
- Previous Article
- Next Article

Research Design and Methods
Article information, literature review of type 2 diabetes management and health literacy.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Rulla Alsaedi , Kimberly McKeirnan; Literature Review of Type 2 Diabetes Management and Health Literacy. Diabetes Spectr 1 November 2021; 34 (4): 399–406. https://doi.org/10.2337/ds21-0014
Download citation file:
- Ris (Zotero)
- Reference Manager
The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs. These challenges can be even more profound among minority populations and non-English speakers in the United States.
A literature search and standard data extraction were performed using PubMed, Medline, and EMBASE databases. A total of 1,914 articles were identified, of which 1,858 were excluded based on the inclusion criteria, and 46 were excluded because of a lack of relevance to both diabetes management and health literacy. The remaining 10 articles were reviewed in detail.
Patients, including ethnic minorities and non-English speakers, who are engaged in diabetes education and health literacy improvement initiatives and ongoing follow-up showed significant improvement in A1C, medication adherence, medication knowledge, and treatment satisfaction. Clinicians considering implementing new interventions to address diabetes care for patients with low health literacy can use culturally tailored approaches, consider ways to create materials for different learning styles and in different languages, engage community health workers and pharmacists to help with patient education, use patient-centered medication labels, and engage instructors who share cultural and linguistic similarities with patients to provide educational sessions.
This literature review identified a variety of interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy.
Diabetes is the seventh leading cause of death in the United States, and 30.3 million Americans, or 9.4% of the U.S. population, are living with diabetes ( 1 , 2 ). For successful management of a complicated condition such as diabetes, health literacy may play an important role. Low health literacy is a well-documented barrier to diabetes management and can lead to poor management of medical conditions, low engagement with health care providers (HCPs), increased hospitalizations, and, consequently, higher health care costs ( 3 – 5 ).
The Healthy People 2010 report ( 6 ) defined health literacy as the “degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” Diabetes health literacy also encompasses a wide range of skills, including basic knowledge of the disease state, self-efficacy, glycemic control, and self-care behaviors, which are all important components of diabetes management ( 3 – 5 , 7 ). According to the Institute of Medicine’s Committee on Health Literacy, patients with poor health literacy are twice as likely to have poor glycemic control and were found to be twice as likely to be hospitalized as those with adequate health literacy ( 8 ). Associations between health literacy and health outcomes have been reported in many studies, the first of which was conducted in 1995 in two public hospitals and found that many patients had inadequate health literacy and could not perform the basic reading tasks necessary to understand their treatments and diagnoses ( 9 ).
Evaluation of health literacy is vital to the management and understanding of diabetes. Several tools for assessing health literacy have been evaluated, and the choice of which to use depends on the length of the patient encounter and the desired depth of the assessment. One widely used literacy assessment tool, the Test of Functional Health Literacy in Adults (TOFHLA), consists of 36 comprehension questions and four numeric calculations ( 10 ). Additional tools that assess patients’ reading ability include the Rapid Estimate of Adult Literacy in Medicine (REALM) and the Literacy Assessment for Diabetes. Tests that assess diabetes numeracy skills include the Diabetes Numeracy Test, the Newest Vital Sign (NVS), and the Single-Item Literacy Screener (SILS) ( 11 ).
Rates of both diabetes and low health literacy are higher in populations from low socioeconomic backgrounds ( 5 , 7 , 12 ). People living in disadvantaged communities face many barriers when seeking health care, including inconsistent housing, lack of transportation, financial difficulties, differing cultural beliefs about health care, and mistrust of the medical professions ( 13 , 14 ). People with high rates of medical mistrust tend to be less engaged in their care and to have poor communication with HCPs, which is another factor HCPs need to address when working with their patients with diabetes ( 15 ).
The cost of medical care for people with diabetes was $327 billion in 2017, a 26% increase since 2012 ( 1 , 16 ). Many of these medical expenditures are related to hospitalization and inpatient care, which accounts for 30% of total medical costs for people with diabetes ( 16 ).
People with diabetes also may neglect self-management tasks for various reasons, including low health literacy, lack of diabetes knowledge, and mistrust between patients and HCPs ( 7 , 15 ).
These challenges can be even more pronounced in vulnerable populations because of language barriers and patient-provider mistrust ( 17 – 19 ). Rates of diabetes are higher among racial and ethnic minority groups; 15.1% of American Indians and Alaskan Natives, 12.7% of Non-Hispanic Blacks, 12.1% of Hispanics, and 8% of Asian Americans have diagnosed diabetes, compared with 7.4% of non-Hispanic Whites ( 1 ). Additionally, patient-provider relationship deficits can be attributed to challenges with communication, including HCPs’ lack of attention to speaking slowly and clearly and checking for patients’ understanding when providing education or gathering information from people who speak English as a second language ( 15 ). White et al. ( 15 ) demonstrated that patients with higher provider mistrust felt that their provider’s communication style was less interpersonal and did not feel welcome as part of the decision-making process.
To the authors’ knowledge, there is no current literature review evaluating interventions focused on health literacy and diabetes management. There is a pressing need for such a comprehensive review to provide a framework for future intervention design. The objective of this literature review was to gather and summarize studies of health literacy–based diabetes management interventions and their effects on overall diabetes management. Medication adherence and glycemic control were considered secondary outcomes.
Search Strategy
A literature review was conducted using the PubMed, Medline, and EMBASE databases. Search criteria included articles published between 2015 and 2020 to identify the most recent studies on this topic. The search included the phrases “diabetes” and “health literacy” to specifically focus on health literacy and diabetes management interventions and was limited to original research conducted in humans and published in English within the defined 5-year period. Search results were exported to Microsoft Excel for evaluation.
Study Selection
Initial screening of the articles’ abstracts was conducted using the selection criteria to determine which articles to include or exclude ( Figure 1 ). The initial search results were reviewed for the following inclusion criteria: original research (clinical trials, cohort studies, and cross-sectional studies) conducted in human subjects with type 2 diabetes in the United States, and published in English between 2015 and 2020. Articles were considered to be relevant if diabetes was included as a medical condition in the study and an intervention was made to assess or improve health literacy. Studies involving type 1 diabetes or gestational diabetes and articles that were viewpoints, population surveys, commentaries, case reports, reviews, or reports of interventions conducted outside of the United States were excluded from further review. The criteria requiring articles to be from the past 5 years and from the United States were used because of the unique and quickly evolving nature of the U.S. health care system. Articles published more than 5 years ago or from other health care systems may have contributed information that was not applicable to or no longer relevant for HCPs in the United States. Articles were screened and reviewed independently by both authors. Disagreements were resolved through discussion to create the final list of articles for inclusion.

PRISMA diagram of the article selection process.
Data Extraction
A standard data extraction was performed for each included article to obtain information including author names, year of publication, journal, study design, type of intervention, primary outcome, tools used to assess health literacy or type 2 diabetes knowledge, and effects of intervention on overall diabetes management, glycemic control, and medication adherence.
A total of 1,914 articles were collected from a search of the PubMed, MEDLINE, and EMBASE databases, of which 1,858 were excluded based on the inclusion and exclusion criteria. Of the 56 articles that met criteria for abstract review, 46 were excluded because of a lack of relevance to both diabetes management and health literacy. The remaining 10 studies identified various diabetes management interventions, including diabetes education tools such as electronic medication instructions and text message–based interventions, technology-based education videos, enhanced prescription labels, learner-based education materials, and culturally tailored interventions ( 15 , 20 – 28 ). Figure 1 shows the PRISMA diagram of the article selection process, and Table 1 summarizes the findings of the article reviews ( 15 , 20 – 28 ).
Findings of the Article Reviews (15,20–28)
SAHLSA, Short Assessment of Health Literacy for Spanish Adults.
Medical mistrust and poor communication are challenging variables in diabetes education. White et al. ( 15 ) examined the association between communication quality and medical mistrust in patients with type 2 diabetes. HCPs at five health department clinics received training in effective health communication and use of the PRIDE (Partnership to Improve Diabetes Education) toolkit in both English and Spanish, whereas control sites were only exposed to National Diabetes Education Program materials without training in effective communication. The study evaluated participant communication using several tools, including the Communication Assessment Tool (CAT), Interpersonal Processes of Care (IPC-18), and the Short Test of Functional Health Literacy in Adults (s-TOFHLA). The authors found that higher levels of mistrust were associated with lower CAT and IPC-18 scores.
Patients with type 2 diabetes are also likely to benefit from personalized education delivery tools such as patient-centered labeling (PCL) of prescription drugs, learning style–based education materials, and tailored text messages ( 24 , 25 , 27 ). Wolf et al. ( 27 ) investigated the use of PCL in patients with type 2 diabetes and found that patients with low health literacy who take medication two or more times per day have higher rates of proper medication use when using PCL (85.9 vs. 77.4%, P = 0.03). The objective of the PCL intervention was to make medication instructions and other information on the labels easier to read to improve medication use and adherence rates. The labels incorporated best-practice strategies introduced by the Institute of Medicine for the Universal Medication Schedule. These strategies prioritize medication information, use of larger font sizes, and increased white space. Of note, the benefits of PCL were largely seen with English speakers. Spanish speakers did not have substantial improvement in medication use or adherence, which could be attributed to language barriers ( 27 ).
Nelson et al. ( 25 ) analyzed patients’ engagement with an automated text message approach to supporting diabetes self-care activities in a 12-month randomized controlled trial (RCT) called REACH (Rapid Education/Encouragement and Communications for Health) ( 25 ). Messages were tailored based on patients’ medication adherence, the Information-Motivation-Behavioral Skills model of health behavior change, and self-care behaviors such as diet, exercise, and self-monitoring of blood glucose. Patients in this trial were native English speakers, so further research to evaluate the impact of the text message intervention in patients with limited English language skills is still needed. However, participants in the intervention group reported higher engagement with the text messages over the 12-month period ( 25 ).
Patients who receive educational materials based on their learning style also show significant improvement in their diabetes knowledge and health literacy. Koonce et al. ( 24 ) developed and evaluated educational materials based on patients’ learning style to improve health literacy in both English and Spanish languages. The materials were made available in multiple formats to target four different learning styles, including materials for visual learners, read/write learners, auditory learners, and kinesthetic learners. Spanish-language versions were also available. Researchers were primarily interested in measuring patients’ health literacy and knowledge of diabetes. The intervention group received materials in their preferred learning style and language, whereas the control group received standard of care education materials. The intervention group showed significant improvement in diabetes knowledge and health literacy, as indicated by Diabetes Knowledge Test (DKT) scores. More participants in the intervention group reported looking up information about their condition during week 2 of the intervention and showed an overall improvement in understanding symptoms of nerve damage and types of food used to treat hypoglycemic events. However, the study had limited enrollment of Spanish speakers, making the applicability of the results to Spanish-speaking patients highly variable.
Additionally, findings by Hofer et al. ( 22 ) suggest that patients with high A1C levels may benefit from interventions led by community health workers (CHWs) to bridge gaps in health literacy and equip patients with the tools to make health decisions. In this study, Hispanic and African American patients with low health literacy and diabetes not controlled by oral therapy benefited from education sessions led by CHWs. The CHWs led culturally tailored support groups to compare the effects of educational materials provided in an electronic format (via iDecide) and printed format on medication adherence and self-efficacy. The study found increased adherence with both formats, and women, specifically, had a significant increase in medication adherence and self-efficacy. One of the important aspects of this study was that the CHWs shared cultural and linguistic characteristics with the patients and HCPs, leading to increased trust and satisfaction with the information presented ( 22 ).
Kim et al. ( 23 ) found that Korean-American participants benefited greatly from group education sessions that provided integrated counseling led by a team of nurses and CHW educators. The intervention also had a health literacy component that focused on enhancing skills such as reading food package labels, understanding medical terminology, and accessing health care services. This intervention led to a significant reduction of 1–1.3% in A1C levels in the intervention group. The intervention established the value of collaboration between CHW educators and nurses to improve health information delivery and disease management.
A collaboration between CHW educators and pharmacists was also shown to reinforce diabetes knowledge and improve health literacy. Sharp et al. ( 26 ) conducted a cross-over study in four primary care ambulatory clinics that provided care for low-income patients. The study found that patients with low health literacy had more visits with pharmacists and CHWs than those with high health literacy. The CHWs provided individualized support to reinforce diabetes self-management education and referrals to resources such as food, shelter, and translation services. The translation services in this study were especially important for building trust with non-English speakers and helping patients understand their therapy. Similar to other studies, the CHWs shared cultural and linguistic characteristics with their populations, which helped to overcome communication-related and cultural barriers ( 23 , 26 ).
The use of electronic tools or educational videos yielded inconclusive results with regard to medication adherence. Graumlich et al. ( 20 ) implemented a new medication planning tool called Medtable within an electronic medical record system in several outpatient clinics serving patients with type 2 diabetes. The tool was designed to organize medication review and patient education. Providers can use this tool to search for medication instructions and actionable language that are appropriate for each patient’s health literacy level. The authors found no changes in medication knowledge or adherence, but the intervention group reported higher satisfaction. On the other hand, Yeung et al. ( 28 ) showed that pharmacist-led online education videos accessed using QR codes affixed to the patients’ medication bottles and health literacy flashcards increased patients’ medication adherence in an academic medical hospital.
Goessl et al. ( 21 ) found that patients with low health literacy had significantly higher retention of information when receiving evidence-based diabetes education through a DVD recording than through an in-person group class. This 18-month RCT randomized participants to either the DVD or in-person group education and assessed their information retention through a teach-back strategy. The curriculum consisted of diabetes prevention topics such as physical exercise, food portions, and food choices. Participants in the DVD group had significantly higher retention of information than those in the control (in-person) group. The authors suggested this may have been because participants in the DVD group have multiple opportunities to review the education material.
Management of type 2 diabetes remains a challenge for HCPs and patients, in part because of the challenges discussed in this review, including communication barriers between patients and HCPs and knowledge deficits about medications and disease states ( 29 ). HCPs can have a positive impact on the health outcomes of their patients with diabetes by improving patients’ disease state and medication knowledge.
One of the common themes identified in this literature review was the prevalence of culturally tailored diabetes education interventions. This is an important strategy that could improve diabetes outcomes and provide an alternative approach to diabetes self-management education when working with patients from culturally diverse backgrounds. HCPs might benefit from using culturally tailored educational approaches to improve communication with patients and overcome the medical mistrust many patients feel. Although such mistrust was not directly correlated with diabetes management, it was noted that patients who feel mistrustful tend to have poor communication with HCPs ( 20 ). Additionally, Latino/Hispanic patients who have language barriers tend to have poor glycemic control ( 19 ). Having CHWs work with HCPs might mitigate some patient-provider communication barriers. As noted earlier, CHWs who share cultural and linguistic characteristics with their patient populations have ongoing interactions and more frequent one-on-one encounters ( 12 ).
Medication adherence and glycemic control are important components of diabetes self-management, and we noted that the integration of CHWs into the diabetes health care team and the use of simplified medication label interventions were both successful in improving medication adherence ( 23 , 24 ). The use of culturally tailored education sessions and the integration of pharmacists and CHWs into the management of diabetes appear to be successful in reducing A1C levels ( 12 , 26 ). Electronic education tools and educational videos alone did not have an impact on medication knowledge or information retention in patients with low health literacy, but a combination of education tools and individualized sessions has the potential to improve diabetes medication knowledge and overall self-management ( 20 , 22 , 30 ).
There were several limitations to our literature review. We restricted our search criteria to articles published in English and studies conducted within the United States to ensure that the results would be relevant to U.S. HCPs. However, these limitations may have excluded important work on this topic. Additional research expanding this search beyond the United States and including articles published in other languages may demonstrate different outcomes. Additionally, this literature review did not focus on A1C as the primary outcome, although A1C is an important indicator of diabetes self-management. A1C was chosen as the method of evaluating the impact of health literacy interventions in patients with diabetes, but other considerations such as medication adherence, impact on comorbid conditions, and quality of life are also important factors.
The results of this work show that implementing health literacy interventions to help patients manage type 2 diabetes can have beneficial results. However, such interventions can have significant time and monetary costs. The potential financial and time costs of diabetes education interventions were not evaluated in this review and should be taken into account when designing interventions. The American Diabetes Association estimated the cost of medical care for people with diabetes to be $327 billion in 2017, with the majority of the expenditure related to hospitalizations and nursing home facilities ( 16 ). Another substantial cost of diabetes that can be difficult to measure is treatment for comorbid conditions and complications such as cardiovascular and renal diseases.
Interventions designed to address low health literacy and provide education about type 2 diabetes could be a valuable asset in preventing complications and reducing medical expenditures. Results of this work show that clinicians who are considering implementing new interventions may benefit from the following strategies: using culturally tailored approaches, creating materials for different learning styles and in patients’ languages, engaging CHWs and pharmacists to help with patient education, using PCLs for medications, and engaging education session instructors who share patients’ cultural and linguistic characteristics.
Diabetes self-management is crucial to improving health outcomes and reducing medical costs. This literature review identified interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy. Clinicians seeking to implement diabetes care and education interventions for patients with low health literacy may want to consider drawing on the strategies described in this article. Providing culturally sensitive education that is tailored to patients’ individual learning styles, spoken language, and individual needs can improve patient outcomes and build patients’ trust.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
Both authors conceptualized the literature review, developed the methodology, analyzed the data, and wrote, reviewed, and edited the manuscript. R.A. collected the data. K.M. supervised the review. K.M. is the guarantor of this work and, as such, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
Portions of this research were presented at the Washington State University College of Pharmacy and Pharmaceutical Sciences Honors Research Day in April 2019.
Email alerts
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Trends in incidence of...
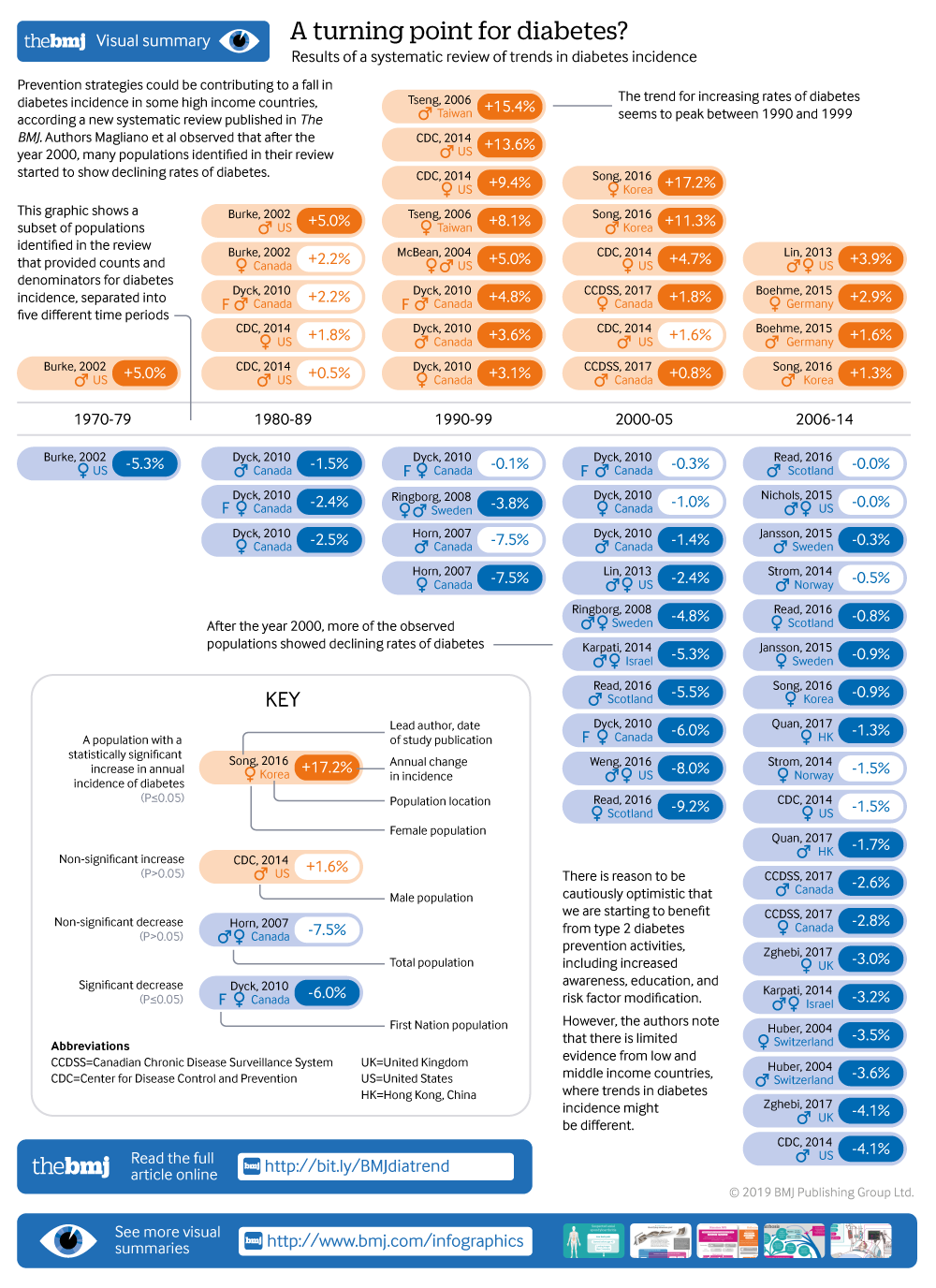
Trends in incidence of total or type 2 diabetes: systematic review
Visual summary available
Showing the turning point in diabetes incidence in 61 populations
Linked editorial
Trends in type 2 diabetes
- Related content
- Peer review
- Dianna J Magliano , laboratory head of diabetes and population health 1 2 ,
- Rakibul M Islam , postdoctoral research fellow 1 2 ,
- Elizabeth L M Barr , postdoctoral research fellow 1 ,
- Edward W Gregg , chair in diabetes and cardiovascular disease epidemiology 3 4 ,
- Meda E Pavkov , physician scientist 3 ,
- Jessica L Harding , research fellow 3 ,
- Maryam Tabesh , research study coordinator 1 2 ,
- Digsu N Koye , postdoctoral research fellow 1 2 ,
- Jonathan E Shaw , deputy director of Baker Heart and Diabetes Institute 1 2
- 1 Baker Heart and Diabetes Institute, Melbourne, VIC 3004, Australia
- 2 School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC 3004, Australia
- 3 Centres for Diseases Control and Prevention, Division of Diabetes Translation, Atlanta, GA, USA
- 4 School of Public Health, Epidemiology and Biostatistics, Imperial College London, London, UK
- Correspondence to: D J Magliano dianna.magliano{at}baker.edu.au
- Accepted 16 July 2019
Objective To assess what proportions of studies reported increasing, stable, or declining trends in the incidence of diagnosed diabetes.
Design Systematic review of studies reporting trends of diabetes incidence in adults from 1980 to 2017 according to PRISMA guidelines.
Data sources Medline, Embase, CINAHL, and reference lists of relevant publications.
Eligibility criteria Studies of open population based cohorts, diabetes registries, and administrative and health insurance databases on secular trends in the incidence of total diabetes or type 2 diabetes in adults were included. Poisson regression was used to model data by age group and year.
Results Among the 22 833 screened abstracts, 47 studies were included, providing data on 121 separate sex specific or ethnicity specific populations; 42 (89%) of the included studies reported on diagnosed diabetes. In 1960-89, 36% (8/22) of the populations studied had increasing trends in incidence of diabetes, 55% (12/22) had stable trends, and 9% (2/22) had decreasing trends. In 1990-2005, diabetes incidence increased in 66% (33/50) of populations, was stable in 32% (16/50), and decreased in 2% (1/50). In 2006-14, increasing trends were reported in only 33% (11/33) of populations, whereas 30% (10/33) and 36% (12/33) had stable or declining incidence, respectively.
Conclusions The incidence of clinically diagnosed diabetes has continued to rise in only a minority of populations studied since 2006, with over a third of populations having a fall in incidence in this time period. Preventive strategies could have contributed to the fall in diabetes incidence in recent years. Data are limited in low and middle income countries, where trends in diabetes incidence could be different.
Systematic review registration Prospero CRD42018092287.
Introduction
Over the past few decades, the prevalence of diabetes in developed and developing countries has risen substantially, making diabetes a key health priority globally. 1 Examination of trends in total burden of diabetes is an essential part of the monitoring of this health priority area, but, to date, it has consisted primarily of studies looking at diabetes prevalence. 1 2 3 4 5 Prevalence estimates suggest that the diabetes burden is still rising in most countries, and this is often interpreted as evidence of increasing risk in the population. However, selective incidence studies 6 7 and some accompanying risk factor data 8 suggest otherwise. Prevalence can be a crude and misleading metric of the trajectory of an epidemic, because increasing prevalence of a disease might be due to either increasing incidence or to improved survival. Furthermore, prevalence cannot be reliably used to study the effects of changes in population risk factors, because their effects are detected earlier with incidence trends than with prevalence trends, and incidence is not affected by changes in survival.
Incidence measures the proportion of people who develop diabetes over a period of time among the population at risk. It is the appropriate measure of population risk, and a valuable way of assessing whether public health campaigns for diabetes prevention are succeeding. While prevalence can rise simply because mortality falls, incidence of diagnosed diabetes is affected only by the risk of the population and the amount of screening undertaken. Changes in prevalence might be an inadequate guide to the effects of prevention activities, and could lead to the inappropriate rejection of effective interventions. It is only by measuring both incidence and prevalence that a better understanding of the extent of diabetes can be achieved.
Among existing diabetes incidence data, a few studies suggest that diabetes incidence could be falling despite rising or stable prevalence, 6 7 9 but not all data are consistently showing the same trends. For example, studies from England and Wales (1994-98), 10 Portugal (1992-2015), 11 and Canada (1995-2007) 12 are reporting increases in diabetes incidence. To understand what is happening at a global level over time, a systematic approach to review all incidence trend data should be undertaken to study patterns and distributions of incidence trends by time, age, and sex. So far, no systematic reviews have reported on trends in the incidence of diabetes. Therefore, we conducted a systematic review of the literature reporting diabetes incidence trends.
Data sources and searches
We conducted a systematic review in accordance with PRISMA guidelines. 13 We searched Medline, Embase, and CINAHL from January 1980 to December 2017 without language restrictions. The full search strategy is available in supplementary table 1.
Study selection
Inclusion and exclusion criteria.
