Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 November 2020

Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis
- Carlos K. H. Wong 1 , 2 na1 ,
- Janet Y. H. Wong 3 na1 ,
- Eric H. M. Tang 1 ,
- C. H. Au 1 &
- Abraham K. C. Wai 4
Scientific Reports volume 10 , Article number: 19765 ( 2020 ) Cite this article
5939 Accesses
47 Citations
3 Altmetric
Metrics details
- Health care
- Medical research
- Microbiology
- Risk factors
This systematic review and meta-analysis investigated the comorbidities, symptoms, clinical characteristics and treatment of COVID-19 patients. Epidemiological studies published in 2020 (from January–March) on the clinical presentation, laboratory findings and treatments of COVID-19 patients were identified from PubMed/MEDLINE and Embase databases. Studies published in English by 27th March, 2020 with original data were included. Primary outcomes included comorbidities of COVID-19 patients, their symptoms presented on hospital admission, laboratory results, radiological outcomes, and pharmacological and in-patient treatments. 76 studies were included in this meta-analysis, accounting for a total of 11,028 COVID-19 patients in multiple countries. A random-effects model was used to aggregate estimates across eligible studies and produce meta-analytic estimates. The most common comorbidities were hypertension (18.1%, 95% CI 15.4–20.8%). The most frequently identified symptoms were fever (72.4%, 95% CI 67.2–77.7%) and cough (55.5%, 95% CI 50.7–60.3%). For pharmacological treatment, 63.9% (95% CI 52.5–75.3%), 62.4% (95% CI 47.9–76.8%) and 29.7% (95% CI 21.8–37.6%) of patients were given antibiotics, antiviral, and corticosteroid, respectively. Notably, 62.6% (95% CI 39.9–85.4%) and 20.2% (95% CI 14.6–25.9%) of in-patients received oxygen therapy and non-invasive mechanical ventilation, respectively. This meta-analysis informed healthcare providers about the timely status of characteristics and treatments of COVID-19 patients across different countries.
PROSPERO Registration Number: CRD42020176589
Similar content being viewed by others
Global prevalence and effect of comorbidities and smoking status on severity and mortality of COVID-19 in association with age and gender: a systematic review, meta-analysis and meta-regression
Santenna Chenchula, Kota Vidyasagar, … Sofia Mudda
Frequency, risk factors, and outcomes of hospital readmissions of COVID-19 patients
Antonio Ramos-Martínez, Lina Marcela Parra-Ramírez, … Carlos Lumbreras Bermejo
Risk factors for severe COVID-19 differ by age for hospitalized adults
Sevda Molani, Patricia V. Hernandez, … Jennifer J. Hadlock
Introduction
Following the possible patient zero of coronavirus infection identified in early December 2019 1 , the Coronavirus Disease 2019 (COVID-19) has been recognized as a pandemic in mid-March 2020 2 , after the increasing global attention to the exponential growth of confirmed cases 3 . As on 29th March, 2020, around 690 thousand persons were confirmed infected, affecting 199 countries and territories around the world, in addition to 2 international conveyances: the Diamond Princess cruise ship harbored in Yokohama, Japan, and the Holland America's MS Zaandam cruise ship. Overall, more than 32 thousand died and about 146 thousand have recovered 4 .
A novel bat-origin virus, 2019 novel coronavirus, was identified by means of deep sequencing analysis. SARS-CoV-2 was closely related (with 88% identity) to two bat-derived severe acute respiratory syndrome (SARS)-like coronaviruses, bat-SL-CoVZC45 and bat-SL-CoVZXC21, but were more distant from SARS-CoV (about 79%) and MERS-CoV (about 50%) 5 , both of which were respectively responsible for two zoonotic human coronavirus epidemics in the early twenty-first century. Following a few initial human infections 6 , the disease could easily be transmitted to a substantial number of individuals with increased social gathering 7 and population mobility during holidays in December and January 8 . An early report has described its high infectivity 9 even before the infected becomes symptomatic 10 . These natural and social factors have potentially influenced the general progression and trajectory of the COVID-19 epidemiology.
By the end of March 2020, there have been approximately 3000 reports about COVID-19 11 . The number of COVID-19-related reports keeps growing everyday, yet it is still far from a clear picture on the spectrum of clinical conditions, transmissibility and mortality, alongside the limitation of medical reports associated with reporting in real time the evolution of an emerging pathogen in its early phase. Previous reports covered mostly the COVID-19 patients in China. With the spread of the virus to other continents, there is an imminent need to review the current knowledge on the clinical features and outcomes of the early patients, so that further research and measures on epidemic control could be developed in this epoch of the pandemic.
Search strategy and selection criteria
The systematic review was conducted according to the protocol registered in the PROSPERO database (CRD42020176589). Following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline throughout this review, data were identified by searches of MEDLINE, Embase and references from relevant articles using the search terms "COVID", “SARS-CoV-2”, and “novel coronavirus” (Supplementary material 1 ). Articles published in English up to 27th March, 2020 were included. National containment measures have been implemented at many countries, irrespective of lockdown, curfew, or stay-at-home orders, since the mid of March 2020 12 , except for China where imposed Hubei province lockdown at 23th January 2020, Studies with original data including original articles, short and brief communication, letters, correspondences were included. Editorials, viewpoints, infographics, commentaries, reviews, or studies without original data were excluded. Studies were also excluded if they were animal studies, modelling studies, or did not measure symptoms presentation, laboratory findings, treatment and therapeutics during hospitalization.
After the removal of duplicate records, two reviewers (CW and CHA) independently screened the eligibility criteria of study titles, abstracts and full-texts, and reference lists of the studies retrieved by the literature search. Disagreements regarding the procedures of database search, study selection and eligibility were resolved by discussion. The second and the last authors (JW and AW) verified the eligibility of included studies.
Outcomes definitions
Signs and symptoms were defined as the presentation of fever, cough, sore throat, headache, dyspnea, muscle pain, diarrhea, rhinorrhea, anosmia, and ageusia at the hospital admission 13 .
Laboratory findings included a complete blood count (white blood count, neutrophil, lymphocyte, platelet count), procalcitonin, prothrombin time, urea, and serum biochemical measurements (including electrolytes, renal-function and liver-function values, creatine kinase, lactate dehydrogenase, C-reactive protein, Erythrocyte sedimentation rate), and treatment measures (i.e. antiviral therapy, antibiotics, corticosteroid therapy, mechanical ventilation, intubation, respiratory support, and renal replacement therapy). Radiological outcomes included bilateral involvement identified and pneumonia identified by chest radiograph.
Comorbidities of patients evaluated in this study were hypertension, diabetes, chronic obstructive pulmonary disease (COPD), cardiovascular disease, chronic kidney disease, liver disease and cancer.
In-patient treatment included intensive care unit admission, oxygen therapy, non-invasive ventilation, mechanical ventilation, Extracorporeal membrane oxygenation (ECMO), renal replacement therapy, and pharmacological treatment. Use of antiviral and interferon drugs (Lopinavir/ritonavir, Ribavirin, Umifenovir, Interferon-alpha, or Interferon-beta), antibiotic drugs, corticosteroid, and inotropes (Nor-adrenaline, Adrenaline, Vasopressin, Phenylephrine, Dopamine, or Dobutamine) were considered.
Data analysis
Three authors (CW, EHMT and CHA) extracted data using a standardized spreadsheet to record the article type, country of origin, surname of first author, year of publications, sample size, demographics, comorbidities, symptoms, laboratory and radiology results, pharmacological and non-pharmacological treatments.
We aggregated estimates across 90 eligible studies to produce meta-analytic estimates using a random-effects model. For dichotomous outcomes, we estimated the proportion and its respective 95% confidence interval. For laboratory parameters as continuous outcomes, we estimated the mean and standard deviation from the median and interquartile range if the mean and standard deviation were not available from the study 14 , and calculated the mean and its respective 95% confidence intervals. Random-effect models on DerSimonian and Laird method were adopted due to the significant heterogeneity, checked by the I 2 statistics and the p values. I 2 statistic of < 25%, 25–75% and ≥ 75% is considered as low, moderate, high likelihood of heterogeneity. Pooled estimates were calculated and presented by using forest plots. Publication bias was estimated by Egger’s regression test. Funnel plots of outcomes were also presented to assess publication bias.
All statistical analyses were conducted using the STATA Version 13.0 (Statacorp, College Station, TX). The random effects model was generated by the Stata packages ‘Metaprop’ for proportions 15 and ‘Metan’ for continuous variables 16 .
The selection and screen process are presented in Fig. 1 . A total of 241 studies were found by our searching strategy (71 in PubMed and 170 in Embase). 46 records were excluded due to duplication. After screening the abstracts and titles, 100 English studies were with original data and included in full-text screening. By further excluding 10 studies with not reporting symptoms presentation, laboratory findings, treatment and therapeutics, 90 studies 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 and 76 studies with more than one COVID-19 case 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 34 , 35 , 36 , 37 , 38 , 39 , 42 , 43 , 44 , 45 , 49 , 50 , 51 , 53 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 67 , 69 , 70 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 98 , 100 , 101 , 102 , 103 , 104 , 105 were included in the current systematic review and meta-analysis respectively. 73.3% 66 studies were conducted in China. Newcastle–Ottawa Quality Assessment Scale has been used to assess study quality of each included cohort study 107 . 30% (27/90) of included studies had satisfactory or good quality. The summary of the included study is shown in Table 1 .
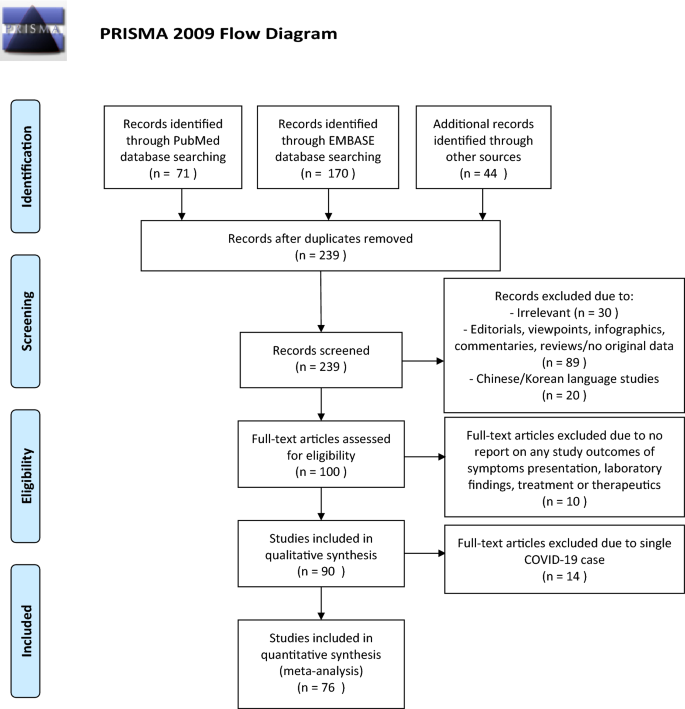
PRISMA flowchart reporting identification, searching and selection processes.
Of those 90 eligible studies, 11,028 COVID-19 patients were identified and included in the systematic review. More than half of patients (6336, 57.5%) were from mainland China. The pooled mean age was 45.8 (95% CI 38.6–52.5) years and 49.3% (pooled 95% CI 45.6–53.0%) of them were male.
For specific comorbidity status, the most prevalent comorbidity was hypertension (18.1%, 95% CI 15.4–20.8%), followed by cardiovascular disease (11.8%, 95% CI 9.4–14.2%) and diabetes (10.4%, 95% CI 8.7–12.1%). The pooled prevalence (95% CI) of COPD, chronic kidney disease, liver disease and cancer were 2.0% (1.3–2.7%), 5.2% (1.7–8.8%), 2.5% (1.7–3.4%) and 2.1% (1.3–2.8%) respectively. Moderate to substantial heterogeneity between reviewed studies were found, with I 2 statistics ranging from 39.4 to 95.9% ( p values between < 0.001–0.041), except for liver disease (I 2 statistics: 1.7%, p = 0.433). Detailed results for comorbidity status are displayed in Fig. 2 .
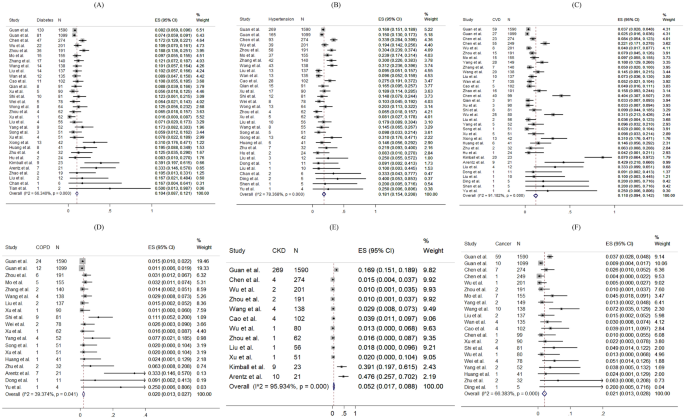
Random-effects meta-analytic estimates for comorbidities. ( A ) Diabetes mellitus, ( B ) Hypertension, ( C ) Cardiovascular disease, ( D ) Chronic obstructive pulmonary disease, ( E ) Chronic kidney disease, ( F ) Cancer.
Regarding the symptoms presented at hospital admission, the most frequent symptoms were fever (pooled prevalence: 72.4%, 95% CI 67.2–77.7%) and cough (pooled prevalence: 55.5%, 95% CI 50.7–60.3%). Sore throat (pooled prevalence: 16.2%, 95% CI 12.7–19.7%), dyspnoea (pooled prevalence: 18.8%, 95% CI 14.7–22.8%) and muscle pain (pooled prevalence: 22.1%, 95% CI 18.6–25.5%) were also common symptoms found in COVID-19 patients, but headache (pooled prevalence: 10.5%, 95% CI 8.7–12.4%), diarrhoea (pooled prevalence: 7.9%, 95% CI 6.3–9.6%), rhinorrhoea (pooled prevalence: 9.2%, 95% CI 5.6–12.8%) were less common. However, none of the included papers reported prevalence of anosmia and ageusia. The I 2 statistics varied from 68.5 to 97.1% (all p values < 0.001), indicating a high heterogeneity exists across studies. Figure 3 shows the pooled proportion of symptoms of patients presented at hospital.
