An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
2021 National Healthcare Quality and Disparities Report [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2021 Dec.

2021 National Healthcare Quality and Disparities Report [Internet].
Disparities in healthcare.
Healthcare delivery is not experienced equitably by all populations. A healthcare disparity is a difference between population groups in the way they access, experience, and receive healthcare. Factors that influence healthcare disparities include social, economic, environmental, and other disadvantages, 1 , 2 some of which are explored in this report.
Unfortunately, Americans too often do not receive care they need, or they receive care that causes harm. Care can be delivered too late or without full consideration of a patient’s preferences and values. Many times, our healthcare system distributes services inefficiently and unevenly across populations. Some Americans receive worse care than others. These disparities may occur for a variety of reasons, including differences in access to care, social determinants, provider biases, poor provider-patient communication, and poor health literacy.
- Research Framework for Health Disparities
The Research Framework in Exhibit 1 was developed by the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities (NIMHD). This framework is based on an evolving conceptualization of factors relevant to the understanding and promotion of minority health and to the understanding and reduction of health disparities.
The framework serves as a vehicle for encouraging NIH-supported research that addresses the complex and multifaceted nature of minority health and health disparities. This research needs to span different domains of influence (Biological, Behavioral, Physical/Built Environment, Sociocultural Environment, Healthcare System) and different levels of influence (Individual, Interpersonal, Community, Societal) within those domains.
The framework also provides a classification structure that facilitates analysis of the NIMHD minority health and health disparities research portfolios to assess progress, gaps, and opportunities. Examples of factors are provided within each cell of the framework (e.g., Family Microbiome within the Interpersonal-Biological cell). These factors are not intended to be exhaustive. Health disparity populations, as well as other features of this framework, may be adjusted over time.
NIMHD Research Framework. * Health Disparity Populations: Race/ethnicity, low socioeconomic status, rural, sexual/gender minority. Other Fundamental Characteristics: Sex/gender, disability, geographic region.
- Role of Research Framework in the NHQDR
The NHQDR reports on progress and opportunities for improving healthcare quality and reducing healthcare disparities. The NIMHD Minority Health and Health Disparities Research Framework highlights factors ranging from individual biology and behavior to social structure that affect disparities. To successfully reduce disparities, it is necessary to address all these factors.
All Americans should have equitable access to high-quality care. Instead, racial and ethnic minorities and poor people often face more barriers to care and receive poorer quality of care when they can get it. 3 In this report, measures were analyzed to assess disparities both by socioeconomic and cultural groups and by settings of care.
An increasing number of healthcare organizations and payers are experimenting with strategies to identify needs and connect patients to resources that address identified needs. The goals are to improve health outcomes, reduce avoidable use of costly health services, and improve health equity. 4
Inequitable health outcomes result from inequities in the distribution of or access to resources that promote good health outcomes. Differences refer to outcomes that result from biological risk or other factors that are not a matter of policy or discrimination in access. A difference may become a disparity when some subgroups and not others are given access to resources to manage their differential risk from biology or other factors and the groups without access have poorer outcomes. Thus, differences and disparities may have different determinants requiring different forms of intervention. 5
The Disparities in Healthcare section of the 2021 NHQDR examines the best and worst performing quality measures among the measures used in the report. These quality measures are analyzed in this section of the report by race and ethnicity, income, insurance status, and residence location. While these categories are broad, each section begins with key definitions to orient readers and includes analyses showing quality measure performance in the latest data year and analyses showing whether disparities were widening or narrowing over time.
More information on the measures included in this section of the report is available through the NHQDR Data Query Tool ( https://datatools.ahrq.gov/nhqdr ). The tool also allows readers to stratify NHQDR data by variables such as education, sex, and age, where available.
- Racial and Ethnic Disparities
Researchers, patients, providers, and policymakers have worked to identify, understand, and eliminate the disparities experienced by different racial and ethnic groups across the healthcare system. In 1985, the Department of Health and Human Services published the Report of the Secretary’s Task Force on Black and Minority Health (Heckler Report), which marked the first comprehensive study of racial and minority health by the U.S. government. 6 Since then, the Department, along with other stakeholders, has continued this work, including throughout the NHQDR. The growing evidence base shows that patients of different racial and ethnic groups experience quality of care inequitably and disparately. 7 , 8
- American Indian or Alaska Native (AI/AN). A person having origins in any of the original peoples of North and South America (including Central America) and maintains tribal affiliation or community attachment.
- Asian. A person having origins in any of the original peoples of the Far East, Southeast Asia, or Indian subcontinent, including, for example, Cambodia, China, India, Japan, Korea, Malaysia, Pakistan, the Philippine Islands, Thailand, and Vietnam.
- Black or African American. A person having origins in any of the Black racial groups of Africa. Terms such as “Haitian” can be used in addition to “Black or African American.”
- Hispanic or Latino. A person of Cuban, Mexican, Puerto Rican, Central or South American, or other Spanish culture or origin, regardless of race. The term “Spanish origin” can be used in addition to “Hispanic or Latino.”
- Native Hawaiian/Pacific Islander (NHPI). A person having origins in any of the original peoples of Hawaii, Guam, Samoa, or other Pacific Islands.
- White. A person having origins in any of the original peoples of Europe, the Middle East, or North Africa.
- Largest disparities for a single data year, focusing on the most recent data year.
- Trends in quality of care (number of measures improving, not changing, and worsening) for the population group.
- Comparison with the reference group, focusing on the change in the gap between the two groups (gap is narrowing, widening, and not changing).
- Overview of Racial and Ethnic Disparities
Figure 1 displays the number of quality measures for which each racial or ethnic group experienced better, same, or worse quality care compared with White populations in the latest data year. Figure 2 shows the number of quality measures with disparities at baseline that were narrowing (improving), widening (worsening), or not changing. xix
Number and percentage of quality measures for which members of selected groups experienced better, same, or worse quality of care compared with White people for the most recent data year, 2015, 2017, 2018, or 2019. Key: n = number of measures; AI/AN = (more...)
- Black populations received worse care than White populations for 43% of quality measures ( Figure 1 ).
- AI/AN populations received worse care than White populations for 40% of quality measures.
- Hispanic populations received worse care than non-Hispanic White populations for 36% of quality measures.
- Asian and NHPI populations received worse care than White populations for about 30% of quality measures but Asian populations also received better care for about 30% of quality measures.
Number and percentage of quality measures with disparity at baseline for which disparities related to race and ethnicity were improving, not changing, or worsening over time, 2000 through 2015, 2016, 2017, 2018, or 2019. Key: n = number of measures; AI/AN (more...)
- For all racial and ethnic groups, at least 90% of measures showed no change in disparities ( Figure 2 ).
- Three measures showed improvement in disparities between AI/AN populations and White populations.
- Black populations and NHPI populations each had two measures that showed improvement in disparities.
- Two measures showed improvement between Hispanic populations and non-Hispanic White populations.
- One measure for Asian populations showed improvement in disparities: People age 13 and over living with HIV who know their HIV status.
- One measure for Asian populations showed worsening disparities: Home health care patients whose management of oral medications improved.
- One measure for Black populations showed worsening disparities: Emergency department visits for asthma, ages 2–19.
- No worsening disparities were observed for AI/AN, Hispanic, or NHPI populations.
- Fewer quality measures are available for select subpopulations overall.
- Disparities for American Indian and Alaska Native Populations
This section presents disparities in quality of care and, new in 2021, access to care for American Indian and Alaska Native (AI/AN) populations. To provide context, findings for other ethnic and racial populations may be included. Additional details on disparities of care for other priority populations are presented in population-specific sections of this report.
Snapshot of Disparities in Access to Care
Number and percentage of access measures for which members of selected racial groups experienced better, same, or worse access to care compared with White people, 2017–2019. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific (more...)
- AI/AN people had worse access to care than White people for 50% of access measures ( Figure 3 ).
Disparities in Quality of Care
American Indian and Alaska Native people experienced worse quality care compared with White people for 40% of all quality measures and 63% of Person-Centered Care measures.
Number and percentage of quality measures for which American Indian and Alaska Native people experienced better, same, or worse quality of care compared with White people for the most recent data year, 2015, 2017, 2018, or 2019. Key: n = number of measures. (more...)
- Data for the most recent year show that quality care was worse for AI/AN people than for White people for 40% of all quality measures and that quality was better for AI/AN people than for White people for 18% of all quality measures ( Figure 4 ).
- Hospital patients who received influenza vaccination.
- Patients with colon cancer who received surgical resection of colon cancer that included at least 12 lymph nodes pathologically examined.
- New HIV cases per 100,000 population age 13 and over.
Influenza Vaccination
Overall, adjusting for age, Black people had the highest flu-associated hospitalization rates across 10 flu seasons, followed by AI/AN and Hispanic people, with similar trends for intensive care admission rates. Among AI/AN children, rates were 3 to 3.5 times higher for all three severe flu-related outcomes. 9
Current clinical guidelines show that people who are 6 months or older should receive an annual flu vaccine, but not all patients can access vaccines or treatment if they become ill. CDC details preventive strategies ( https://www.cdc.gov/flu/prevent/index.html ) to protect against the flu. Moreover, current research shows that influenza vaccination even provides effective flu protection in patients with chronic obstructive pulmonary disease (COPD). 10
Hospital patients who received influenza vaccination, 2018. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander. Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable (more...)
- In 2018, 81.6% of AI/AN hospital patients received influenza vaccinations compared with 92.7% of White patients ( Figure 5 ).
- The 2016 achievable benchmark was 96.6%.
- The top 10% of states that contributed to the achievable benchmark were Florida, Indiana, Maine, Utah, and Virginia.
Patients With Colon Cancer
Healthy People 2020 objectives include reducing the colorectal cancer incidence rate to 40 per 100,000 people and the mortality rate to 14.5 per 100,000 people. 11 Healthy People 2020 also includes an objective for colorectal cancer screening. The USPSTF expanded the recommended ages for colorectal cancer screening to 45 to 75 years (previously, it was 50 to 75 years). The USPSTF continues to recommend selectively screening adults ages 76 to 85 years for colorectal cancer. 12
The American Cancer Society’s newest guidelines recommend that colorectal cancer screenings begin at age 45. The recommended age was lowered from 50 to 45 because colorectal cancer cases are on the rise among young and middle-age people. 13
Patients with colon cancer who received surgical resection of colon cancer that included at least 12 lymph nodes pathologically examined, 2017. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander. Note: The benchmark (more...)
- In 2017, the percentage of patients with colon cancer who received surgical resection of colon cancer that included examination of at least 12 lymph nodes was lower for AI/AN people (83.7%) compared with White people (93%) ( Figure 6 ).
- The 2015 achievable benchmark was 95.5%.
- The top 10% of states that contributed to the achievable benchmark were District of Columbia, Maine, Massachusetts, Rhode Island, and Vermont.
New HIV Infections
Recent CDC data show new HIV infections fell 8% from 2015 to 2019, after a period of general stability in new infections in the United States. 14 AI/AN people represent about 1.3% of the U.S. population and less than 1% (186) of the HIV diagnoses in 2018 in the United States and dependent areas. 15
It is important for everyone to know their HIV status. People who do not know they have HIV cannot take advantage of HIV care and treatment and may unknowingly pass HIV to others.
The United States has 574 federally recognized AI/AN tribes and many different languages. Meaningful engagement with tribal nations is critically important in creating culturally appropriate prevention programs to reduce HIV transmission.
Poverty, including limited access to high-quality housing, directly and indirectly increases the risk of HIV infection and affects the health of people who have and are at risk for HIV infection. Additional structural factors that influence risks of HIV infection in tribal communities are high rates of poverty, lower levels of education, unemployment, and lack of health insurance.
New HIV cases per 100,000 population age 13 and over, 2019. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander. Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable (more...)
- In 2019, the percentage of new HIV cases was higher for AI/AN people (10.5%) compared with White people (5.3%) ( Figure 7 ).
- The 2015 achievable benchmark was 4.2 per 100,000 population.
- The top 10% of states that contributed to the achievable benchmark were Idaho, Iowa, Maine, West Virginia, and Wisconsin.
- Barriers to Care.
- Sensitivity of the Provider.
- Assessment.
- Encounters.
Trends in Quality of Care for American Indian and Alaska Native Populations
Number and percentage of all quality measures that were improving, not changing, or worsening over time, total and by priority area, from 2000 to 2010, 2011, 2012, 2013, 2014, 2015, 2016, 2017, 2018, or 2019. Key: n = number of measures. Note: For each (more...)
- Among the 116 quality measures with data for AI/AN people, 53 (46%) were improving, 55 (47%) were not changing, and 8 (7%) were getting worse from 2000 through 2019 ( Figure 8 ).
- Effective Treatment (52%) and Healthy Living (55%) showed the most improvement.
Changes in Disparities for American Indian and Alaska Native Populations
Number and percentage of quality measures with disparity at baseline for which disparities between AI/AN people and White people were improving, not changing, or worsening over time, total and by priority area, from 2000 to 2010, 2011, 2012, 2013, 2014, (more...)
- Disparities between AI/AN people and White people did not change for most of the quality measures from 2000 through 2019. Of 40 quality measures with a disparity at baseline, 37 (93%) were not changing ( Figure 9 ).
- Adjusted incident rates of end stage renal disease (ESRD) due to diabetes per million population.
- Children ages 2–17 for whom a health provider gave advice within the past 2 years about the amount and kind of exercise, sports, or physically active hobbies they should have.
- Children ages 2–17 for whom a health provider gave advice within the past 2 years about healthy eating.
- No Affordable Care measures with data for AI/AN people were available.
End Stage Renal Disease Due to Diabetes
Diabetes is the leading cause of kidney disease in the United States. According to the National Institute of Diabetes and Digestive and Kidney Diseases, White people experience diabetes and kidney disease at a lower rate than other racial and ethnic groups. 16 , 17
Adjusted incident rates of end stage renal disease due to diabetes per million population, 2001–2018 (lower rates are better). Key: AI/AN = American Indian or Alaska Native.
- From 2001 to 2018, the disparity between AI/AN people and White people decreased for the adjusted incident rate of ESRD due to diabetes. For AI/AN people, the rate decreased from 526 per million population to 273.1 per million, and for White people, there were no statistically significant changes (from 133.3 per million to 152.2 per million) ( Figure 10 ).
- Disparities have been persistent, with AI/AN people having higher incident rates of ESRD due to diabetes than White people in all years.
- Disparities for Asian Populations
This section presents disparities in quality of care and, new in 2021, access to care for Asian populations. To provide context, findings for other ethnic and racial populations may be included. Additional details on disparities of care for other priority populations are presented in population-specific sections of this report.
Number and percentage of access measures for which members of selected racial groups experienced better, same, or worse access to care compared with White people, 2017–2019. Key: AI/AN = American Indian or Alaska Native; NHPI = Native Hawaiian/Pacific (more...)
- Asian people had worse access to care than White people for 29% of access measures and better access to care for 14% of access measures ( Figure 11 ).
Snapshot of Disparities in Quality of Care
For the most recent year, Asian people experienced worse quality care than White people for 28% of all quality measures.
Number and percentage of quality measures for which Asian people experienced better, same, or worse quality of care compared with White people for the most recent data year, 2015, 2017, 2018, or 2019. Key: n = number of measures. Note: The difference (more...)
- Data for the most recent year show that quality care was better for Asian people than for White people on 29% of all quality measures, the same for 43%, and worse for 28% ( Figure 12 ).
Largest Disparities
- Adults with limited English proficiency and usual source of care (USC) whose USC had language assistance.
- Adults who reported that home health care providers always treated them with courtesy and respect in the last 2 months of care.
- Adults who reported that home health care providers always treated them as gently as possible in the last 2 months of care.
Providers With Language Assistance
Current research shows that Asian people continue to experience health disparities in several quality areas, including patient-centered care and satisfaction. 18 Adults who have limited English proficiency may experience disparities in their care and gaps in communication with their healthcare team. 19
According to the Migration Policy Institute, in 2015, an estimated 25.9 million individuals living in the United States reported having limited English proficiency. 20 “More than one in four people aged 5 and over with LEP are born in the U.S.” 21 Language assistance such as access to translation services, health education materials written in a known language, and other resources are required by law, but not all patients have access to these services at their usual source of care. 22
Adults with limited English proficiency and a usual source of care (USC) whose USC had language assistance, 2018.
- In 2018, Asian people with limited English proficiency and a usual source of care were less likely than White people to have a USC with language assistance (68.5% compared with 94.0%) ( Figure 13 ).
The Limited English Proficiency website 23 offers a repository of resources collated by the Department of Justice to support improved communication with patients. AHRQ has also established a Limited English Proficiency module as part of its TeamSTEPPS ® training that shows the importance of language assistance services in keeping patients safe and avoiding adverse events. 24
Treatment by Home Health Care Providers
Home health care providers are committed to delivering high-quality and compassionate care and services to patients in a respectful manner that supports each patient’s dignity. Home health performance is examined through several types of quality measures that look at areas such as efficiency, patient safety, and patient-centered care. Evaluation of patient experience of care is conducted with the Consumer Assessment of Healthcare Providers and Systems Home Health Care Survey. 25
Adults who reported that home health care providers always treated them with courtesy and respect in the last 2 months of care, 2019. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander. Note: The benchmark calculation (more...)
- In 2019, the percentage of adults who reported that home health providers always treated them with courtesy and respect in the last 2 months was lower for Asian people (85.5%) compared with White people (94.4%) ( Figure 14 ).
- The 2015 achievable benchmark was 95.0%.
- The top 10% of states that contributed to the achievable benchmark were Alabama, Louisiana, Mississippi, Rhode Island, South Carolina, and West Virginia. Guam was not included in the benchmark but its percentage was in the benchmark range.
Adults who reported that home health care providers always treated them as gently as possible in the last 2 months of care, 2019. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander. Note: The benchmark calculation takes (more...)
- In 2019, 80.6% of Asian adults reported that home health providers always treated them as gently as possible compared with 91.1% of White adults ( Figure 15 ).
- The 2015 achievable benchmark was 92.5%.
- The top 10% of states that contributed to the achievable benchmark were Alabama, Kentucky, Louisiana, Mississippi, and West Virginia.
Trends in Quality of Care for Asian People
Number and percentage of all quality measures that were improving, not changing, or worsening over time, total and by priority area, from 2000 to 2019. Key: n = number of measures. Note: For each measure with at least four data points over time, the estimates (more...)
- Across the 120 measures of healthcare quality tracked in the report for Asian populations, 58% were improving, 38% were not changing, and 4% were getting worse from 2000 to 2019 ( Figure 16 ). xx
- Affordable Care (no measures) and Effective Treatment (41% of measures) showed the least improvement.
- Healthy Living (66%) and Person-Centered Care (62%) showed the most improvement.
Changes in Disparities for Asian People
Number and percentage of quality measures with disparity at baseline for which disparities between Asian people and White people were improving, not changing, or worsening over time, total and by priority area, from 2000 to 2019. Key: n = number of measures. (more...)
- From 2000 through 2019, disparities in quality of care between Asian people and White people remained the same for most measures. Of 41 quality measures with a disparity at baseline, disparities were not changing for 39 (95%) ( Figure 17 ).
- One measure showed narrowing disparities: People age 13 and over living with HIV who know their HIV status.
- One measure showed a widening disparity: Home health patients whose management of oral medications improved.
- No Affordable Care measures with data for Asian people were available.
Knowledge of HIV Status
HIV and other related stigmas hinder patients from getting tested, which may delay treatment and affect a patient’s health and quality of life. 26 According to CDC, people ages 13–24 are less likely to know their HIV status. 27 Accurate estimates of new HIV infection rates are crucial for preventing the spread of the disease.
People age 13 and over living with HIV who know their HIV status, 2010–2019. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander. Note: The benchmark calculation takes the average of the top 10% of states with (more...)
- Data from 2010 to 2019 show that the disparity between Asian people and White people is narrowing as the percentage of Asian people (68.1% to 86.6%) who know their HIV status increased at a faster rate compared with White people (85.8% to 89.2%) ( Figure 18 ).
- The 2015 achievable benchmark was 90.2%. At the current rate of increase, overall, the benchmark could be achieved in 2 years.
- The top 10% of states that contributed to the achievable benchmark were Connecticut, District of Columbia, Massachusetts, New Hampshire, and New York. Puerto Rico was not included in the benchmark but its percentage was in the benchmark range.
Oral Medication Management
The ability to perform daily activities, such as taking medications correctly, is important to the health status and quality of life of people living in the community. Taking too much or too little can keep the drugs from working properly and may cause unintended harm, including death. The home health team can help teach patients ways to organize medications and to take them properly. If patients get better at taking medications correctly, it means the home health team is doing a good job teaching patients how to take their drugs and about the possible harm if they do not follow these instructions.
Specific items that should be discussed include all the prescriptions and other medications the patient takes, allergic or other adverse reactions to drugs experienced in the past, and actions to take if a medication is not working. This measure shows how often the home health team helped patients get better at taking their medications correctly (including prescription medications, over-the-counter medications, vitamins, and herbal supplements). Only medications the patient takes by mouth are considered.
Home health care patients whose management of oral medications improved, 2013–2018. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander.
- From 2013 to 2018, the percentage of home health care patients whose management of oral medications improved increased for both Asian and White populations. The percentage for White people, however, improved faster than for Asian people, so the disparity between the groups increased ( Figure 19 ).
- The 2015 achievable benchmark was 66.2%. At the current rate of increase, the benchmark could be achieved by Asian people in 2 years; White people have already achieved the benchmark.
- The top 10% of states that contributed to the achievable benchmark were Delaware, Mississippi, New Jersey, North Dakota, and South Carolina.
- Disparities for Black Populations
This section presents disparities in quality of care and, new in 2021, access to care for Black populations. To provide context, findings for other ethnic and racial populations may be included. Additional details on disparities of care for other priority populations are presented in population-specific sections of this report.
- Black people had worse access to care than White people for 53% of access measures ( Figure 20 ).
In 2019, Black people were more than 8 times as likely as White people to have new HIV cases.
Number and percentage of quality measures for which Black people experienced better, same, or worse quality of care compared with White people for the most recent data year, 2015, 2017, 2018, or 2019. Key: n = number of measures. Note: The difference (more...)
- Data for the most recent year show that quality of care was better for Black people than for White people on only 11% of all quality measures and that quality was better for White people than for Black people on 43% of all quality measures ( Figure 21 ).
- For Patient Safety, quality was better for Black people than for White people for 17% of the measures and better for White people than for Black people for 38% of the measures.
- HIV infection deaths per 100,000 population.
- Hospital admissions for hypertension per 100,000 population, adults age 18 and over.
New HIV Cases
According to CDC research, in 2018, Black people accounted for 13% of the nation’s population but represented 42% of all new HIV cases. Most of these cases affect Black male adolescents and adults. 28 The Office of Minority Health reports that in 2019, African Americans were 8.1 times more likely to be diagnosed with HIV infection compared with the White population. 29
New HIV cases per 100,000 population age 13 and over, 2019 (lower rates are better). Note: Black and White are non-Hispanic. Hispanic includes all races. The benchmark calculation takes the average of the top 10% of states with statistically reliable (more...)
- In 2019, Black people reported 45.3 new HIV cases per 100,000 population for people age 13 and over compared with 5.3 per 100,000 cases for White people ( Figure 22 ).
The Department of Health and Human Services has committed to “reducing new infections by 75 percent in the next five years and by 90 percent in the next ten years.” 30 The Department’s website www.hiv.gov also outlines key resources for patients, provides data, and details programs supporting a federal response to the epidemic in the United States.
Deaths From HIV Infection
HIV mortality disproportionately affects some racial and ethnic groups more than others. According to CDC data, in 2019, HIV was the sixth leading cause of death for Black men ages 25–34 and seventh for Black women ages 35–44. 31
HIV infection deaths per 100,000 population, 2018 (lower rates are better). Key: AI/AN = American Indian or Alaska Native. Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable data. U.S. territories are (more...)
- In 2018, Black people had 6.2 HIV infection deaths per 100,000 population compared with 0.9 per 100,000 cases for White people ( Figure 23 ). These cases represent mortality for which HIV was the primary cause of death.
- The 2015 achievable benchmark was 0.8 per 100,000 population.
- The top 10% of states that contributed to the achievable benchmark were Kansas, Kentucky, Minnesota, Missouri, Ohio, and Washington.
Federal efforts to reduce mortality include promotion of treatment therapies, such as antiretroviral therapy, pre-exposure prophylaxis, and postexposure prophylaxis. 32 Several HHS agencies provide a federal response to the HIV epidemic in the United States, including the Health Resources and Services Administration (HRSA) HIV/AIDS Bureau, which administers the Ryan White HIV/AIDS Program (RWHAP). This is the largest federal program focused exclusively on providing HIV care and treatment to patients with inadequate or no insurance. Through RWHAP’s partnerships, nearly 568,000 people receive care annually. 33
Federal efforts to prevent HIV infections include the High-Impact Prevention (HIP) program. HIP is a public health approach to disease prevention in which cost-effective, proven, and scalable interventions are targeted to specific populations based on disease burden. It provides a strategy for using data to maximize the impact of available resources and interventions. The primary goals of HIP are to prevent the largest number of new infections, save life-years, and reduce disparities among populations. In this approach to disease prevention, resources are aligned with disease burden in geographic areas and within populations. 34
Hospital Admissions for Hypertension
Hypertension affects nearly half of all U.S. adults and is responsible for substantial burden of morbidity, mortality, and financial costs on the healthcare system. 35 The cumulative incidence of hypertension by age 55 years was substantially higher for Black men and women compared with White men and women. Based on the 2017 American College of Cardiology/American Heart Association blood pressure guideline definition, 36 75.5% of Black men and 75.7% of Black women developed hypertension compared with 54.5% of White men and 40.0% of White women by age 55 years. 37
Hospital admissions for hypertension per 100,000 population, adults age 18 and over, 2018 (lower rates are better). Key: API = Asian/Pacific Islander. Note: API, Black, and White are non-Hispanic. Hispanic includes all races.
- In 2018, the rate of hospital admissions for hypertension was 212.9 per 100,000 population for Black adults compared with 38.4 per 100,000 cases for White adults ( Figure 24 ).
CDC’s current effort to reduce prevalence and improve control is Hypertension Control Champions. The Million Hearts ® Hypertension Control Champions are clinicians, practices, and health systems that have successfully completed the Million Hearts ® Hypertension Control Challenge. The Challenge is an opportunity for clinicians, practices, and health systems to demonstrate excellence in hypertension control. Hypertension Control Champions must reach 80% control rates among their hypertensive patients.
Trends in Quality of Care for Black People
- Across the 152 measures of healthcare quality tracked in the report for Black people, 49% showed improvement, 45% remained unchanged, and 7% were getting worse from 2000 to 2019 ( Figure 25 ). xxi
- Healthy Living (60% of measures), Care Coordination (44% of measures), Effective Treatment (42% of measures), and Patient Safety (42% of measures) showed more improvement than other priority areas.
Changes in Disparities for Black People
Number and percentage of quality measures with disparity at baseline for which disparities between Black people and White people were improving, not changing, or worsening over time, total and by priority area, 2000–2019. Key: n = number of measures. (more...)
- From 2000 to 2019, disparities between Black people and White people were narrowing in only 3% of measures of quality of care experienced ( Figure 26 ).
- Disparities were not changing for 95% of measures, and disparities were widening for one measure: Emergency department visits for asthma per 10,000 population, ages 2–19.
According to the Office of Minority Health, African American adults are 60 percent more likely than non-Hispanic White adults to have been diagnosed with diabetes by a physician and 3.5 times more likely to be diagnosed with end stage renal disease (ESRD) compared with non-Hispanic White people. During 2018, there were 131,636 newly reported cases of ESRD and diabetes was listed as the primary cause for nearly half (62,012). 38
The U.S. Renal Data System of the National Institute of Diabetes and Digestive and Kidney Diseases tracks cases of ESRD in the ESRD Incident Count.
- Data from 2001 to 2018 show that the disparity between Black people and White people is narrowing, but Black people are still showing a higher rate of ESRD due to diabetes ( Figure 27 ).
- Disparities have been persistent, with Black people having a higher incident rate of ESRD due to diabetes than White people in all years.
New HIV cases per 100,000 population age 13 and over, 2008–2019 (lower rates are better). Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander. Note: All racial groups are non-Hispanic.
- Data from 2008 to 2019 show that the disparity between Black people and White people was narrowing, but Black people are still showing a much higher rate of new HIV cases (45.3 per 100,000 population in 2019) compared with White people (5.3 per 100,000 population in 2019) ( Figure 28 ).
- Disparities for Hispanic Populations
Hispanic groups experienced worse quality care than non-Hispanic White groups for about 40% of Healthy Living measures.
This section presents disparities in quality of care and, new in 2021, access to care for Hispanic populations. To provide context, findings for other ethnic and racial populations may be included. Additional details on disparities of care for other priority populations are presented in population-specific sections of this report.
Snapshot of Disparities in Access to Care for Hispanic Populations
Number and percentage of access measures for which members of selected racial and ethnic groups experienced better, same, or worse access to care compared with White people, 2017, 2018, or 2019. Key: n = number of measures.
- For the most recent year, Hispanic groups had worse access to care than non-Hispanic White groups for 79% of access measures ( Figure 29 ).
Health Insurance
Hispanic populations have the highest uninsured rates of any racial or ethnic group in the United States. Variation occurs among subgroups, with Cubans having the highest percentage and Central Americans the lowest percentage. 39 Disparities in insurance rates by income are also seen in the Hispanic population.
People under age 65 who were uninsured all year, 2018.
- In 2018, poor (20.8%), low-income (21.9%), and middle-income Hispanic people (15.6%) were more likely to be uninsured compared with high-income Hispanic people (7.3%) ( Figure 30 ).
Number and percentage of quality measures for which Hispanic groups experienced better, same, or worse quality of care compared with non-Hispanic White groups for the most recent data year, 2015, 2017, 2018, or 2019. Key: n = number of measures. Note: (more...)
- Data for the most recent year show that quality care was worse for Hispanic groups compared with non-Hispanic White groups for 36% of all quality measures. Quality was better for Hispanic groups than for non-Hispanic White groups on 20% of all quality measures ( Figure 31 ).
- Home health care patients who had influenza vaccination during flu season.
- People without a usual source of care who indicated a financial or insurance reason for not having a source of care.
Approximately 1.2 million people in the United States have HIV and about 13% of them do not know it and need testing. HIV continues to have a disproportionate impact on certain populations, particularly racial and ethnic minorities and gay, bisexual, and other men who have sex with men. New HIV infections declined from 2015 to 2019, after a period of general stability. 40
New HIV cases per 100,000 population age 13 and over, 2019 (lower rates are better). Key: AI/AN = American Indian or Alaska Native; NHPI = Native Hawaiian/Pacific Islander. Note: Racial groups are non-Hispanic. Hispanic includes all races. The benchmark (more...)
- In 2019, the rate of new HIV cases per 100,000 population age 13 and over was higher for Hispanic people (20.0 per 100,000 population) compared with non-Hispanic White people (5.3 per 100,000 population) ( Figure 32 ).
- The top 10% of states that contributed to the benchmark were Idaho, Iowa, Maine, West Virginia, and Wisconsin.
- Federal resources include the Let’s Stop HIV Together campaign (formerly known as Act Against AIDS ), which has resources and partnerships aimed at stopping HIV stigma and promoting HIV testing , prevention , and treatment . This campaign provides Hispanic and Latino people with culturally and linguistically appropriate messages about HIV testing, prevention, and treatment.
- Federal resources also include Ending the HIV Epidemic: A Plan for America , which aims to end the HIV epidemic in the United States by 2030. The plan leverages critical scientific advances in HIV prevention, diagnosis, treatment, and outbreak response by coordinating the highly successful programs, resources, and infrastructure of many HHS agencies and offices.
Influenza Vaccination Among Home Health Care Patients
Medicare defines home health care as a wide range of healthcare services that can be given in the home for an illness or injury. Patients can qualify for this service if they are under the care of a doctor who certifies that they need at least one service such as intermittent skilled nursing care, physical therapy, speech-language pathology, or continued occupational therapy services, and the patient must be home bound.
Home health care is usually less expensive, more convenient, and as effective as care in a hospital or skilled nursing facility. Home health care services include wound care for pressure sores or a surgical wound, patient and caregiver education, intravenous or nutrition therapy, and monitoring of serious illness and unstable health status.
Influenza vaccination is the primary method for preventing the illness and its severe complications, and annual vaccination is recommended for everyone age 6 months and over. 41 All healthcare contacts, including hospitalizations, provide excellent opportunities for vaccination, particularly for people at the highest risk for complications and death from influenza.
Home health care patients who had influenza vaccination during flu season, 2018. Notes: The benchmark calculation takes the average of the top 10% of states with statistically reliable data. U.S. territories are not included in the calculations. Some (more...)
- In 2018, Hispanic home health care patients (90.4%) were less likely than non-Hispanic White home health care patients (96.0%) to receive an influenza vaccine ( Figure 33 ).
- The 2015 achievable benchmark was 94.1%.
- The top 10% of states that contributed to the benchmark were Montana, Nebraska, North Dakota, South Dakota, Vermont, and Wisconsin.
Difficulty Accessing a Usual Source of Care
The AHRQ Medical Expenditure Panel Survey (MEPS) describes usual source of care as the particular medical professional, doctor’s office, clinic, health center, or other place where a person would usually go if sick or in need of advice about his or her health.
According to Healthy People 2020, patients with a usual source of care are more likely to receive recommended preventive services such as flu shots, blood pressure screenings, and cancer screenings. 42
People without a usual source of care who indicate a financial or insurance reason for not having a source of care, 2018 (lower rates are better).
- In 2018, the percentage of people without a usual source of care who indicate a financial or insurance reason for not having a source of care was higher for Hispanic people (26.3%) than for non-Hispanic White people (11.5%) ( Figure 34 ).
Changes in Quality of Care for Hispanic Populations
Number and percentage of all quality measures that were improving, not changing, or worsening over time, total for Hispanic groups and by priority area, from 2000 through 2015, 2017, 2018, or 2019. Key: n = number of measures. Note: For each measure with (more...)
- Of the 120 quality measures with data for Hispanic groups, 66% were improving, 30% were not changing, and 4% were getting worse from 2000 through 2019 ( Figure 35 ). xxii
- Quality was improving for Hispanic groups for about three-fourths of Healthy Living and Patient Safety measures.
- More than half of Effective Treatment measures improved and 10% of measures showed a worsening trend.
Over time, disparities have narrowed in end stage renal disease due to diabetes between Hispanic and non-Hispanic White people but Hispanic people still have a rate more than twice that of non-Hispanic White people.
Changes in Disparities for Hispanic Populations
Number and percentage of all quality measures with disparity at baseline for which disparities related to race and ethnicity were improving, not changing, or worsening over time, total and by priority area, from 2000 through 2015, 2017, 2018, or 2019. (more...)
- Of the 49 quality measures with a disparity at baseline, disparities between Hispanic and non-Hispanic White people did not change for 47 (96%) from 2000 through 2019 ( Figure 36 ).
- Two measures showed narrowing disparities—one Effective Treatment measure and one Healthy Living measure.
- Home health care patients whose shortness of breath decreased.
- No measure showed widening disparities between Hispanic and non-Hispanic White people.
- No Care Coordination measures with data for Hispanic groups were available.
End Stage Renal Disease
Diabetes is the leading cause of kidney disease in the United States. According to the National Institute of Diabetes and Digestive and Kidney Diseases, non-Hispanic White people experience diabetes and kidney disease at a lower rate than other racial and ethnic groups. 43
Adjusted incident rates of end stage renal disease due to diabetes per million population, 2001–2018 (lower rates are better).
- Data from 2001 to 2018 show that the disparity between Hispanic and non-Hispanic White people was narrowing ( Figure 37 ).
- Rates of ESRD due to diabetes decreased for Hispanic people, from 410.0 per million population to 292.7 per million population.
- Disparities have been persistent, with Hispanic populations having higher incident rates of ESRD due to diabetes than White people in all years.
Improved Breathing Among Home Health Care Patients
To assess the quality of care received by home health care patients, measures of wait time to see provider, timely initiation of care, ambulation, ability to get in and out of bed, bathing, toileting, dressing, pain, confusion, management of oral medications, influenza and pneumococcal vaccination, and shortness of breath are tracked.
Shortness of breath is uncomfortable. Many patients with heart or lung problems experience difficulty breathing and may tire easily or be unable to perform daily activities. Doctors and home health staff should monitor shortness of breath and may give advice, therapy, medication, or oxygen to help lessen this symptom.
Home health care patients whose shortness of breath decreased, 2013–2018.
- From 2013 to 2018, the disparity between Hispanic and non-Hispanic White people was narrowing for home health care patients whose shortness of breath decreased ( Figure 38 ).
- Both Hispanic people (53.7% to 74.5%) and non-Hispanic White people (66.7% to 80.9%) showed improvement over time.
- Disparities for Native Hawaiian/Pacific Islander Populations
Native Hawaiian/Pacific Islander populations experienced worse quality care compared with White populations for about 40%of Person-Centered Care measures.
New in 2021, this section presents disparities in access to care for Native Hawaiian and Pacific Islander (NHPI) populations. To provide context, findings for other ethnic and racial populations may be included. Additional details on disparities of care for other priority populations are presented in population-specific sections of this report.
Number and percentage of access measures for which NHPI groups experienced better, same, or worse access to care compared with White groups, 2017–2019. Key: AI/AN = American Indian or Alaska Native, NHPI = Native Hawaiian/Pacific Islander, n = (more...)
- NHPI data were only available for four measures and all four measures showed that NHPI groups had the same access to care as White groups ( Figure 39 ).
Number and percentage of quality measures for which Native Hawaiian/Pacific Islander groups experienced better, same, or worse quality of care compared with White groups for the most recent data year, 2017, 2018, or 2019. Key: n = number of measures. (more...)
- Data for the most recent year show that NHPI groups experienced worse quality care compared with White groups on 28% of all quality measures. Quality was better for NHPI groups than for White groups on 19% of all quality measures ( Figure 40 ).
- No Affordable Care measures with data for NHPI groups were available.
- Home health care patients who had timely initiation of care.
HIV can affect anyone regardless of sexual orientation, race, ethnicity, gender, age, or geographic location. However, in the United States, some racial/ethnic groups are more affected than others, given their percentage of the population. This disparity occurs because some population groups have higher rates of HIV in their communities, thus raising the risk of new infections with each sexual or injection drug use encounter.
In addition, a range of social, economic, and demographic factors such as stigma, discrimination, income, education, and geographic region can affect people’s risk for HIV. In 2018, 42% of new HIV diagnoses were among Black people and 29% were among Hispanic people. 44
While NHPI individuals represent 0.4% of the total population in the United States, their HIV case rate was more than twice that of the White population in 2019.
New HIV cases per 100,000 population age 13 and over, 2019. Key: NHPI = Native Hawaiian or Pacific Islander Note: All racial groups are non-Hispanic. Hispanic includes all races. The benchmark calculation takes the average of the top 10% of states with (more...)
- In 2019, the percentage of new HIV cases per 100,000 population age 13 and over was more than twice as high for NHPI groups (13.9 per 100,000 population) as for White groups (5.3 per 100,000 population) ( Figure 41 ).
Treatment by Home Health Providers
The goal of home health care is to treat an illness or injury; help patients recover, regain independence, become as self-sufficient as possible, and maintain current condition or level of function; and slow decline. 45
Adults who reported that home health care providers always treated them with courtesy and respect in the last 2 months of care, 2019. Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable data. U.S. territories (more...)
- In 2019, the percentage of adults who reported that home health care providers always treated them with courtesy and respect in the last 2 months was lower for NHPI people (90.7%) compared with White people (94.4%) ( Figure 42 ).
- The 2015 achievable benchmark was 95%.
- The top 10% of states that contributed to the benchmark were Alabama, Louisiana, Mississippi, Rhode Island, South Carolina, and West Virginia. Guam was not included in the benchmark but its percentage was in the benchmark range.
Initiation of Home Health Care
Timely initiation of home health care is associated with lower risks of 30-day rehospitalization. Therefore, CMS requires that home health care services be initiated within 2 days of hospital discharge when ordered, except when the physician/provider authorizes a delay in the initiation of services due to an outpatient visit or the patient’s or family’s request. 46
