Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Nature Outlook 08 March 2018

The future of medicine
Modern medicine is affording people longer and healthier lives. But researchers want to take improvements in health even further. With advances in gene editing, technology to overcome paralysis and efforts to address high drug costs, the future of medicine is bright.
This Nature Outlook is editorially independent. It is produced with third party financial support. About this content .

Produced with support from:

This Nature Outlook is editorially independent, produced with financial support from a third party. About this content .
- Nature Outlook content
- Curious2018
Features and comment

Modern medicine has brought huge health benefits. Now researchers want to go further.
- Richard Hodson

Infection forecasts powered by big data
Web searches, medical records and networks of local volunteers are enabling faster control of disease outbreaks.
- Michael Eisenstein

Four stories of antibacterial breakthroughs
Old drugs and new tricks keep researchers one step ahead of antibiotic resistance.
- Natasha Gilbert

How CRISPR is transforming drug discovery
Gene editing is quietly revolutionizing the search for new drugs.
- Andrew Scott

The mind-reading devices that can free paralysed muscles
Technologies that restore movement and the sense of touch are helping people to overcome the physical effects of stroke and spinal-cord injury.
- Neil Savage

Bringing down the cost of cancer treatment
Innovative drugs have the potential to save lives worldwide — if they are affordable.
- Elie Dolgin
The battle to tame autoimmunity
A more tolerant immune system could alleviate, or even prevent, autoimmune disorders such as type 1 diabetes and multiple sclerosis, as well as the rejection of transplanted organs.
- Katherine Bourzac

Fighting the inevitability of ageing
The debilitating loss of muscle and strength that comes with age is being recognized as a disease that could be treated.

How baby’s first microbes could be crucial to future health
Altering the community of bacteria that live in the gut might help infants to thrive or even avoid conditions such as asthma and diabetes.
- Sarah DeWeerdt

Cleaning up pollutants to protect future health
Although the benefits of reducing exposure to toxic chemicals are becoming clearer, the path from evidence to action is not straightforward.
- Karl Gruber
A CRISPR edit for heart disease
A one-off injection to reduce the risk of cardiovascular disease is now a prospect thanks to advances in gene editing.
- Anthony King
More from Nature Research
Functional precision cancer medicine—moving beyond pure genomics
Anthony Letai proposes wider adoption of functional assays in efforts to match the right drug to the right patient and discusses why these assays might be complementary to existing genomics-based approaches.
- Anthony Letai

Making individualized drugs a reality
Magistral drug preparation offers a model to circumvent many of the technological, regulatory and financial challenges that prevent provision of the right drug at the right time to the right patient.
- Huub Schellekens
- Mohammed Aldosari
- Enrico Mastrobattista

Refining strategies to translate genome editing to the clinic
In this Review, Cathomen and colleagues present the latest advances, including improvements in nuclease specificity and delivery, that will expedite the clinical translation of genome editing.
- Tatjana I Cornu
- Claudio Mussolino
- Toni Cathomen

Emerging viral diseases from a vaccinology perspective: preparing for the next pandemic
Emerging viral diseases present a huge and increasingly important global threat to public health systems. Graham and Sullivan discuss the challenges presented by emerging viral diseases and discuss how innovations in technology and policy can address this threat.
- Barney S. Graham
- Nancy J. Sullivan
Predictable response: Finding optimal drugs and doses using artificial intelligence
- Shraddha Chakradhar
The role of vaccines in preventing bacterial antimicrobial resistance
One strategy to counter the rise of antimicrobial resistance is the development of vaccines against resistant pathogens, preventing further infection and spread of antimicrobial resistance.
- Kathrin U Jansen
- Charles Knirsch
- Annaliesa S Anderson

Air pollution and cardiovascular disease: a window of opportunity
The recent publication of The Lancet Commission on pollution and health is a watershed moment for one of the greatest challenges to cardiovascular health. In this Comment article, we discuss the global burden of air pollution on cardiovascular health.
- Michael B. Hadley
- Rajesh Vedanthan
- Valentin Fuster
Advances in subjective well-being research
Diener et al. synthesize findings from psychology and economics on subjective well-being across cultures and identify outstanding questions, priorities for future research and pathways to policy implementation.
- Shigehiro Oishi
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Share full article
Advertisement
Supported by
Guest Essay
The Future of Medicine Is Unfolding Before Us. Are We Nurturing It?