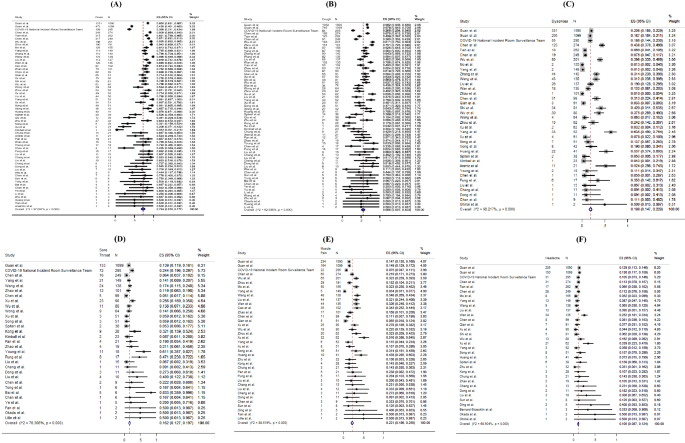
Random-effects meta-analytic estimates for presenting symptoms. ( A ) Fever, ( B ) Cough, ( C ) Dyspnoea, ( D ) Sore throat, ( E ) Muscle pain, ( F ) Headache.
For laboratory parameters, white blood cell (pooled mean: 5.31 × 10 9 /L, 95% CI 5.03–5.58 × 10 9 /L), neutrophil (pooled mean: 3.60 × 10 9 /L, 95% CI 3.31–3.89 × 10 9 /L), lymphocyte (pooled mean: 1.11 × 10 9 /L, 95% CI 1.04–1.17 × 10 9 /L), platelet count (pooled mean: 179.5 U/L, 95% CI 172.6–186.3 U/L), aspartate aminotransferase (pooled mean: 30.3 U/L, 95% CI 27.9–32.7 U/L), alanine aminotransferase (pooled mean: 27.0 U/L, 95% CI 24.4–29.6 U/L) and C-reactive protein (CRP) (pooled mean: 22.0 mg/L, 95% CI 18.3–25.8 mg/L) and D-dimer (0.93 mg/L, 95% CI 0.68–1.18 mg/L) were the common laboratory test taken for COVID-19 patients. Above results and other clinical factors are depicted in Fig. 4 . Same with the comorbidity status and symptoms, high likelihood of heterogeneity was detected by I 2 statistics for a majority of clinical parameters.
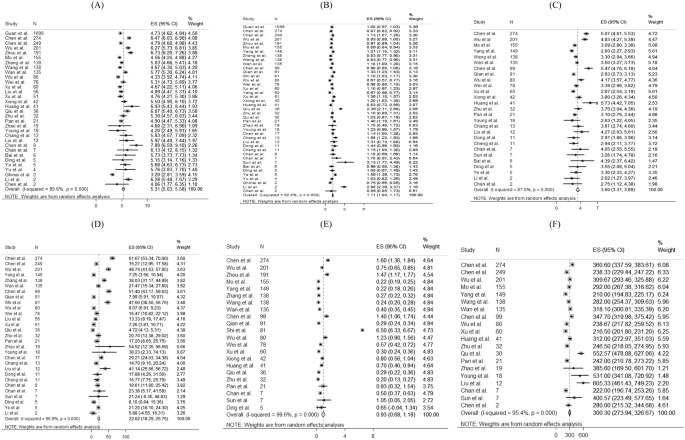
Random-effects meta-analytic estimates for laboratory parameters. ( A ) White blood cell, ( B ) Lymphocyte, ( C ) Neutrophil, ( D ) C-creative protein, ( E ) D-dimer, ( F ) Lactate dehydrogenase.
Figure 5 presents the distribution of the pharmacological treatments received for COVID-19 patients. 10.6% of patients admitted to intensive care units (pooled 95% CI 8.1–13.2%). For drug treatment, 63.9% (pooled 95% CI 52.5–75.3%), 62.4% (pooled 95% CI 47.9–76.8%) and 29.7% (pooled 95% CI 21.8–37.6%) patients used antibiotics, antiviral, and corticosteroid, respectively. 41.3% (pooled 95% CI 14.3–68.3%) and 50.7% (pooled 95% CI 9.2–92.3%) reported using Lopinavir/Ritonavir and interferon-alpha as antiviral drug treatment, respectively. Among 14 studies reporting proportion of corticosteroid used, 7 studies (50%) specified the formulation of corticosteroid as systemic corticosteroid. The remaining one specified the use of methylprednisolone. No reviewed studies reported the proportion of patients receiving Ribavirin, Interferon-beta, or inotropes.
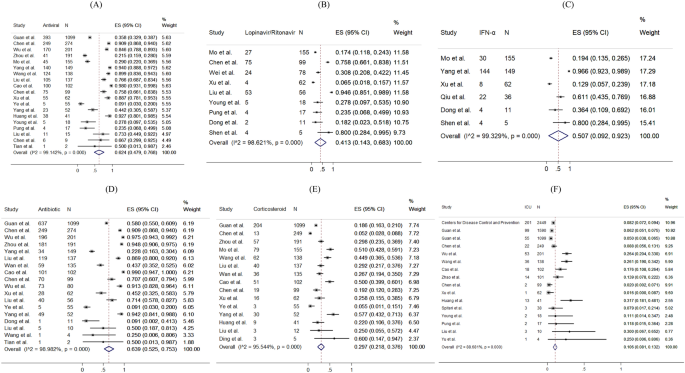
Random-effects meta-analytic estimates for pharmacological treatments and intensive unit care at hospital. ( A ) Antiviral or interferon drugs, ( B ) Lopinavir/Ritonavir, ( C ) Interferon alpha (IFN-α), ( D ) Antibiotic drugs, ( E ) Corticosteroid, ( F ) Admission to Intensive care unit.
The prevalence of radiological outcomes and non-pharmacological treatments were presented in Fig. 6 . Radiology findings detected chest X-ray abnormalities, with 74.4% (95% CI 67.6–81.1%) of patients with bilateral involvement and 74.9% (95% CI 68.0–81.8%) of patients with viral pneumonia. 62.6% (pooled 95% CI 39.9–85.4%), 20.2% (pooled 95% CI 14.6–25.9%), 15.3% (pooled 95% CI 11.0–19.7%), 1.1% (pooled 95% CI 0.4–1.8%) and 4.7% (pooled 95% CI 2.1–7.4%) took oxygen therapy, non-invasive ventilation, mechanical ventilation, ECMO and dialysis respectively.
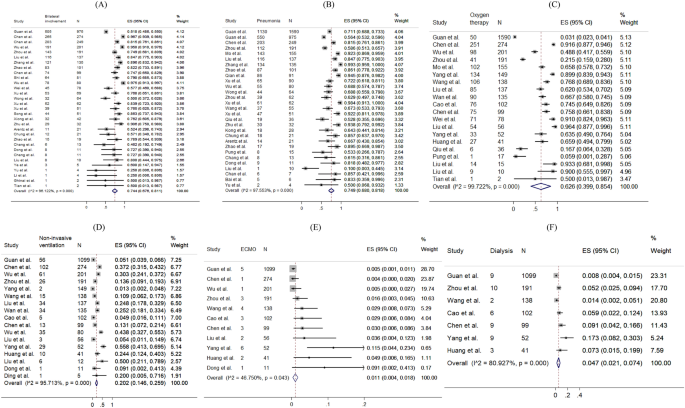
Random-effects meta-analytic estimates for radiological findings and non-pharmacological treatments at hospital. ( A ) Bilateral involvement, ( B ) Pneumonia, ( C ) Oxygen therapy, ( D ) Non-invasive ventilation, ( E ) Extracorporeal membrane oxygenation (ECMO), ( F ) Dialysis.
The funnel plots and results Egger’s test of comorbidity status, symptoms presented, laboratory test and treatment were presented in eFigure 1 – S5 in the Supplement. 63% (19/30) of the funnel plots (eFigure 1 – S5 ) showed significance in the Egger’s test for asymmetry, suggesting the possibility of publication bias or small-study effects caused by clinical heterogeneity.
This meta-analysis reveals the condition of global medical community responding to COVID-19 in the early phase. During the past 4 months, a new major epidemic focus of COVID-19, some without traceable origin, has been identified. Following its first identification in Wuhan, China, the virus has been rapidly spreading to Europe, North America, Asia, and the Middle East, in addition to African and Latin American countries. Three months since Wuhan CDC admitted that there was a cluster of unknown pneumonia cases related to Huanan Seafood Market and a new coronavirus was identified as the cause of the pneumonia 108 , as on 1 April, 2020, there have been 858,371 persons confirmed infected with COVID-19, affecting 202 countries and territories around the world. Although this rapid review is limited by the domination of reports from patients in China, and the patient population is of relative male dominance reflecting the gender imbalance of the Chinese population 109 , it provides essential information.
In this review, the pooled mean age was 45.8 years. Similar to the MERS-CoV pandemic 110 , middle-aged adults were the at-risk group for COVID-19 infections in the initial phase, which was different from the H1N1 influenza pandemic where children and adolescents were more frequently affected 111 . Biological differences may affect the clinical presentations of infections; however, in this review, studies examining the asymptomatic COVID-19 infections or reporting any previous infections were not included. It is suggested that another systematic review should be conducted to compare the age-specific incidence rates between the pre-pandemic and post-pandemic periods, so as to understand the pattern and spread of the disease, and tailor specific strategies in infection control.
Both sexes exhibited clinical presentations similar in symptomatology and frequency to those noted in other severe acute respiratory infections, namely influenza A H1N1 112 and SARS 113 , 114 . These generally included fever, new onset or exacerbation of cough, breathing difficulty, sore throat and muscle pain. Among critically ill patients usually presented with dyspnoea and chest tightness 22 , 29 , 39 , 72 , 141 (4.6%) of them with persistent or progressive hypoxia resulted in the requirement of intubation and mechanical ventilation 115 , while 194 (6.4%) of them required non-invasive ventilation, yielding a total of 11% of patients requiring ventilatory support, which was similar to SARS 116 .
The major comorbidities identified in this review included hypertension, cardiovascular diseases and diabetes mellitus. Meanwhile, the percentages of patients with chronic renal diseases and cancer were relatively low. These chronic conditions influencing the severity of COVID-19 had also been noted to have similar effects in other respiratory illnesses such as SARS, MERS-CoV and influenza 117 , 118 . Higher mortality had been observed among older patients and those with comorbidities.
Early diagnosis of COVID-19 was based on recognition of epidemiological linkages; the presence of typical clinical, laboratory, and radiographic features; and the exclusion of other respiratory pathogens. The case definition had initially been narrow, but was gradually broadened to allow for the detection of more cases, as milder cases and those without epidemiological links to Wuhan or other known cases had been identified 119 , 120 . Laboratory investigations among COVID-19 patients did not reveal specific characteristics—lymphopenia and elevated inflammatory markers such as CRP are some of the most common haematological and biochemical abnormalities, which had also been noticed in SARS 121 . None of these features were specific to COVID-19. Therefore, diagnosis should be confirmed by SARS-CoV–2 specific microbiological and serological studies, although initial management will continue to be based on a clinical and epidemiological assessment of the likelihood of a COVID-19 infection.
Radiology imaging often plays an important role in evaluating patients with acute respiratory distress; however, in this review, radiological findings of SARS-CoV-2 pneumonia were non-specific. Despite chest radiograph usually revealed bilateral involvement and Computed Tomography usually showed bilateral multiple ground-glass opacities or consolidation, there were also patients with normal chest radiograph, implying that chest radiograph might not have high specificity to rule out pneumonia in COVID-19.
Limited clinical data were available for asymptomatic COVID-19 infected persons. Nevertheless, asymptomatic infection could be unknowingly contagious 122 . From some of the official figures, 6.4% of 150 non-travel-related COVID-19 infections in Singapore 123 , 39.9% of cases from the Diamond Princess cruise ship in Japan 124 , and up to 78% of cases in China as extracted on April 1st, 2020, were found to be asymptomatic 122 . 76% (68/90) studies based on hospital setting which provided care and disease management to symptomatic patients had limited number of asymptomatic cases of COVID-19 infection. This review calls for further studies about clinical data of asymptomatic cases. Asymptomatic infection intensifies the challenges of isolation measures. More global reports are crucially needed to give a better picture of the spectrum of presentations among all COVID-19 infected persons. Also, public health policies including social and physical distancing, monitoring and surveillance, as well as contact tracing, are necessary to reduce the spread of COVID-19.
Concerning potential treatment regime, 62.4% of patients received antivirals or interferons (including oseltamivir, lopinavir-ritonavir, interferon alfa), while 63.9% received antibiotics (such as moxifloxacin, and ceftriaxone). In this review, around one-third of patients were given steroid, suggestive as an adjunct to IFN, or sepsis management. Interferon and antiviral agents such as ribavirin, and lopinavir-ritonavir were used during SARS, and the initial uncontrolled reports then noted resolution of fever and improvement in oxygenation and radiographic appearance 113 , 125 , 126 , without further evidence on its effectiveness. At the time of manuscript preparation, there has been no clear evidence guiding the use of antivirals 127 . Further research is needed to inform clinicians of the appropriate use of antivirals for specific groups of infected patients.
Limitations of this meta-analysis should be considered. First, a high statistical heterogeneity was found, which could be related to the highly varied sample sizes (9 to 4226 patients) and study designs. Second, variations of follow-up period may miss the event leading to heterogeneity. In fact, some patients were still hospitalized in the included studies. Third, since only a few studies had compared the comorbidities of severe and non-severe patients, sensitivity analysis and subgroup analysis were not conducted. Fourthly, the frequency and severity of signs and symptoms reported in included studies, primarily based on hospitalized COVID-19 patients were over-estimated. Moreover, different cutoffs for abnormal laboratory findings were applied across countries, and counties within the same countries. Lastly, this meta-analysis reviewed only a limited number of reports written in English, with a predominant patient population from China. This review is expected to inform clinicians of the epidemiology of COVID-19 at this early stage. A recent report estimated the number of confirmed cases in China could reach as high as 232,000 (95% CI 161,000, 359,000) with the case definition adopted in 5th Edition. In this connection, further evidence on the epidemiology is in imminent need.
Oliveira N. Shrimp vendor identified as possible coronavirus ‘patient zero,’ leaked document says. 27 March 2020. New York Daily News. 2020.
World Health Organization. Basic protective measures against the new coronavirus (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 7 Oct 2020.
Google Trend. When will coronavirus end (2020). https://trends.google.com/trends/explore?date=today%203-m&q=when%20will%20coronavirus%20end,%2Fm%2F01cpyy . Accessed 10 Oct 2020.
Worldometer. COVID-19 Coronavirus Pandemic (2020). https://www.worldometers.info/coronavirus/ . Accessed 13 Oct 2020.
Lu, R. et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395 (10224), 565–574 (2020).
