We have a right to die with dignity. The medical profession has a duty to assist
Distinguished Professor of Philosophy and Director: Centre for Applied Ethics, Stellenbosch University

Disclosure statement
Anton van Niekerk is director of the Centre for Applied Ethics and Head of the Unit for Bioethics in that Centre. The Unit receives an annual contribution from Mediclinic, but that is not for the exclusive use of Anton van Niekerk.
Stellenbosch University provides funding as a partner of The Conversation AFRICA.
View all partners

Euthanasia represents one of the oldest issues in medical ethics. It is forbidden in the original Hippocratic Oath, and has consistently been opposed by most religious traditions since antiquity – other than, incidentally, abortion, which has only been formally banned by the Catholic Church since the middle of the 19th century.
Euthanasia is a wide topic with many dimensions. I will limit myself in this article to the issue of assisted death, which seems to me to be one of the most pressing issues of our time.
Desmond Tutu, emeritus archbishop of Cape Town, raised it again on his 85th birthday in an article in the Washington Post. He wrote:
I have prepared for my death and have made it clear that I do not wish to be kept alive at all costs. I hope I am treated with compassion and allowed to pass onto the next phase of life’s journey in the manner of my choice.
Assisted death can take the form of physician assisted suicide (PAS) . Here a suffering and terminal patient is assisted by a physician to gain access to a lethal substance which the patient himself or herself takes or administers. If incapable of doing so, the physician – on request of the patient – administers the lethal substance which terminates the patient’s life.
The latter procedure is also referred to as “voluntary active euthanasia” (VAE). I will not deal with the issue of involuntary euthanasia –where the suffering patient’s life is terminated without their explicit consent -– a procedure which, to my mind, is ethically much more problematic.
Passive form of euthanasia
The term “voluntary active euthanasia” suggests that there also is a passive form of euthanasia. It is passive in the sense that nothing is “actively” done to kill the patient, but that nothing is done to deter the process of dying either, and that the termination of life-support which is clearly futile, is permitted.
However, the moral significance of the distinction between “active” and “passive” euthanasia is increasingly questioned by ethicists. The reason simply is the credibility of arguing that administering a lethal agent is “active”, but terminating life support (for example switching off a ventilator) is “passive”. Both clearly are observable and describable actions, and both are the direct causes of the patient’s death.
There are a number of reasons for the opposition to physician assisted suicide or voluntary active euthanasia. The value bestowed on human life in all religious traditions and almost all cultures, such as the prohibition on murder is so pervasive that it is an element of common, and not statutory, law.
Objections from the medical profession to being seen or utilised as “killers” rather than saviours of human life, as well as the sometimes well-founded fear of the possible abuse of physician assisted suicide or voluntary active euthanasia, is a further reason. The main victims of such possible abuse could well be the most vulnerable and indigent members of society: the poor, the disabled and the like. Those who cannot pay for prolonged accommodation in expensive health care facilities and intensive care units.
Death with dignity
In support of physician assisted suicide or voluntary active euthanasia, the argument is often made that, as people have the right to live with dignity, they also have the right to die with dignity. Some medical conditions are simply so painful and unnecessarily prolonged that the capability of the medical profession to alleviate suffering by means of palliative care is surpassed.
Intractable terminal suffering robs the victims of most of their dignity. In addition, medical science and practice is currently capable of an unprecedented prolongation of human life. It can be a prolongation that too often results in a concomitant prolongation of unnecessary and pointless suffering.
Enormous pressure is placed upon both families and the health care system to spend time and very costly resources on patients that have little or no chance of recovery and are irrevocably destined to die. It is, so the argument goes, not inhumane or irreverent to assist such patients – particularly if they clearly and repeatedly so request – to bring their lives to an end.
I am personally much more in favour of the pro-PAS and pro-VAE positions, although the arguments against do raise issues that need to be addressed. Most of those issues (for example the danger of the exploitation of vulnerable patients) I believe, can be satisfactorily dealt with by regulation.
Argument in favour of assisted suicide
The most compelling argument in favour of physician assisted suicide or voluntary active euthanasia is the argument in support of committing suicide in a democracy. The right to commit suicide is, as far as I am concerned, simply one of the prices we have to be willing to pay as citizens of a democracy.
We do not have the right, and we play no discernible role, in coming into existence. But we do have the right to decide how long we remain in existence. The fact that we have the right to suicide, does not mean that it is always (morally) right to execute that right.
It is hard to deny the right of an 85-year-old with terminal cancer of the pancreas and almost no family and friends left, to commit suicide or ask for assisted death. In this case, he or she both has the right, and will be in the right if exercising that right.
Compare that with the situation of a 40-year-old man, a husband and father of three young children, who has embezzled company funds and now has to face the music in court. He, also, has the right to commit suicide. But, I would argue, it would not be morally right for him to do so, given the dire consequences for his family. To have a right, does not imply that it is always right to execute that right.
My argument in favour of physician assisted suicide or voluntary active euthanasia is thus grounded in the right to suicide, which I think is fundamental to a democracy.
Take the case of a competent person who is terminally ill, who will die within the next six months and has no prospect of relief or cure. This person suffers intolerably and/or intractably, often because of an irreversible dependence on life-support. This patient repeatedly, say at least twice a week, requests that his/her life be terminated. I am convinced that to perform physician assisted suicide or voluntary active euthanasia in this situation is not only the humane and respectful, but the morally justified way to go.
The primary task of the medical profession is not to prolong life or to promote health, but to relieve suffering. We have a right to die with dignity, and the medical profession has a duty to assist in that regard.
- Assisted suicide
- Voluntary euthanasia
- Desmond Tutu
- World Philosophy Day
- Philosophy2021

Project Officer, Student Volunteer Program

Audience Development Coordinator (fixed-term maternity cover)

Lecturer (Hindi-Urdu)

Director, Defence and Security

Opportunities with the new CIEHF
- Dissertation
- PowerPoint Presentation
- Book Report/Review
- Research Proposal
- Math Problems
- Proofreading
- Movie Review
- Cover Letter Writing
- Personal Statement
- Nursing Paper
- Argumentative Essay
- Research Paper
How To Write A Vivid Euthanasia Argumentative Essay?

Table of Contents

Euthanasia (good death from Greek) is the practice of intentional life ending aiming to relieve patients’ pain and suffering. The topic of its use is fiercely debated all over the world.
People have divided into two camps: some say Euthanasia is the matter of choice, even when it comes to choosing death. Another group claims that doctors mustn’t be empowered to offer death to people who may not even realize the decision they make.
Every country where Euthanasia is legal has its own specific legislative base of its use. Nevertheless, there is one aspect of this topic that unites all the people together: the issue is considered from the moral and ethical perspective.
Euthanasia argumentative essay: the basics
The topics for an argumentative essay writing are usually two-sided: voting for or against the topic, agree or disagree with the statement, choose one option or another.
Writing any argumentative assay requires highlighting both possible points of view, no matter what is your own. Remember, you should explain both sides equally correct and impartial.
So let’s take a closer look into the details…
How to write a Euthanasia thesis statement?
Before writing an essay on Euthanasia you have to think about your own attitude towards the topic. It will help you write a good thesis statement.
…Why you need it?
The thesis is the representation of the essay’s main idea. You’ll have to clarify both sides of the topic, sure. Still, you also need to express your own point of view. And that is made with the thesis statement in the first place.
You may clearly state your opinion in the thesis, like:
“Injecting a medication to a hopeless patient is a murder.”
“Taking life from a person who wants to end up sufferings is mercy.”
Also, you can try to intrigue your readers and present your thesis as a question with no answer provided right away. Like:
“Helping people die: is it murder or mercy?”
“Would you personally use your right for euthanasia if there was no chance to get better?”
Variations are welcomed.
Euthanasia essay introduction: general recommendations
Most professional essay writing services agree that writing an introduction is always the hardest thing. You get the fear of the blank paper, writer’s block, and the stress from remembering all the requirements you should ideally follow.
… Sounds familiar?
There are no reasons to be that stressed, actually. The web is full of info, interesting statistics, law variations, and personal stories.
A combination of those would be both, catchy and informative, that’s all you need for a perfect intro.
Start with some background information to help your reader understand the subject better.
What kind of info would be relevant?
- A brief definition of Euthanasia.
- When it might be allowed.
- Laws of the countries where it is permitted.
- Personal stories of friends/relatives.
- Stories of doctors and nurses.
All of that can be easily found online. Your goal here would rewrite it in your style, make it appealing to read and combined logically. End your introduction with the thesis statement. You already know how it’s done.
Specifics of Euthanasia essay main body
The main body for an argumentative essay should consist of two parts, one for each point of view. Once you express your point of view in the introduction, then it would be logical to start the main body from it.
Still, it is far from being obligatory. You may start with whatever you find more comfortable.
Like, f.e., you decide to start by talking about the positive aspects of Euthanasia. List the statements using words “firstly,” “secondly,” “moreover,” etc. Begin with the weakest argument and move up to the most solid one you have.
Provide the reader with some positive examples, including personal stories, if they fit in, try to find shreds of evidence of euthanasia practice in your country.
Here are some ideas for statements in favor of Euthanasia:
- A patient’s life can be worse than death.
- It is better to die from Euthanasia than from suicide.
- Euthanasia can help in saving budget funds. Saved money may help somebody else.
- Some people don’t want to see how their relatives suffer hopelessly.
- Death from Euthanasia can be more humane than natural.
Once you finish with the arguments for the first part, go on representing the opposite point of view. A good idea to begin the second paragraph with phrases like “on the other hand,” “the other side of the coin is,” “however,” etc.
List a couple of statements against Euthanasia. You may also search for some scandals including the illegal activity of doctors who made such decision without consulting the patient’s relatives.
Here are several ideas that might be helpful.
- Life is the primary integral right and can’t be taken away.
- If there are many organizations and measures to prevent suicides, why should we offer death to someone?
- Each aspect of Euthanasia can’t be foreseen in the law.
- It’s impossible to define who may/may not be offered the Euthanasia.
- What if the person who chose Euthanasia could recover and live the life to its fullest?
What to write in Euthanasia essay conclusion?
In conclusion, you sum up all the ideas highlighted in your essay, without adding new ones. Start with phrases like “to sum up,” “to conclude,” “in conclusion,” “on balance,” “in a nutshell,” etc.
Here you should also express your point of view and paraphrase the thesis you used in the introduction. For uttering your point, use inputs like “my point of view is,” “I strongly believe,” “I am convinced,” “to tell you the truth,” and so on.
How to create a Euthanasia essay outline?
An outline is a brief sketch of your essay. If you need to write it, select the main ideas of your work and write them down in a couple of sentences.
The sketch outline for an essay on Euthanasia may be like:
“Th work is about the problem of Euthanasia. I highlight some statements for and against the use of Euthanasia and support them with top examples. In conclusion, I explain my personal position on this question.”
The full version of an outline would look something like this…
Introduction
- Hook sentence
- Thesis statement
- Transition to Main Body
- History of Euthanasia
- Euthanasia statistics in countries where it is legal
- Impact of legal Euthanasia on people’s life
- Negative consequences of illegal Euthanasia
- Transition to Conclusion
- Unexpected twist or a final argument
- Food for thought
The use of Euthanasia argumentative essay example
This topic is pretty vast. It can be both good and bad for you. Due to the variety of topics within the issue of Euthanasia, it might be easy to find something you are genuinely interested in.
On the other hand, there are dozens of various materials, thousands of articles, and billions of opinions you should consider before writing. Sometimes it might be difficult for you to get a full picture.
Therefore, a sample of the essay on this topic is presented here. It follows all the standards of an argumentative essay and shows you how this type of work may be completed.
On balance…
I’d say that it’s great to work with such an ambiguous topic. You’ll definitely benefit from training your persuasive and analytical skills while working on this essay.
Hope you’ve found some inspiration here, good luck!
Not excited to write an essay on euthanasia? Buy argumentative essay instead! Luckily, we’ve got dozens of writers, who are 100% fit for the job. Order an essay and save time for yourself!

Best Tips on How to Write a Descriptive Essay

What Is Spatial Order And How To Use It In Essay?
How to Choose a Strong Compare and Contrast Essay Topic: Ideas for Writing by Grademiners

25,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay on Euthanasia: 100, 200 and 300 Words Samples
- Updated on
- Feb 22, 2024

Essay on Euthanasia: Euthanasia refers to the act of killing a person without any emotions or mercy. Euthanasia is an ethnically complex and controversial topic, with different perspectives and legal regulations on different topics. School students and individuals preparing for competitive exams are given assigned topics like essays on euthanasia. The objective of such topics is to check the candidate’s perspectives and what punishment should be morally and legally right according to them.
If you are assigned an essay on euthanasia, it means your examiner or teacher wants to know your level of understanding of the topic. In this article, we will provide you with some samples of essays on euthanasia. Feel free to take ideas from the essays discussed below.
Master the art of essay writing with our blog on How to Write an Essay in English .
This Blog Includes:
Essay on euthanasia in 150 words, euthanasia vs physician-assisted suicide, euthanasia classification, is euthanasia bad.
Euthanasia or mercy killing is the act of deliberately ending a person’s life. This term was coined by Sir Francis Bacon. Different countries have their perspectives and laws against such harmful acts. The Government of India, 2016, drafted a bill on passive euthanasia and called it ‘The Medical Treatment of Terminally Ill Patient’s Bill (Protection of Patients and Medical Practitioners).
Euthanasia is divided into different classifications: Voluntary, Involuntary and Non-Voluntary. Voluntary euthanasia is legal in countries like Belgium and the Netherlands, with the patient’s consent. On one side, some supporters argue for an individual’s right to autonomy and a dignified death. On the other hand, the opponents raise concerns about the sanctity of life, the potential for abuse, and the slippery slope towards devaluing human existence. The ethical debate extends to questions of consent, quality of life, and societal implications.
Also Read: Essay on National Science Day for Students in English
Essay on Euthanasia in 350 Words
The term ‘Euthanasia’ was first coined by Sir Francis Bacon, who referred to an easy and painless death, without necessarily implying intentional or assisted actions. In recent years, different countries have come up with different approaches, and legal regulations against euthanasia have been put forward.
In 2016, the government of India drafted a bill, where euthanasia was categorised as a punishable offence. According to Sections 309 and 306 of the Indian Penal Code, any attempt to commit suicide and abetment of suicide is a punishable offence. However, if a person is brain dead, only then he or she can be taken off life support only with the help of family members.
Euthanasia is the act of intentionally causing the death of a person to relieve their suffering, typically due to a terminal illness or unbearable pain.
Physician-assisted suicide involves a medical professional providing the means or information necessary for a person to end their own life, typically by prescribing a lethal dose of medication.
In euthanasia, a third party, often a healthcare professional, administers a lethal substance or performs an action directly causing the person’s death.
It is the final decision of the patient that brings out the decision of their death.
Voluntary Euthanasia
It refers to the situation when the person who is suffering explicitly requests or consents to euthanasia. A patient with a terminal illness may express his or her clear and informed desire to end their life to a medical professional.
Involuntary
It refers to the situation when euthanasia is performed without the explicit consent of the person, often due to the individual being unable to communicate their wishes.
Non-Voluntary
In this situation, euthanasia is performed without the explicit consent of the person, and the person’s wishes are unknown.
Active euthanasia refers to the deliberate action of causing a person’s death, such as administering a lethal dose of medication.
It means allowing a person to die by withholding or withdrawing treatment or life-sustaining measures.
Euthanasia and assisted suicide are a defeat for all. We are called never to abandon those who are suffering, never giving up but caring and loving to restore hope. — Pope Francis (@Pontifex) June 5, 2019
Also Read: Essay on Cleanliness
Euthanasia is a subjective term and its perspectives vary from person to person. Different cultures, countries and religions have their own set of values and beliefs. Life is sacred and gifted to us by god or nature. Therefore, intentionally causing death goes against moral and religious beliefs.
However, some people have raised concerns about the potential for a slippery slope, where the acceptance of euthanasia could lead to the devaluation of human life, involuntary euthanasia, or abuse of the practice. Some even argue that euthanasia conflicts with their traditional medical ethics of preserving life and prioritizing the well-being of the patient.
Today, countries like the Netherlands and Belgium have legalised euthanasia. In India, the USA and the UK, it is a punishable offence with varying sentences and fines. Euthanasia is a complex and controversial topic and creating a law against or for it requires a comprehensive study by experts and the opinions of all sections of society.
Ans: Euthanasia refers to the act of killing a person without any emotions or mercy. Euthanasia is an ethnically complex and controversial topic, with different perspectives and legal regulations on different topics.
Ans: The term ‘Euthanasia’ was first coined by Sir Francis Bacon, who referred to an easy and painless death, without necessarily implying intentional or assisted actions. In recent years, different countries have come up with different approaches, and legal regulations against euthanasia have been put forward. In 2016, the government of India drafted a bill, where euthanasia was categorised as a punishable offence. According to Sections 309 and 306 of the Indian Penal Code, any attempt to commit suicide and abetment of suicide is a punishable offence. However, if a person is brain dead, only then he or she can be taken off life support only with the help of family members.
Ans: Belgium and the Netherlands have legalised euthanasia. However, it is banned in India.
Related Articles
For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Shiva Tyagi
With an experience of over a year, I've developed a passion for writing blogs on wide range of topics. I am mostly inspired from topics related to social and environmental fields, where you come up with a positive outcome.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
25,000+ students realised their study abroad dream with us. Take the first step today.

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Doctors' opinions on...
Doctors' opinions on euthanasia, end of life care, and doctor-patient communication: telephone survey in France
- Related content
- Peer review
- P Peretti-Watel , researcher ( peretti{at}marseille.inserm.fr ) 1 ,
- M K Bendiane , researcher 2 ,
- H Pegliasco , chairman 3 ,
- J M Lapiana , director of palliative care centre 4 ,
- R Favre , professor 5 ,
- A Galinier , consultant 6 ,
- J P Moatti , professor 7
- 1 Regional Center for Disease Control of South-Eastern France, 13006 Marseille, France
- 2 Health and Medical Research National Institute, Research Unit 379, Social Sciences Applied to Medical Innovation, Institut Paoli Calmettes, Marseille,
- 3 Departmental Center of Private Health Professionals, Marseille
- 4 La Maison, Gardanne, France
- 5 Assistance Publique Hôpitaux de Marseille, Service of Medical Oncology, Marseille
- 6 Assistance Publique-Hôpitaux de Marseille, Department of Penitentiary Care, Marseille, France
- 7 Department of Economics, University of Aix-Marseille II, France
- Correspondence to: P Peretti-Watel
- Accepted 28 July 2003
Introduction
During the past decade, the debate about legalising euthanasia has grown in many developed countries, including France. Medical journals have reflected this: surveys have assessed doctors' attitudes toward euthanasia and bioethics articles have discussed the pros and cons. Supporters of legalisation argue that euthanasia is a continuation of palliative care and that doctors must respect patients' autonomy, including a wish to die. 1 The latter argument suggests that cultural differences shape opinions about euthanasia, because the emphasis on autonomy is greater in English speaking countries than in other developed countries. 2 3
We assessed French doctors' opinions toward euthanasia and collected data about their attitudes and practices. We compared medical specialties which demand different amounts of palliative care and different amounts of empathy toward and communication with terminally ill patients.
Participants, methods, and results
In 2002, the Regional Center for Disease Control of South-Eastern France and the Health and Medical Research National Institute did a telephone survey of a sample of doctors, stratified by specialty. We selected general practitioners, oncologists, and neurologists randomly from all French doctors, kept on file by the National Health Insurance Fund.
We investigated respondents' involvement in end of life care and palliative care, their attitude toward terminally ill patients, and whether “euthanasia should be legalised, as in the Netherlands.” We compared medical specialties with Pearson's χ 2 .
We contacted 1552 doctors, and 917 (59%) agreed to participate. Response rate was greater for oncologists (217/261; 83%) and neurologists (198/287; 69%) than for general practitioners (502/1004; 50%). Doctors who did not respond were generally too busy; they did not differ in sex, age, or size of town from respondents.
Only a minority of respondents were trained in palliative care, especially neurologists (24/198; 12.1%). Oncologists treated more terminally ill patients during the past year (mean 26.3 patients v 9.4 for neurologists and 7.0 for general practitioners; P < 0.05), and general practitioners practised less often in palliative care units ( table ). Oncologists were less likely to feel uncomfortable with terminally ill patients (7.8% v 16.7% among general practitioners and 27.8% among neurologists; P < 0.001) and more prone to systematically communicate the objectives of treatment (65.9% v 57.2% among general practitioners and 47.0% among neurologists; P < 0.01) and the diagnosis to competent terminally ill patients. Oncologists were also less in favour of legalising euthanasia (35.5% v 44.8% of general practitioners and 46.5% of neurologists; P < 0.05).
French doctors' involvement in end of life care and palliative care, their attitude to and communication with patients, and their opinion on legalising euthanasia, 2002. Values are numbers (percentages) unless otherwise stated
- View inline
Many French doctors want euthanasia to be legalised. This opinion is more common among general practitioners and neurologists than among oncologists, who are more experienced in end of life care, more frequently trained in palliative care, and show greater comfort and better communication with terminally ill patients. Because most proponents of legalisation argue that euthanasia is a continuation of end of life care and that doctors should respect patients' autonomy, including a wish to die, we expected to find the reverse.
Our study has several limitations. Answering questions about a sensitive topic on the telephone can be difficult, a questionnaire with a fixed choice of answers prevented doctors from qualifying or justifying their responses, and we lacked detailed information about doctors who did not respond.
Previous studies found similar patterns, but the French counterparts to Italian general practitioners and US oncologists were more in favour of legalising euthanasia. 3 4 Our findings contradict the argument that opinions on euthanasia are related to cultural differences in English speaking countries; comparative studies are needed. 2 In France, the support shown for euthanasia may be due to a lack of professional knowledge on palliative care. 5 Improving such knowledge would improve end of life care and may also clarify the debate over euthanasia.
Acknowledgments
We thank H Granier, Y Obadia, B Planchet-Barraud, F Ravallec, M Rotily, and O Priolo.
Contributors MKB, HP, JML, RF, and AG designed the survey and reviewed and improved the paper. JPM and PP-W did the statistical analysis and wrote the paper. PP-W is guarantor.
Funding Departmental Centre of Private Health Professionals (grant from the fund for improving ambulatory care), Assistance Publique-Hôpitaux de Marseilles (within the hospital programme for clinical research), and Cancer Research Foundation (ARC).
Competing interests None declared.
Ethical approval Not needed.
- Hermsen MA ,
- ten Have HA
- Magnani K ,
- Emanuel EJ ,
- Fairclough D ,
- Clarridge BC ,
- Penley WC ,
- Ben Diane MK ,
- Pegliasco H ,
- Galinier A ,
- Lapiana JM ,
- Peretti-Watel P ,

