16 Personal Essays About Mental Health Worth Reading
Here are some of the most moving and illuminating essays published on BuzzFeed about mental illness, wellness, and the way our minds work.

BuzzFeed Staff

1. My Best Friend Saved Me When I Attempted Suicide, But I Didn’t Save Her — Drusilla Moorhouse

"I was serious about killing myself. My best friend wasn’t — but she’s the one who’s dead."
2. Life Is What Happens While You’re Googling Symptoms Of Cancer — Ramona Emerson

"After a lifetime of hypochondria, I was finally diagnosed with my very own medical condition. And maybe, in a weird way, it’s made me less afraid to die."
3. How I Learned To Be OK With Feeling Sad — Mac McClelland

"It wasn’t easy, or cheap."
4. Who Gets To Be The “Good Schizophrenic”? — Esmé Weijun Wang
"When you’re labeled as crazy, the “right” kind of diagnosis could mean the difference between a productive life and a life sentence."
5. Why Do I Miss Being Bipolar? — Sasha Chapin
"The medication I take to treat my bipolar disorder works perfectly. Sometimes I wish it didn’t."
6. What My Best Friend And I Didn’t Learn About Loss — Zan Romanoff

"When my closest friend’s first baby was stillborn, we navigated through depression and grief together."
7. I Can’t Live Without Fear, But I Can Learn To Be OK With It — Arianna Rebolini

"I’ve become obsessively afraid that the people I love will die. Now I have to teach myself how to be OK with that."
8. What It’s Like Having PPD As A Black Woman — Tyrese Coleman
"It took me two years to even acknowledge I’d been depressed after the birth of my twin sons. I wonder how much it had to do with the way I had been taught to be strong."
9. Notes On An Eating Disorder — Larissa Pham

"I still tell my friends I am in recovery so they will hold me accountable."
10. What Comedy Taught Me About My Mental Illness — Kate Lindstedt

"I didn’t expect it, but stand-up comedy has given me the freedom to talk about depression and anxiety on my own terms."
11. The Night I Spoke Up About My #BlackSuicide — Terrell J. Starr

"My entire life was shaped by violence, so I wanted to end it violently. But I didn’t — thanks to overcoming the stigma surrounding African-Americans and depression, and to building a community on Twitter."
12. Knitting Myself Back Together — Alanna Okun

"The best way I’ve found to fight my anxiety is with a pair of knitting needles."
13. I Started Therapy So I Could Take Better Care Of Myself — Matt Ortile
"I’d known for a while that I needed to see a therapist. It wasn’t until I felt like I could do without help that I finally sought it."
14. I’m Mending My Broken Relationship With Food — Anita Badejo

"After a lifetime struggling with disordered eating, I’m still figuring out how to have a healthy relationship with my body and what I feed it."
15. I Found Love In A Hopeless Mess — Kate Conger
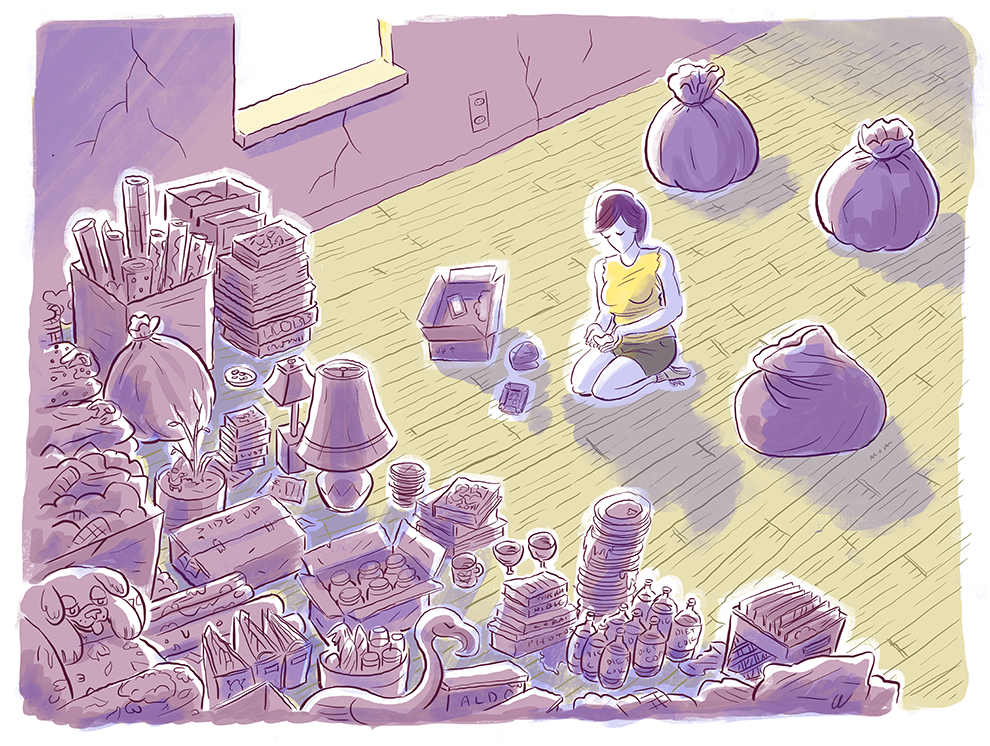
"Dehoarding my partner’s childhood home gave me a way to understand his mother, but I’m still not sure how to live with the habit he’s inherited."
16. When Taking Anxiety Medication Is A Revolutionary Act — Tracy Clayton
"I had to learn how to love myself enough to take care of myself. It wasn’t easy."
Topics in this article
- Mental Health
Greater Good Science Center • Magazine • In Action • In Education
Mind & Body Articles & More
How we’re overcoming the stigma of mental health issues, shame and shunning make mental illness worse. but new studies suggest that attitudes are changing for the better—and that’s largely due to young people..
Today, people in the United States know far more about mental illness than did previous generations. They might know what it looks like: changes in emotions, thinking, or behavior that make function in daily life difficult, if not impossible. They’re much more likely to understand that most of us will experience some form of mental illness in our lifetimes, like depression or anxiety. And they know that smaller numbers of people will experience more severe conditions like bipolar disorder, schizophrenia, or PTSD.
Despite this progress, for decades attitudes toward people with mental disorders have hardly budged. How do we know this? One of the crucial ways we measure prejudice is to ask about “social distance.” In this case, that involves asking: How close would you be willing live to someone with a mental illness? Would you live in the same state? Be in the same classroom or workplace? Participate together on a project? Ride next to them on public transportation? Go out with them? Let your offspring marry them?
When friends, family, and society shame people for their illness, and shun them, that’s stigma. This shaming can take many forms , from stereotypes (“they’re dangerous”) to moral judgments (“you’re just a coward”) to dismissive labeling (“you’re crazy”). There can be real consequences of stigma, such as lost job opportunities and social marginalization, as well as giving up on seeking treatment. Overt discrimination is a big part of stigma, too: People with mental disorders, in many states, cannot run for office, serve on a jury, keep a driver’s license, or retain child custody. Most perniciously, the stigma of mental illness can lead people to hide their troubles and refuse to get help—which is likely to worsen their condition and create a vicious cycle.

Until very recently, studies consistently showed that the desire for social distance from people with mental illness had not improved over the past 50 to 60 years. In fact, in some ways it had actually worsened, as more people than before automatically linked mental illness with aggression and violence.
At the same time, studies also showed that people had greater knowledge of ADHD, depression, bipolar disorder, PTSD, and more—but just “knowing” more facts about mental illness can actually make things worse . For example, if you learn that people with schizophrenia may hear voices and become paranoid, you might consider that to be quite frightening, even threatening. Similarly, understanding that people with severe depression may come to feel that their lives are not worth living—and may therefore consider suicide—can trigger the belief that such individuals are utterly self-centered. What might not be understood is that severe depression can foster the belief, in people affected, that everyone else would be better off without them.
In other words, factual knowledge about mental disorders, alone, can actually fuel stereotypes. In addressing stigma, the missing piece isn’t knowledge—it’s contact, empathy, and humanization.
A recent study published in December by the JAMA Network Open suggests that things may finally be starting to change. But the picture is complicated: Some kinds of illness are becoming less stigmatized, true, but people still want to keep distance from other forms. The good news is that young people are much less likely to stigmatize mental illness than older generations—and that there are specific steps we can take, as individuals and society, to keep making progress.
Generational shifts driving acceptance
In surveying a representative group of U.S. adults during a period of over two decades, sociologist Bernice A. Pescosolido and her colleagues found a significant and important decrease in desire for social distance related to depression over the past few years.
That is unprecedented, and of real importance. However, in the same paper , the researchers found that attitudes related to conditions like schizophrenia and substance-use disorders did not show signs of improvement—and had actually worsened.
Even though the participants in this study were many—over 4,000 adults—it would take even larger groups to understand how socioeconomic, ethnic, or racial characteristics affected changing attitudes toward mental illness. Still, from this study and a number of others, it does appear that improvements are driven mainly by younger people.
In fact, research hints at a massive generational shift in how mental illness is perceived and socially experienced. Multiple other surveys and studies besides the one by Pescosolido and her colleagues suggest that both millennials (those born from the early ’80s to the mid-’90s) and Generation Z (who were mostly born in the 21st century) are much more accepting and knowledgeable about mental illness than previous generations.
Why? Rates of diagnosed mental illness have been rising among young people. For example, one 2019 study found almost half experience depression, peaking at 60% for teens aged 14–17—considerably more than previous generations. More recent work conducted during the COVID-19 pandemic hints at a profound mental health crisis .
When the CDC surveyed almost 8,000 high school students in the first six months of 2021, researchers found that depression, anxiety, and other disorders permeated the lives of adolescents during the pandemic. All groups reported more persistent sadness since spring 2020, though the rate rose faster among white teens than others. Nearly half of lesbian, gay, bisexual, and transgender teens reported seriously thinking about suicide, compared with 14% of heterosexual peers. One in four girls did so, twice the rate of boys.
Did that translate into higher suicide rates? Yes , and decidedly so, especially for girls. Some emergency departments have reported a significant increase in teens coming in for suicide attempts. (Note that these numbers are only provisional and could go up with time.)
What’s responsible for these negative trends? That’s a topic hotly debated by scholars, with most suggesting some combination of factors like the pandemic, climate change , political and economic instability, increased educational competition, and technological changes like phones and social media. Even more, for teenage girls in particular, a toxic “ triple bind ” of impossible expectations (be supportive and nurturing, be super competitive, and do both of the above effortlessly while looking “hot”) plays a key role.
However, as depression and anxiety spread among young people, it does seem as though these conditions are becoming normalized—and that youth are becoming more open and compassionate with one another. And high school clubs, as well as college programs, that focus on reducing stigma with respect to mental disorders have been shown to create real benefits .
All evidence to date suggests that many kinds of mental illness carry less stigma for younger generations. As these young people attain full maturity, the tide could eventually turn even for disorders like schizophrenia—the way it has, convincingly, for issues like same-sex marriage over the past 20 years. There are steps we can take to keep pushing this process forward.
What can create more positive change?
First, from a “top-down” perspective, enforcement of anti-discrimination policies, including the Americans with Disabilities Act, can help to drive acceptance. Title I of the ADA blocks employers from discriminating against people with disabilities, including mental illness, and requires them to make reasonable accommodations. Last week, a man in Kentucky won a half-a-million-dollar judgment against the employer who fired him for having a panic attack at work, which will surely discourage other companies from doing the same.
Beyond employment protection, we need enforcement of laws mandating “parity” for coverage of mental and physical disorders, and there’s much work to do with police and the courts to make a distinction between criminal activity and mental health crises.
Such steps can limit the consequences of stigma, but they can’t erase its existence. Though we’ve learned that information all by itself doesn’t reduce stigma, that doesn’t mean we should stop educating people from early ages about diagnosis and treatment—and there is evidence to suggest public health campaigns can reduce stigma if properly funded and executed.
For example, surveys conducted two years after Scotland’s multiyear, multiplatform “See Me” campaign—which aimed to normalize mental illness— showed a 17% drop in fear of people with serious mental illness, among other good outcomes. A much briefer social media campaign in Canada called “In One Voice” resulted in a “small but significant” decrease in a desire for social distance one year after it ended—though the same study also found that people didn’t feel more motivated to actually help someone in a mental health crisis.
The contrasting results of these two campaigns suggest that size and scope matter when it comes to changing attitudes. Scotland’s much more comprehensive approach made more of an impact than “In One Voice.” And it emphasized personal contact, not just factual knowledge, asking us to “see” real people in all their complexity.
The California Mental Health Services Act is a statewide prevention and early intervention program directly addressing stigma and discrimination, including “a major social marketing campaign; creation of websites, toolkits, and other informational resources; an effort to improve media portrayals of mental illness; and thousands of in-person educational trainings and presentations occurring in all regions of the state.” An independent evaluation found that it succeeded in reducing stigma in California, “with more people reporting a willingness to socialize with, live next door to, and work with people experiencing mental illness.” Participants also reported “providing greater social support to those with mental illness.”
Policies and education do work to reduce stigma, but they alone cannot change human hearts.

The Science of Happiness
What does it take to live a happier life? Learn research-tested strategies that you can put into practice today. Hosted by award-winning psychologist Dacher Keltner. Co-produced by PRX and UC Berkeley’s Greater Good Science Center.
- Apple Podcasts
- Google Podcasts
It has probably helped a lot for more and more people to talk about their experiences with mental illness, on social media and through popular media like magazines and television. In 2013, the New York City chapter of the National Alliance on Mental Illness teamed up with marketing company JWT New York to launch the “I Will Listen” campaign. They asked people to publicly pledge on social media to hear and support individuals struggling with mental illness.
That early effort encouraged others to later speak out about their experience with depression and addiction on platforms like TikTok and Facebook, making private struggles public in a way that previous generations only glimpsed with books like William Styron’s groundbreaking 1990 memoir Darkness Visible . Or, more recently, books like Kay Redfield Jamison’s memoir An Unquiet Mind (1996), Andrew Solomon’s The Noonday Demon (2001), and Brian Broome’s Punch Me Up to the Gods (2021).
It’s important to note that there is little solid evidence to date that talking about mental illness on social media reduces stigma—and, in fact, at least one study found that social media (if it promotes stereotypes) can actually increase stigma. That doesn’t mean people shouldn’t try. It could simply mean that it isn’t enough for people to talk about their own experiences with mental illness; we might also need concerted efforts to limit hate speech and misinformation on social media about people with mental illness. And that personal disclosures of mental disorder need to be grounded in rehearsal, support, and timing, as is the case with stigma expert Pat Corrigan’s program, Honest, Open, and Proud .
Beyond social media, news and entertainment media have a long way to go in representations of mental illness. Many studies through the years have shown that stigmatizing portrayals result in more social stigma and can make suffering much worse in people suffering from mental illnesses. Although more accurate and humanized accounts do appear, the predominant themes are ones of incompetence and violence. We simply need better, more accurate, and more humanized media portrayals—and perhaps that needs to start with targeting journalists and other content creators with specialized education in college, graduate school, and professional development courses. As well, better access to evidence-based treatments is a huge priority for the entire mental health profession. We now understand that many forms of psychotherapy and family-based treatment, as well as medications when needed, can combat some of the most serious symptoms and impairments related to mental disorders. But distressingly low proportions of those in need of such care actually receive evidence-based treatments. For many, even just regular therapy is financially out of reach. At an overall per-capita level, funding for mental health research, via the National Institute of Mental Health, remains far lower than for conditions like cancer.
That is quite ironic. Several generations ago, cancer was highly stigmatized as a disease triggered by one’s loss of will to live. Indeed, if your relative died from cancer, you would instead put in the obituary that she passed away from an unknown illness. Today, though—given the huge spike in disclosure and acceptance—cancer has become a true cause, engendering support and large economic outlays in the battle against it. Understanding that treatment can be effective might help reduce stigma of mental illness, if we can grow to see it as just another human problem that medicine can address, given the time and tools.
Finally, as noted above, young people appear, in many surveys, to be the drivers of changed attitudes and behaviors. A devastating kind of stigma is self-stigma—and the evidence indicates that millennials and Gen Z are turning away from seeing themselves as broken for feeling depressed and anxious, toward seeing themselves as having common illnesses that can be managed and even overcome with treatment, group support, and solidarity.
Young people are the key. Not just because they are always the ones who will shape the future, but because today’s youth are facing formidable mental health challenges. If we can support their mental health through these waves of stressful social change, they might have the compassion and the wisdom to alleviate the suffering of those with mental illness, instead of making it worse with stigma.
About the Authors
Stephen Hinshaw
Stephen Hinshaw, Ph.D., is Distinguished Professor of Psychology at UC Berkeley and Professor of Psychiatry and Behavioral Sciences at UC San Francisco. His focuses on developmental psychopathology, child and adolescent mental health (particularly ADHD), and the use of clinical trials to understand underlying mechanisms. He also actively investigates mental illness stigmatization and attempts to reduce such stigma. Hinshaw has authored over 400 articles, chapters, and commentaries, plus 12 books, including Another Kind of Madness: A Journey through the Stigma and Hope of Mental Illness and The Mark of Shame: Stigma of Mental Illness and an Agenda for Change .
Jeremy Adam Smith
Uc berkeley.
Jeremy Adam Smith edits the GGSC’s online magazine, Greater Good . He is also the author or coeditor of five books, including The Daddy Shift , Are We Born Racist? , and (most recently) The Gratitude Project: How the Science of Thankfulness Can Rewire Our Brains for Resilience, Optimism, and the Greater Good . Before joining the GGSC, Jeremy was a John S. Knight Journalism Fellow at Stanford University.
You May Also Enjoy

