- Case report
- Open access
- Published: 10 May 2021

Alpha-1 antitrypsin deficiency in the elderly: a case report
- Anna Annunziata 1 ,
- Maurizia Lanza 1 ,
- Antonietta Coppola 1 &
- Giuseppe Fiorentino 1
Journal of Medical Case Reports volume 15 , Article number: 231 ( 2021 ) Cite this article
3282 Accesses
2 Altmetric
Metrics details
Generally, alpha-1 antitrypsin deficiency (AATD) is suspected in young patients with pulmonary emphysema or chronic obstructive pulmonary disease (COPD). Patients often suffer from diagnostic gaps and are misdiagnosed with chronic obstructive pulmonary disease (COPD), asthma, and airway hyperresponsiveness (AHR), as AATD may present with nonspecific respiratory symptoms. It is never too late to suspect AATD, especially in a patient with an unusual medical history. In recent years, evidence is beginning to emerge that there may be value in identifying and treating patients who do not already have deterioration of functional parameters.
Case presentation
We describe a case of a 69-year-old Caucasian female patient, late diagnosis of AATD, with both severe bronchial hyperreactivity and numerous exacerbations due to the peculiar clinical history and the presence of a rare mutation; although not presenting forced expiratory volume in 1 second (FEV 1 ) between 30 and 65%, the patient was treated with alpha-1 antitrypsin (AAT) augmentation therapy and achieved clinical and functional improvement.
AATD should always be suspected. The Alpha-1 Foundation recommendations for the diagnosis and management of AATD in adult patients indicate that treatment should be provided for patients with FEV 1 between 30 and 65%. It may be useful to evaluate and treat patients based on clinical symptoms, even outside the established parameters, in particular cases.
Peer Review reports
Alpha-1 antitrypsin deficiency (AATD) causes different respiratory manifestations, including pulmonary emphysema, chronic obstructive pulmonary disease (COPD), asthma and bronchiectasis. AATD is a rare lung disease, with a progressive clinical course, and early diagnosis enables patients to make lifestyle changes and initiate therapy to decelerate or prevent further loss of lung tissue. However, AATD goes largely unrecognized; evidence from screening programs in the United States shows that less than 10% of individuals with AATD are clinically diagnosed with the disorder [ 1 ]. Patients often suffer from diagnostic gaps and are misdiagnosed with COPD, asthma and airway hyperresponsiveness (AHR), as AATD may present with nonspecific respiratory symptoms. Some authors have suggested that AHR, wheezing and dyspnea may be susceptibility phenotypes for the development of respiratory disease, especially in the context of cigarette smoking. In their group of patients, 25% had an increase of at least 10% in forced expiratory volume in 1 second (FEV 1 ), and this reversibility has been associated with lower lung functionality [ 2 ]. Emphysema or COPD may be initially and incorrectly diagnosed as asthma in adults with AATD; a diagnosis of childhood asthma would be unlikely due to emphysema or COPD. In Sweden, individuals with AATD have been identified as part of neonatal screening; 15% were diagnosed with asthma by age 22, and 29% had self-reported recurrent wheezing episodes. The study noted that a medical diagnosis of asthma before age 16 was linked to reduced FEV 1 and severe COPD in adulthood, which could indicate that asthma or asthma-like symptoms may result in a subset of particularly susceptible AATD patients [ 2 ]. Therapeutic diagnostic delay can lead to a complex clinical course.
We describe the case of a 69-year-old Caucasian female patient, housewife and mother of three daughters, in apparent good health, who had never smoked. The patient reported six episodes per year of exacerbation of respiratory failure documented over the previous 10 years. Respiratory symptoms were resolved with steroids and antibiotics. The patient had been hospitalized twice in the last 3 years for acute respiratory failure. She was discharged with a diagnosis of "acute respiratory failure exacerbated by COPD.”
Due to persistence of respiratory symptoms characterized by dyspnea and a dry cough, the patient visited the pulmonary clinic of our department, and a functional assessment was carried out. At a young age, she reported occasional wheezing, sporadic episodes of respiratory exacerbation, especially during the three pregnancies, and intense dyspnea and asthma-like symptoms. She had undergone spirometry several years earlier, for which no written documentation was generated. The patient was being treated with an inhaled corticosteroid and long-acting β2-agonist twice daily, long-acting muscarinic antagonist twice daily, theophylline 200 mg orally twice a day, and montelukast 10 mg per day orally.
The patient complained of worsening dyspnea with wheezing. Spirometry performed at the first visit showed forced vital capacity (FVC) of 2.17 (120%), FEV 1 1.64 (113%) and diffusing capacity for carbon monoxide (DLCO) of 4.11 mmol/(minute KPa), 80%. Spirometry performed at the second visit showed FVC 1.95 (100%), FEV 1 1.44 (100%), Tiffeneau index of 75% and DLCO 4.11 mmol/(minute KPa), 80%. The six-minute walk test was normal. She was subjected to a methacholine challenge test, which was positive for severe hyperreactivity. Allergic skin tests for inhalants and foods were negative. A paper radioimmunosorbent test (PRIST) showed a level of 39 U/mL. The blood tests were normal except for serum alpha-1 antitrypsin (AAT) of 67 mg/L (normal value is 0.90–2.00 g/L). Chest computed tomography scan revealed the presence of small areas of air trapping and diffuse bronchiectasis (Fig. 1 ). Sputum cultures performed to exclude colonization of potentially pathogenic microorganisms that could be the cause of exacerbations were negative.