Home health care patients who had timely initiation of care, 2018. Note: Initiation of care is defined by CMS as home health quality episodes in which the start or resumption of care date was on the physician-specified start or resumption of care date (more...)
- In 2018, NHPI home health patients were less likely than White patients to receive timely initiation of care (91% vs. 94.4%) ( Figure 43 ).
- The 2015 achievable benchmark was 95%. At the current rate of progress, NHPI people should reach the benchmark in 5 years (trend data not shown).
- The top 10% of states that contributed to the benchmark were Louisiana, Nebraska, North Dakota, South Dakota, and West Virginia.
Trends in Quality of Care for Native Hawaiian and Pacific Islander Populations
Nearly 45% of quality measures for NHPI groups showed improvement.
Number and percentage of all quality measures that were improving, not changing, or worsening over time, total and by priority area, from 2001 through 2017, 2018, or 2019. Key: n = number of measures. Note: For each measure with at least four data points (more...)
- Among the 68 quality measures with data for NHPI populations, 30 (44%) were improving, 34 (50%) were not changing, and 4 (6%) were getting worse from 2001 through 2019 ( Figure 44 ).
- No Affordable Care measures with data for NHPI populations were available.
Changes in Disparities for Native Hawaiian and Pacific Islander Populations
Number and percentage of all quality measures with disparity at baseline for which disparities related to race and ethnicity were improving, not changing, or worsening over time, total and by priority area, from 2008 through 2018 or 2019. Key: n = number (more...)
- Disparities between NHPI and White populations did not change for most of the quality measures from 2008 through 2019. Of the 20 quality measures with a disparity at baseline, disparities were not changing for 18 measures (90%) ( Figure 45 ).
- No measure showed widening disparities, and only two measures showed narrowing disparities: People age 13 and over living with HIV who know their HIV status and People age 13 and over living with diagnosed HIV who had at least two CD4 or viral load tests performed at least 3 months apart during the last year.
- No Affordable Care measures with data for NHPI people were available.
It is important for everyone to know his or her HIV status. Getting an HIV test is the first step for people living with HIV to get care and treatment and control the infection. Taking HIV medicine as prescribed helps people living with HIV to live a long, healthy life and protect their sex partners from HIV. About 85% of people with HIV in the United States know they have the virus. However, 15% (162,500) of people with HIV do not know they have the virus, and about 40% of new HIV infections come from them.
Half of people with HIV had the virus 3 years or more before diagnosis. Most people at high risk who did not get tested last year saw a healthcare provider during the year. Everyone should get tested at least once, and people at high risk should be tested at least once a year. Healthcare providers can diagnose HIV sooner if they test more people and test people at high risk more often. 47
People age 13 and over living with HIV who had knowledge of their HIV status, 2010–2019. Note: Data are statistically unreliable for NHPI groups in 2015. The benchmark calculation takes the average of the top 10% of states with statistically reliable (more...)
- Data from 2010 to 2019 show that the disparity between NHPI people and White people was narrowing due to a larger increase in the percentage of NHPI people (69.8% to 83.6%) than White people (85.8% to 89.2%) who are living with HIV and had knowledge of their HIV status ( Figure 46 ).
- The 2015 achievable benchmark was 90.2%.
- The top 10% of states that contributed to the benchmark were Connecticut, District of Columbia, Massachusetts, New Hampshire, and New York.
Viral Load Monitoring
Viral load is the amount of HIV in the blood of a person who has HIV. Viral load is highest during the acute phase of HIV and when HIV is untreated. People with HIV who keep an undetectable viral load (or stay virally suppressed ) can live long, healthy lives. Having an undetectable viral load also helps prevent transmitting the virus to others through sex or sharing needles, syringes, or other injection equipment, and from mother to child during pregnancy, birth, and breastfeeding. Higher viral load increases the risk of transmitting HIV. 48
People age 13 and over living with diagnosed HIV who had at least two CD4 or viral load tests performed at least 3 months apart during the last year, 2014–2018. Note: The benchmark calculation takes the average of the top 10% of states with statistically (more...)
- Data from 2014 to 2018 show that the disparity between NHPI and White populations was narrowing due to a larger increase in the percentage of NHPI people (50.2% to 55.7%) than White people (58.5% to 58.9%) living with diagnosed HIV who had at least two CD4 or viral load tests performed at least 3 months apart during the last year ( Figure 47 ).
- The 2015 achievable benchmark was 66.2%.
- The top 10% of states that contributed to the benchmark were Connecticut, Iowa, Montana, and Oregon.
An example of a Department of Health and Human Services initiative to end the HIV epidemic is the Minority HIV/AIDS Fund (MHAF). This initiative has the goal of transforming HIV prevention, care, and treatment for communities of color by bringing federal, state, and community organizations together to design and test innovative solutions that address critical emerging needs; and by working to improve the efficiency, effectiveness, and impact of federal investments in HIV programs and services for racial and ethnic minorities.
MHAF supports Ending the HIV Epidemic: A Plan for America , a federal initiative designed to reduce the number of new HIV infections in the United States by 75% over 5 years and 90% by 2030.
- Innovation: The Fund designs and tests innovative programs and strategies to improve the efficiency, effectiveness, and impact of HIV programs in racial and ethnic minority communities.
- Systems Change: Successes generated by the Fund are integrated into existing efforts, creating lasting changes across the federal HIV prevention, care, and treatment portfolio.
- Strategic Partnerships and Collaboration: The Fund breaks down program silos and develops new ways for federal, state, and local agencies to work together in the community to improve outcomes for racial and ethnic minorities.
More information can be found at: https://www.hiv.gov/federal-response/smaif/smaif-in-action .
- Disparities by Income
New in 2021, this section presents disparities in access to care by income groups. Additional details on disparities of care for other priority populations are presented in population-specific sections of this report.
Number and percentage of access measures for which members of selected income groups experienced better, same, or worse access to care compared with the high-income group, 2017, 2018, or 2019. Key: n = number of measures.
- People in poor households had worse access to care than people in high-income households for 79% of access measures ( Figure 48 ).
- People in low-income households had worse access to care than people in high-income households for 71% of access measures.
- People in middle-income households had worse access to care than people in high-income households for 50% of access measures.
Number and percentage of access measures for which people in poor households experienced better, same, or worse access to care compared with people in high-income households, by sub-area, 2017, 2018, or 2019. Key: n = number of measures.
- For the most recent year, people in poor households had worse access to care than people in high-income households for 79% of access measures ( Figure 49 ).
- People in poor households had worse access to care than people in high-income households for 100% of health insurance, source of ongoing care, and timely access to care measures.
- People in poor households had worse access to care than people in high-income households for a quarter of patient perception of need measures.
The measure with the largest disparities across all access to care subsections for people in poor households was people under age 65 with any private health insurance.
People under age 65 with any private health insurance, by income and ethnicity, 2019.
- In 2019, among people under age 65, people in poor, low-income, and middle-income families were less likely than people in high-income families to have private health insurance ( Figure 50 ).
- In 2019, among people under age 65, Hispanic people of all income groups were less likely than non-Hispanic White people to have private health insurance.
The relationship between income and healthcare outcomes has been studied for many years, and researchers have shown the positive relationship between more income and better health outcomes. 49 , 50 , 51 , 52 Income is not the same as wealth, which can include assets other than income. Wealth is disproportionately dispersed among higher income categories, and research also shows a positive association between greater wealth and better health outcomes.
- Poor: Less than 100% of FPL.
- Low income: 100% to less than 200% of FPL.
- Middle income: 200% to less than 400% of FPL.
- High income: 400% or more of FPL
The poverty guidelines are issued annually in the Federal Register by the Department of Health and Human Services, Assistant Secretary for Planning and Evaluation. The guidelines vary by family size and there are different family income criteria for the contiguous 48 states, Alaska, and Hawaii. Criteria for U.S. territories are unavailable. 53 For HCUP measures, income is based on median income of the patient’s ZIP Code and is divided into quartiles.
This section shows quality measures with the largest income disparities and trends in disparities.
Quality of care for high-income groups was better than for poor and low-income groups for more than half of all measures.
Number and percentage of quality measures for which income groups experienced better, same, or worse quality of care compared with the high-income group for the most recent data year, 2017, 2018, or 2019. Key: n = number of measures. Note: The most recent (more...)
- Data for the most recent year show that high-income groups experienced better quality care than other income groups on 53% of all measures ( Figure 51 ).
- Poor and low-income groups experienced worse quality care compared with high-income groups on about 57% of the measures. Compared with high-income groups, middle-income groups experienced worse quality care on 44% of the measures.
The measure with the largest income disparities is “children ages 5–17 with untreated dental caries.”
- Children ages 5–17 with untreated dental caries (all income groups).
- People without a usual source of care who indicated a financial or insurance reason for not having a source of care (all income groups).
- People under age 65 whose family’s health insurance premium and out-of-pocket medical expenditures were more than 10% of total family income (middle income)
- Children ages 19–35 months who received 1 or more doses of measles-mumps- rubella vaccine (low income)
- Hospital admissions for short-term complications of diabetes per 100,000 population, adults (first quartile: lowest income).
Pediatric Dental Caries
Dental caries is one of the most common chronic diseases of childhood in the United States. Untreated caries can cause pain and infections that may lead to problems with eating, speaking, playing, and learning. Children who have poor oral health often miss more school and receive lower grades than children who do not . 54
Children ages 5–17 with untreated dental caries, 2015–2018 (lower rates are better). Note: Poor refers to household incomes below the federal poverty level (FPL); low, the FPL to just below 200% of the FPL; middle, 200% to just below 400% (more...)
- In 2015–2018, the measure with the largest income disparities among all income groups was children ages 5–17 with untreated dental caries ( Figure 52 ).
- In 2015–2018, the percentage of children ages 5–17 with untreated dental caries was higher for poor, low-income, and middle-income children compared with high-income children (19.4%, 16.9%, and 12.1%, respectively, vs. 4.5%).
People with lower incomes may experience difficulty accessing affordable care and are less likely to have a usual source of care that is readily accessible. 51 People who are unwell and have low incomes are also more likely to experience poverty. 51
In 2018, the measure with the second largest income disparities among all income groups was people without a usual source of care who indicated a financial or insurance reason for not having a source of care.
People without a usual source of care who indicated a financial or insurance reason for not having a source of care, 2018 (lower rates are better).
- In 2018, the percentage of people without a usual source of care who indicated a financial or insurance reason for not having a source of care was higher for poor, low-income, and middle-income people compared with high-income people (23.6%, 25.9%, and 16.1%, respectively, vs. 7.2%) ( Figure 53 ).
High Family Medical Expenditures
The most prominent barriers to healthcare coverage include affordability, eligibility for public coverage in a person’s state, immigration status, and lack of familiarity with signup procedures. 55 Poor health may require a family to spend more on healthcare, resulting in less income. Costs will vary based on each person or family’s needs and may inhibit a family’s ability to reach other goals. 51
In 2018, the measure with the third largest income disparities among middle-income people was people under age 65 whose family’s health insurance premium and out-of-pocket medical expenditures were more than 10% of total family income
People under age 65 whose family’s health insurance premium and out-of-pocket medical expenditures were more than 10% of total family income, 2018 (lower rates are better).
- In 2018, the percentage of people under age 65 whose family’s health insurance premium and out-of-pocket medical expenditures were more than 10% of total family income was higher for middle-income people compared with high-income people (21.9% vs. 10.7%) ( Figure 54 ).
Childhood Vaccinations
Childhood vaccinations are an important part of preventing disease. Consistently high childhood immunization rates have greatly reduced the rates of death, disability, and illness from communicable diseases such as chicken pox, diphtheria, measles, meningococcal meningitis, mumps, polio, rubella, tetanus, and whooping cough.
In the decade before the measles vaccine became available, an average of 549,000 measles cases and 495 measles deaths were reported annually in the United States. Of the reported cases, approximately 48,000 people were hospitalized from measles and each year, 1,000 people developed chronic disability from acute encephalitis caused by measles. 56
Mumps complications include orchitis, oophoritis, mastitis, meningitis, encephalitis, pancreatitis, and hearing loss. 57
Before the rubella vaccine became available, one noted outbreak infected 12.5 million people, 11,000 pregnant women lost their babies, 2,100 newborns died, and 20,000 babies were born with congenital rubella syndrome . 58
Children ages 19–35 months who received 1 or more doses of measles-mumps-rubella vaccine, 2018. Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable data. U.S. territories are not included in the (more...)
- In 2018, the percentage of children ages 19–35 months who received 1 or more doses of measles-mumps-rubella vaccine was lower for children from poor (90.3%) and low-income (90.3%) families compared with children from high-income families (95.8%) ( Figure 55 ).
- The 2015 achievable benchmark was 96.4%.
- The top 5 states that contributed to the achievable benchmark were Connecticut, Delaware, Iowa, Maine, Nebraska, and Vermont.
Hospital Admissions for Diabetes Complications
More than 100 million people living in the United States have diabetes or are at risk for diabetes. 59 Compared with some other countries, the rate of hospital admissions for short-term complications of diabetes, which include ketoacidosis, hyperosmolarity, and coma, is higher in the United States. 60 Such complications may be related to kidney disease, hypertension, vision problems, pain, or other issues.
Hospital admissions for short-term complications of diabetes per 100,000 population, adults, 2018 (lower rates are better).
- In 2018, the rate of hospital admissions for short-term complications of diabetes was three times as high for adults in the lowest income group (145.3 per 100,000 population) compared with adults in the highest income group (45.0 per 100,000 population) ( Figure 56 ).
Trends in Quality of Care for Income Groups
Poor, low-income, and middle-income people had a higher percentage of improving measures compared with high-income people.
Number and percentage of all quality measures that were improving, not changing, or worsening over time, total and by income group, from 2000 through 2016, 2017, 2018, or 2019. Key: n = number of measures. Note: For each measure with at least four data (more...)
- The percentage of measures that showed improvement was 57% for poor people, low-income people, and middle-income people, and 49% for high-income people ( Figure 57 ).
Changes in Income Disparities
Most disparities by income showed no statistically significant changes over time.
Number and percentage of quality measures with disparity at baseline for which disparities related to income were improving, not changing, or worsening over time, 2000 through 2016, 2017, 2018, or 2019. Key: n = number of measures. Note: Different data (more...)
- Disparities by income were unchanged for about 95% of quality measures ( Figure 58 ).
- Only one measure showed narrowing disparities and five measures showed widening disparities.
- Adolescents ages 16–17 who received 1 or more doses of meningococcal conjugate vaccine (low income).
- Emergency department visits involving opioid-related diagnoses per 100,000 population (first and second quartiles: lowest and second lowest income).
- Hospital inpatient stays involving opioid-related diagnoses per 100,000 population (first, second, and third quartiles: lowest, second lowest, and second highest income).
Adolescent Vaccination
Meningococcal disease refers to any illness caused by bacteria called Neisseria meningitidis , also known as meningococcus. These illnesses are often severe and can be deadly. They include infections of the lining of the brain and spinal cord (meningitis) and bloodstream infections (bacteremia or septicemia). 61
- Meningococcal conjugate or MenACWY vaccines, which help protect against four types of the bacteria that cause meningococcal disease (serogroups A, C, W, and Y).
- Serogroup B meningococcal or MenB vaccines, which help protect against serogroup B meningococcal disease.
According to CDC, all children ages 11 to 12 years old should get a meningococcal conjugate vaccine, with a booster dose at 16 years old. 62
Adolescents ages 16–17 who received 1 or more doses of meningococcal conjugate vaccine, 2008–2018. Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable data. U.S. territories are not included (more...)
- In 2008, 31.9% of low-income adolescents ages 16–17 received 1 or more doses of meningococcal conjugate vaccine, and by 2018, the percentage had increased to 86.4% ( Figure 59 ).
- From 2008 to 2018, the percentage of high-income adolescents ages 16–17 who received 1 or more doses of meningococcal conjugate vaccine increased from 46.8% to 89.8%.
- Data from 2008 to 2018 show that disparities between adolescents in high-income households and in poor households were narrowing over time and both populations were improving.
- The 2015 achievable benchmark was 96.2%. At the current rate of increase, the benchmark could be achieved in 2 years for all income groups.
- The top 5 states that contributed to the achievable benchmark were Indiana, Michigan, New Jersey, Pennsylvania, and Rhode Island.
Emergency Department Visits Involving Opioids
The U.S. opioid overdose epidemic continues to evolve. In 2016, 66.4% of the 63,632 drug overdose deaths involved an opioid. In 2017, among 70,237 drug overdose deaths, 47,600 (67.8%) involved opioids, with increases across age groups, racial and ethnic groups, county urbanization levels, and multiple states. From 2013 to 2017, synthetic opioids contributed to increases in drug overdose death rates in several states. From 2016 to 2017, synthetic opioid-involved overdose death rates increased 45.2%. 63
Emergency department visits related to opioid use per 100,000 population, 2005–2018. Key: 1 st Quartile = <$48000, 2 nd Quartile = $48,000–$60,999, 3 rd Quartile = $61,000–$81,999, and 4 th Quartile = >$82,000. Note: (more...)
- In 2005, the rate of emergency department visits involving opioid-related diagnoses among people in the lowest income group was 104.9 per 100,000 population, and by 2018, the rate had increased to 348.1 per 100,000 population ( Figure 60 ).
- In 2005, the rate of emergency department visits involving opioid-related diagnoses among people in the second lowest income group was 90.2 per 100,000 population, and by 2018, the rate had increased to 231 per 100,000 population.
- In 2005, the rate of emergency department visits involving opioid-related diagnoses among people in the third income group was 83.2 per 100,000 population, and by 2018, the rate had increased to 195.7 per 100,000 population.
- In 2005, the rate of emergency department visits involving opioid-related diagnoses among people in the highest income group was 65.5 per 100,000 population, and by 2018, the rate had increased to 146.8 per 100,000 population.
- Data from 2005 to 2018 show that disparities between high-income and poor and low-income people were widening over time and both populations were worsening.
- The 2015 achievable benchmark was 65.2 per 100,000. No income group showed progress toward the benchmark.
- The top 10% of states contributing to the achievable benchmark were Iowa, Kansas, Nebraska, and South Dakota.
Hospital Stays Involving Opioids
Increased availability and overuse of opioid medications have contributed to adverse outcomes for patients, including increased risk of opioid use disorder, misuse of medication, and overdoses. 64 The National Survey on Drug Use and Health shows that in 2020, nearly 9.5 million people age 12 and over misused opioids in the past year. 65 This treatment measure examines inpatient stays associated with opioid-related diagnoses.
Hospital inpatient stays involving opioid-related diagnoses per 100,000 population, 2005–2018. Key: 1 st Quartile = <$48000, 2 nd Quartile = $48,000–$60,999, 3 rd Quartile = $61,000–$81,999, and 4 th Quartile = >$82,000. (more...)
- In 2005, the rate of hospital inpatient stays involving opioid-related diagnoses among people in the lowest income group was 179.6 per 100,000 population, and by 2018, the rate had increased to 382.1 per 100,000 population ( Figure 61 ).
- In 2005, the rate of hospital inpatient stays involving opioid-related diagnoses among people in the second lowest income group was 125.5 per 100,000 population, and by 2018, the rate had increased to 288.7 per 100,000 population.
- In 2005, the rate of hospital inpatient stays involving opioid-related diagnoses among people in the second highest income group was 117.2 per 100,000 population, and by 2018, the rate had increased to 252.1 per 100,000 population.
- In 2005, the rate of hospital inpatient stays involving opioid-related diagnoses among people in the highest income group was 98.1 per 100,000 population, and by 2018, the rate had increased to 191.6 per 100,000 population.
- Data from 2005 to 2018 show that disparities between people in the highest quartile and people in the other three quartiles were widening over time and all populations were worsening.
- The 2015 achievable benchmark was 102.9 per 100,000. There is no evidence of progress toward the benchmark.
- The top 10% of states that contributed to the achievable benchmark were Georgia, Iowa, Nebraska, Texas, and Wyoming.
- Disparities by Insurance Status
- Increased financial security,
- Access to primary care,
- Adherence to prescription medications,
- Screening for treatable health conditions (such as diabetes, cholesterol, HIV, and breast, prostate, and colon cancer),
- Improved perceptions of health,
- Reduced depression symptoms, and
- Earlier detection of cancer. 66 , 67
This section examines disparities and trends by insurance status among people ages 0–64 years. It focuses on people less than age 65 years because more than 98% of Americans 65 years and over have Medicare. 68 Thus, almost no older adults lack insurance coverage since almost all are covered, at minimum, by public insurance (Medicare).
- Private Insurance : Person has access to insurance from a private insurer.
- Public Insurance : Person receives insurance from one or more government-sponsored sources, including Medicaid, State Children’s Health Insurance Program (S-CHIP), state-sponsored or other government-sponsored health plans, Medicare, and military and veteran health plans.
- Uninsured : Person does not have any health insurance.
It should be noted that the Indian Health Service (IHS) is not considered a health plan for this report. IHS is a healthcare system, which offers comprehensive healthcare services to AI/AN individuals. Currently, IHS serves 2.7 million AI/AN people who belong to 574 federally recognized tribes in 37 states. Non-IHS data sources, including CDC’s National Center for Health Statistics, also track disparities for AI/AN populations and are the source of data for health disparities for this population.
The bar chart ( Figure 62 ) summarizes comparisons between people with private health insurance (the reference group) and people with public health insurance or no insurance for 69 quality of care measures for which data by insurance status are available.
Quality of care for uninsured people was better than quality for those with private insurance on only 7% of measures.
Number and percentage of quality measures for which insurance groups experienced better, same, or worse quality of care compared with reference group (privately insured), 2016, 2017, or 2018. Key: n = number of measures. Note: The difference between two (more...)
- Compared with those with private insurance, people with public insurance experienced better quality care for 10% of measures. Uninsured people experienced better quality care for 7% of measures ( Figure 62 ).
- People under age 65 whose family’s health insurance premium and out-of-pocket medical expenditures were more than 10% of total family income.
- Deaths per 1,000 adult hospital admissions with heart failure.
- Deaths per 1,000 adult hospital admissions with pneumonia.
- Compared with people with private insurance, people with public insurance had worse quality care for 39% of measures, and uninsured people had worse quality care for 61% of measures.
The measures with the largest disparities between people with public health insurance and people with private insurance reflect differences in access to care and in quality of care experienced by patients. The measures with the largest disparities between people with no insurance and those with private insurance reflect differences in access to primary care providers and the routine healthcare services they deliver.
Largest Disparities for People With Public Insurance
Among different public insurance programs, Medicaid and S-CHIP alone cover approximately one-fourth of Americans, 69 of whom nearly two-thirds are seniors, children, or disabled people. 70 While outcomes are often worse for people with public insurance, some of the differences in health outcomes may be explained by factors other than public insurance. For example, injuries, disabilities, and preexisting illnesses that can contribute to negative health outcomes are also reasons many people qualify for public health insurance. 71 Thus, on average, people with public insurance begin with worse baseline health than people with no insurance or those with private insurance. Public insurance serves as a safety net for people with limited options after experiencing disabling injury or illness.
- Women under age 70 treated for breast cancer with breast-conserving surgery who received radiation therapy to the breast within 1 year of diagnosis.
- Adults who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never showed respect for what they had to say.
Having a usual primary care provider is associated with higher likelihood of receiving appropriate care, including preventive care services. Patients with a usual source of care also report better provider-patient communication and increased trust in the provider, both of which are linked to treatment adherence and better health. 72
- In 2018, the percentage of people without a usual source of care who indicated a financial or insurance reason for not having a source of care was more than twice as high for adults with public insurance (17.9%) compared with adults with private insurance (8.7%) ( Figure 63 ).
- In 2018, the percentage of people without a usual source of care who indicated a financial or insurance reason for not having a source of care was more than 5 times as high for uninsured adults (43.8%) compared with adults with private insurance (8.7%).
Receiving Appropriate Treatment After Lumpectomy for Breast Cancer
When women with early stage breast cancer undergo breast-conserving surgery (also called lumpectomy), combining surgical treatment with radiation therapy improves outcomes. 73 Observational studies have reported that adding radiation therapy reduces the risk of recurrence by half and reduces the risk of death from breast cancer by a sixth. 74
Women under age 70 treated for breast cancer with breast-conserving surgery who received radiation therapy to the breast within 1 year of diagnosis, 2017.
- In 2017, the percentage of women who underwent breast-conserving surgery for breast cancer and received radiation therapy within 1 year of surgery was significantly lower for women with public insurance (83.2%) than for women with private insurance (91.3%) ( Figure 64 ).
- The percentage of women who underwent breast-conserving surgery for breast cancer and received radiation therapy within 1 year of surgery was also lower for women with no insurance (88.7%) than for women with private insurance (91.3%).
Providers Who Showed Respect for What Patients Had to Say
Patient-centered care encompasses qualities of compassion, empathy, and responsiveness to the needs, values, and preferences of individuals. It is linked to greater patient participation in their care, lower risk of misdiagnosis due to poor communication, and better patient outcomes. 75 , 76
Adults who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never showed respect for what they had to say, 2017 (lower rates are better).
- In 2017, the percentage of adults who had a doctor’s office or clinic visit in the last 12 months who reported their health providers sometimes or never showed respect for what they had to say was nearly twice as high for people with public insurance (12.2%) compared with people with private insurance (6.4%) ( Figure 65 ).
- The percentage of adults who had a doctor’s office or clinic visit in the last 12 months who reported their health providers sometimes or never showed respect for what they had to say was also higher for people without health insurance (13.3%) than for people with private insurance (6.4%).
Largest Disparities for Uninsured People
- People without a usual source of care who indicated a financial or insurance reason for not having a source of care ( Figure 63 ).
- Children ages 0–17 with a wellness checkup in the past 12 months.
- Adults who received a blood pressure measurement in the last 2 years.
Wellness Visits for Children
Wellness visits are important opportunities to assess the physical, emotional, and social development of children and adolescents, screen for health risks, and influence health behaviors, such as eating habits and physical activity, which often extend into adulthood. 78 Having health insurance facilitates access to providers for recommended well-child visits.
Children ages 0–17 with wellness checkup in the past 12 months, by insurance status, 2019.
- In 2019, children with no insurance (74.1%) were less likely to receive a wellness visit in the preceding 12 months than children with either public (95.2%) or private (94.6%) insurance ( Figure 66 ).
Blood Pressure Screening
Hypertension, also called high blood pressure , affects about one-third of U.S. adults. It can damage the heart, blood vessels, kidneys, and other parts of the body over time, but it is often asymptomatic until complications, such as stroke, heart attack, heart failure, and chronic kidney disease, develop. If hypertension is identified early, providers can offer patients a range of treatment that lowers the risk for complications. 79
Adults without hypertension who had their blood pressure measured in the last 2 years, 2019.
- In 2019, uninsured adults (75.6%) were less likely to receive screening for high blood pressure in the last 2 years than adults covered by public (94.4%) or private (94.1%) insurance ( Figure 67 ).
Changes in Quality of Care by Insurance Status
More than half of quality measures for those with private and public insurance were improving but only one-third of quality measures for uninsured people showed improvement.
Number and percentage of all quality measures that were improving, not changing, or worsening, total and by insurance status, from 2000 through 2015, 2017, 2018, or 2019. Key: n = number of measures. Note: For each measure with at least four data points (more...)
- From 2000 through 2019, for people with private insurance, 54% of measures were improving, 43% of measures were not changing, and 3% of measures were worsening ( Figure 68 ).
- For people with public insurance, 57% of measures were improving, 37% of measures were not changing, and 6% of measures were worsening.
- For people with no insurance, 32% of measures were improving, 62% of measures were not changing, and 6% of measures were worsening.
- Adults who had a doctor’s office or clinic visit in the last 12 months whose health providers always asked them to describe how they will follow the instructions.
- Infants born in the calendar year who received breastfeeding exclusively through 3 months.
- Children who had their height and weight measured by a health provider within the past 2 years.
- Children 41–80 lb for whom a health provider gave advice within the past 2 years about using a booster seat when riding in the car.
- People with a usual source of care who usually asks about prescription medications and treatments from other doctors.
- Adults ages 18 and over who received influenza vaccination in the last flu season.
- Children ages 6 months to 17 years who received influenza vaccination in the last flu season.
- Children ages 2–17 who had a dental visit in the calendar year.
- Children ages 2–17 who received a preventive dental service in the calendar year.
- Adults age 40 and over with diagnosed diabetes who received a flu vaccination in the calendar year.
Changes in Disparities by Insurance
Although many measures of healthcare quality improved over time, disparities between groups by health insurance status changed for only one measure ( Figure 69 ).
Number and percentage of quality measures with disparity at baseline for which disparities related to insurance were improving, not changing, or worsening, 2000 through 2017, 2018, or 2019. Key: n = number of measures.
- Disparities by insurance status for most quality measures did not change ( Figure 69 ).
- Only one measure showed improvement over time in disparities between uninsured people and people with private insurance: Adults age 40 and over with diagnosed diabetes who received a flu vaccination in the calendar year.
Receipt of Flu Vaccine by Patients With Diabetes
The disparity reduction for this measure reflects stagnant outcomes for patients with private insurance while outcomes for uninsured patients showed improvement.
Adults age 40 and over with diagnosed diabetes who received a flu vaccination in the calendar year, 2008–2018. Note: Data for uninsured people did not meet criteria for statistical reliability in 2017 and 2018.
- The percentage of uninsured adults age 40 and over with diabetes who received a flu vaccine increased from 36.7% in 2008 to 49.7% in 2016.
- The percentage of adults with diabetes and public or private insurance who received a flu vaccine showed no statistically significant changes ( Figure 70 ).
CDC has prepared several patient and provider resources, including a web page on flu and diabetes .
- Disparities by Residence Location
Where people live affects their access to healthcare and the quality of services they receive. Research shows that healthcare disparities by residence location exist for both adults and children. 81 , 82 , 83 , 84 , 85 , 86 Socioeconomic differences may contribute to the disparities: residents of inner-city and rural communities are more likely to live in poverty, more likely to engage in unhealthy behaviors (e.g., smoking), and less likely to have health insurance than people who live in suburbs. 87
Differences in population density may also contribute to disparities that are specific to each location. Inner-city residents may live in crowded or inadequate housing that exposes them to higher levels of environmental pollutants, contagious vectors, mental distress, and violence compared with people who live in suburban and rural communities. 88 By contrast, reduced economies of scale, longer travel times to access goods and services, and decreased opportunities for social contact in rural communities may limit the availability of healthcare services and increase risk for diseases related to social isolation. 89 , 90
This section examines disparities in quality of care by residence location.
Residence Location Groups
The analyses in this section use the 2013 National Center for Health Statistics (NCHS) classification, 91 which are the most recent categories used by NCHS.
- That contain the entire population of the largest principal city of the MSA, or
- Whose entire population is contained within the largest principal city of the MSA, or
- That contain at least 250,000 residents of any principal city in the MSA.
- Large Fringe Metropolitan: Counties in MSAs of 1 million or more population that do not qualify as large central areas. xxiii Large Fringe Metropolitan areas are also described as suburban areas. Examples of Large Fringe Metro areas are San Bernardino County, California; Broward County, Florida; and Bergen County, New Jersey.
- Medium Metropolitan: Counties in MSAs of 250,000 to 999,999 population. Examples of Medium Metro areas are Scott County, Kentucky; York County, Maine; and Douglas County, Nebraska.
- Small Metropolitan: Counties in MSAs of less than 250,000 population. Examples of Small Metro areas are Baldwin County, Alabama; Wayne County, North Carolina; and Allen County, Ohio.
- Micropolitan: Nonmetropolitan counties in a “micropolitan statistical area,” which are defined as counties that are less densely populated than MSAs and centered around smaller urban clusters with 2,500–49,999 inhabitants. Examples of Micropolitan areas are Woodward County, Oklahoma; Cherokee County, South Carolina; and Harrison County, West Virginia.
- Noncore: Nonmetropolitan counties that are outside of a micropolitan statistical area. Noncore counties are also described as rural. Examples of Noncore areas are Wallowa County, Oregon; Bedford County, Pennsylvania; and Crane County, Texas.
When examining trends, it is important to recognize that the key differences between the 2013 NCHS Urban-Rural Classification scheme and the earlier 2006 version are in how it describes small metropolitan, micropolitan, and noncore areas. The 2013 classification broadens the inclusion criteria for each of these residence locations. All other definitions are unchanged ( Table 1 ). 92
NCHS Urban-Rural Classification Scheme, 2006 vs. 2013.
Figure 71 shows a map of U.S. county classifications according to the 2013 NCHS Urban-Rural Classification system.
Map showing 2013 NCHS Urban-Rural County Classifications in the United States.
The NHQDR uses the NCHS classification to analyze performance of quality measures that have data available by residence location. Data on state-based performance metrics are also available through the NHQDR State View. 93
With the State View tool, users can explore the quality of their state’s healthcare and compare their state’s data with national data or data from the best performing states. Users can access a state dashboard showing performance compared with benchmarks for more than 80 measures. Some of these measures are also stratified by subpopulations to show disparities.
Overview of Disparities by Residence Location
In the most recent data year, 34% of measures had better performance in large fringe metro areas than in other locations while only 4% of measures showed worse performance ( Figure 72 ). Relative to large fringe metro counties, nonmetropolitan (i.e., micropolitan and noncore) areas had the largest number of measures that showed worse quality care, followed by small metro and large central metro areas. Large central metro and noncore areas had the largest number of measures that showed better quality care.
Nonmetropolitan areas had the largest number of measures showing worse quality care compared with large fringe metropolitan areas, followed by small metropolitan and large central metropolitan areas.
Number and percentage of quality measures for which residents of selected locations experienced better, same, or worse quality of care compared with large fringe metropolitan areas, 2017, 2018, or 2019. Key: n = number of measures. Note: Definitions of (more...)
- Nonmetropolitan (micropolitan and noncore) areas showed worse quality care than large fringe metro areas on 45% and 37% of measures, respectively, and better quality care on 3% and 7% of measures for which data are available by location of residence ( Figure 72 ).
- Large central metro areas showed worse quality care than large fringe metro areas on 22% of measures and better quality care for 5% of measures.
Examining the specific measures where nonmetropolitan areas and large central metro areas experienced better or worse care relative to large fringe metro areas highlights issues where these locations share similar concerns and where they differ. Large central metro, micropolitan, and noncore areas overlapped on six quality of care measures, where all three experienced worse quality than large fringe metro areas. However, they did not overlap in any of the measures for which they experienced better quality of care. Instead, measures where a residence location at one end of the urban-rural spectrum experienced better quality care were frequently the same measure where the residence location at the other end of the spectrum experienced worse quality care.
- Adults who had a doctor’s office or clinic visit in the last 12 months whose health providers sometimes or never listened carefully to them.
- Children over 80 lb for whom a health provider gave advice within the past 2 years about using lap or shoulder belts when riding in a car.
- Hospital admissions for short-term complications of diabetes per 100,000 population, adults.
- Hospital admissions for lower extremity amputations per 1,000 population, adults age 18 and over with diabetes.
- Reclosure of postoperative abdominal wound dehiscence per 1,000 abdominopelvic-surgery admissions of length 2 or more days, adults.
- Emergency department visits with a principal diagnosis related to substance use disorder only, per 100,000 population.
- Hospital admissions for asthma per 100,000 population, adults ages 18–39.
- Hospital admissions for asthma per 100,000 population, children ages 2–17.
- Hospital admissions for community-acquired pneumonia per 100,000 population, adults age 18 and over.
- Lung cancer deaths per 100,000 population per year.
- Suicide deaths among people age 12 and over per 100,000 population.
The three measures with the largest disparities between large fringe metro areas and other locations vary. The differences may reflect differing healthcare needs for each location. In the most recent available data years, the three measures with the largest disparities relative to large fringe metro areas follow for each location.
- HIV infection deaths per 100,000 population
- Hospital admissions for asthma per 100,000 population, children ages 2–17
- Emergency department visits with a principal diagnosis related to substance use disorder only, per 100,000 population
- Hospital admissions for short-term complications of diabetes per 100,000 population, children ages 6–17
- Adults who received a blood cholesterol measurement in the last 5 years
- Infant mortality per 1,000 live births, birth weight 2,500 grams or more
- Children ages 3–5 who ever had their vision checked by a health provider
- Hospitalizations and emergency department encounters for heart failure
- Emergency department visits with a principal diagnosis related to dental conditions
- Hospital admissions for community-acquired pneumonia per 100,000 population, adults age 18 and over
- Deaths per 1,000 hospital admissions with expected low mortality
The following figures these measures in detail.
New HIV diagnoses and HIV prevalence are concentrated primarily in large U.S. metropolitan areas, with Atlanta, Baton Rouge, Miami, New Orleans, and Orlando leading the list of areas with the highest rate of new diagnoses. Atlanta, Baton Rouge, Miami, New Orleans, and New York lead the list of areas with the highest rates of people living with HIV. 94
HIV infection deaths per 100,000 population, 2018 (lower rates are better). Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable data. U.S. territories are not included in the calculations. Some benchmarks (more...)
- In 2018, the death rate from HIV infections was higher in large central metro areas (2.3 per 100,000 population) compared with the rate in large fringe metro areas (1.1 per 100,000 population) ( Figure 73 ).
- The 2015 achievable benchmark was 0.75 per 100,000 population. At the current rate of increase, overall, the benchmark could be achieved in 4 years for large central metro areas and in 2 years for large fringe metro areas (trend data not shown).
An HHS initiative to eliminate new HIV infections is underway. The goal is “to reduce new HIV infections in the United States by 75 percent in five years and by 90 percent by 2030.” 95 Federal efforts to reduce HIV-related mortality include the promotion of treatment therapies such as antiretroviral therapy, as well as pre-exposure prophylaxis and postexposure prophylaxis. 96
Several HHS agencies provide a federal response to the HIV epidemic, including HRSA’s HIV/AIDS Bureau, which administers the Ryan White HIV/AIDS Program (RWHAP). RWHAP is the largest federal program focused exclusively on providing HIV care and treatment to patients with inadequate or no insurance. Through RWHAP’s partnerships, more than 512,000 people receive care annually.
Hospital Admissions for Asthma
Asthma is the most common chronic lung condition among children under 17 years in the United States. 97 Children with asthma may experience debilitating exacerbations triggered by environmental exposures, such as fumes, airborne viruses, and cold air, but appropriate treatment in ambulatory care settings can reduce patients’ risk for exacerbations. 98 , 99
Research has linked access to primary care, continuity of care by a provider, and adherence to preventive care plans to improved quality of care and fewer hospital admissions for chronic conditions such as asthma. 100
Hospital admissions for asthma per 100,000 population, children ages 2–17, 2018 (lower rates are better).
- In 2018, the rate of hospital admissions for children ages 2–17 with asthma was more than 60% higher in large central metro areas (116.3 per 100,000 population) than in large fringe metro areas (71.3 per 100,000 population) ( Figure 74 ).
Emergency Department Visits for Substance Use
Illicit drug use and subsequent overdose deaths have risen in both metropolitan and nonmetropolitan areas over the past two decades. Overdose death rates in rural areas exceeded rates in urban areas between 2007 and 2015, 101 overlapping with the second wave of opioid overdose deaths. 102 However, more recent data show that overdose death rates in the third wave of opioid overdose deaths are highest in urban communities. 103
Emergency department visits with a principal diagnosis related to substance use disorder only per 100,000 population, 2018 (lower rates are better).
- In 2018, the rate of adult emergency department visits with a principal diagnosis related to substance use disorder was 42% higher in large central metro areas (642.8 per 100,000 population) than in large fringe metro areas (452.7 per 100,000 population) ( Figure 75 ).
Hospital Admissions for Short-Term Complications of Diabetes
Type 1 diabetes is one of the most common chronic diseases in childhood. It is caused by insulin deficiency, resulting from an autoimmune reaction that destroys insulin-producing beta-cells in the pancreas. In children and adolescents, the most common complications of diabetes are short-term problems that result from blood sugars going too low or too high: hypoglycemia, ketoacidosis, and diabetic coma. 104 Access to healthcare providers who can prescribe medications and teach patients how to self-manage their health can reduce risks for short-term complications and prevent emergency visits and hospitalizations. 105
Hospital admissions for short-term complications of diabetes per 100,000 population, children 6–17, 2018 (lower rates are better).
- In 2018, the rate of hospitalizations among children ages6–17 years due to short-term complications of diabetes mellitus was 36% higher in medium metro areas (32.1 per 100,000 population) than in large fringe metro areas (23.6 per 100,000 population) ( Figure 76 ).
Cholesterol Check
Medications and lifestyle modifications that lower cholesterol reduce the risk of heart attacks and strokes in people who may have underlying atherosclerosis (i.e., cardiovascular disease). 106 Intermittent laboratory testing for cholesterol by a healthcare provider can identify atherosclerosis in otherwise healthy people and help them make informed treatment decisions to lower their risk of heart attacks and strokes. Thus, access to screening for cholesterol is an important component of efforts to improve cardiovascular health. 107