This article — and everything on this site — is funded by readers like you.
Become a subscribing member today. Help us continue to bring “the science of a meaningful life” to you and to millions around the globe.
Calculate for all schools
Your chance of acceptance, your chancing factors, extracurriculars, should i write about my mental health struggles in my college essay.
I've had some mental health challenges throughout high school and I'm considering writing about them in my college essay. However, I'm worried it might be seen as a red flag by admissions officers. Should I choose a different topic or is it okay to write about my mental health journey?
Writing about mental health challenges can be a deeply personal and meaningful topic for your college essay, but you're right to consider the potential implications. If you decide to write about your mental health journey, it's important to focus primarily on the growth and resilience you've demonstrated despite your challenges. Make sure your essay showcases your strengths and your ability to overcome obstacles.
That being said, it's not a topic without risks. Some admissions officers might be concerned about your ability to handle the stress of college life. So, if you have an alternative topic that reflects your personality and experiences just as well, it might be a safer choice.
Ultimately, the decision is yours and should reflect who you are and what has shaped you through your high school experience. CollegeVine has a helpful blog post about writing about mental health in college essays that may provide you with more guidance: https://blog.collegevine.com/mental-health-college-essays/. Good luck with your essay and college applications!
About CollegeVine’s Expert FAQ
CollegeVine’s Q&A seeks to offer informed perspectives on commonly asked admissions questions. Every answer is refined and validated by our team of admissions experts to ensure it resonates with trusted knowledge in the field.
Appointments at Mayo Clinic
Mental health: overcoming the stigma of mental illness.
False beliefs about mental illness can cause significant problems. Learn what you can do about stigma.
Stigma is when someone views you in a negative way because you have a distinguishing characteristic or personal trait that's thought to be, or actually is, a disadvantage (a negative stereotype). Unfortunately, negative attitudes and beliefs toward people who have a mental health condition are common.
Stigma can lead to discrimination. Discrimination may be obvious and direct, such as someone making a negative remark about your mental illness or your treatment. Or it may be unintentional or subtle, such as someone avoiding you because the person assumes you could be unstable, violent or dangerous due to your mental illness. You may even judge yourself.
Some of the harmful effects of stigma can include:
- Reluctance to seek help or treatment
- Lack of understanding by family, friends, co-workers or others
- Fewer opportunities for work, school or social activities or trouble finding housing
- Bullying, physical violence or harassment
- Health insurance that doesn't adequately cover your mental illness treatment
- The belief that you'll never succeed at certain challenges or that you can't improve your situation
Steps to cope with stigma
Here are some ways you can deal with stigma:
- Get treatment. You may be reluctant to admit you need treatment. Don't let the fear of being labeled with a mental illness prevent you from seeking help. Treatment can provide relief by identifying what's wrong and reducing symptoms that interfere with your work and personal life.
- Don't let stigma create self-doubt and shame. Stigma doesn't just come from others. You may mistakenly believe that your condition is a sign of personal weakness or that you should be able to control it without help. Seeking counseling, educating yourself about your condition and connecting with others who have mental illness can help you gain self-esteem and overcome destructive self-judgment.
- Don't isolate yourself. If you have a mental illness, you may be reluctant to tell anyone about it. Your family, friends, clergy or members of your community can offer you support if they know about your mental illness. Reach out to people you trust for the compassion, support and understanding you need.
- Don't equate yourself with your illness. You are not an illness. So instead of saying "I'm bipolar," say "I have bipolar disorder." Instead of calling yourself "a schizophrenic," say "I have schizophrenia."
- Join a support group. Some local and national groups, such as the National Alliance on Mental Illness (NAMI), offer local programs and internet resources that help reduce stigma by educating people who have mental illness, their families and the general public. Some state and federal agencies and programs, such as those that focus on vocational rehabilitation and the Department of Veterans Affairs (VA), offer support for people with mental illness.
- Get help at school. If you or your child has a mental illness that affects learning, find out what plans and programs might help. Discrimination against students because of a mental illness is against the law, and educators at primary, secondary and college levels are required to accommodate students as best they can. Talk to teachers, professors or administrators about the best approach and resources. If a teacher doesn't know about a student's disability, it can lead to discrimination, barriers to learning and poor grades.
- Speak out against stigma. Consider expressing your opinions at events, in letters to the editor or on the internet. It can help instill courage in others facing similar challenges and educate the public about mental illness.
Others' judgments almost always stem from a lack of understanding rather than information based on facts. Learning to accept your condition and recognize what you need to do to treat it, seeking support, and helping educate others can make a big difference.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- StigmaFree me. National Alliance on Mental Illness. https://www.nami.org/Get-Involved/Take-the-stigmafree-Pledge/StigmaFree-Me. Accessed April 25, 2017.
- What is stigma? Why is it a problem? National Alliance on Mental Illness. https://www.nami.org/stigmafree. Accessed April 25, 2017.
- Stigma and mental illness. Centers for Disease Control and Prevention. https://www.cdc.gov/mentalhealth/basics/stigma-illness.htm. Accessed April 25, 2017.
- Sickel AE, et al. Mental health stigma: Impact on mental health treatment attitudes and physical health. Journal of Health Psychology. http://journals.sagepub.com/doi/pdf/10.1177/1359105316681430. Accessed April 25, 2017.
- Americans with Disabilities Act and mental illness. Womenshealth.gov. https://www.womenshealth.gov/mental-health/your-rights/americans-disability-act.html. Accessed April 25, 2017.
- Picco L, et al. Internalized stigma among psychiatric outpatients: Associations with quality of life, functioning, hope and self-esteem. Psychiatric Research. 2016;246:500.
- The civil rights of students with hidden disabilities under Section 504 of the Rehabilitation Act of 1973. U.S. Department of Education. https://www2.ed.gov/about/offices/list/ocr/docs/hq5269.html. Accessed May 2, 2017.
- Wong EC, et al. Effects of stigma and discrimination reduction trainings conducted under the California Mental Health Services Authority. Rand Health Quarterly. 2016;5:9.
Products and Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Abdominal pain
- Alcohol use disorder
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- Antidepressants: Side effects
- Antidepressants: Selecting one that's right for you
- Antidepressants: Which cause the fewest sexual side effects?
- Are you thinking about suicide? How to stay safe and find treatment
- Atypical antidepressants
- Clinical depression: What does that mean?
- DBS for Tremor
- Deep brain stimulation
- Depression and anxiety: Can I have both?
- Depression, anxiety and exercise
- What is depression? A Mayo Clinic expert explains.
- Depression in women: Understanding the gender gap
- Depression (major depressive disorder)
- Depression: Supporting a family member or friend
- Electroconvulsive therapy (ECT)
- How opioid use disorder occurs
- How to tell if a loved one is abusing opioids
- Intervention: Help a loved one overcome addiction
- Kratom for opioid withdrawal
- Male depression: Understanding the issues
- MAOIs and diet: Is it necessary to restrict tyramine?
- Marijuana and depression
- Mental health providers: Tips on finding one
- Mental health
- Mental illness
- Mental illness in children: Know the signs
- Monoamine oxidase inhibitors (MAOIs)
- Natural remedies for depression: Are they effective?
- Nervous breakdown: What does it mean?
- Opioid stewardship: What is it?
- Pain and depression: Is there a link?
- Passive-aggressive behavior
- Prescription drug abuse
- Psychotherapy
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Suicide: What to do when someone is thinking about suicide
- Suicide and suicidal thoughts
- Tapering off opioids: When and how
- Integrative approaches to treating pain
- Nutrition and pain
- Pain rehabilitation
- Self-care approaches to treating pain
- Thyroid scan
- Transcranial magnetic stimulation
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Vagus nerve stimulation
- Video: Vagus nerve stimulation
- Violinist Still Making Music After DBS Surgery
- Vitamin B-12 and depression
- What are opioids and why are they dangerous?
- Mayo Clinic neurosurgeon Kendall H. Lee, M.D., Ph.D., describes deep brain stimulation research
- Mayo Clinic Minute: Do not share pain medication
- Mayo Clinic Minute: Avoid opioids for chronic pain
- Mayo Clinic Minute: Be careful not to pop pain pills
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Mental health Overcoming the stigma of mental illness
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.

Resilience Is Key to Mitigating Mental Health Challenges
Strategies to boost your resiliency skills..
Posted February 3, 2022 | Reviewed by Vanessa Lancaster
- What Is Resilience?
- Find a therapist near me
- According to recent studies, three out of four adults report that the pandemic has negatively affected their mental health.
- In recognizing a mental disorder, it is essential to assess the level of disruption in various areas of one’s life.
- Biological, psychological, social, and environmental factors can be protective factors for someone experiencing a mental health challenge.
Approximately 52 million people ages 18 and older experience mental health or substance abuse disorder each year. Mental health challenges are the leading cause of disability in the United States and Canada.
Unfortunately, as the COVID-19 pandemic lingers, the risk of mental health-related disorders is more likely to increase, with recent studies revealing that three out of four adults reporting the pandemic has negatively affected their mental health.
It could be difficult to identify someone going through a mental health-related disorder since we might see it as a normal response to tough or traumatic life events. Although this might be a reality, it is also crucial to monitor frequent periods of anxiety and depression since it may indicate a more complex problem.
“A mental health disorder may be present when patterns or changes in thinking, feeling and behaving causes significant distress or disrupts the person’s ability to work" (Mayo Clinic, 2021).
In recognizing a mental disorder, it is important to assess the level of disruption in various areas of one’s life, such as the ability to work, study, care for oneself or others, and maintain successful relationships with friends and families. Nevertheless, identifying a mental disorder is not always an easy task, leading to a resulting delay in diagnosis.
Mental health challenges don’t occur in a vacuum. Often, interacting factors can affect a person’s mental health, such as biological, psychological, social, and environmental, all of which can also act as protective factors for someone experiencing a mental health challenge. These protective factors, along with coping skills, could boost a person’s level of resilience , helping mitigate mental health challenges.
What is resilience? Some think of it as an abundance of optimism or simply a sunny disposition. But resilience is more than that. It is the process of adapting to a higher point than before the hardship (APA, 2020). Resilience is a trait crucial to survival—not just our ability to bounce back but to empower us to continue growing and even improving our lives along the way.
Being resilient does not keep someone from experiencing difficult times or distress. Emotional distress and sadness are common in individuals who have endured major adversities or trauma, and the journey to resilience is prone to the involvement of significant emotional pain. The combination of strong protective factors and the ability to handle emotional distress in a healthy way contributes to long-term resilience.

How You Can Increase Your Resilience
While certain factors might make some individuals more resilient than others, resilience should not be seen as a personality trait that only some people have. On the contrary, resilience entails behaviors, thoughts, and actions that anyone can learn and develop over time. Like developing a muscle, increasing your resilience takes time, motivation , and intentionality.
By understanding what protective factors are essential in building resilience, you can actively support yourself or someone in your life who might be experiencing a mental health or even a substance abuse challenge.
To become more resilient, it is crucial to focus on four main protective factors: connection, wellness, healthy thinking, and meaning, all while empowering others to withstand and learn from tough times.
The following strategies might help boost your resilience skills:
- Build connections. It is important to prioritize relationships, especially with empathetic and understanding people, to provide a reminder you are not alone amid difficulties. Surround yourself with trustworthy and compassionate people who validate your feelings.
- Join a group. People who have suffered traumatic events tend to isolate themselves, but it is important to accept help and support from those who care about you or might have similar experiences. Some people have benefited tremendously from joining groups, whether it is a support group, civic groups, faith-based communities, or any other type of local organization that provides social support.
- Take care of your body. The approach to overcoming a mental health challenge and building resilience must follow a holistic approach. That’s because stress is just as physical as it is emotional. Thus, self-care in all areas is fundamental. For example, proper nutrition , ample sleep, hydration, and regular exercise can support your body to adapt to stress and reduce emotions like anxiety and depression.
- Practice mindfulness . Mindful journaling, yoga, and other spiritual practices like prayer or meditation can also assist you with building connections and re-establishing hope. In turn, this can prime you to deal with situations that require resilience. When you engage in these practices, it is important to reflect on the positive aspects of your life and recall all the things you are grateful for, even during the most demanding times of your life.
- Avoid negative outlets. It may be alluring to try to alleviate your emotional pain by using alcohol or other substances, but this is like putting a bandage on a deep wound. Instead, focus on giving your body the resources it needs to manage stress.
- Help others. Helping others can garner a sense of purpose, foster self-worth , connect with other people and empower you to grow resilient.
- Be proactive. Sometimes we become overwhelmed by just reflecting on the negative and the dimensions of a problem at hand. Thus, if the problem seems too big to tackle, break it down into manageable pieces.
- Move toward your goals. Set realistic goals and do something towards achieving them regularly. Even if it seems like you’re only taking baby steps that will enable you to move toward what you wish to accomplish, instead of putting energy into goals that seem unachievable, ask yourself, what is one thing I can accomplish today that will help me move in the direction I want to go? For example, if you have been recently diagnosed with chronic illness , join a support group in your area and access as much as possible educational resources about your condition.
- Keep things in perspective. It is important to monitor the quality of our self-talk . How you think can play a significant role in how you feel and act. Remember the thinking, feeling, and behaving model. Try to monitor your thinking patterns and identify any irrational thinking, such as the tendency to catastrophize obstacles or assume the world is out to get you. You may not be able to change a highly stressful situation, but you can change how you perceive it and respond to it.
- Accept change. Acceptance plays an important role in building resilience. We have to accept that change is part of life. Accepting circumstances that cannot be changed presently can help you focus on situations you may be able to alter later.
- Learn from your past. By reflecting on what was effective in dealing with a stressful event from the past, we may be able to respond more effectively to new difficult situations. Remind yourself you had the strength to overcome it before and reach for those learning experiences.
American Psychological Association. (2020, February 1). Building your resilience. http://www.apa.org/topics/resilience
Mayo Clinic. (2021, December 14). Mental Health: What’s normal, what’s not. https://www.mayoclinic.org/healhty-lifestyle/adult-health/in-depth/mental-health/art-20044098
Mental Health First Aid USA. (2020). Mental Health First Aid for adults assisting adults. Washington, DC: National Council for Mental Wellbeing.