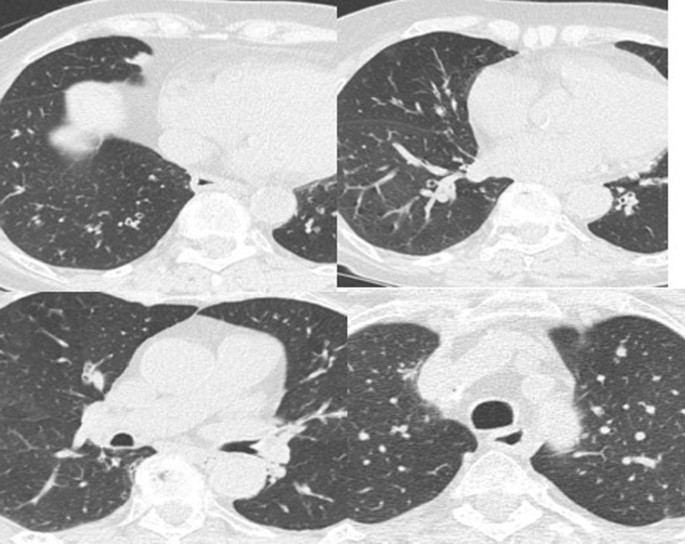
Chest computed tomography scan showed the presence of small areas of air trapping and diffuse bronchiectasis
Genetic screening was performed for the AATD inheritance and showed compound heterozygosity for deficient alleles pis and Pi Lowell .
After informed consent was obtained from the patient, we started intravenous augmentation therapy with human AAT at a dosage of 60 mg/kg every 7 days. At the request of the patient and her family, and after having monitored serum AATD, therapy was performed every 14 days. At 20 months of treatment, the patient showed no exacerbation, dyspnea exertional resolution and stable improvement in respiratory parameters.
After subsequent revaluation diagnostics, this patient, with a rare double heterozygous mutation, was treated with augmentation therapy, obtaining clinical and functional improvement without exacerbation over 2 years of treatment.
A review by Eden [ 3 ] examined the contention that individuals with severe AATD were particularly susceptible to AHR, which was associated with the reactivity of bronchodilators, asthma and allergies. This review summarizes evidence to suggest that the development of AHR related to asthma and reversible bronchospasm in AATD is a risk factor for progression to COPD. Different genetic factors are involved in the development of asthma, such as atopy, and increase the predisposition to the disease [ 3 ]. The different phenotypes of asthma depend on the interaction between heredity and the polygenic environmental complex [ 4 ]. Atopic asthma originates from a genetic predisposition, characterized by allergic manifestations, response to skin tests, eczema and rhinitis, and the response to triggering actors can cause attacks of wheezing and shortness of breath. Gastroesophageal reflux can also trigger AHR in susceptible individuals. AATD as a predisposing factor may contribute to the pathogenesis of asthma due to the lack of anti-neutrophil elastase of the airways; this results in a condition of chronic inflammation which can stimulate an acute reaction in response to various agents [ 5 ]. Asthma exacerbation can be caused by upper respiratory tract infection, obesity or exposure to allergens, including in the workplace [ 6 , 7 ]. With airway inflammation of neutrophils in asthma and chronic bronchitis, both total and active proinflammatory elastase increases in the airways. There is a compensatory development in airway AAT, but an excess of elastase indicates protease/anti-protease imbalance [ 8 ]. Studies have revealed that the presence of asthma with frequent exacerbations is a risk factor for an accelerated decline in FEV 1 [ 9 , 10 ].
For over 10 years, the patient had respiratory symptoms variously diagnosed as episodes of acute bronchitis or chronic bronchitis. There were no professional or lifestyle risk factors, and the patient had never smoked; thus AATD was never suspected. However, despite maximizing drug treatment, the clinical conditions worsened, with an increase in the frequency of episodes of bronchial exacerbation. In the most recent few months, exertional dyspnea had arisen, but the basal functional evaluation and allergology tests carried out on the occasion of different re-evaluations determined nothing pathological. At the time of our first evaluation, the finding of lower than normal serum AAT level necessitated a genetic study documenting the heterozygous presence of a pis and Pi Lowell mutation. The evolution of lung disease in people with AATD would appear to be aggravated by the presence of gene interactions that are not yet clearly understood. Presumably, atopy, modifier genes and extrinsic influences, environmental factors and cigarette smoking work together to increase airway hyperreactivity and asthma, contribute to the decline of lung function in AATD, and play a role in exacerbation [ 11 ].
It is interesting to observe that in our case, the patient at the second evaluation showed a significant reduction in respiratory function compared to her previous parameters, while remaining in the normal range of respiratory function. During the months of augmentation therapy, our patient did not show any bronchial exacerbation; the dyspnea index was reduced as assessed by the six-minute walk test and modified Medical Research Council (mMRC) scale (Table 1 ). The role of the distinct mutations of the gene for AAT and their combination is still an ongoing study. Different clinical pictures of different severity are described in the literature in patients with the same mutation or with rare mutations in combination. Serum AAT levels should be measured at least once in all patients with asthma and COPD, as suggested by the World Health Organization (WHO), as a large number of patients receive the diagnosis too late for effective treatment measures [ 12 ]. The latency time for diagnosis of congenital AATD is greater than 10 years. According to the Italian registry data, the diagnostic delay is about 8–9 years, which is greater than that for the United States and Germany (about 6 years) [ 13 ].