By Elizabeth Currid-Halkett
Dr. Currid-Halkett is a Guggenheim fellow and professor of public policy at the University of Southern California.
On Jan. 8, 2020, as I was parking my car, I got a long-awaited phone call from one of my son’s doctors. She informed me that our 7-month-old son, Eliot, had Duchenne muscular dystrophy, a fatal neuromuscular disease.
I can still remember the way the Los Angeles winter sunlight hit the dashboard. I can see my neighbor walking up her steps with groceries, a leaf falling, oblivious to the devastation below. “Life changes in an instant,” Joan Didion wrote. “The ordinary instant.” Our son had a fatal illness. He would die before us.
D.M.D. prevents the production of dystrophin, a protein needed to protect and repair muscle cells. It is caused by a genetic mutation on the X chromosome, thus the disease almost exclusively affects boys (one in 3,300). Over time, children with D.M.D. lose muscle mass and thus the ability to do basic things like run and walk. Eventually they lose their ability to breathe, and they experience heart failure. There is no known cure. While existing treatments have helped extend the life span of sufferers, they mainly focus on managing symptoms.
In my search for answers for how to save my son, I contacted Dr. Jerry Mendell, a now-retired neurologist at Nationwide Children’s Hospital in Columbus, Ohio, who was running clinical trials for an experimental gene therapy he developed to enable dystrophin production in boys with D.M.D. The treatment, now known as Elevidys, offered the prospect of not merely managing symptoms, but slowing the disease’s progression or even stopping it in its tracks — and potentially, for the first time in the history of this terrible disease, allowing boys with D.M.D. a chance to thrive.
Since I had that first conversation with Dr. Mendell (also a senior adviser for Sarepta, the maker of Elevidys), clinical trials for the gene therapy have had their ups and downs , and some adverse effects have been reported. But in June 2023, based on a two-part clinical trial, the Food and Drug Administration granted accelerated approval for the treatment for 4- and 5-year-olds who do not have other disqualifying conditions. The F.D.A.’s approval was contingent on continuing trials showing evidence of improved motor function, which had not yet been established.
Before Eliot received his treatment, he had difficulty going up stairs. He complained about being tired after walking only a block or two, even on Halloween, when candy ought to have motivated him. Hopping on one foot, a milestone for a 4-year-old, was impossible.
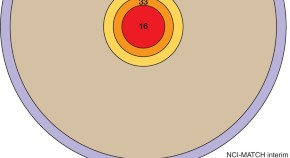
On Aug. 29, he finally received the one-time infusion. Three weeks later, he was marching upstairs and able to jump over and over. After four weeks, he could hop on one foot. Six weeks after treatment, Eliot’s neurologist decided to re-administer the North Star Ambulatory Assessment , used to test boys with D.M.D. on skills like balance, jumping and getting up from the floor unassisted. In June, Eliot’s score was 22 out of 34. In the second week of October, it was a perfect 34 — that of a typically developing , healthy 4-year-old boy. Head in my hands, I wept with joy. This was science at its very best, close to a miracle.
But the goal to offer this possible future to more patients with D.M.D. is in jeopardy. Sarepta is seeking F.D.A. approval to treat boys over 5 . Disagreements over the latest clinical trial’s results threaten to derail that outcome.
Moreover, what the F.D.A. decides to do next with Elevidys could set the tone for how it handles other emerging gene therapies for rare diseases. We can already see roadblocks that prevent more families from gaining access to these new treatments — from high costs and insurance challenges to dissent over how flexible regulators should be in interpreting clinical trial results and taking qualitative improvements into account. What is at stake with the debate around Elevidys is more than just the chance to give other boys with D.M.D. a more normal life. The challenges that we are witnessing with Elevidys are a harbinger of the fights we may see with gene therapies developed for other rare diseases.
There’s an opportunity to reduce those barriers now, while these treatments are still in their early phases. Every child afflicted with a life-threatening disease deserves the chance Eliot has been given.
The biggest obstacle to getting these treatments is cost. Gene therapies cost, on average, $1 million to $2 million . At $3.2 million per patient, Elevidys is the second-most-expensive drug in the world . Insurance companies would probably prefer not to foot the bill, and without full F.D.A. approval, insurance companies can refuse to cover these treatments by claiming they are medically unnecessary or experimental . Before Eliot’s treatment began, my insurance company initially said it would cover the cost but then started stalling on coverage and questioning the urgency of Eliot’s treatment. I was able to call Dana Goldman, the dean of the Sol Price School of Public Policy at the University of Southern California, where I work, to help me navigate the process. I was in the rare position to marshal resources and assistance to pressure my insurance company into covering Elevidys. Across the country, physicians are fighting denials and seeking appeals for their young patients.
Dr. Goldman has argued that one way to incentivize insurance companies to cover the high costs of treatments like gene therapies is to amortize how much the companies pay over time if the effectiveness of such treatments does not last (analogous to a pay-for-performance model). Another option is for pharmaceutical companies to offer a warranty that gives a prorated refund to the insurance company if a patient needs to return to prophylaxis treatment within a certain number of years. Costs are an especially frustrating problem for rare diseases like D.M.D., for which the extremely small patient population deters companies from investing money and resources to develop new treatments. Some experts believe the federal government ought to do more to directly complement research funding for rare diseases , as it has through the Orphan Drug Act for over four decades. The government could also defray the cost to consumers by offering subsidies directly to patients.
There’s another big role the government can play to accelerate gene therapies besides intervening in costs, and that’s to make the wheels of regulatory approval for these drugs less onerous. Flexibility doesn’t have to come at the cost of safety. The F.D.A. acted swiftly to approve an antiretroviral drug for H.I.V. in the 1980s and the Covid vaccines in December 2020, saving millions of lives without putting people in harm’s way.
But Elevidys is a case study in how the F.D.A. can get in its own way. D.M.D. patients 4 or 5 years old received access to the drug under fast-tracked approval, the first time a drug was approved under this new framework. But this was reportedly only because Peter Marks , the director of the F.D.A.’s Center for Biologics Evaluation and Research, disagreed with his own staff’s rejection . Current concern over Elevidys’s approval for boys over 5 focuses on the most recent clinical trial results , which showed older boys, whose muscular decline is further along, did not improve on motor function as measured by the North Star Ambulatory Assessment after treatment. However, as Sarepta has noted, they still saw gains in their ability to rise from the floor and walk 10 meters, indicating possible slowing of the disease that could significantly improve and extend their lives.
Detractors suggest this improvement is not enough to meet the bar for approval. This is a common problem for rare disease trials because they often consist of very few participants. In such cases, a narrow focus on numbers ignores the real quality-of-life benefits doctors, patients and their families see from these treatments. During the advisory committee meeting for Elevidys in May 2023, I listened to F.D.A. analysts express skepticism about the drug after they watched videos of boys treated with Elevidys swimming and riding bikes. These experts — given the highest responsibility to evaluate treatments on behalf of others’ lives — seemed unable to see the forest for the trees as they focused on statistics versus real-life examples.
The F.D.A. can have a more flexible view of treatment efficacy without losing focus on safety. As with any drug, whether for migraines or asthma, there will be a spectrum of effectiveness. The same will be true of all gene therapies, and the F.D.A. should reconsider the metrics it uses to green-light these treatments now, before it potentially leaves thousands of patients in the lurch, out of access to something lifesaving.
Gene therapy is the future of medicine. Our bureaucracy and insurance companies should not hinder patients from receiving pioneering treatments that could transform their lives. As parents, we are not asking for the moon. We just want our children to live.
Elizabeth Currid-Halkett is a Guggenheim fellow and professor of public policy at the University of Southern California.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , X and Threads .
- Open access
- Published: 26 February 2019
Stem cells: past, present, and future
- Wojciech Zakrzewski 1 ,
- Maciej Dobrzyński 2 ,
- Maria Szymonowicz 1 &
- Zbigniew Rybak 1
Stem Cell Research & Therapy volume 10 , Article number: 68 ( 2019 ) Cite this article
557k Accesses
828 Citations
53 Altmetric
Metrics details
In recent years, stem cell therapy has become a very promising and advanced scientific research topic. The development of treatment methods has evoked great expectations. This paper is a review focused on the discovery of different stem cells and the potential therapies based on these cells. The genesis of stem cells is followed by laboratory steps of controlled stem cell culturing and derivation. Quality control and teratoma formation assays are important procedures in assessing the properties of the stem cells tested. Derivation methods and the utilization of culturing media are crucial to set proper environmental conditions for controlled differentiation. Among many types of stem tissue applications, the use of graphene scaffolds and the potential of extracellular vesicle-based therapies require attention due to their versatility. The review is summarized by challenges that stem cell therapy must overcome to be accepted worldwide. A wide variety of possibilities makes this cutting edge therapy a turning point in modern medicine, providing hope for untreatable diseases.
Stem cell classification
Stem cells are unspecialized cells of the human body. They are able to differentiate into any cell of an organism and have the ability of self-renewal. Stem cells exist both in embryos and adult cells. There are several steps of specialization. Developmental potency is reduced with each step, which means that a unipotent stem cell is not able to differentiate into as many types of cells as a pluripotent one. This chapter will focus on stem cell classification to make it easier for the reader to comprehend the following chapters.
Totipotent stem cells are able to divide and differentiate into cells of the whole organism. Totipotency has the highest differentiation potential and allows cells to form both embryo and extra-embryonic structures. One example of a totipotent cell is a zygote, which is formed after a sperm fertilizes an egg. These cells can later develop either into any of the three germ layers or form a placenta. After approximately 4 days, the blastocyst’s inner cell mass becomes pluripotent. This structure is the source of pluripotent cells.
Pluripotent stem cells (PSCs) form cells of all germ layers but not extraembryonic structures, such as the placenta. Embryonic stem cells (ESCs) are an example. ESCs are derived from the inner cell mass of preimplantation embryos. Another example is induced pluripotent stem cells (iPSCs) derived from the epiblast layer of implanted embryos. Their pluripotency is a continuum, starting from completely pluripotent cells such as ESCs and iPSCs and ending on representatives with less potency—multi-, oligo- or unipotent cells. One of the methods to assess their activity and spectrum is the teratoma formation assay. iPSCs are artificially generated from somatic cells, and they function similarly to PSCs. Their culturing and utilization are very promising for present and future regenerative medicine.
Multipotent stem cells have a narrower spectrum of differentiation than PSCs, but they can specialize in discrete cells of specific cell lineages. One example is a haematopoietic stem cell, which can develop into several types of blood cells. After differentiation, a haematopoietic stem cell becomes an oligopotent cell. Its differentiation abilities are then restricted to cells of its lineage. However, some multipotent cells are capable of conversion into unrelated cell types, which suggests naming them pluripotent cells.
Oligopotent stem cells can differentiate into several cell types. A myeloid stem cell is an example that can divide into white blood cells but not red blood cells.
Unipotent stem cells are characterized by the narrowest differentiation capabilities and a special property of dividing repeatedly. Their latter feature makes them a promising candidate for therapeutic use in regenerative medicine. These cells are only able to form one cell type, e.g. dermatocytes.
Stem cell biology
A blastocyst is formed after the fusion of sperm and ovum fertilization. Its inner wall is lined with short-lived stem cells, namely, embryonic stem cells. Blastocysts are composed of two distinct cell types: the inner cell mass (ICM), which develops into epiblasts and induces the development of a foetus, and the trophectoderm (TE). Blastocysts are responsible for the regulation of the ICM microenvironment. The TE continues to develop and forms the extraembryonic support structures needed for the successful origin of the embryo, such as the placenta. As the TE begins to form a specialized support structure, the ICM cells remain undifferentiated, fully pluripotent and proliferative [ 1 ]. The pluripotency of stem cells allows them to form any cell of the organism. Human embryonic stem cells (hESCs) are derived from the ICM. During the process of embryogenesis, cells form aggregations called germ layers: endoderm, mesoderm and ectoderm (Fig. 1 ), each eventually giving rise to differentiated cells and tissues of the foetus and, later on, the adult organism [ 2 ]. After hESCs differentiate into one of the germ layers, they become multipotent stem cells, whose potency is limited to only the cells of the germ layer. This process is short in human development. After that, pluripotent stem cells occur all over the organism as undifferentiated cells, and their key abilities are proliferation by the formation of the next generation of stem cells and differentiation into specialized cells under certain physiological conditions.
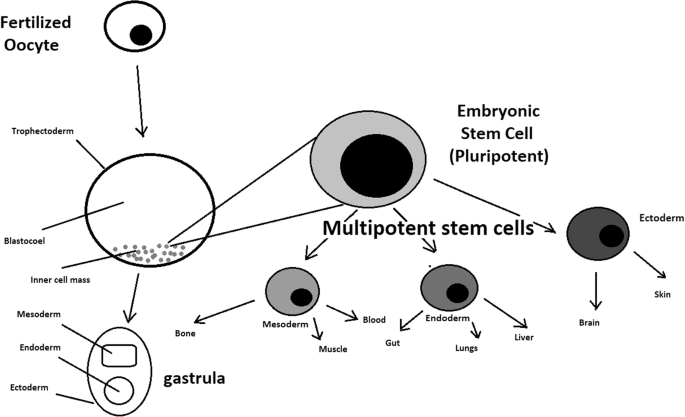
Oocyte development and formation of stem cells: the blastocoel, which is formed from oocytes, consists of embryonic stem cells that later differentiate into mesodermal, ectodermal, or endodermal cells. Blastocoel develops into the gastrula
Signals that influence the stem cell specialization process can be divided into external, such as physical contact between cells or chemical secretion by surrounding tissue, and internal, which are signals controlled by genes in DNA.
Stem cells also act as internal repair systems of the body. The replenishment and formation of new cells are unlimited as long as an organism is alive. Stem cell activity depends on the organ in which they are in; for example, in bone marrow, their division is constant, although in organs such as the pancreas, division only occurs under special physiological conditions.
Stem cell functional division
Whole-body development.
During division, the presence of different stem cells depends on organism development. Somatic stem cell ESCs can be distinguished. Although the derivation of ESCs without separation from the TE is possible, such a combination has growth limits. Because proliferating actions are limited, co-culture of these is usually avoided.
ESCs are derived from the inner cell mass of the blastocyst, which is a stage of pre-implantation embryo ca. 4 days after fertilization. After that, these cells are placed in a culture dish filled with culture medium. Passage is an inefficient but popular process of sub-culturing cells to other dishes. These cells can be described as pluripotent because they are able to eventually differentiate into every cell type in the organism. Since the beginning of their studies, there have been ethical restrictions connected to the medical use of ESCs in therapies. Most embryonic stem cells are developed from eggs that have been fertilized in an in vitro clinic, not from eggs fertilized in vivo.
Somatic or adult stem cells are undifferentiated and found among differentiated cells in the whole body after development. The function of these cells is to enable the healing, growth, and replacement of cells that are lost each day. These cells have a restricted range of differentiation options. Among many types, there are the following:
Mesenchymal stem cells are present in many tissues. In bone marrow, these cells differentiate mainly into the bone, cartilage, and fat cells. As stem cells, they are an exception because they act pluripotently and can specialize in the cells of any germ layer.
Neural cells give rise to nerve cells and their supporting cells—oligodendrocytes and astrocytes.
Haematopoietic stem cells form all kinds of blood cells: red, white, and platelets.
Skin stem cells form, for example, keratinocytes, which form a protective layer of skin.
The proliferation time of somatic stem cells is longer than that of ESCs. It is possible to reprogram adult stem cells back to their pluripotent state. This can be performed by transferring the adult nucleus into the cytoplasm of an oocyte or by fusion with the pluripotent cell. The same technique was used during cloning of the famous Dolly sheep.
hESCs are involved in whole-body development. They can differentiate into pluripotent, totipotent, multipotent, and unipotent cells (Fig. 2 ) [ 2 ].
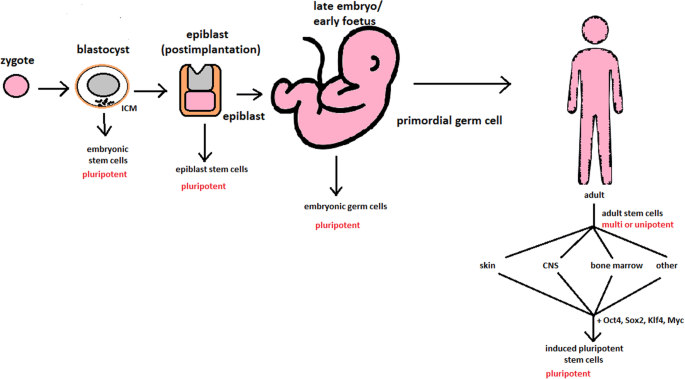
Changes in the potency of stem cells in human body development. Potency ranges from pluripotent cells of the blastocyst to unipotent cells of a specific tissue in a human body such as the skin, CNS, or bone marrow. Reversed pluripotency can be achieved by the formation of induced pluripotent stem cells using either octamer-binding transcription factor (Oct4), sex-determining region Y (Sox2), Kruppel-like factor 4 (Klf4), or the Myc gene
Pluripotent cells can be named totipotent if they can additionally form extraembryonic tissues of the embryo. Multipotent cells are restricted in differentiating to each cell type of given tissue. When tissue contains only one lineage of cells, stem cells that form them are called either called oligo- or unipotent.
iPSC quality control and recognition by morphological differences
The comparability of stem cell lines from different individuals is needed for iPSC lines to be used in therapeutics [ 3 ]. Among critical quality procedures, the following can be distinguished:
Short tandem repeat analysis—This is the comparison of specific loci on the DNA of the samples. It is used in measuring an exact number of repeating units. One unit consists of 2 to 13 nucleotides repeating many times on the DNA strand. A polymerase chain reaction is used to check the lengths of short tandem repeats. The genotyping procedure of source tissue, cells, and iPSC seed and master cell banks is recommended.
Identity analysis—The unintentional switching of lines, resulting in other stem cell line contamination, requires rigorous assay for cell line identification.
Residual vector testing—An appearance of reprogramming vectors integrated into the host genome is hazardous, and testing their presence is a mandatory procedure. It is a commonly used procedure for generating high-quality iPSC lines. An acceptable threshold in high-quality research-grade iPSC line collections is ≤ 1 plasmid copies per 100 cells. During the procedure, 2 different regions, common to all plasmids, should be used as specific targets, such as EBNA and CAG sequences [ 3 ]. To accurately represent the test reactions, a standard curve needs to be prepared in a carrier of gDNA from a well-characterized hPSC line. For calculations of plasmid copies per cell, it is crucial to incorporate internal reference gDNA sequences to allow the quantification of, for example, ribonuclease P (RNaseP) or human telomerase reverse transcriptase (hTERT).
Karyotype—A long-term culture of hESCs can accumulate culture-driven mutations [ 4 ]. Because of that, it is crucial to pay additional attention to genomic integrity. Karyotype tests can be performed by resuscitating representative aliquots and culturing them for 48–72 h before harvesting cells for karyotypic analysis. If abnormalities are found within the first 20 karyotypes, the analysis must be repeated on a fresh sample. When this situation is repeated, the line is evaluated as abnormal. Repeated abnormalities must be recorded. Although karyology is a crucial procedure in stem cell quality control, the single nucleotide polymorphism (SNP) array, discussed later, has approximately 50 times higher resolution.
Viral testing—When assessing the quality of stem cells, all tests for harmful human adventitious agents must be performed (e.g. hepatitis C or human immunodeficiency virus). This procedure must be performed in the case of non-xeno-free culture agents.
Bacteriology—Bacterial or fungal sterility tests can be divided into culture- or broth-based tests. All the procedures must be recommended by pharmacopoeia for the jurisdiction in which the work is performed.
Single nucleotide polymorphism arrays—This procedure is a type of DNA microarray that detects population polymorphisms by enabling the detection of subchromosomal changes and the copy-neutral loss of heterozygosity, as well as an indication of cellular transformation. The SNP assay consists of three components. The first is labelling fragmented nucleic acid sequences with fluorescent dyes. The second is an array that contains immobilized allele-specific oligonucleotide (ASO) probes. The last component detects, records, and eventually interprets the signal.
Flow cytometry—This is a technique that utilizes light to count and profile cells in a heterogeneous fluid mixture. It allows researchers to accurately and rapidly collect data from heterogeneous fluid mixtures with live cells. Cells are passed through a narrow channel one by one. During light illumination, sensors detect light emitted or refracted from the cells. The last step is data analysis, compilation and integration into a comprehensive picture of the sample.
Phenotypic pluripotency assays—Recognizing undifferentiated cells is crucial in successful stem cell therapy. Among other characteristics, stem cells appear to have a distinct morphology with a high nucleus to cytoplasm ratio and a prominent nucleolus. Cells appear to be flat with defined borders, in contrast to differentiating colonies, which appear as loosely located cells with rough borders [ 5 ]. It is important that images of ideal and poor quality colonies for each cell line are kept in laboratories, so whenever there is doubt about the quality of culture, it can always be checked according to the representative image. Embryoid body formation or directed differentiation of monolayer cultures to produce cell types representative of all three embryonic germ layers must be performed. It is important to note that colonies cultured under different conditions may have different morphologies [ 6 ].
Histone modification and DNA methylation—Quality control can be achieved by using epigenetic analysis tools such as histone modification or DNA methylation. When stem cells differentiate, the methylation process silences pluripotency genes, which reduces differentiation potential, although other genes may undergo demethylation to become expressed [ 7 ]. It is important to emphasize that stem cell identity, together with its morphological characteristics, is also related to its epigenetic profile [ 8 , 9 ]. According to Brindley [ 10 ], there is a relationship between epigenetic changes, pluripotency, and cell expansion conditions, which emphasizes that unmethylated regions appear to be serum-dependent.
hESC derivation and media
hESCs can be derived using a variety of methods, from classic culturing to laser-assisted methodologies or microsurgery [ 11 ]. hESC differentiation must be specified to avoid teratoma formation (see Fig. 3 ).
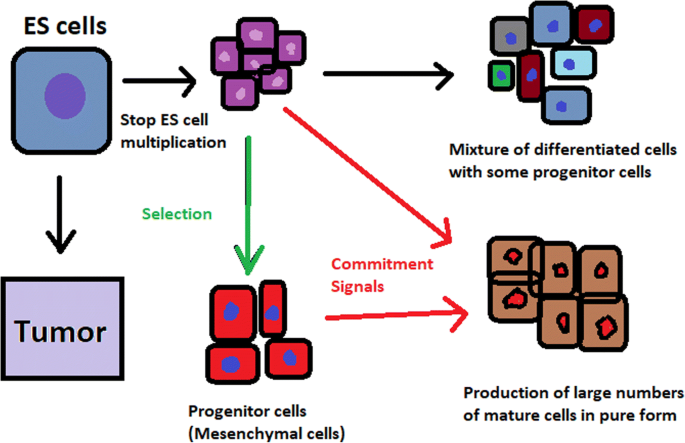
Spontaneous differentiation of hESCs causes the formation of a heterogeneous cell population. There is a different result, however, when commitment signals (in forms of soluble factors and culture conditions) are applied and enable the selection of progenitor cells
hESCs spontaneously differentiate into embryonic bodies (EBs) [ 12 ]. EBs can be studied instead of embryos or animals to predict their effects on early human development. There are many different methods for acquiring EBs, such as bioreactor culture [ 13 ], hanging drop culture [ 12 ], or microwell technology [ 14 , 15 ]. These methods allow specific precursors to form in vitro [ 16 ].
The essential part of these culturing procedures is a separation of inner cell mass to culture future hESCs (Fig. 4 ) [ 17 ]. Rosowski et al. [ 18 ] emphasizes that particular attention must be taken in controlling spontaneous differentiation. When the colony reaches the appropriate size, cells must be separated. The occurrence of pluripotent cells lasts for 1–2 days. Because the classical utilization of hESCs caused ethical concerns about gastrulas used during procedures, Chung et al. [ 19 ] found out that it is also possible to obtain hESCs from four cell embryos, leaving a higher probability of embryo survival. Additionally, Zhang et al. [ 20 ] used only in vitro fertilization growth-arrested cells.
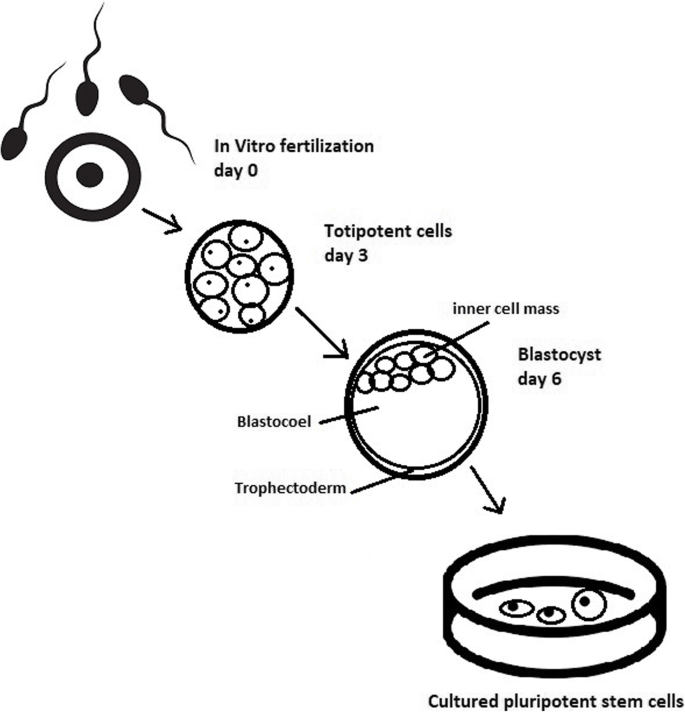
Culturing of pluripotent stem cells in vitro. Three days after fertilization, totipotent cells are formed. Blastocysts with ICM are formed on the sixth day after fertilization. Pluripotent stem cells from ICM can then be successfully transmitted on a dish
Cell passaging is used to form smaller clusters of cells on a new culture surface [ 21 ]. There are four important passaging procedures.
Enzymatic dissociation is a cutting action of enzymes on proteins and adhesion domains that bind the colony. It is a gentler method than the manual passage. It is crucial to not leave hESCs alone after passaging. Solitary cells are more sensitive and can easily undergo cell death; collagenase type IV is an example [ 22 , 23 ].
Manual passage , on the other hand, focuses on using cell scratchers. The selection of certain cells is not necessary. This should be done in the early stages of cell line derivation [ 24 ].
Trypsin utilization allows a healthy, automated hESC passage. Good Manufacturing Practice (GMP)-grade recombinant trypsin is widely available in this procedure [ 24 ]. However, there is a risk of decreasing the pluripotency and viability of stem cells [ 25 ]. Trypsin utilization can be halted with an inhibitor of the protein rho-associated protein kinase (ROCK) [ 26 ].
Ethylenediaminetetraacetic acid ( EDTA ) indirectly suppresses cell-to-cell connections by chelating divalent cations. Their suppression promotes cell dissociation [ 27 ].
Stem cells require a mixture of growth factors and nutrients to differentiate and develop. The medium should be changed each day.
Traditional culture methods used for hESCs are mouse embryonic fibroblasts (MEFs) as a feeder layer and bovine serum [ 28 ] as a medium. Martin et al. [ 29 ] demonstrated that hESCs cultured in the presence of animal products express the non-human sialic acid, N -glycolylneuraminic acid (NeuGc). Feeder layers prevent uncontrolled proliferation with factors such as leukaemia inhibitory factor (LIF) [ 30 ].
First feeder layer-free culture can be supplemented with serum replacement, combined with laminin [ 31 ]. This causes stable karyotypes of stem cells and pluripotency lasting for over a year.
Initial culturing media can be serum (e.g. foetal calf serum FCS), artificial replacement such as synthetic serum substitute (SSS), knockout serum replacement (KOSR), or StemPro [ 32 ]. The simplest culture medium contains only eight essential elements: DMEM/F12 medium, selenium, NaHCO 3, l -ascorbic acid, transferrin, insulin, TGFβ1, and FGF2 [ 33 ]. It is not yet fully known whether culture systems developed for hESCs can be allowed without adaptation in iPSC cultures.
Turning point in stem cell therapy
The turning point in stem cell therapy appeared in 2006, when scientists Shinya Yamanaka, together with Kazutoshi Takahashi, discovered that it is possible to reprogram multipotent adult stem cells to the pluripotent state. This process avoided endangering the foetus’ life in the process. Retrovirus-mediated transduction of mouse fibroblasts with four transcription factors (Oct-3/4, Sox2, KLF4, and c-Myc) [ 34 ] that are mainly expressed in embryonic stem cells could induce the fibroblasts to become pluripotent (Fig. 5 ) [ 35 ]. This new form of stem cells was named iPSCs. One year later, the experiment also succeeded with human cells [ 36 ]. After this success, the method opened a new field in stem cell research with a generation of iPSC lines that can be customized and biocompatible with the patient. Recently, studies have focused on reducing carcinogenesis and improving the conduction system.
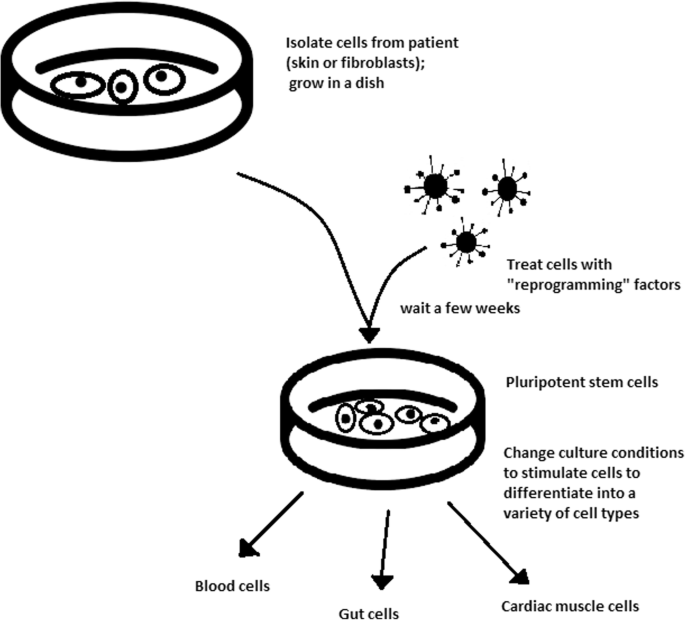
Retroviral-mediated transduction induces pluripotency in isolated patient somatic cells. Target cells lose their role as somatic cells and, once again, become pluripotent and can differentiate into any cell type of human body
The turning point was influenced by former discoveries that happened in 1962 and 1987.
The former discovery was about scientist John Gurdon successfully cloning frogs by transferring a nucleus from a frog’s somatic cells into an oocyte. This caused a complete reversion of somatic cell development [ 37 ]. The results of his experiment became an immense discovery since it was previously believed that cell differentiation is a one-way street only, but his experiment suggested the opposite and demonstrated that it is even possible for a somatic cell to again acquire pluripotency [ 38 ].
The latter was a discovery made by Davis R.L. that focused on fibroblast DNA subtraction. Three genes were found that originally appeared in myoblasts. The enforced expression of only one of the genes, named myogenic differentiation 1 (Myod1), caused the conversion of fibroblasts into myoblasts, showing that reprogramming cells is possible, and it can even be used to transform cells from one lineage to another [ 39 ].
Although pluripotency can occur naturally only in embryonic stem cells, it is possible to induce terminally differentiated cells to become pluripotent again. The process of direct reprogramming converts differentiated somatic cells into iPSC lines that can form all cell types of an organism. Reprogramming focuses on the expression of oncogenes such as Myc and Klf4 (Kruppel-like factor 4). This process is enhanced by a downregulation of genes promoting genome stability, such as p53. Additionally, cell reprogramming involves histone alteration. All these processes can cause potential mutagenic risk and later lead to an increased number of mutations. Quinlan et al. [ 40 ] checked fully pluripotent mouse iPSCs using whole genome DNA sequencing and structural variation (SV) detection algorithms. Based on those studies, it was confirmed that although there were single mutations in the non-genetic region, there were non-retrotransposon insertions. This led to the conclusion that current reprogramming methods can produce fully pluripotent iPSCs without severe genomic alterations.
During the course of development from pluripotent hESCs to differentiated somatic cells, crucial changes appear in the epigenetic structure of these cells. There is a restriction or permission of the transcription of genes relevant to each cell type. When somatic cells are being reprogrammed using transcription factors, all the epigenetic architecture has to be reconditioned to achieve iPSCs with pluripotency [ 41 ]. However, cells of each tissue undergo specific somatic genomic methylation. This influences transcription, which can further cause alterations in induced pluripotency [ 42 ].
Source of iPSCs
Because pluripotent cells can propagate indefinitely and differentiate into any kind of cell, they can be an unlimited source, either for replacing lost or diseased tissues. iPSCs bypass the need for embryos in stem cell therapy. Because they are made from the patient’s own cells, they are autologous and no longer generate any risk of immune rejection.
At first, fibroblasts were used as a source of iPSCs. Because a biopsy was needed to achieve these types of cells, the technique underwent further research. Researchers investigated whether more accessible cells could be used in the method. Further, other cells were used in the process: peripheral blood cells, keratinocytes, and renal epithelial cells found in urine. An alternative strategy to stem cell transplantation can be stimulating a patient’s endogenous stem cells to divide or differentiate, occurring naturally when skin wounds are healing. In 2008, pancreatic exocrine cells were shown to be reprogrammed to functional, insulin-producing beta cells [ 43 ].
The best stem cell source appears to be the fibroblasts, which is more tempting in the case of logistics since its stimulation can be fast and better controlled [ 44 ].
- Teratoma formation assay
The self-renewal and differentiation capabilities of iPSCs have gained significant interest and attention in regenerative medicine sciences. To study their abilities, a quality-control assay is needed, of which one of the most important is the teratoma formation assay. Teratomas are benign tumours. Teratomas are capable of rapid growth in vivo and are characteristic because of their ability to develop into tissues of all three germ layers simultaneously. Because of the high pluripotency of teratomas, this formation assay is considered an assessment of iPSC’s abilities [ 45 ].
Teratoma formation rate, for instance, was observed to be elevated in human iPSCs compared to that in hESCs [ 46 ]. This difference may be connected to different differentiation methods and cell origins. Most commonly, the teratoma assay involves an injection of examined iPSCs subcutaneously or under the testis or kidney capsule in mice, which are immune-deficient [ 47 ]. After injection, an immature but recognizable tissue can be observed, such as the kidney tubules, bone, cartilage, or neuroepithelium [ 30 ]. The injection site may have an impact on the efficiency of teratoma formation [ 48 ].
There are three groups of markers used in this assay to differentiate the cells of germ layers. For endodermal tissue, there is insulin/C-peptide and alpha-1 antitrypsin [ 49 ]. For the mesoderm, derivatives can be used, e.g. cartilage matrix protein for the bone and alcian blue for the cartilage. As ectodermal markers, class III B botulin or keratin can be used for keratinocytes.
Teratoma formation assays are considered the gold standard for demonstrating the pluripotency of human iPSCs, demonstrating their possibilities under physiological conditions. Due to their actual tissue formation, they could be used for the characterization of many cell lineages [ 50 ].
Directed differentiation
To be useful in therapy, stem cells must be converted into desired cell types as necessary or else the whole regenerative medicine process will be pointless. Differentiation of ESCs is crucial because undifferentiated ESCs can cause teratoma formation in vivo. Understanding and using signalling pathways for differentiation is an important method in successful regenerative medicine. In directed differentiation, it is likely to mimic signals that are received by cells when they undergo successive stages of development [ 51 ]. The extracellular microenvironment plays a significant role in controlling cell behaviour. By manipulating the culture conditions, it is possible to restrict specific differentiation pathways and generate cultures that are enriched in certain precursors in vitro. However, achieving a similar effect in vivo is challenging. It is crucial to develop culture conditions that will allow the promotion of homogenous and enhanced differentiation of ESCs into functional and desired tissues.
Regarding the self-renewal of embryonic stem cells, Hwang et al. [ 52 ] noted that the ideal culture method for hESC-based cell and tissue therapy would be a defined culture free of either the feeder layer or animal components. This is because cell and tissue therapy requires the maintenance of large quantities of undifferentiated hESCs, which does not make feeder cells suitable for such tasks.
Most directed differentiation protocols are formed to mimic the development of an inner cell mass during gastrulation. During this process, pluripotent stem cells differentiate into ectodermal, mesodermal, or endodermal progenitors. Mall molecules or growth factors induce the conversion of stem cells into appropriate progenitor cells, which will later give rise to the desired cell type. There is a variety of signal intensities and molecular families that may affect the establishment of germ layers in vivo, such as fibroblast growth factors (FGFs) [ 53 ]; the Wnt family [ 54 ] or superfamily of transforming growth factors—β(TGFβ); and bone morphogenic proteins (BMP) [ 55 ]. Each candidate factor must be tested on various concentrations and additionally applied to various durations because the precise concentrations and times during which developing cells in embryos are influenced during differentiation are unknown. For instance, molecular antagonists of endogenous BMP and Wnt signalling can be used for ESC formation of ectoderm [ 56 ]. However, transient Wnt and lower concentrations of the TGFβ family trigger mesodermal differentiation [ 57 ]. Regarding endoderm formation, a higher activin A concentration may be required [ 58 , 59 ].
There are numerous protocols about the methods of forming progenitors of cells of each of germ layers, such as cardiomyocytes [ 60 ], hepatocytes [ 61 ], renal cells [ 62 ], lung cells [ 63 , 64 ], motor neurons [ 65 ], intestinal cells [ 66 ], or chondrocytes [ 67 ].
Directed differentiation of either iPSCs or ESCs into, e.g. hepatocytes, could influence and develop the study of the molecular mechanisms in human liver development. In addition, it could also provide the possibility to form exogenous hepatocytes for drug toxicity testing [ 68 ].
Levels of concentration and duration of action with a specific signalling molecule can cause a variety of factors. Unfortunately, for now, a high cost of recombinant factors is likely to limit their use on a larger scale in medicine. The more promising technique focuses on the use of small molecules. These can be used for either activating or deactivating specific signalling pathways. They enhance reprogramming efficiency by creating cells that are compatible with the desired type of tissue. It is a cheaper and non-immunogenic method.
One of the successful examples of small-molecule cell therapies is antagonists and agonists of the Hedgehog pathway. They show to be very useful in motor neuron regeneration [ 69 ]. Endogenous small molecules with their function in embryonic development can also be used in in vitro methods to induce the differentiation of cells; for example, retinoic acid, which is responsible for patterning the nervous system in vivo [ 70 ], surprisingly induced retinal cell formation when the laboratory procedure involved hESCs [ 71 ].
The efficacy of differentiation factors depends on functional maturity, efficiency, and, finally, introducing produced cells to their in vivo equivalent. Topography, shear stress, and substrate rigidity are factors influencing the phenotype of future cells [ 72 ].
The control of biophysical and biochemical signals, the biophysical environment, and a proper guide of hESC differentiation are important factors in appropriately cultured stem cells.
Stem cell utilization and their manufacturing standards and culture systems
The European Medicines Agency and the Food and Drug Administration have set Good Manufacturing Practice (GMP) guidelines for safe and appropriate stem cell transplantation. In the past, protocols used for stem cell transplantation required animal-derived products [ 73 ].
The risk of introducing animal antigens or pathogens caused a restriction in their use. Due to such limitations, the technique required an obvious update [ 74 ]. Now, it is essential to use xeno-free equivalents when establishing cell lines that are derived from fresh embryos and cultured from human feeder cell lines [ 75 ]. In this method, it is crucial to replace any non-human materials with xeno-free equivalents [ 76 ].
NutriStem with LN-511, TeSR2 with human recombinant laminin (LN-511), and RegES with human foreskin fibroblasts (HFFs) are commonly used xeno-free culture systems [ 33 ]. There are many organizations and international initiatives, such as the National Stem Cell Bank, that provide stem cell lines for treatment or medical research [ 77 ].
Stem cell use in medicine
Stem cells have great potential to become one of the most important aspects of medicine. In addition to the fact that they play a large role in developing restorative medicine, their study reveals much information about the complex events that happen during human development.
The difference between a stem cell and a differentiated cell is reflected in the cells’ DNA. In the former cell, DNA is arranged loosely with working genes. When signals enter the cell and the differentiation process begins, genes that are no longer needed are shut down, but genes required for the specialized function will remain active. This process can be reversed, and it is known that such pluripotency can be achieved by interaction in gene sequences. Takahashi and Yamanaka [ 78 ] and Loh et al. [ 79 ] discovered that octamer-binding transcription factor 3 and 4 (Oct3/4), sex determining region Y (SRY)-box 2 and Nanog genes function as core transcription factors in maintaining pluripotency. Among them, Oct3/4 and Sox2 are essential for the generation of iPSCs.
Many serious medical conditions, such as birth defects or cancer, are caused by improper differentiation or cell division. Currently, several stem cell therapies are possible, among which are treatments for spinal cord injury, heart failure [ 80 ], retinal and macular degeneration [ 81 ], tendon ruptures, and diabetes type 1 [ 82 ]. Stem cell research can further help in better understanding stem cell physiology. This may result in finding new ways of treating currently incurable diseases.
Haematopoietic stem cell transplantation
Haematopoietic stem cells are important because they are by far the most thoroughly characterized tissue-specific stem cell; after all, they have been experimentally studied for more than 50 years. These stem cells appear to provide an accurate paradigm model system to study tissue-specific stem cells, and they have potential in regenerative medicine.
Multipotent haematopoietic stem cell (HSC) transplantation is currently the most popular stem cell therapy. Target cells are usually derived from the bone marrow, peripheral blood, or umbilical cord blood [ 83 ]. The procedure can be autologous (when the patient’s own cells are used), allogenic (when the stem cell comes from a donor), or syngeneic (from an identical twin). HSCs are responsible for the generation of all functional haematopoietic lineages in blood, including erythrocytes, leukocytes, and platelets. HSC transplantation solves problems that are caused by inappropriate functioning of the haematopoietic system, which includes diseases such as leukaemia and anaemia. However, when conventional sources of HSC are taken into consideration, there are some important limitations. First, there is a limited number of transplantable cells, and an efficient way of gathering them has not yet been found. There is also a problem with finding a fitting antigen-matched donor for transplantation, and viral contamination or any immunoreactions also cause a reduction in efficiency in conventional HSC transplantations. Haematopoietic transplantation should be reserved for patients with life-threatening diseases because it has a multifactorial character and can be a dangerous procedure. iPSC use is crucial in this procedure. The use of a patient’s own unspecialized somatic cells as stem cells provides the greatest immunological compatibility and significantly increases the success of the procedure.
Stem cells as a target for pharmacological testing
Stem cells can be used in new drug tests. Each experiment on living tissue can be performed safely on specific differentiated cells from pluripotent cells. If any undesirable effect appears, drug formulas can be changed until they reach a sufficient level of effectiveness. The drug can enter the pharmacological market without harming any live testers. However, to test the drugs properly, the conditions must be equal when comparing the effects of two drugs. To achieve this goal, researchers need to gain full control of the differentiation process to generate pure populations of differentiated cells.
Stem cells as an alternative for arthroplasty
One of the biggest fears of professional sportsmen is getting an injury, which most often signifies the end of their professional career. This applies especially to tendon injuries, which, due to current treatment options focusing either on conservative or surgical treatment, often do not provide acceptable outcomes. Problems with the tendons start with their regeneration capabilities. Instead of functionally regenerating after an injury, tendons merely heal by forming scar tissues that lack the functionality of healthy tissues. Factors that may cause this failed healing response include hypervascularization, deposition of calcific materials, pain, or swelling [ 84 ].
Additionally, in addition to problems with tendons, there is a high probability of acquiring a pathological condition of joints called osteoarthritis (OA) [ 85 ]. OA is common due to the avascular nature of articular cartilage and its low regenerative capabilities [ 86 ]. Although arthroplasty is currently a common procedure in treating OA, it is not ideal for younger patients because they can outlive the implant and will require several surgical procedures in the future. These are situations where stem cell therapy can help by stopping the onset of OA [ 87 ]. However, these procedures are not well developed, and the long-term maintenance of hyaline cartilage requires further research.
Osteonecrosis of the femoral hip (ONFH) is a refractory disease associated with the collapse of the femoral head and risk of hip arthroplasty in younger populations [ 88 ]. Although total hip arthroplasty (THA) is clinically successful, it is not ideal for young patients, mostly due to the limited lifetime of the prosthesis. An increasing number of clinical studies have evaluated the therapeutic effect of stem cells on ONFH. Most of the authors demonstrated positive outcomes, with reduced pain, improved function, or avoidance of THA [ 89 , 90 , 91 ].
Rejuvenation by cell programming
Ageing is a reversible epigenetic process. The first cell rejuvenation study was published in 2011 [ 92 ]. Cells from aged individuals have different transcriptional signatures, high levels of oxidative stress, dysfunctional mitochondria, and shorter telomeres than in young cells [ 93 ]. There is a hypothesis that when human or mouse adult somatic cells are reprogrammed to iPSCs, their epigenetic age is virtually reset to zero [ 94 ]. This was based on an epigenetic model, which explains that at the time of fertilization, all marks of parenteral ageing are erased from the zygote’s genome and its ageing clock is reset to zero [ 95 ].
In their study, Ocampo et al. [ 96 ] used Oct4, Sox2, Klf4, and C-myc genes (OSKM genes) and affected pancreas and skeletal muscle cells, which have poor regenerative capacity. Their procedure revealed that these genes can also be used for effective regenerative treatment [ 97 ]. The main challenge of their method was the need to employ an approach that does not use transgenic animals and does not require an indefinitely long application. The first clinical approach would be preventive, focused on stopping or slowing the ageing rate. Later, progressive rejuvenation of old individuals can be attempted. In the future, this method may raise some ethical issues, such as overpopulation, leading to lower availability of food and energy.
For now, it is important to learn how to implement cell reprogramming technology in non-transgenic elder animals and humans to erase marks of ageing without removing the epigenetic marks of cell identity.
Cell-based therapies
Stem cells can be induced to become a specific cell type that is required to repair damaged or destroyed tissues (Fig. 6 ). Currently, when the need for transplantable tissues and organs outweighs the possible supply, stem cells appear to be a perfect solution for the problem. The most common conditions that benefit from such therapy are macular degenerations [ 98 ], strokes [ 99 ], osteoarthritis [ 89 , 90 ], neurodegenerative diseases, and diabetes [ 100 ]. Due to this technique, it can become possible to generate healthy heart muscle cells and later transplant them to patients with heart disease.
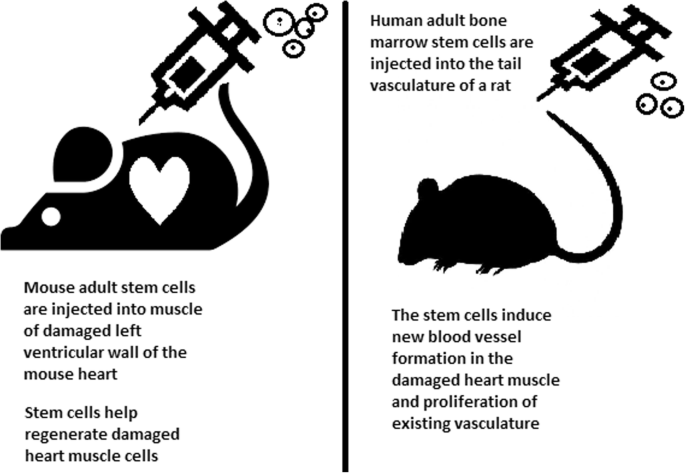
Stem cell experiments on animals. These experiments are one of the many procedures that proved stem cells to be a crucial factor in future regenerative medicine
In the case of type 1 diabetes, insulin-producing cells in the pancreas are destroyed due to an autoimmunological reaction. As an alternative to transplantation therapy, it can be possible to induce stem cells to differentiate into insulin-producing cells [ 101 ].
Stem cells and tissue banks
iPS cells with their theoretically unlimited propagation and differentiation abilities are attractive for the present and future sciences. They can be stored in a tissue bank to be an essential source of human tissue used for medical examination. The problem with conventional differentiated tissue cells held in the laboratory is that their propagation features diminish after time. This does not occur in iPSCs.
The umbilical cord is known to be rich in mesenchymal stem cells. Due to its cryopreservation immediately after birth, its stem cells can be successfully stored and used in therapies to prevent the future life-threatening diseases of a given patient.
Stem cells of human exfoliated deciduous teeth (SHED) found in exfoliated deciduous teeth has the ability to develop into more types of body tissues than other stem cells [ 102 ] (Table 1 ). Techniques of their collection, isolation, and storage are simple and non-invasive. Among the advantages of banking, SHED cells are:
Guaranteed donor-match autologous transplant that causes no immune reaction and rejection of cells [ 103 ]
Simple and painless for both child and parent
Less than one third of the cost of cord blood storage
Not subject to the same ethical concerns as embryonic stem cells [ 104 ]
In contrast to cord blood stem cells, SHED cells are able to regenerate into solid tissues such as connective, neural, dental, or bone tissue [ 105 , 106 ]
SHED can be useful for close relatives of the donor
Fertility diseases
In 2011, two researchers, Katsuhiko Hayashi et al. [ 107 ], showed in an experiment on mice that it is possible to form sperm from iPSCs. They succeeded in delivering healthy and fertile pups in infertile mice. The experiment was also successful for female mice, where iPSCs formed fully functional eggs .
Young adults at risk of losing their spermatogonial stem cells (SSC), mostly cancer patients, are the main target group that can benefit from testicular tissue cryopreservation and autotransplantation. Effective freezing methods for adult and pre-pubertal testicular tissue are available [ 108 ].
Qiuwan et al. [ 109 ] provided important evidence that human amniotic epithelial cell (hAEC) transplantation could effectively improve ovarian function by inhibiting cell apoptosis and reducing inflammation in injured ovarian tissue of mice, and it could be a promising strategy for the management of premature ovarian failure or insufficiency in female cancer survivors.
For now, reaching successful infertility treatments in humans appears to be only a matter of time, but there are several challenges to overcome. First, the process needs to have high efficiency; second, the chances of forming tumours instead of eggs or sperm must be maximally reduced. The last barrier is how to mature human sperm and eggs in the lab without transplanting them to in vivo conditions, which could cause either a tumour risk or an invasive procedure.
Therapy for incurable neurodegenerative diseases
Thanks to stem cell therapy, it is possible not only to delay the progression of incurable neurodegenerative diseases such as Parkinson’s disease, Alzheimer’s disease (AD), and Huntington disease, but also, most importantly, to remove the source of the problem. In neuroscience, the discovery of neural stem cells (NSCs) has nullified the previous idea that adult CNS were not capable of neurogenesis [ 110 , 111 ]. Neural stem cells are capable of improving cognitive function in preclinical rodent models of AD [ 112 , 113 , 114 ]. Awe et al. [ 115 ] clinically derived relevant human iPSCs from skin punch biopsies to develop a neural stem cell-based approach for treating AD. Neuronal degeneration in Parkinson’s disease (PD) is focal, and dopaminergic neurons can be efficiently generated from hESCs. PD is an ideal disease for iPSC-based cell therapy [ 116 ]. However, this therapy is still in an experimental phase ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4539501 /). Brain tissue from aborted foetuses was used on patients with Parkinson’s disease [ 117 ]. Although the results were not uniform, they showed that therapies with pure stem cells are an important and achievable therapy.
Stem cell use in dentistry
Teeth represent a very challenging material for regenerative medicine. They are difficult to recreate because of their function in aspects such as articulation, mastication, or aesthetics due to their complicated structure. Currently, there is a chance for stem cells to become more widely used than synthetic materials. Teeth have a large advantage of being the most natural and non-invasive source of stem cells.
For now, without the use of stem cells, the most common periodontological treatments are either growth factors, grafts, or surgery. For example, there are stem cells in periodontal ligament [ 118 , 119 ], which are capable of differentiating into osteoblasts or cementoblasts, and their functions were also assessed in neural cells [ 120 ]. Tissue engineering is a successful method for treating periodontal diseases. Stem cells of the root apical areas are able to recreate periodontal ligament. One of the possible methods of tissue engineering in periodontology is gene therapy performed using adenoviruses-containing growth factors [ 121 ].
As a result of animal studies, dentin regeneration is an effective process that results in the formation of dentin bridges [ 122 ].
Enamel is more difficult to regenerate than dentin. After the differentiation of ameloblastoma cells into the enamel, the former is destroyed, and reparation is impossible. Medical studies have succeeded in differentiating bone marrow stem cells into ameloblastoma [ 123 ].
Healthy dental tissue has a high amount of regular stem cells, although this number is reduced when tissue is either traumatized or inflamed [ 124 ]. There are several dental stem cell groups that can be isolated (Fig. 7 ).
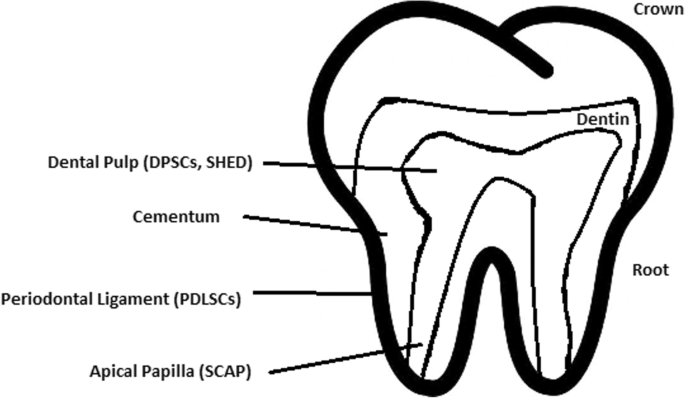
Localization of stem cells in dental tissues. Dental pulp stem cells (DPSCs) and human deciduous teeth stem cells (SHED) are located in the dental pulp. Periodontal ligaments stem cells are located in the periodontal ligament. Apical papilla consists of stem cells from the apical papilla (SCAP)
Dental pulp stem cell (DPSC)
These were the first dental stem cells isolated from the human dental pulp, which were [ 125 ] located inside dental pulp (Table 2 ). They have osteogenic and chondrogenic potential. Mesenchymal stem cells (MSCs) of the dental pulp, when isolated, appear highly clonogenic; they can be isolated from adult tissue (e.g. bone marrow, adipose tissue) and foetal (e.g. umbilical cord) [ 126 ] tissue, and they are able to differentiate densely [ 127 ]. MSCs differentiate into odontoblast-like cells and osteoblasts to form dentin and bone. Their best source locations are the third molars [ 125 ]. DPSCs are the most useful dental source of tissue engineering due to their easy surgical accessibility, cryopreservation possibility, increased production of dentin tissues compared to non-dental stem cells, and their anti-inflammatory abilities. These cells have the potential to be a source for maxillofacial and orthopaedic reconstructions or reconstructions even beyond the oral cavity. DPSCs are able to generate all structures of the developed tooth [ 128 ]. In particular, beneficial results in the use of DPSCs may be achieved when combined with other new therapies, such as periodontal tissue photobiomodulation (laser stimulation), which is an efficient technique in the stimulation of proliferation and differentiation into distinct cell types [ 129 ]. DPSCs can be induced to form neural cells to help treat neurological deficits.
Stem cells of human exfoliated deciduous teeth (SHED) have a faster rate of proliferation than DPSCs and differentiate into an even greater number of cells, e.g. other mesenchymal and non-mesenchymal stem cell derivatives, such as neural cells [ 130 ]. These cells possess one major disadvantage: they form a non-complete dentin/pulp-like complex in vivo. SHED do not undergo the same ethical concerns as embryonic stem cells. Both DPSCs and SHED are able to form bone-like tissues in vivo [ 131 ] and can be used for periodontal, dentin, or pulp regeneration. DPSCs and SHED can be used in treating, for example, neural deficits [ 132 ]. DPSCs alone were tested and successfully applied for alveolar bone and mandible reconstruction [ 133 ].
