- What is Nutritional Psychology?
- Our Mission
- Meet the Team
- CNP Education
- NP 110: Introduction to Nutritional Psychology Methods
- NP 120 Part I
- NP 120 Part II
- NP 150: Mechanisms in the Diet-Mental Health Relationship
- Course Scholarships
- Course login for current students
- Kids Curriculum
- Library Introduction
- NP RESEARCH LIBRARY (NPRL)
- Parent News
- Neurodevelopmental
- CHILD COOKING RESEARCH
- CNP Video Library
- DIET AND MATERNAL MENTAL HEALTH

- CNP Articles
- Related Resources
- Introduction
- Professionals
- Organizations
- Become a Contributor
- Submission Guidelines
- About the Campaign
- Research Announcements

Published on: January 29, 2020 : 2:49 pm.

Micronutrients and Mental Health
The CNP Micronutrients and Mental Health Research Category consolidates research exploring the interdependent relationship between dietary intake and micronutrients. To view each original study on the open internet, click “ Original .” To view the CNP-written abstract summary, click “ CNP Summary .” While only some of the CNP-written abstract summaries are available below for free, all abstract summaries are available to CNP members through the CNP Library Membership .
FEATURED CNP RESEARCH SUMMARY
Dietary creatine intake and depression risk among U.S. adults Original Study -->
Bakian et al. (2020) examined the association between dietary creatine and depression in U.S. adults, using the data on dietary creatine intakes and patient health questionnaires obtained by the 2005 to 2012 National Health and Nutrition Examination Survey (NHANES) on its 22,692 participants (aged ≥20 years). This study compared the depression prevalence in the subjects in the lowest quartile of dietary creatine intake (rate of 10.23/100) to the occurrence in those in the highest quartile of creatine consumption (5.98/100 persons). While an inverse association was confirmed between dietary creatine and depression [adjusted odds ratio (AOR) = 0.68], the strongest correlations were seen in females (AOR = 0.62) and participants not taking antidepressant/anxiolytic medication (AOR = 0.58). These results highlighted a significant negative relationship between creatine intake and depression in a nationally representative cohort. This leaves the role that creatine plays in depression among women and across the lifespan to be investigated in the future.
Efficacy and safety of a vitamin-mineral intervention for symptoms of anxiety and depression in adults: A randomised placebo-controlled trial "NoMAD"
The costs of Depression and anxiety are rising. In an adult community environment, Blampied et al. (2023) looked at whether micronutrients (vitamins and minerals) reduced the symptoms of anxiety and Depression. For ten weeks, participants (n = 150) who reported functionally hindering symptoms of anxiety or Depression received either micronutrients or a placebo. The Generalised Anxiety Disorder Scale-7 (GAD-7), Patient Health Questionnaire-9 (PHQ-9), and Clinical Global Impression-Improvement Scale (CGII) were used as the primary outcome measures. Participants were also monitored online with routine phone calls with a professional psychologist. The authors noted no significant adverse events or increased suicide thoughts throughout the study, and participants showed a low dropout rate (8.7%). Analysis of the results revealed that the micronutrient group improved considerably more quickly on the PHQ-9 and the GAD-7. Further analysis demonstrated that participant characteristics impacted time-by-group interactions; for those from lower socioeconomic categories, younger individuals, and those who had already attempted medical treatment, micronutrients offered the quickest benefit relative to placebo. With 49% of the micronutrient group and 44% of the placebo group being recognized responders on the CGII, there were no group differences at the end-point. Participants taking micronutrients had noticeably more bowel movements than those taking a placebo. The authors recognize the limitations to the generalizability of their results due to the improvement under placebo and the lack of official diagnosis. Nevertheless, all subjects improved despite having little contact with a doctor, albeit changes with micronutrients manifested more rapidly. Participants in particular subgroups responded less well to the placebo, indicating the areas where micronutrients may be most useful as a treatment. [NPID: Anxiety, Depression, micronutrients, mineral, vitamin]
CNP Research Summary can be found in the CNP Library Membership
Vitamin B12 supplementation: Preventing onset and improving prognosis of depression