These data strongly support a recommendation to always suspect AATD in the presence of respiratory symptoms at any age, and above all to promote greater awareness of this genetic condition, which is still under-recognized more than 50 years after its discovery. The exclusion of a genetic component linked to AAT is indicated in all patients with respiratory symptoms, asthma or COPD, and it is important to evaluate each case for the possible indication and potential advantages of AAT augmentation therapy.
The latest Alpha-1 Foundation recommendations for the diagnosis and management of AATD in adult patients supports replacement therapy in individuals with FEV 1 of 30–65% [ 14 ], but emerging data showing that it can be useful for diagnosis and treatment of patients outside of previously established parameters [ 15 ]. Data on these cases need to be collected to better understand the role of augmentation therapy. Large-scale screening in the general population, infants and blood donors, or in targeted populations such as COPD and asthma patients, which can lead to the early identification of patients in need of treatment, would be helpful. Although AAT augmentation therapy is the only treatment available that addresses the underlying cause of AATD, symptomatic therapy and lifestyle changes may be of benefit to all patients.
Availability of supporting data
All data are available c/o UOC Pathophysiology and Respiratory Rehabilitation, Intensive Care Department, Monaldi Hospital, Naples, Italy.
Lascano JE, Campos MA. The important role of primary care providers in the detection of alpha-1 antitrypsin deficiency. Postgrad Med. 2017;129(8):889–95. https://doi.org/10.1080/00325481.2017.1381539 .
Article PubMed Google Scholar
DeMeo DL, Sandhaus RA, Barker AF, et al . Determinants of airflow obstruction in severe alpha-1-antitrypsin deficiency. Thorax. 2007;62(9):806–13. https://doi.org/10.1136/thx.2006.075846 .
Article PubMed PubMed Central Google Scholar
Eden E. Asthma and COPD in alpha-1 antitrypsin deficiency evidence for the Dutch hypothesis. COPD J Chronic Obstr Pulm Dis. 2010;7:366–74.
Article Google Scholar
Postma DS, Bleecker ER, Amelung PJ, Holroyd KJ, Xu J, Panhuysen CI, Meyers DA, Levitt DA. Genetic susceptibility to asthma-bronchial hyperresponsiveness coinherited with a major gene for atopy. N Engl J Med. 1995;333:894–900.
Article CAS Google Scholar
DeMeo DL, Campbell EJ, Barker AF, Brantly ML, Eden E, McElvaney NG, Rennard SI, Sandhaus RA, Stocks JM, Strange C, Turino G, Silverman EK. IL10 Polymorphisms are associated with airflow obstruction in severe alpha1-antitrypsin deficiency. Am J Respir Cell Mol Biol. 2008;38:114–20.
Sook LW, Sablihan NI, Ismail S, Devaraj NK, Mooi CS. Factors associated with the level of physical activities among non-academic staffs in the Faculty of Medicine and Health Sciences of a public university in Selangor, Malaysia. Mal J Med Health Sci. 2019;15(2):47–55.
Google Scholar
Devaraj NK, Rashid AA, Shamsuddin NH, bin Abdullah AA, Han TC, Yee CZ. Occupational asthma as a differential diagnosis of adult-onset asthma—a case report. Mal J Med Health Sci. 2019;15(2):145–7.
Vignola AM, Bonanno A, Profita M, Scichilone N, Spatafora M, Bosquest J, Bonsignore G, Bellia V. Effect of age and asthma duration upon elastase and alpha1-antitrypsin levels in adult asthmatics. Eur Respir J. 2003;22:795–801.
Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15 year follow up study of ventilatory function in adults with asthma. N Engl J Med. 1998;339:1194–200.
Castaldi PJ, DeMeo DL, Kent DM, Campbell EJ, Barker AF, Brantly ML, Eden E, McElvaney NG, Rennard SI, Stocks JM, Stoller JK, Strange C, Turino GM, Sandhaus RA, Griffith JL, Silverman EK. Development of predictive models for airflow obstruction in alpha-1 antitrypsin deficiency. Am J Epidemiol. 2009;17:1005–13.
O’Byrne PM, Pederson S, Lamm CJ, Tan WC, Busse WW, START investigators. Severe exacerbations and decline inlung function in asthma. Am J Respir Crit Care Med. 2009;179:19–24.
Alpha 1-antitrypsin deficiency: memorandum from a WHO meeting. World Health Organization 1997;75(5):397–415.
Ferrarotti I, Baccheschi J, Zorzetto M, et al . Prevalence of rare variants in the Italian Registry for Severe alpha1 antitrypsin deficiency. J Med Genet. 2005;42:282–7.
Sandhaus RA, Turino G, Brantly ML, et al . The diagnosis and management of alpha -1 antitrypsin deficiency in the adult. Chronic Obstr Pulm Dis. 2016;3(3):668–82.
PubMed PubMed Central Google Scholar
Kueppers F. Clinical presentations of four patients with rare alpha 1 antitrypsin variants identified in a single US center. Respir Med Case Rep. 2021;20(32):101345. https://doi.org/10.1016/j.rmcr.2021.101345 .
