Advertisement

How to Prepare an Outstanding Journal Club Presentation
- Request Permissions
Rishi Sawhney; How to Prepare an Outstanding Journal Club Presentation. The Hematologist 2006; 3 (1): No Pagination Specified. doi: https://doi.org/10.1182/hem.V3.1.1308
Download citation file:
- Ris (Zotero)
- Reference Manager
Dr. Sawhney is a member of the ASH Trainee Council and a Fellow at the Medical University of South Carolina.
Journal club presentations provide a forum through which hematology trainees keep abreast of new developments in hematology and engage in informal discussion and interaction. Furthermore, honing presentation skills and mastering the ability to critically appraise the evidence add to our armamentarium as clinicians. Outlined here is a systematic approach to preparing a journal club presentation, with emphasis on key elements of the talk and references for electronic resources. Use of these tools and techniques will contribute to the success of your presentation.
I. ARTICLE SELECTION:
The foundation of an outstanding journal club presentation rests on the choice of an interesting and well-written paper for discussion. Several resources are available to help you select important and timely research, including the American College of Physicians (ACP) Journal Club and the Diffusion section of The Hematologist . McMaster University has created the McMaster Online Rating of Evidence (MORE) system to identify the highest-quality published research. In fact, the ACP Journal Club uses the MORE system to select their articles 1 . Specific inclusion criteria have been delineated in order to distinguish papers with the highest scientific merit 2 . Articles that have passed this screening are then rated by clinicians on their clinical relevance and newsworthiness, using a graded scale 3 . With the help of your mentors and colleagues, you can use these criteria and the rating scale as informal guidelines to ensure that your chosen article merits presentation.
II. ARTICLE PRESENTATION:
Study Background: This section provides your audience with the necessary information and context for a thoughtful and critical evaluation of the article's significance. The goals are 1) to describe the rationale for and clinical relevance of the study question, and 2) to highlight the preclinical and clinical research that led to the current trial. Review the papers referenced in the study's "Background" section as well as previous work by the study's authors. It also may be helpful to discuss data supporting the current standard of care against which the study intervention is being measured.
Study Methodology and Results: Clearly describe the study population, including inclusion/exclusion criteria. A diagrammatic schema is easy to construct using PowerPoint software and will help to clearly illustrate treatment arms in complex trials. Explain the statistical methods, obtaining assistance from a statistician if needed. Take this opportunity to verbally and graphically highlight key results from the study, with plans to expand on their significance later in your presentation.
Author's Discussion: Present the authors' conclusions and their perspective on the study results, including explanations of inconsistent or unexpected results. Consider whether the conclusions drawn are supported by the data presented.
III. ARTICLE CRITIQUE:
This component of your presentation will define the success of your journal club. A useful and widely accepted approach to this analysis has been published in JAMA's series "User's guide to the medical literature." The Centre for Health Evidence in Canada has made the complete full-text set of these user's guides available online 4 . This site offers review guidelines for a menu of article types, and it is an excellent, comprehensive resource to focus your study critique. A practical, user-friendly approach to literature evaluation that includes a worksheet is also available on the ASH Web site for your use 5 .
While a comprehensive discussion of scientific literature appraisal is beyond the scope of this discussion, several helpful tips warrant mention here. In assessing the validity of the study, it is important to assess for potential sources of bias, including the funding sources and authors' affiliations. It is also helpful to look for accompanying editorial commentary, which can provide a unique perspective on the article and highlight controversial issues. You should plan to discuss the trade-offs between potential benefits of the study intervention versus potential risks and the cost. By utilizing the concept of number needed to treat (NNT), one can assess the true impact of the study intervention on clinical practice. Furthermore, by incorporating the incidence rates of clinically significant toxicities with the financial costs into the NNT, you can generate a rather sophisticated analysis of the study's impact on practice.
IV. CONCLUSIONS, IMPLICATIONS, AND FUTURE DIRECTIONS:
Restate the authors' take-home message followed by your own interpretation of the study. Provide a personal perspective, detailing why you find this paper interesting or important. Then, look forward and use this opportunity to "think outside the box." Do you envision these study results changing the landscape of clinical practice or redirecting research in this field? If so, how? In articles about therapy, future directions may include moving the therapy up to first-line setting, assessing the drug in combination regimens or other disease states, or developing same-class novel compounds in the pipeline. Searching for related clinical trials on the NIH Web site 6 can prove helpful, as can consultation with an expert in this field.
Good journal club discussions are integral to the educational experience of hematology trainees. Following the above approach, while utilizing the resources available, will lay the groundwork for an outstanding presentation.
WEB BASED REFERENCES
www.acpjc.org
hiru.mcmaster.ca/more/InclusionCriteria.htm
hiru.mcmaster.ca/more/RatingFormSample.htm
www.cche.net/main.asp
www.hematology.org/Trainees
www.cancer.gov/clinicaltrials
- Previous Article
- Next Article
Email alerts
Affiliations.
- Current Issue
- About The Hematologist
- Advertising in The Hematologist
- Editorial Board
- Permissions
- Submissions
- Email Alerts
- ASH Publications App
American Society of Hematology
- 2021 L Street NW, Suite 900
- Washington, DC 20036
- TEL +1 202-776-0544
- FAX +1 202-776-0545
ASH Publications
- Blood Advances
- Hematology, ASH Education Program
- ASH Clinical News
- The Hematologist
- Publications
- Privacy Policy
- Cookie Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Loading metrics
Open Access
Ten simple rules for effective presentation slides
* E-mail: [email protected]
Affiliation Biomedical Engineering and the Center for Public Health Genomics, University of Virginia, Charlottesville, Virginia, United States of America
- Kristen M. Naegle

Published: December 2, 2021
- https://doi.org/10.1371/journal.pcbi.1009554
- Reader Comments
Citation: Naegle KM (2021) Ten simple rules for effective presentation slides. PLoS Comput Biol 17(12): e1009554. https://doi.org/10.1371/journal.pcbi.1009554
Copyright: © 2021 Kristen M. Naegle. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The author received no specific funding for this work.
Competing interests: The author has declared no competing interests exist.
Introduction
The “presentation slide” is the building block of all academic presentations, whether they are journal clubs, thesis committee meetings, short conference talks, or hour-long seminars. A slide is a single page projected on a screen, usually built on the premise of a title, body, and figures or tables and includes both what is shown and what is spoken about that slide. Multiple slides are strung together to tell the larger story of the presentation. While there have been excellent 10 simple rules on giving entire presentations [ 1 , 2 ], there was an absence in the fine details of how to design a slide for optimal effect—such as the design elements that allow slides to convey meaningful information, to keep the audience engaged and informed, and to deliver the information intended and in the time frame allowed. As all research presentations seek to teach, effective slide design borrows from the same principles as effective teaching, including the consideration of cognitive processing your audience is relying on to organize, process, and retain information. This is written for anyone who needs to prepare slides from any length scale and for most purposes of conveying research to broad audiences. The rules are broken into 3 primary areas. Rules 1 to 5 are about optimizing the scope of each slide. Rules 6 to 8 are about principles around designing elements of the slide. Rules 9 to 10 are about preparing for your presentation, with the slides as the central focus of that preparation.
Rule 1: Include only one idea per slide
Each slide should have one central objective to deliver—the main idea or question [ 3 – 5 ]. Often, this means breaking complex ideas down into manageable pieces (see Fig 1 , where “background” information has been split into 2 key concepts). In another example, if you are presenting a complex computational approach in a large flow diagram, introduce it in smaller units, building it up until you finish with the entire diagram. The progressive buildup of complex information means that audiences are prepared to understand the whole picture, once you have dedicated time to each of the parts. You can accomplish the buildup of components in several ways—for example, using presentation software to cover/uncover information. Personally, I choose to create separate slides for each piece of information content I introduce—where the final slide has the entire diagram, and I use cropping or a cover on duplicated slides that come before to hide what I’m not yet ready to include. I use this method in order to ensure that each slide in my deck truly presents one specific idea (the new content) and the amount of the new information on that slide can be described in 1 minute (Rule 2), but it comes with the trade-off—a change to the format of one of the slides in the series often means changes to all slides.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Top left: A background slide that describes the background material on a project from my lab. The slide was created using a PowerPoint Design Template, which had to be modified to increase default text sizes for this figure (i.e., the default text sizes are even worse than shown here). Bottom row: The 2 new slides that break up the content into 2 explicit ideas about the background, using a central graphic. In the first slide, the graphic is an explicit example of the SH2 domain of PI3-kinase interacting with a phosphorylation site (Y754) on the PDGFR to describe the important details of what an SH2 domain and phosphotyrosine ligand are and how they interact. I use that same graphic in the second slide to generalize all binding events and include redundant text to drive home the central message (a lot of possible interactions might occur in the human proteome, more than we can currently measure). Top right highlights which rules were used to move from the original slide to the new slide. Specific changes as highlighted by Rule 7 include increasing contrast by changing the background color, increasing font size, changing to sans serif fonts, and removing all capital text and underlining (using bold to draw attention). PDGFR, platelet-derived growth factor receptor.
https://doi.org/10.1371/journal.pcbi.1009554.g001
Rule 2: Spend only 1 minute per slide
When you present your slide in the talk, it should take 1 minute or less to discuss. This rule is really helpful for planning purposes—a 20-minute presentation should have somewhere around 20 slides. Also, frequently giving your audience new information to feast on helps keep them engaged. During practice, if you find yourself spending more than a minute on a slide, there’s too much for that one slide—it’s time to break up the content into multiple slides or even remove information that is not wholly central to the story you are trying to tell. Reduce, reduce, reduce, until you get to a single message, clearly described, which takes less than 1 minute to present.
Rule 3: Make use of your heading
When each slide conveys only one message, use the heading of that slide to write exactly the message you are trying to deliver. Instead of titling the slide “Results,” try “CTNND1 is central to metastasis” or “False-positive rates are highly sample specific.” Use this landmark signpost to ensure that all the content on that slide is related exactly to the heading and only the heading. Think of the slide heading as the introductory or concluding sentence of a paragraph and the slide content the rest of the paragraph that supports the main point of the paragraph. An audience member should be able to follow along with you in the “paragraph” and come to the same conclusion sentence as your header at the end of the slide.
Rule 4: Include only essential points
While you are speaking, audience members’ eyes and minds will be wandering over your slide. If you have a comment, detail, or figure on a slide, have a plan to explicitly identify and talk about it. If you don’t think it’s important enough to spend time on, then don’t have it on your slide. This is especially important when faculty are present. I often tell students that thesis committee members are like cats: If you put a shiny bauble in front of them, they’ll go after it. Be sure to only put the shiny baubles on slides that you want them to focus on. Putting together a thesis meeting for only faculty is really an exercise in herding cats (if you have cats, you know this is no easy feat). Clear and concise slide design will go a long way in helping you corral those easily distracted faculty members.
Rule 5: Give credit, where credit is due
An exception to Rule 4 is to include proper citations or references to work on your slide. When adding citations, names of other researchers, or other types of credit, use a consistent style and method for adding this information to your slides. Your audience will then be able to easily partition this information from the other content. A common mistake people make is to think “I’ll add that reference later,” but I highly recommend you put the proper reference on the slide at the time you make it, before you forget where it came from. Finally, in certain kinds of presentations, credits can make it clear who did the work. For the faculty members heading labs, it is an effective way to connect your audience with the personnel in the lab who did the work, which is a great career booster for that person. For graduate students, it is an effective way to delineate your contribution to the work, especially in meetings where the goal is to establish your credentials for meeting the rigors of a PhD checkpoint.
Rule 6: Use graphics effectively
As a rule, you should almost never have slides that only contain text. Build your slides around good visualizations. It is a visual presentation after all, and as they say, a picture is worth a thousand words. However, on the flip side, don’t muddy the point of the slide by putting too many complex graphics on a single slide. A multipanel figure that you might include in a manuscript should often be broken into 1 panel per slide (see Rule 1 ). One way to ensure that you use the graphics effectively is to make a point to introduce the figure and its elements to the audience verbally, especially for data figures. For example, you might say the following: “This graph here shows the measured false-positive rate for an experiment and each point is a replicate of the experiment, the graph demonstrates …” If you have put too much on one slide to present in 1 minute (see Rule 2 ), then the complexity or number of the visualizations is too much for just one slide.
Rule 7: Design to avoid cognitive overload
The type of slide elements, the number of them, and how you present them all impact the ability for the audience to intake, organize, and remember the content. For example, a frequent mistake in slide design is to include full sentences, but reading and verbal processing use the same cognitive channels—therefore, an audience member can either read the slide, listen to you, or do some part of both (each poorly), as a result of cognitive overload [ 4 ]. The visual channel is separate, allowing images/videos to be processed with auditory information without cognitive overload [ 6 ] (Rule 6). As presentations are an exercise in listening, and not reading, do what you can to optimize the ability of the audience to listen. Use words sparingly as “guide posts” to you and the audience about major points of the slide. In fact, you can add short text fragments, redundant with the verbal component of the presentation, which has been shown to improve retention [ 7 ] (see Fig 1 for an example of redundant text that avoids cognitive overload). Be careful in the selection of a slide template to minimize accidentally adding elements that the audience must process, but are unimportant. David JP Phillips argues (and effectively demonstrates in his TEDx talk [ 5 ]) that the human brain can easily interpret 6 elements and more than that requires a 500% increase in human cognition load—so keep the total number of elements on the slide to 6 or less. Finally, in addition to the use of short text, white space, and the effective use of graphics/images, you can improve ease of cognitive processing further by considering color choices and font type and size. Here are a few suggestions for improving the experience for your audience, highlighting the importance of these elements for some specific groups:
- Use high contrast colors and simple backgrounds with low to no color—for persons with dyslexia or visual impairment.
- Use sans serif fonts and large font sizes (including figure legends), avoid italics, underlining (use bold font instead for emphasis), and all capital letters—for persons with dyslexia or visual impairment [ 8 ].
- Use color combinations and palettes that can be understood by those with different forms of color blindness [ 9 ]. There are excellent tools available to identify colors to use and ways to simulate your presentation or figures as they might be seen by a person with color blindness (easily found by a web search).
- In this increasing world of virtual presentation tools, consider practicing your talk with a closed captioning system capture your words. Use this to identify how to improve your speaking pace, volume, and annunciation to improve understanding by all members of your audience, but especially those with a hearing impairment.
Rule 8: Design the slide so that a distracted person gets the main takeaway
It is very difficult to stay focused on a presentation, especially if it is long or if it is part of a longer series of talks at a conference. Audience members may get distracted by an important email, or they may start dreaming of lunch. So, it’s important to look at your slide and ask “If they heard nothing I said, will they understand the key concept of this slide?” The other rules are set up to help with this, including clarity of the single point of the slide (Rule 1), titling it with a major conclusion (Rule 3), and the use of figures (Rule 6) and short text redundant to your verbal description (Rule 7). However, with each slide, step back and ask whether its main conclusion is conveyed, even if someone didn’t hear your accompanying dialog. Importantly, ask if the information on the slide is at the right level of abstraction. For example, do you have too many details about the experiment, which hides the conclusion of the experiment (i.e., breaking Rule 1)? If you are worried about not having enough details, keep a slide at the end of your slide deck (after your conclusions and acknowledgments) with the more detailed information that you can refer to during a question and answer period.
Rule 9: Iteratively improve slide design through practice
Well-designed slides that follow the first 8 rules are intended to help you deliver the message you intend and in the amount of time you intend to deliver it in. The best way to ensure that you nailed slide design for your presentation is to practice, typically a lot. The most important aspects of practicing a new presentation, with an eye toward slide design, are the following 2 key points: (1) practice to ensure that you hit, each time through, the most important points (for example, the text guide posts you left yourself and the title of the slide); and (2) practice to ensure that as you conclude the end of one slide, it leads directly to the next slide. Slide transitions, what you say as you end one slide and begin the next, are important to keeping the flow of the “story.” Practice is when I discover that the order of my presentation is poor or that I left myself too few guideposts to remember what was coming next. Additionally, during practice, the most frequent things I have to improve relate to Rule 2 (the slide takes too long to present, usually because I broke Rule 1, and I’m delivering too much information for one slide), Rule 4 (I have a nonessential detail on the slide), and Rule 5 (I forgot to give a key reference). The very best type of practice is in front of an audience (for example, your lab or peers), where, with fresh perspectives, they can help you identify places for improving slide content, design, and connections across the entirety of your talk.
Rule 10: Design to mitigate the impact of technical disasters
The real presentation almost never goes as we planned in our heads or during our practice. Maybe the speaker before you went over time and now you need to adjust. Maybe the computer the organizer is having you use won’t show your video. Maybe your internet is poor on the day you are giving a virtual presentation at a conference. Technical problems are routinely part of the practice of sharing your work through presentations. Hence, you can design your slides to limit the impact certain kinds of technical disasters create and also prepare alternate approaches. Here are just a few examples of the preparation you can do that will take you a long way toward avoiding a complete fiasco:
- Save your presentation as a PDF—if the version of Keynote or PowerPoint on a host computer cause issues, you still have a functional copy that has a higher guarantee of compatibility.
- In using videos, create a backup slide with screen shots of key results. For example, if I have a video of cell migration, I’ll be sure to have a copy of the start and end of the video, in case the video doesn’t play. Even if the video worked, you can pause on this backup slide and take the time to highlight the key results in words if someone could not see or understand the video.
- Avoid animations, such as figures or text that flash/fly-in/etc. Surveys suggest that no one likes movement in presentations [ 3 , 4 ]. There is likely a cognitive underpinning to the almost universal distaste of pointless animations that relates to the idea proposed by Kosslyn and colleagues that animations are salient perceptual units that captures direct attention [ 4 ]. Although perceptual salience can be used to draw attention to and improve retention of specific points, if you use this approach for unnecessary/unimportant things (like animation of your bullet point text, fly-ins of figures, etc.), then you will distract your audience from the important content. Finally, animations cause additional processing burdens for people with visual impairments [ 10 ] and create opportunities for technical disasters if the software on the host system is not compatible with your planned animation.
Conclusions
These rules are just a start in creating more engaging presentations that increase audience retention of your material. However, there are wonderful resources on continuing on the journey of becoming an amazing public speaker, which includes understanding the psychology and neuroscience behind human perception and learning. For example, as highlighted in Rule 7, David JP Phillips has a wonderful TEDx talk on the subject [ 5 ], and “PowerPoint presentation flaws and failures: A psychological analysis,” by Kosslyn and colleagues is deeply detailed about a number of aspects of human cognition and presentation style [ 4 ]. There are many books on the topic, including the popular “Presentation Zen” by Garr Reynolds [ 11 ]. Finally, although briefly touched on here, the visualization of data is an entire topic of its own that is worth perfecting for both written and oral presentations of work, with fantastic resources like Edward Tufte’s “The Visual Display of Quantitative Information” [ 12 ] or the article “Visualization of Biomedical Data” by O’Donoghue and colleagues [ 13 ].
Acknowledgments
I would like to thank the countless presenters, colleagues, students, and mentors from which I have learned a great deal from on effective presentations. Also, a thank you to the wonderful resources published by organizations on how to increase inclusivity. A special thanks to Dr. Jason Papin and Dr. Michael Guertin on early feedback of this editorial.
- View Article
- PubMed/NCBI
- Google Scholar
- 3. Teaching VUC for Making Better PowerPoint Presentations. n.d. Available from: https://cft.vanderbilt.edu/guides-sub-pages/making-better-powerpoint-presentations/#baddeley .
- 8. Creating a dyslexia friendly workplace. Dyslexia friendly style guide. nd. Available from: https://www.bdadyslexia.org.uk/advice/employers/creating-a-dyslexia-friendly-workplace/dyslexia-friendly-style-guide .
- 9. Cravit R. How to Use Color Blind Friendly Palettes to Make Your Charts Accessible. 2019. Available from: https://venngage.com/blog/color-blind-friendly-palette/ .
- 10. Making your conference presentation more accessible to blind and partially sighted people. n.d. Available from: https://vocaleyes.co.uk/services/resources/guidelines-for-making-your-conference-presentation-more-accessible-to-blind-and-partially-sighted-people/ .
- 11. Reynolds G. Presentation Zen: Simple Ideas on Presentation Design and Delivery. 2nd ed. New Riders Pub; 2011.
- 12. Tufte ER. The Visual Display of Quantitative Information. 2nd ed. Graphics Press; 2001.