Yamila Lezcano, LMHC , is a licensed Mental Health Counselor in private practice in Miami, FL, and Assistant Professor in the Undergraduate Psychology and Education Program at Albizu University.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Is it OK to discuss mental health in an essay?
Mental health struggles can create challenges you must overcome during your education and could be an opportunity for you to show how you’ve handled challenges and overcome obstacles. If you’re considering writing your essay for college admission on this topic, consider talking to your school counselor or with an English teacher on how to frame the essay.
Also Found On
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Strategies to Reduce Mental Illness Stigma: Perspectives of People with Lived Experience and Caregivers
Associated data.
The datasets generated and/or analysed during the current study are not publicly available due institutional policy but are available from the corresponding author upon reasonable request.
Background: Reducing the stigma surrounding mental illness is a global public health priority. Traditionally, anti-stigma campaigns were led by mental health professionals/organisations and had an emphasis on increasing mental health literacy. More recently, it has been argued that people with lived experience have much to contribute in terms of extending and strengthening these efforts. The purpose of this paper was to elicit views and suggestions from people with lived experience (PWLE) as well as from informal caregivers of people with mental health conditions, on effective strategies to combat the stigma surrounding mental illness. Methods: Six focus group discussions (FGDs) were carried out with PWLE recruited at outpatient services at the Institute of Mental Health, Singapore, and five FGDs were carried out with informal caregivers who responded to advertisements for the study between March and November 2018. In all, the sample comprised 42 PWLE and 31 caregivers. All the FGDs were transcribed verbatim and were analysed using thematic analysis. A pragmatic approach was adopted for the study, and the researchers did not assume any particular philosophical orientation. Results: Four overarching themes depicting strategies to combat stigma were identified through thematic analysis. They were (1) raising mental health awareness, (2) social contact, (3) advocacy by influential figures or groups, and (4) the legislation of anti-discriminatory laws. Conclusions: These strategies were in line with approaches that have been used internationally to disrupt the process of stigma. Our study has further identified nuanced details on how these strategies can be carried out as well as possible areas of priority in the Singapore landscape.
1. Introduction
The stigma of living with a mental health condition has been described as being worse than the experience of the illness itself [ 1 ]. The aversive reactions that members of the general population have towards people with mental illness is known as public stigma and can be understood in terms of (i) stereotypes, (ii) prejudice, and (iii) discrimination [ 2 ]. Common stereotypes associated with people with mental health conditions are that they are dangerous, incompetent, and weak in character. Prejudice refers to the agreement with these stereotypes, while discrimination refers to behavioural reactions to these prejudices [ 3 ].
Beyond the interpersonal manifestations of public stigma towards people with mental health conditions, societal-level conditions such as institutional policies and practices and cultural norms have also been found to be biased against people with mental health conditions, resulting in a lack of opportunities and resources being afforded to them [ 4 ]. These socio-political disinclinations, known as structural stigma, result in people with mental health conditions being excluded from employment, living in unstable and unsafe conditions, being disqualified from health insurance, and being subjected to coercive hospitalisation and treatment [ 5 , 6 ]. The deprivation of opportunities and poor-quality resources provided to those with mental health conditions have severe bearings, as evidenced by the gross overrepresentation of individuals with mental health conditions in the criminal justice system and among those living in poverty [ 7 ]. People with mental health conditions also have significantly higher morbidity and mortality rates [ 8 ], and consequent to all the above, have a lower quality of life compared to the general population [ 9 , 10 ].
Through repeated encounters with public and structural stigma, individuals with mental health conditions are inclined to internalise these reactions, a phenomenon known as self-stigma. A systematic review found that exposure to public stigma predicts self-stigma at a later time [ 11 , 12 ]. A person’s own stigmatizing views towards mental illness is associated with lower readiness to appraise his or her own symptoms as potentially indicating a mental health problem and thus reduces help-seeking behaviour [ 13 ]. This could be because the individual seeks to avoid the label of mental illness for him- or herself [ 14 ], fathomably to guard themselves against the negative self-perceptions associated with it and the potential consequences of shame and reduced empowerment [ 15 ]. Indeed, self-stigma decreases one’s self-esteem and self-efficacy, leading to the “why try effect”, where people with mental health conditions question their worthiness and capability to pursue personal goals [ 16 , 17 ], leading to a loss of self-respect and increased shame and hopelessness [ 18 , 19 ]. Over time, higher levels of self-stigma have been found to be associated with suicidal ideation [ 18 , 20 ].
Due to these adverse effects of stigma, stigma-reduction is seen as a global public health priority [ 21 , 22 , 23 , 24 ]. Anti-stigma programmes were traditionally conducted by or in substantial consultation with groups representing psychiatric expertise [ 25 ]. However, several criticisms have been raised towards this approach in the recent years. First, the emphasis on medical understandings of mental health problems and the importance of adhering to psychiatric interventions have been criticised as fulfilling the psychiatric services agenda rather than the interest of people with mental health conditions and eclipsing inputs from other standpoints [ 3 , 26 ]. Next, mental health professionals have been found to be just as likely to stigmatise those with mental health conditions [ 27 , 28 , 29 ]. Thus, is has been argued that the professional expertise that mental health professionals have in providing mental health services may be insufficient in impacting the social spheres in which stigma operate, and it may be timely for them to move to a supporting role [ 30 ].
In recent years, anti-stigma programmes have involved people with lived experience to allow direct or parasocial interactions between target audiences and people with mental health conditions. Contact-based interventions have demonstrated the clearest evidence in reducing stigmatising attitudes, desire for social distancing and discrimination [ 31 , 32 , 33 ]. Contact-based interventions typically involve brief contact between members of a majority group and a stranger representing the stigmatized population who is quite different from a naturally occurring contact. Stigma is reduced by providing an opportunity for interpersonal contact between people who have mental illness and individuals who may hold stigma towards them. A key ingredient of contact-based interventions is the delivery of testimonies by service users [ 34 ]. The efficacy of contact-based education has led to calls for collaborations with individuals with mental health conditions to offer their experiential wisdom in challenging stigma, representing the voice of those who struggle with mental health difficulties and shedding light on blind spots and gaps in previous strategies [ 3 , 35 ]. Corrigan asserted that just as disability rights groups have adopted the slogan of “no policy or action should be taken about a group without full participation of that group”, the same should be applied to alleviate mental health stigma [ 30 ]. Additionally, while we have thus far described the negative processes that arise from stigma, there are people with mental health conditions who do not agree with the hackneyed stereotypes and respond with indignation that seems to empower and energise them to advocate for changes to the ways in which they are treated [ 2 ]. Their inputs towards initiatives that are aimed at improving service delivery and de-stigmatisation programmes have been found to lead to novel results and have been described as a strength of those programmes [ 35 , 36 ].
Singapore is a small, highly urbanised, multi-cultural country located at the Southern tip of the Malayan Peninsula. The resident population is made up of 75.9% Chinese, 15.0% Malay, 7.5% Indian, and 1.6% other ethnicities [ 37 ]. A developed country, the culture of Singapore can be described as a combination of Eastern and Western cultures, and English is the primary language of instruction. Stigma towards mental illness remains prevalent in Singapore today. An earlier nationwide survey revealed that 38.3% of the population believed that people with mental illness are dangerous, and 49.6% felt that people need to be protected from psychiatric patients [ 38 ]. A decade later, another population survey, which used a vignette-based approach, reported that 50.8% of respondents indicated that mental illness was a sign of personal weakness, 42.8% were unwilling to work closely with a person with mental health conditions on a job, and 70.2% were unwilling to have a person with mental health conditions marry into their family [ 39 ]. A recent qualitative study of daily encounters of personal stigma reported themes such as social exclusion, subjection to contemptuous treatment, and rejection by employers following the declaration of a mental health condition [ 40 ].
Anti-stigma activities in Singapore have been conducted by the state psychiatric institution, the Institute of Mental Health (IMH), the National Council of Social Service, the Health Promotion Board (statutory boards), and non-profit organisations such as the Singapore Association for Mental Health and Silver Ribbon Singapore, who have the collective aims of improving mental health literacy, access to mental health care, and improving the reintegration of people with mental health conditions into the community [ 41 , 42 ]. However, the involvement of individuals with mental health conditions in anti-stigma campaigns is lacking. The purpose of this paper was thus to elicit views and suggestions from people with lived experience (PWLE) and informal caregivers of people with mental health conditions on effective strategies to combat stigma.
The present study is part of a larger study that aimed to examine the nature of mental illness stigma in Singapore from the perspectives of five stakeholder groups, namely PWLE, informal caregivers, members of the general public, professionals working in mental health settings, and policy makers. The main purpose of this research was to provide actionable knowledge. It took a pragmatic approach common in health services research and did not assume any particular methodological orientation [ 43 ]. Only data from PWLE and caregivers were used in this analysis. The study was approved by the institutional ethics committee, the National Healthcare Group Domain Specific Review Board. Written informed consent was obtained from all participants before initiating study related procedures.
2.1. Participants
PWLE and caregivers were recruited through referrals by their clinicians or self-referral by learning about the study though poster advertisements placed in waiting areas at the IMH outpatient clinics. The IMH is Singapore’s largest provider of mental health care, providing pharmacological and psychosocial treatments as well as psychosocial rehabilitation for a range of subspecialties, including child and adolescent psychiatry, affective disorders, and psychosis. It has also spearheaded mental health education and anti-stigma events for the public. All the participants were required to be Singapore citizens and permanent residents, aged 21 years old and above, and could not be a student or professional from the mental health field.
PWLE recruitment was limited to two types of psychiatric diagnoses, mood and psychotic disorders, to attain a more homogenous account of encounters with stigma. The groups were also separated by diagnosis to facilitate the identification of members in a group with each other and to provide comfort when expressing themselves. In all, six Focus Group Discussions (FGD) were conducted with PWLE between March to May 2018 (three with individuals with mood disorders, three with those with psychosis-related disorders). Referred and self-referred PWLE were deemed clinically stable by their treating clinicians and were able to provide informed consent.
Although the poster advertisements indicated that the study sought caregivers of individuals with psychosis-related or mood disorders, no attempt was made to confirm the diagnosis of their care recipients with the treating clinicians. The caregiver group was independent of the PWLE group. Unlike the PWLE FGDs, the caregivers were not separated based on the diagnosis of their care recipient. As the initial FGDs did not identify any issue with this approach, the team carried out the rest of the FGDs in a similar manner. In all, five FGDs were conducted with caregivers between June and November 2018.
The PWLE FGDs ranged from 5–8 participants, while the caregiver FGDs ranged from 4–9 participants. The sociodemographic profiles of the PWLE and caregiver participants are presented in Table 1 . Participants received an inconvenience fee at the end of the FGD. All FGDs were conducted in English.
Sociodemographic characteristics.
# 1 missing PWLE response for Highest Completed Education.
2.2. Data Collection
The FGDs were conducted in a closed room that was relatively free from distractions in a community club, which was chosen because it is a neutral venue. Each FGD was conducted by two study team members, who served as the facilitator or the note taker for the day. The facilitators (either MS or SS) were trained and experienced in qualitative research methodologies. CMJG, OWJ, GTTH, SS, and MS took turns as note-takers in the different FGDs.
After individual consent was taken to participate in the research and to audio-record the session, each participant filled out a sociodemographic form that collated information about age, gender, education level, ethnicity, and brief information about their illness (for PWLE) or caregiving relationship (for caregivers), and the completed form was returned to the facilitator. Participants were assured that all of the data collected from them would be kept confidential, the transcripts would be de-identified such that names and other identifying features would be omitted, the audio-recording would be deleted after transcription, and that there were no correct or incorrect answers before the discussion commenced.
The experienced facilitators used a topic guide comprising open-ended questions that had been developed by the research team so that the data collected across the various FGDs would be as uniform as possible. Few specific questions were designed to elicit information that could be best addressed by a particular target group. The topic guide covered areas of mental illness stigma such as encounters of stigma and reasons for stigma. The team formulated the questions in a manner similar to that recommended by Krueger et al. [ 44 ], the recommendations of whom comprised the following: The questions should elicit information that directly relates to the study’s objectives. The questions should be easy for the participants to understand and should be phrased in a neutral manner so as not to bias participant responses. The questions can be answered by all the participants. Questions should be open-ended and not answered with a “yes” or “no” to facilitate descriptive responses. The questions should not make the participants uncomfortable when answering, and they should not trigger defensive responses. The team brainstormed the questions to answer the objectives of the research, and one researcher drafted the questioning route, rephrased, and reordered the questions to form a logical flow. The draft was circulated to the rest of the team, and suggestions were incorporated. The team aimed to keep the final total number of questions between 10–12. Decisions to omit questions were based on importance in addressing the research objectives, with final decisions being made by the lead investigator (MS). The questions were then tested out, using the first focus group as a pilot. The items that were used to elicit responses to the research question addressed in this paper was from the final segment of the topic guide: “How do you think stigma towards people with mental illness can be reduced” and “Have you heard of campaigns to reduce stigma towards those with mental illness? Is there anything that can be done better?”. The facilitator probed for range and depth of responses and sought clarification for responses that were unclear using neutral questions. Attempts were made to encourage responses from all members. The entire duration of each FGD lasted between 1.5–2 h. FGDS were carried out one at a time, first with the PWLE and then with the caregivers. At the end of each FGD, there was a debrief between the facilitator and note-taker, and a comprehensive summary was provided to the rest of the research team soon after to reflect on each session, to ensure that any problems were identified early and addressed, and emerging themes and unique points that had been raised were discussed. The FGDs were later transcribed verbatim for analysis. The decision was made by the team to cease data collection for PWLE and the caregiver groups when no new themes were identified, i.e., when data saturation was reached.
2.3. Analysis
The data were analysed using an inductive thematic analysis method [ 45 ]. Transcripts were first distributed amongst five study team members (SS, CMJG, GTTH, OWJ, and MS) for familiarisation with the collected data. Subsequently, each study team member independently identified preliminary codes from their respective transcripts. The study team members then came together, and through an iterative process of comparing the codes and combining, discarding, and redefining the codes, collaboratively decided on the final list of codes. A codebook was developed by the coders (SS, CMJG, GTTH, OWJ, and MS), in which each code was characterised by a description, inclusion and exclusion criteria, and typical and atypical exemplars to guide the coding process. To ensure coding consistency among the study team members, one transcript was first coded to establish inter-rater reliability. The study team continued to discuss, refine the codebook, and repeat the coding with another transcript until a satisfactory inter-rater reliability score was achieved (Cohen’s Kappa score > 0.75). Transcripts were then distributed among the study team members for coding. Data analysis was completed with Nvivo Version 11.0. (QSR International Pty Ltd. Hawthorn East, Australia).
After coding all transcripts, the codes were sorted such that similar codes were grouped together to form potential themes. Codes that did not seem to fit into any theme at first were revisited as the themes were gradually refined. Relationships between these themes were also examined, and different levels (main theme and sub-themes) were identified. Any remaining codes were compared against the revised themes to determine fit. The initial themes were drafted by SS, JCMG, GTTH, OWJ, and MS and presented to CSA for further refinement before finalisation.
Strategies to ensure the quality of the findings recommended by Anney [ 46 ] were exercised in this research. Data were triangulated from two different informant sources: patients and caregivers. The transcripts were read and re-read by five researchers independently. The interpretations were compared, and regular meetings were held to discuss differences until a consensus was reached. These informant and researcher triangulations aimed to increase the credibility of the findings. To ensure transferability, the participants were sampled in such a way that there was good distribution by age, gender, education level, and ethnicity, and for the caregivers, relationship with the care-recipient. Finally, for confirmability, intentional record keeping of summaries and reflections after each FGD as well as decisions made during the coding and analysis were documented to maintain an audit trail.
Four overarching themes depicting the strategies to combat stigma were identified. They included (1) raising mental health awareness, (2) social contact, (3) advocacy by influential figures or groups, and (4) legislation of anti-discriminatory laws. It was not uncommon for participants to refer to two or more approaches in a single quote. While we have selected quotes to illustrate the main theme, they may cross-cover other themes to some degree. To ensure that standard usage of English was maintained, minimally corrected verbatim of quotes are presented.
3.1. Raising Mental Health Awareness
There were two subthemes pertaining to the strategy of raising mental health awareness, which can be described as the “who and how” and “what” of this approach.
3.1.1. Target Groups/Setting and Methods
Anti-stigma awareness initiatives for the general population were frequently suggested by participants, and they recommended outreach through both traditional and social media as well as popular mass events such as marathons and festivals in order to reach a wide range of members of the public from the young to the old. They also emphasised that these efforts should be carried out repeatedly, reasoning that increased exposure to the topic will lead to greater familiarity and with time, greater acceptance of this taboo subject.
You all have to do a lot of campaigns, running it tends to stick in their minds (Male, 37 years, Psychosis-related disorder, PWLE FGD 5)
Educating the public because it is very important. More on media because there are many people on the internet or computer, TV and all sorts ah, newspaper of course, articles, so that more people will come to know so that lesser, I mean to accept slowly. The stigma will grow weaker and weaker, not that strong. (Female, 65 years, Caregiver FGD 3)
With regards to media portrayal, the participants discouraged the use of drama in and of itself as a means of education. They asserted that such media forms tend to sensationalise mental illness through negative characterizations that further reinforce existing stereotypes. Instead, they prefer coverage through documentaries and talk shows.
I think drama is not a good way to go to raise awareness of mental illness because in drama, it’s drama what. You have to be dramatic, and you have to be dramatic you have to sensationalise. But maybe talk shows are better. Talk show where they invite celebrities together with professionals and then they talk it out. (Male, 28 years, Psychosis-related disorder, PWLE FGD 5)
Raising mental health awareness in two specific target groups was frequently brought up. The first group that the participants wanted to increase mental health awareness in was among school students. The participants rationalised that it would be easier to influence young people whose attitudes are more malleable. They also voiced concerns that youth are a vulnerable group due the heightened challenges they face such as intense academic pressures and societal expectations. Thus, they would benefit from literacy-based interventions to facilitate early recognition and help-seeking behaviours. Some of the participants suggested an incremental approach whereby younger primary school-age students could be primed with information on mental well-being before being introduced to more serious topics on mental health conditions.
Education from, it’s ok for those who are already old enough like us, we can’t like, some people we can’t really unlearn what we learn so we have to teach the new generation and input in what are the more important things, like for example, the major concerns as of now and like how important is mental health so that they won’t grow up to be like their parents or like whoever. So, I think it starts from the younger ones la they will receive fresh information and they won’t have any judgement against us (Female, 22 years, Mood disorder, PWLE FGD 2)
I think it should start across Singapore, like for example, starting from schools, starting from workplaces, meeting the employers you know, the teachers, the, the facilitators, starting from there you know. So, when you have that well-established, designed activities you know, I mean the initiative, we have that initiative to go to, to the schools you know, at a younger age when they already start to understand, so when they come to work, as an maybe an employer, so they can understand further what happens to the subordinates, what happens to the employees who have mental illness. (Female, 48 years, Caregiver FGD 5)
The second target group was employers. The participants commented that in contrast to the recent advances in efforts to raise mental health awareness, workplaces were especially lagging in this regard, and overt stigmatisation continues to occur in workplaces. Legislative measures were also recommended to combat stigma and discrimination in this setting (this will be further elaborated in the fourth theme).
Essentially run multiple small campaigns across companies so we start from the top tier and then you go down to the middle tier and then into the SME like a small, very small enterprises and things like that to do awareness campaign with all their HR [Human Resource], their ops [operations] department and things like that so that they learn. So at least if the managers learn, hopefully they’ll pass that on, not always. It will not always happen, but it might you know, so at least there’s a trickle-down effect and it last longer (Male, 28 years, Mood disorder, PWLE FGD 6)
I think the Singapore government is very effective, and they are respectable, so Ministry of Health or IMH organize talk to the employers, to the unions, trade unions. (Male, 64 years, Caregiver FGD 5)
3.1.2. Types of Content
The participants recommended that messages pertaining to the prevalence of mental illness debunking common myths about mental illness and likening it instead to other chronic illnesses could reduce stigma and demystify mental illness. The participants also recommended disseminating information on where and how mental illness can be managed as well as the efficacy of treatments to emphasise the treatability of mental illnesses.
Get the MP [member of parliament] come and talk, share with them, share with the population, mental illness is common. Especially depression, 1 in 5, in the population will get depression, or even now, now 1 in 4. (Male, 64 years, Caregiver FGD 5)
To me education is the best way to, to erase all these myths (Male, 49 years, Psychosis-related disorder, PWLE FGD 4)
Let them know, no big deal. It is just like any other chronic illness. I say in your whole lifetime anyone can suffer some from of mental illness. (Female, 65 years, Caregiver FGD 3)
The PWLE cautioned that anti-stigma messages should not result in “over-normalisation” or careless over-identification of mental illness and trivialisation among lay members of the public, as it makes light of the disruptions to the lives of those who have been diagnosed with them and the suffering they bring.
You don’t want to reduce stigma so much to the point when somebody likes oh I like to put my water bottle on the right side, oh I’m OCD. You know. Or like oh I had a negative thought that came in, oh I have schizophrenia. You don’t want people to like over-normalise it, cause that does happen in these days. Like when just somebody likes to be neat, they consider themselves OCD. Yeah, it’s so frustrating. The definition of mental illness is it’s supposed to disrupt your natural life. If it doesn’t disrupt your life in any way, it’s not supposed to be considered a mental illness. So, when people are like oh I’m very OCD, or like oh I have depression. Yeah, everybody has depression. (Female, 23 years, Psychosis related disorder, PWLE FGD 5)
They also did not wish for others to take pity on them or treat them differently on account of their mental illness but to instead be supportive in their recovery.
You shouldn’t get them to sympathize with you, more like to understand them. Rather than like say that okay you must be careful of this people, you must just give them information you know (Male, 24 years, Mood disorder, PWLE FGD 6)
We would educate them on how to less stigma, how to know about our condition, then how to actually support us in the recovery process (Female, 34 years, Psychosis-related disorder, PWLE- FGD 4)
3.2. Social Contact
Three kinds of social contact were raised by the participants: celebrity disclosures, testimonies of success stories by people with mental health conditions and opportunities to interact with them.
3.2.1. Celebrity Disclosures
The participants exemplified that the disclosure of mental health struggles by local celebrities as being particularly impactful. They reasoned that Singapore has a celebrity culture in which celebrities have a large following and influence. Sharing their mental health difficulties would drive the message that mental illness does not discriminate, debunk certain stereotypes associated with mental illness, validate the experiences of those coming to terms with their illness, and encourage open and honest discussion about mental illness.
I think it’s good if you can get someone, well known in Singapore, to share about their family members having mental illness or they themselves having mental illness. (Female, 51 years, Caregiver FGD 5)
In Singapore, there is a podcast. That is actually supposed to be a comedy podcast, but every now and then it gets a bit real. And they talk about themselves. So, I think, I don’t know if you guys know Nathan Hartono? He runs a podcast with his friend named Jon Kensey who’s also based in Singapore. He’s Filipino but he’s based in Singapore. He does comedy shows, he does, he’s a comedian. He does all these funny little things but every now and then when we write in, and we are allowed to write in to them it’ll just be like an idea of what would you suggest if we are going through this thing. So, he actually openly talks about his depression. So, he’ll share experiences, he’ll share what he would do, he would make things very clear that it’s not supposedly the only way or the best way to do things but that’s how he would have done it. Yeah, and the thing these little things help knowing that even people who are supposedly seen on a higher pedestal is also facing the same things as you are. Yeah, really changes a lot (Male, 23 years, Mood disorder, PWLE FGD 1)
3.2.2. Sharing Inspirational Recovery Stories
Apart from celebrity figures, the PWLE suggested that inspiring recovery stories of people with lived experiences can be included in anti-stigma efforts. They reasoned that these stories illustrate that mental illness does not need to be a barrier to attaining a meaningful life, that people with mental health conditions could be productive members of society, an embodiment of strength and courage despite adversity, and give hope to those worried about their or their loved one’s future.
I remember that time I was watching the news about lady, she suffered from mental illness but she… she see doctors, follows up regularly, she is recovered in that sense. She secured a job as a lecturer in one of the local polytechnic. She wrote a book. She was very frank with her employer, that was good, and they accept her as she is but she still go back to the hospital like every several months for follow-up and stuff like that. So I find that very enlightening. That there is such people who actually like make good head way in their life despite having mental illness. So I think if you can find more of such people and interview them highlight to the public that is actually… we can also be successful in their own way, it will be good. (Female, 44 years, Psychosis-related disorder, PWLE FGD 3)
3.2.3. Opportunities for Social Contact
The participants opined that it would be beneficial for those without mental illnesses to have opportunities for direct social contact with PWLE. They identified the benefits of this strategy as allowing people to relate to PWLE on a more personal level and debunk extreme examples of mental illness. They added that such a first-hand experience would be more compelling than didactic approaches.
( Another participant: Education is important) And exposure, I think. Because education is like you are telling people you know? But I think exposure for them to experience it, interaction with people with mental illness. It really speaks more than words. How they… because people always have this misconception ‘oh ok, mental illness, violence, negative, crazy, talking to yourself…’ But in fact, in fact most mental patients are not like that, they don’t behave that way. (Female, 39 years, Caregiver FGD 1)
I would emphasize priorities on interaction between the regular population and those with illness. To let them realize there’s no big difference. (Male, 24 years, Mood disorder, PWLE FGD 6)
3.3. Advocacy by Influential Figures or Groups
The participants felt that the question of “who” leads the de-stigmatisation efforts matters. Some participants suggested that mental health experts should partner with organisations that have larger influence, while others asserted that the efforts should be helmed by organisations other than psychiatric experts.
Because like even in my head, the assumption is it’ll probably come from IMH. Which to me is not the most effective method of campaigning because then everybody would be like, yeah they would do this, of course they would do this. So, I think, no. (Male, 23 years, Mood disorder, PWLE FGD 1)
They identified individuals and groups with political affiliations as being particularly suited due to their authoritative influence, networks, and access to funds.
To be effective it has to be nationwide, government-led initiative. It cannot be a little bit here and there, by IMH or by Caregiver Alliance, it doesn’t really work. It has to be nationwide and it has to have the support of the government. First, they have the resources and as what (another FGD participant) said uh, they can be very effective if they are very serious in wanting this campaign to be successful, they can do it. (Female, 51 years, Caregiver FGD 5)
3.4. Legislation of Anti-Discriminatory Laws
3.4.1. removal of declaration of mental illness in job application and scholarship forms.
In virtually all the FGDs, the participants called for the removal of the declaration of mental illness from job application and scholarship application forms. They regarded this requirement as being both irrelevant and discriminatory and believed that their unsuccessful applications were directly due to their disclosure.
Now we talk about the functional ability of a mental illness person, we talk about work. When you work, you need to fill in a lot of forms. There are a lot of things that…why must there be a declaration by the organisation? Why? Why? That is not good, that is not fair. In school, in army or in certain big organisation, there is always a declare, “Are you mentally ill? Do you have a mental problem?” Why is that in the form? It should be out. (Male, 62 years, Caregiver FGD 1)
I hope like whenever you’re applying for a job then you do not need to tick off the, “Do you have a mental illness?” that... that column. But maybe being open about it and talk about it would make the person understand in your shoes (Female, 25 years, Mood disorder, PWLE FGD 6)
3.4.2. Policies That Encourage Employers to Hire and Support PWLE in Workplaces
Although the participants called for the removal of mental illness declarations on application forms, they preferred to be truthful about their condition, as they feared being discovered if they had lied to increase their chances of employment. They also found that concealing their condition and their medical appointments was burdensome. The PWLE suggested that apart from raising awareness among employers, governmental support could be given to encourage employers to hire individuals with known mental health conditions.
The government could perhaps encourage their employers to take on mental patients who are willing to disclose their conditions of their job contracts. I stay in (name of a sheltered home) and the practice of their employment specialist is to have a very honest declaration. Just help… just say we have, this person who is going to help work has a mental condition. So they say that is why I follow them because they do it on a clean cut basis but I feel very upset because I follow suit, I declare my condition, and I loss so many chances of being employed. So government can do, I think government has yet to, have a lot to do. (Female, 55 years, Psychosis-related disorder, PWLE FGD 3)
In line with my unemployment, no money, and at the same time, I feel like I can contribute la to the greater society, ah you know what I’m saying? So that maybe in the future, people will say okay never mind you can work but then like you know, every year got psychiatric evaluation you know that’s even better, you know. A company that’s accepting of your condition. (Male, 24 years, Mood disorder, PWLE FGD 6)
Lastly, several participants shared being caught in awkward situations upon disclosure and the found reactions by their superiors inappropriate. Thus, they suggested that guidelines can be put in place to inform employers on how to respond sensitively to those who choose to disclose.
Maybe you can suggest to MOM [Ministry of Manpower] to remove the questions about health conditions. Have some regulations or advice to employers about how they can react to people who declare or maybe even take it out from the application form. For example, in the US [United States], you’re not actually, it’s kind of discriminatory, you’re not allowed to. It’s against the law to discriminate people based on their orientation or whatever, their conditions. So maybe in Singapore, we can move ahead in that regard. (Male, 28 years, -Psychosis-related disorder, PWLE FGD 5)
4. Discussion
The suggestions by the PWLE and caregivers in tackling stigma can be classified broadly as raising awareness through education, social contact, advocacy, and legislative reform. These strategies are in line with the approaches that have been used internationally to disrupt the process of stigma. Corrigan et al. [ 47 ] have suggested three approaches: education, protest, and contact, while Arboleda-Florez and Stuart [ 22 ] extended Corrigan’s typography with three additional strategies: legislative reform, advocacy, and stigma self-management. Our study has further identified nuanced details on how this can be carried out in the Singapore landscape.
Raising awareness through public education was the most suggested strategy. It is appealing, as it targets lack of awareness and misinformation with the provision of information. Young people in particular were identified as a target group for educational intervention due to the burgeoning pressure they face, the potential they have in changing the future, and the opportunities that school settings have to deliver interventions using a literacy approach, points that have also been described previously [ 48 , 49 ] in the literature. School-friendly literacy approaches have been shown to be effective in improving knowledge about mental health conditions [ 50 ].
The participants suggested various ways of raising awareness for the general population and drew particular attention to the potential problems of media strategies due to their tendency towards presenting stories in a sensational manner. Gottipatti et al. [ 51 ] explored local media portrayals of people with mental disorders in Singapore’s largest media organisations, Singapore Press Holdings and MediaCorp, and reported that mental health-related articles in Singapore were primarily negative in sentiment, with crime-related news accounting for 40% of the corpus. Moreover, mental health experts had unwittingly used stigmatising terms in interviews. The authors suggested that media professionals and editors can also be enlisted to play a more proactive gatekeeping role and to counteract the largely negative portrayal of mental illness by providing articles on well-being and recovery. They also proposed a rule-based solution model based on text mining and natural language processing (NLP) techniques that can automatically identify aspects of stigma in media articles for editing before publication [ 51 ]. Similarly, Stout, Villeges, and Jennings [ 52 ] suggested for informational and educational activities to be arranged for journalists that teach techniques to report on mental health stories in a balanced and responsible way. Other strategies that have been used include SANE Australia’s (a charitable advocacy group) StigmaWatch program, which monitors and responds to the inaccurate or inappropriate media portrayal of mental illness. If problematic reporting is not remedied, then the group may consider taking public action [ 35 ].
The participants also cautioned that messaging should not result in benevolent stigma—an unintended consequence of well-intentioned approaches, where people with mental illness are treated as being unable to competently handle life’s demands and need a benevolent authority to make decisions for them [ 30 ]. This kind of messaging is stigmatizing, as is perpetuates power imbalances by appealing to the public to do good for a seemingly weak, pitiful subordinate group [ 53 ]. Such a response disempowers people with mental health conditions and stunts opportunities for personal growth. The participants in our study, as Corrigan had pointed out, wished for empathy cultivation leading to being treated with parity rather than pity. They also cautioned that efforts at normalising mental illness should not result in the trivialisation of the disorder. Research has suggested that those who accept their mental illness as part of their identity, overcome the challenges of stigma, and who remain resilient, may feel a sense of pride in being able to do so [ 30 ]. Thus, symptoms that are “undeserving” of the diagnosis may be viewed as discrediting their strength and authenticity.
The second theme that the participants identified was an opportunity for members of the general public to have social contact with a PWLE. They believed that many members of the public had never had personal interactions with a person with mental illness and formed attitudes towards people with mental health conditions based on stereotypes. In line with Allport’s [ 54 ] intergroup contact strategy, they proposed that personal contact with individuals with mental health conditions would reduce prejudice towards them. Purely naturalistic contact in everyday settings, however, does not reduce stigma [ 55 ], as high rates of stigma persist amongst mental health service staff who are in contact with individuals with mental health conditions on a daily basis [ 56 ]. Effective contact-based strategies are planned interactions with certain conditions in place. Some of these conditions relate to the credibility of the speaker, the local relevance to the audience, the disclosure of personal struggles due to the illness and “on the way up stories” describing successes in areas of living independently, employment and in having quality relationships [ 21 , 25 , 31 , 57 ] A local study examining the impact of a combined education and face-to-face contact intervention with university students showed that the intervention significantly improved stigma, reduced the desire for social distancing, and improved attitudes towards help-seeking [ 32 , 33 , 58 ]. However, the effects of this intervention was short-term, highlighting our participants’ assertion as well as supporting literature that stigma-reduction efforts should be continuous [ 57 ].
While such planned interactions can be logistically challenging and encumber continuity of exposure, the evidence suggests that non-face-to-face contact can also deliver notable results [ 59 ]. Schiappa et al.’s [ 60 ] “parasocial contact theory”, which was built upon Allport’s hypothesis proposes that sustained mass-mediated contact with a media figure engenders a parasocial relationship where the viewer feels a real, emotional connection with the figure that is akin to that with a close friend. Thus, the revelation of a stigmatised identity from the celebrity with whom a parasocial bond already exists has a greater potential to reduce stigma than an encounter with someone new who reveals the same stigmatised identity [ 61 ]. Indeed, an experimental study among undergraduate students showed that exposure to a video of popular pop singer, Demi Lovato, disclosing her experience with bipolar disorder (BD) significantly reduced negative stereotypes towards BD, and the higher the level of parasocial relationship, the lower their negative stereotypes of people with BD were [ 59 ]. There is also potential for repeated exposure to mass-mediated content to effect long-term change, as demonstrated in a longitudinal study in which college students who were presented with filmed social contact every 2 months over a 12-month period showed significantly positive long-term outcomes (24 months follow-up) in terms of their behavioural intentions for social contact with PWLE compared to the control groups [ 62 ]. Participants highlighted that this approach could serve well in a society such as Singapore, which has a celebrity culture.
The third and fourth themes relate to advocacy by influential figures/groups and the legislation of anti-discriminatory laws. Legislative reform is designed to prohibit discrimination on any grounds, improve the protection of people with mental illness, and offer reasonable accommodations in areas such as employment, education, and housing. Advocacy is designed to ensure that people with mental illness enjoy the rights and freedom offered by legislation and provide avenues of redress for inequitable policies and procedures [ 22 ]. Discussions among participants on these themes highlighted the importance of governmental organisations, grassroots leaders, and other public figures who carry the clout to push for changes in policy and practices to create an environment that is more inclusive and supportive of people with mental health conditions. They argued that mental health experts are not the best people for this task, alluding to the fact that it could be perceived as an act of self-interest to promote the importance of their profession—a point also identified by Clement et al. [ 63 ]. Corrigan [ 30 ] contrasted the service agenda in targeting stigma with the rights agenda, where the former is aimed at removing barriers to professional care, while the latter replaces disenfranchisement with affirming attitudes and behaviours. These agendas, which have different purposes and processes, may compete, and choices need to be made in allocating resources to work towards the chosen endpoint [ 30 ].
The participants in the study commented that mental health awareness has increased in Singapore in the past couple of years, but these advancements have not caught on as quickly, particularly in workplaces. A significant proportion of PWLE remain unemployed despite their desire and ability to work [ 64 ]. At the time when the data were collected, mental illness declarations were still a part of job application processes. In the FGDs, the participants zealously urged for this practice to be put to an end, as it impeded their employability and career ambitions. Further to the removal of this declaration, they suggested that support schemes should be offered to employers for hiring people with mental illnesses. A systematic review of anti-stigma interventions in workplaces showed that targeted interventions could lead to improved employee knowledge and supportive behaviour towards people with mental health problems [ 65 ]. However, due to the methodological shortcomings of the included studies, the heterogeneity of the intervention content and other issues, no efficacious intervention element could be identified. The current evidence suggests that specific workplace messages are more influential than more general workplace messages, and these messages should also be tailored for different stakeholders within the workplace (e.g., supervisors vs. employees) [ 66 ]. Corrigan recommended that identifying specific stigma change goals can be undertaken through a needs assessment conducted together with the target group [ 67 ]. One component of stigma change identified in this study was the inclusion of practice guidelines on responding to disclosure appropriately, fairly, and sensitively in workplaces.
Several mental illness de-stigmatisation endeavours, some of which have incorporated the suggestions identified in this research, have occurred in Singapore. First, Singapore launched its first long-running anti-stigma campaign called Beyond the Label in September 2018, with PWLE fronting the campaign and a strong social media presence. In January 2019, the first insurance policy that covers common mental illnesses, the AIA Beyond Critical Care, was launched by AIA Singapore. In December of the same year, the Tripartite Alliance for Fair and Progressive Employment Practices declared that asking job applicants about their mental health condition without good reason was discriminatory and that employers who do not abide by the updated guidelines may be liable to enforcement actions. As one of the PWLE in our FGD summarised,
“It’s moving, it’s slow…but it is gaining momentum…This is the best time for the mentally ill. People are more able to speak up for themselves even as patients and that is a wonderful thing”.
There are a few limitations to this study. First, the participants were recruited on a voluntary basis. Thus, the findings may not reflect the broader views of PWLE and caregivers. Two FGDs had only four and five participants, which may have made the dynamics of that group different from the larger-sized ones although the analyses did not suggest any specific themes coming up or being omitted in those FGDs. Second, as the researchers were from the IMH, participants have may withheld their critical views of the mental health system and suggestions to improve it, as it was possible that they did not want to offend the researchers affiliated with the institution. Third, the data were analysed from the lens of the researchers—the PWLE and caregivers were not part of the team analysing the data.
Notwithstanding these limitations, this study is one of a few studies in Singapore to have obtained inputs on stigma reduction from the perspectives of those who have been stigmatised. While several positive steps have been taken towards de-stigmatisation, evaluation efforts for these initiatives are currently lacking. It is recommended that scientifically rigorous evaluations of these efforts be undertaken so that outcomes can be tested, and the initiatives can be continually improved. Further, PWLE should be included in future anti-stigma research as well as in the evaluation of these campaigns and programmes.
5. Conclusions
The PWLE and caregivers highlighted that careful deliberation is needed when crafting messages to raise awareness about mental illnesses to avoid the unintended effects of trivialisation of these illnesses and the generation of sympathy. The research also identified how individuals such as community leaders and media figures are in advantageous positions to reduce stigma and advocate for better support for people with mental health conditions. The continued evaluation of new anti-stigma strategies is important to informing the impact of these efforts as well as to fine-tune future initiatives.
Acknowledgments
We would like to thank the participants for sharing their perspectives and making this work possible.
Author Contributions
Project administration, investigation, formal analysis, writing—original draft: S.S.; project administration, investigation, formal analysis, writing—review and editing: C.M.J.G.; investigation; formal analysis, writing—review and editing: G.T.H.T.; investigation, formal analysis, writing—review and editing: W.J.O.; funding acquisition, conceptualization, writing—review and editing: S.A.C.; conceptualization, methodology, investigation, formal analysis, supervision, writing—review and editing: M.S. All authors have read and agreed to the published version of the manuscript.
The study was supported by Tote Board (Singapore) under the Tote Board Strategic Initiative on Mental Health. The funding body of the study had no involvement with the design of the study, collection, data analysis and interpretation, or in the writing of manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by National Healthcare Group Domain Specific Review Board (DSRB Reference No. 2017/01175).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
What are your chances of acceptance?
Calculate for all schools, your chance of acceptance.
Your chancing factors
Extracurriculars.
How to Write the “Overcoming Challenges” Essay + Examples
What’s covered:.
- What is the Overcoming Challenges Essay?
- Real Overcoming Challenges Essay Prompts
- How to Choose a Topic
- Writing Tips
Overcoming Challenges Essay Examples
- Where to Get Your Essay Edited
While any college essay can be intimidating, the Overcoming Challenges prompt often worries students the most. Those students who’ve been lucky enough not to experience trauma tend to assume they have nothing worth saying. On the other hand, students who’ve overcome larger obstacles may be hesitant to talk about them.
Regardless of your particular circumstances, there are steps you can take to make the essay writing process simpler. Here are our top tips for writing the overcoming challenges essay successfully.
What is the “Overcoming Challenges” Essay?
The overcoming challenges prompt shows up frequently in both main application essays (like the Common App) and supplemental essays. Because supplemental essays allow students to provide schools with additional information, applicants should be sure that the subject matter they choose to write about differs from what’s in their main essay.
Students often assume the overcoming challenges essay requires them to detail past traumas. While you can certainly write about an experience that’s had a profound effect on your life, it’s important to remember that colleges aren’t evaluating students based on the seriousness of the obstacle they overcame.
On the contrary, the goal of this essay is to show admissions officers that you have the intelligence and fortitude to handle any challenges that come your way. After all, college serves as an introduction to adult life, and schools want to know that the students they admit are up to the task.
Real “Overcoming Challenges” Essay Prompts
To help you understand what the “Overcoming Challenges” essay looks like, here are a couple sample prompts.
Currently, the Common Application asks students to answer the following prompt in 650 words or less:
“The lessons we take from obstacles we encounter can be fundamental to later success. Recount a time when you faced a challenge, setback, or failure. How did it affect you, and what did you learn from the experience?”
For the past several years, MIT has prompted students to write 200 to 250 words on the following:
“Tell us about the most significant challenge you’ve faced or something important that didn’t go according to plan. How did you manage the situation?”
In both cases, the prompts explicitly ask for your response to the challenge. The event itself isn’t as important as how it pushed you to grow.