- Table of Contents
- Random Entry
- Chronological
- Editorial Information
- About the SEP
- Editorial Board
- How to Cite the SEP
- Special Characters
- Advanced Tools
- Support the SEP
- PDFs for SEP Friends
- Make a Donation
- SEPIA for Libraries
- Entry Contents
Bibliography
Academic tools.
- Friends PDF Preview
- Author and Citation Info
- Back to Top
Voluntary Euthanasia
The entry sets out five conditions often said to be necessary for anyone to be a candidate for legalized voluntary euthanasia (and, with appropriate qualifications, physician-assisted suicide), outlines the moral case advanced by those in favor of legalizing voluntary euthanasia, and discusses the five most important objections made by those who deny that voluntary euthanasia is morally permissible and who are, in consequence, opposed to its being legalized.
1. Introduction
2. five conditions often proposed as necessary for candidacy for voluntary euthanasia, 3. a moral case for voluntary euthanasia, 4. five objections to the moral permissibility of voluntary euthanasia, other internet resources, related entries.
When a person performs an act of euthanasia, she brings about the death of another person because she believes the latter’s present existence is so bad that he would be better off dead, or believes that unless she intervenes and ends his life, his life will very soon become so bad that he would be better off dead. Accordingly, the motive of the person who performs an act of euthanasia is to benefit the one whose death is brought about. (This also holds for many instances of physician-assisted suicide, but use of the latter term is usually restricted to forms of assistance which stop short of the physician ‘bringing about the death’ of the patient, for example, those involving means that have to be activated by the patient.)
It is important to emphasize the motive of benefiting the person who is assisted to die because well-being is a key value in relation to the morality of euthanasia (see Section 3 below). Nonetheless, the defensibility of the contention that someone can be better off dead has been the subject of extensive philosophical deliberation. Those who claim that a person can be better off dead believe this to be true when the life that remains in prospect for that person has no positive value for her (a possibility which is discussed by e.g., Foot, 1977; McMahan 2002; Bradley 2009), whereas some of those who hold that a person’s life is inviolable deny that a person can ever be better off dead (e.g., Keown in Jackson and Keown 2012). A Kant-inspired variant on this latter position has been advanced by Velleman (1999). He considers that a person’s well-being can only matter if she is of intrinsic value and so that it is impermissible to violate a person’s rational nature (the source of her intrinsic value) for the sake of her well-being. Accordingly, he holds that it is impermissible to assist someone to die who judges that she would be better off dead and competently requests assistance with dying. The only exception is when a person’s life is so degraded as to call into question her rational nature, albeit he thinks it unlikely that anyone in that position will remain competent to request assistance with dying. This position appears to be at odds with the well-established right of a competent patient to refuse life-prolonging medical treatment, at least when further treatment is refused because she considers that her life no longer has value for her and further treatment will not restore its value to her. (For further reasons to reject arguments for the inviolability of the life of a person, including Velleman’s, see e.g., McMahan 2002; Young 2007; Sumner 2011, 2017.)
Because our concern will be with voluntary euthanasia – that is, with those instances of euthanasia in which a clearly competent person makes a voluntary and enduring request to be helped to die (or, by extension, when an authorised proxy makes a substituted judgment by choosing in the manner the no-longer-competent person would have chosen had he remained competent) – a second key value is the competence of the person requesting assistance with dying. There will be occasion to mention non-voluntary euthanasia – instances of euthanasia where a person lacks the competence at the time when a decision is to be made to request euthanasia and has not previously competently declared a preference for it via an advance directive (see the entry on advance directives ) – only when consideration is given to the claim that permitting voluntary euthanasia will lead via a slippery slope to permitting non-voluntary euthanasia. Nothing will be said here about involuntary euthanasia , where a competent person’s life is brought to an end despite an explicit expression of opposition to euthanasia, beyond saying that, no matter how honorable the perpetrator’s motive, such a death is, and ought to be, unlawful.
Debate about the morality and legality of voluntary euthanasia has been, for the most part, a phenomenon of the second half of the twentieth century and the beginning of the twenty first century. Certainly, the ancient Greeks and Romans did not believe that life needed to be preserved at any cost and were, in consequence, tolerant of suicide when no relief could be offered to a dying person or, in the case of the Stoics and Epicureans, when a person no longer cared for his life. In the sixteenth century, Thomas More, in describing a utopian community, envisaged such a community as one that would facilitate the death of those whose lives had become burdensome as a result of ‘torturing and lingering pain’. But it has only been in the last hundred years that there have been concerted efforts to make legal provision for voluntary euthanasia. Until quite recently there had been no success in obtaining such legal provision (though assisted suicide, including, but not limited to, physician-assisted suicide, has been legally tolerated in Switzerland for a number of decades). However, the outlook changed dramatically in the 1970s and 80s because of a series of court cases in the Netherlands which culminated in an agreement between the legal and medical authorities to ensure that no physician would be prosecuted for assisting a patient to die as long as certain guidelines were strictly adhered to (see Griffiths, et al., 1998). In brief, the guidelines were established to permit physicians to practise voluntary euthanasia in those instances in which a competent patient had made a voluntary and informed request to be helped to die, the patient’s suffering was unbearable, there was no way of making that suffering bearable that was acceptable to the patient, and the physician’s judgements as to diagnosis and prognosis were confirmed after consultation with another physician.
The first legislative approval for voluntary euthanasia was achieved with the passage in the parliament of Australia’s Northern Territory of a bill enabling physicians to practise voluntary euthanasia. Subsequent to the Act’s proclamation in 1996, it faced a series of legal challenges from opponents of voluntary euthanasia. In 1997 the challenges culminated in the Australian National Parliament overturning the legislation when it prohibited Australian territories from enacting legislation to permit voluntary euthanasia on constitutional grounds. Australia is a federation consisting of six states and two territories. Unlike the territories, the states do have the constitutional right to enact such legislation and in 2017 the state of Victoria did just that. The legislation came into effect in 2019. In 2019, a second state, Western Australia, enacted legislation to enable voluntary medically assisted death. The legislation became effective in 2021. In 2021 three further states, Tasmania, South Australia and Queensland enacted legislation to enable voluntary medically assisted death which came into force in 2022 for the first two, and 2023 for the third. Finally, in 2022 NSW enacted legislation which came into force in 2023 resulting in voluntary medically assisted death being available in each of the states. Attempts are currently being made in both the Australian Capital Territory and the Northern Territory to introduce legislation in favor of voluntary medically assisted death that will avoid being vetoed by the federal parliament.
In November 2000, the Netherlands passed legislation to legalize the practice of voluntary euthanasia. The legislation passed through all the parliamentary stages early in 2001. The Belgian parliament passed similar legislation in 2002 and Luxembourg followed suit in 2009. (For a very helpful comparative study of relevant legislation see Lewis 2007. See also Griffiths, et al. 2008.)
In Oregon in the United States, legislation was introduced in 1997 to permit physician-assisted suicide after a referendum strongly endorsed the proposed legislation. Later in 1997 the Supreme Court of the United States ruled that there is no constitutional right to physician-assisted suicide; however, the Court did not preclude individual states from legislating in favor of physician-assisted suicide (so the Oregon legislation was unaffected). Since that time the Oregon legislation has been successfully utilised by a significant number of people and similar legislation has been passed in the state of Washington in 2009, in Vermont in 2013, and more recently still in California, Colorado, Florida, Hawaii, Iowa, Maine, Maryland, Massachusetts, Minnesota, New Jersey, New Mexico and the District of Columbia. A series of judicial decisions in the state of Montana in 2008 and 2009 established that the state could not prohibit physician-assisted suicide but legislation has not yet been introduced to codify the legal situation. A number of the remaining states are currently considering physician-assisted suicide bills.
A similar legal position to that in Montana obtained in the nation of Colombia from the late 1990s as a result of a majority ruling by its Constitutional Court in favor of the legality of physician-assisted suicide but legislative provision was finally made only quite recently. In 2021, Spain legalized voluntary euthanasia. In Austria and Germany courts have authorised physician-assisted suicide but no legislative backing for the practice has been introduced, while in Italy legislation for voluntary medically assisted death has been passed in one house of the bicameral parliament. In Portugal legislation for physician-assisted suicide was passed but was subsequently rejected by the Constitutional Court.
In Canada, the province of Quebec introduced legislation permitting medical aid in dying in 2014. The legislation came into effect in 2016 at around the same time that the Canadian National Parliament passed legislation permitting both physician-assisted suicide and voluntary euthanasia throughout all of the Canadian federation. (For a brief account of events leading up to the enactment of the various pieces of legislation in Canada see Downie and Schuklenk 2021.)
New Zealand held a referendum in 2019 which resulted in approval for the introduction of legislation for voluntary medically assisted death. The legislation came into effect late in 2021.
In the following countries legislative proposals for voluntary medically assisted death are presently under review: the Czech Republic, France, Ireland, the Isle of Man, Japan, Jersey, South Korea, the Philippines, Slovenia and the United Kingdom.
With that brief sketch of the historical background in place, we will proceed first to consider the conditions that those who have advocated making voluntary medically assisted death legally permissible have typically insisted should be satisfied. Consideration of the proposed conditions will establish a framework for the moral interrogation that will follow in Sections 3 and 4. Section 3 will outline the positive moral case put forward by those who want voluntary euthanasia and physician-assisted suicide to be legally permissible. Section 4 will be devoted to scrutinising the most important of the objections that have been levelled against that case by those opposed to the legalization of voluntary euthanasia and physician-assisted suicide.
Advocates of voluntary euthanasia typically contend that if a person
- is suffering from a terminal illness;
- is unlikely to benefit from the discovery of a cure for that illness during what remains of her life expectancy;
- is, as a direct result of the illness, either suffering intolerable pain, or only has available a life that is unacceptably burdensome (e.g., because the illness has to be treated in ways that lead to her being unacceptably dependent on others or on technological means of life support);
- has an enduring, voluntary and competent wish to die (or has, prior to losing the competence to do so, expressed a wish to be assisted to die in the event that conditions (a)-(c) are satisfied); and
- is unable without assistance to end her life,
there should be legal and medical provision to facilitate her being allowed to die or assisted to die.
It should be acknowledged that these conditions are quite restrictive, indeed more restrictive than many think appropriate. In particular, the first condition restricts access to voluntary euthanasia to those who are terminally ill . While that expression is not free of all ambiguity, for present purposes it can be agreed that it does not include those who are rendered quadriplegic as a result of accidents, or sufferers from chronic diseases, or individuals who succumb to forms of dementia like Alzheimer’s Disease, to say nothing of those afflicted by ‘existential suffering’. Those who consider that cases like these show the first condition to be too restrictive (e.g., Varelius 2014, Braun, 2023) may, nonetheless, agree that including them as candidates for legalized voluntary euthanasia is likely to make it far harder in many jurisdictions to gain sufficient support for legalization (and so to make it harder to help those terminally ill persons who wish to die). Even so, they believe that voluntary euthanasia should be permitted for those who consider their lives no longer worth living, not just for for the terminally ill. Whether those who judge that their lives are no longer worth living, and so believe their lives are in that sense ‘complete’, should be afforded medical assistance with dying, has recently become a pressing concern in Belgium and the Netherlands. Several court cases have affirmed that such assistance may sometimes be provided for individuals in the former category even though the question remains as to whether it is properly a medical responsibility to render assistance with dying to someone who believes her life is complete despite her not suffering from a terminal medical condition (see, e.g., Young 2017). Relatedly, the issues of whether those suffering from a disability which will not reasonably foreseeably lead to death and those suffering because of a mental illness should be able to access medical assistance with dying have recently been the subject of intense debate in Canada. The debate culminated in disabled individuals, whose conditions are the cause of enduring, intolerable and irremediable suffering, being given access to medical assistance with dying as long as they are capable of making a competent request for that assistance. An intention to make a similar arrangement for those whose sole underlying condition is a mental illness was flagged for introduction in 2024, but has been temporarily shelved until further research has been conducted on the issue. It seems likely that the changes that have been made, or mooted, in these jurisdictions to the eligibility conditions for medical assistance with dying will lead to an expansion of the eligibility conditions for voluntary medically assisted death in other jurisdictions.
The fifth condition further restricts access to voluntary euthanasia by excluding those capable of ending their own lives, and so may be thought unduly restrictive by those who would wish to discourage terminally ill patients from attempting suicide. There will be yet others who consider this condition to be too restrictive because competent patients can always refuse nutrition and hydration (see, e.g., Bernat, et al. 1993; Savulescu 2014). Though this is true, many competent dying persons still wish to have access to legalized medically assisted death, rather than having to rely on refusing nutrition and hydration, so that they may retain control over the timing of their deaths and avoid needlessly prolonging the process of dying.
The second condition is intended simply to reflect the fact that it is normally possible to say when someone’s health status is incurable. So-called ‘miracle’ cures may be proclaimed by sensationalist journalists, but progress toward medical breakthroughs is typically painstaking. If there are miracles wrought by God that will be quite another matter entirely, but it is at least clear that not everyone’s death is thus to be staved off.
The third condition recognises what many who oppose the legalization of voluntary euthanasia do not, namely, that it is not only a desire to be released from pain that leads people to request help with dying. In the Netherlands, for example, pain has been found to be a less significant reason for requesting assistance with dying than other forms of suffering like frustration over loss of independence (see e.g., Marquet, et al. 2003; Onwuteaka-Philipsen, et al. 2012; Emanuel, et al. 2016). Sufferers from some terminal conditions may have their pain relieved but have to endure side effects that, for them, make life unbearable. Others may not have to cope with pain but, instead, with having to rely on forms of life support that simultaneously rob their lives of quality (as with, e.g., motor neurone disease). Yet others struggle with psychological distress and various psychiatric conditions and believe these conditions ought to be counted among the forms of suffering that qualify competent individuals to access medical assistance with dying. There has been greater recognition of, and support for, this position in those jurisdictions that make the role of unbearable suffering central to the determination of the eligibility of competent individuals for medical assistance with dying (see the discussion above of the first condition). Even so, inclusion of these forms of suffering highlights legitimate issues to do with the competence of at least some of those who suffer from them. (For a helpful recent study of the handling of requests for assistance with dying by psychiatric patients in the Netherlands see Kim, et al. 2016.)
A final preliminary point is that the fourth condition requires that the choice to die not only be uncoerced and competent but that it be enduring. The choice is one that will require time for reflection, and, almost certainly, discussion with others, so should not be settled in a moment. Nonetheless, as with other decisions affecting matters of importance, adults are presumed to choose voluntarily and to be competent unless the presence of defeating considerations can be established. (See the entry on decision-making capacity .) The burden of proof of establishing lack of voluntariness, or lack of competence, is on those who refuse to accept an adult person’s choice. There is no need to deny that this burden can sometimes be met (e.g., by pointing to the person’s being in a state of clinical depression). The claim is only that the onus falls on those who assert that an adult’s choice is not competent. (There are different issues to be faced when the competence of at least some older children and adolescents is at issue. In the Netherlands, for example, those aged twelve and older have sometimes been found to be competent to make end-of-life decisions for themselves. However, the topic will not be pursued further here because the focus of the entry is on competent adults.)
Clearly the five conditions set out above are likely to require some refinement if complete agreement is to be reached but there is sufficient agreement for us to proceed without further ado to consideration of the cases for and against legalization of voluntary euthanasia. (However, for a fuller discussion of issues concerning the definition of ‘euthanasia’ see, e.g., Beauchamp and Davidson 1979.)
One central ethical contention in support of voluntary euthanasia is that respect for persons demands respect for their autonomous choices as long as those choices do not result in harm to others. Respect for people’s autonomous choices is directly connected with the requirement for competence because autonomy presupposes competence (cf., Brock 1992). People have an interest in making important decisions about their lives in accordance with their own conception of how they want to live. In exercising autonomy, or self-determination, individuals take responsibility for their lives; since dying is a part of life, choices about the manner of their dying and the timing of their death are, for many people, part of what is involved in taking responsibility for their lives. Many are concerned about what the last phase of their lives will be like, not merely because of fears that their dying might involve them in great suffering, but also because of the desire to retain their dignity, and as much control over their lives as possible, during this phase. A second contention in support of voluntary euthanasia was mentioned at the beginning of this entry, namely the importance of promoting the well-being of persons. When someone is suffering intolerable pain or only has available a life that is unacceptably burdensome (see the third condition above), and he competently requests medical assistance with dying, his well-being may best be promoted by affording him that assistance. When harnessed together, the value to individuals of making autonomous choices, and the value to those individuals who make such choices of promoting their own well-being, provide the moral foundation for requests for voluntary euthanasia. Each consideration is necessary for moral justification of the practice, but taken in isolation neither suffices (see, e.g., Young 2007, 2017; Sumner 2011, 2017).
The technological interventions of modern medicine have had the effect of stretching out the time it takes for many people to die. Sometimes the added life this brings is an occasion for rejoicing; sometimes it drags out the period of significant physical and intellectual decline that a person undergoes with the result that life becomes no longer worth living. Many believe there is no single, objectively correct answer as to when, if at all, a person’s life becomes a burden and hence unwanted. If they are right, that simply points up the importance of individuals being able to decide autonomously for themselves whether their own lives retain sufficient quality and dignity to make life worth living. Others maintain that individuals can be in error about whether their lives continue to be worth living (cf., Foot 1977). The conditions outlined above in Section 2 are intended by those who propose them to serve, among other purposes, to safeguard against such error. But it is worth adding that in the event that a person who considers that she satisfies those conditions is judged by her medical attendants to be in error about whether it would be worth her continuing to live, the likely outcome is that those attendants will refuse to provide medical assistance with dying. (Evidence that will be mentioned below shows that this happens more frequently than might be predicted in jurisdictions in which medically assisted dying has been legalized. (There are discussions of the principles at stake in such matters in Young 2007; Wicclair 2011; Sumner 2020.) Unless a patient is able to be transferred to the care of other medical professionals who accept her assessment, she will have to rely on her own resources (e.g., by refusing nutrition and hydration). Even so, other things being equal, as long as a critically ill person is competent, her own judgement of whether continued life is a benefit to her ought to carry the greatest weight in any end-of-life decision making regardless of whether she is in a severely compromised and debilitated state. The idea that a competent individual’s autonomous judgment of the value to her of continued life should trump an assessment by others of her well-being should not be thought surprising because precisely the same happens when a competent patient refuses life-prolonging treatment.
Suppose, for the sake of argument, that it is agreed that we should respect a person’s competent request for medical assistance with dying (e.g., so as to enable her to achieve her autonomously chosen goal of an easeful death). It might be thought that in such an eventuality different moral concerns will be introduced from those that arise in connection with competent refusals. After all, while competent patients are entitled to refuse any form of medical treatment, they are not entitled to insist on the administration of forms of medical treatment that have no prospect of conferring a medical benefit or are not being provided because of a scarcity of medical resources or their affordability. While each of these points is sound, it remains the case that medical personnel have a duty to relieve suffering when that is within their capacity. Accordingly, doctors who regard medical assistance with dying as an element of appropriate medical care will consider it morally permissible to agree to a request for assistance with dying by a competent dying patient who wishes to avoid unbearable suffering. The reason for claiming only that this is morally permissible rather than morally obligatory will be explained in a subsequent paragraph. (For further reflections on the issue of responses to requests for medical assistance see, for instance, Dworkin 1998; Sumner 2011, 2017, 2020; Young 2007, 2017.)
Notwithstanding this response, as was seen earlier, at least some proponents of voluntary medically assisted dying wish to question why medical assistance with dying should be restricted to those covered by, in particular, the first three conditions set out above in Section 2. If people’s competent requests for medically assisted death should be respected why impose any restrictions at all on who may have access to medically assisted death? Why, for example, should those suffering from depression, or forms of dementia, not be eligible for medically assisted dying? Most proponents of voluntary medically assisted dying hold that there are at least two reasons for restricting access to it to those who satisfy the conditions set out earlier (or, a modified set that takes account of the concerns canvassed in the discussion of those proposed conditions). First, they contend that there are political grounds for doing so, namely, that because legalizing medically assisted dying for competent individuals is politically contested, the best hope for its legalization lies in focusing on those forms of suffering most likely to effect law reform. That is why some proponents deny the eligibility even of sufferers from conditions like ‘locked-in’ syndrome, motor neurone disease, and multiple sclerosis for voluntary medically assisted dying since, strictly, they are not terminally ill, and reliance has to be placed in consequence on their claim to be suffering unbearably. Second, and relatedly, most proponents of the legalization of medical assistance with dying have been cautious about supporting medically assisted death for those suffering from, for example, depression and dementia, because not only are they not terminally ill, but their competence to request assistance with dying is apt to be called into question, particularly in instances where they have given no prior indication of their preference for such assistance. Restricting access to medical assistance with dying to those whose suffering is less likely to be disputed avoids becoming embroiled in controversy. As was noted earlier, some critics of the restrictive approach (e.g., Varelius 2014) take a harder line and claim that it should not even be necessary for a person to be suffering from a medical condition to be eligible for medical assistance with dying; it should be enough to be ‘tired of life’. Only in a few jurisdictions, viz., Switzerland, the Netherlands and Belgium, has this issue been seriously broached. Regardless of what may happen in those jurisdictions, those seeking the legal provision of medical assistance with dying in other jurisdictions seem likely to maintain that if such assistance is to be seen as a legitimate form of medical care it has to be provided in response to a medical condition (rather than because someone is ‘tired of life’), and, indeed, restricted to those who satisfy the conditions outlined earlier in Section 2 (or some similar set of conditions). In short, these latter hold that making an autonomous request for assistance with dying is necessary, but should not be sufficient, for triggering such assistance.
There is one final matter of relevance to the moral case for voluntary medically assisted death on which comment must be made. The comment concerns a point foreshadowed in a previous paragraph, but it is also linked with the remark just made about the insufficiency of an autonomous request for assistance with dying to trigger that assistance. It is important to make the point that respect has to be shown not only for the dying person’s autonomy but also for the professional autonomy of any medical personnel asked to lend assistance with dying. The value (or, as some would prefer, the right) of self-determination does not entitle a patient to try to compel medical professionals to act contrary to their own moral or professional values. Hence, if voluntary euthanasia is to be legally permitted, it must be against a backdrop of respect for professional autonomy. Similarly, if a doctor’s view of her moral or professional responsibilities is at odds with her patient’s competent request for euthanasia, she should make provision, where it is feasible to do so, for the transfer of the patient to the care of a doctor who faces no such conflict. Given that, to date, those who contend that no scope should be permitted for conscientious objection within medical practice have garnered very little support for that view, making use of referrals and transfers remains the most effective means of resolving such disagreements.
Opponents of voluntary euthanasia have endeavored in a variety of ways to counter the very straightforward moral case that has been laid out above for its legalization (see, for example, Keown 2002; Foley, et al. 2002; Biggar 2004; Gorsuch 2006). Some of the counter-arguments are concerned only with whether the moral case warrants making the practice of voluntary euthanasia legal, whereas others are concerned with trying to undermine the moral case itself. In what follows, consideration will be given to the five most important counter-arguments. (For more comprehensive discussions of the morality and legality of medically assisted death see Biggar 2004; Gorsuch 2006; Young 2007; Sumner 2011, 2017; Keown 2018).
4.1 Objection 1
It is sometimes said (e.g., Emanuel 1999; Keown in Jackson and Keown 2012) that it is not necessary nowadays for people to die while suffering from intolerable or overwhelming pain because the provision of effective palliative care has improved steadily, and hospice care is more widely available. Some have urged, in consequence, that voluntary euthanasia is unnecessary.
There are several flaws in this contention. First, while both good palliative care and hospice care make important contributions to the care of the dying, neither is a panacea. To get the best palliative care for an individual involves trial and error, with some consequent suffering in the process; moreover, even the best care fails to relieve all pain and suffering. Perhaps even more importantly, high quality palliative care commonly exacts a price in the form of side-effects such as nausea, incontinence, loss of awareness because of semi-permanent drowsiness, and so on. A rosy picture is often painted as to how palliative care can transform the plight of the dying. Such a picture is misleading according to those who have closely observed the effect of extended courses of treatment with drugs like morphine. For these reasons many skilled palliative care specialists acknowledge that palliative care does not enable an easeful death for every patient. Second, even though the sort of care provided through hospices is to be applauded, it is care that is available to only a small proportion of the terminally ill and then usually only in the very last stages of the illness (typically a matter of a few weeks). Notwithstanding that only relatively few of the dying have access to hospice care it is worth drawing attention to the fact that in, Oregon, to cite one example, a high proportion of those who have sought physician-assisted suicide were in hospice care. Third, and of greatest significance for present purposes, not everyone wishes to avail themselves of palliative or hospice care. For those who prefer to die on their own terms and in their own time, neither option may be attractive. As previously mentioned, a major source of distress for many dying patients is the frustration that comes with being unable to satisfy their autonomous wishes. Fourth, as also indicated earlier, the suffering that occasions a desire to end life is not always traceable to pain caused by illness. For some, what is intolerable is their forced dependence on others or on life-supporting machinery; for these patients, the availability of effective pain control is not the primary concern. (In relation to the preceding matters see Rietjens, et al. 2009 and Onwuteaka-Philipsen et al. 2012 for findings for the Netherlands; and, for Oregon, Ganzini, et al. 2009.)
4.2 Objection 2
A second, related objection to the moral and legal permissibility of voluntary euthanasia turns on the claim that we can never have sufficient evidence to be justified in believing that a dying person’s request to be helped to die is competent, enduring and genuinely voluntary.
It is certainly true that a request to die may not reflect an enduring desire to die (just as some attempts to commit suicide may reflect only temporary despair). That is why advocates of the legalization of voluntary euthanasia have argued that a cooling off period should normally be required before euthanasia is permitted to ensure that the request is enduring. That having been said, to claim that we can never be justified in believing that someone’s request to die reflects a settled preference for death is to go too far. If a competent person discusses the issue with others on different occasions over time, and remains steady in her resolve, or privately reflects on the issue for an extended period and does not waver in her conviction, her wish to die surely must be counted as enduring.