Periodontal ligament stem cells (PDLSCs)
These cells are used in periodontal ligament or cementum tissue regeneration. They can differentiate into mesenchymal cell lineages to produce collagen-forming cells, adipocytes, cementum tissue, Sharpey’s fibres, and osteoblast-like cells in vitro. PDLSCs exist both on the root and alveolar bone surfaces; however, on the latter, these cells have better differentiation abilities than on the former [ 134 ]. PDLSCs have become the first treatment for periodontal regeneration therapy because of their safety and efficiency [ 135 , 136 ].
Stem cells from apical papilla (SCAP)
These cells are mesenchymal structures located within immature roots. They are isolated from human immature permanent apical papilla. SCAP are the source of odontoblasts and cause apexogenesis. These stem cells can be induced in vitro to form odontoblast-like cells, neuron-like cells, or adipocytes. SCAP have a higher capacity of proliferation than DPSCs, which makes them a better choice for tissue regeneration [ 137 , 138 ].
Dental follicle stem cells (DFCs)
These cells are loose connective tissues surrounding the developing tooth germ. DFCs contain cells that can differentiate into cementoblasts, osteoblasts, and periodontal ligament cells [ 139 , 140 ]. Additionally, these cells proliferate after even more than 30 passages [ 141 ]. DFCs are most commonly extracted from the sac of a third molar. When DFCs are combined with a treated dentin matrix, they can form a root-like tissue with a pulp-dentin complex and eventually form tooth roots [ 141 ]. When DFC sheets are induced by Hertwig’s epithelial root sheath cells, they can produce periodontal tissue; thus, DFCs represent a very promising material for tooth regeneration [ 142 ].
Pulp regeneration in endodontics
Dental pulp stem cells can differentiate into odontoblasts. There are few methods that enable the regeneration of the pulp.
The first is an ex vivo method. Proper stem cells are grown on a scaffold before they are implanted into the root channel [ 143 ].
The second is an in vivo method. This method focuses on injecting stem cells into disinfected root channels after the opening of the in vivo apex. Additionally, the use of a scaffold is necessary to prevent the movement of cells towards other tissues. For now, only pulp-like structures have been created successfully.
Methods of placing stem cells into the root channel constitute are either soft scaffolding [ 144 ] or the application of stem cells in apexogenesis or apexification. Immature teeth are the best source [ 145 ]. Nerve and blood vessel network regeneration are extremely vital to keep pulp tissue healthy.
The potential of dental stem cells is mainly regarding the regeneration of damaged dentin and pulp or the repair of any perforations; in the future, it appears to be even possible to generate the whole tooth. Such an immense success would lead to the gradual replacement of implant treatments. Mandibulary and maxillary defects can be one of the most complicated dental problems for stem cells to address.
Acquiring non-dental tissue cells by dental stem cell differentiation
In 2013, it was reported that it is possible to grow teeth from stem cells obtained extra-orally, e.g. from urine [ 146 ]. Pluripotent stem cells derived from human urine were induced and generated tooth-like structures. The physical properties of the structures were similar to natural ones except for hardness [ 127 ]. Nonetheless, it appears to be a very promising technique because it is non-invasive and relatively low-cost, and somatic cells can be used instead of embryonic cells. More importantly, stem cells derived from urine did not form any tumours, and the use of autologous cells reduces the chances of rejection [ 147 ].
Use of graphene in stem cell therapy
Over recent years, graphene and its derivatives have been increasingly used as scaffold materials to mediate stem cell growth and differentiation [ 148 ]. Both graphene and graphene oxide (GO) represent high in-plane stiffness [ 149 ]. Because graphene has carbon and aromatic network, it works either covalently or non-covalently with biomolecules; in addition to its superior mechanical properties, graphene offers versatile chemistry. Graphene exhibits biocompatibility with cells and their proper adhesion. It also tested positively for enhancing the proliferation or differentiation of stem cells [ 148 ]. After positive experiments, graphene revealed great potential as a scaffold and guide for specific lineages of stem cell differentiation [ 150 ]. Graphene has been successfully used in the transplantation of hMSCs and their guided differentiation to specific cells. The acceleration skills of graphene differentiation and division were also investigated. It was discovered that graphene can serve as a platform with increased adhesion for both growth factors and differentiation chemicals. It was also discovered that π-π binding was responsible for increased adhesion and played a crucial role in inducing hMSC differentiation [ 150 ].
Therapeutic potential of extracellular vesicle-based therapies
Extracellular vesicles (EVs) can be released by virtually every cell of an organism, including stem cells [ 151 ], and are involved in intercellular communication through the delivery of their mRNAs, lipids, and proteins. As Oh et al. [ 152 ] prove, stem cells, together with their paracrine factors—exosomes—can become potential therapeutics in the treatment of, e.g. skin ageing. Exosomes are small membrane vesicles secreted by most cells (30–120 nm in diameter) [ 153 ]. When endosomes fuse with the plasma membrane, they become exosomes that have messenger RNAs (mRNAs) and microRNAs (miRNAs), some classes of non-coding RNAs (IncRNAs) and several proteins that originate from the host cell [ 154 ]. IncRNAs can bind to specific loci and create epigenetic regulators, which leads to the formation of epigenetic modifications in recipient cells. Because of this feature, exosomes are believed to be implicated in cell-to-cell communication and the progression of diseases such as cancer [ 155 ]. Recently, many studies have also shown the therapeutic use of exosomes derived from stem cells, e.g. skin damage and renal or lung injuries [ 156 ].
In skin ageing, the most important factor is exposure to UV light, called “photoageing” [ 157 ], which causes extrinsic skin damage, characterized by dryness, roughness, irregular pigmentation, lesions, and skin cancers. In intrinsic skin ageing, on the other hand, the loss of elasticity is a characteristic feature. The skin dermis consists of fibroblasts, which are responsible for the synthesis of crucial skin elements, such as procollagen or elastic fibres. These elements form either basic framework extracellular matrix constituents of the skin dermis or play a major role in tissue elasticity. Fibroblast efficiency and abundance decrease with ageing [ 158 ]. Stem cells can promote the proliferation of dermal fibroblasts by secreting cytokines such as platelet-derived growth factor (PDGF), transforming growth factor β (TGF-β), and basic fibroblast growth factor. Huh et al. [ 159 ] mentioned that a medium of human amniotic fluid-derived stem cells (hAFSC) positively affected skin regeneration after longwave UV-induced (UVA, 315–400 nm) photoageing by increasing the proliferation and migration of dermal fibroblasts. It was discovered that, in addition to the induction of fibroblast physiology, hAFSC transplantation also improved diseases in cases of renal pathology, various cancers, or stroke [ 160 , 161 ].
Oh [ 162 ] also presented another option for the treatment of skin wounds, either caused by physical damage or due to diabetic ulcers. Induced pluripotent stem cell-conditioned medium (iPSC-CM) without any animal-derived components induced dermal fibroblast proliferation and migration.
Natural cutaneous wound healing is divided into three steps: haemostasis/inflammation, proliferation, and remodelling. During the crucial step of proliferation, fibroblasts migrate and increase in number, indicating that it is a critical step in skin repair, and factors such as iPSC-CM that impact it can improve the whole cutaneous wound healing process. Paracrine actions performed by iPSCs are also important for this therapeutic effect [ 163 ]. These actions result in the secretion of cytokines such as TGF-β, interleukin (IL)-6, IL-8, monocyte chemotactic protein-1 (MCP-1), vascular endothelial growth factor (VEGF), platelet-derived growth factor-AA (PDGF-AA), and basic fibroblast growth factor (bFGF). Bae et al. [ 164 ] mentioned that TGF-β induced the migration of keratinocytes. It was also demonstrated that iPSC factors can enhance skin wound healing in vivo and in vitro when Zhou et al. [ 165 ] enhanced wound healing, even after carbon dioxide laser resurfacing in an in vivo study.
Peng et al. [ 166 ] investigated the effects of EVs derived from hESCs on in vitro cultured retinal glial, progenitor Müller cells, which are known to differentiate into retinal neurons. EVs appear heterogeneous in size and can be internalized by cultured Müller cells, and their proteins are involved in the induction and maintenance of stem cell pluripotency. These stem cell-derived vesicles were responsible for the neuronal trans-differentiation of cultured Müller cells exposed to them. However, the research article points out that the procedure was accomplished only on in vitro acquired retina.
Challenges concerning stem cell therapy
Although stem cells appear to be an ideal solution for medicine, there are still many obstacles that need to be overcome in the future. One of the first problems is ethical concern.
The most common pluripotent stem cells are ESCs. Therapies concerning their use at the beginning were, and still are, the source of ethical conflicts. The reason behind it started when, in 1998, scientists discovered the possibility of removing ESCs from human embryos. Stem cell therapy appeared to be very effective in treating many, even previously incurable, diseases. The problem was that when scientists isolated ESCs in the lab, the embryo, which had potential for becoming a human, was destroyed (Fig. 8 ). Because of this, scientists, seeing a large potential in this treatment method, focused their efforts on making it possible to isolate stem cells without endangering their source—the embryo.
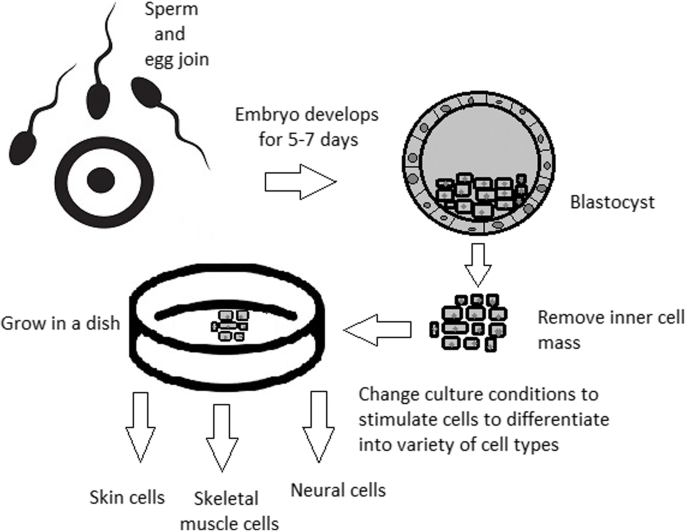
Use of inner cell mass pluripotent stem cells and their stimulation to differentiate into desired cell types
For now, while hESCs still remain an ethically debatable source of cells, they are potentially powerful tools to be used for therapeutic applications of tissue regeneration. Because of the complexity of stem cell control systems, there is still much to be learned through observations in vitro. For stem cells to become a popular and widely accessible procedure, tumour risk must be assessed. The second problem is to achieve successful immunological tolerance between stem cells and the patient’s body. For now, one of the best ideas is to use the patient’s own cells and devolve them into their pluripotent stage of development.
New cells need to have the ability to fully replace lost or malfunctioning natural cells. Additionally, there is a concern about the possibility of obtaining stem cells without the risk of morbidity or pain for either the patient or the donor. Uncontrolled proliferation and differentiation of cells after implementation must also be assessed before its use in a wide variety of regenerative procedures on living patients [ 167 ].
One of the arguments that limit the use of iPSCs is their infamous role in tumourigenicity. There is a risk that the expression of oncogenes may increase when cells are being reprogrammed. In 2008, a technique was discovered that allowed scientists to remove oncogenes after a cell achieved pluripotency, although it is not efficient yet and takes a longer amount of time. The process of reprogramming may be enhanced by deletion of the tumour suppressor gene p53, but this gene also acts as a key regulator of cancer, which makes it impossible to remove in order to avoid more mutations in the reprogrammed cell. The low efficiency of the process is another problem, which is progressively becoming reduced with each year. At first, the rate of somatic cell reprogramming in Yamanaka’s study was up to 0.1%. The use of transcription factors creates a risk of genomic insertion and further mutation of the target cell genome. For now, the only ethically acceptable operation is an injection of hESCs into mouse embryos in the case of pluripotency evaluation [ 168 ].
Stem cell obstacles in the future
Pioneering scientific and medical advances always have to be carefully policed in order to make sure they are both ethical and safe. Because stem cell therapy already has a large impact on many aspects of life, it should not be treated differently.
Currently, there are several challenges concerning stem cells. First, the most important one is about fully understanding the mechanism by which stem cells function first in animal models. This step cannot be avoided. For the widespread, global acceptance of the procedure, fear of the unknown is the greatest challenge to overcome.
The efficiency of stem cell-directed differentiation must be improved to make stem cells more reliable and trustworthy for a regular patient. The scale of the procedure is another challenge. Future stem cell therapies may be a significant obstacle. Transplanting new, fully functional organs made by stem cell therapy would require the creation of millions of working and biologically accurate cooperating cells. Bringing such complicated procedures into general, widespread regenerative medicine will require interdisciplinary and international collaboration.
The identification and proper isolation of stem cells from a patient’s tissues is another challenge. Immunological rejection is a major barrier to successful stem cell transplantation. With certain types of stem cells and procedures, the immune system may recognize transplanted cells as foreign bodies, triggering an immune reaction resulting in transplant or cell rejection.
One of the ideas that can make stem cells a “failsafe” is about implementing a self-destruct option if they become dangerous. Further development and versatility of stem cells may cause reduction of treatment costs for people suffering from currently incurable diseases. When facing certain organ failure, instead of undergoing extraordinarily expensive drug treatment, the patient would be able to utilize stem cell therapy. The effect of a successful operation would be immediate, and the patient would avoid chronic pharmacological treatment and its inevitable side effects.
Although these challenges facing stem cell science can be overwhelming, the field is making great advances each day. Stem cell therapy is already available for treating several diseases and conditions. Their impact on future medicine appears to be significant.
After several decades of experiments, stem cell therapy is becoming a magnificent game changer for medicine. With each experiment, the capabilities of stem cells are growing, although there are still many obstacles to overcome. Regardless, the influence of stem cells in regenerative medicine and transplantology is immense. Currently, untreatable neurodegenerative diseases have the possibility of becoming treatable with stem cell therapy. Induced pluripotency enables the use of a patient’s own cells. Tissue banks are becoming increasingly popular, as they gather cells that are the source of regenerative medicine in a struggle against present and future diseases. With stem cell therapy and all its regenerative benefits, we are better able to prolong human life than at any time in history.
Abbreviations
Basic fibroblast growth factor
Bone morphogenic proteins
Dental follicle stem cells
Dental pulp stem cells
Embryonic bodies
Embryonic stem cells
Fibroblast growth factors
Good Manufacturing Practice
Graphene oxide
Human amniotic fluid-derived stem cells
Human embryonic stem cells
Human foreskin fibroblasts
Inner cell mass
Non-coding RNA
Induced pluripotent stem cells
In vitro fertilization
Knockout serum replacement
Leukaemia inhibitory factor
Monocyte chemotactic protein-1
Fibroblasts
Messenger RNA
Mesenchymal stem cells of dental pulp
Myogenic differentiation
Osteoarthritis
Octamer-binding transcription factor 3 and 4
Platelet-derived growth factor
Platelet-derived growth factor-AA
Periodontal ligament stem cells
Rho-associated protein kinase
Stem cells from apical papilla
Stem cells of human exfoliated deciduous teeth
Synthetic Serum Substitute
Trophectoderm
Vascular endothelial growth factor
Transforming growth factors
Sukoyan MA, Vatolin SY, et al. Embryonic stem cells derived from morulae, inner cell mass, and blastocysts of mink: comparisons of their pluripotencies. Embryo Dev. 1993;36(2):148–58
Larijani B, Esfahani EN, Amini P, Nikbin B, Alimoghaddam K, Amiri S, Malekzadeh R, Yazdi NM, Ghodsi M, Dowlati Y, Sahraian MA, Ghavamzadeh A. Stem cell therapy in treatment of different diseases. Acta Medica Iranica. 2012:79–96 https://www.ncbi.nlm.nih.gov/pubmed/22359076 .
Sullivan S, Stacey GN, Akazawa C, et al. Quality guidelines for clinical-grade human induced pluripotent stem cell lines. Regenerative Med. 2018; https://doi.org/10.2217/rme-2018-0095 .
Amps K, Andrews PW, et al. Screening ethnically diverse human embryonic stem cells identifies a chromosome 20 minimal amplicon conferring growth advantage. Nat. Biotechnol. 2011; 29 (12):1121–44.
Google Scholar
Amit M, Itskovitz-Eldor J. Atlas of human pluripotent stem cells: derivation and culturing. New York: Humana Press; 2012.
Ludwig TE, Bergendahl V, Levenstein ME, Yu J, Probasco MD, Thomson JA. Feeder-independent culture of human embryonic stem cells. Nat Methods. 2006;3:637–46.
CAS PubMed Google Scholar
Kang MI. Transitional CpG methylation between promoters and retroelements of tissue-specific genes during human mesenchymal cell differentiation. J. Cell Biochem. 2007;102:224–39.
Vaes B, Craeye D, Pinxteren J. Quality control during manufacture of a stem cell therapeutic. BioProcess Int. 2012;10:50–5.
Bloushtain-Qimron N. Epigenetic patterns of embryonic and adult stem cells. Cell Cycle. 2009;8:809–17.
Brindley DA. Peak serum: implications of serum supply for cell therapy manufacturing. Regenerative Medicine. 2012;7:809–17.
Solter D, Knowles BB. Immunosurgery of mouse blastocyst. Proc Natl Acad Sci U S A. 1975;72:5099–102.
CAS PubMed PubMed Central Google Scholar
Hoepfl G, Gassmann M, Desbaillets I. Differentiating embryonic stem cells into embryoid bodies. Methods Mole Biol. 2004;254:79–98 https://doi.org/10.1385/1-59259-741-6:079 .
Lim WF, Inoue-Yokoo T, Tan KS, Lai MI, Sugiyama D. Hematopoietic cell differentiation from embryonic and induced pluripotent stem cells. Stem Cell Res Ther. 2013;4(3):71. https://doi.org/10.1186/scrt222 .
Article CAS PubMed PubMed Central Google Scholar
Mohr JC, de Pablo JJ, Palecek SP. 3-D microwell culture of human embryonic stem cells. Biomaterials. 2006;27(36):6032–42. https://doi.org/10.1016/j.biomaterials.2006.07.012 .
Article CAS PubMed Google Scholar
Doetschman TC, Eistetter H, Katz M, Schmidt W, Kemler R. The in vitro development of blastocyst-derived embryonic stem cell lines: formation of the visceral yolk sac, blood islands, and myocardium. J Embryol Exp Morphol. 1985;87:27–45.
Kurosawa HY. Methods for inducing embryoid body formation: in vitro differentiation system of embryonic stem cells. J Biosci Bioeng. 2007;103:389–98.
Heins N, Englund MC, Sjoblom C, Dahl U, Tonning A, Bergh C, Lindahl A, Hanson C, Semb H. Derivation, characterization, and differentiation of human embryonic stem cells. Stem Cells. 2004;22:367–76.
Rosowski KA, Mertz AF, Norcross S, Dufresne ER, Horsley V. Edges of human embryonic stem cell colonies display distinct mechanical properties and differentiation potential. Sci Rep. 2015;5:Article number:14218.
PubMed Google Scholar
Chung Y, Klimanskaya I, Becker S, Li T, Maserati M, Lu SJ, Zdravkovic T, Ilic D, Genbacev O, Fisher S, Krtolica A, Lanza R. Human embryonic stem cell lines generated without embryo destruction. Cell Stem Cell. 2008;2:113–7.
Zhang X, Stojkovic P, Przyborski S, Cooke M, Armstrong L, Lako M, Stojkovic M. Derivation of human embryonic stem cells from developing and arrested embryos. Stem Cells. 2006;24:2669–76.
Beers J, Gulbranson DR, George N, Siniscalchi LI, Jones J, Thomson JA, Chen G. Passaging and colony expansion of human pluripotent stem cells by enzyme-free dissociation in chemically defined culture conditions. Nat Protoc. 2012;7:2029–40.
Ellerström C, Hyllner J, Strehl R. single cell enzymatic dissociation of human embryonic stem cells: a straightforward, robust, and standardized culture method. In: Turksen K, editor. Human embryonic stem cell protocols. Methods in molecular biology: Humana Press; 2009. p. 584.
Heng BC, Liu H, Ge Z, Cao T. Mechanical dissociation of human embryonic stem cell colonies by manual scraping after collagenase treatment is much more detrimental to cellular viability than is trypsinization with gentle pipetting. Biotechnol Appl Biochem. 2010;47(1):33–7.
Ellerstrom C, Strehl R, Noaksson K, Hyllner J, Semb H. Facilitated expansion of human embryonic stem cells by single-cell enzymatic dissociation. Stem Cells. 2007;25:1690–6.
Brimble SN, Zeng X, Weiler DA, Luo Y, Liu Y, Lyons IG, Freed WJ, Robins AJ, Rao MS, Schulz TC. Karyotypic stability, genotyping, differentiation, feeder-free maintenance, and gene expression sampling in three human embryonic stem cell lines deri. Stem Cells Dev. 2004;13:585–97.
Watanabe K, Ueno M, Kamiya D, Nishiyama A, Matsumura M, Wataya T, Takahashi JB, Nishikawa S, Nishikawa S, Muguruma K, Sasai Y. A ROCK inhibitor permits survival of dissociated human embryonic stem cells. Nat Biotechnol. 2007;25:681–6.
Nie Y, Walsh P, Clarke DL, Rowley JA, Fellner T. Scalable passaging of adherent human pluripotent stem cells. 2014. https://doi.org/10.1371/journal.pone.0088012 .
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, Jones JM. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–7.
Martin MJ, Muotri A, Gage F, Varki A. Human embryonic stem cellsexpress an immunogenic nonhuman sialic acid. Nat. Med. 2005;11:228–32.
Smith AG, Heath JK, Donaldson DD, Wong GG, Moreau J, Stahl M, Rogers D. Inhibition of pluripotential embryonic stem cell differentiation by purified polypeptides. Nature. 1988;336(6200):688–90. https://doi.org/10.1038/336688a0 .
Xu C, Inokuma MS, Denham J, Golds K, Kundu P, Gold JD, Carpenter MK. Feeder-free growth of undifferentiated human embryonic stem cells. Nature Biotechnol. 2001;19:971–4. https://doi.org/10.1038/nbt1001-971 .
Article CAS Google Scholar
Weathersbee PS, Pool TB, Ord T. Synthetic serum substitute (SSS): a globulin-enriched protein supplement for human embryo culture. J. Assist Reprod Genet. 1995;12:354–60.
Chen G, Gulbranson DR, Hou Z, Bolin JM, Ruotti V, Probasco MD, Smuga-Otto K, Howden SE, Diol NR, Propson NE, Wagner R, Lee GO, Antosiewicz-Bourget J, Teng JM, Thomson JA. Chemically defined conditions for human iPSC derivation and culture. Nat. Methods. 2011;8:424–9.
Sommer CA, Mostoslavsky G. Experimental approaches for the generation of induced pluripotent stem cells. Stem Cell Res Ther. 2010;1:26.
PubMed PubMed Central Google Scholar
Takahashi K, Yamanaka S. Induced pluripotent stem cells in medicine and biology. Development. 2013;140(12):2457–61 https://doi.org/10.1242/dev.092551 .
Shi D, Lu F, Wei Y, et al. Buffalos ( Bubalus bubalis ) cloned by nuclear transfer of somatic cells. Biol. Reprod. 2007;77:285–91. https://doi.org/10.1095/biolreprod.107.060210 .
Gurdon JB. The developmental capacity of nuclei taken from intestinal epithelium cells of feeding tadpoles. Development. 1962;10:622–40 http://dev.biologists.org/content/10/4/622 .
CAS Google Scholar
Kain K. The birth of cloning: an interview with John Gurdon. Dis Model Mech. 2009;2(1–2):9–10. https://doi.org/10.1242/dmm.002014 .
Article PubMed Central Google Scholar
Davis RL, Weintraub H, Lassar AB. Expression of a single transfected cDNA converts fibroblasts to myoblasts. Cell. 1987;24(51(6)):987–1000.
Quinlan AR, Boland MJ, Leibowitz ML, et al. Genome sequencing of mouse induced pluripotent stem cells reveals retroelement stability and infrequent DNA rearrangement during reprogramming. Cell Stem Cell. 2011;9(4):366–73.
Maherali N, Sridharan R, Xie W, Utika LJ, Eminli S, Arnold K, Stadtfeld M, Yachechko R, Tchieu J, Jaenisch R, Plath K, Hochedlinger K. Directly reprogrammed fibroblasts show global epigenetic remodeling and widespread tissue contribution. Cell Stem Cell. 2007;1:55–70.
Ohi Y, Qin H, Hong C, Blouin L, Polo JM, Guo T, Qi Z, Downey SL, Manos PD, Rossi DJ, Yu J, Hebrok M, Hochedlinger K, Costello JF, Song JS, Ramalho-Santos M. Incomplete DNA methylation underlines a transcriptional memory of somatic cells in human IPS cells. Nat Cell Biol. 2011;13:541–9.
Zhou Q, Brown J, Kanarek A, Rajagopal J, Melton DA. In vivo reprogramming of adult pancreatic exocrine cells to beta-cells. Nature. 2008;455:627–32 https://doi.org/10.1038/nature07314 .
Hilfiker A, Kasper C, Hass R, Haverich A. Mesenchymal stem cells and progenitor cells in connective tissue engineering and regenerative medicine: is there a future for transplantation? Langenbecks Arch Surg. 2011;396:489–97.
Zhang Wendy, Y., de Almeida Patricia, E., and Wu Joseph, C. Teratoma formation: a tool for monitoring pluripotency in stem cell research. StemBook, ed. The Stem Cell Research Community . June 12, 2012. https://doi.org/10.3824/stembook.1.53.1 .
Narsinh KH, Sun N, Sanchez-Freire V, et al. Single cell transcriptional profiling reveals heterogeneity of human induced pluripotent stem cells. J Clin Invest. 2011;121(3):1217–21.
Gertow K, Przyborski S, Loring JF, Auerbach JM, Epifano O, Otonkoski T, Damjanov I, AhrlundRichter L. Isolation of human embryonic stem cell-derived teratomas for the assessment of pluripotency. Curr Protoc Stem Cell Biol . 2007, Chapter 1, Unit 1B 4. 3: 1B.4.1-1B.4.29.
Cooke MJ, Stojkovic M, Przyborski SA. Growth of teratomas derived from human pluripotent stem cells is influenced by the graft site. Stem Cells Dev. 2006;15(2):254–9.
Przyborski SA. Differentiation of human embryonic stem cells after transplantation in immune-deficient mice. Stem Cells. 2005;23:1242–50.
Tannenbaum SE, Turetsky TT, Singer O, Aizenman E, Kirshberg S, Ilouz N, Gil Y, Berman-Zaken Y, Perlman TS, Geva N, Levy O, Arbell D, Simon A, Ben-Meir A, Shufaro Y, Laufer N, Reubinoff BE. Derivation of xeno-free and GMP-grade human embryonic stem cells- platforms for future clinical applications. PLoS One. 2012;7:e35325.
Cohen DE, Melton D. Turning straw into gold: directing cell fate for regenerative medicine. Nat Rev Genet. 2011;12:243–52.
Hwang NS, Varghese S, Elisseeff J. Controlled differentiation of stem cells. Adv Drug Deliv Rev. 2007;60(2):199–214. https://doi.org/10.1016/j.addr.2007.08.036 .
Turner N, Grose R. Fibroblast growth factor signalling: from development to cancer. Nat Rev Cancer. 2010;10:116–29.
Rao TP, Kuhl M. An updated overview on Wnt signaling pathways: a prelude for more. Circ Res. 2010;106:1798–806.
Moustakas A, Heldin CH. The regulation of TGFbeta signal transduction. Development. 2009;136:3699–714.
Efthymiou AG, Chen G, Rao M, Chen G, Boehm M. Self-renewal and cell lineage differentiation strategies in human embryonic stem cells and induced pluripotent stem cells. Expert Opin Biol Ther. 2014;14:1333–44.
Yang L, Soonpaa MH, Adler ED, Roepke TK, Kattman SJ, Kennedy M, Henckaerts E, Bonham K, Abbott GW, Linden RM, Field LJ, Keller GM. Human cardiovascular progenitor cells develop from a KDRþembryonic-stem-cell-derived population. Nature. 2008;453:524–8.
Kroon E, Martinson LA, Kadoya K, Bang AG, Kelly OG, Eliazer S, Young H, Richardson M, Smart NG, Cunningham J, Agulnick AD, D’amour KA, Carpenter MK, Baetge EE. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26(4):443–52. https://doi.org/10.1038/nbt1393 .
Vallier L, Reynolds D, Pedersen RA. Nodal inhibits differentiation of human embryonic stem cells along the neuroectodermal default pathway. Dev Biol. 2004;275:403–21.
Burridge PW, Zambidis ET. Highly efficient directed differentiation of human induced pluripotent stem cells into cardiomyocytes. Methods Mol Biol. 2013;997:149–61.
Cai J, Zhao Y, Liu Y, Ye F, Song Z, Qin H, Meng S, Chen Y, Zhou R, Song X, Guo Y, Ding M, Deng H. Directed differentiation of human embryonic stem cells into functional hepatic cells. Hepatology. 2007;45:1229–39.
Takasato M, Er PX, Becroft M, Vanslambrouck JM, Stanley EG, Elefanty AG, Little MH. Directing human embryonic stem cell differentiation towards a renal lineage generates a selforganizing kidney. Nat Cell Biol. 2014;16:118–26.
Huang SX, Islam MN, O’Neill J, Hu Z, Yang YG, Chen YW, Mumau M, Green MD, VunjakNovakovic G, Bhattacharya J, Snoeck HW. Efficient generation of lung and airway epithelial cells from human pluripotent stem cells. Nat Biotechnol. 2014;32:84–91.
Kadzik RS, Morrisey EE. Directing lung endoderm differentiation in pluripotent stem cells. Cell Stem Cell. 2012;10:355–61.
Wichterle H, Lieberam I, Porter JA, Jessell TM. Directed differentiation of embryonic stem cells into motor neurons. Cell. 2002;110:385–97.
Spence JR, Mayhew CN, Rankin SA, Kuhar MF, Vallance JE, Tolle K, Hoskins EE, Kalinichenko VV, Wells SI, Zorn AM, Shroyer NF, Wells JM. Directed differentiation of human pluripotent stem cells into intestinal tissue in vitro. Nature. 2011;470:105–9.
Oldershaw RA, Baxter MA, Lowe ET, Bates N, Grady LM, Soncin F, Brison DR, Hardingham TE, Kimber SJ. Directed differentiation of human embryonic stem cells toward chondrocytes. Nat Biotechnol. 2010;28:1187–94.
Jun Cai, Ann DeLaForest, Joseph Fisher, Amanda Urick, Thomas Wagner, Kirk Twaroski, Max Cayo, Masato Nagaoka, Stephen A Duncan. Protocol for directed differentiation of human pluripotent stem cells toward a hepatocyte fate. 2012. DOI: https://doi.org/10.3824/stembook.1.52.1 .
Frank-Kamenetsky M, Zhang XM, Bottega S, Guicherit O, Wichterle H, Dudek H, Bumcrot D, Wang FY, Jones S, Shulok J, Rubin LL, Porter JA. Small-molecule modulators of hedgehog signaling: identification and characterization of smoothened agonists and antagonists. J Biol. 2002;1:10.
Oshima K, Shin K, Diensthuber M, Peng AW, Ricci AJ, Heller S. Mechanosensitive hair celllike cells from embryonic and induced pluripotent stem cells. Cell. 2010;141:704–16.
Osakada F, Jin ZB, Hirami Y, Ikeda H, Danjyo T, Watanabe K, Sasai Y, Takahashi M. In vitro differentiation of retinal cells from human pluripotent stem cells by small-molecule induction. J Cell Sci. 2009;122:3169–79.
Kshitiz PJ, Kim P, Helen W, Engler AJ, Levchenko A, Kim DH. Control of stem cell fate and function by engineering physical microenvironments. Intergr Biol (Camb). 2012;4:1008–18.
Amps K, Andrews PW, Anyfantis G, Armstrong L, Avery S, Baharvand H, Baker J, Baker D, Munoz MB, Beil S, Benvenisty N, Ben-Yosef D, Biancotti JC, Bosman A, Brena RM, Brison D, Caisander G, Camarasa MV, Chen J, ChiaoE CYM, Choo AB, Collins D, et al. Screening ethnically diverse human embryonic stem cells identifies a chromosome 20 minimal amplicon conferring growth advantage. Nat Biotechnol. 2011;29:1132–44.
Nukaya D, Minami K, Hoshikawa R, Yokoi N, Seino S. Preferential gene expression and epigenetic memory of induced pluripotent stem cells derived from mouse pancreas. Genes Cells. 2015;20:367–81.
Murdoch A, Braude P, Courtney A, Brison D, Hunt C, Lawford-Davies J, Moore H, Stacey G, Sethe S, Procurement Working Group Of National Clinical H, E. S. C. F, National Clinical H, E. S. C. F. The procurement of cells for the derivation of human embryonic stem cell lines for therapeutic use: recommendations for good practice. Stem Cell Rev. 2012;8:91–9.
Hewitson H, Wood V, Kadeva N, Cornwell G, Codognotto S, Stephenson E, Ilic D. Generation of KCL035 research grade human embryonic stem cell line carrying a mutation in HBB gene. Stem Cell Res. 2016;16:210–2.
Daley GQ, Hyun I, Apperley JF, Barker RA, Benvenisty N, Bredenoord AL, Breuer CK, Caulfield T, Cedars MI, Frey-Vasconcells J, Heslop HE, Jin Y, Lee RT, Mccabe C, Munsie M, Murry CE, Piantadosi S, Rao M, Rooke HM, Sipp D, Studer L, Sugarman J, et al. Setting global standards for stem cell research and clinical translation: the 2016 ISSCR guidelines. Stem Cell Rep. 2016;6:787–97.
Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126(4):663–76. https://doi.org/10.1016/j.cell.2006.07.024 .
Loh YH, Wu Q, Chew JL, Vega VB, Zhang W, Chen X, Bourque G, George J, Leong B, Liu J, et al. The Oct4 and Nanog transcription network regulates pluripotency in mouse embryonic stem cells. Nat Genet. 2006;38:431–40.
Menasche P, Vanneaux V, Hagege A, Bel A, Cholley B, Cacciapuoti I, Parouchev A, Benhamouda N, Tachdjian G, Tosca L, Trouvin JH, Fabreguettes JR, Bellamy V, Guillemain R, SuberbielleBoissel C, Tartour E, Desnos M, Larghero J. Human embryonic stem cell-derived cardiac progenitors for severe heart failure treatment: first clinical case report. Eur Heart J. 2015;36:2011–7.
Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, Hubschman JP, Davis JL, Heilwell G, Spirn M, Maguire J, Gay R, Bateman J, Ostrick RM, Morris D, Vincent M, Anglade E, Del Priore LV, Lanza R. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385:509–16.
Ilic D, Ogilvie C. Concise review: human embryonic stem cells-what have we done? What are we doing? Where are we going? Stem Cells. 2017;35:17–25.
Rocha V, et al. Clinical use of umbilical cord blood hematopoietic stem cells. Biol Blood Marrow Transplant. 2006;12(1):34–4.
Longo UG, Ronga M, Maffulli N. Sports Med Arthrosc 17:112–126. Achilles tendinopathy. Sports Med Arthrosc. 2009;17:112–26.
Tempfer H, Lehner C, Grütz M, Gehwolf R, Traweger A. Biological augmentation for tendon repair: lessons to be learned from development, disease, and tendon stem cell research. In: Gimble J, Marolt D, Oreffo R, Redl H, Wolbank S, editors. Cell engineering and regeneration. Reference Series in Biomedical Engineering. Cham: Springer; 2017.
Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol. 2007;213:626–34.
Widuchowski W, Widuchowski J, Trzaska T. Articular cartilage defects: study of 25,124 knee arthroscopies. Knee. 2007;14:177–82.
Li R, Lin Q-X, Liang X-Z, Liu G-B, et al. Stem cell therapy for treating osteonecrosis of the femoral head: from clinical applications to related basic research. Stem Cell Res Therapy. 2018;9:291 https://doi.org/10.1186/s13287-018-1018-7 .
Gangji V, De Maertelaer V, Hauzeur JP. Autologous bone marrow cell implantation in the treatment of non-traumatic osteonecrosis of the femoral head: five year follow-up of a prospective controlled study. Bone. 2011;49(5):1005–9.
Zhao D, Cui D, Wang B, Tian F, Guo L, Yang L, et al. Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone. 2012;50(1):325–30.
Sen RK, Tripathy SK, Aggarwal S, Marwaha N, Sharma RR, Khandelwal N. Early results of core decompression and autologous bone marrow mononuclear cells instillation in femoral head osteonecrosis: a randomized control study. J Arthroplast. 2012;27(5):679–86.
Lapasset L, Milhavet O, Prieur A, Besnard E, Babled A, Aït-Hamou N, Leschik J, Pellestor F, Ramirez JM, De Vos J, Lehmann S, Lemaitre JM. Rejuvenating senescent and centenarian human cells by reprogramming through the pluripotent state. Genes Dev. 2011;25:2248–53.
Sahin E, Depinho RA. Linking functional decline of telomeres, mitochondria and stem cells during ageing. Nature. 2010;464:520–8.
Petkovich DA, Podolskiy DI, Lobanov AV, Lee SG, Miller RA, Gladyshev VN. Using DNA methylation profiling to evaluate biological age and longevity interventions. Cell Metab. 2017;25:954–60 https://doi.org/10.1016/j.cmet.2017.03.016 .
Gerontology, Rejuvenation by cell reprogramming: a new horizon in. Rodolfo G. Goya, Marianne Lehmann, Priscila Chiavellini, Martina Canatelli-Mallat, Claudia B. Hereñú and Oscar A. Brown. Stem Cell Res Therapy . 2018, 9:349. https://doi.org/10.1186/s13287-018-1075-y .
Ocampo A, Reddy P, Martinez-Redondo P, Platero-Luengo A, Hatanaka F, Hishida T, Li M, Lam D, Kurita M, Beyret E, Araoka T, Vazquez-Ferrer E, Donoso D, Roman JLXJ, Rodriguez-Esteban C, Nuñez G, Nuñez Delicado E, Campistol JM, Guillen I, Guillen P, Izpisua. In vivo amelioration of age-associated hallmarks by partial reprogramming. Cell. 2016;167:1719–33.
de Lázaro I, Cossu G, Kostarelos K. Transient transcription factor (OSKM) expression is key towards clinical translation of in vivo cell reprogramming. EMBO Mol Med. 2017;9:733–6.
Sun S, Li ZQ, Glencer P, Cai BC, Zhang XM, Yang J, Li XR. Bringing the age-related macular degeneration high-risk allele age-related maculopathy susceptibility 2 into focus with stem cell technology. Stem Cell Res Ther. 2017;8:135 https://doi.org/10.1186/s13287-017-0584-4 .
Liu J. Induced pluripotent stem cell-derived neural stem cells: new hope for stroke? Stem Cell Res Ther. 2013;4:115 https://doi.org/10.1186/scrt326 .
Shahjalal HM, Dayem AA, Lim KM, Jeon TI, Cho SG. Generation of pancreatic β cells for treatment of diabetes: advances and challenges. Stem Cell ResTher. 2018;9:355 https://doi.org/10.1186/s13287-018-1099-3 .
Kroon E, Martinson LA, et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26;443–52.
Arora V, Pooja A, Munshi AK. Banking stem cells from human exfoliated deciduous teeth. J Clin Pediatr Dent. 2009;33(4):289–94.
Mao JJ. Stem cells and the future of dental care. New York State Dental J. 2008;74(2):21–4.
Reznick, Jay B. Continuing education: stem cells: emerging medical and dental therapies for the dental Professional. Dentaltown Magazine . 2008, pp. 42–53.
Arthur A, Rychkov G, Shi S, Koblar SA, Gronthos S. Adult human dental pulp stem cells differentiate toward functionally active neurons under appropriate environmental cues. Stem Cells. 2008;26(7):1787–95.
Cordeiro MM, Dong Z, Kaneko T, Zhang Z, Miyazawa M, Shi S, Smith A. Dental pulp tissue engineering with stem cells from exfoliated. J Endod. 2008;34(8):962–9.
Hayashi K, Ohta H, Kurimoto K, Aramaki S, Saitou M. Reconstitution of the mouse germ cell specification pathway in culture by pluripotent stem cells. Cell. 2011;146(4):519–32. https://doi.org/10.1016/j.cell.2011.06.052 .
Sadri-Ardekani H, Atala A. Testicular tissue cryopreservation and spermatogonial stem cell transplantation to restore fertility: from bench to bedside. Stem Cell ResTher. 2014;5:68 https://doi.org/10.1186/scrt457 .
Zhang Q, Xu M, Yao X, Li T, Wang Q, Lai D. Human amniotic epithelial cells inhibit granulosa cell apoptosis induced by chemotherapy and restore the fertility. Stem Cell Res Ther. 2015;6:152 https://doi.org/10.1186/s13287-015-0148-4 .
Ma DK, Bonaguidi MA, Ming GL, Song H. Adult neural stem cells in the mammalian central nervous system. Cell Res. 2009;19:672–82. https://doi.org/10.1038/cr.2009.56 .
Dantuma E, Merchant S, Sugaya K. Stem cells for the treatment of neurodegenerative diseases. Stem Cell ResTher. 2010;1:37 https://doi.org/10.1186/scrt37 .
Wang Q, Matsumoto Y, Shindo T, Miyake K, Shindo A, Kawanishi M, Kawai N, Tamiya T, Nagao S. Neural stem cells transplantation in cortex in a mouse model of Alzheimer’s disease. J Med Invest. 2006;53:61–9. https://doi.org/10.2152/jmi.53.61 .
Article PubMed Google Scholar
Moghadam FH, Alaie H, Karbalaie K, Tanhaei S, Nasr Esfahani MH, Baharvand H. Transplantation of primed or unprimed mouse embryonic stem cell-derived neural precursor cells improves cognitive function in Alzheimerian rats. Differentiation. 2009;78:59–68. https://doi.org/10.1016/j.diff.2009.06.005 .
Byrne JA. Developing neural stem cell-based treatments for neurodegenerative diseases. Stem Cell ResTher. 2014;5:72. https://doi.org/10.1186/scrt461 .
Awe JP, Lee PC, Ramathal C, Vega-Crespo A, Durruthy-Durruthy J, Cooper A, Karumbayaram S, Lowry WE, Clark AT, Zack JA, Sebastiano V, Kohn DB, Pyle AD, Martin MG, Lipshutz GS, Phelps PE, Pera RA, Byrne JA. Generation and characterization of transgene-free human induced pluripotent stem cells and conversion to putative clinical-grade status. Stem Cell Res Ther. 2013;4:87. https://doi.org/10.1186/scrt246 .
Peng J, Zeng X. The role of induced pluripotent stem cells in regenerative medicine: neurodegenerative diseases. Stem Cell ResTher. 2011;2:32. https://doi.org/10.1186/scrt73 .
Wright BL, Barker RA. Established and emerging therapies for Huntington’s disease. 2007;7(6):579–87 https://www.ncbi.nlm.nih.gov/pubmed/17896994/579-87 .
Lin NH, Gronthos S, Bartold PM. Stem cells and periodontal regeneration. Aust Dent J. 2008;53:108–21.
Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J, et al. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet. 2004;364:149–55.
Ramseier CA, Abramson ZR, Jin Q, Giannobile WV. Gene therapeutics for periodontal regenerative medicine. Dent Clin North Am. 2006;50:245–63.
Shi S, Bartold PM, Miura M, Seo BM, Robey PG, Gronthos S. The efficacy of mesenchymal stem cells to regenerate and repair dental structures. OrthodCraniofac Res. 2005;8:191–9.
Iohara K, Nakashima M, Ito M, Ishikawa M, Nakasima A, Akamine A. Dentin regeneration by dental pulp stem cell therapy with recombinant human bone morphogenetic protein. J Dent Res. 2004;83:590–5.
Hu B, Unda F, Bopp-Kuchler S, Jimenez L, Wang XJ, Haikel Y, et al. Bone marrow cells can give rise to ameloblast-like cells. J Dent Res. 2006;85:416–21.
Liu Y, Liu W, Hu C, Xue Z, Wang G, Ding B, Luo H, Tang L, Kong X, Chen X, Liu N, Ding Y, Jin Y. MiR-17 modulates osteogenic differentiation through a coherent feed-forward loop in mesenchymal stem cells isolated from periodontal ligaments of patients with periodontitis. Stem Cells. 2011;29(11):1804–16. https://doi.org/10.1002/stem.728 .
Raspini G, Wolff J, Helminen M, Raspini G, Raspini M, Sándor GK. Dental stem cells harvested from third molars combined with bioactive glass can induce signs of bone formation in vitro. J Oral Maxillofac Res. 2018;9(1):e2. Published 2018 Mar 31. https://doi.org/10.5037/jomr.2018.9102 .
Christodoulou I, Goulielmaki M, Devetzi M, Panagiotidis M, Koliakos G, Zoumpourlis V. Mesenchymal stem cells in preclinical cancer cytotherapy: a systematic review. Stem Cell Res Ther. 2018;9(1;336). https://doi.org/10.1186/s13287-018-1078-8 .
Bansal R, Jain A. Current overview on dental stem cells applications in regenerative dentistry. J Nat Sci Biol Med. 2015;6(1):29–34. https://doi.org/10.4103/0976-9668.149074 .
Article PubMed PubMed Central Google Scholar
Edgar Ledesma-Martínez, Víctor Manuel Mendoza-Núñez, Edelmiro Santiago-Osorio. Mesenchymal stem cells derived from dental pulp: a review. Stem Cells Int . 2016, 4,709,572, p. doi: https://doi.org/10.1155/2016/4709572 ].
Grzech-Leśniak K. Making use of lasers in periodontal treatment: a new gold standard? Photomed Laser Surg. 2017;35(10):513–4.
Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, Shi S. SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci U S A. 2003;100(10):5807–12. https://doi.org/10.1073/pnas.0937635100 .
Yasui T, Mabuchi Y, Toriumi H, Ebine T, Niibe K, Houlihan DD, Morikawa S, Onizawa K, Kawana H, Akazawa C, Suzuki N, Nakagawa T, Okano H, Matsuzaki Y. Purified human dental pulp stem cells promote osteogenic regeneration. J Dent Res. 2016;95(2):206–14. https://doi.org/10.1177/0022034515610748 .
Yamamoto A, Sakai K, Matsubara K, Kano F, Ueda M. Multifaceted neuro-regenerative activities of human dental pulp stem cells for functional recovery after spinal cord injury. Neurosci Res. 2014;78:16–20. https://doi.org/10.1016/j.neures.2013.10.010 .
d’Aquino R, De Rosa A, Lanza V, Tirino V, Laino L, Graziano A, Desiderio V, Laino G, Papaccio G. Human mandible bone defect repair by the grafting of dental pulp stem/progenitor cells and collagen sponge biocomplexes. Eur Cell Mater. 2009;12, PMID: 19908196:75–83.
Wang L, Shen H, Zheng W, Tang L, Yang Z, Gao Y, Yang Q, Wang C, Duan Y, Jin Y. Characterization of stem cells from alveolar periodontal ligament. Tissue Eng. Part A. 2011;17(7–8):1015–26. https://doi.org/10.1089/ten.tea.2010.0140 .
Iwata T, Yamato M, Zhang Z, Mukobata S, Washio K, Ando T, Feijen J, Okano T, Ishikawa I. Validation of human periodontal ligament-derived cells as a reliable source for cytotherapeutic use. J Clin Periodontol. 2010;37(12):1088–99. https://doi.org/10.1111/j.1600-051X.2010.01597.x .
Chen F-M, Gao L-N, Tian B-M, Zhang X-Y, Zhang Y-J, Dong G-Y, Lu H, et al. Treatment of periodontal intrabony defects using autologous periodontal ligament stem cells: a randomized clinical trial. Stem Cell Res Ther. 2016;7:33. https://doi.org/10.1186/s13287-016-0288-1 .
Bakopoulou A, Leyhausen G, Volk J, Tsiftsoglou A, Garefis P, Koidis P, Geurtsen W. Comparative analysis of in vitro osteo/odontogenic differentiation potential of human dental pulp stem cells (DPSCs) and stem cells from the apical papilla (SCAP). Arch Oral Biol. 2011;56(7):709–21. https://doi.org/10.1016/j.archoralbio.2010.12.008 .
Han C, Yang Z, Zhou W, Jin F, Song Y, Wang Y, Huo N, Chen L, Qian H, Hou R, Duan Y, Jin Y. Periapical follicle stem cell: a promising candidate for cementum/periodontal ligament regeneration and bio-root engineering. Stem Cells Dev. 2010;19(9):1405–15. https://doi.org/10.1089/scd.2009.0277 .
Luan X, Ito Y, Dangaria S, Diekwisch TG. Dental follicle progenitor cell heterogeneity in the developing mouse periodontium. Stem Cells Dev. 2006;15(4):595–608. https://doi.org/10.1089/scd.2006.15.595 .
Handa K, Saito M, Tsunoda A, Yamauchi M, Hattori S, Sato S, Toyoda M, Teranaka T, Narayanan AS. Progenitor cells from dental follicle are able to form cementum matrix in vivo. Connect Tissue Res. 2002;43(2–3):406–8 PMID: 12489190.
Guo W, Chen L, Gong K, Ding B, Duan Y, Jin Y. Heterogeneous dental follicle cells and the regeneration of complex periodontal tissues. Tissue Engineering. Part A. 2012;18(5–6):459–70 https://doi.org/10.1089/ten.tea.2011.0261 .
Bai, Yudi et al. Cementum- and periodontal ligament-like tissue formation by dental follicle cell sheets co-cultured with Hertwig’s epithelial root sheath cells. Bone. 2011, 48, Issue 6, pp. 1417–1426, https://doi.org/10.1016/j.bone.2011.02.016 .
Cordeiro MM, Dong Z, Kaneko T, Zhang Z, Miyazawa M, Shi S, et al. Dental pulp tissue engineering with stem cells from exfoliated deciduous teeth. 2008, 34, pp. 962–969.
Dobie K, Smith G, Sloan AJ, Smith AJ. Effects of alginate, hydrogels and TGF-beta 1 on human dental pulp repair in vitro. Connect Tissue Res 2. 2002;43:387–90.
Friedlander LT, Cullinan MP, Love RM. Dental stem cells and their potential role in apexogenesis and apexification. Int Endod J. 2009;42:955–62.
Cai J, Zhang Y, Liu P, Chen S, Wu X, Sun Y, Li A, Huang K, Luo R, Wang L, Liu Y, Zhou T, Wei S, Pan G, Pei D, Generation of tooth-like structures from integration-free human urine induced pluripotent stem cells. Cell Regen (Lond). July 30, 2013, 2(1), pp. 6, doi: https://doi.org/10.1186/2045-9769-2-6 .
Craig J. Taylor, Eleanor M. Bolton, and J. Andrew Bradley 2011 Aug 12 and https://doi.org/10.1098/rstb.2011.0030 ], 366(1575): 2312–2322. [doi:. Immunological considerations for embryonic and induced pluripotent stem cell banking,. Philos Trans R SocLond B Biol Sci. 2011, 366(1575), pp. 2312–2322, doi: https://doi.org/10.1098/rstb.2011.0030 .
T.R. Nayak, H. Andersen, V.S. Makam, C. Khaw, S. Bae, X.F. Xu, P.L.R. Ee, J.H. Ahn, B.H. Hong, G. Pastorin, B. Ozyilmaz, ACS Nano, 5 (6) (2011), pp. 4. Graphene for controlled and accelerated osteogenic differentiation of human mesenchymal stem cells,. ACS Nano. 2011, pp. 4670–4678.
Lee WC, Lim C, Shi H, Tang LAL, Wang Y, Lim CT, Loh KP. Origin of enhanced stem cell growth and differentiation on graphene and graphene oxide. ACS Nano. 2011;5(9):7334–41.
Kenry LWC, Loh KP, Lim CT. When stem cells meet graphene: opportunities and challenges in regenerative medicine. Biomaterials. 2018;155:236–50.
Yuan A, Farber EL, Rapoport AL, Tejada D, Deniskin R, Akhmedov NB, et al. Transfer of microRNAs by embryonic stem cell microvesicles. 2009. 2009, 4(3), p. https://doi.org/10.1371/journal.pone . 0004722.
Oh, Myeongsik, et al. Exosomes derived from human induced pluripotent stem cells ameliorate the aging of skin fibroblasts. Int. J. Mol. Sci. 2018, 19(6), p. 1715.
Ramirez MI. et al. Technical challenges of working with extracellular vesicles. Nanoscale. 2018;10:881–906.
Valadi H, et al. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007;9:654–9.
Mateescu B, et al. Obstacles and opportunities in the functional analysis of extracellular vesicle RNA—an ISEV position paper. J. Extracell. Vesicles. 2017;6(1). https://doi.org/10.1080/20013078.2017.1286095 .
Nawaz M, et al. Extracellular vesicles: evolving factors in stem cell biology. Stem Cells Int. 2016;2016:17. Article ID 1073140.
Helfrich, Y.R., Sachs, D.L. and Voorhees, J.J. Overview of skin aging and photoaging. Dermatol. Nurs. 20, pp. 177–183, https://www.ncbi.nlm.nih.gov/pubmed/18649702 .
Julia Tigges, Jean Krutmann, Ellen Fritsche, Judith Haendeler, Heiner Schaal, Jens W. Fischer, Faiza Kalfalah, Hans Reinke, Guido Reifenberger, Kai Stühler, Natascia Ventura, Sabrina Gundermann, Petra Boukamp, Fritz Boege. The hallmarks of fibroblast ageing, mechanisms of ageing and development, 138, 2014, Pages 26–44. 2014, 138, pp. 26–44, ISSN 0047–6374, https://doi.org/10.1016/j.mad.2014.03.004 .
Huh MI, Kim MS, Kim HK, et al. Effect of conditioned media collected from human amniotic fluid-derived stem cells (hAFSCs) on skin regeneration and photo-aging. Tissue Eng Regen Med. 2014;11:171 https://doi.org/10.1007/s13770-014-0412-1 .
Togel F, Hu Z, Weiss K, et al. Administered mesenchymal stem cells protect against ischemic acute renal failure through differentiation-independent mechanisms. Am J Physiol Renal Physiol. 2005;289:F31.
Liu J, Han G, Liu H, et al. Suppression of cholangiocarcinoma cell growth by human umbilical cord mesenchymal stem cells: a possible role of Wnt and Akt signaling. PLoS One. 2013;8:e62844.
Oh M, et al. Promotive effects of human induced pluripotent stem cell-conditioned medium on the proliferation and migration of dermal fibroblasts. Biotechnol. Bioprocess Eng. 2017;22:561–8.
Chen L, Tredget EE, Wu PY, Wu Y. Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PloS One. 2008;3:e1886.
Bae J-S, Lee S-H, Kim J-E, Choi J-Y, Park R-W, Park JY, Park H-S, Sohn Y-S, Lee D-S, Lee EB. βig-h3 supports keratinocyte adhesion, migration, and proliferation through α3β1 integrin. Biochem. Biophys. Res. Commun. 2002;294:940–8.
Zhou B-R, Xu Y, Guo S-L, Xu Y, Wang Y, Zhu F, Permatasari F, Wu D, Yin Z-Q, Luo D. The effect of conditioned media of adipose-derived stem cells on wound healing after ablative fractional carbon dioxide laser resurfacing. BioMed Res. Int. 2013;519:126.
Peng Y, Baulier E, Ke Y, Young A, Ahmedli NB, Schwartz SD, et al. Human embryonic stem cells extracellular vesicles and their effects on immortalized human retinal Müller cells. PLoS ONE. 2018, 13(3), p. https://doi.org/10.1371/journal.pone.019400 .
Harris MT, Butler DL, Boivin GP, Florer JB, Schantz EJ, Wenstrup RJ. Mesenchymal stem cells used for rabbit tendon repair can form ectopic bone and express alkaline phosphatase activity in constructs. J Orthop Res. 2004;22:998–1003.
Mascetti VL, Pedersen RA. Human-mouse chimerism validates human stem cell pluripotency. Cell Stem Cell. 2016;18:67–72.
Gandia C, Armiñan A, García-Verdugo JM, Lledó E, Ruiz A, Miñana MD, Sanchez-Torrijos J, Payá R, Mirabet V, Carbonell-Uberos F, Llop M, Montero JA, Sepúlveda P. Human dental pulp stem cells improve left ventricular function, induce angiogenesis, and reduce infarct size in rats with acute myocardial infarction. Stem Cells. 2007;26(3):638–45.
Perry BC, Zhou D, Wu X, Yang FC, Byers MA, Chu TM, Hockema JJ, Woods EJ, Goebel WS. Collection, cryopreservation, and characterization of human dental pulp-derived mesenchymal stem cells for banking and clinical use. Tissue Eng Part C Methods. 2008;14(2):149–56.
Garcia-Olmo D, Garcia-Arranz M, Herreros D, et al. A phase I clinical trial of the treatment of Crohn’s fistula by adipose mesenchymal stem cell transplantation. Dis Colon Rectum. 2005;48:1416–23.
de Mendonça CA, Bueno DF, Martins MT, Kerkis I, Kerkis A, Fanganiello RD, Cerruti H, Alonso N, Passos-Bueno MR. Reconstruction of large cranial defects in nonimmunosuppressed experimental design with human dental pulp stem cells. J Craniofac Surg. 2008;19(1):204–10.
Seo BM, Sonoyama W, Yamaza T, Coppe C, Kikuiri T, Akiyama K, Lee JS, Shi S. SHED repair critical-size calvarial defects in mice. Oral Dis. 2008;14(5):428–34.
Abbas, Diakonov I., Sharpe P. Neural crest origin of dental stem cells. Pan European Federation of the International Association for Dental Research (PEF IADR). 2008, Vols. Seq #96 - Oral Stem Cells.
Kerkis I, Ambrosio CE, Kerkis A, Martins DS, Gaiad TP, Morini AC, Vieira NM, Marina P, et al. Early transplantation of human immature dental pulp stem cells from baby teeth to golden retriever muscular dystrophy (GRMD) dogs. J Transl Med. 2008;6:35.
Xianrui Yang, Li Li, Li Xiao, Donghui Zhang. Recycle the dental fairy’s package: overview of dental pulp stem cells. Stem Cell Res Ther . 2018, 9, 1, 1. https://doi.org/10.1186/s13287-018-1094-8 .
Wang J, Wang X, Sun Z, Wang X, Yang H, Shi S, Wang S. Stem cells from human-exfoliated deciduous teeth can differentiate into dopaminergic neuron-like cells. Stem Cells Dev. 2010;19:1375–83.
Wang J, et al. The odontogenic differentiation of human dental pulp stem cells on nanofibrous poly (L-lactic acid) scaffolds in vitro and in vivo. Acta Biomater. 2010;6(10):3856–63.
Davies OG, Cooper PR, Shelton RM, Smith AJ, Scheven BA. A comparison of the in vitro mineralisation and dentinogenic potential of mesenchymal stem cells derived from adipose tissue, bone marrow and dental pulp. J Bone Miner Metab. 2015;33:371–82.
Huang GT-J, Shagramanova K, Chan SW. Formation of odontoblast-like cells from cultured human dental pulp cells on dentin in vitro. J Endod. 2006;32:1066–73.
Shi S, Robey PG, Gronthos S. Comparison of human dental pulp and bone marrow stromal stem cells by cDNA microarray analysis. Bone. 2001;29(6):532–9.
Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A. 2000;97:13625–30.
Nuti N, Corallo C, Chan BMF, Ferrari M, Gerami-Naini B. Multipotent differentiation of human dental pulp stem cells: a literature review. Stem Cell Rev Rep. 2016;12:511–23.
Ferro F, et al. Dental pulp stem cells differentiation reveals new insights in Oct4A dynamics. PloS One. 2012;7(7):e41774.
Conde MCM, Chisini LA, Grazioli G, Francia A, Carvalho RVd, Alcázar JCB, Tarquinio SBC, Demarco FF. Does cryopreservation affect the biological properties of stem cells from dental tissues? A systematic review. Braz Dent J. 2016;1210(6):633-40. https://doi.org/10.1590/0103-6440201600980 .
Papaccio G, Graziano A, d’Aquino R, Graziano MF, Pirozzi G, Menditti D, De Rosa A, Carinci F, Laino G. Long-term cryopreservation of dental pulp stem cells (SBP-DPSCs) and their differentiated osteoblasts: a cell source for tissue repair. J Cell Physiol. 2006;208:319–25.
Alge DL, Zhou D, Adams LL, et. al. Donor-matched comparison of dental pulp stem cells and bone marrow-derived mesenchymal stem cells in a rat model. J Tissue Eng Regen Med. 2010;4(1):73–81.
Jo Y-Y, Lee H-J, Kook S-Y, Choung H-W, Park J-Y, Chung J-H, Choung Y-H, Kim E-S, Yang H-C, Choung P-H. Isolation and characterization of postnatal stem cells from human dental tissues. Tissue Eng. 2007;13:767–73.
Gronthos S, Brahim J, Li W, Fisher LW, Cherman N, Boyde A, DenBesten P, Robey PG, Shi S. Stem cell properties of human dental pulp stem cells. J Dent Res. 2002;81:531–5.
Laino G, d’Aquino R, Graziano A, Lanza V, Carinci F, Naro F, Pirozzi G, Papaccio G. A new population of human adult dental pulp stem cells: a useful source of living autologous fibrous bone tissue (LAB). J Bone Miner Res. 2005;20:1394–402.
Zainal A, Shahrul H, et al. In vitro chondrogenesis transformation study of mouse dental pulp stem cells. Sci World J. 2012;2012:827149.
Wei X, et al. Expression of mineralization markers in dental pulp cells. J Endod. 2007;33(6):703–8.
Dai J, et al. The effect of co-culturing costal chondrocytes and dental pulp stem cells combined with exogenous FGF9 protein on chondrogenesis and ossification in engineered cartilage. Biomaterials. 2012;33(31):7699–711.
Vasandan AB, et al. Functional differences in mesenchymal stromal cells from human dental pulp and periodontal ligament. J Cell Mol Med. 2014;18(2):344–54.
Werle SB, et al. Carious deciduous teeth are a potential source for dental pulp stem cells. Clin Oral Investig. 2015;20:75–81.
Nemeth CL, et al. Enhanced chondrogenic differentiation of dental pulp stem cells using nanopatterned PEG-GelMA-HA hydrogels. Tissue Eng A. 2014;20(21–22):2817–29.
Paino F, Ricci G, De Rosa A, D’Aquino R, Laino L, Pirozzi G, et al. Ecto-mesenchymal stem cells from dental pulp are committed to differentiate into active melanocytes. Eur. Cell Mater. 2010;20:295–305.
Ferro F, Spelat R, Baheney CS. Dental pulp stem cell (DPSC) isolation, characterization, and differentiation. In: Kioussi C, editor. Stem cells and tissue repair. Methods in molecular biology (methods and protocols): Humana Press. 2014;1210.
Ishkitiev N, Yaegaki K, Imai T, Tanaka T, Nakahara T, Ishikawa H, Mitev V, Haapasalo M. High-purity hepatic lineage differentiated from dental pulp stem cells in serum-free medium. J Endod. 2012;38:475–80.
Download references
Acknowledgements
Not applicable.
This work is supported by Wrocław Medical University in Poland.
Availability of data and materials
Please contact author for data requests.
Author information
Authors and affiliations.
Department of Experimental Surgery and Biomaterials Research, Wroclaw Medical University, Bujwida 44, Wrocław, 50-345, Poland
Wojciech Zakrzewski, Maria Szymonowicz & Zbigniew Rybak
Department of Conservative Dentistry and Pedodontics, Krakowska 26, Wrocław, 50-425, Poland
Maciej Dobrzyński
You can also search for this author in PubMed Google Scholar
Contributions
WZ is the principal author and was responsible for the first draft of the manuscript. WZ and ZR were responsible for the concept of the review. MS, MD, and ZR were responsible for revising the article and for data acquisition. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Wojciech Zakrzewski .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Zakrzewski, W., Dobrzyński, M., Szymonowicz, M. et al. Stem cells: past, present, and future. Stem Cell Res Ther 10 , 68 (2019). https://doi.org/10.1186/s13287-019-1165-5
Download citation
Published : 26 February 2019
DOI : https://doi.org/10.1186/s13287-019-1165-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Differentiation
- Pluripotency
- Induced pluripotent stem cell (iPSC)
- Stem cell derivation
- Growth media
- Tissue banks
- Tissue transplantation
Stem Cell Research & Therapy
ISSN: 1757-6512
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
2 Med School Essays That Admissions Officers Loved
Here are tips on writing a medical school personal statement and examples of essays that stood out.
2 Great Med School Personal Statements