Eligible studies needed to report diabetes incidence in two or more time periods. Study populations derived from open, population based cohort studies (that is, with ongoing recruitment over time), diabetes registries, or administrative or health insurance databases based mainly or wholly in primary care (electronic medical records, health insurance databases, or health maintenance organisations). We also included serial, cross sectional, population based studies where incidence was defined as a person reporting the development of diabetes in the 12 months before the survey. Studies were required to report on the incidence of either total diabetes or type 2 diabetes. We excluded studies reporting incidence restricted to select groups (eg, people with heart failure) and studies reporting only on children or youth.
Each title and abstract was screened by at least two authors (DJM, JES, DNK, JLH, and MT) and discrepancies were resolved by discussion. We aimed to avoid overlap of populations between studies. Therefore, if national data and regional data were available from the same country over the same time period, we only included the national data. If multiple publications used the same data source, over the same time period, we chose the publication that covered the longest time period.
Outcome measure
Our outcome was diabetes incidence using various methods of diabetes ascertainment including: blood glucose, glycated haemoglobin (HbA1c), linkage to drug treatment or reimbursement registries, clinical diagnosis by physicians, administrative data (ICD codes (international classification of diseases)), or self report. Several studies developed algorithms based on several of these elements to define diabetes. We categorised the definition of diabetes into one of five groups: clinical diagnosis, diabetes treatment, algorithm derived, glycaemia defined (blood glucose or HbA1c, with or without treatment), and self report.
Data extraction and quality of studies
We extracted crude and standardised incidence by year (including counts and denominators) and the reported pattern of the trends (increasing, decreasing, or stable, (that is, no statistically significant change)) in each time period as well as study and population characteristics. Age specific data were also extracted if available. Data reported only in graphs were extracted by DigitizeIt software (European Organisation for Nuclear Research, Germany). We assessed study quality using a modified Newcastle-Ottawa scale for assessing the risk of bias of cohort studies 14 (supplementary material).
Statistical methods
Data were reported as incidence density (per person year) or yearly rates (percentage per year). From every study, we extracted data from every subpopulation reported, such that a study reporting incidence in men and women separately contributed two populations to this analysis. If studies reported two different trends over different time periods, we considered these as two populations. Further, if the study was over 10 years in duration, we treated these as two separate time periods. To avoid double counting, when the data were reported in the total population as well as by sex and ethnic groups, we only included data once and prioritised ethnicity specific data over sex specific data.
We extracted the age specific incidence data reported for every individual calendar year. These data were then categorised into four age bands (<40, 40-54, 55-69, and ≥70), and were plotted against calendar year. In studies where counts and denominators were reported by smaller age groups than we used, we recalculated incidence across our specified larger age groups. If we found multiple age groups within any of our broader age groups, but with insufficient information to combine the data into a new category, only data from one age group were used. To limit overcrowding on plots, if data were available for men, women, and the total population, only total population data were plotted. Data from populations with high diabetes incidence such as Mauritians 15 and First Nation populations from Canada 16 were plotted separately to allow the examination of most of the data more easily on a common scale (supplementary material). Furthermore, studies reporting data before 1991 or populations with fewer than three data points were not plotted. We also categorised studies into European and non-European populations on the basis of the predominant ethnicity of the population in which they were conducted. Studies conducted in Israel, Canada, and the United States were assigned to the European category.
We took two approaches to analyse trends of diabetes incidence over time. Firstly, we allocated the reported trend (increasing, decreasing, or stable (that is, no statistically significant change)) of each population to the mid-point of each study’s observational period, and then assigned this trend into one of five time periods (1960-79, 1980-89, 1990-99, 2000-05, and 2006-14). Where a test of significance of trends was not reported or when a time period was longer than 10 years, we performed Joinpoint trend analyses 17 18 to observe any significant trends in the data (assuming a constant standard deviation). Joinpoint Trend Analysis Software (version 4.5.0.1) uses permutation tests to identify points where linear trends change significantly in direction or in magnitude, and calculates an annual percentage change for each time period identified. In sensitivity analyses we also tested different cut points in the last two time periods.
The second approach was used to more accurately allocate trends to the prespecified time periods. Among the studies that reported raw counts of diabetes cases and denominators, we examined the association between calendar year and incidence, using Poisson models with the log person years as offset. The midpoints of age and calendar period were used as continuous covariates, and the effects of these were taken as linear functions. We analysed each study separately by prespecified time periods, and reported annual percentage change when the number of data points in the time period was at least four. For studies that did not provide raw data but did report a sufficient number of points, we analysed the relation between year and incidence using Joinpoint regression across the time periods specified above and reported annual percentage change. Analyses were conducted with Stata software version 14.0 (Stata Corporation, College Station, TX, USA), and Joinpoint (Joinpoint Desktop Software Version 4.5.0.1). 17 18
Patient and public involvement
No patients or members of the public were involved in setting the research question or the outcome measures for this study. No patients were asked to advise on interpretation or writing up of results. We intend to disseminate this research through press releases and at research meetings.
We found 22 833 unique abstracts from 1 January 1980 to the end of 2017. Among these, 80 described trends of diabetes incidence, of which 47 met all inclusion criteria. Articles describing trends were excluded for the following reasons: duplicated data (n=21), closed cohorts (n=5), populations included youth only (n=1), occupational cohorts (n=2), or no usable data presented (n=4; fig 1 ).

Flowchart of study selection
- Download figure
- Open in new tab
- Download powerpoint
Table 1 and supplementary material table 2 describe the characteristics of the included studies. Only 19% (9/47) of studies were from predominantly non-Europid populations and 4% (2/47) of studies were from low or middle income countries (China 25 and Mauritius 15 ). Administrative datasets, health insurance data, registry data, survey data, and cohort studies accounted for 38% (n=18), 21% (n=10), 19% (n=9), 11% (n=5), and 11% (n=5) of the 47 data sources, respectively. Among the 47 studies, diabetes was defined by a clinical diagnosis, diabetes treatment (via linkage to drug treatment registers), an algorithm, blood glucose, and self report in 28% (n=13), 9% (n=4), 47% (n=22), 11% (n=5), and 6% (n=3) of studies, respectively. Sample sizes of the populations were greater than 10 000 in every year in 85% (n=40) of the studies, and greater than 130 000 per year in 70% (n=33) of the studies. A total of 62% (n=29) of the 47 included studies exclusively reported on type 2 diabetes, and 38% (n=18) reported on total diabetes.
Characteristics of 47 included studies reporting on diabetes incidence trends, by country
- View inline
Summary of patterns of diabetes incidence trends based on analyses reported in publications in 1960-99
Trends of diabetes incidence
Among the 47 studies, 16 provided information on incidence by age group. Of these 16 studies, 14 were plotted in figure 2 , with those from high incidence countries plotted in supplementary figure 1. In these figures, incidence in most studies increased progressively until the mid-2000s in all age groups. Thereafter, most studies showed a stable or decreasing trend, apart from studies in Denmark 26 27 and Germany 31 and in a US health insurance population 9 where the incidence inflected upwards in the later years for some age groups.

Incidence of diabetes over time for populations aged under 40, 40-54, 55-69, and 70 or more, among studies reporting age specific data. Only populations with at least three points were plotted. NHIS=National Health Interview Survey
Using the first approach to analyse trends of diabetes incidence over time, we separated the data into populations based on sex and ethnicity, and allocated a time period to each population, generating 105 populations for analysis. Seventy four and 31 populations were predominantly Europid and non-Europid, respectively. Table 2 and table 3 show the reported trend for each population. Table 4 summarises the findings in table 2 and table 3 , and shows that the proportion of populations reporting increasing trends peaked in 1990-99 and fell progressively in the two later time periods. Between 1960 and 1989, 36% (8/22) of the populations studied had increasing trends in incidence of diabetes, 55% (12/22) had stable trends, and 9% (2/22) had decreasing trends. In 1990-2005, diabetes incidence increased in 66% (33/50) of populations, was stable in 32% (16/50), and decreased in 2% (1/50). In 2006-14, increasing trends were reported in 33% (11/33) of populations, whereas 30% (10/33) and 36% (12/33) had stable or declining incidence, respectively.
Summary of patterns of diabetes incidence trends based on analyses reported in publications in 2000-14
Summary of incidence trends over time of total or type 2 diabetes
Populations that reported a decrease in incidence after 2005 came from the US, 6 9 Israel, 34 Switzerland, 46 Hong Kong, 32 Sweden, 43 and Korea. 36 Populations reporting increasing incidence after 2005 included Portugal, 11 Denmark, 26 27 and Germany, 31 while populations from Canada, 19 Italy, 35 Scotland, 40 Norway, 39 US (non-Hispanic white), 56 and the United Kingdom 50 showed stable incidence. For two studies (16 populations), 16 29 we could not determine a direction of a trend (increasing, decreasing, or stable), because they showed three phases of change with the trend of the middle phase differing from the trend of the first and last phase. Across the total time period, we observed a higher proportion of populations reporting stable or decreasing trends in predominantly Europid than in non-Europid populations (52% v 41%).
Using the second approach to analyse trends of diabetes incidence over time, we modelled 21 studies (62 populations) that reported diabetes counts and denominators specifically within each time period ( table 5 ). The percentage of populations with a decreased or stable incidence was highest in 1980-89 (88%; 7/8), but this proportion was based on only eight populations in three studies. From 1990 onwards, the percentage with decreasing or stable incidence increased progressively, reaching 83% (19/23) of populations in 2006-14. Eight studies (21 populations) that were analysed by Joinpoint had no data on counts or denominators (supplementary table 3). When these data were considered with the data in table 5 , the percentage of populations in 2006-14 with decreasing or stable incidence fell to 70% (19/27), but this proportion was still the highest of all the time periods, whereas the percentage for 1990-99 remained the lowest at 31% (5/16).
Annual percentage change in diabetes incidence in men (M), women (W), or total population (T) among studies that provided counts and denominators, by time period
In a sensitivity analysis, we tested whether our selection of time periods was driving our results. When we defined the final time periods to be 2000-07 and 2008-14, our results were not altered, with 66% (21/32) of the populations in the last time period showing decreasing or stable trends. We also repeated the analysis in table 4 and excluded cohort studies and surveys, and found that the results were not materially altered, with 65% (20/31) of populations in the last time period (from 2006 onwards) showing decreasing or stable incidence of diabetes.
Quality of studies
The median score for study quality was 10 (interquartile range 8-11; supplementary table 4). We repeated the analyses reported in table 4 after excluding studies that had quality scores in the lowest quarter, and observed similar results to the main findings. For example, in 1960-89, 67% (10/15) of populations reported stable or decreasing incidence, while in the final time period, 67% (18/27) of populations reported stable or decreasing incidence of diagnosed diabetes.
Principal findings
In this systematic review of population based studies on diabetes incidence, we show evidence that the incidence of diagnosed diabetes increased in most populations from the 1960s to the early 2000s, after which a pattern emerged of levelling trends in 30% and declining trends in 36% of the reported populations. Although the lack of data for non-Europid populations leaves global trends in incidence unclear, these findings suggest that trends in the diabetes epidemic in some high income countries have turned in a more encouraging direction compared with previous decades. It is important to note that these results apply predominantly to type 2 diabetes, as even though many studies did not accurately define diabetes type, the incidence of type 2 diabetes in adults is an order of magnitude greater than that of type 1 diabetes.
The countries that showed stable or decreasing trends in the last time period were from Europe and east Asia, with no obvious clustering or commonalities. For the countries showing decreasing or stable diabetes trends, if the prevalence data were used to understand the diabetes epidemic in that country, a different message would be obtained. For example, national data from Korea showed that the prevalence of diabetes increased from 2000 to 2010. 59 Similarly in Sweden, the prevalence of pharmacologically treated diabetes increased moderately from 2006 to 2014. 43 In the US, the prevalence of diabetes reached a plateau when incidence began to decrease. However, we lacked incidence data from many areas of the world where the most steady and substantial increases in prevalence have been reported, including the Pacific Islands, Middle East, and south Asia. Large increases in incidence could still be occurring in these areas. The lack of incidence data for much of the world, combined with the common observation of discordance between incidence and prevalence rates where such data exist, both underscore the importance of using incidence data to understand the direction of the diabetes epidemic.
Incidence could be starting to fall for several reasons. Firstly, we might be starting to benefit from prevention activities of type 2 diabetes, including increased awareness, education, and risk factor modification. These activities have involved both targeted prevention among high risk individuals, similar to that conducted in the Diabetes Prevention study 60 and Diabetes Prevention Programme 61 62 in many countries, 63 and less intensive interventions with broader reach such as telephone counselling in the general community. 64 65 67 Secondly, health awareness and education programmes have also been implemented in schools and work places, and many changes to the physical environment, such as the introduction of bike tracks and exercise parks, have occurred. 68 Thirdly, favourable trends in selected risk factors of type 2 diabetes in some countries provide indirect evidence of positive changes to reduce diabetes incidence. Finally, in the US, there is some evidence in recent years of improved diets and related behaviours, which include reductions in intake of sugar sweetened beverages 69 and fat, 70 small declines in overall energy intake, and declines in some food purchases. 8 71
Similar reduction in consumptions of sugar sweetened beverages have occurred in Norway 72 and Australia 73 and fast food intake has decreased in Korea. 74 Some of these changes could be linked to a fall in diabetes incidence. Some places such as Scotland 75 have also had a plateauing of obesity prevalence, but this is not universal. In the US, despite earlier studies suggesting that the rate of increase in obesity might be slowing down, 76 77 more recent data show a small increase. 78 79 While some evidence supports the hypothesis that these prevention activities for type 2 diabetes and an improved environment could trigger sufficient behaviour change to have an effect on diabetes incidence, other data, such as the continuing rising obesity prevalence in the US, 79 casts some doubt over the explanations underpinning our findings on diabetes incidence trends.
Other factors might have also influenced reported diabetes incidence. Only 11% (n=5) of the studies reported here screened for undiagnosed diabetes, and therefore trends could have been influenced by secular changes in diagnostic behaviour. In 1997, the threshold for fasting plasma glucose for diagnosis of diabetes was reduced from 7.8 to 7.0 mmol/L, which could increase diagnosis of new cases of type 2 diabetes. In 2009-10, HbA1c was then introduced as an alternative way to diagnose diabetes. 80 Evidence from some studies suggests that the HbA1c diagnostic threshold detects fewer people with diabetes than do the thresholds for fasting plasma blood glucose, 80 81 potentially leading to a lowering of incidence estimates. However, across multiple studies, prevalence estimates based on fasting plasma glucose only versus HbA1c definitions are similar. 82 Furthermore, because HbA1c can be measured in the non-fasting state (unlike the fasting blood glucose or oral glucose tolerance test), the number of people who actually undergo diagnostic testing could be higher with HbA1c. Nichols and colleagues 56 reported that among seven million insured US adults, despite a shift towards HbA1c as the diagnostic test in 2010, the incidence of diabetes did not change from 2010 to 2011.
Another potential explanation for declining or stable diabetes incidence after the mid-2000s is a reduction in the pool of undiagnosed diabetes 83 through the intensification of diagnostic and screening activities 83 84 and changing diagnostic criteria during the previous decade. 80 Data from Read and colleagues provide some evidence to support this notion. 41
Among the included studies, two studies specifically examined clinical screening patterns in parallel with incidence trends. These studies reported that the proportion of the population screened for diabetes increased over time, and the incidence of diabetes remained stable 56 or fell. 34 While the Karpati study 34 combined data for glucose testing with HbA1c testing, the study by Nichols and colleagues 56 separated the two, and showed that both glucose testing and HbA1c testing increased over time. A third study, in Korea, 36 also noted that the incidence of diabetes decreased in the setting of an increase in the uptake of the national health screening programme. Despite the introduction of HbA1c for diagnosis of diabetes by the World Health Organization, this practice has not been adopted everywhere. For example, neither Scotland nor Hong Kong have introduced the use of HbA1c for screening or diagnosis of diabetes, and studies in these areas showed a levelling of diabetes incidence trends and decreasing trends, respectively.
Our findings appear to contrast with data showing increasing global prevalence of diabetes. 1 3 However, increasing prevalence could be influenced by improved survival of people with diabetes, because this increases the length of time that each individual remains within the diabetes population. As is shown in several studies in this review, 23 41 mortality from diabetes and incidence of diabetes might both be falling but as long as mortality is lower than incidence, prevalence will rise. Therefore, we argue that prevalence alone is an insufficient measure to track the epidemic of diabetes and other non-communicable diseases.
Strengths and weaknesses of this study
A key strength of this work was the systematic approach and robust methodology to describe trends in diagnosed diabetes incidence. We also presented the reported trends allocated to approximate time periods, as well as conducting our own regression within exact time periods. The following limitations should also be considered. Firstly, we did not formally search the grey literature, because a preliminary grey literature search revealed only low quality studies, with inadequate methodological detail to provide confidence in any observed incidence trends, and thus review could be subject to publication bias. Secondly, we were not able to source age or sex specific data on all populations. Thirdly, it was not possible to adjust for different methods of diabetes diagnosis or ascertain trends by different definitions of diabetes. Fourthly, most data sources reported only on clinically diagnosed diabetes and so were subject to influence from diagnostic behaviour and coding practices. Fifthly, study type changed over time, with large administrative datasets becoming more common and cohort studies becoming less common over time. Nevertheless, the size and absence of volunteer bias in administrative datasets likely make them less biased. Finally, data were limited in low and middle income countries.
Conclusions and unanswered questions
This systematic review shows that in most countries for which data are available, the incidence of diagnosed diabetes was rising from the 1990s to the mid-2000s, but has been stable or falling since. Preventive strategies and public health education and awareness campaigns could have contributed to this recent trend. Data are limited in low and middle income countries where trends in diabetes incidence might be different. Improvement of the collection, availability, and analysis of incidence data will be important to effectively monitor the epidemic and guide prevention efforts into the future.
What is already known on this topic
Monitoring of the diabetes epidemic has mainly focused on reporting diabetes prevalence, which continues to rise; however, increasing prevalence is partly driven by improved medical treatment and declining mortality
Studies on diabetes incidence are scarce, but among those that exist, some report a fall or stabilisation of diabetes incidence;
Whether the proportion of studies reporting falling incidence has changed over time is not known
What this study adds
This systematic review of published data reporting diabetes incidence trends over time shows that in most countries with available data, incidence of diabetes (mainly diagnosed diabetes) increased from the 1990s to the mid-2000s, and has been stable or falling since
Preventive strategies and public health education and awareness campaigns could have contributed to this flattening of rates, suggesting that worldwide efforts to curb the diabetes epidemic over the past decade might have been effective
Published data were very limited in low and middle income countries, where trends in diabetes incidence might be different
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (CDC).
Contributors: MT, DNK, JLH, and RMI are postdoctoral fellows who screened abstracts for selection into the systematic review. JES and DJM also screened abstracts. ELMB applied the quality criteria to the selected articles. RMI extracted data, applied quality criteria to selected articles, and contributed to preparing the manuscript. DJM conceived the project, screened abstracts, extracted the data, analysed the data, and wrote the manuscript. JES, MEP, and EWG conceived the project, edited the manuscript, and provided intellectual input throughout the process. The funder of the study (CDC) was part of the study group and contributed to data collection, data analysis, data interpretation, and writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. DJM is guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: Funded by the CDC. The researchers were independent from the funders.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from the CDC for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required because this work was a systematic review.
Data sharing: Data are available from the corresponding author ([email protected]).
The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Finucane MM ,
- Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose)
- Whiting DR ,
- Guariguata L ,
- International Diabetes Federation
- NCD Risk Factor Collaboration (NCD-RisC)
- Karuranga S ,
- Abraham TM ,
- Pencina KM ,
- Pencina MJ ,
- Slining MM ,
- Kimball ES ,
- Newnham A ,
- de Sousa-Uva M ,
- Antunes L ,
- Johnson JA ,
- Hemmelgarn BR ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- ↵ Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute, 2014. www.ohri.ca/programs/clinical_epidemiology/oxford.asp Last accessed 14 December 2018.
- Söderberg S ,
- Tuomilehto J ,
- ↵ Joinpoint Regression Program. 4.6.0.0 version. Statistical Methodology and Applications Branch, Surveillance Research Program: National Cancer Institute, 2018. https://surveillance.cancer.gov/joinpoint/ .
- Midthune DN
- ↵ Canadian Chronic Disease Surveillance System. Canadian Chronic Disease Surveillance System 2017. https://www.canada.ca/en/public-health.html
- Blanchard JF ,
- Lipscombe LL ,
- Jacobs-Whyte H ,
- Paradis G ,
- Macaulay AC
- Carstensen B ,
- Kristensen JK ,
- Ottosen P ,
- Borch-Johnsen K ,
- Steering Group of the National Diabetes Register
- Jensen PB ,
- Abouzeid M ,
- Wikström K ,
- Peltonen M ,
- Reunanen A ,
- Klaukka T ,
- Maatela J ,
- Michaelis D ,
- Boehme MW ,
- Buechele G ,
- Frankenhauser-Mannuss J ,
- Vilbergsson S ,
- Sigurdsson G ,
- Sigvaldason H ,
- Hreidarsson AB ,
- Sigfusson N
- Karpati T ,
- Cohen-Stavi CJ ,
- Leibowitz M ,
- Feldman BS ,
- Baviera M ,
- Marzona I ,
- Zimmet PZ ,
- Ruwaard D ,
- Bartelds AI ,
- Hirasing RA ,
- Verkleij H ,
- Birkeland KI ,
- Barnett KN ,
- Ogston SA ,
- Kerssens JJ ,
- McAllister DA ,
- Scottish Diabetes Research Network Epidemiology Group
- Stenström G ,
- Sundkvist G
- Jansson SP ,
- Andersson DK ,
- Svärdsudd K
- Ringborg A ,
- Lindgren P ,
- Martinell M ,
- Stålhammar J
- Schwenkglenks M ,
- Holden SH ,
- Barnett AH ,
- Peters JR ,
- Zghebi SS ,
- Steinke DT ,
- Rutter MK ,
- Emsley RA ,
- Ashcroft DM
- Akushevich I ,
- Kravchenko J ,
- Ukraintseva S ,
- O’Brien P ,
- Centers for Disease Control and Prevention (CDC)
- McBean AM ,
- Gilbertson DT ,
- Narayanan ML ,
- Schraer CD ,
- Bulkow LR ,
- Nichols GA ,
- Schroeder EB ,
- Karter AJ ,
- SUPREME-DM Study Group
- Tabaei BP ,
- Chamany S ,
- Driver CR ,
- Pavkov ME ,
- Hanson RL ,
- Knowler WC ,
- Bennett PH ,
- Krakoff J ,
- Lindström J ,
- Eriksson JG ,
- Finnish Diabetes Prevention Study Group
- Barrett-Connor E ,
- Fowler SE ,
- Diabetes Prevention Program Research Group
- Saaristo T ,
- Moilanen L ,
- Korpi-Hyövälti E ,
- Troughton J ,
- Chatterjee S ,
- Schmittdiel JA ,
- Neugebauer R ,
- Solomon LS ,
- Giles-Corti B ,
- Vernez-Moudon A ,
- Bolt-Evensen K ,
- Brand-Miller JC ,
- ↵ Bromley C, Dowling S, L G. The Scottish Health Survey. Scotland: A National Statistics Publication for Scotland, 2013.
- Carroll MD ,
- Flegal KM ,
- Kruszon-Moran D ,
- Freedman DS ,
- American Diabetes Association
- Lorenzo C ,
- Rasmussen SS ,
- Johansen NB ,
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Registered Report Protocol
Registered Report Protocols describe a study’s rationale and methods for which the planned work was peer-reviewed prior to data collection.
See all article types »
Type 1 and type 2 diabetes mellitus: Clinical outcomes due to COVID-19. Protocol of a systematic literature review
Contributed equally to this work with: Juan Pablo Pérez Bedoya, Alejandro Mejía Muñoz
Roles Conceptualization, Investigation, Methodology, Project administration, Writing – original draft
* E-mail: [email protected]
Current address: National Faculty of Public Health, University of Antioquia, Medellin, Antioquia, Colombia
Affiliation Epidemiology Group, National Faculty of Public Health, University of Antioquia, Medellín, Colombia
Affiliation Biology and Control of Infectious Diseases Group, Faculty of Exact and Natural Sciences, University of Antioquia, Medellín, Colombia
Roles Supervision, Validation, Writing – review & editing
¶ ‡ NCB and PADV also contributed equally to this work.
Affiliation Department of Translational Medicine, Herbert Wertheim College of Medicine & Department of Global Health, Robert Stempel College of Public Health and Social Work, Florida International University, Miami, FL, United States of America
- Juan Pablo Pérez Bedoya,
- Alejandro Mejía Muñoz,
- Noël Christopher Barengo,
- Paula Andrea Diaz Valencia

- Published: September 9, 2022
- https://doi.org/10.1371/journal.pone.0271851
- See the preprint
- Peer Review
- Reader Comments
Introduction
Diabetes has been associated with an increased risk of complications in patients with COVID-19. Most studies do not differentiate between patients with type 1 and type 2 diabetes, which correspond to two pathophysiological distinct diseases that could represent different degrees of clinical compromise.
To identify if there are differences in the clinical outcomes of patients with COVID-19 and diabetes (type 1 and type 2) compared to patients with COVID-19 without diabetes.
Observational studies of patients with COVID-19 and diabetes (both type 1 and type 2) will be included without restriction of geographic region, gender or age, whose outcome is hospitalization, admission to intensive care unit or mortality compared to patients without diabetes. Two authors will independently perform selection, data extraction, and quality assessment, and a third reviewer will resolve discrepancies. The data will be synthesized regarding the sociodemographic and clinical characteristics of patients with diabetes and without diabetes accompanied by the measure of association for the outcomes. The data will be synthesized regarding the sociodemographic and clinical characteristics of patients with diabetes and without diabetes accompanied by the measure of association for the outcomes.
Expected results
Update the evidence regarding the risk of complications in diabetic patients with COVID-19 and in turn synthesize the information available regarding type 1 and type 2 diabetes mellitus, to provide keys to a better understanding of the pathophysiology of diabetics.
Systematic review registry
This study was registered at the International Prospective Registry for Systematic Reviews (PROSPERO)— CRD42021231942 .