But, it might be asked, what if a person is racked with pain, or mentally confused because of the measures taken to relieve her pain, and is, in consequence, unable to think clearly and rationally about the alternatives? It has to be agreed that a person in those circumstances who wants to die should not be assumed to have a truly voluntary and enduring desire to die. However, there are at least two important points to make about those in such circumstances. First, they do not account for all of the terminally ill, so even if it is acknowledged that such people are incapable of agreeing to voluntary euthanasia that does not show that no one can ever voluntarily request help to die. Second, it is possible in at least some jurisdictions for a person to indicate, in advance of losing the capacity to give competent consent, how she would wish to be treated should she become terminally ill and suffer either intolerable pain or an unacceptable loss of control over her life (cf., for instance, Dworkin 1993). ‘Living wills’ or ‘advance directives’ are legal instruments for giving voice to people’s wishes while they are capable of giving competent, enduring and voluntary consent, including to their wanting help to die. As long as they are easily revocable in the event of a change of mind (just as civil wills are), they should be respected as evidence of a well thought-out conviction. (For more detailed consideration of these instruments see the entry on advance directives .)
Perhaps, though, what is really at issue in this objection is whether anyone can ever form a competent, enduring and voluntary judgement about being better off dead, rather than continuing to suffer from an illness, prior to suffering such an illness (cf., Keown in Jackson and Keown 2012). If this is what underlies the objection it is surely too paternalistic to be acceptable. Why is it not possible for a person to have sufficient inductive evidence (e.g., based on the experience of the deaths of friends or family) to know her own mind, and act accordingly, without having had direct experience of such suffering?
4.3 Objection 3
According to the traditional interpretation of the ‘doctrine of double effect’ it is permissible to act in a way which it is foreseen will have a bad effect, provided only that
- the bad effect occurs as a side-effect (i.e., indirectly) to the achievement of the act that is directly aimed at;
- the act directly aimed at is itself morally good or, at least, morally neutral;
- the good effect is not achieved by way of the bad, that is, the bad must not be a means to the good; and
- the bad effect must not be so serious as to outweigh the good effect.
Hence, it is permissible, according to the doctrine of double effect, to, for example, alleviate pain (a good effect) by administering a drug such as morphine, knowing that doing so will shorten life, but impermissible to administer the same drug with the direct intention of terminating a patient’s life (a bad effect). This latter claim is said to apply regardless of whether the drug is given at the person’s request.
This is not the appropriate forum for a full consideration of the doctrine, for which see the entry on the doctrine of double effect . However, there is one very important criticism to be made of the application of the doctrine that has direct relevance to the issue of voluntary euthanasia.
On the most plausible reading, the doctrine of double effect can be relevant to the permissibility of voluntary euthanasia only when a person’s death is bad for her or, to put it another way, a harm to her. Sometimes the notion of ‘harm’ is understood simply as damage to a person’s interests whether consented to or not. At other times, it is understood, more strictly, as damage that has been wrongfully inflicted. On either understanding of harm, there can be instances in which death for a person does not constitute a harm for her because it will either render her better off, or, as some would insist, no worse off, when compared with remaining alive. Accordingly, in those instances, the doctrine of double effect can have no relevance to the debate about the permissibility of voluntary euthanasia. (For extended discussions of the doctrine of double effect and its bearing on the moral permissibility of voluntary euthanasia see, e.g., McIntyre 2001; Woodward 2001; Cavanaugh 2006; Young 2007; Sumner 2011, 2017.)
4.4 Objection 4
As was noted earlier in Section 3, there is a widespread belief that so-called passive (voluntary) euthanasia, wherein life-sustaining or life-prolonging measures are withdrawn or withheld in response to a competent patient’s request, is morally permissible. The reason why passive (voluntary) euthanasia is said to be morally permissible is that the patient is simply allowed to die because steps are not taken to preserve or prolong life. This happens, for example, when a dying patient requests the withdrawal or the withholding of measures whose administration would be medically futile, or unacceptably burdensome. By contrast, active (voluntary) euthanasia is said to be morally impermissible because it is claimed to require an unjustifiable intentional act of killing to satisfy the patient’s request (cf., for example, Finnis, 1995; Keown in Jackson and Keown 2012; Keown 2018).
Despite its popularity and widespread use, the distinction between passive and active euthanasia is neither particularly clear nor morally helpful. (For a fuller discussion, see McMahan 2002.) Whether behavior is described in terms of acts or omissions (a distinction which underpins the alleged difference between active and passive voluntary euthanasia and that between killing a person and letting her die), is often a matter of pragmatics rather than anything of deeper moral importance. Consider, for instance, the practice (once common in hospitals) of deliberately proceeding slowly to a ward in response to a request to provide assistance for a patient who has been assigned a ‘not for resuscitation’ code. Or, consider ‘pulling the plug’ on a respirator keeping an otherwise dying patient alive, as against not replacing the oxygen supply when it runs out. Are these acts or omissions? If the answers turn on merely pragmatic considerations the supposed distinction between passive euthanasia and active euthanasia will be hard to sustain.
Even supposing that the distinction between acts and omissions, and the associated distinction between killing and letting die, can be satisfactorily clarified (on which see the entry doing v. allowing harm ), there remains the issue of whether these distinctions have moral significance in every circumstance. Consider a case of a patient suffering from motor neurone disease who is completely respirator dependent, finds her condition intolerable, and competently and persistently requests to be removed from the respirator so that she may die. Even the Catholic Church in recent times has been prepared to agree that it is permissible, in a case like this, to turn off the respirator. No doubt this has been because the Catholic Church considers such a patient is only being allowed to die. Even were it to be agreed, for the sake of argument, that such a death should be regarded as an instance of letting die, this concession would not show that it would have been morally worse had the patient been killed at her request (active voluntary euthanasia) rather than being allowed to die (passive voluntary euthanasia). Indeed, supporters of voluntary medically assisted death maintain that since death is beneficial in such an instance (or, at the very least, leaves the dying person no worse off), actively bringing about the death is morally to be preferred to just allowing it to happen because the desired benefit is achieved sooner and thus with less suffering.
Opponents of voluntary euthanasia claim, however, that the difference between active and passive euthanasia is to be found in the agent’s intention: if someone’s life is intentionally terminated she has been killed, whereas if she is just no longer being aggressively treated, her death should be attributed to the underlying disease. Many physicians would say that their intention in withholding or withdrawing life-sustaining medical treatment in such circumstances is simply to respect the patient’s wishes. This is plausible in those instances where the patient competently requests that aggressive treatment no longer be given (or, the patient’s proxy makes such a request). But it will often be implausible. In many cases the most plausible interpretation of a physician’s intention in withholding or withdrawing life-sustaining measures is that it is to end the patient’s life. Consider the palliative care practice of ‘terminally sedating’ a patient after a decision has been made to cease aggressive treatment. Suppose (as sometimes happens) that this is then followed by withholding artificially supplied nutrition. In these latter instances the best explanation of the physician’s behavior is that the physician intends thereby to end the life of the patient. What could be the point of the action, the goal aimed at, the intended outcome, if not to end the patient’s life? (Cf. Winkler 1995.) No sense can be made of the action as being intended to palliate the patient’s diseased condition, or to keep the patient comfortable. Nor is it appropriate to claim that what kills the patient is the underlying disease. What kills the patient is the act of depriving her of nutrition (i.e., of starving her to death). The point can be generalized to cover many more instances involving either the withdrawal or the withholding of life-sustaining medical treatment. In short, there is no good reason to think that whereas so-called passive voluntary euthanasia is morally acceptable active voluntary euthanasia never can be.
But we can go further. Giving titrated doses of morphine that reach levels beyond those needed to control pain, or removing a respirator from a sufferer from motor neurone disease, seem to many of us to amount to intentionally bringing about the death of the person being cared for. To be sure, as was acknowledged above, there are circumstances in which doctors can truthfully say that the actions they perform, or omissions they make, will bring about the deaths of their patients even though it was not their intention that those patients would die. So, for instance, if a patient refuses life-prolonging medical treatment because she considers it futile, it can be reasonable to say that her doctor’s intention in complying with the request was simply to respect her wishes. Nevertheless, as we have seen, there are other circumstances in which it is highly stilted to claim, as some doctors continue to do, that they had no intention of bringing about death.
These considerations should settle matters but do not do so for those who maintain that killing, in medical contexts, is always morally unjustified – a premise that underwrites much of the debate surrounding this fourth objection. But this underlying assumption is open to challenge and has been challenged by, for instance, Rachels 1986 and McMahan 2002. One of the reasons the challengers have given is that there are cases in which killing a competent dying person when she requests assistance with dying, is morally preferable to allowing her to die, namely, when taking the latter option would serve only to prolong her suffering against her wishes. Further, despite the longstanding legal doctrine that no one can justifiably consent to be killed (on which more later), it surely is relevant to the justification of an act of killing that the person killed has autonomously decided that she would be better off dead and so asks to be helped to die.
4.5 Objection 5
It is sometimes said that if society allows voluntary euthanasia to be legalized, we will then have set foot on a slippery slope that will lead us eventually to support other forms of euthanasia, including, in particular, non-voluntary euthanasia. Whereas it was once the common refrain that that was precisely what happened in Hitler’s Germany, in recent decades the tendency has been to claim that experience with legalized euthanasia in the Netherlands and Belgium, in particular, has confirmed the reality of the slippery slope.
Slippery slope arguments come in various versions. One (but not the only) way of classifying them has been to refer to logical, psychological and arbitrary line versions. The common feature of the different forms is the contention that once the first step is taken on a slippery slope the subsequent steps follow inexorably, whether for logical reasons, psychological reasons, or to avoid arbitrariness in ‘drawing a line’ between a person’s actions. (For further discussion see, e.g., Rachels 1986; Brock 1992; Walton 1992.)
We need first to consider whether, at the theoretical level, any of these forms of argument is powerful enough to refute the case for the legalization of voluntary euthanasia. We will then be in a position to comment on the alleged empirical support from the experiences of Hitler’s Germany and, more recently, of legalized euthanasia in the Netherlands and elsewhere, for the existence of a slippery slope that supposedly comes into being with the legalization of voluntary euthanasia.
To begin with, there is nothing logically inconsistent in supporting voluntary euthanasia while maintaining the moral inappropriateness of non-voluntary euthanasia. (However, for an attempt to press the charge that there is such an inconsistency see, e.g., Keown 2022.) Undoubtedly, some advocates of voluntary euthanasia wish also to lend their support to some acts of non-voluntary euthanasia, for example, for those in persistent vegetative states who have never indicated their wishes about being helped to die, or for certain severely disabled infants for whom the outlook is hopeless. (See, e.g., Kuhse and Singer 1985; Singer 1994; Stingl 2010; Sumner 2017.) Others believe that the consent of the patient is strictly required if euthanasia is appropriately to be legalized. The difference is not a matter of logical acumen; it is to be explained by reference to the importance placed on key values by the respective supporters. Thus, for example, those who insist on the necessity for a competent request by a patient for medical assistance with dying typically believe that such a request is the paramount consideration in end-of-life decision making (even when it is harnessed to the value of individual well-being), whereas those who consider a person’s best interests to be the paramount consideration are more likely to believe in the justifiability of instances of non-voluntary euthanasia like those mentioned above.
Next, it is hard to see why moving from voluntary to non-voluntary euthanasia is supposed to be psychologically inevitable. Why should those who support the legalization of voluntary euthanasia, because they value the autonomy of the individual, find it psychologically easier, in consequence, to endorse the killing of those who are not able competently to request assistance with dying? What reason is there to believe that they will, as a result of their support for voluntary euthanasia, be psychologically driven to endorse a practice of non-voluntary euthanasia?
Finally, since there is nothing arbitrary about distinguishing voluntary euthanasia from non-voluntary euthanasia (because the line between them is based on clear principles), there can be no substance to the charge that only by arbitrarily drawing a line between them could non-voluntary euthanasia be avoided were voluntary euthanasia to be legalized.
What, though, of Hitler’s Germany and the recent experience of legalized voluntary euthanasia in the Netherlands and elsewhere? The former is easily dismissed as an indication of an inevitable descent from voluntary euthanasia to non-voluntary. There never was a policy in favor of, or a legal practice of, voluntary euthanasia in Germany in the 1920s to the 1940s (see, for example, Burleigh 1994). There was, prior to Hitler coming to power, a clear practice of killing some disabled persons. But it was never suggested that their being killed was justified by reference to their best interests; rather, it was said that society would be benefited. Hitler’s later revival of the practice and its widening to take in other groups such as Jews and gypsies was part of a program of eugenics , not euthanasia.
Since the publication of the Remmelink Report in 1991 into the medical practice of euthanasia in the Netherlands, it has frequently been said that the Dutch experience shows that legally protecting voluntary euthanasia is impossible without also affording shelter to the non-voluntary euthanasia that will follow in its train (see, e.g., Keown 2018). In the period since that report there have been regular national studies of the practice of euthanasia in the Netherlands (see, e.g., Rietjens, et al. 2009; Onwuteaka-Philipsen, et al. 2012; van der Heide, et al. 2017). The findings from these national studies have consistently shown that there is no evidence for the existence of such a slippery slope. Among the specific findings the following are worth mentioning: of those terminally ill persons who have been assisted to die about sixty per cent have clearly been cases of voluntary euthanasia as it has been characterised in this entry; of the remainder, the vast majority of cases were of patients who at the time of their medically assisted deaths were no longer competent. It might be thought that these deaths ought to be regarded as instances of non-voluntary euthanasia. But, in fact, it would be inappropriate to regard them as such. Here is why. For the overwhelming majority of these cases, the decisions to end life were taken only after consultation between the attending doctor(s) and close family members, and so can legitimately be thought of as involving substituted judgements. Moreover, according to the researchers, the overwhelming majority of these cases fit within either of two common practices that occur in countries where voluntary euthanasia has not been legalized, namely, that of terminal sedation of dying patients, and that of giving large doses of opioids to relieve pain while foreseeing that this will also end life. In a very few cases, there was no consultation with relatives, though in those cases there were consultations with other medical personnel. The researchers contend that these instances are best explained by the fact that families in the Netherlands strictly have no final legal authority to act as surrogate decision-makers for incompetent persons. For these reasons the researchers maintain that non-voluntary euthanasia is not widely practised in the Netherlands.
That there have only been a handful of prosecutions of Dutch doctors for failing to follow agreed procedures (Griffiths, et al. 1998; Asscher and van de Vathorst 2020), that none of the doctors prosecuted has had a significant penalty imposed, that a significant proportion of requests for medical assistance with dying are rejected as unjustifiable, and that the Dutch public have regularly reaffirmed their support for the agreed procedures suggests that, contrary to the claims of some critics, the legalization of voluntary euthanasia has not increased the incidence of non-voluntary euthanasia. A similar picture to the one in the Netherlands has emerged from studies of the operation of the law concerning physician-assisted suicide in Oregon. Indeed, in a recent wide-ranging study of attitudes and practices of voluntary euthanasia and physician-assisted suicide covering two continents, a prominent critic of these practices has concluded (in agreement with his co-authors) that little evidence exists of abuse, particularly of the vulnerable (see Emanuel, et al., 2016). Unfortunately, insufficient time has elapsed for appropriate studies to be conducted in the other jurisdictions that have legalized either voluntary euthanasia or physician-assisted suicide (but for some relevant evidence see e.g., White, et al. 2022). Finally, some commentators have pointed out that there may, in reality, be more danger of the line between voluntary and non-voluntary euthanasia being blurred if euthanasia is practised in the absence of legal recognition, since there will, in those circumstances, be neither transparency nor monitoring (which cannot be said of the Netherlands, Belgium, Oregon and so on).
None of this is to suggest that it is not necessary to ensure the presence of safeguards against potential abuse of legally protected voluntary euthanasia. This is particularly important for the protection of those who have become incompetent by the time decisions need to be taken about whether to assist them to die. Furthermore, it is, of course, possible that the reform of any law may have unintended effects. However, if the arguments outlined above are sound (and the experience in the Netherlands, Belgium and Luxembourg, along with the more limited experience in several states in the United States and in Canada, is, for the present, not only the best evidence we have that they are sound, but the only relevant evidence), that does not seem very likely.
It is now well-established in many jurisdictions that competent patients are entitled to make their own decisions about life-sustaining medical treatment. That is why they can refuse such treatment even when doing so is tantamount to deciding to end their life. It is plausible to think that the fundamental basis of the right to decide about life-sustaining treatment – respect for a person’s autonomy and her assessment of what will best serve her well-being – has direct relevance to the legalization of voluntary euthanasia (see, e.g., Dworkin 1998; Young 2007, 2017; Sumner 2011, 2017). In consequence, extending the right of self-determination to cover cases of voluntary euthanasia does not require a dramatic shift in legal policy. Nor do any novel legal values or principles need to be invoked. Indeed, the fact that suicide and attempted suicide are no longer criminal offences in many jurisdictions indicates that the central importance of individual self-determination in a closely analogous context has been accepted. The fact that voluntary euthanasia and physician-assisted suicide have not been more widely decriminalized is perhaps best explained along a similar line to the one that has frequently been offered for excluding the consent of the victim as a justification for an act of killing, namely the difficulties thought to exist in establishing the genuineness of the consent. But, the establishment of suitable procedures for giving consent to voluntary euthanasia and physician-assisted suicide is surely no harder than establishing procedures for competently refusing burdensome or otherwise unwanted medical treatment. The latter has already been accomplished in many jurisdictions, so the former should be achievable as well.
Suppose that the moral case for legalizing voluntary euthanasia and physician-assisted suicide does come to be judged more widely as stronger than the case against legalization, and they are made legally permissible in more jurisdictions than at present. Should doctors take part in the practice? Should only doctors perform voluntary euthanasia? These questions ought to be answered in light of the best understanding of what it is to provide medical care. The proper administration of medical care should promote the welfare of patients while respecting their individual self-determination. It is these twin values that should guide medical care, not the preservation of life at all costs, or the preservation of life without regard to whether patients want their lives prolonged should they judge that life is no longer of benefit or value to them. Many doctors in those jurisdictions where medically assisted death has been legalized and, to judge from available survey evidence, in other liberal democracies as well, see the practice of voluntary euthanasia and physician-assisted suicide as not only compatible with their professional commitments but also with their conception of the best medical care for the dying. That being so, doctors of the same conviction in jurisdictions in which voluntary medically assisted death is currently illegal should no longer be prohibited by law from lending their professional assistance to competent terminally ill persons who request assistance with dying because of irremediable suffering or because their lives no longer have value for them.
- Asscher, E. and S. van de Vathorst, 2020, “First Prosecution of a Dutch Doctor Since the Euthanasia Act of 2002: What Does It Mean?”, Journal of Medical Ethics , 46: 71–75.
- Beauchamp, T. and A. Davidson, 1979, “The Definition of Euthanasia”, The Journal of Medicine and Philosophy , 4: 294–312.
- Bernat, J., B. Gert, and R. Mognielnicki, 1993, “Patient Refusal of Hydration and Nutrition: An Alternative to Physician Assisted Suicide or Voluntary Euthanasia”, Archives of Internal Medicine , 153: 2723–2728.
- Biggar, N., 2004, Aiming to Kill: The Ethics of Suicide and Euthanasia , London: Darton, Longman and Todd.
- Bradley, B., 2009, Well-Being and Death , Oxford: Clarendon Press.
- Braun, E., 2023, “An autonomy-based approach to assisted suicide: a way to avoid the expressivist objection against assisted dying laws”, Journal of Medical Ethics , 49: 497–501.
- Brock, D., 1993, “Voluntary Active Euthanasia”, Hastings Center Report , 22(2): 10–22.
- Burleigh, M., 1994, Death and Deliverance: Euthanasia in Germany c. 1900–1945 , Cambridge: Cambridge University Press.
- Cavanaugh, T., 2006, Double-Effect Reasoning: Doing Good and Avoiding Evil , Oxford: Clarendon Press.
- Commission on the Study of Medical Practice Concerning Euthanasia: Medical Decisions Concerning the End of Life , The Hague: SdU, 1991. (This is known as ‘The Remmelink Report’.)
- Downie, J. and U. Schuklenk, 2021, “Social determinants of health and slippery slopes in assisted dying debates: lessons from Canada”, Journal of Medical Ethics , 47: 662–669.
- Dworkin, R., 1993, Life’s Dominion: An Argument About Abortion, Euthanasia, and Individual Freedom , New York: Random House.
- Dworkin, G., 1998, “Public Policy and Physician-Assisted Suicide”, in Dworkin, Frey, & Bok 1998, pp. 64–80.
- Dworkin, G., R. Frey, and S. Bok, 1998, Euthanasia and Physician-Assisted Suicide: For and Against , Cambridge: Cambridge University Press.
- Emanuel, E., 1999, “What Is the Great Benefit of Legalizing Euthanasia or Physician-Assisted Suicide?”, Ethics , 109: 629–642.
- Emanuel, E., B. Onwuteaka-Philipsen, J. Urwin and J. Cohen, 2016, “Attitudes and Practices of Euthanasia and Physician-Assisted Suicide in the United States, Canada and Europe”, Journal of the American Medical Association , 316: 79–90.
- Finnis, J., 1995, “A Philosophical Case Against Euthanasia” in J. Keown (ed.), Euthanasia Examined: Ethical, Clinical and Legal Perspectives , Cambridge: Cambridge University Press.
- Foley, K. and H. Hendin (eds.), 2002, The Case Against Assisted Suicide: For the Right to End-of-Life Care , Baltimore: The Johns Hopkins University Press.
- Foot, P., 1977, “Euthanasia”, Philosophy and Public Affairs , 6: 85–112.
- Ganzini, L., E. Goy and S. Dobscha, 2009, “Oregonians’ Reasons for Requesting Physician Aid in Dying”, Archives of Internal Medicine , 169: 489–492.
- Gorsuch, N., 2006, The Future of Assisted Suicide and Euthanasia , Princeton, New Jersey: Princeton University Press.
- Griffiths, J., A. Bood, and H. Weyers, 1998, Euthanasia and Law in the Netherlands , Amsterdam: Amsterdam University Press.
- Griffiths, J., H. Weyers and M. Adams, 2008, Euthanasia and Law in Europe , Oxford: Hart Publishing.
- Jackson, E. and J. Keown, 2012, Debating Euthanasia , Oxford: Hart Publishing.
- Keown, J., 2018, Euthanasia, Ethics and Public Policy: an argument against legalization , 2nd edition, New York: Cambridge University Press.
- –––, 2022, “The Logical Link Between Voluntary and Non-Voluntary Euthanasia”, Cambridge Law Journal , 81: 84–108.
- Kim, S., R. De Vries and J. Peteet, 2016, “Euthanasia and Assisted Suicide of Patients with Psychiatric Disorders in the Netherlands 2011 to 2014”, Journal of the American Medical Association Psychiatry , 73: 362–368.
- Kuhse, H. and P. Singer, 1985, Should the Baby Live?: The Problem of Handicapped Infants , Oxford: Oxford University Press.
- Lewis, P., 2007, Assisted Dying and Legal Change , Oxford: Oxford University Press.
- Marquet, R., A. Bartelds, G. Visser, P. Spreeuwenberg and L. Peters, 2003, “Twenty Five Years of Requests for Euthanasia and Physician Assisted Suicide in Dutch General Practice: Trend Analysis”, British Medical Journal , 327: 201–202.
- McIntyre, A., 2001, “Doing Away With Double Effect”, Ethics , 111: 219–255.
- McMahan, J., 2002, The Ethics of Killing: Problems at the Margins of Life , New York: Oxford University Press.
- Onwuteaka-Philipsen, B., A. Brinkman-Stoppelenburg, C. Penning, G. Jong-Krul, J. van Delden and A. van der Heide, 2012, “Trends in end-of-life practices before and after the enactment of the euthanasia law in the Netherlands from 1990–2010: A repeated cross-sectional survey”, The Lancet , 380: 908–915.
- Rachels, J., 1986, The End of Life: Euthanasia and Morality , Oxford: Oxford University Press.
- Rietjens, J., P. van der Maas, B. Onwuteaka-Philipsen, J. van Delden and A. van der Heide, 2009, “Two Decades of Research on Euthanasia from the Netherlands: What Have We Learnt and What Questions Remain?”, Journal of Bioethical Inquiry , 6: 271–283.
- Savulescu, J., 2014, “A Simple Solution to the Puzzles of End of Life? Voluntary Palliated Starvation”, Journal of Medical Ethics , 40: 110–113.
- Singer, P. 1994, Rethinking Life and Death: The Collapse of Our Traditional Ethics , Melbourne: Text Publishing.
- Stingl, M., (ed.), 2010, The Price of Compassion: Assisted Suicide and Euthanasia , Peterborough, Ontario: Broadview Press.
- Sumner, L., 2011, Assisted Death: A Study in Ethics and Law , Oxford: Oxford University Press.
- –––, 2017, Physician-Assisted Death: What Everyone Needs to Know , New York: Oxford University Press.
- –––, 2020, “Conscientious Refusal to Provide Medically Assisted Dying”, University of Toronto Law Journal , 71: 1–31.
- van der Heide, A., J.van Delden and B. Onwuteaka-Philipsen, 2017, “End-of-Life Decisions in the Netherlands over 25 Years”, New England Journal of Medicine , 377: 492–494.
- Varelius, J., 2014, “Medical Expertise, Existential Suffering and Ending Life”, Journal of Medical Ethics , 40: 104–107.
- Velleman, J., 1999, “A Right of Self-Termination?”, Ethics , 109: 606–628.
- White, B., L. Willmott, K. Del Villar, J. Hewitt, E. Close, L. Greaves, J. Cameron, R. Meehan and J. Downie, 2022, “Who is Eligible for Voluntary Assisted Death?: Nine Medical Conditions Assessed Against Five Legal Frameworks”, University of New South Wales Law Journal , 45: 401–444.
- Wicclair, M., 2011, Conscientious Objection in Health Care: An Ethical Analysis , Cambridge: Cambridge University Press.
- Winkler, E., 1995, “Reflections on the State of Current Debate Over Physician-Assisted Suicide and Euthanasia”, Bioethics , 9: 313–326.
- Woodward, P., (ed.), 2001, The Doctrine of Double Effect: Philosophers Debate a Controversial Moral Principle , Notre Dame, Indiana: University of Notre Dame Press.
- Young, R., 2007, Medically Assisted Death , Cambridge: Cambridge University Press.
- –––, 2017, “An Argument in Favor of the Morality of Voluntary Medically Assisted Death”, in M. Cholbi (ed.), Euthanasia and Assisted Suicide: Global Views on Choosing to End Life , Santa Barbara: Praeger.
How to cite this entry . Preview the PDF version of this entry at the Friends of the SEP Society . Look up topics and thinkers related to this entry at the Internet Philosophy Ontology Project (InPhO). Enhanced bibliography for this entry at PhilPapers , with links to its database.
- Medically Assisted Dying , an annotated bibliography authored by Robert Young (La Trobe University)
- Eight Reasons Not to Legalize Physician Assisted Suicide , by David Albert Jones, online resource at the Anscombe Bioethics Centre website.
advance directives | decision-making capacity | doing vs. allowing harm | double effect, doctrine of
Copyright © 2024 by Robert Young < robert . young @ iinet . net . au >
- Accessibility
Support SEP
Mirror sites.
View this site from another server:
- Info about mirror sites
The Stanford Encyclopedia of Philosophy is copyright © 2024 by The Metaphysics Research Lab , Department of Philosophy, Stanford University
Library of Congress Catalog Data: ISSN 1095-5054
Accessibility links
- Skip to content
- Skip to local navigation
- Skip to bbc.co.uk navigation
- Skip to bbc.co.uk search
- Accessibility Help
Ethics guide
Pro-euthanasia arguments
This page sets out the arguments in favour of allowing euthanasia in certain cases. Should we accept that euthanasia happens and try to regulate it safely? Do people have the right to arrange their own deaths?
On this page
- Overview of arguments in favour of euthanasia
Regulating euthanasia
People have the right to die, other human rights imply a right to die, libertarian argument, medical resources, moral rules must be universalisable, euthanasia happens anyway, is death a bad thing, page options.
- Print this page
Overview of pro-euthanasia arguments
Arguments in favour of euthanasia can be broken down into a few main categories:
Arguments based on rights
- People have an explicit right to die
- A separate right to die is not necessary, because our other human rights imply the right to die
- Death is a private matter and if there is no harm to others, the state and other people have no right to interfere (a libertarian argument)
Practical arguments
- It is possible to regulate euthanasia
- Allowing people to die may free up scarce health resources (this is a possible argument, but no authority has seriously proposed it)
- Euthanasia happens anyway (a utilitarian or consequentialist argument)
Philosophical arguments
- Euthanasia satisfies the criterion that moral rules must be universalisable
Arguments about death itself
Those in favour of euthanasia think that there is no reason why euthanasia can't be controlled by proper regulation , but they acknowledge that some problems will remain.
For example, it will be difficult to deal with people who want to implement euthanasia for selfish reasons or pressurise vulnerable patients into dying.
This is little different from the position with any crime. The law prohibits theft, but that doesn't stop bad people stealing things.
Human beings have the right to die when and how they want to
In...cases where there are no dependants who might exert pressure one way or the other, the right of the individual to choose should be paramount. So long as the patient is lucid, and his or her intent is clear beyond doubt, there need be no further questions. The Independent, March 2002
Many people think that each person has the right to control his or her body and life and so should be able to determine at what time, in what way and by whose hand he or she will die.
Behind this lies the idea that human beings should be as free as possible - and that unnecessary restraints on human rights are a bad thing.
And behind that lies the idea that human beings are independent biological entities, with the right to take and carry out decisions about themselves, providing the greater good of society doesn't prohibit this. Allied to this is a firm belief that death is the end.

