
Literature Review Basics
- What is a Literature Review?
- Synthesizing Research
- Using Research & Synthesis Tables
- Additional Resources

About the Research and Synthesis Tables
Research Tables and Synthesis Tables are useful tools for organizing and analyzing your research as you assemble your literature review. They represent two different parts of the review process: assembling relevant information and synthesizing it. Use a Research table to compile the main info you need about the items you find in your research -- it's a great thing to have on hand as you take notes on what you read! Then, once you've assembled your research, use the Synthesis table to start charting the similarities/differences and major themes among your collected items.
We've included an Excel file with templates for you to use below; the examples pictured on this page are snapshots from that file.
- Research and Synthesis Table Templates This Excel workbook includes simple templates for creating research tables and synthesis tables. Feel free to download and use!
Using the Research Table

This is an example of a research table, in which you provide a basic description of the most important features of the studies, articles, and other items you discover in your research. The table identifies each item according to its author/date of publication, its purpose or thesis, what type of work it is (systematic review, clinical trial, etc.), the level of evidence it represents (which tells you a lot about its impact on the field of study), and its major findings. Your job, when you assemble this information, is to develop a snapshot of what the research shows about the topic of your research question and assess its value (both for the purpose of your work and for general knowledge in the field).
Think of your work on the research table as the foundational step for your analysis of the literature, in which you assemble the information you'll be analyzing and lay the groundwork for thinking about what it means and how it can be used.
Using the Synthesis Table

This is an example of a synthesis table or synthesis matrix , in which you organize and analyze your research by listing each source and indicating whether a given finding or result occurred in a particular study or article ( each row lists an individual source, and each finding has its own column, in which X = yes, blank = no). You can also add or alter the columns to look for shared study populations, sort by level of evidence or source type, etc. The key here is to use the table to provide a simple representation of what the research has found (or not found, as the case may be). Think of a synthesis table as a tool for making comparisons, identifying trends, and locating gaps in the literature.
How do I know which findings to use, or how many to include? Your research question tells you which findings are of interest in your research, so work from your research question to decide what needs to go in each Finding header, and how many findings are necessary. The number is up to you; again, you can alter this table by adding or deleting columns to match what you're actually looking for in your analysis. You should also, of course, be guided by what's actually present in the material your research turns up!
- << Previous: Synthesizing Research
- Next: Additional Resources >>
- Last Updated: Sep 26, 2023 12:06 PM
- URL: https://usi.libguides.com/literature-review-basics

- Walden University
- Faculty Portal
Common Assignments: Literature Review Matrix
Literature review matrix.
As you read and evaluate your literature there are several different ways to organize your research. Courtesy of Dr. Gary Burkholder in the School of Psychology, these sample matrices are one option to help organize your articles. These documents allow you to compile details about your sources, such as the foundational theories, methodologies, and conclusions; begin to note similarities among the authors; and retrieve citation information for easy insertion within a document.
You can review the sample matrixes to see a completed form or download the blank matrix for your own use.
- Literature Review Matrix 1 This PDF file provides a sample literature review matrix.
- Literature Review Matrix 2 This PDF file provides a sample literature review matrix.
- Literature Review Matrix Template (Word)
- Literature Review Matrix Template (Excel)
Related Resources
Didn't find what you need? Email us at [email protected] .
- Previous Page: Commentary Versus Opinion
- Next Page: Professional Development Plans (PDPs)
- Office of Student Disability Services
Walden Resources
Departments.
- Academic Residencies
- Academic Skills
- Career Planning and Development
- Customer Care Team
- Field Experience
- Military Services
- Student Success Advising
- Writing Skills
Centers and Offices
- Center for Social Change
- Office of Academic Support and Instructional Services
- Office of Degree Acceleration
- Office of Research and Doctoral Services
- Office of Student Affairs
Student Resources
- Doctoral Writing Assessment
- Form & Style Review
- Quick Answers
- ScholarWorks
- SKIL Courses and Workshops
- Walden Bookstore
- Walden Catalog & Student Handbook
- Student Safety/Title IX
- Legal & Consumer Information
- Website Terms and Conditions
- Cookie Policy
- Accessibility
- Accreditation
- State Authorization
- Net Price Calculator
- Contact Walden
Walden University is a member of Adtalem Global Education, Inc. www.adtalem.com Walden University is certified to operate by SCHEV © 2024 Walden University LLC. All rights reserved.

Nursing and Allied Health: Building a Summary Table or Synthesis Matrix
- Nursing Library Services
- Library Support for Nursing Accreditation
- Academic Research Libraries (ACRL) Information Literacy Standards for Science
- ACRL Guidelines for Distance Learning
- AACN Resources: Information Literacy
- The Essentials: Core Competencies for Professional Nursing Education
- Accreditation Commision for Education
- ACEN Learning Resources | Definitions & Standards
- Tutoring: College of Nursing & Allied Health Students
- Technology and Collaboration
- Affordable Learning Louisiana
- NIH Virtual Reality Funding
- Assistive Technology Resources
- Web Accessibility Initiative WC3
- Healthcare Links for Persons With Disabilities
- Accessibility
- Accessibility Tools: Videos
- Braile Institute: Blind and Low Vision Web Accessibility
- Braile Institute: Assistive Technology for the Visually Impaired This link opens in a new window
- Mental Health Resources for Students & Faculty
- Student Activities & Organizations
- Anatomage Video Training
- APA Reference Worksheet With Examples This link opens in a new window
- APA Style and Grammar Guidelines, 7.0
- What's New in APA Guide, 7.0 This link opens in a new window
- APA Instructional Aids for Professors/Instructors
- APA Handouts & Guides This link opens in a new window
- Sample Papers for Students and Instructors
- Academic Writer Tutorial: Basics This link opens in a new window
- APA Styling Your Paper
- When to cite or not cite a database
- Video: A Step-By-Step Guide for APA Style Student Papers
- Video: Citing Works in Text Using APA 7.0 This link opens in a new window
- Video: Creating References Using APA Guide, 7.0 This link opens in a new window
- Journal Article Reporting Standards
- Digital Information Literacy
- Tips Sheet: Copyright Essentials for Higher Education This link opens in a new window
- Citing National Patient Safety Goals (Joint Commission)
- Citing Agency for Healthcare Research and Quality (AHRQ) in APA format
- Best Nursing Apps
- Writing an Abstract for Your PILT or Special Project
- PILT Poster Presentation Archive
- Academic Success
- Healthcare Career Salaries
- Industry Statistics: Healthcare
- Nursing Organizations
- Radiology Organizations
- Controlled Medical Vocabularies
- COVID-19 Current Vaccines (Medscape)
- COVID-19 Current and Candidate Vaccine Landscape and Tracker (WHO)
- COVID-19: Clinical Care (Open Access) This link opens in a new window
- COVID-19: Clinician Care Guidance (CDC.gov) This link opens in a new window
- COVID-19: Coronavirus (NEJM) This link opens in a new window
- COVID -19 Contract Tracing & Patient Privacy (Cornell) This link opens in a new window
- COVID-19: Coronavirus Dashboard (Johns Hopkins Epidemiology)
- COVID-19: Coronavirus Guidelines (Up-To-Date) This link opens in a new window
- COVID-19: Critical Care Evidence (Cochrane) This link opens in a new window
- COVID-19: Diagnosis & Treatment (JAMA) This link opens in a new window
- COVID-19: Free Video Access (Jove) This link opens in a new window
- COVID-19: General Guidance (NSULA)
- COVID-19: Healthcare Hub (Elsevier) This link opens in a new window
- COVID-19 Healthcare Infection Prevention Control (CDC)
- COVID-19: Keeping Up With A Moving Target (Johns Hopkins Nursing Videos)
- COVID-19: LitCovid Daily Update (NLM)
- COVID-19: Literature Links (Massachusetts General Hospital (Epidemiology))
- COVID-19: Louisiana Department of Health
- COVID-19: Novel Coronavirus Information Center (Elsevier) This link opens in a new window
- COVID-19 Nursing Resources (Medscape)
- COVID-19: Open Access Resources (EBSCO)
- COVID-19: Red Book - Recent Pediatric Updates (AAP)
- COVID-19: Resource Center (ECRI Trust) This link opens in a new window
- COVID-19: Twitter Feed (Johns Hopkins)
- COVID-19: Updates (NSULA)
- COVID-19: Washing Your Hands Thoroughly (NHS)
- COVID-19: Well-Being Initiative (ANF)
- COVID-19: Worldwide Map from (Medscape Nursing)
- Properly Putting On Your Facemask & Getting a Good Seal (Dr. Scheiner) This link opens in a new window
- Washing Your Hands the NHS way! (NHS-UK)
- Creating Personal Accounts
- Creating a CINAHL MyFolder Account
- Creating a PubMed | MyNCBI Personal Account
- Creating a ProQuest Nursing & Allied Health Premium | MyResearch Folder
- Creating an OVID MyWorkspace Personal Account
- Mobile APPS | CINAHL for Apple and Android Mobile Devices
- My Circulation Login
- Interlibrary Loan Personal Account
- Data Visualization Products
- International Classification of Diseases (ICD)
- Diagnostic and Statistical Manual of Mental Disorders | DSM-5-TR
- [C1] Infections | Infectious Diseases
- [C04] Neoplasms
- [C05] Musculoskeletal Diseases
- [C06] Digestive System Diseases
- [C07] Stomatognathic Diseases
- [C08] Respiratory Tract Diseases
- [C09] Otorhinolaryngologic Diseases
- [C10] Nervous System Diseases
- [C11] Eye Diseases
- [C12] Urogenital Diseases
- [C14] Cardiovascular Diseases
- [C15] Hemic and Lymphatic Diseases
- [C16] Congenital, Hereditary, and Neonatal Diseases and Abnormalities
- [C17] Skin and Connective Tissue Diseases
- [C18] Nutritional and Metabolic Diseases
- [C19] Endocrine System Diseases
- [C20] Immune System Diseases
- [C21] Disorders of Environmental Origin
- [C22] Animal Diseases [Zoonotic diseases]
- [C23] Pathological Conditions, Signs and Symptoms
- [C24] Occupational Diseases
- [C25] Chemically-Induced Disorders
- [C26] Wounds and Injuries
- WHO Drug Information [Relative to Diseases]
- NDDK Patient Education Tool Kit
- Clinical Tools & Patient Education
- NDDK Resources on Medline Plus
- NDDK Open Research
- Dietary Guidelines for Americans
- Physical Activity Guidelines for Americans
- Move Your Way Community Resources
- National Youth Sports Strategy
- President’s Council on Sports, Fitness & Nutrition
- White House Conference on Hunger, Nutrition, and Health
- Equitable Long-Term Recovery and Resilience
- National Health Observances
- Finding Clinical Trials
- NIH News in Health
- Dosage Calculations & Pharmacology
- PICO - EBM Video This link opens in a new window
- PICO Slides
- Fillable CONSAH Pico Form
- Evidence Based Practice for Nursing
- Evidence-Based Nursing: -Step 2
- Evidence Appraisal - Step 3
- Evidence Application - Step 4
- Outcome Evaluation - Step 5
- Evidence Translation - Step 6
- Google Advanced Search for EBM
- Nursing Research Methods
- Faculty Book Request
- Proctor Request Form
- Peer Reviewed Literature: Assessment Goals
- EBSCO eBooks Anesthesia
- Full Text Finder
- EBSCO e-Books Nursing 2021
- EBSCO eBooks Radiology Science & Allied Health
- EBSCO eBooks: Writing About Nursing and Allied Health
- Alzheimers and Dementia
- Statistics on Aging
- CDC Bibliography: Alzheimers & Aging This link opens in a new window
- Health Conditions
- Health Behaviors
- Populations
- Settings and Systems
- Social Determinants of Health
- ILL Interlibrary Loan
- Gestational Diabetes and Fast Foods (MeSH)
- Mobile Resources
- Full Text eBooks Categories
- Nursing Theory
- Psychiatric Nursing Journals
- Display, sort and; navigate
- Similar articles
- Cite, save and share
- Citations in PubMed
- All About PubMed Filters
- PubMed Quick Tours and Tutorials
- Evidence Based Practice Tutorial (PubMed) This link opens in a new window
- Developing a Clinical Question This link opens in a new window
- Using PubMed to Find Relevant Articles This link opens in a new window
- Next Steps This link opens in a new window
- Scenario (practice) This link opens in a new window
- Radiology Books and e-Books
- History of Radiology & Radiography
- Radiology: Anatomage This link opens in a new window
- Radiology Anatomy Atlas Viewer
- Advanced Radiographic Research
- Diagnostic Imaging Selected Articles
- Faculty and Administrative Resources
- Radiology Tech and MRI Salaries (Bureau of Labor Statistics)
- Radiology Technician Demand by State
- Review Tools for Graduate Students
- Training & Videos
- Register for an Online Meeting
- Joining an Online Meeting
- Training Videos & Search Examples
- Training Survey
- Sources for Health Statistics
- Ebola and Infectious Diseases
- Nursing Sites
Building a Summary Table or Synthesis Matrix