Download references
Acknowledgements
We thank all our nurses, in particular Ida Carrano, Antonella Sabbatino, Grazia Ceraso and Anna Larenza, who help us take care of our patients. The manuscript was proofread by a native English speaker.
No founding source to declare.
Author information
Authors and affiliations.
UOC Pathophysiology and Respiratory Rehabilitation, Intensive Care Department, Monaldi Hospital, Naples, Italy
Anna Annunziata, Maurizia Lanza, Antonietta Coppola & Giuseppe Fiorentino
You can also search for this author in PubMed Google Scholar
Contributions
AA: design, literature review and writing of the manuscript. ML and AC: data collection. GF: supervision. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Anna Annunziata .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Annunziata, A., Lanza, M., Coppola, A. et al. Alpha-1 antitrypsin deficiency in the elderly: a case report. J Med Case Reports 15 , 231 (2021). https://doi.org/10.1186/s13256-021-02847-w
Download citation
Received : 17 August 2020
Accepted : 04 April 2021
Published : 10 May 2021
DOI : https://doi.org/10.1186/s13256-021-02847-w

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Alpha-1 antitrypsin
- Replacement therapy
- Lung disease
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Lung disease patients more likely to develop heart disease independent of any risk factors
Patients with lung disease are more likely to develop heart disease independent of any risk factors, according to new research.
A new study published in Orphanet Journal of Rare Diseases looked at patients who have a rare genetic condition called Alpha-1 antitrypsin deficiency (AATD) which causes lung disease similar to COPD independently of any risk factors such as smoking or age. More than 220 patients with AATD were recruited to the study alongside patients with COPD, and a control non lung disease population; and all were assessed for present cardiovascular disease (CVD) and recognized risk factors, including assessment of vascular stiffness known to increase risk for future events. Patients were then tracked for four years to see whether they developed CVD.
The patients with the rare genetic condition AATD had the highest adjusted scores among all participants for vascular stiffness, but had lowest scores for standard associated risk factors of CVD and nearly half (45%) of patients had discordant scores where one was high and other low.
Meanwhile, COPD and control participants had similar scores across the direct and indirect measures of CVD risk.
Furthermore, despite the AATD participants having lower risk factors associated with developing cardiovascular disease including being younger and a higher proportion who had never smoked, 12.7% of participants developed CVD after four years of follow-up.
This long-term study has enabled us to see the relationship between lung disease and heart disease in a unique way by following a group of patients with this rare genetic disease. Our study has shown that there is an increased risk for people with lung conditions of going on to develop cardiovascular conditions, and that only looking at conventional factors such as age and smoking doesn't give the full picture of the relationship between these two essential systems in the body." Robert Stockley, Professor and Consultant in Acute and Respiratory Medicine at University of Birmingham and senior author of the paper
Potential target for treatment
Participants also gave blood which was tested for an enzyme linked with lung damage in AATD patients.
There was a significantly higher levels of the enzyme Proteinase 3 in the AATD patients, but the study found that there was a link between elevated levels of the enzyme and vascular stiffness and hence CVD risk. The team believe that the Proteinase 3 enzyme may have a more direct impact on the development of heart and lung disease through the breakdown of fibers that support the large arteries and lungs, and that Proteinase 3 inhibitors could be a novel therapeutic to prevent cardiovascular disease especially in AATD patients.
Louise Crowley, Clinical Research Fellow and PhD researcher at the University of Birmingham and corresponding author of the paper said:
"The role of Proteinase 3 acts as a powerful link between lung and heart disease. The action that the enzyme has in attacking elastin fibers found in the lungs and major arteries suggests that inhibiting its action could have a dual effect to slow both lung and cardiovascular diseases."
University of Birmingham
Sapey, E., et al. (2024) Cardiovascular disease in Alpha 1 antitrypsin deficiency: an observational study assessing the role of neutrophil proteinase activity and the suitability of validated screening tools. Orphanet Journal of Rare Diseases . doi.org/10.1186/s13023-024-03124-x .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.44(7); 2019 Jul
Alpha-1 Antitrypsin Replacement in Patients With COPD
Chronic obstructive pulmonary disease can be attributed to genetic conditions and predispositions, among other factors. Alpha-1 antitrypsin deficiency (AATD) is a significant risk factor for COPD development and progression, and aggressive screening for all patients with COPD or adult-onset asthma is encouraged.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a progressive life-threatening disease characterized by airflow limitation that is associated with sporadic episodes of symptomatic decompensation. 1 Airflow limitation typically results from exposure to noxious particles or gases, leading to a chronic inflammatory response in predisposed hosts. The most common source of inflammation is smoking, but other etiologies include environmental or occupational lung exposure. 1 Some people who develop COPD have never smoked and not all people who smoke will develop COPD; this suggests that both host factors and genetics play a role in its development. A small but important number of individuals develop COPD secondary to a genetic deficiency in alpha-1 antitrypsin (AAT). 2
Global Initiative for Chronic Obstructive Lung Disease (GOLD)
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is led by an international group of scientists who collaborate with health care professionals and public health officials to raise awareness of COPD and improve prevention rates and treatment options. 1 Periodically, the group publishes guidelines on diagnostic and treatment strategies based on the best available clinical evidence. As well as providing recommendations for pharmacologic treatment modalities, GOLD provides comprehensive non-pharmacologic prevention and treatment recommendations, such as testing for genetic risk factors for developing COPD, specifically AAT deficiency (AATD).