Citation: Pérez Bedoya JP, Mejía Muñoz A, Barengo NC, Diaz Valencia PA (2022) Type 1 and type 2 diabetes mellitus: Clinical outcomes due to COVID-19. Protocol of a systematic literature review. PLoS ONE 17(9): e0271851. https://doi.org/10.1371/journal.pone.0271851
Editor: Alok Raghav, GSVM Medical College, INDIA
Received: July 7, 2022; Accepted: August 23, 2022; Published: September 9, 2022
Copyright: © 2022 Pérez Bedoya et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: No datasets were generated or analysed during the current study. All relevant data from this study will be made available upon study completion.
Funding: This research was developed within the framework of the project "Repository for the surveillance of risk factors for chronic diseases in Colombia, the Caribbean and the Americas" and has the financial support of the Ministry of Science, Technology and Innovation of Colombia—Minciencias 844 (grant number 111584467754). The opinions expressed are those of the authors and not necessarily of Minciencias.
Competing interests: The authors have declared that no competing interests exist.
The Severe Acute Respiratory Syndrome Coronavirus type 2 (SARS-CoV-2), the causal viral agent of coronavirus disease 2019 (COVID-19), currently has the world in one of the greatest public health crises of recent times since its appearance at the end of 2019 in the city of Wuhan, China [ 1 ]. The infection has a mild or even asymptomatic course in most cases, but in elderly patients (over 60 years-of-age) and in those with pre-existing chronic comorbidities, it can progress severe complications such as pneumonia, acute respiratory distress (ARDS) with hyperinflammatory involvement and multi-organ failure, leading in some cases to death [ 2 ].
Different studies have reported that patients diagnosed with diabetes who suffer from COVID-19 disease have higher morbidity and mortality compared with people without diabetes [ 3 ]. An analysis by Gude Sampedro et al. using prognostic models found that diabetic patients had greater odds of being hospitalized (OR 1.43; 95% CI: 1.18 to 1.73), admitted to the intensive care unit (OR 1.61; 95% CI: 1.12 to 2.31) and dying from COVID-19 (OR 1.79; 95% CI %: 1.38 to 2.32) compared with patients without diabetes [ 4 ]. However, it is difficult to establish whether diabetes alone directly contributed to the increase likelihood of complications.
Several studies using secondary data have emerged during the course of the pandemic that seek to determine the association of diabetes with mortality and other clinical outcomes in patients with COVID-19, such as, for example, a meta-analysis carried out by Shang et al. of severe infection and mortality from COVID-19 in diabetic patients compared with those without diabetes. They reported that patients with COVID-19 and diabetes had higher odds of serious infection (OR = 2.38, 95% CI: 2.05 to 2.78) and mortality (OR = 2, 21, 95% CI: 1.83 to 2.66) than patients without diabetes [ 5 ]. Despite the fact that there are several primary studies that attempt to explain the association between diabetes and COVID-19, most studies lack epidemiological rigor in the design and methodology used [ 6 ]. In addition, many of them did not distinguish between type 1 and type 2 diabetes, which are two very different conditions with different clinical development and pathophysiological mechanisms [ 7 ]. This may lead to different degrees of clinical complications from COVID-19. Currently, there is a gap in knowledge about the complications in patients with COVID-19 according to the type of diabetes. Moreover, only limited information exist how COVID-19 affects type 1 patients [ 8 , 9 ].
The objective of this systematic literature review will be to identify whether there are differences in the clinical outcomes of both type 1 and type 2 diabetes patients diagnosed with COVID-19 compared with patients with COVID-19 without a diagnosis of diabetes. This study will provide scientific evidence regarding the risk of complications in diabetic patients with COVID-19 and, in turn, synthesize the available information regarding to type 1 and type 2 diabetes.
Study design
This systematic literature review protocol was prepared according to the Preferred Reporting Elements for Systematic Review and Meta-Analysis Protocols (PRISMA-P) [ 10 ] ( S1 Appendix ). The results of the final systematic review will be reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA 2020) [ 11 , 12 ]. In the event of significant deviations from this protocol, they will be reported and published with the results of the review.
Eligibility criteria
Participants (population)..
Patients with a confirmed diagnosis of COVID-19 without restriction of geographic region, sex, or age. For the diagnosis of COVID-19, the operational definition of confirmed case of the World Health Organization in its latest update will be used as a reference. Confirmed case of SARS-CoV-2 infection: a person with a positive Nucleic Acid Amplification Test (NAAT), regardless of clinical criteria OR epidemiological criteria or a person meeting clinical criteria AND/OR epidemiological criteria (suspect case A) with a positive professional- use or self-test SARS-CoV-2 Antigen RDT [ 13 ].
Patients with COVID-19 and concomitant diagnosis of unspecified diabetes mellitus, differentiated into type 1 diabetes mellitus or type 2 diabetes mellitus, without restriction of geographic region, gender, or age of the patients, who present definition of clinical criteria and /or paraclinical tests used by researchers to classify patients according to their diabetes status.
The operational definition of a confirmed case of diabetes mellitus provided by the American Diabetes Association will be used as a guide. The reference diagnostic criteria for diabetes are fasting plasma glucose ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 h or 2-h plasma glucose ≥ 200 mg/dL (11.1 mmol/L) during OGTT or hemoglobin A1C ≥6.5% (48 mmol/mol) or in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, at random plasma glucose ≥200 mg/dL [ 14 ].
In selected primary studies, identification of diabetes status may be based on medical history and International Classification of Diseases codes for type 1 or type 2 diabetes, use of antidiabetic medications, or previously defined diagnostic criteria.
Comparator.
Patients with COVID-19 who do not have a concomitant diagnosis of diabetes mellitus.
The main endpoint is all-cause mortality (according to the definitions of each primary study) and the secondary outcomes are hospitalization and admission to the ICU, where the authors specify a clear definition based on clinical practice guidelines and provide a well-defined criteria for patient outcomes.
Type of study.
Primary observational original research studies (prospective or retrospective cohort, case-control design, and cross-sectional studies) will be included in this systematic review.
Exclusion criteria
Clinical trials, editorials, letters to the editor, reviews, case reports, case series, narrative reviews or systematic reviews and meta-analyses, as well as research in the field of basic sciences based on experimental laboratory models, will be excluded. Original research articles that only include other types of diabetes, such as monogenic diabetes, gestational diabetes, latent autoimmune diabetes in adults, ketosis-prone diabetes, among others, or articles with publication status prior to publication will not be considered. In addition, articles whose main hypothesis is not diabetes and do not have the established outcomes will be excluded.
Information sources and search strategy
Electronic bibliographic databases..
For the preparation of the search strategy, the recommendations of the PRISMA-S guide [ 15 ] will be adopted. Relevant articles will be identified by electronic search applying the equation previously developed by the researchers and validated by an expert librarian ( S2 Appendix ). The following electronic bibliographic databases will be used: MEDLINE, EMBASE, LILACS, OVID MEDLINE, WHO (COVID-19 Global literature on coronavirus disease) and SCOPUS with a publication date from December 2019 to August 15, 2022, without language restriction.
The search for potential primary studies published in gray literature will be performed through the World Health Organization database for COVID-19 (WHO COVID-19 Global literature on coronavirus disease). This database contains different electronic bibliographic databases incorporated into its browser, including Web of Science, EuropePMC and Gray literature, among others.
Unlike electronic bibliographic databases.
To identify other potentially eligible studies, the references of relevant publications will be reviewed to perform a snowball manual search. This technique consists of searching for new articles from the primary studies already selected in order to guarantee exhaustiveness in the search.
Study selection process
Two researchers will independently evaluate all the titles and abstracts of the retrieved articles, using the free access Rayyan® software [ 16 ] with previously established selection criteria. Disagreements will be resolved in first instance through discussion and in the second instance through a third reviewer. Subsequently, the full text of the articles selected in the eligibility phase will be read independently by two researchers, both using the same instrument previously validated in Excel according to predefined criteria. Discrepancies will be resolved by discussion or a third reviewer. The process of identification, selection and inclusion of primary studies will be described and presented using the flowchart recommended by the PRISMA statement in its latest version 2020 [ 11 , 12 ].
Data collection and extraction
Standardized and validated forms will be used to collect the data extracted from the primary studies, accompanied by a detailed instruction manual to specify the guiding questions, and avoid the introduction of bias. Data will be extracted from those articles in full text format. If the full text is not available, contact the author or search for the manuscript with the help of the library system. This process will be carried out by two researchers independently. A third investigator will verify the extracted data to ensure the accuracy of the records. The authors of the primary studies will be contacted to resolve any questions that may arise. The reviewers will resolve the disagreements through discussion and one of the two referees will adjudicate the discrepancies presented through discussion and consensus.
In specific terms, the following data will be collected both for the primary studies that report diabetes and COVID-19 and for those that differentiate between DMT1 and DMT2: author, year and country where the study was carried out; study design; general characteristics of the population, sample size, demographic data of the participants (sex, age, ethnicity), percentage of patients with diabetes, percentage of patients with type 1 and/or type 2 diabetes, percentage of patients without diabetes, frequency of comorbidities in diabetics and non-diabetics, percentage of diabetic and non-diabetic patients who presented the outcomes (hospitalization, ICU admission and mortality) and association measures reported for the outcomes. Data extraction will be done using a Microsoft Excel 365 ® spreadsheets.
Quality evaluation
The study quality assessment tool provided by the National Institutes of Health (NIH) [ 17 ] will be used for observational studies such as cohort, case-control, and cross-sectional. Two tools will be sued: one for cohort and cross-sectional studies (14 questions/domains) and one for case-control studies (12 questions/domains). These tools are aimed at detecting elements that allow evaluation of possible methodological problems, including sources of bias (for example, patient selection, performance, attrition and detection), confounding, study power, the strength of causality in the association between interventions and outcomes, among other factors. The different tools that will be used reflect a score of "1" or "0" depending on the answer "yes" or "no", respectively for each question or domain evaluated, or failing that, the indeterminate criterion option. For observational cohort studies, which consist of 14 risk of bias assessment domains, the studies will be classified as having good quality if they obtain ≥10 points, of fair quality if they obtain 8 to 9 points, and of poor quality if they obtain less than 8 points. On the other hand, in the case of case-control studies that consist of 12 bias risk assessment domains, the studies will be classified as good quality if they obtained ≥8 points, regular quality if they obtained 6 to 7 points and of poor quality if they obtained less than 6 points. However, the internal discussion between the research team will always be considered as the primary quality criterion.
Data synthesis
A narrative synthesis with summary tables will be carried out according to the recommendations adapted from the Synthesis Without Meta-analysis (SWiM) guide to describe in a structured way the methods used, and the findings found in the primary studies, as well as the criteria for grouping of the studies [ 18 ]. A narrative synthesis will be presented in two sections, one for patients with COVID-19 and diabetes and another for patients with COVID-19 and type 1 or type 2 diabetes.
Assessment of clinical and methodological heterogeneity will determine the feasibility of the meta-analysis. Possible sources of heterogeneity identified are the clinical characteristics of the study population, the criteria used to define the outcomes in the groups of patients, the time period of the pandemic in which the study was carried out, and the availability of measurement and control for potential confounding factors. For this reason, it is established a priori that this diversity of findings will make it difficult to carry out an adequate meta-analysis [ 19 ]. However, if meta-analysis is considered feasible, the random effects model will be used due to the high probability of heterogeneity between studies. Statistical heterogeneity will be assessed using the X 2 test and the I 2 statistic, and publication bias assessed using funnel plots if there are sufficient (>10) studies [ 20 ].
Exploratory ecological analysis
An exploratory ecological analysis of the association between the frequency of clinical outcomes of diabetic patients with COVID-19 and the indicators related to the health care dimension, reported for the different countries analyzed by means of the correlation coefficient, will be carried out. The open public databases of the World Bank (WB) [ 21 ], the World Health Organization (WHO) [ 22 ] and Our World In Data [ 23 ] will be used to extract population indicators related to health care, among those prioritized, universal health coverage, hospital beds per 1,000 people, doctors per 1,000 people, current health spending as a percentage of gross domestic product (GDP), percentage of complete vaccination coverage for COVID-19.
Since the first epidemiological and clinical reports were released from the city of Wuhan regarding the clinical characteristics of patients with COVID-19, a high incidence of chronic non-communicable diseases has been observed in Covid-19 patients. Current scientific evidence has shown that certain comorbidities increase the risk for hospitalization, severity of illness or death from COVID-19, such as hypertension, cardiovascular disease, chronic kidney disease, chronic respiratory disease, diabetes, among others [ 24 ].
One of the main chronic comorbidities affected by the COVID-19 pandemic is diabetes. Multivariate analysis of several observational epidemiological studies have revealed that COVID-19 patients with diabetes were at increased risk of hospitalization, ICU admission, and mortality compared with patients without diabetes [ 4 ].
For this reason, it is expected that this systematic literature review will provide scientific support regarding the outcomes and complications that patients diagnosed with COVID-19 with type 1 or type 2 diabetes present compared with patients without diabetes. This information will be useful for healthcare personnel, public health professionals and epidemiologists involved in patient care or decision making, generating epidemiological evidence. Thus, highlighting the decisive role of epidemiological research in the context of the pandemic, especially in the field of diabetes epidemiology may improve comprehensive management and care of diabetic patients. This study may also provide important information that can be used to update of clinical practice guidelines.
Limitations
There are some potential limitations to the proposed systematic review. Firstly, both type 1 and type 2 diabetes may have different key search terms and some studies may be missed. To minimize this limitation, different search equations have been designed for each database in an exhaustive and sensitive manner. In addition to reading references and level ball as an additional strategy. Another limitation is that observational studies evaluating the effect of an intervention may be susceptible to significant confounding bias and may present high heterogeneity in the findings. To report these possible biases, an adequate quality assessment will be carried out, with highly sensitive and previously validated tools, exclusive for each type of observational design. The review is intended for publication in a peer-reviewed journal.
The status of the study
The study is in the selection phase of the records by applying the eligibility criteria to the titles and abstracts. Completion of the project is expected in September 2022 with the publication of the results.
Conclusions
This report describes the systematic review protocol that will be utilized to update the evidence regarding the risk of complications in diabetic patients with COVID-19 and in turn synthesize the information available regarding DM1 and DM2, to provide keys to a better understanding of the pathophysiology of diabetics.
Supporting information
S1 appendix. prisma-p (preferred reporting items for systematic review and meta-analysis protocols) 2015 checklist: recommended items to address in a systematic review protocol..
https://doi.org/10.1371/journal.pone.0271851.s001
S2 Appendix. Search string details for each database.
https://doi.org/10.1371/journal.pone.0271851.s002
- View Article
- PubMed/NCBI
- Google Scholar
- 13. World Health Organization. WHO COVID-19 Case definition Updated in Public health surveillance for COVID-19. 2022 July 22. [cited 18 August 2022]. In: World Health Organization [Internet]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2022.1
- 17. National Institutes of Health (NIH) [Internet]. Study Quality Assessment Tools; 2021. [cited 16 June 2022]. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 19. Cochrane Handbook for Systematic Reviews of Interventions; 2022. [cited 16 June 2022]. Available at: https://training.cochrane.org/handbook/current
- 21. World Bank Group [Internet]. World Bank Indicators; 2022. [cited 16 June 2022]. Available at: https://datos.bancomundial.org/indicador
- 22. World Health Organization (WHO) [Internet]. Global Health Observatory Data Repository; 2021. [cited 16 June 2022]. Available at: https://apps.who.int/gho/data/node.home
- 23. Our World In Data [Internet]. Statistics and Research Coronavirus Pandemic (COVID-19); 2022. [cited 16 June 2022]. Available at: https://ourworldindata.org/coronavirus
- 24. Centers for Disease Control and Prevention [Internet]. COVID-19. People with Certain Medical Conditions; 2021. [cited 16 June 2022]. Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html?CDC_AA_refVal=ht
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Diabetes articles within Nature Reviews Endocrinology
Review Article | 22 March 2024
Protein tyrosine phosphatase 1B in metabolic diseases and drug development
This Review summarizes cellular processes and regulation of protein tyrosine phosphatase 1B (PTP1B), discussing evidence from in vivo preclinical and human studies. PTP1B inhibitors, which are being developed for type 2 diabetes mellitus, obesity, rare diseases (such as Rett syndrome) and some cancers, are also discussed.
- Mirela Delibegović
- , Sergio Dall’Angelo
- & Ruta Dekeryte
Correspondence | 21 March 2024
Slowly progressive insulin-dependent diabetes mellitus in type 1 diabetes endotype 2
- Tetsuro Kobayashi
- & Takashi Kadowaki
Reply to ‘Slowly progressive insulin dependent diabetes mellitus in type 1 diabetes endotype 2’
- Maria J. Redondo
- & Noel G. Morgan
Research Highlight | 20 March 2024
Sex differences in diabetic kidney disease explained
- Claire Greenhill
Research Highlight | 07 December 2023
Highlights from SfE BES 2023
Year in Review | 06 December 2023
Type 1 diabetes mellitus: a brave new world
One hundred years after the Nobel prize was bestowed on Banting and McLeod for the ‘discovery’ of insulin, we are again seeing major evolutions in the management of type 1 diabetes mellitus, with the prospect of achieving disease control beyond mere management now becoming real. Here, we discuss the latest, most notable developments.
- Pieter-Jan Martens
- & Chantal Mathieu
Research Highlight | 24 November 2023
β-cells protected from T1DM by early senescence programme
- Olivia Tysoe
Journal Club | 20 November 2023
SGLT inhibitors: a serendipitous glycaemic tale
- Shubham Agarwal
- & Ildiko Lingvay
The metabolic mythos of ketones
- Jonathan Low
- & Kaja Falkenhain
Research Highlight | 26 October 2023
Antivirals in the treatment of new-onset T1DM
Review Article | 16 October 2023
Inter-organ crosstalk during development and progression of type 2 diabetes mellitus
Inter-organ crosstalk is increasingly understood as an important mechanism contributing to insulin resistance and β-cell failure, the key features of type 2 diabetes mellitus. This Review discusses mediators of inter-organ crosstalk in type 2 diabetes mellitus, its pathogenesis and its related complications.
- Georgia Xourafa
- , Melis Korbmacher
- & Michael Roden
Review Article | 02 October 2023
Diabetes mellitus in breast cancer survivors: metabolic effects of endocrine therapy
Evidence indicates an elevated risk of type 2 diabetes mellitus after breast cancer treatment, particularly for endocrine therapy. This Review outlines the evidence for adverse metabolic effects of endocrine therapies in humans. Potential mechanisms, informed by preclinical research, for the increased risk of type 2 diabetes mellitus are discussed.
- Nisha S. Thomas
- , Rebecca L. Scalzo
- & Elizabeth A. Wellberg
Research Highlight | 25 September 2023
GWAS gives insights into glucose regulation
Journal Club | 20 July 2023
The dark side of shift work: circadian misalignment of skeletal muscle
- Ronan Lordan
Journal Club | 10 July 2023
Is combined exercise and incretin-based therapy the way forward for weight-loss maintenance?
- Julie Abildgaard
Review Article | 19 June 2023
Heterogeneity and endotypes in type 1 diabetes mellitus
There is a growing awareness that type 1 diabetes mellitus (T1DM) is a heterogeneous disease that can be characterized into distinct endotypes. This Review discusses the evidence for endotypes in T1DM and explores the implications for clinical practice.
Research Highlight | 07 June 2023
Differences in stem cell-derived islets
Clinical Outlook | 31 May 2023
Therapeutic inertia in type 2 diabetes mellitus: a fine line between advancing and de-intensifying
Type 2 diabetes mellitus is a progressive disease requiring regular monitoring and therapeutic changes. It is important that healthcare professionals embrace both ends of the spectrum of therapeutic inertia, including appropriate advancement and de-intensification of therapies.
- Kamlesh Khunti
- & Alice Y. Y. Cheng
Journal Club | 26 May 2023
A mitochondrial origin for inherited diabetes mellitus
- Brandon J. Berry
Comment | 24 May 2023
Artificial intelligence in diabetes mellitus and endocrine diseases — what can we expect?
Artificial intelligence has already revolutionized various fields in medicine and research. Due to the complex and interconnected nature of the endocrine system, it is an ideal area to further exploit and maximize the potential benefits of artificial intelligence.
- Ioannis T. Oikonomakos
- , Charlotte Steenblock
- & Stefan R. Bornstein
News & Views | 23 May 2023
How can social jetlag affect health?
Our lives are governed by three clocks: the social clock that organizes our lives with others (local time), the biological clock that controls our physiology (circadian time) and the sun clock that defines natural light and darkness. The more misaligned these clocks are, the higher our odds of developing certain diseases. ‘Social jetlag’ quantifies the difference between local and circadian time.
- Till Roenneberg
Research Highlight | 23 May 2023
Gut microbiota influences effectiveness of anti-diabetic drug
Perspective | 22 May 2023
Insulin detection in diabetes mellitus: challenges and new prospects
An urgent need exists for technologies and devices capable of frequent and real-time insulin measurements in patients with diabetes mellitus to guide optimal insulin dosing. This Perspective discusses the advances and challenges in moving insulin assays from laboratory-based assays to frequent and continuous measurements in decentralized settings.
- , Ponnusamy Nandhakumar
- & Joseph Wang
Clinical Outlook | 18 May 2023
Approval of teplizumab: implications for patients
Type 1 diabetes mellitus (T1DM) can be predicted, and immune therapy can alter the progression of the disease. The FDA’s approval of teplizumab as the first disease-modifying therapy for T1DM and the first therapy aimed at delaying the clinical onset of any immune-mediated disease represents a paradigm shift in the treatment of T1DM.
- Cate Speake
- & Carla J. Greenbaum
Perspective | 11 May 2023
Prioritization of genes associated with type 2 diabetes mellitus for functional studies
More genetic variants associated with type 2 diabetes mellitus are being identified. This Perspective article outlines various tools and platforms that can be applied to prioritize candidate genes associated with an increased risk of disease for functional validation.
- Wei Xuan Tan
- , Xueling Sim
- & Adrian K. K. Teo
Review Article | 02 May 2023
Metformin: update on mechanisms of action and repurposing potential
This Review highlights the latest advances in our understanding of the mechanisms of action of metformin. Potential repurposing of metformin for other indications is also discussed.
- Marc Foretz
- , Bruno Guigas
- & Benoit Viollet
Research Highlight | 25 April 2023
A role for the kidney in metformin action
Research Highlight | 19 April 2023
GLP1 receptor agonists for Wolfram syndrome?
- Shimona Starling
Perspective | 18 April 2023
Why does the immune system destroy pancreatic β-cells but not α-cells in type 1 diabetes?
In type 1 diabetes, the immune system destroys pancreatic β-cells but not neighbouring α-cells. Here, the authors describe the key differences between β-cells and α-cells that could account for their differential autoimmune vulnerability, and how these differences could result in the preferential endurance and survival of α-cells over β-cells.
- Decio L. Eizirik
- , Florian Szymczak
- & Roberto Mallone
Research Highlight | 03 April 2023
Variation in metformin pharmacokinetics
Review Article | 20 March 2023
Mammalian models of diabetes mellitus, with a focus on type 2 diabetes mellitus
Small rodents are still the most widely used animal model to study the pathophysiology of diabetes mellitus but non-rodent species can also provide valuable insights. The advantages and disadvantages of selected animal models of diabetes mellitus are outlined in this Review.
- Thomas A. Lutz
Review Article | 17 March 2023
Revisiting the role of glucagon in health, diabetes mellitus and other metabolic diseases
This Review highlights mechanisms of glucagon secretion from pancreatic α-cells, including paracrine actions in islets and α-cell–β-cell crosstalk. Dysregulated glucagon secretion in metabolic diseases is also considered and the clinical potential of targeting glucagon is discussed.
- Sofie Hædersdal
- , Andreas Andersen
- & Tina Vilsbøll
Perspective | 13 March 2023
A perspective on treating type 1 diabetes mellitus before insulin is needed
This Perspective discusses potential approaches to managing patients in the early stages of developing type 1 diabetes mellitus, which could enable the initiation of insulin therapy to be delayed in some patients.
- Danijela Tatovic
- , Parth Narendran
- & Colin M. Dayan
Research Highlight | 10 March 2023
Interventions in people newly diagnosed with type 1 diabetes mellitus
Research Highlight | 07 March 2023
The metabolic benefits of exercise-induced hepatic autophagy
Journal Club | 02 March 2023
GLP1: the early steps of a success story
- Rula Bany Bakar
Research Highlight | 22 February 2023
Sulfonylurea secondary failure mechanism identified
Research Highlight | 13 February 2023
Serine slows diabetic neuropathy in mice
Research Highlight | 10 February 2023
The effect of long-term statin use on diabetic nephropathy
Review Article | 20 January 2023
Towards a better understanding of diabetes mellitus using organoid models
Organoid systems have great potential to improve the study of diseases such as diabetes mellitus. This Review assesses the progress in developing pancreatic organoids and bioengineered systems for modelling diabetes mellitus and its complications.
- Belin Selcen Beydag-Tasöz
- , Siham Yennek
- & Anne Grapin-Botton
Viewpoint | 16 January 2023
Applying the WHO global targets for diabetes mellitus
In May 2022, the WHO released global targets for diabetes mellitus. In this Viewpoint, experts from around the world discuss the challenges and opportunities in applying these targets.
- Alice Y. Y. Cheng
- , Marília Brito Gomes
- & Jonathan E. Shaw
Research Highlight | 06 January 2023

Precision medicine approach improves HbA 1c outcomes in T2DM
News & Views | 04 January 2023
Monogenic diabetes mellitus hidden in autoantibody-negative diabetes mellitus
A considerable proportion of autoantibody-negative children with type 1 diabetes mellitus actually have monogenic forms of diabetes mellitus, which enables tailored treatment. Thus, a diagnosis of monogenic diabetes mellitus should be considered and genetically tested for in this group of patients, even if the clinical criteria for monogenic diabetes mellitus are not met.
- Stepanka Pruhova
- & Petra Dusatkova
Year in Review | 20 December 2022
A spectacular year for islet and stem cell transplantation
The year 2022 has been notable for game-changing early progress in clinical trials with stem cell islets; durable and promising 20-year data with long-term outcomes in clinical islet transplantation; and the development of locally protective or gene-editing-based approaches to avoid long-term immunosuppression.