Quick Links | Nursing & Allied Health

- Library Home
- Campus Computer Labs
- Circulation Policies
- Catalog Search (books/ebooks)
- Contact Your Librarian For Research Assistance (link sends email)
- Database Directory >> Nursing & Allied Health
- Faculty Materials Request Form
- Holidays & University Closures
- Interlibrary Loan Request Form
- Journals Full Text Finder
- LibGuides (Online Help)
- Review My Paper**
- Shreveport Proctor Request Form
- Shreveport Main Phone: (318) 677-3007
- Shreveport Librarian Phone: (318) 677-3013
- Student Help Desk : Phone: (318) 357-6696 [email protected]
- The 20-20-20 Rule
- Training Videos
** Submit your research paper for grammar review
GOOGLE MAP | LINKED

- Simplifying Synthesis | Download the Article PDF Copy
- Writing a Literature Review and Using a Synthesis Matrix
What a Summary Table or Synthesis Matrix looks like
Use the "Literature Review Matrix Template" as a guideline to help you sort through your thoughts, note important points and think through the similarities and differences:
You are organizing the review by ideas and not by sources . The literature review is not just a summary of the already published works. Your synthesis should show how various articles are linked.

A summary table is also called a synthesis matrix. The table helps you organize and compare information for your systematic review, scholarly report, dissertation or thesis
Synthesis Matrix.
A summary table is also called a synthesis matrix . A summary table helps you record the main points of each source and document how sources relate to each other. After summarizing and evaluating your sources, arrange them in a matrix to help you see how they relate to each other, and apply to each of your themes or variables.
Faculty who typically guide students find it challenging to help students learn how to synthesize material (Blondy, Blakesless, Scheffer, Rubenfeld, Cronin, & Luster-Turner, 2016; Kearney, 2015) . Writers can easily summarize material but seem to struggle to adequately synthesize knowledge about their topic and express that in their writing. So, whether you are writing a student papers, dissertations, or scholarly report it is necessary to learn a few tips and tricks to organize your ideas.
Building a summary table and developing solid synthesis skills is important for nurses, nurse practitioners, and allied health researchers. Quality evidence-based practice initiatives and nursing care and medicine are based on understanding and evaluating the resources and research available, identifying gaps, and building a strong foundation for future work.
Good synthesis is about putting the data gathered, references read, and literature analyzed together in a new way that shows connections and relationships. ( Shellenbarger, 2016 ). The Merriam-Webster dictionary defines synthesis as something that is made by combining different things or the composition or combination of parts or elements so as to form a whole (Synthesis, n.d.).
In other words, building a summary table or synthesis matrix involves taking information from a variety of sources, evaluating that information and forming new ideas or insights in an original way. This can be a new and potentially challenging experience for students and researchers who are used to just repeating what is already in the literature.

Visit Our Libraries

Interlibrary Loan | Shreveport Education Center Library | Eugene P. Watson Memorial Library | NSU Leesville Library
Cammie G. Henry Research Center | Prince Music Media Library
- << Previous: Best Nursing Apps
- Next: Writing an Abstract for Your PILT or Special Project >>
- Last Updated: Mar 19, 2024 1:14 PM
- URL: https://libguides.nsula.edu/nursingandalliedhealth
Five tips for developing useful literature summary tables for writing review articles
Affiliations.
- 1 Memorial University of Newfoundland, St John's, Newfoundland, Canada [email protected].
- 2 Swat College of Nursing, Pakistan.
- 3 School of Nursing and Midwifery, University of Sheffield, Sheffield, South Yorkshire, UK.
- 4 Sheffield University Interpersonal Violence Research Group, Sheffield University, Sheffield, UK.
- PMID: 33674415
- DOI: 10.1136/ebnurs-2021-103417
Publication types
- Review Literature as Topic*
- Statistics as Topic*
The Sheridan Libraries
- Write a Literature Review
- Sheridan Libraries
- Find This link opens in a new window
- Evaluate This link opens in a new window
Get Organized
- Lit Review Prep Use this template to help you evaluate your sources, create article summaries for an annotated bibliography, and a synthesis matrix for your lit review outline.
Synthesize your Information
Synthesize: combine separate elements to form a whole.
Synthesis Matrix
A synthesis matrix helps you record the main points of each source and document how sources relate to each other.
After summarizing and evaluating your sources, arrange them in a matrix or use a citation manager to help you see how they relate to each other and apply to each of your themes or variables.
By arranging your sources by theme or variable, you can see how your sources relate to each other, and can start thinking about how you weave them together to create a narrative.
- Step-by-Step Approach
- Example Matrix from NSCU
- Matrix Template
- << Previous: Summarize
- Next: Integrate >>
- Last Updated: Sep 26, 2023 10:25 AM
- URL: https://guides.library.jhu.edu/lit-review
What’s Included: Literature Review Template
This template is structure is based on the tried and trusted best-practice format for formal academic research projects such as dissertations and theses. The literature review template includes the following sections:
- Before you start – essential groundwork to ensure you’re ready
- The introduction section
- The core/body section
- The conclusion /summary
- Extra free resources
Each section is explained in plain, straightforward language , followed by an overview of the key elements that you need to cover. We’ve also included practical examples and links to more free videos and guides to help you understand exactly what’s required in each section.
The cleanly-formatted Google Doc can be downloaded as a fully editable MS Word Document (DOCX format), so you can use it as-is or convert it to LaTeX.
PS – if you’d like a high-level template for the entire thesis, you can we’ve got that too .
FAQs: Literature Review Template
What format is the template (doc, pdf, ppt, etc.).
The literature review chapter template is provided as a Google Doc. You can download it in MS Word format or make a copy to your Google Drive. You’re also welcome to convert it to whatever format works best for you, such as LaTeX or PDF.
What types of literature reviews can this template be used for?
The template follows the standard format for academic literature reviews, which means it will be suitable for the vast majority of academic research projects (especially those within the sciences), whether they are qualitative or quantitative in terms of design.
Keep in mind that the exact requirements for the literature review chapter will vary between universities and degree programs. These are typically minor, but it’s always a good idea to double-check your university’s requirements before you finalize your structure.
Is this template for an undergrad, Master or PhD-level thesis?
This template can be used for a literature review at any level of study. Doctoral-level projects typically require the literature review to be more extensive/comprehensive, but the structure will typically remain the same.
Can I modify the template to suit my topic/area?
Absolutely. While the template provides a general structure, you should adapt it to fit the specific requirements and focus of your literature review.
What structural style does this literature review template use?
The template assumes a thematic structure (as opposed to a chronological or methodological structure), as this is the most common approach. However, this is only one dimension of the template, so it will still be useful if you are adopting a different structure.
Does this template include the Excel literature catalog?
No, that is a separate template, which you can download for free here . This template is for the write-up of the actual literature review chapter, whereas the catalog is for use during the literature sourcing and sorting phase.
How long should the literature review chapter be?
This depends on your university’s specific requirements, so it’s best to check with them. As a general ballpark, literature reviews for Masters-level projects are usually 2,000 – 3,000 words in length, while Doctoral-level projects can reach multiples of this.
Can I include literature that contradicts my hypothesis?
Yes, it’s important to acknowledge and discuss literature that presents different viewpoints or contradicts your hypothesis. So, don’t shy away from existing research that takes an opposing view to yours.
How do I avoid plagiarism in my literature review?
Always cite your sources correctly and paraphrase ideas in your own words while maintaining the original meaning. You can always check our plagiarism score before submitting your work to help ease your mind.
Do you have an example of a populated template?
We provide a walkthrough of the template and review an example of a high-quality literature research chapter here .
Can I share this literature review template with my friends/colleagues?
Yes, you’re welcome to share this template in its original format (no editing allowed). If you want to post about it on your blog or social media, all we ask is that you reference this page as your source.
Do you have templates for the other dissertation/thesis chapters?
Yes, we do. You can find our full collection of templates here .
Can Grad Coach help me with my literature review?
Yes, you’re welcome to get in touch with us to discuss our private coaching services , where we can help you work through the literature review chapter (and any other chapters).

Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Writing a Literature Review

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays). When we say “literature review” or refer to “the literature,” we are talking about the research ( scholarship ) in a given field. You will often see the terms “the research,” “the scholarship,” and “the literature” used mostly interchangeably.
Where, when, and why would I write a lit review?
There are a number of different situations where you might write a literature review, each with slightly different expectations; different disciplines, too, have field-specific expectations for what a literature review is and does. For instance, in the humanities, authors might include more overt argumentation and interpretation of source material in their literature reviews, whereas in the sciences, authors are more likely to report study designs and results in their literature reviews; these differences reflect these disciplines’ purposes and conventions in scholarship. You should always look at examples from your own discipline and talk to professors or mentors in your field to be sure you understand your discipline’s conventions, for literature reviews as well as for any other genre.
A literature review can be a part of a research paper or scholarly article, usually falling after the introduction and before the research methods sections. In these cases, the lit review just needs to cover scholarship that is important to the issue you are writing about; sometimes it will also cover key sources that informed your research methodology.
Lit reviews can also be standalone pieces, either as assignments in a class or as publications. In a class, a lit review may be assigned to help students familiarize themselves with a topic and with scholarship in their field, get an idea of the other researchers working on the topic they’re interested in, find gaps in existing research in order to propose new projects, and/or develop a theoretical framework and methodology for later research. As a publication, a lit review usually is meant to help make other scholars’ lives easier by collecting and summarizing, synthesizing, and analyzing existing research on a topic. This can be especially helpful for students or scholars getting into a new research area, or for directing an entire community of scholars toward questions that have not yet been answered.
What are the parts of a lit review?
Most lit reviews use a basic introduction-body-conclusion structure; if your lit review is part of a larger paper, the introduction and conclusion pieces may be just a few sentences while you focus most of your attention on the body. If your lit review is a standalone piece, the introduction and conclusion take up more space and give you a place to discuss your goals, research methods, and conclusions separately from where you discuss the literature itself.
Introduction:
- An introductory paragraph that explains what your working topic and thesis is
- A forecast of key topics or texts that will appear in the review
- Potentially, a description of how you found sources and how you analyzed them for inclusion and discussion in the review (more often found in published, standalone literature reviews than in lit review sections in an article or research paper)
- Summarize and synthesize: Give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: Don’t just paraphrase other researchers – add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically Evaluate: Mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: Use transition words and topic sentence to draw connections, comparisons, and contrasts.
Conclusion:
- Summarize the key findings you have taken from the literature and emphasize their significance
- Connect it back to your primary research question