Depression is a widespread mental health disease that affects people of all ages, ethnicities, and socioeconomic groups. Depression phenotypes may include hormonal derangements, metabolic disorders, cardiovascular illness, deficiencies, inflammatory disorders, or neurodegenerative disorders. Although there are many different ways to treat depression, it remains a significant worldwide health issue that needs more focus. In this review aimed to demonstrate a link between vitamin B12 and depression, Sangle et al. (2020) gathered relevant articles and papers (n = 35), revealing that supplementing with Vitamin B12 early enough can enhance the impact of anti-depressants and slow down the onset of depression. The authors primarily focused on Vitamin B12 to give concerned professionals a foundation to address this issue with patients prone to depression or who have experienced a major depressive episode, even though other vitamins like Vitamin B6 and folate are known to have a favorable effect on depression. [NPID: Serum vitamin B12, depression prevention, hyperhomocysteinemia, neuropsychiatric]
Zinc supplementation combined with antidepressant drugs for treatment of patients with depression: A systematic review and meta-analysis
Amongst trace elements, zinc is crucial for maintaining healthy neural structure and cerebral functionality. Zinc supplements have been postulated to play a role in preventing and treating depression, as evidenced by a decrease in the symptoms of depression observed in clinical studies following zinc supplementation. In their review, Da Silva et al. (2021) investigated if zinc supplements could prevent or ameliorate symptoms of depression in adults, adolescents, or children. Through searching five electronic databases and reviewing eligible published randomized, controlled, crossover trials dated up to September 2019 (n = 12,322, 5 qualified for meta-analysis), the extrapolated evidence pointed to a reduction of depressive symptoms in participants receiving zinc supplementation compared to placebo. This reduction was more substantial in participants aged 40 or more years, however, a meta-analysis of the eligible studies did not show a significant effect of zinc supplementation on symptoms of depression. In conclusion, the authors comment that zinc supplementation could decrease symptoms of depression in patients receiving antidepressant treatment for clinical depression. [NPID: Depression, depressive symptoms, meta-analysis, zinc]
Vitamin C supplementation promotes mental vitality in healthy young adults: Results from a cross-sectional analysis and a randomized, double-blind, placebo-controlled trial
The overall aim of this 2022 study was to examine if vitamin C levels influence vitality and psychological functions. Firstly, a sample of healthy young adults (aged 20-39 years) were tested on their vitamin C concentrations, vitality, and mood status (stress, depression, and positive and negative affect). Next, those with inadequate levels of vitamin C were randomly selected to take either 500 mg of vitamin C or placebo twice a day for 4 weeks. The data was analyzed to find that serum vitamin C concentration was positively associated with level of attention, but not strongly related to mood and fatigue. Compared to the placebo group, the vitamin D intervention group showed significantly enhanced attention and work absorption. Moreover, adults given vitamin C performed better in the neuropsychological test, Stroop color-word test, compared with the placebo group. However, vitamin D supplementation did not appear to affect mood or serum brain-derived neurotrophic factor (BDNF). The authors concluded that low vitamin C status is related to a low level of mental vitality. Vitamin C supplementation effectively increased work motivation and attentional focus and contributed to better performance on cognitive tasks requiring sustained attention. [NPID: micronutrients, nutrients, diet, vitamin C, supplements, supplementation, cognition, mood, vitality, mental health, attention]
Effect of vitamin D supplementation on outcomes in people with early psychosis: The DFEND randomized clinical trial
