelt, MD, DVM, FACS, Lead, SD
Nipple-Sparing Mastectomy: Use and Indications Raeshell S. Sweeting, MD, Nashville, TN
Troubleshooting Surgical Staple Failure and Malfunction Jon C. Gould, MD, FACS, Milwaukee, WI
Laparoscopic Common Duct Exploration Dana A. Telem, MD, MPH, FACS, Ann Arbor, MI
Extremity Lumps and Bumps Valerie P. Grignol, MD, FACS, Columbus, OH
Update on Tranverse Abdominus Release for Ventral Hernia Bruce Ramshaw, MD, FACS, Knoxville, TN
Recurrent Rectal Prolapse: What to Do? Alexander T. Hawkins, MD, MPH, Nashville, TN
The Case for Robotics in Rural Surgery Jared M. Slater, MD, FACS, Victoria, MN
Optimal Surgical Treatment or Type II Diabetes: Gastric Sleeve or Bypass? Jonathan Carter, MD, San Francisco, CA
Transoral Thyroidectomy: Ready for Prime Time Gustavo G. Fernandez Ranvier, MD, PhD, FACS, Long Island City, NY
Sponsored by the Advisory Council for General Surgery
Learning Objectives
- Apply new knowledge and ideas to improve their surgical practice
- Adapt concepts and quality measures in support of research advancements
- Enhance the quality of patient care
For questions about the course, please contact [email protected] .
- 1.50 AMA PRA Category 1 Credit™
- 1.50 Certificate of Completion
- 1.50 Self Assessment Credit
Disclosure Information
In accordance with the ACCME Accreditation Criteria, the American College of Surgeons must ensure that anyone in a position to control the content of the educational activity (planners and speakers/authors/discussants/moderators) has disclosed all relevant financial relationships with any commercial interest. For additional information, please visit the ACCME website .
The ACCME also requires that ACS manage any reported conflict and eliminate the potential for bias during the educational activity. Any conflicts noted below have been managed to our satisfaction. The disclosure information is intended to identify any commercial relationships and allow learners to form their own judgments. However, if you perceive a bias during a activity, please report it on the evaluation.
(Download the full list of disclosures ).
Faculty and Disclosures
Alexander T. Hawkins MD, MPH - Nothing to Disclose Bruce Ramshaw, MD, FACS - Atrium: Consulting Fee: Consultant; Ethicon (J & J): Honoraria: Consultant; ConMed: Honoraria: Consultant; Medtronic: Honoraria: Speaker; Pacira Pharmaceutical: Honoraria: Consultant, Speaker; WL Gore: Honoraria: Consultant, Speaker E. Christopher Ellison, MD, FACS - McGraw Hill Medical: Royalty: Author; Wolters Kluwer: Royalty: Associate Editor Eric M. Pauli MD, FACS, FASGE - Nothing to Disclose Gustavo G. Fernandez-Ranvier MD, PhD, FACS - Nothing to Disclose Jared M. Slater MD, FACS - Nothing to Disclose John A. Weigelt MD, DVM, FACS - Nothing to Disclose Jon C. Gould, MD, FACS - Gore: Honorarium: Speaker; Torax/Ethicon: Consulting Fee: Consultant and preceptor for LINX Jonathan Carter, MD - VERB Surgical: Consulting Fee: Consultant Kenneth W. Sharp MD, FACS - Nothing to Disclose Raeshell S. Sweeting MD - Nothing to Disclose Valerie P. Grignol MD, FACS - Nothing to Disclose
Program Committee and Disclosures
CHAIR: Henri R. Ford, MD, MHA, FACS, FAAP, FRCSEng(Hon), Miami, FL - Nothing to Disclosure VICE-CHAIR: David T. Cooke, MD, FACS, Sacramento, CA - Nothing to Disclosure
David C. Borgstrom, MD, FACS, Morgantown, WV - Nothing to Disclosure Daniel L. Dent, MD, FACS, San Antonio, TX - Nothing to Disclosure Roger R. Dmochowski, MD, FACS, Nashville, TN - Allergen: Honoraria: Consultant Cynthia D. Downard, MD, FACS, Louisville, KY - Nothing to Disclosure Audra A. Duncan, MD, FACS, London, ON - Nothing to Disclosure Mariam F. Eskander, MD, Boston, MA - Nothing to Disclosure Paula Ferrada, MD, FACS, Richmond, VA - Nothing to Disclosure Neil H. Hyman, MD, FACS, Chicago, IL - Nothing to Disclosure Martin S. Karpeh, Jr., MD, FACS, New York, NY - Nothing to Disclosure Dennis H. Kraus, MD, FACS, New York, NY - Nothing to Disclosure Kenneth W. Sharp, MD, FACS, Nashville, TN - Nothing to Disclosure
Ex-Officios
Daniel M. Herron, MD, FACS, FASBMS, New York, NY - Nothing to Disclosure Edith Tzeng, MD, FACS, Pittsburgh, PA - Nothing to Disclosure
Consultants
Barbara Lee Bass, MD, FACS, FRCSEng(Hon), FRCSI(Hon), FCOSECSA(Hon), Houston, TX - Nothing to Disclosure Quan-Yang Duh, MD, FACS, San Francisco, CA - Nothing to Disclosure B. J. Hancock, MD, FACS, FRCSC, Winnipeg, MB - Nothing to Disclosure Ronald V. Maier, MD, FACS, FRCSEd(Hon), Seattle, WA - Nothing to Disclosure
Continuing Medical Education Credit Information
The American College of Surgeons is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
AMA PRA Category 1 Credits™
The American College of Surgeons designates this enduring activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Of the AMA PRA Category 1 Credits™ listed above, a maximum of 1.5 credits meets the requirements for Self-Assessment.

Note: Residents will receive a Certificate of Completion.
Available Credit
This course is available as part of the Clinical Congress 2019 Webcast Packages
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.183(18); 2011 Dec 13

The art of presenting
The oral case presentation is a time-honoured tradition whereby a trainee presents a new admission to the attending physician. We describe the presentation styles of students, residents and staff physicians and offer pointers on how to present like stereotypical members of each group.
Although the case presentation occurs in nearly all disciplines, internal medicine (especially “team medicine” or Clinical Teaching Units) has a long-standing love–hate relationship with the case presentation and thus will be used throughout the paper to illustrate the ups and downs (mostly downs) of presenting.
Presentation styles
The clinical clerk.
The case presentation can be the most exciting part of the day for the clinical clerk and the most dreaded for the attending physician, or vice-versa. The key feature of a clerk’s presentation is his or her lack of confidence. Overinclusive and unconvincing, the presentation often showcases verbal diarrhea at its finest. The following pointers highlight the techniques best used by clinical clerks.
- Hedge your bets when reporting the physical exam (e.g., “I think I heard a murmur, or it could have been my stethoscope rubbing against his chest hair”).
- Present impossible findings (e.g., “The spleen was almost palpable”).
- Offer creative euphemisms for “I didn’t do that” when asked for physical findings that were not obtained (e.g., “My physical exam did not alter the prior probability of a knee effusion”).
The elective clinical clerk
The elective clinical clerk, unlike other clerks, has declared an interest in pursuing a career in internal medicine. Thus, the case presentation is definitely the most exciting part of his or her day, because it guarantees face time with the staff.
Elective clinical clerks tailor their presentations heavily to impress specific staff physicians in the hope of receiving a positive reference letter. For example, they will list all of the negative findings, not just the pertinent ones, to show that they have left no stone unturned or detail overlooked. Elective clerks are also often hyperaware of their attending’s preferred presentation format and will overindulge in this style. If a staff physician likes a narrative format, the clerk will record the interview to present the case in the patient’s “own words.” Finally, elective clerks who come from other institutions often take the opportunity to promote their own institution in their presentations, usually in backhanded ways.

The following pointers will help elective clerks hone their presentation skills:
- Present a ludicrous number of “pertinent” negatives (e.g., “The patient did not have any neurological symptoms. He denied headache, visual changes, weakness, paresthesias, vertigo, seizure activity, dysarthria, aphasia, alexia, agraphia, ataxia, abulia, akathisia, ageusia, allodynia, anosmia, apraxia, athetosis, astasia and astasia–abasia. Dangit, I forgot to ask about anosognosia”).
- Show knowledge by posing questions you obviously do not need to ask (e.g., “Regarding the woman with recurrent urinary tract infections, would there be any problem with prescribing prophylactic nitrofurantoin … apart from the risk of pulmonary toxicity?”).
- Promote your own institution, preferably in a backhanded way (e.g., “I guess this isn’t the case in Toronto, but here at McMaster we learn to do only physical exam manoeuvres that have been validated in randomized controlled trials”).
The off-service PGY-1 resident
The off-service junior resident on a medicine rotation is the ultimate “fish out of water.” Having begun to develop skills in their specialty of choice, off-service PGY-1 residents leave their comfort zone for cringe-inducing discussions of hyponatremia and eosinophilia. They go to great lengths to avoid the dissertations on diagnosis and management that internists love (e.g., by presenting the case of a patient who has rapid atrial fibrillation with a ventricular rate of 150 beats per minute by speaking at a rate of 150 words per second). Failing that, they seek solace by referencing their own specialty (and not so subtly suggesting its superiority). The following pointers highlight the presentation techniques of off-service residents:
- Avoid discussing “medical issues” by focusing on your own specialty (e.g., “This is an 85-year-old man presenting with shortness of breath. He also has been followed by urology for a remote history of prostate cancer. The cancer was discovered in 1990 and has been inactive since treatment in 1992. It was originally diagnosed by Dr. Thompson, a personal mentor, via transrectal biopsy, and pathology revealed a Gleason score of 5. The biopsy was then stained with [made-up-dye] #2 to determine its malignant potential, although that stain is no longer in use …”).
- Use verbal and nonverbal cues to express the superiority of your own specialty (e.g., “Do you know what type of incision the general surgeon will use to repair the bowel we perforated during the paracentesis?”).
The internal medicine PGY-1 resident
With a background in internal medicine, this first-year resident generally has more medical knowledge and practical knowhow than the other junior residents. The internal medicine trainee will stop at nothing to show his or her prowess in caring for patients, an earnestness that often manifests as a never-ending pursuit of esoteric (and often impossible) diagnoses.
Similarly, the internal medicine trainee goes to great lengths to display his or her burgeoning knowledge base. The goal is to get a “wow” from other junior residents (e.g., by reciting the differential diagnosis of Ortner syndrome) or from clerks (although getting a “wow” from a clerk is not difficult — this can usually be done by pronouncing “syncope” correctly). On occasion, this earnestness can resemble smugness, especially as the resident approaches the end of the internship and begins to think about how he or she will function as the senior resident/team leader.
As a junior resident in internal medicine, you may wish to incorporate the following techniques in your presentations.
- Pursue impossible diagnoses (e.g., “This 87-year-old man with a history of dementia now presents with worsening confusion, diarrhea and occasional arthralgias. Everything has improved with volume repletion and antibiotics, but his constellation of findings raises the possibility of undiagnosed Whipple disease. I’ve already received telephone consent from his third cousin in Florida, so I think we should call GI regarding small-bowel biopsy”).
- Be overly smug regarding the senior resident’s decisions (e.g., “When I run a team, I’ll never …” [this smugness quickly disappears when the senior resident takes a week’s vacation, leaving the PGY-1 resident to function as the “junior senior”]).
The senior medical resident (R2)
The senior resident serves in a supervisory role and must help the junior residents and clinical clerks in their (often futile) attempts to impress the attending physician. As a result, the senior resident is indirectly evaluated every time the junior trainees present. The attending will love a senior resident who can help clerks present cases in a crisp, coherent manner. On the other hand, a poor presentation can raise more questions about the resident than about the clerk. To guard against the latter situation, the senior resident finds ways of showing their own clinical skills. Many do this by interjecting during the presentations of other team members. Unfortunately, these interjections rarely (i.e., never) advance the patient’s care. They are, however, preferable to the “not my fault” approach taken by some senior residents who sit behind a clerk — in the line of sight of the staff — and shake their head in feigned disbelief as the clerk presents.
Below are techniques used by senior medical residents during presentations.
- Interject petty details to show that you are on top of everything (e.g., “I suppose the cardiac exam was ‘normal,’ but there was a physiologically split S 2 over the pulmonic valve”).
- Interject information that serves only to let the team know your desired subspecialty (e.g., “I don’t think we should discount the possibility of brucellosis in this patient. We probably should investigate for tularemia as well … and throw in a VDRL test too”).
The attending physician
As the presentee rather than presenter, the attending physician relies on the information he or she receives to make the final decisions regarding patient care. Knowing this, most trainees assume that attendings want to hear presentations that are comprehensive and error free. They are mistaken. Attending physicians love it when a trainee omits a key detail or misinterprets a key piece of information. Such instances provide attendings with two things they crave: the opportunity to show the clinical acumen achieved through years of experience, and the opportunity to create memorable teaching points. Everything an attending does while hearing a presentation is geared toward fulfilling these two goals (although a third — often unstated — goal is to stay awake). Some attendings simply listen intently and passively recognize subtle deficiencies (these attendings are typically described as “nice,” “approachable” and “boring”). Others have a different approach, actively trying to create gaps they can fill with one of many examples of their clinical expertise, as highlighted in the following pointers.
- Create gaps by preventing the trainee from presenting (e.g., Clerk: “The patient I saw is a 75-year-old male who was referred for chest ...” Attending: “Alright! Let’s go see him! Nice presentation, but I’ll give you some feedback: you’ve got to get to the point a little quicker next time”).
- Create gaps by questioning everything the trainee presents (e.g., Intern: “This 70-year-old male was referred because of a CVA.” Attending: “I think you mean ‘stroke,’ which is not an ‘accident.’” Intern: “Sorry. Anyways, the patient had a positive Babinski reflex on his right.” Attending: “Do you mean that his plantar response was up-going on the right?” Intern: “Of course, I don’t know where I got that from.” Attending: “Did you just end a sentence with a preposition?”).
Presentation styles vary tremendously among trainees. One aspect, however, remains constant: everyone involved is trying to highlight his or her own skills. Clerks want to showcase their ability to compile information, junior residents their diagnostic skills, senior residents their ability to manage complex patients, and attending physicians their clinical reasoning and mentoring skills. Implicit in this is the great strength of the case presentation: trainees at every level not only get to practise their own skills, they also see what they must do at the next level. Fortunately, all trainees provide the team with endless nuggets of entertainment — one just needs to stay awake to hear them.
Acknowledgement
The authors thank Mark Baerlocher for his comments on an earlier draft. Allan Detsky is a member of CMAJ ’s Editorial Board.
Competing interests: None declared.
Contributors: Daniel Rosenfield conceived the idea for the paper while stammering through his internal medicine clerkship presentations. Andrew Smaggus contributed to the design and writing of the paper, although most of what he contributed was subsequently cut or rewritten. Allan Detsky contributed to the overall inspiration for the paper as well as to the design and conceptualization.
Funding: No funding was received for this study. The authors did, however, take advantage of free food from noon rounds, and coffee and doughnuts brought in by clinical clerks.
- Open access
- Published: 06 October 2023
Enhanced perioperative care in emergency general surgery: the WSES position paper
- Marco Ceresoli 1 , 2 ,
- Marco Braga 1 , 2 ,
- Nicola Zanini 3 ,
- Fikri M. Abu-Zidan 4 ,
- Dario Parini 5 ,
- Thomas Langer 1 , 6 ,
- Massimo Sartelli 7 ,
- Dimitrios Damaskos 8 ,
- Walter L. Biffl 9 ,
- Francesco Amico 10 ,
- Luca Ansaloni 11 ,
- Zsolt J. Balogh 12 ,
- Luigi Bonavina 13 ,
- Ian Civil 14 ,
- Enrico Cicuttin 11 ,
- Mircea Chirica 15 ,
- Yunfeng Cui 16 ,
- Belinda De Simone 17 ,
- Isidoro Di Carlo 18 ,
- Andreas Fette 19 ,
- Giuseppe Foti 1 , 20 ,
- Michele Fogliata 1 , 2 ,
- Gustavo P. Fraga 21 ,
- Paola Fugazzola 11 ,
- Joseph M. Galante 22 ,
- Solomon Gurmu Beka 23 ,
- Andreas Hecker 24 ,
- Johannes Jeekel 25 ,
- Andrew W. Kirkpatrick 26 ,
- Kaoru Koike 27 ,
- Ari Leppäniemi 28 , 29 ,
- Ingo Marzi 30 ,
- Ernest E. Moore 31 ,
- Edoardo Picetti 32 ,
- Emmanouil Pikoulis 33 ,
- Michele Pisano 34 ,
- Mauro Podda 35 ,
- Boris E. Sakakushev 36 ,
- Vishal G. Shelat 37 , 38 ,
- Edward Tan 39 ,
- Giovanni D. Tebala 40 ,
- George Velmahos 41 ,
- Dieter G. Weber 42 ,
- Vanni Agnoletti 43 ,
- Yoram Kluger 44 ,
- Gianluca Baiocchi 45 ,
- Fausto Catena 3 &
- Federico Coccolini 46
World Journal of Emergency Surgery volume 18 , Article number: 47 ( 2023 ) Cite this article
4301 Accesses
1 Citations
Metrics details
This article has been updated
Enhanced perioperative care protocols become the standard of care in elective surgery with a significant improvement in patients’ outcome. The key element of the enhanced perioperative care protocol is the multimodal and interdisciplinary approach targeted to the patient, focused on a holistic approach to reduce surgical stress and improve perioperative recovery. Enhanced perioperative care in emergency general surgery is still a debated topic with little evidence available. The present position paper illustrates the existing evidence about perioperative care in emergency surgery patients with a focus on each perioperative intervention in the preoperative, intraoperative and postoperative phase. For each item was proposed and approved a statement by the WSES collaborative group.