- Publication Recognition
How to Make a PowerPoint Presentation of Your Research Paper
- 4 minute read
- 117.5K views
Table of Contents
A research paper presentation is often used at conferences and in other settings where you have an opportunity to share your research, and get feedback from your colleagues. Although it may seem as simple as summarizing your research and sharing your knowledge, successful research paper PowerPoint presentation examples show us that there’s a little bit more than that involved.
In this article, we’ll highlight how to make a PowerPoint presentation from a research paper, and what to include (as well as what NOT to include). We’ll also touch on how to present a research paper at a conference.
Purpose of a Research Paper Presentation
The purpose of presenting your paper at a conference or forum is different from the purpose of conducting your research and writing up your paper. In this setting, you want to highlight your work instead of including every detail of your research. Likewise, a presentation is an excellent opportunity to get direct feedback from your colleagues in the field. But, perhaps the main reason for presenting your research is to spark interest in your work, and entice the audience to read your research paper.
So, yes, your presentation should summarize your work, but it needs to do so in a way that encourages your audience to seek out your work, and share their interest in your work with others. It’s not enough just to present your research dryly, to get information out there. More important is to encourage engagement with you, your research, and your work.
Tips for Creating Your Research Paper Presentation
In addition to basic PowerPoint presentation recommendations, which we’ll cover later in this article, think about the following when you’re putting together your research paper presentation:
- Know your audience : First and foremost, who are you presenting to? Students? Experts in your field? Potential funders? Non-experts? The truth is that your audience will probably have a bit of a mix of all of the above. So, make sure you keep that in mind as you prepare your presentation.
Know more about: Discover the Target Audience .
- Your audience is human : In other words, they may be tired, they might be wondering why they’re there, and they will, at some point, be tuning out. So, take steps to help them stay interested in your presentation. You can do that by utilizing effective visuals, summarize your conclusions early, and keep your research easy to understand.
- Running outline : It’s not IF your audience will drift off, or get lost…it’s WHEN. Keep a running outline, either within the presentation or via a handout. Use visual and verbal clues to highlight where you are in the presentation.
- Where does your research fit in? You should know of work related to your research, but you don’t have to cite every example. In addition, keep references in your presentation to the end, or in the handout. Your audience is there to hear about your work.
- Plan B : Anticipate possible questions for your presentation, and prepare slides that answer those specific questions in more detail, but have them at the END of your presentation. You can then jump to them, IF needed.
What Makes a PowerPoint Presentation Effective?
You’ve probably attended a presentation where the presenter reads off of their PowerPoint outline, word for word. Or where the presentation is busy, disorganized, or includes too much information. Here are some simple tips for creating an effective PowerPoint Presentation.
- Less is more: You want to give enough information to make your audience want to read your paper. So include details, but not too many, and avoid too many formulas and technical jargon.
- Clean and professional : Avoid excessive colors, distracting backgrounds, font changes, animations, and too many words. Instead of whole paragraphs, bullet points with just a few words to summarize and highlight are best.
- Know your real-estate : Each slide has a limited amount of space. Use it wisely. Typically one, no more than two points per slide. Balance each slide visually. Utilize illustrations when needed; not extraneously.
- Keep things visual : Remember, a PowerPoint presentation is a powerful tool to present things visually. Use visual graphs over tables and scientific illustrations over long text. Keep your visuals clean and professional, just like any text you include in your presentation.
Know more about our Scientific Illustrations Services .
Another key to an effective presentation is to practice, practice, and then practice some more. When you’re done with your PowerPoint, go through it with friends and colleagues to see if you need to add (or delete excessive) information. Double and triple check for typos and errors. Know the presentation inside and out, so when you’re in front of your audience, you’ll feel confident and comfortable.
How to Present a Research Paper
If your PowerPoint presentation is solid, and you’ve practiced your presentation, that’s half the battle. Follow the basic advice to keep your audience engaged and interested by making eye contact, encouraging questions, and presenting your information with enthusiasm.
We encourage you to read our articles on how to present a scientific journal article and tips on giving good scientific presentations .
Language Editing Plus
Improve the flow and writing of your research paper with Language Editing Plus. This service includes unlimited editing, manuscript formatting for the journal of your choice, reference check and even a customized cover letter. Learn more here , and get started today!

- Manuscript Preparation
Know How to Structure Your PhD Thesis
- Research Process
Systematic Literature Review or Literature Review?
You may also like.

What is a Good H-index?

What is a Corresponding Author?

How to Submit a Paper for Publication in a Journal
Input your search keywords and press Enter.
Expert Consult
Journal Club: How to Build One and Why
By Michelle Sharp, MD; Hunter Young, MD, MHS
Published April 6, 2022
Journal clubs are a longstanding tradition in residency training, dating back to William Osler in 1875. The original goal of the journal club in Osler’s day was to share expensive texts and to review literature as a group. Over time, the goals of journal clubs have evolved to include discussion and review of current literature and development of skills for evaluating medical literature. The ultimate goal of a journal club is to improve patient care by incorporating evidence into practice.
Why are journal clubs important?
In 2004, Alper et al . reported that it would take more than 600 hours per month to stay current with the medical literature. That leaves residents with less than 5 hours a day to eat, sleep, and care for patients if they want to stay current, and it’s simply impossible. Journal clubs offer the opportunity for residents to review the literature and stay current. Furthermore, Lee et al . showed that journal clubs improve residents’ critical appraisal of the literature.
How do you get started?
The first step to starting a journal club is to decide on the initial goal. A good initial goal is to lay the foundation for critical thinking skills using literature that is interesting to residents. An introductory lecture series or primer on study design is a valuable way to start the journal club experience. The goal of the primer is not for each resident to become a statistician, but rather to lay the foundation for understanding basic study designs and the strengths and weaknesses of each design.
The next step is to decide on the time, frequency, and duration of the journal club. This depends on the size of your residency program and leadership support. Our journal club at Johns Hopkins is scheduled monthly during the lunch hour instead of a noon conference lecture. It is essential to pick a time when most residents in your program will be available to attend and a frequency that is sustainable.
How do you get residents to come?
Generally, if you feed them, they will come. In a cross-sectional analysis of journal clubs in U.S. internal medicine residencies, Sidorov found that providing food was associated with long-lasting journal clubs. Factors associated with higher resident attendance were fewer house staff, mandatory attendance, formal teaching, and an independent journal club (separate from faculty journal clubs).
The design or format of your journal club is also a key factor for attendance. Not all residents will have time during each rotation to read the assigned article, but you want to encourage these residents to attend nonetheless. One way to engage all residents is to assign one or two residents to lead each journal club, with the goal of assigning every resident at least one journal club during the year. If possible, pick residents who are on lighter rotations, so they have more time outside of clinical duties to dissect the article. To enhance engagement, allow the assigned residents to pick an article on a topic that they find interesting.
Faculty leadership should collaborate with residents on article selection and dissection and preparation of the presentation. Start each journal club with a 10- to 20-minute presentation by the assigned residents to describe the article (as detailed below) to help residents who did not have time to read the article to participate.
What are the nuts and bolts of a journal club?
To prepare a successful journal club presentation, it helps for the structure of the presentation to mirror the structure of the article as follows:
Background: Start by briefly describing the background of the study, prior literature, and the question the paper was intended to address.
Methods: Review the paper’s methods, emphasizing the study design, analysis, and other key points that address the validity and generalizability of the results (e.g., participant selection, treatment of potential confounders, and other issues that are specific to each study design).
Results: Discuss the results, focusing on the paper’s tables and figures.
Discussion: Restate the research question, summarize the key findings, and focus on factors that can affect the validity of the findings. What are potential biases, confounders, and other issues that affect the validity or generalizability of the findings to clinical practice? The study results should also be discussed in the context of prior literature and current clinical practice. Addressing the questions that remain unanswered and potential next steps can also be useful.
Faculty participation: At our institution, the faculty sponsor meets with the assigned residents to address their questions about the paper and guide the development of the presentation, ensuring that the key points are addressed. Faculty sponsors also attend the journal club to answer questions, emphasize key elements of the paper, and facilitate the open discussion after the resident’s presentation.
How do you measure impact?
One way to evaluate your journal club is to assess the evidence-based practice skills of the residents before and after the implementation of the journal club with a tool such as the Berlin questionnaire — a validated 15-question survey that assesses evidence-based practice skills. You can also conduct a resident satisfaction survey to evaluate the residents’ perception of the implementation of the journal club and areas for improvement. Finally, you can develop a rubric for evaluation of the resident presenters in each journal club session, and allow faculty to provide feedback on critical assessment of the literature and presentation skills.
Journal clubs are a great tradition in medical training and continue to be a valued educational resource. Set your goal. Consider starting with a primer on study design. Engage and empower residents to be part of the journal club. Enlist faculty involvement for guidance and mentorship. Measure the impact.
Journal Club: How to Prepare Effectively and Smash Your Presentation

