

Counseling Resource Navigation Support Groups Education Financial Assistance
Copelink blog.
Latest news, stories and updates from our blog.
Columbia School of Social Work, Cancer Care and University of Washington School of Social Work Introduce the Handbook of Oncology Social Work
Columbia School of Social Work, Cancer Care and University of Washington School of Social Work applaud the publication of the “ Handbook of Oncology Social Work: Psychosocial Care for People with Cancer ,” published by Oxford University Press.
The development of this inaugural Handbook of Oncology Social Work provides an up-to-date repository of the scope of oncology social workers’ clinical practice, education, research, policy, and program leadership in the psychosocial care of people with cancer and their families. It addresses both the science and art of psychosocial care and identifies the increasing specialization of oncology social work related to its unique knowledge base, skills, role and the progressive complexity of psychosocial challenges for patients with cancer.
The Handbook ’s editors are Grace Christ, DSW/PhD, Professor Emerita, Research Scientist, Columbia School of Social Work; Carolyn Messner, DSW, OSW-C, LCSW-R, Director of Education and Training, Cancer Care ; and Lynn Behar, PhD, LICSW, OSW-C, and Founder, Carol LaMare Program for Oncology and Palliative Social Work, University of Washington School of Social Work.
The “ Handbook of Oncology Social Work: Psychosocial Care for People with Cancer ” includes 109 chapters by 160 authors and is available now for order.
Advance Praise of the Handbook of Oncology Social Work
“This long-awaited volume written by pioneers in the field, provides a wealth of evidence-based information on how to deliver cancer care for the whole person ... a must read for anyone practicing in oncology.”
-- Julia H. Rowland, PhD, Director, Office of Cancer Survivorship, National Cancer Institute, NIH/DHHS
About Columbia School of Social Work Columbia School of Social Work has been a leader in social work education and research since 1898. It joins rigorous academic theory with real-world practice to enhance the welfare of citizens and communities in New York City, the nation and around the world. To learn more, visit www.socialwork.columbia.edu .
About Cancer Care ® Founded in 1944, Cancer Care is the leading national organization providing free, professional support services and information to help people manage the emotional, practical and financial challenges of cancer. Our comprehensive services include counseling and support groups over the phone, online and in-person, educational workshops, publications and financial and co-payment assistance. All Cancer Care services are provided by oncology social workers and world-leading cancer experts. Headquartered in New York, NY, Cancer Care maintains three additional locations in Norwalk, CT, Ridgewood, NJ and Syosset, NY. To learn more, visit www.cancercare.org or call 800-813-HOPE (4673).
About University of Washington School of Social Work Founded in 1934, and celebrating 80 years of impact, the University of Washington School of Social Work is a recognized leader in solving the most demanding social issues of our day through rigorous research, academic innovation and public service. Visit www.socialwork.uw.edu to learn more.
Terms of Use and Privacy Policy
By using our website, you agree to our recently updated Privacy Policy . Here you can read more about our use of cookies which help us make continuous improvements to our website. Privacy Policy .
- Tools and Resources
- Customer Services
- Addictions and Substance Use
- Administration and Management
- Aging and Older Adults
- Biographies
- Children and Adolescents
- Clinical and Direct Practice
- Couples and Families
- Criminal Justice
- Disabilities
- Ethics and Values
- Gender and Sexuality
- Health Care and Illness
- Human Behavior
- International and Global Issues
- Macro Practice
- Mental and Behavioral Health
- Policy and Advocacy
- Populations and Practice Settings
- Race, Ethnicity, and Culture
- Religion and Spirituality
- Research and Evidence-Based Practice
- Social Justice and Human Rights
- Social Work Profession
- Share This Facebook LinkedIn Twitter
Article contents
Oncology social work research.
- Julianne S. Oktay Julianne S. Oktay University of Maryland Baltimore
- and Bradley Zebrack Bradley Zebrack University of Michigan
- https://doi.org/10.1093/acrefore/9780199975839.013.1268
- Published online: 25 June 2018
Oncology social work researchers have made (and continue to make) important contributions to the knowledge base that supports the profession. This article discusses the profession of oncology social work, its roots in medical social work in the United States, the development of cancer treatment, and the body of research that informs its art and practice. Oncology social work research is placed in the broader contexts of the social work profession, the field of oncology, and the specific field of oncology social work.
Through the decades, the profession of oncology social work has grown, gained stability and legitimacy. Oncology social work itself, along with oncology social work research, have made rapid strides in the 21st century and accelerating in impact and relevance. Oncology social work research is stronger now than ever. Recent developments, such as the addition of a research institute at the annual AOSW conference and initiatives to establish a “practice-based research network” are expanding capacity in the field.
Oncology social work researchers bring a unique perspective to their research. Social work’s patient-centered perspective is reflected in research that explores the cancer experience of patients and family members and leads to new interventions based on that experience. Social work’s focus on human development over the life course results in research that reflects a developmental framework or focuses on specific age groups, such as children, adolescents, young adults, or the elderly. Social work’s conceptual model of “Person-in-Environment” is reflected in research on cancer patients in the context of their interpersonal relationships. The values of social justice and cultural competence are reflected in research on health disparities, minority populations, and multicultural perspectives. Finally, the field of oncology social work itself has been the focus of recent research on distress screening and its implementation.
In the 21st century, oncology social work research stands in a pivotal position. Although this type of research is now widely recognized as important, it is still a challenge to access the level of support from major funders of cancer research required to establish and reinforce a strong and vibrant knowledge base for the profession.
- Psychosocial oncology
- Social work
- cancer and oncology social work
Oncology social workers have long served as front-line advocates for the “whole patient,” incorporating psychosocial care into the treatment of patients with cancer and promoting patient- and family-centered care (Hedlund, 2015 ). Several recent developments (discussed later in the article) highlight the importance of social work in quality cancer care. Like all professions, social work relies on empirical research findings to inform psychosocial practice and generate new knowledge. Both oncology social work itself and the research associated with this discipline have made rapid strides in recent years and are on the verge of critical acceleration in terms of its impact and relevance.
This article provides background on the profession of oncology social work, its roots in US medical social work, on cancer treatment, and on the body of research that informs its art and practice. We begin by placing oncology social work research in the broader contexts of (1) the social work profession, (2) the field of oncology, and (3) the specific field of oncology social work.
The Development of the Social Work Profession
The social work profession is rooted in the progressive movement of the early part of the 20th century . Accomplishments from that period included labor laws (especially child labor laws), the integration of large immigrant populations into American society (e.g., settlement houses), voting rights for women, and the building of a basic social network to protect and support vulnerable populations (e.g., the sick, disabled, aged, mentally ill, and children). In the health-care field, pioneers Ida Cannon and Harriett Bartlett at Massachusetts General Hospital and Johns Hopkins Hospital, respectively, developed the first hospital social work departments (Bartlett, 1957 ; Cannon, 1913 ; Gehlert, 2006 ; Fobair et al., 2009 ; Kiegher, 2000 ), while others worked in a variety of public health efforts (e.g., fighting TB, sanitation). The first school of social work was established at Simmons College in 1904 , in part to train social workers to work at Massachusetts General (Simmons, 2016 ). The focus of early health social work was on assisting poor immigrants from Europe struggling with infectious diseases and other maladies attributable to their physical and social environments. As public health advanced, a number of successful programs (vaccination, pubic sanitation, clean water, pasteurization of milk) and the development of antibiotics eliminated many of these health issues; social workers then began to focus on persons struggling with serious chronic and life-threatening conditions such as heart disease, diabetes, and cancer.
By the 1950s, medical social work was a well-established specialty, with its own organization, textbooks, and journal. However, in the mid-1950s, medical social work (and other specialty groups) was absorbed into the new National Association of Social Workers with a broader and more unified vision of the social work profession that emphasized what all social workers have in common, rather than on the skills they had developed in specialty niches. Out of this period came a strong common ideology emphasizing professional ethics, a commitment to social justice, and a strong belief in the importance of professional training and research. Schools of social work grew, as did the importance of the master’s in social work degree and of research. By the mid-1960s, federal dollars became available to fund scholarships for students (NIMH) and to support faculty research in areas of national interest (poverty, health and aging, civil rights/integration).
The creation of Medicare and Medicaid in 1965 led to increased numbers of medical social workers, and once again, knowledge in this field expanded. Two journals in medical social work were established in 1975 , Social Work and Health Care and Health and Social Work , and important textbooks in the field were published (Bracht, 1978 ).
Research in the Social Work Profession
Although many of the very early social work pioneers, such as Jane Addams and Ann Abbott, were involved in research (Zimbalist, 1977 ), research in the social work field did not begin to grow rapidly until the 1950s. Even then, the practice side of the profession expanded much more rapidly, while research activities grew at a much slower pace. New schools of social work strongly emphasized practice, with limited attention to research. Doctoral programs in social work also expanded in the 1960s; however, many of these programs offered a practice-focused doctorate (DSW), instead of the more research-focused PhD. Concerned, the Russell Sage Foundation initiated funding opportunities to encourage and expand research efforts in social work (Austin, 1991 ), and among these was a new doctoral program at the University of Michigan. Despite the emergence of some excellent doctoral programs, by 1988 a National Institute of Mental Health (NIMH) task force declared research in social work to be in crisis. “A sustained and credible program of research is … essential to a profession’s self-respect and to its ability to maintain the positive regard of outsiders whose opinions help support and legitimize the profession’s endeavors (Fanshel, quoted in Austin, 1991 ). They pointed out that research resources in social work had “lagged far behind” the practice aspect of the profession and concluded that social work research “has failed to meet the needs of practitioners.” Also, although new doctoral programs had proliferated, the number of graduates granted doctoral degrees did not increase; and, according to this NIMH report, the quality of research produced by those with social work doctorates was not comparable to that of graduates from other disciplines and professions. The task force identified several major factors limiting a scientific knowledge base in social work, including a lack of strong, research-based doctoral programs, lack of support for social work research at the national level, and a lack of integration of research into practice forums (Austin, 1991 ). The task force recommended increased attention to research in social work education. Research training in many social work doctoral programs was strengthened as a result of the report. Also, a new forum for social work research was established in 1993 , the Society for Social Work Research (SSWR), with its own research journal, the Journal of the Society for Social Work Research (JSSWR).
Also created at the same time was the Institute for the Advancement of Social Work Research (IASWR), designed to strengthen the infrastructure in social work research and to enhance the connections between social work research and practice, education, and policy (Zlotnik, Biegel, & Solt, 2002 ; Zlotnik, & Solt, 2006 , 2008 ). IASWR was funded jointly by major social work organizations such as the NASW, CSWE, and leadership in bachelors and doctoral social work education.
To fully understand social work in oncology, and the role social workers play in the delivery of cancer care, it is helpful to understand the nature of the medical treatment of cancer and how it developed.
The Development of the Field of Oncology
Until the development of effective treatments, cancer was almost always fatal. In the absence of screening and early detection, surgery was often the only treatment. Cancers were not typically discovered until they had grown quite large and patients became symptomatic: as a result, the cancer had already spread throughout the body. At that point, surgery was often ineffective, or it was so extensive that it was deforming (e.g., radical mastectomy). In the earlier days of cancer treatment, it was common practice not to tell patients they had cancer. Often obscure terminology was used, or vague information was given about prognosis.
The introduction of surveillance (Seven Warning Signs program of the ACS), along with advances in treatment such as radiation and chemotherapy meant that more and more cancers were treated successfully. Patients began to live longer, and in some cases, cancers were cured. The first successes were with pediatric cancers, where dramatic increases in survival rates were observed through the 1970s and 1980s.
In breast cancer, the development of mammograms meant that small cancers could be found and treated before they spread (metastasized). In colon cancer, screening allowed polyps to be removed before they become malignant. This has reduced the rate of colon cancer deaths significantly. More recently, the recognition that cancer can arise from environmental or behavioral exposure to carcinogens has reduced the risks for these cancers in the population. The most significant was the connection made between smoking and lung (and other cancers). The long and ultimately successful campaign against smoking has led to a significant reduction in lung cancer and other cancer deaths. The recognition that skin cancers are often related to sun exposure has led to widespread use of sunscreens, and the FDA has recently recommended that tanning salons be off limits for teens.
The successes of early detection and prevention programs gradually led to a significant increase in the number of cancer survivors. A new organization, the National Coalition of Cancer Survivors, founded in 1986 by a group of cancer care providers and patient advocates, helped advance the notion that a cancer experience for patients and families is initiated at the time of diagnosis and contributes through phases of treatment—and, for many, a transition to off-treatment survival. The number of survivors has grown exponentially since then, with over 14 million survivors in the 21st century . In 1996 , partially in response to the political pressure from the cancer survivorship movement, the National Cancer Institute established the Office of Cancer Survivorship, with the primary aim of establishing and advancing a research agenda responsive to the issues and needs of cancer survivors.
There have also been important changes in the way cancer is understood. A national program to study the human genome bolstered our understanding that some cancers are genetically based. That is, vulnerability to some types of cancer can be inherited. This understanding meant that patients who are at higher risk could be identified and treated prophylactically. For example, women with a BRCA1 or BRCA2 mutation can now decide to have prophylactic mastectomies and/or oophorectomies to prevent the development of future cancer. However, the cancers caused by an inherited genetic mutation account for only a small proportion of all cancers. Many more mutations are now thought to be the result of environmental factors interacting with genetic characteristics. Of special interest to social workers is the understanding of “epigenetics,” the interactions occurring among human genes and the physical environment. That is, some cancer risks and associated disparities across demographic sub-groups defined by race, age, or gender can be explained by genomic changes arising from physically or emotionally stressful environments (Werner-Lin, 2015 ). Excess mortality rates for young women (particularly young African American women) with advanced-stage breast cancer may be another example of epigenetics explaining this disparity.
Another new development in cancer prevention is the recognition that screening can lead to over-treatment, especially in cancers that are often slow-growing and in populations (often older) that have high survival rates. Early screening in prostate and early stage breast cancers have become controversial (Brawley, 2017 ).
The most recent developments in cancer treatment include personalization of treatments based on unique characteristics of the individual tumor, and new forms of immunotherapy, also targeted to individual characteristics. Immunotherapy offers great promise for the future, but these treatments are currently so costly that they are often out-of-reach for all but the most wealthy or well-insured patients.
Improved treatments, better screening, and changing demographics are contributing to increases not only in the numbers of oncology patients and survivors but also to changes in the way that patients and their families experience cancer and its treatments, with important implications for the way social work is configured and practiced.
Psychosocial Aspects of Oncology
The increase in the number of survivors, along with a cultural shift that emphasized open communication of cancer diagnosis and prognosis, has led to greater recognition of psychosocial needs of patients as well as the needs of families (IOM, 2006 ). Problems of survivors became visible initially when some survivors of childhood cancers, the first group to respond to new treatments, began to show late effects of initial treatment: including reduced fertility and risks for developing secondary cancers, as they moved into adolescence and young adulthood. Now, it is recognized that cancer survivors of all ages experience problems such as fatigue, sleep difficulties, depression, fear of cancer recurrence, and financial issues (IOM, 2006 ).
New treatments mean that cancer patients are now sometimes faced with difficult treatment decisions. For example, recent research suggests that some early cancers do not progress, even when untreated (e.g., early stage breast and prostate cancers). Also, many of the new treatments are expensive and are not covered by insurance. Patients and families may find themselves choosing prolonged survival but at the cost of bankruptcy as well as physical, psychological, social, and financial distress. Some patients are faced with choosing to know whether they carry genes that predispose them to cancer, with enormous impact not on themselves but on their family members, including children (or future children). In stark contrast to the days when cancer patients were not told that they had cancer, patients in the 21st century have to comprehend and manage an overwhelming amount of information and face daunting choices that require complex negotiations with family members such as issues on when and how to inform children and the need to identify their core values.
Recognizing the increased importance of psychosocial issues in today’s cancer care, the National Comprehensive Cancer Network (NCCN) developed the concept of cancer-related “distress” and published its first guidelines for distress management in 1999 . The NCCN defines “distress” as the “multifactorial unpleasant emotional experience of a psychological (cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment” (NCCN, 2016 ). The NCCN also developed the Distress Thermometer, an instrument to detect distress, and advised performing distress screening in all clinical settings for those diagnosed with cancer. This recommendation was often ignored. Jacobsen and Ransom ( 2007 ) found that of NCCN member institutions that treated adults with cancer only three of the country’s 18 top cancer centers surveyed routinely performed distress screening on all patients.
In 2008 an influential report by the Institute of Medicine (IOM) (now the Academy of Medicine, part of the National Academies of Sciences, Engineering, and Medicine), entitled Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs , concluded that there was sufficient evidence to support the provision of psychosocial health services in cancer care to all patients who need them. Meeting this standard of care, the IOM committee noted, required clinical care protocols that would identify each patient’s psychosocial health needs; link the patient with needed services and coordinate biomedical and psychosocial care; and systematically followed up and adjusted plans as needed. It emphasized that for many patients with cancer, this standard of care was not being met.
Building on the NCCN guidelines and the IOM report, the American College of Surgeons Commission on Cancer (CoC) has mandated distress screening as a clinical activity required for accreditation. The CoC is the primary accrediting body for as many as 1,500 cancer-treating programs serving approximately 70% of all cancer patients in the United States. As of 2015 , CoC-accredited cancer programs must demonstrate compliance with patient-centered standards of care as a condition for cancer center accreditation.
Under this mandate, cancer centers are required to have protocols to screen and identify patients experiencing distress and to refer them, when appropriate, for psychosocial care. Centers must also provide evidence that distress-screening protocols are carried out as intended and result in appropriate referral and follow-up when indicated (ACoS, 2016 ).
Newer research on the contribution of stress and stressful living conditions to cancer development have important implications for social work. Oncology social workers most often focus on the individual and family levels when considering both prevention and treatment. However, the profession’s roots are more closely associated with neighborhood- and community-level interventions (Specht & Courtney, 1994 ). This new understanding of how multiple levels (genetic, biological, environmental, behavioral) interact in cancer development and treatment may lead to more oncology social work intervention at the “macro” levels (Werner-Lin, McCoyd, Doyle, & Gehlert, 2016 ).
Research in Psychosocial Oncology
Psychosocial care for cancer patients and their families reflects developments in the field of oncology, as well as those in mental health care more generally, and this is reflected in psychosocial oncology research. In the earliest days, not surprisingly, the focus of both practice and research was on dealing with death and dying. Early work with cancer patients, a growing interest in the more open way of approaching death promoted by Elizabeth Kubler-Ross, a nurse from England, and the work of sociologists Anselm Strauss (Glaser & Strauss, 1965 , 1968 ) and Barney Glaser focused attention on the negative outcomes of the common practice of withholding a cancer diagnosis to patients. Patients were often isolated and unsupported at the time of death. As open communication became the norm, psychiatrists and other psychosocial providers were able to offer therapies for cancer patients and families.
Early research in the field of psychosocial oncology was conducted primarily by the psychiatrists who had joined the research-focused cancer centers then developing (Holland, 1998 ). One of the earliest centers for psychosocial research on the impact of cancer was the Memorial Sloan-Kettering Cancer Center, under Arthur Sutherland. This group produced a number of studies on the psychological impact of cancer and care of the dying (Holland, 1998 ). Another early center, led by Avery Weisman at the Massachusetts General Hospital in Boston, shed light on patient reaction to a cancer diagnosis (Weisman, Worden, & Sobel, 1980 ). They conducted studies that led to the first tool used to detect distress levels in patients (Zabora & MacMurray, 2012 ).
As cancer treatments improved, psychosocial services and research expanded. A strong leader in the field was Jimmie Holland, now known as the mother of psycho-oncology, who chaired the psychiatry department at Memorial Sloan Kettering, in New York City. Other influential pioneers flourished on the West Coast. David Spiegel (Stanford) and Fawzy Fawzy (UCLA) tested the effect of psychosocial interventions on cancer patients. Working with one of the originators of group psychiatry (Yalom, 1970 ), Speigel applied this type of group therapy for women with Stage III breast cancer. The therapy was based on socio-emotional expression, based on the theory that being open about negative emotions (e.g., fear, depression). To Spiegel’s surprise, the socio-emotional group therapy not only proved to be beneficial to psychological health of the women, as he had expected, but it showed longer survival of the experimental group (Spiegel, Bloom, Kramer, & Gottheil, 1989 ). (This finding was not supported in subsequent research, but it spurred many cancer programs to add psychosocial programs.) Fawzy’s research tested the effect (including biological) of psychoeducation with melanoma patients (Fawzy, 1989 ).