Getty Images
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality.
A personal statement is often a pivotal factor in medical school admissions decisions.
"The essay really can cause me to look more deeply at the entire application," Dr. Stephen Nicholas, former senior associate dean of admissions with the Columbia University Vagelos College of Physicians and Surgeons , told U.S. News in 2017. "So I do think it's pretty important."
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality, according to Dr. Barbara Kazmierczak, director of the M.D.-Ph.D. Program and a professor of medicine and microbial pathogenesis with the Yale School of Medicine.
“The passion that the writer is bringing to this topic tells us about the individual rather than the topic that they’re describing, and the essay is the place for us to learn about the applicant – who they are and what experiences have brought them to this point of applying to medical school,” she told U.S. News in 2017.
Rachel Rudeen, former admissions coordinator for the University of Minnesota Medical School , says personal statements help medical schools determine whether applicants have the character necessary to excel as a doctor. "Grit is something we really look for," she says.
Evidence of humility and empathy , Rudeen adds, are also pluses.
Why Medical Schools Care About Personal Statements
The purpose of a personal statement is to report the events that inspired and prepared a premed to apply to medical school, admissions experts say. This personal essay helps admissions officers figure out whether a premed is ready for med school, and it also clarifies whether a premed has a compelling rationale for attending med school, these experts explain.
When written well, a medical school personal statement conveys a student's commitment to medicine and injects humanity into an admissions process that might otherwise feel cold and impersonal, according to admissions experts.
Glen Fogerty, associate dean of admissions and recruitment with the medical school at the University of Arizona—Phoenix , put it this way in an email: "To me, the strongest personal statements are the ones that share a personal connection. One where a candidate shares a specific moment, the spark that ignited their passion to become a physician or reaffirmed why they chose medicine as a career."
Dr. Viveta Lobo, an emergency medicine physician with the Stanford University School of Medicine in California who often mentors premeds, says the key thing to know about a personal statement is that it must indeed be personal, so it needs to reveal something meaningful. The essay should not be a dry piece of writing; it should make the reader feel for the author, says Lobo, director of academic conferences and continuing medical education with the emergency medicine department at Stanford.
A great personal statement has an emotional impact and "will 'do' something, not just 'say' something," Lobo wrote in an email. Admissions officers "read hundreds of essays – so before you begin, think of how yours will stand out, be unique and different," Lobo suggests.
How to Write a Personal Statement for Medical School
Lobo notes that an outstanding personal statement typically includes all of the following ingredients:
- An intriguing introduction that gets admissions officers' attention.
- Anecdotes that illustrate what kind of person the applicant is.
- Reflections about the meaning and impact of various life experiences .
- A convincing narrative about why medical school is the logical next step.
- A satisfying and optimistic conclusion.
"You should sound excited, and that passion should come through in your writing," Lobo explains.
A personal statement should tie together an applicant's past, present and future by explaining how previous experiences have led to this point and outlining long-term plans to contribute to the medical profession, Lobo said during a phone interview. Medical school admissions officers want to understand not only where an applicant has been but also the direction he or she is going, Lobo added.
When premeds articulate a vision of how they might assist others and improve society through the practice of medicine, it suggests that they aren't self-serving or simply interested in the field because of its prestige, Lobo says. It's ideal when premeds can eloquently describe a noble mission, she explains.
Elisabeth Fassas, author of "Making Pre-Med Count: Everything I Wish I'd Known Before Applying (Successfully) to Medical School," says premeds should think about the doctors they admire and reflect on why they admire them. Fassas, a first-year medical student at the University of Maryland , suggests pondering the following questions:
- "Why can you really only see yourself being a physician?"
- "What is it about being a doctor that has turned you on to this field?"
- "What kind of doctor do you imagine yourself being?"
- "Who do you want to be for your patients?"
- "What are you going to do specifically for your patients that only you can do?"
Fassas notes that many of the possible essay topics a med school hopeful can choose are subjects that other premeds can also discuss, such as a love of science. However, aspiring doctors can make their personal statements unique by articulating the lessons they learned from their life experiences, she suggests.
Prospective medical students need to clarify why medicine is a more suitable calling for them than other caring professions, health care fields and science careers, Fassas notes. They should demonstrate awareness of the challenges inherent in medicine and explain why they want to become doctors despite those difficulties, she says.
Tips on Crafting an Excellent Medical School Personal Statement
The first step toward creating an outstanding personal statement, Fassas says, is to create a list of significant memories. Premeds should think about which moments in their lives mattered the most and then identify the two or three stories that are definitely worth sharing.
Dr. Demicha Rankin, associate dean for admissions at the Ohio State University College of Medicine , notes that a personal statement should offer a compelling portrait of a person and should not be "a regurgitation of their CV."
The most outstanding personal statements are the ones that present a multifaceted perspective of the applicant by presenting various aspects of his or her identity, says Rankin, an associate professor of anesthesiology.
For example, a premed who was a swimmer might explain how the discipline necessary for swimming is analogous to the work ethic required to become a physician, Rankin says. Likewise, a pianist or another type of musician applying to medical school could convey how the listening skills and instrument-tuning techniques cultivated in music could be applicable in medicine, she adds.
Rankin notes that it's apparent when a premed has taken a meticulous approach to his or her personal statement to ensure that it flows nicely, and she says a fine essay is akin to a "well-woven fabric." One sign that a personal statement has been polished is when a theme that was explored at the beginning of the essay is also mentioned at the end, Rankin says, explaining that symmetry between an essay's introduction and conclusion makes the essay seem complete.
Rankin notes that the author of an essay might not see flaws in his or her writing that are obvious to others, so it's important for premeds to show their personal statement to trusted advisers and get honest feedback. That's one reason it's important to begin the writing process early enough to give yourself sufficient time to organize your thoughts, Rankin says, adding that a minimum of four weeks is typically necessary.
Mistakes to Avoid in a Medical School Personal Statement
One thing premeds should never do in an admissions essay is beg, experts say. Rankin says requests of any type – including a plea for an admissions interview – do not belong in a personal statement. Another pitfall to avoid, Rankin says, is ranting about controversial political subjects such as the death penalty or abortion.
If premeds fail to closely proofread their personal statement, the essay could end up being submitted with careless errors such as misspellings and grammar mistakes that could easily have been fixed, according to experts. Crafting a compelling personal statement typically necessitates multiple revisions, so premeds who skimp on revising might wind up with sloppy essays, some experts say.
However, when fine-tuning their personal statements, premeds should not automatically change their essays based on what others say, Fogerty warns.
"A common mistake on personal statements is having too many people review your statement, they make recommendations, you accept all of the changes and then – in the end – the statement is no longer your voice," Fogerty wrote in an email. It's essential that a personal statement sound like the applicant and represent who he or she is as a person, Fogerty says.
Dr. Nicholas Jones, a Georgia-based plastic and reconstructive surgeon, says the worst error that someone can make in the personal statement is to be inauthentic or deceptive.
"Do not lie. Do not fabricate," he warns.
Jones adds that premeds should not include a story in their personal statement that they are not comfortable discussing in-depth during a med school admissions interview . "If it's something too personal or you're very emotional and you don't want to talk about that, then don't put it in a statement."
Medical School Personal Statement Examples
Here are two medical school admissions essays that made a strong, positive impression on admissions officers. The first is from Columbia and the second is from the University of Minnesota. These personal statements are annotated with comments from admissions officers explaining what made these essays stand out.
Searching for a medical school? Get our complete rankings of Best Medical Schools.
Tags: medical school , education , students , graduate schools
Popular Stories
Law Admissions Lowdown