Journal club. It’s so much more than orally dictating a paper to your peers.
It’s an opportunity to get a bunch of intelligent people in one place to share ideas. It’s a means to expand the scientific vocabulary of you and the audience. It’s a way to stimulate inventive research design.
But there are so many ways it can go wrong.
Poorly explained papers dictated blandly to an unengaged audience. Confusing heaps of data shoehorned into long presentations. Everybody stood awkwardly outside a meeting room you thought would be free.
Whether you are unsure what journal club is, are thinking of starting one, or simply want to up your presentation game—you’ve landed on the ultimate journal club guide.
The whats, the whys, and the hows, all in one place.
What Is a Journal Club in Science?
A journal club is a series of meetings in which somebody is elected to present a research paper, its methods, and findings to a group of colleagues.
The broad goal is to stimulate discussion and ideas that the attendees may apply to their own work. Alternatively, someone may choose a paper because it’s particularly impactful or ingenious.
Usually, the presenter alternates per a rota, and attendance may be optional or compulsory.
The presenter is expected to choose, analyze, and present the paper to the attendees with accompanying slides.
The presentation is then followed by a discussion of the paper by the attendees. This is usually in the form of a series of questions and answers directed toward the presenter. Ergo , the presenter is expected to know and understand the paper and subject area to a moderate extent.
Why Have a Journal Club?
I get it. You’re a busy person. There’s a difficult research problem standing between you and your next tenure.
Why bother spending the time and energy participating in a series of meetings that don’t get you closer to achieving your scientific goals?
The answer: journal club does get you closer to achieving your scientific goals!
But it does this in indirect ways that subtly make you a better scientist. For example:
- It probably takes you out of your comfort zone.
- It makes you a better communicator.
- It makes you better at analyzing data.
- It improves your ability to critique research.
- It makes you survey relevant literature.
- It exposes you and your audience to new concepts.
- It exposes your audience to relevant literature.
- It improves the reading habits of you and your audience.
- It gets clever people talking to each other.
- It gives people a break from practical science.
It also provides a platform for people to share ideas based on their collective scientific experience. And every participant has a unique set of skills. So every participant has the potential to provide valuable insight.
This is what a good journal club should illicit.
Think of journal club as reading a book. It’s going to enrich you and add beneficially to the sum of your mental furniture, but you won’t know how until you’ve read it.
Need empirical evidence to convince you? Okay!
In 1988 a group of medical interns was split into two groups. One received journal club teaching and the other received a series of seminars. Approximately 86% of the journal club group reported improved reading habits. This compares to 0% in the group who received seminar-based teaching. [1]
Journal Club Template Structure
So now you know what journal club is, you might wonder, “how is it organized and structured?”
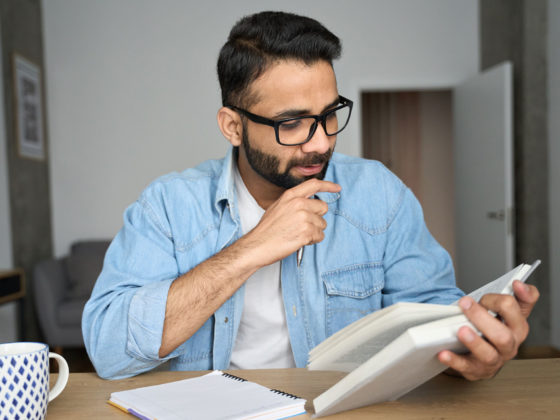
That’s what the rest of this article delves into. If you’re in a rush and need to head back to the lab, here’s a graphical summary (Figure 1).
Nobody likes meetings that flounder around and run over time. And while I have no data to prove it, I reckon people take less away from such meetings. Here’s a basic journal club template that assumes you are the presenter.
Introduce the Paper, Topic, Journal, and Authors
Let your audience know what you will be talking about before diving right in. Remember that repetition (of the important bits) can be a good thing.
Introducing the journal in which the paper is published will give your audience a rough idea of the prestige of the work.
And introducing the authors and their respective institutes gives your audience the option of stowing this information away and following it up with further reading in their own time.
Provide a Reason Why You Chose the Paper
Have the authors managed to circumvent sacrificing animals to achieve a goal that traditionally necessitated animal harm? Have the authors repurposed a method and applied it to a problem it’s not traditionally associated with? Is it simply a monumental feat of work and success?
People are probably more likely to listen and engage with you if they know why, in all politeness, you have chosen to use their time to talk about a given paper.
It also helps them focus on the relevant bits of your presentation and form cogent questions.
Orally Present Key Findings and Methods of the Paper
Simple. Read the paper. Understand it. Make some slides. Present.
Okay, there are a lot of ways you can get this wrong and make a hash of it. We’ll tell you how to avoid these pitfalls later on.
But for now, acknowledge that a journal club meeting starts with a presentation that sets up the main bit of it—the discussion.
Invite Your Audience to Participate in a Discussion
The discussion is the primary and arguably most beneficial component of journal club since it gives the audience a platform to share ideas. Ideas formulated by their previous experience.
And I’ve said already that these contributions are unique and have the potential to be valuable to your work.
That’s why the discussion element is important.
Their questions might concur and elaborate on the contents of the paper and your presentation of it.
Alternatively, they might disagree with the methods and/or conclusions. They might even disagree with your presentation of technical topics.
Try not to be daunted, however, as all of this ultimately adds to your knowledge, and it should all be conducted in a constructive spirit.
Summarize the Meeting and Thank Your Audience for Attending
There’s no particularly enlightening reason as to why to do these things. Summarizing helps people come away from the meeting feeling like it was a positive and rewarding thing to attend.
And thanking people for their time is a simple courtesy.
How Do You Organize It?
Basic steps if you are the organizer.
Okay, we’ve just learned what goes into speaking at the journal club. But presenter or not, the responsibility of organizing it might fall to you.
So, logistically , how do you prepare a journal club? Simply follow these 5 steps:
- Distribute copies of the research article to potential participants.
- Arrange a meeting time and location.
- Organize a speaker.
- Hold the journal club.
- Seek feedback on the quality of the meeting.
Apart from point 5, these are fairly self-explanatory. Regarding point 5, feedback is essential to growing as a scientist and presenter. The easiest way to seek feedback is simply to ask.
Alternatively, you could create a form for all the meetings in the series and ask the audience to complete and return it to you.
Basic Steps If You Are the Speaker
If somebody has done all the logistics for you, great! Don’t get complacent, however.
Why not use the time to elevate your presentation to make your journal club contribution memorable and beneficial?
Don’t worry about the “hows” because we’re going to elaborate on these points, but here are 5 things you can do to ace your presentation:
- Don’t leave it to the last minute.
- Know your audience.
- Keep your presentation slides simple.
- Keep your audience engaged.
- Be open to questions and critiques.
Regarding point 1, giving yourself sufficient time to thoroughly read the article you have chosen to present ensures you are familiar with the material in it. This is essential because you will be asked questions about it. A confident reply is the foundation of an enlightening discussion.
Regarding point 3, we’re going to tell you exactly how to prepare effective slides in its own section later. But if you are in a rush, minimize the use of excessive text. And if you provide background information, stick to diagrams that give an overview of results from previous work. Remember: a picture speaks louder than a thousand words.
Regarding point 4, engagement is critical. So carry out a practice run to make sure you are happy with the flow of your presentation and to give you an idea of your timing. It is important to stick to the time that is allotted for you.
This provides good practice for more formal conference settings where you will be stopped if you run over time. It’s also good manners and shows consideration for the attendees.
And regarding point 5, as the presenter, questions are likely to be directed toward you. So anticipate questions from the outset and prepare for the obvious ones to the best of your ability.
There’s a limit to everyone’s knowledge, but being unable to provide any sort of response will be embarrassing and make you seem unprepared.
Anticipate that people might also disagree with any definitions you make and even with your presentation of other people’s data. Whether or not you agree is a different matter, but present your reasons in a calm and professional manner.
If someone is rude, don’t rise to it and respond calmly and courteously. This shouldn’t happen too often, but we all have “those people” around us.
How Do You Choose a Journal Club Paper?
Consider the quality of the journal.
Just to be clear, I don’t mean the paper itself but the journal it’s published in.
An obscure journal is more likely to contain science that’s either boring, sloppy, wrong, or all three.
And people are giving up their time and hope to be stimulated. So oblige them!
Journal impact factor and rejection rate (the ratio of accepted to rejected articles) can help you decide whether a paper is worth discussing.
Consider the Impact and Scope of the Paper
Similar to the above, but remember, dross gets published in high-impact journals too. Hopefully, you’ve read the paper you want to present. But ask yourself what makes this particular paper stand out from the millions of others to be worth presenting.
Keep It Relevant and Keep It Interesting
When choosing a paper to present, keep your audience in mind. Choose something that is relevant to the particular group you are presenting to. If only you and a few other people understand the topic, it can come off as elitist.
How Do You Break Down and Present the Paper?
Know and provide the background material.
Before you dive into the data, spend a few minutes talking about the context of the paper. What did the authors know before they started this work? How did they formulate their hypothesis? Why did they choose to address it in this way?
You may want to reference an earlier paper from the same group if the paper represents a continuation of it, but keep it brief.
Try to explain how this paper tackles an unanswered question in the field.
Understand the Hypothesis and Methods of the Paper
Make a point of stating the hypothesis or main question of the paper, so everyone understands the goal of the study and has a foundation for the presentation and discussion.
Everyone needs to start on the same foot and remain on the same page as the meeting progresses.
Turn the Paper into a Progression of Scientific Questions
Present the data as a logical series of questions and answers. A well-written paper will already have done the hard work for you. It will be organized carefully so that each figure answers a specific question, and each new question builds on the answer from the previous figure.
If you’re having trouble grasping the flow of the paper, try writing up a brief outline of the main points. Try putting the experiments and conclusions in your own words, too.
Feel free to leave out parts of the figures that you think are unnecessary, or pull extra data from the supplemental figures if it will help you explain the paper better.
Ask Yourself Questions about the Paper Before You Present
We’ve touched on this already. This is to prepare you for any questions that are likely to be asked of you. When you read the paper, what bits didn’t you understand?
Simplify Unfamiliar and Difficult Concepts
Not everyone will be familiar with the same concepts. For example, most biologists will not have a rigorous definition of entropy committed to memory or know its units. The concept of entropy might crop up in a biophysics paper, however.
Put yourself in the audience’s shoes and anticipate what they might not fully understand given their respective backgrounds.
If you are unsure, ask them if they need a definition or include a short definition in your slides.
Sum Up Important Conclusions
After you’ve finished explaining the nitty-gritty details of the paper, conclude your presentation of the data with a list of significant findings.
Every conclusion will tie in directly to proving the major conclusion of the paper. It should be clear at this point how the data answers the main question.
How Do You Present a Journal Club Powerpoint?
Okay, so we’ve just gone through the steps required to break down a paper to present it effectively at journal club. But this needs to be paired with a PowerPoint presentation, and the two bridged orally by your talk. How do you ace this?
Provide Broad Context to the Research
We are all bogged down by minutia and reagents out of necessity.
Being bogged down is research. But it helps to come up for air. Ultimately, how will the research you are about to discuss benefit the Earth and its inhabitants when said research is translated into actual products?
Science can be for its own sake, but funded science rarely is. Reminding the journal club audience of the widest aims of the nominated field provides a clear starting point for the discussion and shows that you understand the efficacy of the research at its most basic level.
The Golden Rule: A Slide per Minute
Remember during lectures when the lecturer would open PowerPoint, and you would see, with dismay, that their slides went up to 90 or something daft? Then the last 20 get rushed through, but that’s what the exam question ends up being based on.
Don’t be that person!
A 10-15 minute talk should be accompanied by? 10-15 slides! Less is more.
Be Judicious about the Information You Choose to Present
If you are present everything in the paper, people might as well just read it in their own time, and we can call journal club off.
Try to abstract only the key findings. Sometimes technical data is necessary for what you are speaking about because their value affects the efficacy of the data and validity of the conclusions.
Most of the time, however, the exact experimental conditions can be left out and given on request. It’s good practice to put all the technical data that you anticipate being asked for in a few slides at the end of your talk.
Use your judgment.
Keep the Amount of Information per Slide Low for Clarity
Your audience is already listening to you and looking at the slides, so they have a limited capacity for what they can absorb. Overwhelming them with visual queues and talking to them will disengage them.
Have only a few clearly related images that apply directly to what you speaking about at the time. Annotate them with the only key facts from your talk and develop the bigger picture verbally.
This will be hard at first because you must be on the ball and confident with your subject area and speaking to an audience.
And definitely use circles, boxes, and arrows to highlight important parts of figures, and add a flowchart or diagram to explain an unfamiliar method.
Keep It Short Overall
The exact length of your meeting is up to you or the organizer. A 15-minute talk followed by a 30-minute discussion is about the right length, Add in tea and coffee and hellos, and you get to an hour.
We tend to speak at 125-150 words per minute. All these words should not be on your slides, however. So, commit a rough script to memory and rehearse it.
You’ll find that the main points you need to mention start to stand out and fall into place naturally. Plus, your slides will serve as visual queue cards.
How Do You Ask a Question in Journal Club?
A well-organized journal club will have clear expectations of whether or not questions should be asked only during the discussion, or whether interruptions during the presentation are allowed.
And I don’t mean literally how do you soliloquize, but rather how do you get an effective discussion going.
Presenters: Ask Questions to the Audience
We all know how it goes. “Any questions?” Silence.
Scientists, by their very nature, are usually introverted. Any ideas they might want to contribute to a discussion are typically outweighed by the fear of looking silly in front of their peers. Or they think everyone already knows the item they wish to contribute. Or don’t want to be publicly disproven. And so on.
Prepare some questions to ask the audience in advance. As soon as a few people speak, everyone tends to loosen up. Take advantage of this.
Audience: Think About Topics to Praise or Critique
Aside from seeking clarification on any unclear topics, you could ask questions on:
- Does the data support the conclusions?
- Are the conclusions relevant?
- Are the methods valid?
- What are the drawbacks and limitations of the conclusions?
- Are there better methods to test the hypothesis?
- How will the research be translated into real-world benefits?
- Are there obvious follow-up experiments?
- How well is the burden of proof met?
- Is the data physiologically relevant?
- Do you agree with the conclusions?
How to Keep It Fun
Make it interactive.
Quizzes and polls are a great way to do this! And QR codes make it really easy to do on-the-fly. Remember, scientists, are shy. So why not seek their participation in an anonymized form?
You could poll your audience on the quality of the work. You could make a fun quiz based on the material you’ve covered. You could do a live “what happened next?” You could even get your feedback this way. Here’s what to do:
- Create your quiz or poll using Google forms .
- Make a shareable link.
- Paste the link into a free QR code generator .
- Put the QR code in the appropriate bit of your talk.
Use Multimedia
Talking to your audience without anything to break it up is a guaranteed way of sending them all to sleep.
Consider embedding demonstration videos and animations in your talk. Or even just pausing to interject with your own anecdotes will keep everyone concentrated on you.
Keep It Informal
At the end of the day, we’re all scientists. Perhaps at different stages of our careers, but we’ve all had similar-ish trajectories. So there’s no need for haughtiness.
And research institutes are usually aggressively casual in terms of dress code, coffee breaks, and impromptu chats. Asking everyone to don a suit won’t add any value to a journal club.
Your Journal Club Toolkit in Summary
Anyone can read a paper, but the value lies in understanding it and applying it to your own research and thought process.
Remember, journal club is about extracting wisdom from your colleagues in the form of a discussion while disseminating wisdom to them in a digestible format.
Need some inspiration for your journal club? Check out the online repositories hosted by PNAS and NASPAG to get your juices flowing.
We’ve covered a lot of information, from parsing papers to organizational logistics, and effective presentation. So why not bookmark this page so you can come back to it all when it’s your turn to present?
While you’re here, why not ensure you’re always prepared for your next journal club and download bitesize bio’s free journal club checklist ?
And if you present at journal club and realize we’ve left something obvious out. Get in touch and let us know. We’ll add it to the article!
- Linzer M et al . (1988) Impact of a medical journal club on house-staff reading habits, knowledge, and critical appraisal skills . JAMA 260 :2537–41
Forgot your password?
Lost your password? Please enter your email address. You will receive mail with link to set new password.
Back to login
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- CAREER GUIDE
- 12 May 2021
Good presentation skills benefit careers — and science
- David Rubenson 0
David Rubenson is the director of the scientific-communications firm No Bad Slides ( nobadslides.com ) in Los Angeles, California.
You can also search for this author in PubMed Google Scholar
You have full access to this article via your institution.

A better presentation culture can save the audience and the larger scientific world valuable time and effort. Credit: Shutterstock
In my experience as a presentation coach for biomedical researchers, I have heard many complaints about talks they attend: too much detail, too many opaque visuals, too many slides, too rushed for questions and so on. Given the time scientists spend attending presentations, both in the pandemic’s virtual world and in the ‘face-to-face’ one, addressing these complaints would seem to be an important challenge.
I’m dispirited that being trained in presentation skills, or at least taking more time to prepare presentations, is often not a high priority for researchers or academic departments. Many scientists feel that time spent improving presentations detracts from research or clocking up the numbers that directly affect career advancement — such as articles published and the amount of grant funding secured. Add in the pressing, and sometimes overwhelming, bureaucratic burdens associated with working at a major biomedical research institute, and scientists can simply be too busy to think about changing the status quo.
Improving presentations can indeed be time-consuming. But there are compelling reasons for researchers to put this near the top of their to-do list.
You’re probably not as good a presenter as you think you are
Many scientists see problems in colleagues’ presentations, but not their own. Having given many lousy presentations, I know that it is all too easy to receive (and accept) plaudits; audiences want to be polite. However, this makes it difficult to get an accurate assessment of how well you have communicated your message.