Since vitamin D deficiency is associated with poorer mental and physical health among patients with psychotic disorders, this 2021 study assessed whether vitamin D supplementation can improve clinical outcomes in first-episode psychosis (FEP). This clinical trial recruited adults (aged between 18 to 65 years) within 3 years of a first presentation with a functional psychotic disorder and no contraindication to vitamin D supplementation. In total, 149 participants were included and randomized to either receive 120,000 international units (UI) of cholecalciferol (vitamin D3) supplement or placebo monthly. After 6 months, 104 of these subjects made up the follow-up data and were examined on their mental health. The primary outcome measure was total Positive and Negative Syndrome Scale (PANSS), which can identify the presence and severity of positive and negative symptoms. There were no differences found in the intention-to-treat analysis in the PANSS between baseline and the 6-month follow-up, or between the 3-month and 6-month scores. Other tests conducted in this trial include the Global Assessment of Function (measures how much a person's symptoms affect their day-to-day life), Calgary Depression Scale score (determines the level of depression), waist circumference, body mass index, and glycated hemoglobin, total cholesterol, and C-reactive protein. There were also no differences in these measures between the baseline and 6-month outcomes. Vitamin D levels were very low in the study participants, particularly in Black participants and those who identified as another minoritized racial and ethnic group. Around 93% of these minority ethnic groups showed low levels of vitamin D. This study did not find an association between vitamin D supplementation and mental health or metabolic outcomes at 6 months. But so few patients had satisfactory vitamin D levels, which suggests that future population health strategies could target and help this group. [NPID: vitamin D, cholecalciferol, supplements, diet, micronutrients, nutrients, ethnic groups, psychosis, schizophrenia, depression]
Superiority of magnesium and vitamin B6 over magnesium alone on severe stress in healthy adults with low magnesemia: A randomized, single-blind clinical trial
This 2018 study was the first randomized trial to measure the influence of combined magnesium and vitamin B6 supplementation on stress in a stressed population with low levels of magnesium. The sample included healthy adults with a serum magnesium concentration within a low range (0.45 mmol/L-0.85 mmol/L), and who scored greater than 18 in the stress subscale of the Depression Anxiety Stress Scales (DASS-42). The participants were firstly randomized to either receive the magnesium-vitamin B6 combination (containing 300mg of magnesium and 30mg of vitamin b6) daily or the 300mg of magnesium alone. The stress subscale score significantly reduced from baseline to Week 8 in both treatment groups. There was no notable difference in stress scores between the magnesium-vitamin B6 combination group and the magnesium group. Further data analysis revealed that individuals with severe or extremely severe stress showed a 24% greater improvement after taking the magnesium-B6 combination for 8 weeks versus magnesium alone. Adverse effects were reported in 12.1% of the combination therapy group and in 17.4% of the monotherapy group. Overall, the data demonstrated that magnesium supplements reduced stress levels in healthy adults with low magnesium, although the combined formula of magnesium and vitamin B6 was not apparently superior to the magnesium alone. The dual therapy did show better results versus magnesium monotherapy among people with severe and extremely severe stress. [NPID: magnesium, vitamin B6, pyridoxine, stress, supplement, supplementation, health, diet, nutrition, nutrients, micronutrients, vitamins, minerals, multivitamins]
Role of magnesium supplementation in the treatment of depression: A randomized clinical trial
Since it is not clear what role magnesium supplementation plays in the management of depressive symptoms, this 2017 trial investigated the effects of over-the-counter magnesium chloride on the symptoms of depression. The study compared 6 weeks of 240mg (milligrams) magnesium per day to 6 weeks of no treatment (control). The participants were adults with an average age of 52, and with mild to moderate depressive symptoms. Symptoms were monitored through twice-weekly phone calls. In addition to depression, everyone was assessed on signs of anxiety, adverse effects, and likelihood to use magnesium supplements in the future. Overall, there was a clinically significant net improvement in Patient Health Questionnaire-9 (PHQ-9) scores and net improvement in Generalized Anxiety Disorders-7 scores, following the 6-week magnesium supplement intervention. These supplements were well tolerated, and participants stated that they would take magnesium again in the future. Similar trends were seen regardless of age, gender, baseline severity of depression, baseline magnesium level, or use of antidepressant treatments. The impact of these supplements were noticed within 2 weeks. Magnesium acts quickly and effectively in improving mild-to-moderate depression in adults, while demonstrating a good safety profile. [NPID: magnesium, nutrients, micronutrients, nutrition, minerals, multivitamins, supplements, supplementation, depression]