Adults who received a blood cholesterol measurement in the last 5 years, 2019.
- In 2019, the percentage of adults who received a blood cholesterol measurement in the last 5 years was lower in micropolitan (83.5%) and medium metropolitan areas (88.1%) than in large fringe metro areas (91.0%) ( Figure 77 ).
Infant Mortality
Infant mortality is the death of infants before their first birthday. It is a key health indicator that reflects baseline maternal and infant health, as well as healthcare services delivered before, during, and immediately after an infant’s birth. In 2018, the five leading causes of infant death were birth defects, preterm birth and low birth weight, injuries (e.g., suffocation), sudden infant death syndrome, and maternal pregnancy complications. 108
Infant mortality per 1,000 live births, birth weight 2,500 grams or more, 2017 (lower rates are better).
- In 2017, the percentage of infant deaths among live births weighing 2,500 grams or more was significantly higher in medium metro (2.2%), small metro (2.4%), micropolitan (2.6%), and noncore (2.9%) areas than in large fringe metro areas (1.7%) ( Figure 78 ).
Pediatric Vision Exams
Pediatric vision screenings are efficient eye examinations that primary care providers, trained laypeople (e.g., in schools), and eye care specialists perform to detect issues that warrant a more comprehensive eye examination by a specialist. They are crucial for identifying conditions that could lead to blindness, life-threatening illness, and problems with school performance if left untreated. 109
Research shows that periodic vision screening in early childhood reduces the risk of vision loss at age 7 years by more than 50%. 110 Thus, access to vision screening throughout childhood is important to ensure children’s health.
Children ages 3–5 who ever had their vision checked by a health provider, 2018. Note: Data for noncore areas are not shown because the data were statistically unreliable.
- In 2018, the percentage of children ages 3–5 years who had their vision checked by a health provider was lower in micropolitan (58.9%) and small metropolitan areas (62.0%) than in large fringe metro areas (77.3%) ( Figure 79 ).
Hospital and Emergency Visits for Heart Failure
Heart failure is an important cause of morbidity and mortality in the United States, accounting for 379,800 deaths in 2018. 111 , 112 It is also the most common and expensive reason for preventable hospitalizations, with more than 1 million admissions and $11.2 billion in total costs in 2017. Access to appropriate treatment in ambulatory care settings can help patients safely avoid emergency visits and hospital admissions for this condition. 113
Hospitalizations and emergency department encounters for heart failure per 100,000 population, 2018 (lower rates are better).
- In 2018, the rate of emergency department visits and hospitalizations per 100,000 population for heart failure was significantly higher in micropolitan (663.6 visits) and noncore (713.3 visits) areas than in large fringe metro areas (434.9 visits) ( Figure 80 ).
Emergency Department Visits for Dental Conditions
Oral health is a vital component of a person’s overall health and well-being. Untreated oral disease can affect appetite, leading to nutritional problems; cause chronic pain, interfering with sleep and work; and has been associated with diabetes, heart and lung disease, stroke, and poor birth outcomes. 114
Preventive dental care, including early detection, treatment, and management of problems, promotes good oral health. When people lack access to a usual source of dental care, they often will seek relief in emergency departments, which are equipped to meet only emergency dental care needs. 115
Emergency department visits with a principal diagnosis related to dental conditions per 100,000 population, 2018 (lower rates are better).
- In 2018, the rate of ED visits related to dental conditions in micropolitan and noncore areas combined (459.7 per 100,000 population) was more than twice the rate in large fringe metro areas (210.3 per 100,000 population) ( Figure 81 ).
Hospital Admissions for Pneumonia
Community-acquired pneumonia (CAP) is an acute lung infection acquired outside of a hospital setting. A person with CAP may present with symptoms that range from mild fever and productive cough to severe infection and inability to breathe without mechanical ventilation. 116
CAP results in substantial morbidity, mortality, and costs in the United States. As the fourth leading reason for hospitalizations in 2018, it accounted for 740,700 admissions and $7.7 billion in healthcare costs. 117 In 2019, it was the underlying cause of death in 43,881 individuals (13.4 deaths per 100,000 population). 118
CAP hospitalizations are often avoidable. Administering pneumococcal vaccines to high-risk groups can prevent infections, and early evaluation and treatment by a healthcare provider can prevent hospitalizations.
Hospital admissions for community-acquired pneumonia per 100,000 population, adults age 18 and over, 2018 (lower rates are better).
- In 2018, the rate of hospital admissions for CAP was nearly twice as high in noncore areas (330.2 per 100,000 population) as in large fringe metro areas (171.2 per 100,000 population) ( Figure 82 ).
Unexpected Deaths After Hospital Admission
Death during a hospital admission may indicate that patients received unsafe or inappropriate care, particularly if a patient dies while being treated for problems with low mortality risk.
Deaths per 1,000 hospital admissions with expected low mortality, 2018 (lower rates are better).
- In 2018, the death rate for conditions with expected low mortality was nearly twice as high in noncore areas (0.81 per 1,000 admission) as in large fringe metro areas (0.45 per 1,000 admission) ( Figure 83 ).
Changes in Quality of Care by Residence Location
The bar chart in Figure 84 summarizes trends in 45 quality of care measures for which data are available by geographic location.
Among the six geographic locations, noncore areas had the fewest improving trends and the most worsening trends.
Number and percentage of all quality measures that were improving, not changing, or worsening, total and by residence location, from 2002 through 2010, 2011, 2013, 2016, 2017, 2018, or 2019. Key: n = number of measures. Note: For each measure with at (more...)
- Noncore areas had the fewest measures with improving trends (33%) and the most measures with worsening trends (14%) ( Figure 84 ).
- Among the remaining geographic locations, large central metro and large fringe metro areas had the most measures with improving trends (51% and 50%, respectively). Large central metro and micropolitan areas had the fewest measures with worsening trends (7%).
Changes in Disparities by Residence Location
The bar chart in Figure 85 summarizes trends in disparities between large fringe metro areas and other locations for 13 measures for which data are available by geographic location. Overall, disparities between large fringe metropolitan counties and other areas did not change during the most recent data year available. The only measure that showed narrowing disparities was “hospital inpatient stays involving opioid-related diagnoses,” which resulted from worsening opioid-related hospitalization rates in large fringe metro areas, instead of improving trends in other locations.
The only disparity that improved was due to a worsening trend for large fringe metropolitan counties instead of improvement in other locations.
In the 2019 NHQDR, two other measures had similarly shown narrowing disparities due to worsening trends in large fringe metro areas: “people unable to get or delayed in getting needed medical care due to financial or insurance reasons” and “people unable to get or delayed in getting needed prescription medicines due to financial or insurance reasons.” These measures are not reported this year due to lack of data availability.
Number and percentage of quality measures with disparity at baseline for which disparities related to residence location were improving or not changing, 2002 through 2015, 2016, 2017, or 2018. Key: n = number of measures. Note: A total of 13 measures (more...)
- Disparities by residence location remained unchanged for most quality measures ( Figure 85 ).
Inpatient Stays Due to Opioid Use
The opioid epidemic constitutes a continuing public health emergency 119 that affects the entire United States. The 2020 National Survey on Drug Use and Health estimates that nearly 9.5 million people misused opioids in the past year, 65 and data from the Centers for Disease Control and Prevention (CDC) indicate that rates of nonfatal and fatal overdose continue to rise in multiple states and territories.
CDC estimates that 49,860 of 70,630 drug overdose deaths (70.6%) involved opioids in 2019, affecting multiple age groups, racial and ethnic groups, and geographic regions. 120 Rising rates of hospital admissions for opioid-related diagnoses echo this trend. They also indicate that narrowing disparities between geographic locations represent worsening trends in large fringe metro areas instead of improving trends in large central metro areas.
Hospital inpatient stays involving opioid-related diagnoses per 100,000 population, 2005–2018 (lower rates are better). Note: The benchmark calculation takes the average of the top 10% of states with statistically reliable data. U.S. territories (more...)
- From 2005 to 2018, the gap in opioid-related hospitalization rates in large central metro areas and in large central fringe metro areas narrowed ( Figure 86 ). However, the reduced disparity was due to rates of opioid-related hospitalizations rising faster in large fringe metro areas. This undesirable trend began to plateau in 2016 but remains well above the 2015 achievable benchmark of 102.9 hospitalizations per 100,000 population. (For this measure, a low value is more desirable, so rates above the achievable benchmark indicate suboptimal quality of care.)
- In 2005, the rate was 111.5 per 100,000 population in large fringe metro areas vs. 195.8 per 100,000 population in large central metro areas. In 2017, rates in both geographic areas had risen to peak 288.4 admissions per 100,000 population in large fringe metro areas and 314.6 admissions per 100,000 population in large central metro areas.
- In 2018, the most recent year for which data are available, hospitalization rates for opioid-related disorders had plateaued at 268.7 per 100,000 population in large fringe metro areas and 307.3 per 100,000 population in large central metro areas, approximately 3 times as high as the achievable benchmark of 102.9 per 100,000 population.
- The top 10% of states that contributed to the achievable benchmark were Georgia, Iowa, Nebraska, Texas, and Wyoming. In 2016–2017, no state reached the benchmark.
In 2017, HHS launched a departmentwide initiative with a five-point strategy to combat the opioid epidemic. Many agencies supported this initiative by establishing specific research opportunities, resources, and data to support providers, patients, and researchers. More information is available at https://www.hhs.gov/opioids/ . Other federal resources are discussed in detail in the Quality of Care – Trends in Effective Treatment section of this report.
Due to a change in the Healthcare Cost and Utilization Project (HCUP) data, the same measures reported in past reports are not represented in this report. HCUP converted all measures from International Classification of Diseases, Ninth Revision (ICD-9) to Tenth Revision (ICD-10) codes in October 2015, thus changing the outcomes of these measures. Therefore, trend data are not directly comparable at this time.
Due to a change in the Healthcare Cost and Utilization Project (HCUP) data, the same measures reported in past reports are not represented in this report. HCUP converted all measures from International Classification of Diseases, Ninth Revision (ICD-9) to Tenth Revision (ICD-10) codes in October 2015, thus changing the outcomes of these measures. Therefore, trend data are not available at this time.
For comparisons across residence locations, large fringe MSAs (large city suburbs) are used as the reference group since these counties have the lowest levels of poverty and typically have the best healthcare quality and access to healthcare.
This document is in the public domain and may be used and reprinted without permission. Citation of the source is appreciated.
- Cite this Page 2021 National Healthcare Quality and Disparities Report [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2021 Dec. DISPARITIES IN HEALTHCARE.
- PDF version of this title (8.0M)
In this Page
Other titles in this collection.
- National Healthcare Quality & Disparities Reports
Recent Activity
- DISPARITIES IN HEALTHCARE - 2021 National Healthcare Quality and Disparities Rep... DISPARITIES IN HEALTHCARE - 2021 National Healthcare Quality and Disparities Report
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health
EDITORIAL — Volume 18 — August 12, 2021
Leonard Jack Jr, PhD, MSc 1 ( View author affiliations )
Suggested citation for this article: Jack L Jr. Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health. Prev Chronic Dis 2021;18:210264. DOI: http://dx.doi.org/10.5888/pcd18.210264 external icon .
Non-Peer Reviewed
Author Information
In June 2017, Preventing Chronic Disease (PCD) invited a panel of 7 nationally recognized experts in scientific publishing to respond to key questions about the journal’s mission, quality of scientific content, scope of operations, intended audience, and future direction (1). PCD and the panel of experts recognized that chronic disease is a major contributor to poor health outcomes, an increase in health care costs, and a reduction in quality of life. Reducing the burden of chronic disease is a challenge requiring diverse collaborations and dissemination and adoption of effective interventions in multiple settings. The expert panel strongly encouraged the journal to focus more on complementing its rich body of published work on epidemiological studies with content that is attentive to evaluating population-based interventions and policies.
Since its inception in 2004, PCD’s mission has been to promote dialogue among researchers, practitioners, and policy makers worldwide on the integration and application of research findings and practical experience to address health disparities, advance health equity, and improve population health. To better advance that mission, PCD used the panel’s recommendations to refine the journal’s focus, addressing 4 main areas of public health research, evaluation, and practice:
Behavioral, psychological, genetic, environmental, biological, and social factors that influence health
Development, implementation, and evaluation of population-based interventions to prevent chronic diseases and control their effect on quality of life, illness, and death
Interventions that reduce the disproportionate incidence of chronic diseases among at-risk populations
Development, implementation, and evaluation of public health law and health policy–driven interventions
Refining the focus on these 4 areas has allowed PCD to receive a wide range of content from authors around the world. In addition to manuscripts received through the journal’s regular submission process, PCD has issued calls for papers on topics that bring to the forefront timely public health issues and targeted public health responses to improve population health.
Advancing health equity and eliminating health disparities have been and continue to be critical factors to PCD in addressing these topic areas. Healthy People 2020 defines health equity as the attainment of the highest level of health for all people (2). According to Healthy People 2020, “Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities” (2). Healthy People 2020 defines health disparities as “a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage” (2).
As part of its mission to address these important issues, PCD is excited to release this collection, “Advancing Health Equity, Eliminating Health Disparities, and Improving Population Health.” Of the 17 articles in the collection, 10 were submitted in response to PCD’s call for papers for the collection and 7 were previously published in the journal. All articles underwent the journal’s rigorous peer-review process. In addition, this collection features a position statement on the journal’s commitment to advancing diversity, equity, and inclusion in its scientific leadership, peer review process, research focus, training, and continuing education (3).
Over the past decade, there has been a range of community-based, technically innovative, and clinically driven prevention strategies in public health to prevent and reduce the burden of chronic conditions among diverse populations worldwide. Articles in this collection describe innovative and successful work to address factors contributing to advancing health equity, eliminating health disparities, and improving population health. They provide the latest information on ways to better understand contextual factors responsible for influencing health outcomes (both negatively and positively) and effective approaches to improve population health among diverse populations in various settings. The 18 articles address these core themes from multiple perspectives:
PCD’s Commitment to Advancing Diversity, Equity, and Inclusion in Its Scientific Leadership, Peer Review Process, Research Focus, Training, and Continuing Education (3)
Engaging With Communities — Lessons (Re)Learned From COVID-19 (4)
Global Perspectives on Improving Chronic Disease Prevention and Management in Diverse Settings (5)
Reaching the Hispanic Community About COVID-19 Through Existing Chronic Disease Prevention Programs (6)
Community Engagement of African Americans in the Era of COVID-19: Considerations, Challenges, Implications, and Recommendations for Public Health (7)
Addressing Racial and Ethnic Disparities in COVID-19 Among School-Aged Children: Are We Doing Enough? (8)
A Framework for Mobilizing Health Care to Respond to the Community Within the COVID-19 Pandemic (9)
Addressing Emotional Wellness During the COVID-19 Pandemic: The Role of Promotores in Delivering Integrated Mental Health Care and Social Services (10)
COVID-19 and Chronic Disease: The Impact Now and in the Future (11)
Screening and Referral Care Delivery Services and Unmet Health-Related Social Needs: A Systematic Review (12)
Community and Research Perspectives on Cancer Disparities in Wisconsin (13)
Urban–Rural Disparities in Access to Low-Dose Computed Tomography Lung Cancer Screening in Missouri and Illinois (14)
Quantification of Potential Inequities in Breast Cancer Incidence in New Mexico Through Bayesian Disease Mapping (15)
HbA 1c Performance in African Descent Populations in the United States With Normal Glucose Tolerance, Prediabetes, or Diabetes: A Scoping Review (16)
Reducing Tobacco Use in Oregon Through Multisector Collaboration: Aligning Medicaid and Public Health Programs (17)
“We’re, Like, the Most Unhealthy People in the Country”: Using an Equity Lens to Reduce Barriers to Healthy Food Access in Rural Appalachia (18)
Oral Health Behaviors in Very Young Children in Low-Income Urban Areas in Chicago, Illinois, 2018–2019 (19)
A Randomized Trial to Improve Adherence to Follow-up Eye Examinations Among People With Glaucoma (20)
Positioning a scientific journal to address matters related to diversity, equity, and inclusion requires careful and intentional thinking and action. Going back to PCD’s inaugural issue in 2004, featuring an essay on social determinants of health by Dr Leonard Symes, professor emeritus of epidemiology at the University of California, Berkeley, the journal has created a space to highlight the importance of these topics in chronic disease prevention and health promotion. Since that first issue, PCD has continued to demonstrate a dedication to these issues at all levels: through its leadership and staff, the content it publishes, its expanding pool of talented volunteers (PCD’s external review panel, editorial board, associate editors, statistics review committee), the rigorous peer-review process, a comprehensive and inclusive variety of article types, calls for papers related to these issues, and more. In its 18 years of publication, PCD has consistently worked to assure the public of its commitment to achieving diversity, equity, and inclusion.
Peer-reviewed journals around the world are also focusing attention on these issues. In keeping with this movement, as PCD’s editor in chief I have authored the first article featured in this collection, which is a position statement on the steps already taken by the journal, steps planned for the next 5 years, and key measurable outcomes (3). PCD hopes to serve as a model in identifying and implementing best practices for diversity, equity, and inclusion to build an even stronger trust with the public.
And trust is needed: mistrust of the health care system has emerged as a primary barrier among members of communities of color to seeking care in health care systems (21). Mistrust stems from historical events, including the Tuskegee syphilis study, and is reinforced by health system issues and discriminatory events that continue to this day (21). This collection includes an article by Michener and colleagues, which posits that COVID-19 has underscored long-standing societal differences in drivers of health (4). The authors offer insights into this historical reality and suggest using a health equity lens to engage communities at risk of poor health outcomes, improve bidirectional communication, establish data sharing, and improve involvement in program implementation, dissemination, and evaluation. Authors share concrete ways these can be achieved by presenting successful examples around the US.
The global impact of COVID-19 among people at risk or living with a chronic condition in multicultural communities necessitates that health communication messages are created and delivered from a health equity perspective (22). Airhihenbuwa and coauthors, in their commentary, discuss the importance of culture in unpacking messages that may be the same globally (eg, physical/social distancing) yet different across cultures and communities (individualist vs collectivist) (5). Authors discuss how use of the PEN-3 framework can facilitate a community-engaged communication response to COVID-19.
Populations with low socioeconomic status and certain racial and ethnic groups (eg, Native American, Hispanic, and African American people) have historically been disproportionately affected by chronic disease, COVID-19 diagnosis, hospitalization, and mortality (23). Calo and associates discuss how COVID-19 has disproportionately affected Hispanic communities throughout the US (6). This commentary describes how Better Together REACH, a community–academic coalition promoting chronic disease prevention, and Project ECHO (a telementoring program based at Penn State University), were adopted to support a coordinated COVID-19 response in the Hispanic community in Pennsylvania. Authors provide insights into how the existing infrastructure of chronic disease programs can be used to leverage resources and provide trusted and continuous services to reach Hispanic populations during the pandemic.
African Americans, like the Hispanic population, are more likely to contract COVID-19, be hospitalized, and die of the disease (24). Akintobi et al describe how psychosocial, sociocultural, and environmental vulnerabilities, compounded by preexisting health conditions, exacerbate the burden of COVID-19 among African Americans (7). Authors share important information based on their years of experience on ways to create and implement approaches to intentionally engage African Americans at higher risk of COVID-19. Insights and recommendations can advance community leadership and be used to prepare public health practitioners, researchers, and evaluators for future pandemics — both assisting in advancing health equity and addressing historical aspects of health disparities among African Americans.
The disproportionate impact of COVID-19 and associated disparities among Hispanic, non-Hispanic Black, and non-Hispanic American Indian/Alaska Native children and teenagers has been widely reported (25). Children from some racial and ethnic minority groups have a higher prevalence of obesity, asthma, type 2 diabetes, and hypertension; were diagnosed more frequently with COVID-19; and had more severe outcomes compared with their non-Hispanic White counterparts (26). In addition, a higher proportion of children from some racial and ethnic minority groups, compared with White children, live in families with incomes less than 200% of the federal poverty level or in households lacking secure employment (8). White et al argue that the COVID-19 pandemic reemphasizes the importance of implementing policy, systems, and environmental changes in school systems to support emergency preparedness and recovery, as well as resilience, through collaborations among local health departments, local school systems, and other public and private organizations (8). Topics addressed in this article include disparities in underlying medical conditions and social determinants of health, inequities in social determinants of health, and community-based approaches to reducing COVID-19 disparities. The article concludes by discussing ways to implement strategies to advance health equity through partnership.
It has long been recognized that disparities in health care access and patient outcomes are associated with factors related to race, sex, gender, sexual orientation, primary language, and socioeconomic status (27). Epps and coauthors recognize that African Americans and other underrepresented racial and ethnic groups are often not included in health decision making and policy development (9). As a result, these public health experts describe steps undertaken to improve participation, joint decision making, and capacity building between an integrated academic health system and a community coalition to address complex health challenges with the aim of increasing the capacity of health systems to reduce the burden of COVID-19. This article describes a call to action by the chair of a health care board of trustees to its board members consisting of clinicians, researchers, educators, and health advocates to identify ways to mitigate disparities and determine how the health care system could play a role in advancing and implementing effective strategies to reduce the disproportionate burden of COVID-19 among communities of color. Authors provide insight into the organizational planning process to generate a community outreach and health disparities collaborative with goals for governance, messaging and education, community partnerships, data, and research and evaluation.
COVID-19 has exacted a tremendous toll on the physical, emotional, and psychological well-being of many Americans, thus requiring a population health response (28). The disproportionate impact of the COVID-19 pandemic on Hispanic communities has resulted in a greater burden of depression, anxiety, and stress along with the need for increased assistance with housing, access to food, and supplemental income (29). Moon and colleagues offer original research that reports findings on demographic characteristics and factors associated with service volume, types of services, and referrals in the pre-COVID-19 and COVID-19 periods (10). They report that referrals shifted from primarily mental health services and disease management during the prepandemic period to affordable housing support, food assistance, and supplemental income during the COVID-19 period. This study presents findings on how a community-based organization with a long-standing presence in the Hispanic community effectively expanded its emotional wellness program, using promotores to provide integrated mental health care and social services to clients disproportionately affected by COVID-19.
Hacker et al discuss the problem of COVID-19 and chronic disease in their essay (11). They describe 3 categories of challenges facing public health professionals and identify solutions needed to improve health outcomes and lessen health inequities among people at risk or living with a chronic disease. Authors also discuss the evolving response by the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion to implement a multipronged approach to enhance access to data at the local level, focus on addressing social determinants of health through a health equity lens, and expand partnerships and communication about the impact of COVID-19 on chronic disease.
Unmet health-related social support needs among people being served by health care systems can contribute to high patient morbidity and poor population health (30,31). However, little is known about the overall impact of screening and referral programs that address unmet health-related social needs on outcomes related to experience of care, population health, and cost. Ruiz Escobar et al conducted a systematic review of peer-reviewed articles in PubMed published over the past 10 years (as of March 2020) to determine the impact of screening and referral care delivery services on unmet health-related social needs (12). Thirty-five articles met the systematic review’s inclusion criteria. After conducting their review, the authors concluded that although evidence exists of a positive influence of screening and referral program outcomes related to experience of care and population health, no definitive conclusions could be made on the overall impact on changes in patient connection to resources, patient satisfaction, and patient-reported outcomes because of the potential high risk of bias across studies. Their findings can inform the use of screening and referral programs in health care organizations, including ways to strengthen future studies to examine their effectiveness.
Qualitative research is an important methodological tool that provides critical insights in identifying subjective meaning in the context of health (32). Qualitative research is a necessary exploratory approach that can be used to better understand and improve health equity research and practice. Olson and her team of researchers conducted 10 listening sessions and 28 interviews with people from diverse backgrounds to identify themes in causes, solutions, and opportunities to collaborate across sectors to address cancer disparities (13). Researchers validated the use of qualitative approaches to engage diverse participants representing many different sectors. Qualitative findings identified medical mistrust, the need for equitable multilevel partnerships, influences of environmental threats on cancer burden, and location of cancer disparities as key concerns among people participating in the listening sessions and interviews. The researchers describe how these findings will be used to form multisector teams to address local social, cultural, and biological influences of cancer disparities and achieve health equity in Wisconsin.
Geographic location continues to be an important contributor in shaping access to timely and necessary screening and treatment options (33). Rohatgi et al conducted original research examining relationships among rurality, sociodemographic characteristics, and access to low-dose computed tomography (LDCT) screening for lung cancer and screening access and lung cancer mortality (14). This study revealed that more than 97% of metropolitan residents had access to LCDT screening, compared with just over 40% of nonmetropolitan residents. Researchers learned that residents of southeastern Missouri, a rural and impoverished area, had low screening access, high smoking prevalence, and high lung cancer mortality. Researchers concluded that targeted strategies to implement rural LDCT screening could reduce geographic disparities in access, and future research could help identify factors that increase access to screening to eliminate rural-related disparities in lung cancer mortality.
Breast cancer is the most frequently diagnosed cancer and a leading cause of cancer mortality among American Indian/Alaska Native (AI/AN) women (34). Despite having a lower incidence of breast cancer than White women, AI/AN women are more likely to be diagnosed at younger ages and later stages (35). Breast cancer incidence among non-AI/AN women has largely been quantified in large geographic regions in the US, and substantial regional variation in breast cancer inequities in non-Hispanic AI/AN populations has been reported. Zahrieh and colleagues conducted research to obtain a deeper understanding at a granular level to identify potential inequities in breast cancer incidence by applying county-level Bayesian disease mapping (a model-based approach that offers a means to improve county-level incidence estimates) to population surveillance data from 2005 through 2014 in New Mexico (30). They found a significant overall disparity effect across New Mexico, evidenced by the age-adjusted rate of breast cancer among non-Hispanic AI/AN women being appropriately 0.38 times the corresponding age-adjusted rate among non-Hispanic White women. Researchers also suggest that findings can be used to facilitate targeted statewide and county-level cancer control interventions to mitigate breast cancer disparities among AI/AN women in New Mexico.
Historically, type 2 diabetes has disproportionately affected racial and ethnic minority groups (31). To ensure accurate detection of type 2 diabetes, we must understand the ability of hemoglobin A 1c (HbA 1c ) to correctly classify type 2 diabetes status and evaluate intra-ethnic variation. Toward this end, Khosla et al conducted a scoping review to determine HbA 1c performance in African descent populations in the US with normal glucose tolerance, prediabetes, and diabetes (16). Results included 7 studies that analyzed HbA 1c performance among African Americans, 1 study that analyzed HbA 1c performance in Afro-Caribbean people, and 4 studies that analyzed HbA 1c performance among Africans. Researchers found that current HbA 1c cutoffs for prediabetes and type 2 diabetes may overestimate glycemic status in African Americans and underestimate glycemic status in Afro-Caribbean and African people. Researchers indicated that alternating testing, such as the oral glucose tolerance test, fasting plasma glucose, and other glycated blood proteins in place of or in combination with HbA 1c may better assess glycemic status in populations of African descent.
Tobacco use remains the leading cause of preventable morbidity and mortality in the US (33). Livingston and colleagues evaluated changes in tobacco cessation benefits, patient access, and cigarette smoking prevalence before and after 16 coordinated care organizations began providing comprehensive cessation benefits for reducing tobacco use prevalence among Medicaid members in Oregon (17). This implementation evaluation identified changes in tobacco cessation benefits, patient–provider discussions of smoking cessation, and cigarette smoking prevalence before and after the introduction of statewide incentives for reducing cigarette smoking. Evaluators reported that statewide effort accelerated progress toward tobacco use reduction among members of coordinated care organizations.
Obesity among adults living in Appalachia continues to be a major problem, and policy, systems, and environmental interventions may help to address long-standing underlying factors that have historically contributed to this persistent public health concern (35). Cardarelli and associates reported findings from a qualitative study that used a grounded theory approach to identify barriers and facilitators for healthy food access in a rural county in Kentucky (18). The goal was to design interventions responsive to social, cultural, and historical contexts from an equity perspective. Focus group participants were asked, for example, if it was easy to get fruits and vegetable at locations where they purchase food, if many people in their community purchase food at farmers markets, and what factors in their community make it easier or harder to eat healthy. The authors concluded that efforts to address food access through policy, systems, and environmental interventions must be sensitive to characteristics of the rural setting, acknowledge social inequities in the region, and proactively engage community members throughout all stages of intervention planning, implementation, and evaluation.
Oral health disparities among children have been linked to socioeconomic inequalities, access to care, health systems barriers, and lack of access to foods that promote optimal oral health outcomes (39). Martin et al conducted original research that explored the frequency of tooth brushing among children with a mean age 21.5 months (19). Their results indicated that the frequency of brushing among children, as reported by guardians, was higher when the correct amount of toothpaste was used, brushing occurred for a longer duration, and other family members helped children with brushing. Their findings strongly suggest that parental and family support for brushing are critically important in promoting and sustaining tooth-brushing behaviors.
According to the Lancet Global Health Commission on Global Eye Health, women, rural populations, and racial/ethnic minority groups are more likely to have vision impairment, a pervasive inequality that needs to be addressed (40). This PCD collection on advancing health equity and reducing health disparities concludes with a research study by Leiby et al investigating the effectiveness of an enhanced intervention among people with glaucoma: using patient navigators and social workers to improve patient adherence to follow-up eye care in community settings (20). The study compared the intervention group with a group of patients in usual care. Participants in usual care were provided with a local ophthalmologist’s contact information and a copy of their eye examination results; they were not provided access to patient navigators or social workers. Study participants, who were randomly assigned to either the enhanced or usual care intervention, were a diverse group of participants aged over 40 with a family history of glaucoma or currently diagnosed with diabetes. Only participants who had not seen an ophthalmologist in the previous 12 months were permitted to enroll in the study. Study participants consisted largely of African Americans, followed by White, Asian American, and Hispanic residents of Philadelphia, Pennsylvania. The study found that the use of patient navigators and social workers doubled the rate of adherence to annual recommended eye care follow-up, compared with participants assigned to the study’s usual care intervention. The study highlights that formalized use of social support in partnership with local ophthalmologists can be an effective approach to increasing access to local ophthalmological services.
At the center of this collection of articles is a shared commitment to the goal of eliminating health disparities, particularly those that continue to persist despite aggressive efforts to ameliorate them. The collection describes a range of diverse and timely examples of efforts to eliminate health disparities and advance health equity among racial and ethnic groups in the US. Articles appearing here represent various types of PCD articles that encompass multiple perspectives, from original research and systematic reviews to implementation evaluation to expert commentaries to tools that can be used in public health practice. As a discipline, we have important work to do, not only to better understand how social determinants of health and other contextual factors impact health but also to design, implement, and evaluate effective multilevel systems approaches that create optimal conditions to promote health for all. PCD will continue to move forward in its commitment to these goals, and we encourage authors to visit the journal’s Author’s Corner website (https://www.cdc.gov/pcd/for_authors/index.htm) to learn more about article types that best fit their research addressing population-based approaches to eliminating health disparities and advancing health equity.
Corresponding Author: Leonard Jack, Jr, PhD, MSc, Editor in Chief, Preventing Chronic Disease: Public Health Research, Practice, and Policy, Office of Medicine and Science, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, 4770 Buford Hwy, NE, Mailstop S107–8, Atlanta, GA 30341. Email: [email protected] .
Author Affiliations: 1 Office of Medicine and Science, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, Georgia.
- Jack L Jr. Using PCD’s first-ever external review to enhance the journal’s worldwide usefulness to researchers, practitioners, and policy makers. Prev Chronic Dis 2018;15:E41. CrossRef external icon PubMed external icon
- US Department of Health and Human Services. Section IV: Advisory Committee findings and recommendation. In: The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: recommendations for the framework and format of Healthy People 2020. http://www.healthypeople.gov/sites/default/files/phaseI_0.pdf. Accessed July 8, 2021.
- Jack L Jr. PCD’s commitment to advancing diversity, equity, and inclusion in its scientific leadership, peer review process, research focus, training, and continuing education. Prev Chronic Dis 2021;18:210269.
- Michener L, Aguilar-Gaxiola S, Alberti PM, Castaneda MJ, Castrucci BC, Harrison LM, et al. Engaging with communities — lessons (re)learned from COVID-19. Prev Chronic Dis 2020;17:E65. CrossRef external icon PubMed external icon
- Airhihenbuwa CO, Tseng TS, Sutton VD, Price L. Global perspectives on improving chronic disease prevention and management in diverse settings. Prev Chronic Dis 2021;18:E33. CrossRef external icon PubMed external icon
- Calo WA, Murray A, Francis E, Bermudez M, Kraschnewski J. Reaching the Hispanic community about COVID-19 through existing chronic disease prevention programs. Prev Chronic Dis 2020;17:E49. CrossRef external icon PubMed external icon
- Akintobi HT, Jacobs T, Sabbs D, Holden K, Braithwaite R, Johnson LN, et al. Community engagement of African Americans in the era of COVID-19: considerations, challenges, implications, and recommendations for public health. Prev Chronic Dis 2020;17:E83. CrossRef external icon PubMed external icon
- White A, Liburd LC, Coronado F. Addressing racial and ethnic disparities in COVID-19 among school-aged children: are we doing enough? Prev Chronic Dis 2021;18:E55. CrossRef external icon PubMed external icon
- Epps F, Wiley Z, Teunis LJ, Johnson TM 2d, Patzer RE, Ofotokun I, et al. A framework for mobilizing health care to respond to the community within the COVID-19 pandemic. Prev Chronic Dis 2021;18:E30. CrossRef external icon PubMed external icon
- Moon KJ, Montiel GI, Cantero PJ, Nawaz S. Addressing emotional wellness during the COVID-19 pandemic: the role of promotores in delivering integrated mental health care and social services. Prev Chronic Dis 2021;18:E53. CrossRef external icon PubMed external icon
- Hacker KA, Briss PA, Richardson L, Wright J, Petersen R. COVID-19 and chronic disease: the impact now and in the future. Prev Chronic Dis 2021;18:210086. CrossRef external icon PubMed external icon
- Ruiz Escobar R, Pathak H, Blanchard C. Screening and referral care delivery services and unmet health-related social needs: a systematic review. Prev Chronic Dis 2021;18:2000569.
- Olson J, Cawthra T, Beyer K, Frazer D, Ignace L, Maurana C, et al. Community and research perspectives on cancer disparities in Wisconsin. Prev Chronic Dis 2020;17:E122. CrossRef external icon PubMed external icon
- Rohatgi KW, Marx CM, Lewis-Thames MW, Liu J, Colditz GA, James AS. Urban–rural disparities in access to low-dose computed tomography lung cancer screening in Missouri and Illinois. Prev Chronic Dis 2020;17:E140. CrossRef external icon PubMed external icon
- Zahrieh D, Golafshar MA, Patel SH, DeWees TA. Quantification of potential inequities in breast cancer incidence in New Mexico through Bayesian disease mapping. Prev Chronic Dis 2021;18:E23. CrossRef external icon PubMed external icon
- Khosla L, Bhat S, Fullington LA, Horlyck-Romanovsky MF. HbA1c performance in African descent populations in the United States with normal glucose tolerance, prediabetes, or diabetes: a scoping review. Prev Chronic Dis 2021;18:E22. CrossRef external icon PubMed external icon
- Livingston CJ, Bartelmann SE, Goff NM, Aird KG. Reducing tobacco use in Oregon through multisector collaboration: aligning Medicaid and public health programs. Prev Chronic Dis 2020;17:E155. CrossRef external icon PubMed external icon
- Cardarelli K, DeWitt E, Gillespie R, Norman-Burgdolf H, Jones N, Mullins JT. “We’re, like, the most unhealthy people in the country”: using an equity lens to reduce barriers to healthy food access in rural Appalachia. Prev Chronic Dis 2020;17:E165. CrossRef external icon PubMed external icon
- Martin M, Pugach O, Avenetti D, Lee H, Salazar S, Rosales G, et al. Oral health behaviors in very young children in low-income urban areas in Chicago, Illinois, 2018–2019. Prev Chronic Dis 2020;17:E152. CrossRef external icon PubMed external icon
- Leiby BE, Hegarty SE, Zhan T, Myers JS, Katz LJ, Haller JA, et al. A randomized trial to improve adherence to follow-up eye examinations among people with glaucoma. Prev Chronic Dis 2021;18:E52. CrossRef external icon PubMed external icon
- Webb Hooper M, Mitchell C, Marshall VJ, Cheatham C, Austin K, Sanders K, et al. Understanding multilevel factors related to urban community trust in healthcare and research. Int J Environ Res Public Health 2019;16(18):3280. CrossRef external icon PubMed external icon
- Finset A, Bosworth H, Butow P, Gulbrandsen P, Hulsman RL, Pieterse AH, et al. Effective health communication — a key factor in fighting the COVID-19 pandemic. Patient Educ Couns 2020;103(5):873–6. CrossRef external icon PubMed external icon
- Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med 2020;9(8):2442. CrossRef external icon PubMed external icon
- Vahidy FS, Nicolas JC, Meeks JR, Khan O, Pan A, Jones SL, et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open 2020;10(8):e039849. CrossRef external icon PubMed external icon
- Bassett MT, Chen JT, Krieger N. The unequal toll of COVID-19 mortality by age in the United States: quantifying racial/ethnic disparities. Working paper. Cambridge (MA): Harvard T.H. Chang School of Public Health; 2020.https://www.hsph.harvard.edu/social-and-behavioral-sciences/2020/06/23/the-unequal-toll-of-covid-19-mortality-by-age-in-the-united-states-quantifying-racial-ethnic-disparities/. Accessed July 13, 2021.
- Kim L, Whitaker M, O’Halloran A, Kambhampati A, Chai SJ, Reingold A, et al. ; COVID-NET Surveillance Team. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 — COVID-NET, 14 states, March 1–July 25, 2020. MMWR Morb Mortal Wkly Rep 2020;69(32):1081–8. CrossRef external icon PubMed external icon
- Okoro CA, Zhao G, Fox JB, Eke PI, Greenlund KJ, Town M. Surveillance for health care access and health services use, adults aged 18–64 years — Behavioral Risk Factor Surveillance System, United States, 2014. MMWR Surveill Summ 2017;66(7):1–42. CrossRef external icon PubMed external icon
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 2020;89:531–42. CrossRef external icon PubMed external icon
- Waitzkin H, Getrich C, Heying S, Rodríguez L, Parmar A, Willging C, et al. Promotoras as mental health practitioners in primary care: a multi-method study of an intervention to address contextual sources of depression. J Community Health 2011;36(2):316–31. CrossRef external icon PubMed external icon
- Tough H, Siegrist J, Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Public Health 2017;17(1):1414. Erratum in BMC Public Health 2017;17(1)580. CrossRef external icon PubMed external icon
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med 2010;7(7):e1000316. CrossRef external icon PubMed external icon
- Mykhalovskiy E, Eakin J, Beagan B, Beausoleil N, Gibson BE, Macdonald ME, et al. Beyond bare bones: critical, theoretically engaged qualitative research in public health. Can J Public Health 2018;109(5-6):613–21. CrossRef external icon PubMed external icon
- Tsui J, Hirsch JA, Bayer FJ, Quinn JW, Cahill J, Siscovick D, et al. Patterns in geographic access to health care facilities across neighborhoods in the United States based on data from the National Establishment Time-Series between 2000 and 2014. JAMA Netw Open 2020;3(5):e205105. CrossRef external icon PubMed external icon
- White MC, Espey DK, Swan J, Wiggins CL, Eheman C, Kaur JS. Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health 2014;104(Suppl 3):S377–87. CrossRef external icon PubMed external icon
- Melkonian SC, Jim MA, Haverkamp D, Wiggins CL, McCollum J, White MC, et al. Disparities in cancer incidence and trends among American Indians and Alaska Natives in the United States, 2010–2015. Cancer Epidemiol Biomarkers Prev 2019;28(10):1604–11. CrossRef external icon PubMed external icon
- Lin J, Thompson TJ, Cheng YJ, Zhuo X, Zhang P, Gregg E, et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metr 2018;16(1):9. CrossRef external icon PubMed external icon
- Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, et al. Tobacco product use and cessation indicators among adults — United States, 2018. MMWR Morb Mortal Wkly Rep 2019;68(45):1013–9. CrossRef external icon PubMed external icon
- Smith LH, Laurent D, Baumker E, Petosa RL. Rates of obesity and obesogenic behaviors of rural Appalachian adolescents: how do they compare to other adolescents or recommendations? J Phys Act Health 2018;15(11):874–81. CrossRef external icon PubMed external icon
- Shen A, Bernabé E, Sabbah W. Systematic review of intervention studies aiming at reducing inequality in dental caries among children. Int J Environ Res Public Health 2021;18(3):1300. CrossRef external icon PubMed external icon
- Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health 2021;9(4):e489–551. CrossRef external icon PubMed external icon
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Research ethics and collaborative research in health and social care: Analysis of UK research ethics policies, scoping review of the literature, and focus group study
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Health Policy and Department of Social Policy, Care Policy and Evaluation Centre, London School of Economics and Political Science, London, United Kingdom
Roles Conceptualization, Methodology, Supervision, Validation, Writing – review & editing
Affiliation Faculty of Health Studies, Jan Oyebode, Centre for Applied Dementia Studies, University of Bradford, Bradford, United Kingdom
- Chiara De Poli,
- Jan Oyebode