- A. M. James Shapiro
- & Kevin Verhoeff
Review Article | 29 November 2022
Cardiorenal diseases in type 2 diabetes mellitus: clinical trials and real-world practice
Cardiorenal diseases are common in patients with type 2 diabetes mellitus (T2DM), with substantial morbidity and premature mortality. This Review discusses how atherosclerotic cardiovascular disease and cardiorenal diseases can be prevented in T2DM, considering evidence from clinical trials and its implementation in clinical practice.
- Lee-Ling Lim
- , Elaine Chow
- & Juliana C. N. Chan
Research Highlight | 21 November 2022
Genomics suggest role for IGF1 resistance in T2DM
Research Highlight | 02 November 2022
Functional HNF1A variants linked with T2DM risk in European-ancestry populations
- Katrin Legg
Research Highlight | 31 October 2022
Engineered T regs prevent diabetes mellitus in mice
Review Article | 31 October 2022
Hypoglycaemia in type 1 diabetes mellitus: risks and practical prevention strategies
Hypoglycaemia is a common occurrence in people with type 1 diabetes mellitus, and can have serious consequences. This Review defines hypoglycaemia in type 1 diabetes mellitus, and also outlines its frequency, risk factors and adverse outcomes. Ways to prevent and treat this complication of insulin therapy are also discussed.
- Jasleen Kaur
- & Elizabeth R. Seaquist
Exercise in adults with type 1 diabetes mellitus
Exercise has many beneficial effects; however, glycaemia needs to be carefully managed in patients with type 1 diabetes mellitus undertaking exercise. This Review characterizes the exercise response in people with type 1 diabetes mellitus and provides clinical management strategies to address glucose control around exercise.
- Michael C. Riddell
- & Anne L. Peters
Browse broader subjects
- Endocrine system and metabolic diseases
- Metabolic diseases
Browse narrower subjects
- Diabetes complications
- Diabetes insipidus
- Gestational diabetes
- Type 1 diabetes
- Type 2 diabetes
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 08 November 2019
Type 2 diabetes and pre-diabetes mellitus: a systematic review and meta-analysis of prevalence studies in women of childbearing age in the Middle East and North Africa, 2000–2018
- Rami H. Al-Rifai ORCID: orcid.org/0000-0001-6102-0353 1 ,
- Maria Majeed 1 ,
- Maryam A. Qambar 2 ,
- Ayesha Ibrahim 2 ,
- Khawla M. AlYammahi 2 &
- Faisal Aziz 1
Systematic Reviews volume 8 , Article number: 268 ( 2019 ) Cite this article
11k Accesses
17 Citations
Metrics details
Investing in women’s health is an inevitable investment in our future. We systematically reviewed the available evidence and summarized the weighted prevalence of type 2 diabetes (T2DM) and pre-diabetes mellitus (pre-DM) in women of childbearing age (15–49 years) in the Middle East and North African (MENA) region.
We comprehensively searched six electronic databases to retrieve published literature and prevalence studies on T2DM and pre-DM in women of childbearing age in the MENA. Retrieved citations were screened and data were extracted by at least two independent reviewers. Weighted T2DM and pre-DM prevalence was estimated using the random-effects model.
Of the 10,010 screened citations, 48 research reports were eligible. Respectively, 46 and 24 research reports on T2DM and pre-DM prevalence estimates, from 14 and 10 countries, were included. Overall, the weighted T2DM and pre-DM prevalence in 14 and 10 MENA countries, respectively, were 7.5% (95% confidence interval [CI], 6.1–9.0) and 7.6% (95% CI, 5.2–10.4). In women sampled from general populations, T2DM prevalence ranged from 0.0 to 35.2% (pooled, 7.7%; 95% CI, 6.1–9.4%) and pre-DM prevalence ranged from 0.0 to 40.0% (pooled, 7.9%; 95% CI, 5.3–11.0%). T2DM was more common in the Fertile Crescent countries (10.7%, 95% CI, 5.2–17.7%), followed by the Arab Peninsula countries (7.6%, 95% CI, 5.9–9.5%) and North African countries and Iran (6.5%, 95% CI, 4.3–9.1%). Pre-DM prevalence was highest in the Fertile Crescent countries (22.7%, 95% CI, 14.2–32.4%), followed by the Arab Peninsula countries (8.6%, 95% CI, 5.5–12.1%) and North Africa and Iran (3.3%, 95% CI, 1.0–6.7%).
Conclusions
T2DM and pre-DM are common in women of childbearing age in MENA countries. The high DM burden in this vital population group could lead to adverse pregnancy outcomes and acceleration of the intergenerational risk of DM. Our review presented data and highlighted gaps in the evidence of the DM burden in women of childbearing age, to inform policy-makers and researchers.
Systematic review registration
PROSPERO CRD42017069231
Peer Review reports
The global burden of type 2 diabetes mellitus (T2DM) is rapidly increasing, affecting individuals of all ages. The global T2DM prevalence nearly doubled in the adult population over the past decade from 4.7% in 1980 to 8.5% in 2014 [ 1 ]. The global burden of T2DM in people 20–79 years is further projected to increase to 629 million in 2045 compared to 425 million in 2017 [ 1 ]. Low- and middle-income countries will be the most affected with the rise in the burden of T2DM. For the period between 2017 and 2045, the projected increase in the prevalence of T2DM in the Middle East and North Africa (MENA) region is 110% compared to 16% in Europe, 35% in North Africa and the Caribbean, and 62% in South and Central America [ 1 ]. Pre-diabetes (pre-DM) or intermediate hyperglycaemia is defined as blood glucose levels above the normal range, but lower than DM thresholds [ 1 ]. The burden of pre-DM is increasing worldwide. By 2045, the number of people aged between 20 and 79 years old with pre-DM is projected to increase to 587 million (8.3% of the adult population) compared to 352.1 million people worldwide in 2017 (i.e., 7.3% of the adult population of adults aged 20 to 79 years) [ 1 ]. About three quarters (72.3%) of people with pre-DM live in low- and middle-income countries [ 1 ].
Pre-DM or T2DM are associated with various unfavorable health outcomes. People with pre-DM are at high risk of developing T2DM [ 1 ]. Annually, it is estimated that 5–10% of people with pre-DM will develop T2DM [ 2 , 3 ]. Pre-DM and T2DM are also associated with early onset of nephropathy and chronic kidney disease [ 4 , 5 , 6 , 7 ], diabetic retinopathy [ 6 , 8 , 9 ], and increased risk of macrovascular disease [ 10 , 11 ]. T2DM is also reported to increase the risk of developing active [ 12 ] and latent tuberculosis [ 13 ]. The rising levels of different modifiable key risk factors, mainly body overweight and obesity, driven by key changes in lifestyle, are the attributes behind the continued burgeoning epidemics of pre-DM and T2DM [ 14 , 15 , 16 ]. Women of childbearing age (15–49 years) [ 17 ] are also affected by the global rise in pre-DM and T2DM epidemics. Rising blood glucose levels in women of childbearing age has pre-gestational, gestational, and postpartum consequences, including increased intergenerational risk of DM [ 18 ].
The total population in 20 countries (Algeria, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Malta, Morocco, Oman, Palestine, Qatar, Saudi Arabia, Syria, Tunisia, the United Arab Emirates, and Yemen) in the Middle East and North Africa region comprises almost 6.7% (~ 421 million people) of the world’s population, with about 200 million females as of July 1, 2015 [ 19 ]. In adults ≥ 18 years, T2DM prevalence rose sharply by 2.3 times in each of the Eastern Mediterranean regions and the African region, between 1980 and 2014 [ 20 ]. This sharp increase in these two regions is higher than that reported in the region of the Americas (1.7 times), the European region (1.4 times), and the Western Pacific Region (1.9 times) [ 20 ].
Key pre-DM and T2DM risk factors, body overweight and obesity, are highly prevalent in people in the MENA countries. In 2013, the age-standardized prevalence of overweight and obesity among women ≥ 20 years was 65.5% (obese 33.9%) [ 21 ]. The high burden of overweight and obesity in several MENA countries attributed to the interrelated economic, dietary, lifestyle behavioral factors. The nutrition transitions and changes in the food consumption habits were supported by the witnessed economic development in most of the MENA countries. For instance, in the past five decades, the economic development in the Arab Gulf countries linked to the discovery of oil and gas reserves led to changes in eating habits towards the consumption of foods rich in fat and calories as well as increasing behavioral habits towards a sedentary lifestyle [ 22 , 23 ]. This is particularly true with the significant shift from the consumption of traditional low-fat food to fat-rich foods, as well as with a major change from an agricultural lifestyle to an urbanized lifestyle that is often accompanied by decreased levels of physical activity. The urbanized lifestyle increases exposure to fast foods through the high penetration of fast food restaurants serving fat-rich foods, the reliance on automobiles for transport, and the increasing penetration of cell phones, all of which facilitate low levels of physical activity. Globally, physical inactivity is estimated to cause around 27% of diabetes cases [ 24 ]. In eight Arab countries, based on national samples, low levels of physical activity in adults ranged from 32.1% of the population in Egypt in 2011–2012 to as high as 67% of the population in Saudi Arabia in 2005 [ 25 ]. Furthermore, fruit and vegetable consumption is inversely associated with weight gain [ 26 ]. Studies indicated a low intake of fruit and vegetables in some of the MENA countries [ 27 , 28 ]. The growing burden of the possible risk factors of body overweight and obesity in women may further affect and exacerbate the burden of DM and its associated complications in the MENA countries.
To develop effective prevention and control interventions, there is a need for understanding the actual burden of pre-DM and T2DM epidemics in vital population groups, such as women of childbearing age (15–49 years), in the MENA region. Thus, individual studies need to be compiled and summarized. According to our previously published protocol (with a slight deviation) [ 29 ], here, we present the results of the systematically reviewed published quantitative literature (systematic review “1”), to assess the burden (prevalence) of T2DM and pre-DM in women of childbearing age in the MENA region, from 2000 to 2018.
Investing in women’s health paves the way for healthier families and stronger economies. Societies that prioritize women’s health are likely to have better population health overall and to remain more productive for generations to come [ 30 ]. Against this background, our review was aimed at characterizing the epidemiology of T2DM and pre-DM in population groups of women of childbearing age in the MENA through (1) systematically reviewing and synthesizing all available published records of T2DM and pre-DM and (2) estimating the mean T2DM and pre-DM prevalence at national, sub-regional, and regional levels, from January 2000 to July 2018. The findings of the review fill an evidence gap to inform policy-makers on the epidemiologic burden of T2DM and pre-DM in women of childbearing age.
Following our published protocol [ 29 ] that is registered with the International Prospective Registry of Systematic Reviews (PROSPERO registration number “CRD42017069231” dated 12/06/2017), we reported here systematic review “1”. This review adheres to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2009 guidelines [ 31 , 32 , 33 ]. The PRISMA checklist is provided in the Additional file 1 .
Data source and search strategy
To identify eligible studies on T2DM and pre-DM prevalence measures in MENA countries, we implemented a comprehensive computerized search of six electronic databases (MEDLINE, EMBASE, Web of Science, SCOPUS, Cochrane library, and Academic Search Complete) from January 1, 2000, to July 12, 2018, using variant Medical Subject Headings (MeSH) and free-text (Text) terms. The detailed search strategy is presented in an additional box file (see Additional file 2 ). We also hand-searched the reference lists of eligible studies for further studies that might have been missed.
We defined the participants, exposure, comparator, outcome(s), and type of study “PECO(T)”. The PECO(T) statement provides the framework for the identification and selection of studies for inclusion [ 34 ]. As we were looking for prevalence studies, we only considered participants and the outcomes.
Inclusion and exclusion criteria
Participants : Women of childbearing age were defined according to the World Health Organization (WHO) as women aged between 15 and 49 years (thereafter, women of childbearing age) [ 35 ]. Pregnant women were also considered in this review as long as they were tested for T2DM and/or pre-DM according to what was reported in the individual studies.
Outcomes : T2DM and pre-DM. The included studies should have reported quantitative or calculable pre-DM or T2DM prevalence estimate(s) in women of childbearing age regardless of the sample size, pregnancy status, or pre-DM/T2DM ascertainment methodology, in any of the 20 MENA region countries [ 36 ]. We excluded studies of self-reported pre-DM/T2DM not supported with either anti-DM medications or a documented diagnosis. We also excluded studies on metabolic syndrome as long as there was no clear information on the proportion of women of childbearing age with pre-DM or T2DM. Studies were also excluded if they pooled women of childbearing age with pre-DM/T2DM with other non-communicable diseases in the same category, or together with males, or for each gender separately but without age stratification. We excluded studies with incalculable pre-DM/T2DM prevalence after attempting to contact the authors at least twice with no response.
Types of studies : We included observational studies if they were cross-sectional, comparative cross-sectional, case-control (not comparing T2DM/pre-DM vs. no T2DM/pre-DM), or cohort study designs. We excluded observational studies of other study designs.
Detailed eligibility criteria are available in the published protocol [ 29 ]. The PRISMA flow chart for the selection of studies is shown in Fig. 1 .
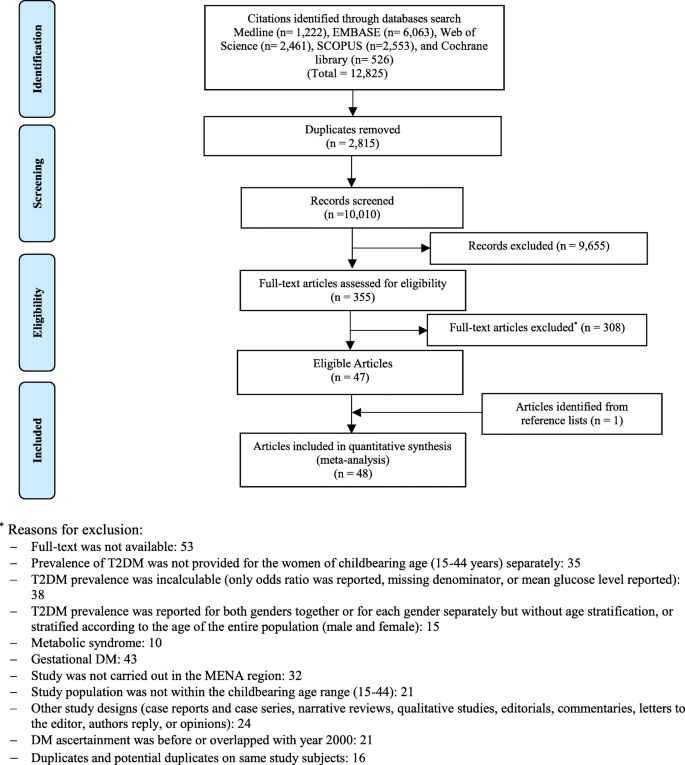
PRISMA flow chart
Identifying eligible studies
Titles and abstracts of the remaining citations were screened independently by four reviewers (AI, KA, MM, and MQ) for any potential study on pre-DM/T2DM in childbearing age women. Full-texts of the identified potentially eligible studies were thoroughly screened and independently assessed by the four reviewers. The qualities of the extracted studies were independently assessed by two other reviewers (RHA and FA). Discrepancies in data extraction were discussed and resolved.
Data extraction
Data from fully eligible studies were extracted into a pre-defined data extraction excel file using a pre-defined list of variables [ 29 ]. Our outcome of interest was the national/regional weighted pooled prevalence of T2DM and pre-DM in women of childbearing age in the MENA. We extracted the following data on the baseline characteristics of the eligible research reports (author names, year of publication, country, city, and study setting), study methodology (design, time period, sampling strategy, and T2DM/pre-DM ascertainment methodology), and study population (age, pregnancy status, co-morbidity, and number of women with the outcomes of interest).
In research reports which provided stratified T2DM/pre-DM prevalence estimates, the prevalence of the total sample was replaced with the stratified estimates keeping the rule of having at least 10 tested subjects per strata, otherwise we extracted information on the whole tested sample. We followed a pre-defined sequential order when extracting stratified prevalence estimates. Outcome measures stratified according to body mass index (BMI) were prioritized, followed by age and year. This prioritization scheme was used to identify the strata with more information on the tested women. When the strata were not prioritized, the overall outcome prevalence measured was extracted. For a research report that stratified the prevalence of the outcome of interest at these different levels (i.e., age and BMI), one stratum per research report was considered and included to avoid double counting. If the outcome measure was ascertained by more than one ascertainment guideline, we extracted relevant information based on the most sensitive and reliable ascertainment assay (i.e., prioritizing fasting blood glucose “FBG” over self-reported DM status), or the most recent and updated criteria (i.e., prioritizing WHO 2006 over WHO 1999 criteria).
We generated a funnel plot to explore the small-study effect on the pooled prevalence estimates. The funnel plot was created by plotting each prevalence measure against its standard error. The asymmetry of the funnel plot was tested using the Egger’s test [ 37 ] (see Additional files 3 and 4 ).
Quality appraisal and risk of bias
We assessed the methodological quality and risk of bias (ROB) of the studies on T2DM or pre-DM prevalence measures using six-quality items adapted from the National Heart, Lung, and Blood Institute (NIH) tool [ 38 ]. Of the 14 items proposed for observational studies on the NIH tool, eight items were not used as they are relevant only for cohort studies assessing the relationship between an exposure and an outcome [ 38 ]. We also assessed the robustness of the implemented sampling methodology and the ascertainment methodology of the measured outcome(s) using three additional quality criteria (sampling methodology, ascertainment methodology, and precision of the estimate). Studies were considered as having “high” precision if at least 100 women tested for T2DM/pre-DM; a reasonable precision, given a pooled prevalence of 7.2% for T2DM or 7.6% for pre-DM estimated in this study, was obtained. We computed the overall proportion of research reports with potentially low risk of bias across each of the nine quality criteria. We also computed the proportion (out of nine) of quality items with potentially a low risk of bias for each of the included research reports.
Quantitative synthesis: meta-analysis
Meta-analyses of the extracted data to estimate the weighted pooled prevalence of T2DM and pre-DM and the corresponding 95% confidence interval (CI) were executed. The variances of prevalence measures were stabilized by the Freeman-Tukey double arcsine transformation method [ 39 , 40 ]. The estimated pooled prevalence measures were weighted using the inverse variance method [ 40 ], and an overall pooled prevalence estimate was generated using a Dersimonian–Laird random-effects model [ 41 ]. Heterogeneity measures were also calculated using the Cochran’s Q statistic and the inconsistency index; I –squared ( I 2 ) [ 42 ]. In addition to the pooled estimates, the prevalence measures were summarized using ranges and medians. The prediction interval, which estimated the 95% interval in which the true effect size in a new prevalence study will lie, was also reported [ 42 , 43 ].
Country-level pooled estimates were generated according to the population group of tested women (general population, pregnant, non-pregnant with history of gestational DM (GDM), and patients with co-morbidity), and the overall country-level pooled prevalence, regardless of the tested population and study period. To assess if the prevalence of T2DM and pre-DM is changing over time, we stratified studies into two time periods: 2000–2009 and 2010–2018. In order not to miss any important data when estimating country-level, sub-regional, and regional prevalence, the period for studies that overlapped these two periods was defined as “overlapping”. In studies with an unclear data collection period, we used the median (~ 2 years) that was obtained from subtracting the year of publication from the year of data collection to estimate the year of data collection in those studies. The “patients with co-morbidity” included women of childbearing age with organ transplant, kidney dialysis, cancer, HIV, chronic obstructive pulmonary disease, polycystic ovarian syndrome (PCOS), or schizophrenia. Categorization of the study period was arbitrary with an aim to estimate the change in T2DM and pre-DM at the country-level and overall, over time.
We also estimated the weighted pooled prevalence, regardless of country, according to the tested women’s population group, study period, T2DM/pre-DM ascertainment guidelines (WHO guidelines, American DM Association (ADA) guidelines, International DM Association (IDF) guidelines, or medical records/anti-DM medications/self-reported), and sample size (< 100 or ≥ 100). The overall weighted pooled prevalence of T2DM and pre-DM regardless of the country, tested population, study period, ascertainment guidelines, and sample size was also generated. Providing pooled estimates regardless of the ascertainment guidelines was justified by the fact that the subject women were defined and treated as T2DM or pre-DM patients following each specific ascertainment guidelines.
To provide prevalence estimates at a more sub-regional level, countries in the MENA region were re-grouped into three sub-regions, namely, “Arab Peninsula, Fertile crescent, and North Africa and Iran.” The pooled prevalence in these three sub-regions was estimated according to the tested population group, study period, ascertainment guidelines, and sample size, as well as overall for each sub-region.
We also estimated the weighted pooled prevalence of T2DM and pre-DM according to age group. We categorized women of childbearing age into three age groups (15–29 years, 30–49 years) and not specified/overlapping. The “not specified/overlapping” category covers women who did fell in the other two age groups. For example, women with an age range of 25–34 years or 18–40 years. The age group weighted pooled prevalence produced regardless of the country, sub-region, and tested population as well as study period.
All meta-analyses were performed using the metaprop package [ 33 ] in Stata/SE v15 [ 44 ].
Sources of heterogeneity: meta-regression
Random-effects univariate and multivariable meta-regression models were implemented to identify sources of between-study heterogeneity and to quantify their contribution to variability in the T2DM and pre-DM prevalence. In univariate meta-regression models, analysis was performed by country, tested population, study period, ascertainment guidelines, and sample size. All variables with a p < 0.1, in the univariate models, were included in the multivariable model. In the final multivariable model, a p value ≤ 0.05 was considered statistically significant, contributing to heterogeneity in prevalence estimates.
All meta-regression analyses were performed using the metareg package in Stata/SE v15 [ 44 ].
Search and eligible research reports
Of the 12,825 citations retrieved from the six databases, 48 research reports were found eligible (Fig. 1 ); 46 reported T2DM prevalence [ 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 ] while 24 reported pre-DM prevalence [ 48 , 49 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 60 , 62 , 63 , 66 , 67 , 70 , 73 , 75 , 81 , 85 , 88 , 89 , 90 ].
Scope of reviewed T2DM reports
The 46 research reports on T2DM prevalence yielded 102 T2DM prevalence studies. The 46 reports were from 14 countries (Algeria, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Morocco, Oman, Qatar, Saudi Arabia, Tunisia, the United Arab Emirates [UAE], and Yemen); ranging by year between 2000 in Saudi Arabia [ 79 ] and 2018 in UAE [ 81 ]. Sixteen (34.9%) research reports were reported in Saudi Arabia [ 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 ], followed by 19.6% in the UAE [ 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 ], and 15.2% in Iran [ 47 , 48 , 49 , 50 , 51 , 52 , 53 ]. Over one third (37.3%) of the yielded 102 T2DM prevalence studies were in Saudi Arabia. Of the 102 T2DM prevalence studies, 79.4% were in women sampled from general populations and 11.8% in pregnant women. Over two thirds (69.6%) of the T2DM prevalence studies were in or before 2009 and 82.4% tested ≥ 100 women (Table 1 ).
Pooled T2DM prevalence
In the 14 countries, the weighted T2DM prevalence in women of childbearing age estimated at 7.5% (95% CI, 6.1–9.0%, I 2 , 98.2%) (Table 2 , Fig. 2 ). The weighted T2DM prevalence was not significantly different ( p = 0.4) in studies reported between 2000 and 2009 (7.9%, 95% CI, 6.2–9.7%, I 2 , 97.9%) and studies reported between 2010 and 2018 (5.8%, 95% CI, 3.4–8.7%, I 2 , 95.4%) (Table 2 ). The weighted T2DM prevalence was higher in women with an age range of 15–19 years (10.9%, 95% CI, 8.8–13.3%, I 2 , 97.9%) than women with an age range of 30–49 years (2.5%, 95% CI, 1.8–3.2%, I 2 , 83.6%) (see Additional file 5 ).
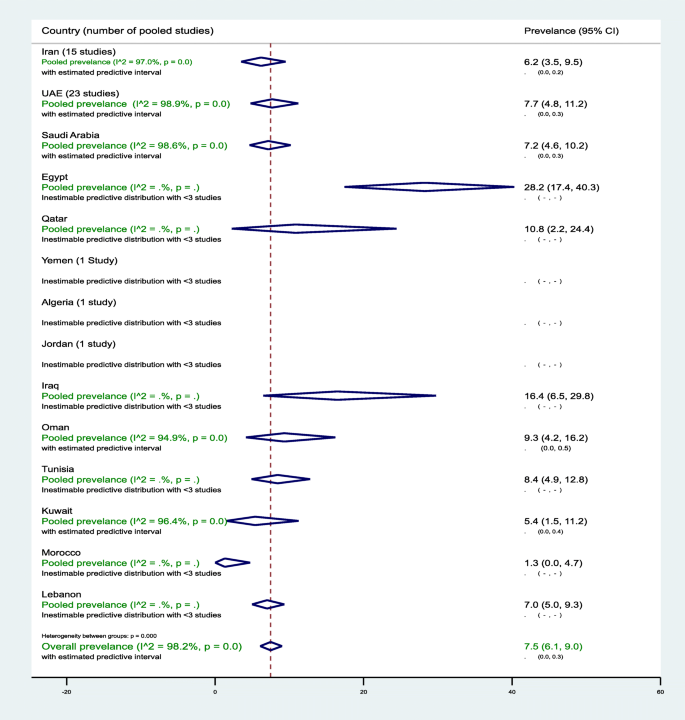
Forest plot of the meta-analyses for the 14 MENA countries’ studies on T2DM
Pooled findings of 102 T2DM prevalence estimates reported in 14 countries in the MENA region. The individual 102 estimates and their 95% confidence interval (CI) omitted to fit the plot. The diamond is centered on the summary effect estimate, and the width indicates the corresponding 95% CI. UAE, United Arab Emirates; T2DM, type 2 diabetes mellitus; MENA, Middle East and Northern Africa
The highest two weighted T2DM estimates were observed in infertile women of childbearing age in Egypt (28.2%, 95% CI, 17.4–40.3%) and in non-pregnant women with a history of GDM in Iran (24.7%, 95% CI, 18.5–31.5%) (Table 2 ). In general populations, the weighted T2DM prevalence ranged between 1.3% (95% CI, 0.0–4.7%) in 2001–2002 in Morocco [ 60 ] and 16.4% (95% CI, 6.5–29.8%, I 2 , 96.5%) in Iraq in 2007 [ 55 ] and in 2011–2012 [ 54 ]. In Saudi Arabia, in women of childbearing age sampled from general populations, the pooled T2DM prevalence estimated at 8.0% (95% CI, 5.3–11.3%, I 2 , 96.5%) (Table 1 ). In Saudi Arabia, the weighted T2DM prevalence in women of childbearing age, regardless of source of population and timeline, estimated at 7.2% (95% CI, 4.6–10.2%, I 2 , 98.6%) (Table 2 ). In Oman, the weighted T2DM prevalence in women of childbearing age sampled from general populations estimated at 8.0% (95% CI, 2.9–15.4%, I 2 , 95.9%) in 2000. In Qatar, the weighted T2DM was prevalence in women of childbearing age sampled from general populations 10.7% (95% CI, 2.2–24.4%, I 2 , 93.7%) between 2007 and 2008. In the UAE, in women of childbearing age sampled from general populations, the pooled T2DM prevalence estimated at 8.0% (95% CI, 4.8–11.9%, I 2 , 98.9%) that declined from 9.4% (95% CI, 5.6–14.1%, I 2 , 95.1%) between 2000 and 2009 to 6.0% (95% CI, 3.3–6.5%, I 2 , 90.5%) between 2010 and 2018 (Table 2 ).