As research in psychosocial oncology expanded, new organizations developed to bring investigators together in influential conferences. In the early stage, existing cancer groups added psychosocial subgroups, such as the Cancer and Leukemia Group (CALGB), NCI’s Psychosocial Collaborative Oncology Group (PSYCOG), and the European Organization for Research in the Treatment of Cancer (EORTC) (Holland, 1998 ). In 1984 the International Psychosocial Oncology Society (IPOS) was formed by the group of scientists (mainly psychiatrists) who were studying the psychosocial aspects of cancer in Europe and the United States. They held their first conference in Beaune, France, in 1994 . Regional societies (e.g., European, American, Canadian, Australian) were formed soon after, creating an international network. The traditional practice of not telling cancer patients the truth about their diagnosis waned around the globe, creating new opportunities for psychosocial services and research. These national, regional, and international societies have grown rapidly as the field of psychosocial oncology has expanded. Meetings of national, regional, and international psychosocial oncology societies and their journal, Psycho-oncology , with Jimmie Holland serving as editor, have been the prime venue for the exchange of scientific information, networking, and training in psychosocial oncology research. In addition, Dr. Holland has edited the Handbook of Psychooncology (with Julia Rowland), and later, Psycho-oncology (Holland, 1998 ), now in its third edition, which serves as the principal reference for researchers in this field.
In the 1990s there was an explosion of research on psychosocial aspects of cancer, including research on the physical, psychological, and social consequences of the disease and its treatments. Also, a body of research developed on interventions, including research on support groups, psychotherapy, problem-solving approaches, cognitive behavioral therapy, mindfulness, and yoga. This reflects the development and testing of measurement instruments that were necessary to study the effectiveness of interventions. These new instruments, targeted to cancer patients rather than those with mental illness, emphasized “quality of life.” Over time, versions of these instruments were developed for specific types and stages of cancer (Cella, 1989 ; Cella et al., 1993 ). Combined with the increasingly sophisticated scales to screen for psychosocial distress (Zabora & MacMurray, 2012 ), these instruments, as well as those that measure mental disorders (anxiety and depression), made it possible for researchers to assess the impact of psychosocial services on patients and families.
By the turn of the century, there was enough research to support review articles and meta-analyses, generally showing the positive effect of psychosocial interventions (Cwikel, Behar, & Rabson-Hare, 2000 ; Faller et al., 2013 ; Graves, 2003 ; McQuellon & Danhauer, 2006 ; Meyer & Mark, 1995 ; Schneider et al., 2010 ), medical cost-offsets (Carlson & Bultz, 2003 , 2004 ), and even survival (Fu et al., 2016 ).
This research led to widening recognition that the psychosocial impact of cancer was significant and that negative consequences could be reduced or avoided by providing evidence-based interventions. Also, it was this research that led to the development of distress screening, and the highly influential IOM report (discussed earlier) on the importance of caring for the “whole patient” and not just the cancer itself (IOM, 2008 ). The IOM report also included a recommendation about research priorities, calling on organizations sponsoring research in oncology care to include as funding priorities “tools and strategies for use by clinical practices to ensure that all patients with cancer receive care that meets the standard of psychosocial care” (IOM, 2008 ).
The Development of Oncology Social Work
The developments discussed in the previous sections have all shaped oncology social work. For example, the Commission on Cancer mandate focused attention on oncology social workers implementing distress screening as well provide appropriate follow-up services. Before discussing these recent developments, however, it is important to place the field of oncology social work in a historical context.
Oncology social work has been impacted by the changes in cancer and its treatment, changes in the health-care system, and by greater recognition of the importance of psychosocial care in the wider professional community (see “Research in Psychosocial Oncology” section) (Hedlund, 2015 ). Although the field has grown and changed in response, a strong foundation had been built many years before.
Following the Second World War, the medical field became increasingly specialized, backed by a strong research base funded by the National Institutes of Health. As a result, the role of medical social workers also became more varied. While the early social work departments employed social workers across many different hospital settings, increased medical specialization and autonomy meant that funding for social work positions shifted to medical departments such as pediatrics, medicine, surgery, oncology, and psychiatry. It became difficult to maintain consistent policies and standards across departments who saw the role (and value) of social workers very differently. For example, many pediatrics departments relied heavily on social workers to work with the families of their patients, while surgery departments typically employed small numbers of social workers, primarily for discharge planning. As cancer treatment began to separate from the broader medical departments (medicine, surgery) and move into standalone centers, oncology social work began to develop as a separate field within medical social work. This new field was strongly affected by the changes in the treatment of oncology patients, which occurred in the late 20th century (see The Development of the Field of Oncology section)
Two early oncology social workers were Eleanor Cockerill (Curran & Cockerill, 1948 ) and Bernice Catherine Harper, from California’s City of Hope National Medical Center (Harper, 1975 , 1977 / 1994 ). As the major cancer centers developed and grew, oncology social work services expanded, initially in the National Cancer Institute (NCI) designated programs. Over time, the scope of oncology social work practice expanded, and oncology social workers began to see themselves as a significant subgroup of hospital-based social workers possessing a specialized skill set. Informal groups of oncology social workers began to form in major cities. These groups often included other professionals, such as nurses and psychiatrists, who were interested in the psychosocial aspect of cancer. By the 1970s, groups were meeting in Boston, New York, San Francisco, and Los Angeles. In 1977 , the Association of Pediatric Oncology Social Workers (APOSW) was formed. This was the first formal organization of social workers dedicated to the support of young cancer patients and their families, and it began to hold annual conferences. Around the same period, the American Cancer Society focused attention on the psychosocial aspect of cancer care, holding “human values conferences” where oncology social workers were invited as both participants and guest speakers. These events also became networking centers for a first generation of oncology social workers (e.g., Joan Herman, Judith Ross, Pat Fobair, Grace Christ, and Marie Lauria) to share knowledge and ideas for research.
With the support the American Cancer Society, a fledging network of oncology social workers took steps to form a professional organization (Fobair et al., 2009 ). Initially (in 1983 ), the ACS formed a national advisory committee on oncology social work and organized a national educational workshop (in 1984 ) to get the ball rolling for a new professional organization, which became the National Association of Oncology Social Workers (NAOSW). In the meantime, Grace Christ, chief of the Social Work Department at Memorial Sloan Kettering Cancer Center in New York, launched the Journal of Psychosocial Oncology —as a publishing outlet for the new organization.
Although the NAOSW held annual meetings and membership grew through the 1980s and 1990s, financial viability was a consistent problem. Membership dues and conference fees did not produce enough income to survive, and the organization had to rely on the support of the cancer centers (usually the employer of the president) for administrative support. By the mid-1990s, the NAOSW was in financial crisis, and under the leadership of presidents Jim Zabora and Hester Hill, it was dissolved and them re-created with a more financially viable structure under the name Association of Oncology Social Work (AOSW). And the Journal of Psychosocial Oncology , under the leadership of editors Grace Christ and Jim Zabora, was offered as an AOSW membership benefit.
The American Cancer Society continued to support AOSW, providing funding for leadership development, strategic planning, and collaboration with national cancer organizations throughout the organization’s history (Fobair et al., 2009 ). The ACS also published two books that became classics in oncology social work, Oncology Social Work: A Clinician’s Guide (Stearns, Lauria, Hermann, & Fogelberg, 1993 ), and Social Work in Oncology: Supporting Survivors, Families and Caregivers (Luria, Clark, Hermann, & Stearns, 2001 ). Also, in 2003 Cancer Support Groups: A Guide for Facilitators (Kraweick & Greer, 2015 ) was published.
AOSW has collaborated with other organizations to advance the field of oncology social work. For example, in 1998 AOSW collaborated with the Oncology Nursing Society (ONS) and the National Coalition of Cancer Survivors (NCCS) to produce the so-called Cancer Survival Toolbox. (The Toolbox project was later joined by the National Association of Social Workers (NASW) (Clark & Collins, 2015 ). During the 1990s and 2000s, AOSW allied with patient advocacy and health-care professional organizations and assumed a position of leadership in a national effort to set a standard for the inclusion of quality psychosocial care for all cancer patients and their families. AOSW members were “at the table” when the National Comprehensive Cancer Network (NCCN) began to develop distress screening tools. When the CoC mandated distress screening (discussed in the section “Research in Psychosocial Oncology” ) oncology social workers, especially those working in cancer centers accredited by the ACoS, began to incorporate distress screening into their practices (Oktay, Nedjat-Haiem, Davis, & Kern, 2012 ; Burg, Adorno, & Hidalgo, 2012 ). This type of screening departs from the more traditional approach in oncology social work, where patients are referred and then fully assessed. However, staffing levels remain too low to allow this approach for every patient in all but a few settings. Distress screening is seen as responsive to the IOM emphasis on treating the whole patient, so that oncology social workers now do a more thorough assessment on patients who screen with high distress scores and/or problems.
Another important 21st-century development in the field of oncology social work is the publication of the Handbook of Oncology Social Work: Psychosocial Care for People with Cancer (Christ, Messner, & Behar, 2015 ). It covers a wide range of topics in over 800 pages, illustrating the extensive knowledge the field has accumulated in its short life.
AOSW has grown to over 1,400 members, holds annual conferences, has an active listserv, many special interest groups, as well as a webpage and Facebook and Twitter accounts; they have also added webinars to continuously spread knowledge throughout the community. AOSW also offers a certification in oncology social work (the OSW-C), now widely recognized in the field (Vaitones, Schutte, & Mattison, 2015 ).
Research in Oncology Social Work
Oncology social workers make up the majority of those offering psychosocial oncology services, but researchers investigating psychosocial outcomes have contributed a disproportionately small portion of research in this field. There are many reasons for this, including the scarcity of oncology social work researchers, lack of funding for social work research, and few opportunities for advanced research training and activities. The issues faced by oncology social work researchers are much the same as those identified by the NIMH Task Force (discussed in Research in the Social Work Profession s ection) 25 years ago.
In spite of these limitations, oncology social work researchers have made important contributions to the knowledge base that supports psychosocial care. In fact, oncology social work research has a long history, as some of the earliest oncology social workers successfully combined research with their clinical practice. One of the first to publish empirical research in a scientific journal was Ruth Abrams, at Massachusetts General Hospital (Abrams & Finesinger, 1953 ; Abrams, 1966 , 1974 ). Abrams later established the Ruth Abrams Interdisciplinary Research Program and hired Barbara Berkman as the first director. Dr. Berkman was interested in cancer in the elderly, since she discovered that cancer was a predictive factor for referral to social work for elderly hospital patients (Berkman & Rehr, 1973 ; Berkman, Rehr, & Rosenberg, 1980 ). Dr. Berkman combined an active research career with professional leadership, advocating for the new profession of oncology social work and eventually establishing the Hartford Geriatric Scholars program for social work education, training, and advocacy. (See the section “American Cancer Society”).
Since the early days, oncology social work leaders have combined practice, leadership, advocacy, and research (Fobair et al., 2009 ). Oncology social work researchers bring a unique perspective to their research in psychosocial oncology. For example, social work is known for “starting where the client is”—a patient-centered perspective. This is reflected in research that explores the cancer experience of patients and family members. One of the earliest examples was the work of a Patricia Fobair, a radiation oncology social worker at Stanford in the early 1980s: her work explored the problems of patients with Hodgkin’s lymphoma who were treated with radiation (Fobair, Hoppe, Bloom, Cox, Varghese, & Spiegal, 1986 ). Other examples include work with children whose parents had terminal cancer (Christ, 2000 ), women whose mothers had breast cancer (Oktay, 2005 ), and women with the BRCA 1 or 2 genes (Werner-Lin, 2007 ). Many of these studies led to new interventions based on the patients’ experience (Abernathy et al., 2010 ; Siegel et al., 1992 ).
As another perspective of social work is human development over the life course, it is not surprising that oncology social work research also reflects a developmental framework (Oktay & Walters, 1991 ) and/or focuses on specific age groups, such as children (Jones, Parker-Raley, & Barczyk, 2011 ; Weiner, Battles, Bernstein, Long, Mansky, & Mackall, 2006 ), adolescents and young adults (Zebrack, 2011 ; Zebrack & Isaacson, 2012 ) or the elderly (Rohan et al., 1995 ; Smith et al., 2008 ).
Social work also applies a conceptual model called the “Person-in-Environment” and this perspective, too, is reflected in oncology social work research. For many of these researchers, this has led to a focus on cancer patients in the context of their interpersonal relationships and families. This work includes studies of couples (Kayser, Feldman, Borstelmann, & Daniels, 2010 ), daughters (Oktay, 2005 ), and mothers (Kayser & Sormanti, 2002 ; Lewis et al., 2000 ).
Social justice and cultural competence are core values of social work. Not surprisingly, oncology social work researchers have engaged in research focusing on health disparities (Ell et al., 2005 ; Ell, Vourlekis, Lee, & Xie, 2007 ; Gehlert et al., 2008 ; Gehlert, Mininger, & Ciriano-Steffens, 2010 ), minority populations (Lee & Vang, 2010 ; Davis, Emerson, & Husaini, 2005 ; Wells et al., 2015 ) and multicultural perspectives (Kayser et al., 2014 ).
With the focus on screening for distress in cancer patients discussed earlier, oncology social work researchers have also focused in this area, including the instruments themselves (Zabora, Smith-Wilson, Fetting, & Enterline, 1990 ) and the prevalence of psychosocial distress (Zabora, Brintzenhofe-Szoc, Curbow, Hooker, & Piantadosi, 2001 ). (Also see the section “A Project to Assure Quality Cancer Care [APAQCC].”)
Finally, the field of oncology social work itself has been the focus of some oncology social work research (Rohan & Bausch, 2009 ). For example, AOSW’s Social Workers in Oncology Research Group (SWORG) conducted a membership survey of oncology social work activities (Zebrack et al., 2008 ). Others have studied the implementation of distress screening (Burg, Adorno, & Hidalgo, 2012 ; Oktay, Nedjat-Haiem, Davis, & Kern, 2012 ; Zebrack et al., 2015 , 2016 ).
In order to build a strong research base for the profession, oncology social work needs a combination of resources. These include support and excellent training for doctoral students, mentoring and funding for researchers, and opportunities for networking and interaction with other researchers—both within the field and in related fields as well. The major sources of support for oncology social work research have been the American Cancer Society (ACS) and the Association for Oncology Social Work (AOSW). Other important support has come from the National Association of Social Work (NASW), which collaborated with ACS and AOSW in several projects discussed below. In addition, in 2002 the National Cancer Institute awarded NASW a grant to investigate barriers to the incorporation of research into oncology social work practice. The expert panel verified that many of the barriers to the use of research in oncology social work practice identified in the past, such as lack of easy access to research results, lack of mentoring, inadequate administrative support, and under-funding remained barriers in 2002 (NASW, 2003 ). The report identified a number of strategies to improve the practice-research linkage. However, most of these required funding, which, unfortunately was not forthcoming (Zlotnik, 2016 , personal communication).
American Cancer Society
The American Cancer Society has contributed significantly to the development of oncology social work researchers through its Health Professional Training Grants in Cancer Control. This program, which began in 1989 under the leadership of Barbara Berkman, provides grants to doctoral students in oncology social work. The program began as a post-master’s clinical training grant, emphasizing advanced clinical practice. By 1999 the program shifted focus to support doctoral student training, and in 2004 it was adapted to allow for support to begin at the start of doctoral education and continue for up to four years. To strengthen the research training of the grantees, funded doctoral scholars and their mentors attend a pre-conference research training institute in conjunction with the annual meeting of the Society for Social Work Research (SSWR), the prime research organization in social work. Over 30 oncology social work doctoral students have received support through this program (Kraweick & Greer, 2015 ).
The AOSW has also recognized and supported research in the field. Several doctorally trained social workers have also served as AOSW president, strengthening the commitment to research in the organization. In the 1990s, oncology social workers recognized the need for research on oncology social work practice and its impact on patient outcomes and cancer-care delivery. Changes in the American health-care system and its financing changed the way social work services were paid for, from the blanket coverage traditionally offered to hospitals, to a managed care approach. As a result, health-care professionals had to demonstrate their effectiveness, especially those not providing traditional medical care. AOSW responded with the development of the social work Oncology Research Group (SWORG). SWORG was approved as a special committee of the board in 1996 , with the goal of development and implementation of research protocols to be used at multiple sites. Other goals were to promote interest in research in the membership, and to generate research proposals for AOSW. It was under the auspices of SWORG that studies of screening, under Zabora’s leadership, of the oncology social work role (Zebrack et al., 2008 ) and of distress screening (Brinzenthof-Socz et al., 2015 ) were conducted. SWORG also published a guide to research for AOSW members (Roberts, Brintzenhofe-Socz, Zebrack, & Behar, 2003 ). AOSW members participated on the committees whose work served as the foundation for the NCCN, IOM, and CoC standards on distress screening. SWORG decided to conduct additional research in distress screening, to help prepare the profession for its expanded role. They used the JPO to share current knowledge, publishing a special issue in the fall of 2012 , edited by Zebrack and Burg. Articles included an overview of distress screening, analysis of screening instruments, qualitative research on how social workers were handling the challenge (Burg, Adorno, & Hidalgo, 2012 ; Oktay, Nedjat-Haiem, Davis, & Kern, 2012 ), among others. The group developed a membership survey to be conducted through the AOSW listserv; this survey was seeking opinions on current experience with distress screening, as well as barriers and facilitating factors. The results of this survey were published in 2015 (Brinzenhof-Socz et al., 2015 ).
Another important resource for networking and strategic planning for oncology social work research has been the development of an annual meeting of the leadership of the field in Louisville. In 2011 Kayser accepted the first endowed professorship in oncology social work (the Dr. Renato LaRocca Chair of Oncology Social Work) at the Kent School of Social Work in Louisville, Kentucky. As a part of her professorship and with funding through the Kent School of Social Work, Kayser has hosted an annual social work research meeting with the purpose of establishing and acting upon a set of priorities for social work research. Important initiatives that have advanced oncology social work research were produced as a result of these meetings, including the aforementioned special issue on distress screening for the JPO, a large-scale survey of AOSW member experiences with implementation of distress screening, and AOSW’s Project to Assure Quality Cancer Care (APAQCC).
In spite of these supportive programs, oncology social work research continues to struggle for funding. This means that most of the research related to psychosocial oncology lacks a social work (let alone patient) perspective. Even now, little is known about the services that social workers offer and their effectiveness. Even basic needs of the profession, such as staffing standards, remain poorly understood.
Recent Developments in Oncology Social Work Research
A project to assure quality cancer care (apaqcc).
Among the responses of oncology social work researchers to the important changes in the field, especially the mandates by the CoC, was the creation of Association of Oncology Social Work’s Project to Assure Quality Cancer Care (APAQCC). Initiated in 2014 , APAQCC involved sixty-five Commission on Cancer (CoC)–accredited cancer programs across the United States (and two in Canada) and academic partners at the University of Michigan School of Social Work and the University of Louisville Kent School of Social Work. Its purpose was twofold. Its first aim was to examine the capacity of cancer programs to provide quality psychosocial support services; and the second aim was to evaluate the implementation of distress screening. The project targeted oncology social workers as the experts on psychosocial care at their institutions and provided them with data necessary to influence change and assume a leadership role at their institutions.
During Phase I, APAQCC participants surveyed cancer-care providers at their respective institutions as a means for assessing the capacity of their cancer program to deliver psychosocial care. In Phase II, APAQCC participants conducted a two-month retrospective review of electronic medical records for patients seen in their cancer program to assess adherence and responsiveness to their institution’s prescribed psychosocial screening protocol, as well as the medical service utilization of those patients.
Research Institutes
Another important development was that the AOSW held its first two-day Post-Conference Research Institute in 2016 , immediately following the AOSW’s 32nd Annual Conference. The effort grew out of the recognition that these forces have set the stage to foster a stronger research agenda for the field and to bridge the gap between research and practice. The research institute, co-chaired by AOSW research director Julianne S. Oktay, and Brad Zebrack, was conceived as a venue for researchers, including established leaders in the field, and oncology social work practitioners interested in conducting research, meeting others with similar interests, and to facilitate mentorship. Mini lectures, panel discussions, and roundtable sessions were designed as opportunities for participants to present and discuss ideas, research topics, and challenges in oncology social work research. These included a keynote address: “Notes from the Data-Mines: Research, Practice and Life Lessons Learned from Personal Encounters with Cancer” presented by Irwin Epstein of Hunter College; a panel discussion on “The Funding Quest: Opportunities, Challenges, and Successes”; expert-led roundtable discussion sessions on identifying research opportunities in social work practice; and a presentation on “Publishing Oncology Social Work Research: New Directions for the Journal of Psychosocial Oncology .” A white paper on the research institute was developed to communicate the recent focus on research within AOSW to members as well as the outside community.
Practice-Based Research Network (PBRN)