Chronic obstructive pulmonary disease is recognized as a major cause of morbidity and mortality. Estimates suggest it causes more than three million deaths each year––accounting for 5% of all deaths globally 3 –– more than 90% of which occur in low- and middle-income countries. The prevalence of the disease largely depends on the population being studied; most information is based on data from developed countries. 1 Worldwide, the incidence of COPD stages 2–4 is believed to be 10% to 12%, 4 , 5 rising to 15% among regular smokers and up to 47% in smokers with a ≥ 15 pack-year history when spirometric screening criteria are used to diagnose the disease. 6 , 7
Genetic factors contribute to COPD’s development, and among those, AATD is of interest as it is both rare and under-recognized. Approximately 2% to 3% of patients diagnosed with COPD have AATD, and severe AATD has been reported in 1% to 2% of patients in the U.S. 8 – 12
Societal Cost of COPD
The greatest determinants of COPD’s cost to society are the severity of illness, presence and frequency of disease exacerbations, and presence and number of comorbid medical conditions. 1 In addition, an under-recognized fourth determinant is the high prevalence of undiagnosed disease. 5 According to GOLD, direct costs exceed $32 billion per year in the U.S. alone; indirect costs are linked to another $20.4 billion per year. 1
A number of studies have evaluated the human and economic costs of this disease. 13 Patients with substantial airflow limitation and moderate-to-severe symptoms experience significant impairments in quality-of-life scores and have excessive rates of disability. The correlation between the severity of the disease and the decrease in quality of health and daily activities appears in many regions throughout the world. 13
The economic costs of COPD vary widely depending on geographic location. 14 This most likely arises from variations in the true cost of the disease, differences in calculation methods, and differences regarding access to routine preventative and urgent medical-care services. The largest number of published economic studies on COPD have been conducted in industrialized countries. A more appropriate assessment would be studies based on an examination of those components that contribute to the overall cost of the disease.
The severity of COPD, the increasing prevalence of comorbid conditions, and patient susceptibility to disease exacerbations are associated with a greater economic burden, 14 , 15 including greater expenditures for direct and indirect medical costs (loss of productivity, home-based care, etc.). In patients with milder forms of COPD, clinic visits and medications comprised the largest component of medical costs, and in patients with severe or very severe COPD, hospitalization costs were the largest component. Patients with more frequent hospitalizations are typically older and have a greater number of comorbid conditions, such as cardiovascular disease, congestive heart failure, diabetes, and depression. These patients also appear to be more susceptible to exacerbations representing a distinct phenotype that is recognized in the new GOLD guidelines. 1
An important component of COPD’s societal cost is the large number of undiagnosed individuals: worldwide, approximately 70% of people with the disease remain undiagnosed. 5 The reasons for under-diagnosis vary, and involve patient and social factors. Individuals may under-report symptoms, making it unlikely that they will seek diagnosis or treatment. Further, they may have no access to health care (particularly in underserved populations) or lack the means to undergo formal testing and evaluation. Studies on the medical costs incurred by patients before receiving a formal COPD diagnosis have found that they exceed those incurred by patients in control groups. 15 The frequency of clinic visits and hospitalizations was 50% greater among patients with a delayed COPD diagnosis. Earlier diagnosis and treatment could slow disease progression and reduce complication rates. 15
A delayed diagnosis may be especially consequential for patients with AATD because new therapies can reduce the risk of irreversible lung damage. 8 , 11 Patients with AATD are under-diagnosed for a number of reasons, but they can be more readily identified when an index of suspicion is present among physicians. Patients with AATD have different patterns of presentation compared to typical patients with COPD. In most cases, they are less likely to have a history of exposure to the usual COPD risk factors (e.g., smoking, biomass-fuel exposure, or chronic exposure to air pollution) and an onset of symptoms occurring at an earlier age. A substantial number of physicians are unaware of the guidelines concerning patient screening for AATD or believe there is no treatment available for this form of COPD, which reduces any perceived urgency of making a diagnosis. 2 Patients with severe AATD are typically evaluated by at least three physicians and experience an average delay of seven years between symptom onset and definitive diagnosis. 2 The lack of familiarity with guidelines and the subtle differences in presentation mean that among the estimated 100,000 cases of AATD in the U.S., approximately 15,000 individuals have been diagnosed. 2 Local, regional, and national education campaigns are critical for expanding awareness and improving identification of this unique patient population.
ALPHA-1 ANTITRYPSIN DEFICIENCY
Alpha-1 antitrypsin deficiency is a genetic disorder characterized by inappropriately low levels of AAT, which inhibits neutrophil elastase––a protease with elastolytic properties that can attack lung elastin and other structural components of the alveolar wall, leading to lung injury and parenchyma destruction. 16 – 18 The disorder can affect multiple organ systems, but primarily affects the lungs and liver. Liver disease in patients with AATD is caused by an alternative mechanism, and is not related to active destruction as in lung disease. Rather, disease is caused by an over-accumulation of abnormal AAT protein in the liver, where it is synthesized. A lack of breakdown of this protein can lead to liver damage, but the process is not universal to all patients with AATD and it can vary greatly. 19
There are multiple genetic variants of AAT. A normal phenotype is a variant of the “M” phenotype, which is present in 99% of the world’s population; deficient phenotypes typically contain the “S” and “Z” variants. These mutant phenotypes result in deficient AAT levels and can cause disease. The null phenotype occurs in patients whose plasma is devoid of AAT. There is also a dysfunctional phenotype in which the plasma carries normal amounts of AAT but the enzyme does not function appropriately. 16 More than 90% of patients with AATD have the deficient PI*ZZ genotype, making it the most common mutation of the disorder. 8 , 17 Patients with AATD are typically homozygous for the autosomal recessive trait. 18 Genotyping and phenotyping of AAT are usually examined simultaneously; genotype evaluation can easily be performed in office with a finger stick or buccal swab, and sent to specialized laboratories for analysis. 10 Results are then submitted to the health care provider and used in further decisions regarding care.