- Published: December 22, 2023
- https://doi.org/10.1371/journal.pone.0296223
- Peer Review
- Reader Comments
Current research ethics frameworks were developed on the footprint of biomedical, experimental research and present several pitfalls when applied to non-experimental social sciences. This work explores how the normative principles underpinning policy and regulatory frameworks of research ethics and the related operational processes work in practice in the context of collaborative health and social care research. The work was organised in three phases. First, UK research ethics policy documents were analysed thematically, with themes further organised under the categories of ‘Principles’ and ‘Processes’. Next, we conducted a scoping review of articles about research ethics in the context of collaborative health and social care research, published in English between 2010 and 2022. We then held an exploratory focus group with ten academic researchers with relevant experience to gather their views on how the research ethics system works in practice in England (UK). The thematic framework developed in the first phase supported the analysis of the articles included in the scoping review and of focus group data. The analysis of policy documents identified twelve themes. All were associated to both a principle and a related operational process. The scoping review identified 31 articles. Across these, some themes were barely acknowledged (e.g., Compliance with legislation). Other themes were extensively covered (e.g., The working of Research Ethics Committees), often to discuss issues and limitations in how, in practice, the research ethics system and its processes deal with collaborative research and to suggest options for improvement. Focus group data were largely consistent with the findings of the scoping review. This work provides evidence of the poor alignment between how the research ethics system is normatively expected to work and how it works in practice and offers options that could make research ethics more fit for purpose when addressing collaborative research in health and social care.
Citation: De Poli C, Oyebode J (2023) Research ethics and collaborative research in health and social care: Analysis of UK research ethics policies, scoping review of the literature, and focus group study. PLoS ONE 18(12): e0296223. https://doi.org/10.1371/journal.pone.0296223
Editor: Alberto Molina Pérez, Spanish National Research Council: Consejo Superior de Investigaciones Cientificas, SPAIN
Received: August 7, 2023; Accepted: December 7, 2023; Published: December 22, 2023
Copyright: © 2023 De Poli, Oyebode. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The Authors were funded by The Health Foundation, grant number 1274233. The funding source had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the articles; and in the decision to submit it for publication.
Competing interests: Chiara De Poli had research grant funding from the National Institute for Health and Care Research, School of Social Care Research, grant number 106152/CBF/LSECDP-IF14. She currently has, as co-applicant, research grant funding by the National Institute of Health and Care Research - Three Schools Dementia Programme, grant number 102645/3SDRP/LSEACH-DP05. Jan Oyebode currently has research grant funding from the National Institute for Health Research, grant number 204266, Social Care for People with Young Onset Dementia.
Introduction
Research ethics and governance represent the regulatory and institutional cornerstones for the conduct of research involving human participants, aiming to oversee its ethical quality and protect research participants from harmful research practices. Since the Nuremberg code (1947) [ 1 ], respect for autonomy, justice, beneficence (i.e., to do good), and non-maleficence (i.e., to do no harm) have been recognised as core ethical principles of biomedical, experimental research involving human participants. These principles were embedded in international guidance and regulation (e.g., the Declaration of Helsinki by the World Medical Association (1964) [ 2 , 3 ], the International Ethical Guidelines for Biomedical Research Involving Human Subjects of the Council for International Organizations of Medical Sciences (CIOMS, 2016) [ 4 ] and in national research ethics frameworks (e.g., the US Belmont Report (1978) [ 5 ], the Canadian Tri-Council Policy Statement [ 6 ], and the UK Policy Framework for Health and Social Care Research [ 7 ]). Over time the application of this research ethics framework has been expanded from regulation of traditional biomedical research to also regulate social sciences, including health and social care research.
Extant research on research ethics has underscored the intrinsic complexity of establishing whether ethics oversight results in ethical research and participant protection. The use of processes and structures as surrogate measures for effectiveness of research ethics has been found particularly unsatisfactory [ 8 – 10 ]. Although there are several reasons to believe that research ethics processes and structures contribute to ensuring ethical research and the protection of research participants, little empirical evidence is available on whether and how research ethics institutions actually achieve these ends [ 9 , 11 , 12 ]. Alongside assumed benefits, negative or unwanted consequences of the research ethics system have been documented. At the procedural level, the apparent arbitrary nature of decision-making, long delays in obtaining research approvals, and the bureaucratic restrictions imposed on the conduct of studies are a frequent source of problems [ 8 , 13 ]. At the organisational level, the establishment of a research ethics industry [ 14 ], with a perceived emphasis on box ticking [ 15 , 16 ] and rule fetishization [ 17 ], ultimately concerned with issues around risk, litigation, and institutional reputation, seems to have contributed to an ‘ethics creep’ [ 17 ]. At an epistemological level, the problems of using a framework rooted in experimental, biomedical research to assess social sciences and research using non-experimental methods (e.g., big data research [ 18 ], social media research [ 19 ], research using machine learning [ 20 ], ethnography [ 21 ] and digital ethnography [ 22 ]) are well documented [ 23 – 26 ].
Research using qualitative or mixed methods [ 27 ] and less codified and predictable designs, such as participatory research (e.g., participatory action research, community-based participatory research) [ 28 ] and research using collaborative approaches (e.g., co-creation, co-design, co-production) [ 29 ], have been particularly affected. As a consequence of the fundamental poor alignment between the biomedical framework of research ethics and qualitative, participatory, and collaborative research, researchers have described their experience of navigating the research ethics system as “jumping through hoops” or “walking a tightrope”, or “something to get through” [ 30 , 31 ]. The requirement to submit a detailed research protocol to prospectively outline research activities clashes with the emergent nature of qualitative, participatory, and collaborative research [ 29 , 30 ]. The bureaucratic practices around consent that are used to operationalise the principle of autonomy are often unworkable for research with a strong relational component [ 17 , 32 – 34 ]. Additionally, research participants and co-researchers may disagree with the way the principle of participant protection is interpreted and risks and benefits are assessed by research ethics institutions [ 29 , 35 , 36 ]. These may be perceived as leaning towards paternalism, in particular in the case of populations with characteristics that are perceived as making them vulnerable [ 37 – 39 ].
If some of these features of qualitative, participatory, and collaborative research result in great scrutiny by research ethics institutions, other features with equally relevant ethical implications are not given due attention. For example, current research ethics frameworks designed to address the principle of justice (which requires the equitable distribution of both the burdens and the benefits of participation in research [ 40 ]) fail to consider how power relations between individuals or groups shape research and do not offer any mechanisms to help address the power differentials intrinsic to research [ 41 ]. Research ethics processes also have a blind spot in relation to gatekeepers, who have a substantial influence on who gets to participate and, conversely, who is excluded from research. There is no mechanism in place to oversee how they perform their role and whether they impact upon free choice of potential participants to take part in studies [ 34 ].
Alongside these issues reported for qualitative, participatory, and collaborative research that reaches the stage of seeking ethics approval, the academic debate has also aired concerns that research which is anticipated to be met with resistance by research ethics institutions is not actually pursued [ 17 , 42 , 43 ]. The perceived or expected barriers might deter researchers from conducting research on sensitive topics, involving vulnerable groups, or using more innovative methods. At best, this could contribute to homogenisation of the research landscape. At worst, it could undermine the role of qualitative, participatory, and collaborative research in promoting research inclusivity and social justice, and in answering research questions that no other research methods could address.
In order to move these debates forward, we conducted a study on research ethics aimed at generating a set of practical recommendations for improving how the research ethics system deals with participatory and collaborative research approaches (collaborative only, hereon). In this context, we used collaborative research as an umbrella term for various research approaches (e.g., participatory action research, community-based participatory research, co-creation, co-design, co-production) where participants are actively involved in shaping the research, beyond simply providing data, and where the primacy of academic knowledge is challenged by other types of knowledge (e.g., based on lived experience).
The study was organised in five consecutive phases. In the first phase, we carried out an analysis of UK research ethics policies, which informed a scoping review of the literature (phase 2). We then held an exploratory focus group with academic researchers in this field to understand their perspectives on the topic (phase 3). Results of these three phases informed a two-round Delphi study, involving academic researchers with experience of conducting participatory and collaborative research involving vulnerable groups in England (UK). The Delphi study aimed to generate consensus on what changes to the research ethics system should be considered to improve the ethics oversight of collaborative research (phase 4). A final focus group with experts was organised to inform the practical recommendations and explore their expected benefit (phase 5). This article reports the results of the first three phases of the work, whilst the remaining phases are reported elsewhere [ 44 ].
Through the analysis of policies (phase 1), we aimed to (i) understand what the UK research ethics system is intended to achieve and how it is designed to work, (ii) identify its underpinning principles, and (iii) map the operational processes and procedures which are designed and implemented to achieve the principles.
Since our work was carried out in the context of a UK-based study, the focus of the analysis was limited to UK research ethics policies, which reflect relevant domestic legislation (as set out in Appendix 2 of the UK Policy Framework for Health and Social Care Research [ 7 ],), but also draw on international standards, governance mechanisms, and good research practice (as per [ 7 ], para 3.4). By design, such policies have a deliberate wide scope: they do not, and possibly cannot, exhaustively compile principles, requirements, and standards that may be relevant for specific types of research, which are left to organisations with responsibilities under the national policy framework. In this sense, the UK system largely shares the bedrock of research ethics principles with other countries [ 45 – 48 ] and can be considered an example of a modern research ethics system. The analysis of policies was also instrumental to the development of the analytical framework of ‘Principles’ and ‘Processes’ that supported the scoping review of the literature that followed (phase 2).
The aim of the review was two-fold. Firstly, we aimed to understand how the normative principles and operational processes of research ethics play out in actual research that adopts participatory or collaborative approaches, often using qualitative methods, in the health and social care field. Secondly, we set out to map the recommendations that the literature had suggested to improve how the research ethics system deals with this type of research. The scoping review approach was deemed fit for the purpose of efficiently gathering and examining the extent, range, and nature of the literature available on this topic.
In phase 3, the exploratory focus group aimed to bring to light actual experiences of navigating the research ethics system from the perspective of active academic researchers with experience of conducting collaborative research in England (UK). By gathering their experiences, we were able to identify current patterns in the English context and to read them against the background of the literature review.
Analysis of UK research ethics policies
The analysis focused on the UK Policy Framework for Health and Social Care Research [ 7 ] and on UK Health Research Authority (HRA) policies publicly available online [ 49 , 50 ]. Policy documents were analysed thematically. The analysis proceeded deductively at first, with themes identified from the research ethics principles stated in the UK Policy Framework for Health and Social Care Research. The initial codebook was then expanded inductively, to include additional themes that were not codified as principles in the UK Policy Framework, but that appeared relevant. To help systematise the data collected, we divided the material under each theme into two categories: ‘Principles’ for data that referred to underpinning principles of the UK research ethics system, and ‘Processes’ for data describing the operational processes and procedures supporting the implementation of the principle ( Table 1 ). The Authors worked collaboratively: CDP started the data extraction and discussed the emerging results with JO as the analysis progressed. Instances of uncertainty or ambiguity were resolved through ongoing discussion.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0296223.t001
Scoping review of the literature
The scoping review was conducted following the Arksey and O’Malley framework [ 51 ] and is reported based on the PRISMA extension for scoping reviews (PRISMA-ScR) [ 52 ]. The review was guided by the following questions: How does the current research ethics system work for collaborative research in health and social care? What are the challenges that the current research ethics framework poses to collaborative research in health and social care? What options have been discussed in the literature to overcome these challenges?
Eligibility criteria.
Articles examining the research ethics and governance systems in the context of collaborative research in the field of health and social care were included. They had to be written in English and published in peer-reviewed journals in the period January 2010-May 2020. The original search was updated in December 2022, to identify articles published between June 2020-December 2022. Three online databases (Web of Science, PubMed/Medline, PsycInfo) were searched in June 2020, using search strings available in S1 File . In December 2022, we re-ran the original search using the same online databases and the same search criteria. Retrieved studies were imported into a reference management software. After removing duplicates, titles, and abstracts of the retrieved results were screened by CDP for eligibility against the inclusion criteria. Full text of all possible eligible articles was retrieved and screened by CDP, with JO screening the articles for which eligibility was uncertain.
Data extraction and analysis.
Data extraction and analysis was conducted by CDP and iteratively discussed and reviewed by JO. The analysis was supported by an analytic framework organised around the themes identified in the analysis of policy documents. At the level of each theme, the analytical framework was organised as a 2X2 matrix. On the first dimension we placed the categories of ‘Principles’ and ‘Processes’, consistently with the way we had analysed the policy documents. On the second dimension, we used the categories of ‘Current system’ and ‘Options for improvement’ ( Table 2 ), to map the debate in relation to how the current research systems deal with collaborative research and to collect suggestions put forward to ensure a better fit of research ethics in the context of collaborative research. The resulting analytic framework was applied to each article. Each article was also charted in relation to its typology, country in which the research was conducted, research approach, and research population(s).
https://doi.org/10.1371/journal.pone.0296223.t002
As recommended by methodological guidance on scoping reviews [ 51 , 53 ], this analytical process allowed us to describe the literature available in this field. It also allowed us to systematically document how the set of a priori themes, derived from the policy documents, had been discussed in the literature. Lastly, it enabled us to identify, in relation to each theme, how the system currently works and opportunities for improvement.
Exploratory focus group.
Following approval by the London School of Economics and Political Science, as per the School’s research ethics policy, the exploratory focus group was conducted online, via Zoom, in May 2020 to discuss actual experiences of navigating the English research ethics system in the context collaborative research in the health and social care field. The emphasis in recruitment of participants was on identifying active researchers with relevant experience of undertaking collaborative research in health and social care, and therefore of having applied for ethical review in England (UK).
Twelve participants were identified or snowballed via the professional networks of the research team and invited by e-mail to take part. Ten academic researchers with different levels of relevant experience, some undertaking research involving populations deemed vulnerable, expressed interest and were sent background information about the study and what their participation would entail. All gave written consent to take part in the study ( Table 3 ).
https://doi.org/10.1371/journal.pone.0296223.t003
The group was facilitated by JO with assistance from CDP, both with similar research interests and experience. The discussion was audio-recorded with consent from participants.
The discussion lasted about two hours and was guided by two broad questions. We started off by asking participants about issues they had encountered in obtaining research governance and ethics approval for studies using collaborative approaches and involving groups deemed vulnerable. The second question invited participants to consider what changes could ensure that research governance and ethics approval processes were better suited for collaborative research with vulnerable groups.
The focus group was transcribed verbatim. Data were imported to Nvivo12 and analysed thematically using a deductive approach supported by the analytical framework developed for the study [ 54 ] ( Table 2 ).
The analysis of the UK Policy Framework [ 7 ] and HRA documents [ 49 , 50 ] resulted in 12 themes ( Table 4 ).
https://doi.org/10.1371/journal.pone.0296223.t004
Theme 1—General ethical principles is a general theme which reflected Principle 3 (Scientific and Ethical Conduct Research) of the UK Policy Framework, by which research projects are expected to be scientifically sound and guided by ethical principles in all their aspects [ 7 ].
We identified both principles and processes for three of the 11 remaining themes: Theme 3—Protection of research participants corresponds to Principle 8 (Benefits and risks) of the UK Policy Framework. The corresponding operational process revolves around the role of Research Ethics Committees (RECs, known as Institutional Review Boards (IRBs) in the US and Canada) to ensure that the rights, safety, dignity, and wellbeing of research participants are adequately protected [ 49 ]. Theme 6—The working of RECs reflects Principle 9 (Approval) of the UK Policy Framework. Operationally, this principle relies on Research Ethics Committees (RECs) providing ethical review of new applications and keeping approved applications under review [ 49 ]. The HRA Standard Operating Procedures for RECs make specific provision regarding the review process (e.g., ‘flagged’ RECs, Proportionate Review Service, expedited review) for different types of research [ 50 ]. Theme 7—The research protocol is equivalent to the Principle 6 (Protocol) of the UK Policy Framework. From an operational perspective, this translates into a requirement to submit the standard protocol for any new research study and a standard Notice of Substantial Amendment when significant changes to the original study are proposed [ 50 ].
The remaining eight themes substantially mirrored principles of the UK Policy Framework, but no corresponding operational process could be identified.
The search conducted in June 2020 yielded 230 references, of which 166 were unique records. After screening titles and abstracts, 109 articles were excluded. The full texts of the remaining 57 papers were retrieved and reviewed. A total of 30 articles were deemed relevant for inclusion. The December 2022 update search identified 23 further references, of which 10 were unique records. After screening titles and abstracts, eight articles were excluded. The full texts of the two remaining papers were retrieved and assessed, and one was included. Combining the two searches, a total of 31 articles were deemed relevant for inclusion in the review ( Table 5 ). The screening process is illustrated in Fig 1 .
https://doi.org/10.1371/journal.pone.0296223.g001
https://doi.org/10.1371/journal.pone.0296223.t005
Seven articles reported research based in Canada [ 28 , 30 , 56 , 61 – 63 , 75 ], seven reported research based in the USA [ 38 , 57 , 60 , 67 , 68 , 73 , 77 ], four in England or the UK [ 35 , 55 , 76 , 78 ], two in Scandinavian countries [ 32 , 71 ], one in Malta [ 69 ], and one in Australia [ 64 ]. Four referred to multiple countries (e.g., low and middle income countries [ 72 ], Ireland and the UK [ 59 ]). Of these, two did not specify the geographical setting in full [ 34 , 58 ]. Five articles did not provide any reference to the geographical setting of their work [ 29 , 65 , 66 , 70 , 74 ].
In terms of research design, 15 articles adopted a single or multiple case study design [ 32 , 34 , 71 , 75 – 78 , 35 , 55 , 56 , 58 , 61 , 64 , 67 , 69 ]. The majority of these presented recommendations for policy and research practice derived from the authors’ experiences of research ethics-related issues they had faced and navigated in their own studies. Six articles were commentaries offering critical reflections on research ethics, without reference to a specific empirical study [ 29 , 30 , 60 , 66 , 68 , 72 ]. Four articles reported on empirical studies that generated primary data: Guta et al’s work discussed the results of a content analysis of ethics review documentation submitted to Research Ethics Boards (REBs) [ 62 ], complemented by a qualitative study based on interviews with REC members, staff, and other key informants [ 28 , 63 ], whereas Shore et al’s article reported the results of a survey of community-engaged research studies reviewed by RECs [ 73 ].
Of the remaining articles, two were methodological and discussed research ethics implications of Community-based participatory research [ 57 ] and Participatory Action Research [ 67 ]. A further two were theoretical in nature: Ross et al presented a research ethics framework to support Community Engaged Research [ 38 ]; Lange et al [ 65 ] discussed the concept of vulnerability and its implications for research ethics. The remaining two were literature reviews. Doyle et al provided a synthesis of the literature that supported the design of a framework to aid the research ethics approval process by RECs [ 59 ]. Tamariz and colleagues’ systematic review identified the most common perceived barriers and facilitators to evaluating research ethics oversight for Community based participatory research [ 74 ].
Research methodologies underpinning the reviewed articles were wide-ranging. Some articles referred to participatory or collaborative research [ 32 , 35 , 72 ] or community engaged research [ 38 , 66 , 73 ] as loosely defined umbrella terms, or emphasised the use of qualitative research methods [ 30 , 34 , 59 , 64 , 68 – 70 , 75 , 76 ]. Other articles were grounded in specific definitions and epistemological traditions, such as Community-based participatory research [ 28 , 57 , 62 , 63 , 67 , 71 , 74 , 77 ] or Participatory Action Research [ 56 , 61 , 78 ]. One article positioned co-design as a collaborative approach to implementation research [ 29 ], one focused on collaborative approaches in quality improvement [ 60 ], and one referred to co-production in the context of participatory organisational research [ 55 ].
Study populations could be classified into two broad groups. About a third of the articles did not describe or provide a definition of their study population [ 28 , 29 , 74 , 30 , 34 , 38 , 57 , 60 , 62 , 63 , 73 ]. Such articles typically focused on a specific methodological approach and discussed its implications for research ethics, regardless of the study population or research setting. Of the remaining studies, three focused on vulnerable individuals broadly defined [ 34 , 65 , 68 ] and the others focused on specific populations deemed vulnerable. In these articles, vulnerability was defined according to demographic characteristics such as age (e.g., young [ 56 , 78 ] or older people [ 55 ]), illness (e.g., mental health problems [ 35 , 70 , 72 ], palliative care patients [ 76 ], people living with HIV/AIDS [ 66 ]) or disability [ 61 ], socio-economic deprivation [ 77 ], geography [ 71 ]. In other cases, vulnerability was framed as situational, being defined by individual circumstances at a specific point in time. These included grandparent caregivers [ 67 ], Lesbian, Gay, Bisexual, Transgender, Queer (LGBTQ) former foster youth [ 67 ], participants from small connected communities, which may pose challenges to the anonymity and confidentiality of research participants [ 58 , 69 ], or people diagnosed with a long-term condition who may move through vulnerable moments in their illness trajectory (such as rheumatoid arthritis [ 75 ]), and clinical staff and patients who had been involved in clinical incidents which made them temporarily vulnerable [ 64 ].
We found wide variation in the level of coverage of the twelve analytical themes ( Table 6 ). A few themes have been sparsely discussed. The theme on compliance with legislation was touched on only by one article. This highlighted the possible tension in decision-making processes about research ethics when pieces of relevant legislation or regulation are broad in scope and require (or allow) some degree of interpretation [ 77 ]. The theme on integrity, quality and transparency of research was discussed only by Øye and colleagues in two different but related articles. In the first, they discussed how gatekeepers may influence the way in which the recruitment of participants is carried out and reported [ 34 ]. In the second, they questioned the principle of scientific integrity and research independence in the context of collaborative research, when stakeholder groups with different interests and agendas, necessarily negotiate research plans and the reporting of research results [ 32 ]. The theme of accessible findings was discussed in two articles, suggesting ways in which RECs could support wider dissemination of research, beyond academic circles [ 57 , 62 ].
https://doi.org/10.1371/journal.pone.0296223.t006
Other themes have been explored more widely, often using the experiences, positive or negative, of their authors as a starting point to discuss how the ethics system currently handles collaborative research, to highlight good practices and identify recommendations for improvement. Several articles highlighted that the biomedical and technocratic approach of research ethics processes and the way in which RECs work are poorly aligned to collaborative research, its relational nature, emergent designs, inclusive approach, and do not allow the flexibility and ongoing adaptations that such research requires [ 28 , 29 ].
The literature has discussed the tension between the involvement of patients, service users, and the public in research–a key feature of collaborative research–and the protection of research participants–a primary concern of research ethics. Although the need for appropriate participant protection was consistently recognised [ 34 , 75 , 76 ], some authors highlighted that, at times, RECs showed an over-protective attitude towards participants, which ultimately could affect agency of individuals and their participation and inclusion in research [ 38 , 61 , 65 , 68 , 72 ]. Therefore, they argued for an overhaul of the way risks and benefits associated with qualitative and collaborative research are framed and assessed, considering that risks are often low (and lower than for biomedical research), whilst benefits from participation are apparent and should not be dismissed [ 38 , 57 , 59 , 60 , 73 , 76 , 78 ]. Moreover, they highlighted that, given the nature of collaborative research, benefits and risks can unfold both at the individual and at the community level and should be assessed accordingly [ 29 ].
Consent-seeking practices can be seen as an example of how research ethics principles are operationalised in the context of collaborative research [ 35 ]. The suitability and appropriateness of traditional consent-seeking procedures, by which participants are requested to give one-off consent in writing, were questioned with specific reference to collaborative research [ 55 , 57 ]. Similarly, traditional research ethics systems were perceived as being uneasy about co-researchers identified from groups labelled or potentially perceived as vulnerable [ 32 , 67 , 78 ].
The role of the researcher and the nature of the research protocol were also recurring themes. Some authors contended that the role of the researcher is relational and constructed continuously on the spot [ 34 ]. They argued that researcher’s skills and experience in attending to ethical relationships with participants and in self-reflection should be integrated into research ethics frameworks [ 72 , 75 ] and considered when defining acceptable levels of risk tolerance [ 59 ].
Several authors commented on the constraints of the biomedical framework that underpins the research protocols required by RECs [ 62 , 74 ]. Standard protocols do not fully allow articulation of the relational nature of collaborative research (e.g., to define the nature of the relationships across participants, co-researchers, and researchers, and establish how their power differentials will be addressed [ 61 ]). They also fail to accommodate its emergent and iterative nature, e.g., when initial research results inform subsequent data gathering and methodological choices [ 64 ], and those layers of everyday ethics which are intrinsic to collaborative research [ 35 ].
Privacy and confidentiality are further themes which have been covered in the literature. The blanket approach to anonymity as the bedrock of confidentiality and privacy was disputed: whilst for some research participants this may be appropriate (e.g., in small connected communities [ 58 , 69 ]), for others, protection of anonymity should be flexed to reflect participants’ preferences (e.g., in the case of young participants, who may perceive the requirement of anonymity as unjust and discriminatory when based on age [ 78 ]). Researchers argued that concepts of privacy and confidentiality are context-specific and culturally-constructed, and research ethics practices should be tailored accordingly.
The literature review highlighted two themes not included in the initial thematic framework. The first was the membership of RECs [ 28 , 29 , 32 , 56 , 57 , 60 , 62 , 74 ]: a recurrent perception was that experience and expertise of qualitative and collaborative research among REC members is minimal, affecting how applications are reviewed and approved. To overcome this, some authors recommend establishing special RECs for collaborative research.
Training was a further additional theme. The literature highlighted the need for REC members to receive training in the full range of research methods and study designs and also recommended that researchers, co-researchers, and gatekeepers engaged in collaborative research should be offered an opportunity to gain a deeper understanding of research ethics, REC culture, and processes [ 29 , 32 , 56 , 57 , 60 , 62 , 74 ].
Exploratory focus group
The analysis of the focus group data identified 9 of the twelve themes of the analytical framework ( Table 7 ).
https://doi.org/10.1371/journal.pone.0296223.t007
At a general level, participants described obtaining ethics approval as a bureaucratic hurdle, particularly burdensome for research involving groups deemed vulnerable by research ethics committees
“I feel the burden of newly found bureaucracy . As we were going through the procedures to prepare for our project , that involved people with dementia , one of the questions that emerged was how much more paperwork will it entail to involve them . Maybe it’s a bit trite , but there was a consideration of how can we involve this group less , so the burden on getting ethics is smaller .” (FG1-4)
They also talked about the poor fit between their research and the underpinnings, practices, and language of the research ethics framework within which they were expected to operate. Participants highlighted how the research ethics approval process posed great emphasis on the approval phase of a study, when the study is appraised prospectively, with less relevance given to the actual conduct of research
“One of the things that I found problematic is the extent to which the whole process is front-loaded . Ethics committees will be very paternalistic in the initial stages of giving approval to a piece of research , but then don’t seem to particularly be interested in monitoring the conduct of the research .” (FG1-3)
In relation to Theme 2—Patient, service user, and public involvement, participants highlighted that there could be scope to engage the public and ask what ethical research means to them
“Some of those concepts [about research ethics] haven’t really been aired , in terms of public contribution and what the public would say are important concepts when we think about ethics . There’s something about unravelling some of those concepts and saying , are they the right ones actually now ? Are they fit for purpose ? (…) And as soon as you start talking about the public , their view of what is ethical conduct around involvement or around research can feel different .” (FG1-6)
In relation to Theme 3—Protection of research participants, the group highlighted the protectionist approach that RECs seem to take towards research participants. They underscored the lack of a proportionality in the way risks and benefits are assessed, at times catastrophising the worst scenarios and discounting (or ignoring) possible benefits of research participation
“What’s interesting about it is (…) the very high level of paternalism that is triggered when you’re trying to organize consent process in a research context (…) which sits rather awkwardly with the idea of empowering members of the public , patients , participants in research , to make their own judgments about their involvement . And here we’re really only talking about studies which involve interviews and questionnaires from highly experienced researchers .” (FG1-5)
In their view, this approach was inconsistent with the ongoing discourse around involvement in health and social care research. In particular, they unravelled the tension between the involvement of groups who are seldom heard in research and the perceptions that RECs may have of these groups (such as homeless people as discussed in the extract below)
“People around the [research ethics] system have a particular view of what homeless people are like , and they’re all horribly vulnerable and we should never approach them . And often they’re not . They have quite a high degree of agency .” (FG1-8)
Alongside highlighting the need to shift towards a more proportionate, risk-based approach to research ethics oversight, participants also underscored the need to design processes better suited to ensure participant protection
“Ethical processes are very important , to make sure that we’re protecting the participants , and they are necessary . It’s just how we implement them in a way that’s most appropriate and acceptable and feasible for the people who are completing them …” (FG1-9)
In relation to Theme 5—Role and competence of researchers, in the experience of participants, the research ethics system seemed to be concerned with protecting participants from possible unethical behaviour of researchers, whose ethos and competencies are undervalued
“I feel sometimes as if I’m a delinquent , who hasn’t yet been found out . The system is geared to treat me as if I’m fundamentally likely to be irresponsible in my dealings with people who are involved in research with me . My experience is that researchers , if anything , are very cautious and careful and thoughtful about the way they engage in this kind of activity .” (FG1-5)
Participants also discussed how the research ethics system is ambivalent in the way the idea of trust towards researchers is framed. On the one hand, the system seems to rely on a front-loaded process that aims to pre-empt ethical issues at the outset of a study and to foresee procedures to mitigate potential issues. On the other, when in the field, researchers operate with substantial degrees of freedom
“Once you get through , there is quite a lot of trust . All the day-to-day ethical decisions we make as researchers… we’re being trusted on those .” (FG1-10)
The group agreed that research ethics policies and institutions should move away from research ethics pivoted around the written word and accept the relational and situated dimension of research ethics
“(Any changes) should be on the basis of trying to introduce more trust into the system . The trustees seem to rely so much on the paperwork rather than on the people with the people , and the trust and responsibilities that people have .” (FG1-8)
Related to Theme 6—The working of RECs, participants described the interactions between research teams and RECs, at times perceived as confrontational and transactional
“It took three iterations of the REC meeting to be able to get approval in the end to involve people who lacked capacity in the research , and then it was at the expense of having to make other concessions .” (FG1-3)
They also highlighted how the review process of research aiming to involve groups deemed vulnerable was in their experience more burdensome than for other populations
“We did eventually get approval for that (i . e ., a study that included people who lacked capacity) . Although it took more times going back to the committee than other projects have .” (FG1-2)
Participants could envision the research ethics approval being handled in a more relational way and as a two-way process, by which RECs and researchers could identify, discuss, and address ethical matters together as the study unfolds. This shift could be beneficial in particular for research with an emergent design, given the expectation that amendments of the research protocol would be required as the research process progresses
“I wish that the whole process could be more collegiate in the way that it’s carried out . That it could be more like a process of mentoring throughout the whole research process , than having to pass an exam at the beginning of it .” (FG1-3)
Participants discussed options to mitigate the uneasiness of some RECs in dealing with collaborative research approaches, specific topics, and research groups that could be perceived as vulnerable
“I wonder if it’s possible to have RECs that are more topic-specific . Or since there are specific consideration for working with vulnerable populations , can there be one or two RECs that specialize on this particular concern ? And they apply the principles in a consistent way across the country .” (FG1-1)
Participants reported several issues in relation to Theme 7—The research protocol. The current protocol template was described as unfit for use in the context of collaborative research using emergent designs
“You find you have to fit your project into a particular kind of language and forms and structure in order to get through .” (FG1-10)
Researchers found the information sheets that they were required to use when recruiting study participants particularly problematic. They felt that these documents looked officious and were hard for the lay public to understand, seemingly protecting the institutions sponsoring the study rather than the participants themselves. Participants suggested that documents supporting participant recruitment could be simplified in many ways
“Information sheets that it’s in one to two pages maximum in decent size font , without all of the sort of legal clauses that are really complicated to understand . (…) I’d really like to see it literally in very easy , accessible everyday language .” (FG1-9)
Relatedly, participants also highlighted that in their experience consent-seeking was operationalised in standardised, one-off procedures heavily reliant on the written word (e.g., completing and signing a consent form) rather than as a relational, continuous process. They also raised issues about how the Mental Capacity Act (MCA) is interpreted by RECs. This resulted in limiting the opportunities for individuals with fluctuating capacity and declining cognitive function to take part in research, or in resorting to secondary consent, in contradiction with the discourse around empowerment, or in research lacking real-world relevance
“During the XX research study , I was put under pressure by a REC to only recruit people who had capacity , even though there would have been a small minority of the people living in that care environment , on the basis that Sections 30–33 of the Mental Capacity Act [which relate to research with people who may lack capacity in England and Wales] say that you can include people who lack capacity only if it’s not possible to answer your research question by including people who do have capacity . And I was told by the Chair of that REC that the representativeness of the research was not an issue , as far as they were concerned . It didn’t matter if the participants who were actually recruited represented the people living in that care environment or not , because they were going by the letter of the Mental Capacity Act .” (FG1-3)
Lastly, they underscored the burden posed to research by current legislation (or its interpretation by RECs, as illustrated by the extract above on the MCA) and how the legal requirements were embedded in the documentation used for research purposes (e.g., to comply with legislation on privacy and confidentiality) (Theme 9 –Compliance with legislation).
No data were collected in relation to themes 4, 11, and 12. One additional theme on local research governance arrangements when carrying out research involving statutory organisations (e.g., NHS hospital trusts) was identified
“The local R&D governance processes raise many of the same issues (…) . The system , certainly at the local level , is still really organized as if everyone’s doing a clinical trial ” (FG1-5)
This article provides an overview of the literature on research ethics in the context of collaborative health and social care research and complements it with the perspectives of active academic researchers with experience of navigating the English research ethics system.
The thematic framework that supported the scoping review and the analysis of the focus group data was organised around the normative principles and operational processes identified with the analysis of UK research ethics policies.
In taking this approach, this work focuses on research ethics as a function of the apparatus of research governance (i.e., the broad range of regulations, principles, and standards of good practice in research) and moves away from previous work conflating the discussion of research ethics requirements and ethical practice in research [ 80 – 82 ].
Importantly, using an analytical framework that stems from a normative standpoint allowed comparison of how the research ethics system is expected to work vs how it works in practice, according to the literature and based on actual experiences of researchers in the field. We applied the framework to the literature identified with the scoping review and updated and improved on a previous review assessing the literature published between 1990 and 2002 against the ethical principles outlined in the Belmont Report (i.e., autonomy, beneficence, and justice) [ 83 ]. We then used the framework to analyse focus group data, generating original empirical evidence about how the research ethics system is currently experienced by active researchers undertaking collaborative research in England.
Our review shows that the literature on this topic is heterogenous (e.g., in terms of language used to identify research using collaborative approaches) and broad in scope. By mapping out how key ethical principles and processes have been dealt with in the literature, it shows that the coverage received by each theme varies substantially. Despite being among the stated principles underpinning research ethics policies, themes around compliance with legislation, integrity, quality and transparency of research, and accessibility of research findings were sparsely covered in the literature. Similarly, they were not discussed by focus group participants as extensively as other topics. Reasons for this are unclear, but it may be that these themes are perceived as peripheral to research ethics per se and are expected to be addressed at different points in the wider research systems (e.g., accessibility of research findings may be addressed prospectively at the point of research funding application and/or at the end of a study, and may be largely seen as a concern of research teams and research funders, not of RECs).
Other themes, such as the working of RECs, the research protocol, and the protection of research participants were found to have received substantial attention in the literature and resonated among focus group participants.
Through the review process, it also became apparent that two themes (‘Training on research ethics’ and ‘REC membership’) discussed in the literature were not captured by the analytical framework we developed from policy documents. The lack of consideration of these two themes seems to reflect the dominant epistemological framework underpinning research ethics policies, at least in the UK context, since international guidance addresses both [ 4 ]. In relation to training, the UK Policy Framework looks exclusively at competencies and qualifications of research teams (Principle 2 Competence [ 7 ]), echoing one of the recommendations of the Helsinki Declaration (“Medical research involving human subjects must be conducted only by individuals with the appropriate ethics and scientific education, training and qualifications” [ 3 ]), taking for granted that REC members are competent to review any type of study regardless of their actual research expertise. Policies do not address REC membership and their expertise either. Historically, this has led to co-option of members with quantitative expertise, well-aligned to the dominant epistemological framework of research ethics, with other types of expertise under-represented [ 30 ]. This issue was also pinpointed by focus group participants who aired the idea of establishing RECs with specialist interest in specific research approaches, topics, or populations.
We note that our review did not find effectiveness of research ethics as an emergent theme across the body of the literature we included. Therefore, this work does not contribute to the ongoing debate about the effectiveness of ethics processes [ 8 , 9 , 11 , 12 ].
Looking at the results across themes, principles, and processes, findings from the literature and from the focus group were highly concordant. The pattern that emerges from both the literature and the focus group converges around issues in how the research ethics system deals with collaborative research and how the research ethics system negatively affects what collaborative research is conducted, and how. On the one hand, this could represent compelling evidence that the positivist underpinnings of research ethics oversight make it unfit for the purpose of reviewing research which does not sit within a positivist paradigm. On the other hand, some of these issues have also been reported in relation to biomedical, experimental research, for example in relation to informed consent [ 84 ], risk-benefit assessments [ 85 ], and the emphasis on procedures and documents to the detriment of day-to-day conduct of research [ 86 ]. Altogether these findings provide empirical corroboration of the concept of ethics creep [ 63 ]: the regulatory structure of the ethics bureaucracy has been expanding outward (e.g., taking over research using collaborative, non-experimental approaches in the social sciences) while at the same time intensifying the regulation of practices deemed to fall within its original scope (i.e., biomedical, experimental research). Consistently with this finding, this work adds to the literature documenting burdens associated with research ethics processes [ 9 , 87 ].
Indeed, the overarching discourse that emerges from both the literature and the focus group points towards the need for an overhaul of the rule-based, procedural approach to ethics threaded throughout current regulatory policies and structures, and endorses processes of ‘micro ethics’ [ 42 ], ‘situated ethics’ [ 34 , 88 , 89 ], relational ethics [ 90 , 91 ], that place emphasis on ‘ethical mindfulness’ [ 92 ] and reflexivity [ 93 ] on the part of individual researchers.
In this vein, this work also offers a rich catalogue of options for improving how the research ethics system could deal with collaborative research. Improvements expressed at the level of principles (e.g., framing consent as an ongoing process or embedding some degree of tolerance around risk, both discussed in the literature and among focus group participants) could open a line of work for research ethics institutions interested in exploring how to translate these principles into institutional processes. Among those expressed at the level of processes, some could be considered for implementation by research ethics institutions (e.g., the creation of specialist RECs, as suggested by focus group participants), others could be used as practical recommendations and advice for researchers navigating the research ethics system.
It is important to recognise strengths and weaknesses of this work. Our analytical framework was based on the analysis of research ethics policies published by UK institutions. However, the themes themselves are consistent with international research ethics frameworks currently in use and the analytical categories of ‘Principles’ and ‘Processes’ are broad enough to ensure that the results of the review are relevant beyond the UK context.
To our knowledge, the scoping review is the first attempt to map the academic literature discussing how the research ethics system deals with collaborative research in the health and social care field. The review identified journal articles published between 2010 and 2022 and indexed in three online academic research databases. Most of the included article were published between 2010 and 2015, when collaborative research approaches became increasingly popular. The academic debate about research ethics flourished at this time [ 29 ], with researchers sharing their experience of navigating the research ethics approval process for collaborative studies and often offering guidance and advice to others with similar research interests. This may have contributed developing a community of practice comfortable with addressing the requirements of research ethics. Perhaps as a result, the scholarly interest in writing about this topic in academic outlets subsequently faded away, to be replaced by methodological and good practice guidance published in the grey literature. Although this was outside the scope of this work, we are aware that resources have been made available by organisations such as those under the WHO umbrella (e.g., [ 94 ]), national research infrastructure (e.g., [ 95 , 96 ]), University-based Research Ethics Committees, and organisations acting as research facilitators and gatekeepers (e.g., [ 97 ]).
The identification of focus group participants began from our professional networks, which may have led to a dominance of participants from certain fields (e.g., dementia care and social care research) and exclusion of others. This could have biased the nature of the discussion towards certain themes or experiences. Also, the focus group was conducted at the beginning of the COVID pandemic, which affected the recruitment of participants.
Conclusions
The need for regulation and ethics oversight of research using collaborative approaches is not questioned. It is clear, however, that the biomedical regulatory framework currently in use presents obstacles to this type of research. This work documents the wide range of issues that researchers may experience when navigating the research ethics system in relation to research adopting a collaborative approach but, more importantly, it also offers options that could help address those issues within the current framework of research ethics.
It would be unrealistic to expect that every option identified could be immediately taken up and seamlessly implemented, and will then deliver positive results. Some practical recommendations could be voluntarily adopted by research teams and RECs alike and could help streamline some elements or procedures of the research ethics system. However, other options would require formal and procedural changes in research ethics processes that should be initiated by relevant institutions. Some of these may need to be accompanied by fundamental changes in the culture that surrounds research ethics, from it being a bureaucratic, prospective, front-loaded process taking place in a confrontational environment to an opportunity to think through ethical issues throughout a study in the context of a formative and collaborative process.
We hope that this work will help move the debate onwards and contribute to an agenda for change of research ethics for collaborative research in the health and social care field, and beyond.
Supporting information
S1 file. scoping review of the literature–search strings..
https://doi.org/10.1371/journal.pone.0296223.s001
S2 File. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist.
https://doi.org/10.1371/journal.pone.0296223.s002
- View Article
- PubMed/NCBI
- Google Scholar
- 2. World Medical Association. Declaration of Helsinki. Helsinki: World Medical Association; 1964. https://doi.org/10.5694/j.1326-5377.1973.tb76647.x
- 5. National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report: ethical principles and guidelines for the protection of human subjects of research. Washington, DC: Department of Health, Education, and Welfare; 1979.
- 15. Spike J. Putting the “ethics” into “research ethics.” American Journal of Bioethics. Taylor & Francis Group; 2005. pp. 51–53. https://doi.org/10.1080/15265160590927822 pmid:16036663
- 31. Van de Hoonard WC. Walking the tightrope: Ethical issues for qualitative researchers. Van de Hoonard WC, editor. Toronto: University of Toronto Press.; 2002.
- 50. Health Research Authority. Standard Operating Procedures for Research Ethics Committees. The Health Research Authority; 2019. Available: https://www.hra.nhs.uk/about-us/committees-and-services/res-and-recs/research-ethics-committee-standard-operating-procedures/ .
- 66. Lavery J V. Wicked problems’, community engagement and the need for an implementation science for research ethics. Journal of Medical Ethics. BMJ Publishing Group; 2018. pp. 163–164. https://doi.org/10.1136/medethics-2016-103573 pmid:27538984
- 81. Wilson E, Kenny A, Dickson-Swift V. Ethical Challenges in Community-Based Participatory Research: A Scoping Review. Qualitative Health Research. SAGE Publications Inc.; 2018. pp. 189–199. https://doi.org/10.1177/1049732317690721 pmid:29235941
- 83. Mikesell L, Bromley E, Khodyakov D. Ethical community-engaged research: A literature review. American Journal of Public Health. American Public Health Association; 2013. p. e7. https://doi.org/10.2105/AJPH.2013.301605 pmid:24134352
- 84. Jefford M, Moore R. Improvement of informed consent and the quality of consent documents. The Lancet Oncology. Elsevier; 2008. pp. 485–493. https://doi.org/10.1016/S1470-2045(08)70128-1 pmid:18452859
- 97. DEEP. The DEEP-Ethics Gold Standards for Dementia Research. DEEP; 2020. Available: https://www.dementiavoices.org.uk/wp-content/uploads/2020/07/The-DEEP-Ethics-Gold-Standards-for-Dementia-Research.pdf .
- Technical Support
- Find My Rep
You are here
Making Sense of Research in Nursing, Health and Social Care
- Pam Moule - University of the West of England, UK
- Description
What is research and how does it work in the context of nursing, health and social care?
Now in its 7 th edition, this introductory guide provides you with a concise overview of the different research methods and terminology that you will come across when undertaking research in any course related to nursing, health and social care. The book’s easy-to-follow structure takes you from research novice to confident researcher, helping you to make sense of research and understand how it is implemented in healthcare practice.
The new edition includes:
- Updates in line with the 2018 NMC standards, with more information on the impact of GDPR, consent and vulnerable groups, Personal and Public Involvement (PPI), and work-based projects.
- Improved case examples of real research, with more on group work, poster presentations, research output and dissemination, literature reviews, and dissertations.
- Upgraded activities that include reflective exercises, critical appraisal tools, a dissemination plan, and a glossary, all in the book.
This is essential reading for undergraduate and postgraduate students within the health and therapy professions, nurses, midwives, physiotherapists, radiographers, occupational therapists, speech and language therapists, and paramedics.
See what’s new to this edition by selecting the Features tab on this page. Should you need additional information or have questions regarding the HEOA information provided for this title, including what is new to this edition, please email [email protected] . Please include your name, contact information, and the name of the title for which you would like more information. For information on the HEOA, please go to http://ed.gov/policy/highered/leg/hea08/index.html .
For assistance with your order: Please email us at [email protected] or connect with your SAGE representative.
SAGE 2455 Teller Road Thousand Oaks, CA 91320 www.sagepub.com
Some books reach their silver anniversary and start to look dated and lose their relevancy. Making Sense of Research in Nursing, Health and Social Care however, has renewed and refreshed at each edition and maintains its applicability for today’s health and social care professionals.
One of the marks of a good textbook is its ability to appeal to readers across professional boundaries and with varying levels of experience in the topic at hand; Moule achieves this both engaging those new to research as well as providing different insights for those with more research knowledge and experience. One of the stated intentions of the book is to make research interesting and in so doing to help practitioners in their adoption of research and evidenced based practice within their work. Moule achieves this with the use of an accessible writing style which is at once both engaging and thought provoking. I would recommend this book as a must have on the shelf for any student of health and social care be they a first year undergraduate or a more experienced individual engaging in post graduate studies.
Evidence-based practice is crucial for the modern healthcare practitioner. Students can often shy away from the topic of research thinking that the subject is too complex for them. However, the benefits of this book in guiding them through the subject include: easy to read short sections with headings, clear key messages at the beginning and end of each chapter and links to current, credible sources of evidence to expand their reading further. Some students find it difficult to seek out credible secondary sources and this book gives them links to guidelines and reports which would be appropriate to inform their assignment work.
Books about the research process are not rare but few authors can clarify the basics with such ease like Pam Moule. This textbook is easy-to-read, speaks to the research novice in accessible language, and leaves the reader feeling well-initiated in research literacy. Without hesitation I would endorse this textbook for undergraduate health and social care students who will draw from it from the first term of study to the last. The chapters take the reader on a journey through critical reading right through to the fundamentals of research project design, and instill habits of systematic thought and process in all elements of research. Included are a number of helpful links and templates as well as examples to aid visualization of new concepts. This book is the perfect springboard to launch health and social care students into evidence-informed practice without overwhelming and scaring them off from what can undoubtedly become a more complex topic with further reading.
This is an informative and easy to read book, which introduces the students to research and directs them through the research process. I have used previous editions of this book and have it on the reading list for research modules I teach to both undergraduate and postgraduate students. The use of practice examples and scenarios clearly demonstrate research in action in health and social care. This new 7th edition will be a valuable addition to the reading list on my modules.
The previous editions of this book have been a steadfast resource and the ‘go to book’ for all levels of paramedic students studying at undergraduate level. The seventh edition of this book does not disappoint and will be the new ‘go to’ edition for current students who want to understand how to make sense of research in health and social care. The format of the book makes it easy to access the information making it a valuable and informative resource for all students in healthcare settings, and especially useful when undertaking a final project/dissertation.
This book is an excellent text that will provide an invaluable resource to health and social care practitioners who are new to research or those undertaking projects. The detailed discussion of the research process is written in an informative and authoritative way that informs the reader and makes the research process and terminology accessible.
Excellent - I will be directing students to this resource to support learning for enquiries into health and social care research.
Such a clear and easy to read text. A seminal volume!
Easy to understand for L5 students, applied examples and clear explanations.
this book is clearly written, easy to read and easy to understand
Preview this book
For instructors, select a purchasing option, related products.

Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.

National Institute for Health and Care Research
We fund, enable and deliver world-leading health and social care research that improves people's health and wellbeing, and promotes economic growth.
Read NIHR news
Read NIHR blog
NIHR launches £50m ‘Challenge’ funding to tackle inequalities in maternity care
The new call will invest in research to tackle inequalities in maternity care. The funding call will establish a diverse research consortium to deliver research and capacity building over five years.
Read the full news story

Project funding
We fund a variety of commissioned, researcher-led and themed call research:
- in health, social care and public health
- in Global Health
Search project funding opportunities
Career development
We support the development of professionals through:
- personal awards including Fellowships
- practitioner academic training
- Global Health Research careers
Find career development opportunities
Making a Difference

Preventing early heart disease in high-risk patients
Use of new software developed with NIHR funding is identifying more patients at high risk of early heart disease and heart attacks. Earlier diagnosis and treatment are saving lives and shaping healthcare policy.

Breaking down barriers to effective cystic fibrosis treatment
In the biggest cystic fibrosis trial in the UK, NIHR-funded research has shown that a personalised web platform, CFHealthHub, could markedly increase adherence to treatment.

NHS programme linked to 20% reduction in risk of diabetes
An NIHR-funded evaluation showed referring people with pre-diabetes to the NHS Diabetes Prevention Programme cut their risk of progressing to diabetes by 20%.
Read our case studies
Applied health and care research on both commissioned and researcher-identified topic areas.
Explore our Programmes
Research Infrastructure
Find out more about our expertise, specialist facilities, research delivery workforce and support services.
Explore our offers
Specialty therapy areas
The NIHR funds and supports research:
- in all specialty therapy areas
- delivered by expert clinical leaders and practitioners
- through effective collaboration
Discover our specialties

Global Health Research
NIHR is a major funder of high quality global health research that directly addresses the diverse health needs of people in low and middle income countries (LMICs).
Explore our Programme
Journals, publications and data
Explore NIHR-supported research projects, their findings and data from our range of resources:
- 5+ journals and publications for the public, care and research professionals
- 3+ open access health research databases
Explore our research

New figures suggest the public's appetite for taking part in research remains remarkably high after an unprecedented period in research history.
Find out more about the NIHR annual statistics
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies

Maximising the benefits of research: Guidance for integrated care systems
England has a vibrant research and development ecosystem, with well-developed research infrastructure and research expertise within our health and care workforce. The value of research in transforming health and care is significant; additionally, staff satisfaction, recruitment and retention is higher among staff who are involved in research. The inception of integrated care systems (ICSs) provides the opportunity for systems to embed research within health and care for the benefit of our population. Supporting this opportunity, a clear research thread runs through ICS strategies and plans, from joint strategic needs assessments and joint health and wellbeing strategies , integrated care strategies , joint forwards plans , integrated care board (ICB) annual reports and the assessment by NHS England of the discharge of duties by ICBs.
The Health and Care Act 2022 (the 2022 Act) sets new legal duties on ICBs around the facilitation and promotion of research in matters relevant to the health service, and the use in the health service of evidence obtained from research. NHS England will assess ICBs for their discharge of these duties. The ICS design framework sets the expectation that in arranging provision of health services, ICBs will facilitate their partners in the health and care system to work together, combining expertise and resources to foster and deploy research and innovations. This guidance supports ICBs in fulfilling their research duties.
ICSs are encouraged to develop a research strategy that aligns to or could be included in their integrated care strategy. This strategy will enable the unification of research across ICS partners, and be consistently embedded to:
- identify and address local research priorities and needs, and work collaboratively to address national research priorities
- improve the quality of health and care and outcomes for all through the evidence generated by research
- increase the quality, quantity and breadth of research undertaken locally
- extend and expand research in settings such as primary care, community care, mental health services, public health and social care
- drive the use of research evidence for quality improvement and evidence-based practice
- influence the national research agenda to better meet local priorities and needs
- improve co-ordination and standardisation within and between localities for the set up and delivery of research
- harness the patient and economic benefits of commercial contract research
- co-ordinate and develop the research workforce across all settings.
1. Introduction
This guidance sets out what good research practice looks like. It supports integrated care systems (ICSs) to maximise the value of their duties around research for the benefit of their population’s health and care and, through co-ordination across ICSs, for national and international impact. It supports integrated care boards (ICBs), integrated care partnerships (ICPs) and their partners to develop a research strategy that aligns to or can be incorporated into their integrated care strategy, and helps them and their workforce to build on existing research initiatives and activities across health and social care to improve sector-wide performance and best practice
- explains the ICB legal duties and other requirements around research and the use of evidence from research, and that research is included in forward planning and reporting
- encourages system leaders to develop a footprint-wide research strategy that aligns to local and national research priorities, develops and supports their workforce, takes the opportunities offered by commercial research and includes plans to embed research in their system’s governance and leadership
- identifies best practice examples and other resources that ICBs may find useful as they develop their research strategies.
This guidance provides comprehensive information for use by:
- those with senior responsibility, including at board level, for research strategy development and/or operationalising research
- managers responsible for developing joint strategic needs assessments, integrated care strategies, joint health and wellbeing strategies, joint forward plans, other linked strategies, or reporting on ICB activities
- research managers
- research and development/innovation leads
- heads of services
- knowledge and library specialists.
It may also be useful to individuals involved in research, education, and partner organisations such as local authorities, social care services, the voluntary, community and social enterprise sector (VCSE) and other providers of healthcare services.
NHS England provides guidance on embedding research in the NHS and secure data environments, and the Office for Life Sciences (OLS ) champions research, innovation and the use of technology to transform health and care service. Other sources of guidance, support and information are signposted in this guidance to support ICSs in aligning to national visions, strategies and plans around research.
1.1 Definition of research
NHS England uses the UK Policy Framework for Health and Social Care Research definition of research:
“… the attempt to derive generalisable or transferable new knowledge to answer or refine relevant questions with scientifically sound methods. This excludes audits of practice and service evaluation. It includes activities that are carried out in preparation for or as a consequence of the interventional part of the research, such as screening potential participants for eligibility, obtaining participants’ consent and publishing results. It also includes non-interventional health and social care research (that is, projects that do not involve any change in standard treatment, care, or other services), projects that aim to generate hypotheses, methodological research and descriptive research”.
This broad definition encompasses the range of types of research:
- clinical trials and other clinical investigations into the safety and effectiveness of medicines, devices and health technologies
- public health research
- observational studies
- discovery science and experimental medicine
- translational research in which results from basic research are developed into results that directly benefit people
- applied research
- research to support policy-making and commissioning
- social care research and research in social care settings
- research into NHS services and care pathways.
1.2 Why research is important
The UK is a world leader for research and invention in healthcare, with around 25% of the world’s top 100 prescription medicines being discovered and developed in the UK ( The impact of collaboration: The value of UK medical research to EU science and health ). Research in the health and care system is important because it underpins all advances in health and care and is the basis for evidence-based practice. Engaging clinicians and healthcare organisations in research is associated with improvements in delivery of healthcare ( Does the engagement of clinicians and organisations in research improve healthcare performance: a three-stage review) . To benefit service users and the public, the NHS and local government, and achieve return on investment, it is vital that research is disseminated, shared and translated into practice.
The National Institute for Health and Care Research (NIHR) is funded by the Department of Health and Social Care (DHSC) to transform research in the health and social care system, including through support for NHS research. Research led to the first proven treatments for Covid, for example the use of dexamethasone, estimated to have saved over a million lives worldwide . This success was in part due to how research is undertaken in the unique environment of the NHS, innovative trial designs, the support provided by the NIHR, frontline staff enabling research, and the awareness and readiness of the public to support research. We need to learn from these and other successes, and translate this across all health and care settings. ICSs will play a vital role in enabling research to be embedded in evolving patient pathways across their footprints.
Example: PRINCIPLE trial – finding treatments for Covid recovery at home
The Platform Randomised Trial of Treatment in the Community for Epidemic and Pandemic Illnesses (PRINCIPLE) was a UK-wide, clinical study to find Covid treatments for recovery at home without the need to attend hospital. The study was open to all with ongoing Covid symptoms, registration was easy, and the trial was run entirely remotely by delivering ‘participant packs’ to people’s homes. It was one of the first trials in the world to show that azithromycin and doxycycline did not benefit patients with Covid and to identify the effectiveness of a commonly used drug – inhaled budesonide –in reducing time to recovery.
The PRINCIPLE study team demonstrated the integral role that primary, secondary and ambulatory care staff can play in the delivery of studies. Local collaborators were trained in good clinical practice to allow them to assess and confirm the eligibility of potential participants, and were commended specifically for their use of patient data to contact people soon after they received a positive test result. It is this network of local staff contributing to research within their healthcare setting that has enabled over 10,000 people to be recruited onto this study so far – one of the largest at home Covid treatment studies worldwide.
This is an example of a study design that incorporates the vital contributions of healthcare providers across the system.
Policy-makers and commissioners need evidence to support their decision-making around the delivery and system-wide transformation of health and care services, including how health inequalities will be reduced.
There is also evidence that:
- staff involved in research have greater job satisfaction and staff turnover is lower in research active trusts ( Academic factors in medical recruitment: evidence to support improvements in medical recruitment and retention by improving the academic content in medical posts)
- research active hospitals have lower mortality rates, and not just among research participants ( Research activity and the association with mortality )
- 83% of people believe that health research is very important ( Survey of the general public: attitudes towards health research)
- healthcare performance improvements have been seen from the creation of academic research placements ( Experiences of hospital allied health professionals in collaborative student research projects: a qualitative study )
- clinical academic research, and in particular the practice changes resulting from it, is associated with improved patient and carer experiences ( A qualitative systematic review and thematic synthesis exploring the impacts of clinical academic activity by healthcare professionals outside medicine ).
Key to having research embedded in health and care is having staff who can understand, undertake, use and generate new research, and share actionable research finding as part of a pro-research culture. Education and training are therefore critical for research to be sustainably embedded within health and care, and for people to develop careers in research and support it in their clinical or care roles.
DHSC, NHS England, the devolved administrations, NIHR and other partners expect to publish a clinical research workforce strategy in 2023/24 to help the UK realise the national clinical research vision outlined in Saving and Improving Lives: The Future of UK Clinical Research Delivery and deliver the Life Sciences Vision to see research embedded in the NHS as part of health and care pathways.
Research will support ICSs to deliver on their four key aims:
Improving outcomes
The NHS 2023/34 priorities and operational planning guidance emphasises the importance of research in improving patient care, outcomes and experience.
Research evidence will inform commissioning decisions to improve experience and outcomes. Research activities should align with the local health priorities identified through local joint strategic needs assessments, and may be best designed and delivered by collaborating with partners. Research priorities may be best addressed by collaborating with partners nationally to design and deliver research.
Tackling inequalities
Research can give a better understanding of local populations and the wider determinants of health, and with this the steps to maintain health and narrow health inequalities.
Enhancing productivity
The development of ICSs creates the opportunity to consider research delivery within the ICS and across ICS boundaries, increasing flexibility of workforce or recruitment while reducing bureaucracy and improving research productivity and value for money.
Supporting social and economic development
An active research ecosystem working in a co-ordinated way and to national standards brings revenue and jobs to regions. The NIHR Clinical Research Network (CRN) supports service users, the public and health and care organisations across England to participate in high-quality research. The 2019 impact and value report detailed the significant income and cost savings that commercial research generates for NHS trusts. Between 2016/17 and 2018/19 the NHS received on average £9,000 per patient recruited to a commercial clinical trial and saved over £5,800 in drug costs for each of these patients. This equates to income of £355 million and cost savings of £26.8 million in 2018/19.
In 2021 150 members of the Association of Medical Research Charities funded £1.55 billion of medical research, including the salaries of 20,000 researchers. Every £1 million spent by charities on medical research in the UK contributes £1.83 million to the economy.
Example: Research that cut problematic prescribing and generated cost savings in general practice – a local health priority
Analysis of routine patient data identified the need for strategies targeting clinicians and patients to curb rising opioid prescribing. From this, the Campaign to Reduce Opioid Prescription (CROP) was launched in 2016, urging GPs across West Yorkshire to ‘think-twice’ before prescribing opioids. This promoted the NICE guidance on chronic pain , which recommends reducing the use of opioids because there is little or no evidence that they make any difference to people’s quality of life, pain or psychological distress, but they can cause harm, including possible addiction.
Over a year 15,000 fewer people were prescribed opioids (a 5.63% relative reduction), a net saving to the NHS of £700,000. The biggest reduction was in people aged over 75, who are at higher risk of opioid-related falls and death, and there was no compensatory rise in the prescribing of other painkillers or referrals to musculoskeletal services.
The CROP campaign, led by researchers at the University of Leeds, has subsequently been rolled out across all ICBs in Yorkshire and the Humber, and the North East and North Cumbria ICB, and the 1,045 practices to which it has been delivered are reporting results similar to the above.
Foy R, Leaman B, McCrorie C, Petty D, House A, Bennett M, et al (2016) Prescribed opioids in primary care: cross-sectional and longitudinal analyses of influence of patient and practice characteristics | BMJ Open 69(5).
Alderson SL, Faragher TM, Willis TA, Carder P, Johnson S, Foy R (2021) The effects of an evidence- and theory-informed feedback intervention on opioid prescribing for non-cancer pain in primary care: A controlled interrupted time series analysis. PLOS Med .
2. ICS, ICP and ICB responsibilities and requirements
ICBs have legal duties and other requirements that relate to research. These are additional to the duties and responsibilities of individual providers within ICS footprints. This section sets out what these duties mean in practical terms and gives examples of how to meet them.
2.1 Legal duties relating to research in the Health and Care Act 2022
Part 1 of the 2022 Act includes specific legal duties for ICBs and NHS England in respect of research. In the Explanatory Notes to the 2022 Act, government sets out how ICBs could discharge their research duty.
Duty to facilitate or otherwise promote research
The ICB duty builds on the previous clinical commissioning group (CCG) duty to promote research, by requiring each ICB, in the exercise of its functions, to facilitate or otherwise promote research on matters relevant to the health service. This duty is intended to include a range of activities to enable research. Section 3 of this guidance outlines ways in which ICBs can do this.
The NHS Constitution also makes clear that patients should be enabled to take part in research: “the NHS pledges … to inform you of research studies in which you may be eligible to participate”.
The Provider Selection Regime (PSR) will be a new set of rules for arranging healthcare services in England, introduced by regulations made under the 2022 Act. The research component should be referred to once the PSR is published.
Duty to facilitate or otherwise promote the use in the health service of evidence obtained from research
This duty similarly builds on the CCG requirement to promote the use of evidence. ICBs must, in the exercise of their functions, facilitate or otherwise promote the use in the health service of evidence obtained from research. For example, ICBs should facilitate or otherwise promote the use of evidence in care, clinical and commissioning decisions.
Duty for ICSs to include research in their joint forward plans and annual reports
Joint forward plans are five-year plans developed by ICBs and their partner NHS trusts and foundation trusts. Systems are encouraged to use the joint forward plan as a shared delivery plan for the integrated care strategy and joint health and wellbeing strategy, aligned to the NHS’s universal commitments. The plan must explain how the ICB will discharge its duties around research, and the ICB must report on the discharge of its research duties in its annual report. These inclusions will raise the profile of research at board level and help embed research as a business-as-usual activity.
The joint forward plan and NHS Oversight Framework guidance set the minimum requirements for what needs to be included in plans and reports.
NHS England duty to include how each ICB is carrying out its duties relating to research in its annual performance assessment of each ICB
NHS England has a new legal duty to annually assess the performance of each ICB and publish a summary of its findings. For 2022/23 NHS England will complete a narrative assessment, identifying areas of good and/or outstanding performance, areas for improvement and any areas that are particularly challenged, drawing on national expertise as required and having regard to relevant guidance. This assessment will include a section considering how effectively the ICB has discharged its duties to facilitate or otherwise promote research and the use of evidence obtained from research.
This, alongside the implementation of the NHS Long Term Plan commitment to develop research metrics for NHS providers, will increase transparency across the system and enable more targeted support for research. Research metrics from NHS England, the Care Quality Commission (CQC) and NIHR will enable the monitoring of progress over time, and are under development with sector colleagues, including providers.
2.2 Legal requirement to work with people and communities
Working with people and communities is a requirement of ICBs, and statutory guidance is available to support them and their partner providers meet this legal duty. A co-ordinated approach across healthcare delivery and research will make it more likely that research reflects what matters to people and communities.
This will also help ICBs to fulfil their legal duty in the 2022 Act to reduce health inequalities in access to health services and the outcomes achieved. Section 3.9 includes links to resources to help guide engagement with underserved communities around research.
The Public Sector Equality Duty also applies and requires equality of opportunities between persons who share a relevant protected characteristic and persons who do not.
2.3 Research governance
While research can address local priorities, it typically operates across ICS boundaries and at national and international levels. Health and social care research is governed by a range of laws, policies, and international, national and professional standards.
The Health Research Authority (HRA ) is responsible for ensuring such regulation is co-ordinated and standardised across the UK to make it easier to do research that people can trust. The HRA is an executive non-departmental public body created by the Care Act 2014 to protect and promote the interests of patients and the public in health and social care research, including by co-ordinating and standardising the practice of research regulation. Local authorities and the NHS are obliged to have regard to its guidance on the management and conduct of research.
Before a research project can start in the NHS in England it must receive approval from the HRA. This includes research taking place in NHS trusts, NHS foundation trusts, ICBs or primary care providers of NHS commissioned services in England, and all research under an NHS duty of care, including that undertaken by NHS staff working in social care or other non-NHS environments.
The HRA schemes indemnify NHS organisations accepting these assurances against any claim covered by the NHS Litigation Authority arising as a result of incorrect assurances. If an NHS organisation duplicates the HRA assessments, it will be liable for any consequences of the decisions it bases on its own checks.
ICBs and partner organisations should have processes for the set up and delivery of research that comply with national laws and systems, and does not duplicate them. Such national systems include confirmation of capacity, National Contract Value Review (NCVR), management of Excess Treatment Costs (ETCs) and contracting arrangements (see section 2.4).
The UK Policy Framework for Health and Social Care sets out the roles and responsibilities of individuals and organisations involved in research.
2.4 Contractual requirements around research
NHS England mandates commissioner use of the NHS Standard Contract for all contracts for healthcare services other than primary care. The contract is updated annually. References to research in the current NHS Standard Contract and service conditions fall into three main areas.
Recruitment of service users and staff into approved research studies
The NHS Standard Contract obliges every provider of NHS-funded services to assist the recruitment of suitable subjects (whether patients or staff) into approved research studies. This requirement aligns to those in the 2022 Act that require ICBs to facilitate or otherwise promote research (see section 2.1). Section 3 considers how this requirement can best be met. Research involving people or their data requires ethical and potentially other approvals (see section 2.3).
National Directive on Commercial Contract Research Studies
Adherence to the National Directive is mandated as part of the NHS Standard Contract. The directive states that providers must:
- Use the unmodified model agreements for sponsor-to-site contracting; HRA and Health and Care Research Wales (HCRW) approval of studies will be dependent on use of these templates.
- Use the standard costing methodology to set prices for commercial contract research undertaken by NHS providers; this is currently in the NIHR interactive costing tool (NIHR iCT).
- Introduce the National Contract Value Review (NCVR) process in line with national rollout. NCVR is a standardised national approach to costing commercial contract research within the NHS. It currently covers acute, specialist and mental health trusts, but the intention is to roll it out to all NHS providers. The creation of ICSs is the ideal opportunity to explore how commercial study set up can be supported across these footprints, reducing the resource needed and time taken.
Comply with HRA/NIHR research reporting guidance
The provider must comply with HRA/NIHR research reporting guidance, as applicable.
2.5 Excess treatment costs
Patients in a research study may receive healthcare that differs from what is standard in the NHS, requires more clinician time or is delivered in a different location. The associated NHS treatment costs may exceed or be less than those of standard treatment. If greater, the difference is referred to as the NHS Excess Treatment Costs (ETCs).
In the case of commercial contract research, the commercial funder will pay the full cost of the study. In the case of non-commercial research, the commissioner of the service in which the study operates is responsible for funding the ETCs.
ICBs as commissioners of services are responsible for ETCs in services that they commission. Guidance for the management of ETCs is available.
DHSC and NIHR are piloting interim arrangements to support non-NHS ETCs for research in public health and social care (non-NHS intervention costs). Please refer to the further detail on the NIHR website .
2.6 Care Quality Commission
The CQC is currently developing its approach for ICS-level assessments, and its new assessment framework will be introduced towards the end of 2023 .
CQC inspection of NHS providers continue, with research assessed as part of the review of the trust-level Well-led framework. Providers are asked:
- Are divisional staff aware of research undertaken in and through the trust, how it contributes to improvement and the service level needed across departments to support it?
- How do senior leaders support internal investigators initiating and managing clinical studies?
- Does the vision and strategy incorporate plans for supporting clinical research activity as a key contributor to best patient care?
- Does the trust have clear internal reporting systems for its research range, volume, activity, safety and performance?
- How are service users and carers given the opportunity to participate in or become actively involved in clinical research studies in the trust?
3. Developing a research strategy
3.1 why develop a research strategy.
Like the health and care system, the research environment is complex. Developing a research strategy will help bring together the legal and other duties around research in a coherent way, and help the ICS understand its local research capability, workforce, activity and needs, set ambitions around research and maximise the benefits associated with commercial research. It will help demonstrate the benefit of research locally, nationally and internationally, and guide the production of clear plans.
Example: Value of research partnerships and integration with ICSs
Bristol Health Partners (BHP) Academic Health Science Centre (AHSC) has a fully integrated relationship as the new Research and Innovation Steering Group for the Bristol, North Somerset and South Gloucestershire (BNSSG) ICS, and reports directly to ICB chief executives.
The group provides the strategic direction and oversight for all research undertaken and delivered across the system. Membership includes directors of research, clinical strategy, public health, social care, senior innovation and education leaders from its core funding partners. It also includes public contributors and senior representatives from primary care, NIHR Applied Research Collaboration West, NIHR CRN West of England, West of England Academic Health Science Network (WEAHSN), Healthier Together ICS, university research institutes and People in Health West of England.
The group has reviewed ICS programmes, identified current and potential research and innovation connections, and begun to establish new connections. It has also supported work with the ICS Ageing Well programme and secured funding for innovative pilots to improve dementia care and increase physical activity for older adults.
Since 2016 BHP has directly contributed an estimated additional £1.1 million to support ICS priorities through Health Integration Team projects and other activities, and has attracted more than £33 million of external research, service redesign and infrastructure into the region.
3.2 General considerations
In developing its research strategy, the ICS may find it helpful to consider these overarching questions alongside the suggested focused content covered in the sections below:
- What do you hope to achieve within a given timeframe?
- Are all the right organisations involved in developing the research strategy?
- How will the health and care workforce be enabled to deliver the research strategy?
- How can research be embedded in existing health and care delivery and pathways?
- What mechanisms are in place to translate actionable research findings into practice and decision-making?
- What inequalities exist in different areas, communities or groups? How will you ensure planning and delivery of research aligns to CORE20plus5 priorities?
- Are you considering equality, diversity and inclusivity and the Public Sector Equality Duty in facilitating and promoting research opportunities for service users and for health and care staff?
- Is the ICS considering the opportunities of developing their commercial research portfolio?
- Is research informing or being informed by population health management?
- How will you plan and deliver research in a sustainable manner, aligning it to the Greener NHS agenda and the ICB’s duties in relation to climate change ?
Buy-in from NHS staff, patients and the public will be vital if ICBs are to discharge their research duties and deliver on their research plans. An important consideration is how to develop sustainable, routine and accessible information flows to ensure the ICB, partners, staff, patients and public can access up-to-date and appropriate information around local research activity, regional, national and international research opportunities and findings, and contact information.
3.3 Leadership and governance across the ICS
Executive leadership.
The Explanatory Notes to the 2022 Act suggest that ICBs have board-level discussions on research activity, the use of the evidence from research, the research workforce and research culture within the ICS. ICSs should refer to the NHS Leadership Competency Framework for board-level leaders at organisation and ICS level for the competencies relating to the research duties of ICSs, once published.
All ICBs are encouraged to have an executive lead responsible for fulfilling the research duties conferred by the 2022 Act. They should help give the ICB a clear understanding of research across the area, regularly reporting on progress towards agreed aims. An executive lead can take responsibility for ensuring clear research ambitions and a research strategy are developed; oversight of organisational research portfolios, diversity in research, alignment to national priorities; promotion of research skills and the need for research skills training; and succession planning.
Senior leaders could engage, consult and be supported by representatives of each registered health and social care professional group when developing strategic plans, and for oversight of training, succession planning, and equality and inclusivity. They could use the capacity and capability of the research and development leads within provider organisations, although established lead roles across social care settings are rare so extra effort may be needed to garner social care research insight.
Research steering group, board or forum
Some CCGs had research steering groups and some of these have expanded with the widening remit of ICBs. ICSs that do not have a such a group should consider adopting a model similar to one in other ICSs where research is effectively embedded in ICS governance structures.
A dedicated steering research group, board and/or forum can:
- provide dedicated time to plan, oversee and report on research
- bring a range of representatives from research infrastructure organisations, patients and the public together with representation from across the ICS, to develop a common aim and objective
- ensure board-level sight of research
- take a cross-ICS approach to research, increasing participation and diversity in research, and reducing bureaucracy.
Example: A dedicated research and innovation subgroup
East and North Hertfordshire Health Care Partnership established a formal research and innovation subgroup to support its objectives to transform services, reduce health inequalities and improve patient health and wellbeing. This subgroup is dedicated to determining and supporting local research priorities and developing an innovation agenda. With effective patient and public involvement, it is working to ensure the local population has access to more research opportunities.
Bringing together the NIHR, academia, industry and local health and care services, the subgroup develops collaborative work plans that support the design, implementation and evaluation of local transformation needs, sharing resources, staff, expertise and facilities. Its work exemplifies a sustainable approach to partnership working and supports Hertfordshire and West Essex ICS’s developing strategy.
HWE ICS Partnership Board 14 September 2021
3.4 Understanding your research activity and working with local and national research infrastructure
Research in NHS and non-NHS settings across an ICS footprint will be supported by different organisations. In some areas networks or collaboratives already exist to bring these organisations together, but in others the links are not as well formed. ICBs would benefit from having a clear map of the research infrastructure and pre-existing local or national investment into research in their area.
It may be valuable to consider:
- Who are the research leaders in your local health and care system, NIHR, higher education institutions, VCSE sector and businesses?
- Are there any pre-existing local or regional research, researcher or research engagement networks?
- What are the opportunities to inform, participate in, collaborate with or lead national and international research efforts in addition to local opportunities?
A list of organisations involved in research including NIHR-funded infrastructure and programmes is included in Annex 1 .
Much of the research undertaken in NHS and other health and care settings is funded though national calls and grants provided by funders such as NIHR, research charities , UK Research and Innovation (UKRI) , including the Medical Research Council (MRC ) and Economic and Social Research Council (ESRC) , and is aligned to national priorities. Other research may include national or international commercial or non-commercial clinical trials funders.
Partners within ICS systems can use NIHR research portfolio data to monitor and plan research activity; however, not all research is included within the NIHR’s portfolio, so this will not give a full picture of the research within the footprint. Mechanisms to map and monitor research more widely could be incorporated in ICB research strategies.
Some local needs may best be addressed through public health or social care research rather than research in primary, secondary or tertiary healthcare settings. Public health and social care research are described in Annex 2 .
Example: Mapping health and care research activity, expertise, interests and infrastructure
The Nottingham and Nottinghamshire Integrated Care System Research Partners Group meets bi-monthly and is chaired by the ICB Head of Research and Evidence. It brings together senior managers from the NHS providers, ICB, two local authorities, two universities and the NIHR CRN East Midlands, providing a forum for ICS-wide research discussions and the development of a system-wide collaborative approach to health and care research across the ICS. Among its aims, the group seeks to increase participation in research at both the organisational and population level, enable equity of access to research opportunities and generate impact on health and care pathways.
The group have mapped health and care research activity, expertise, interests and infrastructure in the constituent organisations. With this the ICS can see the research capabilities, strengths, expertise, and areas of synergy and opportunities for future collaboration that align to its needs and priorities, and also gaps for future development, recognising that organisations are at different stages of research development.
3.5 Understanding local needs
Universal NHS priorities will be reflected in local research needs, and each ICS footprint is likely to have its own specific local research needs. Joint strategic needs assessments (JSNAs) are undertaken jointly by local authorities and ICBs through health and wellbeing boards (HWBs) to identify current health and social care needs of local communities, where more information is needed to do so or to understand how best to address the need. People and communities should be directly involved in identifying local need, including by working with local charities, specific communities or groups who face inequalities in access to, experience of or outcomes from healthcare, eg to target health research at those areas and populations with greatest need.
ICPs are required to develop an integrated care strategy informed by JSNAs and the joint health and wellbeing strategy (JHWS). The integrated care strategy sets out how the assessed needs can be met through the exercise of the functions of the ICB, partner local authorities or NHS England, and is informed by research and practice-based evidence, as stated in the health and wellbeing guidance. In considering where such evidence is lacking, HWBs should identify in JSNAs those research needs that ICBs, local authorities and NHS England could meet through the exercise of their research functions.
Systems are encouraged to use their joint forward plan to develop a shared delivery plan for the Integrated Care Strategy and the JHWS that is supported by the whole system, including local authorities and VCSE partners. ICBs and trusts must also use their Joint Forward Plan to describe how the ICB will discharge its duty in respect of research.
The Explanatory Notes to the 2022 Act suggest how ICBs can discharge their duties around research. These include the articulating local research needs when assessing local needs and how they will be addressed when preparing strategies and plans, and encouraging partner organisations to play an active and collaborative role in pursuing these.
3.6 Supporting delivery of research
Once an ICS has a clear picture of its local research infrastructure it can consider how best to target and support research and the research workforce across its footprint and how research findings will be used. For this, the ICB should ensure that its approaches reflect national approaches to costing, contracting, approvals and information governance, and that they are also informed by learning from effective practices across equivalent ICBs.
As healthcare shifts into communities, ICSs should support the parallel shift in research by embedding research in health and care. Increasing access to research opportunities will give service users earlier access to new treatments, and faster research set up and delivery may provide the evidence needed to support improvements to local care sooner. Inclusive recruitment practices will be needed to ensure that all groups in society have the opportunity to help shape and take part in research, and benefit from research findings.
In developing its research strategy, an ICS has opportunities to reduce bureaucracy, and make research more efficient and effective across its own and with other ICS footprints, and across NHS and non-NHS boundaries, while meeting national regulatory guidance. ICBs will be expected to work with the HRA to co-develop, build on and implement strategies for further co-ordination and standardisation of study set-up and delivery processes. Any regional systems and processes that ICBs do establish must support consistent national practice in relation to the management and regulation of research, and should not duplicate them. The HRA will work with ICBs to address barriers to efficient and rapid study set-up, including model agreements, information governance and R&D office functions.
Other potential areas for streamlining and cross-organisational working include:
- cross-ICS research proposals to identify research needs
- research delivery – identifying how ICS-wide approaches could accelerate patient recruitment and deployment of research delivery staff
- shared data architecture, including the NHS Secure Data Environment for Research Network and its subnational secure data environments (SDEs). Subnational SDEs cover multiple ICSs to achieve access to multimodal data at a scale of approximately 5 million citizens, and over time will achieve technical and governance interoperability
- a greater focus on translation and implementation of research findings into health and care practice, supporting faster improvements
- sharing access to and funding for knowledge and library services
- shared processes and repositories for research assets.
The Explanatory Notes to the 2022 Act suggest that one way an ICB could discharge its research duty would be to have a dedicated research office or team supporting research.
3.7 Enabling cross-provider research
Health and care priorities can often only be addressed with complex, multiorganisational approaches and as such the research to inform these needs to span organisational boundaries. Organisational policies should promote cross-organisational research and dissemination of research findings, including through participation in collaborative research to address national priorities, joint staff posts, honorary contracts, and administratively easier movement of researchers between health and care organisations and other sector partners, including higher education, industry, charities and local authorities.
The HRA and ICS partners are developing national guidance to support cross-provider research.
The NIHR CRN can offer ICSs opportunities to participate in national and international research studies, including those the NIHR, industry and others commission.
3.8 Commercial research
Commercial contract research is research funded solely by industry, where NHS providers are contracted to carry out the research. Most of these research studies in the NHS are interventional clinical trials, such as the NHS-Galleri trial and Astra Zeneca’s COVID-19 vaccine development . Commercial research can give patients access to a wider range of research opportunities, earlier access to novel therapies and treatments, provide drugs free of charge to patients in trials, accelerate the development of new treatments and devices, generate income for providers, and fund NHS staff. It is vitally important for the benefit of patients, the NHS and the UK economy that we create an environment in the NHS that makes it easy and efficient for the NHS to undertake commercial research. This is particularly important when it comes to international commercial research, where companies can place their studies in a number of different countries and consideration of anticipated set up and recruitment times informs where they place trials.
Data gathered during some commercial research is specific to the study and is the property of the company, as is any Intellectual Property (IP) generated. In other cases, where the NHS contributes to the foreground IP – such as through the use of NHS data for research or where NHS expertise provides important contributions to a commercial product – it is important that the NHS shares in the value of IP generated as a consequence of its contributions.
The establishment of ICSs is an ideal opportunity for their creation of ambitions to enable, grow and benefit from commercial research. ICSs should explore how efficient commercial study set up and delivery could be streamlined across sites within their footprint, and should set ambitions around commercial research.
3.9 Involving patients, service users, carers and the public in research
In developing a research strategy ICSs should set out their approach to diverse public and patient involvement (PPI) in relation to research.
Areas where working with people and communities could add value in the context of research include:
- identification of local research needs, including through JSNAs and JHWSs
- designing research proposals in partnership with local or national experts
- raising awareness of research opportunities and recruitment of participants
- developing research outcome reports and identification of how and when participants will be able to access these
- consideration of how members of the public can access the outputs from publicly-funded research
- how volunteers should be involved and what they should be paid.
The UK Standards for Public Involvement sets out the core components of good public involvement. A guide outlining good practice in engaging underserved communities around research is available from NHS England. Resources about good practice around PPI in designing and delivering research, including around incentivisation , are also available from the HRA and NIHR .
It will be useful to link into established community involvement approaches. NIHR infrastructure organisations may have established networks of expert PPI representatives, and ICSs have extensive VCSE Alliances. A co-ordinated community engagement approach across health and care delivery and research will reduce the risk of overburdening communities with organisations wanting to work with them, and will support the identification of under-served communities.
3.10 Ensuring anyone can participate in research
Making research more visible within communities and increasing the public’s understanding of research can ensure greater diversity in research participation. Research findings will then be more generalisable to a broader range of groups or communities, or can be targeted and specific to relevant communities.
ICSs should seek mechanisms to ensure that opportunities to take part in research are available to all. They should consider encouraging patients and members of the public to register on NIHR Be Part of Research (a national registry where people can express their interest in being contacted about research that is relevant to them), widely disseminate research opportunities and make provision for inclusive access for communities to take part in research. Decentralised or virtual trials are remote access trials recruited to and delivered using electronic tools, making it easier for people to participate in some studies without needing to visit a recruiting hospital or attend appointments in person. ICBs should consider ways in which research delivery can increase access to research opportunities for people within their area. ICBs should also advise the public how they can access research outputs.
NIHR and UK Research and Innovation provide resources that help organisations address issues of equality, diversity and inclusion in research settings.
Example: RELIEVE-IBS decentralised trial
In 2020, Newcastle researchers launched RELIEVE-IBS, one of the first interventional decentralised clinical studies in the UK to trial Enterosgel, a new treatment for irritable bowel syndrome with diarrhoea (IBS-D). Decentralised trials are remote access trials that use electronic tools for trial recruitment and delivery, without the patient needing to visit a recruiting hospital site, which could be miles from their homes – a convenient option for patients with IBS-D. By running the trial remotely, researchers could reach beyond the small proportion of those with this condition who attend specialist clinics, as well as save resource for the sponsor.
Not only did this trial embrace technological developments to deliver research, but it empowered more patients to become involved regardless of where they lived. With in-depth patient input, the research team were able to shape the recruitment approach to be highly accessible to participants and were offered feedback on how to refine the trial design by the sponsors. The resulting patient-centric design ensured a good recruitment response when the trial opened.
NIHR (2020) Virtual trial recruits 67% faster led by NIHR Patient Recruitment Centre in Newcastle in collaboration with Enteromed
NIHR (2021) Pushing virtual boundaries to improve patient engagement and accessibility
NIHR (2022) RELIEVE IBS-D trial case study
3.11 Health data in research
Health data generated through care of service users in the NHS can fuel a revolution in the research and development of new diagnostics and treatments, maximising the potential to improve service user outcomes and experiences, support diversity in research, and minimise health inequalities through research. To do this, researchers need access to high quality and timely data to generate insights. The public expect data to be used legally and efficiently to conduct and support research.
National commitments around data for research can be found in Data saves lives: reshaping health and social care with data . This strategy shows how data will be used to bring benefits to all parts of health and social care. To achieve this vision, the NHS will be making a strategic move away from a system of data dissemination to one of data access when making NHS health and social care data available for research and analysis. This will be facilitated by the implementation of secure data environments (SDEs).
SDEs are data storage and access platforms with features that enable organisations to have greater control and oversight over their data. SDEs allow approved users to view and analyse data without it having to leave the environment. The SDE policy guidelines provide a clear signal to the sector that SDEs will become the default way of accessing NHS data for research.
This change is supported by major investments in digital infrastructure through the Data for Research & Development Programme, which is funding the development of national and subnational SDEs. The subnational SDEs will cover the entirety of England and individual platforms will cover several ICS.
ICBs should seek ways to promote and enable the use of these rich data sources for research and include them in their research strategy.
3.12 Using evidence for planning, commissioning and improving health and care
Evidence-based commissioning has advantages for the commissioner, workforce and service users, as it can:
- lead to innovation in service design and delivery
- enhance the quality of health and care provision
- reduce clinical variation between locations and providers
- improve equity of access to services
- improve patient and population outcomes.
As part of the commissioning process, commissioners are expected to use evidence-based clinical policies, as per the Roadmap for integrating specialised services within integrated care systems . Knowledge and library services can help source and interpret evidence.
The Provider Selection Regime will reflect the research duties of the 2022 Act and should be referred to when commissioning provider services, once it has been published.
NHS knowledge and library services provide access to evidence and support for knowledge management; they train people in searching for, handling and publishing information. The Knowledge for Healthcare strategy encourages and equips NHS knowledge and library services to support NHS organisations with the translation of knowledge for the spread and adoption of research and innovation. To fulfil their obligations under the 2022 Act, ICBs could commit to active knowledge translation.
Evidence for commissioning information is available from a number of sources:
- NHS Library and Knowledge Hub
- Health Libraries and Information Services Directory
- NICE guidance
- NIHR evidence
- NHS evidence works toolkit
- Academy of Medical Royal Colleges: Evidence-based Intervention
- A million decisions
The infographic for the role of research and evidence in commissioning also provides sources for evidence-based commissioning.
Example: Evidence mobilisation, knowledge sharing and improving outcomes
The STEMClub (Sustaining Transformation by Evidence Mobilisation) is a network in the North East and North Cumbria that brings together local policy and decision-makers with NHS knowledge and library specialists to facilitate evidence-based decision-making. The input of knowledge specialists ensures timely access to published research and provides knowledge management expertise to shape how soft intelligence is translated into knowledge assets.
As members within the STEMClub network, knowledge and library specialists are providing ongoing detailed evidence reviews and information management expertise to facilitate system-wide working , eg:
- North East North Cumbria Frailty Framework
- North East and North Cumbria Maternity Clinical Network
- a review of optimal patient transfer times in the North East and North Cumbria
- regular evidence summaries for the ICS Mental Health Evidence and Evaluation subgroup.
3.13 The health and care workforce and research
Staff involved in research have greater job satisfaction and research active trusts have lower staff turnover [3] . Clinical academic roles [7] , having research colleagues within services [8] and taking students on research placements [6] are felt to foster an increase in knowledge and skills across the wider staff workforce. The General Medical Council (GMC) and the Royal College of Physicians (RCP) and NIHR have issued position statements and recommendations around research, with additional signatories including UKRI, UKRD, the Academy of Medical Royal Colleges and the Royal College of Surgeons of England. Learning resources, including programmes for ongoing professional development of the research delivery workforce, are available through NIHR Learn.
In developing a research strategy ICSs could ensure that, as part of their people function and approach to workforce planning :
- Staff roles in leading, delivering or facilitating research and in supervising those developing research skills are recognised, supported and enabled across all staff groups and health and care settings as part of a positive research culture.
- The value of evidence is recognised, and education and training around research are facilitated. Opportunities to develop research careers or in overseeing the development of other researchers are enabled; this may include having protected time, inclusion in job plans and joint appointments across health and care providers and academic institutions.
- Ensuring that there is capacity and systems that support research through services like imaging, pathology and pharmacy, as well as finance and human resources.
- Individual organisations do not always have the necessary skills or services to support effective research and its impact, such as IP management, methodological expertise, regulatory compliance, statistical analysis, knowledge mobilisation expertise, genomics expertise, health informatics and data analytics. Mechanisms are needed to ensure that these can readily and rapidly be accessed across other health and care organisations, including from local authorities and other non-NHS care providers.
A UK Clinical Research Workforce Strategy is under development. ICSs should update their approaches to their research workforce once DHSC publishes this in 2023/24.
Example: Investing in the research workforce – developing capacity for chief investigators
Across the West Midlands NIHR CRN, an investment of approximately £750,000 to develop capacity for chief investigators returned additional research grant income of over £18 million in three years. This was achieved primarily by increasing the programme activity for consultants in areas where chief investigators were underrepresented.
The funding was provided through a competitive process and co-supported by the local NIHR CRN, with several local trusts jointly funded these scholars.
Kirk J, Willcocks J, Boyle P, Brocklehurst P, Morris K, Kearney R, et al (2022) Developing chief investigators within the NHS: the West Midlands clinical trials scholars programme. Clin Med 22(2): 149–52.
Kirk J, Reynolds F, Adey E, Boazman M, Brookes M, Brocklehurst P (2022) Developing paediatric chief investigators within the NHS: the Clinical Trials Scholars programme . Arch Dis Child Educ Pract Published online first: 22 February 2022. doi: 10.1136/archdischild-2021-322186
4. References
- Varnai P, Rentel M, Dave A, De Scalzi M, Timmerman W, Rosemberg-Mantes C, Simmonds P, Technopolis Group (2017) The impact of collaboration: The value of UK medical research to EU science and health .
- Boaz A, Hanney S, Jones T, Soper B (2015) Does the engagement of clinicians and organisations in research improve healthcare performance: a three-stage review. BMJ Open 5: e009415. doi:10.1136/ bmjopen-2015-009415 .
- Rees MR, Bracewell M (2019) Academic factors in medical recruitment: evidence to support improvements in medical recruitment and retention by improving the academic content in medical posts. Postgrad Med J 95(1124): 323-327. doi:10.1136/postgradmedj-2019-136501 .
- Ozdemir BA, Karthikesalingham A, Singha S, Poloniecki JD, Hinchliffe RJ, Thompson MM, et al (2015) Research activity and the association with mortality. PLoS ONE 10(2): doi.org/10.1371/journal.pone.0118253 .
- Hunn A (2017) Survey of the general public: attitudes towards health research . Health Research Authority.
- Angus RL, Hattingh HL, Weir KA (2022) Experiences of hospital allied health professionals in collaborative student research projects: a qualitative study. BMC Health Services Research 22(1). Available at: https://doi.org/10.1186/s12913-022-08119-7 .
- Newington L, Wells M, Adonis A, Bolten L, Bolton Saghdaoui L, Coffey M, et al (2021) A qualitative systematic review and thematic synthesis exploring the impacts of clinical academic activity by healthcare professionals outside medicine. BMC Health Serv Res 21(1). Available at: https://doi.org/10.1186/s12913-021-06354-y .
- Wenke RJ, Hickman I, Hulcombe J, Phillips R, Mickan S (2017) Allied health research positions: A qualitative evaluation of their impact. Health Res Policy Syst 15(6). Available at: https://doi.org/10.1186/s12961-016-0166-4
Annex 1 – Organisations that may be involved in regional or local research
- Clinical Research Networks (CRNs) , which will be retendered and renamed regional research delivery networks (RRDNs) from April 2024
- Applied Research Collaborations (ARCs)
- Biomedical Research Centres (BRCs)
- Experimental Cancer Medicine Centres (ECMCs) , jointly funded with Cancer Research UK
- Research Design Services (RDSs) and Clinical Trials Units (CTUs) which will be replaced by the NIHR Research Support Service from 1 October 2023
- Patient Recruitment Centres (PRCs)
- MedTech and In vitro diagnostic Co-operatives (MICs) , which will be replaced with HealthTech research centres from April 2024
- School of Public Health Research, School of Primary Care Research and School of Social Care Research
- Health Determinants Research Collaborations (HDRCs)
- Clinical Research Facilities (CRFs)
- Patient Safety Research Collaborations (PSRCs)
- Translational Research Collaborations (TRCs)
- Academic Health Science Centres (AHSCs)
- university teaching hospitals and all trusts that deliver research activity
- primary care organisations, including GP practices, that deliver research activity
- higher education institutions (HEIs)
- local authorities
- social care partners
- Local Government Association
- local and national charities that fund, collaborate in or support participation in research
- research and development offices in providers or CSUs, including primary care providers and ambulance, community and mental health trusts, and those in the VCSE sector
- UKRD members
- NHS subnational secure data environments for research
- NHS R&D Forum
- NHS Genomic Medicines Service Research Collaborative
- NHS Knowledge and Library Services
- Academic Health Science Networks (AHSNs) are often well linked with research organisations and infrastructure as part of their roles in development, adoption and spread of innovation.
Annex 2 – Public health and social care research
Public health research investigates issues that impact at a population rather than an individual level. This can be done within the NHS with system-level studies, such as secondary prevention of cardiovascular disease and examining the impact on health inequalities of changes to the NHS resource allocation formula, and outside the NHS for the wider determinants of health such as air quality, transport systems and housing. There is a substantial body of public health evidence for the clinical and cost effectiveness of prevention, health protection, health service redesign and addressing health inequalities.
Social care research aims to improve the lives of children and adults who need to draw on personal or practical care and support, and family members or other unpaid carers. It can include research around the introduction, use and impact of technologies, and changing social care interventions, policies and practice. Social care research also examines issues pertaining to the safeguarding of adults and children and workforce, commissioning of services, and questions about organisational and professional practice, including decision-making, training and the quality of care.
Publication reference: PR1662

