- Original article
- Open access
- Published: 23 February 2024

Medico-legal risks of point-of-care ultrasound: a closed-case analysis of Canadian Medical Protective Association medico-legal cases
- Ross Prager ORCID: orcid.org/0000-0001-8145-8141 1 , 2 ,
- Derek Wu 3 ,
- Gary Garber 4 , 5 ,
- P. J. Finestone 4 ,
- Cathy Zang 4 ,
- Rana Aslanova 4 &
- Robert Arntfield 1
The Ultrasound Journal volume 16 , Article number: 16 ( 2024 ) Cite this article
6022 Accesses
102 Altmetric
Metrics details
Point-of-care ultrasound (POCUS) has become a core diagnostic tool for many physicians due to its portability, excellent safety profile, and diagnostic utility. Despite its growing use, the potential risks of POCUS use should be considered by providers. We analyzed the Canadian Medical Protective Association (CMPA) repository to identify medico-legal cases arising from the use of POCUS.
We retrospectively searched the CMPA closed-case repository for cases involving diagnostic POCUS between January 1st, 2012 and December 31st, 2021. Cases included civil-legal actions, medical regulatory authority (College) cases, and hospital complaints. Patient and physician demographics, outcomes, reason for complaint, and expert-identified contributing factors were analyzed.
From 2012 to 2021, there were 58,626 closed medico-legal cases in the CMPA repository with POCUS determined to be a contributing factor for medico-legal action in 15 cases; in all cases the medico-legal outcome was decided against the physicians. The most common reasons for patient complaints were diagnostic error, deficient assessment, and failure to perform a test or intervention. Expert analysis of these cases determined the most common contributing factors for medico-legal action was failure to perform POCUS when indicated (7 cases, 47%); however, medico-legal action also resulted from diagnostic error, incorrect sonographic approach, deficient assessment, inadequate skill, inadequate documentation, or inadequate reporting.
Conclusions
Although the most common reason associated with the medico-legal action in these cases is failure to perform POCUS when indicated, inappropriate use of POCUS may lead to medico-legal action. Due to limitations in granularity of data, the exact number of civil-legal, College cases, and hospital complaints for each contributing factor is unavailable. To enhance patient care and mitigate risk for providers, POCUS should be carefully integrated with other clinical information, performed by providers with adequate skill, and carefully documented.
Point-of-care ultrasound (POCUS) has become a core diagnostic tool for many physicians [ 1 ]. Its portability, excellent safety profile, and ability to make important diagnoses in real-time helps expedite care. The importance of POCUS has been recognized by many undergraduate and post-graduate medical institutions, and it has seen planned or actual integration into core medical curricula [ 2 , 3 , 4 , 5 ]. Additionally, its safety and ability to enhance patient care has led to its endorsement by multiple major clinical societies [ 6 , 7 , 8 , 9 , 10 ]. Despite being an invaluable tool, there is a risk that the rapid uptake of POCUS may outpace development of best practices to safeguard both patients and providers.
Medico-legal analyses can help promote patient safety and improve the quality of healthcare delivery. By analyzing medico-legal cases, we can identify patterns of error, understand the root causes of adverse events, and develop strategies to prevent future occurrences [ 11 ].
The current POCUS medico-legal literature has not identified any cases where performing diagnostic POCUS has resulted in civil-legal action [ 12 , 13 , 14 , 15 , 16 , 17 ]. Instead, all cases have arisen from failure to perform POCUS when clinically indicated [ 12 , 13 , 14 , 15 , 16 , 17 ]. These small studies are limited by sample size, non-comprehensive legal databases, and differences in legal systems between countries, leaving important questions about the medico-legal risk for physicians performing POCUS for Canadian physicians.
The objective of our study was to analyze the Canadian Medical Protective Association (CMPA) closed-case repository to identify medico-legal cases (civil-legal, college complaints, or hospital complaints) related to the use of POCUS. We describe the nature and frequency of medico-legal claims, identify common errors and contributing factors, and discuss strategies for mitigating medico-legal risks when performing POCUS.
In January 2023, the Canadian Medical Protective Association (CMPA), a not-for-profit mutual defense organization, represented over 107,000 physician members. The CMPA offers medico-legal support, advice, and education to physicians, and engages in safe medical care research using medico-legal data from its repository. The repository relies on physician members to voluntarily contact the CMPA and submit materials when seeking advice or support for medico-legal matters. We conducted a 10-year retrospective descriptive analysis of medico-legal cases related to diagnostic POCUS performed in a hospital setting. In this study, cases included civil-legal actions (class action legal cases were excluded), medical regulatory authority cases (College) and hospital complaints. A statistical data analyst searched all cases closed between January 1st, 2012 and December 31st, 2021. Prior to analysis, all cases were de-identified and reported at the aggregate level to ensure confidentiality for both patients and healthcare providers. This means that detailed descriptions of individual cases are not possible and may leave an unavoidable lack of granularity. The Advarra Institutional Review Board provided ethical approval for this study.
CMPA medical analysts, who are experienced registered nurses with training in medico-legal research, used standardized methods to code information retrieved from medico-legal cases, including the case information, patient characteristics, health conditions, complications, peer expert criticisms classified using the CMPA’s contributing factors framework [ 11 ], patient harm classified using an in-house classification of harms, and the court ruling or final regulatory authority or hospital decisions. Peer experts are physicians retained by the parties in a legal action to interpret and provide their opinion on clinical, scientific, or technical issues surrounding the care provided. Clinical coding was applied using the International Statistical Classification of Diseases and Related Health Problems, 10th revision, Canada (ICD-10-CA), the Canadian Classification of Health Interventions, and in-house CMPA coding. To reduce misclassification, nurse-analysts conducted regular quality assurance reviews of coding electronically and as a group.
Closed cases with sufficient information involved various physician specialties caring for patients undergoing diagnostic POCUS. Some cases involved more than one physician and more than one physician specialty per case.
Cases were extracted using word search for point of care ultrasound (see Appendix A for list of terms). We excluded cases involving radiologists, obstetricians performing obstetric ultrasounds, and cardiologists performing echocardiography from the extraction and a manual review excluded cases when POCUS was not the medico-legal issue in the case. A descriptive analysis of the selected cases included an analysis of the contributing factors identified by peer experts as well as analysis of the indications for POCUS, patient harm, care settings, geographical location of care, patient demographics, physician specialty and years in practice.
We report all variables with frequencies and proportions using SAS software, version 9.4 for all statistical analyses (SAS ® Enterprise Guide ® software, Version 9.4. Cary, North Carolina: SAS Institute Inc.; 2013).
From 2012 to 2021, a total of 58,626 medico-legal cases were captured in the CMPA database. Of these, 31 cases met the database search strategy. POCUS was a contributing factor towards medico-legal action in 15/31 (48%) cases. Nine cases were college complaints, the rest were civil-legal actions (five) or hospital complaints. The medico-legal outcomes for physicians were decided against the physician in all 15 cases.
Patient demographics and outcomes
Ten of the 15 patients were female (67%). The age ranges for patients were: 0–18 years old (2, 13%), 19–29 (3, 20%), 30–49 (7, 47%), 50–64 (2, 13%), and 65–79 (1, 7%). Most cases occurred in the emergency department (13, 87%). Thirteen of the 15 cases (87%) resulted from healthcare related harm to the patient, with 2 cases (13.3%) resulting from non-clinical issues (e.g. documentation). Of the 13 patients with healthcare related harm, 5 patients died (33%). For the remaining patients, the harm classification was mild for 4 patients (26.7%), moderate for 2 patients (13%) severe for 1 patient (7%), and 1 patient experienced no harm (7%). See Appendix 2 for the definitions of patient harm.
The most common patient safety indicators were diagnostic error (12/15, 80%), contraindicated procedure or pharmacotherapy (2/15, 13%), and injury associated with healthcare (1/15, 7%). The most common reasons for patient complaints included diagnostic error (14, 93%), deficient assessment (12, 80%), and failure to perform a test or intervention (8, 53%) (Table 1 ).
Physician demographics
The distribution of specialties for physicians involved in the cases (n = 19) were: emergency medicine (9, 47%), resident physician (3,16%), family medicine (3, 16%), obstetrics and gynecology (1, 5%), internal medicine (1, 5%), general surgery (1, 5%), and diagnostic radiology (1, 5%). Note, cases where the POCUS provider was an obstetrician or radiologist were excluded from our search, however, these specialists may have been included in cases if they were listed as co-complainants. Eleven of 19 physicians (58%) were in practice 5 years of less; five of 19 physicians (26%) were in practice 11–20 years; three of 19 physicians (16%) were in practice 21–30 years. Nine cases (60%) occurred in large urban population centers (> 100,000 people), with 3 cases (20%) occurring in medium population centers (30,000 to 100,000 people), and 3 (20%) cases occurring in small population centers (less than 30,000 people).
Expert contributing factor analysis
Expert analysis identified the root cause of medico-legal action for each case. They found that in 7 cases POCUS was not performed when clinically indicated. In 8 cases, POCUS was performed but there was an issue with its application: in 2 cases, inadequate skill; in 1 case, an incorrect approach used (e.g. a surface POCUS instead of an invasive modality); in 1 case, deficient reporting; in 1 case, deficient documentation;, in 1 case, inappropriate use; in 1 case, misdiagnosis; in 1 case, the expert analysis was not recorded. The lack of granularity of the data limits the ability to report how many of the above cases were civil-legal cases, college complaints, or hospital complaints.
For cases involving a diagnostic error (12 cases), 6 (50%) were related to performing POCUS, and 6 (50%) were related to not performing POCUS. For cases of deficient assessment, in one case, the physician relied on serial POCUS exams, disregarding an important physical exam finding that should have prompted additional imaging. In 4 cases (36%) a misinterpretation of the POCUS led to the failure to perform an indicated test or intervention. Notably, whereas only 1 case had inadequate documentation listed as the cause of complaint from the patient or family members, peer expert criticism identified 11 cases where inadequate documentation contributed to the medico-legal outcome. One important note is that not all documentation issues were specific to POCUS; however, failure to document POCUS findings, and failure to use standardized wording for POCUS reports were identified as contributing factors by peer review.
The contributing factor analysis of 14 cases with criticisms related to patient care (not the 1 case related to documentation), identified provider factors in 13/14 case (93%), team factors in 13/14 cases (93%), and system factors in 3/14 cases (21%). The complete list of provider, team, and system factors identified are included in Table 2 ; however, the most common contributing factors included failure to perform a test or intervention, deficient assessment, and misinterpretation of a test. At the team level, these were documentation issues and communication breakdown with a patient. At a system level these were related to resource issues, and protocol, policy, or procedural issues. Of note, the system level issues that arose from lack of resources were not related to lack of POCUS machine access or lack of access to POCUS infrastructure (e.g. image archiving), but rather inadequate staffing of departments in a way that contributed to patient harm.
Interpretation
In this analysis of closed medico-legal cases in the CMPA repository we identified 15 cases where POCUS was a contributing factor towards medico-legal action. Almost half of the cases were due to physicians failing to perform POCUS when indicated. In contrast to previous literature that had not identified POCUS cases that resulted in a medico-legal action [ 12 , 13 , 14 , 15 , 16 , 17 ], we found a number of cases where POCUS use resulted in a medico-legal action due to issues with provider skill, sonographic approach, reporting, documentation, misdiagnosis, and inappropriate use. All cases resulted in findings against the physician involved. Five cases involved patient death.
Contrasting our study to existing literature [ 12 , 13 , 14 , 15 , 16 , 17 ] (which report civil-legal cases only), the increased number of medico-legal cases identified may be accountable by several factors. First, the CMPA repository is a comprehensive database capturing essentially all medico-legal cases against Canadian physicians, with data coded prospectively in a highly searchable way. Additionally, most of the cases were hospital or college complaints, which have a lower barrier to filing compared with civil litigation. This is important as this is the first study to examine hospital and college complaints, in addition to civil litigation. Thus, whereas patients and families may have felt POCUS was applied inappropriately and submitted a hospital or college complaint, it may not have met a threshold to proceed with civil litigation (Fig. 1 ).
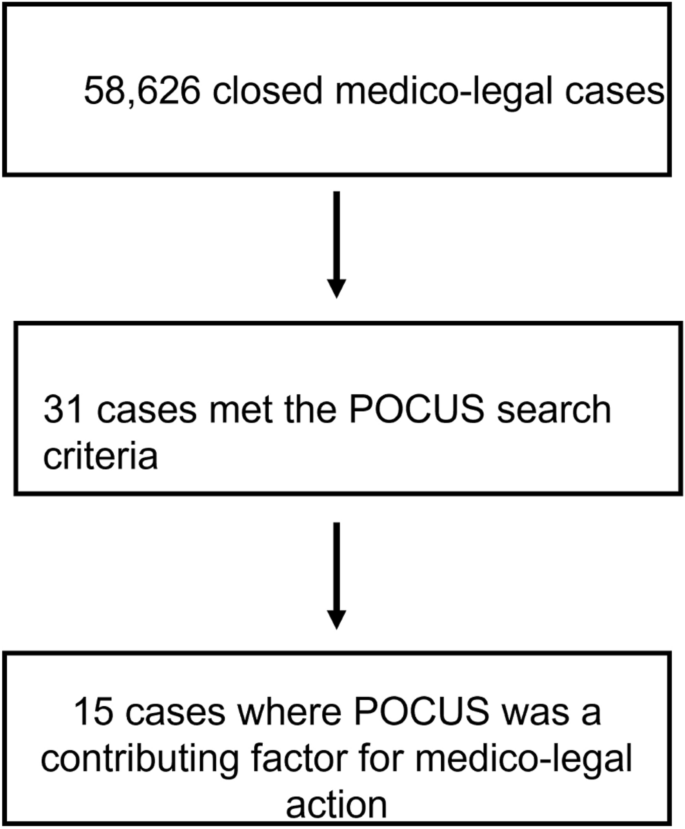
Study flow diagram
Regardless, our study demonstrates an important reality for the twenty-first century acute care physician: failure to perform POCUS when indicated may result in medico-legal action. For some specialties and indications, POCUS may no longer be an adjunct to augment traditional bedside assessment but rather a core part of the diagnostic process itself. While POCUS infrastructure and expertise varies between different settings, as the evidence and use of POCUS grows, so too can the expectation that it is appropriately used when clinically indicated. This may be particularly relevant for specific use cases of POCUS with well-established diagnostic pathways including the Focused Assessment with Sonography in Trauma (FAST) exam during trauma resuscitation, or its use to diagnosis undifferentiated shock [ 18 , 19 , 20 ]. The excellent safety and diagnostic prowess of acute care POCUS has led to its endorsement by various societal guidelines [ 6 , 7 , 8 , 9 , 10 ].
Despite increasing adoption of POCUS in acute care medicine, adequate training and skill is necessary for its safe implementation, and in this analysis was flagged as a contributing factor for medico-legal action in several cases. One systems level approach to POCUS education being implemented at multiple institutions is to teach ultrasound physics, knobology, and anatomy in parallel with traditional medical school curriculum to provide learners with a base skillset that can be built on during further training [ 3 , 4 , 5 ]. Then, specialty specific POCUS training with a focus on interpretation and synthesis can be taught during residency. Although this approach will help ensure future generations of physicians have base competency in POCUS, for clinicians in practice, alternative educational approaches should be considered. These include informal or formal instruction from colleagues with POCUS expertise to help develop core skills. Alternatively, continuing medical education opportunities like POCUS courses, conferences, rotations, or fellowships are an excellent resource, however, may not be feasible for many physicians in practice. Some societies have suggested processes for credentialing and privileging practicing physicians, which may be helpful roadmaps for interested clinicians [ 6 ].
In addition to helping clinicians obtain and interpret POCUS images, formalized training helps clinicians appropriately integrate POCUS findings with other clinical information. In fact, diagnostic errors, deficient assessments, and failure to perform other indicated tests or interventions were the most common reasons for patient complaints in our study, indicating a failure to properly integrate POCUS into the diagnostic workup of patients. Ideally, POCUS findings should be integrated into patient care with a ‘Bayesian mindset’, meaning that the positive or negative finding on POCUS helps change the post-test probability of a pathology being present. This contrasts with an oversimplified view of POCUS where the presence or absence of findings on POCUS dictates whether a disease is present. This dichotomized view of POCUS is potentially dangerous, and in our experience seen more with novice POCUS practitioners. The visual nature of the medium may lend itself to a ‘seeing is believing’ phenomenon, which can lead some clinicians to place inappropriate weight on the POCUS findings, disregarding other competing clinical information.
Inappropriate integration of POCUS into practice may also result from a failure to understand the test characteristics for POCUS in that population. For instance, FAST scan has high specificity (> 98%) to detect intraperitoneal free fluid, however only moderate sensitivity (70–90%) with test characteristics varying between operators [ 18 , 21 , 22 ]. For a trauma patient with a very high pre-test probability for intrabdominal hemorrhage (e.g. 80%), even with a negative FAST scan (assume sensitivity of 70%), the post-test chance of intrabdominal hemorrhage is 55%. Overreliance on POCUS and failure to integrate other clinical information is a crucial pitfall to avoid.
Inadequate documentation led to medico-legal action and was a major theme in the contributing factor analysis. If a POCUS is performed, the indication, views acquired, findings, and interpretation should be recorded in the patient's chart. At a minimum, this should be written as a progress note or included as part of a consultation. A better practice, although not available at many centers, is to save images in an accessible archiving system, and then generate a written report to allow for accountability and communication between providers [ 23 , 24 ]. Ideal practice would have all archived scans undergo quality assurance by a POCUS expert, with the amended reports subsequently uploaded into a patient’s electronic medical record. The practice of "shadow" scans where results are communicated by verbal handover between providers is not acceptable and may expose physicians to medico-legal risk.
Future directions
Although this represents a preliminary analysis of Canadian medico-legal cases involving POCUS, we expect the number of medico-legal cases to grow in parallel with increased POCUS use across. A repeat analysis of this work in 5 or 10 years will be helpful to assess for evolving patterns in POCUS medico-legal risk. Furthermore, this study excluded procedural use of POCUS (e.g. central line insertion) which would be an important area for future research. Additionally, knowledge translation surrounding best practices in POCUS training, clinical integration, and documentation is needed to promote optimal POCUS use among physicians.
Limitations
There are several important limitations: the search terms used may not have retrieved all medico-legal cases related to POCUS. To address this, the CMPA will now prospectively identify POCUS cases to facilitate future research. We omitted granular clinical details from the cases to protect patient and physician privacy, however this limits the analysis of factors leading to poor patient outcomes. This was unavoidable and was done in close collaboration with the CMPA to adhere to their rigorous privacy mandates. We recognize that this leaves unanswered questions, but feel this study still provides actionable take homes to improve patient safety. Finally, we have not included procedural POCUS, as we would lack granularity to distinguish between medico-legal action from the procedure itself, or the POCUS use.
Although failing to perform POCUS when clinically indicated remains an important contributing factor for medico-legal action, in contrast to the existing published literature, we identified cases where the application of POCUS resulted in adverse medico-legal outcomes. Due to limitations in granularity of data, the exact number of civil-legal, College cases, and hospital complaints for each contributing factor is unavailable. Overall, these cases resulted from inadequate skill, misdiagnosis, incorrect approach, deficient patient assessment, and incomplete documentation. The thoughtful and deliberate integration of POCUS into diagnostic pathways will help mitigate risk while allowing patients to experience benefits of this powerful tool.
Availability of data and materials
Data is available on reasonable request to the corresponding author.
Abbreviations
Canadian Medical Protective Association
Focused assessment with sonography in trauma
Point-of-care Ultrasound
Arntfield RT, Millington SJ (2012) Point of care cardiac ultrasound applications in the emergency department and intensive care unit–a review. Curr Cardiol Rev 8(2):98–108
Article PubMed PubMed Central Google Scholar
Micks T, Braganza D, Peng S, McCarthy P, Sue K, Doran P et al (2018) Canadian national survey of point-of-care ultrasound training in family medicine residency programs. Can Fam Physician 64(10):e462–e467
PubMed PubMed Central Google Scholar
Steinmetz P, Dobrescu O, Oleskevich S, Lewis J (2016) Bedside ultrasound education in Canadian medical schools: a national survey. Can Med Educ J 7(1):e78-86
Ma IWY, Steinmetz P, Weerdenburg K, Woo MY, Olszynski P, Heslop CL et al (2020) The Canadian medical student ultrasound curriculum: a statement from the Canadian ultrasound consensus for undergraduate medical education group. J Ultrasound Med 39(7):1279–1287
Weill S, Picard DA, Kim DJ, Woo MY (2023) Recommendations for POCUS curriculum in Canadian undergraduate medical education: consensus from the inaugural Seguin Canadian POCUS Education Conference. POCUS J 8(1):13–18
Lewis D, Rang L, Kim D, Robichaud L, Kwan C, Pham C et al (2019) Recommendations for the use of point-of-care ultrasound (POCUS) by emergency physicians in Canada. CJEM 21(6):721–726
Article PubMed Google Scholar
Bronshteyn YS, Anderson TA, Badakhsh O, Boublik J, Brady MBW, Charnin JE et al (2022) Diagnostic point-of-care ultrasound: recommendations from an expert panel. J Cardiothorac Vasc Anesth 36(1):22–29
Ma IWY, Arishenkoff S, Wiseman J, Desy J, Ailon J, Martin L et al (2017) Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) group. J Gen Intern Med 32(9):1052–1057
Arntfield R, Millington S, Ainsworth C, Arora R, Boyd J, Finlayson G et al (2014) Canadian recommendations for critical care ultrasound training and competency. Can Respir J 21(6):341–345
Meineri M, Arellano R, Bryson G, Arzola C, Chen R, Collins P et al (2021) Canadian recommendations for training and performance in basic perioperative point-of-care ultrasound: recommendations from a consensus of Canadian anesthesiology academic centres. Can J Anaesth 68(3):376–386
McCleery A, Devenny K, Ogilby C, Dunn C, Steen A, Whyte E et al (2019) Using medicolegal data to support safe medical care: a contributing factor coding framework. J Healthc Risk Manag 38(4):11–18
Reaume M, Farishta M, Costello JA, Gibb T, Melgar TA (2021) Analysis of lawsuits related to diagnostic errors from point-of-care ultrasound in internal medicine, paediatrics, family medicine and critical care in the USA. Postgrad Med J 97(1143):55–58
Solomon L, Emma M, Gibbons LM, Kusulas MP (2022) Current risk landscape of point-of-care ultrasound in pediatric emergency medicine in medical malpractice litigation. Am J Emerg Med 58:16–21
Stolz L, O’Brien KM, Miller ML, Winters-Brown ND, Blaivas M, Adhikari S (2015) A review of lawsuits related to point-of-care emergency ultrasound applications. West J Emerg Med 16(1):1–4
Russ B, Arthur J, Lewis Z, Snead G (2022) A review of lawsuits related to point-of-care emergency ultrasound applications. J Emerg Med 63(5):661–672
Blaivas M, Pawl R (2012) Analysis of lawsuits filed against emergency physicians for point-of-care emergency ultrasound examination performance and interpretation over a 20-year period. Am J Emerg Med 30(2):338–341
Nguyen J, Cascione M, Noori S (2016) Analysis of lawsuits related to point-of-care ultrasonography in neonatology and pediatric subspecialties. J Perinatol 36(9):784–786
Article CAS PubMed Google Scholar
Netherton S, Milenkovic V, Taylor M, Davis PJ (2019) Diagnostic accuracy of eFAST in the trauma patient: a systematic review and meta-analysis. CJEM 21(6):727–738
Vieillard-Baron A, Millington SJ, Sanfilippo F, Chew M, Diaz-Gomez J, McLean A et al (2019) A decade of progress in critical care echocardiography: a narrative review. Intensive Care Med 45(6):770–788
Stickles SP, Carpenter CR, Gekle R, Kraus CK, Scoville C, Theodoro D et al (2019) The diagnostic accuracy of a point-of-care ultrasound protocol for shock etiology: a systematic review and meta-analysis. CJEM 21(3):406–417
Lee C, Balk D, Schafer J, Welwarth J, Hardin J, Yarza S et al (2019) Accuracy of focused assessment with sonography for trauma (FAST) in disaster settings: a meta-analysis and systematic review. Disaster Med Public Health Prep 13(5–6):1059–1064
Stengel D, Leisterer J, Ferrada P, Ekkernkamp A, Mutze S, Hoenning A (2018) Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev 12(12):CD012669
PubMed Google Scholar
Aspler A, Wu A, Chiu S, Mohindra R, Hannam P (2022) Towards quality assurance: implementation of a POCUS image archiving system in a high-volume community emergency department. CJEM 24(2):219–223
Lewis D, Alrashed R, Atkinson P (2022) Point-of-care ultrasound image archiving and quality improvement: not “If?” or “When?”…but “How?” and “What Next…?” CJEM 24(2):113–114
Download references
Acknowledgements
We would like to thank Anna MacIntyre for her contributions to the retrieval of cases from the CMPA database.
No funding was obtained for this research.
Author information
Authors and affiliations.
Division of Critical Care, Western University, London, Ontario, Canada
Ross Prager & Robert Arntfield
London Health Sciences Centre, Rm # D2-528, 800 Commissioners Rd. E., London, ON, N6A 5W9, Canada
Ross Prager
Department of Medicine, Western University, London, Ontario, Canada
Department of Safe Medical Care Research, Canadian Medical Protective Association, Ottawa, ON, Canada
Gary Garber, P. J. Finestone, Cathy Zang & Rana Aslanova
Department of Medicine, University of Ottawa, Ottawa, ON, Canada
Gary Garber
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the design, analysis, interpretation, manuscript writing, and revisions of this study.
Corresponding author
Correspondence to Ross Prager .
Ethics declarations
Ethics approval and consent to participate.
The Advarra Institutional Review Board provided ethical approval for this study.
Consent for publication
No patient information is provided in the manuscript.
Competing interests
None of the authors have relevant competing to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
CMPA repository search strategy.
Word search terms:
Bedside ultrasound
Bedside u/s
Point of care
Point of care ultrasound
Point of care u/s
POC ultrasound
Patient harm classification definitions.
The harm classification distinguishes healthcare-associated harm from other medical-legal matters through a reliable method. The system categorizes harm arising from healthcare delivery either from an inherent risk of investigation or treatment, or from three types of patient safety incidents: harmful incident, no harm incident (i.e. incident occurred but did not lead to harm), or a near miss.
Harm classification table.
Based on ASHRM’s Healthcare Associated Preventable Harm Level Classification and Classification of patient safety incidents in primary care.
† Relates to a No harm incident: a patient safety incident that reached a patient but resulted in no discernable harm.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Prager, R., Wu, D., Garber, G. et al. Medico-legal risks of point-of-care ultrasound: a closed-case analysis of Canadian Medical Protective Association medico-legal cases. Ultrasound J 16 , 16 (2024). https://doi.org/10.1186/s13089-024-00364-7
Download citation
Received : 25 July 2023
Accepted : 11 February 2024
Published : 23 February 2024
DOI : https://doi.org/10.1186/s13089-024-00364-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medcio-legal
- Patient safety
- Point-of-care ultrasound
Loading metrics
Open Access
Peer-reviewed
Research Article
Medico-Legal Findings, Legal Case Progression, and Outcomes in South African Rape Cases: Retrospective Review
* E-mail: [email protected]
Affiliations Gender and Health Research Unit, Medical Research Council, Pretoria, South Africa, School of Public Health, University of the Witwatersrand, Johannesburg, South Africa
Affiliation School of Public Health, University of the Witwatersrand, Johannesburg, South Africa
Affiliation Tshwaranang Legal Advocacy Centre, Johannesburg, South Africa
Affiliation Centre for the Study of Violence and Reconciliation, Johannesburg, South Africa
Affiliation Gender and Health Research Unit, Medical Research Council, Pretoria, South Africa
- Rachel Jewkes,
- Nicola Christofides,
- Lisa Vetten,
- Ruxana Jina,
- Romi Sigsworth,
- Lizle Loots