Religious objections
Religious opponents disagree because they believe that the right to decide when a person dies belongs to God.
Secular objections
Secular opponents argue that whatever rights we have are limited by our obligations. The decision to die by euthanasia will affect other people - our family and friends, and healthcare professionals - and we must balance the consequences for them (guilt, grief, anger) against our rights.
We should also take account of our obligations to society, and balance our individual right to die against any bad consequences that it might have for the community in general.
These bad consequences might be practical - such as making involuntary euthanasia easier and so putting vulnerable people at risk.
There is also a political and philosophical objection that says that our individual right to autonomy against the state must be balanced against the need to make the sanctity of life an important, intrinsic, abstract value of the state.
Secular philosophers put forward a number of technical arguments, mostly based on the duty to preserve life because it has value in itself, or the importance of regarding all human beings as ends rather than means.
Without creating (or acknowledging) a specific right to die, it is possible to argue that other human rights ought to be taken to include this right.
The right to life includes the right to die
- The right to life is not a right simply to exist
- The right to life is a right to life with a minimum quality and value
- Death is the opposite of life, but the process of dying is part of life
- Dying is one of the most important events in human life
- Dying can be good or bad
- People have the right to try and make the events in their lives as good as possible
- So they have the right to try to make their dying as good as possible
- People also have obligations - to their friends and family, to their doctors and nurses, to society in general
- These obligations limit their rights
- These obligations do not outweigh a person's right to refuse medical treatment that they do not want
- But they do prevent a patient having any right to be killed
- But even if there is a right to die , that doesn't mean that doctors have a duty to kill , so no doctor can be forced to help the patient who wants euthanasia.
The right not to be killed
The right to life gives a person the right not to be killed if they don't want to be.
Those in favour of euthanasia will argue that respect for this right not to be killed is sufficient to protect against misuse of euthanasia, as any doctor who kills a patient who doesn't want to die has violated that person's rights.
Opponents of euthanasia may disagree, and argue that allowing euthanasia will greatly increase the risk of people who want to live being killed. The danger of violating the right to life is so great that we should ban euthanasia even if it means violating the right to die.
The rights to privacy and freedom of belief include a right to die
This is the idea that the rights to privacy and freedom of belief give a person the right to decide how and when to die.
The European Convention on Human Rights gives a person the right to die
- Not according to Britain's highest court.
- It concluded that the right to life did not give any right to self-determination over life and death, since the provisions of the convention were aimed at protecting and preserving life.
English law already acknowledges that people have the right to die
This argument is based on the fact that the Suicide Act (1961) made it legal for people to take their own lives.
Opponents of euthanasia may disagree:
- The Suicide Act doesn't necessarily acknowledge a right to die;
- it could simply acknowledge that you can't punish someone for succeeding at suicide
- and that it's inappropriate to punish someone so distressed that they want to take their own life.
Euthanasia opponents further point out that there is a moral difference between decriminalising something, often for practical reasons like those mentioned above, and encouraging it.
They can quite reasonably argue that the purpose of the Suicide Act is not to allow euthanasia, and support this argument by pointing out that the Act makes it a crime to help someone commit suicide. This is true, but that provision is really there to make it impossible to escape a murder charge by dressing the crime up as an assisted suicide.
This is a variation of the individual rights argument.
- If an action promotes the best interests of everyone concerned and violates no one's rights then that action is morally acceptable
- In some cases, euthanasia promotes the best interests of everyone involved and violates no one's rights
- It is therefore morally acceptable
Objections to this argument
Opponents attack the libertarian argument specifically by claiming that there are no cases that fit the conditions above:
- The arguments that euthanasia is intrinsically wrong fit in here
- people are sometimes wrong about what's in their best interests
- people may not realise that committing euthanasia may harm other people
- euthanasia may deprive both the person who dies and others of benefits
- euthanasia is not a private act - we cannot ignore any bad effects it may have on society in general
Euthanasia may be necessary for the fair distribution of health resources
This argument has not been put forward publicly or seriously by any government or health authority. It is included here for completeness.
In most countries there is a shortage of health resources.
As a result, some people who are ill and could be cured are not able to get speedy access to the facilities they need for treatment.
At the same time health resources are being used on people who cannot be cured, and who, for their own reasons, would prefer not to continue living.
Allowing such people to commit euthanasia would not only let them have what they want, it would free valuable resources to treat people who want to live.
Abuse of this would be prevented by only allowing the person who wanted to die to intitiate the process, and by regulations that rigorously prevented abuse.
This proposal is an entirely pragmatic one; it says that we should allow euthanasia because it will allow more people to be happy. Such arguments will not convince anyone who believes that euthanasia is wrong in principle.
Others will object because they believe that such a proposal is wide-open to abuse, and would ultimately lead to involuntary euthanasia because of shortage of health resources.
In the end, they fear, people will be expected to commit euthanasia as soon as they become an unreasonable burden on society.
One of the commonly accepted principles in ethics, put forward by Immanuel Kant, is that only those ethical principles that could be accepted as a universal rule (i.e. one that applied to everybody) should be accepted.
So you should only do something if you're willing for anybody to do exactly the same thing in exactly similar circumstances, regardless of who they are.
The justification for this rule is hard to find - many people think it's just an obvious truth (philosophers call such truths self-evident). You find variations of this idea in many faiths; for example "do unto others as you would have them do unto you".
To put it more formally:
A rule is universalisable if it can consistently be willed as a law that everyone ought to obey. The only rules which are morally good are those which can be universalised.
The person in favour of euthanasia argues that giving everybody the right to have a good death through euthanasia is acceptable as a universal principle, and that euthanasia is therefore morally acceptable.
This alone does not justify euthanasia
This is sound, but is not a full justification.
If a person wants to be allowed to commit euthanasia, it would clearly be inconsistent for them to say that they didn't think it should be allowed for other people.
But the principle of universalisability doesn't actually provide any positive justification for anything - genuine moral rules must be universalisable, but universalisability is not enough to say that a rule is a satisfactory moral rule.
Universalisability is therefore only a necessary condition, not a sufficient condition for a rule to be a morally good rule.
So, other than showing that one pre-condition is met, universalisibility doesn't advance the case for euthanasia at all.
How similar can situations be?
Every case is different in some respect, so anyone who is inclined to argue about it can argue about whether the particular differences are sufficent to make this case an exception to the rule.
Universal exceptions to universal rules
Oddly enough, the law of universalisability allows for there to be exceptions - as long as the exceptions are themselves universalisable. So you could have a universal rule allowing voluntary euthanasia and universalise an exception for people who were less than 18 years old.
Euthanasia happens - better to make it legal and regulate it properly
Sounds a bit like "murder happens - better to make it legal and regulate it properly".
When you put it like that, the argument sounds very feeble indeed.
But it is one that is used a lot in discussion, and particularly in politics or round the table in the pub or the canteen.
People say things like "we can't control drugs so we'd better legalise them", or "if we don't make abortion legal so that people can have it done in hospital, people will die from backstreet abortions".
What lies behind it is Utilitarianism : the belief that moral rules should be designed to produce the greatest happiness of the greatest number of people.
If you accept this as the basis for your ethical code (and it's the basis of many people's ethics), then the arguments above are perfectly sensible.
If you don't accept this principle, but believe that certain things are wrong regardless of what effect they have on total human happiness, then you will probably regard this argument as cynical and wrong.
A utilitarian argument for euthanasia
From a utilitarian viewpoint, justifying euthanasia is a question of showing that allowing people to have a good death, at a time of their own choosing, will make them happier than the pain from their illness, the loss of dignity and the distress of anticipating a slow, painful death. Someone who wants euthanasia will have already made this comparison for themselves.
But utilitarianism deals with the total human happiness, not just that of the patient, so that even euthanasia opponents who agree with utilitarianism in principle can claim that the negative effects on those around the patient - family, friends and medical staff - would outweigh the benefit to the patient.
It is hard to measure happiness objectively, but one way to test this argument would be to speak to the families and carers of people who had committed assisted suicide.
Opponents can also argue that the net effect on the whole of society will be a decrease in happiness. The only way to approach this would be to look at countries where euthanasia is legal. However, as no two countries are alike, it seems impossible to extricate the happiness or unhappiness resulting from legal assisted suicide, from any happiness or unhappiness from other sources.
Even if you agree with the utilitarian argument, you then have to deal with the arguments that suggest that euthanasia can't be properly regulated .
Why ask this question?
If death is not a bad thing then many of the objections to euthanasia vanish.
If we put aside the idea that death is always a bad thing, we are able to consider whether death may actually sometimes be a good thing.
This makes it much easier to consider the issue of euthanasia from the viewpoint of someone who wants euthanasia.
Why is death a bad thing?
We tend to regard death as a bad thing for one or more of these reasons:
- because human life is intrinsically valuable
- because life and death are God's business with which we shouldn't interfere
- because most people don't want to die
- because it violates our autonomy in a drastic way
The first two reasons form key points in the arguments against euthanasia , but only if you accept that they are true.
The last two reasons why death is a bad thing are not absolute; if a person wants to die, then neither of those reasons can be used to say that they would be wrong to undergo euthanasia.
People don't usually want to die
People are usually eager to avoid death because they value being alive, because they have many things they wish to do, and experiences they wish to have.
Obviously, this is not the case with a patient who wishes to die - and proper regulation will weed out people who do not really want to die , but are asking for other reasons.
Violation of autonomy
Another reason why death is seen as a bad thing is that it's the worst possible violation of the the wishes of the person who does not want to die (or, to use philosophical language, a violation of their autonomy).
In the case of someone who does want to die, this objection disappears.
Being dead, versus not having been born
Some people say that being dead is no different from not having been born yet, and nobody makes a fuss about the bad time they had before they were born.
There is a big difference - even though being dead will be no different as an experience from the experience of not having yet been born.
The idea is that death hurts people because it stops them having more of the things that they want, and could have if they continued to live.
Someone who makes a request for euthanasia is likely to have a bad quality of life (or a bad prognosis, even if they are not yet suffering much) and the knowledge that this will only get worse. If that is the case, death will not deprive them of an otherwise pleasant existence.
Of course, most patients will still be leaving behind some things that are good: for example, loved ones and things they enjoy. Asking for death does not necessarily mean that they have nothing to live for: only that the patient has decided that after a certain point, the pain outweighs the good things.
« More on Euthanasia
- Religion and Ethics home
Around the BBC
- News - Q&A - Assisted suicide
- Health - Terminal illness
- Health - Palliative care in hospices
- Health - How to Have a Good Death
- Relationships - Coping with grief
Elsewhere on the web
- Care Not Killing
- Compassion in Dying
- Dignity in Dying
- National Council for Palliative Care
Search term:
BBC navigation
- Northern Ireland
- Full A-Z of BBC sites
You're using the Internet Explorer 6 browser to view the BBC website. Our site will work much better if you change to a more modern browser. It's free, quick and easy. Find out more about upgrading your browser here…
- Mobile site
- Terms of Use
- About the BBC
- Contact the BBC
- Parental Guidance
BBC © 2014 The BBC is not responsible for the content of external sites. Read more.
This page is best viewed in an up-to-date web browser with style sheets (CSS) enabled. While you will be able to view the content of this page in your current browser, you will not be able to get the full visual experience. Please consider upgrading your browser software or enabling style sheets (CSS) if you are able to do so.
Euthanasia and Assisted Suicide: A Guide to the Evidence
Introduction
This evidence guide has been written to inform the debate about whether to legalise physician assisted suicide or euthanasia in the United Kingdom. Most of the sources cited here are also relevant to the debates on assisted suicide or euthanasia in other countries.
You can skim to get a sense of the different issues at stake and where to find further information, especially the most reliable information that is freely available online.
This guide aims to be useful for:
- students (especially of the medical professions, law, philosophy, and bioethics)
- research assistants to officials or parliamentarians.
More than this, it is offered to anyone who is concerned about these issues and wishes to assess the evidence.
It is important to remember, as has recently been pointed out , ‘that the medical literature is, in general, favourably disposed toward the empirical and the new [… resultantly] articles defending the ethical status quo (i.e., against PAS) tend to be shut out of the medical literature because they are not reporting anything new and, therefore, cannot have any data. The result is an impression of growing acceptance of PAS, but it really represents an artefact of a scientific bias’. It is hoped that this guide contributes to redressing this scientific bias.
Along with references for the source-data and official reports on assisted suicide and euthanasia in various countries, it identifies some useful articles that have been published in Peer Review Journals (PRJ). Publishing in a PRJ is no guarantee of the truth of an article’s conclusions, for especially in law, ethics and public policy academics frequently argue for opposite conclusions. However, being published in a PRJ is a sign that other academics have considered the argument to be well-structured and the sources of evidence to be clearly identified. This provides a good starting point for debate. Unfortunately, most PRJ material is not free to the general reader but is available only through universities or by subscription. Nevertheless, some PRJ articles are free online and sometimes there are freely available discussions based on the article. At a minimum the abstract of the article will generally be available free online. In this bibliography, all PRJ articles will be identified with an asterisk * . Where the full text of a PRJ is freely available this will be indicated by * (full text available) . Where the published version is not freely available, a pre- or post-print draft occasionally will be. This means that the full text can be read, but the article has none of the publisher’s formatting.
Many articles on euthanasia and assisted suicide have been published since the original version of this evidence guide in 2015. We have updated the guide to include new literature and the changes to legislation regarding euthanasia and assisted suicide throughout the world since that time. The guide is intended to be indicative rather than fully comprehensive, and we intend to update the resources periodically in the future.
DA Jones, R Gay and CM Wojtulewicz
Oxford, April 2022
Abbreviations
EAS = euthanasia and/or assisted suicide.
PAS / AS = physician-assisted suicide / assisted suicide
1. Parliamentary Reports
Since 1990 within the United Kingdom there have been three parliamentary reports on assisted euthanasia or suicide, each of which has been critical of such proposals. The most recent, and the most relevant to the Bills before the House of Lords and the House of Commons, is the 2015 Report of the Health and Sport Committee of the Scottish Parliament.
House of Lords Select Committee on Medical Ethics (HL Paper 21-I of 1993-4). There is no copy of the report available online, but a summary was provided by Lord Walton of Detchant (its chair) in a statement to the House of Lords recorded in Hansard.
House of Lords Assisted Dying for the Terminally Ill Committee 5 April 2005 (Mackay Committee ) On this committee’s findings see also I Finlay, VJ Wheatley, and C Izdebski. ‘The House of Lords Select Committee on the Assisted Dying for the Terminally Ill Bill: implications for specialist palliative care.’ Palliative medicine 19.6 (2005): 444-453 . *
Scottish Parliament Health and Sport Committee 6th Report, 2015 (Session 4): Stage 1 Report on Assisted Suicide (Scotland) Bill . This Committee was ‘not persuaded by the argument that the lack of certainty in the existing law on assisted suicide makes it desirable to legislate to permit assisted suicide... there are ways of responding to suffering (such as increased focus on palliative care and on supporting those with disabilities), which do not raise the kind of concerns about crossing a legal and ethical “Rubicon” that are raised by assisted suicide’. [292, 294]
The House of Lords introduced the Assisted Dying Bill 2021 [HL] , proposed by Baroness Meacher, which was given a second reading on 22 October 2021 .
House of Commons Library Debate Pack 22 January 2020, ‘The Law on Assisted Dying’ , by Elizabeth Rough and Nikki Sutherland.
Current challenges in the culture of healthcare in the UK
If legalised, assisted suicide or euthanasia would be implemented in the context of the NHS. In this regard it is important to be realistic about the current state of healthcare in the UK and failures that can occur and that have occurred, for example, in Mid Staffordshire and in the implementation of the Liverpool Care Pathway for the Dying Patient. These problems were not confined to one Trust or one Pathway but reflect cultural challenges within the NHS. How might assisted suicide or euthanasia be implemented in an environment of targets and ‘tick-boxes’ that sometimes operate to the detriment of patient care?
Mid Staffordshire NHS Foundation Trust Public Inquiry (Francis Report)
Independent Review of the Liverpool Care Pathway: More Care, Less Pathway (Neuberger Report)
2. Official Statistics from Jurisdictions with Assisted Suicide or Euthanasia
Statistics for rates and characteristics of death by assisted suicide or euthanasia are available for fifteen jurisdictions: Canada, the Netherlands, Belgium, Luxembourg, Switzerland, Victoria (Australia) , and, in the USA, the District of Columbia , and the states of California, Colorado, Hawaii, Oregon, Maine, New Jersey, Vermont and Washington . Assisted suicide is legal in Montana and New Mexico, but there are no official reports on the practice.
Such statistics are only as reliable as the questions asked and the means of data collection and in all cases rely on self-reporting. In Flanders (Belgium) it has been shown that official figures underestimate rates by approximately 50% (see section 5.4 below). Official reports tend to gloss the figures and readers should beware of ‘spin.’ Nevertheless, with these caveats, official figures remain an important source of evidence for the impact of legalising assisted suicide or euthanasia.
In Belgium euthanasia was legalised in 2002 and reports have been produced every two years. These are available (in French) here.
In Luxembourg euthanasia was legalised in 2009 and reports are produced every two years. Luxembourg has a small population (less than 1% of the UK population) and thus the number of cases is small. Nevertheless, over 6 years it is possible to see some patterns (a general increase in cases, an increase in non-cancer cases, more cases of women than men). The fifth report (for 2017-2018) is available here. The sixth report (for 2019-2020) was completed in March 2021, but is not available for download.
In the Netherlands euthanasia was effectively decriminalised by a court decision in 1984. This was the basis of a legal statute in 2001 legalising euthanasia and physician assisted suicide. Since 2002 the Netherlands has produced an annual report on the cases notified to the five regional euthanasia committees. These are available (in English once the year is selected).
In Switzerland , since 1942, inciting or assisting suicide has been illegal when it is for selfish motives (such as financial gain). Since 1982 this law has provided legal space for the organisation EXIT to promote assisted suicide for those ‘with unbearable symptoms or with unacceptable disabilities’. There are two government reports from the Federal Statistical Office, one in 2012 and latest, for 2014, published in 2016 and revised in 2017 . There are also statistics for assisted suicide by sex and age for 2003-2019 , published by the Federal Statistical Office. Dignitas has released statistics from 1998-2021 .
North America
Canada passed euthanasia and assisted suicide into law in 2016 (termed ‘medical assistance in dying’ or MAID). Further changes in the law, widening eligibility criteria, were introduced in March 2021 (though not effective until March 2023). The Second Annual Report on Medical Assistance in Dying (2020) shows that ‘MAID’ deaths increased by 34.2% from 2019.
The District of Columbia legalised assisted suicide in 2016 and has produced one statistics report in 2018.
California legalised assisted suicide in 2015 and has produced reports each year since. They can be found here.
Colorado legalised assisted suicide in 2016, and has produced reports each year since. They can be found here.
Hawaii passed assisted suicide into law in 2018, which came into effect in January 2019. The 2019 and 2020 legislative reports can be found here.
Oregon legalised physician assisted suicide in 1997 and produces annual reports. Helpfully the latest report (2021) includes data from previous years. Note that the figure for the number of deaths in the most recent year covered by the report will generally be inaccurate as deaths are recorded against the year of the lethal prescription. For example, if a lethal prescription given in 2012 were used in 2013 the death would be recorded as due to assisted suicide in the 2012 figures. Reports from all individual years can be accessed here.
Maine introduced assisted suicide in 2019 and its reports can be found here.
New Jersey also passed assisted suicide into law in 2019 and its 2019 and 2020 data summaries can be found here.
Vermont legalised physician assisted suicide in 2013 for terminally ill patients. The latest report can be seen here (issued Jan 15 2022).
Washington legalised physician assisted suicide in 2009 following the Oregon model (Washington borders Oregon and to a great extent shares a common culture and history). Washington also produces annual reports.
Victoria (Australia) legalised euthanasia and assisted suicide (under the umbrella term ‘voluntary assisted dying’ or VAD) in 2017, which came into effect in June 2019. Statistics are issued approximately every 6 months, and the data can be found here.
There are common patterns which emerge in each of these jurisdictions: in every jurisdiction numbers have increased over time and continue to do so; there has also been a shift from permitting assisted suicide for cancer victims to include other diseases. In Europe this includes non-terminal conditions such as neuro-psychiatric conditions and multiple co-morbidities (for example, those associated with old age). Supposed safeguards such as psychiatric referral have also declined in frequency (see below for further details). Essentially, the practice has become more widespread and more routine.
3. Public Opinion on Euthanasia and Assisted Suicide
Within the political debate on assisted suicide and euthanasia, both sides, but especially advocates of a change in the law, frequently appeal to surveys of public opinion. In polls, there is a consistent majority of public opinion that expresses support for legalising assisted suicide or euthanasia.
In the UK polls typically show between 70-80% support for legalising assisted suicide. Support drops to around 60% for euthanasia. See for example:
Ipsos-Mori Poll for The Economist (June 2015)
80% believe those accompanying a family member or friend abroad to receive assisted suicide should not be prosecuted. This drops to 74% when informed that current law in England and Wales is that assistance is punishable by up to 14 years in prison. 65% think the law should be changed to permit assistance in travelling abroad, see:
Ipsos-Mori Poll for Dignity in Dying (June 2009)
A 2019 poll commissioned by Dignity in Dying shows net support for assisted suicide law at 84%; but it must be noted that the procedure is referred to as ‘assisted dying’ rather than ‘assisted suicide’ (see the section below on wording of polls):
Populus Poll for Dignity in Dying (March 2019)
Gallup Poll (USA, 2013)
It should be noted that 73% think there ‘ is a difference between a terminally ill adult seeking assistance to end their life and suicide ’, see YouGov / Dignity in Dying (August 2021) . However, the proposed legislation (Assisted Dying Bill [HL] 2021) has the effect of amending the Suicide Act 1961 (as amended by the Coroners and Justice Act 2009) so that it is no longer and offence to ‘encourage or assist’ suicide.
On the issue of correct terminology and the use of euphemism, see:
David Albert Jones, ‘Defining the Terms of the Debate: Euthanasia and Euphemism’, Briefing Papers: Euthanasia and Assisted Suicide (Anscombe Bioethics Centre, Oxford: 2021)
In the UK, 78% are concerned that, as a society, as much as possible ought to be done to reduce suicide rates. 51% are concerned that people would see themselves as a burden and feel pressured into taking their own life if assisted suicide were legal, see:
ComRes Care Not Killing Assisted Suicide Poll (February 2019)
In a 2018 poll, although 75% were in favour of a change in the law, 60% did not know anyone close to them who had died who would have considered assisted suicide had it been available to them, see:
ComRes Daily Mirror Assisted Dying Poll (June 2018)
When participants are exposed to counter arguments to legislation, support wavers. In one poll from 73% to 43%:
Care Not Killing, “‘Assisted Dying’ and Public Opinion” (2014)
ComRes CARE Assisted Suicide Poll (2014)
The Mackay committee produced a very useful critical review on the state of evidence at that time (2005) in relation to public opinion on assisted suicide and euthanasia ( Chapter 6 and Appendix 7 ).
‘ The key conclusion of this report is that, although some idea of the basic attitude of the general public is available through research sources, this does not amount to an authentic picture of public opinion which is in any way comprehensive. Deliberative research techniques, unused so far for this subject, which can produce an account of informed public opinion, are recommended if a proper understanding of public opinion is to be achieved .’ ( Appendix 7 , para 17)
In 2022, it remains the case that ‘ Research sponsors frequently appear to have been more concerned to achieve statistics for media consumption than to work towards achieving a comprehensive understanding of public and health sector attitudes’ (Appendix 7, para 2).
The flaws in most yes/no polls are methodological and are not corrected merely by conducting more polls of a similar kind. Qualitative research is needed to uncover the complexities of the issue and/or the complexities of people’s attitudes to the issue. For example, a study in the Journal of Medical Ethics showed that, if people were given a range of choices (and not just one), more individuals were in favour of legal sanctions against euthanasia than were in support of it.
Hagelin, J, T Nilstun, J Hau, and H-E Carlsson. ‘Surveys on Attitudes towards Legalisation of Euthanasia: Importance of Question Phrasing’. Journal of Medical Ethics 30, no. 6 (1 December 2004): 521–23. https://doi.org/10.1136/jme.2002.002543. * (full text available).
This complexity is also shown in qualitative research with nurses and with dying cancer patients. See here:
Berghs, M, B. Dierckx de Casterlé, and C. Gastmans, ‘The Complexity of Nurses’ Attitudes toward Euthanasia: A Review of the Literature’. Journal of Medical Ethics 31, no. 8 (August 2005): 441–46. https://doi.org/10.1136/jme.2004.009092. * (full text available).
Jaklin, A., N. Olver, and I. Eliott, ‘Dying Cancer Patients Talk about Physician and Patient Roles in DNR Decision Making’. Health Expectations 14, no. 2 (2011): 147–58. https://doi.org/10.1111/j.1369-7625.2010.00630.x * (full text available).
It is worth highlighting the following conclusion from the latter study: ‘ Survey studies showing majority support for euthanasia have typically required individuals to make judgements about hypothetical and abstracted scenarios. Under such conditions, individuals are likely to draw upon the readily available and socially approved discourses of autonomy and compassion, and voice approval. To conclude that this legitimises euthanasia as social policy is to deny the import of other factors that feature when individuals have opportunity to do more than endorse or reject euthanasia ’.
These complexities are by no means peculiar to the issues of assisted suicide and euthanasia, they apply more generally to use of public opinion in ethical debates around public policy. For such reasons government engagement with the public typically employs mixed methods: public events, open online consultations, stakeholder events, and representative opinion polls. The UK government’s Code of Practice on Consultation makes it clear that consideration of public opinion should give particular weight to the views of ‘any groups or sectors... that may be disproportionately affected by the proposals ’ (3.4). [In the case of assisted suicide and euthanasia this would be people who are dying, those who are living with disabilities, their carers, and healthcare professionals, especially doctors who care for the dying.] Consultations should not just ask for conclusions but ‘ the evidence given by consultees to back up their arguments. Analysing consultation responses is primarily a qualitative rather than a quantitative exercise ’ (6.1).
These principles of good practice should apply also when judging the competing claims to how ‘the public’ thinks of assisted suicide and euthanasia.
Wording of polls
Support for euthanasia and assisted suicide in public opinion polls is subject to ‘ over 20% variation in mean support ’ where there are ‘ increasing levels of favourable wording’, and that ‘[a]llusions to hopelessness had an especially strong effect on increasing support for EPAS [euthanasia and physician-assisted suicide] ’:
Grove, Graham, Ian Hughes, Melanie Lovell, and Megan Best. ‘Content Analysis of Euthanasia Polls in Australia and New Zealand: Words Do Matter’. Internal Medicine Journal 51, no. 10 (2021): 1629–35. https://doi.org/10.1111/imj.15377. * (full text available after embargo ).