Risk factors for depression. New evidence on selenium deficiency and depressive
The aim of this 2020 study was to evaluate the effect of selenium deficiency on depressive disorders among a sample of adults. There were 9354 participants recruited by the Polish-Norwegian Study (PONS) cohort, including only men and women aged between 45-65. The average intake of selenium and other nutrients were analyzed against depressive disorders, while also considering possible confounders such as presence of chronic diseases, life problems, pain levels, physical activity, and income. Low selenium, as well as high lipids intake and low iron consumption appeared to significantly affect depressive disorders. There were also non-dietary risk factors that showed strong correlations with depression, including home stress, pain, and low income. Pain was found to mediate a small part of the effect of morbidity too. Furthermore, depressive disorders are associated with work problems and low physical activity. In this analysis model, the effect of dietary risk factors on depressive disorders was moderate compared to non-dietary variables. Among the dietary factors investigated, selenium consumption showed the strongest connection with depression. [NPID: depression, selenium, vitamins, minerals, multi-nutrients, nutrients, nutrition, Polish, Poland, pain, physical activity, income, lipids, iron, stress, income]
An observational preliminary study on the safety of long-term consumption of micronutrients for the treatment of psychiatric symptoms
To test the long-term safety of taking multivitamins, this 2019 study provided patients with psychiatric symptoms with one of two commercially available broad-spectrum micronutrient formulas (EMPowerplus and Daily Essential Nutrients) at doses above the Recommended Dietary Allowances. On average, the micronutrients were consumed for 2.66 years. Participants were examined on their full blood count, coagulation profile, liver, and kidney function, fasting glucose, iron, key nutrients, and prolactin. All but one of the blood tests were within the test reference ranges (B12 was elevated in many of the subjects). One patient was diagnosed with hemochromatosis, which is known as iron overload, but there were no other clinically relevant adverse changes in blood tests performed pre- and post-treatment. Moreover, 85% of the participants were in nonclinical ranges for measures of attention-deficit hyperactivity disorder (ADHD), depression, anxiety, and stress. This article provides preliminary evidence of the long-term safety of commercially available micronutrients, although there remain some unexplained questions. All in all, the psychiatric benefits of these micronutrient formulations appear to outweigh the risk in these patients. Screening for potential medical problems is recommended pre-treatment. [NPID: micronutrients, multivitamins, vitamins, minerals, safety, toxicity, depression, anxiety, stress, ADHD]
A randomised trial of nutrient supplements to minimise psychological stress after a natural disaster
Following the devastating flooding in South Alberta in 2013, residents were invited to take part in this 2015 study investigating the beneficial impact of nutrient supplements after a natural disaster. The researchers wanted to replicate a previous randomized trial conducted in New Zealand that showed multinutrients’ positive effects on mental health after the 2010-11 earthquakes. In Alberta, 56 adults (aged between 23 and 66) were randomized to either receive vitamin D alone, a multivitamin formula (B-complex), or a broad-spectrum mineral/vitamin formula. Although substantial reductions in depression, anxiety and stress were observed in all 3 groups, the B-complex and broad-spectrum mineral/vitamin groups demonstrated significantly greater improvements in stress and anxiety than the vitamin D group. There was no difference to note between the individuals who received the B-complex formula and those who took the broad-spectrum mineral/vitamin formulation. This study becomes the third study to support the use of nutrient formulas with various minerals and vitamins to minimize stress associated with natural disasters. Even still, additional research is encouraged to determine the potential population benefit of distributing these treatments as a post-disaster public health measure. [NPID: natural disasters, New Zealand, Alberta, Canada, depression, anxiety, stress, nutrients, micronutrients, vitamins, multivitamins, minerals]