Why your scientific presentation should not be adapted from a journal article
With few exceptions, biomedical research presentations are less effective than the speaker would believe. And with few exceptions, researchers have little appreciation of what makes for a good presentation. Formal training in presentation techniques (see ‘What do scientists need to learn?’) would help to alleviate these problems.
Improving a presentation can help you think about your own research
A well-designed presentation is not a ‘data dump’ or an exercise in advanced PowerPoint techniques. It is a coherent argument that can be understood by scientists in related fields. Designing a good presentation forces a researcher to step back from laboratory procedures and organize data into themes; it’s an effective way to consider your research in its entirety.
You might get insights from the audience
Overly detailed presentations typically fill a speaker’s time slot, leaving little opportunity for the audience to ask questions. A comprehensible and focused presentation should elicit probing questions and allow audience members to suggest how their tools and methods might apply to the speaker’s research question.
Many have suggested that multidisciplinary collaborations, such as with engineers and physical scientists, are essential for solving complex problems in biomedicine. Such innovative partnerships will emerge only if research is communicated clearly to a broad range of potential collaborators.
It might improve your grant writing
Many grant applications suffer from the same problem as scientific presentations — too much detail and a lack of clearly articulated themes. A well-designed presentation can be a great way to structure a compelling grant application: by working on one, you’re often able to improve the other.
It might help you speak to important, ‘less-expert’ audiences
As their career advances, it is not uncommon for scientists to increasingly have to address audiences outside their speciality. These might include department heads, deans, philanthropic foundations, individual donors, patient groups and the media. Communicating effectively with scientific colleagues is a prerequisite for reaching these audiences.
Collection: Conferences
Better presentations mean better science
An individual might not want to spend 5 hours improving their hour-long presentation, but 50 audience members might collectively waste 50 hours listening to that individual’s mediocre effort. This disparity shows that individual incentives aren’t always aligned with society’s scientific goals. An effective presentation can enhance the research and critical-thinking skills of the audience, in addition to what it does for the speaker.
What do scientists need to learn?
Formal training in scientific presentation techniques should differ significantly from programmes that stress the nuances of public speaking.
The first priority should be to master basic presentation concepts, including:
• How to build a concise scientific narrative.
• Understanding the limitations of slides and presentations.
• Understanding the audience’s time and attention-span limitations .
• Building a complementary, rather than repetitive, relationship between what the speaker says and what their slides show.
The training should then move to proper slide design, including:
• The need for each slide to have an overarching message.
• Using slide titles to help convey that message.
• Labelling graphs legibly.
• Deleting superfluous data and other information.
• Reducing those 100-word text slides to 40 words (or even less) without losing content.
• Using colour to highlight categories of information, rather than for decoration.
• Avoiding formats that have no visual message, such as data tables.
A well-crafted presentation with clearly drawn slides can turn even timid public speakers into effective science communicators.
Scientific leaders have a responsibility to provide formal training and to change incentives so that researchers spend more time improving presentations.
A dynamic presentation culture, in which every presentation is understood, fairly critiqued and useful for its audience, can only be good for science.
Nature 594 , S51-S52 (2021)
doi: https://doi.org/10.1038/d41586-021-01281-8
This is an article from the Nature Careers Community, a place for Nature readers to share their professional experiences and advice. Guest posts are encouraged .
Related Articles

- Conferences and meetings
- Research management

Overcoming low vision to prove my abilities under pressure
Career Q&A 28 MAR 24

How a spreadsheet helped me to land my dream job
Career Column 28 MAR 24

Maple-scented cacti and pom-pom cats: how pranking at work can lift lab spirits
Career Feature 27 MAR 24

China promises more money for science in 2024
News 08 MAR 24

One-third of Indian STEM conferences have no women
News 15 NOV 23

How remote conferencing broadened my horizons and opened career paths
Career Column 04 AUG 23
Superconductivity case shows the need for zero tolerance of toxic lab culture
Correspondence 26 MAR 24
Cuts to postgraduate funding threaten Brazilian science — again

The beauty of what science can do when urgently needed
Career Q&A 26 MAR 24
Expression of Interest – Marie Skłodowska-Curie Actions – Postdoctoral Fellowships 2024 (MSCA-PF)
Academic institutions in Brittany are looking for excellent postdoctoral researchers willing to apply for a Marie S. Curie Postdoctoral Fellowship.
France (FR)
Plateforme projets européens (2PE) -Bretagne
Tenure-track Assistant Professor in Ecological and Evolutionary Modeling
Tenure-track Assistant Professor in Ecosystem Ecology linked to IceLab’s Center for modeling adaptive mechanisms in living systems under stress
Umeå, Sweden
Umeå University
Faculty Positions in Westlake University
Founded in 2018, Westlake University is a new type of non-profit research-oriented university in Hangzhou, China, supported by public a...
Hangzhou, Zhejiang, China
Westlake University

Postdoctoral Fellowships-Metabolic control of cell growth and senescence
Postdoctoral positions in the team Cell growth control by nutrients at Inst. Necker, Université Paris Cité, Inserm, Paris, France.
Paris, Ile-de-France (FR)
Inserm DR IDF Paris Centre Nord
Zhejiang Provincial Hospital of Chinese Medicine on Open Recruitment of Medical Talents and Postdocs
Director of Clinical Department, Professor, Researcher, Post-doctor
The First Affiliated Hospital of Zhejiang Chinese Medical University
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.19(9); 2019 Sep
Seven tips for giving an engaging and memorable presentation
Effective and memorable presentations should be fun, and informative for the presenters and the learners. Engaging presenters stimulate connections with the audience. Excellent presentations not only provide information, but also give opportunities to apply new ideas during and after the talk to ‘real-life’ situations, and add relevant ‘take-home’ messages. 1 In this article we highlight educational techniques that can be used to enhance the impact of a presentation. Although all these techniques can be incorporated in the modified form into large plenary lectures, we suggest that the ‘think-pair-share’, ‘role-playing’, and ‘flipped classroom’ techniques may be more effective in smaller classroom settings.
Tip 1: Know your audience—before and during your talk
Every audience has a different level of interest, knowledge, and experience. A presentation about asthma should be different when given to patients compared with intensivists. The presenter should have a clear a priori idea of why the learners are coming to this lecture, what may motivate them, and what would be valuable to them . Whenever feasible, an assessment of the audience's needs is helpful for the presenter to focus on meaningful points. Sometimes needs-based assessments are prepared in advance, depending on the lecture or meeting, and this information may be available from the organisers of the meeting. However, if the information is not available beforehand, there are methods for collecting real-time assessments that are themselves engaging to learners. Another benefit of engaging audiences in this way is that an audience response system (ARS) can provide real-time feedback before, during, and after a presentation. 2 ARS can range from low-technology (hand raising), to newer generation ‘iClicker’ devices, or online websites such as Poll Everywhere, which can also be used to collect free-text responses. The audience's responses can help learners reinforce the importance of the topic, and provide a gauge for the presenter to customise subsequent information. Furthermore, research has shown that incorporation of multiple-choice questions to allow for ‘test-taking’ is an effective way of solidifying new knowledge. 2 Advantages of web-based ARS programs are that they are free, user-friendly, and accessible by various mobile devices. The potential disadvantages are reliability of Wi-Fi or cell phone carrier connectivity in a lecture theatre. In the absence of connectivity, an invitation to raise hands can engage participants, although without anonymity.
Tip 2: Tell a story
Stories connect people. A story that is personal to the speaker can evoke memories that are relatable and add concrete meaning to the presentation. 3 Consider starting your presentation with a story that shows why the topic is important to you. In addition, stories focus the audience on the speaker, rather than a slideshow. Even when the stories are not based on personal experiences, they can invoke learners to imagine themselves in similar situations applying knowledge to solve a problem. Descriptions of clinical cases that focus on initial presentations of patients allow learners to imagine seeing that patient and stimulate critical thinking. Experiencing the case vicariously makes the learning more memorable.
Tip 3: Trigger videos
Trigger videos are short (ideally 30 s to 3 min) audiovisual clips that represent a case or problem. Videos can be created using a handheld video recorder or smartphone, and edited using movie-editing software. Alternatively, videos can be found online and incorporated into presentations with appropriate attributions. Chosen well, trigger videos can present a thought-provoking dilemma that encourages discussion and debate. 4 They can alter the dynamics of a presentation. Success requires careful linking or embedding the videos into the presentation, making sure they play on the computer and projector, and confirming appropriate loudness of the audio settings.
Tip 4: Think-pair-share
When introducing a novel concept to a small group, consider using the ‘think-pair-share’ technique. In this technique, learners first think quietly about the challenging idea, then pair with neighbours to discuss, and then share their collective thoughts with the audience. 5 This technique gives the audience time to pause, think, and reflect on educational content. Encouraging the audience to come to work with the knowledge in a collaborative way incorporates experiential learning into your presentation. To be successful, allow for extra time in the presentation, ensure the audience's seating arrangement is conducive to small conversations, and display summarised ideas for referencing throughout the presentation. 5 , 6
Tip 5: Role play
When presenting an abstract concept that is controversial or thought-provoking, the use of scripted actors can be helpful. Both exemplary and poor examples can be demonstrated for topics such as obtaining informed consent, speaking up about safety concerns, or giving difficult feedback. Similarly, small group role-play can allow audience members to practice and experiment with actions and language with their peers. 7 The instructor should introduce the exercise in a way that helps assure psychological safety among learners, with an emphasis on deliberate practice rather than perfect performance.
Tip 6: ‘Flip’ the classroom
In situations where homework is assigned, consider ‘flipping’ the classroom experience where work is prepared by the learners before the teaching session. Preparatory work can comprise reading material or watching videos of lectures or demonstrations. This allows for more active collaborative learning, for example learners can solve a diagnostic challenge together, debate the pros and cons of a controversial topic, or practice skills. 8 The classroom experience is enriched by the interaction of many learners, rather than the perspective of a single presenter.
Tip 7: Applying the ‘take-home message’
Many are familiar with the framework of ‘ tell them what you are going to say, say it, and then summarise what you just said. ’ We advocate an additional component in the conclusion, where learners are challenged to commit to a change in their behaviour as a result of something they just learned: ‘ What is something you can do differently and better tomorrow or with your next patient as a result of this presentation? ’ Incorporating this question in the evaluation of a presentation can help facilitate behaviour change by having the learners write an example. Similarly, incentives can be offered for behaviour change: ‘ We have your email addresses, and with your permission we would like to follow-up with you in 2 weeks to see if you have any stories to share about applying this new information. We'll be collecting the responses and having a raffle to select one person to receive a gift card... ’ Not only does this provide an incentive to experimentation, but it also gives valuable and often heart-warming feedback to the presenter.
Dynamic educational techniques increase the engagement of the audience. We emphasise the importance of connecting with the learners and obtaining a commitment to apply the new knowledge for change and improvement. The extent to which these techniques are used will depend on the level of audience expertise, time constraints, and access to audiovisual aids. When used, they can result in a more memorable experience for both learners and presenters.
Declaration of interest
The authors declare that they have no conflicts of interest.
Biographies
Christine Mai MD MS-HPEd is assistant professor of anesthesia at Harvard Medical School and program director of the Pediatric Anesthesia Fellowship at Massachusetts General Hospital. Her clinical and research interests are in simulation education and graduate medical education.
Rebecca Minehart MD MS-HPEd is assistant professor of anesthesia at Harvard Medical School and program director of the Obstetric Anesthesia Fellowship at Massachusetts General Hospital.
May Pian-Smith MD is associate professor of anesthesia at Harvard Medical School and director of quality and safety for the Department of Anesthesia, Critical Care and Pain Medicine at Massachusetts General Hospital.
Matrix codes: 1H02, 2H02, 3J02
Journal Article Presentation
Jul 30, 2014
330 likes | 1.59k Views
A Corpus-based Contrastive Analysis of First Personal Deixis By: Yujie Su ( College of Foreign Studies, Wenzhou University, Wenzhou ). Journal Article Presentation. Group 1: Anik Damaris Maria Rofik. ABSTRACT.
Share Presentation
- friendly relation
- chinese teaching system
- innate defects
- anik damaris maria rofik
- journal article presentation group
- personal deixis

Presentation Transcript
A Corpus-based Contrastive Analysis of First Personal Deixis By: Yujie Su (College of Foreign Studies, Wenzhou University, Wenzhou) Journal Article Presentation Group 1: Anik Damaris Maria Rofik
ABSTRACT • This research centered on comparing the use of first personal deixis in Chinese English Learner Corpus (CLEC) and English-native Speaker Corpus such as FROWN and FLOB. It also made a close investigation into the frequency difference of first nominative personal deixis, that is, “I” and “we”, and their practical use with modal verbs in the three corpora.
Introduction • This investigation was conducted because seeing that Chinese English learners, advanced or primary, wereusually unconsciously influenced by their mother language when learning and using English. They often preferedto use the first personal deixis like “I” or “we” and other alternative forms like “me”, “us”, “my”, “our”, and so on. • Therefore, we wantedto find out the underlying reason. The investigation was conducted into three corpora, Chinese English Learner Corpus, FROWN and FLOB. • We also made comparison of the frequency of the nominative first personal deixis, that is “I” and “we”, as well as the frequency of their practical use with modal verbs in the three corpora.
COMPARISON AND ANALYSIS OF ENGLISH LEARNERS AND NATIVE SPEAKERS CORPORA Definition of Chinese English Learner Corpus (CLEC) • Chinese English Learner Corpus (CLEC), sponsored and constructed by Professor Gui Shichun from Guangdong University of Foreign studies, contains 1 million words of English compositions collected from Chinese learners of English with differing levels of proficiency, covering senior secondary school students, English-major, and non-English-major university students in China.
Freiburg-LOB Corpus of British English (FLOB) and Freiburg-Brown Corpus of American English (FROWN) Corpora of English native speakers ARE
The Purposes of the research: • It can helpto learn about the different way of expression, like the overuse or underuse of certain words or expressions as well as learner’s difficulty when learning or using the language. • It is practically useful for studying learners’ learning strategy and getting teachers of the language to notice learners’ difficulties or problems.
COMPARISON AND ANALYSIS OF ENGLISH LEARNERS AND NATIVE SPEAKERS CORPORA • In English, there is a distinction between nominative and accusative first personal deixis, such as “I” and “me”, “we” and “us”. Their possessive forms are respectively “myself, my” and “ourselves, our”. • However, in Chinese there is only a division between the singular form and plural form of the nominative and accusative first personal deixis. • Comparing with the different variations in English, Chinese first personal deixis has fewer and simpler changes.
TABLE 1 THE FREQUENCY OF THE FIRST PERSONAL DEIXIS IN CLEC, FLOB AND FROWN
The Explanation from the Table • It is clear that thesingular forms of the first personal deixis are much more frequently used by learners than their plural forms. Chinese English learners are more often to use “I” and “we”. The frequency of “I” in CLEC is 16,216, which is almost 3 times larger than that in FLOB and FROWN. The frequency of “we” in CLEC is more than 6 times higher than that in FLOB and FROWN.
In order to know more about the phenomena, detailed investigations are conducted. By means of the software WORDSMITH, modal verbs which Chinese English learners prefer to use together with “we” and “I” are searched according to the key word in context. It is found that the modal verb “must” is used most often, followed by “will”, “would”, “shall”, “can”, “should”, “may”, etc.
ANALYSIS OF THE DATA AND THE POSSIBLE REASONS • Generally speaking, personal deixis refers to the terms the speakers use to convey their message with the words when they call each other during the conversation. There are three types of personal deixis: the first personal deixis, the second deixis and the third deixis. In the research, Chinese and English have a similar division of the personal deixis. However, as for the first personal deixis, the alleged scope in Chinese and English is different. Based on the previous researches who have conducted various studies on personal deixis. Most of their researches is centered on “cultural aspects”.
Still the analysis..... • In English the singular first personal deixis “I” can be used in formal and informal contexts, which has a clear and specific referent. In English, the first person “I” generally refers to the speaker himself or herself, expressing his or her own views. It seldom includes the listener. • This is similar to the first person in Chinese. The plural first person “we” in Chinese has a similar alleged scope as that in English, which refers to the speaker’s side or both the speaker and the listener.
But in conversations when the speaker and the listener are from different ranks, or the speaker wants to persuade or encourage the listener, “we” can be used to refer to the listener. “we” can also refer to the speaker only. • For example, one of the staff says to a friend who does not work at the same department, “We have a kind leader.” Here in this sentence “we” refers to the speaker only.
The Results of the Reseach: • Chinese English learners are frequently under the influence of traditional Chinese culture and values, preferring to use the collective “we” to represent an individual “I”. The reason is that the use of “I” means the feeling when one is isolated from the collective or one endangers the unity of the community. That is why the individual “I” is basically excluded from the collective written culture affected by Confucianism, Taoism, and Buddhism. On the contrary, plural forms of the first personal deixis are much welcomed. Therefore, as for Chinese English learners, the use of the collective “we” can help bring both sides of the communication closer to each other and build an equal and friendly relation. So in their writing they often use “we will”, “we must”, “we can”, etc.
The reasons behind the different using habit of the first personal deixis first go to the difference between the two languages and then lie in the fact that in China English teaching has its innate defects. In other words, in China English is only used or learned as a foreign language. In English classes English is mainly taught by teachers whose first language is Chinese, and who used to be English learners themselves. And the teachers learned the language in a traditional Chinese teaching system. As a result, they often teach what they deem to be true or right.
CONCLUSION • English and Chinese have different language systems. English learners are inevitably under the influence of their mother tongue. • In order to reduce the negative transfer of the mother tongue, the teachers may make use of various corpora and explain to the students the different cognition of the first personal deixis of English-native speakers and English learners by show them the particular examples. • The contrastive analysis of both the English learner corpus and the English native speaker corpus can help the students to understand better so that they can be aware of the negative transfer of Chinese when they say or write something.
- More by User
Birth & Journal Article #1
Birth & Journal Article #1. Lecture 3 Chapter 4 and Cooper & Aslin (1990) Psych 1643. Extra Credit Quiz #1. 1) The researchers found that __________speech had a higher average frequency and a wider frequency range than ________ speech.
604 views • 31 slides
JOURNAL CLUB ARTICLE
Date: February 1, 2006Title
312 views • 0 slides
Outlining the Average Journal Article:
Outlining the Average Journal Article:. A Quick Look at the Sections Taken from Cantor A Guide to Academic Writing with additions. Jennifer L. Bowie . The Title & Abstract. The Title: Make it concise and applicable See Huff & our earlier title discussions for more details The Abstract:
371 views • 11 slides
Critically Appraising a Journal Article
Critically Appraising a Journal Article. What is a Journal Club?. An educational meeting in which a group of individuals read, evaluate and discuss current articles from the biomedical literature A collective forum to provide a venue to keep up with the literature
602 views • 46 slides
Pico journal article presentation Maria Nguyen
Pico journal article presentation Maria Nguyen. BACKGROUND. Asthma is a common, potentially life-threatening condition Accounts for 2 million pediatric ED visits annually 500, 000 hospitalizations ~ $ 6 billion in total healthcare expenditures on an annual basis
703 views • 52 slides