See also: L. Parkinson et al. ‘Cancer patients’ attitudes towards euthanasia and physician-assisted suicide: The influence of question wording and patients’ own definitions on responses’, Journal of Bioethical Enquiry , 2(2) (2005): 82-89 * (full text available).
Aghababaei, Naser, Hojjatollah Farahani, and Javad Hatami. ‘Euthanasia Attitude; A Comparison of Two Scales’. Journal of Medical Ethics and History of Medicine 4 (12 October 2011): 9 . * (full text available).
Another reason to be cautious of such polling (and opinion polls more generally) is that they do not necessarily reflect how people actually vote when given the opportunity. Most ballot initiatives in the USA on this issue have in fact failed , despite opinion polls seeming to show strong support. Those which have passed (Oregon, Washington, and Colorado) only secured modest majorities (51%, 58%, and 65% respectively).
4. Medical Opinion on Euthanasia and Assisted Suicide
Whereas simple yes / no public opinion polls typically find a significant majority in favour of legalising assisted suicide or euthanasia, opinion among the medical profession is generally opposed.
In March 2019, the Royal College of Physicians (RCP) adopted a position of neutrality , based on a survey of fellows’ and members’ views . 43.4% thought the RCP should be opposed to a change in the law, 31.6% thought the RCP should support such a change, and 25% thought the RCP should be neutral. While this shift was interpreted by some in the media as a move in favour of legalisation, they stated that, ‘ So that there can be no doubt, the RCP clarifies that it does not support a change in the law to permit assisted dying at the present time ’.
Although the Royal College of Radiographers (RCR) does not hold a position on ‘assisted dying’, in 2019 they polled their fellows and members , asking what they thought the RCR Faculty of Clinical Oncology’s position should be on whether or not there should be a change in the law on ‘assisted dying’. The response rate was only 34% (540 complete responses), but 42.9% thought the RCR position should be ‘opposed’, 26.9% thought ‘in favour’, and 30.3% thought ‘neutral’.
The 70th General Assembly of the World Medical Association (October 2019) stated that ‘ the WMA is firmly opposed to euthanasia and physician-assisted suicide ’.
In 2020, the Royal College of General Practitioners (RCGP) decided not to change its position of opposition to ‘assisted dying’, and would not review this for five years ‘ unless there are significant developments ’.
The decision was based on a 2019 Savanta ComRes consultation of RCGP members . Only 41% of respondents thought the RCGP should support a change in the law if ‘ there is a regulatory framework and appropriate safeguarding processes in place ’. Only 7% thought ‘ GPs should be responsible for prescribing drugs for assisted dying (provided that a formal verification process is in place) ’. There was also reluctance to the idea of referring a patient (only 46% support) or supporting/counselling whilst a decision is being made (only 42% support).
The British Medical Association (BMA) changed its position on 14th September 2021 from opposition to a position of neutrality on the subject of ‘physician-assisted dying’. This was preceded by a survey of BMA members’ views on the subject (Kantar, February 2020). The response rate was 19.35% (28,986 members out of 152,004).
50% of respondents were personally supportive of ‘physician-assisted dying’ as a practice. But the percentage of those willing to participate in some way in ‘physician-assisted dying’ was only 36%. There is stronger opposition in general to euthanasia than there is for assisted suicide.
The Association for Palliative Medicine of Great Britain and Ireland (APM) urged parliamentarians to reject the Assisted Dying Bill [HL] 2021 in a briefing statement in October 2021 . A 2021 APM member survey found that 67% of respondents thought that ‘ patients and families think they are definitely or probably practicing covert euthanasia ’, showing a prevalence of misconceptions about palliative care among the public. 87% ‘ felt there has not been good enough press coverage of good deaths ’.
A study in New Zealand showed that medical students were less likely to support euthanasia / assisted suicide towards the end of their studies compared with the beginning, which is ‘ most likely due to their time in medical education ’, see:
Nie, Luke, Kelby Smith-Han, Ella Iosua, and Simon Walker. ‘New Zealand Medical Students’ Views of Euthanasia/Assisted Dying across Different Year Levels’. BMC Medical Education 21, no. 1 (23 February 2021): 125. * (full text available).
Research in Norway in 2014 and 2016 shows that only 9.1% of doctors in the Institute for Studies of the Medical Profession ‘strongly agree’ or ‘partially agree’ with PAS:
Gaasø, Ole Marius, Karin Isaksson Rø, Berit Bringedal, and Morten Magelssen. ‘Doctors’ Attitudes to Assisted Dying’. Tidsskrift for Den Norske Laegeforening: Tidsskrift for Praktisk Medicin, Ny Raekke 139, no. 1 (15 January 2019). * (full text available).
Disparity between support and willingness to be involved
Evidence from Canada and Australia show high levels of disparity between those who support euthanasia/assisted suicide in principle, and those who are willing to participate in the procedure.
Sellars, Marcus, Mark Tacey, Rosalind McDougall, Barbara Hayes, Bridget Pratt, Courtney Hempton, Karen Detering, et al. ‘Support for and Willingness to Be Involved in Voluntary Assisted Dying: A Multisite, Cross-Sectional Survey Study of Clinicians in Victoria, Australia’. Internal Medicine Journal 51, no. 10 (2021): 1619-1628 . * ( embargoed until 01/10/2022)
Bouthillier, Marie-Eve, and Lucie Opatrny. ‘A Qualitative Study of Physicians’ Conscientious Objections to Medical Aid in Dying’. Palliative Medicine 33, no. 9 (October 2019): 1212–20. * (full text available).
The RCR poll of fellows and members in 2019 (see above) showed that 37.3% supported a change in the law to permit ‘assisted dying’, with 46.9% opposed. But when asked, regardless of support or opposition, if they would ‘participate directly’ should the law change, 56.1% said ‘no’ and 23.2% said ‘yes’.
Religious views on End-of-Life Issues
Pew Research Center, ‘Religious Groups’ Views on End-of-Life Issues’, November 21 2013.
In the UK, a study of the influence of religious beliefs on medical students’ attitudes to EAS showed that among those surveyed (with 68.5% professing belief in God), ‘ the majority of students did not agree with euthanasia and physician-assisted suicide in the study scenario. Those who had a belief in god were more likely to disagree with actions that hasten death. The findings show that this was particularly the case with students from a Muslim background ’. See:
Pomfret, Suzie, Shaya Mufti, and Clive Seale. ‘Medical Students and End-of-Life Decisions: The Influence of Religion’. Future Healthc J 5, no. 1 (1 February 2018): 25–29. https://doi.org/10.7861/futurehosp.5-1-25 . * (full text available)
5. Causes of Concern where Euthanasia and / or Assisted Suicide (EAS) is Legal (Part 1)
Euthanasia and / or assisted suicide is legal in a number of places in the world. In some cases, legalisation happened nearly 30 years ago, although there has been a rapid growth in the last 10 years in the number of jurisdictions where, in particular, assisted suicide is permitted under certain conditions.
The British Medical Association have produced a map which shows at a glance where euthanasia and / or assisted suicide is legal.
Commonly there is a requirement for reporting data and monitoring of practice in places where EAS is permitted (see section 2 above). Such reports, along with other data and analysis provides a body of evidence which highlights several aspects of the practice, including reasons for concern. This section provides information from such data which highlight problematic aspects of euthanasia and assisted.
Ever increasing number of people dying by EAS following legalisation
Belgium and the Netherlands provide data over a long period of time, and therefore are amongst the most studied jurisdictions. An obvious cause of concern from both places is that EAS have shown large incremental increases over time.
Figures 1 and 2 below show the number of deaths attributed to EAS since the early 2000s in Belgium and the Netherlands, showing the increasing numbers over time. Looking more closely, comparing the number of deaths in each country over the ten-year period between 2008 and 2018, we see significant increases, with EAS making up:
- 0.78% of deaths in Belgium in 2008, rising to 2.4% of deaths by 2018
- 1.7% of deaths in 2008 and 3.9% of deaths in 2018 in the Netherlands (4.1% in 2020)
In other jurisdictions, similar increases are seen. In Canada, for example, the increase in deaths since legalisation of PAS was very steep, rising from 1,018 in 2016 to 7,595 in 2020, a 7.5-fold increase in just four years , representing 0.38% of all deaths in 2016, increasing to 2.5% of all deaths in 2020. In Switzerland, between 2009 and 2019, the number of AS deaths increased more than 4-fold from 297 to 1,196 (see Figure 3 below).
The number of deaths due to AS in Canada in 2020 is the highest total number of deaths due to EAS reported in any country in the world at 7,595, with the Netherlands the next highest number, recording its highest ever number at 6,938 in 2020 . It should be a cause for concern that in places where EAS is legal to practice, increasing numbers of people choose to end their own lives, or to ask for others to end them for them.
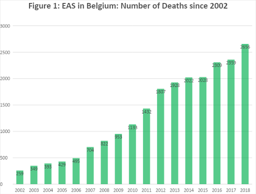
5. Causes of Concern where Euthanasia and / or Assisted Suicide (EAS) is Legal (Part 2)
Terminology of the Legislation
In many places where EAS is legally practised, the language surrounding the legislation could be argued to minimise the reality of the practices employed and the nature of the acts involved; namely a direct act by a medical practitioner with the intention of ending the life of a person (euthanasia), and the writing of a prescription for drugs knowing that they will be used by a person to bring about the end of their own life (physician-assisted suicide).
To accurately assess the ethics and effects of a particular law or practice it is important that terminology is clear and unequivocal in what it describes. ‘Assisted dying’ for example may mean PAS, or EAS. On this point see:
Jones, David Albert. ‘Defining the Terms of the Debate – Euthanasia and Euphemism’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
For an ‘ overview of the terminology, evolution and current legislative picture of assisted dying practices around the globe ’ see:
Mroz, Sarah, Sigrid Dierickx, Luc Deliens, Joachim Cohen, and Kenneth Chambaere. ‘Assisted Dying around the World: A Status Quaestionis’. Annals of Palliative Medicine 10, no. 3 (March 2021): 3540553–553. https://doi.org/10.21037/apm-20-637. * (full text available)
Figure 3 below gives the name for the legislation allowing EAS in various jurisdictions.
Extension of eligibility criteria for EAS
Following legalisation, legislation can extend eligibility from those terminally ill to other non-terminal conditions (children, mentally ill, etc.), see:
Patton, Michaela, and Keith Dobson. ‘Proposal for the Extension of Rights to Medical Assistance in Dying (MAiD) to Mature Minors in Canada’. Canadian Psychology/Psychologie Canadienne 62, no. 3 (2021): 318–25. https://doi.org/10.1037/cap0000219 * (full text available).
The logic of EAS eligibility for the terminally ill can be applied in the same way both to the chronically ill, and to justify non-voluntary euthanasia ( i.e. for those incapable of requesting euthanasia). This is referred to as the ‘slippery slope’. See:
Keown, John. ‘Voluntary Euthanasia & Physician-Assisted Suicide – The Two “Slippery Slope” Arguments’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Keown, John. ‘Euthanasia in the Netherlands: Sliding down the Slippery Slope’. Notre Dame J.L. Ethics & Pub. Pol’y 9, no. 2 (1995): 407–48. * (full text available).
These concerns, including (among others) the EAS for psychiatric indications and evidence in practice of non-voluntary euthanasia are best considered by examining evidence from the four jurisdictions which the longest history of EAS: Switzerland (1982); The Netherlands (1984); Oregon (1997); and Belgium (2002).
5.1 Switzerland
Assisted suicide in Switzerland is performed almost entirely through organisations such as EXIT and Dignitas. Since 1982 (when EXIT was founded) there have been only two official government reports, one in 2012 and another in 2014, and these are dependent on data provided by assisted suicide organisations. Media reporting of UK citizens dying in Switzerland plays a significant role in the UK debate, but it should be noted that most of those individuals would not qualify under current proposals for ‘Assisted Dying’, as they were not expected to die within six months. If the law changed in the UK either people would continue to go to Switzerland (which would have fewer restrictions) or the option of assisted suicide in Switzerland would place pressure on the UK to extend its practice to those who are not terminally ill. Research on the experience of assisted suicide in Switzerland is not reassuring.
In Switzerland, since 1942, inciting or assisting suicide has been illegal when it is for selfish motives (such as financial gain). Since 1982 this law has provided legal space for the organisation EXIT to promote assisted suicide for those ‘with unbearable symptoms or with unacceptable disabilities.’ There are two government reports from the Federal Statistical Office, one in 2012 and latest, for 2014, published in 2016 and revised in 2017 . There are also statistics for assisted suicide by sex and age for 2003-2019 , published by the Federal Statistical Office. Dignitas has released statistics from 1998-2021 .
A systematic study of 43 consecutive cases of assisted suicide in Switzerland from 1992 to 1997 found that in 10 cases (23%), the time between first contact with EXIT and the completed assisted suicide was less than a week and in 4 cases (9%) it was less than a day. In 6 cases (14%) the person had previously been treated in a psychiatric institution. In 11 cases (26%) there was no serious medical condition recorded on file, and in 5 cases (12%) the stated reason for seeking assisted suicide was bereavement. The authors of the study conclude that in the 1990s assisted suicide was ‘performed by lay-people who act without outside control and violate their own rules’.
Frei, Andreas, et al. ‘Assisted suicide as conducted by a “Right-to-Die”-society in Switzerland: a descriptive analysis of 43 consecutive cases.’ Swiss Medical Weekly 131.25-26 (2001): 375-380. * (full text available).
A later study found that between the 1990s and 2001-2004 the rate of assisted suicide for non-fatal diseases increased from 22% to 34% and concluded that ‘ weariness of life rather than a fatal or hopeless medical condition may be a more common reason for older members of Exit Deutsche Schweiz to commit suicide ’.
Fischer, S., Huber, C.A., Imhof, L., Imhof, R.M., Furter, M., Ziegler, S.J., Bosshard, G. ‘Suicide assisted by two Swiss right-to-die organisations’. Journal of Medical Ethics 34, no. 11 (2008): 810-814. * (full text available).
A study in 2014 found that assisted suicide in Switzerland was associated with living alone and divorce and was significantly more frequent among women. In 16% of deaths by assisted suicide no medical condition was listed.
Steck, Nicole, Christoph Junker, Maud Maessen, Thomas Reisch, Marcel Zwahlen, and Matthias Egger. ‘Suicide Assisted by Right-to-Die Associations: A Population Based Cohort Study’. International Journal of Epidemiology 43, no. 2 (April 2014): 614–22. * (full text available).
Research on trends from 1991 to 2008 showed ‘ a tripling of assisted suicide rates in older women, and the doubling of rates in older men ’.
Steck, Nicole, Marcel Zwahlen, and Matthias Egger. ‘Time-Trends in Assisted and Unassisted Suicides Completed with Different Methods: Swiss National Cohort’. Swiss Medical Weekly , no. 25 (14 June 2015). https://doi.org/10.4414/smw.2015.14153 . * (full text available).
Between 2009 and 2019 , the number of assisted suicide deaths increased from 297 to 1196 (an increase of over 400%).
Research showed that requests for assisted suicide were not based on symptom burden but on fear of loss of control. Moreover, those seeking assisted suicide had misconceptions about palliative care.
Gamondi, C., M. Pott, and S. Payne. ‘Families’ Experiences with Patients Who Died after Assisted Suicide: A Retrospective Interview Study in Southern Switzerland’. Annals of Oncology 24, no. 6 (1 June 2013): 1639–44. https://doi.org/10.1093/annonc/mdt033. * (full text available).
Until 2006 assisted suicide had not occurred in Switzerland in a hospital setting. The difficulties of introducing it into hospital and the concerns of the palliative care team are set out below.
Pereira, J, P Laurent, B Cantin, D Petremand, and T Currat. ‘The Response of a Swiss University Hospital’s Palliative Care Consult Team to Assisted Suicide within the Institution’. Palliative Medicine 22, no. 5 (1 July 2008): 659–67. https://doi.org/10.11 . * (full text available).
There is also research from Switzerland on the negative impact on family members of witnessing assisted suicide.
Wagner, B., J. Müller, and A. Maercker. ‘Death by Request in Switzerland: Posttraumatic Stress Disorder and Complicated Grief after Witnessing Assisted Suicide’. European Psychiatry 27, no. 7 (October 2012): 542–46. https://doi.org/10.1016/j.eurpsy.2010.1 *
Assisted suicide in Switzerland is most well known in the UK because of people travelling from the UK to die by assisted suicide. A detailed study of ‘suicide tourism’ shows numbers are increasing, the proportion of cancer is decreasing and the proportion of mental illness and multiple co-morbidities is increasing. Among reasons for assisted suicide the largest single cause, with 223 cases, was cancer, but 37 cited Parkinson’s disease, 37 gave arthritis as a reason, 14 cases were for mental illness, and 40 gave as a reason impairment of eyesight and/or hearing.
Gauthier, Saskia, Julian Mausbach, Thomas Reisch, and Christine Bartsch. ‘Suicide Tourism: A Pilot Study on the Swiss Phenomenon’. Journal of Medical Ethics 41, no. 8 (1 August 2015): 611–17. https://doi.org/10.1136/medethics-2014-102091. * (full text available).
A study from 2016 shows that there has been an increase in the practices of voluntary and non-voluntary euthanasia in Switzerland, which are both illegal. Additionally, there has been a ‘ substantial increase in the use of continuous deep sedation until death, from 4.7% of all deaths in 2001 to 17.5% in 2013 [...] this practice was therefore more common in Switzerland than in either Belgium (12.0% in 2013) or the Netherlands (12.3% in 2010) ’.
Bosshard, Georg, Ueli Zellweger, Matthias Bopp, Margareta Schmid, Samia A. Hurst, Milo A. Puhan, and Karin Faisst. ‘Medical End-of-Life Practices in Switzerland: A Comparison of 2001 and 2013’. JAMA Internal Medicine 176, no. 4 (April 2016): 555–56. * (full text available).
5.2 The Netherlands
In addition to annual reports, based on notified cases of euthanasia there have been a series of studies of end-of-life practices at 5-year intervals since 1990. These were nationwide studies of a stratified sample from the national death registry. Questionnaires were sent to physicians attending these deaths and were returned anonymously. The first is commonly termed the Remmelink Report and subsequent reports followed the same pattern. Both the annual reports and the five yearly studies show incremental increases in deaths by euthanasia over time. Deaths by assisted suicide are less frequent, in part because they are associated with complications.
In the Netherlands euthanasia was effectively decriminalised by a court decision in 1984. This was the basis of a legal statute in 2001 legalising euthanasia and physician assisted suicide. Since 2002 the Netherlands has produced an annual report on the cases notified to the five regional euthanasia committees. These are available (in English once the year is selected) .
The first two reports showed evidence of a number of deaths without explicit patient request (in other words non-voluntary euthanasia). The rates were 0.8% and 0.7% being equivalent to 1,000 and 900 deaths in per year. The reaction of supporters was generally to dismiss the significance of these figures, rather than to see them as a possible cause for concern.
Maas, Paul J. van der, Gerrit van der Wal, Ilinka Haverkate, Carmen L.M. de Graaff, John G.C. Kester, Bregje D. Onwuteaka-Philipsen, Agnes van der Heide, Jacqueline M. Bosma, and Dick L. Willems. ‘Euthanasia, Physician-Assisted Suicide, and Other Medical Practices Involving the End of Life in the Netherlands, 1990-1995’. New England Journal of Medicine 335, no. 22 (28 November 1996): 1699-1705. * (full text available).
Keown, John. ‘Euthanasia in the Netherlands: Sliding down the Slippery Slope’. Notre Dame Journal of Law, Ethics & Public Policy 9, no. 2 (1 January 2012): 407-448. * (full text available).
Van Delden, Johannes J. M., Loes Pijnenborg, and Paul J. Van Der Maas. ‘Reports from The Netherlands. DANCES WITH DATA’. Bioethics 7, no. 4 (1993): 323–29. https://doi.org/10.1111/j.1467-8519.1993.tb00222.x. *
Cohen-Almagor, Raphael. ‘Non-Voluntary and Involuntary Euthanasia in the Netherlands: Dutch Perspectives’. Issues in Law & Medicine 18 (2003): 239-257. * (full text available).
For such reasons the law and practice of euthanasia and assisted suicide in the Netherlands has been criticised several times by the United Nations Human Rights Committee.
UN Human Rights Committee (HRC), UN Human Rights Committee: Concluding Observations: Netherlands, 27 August 2001, CCPR/CO/72/NET
UN Human Rights Committee (HRC), Concluding observations of the Human Rights Committee: Netherlands, 25 August 2009, CCPR/C/NLD/CO/4
The 2019 report expresses its concern by stating ‘ The Committee is concerned, however, at the limited ex ante review of decisions to terminate life, including the legal and ethical implications of such decisions (art. 6) ’. (para. 28). See:
UN Human Rights Committee (HRC), UN Human Rights Committee: ‘Concluding Observations on the 5th Periodic Report of the Netherlands’, 126th session, 22 August 2019. CCPR/C/NLD/CO/5
Results from the most recent 5-yearly study (published in 2017 and providing data from 1990, 1995, 2001, 2005, 2010 and 2015) show that deaths classified as ‘ ending life without explicit patient request ’ have declined from 0.8% in 1990 0.3% in 2015. However, overall numbers of deaths by euthanasia have almost tripled (from 1.7% to 4.5%) Another matter of concern is the steep rise in cases of continuous deep sedation (from 8.2% in 2005to 18.3% in 2015), which is in addition to the rise in deaths by ‘ intensified alleviation of symptoms ’ (from 18.8% of deaths in 1990 to 35.8% of deaths in 2015). The presence of so many deaths with, or by, continuous deep sedation or drugs for intensified alleviations of symptoms confounds the data as either may be used as equivalent to (voluntary) euthanasia or to life ending without request. See:
Van der Heide, Agnes, Johannes JM Van Delden, and Bregje D. Onwuteaka-Philipsen. ‘End-of-life decisions in the Netherlands over 25 years.’ New England Journal of Medicine 377.5 (2017): 492-494. *
The latest annual report (for 2020) shows that the total number of deaths by euthanasia continues to increase. There were 6,938 deaths by euthanasia or assisted suicide notified in 2020, up 9.1% on the previous year, and constituting 4.1% of all deaths in the Netherlands for 2020 (which must be taken in conjunction with the fact that there was an excess of around 15,000 deaths in the Netherlands in 2020). In 2 cases, coronavirus infection was the grounds for euthanasia, and coronavirus infection plus other medical conditions in a further 4 cases.
There are no data on euthanasia for either mental illness or dementia prior to 2012 (before this they are presumably considered under ‘other conditions’). In the 2013 report the category is changed from ‘mental illness’ to ‘mental disorders’, and from 2014 on is referred to as ‘psychiatric disorders’. Figure 1 ( data source ) below shows the figures for these conditions.
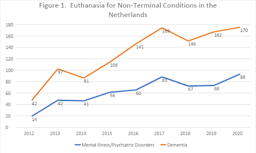
5.2 The Netherlands (cont’d)
From 2012-2020 euthanasia for psychiatric disorders has increased by over 600% and for dementia by over 400%.
This increase in euthanasia or assisted suicide for non-terminal conditions reflects opinion among professionals, with a significant number (between 24% and 39%) in favour of euthanasia or assisted suicide for individuals who experience mental suffering due to loss of control, chronic depression or early dementia. A third of doctors and 58% of nurses were in favour of euthanasia in the case of severe dementia, given the presence of an advance directive.
Kouwenhoven, Pauline SC, Natasja JH Raijmakers, Johannes JM van Delden, Judith AC Rietjens, Maartje HN Schermer, Ghislaine JMW van Thiel, Margo J Trappenburg, et al. ‘Opinions of Health Care Professionals and the Public after Eight Years of Euthanasia Leg i slation in the Netherlands: A Mixed Methods Approach’. Palliative Medicine 27, no. 3 (1 March 2013): 273-80. * (post print text available).
Other research shows a wide variation among general practitioners, consultants and members of the euthanasia committees in their judgement of whether the patient’s suffering is sufficient for euthanasia.
Rietjens, J. a. C., D. G. van Tol, M. Schermer, and A. van der Heide. ‘Judgement of Suffering in the Case of a Euthanasia Request in The Netherlands’. Journal of Medical Ethics 35, no. 8 (1 August 2009): 502–7. https://doi.org/10.1136/jme.2008.028779. *
While euthanasia is defined as ending life on request, the Netherlands has extended life ending without request to newborn infants with disabilities. A description of the protocol (known as the Groningen protocol) is given by two authors who helped develop this practice.
Verhagen, A. A. E., and P. J. J. Sauer. ‘End-of-Life Decisions in Newborns: An Approach From the Netherlands’. Pediatrics 116, no. 3 (1 September 2005): 736–39. https://doi.org/10.1542/peds.2005-0014. * (full text available).
While euthanasia and assisted suicide are requested to secure an easeful death, complications are well documented, especially in assisted suicide. A study in 2000 found that ‘ complications [such as spasm, gasping for breath, cyanosis, nausea or vomiting] occurred in 7% of cases of assisted suicide, and problems with completion [a longer-than-expected time to death, failure to induce coma, or re-awakening of the patient] occurred in 16% ’ because of which ‘ physicians who intend to provide assistance with suicide sometimes end up administering a lethal medication themselves. ’ This is not only a problem of the past; in the 2020 report there were 6,705 cases of euthanasia (‘termination of life on request’), 216 cases of assisted suicide and 17 cases involving a combination of the two ( i.e. , cases which began as assisted suicide, but had to be completed by euthanasia).
Groenewoud, Johanna H., Agnes van der Heide, Bregje D. Onwuteaka-Philipsen, Dick L. Willems, Paul J. van der Maas, and Gerrit van der Wal. ‘Clinical Problems with the Performance of Euthanasia and Physician-Assisted Suicide in the Netherlands’. New England Journal of Medicine 342, no. 8 (24 February 2000): 551–56.
https://doi.org/10.1056/NEJM200002243420805. * (full text available).
Lastly, euthanasia is possible above the age of 12 and below the age of 1. But in 2020, the Netherlands Paediatric Association (Nederlandse Vereinging voor Kindergeneeskunde) expressed the position that the law be extended to allow the termination of life of children between the ages of 1 and 12 under certain conditions. See also the letter to parliament by Hugo de Jonge, the former Minister of Health, Welfare and Sport.
The most important evidence for practice in Oregon is provided by annual reports on the Death with Dignity Act. This section also highlights some aspects that been raised in relation to Oregon practice but are not based on the reports. See also research on the impact of assisted suicide on suicide prevention (section 7, below).
According to the latest official Oregon report, the most frequent end-of-life concern cited by people requesting assisted suicide is not pain but ‘loss of autonomy’ (90.9%), followed by decreased ability ‘to engage in activities making life enjoyable’ (90.2%), ‘loss of dignity’ (73%), ‘burden on family, friends/caregivers’ (48.3%), and ‘losing control of bodily functions’ (43.7%) and only then ‘inadequate pain control or concern about it’ (27.5%), (in each case citing accumulated data for 1998-2021). Evidently, most of these concerns relate to disability and increased dependence. The concern about feeling one is a ‘burden’ on others is significant, much more so than fear of pain (which, also, should not be conflated with actual pain).
From the same report it is clear that in only 14.6% of cases was the prescribing physician present at the time of death (only 11.6% in 2020), that only 3.3% were referred for psychiatric evaluation (only 0.8% in 2021), and that in 56.7% of cases the person was dependent on Medicare/Medicaid insurance or other governmental insurance (up to 78.9% in 2021).
According to Oregon’s Prioritized List of Health Services 2022 cancer treatment is limited according to relative life expectancy, for example, ‘[t]reatment with intent to prolong survival is not a covered service for patients who have progressive metastatic cancer [...]’(Guidance Note 12, GN-5). In contrast ‘It is the intent of the Commission that services under ORS 127.800-127.897 (Oregon Death with Dignity Act) be covered for those that wish to avail themselves to those services’ (Statements of Intent, SI-1).
[N.B. The Statements of Intent and Guidance Notes come after the 160 pages of the prioritised list.]
Health Evidence Review Commission, Prioritized List of Health Services (1 January 2022) .
It should be noted that the drugs that are used for assisted suicide are also used in execution by lethal injection in the United States. This dual use is causing availability problems with supply of the drugs.
Jaquiss, Nigel. ‘Penalized By The Death Penalty’ Willamette Week 21 May 2014.
A good overview of practice in Oregon, including some case studies as well as statistical evidence, shows problems with doctor shopping, suspect coercion and lack of sufficient psychiatric evaluation.
Hendin, Herbert, and Kathleen Foley. ‘Physician-Assisted Suicide in Oregon: A Medical Perspective’. Michigan Law Review 106, no. 8 (2008): 1613–39 . * (full text available).
Kenneth Stevens has shown that from 2001 to 2007 a majority (61%, 165 out of 271) of the lethal prescriptions were written by a minority (18%, 20 out of 109) of the participating physicians. More striking still, just 3 physicians were responsible for 23% of lethal prescriptions (62 out of 271).
Stevens Jr., Kenneth R. ‘Concentration of Oregon’s Assisted Suicide Prescriptions & Deaths from a Small Number of Prescribing Physicians’. Physicians for Compassionate Care Education Foundation, 18 March 2015.
See also ‘Five Oregonians to Remember’ PCCEF, 27 December 2007.
5.4 Belgium
Though Belgium legalised euthanasia in 2002, eighteen years after the Netherlands (in 1984), its number of deaths are near that of the Netherlands. There were 5,015 reported cases in 2019 (more than six times the 822 reported cases in 2009). According to research conducted by Chambaere (see below) these official figures underreport euthanasia by around 50%. What is more worrying is that research indicates that more than 1,000 patients a year (1.7% of all deaths) have their lives ended deliberately without having requested it. This figure has not declined with time. Since legalisation in 2002, reports have been produced every two years. These are available (in French) here.
For a critical analysis of euthanasia in Belgium, see:
Jones, David Albert, Chris Gastmans, and C. MacKellar, eds. Euthanasia and Assisted Suicide: Lessons from Belgium . Cambridge Bioethics and Law. Cambridge, UK and New York, NY: Cambridge University Press, 2017. (This book can be ordered here ).
Devos, Timothy (ed.). Euthanasia: Searching for the Full Story: Experiences and Insights of Belgian Doctors and Nurses , Cham: Springer International Publishing, 2021. https://link.springer.com/book/10.1007/978-3-030-56795-8. (free e-book)
Belgian law came to prominence with the decision in February 2014 to extend euthanasia to children. This caused concern among clinicians and bioethicists in other countries.
Siegel, Andrew M., Dominic A. Sisti, and Arthur L. Caplan. ‘Pediatric Euthanasia in Belgium: Disturbing Developments’. JAMA 311, no. 19 (21 May 2014): 1963–64. https://doi.org/10.1001/jama.2014.4257. *
Carter, Brian S. ‘Why Palliative Care for Children Is Preferable to Euthanasia’. American Journal of Hospice and Palliative Medicine® 33, no. 1 (1 February 2016): 5–7. https://doi.org/10.1177/1049909114542648. * (full text available).
For background to the original 2002 law and its initial implementation see:
Cohen-Almagor, Raphael. ‘Euthanasia Policy and Practice in Belgium: Critical Observations and Suggestions for Improvement’. Issues in Law & Medicine 24, no. 3 (2009): 187–218. * (full text available)
See also a report analysing ten years of euthanasia practice in Belgium.
E de Diesbach, M de Loze, C Brochier and E Monterol. Euthanasia in Belgium: 10 years on European Institute of Bioethics (April 2012).
Research shows that the cases that are not reported are also less likely to involve a written request, less likely to involve specialist palliative care, and more likely to be performed by a nurse.