Assessment of dietary adequacy for important brain micronutrients in patients presenting to a traumatic brain injury clinic for evaluation
This 2014 study analyzed the diet of some patients that were visiting an outpatient traumatic brain injury (TBI) clinic. The patients completed food frequency questionnaires to find out their estimated nutrient intake, while their medical records were also examined to report diagnoses, body mass index, and neurobehavioral subscale scores. Nutrients were assessed individually as well as summarized into summary scores. While the study recognized 14 key micronutrients with defined dietary intake reference ranges that are considered important for brain health, none of the subjects met the recommended dietary allowances (RDAs) for all 14 micronutrients. Ten people met the RDAs for 6 or fewer nutrients, and 10 met the RDAs for 11-12 nutrients. While there were 12 nutrients for which there was sufficient sample size to analyze, eleven of these were associated with lower mean somatic scores, nine were linked with worse cognitive scores, and eight had connections with worse affective scores, when comparing individuals who consumed the least amount of nutrients with those who had the highest nutrient intakes. Only folate, magnesium, vitamin C, and vitamin K were statistically related to the somatic mean score. None of the nutrients was linked with cognitive or affective scores. It was discovered that diets commonly failed to meet recommended dietary allowances for important brain nutrients in an outpatient TBI clinic. Notably, the patients who did not meet the estimated average requirements obtained the worst mean neurobehavioral scores. [NPID: traumatic brain injury, brain, patient, clinic, nutrients, micronutrients, RDA, somatic, cognitive, folate, magnesium, vitamin C, vitamin K, vitamins]
Influence of adjuvant Coenzyme Q10 on inflammatory and oxidative stress biomarkers in patients with bipolar disorders during the depressive episode
Since research studies have increasingly focused its attention on inflammation and oxidative stress to form explanations on the development and maintenance of bipolar disorders, this 2019 study planned to test the effect of coenzyme Q10 on blood levels of inflammatory and oxidative stress biomarkers in patients with bipolar disorder during their depressive phase. The participants with bipolar disorder were randomly chosen to either receive 200 milligrams of the coenzyme Q10 or a placebo daily. While there were 89 subjects at the start of the trial, 69 people completed the entire 8-week study. There was evidence of increased oxidative stress markers and fewer inflammatory biomarkers in the coenzyme Q10 group as time passed and compared with the placebo group. The total antioxidant capacity and level of total thiol groups increased, while tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), nitric oxide, and interleukin-10 (IL-10) dropped. To sum it up, the coenzyme Q10 favorably influenced oxidative stress and inflammatory biomarkers in patients with bipolar disorder during the depressive episode. This adjuvant treatment may represent a safe and effective strategy for treatment of patients with bipolar disorder during the depressive phase. [NPID: bipolar disorder, inflammation, oxidative stress, stress, oxidation, coenzyme Q10, CoQ10, depressive]
Effects of a multivitamin, mineral and herbal supplement on cognition and blood biomarkers in older men: a randomised, placebo-controlled trial
Since nutrition and vitamin intake may have connections to cognitive function and decline in older adults, the aim of this 2012 study was to dive into the effects of nutritional supplementation on cognition in older men. The paper exclusively focused on the multivitamin, mineral and herbal supplement called Swisse Men's Ultivite®, and its impact on cognitive performance in older men. The 51 volunteers of this study were aged between 50 and 74 years, and with an inactive lifestyle. Tests confirmed that contextual recognition memory performance significantly improved after the consumption of the multivitamin, although the subjects’ performances in other cognitive tasks were not affected. Blood samples were also taken to reveal that vitamin B12 and folate levels increased while homocysteine concentrations dropped following supplementation. To conclude, the study found that daily multivitamin supplementation may enhance episodic memory in older men at risk of cognitive decline. [NPID: nutrition, vitamins, multivitamins, supplements, supplementation, minerals, herbal, older, memory, cognition]