Building upon the success of APAQCC, as well as recent recognition of the potential of practice-based research networks to address issues of relevance to social work, particularly health disparities (Gehlert, Walters, Uehara, & Lawlor, 2015 ) research leaders in oncology social work, with support from PCORI, aim to develop a collaborative research group for psychosocial oncology—a sustainable community of cancer patient advocates, oncology social workers, and social work researchers devoted to assuring the delivery of high-quality cancer care for all patients and their families. This cooperative group will draw upon the collective wisdom of oncology social work practitioners, academic researchers, and patient advocates. The group intends to establish an efficient structure within which to answer research questions arising in the practice of social work with cancer patients and their families. Social work researchers will have opportunities to propose and conduct research from within the collaborative, and the lessons learned through conduct of studies undertaken by the cooperative group will inform future studies. At present, vital intellectual capital is lost upon the completion of freestanding studies conducted in silos by individuals or small teams of investigators, which is typically the case in psychosocial oncology research.
The goal is to define and conduct high-impact, clinically relevant research and serve as a venue for ongoing recruitment of new stakeholders and expertise into the field of psychosocial oncology research. The PCRC also will be designed to enhance oncology social workers’ collective knowledge and ability to design and conduct research, disseminate findings, and achieve systems changes that ultimately result in improved patient outcomes and institutional cost savings.
Oncology social work research has contributed to the vibrancy of the field from its earliest days. Through the decades, the profession itself has grown while also gaining stability and legitimacy. Research contributes to the profession by providing knowledge that forms the basis of its professional expertise. As of the early 21st century , oncology social work research is stronger than ever. It is increasingly recognized as critical to understanding the complex interplay of factors that determine the development and outcome of cancer, as evidenced by Sarah Gehlert’s membership on the Board of Scientific Counselors at the National Human Genome Institute of NIH. It has a cadre of well-qualified researchers and outstanding training programs for new PhDs. The continued support of the ACS is critical to this. It also has the support of the AOSW and has been successful in conducting a number of research studies on the membership that have contributed greatly to the knowledge base of the profession. It has successfully secured funding for these research projects and for training in research. The field has greatly benefited from its first endowed professorship at the University of Louisville Kent School of Social Work. Although oncology social work research stands in a pivotal position to conduct much-needed research, now recognized as important by the highest levels in the country (reflected in several reports by the influential IOM), the profession is still challenged in finding the kind of support from major funders of cancer research (e.g., the NCI) required to establish and reinforce a strong knowledge base. Also lacking are vigorous postdoctoral opportunities. While there is some support for early career researchers in psycho-oncology, support that targets oncology social work is lacking. Thus, new PhDs who seek careers in research struggle to find their footing. Attention needs to be paid to these issues if research is to fulfill its promise to the profession.
- Abernathy, A. , Herndon, J. E. , Coan, A. , Staley, T. L. , Wheeler, J. L. , Rowe, K. , et al. (2010). Phase 2 pilot study of Pathfinders: A psychosocial intervention for cancer patients. Supportive Care in Cancer , 18 (7), 893–898.
- Abrams, R. D. (1966). The patient with cancer—his changing pattern of communication. CA: A Cancer Journal for Clinicians , 16 (6), 237.
- Abrams, R. D. (1974). Not alone with cancer: A guide for those who care. What to expect, what to do . New York: Charles C. Thomas.
- Abrams, R. D. & Finesinger, J. E. (1953). Guilt reactions in patients with cancer. Cancer , 6 (3), 474–482.
- ACoS . (2016). American College of Surgeons: Cancer program standards .
- Austin, D. (1991). Building social work knowledge for effective services and policies: A plan for research development . Report of the Task Force on Social Work Research. National Institute of Mental Health. Rockville, MD: NIMH.
- Bartlett, H. (1957). 50 Years of Social Work in the Medical Setting . New York: NASW.
- Berkman, B. & Rehr, H. (1973). Early social service case finding for hospitalized patients: An experiment. Social Service Review , 47 (2), 256–265.
- Berkman, B. , Rehr, H. , & Rosenberg, G. (1980). A social work department develops and test a screening mechanism to identify high social risk situation. Social work in health care , 5 (4), 373–385.
- Bracht, N. F. (1978). Social work in health care: A guide to professional practice . New York: Haworth.
- Brawley, O. W. (2017). Accepting the existence of breast cancer overdiagnosis . Annals of Internal Medicine , 166 (5), 364–365.
- Brintzenthofe-Szoc, K. , Davis, C. , Kayser, K. , Lee, H. Y. , Nedjat-Haiem, F. , Oktay, J. S. , et al. (2015). Screening for psychosocial distress: A national survey of oncology social workers. Journal Psychosocial Oncology , 33 (1), 34–47.
- Burg, M. , Adorno, G. , & Hidalgo . (2012). An analysis of Social Work Oncology Network Listserv postings on the Commission on Cancer’s distress screening guidelines. Journal of Psychosocial Oncology , 30 (6), 636–651.
- Cannon, I. M. (1913). Social work in hospitals: A contribution to progressive medicine . Cambridge, MA: Harvard University Press.
- Carlson, L. E. & Bultz, B. D. (2003) Benefits of psychosocial oncology care: Improved quality of life and medical cost offset. Health and Quality of Life Outcomes , 1 (10), 8 .
- Carlson, L. E. , & Bultz, B. D. (2004). Efficacy and medical cost offset of psychosocial interventions in cancer care: Making the case for economic analyses. Psycho-oncology , 13 , 837–849.
- Cella, D. F. (1989). Quality of life. In J. C. Holland (Ed.), Psycho-oncology (pp. 1135–1146). New York: Oxford University Press.
- Cella, D. F , Tulsky, D. S. , Gray, G. , Sarafin, B. , Linn, E. Bonomi, A. , et al. (1993). The functional assessment of cancer therapy scale: Development and validation of the general measure. Journal Clinical Oncology , 11 (3), 570–579.
- Christ, G. (2000). Healing children’s grief: Surviving a parent’s death from cancer . New York: Oxford University Press.
- Christ, G. H. , Messner, C. & Behar, L. (Eds.). (2015). Handbook of oncology social work: Psychosocial care for people with cancer . New York: Oxford University Press.
- Clark, E. J. & Collins, S. (2015). NASW and oncology social work. In G. H. Christ , C. Messner , & L. Behar (Eds.), Handbook of oncology social work: Psychosocial care for people with cancer (pp. 763–768). New York: Oxford University Press.
- Curran, J. A. & Cockerill, E. (1948). Widening horizons in medical education: A study of the teaching of social and environmental factors in medicine, 1945–1946 . New York, NY: The Commonwealth Fund.
- Cwikel, J. , Behar, L. , & Rabson-Hare, J. (2000). A comparison of a vote count and a meta-analysis review of intervention research with adult cancer patients. Research on Social Work Practice , 10 , 139–158.
- Davis, C. , Emerson, J. S. , & Husaini, B. A. (2005). Breast cancer screening among African American women: Adherence to current recommendations. Journal of Healthcare for the Poor and Underserved , 16 (2), 308–314.
- Ell, K. , Sanchez, K. , Vourlekis, B. , Lee, P. J. , Dwight-Johnson, M. , Lagomasino, I. , et al. (2005). Depression, correlates of depression, and receipt of depression care among low-income women with breast or gynecologic cancer. Journal of Clinical Oncology , 23 (13), 3052–3060.
- Ell, K. , Vourlekis, B. , Lee, P. J. , Xie, B. (2007). Patient navigation and case management following an abnormal mammogram: A randomized clinical trial. Preventive Medicine , 44 (1), 26–33.
- Faller, H. , Schuler, M. , Richard, M. , Heckl, U. , Weis, J. , & Kuffner, R. (2013). Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: Systematic review and meta-analysis. Journal of Clinical Oncology , 31 (6), 782–793.
- Fawzy, F. (1989). Psychoeducational interventions. In J. C. Holland (Ed.), Psycho-oncology (pp. 676–693). New York, NY: Oxford University Press.
- Fobair, P. , Hoppe, R. T. , Bloom, J. , Cox, R. , Varghese, A. , & Spiegal, D. (1986). Psychosocial problems among survivors of Hodgkin’s disease. Journal of Clinical Oncology , 4 (5), 805–814.
- Fobair, P. , Stearns, N. , Christ, G. , Dozier-Hall, D. , Newman, N. , Zabora, J. , et al. (2009). Historical threads in the development of oncology social work. Journal of Psychosocial Oncology , 27 , 155–215.
- Fu, W. W. , Popovic, M. , Agarwal, A. , Milakovic, M. , Fu, T. S. , McDonald, R. , et al. (2016). The impact of psychosocial intervention on survival in cancer: A meta-analysis. Annals of Palliative Medicine , 5 (2), 93–106.
- Gehlert, S. (2006). The conceptual underpinnings of social work in health care. In S. Gehlert & T. A. Browne (Eds.), Handbook of health social work (pp. 3–22). Hoboken, NJ: John Wiley.
- Gehlert, S. , Mininger, C. , & Ciriano-Steffens, T. M. (2010). Placing biology in breast cancer disparities research. In Communities, neighborhoods and health (pp. 57–72). New York: Springer.
- Gehlert, S. , Sohmer, D. , Sacks, T. , Mininger, C. , McClintock, M. , & Olopade, O. (2008). Targeting health disparities: A model linking upstream determinants to downstream interventions. Health Affairs , 27 (2), 339–349.
- Gehlert, S. , Walters, K. , Uehara, E. & Lawlor, E. (2015). The case for a national health social work practice-based research network in addressing health equity. Health and Social Work , 40 (4), 253–255.
- Glaser, B. , & Strauss, A. (1965). Awareness of dying . Chicago: Aldine.
- Glaser, B. , & Strauss, A. (1968). Time for dying . Chicago: Aldine.
- Graves, K. (2003). Social cognitive theory and cancer patients’ quality of life: A meta-analysis of psychosocial intervention components. Health Psychology , 22 , 210–219.
- Harper, B. C. (1975). Social aspects of cancer recovery. Cancer , 3 (1), 1–2.
- Harper, B. C. (1977/1994). Death: The coping mechanisms of the health professional . Greenville, SC: Southeastern University Press.
- Haynes, M. A. , & Smedley, B. D. (1999). The unequal burden of cancer: An assessment of NIH research and programs for ethnic minorities and the medically underserved . Washington, DC: Institute of Medicine, National Academy Press.
- Hedlund, S. (2015). Oncology social work: Past, present, and future. In G. H. Christ , C. Messner , & L Behar (Eds.), Handbook of oncology social work: Psychosocial care for people with cancer (pp. 9–13). New York: Oxford University Press.
- Holland, J. C. (1998). Societal views of cancer and the emergence of psycho-oncology . In J. C. Holland (Ed.), Psycho-oncology (pp. 3–15). New York: Oxford University Press.
- Jacobsen P. B. , & Ransom, S. (2007). Implementation of NCCN distress management guidelines by member institutions. Journal of the National Comprehensive Cancer Network , 5 (1), 99–103.
- Jones, B. L. , Parker-Raley, J. , & Barczyk, A. (2011). Adolescent cancer survivors: Identity paradox and the need to belong. Qualitative Health Research , 21 (8), 1033–1040.
- IOM . (2006). From cancer patient to cancer survivor: Lost in transition . Washington, DC: National Academies Press.
- IOM . (2008). Cancer care for the whole patient: Meeting psychosocial health needs . Washington, DC: National Academies Press.
- IOM . (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis . Washington, DC: National Academies Press.
- Kayser, K. , Cheung, P. K. H. , Rao, N. , Chan, Y. C. L. , Yu Chan, Y. , & Lo, P. (2014). The influence of culture on couples coping with breast cancer: A comparative analysis of couples from China, India, and the United States. Journal of Psychosocial Oncology , 32 (3), 264–288.
- Kayser, K. , Feldman, B. N. , Borstelmann, N. , & Daniels, A. (2010). The effects of a randomized couple-based intervention on the quality of life of breast cancer patients and their partners. Journal of Social Work Research , 34 (1), 20–32.
- Kayser, K. , & Sormanti, M. (2002). Identity and the illness experience: Issues faced by mothers with cancer. Illness, Crisis, and Loss , 10 , 10–26.
- Kiegher, S. M. (2000). Knowledge development in health and social work. Health Social Work , 25 (1), 3–8.
- Kraweick, V. , & Greer, G. (2015). The American Cancer Society’s contributions to oncology social work. In G. H. Christ , C. Messner , L. Behar (Eds.), Handbook of oncology social work: Psychosocial care for people with cancer (pp. 745–750). New York: Oxford University Press.
- Lee, H. Y. & Vang, S. (2010). Barriers to cancer screening among Hmong Americans: The influence of health care accessibility, culture and cancer literacy. Journal of Community Health , 35 , 302.
- Lewis, F. M. , Behar, L. C. , Anderson, K. H. , Shands, M. E. , Zehlis, E. H. , Darby, E. , et al. (2000). Blowing away the myths about the child’s experience with the mother’s breast cancer. Cancer and the Family , 2 , 201–221.
- Luria, M. , Clark, E. , Hermann, J. , & Stearns, N. (2001). Social work in oncology: Supporting survivors, families and caregivers . Atlanta: American Cancer Society.
- McQuellon, R. P. , & Danhauer, S. C. (2006). Psychosocial rehabilitation in cancer care. In A. E. Chang , P. A. Ganz , D. F. Hayes , T. J. Kinsella , H. I. Pass , J. H. Schiller , et al. (Eds.), Oncology (pp. 1942–1954). New York: Springer.
- Meyer, T. J. , & Mark, M. M. (1995). Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychology , 14 (2), 101–108.
- NASW . (2003). Barriers of translating oncology research to social work practice. NASW in partnership with NCI. Washington, DC: NASW.
- NCCN . (2016). National comprehensive cancer network .
- Oktay, J. S. (2005). Breast cancer: Daughters tell their stories . New York: Haworth.
- Oktay, J. S. (2012). Grounded theory . New York: Oxford University Press.
- Oktay, J. S. , Nedjat-Haiem, F. , Davis, C. , & Kern, K. (2012). Distress screening: Experiences of oncology social workers. Journal of Psychosocial Oncology , 30 (6), 652–666.
- Oktay, J. S. , & Volland, P. J. (1987). Foster home care for the frail elderly as an alternative to nursing home care: an experimental evaluation. American Journal of Public Health , 77 (12), 1505–1510.
- Oktay, J. S. , & Volland, P. J. (1990). Post-hospital support program for the frail elderly and their caregivers: A quasi-experimental evaluation. American Journal of Public Health , 80 (1), 39–46.
- Oktay, J. S. , & Walter, C. A. (1991). Breast cancer in the life course: Women’s experiences . New York: Springer.
- Roberts, C. , Brintzenhofe-Socz, K. , Zebrack, B. & Behar, L. (2003). A social work guide to conducting research in psychosocial oncology . Philadelphia: AOSW.
- Rohan, E. A. , & Bausch, J. (2009). Climbing Everest: Oncology work as an expedition in caring. Journal of Psychosocial Oncology , 27 (1), 84–118.
- Rohan, E. A. , Berkman, B. , Walker, S. , & Holmes, W. (1995). The geriatric cancer patient: Ageism in social work practice. Journal of Gerontological Social Work 23 (1–2), 201–222.
- Schneider, S. , Moyer, A. , Knapp-Oliver, S. , Sohl, S. , Cannella, D. , & Targhetta, V. (2010). Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: A meta-analysis. Journal of Behavioral Medicine , 33 , 1–14.
- Siegel, K. , Mesagno, F. P. , Karus, D. , & Christ, G. , Banks, K. , & Moynihan, R. (1992). Psychosocial adjustment of children with a terminally ill parent. Journal of the American Academy of Child & Adolescent Psychiatry , 31 (12), 327–333.
- Simmons School of Social Work . (2016). The evolution of social work: Historical milestones .
- Smith, S. , Zimmerman, S. , Williams, C. S. , Preisser, J. S. , & Clipp, E. C. (2008). Post-traumatic stress outcomes in Non-Hodgkin’s Lymphoma survivors. Journal of Clinical Oncology , 26 (6), 934–941.
- Specht, H. , & Courtney, M. (1994). Unfaithful angels: How social work has abandoned its mission . New York: Free Press.
- Spiegel, D. , Bloom, J. R. , Kramer, H. C. , & Gottheil, E. (1989). Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet , 2 (8668), 888–891.
- Stearns, N. , Lauria, M , Hermann, J. & Fogelberg, P. (1993). Oncology social work: A clinician’s guide . Atlanta: American Cancer Society.
- Vaitones, V. , Schutte, J. , & Mattison, D. (2015). OSW-C: The importance of certification for oncology social workers. In G. H. Christ , C. Messner , L Behar (Eds.), Handbook of oncology social work: Psychosocial care for people with cancer (pp. 757–762). New York: Oxford University Press.
- Weiner, L. , Battles, H. B. , Bernstein, D. , Long, L. , Mansky, P. , & Mackall, C. (2006). Persistent psychological distress in long-term survivors of pediatric sarcoma. Psycho-oncology , 15 , 898–910.
- Weisman, A. D. , Worden, J. W. , & Sobel, H. J. (1980). Psychosocial screening and intervention with cancer patients: A research report . Boston: Harvard Medical School.
- Wells, A. A. , Shon, E. J. , McGowan, K. , & James, A. (2015). Perspectives of low-income African-American women non-adherent to mammography screening: the importance of information, behavioral skills, and motivation . Journal of Cancer Education , 32 (2).
- Werner-Lin, A. (2007). Danger zones: Risk perceptions of young women from families with hereditary breast and ovarian cancer. Family Process , 46 , 335–349.
- Werner-Lin, A. (2015). The oncology social worker and genomics. In G. H. Christ , C. Messner , & L. Behar (Eds.), Handbook of oncology social work: Psychosocial care for people with cancer (pp. 255–260). New York: Oxford University Press.
- Werner-Lin, A. , McCoyd, J. L. , Doyle, M. H. , & Gehlert, S. J. (2016). Leadership, literacy, and translational expertise in genomics: Challenges and opportunities for social work . Health Social Work , 41 (3), e52–e59.
- Yalom, I. D. (1970). The theory and practice of group psychotherapy . New York: Basic Books.
- Zabora, J. R. , Smith-Wilson, R. , Fetting, J. H. , & Enterline, J. P. (1990) An efficient method for psychosocial screening of cancer patients. Psychosomatics , 31 (2), 192–196.
- Zabora, J.R. , Brintzenhofe-Szoc, K. , Curbow, B. , Hooker, C. & Piantadosi, S. (2001) The prevalence of psychological distress by cancer site. Psycho-Oncology 10(1) 19-28.
- Zabora, J. R. & MacMurray, L. (2012). The history of psychosocial screening among cancer patients. Journal of Psychosocial Oncology , 30 (6), 625–635.
- Zebrack, B. (2011). Psychological, social, and behavioral issues for young adults with cancer. Cancer , 117 (S10), 2289–2294.
- Zebrack, B. , & Isaacson, S. (2012). Psychosocial care of adolescent and young adult patients with cancer and survivors. Journal of Clinical Oncology , 30 (11), 1221–1226.
- Zebrack, B. , Kayser, K. , Padgett, L. S. , Sundstrom, L. , Jobin, C. , Nelson, K. , et al. (2016). Institutional capacity to provide psychosocial oncology support services: A report from the Association of Oncology Social Work. Cancer , 122 (12), 1937–1945.
- Zebrack, B. , Kayser, K. , Sundstrom, L. , Savas, S. , Henrickson, C. , Acquati, C. , et al. (2015). Psychosocial distress screening implementation in cancer care: An analysis of adherence, responsiveness, and acceptability. Journal of Clinical Oncology , 33 (10), 1165–1170.
- Zebrack, B , Walsh, K. , Burg, M. A. , Maramaldi, P. , & Lim, J. (2008). Oncology social worker competencies and implications for education and training. Health and Social Work , 47 (4), 355–375.
- Zimbalist, S. E. (1977). Historic themes and landmarks in social welfare research . New York: Harper & Row.
- Zlotnik, J. L. , Biegel, D. , & Solt, B. E. (2002). The Institute for the Advancement of Social Work Research: Strengthening social work research in practice and policy. Research on Social Work Practice , 12 (2), 318–337.
- Zlotnik, J. L. , & Solt, B. E. (2006, September). The Institute for the Advancement of Social Work Research working to increase our practice and policy evidence base. Research on Social Work Practice , 16 (5), 534–539.
- Zlotnik, J. L. , & Solt, B. E. (2008). Developing research infrastructure: The Institute for the Advancement of Social Work Research. Social Work Research , 32 (4), 201–207.
Other Resources
- New & Featured
- Forthcoming Articles
Printed from Encyclopedia of Social Work. Under the terms of the licence agreement, an individual user may print out a single article for personal use (for details see Privacy Policy and Legal Notice).
date: 25 April 2024
- Cookie Policy
- Privacy Policy
- Legal Notice
- Accessibility
- [66.249.64.20|185.80.150.64]
- 185.80.150.64
Character limit 500 /500
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Everything to Know About Oncology Social Workers
- What They Do
- How to Get Help
Frequently Asked Questions
When someone is diagnosed with cancer , the focus is usually on finding the most successful treatment options. But there’s more to dealing with cancer than medical therapies and procedures. Cancer may affect a person emotionally, socially, and financially, too. That’s when oncology social workers can help.
Oncology social workers are skilled professionals who provide emotional, psychological, social, and practical support for cancer patients. They help patients navigate different resources and unpack useful information. These experts address the patient as a whole, instead of only focusing on medical treatment.
This article discusses the role of oncology social workers as advocates for people with cancer.
SDI Productions / Getty Images
What Do Oncology Social Workers Do?
Oncology social workers perform a wide range of services, some of which include:
- Providing information to patients about their disease
- Helping patients explain their cancer diagnosis to family and friends
- Performing counseling services
- Leading or recommending support groups
- Acting as a mediator for patient/caregiver disputes
- Offering resources for financial assistance
- Explaining medical insurance coverage
- Helping patients find transportation to healthcare appointments
- Teaching patients how to perform relaxation and coping strategies
Oncology Social Workers and Research
Oncology social workers are becoming more involved in research, including leading research studies designed to improve patients' quality of life.
Managing Practical Concerns
Oncology social workers can help cancer patients sort out different practical or logistical issues. These professionals are trained to effectively explain a cancer diagnosis and treatments to patients and their family members.
Additionally, they may help patients pay their bills, understand their insurance coverage, or find resources for financial assistance. Sometimes, this involves showing patients how to fill out the necessary paperwork or requesting coverage information from insurance companies.
Oncology social workers can also help patients secure home care services, transportation, and childcare.
Providing Emotional Support
A cancer diagnosis can be psychologically challenging. An oncology social worker helps patients with their emotional needs. They can arrange hospice services (comfort care for patients at the end of life) or provide support for patients who are transitioning to survivorship (care after diagnosis and treatment).
Counseling is one tool social workers use to help patients cope with their stress and anxiety. A counseling session provides a safe space for patients to talk about worries and concerns. Social workers may also teach patients relaxation strategies, such as deep breathing, to help them manage their emotions.
Sometimes, social workers will suggest support groups, so patients can connect with others who are also affected by cancer.
How to Get Help From an Oncology Social Worker
Cancer patients who are interested in working with an oncology social worker might want to first ask their healthcare provider for a recommendation. Many nursing homes or hospice facilities have social workers on staff.
Some resources for finding an oncology social worker include:
- Association of Oncology Social Work
- American Cancer Society
Virtual vs. In-Person Oncology Social Workers
Oncology social workers are available both online or via face-to-face appointments. Your decision will depend on your level of comfort with in-person contact.
How to Become an Oncology Social Worker
Becoming an oncology social worker involves fulfilling many different requirements, which can vary from state to state.
In general, someone who wants to become an oncology social worker might expect to complete the following steps:
- Earn a bachelor’s degree
- Earn a master’s degree in social work (specializing in oncology)
- Complete field work requirements (the number of hours required differs by state)
- Get a state license
Additionally, some universities and programs offer optional certifications that can be added to an individual’s credentials.
Oncology social workers help patients deal with both the practical and emotional side of cancer care. This professional can provide much-needed support for patients and their families.
Oncology social workers earn advanced education degrees and participate in real-life field work before they can practice their trade. Working with an oncology social worker may help improve the quality of life for people with cancer.
A Word From Verywell
Being diagnosed with cancer can be devastating. To help you cope, you may benefit from working with an oncology social worker. This expert can advocate for better care, provide necessary resources, and make sure your emotional needs are met. Ask your healthcare provider if you’re interested in adding an oncology social worker to your medical care team.
An OSW (oncology social work) certification is a type of accreditation for oncology social workers. It signifies an advanced level of expertise and dedication in the field.
Pediatric oncology social workers work with children who have been diagnosed with cancer. They provide support and resources for kids and their families.
Specific credentials are required to become an oncology social worker. You can learn more about the prerequisites here .
American Society of Clinical Oncology. Spotlight on oncology social workers .
Dana-Farber Cancer Institute. How can social workers help cancer patients? .
CancerCare. The value of oncology social workers .
Social Work License Map. How to become an oncology social worker .
Association of Oncology Social Work. OSW-C certification .
By Julie Marks Marks is a Florida-based freelance health writer with a bachelor's degree in broadcast journalism and creative writing.

