📕 Studying HQ
35+ research topics on mental health nursing: fostering wellbeing in psychiatric care, carla johnson.
- August 24, 2023
- Essay Topics and Ideas
Mental health nursing is a critical pillar in nurturing the overall wellness of individuals grappling with psychiatric conditions. Aspiring nursing students, comprehending the nuances of mental health nursing is not only pivotal for your academic voyage but also your future professional practice. In this comprehensive guide, we delve profoundly into mental health nursing. We will explore a range of PICOT questions, propose ideas for evidence-based practice (EBP) projects, furnish you with capstone project ideas, offer a spectrum of research paper topics, present a compilation of research questions, and provide several essay topic concepts. All these facets are intended to equip you holistically for this indispensable domain.
What You'll Learn

Understanding the Essence of Mental Health Nursing
Mental health nursing entails the compassionate care and unwavering support extended to individuals traversing the challenges of mental health issues. The role of a mental health nurse transcends the confines of conventional medical care , encompassing therapeutic communication, emotional bolstering, and fostering an environment conducive to healing. Mental health nurses operate in a myriad of settings including hospitals, community health centers, and outpatient clinics, playing an instrumental role in shaping the lives of their patients.
PICOT Questions on Mental Health Nursing
- Population (P): Adults under psychiatric care ; Intervention (I): Integration of daily RS questionnaire; Comparison (C): Units without daily survey; Outcome (O): Decreased employment of restraint and seclusion; Time (T): 6 months. How does the incorporation of a daily RS (Restraint and Seclusion) questionnaire for adults in psychiatric care, compared to units lacking this daily survey, impact the reduction in the utilization of restraint and seclusion for 6 months?
- P: Adolescents with depressive disorders ; I: Implementation of mindfulness-based intervention; C: Standard therapeutic approach; O: Mitigation of depressive symptoms; T: 8 weeks. Among adolescents diagnosed with depressive disorders, what is the effect of incorporating a mindfulness-based intervention, compared to standard therapy, on alleviating depressive symptoms over an 8-week period?
- P: Elderly residents in long-term care facilities; I: Deployment of pet therapy ; C: Absence of pet therapy; O: Enhancement of mood and social interaction; T: 3 months. In elderly individuals residing within long-term care facilities, does the introduction of pet therapy, as opposed to its absence, result in a noticeable improvement in mood and social interaction over a course of 3 months?
- P: Individuals grappling with schizophrenia ; I: Integration of family psychoeducation; C: Standard care regimen; O: Diminished recurrence rate of episodes; T: 1 year. For individuals diagnosed with schizophrenia, does the inclusion of family psychoeducation within their treatment plan, when compared to standard care, lead to a reduction in the frequency of relapses over a 1-year period?
- P: Veterans afflicted with post-traumatic stress disorder (PTSD); I: Employment of virtual reality exposure therapy; C: Conventional therapeutic methods; O: Reduction in symptoms of PTSD; T: 10 sessions. In veterans struggling with post-traumatic stress disorder (PTSD), does the utilization of virtual reality exposure therapy result in a more pronounced reduction in PTSD symptoms, when contrasted with conventional therapy, across a span of 10 sessions?
- P: Children diagnosed with autism spectrum disorder (ASD); I: Incorporation of equine-assisted therapy; C: Standard interventions; O: Amplification of social skills; T: 12 weeks. Among children with autism spectrum disorder (ASD), does participation in equine-assisted therapy yield an advancement in social skills, in comparison to standard interventions, over a duration of 12 weeks?
- P: Inpatient populace with bipolar disorder ; I: Introduction of a mood tracking application; C: Conventional mood charting techniques; O: Attainment of superior mood stability; T: 6 months. Within inpatients diagnosed with bipolar disorder, does the utilization of a mood tracking application for monitoring moods contribute to enhanced mood stability in comparison to conventional mood charting over a span of 6 months?
- P: Individuals contending with eating disorders; I: Application of cognitive-behavioral therapy (CBT); C: Provision of supportive counseling; O: Reduction in maladaptive eating behaviors; T: 16 sessions. For individuals grappling with eating disorders, does the implementation of cognitive-behavioral therapy (CBT) yield a more substantial reduction in maladaptive eating behaviors, when contrasted with supportive counseling, over 16 sessions?
- P: Patients undergoing substance abuse treatment; I: Integration of music therapy; C: Absence of music therapy; O: Mitigation of anxiety and cravings; T: 8 weeks. Among patients undergoing substance abuse treatment, does engagement in music therapy contribute to a reduction in anxiety and cravings, in comparison to those without exposure to music therapy, over a duration of 8 weeks?
- P: Senior residents of assisted living facilities; I: Implementation of reminiscence therapy; C: Participation in routine activities; O: Elevation in cognitive functioning; T: 3 months.
In senior individuals residing in assisted living facilities, does involvement in reminiscence therapy lead to an improvement in cognitive functioning when juxtaposed with engagement in routine activities across a span of 3 months?
5 EBP Projects on Mental Health Nursing
- Appraising the Efficacy of Art Therapy in Alleviating Anxiety Among Schizophrenia Patients.
- Probing the Influence of Exercise Interventions on Bipolar Disorder Patients’ Depressive Symptoms.
- Unpacking Aromatherapy’s Role in Managing Agitation Among Dementia Patients.
- Evaluating Peer Support Groups’ Contribution to Borderline Personality Disorder Recovery.
- Analyzing Virtual Support Networks’ Role in Mitigating Adolescent Social Anxiety Isolation.
Engaging Capstone Projects on Mental Health Nursing
- Forging a Mental Health Awareness Campaign to Combat Stigma Surrounding Help-Seeking in High Schools.
- Devising an Inclusive Training Module for Nurses Enhancing Communication with Psychosis Patients.
- Crafting a Manual to Empower Families in Supporting Loved Ones with Obsessive-Compulsive Disorder (OCD).
- Establishing a Mindfulness Program for Psychiatric Hospital Personnel to Counter Burnout.
- Designing a Transitional Care Blueprint for Smooth Community Reintegration of Severe Mental Illness Patients Post-Hospitalization.
Research Paper Topics on Mental Health Nursing
- Examining the Role of Trauma-Informed Care in Enhancing Recovery for Domestic Violence Survivors with PTSD.
- Delving into the Nexus Between Childhood Trauma and the Emergence of Dissociative Identity Disorder.
- Surveying the Impact of Sleep Quality on College Students’ Mental Health : A Systematic Review.
- Assessing Telepsychiatry’s Efficacy in Extending Mental Health Services to Rural Regions.
- Navigating Cultural Competency in the Assessment and Treatment of Diverse Depression Patients.
Mental Health Nursing Research Questions
- How Does Early Intervention in Childhood Emotional Dysregulation Shape Mood Disorder Onset in Adulthood?
- What Are the Challenges to Adherence to Medication Among Schizophrenia Patients, and How Can Nursing Strategies Address Them?
- What Is the Impact of Mindfulness-Based Stress Reduction Initiatives on Psychiatric Nurses’ Stress Levels?
- What Factors Contribute to the Overrepresentation of Marginalized Individuals with Coexisting Mental Illness in the Criminal Justice System?
- What Are the Long-Term Effects of Electroconvulsive Therapy (ECT) on Memory and Cognitive Function in Severe Depression Patients?
Essay Topic Ideas & Examples
- Ethical Conundrums in Administering Electroconvulsive Therapy (ECT).
- Exploring the Nexus Between Trauma and Substance Abuse in Individuals with Dual Diagnoses.
- Nurses’ Role in Preventing Suicides: Assessing Risk and Providing Support.
- Cultural Proficiency in Mental Health Nursing: Catering to Multifaceted Patient Requirements.
- COVID-19’s Ripples on Healthcare Providers’ Mental Health: Coping Strategies Amid Challenges.
As you immerse yourself in the tapestry of mental health nursing, myriad opportunities unfold for your contributions to research, evidence-based practices, and compassionate patient care. These PICOT questions, EBP project suggestions, capstone project proposals, research paper topics, research questions, and essay themes constitute the foundation of your journey. Each endeavor you undertake to deepen your comprehension and skills in mental health nursing brings you closer to making a profound difference in the lives entrusted to your care. Should you need additional guidance when crafting essays, research papers, or any scholastic composition related to nursing and mental health, do not hesitate to seek professional aid. Our writing services are tailored to support your academic growth and triumph, ensuring your valuable contributions to mental health nursing are eloquently conveyed and impactful.
- What are the 4 principles of mental health nursing?
The four principles of mental health nursing are: therapeutic relationships, holistic care, patient-centeredness, and evidence-based practice. These principles guide nurses in providing comprehensive and effective care to individuals with mental health conditions.
- What is the role of a nurse in mental health treatment?
Nurses in mental health treatment play a pivotal role in assessing, planning, implementing, and evaluating care for patients with mental health issues. They provide therapeutic support, administer medications, conduct psychoeducation, and collaborate with the multidisciplinary team to promote recovery.
- What are the different types of mental health nurses?
Different types of mental health nurses include psychiatric-mental health nurses, advanced practice psychiatric nurses, child and adolescent mental health nurses, and geriatric mental health nurses. These specialized nurses cater to diverse patient populations and address specific mental health challenges.
- What are the 6 C’s in mental health nursing?
The 6 C’s in mental health nursing stand for Care, Compassion, Competence, Communication, Courage, and Commitment. These core values guide mental health nurses in delivering compassionate and effective care to individuals facing mental health issues.
Mental health nursing stands as a critical pillar in nurturing the overall wellness of individuals grappling with psychiatric conditions. Aspiring nursing students, comprehending the nuances of mental health nursing is not only pivotal for your academic voyage but also for your future professional practice. In this comprehensive guide, we delve profoundly into the realm of mental health nursing. We will explore a range of PICOT questions, propose ideas for evidence-based practice (EBP) projects, furnish you with capstone project ideas, offer a spectrum of research paper topics, present a compilation of research questions, and provide a plethora of essay topic concepts. All these facets are intended to equip you holistically for this indispensable domain.
Mental health nursing entails the compassionate care and unwavering support extended to individuals traversing the challenges of mental health issues. The role of a mental health nurse transcends the confines of conventional medical care, encompassing therapeutic communication, emotional bolstering, and fostering an environment conducive to healing. Mental health nurses operate in a myriad of settings including hospitals, community health centers, and outpatient clinics, playing an instrumental role in shaping the lives of their patients.
- Population (P): Adults under psychiatric care; Intervention (I): Integration of daily RS questionnaire; Comparison (C): Units without daily survey; Outcome (O): Decreased employment of restraint and seclusion; Time (T): 6 months. How does the incorporation of a daily RS (Restraint and Seclusion) questionnaire for adults in psychiatric care, compared to units lacking this daily survey, impact the reduction in the utilization of restraint and seclusion over a span of 6 months?
- P: Adolescents with depressive disorders; I: Implementation of mindfulness-based intervention; C: Standard therapeutic approach; O: Mitigation of depressive symptoms; T: 8 weeks. Among adolescents diagnosed with depressive disorders, what is the effect of incorporating a mindfulness-based intervention, in comparison to standard therapy, on the alleviation of depressive symptoms over an 8-week period?
- P: Elderly residents in long-term care facilities; I: Deployment of pet therapy; C: Absence of pet therapy; O: Enhancement of mood and social interaction; T: 3 months. In elderly individuals residing within long-term care facilities, does the introduction of pet therapy, as opposed to its absence, result in a noticeable improvement in mood and social interaction over a course of 3 months?
- P: Individuals grappling with schizophrenia; I: Integration of family psychoeducation; C: Standard care regimen; O: Diminished recurrence rate of episodes; T: 1 year. For individuals diagnosed with schizophrenia, does the inclusion of family psychoeducation within their treatment plan, when compared to standard care, lead to a reduction in the frequency of relapses over a 1-year period?
- P: Inpatient populace with bipolar disorder; I: Introduction of a mood tracking application; C: Conventional mood charting techniques; O: Attainment of superior mood stability; T: 6 months. Within inpatients diagnosed with bipolar disorder, does the utilization of a mood tracking application for monitoring moods contribute to enhanced mood stability in comparison to conventional mood charting over a span of 6 months?
- Surveying the Impact of Sleep Quality on College Students’ Mental Health: A Systematic Review.
As you immerse yourself in the tapestry of mental health nursing, myriad opportunities unfold for your contributions to research, evidence-based practices, and compassionate patient care. These PICOT questions, EBP project suggestions, capstone project proposals, research paper topics, research questions, and essay themes constitute the foundation of your journey. Each endeavor you undertake to deepen your comprehension and skills in mental health nursing brings you closer to making a profound difference in the lives entrusted to your care. Should you find yourself in need of additional guidance when crafting essays, research papers, or any scholastic composition related to nursing and mental health, do not hesitate to seek professional aid. Our writing services are tailored to support your academic growth and triumph, ensuring your valuable contributions to the realm of mental health nursing are eloquently conveyed and impactful.
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Have a subject expert write for you now, have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, popular topics.
Business StudyingHq Essay Topics and Ideas How to Guides Samples
- Nursing Solutions
- Study Guides
- Free Study Database for Essays
- Privacy Policy
- Writing Service
- Discounts / Offers
Study Hub:
- Studying Blog
- Topic Ideas
- How to Guides
- Business Studying
- Nursing Studying
- Literature and English Studying
Writing Tools
- Citation Generator
- Topic Generator
- Paraphrasing Tool
- Conclusion Maker
- Research Title Generator
- Thesis Statement Generator
- Summarizing Tool
- Terms and Conditions
- Confidentiality Policy
- Cookies Policy
- Refund and Revision Policy
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Contact Us:
📞 +15512677917
2012-2024 © studyinghq.com. All rights reserved
- Research article
- Open access
- Published: 26 April 2019
Mental health nurses’ attitudes, experience, and knowledge regarding routine physical healthcare: systematic, integrative review of studies involving 7,549 nurses working in mental health settings
- Geoffrey L. Dickens ORCID: orcid.org/0000-0002-8862-1527 1 , 2 ,
- Robin Ion 3 ,
- Cheryl Waters 1 ,
- Evan Atlantis 1 &
- Bronwyn Everett 1
BMC Nursing volume 18 , Article number: 16 ( 2019 ) Cite this article
57k Accesses
13 Citations
20 Altmetric
Metrics details
There has been a recent growth in research addressing mental health nurses’ routine physical healthcare knowledge and attitudes. We aimed to systematically review the empirical evidence about i) mental health nurses’ knowledge, attitudes, and experiences of physical healthcare for mental health patients, and ii) the effectiveness of any interventions to improve these aspects of their work.
Systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Multiple electronic databases were searched using comprehensive terms. Inclusion criteria: English language papers recounting empirical studies about: i) mental health nurses’ routine physical healthcare-related knowledge, skills, experience, attitudes, or training needs; and ii) the effectiveness of interventions to improve any outcome related to mental health nurses’ delivery of routine physical health care for mental health patients. Effect sizes from intervention studies were extracted or calculated where there was sufficient information. An integrative, narrative synthesis of study findings was conducted.
Fifty-one papers covering studies from 41 unique samples including 7549 mental health nurses in 14 countries met inclusion criteria. Forty-two (82.4%) papers were published since 2010. Eleven were intervention studies; 40 were cross-sectional. Observational and qualitative studies were generally of good quality and establish a baseline picture of the issue. Intervention studies were prone to bias due to lack of randomisation and control groups but produced some large effect sizes for targeted education innovations. Comparisons of international data from studies using the Physical Health Attitudes Scale for Mental Health Nursing revealed differences across the world which may have implications for different models of student nurse preparation.
Conclusions
Mental health nurses’ ability and increasing enthusiasm for routine physical healthcare has been highlighted in recent years. Contemporary literature provides a base for future research which must now concentrate on determining the effectiveness of nurse preparation for providing physical health care for people with mental disorder, determining the appropriate content for such preparation, and evaluating the effectiveness both in terms of nurse and patient- related outcomes. At the same time, developments are needed which are congruent with the needs and wants of patients.
Peer Review reports
People with a mental disorder diagnosis are at more than double the risk of all-cause mortality than the general population. Most at risk are those with psychosis, mood disorder and anxiety diagnoses. Median length of life lost by this group is 10.1 years greater for people with a diagnosis of mental disorder than for general population controls, but mortality rates are significantly higher in studies which include inpatients [ 1 ]. While risk of unnatural causes of death, notably suicide, are greatly increased in this group, it is death from natural causes that remains responsible for the vast majority of mortality. In people with schizophrenia, for example, cardiovascular disease accounts for about one third of all deaths and cancer for one in six, while other common causes are diabetes mellitus, COPD, influenza, and pneumonia [ 2 ]. A relatively high rate of tobacco smoking in this group is implicated in significant increased mortality [ 3 ], as is obesity [ 4 ], exposure to high levels of antipsychotic pharmacological treatment [ 5 ], and mental disorder itself [ 1 ].
Accordingly, the physical health of patients with mental disorder has been prioritised, becoming the focus of guidelines for practitioners in general [ 6 ] and for mental health nurses and other clinical professionals specifically [ 7 , 8 , 9 ]. However, while policies and guidelines are necessary prerequisites of change they must also be implemented in practice if they are to have a positive effect; one of the key barriers to change implementation for mental health nurses has been identified as lack of confidence, skills, and knowledge [ 10 ]. Robson and Haddad ([ 11 ]: p.74) identified that surprisingly ‘modest attention’ had been paid to the issue of such attitudes and knowledge among nurses related to their role in physical health care provision, and developed the Physical Health Assessment Scale for mental health nurses (PHASe) in order to further investigate the phenomenon. Since then, there has been a tangible and growing response among mental health nursing academics and practitioners. In recent years, published literature reviews have covered a decade of UK-only research on the role of mental health nurses in physical health care [ 12 ], patients’ and professionals’ perceptions of barriers to physical health care for people with serious mental illness [ 13 ], the focus and content of nurse-provided physical healthcare for mental health patients [ 14 ], and the physical health of people with severe mental illness [ 15 ]. There has also been an upsurge in the amount of related empirical research. However, to date, no one has systematically reviewed this growing literature about mental health nurses’ attitudes towards, or their related knowledge and experience about providing routine physical healthcare. Further, studies about the effectiveness of interventions designed to improve their delivery of or attitudes to routine physical healthcare have not been systematically appraised. This is surprising given the known links between nurses’ attitudes and their implementation of evidence-based practice [ 16 , 17 , 18 ] and the centrality of measuring nurses’ attitudes to physical health care delivery in recent mental health nursing research on the topic [ 11 , 19 , 20 ].
In this context we have conducted a systematic review to identify, appraise, and synthesise existing evidence from empirical research literature about i) mental health nurses’ experience of providing physical healthcare for patients and about their related knowledge, skills, educational preparation, and attitudes; ii) the effectiveness of any interventions aimed at improving or changing mental health nurse-related outcomes; and iii) to identify implications for the future provision of relevant training and education, for policy, research, and practice. The specific review question being addressed therefore is: what is known from the international, English language, empirical literature about mental health nurses’ skills, knowledge, attitudes, and experiences regarding provision of physical healthcare.
A systematic review of the literature following the relevant points of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [ 21 ].
Search strategy
Since the review scope encompassed questions about experience and effectiveness a dual literature search strategy was developed. For studies about mental health nurses’ experience of delivering physical healthcare a Population Exposure Outcome (PEO) format review question was developed (Population: mental health nurses; Exposure: physical healthcare provision for patients or related training; Outcomes: experiential, social, educational, knowledge, or attitudinal terms, see Additional file 1 : Table S1). For studies of the effectiveness of interventions to improve or change mental health nurse-related outcomes a Population Intervention Comparator Outcome (PICO) structure was implemented (Population: mental health nurses; Intervention: any intervention including physical health-related education, policy or guideline change; Comparator: any or none; Outcome: any) [ 22 ]. We searched five electronic databases: i) CINAHL, ii) PubMed, iii) MedLine, iv) Scopus, and v) ProQuest Dissertations and Theses using text words and MeSH terms. The references list of all included studies, together with those of relevant literature reviews, and the tables of contents of selected mental health nursing journals were hand searched. The search terms were informed by previous literature reviews on the subject of physical healthcare in mental health. The initial search was conducted in April 2018 and re-run in September 2018.
Inclusion and exclusion criteria
Inclusion criteria for studies were English language accounts of empirical research which investigated mental health nurses’ experience of providing physical health care or examined the effectiveness of any intervention that aimed to improve outcomes related to the provision of physical healthcare. Thus, studies of interventions aimed at changing nursing practice, behaviour, knowledge, attitudes, or experiences were eligible, but not those which solely attempted to determine the effect of an intervention on nurses in terms of patient outcomes. While improvement in patient care and outcomes is clearly the desirable endpoint of any intervention on nurses, previous reviews have indicated that no good quality studies exist [ 23 ]. Additionally, studies were only eligible for inclusion where the practitioners involved comprised or included mental health or psychiatric nurses or mental health nursing students, or registered nurses whose practice was within mental health services. Included studies could have used any design or methodological approach. As in previous reviews, studies solely about mental health nurses providing care for people with alcohol/ drug misuse, or mental disorder/substance misuse dual diagnosis were not eligible. Studies about mental health nurses and the provision of emergency physical care or of their experience of providing care for the seriously deteriorating physical health of a patient were omitted as this is the subject of a separate review (Dickens et al. submitted).
Data extraction
Information about the study title, author, publication year, data collection years, location (country), research objectives, aims or hypotheses, design, population, sample details and size, data sources, study variables (i.e. details of intervention) or other exposure, unit of analysis, and study findings were extracted from full text papers. Corresponding authors of included studies were contacted regarding any issues where clarification or additional data could aid the review.
Studies were categorised as interventional or observational. Intervention studies investigated the impact of an educational, policy, or practice intervention in terms of any mental health nurse- or nursing- related outcome, e.g., knowledge, attitudes, behaviour. Intervention studies were further sub-classified as simulation studies (as defined by Bland et al. ([ 24 ]: p.668) “a dynamic process involving the creation of a hypothetical opportunity that incorporates an authentic representation of reality, facilitates active student engagement and integrates the complexities of practical and theoretical learning with opportunity for repetition, feedback, evaluation and reflection”), traditional educational interventions (e.g., lectures, workshops, workbooks), or policy-level interventions (e.g., requiring nurses to follow some new policy or implement some new practice). Observational studies either described mental health nurse- or nursing- related outcomes and/or utilised case control designs to compare them with those of other occupational or professional groups and/or used qualitative methods.
Study quality appraisal
The likelihood of bias in intervention studies was assessed against criteria described by Thomas et al. [ 25 ] and encompassed assessment of the likelihood of selection bias in the obtained sample, study design, potential confounders, blinding, potential for bias in data collection from invalid instrumentation, and participant retention (see Additional file 2 : Table S2). Relevant items from the US Department of Health & Human Sciences NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [ 26 ] were used to assess cross-sectional observational studies (see Additional file 3 : Table S3). Qualitative descriptive studies were assessed using the Critical Appraisal Skills Programme [ 27 ] tool (See Additional file 4 : Table S4). Multiple papers arising from single studies were quality assessed as a single entity. Study quality was initially undertaken independently by at least two of the team. A good level of inter-rater agreement was achieved (Cohen’s Kappa = 0.742 between pairs of raters). Disputed items were discussed by GD and CW and consensus achieved.
Study synthesis
The available total and subscale data from those studies that conducted data collection via the Physical Healthcare Attitude Scale for mental health nurses (PHASe [ 11 ]), the only scale used across more than two studies, was tabulated and compared across studies using unpaired t-tests in QuickCalcs GraphPad software. Where individual item mean and dispersion scores were unavailable estimates were calculated as follows: the mean mean (i.e., Σ means / n means) and the estimated standard deviation (the square root of the average of the variances [ 28 ]). Also, and where available, dichotomised data (‘Strongly agree’ or ‘agree’ responses versus all other responses) from the multiple studies using the 14-item PHASe scale investigating self-reported current involvement in aspects of physical healthcare was tabulated and subjected to Chi-squared analysis. Significant cross-study differences of means and proportions involved all subscale or item data for each study being compared with the corresponding subscale or item from the original study development sample, ‘the reference group’ [ 11 ].
Where available, effect sizes for correlational, interventional, or difference-related outcomes from studies were extracted or, where sufficient information presented, calculated. Where sufficient information was not presented we attempted to contact the corresponding author for clarification. Appropriate effect size statistics were calculated using an online resource [ 29 ]. All other information from study results was subject to a qualitative synthesis conducted by author 1 and subsequently refined and agreed by all of the authors.
Study settings and participants
The search strategy resulted in the inclusion of 41 study samples published in 51 papers (see Fig. 1 ) involving 7549 ( M [ SD ] = 200.5[374.1], Mdn = 47, range 2 to 1899) mental health nurses and n = 213 mental health nursing students ( Mdn = 33). Thirty-three samples included only nurses, of which 20 drew specifically on mental health nurses or nurses working in mental health settings only; eight samples were multidisciplinary. Four papers drew on two samples (i.e., two papers per study) while one sample featured in nine separate papers [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 ]. Studies were conducted in the UK ( k = 17), Australia ( k = 9), US ( k = 4), Canada ( k = 2), Qatar, Hong Kong, Japan, Jordan, Belgium, Norway, Israel, Turkey, India, and Taiwan (all k = 1); two studies were conducted internationally; first, in Qatar, Hong Kong, and Japan [ 19 ], and the US and Canada [ 39 ]. Studies were published between 1994 and 2018 ( Mdn year of publication 2016, only n = 9 before 2010 and n = 1 before 2000).
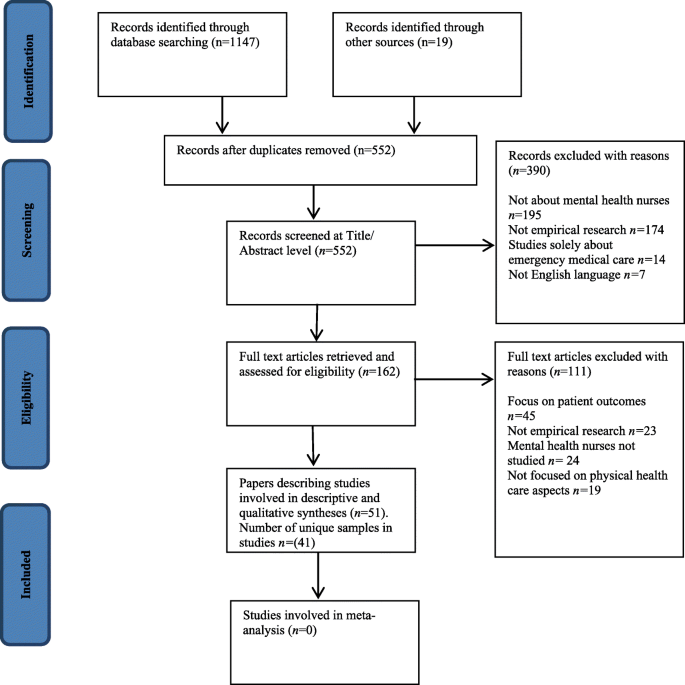
PRISMA study inclusion flowchart
Study design
Eleven studies evaluated an intervention; of these, 10 utilised pre- post AB designs and one adopted a randomised controlled trial design. Other studies used cross-sectional survey or qualitative designs. Intervention studies sometimes incorporated additional qualitative or descriptive elements.
Outcome measures
The most commonly used measure employed was the PHASe or some adaptation of it [ 11 ] in seven studies reported across eight papers [ 11 , 19 , 20 , 40 , 41 , 42 , 43 , 44 ]. The PHASe comprises four factors: 1. Nurses’ attitudes to physical health care; 2. Nurses’ confidence to provide physical health care; 3. Nurses’ perceived barriers in providing physical health care; and 4. Nurses’ attitude towards smoking. Contact with study corresponding authors (Bressington, Chee, Haddad) resulted in acquisition of additional PHASe total and subscale information that was not included in the respective published study papers. Two other outcomes tools were used in two studies each, these being the purpose-designed survey measure of Howard and Gamble [ 45 ] subsequently used by Terry and Cutter [ 46 ], and Happell’s [ 33 ] own questionnaire adapted for use by Clancy et al. [ 40 ]. Most studies used purpose-designed tools. Many reported sufficient information to allow confidence about their internal reliability and face/content validity but there was little information about their measurement reliability, criterion validity, or sensitivity to change (see Additional file 5 : Table S5). A small number of papers used existing validated measures [ 47 , 48 , 49 , 50 , 51 , 52 ] and these were generally the most robust tools (see Additional file 6 : Table S6).
Study quality
All K = 7 qualitative studies were rated very highly in terms of their quality on a 10-point assessment ( Mdn = 9, range 9–10). Cross-sectional observational studies met a median of four of seven quality criteria (range two to six; mean[SD] 4.43[1.33]). Four of these provided an a priori sample size calculation and there was a lack of valid outcome measures in nine of the 21 studies. Overall risk of bias for cross-sectional studies was judged to be low for nine studies, unclear for six and high for six. The quality of interventional studies was generally the poorest ( Mdn = 5, range 2 to 7 of 10 indicators). Only two were judged to be at low risk of bias (see Additional file 2 : Tables S2, Additional file 3 : Table S3, Additional file 4 : Table S4, Additional file 5 : Table S5 and Additional file 6 : Table S6 for further details). Common omissions were, again, sample size justification, lack of repeat pre-baseline and follow up measures, and information about the representativeness of included samples.
Non-intervention studies
Studies examined physical healthcare in general ( k = 24), sexual health ( k = 4), smoking ( k = 6), physical activity and healthy eating, nutrition - in particular the role of Omega-3 in diet, mild brain injury, and breastfeeding (all k = 1; see Table 1 ).
With regards to studies using the PHASe, of all possible comparisons across studies (see Tables 2 and 3 ), the mean score of the study sample differed significantly from the reference sample [ 11 ] on 13 out of 21 (61.9%) subscale and three of four total score combinations (75.0%). Analysis revealed poorer attitudes compared to the reference sample on all three of the significantly poorer attitude scores on 10/17 (58.9%) subscale comparisons, and better attitudes on three (14.3%). However, the reference group only outperformed the other studies on two of the eight possible comparisons on the subscales ‘Physical Healthcare’ and ‘Confidence in Providing Physical Healthcare’ and was poorer for three comparisons. The PHASe total score difference was greatest (large effect size) between the reference sample and Chee et al’s [ 41 ] Australian sample (Cohens d = 1.13) followed by Bressington et al’s [ 19 ] Japanese mental health nurse sub-sample ( d = 0.72). For subscale scores, effect sizes for differences were also largest between the reference sample and that of Chee et al. [ 41 ]. Effect sizes were in favour of the reference sample on the attitudes to smoking and barriers to physical healthcare subscales ( d = 1.48 and 1.78 respectively). Next largest were differences between Haddad et al’s [ 43 ] sample also on the barriers to healthcare ( d = 0.93) and attitudes to smoking subscales ( d = 1.01). On this occasion differences were in favour of Haddad et al’s [ 43 ] sample. Attitudes to smoking were more favourable than the reference sample in two studies, comparable in one and poorer in two.
Regarding the level of self-reported involvement in aspects of physical healthcare the proportion of respondents in PHASe-studies answering ‘strongly agree’ or ‘agree’ to 14 items revealed considerable cross-sample differences. Of 95 possible comparisons between the reference study and others, 70 (73.7%) differed significantly. Of these, 86.7% compared unfavourably with the UK reference study, 13.3% favourably). The number of items per sample differing from the reference sample ranged from 7 to 13 ( Mdn = 10). Japan [ 19 ] provided the only sample of mental health nurses whose responses compared favourably with the reference sample (7/10 significantly differing responses being more favourable in the Japanese sub-sample), while Ganiah et al’s [ 42 ] sample (0/11 favourable comparisons among significantly differing responses), Happell et al’s [ 30 ] (0/14 favourable comparisons), Chee et al’s [ 41 ] Australian sample (1/11 favourable comparisons), Haddad et al’s [ 43 ] UK sample (1/10 favourable comparisons) and Bressington et al’s [ 19 ] Hong Kong sample (2/12 favourable comparisons) all fared poorly. Items relating to checking GP-status, advising on exercise, weight management, healthy eating, contraception, and eyesight checks were all rated less favourably by at least two other samples (range 2 to 6, Mdn = 4) and more favourably by none compared with the reference sample. Only the item about ensuring patients have had their general physical health assessed on first contact with mental health services was rated more favourably by two samples and less favourably by none compared with the reference sample. For all other items there were item-level variations with no clear pattern.