Top Law Schools

Medical School Admissions Doctor

Morse Code: Inside the College Rankings

You May Also Like
What to ask law students and alumni.
Gabriel Kuris April 22, 2024
Find a Strong Human Rights Law Program
Anayat Durrani April 18, 2024
Environmental Health in Medical School
Zach Grimmett April 16, 2024
How to Choose a Law Career Path
Gabriel Kuris April 15, 2024
Questions Women MBA Hopefuls Should Ask
Haley Bartel April 12, 2024

Law Schools With the Highest LSATs
Ilana Kowarski and Cole Claybourn April 11, 2024

MBA Programs That Lead to Good Jobs
Ilana Kowarski and Cole Claybourn April 10, 2024

B-Schools With Racial Diversity
Sarah Wood April 10, 2024

Law Schools That Are Hardest to Get Into
Sarah Wood April 9, 2024

Ask Law School Admissions Officers This
Gabriel Kuris April 9, 2024

10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.
Your Trusted Advisors for Admissions Success
Admissions and test prep resources to help you get into your dream schools
Medical School Secondary Essays: The Complete Guide 2024 (Examples Included)
Proven strategies to write your diversity, challenge, “why us,” gap year, “anything else you’d like us to know,” leadership, and covid medical school secondary essays.

(Note: This article can also be found in our free, 102-page comprehensive guide to medical school applications, Get Into Medical School: 6 Practical Lessons to Stand Out and Earn Your White Coat . )
Part 1: Introduction
Part 2: the medical school diversity essay, part 3: the medical school adversity essay, part 4: the medical school “why us” essay, part 5: the medical school gap year essay, part 6: the medical school leadership essay, part 7: the medical school “anything else you’d like us to know” essay, part 8: the medical school covid essay, appendix: frequently asked questions.
As a medical school applicant, you’ve worked hard on your submitting the best AMCAS application you can. You’ve written a compelling medical school personal statement , a detailed AMCAS Work and Activities section , and more. Now med schools are sending you school-specific secondary applications that require you to write additional essays?
Given that you’ll need to submit multiple essays for most med schools you’ve applied to, the secondary essay writing process can be incredibly grueling, even more so than completing your primary application.
While secondary essay prompts vary in length and topic, there are two pieces of good news:
Secondary essays are typically shorter than your personal statement.
Some topics come up over and over and over again.
You can use this second fact to your advantage by recycling certain “core essays” with a few modifications for multiple schools. Moreover, you can pre-write recurring essays using our medical school secondary essay prompts database .
( WARNING: Make sure to always answer each school's specific prompt, especially when secondary application fatigue inevitably kicks in. In addition, double check that you've referred to the correct medical schools' names in your secondaries. For example, if you're writing an essay for Tufts, be careful not to mistakenly leave in “Emory” if you're recycling your Emory essay for Tufts.)
In our nearly 20 years of experience working with medical school applicants, the following six essays—with varying prompts—come up most often:
Diversity essay
Challenge essay (e.g., “Describe a significant challenge you overcame and what you learned from it.”)
“Why us?” essay (e.g., “Why do you hope to attend [our school]?”)
Gap year essay
Leadership essay
“Anything else you’d like us to know?” essay
Rather than list a bunch of general tips on how to write your secondary application essays, in this guide we’ll provide some background for each essay topic before listing and challenging some common misconceptions that limit students’ thinking. Then we’ll offer fresh ways to write each one, as well as strong samples from students who got into prestigious medical schools.
Struggling to write your med school application essays?
Get our free guide to help you with every step: Get Into Medical School: 6 Practical Lessons to Stand Out and Earn Your White Coat
100% privacy. No spam. Ever.
Thank you! Your guide is on its way. In the meantime, please let us know how we can help you crack the the medical school admissions code . You can also learn more about our 1-on-1 medical school admissions support here .
Part 2: The medical school diversity essay
Example diversity essay prompts.
Example 1: “We seek to train physicians who can connect with diverse patient populations with whom they may not share a similar background. Tell us about an experience that has broadened your own worldview or enhanced your ability to understand those unlike yourself and what you learned from it.” ( Wake Forest School of Medicine )
Example 2: “ The Georgetown University School of Medicine (GUSOM) strives to ensure that its students become respectful physicians, with cultural humility, who embrace all dimensions of caring for the whole person. With our Jesuit values of Cura Personalis, People for Others, and Community in Diversity, we are steadfast in our commitment to racial justice and to addressing the health inequities exacerbated by the recent pandemic. Please describe how your values, life experiences, and your identity will contribute to these GUSOM priorities.” ( Georgetown University School of Medicine )
Diversity essay background
Medical schools love advertising the diversity of their student bodies through their class profile statistics, brochures, and pictures of smiling students from various backgrounds. Is this just for show?
Unlikely. Medicine—and other healthcare fields—are most effectively practiced when clinicians are able to understand and respect whomever is seeking service, regardless of their backgrounds. Thus, having a diverse student body creates a stimulating learning environment that incorporates multiple perspectives.
Before we get into misconceptions about the diversity essay, let’s clarify the meaning of “cultural competency” by first offering the NIH’s definition : “Deliver[ing] services that are respectful of and responsive to the health beliefs, practices and cultural and linguistic needs of diverse patients."
In other words, cultural competency refers to:
The awareness that patients have diverse health beliefs, practices, and needs
The effort and willingness to understand these differences
The effort and willingness to incorporate these differences to provide effective care that fits patients' contexts
On the other hand, cultural competency does not mean:
Believing you know everything about a particular group of people—including your own—and therefore knowing exactly how to treat them
Having to learn everything about a particular group of people before you are able to effectively treat them
Diversity essay misconception 1: “I don’t come from a minority background, so I have nothing to write about.”
Let’s clear this up right away: your diversity essay does not have to be about your or others’ ethnocultural or socioeconomic backgrounds. Moving past this notion will expand your thinking and options for choosing a compelling topic many fold.
Diversity can refer to anything that makes you unique or interesting, including:
Your great qualities (e.g., being a social connector)
Unique experiences (e.g., working as a certified scuba diving instructor)
A commitment to service
Visions and goals (e.g., using artificial intelligence to improve healthcare).
Think about why diversity is interesting in the first place: everyone is different. If all people came to medicine from a certain ethnic minority or low socioeconomic background, that wouldn’t be so interesting, would it?
If you do want to focus on ethnocultural and socioeconomic diversity, strong essay topics include:
Extracurricular activities , pursuits, or organizations committed to diversity and social justice issues
Health disparities
Demonstration of multicultural competence during patient interactions
Navigating your own multicultural identity
Diversity essay misconception 2: “I come from an ethnic minority background that’s already well represented in medicine, so I have nothing unique to share.”
We hear this most often from students of various Asian backgrounds who feel their demographic is so well represented in medicine that they cannot make a case for their uniqueness as a medical school applicant.
However, given Asia's many countries, and the races, cultures, subcultures, languages, religions, and philosophies across and within countries, there's probably a ton you could write about. Although you may feel your background is common in medicine, don’t sell yourself short.
Possible topics include:
(If you’re an immigrant) Your immigration and assimilation experience
(If you’re not an immigrant but your parents immigrated to the U.S.) A thoughtful account about the values/perspectives/goals your parents tried to instill in you, how they may have clashed with your values growing up in a bicultural environment, and how you resolved these differences
Different cultural views on healthcare and how both can be valuable for treating patients
Regardless of the topic you choose, as with all essays, make sure to link it back to your identity and experience by answering these questions:
How did you feel?
What qualities did you demonstrate?
What did you learn?
What do you have yet to learn?
How do you plan to apply these lessons throughout your education and career?
Diversity essay misconception 3: “The more I write the words ‘diversity,’ ‘cultural/multicultural,’ and ‘underserved,’ the more admissions committees will be impressed by my cultural sensitivity/awareness/competence.”
Quite the opposite. These terms, especially when used repeatedly or inappropriately, can be cliché and come off as dishonest. The best essays are those that are written honestly about who you are and your actual perspectives and interactions with diverse individuals.
Medical school diversity essay example
There are many things a girl could be self-conscious about growing up, such as facial hair, body odor, or weight gain. Growing up with a few extra pounds than my peers, I was usually chosen last for team sports and struggled to run a 10-minute mile during P.E. classes. As I started to despise school athletics, I turned towards other hobbies, such as cooking and Armenian dance, which helped me start anew with a healthier lifestyle. Since then, I have channeled my passions for nutrition and exercise into my volunteering activities, such as leading culinary workshops for low-income residents of Los Angeles, organizing community farmer’s markets, or conducting dance sessions with elderly patients. I appreciate not only being able to bring together a range of people, varying in age, socioeconomic status, and ethnicity, but also helping instill a sense of confidence and excitement that comes with making better lifestyle decisions. I have enjoyed encouraging kids in the inner city to combat similar issues of weight gain and low self-esteem through after-school gardening and physical activity lessons. Now, I hope to share my love for culinary nutrition and fitness with fellow medical students at UCLA. As students, we can become better physicians by passing on health and nutrition information to future patients, improving quality of life for ourselves and others.
Part 3: The medical school adversity essay
Example adversity essay prompts.
Example 1: “Share with us a difficult or challenging situation you have encountered and how you dealt with it. In your response, identify both the coping skills you called upon to resolve the dilemma, and the support person(s) from whom you sought advice.” (University of Chicago Pritzker School of Medicine)
Example 2: “Tell us about a challenging problem you faced and how you resolved it. Include how the experience contributed to the person you are today.” ( University of Pittsburgh School of Medicine )
Adversity essay background
Medical school admissions committees ask about adversity simply to understand how you respond to difficult situations. They want to see that you have the maturity, resilience, and capacity for growth to do well in med school.
In other words, medical schools are not trying to start a competition to determine which students have experienced the greatest adversity in their lifetimes.
Rather, they want to know how you:
Manage stress
Attempt to resolve issues
Reflect on challenges
Apply learned lessons in your life
Adversity essay misconception 1: “Nothing really bad has ever happened to me. Neither my family members nor I have suffered a serious illness or death. I also did not overcome poverty or flee to America as a political refugee, etc.”
Let’s say it again: this is not a competition, so it’s perfectly fine if you haven’t experienced an extreme challenge in your life. If you have, you’ll have an obvious topic to discuss, but a significant difficulty alone doesn’t make a great essay.
There are multiple ways to approach adversity essay prompts, including writing about:
Relatable life events (e.g., letting your best friend down, facing major criticism, making new friends after a big move)
Situations beyond your control (e.g., your parents’ divorce, a friend’s drug use).
Adversity essay misconception 2: “Fine. I was able to identify some challenges I’ve faced in life. It still doesn’t matter because none of them are significant enough!”
We get it. Medical school admission is a high stakes process, and you want to stand out in every part of your application.
Remember, however, that the best essays aren’t necessarily the ones with the greatest challenges or sob stories. It's your thoughtfulness and handling of those challenges that will set you apart.
To make this process easier, we ask students to create the following list of 3–4 challenges to help them choose a strong topic. Below we’ve also included a common topic as an example:
Challenge: Difficult academic adjustment from high school to college with corresponding drop in confidence and drive, as well as questioning fitness for medicine
Response: Acknowledged poor study habits and corrected them, humbly asked for help from faculty and classmates
Result: Sustained improvement in study habits and grades, developed mentorships with professors
Lesson: No shame in asking for guidance and help, better to strengthen weakness than rely on false confidence
Once you’ve listed some challenges and their aftermath, choose the one that demonstrates the greatest maturity, thoughtfulness, and growth. Transparency about your hardships and honesty about your growth help to write great essays. It’s also more than acceptable to discuss how you’re still a work in progress and mention the areas you’d like to continue improving on.
Medical school adversity essay example
I named my one-year-old beagle Fitch, after my favorite clothing store. That fact recurred through my mind as I shouted her name for hours at the break of dawn, wondering how I left the door open and where she could have gone. Was she attacked by roaming bands of coyotes? Killed in a hit-and-run? Lost in the desert mountains? I had raised and taken care of Fitch for years, and so I believed I was solely responsible for her loss and her safe return. Yet, my mother admonished me to not let guilt interfere with my judgments and to reach out for help. Therefore, I enlisted the support of the community, including friends, fellow dog owners, and neighbors, some of whom I had never met before, to find my pudgy, spotted beagle.
Over the next two days, this dedicated group helped me create flyers to post in nearby parks, organize teams for day and night searches, and send neighborhood-wide emails. It’s hard to be prepared for difficult situations like these, so between the sleepless nights and uneventful status updates, I found myself learning to be calm and patient like my neighbors, Bill and Susanna, encouraged me to be. Finally, on the third day, a biker found Fitch behind a dumpster, shivering beneath a pile of debris and branches. Although she was eventually safe, I would not be able to hold and feed her to this day had I not knocked on that first neighbor’s door, opening me up to both the physical and mental strength of the surrounding community.