- Cancer Education
How an Oncology Social Worker Can Help
Share this:.
For people diagnosed with cancer, an oncology social worker is an important member of the health care team. An oncology social worker provides counseling, education and information services, referrals to community resources and helps people navigate the health care system.
Taking Care of the Whole Person
For most people, a cancer diagnosis brings new feeling and experiences, and an oncology social worker can help people work through these aspects following a cancer diagnosis. An oncology social worker understands that there are many aspects of a person's life that contribute to his or her cancer experience, such as a person's ethnicity, spirituality, and family situation, and that cancer affects each person in a different way. He or she talks to people about the different aspects of adjusting to the cancer and helps find strategies to adapt to and manage health care concerns. Talking with a professional who has helped other people manage similar situations may help a person find ways to improve his or her quality of life, manage fears, and find hope. This process can happen through individual, couples and family counseling, support groups, and referrals to community agencies that have additional support programs.
Understanding New Roles and Responsibilities
A person with cancer may wonder how parents, children, friends and coworkers will react to the diagnosis. An oncology social worker can help a person cope with these reactions. People may also wonder if there will be changes in their ability and desire to keep up with the many responsibilities of their life, such as a demanding job, taking care of young children, or helping an older parent. A social worker can arrange a meeting to talk about how those roles and responsibilities might change, and explore what kind of support a person may need while going through treatment.
Helping with Relationships
People living with cancer have questions about how their treatment will affect their relationship with their spouse or partner, as well as with their children or other family members. An oncology social worker can provide couples other relationship counseling, during which people with cancer and their partners or family members may talk about the emotional changes they are going through, how they want to handle those changes, and what kind of support they want from each other and from other people.
A Bridge to the Medical Care Team
Another role of an oncology social worker is a liaison between the person with cancer and the medical team. Because an oncology social worker has advanced training in cancer treatment and how these treatments affect a person with cancer, he or she can help people and their families understand the treatment options. For example, an oncology social worker helps gather and organize the information people need to make decisions about their care and arrange a meeting with the patient, family members, and the medical team to discuss the patient's care and treatment options. A social worker can also refer people to additional education resources and to community organizations that have information about cancer and treatment.
Accessing Resources
An oncology social worker helps people connect to the resources they need to find practical help such as transportation, housing, financial assistance, community resources and support groups. For some people, this involves a referral to the financial aid office of the clinic, instructions for applying for disability, or an explanation of rights covered under the Family Medical Leave Act.
Prescription Assistance
Sometimes the cost of medications and cancer treatments can be expensive and at times appear inaccessible. Our social work staff assists patients with location co-pay assistance programs through pharmaceutical companies or foundations. In some situations, a patient's treatment may include a medication that is considered to be off label which is not covered by most insurance companies. Social work staff can assist patients in navigating the off label process as well as exploring available options in making these medications accessible.
Adjusting to Changes
The oncology journey can take many unexpected turns. The oncology social worker is there to provide support to families and patients throughout this journey including end of life issues beyond treatment.
Many find that the months after completing cancer treatment are especially difficult. In addition to a slow physical recovery, there often are intense worries about future health and returning to a more normal life. Oncology social workers can continue to work with individuals through the period of survivorship, and many people find this an ideal time to process the experience. Others may join a support group for survivors and receive understanding and guidance from other people in similar situations.
Advance Care Planning
Advance Care Planning is a resource that is provided to our patients and families at no charge. Trained Advance Care Planning Facilitators provide education and assist patients and families with completing documents as a living will and designation of a health surrogate. Discussion of quality of life and treatment preferences are a very important part of this consult.
The Education of Oncology Social Workers
Oncology social workers have a Masters Degree in Social Work (MSW) from an accredited university. In addition they are licensed clinical social workers which means they have at least two additional years of training and supervision in working with people in a clinical setting. They also have training in cancer care through continuing education and extensive orientation.
If you feel you could benefit from meeting with an oncology social worker, ask your provider for an appointment to meet with one.
Related links:
- Cancer online support group
- Support Group Directory
- Copy link to clipboard
- Report newsfeed post
Interested in more newsfeed posts like this? Go to the Cancer Education blog.