Introduction
Enhanced recovery after surgery (ERAS®) protocol refers to a standardized multimodal approach based on the application of structured protocols in perioperative patients' management. The main goal of these interventions is patient management optimization during the perioperative period under all aspects of perioperative care, not only about the surgical technique, by reducing surgical stress, minimizing the physiological response to surgery, and improving postoperative recovery. The key element of the ERAS protocol is the multimodal and interdisciplinary approach targeted to the patient, focused on a holistic approach [ 1 ].
Perioperative care protocols are structured as a bundle of interventions to be applied during the preoperative, intraoperative and postoperative periods. Each intervention is linked to the others and shares the common goal of reducing the burden of perioperative patient stress (Fig. 1 ). For this reason, it is very difficult to evaluate the efficacy of a single item without considering the effect of all the others, applied as a bundle. Designing studies to evaluate and demonstrate the effect of every single intervention is therefore a major challenge, markedly limiting the available scientific evidence.

Enhanced perioperative care items and interventions
The effectiveness and safety of ERAS protocols in elective surgery are now widely established. Several meta-analyses comparing standard care and fast-track approach show that ERAS protocols in elective surgery lead to a reduction in length of stay and in the rate of postoperative non-surgical complications [ 2 , 3 , 4 , 5 ]. Most of the available studies focused on the postoperative phase, considering the main “surgical” items as study outcomes, with relatively small attention being devoted to preoperative and intraoperative interventions. However, main postoperative items such as oral feeding, urinary drain removal and mobilization should also be considered as compliance indicators rather than only interventions to be implemented [ 6 ]. From a methodological standpoint, there is a clear difference between adherence and compliance to an enhanced recovery protocol. Adherence should identify the percentage of items applied throughout the perioperative care process, while postoperative compliance also reflects how the patient follows the enhanced recovery process. For example, patients’ compliance to a postoperative pathway including early oral feeding and mobilization can be obtained easier if there is good adherence to a preoperative and an intraoperative enhanced pathway (and not only for a medical decision).
Based on the beneficial effect of enhanced perioperative care protocols in elective surgery, the implementation of structured protocols for emergency general surgery patients has also been advocated after the promising results of some studies [ 7 , 8 ]. However, enhanced perioperative care in emergency general surgery remains a “grey area” with little evidence available and great debate.
Patients undergoing elective surgery should be normothermic, euvolemic, clean, and “healthy”, and surgery per se represents their main stressful factor. Emergency surgery represents a more complex scenario where surgery is at the same time a stressful factor but also the key-intervention to solve the pre-existing physiologic imbalance secondary to the acute underlying disease (Fig. 2 ).
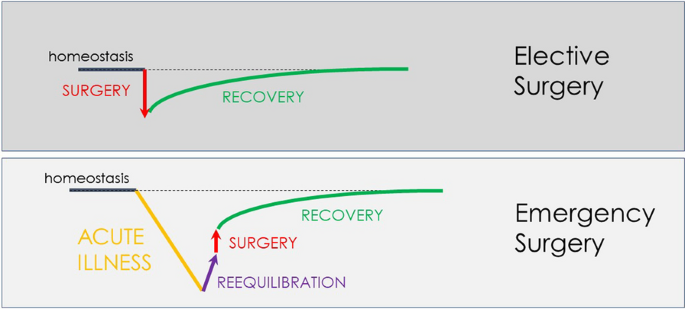
Perioperative diagram of patient’s homeostasis in elective and emergency general surgery
The diagram (Fig. 2 ) shows the impact of the pre-existing acute disorder causing a marked decline of the physiological reserve. The importance of the preoperative phase (re-equilibration) seems intuitive. Despite emergency surgery by definition does not allow schedulable interventions, some preoperative optimization is still possible in the emergency setting, though with much reduced time. The time available between patient presentation and surgery should be optimized to improve the patient’s physiological status to promote post-surgical recovery. In this complex scenario, also the timing of surgery should be carefully evaluated. One of the most intriguing and difficult challenges is to identify the right balance between hastening surgery to directly "face" the acute disease and delaying surgery in trying to improve the patient's condition.
Evidence supporting enhanced perioperative care in emergency general surgery.
Currently, available studies about enhanced perioperative care in emergency general surgery are few, sparse and very heterogeneous. In addition, the perioperative care protocol derived from the elective ERAS protocol but with several and substantial differences [ 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ]. Tables 1 and 2 show in detail the protocols adopted in the evaluated studies. A single perioperative care protocol cannot be identified through the existing literature, and each study applied different interventions.
Huddart et al. demonstrated that the introduction of a bundle evidence care protocol decreased mortality among patients undergoing emergency laparotomy, with a reduction in delayed diagnosis, increased implementation of goal-directed fluid therapy, and improved restoration of biochemical homeostasis [ 29 ]. The bundle protocol consisted in an accurate preoperative assessment with early warning score, early broad-spectrum antibiotics, prompt resuscitation using goal-directed techniques and postoperative ICU admission for all high-risk patients.
Tandberg and colleagues introduced a standardized perioperative care protocol in patients undergoing high-risk emergency abdominal surgery [ 9 ]. The study protocol included consultant-led attention and care, early resuscitation and high-dose antibiotics, surgery within 6 h, perioperative stroke volume-guided volume status optimization, standardized analgesic treatment, early mobilization and early oral feeding. Compared with a historical cohort from the same department, the introduction of the protocol lead to a significant reduction in mortality from 21.8 to 15.5%.
An Italian observational multicentric study demonstrated that adherence to the intraoperative protocol items was low. Major determinants of postoperative compliance were minimally invasive surgery and low intraoperative fluid infusions [ 22 ].
Several other studies investigated the introduction of enhanced perioperative care protocols in emergency general surgery [ 10 , 12 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 22 , 23 , 27 ]. Each study applied a different protocol in different subsets of patients with contrasting results. Some studies adopted a modified ERAS protocol in patients with obstructive colorectal cancer [ 13 , 14 , 16 , 19 ], others on patients with perforated peptic ulcer [ 10 , 15 , 17 ], others on major emergency laparotomy and trauma [ 12 , 18 , 20 , 22 ]. Most of the published enhanced recovery programs in emergency surgery focus on the intra- and postoperative phases of the program, reporting no substantial differences in the preoperative care of patients enrolled in ERAS protocols versus standard “not-ERAS” patients. The majority of the existing studies did not report results on adherence to the protocol items; moreover, also data on compliance to the postoperative pathway were lacking.
The results of some of these studies were included in a meta-analysis published by Hajibandeh et al. published in 2020 [ 30 ]. Despite the great heterogeneity and the poor quality of the evidence, the results showed a reduction in length of stay, pulmonary complications, postoperative ileus and wound infections. No differences were observed in 30-day rehospitalization and 30-day mortality rates.
Despite the promising results, the implementation of an enhanced perioperative care protocol in emergency general surgery may encounter several obstacles. Patients receiving urgent care typically present to medical teams with a complex situation: their conditions at the time of admission are not optimal and they have extremely heterogeneous characteristics [ 31 , 32 ]. The acute illness often leads to several physiological derangements secondary to fasting, vomiting, dehydration, augmented capillary permeability, and metabolic imbalance.
Columbus et al. [ 33 ] have identified two main critical issues concerning the urgent care field: the diversification of patients and the wide range of possible settings and operative contexts (including the hospital organization and the medical team management). Therefore, efforts should focus on improving the structural and organizational aspects. Dedicated medical personnel training and a widespread standardization of the diagnostic and therapeutic process may improve medical performance and, ultimately, the clinical outcome. A recent study demonstrated that the familiarity between surgeon and anesthetist used to work together improve patients’ outcome [ 34 ]. Unfortunately, emergency general surgery is rarely managed by a dedicated staff. Emergency care requires a higher number of specialists and personnel turnover and, therefore, it would lead to wider cross-collaborations and variability in staff composition. In addition, patients undergoing emergency surgery are rarely managed by enhanced recovery-trained anesthetists, surgeons and nurses (working in abdominal surgery), making the development of new treatment protocols very difficult.
The availability of resources is another central tenant to the safe and optimal delivery of surgical care in the emergency setting. For example, laparoscopic facilities or advanced hemodynamic monitoring systems are not universally available, and reported unavailable by some authors, due to logistical issues, timing of surgical interventions (e.g., in office hours vs. after hours), and higher costs [ 18 , 35 ].
The WSES panel promoted the development of this position paper. The work process consisted of two different phases. The first phase was a review of the existing literature about enhanced recovery protocol in emergency general surgery. The second phase was the identification of enhanced recovery protocol items and the development of position statements for each perioperative intervention. This position paper was written according to the WSES methodology [ 36 ]. All the statements contained the level of evidence (LoE) available about the topic, graded according to the GRADE methodology. The consensus on the position paper statements was assessed through a web survey (by Google Form) open to all the members of the steering committee and the experts’ panel, as well as the board of governor members of the WSES. The consensus was reached if a statement was associated with ≥ 70% of the agreement. Otherwise, the statement was re-discussed by email or videoconference, modified, and resubmitted to the experts’ vote until consensus was reached. Table 3 summarizes approved statements.
Preoperative interventions
Education and counseling, patient counseling and education should be encouraged and implemented to explain perioperative risks and post-operative pathway (loe d).
Relieving patient anxiety through preoperative counseling is of utmost importance, especially in an emergent situation. Full preoperative counseling, which is known to reduce post-operative stress, pain and anxiety, may not be possible in the emergency setting. Nevertheless, information such as details of the procedure, possible perioperative complications, the need for the creation of a stoma and length of hospitalization should be communicated with patients and their families before the procedure [ 30 , 37 ]. A recent meta-analysis focusing on the implementation of enhanced recovery protocols in emergency abdominal surgery reported that adapted preoperative counseling was carried out in all of the six included studies. No data about adherence to this counseling were reported [ 30 ]. Depending on the urgency of surgery, preoperative education/counseling may not be possible. However, a recently published multidisciplinary experience reported very high compliance (more than 90% 1 year after implementation) with items such as standardized preoperative patient information and bilateral ostomy marking in patients undergoing emergency general surgery [ 11 , 38 ]. In the case of stoma creation, the implementation of patient education reduced stoma complications and improved postoperative quality of life, reducing the average hospital stay [ 39 ]. However, although it seems feasible and of some utility to appropriately counsel patients before emergency procedures, evidence in support of this hypothesis has not been produced yet and the degree of benefit in terms of postoperative recovery has not been measured.
Fluid balance and volemic status
Volemic status should be evaluated and corrected with goal-directed fluid therapy as soon as possible in the pre-operative phase (loe b).
The majority of emergency general surgery patients present with fluid derangements, mostly related to acute illness, underlying sepsis, prolonged fasting and vomiting. In this setting, preoperative evaluation of the patient should focus on the volemic assessment to rapidly correct alterations in patients' homeostasis, including stress response, gut dysfunction, insulin resistance, electrolyte imbalances, fluid shifts, SIRS and sepsis with varying degrees of organ dysfunction. Although complete optimization of medical conditions cannot be fully achieved in the emergency setting, adequate intravenous fluid resuscitation in emergency general surgery is crucial and feasible, and it should be attempted in all patients. A prospective randomized trial demonstrated better postoperative outcomes when patients were preoperatively managed with a fixed protocol to reach homeostasis [ 40 ]. The adopted protocol defined three targets for the goal-directed crystalloid resuscitation: central venous pressure of 8–12 cmH 2 O, mean arterial pressure > 65 mmHg and urinary output > 0.5 mL/Kg/h. The initial resuscitation should be titrated to the clinical response, such as fluid responsiveness, and not solely guided by a predetermined protocol, with particular attention to the underlying disease. Despite restoring homeostasis should be considered a goal, surgical treatment should not be delayed. According to the indications from the 2016 Surviving Sepsis Guidelines, resuscitation from sepsis-induced hypoperfusion should require at least 30 ml/kg of intravenous crystalloid fluids within the first 3 h [ 41 ]. However, in the updated 2021 version of the Guidelines, the strength of this recommendation was downgraded from “strong” to “weak” (quality of evidence: low) and the recommendation was modified in a suggestion [ 42 ]. Massive fluid therapy has been challenged in the enhanced recovery approach [ 9 ]. Fluid overload should be avoided since it is associated with higher rates of respiratory complications ( i.e., pneumonia, pleural effusion, and respiratory failure) and secondary anastomotic leaks. Early, i.e., preoperative, goal-directed fluid therapy in sepsis was the treatment of the experimental arm in a randomized clinical trial enrolling septic patients published in 2001 [ 43 ]. Excluding patients who needed immediate surgery from the trial, in-hospital mortality was 30.5% in the group assigned to early goal-directed therapy, as compared with 46.5% in the group assigned to standard therapy ( P = 0.009). Tendberg et al. developed a perioperative protocol for emergency high-risk abdominal surgery in which stroke volume-guided hemodynamic optimization before surgery was a key element. The study has shown a significant reduction in mortality as well as postoperative length of ICU stay after the introduction of the standardized protocol [ 9 ]. Therefore, patients should be carefully evaluated and goal-directed fluid resuscitation should be implemented as soon as possible.
Metabolic balance
Glycemic control should be implemented in all emergency surgery patients to prevent both hypo- and hyperglycemia (loe c).
Perioperative hyperglycemia has been demonstrated to be associated with adverse clinical outcomes [ 44 ]. The correction of hyperglycemia with insulin administration and the management of glycemia with the implementation of glycaemic control protocols have been shown to reduce hospital complications and decreases mortality in elective general surgery patients [ 45 ]. Pre-existing diabetes mellitus, acute illness and physiologic changes accompanying a surgical procedure contribute to the worsening of glycemic control. The resulting hyperglycemia due to an abnormal glucose balance is a risk factor for postoperative complications that include poor wound healing and postoperative infections as well as an increase in morbidity, mortality, intensive care unit admission, and hospital length of stay [ 46 ]. Preoperative hyperglycemia has been demonstrated to have a role in postoperative compliance to an enhanced recovery pathway also in emergency surgery patients [ 22 ]. However, in emergency general surgery and in critically ill patients the role of hyperglycemia is more debated and less certain. Hyperglycemia could be considered a marker of organ failure and disease severity. A recent network meta-analysis comparing four different target blood glucose concentrations (< 110, 110–144, 144–180, and > 180 mg/dL) in terms of the benefit and risk of insulin therapy found no significant difference in the risk of mortality and infection among four target blood glucose ranges in critically ill patients, but indicated that target blood glucose levels of below 144 mg/dL were associated with a higher risk of hypoglycemia [ 47 ]. Although a proactive approach to avoid both hyper- and hypoglycemia should be suggested in emergency patients, close glycemic control is advisable and Institutions should develop their own protocols to treat both hyper and hypoglycemia in critically ill patients.
Intraoperative interventions
Postoperative nausea and vomiting (ponv) prevention, ponv prevention with a multimodal approach in an emergency setting should be implemented (loe d).
Prevention of PONV in elective general surgery has become a key element of enhanced recovery protocols [ 48 ]. PONV is very common after general anesthesia and it may negatively impact recovery and short-term outcomes [ 49 ]. Several factors are linked to the occurrence of PONV; however, its exact pathophysiology is still unclear [ 50 ]. Some risk factors are patient-related such as advanced age, female gender, non-smoking status, pain, and anxiety. Other risk factors are related to the type of operative gastro-intestinal manipulation and vagal stimulation, anesthetics, and opioids [ 50 , 51 , 52 ]. Few data are available on emergency patients who frequently complain of nausea and vomiting before surgery in association with anxiety and pain. Several studies investigated the role of different drugs to prevent PONV. The commonest antiemetic drugs are dopamine and serotonin antagonists (e.g., ondansetron) and corticosteroids (e.g., dexamethasone) [ 53 , 54 , 55 , 56 ]. Pre-emptive anesthesia was associated with better pain control and reduction in PONV [ 57 , 58 ].
Other suggested interventions are opioid-sparing anesthesia and avoidance of volatile anesthetics. Unfortunately, the vast majority of evidence is based on elective surgery and very few data are available on emergency general surgery. The emergency setting is associated with more fear, anxiety, pain and, probably, nausea even before surgery. Nevertheless, prevention of PONV should be implemented also in emergency general surgery. Among the interventions suggested, there are opioid-sparing anesthesia, avoidance of volatile anesthetics and a multimodal approach to pharmacological prevention.
Anesthesia and analgesia
General anesthesia warrants proper analgesia, amnesia and muscle relaxation. The ideal general anesthesia protocol should target all these goals, but it should also reduce the need for intraoperative fluids, reduce post-operative residual effects, such as PONV and delirium and it should permit rapid awakening. Several interventions have been implemented to optimize the intraoperative management of the patient. Whether anesthesia should be maintained by a totally intravenous approach or with inhalation drugs still remains uncertain and no recommendations can be made [ 59 ]
Benzodiazepines
Benzodiazepines should be avoided in the emergency anesthetic protocol, in particular in older patients, to reduce delirium risk in the postoperative period (loe c).
The incidence of delirium in the postoperative period has an important impact on clinical outcomes including higher mortality, functional decline, prolonged hospitalizations and risk for institutionalization [ 60 ]. Upon the several risk factors for development, that include acute illness and pain management, medications adopted also for general anesthesia play an important role [ 61 ]. For these reasons, anesthetic protocols should focus on reducing the use of these medications. Benzodiazepines have been linked with the development of delirium in the postoperative period, with a marked effect in elderly and frail patients [ 62 , 63 ]. Despite the potential beneficial effects in treating preoperative anxiety, these drugs should be avoided.
Opioid use should be limited to short-acting drugs in the perioperative period (LoE D)
Opioids are related to several adverse effects such as nausea, vomiting, respiratory depression, sedation and postoperative ileus. Despite their important role in pain management, the undesired effects may impact negatively on patients' recovery. Some experiences exist about opioid-free anesthesia, with the claim of more patient safety [ 64 ]. For this reason, opioids use should be limited to short-acting drugs avoiding morphine to minimize residual effects and to warrant rapid recovery [ 65 ].