How should I organize my lit review?
Lit reviews can take many different organizational patterns depending on what you are trying to accomplish with the review. Here are some examples:
- Chronological : The simplest approach is to trace the development of the topic over time, which helps familiarize the audience with the topic (for instance if you are introducing something that is not commonly known in your field). If you choose this strategy, be careful to avoid simply listing and summarizing sources in order. Try to analyze the patterns, turning points, and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred (as mentioned previously, this may not be appropriate in your discipline — check with a teacher or mentor if you’re unsure).
- Thematic : If you have found some recurring central themes that you will continue working with throughout your piece, you can organize your literature review into subsections that address different aspects of the topic. For example, if you are reviewing literature about women and religion, key themes can include the role of women in churches and the religious attitude towards women.
- Qualitative versus quantitative research
- Empirical versus theoretical scholarship
- Divide the research by sociological, historical, or cultural sources
- Theoretical : In many humanities articles, the literature review is the foundation for the theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You can argue for the relevance of a specific theoretical approach or combine various theorical concepts to create a framework for your research.
What are some strategies or tips I can use while writing my lit review?
Any lit review is only as good as the research it discusses; make sure your sources are well-chosen and your research is thorough. Don’t be afraid to do more research if you discover a new thread as you’re writing. More info on the research process is available in our "Conducting Research" resources .
As you’re doing your research, create an annotated bibliography ( see our page on the this type of document ). Much of the information used in an annotated bibliography can be used also in a literature review, so you’ll be not only partially drafting your lit review as you research, but also developing your sense of the larger conversation going on among scholars, professionals, and any other stakeholders in your topic.
Usually you will need to synthesize research rather than just summarizing it. This means drawing connections between sources to create a picture of the scholarly conversation on a topic over time. Many student writers struggle to synthesize because they feel they don’t have anything to add to the scholars they are citing; here are some strategies to help you:
- It often helps to remember that the point of these kinds of syntheses is to show your readers how you understand your research, to help them read the rest of your paper.
- Writing teachers often say synthesis is like hosting a dinner party: imagine all your sources are together in a room, discussing your topic. What are they saying to each other?
- Look at the in-text citations in each paragraph. Are you citing just one source for each paragraph? This usually indicates summary only. When you have multiple sources cited in a paragraph, you are more likely to be synthesizing them (not always, but often
- Read more about synthesis here.
The most interesting literature reviews are often written as arguments (again, as mentioned at the beginning of the page, this is discipline-specific and doesn’t work for all situations). Often, the literature review is where you can establish your research as filling a particular gap or as relevant in a particular way. You have some chance to do this in your introduction in an article, but the literature review section gives a more extended opportunity to establish the conversation in the way you would like your readers to see it. You can choose the intellectual lineage you would like to be part of and whose definitions matter most to your thinking (mostly humanities-specific, but this goes for sciences as well). In addressing these points, you argue for your place in the conversation, which tends to make the lit review more compelling than a simple reporting of other sources.
- Introduction for Types of Dissertations
- Overview of the Dissertation
- Self-Assessment Exercise
- What is a Dissertation Committee
- Different Types of Dissertations
- Introduction for Overview of the Dissertation Process
- Responsibilities: the Chair, the Team and You
- Sorting Exercise
- Stages of a Dissertation
- Managing Your Time
- Create Your Own Timeline
- Working with a Writing Partner
- Key Deadlines
- Self Assessment Exercise
- Additional Resources
- Purpose and Goals
- Read and Evaluate Chapter 1 Exemplars
- Draft an Introduction of the Study
- Outline the Background of the Problem
- Draft your Statement of the Problem
- Draft your Purpose of the Study
- Draft your Significance of the Study
- List the Possible Limitations and Delimitations
- Explicate the Definition of Terms
- Outline the Organization of the Study
- Recommended Resources and Readings
- Purpose of the Literature Review
- What is the Literature?
- Article Summary Table
- Writing a Short Literature Review
- Outline for Literature Review
- Synthesizing the Literature Review
- Purpose of the Methodology Chapter
- Topics to Include
- Preparing to Write the Methodology Chapter
- Confidentiality
- Building the Components for Chapter Three
- Preparing for Your Qualifying Exam (aka Proposal Defense)
- What is Needed for Your Proposal Defense?
- Submitting Your Best Draft
- Preparing Your Abstract for IRB
- Use of Self-Assessment
- Preparing Your PowerPoint
- During Your Proposal Defense
- After Your Proposal Defense
- Pre-observation – Issues to consider
- During Observations
- Wrapping Up
- Recommended Resources and Readings (Qualitative)
- Quantitative Data Collection
- Recommended Resources and Readings (Quantitative)
- Qualitative: Before you Start
- Qualitative: During Analysis
- Qualitative: After Analysis
- Qualitative: Recommended Resources and Readings
- Quantitative: Deciding on the Right Analysis
- Quantitative: Data Management and Cleaning
- Quantitative: Keep Track of your Analysis
- The Purpose of Chapter 4
- The Elements of Chapter 4
- Presenting Results (Quantitative)
- Presenting Findings (Qualitative)
- Chapter 4 Considerations
- The Purpose of Chapter 5
- Preparing Your Abstract for the Graduate School
- Draft the Introduction for Chapter 5
- Draft the Summary of Findings
- Draft Implications for Practice
- Draft your Recommendations for Research
- Draft your Conclusions
- What is Needed
- What Happens During the Final Defense?
- What Happens After the Final Defense?
Article Summary Table Topic 4: Literature Review
Drafting a summary table
Contributor: Logan Miller
A summary table allows you to compare common research methods, findings, limitations, etc. You can order the entries in any way that you find useful; consider ordering your research alphabetically, by timeliness, or even by grouping similar study aims, models, or results.
Once compiled, you can use this table to compare studies side by side. Such comparison can help you see trends in findings, identify gaps in the research, and rank each study by relative strength. In short, it helps you organize information on a broad topic, which is a crucial first step in synthesizing that information within a research paper.
Summary areas might include
Authors / date : If a paper has numerous authors, consider the level of detail you require to identify a given study.
Aim of study / paper : What were the researchers hoping to learn? This section may include research questions or hypotheses.
Type of study / information : These might be systematic reviews, randomized controlled trials, etc. If you’re less familiar with what these designs entail, writing a short description can be useful.
Main findings / conclusions : The level of detail you employ will come down to necessity and experience, but in listing specific findings, you may see trends or discrepancies across studies.
Strengths / limitations : Strengths may include good research design or data-based conclusions. Remember, a study may mention its limitations explicitly, but many limitations require careful inquiry to uncover.
*Azzopardi, D., Patel, K., Jaunky, T., Santopietro, S., Camacho, O. M., McAughey, J., Gaça, M. (2016). Electronic cigarette aerosol induces significantly less cytotoxicity than tobacco smoke. Toxicology Mechanisms and Methods 26(6), 477-497, doi: 10.1080/15376516.2016.1217112

About Systematic Reviews
Summary of Findings Table in a Systematic Review

Automate every stage of your literature review to produce evidence-based research faster and more accurately.
What is a summary of findings table.
The Cochrane Review defines the “summary of findings table” as a structured tabular format in which the primary findings of a review, particularly information related to the quality of evidence, the magnitude of the effects of the studied interventions, and the aggregate of available data on the main outcomes, are presented. It includes multiple pieces of data derived from both quantitative and qualitative data analysis in systematic reviews . These include information about the main outcomes, the type and number of studies included, the estimates (both relative and absolute) of the effect or association, and important comments about the review, all written in a plain-language summary so that it’s easily interpreted. It also includes a grade of the quality of evidence; i.e., a rating of its certainty.
Most systematic reviews are expected to have one summary of findings table. But some studies may have multiple, if the review addresses more than one comparison, or deals with substantially different populations that require separate tables. The studies in a table can also be grouped in terms of applied intervention type, type of outcome measure, the type of participants, the study design etc..
How Do You Make A Summary Of Findings Table For A Systematic Review?
Learn more about distillersr.
(Article continues below)
What Does A Summary Of Findings Table Include?
A summary of findings table typically includes the following information:
- A description of the population and setting addressed by the available evidence
- A description of comparisons addressed in the table, including all interventions
- A list of the most important outcomes, whether desirable or undesirable (limited to seven)
- A measure of the burdens of each outcome
- The magnitude of effect measured for each outcome (both absolute and relative)
- The participants and studies analyzed for each outcome
- An assessment of the certainty of the evidence for each outcome (typically using GRADE)
- Explanations
It’s best to include evidence profiles, i.e. additional tables that support the data in the summary of findings, to which the review may be linked. It also may be neat to have a study descriptor table different from a results table. The study descriptor table shows information about the characteristics of included studies, like study design, study region, participant information, etc. The results table mostly contains outcomes, outcome measures, study results, etc. These can help provide readers with more context about the review, and its conclusions.
Final Takeaway
3 reasons to connect.
Jump to navigation