Sub-regional pooled T2DM prevalence
The pooled T2DM prevalence measures estimated at 6.5% (95% CI, 4.3–9.1%, I 2 , 96.0%) in North African countries including Iran, 10.7% (95% CI 5.2–17.7%, I 2 , 90.7%) in the Fertile Crescent countries, and 7.6% (95% CI, 5.9–9.5%, I 2 , 98.5%) in the Arabian Peninsula countries (see Additional file 6 ).
Additional file 7 shows figures presenting the sub-regional-weighted prevalence of T2DM (Fig. 1 ) in women of childbearing age from 2000 to 2009 and from 2010 to 2018. Additional file 8 shows figures presenting timeline view of the weighted prevalence of T2DM (Fig. 1 ) by publication year.
Meta-bias in T2DM prevalence
The asymmetry in the funnel plot examining the small-study effects on the pooled T2DM prevalence among women of childbearing age indicates evidence for the presence of a small-study effect (Egger’s test p < 0.0001). The funnel plot is presented in an additional figure file (see Additional file 3 ).
Predictors of heterogeneity in T2DM prevalence
In the univariate meta-regression models, all variables except study period, T2DM ascertainment criteria, and sample size were associated with T2DM prevalence at p value < 0.1. In the adjusted meta-regression model, none of the included variables was significantly associated with T2DM prevalence at p value < 0.05. In two studies in infertile women of childbearing age in Egypt, the T2DM prevalence was higher (adjusted odds ratio (aOR), 5.26, 95% CI, 0.87–32.1) compared to women of childbearing age in Saudi Arabia. Overall, compared to women of childbearing age sampled from general populations, T2DM prevalence in non-pregnant women of childbearing age with a history of GDM was 234% higher (aOR, 3.34%, 95% CI, 0.90–12.41) (see Additional file 9 ).
Scope of reviewed pre-DM reports
The 24 research reports on pre-DM prevalence yielded 52 pre-DM prevalence studies and were from 10 countries (Iran, Iraq, Jordan, Kuwait, Morocco, Oman, Qatar, Saudi Arabia, UAE, and Yemen); ranging by year between 2002 in Oman [ 62 ] and 2018 in Saudi Arabia [ 81 ]. Thirteen (25.0%), 11 (21.2%), and 11 (21.2%) of the pre-DM prevalence studies were from Iran, Saudi Arabia, and UAE, respectively. Approximately 87.0% of the pre-DM prevalence studies tested women of childbearing age sampled from general populations. The pre-DM prevalence estimates ranged from 0.0% in various age groups in multiple countries [ 51 , 60 , 70 ] to 40.0% in Iraq in women aged 20–39 years, recruited from the general population [ 55 ] (Table 1 ).
Pooled pre-DM prevalence
In the 10 countries, the weighted pre-DM prevalence in women of childbearing age was estimated at 7.6% (95% CI, 5.2–10.4%, I 2 , 99.0%) (Table 3 , Fig. 3 ). The weighted pre-DM prevalence in studies reported between 2000 and 2009 (4.8%, 95% CI 4.0–7.8%, I 2 , 97.1%) was significantly lower ( p < 0.001) than the weighted prevalence estimated in studies reported between 2010 and 2018 (9.3%, 95%, 4.7–15.2%, I 2 , 93.9%) (Table 3 ). Weighted pre-DM prevalence was 1.70 times higher in women with an age range of 15–19 years (9.0%, 95% CI, 4.9–14.1%, I 2 , 99.2%) than women with an age range of 30–49 years (5.3%, 95% CI, 1.8–10.3%, I 2 , 99.0%) (see Additional file 5 ).
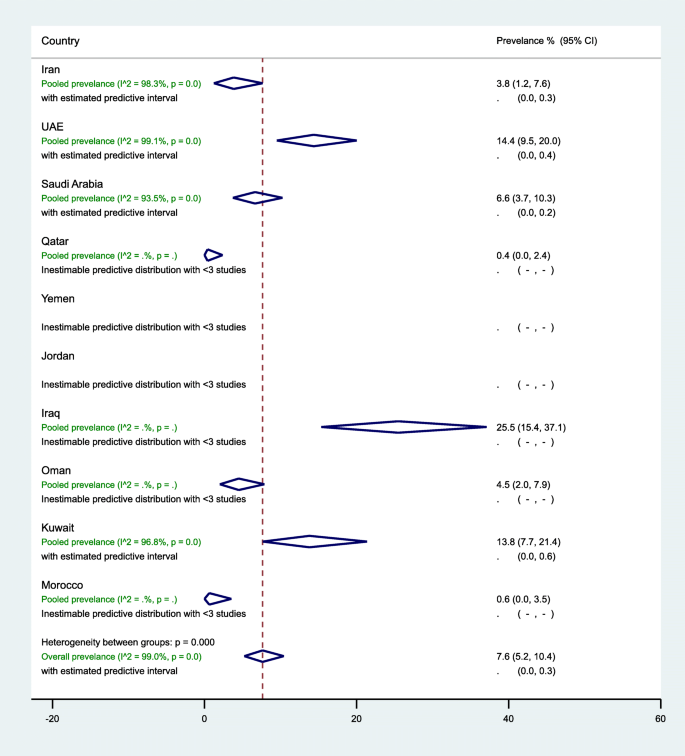
Forest plot of the meta-analyses for the 10 MENA countries’ studies on pre-DM pooled findings of 52 pre-DM prevalence estimates reported in 10 countries in the MENA region. The individual 52 estimates and their 95% confidence interval (CI) omitted to fit the plot. The diamond is centered on the summary effect estimate, and the width indicates the corresponding 95% CI. UAE, United Arab Emirates; pre-DM, pre-diabetes mellitus; MENA, Middle East and Northern Africa
In general populations, the highest three weighted pre-DM prevalence estimates were observed in women of childbearing age in Iraq (25.5%, 95% CI, 15.4–37.1%, I 2 , 92.2%), followed by UAE (15.5%, 95% CI, 10.5–21.2%, I 2 , 99.0%), and Kuwait (13.8%, 95% CI, 7.7–21.4%, I 2 , 96.8%) (Table 3 ). In 13 studies in Iran (7 from the general population), the prevalence of pre-DM ranged from 0.0 to 21.4% with an overall weighted prevalence of 3.8% (95% CI, 1.2–7.6%, I 2 , 98.3%). The 11 pre-DM studies in Saudi Arabia were in women of childbearing age sampled from the general population, with an overall weighted pre-DM prevalence of 6.6% (95% CI, 3.7–10.3%, I 2 , 93.5%) (2000–2009: 9.4% vs. 2010–2018: 4.4%). Regardless of the tested population in UAE, the weighted pre-DM prevalence was 6.6% (95% CI, 5.1–8.3%, I 2 , 65.6%) in studies reported between 2000 and 2009, and 12.0% (95% CI, 8.9–15.5%) in studies reported between 2010 and 2018 with an overall pre-DM prevalence of 14.4% (95% CI, 9.5–20.0%, I 2 , 99.1%) (Table 3 ).
Sub-regional pooled pre-DM prevalence
The pooled pre-DM prevalence estimated at 3.3% (95% CI, 1.0–6.7%, I 2 , 98.1%) in North African countries including Iran, 22.7% (95% CI, 14.2–32.4%, I 2 , 90.0%) in the Fertile crescent countries, and 8.6% (95% CI, 5.5–12.1%, I 2 , 99.1%) in the Arabian Peninsula countries (see Additional files 10 ). Additional file 7 shows figures presenting the sub-regional weighted prevalence of pre-DM (Fig. 2 ) in women of childbearing age from 2000 to 2009 and from 2010 to 2018. Additional file 8 shows figures presenting timeline view of the weighted prevalence of pre-DM (Fig. 2 ) by publication year.
Meta-bias in pre-DM prevalence measures
The asymmetry in the funnel plot examining the small-study effects on the pooled pre-DM prevalence among women of childbearing age indicates evidence for the presence of a small-study effect (Egger’s test p < 0.0001). The funnel plot is presented in an additional figure file (Additional file 4 ).
Predictors of heterogeneity in pre-DM prevalence
Country, study period, and pre-DM ascertainment criteria were associated with a difference in the pre-DM prevalence in the univariate meta-regression models at p value < 0.1. In the univariate meta-regression models, pre-DM prevalence in women of childbearing age in Iraq was 424% higher compared to such women in Saudi Arabia (OR, 5.24, 95% CI, 1.45–18.94%). This significant association turned insignificant in the multivariable model (aOR, 2.20, 95% CI, 0.52–10.82%). In the multivariable model, compared to Saudi Arabia, pre-DM prevalence in women of childbearing age was 70% lower in Iran (aOR, 0.30, 95% CI, 0.11–0.79%) and 88% lower in Morocco (aOR, 0.12, 95% CI, 0.01–0.91%) (see Additional file 11 ).
Quality assessment of the T2DM/pre-DM research reports
Findings of our summarized and research report-specific quality assessments for relevant DM prevalence studies can be found in Additional file 12 . Briefly, all the 48 research reports clearly stated their research questions or objectives, clearly specified and defined their study populations, and selected or recruited the study subjects from the same or similar populations. There was a clear gap in the reporting or justifying of the sample size calculation in 79.2% of the research reports. The majority (87.5%) of the research reports tested ≥ 100 women of childbearing age, and they were classified as having high precision.
Overall, the 48 research reports were of reasonable quality with potentially low ROB in an average of 7.2 items (range, 6–9). Four (8.3%) of the 48 reports had potentially low ROB in all the measured nine quality items [ 66 , 82 , 83 , 86 ] (see Additional file 12 ).
We provided, to our knowledge, the first regional study that comprehensively reviewed and estimated the regional, sub-regional, and country-level burden of T2DM and pre-DM in various populations of women of childbearing age in the MENA. Based on the available data from 14 and 10 studies in MENA countries, the present findings document the comparable burden of T2DM (7.5%, 95% CI 6.9–9.0%) and pre-DM (7.6%, 95% CI 5.2–10.4%) in women of childbearing age. The estimated prevalence of T2DM and pre-DM in 14 countries in the MENA is similar to the estimated worldwide crude diabetes prevalence of 8.2% (95% credible interval (CI) 6.6–9.9%) in adult women in 2014 (age-standardized 7.9%, 95% CI 6.4–9.7%) [ 91 ]. The T2DM and pre-DM prevalence in women of childbearing age varied across the three sub-regions in the MENA, by population group, time period, DM ascertainment criteria, and sample size. The obvious common prevalence of T2DM and pre-DM in women of childbearing age in the MENA countries reflects the highest prevalence of adult diabetes estimated for the MENA [ 91 ]. In this region, the crude diabetes prevalence in adult women increased from 5.0% in 1980 to 9.0% in 2014 [ 91 ]. This increase in diabetes prevalence among adult populations in the MENA over time is higher than many other regions including Europe and Central and West Africa [ 91 ]. The highest national adult diabetes prevalence estimates documented in the MENA is 5–10 times greater than the lowest national prevalence estimates documented in Western European countries [ 91 ].
T2DM is a significant public health problem in both developed and developing countries that can lead to various health complications including increased overall risk of dying prematurely [ 20 ]. The common burden of T2DM and pre-DM in women of childbearing age, which is reflected in the high burden of adult diabetes in this region [ 91 ], might be mainly driven by the sociodemographic changes in this region. In recent decades, there was an increase in median age, sedentary lifestyle, and physical inactivity in the MENA [ 92 ]. These lifestyle changes are linked to an increase in the burden of body overweight and obesity that are shared predisposing factors for pre-DM and T2DM [ 20 ]. At the population level, physical inactivity was very common in many MENA countries (Saudi Arabia 67.6% in 2005; Kuwait 62.6% in 2014; Qatar 45.9% in 2012; Egypt 32.1% in 2011–2012; Iraq 47.0% in 2015) [ 25 ]. The burden of body overweight and obesity is higher in many low-income and middle-income countries in the MENA than in Europe and Asia Pacific countries [ 93 ]. Obesity in women in several Middle Eastern countries was 40–50% [ 93 ]. The age-standardized prevalence of obesity was 32.0% in Egypt, 35.5% in Jordan, 30.4% in Iraq, 32.5% in Libya, and 35.4% in Saudi Arabia [ 94 ]. In Tunisia, 43.7% and 24.1% of 35–70-year-old females in urban and rural areas, respectively, were obese [ 95 ]. In 2016, in almost all of the countries in MENA, the mean BMI for people aged ≥ 18 years was ≥ 25.0 [ 96 ].
To curb the burden of DM and its associated complications in women of childbearing age in the MENA countries, our results suggest three main implications for care. First, based on the estimated 5–10% progression rate from pre-DM to T2DM [ 3 , 10 ], out of the 47,958 tested women of childbearing age for pre-DM (Table 3 ), we estimate that 2398 to 4796 women are expected to progress to T2DM. This risk of progression to T2DM could be reduced through lifestyle and drug-based interventions as it was reported elsewhere [ 97 , 98 , 99 ]. In England, 55–80% of participants with hyperglycemia at baseline had normal glycaemia at 10 year follow-up [ 3 ]. The high burden of DM along with pre-DM in women of childbearing age could accelerate maternal complications including GDM leading to increased intergenerational risk of DM. Programs to halt the growing epidemic of DM among different population groups could start by addressing the key risk factors including sedentary lifestyle and increased body weight. Addressing this problem would require social and public policies and efforts to reduce the national and regional burden of increased body weight and obesity through enhancing healthy eating behaviors and physical activity. Second, there is a critical need for strengthened surveillance systems that match the scale and nature of the DM epidemic in women of childbearing age in the MENA. Enhancing early detection and management of high-risk individuals requires accessible and affordable health care systems, outreach campaigns to raise public awareness, and social and medical support to induce and maintain a healthy lifestyle. Adult people at increased risk of T2DM and pre-DM can be predicted based on good screening tools from the Centers for Disease Control and Prevention (CDC) [ 100 ] and the American Diabetes Association (T2DM Risk Test) [ 101 ]. Early screening and detection will require government-funded prevention programs. Third, controlling the burden of T2DM and pre-DM in MENA countries requires strong and successful partnerships between public health and clinical departments. Physicians have a fundamental role in the care of individual patients to screen, diagnose, and treat both pre-DM and T2DM in clinical settings. In addition, physicians have a fundamental role in working to raise awareness and participating in developing prevention programs and engaging communities. Concerted efforts and partnership between physicians, health departments, and community agencies are needed to strengthen health care services, encouraging and facilitating early screening and detection, and promoting healthy diets and physical activity.
Providing summary estimates and up-to-date mapping gaps-in-evidence of T2DM and pre-DM prevalence in women of childbearing age in different MENA countries provides the opportunities for future public health interventions and research to better characterize the T2DM and pre-DM epidemiology nationally and regionally. Nevertheless, present review findings suggest that the DM burden in women of childbearing age in MENA countries is capturing only the tip of the iceberg. Identifying gaps-in-evidence through systematically reviewing and summarizing the literature has public health research implications. Our review shows that in many countries, the estimation of the burden of T2DM or pre-DM in women of childbearing age in general populations occurred more than a decade ago (Table 1 ). Additionally, the review shows that there was no data on the burden of T2DM and pre-DM in women of childbearing age in several countries in the MENA region. This lack of evidence on a key public heath outcome requires a strongly resourced research capacity and research funding schemes. There is evidence that federally funded research can impact important health issues that affect a large segment of the population [ 102 ].
This robust approach to the literature search and review as well as in retrieving and extracting relevant data from the published literature allowed us to provide summary estimates on the burden of T2DM and pre-DM in women of childbearing age from the 14 and 10 countries in the MENA, respectively. Once the diagnosis was established, regardless of the ascertainment criteria, patients were treated as having diabetes or pre-diabetes. Thus, generating pooled estimates, regardless of the DM ascertainment criteria, stratified according to various population groups, provided more insights into the actual burden of T2DM and pre-DM in various populations of women of childbearing age. The meta-regression analysis identified sources of variations in T2DM and pre-DM prevalence and sources of between-study heterogeneity in prevalence estimates. (Additional files 9 and 11 show these in more detail). The country-stratified and population-stratified T2DM and pre-DM prevalence reports revealed gaps in evidence that can help strengthen research and DM control programs in the most affected countries and populations. The use of probability sampling was very common in the studies included, which may provide broader insights on the representation of our findings to the general or specific group of women of childbearing age at the national, but not at the regional, level.
Limitations
There are important but unavoidable limitations when interpreting the results of our review. Despite the estimated DM prevalence, the actual DM burden could have been underestimated, at country, sub-regional, or regional level, due to several reasons. The inaccessibility of data on pre-DM or T2DM in women of childbearing age from several countries in the MENA may not necessarily mean an actual lack of data. To meet the aim of our review of estimating the burden of pre-DM and T2DM in women of childbearing age, in several published studies reviewed, women of childbearing age were found to have been combined with those of other age groups or with men. The presented overall pooled estimates, regardless of the tested population group, should not be interpreted as the total burden of the outcome at the population level. Utilizing data on T2DM and pre-DM from only 14 and 10 countries may limit the findings from being generalizable to the entire MENA region. Although we followed a thorough and well-defined search strategy, there is a potential of publication bias as shown in funnel plots (Additional files 3 and 4 ). The estimated T2DM and pre-DM prevalence suggest that only the tip of the iceberg was captured. The presented estimates may not be representative of the true prevalence for each population. This underestimation may be particularly true in low-resource settings where necessary resources and capacity in investigating pre-DM at the community level are lacking. The wide array of blood glucose cut-off points and criteria used for T2DM and pre-DM ascertainment also suggests that overestimation and underestimation bias cannot be excluded. Unless estimated from individual population-based studies only, the presented weighted pooled estimates at the country, sub-regional, or regional level should not be interpreted as the burden of the measured outcomes at the population level. Also, the presented pooled estimates according to the two time periods, from 2000 to 2009 and from 2010 to 2018, should not be interpreted as an over-time change in the burden of the measured outcomes. While our meta-analyses revealed substantial heterogeneity across studies, the meta-regression analyses identified the potential sources of between-study heterogeneity within the framework of the present study and the level of detail that can be used in describing these sources (Tables 1 and 2 ). Thus, much of the variability in T2DM and pre-DM prevalence across studies might remain unexplained.
Despite these potential limitations, our study provided a characterization of the scale of T2DM and pre-DM among women of childbearing age in several MENA countries based on the best available evidence. Data presented in this review can be used to (a) understand the burden of T2DM and pre-DM among a vital population group and to identify at high-risk populations within this specific population group; (b) guide the planning, implementation, and evaluation of programs to prevent and control DM; (c) implement immediate public health actions to prioritize the allocation of public health resources; and (d) formulate research hypotheses and provide a basis for epidemiologic studies. Future research opportunities should prioritize large country-level and multicenter comparable studies, to determine the prevalence of T2DM and pre-DM in various population groups of women of childbearing age. A definitive characterization of the burden of DM in women of childbearing age at the regional and sub-regional level would require comparable and empirical studies using standardized methodology and comparable DM ascertainment assays.
In conclusion, women of childbearing age in the MENA region bear an appreciable burden of T2DM and pre-DM. The estimated burden of T2DM and pre-DM was higher in the Arabian Peninsula and Fertile Crescent countries compared to the rest of the MENA countries identified with prevalence estimates in this review. Although both T2DM (7.5%) and pre-DM (7.6%) had similar overall estimated prevalence, there is need for a more focused attention on early detection and control by public health authorities to avoid DM-associated pre-gestational, gestational, and post-gestational complications. Country-level early DM detection and control programs should consider the key risk factors of DM, mainly the growing burden of body overweight and obesity. Furthermore, facilitating high-quality research and surveillance programs in countries with limited data on DM prevalence and reporting of DM prevalence estimates in women of childbearing age warrant focus.
Availability of data and materials
The datasets used and/or analyzed during the current study and its supplementary information files are available from the corresponding author on reasonable request.
Abbreviations
American DM association
Adjusted odds ratio
Confidence interval
Diabetes mellitus
Gestational diabetes mellitus
International Diabetes Mellitus Association
Middle East and North Africa
Medical Subject Headings
National Heart, Lung, and Blood Institute
Participants, exposure, comparator, and outcome
- Pre-diabetes mellitus
Preferred Reporting Items for Systematic Review and Meta-Analysis
Risk of bias
- Type 2 diabetes
United Arab Emirates
World Health Organization
International Diabetes Federation. IDF Diabetes Atlas, 8th edn. Brussels: International Diabetes Federation, 2017. https://diabetesatlas.org/resources/2017-atlas.html Accessed 5 Nov 2018.
Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753–9.
Article CAS PubMed Google Scholar
Forouhi NG, Luan J, Hennings S, Wareham NJ. Incidence of type 2 diabetes in England and its association with baseline impaired fasting glucose: the Ely study 1990-2000. Diabet Med. 2007;24(2):200–7.
Metcalf PA, Baker JR, Scragg RK, Dryson E, Scott AJ, Wild CJ. Microalbuminuria in a middle-aged workforce. Effect of hyperglycemia and ethnicity. Diabetes Care. 1993;16(11):1485–93.
Hoehner CM, Greenlund KJ, Rith-Najarian S, Casper ML, McClellan WM. Association of the insulin resistance syndrome and microalbuminuria among nondiabetic native Americans. The inter-tribal Heart project. J Am Soc Nephrol. 2002;13(6):1626–34.
Gabir MM, Hanson RL, Dabelea D, Imperatore G, Roumain J, Bennett PH, et al. Plasma glucose and prediction of microvascular disease and mortality: evaluation of 1997 American Diabetes Association and 1999 World Health Organization criteria for diagnosis of diabetes. Diabetes Care. 2000;23(8):1113–8.
Plantinga LC, Crews DC, Coresh J, Miller ER 3rd, Saran R, Yee J, et al. Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or prediabetes. Clin J Am Soc Nephrol. 2010;5(4):673–82.
Article PubMed PubMed Central Google Scholar
Nguyen TT, Wang JJ, Wong TY. Retinal vascular changes in pre-diabetes and prehypertension: new findings and their research and clinical implications. Diabetes Care. 2007;30(10):2708–15.
Article PubMed Google Scholar
Wong TY, Klein R, Sharrett AR, Schmidt MI, Pankow JS, Couper DJ, et al. Retinal arteriolar narrowing and risk of diabetes mellitus in middle-aged persons. JAMA. 2002;287(19):2528–33.
Barr EL, Zimmet PZ, Welborn TA, Jolley D, Magliano DJ, Dunstan DW, et al. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, obesity, and lifestyle study (AusDiab). Circulation. 2007;116(2):151–7.
Brunner EJ, Shipley MJ, Witte DR, Fuller JH, Marmot MG. Relation between blood glucose and coronary mortality over 33 years in the Whitehall study. Diabetes Care. 2006;29(1):26–31.
Al-Rifai RH, Pearson F, Critchley JA, Abu-Raddad LJ. Association between diabetes mellitus and active tuberculosis: a systematic review and meta-analysis. PLoS One. 2017;12(11):e0187967. https://doi.org/10.1371/journal.pone.0187967 .
Article CAS PubMed PubMed Central Google Scholar
Lee MR, Huang YP, Kuo YT, Luo CH, Shih YJ, Shu CC, et al. Diabetes mellitus and latent tuberculosis infection: a systematic review and metaanalysis. Clin Infect Dis. 2017;64(6):719–27.
PubMed Google Scholar
Imamura F, O'Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ. 2015;351:h3576.
Ashrafi M, Gosili R, Hosseini R, Arabipoor A, Ahmadi J, Chehrazi M. Risk of gestational diabetes mellitus in patients undergoing assisted reproductive techniques. Eur J Obstet Gynecol Reprod Biol. 2014;176:149–52.
InterAct C, Romaguera D, Norat T, Wark PA, Vergnaud AC, Schulze MB, et al. Consumption of sweet beverages and type 2 diabetes incidence in European adults: results from EPIC-InterAct. Diabetologia. 2013;56:1520–30.
Article CAS Google Scholar
World Health Organisation. Sexual and reproductive health. 2015. http://www.who.int/reproductivehealth/topics/infertility/definitions/en/ . Accessed 5 Feb 2019.
Clausen TD, Mathiesen ER, Hansen T, Pedersen O, Jensen DM, Lauenborg J, et al. High prevalence of type 2 diabetes and pre-diabetes in adult offspring of women with gestational diabetes mellitus or type 1 diabetes: the role of intrauterine hyperglycemia. Diabetes Care. 2008;31(2):340–6.
United Nations. Total Population - Both Sexes. World Population Prospects: The; 2015. pp. Revision 2016. https://esa.un.org/unpd/wpp/Download/Standard/Population/ . .
World Health Organization. Global report on diabetes. 2016. https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=B27DA6B4FB2DCD29CA71FB7C373A17FA?sequence=1 . Accessed 30 Jan 2019.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384:766–81.
Galal O. Nutrition-related health patterns in the Middle East. Asia Pac J Clin Nutr. 2003;12(3):337–43 PubMed PMID: 14505998 .
Ng SW, Zaghloul S, Ali HI, Harrison G, Popkin BM. The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Arabian Gulf States. Obes Rev. 2011;12(1):1–13.
World Health Organization. Health education and promotion. Physical activity. Available at: http://www.emro.who.int/health-education/physical-activity/background.html . Accessed 15 Jan 2019.
Sharara E, Akik C, Ghattas H, Makhlouf OC. Physical inactivity, gender and culture in Arab countries: a systematic assessment of the literature. BMC Public Health. 2018;18(1):639.