Patients with AATD can present in several ways, with dyspnea being the most common manifestation. Other frequent complaints are similar to the classic presentation of COPD: phlegm production, wheezing, cough, and recurrent upper respiratory tract infections. With AATD, the typical age of presentation is one aspect that differs from the typical presentation age with COPD or emphysema: most people with AATD present with symptoms between the ages of 20 and 40, as opposed to people with “traditional” COPD, who tend to present before age 40. 17 Also, people with AATD commonly have a characteristic panacinar emphysema pattern with bullous changes that are more evident at the lung bases than at the apices. 16 Patients with classic COPD emphysema, on the other hand, usually present with more centrilobular disease, often located in the lung’s apical region.
Once a patient has been diagnosed with COPD, testing for AATD should be included. 10 Certain characteristics of individuals who are diagnosed with emphysema should raise suspicions of AATD: < 45 years old; nonsmoker or minimal smoker; chest radiograph with prominent basilar pattern; familial history of AATD––which is important; and adult-onset asthma. 16 In families with multiple members who have obstructive disease but lack the typical risk factors, AATD should also be investigated. Laboratory diagnosis is confirmed with a serum AAT-level test. 20
There is significant under-recognition of AATD as a cause of COPD. 10 , 20 Many clinicians are not intimately familiar with AATD, having little knowledge of the testing and available treatments. 17 Potential nonspecific respiratory symptoms of AATD can be misdiagnosed as classic COPD or asthma. 17 Because patients with AATD show the same clinical features of untreated COPD, the World Health Organization recommends testing all patients who have COPD or adult-onset asthma for AAT. 21 , 22 Diagnostic AAT testing (grade A recommendation) is recommended for symptomatic adults with emphysema, COPD, or asthma with airflow obstruction that is not completely reversible after aggressive treatment with bronchodilators. 8
The Alpha-1 Foundation and the European Respiratory Society (ERS) have formulated guidelines for AATD testing. 11 , 23 By themselves, AAT levels are insufficient for identifying patients with or at risk for the disease: the levels can change with inflammation and with pregnancy. As such, confirmatory testing is strongly recommended via AAT genotyping to identify normal, deficient, or non-functioning alleles. Further, genotyping can enable the identification of more rare AAT alleles, which otherwise would go unrecognized. 23 Both Alpha-1 and ERS recommend an initial baseline lung-function evaluation that includes measurement of diffusing capacity when a diagnosis of AATD is made. 11 , 23 Clinicians can then follow lung function over time to help them decide when or whether to initiate treatment.
The pharmacotherapy of patients with COPD as a result of AATD is the same as that of similar patients with COPD: evidence-based use of a bronchodilator, inhaled steroids, supplemental oxygen, vaccinations, smoking cessation, and pulmonary rehabilitation. 2 Standard COPD treatments may not be as effective for individuals with AATD, and certain patients will require specific treatment with weekly infusions of augmentation therapy. 2 , 24
Alpha-1 Antitrypsin Replacement
Recommendations for initiating AAT replacement therapy vary to some degree by professional society. Replacement therapy in AATD is typically recommended for patients with moderate airflow obstruction (forced expiratory volume in the first second [FEV 1 ], 35–60% of predicted) and AAT levels < 11 μM. 10 Treatment for individuals outside these criteria can be individualized after the patient and care team have discussed the risks and benefits. Alpha-1 antitrypsin therapy, which is derived from human donor plasma, has been available commercially since 1987. Vials of lyophilized alpha-1 proteinase inhibitor and diluent are stored at room temperature before reconstitution; the specific diluents vary with available products. 25 – 28 These products, one of which can be self-administered by the patient/caregiver at home after proper training, 26 are administered by intravenous (IV) infusion only. Although the products are generally well tolerated, vital signs and infusion-related reactions should be monitored continuously during administration, as there is a risk of viral transmission. Alpha-1 proteinase inhibitor levels can be followed with chronic treatment.
The cost of augmentation therapy can be as much as $150,000 annually, depending on such variables as patient weight, frequency of dosing, specific product pricing, line access, and cost of nursing care. 17 , 29 , 30 The most common dose is 60 mg/kg/week, although it may be given biweekly or monthly. Candidates for replacement therapy who do not smoke, are adherent to therapy, and have mild to moderate COPD are more likely to have therapy initiated at established treatment centers. 29 Augmentation therapy is not recommended for patients with the MZ genotype, patients who continue to smoke, or patients with emphysema who do not have airflow obstruction. 22
CASE REPORT
A 70-year-old man who is an avid cyclist presented to the pulmonary clinic with complaints of dyspnea and wheezing while cycling on a recent trip to Europe. He had been followed and treated by primary care providers for years. He has a 1-pack-year history of cigarette smoking but quit 40 years ago. Pulmonary function testing was performed and was notable for mild obstructive lung disease. He was started on an inhaled long-acting muscarinic antagonist, and a computerized tomography (CT) scan of his chest was performed, which revealed emphysematous changes. At follow-up six months later, the patient continued to have intermittent symptoms but was doing well overall. Approximately one year after his initial presentation to the lung specialist, an alpha-1 level was drawn and found to be deficient, at 21 mg/dL. After testing, the genotype was determined to be ZZ. Interestingly, the patient had a gradual decline in his pulmonary-function testing over the year of evaluation and, given his continued decline, the decision was made to initiate augmentation therapy. His lung function has since stabilized but he has developed exercise-induced hypoxia; therefore, he maintains his active lifestyle with supplemental oxygen, and rides his bicycle upward of 15 miles daily.