Article CAS PubMed PubMed Central Google Scholar
Ralph, R. et al. 2019-nCoV (Wuhan virus), a novel Coronavirus: human-to-human transmission, travel-related cases, and vaccine readiness. J. Infect. Dev. Ctries. 14 (1), 3–17 (2020).
Article CAS PubMed Google Scholar
Sun, Z., Thilakavathy, K., Kumar, S. S., He, G. & Liu, S. V. Potential factors influencing repeated SARS outbreaks in China. Int. J. Environ. Res. Public Health 17 (5), 1633 (2020).
Article CAS PubMed Central Google Scholar
Zhao, S. et al. The association between domestic train transportation and novel coronavirus (2019-nCoV) outbreak in China from 2019 to 2020: a data-driven correlational report. Travel Med. Infect. Dis. 33 , 101568 (2020).
Article PubMed PubMed Central Google Scholar
Li, Q. et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 382 (13), 1199–1207 (2020).
Chen, J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 22 (2), 69–71 (2020).
World Health Organization. Database of publications on coronavirus disease (COVID-19) (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov . Accessed 30 Mar 2020.
Wong, C. K. H. et al. Impact of national containment measures on decelerating the increase in daily new cases of COVID-19 in 54 countries and 4 epicenters of the pandemic: comparative observational study. J. Med. Internet Res. 22 (7), e19904 (2020).
Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Symptoms of Coronavirus (2020).
Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 14 (1), 135 (2014).
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch. Public Health 72 (1), 39 (2014).
Harris, R. J. et al. metan: fixed- and random-effects meta-analysis. Stata J. 8 (1), 3–28 (2008).
Article Google Scholar
Xu, X. et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur. J. Nucl. Med. Mol. Imaging 47 (5), 1275–1280 (2020).
Cao, J. et al. Clinical features and short-term outcomes of 18 patients with corona virus disease 2019 in intensive care unit. Intensive Care Med. 46 (5), 851–853 (2020).
Xiong, Y. et al. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest. Radiol. 55 (6), 332–339 (2020).
Arentz, M. et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA 323 (16), 1612–1614 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (10223), 497–506 (2020).
Guan, W. J. et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382 (18), 1708–1720 (2020).
Zhao, D. et al. A comparative study on the clinical features of coronavirus 2019 (COVID-19) pneumonia with other pneumonias. Clin. Infect. Dis. 71 (15), 756–761 (2020).
Xu, X. W. et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 19 (368), m606 (2020).
Chan, J. F. et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395 (10223), 514–523 (2020).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395 (10223), 507–513 (2020).
Pung, R. et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet 395 (10229), 1039–1046 (2020).
Wang, D. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323 (11), 1061–1069 (2020).
Young, B. E. et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 323 (15), 1488–1494 (2020).
Chen, H. et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet 395 (10226), 809–815 (2020).
Huang, W. H. et al. 2019 novel coronavirus disease (COVID-19) in Taiwan: reports of two cases from Wuhan, China. J. Microbiol. Immunol. Infect. 53 (3), 481–484 (2020).
Cheng, S. C. et al. First case of coronavirus disease 2019 (COVID-19) pneumonia in Taiwan. J. Formos. Med. Assoc. 119 (3), 747–751 (2020).
Holshue, M. L. et al. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 382 (10), 929–936 (2020).
Wei, M. et al. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA 323 (13), 1313–1314 (2020).
Bernard Stoecklin, S. et al. First cases of coronavirus disease 2019 (COVID-19) in France: surveillance, investigations and control measures, January 2020. Euro Surveill. 25 (6), 20–26 (2020).
Shi, H. et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 20 (4), 425–434 (2020).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382 (8), 727–733 (2020).
Ghinai, I. et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet 395 (10230), 1137–1144 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395 (10229), 1054–1062 (2020).
Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 8 (5), 475–481 (2020).
Kim, J. Y. et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J. Korean Med. Sci. 35 (5), e61 (2020).
Okada, P. et al . Early transmission patterns of coronavirus disease 2019 (COVID-19) in travellers from Wuhan to Thailand, January 2020. Euro Surveill . 25 (8), 6–10 (2020).
Arashiro, T., Furukawa, K. & Nakamura, A. COVID-19 in 2 persons with mild upper respiratory tract symptoms on a cruise ship, Japan. Emerg. Infect. Dis. 26 (6), 1345–1348 (2020).
Lillie, P. J. et al. Novel coronavirus disease (Covid-19): the first two patients in the UK with person to person transmission. J. Infect. 80 (5), 578–606 (2020).
Tian, S. et al. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J. Thorac. Oncol. 15 (5), 700–704 (2020).
Haveri, A. et al . Serological and molecular findings during SARS-CoV-2 infection: the first case study in Finland, January to February 2020. Euro Surveill . 25 (11), 16–21 (2020).
Nicastri, E. et al . Coronavirus disease (COVID-19) in a paucisymptomatic patient: epidemiological and clinical challenge in settings with limited community transmission, Italy, February 2020. Euro Surveill . 25 (11) (2020).
Van Cuong, L. et al. The first Vietnamese case of COVID-19 acquired from China. Lancet Infect Dis. 20 (4), 408–409 (2020).
Spiteri, G. et al . First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill . 25 (9), 2–7 (2020).
Rothe, C. et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 382 (10), 970–971 (2020).
Tong, Z. D. et al. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg. Infect. Dis. 26 (5), 1052–1054 (2020).
Bai, Y. et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 323 (14), 1406–1407 (2020).
Yu, P., Zhu, J., Zhang, Z. & Han, Y. A familial cluster of infection associated with the 2019 novel coronavirus indicating possible person-to-person transmission during the incubation period. J. Infect. Dis. 221 (11), 1757–1761 (2020).
Li, P. et al. Transmission of COVID-19 in the terminal stages of the incubation period: a familial cluster. Int. J. Infect. Dis. 96 , 452–453 (2020).
Tang, A. et al. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg. Infect. Dis. 26 (6), 1337–1339 (2020).
Kam, K. Q. et al. A well infant with coronavirus disease 2019 with high viral load. Clin. Infect. Dis. 71 (15), 847–849 (2020).
Zhou, S., Wang, Y., Zhu, T. & Xia, L. CT Features of Coronavirus Disease 2019 (COVID-19) Pneumonia in 62 Patients in Wuhan. China. AJR Am J Roentgenol. 214 (6), 1287–1294 (2020).
Article PubMed Google Scholar
Zhao, W., Zhong, Z., Xie, X., Yu, Q. & Liu, J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am. J. Roentgenol. 214 (5), 1072–1077 (2020).
Cheng, Z. et al. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. AJR Am. J. Roentgenol. 215 (1), 121–126 (2020).
Chung, M. et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 295 (1), 202–207 (2020).
Liu, K. et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 133 (9), 1025–1031 (2020).
Chang, L. M. et al. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. JAMA 323 (11), 1092–1093 (2020).
Team C-NIRS. COVID-19, Australia: Epidemiology Report 7 (Reporting week ending 19:00 AEDT 14 March 2020). Commun. Dis. Intell. 44 (2018).
Pan, F. et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology 295 (3), 715–721 (2020).
Wang, S. et al. A case report of neonatal 2019 coronavirus disease in China. Clin. Infect. Dis. 71 (15), 853–857 (2020).
Bastola, A. et al. The first 2019 novel coronavirus case in Nepal. Lancet Infect. Dis. 20 (3), 279–280 (2020).
Qiu, H. et al. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect. Dis. 20 (6), 689–696 (2020).
Zhang, J. J. et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75 (7), 1730–1741 (2020).
Ye, G. et al. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J. Infect. 80 (5), e14–e17 (2020).
Liu, Y. et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 63 (3), 364–374 (2020).
Chen, T. et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 26 (368), m1091 (2020).
Guan, W. J. et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 55 (5), 2000547 (2020).
Wong, H. Y. F. et al. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology 296 (2), E72–E78 (2020).
Xu, T. et al. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int J Infect Dis. 94 , 68–71 (2020).
Shen, C. et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA 323 (16), 1582–1589 (2020).
Kimball, A. et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. Morb. Mortal. Wkly. Rep. 69 (13), 377–381 (2020).
Article CAS Google Scholar
Team CC-R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12-March 16, 2020. Morb. Mortal. Wkly. Rep. 69 (12), 343–346 (2020).
Wu, J. et al. Clinical characteristics of imported cases of coronavirus disease 2019 (COVID-19) in Jiangsu Province: a multicenter descriptive study. Clin. Infect. Dis. 71 (15), 706–712 (2020).
Yang, W. et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J. Infect. 80 (4), 388–393 (2020).
Zhu, L. et al. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am. J. Transplant. 20 (7), 1859–1863 (2020).
Zhu, W. et al. Initial clinical features of suspected coronavirus disease in two emergency departments outside of Hubei, China. J. Med. Virol. 92 , 1525–1532 (2019).
Wu, C. et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 180 (7), 934–943 (2020).
Wang, Z., Chen, X., Lu, Y., Chen, F. & Zhang, W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci. Trends 14 (1), 64–68 (2020).
Wang, Y. et al. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. J. Infect. Dis. 221 (11), 1770–1774 (2020).
Wan, S. et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J. Med.. Virol. 92 (7), 797–806 (2020).
Tian, S. et al. Characteristics of COVID-19 infection in Beijing. J. Infect. 80 (4), 401–406 (2020).
Sun, D. et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J. Pediatr. 16 (3), 251–259 (2020).
Song, F. et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 295 (1), 210–217 (2020).
Hu, Z. et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci. China Life Sci. 63 (5), 706–711 (2020).
Qu, R. et al. Platelet-to-lymphocyte ratio is associated with prognosis in patients with coronavirus disease-19. J. Med. Virol. 92 , 1533–1541 (2020).
Qian, G. Q. et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM 113 (7), 474–481 (2020).
Mo, P. et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin. Infect. Dis . (2020).
Liu, W. et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med. J. (Engl) 133 (9), 1032–1038 (2020).
Liu, K., Chen, Y., Lin, R. & Han, K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J. Infect. 80 (6), e14–e18 (2020).
Liu, F. et al. Patients of COVID-19 may benefit from sustained Lopinavir-combined regimen and the increase of Eosinophil may predict the outcome of COVID-19 progression. Int. J. Infect. Dis. 95 , 183–191 (2020).
Liu, D. et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. AJR Am. J. Roentgenol. 215 (1), 127–132 (2020).
Guillen, E. et al. Case report of COVID-19 in a kidney transplant recipient: does immunosuppression alter the clinical presentation?. Am. J. Transplant. 20 (7), 1875–1878 (2020).
Dong, X. et al. Eleven faces of coronavirus disease 2019. Allergy 75 (7), 1699–1709 (2020).
Fan, C. et al . Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin. Infect. Dis. (2020).
Chen, R. et al. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Can. J. Anaesth. 67 (6), 655–663 (2020).
Chen, L. et al. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg. Microbes Infect. 9 (1), 313–319 (2020).
Chen, J. et al. Clinical progression of patients with COVID-19 in Shanghai, China. J. Infect. 80 (5), e1–e6 (2020).
Ding, Q., Lu, P., Fan, Y., Xia, Y. & Liu, M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan, China. J. Med. Virol. 92 , 1549–1555 (2020).
Covid-19 National Emergency Response Center E & Case Management Team KCfDC, Prevention. Early epidemiological and clinical characteristics of 28 cases of coronavirus disease in South Korea. Osong Public Health Res. Perspect. 11 (1), 8–14 (2020).
Li, Y., Guo, F., Cao, Y., Li, L. & Guo, Y. Insight into COVID-2019 for pediatricians. Pediatr. Pulmonol. 55 (5), E1–E4 (2020).
Ai, J. W., Zhang, Y., Zhang, H. C., Xu, T. & Zhang, W. H. Era of molecular diagnosis for pathogen identification of unexplained pneumonia, lessons to be learned. Emerg Microbes Infect. 9 (1), 597–600 (2020).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 (9), 603–605 (2010).
Khan N. New virus discovered by Chinese scientists investigating pneumonia outbreak. Wall Street J . (2020).
国家统计局 (National Bureau of Statistics). 2019 年国民经济运行总体平稳 发展主要预期目标较好实现 (In 2019, the overall stable development of the national economic operation is expected to achieve the main goals (2020). http://www.stats.gov.cn/tjsj/zxfb/202001/t20200117_1723383.html . Accessed 30 Mar 2020.
Park, J. E., Jung, S., Kim, A. & Park, J. E. MERS transmission and risk factors: a systematic review. BMC Public Health 18 (1), 574 (2018).
Van Kerkhove, M. D. et al. Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Med. 8 (7), e1001053 (2011).
Wang, C. et al. Epidemiological and clinical characteristics of the outbreak of 2009 pandemic influenza A (H1N1) at a middle school in Luoyang, China. Public Health 126 (4), 289–294 (2012).
Lee, N. et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N. Engl. J. Med. 348 (20), 1986–1994 (2003).
Booth, C. M. et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 289 (21), 2801–2809 (2003).
Fowler, R. A. et al. Critically ill patients with severe acute respiratory syndrome. JAMA 290 (3), 367–373 (2003).
Christian, M. D., Poutanen, S. M., Loutfy, M. R., Muller, M. P. & Low, D. E. Severe acute respiratory syndrome. Clin Infect Dis. 38 (10), 1420–1427 (2004).
Mertz, D. et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ 23 (347), f5061 (2013).
Badawi, A. & Ryoo, S. G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int. J. Infect. Dis. 49 , 129–133 (2016).
Tsang, T. K. et al. Effect of changing case definitions for COVID-19 on the epidemic curve and transmission parameters in mainland China: a modelling study. Lancet Public Health. 5 (5), e289–e296 (2020).
国家卫生健康委办公厅 (Office of National Health Comission). 新型冠状病毒肺炎诊疗方案 (试行第七版) (Clinical Guideline for Novel Coronavirus Pneumonia—Interim 7th Edition) (2020).
File, T. M. Jr. & Tsang, K. W. Severe acute respiratory syndrome: pertinent clinical characteristics and therapy. Treat. Respir. Med. 4 (2), 95–106 (2005).
Day, M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ 2 (369), m1375 (2020).
Wei, W. E. et al. Presymptomatic transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. Morb. Mortal. Wkly. Rep. 69 (14), 411–415 (2020).
Mizumoto, K., Kagaya, K., Zarebski, A. & Chowell, G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 25 (10), 2000180 (2020).
Article PubMed Central Google Scholar
Poutanen, S. M. et al. Identification of severe acute respiratory syndrome in Canada. N. Engl. J .Med. 348 (20), 1995–2005 (2003).
Tsang, K. W. et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N. Engl. J. Med. 348 (20), 1977–1985 (2003).