Example “Why us?” essay prompts
Example 1: “What makes LLUSM particularly attractive to you?” (Loma Linda University School of Medicine)
Example 2: “Why have you chosen to apply to the Georgetown University School of Medicine and how do you think your education at Georgetown will prepare you to become a physician for the future?” ( Georgetown University School of Medicine )
“Why us?” essay background
These are everyone’s favorite prompts (we wish our sarcasm could jump through the screen).
The first step to writing an effective “Why us?” essay is to restrain yourself from writing about how great their medical school is or where it's located.
Glad that’s out of the way. Now consider why admissions committees want you to answer this question. After all, they know you’re applying to many other schools and that your GPA and MCAT scores are at least reasonably close to their admission averages.
(Suggested reading: How Many Medical Schools Should I Apply To? Which Ones? and Average GPA and MCAT Score for Every Medical School )
Admissions committees read thousands of essays annually and want to know that you’ve considered them for reasons beyond the obvious (location, prestige, average GPA and MCAT, etc.).
By integrating your qualities, experiences, and aspirations with their specific mission, programs, and resources, you will have a unique opportunity to demonstrate "fit" in your application. Don’t take this for granted!
“Why us?” essay misconception 1: “I should just read a school’s mission statement and research available resources on their website, and then rewrite the same information in essay form.”
The vast majority of students approach the “Why us?” essay this way, so it won’t make your response seem very special.
We basically see the expanded version of the following essay 90+ percent of the time:
I want to go to [School Name] because of their wonderful [program name] and incredible [resources]. {Program] cultivates [attribute] that helps their students become great physicians. In addition, [resources] provide support to help students reach their potential.
You should be able to see how this essay says nothing about why YOU want to go to their school.
Moreover, medical schools already know about all of the programs and resources they offer, so you wouldn’t be providing much value through writing solely about those offerings.
The better approach to this essay would be to look through schools’ websites to find programs and resources that actually interest you and to identify what each school keeps boasting about (e.g., perhaps they mention diversity or early clinical experience multiple times on their homepage). Then consider:
How YOUR experiences fit with their offerings
What YOU could contribute
How YOU would uniquely benefit from their program
For example, if a school focuses a lot on community service and you have similar experiences, mention that. In addition, let the school know how you want to further focus your skills while there. On the other hand, if you have a more research heavy background and are applying to the same school, you could either focus on research or discuss how community service will make you a more well-rounded physician. The more specific you can be, the better.
“Why us?” essay misconception 2: “There’s no other way to find out information about a medical school than by reading their site.”
Looking at a school’s website and demonstrating fit is certainly a tried-and-true approach to answering "Why us?" essay prompts, but it isn’t the only one.
To really impress admissions committees, you could integrate information from current students or recent alumni into your response. Ask these individuals whether they would be willing to share their experiences attending a particular school, and also whether you would be a good fit there given your background and goals.
How do you find these people? The easiest people to contact are those you know personally or through a mutual acquaintance. Otherwise, you could contact a school’s administrative staff and ask whether they could connect you to a current student. While this requires additional work, it will be well worth it for your top school preferences.
If you have to contact a stranger, use the following email template:
Dear [Student Name],
I hope this email finds you well. My name is [Your Name}, and I am currently completing my med school applications. I’m especially interested in attending [School Name] and am therefore hoping to get some more information about the program. [School Name]'s admissions committee gave me your email address as someone who could help me out.
I'd really appreciate it if you would spare 15-20 minutes to answer 3-5 quick questions in the upcoming days. If so, please let me know some days and times that are most convenient for you, your time zone, and the best number to reach you. I’ll do my best to accommodate.
Thanks for your time and consideration. Looking forward to hearing from you soon!
[Your Name]
If you have the opportunity to take a campus tour, you should also make it a priority to meet with students and faculty (the latter may require arranging an appointment in advance). Even a brief conversation might generate some interesting insights that you can refer back to in your secondary essays.
Medical school “Why us?” essay example
Benjamin Franklin once said, “Tell me and I forget, teach me and I may remember, involve me and I learn.” Throughout my undergrad years, I’ve found that working hard to involve myself with others and their unique perspectives is one of the most productive ways in which I can learn. For example, I used to believe that illnesses were just a set of tangible symptoms that resulted solely from maladaptive genes. However, after working closely with families in Boston's inner city, I have come to realize how racial, physical, and social factors, such as a lack of access to fresh produce or primary health services, can influence the likelihood of disease. As I obtained a broader understanding of the many factors that contribute to health, I find myself asking new questions and wanting to learn more. How can we properly assess a community’s needs and design appropriate solutions? How can an understanding of sociocultural factors be used to heal current patients and prevent new ones?
I believe that the answers to these questions and others will come from the Community Health Program at the University of Washington (UW). The year-round lecture series on topics, such as “Health Disparities: An Unequal World's Biggest Challenge,” will allow me to engage closely with faculty and students to work towards developing holistic community-based solutions. Furthermore, the UW PEERS clinic and Friends of UW provide an opportunity to work closely with urban Seattle neighborhoods similar to those I have worked with in Boston.
Having connected with a range of Boston families, varying in age, socioeconomic status, and ethnicity, I have improved my sense of self-awareness and cultural sensitivity, attributes I hope to continue developing with the surrounding Seattle community. I am confident that UW and the Community Health Program can further prepare me to be a physician who not only improves the lives of individual patients, but also addresses the needs of entire communities.
Example gap year essay prompts
Example 1: If you are not attending college during the upcoming academic year, what are your plans? ( Weill Cornell Medical College )
Example 2: Are you planning to matriculate into medical school immediately after completing your undergraduate education? If not, please explain what activities and/or careers you have pursued in the time between your college education and your application. ( Baylor College of Medicine )
Gap year essay background
Essay prompts that ask about gap years tend to be fairly straightforward. Given that the average age of med school matriculants is currently 24, these days, it’s more common than not for applicants to have taken one or more years off between undergrad and med school.
If that describes you, here’s how to think about your gap year essay: medical schools simply want to know what you’ve been up to since graduation and how those activities have prepared you to succeed in med school and beyond.
To approach this essay, begin with the factual. Here are the questions you should try to address in your gap year essay:
What was your goal in taking a gap year?
What did you do during your gap year? Or, if you haven’t taken it yet, what are your plans? Be specific in regard to dates, durations, jobs worked, places traveled to, etc.
How did your gap year experiences enhance your preparedness for medical school, your future skill set as a physician, and enrich your point of view about the world and/or the healthcare field? In other words, what did you learn that you’ll carry with you into medicine?
Bonus points if you can also connect your gap year experience to a specific program or feature of the medical school you're applying to.
Gap year essay misconception 1: “My gap year was unrelated to medicine so I have nothing to write about.”
If you’ve spent your gap year engaged in something directly related to medicine—say you worked in a research lab or were employed as an EMT —it’s easy to argue that you’re better prepared for med school now than when you were right out of college. But what if you’ve spent your gap year doing something else?
Even if your gap year experiences were non-medical in nature, you should still explain how they’ve helped you become a stronger med school candidate.
For example, say your main goal in taking a gap year was to improve your MCAT score, and you spent the year studying for the test while supporting yourself through a bartending job. Not only would you want to talk about much you were able to improve your score, you’d also want to discuss the skills you gained from bartending that are relevant to being a physician, such as social skills, teamwork, and adaptability.
Gap year essay misconception 2: “Writing about how I took a gap year to become a better candidate will make me look bad.”
Sometimes applicants who took a gap year to improve their medical school application profile in some way (a better MCAT score, more clinical experience, completing prerequisites, etc.) worry that talking about this in their essays will make them come off as an underqualified candidate.
This could not be further from the truth. In reality, so long as your time off has yielded meaningful results, medical schools will see your efforts as evidence that you’re resilient, mature, and working towards constant improvement. It doesn’t matter that you weren’t the ideal candidate straight out of college—what matters is that you’re ready for med school now.
Medical school gap year essay example
After graduating from college in May, I moved to Mexico City in order to attend a Spanish language school full-time and volunteer on the weekends at a low-income women’s health clinic. My goals in taking a gap year have been to improve my Spanish language skills to fluency while gaining experience in an international health setting.
I grew up in the suburbs of Los Angeles and plan to return to the area after medical school. While I studied Spanish through the intermediate level in college, given that 45 percent of residents in the LA metropolitan area currently speak Spanish at home, I feel that advancing my Spanish skills beyond the conversational is critical to becoming the best healthcare provider that I can be to patients in LA.
Volunteering at the women’s clinic has also been illuminating. Not only has it accelerated my language acquisition, particularly in that it’s helped me pick up valuable Spanish medical vocabulary, it’s also opened my eyes to how many women do not have adequate access to prenatal care and routine preventative services like cervical cancer screenings. I know that these issues are not unique to Mexico; too many women face the same barriers in the United States.
As the result of my gap year experiences, I am committed to providing compassionate care for all patients, especially those without financial resources or English fluency, and plan to work towards creating greater healthcare access for disadvantaged patients. I look forward to the opportunity to begin this work as a volunteer at Columbia’s student-run free clinics for vulnerable populations in New York City.
Example leadership essay prompts
Example 1: “Describe your most unique leadership, entrepreneurial, or creative activity.” ( UCLA David Geffen School of Medicine )
Example 2: “The pillars of our curriculum are Leadership, Curiosity, and Commitment. Tell us about how you have embodied one or more of these attributes in your path to medicine thus far. In which of these areas do you see the most opportunity for personal growth and why?” (University of Colorado School of Medicine)
Example 3: Please describe your most meaningful leadership positions. ( Columbia University Vagelos College of Physicians and Surgeons )
Leadership essay background
Medical schools are looking for students who are going to drive change in healthcare. They don’t want students who only want to be physicians; they want leaders, too.
Why is leadership important in a medical context? There are several problems that plague the United States healthcare system today, including rising healthcare costs, inequities in access to care, racial discrimination in medicine, and more. Change begins with doctors—think of Paul Farmer, Vivek Murthy, and Atul Gawande. All of these doctors are leaders in their respective fields and have created structural change in specific areas of medicine, whether it was through research, writing, or policy.
Medical schools want students who are going to make an effort to solve problems, like the aforementioned physicians. The leadership essay is an opportunity to show admissions committees that you have what it takes to make a difference by reflecting on your own experiences as a leader.
Over 90% of our students get into med school—the first time.
Leadership essay misconception #1: “i haven’t had any experiences as a leader.”.
One does not have to hold formal leadership positions to be considered a leader. For example, working as a teacher could be considered a leadership position even though a teacher might not have a formal title like “President” or “Treasurer.” Leadership could also entail taking care of a family elder or directing a group project. By reflecting on positions and scenarios in which you have made an impact and demonstrated initiative, you will likely find an example of your own leadership.
Of course, it is to your benefit if you have formal leadership positions—it means that someone thought you were worthy enough to be chosen for some sort of responsibility. But, if you don’t, that’s perfectly okay as well. The most important takeaway of this essay won’t necessarily be the status or level of the experience you describe—it’s what you learned and how you describe it.
Leadership essay misconception #2: “It is enough to just describe my leadership experiences and what I did in them.”
These essays are a place for you to reflect on your experiences as a leader and demonstrate what you’ve learned—simply describing your work isn’t going to cut it.
The idea in this essay is to show growth. If you are applying to medical school, it goes without saying that you have a lot more to learn before you can become a practicing physician. This is true not only when it comes to medical and scientific knowledge, but also when it comes to the personal qualities necessary to be an effective doctor.
In this essay, you will want to discuss your past growth as a leader—highlighting this experience is how you can indicate to medical schools that you will continue to learn and develop as a leader on your road to becoming a physician. Therefore, your essay must be reflective: to discuss past growth, you must deeply analyze your own experiences.
Medical school leadership essay example
During my sophomore year of college, I was selected as the Executive Director of BerkeleyShelter, an undergraduate volunteer organization that operates a shelter for students experiencing houselessness. The next year, I founded HealthGroup, a nonprofit focused on increasing access to affordable medications for individuals with chronic conditions. From these activities, my understanding of what it means to be a leader has begun to change. At HealthGroup, we tried to drive change by drafting legislation, working with elected representatives, and launching campaigns to raise awareness about issues surrounding medication prices. As the founder, I took it upon myself to come up with a plan for other staff and members to follow. I thought it was my job as a leader to direct the organization’s work. But, initially, HealthGroup struggled to create any sort of tangible change in prescription medicine prices; there were too many obstacles generated by pre-existing problems within the American healthcare system. In fact, one year after HealthGroups’s conception, not much had changed. Of course, I wasn’t expecting to fix the healthcare system overnight, but I didn’t expect my efforts to have yielded so little. Before my senior year of college, I began to wonder how I could change HealthGroup: what could I do differently as the leader of the organization? I came to recognize that I hadn’t really given others an opportunity to share their own ideas—I had just assumed that I needed to run the group by myself. Maybe, as a leader, it wasn’t my job to single-handedly decide the organization’s direction but, rather, to create an environment where others could share their thoughts. Today, HealthGroup has written several bills that have created significant changes in prescription drug access—the results of a 40-person collaboration.
Example “Anything else you’d like us to know?” essay prompts
Example 1: “Is there anything else you would like us to know?” ( Columbia University Vagelos College of Physicians and Surgeons )
Example 2: “Please reflect on your primary application and share something not addressed elsewhere that would be helpful to the Admissions Committee as we review your file.” ( Dartmouth Geisel School of Medicine )
“Anything else you’d like us to know?” essay background
The open-ended nature of “Anything else you’d like us to know?” essays tends to cause confusion for many applicants. Being invited to share anything you want can be intimidating!
The good news is that these types of essays allow you to highlight something about yourself that isn’t well represented elsewhere in your application, and you may even be able to use one of your pre-writes to do it.
There are two basic ways to approach “Anything else you’d like us to know?” essays:
You can submit one of the above pre-writes that hasn’t already been asked for. For example, say a medical school asks you for an “Anything else?” essay but not a “Why us?” essay. In that case, you could slot in your “Why us?” essay here. Just be sure the content of the essay doesn’t repeat details and anecdotes that you’ve already mentioned in another essay you’re submitting to that school.
You can write a completely new essay— if time permits you to do it well. For applicants who choose this route, common topics include strengths that haven’t gotten much attention yet, such as:
Extensive volunteer work
A strong research background
Other impressive achievements or skills
If you decide to write a new essay, take care not to treat the space like a catch-all by simply listing a bunch of skills or experiences, which will make your response sound like a résumé rather than an essay. Instead, give your essay focus by first deciding what you want to communicate to adcoms (for instance, your research bona fides), and then choose a few related examples that can together create a through line towards medicine. Despite the vagueness of the “Anything else?” prompt, your essay should still make an argument.
Even if you choose to write about a strength that isn’t explicitly related to medicine, such as an artistic or athletic achievement, you’ll still want to draw a connection to how it has made you a better medical school candidate.
“Anything else you’d like us to know?” essay misconception 1: “I must answer this prompt even though it’s optional.”
“Anything else you’d like us to know?” essays are often optional, which leaves many applicants struggling to determine whether they should answer the question at all. Some applicants erroneously believe that they must answer it, no matter what.
Our advice is to not force it. We generally consider these types of essays as falling somewhere between optional and required.
If you have something to add that would help further differentiate you as an applicant, you should do so, and if you’re able to do this using a pre-write, even better. However, if submitting an essay here would seem completely forced, or if you aren’t able to use a pre-write and don’t have the time to commit to writing a new essay that’s high quality, it probably isn’t worth it.
The bottom line is to always optimize for quality.
“Anything else you’d like us to know?” essay misconception 2: “Any unused pre-write will work here.”
In many cases, you will be able to take advantage of your unused pre-writes to answer “Anything else you’d like us to know?” prompts. However, before shuffling through your already-written essays, consider whether there indeed is something you want adcoms to know beyond what you've been able to communicate through AMCAS or secondaries. In other words, you should ask yourself if the pre-write you want to use adds anything meaningful to your candidacy.
You also don't have to necessarily use your “best” secondary here. Instead, consider which of your answers will best fit with the remainder of your application to that school, based on what you've already written for them and what they're looking for in candidates.
Medical school “Anything else you’d like us to know?” essay example
On the first Sunday of every month, I leave the house at 5:30 AM, coffee in hand, so I can be among a group of 20 volunteers who greet a new group of “bully breed” dogs ready to find loving families. Despite being sensitive, loyal pets, these dogs face pervasive negative stereotypes of aggression that make them among the most vulnerable to abuse and euthanasia. Fortunately, the Paws Please rescue culls bully breeds from high-kill shelters in the greater Houston area to give them a second chance at adoption.
I first became acquainted with Paws Please when my own family adopted an American Staffordshire Terrier, Mary, through them when I was 15. Mary quickly bounded her way into the center of our family, and as a teenager it deeply distressed me whenever I attempted to reconcile the joy she brought us with the fact that she’d come close to being put down. A year later, I decided that I would become a Paws Please volunteer in order to help save dogs like Mary. I began attending the monthly “homecoming day” when I was a junior in high school, and have continued this work through my four years at Rice.
On homecoming day, every new dog receives grooming, vaccines, microchips, and more. For six years, it’s brought me immense gratification to provide these initial moments of care, sometimes for the first time in a dog’s life. While many dogs come from troubling situations and arrive frightened or in need of medical attention, being part of the experienced volunteer team has taught me a great deal about taking stressful or even upsetting moments in stride, not to mention making effective use of teamwork to “process” large numbers of dogs efficiently but with thoroughness and compassion. In fact, as I’ve completed shadowing hours, medical volunteer work, and other clinical experiences as a premed, I’ve frequently found myself leaning on skills that I first developed through Paws Please, and I believe that these experiences will help shape my competence as a physician. I’m grateful for what my work in animal rescue has taught me and for the chance to make a difference in these dogs’ lives.
Example COVID essay prompts:
Example 1: “Describe how the COVID-19 pandemic has impacted your pathway to medical school. Include any academic, personal, financial or professional barriers, as well as other relevant information.” ( UCLA David Geffen School of Medicine )
Example 2: “What have you done during the recent COVID-19 pandemic that will better prepare you to be a medical student and future physician?” (University of Miami Miller School of Medicine)
COVID essay background
During the 2020–2021 application cycle, many medical schools added COVID secondary essay prompts—usually optional—that allowed applicants to discuss how the pandemic had impacted their applications. In the 2021–2022 cycle, as the long-term effects of the pandemic became more evident, many of those formerly optional prompts became required of all applicants.
However, starting in 2023–2024, some schools have reverted to making their COVID prompts optional, and others have removed the prompts from their applications entirely.
Most COVID essay prompts can be divided into the following categories, with some med schools asking for a combination of the two:
Prompts that ask you to explain how the pandemic has negatively affected your medical school applications. In these essays, you can discuss disruptions to your education, test taking, and extracurriculars, plus any relevant personal circumstances that prevented you from presenting your best self to adcoms.
Prompts in which you’re tasked with reflecting more broadly on the pandemic, whether that’s in the realm of personal challenges you’ve faced or medicine in general.
COVID essay misconception 1: “I should make excuses for everything that’s less than ideal about my application.”
It’s likely that the pandemic has thrown plenty of obstacles in the way of your medical school applications, but that doesn’t mean they should all receive equal weight in your COVID essay.
Keep the following in mind, particularly when answering prompts that ask how COVID has affected your preparedness for medical school, and especially if those prompts are optional: the essays are meant to account for appreciable challenges to your application process, allowing you to be seen holistically. Med schools want to understand how you’ve been kept from putting your best foot forward.
“Appreciable challenges” will differ for everyone. For some applicants, they might include illness, the death of a loved one, or financial difficulties. For others, they might mean a lack of access to required extracurriculars, like shadowing or research, or fewer opportunities to take the MCAT.
Whatever circumstances affected you, we suggest trying not to lament relatively insignificant frustrations, like receiving a worse grade in a virtual class than you might have in person or having to complete an extracurricular online. If your essay reads like you’re looking for sympathy regarding something minor, you’ll risk seeming insensitive or out of touch.
That said, it’s fine to write that you found virtual learning challenging or that certain opportunities were unavailable to you. Pick the circumstances that affected you most, stick to the facts, and make sure to talk about how you adapted and what you learned, with the goal of showing that you’re still a strong applicant.
COVID essay misconception 2: “Nothing bad happened to me during the pandemic, so I have nothing to write.”
As we just mentioned, everyone’s pandemic experience has been different, and it’s certainly true that some people have been much more fortunate than others. Nevertheless, COVID has affected everyone, and to reiterate what we wrote in the adversity essay section earlier, it’s not a competition to see who’s suffered the most.
Even if you’ve been relatively fortunate during the pandemic, you can still write about your COVID experience if it’s required of you. Describe the ways that you were affected and what you did to meet those challenges. Again, the key is to remain factual rather than seem like you’re seeking pity for relatively minor inconveniences. It’s also okay to acknowledge that you’ve been fortunate.
Additionally, bear in mind that a COVID essay doesn’t inherently need to describe something difficult. If appropriate to the prompt, you can also discuss:
Unexpected events or silver linings of the pandemic
Ways you’ve changed, lessons you’ve learned, or perspectives you’ve gained
How the pandemic informed your views of medicine
COVID essay example
When my college campus closed in March 2020 due to COVID-19, just a few months before my graduation, the momentum I’d felt propelling me into the future was suddenly put on hold. Nevertheless, I recognized that I was fortunate in many ways, including as a student. Although transitioning to online classes was admittedly disorienting, I’d already completed the vast majority of my coursework in person, including all my premed requirements.
However, my post-graduation plans changed dramatically. I was set to take a gap year, during which time I’d planned to complete my medical school applications while working full-time in the genetics lab I’d been a part of for the past year. Because the lab shut down along with the rest of the university, my position was paused and then a few months later cancelled entirely. As a result of losing this additional research experience, I decided to delay applying to medical school for another year.
Looking for ways to stay busy and help others after graduating, I became a virtual volunteer with a domestic abuse crisis text hotline and an online MCAT tutor. After a few months of job searching, I also began working as an ER scribe in August 2020. Although an intense experience, it was deeply gratifying to work with patients during the pandemic, and my clinical knowledge increased rapidly.
In April 2021, I was invited to come back to the genetics lab, which had reopened months before with just a couple researchers. While I’m grateful that, improbably, I’m now able to complete the gap year I’d envisioned pre-pandemic, I also know that the unexpected experiences of the past 16 months have made me a better future physician and reinforced my certainty that medicine is a field I’m excited and proud to be a part of.
Final thoughts
Secondary applications will likely be one of the most time-consuming, stressful, and exhausting parts of your application process (the other is the medical school admission interview circuit if you’re fortunate to receive multiple invitations).
Nevertheless, you should give yourself some breaks to recharge so that you never rush submissions for the sake of rolling admissions and sacrifice quality.
Like every other piece of written material you submit, aim not only to answer the prompt, but also to give admissions committees deeper insights into what makes YOU so great for their school specifically.