Bes-Rastrollo M, Martinez-Gonzalez MA, Sanchez-Villegas A, de la Fuente AC, Martinez JA. Association of fiber intake and fruit/vegetable consumption with weight gain in a Mediterranean population. Nutrition. 2006;22(5):504–11.
Kelishadi R, Ardalan G, Gheiratmand R, Gouya MM, Razaghi EM, Delavari A, et al. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN study. Bull World Health Organ. 2007;85(1):19–26.
Nasreddine L, Mehio-Sibai A, Mrayati M, Adra N, Hwalla N. Adolescent obesity in Syria: prevalence and associated factors. Child Care Health Dev. 2010;36(3):404–13.
Al-Rifai RH, Aziz F. Prevalence of type 2 diabetes, prediabetes, and gestational diabetes mellitus in women of childbearing age in Middle East and North Africa, 2000-2017: protocol for two systematic reviews and meta-analyses. Syst Rev. 2018;1:96.
Article Google Scholar
Onarheim KH, Iversen JH, Bloom DE. Economic benefits of investing in women's health: a systematic review. PLoS One. 2016;11(3):e0150120.
Article PubMed PubMed Central CAS Google Scholar
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39.
Woodruff TJ, Sutton P. The navigation guide systematic review methodology: a rigorous and transparent method for translating environmental health science into better health outcomes. Environ Health Perspect. 2014;122(10):1007–14.
http://www.who.int/reproductivehealth/topics/infertility/definitions/en/ . .
The World Bank. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lendinggroups . Accessed 10 Nov 2017.
Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–55.
National Heart, Lung, and blood institute. Quality assessment tool for observational cohort and cross-sectional studies https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools . .
Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21(4):607–11.
Miller JJ. The inverse of the freeman –Tukey double arcsine transformation. The American Statistician. 1978;32(4):138
Google Scholar
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Borenstein MHL, Higgins JP, Rothstein HR. Introduction to meta-analysis. Chichester: Wiley; 2009.
Book Google Scholar
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
StataCorp. Stata statistical software: release 15. College Station: StataCorp LLC; 2017.
Salima T, Mounira K, Nadjia D. Assessment of nutritional status of pregnant women attending the City Tebessa PMI (Algeria). Natl J Physiol Pharm Pharmacol. 2011;1(2):97–105.
Eldesoky A-EE, Gad YZ, Ahmed N. Nonalcoholic fatty liver disease in young adult Egyptian women with polycystic ovary syndrome. Egyptian Liver J. 2013;3:15–9.
Ebrahimi H, Emamian MH, Hashemi H, Fotouhi A. High incidence of diabetes mellitus among a middle-aged population in Iran: a longitudinal study. Can J Diabetes. 2016;40(6):570–5.
Valizadeh M, Alavi N, Mazloomzadeh S, Piri Z, Amirmoghadami H. The risk factors and incidence of type 2 diabetes mellitus and metabolic syndrome in women with previous gestational diabetes. Int J Endocrinol Metab. 2015;13(2):e21696.
Hossein-Nezhad A, Mirzaei K, Maghbooli Z, Larijani B. Maternal glycemic status in GDM patients after delivery. Iran J Diabetes Lipid Disorders. 2009;8(1):95–104.
Azimi-Nezhad M, Ghayour-Mobarhan M, Safarian M, Esmailee H, Parizadeh SM, Rajabi-Moghadam M, et al. Anthropometric indices of obesity and the prediction of cardiovascular risk factors in an Iranian population. ScientificWorld J. 2009;9:424–30.
Azimi-Nezhad M, Ghayour-Mobarhan M, Parizadeh MR, Safarian M, Esmaeili H, Parizadeh SM, et al. Prevalence of type 2 diabetes mellitus in Iran and its relationship with gender, urbanisation, education, marital status and occupation. Singap Med J. 2008;49(7):571–6.
CAS Google Scholar
Hadaegh F, Bozorgmanesh MR, Ghasemi A, Harati H, Saadat N, Azizi F. High prevalence of undiagnosed diabetes and abnormal glucose tolerance in the Iranian urban population: Tehran Lipid and Glucose Study. BMC Public Health. 2008;8:176.
Keshavarz M, Cheung NW, Babaee GR, Moghadam HK, Ajami ME, Shariati M. Gestational diabetes in Iran: incidence, risk factors and pregnancy outcomes. Diabetes Res Clin Pract. 2005;69(3):279–86.
Mansour AA, Al-Maliky AA, Kasem B, Jabar A, Mosbeh KA. Prevalence of diagnosed and undiagnosed diabetes mellitus in adults aged 19 years and older in Basrah. Iraq Diabetes Metab Syndr Obes. 2014;7:139–44.
Mansour AA, Wanoose HL, Hani I, Abed-Alzahrea A, Wanoose HL. Diabetes screening in Basrah, Iraq: a population-based cross-sectional study. Diabetes Res Clin Pract. 2008;79(1):147–50.
Abu-Zaiton A, Al-Fawwaz A. Prevalence of diabetes, obesity, hypertension and associated factors among students of Al-albayt University, Jordan. World J Med Sci. 2013;9(1):49–54.
Ahmed F, Waslien C, Al-Sumaie MA, Prakash P, Allafi A. Trends and risk factors of hyperglycemia and diabetes among Kuwaiti adults: National Nutrition Surveillance Data from 2002 to 2009. BMC Public Health. 2013;13:103.
Diejomaoh M, Jirous J, Al-Azemi M, Gupta M, Al-Jaber M, Farhat R, et al. Insulin resistance in women with recurrent spontaneous miscarriage of unknown aetiology. Med Princ Pract. 2007;16(2):114–8.
Tohme RA, Jurjus AR, Estephan A. The prevalence of hypertension and its association with other cardiovascular disease risk factors in a representative sample of the Lebanese population. J Hum Hypertens. 2005;19(11):861–8.
Rguibi M, Belahsen R. Prevalence and associated risk factors of undiagnosed diabetes among adult Moroccan Sahraoui women. Public Health Nutr. 2006;9(6):722–7.
Gowri V, Mathew M, Gravell D, AlFalahi K, Zakwani I, Ganguly SS, et al. Protein Z levels in pregnant Omani women: correlation with pregnancy outcome. J Thromb Thrombolysis. 2011;32(4):453–8.
Al-Lawati JA, Al Riyami AM, Mohammed AJ, Jousilahti P. Increasing prevalence of diabetes mellitus in Oman. Diabet Med. 2002;19(11):954–7.
Bener A, Zirie M, Janahi IM, Al-Hamaq AO, Musallam M, Wareham NJ. Prevalence of diagnosed and undiagnosed diabetes mellitus and its risk factors in a population-based study of Qatar. Diabetes Res Clin Pract. 2009;84(1):99–106.
Al-Nazhan SA, Alsaeed SA, Al-Attas HA, Dohaithem AJ, Al-Serhan MS, Al-Maflehi NS. Prevalence of apical periodontitis and quality of root canal treatment in an adult Saudi population. Saudi Med J. 2017;38(4):413–21.
Saeed AAW. Combined systolic diastolic hypertension among adults in Saudi Arabia: prevalence, risk factors and predictors: results of a national survey. Int J Med Res Health Sci. 2017;6(6):171–6.
Bahijri SM, Jambi HA, Al Raddadi RM, Ferns G, Tuomilehto J. The prevalence of diabetes and prediabetes in the adult population of Jeddah, Saudi Arabia--A Community-Based Survey. PLoS One. 2016;11(4):e0152559. https://doi.org/10.1371/journal.pone.0152559 .
Al-Rubeaan K, Al-Manaa HA, Khoja TA, Ahmad NA, Al-Sharqawi AH, Siddiqui K, et al. Epidemiology of abnormal glucose metabolism in a country facing its epidemic: SAUDI-DM study. J Diabetes. 2015;7(5):622–32.
Serehi AA, Ahmed AM, Shakeel F, Alkhatani K, El-Bakri NK, Buhari BA, et al. A comparison on the prevalence and outcomes of gestational versus type 2 diabetes mellitus in 1718 Saudi pregnancies. Int J Clin Exp Med. 2015;8(7):11502–7.
PubMed PubMed Central Google Scholar
Al-Rubeaan K, Al-Manaa HA, Khoja TA, Youssef AM, Al-Sharqawi AH, Siddiqui K, et al. A community-based survey for different abnormal glucose metabolism among pregnant women in a random household study (SAUDI-DM). BMJ Open. 2014;4(8):e005906.
Amin TT, Al Sultan AI, Mostafa OA, Darwish AA, Al-Naboli MR. Profile of non-communicable disease risk factors among employees at a Saudi university. Asian Pac J Cancer Prev. 2014;15(18):7897–907.
Wahabi HA, Esmaeil SA, Fayed A, Al-Shaikh G, Alzeidan RA. Pre-existing diabetes mellitus and adverse pregnancy outcomes. BMC Res Notes. 2012;5:496.
Saeed AA. Association of tobacco products use and diabetes mellitus-results of a national survey among adults in Saudi Arabia. Balkan Med J. 2012;29(3):247–51. https://doi.org/10.5152/balkanmedj.2012.035 .
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yousef M, Sabico SL, et al. Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (Riyadh cohort 2): a decade of an epidemic. BMC Med. 2011;9:76.
Alqurashi KA, Aljabri KS, Bokhari SA. Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med. 2011;31(1):19–23.
Al-Baghli NA, Al-Ghamdi AJ, Al-Turki KA, Al Elq AH, El-Zubaier AG, Bahnassy A. Prevalence of diabetes mellitus and impaired fasting glucose levels in the Eastern Province of Saudi Arabia: results of a screening campaign. Singap Med J. 2010;51(12):923–30.
Al-Qahtani DA, Imtiaz ML, Saad OS, Hussein NM. A comparison of the prevalence of metabolic syndrome in Saudi adult females using two definitions. Metab Syndr Relat Disord. 2006;4(3):204–14.
Shaaban LA, Al-Saleh RA, Alwafi BM, Al-Raddadi RM. Associated risk factors with ante-partum intra-uterine fetal death. Saudi Med J. 2006;27(1):76–9 PubMed PMID: 16432598.
Habib FA. Incidence of post cesarean section wound infection in a tertiary hospital, Riyadh, Saudi Arabia. Saudi Med J. 2002;23(9):1059–63.
Karim A, Ogbeide DO, Siddiqui S, Al-Khalifa IM. Prevalence of diabetes mellitus in a Saudi community. Saudi Med J. 2000;21(5):438–42.
CAS PubMed Google Scholar
Ben Romdhane H, Ben Ali S, Aissi W, Traissac P, Aounallah-Skhiri H, Bougatef S, et al. Prevalence of diabetes in Northern African countries: the case of Tunisia. BMC Public Health. 2014;14:86.
Sulaiman N, Albadawi S, Abusnana S, Mairghani M, Hussein A, Al Awadi F, et al. High prevalence of diabetes among migrants in the United Arab Emirates using a cross-sectional survey. Sci Rep. 2018;8(1):6862.
Shah SM, Ali R, Loney T, Aziz F, ElBarazi I, Al Dhaheri S, et al. Prevalence of Diabetes among migrant women and duration of residence in the United Arab Emirates: a cross sectional study. PLoS One. 2017;12(1):e0169949.
Al Dhaheri AS, Mohamad MN, Jarrar AH, Ohuma EO, Ismail LC, Al Meqbaali FT, et al. A cross-sectional study of the prevalence of metabolic syndrome among young female Emirati adults. PLoS One. 2016;11(7):e0159378.
Agarwal MM, Dhatt GS, Othman Y. Gestational diabetes mellitus prevalence: effect of the laboratory analytical variation. Diabetes Res Clin Pract. 2015;109(3):493–9.
Hajat C, Harrison O, Al SZ. Weqaya: a population-wide cardiovascular screening program in Abu Dhabi, United Arab Emirates. Am J Public Health. 2012;102(5):909–14.
Baynouna LM, Revel AD, Nagelkerke NJ, Jaber TM, Omar AO, Ahmed NM, et al. High prevalence of the cardiovascular risk factors in Al-Ain, United Arab Emirates. An emerging health care priority. Saudi Med J. 2008;29(8):1173–8.
Saadi H, Carruthers SG, Nagelkerke N, Al-Maskari F, Afandi B, Reed R, et al. Prevalence of diabetes mellitus and its complications in a population-based sample in Al Ain, United Arab Emirates. Diabetes Res Clin Pract. 2007;78(3):369–77.
Malik M, Bakir A, Saab BA, King H. Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: results of a national survey. Diabetes Res Clin Pract. 2005;69(2):188–95.
Agarwal MM, Punnose J, Dhatt GS. Gestational diabetes: implications of variation in post-partum follow-up criteria. Eur J Obstet Gynecol Reprod Biol. 2004;113(2):149–53.
Gunaid AA, Assabri AM. Prevalence of type 2 diabetes and other cardiovascular risk factors in a semirural area in Yemen. East Mediterr Health J. 2008;14(1):42–56.
Collaboration NCDRF. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–30.
Engelhardt H, Schulz F, Büyükkeçeci Z. Demographic and Human Development in the Middle East and North Africa. https://doi.org/10.20378/irbo-50993 . Bamberg: University of Bamberg Press, Universitätsbibliothek Bamberg; 2018. 88 Seiten : Illustrationen, Diagramme p.
Collaboration NCDRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–96.
World health Organization. Global Health Observatory (GHO) data. Overweight and obesity. Noncommunicable diseases. Obesity among adults. 2016. Available at: https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adults/en/.1-8 Accessed 10 Dec 2018.
El Ati J, Traissac P, Delpeuch F, Aounallah-Skhiri H, Beji C, Eymard-Duvernay S, et al. Gender obesity inequities are huge but differ greatly according to environment and socio-economics in a North African setting: a national cross-sectional study in Tunisia. PLoS One. 2012;7(10):e48153.
World health Organization. Global Health Observatory (GHO) data. Overweight and obesity. Noncommunicable diseases. Mean body mass index (BMI) trends among adults. Available at https://www.who.int/gho/ncd/risk_factors/overweight_obesity/bmi_trends_adults/en/ Accessed 10 Dec 2018.
Diabetes Prevention Program Research G, Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–86.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403.
Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–97.
Centers for Disease Control and Prevention. National Diabetes Prevention Program. https://www.cdc.gov/diabetes/prevention/index.html Accessed 10 Mar 2019.
American Diabetes Association. Type 2 Diabetes Risk Test. http://www.diabetes.org/are-you-at-risk/diabetes-risk-test/?loc=atrisk-slabnav Accessed 2 Mar 2019.
Drees BM, Yun S. Reducing the burden of diabetes mellitus in the state of Missouri: a call to action. Mo Med. 2016;113(5):352–7.
Download references
Acknowledgments
Authors are grateful to the Institute of Public Health, College of Medicine and Health Sciences at the United Arab Emirates University for the infrastructure provided.
This systematic review was funded by the Summer Undergraduate Research Experience (SURE) PLUS-Grant of the United Arab Emirates University, 2017 (Research grant: 31M348). The funder had no role in the study design, collection, analysis, or interpretation of the data, nor in writing and the decision to submit this article for publication.
Author information
Authors and affiliations.
Institute of Public Health, College of Medicine and Health Sciences, United Arab Emirates University, P.O. Box 15551, Al Ain, United Arab Emirates
Rami H. Al-Rifai, Maria Majeed & Faisal Aziz
Department of Biology, College of Sciences, United Arab Emirates University, P.O. Box 15551, Al Ain, United Arab Emirates
Maryam A. Qambar, Ayesha Ibrahim & Khawla M. AlYammahi
You can also search for this author in PubMed Google Scholar
Contributions
RHA conceptualized and designed the study. AI, MM, MQ, KA, and FA assessed the eligibility of the retrieved citations in the titles/abstracts and full-text screening phases. RHA, MM, and FA critically assessed the eligible studies and extracted data. RHA analyzed and interpreted the data. RHA drafted the manuscript. All authors critically reviewed the manuscript. RHA read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Rami H. Al-Rifai .
Ethics declarations
Ethics approval and consent to participate.
There are no primary data used in this review. There is no need for any ethical approval or an exemption letter according to the United Arab Emirates University-Human Research Ethics Committee.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
PRISMA checklist.
Additional file 2.
Search strategies for the six databases, from January 1, 2000 to July 12, 2018.
Additional file 3
Funnel plots examining small-study effects on the pooled T2DM prevalence among women of childbearing age. Egger’s test p <0.0001.
Additional file 4
Funnel plots examining small-study effects on the pooled pre-DM prevalence among women of childbearing age. Egger’s test p <0.0001.
Additional file 5.
Weighted prevalence of T2DM and pre-DM in childbearing age women in MENA countries according to age group.
Additional file 6.
Sub-regional weighted prevalence of T2DM in women of childbearing age according to the tested population, data collection period, T2DM ascertainment, sample size, and overall, in 14 MENA countries.
Additional file 7.
Sub-regional weighted prevalence of T2DM (Figure 1 ) and pre-DM (Figure 2 ) in women of childbearing age from 2000 to 2009 and from 2010 to 2018. Square represents the estimated prevalence and lines around the square represent the upper and lower limit of the 95% confidence interval of the prevalence.
Additional file 8.
Timeline view of the weighted prevalence of T2DM (Figure 1 ) and pre-DM (Figure 2 ) in women of childbearing age, by publication year.
Additional file 9.
Univariate and multivariable meta-regression analyses to identify sources of heterogeneity in studies reporting on T2DM prevalence in women of childbearing age by the different measured characteristics.
Additional file 10.
Sub-regional weighted prevalence of pre-DM in childbearing age women according to the tested population, data collection period, Pre-DM ascertainment, sample size, and overall, in the four sub regions of the 10 MENA countries.
Additional file 11.
Univariate and multivariable meta-regression analyses to identify sources of heterogeneity in studies reporting on pre-DM prevalence in women of childbearing age by the different measured characteristics.
Additional file 12.
Quality assessment of the 48 research reports included in the analysis.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Al-Rifai, R.H., Majeed, M., Qambar, M. et al. Type 2 diabetes and pre-diabetes mellitus: a systematic review and meta-analysis of prevalence studies in women of childbearing age in the Middle East and North Africa, 2000–2018. Syst Rev 8 , 268 (2019). https://doi.org/10.1186/s13643-019-1187-1
Download citation
Received : 17 March 2019
Accepted : 07 October 2019
Published : 08 November 2019
DOI : https://doi.org/10.1186/s13643-019-1187-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Women of childbearing age
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 26 March 2024
Treatment approaches and costs associated with diabetes clinical metrics as measured by Healthcare Effectiveness Data and Information Set (HEDIS)
- Jamil Alkhaddo 1 ,
- Jillian M. Rung 2 ,
- Ameer Khowaja 3 ,
- Yue Yin 4 ,
- Shannon B. Richards 2 ,
- Charlotte Drury-Gworek 2 ,
- Samina Afreen 5 ,
- Caitlan Rossi 6 &
- Susan Manzi 6
BMC Health Services Research volume 24 , Article number: 375 ( 2024 ) Cite this article
170 Accesses
Metrics details
The clinical outcomes of diabetes can be influenced by primary care providers’ (PCP) treatment approaches. This study explores the association between PCP approaches to management and performance measured by established diabetes metrics and related costs.
In phase one, Electronic Medical Records were used to extract diabetes related metrics using Healthcare Effectiveness Data and Information Set (HEDIS), for patients with diabetes who had office visits to 44 PCP practices from April 2019 to March 2020. Using those metrics and scoring system, PCP practices were ranked and then categorized into high- and low-performing groups (top and bottom 25%, n = 11 each), with a total of 19,059 clinic visits by patients with a diagnosis of diabetes. Then extensive analysis was performed to evaluate a correlation between treatment approaches and diabetes outcomes across the top and bottom performing practices. In phase 2, patients with diabetes who were attributed to the aforementioned PCP practices were identified in a local health plan claims data base (a total of 3,221 patients), and the allowed amounts from their claims were used to evaluate differences in total and diabetes-related healthcare costs by providers’ performance.
Comparing 10,834 visits in high-performing practices to 8,235 visits in low-performing practices, referrals to certified diabetes care and education specialists and provider-to-provider electronic consults (e-consults) were higher in high-performing practices (Z = 6.06, p < .0001), while traditional referrals were higher in low-performing practices (Z = -6.94, p < .0001). The patient-to-provider ratio was higher in the low-performing group (M = 235.23) than in the high-performing group (M = 153.26) (Z = -2.82, p = .0048). Claims data analysis included 1,825 and 1,396 patients from high- and low-performing providers, respectively. The patient-to-provider ratio was again higher in the low-performing group ( p = .009, V = 0.62). Patients receiving care from lower-performing practices were more likely to have had a diabetes-related hospital observation (5.7% vs. 3.9%, p = .02; V = 0.04) and higher diabetes-related care costs ( p = .002; d = − 0.07); these differences by performance status persisted when controlling for differences in patient and physician characteristics. Patients seeing low-performing providers had higher Charlson Comorbidity Index scores (Mdn = 3) than those seeing high-performing providers (Mdn = 2).
Conclusions
Referrals to the CDCES and e-Consult were associated with better measured diabetes outcomes, as were certain aspects of cost and types of hospital utilization. Higher patients to providers ratio and patients with more comorbidities were observed in low performing group.
Peer Review reports
Although a growing number of patients with diabetes in the U.S. are meeting national quality metrics, only approximately 50% of these patients are able to achieve A1C < 7.0% [ 1 ]. A marked variability in diabetes outcomes at the local and national levels persists despite the availability of new effective treatments, better monitoring tools and increased awareness of the impact of diabetes on healthcare outcomes.
A patient’s unique risk profile and comorbidities may impact glycemic control, and these patient-specific factors likely lead to variation in outcomes among individuals with diabetes. However, the clinical course and outcomes of diabetes can be influenced by providers’ treatment approaches and management decisions, including diabetes and nutrition support, specialty referrals, medication choice, and frequency of follow-up visits [ 1 ]. Previous studies have demonstrated that dedicating resources to train primary care providers (PCPs) in evidence-based diabetes care is associated with positive patient outcomes [ 2 ]. However, little emphasis has been placed on identifying the specific treatment approaches or organizational support that may drive such improvements. To this end, the International Diabetes Federation (IDF) has called for research that explores the implementation of clinical guidelines to inform future best practices and policies in the setting of diabetes. Identifying the treatment approaches associated with positive diabetes outcomes is critical in allowing PCPs and healthcare delivery systems to improve the health of the populations they serve.
Additionally, in pursuit of the triple aim of health care—improved health and better patient experience at lower costs—there has been a great interest in measuring quality of care. The Centers for Medicare & Medicaid Services (CMS) and many healthcare organizations (i.e., National Committee for Quality Assurance [NCQA]) have proposed numerous metrics that align with the trend toward value-based care. Therefore, determining treatment approaches associated with positive diabetes outcomes, particularly those that confer consistent benefits across diverse settings and populations, is critical to achieve such goals. Considering that PCPs manage more than 90% of patients with diabetes, redesigned models of primary care have emphasized team-based diabetes treatment approaches and shared decision making [ 3 – 4 ].
The Allegheny Health Network (AHN), a multifacility academic healthcare system in Western Pennsylvania, has taken many steps toward value-based care to improve population health. To develop innovative treatment models for patients with diabetes, the AHN Division of Endocrinology partnered with the Primary Care Institute to monitor diabetes quality metrics and use these data to identify gaps in the diabetes-related care. In our academic healthcare system, we implemented a novel endocrinology compensation model that encourages collaboration between PCPs and endocrinologists through provider-to-provider electronic consults (e-consult), PCP education sessions, and regular visits to PCP practices by an endocrinologist and certified diabetes care and education specialist (CDCES) every 6 months to discuss practice-specific data and recent updates in diabetes management [ 5 ]. This initiative aims to standardize and improve diabetes care across the network while motivating endocrinologists to take on a supportive role for partnering in primary care services.
In this study, we sought to uncover gaps in treatment approaches that may guide the allocation of future resources and interventions. The objective was to identify treatment approaches that may contribute to the clinical outcomes of patients with diabetes in primary care settings, as well as variation in outcomes across practices within a large integrated health network. We used the Healthcare Effectiveness Data and Information Set (HEDIS), developed and maintained by the National Committee for Quality Assurance (NCQA), to rank primary care practices as high- or low-performing [ 6 ]. The primary outcome was to identify an association between individual treatment approaches and the achievement of established diabetes metrics (performance). In addition, we collected claims data of patients with diabetes managed by high- and low-performing practices to assess cost and other factors associated with potential variations in outcomes.
This study includes two phases of data collection and analysis. In Phase 1, we assessed data directly from the electronic medical record (EMR) and survey data for clinics within a single provider network (Allegheny Health Network, AHN). Phase 2 supplemented these analyses with health insurance claims data for the patients assessed in Phase 1 who were members of Highmark Inc. health plans. The study protocol was reviewed by the AHN Institutional Review Board and was determined to be a clinical quality improvement project and not the human-subjects research, hence protocol was approved and requirement for informed consent was waived.
Phase 1: treatment approaches
Inclusion and Exclusion Criteria of Participating Practices: All AHN primary care practices were included in the initial analysis, and 50 practices adopted HEDIS measures to monitor internal performance and quality improvement. HEDIS measures of all participating PCPs were collected using EMR and updated on a quarterly basis. Practices with fewer than 50 patients with diabetes reported per quarter were excluded. A total of 44 practices were measured against these metrics based on their performance over a one-year period that included the second, third and fourth quarters of 2019 and the first quarter of 2020. HEDIS metrics for diabetes were aggregated over the 12-month period and included in the analysis. Using the scoring system approved by NCQA, each practice was assigned a score (100 being the maximum score) and then ranked based on their score. The top 25% of practices (11 practices) were grouped as top-performing, and the bottom 25% of practices (11 practices) were grouped as low-performing, which comprised the sample of providers used in the analyses. These 22 practices had a total of 19,059 clinic visits by patients with a diagnosis of diabetes during the analysis period.