How to Choose a Topic for an Essay on Overcoming Challenges
When it comes to finding the best topic for your overcoming challenges essays, there’s no right answer. The word “challenge” is ambiguous and could be used to reference a wide range of situations from prevailing over a bully to getting over your lifelong stage fright to appear in a school musical. Here are some suggestions to keep in mind when selecting an essay subject.
1. Avoid trivial or common topics
While there aren’t many hard-and-fast rules for choosing an essay topic, students should avoid overdone topics.
These include:
- Working hard in a challenging class
- Overcoming a sports injury
- Moving schools or immigrating to the US
- Tragedy (divorce, death, abuse)
Admissions officers have read numerous essays on the subject, so it’s harder for you to stand out (see our full list of cliché college essay topics to avoid ). If events like these were truly formative to you, you can still choose to write about them, but you’ll need to be as personal as possible.
It’s also ideal if you have a less traditional storyline for a cliché topic; for example, if your sports injury led you to discover a new passion, that would be a more unique story than detailing how you overcame your injury and got back in the game.
Similarly, students may not want to write about an obstacle that admissions committees could perceive as low stakes, such as getting a B on a test, or getting into a small fight with a friend. The goal of this essay is to illustrate how you respond to adversity, so the topic you pick should’ve been at least impactful on your personal growth.
2. Pick challenges that demonstrate qualities you want to highlight
Students often mistakenly assume they need to have experienced exceptional circumstances like poverty, an abusive parent, or cancer to write a good essay. The truth is that the best topics will allow you to highlight specific personal qualities and share more about who you are. The essay should be less about the challenge itself, and more about how you responded to it.
Ask yourself what personality traits you want to emphasize, and see what’s missing in your application. Maybe you want to highlight your adaptability, for example, but that isn’t clearly expressed in your application. In this case, you might write about a challenge that put your adaptability to the test, or shaped you to become more adaptable.
Here are some examples of good topics we’ve seen over the years:
- Not having a coach for a sports team and becoming one yourself
- Helping a parent through a serious health issue
- Trying to get the school track dedicated to a coach
- Having to switch your Model UN position last-minute
Tips for Writing an Essay About Overcoming Challenges
Once you’ve selected a topic for your essays, it’s time to sit down and write. For best results, make sure your essay focuses on your efforts to tackle an obstacle rather than the problem itself. Additionally, you could avoid essay writing pitfalls by doing the following:
1. Choose an original essay structure
If you want your overcoming challenges essay to attract attention, aim to break away from more traditional structures. Most of these essays start by describing an unsuccessful attempt at a goal and then explain the steps the writer took to master the challenge.
You can stand out by choosing a challenge you’re still working on overcoming, or focus on a mental or emotional challenge that spans multiple activities or events. For example, you might discuss your fear of public speaking and how that impacted your ability to coach your brother’s Little League team and run for Student Council.
You can also choose a challenge that can be narrated in the moment, such as being put on the spot to teach a yoga class. These challenges can make particularly engaging essays, as you get to experience the writer’s thoughts and emotions as they unfold.
Keep in mind that you don’t necessarily need to have succeeded in your goal for this essay. Maybe you ran for an election and lost, or maybe you proposed a measure to the school board that wasn’t passed. It’s still possible to write a strong essay about topics like these as long as you focus on your personal growth. In fact, these may make for even stronger essays since they are more unconventional topics.
2. Focus on the internal
When writing about past experiences, you may be tempted to spend too much time describing specific people and events. With an Overcoming Challenges essay though, the goal is to focus on your thoughts and feelings.
For example, rather than detail all the steps you took to become a better public speaker, use the majority of your essay to describe your mental state as you embarked on the journey to achieving your goals. Were you excited, scared, anxious, or hopeful? Don’t be afraid to let the reader in on your innermost emotions and thoughts during this process.
3. Share what you learned
An Overcoming Challenges essay should leave the reader with a clear understanding of what you learned on your journey, be it physical, mental, or emotional. There’s no need to explicitly say “this experience taught me X,” but your essay should at least implicitly share any lessons you learned. This can be done through your actions and in-the-moment reflections. Remember that the goal is to show admissions committees why your experiences make you a great candidate for admission.
Was I no longer the beloved daughter of nature, whisperer of trees? Knee-high rubber boots, camouflage, bug spray—I wore the g arb and perfume of a proud wild woman, yet there I was, hunched over the pathetic pile of stubborn sticks, utterly stumped, on the verge of tears. As a child, I had considered myself a kind of rustic princess, a cradler of spiders and centipedes, who was serenaded by mourning doves and chickadees, who could glide through tick-infested meadows and emerge Lyme-free. I knew the cracks of the earth like the scars on my own rough palms. Yet here I was, ten years later, incapable of performing the most fundamental outdoor task: I could not, for the life of me, start a fire.
Furiously I rubbed the twigs together—rubbed and rubbed until shreds of skin flaked from my fingers. No smoke. The twigs were too young, too sticky-green; I tossed them away with a shower of curses, and began tearing through the underbrush in search of a more flammable collection. My efforts were fruitless. Livid, I bit a rejected twig, determined to prove that the forest had spurned me, offering only young, wet bones that would never burn. But the wood cracked like carrots between my teeth—old, brittle, and bitter. Roaring and nursing my aching palms, I retreated to the tent, where I sulked and awaited the jeers of my family.
Rattling their empty worm cans and reeking of fat fish, my brother and cousins swaggered into the campsite. Immediately, they noticed the minor stick massacre by the fire pit and called to me, their deep voices already sharp with contempt.
“Where’s the fire, Princess Clara?” they taunted. “Having some trouble?” They prodded me with the ends of the chewed branches and, with a few effortless scrapes of wood on rock, sparked a red and roaring flame. My face burned long after I left the fire pit. The camp stank of salmon and shame.
In the tent, I pondered my failure. Was I so dainty? Was I that incapable? I thought of my hands, how calloused and capable they had been, how tender and smooth they had become. It had been years since I’d kneaded mud between my fingers; instead of scaling a white pine, I’d practiced scales on my piano, my hands softening into those of a musician—fleshy and sensitive. And I’d gotten glasses, having grown horrifically nearsighted; long nights of dim lighting and thick books had done this. I couldn’t remember the last time I had lain down on a hill, barefaced, and seen the stars without having to squint. Crawling along the edge of the tent, a spider confirmed my transformation—he disgusted me, and I felt an overwhelming urge to squash him.
Yet, I realized I hadn’t really changed—I had only shifted perspective. I still eagerly explored new worlds, but through poems and prose rather than pastures and puddles. I’d grown to prefer the boom of a bass over that of a bullfrog, learned to coax a different kind of fire from wood, having developed a burn for writing rhymes and scrawling hypotheses.
That night, I stayed up late with my journal and wrote about the spider I had decided not to kill. I had tolerated him just barely, only shrieking when he jumped—it helped to watch him decorate the corners of the tent with his delicate webs, knowing that he couldn’t start fires, either. When the night grew cold and the embers died, my words still smoked—my hands burned from all that scrawling—and even when I fell asleep, the ideas kept sparking—I was on fire, always on fire.
This essay is an excellent example because the writer turns an everyday challenge—starting a fire—into an exploration of her identity. The writer was once “a kind of rustic princess, a cradler of spiders and centipedes,” but has since traded her love of the outdoors for a love of music, writing, and reading.
The story begins in media res , or in the middle of the action, allowing readers to feel as if we’re there with the writer. One of the essay’s biggest strengths is its use of imagery. We can easily visualize the writer’s childhood and the present day. For instance, she states that she “rubbed and rubbed [the twigs] until shreds of skin flaked from my fingers.”
The writing has an extremely literary quality, particularly with its wordplay. The writer reappropriates words and meanings, and even appeals to the senses: “My face burned long after I left the fire pit. The camp stank of salmon and shame.” She later uses a parallelism to cleverly juxtapose her changed interests: “instead of scaling a white pine, I’d practiced scales on my piano.”
One of the essay’s main areas of improvement is its overemphasis on the “story” and lack of emphasis on the reflection. The second to last paragraph about changing perspective is crucial to the essay, as it ties the anecdote to larger lessons in the writer’s life. She states that she hasn’t changed, but has only shifted perspective. Yet, we don’t get a good sense of where this realization comes from and how it impacts her life going forward.
The end of the essay offers a satisfying return to the fire imagery, and highlights the writer’s passion—the one thing that has remained constant in her life.
“Getting beat is one thing – it’s part of competing – but I want no part in losing.” Coach Rob Stark’s motto never fails to remind me of his encouragement on early-morning bus rides to track meets around the state. I’ve always appreciated the phrase, but an experience last June helped me understand its more profound, universal meaning.
Stark, as we affectionately call him, has coached track at my high school for 25 years. His care, dedication, and emphasis on developing good character has left an enduring impact on me and hundreds of other students. Not only did he help me discover my talent and love for running, but he also taught me the importance of commitment and discipline and to approach every endeavor with the passion and intensity that I bring to running. When I learned a neighboring high school had dedicated their track to a longtime coach, I felt that Stark deserved similar honors.
Our school district’s board of education indicated they would only dedicate our track to Stark if I could demonstrate that he was extraordinary. I took charge and mobilized my teammates to distribute petitions, reach out to alumni, and compile statistics on the many team and individual champions Stark had coached over the years. We received astounding support, collecting almost 3,000 signatures and pages of endorsements from across the community. With help from my teammates, I presented this evidence to the board.
They didn’t bite.
Most members argued that dedicating the track was a low priority. Knowing that we had to act quickly to convince them of its importance, I called a team meeting where we drafted a rebuttal for the next board meeting. To my surprise, they chose me to deliver it. I was far from the best public speaker in the group, and I felt nervous about going before the unsympathetic board again. However, at that second meeting, I discovered that I enjoy articulating and arguing for something that I’m passionate about.
Public speaking resembles a cross country race. Walking to the starting line, you have to trust your training and quell your last minute doubts. When the gun fires, you can’t think too hard about anything; your performance has to be instinctual, natural, even relaxed. At the next board meeting, the podium was my starting line. As I walked up to it, familiar butterflies fluttered in my stomach. Instead of the track stretching out in front of me, I faced the vast audience of teachers, board members, and my teammates. I felt my adrenaline build, and reassured myself: I’ve put in the work, my argument is powerful and sound. As the board president told me to introduce myself, I heard, “runners set” in the back of my mind. She finished speaking, and Bang! The brief silence was the gunshot for me to begin.
The next few minutes blurred together, but when the dust settled, I knew from the board members’ expressions and the audience’s thunderous approval that I had run quite a race. Unfortunately, it wasn’t enough; the board voted down our proposal. I was disappointed, but proud of myself, my team, and our collaboration off the track. We stood up for a cause we believed in, and I overcame my worries about being a leader. Although I discovered that changing the status quo through an elected body can be a painstakingly difficult process and requires perseverance, I learned that I enjoy the challenges this effort offers. Last month, one of the school board members joked that I had become a “regular” – I now often show up to meetings to advocate for a variety of causes, including better environmental practices in cafeterias and safer equipment for athletes.
Just as Stark taught me, I worked passionately to achieve my goal. I may have been beaten when I appealed to the board, but I certainly didn’t lose, and that would have made Stark proud.
While the writer didn’t succeed in getting the track dedicated to Coach Stark, their essay is certainly successful in showing their willingness to push themselves and take initiative.
The essay opens with a quote from Coach Stark that later comes full circle at the end of the essay. We learn about Stark’s impact and the motivation for trying to get the track dedicated to him.
One of the biggest areas of improvement in the intro, however, is how the essay tells us Stark’s impact rather than showing us: His care, dedication, and emphasis on developing good character has left an enduring impact on me and hundreds of other students. Not only did he help me discover my talent and love for running, but he also taught me the importance of commitment and discipline and to approach every endeavor with the passion and intensity that I bring to running.
The writer could’ve helped us feel a stronger emotional connection to Stark if they had included examples of Stark’s qualities, rather than explicitly stating them. For example, they could’ve written something like: Stark was the kind of person who would give you gas money if you told him your parents couldn’t afford to pick you up from practice. And he actually did that—several times. At track meets, alumni regularly would come talk to him and tell him how he’d changed their lives. Before Stark, I was ambivalent about running and was on the JV team, but his encouragement motivated me to run longer and harder and eventually make varsity. Because of him, I approach every endeavor with the passion and intensity that I bring to running.
The essay goes on to explain how the writer overcame their apprehension of public speaking, and likens the process of submitting an appeal to the school board to running a race. This metaphor makes the writing more engaging and allows us to feel the student’s emotions.
While the student didn’t ultimately succeed in getting the track dedicated, we learn about their resilience and initiative: I now often show up to meetings to advocate for a variety of causes, including better environmental practices in cafeterias and safer equipment for athletes.
Overall, this essay is well-done. It demonstrates growth despite failing to meet a goal, which is a unique essay structure. The running metaphor and full-circle intro/ending also elevate the writing in this essay.
Where to Get Your Overcoming Challenges Essay Edited
The Overcoming Challenges essay is one of the trickier supplemental prompts, so it’s important to get feedback on your drafts. That’s why we created our free Peer Essay Review tool , where you can get a free review of your essay from another student. You can also improve your own writing skills by reviewing other students’ essays.
If you want a college admissions expert to review your essay, advisors on CollegeVine have helped students refine their writing and submit successful applications to top schools. Find the right advisor for you to improve your chances of getting into your dream school!
Related CollegeVine Blog Posts