The effects of four-week multivitamin supplementation on mood in healthy older women: A randomized controlled trial
Although taking vitamin supplements have shown ability to alleviate symptoms of mood dysfunction, this 2016 study highlights that healthy older women have rarely been included in these experiments. This present study looked at the effects of multivitamin supplementation for 4 weeks on mood in 76 healthy women aged 50-75 years. Each participant was then assessed on their current mood state and experience of mood over the previous week or longer. Also, mobile phones were used to assess changes in real-time mood ratings twice a week in the home. Although there was no evidence indicating that multivitamins confer benefits using measures of current mood and reflections of recent mood while in the laboratory, the mood assessments conducted at home several hours post-dose demonstrated lower ratings of stress in the multivitamin group. Moreover, it appeared that multivitamins reduce mental fatigue according to the results of these tests taken at home. Overall, we learned that over the 4 weeks of multivitamin supplementation, the subtle swings in stress levels produced by these supplements may not be noticed when examining the pre- and posttreatment mood only. It may be the case that mobile phone-based assessments conducted at home are more sensitive to the influence of nutritional interventions compared with traditional examinations undertaken in the laboratory. [NPID: supplements, supplementation, vitamins, multivitamins, mood, women, older women, nutrition, diet]
The effects of multivitamin supplementation on mood and general well-being in healthy young adults. A laboratory and at-home mobile phone assessment
This 2013 study addresses the limitations of the previous research suggesting a link between multivitamin supplementation with improved mood and general well-being. Previously, the studies have often only recruited male participants, the duration of treatment has typically been less than 90 days, and the acute effects have not been differentiated from chronic effects clearly enough. Therefore in this present article, 138 healthy young adults (aged between 20 and 50 years) each took a multivitamin supplement daily for 16 weeks. A mood rating scale called Bond-Lader VAS was used to assess subjective feelings. There were also several other measures of chronic mood that were administered at baseline, and at the 8- and 16- week mark. In addition, Pipingas et al. examined the changes in Bond-Lader and Visual Analogue Scales (VAS) in response to a multitasking framework (MTF). Some of the participants were also tested on their mood states at home using their mobile phones. The results showed no significant treatment effects for any of the chronic laboratory mood measures. Furthermore, the male participants in the multivitamin group appeared to experience increased levels of stress as time passed. This finding may be explained by the large percentage of the males in the multivitamin group being students. However, the at-home mobile-phone assessments taken post-dose revealed significantly reduced stress, physical fatigue, and anxiety in the multivitamin group, compared with the placebo group across several time points. There is still further research required to absolutely differentiate between the acute and chronic effects of multivitamins. [NPID: supplements, supplementation, vitamins, multivitamins, mood, well-being, mental health, chronic mood, acute mood]
Effects of vitamin and mineral supplementation on stress, mild psychiatric symptoms, and mood in nonclinical samples: A meta-analysis
This 2013 meta-analysis reviewed the literature on the influence of diet supplementation on mood in people without any disease symptoms. It is thought that since mood can be affected by the biochemical processes that occur in the brain, even a minor dietary inadequacy can lead to a small change in enzyme efficiency, and ultimately affect the person’s mood state. Additionally, supplementation is expected to improve mood when the diet does not provide optimal amounts of micronutrients. This review searched for studies that investigated the impact of multivitamin/mineral supplements for at least 28 days, while considering the mood, stress, and mild psychiatric symptoms of the participants (the general population). The research also had to be randomized and placebo-controlled to be included. Ultimately 