Browse all our research projects by topic We have funded more than 150 external research projects across a range of themes over the last five years
- Share on Twitter
- Share on LinkedIn
- Share on Facebook
- Share on WhatsApp
- Share by email
- Link Copy link
Please click below to see the research projects we've funded on the following topics.
- Analytics and data
- Children and young people
- Commissioning
- Community and voluntary
- Digital technology
- Efficiency and productivity
- Emergency medicine
- End of life care
- Funding and sustainability
- Improvement science
- Inequalities
- Integrated care
- Long-term conditions
- Mental health
- Older people
- Patient experience
- Patient safety
- Person-centred care
- Primary care
- Public health
- Quality improvement
- Quality of care
- Social care
- Social determinants of health
Share this page:
Health Foundation @HealthFdn
- Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
The Q community
Q is an initiative connecting people with improvement expertise across the UK.
Quick links
- News and media
- Events and webinars
Hear from us
Receive the latest news and updates from the Health Foundation
- 020 7257 8000
- [email protected]
- The Health Foundation Twitter account
- The Health Foundation LinkedIn account
- The Health Foundation Facebook account
Copyright The Health Foundation 2024. Registered charity number 286967.
- Accessibility
- Anti-slavery statement
- Terms and conditions
- Privacy policy

Cookies on Be Part of Research
We use some essential cookies to make this service work.
We would like to use additional cookies to remember your settings, understand how you use Be Part of Research and improve the service.
We also use cookies set by other sites to help us deliver content via their services.
Keep up to date
Sign up for news and information about taking part and shaping research.
I'm looking for research about
- News and features
- Why take part?
- How to take part
- What happens on a study?
- Volunteering without a condition
- UK research registries
- Information for researchers
- Information for health and care professionals
- Web developer resources
What is health and care research?
- How are studies regulated, approved and funded?
- Frequently asked questions
Search for a study
You already conduct research in your day-to-day life. This research informs and broadens your understanding of things before you make a decision. Health and care research is the same. It seeks to find answers to questions about the best options available. It then uses these discoveries to make decisions about improvements or changes. This is so we can:
- diagnose diseases earlier or more accurately
- provide life-changing treatments
- prevent people from developing conditions
- improve health and care for generations to come
- ensure everyone has a better quality of life
Although health professionals already know a great deal, there are still so many questions that need answers. Sometimes, the outcome of research just confirms that what we have at the moment, is the best available to us right now.
How research contributes to our NHS
This short film explains the important role that research plays in the NHS and how important it is for the future that we all consider taking part ( video transcript ).
Good research is:
- Relevant – it answers questions that are important to the health and care of the public
- High quality – it has to follow strict legal standards
- Safe – it puts people’s safety and dignity first
The first clinical trial

The first clinical trial was conducted by James Lind. He was a Scottish doctor and a pioneer of naval hygiene in the Royal Navy. He conducted the first clinical trial in history in 1747.
James wanted to investigate whether citrus fruits cured scurvy. He selected twelve patients with scurvy on a ship, kept them together and gave them all different diets and monitored them. By the end of the week, the sailors whose daily diet included citrus fruits recovered, therefore proving that citrus fruit could cure scurvy.
We still celebrate this milestone each year on International Clinical Trials Day.
Myths about research
Understanding the facts is really important when deciding whether to take part in research. By clicking on the arrow next to each myth you can reveal the facts.
All health and care research is high risk
All health and social care research has to go through very strict ethical and regulatory checks before it can go ahead. There are lots of different ways to get involved with research . Some involve taking a new medicine or having a new form of treatment, others may be as simple as filling out a questionnaire or leaving a sample. People are very closely monitored while they are taking part in research, so although health and care research is not entirely risk-free, the chances of something going wrong are small.
My doctor will tell me about the research available
Not all health and care professionals will be fully informed about all of the research opportunities available to you. They might also not have the time to discuss it with you in your appointment. However, it is important to ask about opportunities to get involved in research as your healthcare professional will know how to find out what might be available. You can search for studies on this website by using the search bar at the very top of each page by typing in your town, postcode, body part, medicine or health condition. You can also find a condition by pressing the “ view conditions ” button.
Research can only take place in hospital
Health and care research can take place in many different places, from schools to care homes depending on the type of research. It is more common than ever before for research to take place in non-clinical settings. Digital technology provides a way of getting people involved from the comfort of their own homes.
Health and care research means taking lots of drugs
Not all health and care research involves taking drugs. The research may involve testing a new device to help monitor or administer a medicine for an illness. It could be about monitoring how certain changes in our diet and lifestyle could help the health of our nation in the future. Research might simply involve talking to someone, completing a short questionnaire or even using an app on a mobile device. There are also many different ways to be involved in research without being a participant in a research study .
People are treated like guinea pigs
Whatever the type of research, anyone who is involved should be treated with respect. The research is not being done to them but with them. People who participate in research often say that they feel well cared for as they have a dedicated contact within the research staff team. Research teams must follow ethical guidance and before the research can take place, they must seek approval for their plan from a Research Ethics Committee. Research that involves new medicines is not tested on people first. It will have gone through a process to ensure it is ready for use with people.
Health and care research is only about finding a cure
Research aims to prevent diseases as well as cure them. There are a range of factors which can contribute to your health, for example: where you live, what you eat and whether you have a good support network of family and friends. Public health research seeks to answer questions about some of these factors.
Research seeks to find ways for people to live well with long-term conditions. It can help to find out the best ways to care for people living with life-limiting illness and pain, which is known as ’palliative care’. Research can lead to improvements in end-of-life care across all diseases and to help patients to live in comfort and die with dignity.
Health and social care research only involves physical diseases, it cannot help with mental health
People’s health is not limited to physical disease, it includes their mental well being. Research therefore seeks to answer questions about mental health such as is medicine, counselling or a combination of both the best treatment for individuals living with depression? Members of the public can have a role in identifying and prioritising where health research is focused . Given increased awareness of the effects our mental health can have on our physical well being, this is likely to be a growing area of health and social care research. Read about all the research happening within the NIHR specialty for mental health .
Children are not allowed to participate in health and care research
Children can take part in health and care research with the permission of their legal guardian. The research team may meet with the child to make sure they understand what the research is about. They may use pictures to explain the study. Research in child health is vital to help find new and better ways to care for children. You can find studies for children by typing "Children" in the search box at the very top of this page.
Research only benefits the drug companies
Health research is funded by drug companies, charities and the government, although when the NHS undertakes research specifically for drug companies, the company pays the full cost. Everyone benefits from the development of new medicines, and without commercial drug companies there would be less research taking place.
Different types of research

Healthcare research
Sometimes health research studies may be referred to as ‘clinical trials’. They usually involve examining and observing people with different conditions and sometimes comparing them with people who don't have the condition. It can also involve research on samples of blood or other tissues, or tests such as scans or X-rays. Researchers can also analyse information in patient records, or the data from health and lifestyle surveys.

Public health research
Tackles some of the bigger health issues that affect society as a whole, for example, the impact of giving up smoking, how many steps a day for good health etc. It also looks at the benefits, costs, acceptability and the wider impact of treatments.

Social care research
Is about improving the lives of people who receive care and support from our social care sector. Research in social care could be about introducing new devices and technologies such as: lifting equipment to help with residents, exploring the impact of technology driven care environments or changing social care policies and practice.
Important research discoveries
.jpg)
Launched in 1961, the contraceptive pill was initially only prescribed to married women, but the law was relaxed in 1967. The pill works by suppressing fertility with either progesterone or oestrogen or, more commonly, a combination of both.

Penicillin was discovered in 1928 and developed into a drug in the early 1940s. Today it’s used to treat a broad range of bacterial infections accounting for around 45% of the antibiotics prescribed in the NHS in England.

Research in the 1980s and 1990s showed that low doses of blood-thinning drugs such as aspirin and warfarin significantly reduced the number of heart attacks and strokes in people at risk.
Before you go
Research is a team effort. We need members of the public, like you, to take part. Without volunteers, it would not be possible for research to happen.
- Reasons why people take part in research
- How to take part in research
- Learn about how studies are made safe
Mobile Menu Overlay
The White House 1600 Pennsylvania Ave NW Washington, DC 20500
FACT SHEET: President Biden Issues Executive Order and Announces New Actions to Advance Women’s Health Research and Innovation
In his State of the Union address, President Biden laid out his vision for transforming women’s health research and improving women’s lives all across America. The President called on Congress to make a bold, transformative investment of $12 billion in new funding for women’s health research. This investment would be used to create a Fund for Women’s Health Research at the National Institutes of Health (NIH) to advance a cutting-edge, interdisciplinary research agenda and to establish a new nationwide network of research centers of excellence and innovation in women’s health—which would serve as a national gold standard for women’s health research across the lifespan.
It is long past time to ensure women get the answers they need when it comes to their health—from cardiovascular disease to autoimmune diseases to menopause-related conditions. To pioneer the next generation of discoveries, the President and the First Lady launched the first-ever White House Initiative on Women’s Health Research , which aims to fundamentally change how we approach and fund women’s health research in the United States.
Today, President Biden is signing a new Executive Order that will direct the most comprehensive set of executive actions ever taken to expand and improve research on women’s health. These directives will ensure women’s health is integrated and prioritized across the federal research portfolio and budget, and will galvanize new research on a wide range of topics, including women’s midlife health.
The President and First Lady are also announcing more than twenty new actions and commitments by federal agencies, including through the U.S. Department of Health and Human Services (HHS), the Department of Defense (DoD), the Department of Veterans Affairs (VA), and the National Science Foundation (NSF). This includes the launch of a new NIH-wide effort that will direct key investments of $200 million in Fiscal Year 2025 to fund new, interdisciplinary women’s health research—a first step towards the transformative central Fund on Women’s Health that the President has called on Congress to invest in. These actions also build on the First Lady’s announcement last month of the Advanced Research Projects Agency for Health (ARPA-H) Sprint for Women’s Health , which committed $100 million towards transformative research and development in women’s health.
Today, the President is issuing an Executive Order that will:
- Integrate Women’s Health Across the Federal Research Portfolio . The Executive Order directs the Initiative’s constituent agencies to develop and strengthen research and data standards on women’s health across all relevant research and funding opportunities, with the goal of helping ensure that the Administration is better leveraging every dollar of federal funding for health research to improve women’s health. These actions will build on the NIH’s current policy to ensure that research it funds considers women’s health in the development of study design and in data collection and analysis. Agencies will take action to ensure women’s health is being considered at every step in the research process—from the applications that prospective grantees submit to the way that they report on grant implementation.
- Prioritize Investments in Women’s Health Research . The Executive Order directs the Initiative’s constituent agencies to prioritize funding for women’s health research and encourage innovation in women’s health, including through ARPA-H and multi-agency initiatives such as the Small Business Innovation Research Program and the Small Business Technology Transfer Program. These entities are dedicated to high-impact research and innovation, including through the support of early-stage small businesses and entrepreneurs engaged in research and innovation. The Executive Order further directs HHS and NSF to study ways to leverage artificial intelligence to advance women’s health research. These additional investments—across a wide range of agencies—will support innovation and open new doors to breakthroughs in women’s health.
- Galvanize New Research on Women’s Midlife Health . To narrow research gaps on diseases and conditions associated with women’s midlife health or that are more likely to occur after menopause, such as rheumatoid arthritis, heart attack, and osteoporosis, the President is directing HHS to: expand data collection efforts related to women’s midlife health; launch a comprehensive research agenda that will guide future investments in menopause-related research; identify ways to improve management of menopause-related issues and the clinical care that women receive; and develop new resources to help women better understand their options for menopause-related symptoms prevention and treatment. The Executive Order also directs the DoD and VA to study and take steps to improve the treatment of, and research related to, menopause for Service women and women veterans.
- Assess Unmet Needs to Support Women’s Health Research . The Executive Order directs the Office of Management and Budget and the Gender Policy Council to lead a robust effort to assess gaps in federal funding for women’s health research and identify changes—whether statutory, regulatory, or budgetary—that are needed to maximally support the broad scope of women’s health research across the federal government. Agencies will also be required to report annually on their investments in women’s health research, as well as progress towards their efforts to improve women’s health.
Today, agencies are also announcing new actions they are taking to promote women’s health research , as part of their ongoing efforts through the White House Initiative on Women’s Health Research. Agencies are announcing actions to:
Prioritize and Increase Investments in Women’s Health Research
- Launch an NIH-Cross Cutting Effort to Transform Women’s Health Throughout the Lifespan. NIH is launching an NIH-wide effort to close gaps in women’s health research across the lifespan. This effort—which will initially be supported by $200 million from NIH beginning in FY 2025—will allow NIH to catalyze interdisciplinary research, particularly on issues that cut across the traditional mandates of the institutes and centers at NIH. It will also allow NIH to launch ambitious, multi-faceted research projects such as research on the impact of perimenopause and menopause on heart health, brain health and bone health. In addition, the President’s FY25 Budget Request would double current funding for the NIH Office of Research on Women’s Health to support new and existing initiatives that emphasize women’s health research.
This coordinated, NIH-wide effort will be co-chaired by the NIH Office of the Director, the Office of Research on Women’s Health, and the institute directors from the National Institute on Aging; the National Heart, Lung, and Blood Institute; the National Institute on Drug Abuse; the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Institute on Arthritis, Musculoskeletal and Skin Diseases.
- Invest in Research on a Wide Range of Women’s Health Issues. The bipartisan Congressionally Directed Medical Research Program (CDMRP), led out of DoD, funds research on women’s health encompassing a range of diseases and conditions that affect women uniquely, disproportionately, or differently from men. While the programs and topic areas directed by Congress differ each year, CDMRP has consistently funded research to advance women’s health since its creation in 1993. In Fiscal Year 2022, DoD implemented nearly $490 million in CDMRP investments towards women’s health research projects ranging from breast and ovarian cancer to lupus to orthotics and prosthetics in women. In Fiscal Year 2023, DoD anticipates implementing approximately $500 million in CDMRP funding for women’s health research, including in endometriosis, rheumatoid arthritis, and chronic fatigue.
- Call for New Proposals on Emerging Women’s Health Issues . Today, NSF is calling for new research and education proposals to advance discoveries and innovations related to women’s health. To promote multidisciplinary solutions to women’s health disparities, NSF invites applications that would improve women’s health through a wide range of disciplines—from computational research to engineering biomechanics. This is the first time that NSF has broadly called for novel and transformative research that is focused entirely on women’s health topics, and proposals will be considered on an ongoing basis.
- Increase Research on How Environmental Factors Affect Women’s Health. The Environmental Protection Agency (EPA) is updating its grant solicitations and contracts to ensure that applicants prioritize, as appropriate, the consideration of women’s exposures and health outcomes. These changes will help ensure that women’s health is better accounted for across EPA’s research portfolio and increase our knowledge of women’s environmental health—from endocrine disruption to toxic exposure.
- Create a Dedicated, One-Stop Shop for NIH Funding Opportunities on Women’s Health. Researchers are often unaware of existing opportunities to apply for federal funding. To help close this gap, NIH is issuing a new Notice of Special Interest that identifies current, open funding opportunities related to women’s health research across a wide range of health conditions and all Institutes, Centers, and Offices. The NIH Office of Research on Women’s Health will build on this new Notice by creating a dedicated one-stop shop on open funding opportunities related to women’s health research. This will make it easier for researchers and institutions to find and apply for funding—instead of having to search across each of NIH’s 27 institutes for funding opportunities.
Foster Innovation and Discovery in Women’s Health
- Accelerate Transformative Research and Development in Women’s Health. ARPA-H’s Sprint for Women’s Health launched in February 2024 commits $100 million to transformative research and development in women’s health. ARPA-H is soliciting ideas for novel groundbreaking research and development to address women’s health, as well as opportunities to accelerate and scale tools, products, and platforms with the potential for commercialization to improve women’s health outcomes.
- Support Private Sector Innovation Through Additional Federal Investments in Women’s Health Research. The NIH’s competitive Small Business Innovation Research Program and the Small Business Technology Transfer Program is committing to further increasing—by 50 percent—its investments in supporting innovators and early-stage small businesses engaged in research and development on women’s health. These programs will solicit new proposals on promising women’s health innovation and make evidence-based investments that bridge the gap between performance of basic science and commercialization of resulting innovations. This commitment for additional funds builds on the investments the Administration has already made to increase innovation in women’s health through small businesses, including by increasing investments by sevenfold between Fiscal Year 2021 and Fiscal Year 2023.
- Advance Initiatives to Protect and Promote the Health of Women. The Food and Drug Administration (FDA) seeks to advance efforts to help address gaps in research and availability of products for diseases and conditions that primarily impact women, or for which scientific considerations may be different for women, and is committed to research and regulatory initiatives that facilitate the development of safe and effective medical products for women. FDA also plans to issue guidance for industry that relates to the inclusion of women in clinical trials and conduct outreach to stakeholders to discuss opportunities to advance women’s health across the lifespan. And FDA’s Office of Women’s Health will update FDA’s framework for women’s health research and seek to fund research with an emphasis on bridging gaps in knowledge on important women’s health topics, including sex differences and conditions that uniquely or disproportionately impact women.
- Use Biomarkers to Improve the Health of Women Through Early Detection and Treatment of Conditions, such as Endometriosis. NIH will launch a new initiative dedicated to research on biomarker discovery and validation to help improve our ability to prevent, diagnose, and treat conditions that affect women uniquely, including endometriosis. This NIH initiative will accelerate our ability to identify new pathways for diagnosis and treatment by encouraging multi-sector collaboration and synergistic research that will speed the transfer of knowledge from bench to bedside.
- Leverage Engineering Research to Improve Women’s Health . The NSF Engineering Research Visioning Alliance (ERVA) is convening national experts to identify high-impact research opportunities in engineering that can improve women’s health. ERVA’s Transforming Women’s Health Outcomes Through Engineering visioning event will be held in June 2024, and will bring together experts from across engineering—including those in microfluidics, computational modeling, artificial intelligence/imaging, and diagnostic technologies and devices—to evaluate the landscape for new applications in women’s health. Following this event, ERVA will issue a report and roadmap on critical areas where engineering research can impact women’s health across the lifespan.
- Drive Engineering Innovations in Women’s Health Discovery . NSF awardees at Texas A&M University will hold a conference in summer 2024 to collectively identify challenges and opportunities in improving women’s health through engineering. Biomedical engineers and scientists will explore and identify how various types of engineering tools, including biomechanics and immuno-engineering, can be applied to women’s health and spark promising new research directions.
Expand and Leverage Data Collection and Analysis Related to Women’s Health
- Help Standardize Data to Support Research on Women’s Health. NIH is launching an effort to identify and develop new common data elements related to women’s health that will help researchers share and combine datasets, promote interoperability, and improve the accuracy of datasets when it comes to women’s health. NIH will initiate this process by convening data and scientific experts across the federal government to solicit feedback on the need to develop new NIH-endorsed common data elements—which are widely used in both research and clinical settings. By advancing new tools to capture more data about women’s health, NIH will give researchers and clinicians the tools they need to enable more meaningful data collection, analysis, and reporting and comprehensively improve our knowledge of women’s health.
- Reflect Women’s Health Needs in National Coverage Determinations. The Centers for Medicare & Medicaid Services (CMS) will strengthen its review process, including through Coverage with Evidence Development guidance, to ensure that new medical services and technologies work well in women, as applicable, before being covered nationally through the Medicare program. This will help ensure that Medicare funds are used for treatments with a sufficient evidence base to show that they actually work in women, who make up more than half of the Medicare population.
- Leverage Data and Quality Measures to Advance Women’s Health Research. The Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration (HRSA) are building on existing datasets to improve the collection, analysis, and reporting of information on women’s health. The CDC is expanding the collection of key quality measures across a woman’s lifespan, including to understand the link between pregnancy and post-partum hypertension and heart disease, and plans to release the Million Hearts Hypertension in Pregnancy Change Package. This resource will feature a menu of evidence-informed strategies by which clinicians can change care processes. Each strategy includes tested tools and resources to support related clinical quality improvement. HRSA is modernizing its Uniform Data System in ways that will improve the ability to assess how women are being served through HRSA-funded health centers. By improving the ability to analyze data on key clinical quality measures, CDC and HRSA can help close gaps in women’s health care access and identify new opportunities for high-impact research.
Strengthen Coordination, Infrastructure, and Training to Support Women’s Health Research
- Launch New Joint Collaborative to Improve Women’s Health Research for Service Members and Veterans. DoD and VA are launching a new Women’s Health Research collaborative to explore opportunities that further promote joint efforts to advance women’s health research and improve evidence-based care for Service members and veterans. The collaborative will increase coordination with the goal of helping improve care across the lifespan for women in the military and women veterans. The Departments will further advance research on key women’s health issues and develop a roadmap to close pressing research gaps, including those specifically affecting Service women and women veterans.
- Coordinate Research to Advance the Health of Women in the Military. DoD will invest $10 million, contingent on available funds, in the Military Women’s Health Research Partnership. This Partnership is led by the Uniformed Services University and advances and coordinates women’s health research across the Department. The Partnership is supporting research in a wide range of health issues affecting women in the military, including cancers, mental and behavioral health, and the unique health care needs of Active Duty Service Women. In addition, the Uniformed Services University established a dedicated Director of Military Women’s Health Research Program, a role that is responsible for identifying research gaps, fostering collaboration, and coordinating and aligning a unified approach to address the evolving needs of Active Duty Service Women.
- Support EPA-Wide Research and Dissemination of Data on Women’s Health. EPA is establishing a Women’s Health Community of Practice to coordinate research and data dissemination. EPA also plans to direct the Board of Scientific Counselors to identify ways to advance EPA’s research with specific consideration of the intersection of environmental factors and women’s health, including maternal health.
- Expand Fellowship Training in Women’s Health Research. CDC, in collaboration with the CDC Foundation and American Board of Obstetrics and Gynecology, is expanding training in women’s health research and public health surveillance to OBGYNs, nurses and advanced practice nurses. Through fellowships and public health experiences with CDC, these clinicians will gain public health research skills to improve the health of women and children exposed to or affected by infectious diseases, mental health and substance use disorders. CDC will invite early career clinicians to train in public health and policy to become future leaders in women’s health research.
Improve Women’s Health Across the Lifespan
- Create a Comprehensive Research Agenda on Menopause. To help women get the answers they need about menopause, NIH will launch its first-ever Pathways to Prevention series on menopause and the treatment of menopausal symptoms. Pathways to Prevention is an independent, evidence-based process to synthesize the current state of the evidence, identify gaps in existing research, and develop a roadmap that can be used to help guide the field forward. The report, once completed, will help guide innovation and investments in menopause-related research and care across the federal government and research community.
- Improve Primary Care and Preventive Services for Women . The Agency for Healthcare Research and Quality (AHRQ) will issue a Notice of Intent to publish a funding opportunity announcement for research to advance the science of primary care, which will include a focus on women’s health. Through this funding opportunity, AHRQ will build evidence about key elements of primary care that influence patient outcomes and advance health equity—focusing on women of color—such as care coordination, continuity of care, comprehensiveness of care, person-centered care, and trust. The results from the funding opportunity will shed light on vital targets for improvements in the delivery of primary healthcare across a woman’s lifespan, including women’s health preventive services, prevention and management of multiple chronic diseases, perinatal care, transition from pediatric to adult care, sexual and reproductive health, and care of older adults.
- Promote the Health of American Indian and Alaska Native Women. The Indian Health Service is launching a series of engagements, including focus groups, to better understand tribal beliefs related to menopause in American Indian and Alaska Native Women. This series will inform new opportunities to expand culturally informed patient care and research as well as the development of new resources and educational materials.
- Connect Research to Real-World Outcomes to Improve Women’s Mental and Behavioral Health. The Substance Abuse and Mental Health Services Administration (SAMHSA) is supporting a range of health care providers to address the unique needs of women with or at risk for mental health and substance use disorders. Building on its current efforts to provide technical assistance through various initiatives , SAMHSA intends, contingent on available funds, to launch a new comprehensive Women’s Behavioral Health Technical Assistance Center. This center will identify and improve the implementation of best practices in women’s behavioral health across the life span; identify and fill critical gaps in knowledge of and resources for women’s behavioral health; and provide learning opportunities, training, and technical assistance for healthcare providers.
- Support Research on Maternal Health Outcomes. USDA will fund research to help recognize early warning signs of maternal morbidity and mortality in recipients of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and anticipates awarding up to $5 million in Fiscal Year 2023 to support maternal health research through WIC. In addition, research being conducted through the Agricultural Research Service’s Human Nutrition Research Centers is focusing on women’s health across the lifespan, including the nutritional needs of pregnant and breastfeeding women and older adults.
Stay Connected
We'll be in touch with the latest information on how President Biden and his administration are working for the American people, as well as ways you can get involved and help our country build back better.
Opt in to send and receive text messages from President Biden.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
How Health Care Organizations Should Support Social Services
- 1 The Brookings Institution, Washington, DC
In a recent JAMA Health Forum article, Glied and D’Aunno ask whether health sector investment in social services is “a bridge too far” and raise concerns about differing priorities, skills, finances, and functions of the 2 sectors that question whether this is a good match for collaboration. 1
As health care organizations ponder their role, if any, in supporting social services, there is growing evidence of health benefits from certain investments in social services (including housing and nutrition). But it is hard to make a traditional return-on-investment (ROI) case for many instances of health systems funding social service programs. For instance, to the extent that this “upstream” social funding helps improve household and community health, it means reduced revenues to hospitals and fee-for-service medical practices—so, not good for business. Managed care organizations do have a stronger business incentive to address their enrollees’ health-influencing social conditions. Still, although there is evidence that certain investments in housing, nutrition, etc do yield health care savings , the direct ROI to the health sector is often questionable. 2
The ROI Conundrum
This does not actually mean such investments have a poor return; it’s just that the principal returns often do not accrue to the investor. Health organization investments typically have positive spillover effects in areas beyond immediate health savings, such as economic improvement, better school graduation rates, and better long-term community health. But this form of value-added is not captured as revenue or savings by the health sector investor—a classic “ wrong pockets ” problem. In the same way, improvements in housing conditions financed by a housing authority, or a reduction in violence-caused injuries from new policing programs, can generate large spillover health care savings, yet the financial value of those health benefits do not accrue to the budget bottom line of housing authorities or police departments. The result in each case is usually suboptimal levels of investment in the general well-being of a community.
The key to achieving an optimal level of health system funding of social services, in which public funding is supplemented with health sector funding aimed at improving health, is to organize these investments through multisector partnerships in a community, with each partner strategically investing in community needs that generate spillover benefits to all partners. If designed and implemented well, this partnership approach encourages investments by all community partners to create a strong social return on investment ( SROI ), with benefits and savings shared by each partner as it advances its goal. Of course, reaching that result requires the investing partners to agree on their shares. That can easily lead to difficult negotiations and heightened distrust. Nichols and Taylor are among those testing procedures in communities to create a positive climate, in their case through an innovative bidding process run by a neutral broker and designed to align each partner’s investment commitment with the benefits it will receive from joint action.
Government Encouragement
There are several ways to encourage appropriate health sector investments in social services.
Government initiatives can help in several ways. At the state and local level, the government can act as an honest broker to foster joint investments within communities; states can use Medicaid contracts to require managed care plans to include community engagement, with community partners involved from the beginning. Tweaking community benefit requirements is another way. As a condition of their tax exemption, nonprofit hospitals are already required by law to invest in their communities to improve general health. The Internal Revenue Service (IRS) establishes the rules and over many years has broadened the types of community investments that qualify, including “community building activities.” The IRS could and should encourage nonprofit hospitals to be more creative in supporting innovative social service investments that appear to improve the long-term health and vitality of their communities.
The federal government can provide much clearer guidance on how programs can be used to foster local partnerships with braided funds . It can also help the development of community-level referral systems between health and social services through pilots and more grants to states and communities. More sophisticated referral infrastructure would help facilitate better coordination of social and medical care for households. It would also create important data to help improve our ability to quantify the multisector impacts of investments. In addition, analyzing the impact of recent Medicaid 1115 waivers allowing states, such as Arkansas and New Jersey , more flexibility to mix medical and social services to improve health outcomes will also generate valuable insights on how to best structure health sector investments in social services that will improve community health.
Taking a Back Seat in Partnerships
Effective partnerships require trust, understanding, and the effective use of complementary skills. Indeed, a review of health-human services partnerships suggests that the quality of the relationship is key. This is not easy to achieve between health and social service organizations when communities often doubt the motives and commitment of large health institutions that, in turn, can be skeptical of the expertise of community organizations.
Health systems need to adapt to this reality for their investments to be most beneficial. In 2017, Kaiser Permanente considered supporting a public health and economic development project in Baltimore, Maryland; however, the organization was not then well known in the mid-Atlantic area. So it first partnered with Bon Secours hospital , a very small but highly respected institution in the community; essentially, Bon Secours “credentialled” Kaiser within the community.
CommonSpirit Health has been a pioneer in developing trusted partnerships with social service organizations in communities. CommonSpirit recognizes that there is a critically important difference between functioning as a catalyst for action and being in the driver’s seat. It has partnered with the Pathways Community HUB Institute (PCHI) in 6 communities. In the PCHI model, a neutral hub operated by a local entity links a network of community organizations, health systems, and community health workers to help coordinate care and address health-related social needs. CommonSpirit, along with competing health systems in each area, funds a “community bank” that helps fund the hub’s operating costs and covers otherwise nonreimbursable service costs. It is an intriguing example of how a community partnership can function and how competing health systems can collaborate in a “co-opetition” model for their common benefit. 3
We have come to appreciate that achieving healthier communities requires a larger focus on social factors contributing to ill health. For that to happen, we need to design better SROI techniques and ways in which community savings are distributed. Health systems need to deploy investment resources in ways that prevent illness as well as treat it. Their levels and type of investment should also reflect the broad economic value of prevention and better health. And they must appreciate the importance of sharing control of decision-making over the use of their own investments.
That is not an easy equation to get right. But we have been making steady progress and should be encouraging health systems to explore more partnerships.
Published: November 9, 2023. doi:10.1001/jamahealthforum.2023.4569
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Butler SM. JAMA Health Forum .
Corresponding Author: Stuart M. Butler, PhD, The Brookings Institution, Economic Studies, 1775 Massachusetts Ave NW, Washington, DC, 20036 ( [email protected] ).
Conflict of Interest Disclosures: None reported.
See More About
Butler SM. How Health Care Organizations Should Support Social Services. JAMA Health Forum. 2023;4(11):e234569. doi:10.1001/jamahealthforum.2023.4569
Manage citations:
© 2024
Artificial Intelligence Resource Center
Best of JAMA Network 2022
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Health-Related Social Needs: Three Trends in Leveraging Community Partnerships
Payor/provider blog series: article 6.

Leading health authorities have increasingly emphasized how non-medical factors such as socioeconomic status, education, employment, housing, food security, and community support have an outsized impact on health outcomes. By some recent U.S. estimates , clinical care accounts for only 20% of county-level variation of health outcomes in the United States, with the social determinants of health (SDOH) responsible for as much as 50%. SDOH are now widely acknowledged as critical not only to improving individual health and population health, but also to meeting federal health equity goals . Yet conventional models of health care delivery still struggle with interventions to impact individuals’ health-related social needs (HRSN). One reason is that health plans and health care providers must look to nontraditional partnerships with organizations that have not historically been part of the health care industry to meet these needs.
We highlight three trends associated with partnerships to address HRSNs:
- Medicaid and Medicare health plan initiatives;
- Local and regional data sharing efforts; and
- Risk mitigation in collaborations between health care providers and community partners.
Health care providers and health plans involved in any of these trends — or looking to become involved — must navigate complex and interrelated reimbursement, privacy, compliance, and fraud and abuse issues. It is critical to consult with counsel when developing new initiatives targeting the SDOH and HRSNs to ensure legal concerns are evaluated and addressed.
Medicaid and Medicare Health Plan Initiatives
The Centers for Medicare & Medicaid Services (CMS) have begun to incorporate new tools to foster “whole person” care for Medicaid and Medicare beneficiaries and have implemented policies to encourage and pay for appropriate community partnerships.
Late last year, CMS published an informational bulletin discussing opportunities for states to cover services and supports to address health-related social needs in Medicaid and the Children’s Health Insurance Program. Accompanying guidance describes the authority for health plans in a state’s Medicaid managed care delivery system to cover “in lieu of services” that address HRSN. For example, “in lieu of services” may address housing and the home environment by covering a tenant’s first month’s rent, caregiver respite services, home remediations, and sobering centers, and may address nutrition needs by covering nutrition counseling and home-delivered meals. The bulletin highlights recent CMS approvals in seven states for evidence-based housing and nutritional services designed to mitigate the negative health impacts of unmet social needs. Since the bulletin was published, CMS approved New York’s section 1115 demonstration , which includes Medicaid opportunities for New York to address HRSN by covering similar housing supports, enhanced case management, nutrition supports, cooking supplies, and private and public transportation to HRSN services.
Interested parties should also consult CMS’ comprehensive 2021 guidance on SDOH opportunities in Medicaid, which trumpets Medicaid’s flexibility while cautioning that federal principles require services to be provided based on individual assessments of need, typically making Medicaid the payor of last resort (states must assess all available public and private funding streams before using Medicaid to cover unmet social needs), and require that services addressing SDOH be economic and efficient. CMS specifically identifies how state Medicaid programs may address SDOH through managed care, such as by sharing managed care savings with Medicaid beneficiaries in the form of additional health-related services, directing health plans to implement alternative payment models rewarding improvements in SDOH, offering incentive payments for health plans that make investments in SDOH, and using waiver authorities to incorporate SDOH services into the managed care contract and plan capitation rates. A 2023 CMS rule also proposed to make significant changes to Medicaid managed care authorities to cover “in-lieu of services,” and its finalization is expected later this year.
A 2023 CMS Final Rule for Medicare Advantage (MA) also addresses how MA plans may impact the SDOH . Over the last five to ten years, CMS has revised MA regulations to give health plans more discretion to cover services that compensate for physical impairments, reduce avoidable emergency room visits, and address SDOH-related needs for chronically ill enrollees. In some circumstances, MA plans may offer supplemental benefits covering non-medical services such as home-delivered meals, transportation, pest control, access to community-sponsored programs, and home modifications. These changes have allowed MA plans to take a more holistic approach and connect enrollees to interventions targeting social factors impacting their health.
Local and Regional Data Sharing Efforts Implicate Privacy Laws
Leveraging data is critical for both health plans and health care providers to identify and address HRSN. While some data may be available from public sources such as census records and community needs assessments, key information that is confidential and protected by privacy laws is likely to be controlled by health care organizations, governmental service providers, and community partners. Integrating and analyzing this information can be essential to quantify the prevalence of issues like food insecurity, housing instability, and transportation barriers. Integration across health and social service sectors also enables a comprehensive view of individuals’ needs and supports targeted interventions to high-risk populations. This makes data partnerships between health care entities and community organizations especially critical.
Efforts to collect and share data related to SDOH implicate a range of privacy laws. At the federal level, health care providers and plans must navigate the complex and ever-evolving landscape of laws such as the Health Insurance Portability and Accountability Act (HIPAA) and substance-use disorder confidentiality law (frequently known as Part 2). Many states also impose their own health information privacy laws, which may exceed the floors set by federal minimum requirements. In some cases, health care privacy restrictions must be balanced against an evolving set of federal and state legal requirements to share health information, such as the federal information blocking rule and California’s recent statewide data sharing framework . And because SDOH extend well beyond health information, other privacy laws addressing information such as education records and social services records must be considered. Addressing privacy laws may involve data use agreements, patient authorizations, de-identification techniques, and the design of physical, technical, and administrative safeguards to secure data and appropriately restrict the sharing of identifiable information.
Risk Mitigation in Collaborations between Health Care Providers and Community Partners
Health care providers and plans also need to collaborate with community partners to address HRSN by coordinating care and resources for individuals served by multiple providers and partners (who are also often high utilizers with high costs). Collaboration could involve multi-party arrangements with partners such as housing agencies, food banks, transportation services, government agencies, and social service organizations.
One legal challenge in developing such partnerships is adherence to health care fraud and abuse laws. For example, the federal Anti-Kickback Statute (AKS) and physician self-referral law (Stark) may be implicated by any exchange of remuneration, including in-kind services, between health care entities and community partners who work with Medicaid and Medicare patients.
In addition, Medicare and Medicaid anti-supplementation provisions must be considered when designing payments to incentivize the use of health care services, including non-traditional services. Health care partnerships must be carefully designed to fit within regulatory exceptions and safe harbors to mitigate these risks.
When addressing HRSN for federal health care program beneficiaries, risk mitigation may involve leveraging the recent value-based exceptions promulgated by CMS and the Office of Inspector General for the Department of Health and Human Services (OIG). Value-based exceptions can shield from AKS and Stark liability certain arrangements between partners who are jointly pursuing value-based purposes such as coordinating and managing care, improving quality of care, and appropriately reducing health care costs. As with any fraud and abuse issue, it is important to consult legal counsel and establish robust compliance safeguards.
Payor/Provider Convergence Blog Series
For additional resources on the intersection of payor/provider convergence and the issues that plague insurance and health companies, payors, and providers, click here to read the other articles in our series.
Foley is here to help you navigate the complex legal issues involved in addressing the social determinants of health. To learn more, please reach out to the authors, your Foley relationship partner, our Payor/Provider Convergence Area of Focus , or to our Health Care Practice Group with any questions.