Cao, B. et al. A trial of Lopinavir–Ritonavir in adults hospitalized with severe covid-19. N. Engl. J. Med. 382 (19), 1787–1799 (2020).
Download references
Acknowledgements
There was no funding source for this study.
Author information
These authors contributed equally: Carlos K. H. Wong and Janet Y. H. Wong.
Authors and Affiliations
Department of Family Medicine and Primary Care, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Carlos K. H. Wong, Eric H. M. Tang & C. H. Au
Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Carlos K. H. Wong
School of Nursing, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Janet Y. H. Wong
Emergency Medicine Unit, Li Ka Shing, Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Abraham K. C. Wai
You can also search for this author in PubMed Google Scholar
Contributions
C.W., J.W. and A.W. contributed equally to all aspects of study design, conduct, data interpretation, and the writing of the manuscript. C.W., E.T. and C.H.A. contributed to eligibility screening, data extraction from eligible studies, and data analysis and interpretation.
Corresponding author
Correspondence to Abraham K. C. Wai .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary figure 1., supplementary figure 2., supplementary figure 3., supplementary figure 4., supplementary figure 5., supplementary material 6., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wong, C.K.H., Wong, J.Y., Tang, E.H.M. et al. Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis. Sci Rep 10 , 19765 (2020). https://doi.org/10.1038/s41598-020-74988-9
Download citation
Received : 04 May 2020
Accepted : 25 September 2020
Published : 13 November 2020
DOI : https://doi.org/10.1038/s41598-020-74988-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Comorbidity genetic risk and pathways impact sars-cov-2 infection outcomes.
- Rachel K. Jaros
- Tayaza Fadason
- Justin M. O’Sullivan
Scientific Reports (2023)
Adrenal function in relation to cytokines and outcome in non-critically ill patients with COVID-19
- N. Athanasiou
- A. Diamantopoulos
- D. A. Vassiliadi
Journal of Endocrinological Investigation (2023)
The Role of Multidimensional Prognostic Index to Identify Hospitalized Older Adults with COVID-19 Who Can Benefit from Remdesivir Treatment: An Observational, Prospective, Multicenter Study
- Carlo Custodero
- Nicola Veronese
- Julia Schlotmann
Drugs & Aging (2023)
Prevalence of hypertension and associated risks in hospitalized patients with COVID-19: a meta-analysis of meta-analyses with 1468 studies and 1,281,510 patients
- Yousof Khairy
- Deniz Naghibi
- Saber Azami-Aghdash
Systematic Reviews (2022)
An alternative approach to determination of Covid-19 personal risk index by using fuzzy logic
- Hakan Şimşek
- Elifnaz Yangın
Health and Technology (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Microbiology newsletter — what matters in microbiology research, free to your inbox weekly.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present...
How to present clinical cases
- Related content
- Peer review
- Ademola Olaitan , medical student 1 ,
- Oluwakemi Okunade , final year medical student 1 ,
- Jonathan Corne , consultant physician 2
- 1 University of Nottingham
- 2 Nottingham University Hospitals
Presenting a patient is an essential skill that is rarely taught
Clinical presenting is the language that doctors use to communicate with each other every day of their working lives. Effective communication between doctors is crucial, considering the collaborative nature of medicine. As a medical student and later as a doctor you will be expected to present cases to peers and senior colleagues. This may be in the setting of handovers, referring a patient to another specialty, or requesting an opinion on a patient.
A well delivered case presentation will facilitate patient care, act a stimulus for timely intervention, and help identify individual and group learning needs. 1 Case presentations are also used as a tool for assessing clinical competencies at undergraduate and postgraduate level.
Medical students are taught how to take histories, examine, and communicate effectively with patients. However, we are expected to learn how to present effectively by observation, trial, and error.
Principles of presentation
Remember that the purpose of the case presentation is to convey your diagnostic reasoning to the listener. By the end of your presentation the examiner should have a clear view of the patient’s condition. Your presentation should include all the facts required to formulate a management plan.
There are no hard and fast rules for a perfect presentation, rather the content of each presentation should be determined by the case, the context, and the audience. For example, presenting a newly admitted patient with complex social issues on a medical ward round will be very different from presenting a patient with a perforated duodenal ulcer who is in need of an emergency laparotomy.
Whether you’re presenting on a busy ward round or during an objective structured clinical examination (OSCE), it is important that you are concise yet get across all the important points. Start by introducing patients with identifiers such as age, sex, and occupation, and move on to the complaint that they presented with or the reason that they are in hospital. The presenting complaint is an important signpost and should always be clearly stated at the start of the presentation.
Presenting a history
After you’ve introduced the patient and stated the presenting complaint, you can proceed in a chronological approach—for example, “Mr X came in yesterday with worsening shortness of breath, which he first noticed four days ago.” Alternatively you can discuss each of the problems, starting with the most pertinent and then going through each symptom in turn. This method is especially useful in patients who have several important comorbidities.
The rest of the history can then be presented in the standard format of presenting complaint, history of presenting complaint, medical history, drug history, family history, and social history. Strictly speaking there is no right or wrong place to insert any piece of information. However, in some instances it may be more appropriate to present some information as part of the history of presenting complaints rather than sticking rigidly to the standard format. For example, in a patient who presents with haemoptysis, a mention of relevant risk factors such as smoking or contacts with tuberculosis guides the listener down a specific diagnostic pathway.
Apart from deciding at what point to present particular pieces of information, it is also important to know what is relevant and should be included, and what is not. Although there is some variation in what your seniors might view as important features of the history, there are some aspects which are universally agreed to be essential. These include identifying the chief complaint, accurately describing the patient’s symptoms, a logical sequence of events, and an assessment of the most important problems. In addition, senior medical students will be expected to devise a management plan. 1
The detail in the family and social history should be adapted to the situation. So, having 12 cats is irrelevant in a patient who presents with acute appendicitis but can be relevant in a patient who presents with an acute asthma attack. Discerning the irrelevant from the relevant is not always easy, but it comes with experience. 2 In the meantime, learning about the diseases and their associated features can help to guide you in the things you need to ask about in your history. Indeed, it is impossible to present a good clinical history if you haven’t taken a good history from the patient.
Presenting examination findings
When presenting examination findings remember that the aim is to paint a clear picture of the patient’s clinical status. Help the listener to decide firstly whether the patient is acutely unwell by describing basics such as whether the patient is comfortable at rest, respiratory rate, pulse, and blood pressure. Is the patient pyrexial? Is the patient in pain? Is the patient alert and orientated? These descriptions allow the listener to quickly form a mental picture of the patient’s clinical status. After giving an overall picture of the patient you can move on to present specific findings about the systems in question. It is important to include particular negative findings because they can influence the patient’s management. For example, in a patient with heart failure it is helpful to state whether the patient has a raised jugular venous pressure, or if someone has a large thyroid swelling it is useful to comment on whether the trachea is displaced. Initially, students may find it difficult to know which details are relevant to the case presentation; however, this skill becomes honed with increasing knowledge and clinical experience.
Presenting in an exam
Although the same principles as presenting in other situations also apply in an exam setting, the exam situation differs in the sense that its purpose is for you to show your clinical competence to the examiner.
It’s all about making a good impression. Walk into the room confidently and with a smile. After taking the history or examining the patient, turn to the examiner and look at him or her before starting to present your findings. Avoid looking back at the patient while presenting. A good way to avoid appearing fiddly is to hold your stethoscope behind your back. You can then wring to your heart’s content without the examiner sensing your imminent nervous breakdown.
Start with an opening statement as you would in any other situation, before moving on to the main body of the presentation. When presenting the main body of your history or examination make sure that you show the examiner how your findings are linked to each other and how they come together to support your conclusion.
Finally, a good summary is just as important as a good introduction. Always end your presentation with two or three sentences that summarise the patient’s main problem. It can go something like this: “In summary, this is Mrs X, a lifelong smoker with a strong family history of cardiovascular disease, who has intermittent episodes of chest pain suggestive of stable angina.”
Improving your skills
The RIME model (reporter, interpreter, manager, and educator) gives the natural progression of the clinical skills of a medical student. 3 Early on in clinical practice students are simply reporters of information. As the student progresses and is able to link together symptoms, signs, and investigation results to come up with a differential diagnosis, he or she becomes an interpreter of information. With further development of clinical skills and increasing knowledge students are actively able to suggest management plans. Finally, managers progress to become educators. The development from reporter to manager is reflected in the student’s case presentations.
The key to improving presentation skills is to practise, practise, and then practise some more. So seize every opportunity to present to your colleagues and seniors, and reflect on the feedback you receive. 4 Additionally, by observing colleagues and doctors you can see how to and how not to present.
Remember the purpose of the presentation
Be flexible; the context should dictate the content of the presentation
Always include a presenting complaint
Present your findings in a way that shows understanding
Have a system
Use appropriate terminology
Additional tips for exams
Start with a clear introductory statement and close with a brief summary
After your summary suggest a working diagnosis and a management plan
Practise, practise, practise, and get feedback
Present with confidence, and don’t be put off by an examiner’s poker face
Be honest; do not make up signs to fit in with your diagnosis
Originally published as: Student BMJ 2010;18:c1539
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
See “Medical ward rounds” ( Student BMJ 2009;17:98-9, http://archive.student.bmj.com/issues/09/03/life/98.php ).
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: Opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 -3. OpenUrl CrossRef PubMed Web of Science
- ↵ Lingard LA, Haber RJ. What do we mean by “relevance”? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format. Acad Med 1999 ; 74 : S124 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med 1999 ; 74 : 1203 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Haber RJ, Lingard LA. Learning oral presentation skills: a rhetorical analysis with pedagogical and professional implications. J Gen Intern Med 2001 ; 16 : 308 -14. OpenUrl CrossRef PubMed Web of Science
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
Clinical Presentation
Clinical considerations for care of children and adults with confirmed COVID-19
‹ View Table of Contents
- The clinical presentation of COVID-19 ranges from asymptomatic to critical illness.
- An infected person can transmit SARS-CoV-2, the virus that causes COVID-19, before the onset of symptoms. Symptoms can change over the course of illness and can progress in severity.
- Uncommon presentations of COVID-19 can occur, might vary by the age of the patient, and are a challenge to recognize.
- In adults, age is the strongest risk factor for severe COVID-19. The risk of severe COVID-19 increases with increasing age especially for persons over 65 years and with increasing number of certain underlying medical conditions .
Incubation Period
Data suggest that incubation periods may differ by SARS-CoV-2 variant. Meta-analyses of studies published in 2020 identified a pooled mean incubation period of 6.5 days from exposure to symptom onset. (1) A study conducted during high levels of Delta variant transmission reported an incubation period of 4.3 days, (2) and studies performed during high levels of Omicron variant transmission reported a median incubation period of 3–4 days. (3,4)
Presentation
People with COVID-19 may be asymptomatic or may commonly experience one or more of the following symptoms (not a comprehensive list) (5) :
- Fever or chills
- Shortness of breath or difficulty breathing
- Myalgia (Muscle or body aches)
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
The clinical presentation of COVID-19 ranges from asymptomatic to severe illness, and COVID-19 symptoms may change over the course of illness. COVID-19 symptoms can be difficult to differentiate from and can overlap with other viral respiratory illnesses such as influenza(flu) and respiratory syncytial virus (RSV) . Because symptoms may progress quickly, close follow-up is needed, especially for:
- older adults
- people with disabilities
- people with immunocompromising conditions, and
- people with medical conditions that place them at greater risk for severe illness or death.
The NIH COVID-19 Treatment Guidelines group SARS-CoV-2 infection into five categories based on severity of illness:
- Asymptomatic or pre-symptomatic infection : people who test positive for SARS-CoV-2 using a virologic test (i.e., a nucleic acid amplification test [NAAT] or an antigen test) but who have no symptoms that are consistent with COVID-19.
- Mild illness : people who may have any of the various signs and symptoms of COVID-19 but who do not have shortness of breath, dyspnea, or abnormal chest imaging.
- Moderate illness : people who have evidence of lower respiratory disease during clinical assessment or imaging and who have an oxygen saturation (SpO 2 ) ≥94% on room air at sea level.
- Severe illness : people who have oxygen saturation <94% on room air at sea level, a ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO 2 /FiO 2 ) <300 mm Hg, a respiratory rate >30 breaths/min, or lung infiltrates >50%
- Critical illness : people who have respiratory failure, septic shock, or multiple organ dysfunction.
Asymptomatic and presymptomatic presentation
Studies have documented SARS-CoV-2 infection in people who never develop symptoms (asymptomatic presentation) and in people who are asymptomatic when tested but develop symptoms later (presymptomatic presentation). ( 6,7 ) It is unclear what percentage of people who initially appear asymptomatic progress to clinical disease. Multiple publications have reported cases of people with abnormalities on chest imaging that are consistent with COVID-19 very early in the course of illness, even before the onset of symptoms or a positive COVID-19 test. (9)

Radiographic Considerations and Findings
Chest radiographs of patients with severe COVID-19 may demonstrate bilateral air-space consolidation. (23) Chest computed tomography (CT) images from patients with COVID-19 may demonstrate bilateral, peripheral ground glass opacities and consolidation. (24,25) Less common CT findings can include intra- or interlobular septal thickening with ground glass opacities (hazy opacity) or focal and rounded areas of ground glass opacity surrounded by a ring or arc of denser consolidation (reverse halo sign). (24)
Multiple studies suggest that abnormalities on CT or chest radiograph may be present in people who are asymptomatic, pre-symptomatic, or before RT-PCR detection of SARS-CoV-2 RNA in nasopharyngeal specimens. (25)
Common COVID-19 symptoms
Fever, cough, shortness of breath, fatigue, headache, and myalgia are among the most commonly reported symptoms in people with COVID-19. (5) Some people with COVID-19 have gastrointestinal symptoms such as nausea, vomiting, or diarrhea, sometimes prior to having fever or lower respiratory tract signs and symptoms. (10) Loss of smell and taste can occur, although these symptoms are reported to be less common since Omicron began circulating, as compared to earlier during the COVID-19 pandemic. (11,19-21) People can experience SARS-CoV-2 infection (asymptomatic or symptomatic), even if they are up to date with their COVID-19 vaccines or were previously infected. (8)
Several studies have reported ocular symptoms associated with SARS-CoV-2 infection, including redness, tearing, dry eye or foreign body sensation, discharge or increased secretions, and eye itching or pain. (13)
A wide range of dermatologic manifestations have been associated with COVID-19; timing of skin manifestations in relation to other COVID-19 symptoms and signs is variable. (14) Some skin manifestations may be associated with increased disease severity. (15) Images of cutaneous findings in COVID-19 are available from the American Academy of Dermatology .