Chronic obstructive pulmonary disease is a preventable, heterogeneous disease that can be attributed to multiple risk factors, including genetic conditions and predispositions. Alpha-1 antitrypsin deficiency is a significant, under-recognized risk factor for the development and progression of the disease. Aggressive guideline-based AAT screening for all patients with COPD or adult-onset asthma is encouraged. Identifying patients with deficient, null, or dysfunctional phenotypes of AATD will enable clinicians to initiate individualized treatments to prevent further lung-function decline. Although AATD infusion-replacement therapy may be beneficial, it must be administered in conjunction with other important guideline-based approaches and treatments, such as smoking cessation.
The data supporting AATD replacement therapy were generated by multiple small studies. Recruiting large AATD populations is challenging because of the limited number of patients who have been identified with the disease. Replacement therapy raises plasma AAT levels, but the clinical impact of enzyme replacement remains difficult to quantify. Small studies have shown a reduction in the rate of lung-function decline, with a corresponding decrease in mortality. Continuing research is needed into additional or new modalities for quantifying disease progression or regression in patients with AATD and COPD. One such modality is more specialized imaging via CT scans, which could improve our understanding of the impact of replacement therapy among patients with AATD.
Disclosure: The authors report no commercial or financial interest in regard to this article.
Infantile alpha 1 antitrypsin deficiency: a case report
- PMID: 7727562
- DOI: 10.1097/00001610-199501000-00005
Using a case study format, the authors describe an infant with an unusual metabolic disorder, Alpha 1 Antitrypsin Deficiency. It is rare to find an infant in whom such significant liver and pulmonary disease develops before his first birthday. In this article the authors describe the pathophysiology, genetics, diagnosis, and treatment of this disorder. The nursing diagnoses alteration in nutrition, alteration in skin integrity, ineffective airway clearance, and potential for ineffective family coping are the framework used to describe the nursing care.
Publication types
- Case Reports
- Genetic Diseases, Inborn / diagnosis
- Genetic Diseases, Inborn / nursing*
- Infant, Newborn
- Nursing Diagnosis
- alpha 1-Antitrypsin Deficiency*

IMAGES
VIDEO
COMMENTS
Background Generally, alpha-1 antitrypsin deficiency (AATD) is suspected in young patients with pulmonary emphysema or chronic obstructive pulmonary disease (COPD). Patients often suffer from diagnostic gaps and are misdiagnosed with chronic obstructive pulmonary disease (COPD), asthma, and airway hyperresponsiveness (AHR), as AATD may present with nonspecific respiratory symptoms. It is never ...
A diagnostic dilemma: case study of a 36-year-old female with alpha-1-antitrypsin deficiency. 2005 Mar-Apr;101 (2):73-4. James P Clark 2nd. Dept. of Pediatrics, West Virginia University School of Medicine, Charleston Division, USA. Alpha-1-antitrypsin deficiency is a genetic disorder that presents as early-onset emphysema in its most severe ...
Alpha-1 antitrypsin deficiency (AATD) is an autosomal dominant genetic disorder that presents with pulmonary complications and is most commonly manifested by panacinar emphysema and chronic obstructive pulmonary disease. A 49-year-old Caucasian female with a history of AATD and chronic tobacco use was referred to both infectious disease and ...
Interim results of a large case-control study. J Pediatr Gastroenterol Nutr 2006;43: Suppl 1: S30-S35. ... Diagnostic Tests for Alpha 1-Antitrypsin (AAT) Deficiency and Associated Disease Risks.
Abstract. Clinical heterogeneity has been demonstrated in alpha-1 antitrypsin deficiency (AATD), such that clinical suspicion plays an important role in its diagnosis. The PiZZ genotype is the most common severe deficiency genotype and so tends to result in the worst clinical presentation, hence it has been the major focus of research.
Alpha 1 Antitrypsin Deficiency (AATD) is a rare condition primarily associated with lung complications and liver disease. As disease symptoms are similar to those in other respiratory conditions, patients generally experience long delays before receiving an accurate diagnosis and treatment. ... Case series. This study, investigating rare/novel ...
Figure. Alpha-1 antitrypsin (AAT) deficiency is a common genetic condition characterized by low serum levels of AAT, which is a major circulating serine protease inhibitor (PI). 1 AAT is synthesized in the liver, and has a key role in inhibiting neutrophil elastase, thereby protecting tissues, particularly the lungs, from degradation.AAT deficiency occurs as a result of mutations in the ...
