- AERA Open Editors
- AERJ Editors
- EEPA Editors
- ER Issues and Archives
- JEBS Editors
- JSTOR Online Archives
- RER Editors
- RRE Editors
- AERA Examination and Desk Copies
- Mail/Fax Book Order Form
- International Distribution
- Books & Publications
- Merchandise
- Search The Store
- Online Paper Repository
- Inaugural Presentations in the i-Presentation Gallery
- Research Points
- AERA Journal Advertising Rate Cards
- Publications Permissions
- Publications FAQs


Share

The Review of Educational Research ( RER , bimonthly, begun in 1931) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. RER encourages the submission of research relevant to education from any discipline, such as reviews of research in psychology, sociology, history, philosophy, political science, economics, computer science, statistics, anthropology, and biology, provided that the review bears on educational issues. RER does not publish original empirical research unless it is incorporated in a broader integrative review. RER will occasionally publish solicited, but carefully refereed, analytic reviews of special topics, particularly from disciplines infrequently represented.
Impact Factor : 11.2 5-Year Impact Factor : 16.6 Ranking : 1/263 in Education & Educational Research

- Open Access
- © 2020
Systematic Reviews in Educational Research
Methodology, Perspectives and Application
- Olaf Zawacki-Richter 0 ,
- Michael Kerres 1 ,
- Svenja Bedenlier 2 ,
- Melissa Bond 3 ,
- Katja Buntins 4
Oldenburg, Germany
You can also search for this editor in PubMed Google Scholar
Essen, Germany
With contributions from international experts
First volume with a special focus on systematic reviews in educational research
Contains practical examples
Takes ethical considerations into account
502k Accesses
350 Citations
222 Altmetric
- Table of contents
About this book
Editors and affiliations, about the editors, bibliographic information.
- Publish with us
Buying options
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Other ways to access
Table of contents (9 chapters), front matter, methodological considerations, systematic reviews in educational research: methodology, perspectives and application.
- Mark Newman, David Gough
Reflections on the Methodological Approach of Systematic Reviews
- Martyn Hammersley
Ethical Considerations of Conducting Systematic Reviews in Educational Research
Teaching systematic review.
- Melanie Nind
Why Publish a Systematic Review: An Editor’s and Reader’s Perspective
- Alicia C. Dowd, Royel M. Johnson
Examples and Applications
Conceptualizations and measures of student engagement: a worked example of systematic review.
- Joanna Tai, Rola Ajjawi, Margaret Bearman, Paul Wiseman
Learning by Doing? Reflections on Conducting a Systematic Review in the Field of Educational Technology
- Svenja Bedenlier, Melissa Bond, Katja Buntins, Olaf Zawacki-Richter, Michael Kerres
Systematic Reviews on Flipped Learning in Various Education Contexts
- Chung Kwan Lo
The Role of Social Goals in Academic Success: Recounting the Process of Conducting a Systematic Review
- Naska Goagoses, Ute Koglin
- Systematic Reviews
- Educational Research
- Practical Examples for Systematic Reviews
- Student Engagement
- Educational Technology
- Academic Success
- Education Research
Olaf Zawacki-Richter, Svenja Bedenlier, Melissa Bond
Michael Kerres, Katja Buntins
Prof. Dr. Olaf Zawacki-Richter, Professor of Educational Technology, Center for Open Education Research (COER), Faculty of Education and Social Science, Carl von Ossietzky University of Oldenburg, Germany.
Prof. Dr. Michael Kerres, Professor of Educational Science | Learning Technology & Innovations, Learning Lab, University of Duisburg-Essen, Essen, Germany.
Dr. Svenja Bedenlier, Research Associate, Center for Open Education Research (COER), Faculty of Education and Social Science, Carl von Ossietzky University of Oldenburg, Germany.
Katja Buntins, Research Associate, Learning Lab, University of Duisburg-Essen, Essen, Germany.
Book Title : Systematic Reviews in Educational Research
Book Subtitle : Methodology, Perspectives and Application
Editors : Olaf Zawacki-Richter, Michael Kerres, Svenja Bedenlier, Melissa Bond, Katja Buntins
DOI : https://doi.org/10.1007/978-3-658-27602-7
Publisher : Springer VS Wiesbaden
eBook Packages : Education , Education (R0)
Copyright Information : The Editor(s) (if applicable) and The Author(s) 2020
License : CC BY
Hardcover ISBN : 978-3-658-27601-0 Published: 02 December 2019
Softcover ISBN : 978-3-658-27604-1 Published: 11 September 2020
eBook ISBN : 978-3-658-27602-7 Published: 21 November 2019
Edition Number : 1
Number of Pages : XXI, 161
Number of Illustrations : 4 b/w illustrations
Topics : Research Methods in Education
Policies and ethics
- Find a journal
- Track your research
Review of Educational Research
Subject Area and Category
SAGE Publications Inc.
Publication type
00346543, 19351046
Information
How to publish in this journal
The set of journals have been ranked according to their SJR and divided into four equal groups, four quartiles. Q1 (green) comprises the quarter of the journals with the highest values, Q2 (yellow) the second highest values, Q3 (orange) the third highest values and Q4 (red) the lowest values.
The SJR is a size-independent prestige indicator that ranks journals by their 'average prestige per article'. It is based on the idea that 'all citations are not created equal'. SJR is a measure of scientific influence of journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from It measures the scientific influence of the average article in a journal, it expresses how central to the global scientific discussion an average article of the journal is.
Evolution of the number of published documents. All types of documents are considered, including citable and non citable documents.
This indicator counts the number of citations received by documents from a journal and divides them by the total number of documents published in that journal. The chart shows the evolution of the average number of times documents published in a journal in the past two, three and four years have been cited in the current year. The two years line is equivalent to journal impact factor ™ (Thomson Reuters) metric.
Evolution of the total number of citations and journal's self-citations received by a journal's published documents during the three previous years. Journal Self-citation is defined as the number of citation from a journal citing article to articles published by the same journal.
Evolution of the number of total citation per document and external citation per document (i.e. journal self-citations removed) received by a journal's published documents during the three previous years. External citations are calculated by subtracting the number of self-citations from the total number of citations received by the journal’s documents.
International Collaboration accounts for the articles that have been produced by researchers from several countries. The chart shows the ratio of a journal's documents signed by researchers from more than one country; that is including more than one country address.
Not every article in a journal is considered primary research and therefore "citable", this chart shows the ratio of a journal's articles including substantial research (research articles, conference papers and reviews) in three year windows vs. those documents other than research articles, reviews and conference papers.
Ratio of a journal's items, grouped in three years windows, that have been cited at least once vs. those not cited during the following year.
Leave a comment
Name * Required
Email (will not be published) * Required
* Required Cancel
The users of Scimago Journal & Country Rank have the possibility to dialogue through comments linked to a specific journal. The purpose is to have a forum in which general doubts about the processes of publication in the journal, experiences and other issues derived from the publication of papers are resolved. For topics on particular articles, maintain the dialogue through the usual channels with your editor.
Follow us on @ScimagoJR Scimago Lab , Copyright 2007-2022. Data Source: Scopus®
Cookie settings
Cookie Policy
Legal Notice
Privacy Policy

On The Site
Harvard educational review.
Edited by Maya Alkateb-Chami, Jane Choi, Jeannette Garcia Coppersmith, Ron Grady, Phoebe A. Grant-Robinson, Pennie M. Gregory, Jennifer Ha, Woohee Kim, Catherine E. Pitcher, Elizabeth Salinas, Caroline Tucker, Kemeyawi Q. Wahpepah

Individuals
Institutions.
- Read the journal here
Journal Information
- ISSN: 0017-8055
- eISSN: 1943-5045
- Keywords: scholarly journal, education research
- First Issue: 1930
- Frequency: Quarterly
Description
The Harvard Educational Review (HER) is a scholarly journal of opinion and research in education. The Editorial Board aims to publish pieces from interdisciplinary and wide-ranging fields that advance our understanding of educational theory, equity, and practice. HER encourages submissions from established and emerging scholars, as well as from practitioners working in the field of education. Since its founding in 1930, HER has been central to elevating pieces and debates that tackle various dimensions of educational justice, with circulation to researchers, policymakers, teachers, and administrators.
Our Editorial Board is composed entirely of doctoral students from the Harvard Graduate School of Education who review all manuscripts considered for publication. For more information on the current Editorial Board, please see here.
A subscription to the Review includes access to the full-text electronic archives at our Subscribers-Only-Website .
Editorial Board
2023-2024 Harvard Educational Review Editorial Board Members
Maya Alkateb-Chami Development and Partnerships Editor, 2023-2024 Editor, 2022-2024 [email protected]
Maya Alkateb-Chami is a PhD student at the Harvard Graduate School of Education. Her research focuses on the role of schooling in fostering just futures—specifically in relation to language of instruction policies in multilingual contexts and with a focus on epistemic injustice. Prior to starting doctoral studies, she was the Managing Director of Columbia University’s Human Rights Institute, where she supported and co-led a team of lawyers working to advance human rights through research, education, and advocacy. Prior to that, she was the Executive Director of Jusoor, a nonprofit organization that helps conflict-affected Syrian youth and children pursue their education in four countries. Alkateb-Chami is a Fulbright Scholar and UNESCO cultural heritage expert. She holds an MEd in Language and Literacy from Harvard University; an MSc in Education from Indiana University, Bloomington; and a BA in Political Science from Damascus University, and her research on arts-based youth empowerment won the annual Master’s Thesis Award of the U.S. Society for Education Through Art.
Jane Choi Editor, 2023-2025
Jane Choi is a second-year PhD student in Sociology with broad interests in culture, education, and inequality. Her research examines intra-racial and interracial boundaries in US educational contexts. She has researched legacy and first-generation students at Ivy League colleges, families served by Head Start and Early Head Start programs, and parents of pre-K and kindergarten-age children in the New York City School District. Previously, Jane worked as a Research Assistant in the Family Well-Being and Children’s Development policy area at MDRC and received a BA in Sociology from Columbia University.
Jeannette Garcia Coppersmith Content Editor, 2023-2024 Editor, 2022-2024 [email protected]
Jeannette Garcia Coppersmith is a fourth-year Education PhD student in the Human Development, Learning and Teaching concentration at the Harvard Graduate School of Education. A former public middle and high school mathematics teacher and department chair, she is interested in understanding the mechanisms that contribute to disparities in secondary mathematics education, particularly how teacher beliefs and biases intersect with the social-psychological processes and pedagogical choices involved in math teaching. Jeannette holds an EdM in Learning and Teaching from the Harvard Graduate School of Education where she studied as an Urban Scholar and a BA in Environmental Sciences from the University of California, Berkeley.
Ron Grady Editor, 2023-2025
Ron Grady is a second-year doctoral student in the Human Development, Learning, and Teaching concentration at the Harvard Graduate School of Education. His central curiosities involve the social worlds and peer cultures of young children, wondering how lived experience is both constructed within and revealed throughout play, the creation of art and narrative, and through interaction with/production of visual artifacts such as photography and film. Ron also works extensively with educators interested in developing and deepening practices rooted in reflection on, inquiry into, and translation of the social, emotional, and aesthetic aspects of their classroom ecosystems. Prior to his doctoral studies, Ron worked as a preschool teacher in New Orleans. He holds a MS in Early Childhood Education from the Erikson Institute and a BA in Psychology with Honors in Education from Stanford University.
Phoebe A. Grant-Robinson Editor, 2023-2024
Phoebe A. Grant-Robinson is a first year student in the Doctor of Education Leadership(EdLD) program at the Harvard Graduate School of Education. Her ultimate quest is to position all students as drivers of their destiny. Phoebe is passionate about early learning and literacy. She is committed to ensuring that districts and school leaders, have the necessary tools to create equitable learning organizations that facilitate the academic and social well-being of all students. Phoebe is particularly interested in the intersection of homeless students and literacy. Prior to her doctoral studies, Phoebe was a Special Education Instructional Specialist. Supporting a portfolio of more than thirty schools, she facilitated the rollout of New York City’s Special Education Reform. Phoebe also served as an elementary school principal. She holds a BS in Inclusive Education from Syracuse University, and an MS in Curriculum and Instruction from Pace University.
Pennie M. Gregory Editor, 2023-2024
Pennie M. Gregory is a second-year student in the Doctor of Education Leadership (EdLD) program at the Harvard Graduate School of Education. Pennie was born in Incheon, South Korea and raised in Gary, Indiana. She has decades of experience leading efforts to improve outcomes for students with disabilities first as a special education teacher and then as a school district special education administrator. Prior to her doctoral studies, Pennie helped to create Indiana’s first Aspiring Special Education Leadership Institute (ASELI) and served as its Director. She was also the Capacity Events Director for MelanatED Leaders, an organization created to support educational leaders of color in Indianapolis. Pennie has a unique perspective, having worked with members of the school community, with advocacy organizations, and supporting state special education leaders. Pennie holds an EdM in Education Leadership from Marian University.
Jennifer Ha Editor, 2023-2025
Jen Ha is a second-year PhD student in the Culture, Institutions, and Society concentration at the Harvard Graduate School of Education. Her research explores how high school students learn to write personal narratives for school applications, scholarships, and professional opportunities amidst changing landscapes in college access and admissions. Prior to doctoral studies, Jen served as the Coordinator of Public Humanities at Bard Graduate Center and worked in several roles organizing academic enrichment opportunities and supporting postsecondary planning for students in New Haven and New York City. Jen holds a BA in Humanities from Yale University, where she was an Education Studies Scholar.
Woohee Kim Editor, 2023-2025
Woohee Kim is a PhD student studying youth activists’ civic and pedagogical practices. She is a scholar-activist dedicated to creating spaces for pedagogies of resistance and transformative possibilities. Shaped by her activism and research across South Korea, the US, and the UK, Woohee seeks to interrogate how educational spaces are shaped as cultural and political sites and reshaped by activists as sites of struggle. She hopes to continue exploring the intersections of education, knowledge, power, and resistance.
Catherine E. Pitcher Editor, 2023-2025
Catherine is a second-year doctoral student at Harvard Graduate School of Education in the Culture, Institutions, and Society program. She has over 10 years of experience in education in the US in roles that range from special education teacher to instructional coach to department head to educational game designer. She started working in Palestine in 2017, first teaching, and then designing and implementing educational programming. Currently, she is working on research to understand how Palestinian youth think about and build their futures and continues to lead programming in the West Bank, Gaza, and East Jerusalem. She holds an EdM from Harvard in International Education Policy.
Elizabeth Salinas Editor, 2023-2025
Elizabeth Salinas is a doctoral student in the Education Policy and Program Evaluation concentration at HGSE. She is interested in the intersection of higher education and the social safety net and hopes to examine policies that address basic needs insecurity among college students. Before her doctoral studies, Liz was a research director at a public policy consulting firm. There, she supported government, education, and philanthropy leaders by conducting and translating research into clear and actionable information. Previously, Liz served as a high school physics teacher in her hometown in Texas and as a STEM outreach program director at her alma mater. She currently sits on the Board of Directors at Leadership Enterprise for a Diverse America, a nonprofit organization working to diversify the leadership pipeline in the United States. Liz holds a bachelor’s degree in civil engineering from the Massachusetts Institute of Technology and a master’s degree in higher education from the Harvard Graduate School of Education.
Caroline Tucker Co-Chair, 2023-2024 Editor, 2022-2024 [email protected]
Caroline Tucker is a fourth-year doctoral student in the Culture, Institutions, and Society concentration at the Harvard Graduate School of Education. Her research focuses on the history and organizational dynamics of women’s colleges as women gained entry into the professions and coeducation took root in the United States. She is also a research assistant for the Harvard and the Legacy of Slavery Initiative’s Subcommittee on Curriculum and the editorial assistant for Into Practice, the pedagogy newsletter distributed by Harvard University’s Office of the Vice Provost for Advances in Learning. Prior to her doctoral studies, Caroline served as an American politics and English teaching fellow in London and worked in college advising. Caroline holds a BA in History from Princeton University, an MA in the Social Sciences from the University of Chicago, and an EdM in Higher Education from the Harvard Graduate School of Education.
Kemeyawi Q. Wahpepah Co-Chair, 2023-2024 Editor, 2022-2024 [email protected]
Kemeyawi Q. Wahpepah (Kickapoo, Sac & Fox) is a fourth-year doctoral student in the Culture, Institutions, and Society concentration at the Harvard Graduate School of Education. Their research explores how settler colonialism is addressed in K-12 history and social studies classrooms in the United States. Prior to their doctoral studies, Kemeyawi taught middle and high school English and history for eleven years in Boston and New York City. They hold an MS in Middle Childhood Education from Hunter College and an AB in Social Studies from Harvard University.
Submission Information
Click here to view submission guidelines .
Contact Information
Click here to view contact information for the editorial board and customer service .
Subscriber Support
Individual subscriptions must have an individual name in the given address for shipment. Individual copies are not for multiple readers or libraries. Individual accounts come with a personal username and password for access to online archives. Online access instructions will be attached to your order confirmation e-mail.
Institutional rates apply to libraries and organizations with multiple readers. Institutions receive digital access to content on Meridian from IP addresses via theIPregistry.org (by sending HER your PSI Org ID).
Online access instructions will be attached to your order confirmation e-mail. If you have questions about using theIPregistry.org you may find the answers in their FAQs. Otherwise please let us know at [email protected] .
How to Subscribe
To order online via credit card, please use the subscribe button at the top of this page.
To order by phone, please call 888-437-1437.
Checks can be mailed to Harvard Educational Review C/O Fulco, 30 Broad Street, Suite 6, Denville, NJ 07834. (Please include reference to your subscriber number if you are renewing. Institutions must include their PSI Org ID or follow up with this information via email to [email protected] .)
Permissions
Click here to view permissions information.
Article Submission FAQ
Closing the open call, question: “i have already submitted an article to her and i am awaiting a decision, what can i expect”.
Answer: First, any manuscripts already submitted through the open call and acknowledged by HER, as well as all invited manuscripts, R&R’d manuscripts, and manuscripts currently in production are NOT affected in any way by our pause in open calls. Editors are working to move through all current submissions and you can expect to receive any updates or decisions as we move through each step of our production process. If you have any questions, please contact the Co-Chairs, Caroline Tucker and Kemeyawi Wahpepah at [email protected] .
Question: “Can you share more about why you are closing the open call?”
Answer: As a graduate student run journal, we perform our editorial tasks in addition to our daily lives as doctoral students. We have been (and continue to be) incredibly grateful for the authors who share their work with us. In closing the open call, we hope to give ourselves time to review each manuscript in the best manner possible.
Submissions
Question: “what manuscripts are a good fit for her ”.
Answer: As a generalist scholarly journal, HER publishes on a wide range of topics within the field of education and related disciplines. We receive many articles that deserve publication, but due to the restrictions of print publication, we are only able to publish very few in the journal. The originality and import of the findings, as well as the accessibility of a piece to HER’s interdisciplinary, international audience which includes education practitioners, are key criteria in determining if an article will be selected for publication.