Cochrane Training
Chapter 14: completing ‘summary of findings’ tables and grading the certainty of the evidence.
Holger J Schünemann, Julian PT Higgins, Gunn E Vist, Paul Glasziou, Elie A Akl, Nicole Skoetz, Gordon H Guyatt; on behalf of the Cochrane GRADEing Methods Group (formerly Applicability and Recommendations Methods Group) and the Cochrane Statistical Methods Group
Key Points:
- A ‘Summary of findings’ table for a given comparison of interventions provides key information concerning the magnitudes of relative and absolute effects of the interventions examined, the amount of available evidence and the certainty (or quality) of available evidence.
- ‘Summary of findings’ tables include a row for each important outcome (up to a maximum of seven). Accepted formats of ‘Summary of findings’ tables and interactive ‘Summary of findings’ tables can be produced using GRADE’s software GRADEpro GDT.
- Cochrane has adopted the GRADE approach (Grading of Recommendations Assessment, Development and Evaluation) for assessing certainty (or quality) of a body of evidence.
- The GRADE approach specifies four levels of the certainty for a body of evidence for a given outcome: high, moderate, low and very low.
- GRADE assessments of certainty are determined through consideration of five domains: risk of bias, inconsistency, indirectness, imprecision and publication bias. For evidence from non-randomized studies and rarely randomized studies, assessments can then be upgraded through consideration of three further domains.
Cite this chapter as: Schünemann HJ, Higgins JPT, Vist GE, Glasziou P, Akl EA, Skoetz N, Guyatt GH. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. Available from www.training.cochrane.org/handbook .
14.1 ‘Summary of findings’ tables
14.1.1 introduction to ‘summary of findings’ tables.
‘Summary of findings’ tables present the main findings of a review in a transparent, structured and simple tabular format. In particular, they provide key information concerning the certainty or quality of evidence (i.e. the confidence or certainty in the range of an effect estimate or an association), the magnitude of effect of the interventions examined, and the sum of available data on the main outcomes. Cochrane Reviews should incorporate ‘Summary of findings’ tables during planning and publication, and should have at least one key ‘Summary of findings’ table representing the most important comparisons. Some reviews may include more than one ‘Summary of findings’ table, for example if the review addresses more than one major comparison, or includes substantially different populations that require separate tables (e.g. because the effects differ or it is important to show results separately). In the Cochrane Database of Systematic Reviews (CDSR), all ‘Summary of findings’ tables for a review appear at the beginning, before the Background section.
14.1.2 Selecting outcomes for ‘Summary of findings’ tables
Planning for the ‘Summary of findings’ table starts early in the systematic review, with the selection of the outcomes to be included in: (i) the review; and (ii) the ‘Summary of findings’ table. This is a crucial step, and one that review authors need to address carefully.
To ensure production of optimally useful information, Cochrane Reviews begin by developing a review question and by listing all main outcomes that are important to patients and other decision makers (see Chapter 2 and Chapter 3 ). The GRADE approach to assessing the certainty of the evidence (see Section 14.2 ) defines and operationalizes a rating process that helps separate outcomes into those that are critical, important or not important for decision making. Consultation and feedback on the review protocol, including from consumers and other decision makers, can enhance this process.
Critical outcomes are likely to include clearly important endpoints; typical examples include mortality and major morbidity (such as strokes and myocardial infarction). However, they may also represent frequent minor and rare major side effects, symptoms, quality of life, burdens associated with treatment, and resource issues (costs). Burdens represent the impact of healthcare workload on patient function and well-being, and include the demands of adhering to an intervention that patients or caregivers (e.g. family) may dislike, such as having to undergo more frequent tests, or the restrictions on lifestyle that certain interventions require (Spencer-Bonilla et al 2017).
Frequently, when formulating questions that include all patient-important outcomes for decision making, review authors will confront reports of studies that have not included all these outcomes. This is particularly true for adverse outcomes. For instance, randomized trials might contribute evidence on intended effects, and on frequent, relatively minor side effects, but not report on rare adverse outcomes such as suicide attempts. Chapter 19 discusses strategies for addressing adverse effects. To obtain data for all important outcomes it may be necessary to examine the results of non-randomized studies (see Chapter 24 ). Cochrane, in collaboration with others, has developed guidance for review authors to support their decision about when to look for and include non-randomized studies (Schünemann et al 2013).
If a review includes only randomized trials, these trials may not address all important outcomes and it may therefore not be possible to address these outcomes within the constraints of the review. Review authors should acknowledge these limitations and make them transparent to readers. Review authors are encouraged to include non-randomized studies to examine rare or long-term adverse effects that may not adequately be studied in randomized trials. This raises the possibility that harm outcomes may come from studies in which participants differ from those in studies used in the analysis of benefit. Review authors will then need to consider how much such differences are likely to impact on the findings, and this will influence the certainty of evidence because of concerns about indirectness related to the population (see Section 14.2.2 ).
Non-randomized studies can provide important information not only when randomized trials do not report on an outcome or randomized trials suffer from indirectness, but also when the evidence from randomized trials is rated as very low and non-randomized studies provide evidence of higher certainty. Further discussion of these issues appears also in Chapter 24 .
14.1.3 General template for ‘Summary of findings’ tables
Several alternative standard versions of ‘Summary of findings’ tables have been developed to ensure consistency and ease of use across reviews, inclusion of the most important information needed by decision makers, and optimal presentation (see examples at Figures 14.1.a and 14.1.b ). These formats are supported by research that focused on improved understanding of the information they intend to convey (Carrasco-Labra et al 2016, Langendam et al 2016, Santesso et al 2016). They are available through GRADE’s official software package developed to support the GRADE approach: GRADEpro GDT (www.gradepro.org).
Standard Cochrane ‘Summary of findings’ tables include the following elements using one of the accepted formats. Further guidance on each of these is provided in Section 14.1.6 .
- A brief description of the population and setting addressed by the available evidence (which may be slightly different to or narrower than those defined by the review question).
- A brief description of the comparison addressed in the ‘Summary of findings’ table, including both the experimental and comparison interventions.
- A list of the most critical and/or important health outcomes, both desirable and undesirable, limited to seven or fewer outcomes.
- A measure of the typical burden of each outcomes (e.g. illustrative risk, or illustrative mean, on comparator intervention).
- The absolute and relative magnitude of effect measured for each (if both are appropriate).
- The numbers of participants and studies contributing to the analysis of each outcomes.
- A GRADE assessment of the overall certainty of the body of evidence for each outcome (which may vary by outcome).
- Space for comments.
- Explanations (formerly known as footnotes).
Ideally, ‘Summary of findings’ tables are supported by more detailed tables (known as ‘evidence profiles’) to which the review may be linked, which provide more detailed explanations. Evidence profiles include the same important health outcomes, and provide greater detail than ‘Summary of findings’ tables of both of the individual considerations feeding into the grading of certainty and of the results of the studies (Guyatt et al 2011a). They ensure that a structured approach is used to rating the certainty of evidence. Although they are rarely published in Cochrane Reviews, evidence profiles are often used, for example, by guideline developers in considering the certainty of the evidence to support guideline recommendations. Review authors will find it easier to develop the ‘Summary of findings’ table by completing the rating of the certainty of evidence in the evidence profile first in GRADEpro GDT. They can then automatically convert this to one of the ‘Summary of findings’ formats in GRADEpro GDT, including an interactive ‘Summary of findings’ for publication.
As a measure of the magnitude of effect for dichotomous outcomes, the ‘Summary of findings’ table should provide a relative measure of effect (e.g. risk ratio, odds ratio, hazard) and measures of absolute risk. For other types of data, an absolute measure alone (such as a difference in means for continuous data) might be sufficient. It is important that the magnitude of effect is presented in a meaningful way, which may require some transformation of the result of a meta-analysis (see also Chapter 15, Section 15.4 and Section 15.5 ). Reviews with more than one main comparison should include a separate ‘Summary of findings’ table for each comparison.
Figure 14.1.a provides an example of a ‘Summary of findings’ table. Figure 15.1.b provides an alternative format that may further facilitate users’ understanding and interpretation of the review’s findings. Evidence evaluating different formats suggests that the ‘Summary of findings’ table should include a risk difference as a measure of the absolute effect and authors should preferably use a format that includes a risk difference .
A detailed description of the contents of a ‘Summary of findings’ table appears in Section 14.1.6 .
Figure 14.1.a Example of a ‘Summary of findings’ table
Summary of findings (for interactive version click here )
a All the stockings in the nine studies included in this review were below-knee compression stockings. In four studies the compression strength was 20 mmHg to 30 mmHg at the ankle. It was 10 mmHg to 20 mmHg in the other four studies. Stockings come in different sizes. If a stocking is too tight around the knee it can prevent essential venous return causing the blood to pool around the knee. Compression stockings should be fitted properly. A stocking that is too tight could cut into the skin on a long flight and potentially cause ulceration and increased risk of DVT. Some stockings can be slightly thicker than normal leg covering and can be potentially restrictive with tight foot wear. It is a good idea to wear stockings around the house prior to travel to ensure a good, comfortable fit. Participants put their stockings on two to three hours before the flight in most of the studies. The availability and cost of stockings can vary.
b Two studies recruited high risk participants defined as those with previous episodes of DVT, coagulation disorders, severe obesity, limited mobility due to bone or joint problems, neoplastic disease within the previous two years, large varicose veins or, in one of the studies, participants taller than 190 cm and heavier than 90 kg. The incidence for the seven studies that excluded high risk participants was 1.45% and the incidence for the two studies that recruited high-risk participants (with at least one risk factor) was 2.43%. We have used 10 and 30 per 1000 to express different risk strata, respectively.
c The confidence interval crosses no difference and does not rule out a small increase.
d The measurement of oedema was not validated (indirectness of the outcome) or blinded to the intervention (risk of bias).
e If there are very few or no events and the number of participants is large, judgement about the certainty of evidence (particularly judgements about imprecision) may be based on the absolute effect. Here the certainty rating may be considered ‘high’ if the outcome was appropriately assessed and the event, in fact, did not occur in 2821 studied participants.
f None of the other studies reported adverse effects, apart from four cases of superficial vein thrombosis in varicose veins in the knee region that were compressed by the upper edge of the stocking in one study.
Figure 14.1.b Example of alternative ‘Summary of findings’ table
14.1.4 Producing ‘Summary of findings’ tables
The GRADE Working Group’s software, GRADEpro GDT ( www.gradepro.org ), including GRADE’s interactive handbook, is available to assist review authors in the preparation of ‘Summary of findings’ tables. GRADEpro can use data on the comparator group risk and the effect estimate (entered by the review authors or imported from files generated in RevMan) to produce the relative effects and absolute risks associated with experimental interventions. In addition, it leads the user through the process of a GRADE assessment, and produces a table that can be used as a standalone table in a review (including by direct import into software such as RevMan or integration with RevMan Web), or an interactive ‘Summary of findings’ table (see help resources in GRADEpro).
14.1.5 Statistical considerations in ‘Summary of findings’ tables
14.1.5.1 dichotomous outcomes.
‘Summary of findings’ tables should include both absolute and relative measures of effect for dichotomous outcomes. Risk ratios, odds ratios and risk differences are different ways of comparing two groups with dichotomous outcome data (see Chapter 6, Section 6.4.1 ). Furthermore, there are two distinct risk ratios, depending on which event (e.g. ‘yes’ or ‘no’) is the focus of the analysis (see Chapter 6, Section 6.4.1.5 ). In the presence of a non-zero intervention effect, any variation across studies in the comparator group risks (i.e. variation in the risk of the event occurring without the intervention of interest, for example in different populations) makes it impossible for more than one of these measures to be truly the same in every study.
It has long been assumed in epidemiology that relative measures of effect are more consistent than absolute measures of effect from one scenario to another. There is empirical evidence to support this assumption (Engels et al 2000, Deeks and Altman 2001, Furukawa et al 2002). For this reason, meta-analyses should generally use either a risk ratio or an odds ratio as a measure of effect (see Chapter 10, Section 10.4.3 ). Correspondingly, a single estimate of relative effect is likely to be a more appropriate summary than a single estimate of absolute effect. If a relative effect is indeed consistent across studies, then different comparator group risks will have different implications for absolute benefit. For instance, if the risk ratio is consistently 0.75, then the experimental intervention would reduce a comparator group risk of 80% to 60% in the intervention group (an absolute risk reduction of 20 percentage points), but would also reduce a comparator group risk of 20% to 15% in the intervention group (an absolute risk reduction of 5 percentage points).
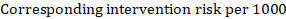
‘Summary of findings’ tables are built around the assumption of a consistent relative effect. It is therefore important to consider the implications of this effect for different comparator group risks (these can be derived or estimated from a number of sources, see Section 14.1.6.3 ), which may require an assessment of the certainty of evidence for prognostic evidence (Spencer et al 2012, Iorio et al 2015). For any comparator group risk, it is possible to estimate a corresponding intervention group risk (i.e. the absolute risk with the intervention) from the meta-analytic risk ratio or odds ratio. Note that the numbers provided in the ‘Corresponding risk’ column are specific to the ‘risks’ in the adjacent column.
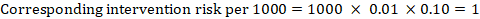
For the meta-analytic risk ratio (RR) and assumed comparator risk (ACR) the corresponding intervention risk is obtained as:
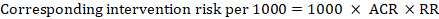
As an example, in Figure 14.1.a , the meta-analytic risk ratio for symptomless deep vein thrombosis (DVT) is RR = 0.10 (95% CI 0.04 to 0.26). Assuming a comparator risk of ACR = 10 per 1000 = 0.01, we obtain:
For the meta-analytic odds ratio (OR) and assumed comparator risk, ACR, the corresponding intervention risk is obtained as:
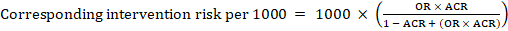