JOURNAL ARTICLE
JOURNAL ARTICLE . BY: ASHLEY PATTON HUMN240-E2WW PROFESSOR, JENNIFER KRASNO. JOURNAL ARTICLE. CLASS ON FIRE: USING THE HUNGER GAMES TRILOGY TO ENCOURAGE SOCIAL ACTION AUTHOR: AMBER SIMMONS. MAIN POINTS .
719 views • 9 slides
JOURNAL PRESENTATION
JOURNAL PRESENTATION. Al Jadidi Bin Sulaiman Moderator : Dr Abdul Karim. Introduction. Rapid sequence induction and intubation (RSII) is performed when there is an increased risk of pulmonary aspiration of gastric contents Consists of following:
660 views • 51 slides

Writing a Journal Article
Writing a Journal Article. Sections of a Journal Article. Introduction or Statement of Purpose Literature Review Specific Statement of Hypothesis( es ) Description of Methods Results Summary and Conclusions Abstract. Statement of Purpose. The statement of purpose should
463 views • 13 slides
Journal Article, Name of Journal Journal Article, Name of Journal
Poster Title Researchers ’ /Presenters ’ Names Department(s). General formatting tips: Retain a border on the sides of the slide that is a minimum of 1/32 ” (this slide has 1/32” borders). Use at least an 18 point font. Dark text on a light background is most legible.
192 views • 1 slides
Article Presentation
Article Presentation. By : Jaquella Alston. Teacher-Created Electronic Books: Integrating Technology to Support Readers with Disabilities. By Joan A. Rhodes, Tammy Milby.
483 views • 7 slides
The Scholarly Journal Article
The Scholarly Journal Article . Writing in CSD. Title . Should be brief, informative, and descriptive of the subject matter. Should contain keywords/variables. Abstract . Short summary of the entire article: purpose, method, results, and conclusions.
329 views • 10 slides
Journal Article Search
Journal Article Search. Go to the Newman Library webpage ( www.lib.vt.edu ) Select All Databases, A-Z which opens a second page. A large list of databases then opens with those beginning with A shown.
345 views • 20 slides
Journal article reading
Journal article reading. Student: Louis Instructor: Joni Chao. The Journal Article. Article title: Bricks or mortar: which parts of the input does a second language listener rely on? Article source: TESOL Quarterly , vol.42(33), 411-432 . . Authors: John Field
550 views • 15 slides
AWWA Journal Article Review
AWWA Journal Article Review. Peter Greiner, NSF International DWAJC Meeting December, 2011. AWWA Journal Article Review. Group from Lead Task Group established to review article and determine whether there are any research findings that should be acted on. Aggressiveness of test waters:
968 views • 2 slides

JOURNAL PRESENTATION. By: Nur Izzatul Ashikin Harun Moderator: Dr Abdul Karim Othman. Complications and mortality in older surgical patients in Australia and New Zealand (the REASON study): a multicentre, prospective, observational study. Summary.
522 views • 28 slides
Reading a Scientific Journal Article
Reading a Scientific Journal Article. Dr. C.’s AP Chemistry Lake Dallas High School Fall 2014. Now some do’s. First skim the article Identify the article’s structure and features Look for the author’s main points Generate questions
766 views • 18 slides
Evidence-Based Journal Article Presentation
Evidence-Based Journal Article Presentation. [Insert your name here] [Insert your designation here] [Insert your institutional affiliation here]. Department of Obstetrics & Gynecology Greenville Hospital System University Medical Center Greenville, South Carolina. Citation.
1.26k views • 16 slides
journal article analysis sample
1.11k views • 4 slides

Research academic journal article
Find the most well written and thoroughly researched academic journal article on the internet, written by experts having years of experience.
145 views • 5 slides
journal article Perfect Education/tutorialoutletdotcom
FOR MORE CLASSES VISIT www.tutorialoutlet.com Find a legal case, journal article, or detailed news article that describes a recent criminal case involving the kind of health care facility in which you are interested in working. As you analyze your case and prepare for the Discussion, consider possible motivations behind this criminal act. What could an administrator do to prevent this from happening or to address it effectively once it is detected? Briefly describe the case you selected. Evaluate the state and/or federal laws that are involved in your case
65 views • 3 slides
Evaluating a journal article
Evaluating a journal article. Overview:. Start with a brief summary of the article. Give the listener an overview of what was done, what was found, and the author's conclusions. Rationale:. Why was the study done? What research question did it attempt to address?
116 views • 10 slides
Evidence-Based Journal Article Presentation. [Insert your name here] [Insert your designation here] [Insert your institutional affiliation here]. Department of [Insert your department name] Tabriz University of Medical Sciences. Citation. Insert Article Title Insert Author Names
222 views • 16 slides
CEE Comm Lab helps first-year undergraduates present scientific research
The following is a modified excerpt from the MIT News article, “ First-year MIT students gain hands-on research experience in supportive peer community ” by Callie Ayoub.
During MIT’s Independent Activities Period (IAP) this January, first-year students interested in civil and environmental engineering (CEE) participated in a four-week undergraduate research opportunities program known as the mini-UROP (1.097). The six-unit subject pairs first-year students with a CEE graduate student or postdoc mentor, providing them with an inside look at the research being conducted in the department. The program culminates with a presentation event open to the entire CEE community.
Overall, eight labs in the department opened their doors to the 2024 cohort, who were eager to take advantage of the opportunity to collaborate with current students and build a community around their interests. The interdisciplinary nature of the department’s research offered participants a wide range of projects to work on, from redefining autonomous vehicle deployment to mitigating the effects of drought on crops.
Mini-UROP participant Iraira Rivera Rojas works in the Marelli Lab in CEE.
Throughout the duration of the mini-UROP, participants attended three workshops led by Jared Berezin , the manager of the Civil and Environmental Engineering Communication Lab (CEE Comm Lab). The communication lab is a free resource to undergraduates, graduates, and postdocs in the CEE community, providing one-on-one coaching and interactive workshops. Held on Fridays during IAP, the workshops focused on visual and oral communication strategies to help students contextualize their projects, explain scientific concepts, describe their methodologies, and present their results.
“Students were fortunate to have research mentors in the lab, and my goal was to provide communication mentorship outside of the lab,” says Berezin. “Our weekly workshops focused on scientific communication strategies, but perhaps more importantly I’d prompt them to talk about their projects, ask questions, and brainstorm together. They really embraced the opportunity to foster a supportive peer community, which I think is a core part of the CEE experience.”

Mini-UROP participants present their research to fellow students, staff, and faculty.
A significant challenge students face while completing the program is condensing their research down to a clear and concise two-minute presentation. To assist with this task, the workshops also featured presentations by CEE Communication Fellows Ignacio Arzuaga and Matthew Goss , providing students with a preview of how their own presentations may take shape. Before the final presentation event, students also had the option to meet with Comm Fellows to receive feedback, rehearse their talks, and practice responding to questions about their work.
“The final talks were impressive, and I was proud of the students for approaching both their research and communication challenges with such curiosity and thoughtfulness,” Berezin remarks.
To learn more about the experiences of students and mentors during the 2024 mini-UROP, you can read the full MIT News article .
- Case Report
- Open access
- Published: 28 March 2024
Unusual presentation and delayed diagnosis of cardiac angiosarcoma
- Salman Zaheer 1 ,
- Alice L. Zhou 1 ,
- John M. Gross 2 &
- Ahmet Kilic 1
Journal of Cardiothoracic Surgery volume 19 , Article number: 161 ( 2024 ) Cite this article
53 Accesses
Metrics details
Primary cardiac angiosarcomas are very rare and present aggressively with high rates of metastasis. Given the poor prognosis, particularly once disease has spread, early diagnosis and multidisciplinary treatment is essential.
Case presentation
We present the case of a 46-year-old male who presented with chest pain, intermittent fevers, and dyspnea. Workup with computed tomography scan and transesophageal echocardiography demonstrated a right atrial pseudoaneurysm. Given the concern for rupture, the patient was taken to the operating room, where resection of the pseudoaneurysm and repair using a bovine pericardial patch was performed. Histopathology report initially demonstrated perivascular lymphocyte infiltrate. Six weeks later, the patient represented with chest pain and new word finding difficulty. Workup revealed multiple solid lung, pericardial, brain, and bone nodules. Eventual biopsy of a cardiophrenic nodule demonstrated angiosarcoma, and rereview of the original pathology slides confirmed the diagnosis of primary cardiac angiosarcoma.
Conclusions
Primary cardiac angiosarcomas are often misdiagnosed given the rarity of these tumors, but early diagnosis and initiation of treatment is essential. The unique presentation of our case demonstrates that clinical suspicion for cardiac angiosarcoma should be maintained for spontaneous pseudoaneurysm originating from the right atrium.
Peer Review reports
Primary cardiac angiosarcomas are very aggressive tumors that often present after metastatic spread. Given the aggressive nature of the disease, early diagnosis is essential. We describe the case of a patient with primary cardiac angiosarcoma who initially presented with a right atrial pseudoaneurysm.
We present a case of 46-year-old male with no pertinent past medical history who presented to the emergency department with ongoing chest pain for 9 days associated with intermittent fevers and shortness of breath. On examination, the patient had a heart rate of 88 beats per minute and blood pressure of 143/72 mmHg. There were no audible murmurs or rubs on auscultation. He endorsed ongoing chest pain and shortness of breath.
The patient underwent contrast computed tomography (CT) angiography pulmonary embolism with pulmonary arterial phase timing that showed no evidence of pulmonary embolism, but demonstrated a moderate sized pericardial effusion with high density concerning for hemopericardium, along with an outpouching on the right atrial wall with a narrow neck concerning for a pseudoaneurysm (Fig. 1 ). Further workup, including lab work and an electrocardiogram, were unremarkable. Transesophageal echocardiogram (TEE) redemonstrated the pericardial effusion and right atrial pseudoaneurysm (Fig. 2 ).
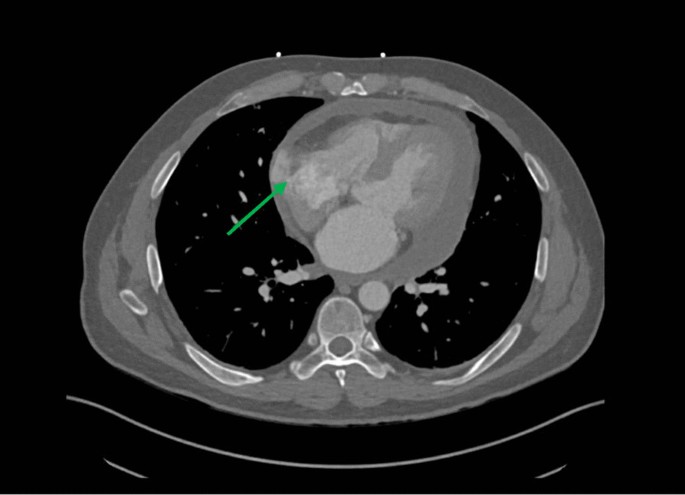
Computed tomography angiogram of the chest. Computed tomography angiogram showing a right atrial pseudoaneurysm. Neck of the pseudoaneurysm is shown by the green arrow. Attenuation of the pericardial fluid was 28.4 Hounsfield units
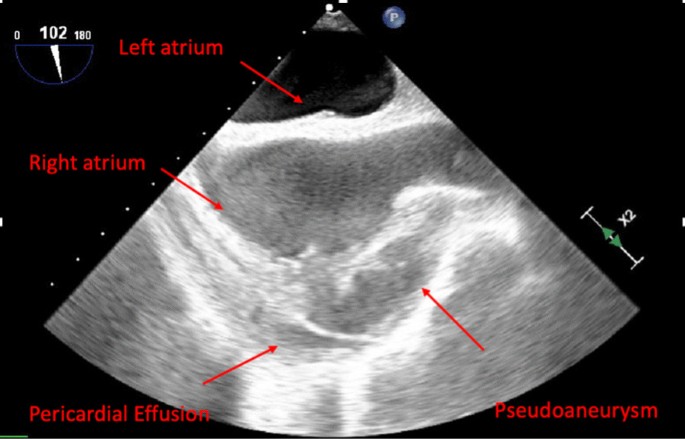
Transesophageal echocardiogram of pseudoaneurysm. Pseudoaneurysm with pericardial effusion redemonstrated on transesophageal echocardiogram arising from right atrium
The case was discussed at the multidisciplinary cardiac conference and the decision was made to take the patient to the operating room given his ongoing symptoms as well as concern for hemopericardium and rupture of pseudoaneurysm into the pericardial space. Cardiac magnetic resonance imaging (MRI) and positron emission tomography (PET) CT were not performed given time-sensitive nature of the case and the desire for tissue diagnosis. The operation was performed via median sternotomy with cardiopulmonary bypass. A pericardial effusion and dense pericardial adhesions were found intraoperatively. After meticulous lysis of adhesions, central cannulation was performed, and the aorta and right atrium were cannulated. Right atrial pseudoaneurysm was identified (Fig. 3 ) and excised with the surrounding atrial wall. The defect in the atrial wall was closed using a bovine pericardial patch. Full exploration of the chest revealed no other lesions. The resected specimen was sent for pathology to try to establish tissue diagnosis and the patient was closed. The patient’s post-operative course was unremarkable, and he was discharged home on post operative day 4. Operative cultures showed no growth. Pericardial fluid cytopathology demonstrated abundant mixed inflammation with eosinophils, reactive mesothelial cells, histiocytes, and lymphocytes, with no malignant neoplasm identified. Tissue histopathology demonstrated granulation tissue, perivascular lymphocyte infiltrate, dense fibrous tissue, focal calcification, and organizing fibrin thrombus, but no evidence of malignancy.
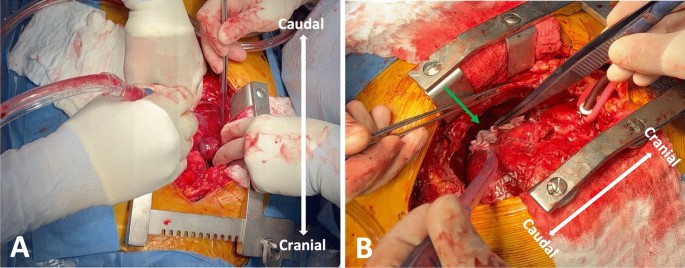
Intra-operative photos of pseudoaneurysm. Pseudoaneurysm demonstrated by green arrow. A Blue arrow indicates pseudoaneurysm. B Green arrow indicates bovine pericardial patch used to repair defect in atrial wall after pseudoaneurysm resection
Six weeks postoperatively, the patient presented to emergency department with chest pain, new word finding difficulty, clumsiness, gait instability, and intermittent low-grade fevers. A CT chest scan showed multiple halo-like solid lung, pericardial, and bone nodules (Fig. 4 A, B ). The CT head scan showed 1–1.5 cm left anterior thalamic and left temporal lobe hemorrhagic lesions. Magnetic resonance imaging of the brain demonstrated multiple enhancing lesions in the left temporal lobe, left anterior thalamus, and right parietal lobe (Fig. 4 C). Together, the findings were suspicious for hemorrhagic metastasis, invasive fungal infection (such as invasive aspergillosis), or septic emboli. Given the concern for metastatic process, a biopsy of a lung nodule was performed and showed focal organizing exudative and fibrotic pneumonia negative for carcinoma. A lumbar puncture was also performed and showed no malignant neoplasm. Given the repeated surgical specimens that were negative for malignancy, an extensive infectious and rheumatologic workup was pursued. He was discharged with outpatient infectious disease follow-up, as the most likely diagnosis on the differential was thought to be invasive fungal infection and cultures would take several weeks to result.