We strongly recommend that prospective authors review the current and past issues of HER to see the types of articles we have published recently. If you are unsure whether your manuscript is a good fit, please reach out to the Content Editor at [email protected] .
Question: “What makes HER a developmental journal?”
Answer: Supporting the development of high-quality education research is a key tenet of HER’s mission. HER promotes this development through offering comprehensive feedback to authors. All manuscripts that pass the first stage of our review process (see below) receive detailed feedback. For accepted manuscripts, HER also has a unique feedback process called casting whereby two editors carefully read a manuscript and offer overarching suggestions to strengthen and clarify the argument.
Question: “What is a Voices piece and how does it differ from an essay?”
Answer: Voices pieces are first-person reflections about an education-related topic rather than empirical or theoretical essays. Our strongest pieces have often come from educators and policy makers who draw on their personal experiences in the education field. Although they may not present data or generate theory, Voices pieces should still advance a cogent argument, drawing on appropriate literature to support any claims asserted. For examples of Voices pieces, please see Alvarez et al. (2021) and Snow (2021).
Question: “Does HER accept Book Note or book review submissions?”
Answer: No, all Book Notes are written internally by members of the Editorial Board.
Question: “If I want to submit a book for review consideration, who do I contact?”
Answer: Please send details about your book to the Content Editor at [email protected].
Manuscript Formatting
Question: “the submission guidelines state that manuscripts should be a maximum of 9,000 words – including abstract, appendices, and references. is this applicable only for research articles, or should the word count limit be followed for other manuscripts, such as essays”.
Answer: The 9,000-word limit is the same for all categories of manuscripts.
Question: “We are trying to figure out the best way to mask our names in the references. Is it OK if we do not cite any of our references in the reference list? Our names have been removed in the in-text citations. We just cite Author (date).”
Answer: Any references that identify the author/s in the text must be masked or made anonymous (e.g., instead of citing “Field & Bloom, 2007,” cite “Author/s, 2007”). For the reference list, place the citations alphabetically as “Author/s. (2007)” You can also indicate that details are omitted for blind review. Articles can also be blinded effectively by use of the third person in the manuscript. For example, rather than “in an earlier article, we showed that” substitute something like “as has been shown in Field & Bloom, 2007.” In this case, there is no need to mask the reference in the list. Please do not submit a title page as part of your manuscript. We will capture the contact information and any author statement about the fit and scope of the work in the submission form. Finally, please save the uploaded manuscript as the title of the manuscript and do not include the author/s name/s.
Invitations
Question: “can i be invited to submit a manuscript how”.
Answer: If you think your manuscript is a strong fit for HER, we welcome your request for invitation. Invited manuscripts receive one round of feedback from Editors before the piece enters the formal review process. To submit information about your manuscript for the Board to consider for invitation, please fill out the Invitation Request Form. Please provide as many details as possible. Whether we could invite your manuscript depends on the interest and availability of the current Board. Once you submit the form, we will give you an update in about 2–3 weeks on whether there are Editors who are interested in inviting your manuscript.
Review Timeline
Question: “who reviews manuscripts”.
Answer: All manuscripts are reviewed by the Editorial Board composed of doctoral students at Harvard University.
Question: “What is the HER evaluation process as a student-run journal?”
Answer: HER does not utilize the traditional external peer review process and instead has an internal, two-stage review procedure.
Upon submission, every manuscript receives a preliminary assessment by the Content Editor to confirm that the formatting requirements have been carefully followed in preparation of the manuscript, and that the manuscript is in accord with the scope and aim of the journal. The manuscript then formally enters the review process.
In the first stage of review, all manuscripts are read by a minimum of two Editorial Board members. During the second stage of review, manuscripts are read by the full Editorial Board at a weekly meeting.
Question: “How long after submission can I expect a decision on my manuscript?”
Answer: It usually takes 6 to 10 weeks for a manuscript to complete the first stage of review and an additional 12 weeks for a manuscript to complete the second stage. Due to time constraints and the large volume of manuscripts received, HER only provides detailed comments on manuscripts that complete the second stage of review.
Question: “How soon are accepted pieces published?”
Answer: The date of publication depends entirely on how many manuscripts are already in the queue for an issue. Typically, however, it takes about 6 months post-acceptance for a piece to be published.
Submission Process
Question: “how do i submit a manuscript for publication in her”.
Answer: Manuscripts are submitted through HER’s Submittable platform, accessible here. All first-time submitters must create an account to access the platform. You can find details on our submission guidelines on our Submissions page.
Rick Hess Straight Up
Education policy maven Rick Hess of the American Enterprise Institute think tank offers straight talk on matters of policy, politics, research, and reform. Read more from this blog.
Is Education Research Too Political?

- Share article
On Monday, I talked with departing Institute of Education Sciences Director Mark Schneider, who just wrapped up his six-year term. In our conversation, he argued for newer and better research centers at IES, along with a heightened commitment to producing timely and accessible reports. Well, as anyone who knows Mark well can attest, he almost always has more to say. I thought I’d reach back out and see if he had anything else he wanted to get off his mind. Here is Part Two of our conversation.
Rick: On Monday, you mentioned that Marguerite Roza, Emily Oster, and Sean Reardon are doing good, serious work on education topics and releasing it in a timely fashion. Can you say a bit about what they’re doing right and why NCES isn’t meeting that need?
Mark : As noted on Monday, the most telling example is the collection of school-level finance data. Not only are these data required by law, they are also among the most important pieces of information needed to understand the distribution of resources and to relate detailed expenditure data to school outcomes. But despite years of pressure—from Jim Blew, who headed the policy division of ED during the last few years of the DeVos era, from me, and from many others—NCES has never produced timely district financial data and has yet to produce complete school-by-school financials. District financials are released more than two years after the close of the fiscal year, and school-by-school financial pilot data dating back to FY18 have not yet been released. Looking ahead, NCES has promised to release its first set of complete FY22 school-level financials at the end of 2024—again, over two years after the close of the fiscal year . Assuming NCES meets its promise—a risky bet, given past missed deadlines—this would be “fast” by government standards—but far too slow to meet real-world needs.
Rick : What’s responsible for this?
Mark: Much of the problem is that NCES uses an antiquated approach to data collection, issuing a uniform survey that doesn’t match up to different state systems and then waiting for all submissions before releasing datasets. In contrast, teams from Georgetown, Brown, Stanford, and others grab data directly from the source and then convert them into a more standardized format. Teams then release the state-by-state files as they are available instead of holding it all until the very last state has a clean file. The process is far faster. For instance, Georgetown’s NERD$ site—run by Roza—is posting FY23 school-by-school financial files for some states in as few as six to eight months after the close of the fiscal year. With the quick turnaround, district leaders can, for example, marry the finance data with Stanford’s SEDA performance data and use it to inform decisions during the next budget season.
Rick : OK. So, what’s some of this other work that you flagged?
Mark : Similarly, Emily Oster’s work on school closures during the pandemic was released faster than NCES’s and its coverage was more comprehensive. In part because of NCES’s lagging performance, I was able to get additional money from Congress to set up the School Pulse Survey, which has finally given NCES a tool for gathering close to real-time information about conditions in schools. Fair warning, though: NCES calls it “experimental,” which means they are lying in wait to encumber it with more and more statistical tests that will likely delay the release of the data.
Oster and Sean Reardon have also been far ahead of NCES in gathering and releasing detailed data on student performance. Reardon’s Educational Opportunity Project presents detailed and timely information about COVID-related learning loss and recovery. Oster is also working on releasing more detailed and extensive data on student assessment from all states. To this point, they have released data through 2023. In contrast, NCES’s EdFacts promised the 2022 data in December 2023, but it’s not been released yet. Here’s an additional wrinkle: Oster did her work with one salaried employee and a team of undergrads. EdFacts costs around $13 million per year.
Rick : I’ve been struck that, during Secretary Cardona’s tenure, political appointees have gotten far more involved in the release of NAEP results and used the releases to promote administration talking points more than they have in past administrations. How concerned should we be about IES getting caught up in our partisan divides?
Mark: I was both lucky and happy to serve during both the Trump and Biden administrations. Although appointed by Trump, I have found that most of my dealings with senior leaders appointed by Biden have been quite good. But will that political distance and professionalism hold in a second administration of either major candidate? The signs are not good. For instance, IES has an advisory board called the National Board of Education Sciences, or NBES. When the Obama administration was on its way out the door, it tried to fill NBES with their appointees. However, the commissions were never fully executed, and the Trump administration refused to honor the unfinished appointments. Both administrations were within their legal rights to take these actions—but we will still need to see what political ramifications follow.
When I assumed the IES director’s role about halfway through the Trump administration, there were few people on the board, all holdovers from the Obama administration. It was very hard to get the White House to pay attention to the open seats, and I was only able to get three people, all high quality, appointed to the board. At the end of 2020, on his way out the door, Trump appointed a whole bunch of people to the board, many of whose qualifications raised eyebrows. When Biden took office, those commissions had not been finalized, leaving the board consisting of the three people I was able to get appointed. One morning, each of them received an email saying that they had to resign by the end of the day or be fired. The administration then appointed 14 people to the 15-person board. I fear that if the Republicans win the presidency this fall, they will fire the board and replace it with people more to their liking, making what should be a nonpartisan science board highly politicized. I can’t help but wonder if that will lead to the politicization of the director’s tenure.
Rick: Looking outside of IES, it certainly feels to me like the professional education research organizations have become increasingly ideological over the years. Is that a valid criticism? If so, what might help?
Mark: I agree. In 1996, mathematics professor Alan Sokal published the paper “ Transgressing the Boundaries: Towards a Transformative Hermeneutics of Quantum Gravity ” as a hoax to show the shallowness of postmodern critical theory. When he wrote it, I’m sure he was hoping to put an end to that line of work. But, as James Meigs notes in a 2021 Commentary piece: “Sokal meant his essay as a parodic warning. Twenty-five years later, it appears that the Sokal Hoax was actually an instruction manual.” Rick, as you recall, for years, as the AERA annual conference approached, you would go through the program and identify what you considered the most bizarre takes on education. I’m not sure that you could do this today, since you’d have to publish just about the entire program.
Rick: Oh, man, that takes me back. Yeah, I eventually gave that up. I’d hoped that shame could help discourage some of the sillier stuff, but it felt, like you note, that the silly stuff won out. Why is that?
Mark: Education research is highly ideologically driven. If DEI has affected more established and rigorous sciences, which it has, then what can we expect from a far weaker scientific field such as ours? As Meigs noted about Sokal’s paper turning into an instruction manual, I guess your lists could be viewed as a guide to the future work in education.
Rick: Here’s a final question. If you could leave your successor at IES with one piece of advice, what would it be?
Mark: My daughter told me that she learned this parable while in business school.
A new executive is meeting with the executive she is replacing and asks for advice. The outgoing exec says, “I left three envelopes in the desk drawer. Open them sequentially as crises emerge.”
Sure enough, at the inevitable first crisis, the new exec opened the first envelop, which read: “Blame your predecessor.” At the second crisis, the exec opened the second envelop, which read: “Apologize and swear to do better.” Then the third crisis showed up, and the third envelop read: “Write three letters.”
When I pass the baton, I hope that I have gotten IES a little further down the track than people expected. But the race is long, there’s a lot of work left unfinished, and the demand for accountability and innovation won’t go away any time soon.
Oh, and finally, the next director should pray that we don’t have another pandemic. While there are many reasons we should hope never to see a pandemic again, from a narrow perspective, COVID punched a two-year hole in my tenure, limiting what I was able to accomplish.
The opinions expressed in Rick Hess Straight Up are strictly those of the author(s) and do not reflect the opinions or endorsement of Editorial Projects in Education, or any of its publications.
Sign Up for EdWeek Update
Edweek top school jobs.

Sign Up & Sign In

- Frontiers in Medicine
- Healthcare Professions Education
- Research Topics
Impact of Technology on Human Behaviors in Medical Professions Education
Total Downloads
Total Views and Downloads
About this Research Topic
Human behaviors are essential in understanding how individuals engage in medical science academic activities. Healthcare systems across the globe have witnessed a significant shift in recent years by integrating technology in innovating new methods and practices to improve educational practices. Therefore, ...
Keywords : healthcare education, medical education, teachers’ behavior, students’ behavior, human behavior, technology in medical sciences, program development, curriculum development, teacher and student performance
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines, participating journals.
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
- Open access
- Published: 05 December 2023
A scoping review to identify and organize literature trends of bias research within medical student and resident education
- Brianne E. Lewis 1 &
- Akshata R. Naik 2
BMC Medical Education volume 23 , Article number: 919 ( 2023 ) Cite this article
829 Accesses
1 Citations
2 Altmetric
Metrics details
Physician bias refers to the unconscious negative perceptions that physicians have of patients or their conditions. Medical schools and residency programs often incorporate training to reduce biases among their trainees. In order to assess trends and organize available literature, we conducted a scoping review with a goal to categorize different biases that are studied within medical student (MS), resident (Res) and mixed populations (MS and Res). We also characterized these studies based on their research goal as either documenting evidence of bias (EOB), bias intervention (BI) or both. These findings will provide data which can be used to identify gaps and inform future work across these criteria.
Online databases (PubMed, PsycINFO, WebofScience) were searched for articles published between 1980 and 2021. All references were imported into Covidence for independent screening against inclusion criteria. Conflicts were resolved by deliberation. Studies were sorted by goal: ‘evidence of bias’ and/or ‘bias intervention’, and by population (MS or Res or mixed) andinto descriptive categories of bias.
Of the initial 806 unique papers identified, a total of 139 articles fit the inclusion criteria for data extraction. The included studies were sorted into 11 categories of bias and showed that bias against race/ethnicity, specific diseases/conditions, and weight were the most researched topics. Of the studies included, there was a higher ratio of EOB:BI studies at the MS level. While at the Res level, a lower ratio of EOB:BI was found.

Conclusions
This study will be of interest to institutions, program directors and medical educators who wish to specifically address a category of bias and identify where there is a dearth of research. This study also underscores the need to introduce bias interventions at the MS level.
Peer Review reports
Physician bias ultimately impacts patient care by eroding the physician–patient relationship [ 1 , 2 , 3 , 4 ]. To overcome this issue, certain states require physicians to report a varying number of hours of implicit bias training as part of their recurring licensing requirement [ 5 , 6 ]. Research efforts on the influence of implicit bias on clinical decision-making gained traction after the “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care” report published in 2003 [ 7 ]. This report sparked a conversation about the impact of bias against women, people of color, and other marginalized groups within healthcare. Bias from a healthcare provider has been shown to affect provider-patient communication and may also influence treatment decisions [ 8 , 9 ]. Nevertheless, opportunities within medical education curriculum are created to evaluate biases at an earlier stage of physician-training and provide instruction to intervene them [ 10 , 11 , 12 ]. We aimed to identify trends and organize literature on bias training provided during medical school and residency programs since the meaning of ‘bias’ is broad and encompasses several types of attitudes and predispositions [ 13 ].
Several reviews, narrative or systematic in nature, have been published in the field of bias research in medicine and healthcare [ 14 , 15 , 16 ]. Many of these reviews have a broad focus on implicit bias and they often fail to define the patient’s specific attributes- such as age, weight, disease, or condition against which physicians hold their biases. However, two recently published reviews categorized implicit biases into various descriptive characteristics albeit with research goals different than this study [ 17 , 18 ]. The study by Fitzgerald et al. reviewed literature focused on bias among physicians and nurses to highlight its role in healthcare disparities [ 17 ]. While the study by Gonzalez et al. focused on bias curricular interventions across professions related to social determinants of health such as education, law, medicine and social work [ 18 ]. Our research goal was to identify the various bias characteristics that are studied within medical student and/or resident populations and categorize them. Further, we were interested in whether biases were merely identified or if they were intervened. To address these deficits in the field and provide clarity, we utilized a scoping review approach to categorize the literature based on a) the bias addressed and b) the study goal within medical students (MS), residents (Res) and a mixed population (MS and Res).
To date no literature review has organized bias research by specific categories held solely by medical trainees (medical students and/or residents) and quantified intervention studies. We did not perform a quality assessment or outcome evaluation of the bias intervention strategies, as it was not the goal of this work and is standard with a scoping review methodology [ 19 , 20 ]. By generating a comprehensive list of bias categories researched among medical trainee population, we highlight areas of opportunity for future implicit bias research specifically within the undergraduate and graduate medical education curriculum. We anticipate that the results from this scoping review will be useful for educators, administrators, and stakeholders seeking to implement active programs or workshops that intervene specific biases in pre-clinical medical education and prepare physicians-in-training for patient encounters. Additionally, behavioral scientists who seek to support clinicians, and develop debiasing theories [ 21 ] and models may also find our results informative.
We conducted an exhaustive and focused scoping review and followed the methodological framework for scoping reviews as previously described in the literature [ 20 , 22 ]. This study aligned with the four goals of a scoping review [ 20 ]. We followed the first five out of the six steps outlined by Arksey and O’Malley’s to ensure our review’s validity 1) identifying the research question 2) identifying relevant studies 3) selecting the studies 4) charting the data and 5) collating, summarizing and reporting the results [ 22 ]. We did not follow the optional sixth step of undertaking consultation with key stakeholders as it was not needed to address our research question it [ 23 ]. Furthermore, we used Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) that aided in managing steps 2–5 presented above.
Research question, search strategy and inclusion criteria
The purpose of this study was to identify trends in bias research at the medical school and residency level. Prior to conducting our literature search we developed our research question and detailed the inclusion criteria, and generated the search syntax with the assistance from a medical librarian. Search syntax was adjusted to the requirements of the database. We searched PubMed, Web of Science, and PsycINFO using MeSH terms shown below.
Bias* [ti] OR prejudice*[ti] OR racism[ti] OR homophobia[ti] OR mistreatment[ti] OR sexism[ti] OR ageism[ti]) AND (prejudice [mh] OR "Bias"[Mesh:NoExp]) AND (Education, Medical [mh] OR Schools, Medical [mh] OR students, medical [mh] OR Internship and Residency [mh] OR “undergraduate medical education” OR “graduate medical education” OR “medical resident” OR “medical residents” OR “medical residency” OR “medical residencies” OR “medical schools” OR “medical school” OR “medical students” OR “medical student”) AND (curriculum [mh] OR program evaluation [mh] OR program development [mh] OR language* OR teaching OR material* OR instruction* OR train* OR program* OR curricul* OR workshop*
Our inclusion criteria incorporated studies which were either original research articles, or review articles that synthesized new data. We excluded publications that were not peer-reviewed or supported with data such as narrative reviews, opinion pieces, editorials, perspectives and commentaries. We included studies outside of the U.S. since the purpose of this work was to generate a comprehensive list of biases. Physicians, regardless of their country of origin, can hold biases against specific patient attributes [ 17 ]. Furthermore, physicians may practice in a different country than where they trained [ 24 ]. Manuscripts were included if they were published in the English language for which full-texts were available. Since the goal of this scoping review was to assess trends, we accepted studies published from 1980–2021.