8 studies met the inclusion criteria, and the meta-analysis revealed that supplementation significantly reduced the levels of perceived stress, mild psychiatric symptoms, and anxiety in the subjects. Reduced fatigue and confusion were also observed in the participants, but there was no reduction in cases of depression. Nevertheless, micronutrient supplementation had positive effects on perceived stress, mild psychiatric symptoms, and aspects of everyday mood in healthy adults with no disease symptoms. It should be added that supplements containing high doses of B vitamins may be more effective in improving mood states. Areas that require further investigation include the optimal levels of micronutrient consumption, optimal doses, and the most appropriate active ingredients. [NPID: supplements, supplementation, mood, depression, stress, anxiety, fatigue, tired, confusion, micronutrients, nutrients, vitamins, B vitamins]
The effect of multivitamin supplementation on mood and stress in healthy older men
It has been established that diets lacking in micronutrients are correlated with poorer health, this 2011 paper states. Since multivitamins contain a wide range of nutrients, these supplements may be effective in enhancing mood. Few studies have explored this potential link in randomized controlled trials, which is why this present study examined if multivitamins, minerals, and herbal supplements affect mood and stress in a group of healthy, older men. These 50–69-year-old volunteers were given either a placebo capsule or a multivitamin formulation consisting of vitamins (at levels above recommended daily intakes), minerals, antioxidants, and herbal extracts. Questionnaires were completed at baseline and after supplementation, to assess the participants’ mood and stress levels. Compared with the placebo control group, the individuals that received the multivitamins showed increased alertness, better general functioning, and significantly lower overall scores on depression, anxiety, and stress scales. This study therefore deduced that consuming supplements containing multivitamins, minerals, and herbal components can potentially enhance alertness, reduce negative mood symptoms, and improve feelings of general day-to-day well-being. [NPID: supplements, supplementation, vitamins, multivitamins, minerals, herbs, herbal, health, diet, nutrition, mood, stress, antioxidants, depression, anxiety]
Effects of high-dose B vitamin complex with vitamin C and minerals on subjective mood and performance in healthy males
This 2010 trial investigated the effects of a high-dose B-complex vitamin and mineral supplement (Berocca) on the cognition and mood of adult men (aged 30-55) in full-time employment. Few studies have examined the influential role of vitamins and minerals on psychological functioning in healthy non-elderly adults, although much of the general population take vitamins and minerals as dietary supplements with the goal of ameliorating stress and fatigue and enhancing mental functioning. In this present article, supplementation with vitamins or minerals resulted in significant improvements in perceived stress levels, answers to the General Health Questionnaire, and in the ‘vigor’ subscale of the mood assessment called Profile of Mood States (POMS). Moreover, the group that received vitamin/mineral supplements performed better in the Serial 3’s subtractions task (a test of mental health) compared with the control group. The intervention group also reported being less “mentally tired” both before and after completing the cognitive demand battery. The study found that healthy adults may benefit from taking vitamins/minerals, as supplementation led to less stress, better mental health, higher vigor, and enhanced cognitive performance while performing intense mental tasks. [NPID: cognitive, cognition, vigor, stress, health, vitamins, minerals, vitamin C, vitamin B, mood, supplements, supplementation, fatigue]
Higher vitamin B 6 intake is associated with lower depression and anxiety risk in women but not in men: A large cross-sectional study
Multinutrients for the treatment of psychiatric symptoms in clinical samples: A systematic review and meta-analysis of randomized controlled trials