- Published: October 13, 2009
- https://doi.org/10.1371/journal.pmed.1000164
- Reader Comments
Health services for victims of rape are recognised as a particularly neglected area of the health sector internationally. Efforts to strengthen these services need to be guided by clinical research. Expert medical evidence is widely used in rape cases, but its contribution to the progress of legal cases is unclear. Only three studies have found an association between documented bodily injuries and convictions in rape cases. This article aims to describe the processing of rape cases by South African police and courts, and the association between documented injuries and DNA and case progression through the criminal justice system.
Methods and Findings
We analysed a provincially representative sample of 2,068 attempted and completed rape cases reported to 70 randomly selected Gauteng province police stations in 2003. Data sheets were completed from the police dockets and available medical examination forms were copied. 1,547 cases of rape had medical examinations and available forms and were analysed, which was at least 85% of the proportion of the sample having a medical examination. We present logistic regression models of the association between whether a trial started and whether the accused was found guilty and the medico-legal findings for adult and child rapes. Half the suspects were arrested ( n = 771), 14% (209) of cases went to trial, and in 3% (31) of adults and 7% (44) of children there was a conviction. A report on DNA was available in 1.4% (22) of cases, but the presence or absence of injuries were documented in all cases. Documented injuries were not associated with arrest, but they were associated with children's cases (but not adult's) going to trial (adjusted odds ratio [AOR] for having genital and nongenital injuries 5.83, 95% confidence interval [CI] 1.87–18.13, p = 0.003). In adult cases a conviction was more likely if there were documented injuries, whether nongenital injuries alone AOR 6.25 (95% CI 1.14–34.3, p = 0.036), ano-genital injuries alone (AOR 7.00, 95% CI 1.44–33.9, p = 0.017), or both nongenital and ano-genital injuries (AOR 12.34, 95% CI 2.87–53.0, p = 0.001). DNA was not associated with case outcome.
Conclusions
This is the first study, to our knowledge, to show an association between documentation of ano-genital injuries, trials commencing, and convictions in rape cases in a developing country. Its findings are of particular importance because they show the value of good basic medical practices in documentation of injuries, rather than more expensive DNA evidence, in assisting courts in rape cases. Health care providers need training to provide high quality health care responses after rape, but we have shown that the core elements of the medico-legal response require very little technology. As such they should be replicable in low- and middle-income country settings. Our findings raise important questions about the value of evidence that requires the use of forensic laboratories at a population level in countries like South Africa that have substantial inefficiencies in their police services.
Please see later in the article for the Editors' Summary
Citation: Jewkes R, Christofides N, Vetten L, Jina R, Sigsworth R, Loots L (2009) Medico-Legal Findings, Legal Case Progression, and Outcomes in South African Rape Cases: Retrospective Review. PLoS Med 6(10): e1000164. https://doi.org/10.1371/journal.pmed.1000164
Academic Editor: Chris Beyrer, John Hopkins University, United States of America
Received: January 27, 2009; Accepted: September 3, 2009; Published: October 13, 2009
Copyright: © 2009 Jewkes et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: Funding was provided by the Norwegian Centre for Human Rights, the Open Society Foundation, the Ford Foundation and the Medical Research Council of South Africa. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval
Editors' Summary
Sexual violence has significant short- and long-term mental and physical health consequences for the victim. Estimates of how common rape is vary within and between countries. The World Health Organization (WHO) estimates that between 1% and 12% of women aged 15 or over have experienced sexual violence by a nonpartner. It has also been used as a weapon of war.
The WHO recognises that rape may be committed by a spouse, partner, or acquaintance as well as a stranger, that men can be victims as well as perpetrators, and that coercion need not be physical. It advocates preventing sexual violence through better support for victims, legal and policy changes, educational programmes, and campaigns to change attitudes, and better health care services and training for health care workers.
Health services for victims of rape have two important roles: to assist the victim and to gather evidence for the police and courts. Nonetheless, health services for victims of rape are often poor. Over the last decade, the South African government has taken steps to reduce particularly high rates of sexual violence by broadening the legal definition of rape and improving health services.
Why Was This Study Done?
Previous studies into how useful expert medical evidence is for the police and courts have focused almost exclusively on high-income countries. It is not clear what interventions work best in countries with fewer resources. The researchers wanted to know the impact of medical evidence on how the South African criminal justice system handled cases of rape and attempted rape.
What Did the Researchers Do and Find?
The authors analysed data from police and court files of 1,547 cases of rape or attempted rape first reported in 2003 to a random sample of police stations in Gauteng province, South Africa. They looked for associations between case data and the arrest, charge, trial, and conviction or acquittal of the alleged perpetrator. They included only cases that were closed when they collected data in 2006 and only cases that contained a record of a medical examination of the victim. The researchers used South Africa's then legal definition of rape as “intentional and unlawful vaginal sex with woman without consent.” They analysed cases involving adults and children (aged 0–17 years) separately. They found that the overall conviction rate was very low, with only 3% of adult cases and 7.4% of children's cases resulting in a guilty verdict. Many cases were dropped at each stage of the legal process and DNA evidence was often not collected or, if collected, not analysed. DNA reports were rarely available for the courts. Injuries were not associated with arrests for either adult or children's cases; an arrest took place in 40% of cases without injuries. Child cases were more likely to come to trial if injuries were present, although a guilty verdict was not more likely. The reverse was true in adult cases: the presence or absence of injury was not linked to cases being brought to trial, but if injuries were present, whether genital, nongenital, or both, a conviction was more likely.
What Do These Findings Mean?
One limitation of the research is that the researchers identified statistical associations of events, but this does not prove that one event caused the other. Other possible limitations of the study are that the researchers had access only to cases closed by the police, which may have biased their results, and the quality of the recorded data was very variable. In addition, the research did not consider other factors that may have affected case outcomes, such as how witnesses are perceived in court.
The system to collect and analyse DNA was rarely effective in making evidence available to the courts. It is known from other countries with effective systems that DNA evidence is of no value if the basis of defence is consent; for instance in cases where the accused is an intimate partner of the victim. Injuries appear not to be necessary to secure a conviction but may be seen as useful by the South African courts in corroborating the victim's testimony, at least in adult cases.
The authors conclude that in poor countries, training for nurses and/or doctors who act as forensic medical examiners in how to record injuries and present their evidence in court will be more effective than investing in costly systems for DNA analysis. However, they argue that in South Africa, as a middle-income country with a high proportion of nonintimate partner rapes, there would be benefit in improving the system to collect and analyse DNA evidence rather than abandoning it entirely.
Additional Information
Please access these Web sites via the online version of this summary at http://dx.doi.org/10.1371/journal.pmed.1000164 .
- Further information on rape in South Africa is available from the Tshwaranang Legal Advocacy Centre
- Information on rape is also available from the Rape Crisis Cape Town Trust
- Emergency rape information, facts about rape, events, legal services, and medical care can be found at the Speakout Web site
- The World Health Organization publishes a factsheet on sexual violence , a report on violence and health , as well as guidelines on medico-legal care for victims of sexual violence
Introduction
In 2008 the United Nations Security Council adopted Resolution 1820 (2008), which declared rape to be a threat to global security—an act recognising that rape violates its victims' human rights and has particularly destructive social consequences. The Council also recognised that rape may cause considerable physical and psychological morbidity. Health systems have a critical role in responses to rape, yet in most countries the health sector response is underdeveloped [1] . Post-rape services generally receive few resources, service providers often lack specific training for and confidence in examining victims and interpreting their findings for the courts, and the health needs of victims often remain unmet [2] , [3] . In most countries rape services need resources and development, and research has a valuable role to play in guiding efforts to appropriately focus post-rape health services.
Expert medical evidence is widely used in rape cases, but its contribution to the progression of cases through the legal system and to legal case outcomes is unclear. A recent review [2] found 35 studies exploring the association, all but two from high-income countries, and two others have since been published. In just two studies, both from the United States, having a documented ano-genital injury was associated with filing charges [4] , [5] . Thirteen studies examined the association between the documentation of bodily injuries generally and case outcomes, with only two studies from the United States [6] , [7] and one from Canada [8] finding an association. Many of the studies were very small and dated, which influenced the analyses performed and power thereof [2] .
South Africa has an especially high prevalence of rape [9] , and as such, it is a particularly important context in which to conduct research on health sector responses to rape. Although in this country these responses have historically been poor, in the last decade there have been great efforts for improvement with a new national policy on sexual assault care [10] and clinical management guidelines [11] . The policy includes offering HIV testing and the provision of postexposure prophylaxis for HIV to rape survivors. There have been many different initiatives to train health providers in the provision of post-rape health care and forensic medical examination, which have culminated in the development of a national curriculum [12] . There have also been many efforts to improve the environment of rape facilities, including by identifying and furnishing dedicated rape care rooms. A forensic kit for collecting evidence, chiefly for genotyping, has been in use since 2000 and its completion is a standard part of the medical forensic examination [10] , [13] . The forensic kit enables collection of material that can form part of the evidence presented in court, as in rape cases medical evidence consists of both the observations about the victim at the time of the medical examination (including her or his physical and emotional state and sobriety), observations of injuries on her or his body generally and in the ano-genital region, and results of analysis of specimens taken for DNA. Examination findings are usually presented by the medical examiner (doctor or nurse) in person in a court room as an expert witness, whose testimony consists of the description of these observations and their interpretation. The DNA results are presented by an analyst from the Forensic Science Laboratory. The South African legal system is an adversarial system based on Roman Dutch law.
Given the growth of initiatives to strengthen the post-rape health care and the dual role of the health sector in providing care for victims as well as collection of evidence to assist the courts, it is important to understand the contribution of forensic medical evidence and the role of DNA evidence in case outcomes. To our knowledge, these two considerations have not previously been explored in a developing country. This article reports findings of a study that aimed to describe the processing of rape cases by South African police and courts and the association between medico-legal findings and case progression through the criminal justice system.
Ethics approval was given by the University of Witwatersrand, Faculty of Health Sciences Ethics Committee.
In terms of South African law from 1959 to 2007, rape was defined as occurring when a man had “intentional & unlawful vaginal sex with woman without consent,” and anal and oral penetration without consent were deemed “indecent assaults.” In December 2007 this definition was changed to include anal and oral penetration and encompassed the rape of men. This article presents a study of legally defined rape, based on a provincially representative sample of cases of rape and attempted rape opened at Gauteng province police stations between 00:00 on 1 January 2003 and 23:59 on 31 December 2003, and which had been closed by the police at the time of data collection in 2006 [14] .
A total of 11,926 rapes were reported at the 128 police stations in the province that year. A sample was drawn for the study using a two-stage procedure. The first stage drew a random sample of 70 police stations using probability proportional to size, where size was based on the number of rape cases that year. Within each police station all the closed rape cases for the year were identified and a systematic sample of 30 dockets was selected (or all cases were taken if the number was less than 30). Dockets selected that were not available were not replaced. The proportion of dockets opened from which we were about to draw the sample was 70.1%. We were not able to ascertain how many dockets were unavailable because they were still open and how many were missing for other reasons. This procedure provided a sample of 2,068 cases for the study. If cases went to court, we obtained court records from both High Courts in the province, as well as all 30 magistrates' courts.
The police dockets included the witness statements, police investigation diary, the form on which the findings of the medical examination were documented by the medical examiner, and any other reports, including any from the Forensic Science Laboratory (if available). Data were abstracted by a team of trained fieldworkers using a standardised data coding sheet. Information gathered included the details of the complainant (age, race, occupation, in the case of children the carer), the circumstances of the rape (when it occurred, where, what the victim was doing, use of weapons, victim responses after the rape), information on the suspect (age and relationship to victim), and on the case outcome. Medico-legal forms found in dockets were copied verbatim onto a blank form in the data capture sheet by the fieldworker, whereas those found in court records were photocopied. The information from these was abstracted onto a form for data entry by health professionals on the study team (NC, RJ, and RJ).
Permission to review closed rape dockets was obtained from the police nationally, provincially, and at the stations. Court documents are a matter of public record. No identifying information related to rape victims was collected during fieldwork and any found on documents that were photocopied was erased.
Data Analysis
The analysis was undertaken using Stata 10 and the svy commands used to take into account the structure of the sample. All cases without a medico-legal form, including those for attempted or suspected rape, were excluded from the analysis. Among these, no medical examination was done in 250 cases (50%), in three cases the form had been destroyed with court records, and in a further 252 the reason for nonavailability was unknown. Sixteen cases were dropped because very basic information was unavailable. The remaining 1,547 cases were analysed (85% of those that may have had medical examinations). The analysis is presented according to the age group of the victim (0–17 y and ≥18 y), because the variables operated differently in different age groups. We examined the findings for the 0–11-y-old and 12–17-y-old age groups separately, but combined them because no additional information was gained by their separation.
For Table 1 , we calculated the number and proportion of the cases opened by the police where the perpetrator was arrested (or asked to appear in court), charged, brought to trial, found guilty of a sexual offence (rape, attempted rape, or indecent assault), and imprisoned. We calculated the proportion of the cases that had a forensic evidence kit completed, sent to laboratory, where the suspect's blood was drawn, and where a report on DNA was available from the Forensic Science Laboratory. We also calculated the proportion attaining the previous stage in this process that progressed to the next stage (attrition by stage). We compared the proportion of cases reaching each stage between adults and children using a Pearson Chi-squared test.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1000164.t001
For Tables 2 and 3 , we calculated the column percentage or mean for variables according to whether the suspect was arrested or not, brought to trial, and convicted of a sexual offence. The variables presented in these tables are those potential confounding variables for the relationship between the medical evidence variables and the outcomes. The survey regression command was used to compare the ages of victim and perpetrator between the two subgroups. A Pearson Chi-squared test was used to compare the proportion of cases at each level of the variable between the two subgroups for categorical variables.
https://doi.org/10.1371/journal.pmed.1000164.t002
https://doi.org/10.1371/journal.pmed.1000164.t003