Our inclusion criteria also considered the goal and the population of the study. We defined the study goal as either that documented evidence of bias or a program directed bias intervention. Evidence of bias (EOB) had to originate from the medical trainee regarding a patient attribute. Bias intervention (BI) studies involved strategies to counter biases such as activities, workshops, seminars or curricular innovations. The population studied had to include medical students (MS) or residents (Res) or mixed. We defined the study population as ‘mixed’ when it consisted of both MS and Res. Studies conducted on other healthcare professionals were included if MS or Res were also studied. Our search criteria excluded studies that documented bias against medical professionals (students, residents and clinicians) either by patients, medical schools, healthcare administrators or others, and was focused on studies where the biases were solely held by medical trainees (MS and Res).
Data extraction and analysis
Following the initial database search, references were downloaded and bulk uploaded into Covidence and duplicates were removed. After the initial screening of title and abstracts, full-texts were reviewed. Authors independently completed title and abstract screening, and full text reviews. Any conflicts at the stage of abstract screening were moved to full-text screening. Conflicts during full-text screening were resolved by deliberation and referring to the inclusion and exclusion criteria detailed in the research protocol. The level of agreement between the two authors for full text reviews as measured by inter-rater reliability was 0.72 (Cohen’s Kappa).
A data extraction template was created in Covidence to extract data from included full texts. Data extraction template included the following variables; country in which the study was conducted, year of publication, goal of the study (EOB, BI or both), population of the study (MS, Res or mixed) and the type of bias studied. Final data was exported to Microsoft Excel for quantification. For charting our data and categorizing the included studies, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews(PRISMA-ScR) guidelines [ 25 ]. Results from this scoping review study are meant to provide a visual synthesis of existing bias research and identify gaps in knowledge.
Study selection
Our search strategy yielded a total of 892 unique abstracts which were imported into ‘Covidence’ for screening. A total of 86 duplicate references were removed. Then, 806 titles and abstracts were screened for relevance independently by the authors and 519 studies were excluded at this stage. Any conflicts among the reviewers at this stage were resolved by discussion and referring to the inclusion and exclusion criteria. Then a full text review of the remaining 287 papers was completed by the authors against the inclusion criteria for eligibility. Full text review was also conducted independently by the authors and any conflicts were resolved upon discussion. Finally, we included 139 studies which were used for data extraction (Fig. 1 ).
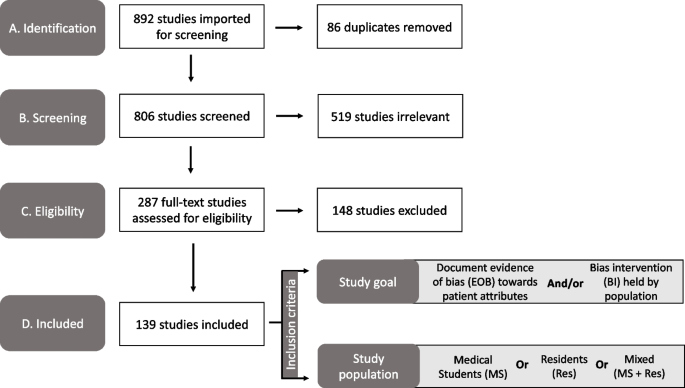
PRISMA diagram of the study selection process used in our scoping review to identify the bias categories that have been reported within medical education literature. Study took place from 2021–2022. Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Publication trends in bias research
First, we charted the studies to demonstrate the timeline of research focused on bias within the study population of our interest (MS or Res or mixed). Our analysis revealed an increase in publications with respect to time (Fig. 2 ). Of the 139 included studies, fewer studies were published prior to 2001, with a total of only eight papers being published from the years 1985–2000. A substantial increase in publications occurred after 2004, with 2019 being the peak year where most of the studies pertaining to bias were published (Fig. 2 ).
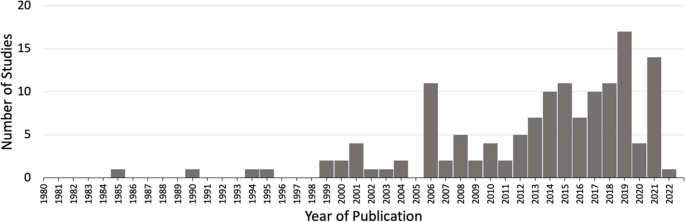
Studies matching inclusion criteria mapped by year of publication. Search criteria included studies addressing bias from 1980–2021 within medical students (MS) or residents (Res) or mixed (MS + Res) populations. * Publication in 2022 was published online ahead of print
Overview of included studies
We present a descriptive analysis of the 139 included studies in Table 1 based on the following parameters: study location, goal of the study, population of the study and the category of bias studied. All of the above parameters except the category of bias included a denominator of 139 studies. Several studies addressed more than one bias characteristic; therefore, we documented 163 biases sorted in 11 categories over the 139 papers. The bias categories that we generated and their respective occurrences are listed in Table 1 . Of the 139 studies that were included, most studies originated in the United States ( n = 89/139, 64%) and Europe ( n = 20/139, 20%).
Sorting of included research by bias category
We grouped the 139 included studies depending on the patient attribute or the descriptive characteristic against which the bias was studied (Table 1 ). By sorting the studies into different bias categories, we aimed to not only quantitate the amount of research addressing a particular topic of bias, but also reveal the biases that are understudied.
Through our analysis, we generated 11 descriptive categories against which bias was studied: Age, physical disability, education level, biological sex, disease or condition, LGBTQ + , non-specified, race/ethnicity, rural/urban, socio-economic status, and weight (Table 1 ). “Age” and “weight” categories included papers that studied bias against older population and higher weight individuals, respectively. The categories “education level” and “socio-economic status” included papers that studied bias against individuals with low education level and individuals belonging to low socioeconomic status, respectively. Within the bias category named ‘biological sex’, we included papers that studied bias against individuals perceived as women/females. Papers that studied bias against gender-identity or sexual orientation were included in its own category named, ‘LGBTQ + ’. The bias category, ‘disease or condition’ was broad and included research on bias against any patient with a specific disease, condition or lifestyle. Studies included in this category researched bias against any physical illnesses, mental illnesses, or sexually transmitted infections. It also included studies that addressed bias against a treatment such as transplant or pain management. It was not significant to report these as individual categories but rather as a whole with a common underlying theme. Rural/urban bias referred to bias that was held against a person based on their place of residence. Studies grouped together in the ‘non-specified bias’ category explored bias without specifying any descriptive characteristic in their methods. These studies did not address any specific bias characteristic in particular but consisted of a study population of our interest (MS or Res or mixed). Based on our analysis, the top five most studied bias categories in our included population within medical education literature were: racial or ethnic bias ( n = 39/163, 24%), disease or condition bias ( n = 29/163, 18%), weight bias ( n = 22/163, 13%), LGBTQ + bias ( n = 21/163, 13%), and age bias ( n = 16/163, 10%) which are presented in Table 1 .
Sorting of included research by population
In order to understand the distribution of bias research based on their populations examined, we sorted the included studies in one of the following: medical students (MS), residents (Res) or mixed (Table 1 ). The following distributions were observed: medical students only ( n = 105/139, 76%), residents only ( n = 19/139, 14%) or mixed which consisted of both medical students and residents ( n = 15/139, 11%). In combination, these results demonstrate that medical educators have focused bias research efforts primarily on medical student populations.
Sorting of included research by goal
A critical component of this scoping review was to quantify the research goal of the included studies within each of the bias categories. We defined the research goal as either to document evidence of bias (EOB) or to evaluate a bias intervention (BI) (see Fig. 1 for inclusion criteria). Some of the included studies focused on both, documenting evidence in addition to intervening biases and those studies were grouped separately. The analysis revealed that 69/139 (50%) of the included studies focused exclusively on documenting evidence of bias (EOB). There were fewer studies ( n = 51/139, 37%) which solely focused on bias interventions such as programs, seminars or curricular innovations. A small minority of the included studies were more comprehensive in that they documented EOB followed by an intervention strategy ( n = 19/139, 11%). These results demonstrate that most bias research is dedicated to documenting evidence of bias among these groups rather than evaluating a bias intervention strategy.
Research goal distribution
Our next objective was to calculate the distribution of studies with respect to the study goal (EOB, BI or both), within the 163 biases studied across the 139 papers as calculated in Table 1 . In general, the goal of the studies favors documenting evidence of bias with the exception of race/ethnic bias which is more focused on bias intervention (Fig. 3 ). Fewer studies were aimed at both, documenting evidence then providing an intervention, across all bias categories.
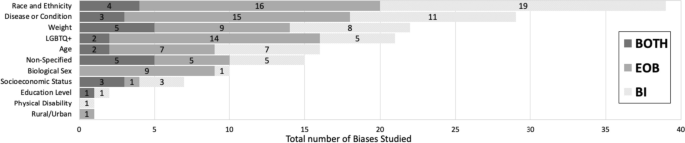
Sorting of total biases ( n = 163) within medical students or residents or a mixed population based on the bias category . Dark grey indicates studies with a dual goal, to document evidence of bias and to intervene bias. Medium grey bars indicate studies which focused on documenting evidence of bias. Light grey bars indicate studies focused on bias intervention within these populations. Numbers inside the bars indicate the total number of biases for the respective study goal. * Non-specified bias includes studies which focused on implicit bias but did not mention the type of bias investigated
Furthermore, we also calculated the ratio of EOB, BI and both (EOB + BI) within each of our population of interest (MS; n = 122, Res; n = 26 and mixed; n = 15) for the 163 biases observed in our included studies. Over half ( n = 64/122, 52%) of the total bias occurrences in MS were focused on documenting EOB (Fig. 4 ). Contrastingly, a shift was observed within resident populations where most biases addressed were aimed at intervention ( n = 12/26, 41%) rather than EOB ( n = 4/26, 14%) (Fig. 4 ). Studies which included both MS and Res (mixed) were primarily focused on documenting EOB ( n = 9/15, 60%), with 33% ( n = 5/15) aimed at bias intervention and 7% ( n = 1/15) which did both (Fig. 4 ). Although far fewer studies were documented in the Res population it is important to highlight that most of these studies were focused on bias intervention when compared to MS population where we documented a majority of studies focused on evidence of bias.
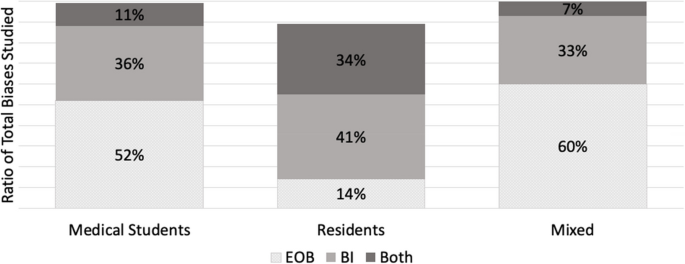
A ratio of the study goal for the total biases ( n = 163) mapped within each of the study population (MS, Res and Mixed). A study goal with a) documenting evidence of bias (EOB) is depicted in dotted grey, b) bias intervention (BI) in medium grey, and c) a dual focus (EOB + BI) is depicted in dark grey. * N = 122 for medical student studies. b N = 26 for residents. c N = 15 for mixed
Addressing biases at an earlier stage of medical career is critical for future physicians engaging with diverse patients, since it is established that bias negatively influences provider-patient interactions [ 171 ], clinical decision-making [ 172 ] and reduces favorable treatment outcomes [ 2 ]. We set out with an intention to explore how bias is addressed within the medical curriculum. Our research question was: how has the trend in bias research changed over time, more specifically a) what is the timeline of papers published? b) what bias characteristics have been studied in the physician-trainee population and c) how are these biases addressed? With the introduction of ‘standards of diversity’ by the Liaison Committee on Medical Education, along with the Association of American Medical Colleges (AAMC) and the American Medical Association (AMA) [ 173 , 174 ], we certainly expected and observed a sustained uptick in research pertaining to bias. As shown here, research addressing bias in the target population (MS and Res) is on the rise, however only 139 papers fit our inclusion criteria. Of these studies, nearly 90% have been published since 2005 after the “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care” report was published in 2003 [ 7 ]. However, given the well documented effects of physician held bias, we anticipated significantly more number of studies focused on bias at the medical student or resident level.
A key component from this study was that we generated descriptive categories of biases. Sorting the biases into descriptive categories helps to identify a more targeted approach for a specific bias intervention, rather than to broadly intervene bias as a whole. In fact, our analysis found a number of publications (labeled “non-specified bias” in Table 1 ) which studied implicit bias without specifying the patient attribute or the characteristic that the bias was against. In total, we generated 11 descriptive categories of bias from our scoping review which are shown in Table 1 and Fig. 3 . Furthermore, our bias descriptors grouped similar kinds of biases within a single category. For example, the category, “disease or condition” included papers that studied bias against any type of disease (Mental illness, HIV stigma, diabetes), condition (Pain management), or lifestyle. We neither performed a qualitative assessment of the studies nor did we test the efficacy of the bias intervention studies and consider it a future direction of this work.
Evidence suggests that medical educators and healthcare professionals are struggling to find the appropriate approach to intervene biases [ 175 , 176 , 177 ] So far, bias reduction, bias reflection and bias management approaches have been proposed [ 26 , 27 , 178 ]. Previous implicit bias intervention strategies have been shown to be ineffective when biased attitudes of participants were assessed after a lag [ 179 ]. Understanding the descriptive categories of bias and previous existing research efforts, as we present here is only a fraction of the challenge. The theory of “cognitive bias” [ 180 ] and related branches of research [ 13 , 181 , 182 , 183 , 184 ] have been studied in the field of psychology for over three decades. It is only recently that cognitive bias theory has been applied to the field of medical education medicine, to explain its negative influence on clinical decision-making pertaining only to racial minorities [ 1 , 2 , 15 , 16 , 17 , 185 ]. In order to elicit meaningful changes with respect to targeted bias intervention, it is necessary to understand the psychological underpinnings (attitudes) leading to a certain descriptive category of bias (behaviors). The questions which medical educators need to ask are: a) Can these descriptive biases be identified under certain type/s of cognitive errors that elicits the bias and vice versa b) Are we working towards an attitude change which can elicit a sustained positive behavior change among healthcare professionals? And most importantly, c) are we creating a culture where participants voluntarily enroll themselves in bias interventions as opposed to being mandated to participate? Cognitive psychologists and behavioral scientists are well-positioned to help us find answers to these questions as they understand human behavior. Therefore, an interdisciplinary approach, a marriage between cognitive psychologists and medical educators, is key in targeting biases held by medical students, residents, and ultimately future physicians. This review may also be of interest to behavioral psychologists, keen on providing targeted intervening strategies to clinicians depending on the characteristics (age, weight, sex or race) the portrayed bias is against. Further, instead of an individualized approach, we need to strive for systemic changes and evidence-based strategies to intervene biases.
The next element in change is directing intervention strategies at the right stage in clinical education. Our study demonstrated that most of the research collected at the medical student level was focused on documenting evidence of bias. Although the overall number of studies at the resident level were fewer than at the medical student level, the ratio of research in favor of bias intervention was higher at the resident level (see Fig. 3 ). However, it could be helpful to focus on bias intervention earlier in learning, rather than at a later stage [ 186 ]. Additionally, educational resources such as textbooks, preparatory materials, and educators themselves are potential sources of propagating biases and therefore need constant evaluation against best practices [ 187 , 188 ].
This study has limitations. First, the list of the descriptive bias categories that we generated was not grounded in any particular theory so assigning a category was subjective. Additionally, there were studies that were categorized as “nonspecified” bias as the studies themselves did not mention the specific type of bias that they were addressing. Moreover, we had to exclude numerous publications solely because they were not evidence-based and were either perspectives, commentaries or opinion pieces. Finally, there were overall fewer studies focused on the resident population, so the calculated ratio of MS:Res studies did not compare similar sample sizes.
Future directions of our study include working with behavioral scientists to categorize these bias characteristics (Table 1 ) into cognitive error types [ 189 ]. Additionally, we aim to assess the effectiveness of the intervention strategies and categorize the approach of the intervention strategies.
The primary goal of our review was to organize, compare and quantify literature pertaining to bias within medical school curricula and residency programs. We neither performed a qualitative assessment of the studies nor did we test the efficacy of studies that were sorted into “bias intervention” as is typical of scoping reviews [ 22 ]. In summary, our research identified 11 descriptive categories of biases studied within medical students and resident populations with “race and ethnicity”, “disease or condition”, “weight”, “LGBTQ + ” and “age” being the top five most studied biases. Additionally, we found a greater number of studies conducted in medical students (105/139) when compared to residents (19/139). However, most of the studies in the resident population focused on bias intervention. The results from our review highlight the following gaps: a) bias categories where more research is needed, b) biases that are studied within medical school versus in residency programs and c) study focus in terms of demonstrating the presence of bias or working towards bias intervention.
This review provides a visual analysis of the known categories of bias addressed within the medical school curriculum and in residency programs in addition to providing a comparison of studies with respect to the study goal within medical education literature. The results from our review should be of interest to community organizations, institutions, program directors and medical educators interested in knowing and understanding the types of bias existing within healthcare populations. It might be of special interest to researchers who wish to explore other types of biases that have been understudied within medical school and resident populations, thus filling the gaps existing in bias research.
Despite the number of studies designed to provide bias intervention for MS and Res populations, and an overall cultural shift to be aware of one’s own biases, biases held by both medical students and residents still persist. Further, psychologists have recently demonstrated the ineffectiveness of some bias intervention efforts [ 179 , 190 ]. Therefore, it is perhaps unrealistic to expect these biases to be eliminated altogether. However, effective intervention strategies grounded in cognitive psychology should be implemented earlier on in medical training. Our focus should be on providing evidence-based approaches and safe spaces for an attitude and culture change, so as to induce actionable behavioral changes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- Medical student
Evidence of bias
- Bias intervention
Hagiwara N, Mezuk B, Elston Lafata J, Vrana SR, Fetters MD. Study protocol for investigating physician communication behaviours that link physician implicit racial bias and patient outcomes in Black patients with type 2 diabetes using an exploratory sequential mixed methods design. BMJ Open. 2018;8(10):e022623.
Article Google Scholar
Haider AH, Schneider EB, Sriram N, Dossick DS, Scott VK, Swoboda SM, Losonczy L, Haut ER, Efron DT, Pronovost PJ, et al. Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. JAMA Surg. 2015;150(5):457–64.
Penner LA, Dovidio JF, Gonzalez R, Albrecht TL, Chapman R, Foster T, Harper FW, Hagiwara N, Hamel LM, Shields AF, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol. 2016;34(24):2874–80.
Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–26.
Garrett SB, Jones L, Montague A, Fa-Yusuf H, Harris-Taylor J, Powell B, Chan E, Zamarripa S, Hooper S, Chambers Butcher BD. Challenges and opportunities for clinician implicit bias training: insights from perinatal care stakeholders. Health Equity. 2023;7(1):506–19.
Shah HS, Bohlen J. Implicit bias. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Copyright © 2023, StatPearls Publishing LLC.