Anesthesia depth monitoring
Anesthesia depth monitoring should be implemented in the emergency setting, to minimize anesthesia side effects such intra-operative hypotension, increased need for fluids and postoperative delirium (loe c).
To reduce all the detrimental effects of general anesthetics, such as cognitive effects and vasoactive depressing activity, titrating the minimal needed drug dose guided by the depth of anesthesia monitoring has been recommended. Monitoring of anesthesia depth could be guided by the bispectral index (BIS) or other techniques based on electrical brain activity (EEG). Anesthesia depth monitoring has been demonstrated to be associated with a lower incidence of postoperative delirium and with decreased morbidity [ 66 , 67 , 68 ]. Moreover, depth monitoring has been demonstrated to be associated also with a higher intraoperative mean arterial pressure, possibly reducing the need for fluid administration to maintain adequate systemic perfusion [ 69 ].
Neuromuscular blockade monitoring
Neuromuscular blockade monitoring should be implemented to reduce post-operative morbidity (loe c).
Neuromuscular blockade is needed during abdominal surgery to improve surgical exposure. A post-operative residual neuromuscular block is a risk factor for morbidity and mortality, conditioning weakness of airway muscles, airway obstruction and aspiration with consequent increased postoperative pulmonary complications [ 70 ]. Residual neuromuscular block has been reported in up to 40% of patients treated with neuromuscular blocking agents [ 71 ]. Adopting strategies such as the qualitative monitoring of the peripheral muscular blockade as the train of four (TOF) has been demonstrated to significantly reduce the residual blockade at the end of anesthesia [ 72 ]. Monitoring of the neuromuscular blockade is therefore recommended to avoid potential side effects.
Multimodal pain control
Multimodal analgesia, with a combination of systemic and loco-regional approaches, should be encouraged in the emergency setting to improve pain control and reduce the need for analgesics and opioids (loe c).
Pain is one of the limitations to patient recovery after surgery. Standard general anesthesia warrants analgesia during surgery, but has no effect on pain control after surgery, requiring drug administration with possible detrimental effects such as opioids. Multimodal analgesia has been proposed to manage pain with several different treatments reducing the need for systemic opioids and avoiding their potential side effects [ 73 ]. The association of general and locoregional analgesia has been demonstrated also to reduce the incidence of postoperative delirium [ 74 ].
Thoracic epidural analgesia (TEA) has been demonstrated to be superior to systemic opioids in pain management in open elective abdominal surgery [ 75 ]. A recent Scandinavian population study reported that epidural analgesia was adopted in emergency general surgery in less than one third of patients; epidural analgesia was associated with lower 90-day mortality probably due to a reduction in paralytic ileus and pain that most likely allowed an early mobilization and coughing [ 76 ]. TEA was included in an emergency general surgery enhanced recovery protocol that demonstrated a significant reduction in mortality, despite the adherence to this specific item was not reported [ 9 ]. Spinal analgesia has been proposed as an alternative to epidural analgesia in patients treated with minimally invasive colorectal surgery: the administration of long-acting local anesthetics and opioids warrant pain control in the first postoperative hours allowing early mobilization. Moreover, it has been associated with a lower risk of hypotension and fluid overload [ 77 ]. However, spinal and epidural anesthesia should be considered with caution in septic patients.
Surgical incision is one of the main responsible of postoperative pain. To manage this pain, abdominal wall blockade such as the Transversus abdominis plane (TAP) block has been proposed. The adjunct of abdominal wall blocks to general anesthesia has been demonstrated to have beneficial effects on pain control during the first 24 h and to allow faster recovery and better hemodynamic control in elective abdominal surgery [ 78 , 79 , 80 , 81 ]. Of note, the TAP block can be performed both ultrasound-guided and laparoscopy-guided [ 82 ]. Currently, no studies focus on the performance of the TAP block in emergency general surgery. However, abdominal wall blocks should be considered in a multimodal analgesic approach.
Active warming
Active warming and body temperature monitoring should be encouraged in the emergency setting to reduce postoperative morbidity (loe c).
Body temperature plays an important role in several pathophysiologic mechanisms Hypothermia typically occurs during general and locoregional anesthesia due to vasodilatation and a rapid redistribution of heat from the core to peripheral districts. Moreover, several anesthetic drugs impair thermoregulatory control, further contributing to the maintenance of hypothermia. Finally, the development of hypothermia is facilitated by direct heat loss deriving from the surgical exposure of the abdominal cavity and by the low operating theater temperature. Importantly, perioperative hypothermia implicates an increased risk of surgical site infection, morbidity and mortality. Moreover, hypothermia may alter drug metabolism and it is also associated with an increased risk for coagulopathy and a consequent increased blood loss [ 83 ]. Body temperature monitoring is therefore mandatory and allows temperature correction with active warming. Active warming, ideally starting before the entrance to the operating room, has been recognized as one of the core items of the enhanced recovery pathway and its implementation significantly reduced postoperative morbidity [ 84 , 85 ].
Fluid management
Fluids should be managed within a goal-directed fluid therapy strategy to target the amount of given fluids on patient needs (loe c).
General anesthetics lead to dose-depend myocardial depression and systemic vasodilatation. The associated increased venous capacitance leads to a relative hypovolemia that, along with myocardial depression, might lead to hypotension, and organ hypoperfusion with the related consequences. Therefore, during surgery, fluids are frequently administered to maintain an adequate intravascular volume status and systemic perfusion. However, both hypovolemia and hypervolemia are associated with postoperative morbidity and several studies demonstrated the J-shaped relation between intraoperative fluids administered and postoperative morbidity [ 86 , 87 , 88 ]. Intraoperative fluid management should therefore be balanced, giving the needed amounts of fluids to warrant euvolemia and systemic perfusion, but avoiding fluid overload [ 89 , 90 ]. Fluid overload is associated with several detrimental effects related to tissue edema. Increased interstitial fluids might impair gas exchange with consequent respiratory failure and foster the development of pneumonia. Moreover, fluid overload is associated with bowel edema and postoperative ileus, conditioning a delayed recovery of GI function [ 91 ]. For these reasons in elective surgery, a restrictive fluid strategy has been proposed, with the target of a near-zero fluid balance during surgery and a limited amount of fluids given (generally around 3 mL/Kg/h) [ 92 ]. This approach is valid under the condition that patients arrive at the surgery in perfect homeostasis without fluid derangements.
Several factors may worsen and make fluid management in emergency surgery patients more difficult. Increased vascular permeability related to acute illness, preoperative fasting, preoperative dehydration and blood loss may dramatically increase the need for intraoperative fluids compared to elective surgical patients. In this complex scenario, goal-directed fluid therapy has been proposed to titrate and balance the amount of fluids. Fluid therapy should be guided by hemodynamic monitoring systems, ideally capable of monitoring dynamic parameters, such as cardiac output, stroke volume variation, pulse pressure variation and stroke volume variation [ 93 , 94 ]. The implementation of an intraoperative goal-directed fluid strategy, associated with restrictive fluid regimens and the early adoption of vasopressors to maintain adequate circulating volumes has been demonstrated to significantly reduce perioperative morbidity [ 94 ]. While only few studies exist on fluid management during general emergency surgery, available evidence derived from elective surgery and current pathophysiological understanding strongly underlines the importance of reasoned fluid management during emergency surgery. In the emergency setting, a recent study highlighted the importance of fluid therapy, with a negative correlation between increasing intraoperative fluids given and patients' recovery [ 22 ].
Minimally invasive surgery
Minimally invasive surgery approach in emergency surgery should be encouraged whenever possible and needed skills are available (loe c).
Reducing surgical stress is the cornerstone of an enhanced perioperative care protocol. The use of minimally invasive surgery in elective major surgery has been demonstrated to reduce inflammation, improve pulmonary function, and facilitate GI function with a consequent reduction in morbidity and length of stay [ 95 , 96 , 97 ]. Minimally invasive surgery, even within an enhanced recovery pathway, has been associated with a faster recovery when compared with open surgery [ 98 ]. In emergency major abdominal surgery, such as repair for perforated peptic ulcer and colorectal surgery invasive minimally techniques have been associated with better clinical outcomes with a lower mortality and length of stay [ 99 , 100 , 101 ]. A population study on the commonest abdominal surgical emergencies in the USA demonstrated an increasing trend of a laparoscopic approach. Minimally invasive surgery was associated with lower mortality, surgical site infection rate and length of stay. However, minimally invasive surgery in major interventions such as peptic ulcer repair and small bowel obstruction was adopted in less than 40% and 10%, respectively [ 102 ]. Data from the national emergency laparotomy audit (NELA) from the U.K. demonstrated that laparoscopy is adopted in less than 20% of major surgeries [ 99 ]. Existing data demonstrated the beneficial effect of minimally invasive surgery but also its poor diffusion among surgeons with several difficulties [ 103 ]. A recent prospective study identified minimally invasive surgery as the major determinant of postoperative compliance to an enhanced recovery protocol [ 22 ]. Efforts should be made to implement laparoscopy in emergency general surgery daily practice.
Abdominal drains should be placed for limited indications, including in the presence of gross bacterial contamination and inadequate source control (LoE D)
The routine positioning of a peritoneal drain after elective major colorectal surgery has been demonstrated to be ineffective in preventing surgical complications and is not recommended [ 104 ]. Moreover, the presence of a drain has been identified as one of the main failure predictors of an enhanced recovery pathway, both in elective and emergency surgery [ 22 , 105 ]. Drain in emergency general surgery is justified by a clear rationale, in case of contaminated surgical field and intra-abdominal infections. Few experiences exist about avoiding drains in emergency general surgery: some studies focused on the introduction of enhanced perioperative care protocol on colorectal emergencies (obstructions) demonstrated better results avoiding the drain (along with other interventions) [ 13 , 14 , 16 ]; other studies demonstrated the safety of an early removal in perforated peptic ulcer and trauma [ 15 , 20 ]. Evidence quality is very low to recommend avoiding abdominal drains, but we believe drains should be placed only in case of gross abdominal contamination and high risk for collection and abdominal abscess.
Postoperative care
Multimodal analgesia, using different classes of analgesics and avoiding long-acting opioids, should be recommended in the postoperative phase (loe c).
Proper analgesia and pain control are key elements of a patient’s recovery after surgery. The control of pain in the postoperative period is the result of many several factors related to patients' characteristics, invasiveness of surgical intervention, the underlying diagnosis and adopted intra- and post-operative analgesia techniques. Perioperative management should be focused on maximizing the effect of pain control and avoiding the side effects of drugs. The use of long-acting opioids, such as morphine, should be ideally avoided also in the postoperative period. Indeed, avoiding opioids has been demonstrated to facilitate mobilization and to fasten GI function recovery [ 65 ]. The treatment of pain should be multimodal and tailored to patients’ conditions, according to available skills [ 106 ].
Early nasogastric tube removal
The nasogastric tube should be removed as soon as possible, even at the end of surgery (loe d).
According to a reactive policy, the nasogastric tube (NGT) was traditionally removed after GI function recovery to prevent PONV and inhalation. Enhanced recovery protocols recommend the removal of NGT at the end of elective surgery. This practice reduced pulmonary complications and promoted GI function recovery [ 107 ]. Preliminary studies carried out in patients with obstructive colorectal cancer or perforated peptic ulcer reported a high patient compliance to NGT removal at the end of surgery [ 17 , 19 , 108 ]. Other studies suggested removing the NGT when the output was less than 300 ml [ 15 , 18 ]. When patients are managed according to enhanced recovery protocols, the early removal of NGT is safe and should be implemented in clinical practice.
Early mobilization
Early mobilization should be encouraged and stimulated as soon as possible to reduce post-operative morbidity (loe c).
Prolonged immobilization is associated with insulin resistance, thromboembolic events and respiratory complications [ 109 ]. Several studies reported that early mobilization after surgery reduced overall morbidity and shortened the length of hospital stay [ 110 , 111 , 112 , 113 ]. Several factors can negatively impact on patient’s mobilization such as abdominal drain, urinary catheter, suboptimal pain control, prolonged i.v fluids, and patient's motivation. In emergency surgery, different protocols have been proposed targeting mobilization the same day of surgery [ 15 , 18 ] or on postoperative day 1 [ 14 , 16 , 19 ]. According to existing evidence, patient mobilization should be encouraged as early as possible, along with all the interventions that could facilitate it, such as proper pain control, and the early removal of urinary catheter and drains.
Nutrition and early oral feeding
Early oral feeding should be encouraged and promoted as soon as tolerated by patients (loe c).
The close relationship between preoperative nutritional status and surgical outcomes has been extensively reported in elective surgery, where tailored nutritional and prehabilitation programs can be planned before the operation [ 114 ]. Postoperative fasting has been demonstrated to be harmful in elective surgery with delayed recovery and increased complications[ 2 , 115 , 116 ]. Oral feeding can be resumed early after surgery regardless of bowel canalization, whether removal of the nasogastric tube, PONV prophylaxis, near zero fluid balance, early mobilization, and pain control have been carried out according to enhanced recovery protocol. Patients undergoing emergency surgery often have an altered metabolic status, with dehydration and several derangements such as prolonged fasting, vomiting, impairment of GI function, and fluid loss related to the acute illness. The great condition's heterogeneity in emergency surgery patients makes quite impossible to standardize the timing of oral feeding recovery. However, studies carried out in patients with perforated peptic ulcer or obstructive colorectal cancer demonstrated both feasibility and safety of early oral feeding [ 19 , 20 , 117 ]. Perioperative nutritional intervention should be therefore tailored to the patient's conditions adopting as the target the earliest possible recovery.
Urinary catheter removal
Urinary catheter should be removed as soon as possible when urinary output no longer needs to be monitored (loe c).
Urinary output monitoring is a key element to assess patients' volemic status and to guide goal-directed fluid therapy. In emergency surgery patients, the urine output target should be 0.5 ml/Kg/h. Different policies about the timing of catheter removal have been proposed: immediately after surgery in a randomized study on perforated peptic ulcer patients [ 17 ], on postoperative day 1 [ 19 , 20 ] or according to urinary output (> 1 ml/Kg/h) [ 15 , 18 ]. Regardless, the urinary catheter should be removed as early as possible after reaching the minimum urinary output target to facilitate mobilization and reduce infections.
Postoperative fluids
Postoperative intravenous fluids should be minimized and maintained until oral fluid intake is adequate (loe c).
Fluid therapy should be targeted to restore the euvolemic status and to maintain adequate hydration and tissue perfusion until the oral intake can be restarted. As reported for operative management, fluid therapy can be harmful if too many or too few fluids are given [ 86 , 87 , 88 ]. Following elective colorectal surgery i.v. fluids should be stopped on postoperative day one. Studies performed on emergency surgery patients did not report on timing to stop i.v fluids; however, infusions should be tailored to patient conditions, giving the minimum fluid amount to restore and maintain euvolemia and to obtain adequate perfusion.
Antibiotic therapy
Antibiotic therapy should not be continued in case of non-complicated intra-abdominal infections, while a short course antibiotic therapy is indicated in case of complicated infection (LoE A).
A large part of emergency patients undergo surgery for intra-abdominal infections; therefore, antibiotic therapy is a cornerstone of treatment along with surgical source control . The need for antibiotics during the postoperative period may contribute to delaying patient recovery, as an obstacle to active mobilization and i.v. infusions suspension; moreover, prolonged antibiotic therapies may have a role in delaying home return. Postoperative antibiotic therapy should be reserved for patients with complicated intra-abdominal infections. In these patients, a short therapy (3–5 days) after adequate surgical source control is not inferior when compared to longer therapy [ 118 , 119 , 120 ]. In non-complicated infections, antibiotic therapy should be stopped at the end of surgery if the source control is adequate.
The majority of patients presenting with a severe infection who initially require IV therapy can be switched to oral therapy after 24–48 h provided that they are improving clinically and can tolerate an oral formulation. The switch from IV to oral route should be encouraged.
Research agenda
The present position paper highlights the great heterogeneity of protocols adopted and the lack of good-quality evidence supporting the implementation of enhanced recovery pathway in emergency general surgery. Further studies on this topic should address:
The definition of the safety, feasibility and effectiveness of each perioperative intervention.
The definition of a standardized enhanced recovery protocol for emergency general surgery procedures
The selection of patients who may benefit from an enhanced recovery pathway and the clinical scenarios in which enhanced recovery pathway could be applied.
Conclusions
Enhanced perioperative care, similar to elective surgery, should be implemented in emergency general surgery. One of the key elements for the success of the enhanced pathways is the multimodal approach involving surgeons, anesthetists, ICU physicians, nurses, patients and patient families. Available evidence suggests future required research on the implementation of enhanced recovery pathways in clinical practice.
Availability of data and materials
Data are available under request to the corresponding author.
Change history
15 october 2023.
The CRUE CSIC TA funding note has been removed
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg [Internet]. 2017;152:292–8.
PubMed Google Scholar
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg [Internet]. 2014;38:1531–41.
Lee Y, Yu J, Doumouras AG, Li J, Hong D. Enhanced recovery after surgery (ERAS) versus standard recovery for elective gastric cancer surgery: a meta-analysis of randomized controlled trials. Surg Oncol. 2020;32:75–87.
Ni X, Jia D, Chen Y, Wang L, Suo J. Is the enhanced recovery after surgery (ERAS) program effective and safe in laparoscopic colorectal cancer surgery? A meta-analysis of randomized controlled trials. J Gastrointest Surg [Internet]. 2019;23:1502–12.
Ni X, Jia D, Guo Y, Sun X, Suo J. The efficacy and safety of enhanced recovery after surgery (ERAS) program in laparoscopic digestive system surgery: a meta-analysis of randomized controlled trials. Int J Surg. 2019;69:108–15.
Ceresoli M, Braga M. Reply to: Early non compliance to enhanced recovery pathway might be an alert for underlying complications following colon surgery. Eur J Surg Oncol. 2023;49:526.