The remaining non-intervention studies provide a mixed and sometimes contradictory picture. First, in terms of reported use of physical health care skills, Osborn et al’s [ 47 ] study revealed that nurses working in mental health settings in one large hospital were less likely to use physical healthcare skills than colleagues in medical, oncology, maternity and surgical settings. Further, they reported using a smaller range of relevant skills. In Howard and Gamble’s [ 45 ] survey, nurses’ responses indicated a gap between their perceived responsibilities for physical healthcare and their practice. Elsewhere, compared with those responding on behalf of healthcare and educational organisations, nurses were less likely to endorse their role in physical healthcare provision [ 53 ] and they reported very low levels of endorsement of related skills training need [ 54 ]. However, for others in more recent studies, they displayed a clear commitment to the physical healthcare role [ 55 ], and said they want more training [ 31 , 56 ]. Further, nurses strongly endorsed their own role in physical health, sexual health, and substance abuse related care and were supported strongly by other healthcare professionals [ 40 ]. Across a series of linked surveys and qualitative studies, Happell et al. [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 57 ] reported associations between nurses’ positive evaluation of the physical healthcare role and practicing aspects of it more commonly. In studies of nurses and specific physical healthcare-related activities there was a suggestion that respondents’ own values or beliefs might be more influential in determining their health-giving or advising behaviour in relation to smoking cessation [ 50 , 58 ]. In relation to sexual health, both Dorsay and Forchuk [ 59 ] and Quinn et al. [ 60 ] have reported that nurses cite patient embarrassment as a reason for not asking patients about sexual side effects of antipsychotic medications. Lack of time, resources and knowledge were reported as barriers to providing advice and interventions regarding exercise and physical activity [ 61 ], Omega-3 [ 62 ]. Knowledge and attitudes to HIV/AIDS were generally good [ 63 ]. Finally, smoking-cessation training was associated with more smoking-cessation helping behaviour [ 64 ] though, counter-inuitively, training was negatively associated with attitudes to smoking cessation in a single study [ 65 ]. Further, Sharma et al’s [ 64 ] study compared the attitudes of mental health trained nurses and comprehensive/ generalist trained nurses working in mental health services: the most marked differences between the groups were on the smoking-related items with the former group expressing significantly more liberal views about smoking restrictions, more worrying attitudes about the benefits and utility of cigarette use as a therapeutic tool, and less confidence in the ability of mental health patients to quit smoking. This was particularly concerning in the study context which was about attitudes to physical healthcare with younger, first episode psychosis patients.
Intervention studies
Five studies focused on physical healthcare in general and six on specific issues (diabetes n = 3; sexual health, cardiometabolic health, obesity all n = 1). Ten evaluated an educational innovation, the exception being Happell et al. [ 35 ], who examined attitudes among nurses to the introduction of a specialist cardiometabolic health nurse role. Haddad et al. [ 43 ] examined the impact of the introduction of personal physical health care plans for patients on nurses’ physical healthcare attitudes alongside the delivery of a single educational session on physical healthcare assessment. The remaining nine studies evaluated educational interventions including three involving simulation and six involving didactic teaching, workshop-format or blended-learning approaches.
Simulation studies
Duration of interventions was 30 min [ 49 ] and1-day [ 66 ], while information was not provided by Wynn [ 52 ]. The mode of simulation delivery involved manikins [ 66 ], human actor as patient [ 66 ], software-based Human Person Simulator [ 52 ], and participant as ‘patient’ in which student participants wore a 15 kg bariatric empathy suit while undertaking everyday tasks in order to help them appreciate the experience of obesity [ 49 ]. Other simulations involved diabetes care [ 52 ], fractured leg in the context of a jump or fall in a patient with first episode psychosis, medical deterioration in the same patient following transfer to a psychiatric ward, and delirium [ 66 ]. Results indicated improved clinical judgement and reduced diabetes-related medical emergency reports [ 52 ], improved knowledge, attitudes, and confidence about physical healthcare [ 66 ], improved response to obese patients, characteristics of obese patients and supportive roles in caring for obese patients [ 49 ].
Non-simulation studie
Study duration ranged from a 2.5-h workshop on physical health [ 67 ] to a 20-credit bachelor’s degree level (equivalent to 200-h of taught and self-directed study and assessment completion) module on physical healthcare in mental health [ 46 ]. Non-simulation studies evaluated the introduction of personal health plans for patients in a low secure forensic unit together with a single educational session on physical health care for nursing staff [ 43 ]. Specific topics addressed included diabetes [ 68 , 69 ], health assessment [ 46 , 67 ], oral health, IM injectables [ 68 ], vital signs, blood readings, BMI measurement [ 46 ], and cardio-metabolic health [ 35 , 57 ].
In Sung et al’s [ 51 ] RCT, nurses were allocated in a random stratified design to attend 8 × 2-h session about sexual healthcare over a period of 4-w or no intervention. Significant effects were detected in the experimental group relative to the control group for improvements in related knowledge and in attitudes, but not in self-efficacy. The study involved nurses employed both in medical and psychiatric wards (stratified allocation from both) and there was no reported effect of ward-type on outcomes. Pretest- posttest design intervention studies targeted at diabetes found greatly improved clinical judgment in relation to diabetes care and reduced diabetes-related emergency referrals [ 52 ] and similarly impressive improved diabetes-related knowledge [ 69 , 70 ]. Improved attitudes to obesity, obese patients, and supportive roles in caring for obese individuals have been reported across a mixed group of participants and did not differ between mental health and other nurses [ 49 ]. and physical healthcare in general. Happell et al. [ 57 ] reported improved support for a specialist cardiometabolic nurse role following its introduction, however we find this conclusion is unwarranted since it is derived from statistical testing of 14-questionnaire items only one of which was found significant. Interventions aimed at physical healthcare in general found some impressive post- group improvements in knowledge [ 66 , 67 , 68 ], attitudes [ 66 ], and confidence [ 46 , 66 ].
We have conducted a systematic review of the empirical literature about mental health nurses and their attitudes towards, knowledge about, and experiences of physical health care for patients. We took a broad approach to searching the literature and included interventional and observational studies involving real or simulated situations. We included studies involving mental health nursing students and multidisciplinary professional groups in addition to those including only mental health nurses. We contacted study authors to gain additional information and, for the studies using the PHASe [ 11 ] and this elicited significant, previously unpublished information. While we applied no time limits to our comprehensive search we found studies only from as early as 1994, only nine from before 2000, and the median year of publication was 2016. This means that there has been a welcome increase, which we described as a ‘mini-explosion’ in the Introduction, in related empirical work in recent years. The total number of nurses involved in studies, 7549, makes this to our knowledge one of the largest amalgamations of evidence gathered directly from mental health nurses.
However, the overall methodological quality of studies was somewhat limited, particularly interventional studies to improve mental health nurses’ physical healthcare assessment practices and skills. Nevertheless, while many of the included studies examine mental health nurses, and nurses working in mental health settings, this group comprises a heterogeneous collection of individuals of vastly differing experience, preparation, knowledge, and roles. As a result, it is not too surprising that some less well-researched areas have thrown up starkly different results. However, there is consistent evidence that there is a strong association between mental health nurses’ reported attitudes and their reported involvement in physical health care [ 19 , 20 , 42 ]. Similarly, that the nurses who value physical health care also report that they deliver more of it [ 30 ] and those who talk to at least one other discipline about their patients’ physical health do so with multiple professional groups [ 33 ]. Accordingly, fewer resources could be expended on answering these sorts of associational questions in the future.
Our conclusion is that it is now time for a new phase for mental health nursing research related to physical healthcare: efforts must be redoubled to focus on developing and testing interventions to improve nurses’ attitudes, knowledge, and skills. We must ensure that new studies are well-designed and rigorously conducted. More specifically, further research is required to build knowledge about whether the supposed benefits arising from this relationship translate into objectively better practice and indeed better patient outcomes. This would strengthen the case for training to improve attitudes and provide some urgency to better understand what interventions might deliver that outcome. Further, it appears that mental health nurses well-recognise that they require further skills and knowledge related to physical health care across a wide range of areas [ 19 , 30 , 31 , 57 , 71 ]. However, ambivalence and reluctance remains about embracing the change needed to achieve this [ 61 ].
The PHASe was used across multiple studies which allowed for some international and setting-specific comparison of nurses’ attitudes. We found that nurses’ self-perceived practices and attitudes differed significantly between samples from across the world. This, of course, may well reflect different approaches to mental health nurse preparation; for example, in Australia, all pre-registration nurses undergo the same core programme whereas in the UK mental health nursing is a specialist branch of pre-registration training. Therefore, results from Chee et al’s [ 41 ] recent study are enlightening since they reveal equivalent attitudes to physical healthcare specifically, more confidence in delivering physical healthcare but poorer scores in relation to barriers to physical healthcare delivery and smoking cessation. Given the non-equivalence of results on the attitudes to smoking subscale between Chee et al. [ 41 ] and Wynaden et al. [ 44 ], both conducted in Western Australia by related research teams, there are questions about the extent to which results are sample specific. Larger scale, representative data collection in Australia and New Zealand could therefore add significantly to the debate about nurses’ preparation for physical healthcare skills under different preparation regimes. As the PHASe authors’ note, the tool has not been subjected to tests of its stability or criterion validity and improvements in evidence for this would add significantly to the ability to draw sound conclusions from research using the tool. Findings from Osborne et al’s [ 47 ] large hospital-wide survey indicate that the gap in the physical health-related skills addressed by the PHASe is real and of concern.
Apart from the PHASe the literature is peppered with outcomes tools designed for single studies and with little evidence of anything other than face validity and internal consistency. Is it possible, we must ask, that this reflects that researchers are asking the wrong questions i.e., focusing overly on mental health nurses’ attitudes and self-proclaimed knowledge and efficacy when what is now required is a more robust approach to examining their actual knowledge and performance and, crucially, their impact on patient outcomes. Little seems to have been added to the literature on this since Hardy et al. [ 23 ] found no studies to include in their systematic review. Further, Haddad et al’s [ 43 ] study in a low secure forensic setting found nurses scoring favourably on PHASe subscales about attitudes to physical healthcare and to smoking compared with non-forensic nurses in the reference sample, suggesting perhaps that in a setting where length of stay is considerably longer then nurses have more opportunity to engage with patients in this aspect of care. Notably, however, nurses in the same sample compared unfavourably with the reference sample in terms of perceived involvement in actual physical healthcare, a somewhat contradictory finding.
For intervention studies, effect sizes were generally largest, and were in fact sometimes startlingly large, where interventions were targeted and outcomes were knowledge based (e.g., educational studies). This is unsurprising since educational interventions are generally evaluated against criteria that are specifically and directly addressed in the intervention. Outcomes tended to be measured immediately following the training [ 46 , 52 ], but their long term retention is generally not known and neither is any practical beneficial change to practice. The apparent potency of these interventions requires further testing in randomized designs with appropriate follow-up periods.
Some study samples in the current review included non-nursing staff; though their occurrence and representativeness was too limited to allow robust conclusions to be drawn about the relative state of nurses’ knowledge and attitudes within the multidisciplinary team context. Given the current review explicitly focused on mental health nurses then further research exploring the multidisciplinary aspects of physical health care provision is warranted.
Mental health nurses’ ability to provide routine physical healthcare has been highlighted in recent years. Recent literature provides a starting point for future research which must now concentrate on determining the effectiveness of nurse preparation for providing physical health care for people with mental disorder, determining the appropriate content for such preparation, and evaluating the effectiveness both in terms of nurse and patient- related outcomes. At the same time, developments are needed which are congruent with the needs and wants of patients. Perhaps what the included studies best demonstrate is that mental health nurses seem to realise that physical health care is part of their role.
Abbreviations
Medical Subject Headings
Physical Health Attitudes Scale for mental health nurses
Population Intervention Comparator Outcome
Preferred Reporting Items for Systematic Reviews and Meta Analyses
Walker ER, McGee E, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. 2015;72(4):334–41. https://doi.org/10.1001/jamapsychiatry.2014.2502 .
Article Google Scholar
Olfson M, Gerhard T, Huang C. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiat. 2015;72(12):1172–81. https://doi.org/10.1001/jamapsychiatry.2015.1737 .
Drope J, Liber AC, Cahn Z, Stoklosa M, Kennedy R, Douglas CE, Henson R, Drope J. Who's still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018;68(2):106–15. https://doi.org/10.3322/caac.21444 .
Article PubMed Google Scholar
Annamalai A, Kosir U, Tek C. Prevalence of obesity and diabetes in patients with schizophrenia. World J Diabetes. 2017;8(8):390–6. https://doi.org/10.4239/wjd.v8.i8.390 .
Article PubMed PubMed Central Google Scholar
Tomiainen M, Mittendorfer-Rutz E, Bjӧrkenstam C, Suvisaari J, Alexanderson K, Tiihonen J. Antipsychotic treatment and mortality in schizophrenia. Schizophr Bull. 2016;41(3):656–63. https://doi.org/10.1093/schbul/sbu164 .
World Health Organisation. Guidelines for the management of physical health conditions in adults with severe mental disorders. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO
Google Scholar
New South Wales Government. Physical Health Care of Mental Health Consumers. North Sydney: NSW Ministry of Health; 2017. Accessed 29 Jan 2019: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2017_019.pdf
Nursing, Midwifery and Allied Health Professions Policy Unit. Improving the physical health of people with mental health problems: Actions for mental health nurses. London: Department of Health; 2016. Accessed 4 Jan 2019 at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/532253/JRA_Physical_Health_revised.pdf
Royal Australian and New Zealand College of Psychiatrists. Keeping Body and Mind Together: Improving the physical health and life expectancy of people with serious mental illness. Melbourne: Victoria; 2015. Accessed 29 Jan 2019 at: https://www.ranzcp.org/files/resources/reports/ranzcp-keeping-body-and-mind-together.aspx
Department of Health. From values to action: the chief nursing Officer’s review of mental health nursing. London: DOH; 2006.
Robson D, Haddad M. Mental health nurses' attitudes towards the physical health care of people with severe and enduring mental illness: the development of a measurement tool. Int J Nurs Stud. 2012;49(1):72–83. https://doi.org/10.1016/j.ijnurstu.2011.07.011 .
Blythe J, White J. Role of the mental health nurse towards physical health care in serious mental illness: an integrative review of 10 years of UK literature. Int J Ment Health Nurs. 2012;21(3):193–201. https://doi.org/10.1111/j.1447-0349.2011.00792.x .
Happell B, Scott D, Platania-Phung C. Perceptions of barriers to physical health care for people with serious mental illness: a review of the international literature. Issues Ment Health Nurs. 2012;33(11):752–61. https://doi.org/10.3109/01612840.2012.708099 .
Happell B, Platania-Phung C, Scott D. A systematic review of nurse physical healthcare for consumers utilizing mental health services. J Psychiatr Ment Health Nurs. 2014;21(1):11–22. https://doi.org/10.1111/jpm.12041 .
Article CAS PubMed Google Scholar
Collins E, Tranter S, Irvine F. The physical health of the seriously mentally ill: an overview of the literature. J Psychiatr Ment Health Nurs. 2012;19(7):638–46. https://doi.org/10.1111/j.1365-2850.2011.01831.x .
Estabrooks CA, Floyd JA, Scott-Findlay S, O’Leary KA, Gushta M. Individual determinants of research utilization: a systematic review. J Adv Nurs. 2003;43(5):506–20. https://doi.org/10.1046/j.1365-2648.2003.02748.x .
Melnyk BM, Fineout-Overholt E, Feinstein NF, Li H, Wilcox L, Kraus R. Nurses’ perceived knowledge, beliefs, skills and needs regarding evidence-based practice: implications for accelerating the paradigm shift. Worldviews Evid-Based Nurs. 2004;1(4):185193. https://doi.org/10.1111/j.1524-475X.2004.04024.x .
Varnell G, Haas B, Duke G, Hudson K. Effect of an educational intervention on attitudes toward and implementation of evidence-based practice. Worldviews Evid-Based Nurs. 2008;5(4):172–81. https://doi.org/10.1111/j.1741-6787.2008.00124.x .
Bressington D, Badnapurkar A, Inoue S, Ma HY, Chien WT, Nelson D, Gray R. Physical health care for people with severe mental illness. Int J Environ Res Public Health. 2018;15(343). https://doi.org/10.3390/ijerph15020343 .
Robson D, Haddad M, Gray R, Gournay K. Mental health nursing and physical health care: a cross-sectional study of nurses' attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int J Ment Health Nurs. 2013;22(5):409–17. https://doi.org/10.1111/j.1447-0349.2012.00883.x .
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097 .
Munn Z, Srtern C, Aromataris E, Lockwood C, Jordan Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol. 2018;18(5):1–9. https://doi.org/10.1186/s12874-017-0468-4 .
Hardy S, White J, Deane K, Gray R. Educating healthcare professionals to act on the physical health needs of people with serious mental illness: a systematic search for evidence. J Psychiatr Ment Health Nurs. 2011;18(8):721–7. https://doi.org/10.1111/j.13652850.2011.01722.x .
Bland AJ, Topping A, Wood B. A concept analysis of simulation as a learning strategy in the education of undergraduate nursing students. Nurse Educ Today. 2011;31:664–70. https://doi.org/10.1016/j.nedt.2010.10.013 .
Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid-Based Nurs. 2004;1(3):176–84. https://doi.org/10.1111/j.1524-475X.2004.04006.x .
NIH National Heart, Lung and Blood Institute (n.d.). Study Quality Assessment Tools: Quality Assessment Tool for Observational Cohort and Cross Sectional Studies. Accessed 28 Apr 2018: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools
Critical Appraisal Skills Programme (n.d.). CASP checklist: 10 questions to help you make sense of qualitative research. Oxford: CASP. Available at: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf . Accessed 16 Apr 2019.
Campbell MJ. Statistics at square one (9th edition) T.D.V. Swinscow [revised by M.J. Campbell]: University of Southampton: BMJ publishing group; 1997. Accessed 14 Jun 2018: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/
Wilson, D.B. (n.d.). Practical meta-analysis effect size calculator. Accessed 11 Mar 2019 https://campbellcollaboration.org/escalc/html/EffectSizeCalculator-SMD-main.php .
Happell B, Platania-Phung C, Scott D. Are nurses in mental health services providing physical health care for people with serious mental illness? An Australian perspective. Issues Ment Health Nurs. 2013;34(3):198–207. https://doi.org/10.3109/01612840.2012.733907 .
Happell B, Platania-Phung C, Scott D. Physical health care for people with mental illness: training needs for nurses. Nurse Educ Today. 2013;33:396–401. https://doi.org/10.1016/j.nedt.2013.01.015 .
Happell B, Platania-Phung C, Scott D. Proposed nurse-led initiatives in improving physical health of people with serious mental illness: a survey of nurses in mental health. J Clin Nurs. 2013;23:1018–29. https://doi.org/10.1111/jocn.12371 .
Happell B, Platania-Phung C, Scott D, Nankivell J. Communication with colleagues: frequency of collaboration regarding physical health of consumers with mental illness. Perspect Psychiatr Care. 2014;50(1):33–43. https://doi.org/10.1111/ppc.12021 .
Happell B, Platania-Phung C, Scott D. What determines whether nurses provide physical health care to consumers with serious mental illness? Arch Psychiatr Nurs. 2014;28:87–93. https://doi.org/10.1016/j.apnu.2013.11.001 .
Happell B, Platania-Phung C, Scott D, Stanton R. Predictors of nurse support for the introduction of the cardiometabolic health nurse in the Australian mental health sector. Perspect Psychiatr Care. 2015;51(3):162–70. https://doi.org/10.1111/ppc.12077 .
Happell B, Platania-Phung C. Cardiovascular health promotion and consumers with mental illness in Australia. Issues Ment Health Nurs. 2015;36:286–93. https://doi.org/10.3109/01612840.2014.981770 .
Happell B, Platania-Phung C, Stanton R, Millar F. Exploring the views of nurses on the cardiometabolic health nurse in mental health services in Australia. Issues Ment Health Nurs. 2015;36:135–44. https://doi.org/10.3109/01612840.2014.901449 .
Happell B, Platania-Phung C, Scott D, Hanley C. Access to dental care and dental ill-health of people with serious mental illness: views of nurses working in mental health settings in Australia. Aust J Prim Health. 2015;21(1):32–7. https://doi.org/10.1071/PY13044 .
Klein TA, Graves JM. A comparison of psychiatric and non-psychiatric nurse practitioner knowledge and management recommendations regarding adolescent mild traumatic brain injury. J Am Psychiatr Nurses Assoc. 2017;23(1):37–49. https://doi.org/10.1177/1078390316668992 .
Clancy R, Lewin TJ, Bowman JA, Kelly BJ, Mullen AD, Flanagan K, Hazelton MJ. Providing physical health care for people accessing mental health services: clinicians’ perceptions of their role. Int J Ment Health Nurs. 2018;28(1):256–67. https://doi.org/10.1111/inm.12529 .
Chee G, Wynaden D, Heslop K. The provision of physical health care by nurses to young people with first episode psychosis: a cross-sectional study. J Psychiatr Ment Health Nurs. 2018;25(7):411–22.
Ganiah AN, Al-Hussami M, Alhadidi M. Mental health nurses’ attitudes and practice toward physical health care in Jordan. Community Ment Health J. 2017;53(6):725–35. https://doi.org/10.1007/s10597-017-0143-6 .
Haddad M, Llewellyn-Jones S, Yarnold S, Simpson A. Improving the physical health of people with severe mental illness in a low secure forensic unit: an uncontrolled evaluation study of staff training and physical health care plans. Int J Ment Health Nurs. 2016;25(6):554–65. https://doi.org/10.1111/inm.12246 .
Wynaden D, Heslop B, Heslop K, Barr L, Lim E, Chee GL, Murdock J. The chasm of care: where does the mental health nursing responsibility lie for the physical health care of people with severe mental illness? Int J Ment Health Nurs. 2016;25(6):516–25. https://doi.org/10.1111/inm.12242 .
Howard L, Gamble C. Supporting mental health nurses to address the physical health needs of people with serious mental illness in acute inpatient care settings. J Psychiatr Ment Health Nurs. 2010;18(2):105112. https://doi.org/10.1111/j.1365-2850.2010.01642.x .
Terry J, Cutter J. Does education improve mental health practitioners' confidence in meeting the physical health needs of mental health service users? A mixed methods pilot study. Issues Ment Health Nurs. 2013;34(4):249–55. https://doi.org/10.3109/01612840.2012.740768 .
Osborn S, Douglas C, Reid C, Jones L, Gardner G. The primacy of vital signs – acute care nurses’ and midwives’ use of physical assessment skills: a cross sectional study. Int J Nurs Stud. 2015;52:952–62 https://doi.org/10.1016/j.ijnurstu.2015.01.014 .
Artzi-Medvedik R, Chertok IRA, Romem Y. Nurses' attitudes towards breastfeeding among women with schizophrenia in southern Israel. J Psychiatr Ment Health Nurs. 19(8):702–8. https://doi.org/10.1111/j.1365-2850.2011.01846.x .
Hunter J, Rawlings-Anderson K, Lindsay T, Bowden T, Aitken LM. Exploring student nurses' attitudes towards those who are obese and whether these attitudes change following a simulated activity. Nurse Educ Today. 2018;65:225–31. https://doi.org/10.1016/j.nedt.2018.03.013 .
Magor-Blatch LE, Rugendyke AR. Going smoke-free: attitudes of mental health professionals to policy change. J Psychiatr Ment Health Nurs. 2016;23(5):290–302. https://doi.org/10.1111/jpm.12309 .
Sung SC, Jiang HH, Chen RR, Chao JK. Bridging the gap in sexual healthcare in nursing practice: implementing a sexual healthcare training programme to improve outcomes. J Clin Nurs. 2016;25:19–20. https://doi.org/10.1111/jocn.13441 2989-3000.
Wynn SD. Improving the quality of care of veterans with diabetes: a simulation intervention for psychiatric nurses. J Psychosoc Nurs Ment Health Serv. 2011;49(2):38–45. https://doi.org/10.3928/02793695-20110111-01 .
Brimblecombe N, Tingle A, Tunmore R, Murrells T. Implementing holistic practices in mental health nursing: a national consultation. Int J Nurs Stud. 2007;44(3):339–48. https://doi.org/10.1016/j.ijnurstu.2006.07.021 .
Delaney KR, Hamera E, Drew BL. Health advanced practice nursing: the adequacy of educational preparation: voices of our graduates. J Am Psychiatr Nurses Assoc. 2009;15(6):383–92. https://doi.org/10.1177/1078390309353070 .
Mwebe H. Physical health monitoring in mental health settings: a study exploring mental health nurses' views of their role. J Clin Nurs. 2017;26(19/20):3067–78. https://doi.org/10.1111/jocn.13653 .
Çelik Ince S, Partlak Günüşen N, Serçe Ö. The opinions of Turkish mental health nurses on physical health care for individuals with mental illness: a qualitative study. J Psychiatr Ment Health Nurs. 2018;25(4):245–57.
Happell B, Stanton R, Hoey W, Scott D. Reduced ambivalence to the role of the cardiometabolic health nurse following a 6-month trial. Perspect Psychiatr Care. 2015;51(2):80–5. https://doi.org/10.1111/ppc.12066 .
Sharp DL, Blaakman SW, Cole RE, Evinger JS. Report from a national tobacco dependence survey of psychiatric nurses. J Am Psychiatr Nurses Assoc. 2009;15(3):172–81. https://doi.org/10.1177/1078390309336746 .
Dorsay JP, Forchuk C. Assessment of the sexuality needs of individuals with psychiatric disability. J Psychiatr Ment Health Nurs. 2009;1(2):93–7. https://doi.org/10.1111/j.1365-2850.1994.tb00025.x .
Quinn C, Platania-Phung C, Bale C, Happell B, Hughes E. Understanding the current sexual health service provision for mental health consumers by nurses in mental health settings: findings from a survey in Australia and England. Int J Ment Health Nurs. 2018;27(5):1522–34. https://doi.org/10.1111/inm.12452 .
Verhaege N, De Maeseneer J, Maes L, Van Heeringen C, Annemans L. Health promotion in mental health care: perceptions from patients and mental health nurses. J Clin Nurs. 2013;22(11–12):1569–78. https://doi.org/10.1111/jocn.12076 .
Johannessen B, Skagestad I, Bergkaasa AM. Food as medicine in psychiatric care: which profession should be responsible for imparting knowledge and use of omega-3 fatty acids in psychiatry. Complement Ther Clin Pract. 2011;17(2):107–12. https://doi.org/10.1016/j.ctcp.2010.08.001 .
Hughes E, Gray R. HIV prevention for people with serious mental illness: a survey of mental health workers' attitudes, knowledge and practice. J Clin Nurs. 2009;18(4):591–600. https://doi.org/10.1111/j.1365-2702.2007.02227.x .
Sharma R, Meurk C, Bell S, Ford P, Gartner C. Australian mental health care practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm reduction in smokers with severe mental illness. Int J Ment Health Nurs. 2018;27:247–57. https://doi.org/10.1111/inm.12314 .
Parel JT, Khakha DC, Balhara YPS. Do psychiatric nurses have favourable knowledge and attitude towards tobacco prevention among their patients? A cross-sectional study from national capital of India. Asian J Nurs Educ Res. 2018;8(1):01–4. https://doi.org/10.5958/2349-2996.2018.00001.0 .
Fernando A, Attoe C, Jaye P, Cross S, Pathan J, Wessely S. Improving interprofessional approaches to physical and psychiatric comorbidities through simulation. Clin Simul Nurs. 2017;13(4):186193. https://doi.org/10.1016/j.ecns.2016.12.004 .
White J, Hemingway S, Stephenson J. Training mental health nurses to assess the physical health needs of mental health service users: a pre- and post-test analysis. Perspect Psychiatr Care. 2014;50(4):243–50. https://doi.org/10.1111/ppc.12048 .
Hemingway S, Clifton A, Stephenson J, Edward KL. Facilitating knowledge of mental health nurses to undertake physical health interventions: a pre-test/post-test evaluation. J Nurs Manag. 2014;22(3):383–93. https://doi.org/10.1111/jonm.12220 .
Hemingway S, Stephenson J, Trotter F, Clifton A, Holdich P. Increasing the health literacy of learning disability and mental health nurses in physical care skills: a pre and post-test evaluation of a workshop on diabetes care. Nurse Educ Pract. 2015;15(1):30–7. https://doi.org/10.1016/j.nepr.2014.08.003 .
Hemingway S, Trotter F, Stephenson J, Holdich P. Diabetes: Increasing the knowledge base of mental health nurses. Br J Nurs. 2013;22(17):991–5. https://doi.org/10.12968/bjon.2013.22.17.991 .
Nash M. Physical care skills: a training needs analysis of inpatient and community mental health nurses. Ment Health Pract. 2005;9(4):20–3. https://doi.org/10.7748/mhp2005.12.9.4.20.c1896 .
Happell B, Scott D, Nankivell J, Platania-Phung C. Nurses’ views on training needs to increase provision of primary care for consumers with serious mental illness. Perspect Psychiatr Care. 2013;49:210–7. https://doi.org/10.1111/j.1744-6163.2012.00351.x .
Happell B, Scott D, Nankivell J, Platania-Phung C. Screening physical health? Yes! But…: nurses’ views on physical health screening in mental health care. J Clin Nurs. 2013;22:2286–97. https://doi.org/10.1111/j.1365-2702.2012.04325.x .
Birks M, Cant R, James A, Chung C, Davis J. The use of physical assessment skills by registered nurses in Australia: issues for nursing education. Collegian. 2012;20:27–33. https://doi.org/10.1016/j.colegn.2012.02.004 .
Giddens JF. A survey of physical assessment techniques performed by RNs: lessons for nursing education. J Nurs Educ. 2007;46:83–7.
PubMed Google Scholar
Douglas C, Osborne S, Reid C, Batch M, Hollingdrake O, Gardner G. What factors influence nurses’ assessment practices? Development of the barriers to nurses’ use of physical assessment scale. J Adv Nurs. 2014;70:2683–94. https://doi.org/10.1111/jan.12408 .
Phelan M, Stradins L, Amin D, Isadore R, Hitrov C, Doyle A, Inglis R. The physical health check: a tool for mental health workers. J Ment Health. 2004;13(3):277–85. https://doi.org/10.1080/09638230410001700907 .
Shuel F, White J, Jones M, Gray R. Using the serious mental illness health improvement profile [HIP] to identify physical problems in a cohort of community patients: a pragmatic case series evaluation. Int J Nurs Stud. 2010;47(2):136–45. https://doi.org/10.1016/j.ijnurstu.2009.06.003 .
Freed GL, Clark SJ, Sorensen J, Lohr JA, Cefalo R, Curtis P. National assessment of physicians’ breastfeeding knowledge, attitudes, training, and experience. JAMA. 1995;273:472–6.
Corrigan P, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44(2):162–79.
Shore TH, Tashchian A, Adams JS. Development and validation of a scale measuring attitudes toward smoking. J Soc Psychol. 2000;140(5):615–23.
Nash M. Mental health nurses' diabetes care skills - a training needs analysis. Br J Nurs. 2009;18(10):626–30. https://doi.org/10.12968/bjon.2009.18.10.42472 .
Quinn C, Happell B, Browne G. Opportunity lost? Psychiatric medications and problems with sexual function: a role for nurses in mental health. J Clin Nurs. 2011;21:415–23. https://doi.org/10.1111/j.1365-2702.2011.03908.x .
Ford P, Tran P, Keen B, Gartner C. Survey of Australian oral health practitioners and their smoking cessation practices. Aust Dent J. 2015;60:43–51.
Morris C, Waxmonsky J, May M, Giese A, Martin L. Smoking cessation for persons with mental illness: a toolkit for mental health providers: University pf Colorado Denver, CO; 2009. Accessed 19 Mar 2019: https://www.integration.samhsa.gov/Smoking_Cessation_for_Persons_with_MI.pdf
Watson L, Oberle K, Deutscher D. Development and psychometric testing of the Nurses' attitudes toward obesity and obese patients scale (NATOOPS). Res Nurs Health. 2008;31(6):586–93. https://doi.org/10.1002/nur.20292 .
Lasater K. Clinical judgment development: using simulation to create an assessment rubric. J Nurs Educ. 2007;46(11):496–503. https://doi.org/10.1097/NND.0000000000000209 .
Download references
Acknowledgements
The study was partly funded as part of the CUBIC Capability, Capacity and Cultural Change project funded by Nursing and Midwifery Office (NaMO) New South Wales
‘The funding body played no part in the in the design of the study, collection, analysis, interpretation of data, and in writing the manuscript.’
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files] and, where applicable data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and affiliations.
Professor Mental Health Nursing, Centre for Applied Nursing Research (CANR), Western Sydney University, Sydney, Australia
Geoffrey L. Dickens, Cheryl Waters, Evan Atlantis & Bronwyn Everett
South West Sydney Local Health District, Sydney, Australia
Geoffrey L. Dickens
Division of Mental Health Nursing and Counselling, Abertay University, Dundee, Scotland
You can also search for this author in PubMed Google Scholar
Contributions
GLD conceived of and designed the study. GLD, RI, CW, EA, BE contributed to acquisition of data, analysis and interpretation of data. GLD, RI, CW, EA, BE contributed to drafting the manuscript or revising it critically for important intellectual content. GLD, RI, CW, EA, BE gave final approval of the version to be published. GLD, RI, CW, EA, BE agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Geoffrey L. Dickens .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Table S1. Example PICO-style electronic literature search. Example literature search (DOCX 13 kb)
Additional file 2:
Table S2. Controlled intervention evaluation study quality assessment. Study Quality Assessment (controlled intervention study) (DOCX 13 kb)
Additional file 3:
Table S3. Cross-sectional, observational studies quality assessment (adapted from National Heart, Lung, and Blood Institute [ 26 ]. Study Quality Assessment (Cross-sectional and observational studies) (DOCX 16 kb)
Additional file 4:
Table S4. Longitudinal uncontrolled intervention study quality assessment. Study Quality Assessment (uncontrolled intervention studies) (DOCX 14 kb)
Additional file 5:
Table S5. Qualitative study quality assessment. Study Quality Assessment. (Qualitative studies) (DOCX 14 kb)
Additional file 6:
Table S6. Outcome measure content and quality assessment. Quality assessment of outcomes measures used in studies. (DOCX 25 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Dickens, G.L., Ion, R., Waters, C. et al. Mental health nurses’ attitudes, experience, and knowledge regarding routine physical healthcare: systematic, integrative review of studies involving 7,549 nurses working in mental health settings. BMC Nurs 18 , 16 (2019). https://doi.org/10.1186/s12912-019-0339-x
Download citation
Received : 30 October 2018
Accepted : 01 April 2019
Published : 26 April 2019
DOI : https://doi.org/10.1186/s12912-019-0339-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health nurses
- Emergency medicine
- Deteriorating patient
- Educational interventions
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Psychiatric-Mental Health Nursing Research Paper Topics