Uncommon COVID-19 symptoms
Less common presentations of COVID-19 can occur. Older adults may present with different symptoms than children and younger adults. Some older adults can experience SARS-CoV-2 infection accompanied by delirium, falls, reduced mobility or generalized weakness, and glycemic changes. ( 12)
Transmission
People infected with SARS-CoV-2 can transmit the virus even if they are asymptomatic or presymptomatic. ( 16) Peak transmissibility appears to occur early during the infectious period (prior to symptom onset until a few days after), but infected persons can shed infectious virus up to 10 days following infection. (22 ) Both vaccinated and unvaccinated people can transmit SARS-CoV-2. ( 17,18) Clinicians should consider encouraging all people to take the following prevention actions to limit SARS-CoV-2 transmission:
- stay up to date with COVID-19 vaccines,
- test for COVID-19 when symptomatic or exposed to someone with COVID-19, as recommended by CDC,
- wear a high-quality mask when recommended,
- avoiding contact with individuals who have suspected or confirmed COVID-19,
- improving ventilation when possible,
- and follow basic health and hand hygiene guidance .
Clinicians should also recommend that people who are infected with SARS-CoV-2, follow CDC guidelines for isolation.
Table of Contents
- › Clinical Presentation
- Clinical Progression, Management, and Treatment
- Special Clinical Considerations
- Bhaskaran K, Bacon S, Evans SJ, et al. Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg Health Eur. Jul 2021;6:100109. doi:10.1016/j.lanepe.2021.100109
- Kim L, Garg S, O'Halloran A, et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality among Hospitalized Adults Identified through the U.S. Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin Infect Dis. Jul 16 2020;doi:10.1093/cid/ciaa1012
- Kompaniyets L, Pennington AF, Goodman AB, et al. Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020-March 2021. Preventing chronic disease. Jul 1 2021;18:E66. doi:10.5888/pcd18.210123
- Ko JY, Danielson ML, Town M, et al. Risk Factors for COVID-19-associated hospitalization: COVID-19-Associated Hospitalization Surveillance Network and Behavioral Risk Factor Surveillance System. Clin Infect Dis. Sep 18 2020;doi:10.1093/cid/ciaa1419
- Wortham JM, Lee JT, Althomsons S, et al. Characteristics of Persons Who Died with COVID-19 - United States, February 12-May 18, 2020. MMWR Morb Mortal Wkly Rep. Jul 17 2020;69(28):923-929. doi:10.15585/mmwr.mm6928e1
- Yang X, Zhang J, Chen S, et al. Demographic Disparities in Clinical Outcomes of COVID-19: Data From a Statewide Cohort in South Carolina. Open Forum Infect Dis. Sep 2021;8(9):ofab428. doi:10.1093/ofid/ofab428
- Rader B.; Gertz AL, D.; Gilmer, M.; Wronski, L.; Astley, C.; Sewalk, K.; Varrelman, T.; Cohen, J.; Parikh, R.; Reese, H.; Reed, C.; Brownstein J. Use of At-Home COVID-19 Tests — United States, August 23, 2021–March 12, 2022. MMWR Morb Mortal Wkly Rep. April 1, 2022;71(13):489–494. doi:http://dx.doi.org/10.15585/mmwr.mm7113e1
- Pingali C, Meghani M, Razzaghi H, et al. COVID-19 Vaccination Coverage Among Insured Persons Aged >/=16 Years, by Race/Ethnicity and Other Selected Characteristics - Eight Integrated Health Care Organizations, United States, December 14, 2020-May 15, 2021. MMWR Morb Mortal Wkly Rep. Jul 16 2021;70(28):985-990. doi:10.15585/mmwr.mm7028a1
- Wiltz JL, Feehan AK, Molinari NM, et al. Racial and Ethnic Disparities in Receipt of Medications for Treatment of COVID-19 - United States, March 2020-August 2021. MMWR Morb Mortal Wkly Rep. Jan 21 2022;71(3):96-102. doi:10.15585/mmwr.mm7103e1
- Murthy NC, Zell E, Fast HE, et al. Disparities in First Dose COVID-19 Vaccination Coverage among Children 5-11 Years of Age, United States. Emerg Infect Dis. May 2022;28(5):986-989. doi:10.3201/eid2805.220166
- Saelee R, Zell E, Murthy BP, et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties - United States, December 14, 2020-January 31, 2022. MMWR Morb Mortal Wkly Rep. Mar 4 2022;71(9):335-340. doi:10.15585/mmwr.mm7109a2
- Burki TK. The role of antiviral treatment in the COVID-19 pandemic. Lancet Respir Med. Feb 2022;10(2):e18. doi:10.1016/S2213-2600(22)00011-X
- Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients. N Engl J Med. Feb 10 2022;386(6):509-520. doi:10.1056/NEJMoa2116044
- Sjoding MW, Dickson RP, Iwashyna TJ, Gay SE, Valley TS. Racial Bias in Pulse Oximetry Measurement. N Engl J Med. Dec 17 2020;383(25):2477-2478. doi:10.1056/NEJMc2029240
- Jordan TB, Meyers CL, Schrading WA, Donnelly JP. The utility of iPhone oximetry apps: A comparison with standard pulse oximetry measurement in the emergency department. Am J Emerg Med. May 2020;38(5):925-928. doi:10.1016/j.ajem.2019.07.020
- Iuliano AD, Brunkard JM, Boehmer TK, et al. Trends in Disease Severity and Health Care Utilization During the Early Omicron Variant Period Compared with Previous SARS-CoV-2 High Transmission Periods - United States, December 2020-January 2022. MMWR Morb Mortal Wkly Rep. Jan 28 2022;71(4):146-152. doi:10.15585/mmwr.mm7104e4
- Taylor CA, Whitaker M, Anglin O, et al. COVID-19-Associated Hospitalizations Among Adults During SARS-CoV-2 Delta and Omicron Variant Predominance, by Race/Ethnicity and Vaccination Status - COVID-NET, 14 States, July 2021-January 2022. MMWR Morb Mortal Wkly Rep. Mar 25 2022;71(12):466-473. doi:10.15585/mmwr.mm7112e2
- Johnson AG, Amin AB, Ali AR, et al. COVID-19 Incidence and Death Rates Among Unvaccinated and Fully Vaccinated Adults with and Without Booster Doses During Periods of Delta and Omicron Variant Emergence - 25 U.S. Jurisdictions, April 4-December 25, 2021. MMWR Morb Mortal Wkly Rep. Jan 28 2022;71(4):132-138. doi:10.15585/mmwr.mm7104e2
- Danza P, Koo TH, Haddix M, et al. SARS-CoV-2 Infection and Hospitalization Among Adults Aged >/=18 Years, by Vaccination Status, Before and During SARS-CoV-2 B.1.1.529 (Omicron) Variant Predominance - Los Angeles County, California, November 7, 2021-January 8, 2022. MMWR Morb Mortal Wkly Rep. Feb 4 2022;71(5):177-181. doi:10.15585/mmwr.mm7105e1
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
The Clinical Presentation of CLL
- First Online: 25 April 2019
Cite this chapter
- Daniel Catovsky 5 ,
- Monica Else 5 &
- David Oscier 6
Part of the book series: Hematologic Malignancies ((HEMATOLOGIC))
1045 Accesses
2 Citations
This chapter deals with the basic demographics and the presenting features of CLL and how to assess patients once a diagnosis has been made. CLL is predominantly a disease of the elderly with a preponderance of male patients. New evidence suggests that there are variations in gender incidence according to the clinical status of patients, with a higher male:female ratio in the groups with worse prognosis.
Full blood counts and a physical examination are the basis of the existing staging systems of Rai and Binet. Establishing the patient’s clinical stage sets the scene for the frequency of follow-up, the possible need for therapy and the need for cytogenetic and molecular investigations. Examination of blood films is still important, to identify the presence of prolymphocytes and to consider alternative diagnostic possibilities. In addition, biochemical tests such as beta-2 microglobulin and lactate dehydrogenase are a valuable part of the prognostic evaluation.
Patients may need support to deal with the psychological and quality of life issues arising from their disease.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, et al., editors. SEER cancer statistics review, 1975–2013. Bethesda: National Cancer Institute; 2016. https://seer.cancer.gov/statfacts/html/clyl.html .
Lifetime risk estimates calculated by the Statistical Information Team at Cancer Research UK. Based on data provided by the Office of National Statistics, ISD Scotland, the Welsh Cancer Intelligence and Surveillance Unit and the Northern Ireland Cancer Registry, on request. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/leukaemia-cll/incidence .
Yang SM, Li JY, Gale RP, Huang XJ. The mystery of chronic lymphocytic leukemia (CLL): why is it absent in Asians and what does this tell us about etiology, pathogenesis and biology? Blood Rev. 2015;29:205–13.
Article PubMed Google Scholar
Liang XS, Caporaso N, McMaster ML, Ng D, Landgren O, Yeager M, et al. Common genetic variants in candidate genes and risk of familial lymphoid malignancies. Br J Haematol. 2009;146:418–23.
Article CAS PubMed Google Scholar
Cerhan JR, Slager SL. Familial predisposition and genetic risk factors for lymphoma. Blood. 2015;126:2265–73.
CAS PubMed PubMed Central Google Scholar
Law PJ, Berndt SI, Speedy HE, Camp NJ, Sava GP, Skibola CF, et al. Genome-wide association analysis implicates dysregulation of immunity genes in chronic lymphocytic leukaemia. Nat Commun. 2017;8:14175.
Article CAS PubMed PubMed Central Google Scholar
International CLL-IPI working group. An international prognostic index for patients with chronic lymphocytic leukaemia (CLL-IPI): a meta-analysis of individual patient data. Lancet Oncol. 2016;17:779–90.
Article Google Scholar
Da Cunha-Bang C, Christiansen I, Niemann CU. The CLL-IPI applied in a population-based cohort. Blood. 2016;128:2181–3.
Catovsky D, Wade R, Else M. The clinical significance of patients’ sex in chronic lymphocytic leukemia. Haematologica. 2014;99:1088–94.
Article PubMed PubMed Central Google Scholar
Al-Sawaf O, Robrecht S, Bahlo J, Fink AM, Cramer P, von Tresckow J, et al. Impact of gender on outcome after chemoimmunotherapy in patients with chronic lymphocytic leukemia: a meta-analysis by the German CLL study group. Leukemia. 2017;31(10):2251–3. https://doi.org/10.1038/leu.2017.221 .
Abrisqueta P, Pereira A, Rozman C, Aymerich M, Giné E, Moreno C, et al. Improving survival in patients with chronic lymphocytic leukemia (1980-2008): the Hospital Clinic of Barcelona experience. Blood. 2009;114:2044–50.
Stauder R, Eichhorst B, Hamaker ME, Kaplanov K, Morrison VA, Österborg A, et al. Management of chronic lymphocytic leukemia (CLL) in the elderly: a position paper from an international Society of Geriatric Oncology (SIOG) Task Force. Ann Oncol. 2017;28(2):218–27. https://doi.org/10.1093/annonc/mdw547 .
Rai KR, Sawitsky A, Cronkite EP, Chanana AD, Levy RN, Pasternack BS. Clinical staging of chronic lymphocytic leukemia. Blood. 1975;46:219–34.
CAS PubMed Google Scholar
Binet JL, Auquier A, Dighiero G, Chastang C, Piguet H, Goasguen J, et al. A new prognostic classification of chronic lymphocytic leukemia derived from a multivariate survival analysis. Cancer. 1981;48:198–206.
Ratterman M, Kruczek K, Sulo S, Shanafelt TD, Kay NE, Nabhan C. Extramedullary chronic lymphocytic leukemia: systematic analysis of cases reported between 1975 and 2012. Leuk Res. 2014;38:299–303.
Strati P, Uhm JH, Kaufmann TJ, Nabhan C, Parikh SA, Hanson CA, et al. Prevalence and characteristics of central nervous system involvement by chronic lymphocytic leukemia. Haematologica. 2016;101:458–65.
Cramer P, Bahlo J, Eichhorst B, Fischer K, Hallek M. Extramedullary manifestations of chronic lymphocytic leukaemia are not unusual. Leuk Res. 2014;38:284–5.
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, et al. International Workshop on Chronic Lymphocytic Leukemia. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111:5446–56.
Jain P, Keating M, Renner S, Cleeland C, Xuelin H, Gonzalez GN, et al. Ruxolitinib for symptom control in patients with chronic lymphocytic leukaemia: a single-group, phase 2 trial. Lancet Haematol. 2017;4:e67–74.
Hisada M, Biggar RJ, Greene MH, Fraumeni JF Jr, Travis LB. Solid tumors after chronic lymphocytic leukemia. Blood. 2001;98:1979–81.
Tsimberidou AM, Wen S, McLaughlin P, O’Brien S, Wierda WG, Lerner S, et al. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. J Clin Oncol. 2009;27:904–10.
Maurer C, Langerbeins P, Bahlo J, Cramer P, Fink AM, Pflug N, et al. Effect of first-line treatment on second primary malignancies and Richter’s transformation in patients with CLL. Leukemia. 2016;30:2019–25.
Solomon BM, Rabe KG, Slager SL, Brewer JD, Cerhan JR, Shanafelt TD. Overall and cancer-specific survival of patients with breast, colon, kidney, and lung cancers with and without chronic lymphocytic leukemia: a SEER population-based study. J Clin Oncol. 2013;31:930–7.
Kleinstern G, Rishi A, Achenbach SJ, Chaffee KR, Kay NE, Shanafelt TD, et al. Skin cancers among chronic lymphocytic leukemia (CLL) patients - the effect of UV radiation and CLL clinical characteristics. Blood. 2016;128:4772.
Google Scholar
Oscier D, Else M, Matutes E, Morilla R, Strefford JC, Catovsky D. The morphology of CLL revisited: the clinical significance of prolymphocytes and correlations with prognostic/molecular markers in the LRF CLL4 trial. Br J Haematol. 2016;174:767–75.
Autore F, Strati P, Innocenti I, Corrente F, Trentin L, Cortelezzi A, et al. LDH levels predict progression-free survival in treatment-NaÏVe patients with trisomy 12 chronic lymphocytic leukemia. Blood. 2016;128:3211. Abstract.
Giné E, Martinez A, Villamor N, López-Guillermo A, Camos M, Martinez D, et al. Expanded and highly active proliferation centers identify a histological subtype of chronic lymphocytic leukemia (“accelerated” chronic lymphocytic leukemia) with aggressive clinical behavior. Haematologica. 2010;95:1526–33.