Upper and lower confidence limits for the corresponding intervention risk are obtained by replacing RR or OR by their upper and lower confidence limits, respectively (e.g. replacing 0.10 with 0.04, then with 0.26, in the example). Such confidence intervals do not incorporate uncertainty in the assumed comparator risks.
When dealing with risk ratios, it is critical that the same definition of ‘event’ is used as was used for the meta-analysis. For example, if the meta-analysis focused on ‘death’ (as opposed to survival) as the event, then corresponding risks in the ‘Summary of findings’ table must also refer to ‘death’.
In (rare) circumstances in which there is clear rationale to assume a consistent risk difference in the meta-analysis, in principle it is possible to present this for relevant ‘assumed risks’ and their corresponding risks, and to present the corresponding (different) relative effects for each assumed risk.
The risk difference expresses the difference between the ACR and the corresponding intervention risk (or the difference between the experimental and the comparator intervention).
For the meta-analytic risk ratio (RR) and assumed comparator risk (ACR) the corresponding risk difference is obtained as (note that risks can also be expressed using percentage or percentage points):
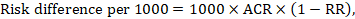
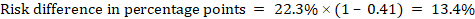
As an example, in Figure 14.1.b the meta-analytic risk ratio is 0.41 (95% CI 0.29 to 0.55) for diarrhoea in children less than 5 years of age. Assuming a comparator group risk of 22.3% we obtain:
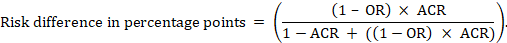
For the meta-analytic odds ratio (OR) and assumed comparator risk (ACR) the absolute risk difference is obtained as (percentage points):
Upper and lower confidence limits for the absolute risk difference are obtained by re-running the calculation above while replacing RR or OR by their upper and lower confidence limits, respectively (e.g. replacing 0.41 with 0.28, then with 0.55, in the example). Such confidence intervals do not incorporate uncertainty in the assumed comparator risks.
14.1.5.2 Time-to-event outcomes
Time-to-event outcomes measure whether and when a particular event (e.g. death) occurs (van Dalen et al 2007). The impact of the experimental intervention relative to the comparison group on time-to-event outcomes is usually measured using a hazard ratio (HR) (see Chapter 6, Section 6.8.1 ).
A hazard ratio expresses a relative effect estimate. It may be used in various ways to obtain absolute risks and other interpretable quantities for a specific population. Here we describe how to re-express hazard ratios in terms of: (i) absolute risk of event-free survival within a particular period of time; (ii) absolute risk of an event within a particular period of time; and (iii) median time to the event. All methods are built on an assumption of consistent relative effects (i.e. that the hazard ratio does not vary over time).
(i) Absolute risk of event-free survival within a particular period of time Event-free survival (e.g. overall survival) is commonly reported by individual studies. To obtain absolute effects for time-to-event outcomes measured as event-free survival, the summary HR can be used in conjunction with an assumed proportion of patients who are event-free in the comparator group (Tierney et al 2007). This proportion of patients will be specific to a period of time of observation. However, it is not strictly necessary to specify this period of time. For instance, a proportion of 50% of event-free patients might apply to patients with a high event rate observed over 1 year, or to patients with a low event rate observed over 2 years.
As an example, suppose the meta-analytic hazard ratio is 0.42 (95% CI 0.25 to 0.72). Assuming a comparator group risk of event-free survival (e.g. for overall survival people being alive) at 2 years of ACR = 900 per 1000 = 0.9 we obtain:
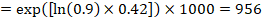
so that that 956 per 1000 people will be alive with the experimental intervention at 2 years. The derivation of the risk should be explained in a comment or footnote.
(ii) Absolute risk of an event within a particular period of time To obtain this absolute effect, again the summary HR can be used (Tierney et al 2007):
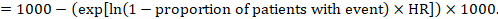
In the example, suppose we assume a comparator group risk of events (e.g. for mortality, people being dead) at 2 years of ACR = 100 per 1000 = 0.1. We obtain:
so that that 44 per 1000 people will be dead with the experimental intervention at 2 years.
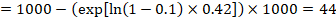
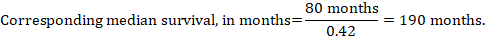
(iii) Median time to the event Instead of absolute numbers, the time to the event in the intervention and comparison groups can be expressed as median survival time in months or years. To obtain median survival time the pooled HR can be applied to an assumed median survival time in the comparator group (Tierney et al 2007):
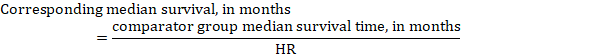
In the example, assuming a comparator group median survival time of 80 months, we obtain:
For all three of these options for re-expressing results of time-to-event analyses, upper and lower confidence limits for the corresponding intervention risk are obtained by replacing HR by its upper and lower confidence limits, respectively (e.g. replacing 0.42 with 0.25, then with 0.72, in the example). Again, as for dichotomous outcomes, such confidence intervals do not incorporate uncertainty in the assumed comparator group risks. This is of special concern for long-term survival with a low or moderate mortality rate and a corresponding high number of censored patients (i.e. a low number of patients under risk and a high censoring rate).
14.1.6 Detailed contents of a ‘Summary of findings’ table
14.1.6.1 table title and header.
The title of each ‘Summary of findings’ table should specify the healthcare question, framed in terms of the population and making it clear exactly what comparison of interventions are made. In Figure 14.1.a , the population is people taking long aeroplane flights, the intervention is compression stockings, and the control is no compression stockings.
The first rows of each ‘Summary of findings’ table should provide the following ‘header’ information:
Patients or population This further clarifies the population (and possibly the subpopulations) of interest and ideally the magnitude of risk of the most crucial adverse outcome at which an intervention is directed. For instance, people on a long-haul flight may be at different risks for DVT; those using selective serotonin reuptake inhibitors (SSRIs) might be at different risk for side effects; while those with atrial fibrillation may be at low (< 1%), moderate (1% to 4%) or high (> 4%) yearly risk of stroke.
Setting This should state any specific characteristics of the settings of the healthcare question that might limit the applicability of the summary of findings to other settings (e.g. primary care in Europe and North America).
Intervention The experimental intervention.
Comparison The comparator intervention (including no specific intervention).
14.1.6.2 Outcomes
The rows of a ‘Summary of findings’ table should include all desirable and undesirable health outcomes (listed in order of importance) that are essential for decision making, up to a maximum of seven outcomes. If there are more outcomes in the review, review authors will need to omit the less important outcomes from the table, and the decision selecting which outcomes are critical or important to the review should be made during protocol development (see Chapter 3 ). Review authors should provide time frames for the measurement of the outcomes (e.g. 90 days or 12 months) and the type of instrument scores (e.g. ranging from 0 to 100).
Note that review authors should include the pre-specified critical and important outcomes in the table whether data are available or not. However, they should be alert to the possibility that the importance of an outcome (e.g. a serious adverse effect) may only become known after the protocol was written or the analysis was carried out, and should take appropriate actions to include these in the ‘Summary of findings’ table.
The ‘Summary of findings’ table can include effects in subgroups of the population for different comparator risks and effect sizes separately. For instance, in Figure 14.1.b effects are presented for children younger and older than 5 years separately. Review authors may also opt to produce separate ‘Summary of findings’ tables for different populations.
Review authors should include serious adverse events, but it might be possible to combine minor adverse events as a single outcome, and describe this in an explanatory footnote (note that it is not appropriate to add events together unless they are independent, that is, a participant who has experienced one adverse event has an unaffected chance of experiencing the other adverse event).
Outcomes measured at multiple time points represent a particular problem. In general, to keep the table simple, review authors should present multiple time points only for outcomes critical to decision making, where either the result or the decision made are likely to vary over time. The remainder should be presented at a common time point where possible.
Review authors can present continuous outcome measures in the ‘Summary of findings’ table and should endeavour to make these interpretable to the target audience. This requires that the units are clear and readily interpretable, for example, days of pain, or frequency of headache, and the name and scale of any measurement tools used should be stated (e.g. a Visual Analogue Scale, ranging from 0 to 100). However, many measurement instruments are not readily interpretable by non-specialist clinicians or patients, for example, points on a Beck Depression Inventory or quality of life score. For these, a more interpretable presentation might involve converting a continuous to a dichotomous outcome, such as >50% improvement (see Chapter 15, Section 15.5 ).
14.1.6.3 Best estimate of risk with comparator intervention
Review authors should provide up to three typical risks for participants receiving the comparator intervention. For dichotomous outcomes, we recommend that these be presented in the form of the number of people experiencing the event per 100 or 1000 people (natural frequency) depending on the frequency of the outcome. For continuous outcomes, this would be stated as a mean or median value of the outcome measured.
Estimated or assumed comparator intervention risks could be based on assessments of typical risks in different patient groups derived from the review itself, individual representative studies in the review, or risks derived from a systematic review of prognosis studies or other sources of evidence which may in turn require an assessment of the certainty for the prognostic evidence (Spencer et al 2012, Iorio et al 2015). Ideally, risks would reflect groups that clinicians can easily identify on the basis of their presenting features.
An explanatory footnote should specify the source or rationale for each comparator group risk, including the time period to which it corresponds where appropriate. In Figure 14.1.a , clinicians can easily differentiate individuals with risk factors for deep venous thrombosis from those without. If there is known to be little variation in baseline risk then review authors may use the median comparator group risk across studies. If typical risks are not known, an option is to choose the risk from the included studies, providing the second highest for a high and the second lowest for a low risk population.
14.1.6.4 Risk with intervention
For dichotomous outcomes, review authors should provide a corresponding absolute risk for each comparator group risk, along with a confidence interval. This absolute risk with the (experimental) intervention will usually be derived from the meta-analysis result presented in the relative effect column (see Section 14.1.6.6 ). Formulae are provided in Section 14.1.5 . Review authors should present the absolute effect in the same format as the risks with comparator intervention (see Section 14.1.6.3 ), for example as the number of people experiencing the event per 1000 people.
For continuous outcomes, a difference in means or standardized difference in means should be presented with its confidence interval. These will typically be obtained directly from a meta-analysis. Explanatory text should be used to clarify the meaning, as in Figures 14.1.a and 14.1.b .
14.1.6.5 Risk difference
For dichotomous outcomes, the risk difference can be provided using one of the ‘Summary of findings’ table formats as an additional option (see Figure 14.1.b ). This risk difference expresses the difference between the experimental and comparator intervention and will usually be derived from the meta-analysis result presented in the relative effect column (see Section 14.1.6.6 ). Formulae are provided in Section 14.1.5 . Review authors should present the risk difference in the same format as assumed and corresponding risks with comparator intervention (see Section 14.1.6.3 ); for example, as the number of people experiencing the event per 1000 people or as percentage points if the assumed and corresponding risks are expressed in percentage.
For continuous outcomes, if the ‘Summary of findings’ table includes this option, the mean difference can be presented here and the ‘corresponding risk’ column left blank (see Figure 14.1.b ).
14.1.6.6 Relative effect (95% CI)
The relative effect will typically be a risk ratio or odds ratio (or occasionally a hazard ratio) with its accompanying 95% confidence interval, obtained from a meta-analysis performed on the basis of the same effect measure. Risk ratios and odds ratios are similar when the comparator intervention risks are low and effects are small, but may differ considerably when comparator group risks increase. The meta-analysis may involve an assumption of either fixed or random effects, depending on what the review authors consider appropriate, and implying that the relative effect is either an estimate of the effect of the intervention, or an estimate of the average effect of the intervention across studies, respectively.
14.1.6.7 Number of participants (studies)
This column should include the number of participants assessed in the included studies for each outcome and the corresponding number of studies that contributed these participants.
14.1.6.8 Certainty of the evidence (GRADE)
Review authors should comment on the certainty of the evidence (also known as quality of the body of evidence or confidence in the effect estimates). Review authors should use the specific evidence grading system developed by the GRADE Working Group (Atkins et al 2004, Guyatt et al 2008, Guyatt et al 2011a), which is described in detail in Section 14.2 . The GRADE approach categorizes the certainty in a body of evidence as ‘high’, ‘moderate’, ‘low’ or ‘very low’ by outcome. This is a result of judgement, but the judgement process operates within a transparent structure. As an example, the certainty would be ‘high’ if the summary were of several randomized trials with low risk of bias, but the rating of certainty becomes lower if there are concerns about risk of bias, inconsistency, indirectness, imprecision or publication bias. Judgements other than of ‘high’ certainty should be made transparent using explanatory footnotes or the ‘Comments’ column in the ‘Summary of findings’ table (see Section 14.1.6.10 ).
14.1.6.9 Comments
The aim of the ‘Comments’ field is to help interpret the information or data identified in the row. For example, this may be on the validity of the outcome measure or the presence of variables that are associated with the magnitude of effect. Important caveats about the results should be flagged here. Not all rows will need comments, and it is best to leave a blank if there is nothing warranting a comment.
14.1.6.10 Explanations
Detailed explanations should be included as footnotes to support the judgements in the ‘Summary of findings’ table, such as the overall GRADE assessment. The explanations should describe the rationale for important aspects of the content. Table 14.1.a lists guidance for useful explanations. Explanations should be concise, informative, relevant, easy to understand and accurate. If explanations cannot be sufficiently described in footnotes, review authors should provide further details of the issues in the Results and Discussion sections of the review.
Table 14.1.a Guidance for providing useful explanations in ‘Summary of findings’ (SoF) tables. Adapted from Santesso et al (2016)
14.2 Assessing the certainty or quality of a body of evidence
14.2.1 the grade approach.
The Grades of Recommendation, Assessment, Development and Evaluation Working Group (GRADE Working Group) has developed a system for grading the certainty of evidence (Schünemann et al 2003, Atkins et al 2004, Schünemann et al 2006, Guyatt et al 2008, Guyatt et al 2011a). Over 100 organizations including the World Health Organization (WHO), the American College of Physicians, the American Society of Hematology (ASH), the Canadian Agency for Drugs and Technology in Health (CADTH) and the National Institutes of Health and Clinical Excellence (NICE) in the UK have adopted the GRADE system ( www.gradeworkinggroup.org ).