This page provides a comprehensive list of psychiatric-mental health nursing research paper topics , which serves as a crucial resource for nursing students assigned to write research papers. The field of psychiatric-mental health nursing is vast, encompassing a wide variety of topics related to mental health care. This extensive list has been carefully curated to include a diverse range of topics divided into ten distinct categories, making it easier for students to find a subject of interest and relevance to their studies. In addition to the list of topics, the page also includes a detailed article discussing the significance of psychiatric-mental health nursing and the various aspects it covers. Additionally, the page offers information on iResearchNet’s writing services, providing an opportunity for students to order custom-written research papers if needed. Ultimately, this page serves as a one-stop resource for students, aiding them in selecting a topic, understanding the importance of psychiatric-mental health nursing, and, if necessary, ordering a custom research paper.
100 Psychiatric-Mental Health Nursing Research Paper Topics
The field of psychiatric-mental health nursing is incredibly diverse, providing a wide range of research opportunities. Understanding the various aspects of psychiatric-mental health nursing is crucial for providing comprehensive care to patients with mental health issues. This section provides a comprehensive list of psychiatric-mental health nursing research paper topics, categorized into ten different areas of focus. These topics are carefully selected to cover the most pertinent issues and trends in the field, encouraging students to explore and contribute to the existing body of knowledge.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
Understanding Mental Health Disorders
- The role of genetic factors in the development of schizophrenia.
- The impact of childhood trauma on adult mental health.
- The relationship between anxiety disorders and cardiovascular diseases.
- The link between depression and chronic pain.
- The effect of sleep disorders on mental health.
- The role of nutrition in managing mental health disorders.
- The impact of substance abuse on mental health.
- The relationship between personality disorders and criminal behavior.
- The role of social support in managing bipolar disorder.
- The impact of post-traumatic stress disorder on quality of life.
Psychopharmacology in Mental Health Nursing
- The effectiveness of antidepressants in managing major depressive disorder.
- The side effects of antipsychotic medications.
- The role of mood stabilizers in managing bipolar disorder.
- The impact of benzodiazepines on cognitive function.
- The effectiveness of non-pharmacological interventions in managing anxiety disorders.
- The role of psychostimulants in managing attention deficit hyperactivity disorder (ADHD).
- The impact of medication adherence on treatment outcomes in schizophrenia.
- The role of pharmacogenomics in personalized treatment of mental health disorders.
- The effectiveness of electroconvulsive therapy in treatment-resistant depression.
- The impact of polypharmacy on treatment outcomes in elderly patients with mental health disorders.
Therapeutic Communication in Mental Health Nursing
- The impact of therapeutic communication on patient outcomes in mental health care.
- The role of non-verbal communication in building therapeutic relationships with patients.
- The effectiveness of motivational interviewing in substance abuse treatment.
- The impact of active listening on patient satisfaction and adherence to treatment.
- The role of empathy in mental health nursing.
- The effectiveness of group therapy in managing social anxiety disorder.
- The impact of family therapy on the mental health of adolescents.
- The role of cognitive-behavioral therapy in managing depression.
- The effectiveness of dialectical behavior therapy in managing borderline personality disorder.
- The impact of psychoeducation on the management of schizophrenia.
Mental Health Promotion and Prevention
- The role of school-based mental health programs in preventing adolescent depression.
- The effectiveness of community-based mental health promotion programs.
- The impact of workplace mental health promotion programs on employee well-being.
- The role of physical activity in preventing mental health disorders.
- The effectiveness of mindfulness-based stress reduction in preventing anxiety and depression.
- The impact of social support on the prevention of mental health disorders.
- The role of early intervention programs in preventing the development of psychosis.
- The effectiveness of suicide prevention programs in reducing suicide rates.
- The impact of anti-stigma campaigns on public attitudes towards mental health.
- The role of primary care providers in mental health promotion and prevention.
Legal and Ethical Issues in Mental Health Nursing
- The impact of involuntary hospitalization on the mental health of patients.
- The role of advanced directives in mental health care.
- The effectiveness of mental health courts in reducing recidivism rates.
- The impact of confidentiality breaches on the therapeutic relationship.
- The role of informed consent in mental health care.
- The effectiveness of restraint and seclusion in managing aggressive behavior.
- The impact of medication refusal on treatment outcomes.
- The role of ethics committees in resolving ethical dilemmas in mental health care.
- The effectiveness of de-escalation techniques in managing aggressive behavior.
- The impact of legal and ethical issues on the role of the mental health nurse.
Mental Health Nursing Across the Lifespan
- The impact of developmental stages on the mental health of individuals.
- The role of mental health nursing in the care of children and adolescents.
- The effectiveness of mental health interventions for older adults.
- The impact of life transitions on mental health.
- The role of mental health nursing in the care of pregnant and postpartum women.
- The effectiveness of mental health interventions for individuals with intellectual disabilities.
- The impact of aging on mental health.
- The role of mental health nursing in the care of individuals with dementia.
- The effectiveness of mental health interventions for adolescents with eating disorders.
- The impact of end-of-life care on the mental health of patients and their families.
Cultural Competence in Mental Health Nursing
- The impact of cultural competence on patient satisfaction and outcomes in mental health care.
- The role of cultural competence in building therapeutic relationships with patients from diverse backgrounds.
- The effectiveness of culturally tailored interventions in managing mental health disorders.
- The impact of language barriers on access to mental health care.
- The role of cultural competence in the assessment and diagnosis of mental health disorders.
- The effectiveness of cultural competence training for mental health professionals.
- The impact of cultural beliefs and practices on mental health.
- The role of cultural competence in the prevention of mental health disorders.
- The effectiveness of culturally adapted cognitive-behavioral therapy in managing depression.
- The impact of cultural competence on the delivery of mental health services to immigrant and refugee populations.
Psychiatric-Mental Health Nursing in Various Settings
- The role of mental health nursing in primary care settings.
- The effectiveness of mental health nursing interventions in acute care settings.
- The impact of mental health nursing on patient outcomes in long-term care settings.
- The role of mental health nursing in community mental health services.
- The effectiveness of mental health nursing interventions in correctional facilities.
- The impact of mental health nursing on patient outcomes in home health care.
- The role of mental health nursing in school-based mental health services.
- The effectiveness of mental health nursing interventions in emergency departments.
- The impact of mental health nursing on patient outcomes in psychiatric hospitals.
- The role of mental health nursing in substance abuse treatment centers.
Technological Advances in Mental Health Nursing
- The impact of telepsychiatry on access to mental health care in rural areas.
- The role of electronic health records in improving the quality of mental health care.
- The effectiveness of online support groups in managing mental health disorders.
- The impact of mobile applications on medication adherence in patients with mental health disorders.
- The role of virtual reality in the treatment of phobias.
- The effectiveness of online cognitive-behavioral therapy in managing anxiety disorders.
- The impact of teletherapy on patient satisfaction and outcomes in mental health care.
- The role of technology in enhancing communication between mental health professionals and patients.
- The effectiveness of online psychoeducation in the management of bipolar disorder.
- The impact of technology on the role of the mental health nurse.
Emerging Trends in Psychiatric-Mental Health Nursing
- The impact of the COVID-19 pandemic on the mental health of healthcare workers.
- The role of psychiatric-mental health nurses in addressing the opioid crisis.
- The effectiveness of trauma-informed care in managing post-traumatic stress disorder.
- The impact of the integration of mental health and primary care services on patient outcomes.
- The role of psychiatric-mental health nurses in addressing the mental health needs of LGBTQ+ populations.
- The effectiveness of peer support in the management of mental health disorders.
- The impact of climate change on mental health.
- The role of psychiatric-mental health nurses in addressing the mental health needs of immigrant and refugee populations.
- The effectiveness of mindfulness-based interventions in managing stress and burnout among mental health professionals.
- The impact of social media on mental health.
The psychiatric-mental health nursing field offers a vast array of research opportunities, as evident from the extensive list of topics provided above. These topics encompass various aspects of mental health care, from understanding mental health disorders to exploring the ethical and legal considerations in psychiatric-mental health nursing. It is crucial for students and professionals in the field to engage in research to contribute to the advancement of knowledge and improvement of mental health care. This list of psychiatric-mental health nursing research paper topics serves as a starting point for students to explore and contribute to this vital field of nursing.
The Range of Psychiatric-Mental Health Nursing Research Paper Topics
Psychiatric-mental health nursing is a specialized field of nursing that is dedicated to promoting mental health through the assessment, diagnosis, and treatment of mental health disorders and conditions. This field of nursing is incredibly important, as mental health disorders are prevalent and can have a significant impact on individuals’ overall health and well-being. According to the World Health Organization, approximately one in four people in the world will be affected by mental or neurological disorders at some point in their lives. This staggering statistic underscores the critical need for skilled psychiatric-mental health nurses who can provide comprehensive and compassionate care to individuals with mental health needs.
The significance of psychiatric-mental health nursing is multifaceted. First and foremost, psychiatric-mental health nurses play a crucial role in providing care and support to individuals with mental health disorders. They are often the first point of contact for individuals seeking help for mental health issues and play a key role in the assessment and diagnosis of mental health disorders. Psychiatric-mental health nurses also develop and implement treatment plans, provide psychoeducation to patients and their families, and offer support and counseling. Additionally, they play a vital role in crisis intervention and the management of acute mental health episodes.
Furthermore, psychiatric-mental health nurses also play a critical role in promoting mental health and preventing mental health disorders. They work in a variety of settings, including community mental health centers, schools, and primary care clinics, where they provide mental health education and promote strategies for maintaining good mental health. Additionally, psychiatric-mental health nurses often work in interdisciplinary teams, collaborating with other healthcare professionals, such as psychiatrists, psychologists, and social workers, to provide comprehensive care to individuals with mental health needs.
Various aspects of psychiatric-mental health nursing offer a wide range of psychiatric-mental health nursing research paper topics. One critical area of focus is mental health assessment. This involves the evaluation of an individual’s mental health status through the use of various assessment tools and techniques. Research in this area might explore the validity and reliability of different mental health assessment tools, the impact of cultural differences on mental health assessment, or the development of new assessment tools and techniques.
Another important aspect of psychiatric-mental health nursing is treatment and intervention strategies. This encompasses a wide range of approaches, from psychopharmacology to psychotherapy to lifestyle interventions. Psychiatric-mental health nursing research paper topics in this area might include the effectiveness of different treatment approaches for specific mental health disorders, the impact of treatment adherence on treatment outcomes, or the development of new intervention strategies.
The role of the psychiatric-mental health nurse is another crucial aspect of this field. Psychiatric-mental health nurses have a unique set of skills and competencies that enable them to provide comprehensive care to individuals with mental health needs. Research topics in this area might explore the impact of nurse-patient relationships on treatment outcomes, the role of psychiatric-mental health nurses in interdisciplinary teams, or the development of new competencies and skills for psychiatric-mental health nurses.
In addition to these areas, there are many other aspects of psychiatric-mental health nursing that offer a wealth of research opportunities. For example, legal and ethical issues in psychiatric-mental health nursing, the role of technology in mental health care, and the mental health needs of specific populations, such as the elderly, children, or individuals with co-occurring disorders, are all important areas of focus.
Overall, the field of psychiatric-mental health nursing offers a wide range of research opportunities. From mental health assessment to treatment and intervention strategies to the role of the psychiatric-mental health nurse, there are numerous psychiatric-mental health nursing research paper topics to explore. Engaging in research in this field is crucial for the advancement of knowledge and the improvement of mental health care for individuals around the world.
In conclusion, psychiatric-mental health nursing is a vital field that plays a crucial role in promoting mental health and providing care and support to individuals with mental health needs. The various aspects of psychiatric-mental health nursing offer a wide range of psychiatric-mental health nursing research paper topics, from mental health assessment to treatment and intervention strategies to the role of the psychiatric-mental health nurse. Engaging in research in this field is essential for advancing knowledge and improving mental health care worldwide.
iResearchNet’s Custom Writing Services
iResearchNet is a leading provider of custom writing services, designed to assist students in achieving academic excellence. Our team of expert writers is committed to providing top-quality academic papers, tailored to meet your specific requirements. Whether you need help with a research paper, essay, dissertation, or any other academic assignment, iResearchNet is here to provide you with the support you need.
Features of iResearchNet’s Writing Services
- Expert Degree-Holding Writers: Our team consists of highly qualified writers, each holding a minimum of a Master’s degree in their respective fields. This ensures that your paper is written by an expert with a deep understanding of your subject matter.
- Custom Written Works: Each paper is crafted from scratch, according to your specific instructions. This ensures that your paper is unique, original, and tailored to your requirements.
- In-depth Research: Our writers conduct thorough research on each topic, using a variety of reliable sources. This ensures that your paper is well-researched, accurate, and comprehensive.
- Custom Formatting: Your paper will be formatted according to your preferred style guide, whether it is APA, MLA, Chicago/Turabian, or Harvard. This ensures that your paper meets the specific formatting requirements of your institution.
- Top Quality: We are committed to providing top-quality work. Each paper is carefully reviewed by our quality assurance team to ensure that it meets our high standards.
- Customized Solutions: We understand that each student has unique needs. Therefore, we offer customized solutions to meet your specific requirements. Whether you need a paper written from scratch, editing and proofreading services, or assistance with a specific part of your paper, we are here to help.
- Flexible Pricing: We offer flexible pricing options to suit your budget. Our prices are competitive, and we provide a detailed price quote upfront, with no hidden fees.
- Short Deadlines up to 3 hours: We understand that sometimes you may need your paper urgently. We offer short deadlines up to 3 hours for certain types of assignments.
- Timely Delivery: We are committed to delivering your paper on time, every time. You can count on us to meet your deadline.
- 24/7 Support: Our customer support team is available 24/7 to assist you with any questions or concerns you may have. You can contact us via phone, email, or live chat.
- Absolute Privacy: We respect your privacy and take all necessary measures to protect your personal information. Your personal details will never be shared with any third party.
- Easy Order Tracking: Our user-friendly online platform allows you to easily track the progress of your order. You can also communicate directly with your writer through our messaging system.
- Money-Back Guarantee: We are confident in the quality of our services. However, if you are not satisfied with the final product, we offer a money-back guarantee.
iResearchNet is committed to providing top-quality writing services to help students achieve academic success. Our expert degree-holding writers, custom written works, in-depth research, and custom formatting ensure that your paper is of the highest quality. Our customized solutions, flexible pricing, and short deadlines cater to your specific needs. With our timely delivery, 24/7 support, absolute privacy, easy order tracking, and money-back guarantee, you can have complete peace of mind when you choose iResearchNet for your academic writing needs.
Secure Your Success with iResearchNet
Are you feeling overwhelmed by the multitude of assignments and deadlines looming over your head? You are not alone. Many nursing students struggle to find the time and resources necessary to complete their psychiatric-mental health nursing research papers. That’s where iResearchNet comes in. We are here to provide you with top-quality, custom-written research papers that will not only help you to achieve your academic goals but also to deepen your understanding of psychiatric-mental health nursing.
Our team of expert writers is highly qualified and experienced in the field of psychiatric-mental health nursing. They are adept at conducting in-depth research and creating comprehensive, well-structured, and meticulously referenced research papers. When you order a custom research paper from iResearchNet, you can be confident that you are receiving a paper of the highest quality, tailored to your specific requirements and formatted according to your preferred style guide.
Submitting a high-quality research paper is crucial for your academic success. It demonstrates your understanding of the subject matter, your ability to conduct thorough research, and your skill in organizing and presenting information in a clear and coherent manner. A well-crafted research paper can significantly impact your final grade and your future career prospects in the field of psychiatric-mental health nursing. Don’t take chances with your academic and professional future. Trust iResearchNet to provide you with the top-quality research paper you need to succeed.
Take the First Step Towards Your Success
Don’t wait until the last minute to start your psychiatric-mental health nursing research paper. Take the first step towards your academic success by ordering a custom research paper from iResearchNet today. Our user-friendly online platform makes it easy to place your order, and our 24/7 customer support team is always here to assist you with any questions or concerns you may have. With our absolute privacy policy, you can be assured that your personal information will be kept confidential. And with our money-back guarantee, you can have complete peace of mind knowing that your satisfaction is our top priority. Invest in your future by choosing iResearchNet for your academic writing needs.
ORDER HIGH QUALITY CUSTOM PAPER