Imaging findings on representation. A Computed tomography (CT) of chest showing multiple lung nodules (green arrows). B CT of chest showing nodular appearance of pericardial effusion and outpouching of the right atrium. C Head magnetic resonance imaging (MRI) demonstrating peripherally enhancing lesions (red arrow)
He represented one week later with returned right-sided chest pain, intermittent headaches, and abdominal pain. Repeat CT scan demonstrated increased number of pulmonary and pericardial nodules. Given the patient’s diagnostic dilemma and ongoing symptoms, a cardiophrenic nodule was biopsied with image guidance. Pathology demonstrated atypical cells, anaplasia, and poorly-formed vascular lumina, suggestive of angiosarcoma (Fig. 5 ).
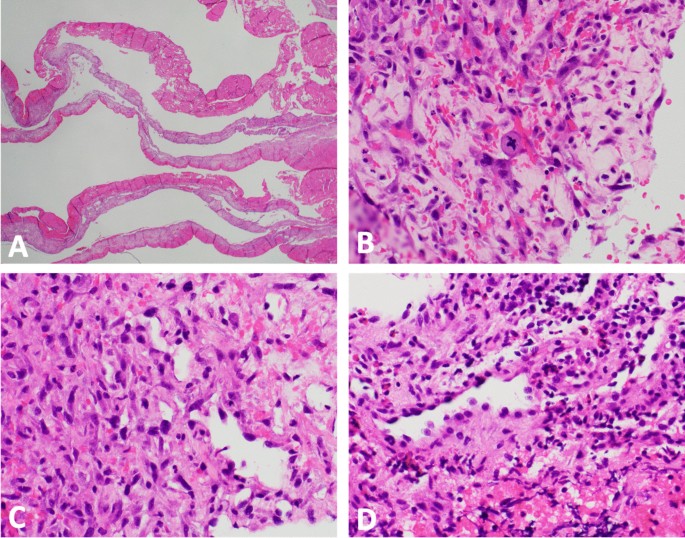
Pathology findings demonstrating angiosarcoma. A low power magnification (× 12.5) hematoxylin and eosin staining of pseudoaneurysm reveals fibrin and organizing hematoma with a variably cellular fibrous cyst wall. B High power magnification (× 400) of pseudoaneurysm reveals scattered enlarged pleomorphic tumor cells with rare atypical mitoses in the background of abundant reactive granulation tissue. C Cardiophrenic nodule (× 400) shows similar atypical cells with unequivocal anaplasia and poorly-formed vascular lumina. D Cardiophrenic nodule (× 400) shows malignant endothelial cells with endothelial hobnailing into the vascular lumen
The patient’s tissue biopsy from his initial right atrial pseudoaneurysm resection was retrospectively reviewed and similar atypical cells were noted in the background of granulation tissue and organizing thrombus (Fig. 5 ). A diagnosis of primary cardiac angiosarcoma was made. The patient is currently undergoing chemotherapy with weekly paclitaxel for metastatic cardiac angiosarcoma.
Discussion and conclusions
Primary tumors of the heart are very rare and are identified in only 1 in 500 cardiac surgical cases. Of these, malignant tumors make up only 25%, the majority (95%) of which are cardiac sarcomas [ 1 ]. Angiosarcomas are the most common histologic subtype of cardiac sarcomas (30%) and are very aggressive in nature with high rates of metastasis [ 2 ].
Cardiac angiosarcomas more frequently present in males (2–3:1 male:female ratio) and most commonly arise from the right atrium [ 3 ]. Patients often present with nonspecific symptoms such as chest pain, dyspnea, weight loss, and fatigue [ 1 ]. Later in the disease course, patients may present with more specific symptoms, such as pericardial effusion, due to local infiltration into the myocardium and neighboring structures. Over half of patients present with metastatic disease, with spread to the lungs or pleura being most common [ 3 ]. Imaging can aid in the diagnosis of cardiac angiosarcomas. CT scan often shows a large multilobular mass that comprises the majority of the right atrium [ 4 ]. Transthoracic echocardiography (TTE) often shows a large echogenic mass with poorly defined borders and can be used to understand the size and location of the mass, understand its relation to other structures, and determine if cardiac function is affected [ 5 ]. Magnetic resonance imaging (MRI) can be used to differentiate between thrombus and tumor [ 6 ]. Histopathologically, angiosarcomas are difficult to diagnose due to the cellular heterogeneity. Common tumor markers include CD34, CD31, and factor VIII [ 1 ].
Due to the aggressive nature of this cancer, early diagnosis is essential. Our case represented a diagnostic challenge and initially presented on imaging as a right atrial pseudoaneurysm with a narrow neck, as opposed to a large multilobular mass with broad-based attachment typically described for cardiac angiosarcoma [ 4 , 5 ]. Diagnosis was further delayed by the challenging histologic presentation in the context of low clinical suspicion, with malignant cells being obscured by extensive fibrin, granulation tissue, and organizing thrombus. Given these difficulties, diagnosis was not made until after distant metastatic spread and a cardiophrenic metastatic lesion was biopsied.
Given the rarity of this tumor and high mortality rate, there is no standardized approach to treatment. Without surgical resection, average survival is about 4 months [ 1 ]. The mainstay of treatment involves complete surgical resection, with a median post-operative survival of about 14 months [ 1 , 3 ]. However, achieving complete resection with negative margins is often difficult given the diagnostic delay and proximity to vascular structures and propensity for distant microscopic spread at time of diagnosis. Chemotherapy and radiation are often used in the treatment either as neoadjuvant or adjuvant therapy, but the exact role of these modalities remains unknown [ 7 , 8 ]. Overall, a multidisciplinary approach involving local resection, systemic chemotherapy, and radiation therapy seems to be the most favorable strategy.
Primary cardiac angiosarcomas are often misdiagnosed given the rarity of these tumors. Cardiac angiosarcoma presenting initially on imaging as either a right atrial pseudoaneurysm or a right coronary artery aneurysm has only been reported in a handful of case reports [ 9 , 10 , 11 , 12 , 13 , 14 ]. The unique presentation of this case demonstrates that clinical suspicion for cardiac angiosarcoma should be maintained for spontaneous pseudoaneurysm originating from the right atrium. With an aggressive disease course, early diagnosis is vital and allows for multidisciplinary care with medical and radiation oncology to offer patients the best chances of survival.
Availability of data and materials
Not applicable.
Abbreviations
Computed tomography
Magnetic resonance imaging
Positron emission tomography
Transesophageal echocardiogram
Transthoracic echocardiography
Patel SD, Peterson A, Bartczak A, et al. Primary cardiac angiosarcoma—a review. Med Sci Monit. 2014;20:103–9. https://doi.org/10.12659/MSM.889875 .
Article CAS PubMed PubMed Central Google Scholar
Ferguson PC. Surgical considerations for management of distal extremity soft tissue sarcomas. Curr Opin Oncol. 2005;17(4):366–9. https://doi.org/10.1097/01.cco.0000166651.38417.c8 .
Article PubMed Google Scholar
Look Hong NJ, Pandalai PK, Hornick JL, et al. Cardiac angiosarcoma management and outcomes: 20-year single-institution experience. Ann Surg Oncol. 2012;19(8):2707–15. https://doi.org/10.1245/s10434-012-2334-2 .
Kassop D, Donovan MS, Cheezum MK, et al. Cardiac masses on cardiac CT: a review. Curr Cardiovasc Imaging Rep. 2014;7(8):9281. https://doi.org/10.1007/s12410-014-9281-1 .
Article PubMed PubMed Central Google Scholar
Luo L, Zhao W, Wang Y, Liu K. Cardiac angiosarcoma: a case report and review of the literature. Echocardiography. 2021;38(12):2083–90. https://doi.org/10.1111/echo.15221 .
Riles E, Gupta S, Wang DD, Tobin K. Primary cardiac angiosarcoma: a diagnostic challenge in a young man with recurrent pericardial effusions. Exp Clin Cardiol. 2012;17(1):39–42.
PubMed PubMed Central Google Scholar
Penel N, Bui BN, Bay JO, et al. Phase II trial of weekly paclitaxel for unresectable angiosarcoma: the ANGIOTAX study. JCO. 2008;26(32):5269–74. https://doi.org/10.1200/JCO.2008.17.3146 .
Article CAS Google Scholar
Blackmon SH, Reardon MJ. Surgical treatment of primary cardiac sarcomas. Tex Heart Inst J. 2009;36(5):451–2.
Sawamura T, Takiya H, Yamada T, Sugimoto H, Kawai H. A case of cardiac angiosarcoma with a pseudoaneurysm formed in the right coronary artery. Kyobu Geka. 1994;47(7):565–8.
CAS PubMed Google Scholar
Serra V, Moura L, Almería C, Pérez de Isla L, Zamorano J. Right atrial rupture. Rev Port Cardiol. 2004;23(5):731–6.
PubMed Google Scholar
Berry MF, Williams M, Welsby I, Lin S. Cardiac angiosarcoma presenting with right coronary artery pseudoaneurysm. J Cardiothorac Vasc Anesth. 2010;24(4):633–5. https://doi.org/10.1053/j.jvca.2009.04.002 .
Chaturvedi A, Vummidi D, Shuman WP, Dubinsky TJ, Maki JH. Cardiac angiosarcoma: an unusual cause of coronary artery pseudoaneurysm. J Thorac Imaging. 2012;27(1):W8. https://doi.org/10.1097/RTI.0b013e3182078187 .
Kimura S, Yonekura R, Umesue M. Angiosarcoma mimicking an infected pseudoaneurysm after graft replacement. Ann Thorac Surg. 2015;100(3):1114. https://doi.org/10.1016/j.athoracsur.2015.05.084 .
Murthy JSN, Gorantla R, Periyasamy T, et al. Right atrial angiosarcoma presenting as giant pseudoaneurysm with impending rupture. IHJ Cardiovasc Case Rep. 2017;1(3):165–8. https://doi.org/10.1016/j.ihjccr.2016.09.002 .
Article Google Scholar
Download references
Acknowledgements
Author information, authors and affiliations.
Division of Cardiac Surgery, Department of Surgery, The Johns Hopkins Hospital, Baltimore, MD, USA
Salman Zaheer, Alice L. Zhou & Ahmet Kilic
Bone and Soft Tissue Pathology, The Johns Hopkins Hospital, 1800 Orleans Street, Zayed Tower Suite 7107, Baltimore, MD, 21287, USA
John M. Gross
You can also search for this author in PubMed Google Scholar
Contributions
SZ: Concept/design, drafting article, critical revision of article, approval of article. AZ: Drafting article, critical revision of article, approval of article. JG: pathological examination of the tumor sample, drafting of the article, critical revision of the article, and approval of the article. AK: Concept/design, critical revision of article, approval of article. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Salman Zaheer or Ahmet Kilic .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Consent was obtained from the patient for the publication of this report.
Competing interests
Additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zaheer, S., Zhou, A.L., Gross, J.M. et al. Unusual presentation and delayed diagnosis of cardiac angiosarcoma. J Cardiothorac Surg 19 , 161 (2024). https://doi.org/10.1186/s13019-024-02555-8
Download citation
Received : 21 April 2023
Accepted : 30 January 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s13019-024-02555-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cardiac tumor
- Pseudoaneurysm
- Angiosarcoma
- Tumor resection
- Case report
Journal of Cardiothoracic Surgery
ISSN: 1749-8090
- General enquiries: [email protected]
- Search Menu
- Advance Articles
- Case of the Year
- Competition Winners
- Grand Rounds
- ESC Content Collections
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About European Heart Journal - Case Reports
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Editor and Reviewer Programmes
- Advertising & Corporate Services
- Journals Career Network
- Code of Conduct
- Publons: Recognising Review
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, summary figure, case presentation, lead author biography, supplementary material, acknowledgements, data availability, a missing coronary guidewire mimicking aortic dissection—a case report.
Conflict of interest : none.
- Article contents
- Figures & tables
- Supplementary Data
Ziad Arow, Avigdor Bar Sef, Abid Assali, Yoav Arnson, A missing coronary guidewire mimicking aortic dissection—a case report, European Heart Journal - Case Reports , Volume 8, Issue 4, April 2024, ytae100, https://doi.org/10.1093/ehjcr/ytae100
- Permissions Icon Permissions
A retained coronary guidewire following coronary angiography is an extremely rare complication. We present a case of a retained coronary guidewire from a percutaneous coronary intervention done 2 years ago.
An 80-year-old asymptomatic man with a history of ischemic heart disease and moderate aortic stenosis presented to the echocardiography lab for routine follow-up. Transthoracic echocardiography showed Moderate aortic stenosis and a suspected linear echogenic structure in the ascending aorta. trans-esophageal echocardiography was performed to reveal a mobile and linear echogenic structure originating from the sinuses of Valsalva/Sinotubular junction and extending to the ascending aorta. An electrocardiogram gated cardiac computed tomography was performed and showed A linear well-defined structure originating from the ostium of the left main coronary artery and extending to the ascending aorta—a coronary guidewire from an earlier procedure. A second look at the last invasive coronary angiography record demonstrated the same finding. A multidisciplinary heart team discussion was obtained and concluded that the risk of surgical or endovascular intervention outweighed the potential benefit. The patient was discharged home for a close clinical and echocardiographic follow-up.
A retained coronary guidewire is a rare complication that operators should be aware of. Management should be case-specific depending on clinical presentation.
A retained coronary guidewire is a rare complication that operators should be aware of following percutaneous coronary intervention (PCI).
The use of multi-modality imaging is essential for accurate diagnosis and a multidisciplinary heart team discussion is important for appropriate treatment decisions.
Invasive coronary angiography and percutaneous coronary intervention (PCI) have become the standard of care for all non-ST segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI) as well as for part of the patients with chronic coronary syndromes. 1 , 2 , 3 Complications may occur during percutaneous coronary procedures or subsequently. Some of the common complications include coronary artery dissection or perforation, hyper-acute stent thrombosis, contrast-induced nephropathy or anaphylaxis, and vascular access site-related complications. 4 , 5 A retained coronary guidewire is an extremely rare complication. We present a case of a retained coronary guidewire from a PCI done 2 years ago.