Quiney N, Aggarwal G, Scott M, Dickinson M. Survival after emergency general surgery: what can we learn from enhanced recovery programmes? World J Surg [Internet]. 2016;40:1283–7. https://doi.org/10.1007/s00268-016-3418-0 .
Article CAS PubMed Google Scholar
Aggarwal G, Peden CJ, Mohammed MA, Pullyblank A, Williams B, Stephens T, et al. Evaluation of the collaborative use of an evidence-based care bundle in emergency laparotomy. JAMA Surg [Internet]. 2019;154:e190145.
Tengberg LT, Bay-Nielsen M, Bisgaard T, Cihoric M, Lauritsen ML, Foss NB, et al. Multidisciplinary perioperative protocol in patients undergoing acute high-risk abdominal surgery. Br J Surg [Internet]. 2017;104:463–71.
CAS PubMed Google Scholar
Møller MH, Adamsen S, Thomsen RW, Møller AM. Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg. 2011;98:802–10.
Burcharth J, Falkenberg A, Oreskov JO, Ekeloef S, Gögenur I. Patients’ perceptions of barriers to enhanced recovery after emergency abdominal surgery. Langenbecks Arch Surg. 2021;406:405–12.
Wisely JC, Barclay KL. Effects of an Enhanced Recovery After Surgery programme on emergency surgical patients. ANZ J Surg. 2016;86:883–8.
Lohsiriwat V. Enhanced recovery after surgery for emergency colorectal surgery: Are there any differences between intra-abdominal infection and other indications? J Visc Surg [Internet]. 2019;156:489–96.
Lohsiriwat V. Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol [Internet]. 2014;20:13950.
Mohsina S, Shanmugam D, Sureshkumar S, Kundra P, Mahalakshmy T, Kate V. Adapted ERAS pathway vs. standard care in patients with perforated duodenal ulcer—a randomized controlled trial. J Gastrointest Surg [Internet]. 2018;22:107–16. https://doi.org/10.1007/s11605-017-3474-2 .
Article PubMed Google Scholar
Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer. Medicine [Internet]. 2018;97:e12348. Available from: https://journals.lww.com/00005792-201809280-00034 .
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU, et al. Enhanced postoperative recovery pathways in emergency surgery: a randomised controlled clinical trial. Am J Surg [Internet]. 2014;207:807–14. https://doi.org/10.1016/j.amjsurg.2013.07.025 .
Pranavi AR, Sureshkumar S, Mahalakshmy T, Kundra P, Kate V. Adapted ERAS pathway versus standard care in patients undergoing emergency surgery for perforation peritonitis—a randomized controlled trial. J Gastrointest Surg [Internet]. 2022;26:39–49. https://doi.org/10.1007/s11605-021-05184-x .
Roulin D, Blanc C, Muradbegovic M, Hahnloser D, Demartines N, Hübner M. Enhanced recovery pathway for urgent colectomy. World J Surg [Internet]. 2014;38:2153–9. https://doi.org/10.1007/s00268-014-2518-y .
Purushothaman V, Priyadarshini P, Bagaria D, Joshi M, Choudhary N, Kumar A, et al. Enhanced recovery after surgery (ERAS) in patients undergoing emergency laparotomy after trauma: a prospective, randomized controlled trial. Trauma Surg Acute Care Open [Internet]. 2021;6:e000698.
Nechay T, Titkova S, Tyagunov A, Anurov M, Sazhin A. Modified enhanced recovery after surgery protocol in patients with acute cholecystitis: efficacy, safety and feasibility. Multicenter randomized control study. Updates Surg. 2021;73:1407–17.
Ceresoli M, Biloslavo A, Bisagni P, Ciuffa C, Fortuna L, La Greca A, et al. Implementing enhanced perioperative care in emergency general surgery: a prospective multicenter observational study. World J Surg [Internet]. 2023. https://doi.org/10.1007/s00268-023-06984-9 .
Sharma J, Kumar N, Huda F, Payal YS. Enhanced recovery after surgery protocol in emergency laparotomy: a randomized control study. Surg J. 2021;07:e92–9.
Google Scholar
Masood A, Viqar S, Zia N, Ghani M usman. Early oral feeding compared with traditional postoperative care in patients undergoing emergency abdominal surgery for perforated duodenal ulcer. Cureus. 2021.
Chndan MN, Khakholia M, Bhuyan K. Enhanced recovery after surgery (ERAS) versus standard care in patients undergoing emergency surgery for perforated peptic ulcer. Indian J Surg. 2020;82:1044–9.
Ruiz-Tovar J, Llavero C, Perez-Lopez M, Garcia-Marin A. Implementation of an enhanced recovery after surgery (ERAS) protocol for acute complicated and uncomplicated appendicitis. Tech Coloproctol. 2021;25:1073–8.
Saurabh K, Sureshkumar S, Mohsina S, Mahalakshmy T, Kundra P, Kate V. Adapted ERAS pathway versus standard care in patients undergoing emergency small bowel surgery: a randomized controlled trial. J Gastrointest Surg [Internet]. 2020;24:2077–87.
Pathrikar SG, Jadhav GS, Adhikari GR. The application of enhanced recovery after surgery protocols in patients with perforated duodenal ulcer. Cureus. 2023.
Huddart S, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA, et al. Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg [Internet]. 2015;102:57–66.
Hajibandeh S, Hajibandeh S, Bill V, Satyadas T. Meta-analysis of enhanced recovery after surgery (ERAS) protocols in emergency abdominal surgery. World J Surg [Internet]. 2020;44:1336–48. https://doi.org/10.1007/s00268-019-05357-5 .
Lee KC, Sturgeon D, Lipsitz S, Weissman JS, Mitchell S, Cooper Z. Mortality and health care utilization among medicare patients undergoing emergency general surgery vs those with acute medical conditions. JAMA Surg. 2020;155:216.
Quiney N, Aggarwal G, Scott M, Dickinson M. Survival after emergency general surgery: what can we learn from enhanced recovery programmes? World J Surg. 2016;40:1283–7.
Columbus AB, Morris MA, Lilley EJ, Harlow AF, Haider AH, Salim A, et al. Critical differences between elective and emergency surgery: identifying domains for quality improvement in emergency general surgery. Surgery [Internet]. 2018;163:832–8.
Hallet J, Sutradhar R, Jerath A, Perez D’empaire P, Carrier F, Turgeon A, et al. Association between familiarity of the surgeon-anesthesiologist dyad and postoperative patient outcomes for complex gastrointestinal cancer surgery. JAMA Surg [Internet]. 2023.
Puccetti F, Elmore U, Rosati R. Application of ERAS protocols in esophagogastric emergency surgery: is it feasible and does it make sense? Updates Surg. 2023;75:383–7.
Bala M, Kashuk J, Moore EE, Catena F, Leppaniemi A, Ansaloni L, et al. Establishing position papers by the WSES. World J Emerg Surg. 2018;13:1.
CAS PubMed PubMed Central Google Scholar
Shuldham C. A review of the impact of pre-operative education on recovery from surgery. Int J Nurs Stud. 1999;36:171–7.
Burcharth J, Abdulhady L, Danker J, Ekeloef S, Jørgensen T, Lauridsen H, et al. Implementation of a multidisciplinary perioperative protocol in major emergency abdominal surgery. Eur J Trauma Emerg Surg [Internet]. 2021;47:467–77. https://doi.org/10.1007/s00068-019-01238-7 .
Ferrara F, Parini D, Bondurri A, Veltri M, Barbierato M, Pata F, et al. Italian guidelines for the surgical management of enteral stomas in adults. Tech Coloproctol. 2019;23:1037–56.
Sethi A, Debbarma M, Narang N, Saxena A, Mahobia M, Tomar GS. Impact of targeted preoperative optimization on clinical outcome in emergency abdominal surgeries: a prospective randomized trial. Anesth Essays Res [Internet]. 2018;12:149.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign. Crit Care Med. 2017;45:486–552.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49:e1063–143.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med [Internet]. 2001;345:1368–77. https://doi.org/10.1056/NEJMoa010307 .
Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management. Anesthesiology. 2017;126:547–60.
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 Surgery). Diabetes Care. 2011;34:256–61.
Jehan F, Joseph B. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of HbA1c? J Trauma Acute Care Surg. 2019;86:379–379.
Yatabe T, Inoue S, Sakaguchi M, Egi M. The optimal target for acute glycemic control in critically ill patients: a network meta-analysis. Intensive Care Med. 2017;43:16–28.
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg [Internet]. 2019;43:659–95.
Koivuranta M, Läärä E, Snåre L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia [Internet]. 1997;52:443–9.
Horn CC, Wallisch WJ, Homanics GE, Williams JP. Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting. Eur J Pharmacol [Internet]. 2014;722:55–66.
Veiga-Gil L, Pueyo J, López-Olaondo L. Postoperative nausea and vomiting: physiopathology, risk factors, prophylaxis and treatment. Rev Esp Anestesiol Reanim [Internet]. 2017;64:223–32.
Cozza V, Barberis L, Altieri G, Donatelli M, Sganga G, Greca A la. Prediction of postoperative nausea and vomiting by point-of-care gastric ultrasound: can we improve complications and length of stay in emergency surgery? A cohort study. 2021. https://doi.org/10.1186/s12871-021-01428-0 .
de Oliveira GS, Castro-Alves LJS, Ahmad S, Kendall MC, McCarthy RJ. Dexamethasone to prevent postoperative nausea and vomiting: an updated meta-analysis of randomized controlled trials. Anesth Analg [Internet]. 2013;116:58–74.
Eberhart LHJ, Mauch M, Morin AM, Wulf H, Geldner G. Impact of a multimodal anti-emetic prophylaxis on patient satisfaction in high-risk patients for postoperative nausea and vomiting. Anaesthesia [Internet]. 2002;57:1022–7.
Apfel CC, Bacher A, Biedler A, Danner K, Danzeisen O, Eberhart LHJ, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. Anaesthesist [Internet]. 2005;54:201–9.
Polderman JA, Farhang-Razi V, van Dieren S, Kranke P, DeVries JH, Hollmann MW, et al. Adverse side effects of dexamethasone in surgical patients. Cochrane Database Syst Rev [Internet] 2018;11.
Doleman B, Leonardi-Bee J, Heinink TP, Boyd-Carson H, Carrick L, Mandalia R, et al. Pre-emptive and preventive NSAIDs for postoperative pain in adults undergoing all types of surgery. Cochrane Database Syst Rev [Internet] 2021;6.
Apfel CC, Turan A, Souza K, Pergolizzi J, Hornuss C. Intravenous acetaminophen reduces postoperative nausea and vomiting: a systematic review and meta-analysis. Pain [Internet]. 2013;154:677–89.
Miller D, Lewis SR, Pritchard MW, Schofield-Robinson OJ, Shelton CL, Alderson P, et al. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst Rev [Internet] 2018;8.
Saljuqi AT, Hanna K, Asmar S, Tang A, Zeeshan M, Gries L, et al. Prospective evaluation of delirium in geriatric patients undergoing emergency general surgery. J Am Coll Surg [Internet]. 2020;230:758–65.
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, et al. Long-term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. Lancet [Internet]. 1998;351:857–61.
Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing [Internet]. 2011;40:23–9.
Duprey MS, Devlin JW, Griffith JL, Travison TG, Briesacher BA, Jones R, et al. Association between perioperative medication use and postoperative delirium and cognition in older adults undergoing elective noncardiac surgery. Anesth Analg [Internet]. 2022;134:1154–63.
McLott J, Stahel PF. Opioid-free anesthesia: the next frontier in surgical patient safety. Patient Saf Surg. BioMed Central Ltd; 2022.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg [Internet]. 2017;152:691–7.
Chan MTV, Cheng BCP, Lee TMC, Gin T. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol [Internet]. 2013;25:33–42.
Zorrilla-Vaca A, Healy RJ, Wu CL, Grant MC. Relation between bispectral index measurements of anesthetic depth and postoperative mortality: a meta-analysis of observational studies. Can J Anaesth [Internet]. 2017;64:597–607.
Evered LA, Chan MTV, Han R, Chu MHM, Cheng BP, Scott DA, et al. Anaesthetic depth and delirium after major surgery: a randomised clinical trial. Br J Anaesth [Internet]. 2021;127:704–12.
Short TG, Campbell D, Frampton C, Chan MTV, Myles PS, Corcoran TB, et al. Anaesthetic depth and complications after major surgery: an international, randomised controlled trial. Lancet [Internet]. 2019;394:1907–14.
Berg H, Viby-Mogensen J, Roed J, Mortensen CR, Engbæk J, Skovgaard LT, et al. Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand [Internet]. 1997;41:1095–103.
Naguib M, Kopman AF, Ensor JE. Neuromuscular monitoring and postoperative residual curarisation: a meta-analysis. Br J Anaesth [Internet]. 2007;98:302–16.
Carvalho H, Verdonck M, Cools W, Geerts L, Forget P, Poelaert J. Forty years of neuromuscular monitoring and postoperative residual curarisation: a meta-analysis and evaluation of confidence in network meta-analysis. Br J Anaesth [Internet]. 2020;125:466–82.
Carli F, Kehlet H, Baldini G, Steel A, McRae K, Slinger P, et al. Evidence basis for regional anesthesia in multidisciplinary fast-track surgical care pathways. Reg Anesth Pain Med [Internet]. 2011;36:63–72.
Li YW, Li HJ, Li HJ, Zhao BJ, Guo XY, Feng Y, et al. Delirium in older patients after combined epidural-general anesthesia or general anesthesia for major surgery: a randomized trial. Anesthesiology [Internet]. 2021;135:218–32.
Werawatganon T, Charuluxananan S. Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev [Internet]. 2013. https://doi.org/10.1002/14651858.CD004088.pub3/full .
Vester-Andersen M, Lundstrøm LH, Møller MH. The association between epidural analgesia and mortality in emergency abdominal surgery: a population-based cohort study. Acta Anaesthesiol Scand [Internet]. 2020;64:104–11.
Hübner M, Blanc C, Roulin D, Winiker M, Gander S, Demartines N. Randomized clinical trial on epidural versus patient-controlled analgesia for laparoscopic colorectal surgery within an enhanced recovery pathway. Ann Surg [Internet]. 2015;261:648–53.
Tsuchiya M, Takahashi R, Furukawa A, Suehiro K, Mizutani K, Nishikawa K. Transversus abdominis plane block in combination with general anesthesia provides better intraoperative hemodynamic control and quicker recovery than general anesthesia alone in high-risk abdominal surgery patients. Minerva Anestesiol [Internet]. 2012;78:1241–7.
McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg [Internet]. 2007;104:193–7.
Walter CJ, Maxwell-Armstrong C, Pinkney TD, Conaghan PJ, Bedforth N, Gornall CB, et al. A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc [Internet]. 2013;27:2366–72.
Tikuisis R, Miliauskas P, Lukoseviciene V, Samalavicius N, Dulskas A, Zabuliene L, et al. Transversus abdominis plane block for postoperative pain relief after hand-assisted laparoscopic colon surgery: a randomized, placebo-controlled clinical trial. Tech Coloproctol [Internet]. 2016;20:835–44.
Hamid HK, Emile SH, Saber AA, Ruiz-Tovar J, Minas V, Cataldo TE. Laparoscopic-guided transversus abdominis plane block for postoperative pain management in minimally invasive surgery: systematic review and meta-analysis. J Am Coll Surg [Internet]. 2020;231:376-386.e15.
Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery [Internet]. 2014;156:1245–52.
Braga M, Scatizzi M, Borghi F, Missana G, Radrizzani D, Gemma M, et al. Identification of core items in the enhanced recovery pathway. Clin Nutr ESPEN. 2018;25:139–44.
Balki I, Khan JS, Staibano P, Duceppe E, Bessissow A, Sloan EN, et al. Effect of perioperative active body surface warming systems on analgesic and clinical outcomes: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2020;131:1430–43.
Bellamy MC. Wet, dry or something else? Br J Anaesth [Internet]. 2006;97:755–7.
Shin CH, Long DR, McLean D, Grabitz SD, Ladha K, Timm FP, et al. Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg [Internet]. 2018;267:1084–92.
Thacker JKM, Mountford WK, Ernst FR, Krukas MR, Mythen MG. Perioperative fluid utilization variability and association with outcomes: considerations for enhanced recovery efforts in sample US surgical populations. Ann Surg [Internet]. 2016;263:502–10.
Lowell JA, Schifferdecker C, Driscoll DF, Benotti PN, Bistrian BR. Postoperative fluid overload: not a benign problem. Crit Care Med [Internet]. 1990;18:728–33.
Nisanevich V. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology [Internet]. 2005;103:25–32.
Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. Br J Anaesth [Internet]. 2002;89:622–32.
Brandstrup B. Fluid therapy for the surgical patient. Best Pract Res Clin Anaesthesiol [Internet]. 2006;20:265–83.
Bundgaard-Nielsen M, Holte K, Secher NH, Kehlet H. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand [Internet]. 2007;51:331–40.
Jessen MK, Vallentin MF, Holmberg MJ, Bolther M, Hansen FB, Holst JM, et al. Goal-directed haemodynamic therapy during general anaesthesia for noncardiac surgery: a systematic review and meta-analysis. Br J Anaesth. 2022;128:416–33.
Mamidanna R, Burns EM, Bottle A, Aylin P, Stonell C, Hanna GB, et al. Reduced risk of medical morbidity and mortality in patients selected for laparoscopic colorectal resection in England: a population-based study. Arch Surg [Internet]. 2012;147:219–27.
Kehlet H. Surgical stress response: does endoscopic surgery confer an advantage? World J Surg [Internet]. 1999;23:801–7.
Novitsky YW, Litwin DEM, Callery MP. The net immunologic advantage of laparoscopic surgery. Surg Endosc [Internet]. 2004;18:1411–9.