About the Author
Dr. Shirag Shemmassian is the Founder of Shemmassian Academic Consulting and one of the world's foremost experts on medical school admissions. For nearly 20 years, he and his team have helped thousands of students get into medical school using his exclusive approach.
Enjoyed this article? Get the FREE, 102-page guide we use to help over 90% of our students get into med school—the first time.
Get into medical school: 6 practical lessons to stand out and earn your white coat.
Below is a list of the most frequently asked questions (FAQ) we receive about medical school secondary essays that are not answered in this guide.
We encourage you to ask any other questions you have about secondary essays in the comments section below. We’ll make sure to answer your questions ASAP and add some of them to this FAQ section to make it easier for other students to find this information.
When should I expect to receive secondary applications?
Once you certify and submit your primary application and AMCAS receives your official transcripts, they begin verifying your application. You will receive your secondary applications after AMCAS completes verification and releases your primary applications to medical schools.
Because the verification process can take several weeks, it's important to submit your primary application as soon as possible after AMCAS opens submission on May 28. Students who submit AMCAS by early June can expect to begin receiving their secondary applications in late June to early July, positioning themselves to take full advantage of rolling admissions.
Note: Some DO schools send out secondaries as early as mid- to late-June.
(Further reading: The Ideal Medical School Application Timeline )
Will all medical schools send me a secondary application?
The majority will. However, whereas most schools send secondary applications without screening your primary application, some competitive schools will screen. You may experience a slight delay in receiving secondary applications from schools that screen.
How soon after receiving a secondary application should I aim to submit it?
As soon as possible, without sacrificing quality. While you should aim to submit secondaries within two weeks after receiving them, this is not required and you should never forfeit essay quality to do so. Many students believe there is a two-week “rule,” but very few schools actually expect the secondary to come back within two weeks. Moreover, the schools that have this expectation will make this explicit. In the grand scheme, a few days to a week later won’t make a huge difference.
Is it really a good idea to pre-write secondary essays? What if a school changes their secondary prompts during my admissions cycle?
Yes, you should absolutely pre-write secondary essays whenever possible because medical schools rarely change their prompts. In the event that a medical school does change their prompt, you'll likely be able to recycle your already-written essay for other schools.
Are “optional” essays really optional?
Yes. You should only answer an optional prompt when you have appropriate information to discuss. Forced responses will annoy admissions committees and can cast a negative light on the rest of your application.
Which secondaries should I work on first?
We recommend prioritizing your target schools, and specifically those that have the longest secondaries (so you can recycle more material for future applications) and those that you're most interested in attending. (so you can maximize the rolling admissions process at those institutions)
Do I need to submit my secondary essays two weeks after I receive my secondary applications?
Try not to get too caught up on the idea of a “two week” submission deadline. Unless a school has explicitly set a deadline of two weeks, your goal should just be to submit your essays as early as possible while still maintaining the quality of your essays.
If a secondary prompt asks me to explain my preference for a particular location, can I be honest about my reasons?
Various factors impact a med school applicant’s decisions about where to apply. Many applicants make these decisions based on proximity to family or home, for example. There’s nothing wrong with being transparent about your desire to stay close to home, but don’t leave it at that. You don’t want to give adcoms any reason to think that you might have only chosen their school out of convenience, so be sure to also describe how your connection to the local community will make you a great fit on the campus and vice versa. How will you utilize your existing networks and cultural knowledge of the local area to benefit the school?
Is it okay to repeat some information from my primary application on my secondary applications?
As a rule of thumb, you shouldn’t be repeating the same anecdotes or details in your secondary essays that you used in your personal statement. However, the experiences listed in the Work & Activities Section of your primary application will almost certainly reappear in your secondary essays. You’ll want to use your secondary essays to provide additional context, so it may help to think of the Work & Activities Section as the movie trailer and the secondary essays as the feature film.
Enjoyed this article? Get the FREE guide we use to help over 90% of our students get into med school—the first time.
Introducing the Dr. Kent Reifschneider Scholarship for Pediatric Medicine: Nurturing Future Leaders in Healthcare
Norfolk's Kent Reifschneider Gives Back With Scholarship Fund
Norfolk-Portsmouth-Newport News, VA, United States - April 22, 2024 —

Dr. Kent Reifschneider , a distinguished figure in the realm of pediatric medicine, announces the establishment of the prestigious Dr. Kent Reifschneider Scholarship for Pediatric Medicine. This scholarship aims to recognize and support outstanding undergraduate students who exhibit a fervent dedication to advancing pediatric healthcare.
Named in honor of its founder, Dr. Kent Reifschneider , the scholarship seeks to empower aspiring healthcare professionals with a passion for pediatric medicine. With a one-time award of $1,000, this scholarship is designed to assist deserving students in their pursuit of academic excellence and leadership in the field of pediatric healthcare.
"The Dr. Kent Reifschneider Scholarship for Pediatric Medicine represents a commitment to fostering the next generation of leaders in pediatric healthcare," says Dr. Kent Reifschneider, THE FOUNDER of the scholarship. "By supporting promising students who demonstrate a genuine passion for pediatric medicine, we aim to make a meaningful impact on the future of healthcare for children."
To be eligible for the Dr. Kent Reifschneider Scholarship for Pediatric Medicine, applicants must meet rigorous criteria designed to identify individuals who show exceptional promise in the field. Eligible candidates must be enrolled in an accredited undergraduate program in healthcare, medicine, or related fields, with a specific focus on pediatric medicine. Additionally, applicants must demonstrate a genuine passion for pediatric healthcare and a strong commitment to making a positive impact in the field.
Applicants are required to submit an original essay addressing a specific prompt that encourages reflection on their motivations for pursuing a career in pediatric medicine and the challenges that have influenced their journey. Moreover, applicants should provide evidence of academic excellence, leadership roles, extracurricular activities, and community involvement relevant to pediatric healthcare. At least one letter of recommendation from a faculty member, mentor, or healthcare professional is also required.
The selection committee will evaluate applications based on the quality and depth of the essay, academic achievements, and demonstrated commitment to pediatric healthcare. The deadline to apply for the scholarship is December 15, 2024, with the winner announced on January 15, 2025.
"As an Associate Professor of Pediatrics at Eastern Virginia Medical School, I am deeply committed to nurturing the next generation of healthcare professionals," says Dr. Kent Reifschneider. "Through the Dr. Kent Reifschneider Scholarship for Pediatric Medicine, I hope to inspire and support talented individuals who share my passion for pediatric healthcare."
For more information about the Dr. Kent Reifschneider Scholarship for Pediatric Medicine and to apply, please visit https://drkentreifschneiderscholarship.com/.
[About Dr. Kent Reifschneider]
Dr. Kent Reifschneider, M.D., is a prominent figure in pediatric medicine, known for his unwavering commitment to advancing healthcare for children. With extensive experience in Pediatric Endocrinology and a strong dedication to education and mentorship, Dr. Reifschneider continues to make significant contributions to the medical community. As the founder of the Dr. Kent Reifschneider Scholarship for Pediatric Medicine, he remains deeply invested in supporting aspiring healthcare professionals in their journey to make a positive impact in pediatric healthcare.
Contact Info: Name: Dr. Kent Reifschneider Email: Send Email Organization: Dr. Kent Reifschneider Scholarship Website: https://drkentreifschneiderscholarship.com
Release ID: 89127657
Should you come across any errors, concerns, or inconsistencies within this press release's content, we urge you to reach out without delay by contacting [email protected]. Our committed team will promptly address your feedback within 8 hours and take appropriate measures to resolve any identified issues or guide you through the removal process. Providing accurate and dependable information remains our utmost priority.

Opioid epidemic: How are we teaching future doctors to treat pain?
Uc davis school of medicine takes comprehensive approach to relieve pain with and without opioids.
Pain is the most common reason that people go to the doctor. Yet, amid the growing need for the treatment of pain, physicians and medical students in the United States have limited training in pain management and prescribing opioids.
The UC Davis School of Medicine , however, has taken a different approach – it has re-examined how pain management is taught, and adopted a new pain curriculum throughout medical education.
UC Davis medical students undergo more than 100 hours of required and dedicated total pain medicine educational content during their four years of training. The School of Medicine is now among the leading medical schools in the world for pain management education.
Need for increased training in pain management
A recent report from the Centers for Disease Control and Prevention (CDC) estimated 51.6 million United States adults (20.9%) experienced chronic pain, and 17.1 million (6.9%) had high-impact chronic pain that results in substantial restriction to daily activities and unnecessary suffering.
Despite the number of patients experiencing chronic pain, many doctors have not been adequately trained in pain management because medical schools traditionally don’t dedicate much time to teaching future physicians about it.
A 2018 study of pain medicine curriculum in 383 medical schools internationally and found 96% of schools in the United Kingdom and United States, and nearly 80% of schools in Europe had no required dedicated teaching in pain medicine.
Additionally, the study showed U.S. medical students received the lowest number of hours (fewer than 10) allocated to pain management training.
“The data clearly showed that pain medicine education at medical schools internationally was not adequately responding to societal needs in terms of the prevalence,” said Naileshni Singh , professor of anesthesiology and pain medicine. “Therefore, we decided to expand the curriculum at UC Davis School of Medicine to include more education on pain management to better prepare tomorrow’s doctors for the growing need to treat pain and address the opioid epidemic.”
We decided to expand the curriculum at UC Davis School of Medicine to include more education on pain management to better prepare tomorrow’s doctors for the growing need to treat pain and address the opioid epidemic.” — Naileshni Singh
Shift in landscape – opioid epidemic
Another factor that created a shift in the landscape of pain management and a call for action was the opioid epidemic.
Over a 15-year period, from 1999 to 2014, the number of U.S. prescriptions for opioids nearly doubled from 105 million to 207 million. During that same period, fatal overdoses from opioids, prescription and non-prescription such as fentanyl, soared almost five-fold, from 4,000 to 19,000 deaths a year.
“Part of what contributed to this opioid epidemic was poorly understood prescription paradigms for pain treatment and limited education on pain management in medical and other health professional schools,” Singh explained.
In response to the opioid epidemic, administrators of the six University of California medical schools co-authored a paper calling for a coordinated response to the opioid epidemic in California. The article detailed the UC’s urgent need to develop core competencies for pain, substance use disorder and safer opioid prescribing.
“The article outlined the approach that should be taken, the resulting competencies and related work focusing on pain medicine and substance use disorder from clinical and public health perspectives throughout the extensive University of California academic health system,” Singh said.
UC Davis School of Medicine pain education curriculum
Around the same time, the UC Davis School of Medicine was in the process of implementing a new, competency-based medical education curriculum I-EXPLORE (Integrated EXplorative Patient and Learner ORiented Education) that was launched in 2021. The school began to integrate into I-EXPLORE an entire pain curriculum through multiple aspects of the educational curriculum.
A major aspect of I-EXPLORE was the implementation of threads or core competencies that would be taught across all four years of school, including:
- Diagnostic medicine
- Preventive medicine
- Pain medicine
- Stages of life
- Care for vulnerable populations
- Behavioral health
“The inclusion of a pain medicine thread was an incredible step taken at UC Davis to recognize the importance of pain management in the curriculum,” said Chinar Daivesh Sanghvi , assistant clinical professor of anesthesiology and pain medicine.
The inclusion of a pain medicine thread was an incredible step taken at UC Davis to recognize the importance of pain management in the curriculum.” — Chinar Daivesh Sanghvi
Starting in the first few months of medical school, UC Davis students begin studying pain-specific curriculum incorporated into lectures, problem-based learning sessions, peer-teaching sessions, self-directed learning and clinical experiences. During their first and second years, students can learn unique integrated topics taught by a variety of instructors during pre-clerkship intersessions. One of the topics explores how childhood trauma can affect the experience of pain years later.
During their third and fourth years, students experience integrated lectures in their OB-GYN and surgery clinical rotations. They also learn about deprescribing medications and palliative medicine in a weeklong intersession before students enter their clinical experience phase. .
In addition, shortly before starting residencies, students take a course on opioid medications for pain management and alternatives to opioids for pain management.
“We know that it’s important to know about opioid management given that the most common reason patients present to the hospital is due to pain and it’s crucial as an intern to know medication transitions as patients travel through various areas of the hospital, whether it’s in the ER, post-surgery, ICU, or the wards,” added Sanghvi. “In addition, we want students to appreciate that pain medicine requires an integrated multidisciplinary approach, which includes pharmacists, physical therapists, pain psychologists, acupuncturists and many other clinicians to deliver comprehensive care.”
With the curricula evolving each year, Singh and Sanghvi are also incorporating the effects of disparities in pain care. Lessons about health inequities based on demographic and socioeconomic factors such as gender, ethnicity, and race are being incorporated into the programming so students can better understand patients who come from a wide variety of backgrounds.
New training on the horizon
The School of Medicine has also created two chronic pain electives for fourth-year medical students: A four-week immersive rotation in the Division of Pain Medicine and a two-week hybrid online and in-person course on the assessment and management of spinal pain.
Additionally, the school has recognized that a multidisciplinary approach is important to pain management. A new clinical rotation is being developed to expose third- and fourth-year medical students to complementary medicine in relation to:
- Physical therapy
- Occupational therapy
- Hand therapy
- Integrative medicine
- Pain psychology
- Pain pharmacy
- Acupuncture
“I am extremely proud of the pioneering work we have done and are continuing to do to provide our students with a strong foundation of education on pain management and the use of opioids,” added Singh. “I feel like we are preparing our students with the foundational knowledge that they need to meet the needs of the patients they will serve.”
Explore related topics

Four School of Medicine researchers elected as AAAS fellows

UC Davis and Cal Poly Humboldt launch program to attract Native Americans into medical school

Free cancer screening day to mark Head & Neck Cancer Awareness Month
Connect with us.

- Center Reports
- Advisory Board
- Executive Committee
- Faculty & Fellows
- Graduate Students
- Postdoctoral Researchers
- Research Associates
- Visiting Scholars & Students
- Alumni Spotlight
- Past Graduate Students
- Past Postdoctoral Researchers
- Past Visiting Scholars & Students
- Algorithms in Culture
- Art+Science in Residence Program
- Workshop: Advancing Science for Policy Through Interdisciplinary Research in Regulation (ASPIRR)
- Berkeley Papers in History of Science
- Historical Studies in the Natural Sciences
- Quantum Physics Collections and Databases
- The Cloud and the Crowd
- Nuclear Engineering & Society
- Nuclear Futures
- Epistemic Jurisdiction in Biofuels and Geoengineering
- PhD Graduate Field in History of Science
- PhD Designated Emphasis in STS
- Undergraduate Minor in STS
- Undergraduate Course Thread
- Current Events
- Conferences & Workshops
Other Events of Interest
- Past Brownbags
- Past Colloquia
- Past Conferences & Workshops
- Become a part of the Center
- Apply to become a Visiting Scholar or Student
- Past Working Groups
- Rent 470 Stephens
HSNS 54.1: A Special Issue of Essays: Pedagogy in the History of Science and Medicine
April 22nd, 2024 | Published in Latest news

The HSNS February 2024 Issue marks the first for a new “Essays and Reviews” editorial team: Melinda Baldwin and Brigid Vance.
From the Editorial Team:
Henry Cowles and Chitra Ramalingam have left us big shoes to fill, and we want to express our appreciation for everything they have done for both HSNS and us during this editorial transition.
The February 2024 special section focuses on the theme of “Pedagogy in the History of Science.” Like most of our colleagues, the two of us found ourselves navigating a new teaching environment during the COVID-19 pandemic. Our classes moved online; many students fell ill and needed extra support; faculty and students alike had to find ways to cope with and work through the anxiety, stress, and loneliness of social distancing. In this new environment, we reconsidered learning goals for our students, revised policies on absences and late work, and examined how our field could speak to this moment in history.
That experience led us to solicit essays on pedagogy in the history of science and medicine. Classes at most universities have now resumed in person, but we have heard from many colleagues whose pandemic experiences shifted what and how they teach. The essays in this special section reflect caring, innovative, and rigorous pedagogical approaches that teach not just historical content, but analytical thinking, key academic skills, and new approaches to collaborative and individual work.
The authors of our essays work in a variety of educational contexts, not all of which are university settings. Matthew Shindell and Samantha Thompson of the Smithsonian National Air and Space Museum share reflections on pedagogy in a museum environment, and Shireen Hamza’s essay recounts her experience teaching at Statesville Prison in Crest Hill, Illinois. Nor are all of the essays about teaching in North America. John DiMoia writes about his experience building a history of computing syllabus for a large course at Seoul National University, and Jongsik Yi shares her work building an innovative syllabus on the history of science in Korea. Many of the essays address efforts to decolonize the way we teach our field, or ways to put the history of science into conversation with other fields. Honghong Tinn’s course on “Ethics and Science and Technology” pushes students to consider case studies of indigenous technology, invisible labor, and exploitation in the East Asian context, and David Dunning and Judith Kaplan share their experience contributing to an interdisciplinary team-taught freshman program.
For the complete text, please read “Introduction: Pedagogy in the History of Science and Medicine” by Melinda Baldwin and Brigid Vance.
Share this:
- See All Events
International Careers Panel: Professionals Across Sectors Share Their Stories
DISCO Summit 2024
06/14/2024 - 06/15/2024
Search Icon
Events See all →
Creating canopy 2024.

Various locations
Earth Week 2024

This is a campuswide week of events, lectures, and volunteer opportunities designed to educate and inspire action related to environmental justice, climate, and nature-based solutions. This year’s theme is Restore & Regenerate.
Take Our Children to Work Day

Excellence in Graduate Teaching Reception

5:00 p.m. - 6:30 p.m.
Penn Graduate Student Center, 3615 Locust Walk
Health Sciences
How Penn Medicine is going green for good health
The university of pennsylvania health system prioritizes sustainability in its day-to-day practices, while envisioning novel approaches to greening efforts..

The health care sector has an outsized impact on the Earth’s changing climate, responsible for an estimated 8.5% of all greenhouse gas emissions in the United States. At the same time, the mission of health care—to improve an individual’s health—sits at odds with its negative contributions to the environment and public health.
But does providing health care to patients have to contribute to worsening the health of other people and the planet?
Increasingly, health care professionals and organizations are saying no. A green health care system is attainable, and a three-way win: a win for a patient’s health, a win for the health of the planet and public health, and a win in the form of cost savings.
For example, an initiative from Penn Medicine anesthesiologists to reduce the flow rate of anesthesia gases for patients—while still delivering safe care—slashed greenhouse gas emissions by the equivalent of 30 metric tons of carbon in the space of only three months at the Hospital of the University of Pennsylvania last year.
Surgery and anesthesia teams address climate impacts in the OR : From anesthesia gases that have outsized greenhouse effects, to medical waste disposal, operating rooms at Penn Medicine are greening health care.
Health care teams ‘act locally’ to support Penn Medicine sustainability goals : Teams across Penn Medicine are working hard to “think globally, act locally” when making environmentally friendly changes in their day-to-day operations.
Health research on a warming planet : Climate change affects human health, from viral transmission to the effectiveness of medications. Researchers at Penn Medicine are discovering how and seeking solutions.
How the next generation of physicians will combat climate change: Through a new Planetary Health curriculum, Penn medical students are learning about the impact of climate change on human health.
From large-scale efforts, like a commitment to sustainable building design and a massive renewable power purchase agreement in collaboration with the University, to more localized initiatives in hospital operating rooms and offices, the changes are meant to move toward the same goal, articulated in the organization’s recent strategic plan : making Penn Medicine the most environmentally friendly health care organization in the nation.
“Health care is dedicated to healing, but the industry has played a role in the changing climate,” says Kevin B. Mahoney , chief executive officer of the University of Pennsylvania Health System (UPHS). “It’s our responsibility now to balance health care with impact. We can do this by fostering engagement around climate-related initiatives, improving sustainability within our own health systems and beyond, and setting an example for the field. It’s the right thing to do for our patients, the community, and the generations to come.”
Penn Medicine, which encompasses UPHS and the Perelman School of Medicine , currently has a climate footprint that rivals the rest of the University combined. The health system has committed to the University’s Climate and Sustainability Action Plan , which includes adopting the “audacious yet achievable” goal of reaching 100% carbon neutrality by 2042, says Greg Evans, UPHS corporate director of sustainability.
Read more at Penn Medicine News .
Picturing artistic pursuits

Campus & Community
Penn celebrates operation and benefits of largest solar power project in Pennsylvania
Solar production has begun at the Great Cove I and II facilities in central Pennsylvania, the equivalent of powering 70% of the electricity demand from Penn’s academic campus and health system in the Philadelphia area.

Education, Business, & Law
Investing in future teachers and educational leaders
The Empowerment Through Education Scholarship Program at Penn’s Graduate School of Education is helping to prepare and retain teachers and educational leaders.

Arts, Humanities, & Social Sciences
‘The Illuminated Body’ fuses color, light, and sound
A new Arthur Ross Gallery exhibition of work by artist Barbara Earl Thomas features cut-paper portraits reminiscent of stained glass and an immersive installation constructed with intricately cut material lit from behind.

25 years of ‘LOVE’
The iconic sculpture by pop artist Robert Indiana arrived on campus in 1999 and soon became a natural place to come together.

NIH grant will help researchers follow a virus on its path to the nucleus
A University of Arizona College of Medicine – Tucson virologist’s work on human papillomavirus has been recognized by the National Institutes of Health for its enormous potential.
Chaz DeCoteau (left), an undergraduate double-majoring in biochemistry and pharmaceutical sciences, untangles the mysteries of human papillomavirus under the mentorship of Samuel Campos, PhD (right), associate professor of immunobiology.
Deanna R. Sanchez, BIO5 Institute
Human papillomavirus (HPV) can cause warts and certain cancers, and has been with us since the dawn of humanity. This tightknit relationship makes HPV an important source of information about our own biology, according to Samuel K. Campos, PhD, associate professor of immunobiology at the University of Arizona College of Medicine – Tucson and member of the BIO5 Institute.

Samuel Campos, PhD
“These viruses take advantage of pathways the cell has and tweak them. What better cell biologists to teach us how cells work than the viruses that have evolved with us for eons?” Dr. Campos said about how HPV illuminates the innerworkings of our bodies. “Follow the biology of the virus, and we’ll learn some cool new cell biology.”
To delve deeper into their research on HPV, the Campos Lab was awarded a five-year $1.8 million R35 grant from the National Institutes of Health. This type of grant provides long-term funding that gives investigators flexibility to follow their research in whatever direction it takes them, and is reserved for scientists with outstanding research records and potential to make major contributions to their fields.
‘Constantly shedding’
Dr. Campos says there are more than 600 known strains of human papillomavirus, with more yet to be discovered. His lab mainly focuses on HPV16, the type that causes the majority of cervical, anal and head-and-neck cancers.
“Most HPV infections are cleared by the immune system, but there are so many infections out there that even the tiny fraction that aren’t cleared in a timely manner cause about 5% of cancers worldwide,” Dr. Campos said.
HPV has found its niche in certain types of epithelial cells, which cover our body as skin and line our body cavities as mucous membranes. The virus moves from the lower layers of the epithelium to the upper layers, and once it’s close to the surface, replication kicks into high gear as it prepares to leave one body and infect another.
“We are constantly shedding dead skin — it just comes off our body,” Dr. Campos said. “That is how they’ve so successfully spread throughout the human population.”
‘A wolf in sheep’s clothing’
HPV’s genes are packaged in a protein shell. The Campos Lab focuses on the role of one of these shell proteins, called L2, which can insert itself into the membranes of our cells, like a key into a lock, and let itself inside. Upon entry, the virus is escorted along a twisted path to the nucleus, where it hijacks the cell to make copies of itself.

Isabelle Tobey (left), a doctoral student in cancer biology, helps to move the Campos Lab’s research forward.
Dr. Campos says his lab’s prior research revealed that, from the cell’s point of view, L2 looks like another part of the cell.
“We learned that the virus is really sneaky,” Dr. Campos said. “L2 can actually stick through the cell membrane without rupturing it, and HPV stays hidden behind these membranes. It’s able to avoid sensors that detect danger signals, like a wolf in sheep’s clothing.”
Previous research published by the Campos Lab and other groups suggested that HPV may be able to hide out until the cell’s machinery whirs into action during cell division, at which point it sheds its “sheep’s clothing” and hitches a ride to the nucleus.
“Once the virus has successfully delivered its DNA genome into the nucleus, it can begin expressing its own genes to take over the cell,” Dr. Campos said. “That will lead to immune evasion, alteration of the cell cycle, the generation of new viral particles, and transmission to another host. If the virus sticks around long enough, these infections can sometimes alter the cell in a way that leads to cancer.”
The grant will support the Campos Lab as they uncover how HPV takes advantage of cell division to move from its hiding place in the cell to the nucleus.
“It’s a complete black box. It’d be really neat to figure that out,” Dr. Campos said, adding that following the virus’s path will shed light on the intricacies of cell division and how things move in and out of cells.
‘A potent inhibitor’
The Campos Lab will use SNX-1.3, a type of small molecule known as a peptide, to explore how HPV initiates infection. Their previous work found that the peptide interferes with the virus’s ability to enter the cell.
“The peptide turned out to be a really potent inhibitor of HPV — it actually blocked the ability of L2 to stick through cell membranes in the first place,” he said. “We don’t understand how.”
Their hypothesis is that the peptide makes cell membranes less bendy and flexible, preventing L2 from creating weak spots through which to enter the cell. The grant will help them test this idea, which Dr. Campos hopes will uncover details of our own biology, though he doesn’t see potential in developing the peptide into a therapeutic to prevent HPV because there is already an excellent vaccine to block infection.
The lab’s use of SNX-1.3 arose from a chance encounter with Joyce Schroeder, PhD, professor of molecular and cellular biology and member of the UArizona Cancer Center. As she gave a presentation on this peptide, which her lab discovered while researching breast cancer, Dr. Campos’ ears perked up when she mentioned that it blocked the same pathway HPV uses to reach the nucleus.
“I was like, ‘Joyce, can I have some of your peptide to see if it would inhibit HPV?’ She was happy to give me her peptide to try,” he recalled. “That’s how most basic scientists are. We’re interested in getting answers to basic questions, and we’re usually happy to help each other out.”
‘Scratching my head about basic biology’
As a graduate student at Rice University, Dr. Campos conducted translational research aimed at creating new clinical procedures and therapeutics. But his work using viruses in gene therapy made him more interested in basic science — the foundational knowledge upon which translational science is built.

Under the mentorship of Samuel Campos, PhD (right), molecular and cellular biology doctoral students Ashlin Schaefbauer (left) and Zach Williamson (center) hope to learn how HPV travels to the center of the cell.
“That gene therapy work was cool, but it got me scratching my head about the basic biology of how these viruses work,” he said. “There are so many facets of our own cell biology that have been illuminated by viruses.”
Dr. Campos says discoveries in basic science may not immediately lead to vaccines or cures, but those discoveries can lead other researchers down investigative pathways that may ultimately benefit patients.
For example, discoveries about HPV’s protein shell helped scientists develop the HPV vaccine, which primes the immune system to recognize another viral protein, L1, and neutralize the virus before it can infect a cell.
“We’re just trying to understand the basics of how cells work, how viruses work, and how they interplay together,” Dr. Campos said. “Who knows where this stuff will lead? Maybe it would lead to a great Ebola antiviral, who knows?”
These unknowns are what keep Dr. Campos coming to work each day.
“It’s tough and it’s frustrating, but it’s also satisfying — like solving a puzzle,” he said. “You don’t know where the science will take you. You don’t know what the ending is going to be. That’s exciting.”
This research is supported by the National Institute of General Medical Sciences, a division of the National Institutes of Health, under award No. 1R35GM152143-01.
Essay For Future Plan In Medicine
Respected Madam,
I am an international medical graduate from WHO medical school directory listed institute –SMIMER (Surat Municipal Institute of Medical Education & Research) during year 2013. During next 10 years, I dream to become Infectious Diseases specialist, as hospitalist as well as academician who serve all the time for better health of patient and society. I believe it is important to learn advanced practice and systemic approach in the field of Internal Medicine of developed country. In several under-developed and developing countries, in remote and suburban areas, population is increasing fast which will be in dire need of better and affordable health care.
Order custom essay Essay For Future Plan In Medicine with free plagiarism report
Residency & post graduate program will fulfill my thrust in research field which is totally ignored area in home country. The opportunity will also boost my performance and prospect of getting a “INTERNAL MEDICINE” residency match when I apply next September. I will be obliged to become part of one world’s most advanced healthcare systems. I understand that the observership program does not involve direct patient interaction and it may not be remunerated. I am willing to follow any instructions and regulations you deem necessary. I will be very grateful if you can place me for a month of JULY-AUGUST 2014 observership rotation in the internal medicine department.
Yours Sincerely, Jugal Chahwala
Cite this Page
Essay For Future Plan In Medicine. (2016, Aug 18). Retrieved from https://phdessay.com/essay-for-future-plan-in-medicine/
Run a free check or have your essay done for you

More related essays
Abstract This paper is going to educate the reader about Alternative and Complementary Medicine which is also known as CAM. The paper will define Alternative and Complementary Medicine or CAM.
A life with purpose is a life without misery. While yet many choose purpose out of a mere likeness, I have chosen mine out of interest, vision and passion. To.
Being a part of alternative medicine, herbalism is often opposed to orthodox medicine. I believe that herbalism can make a good competition to conventional medicine as it has not only.
This study was undertaken to research behavioral medicine in psychology. In summary, this research examines the origins of behavioral medicine, reviews the psychosocial and behavioral mechanisms, and describes concrete and.
Review of Literature How is health promotion defined? Health promotion is a process of enabling people to increase control over and improve their health (WHO, 2013). People involved in health promotion.
Medicine in Colonial America was much different from today, but gave us a lot of insight in the human body’s needs. Due to lack of education, experience, proper tools, and.
The Limba people of Africa live in different villages, and each village puts its own spin on the myths that are passed down from generation to generation. One of these.
Diabetes is one of the public health concerns which have affected many people all over the world, despite the recent advances in the field of medicine, care and management. It.
We use cookies to give you the best experience possible. By continuing we’ll assume you’re on board with our cookie policy
Save time and let our verified experts help you.
Wait a second!
More handpicked essays just for you.