Recent Posts

- Behavioral Health
- Children's Health (Pediatrics)
- Exercise and Fitness
- Heart Health
- Men's Health
- Neurosurgery
- Obstetrics and Gynecology
- Orthopedic Health
- Weight Loss and Bariatric Surgery
- Women's Health

Overcoming stigmas, barriers to mental health care

The COVID-19 pandemic shined a glaring light on the deep underlying need for mental health care — and the barriers and stigmas surrounding access to care. These barriers and stigmas aren't new. They affect people of all ages, genders, races and ethnicities, and socioeconomic levels, as well as those from cultures and religions who view mental health according to their traditions. But they particularly affect people of color and those with fewer resources.
One of the biggest barriers to care is navigating the system. It's not easy. And, for many, they're already navigating health care, education, employment and other systems. It's just one more, and it can be overwhelming. Once they do make progress, they still may not be matched with the right care at the right time.
Fear is another barrier, including fear of seeking unfamiliar care and of unfamiliar conditions; fear of how they'll be viewed if friends and family know they're receiving mental health support; fear of appearing weak or not capable enough to cope; fear of fallout from what a child may share with a mental health professional; fear of the cost; and fear of further stress on an already fragile family.
Cultures and religions may have differing views of mental health. There may be pressure to be as strong and capable as previous generations. Not living up to that standard may make people feel "less than" and that they need to be better.
Breaking barriers, building relationships
Sometimes it may take a heartfelt talk with a friend or a crisis to break a barrier and take that first step toward mental health care. Once a connection is made with a trained professional, treatment is most effective when a trusting relationship forms.
The same barriers and stigmas affect kids, too. They also have the 24/7 pressure of social media, just at a time when their social status is tied to their self-worth.
But most children have a parent, relative, caregiver, teacher or other trusted adult to take the initial step for them. Changes in behavior, acting out, not able to focus, being withdrawn, not doing well in school and other easily-observed clues can be indicators of underlying mental health concerns, such as depression or anxiety.
When adults see children struggling, they'll seek the avenues to help them. That also may mean seeking mental health care for the entire family to ensure struggling children have a wraparound, supportive environment.
The main thing is for adults and kids to get the help they need to manage symptoms and make progress along their mental health journey.
The glaring light of the pandemic significantly raised awareness and acceptance of mental health care. And with that awareness has come funding, especially for children, to increase the number of counselors and overall access to care.
Laquita Becker is a clinical therapist in Psychiatry & Psychology in La Crosse , Wisconsin, and Youth and Family Services director for Boys & Girls Clubs of Greater La Crosse.
Related Posts