Smets, T., J. Bilsen, J. Cohen, M. L. Rurup, F. Mortier, and L. Deliens. ‘Reporting of Euthanasia in Medical Practice in Flanders, Belgium: Cross Sectional Analysis of Reported and Unreported Cases’. BMJ 341, no. oct05 2 (5 October 2010): c5174–c5174. * (full text available).
Research on nurses in Belgium in 2007 showed that cases of life-ending without request were almost as common as cases of euthanasia, and that in 12% of euthanasia cases and 45% of life-ending without request it was a nurse who administered the lethal dose, actions which went ‘beyond the legal margins of their profession’.
Inghelbrecht, E., J. Bilsen, F. Mortier, and L. Deliens. ‘The Role of Nurses in Physician-Assisted Deaths in Belgium’. Canadian Medical Association Journal 182, no. 9 (15 June 2010): 905–10. https://doi.org/10.1503/cmaj.091881. * (full text available).
On the ongoing issue of high levels of intentional life-ending without consent in Belgium see:
Cohen-Almagor, Raphael. ‘First Do No Harm: Intentionally Shortening Lives of Patients Without Their Explicit Request in Belgium’. Journal of Medical Ethics , 4 June 2015. https://papers.ssrn.com/abstract=2614587. * (full text available).
Research has also shown that, in Belgium, continuous deep sedation is used with the intention or co-intention to shorten life in 17% of cases, but that it is rarely instituted at the request of the patient (only in 12.7% of cases).
Papavasiliou, Evangelia, Kenneth Chambaere, Luc Deliens, Sarah Brearley, Sheila Payne, Judith Rietjens, Robert Vander Stichele, and Lieve Van den Block. ‘Physician-Reported Practices on Continuous Deep Sedation until Death: A Descriptive and Comparative Study’. Palliative Medicine 28, no. 6 (1 June 2014): 491-500. https://doi.org/10.1177/0269216314530768 * (full text available).
Recent research (published in 2015) shows that while rates of euthanasia increase there has been no improvement in reporting and no reduction in cases of life-ending without request.
Chambaere, Kenneth, Robert Vander Stichele, Freddy Mortier, Joachim Cohen, and Luc Deliens. ‘Recent Trends in Euthanasia and Other End-of-Life Practices in Belgium’. The New England Journal of Medicine 372, no. 12 (19 March 2015): 1179–81 . * (full text available).
In the face of evidence of widespread ending of life without request some researchers have sought to excuse these actions because a third of such patients had, ‘at some point’ in the past, either explicitly or ‘implicitly’ expressed a wish that their lives be ended. However, the very attempt to downplay concerns about deaths deliberately brought about without an explicit request itself illustrates the degree to which non-voluntary euthanasia in Belgium is tolerated and is not regarded as shocking or as a practice in urgent need of correction.
Chambaere, K., J. L. Bernheim, J. Downar, and L. Deliens. ‘Characteristics of Belgian “Life-Ending Acts without Explicit Patient Request”: A Large-Scale Death Certificate Survey Revisited’. CMAJ Open 2, no. 4 (2 December 2014): E262–67. * (full text available).
On the distinction between expressing a wish to die, a wish to hasten death, and a request, see:
Monforte-Royo, Cristina, Christian Villavicencio-Chávez, Joaquín Tomás-Sábado, and Albert Balaguer. ‘The Wish to Hasten Death: A Review of Clinical Studies’. Psycho-Oncology 20, no. 8 (2011): 795–804. https://doi.org/10.1002/pon.1839. * (full text available).
Data from the annual reports shows that an increasing percentage of those dying by euthanasia mention a combination of physical and psychical suffering (78.8% in 2018 and 82.8% in 2019), with figures for solely physical pain reducing (17.7% in 2018 and 12.8% in 2019) and suffering for solely psychic reasons increasing (3.5% in 2018 and 4.3% in 2019).
Stories of individual cases are no substitute for quantitative research, but they help show the possible human meaning behind these statistics. Some illustrative examples are given below.
‘Marc and Eddy Verbessem, Deaf Belgian Twins, Euthanized’ The World Post 15 January 2013 .
Waterfield, ‘Belgian killed by euthanasia after a botched sex change operation’ Telegraph 01 Oct 2013.
E O’Gara ‘Physically healthy 24-year-old granted right to die in Belgium’ Newsweek 29 June 2015.
Associated Press, ‘Belgian Court Acquits 3 Doctors in Landmark Euthanasia Case’ Courthouse News Service 31 January 2020.
Further example cases from Belgium are described here:
Beuselinck, Benoit. ‘Euthanasia Case Studies from Belgium: Concerns about Legislation and Hope for Palliative Care’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
6. Disability and the Impact of Assisted Suicide and Euthanasia
Groups representing people with disabilities have been at the forefront of opposition to the legalisation of assisted suicide and euthanasia. Arguments from this perspective, especially in popular publications and comment pieces, have been criticised as reflecting and/or feeding on fears without showing that these fears are reasonable. However, there is also more critical reflection from this perspective, including discussion of empirical evidence relevant to assessing these concerns.
Some opinion polls among disabled people find considerable support for legalising ‘assisted dying’ .
These results are similar to opinion polls in the general population and should be treated with the same caution (see above on the wording of polls). It is important also to take into account polls that identify concerns among disabled people that legal changes could put pressure on disabled people to end their lives prematurely .
An interesting exchange on this issue by two people with disabilities was conducted by Carol Gill and Andrew Batavia. Batavia argues that empirical data is irrelevant to the issue which, in his view, is about values, and centrally the value of autonomy. He is in favour of legalising assisted suicide.
Batavia, A. I. ‘The Relevance of Data on Physicians and Disability on the Right to Assisted Suicide: Can Empirical Studies Resolve the Issue?’ Psychology, Public Policy, and Law: An Official Law Review of the University of Arizona College of Law and the University of Miami School of Law 6, no. 2 (June 2000): 546-58. *
In response Gill presents data, which is relevant to the perception of disability and its role (implicitly or explicitly) in decisions to grant requests for assistance in suicide. For example, she cites research that shows that among 153 emergency care providers, only 18% of physicians, nurses, and technicians imagined they would be glad to be alive with a severe spinal cord injury. In contrast, 92% of a group of 128 persons with high-level spinal cord injuries said they were glad to be alive.
Gill, CJ. ‘Health professionals, disability, and assisted suicide: An examination of relevant empirical evidence and reply to Batavia (2000).’ Psychology, Public Policy, and Law 6.2 (2000): 526-45. *
Unfortunately, neither of these papers is freely available online. However, another very interesting paper by Gill provides a good sense of what a critical and empirically informed disability perspective looks like. More generally, the Disability and Health Journal (in which this paper appears) is a useful source for articles on disability and assisted suicide.
Gill, CJ. ‘No, we don't think our doctors are out to get us: Responding to the straw man distortions of disability rights arguments against assisted suicide’. Disability and Health Journal 3.1 (2010): 31-38 . * (full text available)
Probably the most influential article arguing that the evidence shows no negative impact of assisted suicide or euthanasia on vulnerable groups (including people with disabilities) is by Margaret Battin.
Battin, Margaret P, Agnes van der Heide, Linda Ganzini, and Gerrit van der Wal. ‘Legal Physician‐assisted Dying in Oregon and the Netherlands: Evidence Concerning the Impact on Patients in “Vulnerable” Groups’. Journal of Medical Ethics 33, no. 10 (October 2007):591-597. * (full text available)
The methodology and conclusions of this paper have been criticised by Ilora Finlay and Rob George.
Finlay, I. G., and R. George. ‘Legal Physician-Assisted Suicide in Oregon and The Netherlands: Evidence Concerning the Impact on Patients in Vulnerable Groups--Another Perspective on Oregon’s Data’. Journal of Medical Ethics 37, no. 3 (March 2011): 171–74 . https://doi.org/10.1136/jme.2010.037044 . *
A detailed discussion of Battin’s evidence and counter-evidence from other expert witnesses is found in the Irish Divisional Court case Fleming v Ireland [2013] IEHC 2 (especially para 67) .
‘ [T]he the expert evidence offered by Dr. O’Brien and Professor George to the effect that relaxing the ban on assisted suicide would bring about a paradigm shift with unforeseeable (and perhaps uncontrollable) changes in attitude and behaviour to assisted suicide struck the Court as compelling and deeply worrying… The Court finds the evidence of these witnesses, whether taken together or separately, more convincing than that tendered by Professor Battin, not least because of the somewhat limited nature of the studies and categories of person studied by Professor Battin… ’
Battin’s argument is also criticised by Pereira on the basis that “safeguards” are largely illusory.
Pereira, J. ‘Legalizing Euthanasia or Assisted Suicide: The Illusion of Safeguards and Controls’. Current Oncology 18, no. 2 (April 2011): e38. https://doi.org/10.3747/co.v18i2.883. * (full text available).
Similarly, a detailed discussion of the evidence from Oregon from a disability perspective concludes that ‘ Battin et al.’s interpretation that people with physical disabilities or chronic illnesses are not at increased risk for DWD does not seem to be supportable given available data’ .
CE Drum, G White, G Taitano and W Horner-Johnson, ‘The Oregon Death with Dignity Act: results of a literature review and naturalistic inquiry’. Disability and health journal , 2010, 3(1): 3-15 . * (full text available).
If disability includes mental illness, then there is clearly a group of patients who are prima facie endangered by assisted suicide. In Oregon there has been a decline in the “safeguard” of referral for psychiatric evaluation whereas in Belgium and Switzerland mental illness can itself be a basis for euthanasia or assisted suicide. A study published in the BMJ shows how far the euthanising of psychiatric patients has progressed in Belgium: of 100 patients who requested euthanasia for psychiatric reasons, 73 ‘ were medically unfit for work (they were either receiving disability living allowances or had taken early retirement) ’, i.e. most were categorised as having a disability. Of the 100, 38 were referred for further psychiatric evaluation, after which 17 were approved for euthanasia and 10 died by euthanasia during the study period. Of the 62 people not referred, 31 were approved for euthanasia and 25 died by euthanasia during the study period. These patients suffered from a variety of conditions including mood disorders (58 including 10 who were bipolar), borderline personality disorder (27), schizophrenia and other psychotic disorders (14), post-traumatic stress disorder (13), eating disorders (10), autism spectrum disorder (7), attention deficit hyperactivity (1) as well as other diagnoses, often combining diagnoses ( e.g. , a mood disorder and personality disorder). During the period of the study 6 participants died by (non-assisted) suicide, one from anorexia nervosa and one from palliative sedation. None were terminally ill.
Thienpont L, Verhofstadt M, Van Loon T, et al. ‘Euthanasia requests, procedures and outcomes for 100 Belgian patients suffering from psychiatric disorders: a retrospective, descriptive study’. BMJ Open 2015;5: e007454. doi:10.1136/bmjopen-2014-007454 * (full text available).
Disability makes assessment of ‘ decisional capacity ’ difficult. A study of cases in the Netherlands shows that the ‘ Dutch EAS due care criteria are not easily applied to people with intellectual disabilities and/or autism spectrum disorder, and do not appear to act as adequate safeguards. ’ See:
Tuffrey-Wijne, Irene et al. “Euthanasia and assisted suicide for people with an intellectual disability and/or autism spectrum disorder: an examination of nine relevant euthanasia cases in the Netherlands (2012-2016).” BMC medical ethics vol. 19,1 17. 5 Mar. 2018, doi:10.1186/s12910-018-0257-6 * (full text available).
Tuffrey-Wijne, Irene et al. “‘Because of His Intellectual Disability, He Couldn’t Cope.’ Is Euthanasia the Answer?”. Journal of Policy and Practice in Intellectual Disabilities , vol. 16, no. 2 (June 2019):113-116, https://doi.org/10.1111/jppi.12307 * (post-print draft version available).
EAS in the Netherlands for psychiatric disorders shows that patients are ‘ mostly women, of diverse ages, with complex and chronic psychiatric, medical, and psychosocial histories ’. See:
Kim, Scott Y H et al. “Euthanasia and Assisted Suicide of Patients With Psychiatric Disorders in the Netherlands 2011 to 2014.” JAMA Psychiatry vol. 73,4 (2016): 362-8. doi:10.1001/jamapsychiatry.2015.2887 * (full text available).
Concern is also expressed over safeguards for the disabled, stemming from the myriad of problems the disabled face, such as ‘ subtle pressure, despair at living in a world where their daily existence is seen as one of inevitable suffering or, exhaustion from fighting for the accommodations required to live a life of dignity and pursue their chosen lifestyle and purposes ’. See:
Stainton, Tim. “Disability, vulnerability and assisted death: commentary on Tuffrey-Wijne, Curfs, Finlay and Hollins.” BMC Medical Ethics vol. 20,1 89. 27 (Nov. 2019), doi:10.1186/s12910-019-0426-2 * (full text available).
With respect to more recent developments in Canada regarding EAS for mentally ill patients, see:
Komrad, Mark S. ‘First, Do No Harm: How Canadian Law Allows for Euthanasia and Assisted Suicide for Patients with Psychiatric Disorders’. Briefing Papers: Euthanasia and Assisted Suicide (Anscombe Bioethics Centre, Oxford: 2021).
On the changing social attitude to those living with dementia and how euthanasia poses a threat to living and dying well with dementia, see:
Matthews, Pia. ‘Dignity in Living: Addressing Euthanasia by Affirming Patient Personhood in Dementia’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
7. Suicide Prevention and the Impact of Assisted Suicide
Sometimes advocates of assisted suicide are happy to use this terminology, as for example in the ‘Assisted Suicide (Scotland) Bill’ (introduced in 2011), which was rejected by the Scottish Parliament in 2015. Other proponents avoid this language and prefer ‘dying / death with dignity’, ‘assisted dying/death’ or ‘medical aid in dying’. However, evidence indicates no sharp distinction between assisted suicide and non-assisted suicide. Evidence also suggests legalising assisted suicide ‘normalises’ suicide and is associated with increases in suicide.
Evidence from the USA shows that the legalisation of ‘ assisted suicide is associated with a significant increase in total suicide (inclusive of assisted suicide) and no reduction in non-assisted suicide .’
Jones, David Albert and David Paton ‘How does legalization of physician-assisted suicide affect rates of suicide?, Southern Medical Journal , 108.10 (2015): 599-604. * (pre-print draft available).
The association of legalising assisted suicide and a ‘ significant increase in total suicides ’ is also supported by more recent research on data from the USA. Paton and Sourafel also conclude that ‘ [i]t is possible that there is some substitution from unassisted suicide to assisted suicide but that this is balanced out by an increase in unassisted suicide arising from, for example, a reduction in societal taboos associated with suicide ’. See:
Sourafel, Girma, and David Paton. ‘Is Assisted Suicide a Substitute for Unassisted Suicide?’ European Economic Review , 9 April 2022, 104113. https://doi.org/10.1016/j.euroecorev.2022.104113. * (pre-proof text available).
In Europe, the introduction of euthanasia and assisted suicide has resulted in ‘ considerable increases in suicide (inclusive of assisted suicide) and in intentional self-initiated death ’. See:
Jones, David Albert. ‘Euthanasia, Assisted Suicide, and Suicide Rates in Europe’, Journal of the Ethics of Mental Health 11 (2022):1-35. * (full text available).
Restricting access to means of suicide appear to be ‘ particularly effective in contexts where the method is popular, highly lethal, widely available, and/or not easily substituted by other similar methods ’. See:
Sarchiapone, Marco, Laura Mandelli, Miriam Iosue, Costanza Andrisano, and Alec Roy. ‘Controlling access to suicide means.’ International journal of environmental research and public health 8, no. 12 (2011): 4550-4562, doi: 10.3390/ijerph8124550 * (full text available).
It is argued that ‘assisted death’ of a kind legalised in Oregon, is not assisted suicide because (1) with ‘assisted death’ the person is terminally ill and (2) (non-assisted) suicide is typically the result of depression. However, according to one UK study, ‘at least 10 percent of [non-assisted] suicides nationally involve[ed] some form of serious physical illness (either chronic or terminal)’. See:
Bazalgette, L., W Bradley, J Ousbey. The Truth about Suicide (London: Demos, 2011)
Similarly in Switzerland ‘ In 53% of cases, causes of death registrations for [non-assisted] suicide do not contain any information about concomitant diseases. If no information is available, this may mean various things: either no disease was present or it was unknown. If information is available, 56% of entries cite depression. In the remaining 44% of entries, a physical disease is mentioned. Physical diseases include a range similar to that of assisted suicide (G11). ’ (emphasis added)
Similarly, a report on suicide in Oregon found that 25% of men and 26% of women who died by suicide had had physical health problems, and in the over-65 cohort, 66% of men and 56% of women had physical health problems, including conditions such as cancer, heart disease, and chronic pain.
Shen, X., L Millet. Suicide in Oregon: Trends and Risk Factors 2012 Report . Oregon Health Authority, Portland, Oregon.
The vulnerability of older people, those living alone and those with physical illness was highlighted in a report by the New York Task Force in 1994. The Task Force also found that depression was prevalent in this population, but largely undiagnosed and untreated (see especially chapter 2 of the report).
New York State Task Force on Life and the Law, ‘When Death is Sought: Assisted Suicide and Euthanasia in the Medical Context’ (1994).
Similarly, in a study of 178 Compassion & Choices clients, of those who, in the study period, obtained lethal medication 3 out of 18 (17%) fulfilled the criteria for depression and of those who died by assisted suicide by the end of the study 3 out of 9 (33%) met the criteria for depression.
Ganzini, L., E. R Goy, and S. K Dobscha. ‘Prevalence of Depression and Anxiety in Patients Requesting Physicians’ Aid in Dying: Cross Sectional Survey’. BMJ 337, no. 2 (7 October 2008): a1682–a1682. https://doi.org/10.1136/bmj.a1682. * (full text available).
It has been argued that legalising assisted suicide could, paradoxically, delay or inhibit suicide. This has been argued by Lord Falconer and others, but a particularly clear statement is provided by EXIT.
However, in Oregon between 1999 (two years after PAS was introduced) and 2010 the suicide rate among those aged 35-64 increased by almost 50% (compared to 28% nationally).
See also the report on high rates of suicide in Portland, Oregon. This increase is without counting assisted suicides, which rose in Oregon by 44% in 2013 alone .
According to the Swiss government report , ‘ From 1995 to 2003, the absolute number of suicides fell considerably. Since then, it has more or less remained stable while cases of assisted suicide have increased considerably since 2008 in particular. In 2014, for 7 cases of suicide observed, 5 cases of assisted suicide were seen (G7) ’.
Determination of eligibility for EAS may also have an effect on vulnerability. Looking at the situation in Canada, Isenberg-Grzeda et al conclude that ‘ Clinicians must be vigilant and prepared for the possibility of heightened risk, including risk of self-harm, after a finding of ineligibility for assisted death ’. See:
Isenberg-Grzeda, E., S. Bean, C. Cohen, and D. Selby, ‘Suicide attempt after determination of ineligibility for assisted death: A case series’ Journal of pain and symptom management 60, no. 1 (2020): 158-163 *
It must be noted that if suicide follows on from a determination of ineligibility for EAS, that person’s death would be considered suicide. However, it would not be considered ‘suicide’ if he or she had been eligible and died as a result of the provision of EAS. This highlights the broader point that euphemistic expressions such a ‘assisted dying’ or ‘medical aid in dying’ simply rename what is correctly termed ‘suicide’.
Suicide Contagion
A Swiss study indicates evidence for suicide contagion following media reports of assisted suicide:
Frei, Andreas, Tanja Schenker, Asmus Finzen, Volker Dittmann, Kurt Kraeuchi, and Ulrike Hoffmann-Richter. ‘The Werther Effect and Assisted Suicide’. Suicide and Life-Threatening Behavior 33, no. 2 (June 2003): 192–200. https://doi.org/10.1521/suli.33.2.19 *
Research on the impact of reporting assisted suicide in Oregon has also suggested such an effect.
Stark, Paul. ‘Assisted suicide and contagion’ MCCL White Paper, May 2015 .
This evidence coheres with what is known about suicide, that it increases if the means are more widely available and if it is normalised, see for example, Euregenas (European Regions Enforcing Actions Against Suicide) Suicide Prevention Toolkit for Media Professionals .
See also Preventing Suicide: A Resource for Media Professionals, Update 2017 . Geneva: World Health Organization; 2017 (WHO/MSD/MER/17.5). Licence: CC BY-NC-SA 3.0 IGO.
Evidence of suicide rates among veterinarians (which are significantly higher than the average among the population) is generally understood to be due to access to lethal drugs.
Witte, T.K., E.G. Spitzer, N. Edwards, K.A. Fowler, and R. J. Nett. ‘Suicides and Deaths of Undetermined Intent among Veterinary Professionals from 2003 through 2014’. Journal of the American Veterinary Medical Association 255, no. 5 (2019):595-608. * (full text available).
Research also shows that positive ‘suicide role models’ reinforce high rates of suicide in a population:
Stack, Steven, and Augustine J. Kposowa. ‘The Association of Suicide Rates with Individual-Level Suicide Attitudes: A Cross-National Analysis*’. Social Science Quarterly 89, no. 1 (2008): 39–59. https://doi.org/10.1111/j.1540-6237.2008.00520.x . * (full text available).
Werther and Papageno Effects
Suicides are also associated with the way that suicide is presented in the media. The ‘Werther effect’ refers to media presentations of suicides (fictional and real) and their effect on an increase in suicide rates. The ‘Papageno effect’ refers instead to the preventative effect of media portrayals which depict people coping despite difficult life circumstances and suicidal ideation.
A survey of studies on the two effects shows that ‘ suicide contagion is more likely to occur after extensive media coverage with a content rich in positive definitions of suicide ’. Factors that increase the likelihood of imitation are, for example, ‘ the celebrity status of the suicide victim, similar demographic characteristics and the media audience, and media reports on a new suicide method’ . At the same time, different media portrayals can ‘ have an educative or preventative effect and can reduce the risk of contagion ’. See:
Domaradzki, J. ‘The Werther Effect, the Papageno Effect or No Effect? A Literature Review’. International Journal of Environmental Research and Public Health 18, no. 5 (1 March 2021): 2396. https://doi.org/10.3390/ijerph18052396 . * (full text available).
Studies of the Werther and Papageno effects focus on media portrayals of suicide, but ‘ [g]uidance is needed for media reporting of assisted suicide ’ as well. See:
Jones, David Albert. ‘Assisted dying and suicide prevention’ Journal of Disability & Religion , 22.3 (2018): 298-316 . * (pre print text available online).
A 2021 survey of members of the Association for Palliative Medicine of Great Britain and Ireland showed that ‘ There is also a significant degree of frustration at the media narrative regarding end of life care, which clinicians view as being driven by assisted suicide lobbying. There is concern that poor portrayal of palliative care in the media has led patients and families to have a skewed understanding of palliative care, and there is fear that patients are in a position of ignorance at a vulnerable moment in their lives ’.
8. Gender and the Impact of Assisted Suicide and Euthanasia
Proponents of a change in the law frequently invoke choice (for example the US organisation ‘Compassion & Choices’ or the Scottish organisation ‘My Life, My Death, My Choice’). This language is very similar to ‘pro-choice’ language in relation to abortion, and so it might seem that feminists who are in favour of increased access to legal abortion would also support legalisation of EAS. This argument is indeed accepted by some feminists; however, it has been challenged by a number of feminists who argue that EAS would have a disproportionately negative impact on women.
Wolf, SM. ‘Gender, Feminism, and Death: Physician-Assisted Suicide and Euthanasia’ in Feminism & Bioethics: Beyond Reproduction . New York: Oxford University Press, 1996, pp. 282-317.
Wolf argues that a legal right to abortion (which she supports) does not imply a legal right to assisted suicide.
Wolf, SM. ‘Physician-assisted suicide, abortion, and treatment refusal: Using gender to analyze the difference’ in R Weir, ed. Physician-Assisted Suicide . Indiana University Press, 1997, pp. 167-201 .
On this point see also:
Spindelman, Marc. ‘Are the Similarities between a Woman’s Right to Choose an Abortion and the Alleged Right to Assisted Suicide Really Compelling?’ U. Mich. J. L. Reform 29, no. 775 (1996): 775-856. * (full text available).
Whereas, in the West, the rate of suicide is much higher among men than women (roughly four times), PAS (in Oregon and Washington) is roughly equal between men and women, and rates of assisted suicide in Switzerland reveal a higher proportion of women; this is also true of the suicides assisted by Kervorkian.
Canetto, Silvia Sara, and Janet D. Hollenshead. ‘Gender and Physician-Assisted Suicide: An Analysis of the Kevorkian Cases, 1990–1997’. OMEGA - Journal of Death and Dying 40, no. 1 (2000): 165–208. *
Kohm, Lynne Marie, and Britney N. Brigner. ‘Women and Assisted Suicide: Exposing the Gender Vulnerability to Acquiescent Death’. Cardozo Women’s Law Journal 4 (1997): 241. * (full text available).
Canetto, Silvia Sara, and Janet D. Hollenshead. ‘Older Women and Mercy Killing’. OMEGA - Journal of Death and Dying 42, no. 1 (1 February 2001): 83–99. https://doi.org/10.2190/NRB4-JH8B-VBCW-WM7J. *
Canetto, Silvia Sara, and John L. McIntosh. ‘A Comparison of Physician-Assisted/Death-With-Dignity-Act Death and Suicide Patterns in Older Adult Women and Men’. The American Journal of Geriatric Psychiatry , June 2021, S1064748121003559. https://doi.org/10.1016/j.jagp.2021.06.003 *
George, Katrina. ‘A Woman’s Choice? The Gendered Risks of Voluntary Euthanasia and Physican-Assisted Suicide’. Medical Law Review 15, no. 1 (1 March 2007): 1–33. https://doi.org/10.1093/medlaw/fwl017. *
It has also been argued that a feminist account of relational autonomy gives more ground to be cautious about permitting assisted suicide.
Donchin, Anne. ‘Autonomy, Interdependence, and Assisted Suicide: Respecting Boundaries/Crossing Lines’. Bioethics 14, no. 3 (2000): 187–204. https://doi.org/10.1111/1467-8519.00190. *
Canetto, Sylvia Sara. ‘If Physician-Assisted Suicide Is the Modern Woman’s Last Powerful Choice, Why Are White Women Its Leading Advocates and Main Users?’ Professional Psychology: Research and Practice 50, no. 1 (2019): 39–50. *
For a study of the larger number of women who receive EAS for a psychiatric condition in Belgium and the Netherlands, and its relation to questions of suicide prevention, see:
Nicolini, Marie E., Chris Gastmans, and Scott Y. H. Kim. ‘Psychiatric Euthanasia, Suicide and the Role of Gender’. The British Journal of Psychiatry 220, no. 1 (January 2022): 10–13. https://doi.org/10.1192/bjp.2021.95. *
Data from Switzerland demonstrates not only an increase in total assisted suicides year on year, but also the disproportionately large number of women dying by assisted suicide.
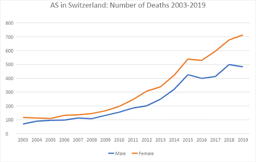
9. Links to Some Campaign Organisations and Further Resources
Whichever side of the argument you find more cogent, it is useful to look at the opposite view and the counter-arguments and evidence they produce, such as it is. Campaign organisations are, by their nature, one sided, but at the very least they raise questions and identify some relevant evidence.
Organisations in favour of legalising assisted suicide or euthanasia
In 2005 the Voluntary Euthanasia Society (founded 1935) changed its name to ‘Dignity in Dying.’ Its immediate aim is legalising physician assisted suicide for the terminally ill not, currently, euthanasia.
http://www.dignityindying.org.uk/
In 2009 Michael Irwin left the Dignity in Dying to found the Society for Old Age Rational Suicide which campaigns for assisted suicide for people who are not dying, but are tired of living. In 2015, the organisation changed its name to ‘My Death, My Decision’.
https://www.mydeath-mydecision.org.uk/
The largest organisation in the USA to campaign in favour of assisted suicide is Compassion & Choices (successor to the Hemlock Society which was founded in 1980).
http://www.compassionandchoices.org/
Also founded in 1980, The World Federation of Right to Die Societies no longer counts Dignity in Dying or Compassion & Choices as ‘members,’ but has links to them as ‘other right to die societies’.
https://wfrtds.org
EXIT founded in 1982 is the main organisation that arranges assisted suicide for Swiss citizens.
http://www.exit.ch/en/
Organisations opposed to legalising assisted suicide and euthanasia
Founded in 2005, Care Not Killing is a UK-based alliance of individuals, disability and human rights groups, healthcare providers, and faith-based bodies opposed to assisted suicide and euthanasia.
http://www.carenotkilling.org.uk/
In 2021 the Better Way campaign was founded to oppose assisted suicide and to set out a positive, alternative vision for the UK. Its website contains information about the Canadian experience of euthanasia and assisted suicide.
https://www.betterwaycampaign.co.uk/canada/
The Euthanasia Prevention Coalition (EPC) has an international scope. There is also a European arm.
https://www.epcc.ca/
https://www.epce.eu/
For a disability perspective see Not Dead Yet and the rather more British (and understated) Not Dead Yet UK.
http://www.notdeadyet.org/
http://notdeadyetuk.org/
For an American perspective critical of assisted suicide see the websites of Physicians for Compassionate Care Education Foundation, the Patients’ Rights Council and ‘Choice’ is an Illusion.
https://www.pccef.org/
https://www.patientsrightscouncil.org/site/
https://www.choiceillusion.org/
News and comment
The excellent and free bioethics news service Bioedge frequently includes stories on these issues.
https://bioedge.org/end-of-life-issues/euthanasia/
Alex Schadenberg (chair of EPC) has a blog, which is also very useful for news stories.
https://alexschadenberg.blogspot.co.uk/
Living and dying well is not a campaign organisation, but presents research and analysis of evidence relevant to (and critical of) assisted suicide and euthanasia.
https://www.livinganddyingwell.org.uk/
Further academic resources
This guide is intended only as an introduction to some of the resources for assessing the evidence and arguments for and against assisted suicide and euthanasia. It is, of necessity, selective as there are many hundreds of official reports, legal cases and journal articles on these topics. Students should research independently making use of academic indices and databases such as EBSCO, Lexis Nexis, Philosophers’ Index, PhilPapers and MEDLINE. You should also ‘follow the footnotes’ reading the sources invoked by or criticised by the article you are reading.
The search engine Pubmed gives access to the MEDLINE database, which includes very many medical journals and also journals of medical ethics, and medically related humanities and social sciences. Unlike other indices it is freely accessible and is a good place for the non-specialist to begin more serious research.
https://www.ncbi.nlm.nih.gov/pubmed
Anscombe Bioethics Centre Briefing Papers
Beuselinck, Benoit. ‘Euthanasia Case Studies from Belgium: Concerns About Legislation and Hope for Palliative Care’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Jones, David Albert. ‘Defining the Terms of the Debate: Euthanasia and Euphemism’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Keown, John. ‘Voluntary Euthanasia & Physician-assisted Suicide: The Two “Slippery Slope” Arguments’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2022.
Komrad, Mark. ‘First, Do No Harm: How Canadian Law Allows for Euthanasia and Assisted Suicide for Patients with Psychiatric Disorders’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2021.
Pontifical Academy for Life. ‘Position Paper of the Abrahamic Monotheistic Religions on Matters Concerning the End of Life (28 October 2019)’.
Symons, Xavier. ‘The Principle of Autonomy – Does it Support the Legalisation of Euthanasia and Assisted Suicide?’. Briefing Papers: Euthanasia and Assisted Suicide. Oxford: The Anscombe Bioethics Centre, 2022.
Most recent