Braga M, Borghi F, Scatizzi M, Missana G, Guicciardi MA, Bona S, et al. Impact of laparoscopy on adherence to an enhanced recovery pathway and readiness for discharge in elective colorectal surgery: results from the PeriOperative Italian Society registry. Surg Endosc [Internet]. 2017;31:4393–9. https://doi.org/10.1007/s00464-017-5486-0 .
Pucher PH, Mackenzie H, Tucker V, Mercer SJ. A national propensity score-matched analysis of emergency laparoscopic versus open abdominal surgery. Br J Surg [Internet]. 2021;108:934–40.
Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, Jiang Y, et al. Laparoscopic versus open repair for perforated peptic ulcer: a meta analysis of randomized controlled trials. Int J Surg. 2016;33:124–32.
Warps A-LK, Zwanenburg ES, Dekker JWT, Tollenaar RAEM, Bemelman WA, Hompes R, et al. Laparoscopic versus open colorectal surgery in the emergency setting. Ann Surg Open. 2021;2:e097.
PubMed PubMed Central Google Scholar
Arnold M, Elhage S, Schiffern L, Lauren Paton B, Ross SW, Matthews BD, et al. Use of minimally invasive surgery in emergency general surgery procedures. Surg Endosc [Internet]. 2020;34:2258–65. https://doi.org/10.1007/s00464-019-07016-1 .
Ceresoli M, Pisano M, Abu-Zidan F, Allievi N, Gurusamy K, Biffl WL, et al. Minimally invasive surgery in emergency surgery: a WSES survey. World J Emerg Surg. 2022;17:18.
Zhang HY, Zhao CL, Xie J, Ye YW, Sun JF, Ding ZH, et al. To drain or not to drain in colorectal anastomosis: a meta-analysis. Int J Colorectal Dis [Internet]. 2016;31:951–60.
Chen JS, da Sun S, Wang ZS, Cai TH, Huang LK, Sun WX, et al. The factors related to failure of Enhanced Recovery after Surgery (ERAS) in colon cancer surgery. Langenbecks Arch Surg [Internet]. 2020;405:1025–30.
Coccolini F, Corradi F, Sartelli M, Coimbra R, Kryvoruchko IA, Leppaniemi A, et al. Postoperative pain management in non-traumatic emergency general surgery: WSES-GAIS-SIAARTI-AAST guidelines. World J Emerg Surg [Internet]. 2022;17:1–15.
Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev [Internet]. 2007;10:50. https://doi.org/10.1002/14651858.CD004929.pub3/full .
Article Google Scholar
Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer. Medicine [Internet]. 2018;97:e12348.
Brower RG. Consequences of bed rest. Crit Care Med. 2009;37:S422–8.
Wren SM, Martin M, Yoon JK, Bech F. Postoperative pneumonia-prevention program for the inpatient surgical ward. J Am Coll Surg. 2010;210:491–5.
Haines KJ, Skinner EH, Berney S. Association of postoperative pulmonary complications with delayed mobilisation following major abdominal surgery: an observational cohort study. Physiotherapy. 2013;99:119–25.
Castelino T, Fiore JF, Niculiseanu P, Landry T, Augustin B, Feldman LS. The effect of early mobilization protocols on postoperative outcomes following abdominal and thoracic surgery: a systematic review. Surgery. 2016;159:991–1003.
Rosowicz A, Brody JS, Lazar DJ, Bangla VG, Panahi A, Nobel TB, et al. Early ambulation is associated with improved outcomes following colorectal surgery. Am Surg. 2022. https://doi.org/10.1177/00031348221142 .
Gillis C, Carli F. Promoting perioperative metabolic and nutritional care. Anesthesiology. 2015;123:1455–72.
Zhuang C-L, Ye X-Z, Zhang C-J, Dong Q-T, Chen B-C, Yu Z. Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg. 2013;30:225–32.
Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev. 2006.
Gonenc M, Gemici E, Kalayci MU, Karabulut M, Turhan AN, Alis H. Intracorporeal knotting versus metal endoclip application for the closure of the appendiceal stump during laparoscopic appendectomy in uncomplicated appendicitis. J Laparoendosc Adv Surg Tech. 2011;22:231–5.
Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med [Internet]. 2015;372:1996–2005.
Sartelli M, Catena F, Ansaloni L, Coccolini F, di Saverio S, Griffiths EA. Duration of antimicrobial therapy in treating complicated intra-abdominal infections: a comprehensive review. Surg Infect. 2016;17:9–12. https://doi.org/10.1089/sur.2015.130 .
Sartelli M, Coccolini F, Kluger Y, Agastra E, Abu-Zidan FM, Abbas AES, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emerg Surg. 2021;16:1–48. https://doi.org/10.1186/s13017-021-00387-8 .
Download references
No fundings were received for this paper.

Author information
Authors and affiliations.
School of Medicine and Surgery, Milano-Bicocca University, Monza, Italy
Marco Ceresoli, Marco Braga, Thomas Langer, Giuseppe Foti & Michele Fogliata
General and Emergency Surgery Department, Fondazione IRCCS San Gerardo dei Tintori, Via Pergolesi 33, 20900, Monza, Italy
Marco Ceresoli, Marco Braga & Michele Fogliata
General Surgery Department, Bufalini Hospital, Cesena, Italy
Nicola Zanini & Fausto Catena
The Research Office, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, UAE
Fikri M. Abu-Zidan
General Surgery Department - Santa Maria Della Misericordia Hospital, Rovigo, Italy
Dario Parini
Department of Anesthesia and Critical Care, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy
Thomas Langer
General Surgery, Macerata Hospital, Macerata, Italy
Massimo Sartelli
Department of General Surgery, Royal Infirmary of Edinburgh, Edinburgh, UK
Dimitrios Damaskos
Scripps Memorial Hospital La Jolla, La Jolla, CA, USA
Walter L. Biffl
John Hunter Hospital Trauma Service and School of Medicine and Public Health, The University of Newcastle, Newcastle, AU, Australia
Francesco Amico
General Surgery, Fondazione IRCCS San Matteo, Pavia, Italy
Luca Ansaloni, Enrico Cicuttin & Paola Fugazzola
Department of Traumatology, John Hunter Hospital and University of Newcastle, Hunter Medical Research Institute, Newcastle, NSW, Australia
Zsolt J. Balogh
Division of General and Foregut Surgery, Department of Biomedical Sciences for Health, IRCCS Policlinico San Donato, University of Milan, Milan, Italy
Luigi Bonavina
University of Auckland, Auckland, New Zealand
Department of Digestive Surgery, CHU Grenoble Alpes, Grenoble, France
Mircea Chirica
Department of Surgery, Tianjin Nankai Hospital, Nankai Clinical School of Medicine, Tianjin Medical University, Tianjin, China
Yunfeng Cui
Unit of Emergency and Trauma Surgery, Villeneuve St Georges Academic Hospital, Villeneuve St Georges, France
Belinda De Simone
Department of Surgical Sciences and Advanced Technologies, General Surgery Cannizzaro Hospital, University of Catania, Catania, Italy
Isidoro Di Carlo
PS_SS Weissach im Tal, Weissach im Tal, Germany
Andreas Fette
Department of Critical Care and Anesthesia, Fondazione IRCCS San Gerardo Dei Tintori, Monza, Italy
Giuseppe Foti
Division of Trauma Surgery, School of Medical Sciences (FCM), University of Campinas (Unicamp), Campinas, Brazil
Gustavo P. Fraga
University of California, Davis, Sacramento, CA, USA
Joseph M. Galante
University of Otago, Dunebin, New Zealand
Solomon Gurmu Beka
Department of General and Thoracic Surgery, University Hospital of Giessen, Gießen, Germany
Andreas Hecker
Erasmus MC University, Rotterdam, The Netherlands
Johannes Jeekel
General, Acute Care, Abdominal Wall Reconstruction, and Trauma Surgery, Foothills Medical Centre, Calgary, AB, Canada
Andrew W. Kirkpatrick
Department of Primary Care and Emergency Medicine, Kyoto University Graduate School of Medicine, Kyoto, Japan
Kaoru Koike
Helsinki University Hospital and University of Helsinki, Helsinki, Finland
Ari Leppäniemi
Andrei Litvin, CEO AI Medica Hospital Center, Kaliningrad, Russia
Department of Trauma, Hand, and Reconstructive Surgery, Goethe University, Frankfurt University Hospital, Frankfurt am Main, Germany
Director of Surgery Research, Ernest E. Moore Shock Trauma Center, Distinguished Professor of Surgery, University of Colorado, Denver, CO, USA
Ernest E. Moore
Department of Anesthesia and Intensive Care, Parma University Hospital, Parma, Italy
Edoardo Picetti
Third Department of Surgery, Attikon University Hospital, Athene, Greece
Emmanouil Pikoulis
General Surgery, ASST Papa Giovanni XXIII, Bergamo, Italy
Michele Pisano
Department of Surgical Science, University of Cagliari, Cagliari, Italy
Mauro Podda
RIMU Plovdiv/UMHAT St George Plovdiv, Plovdiv, Bulgaria
Boris E. Sakakushev
Department of General Surgery, Tan Tock Seng Hospital, Singapore, Singapore
Vishal G. Shelat
Department of Surgery, Brody School of Medicine, East Carolina University, Greenville, NC, USA
Former Chair Department of Emergency Medicine, HEMS Physician, Radboud University Medical Center, Nijmegen, The Netherlands
Digestive and Emergency Surgery Department, Azienda Ospedaliera S.Maria, Terni, Italy
Giovanni D. Tebala
Harvard Medical School - Massachusetts General Hospital, Boston, USA
George Velmahos
Department of General Surgery, Royal Perth Hospital, Head of Service and Director of Trauma, Royal Perth Hospital, The University of Western Australia, Perth, Australia
Dieter G. Weber
Anesthesia and Critical Care Department, Bufalini Hospital, Cesena, Italy
Vanni Agnoletti
Department of General Surgery, The Rambam Academic Hospital, Haifa, Israel
Yoram Kluger
General Surgery, University of Brescia, ASST Cremona, Cremona, Italy
Gianluca Baiocchi
Emergency Surgery, University of Pisa, Pisa, Italy
Federico Coccolini
You can also search for this author in PubMed Google Scholar
Contributions
All the authors contributed to the conception, writing, discussion and approval of the present manuscript.
Corresponding author
Correspondence to Marco Ceresoli .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not required for this review and position paper.
Competing interests
All the authors have no conflict of interest to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ceresoli, M., Braga, M., Zanini, N. et al. Enhanced perioperative care in emergency general surgery: the WSES position paper. World J Emerg Surg 18 , 47 (2023). https://doi.org/10.1186/s13017-023-00519-2
Download citation
Received : 13 September 2023
Accepted : 30 September 2023
Published : 06 October 2023
DOI : https://doi.org/10.1186/s13017-023-00519-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
World Journal of Emergency Surgery
ISSN: 1749-7922
- Submission enquiries: [email protected]
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

Landmark Papers in General Surgery
- Cite Icon Cite
- Permissions Icon Permissions
Critiquing key papers in the field, Landmark Papers in General Surgery gives surgeons and trainees an expert appraisal and contextual discussion of the evidence base behind current clinical practice.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Quick Links
Tools & Resources
- Events Calendar
- Strauss Health Sciences Library
- Department A-Z Directory
- Campus Directory
- Faculty & Staff Resources
- Supporter & Alumni Resources
- Student Resources
- Mental Health Resources
- University Policies
CU Campuses
Cu anschutz medical campus.
- CU Colorado Springs
- School of Dental Medicine
- Graduate School
- School of Medicine
- College of Nursing
- Skaggs School of Pharmacy and Pharmaceutical Sciences
- Colorado School of Public Health
Department of Surgery
Resident presentations.
Our Residents regularly present at national and international meetings, as well as participating in our on-campus research symposium each May. See below for some of their recent activities.
2023 AAS Academic Surgical Conference (Houston, TX)
Presentation lists from recent conferences.
- pdf 2023 AAS Academic Surgical Congress Presentations (pdf) Download 2023 AAS Academic Surgical Congress Presentations (134 KB)
- pdf 2022 ACS Clinical Congress Presentations (pdf) Download 2022 ACS Clinical Congress Presentations (534 KB)
- pdf 2020 ACS Virtual Clinical Congress Presentations (pdf) Download 2020 ACS Virtual Clinical Congress Presentations (110 KB)
- pdf 2019 ACS Clinical Congress Presentations (Residents Only) (pdf) Download 2019 ACS Clinical Congress Presentations (Residents Only) (135 KB)
- pdf 2018 ACS Clinical Congress Presentations (Residents Only) (pdf) Download 2018 ACS Clinical Congress Presentations (Residents Only) (106 KB)
2020-2021 Presentations
Adam dyas (research year 2).
.jpg?sfvrsn=c481c2ba_2)
- Dyas A.R., Rozeboom P.D., Bronsert M.R., et al. Accurate Preoperative Prediction of Need for Postoperative Intensive Care. Academic Surgical Congress 16 th Annual Conference. Virtual, 2/2021.
- Dyas A.R. Implementation of an Evidence-Based Thoracic Enhanced Recovery After Surgery Protocol in a Diverse, Multi-Hospital Health System. 15 th Annual Pomerantz Visiting Professor Lectureship, Resident Research Presentations. Virtual, 3/2021.
- Dyas A.R. Implementation of an Evidence-Based Thoracic Enhanced Recovery After Surgery Protocol in a Diverse, Multi-Hospital Health System. University of Colorado Quality Outcomes Committee Meeting. Virtual, 4/2021.
- Dyas A.R., Bronsert M.R., Meguid R.A., et. al. Using the Surgical Risk Preoperative Assessment System to Define the “High Risk” Surgical Patient. University of Colorado 8 th Annual Department of Surgery Research Symposium. Aurora, CO, 5/2021.
Alex Suarez-Pierre (PGY-3)
.jpg?sfvrsn=cc81c2ba_2)
Suarez-Pierre A , Halpern AL, Valero V III, Gergen AK, Vigneshwar NG, Bartley M, Ghincea C, Mitchell JD, Fullerton DA, Weyant MJ, Meguid RA, Scott C. Survival Following Lung Transplantation: A Population-based Nested Case Control Study. EACTS 34th Annual Meeting 2020. Barcelona, Spain.
Anna Gergen (PGY-3)
.jpg?sfvrsn=bf81c2ba_2)
- Secretory Phospholipase A2 Inhibition Downregulates Intercellular Adhesion Molecule-1 in Human Esophageal Barrett’s Cells. Oral presentation at: American College of Surgeons Clinical Congress. 2020 Oct 4-8; Virtual.
- Impact of Introduction of Robotic Surgery on a Cardiothoracic Fellowship Program. Oral presentation at: Southern Thoracic surgical Association. 2020 Nov 4-7; Orlando, FL. Cancelled due to COVID-19.
- Expression of Adhesion Molecules in a Surgical Gastroduodenal Reflux Model. Oral presentation at: Society of Thoracic Surgeons. 2021 Jan 29-31; Virtual.
- An Assessment of Discharge Analgesic Prescription Patterns for Hospitalized Patients with Rib Fractures. Oral presentation at: Chest Wall Injury Summit. 2021 Apr 22-24; Denver, CO.
- Toll-like Receptor 4 Mediates Reflux-induced Inflammatory Responses in a Murine Reflux Model. Oral presentation at: American Association for Thoracic Surgery. 2021 Apr 30-May 2; Virtual.
- Expression of Adhesion Molecules in a Gastroduodenal Reflux Murine Model. Oral presentation at: 8 th Annual University of Colorado Department of Surgery Research Symposium. 2021 May 24; Aurora, CO.
- Efficacy of Combined Hiatal Hernia Repair and Transoral Fundoplication for Large Paraesophageal Hernias. Poster presentation at: Society of American Gastrointestinal and Endoscopic Surgeons. 2021 Aug 31-Sept 3; Las Vegas, NV.
- Novel Robotic Transabdominal Preperitoneal Reversed Falciform Ligament Flap for Repair of Recurrent Incisional Hernias. Poster presentation at: Society of American Gastrointestinal and Endoscopic Surgeons. 2021 Aug 31-Sept 3; Las Vegas, NV.
- Robotic-Assisted Giant Epiphrenic Esophageal Diverticulectomy with Myotomy. “Video Loop” presentation at: Society of American Gastrointestinal and Endoscopic Surgeons. 2021 Aug 31-Sept 3; Las Vegas, NV.
- Is Early Administration of Parenteral Nutrition Safe in Elderly Emergency General Surgery Patients? Poster presentation at: American College of Surgeons Clinical Congress. 2021 Oct 24-28; Virtual.
- Simvastatin Inhibits Histologic Changes Associated with Gastroduodenal Reflux in a Murine Model. Oral presentation at: Southern Thoracic Surgical Association. 2021 Nov 3-6. Atlanta, GA.
Tori Huynh (PGY-3)
.jpg?sfvrsn=d081c2ba_2)
- Huynh V , Ludwigson A, Romandetti K, Ahrendt G, Afghahi A, Tevis S. Characterizing informational needs in breast cancer patients. Oral presentation at the American College of Surgeons Clinical Congress, October 2021.
- Huang J, Huynh V , Ahrendt G, Afghahi A, Sams S, Tevis S. A call to re-evaluate receptor statuses for breast cancer patients after neoadjuvant chemotherapy. Oral presentation at the American College of Surgeons Clinical Congress, October 2021.
- Leonard L, Shaw M, Cunniff K, Huynh V , Yi J, Patton C, Weitzel N, Ballou M, Cumbler E, Tevis S. Pointing fingers over the drape: Perceptions of operating room delays differ by provider type. Poster presentation at the American College of Surgeons Clinical Congress, October 2021.
- Huynh V , Leonard L, Kaoutzanis C, Ahrendt G, Cumbler E, Tamm-Daniels I, Tevis S. First start operative delays in breast surgery: What are the contributing factors? Oral presentation at the Southwest Surgical Congress, September 2021; Maui, HI.