Potential confounders included those related to the circumstances of the rape and possibility of apprehending the rapist: the involvement of more than one perpetrator, the suspect having previous convictions, the suspect's age, and the victim–perpetrator relationship. Some variables that may have influenced the violence of the rape as well as those that might have been in keeping stereotypical myths about what constitutes a “real rape” were examined: whether the victim resisted physically or verbally, weapons, and abduction, and whether the case was reported within 72 h was included as it could influence detection of injury and the presence of DNA. As an indicator of the quality of the investigation we included whether the first report statement was taken by the police or not. This statement is taken from the first person who the victim told about the rape and is often used as corroboration of aspects of the account of events and the victim's emotional and physical state at the time.
Nongenital (or anal) injuries included incised wounds, lacerations, grazes, bruises, and areas of tenderness and observations are intended to include the whole body except the ano-genital region. Ano-genital injuries were defined as those that may have been found on the mons pubis, frenulum, clitoris, labia majora, labia minora, perineum, fossa navicularis, hymen, vagina, clitoris, or anus. The injuries recorded ranged from lacerations to bruising, redness, inflammation, or tenderness. The variable “injury to the genitals with a skin break” only included genital injury that took the form of an incised wound, scratch, abrasion or laceration, if bleeding was seen, or if there was scarring that was believed to be from injuries caused by the rape. This variable was examined as an indicator of somewhat greater severity of injury. A four-level injury variable was derived with the referent group being no injury, and comparison groups being nongenital injury only, genital injury with a skin break only, both nongenital and genital injuries with a skin break.
Six logistic regression models were built using the Stata 10 svylogit command to describe factors associated with there being an arrest, having the trial commence (among those arrested or asked to appear in court), and being found guilty of a sexual offence (among those going to trial). Models for adults and children are presented separately. For each model the variables in Tables 2 and 3 were considered and those associated with the outcome at p <0.1 were entered into the model with the victim's age and the four-level exposure variable for injury. For the models for conviction, the presence of a DNA report was included; this was not included for the earlier models as DNA analysis is often only completed on a prosecutor's request because a case is about to go to trial. Stepwise backwards elimination was used to reach the parsimonious model from the variables tested. The associations between the outcome and the injury (and DNA) variables are presented for each model, adjusted for age and in the trial models, having a first report statement taken, which significantly associated with the outcome ( p ≤0.05). No other tested variables were significantly associated in these models; these are presented in Table 4 .
https://doi.org/10.1371/journal.pmed.1000164.t004
Table 1 shows the proportion of cases of rape reported to the police and reaching each stage of the criminal justice system process for adults and children. Although an arrest was made in almost half of cases, there was only a conviction for a sexual offence in 3% of adult and 7.4% of children's cases. Examining attrition by stage we see that a trial was commenced in only 27% of adult and 38% of child cases where the suspect was arrested and charged in court. Convictions for sexual offences were achieved in a similar proportion of adult and child cases (30% and 41%) commencing trial.
A forensic evidence kit was completed much more often in adults than children (91% versus 63%). Whereas children were much more likely than adults to present more than 72 h after the rape (17.8% versus 3.4%), kits were still not completed on 23.8% of children and 6.3% of adults presenting within 72 h. Completed kits were often not sent to the laboratory for analysis and, in 71.5% of cases that were prosecuted, the suspect's blood was never drawn. Even when blood was drawn, reports on DNA found were rarely available for the courts.
Some of the features of the adult cases are presented in Table 2 and of child cases in Table 3 , by whether the suspect was arrested, brought to trial, and convicted. Arrest was more common when older children were raped and there was a suggestion that convictions were more common when adult victims were older ( p = 0.07). Otherwise a victim's age was not associated with case outcomes.
Arrest was less likely in rapes of adults involving multiple perpetrators ( p = 0.0003), but otherwise there was no significant difference in this by outcome. The suspect's age was not associated with case outcome. In adult cases, there is some evidence that trials may have been more likely to start if there were previous convictions ( p = 0.08), but conviction for a sexual offence occurred less frequently in this group ( p = 0.05). Arrests in both adult and child cases were much more common if the accused was known to the victim ( p <0.0001).
There was no association between whether the victim resisted the rape or abduction and any of the outcomes, for adults or children. Abducted adult and child victims were less likely to see the suspect arrested, but if there was an arrest, the trial was more likely to commence in adult cases. Armed perpetrators were less likely to be arrested. In cases where there was both an arrest and a trial, a statement from the first witness was much more likely to be in the docket.
Injuries in adults and children did not appear to have any influence over arrests. A notable finding was the high proportion (approximately 40%) of cases where an arrest was effected in rape cases of adults and children where no injuries were described. In children, nongenital injuries were uncommon. In child cases, genital injuries were more often found in cases that were brought to trial. In adults, they were more prevalent in cases where there was a conviction. A DNA report was only available for ten adults and 12 children. There was a conviction in three adult cases and two child cases that had a DNA report. The DNA report more often it led to an acquittal when in five adult and five child cases the short tandem repeat (STR) profile did not match that of the suspect. A match did not assure conviction, the accused having been acquitted in three children's cases and one adult case where the profile did match.
There was no statistically significant association between the presence of injuries and whether the suspect was arrested in adult or child cases (models not shown). Table 4 shows the four multiple variable models for factors associated with going to trial and convictions for a sexual offence in adult and child cases. After an arrest, a trial was significantly more likely to commence in children with both nongenital and genital injuries causing a skin break and there was some evidence that documented genital injuries alone also increased the likelihood of a case going to trial. In children, convictions for sexual offences were not more common in cases where there was evidence of injury. In adults, on the other hand, finding injuries was not associated with case progression to trial. However, having nongenital or genital injury, and having both, were all strongly associated with a conviction. The presence of a DNA report was not associated with conviction in either age group.
We examined a subset of rape cases where there was a forensic medical examination of the victim and have shown a precipitous decline in the proportion of cases reaching each sequential stage in the criminal justice system, with suspects only being convicted in about one in 20 of the documented rape cases. We described a parallel decline in the proportion of cases in which the chain of activities were performed to enable specimens to be collected and sent to a laboratory so that a report on the presence and analysis of DNA would be potentially available for use in trials. Substantial flaws in the system were evident, with forensic evidence collection kits not always being completed, when indicated; those completed often not being sent to the laboratory for analysis; and the suspect's blood infrequently being drawn. As a result of this, DNA reports were almost never available to be used in court cases. Although DNA is often presented as a key to solving cases and convicting offenders, we have shown that when available, DNA more certainly led the courts to acquit [15] , usually because no match to the accused was established, although medical evidence of injuries may have been available. This is not a positive outcome for a rape complainant, but in a criminal justice system that determines cases on absence of reasonable doubt, it would establish “reasonable doubt” that the accused was the culprit and thus assist the court.
We have shown that the presence of ano-genital injuries was associated with children's cases going to trial, and in adult cases a conviction was very much more likely if injuries were documented. It is notable that in a quarter of child cases where there was a conviction there were no documented injuries, which was also the case in 10% of adult cases. These data confirm that the presence of injury is not essential for a conviction in rape cases in South Africa, but at the same time it seems to suggest that courts may like to use the presence of injuries, at least in adult cases, as corroboration of the victim's testimony.
The attrition of cases in the criminal justice system is similar to that found in previous research [16] , and our findings about the nonavailability of DNA confirms those of an earlier small case series [17] . In South Africa, considerable resources have been invested in establishing a system that potentially enables the use of DNA in rape cases, yet it has clearly not been operating properly. It seems that the police are not able to respond appropriately in sending kits to laboratories and ensuring blood is taken from suspects. The police not sending kits to the laboratory was not explained by failure to make an arrest or the police withdrawing the case, but depended primarily on which police station or district the case was opened in. In most cases where suspect's blood was sent to the laboratory the kits were still not analysed. In 2005 the South African Forensic Science Laboratories had backlogs of about 20,000 unanalysed kits [18] , a number proportionately somewhat similar to that reported in the United States, but they were much slower at completing analysis than the average time in the United States [19] . As a result, few kits sent to them are processed, and only children's kits are analysed routinely, rather than on a request from a prosecutor.
This study has shown that in this setting medical documentation of injury and expert testimony in court may have influenced case progression and outcomes. In some individual cases DNA may be of value, but when the system is viewed as a whole this is not evident. It seems likely that this is chiefly because health and police systems in South Africa simply do not work well enough to enable DNA and forensic evidence collection and analysis to realise its potential. Although we know that in some countries even where DNA and forensic evidence systems work more effectively, they are still not associated with a positive legal outcome [8] , as DNA is of no value if the basis of the defence is consent. Nonetheless we believe that as a middle-income country South African forensic laboratories are affordable and a high proportion of South African rape cases are not intimate partner rapes, therefore DNA has the potential to contribute. On the basis of current information, efforts should be made to improve the system and the proportion of cases in which DNA is available rather than dispensing with it entirely.
This study is, to our knowledge, the first from a developing country to examine the association between findings on medico-legal examination and rape case progression and outcomes. Its strengths are its size and the fact that it is based on a random sample of cases from a broad geographic region. There may be limitations to the generalisablity of the findings since we only had access to closed cases and are not sure what proportion of eligible dockets were available for the sample or what biases could have ensued from this. The study relied on routine data, which are often flawed. We enhanced the validity of case outcomes data by using data from courts as well as the dockets. We are aware that the quality of documentation of the dockets and medical findings was very variable, but since this is what is used in the criminal justice system it is still valid to see how it may be associated with the progression of cases. In the analysis here we have only adjusted for a small set of potential confounding factors. We recognise that there could have been other factors influencing whether cases go to trial and convictions, notably how witnesses come across in court, willingness to accept children's testimony in court, and bias from judges. Further research with large datasets is needed to explore these areas in more detail.
This is the first study, to our knowledge, to show an association between documentation of ano-genital injuries, trials commencing, and convictions in rape cases in a developing country. Its findings are of particular importance because they point to the value of good basic, forensic medical practices in assisting courts in rape cases. Health care providers need to be trained to provide high quality health care responses after rape, and we have shown that the core elements of the medico-legal response require very little technology. As such they should be replicable in low- and middle-income country settings, providing forensic medical examiners are trained in examination and documentation of injuries, and the presentation and interpretation of findings in court. Our findings raise important questions about the value of evidence that requires the use of forensic laboratories at a population level in countries like South Africa that have substantial inefficiencies in their police services. They suggest that in a resource constrained setting far more benefit may be accrued to rape victims and the criminal justice system by establishing policy, guidelines, and training for forensic medical examiners (be they nurses or doctors) and ensuring that they are equipped to provide good basic health care, including the forensic medical examination, than by focusing on complex and expensive systems to allow for DNA analysis. Further research is needed to deepen understandings of the use of medical evidence in court in a range of settings, and more health systems research is needed in both developed and developing countries to evaluate health systems interventions in post-rape care and their impact on victim/survivor health outcomes as well as the processes of justice.
Acknowledgments
We would like to thank the South African Police Services for giving us access for the study; Olivia Dunseith and Collet Ngwane who supervised fieldwork and the fieldworkers; Jonathan Levin for drawing the sample; and Samuel Manda for statistical review of the paper.
Author Contributions
ICMJE criteria for authorship read and met: R Jewkes, N Christofides, L Vetten, R Jina, R Sigsworth, L Loots. Agree with the manuscript's results and conclusions: R Jewkes, N Christofides, L Vetten, R Jina, R Sigsworth, L Loots. Designed the experiments/the study: R Jewkes, N Christofides, L Vetten, R Jina, R Sigsworth. Analyzed the data: R Jewkes, L Vetten, R Sigsworth. Collected data/did experiments for the study: R Jewkes, L Vetten, R Sigsworth, L Loots. Wrote the first draft of the paper: R Jewkes. Contributed to the writing of the paper: N Christofides, L Vetten, R Jina. Contributed to data coding of medico-legal forms: N Christofides. Principal investigator: L Vetten. Developed the data schedule collecting court information: L Vetten.
- 1. Jewkes R, Sen P, Garcia Moreno C (2002) Sexual violence. In: Krug EG, Mercy J, Zwi A, Lozano R, editors. World Health Report on Violence and Health. Geneva: World Health Organization. pp. 148–181.
- 2. Du Mont J, White D (2007) The uses and impacts of medico-legal evidence in sexual assault cases: a global review. Geneva: World Health Organisation.
- 3. Wang SK, Rowley E (2008) Rape: responses from women and health providers. Geneva: Sexual Violence Research Initiative, World Health Organisation.
- View Article
- Google Scholar
- 5. Lindsay SP (1998) An epidemiologic study of the influence of victim age and relationship to the suspect on the results of evidentiary examinations and law enforcement outcomes in cases of reported sexual assault [PhD dissertation]. San Diego: San Diego State University.
- 10. Department of Health (2005) National sexual assault policy. Pretoria: National Department of Health.
- 11. Department of Health (2004) National management guidelines for sexual assault care. Pretoria: National Department of Health.
- 12. Jina R, Jewkes R, Christofides N, Loots L, editors. (2008) Caring for survivors of sexual assault. A training programme for health care providers in South Africa. Pretoria: Department of Health.
- 13. Biology Training Section (2000) Evidence collection kits: the new series of ECK for biological evidence. Pretoria: DNA Unit SAPS Forensic Science Laboratory.
- 14. Vetten L, Jewkes R, Fuller R, Christofides N (2008) Tracking justice: the attrition of rape cases through the criminal justice system in Gauteng. Johannesburg: Tshwaranang Legal Advocacy Centre.
- 16. Sidiropoulos E (1998) South Africa survey 1997/98. Johannesburg: South African Institute of Race Relations.
- 17. Blass L (2004) The responses of the criminal justice system to sexual violence crimes in the Kathorus region. South Africa. Johannesburg: Centre for Applied Legal Studies, University of the Witswatersrand.
- 18. Jina R (2006) Assessing the use of sexual assault evidence collection kits from six provinces in South Africa [unpublished MMed thesis]. Johannesburg: University of the Witwatersrand.
- 19. Lovrich NP, Pratt TC, Gaffney MJ, Johnson CL, Asplen CH, et al. (2003) National forensic DNA study report. Pullman (Washington): Division of Governmental Studies and Services, Washington State University; Tacoma (Washington): Smith Alling Lane, P.S. Report No: 203970.
Advertisement
Medico-Legal Issues Related to Hip and Knee Arthroplasty: A Literature Review Including the Indian Scenario
- Review Article
- Published: 30 March 2021
- Volume 55 , pages 1286–1294, ( 2021 )
Cite this article
- Satvik Pai ORCID: orcid.org/0000-0002-3621-150X 1
1617 Accesses
8 Citations
Explore all metrics
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are commonly performed surgeries worldwide. The number of joint replacement surgeries being performed has increased considerably over the past two decades, but it has also seen an increase in litigation associated with it. The purpose of our study was to review and consolidate literature regarding medico-legal issues pertaining to THA and TKA cases. We looked at the causes of litigation, medico legal aspects of pre-operative requirements, optimisation of medical condition, indications and contraindications for arthroplasty, informed consent, implants, mixing of components from different manufacturers and post-operative rehabilitation. We also wanted to analyse available literature and legal proceedings regarding these cases in India specifically.
Similar content being viewed by others