‘Marathon of crisis’: Nurses’ mental health in forefront of new study
By Tim Brouk, [email protected]

A new Purdue University College of Health and Human Sciences study reveals the stress, psychological trauma and, at times, system failures, that occurred in healthcare facilities during the COVID-19 pandemic as reported by the frontline critical-care nurses themselves.
The research project, “Nurses’ Psychological Trauma and Cognitive Control in the COVID-19 Pandemic,” surveyed more than 100 nurses around the United States and Canada, including several Purdue School of Nursing alumni. The questionnaire covered vital mental health topics such as depression, anxiety, PTSD, and drug and alcohol use during the height of the pandemic.
“Nurses have gone through incredible psychological distress and trauma,” said Karen Foli, associate professor of nursing and co-principal investigator on the project with Department of Psychological Sciences assistant professor Yu-Chin Chiu. “They’re not soldiers; they are professional nurses who were put in extraordinary situations that sometimes overwhelmed them on a chronic basis.”

Yu-Chin Chiu
Funded by the College of Health and Human Sciences’ Rapid Response Grant program , the research results were published in the Journal of Advanced Nursing . A second paper from this study will concentrate on nurses’ ability to complete cognitive control tasks after experiencing COVID-19-related trauma. This study is still ongoing. Lingsong Zhang, associate professor in the Department of Statistics and Regenstrief Center for Healthcare Engineering, is also a co-investigator on this research.
Foli paid particular attention to the responses to a pair of open-ended questions in the survey. Not all nurses responded but more than 70 participants filled out at least one, which allowed them to pour out their experiences during their shifts and at home.
“They talked about this tsunami of death, just this wave upon wave,” Foli said. “Often the patients would die alone or only with the nurse at the bedside, and that was a major contributor to secondary traumatic stress on the nurse.”
The qualitative data “puts muscle on the bones” of the quantitative data collected by Foli and Chiu. The narratives and themes reveal what can be done to improve the mental health of these vital nurses as well as the care of patients during the next pandemic. One nurse’s long response inspired Foli to call nurses’ experiences during the pandemic a “marathon of crisis.”
Foli shared some of this unidentified nurse’s response: “The hospital did not have enough critical care-trained nurses to care for the amount of patients we were seeing. I agreed to help, despite the fact that I had a 6-month-old baby at home. My very first shift at the sister hospital, I had three intubated, sedated, paralyzed, prone, unstable patients.”
“The nurses were concerned about getting their family sick,” Foli said. “They would isolate themselves, which would compound what they were experiencing. Their peers also began to provide less support, further exacerbating the trauma they were experiencing.”
One recurring problem reported by the nurses was the shortage of personal protective equipment (PPE) at the beginning of the pandemic. This unfortunate phenomenon made headlines , but Foli said it was an issue before the first COVID-19 cases began rolling in. She coined the phrase “insufficient resource trauma” in a paper published pre-pandemic in the Archives of Psychiatric Nursing (Foli, Reddick, Zhang, & Krcelich, 2020).
The nurses in the study reported another grave issue surrounding insufficient resources: lack of staffing. Foli said due to many hospitals losing money during the pandemic — a decrease in elective surgeries, for example — nursing corps are being short-staffed. Anecdotal reports in daily professional newsletters describe open positions not being filled or departments in need of more nurses being denied.
“That’s the worst thing they could do,” Foli said. “If true, it’s a very uninformed, bad call in my opinion. … Nurses are seen as a cost instead of an income generator. I think if they are going to be short-sighted about nurse-staffing, they need to realize that nurses aren’t going to be able to render the quality care patients need.”
Nurses weren’t the only health workers to experience trauma during the pandemic. Doctors, EMTs and other staff all experienced the brunt of the historic event, but Foli said nurses had especially trying times because they were at the bedside 24/7.
“Those folks who think the pandemic is over, they have to understand what nurses went through,” Foli said. “We need to give them resources in the form of mental health support, not just in the short term, and we need make sure it’s accessible and trauma-informed.”
With Foli and Chiu’s research, other research, and the American Nurses Association Enterprise COVID-19 Well-Being Initiative , there is growing awareness of the mental health and well-being of nurses. The work could help bolster the ranks of the nursing corps, too. According to a May 2021 McKinsey Global Institute study , 22% of nurses polled said they are thinking of leaving their current position. These initiatives could encourage nurses to stay in their profession.
Hannah McKinney’s (NUR ‘20) career has been parallel with the pandemic. At Eskenazi Hospital in downtown Indianapolis, she was a student tech in March 2020 when the first COVID-19 patients began trickling in. She was hired immediately after her May graduation as a nurse in the ER trauma unit. By then, the COVID-19 patients far exceeded the patients who needed lifesaving treatments from crashes, shootings or stabbings.

Hannah McKinney (NUR ’20) has treated COVID-19 patients for her entire young career so far. Photo provided
McKinney said she still suffers from the trauma she experienced during her first few months at Eskenazi. The patient deaths, the unknown variables of the new coronavirus and the often-changing guidelines from the Centers for Disease Control and Prevention weighed heavily on the young nurse and her colleagues. A near breaking point occurred when PPE namely N95 masks, became scarce for her and her fellow nurses. They had to make their lone N95 mask last for a month at least.
“That’s when it stated to feel almost apocalyptic. Are we being led to our deaths basically?” McKinney remembered. “It got to the point where I stopped going to the grocery store because I would have a really hard time whenever I saw a person wearing an N95, thinking I’m not allowed. I’m going into situations where I could get sick because I wasn’t allowed access to a new N95. It just felt very isolating and lonely.”
McKinney reports that conditions are better now than they were the first few months of the pandemic. Much more is now known as she has started to assist in intubating patients again during the delta variant surge. However, reading about experiences from fellow nurses across the country on social media has helped her mental well-being. She knows she is not alone and there is help out there for her and her colleagues.