An 80-year-old male presented to the echocardiography lab for routine follow-up for moderate aortic stenosis (AS). His medical comorbidities included hyperlipidaemia, hypertension, and type 2 diabetes mellitus. In the past, the patient underwent multiple PCI’s due to ischemic heart disease (IHD). His last coronary intervention involved implanting a drug eluting stent (DES) to the left main (LM) and proximal left anterior descending (LAD) coronary arteries, at an outside institution 2 years ago.
The patient was hemodynamically stable and reported no chest pain, back pain, or dyspnoea. Cardiac auscultation demonstrated regular heart sounds with crescendo-decrescendo systolic murmur heard best at the right upper sternal border, radiating to the neck. His lungs were clear and he had no signs of heart failure. Initial Transthoracic echocardiography (TTE) showed normal left ventricular systolic function with moderate AS (aortic valve area: 1.1 cm², max and mean aortic gradients: 46 and 30 mmHg, respectively), moreover, a suspected linear echogenic structure was noted in the ascending aorta, which was suspicious for a dissection flap or an artefact ( Figure 1 , Supplementary material online , Videos S1 and S2 ). As mentioned above, the patient was completely asymptomatic and for better visualization, evaluation, and characterization of the findings seen on TTE, trans-esophageal echocardiography (TEE) was immediately performed to reveal a mobile and linear echogenic structure originating from the sinuses of Valsalva/Sinotubular junction (STJ) and extending to the ascending aorta and the aortic arch ( Figure 2 , Supplementary material online , Video S3 ), highly suspicious for Stanford type A aortic dissection. No aortic regurgitation was noted (see Supplementary material online , Video S4 ). Electrocardiogram (ECG) showed normal sinus rhythm with no signs of acute ischaemia ( Figure 3 ). Blood tests for high-sensitivity cardiac Troponin T (hs-cTnT) and Creatine Kinase-Myocardial Band (CK-MB) were negative. Immediate ECG-gated cardiac computed tomography (CT) was performed. In CT images the aortic endothel was intact and no false lumen was noticed, thus ruling out aortic dissection. A linear well-defined structure was noted originating from the ostium of the LM coronary artery and extending to the ascending aorta, aortic arch, and descending aorta, most probably a coronary guidewire from an earlier procedure ( Figure 4 ). A second look at the last invasive coronary angiography record demonstrated the same finding at the end of the procedure—a coronary guidewire originating from the LM coronary artery and extending to the ascending aorta (see Supplementary material online , Video S5 ). A multidisciplinary heart team discussion, including an invasive cardiologist, a cardiothoracic surgeon, and a cardiac imaging specialist, was obtained, and concluded that the risk of surgical or endovascular intervention outweighed the potential benefit, particularly since the patient was completely asymptomatic, at advanced age and with multiple comorbidities. Discharge home followed several detailed explanations to the patient and his family regarding his condition and a recommendation for a close clinical and echocardiographic follow-up.

Transthoracic echocardiography.

Trans-esophageal echocardiography.

Twelve lead electrocardiogram.

Electrocardiogram gated cardiac computed tomography.
A retained coronary guidewire is an extremely rare complication that occurs in 0.1–0.2% of PCI procedures. 6 In some cases of wire entrapment, over-rotation, or excessive bending—a wire fracture may occur. 7 A retained coronary guidewire or guidewire remnants can lead to various complications including acute thrombosis or perforation of the coronary artery involved and systemic thrombo-embolization, leading to cerebrovascular accident (CVA). 8 , 9
Most reported cases of entrapped guidewires were cases discovered during PCI. 10 This is a rare case of a jailed wire behind the LM stent struts protruding the aorta, discovered years after the procedure. The use of multi-modality imaging was essential for accurate diagnosis and for further risk stratification. Management of patients with retained fractured guidewire fragments during PTCA remains particularly challenging due to the lack of data regarding clinical outcomes. There are no specific guidelines as to how this complication should be managed. Treatment options include conservative treatment and close follow-up (if the patient is completely asymptomatic), medical treatment with anticoagulation (in case of systemic embolization), 11 and endovascular retrieval or surgical extraction (in case of acute thrombosis, perforation, or embolic phenomena threatening coronary artery occlusion). 10
In conclusion, a retained coronary guidewire is a rare complication that operators should be aware of. Management should be case-specific depending on clinical presentation.

Supplementary material is available at European Heart Journal – Case Reports online.
The authors thank Osnat Benvenisti for her support in the image acquisition and processing.
Consent: The authors confirm that written consent for the submission and publication of this case report, including images, Videos, and associated text, was obtained from the patient in accordance with COPE guidance.
Funding : This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The data underlying this article will be shared on reasonable request to the corresponding author.
Ibanez B , James S , Agewall S , Antunes MJ , Bucciarelli-Ducci C , Bueno H , et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC) . Eur Heart J 2018 ; 39 : 119 – 177 .
Google Scholar
Collet JP , Thiele H , Barbato E , Barthélémy O , Bauersachs J , Bhatt DL , et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation . Eur Heart J 2021 ; 42 : 1289 – 1367 .
Knuuti J , Wijns W , Saraste A , Capodanno D , Barbato E , Funck-Brentano C , et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes . Eur Heart J 2020 ; 41 : 407 – 477 .
Neumann FJ , Sousa-Uva M , Ahlsson A , Alfonso F , Banning AP , Benedetto U , et al. 2018 ESC/EACTS guidelines on myocardial revascularization . Eur Heart J 2019 ; 40 : 87 – 165 .
Kandan SR , Johnson TW . Management of percutaneous coronary intervention complications . Heart 2019 ; 105 : 75 – 86 .
Hartzler GO , Rutherford BD , McConahay DR . Retained percutaneous transluminal coronary angioplasty equipment components and their management . Am J Cardiol 1987 ; 60 : 1260 – 1264 .
Lotan C , Hasin Y , Stone D , Meyers S , Applebaum A , Gotsman MS . Guide wire entrapment during PTCA: a potentially dangerous complication . Cathet Cardiovasc Diagn 1987 ; 13 : 309 – 312 .
Ghosh PK , Alber G , Schistek R , Unger F . Rupture of guide wire during percutaneous transluminal coronary angioplasty. Mechanics and management . J Thorac Cardiovasc Surg 1989 ; 97 : 467 – 469 .
Khonsari S , Livermore J , Mahrer P , Magnusson P . Fracture and dislodgment of floppy guidewire during percutaneous transluminal coronary angioplasty . Am J Cardiol 1986 ; 58 : 855 – 856 .
Al-Moghairi AM , Al-Amri HS . Management of retained intervention guide-wire: a literature review . Curr Cardiol Rev 2013 ; 9 : 260 – 266 .
Karan A , Omar M , Velarde G , Sattiraju S . An unusual case of an incidentally detected angioplasty wire in the aorta . AIM Clinical Cases 2022 ; 1 : e220047 .
Author notes
- dissection of aorta
- percutaneous coronary intervention
- echocardiography
- catheter guide wires
Supplementary data
Email alerts, more on this topic, related articles in pubmed, citing articles via.
- General Instructions
- Advertising and Corporate Services
Affiliations
- Online ISSN 2514-2119
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
What is Good Friday? What the holy day means for Christians around the world

Christians around the world observe Good Friday two days before Easter, but what is it, and why do they commemorate the holy day?
The holiday is part of Holy Week, which leads up to Easter Sunday. Palm Sunday kicks off the series of Christian holy days that commemorate the Crucifixion and celebrate Jesus Christ's resurrection.
"Good Friday has been, for centuries now, the heart of the Christian message because it is through the death of Jesus Christ that Christians believe that we have been forgiven of our sins," Daniel Alvarez, an associate teaching professor of religious studies at Florida International University, told USA TODAY.
What is Holy Saturday? What the day before Easter means for Christians around the world
When is Good Friday?
Good Friday is always the Friday before Easter. It's the second-to-last day of Holy Week.
In 2024, Good Friday will fall on March 29.
What is Good Friday?
Good Friday is the day Christ was sacrificed on the cross. According to Britannica , it is a day for "sorrow, penance, and fasting."
"Good Friday is part of something else," Gabriel Radle, an assistant professor of theology at the University of Notre Dame, previously told USA TODAY. "It's its own thing, but it's also part of something bigger."
Are Good Friday and Passover related?
Alvarez says that Good Friday is directly related to the Jewish holiday, Passover.
Passover , or Pesach, is a major Jewish holiday that celebrates the Israelites’ exodus from Egypt.
"The whole Christian idea of atoning for sin, that Jesus is our atonement, is strictly derived from the Jewish Passover tradition," said Alvarez.
How is that possible?
According to the professor, Passover celebrates the day the "Angel of Death" passed over the homes of Israelites who were enslaved by the Egyptians. He said that the Bible states when the exodus happened, families were told to paint their doors with lamb's blood so that God would spare the lives of their firstborn sons.
Alvarez says this is why Christians call Jesus the "lamb of God." He adds that the symbolism of the "blood of the lamb" ties the two stories together and is why Christians believe God sacrificed his firstborn son. Because, through his blood, humanity is protected from the "wrath of a righteous God that cannot tolerate sin."
He adds that the stories of the exodus and the Crucifixion not only further tie the stories together but also emphasize just how powerful the sacrifice of the firstborn and the shedding of blood are in religion.
"Jesus is the firstborn, so the whole idea of the death of the firstborn is crucial," said Alvarez.
He adds that the sacrifice of the firstborn, specifically a firstborn son, comes from an ancient and "primitive" idea that the sacrifice unleashes "tremendous power that is able to fend off any kind of force, including the wrath of God."
Why Is Good Friday so somber?
Alavarez says people might think this holiday is more depressing or sad than others because of how Catholics commemorate the Crucifixion.
"I think [it's] to a level that some people might think is morbid," said Alvarez.
He said Catholics not only meditate on Jesus' death, but primarily focus on the suffering he faced in the events that led up to his Crucifixion. That's what makes it such a mournful day for people.
But, the professor says that Jesus' suffering in crucial to Christianity as a whole.
"The suffering of Christ is central to the four Gospels," said Alvarez. "Everything else is incidental."
According to the professor, statues that use blood to emphasize the way Jesus and Catholic saints suffered is very common in Spanish and Hispanic Countries, but not as prevalent in American churches.
Do you fast on Good Friday?
Father Dustin Dought, the executive director of the Secretariat of Divine Worship of the United States Conference of Catholic Bishops, previously told USA TODAY that Good Friday and Ash Wednesday are the two days in the year that Roman Catholics are obliged to fast.
"This practice is a way of emptying ourselves so that we can be filled with God," said Dought.
What do you eat on Good Friday?
Many Catholics do not eat meat on any Friday during Lent. Anything with flesh is off-limits. Dought says this practice is to honor the way Jesus sacrificed his flesh on Good Friday.
Meat that is off limits includes:
Instead, many Catholics will eat fish. According to the Marine Stewardship Council , this is allowed because fish is considered to be a different type of flesh.
Contributing: Jordan Mendoza ; USA TODAY
- Case report
- Open access
- Published: 30 March 2024
Conventional herniorrhaphy followed by laparoscopic appendectomy for a variant of Amyand’s hernia: a case report
- Yau-Ren Chang ORCID: orcid.org/0000-0003-4968-2746 1 ,
- Yu-Tung Wu 1 &
- Chi-Hsun Hsieh 1
Journal of Medical Case Reports volume 18 , Article number: 194 ( 2024 ) Cite this article
35 Accesses
Metrics details
Amyand’s hernia (AH) is an appendix (with or without acute inflammation) trapped within an inguinal hernia. Most AH with acute appendicitis had a preexisting appendix within the hernia sac. We herein report a variant of AH that has never been described before. An inflamed appendix that was managed conservatively was found to have migrated and trapped in the sac of a previously unrecognized right inguinal hernia 6 weeks after the index admission, resulting in a secondary Amyand’s hernia.
Case presentation
A 25-year-old healthy Taiwanese woman had persistent right lower abdominal pain for 1 week and was diagnosed with perforated appendicitis with a localized abscess by abdominal computed tomography (CT). No inguinal hernia was noted at that time. Although the inflamed appendix along with the abscess was deeply surrounded by bowel loops so that percutaneous drainage was not feasible, it was treated successfully with antibiotics. However, she was rehospitalized 6 weeks later for having a painful right inguinal bulging mass for a week. Abdominal CT revealed an inflamed appendix with abscess formation in an indirect inguinal hernia raising the question of a Amyand’s hernia with a perforated appendicitis. Via a typical inguinal herniorrhaphy incision, surgical exploration confirmed the diagnosis, and it was managed by opening the hernial sac to drain the abscess and reducing the appendix into the peritoneal cavity, followed by conventional tissue-based herniorrhaphy and a laparoscopic appendectomy. She was then discharged uneventfully and remained well for 11 months.
Conclusions
Unlike the traditional definition of Amyand’s hernia, where the appendix is initially in the hernia sac, the current case demonstrated that Amyand’s hernia could be a type of delayed presentation following initial medical treatment of acute appendicitis. However, it can still be managed successfully by a conventional tissue-based herniorrhaphy followed by laparoscopic appendectomy.
Peer Review reports
Amyand’s hernia (AH) is defined as an inguinal hernia containing an inflamed or noninflamed appendix within the hernia sac [ 1 ]. AH can be seen in patients of all ages and consists of much less than 1% of all inguinal hernias [ 2 , 3 ].
The symptoms and signs of AH with concomitant appendicitis generally present as nausea, vomiting and a nonreducible inguinal bulging mass with local tenderness and swelling. Typical signs of acute appendicitis, such as tenderness over McBurney’s point, psoas sign, and Rovsing sign, are absent in these patients due to the unique positioning of appendicitis [ 4 , 5 ].
Although the exact mechanism of AH with concomitant appendicitis is not well clarified, several common hypotheses have been reported in the literature, including adhesion between the appendix and the inguinal sac followed by venostasis and hypoperfusion of appendix due to contraction of abdominal wall muscle [ 6 , 7 ]; incarceration of the appendix leading to inflammation and swelling, which turns AH into a nonreducible hernia [ 8 ]. All the hypotheses of AH with simultaneous appendicitis have one thing in common: the preexistence of an inflamed appendix within the inguinal sac. Herein, we report one case of incarcerated AH which is caused by migration of a ruptured appendicitis 6 weeks after conservative treatment.
A 25-year-old healthy Taiwanese woman without any underlying medical disease or inguinal hernia history had experienced persistent right lower abdominal pain for 1 week. The pain was dull, progressive, and not related to food intake. Associated symptoms included anorexia and nausea. She was brought to the emergency department (ED) due to progressive symptoms, including a positive McBurney’s point tenderness, mild muscle guarding, mild leukocytosis with a left shift, and elevated CRP levels. Abdominal computed tomography (CT) showed an engorged appendix with wall thickening, appendicolith along with small amount of abscess (Fig. 1 ). No inguinal hernia was noted by CT, and the appendix was located in the paracecal position. Percutaneous drainage was contraindicated because of the engulfing surrounding intestinal loops and the more minimal volume of abscess. Therefore, she was treated with empiric antibiotics for a week and was discharged uneventfully.