Litigation analysis of medical damage after total knee arthroplasty: a case study based on Chinese legal database in the past ten years
Shuai Liu, Jilong Zou, … Shuo Geng

Litigation after primary total hip and knee arthroplasties in France: review of legal actions over the past 30 years
Grégoire Rougereau, Thibaut Marty-Diloy, … Philippe Boisrenoult

Knee arthroplasty and lawsuits: the experience in France
Emmanuel Gibon, Thierry Farman & Simon Marmor
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are commonly performed surgeries worldwide. The number of joint replacement surgeries being performed has increased considerably over the past two decades, but it has also seen an increase in litigation associated with it [ 1 ]. In fact orthopaedic adult reconstruction subspecialists are sued for alleged medical malpractice at a rate over twice that of the physician population as a whole [ 2 ]. A survey of the American Association of Hip and Knee Surgeons found that 78% of responding surgeons had been named as a defendant in at least one lawsuit alleging medical malpractice [ 3 ]. The purpose of our study was to review and consolidate literature regarding medico-legal issues pertaining to THA and TKA cases. With respect to THA, TKA cases we looked at the causes of litigation, medico-legal aspects of pre-operative requirements, optimization of medical condition, indications and contraindications for arthroplasty, informed consent, implants, mixing of components from different manufacturers and post-operative rehabilitation. We also wanted to analyse available literature and legal proceedings regarding these cases in India specifically.
Materials and Methods
An extensive literature search was conducted to identify studies pertaining to medico-legal issues in relation to total hip arthroplasty (THA) and total knee arthroplasty (TKA). The electronic databases of PubMed and Cochrane Library were explored using the following search terms and Boolean operators: ‘medico-legal’ OR ‘lawsuit’ OR ‘malpractice’ OR ‘litigation’ AND ‘total hip arthroplasty’ OR ‘total knee arthroplasty’ OR ‘total hip replacement’ OR ‘total knee replacement’ OR ‘THA’ OR ‘TKA’. No restriction in publication date was applied. Manuscript language was restricted to English. In addition, a comprehensive search of reference lists of all identified articles was conducted to find additional studies. Information about specific medico-legal proceedings involving THA/TKA cases in Indian legal courts, state and national consumer dispute redressal forums, and state medical councils were obtained from different books having compendium of medico-legal judgements.
Causes for Litigation
It is important to know the causes of litigation and common allegations in malpractice lawsuits involving hip and knee arthroplasty, so that measures can be taken to prevent such complications occurring and the orthopaedic surgeon can be better prepared in the event of such complications happening. Patterson et al. [ 4 ] analysed 115 malpractice claims filed for alleged neglectful primary and revision THA surgeries. They found that in primary cases, nerve injury (“foot drop”) was the most frequent allegation with 27 claims. Negligent surgery causing dislocation was alleged in 18 and leg length discrepancy in 14. Medical complications were also reported, including three thromboembolic events and six deaths. In revision cases, dislocation and infection were the most common source of suits. The data pertaining to causes of litigation following THA in various studies is represented in Table 1 . Patterson et al. [ 5 ] also studied the malpractice claims filed for alleged neglectful primary and revision TKA surgeries. The analysed 69 primary and eight revision TKAs which were involved in malpractice lawsuits and found that the most frequent factor leading to lawsuits for primary TKA was chronic pain or dissatisfaction in 12 cases, followed by nerve palsy in eight, postoperative in-hospital falls in five, and deep vein thrombosis or pulmonary embolism in three. Medical complications included acute respiratory distress syndrome, cardiac arrest, and decubitus ulcers. Contracture was most common after revision TKA (three of eight cases). They concluded that pre-operative counselling regarding the risks of incomplete pain relief could reduce substantially the number of suits relating to primary TKAs. The data pertaining to causes of litigation following TKA in various studies is represented in Table 2 .
Bokshan et al. [ 6 ] analysed 213 lawsuits pertaining to THA/TKAs and found that 15.0% of cases ended in settlement, 29.6% ended in a verdict in favour of the patient. The average payment for cases lost in court was significantly larger than cases that ended in settlement. They noted that while complications such as “pain and weakness” are less likely to result in favourable litigation for patients, the presence of an objective technical complication or nerve injury was associated with an increased risk for a physician loss and a higher payment. Jarvelin et al. [ 13 ] analysed factors predisposing to claims and compensations for patient injuries following total hip and knee arthroplasty. They found that patients over 65 years of age were less likely to file a claim than patients under the age of 65 years, patients with increased comorbidity were more likely to file a claim. Following THA, male sex and cemented prosthesis reduced the odds of a claim. Following TKA, a volume of over 300 operations reduced the probability of compensation for certain injury types. Thus they suggested that centralisation of TKA to hospitals with higher volume may reduce the rate of compensable patient injuries. Novi et al. [ 7 ] analysed 40 lawsuits pertaining to THA and found that some complications such as nerve injuries and infection are almost always considered directly dependent on physician’s errors, and especially in these cases, hospitals try to settle the claim out of court. They suggest that possible strategies to reduce malpractice claims are diligent execution of the surgical procedure and of a proper postoperative management, the correct compilation of a procedure-specific informed consent and adequate doctor–patient communication to provide the necessary explanations, possible risks and realistic expectations. Gibon et al. [ 12 ] analysed 107 lawsuits pertaining to TKA and found that frequent complications are not those which raise most of the claims. Patients sue the surgeon when the outcome of the surgery is different from what they were expecting. They also noted that in court judgements or proceeding it is often stated that delay in diagnosis or treatment of a complication involves the personal responsibility of the surgeon. Therefore, the best practice in handling complications or errors in knee arthroplasty is to quickly recognise and to treat them properly as well as to provide the patient comprehensible information. Chen et al. [ 14 ] analysed 298 lawsuits following TKA and found that litigation success rates for TKA were higher when involving a technical error such as malalignment, as compared to events less under the surgeon's control such as infection or venous thromboembolism. The number of incorrect prosthesis/prosthesis size claims was concerning. They suggest that these may be addressed with strict use of pre-operative templating, the WHO Surgical Safety checklist and repeat intra-operative checking of the implant. Mcgrory et al. [ 2 ] analysed the relationship between surgeon demographics and malpractice lawsuits for joint reconstruction surgeons. They found that the overall risk of a malpractice claim is related to years spent in practice. After 30 years in an adult reconstruction practice, the cumulative rate of being sued at least once is over 90%. They were unable to identify any relationship between the type, size, or location of practice, fellowship training, or surgery volume and the risk of an adult reconstruction surgeon being named as a defendant in a malpractice suit.
Indications and Contraindications for THA/TKA
There are various indications for THA/TKA in patients with osteoarthritis of the joint, rheumatoid arthritis, intra articular fractures which cannot be reconstructed by internal fixation, destruction of joint by infection or malignancy, avascular necrosis of femoral head, among others. The decision of arthroplasty is usually taken after trial of non-surgical management or when other surgical procedures are deemed insufficient. The legal importance of the indication for arthroplasty arises when a patient claims that arthroplasty was not indicated in the patient or not appropriate for the patient. It is also important to discuss the indication for the arthroplasty with the patients to ensure that they understand the primary reason why the procedure is being done, so as to avoid unrealistic expectations of post-surgical outcomes. Gademan et al. [ 15 ] performed a systematic review of the indication criteria for THA, TKA in literature and found that they could be divided into four main domains of pain, function, radiological changes and failed conservative therapy. However, they noted that specific cut-off values or ranges in the domains were lacking and the level of evidence was low. Cross et al. [ 16 ] studied the consensus among orthopaedic surgeons and found that there no agreement regarding the indications for total knee arthroplasty. They also studied the agreement between orthopaedic surgeons, rheumatologists, and primary care providers and found that ‘pain not responsive to drug therapy’ was the only indication for TKA which had sufficient agreement. ‘Major psychiatric disorder, including dementia’ was the only contraindication for TKA which had consensus. This we believe, increases the importance of documentation of indication for arthroplasty by the orthopaedic surgeon. In the case of KS Sridhar vs Rajkumar (I(07)CPJ 362) [ 17 ], a 40-year-old patient filled a lawsuit alleging that the total hip arthroplasty he underwent was not the appropriate procedure for his fracture around the hip joint in view of his age. The court ruled in favour of the patient, stating the total hip replacement was not indicated in the patient considering his younger age.
Pre-operative Requirements and Optimization of Medical Condition
THA, TKA are elective procedures. This warrants the patients’ medical condition to be optimized before undergoing the procedure. Clelland et al. [ 18 ] found that conditions necessitating postponement or cancellation of total joint arthroplasty were present in approximately 4% of patients. Vincent et al. [ 19 ] provides comprehensive guidelines for the pre-operative risk stratification and risk reduction for joint arthroplasty. Factors which increase the rates of post-operative complications should be identified and managed prior to joint replacement. Peersman et al. [ 20 ] identified the comorbidities that were statistically significant in increasing the risk of infection were prior open surgical procedures, immunosuppressive therapy, poor nutrition, hypokalaemia, diabetes mellitus, obesity, and a history of smoking. Baek et al. [ 21 ] recommend correction of modifiable risk factors to decrease the rate of peri-prosthetic joint infection. Jamsen et al. [ 22 ] found that pre-operative reduction of glucose levels to less than 124 mg/dL decreases the rate of peri-prosthetic joint infection. Rasouli et al. [ 23 ] recommends a pre-operative correction of haemoglobin levels prior to joint arthroplasty. Huang et al. [ 24 ] identified malnutrition to also increase the rate of complications postoperatively. Ragni et al. [ 25 ] found that rate of postoperative infection in human immunodeficiency virus-positive haemophiliacs with CD4 counts of 200/mm 3 or less appears to be high, when compared with the general population and recommends early, vigorous treatment should be instituted for suspected infection, antibiotic prophylaxis considered for invasive procedures, and surgical intervention individualised based on the balance of risks and benefits. Sendi et al. [ 26 ] recommends antimicrobial treatment of symptomatic bacteriuria, but not for asymptomatic bacteriuria prior to arthroplasty. They also found that indwelling urinary catheters are the most frequent reason for healthcare-associated urinary tract infections and should be avoided or removed as soon as possible. Thus patients should be carefully selected for arthroplasty and medical evaluation should be performed in collaboration with the internists. In the Sheuli Das vs. Dr. Kanchan Bhattacharya case (7MLCDa13; j26 January 2014) [ 17 ] the patient alleged that the orthopaedic surgeon was negligent in performing a total hip replacement when the patient’s medical condition was not suitable for the procedure. The doctor successfully defended his actions by proving necessary pre-operative investigations were done, opinions of relevant specialists were obtained, and only after obtaining fitness for the procedure from all specialists was the arthroplasty performed.
The elective nature of arthroplasty also warrants the procedure to be done by an orthopaedic surgeon who is trained in arthroplasty and has sufficient experience. It is a major surgery, which should be performed in a setup which has the required infrastructure including an orthopaedic surgeon trained in arthroplasty [ 27 ]. In the RR Dobhal vs. Dr. SK Gupta case [ 17 ] the prosecution was successful in obtaining a verdict in their favour after they proved that they had requested the orthopaedic surgeon for referral to a higher medical centre for TKA but was refused.
Informed Consent
Informed consent is meant to protect the rights of the patients and provide them with adequate information before undergoing the procedure. Its importance has risen significantly in the past few decades with it being the crux of several malpractice lawsuits. Hence, it is vital for orthopaedic surgeons to be aware of what needs to be included in the informed consent document. Improving patient education and counselling during the process of obtaining an informed consent decreases the incidence of malpractice claims [ 28 ]. For example, patient education in terms of realistic expectations after THA may be effective in reducing claims related to limb length discrepancy after THA [ 29 ].The informed consent document should not be seen as a formality, rather given its due importance as it can often be the most vital document in defence of a malpractice lawsuit. The informed consent documentation should be comprehensive and include name, age, sex, hospital number of the patient; diagnosis; surgical procedure planned including which limb, side of body is being operated upon; the date of planned surgery; name of the chief operating surgeon; common complications of the procedure, few serious complications of the procedure; alternative treatment options with pros and cons of such alternatives; specific implants to be used; the consent for anaesthesia including type of anaesthesia and its complications; the signatures of the patient, person obtaining the consent and of the chief operating surgeon. However, it is often found that the informed consent is lacking in some of these aspects. Beresford et al. [ 30 ] reviewed the consent process of 47 THR and 53TKR patients performed by 11 different surgeons and compared the complications listed in this informed consent to those recommended by the British Orthopaedic Association (BOA). They found that in 23% of THR and 32% of TKR patients, none of the BOA-listed complications was documented; in 13% of THR and 15% of TKR patients, no complications were documented; in 13% of THR and 17% of TKR patients, only non-specific descriptions of complications (e.g. morbidity, mortality and medical complications) were used in their consent forms. A study involving 50 patients undergoing TKA revealed only 28% received information regarding possible complications of TKA and 85% were not given any information about the alternative treatments [ 31 ]. In another study of informed consent in THA, TKA patients, it was found that documentation of all clinically significant complications was insufficient when generic informed consent forms with blank spaces were used, hence the use of standardised procedure-specific consent forms is recommended [ 32 ].
Section 87 of the Indian Penal Code (IPC) [ 33 ] states that an “Act not intended and not known to be likely to cause death or grievous hurt, done by consent of a person above 18 years of age” is not considered an offence, while Sect. 88 of IPC [ 33 ] states that an “Act not intended to cause death, done by consent in good faith for person’s benefit” is not an offence. Thus these are important IPC’s that are the vital in the defence of a lawsuit filed when complications occur following an arthroplasty. The Samira Kohli case is a landmark judgement in relation to informed consent, where in its judgement the Supreme Court of India laid down guidelines for informed consent [ 33 ], stating that adequate information to be furnished by the doctor (or a member of his team) who treats the patient, should enable the patient to make a balanced judgement as to whether he should submit to the particular treatment or not. This means that the doctor should disclose: the nature and procedure of the treatment, its purpose, benefits and effects; alternatives, if any available; an outline of the substantial risk; adverse consequences of refusing treatment. But there is no need to explain remote theoretical risks involved, which may frighten or confuse a patient and result in refusal of consent for the necessary treatment.
The decision regarding which implant is to be used in the arthroplasty is one that is often made by the surgeon. This could be effected by several factors, including the surgeon’s familiarity with the implant, requirement of the patient’s condition, availability, and cost. For these reasons, the surgeon is often the person making the choice regarding the implant to be used. However, we must remember that ultimately the patient should have a say in what implant will be used in their body. Hence, the decision regarding implant to be used has to be shared decision after discussion between the surgeon and patient. Prokopetz et al. [ 34 ] discuss the guidelines for shared decision-making for implants in arthroplasty. They advise prior to arthroplasty, the orthopaedic surgeon discusses with the patient regarding the implant options available, the implant the surgeon feels most appropriate for the patient and the reasons for the same, the scientific evidence present regarding the implant, and also disclose any financial relationships or conflicts of interest for the surgeon. This is recommended to be a part of the informed consent obtained from the patient prior to surgery. A useful and impartial source for information regarding the various implant-specific estimates of complications and their outcomes are arthroplasty registries [ 35 ]. There are several arthroplasty registries maintained worldwide. The Mayo registry of USA is the oldest continuing registry for arthroplasty [ 36 ]. The Indian Society of Hip and Knee Surgeons (ISHKS) has established an arthroplasty registry in India and has been collecting data since 2006 [ 37 ], which can be accessed at http://www.ishks.com . It is important for an orthopaedic surgeon to verify the licences of an implant and manufacturer, and the outcomes of the implant is these registries prior to recommendation or use in a patient. This will be useful in the chance a lawsuit is filed in relation to the implant that was used. In the Anusuya vs. Bone and Joint Clinic case presented before the Tamil Nadu State Consumer Dispute Redressal Commission, Chennai {first appeal No. 160/2006} [ 17 ], the implant used in total hip replacement was found to have broken. The patient alleged that this occurred due to an inferior quality implant being used. However, the verdict was in favour of the surgeon as he provided evidence that the implant used was of international quality. In the Vijaya Menon vs. BK Thampi case [ 17 ] as well the patient alleged an implant of inferior quality was used. However, the hospital produced attested copies of International Organisation of Standardization (ISO) certificate, licence for manufacturing the implant, proving the implants were nationally and internationally approved.
Mixing of Components in Arthroplasty/Mixing of Components from Different Manufacturers
The routine practice is to use components of the same manufacturer while performing an arthroplasty. However, certain situations might arise where the surgeon wishes to use components from different manufacturers in the same joint reconstruction. Mixed THAs are defined as THAs (stem, head, and cup) comprising components made by different manufactures. This mixing of components is usually done the interest of the patient in mind. For example, a patient with THA requiring acetabular cup revision, would be subject to lesser morbidity if only the acetabular cup is replaced with an appropriate alternative, with the stem of the original manufacturer left in place if it is stable and well fit. This practice is, however, against the recommendation of all implant manufacturers. The benefit and drawbacks of performing such mixed THAs have been studied. Certain studies have reported complications from the use of components of different manufacturers [ 38 , 39 ]. However, most studies have actually found mixed THAs have similar or better outcomes and implant survival than non-mixed THAs. Tucker et al. [ 40 ] found that mixing of stems from one manufacturer with cups from another was associated with a lower revision rate. At 8 years, the cumulative percentage of revisions was 1.9% (95% CI 1.7–2.1) in the mixed group as compared to 2.4% (2.3–2.5) in the matched group ( p = 0.001). However, they also found that, mixing of heads from one manufacturer with stems from another was associated with a higher revision rate ( p < 0.001). Peters et al. [ 41 ] found that 6 year revision rates for mixed THAs (3.4% [95% CI 3.1–3.7]) were similar to that of non-mixed THAs (3.5% [95% CI 3.4–3.7]). The occurrence of complications, including infection, periprosthetic fracture, dislocation, loosening of femoral component and liner wear were similar in mixed and non-mixed THAs. However, they noted that loosening of the acetabular cup was more common in mixed THAs (16 vs. 12%). Taylor et al. [ 42 ] performed a survival analysis of 108,613 primary THAs, which showed 17-year survival of matched components and unmatched components to be similar. They also found a small, statistically significant improvement in Oxford Hip Scores for the unmatched group compared with the matched group. Thus, the mixing of components from different manufacturers may yield similar or better outcomes if it is performed when indicated as long as mixing of stem of one manufacturer with head of another manufacturer is avoided.
While the safety of mixing of components from different manufacturers may be satisfactory, the legal implications of mixing of components is another important aspect that has to be taken into consideration. Mixing of components from different manufacturers is against the guidelines of all manufacturers. This could absolve the manufacturer of complications relating to the implant use, and transfer the responsibility of manufacturer of implant to the orthopaedic surgeon. The approval from the regulatory body for the use of an implant after assessing its safety, may no longer be valid as the implant was not designed or tested for use with an implant from a different manufacturer. This opens the door for claims of medical negligence against the orthopaedic surgeon for the use of a defective and unauthorised implant. If a situation does require the use of mixed components, it is advisable to inform the patient about the need for mixed components, the benefits and drawbacks of mixing components, and to obtain an informed consent for the use of mixed components from the patient. Till date, no orthopaedic surgeon has been held legally responsible or ended up in a lawsuit for the use of mixed components, based on case law review in the United Kingdom, Germany, and the Netherlands [ 43 ]. We were unable to find any lawsuit in India pertaining to the issue of mixing of components from different manufactures for an arthroplasty. Peters et al. [ 43 ] suggests that if an orthopaedic surgeon desires to use mixed components, they are advised to avoid mixing across the fixed articulation (i.e., use a head from the same manufacturer as the stem), appropriately match sizes across the mobile articulation in hard-on-soft THAs and to avoid mixing of components in hard-on-hard bearings. In summary, despite mixing of components yielding satisfactory outcomes, it is best avoided for the risk of legal implications.