Kaley Butler credits her colleagues for helping her persevere as an ICU COVID-19 nurse in Mishawaka, Indiana. Photo provided
“COVID is still so defeating,” McKinney said. “But every time I would see a post on Facebook or something from another nurse’s perspective, to see my experiences expressed by someone else so that others can hear it, I think that’s so impactful and so helpful.”
Kaley Butler (NUR ’20) was hired at an ICU in Mishawaka, just a few months before COVID-19 terrorized northeast Indiana. Like McKinney, she suffered mentally and physically in 2020 due to the overwhelming number of patients, lack of PPE, understaffing and emotions of family members not being able to see their sick loved ones. She credits her colleagues as the reason she returns to work every shift. Support from fellow nurses helps Butler to soldier through as they now battle the COVID-19 delta variant.
“My mindset during the delta variant is to just keep pushing to get through it. I try to look at the positives — like how we know more about how to treat the virus,” Butler said. “Keeping that in mind along with knowing that my coworkers have my back is what keeps me going back to work.”
Nursing Perspectives in Mental Health and Psychiatric Disorders in All Patients
Loading... Editorial Frontiers in Psychology Nursing Perspectives in Mental Health and Psychiatric Disorders in All Patients Elsa Vitale , Selmin Köse and Yun-Chen Chang 829 views 0 citations
Loading... Original Research 24 April 2023 Depression and quality of life among Macau residents in the 2022 COVID-19 pandemic wave from the perspective of network analysis Tong Leong Si , 13 more and Yu-Tao Xiang 2,478 views 3 citations
Loading... Original Research 24 February 2023 Social support mediates the relationship between illness perception and psychosocial adaptation among young and middle-aged kidney transplant recipients in China Na Hu , 1 more and Tiantian Chang 2,062 views 4 citations
Original Research 23 February 2023 Why do pregnant women with fear of birth prefer vaginal birth? A qualitative study in China Tieying Zeng , 3 more and Ke Zhang 2,067 views 0 citations
Loading... Original Research 06 January 2023 The quality of life in patients with multiple sclerosis – Association with depressive symptoms and physical disability: A prospective and observational study Aleksandra Kołtuniuk , 2 more and Justyna Chojdak-Łukasiewicz 3,544 views 4 citations
Loading... Original Research 22 December 2022 The role of parents in the care for adolescents suffering from emotional and behavioral problems Jaroslava Mackova , 4 more and Sijmen A. Reijneveld 4,301 views 3 citations
- Open access
- Published: 24 April 2024
Association between body mass index and mental health among nurses: a cross-sectional study in China
- Bonan Luan ORCID: orcid.org/0000-0003-2703-3390 1 ,
- Xueyan Tian ORCID: orcid.org/0000-0002-7933-5844 2 ,
- Chao Wang ORCID: orcid.org/0000-0001-6097-7719 2 ,
- Ming Cao ORCID: orcid.org/0009-0001-4858-838X 2 &
- Dongmei Liu ORCID: orcid.org/0000-0003-1822-7580 2
BMC Health Services Research volume 24 , Article number: 506 ( 2024 ) Cite this article
Metrics details
To examine the correlation between body mass index (BMI) and mental well-being in Chinese nurses during the COVID-19 epidemic.
This study was conducted in a tertiary hospital using a cross-sectional design. A total of 2,811 nurses were enlisted at Shengjing Hospital in China during the period from March to April, 2022. Information was gathered through a questionnaire that individuals completed themselves. The mental health of the participants was assessed using the Patient Health Questionnaire-9 and the Generalized Anxiety Disorder Assessment-7. Binary logistic regression was used to calculate adjusted odds ratios (ORs) and their corresponding 95% confidence intervals.
The prevalence of nurses experiencing depression and anxiety was 7.8% (219) and 6.7% (189), respectively. Regarding depression after adjustment, the odds ratios (ORs) for each quartile, compared to the lowest quartile, were as follows: 0.91 (95% confidence interval [CI]: 0.53, 1.56), 2.28 (95% CI: 0.98, 3.77), and 2.32 (95% CI: 1.41, 3.83). The p-value for trend was found to be 0.001. The odds ratios (ORs) for anxiety after adjustment were 2.39 (0.83, 4.36), 4.46 (0.51, 7.93), and 2.81 (1.56, 5.08) when comparing the highest quartiles to the lowest quartile. The p -value for trend was 0.009.
This study found a positive association between BMI and poor mental health among nurses during the COVID-19 pandemic, particularly in those who were overweight or obesity. The findings could assist in developing interventions and help policy-makers establish appropriate strategies to support the mental health of frontline nurses, especially those who are overweight or obesity.
Peer Review reports
Introduction
Depression and anxiety are the most common mental health illnesses worldwide [ 1 ]. Depression is a mood disorder that affects an individual’s thoughts and feelings and leads to persistent feelings of sadness and disinterest [ 2 ]. Anxiety is a group of mental disorders characterized by nervousness, apprehension, and fear [ 3 ]. Depression and anxiety disorders are major contributors to the mental health burden of adults [ 4 ]. Poor mental health often affects regular activities and probably results in poor professional performance. Given the detrimental effects of depression and anxiety on physical and mental health, it is important to explore the relevant factors, and to thereby contribute toward preventing the development of mental health disorders [ 5 ].
According to the National Institute of Health of America, body mass index (BMI) is a measure that defines individuals as underweight, normal weight, or overweight, that is calculated using their weight and height [ 6 ]. Recent research indicates that high BMI and obesity continue to relentlessly increase globally, with approximately two billion people being overweight or obese [ 7 ]. In a meta-analysis including 57 prospective studies and 900,000 adults, they found that above 25 kg/m 2 , positive associations between BMI and cardiovascular disease, hypertension, diabetes mellitus, stroke, and cancer were recorded in both sexes. Moreover, each 5 kg/m 2 higher BMI was associated with about 30% higher overall mortality [ 8 ]. Obesity-related diseases have become the fifth leading cause of death worldwide [ 9 ].
A systematic review and meta-analysis on the longitudinal relationship between BMI and mental health, they found that obesity at baseline increased the risk of onset of depression and the unadjusted ORs were 1.55 (including 15 included studies and 58,745 participants) [ 10 ]. Moreover, another meta-analysis of 8 Mendelian randomization studies indicated that obesity is a causal risk factor for elevated risk of depression (OR = 1.33) [ 11 ]. Previous studies also demonstrate a bi-directional relationship between obesity and mental health [ 12 ]. Although these existing studies address the issue of obesity and mental health, none of these studies address this issue among nurses.
As nurses fulfill an essential role among healthcare workers, they experienced a particularly high occupational burden during the peak of coronavirus disease (COVID-19) pandemic [ 13 ]. In a multi-center cross-sectional online survey, among 395 healthcare workers, there were 42.28% and 56.2% were found to have depression, and anxiety during the COVID-19 pandemic, respectively [ 14 ]. A recent study conducted in 2020 from China shows that nurses experienced more unfavorable mental health outcomes than other healthcare workers during the pandemic [ 15 ]. Furthermore, for nurses, poor mental health may influence not only themselves but also their professional performance and the quality of the health care provided, even affecting patient safety [ 16 , 17 ]. A growing body of evidence suggests that individuals with changes in BMI have experienced deteriorating symptoms, such as isolation, anxiety and depression as a result of the COVID-19 pandemic compared to previous timepoints. The increasing obesity rates may have modestly increased the prevalence of depressive symptoms in the general population [ 18 ]. However, there is currently no data to explore the association between BMI and mental health among nurses during the COVID-19 pandemic. To fill this gap, we conducted a large cross-sectional study to explore the association between BMI and mental health among nurses in China during the COVID-19 pandemic.
Study design
The present cross-sectional investigation was carried out at a Chinese hospital throughout the period from March 2022 to April 2022. The survey was conducted by the nursing department, and it included a total of 3,450 nurses who were employed at the hospital. In the end, a grand total of 2,811 individuals supplied valid and useful responses, leading to an effective response rate of 81.49%. An ensemble of web-based surveys that individuals completed themselves was utilized. Participants successfully filled out a well-organized questionnaire within a time frame of 20 to 25 min. Figure 1 provides a visual representation of the specific information using a flow chart.
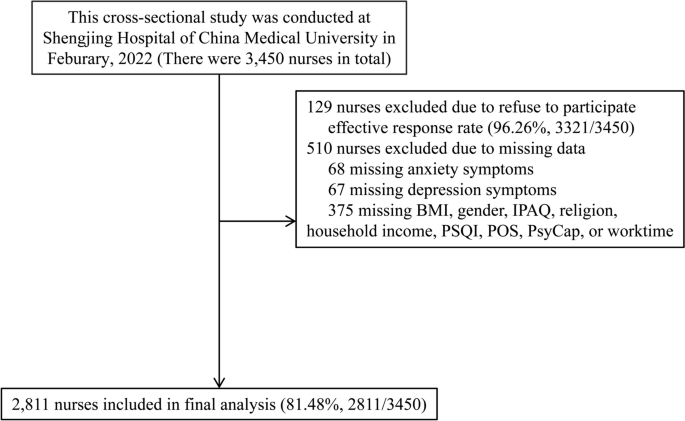
Flowchart of this study
The Ethics Committee of Shengjing Hospital Affiliated China Medical University granted ethical permission (2022PS753K). All participants provided written informed consent. The procedures were carried out in accordance with the ethical guidelines outlined in the 1975 Declaration of Helsinki.
Inclusion and exclusion criteria
The criteria for inclusion were as follows: nurses who were currently employed in hospitals and actively working. The study employed the following exclusion criteria: nurses who had engaged in employment for less than three months or had not completed the psychological questionnaire in its whole were disqualified.
Measurement of covariates characteristics
This study gathered data from the nursing staff on various aspects, including demographic characteristics, dietary habits, life-related factors, work-related factors, experienced important life events, history of physical sickness, exposure to the COVID-19 pandemic, and psychological assessments.
The demographic data encompassed age, gender, and body mass index (BMI), which was self-reported by the participants and measured in kg/m 2 . The individual's dietary habits encompassed their smoking status, alcohol consumption patterns, and coffee consumption patterns. Smoking behavior was classified into three categories: current smokers (those who smoked at least one cigarette per day and had done so for at least six months), former smokers (those who had stopped smoking for at least six months), and non-smokers. Alcohol and coffee consumption patterns are classified into three categories: current drinkers (those who use alcohol or coffee at least once a day and have been doing so for at least six months), former drinkers (those who have stopped consuming alcohol or coffee for at least six months), and non-drinkers (those who do not consume alcohol or coffee).
Life-related factors encompassed various aspects such as sleep quality (measured by PSQI, Pittsburgh Sleep Quality Index scores), physical activity (assessed using IPAQ, International Physical Activity Questionnaire, in terms of Mets × hour/week), religious affiliation, marital status, presence of siblings, monthly household income (in RMB, yuan), occurrence of major life events, history of chronic disease, and frequency of visiting friends.The researchers evaluated the level of physical activity (PA) in the past week using the abbreviated version of the International Physical Activity Questionnaire [ 19 ]. The Pittsburgh sleep quality index (PSQI) [ 20 ] was used to assess sleep quality.
Work-related variables including employment, field of expertise, weekly working hours, and night shifts. Exposure to the COVID-19 pandemic pertains to nurses who may come into touch with patients suspected or confirmed to have COVID-19, or find themselves in a situation that necessitates COVID-19 quarantine.
Measurements of psychological variates
The level of organization support was measured using the Chinese version of the Perceived Organization Support Questionnaire (POS) [ 21 ]. The Cronbach's α coefficient for POS was 0.921. The Chinese version of the 24-item Psychological Capital Questionnaire (PCQ) [ 22 , 23 ] was used to assess PsyCap. The Cronbach's α coefficients for self-efficacy, hope, resilience, and optimism were 0.921, 0.936, 0.920, and 0.900, respectively.
Measurement of depression and anxiety
The assessment of depressive symptoms was conducted using clinically validated measures, specifically the PHQ09 [ 24 ]. The PHQ09 scale consists of nine items, each with a 4-point Likert-type scale answer. These responses indicate the frequency of individuals' feelings during the preceding two weeks, ranging from 0 to 3. The cumulative score spans from 0 to 27, with a higher value denoting a greater intensity of depression symptoms. A PHQ09 score of 10 or more was used to determine the presence of serious depression.
The Chinese version of the GAD07 [ 25 ] was used to assess anxiety symptoms. The GAD07 questionnaire comprises 7 items, with each item being responded to on a 4-point Likert-type scale ranging from 0 (indicating never) to 3 (indicating always). A greater score indicates a higher level of anxiety symptoms. A GAD07 standardized score of 10 or higher was used to characterize the presence of significant anxiety symptoms. The Cronbach's α coefficients for the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) were 0.951 and 0.928, respectively.
Sample size calculation
The confidence level (1-α) was 0.95; the proportion of main outcome (depression and anxiety) was 0.1; The confidence interval width (two sided) was 0.03. The confidence interval formula was Exact (Clopper-Pearson); the 2-tailed P value was 0.05. The sample size was 1,603. It was calculated by PASS 11.0 (Power Analysis and Sample Size 11.0, NCSS Inc., USA) [ 8 , 10 , 18 ].
Statistical analysis
The data were analyzed using SPSS 22.0 for Windows, developed by SPSS Inc. in Chicago, IL, USA. The continuous variables were reported as the median together with the interquartile range. The categorical variables were presented as the count (proportion). Discrete sets of data that are neither related or dependent on each other. The mean of two continuous variables that follow a normal distribution was compared using the Student's t-test. The Mann–Whitney U test was employed to compare the average values of two continuous variables that do not follow a normal distribution. On the other hand, the χ2 test or Fisher's exact test were utilized for categorical variables.
The quartiles were determined by categorizing the BMI values of all participants depending on their distribution, and these quartiles were then utilized for subsequent research. The study investigated the association between quartile categories of BMI and the presence of poor mental health, specifically depression and anxiety, using binary unconditional logistic regression analysis. The dependent variable in this study was the individual's mental health state, whereas the independent variable was their BMI. The crude odds ratio (OR) was calculated using crude data, and model 1 was further modified for age and gender. Model 2 further accounted for baseline variables that were deemed clinically significant or had a p -value < 0.10 in the univariate analysis. These variables included alcohol consumption, sleep quality, number of siblings, experience of major life events, frequency of visiting friends, years of employment, duration of work hours, psychological characteristics related to depression, age, physical activity, marital status, history of chronic disease, specialty, and psychological characteristics related to anxiety. The Model 3 was modified to account for all baseline variables. Adjusted OR and their corresponding 95% confidence intervals (95% CI) were calculated using binary unconditional logistic regression, taking into account any confounding factors. The study examined the presence of a linear trend by analyzing the median value of each quartile as a continuous variable. All P values were calculated using a two-tailed test, and the observed difference was considered statistically significant when the P value was less than 0.05.
A total of 2,811 nurses were ultimately enrolled in the study, with a median age of 35 years and a median BMI of 21.83 kg/m 2 . Female participants constituted the majority (94.20%). Out of the total, 69.9% (1,965) of the nurses had a normal weight, 6.3% (177) were underweight, 19.9% (558) were overweight, and 3.9% (111) were obese. The occurrence of depression and anxiety among nurses was 7.8% (219 out of 2,811) and 6.7% (189 out of 2,811), respectively; see details in Table 1 (the distribution of characters by outcome status) and supplementary Table 1 ( the distribution of characters by BMI status ) .
Participants with elevated BMI, impaired sleep quality, and diminished scores in perceived organizational support, efficacy, hope, resiliency, and optimism exhibited an increased likelihood of developing depression, as indicated by the univariate analysis. A greater proportion of individuals with depression exhibited concurrent alcohol consumption, had siblings, encountered significant life events, had infrequent social interactions with friends, had employment tenure exceeding five years, and worked in excess of 40 h per week. Individuals who were older, had a higher BMI, experienced poor sleep quality, engaged in lower levels of weekly physical activity, and had lower scores in perceived organizational support, efficacy, hope, resiliency, and optimism were found to have a higher likelihood of developing anxiety. A greater proportion of individuals with anxiety engaged in marriage or cohabitation, had siblings, experienced significant life events, had a background of chronic illnesses, had infrequent social interactions with friends, had a job history exceeding five years, worked for more than 40 h per week, and were employed in the surgical department. The factors stated above exhibited statistical significance in the univariate analysis, as shown in detail in Table 1 .
In order to investigate the correlation between BMI and depression, the BMI was divided into four categories based on quartiles. In comparison to the lowest quartile, the odds ratios (ORs) for the other quartiles were as follows: 0.91 (0.53, 1.56), 2.28 (0.98, 3.77), and 2.32 (1.41, 3.83) after making adjustments. Additionally, the p-value for the trend was found to be 0.001. In relation to anxiety, the odds ratios (ORs) for each quartile were as follows: 2.39 (0.83, 4.36), 4.46 (0.51, 7.93), and 2.81 (1.56, 5.08) after adjusting for other factors. Furthermore, there was a significant trend with a p -value of 0.009. Refer to the comprehensive information provided in Table 2 . We also did sensitivity analysis by excluding participants who were underweight (BMI < 18.5) and only including participants who exposed to the COVID-19 pandemic, these results were consistent with the main outcome; see details in supplementary Tables 2 and 3 .
Obesity is a major contributor to morbidity and mortality. However, no existing study has focused on the relationship between BMI and mental health among nurses during COVID-19 pandemic. Therefore, we performed a cross-sectional study on a large population of nurses in China. This study showed a positive association between BMI and poor mental health (anxiety and depression) among Chinese nurses during the COVID-19 pandemic, particularly in those who were overweight or obesity.
In line with this, A systematic review and meta-analysis on the longitudinal relationship between BMI and mental health, they found that obesity at baseline increased the risk of onset of depression and the unadjusted ORs were 1.55 (including 15 included studies and 58,745 participants) [ 10 ]. Another population-based cross-sectional study enrolled 4,361 Iranian healthcare staff; their results indicate that abdominal obesity was significantly associated with anxiety among females but not among males. It is worth noting that in the current study, most participants were female. At the same time, no significant association was discovered between abdominal obesity and psychological distress in either gender. There was, however, a weak positive association between BMI and depression [ 26 ]. Further, a meta-analysis reviewed 25 prospective studies and provided solid evidence of the link between obesity and depression, indicating a bi-directional relationship between BMI and depression [ 27 ]. A possible mechanism is the adoption of an unhealthy lifestyle, such as insufficient physical exercise and unhealthy dietary preferences, possibly leading to obesity [ 27 ].
The exact underlying pathophysiological mechanism between being overweight and poor mental health is unknown. It has been shown that immune inflammation disorder plays an essential role in mental health disorders such as depression and anxiety. Moreover, a high BMI status can lead to many pro-inflammatory factors in the peripheral circulation system crossing the blood–brain barrier, subsequently inducing depressive-like behaviors. In such cases, the risk of depression and anxiety gradually increases [ 28 , 29 ]. The association between obesity and disorders such as depression and anxiety may also be explained by hypothalamic–pituitary–adrenal (HPA) axis disorder, leptin, or microbial mechanisms [ 30 , 31 , 32 , 33 , 34 , 35 ]. The obesity might involve HPA-axis dysregulation and HPA-axis dysregulation is also well known to be involved in depression. Through HPA axis dysregulation, obesity might cause development to depression. Leptin play an important role in the signaling pathway of glutamatergic neurons for regulating depression-related behaviors, suggesting a possible association between synaptic depression and behavioral manifestations of depression. Depression is associated with decreased gut microbiota richness and diversity. Fecal microbiota transplantation from depressed patients to microbiota-depleted rats can induce behavioural and physiological features characteristic of depression in the recipient animals, including anhedonia and anxiety-like behaviours, as well as alterations in tryptophan metabolism. This suggests that the gut microbiota may play a causal role in the development of features of depression.
While this study provides interesting insights, it is important to acknowledge its various limitations. First, since this study is cross-sectional, there is a concern for reverse causation, where mental health problems may contribute to increased BMI. Future studies with a longitudinal framework are warranted to address this issue. Second, the data were gathered by self-reported questionnaires, specifically pertaining to measurements such as height and weight. It is important to note that this method may be susceptible to recall bias. In addition, given that the majority of the study sample consists of young women, there is a possibility that they may be tempted to falsely report their height and weight. Therefore, this social desirability bias is another limitation of this study. Third, it is important to note that the GAD-7 and PHQ-9 are screening questionnaires that lack the ability to provide clinical diagnosis. This limitation may have had an impact on the outcomes of our study. However, this study is the first to examine the connection between BMI and mental health in nurses during the COVID-19 epidemic while accounting for several influential factors.
Availability of data and materials
No datasets were generated or analysed during the current study.
Naser AY, Alwafi H, Amara NA, et al. Epidemiology of depression and anxiety among undergraduate students. Int J Clin Pract. 2021;75(9):e14414.
Article PubMed Google Scholar
Durisko Z, Mulsant BH, Andrews PW. An adaptationist perspective on the etiology of depression. J Affect Disord. 2015;172:315–23.
Amu H, Osei E, Kofie P, et al. Prevalence and predictors of depression, anxiety, and stress among adults in Ghana: a community-based cross-sectional study. PLoS ONE. 2021;16(10):e0258105.
Article CAS PubMed PubMed Central Google Scholar
mhGAP: Mental Health Gap Action Programme: Scaling Up Care for Mental, Neurological and Substance Use Disorders. Geneva: World Health Organization; 2008.
Salari N, Khazaie H, Hosseinian-Far A, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18(1):100.
Article PubMed PubMed Central Google Scholar
Weir CB, Jan A. BMI Classification Percentile And Cut Off Points. In: In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
Google Scholar
Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes (Lond). 2008;32(Suppl 3):S56–9.
Prospective Studies Collaboration, Whitlock G, Lewington S, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96.
Article PubMed Central Google Scholar
Lopez-Jimenez F. Speakable and unspeakable facts about BMI and mortality. Lancet. 2009;373(9669):1055–6.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–9.
Jokela M, Laakasuo M. Obesity as a causal risk factor for depression: systematic review and meta-analysis of mendelian randomization studies and implications for population mental health. J Psychiatr Res. 2023;163:86–92.
Hruby A, Lieberman HR, Smith TJ. Symptoms of depression, anxiety, and post-traumatic stress disorder and their relationship to health-related behaviors in over 12,000 US military personnel: bi-directional associations. J Affect Disord. 2021;283:84–93.
Phillips CS, Becker H, Gonzalez E. Psychosocial well-being: an exploratory cross-sectional evaluation of loneliness, anxiety, depression, self-compassion, and professional quality of life in oncology nurses. Clin J Oncol Nurs. 2021;25(5):530–8.
Nayak BS, Sahu PK, Ramsaroop K, Maharaj S, Mootoo W, Khan S, Extravour RM. Prevalence and factors associated with depression, anxiety and stress among healthcare workers of Trinidad and Tobago during COVID-19 pandemic: a cross-sectional study. BMJ Open. 2021;11(4):e044397.
Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976.
Maharaj S, Lees T, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of australian nurses. Int J Environ Res Public Health. 2018;16(1):61.
Abbas A, Al-Otaibi T, Gheith OA, et al. Sleep quality among healthcare workers during the COVID-19 pandemic and its impact on medical errors: Kuwait experience. Turk Thorac J. 2021;22(2):142–8.
J Devoe D, Han A, Anderson A, Katzman DK, Patten SB, Soumbasis A, Flanagan J, Paslakis G, Vyver E, Marcoux G, Dimitropoulos G. The impact of the COVID-19 pandemic on eating disorders: a systematic review. Int J Eat Disord. 2023;56(1):5–25.
Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Article CAS PubMed Google Scholar
Eisenberger R, Stinglhamber F, Vandenberghe C, et al. Perceived supervisor support: contributions to perceived organizational support and employee retention. J Appl Psychol. 2002;87(3):565–73.
Avey JB, Luthans F, Smith RM, et al. Impact of positive psychological capital on employee well-being over time. J Occup Health Psychol. 2010;15(1):17–28.
Wu S, Xu Z, Zhang Y, et al. Relationship among psychological capital, coping style and anxiety of Chinese college students. Riv Psichiatr. 2019;54(6):264–8.
PubMed Google Scholar
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Heidari-Beni M, Azizi-Soleiman F, Afshar H, et al. Relationship between obesity and depression, anxiety and psychological distress among Iranian health-care staff. East Mediterr Health J. 2021;27(4):327–35.
Kasen S, Cohen P, Chen H, Must A. Obesity and psychopathology in women: a three decade prospective study. Int J Obes (Lond). 2008;32(3):558–66.
Valkanova V, Ebmeier KP, Allan CL. CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2013;150(3):736–44.
Amer SAAM, Fouad AM, El-Samahy M, et al. Mental stress, anxiety and depressive symptoms and interleuken-6 level among healthcare workers during the COVID-19 pandemic. J Prim Care Community Health. 2021;12:21501327211027430.
Wang P, Loh KH, Wu M, et al. A leptin-BDNF pathway regulating sympathetic innervation of adipose tissue. Nature. 2020;583(7818):839–44.
Guo M, Lu Y, Garza JC, et al. Forebrain glutamatergic neurons mediate leptin action on depression-like behaviors and synaptic depression. Transl Psychiatry. 2012;2(2):e83.
Martin KA, Mani MV, Mani A. New targets to treat obesity and the metabolic syndrome. Eur J Pharmacol. 2015;763(Pt A):64–74.
Kelly JR, Borre Y, O’ Brien C, et al. Transferring the blues: depression-associated gut microbiota induces neurobehavioural changes in the rat. J Psychiatr Res. 2016;82:109–18.
Choi KW, Kim YK, Jeon HJ. Comorbid anxiety and depression: clinical and conceptual consideration and transdiagnostic treatment. Adv Exp Med Biol. 2020;1191:219–35.
Rosmond R, Dallman MF, Björntorp P. Stress-related cortisol secretion in men: relationships with abdominal obesity and endocrine, metabolic and hemodynamic abnormalities. J Clin Endocrinol Metab. 1998;83(6):1853–9.
CAS PubMed Google Scholar
Download references
Acknowledgements
We give special thanks to all the colleagues of Shengjing Hospital for their help and support. We thank International Science Editing ( http://www.internationalscienceediting.com ) for editing this manuscript. The authors would like to thank all of the study participants.
Conflict of interest
There is no conflict of interest.
This study was financially supported by The 345 Talent Project of Shengjing Hospital (grant number: N/A).
These sponsors had no role in the study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and affiliations.
Department of Operating Room, Shengjing Hospital of China Medical University, Shenyang, P.R. China
Department of Urology, Shengjing Hospital of China Medical University, 36 Sanhao Street, Shenyang, Liaoning, 110004, P.R. China
Xueyan Tian, Chao Wang, Ming Cao & Dongmei Liu
You can also search for this author in PubMed Google Scholar
Contributions
B.L and M.C had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. D.L and M.C: Protocol/project development. B.L, C.W, X. T, M.C, and D.L: Data collection or management. B.L, C.W, and X.T: Data analysisBonan Luan: Manuscript writing/editing.
Corresponding author
Correspondence to Dongmei Liu .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval (2022PS753K) was offered by the Ethics Committee of Shengjing hospital Affiliated China Medical University. All informed consent of these patients in this study has been obtained. The research program is in line with the ethical guidelines of the 1975 Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Luan, B., Tian, X., Wang, C. et al. Association between body mass index and mental health among nurses: a cross-sectional study in China. BMC Health Serv Res 24 , 506 (2024). https://doi.org/10.1186/s12913-024-11006-y
Download citation
Received : 31 January 2024
Accepted : 18 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12913-024-11006-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Best Nursing Research Topics for Students
What is a nursing research paper.
- What They Include
- Choosing a Topic
- Best Nursing Research Topics
- Research Paper Writing Tips

Writing a research paper is a massive task that involves careful organization, critical analysis, and a lot of time. Some nursing students are natural writers, while others struggle to select a nursing research topic, let alone write about it.
If you're a nursing student who dreads writing research papers, this article may help ease your anxiety. We'll cover everything you need to know about writing nursing school research papers and the top topics for nursing research.
Continue reading to make your paper-writing jitters a thing of the past.
A nursing research paper is a work of academic writing composed by a nurse or nursing student. The paper may present information on a specific topic or answer a question.
During LPN/LVN and RN programs, most papers you write focus on learning to use research databases, evaluate appropriate resources, and format your writing with APA style. You'll then synthesize your research information to answer a question or analyze a topic.
BSN , MSN , Ph.D., and DNP programs also write nursing research papers. Students in these programs may also participate in conducting original research studies.
Writing papers during your academic program improves and develops many skills, including the ability to:
- Select nursing topics for research
- Conduct effective research
- Analyze published academic literature
- Format and cite sources
- Synthesize data
- Organize and articulate findings
About Nursing Research Papers
When do nursing students write research papers.
You may need to write a research paper for any of the nursing courses you take. Research papers help develop critical thinking and communication skills. They allow you to learn how to conduct research and critically review publications.
That said, not every class will require in-depth, 10-20-page papers. The more advanced your degree path, the more you can expect to write and conduct research. If you're in an associate or bachelor's program, you'll probably write a few papers each semester or term.
Do Nursing Students Conduct Original Research?
Most of the time, you won't be designing, conducting, and evaluating new research. Instead, your projects will focus on learning the research process and the scientific method. You'll achieve these objectives by evaluating existing nursing literature and sources and defending a thesis.
However, many nursing faculty members do conduct original research. So, you may get opportunities to participate in, and publish, research articles.
Example Research Project Scenario:
In your maternal child nursing class, the professor assigns the class a research paper regarding developmentally appropriate nursing interventions for the pediatric population. While that may sound specific, you have almost endless opportunities to narrow down the focus of your writing.
You could choose pain intervention measures in toddlers. Conversely, you can research the effects of prolonged hospitalization on adolescents' social-emotional development.
What Does a Nursing Research Paper Include?
Your professor should provide a thorough guideline of the scope of the paper. In general, an undergraduate nursing research paper will consist of:
Introduction : A brief overview of the research question/thesis statement your paper will discuss. You can include why the topic is relevant.
Body : This section presents your research findings and allows you to synthesize the information and data you collected. You'll have a chance to articulate your evaluation and answer your research question. The length of this section depends on your assignment.
Conclusion : A brief review of the information and analysis you presented throughout the body of the paper. This section is a recap of your paper and another chance to reassert your thesis.
The best advice is to follow your instructor's rubric and guidelines. Remember to ask for help whenever needed, and avoid overcomplicating the assignment!
How to Choose a Nursing Research Topic
The sheer volume of prospective nursing research topics can become overwhelming for students. Additionally, you may get the misconception that all the 'good' research ideas are exhausted. However, a personal approach may help you narrow down a research topic and find a unique angle.
Writing your research paper about a topic you value or connect with makes the task easier. Additionally, you should consider the material's breadth. Topics with plenty of existing literature will make developing a research question and thesis smoother.
Finally, feel free to shift gears if necessary, especially if you're still early in the research process. If you start down one path and have trouble finding published information, ask your professor if you can choose another topic.