Google Scholar
Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. In: Smedley BD, Stith AY, Nelson AR, editors. Washington (DC): National Academies Press (US); 2003. PMID: 25032386.
Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S. A systematic review of the impact of physician implicit racial bias on clinical decision making. Acad Emerg Med. 2017;24(8):895–904.
Oliver MN, Wells KM, Joy-Gaba JA, Hawkins CB, Nosek BA. Do physicians’ implicit views of African Americans affect clinical decision making? J Am Board Fam Med. 2014;27(2):177–88.
Rincon-Subtirelu M. Education as a tool to modify anti-obesity bias among pediatric residents. Int J Med Educ. 2017;8:77–8.
Gustafsson Sendén M, Renström EA. Gender bias in assessment of future work ability among pain patients - an experimental vignette study of medical students’ assessment. Scand J Pain. 2019;19(2):407–14.
Hardeman RR, Burgess D, Phelan S, Yeazel M, Nelson D, van Ryn M. Medical student socio-demographic characteristics and attitudes toward patient centered care: do race, socioeconomic status and gender matter? A report from the medical student CHANGES study. Patient Educ Couns. 2015;98(3):350–5.
Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
Kruse JA, Collins JL, Vugrin M. Educational strategies used to improve the knowledge, skills, and attitudes of health care students and providers regarding implicit bias: an integrative review of the literature. Int J Nurs Stud Adv. 2022;4:100073.
Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit bias in health care: a narrative review. Group Process Intergroup Relat. 2016;19(4):528–42.
Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, Eng E, Day SH, Coyne-Beasley T. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):E60–76.
FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
Gonzalez CM, Onumah CM, Walker SA, Karp E, Schwartz R, Lypson ML. Implicit bias instruction across disciplines related to the social determinants of health: a scoping review. Adv Health Sci Educ. 2023;28(2):541–87.
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–85.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
Pat C, Geeta S, Sílvia M. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf. 2013;22(Suppl 2):ii58.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Thomas A, Lubarsky S, Durning SJ, Young ME. Knowledge syntheses in medical education: demystifying scoping reviews. Acad Med. 2017;92(2):161–6.
Hagopian A, Thompson MJ, Fordyce M, Johnson KE, Hart LG. The migration of physicians from sub-Saharan Africa to the United States of America: measures of the African brain drain. Hum Resour Health. 2004;2(1):17.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Teal CR, Shada RE, Gill AC, Thompson BM, Frugé E, Villarreal GB, Haidet P. When best intentions aren’t enough: Helping medical students develop strategies for managing bias about patients. J Gen Intern Med. 2010;25(Suppl 2):S115–8.
Gonzalez CM, Walker SA, Rodriguez N, Noah YS, Marantz PR. Implicit bias recognition and management in interpersonal encounters and the learning environment: a skills-based curriculum for medical students. MedEdPORTAL. 2021;17:11168.
Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–301.
Mayfield JJ, Ball EM, Tillery KA, Crandall C, Dexter J, Winer JM, Bosshardt ZM, Welch JH, Dolan E, Fancovic ER, et al. Beyond men, women, or both: a comprehensive, LGBTQ-inclusive, implicit-bias-aware, standardized-patient-based sexual history taking curriculum. MedEdPORTAL. 2017;13:10634.
Morris M, Cooper RL, Ramesh A, Tabatabai M, Arcury TA, Shinn M, Im W, Juarez P, Matthews-Juarez P. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC Med Educ. 2019;19(1):325.
Perdomo J, Tolliver D, Hsu H, He Y, Nash KA, Donatelli S, Mateo C, Akagbosu C, Alizadeh F, Power-Hays A, et al. Health equity rounds: an interdisciplinary case conference to address implicit bias and structural racism for faculty and trainees. MedEdPORTAL. 2019;15:10858.
Sherman MD, Ricco J, Nelson SC, Nezhad SJ, Prasad S. Implicit bias training in a residency program: aiming for enduring effects. Fam Med. 2019;51(8):677–81.
van Ryn M, Hardeman R, Phelan SM, Burgess DJ, Dovidio JF, Herrin J, Burke SE, Nelson DB, Perry S, Yeazel M, et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a medical student CHANGES study report. J Gen Intern Med. 2015;30(12):1748–56.
Chary AN, Molina MF, Dadabhoy FZ, Manchanda EC. Addressing racism in medicine through a resident-led health equity retreat. West J Emerg Med. 2020;22(1):41–4.
DallaPiazza M, Padilla-Register M, Dwarakanath M, Obamedo E, Hill J, Soto-Greene ML. Exploring racism and health: an intensive interactive session for medical students. MedEdPORTAL. 2018;14:10783.
Dennis SN, Gold RS, Wen FK. Learner reactions to activities exploring racism as a social determinant of health. Fam Med. 2019;51(1):41–7.
Gonzalez CM, Walker SA, Rodriguez N, Karp E, Marantz PR. It can be done! a skills-based elective in implicit bias recognition and management for preclinical medical students. Acad Med. 2020;95(12S Addressing Harmful Bias and Eliminating Discrimination in Health Professions Learning Environments):S150–5.
Motzkus C, Wells RJ, Wang X, Chimienti S, Plummer D, Sabin J, Allison J, Cashman S. Pre-clinical medical student reflections on implicit bias: Implications for learning and teaching. PLoS ONE. 2019;14(11):e0225058.
Phelan SM, Burke SE, Cunningham BA, Perry SP, Hardeman RR, Dovidio JF, Herrin J, Dyrbye LN, White RO, Yeazel MW, et al. The effects of racism in medical education on students’ decisions to practice in underserved or minority communities. Acad Med. 2019;94(8):1178–89.
Zeidan A, Tiballi A, Woodward M, Di Bartolo IM. Targeting implicit bias in medicine: lessons from art and archaeology. West J Emerg Med. 2019;21(1):1–3.
Baker TK, Smith GS, Jacobs NN, Houmanfar R, Tolles R, Kuhls D, Piasecki M. A deeper look at implicit weight bias in medical students. Adv Health Sci Educ Theory Pract. 2017;22(4):889–900.
Eymard AS, Douglas DH. Ageism among health care providers and interventions to improve their attitudes toward older adults: an integrative review. J Gerontol Nurs. 2012;38(5):26–35.
Garrison CB, McKinney-Whitson V, Johnston B, Munroe A. Race matters: addressing racism as a health issue. Int J Psychiatry Med. 2018;53(5–6):436–44.
Geller G, Watkins PA. Addressing medical students’ negative bias toward patients with obesity through ethics education. AMA J Ethics. 2018;20(10):E948-959.
Onyeador IN, Wittlin NM, Burke SE, Dovidio JF, Perry SP, Hardeman RR, Dyrbye LN, Herrin J, Phelan SM, van Ryn M. The value of interracial contact for reducing anti-black bias among non-black physicians: a Cognitive Habits and Growth Evaluation (CHANGE) study report. Psychol Sci. 2020;31(1):18–30.
Poustchi Y, Saks NS, Piasecki AK, Hahn KA, Ferrante JM. Brief intervention effective in reducing weight bias in medical students. Fam Med. 2013;45(5):345–8.
Ruiz JG, Andrade AD, Anam R, Taldone S, Karanam C, Hogue C, Mintzer MJ. Group-based differences in anti-aging bias among medical students. Gerontol Geriatr Educ. 2015;36(1):58–78.
Simpson T, Evans J, Goepfert A, Elopre L. Implementing a graduate medical education anti-racism workshop at an academic university in the Southern USA. Med Educ Online. 2022;27(1):1981803.
Wittlin NM, Dovidio JF, Burke SE, Przedworski JM, Herrin J, Dyrbye L, Onyeador IN, Phelan SM, van Ryn M. Contact and role modeling predict bias against lesbian and gay individuals among early-career physicians: a longitudinal study. Soc Sci Med. 2019;238:112422.
Miller DP Jr, Spangler JG, Vitolins MZ, Davis SW, Ip EH, Marion GS, Crandall SJ. Are medical students aware of their anti-obesity bias? Acad Med. 2013;88(7):978–82.
Gonzalez CM, Deno ML, Kintzer E, Marantz PR, Lypson ML, McKee MD. A qualitative study of New York medical student views on implicit bias instruction: implications for curriculum development. J Gen Intern Med. 2019;34(5):692–8.
Gonzalez CM, Kim MY, Marantz PR. Implicit bias and its relation to health disparities: a teaching program and survey of medical students. Teach Learn Med. 2014;26(1):64–71.
Gonzalez CM, Nava S, List J, Liguori A, Marantz PR. How assumptions and preferences can affect patient care: an introduction to implicit bias for first-year medical students. MedEdPORTAL. 2021;17:11162.
Hernandez RA, Haidet P, Gill AC, Teal CR. Fostering students’ reflection about bias in healthcare: cognitive dissonance and the role of personal and normative standards. Med Teach. 2013;35(4):e1082-1089.
Kushner RF, Zeiss DM, Feinglass JM, Yelen M. An obesity educational intervention for medical students addressing weight bias and communication skills using standardized patients. BMC Med Educ. 2014;14:53.
Nazione S, Silk KJ. Patient race and perceived illness responsibility: effects on provider helping and bias. Med Educ. 2013;47(8):780–9.
Ogunyemi D. Defeating unconscious bias: the role of a structured, reflective, and interactive workshop. J Grad Med Educ. 2021;13(2):189–94.
Phelan SM, Burke SE, Hardeman RR, White RO, Przedworski J, Dovidio JF, Perry SP, Plankey M, A Cunningham B, Finstad D, et al. Medical school factors associated with changes in implicit and explicit bias against gay and lesbian people among 3492 graduating medical students. J Gen Intern Med. 2017;32(11):1193–201.
Phelan SM, Puhl RM, Burke SE, Hardeman R, Dovidio JF, Nelson DB, Przedworski J, Burgess DJ, Perry S, Yeazel MW, et al. The mixed impact of medical school on medical students’ implicit and explicit weight bias. Med Educ. 2015;49(10):983–92.
Barber Doucet H, Ward VL, Johnson TJ, Lee LK. Implicit bias and caring for diverse populations: pediatric trainee attitudes and gaps in training. Clin Pediatr (Phila). 2021;60(9–10):408–17.
Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, Nelson DB, Burgess DJ, Yeazel MW, van Ryn M. Do contact and empathy mitigate bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
Johnston B, McKinney-Whitson V, Garrison V. Race matters: addressing racism as a health issue. WMJ. 2021;120(S1):S74–7.
Kost A, Akande T, Jones R, Gabert R, Isaac M, Dettmar NS. Use of patient identifiers at the University of Washington School of Medicine: building institutional consensus to reduce bias and stigma. Fam Med. 2021;53(5):366–71.
Madan AK, Aliabadi-Wahle S, Beech DJ. Ageism in medical students’ treatment recommendations: the example of breast-conserving procedures. Acad Med. 2001;76(3):282–4.
Marbin J, Lewis L, Kuo AK, Schudel C, Gutierrez JR. The power of place: travel to explore structural racism and health disparities. Acad Med. 2021;96(11):1569–73.
Phelan SM, Dovidio JF, Puhl RM, Burgess DJ, Nelson DB, Yeazel MW, Hardeman R, Perry S, van Ryn M. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring). 2014;22(4):1201–8.
Van J, Aloman C, Reau N. Potential bias and misconceptions in liver transplantation for alcohol- and obesity-related liver disease. Am J Gastroenterol. 2021;116(10):2089–97.
White-Means S, Zhiyong D, Hufstader M, Brown LT. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students: implications for addressing health disparities. Med Care Res Rev. 2009;66(4):436–55.
Williams RL, Vasquez CE, Getrich CM, Kano M, Boursaw B, Krabbenhoft C, Sussman AL. Racial/gender biases in student clinical decision-making: a mixed-method study of medical school attributes associated with lower incidence of biases. J Gen Intern Med. 2018;33(12):2056–64.
Cohen RW, Persky S. Influence of weight etiology information and trainee characteristics on physician-trainees’ clinical and interpersonal communication. Patient Educ Couns. 2019;102(9):1644–9.
Haider AH, Sexton J, Sriram N, Cooper LA, Efron DT, Swoboda S, Villegas CV, Haut ER, Bonds M, Pronovost PJ, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306(9):942–51.
Lewis R, Lamdan RM, Wald D, Curtis M. Gender bias in the diagnosis of a geriatric standardized patient: a potential confounding variable. Acad Psychiatry. 2006;30(5):392–6.
Matharu K, Shapiro JF, Hammer RR, Kravitz RL, Wilson MD, Fitzgerald FT. Reducing obesity prejudice in medical education. Educ Health. 2014;27(3):231–7.
McLean ME, McLean LE, McLean-Holden AC, Campbell LF, Horner AM, Kulkarni ML, Melville LD, Fernandez EA. Interphysician weight bias: a cross-sectional observational survey study to guide implicit bias training in the medical workplace. Acad Emerg Med. 2021;28(9):1024–34.
Meadows A, Higgs S, Burke SE, Dovidio JF, van Ryn M, Phelan SM. Social dominance orientation, dispositional empathy, and need for cognitive closure moderate the impact of empathy-skills training, but not patient contact, on medical students’ negative attitudes toward higher-weight patients. Front Psychol. 2017;8:15.
Stone J, Moskowitz GB, Zestcott CA, Wolsiefer KJ. Testing active learning workshops for reducing implicit stereotyping of Hispanics by majority and minority group medical students. Stigma Health. 2020;5(1):94–103.
Symons AB, Morley CP, McGuigan D, Akl EA. A curriculum on care for people with disabilities: effects on medical student self-reported attitudes and comfort level. Disabil Health J. 2014;7(1):88–95.
Ufomata E, Eckstrand KL, Hasley P, Jeong K, Rubio D, Spagnoletti C. Comprehensive internal medicine residency curriculum on primary care of patients who identify as LGBT. LGBT Health. 2018;5(6):375–80.
Aultman JM, Borges NJ. A clinical and ethical investigation of pre-medical and medical students’ attitudes, knowledge, and understanding of HIV. Med Educ Online. 2006;11:1–12.
Bates T, Cohan M, Bragg DS, Bedinghaus J. The Medical College of Wisconsin senior mentor program: experience of a lifetime. Gerontol Geriatr Educ. 2006;27(2):93–103.
Chiaramonte GR, Friend R. Medical students’ and residents’ gender bias in the diagnosis, treatment, and interpretation of coronary heart disease symptoms. Health Psychol. 2006;25(3):255–66.
Friedberg F, Sohl SJ, Halperin PJ. Teaching medical students about medically unexplained illnesses: a preliminary study. Med Teach. 2008;30(6):618–21.
Gonzales E, Morrow-Howell N, Gilbert P. Changing medical students’ attitudes toward older adults. Gerontol Geriatr Educ. 2010;31(3):220–34.
Hinners CK, Potter JF. A partnership between the University of Nebraska College of Medicine and the community: fostering positive attitudes towards the aged. Gerontol Geriatr Educ. 2006;27(2):83–91.
Lee M, Coulehan JL. Medical students’ perceptions of racial diversity and gender equality. Med Educ. 2006;40(7):691–6.
Schmetzer AD, Lafuze JE. Overcoming stigma: involving families in medical student and psychiatric residency education. Acad Psychiatry. 2008;32(2):127–31.
Willen SS, Bullon A, Good MJD. Opening up a huge can of worms: reflections on a “cultural sensitivity” course for psychiatry residents. Harv Rev Psychiatry. 2010;18(4):247–53.
Dogra N, Karnik N. First-year medical students’ attitudes toward diversity and its teaching: an investigation at one U.S. medical school. Acad Med. 2003;78(11):1191–200.
Fitzpatrick C, Musser A, Mosqueda L, Boker J, Prislin M. Student senior partnership program: University of California Irvine School of Medicine. Gerontol Geriatr Educ. 2006;27(2):25–35.
Hoffman KG, Gray P, Hosokawa MC, Zweig SC. Evaluating the effectiveness of a senior mentor program: the University of Missouri-Columbia School of Medicine. Gerontol Geriatr Educ. 2006;27(2):37–47.
Kantor BS, Myers MR. From aging…to saging-the Ohio State Senior Partners Program: longitudinal and experiential geriatrics education. Gerontol Geriatr Educ. 2006;27(2):69–74.
Klamen DL, Grossman LS, Kopacz DR. Medical student homophobia. J Homosex. 1999;37(1):53–63.
Kopacz DR, Grossman LS, Klamen DL. Medical students and AIDS: knowledge, attitudes and implications for education. Health Educ Res. 1999;14(1):1–6.
Leiblum SR. An established medical school human sexuality curriculum: description and evaluation. Sex Relatsh Ther. 2001;16(1):59–70.
Rastegar DA, Fingerhood MI, Jasinski DR. A resident clerkship that combines inpatient and outpatient training in substance abuse and HIV care. Subst Abuse. 2004;25(4):11–5.
Roberts E, Richeson NA, Thornhill JTIV, Corwin SJ, Eleazer GP. The senior mentor program at the University of South Carolina School of Medicine: an innovative geriatric longitudinal curriculum. Gerontol Geriatr Educ. 2006;27(2):11–23.
Burgess DJ, Burke SE, Cunningham BA, Dovidio JF, Hardeman RR, Hou YF, Nelson DB, Perry SP, Phelan SM, Yeazel MW, et al. Medical students’ learning orientation regarding interracial interactions affects preparedness to care for minority patients: a report from medical student CHANGES. BMC Med Educ. 2016;16:254.
Burgess DJ, Hardeman RR, Burke SE, Cunningham BA, Dovidio JF, Nelson DB, Perry SP, Phelan SM, Yeazel MW, Herrin J, et al. Incoming medical students’ political orientation affects outcomes related to care of marginalized groups: results from the medical student CHANGES study. J Health Pol Policy Law. 2019;44(1):113–46.
Kurtz ME, Johnson SM, Tomlinson T, Fiel NJ. Teaching medical students the effects of values and stereotyping on the doctor/patient relationship. Soc Sci Med. 1985;21(9):1043–7.
Matharu K, Kravitz RL, McMahon GT, Wilson MD, Fitzgerald FT. Medical students’ attitudes toward gay men. BMC Med Educ. 2012;12:71.
Pearl RL, Argueso D, Wadden TA. Effects of medical trainees’ weight-loss history on perceptions of patients with obesity. Med Educ. 2017;51(8):802–11.
Perry SP, Dovidio JF, Murphy MC, van Ryn M. The joint effect of bias awareness and self-reported prejudice on intergroup anxiety and intentions for intergroup contact. Cultur Divers Ethnic Minor Psychol. 2015;21(1):89–96.
Phelan SM, Burgess DJ, Burke SE, Przedworski JM, Dovidio JF, Hardeman R, Morris M, van Ryn M. Beliefs about the causes of obesity in a national sample of 4th year medical students. Patient Educ Couns. 2015;98(11):1446–9.
Phelan SM, Puhl RM, Burgess DJ, Natt N, Mundi M, Miller NE, Saha S, Fischer K, van Ryn M. The role of weight bias and role-modeling in medical students’ patient-centered communication with higher weight standardized patients. Patient Educ Couns. 2021;104(8):1962–9.