Adam J. Hepworth

Anil Shankar

Jordan H. Smiley
Related insights, hhs updates pixels and trackers guidance for hipaa regulated entities, clinical research: fda issues draft guidance on informed consent, clinical trials: fda issues finalized charging guidance for investigational drug use .
Social Justice in Modern Health Care
How personal experience inspired u.s. health care leaders, published march 25, 2024, courses mentioned in this post: reducing racial disparities in health care series mentioned in this post: health care leadership.
Understanding health care disparities is personal for Aswita Tan-McGrory , Director of the Disparities Solutions Center and Director of Equity and Care Implementation at Massachusetts General Hospital (MGH). Inspired by her work at MGH and her own life experiences, Tan-McGrory co-leads our Harvard Online course Reducing Racial Disparities in Health Care to educate other industry leaders on inequalities in health care and how to address social justice issues.
To dive deeper into these complex topics, Tan-McGrory gathered with health care leaders from across the U.S. on a 45-minute webinar . Featured panelists included Dr. Lenny Lopez , Chief of Hospital Medicine and Associate Professor of Medicine at the University of California, San Francisco; Andrea Madu , Consultant at The Bridgespan Group; and Dr. Esteban Barreto , Director of Evaluation of Equity and Community Health at Massachusetts General Hospital.
The panelists shared how their personal experiences have led them to research and address health care disparities. Andrea Madu shared the story of her family emigrating from Nigeria and how she remembers “going to the hospital as a child and seeing how doctors treated my non-English-speaking grandmother very differently from me and my siblings… I've seen how this poor treatment can translate to poor outcomes for patients.”
Dr. Esteban Barreto shared his similar experiences as an immigrant to the U.S., often watching family members with language barriers try to deal with different systems. Dr. Barreto noted, “It's a combination of both lived experience and also early professional experience, I was able to explore barriers in a more tailored way and hear from those voices who may otherwise be excluded from different assessments.”
To summarize in Tan-McGrory’s words, “This is personal to us. Very personal. Not only are we motivated because, as many people say, it's the right thing to do, but it also resonates with many of us. It's the people that we love that we see as patients.”
Helping people get the care they need is the essence of health care. Unfortunately, too often, modern health care systems are selective about both the people and type of care based on racial bias. How can health care leaders address these inequitable practices in health care, regardless of whether they have relevant, lived experiences like our webinar panelists mentioned?
In her course , Tan-McGrory aims to answer this question and provide tools for industry leaders to tackle health care equality. And it truly does take a village—not just those new to the industry. Dr. Lopez shared, “Even after 20 years of working in the field of equity and health care disparities, I’m constantly learning. I'm constantly being pushed. I’m constantly needing to reflect on my own implicit biases… it’s key to realize that you don’t know everything.”
While the panelists highlighted the value of taking a course to learn about social justice in health care, they also provided some immediate solutions for health care workers to take towards addressing disparities:
- Have an honest and open dialogue about historical missteps that could damage the community’s trust in medical providers. Madu noted, “Understand the medical mistrust that has happened over decades or centuries, and why some people might not want to come to the doctor or adhere to treatments. There are reasons behind it, and it’s important to come to it with humility and empathy for patients.”
- Establish networks of passionate health care providers that reflect the community's varied backgrounds. Madu added, “What’s needed is a pipeline of doctors who look like the communities they’re serving and have that lived experience to understand the cultural context of what patients are saying.”
- Practice listening to patients and inviting them into the solution process. From Madu, “Treat patients as the subject matter experts of their lives. Build trust within the community to recognize where the core issues and root causes are before going into treatment planning.”
- Focus intentionally on specific areas to make forward progress. Dr. Lopez shared, “That’s where the change happens. We oftentimes have grandiose ideas about how the world is going to change, and often, it’s much smaller victories that add up over time. Those small things are what give you strength, courage, and energy to keep doing the work.”
As Andrea Madu puts it, the key to all of this vital work is this: “Equity is not something that we’re going to solve in our lifetime. But there are pieces of it that we can move along—a journey we’re working toward.”
To hear the full conversation between our panelists and Aswita Tan-McGrory, view the full webinar here .
To learn more about these solutions and other tools for addressing racial disparities in our health care system, check out our Reducing Racial Disparities in Health Care course here.
Related Blog Posts
The business of health care in the united states.
How can we ensure that patients have access to care while still adopting important, life-saving innovations that have the potential to improve health and health care?
How To Earn CME Credits with Harvard Online Courses On Health
Harvard University faculty guide you through topics with a focus on the current state of the US health care system and how you can apply innovative approaches to make improvements within your organization.
Aswita Tan-McGrory Examines Why Disparities Exist in Health Care Systems
While quality and access to health care in the U.S. has been improving in recent years, there’s still significant work to do. Aswita Tan-McGrory is one of the leaders at the helm of this transformative work.
This site uses session cookies and persistent cookies to improve the content and structure of the site.
By clicking “ Accept All Cookies ”, you agree to the storing of cookies on this device to enhance site navigation and content, analyse site usage, and assist in our marketing efforts.
By clicking ' See cookie policy ' you can review and change your cookie preferences and enable the ones you agree to.
By dismissing this banner , you are rejecting all cookies and therefore we will not store any cookies on this device.
UK Policy Framework for Health and Social Care Research
This policy framework sets out principles of good practice in the management and conduct of health and social care research in the UK.
These principles protect and promote the interests of patients, service users and the public in health and social care research, by describing ethical conduct and proportionate, assurance-based management of health and social care research, so as to support and facilitate high-quality research in the UK that has the confidence of patients, service users and the public.
It is for organisations and individuals that have responsibilities for health and social care research. This includes funders, sponsors, researchers and their employers, research sites and care providers.
The policy framework applies to health and social care research involving patients, service users or their relatives or carers. This includes research involving them indirectly, for example using information that the NHS or social care services have collected about them.
The Health Research Authority and the health departments in Northern Ireland, Scotland and Wales have developed the policy framework following public consultation . It replaces the separate Research Governance Frameworks in each UK country with a single, modern set of principles for the whole UK.
Read the policy framework
You can read the UK Framework for Health and Social Care Research in full on our website or download the UK Framework for Health and Social Care Research (PDF) .
We welcome your comments on the framework, which will help us improve future versions; and any examples of where you have used the framework as part of your work.

"I welcome publication of the UK Policy Framework for Health and Social Care Research which sets out the principles of good practice in the management and conduct of health and social care research across the UK. The Framework will ensure that the public will continue to feel safe when they take part in research and it will enable researchers to develop innovations which will help to improve the quality of health and care in the UK."
Related links
- Replacing the Research Governance Framework
- New framework for UK health and social care research launched
- UK Policy Framework for Health and Social Care Research: consultation
- Privacy notice
- Terms & conditions
- Accessibility statement
- Feedback or concerns
Australian Government Department of Health and Aged Care
Final report of the Aged Care Taskforce
This report examines the recommendations proposed by the Aged Care Taskforce to support an aged care system that is sustainable, fair and facilitates greater innovation in the sector.
Scroll down to access downloads and media.
Download [Publication] Final report of the Aged Care Taskforce (PDF) as PDF - 1.36 MB - 64 pages
Download [Publication] Final report of the Aged Care Taskforce (Word) as Word - 1.89 MB - 64 pages
We aim to provide documents in an accessible format. If you're having problems using a document with your accessibility tools, please contact us for help .
We held a presentation on the Aged Care Taskforce report on Tuesday 12 March 2024. A recording of this presentation will be available soon. You can still submit questions by email .
Is there anything wrong with this page?
Help us improve health.gov.au
If you would like a response please use the enquiries form instead.
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries
What the data says about abortion in the u.s..
Pew Research Center has conducted many surveys about abortion over the years, providing a lens into Americans’ views on whether the procedure should be legal, among a host of other questions.
In a Center survey conducted nearly a year after the Supreme Court’s June 2022 decision that ended the constitutional right to abortion , 62% of U.S. adults said the practice should be legal in all or most cases, while 36% said it should be illegal in all or most cases. Another survey conducted a few months before the decision showed that relatively few Americans take an absolutist view on the issue .
Find answers to common questions about abortion in America, based on data from the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, which have tracked these patterns for several decades:
How many abortions are there in the U.S. each year?
How has the number of abortions in the u.s. changed over time, what is the abortion rate among women in the u.s. how has it changed over time, what are the most common types of abortion, how many abortion providers are there in the u.s., and how has that number changed, what percentage of abortions are for women who live in a different state from the abortion provider, what are the demographics of women who have had abortions, when during pregnancy do most abortions occur, how often are there medical complications from abortion.
This compilation of data on abortion in the United States draws mainly from two sources: the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, both of which have regularly compiled national abortion data for approximately half a century, and which collect their data in different ways.
The CDC data that is highlighted in this post comes from the agency’s “abortion surveillance” reports, which have been published annually since 1974 (and which have included data from 1969). Its figures from 1973 through 1996 include data from all 50 states, the District of Columbia and New York City – 52 “reporting areas” in all. Since 1997, the CDC’s totals have lacked data from some states (most notably California) for the years that those states did not report data to the agency. The four reporting areas that did not submit data to the CDC in 2021 – California, Maryland, New Hampshire and New Jersey – accounted for approximately 25% of all legal induced abortions in the U.S. in 2020, according to Guttmacher’s data. Most states, though, do have data in the reports, and the figures for the vast majority of them came from each state’s central health agency, while for some states, the figures came from hospitals and other medical facilities.
Discussion of CDC abortion data involving women’s state of residence, marital status, race, ethnicity, age, abortion history and the number of previous live births excludes the low share of abortions where that information was not supplied. Read the methodology for the CDC’s latest abortion surveillance report , which includes data from 2021, for more details. Previous reports can be found at stacks.cdc.gov by entering “abortion surveillance” into the search box.
For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. In computing those figures, we excluded abortions listed in the report under the categories “spontaneous or unspecified” or as “other.” (“Spontaneous abortion” is another way of referring to miscarriages.)
Guttmacher data in this post comes from national surveys of abortion providers that Guttmacher has conducted 19 times since 1973. Guttmacher compiles its figures after contacting every known provider of abortions – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, and it provides estimates for abortion providers that don’t respond to its inquiries. (In 2020, the last year for which it has released data on the number of abortions in the U.S., it used estimates for 12% of abortions.) For most of the 2000s, Guttmacher has conducted these national surveys every three years, each time getting abortion data for the prior two years. For each interim year, Guttmacher has calculated estimates based on trends from its own figures and from other data.
The latest full summary of Guttmacher data came in the institute’s report titled “Abortion Incidence and Service Availability in the United States, 2020.” It includes figures for 2020 and 2019 and estimates for 2018. The report includes a methods section.
In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion.
An exact answer is hard to come by. The CDC and the Guttmacher Institute have each tried to measure this for around half a century, but they use different methods and publish different figures.
The last year for which the CDC reported a yearly national total for abortions is 2021. It found there were 625,978 abortions in the District of Columbia and the 46 states with available data that year, up from 597,355 in those states and D.C. in 2020. The corresponding figure for 2019 was 607,720.
The last year for which Guttmacher reported a yearly national total was 2020. It said there were 930,160 abortions that year in all 50 states and the District of Columbia, compared with 916,460 in 2019.
- How the CDC gets its data: It compiles figures that are voluntarily reported by states’ central health agencies, including separate figures for New York City and the District of Columbia. Its latest totals do not include figures from California, Maryland, New Hampshire or New Jersey, which did not report data to the CDC. ( Read the methodology from the latest CDC report .)
- How Guttmacher gets its data: It compiles its figures after contacting every known abortion provider – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, then provides estimates for abortion providers that don’t respond. Guttmacher’s figures are higher than the CDC’s in part because they include data (and in some instances, estimates) from all 50 states. ( Read the institute’s latest full report and methodology .)
While the Guttmacher Institute supports abortion rights, its empirical data on abortions in the U.S. has been widely cited by groups and publications across the political spectrum, including by a number of those that disagree with its positions .
These estimates from Guttmacher and the CDC are results of multiyear efforts to collect data on abortion across the U.S. Last year, Guttmacher also began publishing less precise estimates every few months , based on a much smaller sample of providers.
The figures reported by these organizations include only legal induced abortions conducted by clinics, hospitals or physicians’ offices, or those that make use of abortion pills dispensed from certified facilities such as clinics or physicians’ offices. They do not account for the use of abortion pills that were obtained outside of clinical settings .
(Back to top)
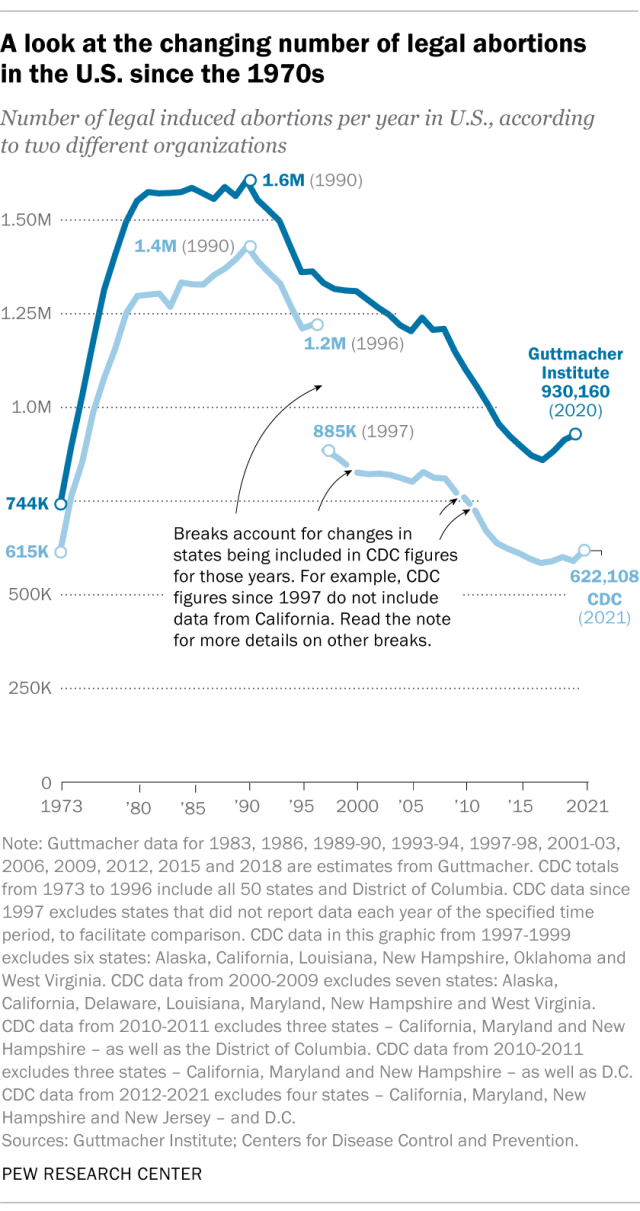
The annual number of U.S. abortions rose for years after Roe v. Wade legalized the procedure in 1973, reaching its highest levels around the late 1980s and early 1990s, according to both the CDC and Guttmacher. Since then, abortions have generally decreased at what a CDC analysis called “a slow yet steady pace.”
Guttmacher says the number of abortions occurring in the U.S. in 2020 was 40% lower than it was in 1991. According to the CDC, the number was 36% lower in 2021 than in 1991, looking just at the District of Columbia and the 46 states that reported both of those years.
(The corresponding line graph shows the long-term trend in the number of legal abortions reported by both organizations. To allow for consistent comparisons over time, the CDC figures in the chart have been adjusted to ensure that the same states are counted from one year to the next. Using that approach, the CDC figure for 2021 is 622,108 legal abortions.)
There have been occasional breaks in this long-term pattern of decline – during the middle of the first decade of the 2000s, and then again in the late 2010s. The CDC reported modest 1% and 2% increases in abortions in 2018 and 2019, and then, after a 2% decrease in 2020, a 5% increase in 2021. Guttmacher reported an 8% increase over the three-year period from 2017 to 2020.
As noted above, these figures do not include abortions that use pills obtained outside of clinical settings.
Guttmacher says that in 2020 there were 14.4 abortions in the U.S. per 1,000 women ages 15 to 44. Its data shows that the rate of abortions among women has generally been declining in the U.S. since 1981, when it reported there were 29.3 abortions per 1,000 women in that age range.
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher’s data, the CDC’s figures also suggest a general decline in the abortion rate over time. In 1980, when the CDC reported on all 50 states and D.C., it said there were 25 abortions per 1,000 women ages 15 to 44.
That said, both Guttmacher and the CDC say there were slight increases in the rate of abortions during the late 2010s and early 2020s. Guttmacher says the abortion rate per 1,000 women ages 15 to 44 rose from 13.5 in 2017 to 14.4 in 2020. The CDC says it rose from 11.2 per 1,000 in 2017 to 11.4 in 2019, before falling back to 11.1 in 2020 and then rising again to 11.6 in 2021. (The CDC’s figures for those years exclude data from California, D.C., Maryland, New Hampshire and New Jersey.)
The CDC broadly divides abortions into two categories: surgical abortions and medication abortions, which involve pills. Since the Food and Drug Administration first approved abortion pills in 2000, their use has increased over time as a share of abortions nationally, according to both the CDC and Guttmacher.
The majority of abortions in the U.S. now involve pills, according to both the CDC and Guttmacher. The CDC says 56% of U.S. abortions in 2021 involved pills, up from 53% in 2020 and 44% in 2019. Its figures for 2021 include the District of Columbia and 44 states that provided this data; its figures for 2020 include D.C. and 44 states (though not all of the same states as in 2021), and its figures for 2019 include D.C. and 45 states.
Guttmacher, which measures this every three years, says 53% of U.S. abortions involved pills in 2020, up from 39% in 2017.
Two pills commonly used together for medication abortions are mifepristone, which, taken first, blocks hormones that support a pregnancy, and misoprostol, which then causes the uterus to empty. According to the FDA, medication abortions are safe until 10 weeks into pregnancy.
Surgical abortions conducted during the first trimester of pregnancy typically use a suction process, while the relatively few surgical abortions that occur during the second trimester of a pregnancy typically use a process called dilation and evacuation, according to the UCLA School of Medicine.
In 2020, there were 1,603 facilities in the U.S. that provided abortions, according to Guttmacher . This included 807 clinics, 530 hospitals and 266 physicians’ offices.
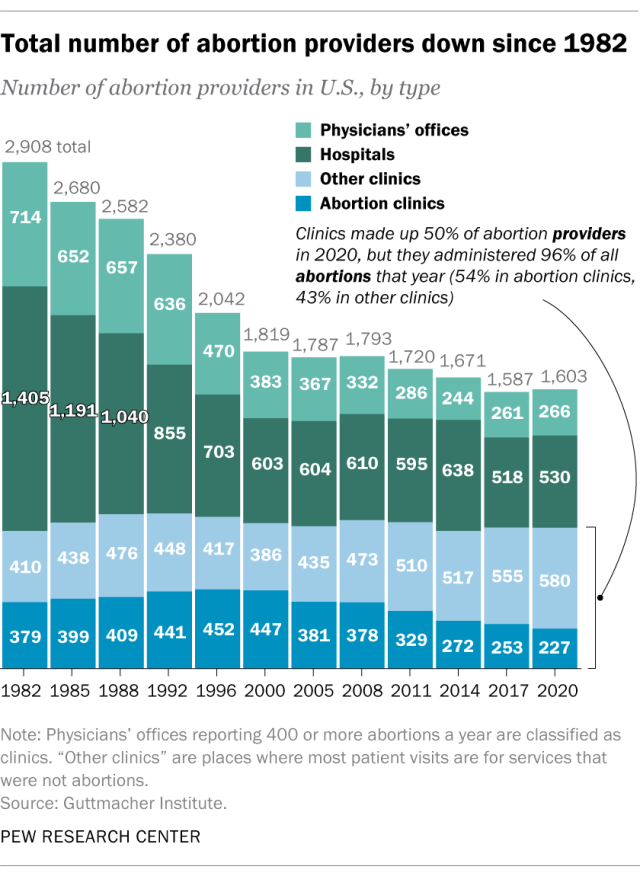
While clinics make up half of the facilities that provide abortions, they are the sites where the vast majority (96%) of abortions are administered, either through procedures or the distribution of pills, according to Guttmacher’s 2020 data. (This includes 54% of abortions that are administered at specialized abortion clinics and 43% at nonspecialized clinics.) Hospitals made up 33% of the facilities that provided abortions in 2020 but accounted for only 3% of abortions that year, while just 1% of abortions were conducted by physicians’ offices.
Looking just at clinics – that is, the total number of specialized abortion clinics and nonspecialized clinics in the U.S. – Guttmacher found the total virtually unchanged between 2017 (808 clinics) and 2020 (807 clinics). However, there were regional differences. In the Midwest, the number of clinics that provide abortions increased by 11% during those years, and in the West by 6%. The number of clinics decreased during those years by 9% in the Northeast and 3% in the South.
The total number of abortion providers has declined dramatically since the 1980s. In 1982, according to Guttmacher, there were 2,908 facilities providing abortions in the U.S., including 789 clinics, 1,405 hospitals and 714 physicians’ offices.
The CDC does not track the number of abortion providers.
In the District of Columbia and the 46 states that provided abortion and residency information to the CDC in 2021, 10.9% of all abortions were performed on women known to live outside the state where the abortion occurred – slightly higher than the percentage in 2020 (9.7%). That year, D.C. and 46 states (though not the same ones as in 2021) reported abortion and residency data. (The total number of abortions used in these calculations included figures for women with both known and unknown residential status.)
The share of reported abortions performed on women outside their state of residence was much higher before the 1973 Roe decision that stopped states from banning abortion. In 1972, 41% of all abortions in D.C. and the 20 states that provided this information to the CDC that year were performed on women outside their state of residence. In 1973, the corresponding figure was 21% in the District of Columbia and the 41 states that provided this information, and in 1974 it was 11% in D.C. and the 43 states that provided data.
In the District of Columbia and the 46 states that reported age data to the CDC in 2021, the majority of women who had abortions (57%) were in their 20s, while about three-in-ten (31%) were in their 30s. Teens ages 13 to 19 accounted for 8% of those who had abortions, while women ages 40 to 44 accounted for about 4%.
The vast majority of women who had abortions in 2021 were unmarried (87%), while married women accounted for 13%, according to the CDC , which had data on this from 37 states.
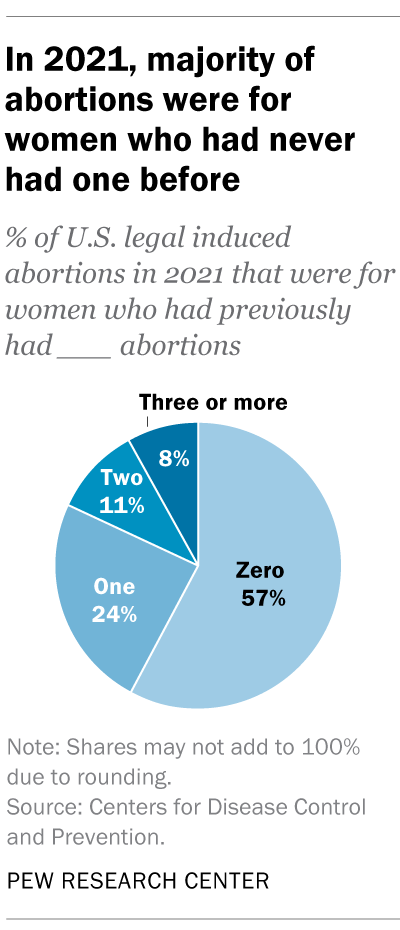
In the District of Columbia, New York City (but not the rest of New York) and the 31 states that reported racial and ethnic data on abortion to the CDC , 42% of all women who had abortions in 2021 were non-Hispanic Black, while 30% were non-Hispanic White, 22% were Hispanic and 6% were of other races.
Looking at abortion rates among those ages 15 to 44, there were 28.6 abortions per 1,000 non-Hispanic Black women in 2021; 12.3 abortions per 1,000 Hispanic women; 6.4 abortions per 1,000 non-Hispanic White women; and 9.2 abortions per 1,000 women of other races, the CDC reported from those same 31 states, D.C. and New York City.
For 57% of U.S. women who had induced abortions in 2021, it was the first time they had ever had one, according to the CDC. For nearly a quarter (24%), it was their second abortion. For 11% of women who had an abortion that year, it was their third, and for 8% it was their fourth or more. These CDC figures include data from 41 states and New York City, but not the rest of New York.
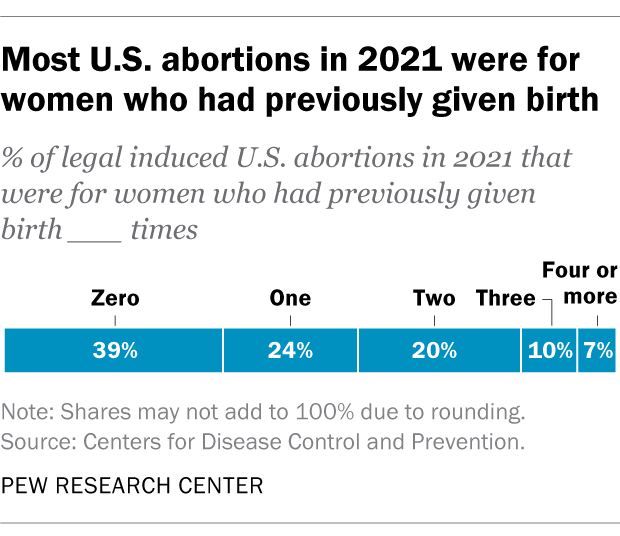
Nearly four-in-ten women who had abortions in 2021 (39%) had no previous live births at the time they had an abortion, according to the CDC . Almost a quarter (24%) of women who had abortions in 2021 had one previous live birth, 20% had two previous live births, 10% had three, and 7% had four or more previous live births. These CDC figures include data from 41 states and New York City, but not the rest of New York.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester – that is, at or before 13 weeks of gestation, according to the CDC . An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation. These CDC figures include data from 40 states and New York City, but not the rest of New York.
About 2% of all abortions in the U.S. involve some type of complication for the woman , according to an article in StatPearls, an online health care resource. “Most complications are considered minor such as pain, bleeding, infection and post-anesthesia complications,” according to the article.
The CDC calculates case-fatality rates for women from induced abortions – that is, how many women die from abortion-related complications, for every 100,000 legal abortions that occur in the U.S . The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions. During the five-year periods in between, the figure ranged from 0.52 (from 1993 to 1997) to 0.78 (from 1978 to 1982).
The CDC calculates death rates by five-year and seven-year periods because of year-to-year fluctuation in the numbers and due to the relatively low number of women who die from legal induced abortions.
In 2020, the last year for which the CDC has information , six women in the U.S. died due to complications from induced abortions. Four women died in this way in 2019, two in 2018, and three in 2017. (These deaths all followed legal abortions.) Since 1990, the annual number of deaths among women due to legal induced abortion has ranged from two to 12.
The annual number of reported deaths from induced abortions (legal and illegal) tended to be higher in the 1980s, when it ranged from nine to 16, and from 1972 to 1979, when it ranged from 13 to 63. One driver of the decline was the drop in deaths from illegal abortions. There were 39 deaths from illegal abortions in 1972, the last full year before Roe v. Wade. The total fell to 19 in 1973 and to single digits or zero every year after that. (The number of deaths from legal abortions has also declined since then, though with some slight variation over time.)
The number of deaths from induced abortions was considerably higher in the 1960s than afterward. For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965 , according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services.
Note: This is an update of a post originally published May 27, 2022, and first updated June 24, 2022.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
Key facts about the abortion debate in America
Public opinion on abortion, three-in-ten or more democrats and republicans don’t agree with their party on abortion, partisanship a bigger factor than geography in views of abortion access locally, do state laws on abortion reflect public opinion, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .

IMAGES
COMMENTS
A healthcare disparity is a difference between population groups in the way they access, experience, and receive healthcare. Factors that influence healthcare disparities include social, economic, environmental, and other disadvantages, 1, 2 some of which are explored in this report. Unfortunately, Americans too often do not receive care they ...
"Learning from Massachusetts Hospitals on Programs to Address Social Determinants of Health" by David E. Velasquez, BS, and Jose F. Figueroa, MD, MPH, both of Harvard Medical School, helps clarify the current landscape, showing that health care executives in that state strongly endorse the importance of addressing SDOH in their patients, and that their hospitals often use community benefit ...
Health care today is often characterized by mediocre quality, poor safety, and high costs. 1 Though change usually comes slowly, the Covid-19 pandemic has demonstrated that it is possible to rapidly retool our systems if there is a strong enough stimulus. 2 In this article, we examine the future of health care — how it should change over the next 10 years, and the key drivers to enable our ...
This PCD collection on advancing health equity and reducing health disparities concludes with a research study by Leiby et al investigating the effectiveness of an enhanced intervention among people with glaucoma: using patient navigators and social workers to improve patient adherence to follow-up eye care in community settings (20).
1 INTRODUCTION. Over the past decade, an increased focus on the way that integrated health and social care (IHSC) services are delivered and a growing demand for improved service user experience have driven forward improvements in worldwide health and social care (HSC; World Health Organization, 2016a).Person-centred IHSC systems aim to follow principles of participatory care and governance ...
Health research entails systematic collection or analysis of data with the intent to develop generalizable knowledge to understand health challenges and mount an improved response to them. The full spectrum of health research spans five generic areas of activity: measuring the health problem; understanding its cause(s); elaborating solutions; translating the solutions or evidence into policy ...
Suzanne Sayuri Ii is a Qualitative Researcher in the Medical Sociology & Health Experiences Research Group (MS&HERG), in the Nuffield Department of Primary Care Health Sciences, University of Oxford. Her research interests include issues in social care, knowledge mobilisation, mixed methods, and patient and public involvement.
Current research ethics frameworks were developed on the footprint of biomedical, experimental research and present several pitfalls when applied to non-experimental social sciences. This work explores how the normative principles underpinning policy and regulatory frameworks of research ethics and the related operational processes work in practice in the context of collaborative health and ...
What is research and how does it work in the context of nursing, health and social care? Now in its 7 th edition, this introductory guide provides you with a concise overview of the different research methods and terminology that you will come across when undertaking research in any course related to nursing, health and social care. The book's easy-to-follow structure takes you from research ...
We fund, enable and deliver world-leading health and social care research that improves people's health and wellbeing, and promotes economic growth. News. Scientists close in on blood test to stop spread of tuberculosis. £17.9m for Advanced Therapy Treatment Centre network to bolster clinical trial infrastructure in the UK.
Evidence from trials without randomisation or from single before-and-after studies, cohort, time series or matched case-controlled studies or observational studies. Evidence from well-designed descriptive studies or qualitative research. Opinions from expert committees or formal consensus methods. Expert opinion.
Annex 2 - Public health and social care research. Public health research investigates issues that impact at a population rather than an individual level. This can be done within the NHS with system-level studies, such as secondary prevention of cardiovascular disease and examining the impact on health inequalities of changes to the NHS ...
Early in the pandemic, psychologists helped document an increase in anxiety and depression among health care providers. Now, that acute stress has transformed into ongoing frustration, fatigue, and burnout as medical workers face surging cases, overflowing hospitals, nursing shortages, protests against vaccination mandates, and other ...
Health research is critical to making sure that we're providing the best possible care for everyone - both today, and in the future. Whether our knowledge is gained through clinical trials, equipment testing, surveys, questionnaires or data analysis, the answers we find help us improve our processes, healthcare and make positive change.
Browse all our research projects by topic We have funded more than 150 external research projects across a range of themes over the last five years. Browse all our research projects by topic. Copy link. Please click below to see the research projects we've funded on the following topics.
Oral health: Approximately one in seven people were unable to get or delayed getting needed dental care due to cost in 2019, a rate far higher than the percentage of people unable to get or get needed medical care due to cost. The data also indicate that access to oral healthcare and outcomes has improved for children, not adults.
Social care research. Is about improving the lives of people who receive care and support from our social care sector. Research in social care could be about introducing new devices and technologies such as: lifting equipment to help with residents, exploring the impact of technology driven care environments or changing social care policies and ...
These actions will build on the NIH's current policy to ensure that research it funds considers women's health in the development of study design and in data collection and analysis ...
In a recent JAMA Health Forum article, Glied and D'Aunno ask whether health sector investment in social services is "a bridge too far" and raise concerns about differing priorities, skills, finances, and functions of the 2 sectors that question whether this is a good match for collaboration. 1. As health care organizations ponder their role, if any, in supporting social services, there ...
Leading health authorities have increasingly emphasized how non-medical factors such as socioeconomic status, education, employment, housing, food security, and community support have an outsized impact on health outcomes. By some recent U.S. estimates, clinical care accounts for only 20% of county-level variation of health outcomes in the United States, with the social determinants of health ...
Understanding health care disparities is personal for Aswita Tan-McGrory, Director of the Disparities Solutions Center and Director of Equity and Care Implementation at Massachusetts General Hospital (MGH).Inspired by her work at MGH and her own life experiences, Tan-McGrory co-leads our Harvard Online course Reducing Racial Disparities in Health Care to educate other industry leaders on ...
Special Issue Information. Dear Colleagues, The development of effective health and social care policy is becoming essential, especially in eras of unexpected health crises and social changes like the current situation. Vulnerable social groups, specific patient groups and people in need are being negatively affected as health and welfare ...
Last updated on 6 Sep 2023. This policy framework sets out principles of good practice in the management and conduct of health and social care research in the UK. These principles protect and promote the interests of patients, service users and the public in health and social care research, by describing ethical conduct and proportionate ...
The Department of Health and Aged Care acknowledges the traditional owners of country throughout Australia, and their continuing connection to land, sea and community. We pay our respects to them and their cultures, and to elders both past and present.
For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965, according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services. (Back to top)