Treatment approaches: Five components of treatment approaches (variables) were collected using a combination of EMR and facility information. The 5 components included (1) the rate of traditional endocrine consults; (2) the rate of electronic provider to provider endocrine consults (e-consults), which is a service that is available to all practices included in the analysis; (3) the rate of CDCES referral orders (this service was equally available to all practices); (4) the utilization of insulin and noninsulin injectable medications (glucagon-like peptide-1 receptor agonists) among patients with diabetes; and (5) the PCP practice location and its proximity to the endocrine office (distance in miles) as it may impact treatment approaches, like referrals. Selection rates were based on the ratio of selected treatment approaches relative to PCP annual office visits of patients with diabetes. The 5 components chosen were based on their hypothesized effects on functional and clinical outcomes associated with diabetes management.
Data Analyses: Both descriptive and inferential statistics were computed for the treatment approaches. For continuous variables, t tests were conducted. For rate- and proportion-based variables (all referral- and medication-related variables), generalized linear models were used. Patients’ visit volume across performance status groups (ratio of patients to practitioners) was tested using a negative binomial model.
Phase 2: insurance claims data
Data Source: The database used contained health plan claims for insurance products offered by Highmark Inc., an independent Blue Cross Blue Shield licensee. Both AHN and Highmark Inc. are owned by Highmark Health and are headquartered in Western Pennsylvania. Highmark Inc. offers independent, group, and Medicare Advantage health plans, and insured 5 + million members in Pennsylvania, Delaware, and West Virginia during the years of focus for analysis [ 7 , 8 ].
Inclusion and Exclusion Criteria: We identified a total of 3,221 members with diabetes who were seen by the 78 physicians (MDs and DOs) that belonged to the top 11 and bottom 11 performing practices that were ranked in Phase 1. These members were identified using the criteria of (i) at least one approved claim with a primary diagnosis of diabetes (ICD 10: E08.xx, E09.xx, E10.xx, E11.xx, E12.xx, or E13.xx.) between April 1st, 2019, and March 31st, 2020, (ii) twelve months of continuous enrollment during the aforementioned timeframe, and (iii) receiving treatment from one of the aforementioned 78 AHN providers.
Member Characteristics, Physician Characteristics and Patient Load: Demographic and insurance plan types were obtained from members’ enrollment information. Insurance plan type was categorized as commercial (e.g., plans purchased individually or through participating employers), senior (e.g., Medicare Advantage), or other (e.g., federal employee). We defined patients’ health status using the Charlson Comorbidity Index (CCI), which quantifies long-term mortality in individuals with multiple comorbidities [ 9 – 10 ]. The CCI for each member was calculated using ICD-10 codes appearing on members’ claims from the study period. Type of diabetes diagnosis (type 1, type 2, secondary, both type 1 and type 2) and insulin use were derived from the presence of corresponding diagnosis codes and national drug codes (NDCs) in a member’s claims throughout the 12-month period. In addition to member characteristics, physician characteristics were extracted from standard information maintained within the claims database (e.g., age, sex, degree type). The patient-level data, along with linked practice/physician information from the claims, were used to calculate the number of patients seen within each practice and by each physician. Note that due to the nature of using claims data, these patient load estimates reflect the number of patients who are Highmark members and not the total number of patients.
Cost and Utilization: Allowed amounts (i.e., negotiated costs for service) were used to calculate the total cost of diabetes-related care and all other healthcare for the twelve-month study period. Diabetes-related cost of care was calculated as the sum of all claims costs that fell into one of the following categories: medical claims that had diabetes as the primary or admitting diagnosis (ICD 10 E08.xx – E13.xx), diabetes medication claims, or claims for diabetes-related durable medical equipment (DME), i.e., glucose monitoring supplies. All claims not meeting the diabetes-related criteria were summed to create the total cost of other care. Details on medications, DME, and CPTs used for categorization of diabetes-related spending and utilization are provided in the Supplementary Materials (eTables 1 – 3 ). Diabetes-related hospital utilization was identified using a combination of diagnosis codes, claim type codes (e.g., inpatient vs. professional claims), and CPTs from individual claims. Three types of diabetes-related hospital utilizations over the 12-month period were identified (coded as any vs. none per member): hospital observations, inpatient admissions, and emergency department use (eTable 3 ). Determination of hospitalizations as diabetes-related followed the same coding strategy described above for costs.
Data Analysis: Descriptive statistics were computed for patient and physician characteristics (e.g., demographics, type of diabetes diagnoses) as a function of performance status (high vs. low). Differences in patient and physician characteristics were evaluated using Wilcoxon rank sum tests, chi-squared tests, and Fisher’s exact tests as appropriate. Cohen’s d and Cramer’s V are provided to quantify the magnitude of performance group differences. Follow-up analyses to determine factors that may underlie differences in practices’ performance status consisted of comparisons of the number of physicians within practices, the number of patients seen per physician, patient’s health status (CCI scores), diabetes-related care costs, and diabetes-related hospital utilization (stratified by type). These patient and care-related factors were compared using Wilcoxon rank-sum tests (continuous variables) and Fisher’s exact tests (categorical variables).
Cost and utilization measures that differed by performance status were compared using logistic and quantile regression to evaluate differences while controlling for patient and physician factors. Quantile regression was selected to relax assumptions of normality and allow specification of the part(s) of the outcome distribution to predict using percentiles. For example, specifying the 50th percentile allows prediction of the median. Quantile regression was well designed for the cost data because the distribution was both skewed and bimodal. The percentiles chosen for modeling corresponded to the two modes for the high-performance group. In all models, the primary predictor of interest was performance status; control variables included patient age (centered), physician age (centered), patient sex, physician sex, plan type (commercial, senior, or other), CCI score, presence of type 1 diabetes diagnosis (yes/no), insulin use (any/none), and members’ spend on non-diabetes-related care (in $100 units). Cost and utilization measures of interest in these adjusted analyses had low correlations within physicians (intraclass correlation coefficients between 0.00 and 0.02), and as such analysis methods that allowed for modeling individual physician-level variance were not pursued (e.g., mixed effects modeling).
Analyses were conducted using RStudio Workbench (version 1.4.1717-3) running R version 3.6.3 with an alpha level of 0.05 for significance. Analyses, tables, and figures were created using the following packages: ggplot2, ggridges, effsize, rstatix, quantreg, marginaleffects, performance, and gtsummary [ 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 ].
Treatment approaches that differed between groups were the rate of CDCES referrals (Z = 6.06, p < .0001), e-consults (Z = 3.76, p = .0002), and traditional referrals (Z = − 6.94, p < .0001). CDCES referrals (M = 0.06) and e-consults (M = 0.006) were higher in the high-performing group than in the low-performing group (M = 0.04 for CDCES referrals, M = 0.0020 for e-consults). In contrast, the low-performing group (M = 0.08) had more traditional referrals than the high-performing group (M = 0.05). The ratio of patients to providers between groups was significantly different (Z = -2.82, p = .0048). The ratio of patients to providers for the low-performing group (M = 235.23) was higher than that of the high-performing group (M = 153.26). Tables 1a and 1b contain descriptive statistics and a comparison of treatment approaches between high- and low-performing groups.
Most demographic and health characteristics of patients receiving care from high- versus low-performing practices were similar; in instances where they did differ, the effects were typically small (e.g., Cohen’s d < |0.18|). The largest of these differences was in comorbidities: patients seeing physicians at low-performing practices had higher Charlson Comorbidity Index (CCI) scores (Mdn = 3) than those seeing physicians at high-performing practices (Mdn = 2); details are provided in Table 2 , and eFigure 2 depicts the distributions of CCI scores. The second largest difference was in plan type that patients were enrolled in; patients seeing physicians at high-performing practices were more likely to be enrolled in commercial (52% vs. 44% for high vs. low performing) and senior plans (6.5% vs. 4.9% for high vs. low performing). See Table 2 for details of tests performed and results of all comparisons.
Physicians at low and high performing practices differed in respect to several demographic characteristics, as well as in considerations of patient load. Specifically, physicians at high performing practices were significantly younger (Mdn age = 41) than those at low-performing practices (Mdn age = 53), and the effect was large ( d = -0.83; see Table 2 for details). There was also a significantly larger percentage of physicians identifying as female at high performing practices (57%) than at low performing practices (30%), although this effect was smaller. In agreement with the results of phase 1 analysis, physicians at low-performing practices had significantly higher patient loads (median = 52 patients per physician, Q1 = 32, Q3 = 72) than those at high-performing practices (median = 32 patients per physician, Q1 = 22, Q3 = 46; p = .009, V = 0.62). Figure 1 shows the distributions of patient counts per physician by performance status. Among low-performing practices, there were also significantly fewer physicians (high-performing median = 5, low-performing median = 3; p < .001, V = 0.95).
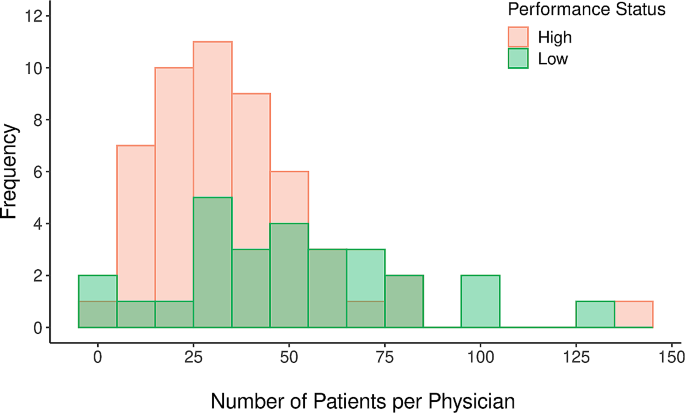
Frequency histogram of the number of patients with diabetes seen per physician who received diabetes-related care during the study period, with the color of bars corresponding to physicians within high (coral) versus low (green) performing practices
The unadjusted analyses of cost and utilization revealed several differences as a function of performance status, as shown in Table 3 . However, the differences that did emerge were small: overall, those receiving care from lower-performing practices were more likely to have had a diabetes-related outpatient hospital observation (5.7% vs. 3.9%, p = .02; V = 0.04) and higher diabetes-related care costs (median difference = $552, p = .002; d = − 0.07). In follow-up analyses controlling for patient and physician characteristics, the difference in the likelihood of diabetes-related hospital observations as a function of performance status remained significant ( p = .04; see Table 4 ). Visual analysis of the cost distribution indicated that the modes for the high-performance group were at values of $325 and $6,800, which corresponded to the 30th and 79th percentiles (see Fig. 1 ). The quantile regression predicting costs at these modal percentiles clarified that significant differences in cost were confined to the higher ends of the cost distribution. At the 79th percentile, low performance status was associated with increased diabetes care cost (b = $847.43, p = .01; see Table 4 ). In other words, the cost of diabetes care was similar across performance status groups at the lower end of the cost distribution; however, this changed as low-performing providers have higher costs at the high end of the distribution.
In this study, we ranked primary care practices based on NCQA-HEDIS measures for diabetes outcomes and then analyzed treatment approaches to identify the practices that are associated with better outcomes. Our findings indicated that, relative to low-performing practices, high-performing practices had higher e-Consult utilization rates, while low-performing practices had higher traditional referral rates.
E-consults are asynchronous consultative communications between clinicians, during which a PCP typically asks an endocrinologist to review the patient’s records and answer specific questions related to the patient’s diabetes management or endocrine disorders using a note that is placed in the patient’s records. The use of e-consults has improved access to care by facilitating the timeliness of specialist input [ 19 ]. In contrast, in-person consultations require administrative assistance to schedule and consult completion depending on clinic access [ 20 ]. E-Consults not only provide timely access to specialist input but also likely reflect PCP engagement in network initiatives and openness to partner with specialists to coordinate care. In this study, low-performing practices placed more traditional (face-to-face) endocrine referrals than high-performing PCPs. It is plausible that such a higher frequency of traditional consults may not necessarily lead to completion of endocrine consult, considering administrative barriers as well as low engagement in the network’s initiatives or limited motivation to partner with specialists.
We observed in this study that high-performing PCPs also had higher rates of CDCES referrals. Appropriate diabetes management requires daily monitoring of blood sugars and changes in diet and activity level, which in turn demands a patient’s active, continuous role [ 21 ]. CDCES not only make themselves available to advise patients on self-management but also facilitate care coordination and support providers by reducing administrative tasks such as collecting and reporting data, especially in complex cases [ 22 – 23 ]. Studies have demonstrated dismal utilization of CDCES [ 22 , 23 , 24 ]. In this study, high-performing practices more frequently made use of external support in the form of diabetes education and nutrition referrals. Developing management algorithms that prompt CDCES referrals, as well as tracking such referrals, have been suggested as strategies to improve uptake [ 22 , 23 , 24 , 25 ].
Higher-performing practices had lower patient-to-provider ratios (derived from the ratio of total annual visits to number of providers). This may represent a significant factor impacting provider performance, as high patient volumes limit providers’ ability to invest time in lifestyle and behavior counseling [ 21 ]. Numerous studies have shown that high-volume surgeons have better patient outcomes, but this trend is unlikely to translate to the primary care setting [ 26 ]. Higher patient volume often forces PCPs to spend less time per patient and hence compromises quality of visit and focus on more acute issues during visits and follow-up (i.e., adjusting insulin doses in between visits based on blood sugar readings), thereby potentially affecting diabetes-related outcomes. In our network, low-performing practices were found to have relatively fewer providers per practice (eFigure 3 ), perhaps indicating suboptimal support staff, which could also impact patient care and outcomes. Low-performing PCPs may not have the requisite support to care for complex diabetic cases compared to larger practices with more providers. Future studies exploring the optimal size of patient panels for PCPs and support in practice would likely help improve the quality of diabetes care.
Using the CCI, a weighted index that considers the number and seriousness of co-occurring diseases and a widely used predictor of prognosis [ 9 ], we found a relatively higher index in the low-performing group. This finding indicates that patients in low-performing practices may have more comorbidities, thereby partially explaining the variation in outcomes. In the setting of diabetes, PCPs manage patients with more medications and co-occurring diseases than ever before, which has made it challenging to provide optimal care as “first contact” providers [ 27 ]. Studies have shown that the type, number and severity of comorbid conditions can cause patients to deprioritize diabetes self-management, a factor that might have been responsible for higher A1cs among these patients [ 28 ]. Moreover, according to ADA guidelines, less stringent A1c targets are recommended for appropriate patients who have comorbidities that decrease life expectancy. Therefore, the “low performing” PCPs in this study who manage patients with high CCI indexes might in fact be appropriately pursuing less stringent A1c targets in accordance with guidelines [ 29 ]. In this manner, it highlights the limitations of the HEDIS system that need to be acknowledged. Our results indicate that patients with diabetes attributed to low-performing providers had slightly higher diabetes-related costs and hospital observations. We cannot ignore the likely impact of a higher CCI index on this finding, illustrating the difficulty of uncovering ties between cost and outcomes.
There is an urgent need for health care leaders to identify cost-effective, evidence-based solutions that meet quality standards [ 22 ]. The importance of innovative ways to support PCPs (i.e., diabetes education and the use of e-consults) to reduce workload and improve overall performance should be emphasized. In addition, while moving toward pay-for-performance is a step in the right direction and using metrics will likely help coordinate the actions and behaviors of providers, we must be aware of the shortcomings and possible adverse effects of this approach [ 30 ].
Limitations
We acknowledge the many limitations that surround research relying on Electronic Medical Records and claims data, such as incomplete data and limited capture of relevant information. In particular with our study, all data were extracted from a single health care system (Phase 1) and a single health insurance provider (Phase 2) that are headquartered in the same region of the United States (Western Pennsylvania). In addition to these geographical considerations, the sample in Phase 2 likely contains greater proportions of individuals who work for select employers within the region (i.e., offer Highmark coverage to their employees) and those who enroll in Medicare Advantage and other senior plans. In sum, it is possible these results may not generalize to healthcare systems and patient populations in disparate regions, share idiosyncrasies associated with enrollment in Highmark plans in particular, or to those who do not need, or cannot afford Medicare Advantage coverage.
In addition to considerations surrounding our data source, there are limitations of HEDIS measures in assessing diabetes care quality, which we have tried to highlight in conducting this study. The definition of control, as mentioned, may vary with respect to HbA1c goals in patients with comorbidities. Finally, our claims-based analyses helped clarify what factors at the patient level—and some limited characteristics at the physician level—are associated with higher and lower performance on outcomes, which afforded the ability to control for characteristics in select analyses. However, we were not able to adjust for certain patient characteristics that are known to impact diabetes outcomes such as socioeconomic status, access care and other barriers to care, etc.
This study highlights treatment approaches that may improve diabetes care in the primary care setting, likely impacting outcomes and costs downstream. High-performing practices more frequently used e-consults than traditional consultations. PCPs in the high-performance group also placed more CDCES referrals. Our findings indicate that more support and coordination are needed among PCPs to care for patients with diabetes and that providers’ patient panels should be optimized to allow for the time and resources needed to care for this population. In addition, while the use of quality metrics seems to be essential in monitoring performance and moving away from the fee-for-service model, our results underscore that these metrics should account for complex cases, comorbidities, patient panels and available resources (such as diabetes education).
Data availability
The dataset used and/or analyzed during the current study is available from the corresponding author upon reasonable request.
Abbreviations
Healthcare Effectiveness Data and Information Set
Certified diabetes care and education specialist
Consults-Electronic Consults
Allegheny Health Network
Primary Care Providers
International Diabetes Federation
Center for Medicare and Medicaid Services
National Committee for Quality Assurance
Pantalone K, Misra-Hebert A, Hobbs T, et al. The probability of A1C goal attainment in patients with uncontrolled type 2 diabetes in a large Integrated Delivery System: a prediction model. Diabetes Care. 2020;43(8):1910–9.
Article CAS PubMed PubMed Central Google Scholar
Siminerio LM, Piatt G, Zgibor JC. Implementing the chronic care model for improvements in diabetes care and education in a rural primary care practice. Diabetes Educ. 2005;31(2):225–34.
Article PubMed Google Scholar
Janes GR. Ambulatory medical care for diabetes. In: Group NDD, editor. Diabetes in America. Bethesda, Md: National Institutes of Health; 1995. pp. 95–1468.
Google Scholar
Peterson KA, Brown MT, Warren-Boulton E. Responding to the challenges of primary diabetes care through the National Diabetes Education Program. Diabetes Care. 2015;38:343–4.
Alkhaddo J, Bhargava A, Rossi C, Custodio P, Bononi P, Kramer E, Stanescu I. Piloting a new compensation model for endocrinologists to improve diabetes care. Diabetes Epidemiol Manage. 2022;7:100071. https://doi.org/10.1016/j.deman.2022.100071 . ISSN 2666–9706.
Article Google Scholar
National Committee for Quality Assurance. HEDIS and performance measurement. https://www.ncqa.org/hedis/ .
Highmark Health. 2019 Annual Report | Highmark Health Plans [Internet]. www.highmarkhealth.org. [cited 2024 Jan 22]. Available from: https://www.highmarkhealth.org/annualreport2019/highlights/healthplans/index.shtml .
Highmark Health. 2020 Annual Report | Highmark Health Plans [Internet]. www.highmarkhealth.org. [cited 2024 Jan 22]. Available from: https://www.highmarkhealth.org/annualreport2020/highlights/healthplans/index.shtml .
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Article CAS PubMed Google Scholar
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82.
H. Wickham. ggplot2: elegant graphics for data analysis. Springer- New York, 2016.
Claus O, Wilke. (2022). ggridges: Ridgeline Plots in ‘ggplot2’. R package version 0.5.4. https://wilkelab.org/ggridges/ .
Torchiano M. Effsize: efficient effect size computation. R Package Version 0 8 1. 2020. https://doi.org/10.5281/zenodo.1480624 . https://CRAN.R-project.org/package=effsize .
Alboukadel K. (2022). rstatix: Pipe-Friendly Framework for Basic Statistical Tests. R package version 0.7.1. https://rpkgs.datanovia.com/rstatix/ .
Roger Koenker. (2022). quantreg: Quantile Regression. R package version 5.94. https://www.r-project.org .
Vincent Arel-Bundock. (2022). marginaleffects: Marginal Effects, Marginal Means, Predictions, and Contrasts. R package version 0.8.1. https://vincentarelbundock.github.io/marginaleffects/ .
Lüdecke, et al. Performance: an R Package for Assessment, comparison and testing of statistical models. J Open Source Softw. 2021;6(60):3139. https://doi.org/10.21105/joss.03139 .
Sjoberg DD, Whiting K, Curry M, Lavery JA, Larmarange J. Reproducible summary tables with the gtsummary package. R J. 2021;13:570–80. https://doi.org/10.32614/RJ-2021-053 .
Vimalananda VG, et al. Electronic consultations (E-consults) and their outcomes: a systematic review. J Am Med Inf Assoc. 2020;27(3):471–9.
Patel PS, et al. Electronic Consultation: an effective alternative to In-Person clinical care for patients with diabetes Mellitus. J Diabetes Sci Technol. 2019;13(1):152–3.
Ashrafzadeh S, Hamdy O. Patient-driven Diabetes Care of the future in the Technology era. Cell Metab. 2019;29(3):564–75.
Rodriguez K, et al. Improving Quality outcomes: the value of Diabetes Care and Education specialists. Clin Diabetes. 2022;40(3):356–65.
Article PubMed PubMed Central Google Scholar
Powers MA, et al. Diabetes self-management education and support in adults with type 2 diabetes: a Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American pharmacists Association. Diabetes Educ. 2020;46(4):350–69.
Li R, Shrestha SS, Lipman R, et al. Diabetes self-management education and training among privately insured persons with newly diagnosed diabetes–United States, 2011–2012. MMWR Morb Mortal Wkly Rep. 2014;63(46):1045–9.
James TL. Improving referrals to Diabetes Self-Management Education in Medically Underserved adults. Diabetes Spectr. 2021;34(1):20–6.
Morche J, Mathes T, Pieper D. Relationship between surgeon volume and outcomes: a systematic review of systematic reviews. Syst Rev. 2016;5(1):204. https://doi.org/10.1186/s13643-016-0376-4 . Published 2016 Nov 29.
Bodenheimer T. Coordinating Care—A perilous journey through the Health Care System. N Engl J Med. 2008;358:1064–71.
Kerr EA, et al. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22(12):1635–40.
Glycemic Targets. Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S73–s84.
Harris J, Haltbakk J, Dunning T, et al. How patient and community involvement in diabetes research influences health outcomes: a realist review. Health Expect. 2019;22(5):907–20.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Allegheny Health Network, Division of Endocrinology, Pittsburgh, PA, USA
Jamil Alkhaddo
Highmark Health Enterprise Data & Analytics, Pittsburgh, PA, USA
Jillian M. Rung, Shannon B. Richards & Charlotte Drury-Gworek
Northeast Endocrinology Associates, San Antonio, TX, USA
Ameer Khowaja
Allegheny-Singer Research Institute, Pittsburgh, PA, USA
Division of Endocrinology, University of Virginia, Charlottesville, VA, USA
Samina Afreen
Allegheny Health Network Medicine Institute, Pittsburgh, PA, USA
Caitlan Rossi & Susan Manzi
You can also search for this author in PubMed Google Scholar
Contributions
JA – Conceived the project and participated in data extraction, analysis and manuscript editing, JMR, YY, SBR, CDG and CR participated in data extraction, analysis and review, AK reviewed the results and edited manuscript, SA and SM participated in literature and manuscript review.
Corresponding author
Correspondence to Jamil Alkhaddo .
Ethics declarations
Ethics approval and consent to participate.
The study protocol was reviewed by the Allegheny Health Network (AHN) Institutional Review Board and was determined to be a clinical quality improvement project and not the human-subjects research, hence protocol was approved and requirement for informed consent was waived. Furthermore, authors confirm that all methods were carried out in accordance with relevant guidelines and regulations (declarations of Helsinki).
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Alkhaddo, J., Rung, J.M., Khowaja, A. et al. Treatment approaches and costs associated with diabetes clinical metrics as measured by Healthcare Effectiveness Data and Information Set (HEDIS). BMC Health Serv Res 24 , 375 (2024). https://doi.org/10.1186/s12913-024-10745-2
Download citation
Received : 07 September 2023
Accepted : 18 February 2024
Published : 26 March 2024
DOI : https://doi.org/10.1186/s12913-024-10745-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Healthcare Effectiveness Data and Information Set (HEDIS)
- Certified diabetes care and education specialist (CDCES)
- Electronic consults (E-consults)
- Patients-to-providers
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Severe hyponatremia and diabetes insipidus caused by low-dose cyclophosphamide in breast cancer patients: A case report and literature review
Affiliations.
- 1 Department of General Surgery, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
- 2 Guangdong Provincial Key Laboratory of Major Obstetric Diseases, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
- 3 Guangdong Provincial Clinical Research Center for Obstetrics and Gynecology, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.
- PMID: 38552085
- PMCID: PMC10977568
- DOI: 10.1097/MD.0000000000037572
Rationale: Cyclophosphamide (CTX) is widely used in the treatment of malignancies and autoimmune diseases. Although severe hyponatremia caused by low-dose CTX chemotherapy is uncommon, it can lead to serious complications and even death.
Patient concerns: A 44-year-old woman with left-sided breast cancer suddenly experienced headaches, disorientation and weakness after receiving low-dose neoadjuvant chemotherapy combined with CTX and doxorubicin.
Diagnoses: The patient pathology showed invasive breast carcinoma. She developed severe hyponatremia and a generalized seizure after completing the first cycle of neoadjuvant chemotherapy with CTX and doxorubicin. Laboratory tests showed a serum sodium of 118 mmol/L (normal range 135-145 mmol/L) and potassium sodium 3.16 mmol/L (normal range 3.5-5.5 mmol/L). Subsequently, the patient developed secondary diabetes insipidus 4 hours after sodium supplementation, her 24-hour urine volume was 4730 mL (normal range 1000-2000 mL/24 hours), and the urine specific gravity decreased to 1.005.
Interventions: The patient was given intravenous sodium chloride (500 mL of 3%NaCl, 100 mL/hour) and potassium chloride (500 mL of 0.3%KCl, 250 mL/hour). Meanwhile, she was advised to reduce her water intake, and pituitrin was administered to prevent dehydration caused by diabetes insipidus.
Outcomes: The patient completely recovered after correcting of the serum sodium concentration (137 mmol/L) without any neurological deficits. After discontinuing pituitrin, her 24-hour urine volume was 2060 mL and the urine specific gravity was 1.015.
Lessons: This is a typical case of severe hyponatremia induced by low-dose CTX. Clinicians and healthcare providers should be aware of this potential toxicity, and appropriate monitoring should be implemented.
Copyright © 2024 the Author(s). Published by Wolters Kluwer Health, Inc.