Polan HJ, Auerbach MI, Viederman M. AIDS as a paradigm of human behavior in disease: impact and implications of a course. Acad Psychiatry. 1990;14(4):197–203.
Reuben DB, Fullerton JT, Tschann JM, Croughan-Minihane M. Attitudes of beginning medical students toward older persons: a five-campus study. J Am Geriatr Soc. 1995;43(12):1430–6.
Tsai J. Building structural empathy to marshal critical education into compassionate practice: evaluation of a medical school critical race theory course. J Law Med Ethics. 2021;49(2):211–21.
Weyant RJ, Bennett ME, Simon M, Palaisa J. Desire to treat HIV-infected patients: similarities and differences across health-care professions. AIDS. 1994;8(1):117–21.
Ross PT, Lypson ML. Using artistic-narrative to stimulate reflection on physician bias. Teach Learn Med. 2014;26(4):344–9.
Calabrese SK, Earnshaw VA, Krakower DS, Underhill K, Vincent W, Magnus M, Hansen NB, Kershaw TS, Mayer KH, Betancourt JR, et al. A closer look at racism and heterosexism in medical students’ clinical decision-making related to HIV Pre-Exposure Prophylaxis (PrEP): implications for PrEP education. AIDS Behav. 2018;22(4):1122–38.
Fitterman-Harris HF, Vander Wal JS. Weight bias reduction among first-year medical students: a quasi-randomized, controlled trial. Clin Obes. 2021;11(6):e12479.
Madan AK, Cooper L, Gratzer A, Beech DJ. Ageism in breast cancer surgical options by medical students. Tenn Med. 2006;99(5):37–8, 41.
Bikmukhametov DA, Anokhin VA, Vinogradova AN, Triner WR, McNutt LA. Bias in medicine: a survey of medical student attitudes towards HIV-positive and marginalized patients in Russia, 2010. J Int AIDS Soc. 2012;15(2):17372.
Dijkstra AF, Verdonk P, Lagro-Janssen AL. Gender bias in medical textbooks: examples from coronary heart disease, depression, alcohol abuse and pharmacology. Med Educ. 2008;42(10):1021–8.
Dobrowolska B, Jędrzejkiewicz B, Pilewska-Kozak A, Zarzycka D, Ślusarska B, Deluga A, Kościołek A, Palese A. Age discrimination in healthcare institutions perceived by seniors and students. Nurs Ethics. 2019;26(2):443–59.
Hamberg K, Risberg G, Johansson EE, Westman G. Gender bias in physicians’ management of neck pain: a study of the answers in a Swedish national examination. J Womens Health Gend Based Med. 2002;11(7):653–66.
Magliano L, Read J, Sagliocchi A, Oliviero N, D’Ambrosio A, Campitiello F, Zaccaro A, Guizzaro L, Patalano M. “Social dangerousness and incurability in schizophrenia”: results of an educational intervention for medical and psychology students. Psychiatry Res. 2014;219(3):457–63.
Reis SP, Wald HS. Contemplating medicine during the Third Reich: scaffolding professional identity formation for medical students. Acad Med. 2015;90(6):770–3.
Schroyen S, Adam S, Marquet M, Jerusalem G, Thiel S, Giraudet AL, Missotten P. Communication of healthcare professionals: Is there ageism? Eur J Cancer Care (Engl). 2018;27(1):e12780.
Swift JA, Hanlon S, El-Redy L, Puhl RM, Glazebrook C. Weight bias among UK trainee dietitians, doctors, nurses and nutritionists. J Hum Nutr Diet. 2013;26(4):395–402.
Swift JA, Tischler V, Markham S, Gunning I, Glazebrook C, Beer C, Puhl R. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6(1):91–102.
Yertutanol FDK, Candansayar S, Seydaoğlu G. Homophobia in health professionals in Ankara, Turkey: developing a scale. Transcult Psychiatry. 2019;56(6):1191–217.
Arnold O, Voracek M, Musalek M, Springer-Kremser M. Austrian medical students’ attitudes towards male and female homosexuality: a comparative survey. Wien Klin Wochenschr. 2004;116(21–22):730–6.
Arvaniti A, Samakouri M, Kalamara E, Bochtsou V, Bikos C, Livaditis M. Health service staff’s attitudes towards patients with mental illness. Soc Psychiatry Psychiatr Epidemiol. 2009;44(8):658–65.
Lopes L, Gato J, Esteves M. Portuguese medical students’ knowledge and attitudes towards homosexuality. Acta Med Port. 2016;29(11):684–93.
Papadaki V, Plotnikof K, Gioumidou M, Zisimou V, Papadaki E. A comparison of attitudes toward lesbians and gay men among students of helping professions in Crete, Greece: the cases of social work, psychology, medicine, and nursing. J Homosex. 2015;62(6):735–62.
Papaharitou S, Nakopoulou E, Moraitou M, Tsimtsiou Z, Konstantinidou E, Hatzichristou D. Exploring sexual attitudes of students in health professions. J Sex Med. 2008;5(6):1308–16.
Roberts JH, Sanders T, Mann K, Wass V. Institutional marginalisation and student resistance: barriers to learning about culture, race and ethnicity. Adv Health Sci Educ. 2010;15(4):559–71.
Wilhelmi L, Ingendae F, Steinhaeuser J. What leads to the subjective perception of a ‘rural area’? A qualitative study with undergraduate students and postgraduate trainees in Germany to tailor strategies against physician’s shortage. Rural Remote Health. 2018;18(4):4694.
Herrmann-Werner A, Loda T, Wiesner LM, Erschens RS, Junne F, Zipfel S. Is an obesity simulation suit in an undergraduate medical communication class a valuable teaching tool? A cross-sectional proof of concept study. BMJ Open. 2019;9(8):e029738.
Ahadinezhad B, Khosravizadeh O, Maleki A, Hashtroodi A. Implicit racial bias among medical graduates and students by an IAT measure: a systematic review and meta-analysis. Ir J Med Sci. 2022;191(4):1941–9. https://doi.org/10.1007/s11845-021-02756-3 .
Hsieh JG, Hsu M, Wang YW. An anthropological approach to teach and evaluate cultural competence in medical students - the application of mini-ethnography in medical history taking. Med Educ Online. 2016;21:32561.
Poreddi V, Thimmaiah R, Math SB. Attitudes toward people with mental illness among medical students. J Neurosci Rural Pract. 2015;6(3):349–54.
Mino Y, Yasuda N, Tsuda T, Shimodera S. Effects of a one-hour educational program on medical students’ attitudes to mental illness. Psychiatry Clin Neurosci. 2001;55(5):501–7.
Omori A, Tateno A, Ideno T, Takahashi H, Kawashima Y, Takemura K, Okubo Y. Influence of contact with schizophrenia on implicit attitudes towards schizophrenia patients held by clinical residents. BMC Psychiatry. 2012;12:8.
Banwari G, Mistry K, Soni A, Parikh N, Gandhi H. Medical students and interns’ knowledge about and attitude towards homosexuality. J Postgrad Med. 2015;61(2):95–100.
Lee SY. Obesity education in medical school curricula in Korea. J Obes Metab Syndr. 2018;27(1):35–8.
Aruna G, Mittal S, Yadiyal MB, Acharya C, Acharya S, Uppulari C. Perception, knowledge, and attitude toward mental disorders and psychiatry among medical undergraduates in Karnataka: a cross-sectional study. Indian J Psychiatry. 2016;58(1):70–6.
Wong YL. Review paper: gender competencies in the medical curriculum: addressing gender bias in medicine. Asia Pac J Public Health. 2009;21(4):359–76.
Earnshaw VA, Jin H, Wickersham JA, Kamarulzaman A, John J, Lim SH, Altice FL. Stigma toward men who have sex with men among future healthcare providers in Malaysia: would more interpersonal contact reduce prejudice? AIDS Behav. 2016;20(1):98–106.
Larson B, Herx L, Williamson T, Crowshoe L. Beyond the barriers: family medicine residents’ attitudes towards providing Aboriginal health care. Med Educ. 2011;45(4):400–6.
Wagner AC, Girard T, McShane KE, Margolese S, Hart TA. HIV-related stigma and overlapping stigmas towards people living with HIV among health care trainees in Canada. AIDS Educ Prev. 2017;29(4):364–76.
Tellier P-P, Bélanger E, Rodríguez C, Ware MA, Posel N. Improving undergraduate medical education about pain assessment and management: a qualitative descriptive study of stakeholders’ perceptions. Pain Res Manage. 2013;18(5):259–65.
Loignon C, Boudreault-Fournier A, Truchon K, Labrousse Y, Fortin B. Medical residents reflect on their prejudices toward poverty: a photovoice training project. BMC Med Educ. 2014;14:1050.
Phillips SP, Clarke M. More than an education: the hidden curriculum, professional attitudes and career choice. Med Educ. 2012;46(9):887–93.
Jaworsky D, Gardner S, Thorne JG, Sharma M, McNaughton N, Paddock S, Chew D, Lees R, Makuwaza T, Wagner A, et al. The role of people living with HIV as patient instructors—Reducing stigma and improving interest around HIV care among medical students. AIDS Care. 2017;29(4):524–31.
Sukhera J, Wodzinski M, Teunissen PW, Lingard L, Watling C. Striving while accepting: exploring the relationship between identity and implicit bias recognition and management. Acad Med. 2018;93(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 57th Annual Research in Medical Education Sessions):S82-s88.
Harris R, Cormack D, Curtis E, Jones R, Stanley J, Lacey C. Development and testing of study tools and methods to examine ethnic bias and clinical decision-making among medical students in New Zealand: the Bias and Decision-Making in Medicine (BDMM) study. BMC Med Educ. 2016;16:173.
Cormack D, Harris R, Stanley J, Lacey C, Jones R, Curtis E. Ethnic bias amongst medical students in Aotearoa/New Zealand: findings from the Bias and Decision Making in Medicine (BDMM) study. PLoS ONE. 2018;13(8):e0201168.
Harris R, Cormack D, Stanley J, Curtis E, Jones R, Lacey C. Ethnic bias and clinical decision-making among New Zealand medical students: an observational study. BMC Med Educ. 2018;18(1):18.
Robinson EL, Ball LE, Leveritt MD. Obesity bias among health and non-health students attending an Australian university and their perceived obesity education. J Nutr Educ Behav. 2014;46(5):390–5.
Sopoaga F, Zaharic T, Kokaua J, Covello S. Training a medical workforce to meet the needs of diverse minority communities. BMC Med Educ. 2017;17:19.
Parker R, Larkin T, Cockburn J. A visual analysis of gender bias in contemporary anatomy textbooks. Soc Sci Med. 2017;180:106–13.
Gomes MdM. Doctors’ perspectives and practices regarding epilepsy. Arq Neuropsiquiatr. 2000;58(2):221–6.
Caixeta J, Fernandes PT, Bell GS, Sander JW, Li LM. Epilepsy perception amongst university students - A survey. Arq Neuropsiquiatr. 2007;65:43–8.
Tedrus GMAS, Fonseca LC, da Câmara Vieira AL. Knowledge and attitudes toward epilepsy amongst students in the health area: intervention aimed at enlightenment. Arq Neuropsiquiatr. 2007;65(4-B):1181–5.
Gomez-Moreno C, Verduzco-Aguirre H, Contreras-Garduño S, Perez-de-Acha A, Alcalde-Castro J, Chavarri-Guerra Y, García-Lara JMA, Navarrete-Reyes AP, Avila-Funes JA, Soto-Perez-de-Celis E. Perceptions of aging and ageism among Mexican physicians-in-training. Clin Transl Oncol. 2019;21(12):1730–5.
Campbell MH, Gromer J, Emmanuel MK, Harvey A. Attitudes Toward Transgender People Among Future Caribbean Doctors. Arch Sex Behav. 2022;51(4):1903-11. https://doi.org/10.1007/s10508-021-02205-3 .
Hatala R, Case SM. Examining the influence of gender on medical students’ decision making. J Womens Health Gend Based Med. 2000;9(6):617–23.
Deb T, Lempp H, Bakolis I, et al. Responding to experienced and anticipated discrimination (READ): anti -stigma training for medical students towards patients with mental illness – study protocol for an international multisite non-randomised controlled study. BMC Med Educ. 2019;19:41. https://doi.org/10.1186/s12909-019-1472-7 .
Morgan S, Plaisant O, Lignier B, Moxham BJ. Sexism and anatomy, as discerned in textbooks and as perceived by medical students at Cardiff University and University of Paris Descartes. J Anat. 2014;224(3):352–65.
Alford CL, Miles T, Palmer R, Espino D. An introduction to geriatrics for first-year medical students. J Am Geriatr Soc. 2001;49(6):782–7.
Stone J, Moskowitz GB. Non-conscious bias in medical decision making: what can be done to reduce it? Med Educ. 2011;45(8):768–76.
Nazione S. Slimming down medical provider weight bias in an obese nation. Med Educ. 2015;49(10):954–5.
Dogra N, Connin S, Gill P, Spencer J, Turner M. Teaching of cultural diversity in medical schools in the United Kingdom and Republic of Ireland: cross sectional questionnaire survey. BMJ. 2005;330(7488):403–4.
Aultman JM, Borges NJ. A clinical and ethical investigation of pre-medical and medical students’ attitudes, knowledge, and understanding of HIV. Med Educ Online. 2006;11(1):4596.
Deb T, Lempp H, Bakolis I, Vince T, Waugh W, Henderson C, Thornicroft G, Ando S, Yamaguchi S, Matsunaga A, et al. Responding to experienced and anticipated discrimination (READ): anti -stigma training for medical students towards patients with mental illness – study protocol for an international multisite non-randomised controlled study. BMC Med Educ. 2019;19(1):41.
Gonzalez CM, Grochowalski JH, Garba RJ, Bonner S, Marantz PR. Validity evidence for a novel instrument assessing medical student attitudes toward instruction in implicit bias recognition and management. BMC Med Educ. 2021;21(1):205.
Ogunyemi D. A practical approach to implicit bias training. J Grad Med Educ. 2021;13(4):583–4.
Dennis GC. Racism in medicine: planning for the future. J Natl Med Assoc. 2001;93(3 Suppl):1S-5S.
Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219–29.
Blair IV, Steiner JF, Hanratty R, Price DW, Fairclough DL, Daugherty SL, Bronsert M, Magid DJ, Havranek EP. An investigation of associations between clinicians’ ethnic or racial bias and hypertension treatment, medication adherence and blood pressure control. J Gen Intern Med. 2014;29(7):987–95.
Stanford FC. The importance of diversity and inclusion in the healthcare workforce. J Natl Med Assoc. 2020;112(3):247–9.
Education LCoM. Standards on diversity. 2009. https://health.usf.edu/~/media/Files/Medicine/MD%20Program/Diversity/LCMEStandardsonDiversity1.ashx?la=en .
Onyeador IN, Hudson STJ, Lewis NA. Moving beyond implicit bias training: policy insights for increasing organizational diversity. Policy Insights Behav Brain Sci. 2021;8(1):19–26.
Forscher PS, Mitamura C, Dix EL, Cox WTL, Devine PG. Breaking the prejudice habit: mechanisms, timecourse, and longevity. J Exp Soc Psychol. 2017;72:133–46.
Lai CK, Skinner AL, Cooley E, Murrar S, Brauer M, Devos T, Calanchini J, Xiao YJ, Pedram C, Marshburn CK, et al. Reducing implicit racial preferences: II. Intervention effectiveness across time. J Exp Psychol Gen. 2016;145(8):1001–16.
Sukhera J, Watling CJ, Gonzalez CM. Implicit bias in health professions: from recognition to transformation. Acad Med. 2020;95(5):717–23.
Vuletich HA, Payne BK. Stability and change in implicit bias. Psychol Sci. 2019;30(6):854–62.
Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biases. Science. 1974;185(4157):1124–31.
Miller DT, Ross M. Self-serving biases in the attribution of causality: fact or fiction? Psychol Bull. 1975;82(2):213–25.
Nickerson RS. Confirmation bias: a ubiquitous phenomenon in many guises. Rev Gen Psychol. 1998;2(2):175–220.
Suveren Y. Unconscious bias: definition and significance. Psikiyatride Guncel Yaklasimlar. 2022;14(3):414–26.
Dietrich D, Olson M. A demonstration of hindsight bias using the Thomas confirmation vote. Psychol Rep. 1993;72(2):377–8.
Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–8.
Rushmer R, Davies HT. Unlearning in health care. Qual Saf Health Care. 2004;13 Suppl 2(Suppl 2):ii10-15.
Vu MT, Pham TTT. Gender, critical pedagogy, and textbooks: Understanding teachers’ (lack of) mediation of the hidden curriculum in the EFL classroom. Lang Teach Res. 2022;0(0). https://doi.org/10.1177/13621688221136937 .
Kalantari A, Alvarez A, Battaglioli N, Chung A, Cooney R, Boehmer SJ, Nwabueze A, Gottlieb M. Sex and race visual representation in emergency medicine textbooks and the hidden curriculum. AEM Educ Train. 2022;6(3):e10743.
Satya-Murti S, Lockhart J. Recognizing and reducing cognitive bias in clinical and forensic neurology. Neurol Clin Pract. 2015;5(5):389–96.
Chang EH, Milkman KL, Gromet DM, Rebele RW, Massey C, Duckworth AL, Grant AM. The mixed effects of online diversity training. Proc Natl Acad Sci U S A. 2019;116(16):7778–83.
Download references
Acknowledgements
The authors would like to thank Dr. Misa Mi, Professor and Medical Librarian at the Oakland University William Beaumont School of Medicine (OWUB) for her assistance with selection of databases and construction of literature search strategies for the scoping review. The authors also wish to thank Dr. Changiz Mohiyeddini, Professor in Behavioral Medicine and Psychopathology at Oakland University William Beaumont School of Medicine (OUWB) for his expertise and constructive feedback on our manuscript.
Author information
Authors and affiliations.
Department of Foundational Sciences, Central Michigan University College of Medicine, Mt. Pleasant, MI, 48859, USA
Brianne E. Lewis
Department of Foundational Medical Studies, Oakland University William Beaumont School of Medicine, 586 Pioneer Dr, Rochester, MI, 48309, USA
Akshata R. Naik
You can also search for this author in PubMed Google Scholar
Contributions
A.R.N and B.E.L were equally involved in study conception, design, collecting data and analyzing the data. B.E.L and A.R.N both contributed towards writing the manuscript. A.R.N and B.E.L are both senior authors on this paper. All authors reviewed the manuscript.
Corresponding author
Correspondence to Akshata R. Naik .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lewis, B.E., Naik, A.R. A scoping review to identify and organize literature trends of bias research within medical student and resident education. BMC Med Educ 23 , 919 (2023). https://doi.org/10.1186/s12909-023-04829-6
Download citation
Received : 14 March 2023
Accepted : 01 November 2023
Published : 05 December 2023
DOI : https://doi.org/10.1186/s12909-023-04829-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preclinical curriculum
- Evidence of bis
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Find My Rep
You are here
Review of Educational Research
Preview this book.