Dearden C, Wade R, Else M, Richards S, Milligan D, Hamblin T, et al. The prognostic significance of a positive direct antiglobulin test in chronic lymphocytic leukemia: a beneficial effect of the combination of fludarabine and cyclophosphamide on the incidence of hemolytic anemia. Blood. 2008;111:1820–6.
Rogers KA, Ruppert AS, Bingman A, Andritsos LA, Awan FT, Blum KA, et al. Incidence and description of autoimmune cytopenias during treatment with ibrutinib for chronic lymphocytic leukemia. Leukemia. 2016;30:346–50.
Muntañola A, Bosch F, Arguis P, Arellano-Rodrigo E, Ayuso C, Giné E, et al. Abdominal computed tomography predicts progression in patients with Rai stage 0 chronic lymphocytic leukemia. J Clin Oncol. 2007;25:1576–80.
Rai KR. A critical analysis of staging in CLL. In: Gale RP, Rai KR, editors. Chronic lymphocytic leukemia: recent progress and future directions. New York: Alan R. Liss; 1987. p. 253–64.
Binet J-L, Catovsky D, Chandra P, Dighiero G, Montserrat E, Rai KR, et al. Chronic lymphocytic leukaemia: proposals for a revised prognostic staging system. Br J Haematol. 1981;48:365–7.
International Workshop on Chronic Lymphocytic Leukemia. Chronic lymphocytic leukemia: recommendations for diagnosis, staging, and response criteria. Ann Intern Med. 1989;110:236–8.
French Cooperative Group on Chronic Lymphocytic Leukaemia. Natural history of stage A chronic lymphocytic leukaemia untreated patients. Br J Haematol. 1990;76:45–57.
Binet J-L, Catovsky D, Chastang C, Dighiero G, Fooks J, Galton DAG, et al. Workshop: prognostic features of early CLL. Lancet. 1989;334:968–9.
Catovsky D, Richards S, Matutes E, Oscier D, Dyer MJ, Bezares RF, et al. Assessment of fludarabine plus cyclophosphamide for patients with chronic lymphocytic leukaemia (the LRF CLL4 Trial): a randomised controlled trial. Lancet. 2007;370:230–9.
Zent CS, Ding W, Schwager SM, Reinalda MS, Hoyer JD, Jelinek DF, et al. The prognostic significance of cytopenia in chronic lymphocytic leukaemia/small lymphocytic lymphoma. Br J Haematol. 2008;141:615–21.
Else M, Cocks K, Crofts S, Wade R, Richards SM, Catovsky D, et al. Quality of life in chronic lymphocytic leukemia: 5-year results from the multicenter randomized LRF CLL4 trial. Leuk Lymphoma. 2012;53:1289–98.
Shanafelt TD, Bowen D, Venkat C, Slager SL, Zent CS, Kay NE, et al. Quality of life in chronic lymphocytic leukemia: an international survey of 1482 patients. Br J Haematol. 2007;139:255–64.
Download references
Author information
Authors and affiliations.
Division of Molecular Pathology, The Institute of Cancer Research, London, UK
Daniel Catovsky & Monica Else
Department of Molecular Pathology, Royal Bournemouth Hospital, Bournemouth, UK
David Oscier
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Daniel Catovsky .
Editor information
Editors and affiliations.
Department I of Internal Medicine, University of Cologne, Cologne, Nordrhein-Westfalen, Germany
Michael Hallek
Barbara Eichhorst
Daniel Catovsky
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Catovsky, D., Else, M., Oscier, D. (2019). The Clinical Presentation of CLL. In: Hallek, M., Eichhorst, B., Catovsky, D. (eds) Chronic Lymphocytic Leukemia. Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-11392-6_3
Download citation
DOI : https://doi.org/10.1007/978-3-030-11392-6_3
Published : 25 April 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-11391-9
Online ISBN : 978-3-030-11392-6
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

HelpLine : 1-866-507-7222 or [email protected]
Behavioral Variant FTD
- Primary Progressive Aphasia (PPA)
- ALS and Frontotemporal Degeneration
- Progressive Supranuclear Palsy
- Corticobasal Syndrome
- FTD & Genetics
- Find a Medical Center
- Glossary of FTD Terms
- AFTD HelpLine
- Find Support Near You
- Newly Diagnosed
- Coordinating Care
- Support for People with FTD
- Support for Kids and Teens
- Legal and Financial Planning
- Ways to Participate
- Studies Seeking Participants
- FTD Disorders Registry
- For Researchers
- Ways to Give
- Host an Event
- Volunteer With Us
- Advocacy Action Center
- Calendar of Events
- Diagnosing FTD
- Treating FTD
- Partners in FTD Care
- Healthcare Webinars
- Mission, Vision & Values
- AFTD is Hiring
- Our History
- Board of Directors
- Medical Advisory Council
- Persons With FTD Advisory Council
- AFTD Ambassadors
- Strategic Plan
- Impact Reports
- FTD in the News
- Press Releases
- AFTD Insights
- Help & Hope
- Contact our Newsroom
For Health Professionals
Ftd is frequently misdiagnosed as alzheimer’s, depression, parkinson’s disease, or a psychiatric condition. on average, it currently takes 3.6 years to get an accurate diagnosis., clinical presentations.
Frontotemporal degeneration (FTD) is a spectrum of neurodegenerative conditions that often occur in individuals younger than 65 years of age. ( Knopman and Roberts, 2011 ). Many cases are familial, but sporadic cases suggest that environmental triggers also exist. Several genetic etiologies are known, but environmental triggers remain largely undefined.
FTD disorders are identified by their clinical symptoms which present as behavioral/cognitive changes, or language deficits, or decline in motor function. The underlying biology of these clinical diagnoses are diverse. Many affected individuals have overlapping symptoms, particularly as the disease progresses.
Two proteins most commonly aggregate in nerve cells in FTD disorders— tau protein or TDP-43 protein. These are the defining pathological hallmark of FTD.
The most common FTD subtype is behavioral variant FTD (bvFTD), characterized by changes in affect (emotional presentation of the individual), personality and social comportment. People with bvFTD typically have little insight into this change, though it is obvious to those around them. The key is that their behavior is clearly different from their prior functioning and inappropriate based on social norms. They are often disinhibited and impulsive, saying things and acting in ways that are incongruous with the situation. Childishness, lack of empathy, and an insensitive, self-centered demeanor are common features of the behavioral variant. Patients are sometimes apathetic. Obsessive-compulsive behaviors, changes in sexual drive, food cravings (especially carbohydrates, sweets or a specific food), and criminal or violent behavior can also occur.
In 2011, a multidisciplinary group expanded the specific clinical criteria for the diagnosis of bvFTD which both improved diagnostic accuracy and now allows for earlier diagnosis of “possible” as opposed to “probable” bvFTD ( Rascovsky et al.,2011 ).
Primary Progressive Aphasia
Primary progressive aphasia (PPA) is the FTD subtype characterized by progressive loss of oral and written language skills. Comprehension and language expression may be involved. Consensus criteria for diagnosing the PPA variants was published in 2011 (Gorno-Tempini et al, 2011). When the problem is primarily with anomia and loss of word meaning, it is referred to as the semantic variant of PPA . Here, the meaning of specific words is lost, and both comprehension of the word and the ability to retrieve the name of an object may be lost. The patient retains fluent speech and proper grammar; however, paraphasias (word substitution errors) are common. This subtype of PPA is usually associated with TDP-43 pathology.
On the other end of the spectrum, the nonfluent/agrammatic variant of PPA primarily affects speech production. In this case, individuals lose proper grammar (especially their ability to use small connecting words) but have preserved language comprehension for specific items/objects. This causes speech to become effortful and hesitant; sentence length becomes progressively truncated. Writing and language comprehension may be affected in the same manner. This subtype of PPA is usually associated with tau pathology.
Logopenic PPA is the third major PPA variant. In this variant, speech is slow, but grammar and comprehension are less affected. Impairment in the repetition of multisyllabic words and particularly phrases is a key feature. Sound substitution (phonemic) paraphasias are also seen in this group, as in a false word that rhymes with the intended word. Logopenic aphasia is usually associated with an underlying Alzheimer’s pathology.
As many as 20% of FTD patients develop signs of motor neuron disease (MND), often called ALS in North America for Lou Gehrig’s disease. Likewise, approximately half of individuals diagnosed with the most common form of MND, amyotrophic lateral sclerosis (ALS) exhibit neuropsychological symptoms or cognitive decline ( Strong, et al 2016, Elahi & Miller, 2017 ). A growing number of experts believe that ALS and FTD fall on a clinical continuum ( Strong, et al, 2016 ). A smaller number of these patients develop full-blown FTD withALS. The most common genetic cause of familial FTD-ALS results from a mutation resulting in expanded repeats the C9orf72 gene.
With or without the C9 gene expansion, the addition of motor neuron disease to FTD is a compromising factor that greatly reduces median survival to less than three years ( Olney, et. al 2005 ). Behavioral symptoms complicate the management of dysphagia (difficulty swallowing) as well as respiratory dysfunction as respiration therapy and percutaneous endoscopic gastrostomy (PEG) feeding tubes are not well tolerated by the patient. ( Alagiakrishnan et al. 2013 ).
Although significant phenotypic heterogeneity exists among C9orf72 carriers, the majority present with either bvFTD or FTD-ALS. PPA variants, including nonfluent/agrammatic and semantic, are rare. Prominent psychosis with delusions and hallucinations are relatively common (Boeve et al. 2012). Research into the clinical features associated with the C9orf72 mutation is active and ongoing.
For more information on FTD and MND, consider this resource for general practitioners , offered by the UK-based MNDA.
Parkinsonian-like FTD Syndromes
FTD subtypes may also be associated with the Parkinson’s-plus syndromes of progressive supranuclear palsy (PSP) or corticobasal syndrome (CBS). Frontal lobe degeneration and the presence of Tau protein aggregates in the brain have classified these as FTD disorders. PSP and CBS both demonstrate motor deficits as the dominant clinical symptom at diagnosis. PSP patients show early signs of postural instability and vertical gaze impairments. Some PSP patients can show clinical signs of bvFTD prior to the motor deficits. CBS-like symptoms of asymmetrical movement problems, abnormal muscle tone, complex tremors, myoclonus and limb apraxia form the core CBS phenotype. Like PSP, some CBS patients may present with bvFTD symptoms first. Five phenotypic presentations of CBS have recently been defined to support more accurate diagnosis ( Armstrong et al., 2013 ).
Key References
- Clinical Criteria of Behavioral Variant FTD – In 2011, an international consortium developed and published revised guidelines for the diagnosis of behavioral variant frontotemporal dementia.
- Rascovsky K et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia . Brain . 2011 Sep, 134(pt9): 2456-77. Epub 2011 Aug 2.
- Gorno-Tempini, ML, Hillis, AE, Weintraub, S, et al. Classification of primary progressive aphasia and its variants . Neurology . 2011 Mar 15;76(11):1006-14. Epub 2011 Feb 16.
- Boeve BF, Boylan KB, Graff-Radford NR, DeJesus-Hernandez M, Knopman DS, Pedraza O, Vemuri P, Jones D, Lowe V, Murray ME, Dickson DW, Josephs KA, Rush BK, Machulda MM, Fields JA, Ferman TJ, Baker M, Rutherford NJ, Adamson J, Wszolek ZK, Adeli A, Savica R, Boot B, Kuntz KM, Gavrilova R, Reeves A, Whitwell J, Kantarci K, Jack CR Jr, Parisi JE, Lucas JA, Petersen RC. Rademakers R. Characterization of frontotemporal dementia and/or amyotrophic lateral sclerosis associated with the GGGGCC repeat expansion in C9ORF72 . Brain . 2012 Mar;135 (Pt 3):765-83.)
- Frontotemporal dementia: diagnosis, deficits and management Nicholas T Bott*,1, Anneliese Radke1, Melanie L Stephens1, and Joel H Kramer1
- Neurodegener Dis Manag. 2014 ; 4(6): 439–454. doi:10.2217/nmt.14.34.
- Diagnostic Accuracy of the Frontotemporal Dementia Consensus Criteria in the Late-Onset Frontal Lobe Syndrome. Vijverberg EG 1 , Dols A , Krudop WA , Peters A , Kerssens CJ , van Berckel BN , Wattjes MP , Barkhof F , Gossink F , Prins ND , Stek ML , Scheltens P , Pijnenburg YA . Dement Geriatr Cogn Disord. 2016;41(3-4):210-9. doi: 10.1159/000444849. Epub 2016 May 5.
- Elahi, FM and Miller, BL. A clinicopathological approach to the diagnosis of dementia. Nature Reviews Neurology 2017 Aug; 13: 457 – 476.
- Strong, MJ, Abrahams, S, Goldstein, LH, et al. Amyotrophic lateral sclerosis – frontotemporal spectrum disorder (ALS-FTSD): Revised diagnostic criteria. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. 2016 Nov 18; 18: 153-174.
- Finger, EC. Frontotemporal dementias. Continuum, 2016; 22 (2): 464-489.
- Wollacott, IOC and Rohrer, JD. The clinical spectrum of sporadic and familial forms of frontotemporal dementia. Journal of Neurochemistry, 2016. 10.1111/jnc.13654.
Privacy Overview
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My Portfolio
- Stock Market
- Biden Economy
- Stocks: Most Actives
- Stocks: Gainers
- Stocks: Losers
- Trending Tickers
- World Indices
- US Treasury Bonds
- Top Mutual Funds
- Highest Open Interest
- Highest Implied Volatility
- Stock Comparison
- Advanced Charts
- Currency Converter
- Investment Ideas
- Research Reports
- Basic Materials
- Communication Services
- Consumer Cyclical
- Consumer Defensive
- Financial Services
- Industrials
- Real Estate
- Mutual Funds
- Credit Cards
- Balance transfer cards
- Cash-back cards
- Rewards cards
- Travel cards
- Personal Loans
- Student Loans
- Car Insurance
- Options 101
- Good Buy or Goodbye
- Options Pit
- Yahoo Finance Invest
- EV Deep Dive
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Yahoo Finance
Coherus announces presentation at the 2024 american society of clinical oncology (asco) annual meeting.
REDWOOD CITY, Calif., April 24, 2024 (GLOBE NEWSWIRE) -- Coherus BioSciences, Inc. (Coherus, Nasdaq: CHRS) today announced the first presentation of clinical data for CHS-114, a highly selective cytolytic anti-CCR8 antibody, at the upcoming ASCO Annual Meeting, which will be held from May 31 to June 4, 2024, at McCormick Place in Chicago.