Post-operative Rehabilitation Protocol
Following a THA/TKA rehabilitation plays a vital role in the outcome of the surgery. There remain uncertainty regarding the post-operative rehabilitation and mobilisation protocols to be followed and is often patient-specific. Early mobilisation decreases length of hospital stay and cost [ 44 ]; however, increases the chances of fall, implant breakage and is dependent on patient’s pain tolerance. The length of hospital stay post arthroplasty for rehabilitation is also debatable. The usual indications for inpatient multidisciplinary rehabilitation are: two simultaneous arthroplasties, revision of a previous hip or knee arthroplasty, postsurgical complications, advanced age, comorbidities influencing the rehabilitation process, social difficulties, necessity for adaptation of the environment, insufficient or unadapted out-patient (para)medical care [ 45 ]. Surgeons and hospitals might have their own protocol regarding mobilisation and physiotherapy following arthroplasty. While this is left to the discretion of the surgeon, it is important for legal purposes that the advice given regarding mobilisation and physiotherapy be documented, as well as document whether the patient is following such advice. In the Rohini Morghade vs. Dr. AV Spare (7MLCDa118; j313–August 2014) [ 17 ], the patient developed a complication following arthroplasty. The patient was adviced by the orthopaedic surgeon for bed rest and the same was documented in the discharge summary. The fact the patient was not following this advice was used in the defence of the lawsuit by the doctor. In the Asthana vs. Sh Ramsingh Hospital Case (I(09)CPJ132) [ 17 ], an in-patient following arthroplasty who was advised bed rest, requested for a bed pan, but was refused by the hospital attendant. The patient slipped while walking and ended up fracturing her tibia and fibula. The administrative deficiency to follow post-operative rehabilitation protocol was proved and compensation was awarded. A summary of the precautions to be taken to prevent lawsuits in THA, TKA cases has been listed in Table 3 .
Lawsuits involving THA, TKAs are on the rise, and it is increasingly important for orthopaedic surgeons to be aware of medico-legal issues related to it. Understanding these matters, we believe will help avoid malpractice lawsuits, improve planning and protocols of orthopaedic surgeons, and help in the defence of lawsuits. Further studies on this matter should be promoted in developing countries such as India where there is deficiency of published literature on this matter.
McWilliams, A. B., Douglas, S. L., Redmond, A. C., Grainger, A. J., O’Connor, P. J., Stewart, T. D., & Stone, M. H. (2013). Litigation after hip and knee replacement in the National Health Service. Bone Joint Journal, 95 (1), 122–126. https://doi.org/10.1302/0301-620X.95B1.30908.2 .
Article PubMed Google Scholar
McGrory, B. J., Bal, B. S., York, S., Macaulay, W., & McConnell, D. B. (2009). Surgeon demographics and medical malpractice in adult reconstruction. Clinical Orthopaedics and Related Research, 467 (2), 358–366. https://doi.org/10.1007/s11999-008-0581-0 .
Upadhyay, A., York, S., Macaulay, W., McGrory, B., Robbennolt, J., & Bal, B. S. (2007). Medical malpractice in hip and knee arthroplasty. Journal of Arthroplasty, 22 (6 Suppl 2), 2–7. https://doi.org/10.1016/j.arth.2007.05.003 .
Article Google Scholar
Patterson, D. C., Grelsamer, R. P., Bronson, M. J., & Moucha, C. S. (2017). Lawsuits after primary and revision total hip arthroplasties: A malpractice claims analysis. Journal of Arthroplasty, 32 (10), 2958–2962. https://doi.org/10.1016/j.arth.2017.04.044 .
Patterson, D. C., Grelsamer, R., Bronson, M. J., & Moucha, C. S. (2017). Lawsuits After Primary And Revision Total Knee Arthroplasty: A malpractice claims analysis. Journal of American Academy of Orthopaedic Surgeons, 25 (10), e235–e242. https://doi.org/10.5435/JAAOS-D-16-00736 .
Bokshan, S. L., Ruttiman, R. J., DePasse, J. M., Eltorai, A. E. M., Rubin, L. E., Palumbo, M. A., & Daniels, A. H. (2017). Reported litigation associated with primary hip and knee arthroplasty. Journal of Arthroplasty, 32 (12), 3573-3577.e1. https://doi.org/10.1016/j.arth.2017.07.001 .
Novi, M., Vanni, C., Parchi, P. D., Di Paolo, M., Piolanti, N., & Scaglione, M. (2020). Claims in total hip arthroplasty: Analysis of the instigating factors, costs and possible solution. Musculoskeletal Surgery, 104 (1), 43–48. https://doi.org/10.1007/s12306-019-00590-6 .
Article CAS PubMed Google Scholar
Kheir, M. M., Rondon, A. J., Woolsey, A., Hansen, H., Tan, T. L., & Parvizi, J. (2018). Infection following total joint arthroplasty is the main cause of litigation: Data from one metropolitan area. Journal of Arthroplasty, 33 (5), 1520–1523. https://doi.org/10.1016/j.arth.2017.12.007 .
Samuel, L. T., Sultan, A. A., Rabin, J. M., Surace, P. A., Yao, B., Moskal, J. T., & Mont, M. A. (2019). Medical malpractice litigation following primary total joint arthroplasty: A comprehensive, nationwide analysis of the past decade. Journal of Arthroplasty, 34 (7S), S102–S107. https://doi.org/10.1016/j.arth.2019.02.066 .
Bhutta, M. A., Arshad, M. S., Hassan, S., & Henderson, J. J. (2011). Trends in joint arthroplasty litigation over five years: The British experience. Annals of the Royal College of Surgeons of England, 93 (6), 460–464. https://doi.org/10.1308/003588411X587226 .
Article CAS PubMed PubMed Central Google Scholar
Zengerink, I., Reijman, M., Mathijssen, N. M., Eikens-Jansen, M. P., & Bos, P. K. (2016). Hip arthroplasty malpractice claims in the Netherlands: Closed claim study 2000–2012. Journal of Arthroplasty, 31 (9), 1890-1893.e4. https://doi.org/10.1016/j.arth.2016.02.055 .
Gibon, E., Farman, T., & Marmor, S. (2015). Knee arthroplasty and lawsuits: The experience in France. Knee Surgery, Sports Traumatology, Arthroscopy, 23 (12), 3723–3728. https://doi.org/10.1007/s00167-014-3292-y .
Järvelin, J., Häkkinen, U., Rosenqvist, G., & Remes, V. (2012). Factors predisposing to claims and compensations for patient injuries following total hip and knee arthroplasty. Acta Orthopaedica, 83 (2), 190–196. https://doi.org/10.3109/17453674.2012.672089 .
Article PubMed PubMed Central Google Scholar
Chen, A., Patel, N. K., Khan, Y., Cobb, J. P., & Gupte, C. M. (2015). The cost of adverse events from knee surgery in the United Kingdom: An in-depth review of the National Health Service Litigation Authority database. The Knee, 22 (4), 286–291. https://doi.org/10.1016/j.knee.2015.04.011 .
Gademan, M. G., Hofstede, S. N., Vliet Vlieland, T. P., Nelissen, R. G., & Marang-van de Mheen, P. J. (2016). Indication criteria for total hip or knee arthroplasty in osteoarthritis: A state-of-the-science overview. BMC Musculoskeletal Disorders, 17 (1), 463. https://doi.org/10.1186/s12891-016-1325-z .
Cross, W. W., 3rd., Saleh, K. J., Wilt, T. J., & Kane, R. L. (2006). Agreement about indications for total knee arthroplasty. Clinical Orthopaedics and Related Research, 446 , 34–39. https://doi.org/10.1097/01.blo.0000214436.49527.5e .
Tiwari, S., Baldwa, M., Tiwari, M., & Kuthe, A. (2019). Textbook on medico legal issues related to various medical specialities . (1st ed., p. 291). Jaypee Brothers 301–306.
Google Scholar
Clelland, C., Worland, R. L., Jessup, D. E., & East, D. (1996). Preoperative medical evaluation in patients having joint replacement surgery: Added benefits. Southern Medical Journal, 89 (10), 958–960. https://doi.org/10.1097/00007611-199610000-00004 .
Ng, V. Y., Lustenberger, D., Hoang, K., Urchek, R., Beal, M., Calhoun, J. H., & Glassman, A. H. (2013). Preoperative risk stratification and risk reduction for total joint reconstruction: AAOS exhibit selection. Journal of Bone and Joint Surgery American Volume, 95 (4), e191–e215. https://doi.org/10.2106/JBJS.L.00603 .
Peersman, G., Laskin, R., Davis, J., & Peterson, M. (2001). Infection in total knee replacement: A retrospective review of 6489 total knee replacements. Clinical Orthopaedics and Related Research, 392 , 15–23.
Baek, S. H. (2014). Identification and preoperative optimization of risk factors to prevent periprosthetic joint infection. World Journal of Orthopedics., 5 (3), 362–367. https://doi.org/10.5312/wjo.v5.i3.362 .
Jämsen, E., Nevalainen, P., Eskelinen, A., Huotari, K., Kalliovalkama, J., & Moilanen, T. (2012). Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: A single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. Journal of Bone and Joint Surgery American Volume, 94 (14), e101. https://doi.org/10.2106/JBJS.J.01935 .
Rasouli, M. R., Restrepo, C., Maltenfort, M. G., Purtill, J. J., & Parvizi, J. (2014). Risk factors for surgical site infection following total joint arthroplasty. Journal of Bone and Joint Surgery American Volume, 96 (18), e158. https://doi.org/10.2106/JBJS.M.01363 .
Huang, R., Greenky, M., Kerr, G. J., Austin, M. S., & Parvizi, J. (2013). The effect of malnutrition on patients undergoing elective joint arthroplasty. Journal of Arthroplasty, 28 (8 Suppl), 21–24. https://doi.org/10.1016/j.arth.2013.05.038 .
Ragni, M. V., Crossett, L. S., & Herndon, J. H. (1995). Postoperative infection following orthopaedic surgery in human immunodeficiency virus-infected haemophiliacs with CD4 counts ≤ 200/mm 3 . Journal of Arthroplasty, 10 (6), 716–721. https://doi.org/10.1016/s0883-5403(05)80065-8 .
Article CAS Google Scholar
Sendi, P., Borens, O., Wahl, P., Clauss, M., & Uçkay, I. (2017). Management of asymptomatic bacteriuria, urinary catheters and symptomatic urinary tract infections in patients undergoing surgery for joint replacement: A position paper of the expert group “Infection” of swissorthopaedics . Journal of Bone and Joint Infection, 2 (3), 154–159. https://doi.org/10.7150/jbji.20425 .
Bleß, H. H. (2018). Requirements for adequate arthroplasty care (expert opinions). In: Bleß HH, Kip M, editors. White paper on joint replacement: Status of hip and knee arthroplasty care in Germany [Internet]. Springer. Chapter 6. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546139/ . https://doi.org/10.1007/978-3-662-55918-5_6 .
Bhattacharyya, T., Yeon, H., & Harris, M. B. (2005). The medical-legal aspects of informed consent in orthopaedic surgery. Journal of Bone and Joint Surgery American Volume, 87 (11), 2395–2400. https://doi.org/10.2106/JBJS.D.02877 .
Clark, C. R., Huddleston, H. D., Schoch, E. P., 3rd., & Thomas, B. J. (2006). Leg-length discrepancy after total hip arthroplasty. Journal of American Academy of Orthopaedic Surgeons, 14 (1), 38–45. https://doi.org/10.5435/00124635-200601000-00007 .
Beresford-Cleary, N. J., Halliday, J., Breusch, S. J., & Biant, L. C. (2011). Consent process for elective total hip and knee arthroplasty. Journal of Orthopaedic Surgery (Hong Kong), 19 (3), 274–278. https://doi.org/10.1177/230949901101900302 .
Ekmekci, P. E., Ekmekci, A. B., Karakaş, Ö., Kulduk, A., & Arda, B. (2016). Evaluation of the informed consent procedure for total knee arthroplasty patients in Turkey. Acta Orthopaedica et Traumatologica Turcica, 50 (4), 400–404. https://doi.org/10.1016/j.aott.2016.06.003 .
Mussa, M. A., Sweed, T. A., & Khan, A. (2014). Informed consent documentation for total hip and knee replacement using generic forms with blank spaces. Journal of Orthopaedic Surgery (Hong Kong), 22 (2), 214–217. https://doi.org/10.1177/230949901402200220 .
Singh, V. P. (Ed.). (2016). Legal issues in medical practice: Medicolegal guidelines for safe practice . (1st ed., pp. 55–58). Jaypee Brothers.
Prokopetz, J. J., Katz, J. N., Losina, E., Thornhill, T. S., Wright, J., & Lehmann, L. S. (2013). Preceding the procedure: medical devices and shared decision making. Arthritis Care and Research (Hoboken)., 65 (1), 148–151. https://doi.org/10.1002/acr.21826 .
Hughes, R. E., Batra, A., & Hallstrom, B. R. (2017). Arthroplasty registries around the world: Valuable sources of hip implant revision risk data. Current Reviews in Musculoskeletal Medicine, 10 (2), 240–252. https://doi.org/10.1007/s12178-017-9408-5 .
Malchau, H., Garellick, G., Berry, D., Harris, W. H., Robertson, O., Kärrlholm, J., Lewallen, D., Bragdon, C. R., Lidgren, L., & Herberts, P. (2018). Arthroplasty implant registries over the past five decades: Development, current, and future impact. Journal of Orthopaedic Research, 36 (9), 2319–2330. https://doi.org/10.1002/jor.24014 .
Pachore, J. A., Vaidya, S. V., Thakkar, C. J., Bhalodia, H. K., & Wakankar, H. M. (2013). ISHKS joint registry: A preliminary report. Indian Journal of Orthopaedics., 47 (5), 505–509. https://doi.org/10.4103/0019-5413.118208 .
Higgs, G. B., Hanzlik, J. A., MacDonald, D. W., Gilbert, J. L., Rimnac, C. M., Kurtz, S. M., & Implant Research Center Writing Committee. (2013). Is increased modularity associated with increased fretting and corrosion damage in metal-on-metal total hip arthroplasty devices?: A retrieval study. Journal of Arthroplasty, 28 (8 Suppl), 2–6. https://doi.org/10.1016/j.arth.2013.05.040 .
Mistry, J. B., Chughtai, M., Elmallah, R. K., Diedrich, A., Le, S., Thomas, M., & Mont, M. A. (2016). Trunnionosis in total hip arthroplasty: A review. Journal of Orthopaedics and Traumatology, 17 (1), 1–6. https://doi.org/10.1007/s10195-016-0391-1 .
Tucker, K., Pickford, M., Newell, C., Howard, P., Hunt, L. P., & Blom, A. W. (2015). Mixing of components from different manufacturers in total hip arthroplasty: Prevalence and comparative outcomes. Acta Orthopaedica, 86 (6), 671–677. https://doi.org/10.3109/17453674.2015.1074483 .
Peters, R. M., van Steenbergen, L. N., Bulstra, S. K., Zeegers, A. V., Stewart, R. E., Poolman, R. W., & Hosman, A. H. (2016). Nationwide review of mixed and non-mixed components from different manufacturers in total hip arthroplasty. Acta Orthopaedica, 87 (4), 356–362. https://doi.org/10.1080/17453674.2016.1194128 .
Taylor, J. W., Frampton, C., & Rothwell, A. G. (2017). Long term survival of total hip arthroplasty using implants from different manufacturers. The Journal of Arthroplasty . https://doi.org/10.1016/j.arth.2017.09.047 .
Peters, R. M., Hiemstra, J. T., Zijlstra, W. P., Bulstra, S. K., & Stevens, M. (2020). To mix or not to mix? Medicolegal implications of mixed components in total hip arthroplasty. Acta Orthopaedica, 91 (6), 624–626. https://doi.org/10.1080/17453674.2020.1822066 .
Masaracchio, M., Hanney, W. J., Liu, X., Kolber, M., & Kirker, K. (2017). Timing of rehabilitation on length of stay and cost in patients with hip or knee joint arthroplasty: A systematic review with meta-analysis. PLoS ONE, 12 (6), e0178295. https://doi.org/10.1371/journal.pone.0178295 .
Jansen, E., Brienza, S., Gierasimowicz-Fontana, A., Matos, C., Reynders-Frederix-Dobre, C., & Hatem, S. M. (2015). Revalidation après les arthroplasties de hanche et de genou [Rehabilitation after total knee arthroplasty of hip and knee]. Revue Médicale de Bruxelles, 36 (4), 313–320.
CAS PubMed Google Scholar
Download references
Author information
Authors and affiliations.
Department of Orthopaedic Surgery, Sri Ramachandra Medical College and Research Institute, Ramachandra Nagar, Porur, Chennai, Tamil Nadu, 600116, India
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Satvik Pai .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Pai, S. Medico-Legal Issues Related to Hip and Knee Arthroplasty: A Literature Review Including the Indian Scenario. JOIO 55 , 1286–1294 (2021). https://doi.org/10.1007/s43465-021-00398-2
Download citation
Received : 29 January 2021
Accepted : 22 March 2021
Published : 30 March 2021
Issue Date : October 2021
DOI : https://doi.org/10.1007/s43465-021-00398-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medico-legal
- Arthroplasty
- Joint replacement
- Find a journal
- Publish with us
- Track your research
- Publisher Home