The Best Research Topics for Nursing Students
You have endless subject choices for nursing research papers. This non-exhaustive list just scratches the surface of some of the best nursing research topics.
1. Clinical Nursing Research Topics
- Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties.
- Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings.
- Explore the effectiveness of pain management protocols in pediatric patients.
2. Community Health Nursing Research Topics
- Assess the impact of nurse-led diabetes education in Type II Diabetics.
- Analyze the relationship between socioeconomic status and access to healthcare services.
3. Nurse Education Research Topics
- Review the effectiveness of simulation-based learning to improve nursing students' clinical skills.
- Identify methods that best prepare pre-licensure students for clinical practice.
- Investigate factors that influence nurses to pursue advanced degrees.
- Evaluate education methods that enhance cultural competence among nurses.
- Describe the role of mindfulness interventions in reducing stress and burnout among nurses.
4. Mental Health Nursing Research Topics
- Explore patient outcomes related to nurse staffing levels in acute behavioral health settings.
- Assess the effectiveness of mental health education among emergency room nurses .
- Explore de-escalation techniques that result in improved patient outcomes.
- Review the effectiveness of therapeutic communication in improving patient outcomes.
5. Pediatric Nursing Research Topics
- Assess the impact of parental involvement in pediatric asthma treatment adherence.
- Explore challenges related to chronic illness management in pediatric patients.
- Review the role of play therapy and other therapeutic interventions that alleviate anxiety among hospitalized children.
6. The Nursing Profession Research Topics
- Analyze the effects of short staffing on nurse burnout .
- Evaluate factors that facilitate resiliency among nursing professionals.
- Examine predictors of nurse dissatisfaction and burnout.
- Posit how nursing theories influence modern nursing practice.
Tips for Writing a Nursing Research Paper
The best nursing research advice we can provide is to follow your professor's rubric and instructions. However, here are a few study tips for nursing students to make paper writing less painful:
Avoid procrastination: Everyone says it, but few follow this advice. You can significantly lower your stress levels if you avoid procrastinating and start working on your project immediately.
Plan Ahead: Break down the writing process into smaller sections, especially if it seems overwhelming. Give yourself time for each step in the process.
Research: Use your resources and ask for help from the librarian or instructor. The rest should come together quickly once you find high-quality studies to analyze.
Outline: Create an outline to help you organize your thoughts. Then, you can plug in information throughout the research process.
Clear Language: Use plain language as much as possible to get your point across. Jargon is inevitable when writing academic nursing papers, but keep it to a minimum.
Cite Properly: Accurately cite all sources using the appropriate citation style. Nursing research papers will almost always implement APA style. Check out the resources below for some excellent reference management options.
Revise and Edit: Once you finish your first draft, put it away for one to two hours or, preferably, a whole day. Once you've placed some space between you and your paper, read through and edit for clarity, coherence, and grammatical errors. Reading your essay out loud is an excellent way to check for the 'flow' of the paper.
Helpful Nursing Research Writing Resources:
Purdue OWL (Online writing lab) has a robust APA guide covering everything you need about APA style and rules.
Grammarly helps you edit grammar, spelling, and punctuation. Upgrading to a paid plan will get you plagiarism detection, formatting, and engagement suggestions. This tool is excellent to help you simplify complicated sentences.
Mendeley is a free reference management software. It stores, organizes, and cites references. It has a Microsoft plug-in that inserts and correctly formats APA citations.
Don't let nursing research papers scare you away from starting nursing school or furthering your education. Their purpose is to develop skills you'll need to be an effective nurse: critical thinking, communication, and the ability to review published information critically.
Choose a great topic and follow your teacher's instructions; you'll finish that paper in no time.

Joleen Sams is a certified Family Nurse Practitioner based in the Kansas City metro area. During her 10-year RN career, Joleen worked in NICU, inpatient pediatrics, and regulatory compliance. Since graduating with her MSN-FNP in 2019, she has worked in urgent care and nursing administration. Connect with Joleen on LinkedIn or see more of her writing on her website.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

- 1.866.411.2159
- Online Master’s Degrees Overview
- Master’s in Applied Behavior Analysis
- Online Master of Science in Product Management
- Online Master of Science in Nursing
- Online Master of Social Work
- Online Doctoral Degrees Overview
- Online BSN to Doctor of Nursing Practice
- Online MSN to Doctor of Nursing Practice
- Online Certificate Programs Overview
- Online ABA Certificate
- Online Introduction to Product Management Certificate
- Online Nursing Certificate Programs
- About Regis College
- Corporate Partners Tuition Discount
- Federal Employee Program
- Military & Veterans Tuition Discount Program
- Faculty Directory
Evidence-Based Practice in Nursing for Mental Health Nurses
March 8, 2023
View all blog posts under Articles | View all blog posts under Doctor of Nursing Practice | View all blog posts under Master of Science in Nursing