Do most hospitals and oncology practices have an oncology social worker? If not, where can a patient find one?
- Report comment

Jump to this post
Becky, social workers who specialize in oncology are commonly a member of the cancer care team at cancer centers and large oncology department.
@michellewalsh , can you share how patients get referred or can self-refer to an oncology social worker at Mayo Clinic?

Hello Becky, Thank you for your question. The role of the social worker many times depends on the provider and location. Hospitals usually have social workers on staff to assist with discharge planning when patients need further assistance. Many larger oncology centers have licensed clinical social workers on staff to assist patients for a variety of reasons during and after treatments. Patients and caregivers should ask if this service is available in their center and request a consult if needed. If your center does not have a social worker on staff, some organizations can assist you with locating a counselor or social worker that is covered by your insurance and can meet your needs. The Association of Oncology Social Workers provides a list of resources for patients and their families. Many non-profit organizations offer free services online and by phone/video.
Some of the non-profit organizations that can provide assistance in locating a counselor or providing free services include: Cancer Support Community ( https://www.cancersupportcommunity.org/cancer-support-helpline ) Cancer Care ( https://www.cancercare.org/casemanagement ) Be The Match ( https://bethematch.org/patients-and-families/support-for-you-and-your-family/one-on-one-support/counseling-services/ ) Leukemia and Lymphoma Society ( http://https.org/support/other-helpful-://www.llsorganizations/patient-and-caregiver-resources-support-and-counseling )
I hope these resources are helpful. Michelle Walsh, LCSW Oncology Social Worker
@michellewalsh , such a wealth of information. Thank you. I also want to underline your point that social work services are available not only to the patient, but also for the caregivers or care partners support the patient. So important for family members to know.
Thanks, but cancer is not the problem now...only complications from radiation damage in the 80's. Now it is drastic heart failure. My 66 year old daughter takes handfuls of medications, but still breath getting shorter, energy lower. Needs heart transplant, but radiation scarring makes operation too risky, according to Oklahoma Heart Institute. Am hoping research on right ventricle insert (?) might be able to help. Thanks for listening. Ida Lundy
Thanks for posting this article. I feel like I have been holding my breath since Oct 2019. My treatments were working for a while and then in March 2020 same time as COVID hit my treatments stopped working. Started another treatment, while on that one everything was going well. Then a few months later that treatment also stopped working. Now on yet another treatment plan. At the Mayo Clinic that I go to I was given a list of groups, however none of them seem to fit my cancer diagnosis. I do not recall there being an Oncology Social Worker being offered, there may have been. I feel I need someone to talk to to help me thru all of this.
Hi Ida, I'm sorry to hear that your daughter is still dealing with radiation damage from cancer treatments, resulting in drastic heart failure. Cancer treatment-induced heart disease does happen. There is a discussion on Mayo Clinic Connect dedicated to it here: - Cancer Treatment Induced Heart Disease https://connect.mayoclinic.org/discussion/radiation-induced-heart-disease/
The cancer education team also posted a related blog and video here on Mayo Clinic Connect. See – Cancer Treatment and the Heart https://connect.mayoclinic.org/page/cancer-education-center/newsfeed-post/cancer-treatment-and-the-heart-1/
Has your daughter been seen at a Cardio-Oncology clinic? Have you and your daughter considered a second opinion regarding her qualification for a heart transplant? May I ask what type of cancer your daughter had?
Mayo Clinic patients or family members can ask their provider, nursing staff or front desk staff to send the social work department a note that they would like to see a social worker and we will schedule a consult.
You can also call the social work department directly at the location where you are seen at Mayo Clinic Mayo Clinic Florida: 904-953-6831 Mayo Clinic Minnesota: 507-284-2131 Mayo Clinic Health System: 715-838-3139
She goes to the advanced heart failure clinic in the Oklahoma Heart Institute. Have not had a second opinion. Type of cancer was breast cancer. Radiation protocol at the time was irradiating the medialstinal nodes and subclavicular nodes. She had an aortic valve replacement, biological, in 2015 and shortly thereafter went into right heart failure. Multiple pleural effusions with chest tubes that caused more scarring. Oklahoma Heart says there is too much scar tissue for a heart transplant. She has a mitral clip to reduce regurgitation, a synchronizing pacemaker with a defibrillator and cardio-mem in the pulmonary artery. If you feel that it would be worth pursuing, we would like to hear from you. We are also very interested in research on right-heart pump. Thank you.
As an addendum to our previous comments.... . Being a retired nurse she can speak way better about medical issues than I can at my 91 years. Thanks so much for your reply.