Presentation Details
Abstract: 2664 Title: Preliminary Results of a Phase 1, First-in-human, Dose Escalation Study of the Anti-CCR8 Cytolytic Antibody, CHS-114 (formerly SRF114) in Patients with Advanced Solid Tumors. Poster Session– Developmental Therapeutics - Immunotherapy Date and Time: Saturday, June 1, 2024, 9:00 a.m. – 12:00 p.m. Central Daylight Time
About CHS-114
CHS-114, a human, afucosylated anti-CCR8 monoclonal antibody, is designed to selectively target human CCR8 and preferentially deplete CCR8+ regulatory T cells (Tregs) within the tumor microenvironment, not effector T (Teff) cells in tumors or Tregs in normal tissue. In preclinical studies, CHS-114 induced antibody-dependent cellular cytotoxicity (ADCC) and/or antibody-dependent cellular phagocytosis (ADCP) to deplete tumoral CCR8+ Tregs. In addition, treatment with CHS-114 alone reduced tumor growth in murine models, and enhanced antitumor activity was observed in combination with anti-PD-1 treatment.
CHS-114 is currently being evaluated in a Phase 1 clinical trial ( NCT05635643 ) as a monotherapy and in combination with toripalimab in advanced solid tumors, including head and neck cancer. As reported in June 2023, early evidence of biological effect has been seen with CCR8+ Tregs depletion in blood following treatment with CHS-114, with no effect observed on non-CCR8+ Tregs. Clinical data from the CHS-114 single agent dose escalation stage of the Phase 1 study will be presented at the 2024 ASCO Annual Meeting.
About Coherus BioSciences
Coherus is a commercial-stage biopharmaceutical company focused on researching, developing, and commercializing innovative therapies to treat cancer. Coherus is developing an innovative immuno-oncology pipeline expected to synergize with its proven commercial capabilities in oncology.
Coherus’ immuno-oncology pipeline includes multiple antibody immunotherapy candidates focused on enhancing the innate and adaptive immune responses to enable a robust antitumor immunologic response and enhance outcomes for patients with cancer. Casdozokitug is a novel IL-27 antagonistic antibody currently being evaluated in two ongoing clinical studies: a Phase 1/2 study in advanced solid tumors and a Phase 2 study in hepatocellular carcinoma. CHS-114 is a highly selective, competitively positioned, cytolytic anti-CCR8 antibody currently in a Phase 1 study in patients with advanced solid tumors. CHS-1000 is a preclinical candidate targeting immune-suppressive mechanisms via the pathway ILT4, with an IND filing planned in Q2 2024.
Coherus markets LOQTORZI ® (toripalimab-tpzi), a novel next-generation PD-1 inhibitor, UDENYCA ® (pegfilgrastim-cbqv), a biosimilar of Neulasta ® , and YUSIMRY ® (adalimumab-aqvh), a biosimilar of Humira ® .
Neulasta ® is a registered trademark of Amgen, Inc. Humira ® is a registered trademark of AbbVie Inc.
Forward-Looking Statements
Except for the historical information contained herein, the matters set forth in this press release are forward-looking statements within the meaning of the "safe harbor" provisions of the Private Securities Litigation Reform Act of 1995, including, but not limited to, statements regarding Coherus’ ability to identify synergies between its I-O pipeline and its commercial capabilities; Coherus’ expected timing for filing an IND for CHS-1000; Coherus’ expectations to be able to advance its candidates through clinical trials; and Coherus’ expectations that its immunotherapy candidates will enhance outcomes for patients with cancer.
Such forward-looking statements involve substantial risks and uncertainties that could cause Coherus’ actual results, performance, or achievements to differ significantly from any future results, performance, or achievements expressed or implied by the forward-looking statements. Such risks and uncertainties include, among others, the risks and uncertainties inherent in the preclinical and clinical drug development process; risks related to Coherus’ existing and potential collaboration partners; risks of Coherus’ competitive position; the risks and uncertainties of the regulatory approval process, including the speed of regulatory review and the timing of Coherus’ regulatory filings; the risks of competition; the risk that Coherus is unable to complete commercial transactions; and the risks and uncertainties of possible litigation. All forward-looking statements contained in this press release speak only as of the date of this press release. Coherus undertakes no obligation to update or revise any forward-looking statements. For a further description of the significant risks and uncertainties that could cause actual results to differ from those expressed in these forward-looking statements, as well as risks relating to Coherus’ business in general, see Coherus’ Annual Report on Form 10-K for the fiscal year ended December 31, 2023 filed with the Securities and Exchange Commission on March 15, 2024, including the section therein captioned “Risk Factors” and in other documents Coherus files with the Securities and Exchange Commission.
UDENYCA ® , YUSIMRY ® , and LOQTORZI ® , whether or not appearing in large print or with the trademark symbol, are trademarks of Coherus, its affiliates, related companies or its licensors or joint venture partners unless otherwise noted. Trademarks and trade names of other companies appearing in this press release are, to the knowledge of Coherus, the property of their respective owners.
Coherus Contact Information: For Investors: Jami Taylor Head of Investor Relations [email protected]
For Media: Jodi Sievers VP, Corporate Communications [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.183(18); 2011 Dec 13

The art of presenting
The oral case presentation is a time-honoured tradition whereby a trainee presents a new admission to the attending physician. We describe the presentation styles of students, residents and staff physicians and offer pointers on how to present like stereotypical members of each group.
Although the case presentation occurs in nearly all disciplines, internal medicine (especially “team medicine” or Clinical Teaching Units) has a long-standing love–hate relationship with the case presentation and thus will be used throughout the paper to illustrate the ups and downs (mostly downs) of presenting.
Presentation styles
The clinical clerk.
The case presentation can be the most exciting part of the day for the clinical clerk and the most dreaded for the attending physician, or vice-versa. The key feature of a clerk’s presentation is his or her lack of confidence. Overinclusive and unconvincing, the presentation often showcases verbal diarrhea at its finest. The following pointers highlight the techniques best used by clinical clerks.
- Hedge your bets when reporting the physical exam (e.g., “I think I heard a murmur, or it could have been my stethoscope rubbing against his chest hair”).
- Present impossible findings (e.g., “The spleen was almost palpable”).
- Offer creative euphemisms for “I didn’t do that” when asked for physical findings that were not obtained (e.g., “My physical exam did not alter the prior probability of a knee effusion”).
The elective clinical clerk
The elective clinical clerk, unlike other clerks, has declared an interest in pursuing a career in internal medicine. Thus, the case presentation is definitely the most exciting part of his or her day, because it guarantees face time with the staff.
Elective clinical clerks tailor their presentations heavily to impress specific staff physicians in the hope of receiving a positive reference letter. For example, they will list all of the negative findings, not just the pertinent ones, to show that they have left no stone unturned or detail overlooked. Elective clerks are also often hyperaware of their attending’s preferred presentation format and will overindulge in this style. If a staff physician likes a narrative format, the clerk will record the interview to present the case in the patient’s “own words.” Finally, elective clerks who come from other institutions often take the opportunity to promote their own institution in their presentations, usually in backhanded ways.

The following pointers will help elective clerks hone their presentation skills:
- Present a ludicrous number of “pertinent” negatives (e.g., “The patient did not have any neurological symptoms. He denied headache, visual changes, weakness, paresthesias, vertigo, seizure activity, dysarthria, aphasia, alexia, agraphia, ataxia, abulia, akathisia, ageusia, allodynia, anosmia, apraxia, athetosis, astasia and astasia–abasia. Dangit, I forgot to ask about anosognosia”).
- Show knowledge by posing questions you obviously do not need to ask (e.g., “Regarding the woman with recurrent urinary tract infections, would there be any problem with prescribing prophylactic nitrofurantoin … apart from the risk of pulmonary toxicity?”).
- Promote your own institution, preferably in a backhanded way (e.g., “I guess this isn’t the case in Toronto, but here at McMaster we learn to do only physical exam manoeuvres that have been validated in randomized controlled trials”).
The off-service PGY-1 resident
The off-service junior resident on a medicine rotation is the ultimate “fish out of water.” Having begun to develop skills in their specialty of choice, off-service PGY-1 residents leave their comfort zone for cringe-inducing discussions of hyponatremia and eosinophilia. They go to great lengths to avoid the dissertations on diagnosis and management that internists love (e.g., by presenting the case of a patient who has rapid atrial fibrillation with a ventricular rate of 150 beats per minute by speaking at a rate of 150 words per second). Failing that, they seek solace by referencing their own specialty (and not so subtly suggesting its superiority). The following pointers highlight the presentation techniques of off-service residents:
- Avoid discussing “medical issues” by focusing on your own specialty (e.g., “This is an 85-year-old man presenting with shortness of breath. He also has been followed by urology for a remote history of prostate cancer. The cancer was discovered in 1990 and has been inactive since treatment in 1992. It was originally diagnosed by Dr. Thompson, a personal mentor, via transrectal biopsy, and pathology revealed a Gleason score of 5. The biopsy was then stained with [made-up-dye] #2 to determine its malignant potential, although that stain is no longer in use …”).
- Use verbal and nonverbal cues to express the superiority of your own specialty (e.g., “Do you know what type of incision the general surgeon will use to repair the bowel we perforated during the paracentesis?”).
The internal medicine PGY-1 resident
With a background in internal medicine, this first-year resident generally has more medical knowledge and practical knowhow than the other junior residents. The internal medicine trainee will stop at nothing to show his or her prowess in caring for patients, an earnestness that often manifests as a never-ending pursuit of esoteric (and often impossible) diagnoses.
Similarly, the internal medicine trainee goes to great lengths to display his or her burgeoning knowledge base. The goal is to get a “wow” from other junior residents (e.g., by reciting the differential diagnosis of Ortner syndrome) or from clerks (although getting a “wow” from a clerk is not difficult — this can usually be done by pronouncing “syncope” correctly). On occasion, this earnestness can resemble smugness, especially as the resident approaches the end of the internship and begins to think about how he or she will function as the senior resident/team leader.
As a junior resident in internal medicine, you may wish to incorporate the following techniques in your presentations.
- Pursue impossible diagnoses (e.g., “This 87-year-old man with a history of dementia now presents with worsening confusion, diarrhea and occasional arthralgias. Everything has improved with volume repletion and antibiotics, but his constellation of findings raises the possibility of undiagnosed Whipple disease. I’ve already received telephone consent from his third cousin in Florida, so I think we should call GI regarding small-bowel biopsy”).
- Be overly smug regarding the senior resident’s decisions (e.g., “When I run a team, I’ll never …” [this smugness quickly disappears when the senior resident takes a week’s vacation, leaving the PGY-1 resident to function as the “junior senior”]).
The senior medical resident (R2)
The senior resident serves in a supervisory role and must help the junior residents and clinical clerks in their (often futile) attempts to impress the attending physician. As a result, the senior resident is indirectly evaluated every time the junior trainees present. The attending will love a senior resident who can help clerks present cases in a crisp, coherent manner. On the other hand, a poor presentation can raise more questions about the resident than about the clerk. To guard against the latter situation, the senior resident finds ways of showing their own clinical skills. Many do this by interjecting during the presentations of other team members. Unfortunately, these interjections rarely (i.e., never) advance the patient’s care. They are, however, preferable to the “not my fault” approach taken by some senior residents who sit behind a clerk — in the line of sight of the staff — and shake their head in feigned disbelief as the clerk presents.
Below are techniques used by senior medical residents during presentations.
- Interject petty details to show that you are on top of everything (e.g., “I suppose the cardiac exam was ‘normal,’ but there was a physiologically split S 2 over the pulmonic valve”).
- Interject information that serves only to let the team know your desired subspecialty (e.g., “I don’t think we should discount the possibility of brucellosis in this patient. We probably should investigate for tularemia as well … and throw in a VDRL test too”).
The attending physician
As the presentee rather than presenter, the attending physician relies on the information he or she receives to make the final decisions regarding patient care. Knowing this, most trainees assume that attendings want to hear presentations that are comprehensive and error free. They are mistaken. Attending physicians love it when a trainee omits a key detail or misinterprets a key piece of information. Such instances provide attendings with two things they crave: the opportunity to show the clinical acumen achieved through years of experience, and the opportunity to create memorable teaching points. Everything an attending does while hearing a presentation is geared toward fulfilling these two goals (although a third — often unstated — goal is to stay awake). Some attendings simply listen intently and passively recognize subtle deficiencies (these attendings are typically described as “nice,” “approachable” and “boring”). Others have a different approach, actively trying to create gaps they can fill with one of many examples of their clinical expertise, as highlighted in the following pointers.
- Create gaps by preventing the trainee from presenting (e.g., Clerk: “The patient I saw is a 75-year-old male who was referred for chest ...” Attending: “Alright! Let’s go see him! Nice presentation, but I’ll give you some feedback: you’ve got to get to the point a little quicker next time”).
- Create gaps by questioning everything the trainee presents (e.g., Intern: “This 70-year-old male was referred because of a CVA.” Attending: “I think you mean ‘stroke,’ which is not an ‘accident.’” Intern: “Sorry. Anyways, the patient had a positive Babinski reflex on his right.” Attending: “Do you mean that his plantar response was up-going on the right?” Intern: “Of course, I don’t know where I got that from.” Attending: “Did you just end a sentence with a preposition?”).
Presentation styles vary tremendously among trainees. One aspect, however, remains constant: everyone involved is trying to highlight his or her own skills. Clerks want to showcase their ability to compile information, junior residents their diagnostic skills, senior residents their ability to manage complex patients, and attending physicians their clinical reasoning and mentoring skills. Implicit in this is the great strength of the case presentation: trainees at every level not only get to practise their own skills, they also see what they must do at the next level. Fortunately, all trainees provide the team with endless nuggets of entertainment — one just needs to stay awake to hear them.
Acknowledgement
The authors thank Mark Baerlocher for his comments on an earlier draft. Allan Detsky is a member of CMAJ ’s Editorial Board.
Competing interests: None declared.
Contributors: Daniel Rosenfield conceived the idea for the paper while stammering through his internal medicine clerkship presentations. Andrew Smaggus contributed to the design and writing of the paper, although most of what he contributed was subsequently cut or rewritten. Allan Detsky contributed to the overall inspiration for the paper as well as to the design and conceptualization.
Funding: No funding was received for this study. The authors did, however, take advantage of free food from noon rounds, and coffee and doughnuts brought in by clinical clerks.
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
- Search Results
- Study Record Detail

An Open Comparative Study of the Effectiveness and Incomparable Study of the Immunogenicity and Safety of the Vaccine (CoviVac) for Adults Aged 60 Years and Older
- Study Details
- Tabular View
- No Results Posted

Inclusion Criteria:
Volunteers must meet the following inclusion criteria:
Type of participants
• Healthy volunteers or volunteers with a history of stable diseases that do not meet any of the criteria for non-inclusion in the study.