- Leonard L, Himelhoch B, Huynh V , Wolverton D, Ahrendt G, Jaiswal K, Sams S, Cumbler E, Schulick R, Tevis S. Patient and provider perceptions of the immediate release of electronic health information. Oral presentation at the Southwest Surgical Congress, September 2021; Maui, HI.
- Huynh V , Fasano M, Hampanda K, Rojas K, Pettigrew J, Coons H, Afghahi A, Tevis S. When to bring up sexual health during breast cancer treatment? Early and often. Poster presentation at the Virtual Scientific Session of the Scientific Network on Female Sexual Health and Cancer, April 2021.
- Huynh V , Christian N, Tuthill K, Colborn K, Tevis S. Development of a surgical research program for medical students and its short-term impact on academic productivity. Oral presentation at the Association of Program Directors in Surgery Annual Meeting, April 2021; Boston, MA.
- Huynh V , Tevis S, Cumbler E, Nehler M, Christian N. Sustainability of lecture-based educational interventions in improving surgical resident opioid prescribing. Poster presentation at the Association for Surgical Education Annual Meeting, April 2021.
- Huynh V , Colborn K, Bonnell L, Ahrendt G, Christian N, Kim S, Kukreja J, Borges V, Tevis S. Longitudinal trajectories of patient reported outcomes in breast cancer patients undergoing lumpectomy versus mastectomy. Poster presentation at the American Society of Breast Surgeons Annual Meeting, April 2021; Orlando, FL.
- Yang J, Huynh V , Bronsert M, Ludwigson A, Ahrendt G, Hampanda K, Tevis S. Choosing between mastectomy and breast conserving therapy: Is patient distress an influencing factor? Poster presentation at the American Society of Breast Surgeons Annual Meeting, April 2021; Orlando, FL.
- Ludwigson A, Huynh V , Myers S, Hampanda K, Borges V, Romandetti K, Tevis S. Patient perception of changes in breast cancer care during the COVID-19 pandemic. Poster presentation at the American Society of Breast Surgeons Annual Meeting, April 2021; Orlando, FL.
- Paton M, Huynh V , Bronsert M, Ahrendt G, Sams S, McLemore L, Berning A, Wolverton D, Tevis S. Margin re-excision and complication rates in patients undergoing breast conserving surgery using shave margin protocol following neoadjuvant chemotherapy. Poster presentation at the American Society of Breast Surgeons Annual Meeting, April 2021; Orlando, FL.
- Kalluri R, Huynh V , Carter T, Wolverton D, Tevis S, Ahrendt G. Second opinion review of outside breast imaging: an analysis of the frequency that additional testing is recommended and radiology/pathology outcomes. Poster presentation at the American Society of Breast Surgeons Annual Meeting, April 2021; Orlando, FL.
- Leonard L, Cuniff K, Shaw M, Huynh V , Yi J, Cumbler E, Tevis S. Staff perceptions of operating room delays. Poster presentation at the Virtual Perioperative Medicine Summit, March 2021.
- Su M, Huynh V , Su E, Goode J, Lock A, Banden S, Ahrendt G, Afghahi A, Arruda J, Tevis S. Patterns of care in patients with increased breast cancer risk. Oral presentation at the Academic Surgical Congress, Feb 2021.
- Vossler K, Huynh V , Ahrendt G, Arruda J, Kaoutzanis C, Tevis S. Postoperative complications in coordinated versus staged breast and gynecologic surgeries. Oral presentation at the Academic Surgical Congress, Feb 2021.
- Neilson T, Huynh V , MacDonald A, Romandetti K, Ahrendt G, Tevis S. Bills, bills, bills: A characterization of financial burden in breast cancer care and strategies used to address it. Oral presentation at the Academic Surgical Congress, Feb 2021.
- Huynh V , Colborn K, Rojas K, Christian N, Ahrendt G, Cumbler E, Schulick R, Tevis S. An evaluation of opioid prescribing preferences in surgical residents and faculty at a large academic medical center. Oral presentation at the American College of Surgeons Clinical Congress, October 2020.
- Yang J, Kovar A, Huynh V , Bronsert M, Ahrendt G, Christian N, Murphy C, Jaiswal K, Wolverton D, Tevis S. Delays in breast cancer diagnoses: Do patients have higher distress? Poster presentation at the American College of Surgeons Clinical Congress, October 2020.
- Huynh V , Parris H, Ahrendt G, Christian N, Jaiswal K, Murphy C, Borges V, Tevis S. Breast-Q: A launching point for discussion. Oral presentation for the Association of Women Surgeons Resident Research Madness 2020.
- Huynh V , Ahrendt G, Cumbler E, Tamm-Daniels, I, Tevis S. Preoperative blocks: Do they delay operative start times? Oral presentation at the American College of Surgeons Quality and Safety Virtual Conference, August 2020.
- Huynh V , Ahrendt G, Cumbler E, Kaoutzanis C, Cohen J, Tevis S. Improving consistency in patient messaging following breast surgery at a large academic medical center. Oral presentation at the American College of Surgeons Quality and Safety Virtual Conference, August 2020.
Janet Lee (Research Year 2)
.jpg?sfvrsn=c081c2ba_2)
- Lee J , Khan A, Dolac C, Dunn J, McIntyre R, Wright F, Platnick B, Brockman V, Vega S, Cofran J, Duero C, Schroeppel T. Your voice matters: The impact of advance directives on elderly trauma patients. Western Trauma Association Annual Meeting, March 2021; Virtual.
- Lee J, Khan A, Wright F, McIntyre R, Dorlac W, Cribari C, Schroeppel T. Is the whole better than the sum of the individual components? A multi-center analysis of whole blood use in trauma patients. Southeastern Surgical Congress Annual Meeting, August 2021; Atlanta, GA***
- Lee J, Khan A, Cribari C, Dorlac W, McIntyre R, Wright F, Schroeppel T. Is the century mark the new gold standard? The impact of the systolic blood pressure activation criteria on the need for trauma intervention in elderly trauma. Southwestern Surgical Congress Annual Meeting, September 2021; Maui, HI.***
- Lee J, Finch H, Higa K, Khan A, Brockman V, Schroeppel T. STRAUMA Alert: a novel alert system for a combined stroke and trauma. American College of Surgeons Clinical Congress, October, 2021; Virtual.***
Jason Samuels (PGY-5)
- Jason M Samuels MD , Ernest E Moore MD, Julia R Coleman MD MPH, Matt Bartley MD MS, Navin Vigneshwar MD, Anirban Banerjee PhD, Christopher C Silliman MD PhD, Angela Sauaia MD PhD. Obesity Is Independently Associated with Postinjury Fibrinolysis Shutdown. 20th European Congress of Trauma & Emergency Surgery, Prague, Czechia *2 nd place, Best oral presentation
- Samuels JM, Ernest E Moore MD, Julia R Coleman MD MPH, Anirban Banerjee PhD, Christopher C Silliman MD PhD, Arsen Ghasabyan, James Chandler, Angela Sauaia MD PhD. American College of Surgeon Clinical Congress, San Francisco CA, October 2020.
- Samuels JM , Carmichael H, Kovar A, Urban S, Vega S, Velopulos C, McIntyre RC, Jr. Reevaluation of Hepatic Angioembolization for Trauma in Stable Patients: Weighing the Risk. 127 th Western Surgical Association Annual Meeting, Las Vegas, NV.
Allie Kovar (PGY-4)
.jpg?sfvrsn=d881c2ba_2)
- Lane M, Kirsch M, Sluiter E, Hamill J, Kuzon W, Cederna P, Gilman R, Wilkins E. Impact of Gender-Affirming Mastectomy on Depression, Anxiety, and Body Image in Transmen. EPATH 2021. August 2021.
- Kirsch M, Wixon M, Kim G, Hughes D. Determining High Yield Content for a Residency Preparation Course. American College of Surgeons Clinical Congress 2020. October 2020.
- Robinson TN, Kovar A, Carmichael H, Overbey DM, Goode CM, Jones TS. Postoperative Delirium is Associated with Decreased Recovery of Ambulation One-Month after Surgery. American College of Surgeons Clinical Congress. October 2020; Virtual Forum.
- Kovar A, Horney C, Franklin J, Finley J, Robinson T, Jones E, Moore JT, Jones TS. The Aging Veterans Surgical Wellness Program Improves the Care and Outcomes for Geriatric Patients at the Rocky Mountain Regional VA Medical Center. American College of Surgeons Clinical Congress. October 2020; Virtual Forum.
Media/Press Related to Scholarship
- American College of Surgeons 2019 Daily Highlight — The waiting game: How long are breast cancer patients waiting for definitive diagnosis and treatment? https://www.facs.org/clincon2019/resources/highlights/wed/videos1#breast
- American College of Surgeons 2020- Program to improve outcomes for geriatric surgery patients shows promise in a hospital setting. https://www.facs.org/media/press-releases/2020/kovar-robinson100320
Laura Leonard (Research Year 2)
Invited presentations.
- Leonard LD , Billings J, Marks J, Cumbler E. Event Reporting and Adverse Event Analysis. Invited Grand Rounds. Department of Surgery, Division of Urology. (2021). Aurora, CO.
National Presentations
- Leonard LD , Shaw M, Cunniff K, Huynh V, Yi J, Patton C, Weitzel N, Ballou M, Cumbler E, Tevis SE. Pointing Fingers Over The Drape: Perceptions Of Operating Room Delays Differ By Provider Type. American College of Surgeons Clinical Congress (2021). Virtual.
- Leonard LD , Shaw M, Tevis S, Schulick R, Ballou M, Reiter K, Wiler J, Meacham R, Cumbler E, Steward L. Barriers to the Completion of a Multidisciplinary Surgical Debrief. American College of Surgeons Clinical Congress (2021). Virtual.
- Burges B, Leonard LD , Tevis S, Billings J, Kovar A, Kim S and Cumbler E. Surgeon Perceptions of Integrating Patient Reported Outcome Measures (PROMs) into Clinical Practice . American College of Surgeons Clinical Congress (2021). Virtual.
- Leonard LD , Himelhoch B, Huynh V, Wolverton D, Ahrendt G, Jaiswal K, Sams S, Cumbler E, Schulick R, Tevis SE. Patient and Provider Perceptions of the Immediate Release of Electronic Health Information. Southwest Surgical Congress Annual Meeting (2021). Maui, HI
- Leonard LD , Torphy R, Beaty L, de Araujo TB, Colborn K, Ho F, Albuquerque A, Lewis K, Gonzalez R, Medina T, Robinson W, McCarter M, Stewart C, Gleisner A. Unmeasured Contextual Effects are the Major Drivers Associated with De-implementation of CLND for Melanoma. Southwest Surgical Congress Annual Meeting (2021). Maui, HI
- Tilva K, Leonard LD , McIntyre R, Nehler M, Christian N. An Evaluation of the Effect of Virtual Learning on Educational Conference Attendance. Southwest Surgical Congress Annual Meeting (2021). Maui, HI
- Huynh V, Leonard LD , Kaoutzanis C, Ahrendt G, Cumbler E, Tamm-Daniels I, Tevis SE. Contributors to Operative Delay in Breast Surgery at a Single Academic Institution. Southwest Surgical Congress Annual Meeting (2021). Maui, HI
- Leonard LD , Torphy R, Beaty L, de Araujo TB, Colborn K, Ho F, Albuquerque A, Lewis K, Gonzalez R, Medina T, McCarter M, Stewart C, Gleisner A. Facility contextual effects influence the use of adjuvant immunotherapy in stage III melanoma . American Society of Clinical Oncology Annual Meeting; (2021).
- Barrett JR, Leonard LD , Kovar A, McCarthy DP, Harms B, Tevis S. Medically Smart, Fiscally Illiterate: Lack of Financial Education Leads to Poor Retirement Savings Strategies in Surgical Trainees . The Association for Surgical Education Annual Meeting; (2021). Virtual.
- Leonard LD , Cuniff K, Shaw M, Huynh V, Yi J, Cumbler E, Tevis SE. Staff Perceptions of Operating Room Delays. The 2021 Virtual PeriOperative Medicine Summit; (2021). Virtual.
- Leonard LD, Burges B, Tevis SE, Kovar A, Billings J, Kim S, Lin CT, Cumbler E. Surgeon Perceived Requirements for a Platform to Integrate Patient Reported Outcome Measures (PROMs) into Clinical Practice. Poster- American Medical Informatics Association (AMIA) Clinical Informatics Conference; (2021). Virtual.
Helen Madsen (Research Year 2)
- Madsen, H. , Carmichael, H., Gleisner, A., Del Chiaro, M., Schulick, R., Stewart, C. Cannabis Use and Post-Operative Complications in Patients Undergoing Pancreatic Resection. (2021). Oral Presentation at the Virtual Cannabis Research Conference.
- Madsen, H. , Carmichael, H., Gleisner, A., Del Chiaro, M., Schulick, R., Stewart, C. Cannabis Use and Post-Operative Complications in Patients Undergoing Pancreatic Resection. (2021). On-Demand Presentation at The Americas Hepato-Pancreato-Biliary Association Annual Meeting [Virtual meeting]
- Gergen, A., Madsen, H. , Li, A., Cheng, L., Meng, X., Fullerton, D., Pratap, A., Weyant, M. Simvastatin Inhibits Histologic Changes Associated with Gastroduodenal Reflux in a Murine Model. (2021). Oral Presentation at the Southern Thoracic Surgical Association Annual Meeting.
- Moyer, A., Smalley, B., Madsen, H. , Stewart, C., Johnson, J., Del Chiaro, M., Gleisner, A., Lieu, C., Tevis, S. Understanding Types and Sources of Information Sought Out by Patients with Cancer through a Prospective Cross-Sectional Patient Survey. (2021) Oral presentation at the American College of Surgeons Annual Meeting.
Poster Presentations
- Madsen, H. , Meguid, R., Bronsert, M., Dyas, A., Colborn, K., Lambert-Kerzner, A., Henderson, W. Associations between Preoperatively Predicted Postoperative Complications in American College of Surgeon’s National Surgical Quality Improvement Program (ACS-NSQIP) Patients. (2021). E-poster at the American College of Surgeons Annual Meeting [Virtual meeting]
- Dyas, A., Carmichael, H., Bronsert, M., Henderson, W., Madsen, H., Colborn, K., Velopulos, C., Meguid, R. Integrating a Measure of Social Vulnerability into a Parsimonious Surgical Risk Calculator Does Not Improve Model Performance. (2021). E-poster at the American College of Surgeons Annual Meeting [Virtual meeting]
Julia Coleman (PGY-5)
Research presentations and related awards.
- Coleman JR, et al. A mechanistic exploration of sex dimorphisms in coagulation: Calcium signaling drives female-specific hyperactivity. American College of Surgeons Committee on Trauma National Resident Paper Competition. November 18, 2020, virtual. * First Place in Basic Science Category in State Resident Paper Competition
- Coleman JR, et al. Whole blood thrombin generation is depressed in severely injured patients requiring massive transfusion. American College of Surgeons Committee on Trauma National Resident Paper Competition. October 1, 2020, virtual. * First Place in Basic Science Category in National Resident Paper Competition
- Coleman JR, et al. Calcium Signaling Drives Female-Specific Platelet Hyperactivity: A Mechanistic Exploration of Sex Dimorphisms in Platelet Function. American Association for the Surgery of Trauma. September 18, 2020, virtual.
- Burlew CC, Coleman JR, et al. Inflate and Pack! Pelvic Packing Combined with REBOA Deployment Prevents Hemorrhage Related Deaths in Unstable Pelvic Fractures. American Association for the Surgery of Trauma September 8, 2020, virtual.
- Coleman JR, et al. Whole blood thrombin generation is depressed in severely injured patients requiring massive transfusion. American College of Surgeons Committee on Trauma National Resident Paper Competition. September 9, 2020, virtual.
Invited Talks
- Maintaining Trauma Care Access During the COVID-19 Pandemic: An Urban, Level-1 Trauma Center’s Experience. Qatar 2020. January 20, 2021, virtual.
- Sex Dimorphisms in Coagulation. Center for COMBAT Research Symposium 2020. October 30, 2020, virtual.
Heather Carmichael (PGY-3)
Abstracts/national meeting presentations.
- *Carmichael H, Coleman JR, Velopulos CG. Discharge Against Medical Advice After Trauma: Risk Factors and Opportunity for Intervention. In: Southwest Surgical Congress Annual Meeting. 2020 [Abstract accepted for presentation – meeting cancelled].
- *Carmichael H, Jones TS, Hosokawa P, Goode CM, Overbey DM, Kovar A, Jones EL, Robinson TN. Identifying Patients at Risk of Delayed Recovery After Elective Surgery. In: Association of Veterans’ Affairs Surgeons Annual Meeting. 2020 [Abstract accepted for presentation – meeting cancelled].
- Dyamenahalli K, Carmichael H, Niemiec S, Buenting Gritton C, Ghincea C, Torphy R, Louiselle A, Royer D.Influence of Resident-Led “Bedside Anatomy” Cases on Medical Student Interest and Perceptions Surrounding Surgical Careers. In: Annual Meeting of the Association for Surgical Education. 2020 [Abstract accepted for presentation – meeting cancelled].
- *Carmichael H, Altieri MS, Jones E, Robinson T, Pryor A, Madani A. Educational value of telementoring for a simulation-based fundamental use of surgical energy TM (FUSE) curriculum: a randomized controlled trial in surgical trainees. In: Society of American Gastrointestinal and Endoscopic Surgeons Annual Meeting and World Endoscopic Congress. Virtual Meeting, 2020.
- *Carmichael H, Overbey DM, Goode CM, Jones EL, Robinson TN. Does Approach to Inguinal Hernia Repair Impact Postoperative Recovery of Activity? In: Society of American Gastrointestinal and Endoscopic Surgeons Annual Meeting and World Endoscopic Congress. Virtual Meeting, 2020
- Royer D, Buenting Gritton C, Carmichael H, Kondo K, Lee LL. Let Students SOAR: Impact of Early Clinical Interactions on Perceptions of Specialties and Anatomy. In: Experimental Biology Annual Conference. San Diego, 2020 [Abstract accepted for presentation – meeting cancelled].