Alpha-1 antitrypsin deficiency and risk of lung cancer in never-smokers: a multicentre case-control study BMC Cancer. 2022 Jan 19;22(1) :81. doi: 10 ... Methods: A multicentre case-control study was conducted in Spain across the period January 2011 to August 2019. Cases were non-smokers diagnosed with LC, and controls were composed of never ...
In alpha-1 antitrypsin deficiency (AATD)-associated chronic obstructive pulmonary disease (COPD), HRQoL research remains scarce. ... Methods: Our study included participants of AlphaNet (2008-2019), a health management organization for people with AATD in the US who are prescribed augmentation therapy. Norm-based SF-36 scores for the mental and ...
Asthma and alpha-1 antitrypsin deficiency (AATD) differ in pathogenesis but can present with similar clinical symptoms, such as dyspnea, wheezing and cough. The similarity of symptoms can often lead to delayed or missed diagnosis of AATD in patients with concurrent asthma. Our abstract focuses on the importance of assessing for AATD in those ...
This public archive of the Alphal-Antitrypsin Deficiency Registry Database was developed by the Cleveland Clinic Foundation's Department of Biostatistics and Epidemiology and is being distributed by the Registry's sponsor, the National Heart Lung and Blood Institute (NHLBI). We have strived to make the CD complete and self-documenting.
Case presentation. We describe a case of a 69-year-old Caucasian female patient, late diagnosis of AATD, with both severe bronchial hyperreactivity and numerous exacerbations due to the peculiar clinical history and the presence of a rare mutation; although not presenting forced expiratory volume in 1 second (FEV 1) between 30 and 65%, the patient was treated with alpha-1 antitrypsin (AAT ...
Brief Summary of Findings on the Association Between Alpha-1 Antitrypsin Deficiency and Severe COVID-19 Outcomes . Six studies were included for analysis. Three cohort studies, two ecological studies, and one case report were retrieved that reported data on underlying Alpha-1 Antitrypsin Deficiency ( A1AT) and severe COVID-19 outcomes.
Alpha-1 antitrypsin (AAT) deficiency is a clinically under-recognized genetic disorder that causes the defective production of alpha-1 antitrypsin protein. AAT protein protects the body from the neutrophil elastase enzyme which is released from white blood cells to fight infection. This inherited disorder leads to decreased AAT activity in the blood and lung and deposition of excessive ...
Identifying AATD cases. Alpha-1-antitrypsin deficiency (AATD) is an autosomal genetic disorder and one of the most frequent genetic causes of liver and lung diseases Citation (1).Inherited low concentrations of alpha-1-antitrypsin lead to unopposed proteolysis in the lungs, predisposing individuals to early-onset emphysema, which predominantly affects the lower zones of the lungs.
Alpha-1 antitrypsin deficiency is a genetic condition that can cause lung and liver damage. Lung symptoms are usually similar to emphysema, including chronic cough, shortness of breath and wheezing. Treatments can reduce your risk of lung damage. Not smoking is the best way to reduce your risk of serious complications.
Panniculitis represents a rare and potentially lethal manifestation of alpha-1 antitrypsin deficiency (AATD). Evidence regarding management is limited to case reports and small case series. We sought to clarify typical features and investigation of AATD-associated panniculitis and assess the evidence regarding therapeutic options.
Through this case study, we present some challenges and limitations of a BIA of managing patients affected with alpha-1 antitrypsin deficiency (AATD). We explored a conceptual basis and barriers for health services researchers interested in quantifying budget impacts of rare disease management program (DMP).
Casas F, Blanco I, Martínez MT, Bustamante A, Miravitlles M, Cadenas S, et al. Indications for active case searches and intravenous alpha-1 antitrypsin treatment for patients with alpha-1 antitrypsin deficiency chronic pulmonary obstructive disease: an update. Arch Bronconeumol. 2015; 51 (4):185-192. doi: 10.1016/j.arbres.2014.05.008.
Through this case study, we present some challenges and limitations of a BIA of managing patients affected with alpha-1 antitrypsin deficiency (AATD). We explored a conceptual basis and barriers for health services researchers interested in quantifying budget impacts of rare disease management program (DMP).
A new study published in Orphanet Journal of Rare Diseases looked at patients who have a rare genetic condition called Alpha-1 antitrypsin deficiency (AATD) which causes lung disease similar to ...
Alpha-1 antitrypsin deficiency is a genetic disorder characterized by ... a systematic analysis for the Global Burden of Disease Study 2015 [published online August 16, 2017] Lancet Respir Med ... et al. Early detection of COPD: a case finding study in general practice [published online August 14, 2006] Respir Med. 2007; 101 (3):525-530 ...
Alpha-1 antitrypsin deficiency, or AATD, is an inherited disease that affects the lung, liver, and skin. ... A Phase 2 ASTRAEUS study in augmentation-naive patients, showed a statistically ...
Case study: alpha 1-antitrypsin deficiency in a burn patient. Case study: alpha 1-antitrypsin deficiency in a burn patient J Burn Care Rehabil. Jul-Aug 1985;6(4):369-71. doi: 10.1097/00004630-198507000-00013. Authors M Cole, D N Herndon. PMID: 3879939 DOI: 10.1097 ...
Using a case study format, the authors describe an infant with an unusual metabolic disorder, Alpha 1 Antitrypsin Deficiency. It is rare to find an infant in whom such significant liver and pulmonary disease develops before his first birthday. In this article the authors describe the pathophysiology …