- Description
- Aims and Scope
- Editorial Board
- Abstracting / Indexing
- Submission Guidelines
The Review of Educational Research ( RER , quarterly, begun in 1931; approximately 640 pp./volume year) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. RER encourages the submission of research relevant to education from any discipline, such as reviews of research in psychology, sociology, history, philosophy, political science, economics, computer science, statistics, anthropology, and biology, provided that the review bears on educational issues. RER does not publish original empirical research unless it is incorporated in a broader integrative review. RER will occasionally publish solicited, but carefully refereed, analytic reviews of special topics, particularly from disciplines infrequently represented.
The Review of Educational Research publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. RER encourages the submission of research relevant to education from any discipline, such as reviews of research in psychology, sociology, history, philosophy, political science, economics, computer science, statistics, anthropology, and biology, provided that the review bears on educational issues. RER does not publish original empirical research, and all analyses should be incorporated in a broader integrative review. RER will occasionally publish solicited, but carefully refereed, analytic reviews of special topics, particularly from disciplines infrequently represented. The following types of manuscripts fall within the journal’s purview:
Integrative reviews pull together the existing work on an educational topic and work to understand trends in that body of scholarship. In such a review, the author describes how the issue is conceptualized within the literature, how research methods and theories have shaped the outcomes of scholarship, and what the strengths and weaknesses of the literature are. Meta-analyses are of particular interest when they are accompanied by an interpretive framework that takes the article beyond the reporting of effect sizes and the bibliographic outcome of a computer search.
Theoretical reviews should explore how theory shapes research. To the extent that research is cited and interpreted, it is in the service of the specification, explication, and illumination of a theory. Theoretical reviews and integrative reviews have many similarities, but the former are primarily about how a theory is employed to frame research and our understandings, and refer to the research as it relates to the theory.
Methodological reviews are descriptions of research design, methods, and procedures that can be employed in literature reviews or research in general. The articles should highlight the strengths and weaknesses of methodological tools and explore how methods constrain or open up opportunities for learning about educational problems. They should be written in a style that is accessible to researchers in education rather than methodologists.
Historical reviews provide analyses that situate literature in historical contexts. Within these reviews, explanations for educational phenomena are framed within the historical forces that shape language and understanding.
Commissioned reviews and thematic issues. The editors may commission and solicit authors to review areas of literature. In all other respects, commissioned reviews are subject to the same review process as submitted reviews. The editors also encourage readers to propose thematic topics for special issues and, as potential guest editors, to submit plans for such issues.
In addition to review articles, RER will occasionally publish notes and responses which are short pieces of no more than 1,200 words on any topic that would be of use to reviewers of research. Typically, they point out shortcomings and differences in interpretation in RER articles and policy.
The standards and criteria for review articles in RER are the following:
1. Quality of the Literature. Standards used to determine quality of literature in education vary greatly. Any review needs to take into account the quality of the literature and its impact on findings. Authors should attempt to review all relevant literature on a topic (e.g., international literature, cross-disciplinary work, etc.).
2. Quality of Analysis. The review should go beyond description to include analysis and critiques of theories, methods, and conclusions represented in the literature. This analysis should also examine the issue of access—which perspectives are included or excluded in a body of work? Finally, the analysis should be reflexive—how does the scholars’ framework constrain what can be known in this review?
3. Significance of the Topic. The review should seek to inform and/or illuminate questions important to the field of education. While these questions may be broad-based, they should have implications for the educational problems and issues affecting our national and global societies.
4. Impact of the Article. The review should be seen as an important contribution and tool for the many different educators dealing with the educational problems and issues confronting society.
5. Advancement of the Field. The review should validate or inform the knowledge of researchers and guide and improve the quality of their research and scholarship.
6. Style. The review must be well written and conform to style of the Publication Manual of the American Psychological Association (6th edition). Authors should avoid the use of unexplained jargon and parochialism.
7. Balance and Fairness. The review should be careful not to misrepresent the positions taken by others, or be disrespectful of contrary positions.
8. Purpose. Any review should be accessible to the broad readership of RER. The purpose of any article should be to connect the particular problem addressed by the researcher(s) to a larger context of education.
We also encourage all authors interested in submitting a manuscript to RER to read our Editorial Vision for more information on our publication aims.
- Academic Search - Premier
- Academic Search Alumni Edition
- Academic Search Elite
- Clarivate Analytics: Current Contents - Physical, Chemical & Earth Sciences
- EBSCO: MasterFILE Elite
- EBSCO: MasterFILE Premier
- EBSCO: Professional Development Collection
- EBSCO: Sales & Marketing Source
- EBSCOhost: Current Abstracts
- ERIC (Education Resources Information Center)
- Educational Research Abstracts Online (T&F)
- Higher Education Abstracts
- MasterFILE Select - EBSCO
- ProQuest Education Journals
- Social SciSearch
- Social Sciences Citation Index (Web of Science)
- Teacher Reference Center
- Wilson Education Index/Abstracts
1. Publication Standards 2. Submission Preparation Checklist 3. How to Get Help With the Quality of English in Your Submission 4. Copyright Information 5. For authors who use figures or other materials for which they do not own copyright 6. Right of Reply 7. Sage Choice and Open Access
The Review of Educational Research (RER) publishes comprehensive reviews of literature related to education and does not publish new empirical work, except in the context of meta-analytic reviews of an area. Please check the journal’s Aims and Scope to see if your manuscript is appropriate to submit to RER.
All manuscripts should be submitted electronically to the editorial team at http://mc.manuscriptcentral.com/rer . For questions or inquiries about manuscripts, email us at [email protected] . Manuscripts may not be submitted via e-mail.
Publication Standards
Researchers who intend to submit studies for publication should consult the Standards for Research Conduct adopted by the AERA Council. We also recommend consulting (a) the Guidelines for Reviewers , which outline the criteria under which manuscripts are reviewed for publication by AERA and (b) recent previous editions of the journal. Individuals submitting systematic reviews or meta-analyses should also consult The PRISMA Statement ( http://www.prisma-statement.org ) as well the article on “Reporting Standards for Research in Psychology” in American Psychologist, 63 , 839 – 851 (doi:10.1037/0003-066X.63.9.839).
Submission Preparation Checklist
When you upload your initial submission, upload (1) a separate title page that is not anonymized. Please format the title page as described by the 7th edition of the APA Manual and (2) the main manuscript, which includes an ANONYMIZED title page, an abstract with keywords at the bottom, and the rest of the document including tables and figures, and finally (c) Author Bios.
Please ensure that your manuscript complies with the “ RER Formatting Requirements and Common Formatting Errors ” (see PDF on the RER website). If your submission does not meet these requirements, it will be returned to you.
Additionally, your submission should meet the following guidelines:
1. The submission has not been previously published and is not under consideration for publication elsewhere; or an explanation has been provided in the Cover Letter. Authors should indicate in the Author Note on the separate title page if sections of the manuscript have been published in other venues.
2. THE MANUSCRIPT CONTAINS NO IDENTIFYING INFORMATION, EVEN ON THE ANONYMIZED TITLE PAGE. Please anonymize any work of limited circulation (e.g., in press papers, manuscripts under submission) that would point to the author, both in the body of the manuscript and the reference list. More information on anonymizing is described subsequently. Please double check that the author’s name has been removed from the document’s Properties, which in Microsoft Word is found in the File menu (select “File,” “Properties,” “Summary,” and remove the author’s name; select “OK” to save).
3. The text conforms to APA style (currently the 7th ed.). Consult the guidelines spelled out under “Manuscript Style, Length, and Format” on this webpage and in the RER Formatting Requirements PDF included on our website.
4. The submission must be in Microsoft Word format (.doc or .docx), which will be converted into a PDF file. Please do not upload PDF files, or they will be returned to you.
5. All URL addresses and DOIs in the manuscript (e.g., http://www.aera.net ) should be activated and ready to click.
6. An abstract of 150 words maximum is included (both separately and on the second page of the main document after the ANONYMIZED title page). Please also include three to five keywords—the terms that researchers will use to find your article in indexes and databases.
Manuscript Style, Length, and Format
The style guide for the Review of Educational Research and all AERA journals is the Publication Manual of the American Psychological Association, 7th ed., 2020. The manual is available for purchase here . Guidelines are also available on the APA website .
Manuscripts should NOT exceed 65 pages (or 15,000 words), including tables, figures, appendices, notes, and references, but excluding anonymized title page, abstract, and any supplementary files. Pages should be numbered consecutively in the top right-hand corner, with a fully capitalized running head in the top-left corner. All manuscripts should begin with the anonymized title page (p.1). Manuscripts should be typed for 8½” x 11” paper, in upper and lower case, with 1-inch margins on all sides. Manuscripts should be typed in 12-point Times New Roman font. Manuscripts that exceed 65 pages may be returned without review.
All text, from the title page to the end of the manuscript should be double-spaced , including the abstract, block quotations, bulleted text, and the reference list. Single-spacing is allowed in tables when it is useful in making the table clearer. Do not leave blank lines after paragraphs or before sub-headings. However, if a heading or subheading is the last line on a page, use a page break to move it to the top of the next page. The Abstract, Introduction (beginning with the title), the References, and all tables and figures begin on new pages.
Please use the five subheadings as appropriate based on the 7th edition of the APA style manual. In addition to being on the title page, the title should also be placed at the beginning of the Introduction (in lieu of the word, “Introduction,” which should not appear) and the title at the beginning of the Introduction should be a Level 1 heading.
Tables and figures are to be placed after the references—all tables precede all figures—and should not be included in the body of the text. Each figure and table should begin on a separate page. Do NOT use the “Place Table 5 here” or “Place Figure 1 here” convention. The tables and figures will be placed nearest to where they are mentioned as appropriate when copyediting is done.
Figures and tables should present data to the reader in a clear and unambiguous manner, and should be referred to in the text. If the illustration/table/figure and text are redundant, eliminate the illustration or reduce the amount of detail provided in text. The use of lines in tables is limited (please consult the APA style manual for formatting guidelines ). Figure captions should be placed at the bottom of the figure. One high-quality electronic version of each figure must be submitted with the manuscript. Tables will be typeset. Note that any figures and tables uploaded separately from the main manuscript will still count toward the total 65-page limit.
Italics can be used for emphasis or contrast in special situations but should be used sparingly. Ideally, sentence structure should be used for these issues. All words to be set in italics (e.g., book titles, journal names) should be typed in italics. There should be no underlined text . Abbreviations and acronyms should be spelled out the first time they are mentioned unless they are found as entries in their abbreviated form in Merriam-Webster’s Collegiate Dictionary , 11th ed., 2003 (e.g., “IQ” can be used without being spelled out). Mathematical symbols and symbols for vectors should be clearly formatted in italics and boldface, respectively.
You can use the footnote or endnote feature of Microsoft Word. However, notes are only for explanations or amplifications of textual material that cannot be incorporated into the regular text; they are not for reference information. Moreover, notes are distracting to readers and expensive to produce and should be used sparingly and avoided whenever possible.
The reference list should contain only references that are cited in the text. Its accuracy and completeness are the responsibility of the authors. Reference each publicly available dataset with its title, author, date, and a persistent Web identifier such as a digital object identifier (doi), a handle, or a uniform resource name (URN). If necessary, this last element may be replaced by a web address. Additionally, any references that were included in the analysis but not cited in-text in the main manuscript can be included in a separate reference list that is uploaded as a Supplementary File for Review (this may assist in meeting the page limit).
Authors should anonymize their manuscripts for review . Anonymizing does not mean removing all self-citations. Authors should only anonymize citations of limited circulation (e.g., forthcoming, in press, unpublished) that point to the author. Publications already in the extant literature (e.g., books, book chapters, journal articles) should be cited normally, but authors should include self-citations judiciously . When anonymizing, please use “Author” or “Authors” as in the examples below and place this alphabetically in the reference list and not where the author’s actual name would typically appear.
For examples of common types of references, consult the APA 7th edition manual, or visit the webpage here: https://apastyle.apa.org/style-grammar-guidelines/references
How to Get Help with the Quality of English in Your Submission
Authors who would like to refine the use of English in their manuscripts might consider using the services of a professional English-language editing company. We highlight some of these companies at https://languageservices.sagepub.com/en/ .
Please be aware that Sage has no affiliation with these companies and makes no endorsement of them. An author's use of these services in no way guarantees that his or her submission will ultimately be accepted. Any arrangement an author enters into will be exclusively between the author and the particular company, and any costs incurred are the sole responsibility of the author.
Copyright Information Accepted authors will be asked to assign copyright to AERA, in return for which AERA grants several rights to authors.
Permission to reproduce your own published material
No written or oral permission is necessary to reproduce a table, a figure, or an excerpt of fewer than 500 words from this journal, or to make photocopies for classroom use. Authors are granted permission, without fee, to photocopy their own material or make printouts from the final pdf of their article. Copies must include a full and accurate bibliographic citation and the following credit line: “Copyright [year] by the American Educational Research Association; reproduced with permission from the publisher.” Written permission must be obtained to reproduce or reprint material in circumstances other than those just described. Please review Sage Publishing’s Journal Permissions for further information on policies and fees.
Permission to submit material for which you do not own copyright
Authors who wish to use material, such as figures or tables, for which they do not own the copyright must obtain written permission from the copyright holder (usually the publisher) and submit it along with their manuscript. However, no written or oral permission is necessary to reproduce a table, a figure, or an excerpt of fewer than 500 words from an AERA journal.
Copyright transfer agreements for accepted works with more than one author
This journal uses a transfer of copyright agreement that requires just one author (the corresponding author) to sign on behalf of all authors. Please identify the corresponding author for your work when submitting your manuscript for review. The corresponding author will be responsible for the following:
1. Ensuring that all authors are identified on the copyright agreement, and notifying the editorial office of any changes in the authorship.
2. Securing written permission (by letter or e-mail) from each co-author to sign the copyright agreement on the co-author’s behalf.
3. Warranting and indemnifying the journal owner and publisher on behalf of all co-authors. Although such instances are very rare, you should be aware that in the event that a co-author has included content in his or her portion of the article that infringes the copyright of another or is otherwise in violation of any other warranty listed in the agreement, you will be the sole author indemnifying the publisher and the editor of the journal against such violation.
Please contact the publications office at AERA if you have questions or if you prefer to use a copyright agreement for all coauthors to sign.
Right of Reply
The right of reply policy encourages comments on recently published articles in AERA publications. They are, of course, subject to the same editorial review and decision process as articles. If the comment is accepted for publication, the editor shall inform the author of the original article. If the author submits a reply to the comment, the reply is also subject to editorial review and decision. The editor may allot a specific amount of journal space for the comment (ordinarily about 1,500 words) and for the reply (ordinarily about 750 words). The reply may appear in the same issue as the comment or in a later issue (Council, June 1980).
If an article is accepted for publication in an AERA journal that, in the judgment of the editor, has as its main theme or thrust a critique of a specific piece of work or a specific line of work associated with an individual or program of research, then the individual or representative of the research program whose work is critiqued should be notified in advance about the upcoming publication and given the opportunity to reply, ideally in the same issue. The author of the original article should also be notified. Normal guidelines for length and review of the reply and publication of a rejoinder by the original article’s author(s) should be followed. Articles in the format “an open letter to …” may constitute prototypical exemplars of the category defined here, but other formats may well be used, and would be included under the qualifications for response prescribed here (Council, January 2002).
Sage Choice and Open Access
If you or your funder wish your article to be freely available online to nonsubscribers immediately upon publication (gold open access), you can opt for it to be included in Sage Choice, subject to payment of a publication fee. The manuscript submission and peer review procedure is unchanged. On acceptance of your article, you will be asked to let Sage know directly if you are choosing Sage Choice. To check journal eligibility and the publication fee, please visit Sage Choice . For more information on open access options and compliance at Sage, including self author archiving deposits (green open access) visit Sage Publishing Policies on our Journal Author Gateway.
- Read Online
- Sample Issues
- Current Issue
- Email Alert
- Permissions
- Foreign rights
- Reprints and sponsorship
- Advertising
Individual Subscription, Combined (Print & E-access)
Institutional Subscription, E-access
Institutional Subscription & Backfile Lease, E-access Plus Backfile (All Online Content)
Institutional Subscription, Print Only
Institutional Subscription, Combined (Print & E-access)
Institutional Subscription & Backfile Lease, Combined Plus Backfile (Current Volume Print & All Online Content)
Institutional Backfile Purchase, E-access (Content through 1998)
Individual, Single Print Issue
Institutional, Single Print Issue
Subscription Information
To purchase a non-standard subscription or a back issue, please contact SAGE Customer Services for availability.
[email protected] +44 (0) 20 7324 8701
- Open access
- Published: 07 April 2024
Efficacy of a virtual nursing simulation-based education to provide psychological support for patients affected by infectious disease disasters: a randomized controlled trial
- Eunjung Ko 1 &
- Yun-Jung Choi 1
BMC Nursing volume 23 , Article number: 230 ( 2024 ) Cite this article
81 Accesses
1 Altmetric
Metrics details
Virtual simulation-based education for healthcare professionals has emerged as a strategy for dealing with infectious disease disasters, particularly when training at clinical sites is restricted due to the risk of infection and a lack of personal protective equipment. This research evaluated a virtual simulation-based education program intended to increase nurses’ perceived competence in providing psychological support to patients affected by infectious disease disasters.
The efficacy of the program was evaluated via a randomized controlled trial. We recruited 104 nurses for participation in the study and allocated them randomly and evenly to an experimental group and a control group. The experimental group was given a web address through which they could access the program, whereas the control group was provided with a web address that directed them to text-based education materials. Data were then collected through an online survey of competence in addressing disaster mental health, after which the data were analyzed using the Statistical Package for the Social Sciences(version 23.0).
The analysis showed that the experimental group’s disaster mental health competence (F = 5.149, p =.026), problem solving process (t = 3.024, p =.003), self-leadership (t = 2.063, p =.042), learning self-efficacy (t = 3.450, p =.001), and transfer motivation (t = 2.095, p =.039) significantly statistically differed from those of the control group.
Conclusions
A virtual nursing simulation-based education program for psychological support can overcome limitations of time and space. The program would also be an effective learning resource during infectious disease outbreaks.
Clinical trial registration
This Korean clinical trial was retrospectively registered (21/11/2023) in the Clinical Research Information Service ( https://cris.nih.go.kr ) with trial registration number KCT0008965.
Peer Review reports
The last two decades have confronted the world with a variety of infectious diseases, such as severe acute respiratory syndrome, which first occurred in Asia in 2003 before spreading worldwide, including Korea, in only a few months. Since then, infectious disease outbreaks began to be recognized as severe disasters. Other examples include the 2009 H1N1 influenza outbreak, which caused more than 10,000 deaths worldwide and 140 deaths in Korea; the proliferation of the Ebola virus, which resulted in a fatality rate of more than 90% in Africa in 2014; and the outbreak of Middle East respiratory syndrome in 2015, Zika virus disease in 2016, and coronavirus disease (COVID-19) in 2019 [ 1 ]. The COVID-19 pandemic, in particular, has caused infections among approximately 64 million people and the deaths of 1.5 million individuals as of December 2020 [ 2 ].