Home — Essay Samples — Nursing & Health — Psychiatry & Mental Health — Mental Health
Argumentative Essays About Mental Health
Hook examples for mental health essays, the personal experience hook.
Share a personal anecdote or experience related to mental health. Describe your journey or the experiences of someone close to you, highlighting the challenges and the importance of mental well-being.
The Stigma-Breaking Hook
Begin by discussing the stigma surrounding mental health. Explain how society's perceptions can hinder individuals from seeking help and why it's crucial to challenge these stereotypes.
The Statistics and Prevalence Hook
Start with shocking statistics or data on the prevalence of mental health issues. Highlight the scale of the problem and its impact on individuals and communities.
The Historical Perspective Hook
Explore the historical treatment of mental health. Discuss how society's understanding of mental illnesses has evolved over time and the significance of these changes.
The Celebrities and Advocacy Hook
Highlight the advocacy efforts of well-known figures who have openly discussed their mental health struggles. Explain how their stories have helped reduce stigma and raise awareness.
The Impact on Daily Life Hook
Discuss how mental health issues affect everyday life, including relationships, work, and overall well-being. Share relatable scenarios to engage readers emotionally.
The Psychological Insights Hook
Introduce a psychological concept or theory related to mental health. Explain its relevance and how it can provide valuable insights into human behavior and emotions.
The Global Mental Health Hook
Examine mental health on a global scale. Discuss disparities in access to mental health care and the impact of cultural factors on mental well-being.
The Resilience and Recovery Hook
Share stories of individuals who have overcome mental health challenges and emphasize the themes of resilience, recovery, and hope. Showcase the importance of seeking help and support.
The Call to Action Hook
Conclude your essay with a compelling call to action. Encourage readers to prioritize their mental health, seek help when needed, and advocate for better mental health care and awareness.
Mental Health Challenges in Higher Education
Marina joyce research paper, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Health Benefits of Basketball Essay
Mental illness as a social problem: essay, the stigma of mental illness and forms of treatment, overview of biological predispositions and risk factors associated with depression, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
The Effects of Mental Health on Our Life
Teenage mental health: the increase in mental illnesses, how to overcome teenage depression, mental health awareness: importance and impact, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
The Importance of Understanding of Self-knowledge and The Subconscious Mind
Mental illness that affect millions of people, the topic of mental disorders in winnie the pooh, the importance of mental health awareness, mental illnesses: definition, kinds and its effects on society, the effects of the stigmatization of mental illness on the society, the theme of mental illness in "the woman in the window" written by a.j. finn, research of stigmatization of mental illness, the history of the treatment of mental illness in the middle ages, the cultural beliefs concerning mental illnesses in the south asian community, the effect of mental illnesses on art throughout different time periods, the perception of mental illnesses by senegalese people, supportive homes for people with serious mental illness, the problem of ignorance about mental illness, an examination of the six mental illnesses and its impact on human life, the special needs of the criminal justice on mental illness cases, serial killers with mental illnesses, the interrelation between mental illness and drug addiction, child abuse as a reason for childhood mental illness, bridging the gap between police officers and citizens with mental illnesses in canada.
A mental illness, referred to as a mental disorder or psychiatric disorder, is a condition characterized by disrupted behavioral or mental patterns that result in considerable distress or impairment to an individual's personal functioning.
Anxiety disorders, mood disorders, psychotic disorders, personality disorders, eating disorders, sleep disorders, sexuality related disorders, other disorders.
Genetic and biological factors: Having a family history of mental illness can elevate the likelihood of experiencing such conditions. Additionally, specific genetic variations and imbalances in brain chemistry can contribute to an individual's susceptibility to mental health disorders. Environmental factors: Adverse childhood experiences, including trauma, abuse, neglect, or growing up in a stressful and unstable environment, increase the vulnerability to developing mental health issues. Psychological factors: Certain traits like high levels of neuroticism or low self-esteem can also contribute to an individual's susceptibility to mental health problems. Substance abuse: Alcohol and drug abuse is strongly associated with an increased risk of mental health disorders. Medical conditions: Certain medical conditions and chronic illnesses, such as cardiovascular disease, cancer, or neurological disorders, can be linked to a heightened risk of mental illness.
Emotional disturbances: persistent sadness, anxiety, irritability, mood swings, or a general sense of emptiness. Cognitive impairments: mental health disorders can affect cognitive processes such as thinking, concentration, memory, and decision-making. Individuals may experience difficulties in focusing, problem-solving, or retaining information. Behavioral changes: withdrawal from social activities, changes in sleep patterns, appetite fluctuations, increased substance use, self-harm, or engaging in risky behaviors. Distorted perceptions: hallucinations (perceiving things that are not there) or delusions (strongly held beliefs that are not based on reality). Impairment in functioning: mental illness often interferes with an individual's ability to function effectively in their daily life. This can include challenges in personal relationships, occupational difficulties, impaired academic performance, or a decline in overall quality of life. Physical symptoms: headaches, digestive problems, fatigue, or unexplained aches and pains.
Psychotherapy: also referred to as talk therapy, involves collaborating with a trained therapist to explore thoughts, emotions, and behaviors. Its purpose is to gain insights, develop coping skills, and foster positive transformations. Medication: certain mental disorders can be aided by medication, such as antidepressants, antianxiety drugs, or mood stabilizers. These medications assist in regulating brain chemistry and alleviating symptoms. Lifestyle changes: adopting a healthy lifestyle, including regular exercise, balanced nutrition, sufficient sleep, and effective stress management, can contribute to enhancing mental well-being. Support groups: becoming part of support groups or engaging in group therapy can provide a sense of community and empathy, allowing for the exchange of experiences and receiving support from peers. Alternative therapies: some individuals find alternative treatments like yoga, meditation, art therapy, or acupuncture beneficial. These practices can reduce stress, promote relaxation, and enhance emotional well-being. Hospitalization or intensive treatment programs: in severe cases or during mental health emergencies, hospitalization or intensive treatment programs may be required to ensure safety, stabilization, and access to specialized care.
The significance of the subject of mental illness cannot be overstated, as it holds profound relevance for individuals, families, and society at large. The far-reaching impact of mental health conditions on countless people globally necessitates attention and understanding. These conditions impose substantial suffering, impair daily functioning, and tragically, may even lead to loss of life. Recognizing and comprehending mental illness is imperative to foster awareness, combat societal stigma, and enable timely intervention. Prioritizing mental health enables the enhancement of overall well-being and life quality for those affected, while also driving the development of effective treatment methods, improved accessibility to resources, and the cultivation of supportive environments that nurture healing and resilience.
The topic of mental illness is immensely deserving of an essay due to its profound significance in today's society. Exploring mental illness provides an opportunity to raise awareness, challenge misconceptions, and promote understanding. By delving into this subject, one can shed light on the experiences of individuals facing mental health challenges, the impact on their lives, and the broader societal implications. It allows for an examination of the available resources, treatment approaches, and the need for improved mental healthcare systems. Addressing mental illness in an essay contributes to reducing stigma, fostering empathy, and inspiring action to create a more compassionate and supportive environment for those affected.
1. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. 2. World Health Organization. (2019). Mental disorders. Retrieved from https://www.who.int/news-room/fact-sheets/detail/mental-disorders 3. Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry, 62(6), 617-627. 4. National Institute of Mental Health. (n.d.). Mental health information. Retrieved from https://www.nimh.nih.gov/health/topics/index.shtml 5. Substance Abuse and Mental Health Services Administration. (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. 6. Greenberg, G. (2013). The book of woe: The DSM and the unmaking of psychiatry. New York, NY: Penguin Books. 7. Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest, 15(2), 37-70. 8. Pincus, H. A., Davis, W. W., & McQueen, L. E. (2017). "Subthreshold" mental disorders: A review and synthesis of studies on minor depression and other "brand names." British Journal of Psychiatry, 190(4), 288-294. 9. Sartorius, N. (2017). Stigma and mental health. Lancet Psychiatry, 4(10), 777-778. 10. Patel, V., Saxena, S., Lund, C., Thornicroft, G., Baingana, F., Bolton, P., ... & Unützer, J. (2018). The Lancet Commission on global mental health and sustainable development. The Lancet, 392(10157), 1553-1598.
Relevant topics
- Eating Disorders
- Drug Addiction
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Bibliography
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
434 Depression Essay Titles & Research Topics: Argumentative, Controversial, and More
Depression is undeniably one of the most prevalent mental health conditions globally, affecting approximately 5% of adults worldwide. It often manifests as intense feelings of hopelessness, sadness, and a loss of interest in previously enjoyable activities. Many also experience physical symptoms like fatigue, sleep disturbances, and appetite changes. Recognizing and addressing this mental disorder is extremely important to save lives and treat the condition.
In this article, we’ll discuss how to write an essay about depression and introduce depression essay topics and research titles for students that may be inspirational.
- 🔝 Top Depression Essay Titles
- ✅ Essay Prompts
- 💡 Research Topics
- 🔎 Essay Titles
- 💭 Speech Topics
- 📝 Essay Structure
🔗 References
🔝 top 12 research titles about depression.
- How is depression treated?
- Depression: Risk factors.
- The symptoms of depression.
- What types of depression exist?
- Depression in young people.
- Differences between anxiety and depression.
- The parents’ role in depression therapy.
- Drugs as the root cause of depression.
- Dangerous consequences of untreated depression.
- Effect of long-term depression.
- Different stages of depression.
- Treatment for depression.
✅ Prompts for Essay about Depression
Struggling to find inspiration for your essay? Look no further! We’ve put together some valuable essay prompts on depression just for you!
Prompt for Personal Essay about Depression
Sharing your own experience with depression in a paper can be a good idea. Others may feel more motivated to overcome their situation after reading your story. You can also share valuable advice by discussing things or methods that have personally helped you deal with the condition.
For example, in your essay about depression, you can:
- Tell about the time you felt anxious, hopeless, or depressed;
- Express your opinion on depression based on the experiences from your life;
- Suggest a way of dealing with the initial symptoms of depression ;
- Share your ideas on how to protect mental health at a young age.
How to Overcome Depression: Essay Prompt
Sadness is a common human emotion, but depression encompasses more than just sadness. As reported by the National Institute of Mental Health, around 21 million adults in the United States, roughly 8.4% of the total adult population , faced at least one significant episode of depression in 2020. When crafting your essay about overcoming depression, consider exploring the following aspects:
- Depression in young people and adolescents;
- The main causes of depression;
- The symptoms of depression;
- Ways to treat depression;
- Help from a psychologist (cognitive behavioral therapy or interpersonal therapy ).
Postpartum Depression: Essay Prompt
The birth of a child often evokes a spectrum of powerful emotions, spanning from exhilaration and happiness to apprehension and unease. It can also trigger the onset of depression. Following childbirth, many new mothers experience postpartum “baby blues,” marked by shifts in mood, bouts of tears, anxiety, and sleep disturbances. To shed light on the subject of postpartum depression, explore the following questions:
- What factors may increase the risk of postpartum depression?
- Is postpartum depression predictable?
- How to prevent postpartum depression?
- What are the symptoms of postpartum depression?
- What kinds of postpartum depression treatments exist?
Prompt for Essay about Teenage Depression
Teenage depression is a mental health condition characterized by sadness and diminishing interest in daily activities. It can significantly impact a teenager’s thoughts, emotions, and behavior, often requiring long-term treatment and support.
By discussing the primary symptoms of teenage depression in your paper, you can raise awareness of the issue and encourage those in need to seek assistance. You can pay attention to the following aspects:
- Emotional changes (feelings of sadness, anger, hopelessness, guilt, etc.);
- Behavioral changes (loss of energy and appetite , less attention to personal hygiene, self-harm, etc.);
- New addictions (drugs, alcohol, computer games, etc.).
💡 Research Topics about Depression
- The role of genetics in depression development.
- The effectiveness of different psychotherapeutic interventions for depression.
- Anti-depression non-pharmacological and medication treatment .
- The impact of childhood trauma on the onset of depression later in life.
- Exploring the efficacy of antidepressant medication in different populations.
- The impact of exercise on depression symptoms and treatment outcomes.
- Mild depression: pharmacotherapy and psychotherapy .
- The relationship between sleep disturbances and depression.
- The role of gut microbiota in depression and potential implications for treatment.
- Investigating the impact of social media on depression rates in adolescents.
- Depression, dementia, and delirium in older people .
- The efficacy of cognitive-behavioral therapy in preventing depression relapse.
- The influence of hormonal changes on depression risk.
- Assessing the effectiveness of self-help and digital interventions for depression.
- Herbal and complementary therapies for depression .
- The relationship between personality traits and vulnerability to depression.
- Investigating the long-term consequences of untreated depression on physical health.
- Exploring the link between chronic pain and depression.
- Depression in the elderly male .
- The impact of childhood experiences on depression outcomes in adulthood.
- The use of ketamine and other novel treatments for depression.
- The effect of stigma on depression diagnosis and treatment.
- The conducted family assessment: cases of depression .
- The role of social support in depression recovery.
- The effectiveness of online support groups for individuals with depression.
- Depression and cognitive decline in adults.
- Depression: PICOT question component exploration .
- Exploring the impact of nutrition and dietary patterns on depression symptoms.
- Investigating the efficacy of art-based therapies in depression treatment.
- The role of neuroplasticity in the development and treatment of depression.
- Depression among HIV-positive women .
- The influence of gender on depression prevalence and symptomatology.
- Investigating the impact of workplace factors on depression rates and outcomes.
- The efficacy of family-based interventions in reducing depression symptoms in teenagers.
- Frontline nurses’ burnout, anxiety, depression, and fear statuses .
- The role of early-life stress and adversity in depression vulnerability.
- The impact of various environmental factors on depression rates.
- Exploring the link between depression and cardiovascular health .
- Depression detection in adults in nursing practice .
- Virtual reality as a therapeutic tool for depression treatment.
- Investigating the impact of childhood bullying on depression outcomes.
- The benefits of animal-assisted interventions in depression management.
- Depression and physical exercise .
- The relationship between depression and suicidal behavior .
- The influence of cultural factors on depression symptom expression.
- Investigating the role of epigenetics in depression susceptibility.
- Depression associated with cognitive dysfunction .
- Exploring the impact of adverse trauma on the course of depression.
- The efficacy of acceptance and commitment therapy in treating depression.
- The relationship between depression and substance use disorders .
- Depression and anxiety among college students .
- Investigating the effectiveness of group therapy for depression.
- Depression and chronic medical conditions .
Psychology Research Topics on Depression
- The influence of early attachment experiences on the development of depression.
- The impact of negative cognitive biases on depression symptomatology.
- Depression treatment plan for a queer patient .
- Examining the relationship between perfectionism and depression.
- The role of self-esteem in depression vulnerability and recovery.
- Exploring the link between maladaptive thinking styles (e.g., rumination, catastrophizing) and depression.
- Investigating the impact of social support on depression outcomes and resilience.
- Identifying depression in young adults at an early stage .
- The influence of parenting styles on the risk of depression in children and adolescents.
- The role of self-criticism and self-compassion in depression treatment.
- Exploring the relationship between identity development and depression in emerging adulthood.
- The role of learned helplessness in understanding depression and its treatment.
- Depression in the elderly .
- Examining the connection between self-efficacy beliefs and depression symptoms.
- The influence of social comparison processes on depression and body image dissatisfaction .
- Exploring the impact of trauma-related disorders on depression.
- The role of resilience factors in buffering against the development of depression.
- Investigating the relationship between personality traits and depression.
- Depression and workplace violence .
- The impact of cultural factors on depression prevalence and symptom presentation.
- Investigating the effects of chronic stress on depression risk.
- The role of coping strategies in depression management and recovery.
- The correlation between discrimination/prejudice and depression/anxiety .
- Exploring the influence of gender norms and societal expectations on depression rates.
- The impact of adverse workplace conditions on employee depression.
- Investigating the effectiveness of narrative therapy in treating depression.
- Cognitive behavior and depression in adolescents .
- Childhood emotional neglect and adult depression.
- The influence of perceived social support on treatment outcomes in depression.
- The effects of childhood bullying on the development of depression.
- The impact of intergenerational transmission of depression within families.
- Depression in children: symptoms and treatments .
- Investigating the link between body dissatisfaction and depression in adolescence.
- The influence of adverse life events and chronic stressors on depression risk.
- The effects of peer victimization on the development of depression in adolescence.
- Counselling clients with depression and addiction .
- The role of experiential avoidance in depression and its treatment.
- The impact of social media use and online interactions on depression rates.
- Depression management in adolescent .
- Exploring the relationship between emotional intelligence and depression symptomatology.
- Investigating the influence of cultural values and norms on depression stigma and help-seeking behavior.
- The effects of childhood maltreatment on neurobiological markers of depression.
- Psychological and emotional conditions of suicide and depression .
- Exploring the relationship between body dissatisfaction and depression.
- The influence of self-worth contingencies on depression vulnerability and treatment response.
- The impact of social isolation and loneliness on depression rates.
- Psychology of depression among college students .
- The effects of perfectionistic self-presentation on depression in college students.
- The role of mindfulness skills in depression prevention and relapse prevention.
- Investigating the influence of adverse neighborhood conditions on depression risk.
- Personality psychology and depression .
- The impact of attachment insecurity on depression symptomatology.
Postpartum Depression Research Topics
- Identifying risk factors for postpartum depression.
- Exploring the role of hormonal changes in postpartum depression.
- “Baby blues” or postpartum depression and evidence-based care .
- The impact of social support on postpartum depression.
- The effectiveness of screening tools for early detection of postpartum depression.
- The relationship between postpartum depression and maternal-infant bonding .
- Postpartum depression educational program results .
- Identifying effective interventions for preventing and treating postpartum depression.
- Examining the impact of cultural factors on postpartum depression rates.
- Investigating the role of sleep disturbances in postpartum depression.
- Depression and postpartum depression relationship .
- Exploring the impact of a traumatic birth experience on postpartum depression.
- Assessing the impact of breastfeeding difficulties on postpartum depression.
- Understanding the role of genetic factors in postpartum depression.
- Postpartum depression: consequences .
- Investigating the impact of previous psychiatric history on postpartum depression risk.
- The potential benefits of exercise on postpartum depression symptoms.
- The efficacy of psychotherapeutic interventions for postpartum depression.
- Postpartum depression in the twenty-first century .
- The influence of partner support on postpartum depression outcomes.
- Examining the relationship between postpartum depression and maternal self-esteem.
- The impact of postpartum depression on infant development and well-being.
- Maternal mood symptoms in pregnancy and postpartum depression .
- The effectiveness of group therapy for postpartum depression management.
- Identifying the role of inflammation and immune dysregulation in postpartum depression.
- Investigating the impact of childcare stress on postpartum depression.
- Postpartum depression among low-income US mothers .
- The role of postnatal anxiety symptoms in postpartum depression.
- The impact of postpartum depression on the marital relationship.
- The influence of postpartum depression on parenting practices and parental stress.
- Postpartum depression: symptoms, role of cultural factors, and ways to support .
- Investigating the efficacy of pharmacological treatments for postpartum depression.
- The impact of postpartum depression on breastfeeding initiation and continuation.
- The relationship between postpartum depression and post-traumatic stress disorder .
- Postpartum depression and its identification .
- The impact of postpartum depression on cognitive functioning and decision-making.
- Investigating the influence of cultural norms and expectations on postpartum depression rates.
- The impact of maternal guilt and shame on postpartum depression symptoms.
- Beck’s postpartum depression theory: purpose, concepts, and significance .
- Understanding the role of attachment styles in postpartum depression vulnerability.
- Investigating the effectiveness of online support groups for women with postpartum depression.
- The impact of socioeconomic factors on postpartum depression prevalence.
- Perinatal depression: research study and design .
- The efficacy of mindfulness-based interventions for postpartum depression.
- Investigating the influence of birth spacing on postpartum depression risk.
- The role of trauma history in postpartum depression development.
- The link between the birth experience and postnatal depression .
- How does postpartum depression affect the mother-infant interaction and bonding ?
- The effectiveness of home visiting programs in preventing and managing postpartum depression.
- Assessing the influence of work-related stress on postpartum depression.
- The relationship between postpartum depression and pregnancy-related complications.
- The role of personality traits in postpartum depression vulnerability.
🔎 Depression Essay Titles
Depression essay topics: cause & effect.
- The effects of childhood trauma on the development of depression in adults.
- The impact of social media usage on the prevalence of depression in adolescents.
- “Predictors of Postpartum Depression” by Katon et al.
- The effects of environmental factors on depression rates.
- The relationship between academic pressure and depression among college students.
- The relationship between financial stress and depression.
- The best solution to predict depression because of bullying .
- How does long-term unemployment affect mental health ?
- The effects of unemployment on mental health, particularly the risk of depression.
- The impact of genetics and family history of depression on an individual’s likelihood of developing depression.
- The relationship between depression and substance abuse .
- Child abuse and depression .
- The role of gender in the manifestation and treatment of depression.
- The effects of chronic stress on the development of depression.
- The link between substance abuse and depression.
- Depression among students at Elon University .
- The influence of early attachment styles on an individual’s vulnerability to depression.
- The effects of sleep disturbances on the severity of depression.
- Chronic illness and the risk of developing depression.
- Depression: symptoms and treatment .
- Adverse childhood experiences and the likelihood of experiencing depression in adulthood.
- The relationship between chronic illness and depression.
- The role of negative thinking patterns in the development of depression.
- Effects of depression among adolescents .
- The effects of poor body image and low self-esteem on the prevalence of depression.
- The influence of social support systems on preventing symptoms of depression.
- The effects of child neglect on adult depression rates.
- Depression caused by hormonal imbalance .
- The link between perfectionism and the risk of developing depression.
- The effects of a lack of sleep on depression symptoms.
- The effects of childhood abuse and neglect on the risk of depression.
- Social aspects of depression and anxiety .
- The impact of bullying on the likelihood of experiencing depression.
- The role of serotonin and neurotransmitter imbalances in the development of depression.
- The impact of a poor diet on depression rates.
- Depression and anxiety run in the family .
- The effects of childhood poverty and socioeconomic status on depression rates in adults.
- The impact of divorce on depression rates.
- The relationship between traumatic life events and the risk of developing depression.
- The influence of personality traits on susceptibility to depression.
- The impact of workplace stress on depression rates.
- Depression in older adults: causes and treatment .
- The impact of parental depression on children’s mental health outcomes.
- The effects of social isolation on the prevalence and severity of depression.
- The role of cultural factors in the manifestation and treatment of depression.
- The relationship between childhood bullying victimization and future depressive symptoms.
- The impact of early intervention and prevention programs on reducing the risk of postpartum depression.
- Treating mood disorders and depression .
- How do hormonal changes during pregnancy contribute to the development of depression?
- The effects of sleep deprivation on the onset and severity of postpartum depression.
- The impact of social media on depression rates among teenagers.
- The role of genetics in the development of depression.
- The impact of bullying on adolescent depression rates.
- Mental illness, depression, and wellness issues .
- The effects of a sedentary lifestyle on depression symptoms.
- The correlation between academic pressure and depression in students.
- The relationship between perfectionism and depression.
- The correlation between trauma and depression in military veterans.
- Anxiety and depression during childhood and adolescence .
- The impact of racial discrimination on depression rates among minorities.
- The relationship between chronic pain and depression.
- The impact of social comparison on depression rates among young adults.
- The effects of childhood abuse on adult depression rates.
Depression Argumentative Essay Topics
- The role of social media in contributing to depression among teenagers.
- The effectiveness of antidepressant medication: an ongoing debate.
- Depression treatment: therapy or medications ?
- Should depression screening be mandatory in schools and colleges?
- Is there a genetic predisposition to depression?
- The stigma surrounding depression: addressing misconceptions and promoting understanding.
- Implementation of depression screening in primary care .
- Is psychotherapy more effective than medication in treating depression?
- Is teenage depression overdiagnosed or underdiagnosed: a critical analysis.
- The connection between depression and substance abuse: untangling the relationship.
- Humanistic therapy of depression .
- Should ECT (electroconvulsive therapy) be a treatment option for severe depression?
- Where is depression more prevalent: in urban or rural communities? Analyzing the disparities.
- Is depression a result of chemical imbalance in the brain? Debunking the myth.
- Depression: a serious mental and behavioral problem .
- Should depression medication be prescribed for children and adolescents?
- The effectiveness of mindfulness-based interventions in managing depression.
- Should depression in the elderly be considered a normal part of aging?
- Is depression hereditary? Investigating the role of genetics in depression risk.
- Different types of training in managing the symptoms of depression .
- The effectiveness of online therapy platforms in treating depression.
- Should psychedelic therapy be explored as an alternative treatment for depression?
- The connection between depression and cardiovascular health: Is there a link?
- The effectiveness of cognitive-behavioral therapy in preventing depression relapse.
- Depression as a bad a clinical condition .
- Should mind-body interventions (e.g., yoga , meditation) be integrated into depression treatment?
- Should emotional support animals be prescribed for individuals with depression?
- The effectiveness of peer support groups in decreasing depression symptoms.
- The use of antidepressants: are they overprescribed or necessary for treating depression?
- Adult depression and anxiety as a complex problem .
- The effectiveness of therapy versus medication in treating depression.
- The stigma surrounding depression and mental illness: how can we reduce it?
- The debate over the legalization of psychedelic drugs for treating depression.
- The relationship between creativity and depression: does one cause the other?
- Cognitive-behavioral therapy for generalized anxiety disorder and depression .
- The role of childhood trauma in shaping adult depression: Is it always a causal factor?
- The debate over the medicalization of sadness and grief as forms of depression.
- Alternative therapies, such as acupuncture or meditation, are effective in treating depression.
- Depression as a widespread mental condition .
Controversial Topics about Depression
- The existence of “chemical imbalance” in depression: fact or fiction?
- The over-reliance on medication in treating depression: are alternatives neglected?
- Is depression overdiagnosed and overmedicated in Western society?
- Measurement of an individual’s level of depression .
- The role of Big Pharma in shaping the narrative and treatment of depression.
- Should antidepressant advertisements be banned?
- The inadequacy of current diagnostic criteria for depression: rethinking the DSM-5.
- Is depression a biological illness or a product of societal factors?
- Literature review on depression .
- The overemphasis on biological factors in depression treatment: ignoring environmental factors.
- Is depression a normal reaction to an abnormal society?
- The influence of cultural norms on the perception and treatment of depression.
- Should children and adolescents be routinely prescribed antidepressants?
- The role of family in depression treatment .
- The connection between depression and creative genius: does depression enhance artistic abilities?
- The ethics of using placebo treatment for depression studies.
- The impact of social and economic inequalities on depression rates.
- Is depression primarily a mental health issue or a social justice issue?
- Depression disassembling and treating .
- Should depression screening be mandatory in the workplace?
- The influence of gender bias in the diagnosis and treatment of depression.
- The controversial role of religion and spirituality in managing depression.
- Is depression a result of individual weakness or societal factors?
- Abnormal psychology: anxiety and depression case .
- The link between depression and obesity: examining the bidirectional relationship.
- The connection between depression and academic performance : causation or correlation?
- Should depression medication be available over the counter?
- The impact of internet and social media use on depression rates: harmful or beneficial?
- Interacting in the workplace: depression .
- Is depression a modern epidemic or simply better diagnosed and identified?
- The ethical considerations of using animals in depression research.
- The effectiveness of psychedelic therapies for treatment-resistant depression.
- Is depression a disability? The debate on workplace accommodations.
- Polysubstance abuse among adolescent males with depression .
- The link between depression and intimate partner violence : exploring the relationship.
- The controversy surrounding “happy” pills and the pursuit of happiness.
- Is depression a choice? Examining the role of personal responsibility.
Good Titles for Depression Essays
- The poetic depictions of depression: exploring its representation in literature.
- The melancholic symphony: the influence of depression on classical music.
- Moderate depression symptoms and treatment .
- Depression in modern music: analyzing its themes and expressions.
- Cultural perspectives on depression: a comparative analysis of attitudes in different countries.
- Contrasting cultural views on depression in Eastern and Western societies.
- Diagnosing depression in the older population .
- The influence of social media on attitudes and perceptions of depression in global contexts.
- Countries with progressive approaches to mental health awareness.
- From taboo to acceptance: the evolution of attitudes towards depression.
- Depression screening tool in acute settings .
- The Bell Jar : analyzing Sylvia Plath’s iconic tale of depression .
- The art of despair: examining Frida Kahlo’s self-portraits as a window into depression.
- The Catcher in the Rye : Holden Caulfield’s battle with adolescent depression.
- Music as therapy: how jazz artists turned depression into art.
- Depression screening tool for a primary care center .
- The Nordic paradox: high depression rates in Scandinavian countries despite high-quality healthcare.
- The Stoic East: how Eastern philosophies approach and manage depression.
- From solitude to solidarity: collective approaches to depression in collectivist cultures.
- The portrayal of depression in popular culture: a critical analysis of movies and TV shows.
- The depression screening training in primary care .
- The impact of social media influencers on depression rates among young adults.
- The role of music in coping with depression: can specific genres or songs help alleviate depressive symptoms?
- The representation of depression in literature: a comparative analysis of classic and contemporary works.
- The use of art as a form of self-expression and therapy for individuals with depression.
- Depression management guidelines implementation .
- The role of religion in coping with depression: Christian and Buddhist practices.
- The representation of depression in the video game Hellblade: Senua’s Sacrifice .
- The role of nature in coping with depression: can spending time outdoors help alleviate depressive symptoms?
- The effectiveness of dance/movement therapy in treating depression among older adults.
- The National Institute for Health: depression management .
- The portrayal of depression in stand-up comedy: a study of comedians like Maria Bamford and Chris Gethard.
- The role of spirituality in coping with depression: Islamic and Hindu practices .
- The portrayal of depression in animated movies : an analysis of Inside Out and The Lion King .
- The representation of depression by fashion designers like Alexander McQueen and Rick Owens.
- Depression screening in primary care .
- The portrayal of depression in documentaries: an analysis of films like The Bridge and Happy Valley .
- The effectiveness of wilderness therapy in treating depression among adolescents.
- The connection between creativity and depression: how art can help heal.
- The role of Buddhist and Taoist practices in coping with depression.
- Mild depression treatment research funding sources .
- The portrayal of depression in podcasts: an analysis of the show The Hilarious World of Depression .
- The effectiveness of drama therapy in treating depression among children and adolescents.
- The representation of depression in the works of Vincent van Gogh and Edvard Munch.
- Depression in young people: articles review .
- The impact of social media on political polarization and its relationship with depression.
- The role of humor in coping with depression: a study of comedians like Ellen DeGeneres.
- The portrayal of depression in webcomics: an analysis of the comics Hyperbole and a Half .
- The effect of social media on mental health stigma and its relationship with depression.
- Depression and the impact of human services workers .
- The masked faces: hiding depression in highly individualistic societies.
💭 Depression Speech Topics
Informative speech topics about depression.
- Different types of depression and their symptoms.
- The causes of depression: biological, psychological, and environmental factors.
- How depression and physical issues are connected .
- The prevalence of depression in different age groups and demographics.
- The link between depression and anxiety disorders .
- Physical health: The effects of untreated depression.
- The role of genetics in predisposing individuals to depression.
- What you need to know about depression .
- How necessary is early intervention in treating depression?
- The effectiveness of medication in treating depression.
- The role of exercise in managing depressive symptoms.
- Depression in later life: overview .
- The relationship between substance abuse and depression.
- The impact of trauma on depression rates and treatment.
- The effectiveness of mindfulness meditation in managing depressive symptoms.
- Enzymes conversion and metabolites in major depression .
- The benefits and drawbacks of electroconvulsive therapy for severe depression.
- The effect of gender and cultural norms on depression rates and treatment.
- The effectiveness of alternative therapies for depression, such as acupuncture and herbal remedies .
- The importance of self-care in managing depression.
- Symptoms of anxiety, depression, and peritraumatic dissociation .
- The role of support systems in managing depression.
- The effectiveness of cognitive-behavioral therapy in treating depression.
- The benefits and drawbacks of online therapy for depression.
- The role of spirituality in managing depression.
- Depression among minority groups .
- The benefits and drawbacks of residential treatment for severe depression.
- What is the relationship between childhood trauma and adult depression?
- How effective is transcranial magnetic stimulation (TMS) for treatment-resistant depression?
- The benefits and drawbacks of art therapy for depression.
- Mood disorder: depression and bipolar .
- The impact of social media on depression rates.
- The effectiveness of dialectical behavior therapy (DBT) in treating depression.
- Depression in older people .
- The impact of seasonal changes on depression rates and treatment options.
- The impact of depression on daily life and relationships, and strategies for coping with the condition.
- The stigma around depression and the importance of seeking help.
Persuasive Speech Topics about Depression
- How important is it to recognize the signs and symptoms of depression ?
- How do you support a loved one who is struggling with depression?
- The importance of mental health education in schools to prevent and manage depression.
- Social media: the rise of depression and anxiety .
- Is there a need to increase funding for mental health research to develop better treatments for depression?
- Addressing depression in minority communities: overcoming barriers and disparities.
- The benefits of including alternative therapies , such as yoga and meditation, in depression treatment plans.
- Challenging media portrayals of depression: promoting accurate representations.
- Two sides of depression disease .
- How social media affects mental health: the need for responsible use to prevent depression.
- The importance of early intervention: addressing depression in schools and colleges.
- The benefits of seeking professional help for depression.
- There is a need for better access to mental health care, including therapy and medication, for those suffering from depression.
- Depression in adolescents and suitable interventions .
- How do you manage depression while in college or university?
- The role of family and friends in supporting loved ones with depression and encouraging them to seek help.
- The benefits of mindfulness and meditation for depression.
- The link between sleep and depression, and how to improve sleep habits.
- How do you manage depression while working a high-stress job?
- Approaches to treating depression .
- How do you manage depression during pregnancy and postpartum?
- The importance of prioritizing employee mental health and providing resources for managing depression in the workplace.
- How should you manage depression while caring for a loved one with a chronic illness?
- How to manage depression while dealing with infertility or pregnancy loss.
- Andrew Solomon: why we can’t talk about depression .
- Destigmatizing depression: promoting mental health awareness and understanding.
- Raising funds for depression research: investing in mental health advances.
- The power of peer support: establishing peer-led programs for depression.
- Accessible mental health services: ensuring treatment for all affected by depression.
- Evidence-based screening for depression in acute care .
- The benefits of journaling for mental health: putting your thoughts on paper to heal.
- The power of positivity: changing your mindset to fight depression .
- The healing power of gratitude in fighting depression.
- The connection between diet and depression: eating well can improve your mood.
- Teen depression and suicide in Soto’s The Afterlife .
- The benefits of therapy for depression: finding professional help to heal.
- The importance of setting realistic expectations when living with depression.
📝 How to Write about Depression: Essay Structure
We’ve prepared some tips and examples to help you structure your essay and communicate your ideas.
Essay about Depression: Introduction
An introduction is the first paragraph of an essay. It plays a crucial role in engaging the reader, offering the context, and presenting the central theme.
A good introduction typically consists of 3 components:
- Hook. The hook captures readers’ attention and encourages them to continue reading.
- Background information. Background information provides context for the essay.
- Thesis statement. A thesis statement expresses the essay’s primary idea or central argument.
Hook : Depression is a widespread mental illness affecting millions worldwide.
Background information : Depression affects your emotions, thoughts, and behavior. If you suffer from depression, engaging in everyday tasks might become arduous, and life may appear devoid of purpose or joy.
Depression Essay Thesis Statement
A good thesis statement serves as an essay’s road map. It expresses the author’s point of view on the issue in 1 or 2 sentences and presents the main argument.
Thesis statement : The stigma surrounding depression and other mental health conditions can discourage people from seeking help, only worsening their symptoms.
Essays on Depression: Body Paragraphs
The main body of the essay is where you present your arguments. An essay paragraph includes the following:
- a topic sentence,
- evidence to back up your claim,
- explanation of why the point is essential to the argument;
- a link to the next paragraph.
Topic sentence : Depression is a complex disorder that requires a personalized treatment approach, comprising both medication and therapy.
Evidence : Medication can be prescribed by a healthcare provider or a psychiatrist to relieve the symptoms. Additionally, practical strategies for managing depression encompass building a support system, setting achievable goals, and practicing self-care.
Depression Essay: Conclusion
The conclusion is the last part of your essay. It helps you leave a favorable impression on the reader.
The perfect conclusion includes 3 elements:
- Rephrased thesis statement.
- Summary of the main points.
- Final opinion on the topic.
Rephrased thesis: In conclusion, overcoming depression is challenging because it involves a complex interplay of biological, psychological, and environmental factors that affect an individual’s mental well-being.
Summary: Untreated depression heightens the risk of engaging in harmful behaviors such as substance abuse and can also result in negative thought patterns, diminished self-esteem, and distorted perceptions of reality.
We hope you’ve found our article helpful and learned some new information. If so, feel free to share it with your friends. You can also try our free online topic generator !
- Pain, anxiety, and depression – Harvard Health | Harvard Health Publishing
- Depression-related increases and decreases in appetite reveal dissociable patterns of aberrant activity in reward and interoceptive neurocircuitry – PMC | National Library of Medicine
- How to Get Treatment for Postpartum Depression – The New York Times
- What Is Background Information and What Purpose Does It Serve? | Indeed.com
- Thesis | Harvard College Writing Center
- Topic Sentences: How Do You Write a Great One? | Grammarly Blog
725 Research Proposal Topics & Title Ideas in Education, Psychology, Business, & More
414 proposal essay topics for projects, research, & proposal arguments.