Essay on technology in the healthcare industry today and its impact
Impact of technology on health care
Essay on impact of technology on healthcare

Don’t take our word for it - see why 10 million students trust us with their essay needs.

Medicine in the Future
As time goes by and human civilization continues to evolve, so do the careers that we partake in. Whether it be a plumber no longer having to bend over or a teacher not having to be face to face with their students, changes have a been an essential factor in pushing our society towards being a more efficient place. One of the most important fields that is changing today is medicine . Medicine's goal is to not only increase the longevity of a person's life but also the quality so that they can enjoy the moments they have with their loved ones on this planet. In the future the medical field will become more technologically advanced through the new frontiers provided by genetics , bio-medical engineering, and nanotechnology in pharmaceuticals. In the past 30 years the foundation of medicine has been shaken by the discovery of the human genome. The genome consists of genes that are essentially the blueprints for how a person develops as the grow up. This can range from eye color to height and even to the ability to tap into more of the brain's capacity to function. The entire ...
Analysis Of The Article: The Shifting Engines Of Medicalization
The concepts discussed within the article regarding medicalization and changes within the field of medicine served to be new knowledge for me as the article addressed multiple different aspects regarding the growth of medicalization from a sociological standpoint. Furthermore, the article “The Shifting Engines of Medicalization” discussed the significant changes regarding medicalization that have evolved and are evidently practiced within the contemporary society today. For instance, changes have occurred within health policies, corporatized medicine, clinical freedom, authority and sovereignty exercised by physicians has reduced as other factors began to grow that gained importance within medical care (Conrad 4). Moreover, the article emphasized
Ethical Issues Surrounding Genetic Screening and Genetic Engineering
In 1990, the first great stride of genetics took place. This was called the Human Genome Project, a large-scale operation that was designed to understand the human genome (genetic structure). Since its commencement, there have been many leaps and bounds that have taken place. For certain genetic issues that we once knew nothing about, we no...
Checking Should Not Be Banned in Hockey
"10 Medical Breakthroughs Expected in the Next 10 Years." n. pag. Web. 31 Jul 201
Dealing with My Bipolar Sister
-Reilly Philip. Is It In Your Genes. Cold Spring Harbor Laboratory Press. 2004: 223-228. Print
Stone Man Syndrome Research Paper
Medical science has undergone a great revolution, it is getting better and more advanced than it was some decades back. In spite of such breakthrough advancement there are several diseases that don’t have a cure yet. A very hefty amount is being spent every day
Race for the Double Helix: An Analysis
...hich inherited traits, such as those for genetic disease, can be tracked over generations. Throughout out the course of human development, scientists will continue to find new new ways to help the human race through the discovery of the human gene inside of each of us, its uses, as well as complications, that can help the survival of our species.
The Ever-changing World of Healthcare
Healthcare is a dynamic, ever-changing environment. The complex circumstances around daily conversations that encompass life-threatening decisions are critical. In order to deliver high quality care, individuals must be able to communicate effectively. In the perfect world of communication, everyone receives the exact same information and is able to respond the exact same way. Unfortunately, communication breakdown is a prevalent issue among hospitals. On any given day of the hospital arena, multiple interactions take place. Some of the dialogue is planned, and some is not. While hospital departments are living in different silos within the same organization, the cultures may vary among the employees. Hospital leadership fosters the importance of collaboration within the organization and depends on the employees to ultimately drive the process. In order to overcome communication barriers in the workplace, conversations must occur. Engaging in daily face-to-face meetings with employees increases positive work culture, morale and overall productivity.
The Rising Cost of Health Care
Over the past decade, scientists have made significant advancements in the treatment of certain diseases. Unfortunately, just like any new product, the cost of developing these new technologies and treatments is extremely high. Plus, unlike other technology, heath technolo...
The Genome Revolution
For numerous years, the world’s most prestigious geneticists have been trying to crack the human genetic code, the intricate puzzle that defines each and every one of us as individuals. With the monumental success of the Human Genome Project, a new and exciting biological frontier is ready for exploration. The ramifications of the knowledge derived from this endeavor will no doubt be staggering for residents of the Rio Grande Valley and the world at large.
Genetic Engineering Essay
With today’s technology, we are capable of doing countless features such as coming up with new medical innovations to treat diseases and other medical related issues. Since we now
I Will Become a Physician
With the ever-changing field of medicine, many people wonder what medicine will be like in the future. For example, will we still have to live in fear of contracting an incurable and deadly disease, like AIDS? Or will medicine in the future have the capability of handling such threats to our lives? Answering these questions and having the proper education and training to help prevent such threats has been my major ambition. I feel that I can best fulfill this ambition by becoming a physician.
Medical Advances
Besides the computer revolution, medical advances have caused tension between faith and reason. The medical advances of the Twentieth Century have many beneficial effects for humanity. Diseases that used to be dangerous or life threatening, like mumps, measles, and whooping cough, are no longer worries in todays medical world. Tetanus, typhoid, and the bubonic plaque can now be treated with antibiotics or other medicines. Vaccines, especially the polio vaccine, freed many people from the effects of a disease. Advances in heart surgery and organ transplants have saved many lives. Anesthetics and painkillers have been made to reduce or eliminate pain during surgery or a painful disease. Advances in cancer and AIDS have also been made, although many of the details of these diseases are yet to be learned.
The Benefits of Modern Medicine
After the industrial revolution in the 18th century in Europe and America, there was the rapid industrial and economic growth in the 19th century, which in turn caused various scientific discoveries and various invention therefore making more progress in identifying illnesses and developing modes of treatment and cure, this was where modern medicine started. After the industrial revolution there were more industries, which in turn created a lot of work-related diseases and poor hygiene, also as the cities began to grow larger, more communicable diseases began to increase, cases like typhoid and cholera became epidemics. As well, due to the changes occurring, more and more people became more aware and since there was democracy there became an increase in demand for health care. There were also the wars that occurred, causing injuries which needed to be treated. Modern medicine evolves to solve the problems of the society at a given time and various advances in this mode of health care has occurred over the years. It has been seen that modern medicine is a positive influence in the society today for various reasons, the goal of the modern medicine is to achieve good health of the citizens, and modern medicine is experimental which is capable of advanced diagnosis. Likewise, modern medicine has an effect on the social and economic state of the modern society. Modern medicine is understood as the science of treating, diagnosing or even preventing illnesses using improved sophisticated technology. This mode of treatment involves a variety of methods, using diet, exercise, treatment by drugs or even surgery.
Essay On Us Healthcare 2050
What will US healthcare look like in 2050? According to Getzen (2013), trends in better health will lead to greater need for long-term care and chronic care for the aging population while correspondingly trending toward less acute illnesses (p. 438). Personalized prognostic healthcare will lead to healthier longer lives (Lawrence, 2010). Physicians will become leaders of teams within healthcare organizations rather than the independent practitioners we are familiar with today (Getzen, 2013, p. 438). Thus, the concept of the primary care physician will become a thing of the past (Lawrence, 2010).
Technology and Medicine
Technology has had a great impact on society when it comes to medicine. Medical technology has been around since the cave man began using rocks as tools to perform trephening. Since then there has been many new advancements in medicine due to technology. From painless needles to robots used for surgeries technology is around to stay.
More about Medicine in the Future
Related topics.
- Human Genome Project
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.90(2); 2017
History of Medicine between tradition and modernity
History of medicine is an extensive and very complex science. In a simple and classical understanding, it has an informative and associative role. Although it is not easy for students to understand the multiple implications of the history of medicine, its importance becomes more evident during their academic formation. The students must be persuaded particularly about the ethical and cultural values that history of medicine has in their training. Furthermore, history of medicine participates in creating the necessary perspective for shaping the future of medicine in the next decades. This is, perhaps, the most interesting role that the history of medicine should play from the modern point of view of students and young physicians. This paper presents different ways of understanding the roles of the history of medicine regarded from the traditional perspective to the contemporary point of view.
Introduction
History of medicine is an extensive and a very complex science, with many interesting and even fascinating aspects, which should be studied carefully and with no partisan bias. This paper is a plea for studying history of medicine in the higher medical education.
As 2017 marks 125 years since Valeriu Lucian Bologa (1892–1971) – the first Romanian professor of history of medicine – was born, we bring thus a homage to his memory.
We publish this paper in “Clujul Medical” journal, because Bologa was professor and head of Department of the History of Medicine at the Cluj Faculty of Medicine for more than three decades (1930–1962) and also a member of the editorial board of this publication.
The history of medicine between positive and negative understanding
The evolution of medicine has interested many historians of medicine in the past and new arguments continue to be brought about the need of its study [ 1 ].
It is necessary to show that the formative role of the history of medicine has been discussed since the second half of the nineteenth century. After a century, emphasizing the significance of the history of medicine in the training of the future doctors, V. L. Bologa evidenced several objectives: to give to physician the possibility to refresh and enlarge his general culture; to focus his attention on one of the most beautiful chapters from the history of civilization and to promote respect for the past of medicine for its outstanding protagonists [ 2 ].
However, it is strange to observe that the interest of some students is not sufficiently developed for learning the history of medicine. There could be different reasons for this situation.
One reason is the fact that the present time has its focus on “what is” – the immediate present – and “what is to be” – the future. In this context, Farokh Erach Udwadia put the question “it is therefore worthwhile to give the reader a glimpse of the recent past?” His answer is significant: “I do believe so, for the past in any field of endeavour permeates the present and lies buried within the future” [ 3 ]. Referring to history of medicine, he added: “to gain a proper perspective, the never-ending canvas of medicine is best viewed in its entirety – the past, the present, the changing unfinished future” [ 3 ].
The misunderstanding regarding the formative role of history of medicine for students can be explained in another way. The period of accelerated progress involves the appearance of many professional notions, new conceptions etc. Their consequence is the need to introduce new topics or types of lectures in the academic curricula. Implicitly, they lead to a compression of classical subjects of study, although they could be important for the professional training of students or for their general culture.
Referring directly to the history of medicine, the study of the past of medicine permits a better understanding of its present and gives the possibility to do develop strategies for its future.
Studying history of medicine, students learn how to understand and to think different medical events from various perspectives: how to correlate various medical profiles apparently without connection with each other, or how the same discovery may occur several times at intervals of centuries and without continuity in time. For example, students can understand how the important anatomist Giovanni Battista Morgagni (1682–1771) can be regarded as the father of modern pathology. Another significant example is that students learn that the cataract surgery – which is considered an operation specific for modern times – was practiced in antiquity and mentioned by Aulus Cornelius Celsus (c. 25 BC – c. 50 AD) [ 4 ] and later, in the Middle Ages, by Abulcasis (936–1013). Learning the history of medicine, students reach a certain level of understanding, like how it was possible that Galen’s influence on European medicine lasted nearly fifteen centuries after his death.
The correct analysis of the past of medical science allows us to understand not only the progressive phases of medicine, but also the periods of stagnation or regression. This is a significant advantage, because knowing the negative experiences of the past, future errors can be avoided.
An interesting point of view was discussed by Jacalyn Duffin (b. 1950): the history of medicine offers a “conceptual tool for learning about medicine”. She added: “medical students are intelligent. Even if they last studied humanities in high school, they soon grasp the thrill and an adventure of a debate over questions and context. In reaching for this modest goal, students learn something about the past; however, they can select the events that seem more relevant for their own personal lives and career goal” [ 5 ].
Why should students memorize different names and data from the past of medicine? The effort to memorize is useful, because it will help students to learn easier some diseases and syndromes having proper names. Certainly, not all historical data have the same significance. It is more useful to remember the century or the historical period in which different personalities lived, rather than their years of birth and death. Also, not all titles of books they wrote are important to be kept in mind, but only those that marked the progress of medicine. For example, is very useful to memorize the title “De humani corporis fabrica” of Andreas Vesalius (sixteen century), because it marked a turning point in the evolution of anatomy.
Although very few, there are students who consider history as a boring and unimportant subject. This is due to the fact that they are not convinced by what means history. This is a consequence that during school years, history is presented in a thematic approach. Thus, it is difficult for future students to understand that the correct study of the history is “the past of mankind since ancient times till today, according to the specifics of geographic areas and of communities” [ 6 ]. Ioan-Aurel Pop (b. 1955) shows that: “the facts of the past, removed from space and time have no historical relevance. Being dispersed, they serve the political discourse, the writer, the musician, filmmaker, essayist, philosopher, etc., but these are not history” [ 6 ].
How medical history should be presented in order to be clearly understood?
To teach the history of medicine is a great responsibility, being necessary to analyze every medico-historical aspect in various ethical, socio-economic, cultural etc. perspectives. As Giorgio Zanchin (b. 1945) puts into evidence: “if history is understood as a succession of events determined by specific causes, with specific consequences that vary according to social, economic, and political conditions, a historical analysis is essential for a dynamic interpretation of scientific theories in a social-cultural context of reference” [ 7 ].
In a book exploring the continuities and discontinuities in medical thought and practice, Keir Waddington shows that “this approach encouraged readers to think about how medicine has been used to fashion and refashion views of the body and disease; how it informed access to healthcare and welfare policies; and how this was related to different political, cultural, intellectual and socioeconomic contexts” [ 8 ]. About his volume entitled “An Introduction to the Social History of Medicine” he noted that it “focuses not on individuals, institutions or discoveries, but on a comparative examination of key theme in the social history in Europe” [ 8 ].
There is also the approach of history of medicine in terms of the conditions in which the discoveries were made. Michael T. Kennedy (b. 1938) noted in the introduction of his book entitled “A brief history of disease, science and medicine” that much of what medical students learned from the past has now been shown to be in error. For that reason, his concept of history of medicine includes other subjects than those in a «classical» account. Thus, he gave explanations about his interest “in how infectious diseases evolved and [I] think it important to understand this aspect of science to make sense of the story of smallpox in the New World and syphilis in the old” [ 9 ].
Regarding the history of medicine presented in essays we consider that it can be correctly understood only by those who have a solid knowledge of history. For example, this type of approach can be used with certain intentions, as Olivier Faure (b. 1953) did, gathering his articles previously published in various journals. However, this approach is limited only for shorter periods of time and is focused on some social aspects of medicine. Faure used a certain style of presentation, as he noted: “an absence of mastery of academic codes or contempt for them, this propensity to direct language is the sign of the enthusiasm and passion with which I have always approached the subjects I have dealt with” [ 10 ].
A book of history of medicine that aims to include more subjects, such as the evolution of different medical discoveries, the evolution of techniques and medical innovations, controversies in medicine etc. is difficult to be elaborated and published in only one comprehensive volume. It should be written by several authors. This gives the authors the responsibility, but also the opportunity to approach the problems in their own way. This multiple approach can have, as result, a book which is it not unitarily written. Moreover, this type of book exceeds the requirements of medical students in higher education. Furthermore it could give rise to heated debates on issues related to these thematic problems [ 11 ].
Discussing the importance of the scientific research in history of medicine, John L. Thorthon reveals that “The history of medicine has been studied for centuries, but remains a fluid subject. Fresh facts can reveal new fields of research, and even result in a re-evaluation of the subject. A misinterpretation may have led to false assumptions which in turn have misled later writers, resulting in errors which have been perpetuated for centuries. Only comparatively recently have professional medical historians, armed with an appreciation of both medical knowledge and a background of social history, attempted to unravel the intricacies of the development of medical progress” [ 12 ].
At the end of our paper, we consider adequate to remember some ideas of Nicolae Vătămanu (1897–1977) and Gheorghe Brătescu (b. 1923): “knowing the past of this exciting science [history of medicine] is meant to attract alike the young man who strives to embrace the medical profession, and the one that deepens it with passion: it [history of medicine] is useful for the physician who needs a [...] quick and safe orientation, as for the inexperienced scholar, sensitive to all what is noble, profound and useful in human activity” [ 13 ].
Conclusions
- The study of the past of medicine permits a better understanding of its present and gives the possibility to develop adequate strategies for its future.
- The study of the history of medicine offers the students the possibility to correlate various medical profiles seemingly without connection with each other.
- To teach history of medicine is a great responsibility, being necessary to analyze medico-historical aspects in various ethical, socio-economic and cultural perspectives.
- There are different ways of understanding the roles of the history of medicine regarded from the traditional perspective to the contemporary point of view.
- Fresh medico-historical facts can reveal new fields of research, and even a re-evaluation of the same subject.
Future leaders in medicine and beyond: Vote for the Student of the Week for April 22-26
Student of the Week offers schools the chance to celebrate teens who have placed in an art, dance or music competition, excelled in a science fair, won an essay contest, received a scholarship, were recognized for their volunteer service or have shined in some other way.
All high schools in Arizona are invited to nominate students to be included in an online poll where azcentral.com readers vote to choose the Student of the Week.
Student of the Week voting is open from 6 a.m. Monday through noon Thursday. Each week's winner is announced online Friday at 6 a.m.
Meet this week's nominees!
How to nominate: Know a teen we should celebrate? Choose them for Arizona Student of the Week
Lydia Luehrs, sophomore, Great Hearts Anthem
Lydia had a goal last summer to collect 1,000 books to create a dedicated library for her campus. Through donations and community support, she was able to reach this goal and gift the books to Great Hearts Anthem for student use. Lydia was elected unanimously by her teachers to be a student mentor on campus and has proven this decision with her skills in leadership, teamwork, and perseverance through driving the library project. Having spent over 100 hours on the project and coordinating with administration this school year to help make the library a success!
Nomination submitted by Riley Chaisson, Marketing Coordinator for Great Hearts Academies.
Julio Arreguin Hernandez, senior, Sunnyslope High School
Julio is a senior at Sunnyslope High School and is in his second year of the Medical Assisting program at Western Maricopa Education Center’s (West-MEC) Northeast Campus. Julio is a leader inside and outside of the classroom. He is the HOSA class president, and he placed first in the phlebotomy competition this year at the state competition. He will participate in the HOSA internationals in June.
Julio is constantly a spokesperson for West-MEC, whether it be giving campus tours to the Mayor’s office or visiting local elementary schools to advocate for the power of West-MEC. Julio will head to the University of Arizona this fall, pursuing a bachelor’s degree in biochemistry with a minor in Spanish. He aspires to become a surgeon in the future.
Submitted by Maria Romero, Medical Assisting Instructor, West-MEC Northeast Campus.
For more information on Student of the Week, email [email protected] .
Get the best experience and stay connected to your community with our Spectrum News app. Learn More
Continue in Browser
Get hyperlocal forecasts, radar and weather alerts.
Please enter a valid zipcode.

Florida hemp industry could face an uncertain future
CLEARWATER, Fla. — Gov. Ron DeSantis could soon sign SB 1698 into law.
It caps the potency of THC in hemp products, prohibits businesses from manufacturing or selling products that contain more than .3% Delta-9 and places limits on other cannabinoids .
State Rep. Tommy Gregory is one of the bill sponsors and says it’s about safety.
“I think that the overall limit, in terms of per container, is based on that logic to say ‘if you took everyone in this container and you were an adult who didn’t normally use Delta-9 THC, marijuana or synthetic cannabinoids,’” Gregory said. “That would get you to a place you probably don’t want to go beyond.”
What You Need To Know
Gov. ron desantis could soon sign a sb-1698 into law; it caps the potency of thc in hemp products state representative tommy gregory is one of the bill sponsors and says it’s about safety matt wetzel, who runs a hemp shop in clearwater beach, said his son's condition was helped by hemp.
One hemp shop owner, Matt Wetzel, has a store in Clearwater Beach.
He isn’t just worried about the future of his hemp shop, but about the entire industry in the state and how the bill would limit CBD products for people who use them for health issues. His own son uses CBD without THC for a very rare medical condition.

Wetzel’s son Jameson Wetzel had a rough start in life. When he was a baby, he would overheat to the point of having seizures and even stopped breathing. His mother, Emma Wetzel, recalled how terrifying it was.
“He got really warm, lethargic when I went to put him in bed,” Emma Wetzel said. “He curled up in a ball and then he breathed really loud and let the breath out and he stopped breathing.”
Eventually, they would learn that the boy was suffering from Febrile Status Epilepticus. It’s a condition where seizures caused by a fever last 30 minutes or longer. He also had a hard time regulating his body heat. His parents say he has had fevers as high as 105 degrees.
One day, Matt Wetzel heard a news report about CBD, made from a cannabis plant, but it’s not psychoactive, meaning it doesn’t make you high.
It was being used to help people with seizures. The family lived in Wisconsin then, where it wasn’t legal, but in Colorado it was. The parents made the desperate move to help their son. Eventually, they started giving him CBD.
“After a couple of days, we saw an immediate transformation,” Matt Wetzel said. “It was like…he was running, he was chasing birds, he was our little boy again.”
They eventually moved to Florida and now worry about the new legislation and that it might destroy hemp shop owners across the state.
“Gov. DeSantis needs to make a decision. Is he going to let something like this from happening again to another family because we are going to go right back to when Jameson was 1-year-old?” Matt said.
The parents say CBD is the reason their son is here today, flourishing and living life to the fullest.
Wetzel said if the legislation goes into effect in October, they might have to move to a more CBD friendly state like Georgia.

IMAGES
VIDEO
COMMENTS
What Will Health and Medicine Look Like in 2050? No one can see the future, but that won't stop us from trying. We asked UCSF faculty and alumni to score these predictions for likelihood and impact. By UCSF Faculty and Alumni UCSF Magazine Winter 2020. Tap the plus sign to open popups with background and related links.
Between 2009 and 2025, the global market value for nanomedicine is projected to grow from $53 billion to $334 billion USD — an average of 17.5% growth per year. At this rate of increase, the ...
But let's try. Over the next 25 years, genomic-driven analysis will continue to broaden the impact of personalized medicine in healthcare globally. Precision medicine will continue to deliver ...
Future scientists will likely be manipulating cells at the molecular level, and this will further tap into opportunities for a personalized approach to medicine.
Recently, advances in wearable technologies, data science and machine learning have begun to transform evidence-based medicine, offering a tantalizing glimpse into a future of next-generation ...
Health care today is often characterized by mediocre quality, poor safety, and high costs. 1 Though change usually comes slowly, the Covid-19 pandemic has demonstrated that it is possible to rapidly retool our systems if there is a strong enough stimulus. 2 In this article, we examine the future of health care — how it should change over the next 10 years, and the key drivers to enable our ...
Over the past year, the Journal has commemorated 200 years of publication and the astonishing progress made since 1812 in the science and practice of medicine. Thanks to digital technology, our ...
The future of medicine. Modern medicine is affording people longer and healthier lives. But researchers want to take improvements in health even further. With advances in gene editing, technology ...
But the goal to offer this possible future to more patients with D.M.D. is in jeopardy. Sarepta is seeking F.D.A. approval to treat boys over 5. Disagreements over the latest clinical trial's ...
As part of the celebration of Lawrence Bacow's inauguration as Harvard University's 29th president, six world-renowned life scientists from across the university came together to discuss their vision for what is possible in life science, medicine, global health and care delivery in an Oct. 5 symposium, "Life Sciences and the Future of Medicine."
2. Current Contributions. The goal of this special issue of Medicina was to address these gaps in collective understanding and to promote the integration of TCIM into contemporary medicine and public health. This collection of articles will stimulate further research and support healthcare professionals, consumers, and policy makers to make informed decisions about the utilization of evidence ...
The future of medicine is here. An essay by Vas Narasimhan, CEO of Novartis about the historical context and coming innovations in medicine with an introduction by Goran Mijuk. When Novartis was founded in 1996, the company's creation out of the merger between Sandoz and Ciba-Geigy was hailed as an industrial milestone.
Citations are an informative indication for determining the impact of a published article. A special mention goes to our top three most cited articles from Regenerative Medicine in 2023.. The aforementioned perspective article by Fabbri et al. from our February issue titled "Modeling policy development: examining national governance of stem cell-based embryo models" [].
In recent years, stem cell therapy has become a very promising and advanced scientific research topic. The development of treatment methods has evoked great expectations. This paper is a review focused on the discovery of different stem cells and the potential therapies based on these cells. The genesis of stem cells is followed by laboratory steps of controlled stem cell culturing and derivation.
Lobo notes that an outstanding personal statement typically includes all of the following ingredients: An intriguing introduction that gets admissions officers' attention. Anecdotes that ...
Over the next 25 years, the development and integration of these tools into an early-warning system embedded into healthcare systems around the world could revolutionize infectious disease detection and response. But this will only happen with a commitment from the global community. Go to: Els Torreele.
REVIEW. In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better ...
AI will support the future needs of medicine by analyzing the vast amounts and various forms of data that patients and healthcare institutions record in every moment. AI is likely to support and augment physicians by taking away the routine parts of a physician's work hopefully enabling the physician to spend more precious time with their ...
How the pandemic informed your views of medicine. COVID essay example. When my college campus closed in March 2020 due to COVID-19, just a few months before my graduation, the momentum I'd felt propelling me into the future was suddenly put on hold. Nevertheless, I recognized that I was fortunate in many ways, including as a student.
Norfolk-Portsmouth-Newport News, VA, United States - April 22, 2024 — Dr. Kent Reifschneider, a distinguished figure in the realm of pediatric medicine, announces the establishment of the ...
Transforming the Future of Medicine. Advancing human health is at the heart of Washington University's plans for the future. Through a strategic planning process that began in 2006, the university identified improvements in human health as one of four key themes, together with preparing the leaders of tomorrow, inspiring innovation and ...
UC Davis School of Medicine pain education curriculum. Around the same time, the UC Davis School of Medicine was in the process of implementing a new, competency-based medical education curriculum I-EXPLORE (Integrated EXplorative Patient and Learner ORiented Education) that was launched in 2021. The school began to integrate into I-EXPLORE an ...
The HSNS February 2024 Issue marks the first for a new "Essays and Reviews" editorial team: Melinda Baldwin and Brigid Vance. ... That experience led us to solicit essays on pedagogy in the history of science and medicine. Classes at most universities have now resumed in person, but we have heard from many colleagues whose pandemic ...
From Penn Medicine News Surgery and anesthesia teams address climate impacts in the OR: From anesthesia gases that have outsized greenhouse effects, to medical waste disposal, operating rooms at Penn Medicine are greening health care.. Health care teams 'act locally' to support Penn Medicine sustainability goals: Teams across Penn Medicine are working hard to "think globally, act locally ...
Human papillomavirus (HPV) can cause warts and certain cancers, and has been with us since the dawn of humanity. This tightknit relationship makes HPV an important source of information about our own biology, according to Samuel K. Campos, PhD, associate professor of immunobiology at the University of Arizona College of Medicine - Tucson and member of the BIO5 Institute.
Order custom essay Essay For Future Plan In Medicine with free plagiarism report. 450+ experts on 30 subjects Starting from 3 hours delivery. Get Essay Help. Residency & post graduate program will fulfill my thrust in research field which is totally ignored area in home country. The opportunity will also boost my performance and prospect of ...
In the future the medical field will become more technologically advanced through the new frontiers provided by genetics, bio-medical engineering, and nanotechnology in pharmaceuticals. In the past 30 years the foundation of medicine has been shaken by the discovery of the human genome. The genome consists of genes that are essentially the ...
History of medicine is an extensive and a very complex science, with many interesting and even fascinating aspects, which should be studied carefully and with no partisan bias. This paper is a plea for studying history of medicine in the higher medical education. As 2017 marks 125 years since Valeriu Lucian Bologa (1892-1971) - the first ...
Future leaders in medicine and beyond: Vote for the Student of the Week for April 22-26 ... won an essay contest, received a scholarship, were recognized for their volunteer service or have shined ...
Florida hemp industry could face an uncertain future. By Jeff Van Sant Florida. UPDATED 12:49 PM ET Apr. 22, 2024 PUBLISHED 8:58 PM ET Apr. 21, 2024 PUBLISHED 8:58 PM EDT Apr. 21, 2024.