Connect with thousands of patients and caregivers for support and answers.
- Hosted and moderated by Mayo Clinic.
- Safe and secure.
Already have an account? Sign In

Scope and Standards of Practice
Scope of practice in oncology social work.
The scope of practice in oncology social work, as identified in the AOSW Standards of Practice, includes:
- Services to cancer survivors, families and caregivers through clinical practice providing comprehensive psychosocial services and programs through all phases of the cancer experience
- Services to institutions and agencies to increase their knowledge of the psychosocial, social, cultural and spiritual factors that impact coping with cancer and its effects, and to insure provision of quality psychosocial programs and care
- Services to the community through education, consultation, research and volunteering to utilize, promote or strengthen the community services, programs and resources available to meet the needs of cancer survivors
- Services to the profession to support the appropriate orientation, supervision and evaluation of clinical social workers in oncology; participate in and promote student training and professional education in oncology social work; and advance knowledge through clinical and other research
Oncology social workers are knowledgeable about cancer and about the psychosocial and other effects of disease, treatment, and survivorship. They are generally masters prepared and often have experience and training in oncology and other life-threatening illnesses. They practice in accord with the values of the profession using the guidelines offered in the National Association of Social Work’s Code of Ethics . Oncology social workers have goals in each area of practice and carry out critical functions to achieve those goals. What follows is a listing of common goals and functions.
1. Services to Survivors, Families, and Caregivers
The goals of clinical practice with survivors, families and caregivers are:
- Fostering coping and adaptation to cancer and its effects in order to help cancer survivors maintain or improve quality of life
- Assisting survivors in navigating through health care systems to help them achieve quality care
- Mobilizing new or existing family, system and community resources to provide social and emotional support to cancer survivors
- Conducting research to advance clinical knowledge or evaluate practice effectiveness
- Advocating with, or on behalf of, survivors, families and caregivers to address their needs or for policies and programs that will benefit them
The functions of clinical practice are:
- Use of high risk screening criteria to identify survivors and families in need of Social Work services.
- Completion of a psychosocial assessment to determine survivor and family’s strengths and needs relative to coping effectively with cancer diagnosis, treatment and follow-up cares.
- Development of a multidisciplinary care plan with survivor and family input and based on mutual goals.
- Use of a range of therapeutic and other interventions, including supportive counseling, group work, and education to address issues in each phase of the illness.
- Provision of pre-admission, transfer, and discharge planning.
- Provision of case management services.
- Provision of direct assistance to meet financial, transportation, lodging and other needs.
- Advocacy to remove barriers to quality care, to address gaps in service, to help survivors and families secure the protection of existing laws, and to work for any changes needed to policies, programs and legislation.
- Involvement conducting and publishing research to advance knowledge about the impact of cancer, refine interventions, and evaluate practice outcomes.
2. Services to Institutions and Agencies
The goals of practice in providing to institutions and agencies are:
- To insure that the agencies and institutions are responsive to the needs of both individual cancer survivors, families and caregivers, as well as groups
- To contribute the multidisciplinary effort to provide quality medical psychosocial care to oncology survivors
- To assist social work colleagues and members of other disciplines to manage the stress of clinical practice
The functions necessary to such services are:
- Education and consultation to professionals and staff regarding the biopsychosocial, environmental, spiritual, and cultural factors affecting cancer care.
- Collaboration with other professionals in the delivery of quality psychosocial care, education and research.
- Recording, statistical reporting, and evaluation to improve services, assist in identifying gaps in services and programs, and assure quality care.
- Development of programs and resources to address the needs of cancer survivors.
- Provision of support services to aid in stress management.
3. Services to the Community
The goals of oncology social work practice related to the community are:
- To assure that community programs and resources address and are responsive to the needs of cancer survivors, families, and caregivers.
- To provide oncology social work expertise to communities as they work to assist cancer survivors.
The functions of oncology social workers working with communities are:
- Education of communities to increase awareness of the psychosocial needs of cancer survivors, families, and caregivers.
- Collaboration with community agencies to remove barriers to cancer prevention, screening and early detection, and access to care.
- Collaboration in the development of special programs and resources to address community-based needs.
- Consultation with voluntary cancer agencies, such as the American Cancer Society and the Leukemia and Lymphoma Society to provide community education and develop programs to benefit cancer survivors.
4. Services to the Profession
The goals of providing services to the profession are:
- To assure that oncology social workers have the necessary knowledge, skills, resources, time, funding and support to deliver quality psychosocial services to all cancer survivors, families and caregivers.
The functions of oncology social workers working to serve the profession are:
- Teaching oncology social work trainees in the classroom or in clinical settings.
- Orientation, supervision and evaluation of practitioners in oncology social work.
- Consultation with colleagues via telephone networking, conferences, or on listservs.
- Presentation of or participation in continuing professional education specific to oncology social work practice.
- Publishing research findings and clinical observations.
- Clinical practice and research in accord with NASW’s Code of Ethics .
- Participation in oncology and social work organizations.
Standards of Practice in Oncology Social Work
Oncology social work is the primary professional discipline that provides psychosocial services to patients, families and significant others facing the impact of a potential or actual diagnosis of cancer. The scope of oncology social work includes clinical practice, education, advocacy, administration, policy and research. The standards of practice provided in this document are intended for clinical social workers practicing in the specialty of oncology social work.
The Masters in Social Work degree provides oncology social workers with theoretical knowledge, clinical expertise and practical significant others. In addition, oncology social workers often receive specialized training in cancer care through clinical supervision, continuing education, in-service training and on-the-job experience.
Psychosocial services provided by oncology social workers include individual, family and group counseling, education, advocacy, discharge planning, case management, patient-navigation and program development. These services are designed to maximize the patient’s utilization of the health care system, foster coping, mobilize community resources in order to support optimal functioning, and empower the patient and family to be active participants in health care decisions and management.
Oncology social work services are available to patients and families throughout all phases of the cancer continuum, including prevention, diagnosis, treatment, survivorship, palliative care, end-of-life care and bereavement. Services are delivered in a wide variety of settings including specialty cancer centers, community hospitals and health systems, ambulatory centers, home health and hospice programs, community-based agencies and private practice settings.
Oncology social workers are an integral part of the health care team and contribute to the development and coordination of the overall treatment plan. In collaboration with the patient and family and other health care disciplines, oncology social workers provide counseling, education, discharge planning, case management and navigation, linking patients with a variety of services necessary to meet the person’s multiple needs.
In addition to services to patients and families, oncology social workers address organizational and community needs through professional practice. Services are provided to institutions, voluntary health organizations, and community agencies with the overall aim of promoting health and safety, and improving the delivery of care to individuals at risk for or affected by cancer.
Oncology social workers embrace patient- and family-centered care at all levels of practice. Social work training and professional values are congruent with this approach at the clinical level and position oncology social workers to substantially contribute the development of a health care environment that embodies the core concepts of patient- and family-centered care organizationally. This approach includes: respect for patients’ values, preferences and expressed needs; coordinated and integrated culturally competent care; timely, affirming and useful information, communication and education; individualized care; physical comfort, emotional support, involvement of family and friends, shared decision-making and collaboration with patients and families in the evaluation, planning and delivery of care.
Standard I. Qualifications
Oncology social workers shall be knowledgeable about oncologic diseases and their treatments, psychosocial implications for individuals and families, appropriate interventions and available community and governmental resources. Oncology social workers must have knowledge of the usual course of cancer and its treatment, including genetics, so that patients and families can be helped to anticipate and deal with changes in individual and family life.
The oncology social worker shall be masters prepared from a graduate program accredited by the Council on Social Work Education. It is preferred that the graduate have had prior employment or field placement experience in a health care setting.
Standard II. Services to Patients and Families
Oncology social work programs shall provide the following clinical and programmatic services:
B. Completion of a psychosocial assessment of the patient and family’s response to the cancer diagnosis and treatment to include:
2. Knowledge about cancer and its treatment including level of understanding, reactions, goals for care and expectations.
3. Characteristics of the patient’s support system, including family, related biologically, legally, or emotionally.
4. Patient and family psychosocial functioning including strengths, limitations and coping skills.
5. Race, ethnicity, religion, culture, language, physical or mental disability, socioeconomic status, sex sexual orientation, and gender identity or expression.
6. Identification of barriers to care.
7. The source, availability, and adequacy of community resources.
8. Patient and family level of interest in participation in care and decision-making.
9. Development of a case plan with patient and family based on mutually agreed upon goals to enhance, maintain and promote optimal psychosocial functioning throughout cancer treatment and its outcome.
C. Utilization of a wide range of clinical interventions designed to address current and/or future problems as the patient’s medical and psychosocial needs evolve.
D. Outreach activities to vulnerable populations.
E. Maintenance of knowledge of community resources and governmental programs available from local, state, and national health and social service agencies including expertise in accessing these for patients and families.
F. Organization and facilitation of patient and family education.
G. Utilization of knowledge and clinical skills in assisting the patient and family with advance care planning and advance directives.
H. Pro-active provision of services to at-risk populations, including assistance with negotiating barriers to cancer information, screening, treatment and resources within the institution and in the community.
I. Collaboration with patients and family members who serve as advisors in policy and program development, implementation and evaluation; health care facility design; professional education, and the delivery of care.
J. Collaboration with other professional disciplines in the planning and provision of timely and efficient clinical services to cancer patients and their families.
K. Advocacy for and protection of patients’ dignity, confidentiality, rights, and access to care.
L. Development and utilization of research to improve clinical practice and implement evidence-based psychosocial support programs, services and interventions.
Standard III. Services to Institutions and Agencies
Oncology social work programs shall address institutional and agency needs including the following:
B. Collaboration with other disciplines and staff in the areas of psychosocial clinical services, patient-and family-centered care, research and education.
C. Provision of services to professional caregivers which are designed to assist staff in the management of stresses inherent in clinical practice.
D. Utilization of clinical documentation, statistical reporting, and evaluation to improve services, assure quality and develop programs.
E. The advancement of the practice of patient-and family-centered care at the clinical and organizational levels.
F. Representation on Cancer Care and other related hospital committees.
Standard IV. Services to the Community
Oncology social work programs shall address community needs including the following:
B. Provision of services to at-risk populations, including navigation assistance with access to cancer information, screening, treatment and resources.
C. Provision of consultation and volunteer services to institutions, voluntary health organizations and community agencies to promote health, provide education, and develop programs to better serve the community.
Standard V. Services to the Profession
Oncology social work programs shall address the following needs of the profession and its practitioners:
B. Commitment to continuing professional education.
C. Promotion of professional practice in accord with the National Association of Social Workers (NASW) Code of Ethics .
D. Participation in student and professional training and education in the area of oncology social work.
E. Contribution to oncology social work through participation in professional associations.
F. Contribution to oncology social work knowledge base through psychosocial research, publications, presentations and evidence-based practice.
G. Pro-active provision of patient navigation services to at-risk populations, including assistance.
H. Collaboration with other professional disciplines in the planning and provision of timely and efficient clinical services to cancer patients and their families.
I. Development of research based knowledge that relates to clinical issues, interventions and outcomes.
Cancer and Oncology Social Work
- First Online: 15 July 2023