- Buenting Gritton C, Carmichael H, Kondo K, Lee LL, Royer D. SOARing Achievements: Do Medical Students Think our New Teaching Strategy Achieved Its Goals? In: Experimental Biology Annual Conference. San Diego, 2020 [Abstract accepted for presentation – meeting cancelled].
- Monahan AM, Dyamenahalli KU, Barron MA, Duffy P, Carmichael H, Wagner AL, Wiktor AJ. Relationship of Microbiome, Antimicrobial Resistance and Wound Closure in ³90% Burn Patients. In: Academic Burn Association Annual Meeting . Virtual Meeting 2020.
- Wiktor AJ, Carmichael H, Weber EB, Duffy, P, Lambert Wagner A. Triage and Transfer to a Regional Burn Center – Impact of a Mobile Phone App. In: Academic Burn Association Annual Meeting . Virtual Meeting 2020.
- *Carmichael H, Dyamenahalli K, Duffy P, Lambert Wagner A, Wiktor AJ. Triage and Transfer to a Regional Burn Center – Impact of a Mobile Phone App. In: Academic Burn Association Annual Meeting . Virtual Meeting 2020.
- Carmichael H, Moore A, Steward L, Velopulos CG. Disparities in Emergent vs. Elective Surgery: Comparing Measures of Neighborhood Social Vulnerability. In: Academic Surgical Congress . Orlando, 2020.
- Kovar A, Carmichael H, Harms B, Nehler M, Tevis S. Overworked and Underpaid: How Resident Finances Impact Burnout, Career Choices, and Family Life. In: Academic Surgical Congress . Orlando, 2020.
- *Carmichael H, Samuels JM, Jamison EC, Bol KA, Coleman JJ, Campion EM, Velopulos CG. Finding the Elusive Trauma Denominator: Feasibility of Combining Data Sets to Quantify the True Burden of Firearm Trauma. In: Annual Meeting of the Eastern Association for the Surgery of Trauma. Orlando, 2020.
- Zangara T, Coleman JR, Carmichael H, Sauaia A, Moore EE, Dunn J, Schroeppel T, Campion E, Ferrigno L.
- Missed chemoprophylaxis doses matter: a multicenter analysis of venous thromboembolism chemoprophylaxis in traumatic brain injury patients. In: Western Medical Research Conference. Carmel, 2020.
Paul Rozeboom (PGY-4)
.jpg?sfvrsn=a381c2ba_2)
- Rozeboom, P.D., Bronsert, M.R., Henderson, W.G., Colborn, K.L., Lambert-Kerzner, A., McIntyre, R.C., Meguid, R.A. “A New, Parsimonious Preoperative Risk Assessment Tool SURPAS Accurately Predicts Outcomes in Emergency Surgery” , Poster presentation at The 79 th annual meeting of the American Association for the Surgery of Trauma, Waikoloa, HI (virtual meeting due to COVID-19 pandemic, September 2020.
2019 ACS Clinical Congress (San Francisco, CA)
Video: resident allie kovar, md, at the 2019 acs clinical congress.
Other Recent Conferences
CU Anschutz
Academic Office One
12631 East 17th Avenue
Aurora, CO 80045
303-724-2750
- Find a Doctor
- Find a Researcher
- Make a Gift
- Graduate Medical Education
- Center for Surgical Innovation
- Health Sciences Library
- CU Department Websites
- CU Anschutz Campus Directory
- Parking and Maps
- Paper Presentations
Presented paper on on comparative study between 0.5 % Ropivacaine with Fentanyl and 0.5 % bupivacaine with fentanyl in USG guided supraclavicular Block in Upper Limb Surgeeries
Presented e-paper on the effect of ketamine in lowering the incidence and severity of post op sore throat after endotrttacheal in patients receiving GA on 19 DEC 2020 at TNISA PG Conclave
Ashish , Logeshwari P
Presented an e-poster on’A randomised control study comparing effect of intravenous dexmedetomidine vs IV esmolol omn attenuation of pressor response to laryngoscopy and endotracheal intubatiion’ and e-paper on ‘the effectiven3ess of dexmedetomidine as an additive to Ropivacaine in supraclavicular brachial plexus block.
Presented e-paper on MAHAYUVAISACON 21 on 20 th Feb 2021 titled as “the effect of nebulised ketamine in decreasing the incidence and severity of post operative sore throat after endotracheal intubation in patients receiving general anaesthesia.
Biochemistry
Made presentation on scientists and clinicians preceptorship for translational research in Webinar 'Biology to Omics' organized by TMS-ACTREC, Navi Mumbai during March 10-12, 2021
Community Medicine
Sero Surveillance in the Wardha District of central India to monitor
SARS Cov 2 infection status among asymptomatic General population
International conference Conquering COVID-19 , at Kasibai Navle
Medical College, Pune.18-19 December 2020
Participated in 5th National IAPSM postgraduate quiz Competition 48th Annual National Conference of Indian Association of Preventive and Social Medicine (IAPSMCON),PGIMER, Chandigarh,19-21 March 2021
Kolhe R , Gupta SS
Relationship of Father's engagement in responsive caregiving with child development a cohort study - presented at IAPSMCON 2021, PGIMER, Chandigarh, 19-21 March,21(poster presentation)
48th Annual National Conference of Indian Association of Preventive and Social Medicine (IAPSMCON),PGIMER, Chandigarh,19-21 March 2021 - Participated in (WAR OF VIDEO COMPETITION) “MAHASANGAM”
2nd IAPSM Young Leaders National Conclave,26-27 March 2021 Participated in (Worth A Thousand Word: Public Health Photography Competition)
Forensic Medicine
Moderate a session topic- crime scene examination-role of doctor in state conference of MLAM“forensicon 2020 on 10 th april 2021 Organized by Department of Forensic Medicine &Toxicology, TNMC & BYL charitable , hospital, Mumbai
Khandekar I L
Chaired a session in 42 nd Annual National conference of IAFM “FORENSIC MEDICON 2021” organized at SCB medical college cuttack, odisha from 23 rd - 24 th Jan 2021,
Moderate a session topic- Non uniformity of medical & medicolegal certificates in state. in state conference of MLAM“ forensicon 2020 on 10 th april 2021 Organized by Department of Forensic Medicine &Toxicology, TNMC & BYL charitable , hospital, Mumbai
Politics of Science in a Pandemic: Impact of Evidence Based Medicine (Guest Speaker)
8 th National Bioethics Conference, 12 December 2020
SP Kalantri
Predictors of Mortality in Venomous Snakebites: Sevagram Story (Guest Speaker)
Amrita Institute of Medical Science (AIMS) Kochi. Amrita National Conference on Snakebite. 22 November 2020
How Covid Vaccines Are Being Developed: Clinical Trials in India (Guest Speaker)
BOOM, 6 August 2020
Aarupadai Veedu Medical College & Hospital. AVMC Webinar Series – ‘Forefront of Future Frontiers’ (Guest Speaker)
Clinical Trials in COVID -19: The Science and Ethics’, 31 July 2020
The Need for Evidence Based Medicine in Treating Covid19 (Guest Speaker)
20 July 2020
14th National Cancer Grid webinar on COVID19 Preparedness (Guest Speaker)
Research Priorities for COVID-19, 18 July 2020
Can Alternative Medicine Be Subject To Modern Rigour? (Guest Speaker)
The Hindu Podcast by Jacob Koshy,3 July 2020
Webinar: Ethical Challenges of Research in a Pandemic (Guest Speaker)
Sunoindia podcast, 27 June 2020
The Why, How & What of Research during COVID era (Guest Speaker)
11 th National Cancer Grid webinar on COVID-19 preparedness, 20 June 2020
Covid and Rural India: Wardha Story (Guest Speaker)
Podcast: SoundCloud by Rukmini S, 10 June 2020
Hydroxychloroquine: More Questions than Answers (Guest Speaker)
BOOM, 5 June 2020
TheEvidence and/or Lack of Evidence for the Effectiveness of Hydroxychloroquinein Treating COVID-19
BBC (British Broadcasting Corporation) Talk , 20 May 2020
Dr. Amrish Saxena
Poster Presentation on Magnitude and determinants of depression in chronic kidney disease patients on maintenance hemodialysis in rural tertiary care hospital at ISN-WZ 2020, 36 th Annual ISN West Zone Conference, Nagpur, 19 th & 20 th September, 26 th & 27 th September 2020.
Microbiology
Presented a paper (Oral Presentation) on “Co infection of pneumocystis
carinii and cryptococcus neoformans” in the 2 nd Annual Conference of
Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021
Maraskolhe D
Presented a paper (Oral Presentation) on “Are tuberculosis patients at greater risk of acquiring COVID-19 MGIMS data and Review of literature” in the 2 nd Annual Conference of Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021 and received Dr. Ashok Pathak Junior Best Oral Paper Award
Obstetrics and Gynaecology
Presentation on Elderly Girls and How can we keep the rural work force we have ?” Unwanted pregnancies in adolescent girls – Global Challenges
Virtual 17 th WONCA World Health Rural Conference (Speaker)
Primary Care and Rural Health Bangladesh (PCRHB), Bangladesh, 15 th -18 th April, 2020
Critical Obstetric Care (Transfusion protocol, use of anticoagulants, Labour and Delivery in ICU training Webcast conference ( Panelist)
FOGSI 26 th April, 2020
4 th Global Virtual summit featuring wizard of endoscopy
Indian association of Gynaecology Endoscopist 21 st June, 2020
Mid Life Health Issue (Panelist)
Mid life Health committee Online conference (Chairperson nominee) Amravati Obstetrics and Gynaecology Society, Amravati, 12 th August, 2020
Management of worst Obstetric emergencies, PPH Online workshop on “ PPH Management” ( Panelist)
Ghaziabad Obstetrics and Gynaecological Society 13 th August, 2020
Hypertensive DS of Pregnancy Online Conference on “Hypertensive Pregnancy” (Panelist)
Nagpur Obstetrics and Gynaecological Society, Nagpur, 18 th August, 2020
USG in Infertility E-conference on “USG in Infertility “The Third Eye” ( Guest lecture)
Revari Obstetrics and Gynaecological Society, Rewari, Haryana, 4 th Sept, 2020
Classic For Clinician - RH Incompatibility in Obstetrics
Classic for Clinician Webinar Series 2, 25th November, 2020
NHM-UNICEF-NQOCN Webinar on Management of Post Partum Haemorrhage With Bundle Approach -Management Of Mother And Newborn In Labour Room
NQOCN with support of UNICEF, 28th November, 2020
Family Integrated Care
NQOCN 14 th December, 2020
Gestational Diabetes – Early intervention key to best Outcome
Rewari Obst & Gynaec Society, 11th January, 2021
Virtual conference on High risk pregnancy, infertility and Gynaecologic
Pune Obstetric and Gynaecology Society, 5 th -7 th March, 2021
Appropriate Blood and Blood Product Transfusion Guidelines PPH- Prevent the Catastrophe Part -5
Association of Madhya Pradesh Obst & Gynae Society and Raipur Obst & Gynae society 9th March, 2021
Amenorrhoea - Clinician's Perspective 29 th Annual POGS Conference “REEDIFY 2021” (Panelist)
Organised by Pune Obstetrics and Gynaecological Society, Pune, 5 th -7 th March, 2021
Maternal Health Care Bundles Classic for Clinician Webinar Series
25th March, 2021
Case Presentation & Table Viva Orator- Respectful Maternity Care (Late Dr. Leela Dube Oration) Virtual PG Force-2021 Nagpur Obstetrics and Gynaecology (Faculty)
Organized by Dept of OBGY, NKP Salve Institute of Medical Sciences & Research Centre & Lata Mangeshkar Hospital, Nagpur in Association with Nagpur Obstetrics and Gynaecology Society, Nagpur 16 th -21 st March, 2021
PMNCH Call to action on COVID 19 Webinar on PMNCH Stratergry outline
WHO 30th March, 2021
Infertility E-conference on “Roll of USG in Pregnancy” ( Chief Guest) Rewari Obst & Gynaec Society Rewari, Haryana 4 th September, 2020
Unwanted Pregnancies in Adolescent Girl, Global Challenges For Safe Baby, Safe Childhood, Safe Motherhood, Safe Womenhood, Maternity Violence must stop. How?
Rural Tribal Elderly Women’s suffering in a low resource region
Workshop-How Can We Keep the Rural Workforce We Have?”: A
Workshop on Rural Workforce Retention
TUFH Network : Primary Health Care: A Path towards Social Justice-
System and Community Based response to Covid-19,
Mexico, 23 rd -25 th September,2020
"Partograph and its interpretation: Risk for mother and Newborn"
NQOCN for Madhya Pradesh 15 th September, 2020
Developing prospective authors from QI teams across India for preparing QI reports for publication in peer reviewed journals
NQOCN 27 th October, 2020
Checklist For Immediate Postpartum Vigilence- For Mother And Newborn
Nqocn 10 th December, 2020
The Nuances of Infertility Webinar on The Nuances of Infertility ( Chaired the Session)
Nagpur Obstetrics and Gynaecology Society, Nagpur, 23 rd December, 2020
Triaging and Emergency Management in Obstetrics emergency (Guest Speaker) Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era: Pregnant Women deserves the Quality Care in any Situation
13th February, 2021
Post natal care – recent advances (Guest speaker) Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era: Pregnant Women deserves the Quality Care in any Situation - Day 4
27th February, 2021
Infection Prevention Practices- Covid/ Non Covid Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era:
Pregnant Women deserves the Quality Care in any Situation
31st March, 2021
Ophthalmology
Diabetic Retinopathy Screening by Teleophthalmology (Guest Speaker)
Annual Delhi Ophthalmic Society International Hybrid Conference of 19 th December, 2020
Enhancing Clincal Skills in Ophthalmology using OSCE’s (Guest Speaker)
Annual Delhi Ophthalmic Society International Hybrid Conference of 18 th December, 2020
Lens Induced Glaucoma
Annual Delhi Ophthalmic Society International Hybrid Conference of
19 th December, 2020
Tayde D , Shukla A K, Singh S, Sheikh A, Lilhare K
Correlation between ablation depth and change in corneal curvature after
LASIK surgery”
45 th Virtual Annual Conference VOS-VRCON 2020 of the Vidarbha Ophthalmic Society from 26 th & 27 th December, 2020
More A , Shukla A K, Singh S, Sheikh A, Bhosale N
Management of Diabetic Patients with Vision Threatening Diabetic
Retinopathy in Rural Vidarbha region”
Peddawad S , Shukla A K, Singh S, Sheikh A, Bhosale N
Screening for vitamin A deficiency in tribal Maharashtra (Melghat)”
Bhosale N , Shukla A K, Singh S, More A
Visual outcome after small incision cataract surgery (SICS) in diabetic and non-diabetic patients”
Rathi N , Singh S, Shukla A K, Tayde D
Corneal topographic patterns in myopic eyes”
Taneshwari S , Dhabarde A, Shukla A K, Pednekar N, Sarode K
Analysis of Causes of Protposis in a Rural Based Tertiary Care Hospital
Tejashree B , Shukla A K, Singh S, Bang P, Peddawad S
An Insight into the Burden of Concomitant Strabismus among Primary School Children in Central India”
Yadav V , Shukla A K, Singh S, Tayde D, Malwe G
A case of lid ptosis and total ophthalmoplegia Annual Delhi Ophthalmic
Society International Hybrid Conference of 18 th December, 2020
Study of change in contrast sensitivity and corneal aberration in eyes
undergoing LASIK (Laser in situ Keratomileusis)
Bhosale N , Shukla A K, Singh S, More A, Malwe G
Bilateral Optic neuropathy: a rare presentation of Systemic lupus erythematosus ( e Poster)
Rosai Dorfmann Disease of Orbit” ( e Poster)
A case of optic nerve head drusens mimicking optic disc oedema” ( e Poster)
Yadav V , Shukla A K, Singh S, Tayde D, Chauragade S
An unusual presentation of mucormycosis in a known diabetic 45 th Virtual
Annual Conference VOS-VRCON 2020 of the Vidarbha Ophthalmic Society from 26 th & 27 th December, 2020
CISP II Workshop (Convener and Resource Person)
28—29 August 2020 at MGIMS, Sevagram
Graduate Medical Education Regulation (2019) on 28 th August 2020
Alignment & Integration on 29 th August 2020
Skills training on 29 th August 2020
Panel discussion on the impact of the corona pandemic on medical
education in the country. ( Panelist )
The Indian Medical Association- Indian Medical Students Network and the Medical Students Association of India, 14 Jun 2020
Enhancing learner engagement in online sessions. (Guest speaker)
Medical Education Unit, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, 27 May 2020
Case based learning in Pathology . (Resource person)
E-course on Competency based learning in Pathology. 6 May 2020
Online teaching learning: Modalities for student engagement. (Guest speaker)
Webinar by Indian Association of Public Health Dentistry, 16 May 2020
Anshu Attention please: Tips for enhancing learner engagement online. (Guest speaker)
Webinar organized by Academy of Health Professions Educators, 19 April 2020
MGIMS Sevagram's Village Adoption Scheme and Social Service Camp for medical students. (Guest speaker)
Organized by the Network Towards Unity for Health (TUFH) Social Accountability Institute. 14 Apr 2020
Enhancing student engagement in online teaching. (Guest speaker)
Medical Education Unit, MGIMS, Sevagram, 17 Aug 2020
Enhancing student engagement in online teaching: Tips and tools (Guest speaker)
Centre for Continuing Education and Inter professional Development (CCEID), Manipal Academy of Higher Education, 25 Jul 2020.