Other inclusion criteria
- Written informed consent of volunteers to participate in a clinical trial
- Volunteers who are able to fulfill the Protocol requirements (i.e., fill out a self-observation Diary, come to control visits).
Exclusion Criteria:
SARS-CoV-2 infection • A case of established COVID-19 disease confirmed by PCR and/or ELISA in the last 6 months.
Diseases or medical conditions
- Serious post-vaccination reaction (temperature above 40 C, hyperemia or edema more than 8 cm in diameter) or complication (collapse or shock-like condition that developed within 48 hours after vaccination; convulsions, accompanied or not accompanied by a feverish state) to any previous vaccination.
- Burdened allergic history (anaphylactic shock, Quincke's edema, polymorphic exudative eczema, serum sickness in the anamnesis, hypersensitivity or allergic reactions to the introduction of any vaccines in the anamnesis, known allergic reactions to vaccine components, etc.).
- Guillain-Barre syndrome (acute polyradiculitis) in the anamnesis.
- The axillary temperature at the time of vaccination is more than 37.0 ° C.
- Acute infectious diseases (recovery earlier than 4 weeks before vaccination) according to anamnesis.
- Donation of blood or plasma (in the amount of 450 ml or more) less than 2 months before inclusion in the study.
- Severe and/or uncontrolled diseases of the cardiovascular, bronchopulmonary, neuroendocrine systems, gastrointestinal tract, liver, kidneys, hematopoietic, immune systems.
- Is registered at the dispensary for tuberculosis, leukemia, oncological diseases, autoimmune diseases.
- Any confirmed or suspected immunosuppressive or immunodeficiency condition in the anamnesis.
- Splenectomy in the anamnesis.
- Neutropenia (decrease in the absolute number of neutrophils less than 1000/mm3), agranulocytosis, significant blood loss, severe anemia (hemoglobin less than 80 g/l) according to anamnesis.
- Anorexia according to anamnesis.
Prior or concomitant therapy
- Vaccination with any vaccine carried out within 30 days before vaccination / the first dose of the studied vaccine or planned administration within 30 days after vaccination / the last dose of the studied vaccine.
- Prior vaccination with an experimental or registered vaccine that may affect the interpretation of the study data (any coronavirus or SARS vaccines).
- Long-term use (more than 14 days) of immunosuppressants or other immunomodulatory drugs (immunoregulatory peptides, cytokines, interferons, immune system effector proteins (immunoglobulins), interferon inducers (cycloferon) during the six months preceding the study, according to anamnesis.
- Treatment with systemic glucocorticosteroids (≥ 20 mg of prednisone, or an analog, for more than 15 days during the last month).
- Volunteers who received immunoglobulin preparations or blood transfusion during the last 3 months prior to the start of the study according to anamnesis.
Other non-inclusion criteria
• Participation in any other clinical trial within the last 3 months.
Exclusion criteria:
- Withdrawal of Informed consent by a volunteer;
- The volunteer was included in violation of the inclusion/non-inclusion criteria of the Protocol;
- Any condition of a volunteer that requires, in the reasoned opinion of a medical researcher, the withdrawal of a volunteer from the study;
- Taking unauthorized medications (see section 6.2);
- The volunteer refuses to cooperate or is undisciplined (for example, failure to attend a scheduled visit without warning the researcher and/or loss of communication with the volunteer), or dropped out of observation;
- For administrative reasons (termination of the study by the Sponsor or regulatory authorities), as well as in case of gross violations of the Protocol that may affect the results of the study.
- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services
- Victor Mukhin

Victor M. Mukhin was born in 1946 in the town of Orsk, Russia. In 1970 he graduated the Technological Institute in Leningrad. Victor M. Mukhin was directed to work to the scientific-industrial organization "Neorganika" (Elektrostal, Moscow region) where he is working during 47 years, at present as the head of the laboratory of carbon sorbents. Victor M. Mukhin defended a Ph. D. thesis and a doctoral thesis at the Mendeleev University of Chemical Technology of Russia (in 1979 and 1997 accordingly). Professor of Mendeleev University of Chemical Technology of Russia. Scientific interests: production, investigation and application of active carbons, technological and ecological carbon-adsorptive processes, environmental protection, production of ecologically clean food.
Title : Active carbons as nanoporous materials for solving of environmental problems
Quick links.
- Conference Brochure
- Tentative Program

Ultimovacs Announces Poster Presentation at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting
NON-REGULATORY PRESS RELEASE
Oslo, April 24, 2024: Ultimovacs ASA ("Ultimovacs") (OSE ULTI), aclinical-stagebiotechnology company developing immunotherapeutic cancer vaccines, todayannounces that the data from the Phase II clinical trial INITIUM(NCT04382664(https://clinicaltrials.gov/study/NCT04382664?term=ultimovacs&rank=2)), willbepresented in a poster session at the 2024 ASCO Annual Meeting, taking placeMay31 - June 4, 2024, in Chicago, IL & Online.
INITIUM is an Ultimovacs-sponsored randomized, comparative, multicenter PhaseIItrial evaluating the company's therapeutic cancer vaccine candidate UV1incombination with the checkpoint inhibitors ipilimumab and nivolumab asfirst-line treatment in unresectable or metastatic malignant melanoma. The trialwasconducted at 39 hospitals across the U.S., U.K., Belgium, and Norway, and156patients were enrolled between June 2020 and July 2022.
The poster presentation features key findings and analyses after a minimum18-month follow-up of the patients in the trial.
Presentation Details:
Abstract Number: LBA9519Abstract Title: Ipilimumab and nivolumab plus UV1, an anticancervaccinationagainst telomerase, in advanced melanoma.
Session Title: Poster Session - Melanoma/Skin CancersPoster Board: 303Date and Time: June 1, 2024 1:30 PM - 4:30 PM (CT)Presenter: Paul Lorigan, Professor of Medical Oncology at the UniversityofManchester and Investigator in the INITIUM study
Late-Breaking Abstracts are under embargo and will be released at 7:00AM(CT)/8:00 AM (ET) on the day of the presentation.
About UltimovacsUltimovacs is a clinical-stage biotechnology leader in novel immunotherapeuticcancer vaccines. The lead cancer vaccine candidate UV1 is an off-the-shelfvaccine directed against human telomerase (hTERT), an antigen present in85-90%of cancers in all stages of tumor growth. A broad clinical program, with PhaseII trials in five cancer indications enrolling more than 670 patients, aims toinvestigate UV1's impact in combination with other immunotherapies in multiplecancer types. UV1 is a patented technology owned by Ultimovacs. In addition,Ultimovacs holds all rights to the proprietary TET technology platform for anypossible future use of formulations in various solid tumor indications.
The Company is listed on the Euronext Oslo Stock Exchange (ULTI).
For further information, please contact:
Carlos de Sousa, CEOEmail: [email protected] (mailto:[email protected])Phone: +47 908 92507
Anne Worsøe, Head of Investor RelationsEmail: [email protected] (mailto:[email protected])Phone: +47 90686815
This stock exchange announcement was published by Anne Worsøe, Head ofInvestorRelations at Ultimovacs ASA, on April 24, 2024, at 16:15 CET.
https://newsweb.oslobors.no/message/616670

IMAGES
VIDEO
COMMENTS
There are a multitude of presentation formats for sharing and discussing clinical cases, diagnostic formulations or dilemmas, treatment approaches, and ethical issues. These presentation formats vary in terms of the number and type of participants, the use of multimedia , the availability of continuing medical education credits, etc. (Hull et ...
The clinical presentations that arise from exposure to novel stimulants and their drug relatives are discussed further, below. Particular difficulties arise when a stimulant-intoxicated child is accompanied by a stimulant-intoxicated guardian. The paranoia and propensity to violence that characterise adult stimulant intoxication can badly ...
Here, we provide an overview of the epidemiology, pathogenesis, clinical presentation, diagnosis, and treatment of COVID-19. Areas covered. Direct person-to-person respiratory transmission has rapidly amplified the spread of coronavirus. In the absence of any clinically proven treatment options, the current clinical management of COVID-19 ...
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence.1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Both sexes exhibited clinical presentations similar in symptomatology and frequency to those noted in other severe acute respiratory infections, namely influenza A H1N1 112 and SARS 113,114. These ...
The clinical presentation of COVID-19 can be indistinguishable from other viral causes of pneumonia and include fever (83-98%), dry cough (76-82%), and fatigue or myalgia (11-44%) (74, 75). The median age of confirmed COVID-19 cases is in the 6th decade of life with a slight male predominance. Twenty-five percent of patients have severe ...
Presenting a patient is an essential skill that is rarely taught Clinical presenting is the language that doctors use to communicate with each other every day of their working lives. Effective communication between doctors is crucial, considering the collaborative nature of medicine. As a medical student and later as a doctor you will be expected to present cases to peers and senior colleagues ...
The clinical presentation of COVID-19 ranges from asymptomatic to critical illness. An infected person can transmit SARS-CoV-2, the virus that causes COVID-19, before the onset of symptoms. Symptoms can change over the course of illness and can progress in severity. Uncommon presentations of COVID-19 can occur, might vary by the age of the ...
Clinical presentation (CP) is a relatively new and innovative approach to teaching medicine. CP engages medical students in their understanding of the disease process from clinical feature to diagnosis. Students begin studying abnormalities of complaints, examination, and laboratory findings; i.e., signs, symptoms, and laboratory investigations ...
Clinical presentation MS is a CNS disease characterised by demyelinating lesions in regions including the optic nerves, brainstem, cerebellum, periventricular and spinal cord. Histopathology also shows widespread involvement of the cerebral grey matter, although this is not well appreciated on conventional MRI.
Notes. Notes. 12.4 Disorders of purine and pyrimidine metabolism. Notes. Notes. 12.5 The porphyrias. AbstractRespiratory disease can present in many ways, with variations attributable to many factors. The clinical presentation directs diagnostic hypothesis.
The clinical presentation and clinical signs are dependent on the site of infection and may cause organ specific symptoms (for example cough) or generalised, non-specific symptoms such as fever and weight loss. The less common manifestations of TB such as erythema induratum or ocular TB can be extremely challenging in the setting of ...
A clinical presentation is the mode by which a patient presents to a physician and represents the clinical problem a physician is expected to manage. Big picture: The curriculum begins and ends with a focus on the patient, specifically the patient's clinical presentation. Deconstruct and independent learning: Each clinical presentation is ...
4 The Clinical Presentation R. E. BARRY P. BAKER A. E. READ For the purpose of this paper, coeliac disease is defined as a malabsorptive disorder of the small intestine in which the histological abnormalities of structure and the clinical features they are associated with are reversed by gluten withdrawal. The incidence of coeliac disease in ...
1 Introduction. CLL is predominantly a disease of the elderly and has a variable clinical presentation and subsequent evolution. Clinical features and laboratory investigations are important for making decisions about patient management and for predicting outcomes, which are very variable in this disease.
Clinical Presentations. Frontotemporal degeneration (FTD) is a spectrum of neurodegenerative conditions that often occur in individuals younger than 65 years of age. ( Knopman and Roberts, 2011 ). Many cases are familial, but sporadic cases suggest that environmental triggers also exist. Several genetic etiologies are known, but environmental ...
REDWOOD CITY, Calif., April 24, 2024 (GLOBE NEWSWIRE) -- Coherus BioSciences, Inc. (Coherus, Nasdaq: CHRS) today announced the first presentation of clinical data for CHS-114, a highly selective ...
Clinical presentation. Similar to other coronaviruses, SARS‐CoV‐2 is predominantly spread by respiratory droplets, although spread by contact with contaminated fomites also occurs, as does transmission by aerosols in certain circumstances.1 Based on the experience in China, the typical incubation period of COVID‐19 infection has been estimated to be a median of 5.1 days (95% CI, 4.5-5. ...
Replicate Bioscience, an Apple Tree Partners portfolio company, is a clinical-stage company amplifying the power of RNA therapeutics by pioneering its novel self-replicating RNA (srRNA) technology ...
Tirzepatide achieved a mean apnea-hypopnea index reduction of up to 63% (about 30 fewer events per hour), meeting all primary and key secondary endpoints in two phase 3 clinical trials Tirzepatide meaningfully improved sleep apnea symptoms in those with moderate-to-severe OSA and obesity with and without PAP therapy, and based on these results ...
Presentations. FT819-102: Clinical translation of off-the-shelf, TCR-less, CD8αβ+ anti-CD19 CAR-T cells for the treatment of B cell-mediated autoimmune disorders Abstract Number: 1415
Randomized, double-blind, placebo controlled, multi-center clinical trials of the tolerability, safety and immunogenicity of the inactivated whole-virion concentrated purified vaccine against COVID-19, manufactured by FSBSI "Chumakov FSC R&D IBP RAS", of childrens aged 12-17" (Clinical trials, phase III).
The clinical clerk. The case presentation can be the most exciting part of the day for the clinical clerk and the most dreaded for the attending physician, or vice-versa. The key feature of a clerk's presentation is his or her lack of confidence. Overinclusive and unconvincing, the presentation often showcases verbal diarrhea at its finest.
Written informed consent of volunteers to participate in a clinical trial; Volunteers who are able to fulfill the Protocol requirements (i.e., fill out a self-observation Diary, come to control visits). Exclusion Criteria: SARS-CoV-2 infection • A case of established COVID-19 disease confirmed by PCR and/or ELISA in the last 6 months.
An Clinical Trials Manager at Qureight Ltd and a recent graduate from the University of Cambridge. Throughout my studies and work experience, I have demonstrated that I am a keen and quick learner and a highly motivated individual. I have experience in imaging research and in managing multicentral and multination imaging studies and working with both academic and industrial partners.
Catalysis Conference is a networking event covering all topics in catalysis, chemistry, chemical engineering and technology during October 19-21, 2017 in Las Vegas, USA. Well noted as well attended meeting among all other annual catalysis conferences 2018, chemical engineering conferences 2018 and chemistry webinars.
REDWOOD CITY, Calif., April 24, 2024 (GLOBE NEWSWIRE) -- Coherus BioSciences, Inc. (Coherus, Nasdaq: CHRS) today announced the first presentation of clinical data for CHS-114, a highly selective cytolytic anti-CCR8 antibody, at the upcoming ASCO Annual Meeting, which will be held from May 31 to June 4, 2024, at McCormick Place in Chicago. Presentation Details
Late-Breaking Abstracts are under embargo and will be released at 7:00AM(CT)/8:00 AM (ET) on the day of the presentation. ==ENDS== About UltimovacsUltimovacs is a clinical-stage biotechnology leader in novel immunotherapeuticcancer vaccines.