Cite this chapter
- Linda Mathew DSW 4 ,
- Jacob Maier 4 &
- Annamma Abraham Kaba 4
Part of the book series: Essential Clinical Social Work Series ((ECSWS))
254 Accesses
1 Citations
Cancer is a broad term that comprises dozens, if not hundreds, of diagnoses and illnesses. It is one of the leading causes of death worldwide. Cancer can be emotionally and physically devastating and the treatment process can be confusing and overwhelming. The role of the oncology social worker is to support patients and families as they process the diagnosis and make difficult decisions about treatment. This chapter aims to address the challenges oncology social workers face while working with patients with cancer. It will examine the complex emotions experienced by cancer patients at each phase of disease treatment, in bereavement, and in complex grief. It will also discuss social justice issues and healthcare disparities, and how the oncology social worker provides clinical interventions at all of these points.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
All names and other personal identifiers in the case are fictitious. Any similarity to actual persons, living or dead, or actual events is purely coincidental.
Abdalla, E., Troy, R., Fall, S., Elhussin, I., Egiebor-Aiwan, O., & Nganwa, D. (2020). Racial differences in 5-year relative survival rates of cervical cancer by stage at diagnosis, between African American (black) and white women, living in the state of Alabama, USA. BMC Cancer, 20 (1), 1–12. https://doi.org/10.1186/s12885-020-07338-7
Article Google Scholar
Al Hadidi, S., Mims, M., Miller-Chism, C. N., & Kamble, R. (2020). Participation of African American persons in clinical trials supporting US Food and Drug Administration approval of cancer drugs. Annals of Internal Medicine, 173 (4), 320–322. https://doi.org/10.7326/M20-0410
Article PubMed PubMed Central Google Scholar
Altillo, T., & Tropeano, L. E. (2015). Pain and symptom management. In G. Christ, C. Messner, & L. Behar (Eds.), Handbook of oncology social work: Psychosocial care of people with cancer (pp. 239–246). Oxford University Press.
Google Scholar
Arch, J. J., Vanderkruik, R., Kirk, A., & Carr, A. L. (2018). A closer lens: Cancer survivors’ supportive intervention preferences and interventions received. Psychooncology, 27 (5), 1434–1441. https://doi.org/10.1002/pon.4526
Article PubMed Google Scholar
Bahrami, M., Mohamadirizi, M., Mohamadirizi, S., & Hosseini, S. A. (2017). Evaluation of body image in cancer patients and its association with clinical variables. Journal of education and health promotion, 6 , 81. https://doi.org/10.4103/jehp.jehp_4_15
Bernstein, D. M. (2001). Therapist-patient relations and ethnic transference. In W.-S. Tseng & J. Streltzer (Eds.), Culture and psychotherapy: A guide to clinical practice (pp. 103–121). American Psychiatric Press.
Blacker, S., & Christ, G. H. (2011). Defining social work’s role and leadership contributions in palliative care. In T. A. S. Otis-Green (Ed.), Oxford textbook of palliative social work (pp. 21–30). Oxford University Press.
Chapter Google Scholar
Boerger-Knowles, K., & Ridley, T. (2014). Chronic cancer: Counseling the individual. Social Work in Health Care, 53 (1), 11–30.
Breitbart, W., Rosenfeld, B., Gibson, C., Pessin, H., Poppito, S., Nelson, C., et al. (2010). Meaning-centered group psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psychooncology, 19 (1), 21–28. https://doi.org/10.1002/pon.1556
Breitbart, W., Pessin, H., Rosenfeld, B., Applebaum, A. J., Lichtenthal, W. G., Li, Y., et al. (2018). Individual meaning-centered psychotherapy for the treatment of psychological and existential distress: A randomized controlled trial in patients with advanced cancer. Cancer, 124 (15), 3231–3239. https://doi.org/10.1002/cncr.31539
Cameron, M. (2014). This is common factors. Clinical Social Work Journal, 42 (2), 151–160.
Charlton, M., Schlichting, J., Chioreso, C., Ward, M., & Vikas, P. (2015). Challenges of Rural Cancer Care in the United States. Oncology (Williston Park, N.Y.), 29(9), 633–640.
Chu Foy, K., Fisher, J. L., Lustberg, M. B., Gray, D. M., DeGraffinreid, C. R., & Paskett, E. D. (2018). Disparities in breast cancer tumor characteristics, treatment, time to treatment, and survival probability among African American and white women. NPJ Breast Cancer, 4 (1), 1–6. https://doi.org/10.1038/s41523-018-0059-5
Damaskos, P., & Gerbino, S. (2014). Introduction to the special issue: Coping with chronic cancer: Clinical approaches for oncology social work practice. Social Work in Health Care, 53 (1), 1–4.
Damaskos, P., & Parry, C. (2015). Cancer survivorship: Concepts, interventions, and research. In G. Christ, C. Messner, & L. Behar (Eds.), Handbook of oncology social work: Psychosocial care of people with cancer (pp. 57–64). Oxford University Press.
Damaskos, P., Amaya, B., Gordon, R., & Walters, C. B. (2018). Intersectionality and the LGBT cancer patient. Seminars in Oncology Nursing, 34 (1), 30–36.
Daniels, J., & Kissane, D. W. (2008). Psychosocial interventions for cancer patients. Current Opinion in Oncology, 20 (4), 367–371. https://doi.org/10.1097/CCO.0b013e3283021658
Dougherty, L. (2007). Using nursing diagnoses in prevention and management of chemotherapy-induced alopecia in the cancer patient. International Journal of Nursing Terminologies and Classifications: The Official Journal of NANDA International, 18 (4), 142–149. https://doi.org/10.1111/j.1744-618X.2007.00069.x
Ernstmann, N., Neumann, M., Ommen, O., Galushko, M., Wirtz, M., Voltz, R., et al. (2009). Determinants and implications of cancer patients’ psychosocial needs. Supportive Care in Cancer, 17 (11), 1417–1423. https://doi.org/10.1007/s00520-009-0605-7
Ezra, E., & Chi, M. (2015). When the other shoe drops: Unique fears and challenges of recurrent disease. In G. Christ, C. Messner, & L. Behar (Eds.), Handbook of oncology social work: Psychosocial care of people with cancer (p. 107). Oxford University Press.
Fleishman, S. B., & Messner, C. (2015). Cancer in contemporary society: Grounding in oncology and psychosocial care. In G. Christ, C. Messner, & L. Behar (Eds.), Handbook of oncology social work: Psychosocial care of people with cancer (p. 1). Oxford University Press.
Floríndez, L. I., Floríndez, D. C., Como, D. H., Secola, R., & Duker, L. I. S. (2020). Differing interpretations of health care encounters: A qualitative study of non-Latinx health care providers’ perceptions of Latinx patient behaviors. Plos One, 15 (8), e0236706.
Godofredo, A. V. (2020). Racism, discrimination, and the practice of oncology. Lancet, 395 , 1813.
Hall, D. L., Luberto, C. M., Philpotts, L. L., Song, R., Park, E. R., & Yeh, G. Y. (2018). Mind-body interventions for fear of cancer recurrence: A systematic review and meta-analysis. Psychooncology, 27 (11), 2546–2558. https://doi.org/10.1002/pon.4757
Harley, C., Pini, S., Bartlett, Y. K., & Velikova, G. (2012). Defining chronic cancer: Patient experiences and self-management needs. BMJ Supportive & Palliative Care, 2 (3), 248–255.
Hartman, K. K. (2015). Diagnosis and initiation of cancer treatment. In G. Christ, C. Messner, & L. Behar (Eds.), Handbook of oncology social work: Psychosocial care of people with cancer (pp. 43–50). Oxford University Press.
Holland, J. C. (2002). History of psycho-oncology: Overcoming attitudinal and conceptual barriers. Psychosomatic Medicine, 64 (2), 206–221.
Kissane, D. W., McKenzie, M., Block, S., Moskowitz, C., McKenzie, D. P., & O’Neill, I. (2006). Family focused grief therapy: A randomized, controlled trial in palliative care and bereavement. The American Journal of Psychiatry, 163(7), 1208–1218.
Klitzman, R. L., & Greenberg, J. D. (2002). Patterns of communication between gay and lesbian patients and their health care providers. Journal of Homosexuality, 42 (4), 65–75. https://doi.org/10.1300/J082v42n04_04
Kyngäs, H., Mikkonen, R., Nousiainen, E. M., Rytilahti, M., Seppänen, P., Vaattovaara, R., & Jämsä, T. (2001). Coping with the onset of cancer: Coping strategies and resources of young people with cancer. European Journal of Cancer Care, 10 (1), 6–11.
Lawson, K. C., & Lawson, D. H. (2018). Insights into the psychology of trauma should inform the practice of oncology. The Oncologist, 23 (7), 750.
Le, M. N., Nguyen, G. T., Pan, Z., Maglalang, D. D., Butt, F., Bautista, R., et al. (2017). Unmet needs of Asian American and Pacific Islander cancer survivors. Journal of Cancer Education, 32 (2), 374–381. https://doi.org/10.1007/s13187-015-0952-7
Mathew, L., & Fulton, C. (2017). Chapter 12: Social isolation and caregiver burden. In B. Korc-Grodzicki & W. P. Tew (Eds.), Handbook of geriatric oncology (pp. 99–103). Demos Medical.
McClement, S. E., & Chochinov, H. M. (2008). Hope in advanced cancer patients. European Journal of Cancer, 44 (8), 1169–1174. https://doi.org/10.1016/j.ejca.2008.02.031
McClement, S., Chochinov, H. M., Hack, T., Hassard, T., Kristjanson, L. J., & Harlos, M. (2007). Dignity therapy: Family member perspectives. Journal of Palliative Medicine, 10 (5), 1076–1082.
National Association of Social Workers. (2021). Code of ethics . https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-Ethics-English
National Cancer Institute. (2021a, May 5) What is cancer? https://www.cancer.gov/about-cancer/understanding/what-is-cancer
National Cancer Institute. (2021b, August 6). Depression (PDQ)-Health professional version . https://www.cancer.gov/about-cancer/coping/feelings/depression-hp-pdq
Nguyen, T. U. N., & Kagawa-Singer, M. (2008, November). Overcoming barriers to cancer care through health navigation programs. Seminars in oncology nursing, 24 (4), 270–278.
Ore, M. L., & Foli, K. J. (2020). Reintegration for Post-treatment Cancer Survivors: A Concept Analysis. Journal of holistic nursing: official journal of the American Holistic Nurses’ Association, 38(3), 300–317. https://doi.org/10.1177/0898010119883760
Panganiban, J. M., & O’Neil, J. (2021). Breast cancer and gynecologic risks in lesbian and bisexual women. Nursing, 51 (3), 58–62.
Quach, T., Nuru-Jeter, A., Morris, P., Allen, L., Shema, S. J., Winters, J. K., et al. (2012). Experiences and perceptions of medical discrimination among a multiethnic sample of breast cancer patients in the Greater San Francisco Bay Area, California. American Journal of Public Health, 102 (5), 1027–1034. https://doi.org/10.2105/AJPH.2011.300554
Sánchez-Díaz, C. T., Strayhorn, S., Tejeda, S., Vijayasiri, G., Rauscher, G. H., & Molina, Y. (2021). What mediates the racial/ethnic disparity in psychosocial stress among breast cancer patients? Cancer Causes & Control, 32 (4), 357–367. https://doi.org/10.1007/s10552-021-01392-7
Scharff, D. P., Mathews, K. J., Jackson, P., Hoffsuemmer, J., Martin, E., & Edwards, D. (2010). More than Tuskegee: Understanding mistrust about research participation. Journal of Health Care for the Poor and Underserved, 21 (3), 879. https://doi.org/10.1353/hpu.0.0323
Siegel, R. L., Miller, K. D., & Jemal, A. (2018). Cancer statistics, 2018. CA: A Cancer Journal for Clinicians, 68 (1), 7–30. https://doi.org/10.3322/caac.21442
Stump-Sutliff, K., Watson, L. R., & Gersten, T. (n.d.). Cancer risks for gay and bisexual men . https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=134&contentid=131
Tamargo, C. L., Quinn, G. P., Sanchez, J. A., & Schabath, M. B. (2017). Cancer and the LGBTQ population: Quantitative and qualitative results from an oncology providers’ survey on knowledge, attitudes, and practice behaviors. Journal of Clinical Medicine, 6 (10), 93.
Thetford, K., Gillespie, T. W., Kim, Y.-I., Hansen, B., & Scarinci, I. C. (2021). Willingness of Latinx and African Americans to participate in non therapeutic trials: It depends on who runs the research. Ethnicity & Disease, 31 (2), 263–272. https://doi.org/10.18865/ed.31.2.263
Treanor, C. J. (2020). Psychosocial support interventions for cancer caregivers: Reducing caregiver burden. Current Opinion in Supportive and Palliative Care, 14 (3), 247–262.
Wall, L. L. (2006). The medical ethics of Dr J Marion Sims: A fresh look at the historical record. Journal of Medical Ethics, 32 (6), 346–350. https://doi.org/10.1136/jme.2005.012559
Wallace, K., Li, H., Brazeal, J. G., Lewin, D. N., Sun, S., Ba, A., Paulos, C. M., Rachidi, S., Li, Z., & Alekseyenko, A. V. (2020). Platelet and hemoglobin count at diagnosis are associated with survival in African American and Caucasian patients with colorectal cancer. Cancer Epidemiology, 67 . https://doi.org/10.1016/j.canep.2020.101746
Williams, I. (2014). Psychosocial burden of family caregivers to adults with cancer. In U. Goerling (Ed.), Psycho-oncology. Recent results in cancer research (Vol. 197, pp. 73–85). Springer. https://doi.org/10.1007/978-3-642-40187-9_6
Download references
Author information
Authors and affiliations.
Memorial Sloan Kettering Cancer Center, New York, NY, USA
Linda Mathew DSW, Jacob Maier & Annamma Abraham Kaba
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Linda Mathew DSW .
Editor information
Editors and affiliations.
City Center Psychotherapy, New York, NY, USA
Meredith Hemphill
Silver School of Social Work, New York University, New York, NY, USA
Abigail Nathanson
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Mathew, L., Maier, J., Kaba, A.A. (2023). Cancer and Oncology Social Work. In: Hemphill, M., Nathanson, A. (eds) The Practice of Clinical Social Work in Healthcare. Essential Clinical Social Work Series. Springer, Cham. https://doi.org/10.1007/978-3-031-31650-0_2
Download citation
DOI : https://doi.org/10.1007/978-3-031-31650-0_2
Published : 15 July 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-31649-4
Online ISBN : 978-3-031-31650-0
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
News Details
First-Ever Program in Oncology Social Work Prepares New Generation of Cancer Care Leaders

Authored by: Alina Ladyzhensky
Photography by: Provided
Faculty & Research, Student Life
When an individual is diagnosed with cancer, their course of medical care– scheduling tests and doctor’s appointments, managing treatments and their side-effects – undoubtedly becomes a primary focus. Beyond one’s physical well-being, a cancer diagnosis can also upset virtually every other aspect of a person’s life. Patients face emotional, psychosocial, and financial distress in addition to the side effects of the disease and its treatment– not to mention the ripple effect that cancer has on their loved ones and broader communities.
While their doctors and nurses focus on providing medical care, cancer patients often require additional guidance, advocacy, and support in coping with their diagnoses and the myriad, often complex issues that consequently arise. This is precisely where oncology social workers come in.
“All across different systems levels, social workers are involved– from even before diagnoses happen, as people are waiting for diagnoses or trying to prevent diagnoses, through all different levels of cancer care,” explained Allison Werner-Lin , PhD, a practicing oncology social worker and Assistant Professor at Penn’s School of Social Policy & Practice (SP2). “Social workers are doing crisis intervention.”
According to Werner-Lin, the role of social workers within communities impacted by cancer is both critical and wide-ranging. “We work in cancer centers, in palliative care, and in community health clinics. We do bedside visits, home visits, and help people make treatment decisions or decisions about terminating treatment. We run support groups for parents, aging caregivers, children, and adolescents who won’t talk to anybody about what’s going on at home, who won’t have people over because they don’t want anyone to know that they’re different.”
“We go into schools and talk about what re-entry is like for a child who is coming off treatment, or a beloved teacher who has just died after a late-stage diagnosis. We go into churches and talk about screening and prevention programs with populations that are hard to reach,” she continued. “We go into policy settings and talk to government officials and aids about why we need better access to preventative care and research funding.”
Despite this compelling need for oncological social workers on both individual and community-wide levels, a post-masters social work training specifically focused on oncology did not exist until very recently. In fall 2018, Werner-Lin launched the Penn Advanced Certificate in Oncology Social Work , for which she serves as Program Director. The 12-month program, which includes monthly sessions taught at the Perelman School of Medicine, is the first of its kind in the world. The Advanced Certificate in Oncology Social Work is offered as part of the new OpenSP2 learning division, which provides learners with continuing education opportunities and transferable skills to advance their careers, or to apply in their current places of work.
Werner-Lin’s social work practice focuses on parentally bereaved children and teens, and her internationally-recognized research addresses the intersection of genomic discovery and family life. This has given her a particularly profound view of how everything from family genetic history to making decisions about engagement with preventative technology is part of the constellation of issues that families affected by cancer must face.
“The current landscape is completely different in terms of decision-making than even 20 years ago. A lot of technologies are rolled out before we really understand what some of the psychosocial concerns are,” Werner-Lin said. “We are just starting to understand what it means for kids to grow up in a family with a known genetic mutation, or for someone to consider prophylactic mastectomy without a cancer diagnosis —what does that mean for a family? Some of these issues are novel in the social work world, and we need our teams on board.”
Werner-Lin’s SP2 colleague, Christina Bach, MBE, MSW, LCSW, OSW-C, serves as Program Associate Director of the Penn Advanced Certificate in Oncology Social Work. A nationally-known oncology social work leader, Bach believes that the decision to offer a social work certificate program in oncology care couldn’t be more well-timed.
“Need is increasing exponentially in terms of psychosocial issues, an aging population, financial distress, lack of access to care, understanding social determinants of health and disparities in disease burden and survival,” said Bach. “We need to prepare folks for these challenges going forward, to meet them head-on, and train others to do this, too. Oncology nurses and oncologists have been doing this type of specialized training for years, and now it’s time for us to step up our professional practice.”
According to Bach and Werner-Lin, the practice of social work is becoming more robust, and post-masters education in social work is becoming increasingly popular. Simultaneously, the decisions that individuals and parents must make are becoming more complicated. While a number of existing social work programs address practice in end-of-life and palliative care settings, there were none specific to practice in oncology.
Werner-Lin lead design of the Penn Advanced Certificate in Oncology Social Work program to teach practicing social workers how to address, and keep up with, the emotional needs, treatment, financial issues, family dynamics, and other matters surrounding cancer care. The program is geared toward social workers who have completed a master’s program and are now looking to advance their careers, specialize in oncology, or move into oncology from other health settings.
“Social work is involved in every way, from the beginning diagnosis through lifelong or long-term survivorship, and working with end-of-life decision-making and bereavement,” said Werner-Lin. “We’ve designed a program that really covers the gamut, so social workers can be involved with families all across the cancer trajectory.”
A Mechanism for Outstanding Learning, Teaching, and Networking
The program’s Advisory Board, which helped Werner-Lin develop the curriculum, and where Bach first distinguished herself as a dedicated ally in delivering high-quality programming, consists of leading oncology social work practitioners and allied health and mental health professionals from around the country, many of whom have also become instructors in the program. Werner-Lin was mindful of being both contemporary and broad in the curriculum’s coverage of various topics related to oncology care. Through the program, learners will be exposed to top researchers in the areas of survivorship; program development and leadership, genetic testing and cancer prevention, sex and sexuality; pediatric and adolescent/young adult cancer; and methodological innovations in cancer research, in addition to a variety of master clinicians who have worked extensively in cancer clinics and centers.
Werner-Lin envisions the program as a venue and mechanism for “really outstanding learning, teaching, and networking,” bringing experts in the field together to develop the next generation of expert oncology social work practitioners and research scholars, and building a robust network of alumni as the cohorts grow over time. She views the network-building aspect of the program as particularly important.
“Some participants who are in smaller cancer care settings do not have a way to network, they don’t have the resources, they don’t have the colleagues, they don’t have the supervision, and they certainly don’t have the opportunity to work alongside a team, which can validate or normalize some of the distress that comes from working with people with cancer, at the end of life, and suffering through treatments on a regular basis,” she explained. “These learners will be building a local and national network of colleagues with their instructors, but also in the room together. The hope is that we grow expert oncology social workers from the program while feeding into the leadership of national organizations, into doctoral study, or diffused out into the broader world of social work practice.”
Bach further highlighted the career advancement opportunities that the Penn Advanced Certificate in Oncology Social Work offers to learners, noting that the program ends with a capstone or demonstration project that students can take back to their place of work to elevate their practice, grow programmatic offerings, and help their own career development and growth. Moreover, in the second month of the program, students learn about program development, as well as administration supervising and teaching. Bach and Werner-Lin are hopeful that individuals from the cohort will go on to become field instructors for MSW students at SP2 or for social work programs in their own geographic regions, thereby giving back to the community of learners.
While the program has only recently gotten underway, Werner-Lin is already heartened by the first cohort of learners, noting that participants run the gamut from recent graduates to those who have been in the field for many years and are looking to make their positions more robust. Some learners hail from well-funded teaching and research hospitals, while others come from small community hospital settings, or the national network of cancer wellness centers. According to Werner-Lin, all 12 participants in the program’s first cohort have shown enormous enthusiasm and dedication to continuing education and lifelong learning.
That dedication and enthusiasm will certainly be needed in the difficult— but immensely impactful and rewarding— field of oncology social work. There is no shortage of ways in which this first cohort, and those who follow them, will be able to make a difference for individuals whose lives have been affected by cancer.
“Our role is limitless. It’s way beyond arranging transportation and getting people to their appointments, but actually, ‘How do I live with this, and after this disease, or tolerate knowing that it might come back and end my life?’” said Bach. “There is so much we can do, and I feel that we’ve barely scratched the surface of the impact we can make.”