- About the Journal
- Editorial Team
- Article Processing Fee
- Privacy Statement
- Crossmark Policy
- Copyright Statement
- GDPR Policy
- Open Access Policy
- Publication Ethics Statement
- Author Guidelines
- Announcements
Profile of Medico-Legal Cases in Accident & Emergency Department of SSKH, LHMC, New Delhi During Pre-Covid-19 and Covid-19 Periods
- Rajesh Kumar
Rajesh Kumar
Search for the other articles from the author in:
- Satyakam Jena
Satyakam Jena
- Mukesh Singh
Mukesh Singh
- Shrabana Naik
Shrabana Naik
- Anupam Prakash
Anupam Prakash
- Sukhdeep Singh
Sukhdeep Singh
Abstract Views 265
Downloads 137
##plugins.themes.bootstrap3.article.sidebar##
##plugins.themes.bootstrap3.article.main##
Medico-legal cases presented to the Accident & Emergency department vary from hospital to hospital. Profiling these cases from time to time provides an insight into the workload of medico-legal cases as well as what is going on in and around the locality. The present study was conducted at LHMC, New Delhi from January 2021 to June 2022 from the available records of MLCs from 1st January 2019 to 31st December 2021. Out of a total of 5702 MLCs, males were 85.77%. Victims of the age group 21–30 years formed the majority (36.30%) of the cases followed by age groups 31–40 years (25.44%). The time of incidence was between 6 p.m. and 11.59 p.m. in the majority (42.00%) cases. The time of reporting was between 6 p.m. and 11.59 p.m. in the majority (40.05%) of cases. A majority (56.92%) of the victims had reported within 1 hour of the incident. The cause was blunt force trauma in more than half (51.05%) cases, followed by RTA (17.93%) and poisoning (17.84%). In more than half (56.51%) cases, the manner was homicidal, followed by accidental including RTA (23.95%) and suicidal (19.35%). The surgery department was found involved in more than 2/3 (69.15%) cases, followed by Orthopaedics (31.85%), Medicine (20.199%) and ENT (19.52%). In 85.50% of cases, the victims were discharged within 24 hours. Hospital death in MLCs was 4.15% whereas 1.87% of victims were referred to other hospitals for further management.
Introduction
Analysis of the medico-legal cases presented to the casualty of a hospital gives an understanding of what unnatural things are happening to human beings in and around the particular locality. Lady Hardinge Medical College & Smt. S.K. Hospital is situated in the heart of Delhi, adjacent to Connaught Place catering for the people of New Delhi and central Delhi districts. However, two other large government hospitals, LNJP Hospital and Dr RML Hospital are also lying within a distance of 2–5 km. Therefore, patients turn to these hospitals because of their convenience and the kind of services available in these hospitals. In case of emergency medical needs, odd hours or medico-legal cases, the casualty remains the target place for the patients and police. Thus analysis of the medico-legal cases of a hospital from time to time helps to fulfill the medical needs of the nearby patients with the development of proper infrastructures, manpower, strategy and policies.
Aim and Objectives
- To analyze the profile of medico-legal cases presented to the Accident & Emergency Department, SSKH, New Delhi.
- To compare the volume of medico-legal cases during the 2019 non-Covid and 2020–2021 Covid periods.
- To analyze the nature, manner and outcome of the medico-legal cases.
Materials and Methods
After obtaining ethical clearance from the institutional ethics committee, the present 2-year retrospective (from 1 st January 2019 to 31 st December 2020) and 1-year prospective study (from 1 st January 2021 to 31 st December 2021) study was conducted in the Department of Forensic Medicine, Department of Accident & Emergency and Medical Record Department at Lady Hardinge Medical College & Smt. S.K. Hospital, New Delhi from January 2021 to June 2022 by collecting all the relevant data available in the MLC records of the study period using pre-designed pro forma, then transferred to MS Excel sheet and analysed.
Results and Discussion
Magnitude of mlcs at lhmc, new delhi.
The total number of MLCs registered from 1 st January 2019 till 31 st December 2021 was 5702. Out of those, 2581 (45.26%) MLCs were found registered in the year 2019 (Pre-Covid year), 1955 (34.28%) MLCs were registered in the year 2020 and 1166 (20.44%) MLCs were registered in the year 2021 ( Table I ). Hence, there was a significant drop in MLCs during the Covid-19 period.
Out of a total of 5702 cases, males were found in 4891 (85.77%) MLCs whereas females were found in 810 (14.20%) MLCs. Only one transgender individual was involved in MLC as a case of RTA in the year 2021 ( Table II ). Our findings were similar to the studies reported by references [ 1 ]–[ 38 ].
Out of a total of 5702 MLCs, victims of the age group 21–30 years (N = 2070; 36.30%) form the majority of the cases followed by age groups 31–40 years (N = 1451; 25.44%), and 41–50 years (N = 918; 16.09%), respectively ( Table III ). The age range was from Newborn baby to 95 years old. The average age of the victims was 34.53 years and the median age was 32 years. Our findings were similar to the studies reported by references [ 1 ], [ 3 ]–[ 9 ], [ 11 ], [ 13 ], [ 15 ], [ 16 ], [ 18 ]–[ 25 ], and [ 27 ]–[ 38 ].
However, the medico-legal cases in the paediatric age group in our study do not reflect the true figures as the data were collected from Sucheta Kripalini Hospital only. Lady Hardinge Medical College has a separate Kalavati Saran Children’s Hospital to deal with paediatric age group patients.
Time of Incidence
Barring 93 MLCs where details were not available and 469 cases where natural disease cases were registered under MLCs, among the rest 5140 MLCs, the time of incidence was between 6 p.m.–11.59 p.m. in majority (N = 2159; 42.00%) cases, followed by 12 p.m.–5.59 p.m. (N = 1313; 25.54%) and 6 a.m.–11.59 a.m. (N = 943; 18.34%), respectively ( Table IV ).
Reference [ 6 ] has reported that the majority (29.49%) of the incidents occurred between 12 p.m. to 4 p.m., followed by 27.29% between 4 p.m. to 8 p.m. Reference [ 9 ] reported that the majority of the incidents occurred during the evening. Reference [ 24 ] reported that the majority (37.6%) occurred between 12 p.m. to 6 p.m., followed by 34.3% between 6 p.m. to 12 a.m. Reference [ 36 ] reported that the peak time of incidence was between 4 p.m. to 8 p.m. (33.5%).
Time of Reporting
Among the 5140 MLCs, the time of reporting was between 6 p.m.–11.59 p.m. in the majority (N = 2059; 40.05%) cases, followed by 12 p.m.–5.59 p.m. (N = 1327; 25.81%) and 12 a.m.–5.59 a.m. (N = 971; 18.89%), respectively ( Table V ). Thus evening hour was the busiest period to deal with medico-legal cases at the Accident & Emergency Department at SSKH.
Reference [ 5 ] reported that the peak time of reporting was between 12 p.m. to 6 p.m. Reference [ 15 ] reported that the majority (36.9%) of victims reported between 12 p.m. to 6 p.m., followed by 35% between 6 p.m. to 12 a.m. Reference [ 19 ] has reported that majority (31.18%) of victims reported between 6 p.m. to 12 a.m., followed by 30.59% between 12 p.m. to 6 p.m. Reference [ 21 ] has reported that the majority (40.8%) of victims reported between 8 p.m. to 8 a.m., followed by 32.8% between 2 p.m. to 8 p.m. Reference [ 23 ] reported that the majority (37.44%) of victims reported between 12 p.m. to 6 p.m. Reference [ 24 ] reported that the majority (36.7%) of victims reported between 12 p.m. to 6 p.m., followed by 34.3% between 6 p.m. to 12 a.m. Reference has reported that the majority (40.5%) of victims reported between 6 p.m. to 12 a.m., followed by 32.5% between 12 p.m. to 6 p.m. Reference [ 37 ] reported that most of the cases reported between 12 p.m. to 6 p.m. (35.61%) followed by 6 p.m. to 12 a.m. (35.23%).
The Time Gap between the Incidence and Reporting
Out of 5140 MLCs, the victims had reported within 1 hour of the incidence in the majority (N = 2926; 56.92%) of cases, followed by within 1–2 hours (N = 1368; 26.61%) ( Table VI ). Our findings were similar to the studies reported in References [ 5 ], [ 14 ], [ 20 ], [ 22 ], [ 23 ], [ 30 ]–[ 32 ], and [ 38 ].
Person Presented the MLCs to the Hospital
The MLCs were presented to the hospital by the police in the majority (N = 1810; 31.74%) cases, followed by relatives (N = 1577; 27.65%), self (N = 1269; 22.25%) and by unknown person (N = 953; 16.71%) ( Table VII ). No other study was found to compare these findings.
Alleged History of the Causes of MLCs
Out of 5140 MLCs, the alleged history of a causative factor was blunt force trauma in more than half (N = 2624; 51.05%) cases, followed by RTA (N = 922; 17.93%) and poisoning (N = 917; 17.84%), respectively ( Table VIII ). Our findings were similar to the studies reported by references [ 10 ], [ 25 ]–[ 27 ], and [ 29 ].
However, references [ 3 ]–[ 8 ], [ 11 ]–[ 13 ], [ 15 ]–[ 17 ], [ 18 ], [ 20 ], [ 22 ]–[ 24 ], [ 28 ], [ 30 ], [ 32 ]–[ 37 ] have reported that Road Traffic Accidents were major causes of medico-legal cases presented to the hospitals. Reference [ 38 ] reported that poisoning was the major cause of admission to the casualty.
Manner of Causation in MLCs
Out of 5140 MLCs, more than half (N = 2905: 56.51%) of victims the manner was homicidal, followed by accidental including RTA (N = 1232; 23.95%) and suicidal (N = 995; 19.35%), respectively ( Table IX ).
Reference [ 5 ] has reported that in the majority (69.03%) of MLCs, the manner was accidental. Reference [ 4 ] has reported that the manners were accidental-75.4%, suicidal-15.5% and homicidal-5.9%. Similarly, reference [ 31 ] reported that the manners were accidental-52.4%, suicidal-41.41% and homicidal-5.03%. Reference [ 32 ] reported that the manner was accidental in 79.9%. Reference [ 38 ] reported that the manner was an assault in the majority (39.6%) of cases.
Department Involved in Managing the MLCs
Out of a total of 5609 MLCs (5702-93), where details were available, the Surgery department was found involved in more than 2/3 (N = 3879; 69.15%) cases, followed by the departments of Orthopaedics (N = 1787; 31.85%), Medicine (N = 1133; 20.199%), ENT (N = 1095; 19.52%), respectively. The Department of Forensic Medicine was found involved only in 1 (0.01%) case ( Table X ).
Reference [ 12 ] reported that the majority (52.94%) of the MLCs were managed by the Surgery department, followed by 43.28% by the Orthopaedics department. Reference [ 21 ] also reported that the majority (93%) of MLCs were managed by the Surgery department, followed by the Orthopaedics and Neurosurgery departments, respectively. Reference [ 32 ] reported that the majority (69.96%) of the MLCs were managed by the Surgery department, followed by Orthopaedics (58.99%) and Medicine (35.88%), respectively.
Number of Department(s) Involved in Managing the MLCs
Out of a total of 5609 MLCs (5702-93), where details were available, the majority (N = 2562; 45.67%) cases were handled and managed by a single department whereas in 2299 (40.98%) cases, they were managed by two departments and in 748 (13.33%) cases, they were managed by more than two departments ( Table XI ). Reference [ 32 ] reported that in the majority (64.93%) of MLCs, opinions were sought from a single department, followed by two departments (26.72%) and more than two departments (8.35%), respectively.
Radiological Investigations Required in MLCs
Out of a total of 5609 MLCs (5702-93), where details were available, a radiological investigation was advised in the majority (n = 3038; 54.16%) cases followed by CT scan (N = 1883; 33.57%), USG (N = 1655; 29.50%) and MRI (N = 39; 0.69%), respectively ( Table XII ). No other study was found to compare these findings.
Duration of Stay in the Hospital in MLCs
Out of a total of 5609 MLCs (5702-93), where details were available, in 4796 (85.50%) cases, the stay of the victims in the hospital was less than 24 hours whereas in 813 (14.49%) cases, the stay in the hospital was more than 24 hours and maximum up to 97 days ( Table XIII ). Most of the patients who stayed in the hospital for longer durations were victims of RTA with bone fractures.
Reference [ 23 ] reported that the majority (90.89%) of the victims of MLCs were discharged from the hospital within 1 week of admission to the hospital.
Outcome in the MLCs
Out of a total of 5702 MLCs, about 1/3 i.e., 3789 (66.45%) victims were discharged followed by those who absconded from the hospital (N = 1544; 27.07%), death (N = 237; 4.15%) and referred for further management (N = 107; 1.87%), respectively ( Table XIV ).
Reference [ 13 ] reported that 0.6% of victims of MLCs were referred to other higher hospitals for treatment and LA.M.A cases were 1.63%. Reference [ 14 ] reported that 85.71% of MLCs in the paediatric age group were discharged, 1.68% absconded, 5.04% were referred to other hospitals for further management and deaths were 2.06%. Reference [ 20 ] reported that 80.69% of MLCs were discharged, deaths were 9.68% whereas 4.45% of MLCs were referred to other hospitals for further management. Reference [ 24 ] reported that 66.1% of MLCs were discharged, deaths were 9.9% whereas 11.6% of MLCs were LA.M.A. Reference [ 30 ] reported that 78.4% of MLCs were discharged, deaths were 9.59% whereas 4.69% MLCs were referred to other hospitals for further management. Reference reported that 81.84% of MLCs were discharged, 12.03% were referred to other hospitals for further management whereas deaths were 5.9%.
The Accident & Emergency Department of SSKH, Lady Hardinge Medical College deals with a reasonable number of MLCs due to the large urban population and easy accessibility from nearby areas. There was a significant drop in MLCs during Covid periods 2020 & 2021 from non-Covid period 2019. As the busiest hours to deal with MLCs were found between 6 p.m. and 11.59 p.m., hence, the concerned Surgery, Orthopaedics, Medicine and ENT departments should remain vigilant with well-trained manpower during those hours. The majority of the MLCs were found blunt force trauma caused by homicidal assault, followed by RTA and poisoning respectively that reflected the mindset of the people living in the region. Referral of 1.87% MLCs to other hospitals for further management and death of 4.15% victims of MLCs need to be addressed properly with the overall augmentation of medical facilities and services. The clinical forensic medicine branch should be developed well to deal with MLC documentation for the administration of proper justice in the court of law at a later stage.
Most read articles by the same author(s)
- Rajesh Kumar, Shrabana Naik, Anupam Prakash, Sukhdeep Singh, Impact of COVID-19 Pandemic on Magnitude, Cause and Manner of Medico-legal Cases in A Tertiary Care Hospital, New Delhi , European Journal of Medical and Health Sciences: Vol. 5 No. 3 (2023)
- Satyakam Jena, Mukesh Singh, Kuldeep Singh, Shrabana Naik, Thejaswi Hiriyur Thipperudrappa, Critical Analysis of Firearm Wound Characteristics in Victims Brought for Autopsy at LHMC, New Delhi: A 20-Year Retrospective Study , European Journal of Medical and Health Sciences: Vol. 5 No. 4 (2023)
- Nisha Nupur, Satyakam Jena, Mukesh Singh, Shrabana Kumar Naik, Thejaswi Hiriyur Thipperudrappa, Sachin Mittal, Position and Length of Appendix among Delhi Population-An Autopsy Based Study , European Journal of Medical and Health Sciences: Vol. 6 No. 1 (2024)


- Leadership Crisis
- Editor's Pick

Broad, Boston Children’s Provide Research Integrity Tools Following Longwood Data Manipulation Allegations

‘Message of Hope’: 11 Harvard Affiliates Visit Israel in Solidarity Trip

Campaign to Fire Graham & Parks Principal Causes Rift Among Parents

Class of 2028 Results Will Offer the First Clues About Harvard’s Post-Affirmative Action Admissions

Harvard College Women’s Center Kicks Off 2024 Women’s Week With ‘Rooted’ Theme
Harvard Law School Digitization Project Publishes Nearly 7 Million Court Cases Online

The Caselaw Access Project published nearly seven million cases from the Harvard Law School’s collections online on March 8, concluding a nine-year process to digitize the HLS Library’s archive of court cases.
The Caselaw Access Project, also known as CAP, aimed “to make all published U.S. court decisions freely available to the public online in a consistent format, digitized from the collection of the Harvard Law School Library,” according to the project’s website.
The recent release of cases has culminated in “360 years of United States caselaw” accessible to the public, according to the project’s website. This includes all “official, book-published state and federal United States caselaw through 2020,” with the first case dating back to 1658.
Jack Cushman, the project’s director, said that the impetus behind the effort was a desire to make caselaw more accessible to the public. In the past, few people beyond lawyers had access to expensive caselaw databases and could view important legal decisions.
This project, according to Cushman, sought to level the playing field.
Cushman said he believed it was important “for everyone to have access to the law of the land.”
CAP launched in 2015 through a partnership with Ravel Law, a legal research and analytics startup company. Per the terms of the partnership, CAP received financial support in exchange for Ravel obtaining eight years of exclusivity with the caselaw documents, according to Harvard Law Today, a school-run publication.
This project falls under the initiatives of the Law School’s Library Innovation Lab, “a forward-looking group of thinkers and doers working at the intersection of libraries, technology, and law,” according to the organization's website. The LIL facilitated the delicate process of digitizing case files for the project.
As part of the process, 40,000 books containing case files were retrieved from Harvard Law School’s collection in the HLS Library and a repository in Southborough, Mass. The CAP team then used a variety of tools to de-bind the books, effectively scan case files at a rate of 500,000 pages per week, and wrap the books in plastic to be sent to a limestone mine in Kentucky for preservation.
The scanned files were then translated into machine-readable documents and uploaded to the Ravel website. Ravel’s website made sifting through documents easier with their “data science, machine learning, and visualization” systems, according to Harvard Law Today.
Cushman said it was essential to not rush the process, as CAP was dealing with delicate documents that were both culturally and historically important.
“I think one lesson is just, it’s okay if it takes a long time,” he said. “For cultural preservation and cultural heritage — we’re in this for the long run.”
Now that the case files have been digitized, CAP aims to further improve search functionality to make the platform “practically usable,” furthering their mission to increase caselaw accessibility for all. With this forward-looking approach to law accessibility, CAP’s next goal is to strengthen its institutional collaborations with AI model makers interested in high quality datasets.
Cushman said that the digital archive could be useful for “Harvard students who are looking for projects or ways to make their mark with civic technology and big datasets.”
“We’ve only scratched the surface of what you can do with it,” Cushman added.
Want to keep up with breaking news? Subscribe to our email newsletter.
Advertisement
Supported by
Erin Hawley: The Woman Arguing Against the Abortion Pill
Erin Hawley, a law professor and wife of Senator Josh Hawley, is arguing the Supreme Court case.
- Share full article