The nursing profession has long taken the lead in practicing evidence-based care. Evidence-based care relies on nurses’ clinical expertise, critical thinking, and research knowledge. Nurses use this skill set to support patient care decisions and as a lens through which to view patient outcomes.
Evidence-based practice in nursing may be even more crucial for mental health nurse practitioners . Mental and behavioral health disorders are complex, as patients may suffer from two or more diagnoses. Additionally, patients may be homeless or incarcerated, making treatment even more difficult.
An advanced degree program that supplies a rigorous background in evidence-based practice is essential for any nurse planning a career in mental and behavioral health.
What Are Evidence-Based Mental Health Services?
Evidence-based mental health services recognize that patients don’t just need therapeutic care; they may also suffer from loss of housing and income, among other basic needs. They may live in high-crime areas and are more likely to be incarcerated. Evidence-based mental health services often combine psychiatric and therapeutic treatment with services that include helping patients find housing, employment, and other support.
The following are some examples of evidence-based practices and treatments supported by SAMHSA. Mental health nurses engaged in evidence-based nursing practice may employ these treatments to support individuals dealing with mental and behavioral health issues.
Assertive Community Treatment (ACT)
Assertive community treatment seeks to provide behavioral health services in the community setting. The framework serves conditions such as schizophrenia, bipolar disorder, and depression. ACT services seek to maintain outpatient treatments and ensure regular, ongoing therapies.
Using the framework, various health care practitioners provide services such as assistance with activities of daily living (ADL), help managing family responsibilities, and support in securing important needs such as food and housing.
Integrated Treatment for Co-Occurring Disorders
Integrated treatment delivers dual treatments for patients diagnosed with behavioral health and substance abuse disorders. By combining the two services, patients usually have a better chance of making a full, long-term recovery.
Practitioners provide patients with services and resources such as case management, outreach, housing, and employment assistance. The framework aids the high-risk dual diagnoses population, who are more likely to relapse and resume substance use, suffer from poor health, or face homelessness.
Illness Management and Recovery (IMR)
Illness management and recovery is an evidence-based psychiatric treatment framework for patients with a severe mental illness, such as schizophrenia. It’s designed to allow patients to participate actively in their own recoveries. During ongoing weekly sessions, behavioral health practitioners help patients develop treatment plans and identify goals. This may encompass teaching recovery methodologies, behavioral health facts, and stress management techniques.
Practitioners also teach patients how to build and maintain social support networks, reduce the chances of resuming drug use, and use prescribed medications effectively. The teaching techniques of this framework might also include cognitive behavioral therapy and motivational sessions.
Permanent Supportive Housing
Homelessness is a complex challenge in treating people with mental health and substance use disorders. Not only can homelessness worsen a patient’s mental health condition, but it also makes them physically vulnerable to violence, disease, and incarceration. According to SAMHSA, the longer a person experiences homelessness, the harder it is to get them the treatment they need. The agency recommends moving people to permanent housing, with additional support services including therapy, treatment, financial support, and training services, without requiring transitional steps such as getting sober first.
Screening for Postpartum Depression
A study in BMC Psychiatry found nearly 20% of mothers experience postpartum depression, which can impact the health of the mother and the child. Screening and treating pregnant mothers for perinatal depression (depression during pregnancy) can help reduce instances of postpartum depression and in some cases improve the physical and mental health of babies.
Additional Treatments for Mental and Behavioral Health
Many mental health treatment practices are evidence-based and numerous studies have reinforced their effectiveness. Some of the most common evidence-based techniques for treating mental health, behavioral health, and substance use include:
- Cognitive behavioral therapy (CBT) , helps patients change patterns of behavior.
- Dialectical behavior therapy (DBT) , is based on CBT practices, while also focusing on emotion regulation and mindfulness, among other techniques. It is shown to be effective in treating various mental health disorders.
- Motivational interviewing , uses open questions, affirmations, reflection, and summarizing to help people overcome substance use disorders.
Some therapies are not considered evidence-based, even though they may be popular and effective, such as:
- 12-step programs : Alcoholics Anonymous (AA) pioneered the 12-step process. Some aspects of 12-step programs can be very effective in helping individuals deal with substance use.
- Talk therapy : A traditional form of therapy, talk therapy is widely used on its own and in conjunction with other treatments.
The Role of Doctors of Nursing Practice (DNPs) in Evidence-Based Practice
In the United States, more Doctor of Nursing Practice (DNP) programs are emerging to fill the anticipated shortage of health care talent. The nation needs these professionals to fill the service gaps faced by underserved populations in settings such as rural communities, schools, prisons, and urgent care facilities.
DNP-educated nurses are well-positioned to bring the evidence-based nursing practice to the communities they serve. With their background in research and clinical practice, they can lead the establishment of evidence-based plans and criteria at hospitals, clinics, and government agencies.
Become a Leader in Evidence-Based Nursing
Are you eager to become a leader in the field of mental health nursing? The Regis College online MSN to Doctor of Nursing Practice program offers an excellent foundation in evidence-based nursing practice, equipping you with the tools to embrace the exciting challenges of delivering best-in-class mental and behavioral health services. The curriculum includes classes in advanced research, informatics and statistics, cultural perspectives in health care, and more. Explore your options and take your first steps to make a difference in nursing.
Recommended Reading
What Is a Psychiatric Mental Health Nurse Practitioner?
How Nurse Practitioners Can Become Community Advocates
10 Best Practices to Promote Cultural Awareness in the Nursing Profession
Behavioral Health Resources, “PACT: Program for Assertive Community Treatment”
BMC Psychiatry , “Screening Programs for Common Maternal Mental Health Disorders Among Perinatal Women: Report of the Systematic Review of Evidence”
Frontiers in Psychiatry, “Effects of Illness Management and Recovery: A Multicenter Randomized Controlled Trial”
Psychology Today , “From Evidence-Based Practice to Practice-Based Evidence”
THERAPlatform, “ Evidence-Based Practices for Mental Health”
Substance Abuse and Mental Health Services Administration, “ About the Evidence-Based Practices Resource Center”
Substance Abuse and Mental Health Services Administration, “The Case for Screening and Treatment of Co-Occurring Disorders”
Substance Abuse and Mental Health Services Administration. “Homelessness Resources: Housing and Shelter”
U.S. Department of Health & Human Services, “Mental Health Myths and Facts”
Let’s move forward
Wherever you are in your career and wherever you want to be, look to Regis for a direct path, no matter your education level. Fill out the form to learn more about our program options or get started on your application today.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Nurses’ Work-Related Mental Health in 2017 and 2020—A Comparative Follow-Up Study before and during the COVID-19 Pandemic
Cicilia nagel.
1 Division of Occupational and Environmental Medicine, Department of Laboratory Medicine, Lund University, 22184 Lund, Sweden
2 Division of Public Health, Kristianstad University, 29128 Kristianstad, Sweden
Kerstin Nilsson
Associated data.
Not applicable.
The COVID-19 pandemic put a lot of strain on healthcare organizations. Nurses account for over 50% of healthcare staff, and how nurses perform in their work is influenced by a number of human and work environmental factors. However, to our knowledge, there has not been a previous study with the intention to look at all areas that affect a sustainable working life and how these impact nurses’ mental well-being. The aim of this study is to investigate the association between, and the effect of, different factors in nurses’ work situations associated with nurses’ work-related mental-health diagnoses, before and during the COVID-19 pandemic. A questionnaire was sent out to all 9219 nurses in the Swedish county of Skane in the spring of 2017 and during wave two of the COVID-19 pandemic in the fall of 2020. The data were analyzed through logistic regression analysis. The results showed that lack of joy in the daily work, an increased workload and lack of support from co-workers had an increased association with work-related mental-health diagnoses. Future research regarding the long-term impact of COVID-19 on all areas of nurses’ professional and personal lives is needed.
1. Introduction
Healthcare workers around the world, primarily the nurses, were on the frontline of the Coronavirus pandemic that started in 2019 [ 1 ]. The second wave of the pandemic in Sweden occurred during the fall/winter 2020, the most serious wave of the pandemic regarding the burden on the healthcare sector. The pandemic has been described as a gigantic strain experiment on healthcare organizations, especially on healthcare staff due to exposure to hazards, such as psychological distress, fatigue, and trauma [ 1 , 2 , 3 , 4 , 5 ]. Healthcare workers had to perform their duties and face higher risks to their own health, such as the risk of infection [ 1 ]. Many nurses were afraid to become ill and die of COVID-19, which was incredibly stressful [ 6 ].
Nurses comprise half of the global health workforce [ 7 , 8 ]; however, for much of the general public, it is not fully understood what nurses do. Being a nurse includes promoting health, preventing illness as well as caring for people who are ill, disabled and dying. Advocating patients’ rights, promoting a safe environment, conducting and/or taking part in research and education are also key nursing roles [ 9 ]. Nurses are often the first healthcare staff that the patient encounters. Their roles may vary depending on workplace, but often include triage, early recognition of life-threatening conditions, administration of medications, performance of life-saving procedures and initiation of early referral [ 7 ]. Despite nurses being a common profession in healthcare, there is an increasing demand for nurses worldwide [ 8 ]. According to the World Health Organization (WHO) [ 7 ], one out of six of the world’s nurses are expected to retire in the next 10 years. Several countries experienced a lack of healthcare workers prior to the pandemic and many nurses are considering leaving the profession [ 10 ]. There is a serious nursing shortage in most European countries, which is insufficient to meet current healthcare demands [ 11 , 12 ]. Due to an ageing population, healthcare demands are predicted to increase, resulting in an estimated worldwide shortage of almost 6 million nurses by 2035 [ 7 ]. The ageing segment of the population is rapidly expanding and, thus, consuming more health services. Unfortunately, fewer new nurses are entering the work force; therefore, providing a healthy work environment to retain nurses in their workplace is essential for sustaining the profession [ 13 ].
Being able to work has a significant positive impact on people’s health, and healthy workplaces are beneficial not only for employees but also for organizations and for society [ 14 ]. Decent work is one of the UN Global Goals for sustainable society development [ 15 ]. A sustainable work situation for employees is significant for a healthy organization that attracts people to work as well as promoting better health for employees, thus, also giving a better possibility for employability to an increased age [ 16 , 17 , 18 , 19 ]. Working in a hospital can be complicated due to the interaction between patients, nurses and the organization. This can, under normal circumstances, cause problematic work situations, but during the pandemic this was likely even more of a factor. It is, therefore, important to detect problems and shortcomings in the work situation in order to improve and support healthy and sustainable employability and understand what measures need to be taken. Areas of employability, and whether individuals can and want to work or not, has been stated as nine impact and determinant areas connected to sustainable healthy working life in the SwAge-model [ 6 , 16 , 17 , 18 , 19 ], i.e., (1) the employees self-rated health and diagnoses; (2) factors in the physical work environment; (3) factors in the mental work environment; (4) having time for recuperation within the employees’ working hours, breaks and work pace; (5) the personal financial situation; (6) the employees’ personal social environment outside of work; (7) the work social environment at the workplace, with leadership, colleagues, etcetera; (8) factors related to whether the employee experiences stimulation and motivation within work tasks and appreciation from the organization/work place regarding their performed tasks; (9) if the employees’ have the right competence, skills and possibility for knowledge development in work.
As earlier mentioned, nurses play a key role in delivering care to patients [ 11 ]. How the nurses perform in their work environment is influenced by a number of human and environmental factors, including the type of information available, work experience, ambiguity, unpredictability, conflicting goals and time pressure [ 20 ]. Nurses face a higher risk of developing negative mental states, such as depression, anxiety and stress [ 21 ], due to the nature of their work. Unlike depression, burnout is specific to an individual’s relationship to his or her occupation and usually results from long-term exposure to occupational stress [ 22 ]. Burnout may lead to adverse outcomes, such as medical errors, suicide, depression and absenteeism [ 23 , 24 ]. It is known that stress and burnout are factors that can contribute to a decreased mental health [ 10 , 25 ]. The ICN [ 26 ] states that long and stressful shifts severely impact nurses’ mental health, resulting in nurses leaving or planning to leave the profession. Stress and burnout were recognized internationally as work hazards for nurses even before the pandemic [ 27 ]. Some argue that burnout in itself is a form of mental illness. However, a more common assumption has been that burnout causes mental dysfunction, such as anxiety and depression [ 28 ]. Temporal, physical, emotional and mental workloads, as well as job stressors such as time pressure, have in previous studies been positively associated with negative stress and burnout symptoms [ 28 , 29 ]. Previous studies have stated that nurses’ work environments contribute to high stress, job dissatisfaction and burnout [ 30 , 31 ]. Additionally, a previous study also stated that healthcare professionals (HCPs) in hospitals engage in many work-related tasks and experience relatively high levels of mental stress while caring for patients [ 32 ], while another study showed that workload and work pressure have an impact on job outcomes and quality of care [ 33 ]. Problems within the nurses’ working environments are described as concerns over inadequate staffing, ability to provide safe care, working long hours with high levels of fatigue and a sense of not being valued or involved in decision-making processes concerning patients [ 34 , 35 , 36 ]. Mental ill health has, in previous studies, been associated with different factors, such as long hours worked, work overload and work pressure, lack of control over work, lack of participation in decision making, poor social support as well as poor support from managers and an unclear work role [ 10 , 28 , 37 ]. Repeated exposure to stressful patient-related situations makes nurses especially susceptible to stress-related outcomes, such as emotional exhaustion and post-traumatic stress disorder (PTSD) [ 38 ]. Stress-related outcomes in nurses can lead to grave consequences, including depression, lower job satisfaction, increased risk of medical errors, lower productivity and higher turnover intentions [ 28 ]. Ignoring the signs of anxiety and depression presented by nursing professionals could increase physical and emotional stress for the individual but could also result in low quality patient care and higher work burden on the organizations [ 18 ].
However, even though there are investigations into nurses’ stress related to health and work environment, to our knowledge, there are no previous investigations on nurses´ total work situation, i.e., that investigates all areas of impact and determination for a sustainable working life, before and during the COVID-19 pandemic. It is, therefore, important to investigate what effect the COVID-19 pandemic had on healthcare organizations’ impact and determinant areas associated with nurses´ work-related mental health diagnoses.
The objective of this present study is to investigate the association between work-related mental-health diagnoses and different factors in nurses’ work situations before and during the COVID-19 pandemic. We want to test the hypothesis that there are no differences in nurses’ work related mental-health diagnoses in 2017 and 2020. The specific research questions are:
- Is there a difference between 2017 and 2020 regarding nurses’ work-related mental health?
- What associations are there between nurses’ work-related mental health and their work situation in 2017?
- What associations are there between nurses’ work-related mental health and their work situation in 2020, that is, during the COVID-19 pandemic?
This study also wants to increase knowledge and suggest measures against staff shortages and future challenges in healthcare.
2. Materials and Methods
2.1. design.
This longitudional study is part of a greater research programme, “Sustainable working life for all ages” [ 19 , 39 ]. In the spring of 2017, a baseline survey was performed where links to an online survey were sent out to all healthcare staff in the Swedish Region of Skane via their work e-mail. The follow-up study was performed in the fall of 2020, where all healthcare staff who were employed in 2017 and that were still employed in 2020 were invited to partake in the online survey.
2.2. Study Population
A link to a web survey was sent out via work e-mail to all employees in the Healthcare sector in the Swedish region of Skane, that is to all physiotherapists, occupational therapists, doctors, psychologists, nurses (including specialties such as midwife, CRNA, O.R nurse), nurse aids, etc. In total, the link to the 2017 survey was sent out to 22,935 employees, out of which 11,902 completed the survey. In this study, we will look specifically at nurses. In 2017 there were 9219 nurses (including specialist nurses) employed in the region, out of which 4692 completed the survey (50.9%). Some of the reasons for not answering the survey were wrong e-mail address, absence from work, lack of time and concerns about the manager finding out what they wrote. In 2020, data was collected via web-survey from the same study group during the second Covid 19-pandemic wave in Sweden, i.e., from September to December. Again, all healthcare staff who were employed in 2017 and that were still employed in 2020 were invited by e-mail to partake in the study. The survey link was sent out to all 18,143 staff, out of which 7781 participants responded. The number of nurses completing the web survey in 2020 was 3107 (40.1%). Some of the reasons for not responding to the survey were the same as in 2017, but there were also many nurses who stated that they wanted to prioritize their work and some nurses that had left the region.
Of the 4692 participants in the 2017 survey, the median age of the participants was 48 (23–67) and among the 3107 participants in 2020 it was 52 (26–70). In 2017, 90.4% who answered the questionnaire were women and in 2020 that number was 90.5%. A large majority (54.1% vs. 59.4% respectively in 2017 and 2020) of participants had worked as nurses for more than 16 years.
2.3. Themes in the Analysis Model
The theoretical SwAge-model (sustainable working life for all ages) [ 17 , 18 , 19 ] was used as the theme areas in the analysis with the intention of investigating factors concerning the complexity of the nurses’ work situations that could relate to their mental diagnoses caused by their work life and work environment. The SwAge-model consists of nine different impact and determinant areas that are important for a healthy and sustainable working life for all ages, and the four spheres of determination regarding employability. These four spheres and the nine impact and determinant areas are:
- (1) Self-rated health, diagnoses and diverse physical and mental health functionality in work;
- (2) Physical work environment with unilateral movements, heavy lifting, risk of accidents, climate, chemical exposure and risk of contagion;
- (3) Mental work environment: stress and fatigue syndrome, threats and violence;
- (4) Working hours, work pace and possibility of recuperation during and between work shifts.
- (5) The personal financial situation’s effects on individuals’ needs and willingness to work. Issues with employability due to ill health and lack of support can jeopardize inclusion in working life and cause an inferior financial situation for the individual, e.g., through sick leave, unemployment and early retirement.
- (6) The effects of the personal social environment with family, friends and in the leisure context;
- (7) The social work environment with leadership, discrimination and the significance of the employment relationship context for individuals’ work.
- (8) Motivation, appreciation, satisfaction and stimulation when performing the work tasks;
- (9) Knowledge, skills, competence and competence development.
Seven out of the nine impact and determinate areas in the SwAge-model were used as independent variables in this investigation to analyze factors in the nurses’ work situation associated with work-related mental health diagnoses. The Health (1) area was used as the outcome/dependent variable in the analysis, i.e., mental health diagnoses caused by the work situation. However, the Personal finances (5) area was excluded since there were no data on the nurses’ private economic situation related to the work situation that could be used in the analysis.
2.4. Outcome Measures
The dependent variable was initially two individual statements: “I have a current diagnosis of exhaustion/stress” and “I have a current diagnosis of depression/anxiety”. These individual statements were put together into one variable regarding their work-related mental-health diagnoses as an outcome measure. The self-reported doctor’s diagnoses included in mental health were depression, anxiety, exhaustion and stress. The response options in the survey regarding diagnoses were taken from WHO’s ICD-10 codes.
The independent variables used in the univariate estimates and multivariate models were calculated using a categorical variable of diagnoses caused by work, i.e., mental health, as the outcome measures in association with the seven determinate areas for a healthy and sustainable worklife and employability in the SwAge-model that have been used in previous studies investigating factors associated to a sustainable working life (see above).
2.5. Questionns and Statments
The questionnaires were written in Swedish and contained 158 questions based on the SwAge-model that has been used in different investigations since 2004 [ 19 ]. However, in the questionnaire that was sent out in the second pandemic wave in 2020, additional questions about the COVID-19 situation were added. Some questions were simple yes/no questions and some were open answer questions where the participants could write freely. Most questions were designed as statements, a validated Lickert scale was used, and the participants had four answer options ranging from fully agree (1–2, i.e., Fully agree, partly agree) to fully disagree (3–4, i.e., partly disagree, fully disagree). The sample data was collected and handled by researcher KN. In the present study, 24 statements sorted into seven of the determinate areas of the SwAge-model were used.
2.6. Statistical Analyses
Logistic regression analysis was used to test models to predict categorial outcomes and to assess how well a predictor variable associates with a categorial dependent variable [ 40 ]. The material was analyzed with the IBM SPSS software, version 27. Data are presented as odds ratios (ORs) with their 95% confidence intervals (CIs). Questions with four answer options were dichotomized for clear distinction of the participants’ experiences. A multivariate analysis of variance (MANOVA) was performed comparing and testing the statistical significance of the multivariate sample mean differences to see which statements in the multivariate model saw the most increase between 2017 and 2020. Mental health was the dependent variable and the 24 statements in the seven impact and determinate areas were the independent variables. As with the logistic regression analysis, the MANOVA was analyzed with the IBM SPSS software, version 27.
2.6.1. Analyses within Each of the Seven Determinate Areas in the SwAge Analysis Model
Univariate logistic regression analysis was the first step to building multivariate models in each determinate area as well as for all determinate areas together. The univariate logistic regression analysis estimated for all statements within each of the seven determinate areas of the SwAge-model to investigate the association between the independent and the dependent variables. Initially, the associations for each statement were evaluated and the statements with p -values < 0.05, considered as the statistically significant level, were evaluated with other statements from the same determinate area. After this, the statements that continued to have a p -value < 0.05 were tested against the remaining statements one at a time. This continued for as long as the p -values for all included statements were <0.05.
2.6.2. Analyses including the Seven Determinate Areas in the SwAge Analysis Model
After the initial univariate analysis, a modulation was made for each determinate area in the SwAge-model. All the selected statements from the seven included determinate areas of the SwAge-model were analyzed in a logistical regression model. Thereafter, the analysis moved to step 2, where the statistically significantly statements ( p -values < 0.05) from each determinate area was added, one determinate area at a time. These statements were tested to form the final model. In step 3, the out-sorted statements from step 2 and from each of the seven determinate areas were added one at a time to test the robustness of the model [ 41 ]. The multivariate models were tested for collinearity.
2.7. Ethical Considerations
The study was performed in accordance with the Helsinki declaration [ 42 ] and Swedish laws [ 43 ]. The benefits the knowledge this study would generate was considered to outweigh the potential risks that the study could bring. Rules for the handling and storage of data was and will be followed in accordance with university policies as well as guidelines for handling sensitive data according to GDPR [ 44 ]. The study was approved by the Swedish Ethical Review Agency (number 2016/867 and 2020-01897).
3.1. Findings
There was an increase in diagnosis for both examined areas, i.e., exhaustion/stress and depression/anxiety between 2017 and 2020 (see Table 1 ). Of note, 128 nurses that previously reported no mental health diagnosis stated that they had been diagnosed with exhaustion/stress and/or depression/anxiety in 2020. In the logistic regression analysis, these diagnoses were combined into one variable: “mental health diagnoses”.
Percentage of nurses diagnosed with exhaustion/stress and/or depression/anxiety in 2017 and 2020.
3.2. Univariate Estimates and Multivariate Models for Work-Related Mental Health Diagnoses and Each of the Statements in the Analysed Areas
A logistic regression analysis was used to investigate which of the areas of importance for a healthy and sustainable work situation had the highest association with nurses’ work-related mental health diagnoses in 2017 and in the second wave of COVID-19 in 2020. The statements in each impact and determinate area were analyzed by area. There were seven impact and determinant areas included in the study, which were physical work environment (2); mental work environment (3); work pace, work time, recuperation (4); private social environment (6); work social environment, organization, leadership (7); motivation and satisfaction of and to work tasks (8); knowledge and competency (9).
In the impact and determinant area “physical work environment”, both included statements had a statistical association with nurses´ mental health diagnoses caused by their work for both 2017 and 2020 in the univariate estimates and in the multivariate model in 2017. However, the statement “For the most part I cannot cope with the physical work demands” also showed an association in the 2020 multivariate model.
All five statements in the impact and determinant area “Mental work environment” were statistically significant in the univariate estimates. In the 2017 multivariate model three statements were significant, which were “My work involves many psychologically heavy work tasks” (OR 1.78), “My work tasks usually clump together to the extent that I get frustrated” (OR 1.78) and “I wish for more opportunities to determine how to perform my work” (OR 1.60). In 2020, “My work tasks usually clump together to the extent that I get frustrated” (OR 2.05), “My work involves many psychologically heavy work tasks” (OR 1.76) and “I wish for greater control over my work (OR 1.75) showed significance.
All three of the investigated statements in the impact and determinant area “Work pace, work time, recuperation” showed an association in both the univariate estimates and the multivariate model for a healthy and sustainable working life.
In the impact and determinant area “Private social environment”, both statements were statistically significant in the univariate estimates of 2017. The statement “I need to work more at home/care for relatives and will probably therefore work less in the future” showed an association in the multivariate model of 2017, whereas the statement “I want to spend more time enjoying leisure activities and will therefore work less in the future” showed an association in both the univariate estimates and multivariate model of 2020.
The area “Work social environment, organization, leadership” consisted of six statements that all indicated an association in the univariate estimates of 2017 and 2020. In 2017, three statements showed significance, which were “Not having enough staff means that I cannot perform my work in the way I want” (OR 2.04), “Big changes in my work situation causes me to want to leave” (OR 1.41) and “The social community at my workplace does not make me want to stay” (OR 1.33). In 2020, only two statements showed significance, including “I do not feel I have enough support from my co-workers” (OR 3.14) and “Big changes in my work situation causes me to want to leave” (OR 1.73).
Similar to the previous determinant area, all statements in the impact and determinate area “Motivation and satisfaction of and to work tasks” indicated an association in the univariate estimates of both 2017 and 2020. However, only two statements showed association in the 2017 and 2020 multivariate models: “I do not experience joy in my daily work” and “I do not experience satisfaction in my daily work”.
The impact and determinant area “Knowledge and Competency” consisted of two statements that were both found to be statistically significant in the univariate estimates of 2017 and 2020, but only the statement “I do not feel like my competencies are being utilized in a satisfactory way” showed association with nurses’ work-related mental health diagnoses in the 2017 and 2020 multivariate model ( Table 2 ).
Univariate and multivariate variables 2017 and 2020. Univariate estimates and multivariate models in each of the analyzed areas between the statements (agree vs. disagree) and work-related mental health diagnoses and other factors. OR = Odds ratio; CI = Confidence interval. * The variable shows no statistical significance in the multivariate modelling and is, therefore, not included in the final multivariate model shown in this column.
A multivariate analysis of variance (MANOVA) was performed in the multivariate model in order to see which of the 24 statements showed the most increase between 2017 and 2020. MANOVA was used since it does not affect the Type I error rate to the same extent as other independent tests. The results of the MANOVA mirrored the logistic regression analysis and the four statements that saw the most increase were “I do not have the time to perform the work duties I have planned for the day”, “I want to spend more time enjoying leisure activities and will therefore work less in the future”, “I do not feel I have enough support from co-workers” and “I do not experience joy in my daily work”. Results of the MANOVA showed that there was a statistical difference between the combined dependent variables. Wilks´Λ = 0.09, F(40,1582) = 4.200, p < 0.001, partial η 2 = 0.096, observed power = 1.00. Based on the low Wilks´Λ, we want to be careful rejecting the null hypothesis. The observed power was 1.00, indicating that there was a 100% chance that the results could have been significant.
3.3. Multivariate Model of all Impact and Determinant Areas in the Work Situation in Association with Nurses’ Mental Health Diagnoses Caused by the Work Situation in 2017 and in 2020
In real life, nurses are not only affected by one of the impact and determinant areas from the SwAge-model, there is impact from all nine areas. Therefore, in the next step of the analysis we aimed to make a collected analysis of the seven relevant impact and determinate areas in this study. Hence, all the statements from the seven deteminant and impact areas for a sustainable healthy working life (the swAge-model) included in this investigation were modelled into a single multivariate model for each year, i.e., 2017 and for the second wave of COVID-19 in 2020. The variables that were statistically significant ( p -value < 0.05) from each area were used in the modelling, and each of the eliminated statements (i.e., the variables not statistic significant in the earlier analysis of each area) were added once more one at a time to test the robustness of the model.
In the 2017 multivariate model, six statements showed significance: “I do not experience joy in my daily work” (OR 1.97), “My work involves many psychologically heavy work tasks” (OR 1.66), “The work pace in my daily work is too high” (OR 1.37), “I wish for more opportunities to determine how to perform my work” (OR 1.37), “My work tasks usually clump together to the extent that I get frustrated” (OR 1.34) and “I need to work more at home/care for relatives and will probably therefore work less in the future” (OR 1.27). In 2020, five statements showed significance: “I do not experience joy in my daily work” (OR 2.17), “I do not feel enough support from my co-workers” (OR 2.00), “My work tasks usually clump together to the extent that I get frustrated” (OR 1.81), “My work involves many psychologically heavy work tasks” (OR 1.69) and “I do not get enough rest/recuperation between work shifts (OR 1.41). There were no statistically significant statements in 2017 or in 2020 from the area “physical work environment” and “knowledge and competency” in the final total multivariate model, including all relevant impact and determinant areas for a healthy and sustaniable working life ( Table 3 ).
The final multivariate model for all areas and statement together for 2017 and for 2020. Statistically significant variables in relation to nurses’ work-related mental health diagnosis in 2017 and 2020. OR = Odds ratio; CI = Confidence intervl. Nagelkerke R square 0.073. * The variable shows no statistical significance in the multivariate modelling and is, therefore, not included in the final multivariate model shown in this column.
3.4. Multivariate Model of the Work Situation in the Second Wave of COVID-19 in Association with Nurses’ Mental Diagnoses Caused by the Work Situation, including COVID-19-Specific Questions
COVID-19 had a significant impact on the healthcare systems in Sweden, particularly during the fall/winter of 2020. COVID-19-specific questions were, therefore, added to the investigation during the second wave of COVID-19 in 2020. Therefore, 25 COVID-19-specific variables in the seven impact and determinant areas were included in the next step of the analysis of the multivariate model regarding the second wave of COVID-19 in 2020 to see whether there were particular areas that affected the nurses. The statements in each impact and determinant area were analyzed within that particular determinant area. All statements showed significance in the univariate model. Sixteen statements remained significant in the multivariate model; out of these, five showed a slightly higher OR, which were “I do not feel enough support from my co-workers” (OR 2.86), “I do not experience joy in my daily work” (OR 2.46), “My workload has been higher during COVID-19 compared to my average workload” (OR 2.33), “My work tasks usually clump together to the extent that I get frustrated” (OR 2.07) and “I do not feel like my competencies are being utilized in a satisfactory way” (OR 2.02) ( Table 4 ).
Univariate estimates and the total multivariate model including all seven investigated areas in 2020 with COVID-19-specific questions. Statistically significant variables in relation to work-related mental health diagnoses in 2020. OR = Odds ratio; CI = Confidence interval. Nagelkerke R square 0.115. * The variable shows no statistical significance in the multivariate modelling and is, therefore, not included in the final multivariate model shown in this column.
3.5. Final Multivariate Model with COVID-19-Specific Variables of the Work Situation in Association with Nurses’ Mental Health Diagnoses Caused by the Work Situation
We wanted to see which of the variables were most likely to impact nurses’ mental health and, therefore, be chosen for a final multivariate model. All statistically significant variables from Table 4 were added one at a time to form a multivariate model. The discarded statements were then added to the model one at a time to test the robustness of the model. In the end, the model consisted of eight statements that showed a connection with nurses’ mental health diagnoses ( Table 5 ).
Final multivariate model with COVID-19-specific variables. Statistically significant variables in relation to work-related mental health diagnoses in 2020. OR = Odds ratio; CI = Confidence interval. Cox and Snell R Square 0.058; Nagelkerke R square 0.121.
4. Discussion
Nurses are one of the biggest workgroups within the healthcare sector, and nursing is an important social security profession [ 7 , 8 ]. Unfortunately, many nurses are currently on short- or long-term sick leave, and too many nurses choose to leave the profession in the beginning of their educational training or a short time after their entry into the profession [ 10 ]. During the COVID-19 pandemic, nurses’ work situations were tested to the limit [ 1 , 2 , 3 , 4 , 5 ]. The aim of the study was, therefore, to investigate the association between work-related mental health diagnoses and nurses’ work situations in 2017 and 2020, i.e., before and during the second wave of the COVID-19 pandemic. With the intention of investigating the complexity of the nurses’ work situations, the swAge-model was used as the theme model in the analysis. In the results, we could see that the percentage of nurses having a diagnosis for exhaustion/stress had tripled between 2017 and 2020, and the percentage of nurses with a diagnosis of depression/anxiety had doubled. These are alarming numbers, and the fact that so many nurses suffer from work-related mental health issues is something that needs to be addressed and dealt with.
4.1. Impact and Determinant Areas Important for Nurses’ Mental Health Diagnoses Caused by Their Work
The seven different impact and determinant areas of importance for a healthy and sustainable working life were analyzed one at a time before multivariate modelling to understand the wider complexity of the nurses´ work situations in relation to mental health diagnoses caused by their work. Earlier studies stated the importance of investigating the total complexity of the work situation and not only one or two areas of importance for a sustainable working life if the intention is to develop practically important knowledge for measured activities [ 16 , 17 , 18 , 19 , 20 , 21 ]. The result of this investigation showed that all seven of the impact and determinant areas appeared to have an association with nurses’ mental health diagnoses caused by work.
According to the result of the univariate estimates, the nurses felt unable to cope with the physical work demands in both 2017 and in 2020. A too demanding physical work environment is problematic for a sustainable working life [ 16 , 17 , 18 ]. A lot of nurses’ physical activity is spent standing and/or walking [ 45 , 46 , 47 ]; however, depending on where you work, the physical activity can also consist of working in strenuous work postures or moving patients from bed to wheelchair or on/off operating tables [ 48 , 49 , 50 , 51 ]. A physically demanding work environment could contribute to stress since people tend to get more tired from a physically demanding work environment, and if you are tired, you tend to not keep up with the work pace and be more sensitive to stressful situations, thus, increasing a vulnerability to mental health diagnoses, such as burnout [ 19 , 20 ].
The mental work environment was earlier described as a very important area for employees’ mental health [ 16 , 17 , 18 , 52 ]. In the nurses´ mental work environment area, all five statements were statistically significant in 2017 with “psychologically heavy work task” having a strong connection; in 2020, this statement was still significant but the “I wish for more opportunities to determine how to perform my work” statement showed a slightly higher association. Having a perceived sense of control is identified as important for the well-being and mental health of nurses [ 53 ]. Previous studies state that the more nurses are exposed to stressful situations, the more likely it is that it will drain their psychological resources and they will experience stress-related outcomes, i.e., their job demands exceed their job resources and the result can be poor mental health [ 54 , 55 ].
Rest and recuperation are important to the individual’s health and vital in a sustainable working life [ 16 , 17 , 18 ]. In the “work pace, work time, recuperation area” in the analysis, it was a “lack of time to perform work duties” that showed a high association in 2017 and it was still significant in the regression analysis in 2020; however, in 2020, it was the “accumulation of work tasks” that seemed to have a stronger association. Not having enough time for work tasks or feeling like the work tasks are piling up can cause frustration and ultimately lead to certain work tasks not being carried out and a wish to leave the profession [ 16 , 17 , 18 ]. A recent study found a strong negative association between high work time demands and emotional exhaustion [ 56 ]. A worst-case scenario is that lack of time can affect quality of care and/or affect nurses’ health [ 57 , 58 ]. A British survey [ 59 ] showed that, in some cases, this time constraint can result in malpractice and the neglect of patients. Recuperation between work shifts is important for all aspects of an individual’s well-being. Recovery is necessary for the body to reverse changes in the psychobiological system (such as increased heartrate from stressful work situations) [ 60 ].
In the impact and determinant area of “private social environment for a sustainable working life”, it was interesting that it was the “need to work more from home/care for relatives” that was statistically significant in 2017, whereas “wanting to spend more time enjoying leisure activities” showed as not being significant; however, in 2020, the roles were reversed. The balance between the work and the private social situation is important for employees’ sustainable working life [ 16 , 17 , 18 ]. Sweden, as a country, did not enforce lock-down during the COVID-19 pandemic. There were restrictions as to how and when you could go to gyms, for example, and a lot of activities were held on-line instead of in person. However, could the fact that there were restrictions in place influence the respondents’ feelings? A recent study showed that nurses felt it was important to leave all their experiences from working during the pandemic behind at work and when at home to focus on being at home cooking and cleaning as well as practicing self-care by exercising, walking, or spending time in nature [ 61 ].
Concerning the social environment at work, the organization and leadership are very important factors for a healthy and sustainable working life. In our study, the data from 2017 showed that lack of support from managers and co-workers seemed to have the least connection with nurses’ work-related mental health diagnoses. However, in 2020, lack of support from co-workers had one of the highest connections. Our study did not show any statistical significance regarding lack of support from managers in 2017 or in 2020. It is interesting that lack of support from co-workers changed from a low connection to having one of the highest connections with work-related mental health diagnoses. Is this due to the fact that nurses relied on support from colleagues more during the COVID-19 pandemic or has the pandemic simply put the spotlight on what was always there? Previous studies have shown that collegial support affects communication, organizational commitment, teamwork, stress, negative interaction, human relations, job satisfaction and the hierarchy in the workplace [ 16 , 17 , 18 , 62 ]. Positive social relations at work can ease the burden of emotional demands and work time demands [ 16 , 17 , 18 , 63 ].
Motivation and satisfaction regarding work tasks are important in order to have a healthy and sustainable working life. Our results show that in 2017, both lack of joy in the daily work as well as having no job satisfaction seemed to have high associations with mental health and work-related diagnoses. Lack of joy in the daily work continues to have increased association with work-related diagnoses both in the 2017 and the 2020 multivariate model. According to a study [ 64 ], experiencing joy at work is important both for the nurse and for healthcare in general. Several studies [ 65 , 66 , 67 ] show that job satisfaction is a vital component in nursing and that it is strongly related to factors such as job stress [ 16 , 17 , 18 , 67 ], intention to leave [ 16 , 17 , 18 , 65 , 67 , 68 ], quality of care [ 69 ] and patient satisfaction [ 67 ]. Studies have shown that nurses reported higher levels of job satisfaction when they felt high levels of support from their manager [ 17 , 70 ].
When it came to the impact and determinant area “knowledge and competency”, only the feeling of not having their competencies utilized showed to be statistically significant to nurses´ work-related mental health diagnoses. An earlier study [ 71 ] showed that good interaction between colleagues was a resource for high quality of care, which allowed everyone to use their competence well. Additionally, not being able to use their skills could most likely affect nurses’ willingness to stay in their workplace.
4.2. Multivariate Analysis of the Total Complexity in the Nurses’ Work Situation in Association with Work-Related Mental Diagnoses in 2017 and in 2020
In reality, each impact and determinant area is not operated separately. Therefore, all impact and determinant areas involved in this investigation were analyzed together in a total multivariate model to investigate the association between nurses’ work situations and nurses´ mental health diagnoses. Out of the original seven included impact and determinant areas, only five remained statistically significant and were, therefore, included in the final multivariate models for 2017 and 2020. The included areas were ”mental work environment”, ”work time, work pace, recuperation”, “private social environment”, “work social environment, organization, leadership” and “motivation and satisfaction of and to work tasks”. Only three statements showed an association with nurses’ work-related mental health diagnoses in both 2017 and 2020, they were “My work involves many psychologically heavy work tasks”, “My work tasks usually clump together to the extent that I get frustrated” and “I do not experience joy in my daily work”. Two additional statements showed significance in the 2020 model, which were “I do not feel that I get enough rest/recuperation between work shifts” and “I do not feel enough support from my co-workers”. Feeling that you are unable to provide proper care to patients can lead to ethical and moral stress among nurses, which, in turn, can affect their health and psychological well-being [ 72 , 73 ] and cause job dissatisfaction [ 73 ]. Nurses and other healthcare workers’ mental health diagnoses have been shown to threaten the quality of care and patient safety [ 74 , 75 , 76 ]; this adds further importance to the fact that healthcare organizations must take the nurses’ work situation very seriously.
4.3. The COVID-19 Pandemics Effect on Nurses’ Work Situation
Several studies have shown that many healthcare workers have experienced anxiety, depression [ 77 , 78 , 79 ] and burnout [ 79 ] during the COVID-19 pandemic. The final multivariate model showed that anxiety over being seriously ill can be associated with nurses’ work-related mental health diagnosis. The COVID-19 pandemic had a huge impact on the healthcare organizations, with many millions of people, including nurses, becoming infected by the virus, thus, causing an increased workload for nurses [ 1 , 2 , 3 , 4 , 5 ]. Being at risk of being infected by COVID-19, becoming seriously ill, dying or infecting others has been cited as a major risk for work-related mental illness for healthcare workers during the COVID-19 pandemic. In this investigation, some of the variables have not shown a change between 2017 and 2020, most likely indicating that the COVID-19 pandemic did not impact these particular variables. The result in the final multivariate model did show that the nurses‘ increased risk of being infected by COVID-19 in their workplace was associated with work-related mental health illness. However, issues related to personal protective equipment was not statistically significant. Instead, the result showed that especially lack of support from co-workers, lack of joy in their daily work as well as an increased workload and the accumulation of work tasks showed increased associations with nurses’ work-related mental health diagnoses during the COVID-19 pandemic. A previous systematic review stated that the COVID-19 pandemic forced nurses to have a greater workload, but also that many nurses had trouble falling asleep and/or not getting enough sleep, which they attributed to lack of time to decompress mentally between work shifts [ 10 ]. Additionally, nurses felt like their competencies were not utilized in a satisfactory way. Not being given the opportunity to use their skills or feeling that the organization does not utilize or appreciate the skills and knowledge that the employees possess has, in previous studies, been associated with a lack of job satisfaction and motivation and could lead to employees not wanting to continue working at the workplace [ 16 , 17 , 18 ].
The pandemic put the spotlight on nurses’ work situations, but is the spotlight pointing in the right place? Many healthcare organizations had problems in their work environment prior to the pandemic (including lack of staff and the work situation). Have certain aspects of the nurses’ work situation become more important during the COVID-19 pandemic or has the pandemic simply shown cracks in the façade? Perhaps only the future can tell since we are still living with the pandemic.
4.4. Limitations
One limitation of the study is that we had a large percentage of non-responders, the answer rate was 50.1% and 40.1% in 2017 and 2020, respectively. However, considering that it was a survey, the low response rate was expected, and we are very grateful to those nurses who took the time and answered the survey, especially in 2020 when there was an on-going pandemic. Another limitation is that when you use dichotomization, there is always a risk of losing valuable information. The dichotomization was made by an experienced researcher who thoroughly made considerations in which response choice dichotomization was used. The fifth impact and determinate area, i.e., "personal finances” was not included in the study since there was no data on the nurses’ private economic situation related to the work situation that could be used in the analysis. However, this area could have an impact on the results, for instance, if nurses went to work despite being sick due to not being able to afford the loss in pay. This, in turn, could contribute an added stress. In this study, we have used the respondents’ self-reported doctors’ diagnoses that they felt were caused by their work. One opportunity could have been to use registers with reported work-related illnesses. However, in these registers there are only those diagnoses that have been deemed as work injuries and, therefore, the diagnoses in our study would probably not have been reported. It is also well known that the number of reported work-related illnesses is underreported [ 80 ]. Therefore, we found it more valuable to ask the nurses about which of their diagnoses they felt had been caused by their work. One limitation is the possibility of responders misunderstanding the questions regarding their current mental health diagnoses since no specific timeframe was given, i.e., “I was diagnosed with exhaustion/stress or depression/anxiety within the last six months”. Another limitation is the low score on Wilks´Λ, which would mean that we cannot rule out the possibility of other factors influencing nurses’ work-related mental health other than those we have presented.
5. Conclusions
Based on the results of this survey, there were some differences in what was associated with the nurses’ work-related mental health diagnoses in 2017 and in 2020. The COVID-19 pandemic put nurses’ working situations to a severe test. The result from this comparative analysis, where we examined the work situations and work-related mental health diagnoses before and during the second wave of the COVID-19 pandemic, showed that increased workload and experiencing a lack of joy in the nurses´ daily work as well as experiencing a perceived lack support from their co-workers had the strongest association with nurses’ work-related mental health diagnoses in 2020. It is hard to get around the fact that nurses will continue to face psychologically and physically heavy work tasks, but it is important for organizations to have an open climate so that nurses can talk about their experiences. For nurses to have more opportunities to determine how to perform their work tasks, it is important that they feel like they have a safe work environment and that they have adequate staff and resources and feel involved in decision-making. This study’s analysis model is based on theories about factors that influence a healthy and sustainable working life, and the results are consistent with what the SwAge-model has previously shown [ 16 , 17 , 18 ].
Nurses and other healthcare workers’ mental health diagnoses have been shown to threaten the quality of care and patient safety [ 74 , 75 ]. Therefore, the result from this study investigating nurses’ work-related mental health diagnoses could be important knowledge for the future development of healthcare organizations. The results from this study could also be used by hospitals and ministries of health, etc. as a template to improve the working conditions and quality of life at work for nurses. If these two things improve, perhaps nurses would be more inclined to remain in their current workplace/profession. Future research regarding the long-term impact from COVID-19 on all areas of nurses’ professional and personal lives is needed.
Acknowledgments
The authors wish to acknowledge the valuable input given to us by Lars Rylander, Jens Peter Ellekilde Bonde, Sandra Sögaard Töttenborg, Esben Meulengracht Flachs, Kajsa Kirstine Ugelvig Petersen and Christel Nielsen.
Funding Statement
This research was funded by Interreg (European Regional Development Fund, EU), grant number NYPS20303383; FORTE FORMAS, grant number 2020-02746 and the Research Platform for Collaboration for Health, Kristianstad University, Sweden, funding number 9/2021.
Author Contributions
Conceptualization, C.N. and K.N.; methodology, C.N. and K.N.; software, C.N.; formal analysis, C.N.; writing—original draft preparation, C.N.; writing—review and editing, All authors; supervision, K.N.; project administration, K.N.; funding acquisition, K.N. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Swedish Ethical Review Agency (2016/867 approved 07 December 2016 and 2020-01897 approved 29 April 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Research: More People Use Mental Health Benefits When They Hear That Colleagues Use Them Too
- Laura M. Giurge,
- Lauren C. Howe,
- Zsofia Belovai,
- Guusje Lindemann,
- Sharon O’Connor