Publication types
- Case Reports
- Breast Neoplasms* / complications
- Breast Neoplasms* / drug therapy
- Cyclophosphamide / adverse effects
- Diabetes Insipidus*
- Diabetes Mellitus*
- Doxorubicin / adverse effects
- Hyponatremia* / chemically induced
- Hyponatremia* / complications
- Pituitary Hormones, Posterior* / adverse effects
- Cyclophosphamide
- Doxorubicin
- Pituitary Hormones, Posterior
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Nephropharmacol
- v.5(2); 2016

Effectiveness of diabetes education and awareness of diabetes mellitus in combating diabetes in the United Kigdom; a literature review
Chaudhary muhammad junaid nazar.
1 Department of Nephrology, Shifa International Hospital, Islamabad, Pakistan
Micheal Mauton Bojerenu
2 Department of Internal Medicine, Sickle Cell Unit, Harvard University Hospital, Washington DC, USA
Muhammad Safdar
Jibran marwat.
Diabetes mellitus is a metabolic disorder that is characterized by high blood glucose level, and body cannot produce enough insulin, or does not respond to the produced insulin. In spite of the diabetes education campaigns and programmes, a large number of people in the United Kingdom are living with diabetes. The main objective of the study is to evaluate the role of knowledge and awareness of diabetes in fighting against diabetes and to interpret to which extent is diabetes education successful. The systematic review to be carried out will include literature from 2001 to 2011 in the United Kingdom regarding awareness of diabetes among UK population and effectiveness of diabetes education. Literature will be accessed using search database, British medical journals, and library. Good quality papers will be used for the systematic review. Previous studies about diabetes education will consulted and assessed. This study is going to summarize the efficacy of diabetes education campaigns and programmes which are promising to enhance the awareness The outcome of the review will be the guideline for the government, education centres, researchers, and campaigns to implement more diabetic education programmes and easily accessible diabetes services and education interventions to increase the awareness of risk factors and complications of diabetes to overcome the increasing epidemic of diabetes in the United Kingdom.
Implication for health policy/practice/research/medical education:
Diabetes mellitus is a metabolic disorder, in which there is high blood glucose level, and body cannot produce enough insulin, or the body does not respond to the insulin produced. In spite of the diabetes education campaigns and programmes, a large number of people in the United Kingdom are living with diabetes. The main objective of the study is to evaluate the role of knowledge and awareness of diabetes in fighting against diabetes and to interpret to which extent is diabetes education successful. The outcome of the review will be the guideline for the government, education centres, researchers, and campaigns to implement more diabetic education programmes and easily accessible diabetes services and education interventions to increase the awareness of risk factors and complications of diabetes to overcome the increasing epidemic of diabetes in in the United Kingdom.
Introduction
Diabetes is a serious and life-threatening disease, however it can be managed very well through proper treatment and controlling. Diabetes self-management training and education plays a vital role in the management of diabetes ( 1 ). It is crucial for diabetic patients to be aware of nature, treatment, risk factors and complication of disease due to providing suitable modality to attenuate following complications. In a study to detect the relation between health literacy, complication awareness and diabetic control among patients with type 2 diabetes mellitus, it was concluded that patient awareness scores and health literacy was negatively related to diabetes control ( 2 ). This study was 6 months study, carried out from September 2005 to February 2006 with about 150 Chinese patients.
Materials and Methods
For this review, we used a variety of sources by searching through PubMed, EMBASE, Scopus and directory of open access journals (DOAJ). The search was performed by using combinations of the following key words and or their equivalents; Prevalence of diabetes mellitus, awareness and knowledge about diabetes and its management, diabetes education programmes, effectiveness of diabetes education.
Looking at the study carried out to explore the total prevalence of diabetes mellitus in 2001 in England to support delivery of healthcare services it was estimated that in 2001 the prevalence of diabetes (diagnosed as well as undiagnosed) in England was about 4.5%, affecting more than 2 million persons ( 3 ). It was found that the prevalence of type 2 diabetes was 92% affecting 2000000 persons and the prevalence of type 1 diabetes was nearly 8% affecting 160000 persons. The prevalence of diabetes was estimated to be more in women (5.2%) than men (3.6%). It was also estimated that the prevalence of diabetes was higher in the people from ethnic minority groups than the white people. The estimated prevalence rates are 4.3 for white people, 5.7 for black African/Caribbean, and 6.6 for South Asians and 2.1% for other groups. The prevalence of diabetes was found to be increased rapidly with age as the prevalence was found to be 0.3 in people aged 0–29, 3.3 in those 30–59 and 14% in people over 60 years age.
According to Diabetes UK (2010) in 2009, the prevalence of diabetes in adults over 17 years old is estimated to be 5.1% in England affecting 2213138, 4.5% in Northern Ireland affecting 65066, 4.6% in Wales affecting 146173 and 3.9% in Scotland affecting 209886 people. The total average prevalence of diabetes in 2009 in the United Kingdom is estimated to be 4.26%.
A systematic review was conducted to estimate the age- and sex-specific diabetes prevalence worldwide for years 2010 and 2030 ( 4 ). Studies from 91 countries were selected and it was found from the review findings that the incidence of diabetes among people aged 20–80 years will be 6.5% in 2010 and 286 million adults will be affected in 2010. The prevalence of diabetes will increase to 7.8%, and nearly 440 million adults will be affected by 2030. It was suggested that there will be a 70% increase in the prevalence of diabetes in adults of developing countries and about 21% rise in developed countries. By looking at CHASE study, a cross-sectional survey carried out involving nearly 4800 children aged 9-10 years old recruited from London, Birmingham and Leicester, it is found that South Asians adults, residents of UK are 3 times more prone to develop type 2 diabetes than white Europeans ( 5 , 6 ). These people have higher blood levels of glycated haemoglobin (HbA1c), higher level of C-reactive proteins in the blood, lower level of High-density lipoprotein -cholesterol (HDL-C) and high triglyceride levels than white people. Black African-Caribbean adults residing in the United Kingdom have also most of these diabetic risk factors but these people have high HDL-C levels and low triglyceride levels.
Better diabetic education and knowledge to control and treat diabetes at right time can minimize the chances to develop complications of diabetes and thus reduce morbidity and mortality in diabetics ( 7 , 8 ). It suggests that as the rising figures of people diagnosed with diabetes is becoming a challenge in the United Kingdom so a randomised clinical trial will be run by independent research teams to interpret effective delivery and cost effectiveness of CASCADE (Child and Adolescent Structured Competencies Approach to Diabetes Education) for children and young people involved in this trial. As we know that if diabetes is diagnosed in childhood and bitterly controlled, the chances to develop long-term complications become less. The CASCADE is a multi-centre randomised control trial involving 26 clinics randomly selected as control/intervention groups, including 572 children and young people ( 7 ). Despite of the advanced medications and their delivery systems there is less improvement in control of diabetes in children and young people in the United Kingdom in last decade ( 8 ). So new health delivery systems are needed for children and young people to improve and control the diabetes.
With regards to this, in 2010, fifth national survey was carried out to assess the delivery of UK diabetes services to children and young people and identified changes in service delivery systems since 2002 ( 9 ). One hundred twenty-nine services took part in the survey involving 220 clinics. Ninety-eight percent of paediatric consultants were found having special interest in diabetes whereas in 2002 about 89% of consultants were interested in diabetes. In 88% of services, the diabetes specialist nurse worked alone in paediatric diabetes compared to 53% of the services in 2002. So overall it was concluded that there is much improvement in diabetes services for children providing high quality care, but serious deficiencies still remains.
According to Diabetes UK (2010) most of the people with diabetes type 2 in the United Kingdom are over 60; their level of diabetes knowledge tends to be poorer. According to Diabetes UK (2010) report, the residents of care homes fail to receive diabetes education and screening. A care home resident gets admitted to the hospital for screening and diagnosis of diabetes due to the lack of screening facilities and lack of diabetes education. There are diabetic residents in 6 out of 10 care homes that cannot provide special education ( 10 ).
UK prospective diabetes study has shown that adapting the effective therapy to reduce high blood pressure and high blood glucose level will result in reducing the diabetes complications ( 11 ). Diabetes UK invested more than 2 million on this study ( 11 ). The UK Prospective Diabetes Study, the 20-year study involving 5000 patients with diabetes in the United Kingdom, has revealed that intensive blood glucose level control and adopting better treatment methods can reduce the risk of diabetic retinopathy by a quarter and early renal damage by a third ( 11 ). Intensive management and control of blood pressure in hypertensive patients can reduce the risk of death resulting from life threatening long-term complications of diabetes by a third, vision loss by more than a third and cardiovascular disease by more than a third ( 10 ).
By looking at the data collected between 1st April 2008 and 31st March 2010 from 1421 weight reducing operations carried out, it is found that before surgery 379 of these 1421 patients were having type 2 diabetes ( 11 ). After 1 year of surgery it was found that this number of diabetic patients was decreased to 188 from 379 ( 11 ). Therefore by providing knowledge of advance treatment methods to people helps in controlling the diabetes as educating people about the weight loss surgeries (gastric bypass and gastric bands) can tackle type 2 diabetes as seen in this study.
Diabetes education can improve the quality of life of diabetic patients and can also prevent the costs of long-term complications of diabetes in the patients ( 10 ). As amputation of lower limb in a diabetic patient, a long-term complication of diabetes is a costly intervention, the diabetes education can help in reducing the amputation rate that can lead to large cost savings ( 10 ). Diabetic foot ulcers can develop in patients having diabetes both in type 1 and type 2 diabetes ( 11 ). It has been found, 10% of diabetic individuals may suffer from foot ulcer during their lifetime. Foot ulcer often occurs in the people who develop peripheral diabetic neuropathy and also by wearing tight shoes, by walking on tread mill, having cuts, blisters and also having narrowed arteries; atherosclerotic peripheral arterial disease. The diabetic foot ulcers should not be avoided and diabetic foot needs a special care, otherwise the diabetic foot ulcer can result in the amputation of the foot even the whole lower limb ( 11 ). The risk of lower limb amputation in diabetic patients is 15 to 45 times more than in people with no diabetes ( 10 ). About 25% of hospital admissions of diabetic people in United States and Great Britain are due to diabetic foot complications ( 10 ). The annual incidence of diabetic foot ulcers and amputation are 2.5% to 10.7% and 0.25% to 1.8%, respectively ( 12 ).
In the United States an estimated more than 130 billion dollars in 2002 is the cost of diabetes ( 13 ). Because of these devastating numbers, the cost-efficacy of preventing and treating diabetes, and the cost-effectiveness of diabetes self-management training and medical nutrition therapy to treat diabetes are receiving much attention ( 13 ). While in the United Kingdom, the cost of diabetes to the National Health Service (NHS) stands at approximately £1 million per hour, and is increasing rapidly. Diabetes accounts for approximately a tenth of NHS budget each year, a total exceeding £9 billion ( 11 ). With regards to this a systematic review was carried out involving 26 articles including randomized controlled trials, retrospective database analyses, meta-analysis, prospective, quasi-experimental and, to evaluate the cost-effectiveness of diabetes education. The results of more than half of the studies reviewed were indicated positive association between diabetes education and decreased cost. The findings of these studies indicate that diabetes self-management education (DSME) has more benefits in reducing the costs associated with diabetes intervention. Study agreed with this finding by conducting a 12-month study involving primary care trusts in the United Kingdom to assess the long-term clinical and cost-effectiveness of the diabetes education and self-management for ongoing and newly diagnosed (DESMOND) intervention ( 14 ). The cost-utility analysis was undertaken using data from a 12-month, multicentre, cluster randomised controlled trial and the study resulted that the DESMOND intervention is considered to be cost effective compared with usual care, especially with respect to the real world cost of the intervention to primary care trusts, with reductions in Cardiovascular disease (CVD) risk especially reduction in weight and smoking ( 14 ).
According to a cohort study, conducted in 2005 by Diabetes UK, The cancer risk and mortality is progressively elevating in insulin treated diabetic individuals ( 15 ). This study involved 28900 UK resident patients with insulin-treated diabetes who were less than 50 years old at the diagnosis of diabetes. However, the results showed, risks of some cancers such as liver, pancreatic, endometrial, renal and colorectal cancer slightly are raising in patients with prime type 2 diabetes but some cancer incidence including gall bladder, breast cancers and non-Hodgkin lymphoma (NHL) have not changed or prostate cancer risk has been reduced ( 15 ).
Celiac disease, as a chronic immune mediated disorder, is triggered by gluten intake in predisposed patients ( 16 ). Type 1 diabetes is one of the diseases associated with celiac disease ( 18 ). Both diseases have a common genetic predisposition. In one Turkish study involving 100 diabetic patients (51 female, 49 male, mean age 26 ±9 years, and 80 control subjects - 40 female, 40 male, mean age 27 ± 8 years), it was estimated that the prevalence of celiac disease is more in diabetic patients than the general people and celiac disease in diabetic patients can only be diagnosed by screening tests for celiac disease as CD is mostly seen as asymptomatic in these patients. The most sensitive and specific test for the diagnosis of CD is the anti-endomysial IgA antibody (IgA-EMA) test with a sensitivity of more than 90% and a specificity about 100%. This is a screening method in patients at high risk for CD. Anti-endomysium IgA was tested by indirect immunofluorescence using sections of human umbilical cord for screening. Some investigators predicted that the complications of diabetes are increased in the presence of celiac disease and worsens the metabolic control in these diabetic patients ( 17 ).
High blood glucose level can lead to microvascular and macrovascular complications ( 18 ). For examining this, a prospective observational study (UKPDS 35) was conducted by Stratton et al ( 18 ). To report positive correlation between hyperglycaemia and macro/micro-vascular insults in type 2 diabetic patients. This study involved 23 hospital-based clinics in England, Scotland and Northern Ireland. About 4600 patients including white, Asian Indian and African-Caribbean patients were participated in incidence rates analysis. Risk factors related macro-vascular complication were noticed in about 3600 of the total patient. The results of the study indicated that there is a direct relation between hyperglycemia, micro-vascular and macro-vascular complications ( 18 ). This is also clear by examining a cohort study, conducted by Fuller et al to assess cardiovascular disease associated risk in type 1 diabetic patients in the United Kingdom ( 19 ). This study consisted of group of 7500 patients with type 1 diabetes and 5 age- and gender-matched controls per non-diabetic individuals comparison group (nearly 38200) selected from the General Practice Research Database (GPRD). The cardiovascular events in these two groups were apprehended between1992-1999. These high CVD risks were seen for strokes, acute coronary disorders, and for coronary revascularizations. Results showed that women having type 1 diabetes continue to experience greater relative risks of cardiovascular disease than men compared with those without diabetes ( 19 ). Hence, there is increased absolute and relative risk of mortality due to CVD in patients with type 1diabetes compared with those without diabetes in the United Kingdom ( 19 ).
Blood glucose awareness training and cognitive behavioural therapy have been able to balance blood glucose level in type 1 diabetic patients ( 20 ). To support this evidence, a systematic review was completed ( 20 ) in Oxford to assess fear of hypoglycaemia in the patients having diabetes. About 36 papers were reviewed. And it was implicated from the review that fear of hypoglycaemia can have negative impact on diabetes management and awareness training is needed to reduce this fear of hypoglycaemia. This was further supported by a randomised control trial, carried out ( 21 ) on 650 randomly selected diabetic patients from Bournemouth Diabetes and Endocrine Centre’s diabetes register to determine the relationship between numeracy skills and glycaemic control in type 1 diabetes. Out of 650 patients 112 patients completed the study. Forty-seven percent were the male patients and it was found that low numeracy skills were badly associated with glycaemic control in diabetes and literacy was also badly associated with glycaemic control in diabetes and also relationship between literacy and glycaemic control was found to be independent of the duration of diabetes and socio-economic status of the patients.
Diabetic patients can develop hyperglycaemia and hypoglycaemia in the critical care setting while hospitalized due to various factors including infection, poor diet, and drugs ( 22 ). Hospitalized patients can develop hyperglycaemia even in the absence of family history of diabetes ( 22 ). The blood glucose level range of 100–200 mg/dl is the target of glycaemic control in the hospitalized patients. Insulin infusion is done in hospitalized patients having type 1 diabetes and in type 2 diabetic patients, oral drugs are stopped and insulin is started for glycaemic control ( 22 ).
Educational and psychosocial interventions are able to approximately improve diabetes management. ( 23 , 24 ). A systematic review was completed by Hampson et al ( 23 ) to investigate the educational and psychosocial intervention efficacy on improvement of diabetes management in adolescents type 1 diabetes patients. About 60 articles were reviewed. This systematic review gave the result that educational and psychosocial interventions have beneficial impacts on various diabetes management consequences. Similarly a systematic review was conducted by Norris et al ( 24 ) to assess the effectiveness of self-management education on glycosylated hemoglobin in adults having type 2 diabetes. Total 31 articles on randomized control trials were reviewed and it was found that DSME improves glycated hemoglobin levels at immediate follow-up by 0.76%, that long-lasting interventions may be needed to maintain the improved glycaemic control brought about by DSME programs as the more contact time between patient and educator enhances the efficacy of the result and that the improvement in glycosylated hemoglobin level drops 1–3 months after the intervention ceases ( 24 ). Further supporting this, another systematic review was conducted by Hawthorne et al ( 25 ) to determine the efficacy of various diabetic diet advice on balancing blood glucose level and weight in type 2 diabetic individuals. Only randomized controlled trials of 6 months or longer, were selected for the review and total 36 articles were reviewed. In this review study, some parameters such as weight, mortality, maximal exercise capacity and compliance various lipoproteins levels and blood pressure were measured. The review indicated that dietary advice is effective in the glycaemic control in type 2 diabetes mellitus ( 25 ) further supported all these reviews by conducting a systematic review to assess the effectiveness of culturally appropriate diabetes health education on type 2 diabetes mellitus as prevalence of type 2 diabetes mellitus is higher in ethnic minorities in the developed countries like the United Kingdom ( 25 ). Eleven randomised control trials of culturally appropriate diabetes health education on people having type 2 diabetes over 15 years from defined ethnic minority groups of developed countries were reviewed. The trials indicated both glycaemic control as well as improvement in knowledge after culturally appropriate diabetes education interventions. It was suggested from the review that culturally appropriate diabetes health education is effective in glycaemic control in type 2 diabetes and improving the knowledge score and changing the lifestyles and attitudes of the people.
Various diabetes education courses are being carried out in the United Kingdom, including DAFNE, DESMOND and X-PERT in order to increase awareness and knowledge of diabetes among people. These diabetes courses are designed to empower diabetic patients to manage their own condition effectively. Various factors like cost, distance, shortage of enough educators or centres, lack of appropriate services affect many people with diabetes to get access to diabetes knowledge. Educating the patients regarding diabetes have a key role in encouraging and supporting them to assume active responsibility for the day to day control of their situation. The review depicts that illiteracy and lack of knowledge poses a great challenge to effective health education. The review demonstrates that south Asian patients face problems regarding diet aspect and show poor level of knowledge about diabetes and also are discouraged to join educational sessions. The review indicates that impaired awareness of the diabetes increases the chances to develop complications of diabetes as the severe hypoglycaemia is becoming more common in insulin treated type 2 diabetes than previously recognized and with increased duration of insulin therapy may increase to meet that observed in type 1 diabetes. The risk of severe hypoglycaemia increases with having impaired awareness of hypoglycaemia. The authors has concluded that diabetes associated complications and psychological insults is usual in diabetic individuals. The study indicates that many providers involved in the study are aware of the diabetes related psychological problems but lack confidence in their ability to evaluate these problems and to support these patients. So, there is a need for manipulating models of care that provide essential psychosocial services. There is also need of integrating mental health professionals into the diabetes care team. This study will help the government to implement the diabetes education programmes that are cost effective and attractive to the public, easy to get access. Any diabetes service should provide highly structured diabetes education programme. In spite of the advanced medications and their delivery systems there is less improvement in control of diabetes in children and young people in UK in last decade. Better diabetic education and knowledge to control and treat diabetes at right time can reduce the risk factors and minimize the chances to develop complications of diabetes and thus reduce morbidity and mortality in diabetics.
Authors’ contribution
CMJN completed the article, MS and MMB reviewed the article, and JM completed the draft.
Conflicts of interest
The authors declared no competing interests.
Ethical considerations
Ethical issues (including plagiarism, data fabrication, double publication) have been completely observed by the authors.
Funding/Support
Please cite this paper as: Nazar CMJ, Bojerenu MM, Safdar M, Marwat J. Effectiveness of diabetes education and awareness of diabetes mellitus in combating diabetes in the United Kigdom; a literature review. J Nephropharmacol. 2016;5(2):110-115.

IMAGES
COMMENTS
Additionally, this literature review did not focus on A1C as the primary outcome, although A1C is an important indicator of diabetes self-management. A1C was chosen as the method of evaluating the impact of health literacy interventions in patients with diabetes, but other considerations such as medication adherence, impact on comorbid ...
Abstract. Objective: The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs. These challenges ...
Abstract. Diabetes mellitus arises as a result of insulin resistance or a decrease in its production. This work consists of analyzing the various immunological and pathophysiological factors of ...
In this paper, we present a systematic review of the literature on the association of these risk factors with the incidence/prevalence of type 2 diabetes. We give insights on the contribution of independent risk factors in the development of type 2 diabetes along with possible solutions towards a preventive approach.
Introduction. Insulin resistance and β-cell dysfunction are the 2 major hallmarks of type 2 diabetes mellitus (T2DM) that appear as the result of disturbed homeostasis [].Failure of β-cells (∼80% of their β-cell function) and insulin resistance in muscles and the liver is a vicious triumvirate responsible for the core physiological defects.
In a systematic review, diabetes mellitus distress was ... Ludwig, C. & Panton, U. H. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence ...
The present review indicates that the rate of published qualitative research on lived experience of diabetes has increased dramatically over the last 25 years. We developed an innovative Next-Generation mixed-method approach to qualitative secondary analysis and used it to review this literature, derived from a systematic search of PubMed.
Type 2 diabetes mellitus (T2DM) is an expanding global health problem, closely linked to the epidemic of obesity. Individuals with T2DM are at high risk for both microvascular complications ...
Objective To assess what proportions of studies reported increasing, stable, or declining trends in the incidence of diagnosed diabetes. Design Systematic review of studies reporting trends of diabetes incidence in adults from 1980 to 2017 according to PRISMA guidelines. Data sources Medline, Embase, CINAHL, and reference lists of relevant publications. Eligibility criteria Studies of open ...
The objective of this systematic literature review will be to identify whether there are differences in the clinical outcomes of both type 1 and type 2 diabetes patients diagnosed with COVID-19 compared with patients with COVID-19 without a diagnosis of diabetes.
This Review defines hypoglycaemia in type 1 diabetes mellitus, and also outlines its frequency, risk factors and adverse outcomes. Ways to prevent and treat this complication of insulin therapy ...
The global burden of type 2 diabetes mellitus (T2DM) is rapidly increasing, affecting individuals of all ages. The global T2DM prevalence nearly doubled in the adult population over the past decade from 4.7% in 1980 to 8.5% in 2014 [].The global burden of T2DM in people 20-79 years is further projected to increase to 629 million in 2045 compared to 425 million in 2017 [].
This is a literature review aiming to overview, summarise and discuss the role and effect of patient empowerment, self-management education and lifestyle modification in the management of people with DM. ... Kelly JT, et al. Effectiveness of group-based self-management education for individuals with Type 2 diabetes: A systematic review with ...
Introduction. Diabetes mellitus (DM) is probably one of the oldest diseases known to man. It was first reported in Egyptian manuscript about 3000 years ago. 1 In 1936, the distinction between type 1 and type 2 DM was clearly made. 2 Type 2 DM was first described as a component of metabolic syndrome in 1988. 3 Type 2 DM (formerly known as non-insulin dependent DM) is the most common form of DM ...
This systematic literature review aims to identify diabetes self-management education (DSME) features to improve diabetes education for Black African/Caribbean and Hispanic/Latin American women with Type 2 diabetes mellitus. ... Given the results from our systematic literature review, we propose that the balance between tailoring care and ...
Introduction. The Vermont Department of Health has been charged with conducting a literature review on behalf of the Vermont Blueprint for Health and OneCare Vermont with the goal of identifying effective and scalable self-management or community-based programs to address the underlying health behaviors for prediabetes and diabetes.
Based on this phenomenon, a literature review was prepared to highlight effectiveness of DSME on T2DM. Design and Methods. ... Descriptive, retrospective chart review: 100 participants: 8: Effect of diabetes self-management education (DSME) on glycated hemoglobin (HbA1c) level among patients with T2DM: Systematic review and meta-analysis of ...
The clinical outcomes of diabetes can be influenced by primary care providers' (PCP) treatment approaches. This study explores the association between PCP approaches to management and performance measured by established diabetes metrics and related costs. In phase one, Electronic Medical Records were used to extract diabetes related metrics using Healthcare Effectiveness Data and Information ...
Arif Mohiddin. Diabetes is the disease or disorder of pancreas by which pancreas stop the secretion of insulin in the body. Insulin allows the glucose enter in to the cells which provide energy to ...
This prompted a literature review of best practice guidelines for long-term management of checkpoint-inhibitor induced T1DM including oral steroids as a treatment option similar to other ICI adverse effects. ... Kilari D, et al. Immune checkpoint inhibitor-associated type 1 diabetes mellitus: case series, review of the literature, and optimal ...
Diabetes puts a burden on patients and their families . The burden of diabetes and its management on other family members can include emotional, financial, logistical and physical impacts. For example, parents of children with diabetes and spouses of adults with diabetes may lose sleep to help manage their loved one's blood glucose overnight.
The purpose of this literature review is to describe the concept, model or theory that can be used in improving the management of diabetes mellitus ... Diabetes; Theory; Model; Concept; Management; Health Care . Introduction . Diabetes is a lifelong chronic disease, usually divided into type 1 and
Severe hyponatremia and diabetes insipidus caused by low-dose cyclophosphamide in breast cancer patients: A case report and literature review Medicine (Baltimore) . 2024 Mar 29;103(13):e37572. doi: 10.1097/MD.0000000000037572.
The systematic review to be carried out will include literature from 2001 to 2011 in the United Kingdom regarding awareness of diabetes among UK population and effectiveness of diabetes education. Literature will be accessed using search database, British medical journals, and library. Good quality papers will be used for the systematic review.