By Elizabeth Dias and Abbie VanSickle
It was 2014, and Erin Morrow Hawley was fighting against the egg-laying hens of Missouri. Specifically, a new requirement that chicken cages have enough space for the hens to stand up, turn around and stretch out.
A law professor from five generations of ranchers and the wife of Senator Josh Hawley, Ms. Hawley joined a challenge to California, which required more spacious enclosures for hens laying eggs to be sold there. The state where she taught, Missouri, sold a third of its eggs to California, and Ms. Hawley believed that a blue state had no right to impose its values and rules on Missouri’s farmers.
She joined in a lawsuit against California’s attorney general at the time, Kamala Harris. A judge found that the challengers could show no direct injury and dismissed the case. Ms. Hawley continued teaching, and Ms. Harris became Joe Biden’s vice president.
Ten years later, Ms. Hawley, 44, is now at the center of one of the country’s most heated cultural battles about bodily autonomy, gender roles and abortion. On Tuesday, for the first time since the overturning of Roe v. Wade, the Supreme Court considered a case involving nationwide limits on abortion access. And Ms. Hawley was the woman standing before the justices, arguing to sharply curtail access to the abortion pill.
The case centers on the Food and Drug Administration’s approval of mifepristone, a commonly available drug used in the majority of abortions in the country. Limiting medication abortion is a next frontier for the anti-abortion movement in the post-Roe era.
Ms. Hawley represents a group of anti-abortion doctors and an umbrella group of conservative medical associations that claim that the abortion pill — approved more than two decades ago — is a danger to women. The F.D.A. has pointed to substantial scientific evidence that the medication abortion is safe .
Ms. Hawley views the cause as similar to her fights against government interference, rooted in her experience of ranch life.
“You see how those regulations impact people that are really living on the ground, and sometimes for good and sometimes maybe not for good,” she said in an interview with The Times earlier this month. “And so being pro-life, and believing that every child, no matter how small, no matter if they’re not yet born, is invested with inherent dignity and worth — government action can have a lot to say about that as well.”
She argues that federal approval of the abortion pill went forward without enough consideration of possible side effects and dangers, and that subsequent changes to enable greater access have ignored health risks to women.
The government lawyers in this case, led by Solicitor General Elizabeth B. Prelogar, have argued in court filings that Ms. Hawley and her legal team offered scant evidence of real injury, and that declarations from “seven identified doctors” were “often vague or conclusory.”
Ms. Hawley’s particular background makes her ideal for this moment. Her longtime interest in limiting the power of the administrative state is well suited to speak to the current court’s conservative supermajority, which has welcomed cases challenging regulations on everything from herring fish to machine guns and, now, abortion.
Ms. Hawley brings her credentials not only as a former clerk to Chief Justice John G. Roberts Jr. but as a millennial Christian mother. An evangelical believer who forefronts her identity as a wife and mother of three, Ms. Hawley works for the Alliance Defending Freedom, a powerful conservative Christian legal group. She represents the ideals of womanhood many in the anti-abortion and conservative Christian movement seek to elevate.
Until now, Ms. Hawley has been best known as the wife of Senator Hawley, Republican of Missouri, who actively sought the overturning of Roe and has supported anti-abortion legislation.
In a campaign ad for him, Ms. Hawley starred as an everyday mom, playing with their children in the kitchen, while he took the spotlight. But she will be one of a few women to argue a prominent abortion case at the Supreme Court for the anti-abortion side.
Even anti-abortion leaders often said “who?” or “Josh’s wife?” when asked about Ms. Hawley. Penny Nance, president of Concerned Women for America, has met her at events supporting Senator Hawley but did not realize that Ms. Hawley was arguing the mifepristone case.
“There are millions of conservative women all over our country who are educated and powerful and love their families, similar to Erin Hawley,” Ms. Nance said. “She is actually fairly typical of young millennial conservative Christian women coming up through the ranks.”
But it may be Ms. Hawley, not Sen. Hawley, whose work will most power the anti-abortion cause.
“I think it may be more accurate to say that he’s Erin Hawley’s husband,” Mary Ziegler, a law professor and historian at University of California, Davis, said of the senator. “I think people are just beginning to see how influential she is.”
Erin Morrow was born into a family of frontier women and grew up on a cattle ranch near Folsom, N.M., population roughly 50. The foundation of her great-great-great grandmother’s homestead is still visible on the land, where family lore says that as a young widow, she outwitted marauding bandits.
The oldest of three daughters, Ms. Hawley was raised mainly by her mother after her parents divorced. Her father, a former national rodeo champion who struggled with alcoholism and depression, died by suicide when she was in high school, a pivotal moment she has spoken about on her podcast . Her mother, Shari Morrow, ran the family’s ranch, WineCup, and started teaching Erin to ride horses before she could walk.
“She was there when the bus came home, and often she’d throw us on horseback, and we’d help her move cattle, and we were able to sort of participate in her job in a small way,” Ms. Hawley said in the interview with Times reporters. “She was just a wonderful example of putting her family first but also doing something she loved and cared about.”
Her mother, a registered Democrat in the 1990s, had wanted to be a veterinarian, and for a while her daughter did too. Ms. Hawley studied animal science at Texas A&M University and considered a doctorate in genetics. But an internship for the House Committee on Agriculture sparked her interest in regulatory law.
Ms. Hawley started law school at the University of Texas in Austin, then transferred to Yale Law School, where she was a senior editor on the law review.
She clerked for J. Harvie Wilkinson III, a Reagan appointee on the U.S. Court of Appeals for the Fourth Circuit, and for Chief Justice Roberts in 2007.
There, her desk faced that of another clerk from Yale, Josh Hawley, and they secretly dated. He persuaded her to get married, when she was skeptical after having grown up “in a home with a marriage that wasn’t ideal,” she said in a podcast, and they moved back to his home state of Missouri.
When they searched for jobs, she impressed the faculty at the University of Missouri’s School of Law and expressed interest in filling a need to teach tax law. The school offered jobs to both of them.
Together they started the Missouri Liberty Project, “dedicated to promoting constitutional liberty and limited government.” But her husband’s career soon took the lead in their lives. As he campaigned for the U.S. Senate, she wrote a devotional book for mothers, drawing spiritual lessons from the lives of her children while comfortably weaving in references to modern theologians like Stanley Hauerwas. Her light textual analysis of original Greek words in the Bible echoes her approach to interpreting the Constitution in her legal work.
“Why can’t a high-powered lawyer also share that side of her life? Why not? That is her foundation, that is who she is,” said Julie Holmquist, who edited the book.
Ms. Hawley had expected her husband to pursue a political career after their children were grown. When they felt God calling him to run for office, she packed the family onto the campaign bus. The couple voted at their home church, The Crossing Church, an evangelical Presbyterian congregation, and the Hawleys moved to Washington.
Only a few months into her role as a lawyer for the conservative Christian legal advocacy group A.D.F. in 2021, Ms. Hawley flew to Mississippi to strategize on the Dobbs case, which overturned Roe v. Wade.
Ms. Hawley and her infant daughter arrived on time, but her babysitter did not. In the middle of the meeting, the baby let out a wail.
As Ms. Hawley tells it, this moment encapsulated her purpose, both as a Christian mom and as a lawyer aimed at dismantling the right to abortion. On the couple’s podcast, she described her baby’s crying as “a tangible reminder of why the Dobbs case might matter so much.”
At a speech after the Dobbs oral argument, Ms. Hawley said she had “been blessed to have a front-row seat on this case.” She added, “As a conservative mother, I can tell you it has been the project of a lifetime.”
Ms. Hawley has notched other legal victories, becoming synonymous with conservative social-issue cases. She worked on 303 Creative, the case in which the Supreme Court justices ruled in favor of a Colorado web designer who cited the First Amendment in refusing to serve same-sex couples.
Ms. Hawley is currently helping the Idaho attorney general defend the state’s abortion ban from a challenge by the Biden administration.
At the Supreme Court on Tuesday, her unique background was on display, even as most justices seemed skeptical of her argument. She answered a question from Justice Samuel A. Alito Jr. about determining standing — whether the anti-abortion doctors could show direct harm — by referencing how the court considered the issue in a case about genetically engineered crops. In that case, Ms. Hawley said, the court looked at “the distance that bees might fly in order to pollinate seed farms,” she said. She had the support of her husband, who was present in the courtroom.
Even with the pressure of a first-time oral argument, she said in the interview that she remained calm because the decision was ultimately up to God.
“Christians are called to work with excellence but also to rest in the knowledge that God is sovereign, and that we can trust the results to Him,” she said. “To have the faith that all of it is in His hands, I think does help.”
The justices are expected to make a decision in June.
Julie Tate and Kitty Bennett contributed research.
Elizabeth Dias is The Times’s national religion correspondent, covering faith, politics and culture. More about Elizabeth Dias
Abbie VanSickle covers the United States Supreme Court for The Times. She is a lawyer and has an extensive background in investigative reporting. More about Abbie VanSickle
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries
What the data says about abortion in the u.s..
Pew Research Center has conducted many surveys about abortion over the years, providing a lens into Americans’ views on whether the procedure should be legal, among a host of other questions.
In a Center survey conducted nearly a year after the Supreme Court’s June 2022 decision that ended the constitutional right to abortion , 62% of U.S. adults said the practice should be legal in all or most cases, while 36% said it should be illegal in all or most cases. Another survey conducted a few months before the decision showed that relatively few Americans take an absolutist view on the issue .
Find answers to common questions about abortion in America, based on data from the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, which have tracked these patterns for several decades:
How many abortions are there in the U.S. each year?
How has the number of abortions in the u.s. changed over time, what is the abortion rate among women in the u.s. how has it changed over time, what are the most common types of abortion, how many abortion providers are there in the u.s., and how has that number changed, what percentage of abortions are for women who live in a different state from the abortion provider, what are the demographics of women who have had abortions, when during pregnancy do most abortions occur, how often are there medical complications from abortion.
This compilation of data on abortion in the United States draws mainly from two sources: the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, both of which have regularly compiled national abortion data for approximately half a century, and which collect their data in different ways.
The CDC data that is highlighted in this post comes from the agency’s “abortion surveillance” reports, which have been published annually since 1974 (and which have included data from 1969). Its figures from 1973 through 1996 include data from all 50 states, the District of Columbia and New York City – 52 “reporting areas” in all. Since 1997, the CDC’s totals have lacked data from some states (most notably California) for the years that those states did not report data to the agency. The four reporting areas that did not submit data to the CDC in 2021 – California, Maryland, New Hampshire and New Jersey – accounted for approximately 25% of all legal induced abortions in the U.S. in 2020, according to Guttmacher’s data. Most states, though, do have data in the reports, and the figures for the vast majority of them came from each state’s central health agency, while for some states, the figures came from hospitals and other medical facilities.
Discussion of CDC abortion data involving women’s state of residence, marital status, race, ethnicity, age, abortion history and the number of previous live births excludes the low share of abortions where that information was not supplied. Read the methodology for the CDC’s latest abortion surveillance report , which includes data from 2021, for more details. Previous reports can be found at stacks.cdc.gov by entering “abortion surveillance” into the search box.
For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. In computing those figures, we excluded abortions listed in the report under the categories “spontaneous or unspecified” or as “other.” (“Spontaneous abortion” is another way of referring to miscarriages.)
Guttmacher data in this post comes from national surveys of abortion providers that Guttmacher has conducted 19 times since 1973. Guttmacher compiles its figures after contacting every known provider of abortions – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, and it provides estimates for abortion providers that don’t respond to its inquiries. (In 2020, the last year for which it has released data on the number of abortions in the U.S., it used estimates for 12% of abortions.) For most of the 2000s, Guttmacher has conducted these national surveys every three years, each time getting abortion data for the prior two years. For each interim year, Guttmacher has calculated estimates based on trends from its own figures and from other data.
The latest full summary of Guttmacher data came in the institute’s report titled “Abortion Incidence and Service Availability in the United States, 2020.” It includes figures for 2020 and 2019 and estimates for 2018. The report includes a methods section.
In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion.
An exact answer is hard to come by. The CDC and the Guttmacher Institute have each tried to measure this for around half a century, but they use different methods and publish different figures.
The last year for which the CDC reported a yearly national total for abortions is 2021. It found there were 625,978 abortions in the District of Columbia and the 46 states with available data that year, up from 597,355 in those states and D.C. in 2020. The corresponding figure for 2019 was 607,720.
The last year for which Guttmacher reported a yearly national total was 2020. It said there were 930,160 abortions that year in all 50 states and the District of Columbia, compared with 916,460 in 2019.
- How the CDC gets its data: It compiles figures that are voluntarily reported by states’ central health agencies, including separate figures for New York City and the District of Columbia. Its latest totals do not include figures from California, Maryland, New Hampshire or New Jersey, which did not report data to the CDC. ( Read the methodology from the latest CDC report .)
- How Guttmacher gets its data: It compiles its figures after contacting every known abortion provider – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, then provides estimates for abortion providers that don’t respond. Guttmacher’s figures are higher than the CDC’s in part because they include data (and in some instances, estimates) from all 50 states. ( Read the institute’s latest full report and methodology .)
While the Guttmacher Institute supports abortion rights, its empirical data on abortions in the U.S. has been widely cited by groups and publications across the political spectrum, including by a number of those that disagree with its positions .
These estimates from Guttmacher and the CDC are results of multiyear efforts to collect data on abortion across the U.S. Last year, Guttmacher also began publishing less precise estimates every few months , based on a much smaller sample of providers.
The figures reported by these organizations include only legal induced abortions conducted by clinics, hospitals or physicians’ offices, or those that make use of abortion pills dispensed from certified facilities such as clinics or physicians’ offices. They do not account for the use of abortion pills that were obtained outside of clinical settings .
(Back to top)
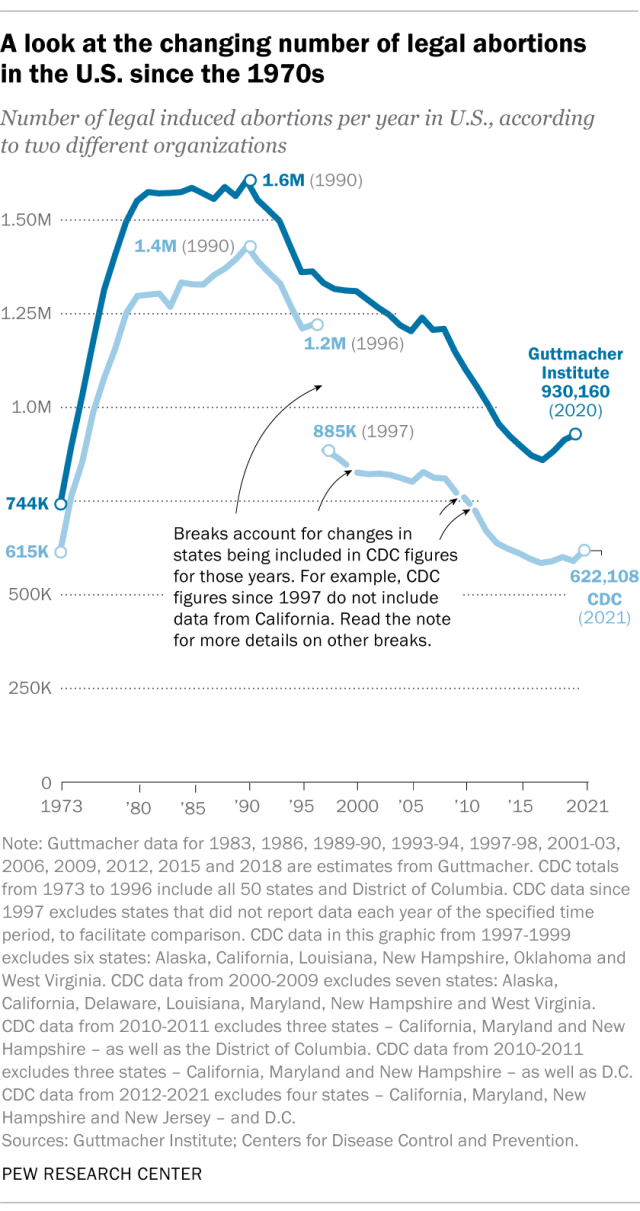
The annual number of U.S. abortions rose for years after Roe v. Wade legalized the procedure in 1973, reaching its highest levels around the late 1980s and early 1990s, according to both the CDC and Guttmacher. Since then, abortions have generally decreased at what a CDC analysis called “a slow yet steady pace.”
Guttmacher says the number of abortions occurring in the U.S. in 2020 was 40% lower than it was in 1991. According to the CDC, the number was 36% lower in 2021 than in 1991, looking just at the District of Columbia and the 46 states that reported both of those years.
(The corresponding line graph shows the long-term trend in the number of legal abortions reported by both organizations. To allow for consistent comparisons over time, the CDC figures in the chart have been adjusted to ensure that the same states are counted from one year to the next. Using that approach, the CDC figure for 2021 is 622,108 legal abortions.)
There have been occasional breaks in this long-term pattern of decline – during the middle of the first decade of the 2000s, and then again in the late 2010s. The CDC reported modest 1% and 2% increases in abortions in 2018 and 2019, and then, after a 2% decrease in 2020, a 5% increase in 2021. Guttmacher reported an 8% increase over the three-year period from 2017 to 2020.
As noted above, these figures do not include abortions that use pills obtained outside of clinical settings.
Guttmacher says that in 2020 there were 14.4 abortions in the U.S. per 1,000 women ages 15 to 44. Its data shows that the rate of abortions among women has generally been declining in the U.S. since 1981, when it reported there were 29.3 abortions per 1,000 women in that age range.
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher’s data, the CDC’s figures also suggest a general decline in the abortion rate over time. In 1980, when the CDC reported on all 50 states and D.C., it said there were 25 abortions per 1,000 women ages 15 to 44.
That said, both Guttmacher and the CDC say there were slight increases in the rate of abortions during the late 2010s and early 2020s. Guttmacher says the abortion rate per 1,000 women ages 15 to 44 rose from 13.5 in 2017 to 14.4 in 2020. The CDC says it rose from 11.2 per 1,000 in 2017 to 11.4 in 2019, before falling back to 11.1 in 2020 and then rising again to 11.6 in 2021. (The CDC’s figures for those years exclude data from California, D.C., Maryland, New Hampshire and New Jersey.)
The CDC broadly divides abortions into two categories: surgical abortions and medication abortions, which involve pills. Since the Food and Drug Administration first approved abortion pills in 2000, their use has increased over time as a share of abortions nationally, according to both the CDC and Guttmacher.
The majority of abortions in the U.S. now involve pills, according to both the CDC and Guttmacher. The CDC says 56% of U.S. abortions in 2021 involved pills, up from 53% in 2020 and 44% in 2019. Its figures for 2021 include the District of Columbia and 44 states that provided this data; its figures for 2020 include D.C. and 44 states (though not all of the same states as in 2021), and its figures for 2019 include D.C. and 45 states.
Guttmacher, which measures this every three years, says 53% of U.S. abortions involved pills in 2020, up from 39% in 2017.
Two pills commonly used together for medication abortions are mifepristone, which, taken first, blocks hormones that support a pregnancy, and misoprostol, which then causes the uterus to empty. According to the FDA, medication abortions are safe until 10 weeks into pregnancy.
Surgical abortions conducted during the first trimester of pregnancy typically use a suction process, while the relatively few surgical abortions that occur during the second trimester of a pregnancy typically use a process called dilation and evacuation, according to the UCLA School of Medicine.
In 2020, there were 1,603 facilities in the U.S. that provided abortions, according to Guttmacher . This included 807 clinics, 530 hospitals and 266 physicians’ offices.
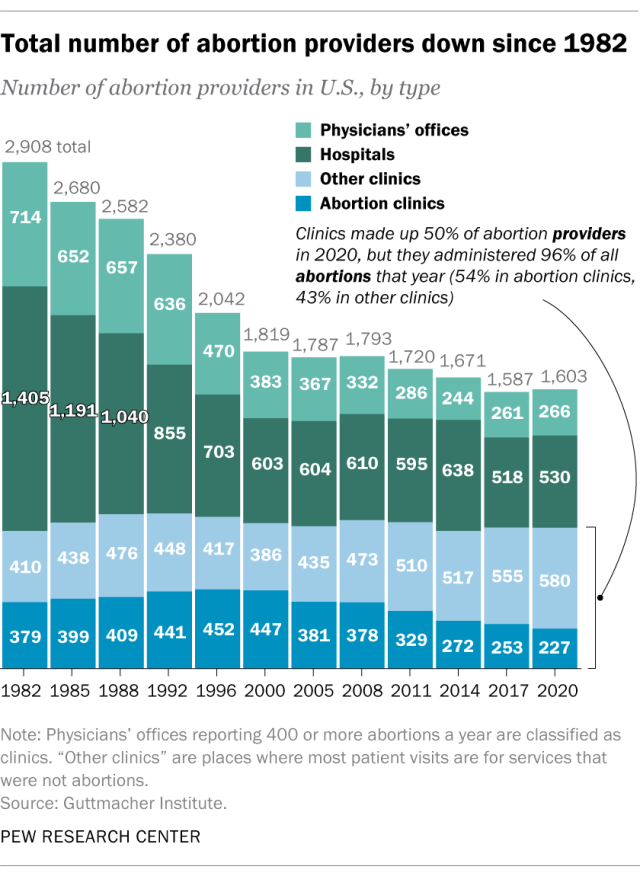
While clinics make up half of the facilities that provide abortions, they are the sites where the vast majority (96%) of abortions are administered, either through procedures or the distribution of pills, according to Guttmacher’s 2020 data. (This includes 54% of abortions that are administered at specialized abortion clinics and 43% at nonspecialized clinics.) Hospitals made up 33% of the facilities that provided abortions in 2020 but accounted for only 3% of abortions that year, while just 1% of abortions were conducted by physicians’ offices.
Looking just at clinics – that is, the total number of specialized abortion clinics and nonspecialized clinics in the U.S. – Guttmacher found the total virtually unchanged between 2017 (808 clinics) and 2020 (807 clinics). However, there were regional differences. In the Midwest, the number of clinics that provide abortions increased by 11% during those years, and in the West by 6%. The number of clinics decreased during those years by 9% in the Northeast and 3% in the South.
The total number of abortion providers has declined dramatically since the 1980s. In 1982, according to Guttmacher, there were 2,908 facilities providing abortions in the U.S., including 789 clinics, 1,405 hospitals and 714 physicians’ offices.
The CDC does not track the number of abortion providers.
In the District of Columbia and the 46 states that provided abortion and residency information to the CDC in 2021, 10.9% of all abortions were performed on women known to live outside the state where the abortion occurred – slightly higher than the percentage in 2020 (9.7%). That year, D.C. and 46 states (though not the same ones as in 2021) reported abortion and residency data. (The total number of abortions used in these calculations included figures for women with both known and unknown residential status.)
The share of reported abortions performed on women outside their state of residence was much higher before the 1973 Roe decision that stopped states from banning abortion. In 1972, 41% of all abortions in D.C. and the 20 states that provided this information to the CDC that year were performed on women outside their state of residence. In 1973, the corresponding figure was 21% in the District of Columbia and the 41 states that provided this information, and in 1974 it was 11% in D.C. and the 43 states that provided data.
In the District of Columbia and the 46 states that reported age data to the CDC in 2021, the majority of women who had abortions (57%) were in their 20s, while about three-in-ten (31%) were in their 30s. Teens ages 13 to 19 accounted for 8% of those who had abortions, while women ages 40 to 44 accounted for about 4%.
The vast majority of women who had abortions in 2021 were unmarried (87%), while married women accounted for 13%, according to the CDC , which had data on this from 37 states.
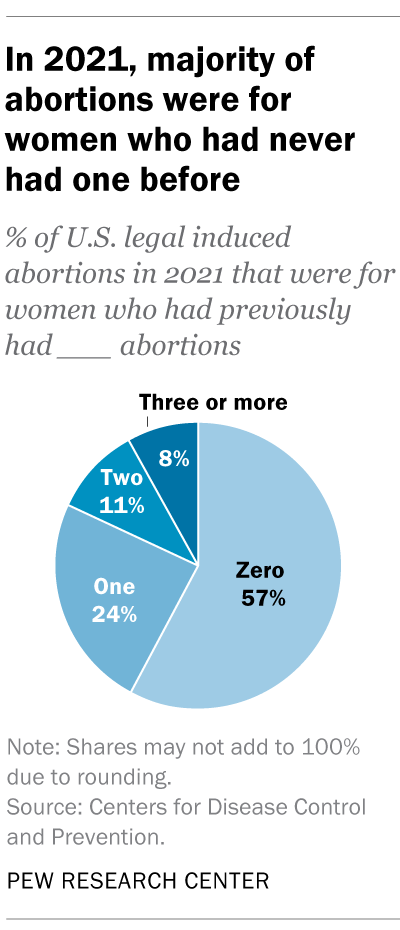
In the District of Columbia, New York City (but not the rest of New York) and the 31 states that reported racial and ethnic data on abortion to the CDC , 42% of all women who had abortions in 2021 were non-Hispanic Black, while 30% were non-Hispanic White, 22% were Hispanic and 6% were of other races.
Looking at abortion rates among those ages 15 to 44, there were 28.6 abortions per 1,000 non-Hispanic Black women in 2021; 12.3 abortions per 1,000 Hispanic women; 6.4 abortions per 1,000 non-Hispanic White women; and 9.2 abortions per 1,000 women of other races, the CDC reported from those same 31 states, D.C. and New York City.
For 57% of U.S. women who had induced abortions in 2021, it was the first time they had ever had one, according to the CDC. For nearly a quarter (24%), it was their second abortion. For 11% of women who had an abortion that year, it was their third, and for 8% it was their fourth or more. These CDC figures include data from 41 states and New York City, but not the rest of New York.
Nearly four-in-ten women who had abortions in 2021 (39%) had no previous live births at the time they had an abortion, according to the CDC . Almost a quarter (24%) of women who had abortions in 2021 had one previous live birth, 20% had two previous live births, 10% had three, and 7% had four or more previous live births. These CDC figures include data from 41 states and New York City, but not the rest of New York.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester – that is, at or before 13 weeks of gestation, according to the CDC . An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation. These CDC figures include data from 40 states and New York City, but not the rest of New York.
About 2% of all abortions in the U.S. involve some type of complication for the woman , according to an article in StatPearls, an online health care resource. “Most complications are considered minor such as pain, bleeding, infection and post-anesthesia complications,” according to the article.
The CDC calculates case-fatality rates for women from induced abortions – that is, how many women die from abortion-related complications, for every 100,000 legal abortions that occur in the U.S . The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions. During the five-year periods in between, the figure ranged from 0.52 (from 1993 to 1997) to 0.78 (from 1978 to 1982).
The CDC calculates death rates by five-year and seven-year periods because of year-to-year fluctuation in the numbers and due to the relatively low number of women who die from legal induced abortions.
In 2020, the last year for which the CDC has information , six women in the U.S. died due to complications from induced abortions. Four women died in this way in 2019, two in 2018, and three in 2017. (These deaths all followed legal abortions.) Since 1990, the annual number of deaths among women due to legal induced abortion has ranged from two to 12.
The annual number of reported deaths from induced abortions (legal and illegal) tended to be higher in the 1980s, when it ranged from nine to 16, and from 1972 to 1979, when it ranged from 13 to 63. One driver of the decline was the drop in deaths from illegal abortions. There were 39 deaths from illegal abortions in 1972, the last full year before Roe v. Wade. The total fell to 19 in 1973 and to single digits or zero every year after that. (The number of deaths from legal abortions has also declined since then, though with some slight variation over time.)
The number of deaths from induced abortions was considerably higher in the 1960s than afterward. For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965 , according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services.
Note: This is an update of a post originally published May 27, 2022, and first updated June 24, 2022.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
Key facts about the abortion debate in America
Public opinion on abortion, three-in-ten or more democrats and republicans don’t agree with their party on abortion, partisanship a bigger factor than geography in views of abortion access locally, do state laws on abortion reflect public opinion, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Radiol Imaging
- v.18(2); 2008 May