A study of 2,400 Novartis employees around the world found that simply hearing about others’ struggles can normalize accessing support at work.
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program remains low. To understand why, a team of researchers conducted a randomized controlled trial with 2,400 Novartis employees who worked in the UK, Ireland, India, and Malaysia. Employees were shown one of six framings that were designed to overcome two key barriers: privacy concerns and usage concerns. They found that employees who read a story about their colleague using the service were more likely to sign up to learn more about the program, and that emphasizing the anonymity of the program did not seem to have an impact. Their findings suggest that one way to encourage employees to make use of existing mental health resources is by creating a supportive culture that embraces sharing about mental health challenges at work.
“I almost scheduled an appointment about a dozen times. But no, in the end I never went. I just wasn’t sure if my problems were big enough to warrant help and I didn’t want to take up someone else’s time unnecessarily.”
- Laura M. Giurge is an assistant professor at the London School of Economics, and a faculty affiliate at London Business School. Her research focuses on time and boundaries in organizations, workplace well-being, and the future of work. She is also passionate about translating research to the broader public through interactive and creative keynote talks, workshops, and coaching. Follow her on LinkedIn here .
- Lauren C. Howe is an assistant professor in management at the University of Zurich. As head of research at the Center for Leadership in the Future of Work , she focuses on how human aspects, such as mindsets, socioemotional skills, and leadership, play a role in the changing world of work.
- Zsofia Belovai is a behavioral science lead for the organizational performance research practice at MoreThanNow, focusing on exploring how employee welfare can drive KPIs.
- Guusje Lindemann is a senior behavioral scientist at MoreThanNow, in the social impact and organizational performance practices, working on making the workplace better for all.
- Sharon O’Connor is the global employee wellbeing lead at Novartis. She is a founding member of the Wellbeing Executives Council of The Conference Board, and a guest lecturer on the Workplace Wellness postgraduate certificate at Trinity College Dublin.
Partner Center
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
In CDC survey, 37% of U.S. high school students report regular mental health struggles during COVID-19 pandemic

Many high school students have reported experiencing mental health challenges during the coronavirus outbreak, according to recently published survey findings from the Centers for Disease Control and Prevention (CDC). High school students who are gay, lesbian or bisexual, as well as girls, were especially likely to say their mental health has suffered during the pandemic.
This analysis explores U.S. high school students’ self-reported mental health challenges during the COVID-19 pandemic. It expands on Pew Research Center surveys that have explored U.S. adults’ mental health difficulties during this time. Not all of the survey questions asked specifically about mental health during the pandemic.
This analysis relies on the Center for Disease Control and Prevention’s Adolescent Behaviors and Experiences Survey (ABES), which was conducted from January to June 2021 to assess students’ health-related behaviors and experiences during the COVID-19 pandemic. ABES surveyed high school students in grades 9-12 attending U.S. public and private schools. More information about the survey and its methodology can be found on the CDC’s website.
The results from this one-time survey are not directly comparable to previous CDC surveys on these topics.
Overall, 37% of students at public and private high schools reported that their mental health was not good most or all of the time during the pandemic, according to the CDC’s Adolescent Behaviors and Experiences Survey , which was fielded from January to June 2021. In the survey, “poor mental health” includes stress, anxiety and depression. About three-in-ten high school students (31%) said they experienced poor mental health most or all of the time in the 30 days before the survey. In addition, 44% said that, in the previous 12 months, they felt sad or hopeless almost every day for at least two weeks in a row such that they stopped doing some usual activities. (Not all of the survey questions asked specifically about mental health during the pandemic.)
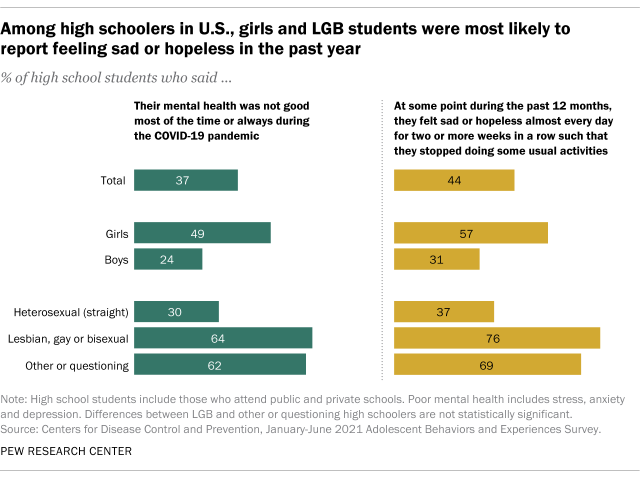
High school students who are gay, lesbian or bisexual reported higher rates of mental health stresses than their heterosexual (straight) peers. The share of LGB high schoolers who said their mental health was not good most of the time or always during the pandemic was more than double that of heterosexual students (64% vs. 30%). More than half of LGB students (55%) said they experienced poor mental health at least most of the time in the 30 days before the survey, while 26% of heterosexual teens said the same. And about three-quarters of LGB high schoolers (76%) said they felt sad or hopeless almost daily for at least two weeks such that they stopped doing some of their usual activities, compared with 37% of heterosexual students.
There were also differences by gender. About half of high school girls (49%) said their mental health was not good most of the time or always during the COVID-19 outbreak – roughly double the share of boys who said this (24%). And roughly four-in-ten girls (42%) reported feeling this way in the 30 days before the survey; 20% of boys said the same. About six-in-ten high school girls (57%) reported that at some point in the 12 months before taking the survey (in the first half of 2021) they felt sad or hopeless almost every day for at least two weeks in a row such that they stopped doing some usual activities, compared with 31% of high school boys who said this.
LGB high schoolers were also more likely than their heterosexual peers to have sought mental health care – including treatment or counseling for alcohol or drug use – via telemedicine during the COVID-19 pandemic. Around one-in-five LGB students (19%) said they received treatment this way at some point during the pandemic, compared with 6% of heterosexual students. Girls were more likely than boys to have received mental health care through telemedicine (10% vs. 7%, respectively).
Pandemic-related disruptions to schooling, socializing and family life have created a situation that the U.S. surgeon general has described as a “ youth mental health crisis ,” with high rates of teens experiencing distress. But public health experts had called attention to teen mental health even before the coronavirus outbreak. For instance, a separate CDC survey conducted in 2015 found that LGB teens were at greater risk of depression than their heterosexual peers. And a Pew Research Center analysis of pre-pandemic data from the National Survey for Drug Use and Health showed teenage girls were more likely than their male peers to report recent experiences with depression , as well as to receive treatment for it.
- Coronavirus (COVID-19)
- Generation Z
- Happiness & Life Satisfaction
- LGBTQ Attitudes & Experiences
- Teens & Youth

Katherine Schaeffer is a research analyst at Pew Research Center
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 23, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Social media affects people's views on mental illness, study finds
by Jeff Grabmeier, The Ohio State University

Even subtle differences in the wording of social media messages may be enough to sway young people's beliefs about depression and anxiety and their treatment.
In a new study, researchers found that college students were more optimistic about the possibility of successfully treating mental health problems after they read social media messages conveying what is called a " growth mindset ."
But social media posts written with a "fixed mindset" led young people to feel that depression and anxiety were more stable and innate, and not so easy to treat.
Growth mindset is the belief that a feature, such as mental health, can be improved with effort. A fixed mindset is the belief that a feature can't change, no matter how hard you try.
The results are important because young people spend a lot of time on social media and those with depression and anxiety may be encountering a lot of messages about their condition, said Whitney Whitted, lead author of the study and a doctoral student in psychology at The Ohio State University.
"These relatively subtle messages may be influencing whether they believe they have any possibility of working through their depression and anxiety and getting better," Whitted said.
The study, published recently in the Journal of Clinical Psychology , involved 322 undergraduate students.
Participants viewed a series of messages (tweets) from the social media site X, formerly Twitter. They were randomly assigned to view tweets about mental health with a growth mindset or a fixed mindset, or a control condition in which the tweets did not involve mental health at all.
In the fixed mindset condition, the tweets portrayed mental health as a fixed condition that does not change. (For example, one tweet said, "I can't wait for my seasonal depression to be over so that I can get back to my regular depression.")
Participants in the growth mindset condition read tweets that emphasized the fluid nature of mental health and the ability to recover from and take control of mental illness. (In one tweet, the user captioned "I got this" to a meme that read "telling those anxious thoughts who's really in control.")
After reading the tweets, participants completed a survey assessing their beliefs about how long depression and anxiety normally last and whether they ever go away; the effectiveness of treatment for depression and anxiety; and beliefs about how much control people have in recovering from mental illness.
Results showed that participants who read the growth mindset tweets were more likely than others to say depression and anxiety don't have to be permanent conditions and that people can take steps to alleviate the symptoms.
In contrast, those who read the fixed mindset tweets had less optimistic views about the permanence of mental illness and the ability of people to treat it.
It is notable that this short intervention had an impact, said study co-author Jennifer Cheavens, professor of psychology at The Ohio State University.
"It was just a few minutes of people reading these tweets with small variations in how the messages about mental illness were framed," Cheavens said. "But it made a difference in what these participants reported they believed."
Of course, it is not known how long the changes connected to reading the social media messages will last. But the results could be encouraging for several reasons.
For one, it suggests that growth mindset social media messages may help persuade people with depression or anxiety that it is worthwhile to seek help, the researchers said.
It can also help with people who are already in therapy.
"We want our clients to put in the hard work necessary to overcome their problems—but they have to believe it is possible," Cheavens said.
"This study suggests there may be ways to give them a boost, to help persuade them that working hard in therapy can pay off in the end."
Whitted said the findings are especially important now, given how much time young people spend on social media. Participants in this study reported using social media one to three hours a day.
"What we found is that what young adult college students view on social media has the potential to impact what they believe about mental illness," Whitted said.
"It is important that the messages they receive accurately reflect what we know about mental illness, especially the fact that it is treatable."
Other co-authors were Matthew Southward of the University of Kentucky; Kristen Howard of the Milwaukee VA Medical Center/Medical College of Wisconsin; Samantha Wick of Miami University; and Daniel Strunk of Ohio State.
Explore further
Feedback to editors

The consumption of certain food additive emulsifiers could be associated with the risk of developing type 2 diabetes
7 hours ago

Perinatal transmission of HIV can lead to cognitive deficits

Study finds suicidal behaviors increased by over 50% in Catalonia, Spain after the COVID-19 pandemic
8 hours ago

Why do we move slower the older we get? New study delivers answers
9 hours ago

Stress activates brain regions linked to alcohol use disorder differently for women than men, finds study

Chemical tool illuminates pathways used by dopamine, opioids and other neuronal signals

Gentle defibrillation for the heart: A milder method developed by researchers for cardiac arrhythmias
10 hours ago

Q&A: Research shows neural connection between learning a second language and learning to code

Gut microbiota acts like an auxiliary liver, study finds

Higher light levels may improve cognitive performance
Related stories.

Stigmatizing content on social media affects perceptions of mental health care, study reveals
Nov 30, 2023

Teachers' growth mindset appears more important than warmth, research suggests
Feb 21, 2024

Young Britons increasingly face mental illness: study
Feb 26, 2024

Social media can reveal who needs the most help
Feb 8, 2024

Social media use interventions alleviate symptoms of depression
Aug 11, 2023

High volumes of mental health-related tweets associated with crisis referrals
Feb 6, 2020
Recommended for you

Study suggests that living near green spaces reduces the risk of depression and anxiety
15 hours ago

Magic mushrooms can treat medication-resistant depression—but are they safe?
13 hours ago

Charting brain synchronization patterns during social interactions

Image viewing experiments challenge theory of universal internal clock
16 hours ago

Would you be happy as a long-term single? The answer may depend on your attachment style
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
35+ Research Topics on Mental Health Nursing: Fostering Wellbeing in Psychiatric Care. Mental health nursing is a critical pillar in nurturing the overall wellness of individuals grappling with psychiatric conditions. Aspiring nursing students, comprehending the nuances of mental health nursing is not only pivotal for your academic voyage but ...
Examples of Mental Health Nursing Research Topics The Effectiveness of Mindfulness Practices on Mental Health Outcomes. Mindfulness practices, such as meditation and yoga, have become increasingly popular in recent years as a way to reduce stress and improve overall well-being. Research has shown that these practices may also effectively treat ...
Background There has been a recent growth in research addressing mental health nurses' routine physical healthcare knowledge and attitudes. We aimed to systematically review the empirical evidence about i) mental health nurses' knowledge, attitudes, and experiences of physical healthcare for mental health patients, and ii) the effectiveness of any interventions to improve these aspects of ...
The Journal of Psychiatric & Mental Health Nursing is pleased to present this very special Virtual Issue. This is a collection of people's mental health and mental illness narratives from this section's inception, in one place. This collection is free to access and all lived experience narratives are free to view.
We aimed to include any potentially relevant research on the topic of interest; therefore, the inclusion criteria were as follows: (1) observational studies carried out in any setting (primary care centres, hospitals and nursing homes); and (2) studies that measured the levels of mental health burden in terms of anxiety, depression ...
The Journal of the American Psychiatric Nurses Association (JAPNA) is a peer-reviewed bi-monthly journal publishing up-to-date information to promote psychiatric nursing, improve mental health care for culturally diverse individuals, families, groups, and … | View full journal description. This journal is a member of the Committee on ...
An initial email discussion was held with a university librarian and informatic expert in February 2021 to outline the research topic, aim, and research question, as well as suggested key terms. ... Lost in Translation, or the True Text: Mental Health Nursing Representations of Psychology. Qualitative Health Research, 17 (4), 471-479. 10.1177 ...
1. Introduction. Nursing staff are the core of the caring profession and central to their role is the development of effective relationships with the individuals they support (Hoeve et al., 2014; Zugai et al., 2015).In the United Kingdom, engaging meaningfully with patients (rather than 'doing to') runs through the principles of the nursing profession (Royal College of Nursing, 2010 ...
This page provides a comprehensive list of psychiatric-mental health nursing research paper topics, which serves as a crucial resource for nursing students assigned to write research papers. The field of psychiatric-mental health nursing is vast, encompassing a wide variety of topics related to mental health care.
For anyone requiring immediate crisis intervention or assistance finding a local mental health provider, the following resources are available: Mental Health America: 1-866-400-6428 for referrals, 1-800-273-8255 for crisis. National Alliance on Mental Illness HelpLine 1-800-950-6264. National Suicide Prevention Helpline 1-800-273-8255.
The research project, "Nurses' Psychological Trauma and Cognitive Control in the COVID-19 Pandemic," surveyed more than 100 nurses around the United States and Canada, including several Purdue School of Nursing alumni. The questionnaire covered vital mental health topics such as depression, anxiety, PTSD, and drug and alcohol use during ...
A focus on the mental health of children and young people is vital, the foundations for positive development and good health are laid during childhood and adolescence (United Nations Children's Fund [UNICEF], 2021).The World Health Organization (WHO) defined mental health as "a state of well-being in which each individual can realize his own potential, cope with ordinary stresses, work ...
Since mental health is nowadays a fundamental topic for public health and nurses due to improving mental health in patients, of all ages, the present Research Topic aims to collect all manuscripts dealing with psychiatric disorders in all ages and in all patient typologies, by highlighting nursing diagnoses, interventions, and outcomes in this ...
The future of nursing: A guide for advancement in the US. Two publications, The Future of Nursing: Leading Change, Advancing Health (IOM, Citation 2011) and The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (NASEM, Citation 2021) have focused on how the discipline of nursing can engage with individuals, families, and communities in the US.
Purpose To examine the correlation between body mass index (BMI) and mental well-being in Chinese nurses during the COVID-19 epidemic. Method This study was conducted in a tertiary hospital using a cross-sectional design. A total of 2,811 nurses were enlisted at Shengjing Hospital in China during the period from March to April, 2022. Information was gathered through a questionnaire that ...
Challenges of mental health care delivery. Care of patients in psychiatric intensive care (PICU), a challenging environment for humanistic psychiatric nursing practice, was the topic of an integrative review article by Swedish author Martin Salzmann-Erikson (Citation 2023, this issue).The author sought to synthesize research conducted within the past 5 years.
Keyword cluster analysis revealed that critical care, oncology care, long-term care, emotional mental health of nurses, quality of life of nurses were currently the key research directions in this field. Additionally, "mental health", "job satisfaction", "stress", and "covid-19" were the current hot topics in this field.
1. Clinical Nursing Research Topics. Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties. Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings. Explore the effectiveness of pain management protocols in pediatric patients. 2.
Evidence-based care relies on nurses' clinical expertise, critical thinking, and research knowledge. Nurses use this skill set to support patient care decisions and as a lens through which to view patient outcomes. Evidence-based practice in nursing may be even more crucial for mental health nurse practitioners.
Objective: To explore nurses' knowledge, attitudes, and perceived social norms about psychedelic use to address mental health conditions. Methods: Data were collected through an anonymous e-survey of Minnesota registered nurses, advanced practice registered nurses, and psychiatric-mental health nurse practitioners in Spring 2023; the pool was randomly selected from the Minnesota Board of ...
2.1. Design. This longitudional study is part of a greater research programme, "Sustainable working life for all ages" [19,39].In the spring of 2017, a baseline survey was performed where links to an online survey were sent out to all healthcare staff in the Swedish Region of Skane via their work e-mail.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022. Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began ...
Yaroslav Danylchenko/Stocksy. Summary. Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager ...
Student nurse wins recognition for research on ketamine for depression | Nursing Times. A student nurse has won a national research award for her work on a trial on using ketamine as a treatment for severe depression. Read more.
Severe heavy rains caused by linear precipitation systems are occurring more frequently in Japan owing to climate change, and residents are being asked to evacuate more often. The purpose of this study was to identify factors associated with the willingness of people with mental health illness (PMHI) in group homes to disclose their illness when being evacuated. Participants were PMHI living ...
Overall, 37% of students at public and private high schools reported that their mental health was not good most or all of the time during the pandemic, according to the CDC's Adolescent Behaviors and Experiences Survey, which was fielded from January to June 2021. In the survey, "poor mental health" includes stress, anxiety and depression.
Credit: DOI: 10.3386/w32354. Mental illness costs the U.S. economy $282 billion annually, which is equivalent to the average economic recession, according to a new study co-authored by Yale ...
Alla Kholmogorova currently works at the Moscow State University of Psychology and Education (dean of the faculty of Counseling and Clinical Psychology). Alla does research in Health Psychology ...
Stigmatizing content on social media affects perceptions of mental health care, study reveals Nov 30, 2023 Teachers' growth mindset appears more important than warmth, research suggests