Cochrane has also formally adopted this approach, and all Cochrane Reviews should use GRADE to evaluate the certainty of evidence for important outcomes (see MECIR Box 14.2.a ).
MECIR Box 14.2.a Relevant expectations for conduct of intervention reviews
For systematic reviews, the GRADE approach defines the certainty of a body of evidence as the extent to which one can be confident that an estimate of effect or association is close to the quantity of specific interest. Assessing the certainty of a body of evidence involves consideration of within- and across-study risk of bias (limitations in study design and execution or methodological quality), inconsistency (or heterogeneity), indirectness of evidence, imprecision of the effect estimates and risk of publication bias (see Section 14.2.2 ), as well as domains that may increase our confidence in the effect estimate (as described in Section 14.2.3 ). The GRADE system entails an assessment of the certainty of a body of evidence for each individual outcome. Judgements about the domains that determine the certainty of evidence should be described in the results or discussion section and as part of the ‘Summary of findings’ table.
The GRADE approach specifies four levels of certainty ( Figure 14.2.a ). For interventions, including diagnostic and other tests that are evaluated as interventions (Schünemann et al 2008b, Schünemann et al 2008a, Balshem et al 2011, Schünemann et al 2012), the starting point for rating the certainty of evidence is categorized into two types:
- randomized trials; and
- non-randomized studies of interventions (NRSI), including observational studies (including but not limited to cohort studies, and case-control studies, cross-sectional studies, case series and case reports, although not all of these designs are usually included in Cochrane Reviews).
There are many instances in which review authors rely on information from NRSI, in particular to evaluate potential harms (see Chapter 24 ). In addition, review authors can obtain relevant data from both randomized trials and NRSI, with each type of evidence complementing the other (Schünemann et al 2013).
In GRADE, a body of evidence from randomized trials begins with a high-certainty rating while a body of evidence from NRSI begins with a low-certainty rating. The lower rating with NRSI is the result of the potential bias induced by the lack of randomization (i.e. confounding and selection bias).
However, when using the new Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool (Sterne et al 2016), an assessment tool that covers the risk of bias due to lack of randomization, all studies may start as high certainty of the evidence (Schünemann et al 2018). The approach of starting all study designs (including NRSI) as high certainty does not conflict with the initial GRADE approach of starting the rating of NRSI as low certainty evidence. This is because a body of evidence from NRSI should generally be downgraded by two levels due to the inherent risk of bias associated with the lack of randomization, namely confounding and selection bias. Not downgrading NRSI from high to low certainty needs transparent and detailed justification for what mitigates concerns about confounding and selection bias (Schünemann et al 2018). Very few examples of where not rating down by two levels is appropriate currently exist.
The highest certainty rating is a body of evidence when there are no concerns in any of the GRADE factors listed in Figure 14.2.a . Review authors often downgrade evidence to moderate, low or even very low certainty evidence, depending on the presence of the five factors in Figure 14.2.a . Usually, certainty rating will fall by one level for each factor, up to a maximum of three levels for all factors. If there are very severe problems for any one domain (e.g. when assessing risk of bias, all studies were unconcealed, unblinded and lost over 50% of their patients to follow-up), evidence may fall by two levels due to that factor alone. It is not possible to rate lower than ‘very low certainty’ evidence.
Review authors will generally grade evidence from sound non-randomized studies as low certainty, even if ROBINS-I is used. If, however, such studies yield large effects and there is no obvious bias explaining those effects, review authors may rate the evidence as moderate or – if the effect is large enough – even as high certainty ( Figure 14.2.a ). The very low certainty level is appropriate for, but is not limited to, studies with critical problems and unsystematic clinical observations (e.g. case series or case reports).
Figure 14.2.a Levels of the certainty of a body of evidence in the GRADE approach. *Upgrading criteria are usually applicable to non-randomized studies only (but exceptions exist).
14.2.2 Domains that can lead to decreasing the certainty level of a body of evidence
We now describe in more detail the five reasons (or domains) for downgrading the certainty of a body of evidence for a specific outcome. In each case, if no reason is found for downgrading the evidence, it should be classified as 'no limitation or not serious' (not important enough to warrant downgrading). If a reason is found for downgrading the evidence, it should be classified as 'serious' (downgrading the certainty rating by one level) or 'very serious' (downgrading the certainty grade by two levels). For non-randomized studies assessed with ROBINS-I, rating down by three levels should be classified as 'extremely' serious.
(1) Risk of bias or limitations in the detailed design and implementation
Our confidence in an estimate of effect decreases if studies suffer from major limitations that are likely to result in a biased assessment of the intervention effect. For randomized trials, these methodological limitations include failure to generate a random sequence, lack of allocation sequence concealment, lack of blinding (particularly with subjective outcomes that are highly susceptible to biased assessment), a large loss to follow-up or selective reporting of outcomes. Chapter 8 provides a discussion of study-level assessments of risk of bias in the context of a Cochrane Review, and proposes an approach to assessing the risk of bias for an outcome across studies as ‘Low’ risk of bias, ‘Some concerns’ and ‘High’ risk of bias for randomized trials. Levels of ‘Low’. ‘Moderate’, ‘Serious’ and ‘Critical’ risk of bias arise for non-randomized studies assessed with ROBINS-I ( Chapter 25 ). These assessments should feed directly into this GRADE domain. In particular, ‘Low’ risk of bias would indicate ‘no limitation’; ‘Some concerns’ would indicate either ‘no limitation’ or ‘serious limitation’; and ‘High’ risk of bias would indicate either ‘serious limitation’ or ‘very serious limitation’. ‘Critical’ risk of bias on ROBINS-I would indicate extremely serious limitations in GRADE. Review authors should use their judgement to decide between alternative categories, depending on the likely magnitude of the potential biases.
Every study addressing a particular outcome will differ, to some degree, in the risk of bias. Review authors should make an overall judgement on whether the certainty of evidence for an outcome warrants downgrading on the basis of study limitations. The assessment of study limitations should apply to the studies contributing to the results in the ‘Summary of findings’ table, rather than to all studies that could potentially be included in the analysis. We have argued in Chapter 7, Section 7.6.2 , that the primary analysis should be restricted to studies at low (or low and unclear) risk of bias where possible.
Table 14.2.a presents the judgements that must be made in going from assessments of the risk of bias to judgements about study limitations for each outcome included in a ‘Summary of findings’ table. A rating of high certainty evidence can be achieved only when most evidence comes from studies that met the criteria for low risk of bias. For example, of the 22 studies addressing the impact of beta-blockers on mortality in patients with heart failure, most probably or certainly used concealed allocation of the sequence, all blinded at least some key groups and follow-up of randomized patients was almost complete (Brophy et al 2001). The certainty of evidence might be downgraded by one level when most of the evidence comes from individual studies either with a crucial limitation for one item, or with some limitations for multiple items. An example of very serious limitations, warranting downgrading by two levels, is provided by evidence on surgery versus conservative treatment in the management of patients with lumbar disc prolapse (Gibson and Waddell 2007). We are uncertain of the benefit of surgery in reducing symptoms after one year or longer, because the one study included in the analysis had inadequate concealment of the allocation sequence and the outcome was assessed using a crude rating by the surgeon without blinding.
(2) Unexplained heterogeneity or inconsistency of results
When studies yield widely differing estimates of effect (heterogeneity or variability in results), investigators should look for robust explanations for that heterogeneity. For instance, drugs may have larger relative effects in sicker populations or when given in larger doses. A detailed discussion of heterogeneity and its investigation is provided in Chapter 10, Section 10.10 and Section 10.11 . If an important modifier exists, with good evidence that important outcomes are different in different subgroups (which would ideally be pre-specified), then a separate ‘Summary of findings’ table may be considered for a separate population. For instance, a separate ‘Summary of findings’ table would be used for carotid endarterectomy in symptomatic patients with high grade stenosis (70% to 99%) in which the intervention is, in the hands of the right surgeons, beneficial, and another (if review authors considered it relevant) for asymptomatic patients with low grade stenosis (less than 30%) in which surgery appears harmful (Orrapin and Rerkasem 2017). When heterogeneity exists and affects the interpretation of results, but review authors are unable to identify a plausible explanation with the data available, the certainty of the evidence decreases.
(3) Indirectness of evidence
Two types of indirectness are relevant. First, a review comparing the effectiveness of alternative interventions (say A and B) may find that randomized trials are available, but they have compared A with placebo and B with placebo. Thus, the evidence is restricted to indirect comparisons between A and B. Where indirect comparisons are undertaken within a network meta-analysis context, GRADE for network meta-analysis should be used (see Chapter 11, Section 11.5 ).
Second, a review may find randomized trials that meet eligibility criteria but address a restricted version of the main review question in terms of population, intervention, comparator or outcomes. For example, suppose that in a review addressing an intervention for secondary prevention of coronary heart disease, most identified studies happened to be in people who also had diabetes. Then the evidence may be regarded as indirect in relation to the broader question of interest because the population is primarily related to people with diabetes. The opposite scenario can equally apply: a review addressing the effect of a preventive strategy for coronary heart disease in people with diabetes may consider studies in people without diabetes to provide relevant, albeit indirect, evidence. This would be particularly likely if investigators had conducted few if any randomized trials in the target population (e.g. people with diabetes). Other sources of indirectness may arise from interventions studied (e.g. if in all included studies a technical intervention was implemented by expert, highly trained specialists in specialist centres, then evidence on the effects of the intervention outside these centres may be indirect), comparators used (e.g. if the comparator groups received an intervention that is less effective than standard treatment in most settings) and outcomes assessed (e.g. indirectness due to surrogate outcomes when data on patient-important outcomes are not available, or when investigators seek data on quality of life but only symptoms are reported). Review authors should make judgements transparent when they believe downgrading is justified, based on differences in anticipated effects in the group of primary interest. Review authors may be aided and increase transparency of their judgements about indirectness if they use Table 14.2.b available in the GRADEpro GDT software (Schünemann et al 2013).
(4) Imprecision of results
When studies include few participants or few events, and thus have wide confidence intervals, review authors can lower their rating of the certainty of the evidence. The confidence intervals included in the ‘Summary of findings’ table will provide readers with information that allows them to make, to some extent, their own rating of precision. Review authors can use a calculation of the optimal information size (OIS) or review information size (RIS), similar to sample size calculations, to make judgements about imprecision (Guyatt et al 2011b, Schünemann 2016). The OIS or RIS is calculated on the basis of the number of participants required for an adequately powered individual study. If the 95% confidence interval excludes a risk ratio (RR) of 1.0, and the total number of events or patients exceeds the OIS criterion, precision is adequate. If the 95% CI includes appreciable benefit or harm (an RR of under 0.75 or over 1.25 is often suggested as a very rough guide) downgrading for imprecision may be appropriate even if OIS criteria are met (Guyatt et al 2011b, Schünemann 2016).
(5) High probability of publication bias
The certainty of evidence level may be downgraded if investigators fail to report studies on the basis of results (typically those that show no effect: publication bias) or outcomes (typically those that may be harmful or for which no effect was observed: selective outcome non-reporting bias). Selective reporting of outcomes from among multiple outcomes measured is assessed at the study level as part of the assessment of risk of bias (see Chapter 8, Section 8.7 ), so for the studies contributing to the outcome in the ‘Summary of findings’ table this is addressed by domain 1 above (limitations in the design and implementation). If a large number of studies included in the review do not contribute to an outcome, or if there is evidence of publication bias, the certainty of the evidence may be downgraded. Chapter 13 provides a detailed discussion of reporting biases, including publication bias, and how it may be tackled in a Cochrane Review. A prototypical situation that may elicit suspicion of publication bias is when published evidence includes a number of small studies, all of which are industry-funded (Bhandari et al 2004). For example, 14 studies of flavanoids in patients with haemorrhoids have shown apparent large benefits, but enrolled a total of only 1432 patients (i.e. each study enrolled relatively few patients) (Alonso-Coello et al 2006). The heavy involvement of sponsors in most of these studies raises questions of whether unpublished studies that suggest no benefit exist (publication bias).
A particular body of evidence can suffer from problems associated with more than one of the five factors listed here, and the greater the problems, the lower the certainty of evidence rating that should result. One could imagine a situation in which randomized trials were available, but all or virtually all of these limitations would be present, and in serious form. A very low certainty of evidence rating would result.
Table 14.2.a Further guidelines for domain 1 (of 5) in a GRADE assessment: going from assessments of risk of bias in studies to judgements about study limitations for main outcomes across studies
Table 14.2.b Judgements about indirectness by outcome (available in GRADEpro GDT)
Intervention:
Comparator:
Direct comparison:
Final judgement about indirectness across domains:
14.2.3 Domains that may lead to increasing the certainty level of a body of evidence
Although NRSI and downgraded randomized trials will generally yield a low rating for certainty of evidence, there will be unusual circumstances in which review authors could ‘upgrade’ such evidence to moderate or even high certainty ( Table 14.3.a ).