Allison Werner-Lin, PhD, LCSW
Associate Professor
awer@upenn.edu
Please read our guidelines before visiting Rutgers Cancer Institute. | COVID-19: What Cancer Patients Should Know
- About Rutgers Cancer Institute of New Jersey
- Consortium Cancer Center
- Why Choose a Comprehensive Cancer Center?
Skip to Content
- Conquer Cancer
- ASCO Journals
- f Cancer.net on Facebook
- t Cancer.net on Twitter
- q Cancer.net on YouTube
- g Cancer.net on Google
- Types of Cancer
- Navigating Cancer Care
- Coping With Cancer
- Research and Advocacy
- Survivorship
Social worker
A professional who helps patients with cancer and their family members cope with everyday tasks and challenges before, during, and after treatment. Social workers, who may work for a hospital, a service agency, or a local government, can help address financial problems, explain insurance benefits, provide access to counseling, and more.
Timely. Trusted. Compassionate.
Comprehensive information for people with cancer, families, and caregivers, from the American Society of Clinical Oncology (ASCO), the voice of the world's oncology professionals.
Find a Cancer Doctor

How Can Social Workers Help Cancer Patients?

A cancer diagnosis affects every area of a person’s life. The journey is both challenging and costly, and many experiencing it for the first time feel lost about how they should handle the changes cancer brings. That’s where social workers step in.
“Our role is to help patients think through the impacts of their diagnosis, whether it’s work situations, telling their children, anxiety and depression, or other changes that cause concern,” says Nancy Borstelmann, MPH, MSW, LICSW, director of Social Work at Dana-Farber, a division of Psychosocial Oncology and Palliative Care . Borstelmann has been a social worker at Dana-Farber for 18 years, during which she has helped guide countless patients and caregivers through their cancer experiences. “Our job is to help them so they can focus on their treatment and have the best possible quality of life.”
Social workers help with a wide variety of issues and are a wealth of knowledge when it comes to resources that can help patients and caregivers during treatment. Some of the areas they can help with include:
- Recommending and facilitating support groups
- Counseling for anxiety and depression, and, on the deepest level of face-to-face contact, help with all the complicated emotional and psychosocial aspects of cancer diagnosis, treatment, and survivorship. These emotions are unique to every patient, just as every patient’s cancer is unique.
- Explaining diagnoses to friends and family
- Mediating patient-caregiver conflicts
- Referrals to financial assistance organizations
- Information on spiritual counseling
- Transportation to and from treatment
- Counseling for physical changes and body image and identity issues
- Providing information about a patient’s disease
“My social worker is my lifeline,” says Dana-Farber patient Carol Halberstadt. “When I walk into her office it’s a safe haven.”
Social workers have helped Halberstadt with many aspects of her cancer journey; they assisted her with referrals for patient assistance programs and gave her the opportunity help other patients through Dana-Farber’s Living with Lung Cancer Forum and a program for palliative care and psychosocial oncology caregivers. Social workers also encouraged her poetry, with some of her poems published in the Journal of the American Medical Association.
“Sometimes your close friends and family don’t want to talk about cancer,” says Halberstadt, “but I can talk about anything with my social workers.”
- Tips for Communicating with Your Care Team
- How a Stem Cell Transplant Changed My Outlook — and My Career
- Depression and Cancer: What You Need to Know
During one of her first appointments at Dana-Farber, Sandra Edwards entrusted her social worker to take care of her 10-year-old son, Atticus, while she spoke with her care team.
“It immediately made me feel like my family and I were in good hands,” says Edwards.
When it became clear that Sandra and her son would have to stay in Boston while Sandra underwent treatment, her social worker found her housing as well as a nearby school for her son.
“The social work team gently guides me through all of the decisions that I have to make; they help me care for my spirit which is just as important as caring for my body.”
A major part of the social work role at Dana-Farber involves end-of-life and grief counseling for patients and their loved ones. Meeting with a social worker can help a patient plan how they can explain their diagnosis and prognosis to friends and family as well as how to make arrangements for the future.
“We as social workers are very interested in helping patients in their whole life – during and after cancer,” Borstelmann says.
If you or a loved one may benefit from speaking with a social worker, talk to your care team, who will be able to refer you to a social worker who will best fit your needs.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Latest science news, discoveries and analysis

The Maldives is racing to create new land. Why are so many people concerned?

Mini-colon and brain 'organoids' shed light on cancer and other diseases
Retractions are part of science, but misconduct isn’t — lessons from a superconductivity lab
Monkeypox virus: dangerous strain gains ability to spread through sex, new data suggest
Dna from ancient graves reveals the culture of a mysterious nomadic people, atomic clock keeps ultra-precise time aboard a rocking naval ship, who redefines airborne transmission: what does that mean for future pandemics, ecologists: don’t lose touch with the joy of fieldwork chris mantegna, european ruling linking climate change to human rights could be a game changer — here’s how charlotte e. blattner.

Lethal AI weapons are here: how can we control them?
Living on Mars would probably suck — here's why

Dozens of genes are linked to post-traumatic stress disorder

What toilets can reveal about COVID, cancer and other health threats
How gliding marsupials got their ‘wings’, plastic pollution: three numbers that support a crackdown, first glowing animals lit up the oceans half a billion years ago, how to freeze a memory: putting worms on ice stops them forgetting.

Any plan to make smoking obsolete is the right step

Will AI accelerate or delay the race to net-zero emissions?

Citizenship privilege harms science
We must protect the global plastics treaty from corporate interference martin wagner, un plastics treaty: don’t let lobbyists drown out researchers, current issue.

Surprise hybrid origins of a butterfly species
Stripped-envelope supernova light curves argue for central engine activity, optical clocks at sea, research analysis.
A chemical method for selective labelling of the key amino acid tryptophan
Charles Darwin investigates: the curious case of primrose punishment
Nanoparticle fix opens up tricky technique to forensic applications
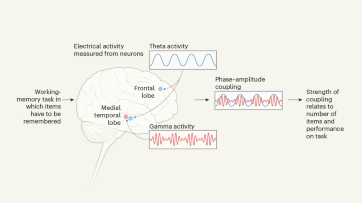
Coupled neural activity controls working memory in humans
Robust optical clocks promise stable timing in a portable package, targeting rna opens therapeutic avenues for timothy syndrome, bioengineered ‘mini-colons’ shed light on cancer progression, ancient dna traces family lines and political shifts in the avar empire.

Breaking ice, and helicopter drops: winning photos of working scientists

Shrouded in secrecy: how science is harmed by the bullying and harassment rumour mill

Londoners see what a scientist looks like up close in 50 photographs
How ground glass might save crops from drought on a caribbean island, deadly diseases and inflatable suits: how i found my niche in virology research, books & culture.

How volcanoes shaped our planet — and why we need to be ready for the next big eruption
Dogwhistles, drilling and the roots of Western civilization: Books in brief

Cosmic rentals
Las boriqueñas remembers the forgotten puerto rican women who tested the first pill, dad always mows on summer saturday mornings, nature podcast.

Latest videos
Nature briefing.
An essential round-up of science news, opinion and analysis, delivered to your inbox every weekday.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
COMMENTS
Social workers are key members of the health care team and intervene at multiple levels and in multiple systems to optimize quality of life and quality of care. Beyond direct practice, social workers are engaged in research that address many of the priority areas outlined in The Nation's Investment in Cancer Research (2002) including: Health ...
Oncology social workers have historically performed a wide range of services to support cancer patients from diagnosis through long-term survival. 1,2 Working within frameworks informed by the biopsychosocial model and person-in-environment ecological theory, oncology social workers have supported cancer patients and their families via screening and assessment of cancer-related problems ...
The development of this inaugural Handbook of Oncology Social Work provides an up-to-date repository of the scope of oncology social workers' clinical practice, education, research, policy, and program leadership in the psychosocial care of people with cancer and their families. It addresses both the science and art of psychosocial care and ...
This special issue is the culmination of work undertaken in a long-term, academic-practitioner partnership that began over a decade ago. Supported by interdisciplinary oncology networks and long careers in hospital social work and later in academia, a research agenda has been pursued that explored the scope of oncology social work practice in Australia.
Oncology social work researchers bring a unique perspective to their research in psychosocial oncology. For example, social work is known for "starting where the client is"—a patient-centered perspective. This is reflected in research that explores the cancer experience of patients and family members.
Oncology social workers are skilled professionals who provide emotional, psychological, social, and practical support for cancer patients. They help patients navigate different resources and unpack useful information. These experts address the patient as a whole, instead of only focusing on medical treatment.
An oncology social worker provides counseling, education and information services, referrals to community resources and helps people navigate the health care system. Taking Care of the Whole Person. For most people, a cancer diagnosis brings new feeling and experiences, and an oncology social worker can help people work through these aspects ...
Oncology social work is the primary professional discipline that provides psychosocial services to patients, families and significant others facing the impact of a potential or actual diagnosis of cancer. The scope of oncology social work includes clinical practice, education, advocacy, administration, policy and research.
Abstract. Cancer is a broad term that comprises dozens, if not hundreds, of diagnoses and illnesses. It is one of the leading causes of death worldwide. Cancer can be emotionally and physically devastating and the treatment process can be confusing and overwhelming. The role of the oncology social worker is to support patients and families as ...
"Social work is involved in every way, from the beginning diagnosis through lifelong or long-term survivorship, and working with end-of-life decision-making and bereavement," said Werner-Lin. "We've designed a program that really covers the gamut, so social workers can be involved with families all across the cancer trajectory."
This chapter introduces the foundations of oncology social work and highlights social work's unique contributions to comprehensive and integrated cancer care with global perspectives. It provides an introduction of cancer epidemiology, screening, and treatment, and the psychosocial, behavioral, cultural, and spiritual impact of the disease on ...
Recent research by Pockett et al. (2020) noted the limited research into the role of oncology social workers in the Australian context and found that social workers have a significant role to play in the provision of psychosocial care for cancer patients and their families. Credentialing of oncology social workers was implemented in the USA to ...
And, if you're a patient or caregiver at MD Anderson, your clinic has social work counselors available ready to support you. Here are six ways social work counselors can help MD Anderson cancer patients and their caregivers navigate cancer - from diagnosis through survivorship. 1. Understanding your diagnosis.
Spotlight On: Oncology Social Workers - Part I, a Q&A. If you've been diagnosed with cancer, you will interact with a number of different members of the health care team at various times during treatment. When you walk into a doctor's office, hospital, or cancer center, you may encounter nurses, physician assistants, social workers ...
732-507-8307. [email protected]. For patient appointments/inquiries - contact: 844-CANCERNJ (844-226-2376) New Brunswick, N.J., March 1, 2022 - Cancer is a challenging disease with many aspects. Psychosocial support services have powerful benefits on the success of a patient's treatment and recovery.
Primarily, our results reveal the lack of high-quality research on the evaluation of psychosocial cancer support services—specifically in form of RCTs. The lack of studies with RCT designs may be due to the lack of standardized interventions offered in psychosocial support, which may hamper comparability.
If you have any questions or feel that you could benefit from additional support, please contact the Department of Social Work at 713-792-6195, or ask your nurse or doctor to speak with a social work counselor. Topics. Support. Read More by Traci Newsom. Traci Newsom speaks with a patient.
Social worker. A professional who helps patients with cancer and their family members cope with everyday tasks and challenges before, during, and after treatment. Social workers, who may work for a hospital, a service agency, or a local government, can help address financial problems, explain insurance benefits, provide access to counseling ...
Compliance: Billing for Social Workers. By Cindy Parman, CPC, CPC-H, RCC. Social workers in cancer centers typically provide psychosocial services to patients, families, and caregivers facing the impact of a cancer diagnosis. Growing a Patient Transportation Program. Sherry Laniado, MSW, LCSW, OSW-C.
Social workers help with a wide variety of issues and are a wealth of knowledge when it comes to resources that can help patients and caregivers during treatment. Some of the areas they can help with include: Recommending and facilitating support groups. Counseling for anxiety and depression, and, on the deepest level of face-to-face contact ...
Contact Us. Connect with Us. UT Health San Antonio. MD Anderson Cancer Center. (210) 450-1000. Social and Emotional Impacts of Cancer. Cancer and cancer treatment can bring social and emotional difficulties. But you don't have to face them alone. About Us.
By Melinda Krigel. Leading cancer researchers from UC San Francisco presented talks about advances in targeted therapy, cancer genomics, eliminating treatment disparities and other cancer research topics at this year's annual meeting of the American Association for Cancer Research (AACR) conference, which was held April 5-10 in San Diego.
Research indicates that receiving support from family and friends including calmness, comfort, and problem-solving in the post-diagnosis period is an important resource that can help cancer survivors find positive meaning in their cancer experience . Social support was also mentioned as a factor that significantly contributed to disease ...
Who Can Apply: Current and past American Cancer Society grantees, including former ACS Postdoctoral Fellows Purpose: Enables transition of patient-focused research to accelerate clinical impact Funding, Stage I: 2 years with $135K a year direct costs, plus 10% allowable indirect costs Funding, Stage II: 1.5 years with $545K total direct costs, plus 10% allowable indirect costs
Women's health is a significant topic of discussion in Pink October campaigns. These campaigns seek to increase awareness of both breast cancer and women's general health. This study aims to examine the textual strategies in health communication. This is achieved by applying corpus stylistic tools to investigate linguistic patterns in Pink ...
Latest science news and analysis from the world's leading research journal ... the marriage habits and social norms of the Avar people of central Europe. ... in the frontal and temporal lobes work ...