Initial contrast-enhanced abdominal CT revealed an engorged appendix with wall thickening, appendicolith and surrounding tumor formation, compatible with ruptured appendicitis with local abscess formation. (Arrow: Appendicolith with local abscess formation)
Throughout the course of hospitalization, she did not complain of a bulging inguinal mass or inguinal pain. An interval appendectomy was scheduled at about three months after discharge.
However, she came to the ED a month later due to a persistent painful right inguinal bulging mass for one week. It was firm, tender and nonreducible. No recent history of coughing or constipation was mentioned. Pelvic CT was then arranged and revealed an inflamed appendix with abscess formation in an indirect inguinal hernia raising the question of an Amyand’s hernia with a perforated appendicitis. (Fig. 2 ), including the preperitoneal region and right inguinal canal. It was most likely due to a perforated appendix incarcerated in the hernia sac. After thorough irrigation and debridement of the infected right inguinal region, right inguinal herniorrhaphy with McVay repair was performed by opening the sac, reducing the inflamed appendix into abdominal cavity, carefully avoiding contamination of the surgical field at inguinal region, and conducting high ligation of the sac. Use of a mesh-based repair was contraindicated because of the associated abscess. The reasons not to perform appendectomy in situ was that the cecal-appendiceal junction was still inside the peritoneal cavity and the appendiceal stump could not be safely secured if appendectomy was to be performed through the narrow opening of the sac. Furthermore, the peritoneal cavity had to be irrigated and cleared anyway. Therefore, closing the inguinal wound followed by laparoscopic appendectomy seemed to be the best choice under those circumstances. A laparoscopic appendectomy as well as irrigation of intra-abdominal abscess was then performed successfully (Fig. 3 ), with one Jackson Pratt drain left at the cul-de sac. The drain was successfully removed 5 days after the operation. (Fig. 3 ). The postoperative course was smooth without complications and the patient was discharged 5 days after the operation.

The follow-up contrast-enhanced abdominal CT revealed interval progression of the right lower abdominal abscess with transcompartment involvement, including the preperitoneal region and right inguinal canal, highly suspicious of incarcerated AH, secondary to ruptured appendicitis. (Arrow: Transcompartment inflammation into right inguinal canal)
After detachment of the appendix from the inguinal canal, laparoscopic inspection clearly showed the internal ring of the right inguinal hernia (asterisk)
Discussion and conclusions
AH is an uncommon but complicated type of inguinal hernia, arising in much less than 1% of all inguinal hernia cases [ 2 ]. It is an appendix inside the hernia sac (usually not inflamed). However, the trapped appendix in the hernia sac can become inflamed and the incidence of appendicitis within the inguinal hernia sac is reported to range from 0.07% to 0.13% of all inguinal hernias [ 9 , 10 , 11 ].
We herein reported an atypical type of AH that the inflamed appendix was initially located in the abdominal cavity and there was no history or physical findings of an inguinal bulge or an inguinal hernia. However, following conservative antibiotic-treated treatment for the perforated appendicitis, the appendix then migrated and trapped in a previous undiagnosed inguinal hernia. The likely pathophysiology might be that the local inflammation and surrounding intraperitoneal abscess has led to subsequent adhesions between the inflamed appendix and peritoneum. The peritoneum then became part of the hernia sac with the appendix trapped in it. When the appendicitis deteriorated, the incarcerated AH then became symptomatic.
A noninflamed AH can be treated with inguinal incision followed by inguinal herniorrhaphy, and the appendix is reduced into abdominal cavity with or without subsequent appendectomy [ 3 , 12 ]. It is believed that such approach may keep the herniorrhaphy to be a clean surgery rather than a clean-contaminated surgery [ 2 ]. Although our case is a secondary Amyand’s hernia that was noted following initially conservative treatment of a perforated appendicitis, we took a similar approach to avoid extensive contamination of the operative field for herniorrhaphy. For our case, an additional advantage that appendectomy is performed after herniorrhaphy but not simultaneously with herniorrhaphy is that it is easier to clear intra-abdominal abscess via this approach. Furthermore, we chose laparoscopic appendectomy rather than open appendectomy for this patient because laparoscopic appendectomy is no longer a contraindication for perforated appendicitis at modern era [ 13 ].
In conclusion, our patient had a variant of AH that has never been reported before. The likely pathophysiology of this secondary AH was inflammation and adhesion of appendix to the part of peritoneum that subsequently became part of the indirect inguinal hernia sac. Herniorrhaphy followed by laparoscopic appendectomy provided good outcome for this patient.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- Amyand’s hernia
Computed tomography
Emergency department
Orr KB. Perforated appendix in an inguinal hernial sac: Amyand’s hernia. Med J Aust. 1993;159(11–12):762–3.
Article CAS PubMed Google Scholar
Patoulias D, Kalogirou M, Patoulias I. Amyand’s hernia: an up-to-date review of the literature. Acta Medica (Hradec Kralove). 2017;60(3):131–4.
Article PubMed Google Scholar
Singhal S, Singhal A, Negi SS, Tugnait R, Arora PK, Tiwari B, et al . Amyand’s hernia: rare presentation of a common ailment. Case Rep Gastrointest Med. 2015;2015: 629127.
PubMed PubMed Central Google Scholar
Quartey B, Ugochukwu O, Kuehn R, Ospina K. Incarcerated recurrent Amyand’s hernia. J Emerg Trauma Shock. 2012;5(4):344–6.
Article PubMed PubMed Central Google Scholar
Laermans S, Aerts R, De Man R. Amyand’s hernia: inguinal hernia with acute appendicitis. JBR-BTR. 2007;90(6):524–5.
CAS PubMed Google Scholar
Abu-Dalu J, Urca I. Incarcerated inguinal hernia with a perforated appendix and periappendicular abscess: report of a case. Dis Colon Rectum. 1972;15(6):464–5.
Solecki R, Matyja A, Milanowski W. Amyand’s hernia: a report of two cases. Hernia. 2003;7(1):50–1.
Ash L, Hatem S, Ramirez GA, Veniero J. Amyand’s hernia: a case report of prospective ct diagnosis in the emergency department. Emerg Radiol. 2005;11(4):231–2.
Ivanschuk G, Cesmebasi A, Sorenson EP, Blaak C, Loukas M, Tubbs SR. Amyand’s hernia: a review. Med Sci Monit. 2014;20:140–6.
Sharma H, Gupta A, Shekhawat NS, Memon B, Memon MA. Amyand’s hernia: a report of 18 consecutive patients over a 15-year period. Hernia. 2007;11(1):31–5.
Erdogan D, Karaman I, Aslan MK, Karaman A, Cavusoglu YH. Analysis of 3,776 pediatric inguinal hernia and hydrocele cases in a tertiary center. J Pediatr Surg. 2013;48(8):1767–72.
Cankorkmaz L, Ozer H, Guney C, Atalar MH, Arslan MS, Koyluoglu G. Amyand’s hernia in the children: a single center experience. Surgery. 2010;147(1):140–3.
Talha A, El-Haddad H, Ghazal AE, Shehata G. Laparoscopic versus open appendectomy for perforated appendicitis in adults: randomized clinical trial. Surg Endosc. 2020;34(2):907–14.
Download references
Acknowledgements
The authors gratefully acknowledge that all team members dedicate their best efforts to care for patients with acute abdominal diseases.
This research received no funding or grant support.
Author information
Authors and affiliations.
Division of Trauma and Emergency Surgery, Department of Surgery, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
Yau-Ren Chang, Yu-Tung Wu & Chi-Hsun Hsieh
You can also search for this author in PubMed Google Scholar
Contributions
YC was a major contributor in writing the manuscript. YW was the operator of the surgery in this case and the main medical provider to the patient. CH was in charge of the therapeutic planning for the patient and revised the whole manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yau-Ren Chang .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted in accordance with the fundamental principles of the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chang, YR., Wu, YT. & Hsieh, CH. Conventional herniorrhaphy followed by laparoscopic appendectomy for a variant of Amyand’s hernia: a case report. J Med Case Reports 18 , 194 (2024). https://doi.org/10.1186/s13256-023-04340-y
Download citation
Received : 10 June 2022
Accepted : 26 December 2023
Published : 30 March 2024
DOI : https://doi.org/10.1186/s13256-023-04340-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ruptured appendicitis
- Incarcerated inguinal hernia
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The foundation of an outstanding journal club presentation rests on the choice of an interesting and well-written paper for discussion. Several resources are available to help you select important and timely research, including the American College of Physicians (ACP) Journal Club and the Diffusion section of The Hematologist.McMaster University has created the McMaster Online Rating of ...
The "presentation slide" is the building block of all academic presentations, whether they are journal clubs, thesis committee meetings, short conference talks, or hour-long seminars. A slide is a single page projected on a screen, usually built on the premise of a title, body, and figures or tables and includes both what is shown and what ...
Here are some simple tips for creating an effective PowerPoint Presentation. Less is more: You want to give enough information to make your audience want to read your paper. So include details, but not too many, and avoid too many formulas and technical jargon. Clean and professional: Avoid excessive colors, distracting backgrounds, font ...
Some programs do not use powerpoints or want your presentation under 5 mins. Regardless of the timing and format, every journal club presentation can be approached in this general format: Step 1: Introduction Explain the clinical question that prompted you to consult the literature and what drew you to the article.
Faculty leadership should collaborate with residents on article selection and dissection and preparation of the presentation. Start each journal club with a 10- to 20-minute presentation by the assigned residents to describe the article (as detailed below) to help residents who did not have time to read the article to participate. ...
The exact length of your meeting is up to you or the organizer. A 15-minute talk followed by a 30-minute discussion is about the right length, Add in tea and coffee and hellos, and you get to an hour. We tend to speak at 125-150 words per minute. All these words should not be on your slides, however.
Delivery. It is important to dress appropriately, stand up straight, and project your voice towards the back of the room. Practise using a microphone, or any other presentation aids, in advance. If you don't have your own presenting style, think of the style of inspirational scientific speakers you have seen and imitate it.
imprecise case presentations on clinical clerkships to brief, utilitarian sign-outs as senior residents, journal club pre-senters can learn to efficiently convey the essence of an article. We introduce this model of journal club presentation to medical residents in a small group workshop early during
What is a journal club? How do your prepare for it? And how do you present it? In this video, I will guide you on how to prepare a journal club presentation....
Why your scientific presentation should not be adapted from a journal article With few exceptions, biomedical research presentations are less effective than the speaker would believe.
A Template for Journal Club Presentations, Celia M. Elliott If you feel compelled to provide an outline, make it content‐rich Today we'll discuss Majorana fermions (MFs), theory background InSb nanowires used as "colliders" Zero‐energy peaks observed; believed to be electrons scattering off MFs
PROOFREADING / ACADEMIC ESSAY SERVICE (£/$)For all academic proofreading and mentoring services, send a request on https://www.thepagedoctor.comChapter Times...
In this video, I will show you how to create a research article or journal article presentation quickly in PowerPoint.Get the 30-day Research Jumpstart Guide...
The tools provided in this article can help you develop a presentation that will be meaningful and impactful to your audience. It is a great feeling when audience members come to you after your presentation to share with you how much they enjoyed and learned from your talk. ... Journal of Voice. 2016; 31 (1):127.e7-127.e11. [Google Scholar] 4 ...
Be 'pointer aware', that is don't point it at the audience. Try to control wild tremors by, if necessary, leaning on the podium to support your arm. The aim should be to inspire confidence in the paper being presented. The audience should be watching and listening to you, not just staring at the screen. 9.4.
The list of presentation items (i.e. areas to consider when delivering oral presentations) was retrieved and modified from the following: (1) presentation assessment criteria in some journal articles such as Al-Issa and Al-Qubtan (2010), Langan et al. (2005) and Živković (2014), (2) practical advice from websites and chapters from books, most ...
Creating the Visual. Stick with 1 to 3 learning objectives, and focus the talk on them. The key is to know the message of the presentation upfront. Build the visuals of the lecture to include the background, evidence, and conclusions for those specific messages. Too much text is overwhelming.
It is important not to clutter your slides with too much text or too many pictures. An easy way to do this is by using the 5×5 rule. This means using no more than 5 bullet points per slide, with no more than 5 words per bullet point. It is also good to break up the text-heavy slides with ones including diagrams or graphs.
Excellent presentations not only provide information, but also give opportunities to apply new ideas during and after the talk to 'real-life' situations, and add relevant 'take-home' messages. 1 In this article we highlight educational techniques that can be used to enhance the impact of a presentation. Although all these techniques can ...
Abstract. This article aims to provide an overview of the form, structure and content of conference posters for researchers who intend to submit an academic poster to a conference. It focuses in particular on the design and layout of academic conference posters, making some suggestions for possible poster layouts.
The Slidesgo Journal is back with more news that will fill your day with knowledge! These Google Slides & PowerPoint templates about journals will bring your content to the headline after you edit them. What is happening now at the world? Share the best themes with your readers with cool, creative presentations!
Pico journal article presentation Maria Nguyen. Pico journal article presentation Maria Nguyen. BACKGROUND. Asthma is a common, potentially life-threatening condition Accounts for 2 million pediatric ED visits annually 500, 000 hospitalizations ~ $ 6 billion in total healthcare expenditures on an annual basis. 703 views • 52 slides
More from the blog. From Paper to Presentation: Redesigning Existing Figures for Slides January 15, 2024 Scientific figures do not equally suit all contexts. A figure designed for a paper will often be information-dense; multiple panels illustrate multiple ideas, multiple axes and color bars show the impact of numerous variables, annotations highlight specific caveats, and an extensive caption ...
Over its 200-plus years, the Journal has sometimes published articles that have perpetuated injustices against various groups of people. A new Perspective series explores that history and its lessons.
Background Primary cardiac angiosarcomas are very rare and present aggressively with high rates of metastasis. Given the poor prognosis, particularly once disease has spread, early diagnosis and multidisciplinary treatment is essential. Case presentation We present the case of a 46-year-old male who presented with chest pain, intermittent fevers, and dyspnea. Workup with computed tomography ...
Journal Article. A missing coronary guidewire mimicking aortic dissection—a case report Ziad Arow, Ziad Arow Cardiology Department, Meir Medical Center ... Management should be case-specific depending on clinical presentation. Lead author biography. Ziad Arow is currently a resident in the cardiology department at Meir Medical Center in ...
Alvarez says this is why Christians call Jesus the "lamb of God." He adds that the symbolism of the "blood of the lamb" ties the two stories together and is why Christians believe God sacrificed ...
In a presentation to staff of the brain-computer startup company, a quadriplegic Arizona man details his improvements after the procedure.
Amyand's hernia (AH) is defined as an inguinal hernia containing an inflamed or noninflamed appendix within the hernia sac [].AH can be seen in patients of all ages and consists of much less than 1% of all inguinal hernias [2, 3].The symptoms and signs of AH with concomitant appendicitis generally present as nausea, vomiting and a nonreducible inguinal bulging mass with local tenderness and ...
Bills fans experience 'major sticker shock' from presentation of PSL prices 3.25.2024 The first PSL prices for seats at the Bills' news stadium have "come with major sticker shock," as some fans have said that they were presented with prices between $15,000 to $50,000 per seat for PSLs in the club sections, according to Michael Petro of the ...