A Briefing on the Human Fertilisation & Embryology Authority (HFEA) consultation, ‘Modernising the regulation of fertility treatment and research involving human embryos’
27 March 2023
Our Briefing on the March-April 2023 HFEA consultation into the potential revision of Human Fertilis...

Anscombe Centre Submission to Isle of Man Consultation on Private Member’s Bill for Euthanasia and Assisted Suicide (EAS)
25 January 2023
From 01 December 2022 to 26 January 2023, a Consultation was held on a Private Member’s Bill introdu...
Anscombe Centre Submission to Government of Jersey Consultation on Euthanasia and Assisted Suicide (EAS)
16 January 2023
From 17 October 2022 to 14 January 2023, the Government of Jersey held a consultation on proposals t...
The Anscombe Bioethics Centre is supported by the Catholic Church in England and Wales, Scotland, and Ireland, but has also always relied on donations from generous individuals, friends and benefactors.
FIND OUT MORE MAKE A DONATION
Cookie notice
We use cookies on our website. They help us to know a little bit about you and how you use our website. They are stored locally on your computer or mobile device. If you continue without changing your settings, we’ll assume that you are happy to receive all cookies. However, you can change your cookie settings at any time. Go to the cookie policy for more information and to update your preferences.
Your cookie preferences
We use cookies and similar technologies on our website. Cookies are text files containing small amounts of information, which your computer or mobile device downloads when you visit a website. When you return to websites, or visit websites that use the same cookies, they recognise these cookies and therefore your browsing device.
We use different types of cookies for different things, such as:
- Analysing how you use our website
- Giving you a better, more personalised experience
- Recognising when you’ve sign in
We split our cookies into three distinct categories. You can turn Functional and Performance cookies on and off right here. Strictly necessary cookies can’t be turned off.
Strictly necessary cookies
These cookies are essential in order to enable you to move around the website and use its features. Without these cookies services you have asked for cannot be provided.
Some examples of how we use these cookies are:
- Signing into our website
- Remembering previous actions such as text entered into a form when navigating back to a page in the same session
- Remembering security settings
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Arguments in Favor of Right-to-Die Legislation
There are many arguments about whether people should have the right to die when they choose, intentionally and by design, to end their own perceived pain and suffering .
Differences of Opinion
Most of the arguments for and against the right to die are ideological, based on many important aspects of civility: the law, religion or spiritual beliefs, ethics, and social mores. Opinions vary based on personal experiences, belief systems, age, culture, and other aspects of humankind that influence how we think about important aspects of life.
Where the Right to Die Is Legal
In the United States, with the exception of a small number of states which have passed right-to-die legislation, a doctor who injects a patient who wants to die with a lethal drug and kills him would technically have committed murder. Proponents of right-to-die legislation desire a legal remedy for doctors who assist their suffering patients in ending their lives. Outside of the United States, euthanasia is the law of the land in Canada, the Netherlands, Colombia, Belgium, Luxembourg, and Switzerland.
Understanding Right-to-Die Laws
Right-to-Die legislation, also known as physician-assisted death or aid in dying, gives mentally competent adult patients with a terminal illness and a prognosis of six months or less to have the ability to request and receive a prescription medication to bring about their death. Most statutes under consideration at the state level are modeled after Oregon’s Death with Dignity Act, which requires two physicians to confirm the patient’s residence, diagnosis, prognosis, mental competence, and voluntariness of the request to die. In addition, two waiting periods are required.
The Pros for Right-to-Die Laws
Here are some arguments in favor of giving patients the right to die and protecting healthcare providers who carry out those wishes. Compare these arguments in favor of death with dignity and the right to die against the cons .
- A patient's death brings him or her the end of pain and suffering.
- Patients have an opportunity to die with dignity, without fear that they will lose their physical or mental capacities.
- The overall healthcare financial burden on the family is reduced.
- Patients can arrange for final goodbyes with loved ones.
- If planned for in advance, organs can be harvested and donated .
- With physician assistance , patients have a better chance of experiencing a painless and less traumatic death (death with dignity).
- Patients can end pain and suffering when there is no hope for relief.
- Some say assisted death with dignity is against the Hippocratic Oath; however, the statement “first do no harm” can also apply to helping a patient find the ultimate relief from pain through death.
- Medical advances have enabled life beyond what nature might have allowed, but that is not always in the best interest of the suffering patient with no hope of recovery.
- A living will, considered a guiding document for a patient's healthcare wishes, can provide clear evidence of a patient's decisions regarding end-of-life care.
Pereira J. Legalizing euthanasia or assisted suicide: the illusion of safeguards and controls . Curr Oncol . 2011;18(2):e38-45. doi:10.3747/co.v18i2.883
Battin MP, Van der heide A, Ganzini L, Van der wal G, Onwuteaka-philipsen BD. Legal physician-assisted dying in Oregon and the Netherlands: evidence concerning the impact on patients in "vulnerable" groups . J Med Ethics . 2007;33(10):591-7. doi:10.1136/jme.2007.022335
By Trisha Torrey Trisha Torrey is a patient empowerment and advocacy consultant. She has written several books about patient advocacy and how to best navigate the healthcare system.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.3(4); Oct-Dec 2014
‘Euthanasia: Right to Die with Dignity’
Kalaivani annadurai.
Department of Community Medicine, Shri Sathya Sai Medical College and Research Institute, Kancheepuram district, Tamil Nadu, India
Raja Danasekaran
Geetha mani.
Dear Editor,
The concept of Euthanasia has been a controversial topic since its inception. The word ‘Euthanasia’ is derived from Greek, ‘Eu’ meaning ‘good’ and ‘thanatos’ meaning ‘death’, put together it means ‘good death’. Euthanasia is defined as the hastening of death of a patient to prevent further sufferings. Active euthanasia refers to the physician deliberate act, usually the administration of lethal drugs, to end an incurably or terminally ill patient’s life. Passive euthanasia refers to withholding or withdrawing treatment which is necessary for maintaining life. There are three types of active euthanasia, in relation to giving consent for euthanasia, namely voluntary euthanasia – at patient request, nonvoluntary – without patient consent, involuntary euthanasia – patient is not in a position to give consent. [ 1 ]
Other terminology like assisted suicide and physician-assisted suicide are not synonyms of euthanasia. [ 1 ] Do not resuscitate (DNR) order means the attending doctor is not required to resuscitate a patient if their heart stops and is designed to prevent unnecessary suffering. Even though DNR is considered as passive euthanasia, it is practiced in most part of the world without much legal issues. [ 2 ]
Common conditions which make patients to seek euthanasia are terminally ill cancer patients, acquired immune deficiency syndrome (AIDS) and other terminally ill conditions where there is no active treatment. Factors which are responsible for decision making are classified into physical and psychological factors. Physical conditions that affect the quality of life in these patients are unbearable pain, nausea and vomiting, difficulty in swallowing, paralysis, incontinence, and breathlessness. Psychological factors include depression, feeling a burden, fearing loss of control or dignity, or dislike of being dependent. [ 2 ] But some argues that suicidal ideation and inadequate palliative care might also be the underlying reasons for seeking euthanasia. [ 3 ]
Passive euthanasia is generally accepted worldwide. Active involuntary euthanasia is illegal in almost all countries. Practicing active voluntary euthanasia is illegal and considered as criminal homicide in most of the countries and will faces punishment up to imprisonment for 14 years. While active involuntary euthanasia is legal in countries such as Netherland, Belgium, and Luxembourg, assisted suicide is legal in Switzerland and the United States of Oregon, Washington, and Montana. [ 4 ]
Previously there was an age restriction for euthanasia in Belgium, but recently the country has passed a bill in the parliament which lifts ban on all age restriction on euthanasia. In Belgium alone, there are 1400 cases of euthanasia practiced. The concept of death tourism or euthanasia tourism is slowly increasing in which patients who want to seek euthanasia or other assisted suicide services will travel to countries where it is legalized to avail those services. Switzerland is known for death tourism, where every year patients primarily from British, German, and French travel there to end their lives. [ 5 ] In Netherland, euthanasia accounts for 2% of all deaths. [ 6 ]
Many activists against euthanasia feel that legalizing euthanasia will leads to ‘slippery slope’ phenomenon which leads on to more number of nonvoluntary euthanasia. To conclude, strict standard guidelines should be formulated to practice euthanasia in countries where it is legalized, regulation of death tourism and other practices like mandatory reporting of all cases of euthanasia, consultation with psychiatrist, obtaining second opinion, improved hospice care have to be followed for standardization of euthanasia.
The Euthanasia in Humans Essay
The right to choose how to die, potential contradictions and ambiguities, real-life examples and justifications.
The moral and ethical aspects of medical practice include not only the features of interaction with patients and other interested parties but also deeper nuances. In particular, one of the controversial and acute topics is euthanasia and its acceptability from different perspectives, including both patients’ and healthcare employees’ positions. In addition, religious issues are involved, which makes it difficult to enact uniform legislation on this topic. From a medical standpoint, euthanasia is associated with a number of restrictions and obstacles, and, despite the freedom of choice as an inalienable right of any citizen, the practice of ending a life is not perceived unambiguously. In general, death is a natural human outcome, and although life is manageable, the choice of how to die is still not possible in many healthcare systems, which is a conservative and outdated practice.
The provision of medical services to people with disabilities is a prerequisite for any healthcare system. However, regarding the issue of assisting patients in their death, obstacles and barriers arise, which are caused by legal, religious, and other conventions. Riddle (2017) analyzes this topic from the perspective of the freedom of choice. In accordance with the study the author conducts, the predominant number of terminally ill patients expresses approval of the practice of euthanasia (Riddle, 2017). In addition to ethical aspects, for instance, the desire to reduce torment and get rid of a protracted and persistent disease, some social issues are raised. Riddle (2017) describes the desire of patients to help relatives and remove the heavy burden of carers from them. Also, the high financial costs of meaningless help and maintenance of a life that will soon end inevitably are the reasons for euthanasia approval. Moreover, the right to choose death can be regarded as standard and natural freedom. There are no laws prohibiting a person from developing financially, intellectually, and morally. Therefore, limiting an opportunity to die for objective reasons may be considered the infringement of human rights.
The objectivity of the widespread legalization of euthanasia may be due to not only ethical but also legal aspects. Dresser (2017) considers the possibility of physicians’ assistance in death as a patient’s right to interrupt one’s life. The author analyzes the examples of people with irreversible dementia and notes that although at the final stage of this disease, people’s minds are damaged, temporary legal capacity allows them to participate in deciding their fate (Dresser, 2017). If a patient is able to respond to direct calls and draw conclusions on one’s own, this may be an incentive to take his or her opinions into account. As Rudnev and Savelkaeva (2018) state, tendencies towards a decrease in the significance of religion and an increase in the role of autonomy values contribute to supporting euthanasia as an inalienable right of any person. In the context of an approaching death, a patient can rethink one’s priorities, which, however, should not affect the freedom of choice. Therefore, the right to euthanasia as a natural procedure may be considered an objective and inalienable attribute of a democratic and humane society with a liberal approach to care.
Despite the approval of the widespread legalization of euthanasia in healthcare, some contradictions impede this practice and may be considered objective obstacles. In the study by Murphy (2017), the author discusses the possibility of obtaining information from physicians and nurses as stakeholders. According to the researcher, the empirical method of data collection is hampered by the inability to engage a large sample (Murphy, 2017). Additional contradictions are due to the interaction of legislation with other life sectors. Murphy (2017) argues that any legalization process “occurs within a specific cultural and social framework,” and conventions in these areas may contradict with laws (p. 337). Religious reasoning is included in the spectrum of the most significant barriers in the context of the issue of euthanasia. The arguments of people regarding the inadmissibility of physician-assisted deaths are confirmed by representatives of different religious movements, and, as Rudnev and Savelkaeva (2018) state, for a large number of believers, these opinions are dominant. As a result, the idea that no one has the right to terminate life consciously against God’s will is the reason for preventing the legalization of euthanasia in the world medical practice.
When analyzing potentially objective reasons for the ban on euthanasia, one should take into account the peculiarities of the healthcare sector. Parmar, Rathod, and Parikh (2016), who analyze people’s opinions on the possibility of introducing such a procedure into general practice, note that many respondents consider physician-assisted deaths a crime. Potential errors made by medical specialists in diagnosing incurable diseases are an argument that determines the inadmissibility of euthanasia as a common activity. From this perspective, the voluntary interruption of life is perceived as a real threat to people who could live longer. Thus, the aforementioned nuances are reasons for discussing the bias of legalizing euthanasia as an inalienable right of any terminally ill patient.
Although death is a natural phenomenon and an inevitable outcome of people’s lives, discussing it as a culture makes it possible to explain the groundlessness of the arguments against euthanasia. Legalization implying unlimited freedom is contrary to both legislative and moral ethics. Weikart (2017) gives an example of the Swiss system in which any person has the right to interrupt one’s life for any reason. This practice cannot be called objective due to the ambiguity of the approach. At the same time, religious arguments against euthanasia may be interpreted distinctively. The interruption of the torment and pain of a patient suffering from an incurable disease can be considered a blessing. Therefore, even strict principles of spirituality may help explain a person’s desire to alleviate suffering for oneself and one’s family.
Regarding the arguments about potential medical errors, this nuance should be considered an unrealistic opportunity in the current conditions of the development of the healthcare industry. Decisions about the incurability of a particular disease are not made by one person on the basis of a one-time diagnosis. As Parmar et al. (2016) state, the decision-making process lies largely with physicians, and this responsibility encourages medical professionals to use the latest developments to identify and predict ailments. In case a particular diagnosis is confirmed by numerous clinical studies and approved at general meetings, the objectivity of such an opinion cannot be questioned. As a result, possible arguments against euthanasia are an individual rejection of the issue and cannot be involved as a common public opinion.
Although human life is manageable, the choice of how to die is not always available, which is a restriction of freedom and a conservative practice that explains the importance of accepting euthanasia. An inalienable right to decide one’s fate individually should be granted to a person in a difficult situation, and the incurability of a specific disease is a reasonable argument in support of a physician-assisted death. Despite possible arguments about its inadmissibility from a religious perspective or due to potential medical errors, the interpretation of euthanasia may be different, and the participation of medical personnel in this decision is conditional. Providing opportunities for interrupting suffering to terminally ill patients is a humane practice in a democratic world.
Dresser, R. (2017). On legalizing physician-assisted death for dementia . Hastings Center Report, 47 (4), 5-6. Web.
Murphy, S. (2017). Legalization of assisted suicide and euthanasia: Foundational issues and implications. BYU Journal of Public Law, 31 (2), 333-394.
Parmar, P., Rathod, S., & Parikh, A. (2016). Perceptions of patients’ towards euthanasia – A medico-legal perspective. International Archives of Integrated Medicine, 3 (5), 20-23.
Riddle, C. A. (2017). Assisted dying & disability . Bioethics, 31 (6), 484-489. Web.
Rudnev, M., & Savelkaeva, A. (2018). Public support for the right to euthanasia: Impact of traditional religiosity and autonomy values across 37 nations. International Journal of Comparative Sociology , 59 (4), 301-318. Web.
Weikart, R. (2017). Upholding the sanctity of life in a culture of death. Issues in Law & Medicine, 32 (2), 269-275.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 24). The Euthanasia in Humans. https://ivypanda.com/essays/the-euthanasia-in-humans/
"The Euthanasia in Humans." IvyPanda , 24 Mar. 2024, ivypanda.com/essays/the-euthanasia-in-humans/.
IvyPanda . (2024) 'The Euthanasia in Humans'. 24 March.
IvyPanda . 2024. "The Euthanasia in Humans." March 24, 2024. https://ivypanda.com/essays/the-euthanasia-in-humans/.
1. IvyPanda . "The Euthanasia in Humans." March 24, 2024. https://ivypanda.com/essays/the-euthanasia-in-humans/.
Bibliography
IvyPanda . "The Euthanasia in Humans." March 24, 2024. https://ivypanda.com/essays/the-euthanasia-in-humans/.
- Physician-Assisted Suicide
- Physician-Assisted Suicide: Different Ethics Perspectives
- Physician-Assisted Suicide and Ethical Theories
- Physician-Assisted Suicide, Alzheimer's Disease, and Genetics
- Consequentialism: Euthanasia and Physician-Assisted Suicide
- Euthanasia and Physician-Assisted Suicide Articles
- Attitudes Related to Euthanasia and Physician-Assisted Suicide Among Terminally Ill Patients
- Why Physician-Assisted Death on the Terminally Ill lacks Justification
- Discussion of Physician-Assisted Suicide
- Terminal Sedation and Physician-Assisted Suicide
- The Problem of Food Safety and the Spread of Various Diseases
- Elimination of Religious Exemptions to Childhood Vaccines in New Jersey
- Sexually Transmitted Diseases: Statistics in the New Jersey
- The Vaping Ages 13 and Up
- Tuberculosis as the Health Problem in New Jersey
Vatican rejects gender-affirming surgery and surrogacy in new document