Direct victims of infectious disease disasters, infected patients, and quarantined individuals suffer from a fear of stigma or social blame and guilt, but even people who are unexposed to sources of infection experience psychological distress from anxiety and fear of disease or possible death [ 3 ]. They also blame infected people and harbor hatred toward them [ 3 ]. This assertion is supported by an examination of web search behaviors and infodemic attitudes toward COVID-19, which identified superficial and racist attitudes [ 4 ]. Additionally, in research using a health stigma and discrimination framework related to communicable diseases, the authors found that people exhibit negative stereotypes, biases, and discriminatory conduct toward infected groups owing to fears of contagion, concerns about potential harm, and perceptions that individuals violate central values [ 5 ]. Stigmatized individuals experience adverse effects on their health because of both the stress induced by stigma and the decreased use of available services [ 5 ].
Severe and prolonged anxiety, fear, blame, and aggression can lead to mental health problems, including depression, anxiety, panic attacks, somatic symptoms, post-traumatic stress disorder, psychosis, and even suicide and life-threatening behaviors [ 6 ]. Therefore, recovery from the psychological trauma caused by a disaster should be regarded as equally necessary as physical recovery, with emphasis placed on psychological support activities that prevent the deterioration of mental health [ 7 ].
Disasters pose a significant threat to mental health support systems, wherein the lack of healthcare professionals or psychologists trained to address these conditions exacerbates the psychological distress and psychopathological risk experienced by society [ 8 ]. When training at clinical sites is restricted due to infection risks and a lack of personal protective equipment (PPE), an emerging solution is virtual simulation [ 9 ].
A virtual simulation is a simulation modality developed on the basis of video or graphic recordings featuring virtual patients and delivered via either a static or mobile device. It replicates real-world clinical situations and affords learners an interactive experience [ 10 ]. Virtual simulation-based education provides an immersive clinical environment, as virtual patients respond to a learner’s assessments and interventions [ 11 , 12 ]. It enables two-way communication, and allows medical professionals to practice making clinical decisions [ 10 ]. Virtual patients are equipped with voice, intonation, and expressions that reinforce the educational narrative within the virtual environment, thereby enhancing the effectiveness of the learning experience [ 13 ]. One of the primary advantages of virtual simulation-based education is its provision of a safe and non-threatening environment in which learners can practice. It also offers flexible and reproducible learning experiences, thus catering to the diverse needs of learners [ 14 ].
Self-assessment is the most commonly used competence evaluation tool, as it is cost-effective and helps nurses improve their practice by identifying their strengths and weaknesses for development [ 15 ]. Self-assessed competence is also related to the quality of patient care because nurses promote continuous learning by determining educational needs through such evaluations [ 16 ]. The competence perceived by a nurse is inherently subjective given its self-reported nature and poses a challenge in establishing a direct correlation with the actual care of patients [ 17 , 18 ]. However, studies have indicated that increased levels of self-perceived competence are associated with a significant increase in core competencies related to patient care and frequent use of clinical skills [ 19 , 20 ]. Perceived competence likewise influences the job satisfaction and organizational citizenship behavior of nurses and is significantly related to absenteeism, one of the deterrents to the delivery of quality care [ 21 , 22 ].
Competence refers to the possession of qualifications and abilities to satisfy professional standards, as well as the capability to perform tasks and duties in a suitable and effective manner [ 23 ]. Competencies for disaster mental health are crucial for enhancing disaster response capabilities. These competencies encompass a range of skills, knowledge, and attitudes necessary for mental health professionals to effectively support individuals and communities affected by disasters [ 24 ]. Such competencies and how they are affected by simulation-based training have been explored in some studies, which reported a significant increase in competence after exposure to the aforementioned education [ 25 , 26 ].
The simulation education defined in mock training designs based on real situations provides opportunities to exercise problem-solving through various strategies. Problem-solving process is considered key competency through which learners are expected to enhance their relevant knowledge and clinical performance abilities [ 27 ]. In particular, problem-solving processes for identifying and assessing problems and finding solutions are psychological strategies that help people cope and recover after a disaster [ 28 ]. A scoping review on the effect of simulation-based education on the problem-solving process indicated that out of 32 studies reviewed, 21 demonstrated statistically significant improvement in people’s ability to resolve problems [ 29 ].
Simulation training can also address self-leadership, which is an essential self-learning quality that aids individuals in staying motivated and focused on their learning goals. It is also required as a basic qualification of professional nurses, who must be able to take initiative and make responsible decisions [ 30 , 31 ]. Previous studies have reported statistically significant improvements in self-leadership following simulation training [ 32 , 33 ].
Another aspect that benefits from simulation-driven education is learning self-efficacy, which plays a crucial role in predicting learners’ levels of engagement and academic success in online education. It reflects learners’ confidence in their ability to manage their own learning process. It is a significant predictor of both learners’ participation levels and their academic achievements in online education settings [ 34 , 35 ]. Several studies have demonstrated virtual simulation- or online education-induced significant improvements in learning self-efficacy [ 36 , 37 ]. Finally, virtual simulation-based education can also improve the motivation to transfer new knowledge and skills learned through education to clinical practice [ 38 ]. This motivation is considered an essential measure of effective learning for nurses working in the clinical field [ 38 ]. A previous study reported that psychiatric nursing simulation training combined with post-course debriefing significantly increases participants’ level of motivation to transfer [ 38 ].
On the basis of the discussion above, this study evaluated a virtual nursing simulation-based education program on disaster psychology designed to provide psychological support to patients affected by infectious disease disasters.
Study design
This study conducted a randomized controlled trial (RCT) to test the virtual nursing simulation-based education program of interest. The RCT protocol used was based on CONSORT guidelines.
Participants
We recruited nurses working at general hospitals in South Korea. With permission from the nurse managers of these hospitals, a participation notice was posted on the institutions’ internet bulletin boards for nurses for a week. The two-sided test criterion, with a significance level (α) of 0.05, a power (1-β) of 0.80, and a medium effect size of 0.6, dictates that the minimum number of participants per group be 90. The effect size was based on a virtual simulation intervention study conducted by Kim and Choi [ 36 ]. Taking the dropout rate into consideration, we recruited 104 nurses, who were assigned to an experimental group and a control group using the random sampling functionality of the Statistical Package for the Social Sciences (SPSS version 23.0). Out of the initial sample, 11 participants were excluded because they were on vacation, could not be contacted, or provided incomplete responses during data collection (Fig. 1 ).
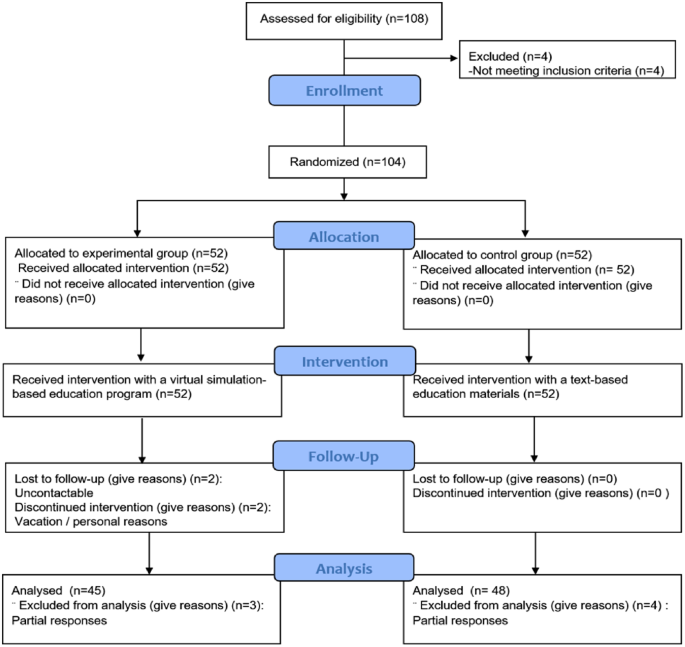
Flowchart of the randomized controlled trial
The virtual nursing simulation-based education program
This study probed into the virtual nursing simulation-based education program developed by Ko [ 39 ]. The program is implemented using an e-learning development platform, Articulate Storyline, whose operating environment is compatible with all web browsers (Internet Explorer, Microsoft Edge, Firefox, Google Chrome, etc.). It is a mobile-friendly application that can run in devices with Android and iOS operating systems. When an individual uses their smartphone or personal computer to access the server via the web address corresponding to the education program, the content functions execute. Ko’s [ 39 ] program involves five stages of learning completed in 100 min: (1) preparatory learning (30 min), (2) pre-test (5 min), (3) pre-briefing (5 min), (4) simulation game (30 min), and (5) structured self-debriefing (30 min) (Fig. 2 ).
Preparatory learning comes with lecture materials on guidelines for providing psychological support to victims of infectious disease disasters, administering psychological first aid, donning and doffing PPE, and exercising mindfulness through videos and pictures. In the pretest stage, a learner answers five questions and can immediately check the correct responses, which come with detailed explanations. In the prebriefing stage, an overview of a nursing simulation scenario, patient information, learning objectives, and instructions on using the virtual simulation are provided. During the simulation game, a video of the simulation is presented. It starts with a 39-year-old female, a standardized patient who is age- and gender-matched to the scenario, confirmed to have contracted COVID-19 and transferred to a negative pressure isolation room. The patient presents with extreme anxiety and feeling of tightness in her chest. During the game, learners are expected to complete 12 quizzes. In the debriefing stage, a summary of the simulation quiz results and self-debriefing questions are provided, and the comments made by learners are saved in the Naver cloud platform.
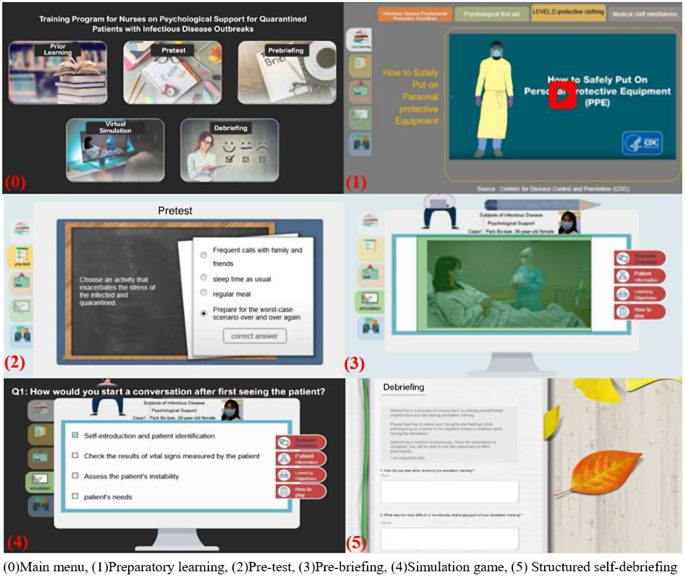
The evaluated virtual nursing simulation-based education program (examples are our own work)
Measurements
Disaster mental health competence.
Disaster mental health competence was measured using the perceived competence scale for disaster mental health workforce (PCS-DMHW), which was developed by Yoon and Choi [ 40 ]. This tool consists of 24 questions related to knowledge (6 questions), attitudes (9 questions), and skills (9 questions). Each item is rated using a five-point Likert scale (0 = strongly disagree, 4 = strongly agree), and the responses are summed. The higher the score, the greater the perception of competence in a relevant area [ 40 ]. The Cronbach’s α values of the PCS-DMHW were 0.95 and 0.94 at the time of tool development and the present study, respectively.
Problem solving process
Problem solving process was determined using a tool modified and supplemented by Park and Woo [ 41 ] on the grounds of the problem solving process and behavior survey developed by Lee [ 42 ]. This tool is composed of 25 questions on five factors, namely, problem discovery, problem definition, problem solution design, problem solution execution, and problem solving review [ 41 ]. The reliability of the tool was 0.89 at the time of development [ 41 ], but the Cronbach’s α found in the current research was 0.94.
Self-leadership
Self-leadership was measured using a tool developed by Manz [ 43 ] and modified by Kim [ 44 ]. The tool consists of 18 questions distributed over six factors (three questions each): self-defense, rehearsal, goal setting, self-compensation, self-expense edition, and constructive thinking. The reliability of the tool at the time of development and the present research was (Cronbach’s α) 0.87 and 0.82, respectively.
Learning self-efficacy
To ascertain learning self-efficacy, we used the tool developed by Ayres [45] and translated by Park and Kweon [ 38 ]. This tool consists of 10 questions, and it had a reliability (Cronbach’s ⍺) of 0.94 and 0.93 at the time of development and the current study, respectively.
Motivation to transfer
We used Ayres’s [45] motivation to transfer scale, which was translated by Park and Kweon [ 38 ]. Its reliability at the time of development and the present research was (Cronbach’s ⍺) 0.80 and 0.93, respectively.
Data collection
The experimental and control groups were administered a pretest through an online survey. The web address through which the evaluated virtual simulation-based education program could be accessed was provided to the experimental group, whereas text-based education materials on psychological support for victims of infectious disease disasters were given to the control group. The groups were simultaneously sent the program’s instruction manual, and their inquiries were answered through chat. After the interventions, each participant was administered a posttest through another online survey.
Data analysis
The collected data were analyzed using SPSS version 23.0. The homogeneity test for general characteristics between the experimental and control groups was analyzed using a t-test, a chi-square test, and Fisher’s exact test. The normality of the dependent variables was analyzed using the Kolmogorov-Smirnov test. Changes in the dependent variables between the pretest and posttest were analyzed using a paired t-test. Differences in the dependent variables before and after the groups’ use of the interventions were examined via a t-test and ANCOVA.
Ethical considerations
We completed education in bioethics law prior to the research and obtained approval of the research proposal and questionnaire from the Institutional Review Board of the affiliated university (IRB approval number 1041078-202003-HRSB-070-01CC). A signed consent form was also obtained from each participant after the purpose and methods of the research, the confidentiality of personal information, and the voluntary nature of participation or their right to withdraw from the study were explained to them. All collected data were kept in a lockable cabinet, and electronic data were encrypted and stored. These data are to be discarded after three years.
A total of 93 participants (45 in the experimental group and 48 in the control group) were left after the exclusion of unsuitable respondents. of the between-group comparisons of the subjects indicated no significant differences between them (5% significance level) in terms of general characteristics, such as gender, age, work unit, and clinical experience (Table 1 ).
The score of the experimental group on disaster mental health competence increased from 48.13 in the pretest to 70.51 in the posttest (+ 22.38), whereas that of the control group increased from 53.33 in the pretest to 68.38 in the posttest (+ 15.04). These findings reflect a statistically significant difference in competence between the groups (F = 5.149, p =.026). The scores of the experimental and control groups on problem solving process increased from 73.07 in the pretest to 88.24 in the posttest (+ 15.18) and from 75.75 in the pretest to 83.77 in the posttest (+ 8.02), respectively. As with the competence findings, these point to a significant difference between the groups in terms of the ability to resolve problems (t = 3.024, p =.003) (Table 2 ).
The score of the experimental group on self-leadership increased from 54.87 in the pretest to 59.58 in the posttest (+ 4.71), and that of the control group increased from 57.48 in the pretest to 60.10 in the posttest (+ 2.63). These results denote a statistically significant difference in this ability between the groups (t = 2.063, p =.042). The scores of the experimental and control participants on learning self-rose from 55.40 in the pretest to 58.84 in the posttest (+ 3.44) and from 56.81 in the pretest to 57.13 in the posttest (+ 0.31), respectively. Again, a statistically significant difference was found between the groups (t = 3.450, p =.001). Their scores on motivation to transfer rose from 49.31 in the pretest to 54.29 in the posttest (+ 4.98) (experimental group) and the score increased from 50.50 in the pretest to 51.85 in the posttest (+ 1.35) (control group), pointing to a significant difference between the groups (t = 2.095, p =.039).
As previously stated, this research was evaluated a virtual nursing simulation-based education program designed to provide psychological support to patients affected by infectious disease disasters. The results showed statistically significant increases in the experimental group’s pretest and posttest scores on disaster mental health competence, problem solving process, self-leadership, learning self-efficacy, and motivation to transfer.
The experimental group achieved more statistically significant improvements in disaster mental health competence than did the control group. This finding is similar to the statistically significant increase in the average disaster mental health competence shown by providers of disaster mental health services providers and non-expert groups after PFA training involving lecture and practice [ 46 ]. It is also consistent with the significant increase in the scores of school counselors on disaster mental health competence after a lecture and simulation on PFA [ 25 ]. In their study on disaster relief workers, Kang and Choi [ 26 ] measured the participants’ performance competence in PFA after the delivery of a lecture and simulation-based education using a standardized patient. The authors found a significant increase in PFA performance competence, consistent with the present research. Since there are currently no other virtual simulation-based education programs for disaster psychological support available, we compared the effectiveness of various PFA training methods with the program assessed in the present work.
In the current research, the posttest scores of the experimental group on problem solving process significantly increased, similar to the results of Kim et al.’s study on virtual simulation- and blended simulation-based education on asthmatic child nursing [ 47 ]. Both the control and experimental groups (virtual simulation only and blended simulation featuring high-fidelity and virtual simulations, respectively) showed an increase in their problem solving process scores. These results and those derived in the present work are similar because reading and pretest phases were incorporated into the design of the previous study. Given that researchers have used commercial virtual simulations featuring avatars rather than standardized patient videos available through English-based platforms, user experiences may differ, thus requiring a qualitative analysis to identify differences. However, Kim et al. [ 47 ] did not implement a debriefing after the virtual simulation program, rendering comparison impossible. Another research reported that a multimodality simulation education that combines such methods as virtual simulation, the use of mannequins, and part-task training increase increased the scores of hospital nurses’ on problem solving process [ 48 ].
In the present work, the experimental group’s self-leadership scores increased after they used the program, and these scores were higher [ 49 , 50 ]. This difference can be explained by the fact that our respondents voluntarily participated in our research given their interest in self-learning programs for disaster psychological support; even in the comparison studies, participants with stronger interest in leadership education typically exhibited heightened degrees of self-leadership [ 51 ]. The increase in self-leadership scores in the current research is consistent with a previous study involving a two-hour simulation education about PPE donning and doffing, medication administration, and medical specimen treatment in a scenario of patients suspected of having infectious diseases [ 32 ]. Another research showed that simulation education on high-risk pregnancy enhances nursing students’ problem-solving processes and self-leadership [ 52 ].