Erasing Mental Health Stigma in the Black Community
By Brakeyshia R. Samms

As a Black woman living with mental illness, I’ve been told plenty of times by other Black people that I should not talk about my experience managing my mental health condition. That sentiment is always frustrating and discouraging to hear.
The pervasive stigma surrounding mental illness in the Black community often makes me feel like my life is embarrassing and that I must hide a major part of myself. Sometimes, this shame can be too much to bear. But it also led me to wonder: How widespread is mental illness itself in the Black community? I figured that understanding the statistics would make it easier to erase the stigma.
I did some research, and as it turns out, I am certainly not the only Black person experiencing mental illness. Among the nearly 5 million Black people living with a mental illness, nearly a quarter reported having a serious condition, including schizophrenia, bipolar disorder and depression, among many others.
Despite that sizeable number, only 1 out of every 3 seek suitable treatment, which could include meeting with a mental health professional, such as a social worker, therapist or psychiatrist. While there are many factors contributing to the discrepancy between prevalence and people seeking adequate treatment — ranging from the prevalence of misdiagnosis to the lack of access to adequate medical care — stigma in the Black community still remains an insidious culprit.
The Black community, and truly all communities, can engage in four activities to help get rid of stigma around mental illness.
1) Gather Information
Stigma stems from a lack of knowledge, and the best way to fight a gap in information is by educating others in our community. There are numerous public resources on the different types of mental illnesses. Personally, I turned to resources on websites for the Depression and Bipolar Support Alliance , National Alliance on Mental Illness and Mental Health America .
These were helpful places to start because they provided me with basic information and helped me recognize the negative preconceived notions I had about mental illness. They also directed me to places where I could learn even more. I also sought advice on what to read from the mental health professionals in my life, which I suggest everyone do as well. I read so many books and articles that, eventually, I had the language I needed to speak about my mental illness.
2) Speak Up
I have noticed that, in our community, we often equate strength with being silent and stoic — and that speaking up and asking for help is weakness. I believe the opposite is true. That’s why I have chosen to be open with my family and friends about living with a mental illness — and I emphasize the fact that I have won prestigious fellowships, scholarships and awards in spite of it all. I’ve also written about seeking help after experiencing a traumatic event.
Living with a mental illness doesn’t define anyone, nor does it limit anyone’s abilities. Showcasing our best selves — with mental health issues and all — reveals to some that we are just as capable as anyone else when it comes to leading a successful life.
3) Remain Open
As more Black people open up about living with a mental illness, the closer we will get to dismantling the stigma in our community. There is genuine comradery found in knowing that I am not the only Black person living with a mental illness. Celebrities like Taraji P. Henson, Jenifer Lewis and Janet Jackson, among many others , have opened up about their experiences with mental illnesses ranging from depression to bipolar disorder. Henson even founded The Boris Lawrence Henson Foundation in 2018 in memory of her late father. The more we recognize that mental illness can affect anyone, from your next-door neighbor to your personal hero, the more real and less frightening mental illness becomes to our community.
4) Believe People
Believing people when they say they have a mental illness is vital to eradicating stigma. When someone has a mental health crisis or expresses emotional distress, telling them to simply “pray it away” or to “fix your attitude” isn’t helpful. Failing to consider that people do, in fact, live with mental illness — and being dismissive in our advice — dissuades people from coming forward with how they are truly feeling. This sometimes causes people to not seek appropriate medical help.
These suggestions are just first steps when it comes to overcoming mental health stigma in the Black community. We must do better and be better when it comes to supporting other Black people living with mental illnesses, myself included. I hope my thoughts push discussions further and foster a more productive and positive dialogue. While not everyone in the Black community has a diagnosis, it’s important to keep in mind that mental illness can affect anyone, including our community.
Brakeyshia R. Samms is a writer who lives with a mental illness and works as a policy analyst. She has previously published essays in The Huffington Post, The Dallas Morning News, The Austin American-Statesman and Invisible Illness. All opinions expressed here do not reflect the views of her affiliations.
Submit to the NAMI Blog
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
Recent Posts
- From Gang Member to Mental Health Advocate
- How EMDR Healed My Trauma
- How Research Is Advancing Our Understanding of OCD
- Finding Treatment and Breaking the Cycle of Intergenerational Depression
- African American
- Mental Health professionals
- Treatment Settings
- December 2023
- October 2023
- September 2023
- August 2023
Find Your Local NAMI

- Mission and Vision
- Scientific Advancement Plan
- Science Visioning
- Research Framework
- Minority Health and Health Disparities Definitions
- Organizational Structure
- Staff Directory
- About the Director
- Director’s Messages
- News Mentions
- Presentations
- Selected Publications
- Director's Laboratory
- Congressional Justification
- Congressional Testimony
- Legislative History
- NIH Minority Health and Health Disparities Strategic Plan 2021-2025
- Minority Health and Health Disparities: Definitions and Parameters
- NIH and HHS Commitment
- Foundation for Planning
- Structure of This Plan
- Strategic Plan Categories
- Summary of Categories and Goals
- Scientific Goals, Research Strategies, and Priority Areas
- Research-Sustaining Activities: Goals, Strategies, and Priority Areas
- Outreach, Collaboration, and Dissemination: Goals and Strategies
- Leap Forward Research Challenge
- Future Plans
- Research Interest Areas
- Research Centers
- Research Endowment
- Community Based Participatory Research Program (CBPR)
- SBIR/STTR: Small Business Innovation/Tech Transfer
- Solicited and Investigator-Initiated Research Project Grants
- Scientific Conferences
- Training and Career Development
- Loan Repayment Program (LRP)
- Data Management and Sharing
- Social and Behavioral Sciences
- Population and Community Health Sciences
- Epidemiology and Genetics
- Medical Research Scholars Program (MRSP)
- Coleman Research Innovation Award
- Health Disparities Interest Group
- Art Challenge
- Breathe Better Network
- Healthy Hearts Network
- DEBUT Challenge
- Healthy Mind Initiative
- Mental Health Essay Contest
- Science Day for Students at NIH
- Fuel Up to Play 60 en Español
- Brother, You're on My Mind
- Celebrating National Minority Health Month
- Reaching People in Multiple Languages
- Funding Strategy
- Active Funding Opportunities
- Expired Funding Opportunities
- Technical Assistance Webinars

- Community Health and Population Sciences
- Clinical and Health Services Research
- Integrative Biological and Behavioral Sciences
- Intramural Research Program
- Training and Diverse Workforce Development
- Inside NIMHD
- ScHARe HDPulse PhenX SDOH Toolkit Understanding Health Disparities For Research Applicants For Research Grantees Research and Training Programs Reports and Data Resources Health Information for the Public Science Education

- NIMHD Programs
- NIMHD Education and Outreach
- NIH Teen Mental Health Essay Contest
- Extramural Research
- Intramural Research
- NIMHD Collaborations
- Fuel Up to Play 60 en Espanol
- COVID-19 Information and Resources
Speaking Up About Mental Health
National essay contest.
SUBMIT YOUR ESSAY The contest is open to high school students ages 16-18
PROMOTION TOOLKIT Help spread the word with social media and email tools
December 1, 2023
Dec. 1, 2023
January 16, 2024
Jan. 16, 2024
May 31, 2024
Mental health is an important part of overall health across all life stages. However, far too often, symptoms are not addressed or recognized among teens.
Speaking Up About Mental Health is an essay contest that challenges high school students ages 16-18 to raise awareness of mental health. The contest gives students a platform to share ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities.
This contest is soliciting essays that:
- Discuss ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities
- Share resilience and coping strategies to overcome mental health issues such as social isolation and loneliness, depression, and anxiety
- Address mental health stigma
- Encourage conversations about mental health, social media, and/or technology
- Suggest school policies or practices that could help reduce stigma
- Describe barriers to mental health treatment
- Cover other areas of concern to individuals and their communities with respect to mental health
Get details on contest rules and submit your entry on Challenge.gov
Promotion toolkit : Help promote the Speaking Up About Mental Health essay contest
The contest is led by:
National Institute of Mental Health
National Institute on Minority Health and Health Disparities
Eunice Kennedy Shriver National Institute of Child Health and Human Development
Page updated Jan. 23, 2024
September 2022: NIH Announces Winners of High School Mental Health Essay Contest
2022 Essay Awardees
2019 Essay Awardees

Staying Connected
- Funding Opportunities
- News & Events
- HHS Vulnerability Disclosure
- Privacy/Disclaimer/Accessibility Policy
- Viewers & Players
Talk to our experts
1800-120-456-456
- Mental Health Essay

Essay on Mental Health
According to WHO, there is no single 'official' definition of mental health. Mental health refers to a person's psychological, emotional, and social well-being; it influences what they feel and how they think, and behave. The state of cognitive and behavioural well-being is referred to as mental health. The term 'mental health' is also used to refer to the absence of mental disease.
Mental health means keeping our minds healthy. Mankind generally is more focused on keeping their physical body healthy. People tend to ignore the state of their minds. Human superiority over other animals lies in his superior mind. Man has been able to control life due to his highly developed brain. So, it becomes very important for a man to keep both his body and mind fit and healthy. Both physical and mental health are equally important for better performance and results.
Importance of Mental Health
An emotionally fit and stable person always feels vibrant and truly alive and can easily manage emotionally difficult situations. To be emotionally strong, one has to be physically fit too. Although mental health is a personal issue, what affects one person may or may not affect another; yet, several key elements lead to mental health issues.
Many emotional factors have a significant effect on our fitness level like depression, aggression, negative thinking, frustration, and fear, etc. A physically fit person is always in a good mood and can easily cope up with situations of distress and depression resulting in regular training contributing to a good physical fitness standard.
Mental fitness implies a state of psychological well-being. It denotes having a positive sense of how we feel, think, and act, which improves one’s ability to enjoy life. It contributes to one’s inner ability to be self-determined. It is a proactive, positive term and forsakes negative thoughts that may come to mind. The term mental fitness is increasingly being used by psychologists, mental health practitioners, schools, organisations, and the general population to denote logical thinking, clear comprehension, and reasoning ability.
Negative Impact of Mental Health
The way we physically fall sick, we can also fall sick mentally. Mental illness is the instability of one’s health, which includes changes in emotion, thinking, and behaviour. Mental illness can be caused due to stress or reaction to a certain incident. It could also arise due to genetic factors, biochemical imbalances, child abuse or trauma, social disadvantage, poor physical health condition, etc. Mental illness is curable. One can seek help from the experts in this particular area or can overcome this illness by positive thinking and changing their lifestyle.
Regular fitness exercises like morning walks, yoga, and meditation have proved to be great medicine for curing mental health. Besides this, it is imperative to have a good diet and enough sleep. A person needs 7 to 9 hours of sleep every night on average. When someone is tired yet still can't sleep, it's a symptom that their mental health is unstable. Overworking oneself can sometimes result in not just physical tiredness but also significant mental exhaustion. As a result, people get insomnia (the inability to fall asleep). Anxiety is another indicator.
There are many symptoms of mental health issues that differ from person to person and among the different kinds of issues as well. For instance, panic attacks and racing thoughts are common side effects. As a result of this mental strain, a person may experience chest aches and breathing difficulties. Another sign of poor mental health is a lack of focus. It occurs when you have too much going on in your life at once, and you begin to make thoughtless mistakes, resulting in a loss of capacity to focus effectively. Another element is being on edge all of the time.
It's noticeable when you're quickly irritated by minor events or statements, become offended, and argue with your family, friends, or co-workers. It occurs as a result of a build-up of internal irritation. A sense of alienation from your loved ones might have a negative influence on your mental health. It makes you feel lonely and might even put you in a state of despair. You can prevent mental illness by taking care of yourself like calming your mind by listening to soft music, being more social, setting realistic goals for yourself, and taking care of your body.
Surround yourself with individuals who understand your circumstances and respect you as the unique individual that you are. This practice will assist you in dealing with the sickness successfully. Improve your mental health knowledge to receive the help you need to deal with the problem. To gain emotional support, connect with other people, family, and friends. Always remember to be grateful in life. Pursue a hobby or any other creative activity that you enjoy.
What does Experts say
Many health experts have stated that mental, social, and emotional health is an important part of overall fitness. Physical fitness is a combination of physical, emotional, and mental fitness. Emotional fitness has been recognized as the state in which the mind is capable of staying away from negative thoughts and can focus on creative and constructive tasks.
He should not overreact to situations. He should not get upset or disturbed by setbacks, which are parts of life. Those who do so are not emotionally fit though they may be physically strong and healthy. There are no gyms to set this right but yoga, meditation, and reading books, which tell us how to be emotionally strong, help to acquire emotional fitness.
Stress and depression can lead to a variety of serious health problems, including suicide in extreme situations. Being mentally healthy extends your life by allowing you to experience more joy and happiness. Mental health also improves our ability to think clearly and boosts our self-esteem. We may also connect spiritually with ourselves and serve as role models for others. We'd also be able to serve people without being a mental drain on them.
Mental sickness is becoming a growing issue in the 21st century. Not everyone receives the help that they need. Even though mental illness is common these days and can affect anyone, there is still a stigma attached to it. People are still reluctant to accept the illness of mind because of this stigma. They feel shame to acknowledge it and seek help from the doctors. It's important to remember that "mental health" and "mental sickness" are not interchangeable.
Mental health and mental illness are inextricably linked. Individuals with good mental health can develop mental illness, while those with no mental disease can have poor mental health. Mental illness does not imply that someone is insane, and it is not anything to be embarrassed by. Our society's perception of mental disease or disorder must shift. Mental health cannot be separated from physical health. They both are equally important for a person.
Our society needs to change its perception of mental illness or disorder. People have to remove the stigma attached to this illness and educate themselves about it. Only about 20% of adolescents and children with diagnosable mental health issues receive the therapy they need.
According to research conducted on adults, mental illness affects 19% of the adult population. Nearly one in every five children and adolescents on the globe has a mental illness. Depression, which affects 246 million people worldwide, is one of the leading causes of disability. If mental illness is not treated at the correct time then the consequences can be grave.
One of the essential roles of school and education is to protect boys’ and girls' mental health as teenagers are at a high risk of mental health issues. It can also impair the proper growth and development of various emotional and social skills in teenagers. Many factors can cause such problems in children. Feelings of inferiority and insecurity are the two key factors that have the greatest impact. As a result, they lose their independence and confidence, which can be avoided by encouraging the children to believe in themselves at all times.
To make people more aware of mental health, 10th October is observed as World Mental Health. The object of this day is to spread awareness about mental health issues around the world and make all efforts in the support of mental health.
The mind is one of the most powerful organs in the body, regulating the functioning of all other organs. When our minds are unstable, they affect the whole functioning of our bodies. Being both physically and emotionally fit is the key to success in all aspects of life. People should be aware of the consequences of mental illness and must give utmost importance to keeping the mind healthy like the way the physical body is kept healthy. Mental and physical health cannot be separated from each other. And only when both are balanced can we call a person perfectly healthy and well. So, it is crucial for everyone to work towards achieving a balance between mental and physical wellbeing and get the necessary help when either of them falters.


Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- About the Director
- Advisory Boards and Groups
- Strategic Plan
- Offices and Divisions
- Careers at NIMH
- Staff Directories
- Getting to NIMH

Decoding the Mind: Basic Science Revolutionizes Treatment of Mental Illnesses
By Linda Brady, Margaret Grabb, Susan Koester, Yael Mandelblat-Cerf, David Panchision, Jonathan Pevsner, Ashlee Van’t-Veer, and Aleksandra Vicentic on behalf of the NIMH Division of Neuroscience and Basic Behavioral Science
March 21, 2024 • 75th Anniversary
Follow the NIMH Director on
For 75 years, NIMH has transformed the understanding and treatment of mental illnesses through basic and clinical research—bringing hope to millions of people. This Director’s Message, guest written by NIMH’s Division of Neuroscience and Basic Behavioral Science , is part of an anniversary series celebrating this momentous milestone.
The Division of Neuroscience and Basic Behavioral Science (DNBBS) at the National Institute of Mental Health (NIMH) supports research on basic neuroscience, genetics, and basic behavioral science. These are foundational pillars in the quest to decode the human mind and unravel the complexities of mental illnesses.
At NIMH, we are committed to supporting and conducting genomics research as a priority research area . As the institute celebrates its 75th Anniversary , we are spotlighting DNBBS-supported efforts connecting genes to cells to circuits to behavior that have led to a wealth of discoveries and knowledge that can improve the diagnosis, treatment, and prevention of mental illnesses.
Making gene discoveries
Medical conditions often run in families. For instance, if someone in your immediate family has high blood pressure, you are more likely to have it too. It is the same with mental disorders—often they run in families. NIMH is supporting research into human genetics to better understand why this occurs. This research has already led to the discovery of hundreds of gene variants that make us more or less likely to develop a mental disorder.
There are two types of genetic variation: common and rare. Common variation refers to DNA changes often seen in the general population, whereas rare variation is DNA changes found in only a small proportion of the population. Individually, most common gene variants have only a minor impact on the risk for a mental disorder. Instead, most disorders result from many common gene variants that, together, contribute to the risk for and severity of that disorder.
NIMH is committed to uncovering the role of genes in mental disorders with the aim of improving the lives of people who experience them. One of the many ways NIMH contributes to the discovery of common gene variants is by supporting the Psychiatric Genomics Consortium (PGC) . The consortium of almost 1,000 scientists across the globe, including ones in the NIMH Intramural Research Program and others conducting NIMH-supported research, is one of the largest and most innovative biological investigations in psychiatry.
Global collaborations such as the PGC are critical to amassing the immense sample sizes needed to identify common gene variants. Data from the consortium’s almost one million participants have already led to transformative insights about genetic contributors to mental illnesses and the genetic relationships of these illnesses to each other. To date, studies conducted as part of the consortium have uncovered common variation in over a dozen mental illnesses.
In contrast to common gene variants, rare gene variants are very uncommon in the general population. When they do occur, they often have a major impact on the occurrence of an illness, particularly when they disrupt gene function or regulation. Rare variants involving mutations in a single gene have been linked to several mental disorders, often through NIMH-supported research. For instance, a recent NIMH-funded study found that rare variation in 10 genes substantially increased the risk for schizophrenia. However, it is important to note that genetics is not destiny; even rare variants only raise the risk for mental disorders, but many other factors, including your environment and experiences, play important roles as well.
Because of the strong interest among researchers and the public in understanding how genes translate to changes in the brain and behavior, NIMH has developed a list of human genes associated with mental illnesses. These genes were identified through rare variation studies and are meant to serve as a resource for the research community. The list currently focuses on rare variants, but NIMH plans to continue expanding it as evidence accumulates for additional gene variants (rare or common).
Moreover, mental illnesses are a significant public health burden worldwide . For this reason, NIMH investments in genomics research extend across the globe. NIMH has established the Ancestral Populations Network (APN) to make genomics studies more diverse and shed light on how genetic variation contributes to mental disorders across populations. APN currently includes seven projects with more than 100 researchers across 25 sites worldwide.
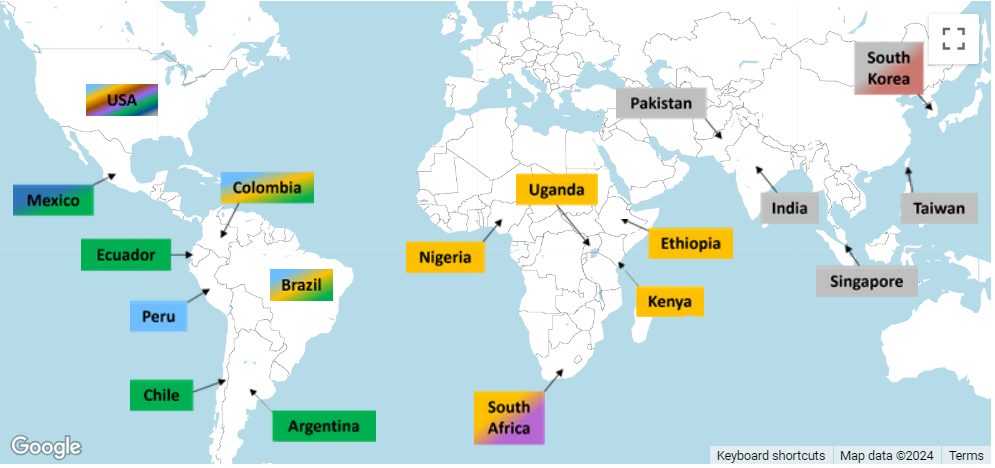
Connecting biology to behavior
While hundreds of individual genes have been linked to mental illnesses, the function of most of these genes in the brain remains poorly understood. But high-tech advances and the increased availability of computational tools are enabling researchers to begin unraveling the intricate roles played by genes.
In addition to identifying genetic variation that raises the risk for mental illnesses, NIMH supports research that will help us understand how genes contribute to human behavior. This information is critical to discovering approaches to diagnose, treat, and ultimately prevent or cure mental illnesses.
An NIMH-funded project called the PsychENCODE consortium focuses on understanding how genes impact brain function. PsychENCODE is furthering knowledge of how gene risk maps onto brain function and dysfunction by cataloging genomic elements in the human brain and studying the actions of different cell types. The PsychENCODE dataset currently includes multidimensional genetic data from the postmortem brains of thousands of people with and without mental disorders.
Findings from the first phase of PsychENCODE were published as a series of 11 papers examining functional genomics in the developing and adult brains and in mental disorders. A second batch of PsychENCODE papers will be published later this year. These findings help clarify the complex relationships between gene variants and the biological processes they influence.
PsychENCODE and other NIMH-supported projects are committed to sharing biospecimens quickly and openly to help speed research and discovery.

Facilitating these efforts is the NIMH Repository and Genomics Resource (NRGR) , where samples are stored and shared. NRGR includes hundreds of thousands of samples, such as DNA, RNA, and cell lines, from people with and without mental disorders, along with demographic and diagnostic information.

Another NIMH initiative to connect risk genes to brain function is Scalable and Systematic Neurobiology of Psychiatric and Neurodevelopmental Disorder Risk Genes (SSPsyGene) . This initiative uses cutting-edge techniques to characterize the biological functions of 250 mental health risk genes—within the cells where they are expressed—to better understand how those genes contribute to mental illnesses. By systematically characterizing the biological functions of risk genes in cells, SSPsyGene will empower researchers to learn about biological pathways that may serve as new targets for treatment.
Genes also affect behavior by providing the blueprint for neurons, the basic units of the nervous system. Neurons communicate with each other via circuits in the brain, which enables us to process, integrate, and convey information. NIMH supports many initiatives to study the foundational role of neural networks and brain circuits in shaping diverse mental health-related behaviors like mood, learning, memory, and motivation.
For instance, studies supported through a basic-to-translational science initiative at NIMH focus on modifying neural activity to improve cognitive, emotional, and social processing . Similarly, another new funding opportunity encourages studies in humans and animals examining how emotional and social cues are represented across brain circuits to help address a core deficit in many mental disorders. These studies will increase understanding of the biological mechanisms that support behavior throughout life and offer interventions to improve these functions in healthy and clinical populations.
Developing treatments and therapeutics
The gene discovery and biology-to-behavior programs described here will lay the foundation for delivering novel therapeutics. To be prepared to rapidly implement findings from this research, NIMH supports several initiatives to identify behavioral and biological markers for use in clinical studies and increase our ability to translate research into practice.
Through its therapeutics discovery research programs , NIMH advances early stage discovery and development studies in humans and early efficacy trials for mental disorders. Taking these efforts a step further, NIMH supports the National Cooperative Drug Discovery/Development Groups for the Treatment of Mental Disorders , which encourage public–private partnerships to accelerate the discovery and development of novel therapeutics and new biomarkers for use in human trials. Moreover, NIMH is one of several institutes and centers in the NIH Blueprint Neurotherapeutics Network , launched to enable neuroscientists in academia and biotechnology companies to develop new drugs for nervous system disorders.
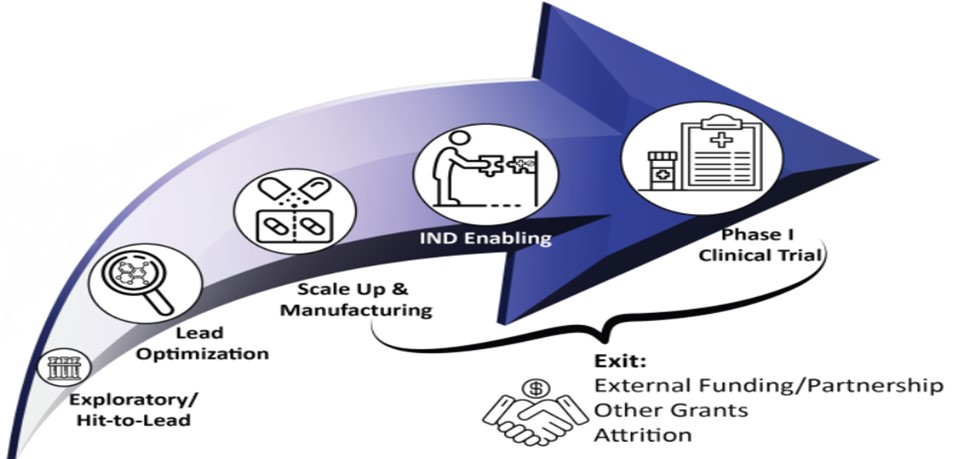
For the treatments of tomorrow, NIMH is building a new research program called Pre-Clinical Research on Gene Therapies for Rare Genetic Neurodevelopmental Disorders , which encourages early stage research to optimize gene therapies to treat disorders with prominent cognitive, social, or affective impairment. In parallel, NIMH’s Planning Grants for Natural History Studies of Rare Genetic Neurodevelopmental Disorders encourage the analysis of pre-existing data from people with rare disorders to learn about disease progression and enable future clinical trials with these populations.
NIMH's Division of Neuroscience and Basic Behavioral Science supports many different research projects that help us learn about genes and gene functions, how the brain develops and works, and impacts on behavior. By investing in basic neuroscience, genetics, and behavioral research, we're trying to find new targets for treatment and develop better therapies for mental disorders. We're hopeful these efforts will lead to new ways to treat and prevent mental illnesses in the near future and, ultimately, improve the lives of people in this country and across the globe.

IMAGES
VIDEO
COMMENTS
16 Personal Essays About Mental Health Worth Reading. Here are some of the most moving and illuminating essays published on BuzzFeed about mental illness, wellness, and the way our minds work. ... But I didn't — thanks to overcoming the stigma surrounding African-Americans and depression, and to building a community on Twitter." 12.
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life.
An independent evaluation found that it succeeded in reducing stigma in California, "with more people reporting a willingness to socialize with, live next door to, and work with people experiencing mental illness.". Participants also reported "providing greater social support to those with mental illness.".
Mental illness is stigmatized in general, and ECT is so stigmatized that many people are afraid to even mention the treatment that helped us get better. ... can help with overcoming addiction and ...
Living with depression. A part of managing my depression is accepting it, as with any other illness. It is a lifelong healing journey that requires changes to my treatment plan, patience, and most importantly loving kindness to myself. Learning to understand my feelings, stressors, and triggers has helped me to manage my symptoms.
Mental health stigma is a complex issue rooted in societal attitudes and beliefs about mental illness. It encompasses both public stigma, where society holds negative stereotypes about individuals with mental health conditions, and self-stigma, where individuals internalize these negative beliefs, leading to feelings of shame and low self-esteem.
5 months ago. Writing about mental health challenges can be a deeply personal and meaningful topic for your college essay, but you're right to consider the potential implications. If you decide to write about your mental health journey, it's important to focus primarily on the growth and resilience you've demonstrated despite your challenges.
Stigma is when someone views you in a negative way because you have a distinguishing characteristic or personal trait that's thought to be, or actually is, a disadvantage (a negative stereotype). Unfortunately, negative attitudes and beliefs toward people who have a mental health condition are common. Stigma can lead to discrimination ...
The approach to overcoming a mental health challenge and building resilience must follow a holistic approach. That's because stress is just as physical as it is emotional. Thus, self-care in all ...
Mental health struggles can create challenges you must overcome during your education and could be an opportunity for you to show how you've handled challenges and overcome obstacles. If you're considering writing your essay for college admission on this topic, consider talking to your school counselor or with an English teacher on how to frame the essay.
While You Were Out. By Meg Kissinger. Award-winning journalist Meg Kissinger delivers a stirring and surprisingly humorous personal history of her family's struggles with mental illness and suicide in her new memoir. At first glance, the Kissingers appeared healthy and happy, a boisterous bunch of eight children in the 1960s Chicago suburbs.
1. Introduction. The stigma of living with a mental health condition has been described as being worse than the experience of the illness itself [].The aversive reactions that members of the general population have towards people with mental illness is known as public stigma and can be understood in terms of (i) stereotypes, (ii) prejudice, and (iii) discrimination [].
Overcoming stigma: Three strategies toward better mental health in the workplace by Erica Coe, Jenny Cordina, Kana Enomoto, and Nikhil Seshan July 2021 1 "World Mental Health Day: An opportunity to kick-start a massive scale-up in investment in mental health," WHO, August 27, 2020, who.int.
1. Avoid trivial or common topics. While there aren't many hard-and-fast rules for choosing an essay topic, students should avoid overdone topics. These include: Working hard in a challenging class. Overcoming a sports injury. Moving schools or immigrating to the US. Tragedy (divorce, death, abuse)
Depending on the type, severity and doctor's opinion, there are several treatments that can be prescribed for mental illness. Mostly, a combination of the medications brings the best results. Medications. Medications which can be prescribed include; antidepressants, mood-stabilizers, anti-anxiety, and antipsychotic medications (Mayo Clinic ...
Overcoming stigmas, barriers to mental health care. The COVID-19 pandemic shined a glaring light on the deep underlying need for mental health care — and the barriers and stigmas surrounding access to care. These barriers and stigmas aren't new. They affect people of all ages, genders, races and ethnicities, and socioeconomic levels, as well ...
Mental health essay topics listed in this category focus on: forms of mental illness, mental illness as a social issue (especially considering its increasing rates), stigmatization of people affected by it in different cultures, examples, and representation of mental illness in literature and pop culture, correlation with other aspects/ phenomena (e.g. drug addiction), current and past ...
1. Our Experts. can deliver a custom essay. for a mere 11.00 9.35/page 304 qualified. specialists online Learn more. Depression is undeniably one of the most prevalent mental health conditions globally, affecting approximately 5% of adults worldwide. It often manifests as intense feelings of hopelessness, sadness, and a loss of interest in ...
In conclusion, mental illness stigma is a complex issue. The pressure of mental health stigma can come from family, friends, coworkers, and society on a broader level. Groups can also politicize stigma. A lack of awareness, education, perception, and a fear of people with mental illness can all lead to increased stigma.
Among the nearly 5 million Black people living with a mental illness, nearly a quarter reported having a serious condition, including schizophrenia, bipolar disorder and depression, among many others. Despite that sizeable number, only 1 out of every 3 seek suitable treatment, which could include meeting with a mental health professional, such ...
This contest is soliciting essays that: Discuss ways to eliminate and/or reduce mental health stigma faced by young people, especially in diverse communities. Share resilience and coping strategies to overcome mental health issues such as social isolation and loneliness, depression, and anxiety. Encourage conversations about mental health ...
Mental health refers to a person's psychological, emotional, and social well-being; it influences what they feel and how they think, and behave. The state of cognitive and behavioural well-being is referred to as mental health. The term 'mental health' is also used to refer to the absence of mental disease. Mental health means keeping our minds ...
Break the stigma around mental health in minority communities. Learn how cultural competence, education, community support and access can make a difference. Español. ... With the help of Dr. Taylor, here are a few of the stigmas surrounding mental health and how we can overcome these barriers together. Factors contributing to stigma.
Essay, Pages 6 (1354 words) Views. 1075. According to the information found in the literature and theoretical formulations, it is commonly suggested that the most common mental health stigma in the psychological domain is associated with seeking help from professionals or psychiatrists. Mental illness can be defined as medical conditions that ...
The Division of Neuroscience and Basic Behavioral Science (DNBBS) at the National Institute of Mental Health (NIMH) supports research on basic neuroscience, genetics, and basic behavioral science. These are foundational pillars in the quest to decode the human mind and unravel the complexities of mental illnesses. At NIMH, we are committed to supporting and conducting genomics research as a ...
" Sé que hablar de salud mental es difícil, pero tus sentimientos son importantes". "Estoy aquí para ti." "No estás solo". "Cuidar la salud mental es importante". No digas: "Simplemente sal de ahí". "Todo está en tu cabeza." "Solo piensa en positivo". "No necesitas terapia. Simplemente esfuérzate más".