'GENDER THEORY'
Abortion, euthanasia, death penalty.
The Reuters Daily Briefing newsletter provides all the news you need to start your day. Sign up here.
Reporting by Alvise Armellini; Editing by Kevin Liffey and Lisa Shumaker
Our Standards: The Thomson Reuters Trust Principles. , opens new tab

Russia, China to maintain fight against terrorism, Lavrov says
Russia and China will continue to cooperate in the fight against terrorism as part of their ever-strengthening relationship, Russian Foreign Minister Sergei Lavrov said in Beijing on Tuesday after talks with Chinese Foreign Minister Wang Yi.

- Share full article
Advertisement
Supported by
Vatican Document Casts Gender Change and Fluidity as Threat to Human Dignity
The statement is likely to be embraced by conservatives and stir consternation among L.G.B.T.Q. advocates who fear it will be used as a cudgel against transgender people.

By Jason Horowitz and Elisabetta Povoledo
Reporting from Rome
The Vatican on Monday issued a new document approved by Pope Francis stating that the church believes that gender fluidity and transition surgery, as well as surrogacy, amount to affronts to human dignity.
The sex a person is assigned at birth, the document argued, was an “irrevocable gift” from God and “any sex-change intervention, as a rule, risks threatening the unique dignity the person has received from the moment of conception.” People who desire “a personal self-determination, as gender theory prescribes,” risk succumbing “to the age-old temptation to make oneself God.”
Regarding surrogacy, the document unequivocally stated the Roman Catholic Church’s opposition, whether the woman carrying a baby “is coerced into it or chooses to subject herself to it freely.” Surrogacy makes the child “a mere means subservient to the arbitrary gain or desire of others,” the Vatican said in the document, which also opposed in vitro fertilization.
The document was intended as a broad statement of the church’s view on human dignity, including the exploitation of the poor, migrants, women and vulnerable people. The Vatican acknowledged that it was touching on difficult issues, but said that in a time of great tumult, it was essential, and it hoped beneficial, for the church to restate its teachings on the centrality of human dignity.
Even if the church’s teachings on culture war issues that Francis has largely avoided are not necessarily new, their consolidation now was likely to be embraced by conservatives for their hard line against liberal ideas on gender and surrogacy.
The document, five years in the making, immediately generated deep consternation among advocates for L.G.B.T.Q. rights in the church, who fear it will be used against transgender people. That was so, they said, even as the document warned of “unjust discrimination” in countries where transgender people are imprisoned or face aggression, violence and sometimes death.
“The Vatican is again supporting and propagating ideas that lead to real physical harm to transgender, nonbinary and other L.G.B.T.Q.+ people,” said Francis DeBernardo, the executive director of New Ways Ministry, a Maryland-based group that advocates for gay Catholics, adding that the Vatican’s defense of human dignity excluded “the segment of the human population who are transgender, nonbinary or gender nonconforming.”
He said it presented an outdated theology based on physical appearance alone and was blind to “the growing reality that a person’s gender includes the psychological, social and spiritual aspects naturally present in their lives.”
The document, he said, showed a “stunning lack of awareness of the actual lives of transgender and nonbinary people.” Its authors ignored the transgender people who shared their experiences with the church, Mr. DeBernardo said, “cavalierly,” and incorrectly, dismissing them as a purely Western phenomenon.
Though the document is a clear setback for L.G.B.T.Q. people and their supporters, the Vatican took pains to strike a balance between protecting personal human dignity and clearly stating church teaching, a tightrope Francis has tried to walk in his more than 11 years as pope.
Francis has made it a hallmark of his papacy to meet with gay and transgender Catholics and has made it his mission to broadcast a message for a more open, and less judgmental, church. Just months ago, Francis upset more conservative corners of his church by explicitly allowing L.G.B.T.Q. Catholics to receive blessings from priests and by allowing transgender people to be baptized and act as godparents .
But he has refused to budge on the church rules and doctrine that many gay and transgender Catholics feel have alienated them, revealing the limits of his push for inclusivity.
“In terms of pastoral consequences,” Cardinal Víctor Manuel Fernández, who leads the Vatican’s office on doctrine, said in a news conference Monday, “the principle of welcoming all is clear in the words of Pope Francis.”
Francis, he said, has repeatedly said that “all, all, all” must be welcomed. “Even those who don’t agree with what the church teaches and who make different choices from those that the church says in its doctrine, must be welcomed,” he said, including “those who think differently on these themes of sexuality.”
But Francis’ words were one thing, and church doctrine another, Cardinal Fernández made clear, drawing a distinction between the document, which he said was of high doctrinal importance, as opposed to the recent statement allowing blessings for same-sex Catholics. The church teaches that “homosexual acts are intrinsically disordered.”
In an echo of the tension between the substance of church law and Francis’ style of a papal inclusivity, Cardinal Fernández said on Monday that perhaps the “intrinsically disordered” language should be modified to better reflect that the church’s message that homosexual acts could not produce life.
“It’s a very strong expression and it requires explanation,” he said. “Maybe we could find an expression that is even clearer to understand what we want to say.”
Though receptive to gay and transgender followers, the pope has also consistently expressed concern about what he calls “ideological colonization,” the notion that wealthy nations arrogantly impose views — whether on gender or surrogacy — on people and religious traditions that do not necessarily agree with them. The document said “gender theory plays a central role” in that vision and that its “scientific coherence is the subject of considerable debate among experts.”
Using “on the one hand” and “on the other hand,” language, the Vatican’s office on teaching and doctrine wrote that “it should be denounced as contrary to human dignity the fact that, in some places, not a few people are imprisoned, tortured, and even deprived of the good of life solely because of their sexual orientation.”
“At the same time,” it continued, “the church highlights the definite critical issues present in gender theory.”
On Monday, Cardinal Fernández also struggled to reconcile the two seemingly dissonant views.
“I am shocked having read a text from some Catholics who said, ‘Bless this military government of our country that created these laws against homosexuals,’” Cardinal Fernández said on Monday. “I wanted to die reading that.”
But he went on to say that the Vatican document was itself not a call for decriminalization, but an affirmation of what the church believed. “We shall see the consequences,” he said, adding that the church would then see how to respond.
In his presentation, Cardinal Fernández described the long process of the drafting of a document on human dignity, “Infinite Dignity,” which began in March 2019, to take into account the “latest developments on the subject in academia and the ambivalent ways in which the concept is understood today.”
In 2023, Francis sent the document back with instructions to “highlight topics closely connected to the theme of dignity, such as poverty, the situation of migrants, violence against women, human trafficking, war, and other themes.” Francis signed off on the document on March 25.
The long road, Cardinal Fernández wrote, “reflects the gravity” of the process.
In the document, the Vatican embraced the “clear progress in understanding human dignity,” pointing to the “desire to eradicate racism, slavery, and the marginalization of women, children, the sick, and people with disabilities.”
But it said the church also sees “grave violations of that dignity,” including abortion, euthanasia, the death penalty, polygamy, torture, the exploitation of the poor and migrants, human trafficking and sex abuse, violence against women, capitalism’s inequality and terrorism.
The document expressed concern that eliminating sexual differences would undercut the family, and that a response “to what are at times understandable aspirations,” will become an absolute truth and ideology, and change how children are raised.
The document argued that changing sex put individualism before nature and that human dignity as a subject was often hijacked to “justify an arbitrary proliferation of new rights,” as if “the ability to express and realize every individual preference or subjective desire should be guaranteed.”
Cardinal Fernández on Monday said that a couple desperate to have a child should turn to adoption, rather than surrogacy or in vitro fertilization because those practices, he said, eroded human dignity writ large.
Individualistic thinking, the document argues, subjugates the universality of dignity to individual standards, concerned with “psycho-physical well-being” or “individual arbitrariness or social recognition.” By making dignity subjective, the Vatican argues, it becomes subject to “arbitrariness and power interests.”
Jason Horowitz is the Rome bureau chief for The Times, covering Italy, the Vatican, Greece and other parts of Southern Europe. More about Jason Horowitz
Elisabetta Povoledo is a reporter based in Rome, covering Italy, the Vatican and the culture of the region. She has been a journalist for 35 years. More about Elisabetta Povoledo
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.

COMMENTS
3. Evolution of euthanasia and assisted suicide: digging into historical events. To understand the evolution and relevance of these concepts should analyze the history of euthanasia and assisted suicide; from the emergence of the term, going through its first manifestations in antiquity; mentioning the conceptions of great thinkers such as Plato and Hippocrates; going through the role of the ...
1. Legalization. "The right to die should be a matter of personal choice. We are able to choose all kinds of things in life from who we marry to what kind of work we do and I think when one comes to the end of one's life, whether you have a terminal illness or whether you're elderly, you should have a choice about what happens to you….
The most compelling argument in favour of physician assisted suicide or voluntary active euthanasia is the argument in support of committing suicide in a democracy. The right to commit suicide is ...
The phenomenon about both the morality and legality of euthanasia and physician assisted death have been a significant debates of the last decades of the twentieth century and they will remain further a source of controversies. This paper explores and analyze the arguments in support and against e uthanasia and physician assisted suicide.
As a medical doctor I have, with some worry, followed the assisted dying debate that regularly hits headlines in many parts of the world. The main arguments for legalisation are respecting self-determination and alleviating suffering. Since those arguments appear self-evident, my book Euthanasia and the Ethics of a Doctor's Decisions—An Argument Against Assisted Dying 1 aimed to contribute ...
The sketch outline for an essay on Euthanasia may be like: "Th work is about the problem of Euthanasia. I highlight some statements for and against the use of Euthanasia and support them with top examples. In conclusion, I explain my personal position on this question." The full version of an outline would look something like this ...
It has been a pertinent issue in human rights discourse as it also affects ethical and legal issues pertaining to patients and health care providers. This paper discusses the legal and ethical ...
Essay on Euthanasia in 150 Words. Euthanasia or mercy killing is the act of deliberately ending a person's life. This term was coined by Sir Francis Bacon. Different countries have their perspectives and laws against such harmful acts. The Government of India, 2016, drafted a bill on passive euthanasia and called it 'The Medical Treatment ...
The whole family or support group talks not just about this particular way of dying, but about all the issues related to how they feel about the death and what they will do later. It's an enormous benefit," Gordon says. End-of-life inequity. Despite those potential benefits, critics express concerns about the possible harms of assisted death. ...
During the past decade, the debate about legalising euthanasia has grown in many developed countries, including France. Medical journals have reflected this: surveys have assessed doctors' attitudes toward euthanasia and bioethics articles have discussed the pros and cons. Supporters of legalisation argue that euthanasia is a continuation of palliative care and that doctors must respect ...
4.4 Objection 4. As was noted earlier in Section 3, there is a widespread belief that so-called passive (voluntary) euthanasia, wherein life-sustaining or life-prolonging measures are withdrawn or withheld in response to a competent patient's request, is morally permissible.
Arguments based on rights. People have an explicit right to die. A separate right to die is not necessary, because our other human rights imply the right to die. Death is a private matter and if ...
These principles of good practice should apply also when judging the competing claims to how 'the public' thinks of assisted suicide and euthanasia. Wording of polls. Support for euthanasia and assisted suicide in public opinion polls is subject to 'over 20% variation in mean support' where there are 'increasing levels of favourable ...
Assisted dying is a general term that incorporates both physician-assisted dying and voluntary active euthanasia.Voluntary active euthanasia includes a physician (or third person) intentionally ending a person's life normally through the administration of drugs, at that person's voluntary and competent request. 2,3 Facilitating a person's death without their prior consent incorporates ...
Currently, interest in the topics of euthanasia and assisted suicide is substantial. The success of books by Derek Humphrey and the notoriety of Jack Kevorkian are as much a reflection of changing societal values as they are a stimulus to public discussion. The magnitude of public interest is demonstrated in legislation to legalize assisted suicide, an issue that has been included on the ...
The Pros for Right-to-Die Laws. Here are some arguments in favor of giving patients the right to die and protecting healthcare providers who carry out those wishes. Compare these arguments in favor of death with dignity and the right to die against the cons . A patient's death brings him or her the end of pain and suffering.
Currently, nine states and the District of Columbia allow doctors to help patients who meet well-defined criteria and are on the threshold of dying choose when and how to end their lives. The laws ...
The word 'Euthanasia' is derived from Greek, 'Eu' meaning 'good' and 'thanatos' meaning 'death', put together it means 'good death'. Euthanasia is defined as the hastening of death of a patient to prevent further sufferings. Active euthanasia refers to the physician deliberate act, usually the administration of lethal ...
Here are some examples of euthanasia essay topics and titles we can suggest: The benefits and disadvantages of a physician-assisted suicide. Ethical dilemmas associated with euthanasia. An individual's right to die. Euthanasia as one of the most debatable topics in today's society.
The Euthanasia in Humans Essay. The moral and ethical aspects of medical practice include not only the features of interaction with patients and other interested parties but also deeper nuances. In particular, one of the controversial and acute topics is euthanasia and its acceptability from different perspectives, including both patients ...
The Vatican on Monday reaffirmed its opposition to sex changes, gender theory and surrogate parenthood, as well as abortion and euthanasia, four months after supporting blessings for same-sex couples.
Send your letters to the editor: [email protected] more >. Print. Commentary. OPINION: I am glad to see that Pope Francis is taking a stand against some of the 'wedge' issues in ...
April 8, 2024, 7:17 a.m. ET. The Vatican on Monday issued a new document approved by Pope Francis stating that the church believes that sex-change operations, gender fluidity and surrogacy all ...
The Vatican declared Monday that gender-transition surgery and surrogacy are grave violations of human dignity. It put them on par with abortion and euthanasia as practices that reject God's plan ...
Federal prosecutors claim the apartment, on the 32nd floor of the Trump International Hotel and Tower, near the southwest corner of Central Park, was bought in 2014 for $7.1 million and was traced ...