Learning self-efficacy is a key variable that enables the prediction of learners’ degrees of participation in online education and the prediction of their academic achievements, as it points to the ability to manage their learning processes [ 34 , 53 ]. The results of the current research in this regard are consistent with those of a study on the online practice of basic nursing skills, which increased participants’ learning self-efficacy [ 54 ]. The researchers included an online quiz about basic nursing skills and feedback sections for learners’ self-evaluations of their performance as avenues through which to encourage autonomy in learning. A similar approach was used in the present study, which involved both a pretest for self-evaluation, direct feedback on the virtual simulation, and a self-debriefing session, enabling the participants to reflect on their simulation experiences while reviewing other participants’ answers during self-debriefing. These functions of the evaluated program were expected to factor importantly in the significant increase in the participants’ learning self-efficacy scores.
Many studies on practice education have examined participants’ motivations to transfer knowledge and skills alongside their learning self-efficacies. In the current research, the motivation to transfer scores of the experimental increased, and the difference between the two groups was statistically meaningful. This result is consistent with the findings of Park and Kweon on the simulation education about psychiatric nursing, during which post-course debriefing increased the participants’ average scores on motivation to transfer and learning self-efficacy [ 38 ]. Conversely, Kang and Kim found that a six-week simulation program for alcoholic patient care did not generate a significant increase in the participants’ motivation to transfer and learning self-efficacy scores [ 55 ]. This finding was attributed to the unfamiliarity of the local community scenario used in the research to the participants, who were in their senior year of nursing school [ 55 ]. This limitation was overcome in the current research by administering a qualitative survey of nurses’ actual demand for education on psychological support for infectious disease patients. That is, the survey presented scenarios that the participants needed.
As with other studies, the present research was encumbered by several limitations. First, the self-assessment measures used in this study may be unreliable, because they are based on individuals’ subjective perceptions and interpretations of their abilities. There is also the possibility of respondent fatigue given that the participants were compelled to answer numerous questions. Future studies should incorporate both subjective and objective measures into data collection and consider as concise an evaluation method as possible to prevent respondent fatigue. Second, this study did not establish a direct link between the obtained results and actual changes in practice or improvements in patient outcomes. We propose a follow-up study to investigate the impact of the education program examined in this study on either the mental health of patients or the quality of patient care. Third, simulation-based education tends to be accompanied with more guidance than text-based program because the former has diverse components, including quiz games, and participants are predisposed to allocate more time to simulation-based education. These may potentially influence the results. In the future, we propose to conduct research by modifying education under the same time and guided condition.
This study proposed that a well-designed virtual nursing simulation-based education program can be an effective modality with which to satisfy the educational needs of nurses in the context of infectious disease outbreaks. Such programs can be easily used by nurses anywhere and anytime before they are deployed to provide psychological support to patients with infectious diseases. They are also expected to contribute to enhancing competence in addressing disaster mental health and improving the quality of care of patients afflicted with infectious diseases.
Data availability
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
Abbreviations
Coronavirus disease 2019
Randomized controlled trial
Personal protective equipment
Statistical Package for the Social Sciences
Analysis of covariance
Psychological first aid
World Health Organization. WHO coronavirus disease (COVID-19) dashboard. 2020.
Oh EG, Yu SH, Kang JH, Oh YJ, Cha KI, Jeon YH, et al. Perspectives on nursing profession for a post-COVID-19 new normal. Korean J Adult Nurs. 2020;32(3):221–2.
Article Google Scholar
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. Rapid review. Lancet. 2020;395:912–20.
Article CAS PubMed PubMed Central Google Scholar
Çalışkan C, Özsezer G, Pay M, Demir G, Çelebi I, Koçak H. Web search behaviors and infodemic attitudes regarding COVID-19 in Turkey: a framework study for improving response and informing policy on the COVID-19 infodemic. Front Public Health. 2022;10:948478.
Article PubMed PubMed Central Google Scholar
Stangl AL, Earnshaw VA, Logie CH, Van Brakel WC, Simbayi L, Barré I, et al. The health stigma and discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17:1–13.
Tucci V, Moukaddam N, Meadows J, Shah S, Galwankar SC, Kapur GB. The forgotten plague: psychiatric manifestations of Ebola, Zika, and emerging infectious diseases. J Global Infect Dis. 2017;9(4):151.
Korea Mental Health Technology R&D Project. (2017). Korean Disaster and Mental Health Support Guidelines.
Zhang J, Wu W, Zhao X, Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precision Clin Med. 2020;3(1):3–8.
Liu W. The effects of virtual simulation on undergraduate nursing students’ mental health literacy: a prospective cohort study. Issues Ment Health Nurs. 2020:1–10.
Cant R, Cooper S, Sussex R, Bogossian F. What’s in a name? Clarifying the nomenclature of virtual simulation. Clin Simul Nurs. 2019;27:26–30.
Foronda C, Bauman EB. Strategies to incorporate virtual simulation in nurse education. Clin Simul Nurs. 2014;10(8):412–812.
Berman NB, Durning SJ, Fischer MR, Huwendiek S, Triola MM. The role for virtual patients in the future of medical education. Acad Med. 2016;91(9):1217–22.
Article PubMed Google Scholar
Verkuyl M, Hughes M, Tsui J, Betts L, St-Amant O, Lapum JL. Virtual gaming simulation in nursing education: a focus group study. J Nurs Educ. 2017;56(5):274–80.
Cobbett S, Snelgrove-Clarke E. Virtual versus face-to-face clinical simulation in relation to student knowledge, anxiety, and self-confidence in maternal-newborn nursing: a randomized controlled trial. Nurse Educ Today. 2016;45:179–84.
Bahreini M, Shahamat S, Hayatdavoudi P, Mirzaei M. Comparison of the clinical competence of nurses working in two university hospitals in Iran. Nurs Health Sci. 2011;13(3):282–8.
Goliroshan S, Babanataj R, Aziznejadroshan P. Investigating the self-assessment of clinical competency of nurses working in Babol University of Medical Sciences hospitals. Middle East J Family Med. 2018;7(10):279.
Google Scholar
Bam V, Diji AKA, Asante E, Lomotey AY, Adade P, Akyeampong BA. Self-assessed competencies of nurses at an emergency department in Ghana. Afr J Emerg Med. 2020;10(1):8–12.
O’Leary J. Comparison of self-assessed competence and experience among critical care nurses. J Nurs Adm Manag. 2012;20(5):607–14. https://doi.org/10.1111/j.1365-2834.2012.01394.x .
Kim KM, Choi JS. Self-perceived competency of infection control nurses based on Benner’s framework: a nationwide survey in Korea. Appl Nurs Res. 2015;28(2):175–9.
Hassankhani H, Hasanzadeh F, Powers KA, Dadash Zadeh A, Rajaie R. Clinical skills performed by Iranian emergency nurses: perceived competency levels and attitudes toward expanding professional roles. J Emerg Nurs. 2018;44(2):156–63. https://doi.org/10.1016/j.jen.2017.06.007 .
Biagioli V, Prandi C, Nyatanga B, Fida R. The role of professional competency in influencing job satisfaction and organizational citizenship behavior among palliative care nurses. J Hospice Palliat Nurs. 2018;20(4):377–84.
Alreshidi NM, Alaseeri R, Garcia M. Factors influencing absenteeism among nursing staff in the primary health care centers in hail: a preliminary study for enhancing staff commitment. Health Sci J. 2019;13(3):658–1.
Rodolfa E, Bent R, Eisman E, Nelson P, Rehm L, Ritchie P. A cube model for competency development: implications for psychology educators and regulators. Prof Psychology: Res Pract. 2005;36(4):347.
King RV, Burkle FM, Walsh LE, North CS. Competencies for disaster mental health. Curr Psychiatry Rep. 2015;17(3).
Lee JS, You S, Choi YK, Youn Hy SH. A preliminary evaluation of the training effects of a didactic and simulation-based psychological first aid program in students and school counselors in South Korea. PLoS ONE. 2017;12(7):e0181271.
Kang JY, Choi YJ. Effects of a psychological first aid simulated training for pregnant flood victims on disaster relief worker’s knowledge, competence, and self-efficacy. Appl Nurs Res. 2020:1513.
Park S, Kim S. The effects of team-based simulation education on problem solving process. Korean J Health Communication. 2019;14(2):165–72.
Australian Psychological Society. Useful skills for disaster recovery: Problem solving. 2016.
Lim A, Song Y. A scoping review of instruments for measuring problem-solving ability in simulation nursing education in Korea: a focus on process behavior survey. J Korean Acad Fundamentals Nurs. 2022;29(3):269–83.
Lee M, Lee M, Kim S. A study on nursing students’ self-leadership and their perception of learning. J Korean Acad Soc Nurs Educ. 2015;21(3):417–25. https://doi.org/10.5977/jkasne.2015.21.3.417 .
Goldsby E, Goldsby M, Neck CB, Neck CP. Under pressure: time management, self-leadership, and the nurse manager. Administrative Sci. 2020;10(3):38.
Kim JK, Song MS. Effects of respiratory infectious disease simulation-based education on nursing students of clinical competency, self-leadership and critical thinking. J Korea Academia-Industrial Cooperation Soc. 2019;20(8):93–101.
Cho GY, Seo MK. Influencing factors of learning flow, self-leadership and debriefing satisfaction on problem solving ability of nursing students in simulation learning. J Fisheries Mar Sci Educ. 2020;32(2):409–19.
Artino AR. Motivational beliefs and perceptions of instructional quality: Predicting satisfaction with online training. J Comput Assist Learn. 2008;24(3):260–70.
Yu BM, Jeon JC, Park HJ. The effects on learning motivation and self-efficacy according to the type of reflection. J Educational Inform Media. 2013;19(4):837–59.
Kim KA, Choi DW. The effect of virtual simulation in nursing education: an application of care for acute heart disease patients. J Korean Soc Simul Nurs. 2018;6(2):1–13.
Sapiano AB, Sammut R, Trapani J. The effectiveness of virtual simulation in improving student nurses’ knowledge and performance during patient deterioration: a pre and post test design. Nurse Educ Today. 2018;62:128–33.
Park SY, Kweon YR. The effect of using standardized patients in psychiatric nursing practical training for nursing college students. J Korean Acad Psychiatric Mental Health Nurs. 2012;21(1):79–88.
Ko E. Development of a virtual simulation-based nurse education program to provide psychological support for patients affected by infectious disease disasters [dissertation]. [Seoul, Korea]: Chung-Ang University.
Yoon HY, Choi YK. The development and validation of the perceived competence scale for disaster mental health workforce. Psychiatry Invest. 2019;16(11):816.
Park JW, Woo OH. The effects of PBL (problem-based learning) on problem solving process by learner’s metacognitive level. J Educational Technol. 1999;15(3):55–81.
Lee JS. The effects of process behaviors on problem-solving performance in various tests. Dissertation Abstracts International Section A: Humanities and Social Sciences. 1978;39(4-A):2149.
Manz CC. The art of self-leadership: strategies for personal effectiveness in your life and work. Prentice-Hall; 1983.44. Kim HS. The relationship between self-leadership and job satisfaction of middle school teacher [master’s thesis]. [Seoul]: Soongsil University; 2003. 83 p. 45. Ayres HW. Factors related to motivation to learn and motivation to transfer learning in a nursing population [dissertation]. [Raleigh]: North Carolina State University.
Kim HS. The relationship between self-leadership and job satisfaction of middle school teacher [master?s thesis]. [Seoul]: Soongsil University; 2003. 83 p.
Ayres HW. Factors related to motivation to learn and motivation to transfer learning in a nursing population [dissertation]. [Raleigh]: North Carolina State University.
Park H, Choi S, Choi Y, Park S, You S, Baik M, et al. Effect of Korean version of psychological first aid training program on training disaster mental health service provider. J Korean Neuropsychiatric Association. 2020;59(2):123–35.
Kim M, Kim S, Lee WS. Effects of a virtual reality simulation and a blended simulation of care for pediatric patient with asthma. Child Health Nurs Res. 2019;25(4):496–506.
Noh J, Oh EG, Kim SS, Jang YS, Chung HS, Lee O. Development and evaluation of a multimodality simulation disaster education and training program for hospital nurses. Int J Nurs Pract. 2020:e12810.
Cho JL. The effect of self-leadership and communication barriers on nursing performance in hospital nurses. J Convergence Cult Technol. 2019;5(2):239–46.
Kwon SN, Park HJ. Effects of nurses’ positive psychological capital, self-leadership, and relational bonds on organizational commitment. J Korean Acad Nurs Adm. 2020;26(3):241–50.
Yoo JY, Lee YH, Ha YK. A convergence study on the effects of self-leadership and job satisfaction on nursing performance in general hospital nurses. J Convergence Inform Technol. 2019;9(10):28–38.
Park SY, Shim CS. Effects of a simulator-based delivery education on the major satisfaction, nursing professionalism and clinical competence of the nursing students. J Korea Entertainment Ind Association (JKEIA). 2018;12(5):199.
Jeon JC. The effects on learning motivation and self-efficacy according to the type of reflection. J Educational Inform Media. 2013;19(4):837–59.
Kim S, Cho Y. Proliferation of online learning and the implications for teaching and learning in future university education. J Lifelong Learn Soc. 2018;14(4):51–78.
Kang GS, Kim Y. Development and application of integrated-simulation practice program using standardized patients: caring for alcoholism with diabetes mellitus in the community. J Korea Academia-Industrial Cooperation Soc. 2016;17(8):662–72.
Download references
Acknowledgements
The authors would like to thank Eun-Joo Choi and Dong-Hee Cho for their contributions to the development of the simulation program.
This work was supported by the National Research Foundation of Korea (NRF) through a grant funded by the Korean government (Ministry of Science and ICT) (NRF-2020R1A2B5B0100208).
Author information
Authors and affiliations.
Chung-Ang University, Red Cross College of Nursing, Seoul, South Korea
Eunjung Ko & Yun-Jung Choi
You can also search for this author in PubMed Google Scholar
Contributions
K.E. and Y.C. wrote the design, collected data, data analysis, results, discussion, and conclusion.
Corresponding author
Correspondence to Yun-Jung Choi .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted in accordance with the Declaration of Helsinki (Association World Medical, 2013) and was part of a larger study. It was approved by the Institutional Review Board of Chung-Ang University (IRB approval number 1041078-202003-HRSB-070-01CC) and retrospectively registered (21/11/2023) in the Clinical Research Information Service ( https://cris.nih.go.kr ) with trial registration number KCT0008965. All the participants provided written informed consent and were informed of the right to withdraw from participation at any time during the research until publication. Data confidentiality was ensured, and the results were provided to the participants at their request.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ko, E., Choi, YJ. Efficacy of a virtual nursing simulation-based education to provide psychological support for patients affected by infectious disease disasters: a randomized controlled trial. BMC Nurs 23 , 230 (2024). https://doi.org/10.1186/s12912-024-01901-4
Download citation
Received : 01 November 2023
Accepted : 29 March 2024
Published : 07 April 2024
DOI : https://doi.org/10.1186/s12912-024-01901-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Virtual simulation
- Psychological support
- Infectious diseases disaster
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

COMMENTS
The Review of Educational Research (RER) publishes critical, integrative reviews of research literature bearing on education, including conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. View full journal description.
Educational Research Review is an international journal addressed to researchers and various agencies interested in the review of studies and theoretical papers in education at any level. The journal accepts high quality articles that are solving educational research problems by using a review approach. This may include thematic or ...
The Review of Educational Research ( RER, bimonthly, begun in 1931) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research.
Review of Educational Research (RER) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field. RER encourages the submission of research relevant to education from any discipline, such as reviews ...
2006 — Volume 1. ISSN: 1747-938X. Read the latest articles of Educational Research Review at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature.
Adolescent psychosocial factors and participation in education and employment in young adulthood: A systematic review and meta-analyses. Sümeyra N. Tayfur, Susan Prior, Anusua Singh Roy, Linda Irvine Fitzpatrick, Kirsty Forsyth. Article 100404. View PDF.
The Review of Educational Research is a bimonthly peer-reviewed review journal published by SAGE Publications on behalf of the American Educational Research Association.It was established in 1931 and covers all aspects of education and educational research.The journal's co-editors are Mildred Boveda, Karly Sarita Ford, Erica Frankenberg, and Francesca López (Pennsylvania State University).
In this open access edited volume, international researchers of the field describe and discuss the systematic review method in its application to education research. Reflections and practical examples are included and provide an introduction and overview on systematic reviews in education research.
Review of Education is the only journal outlet for publication of both major studies and substantial reviews in education, and comprehensive Research Syntheses (8,000 to 20,000 words). Review of Education publishes supplementary materials alongside articles, such as video abstracts and teaching resources, allowing you to maximize the impact of ...
The Review of Educational Research publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. RER encourages the submission of research ...
Description. The Harvard Educational Review (HER) is a scholarly journal of opinion and research in education. The Editorial Board aims to publish pieces from interdisciplinary and wide-ranging fields that advance our understanding of educational theory, equity, and practice. HER encourages submissions from established and emerging scholars, as ...
Educational Review is a leading research journal for generic educational scholarship. For almost seventy-five years it has offered cutting-edge scholarly analyses of global issues in all phases of education, formal and informal, in order to rethink and shape the future of education. It publishes peer-reviewed papers from international ...
Establishing a dynamic understanding of factors that influence university students' leadership approaches, perceptions, and skills through a systematic literature review. Katherine K.W. Lee, Cecilia K.Y. Chan. Article 100570. View PDF. Article preview. Read the latest articles of Educational Research Review at ScienceDirect.com, Elsevier's ...
Education policy maven Rick Hess of the American Enterprise Institute think tank offers straight talk on matters of policy, politics, research, and reform. Read more from this blog.
Keywords: healthcare education, medical education, teachers' behavior, students' behavior, human behavior, technology in medical sciences, program development, curriculum development, teacher and student performance . Important Note: All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements.
A systematic review of immersive technology applications for medical practice and education - Trends, application areas, recipients, teaching contents, evaluation methods, and performance. Yuk Ming Tang, Ka Yin Chau, Alex Pak Ki Kwok, Tongcun Zhu, Xiangdong Ma. Article 100429. View PDF.
We conducted an exhaustive and focused scoping review and followed the methodological framework for scoping reviews as previously described in the literature [20, 22].This study aligned with the four goals of a scoping review [].We followed the first five out of the six steps outlined by Arksey and O'Malley's to ensure our review's validity 1) identifying the research question 2 ...
The Review of Educational Research (RER, quarterly, begun in 1931; approximately 640 pp./volume year) publishes critical, integrative reviews of research literature bearing on education.Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research.
A systematic review was conducted of the literature published between 2010 and 2023 in the PsycINFO, ERIC, Education, and Psychology databases. An initial 1176 studies were reviewed by abstract, of which 485 were read in full text, leading to the selection and analysis of 22 studies. ... American Educational Research Association (AERA ...
Educational Research Review Educational Research Review is an international journal addressed to researchers and various agencies interested in the review of studies and theoretical papers in education at any level. The journal accepts high quality articles that are solving educational research problems by using a review approach. This may ...
Virtual simulation-based education for healthcare professionals has emerged as a strategy for dealing with infectious disease disasters, particularly when training at clinical sites is restricted due to the risk of infection and a lack of personal protective equipment. This research evaluated a virtual simulation-based education program intended to increase nurses' perceived competence in ...