- Large effects On rare occasions when methodologically well-done observational studies yield large, consistent and precise estimates of the magnitude of an intervention effect, one may be particularly confident in the results. A large estimated effect (e.g. RR >2 or RR <0.5) in the absence of plausible confounders, or a very large effect (e.g. RR >5 or RR <0.2) in studies with no major threats to validity, might qualify for this. In these situations, while the NRSI may possibly have provided an over-estimate of the true effect, the weak study design may not explain all of the apparent observed benefit. Thus, despite reservations based on the observational study design, review authors are confident that the effect exists. The magnitude of the effect in these studies may move the assigned certainty of evidence from low to moderate (if the effect is large in the absence of other methodological limitations). For example, a meta-analysis of observational studies showed that bicycle helmets reduce the risk of head injuries in cyclists by a large margin (odds ratio (OR) 0.31, 95% CI 0.26 to 0.37) (Thompson et al 2000). This large effect, in the absence of obvious bias that could create the association, suggests a rating of moderate-certainty evidence. Note : GRADE guidance suggests the possibility of rating up one level for a large effect if the relative effect is greater than 2.0. However, if the point estimate of the relative effect is greater than 2.0, but the confidence interval is appreciably below 2.0, then some hesitation would be appropriate in the decision to rate up for a large effect. Another situation allows inference of a strong association without a formal comparative study. Consider the question of the impact of routine colonoscopy versus no screening for colon cancer on the rate of perforation associated with colonoscopy. Here, a large series of representative patients undergoing colonoscopy may provide high certainty evidence about the risk of perforation associated with colonoscopy. When the risk of the event among patients receiving the relevant comparator is known to be near 0 (i.e. we are certain that the incidence of spontaneous colon perforation in patients not undergoing colonoscopy is extremely low), case series or cohort studies of representative patients can provide high certainty evidence of adverse effects associated with an intervention, thereby allowing us to infer a strong association from even a limited number of events.
- Dose-response The presence of a dose-response gradient may increase our confidence in the findings of observational studies and thereby enhance the assigned certainty of evidence. For example, our confidence in the result of observational studies that show an increased risk of bleeding in patients who have supratherapeutic anticoagulation levels is increased by the observation that there is a dose-response gradient between the length of time needed for blood to clot (as measured by the international normalized ratio (INR)) and an increased risk of bleeding (Levine et al 2004). A systematic review of NRSI investigating the effect of cyclooxygenase-2 inhibitors on cardiovascular events found that the summary estimate (RR) with rofecoxib was 1.33 (95% CI 1.00 to 1.79) with doses less than 25mg/d, and 2.19 (95% CI 1.64 to 2.91) with doses more than 25mg/d. Although residual confounding is likely to exist in the NRSI that address this issue, the existence of a dose-response gradient and the large apparent effect of higher doses of rofecoxib markedly increase our strength of inference that the association cannot be explained by residual confounding, and is therefore likely to be both causal and, at high levels of exposure, substantial. Note : GRADE guidance suggests the possibility of rating up one level for a large effect if the relative effect is greater than 2.0. Here, the fact that the point estimate of the relative effect is greater than 2.0, but the confidence interval is appreciably below 2.0 might make some hesitate in the decision to rate up for a large effect
- Plausible confounding On occasion, all plausible biases from randomized or non-randomized studies may be working to under-estimate an apparent intervention effect. For example, if only sicker patients receive an experimental intervention or exposure, yet they still fare better, it is likely that the actual intervention or exposure effect is larger than the data suggest. For instance, a rigorous systematic review of observational studies including a total of 38 million patients demonstrated higher death rates in private for-profit versus private not-for-profit hospitals (Devereaux et al 2002). One possible bias relates to different disease severity in patients in the two hospital types. It is likely, however, that patients in the not-for-profit hospitals were sicker than those in the for-profit hospitals. Thus, to the extent that residual confounding existed, it would bias results against the not-for-profit hospitals. The second likely bias was the possibility that higher numbers of patients with excellent private insurance coverage could lead to a hospital having more resources and a spill-over effect that would benefit those without such coverage. Since for-profit hospitals are likely to admit a larger proportion of such well-insured patients than not-for-profit hospitals, the bias is once again against the not-for-profit hospitals. Since the plausible biases would all diminish the demonstrated intervention effect, one might consider the evidence from these observational studies as moderate rather than low certainty. A parallel situation exists when observational studies have failed to demonstrate an association, but all plausible biases would have increased an intervention effect. This situation will usually arise in the exploration of apparent harmful effects. For example, because the hypoglycaemic drug phenformin causes lactic acidosis, the related agent metformin was under suspicion for the same toxicity. Nevertheless, very large observational studies have failed to demonstrate an association (Salpeter et al 2007). Given the likelihood that clinicians would be more alert to lactic acidosis in the presence of the agent and over-report its occurrence, one might consider this moderate, or even high certainty, evidence refuting a causal relationship between typical therapeutic doses of metformin and lactic acidosis.
14.3 Describing the assessment of the certainty of a body of evidence using the GRADE framework
Review authors should report the grading of the certainty of evidence in the Results section for each outcome for which this has been performed, providing the rationale for downgrading or upgrading the evidence, and referring to the ‘Summary of findings’ table where applicable.
Table 14.3.a provides a framework and examples for how review authors can justify their judgements about the certainty of evidence in each domain. These justifications should also be included in explanatory notes to the ‘Summary of Findings’ table (see Section 14.1.6.10 ).
Chapter 15, Section 15.6 , describes in more detail how the overall GRADE assessment across all domains can be used to draw conclusions about the effects of the intervention, as well as providing implications for future research.
Table 14.3.a Framework for describing the certainty of evidence and justifying downgrading or upgrading
14.4 Chapter information
Authors: Holger J Schünemann, Julian PT Higgins, Gunn E Vist, Paul Glasziou, Elie A Akl, Nicole Skoetz, Gordon H Guyatt; on behalf of the Cochrane GRADEing Methods Group (formerly Applicability and Recommendations Methods Group) and the Cochrane Statistical Methods Group
Acknowledgements: Andrew D Oxman contributed to earlier versions. Professor Penny Hawe contributed to the text on adverse effects in earlier versions. Jon Deeks provided helpful contributions on an earlier version of this chapter. For details of previous authors and editors of the Handbook , please refer to the Preface.
Funding: This work was in part supported by funding from the Michael G DeGroote Cochrane Canada Centre and the Ontario Ministry of Health.
14.5 References
Alonso-Coello P, Zhou Q, Martinez-Zapata MJ, Mills E, Heels-Ansdell D, Johanson JF, Guyatt G. Meta-analysis of flavonoids for the treatment of haemorrhoids. British Journal of Surgery 2006; 93 : 909-920.
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O'Connell D, Oxman AD, Phillips B, Schünemann HJ, Edejer TT, Varonen H, Vist GE, Williams JW, Jr., Zaza S. Grading quality of evidence and strength of recommendations. BMJ 2004; 328 : 1490.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011; 64 : 401-406.
Bhandari M, Busse JW, Jackowski D, Montori VM, Schünemann H, Sprague S, Mears D, Schemitsch EH, Heels-Ansdell D, Devereaux PJ. Association between industry funding and statistically significant pro-industry findings in medical and surgical randomized trials. Canadian Medical Association Journal 2004; 170 : 477-480.
Brophy JM, Joseph L, Rouleau JL. Beta-blockers in congestive heart failure. A Bayesian meta-analysis. Annals of Internal Medicine 2001; 134 : 550-560.
Carrasco-Labra A, Brignardello-Petersen R, Santesso N, Neumann I, Mustafa RA, Mbuagbaw L, Etxeandia Ikobaltzeta I, De Stio C, McCullagh LJ, Alonso-Coello P, Meerpohl JJ, Vandvik PO, Brozek JL, Akl EA, Bossuyt P, Churchill R, Glenton C, Rosenbaum S, Tugwell P, Welch V, Garner P, Guyatt G, Schünemann HJ. Improving GRADE evidence tables part 1: a randomized trial shows improved understanding of content in summary of findings tables with a new format. Journal of Clinical Epidemiology 2016; 74 : 7-18.
Deeks JJ, Altman DG. Effect measures for meta-analysis of trials with binary outcomes. In: Egger M, Davey Smith G, Altman DG, editors. Systematic Reviews in Health Care: Meta-analysis in Context . 2nd ed. London (UK): BMJ Publication Group; 2001. p. 313-335.
Devereaux PJ, Choi PT, Lacchetti C, Weaver B, Schünemann HJ, Haines T, Lavis JN, Grant BJ, Haslam DR, Bhandari M, Sullivan T, Cook DJ, Walter SD, Meade M, Khan H, Bhatnagar N, Guyatt GH. A systematic review and meta-analysis of studies comparing mortality rates of private for-profit and private not-for-profit hospitals. Canadian Medical Association Journal 2002; 166 : 1399-1406.
Engels EA, Schmid CH, Terrin N, Olkin I, Lau J. Heterogeneity and statistical significance in meta-analysis: an empirical study of 125 meta-analyses. Statistics in Medicine 2000; 19 : 1707-1728.
Furukawa TA, Guyatt GH, Griffith LE. Can we individualize the 'number needed to treat'? An empirical study of summary effect measures in meta-analyses. International Journal of Epidemiology 2002; 31 : 72-76.
Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine 2007; 32 : 1735-1747.
Guyatt G, Oxman A, Vist G, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann H. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336 : 3.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011a; 64 : 383-394.
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, Devereaux PJ, Montori VM, Freyschuss B, Vist G, Jaeschke R, Williams JW, Jr., Murad MH, Sinclair D, Falck-Ytter Y, Meerpohl J, Whittington C, Thorlund K, Andrews J, Schünemann HJ. GRADE guidelines 6. Rating the quality of evidence--imprecision. Journal of Clinical Epidemiology 2011b; 64 : 1283-1293.
Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B, McGinn T, Hayden J, Williams K, Shea B, Wolff R, Kujpers T, Perel P, Vandvik PO, Glasziou P, Schünemann H, Guyatt G. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ 2015; 350 : h870.
Langendam M, Carrasco-Labra A, Santesso N, Mustafa RA, Brignardello-Petersen R, Ventresca M, Heus P, Lasserson T, Moustgaard R, Brozek J, Schünemann HJ. Improving GRADE evidence tables part 2: a systematic survey of explanatory notes shows more guidance is needed. Journal of Clinical Epidemiology 2016; 74 : 19-27.
Levine MN, Raskob G, Landefeld S, Kearon C, Schulman S. Hemorrhagic complications of anticoagulant treatment: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126 : 287S-310S.
Orrapin S, Rerkasem K. Carotid endarterectomy for symptomatic carotid stenosis. Cochrane Database of Systematic Reviews 2017; 6 : CD001081.
Salpeter S, Greyber E, Pasternak G, Salpeter E. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2007; 4 : CD002967.
Santesso N, Carrasco-Labra A, Langendam M, Brignardello-Petersen R, Mustafa RA, Heus P, Lasserson T, Opiyo N, Kunnamo I, Sinclair D, Garner P, Treweek S, Tovey D, Akl EA, Tugwell P, Brozek JL, Guyatt G, Schünemann HJ. Improving GRADE evidence tables part 3: detailed guidance for explanatory footnotes supports creating and understanding GRADE certainty in the evidence judgments. Journal of Clinical Epidemiology 2016; 74 : 28-39.
Schünemann HJ, Best D, Vist G, Oxman AD, Group GW. Letters, numbers, symbols and words: how to communicate grades of evidence and recommendations. Canadian Medical Association Journal 2003; 169 : 677-680.
Schünemann HJ, Jaeschke R, Cook DJ, Bria WF, El-Solh AA, Ernst A, Fahy BF, Gould MK, Horan KL, Krishnan JA, Manthous CA, Maurer JR, McNicholas WT, Oxman AD, Rubenfeld G, Turino GM, Guyatt G. An official ATS statement: grading the quality of evidence and strength of recommendations in ATS guidelines and recommendations. American Journal of Respiratory and Critical Care Medicine 2006; 174 : 605-614.
Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, Williams JW, Jr., Kunz R, Craig J, Montori VM, Bossuyt P, Guyatt GH. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008a; 336 : 1106-1110.
Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Bossuyt P, Chang S, Muti P, Jaeschke R, Guyatt GH. GRADE: assessing the quality of evidence for diagnostic recommendations. ACP Journal Club 2008b; 149 : 2.
Schünemann HJ, Mustafa R, Brozek J. [Diagnostic accuracy and linked evidence--testing the chain]. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen 2012; 106 : 153-160.
Schünemann HJ, Tugwell P, Reeves BC, Akl EA, Santesso N, Spencer FA, Shea B, Wells G, Helfand M. Non-randomized studies as a source of complementary, sequential or replacement evidence for randomized controlled trials in systematic reviews on the effects of interventions. Research Synthesis Methods 2013; 4 : 49-62.
Schünemann HJ. Interpreting GRADE's levels of certainty or quality of the evidence: GRADE for statisticians, considering review information size or less emphasis on imprecision? Journal of Clinical Epidemiology 2016; 75 : 6-15.
Schünemann HJ, Cuello C, Akl EA, Mustafa RA, Meerpohl JJ, Thayer K, Morgan RL, Gartlehner G, Kunz R, Katikireddi SV, Sterne J, Higgins JPT, Guyatt G, Group GW. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. Journal of Clinical Epidemiology 2018.
Spencer-Bonilla G, Quinones AR, Montori VM, International Minimally Disruptive Medicine W. Assessing the Burden of Treatment. Journal of General Internal Medicine 2017; 32 : 1141-1145.
Spencer FA, Iorio A, You J, Murad MH, Schünemann HJ, Vandvik PO, Crowther MA, Pottie K, Lang ES, Meerpohl JJ, Falck-Ytter Y, Alonso-Coello P, Guyatt GH. Uncertainties in baseline risk estimates and confidence in treatment effects. BMJ 2012; 345 : e7401.
Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JPT. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355 : i4919.
Thompson DC, Rivara FP, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database of Systematic Reviews 2000; 2 : CD001855.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007; 8 .
van Dalen EC, Tierney JF, Kremer LCM. Tips and tricks for understanding and using SR results. No. 7: time‐to‐event data. Evidence-Based Child Health 2007; 2 : 1089-1090.
For permission to re-use material from the Handbook (either academic or commercial), please see here for full details.
Library FAQs
- Capella FAQs Home
- Capella FAQs
Q. How do I find the Literature Review Summary Table?
- Career Center
- Disability Support
- Doctoral Support
- Learner Records
- Military Support
- Office of Research & Scholarship
- Quantitative Skills Center
- Scholarships & Grants
- Technical Support
- Writing Center
- 8 About the library
- 2 Alumni Library
- 19 Articles
- 8 Bookstore
- 11 Business
- 7 Comprehensive Exams
- 4 Counseling
- 17 Course Readings
- 37 Databases
- 21 Dissertation
- 7 Dissertation Writing
- 5 Education
- 9 Evaluating Sources
- 3 Health Administration
- 8 How do I...
- 2 Human Services
- 2 Information Literacy
- 2 Information Technology
- 8 Interlibrary Loan
- 8 Internet Research
- 13 Journal & Book Locator
- 3 Legal Research
- 14 Library Help
- 4 Literature Reviews
- 2 Methodology
- 2 Non-Library
- 16 Psychology
- 3 Public Health
- 1 Public Safety
- 8 Public Service Leadership
- 12 RefWorks
- 38 Searching
- 1 Social Work
- 14 Technical Issues
Search Library FAQs
Search All FAQs
Answer Last Updated: Jun 28, 2023 Views: 940
Here are some examples of a literature review summary table: literature review summary table - with examples .
Researchers use literature review summary tables to organize a number of articles in a small space, based on selected criteria.
If you have the need to summarize and organize a lot of literature in a small space, you may want to ask your faculty whether a literature review summary table would be appropriate.
This resource and other tools can also be found in this library guide: Staying Organized & Keeping Track: Research Tools
- Share on Facebook
Was this helpful? Yes 0 No 0
Need Help? Ask a Librarian
SEND US YOUR QUESTION Learner Request Form Faculty & Staff Request Form
MAKE A PHONE APPOINTMENT Schedule a Phone Call with a Librarian
Related Topics
- Dissertation
- Dissertation Writing
PREPUBLICATION COPY: UNCORRECTED PROOFS