Radiology medico-legal cases
From medical law cases - for doctors, vol 1: 1; pgs 34, 35, case 1: medical literature in aid to justify medical action.
Editor's note: The article has been modified from the original to protect the identities of those concerned.
Dr. A and Ors versus Patient Z; Judgment in favor of: Doctor.
Facts of the case
The patient underwent a USG examination of the abdomen, performed by the sonologist (Opposite Party - OP) and the report read, “gall bladder …. contains multiple echogenic shadows of stones accompanied by P-A shadowing in the neck region.” Relying on the report, the patient was operated for removal of stones but no stones were found.
Patient's allegation/s of medical negligence
The allegation was that a wrong report was given by the sonologist (OP) and relying on the same, the patient underwent surgery. It was alleged that it was unconvincing that stones could have disappeared within a period of 18 days of the USG, i.e., when the surgery done.
Doctor's Defense
- The doctor in his defense produced medical literature wherein it was categorically stated, “Finally small gallstones are occasionally seen to disappear…. This can happen at any time and is not necessarily accompanied by symptoms.”
- Further, the operational notes of surgeon recorded, “Gall bladder had few adhesions with omentum and the cut surface showed thickened mucosa with few tiny whitish spots? Calcareous deposits, but did not contain any calculi” were also pointed out in defense.
Findings of the Court
- The court in view of the medical literature, the operating surgeon's statement in court and findings recorded in the operation notes, held that it was possible for stones to disappear within 18 days.
- Hence, the sonologist (OP) was not found to be negligent.
Detailed Discussion
- The appellants were the opposite parties before the State Commission, where the respondent/complainant, patient Z had filed a complaint alleging a case of medical negligence against the appellants.
“The gall bladder is normal in size and shape. Its wall thickness is 3 mm. It contains multiple echogenic shadows of stones accompanied by P-A shadowing in the neck region. No mass seen. No perifocal edema seen. No stone seen in the CBD or cystic duct.”
- Because this report showed multiple shadows of stones, the complainant got herself admitted for removal of stones and operation was carried on, on 11.6.1996 by one Dr. B, but in reality, no stones were found. Thus, alleging a case of medical negligence, a case was filed before the State Commission, who after hearing the parties allowed the complaint and directed the appellants to refund Rs. 400 charged for the examination along with cost of Rs. 1,000. Aggrieved by this order, this appeal has been filed before us.
- Despite service of notice, none appears for the respondent/complainant, hence proceeded ex parte . We heard the appellant Dr. C on behalf of the appellants.
- After hearing appellant and perusal of material on record as well as the medical literature brought on record, we find that the State Commission has held the appellants guilty of medical negligence on account of the fact that while the USG test carried out on 24.5.1996 by the appellants showed multiple echogenic shadows of stones in gall bladder by P-A shadowing in the neck region, the State Commission found it unconvincing that it could have disappeared within a period of 18 days, i.e., when the surgery done by Dr. B on 11.6.1996, the stones were not seen.
“Finally small gallstones are occasionally seen to disappear. This is usually due to their passage into b the common duct where they mayor may not be retained. This can happen at any time [Figure 37.6] and is not necessarily accompanied by symptoms. This is one of the main justifications for operative choledochography.”
“Gall bladder had few adhesions with omentum and the cut surface showed thickened mucosa with few tiny whitish spots? Calcareous deposits, but did not contain any calculi. Liver and other adjacent viscera normal. CBD normal. Gall bladder sent for HPE (Histopathological examination).”
- We have also seen the cross-examination of the concerned surgeon, wherein he has clearly admitted, “…if the stone is of very small size or few in number, there could be its passing out during the period between 24.5.96 and 11.6.1996.”
- In view of the medical literature brought on record cited above and what the operating surgeon stated in his cross-examination, along with his findings referred to in the operation notes, we are of the view that in the light of this material, the order passed by the State Commission cannot be sustained. There is neither any other expert evidence nor material brought on record by the respondent/complainant in support of the allegations of medical negligence on the part of the appellants. Only, deemed to be expert, Dr. B has admitted that these stones could have passed out during this period. In view of this, according to us, the State Commission could not have held the statement of the appellants “not at all convincing”.
- In the aforementioned circumstances, we are unable to sustain the order passed by the State Commission, which is set aside. The appeal is allowed and the complaint stands dismissed.
- No order as to costs.
- Appeal allowed.
Source of Support: Nil
Conflict of Interest: None declared.

IMAGES
VIDEO
COMMENTS
Cases that are to be treated as medicolegal are: [ 3] (1) All cases of injuries and burns - the circumstances of which suggest commission of an offense by somebody (irrespective of suspicion of foul play); (2) all vehicular, factory, or other unnatural accident cases specially when there is a likelihood of patient's death or grievous hurt; (3 ...
The physician was responsible for $750,000, and the pharmacist was responsible for $250,000.2. Case 2 - Anonymous v Miller Pharmacy. A 67-year-old cancer survivor picked up her regular prescription for methadone that was prescribed as 15 mg (three 5 mg tablets) twice daily. Four days later, she was found dead.
Introduction. A medico-legal case (MLC) applies to any case of injury or medical condition in which law enforcement agencies seek to investigate and fix the responsibility regarding the said injury or medical condition. 1 From a physician's perspective, a MLC is a medical or clinical case with legal implications. In such cases presented directly to the hospital, after obtaining a detailed ...
A medico-legal case (MLC) involves any injury or medical condition in which law enforcement agencies investigate and fix the responsibility regarding of an injury or medical condition. Incorrect or incomplete medico-legal reports (MLRs) may trigger a pause or delay in legal proceedings and patients' rights could be violated.
We conducted a descriptive study and content analysis of medico-legal cases involving emergency department physicians from a national repository at the Canadian Medical Protective Association. Cases with peer expert criticism of an emergency physician's documentation, which were closed between 2016 and 2020, and occurred in an emergency ...
In our study, there was a very low percentage of external ADR mechanisms utility (1.3%; n = 3), suggesting that the in-built dispute resolution mechanisms for early intervention and engagement was effective and well accepted by patients for most medico-legal cases. In our study, a significant association was found between PRS' engagement of ...
A study was conducted in a rural hospital to assess profile, types, and the frequency with an incident rate of different types of medico-legal cases (MLC). Medicolegal case concentrates on ...
For inclusion in our study, cases must have involved a physician named in the medico-legal matter who self-reported cardiology as their specialty when obtaining membership with the CMPA. Additionally, cases must have closed (defined in Supplemental Table S1 ) by the CMPA between January 1, 2009 and December 31, 2018 inclusive.
Abstract. Abortion has always been a vital issue in reproductive and legal medicine. Globally, medical termination of pregnancy (MTP) is allowed primarily on six grounds: (1) to save the life of a woman, (2) risk to the physical and mental health of a woman, (3) ... Restricted accessReview articleFirst published April 5, 2023pp. 34-42.
The study comprised a 15-year medicolegal trend analysis and a 5-year contributing factors analysis of cases (civil legal and regulatory authority matters) from the Canadian Medical Protective Association (CMPA), representing an estimated 95% of physicians in Canada. Included cases were closed by the CMPA between 2004 and 2018 (trends) or 2014 ...
Top of FormTripathy K, Chawla R, Venkatesh P, et al. Clinical profile of medicolegal cases presenting to the eye casualty in a tertiary care center in India. Indian J of Ophthalmol. 2016;64 (6 ...
Medico Legal Case Study Collection. Invaluable insights. Undeniable expertise. Our board certified, actively practicing medical witnesses bring unparalleled expertise to your case. Read these in-depth medico legal case studies, each authored by an AMFS medical expert witness, for a glimpse into the value our experts deliver for the nation's ...
Background Point-of-care ultrasound (POCUS) has become a core diagnostic tool for many physicians due to its portability, excellent safety profile, and diagnostic utility. Despite its growing use, the potential risks of POCUS use should be considered by providers. We analyzed the Canadian Medical Protective Association (CMPA) repository to identify medico-legal cases arising from the use of ...
Thirteen studies examined the association between the documentation of bodily injuries generally and case outcomes, with only two studies from the United States , and ... All cases without a medico-legal form, including those for attempted or suspected rape, were excluded from the analysis. Among these, no medical examination was done in 250 ...
Medico-legal helpline 0800 716 646 Search MDU Search. Menu Back ... Case studies. GMC interview. An SHO faced a dilemma when the GMC wanted to interview them about a colleague's alleged misconduct. The perils of poor communication . 30 January 2024.
Medico-Legal Journal. Medico-Legal Journal is dedicated to promoting Medico-Legal knowledge in all its aspects. It provides an official record of the proceedings of the Medico-Legal Society. The journal seeks to further the society's aim to expand knowledge of medico-legal matters by commissioning articles on topics from across this diverse ...
The purpose of our study was to review and consolidate literature regarding medico-legal issues pertaining to THA and TKA cases. We looked at the causes of litigation, medico legal aspects of pre-operative requirements, optimisation of medical condition, indications and contraindications for arthroplasty, informed consent, implants, mixing of ...
This chapter considers the legal case of Stamford Hospital vs. Nelly E. Vega, 674 A. 2d 821 (Conn., 1996). In this matter, an obstetrical patient was given blood transfusions against her will ...
Categories of Medico legal cases documented at casualty department. In our study out of 3105 cases, maximum number of cases 1283 (42%) were reported having predilection of age during third decade of life i.e., in the age group 21-30 years followed by age group 11-20 years which showed 955 (31%) cases. Almost three quarter of victims (73%) were ...
Medico-legal cases presented to the Accident & Emergency department vary from hospital to hospital. Profiling these cases from time to time provides an insight into the workload of medico-legal cases as well as what is going on in and around the locality. The present study was conducted at LHMC, New Delhi from January 2021 to June 2022 from the available records of MLCs from 1st January 2019 ...
This article was written by Adhila Muhammed Arif, a student of Government Law College, Thiruvananthapuram. This article seeks to explain what a medico-legal case is, some important laws related to it, and what medical practitioners must keep in mind while dealing with a medico-legal cases. It has been published by Rachit Garg. Introduction The legal […]
The Caselaw Access Project published nearly seven million cases from the Harvard Law School's collections online on March 8, concluding a nine-year process to digitize the HLS Library's ...
F.D.A. data has found that hospitalization occurs in less than 0.7 percent of cases of women taking abortion pills, that serious infections occurs in less than 0.2 percent of cases and that ...
A medico-legal case can be defined as "a case of injury or illness that requires investigation by law-enforcing agencies to fix the responsibility regarding the causation of the injury or illness". ... which may have been due to minimal exposure or lack of training in handling medico-legal cases. In the present study, 42.4% of the emergency ...
Ms. Hawley has notched other legal victories, becoming synonymous with conservative social-issue cases. She worked on 303 Creative, the case in which the Supreme Court justices ruled in favor of a ...
The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions.
Very briefly the facts of the case are that the respondent/complainant got a USG examination of the abdomen done by the appellants for a consideration and report was supplied to the complainant. The report reads as follows: "The gall bladder is normal in size and shape. Its wall thickness is 3 mm. It contains multiple echogenic shadows of ...