Effective strategies for online learning. (Resource person)
Personal and Professional Development Group of Melaka Manipal Medical College for Malaysian students of I MBBS, 11 Jul 2020
Should a pathologist be a jack of all trades or a master of one? (Debate,
Invited speaker)
Vidarbha Association of Pathologists and Microbiologists, Nagpur, 20 Dec 2020
Pharmacology
National Level e-poster competition
Dr. P.R. Pote Patil College of Pharmacy, Amravati, June 2020
Gorjelwar P
Transfusion-Related Adverse Reactions in patients admitted in medicine department at Tertiary Care Teaching Hospital of Central India
Virtually Online, IPCON 2021 Date: 25 Feb 2021
Gorjelwar P & Kale R
Poster presentation in National Level e poster competition on Proposed
treatment of Covid 19
PR Pote Patil College of Pharmacy, Amravati, 31 st May 2020
Singh Rajput A
To study the effect of wound healing activity of Musa Balbisiana Sp.peel as anti-inflamatory activity on wistar Rats
2 nd World Congress on infectious Disease & Antibiotics 2020
J.N. Tata Auditorium, Indian institute of Science, Bengluru, 17 th Oct 2020
Knowledge attitude and practice towards covid 19 among medical students: a questionnaire based study (Poster Presentation)
Asian ACPCON 2021 organised by American college of physician- india chapter supported by acp chapters, 6 th 7 th feb 2021
International Webinar on Cardiovascular & VO 2 Max Assessment”
AD Instruments, South East Asia, 9 Sep 2020
Webinar : IPS community psychiatry seminar “Healthy eating, under nutrition and obesity among Indian children and adolescent (Guest Speaker)
Organized by : Dr.KS Shubrata, 2 nd May 2020
Annual National CME of industrial Psychiatry of India “Mental Health Issues in IT Industry” Theme - Current and emerging mental health issues in different industries, on 12/12/2020 (Guest Speaker)
KK Mishra, Ahmed
Title – ‘Absenteeism in Health Care Industries’ (Award Paper)
18 th ANCAIPI” held at DY Patil, Pune on 4 th to 6 th March 2021.
“IK Mujawar Award Poster”
Annual Conference IPS West Zone 2 nd & 4 th Oct. 2020.(Webinar)
Radiotherapy
Palliative radiotherapy to triage patients for radical treatment in locally
advanced oral cavity cancer during COVID CRISIS’ Annual Conference of
Association of Radiation Oncologist of Maharashtra, 19 Dec 2020
Clinical outcomes of reirradiation of brain metastasis with erlotinib in
metastatic adenocarcinoma lung’ 10 th Annual Conference of Indian Society
for study of lung cancer, Association of Radiation Oncologist, 26 Sept 2020
Covid 19 a double edge sword for cancer patients’
The Federation of Obstetric & Gynecological Societies of India and POGS international Conference of Indian society for study of lung cancer, Association of Radiation Oncologist, 11 Dec 2020
Efficacy and outcomes of hypofractionation in locally advanced head and neck cancer’
Annual Conference of Association of Radiation Oncologist of India North zone, 2 Oct 2020
Evaluation of nasogastric tube feeding during radiotherapy in head and neck cancer patients’
Annual Conference of Association of Oncologist of North East India, 19 Jan 2021
Left Coronary Artery Dose Exposure Predicts Major Adverse Cardiac Events in Coronary Heart Disease Negative Lung Cancer Patients’
Best of ASTRO 2020, 15 Aug 2020
The Dutch Lung Cancer Audit-Radiotherapy (DLCA-R): Real-World Data on
Elderly Stage III Non-Small Cell Lung Cancer Treated with Definitive
Chemoradiation
Best of ASTRO 2020 16 Aug 2020
Changing Paradigm in Radiotherapy of Postmastectomy Breast Cancer patients A comparative study of 3DCRT vs IMRT : Dosimetry,Toxicity and Outcome at the end of 4 years’
Annual Conference of Indian Society of Medical and Paediatric Oncology, 6 Nov 2020
How to optimally utilize the waiting time/area of patients while they are in
waiting hall before their RT commences for the purpose of patient education 43rd Indian Cooperative Oncology Network Virtual Conference, 9 Oct 2020
Role of prophylactic nasogastric feeding tube to maintain nutrition during
radiotherapy in head and neck cancer patients” Virtual Symposium on
Nutrition in Cancer Care & Management of Mucositis to be held on Friday,
26th February 2021
Kale P, Kalbande P , Rangari P , Datta NR
An evaluation of cost-effective nutrition supplement using homemade recipes vs commercially available formulations in cancer patients on liquid diet from low-middle-income group countries”
Virtual Symposium on Nutrition in Cancer Care & Management of Mucositis to be held on Friday, 26th February 2021
Skin & VD
Puzzling papules on the neck: Cutaneous metastasis from the breast ( e-Poster)
49th National Conference of IADVL, 5th to 7th February, 2021
Patrick S , Kar S, Gangane N, Deshmukh A
Lepromatous Hansen’s disease simulating Still’s Disease: a parodying case
report with diagnostic conundrum (e-Poster)
Manwar P , Kar S, Sawant A, Patrick S, Nandwani S
Blaschkolinear Atrophoderma of Pasini and Pierni with shortening of foot –A
Rare Entity ( e-Poster)
Nandwani S , Kar S, Sawant A, Patrick S, Manwar P
Leprosy presenting as a diagnostic challenge in a case of HIV with Pulmonary Tuberculosis at a rural tertiary care hospital (e-Poster)
Approach to obstructive Jaundice (Guest Lecture)
ASICON-2020 (virtual) from 14 - 19 th Dec. 2020
- Departments
- NAAC Cycle 3
- Courses Attended
- Academic Activities Conducted
- CME Attended
- Conference Attended
- Students Activities
- Student Awards
- Academy of Medical Sciences
- Medical Education Unit
- Institutional Ethics Committee
- Internal Quality Assurance Cell
- Dr Sushila Nayar School of Public Health
- UG Students
- PG Students
- Teaching Staff
- Non-Teaching Staff
- Senior Residents
- Non PG Junior Residents
- Outpatient Services
- Inpatient Services
- Accident and Emergency
- Investigation Facilities
- Information Technology
- Hospital in Numbers
- Hospital Charges
- Life Saving Equipment
- Bio Medical Waste
- Institutional Research
- Student Research
- In-house Publication
- Journal of MGIMS
- Publications
- Community Activities
- Community Based Medical Education
- Social Impact
- Government Approval
- History and Heritage
- Our Founder
- Administration
- Citizen Charter
- Life at Sevagram
- Anti-Ragging
- Right to Information
- Women's Complaints Committee
- Annual Report
- Employe's Information
- Audited Statements
- Foreign Contributions
- Human Rights Complaints
- Mandatory Disclosure
- Getting Here
- NMC Disclosure
- MUHS Mandate
- Harvard Library
- Research Guides
- Countway Library – Health Sciences
Surgery Clerkship
- Finding Classic Papers
- Finding Information
- Online Books
- Visuals/Video
- Board/Exam Info
- Anatomy/Physiology
- Procedures/Instruments/the OR
- Core Journals
How to find a "classic" or "watershed" paper
Here are some suggestions on finding "watershed" or classic papers for your presentation:
- Check the list of Surgical Milestone Papers on to see if it includes your topic. The times an article has been cited is noted when available. Citation indexing became available with the publication of Science Citation Index in 1964. A number of these articles are too early to be included in the SCI database that goes back to 1900 and some of the journals are not indexed in SCI.
- Look at relevant sections of the text Surgery: Basic Science and Clinical Evidence - online and on reserve at Call# WO 100 S9613 2008 . This book is a gold mine. Each chapter gives a summary of the history of surgery for a particular indication including historical vignettes, and an excellent bibliography!
- Other books:
Sabiston's Textbook of Surgery (online) Find the chapter on your topic; some include a brief section on history, look especially at the Selected References at the end of each chapter. As a bonus, these are annotated to explain their value and importance to surgery in this field.
Landmark papers in general surgery (Online) / edited by Graham J. MacKay, Richard G. Molloy, Patrick J. O'Dwyer. Oxford : Oxford University Press, 2013.
Great Ideas in the History of Surgery. Countway WO11 Z5q There is a bibliography is on page 548, but you will need to read the related section of text on your topic for background on the significance of entry. Use the Index.
Operations that Made History Countway WO11.1 E470 This slim volume covers only 18 surgical procedures but if your topic is there you will find a very concise bibliographies after each.
Surgical Case Histories from the Past. Countway WO11.1 E47s Each case history describes a case which leads to a surgical breakthrough. If you topic is in here the 3-4 references of your section will be valuable.
Surgical oncology : fundamentals, evidence-based approaches, and new technology Countway QZ 268 S961 2012 - superb for oncology topics includes list of "landmark papers" and tables of evidence.
- You can consult other authoritative textbooks on your topic and look at the references to the most relevant chapter . If the authors have done a good job writing the background section of the chapter they should reference the "watershed" papers. Try searching the HOLLIS catalog and/or ask a librarian for help identifying books . It's good to give the "big names" (Schwartz or Sabiston), but also think about texts on the specific topic. For example, Principles and practice of surgical oncology : multidisciplinary approach to difficult problems . OR 50 Studies Every Plastic Surgeon Should Know .
- Search in Science Citation Index (aka Web of Science) which allows you to search on a topic and then rank articles by the most cited. Be sure to search multiple synonyms since this database has no indexing. It is computer generated so the keywords the author used are what is found. For example if you topic is gastric cancer, I would suggest entering "gastric cancer" OR "stomach neoplasms" OR "stomach cancer" OR "gastric neoplasms" as a start. Be sure to put the phrases in quotes so it will be searched as a unit and to change the field searched to topic.
When you have the search results, on the right hand side of the screen change the "Sort by" option to "Times Cited" on the drop down menu. This will bring the most cited studies to the top of the list. - Search HOLLIS for works that end with "collected works" OR look for "classic papers" in the title. You might search for "gastrointestinal surgery-collected works to find collections of papers.
Stuck? Not finding what you need? Ask a Librarian for help!
Tips for Specific Presentation Topics
In addition to the broad strategies listed above, here are some suggested sources to consult in your search for classic papers for your presentations. Definitely try the broad strategies in addition to looking at these titles. The suggestions are not comprehensive but they should give you a good start. Please, if you find other valuable sources, let me know so we can expand these lists.
- Acute Abdomen - Sources for classic paper references
- Bariatric Surgery - Finding Important Papers
- Cholangiocarcinoma and Hepatocellular Carcinoma
- ClassisPapersBreastCancerSurgery Tips to help surgery clerkship students find classic papers for Dr. Osteen's presentations
- Gastric Cancer Classic Articles
- Soft Tissue Sarcomas - Suggested sources for classic papers
- Pancreatic Cancer
- Surgical Treatment for Peripheral Artery Disease
- Thyroid Cancer- Sources for Classic Paper
Using PubMed to Find Historical Stuff
PubMed doesn't have any tools to help you find specific landmark papers, but there are specific tools to help you find historical works:
Use the History subset . You can access this search limit by choosing "Show Additional Filters" from the column to the left of your PubMed results. Choose "Subjects" then at the bottom of the new Subjects box, choose customize. Here you can select History to limit your search to historical articles.
With less fuss, you can just append AND history[sb] to your search. For example
cholecystectomy AND history[sb]
If that returns to much stuff, you can use the history subheading , either on its own or appended to a MeSH term:
cholecystectomy AND history[subheading]
"Cholecystectomy/history"[Majr]
Need more help? Check the PubMed User Guide .
- << Previous: Finding Information
- Next: Online Books >>
- Last Updated: Dec 15, 2020 1:53 PM
- URL: https://guides.library.harvard.edu/surgery
General Surgery: Clinical Resources
- Clinical Resources
- Other eBooks
- Plastic Surgery
- Pharmacology
- Patient Education
Point of Care
- Quick Answers Surgery | Access Surgery
- Topics General Surgery | UpToDate
Calculators
- GuidelineCentral Surgery, General
- UpToDate General Surgery
- ClinicalKey Surgery
- UpToDate Society Guidelines General Surgery
Research Tools
Core ebooks.
Search eBooks
Clinical Trials
Please let us know if you have any suggestions , questions, or find broken links
Mayo Clinic Libraries
Mayo Clinic Libraries Services
Mayo clinic resources.
- Procedural Videos | ClinicalKey Surgery
- Videos | AccessSurgery
https://libraryguides.mayo.edu/generalsurgery
- Next: Other eBooks >>
- Last Updated: Mar 29, 2024 11:01 AM
- URL: https://libraryguides.mayo.edu/generalsurgery

IMAGES
VIDEO
COMMENTS
General Surgery articles covering presentation, surgical treatment, prognosis, and follow-up. Peer reviewed and up-to-date recommendations written by leading experts.
Presentations are generally short and sharp, and careful preparation is key to ensure that the premise, findings, and relevance of your work are successfully conveyed. For most conference papers, the structure will mirror that of a scientific manuscript, with an introduction, materials and methods, results, discussion, and conclusions.
For example, if a reviewer is a surgical oncologist, it is probably appropriate to review manuscripts for general surgery and oncology topics, whereas vascular surgery topics may be outside their scope of knowledge. Similarly, if a reviewer is familiar with surgical outcomes research but has never spent any time in a basic science lab, it is ...
Join us for the only multidisciplinary congress for General Surgery including Endocrine, Trauma, Digestive, Breast, Nutrition and Anesthesia Surgery. ... The 6 best abstracts intended for a Free Paper presentation in the program of the International Society of Surgery ISS/SIC are presented in the "Lloyd M. Nyhus Prize Session" and are awarded a ...
The objective of this article is to provide surgery trainees with an overview of how to report to the scienti c literature through. fi. peer-reviewed publications. While there are many published manuscripts that address paper writing in general, there is less information that speci cally targets the surgery trainee.
Within general surgery, there are a wide range of clinical presentations that patients can present with, and the underlying pathologies are even wider. The most common of these is acute abdominal pain, often termed the "acute abdomen" and is essential to know how to approach this presentation and potential investigations required.
Population was limited to general surgery and subspecialties with emphasis on emergency general surgery; intervention included all format changes to an existing MMC model; comparison was the prior MMC format of each study; and outcomes included any demonstrated improvement in MMC, such as perceived increase in presentation quality, practice ...
Abstract. General surgery continues to evolve with advancements in techniques and strategies, presenting both opportunities and challenges for surgical practitioners. This comprehensive review ...
In this popular session, the panelists review 10 of the hottest topics in general surgery selected from the ACS General Surgery Communities, recent surgery meetings, and the literature. Course Outline. Approaches to Femoral Hernia Benjamin K. Poulose, MD, MPH, FACS, Nashville, TN; Pure Tissue Repair of Inguinal Hernia: Resurrection of a Lost Art
This rapid-fire/quick-shot session will cover ten currently popular issues in general surgery. Moderator: Kenneth W ... Presentations. Bullet Removal: Pros and Cons John A. Weigelt, MD, DVM, FACS, Lead, SD. Nipple-Sparing Mastectomy: Use and Indications Raeshell S. Sweeting, MD, Nashville, TN. Troubleshooting Surgical Staple Failure and Malfunction
The art of presenting. The oral case presentation is a time-honoured tradition whereby a trainee presents a new admission to the attending physician. We describe the presentation styles of students, residents and staff physicians and offer pointers on how to present like stereotypical members of each group. Although the case presentation occurs ...
The effectiveness and safety of ERAS protocols in elective surgery are now widely established. Several meta-analyses comparing standard care and fast-track approach show that ERAS protocols in elective surgery lead to a reduction in length of stay and in the rate of postoperative non-surgical complications [2,3,4,5].Most of the available studies focused on the postoperative phase, considering ...
GJ MacKay, RJ Molloy, PJ O'Dwyer (eds). Oxford University Press, First edition 2013. 399pp (hardback). ISBN: 978--19-964425-4 ![Graphic][1] As a trainee approaching my final years and revising for the Fellow of the Royal College of Surgeons (FRCS), the prospect of a book that contains the
The contents follow the usual format of paper surgery textbooks and classify the chapters according to the diseased organ. At the end of each section, a … But now the internet contains lots of resources including several surgical textbooks that are available free of charge.
Surgery. Transplant Surgery. Trauma and Orthopaedic Surgery. Upper Gastrointestinal Surgery. Vascular Surgery. Books. Journals. Abstract. Critiquing key papers in the field, Landmark Papers in General Surgery gives surgeons and trainees an expert appraisal and contextual discussion of th.
Dyas A.R., Rozeboom P.D., Bronsert M.R., et al. Accurate Preoperative Prediction of Need for Postoperative Intensive Care. Academic Surgical Congress 16 th Annual Conference. Virtual, 2/2021. Dyas A.R. Implementation of an Evidence-Based Thoracic Enhanced Recovery After Surgery Protocol in a Diverse, Multi-Hospital Health System. 15 th Annual Pomerantz Visiting Professor Lectureship, Resident ...
Deotale V. Presented a paper (Oral Presentation) on "Co infection of pneumocystis. carinii and cryptococcus neoformans" in the 2 nd Annual Conference of. Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021.
How to find a "classic" or "watershed" paper. Here are some suggestions on finding "watershed" or classic papers for your presentation: - Check the list of Surgical Milestone Papers on to see if it includes your topic. The times an article has been cited is noted when available. Citation indexing became available with the publication of Science ...
Sabiston Textbook of Surgery, 21st ed. by Courtney M. Townsend, 2022 For more than 80 years, Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice has been the go-to text for trainees and surgeons at all levels of experience for definitive guidance on every aspect of general surgery. As the oldest continuously published textbook of surgery in North America, this fully ...
General surgery revision notes. General surgery. A collection of articles relating to general surgery, including abdominal incision types, common general surgical presentations and more. Latest. Latest. Oldest. Random. A to Z.
Our latest template at Slidesgo is a medical-inspired one that's perfect for clinical case presentations. The topic in particular is surgery-related and it's structured to optimize the way useful information is provided. There's heavy use of pictures in the slides with images of doctors and surgeons hard at work. For color, we've used a ...