IMAGES
VIDEO
COMMENTS
A literature summary table provides a synopsis of an included article. It succinctly presents its purpose, methods, findings and other relevant information pertinent to the review. The aim of developing these literature summary tables is to provide the reader with the information at one glance.
This is an example of a research table, in which you provide a basic description of the most important features of the studies, articles, and other items you discover in your research.The table identifies each item according to its author/date of publication, its purpose or thesis, what type of work it is (systematic review, clinical trial, etc.), the level of evidence it represents (which ...
in the summary tables (see figure 1) demonstrates to. the readers that a robust method of data extraction and. synthesis has been followed. Tip 5: create your person alised template for lit ...
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
Literature Review Matrix. As you read and evaluate your literature there are several different ways to organize your research. Courtesy of Dr. Gary Burkholder in the School of Psychology, these sample matrices are one option to help organize your articles. These documents allow you to compile details about your sources, such as the foundational ...
Annotated Bibliographies. Annotated bibliographies can help you clearly see and understand the research before diving into organizing and writing your literature review. Although typically part of the "summarize" step of the literature review, annotations should not merely be summaries of each article - instead, they should be critical ...
John's, NL A1C 5C4, Canada; various approaches for developing literature summary a y6133@ mun. ac Five tips for developing useful literature summary tables for writing review articles Ahtisham Younas ,1,2 Parveen Ali 3,4 Research made simple 10.1136/ebnurs-2021-103417 Introduction Literature reviews offer a critical synthesis of empir-
When writing a literature review it is important to start with a brief introduction, followed by the text broken up into subsections and conclude with a summary to bring everything together. A summary table including title, author, publication date and key findings is a useful feature to present in your review (see Table 1 for an example). This ...
A summary table is also called a synthesis matrix. The table helps you organize and compare information for your systematic review, scholarly report, dissertation or thesis. Synthesis Matrix. A summary table is also called a synthesis matrix. A summary table helps you record the main points of each source and document how sources relate to each ...
Five tips for developing useful literature summary tables for writing review articles. Five tips for developing useful literature summary tables for writing review articles. Evid Based Nurs. 2021 Apr;24 (2):32-34. doi: 10.1136/ebnurs-2021-103417. Epub 2021 Mar 4.
A synthesis matrix helps you record the main points of each source and document how sources relate to each other. After summarizing and evaluating your sources, arrange them in a matrix or use a citation manager to help you see how they relate to each other and apply to each of your themes or variables. By arranging your sources by theme or ...
This video shows you exactly how to create a summary table for your research articles. It outlines what information should go in the table and provides helpf...
The literature review template includes the following sections: Before you start - essential groundwork to ensure you're ready. The introduction section. The core/body section. The conclusion /summary. Extra free resources. Each section is explained in plain, straightforward language, followed by an overview of the key elements that you ...
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays).
Topic 4: Literature Review. An article summary table is a tool that can help you organize and summarize what you've read. Moreover, it can provide you with a quick glance as to how you might organize articles when you begin to write your literature review. Once you know your variables and concepts and you start to find articles, it is ...
Organizing principle(s) - C are pathway. Clarke (2007) 3 Not specific: One author read each record and categorized it on the basis of whether a recommendation was made as to the need for more research and, if so, whether suggestions were made regarding the specific types of intervention, participant, or outcome measures that should be assessed or included in future research.
A summary table allows you to compare common research methods, findings, limitations, etc. You can order the entries in any way that you find useful; consider ordering your research alphabetically, by timeliness, or even by grouping similar study aims, models, or results. Once compiled, you can use this table to compare studies side by side.
Conclusions: Publishing a search summary table in all systematic reviews would add to the growing evidence base about information retrieval, which would help in determining which databases to search for which type of review (in terms of either topic or scope), what supplementary search methods are most effective, what type of literature is being included, and where it is found.
A summary of findings table is an essential component of a systematic review. This comprehensive synthesis of data analysis provides a simple, and transparent presentation of data, which makes it easier for readers to understand the study, the assessment of its reviewed literature, and the conclusions derived from its methodology.
If there are more outcomes in the review, review authors will need to omit the less important outcomes from the table, and the decision selecting which outcomes are critical or important to the review should be made during protocol development (see Chapter 3). Review authors should provide time frames for the measurement of the outcomes (e.g ...
http://youstudynursing.com/ A Quick guide to creating a table in Microsoft Word for your literature reviewMusic By http://instrumentalsfree.com
Researchers use literature review summary tables to organize a number of articles in a small space, based on selected criteria. If you have the need to summarize and organize a lot of literature in a small space, you may want to ask your faculty whether a literature review summary table would be appropriate. This resource and other tools can ...
TABLE B-1 Systematic Reviews Study Study Purpose Relevant Findings Health IT Component Time Frame Sample Size Outcome Measures Black, A. D., J. Car, C Pagliari, C. ... review of the literature. Drug Safety 30(12):1111-1125. CDS e-prescribing - Pre August 2004; - September 2004 to October