Johnstone et al. (2020) conducted a systematic review on randomized controlled trials (RCTs) involving multinutrient interventions consisting of at least 4 vitamins and/or minerals in people with psychiatric symptoms, producing 16 RCTs (total 1719 participants) that met the inclusion criteria. The trials were related to various psychiatric categories including depression, post-disaster stress, antisocial behavior, behavioral deficits in dementia, attention-deficit/hyperactivity disorder, and autism. Grading of Recommendations, Assessment, Development and Evaluations (GRADE) assisted with the rating of evidence base, while significant clinical benefit was determined by using minimal clinically important differences (MIDs). The meta-analysis was performed on the trials in the Attention-Deficit/Hyperactivity Disorder (ADHD) category only because of the heterogeneity in participants, multinutrient formulas, outcome measures, and the absence of complete data. In samples with ADHD, the multinutrient intervention significantly improved (statistically and clinically) global functioning [mean difference (MD) −3.3, p = 0.001, MID −3.26; Standardized Mean Difference (SMD) −0.49 p = 0.001 MD −0.5), clinician ratings of global improvement (MD −0.58, p = 0.001, MID −0.5) and ADHD improvement (MD −0.54, p = 0.002, MID −0.5), and clinician (but not observer) measures of ADHD inattentive symptoms (MD −1.53, p = 0.05, MID −0.5)]. Narrative synthesis also revealed an improving trend of global measures among those subjects with autism and those with behavioral deficits in dementia. Furthermore, multinutrient interventions were associated with improvements in anxiety experienced post-natural disaster, and in the number of violent incidents among prisoners. According to this review, broad-spectrum formulas containing both vitamins and minerals had more substantial impacts than other formulas with fewer ingredients. Importantly, the reviewers have exposed the need for robust RCTs with full data (means and standard deviations for all outcomes) in order to find strong evidence for the role of multinutrients in psychiatric disorders. [NPID: micronutrients, nutritional supplements, depression, stress, antisocial behavior, autism, ADHD, dementia]
Serum vitamin D concentrations are associated with depressive symptoms in men: The sixth Korea national health and nutrition examination survey 2014
The aim of this 2020 study was to investigate the correlation between serum vitamin D concentrations and specific domains of depressive symptoms by each sex in the Korean general population. Rhee, Lee, and Ahn (2020) retrieved data from the Korea National Health and Nutrition Examination Survey of 2014 to gather their sample size of 820 men and 916 women (aged 19-76) who had completed health interviews and health examinations. These examinations provided data for serum 25-hydroxyvitamin [25(OH)D] concentrations, the Patient Health Questionnaire-9 (PHQ-9), and certain covariates. A statistically significant association between log-transformed serum 25(OH)D concentrations and total PHQ-9 scores in men (incidence rate ratio [IRR] = 0.74) was identified after multiple covariate adjustments. In men, log-transformed serum 25(OH)D concentrations were significantly associated with the PHQ-9 cognitive/affective subscore (IRR = 0.56). The findings show that serum vitamin D levels were inversely associated with cognitive/affective depressive symptoms in men. [NPID: micronutrients, nutritional supplements, vitamin D, Korea, cognition, affect, depression]
Creatine for the treatment of depression
As various studies have determined that the disturbances in the production, storage and utilization of brain energy are relevant in the development and maintenance of depression, Kious et al. (2019) proposes creatine as a nutritional supplement as it can possibly help correct this dyshomeostasis and has shown potential as an antidepressant in early clinical trials. [NPID: micronutrients, nutritional supplements, depression, dyshomeostasis, creatine, antidepressants]
Alterations of serum macro-minerals and trace elements are associated with major depressive disorder: A case-control study
The aim of this 2018 study was to evaluate the differences between 247 patients with major depressive disorder (MDD) and 248 healthy individuals (matched by age and sex) in their serum levels of the macro-minerals (MM) calcium and magnesium, and of the trace elements (TE) copper, iron, manganese, selenium, and zinc. Another objective was to assess the prevalence of depression associated with these MMs and TEs [both analyzed by atomic absorption spectroscopy (AAS)]. The data indicated significantly higher concentrations of copper and lower levels of calcium and magnesium, iron, manganese, selenium, and zinc in MDD patients compared with control subjects (both p-values < 0.05). A disturbance in the element homeostasis was strongly suspected, possibly signifying that abnormal serum concentrations of MM and TE may contribute substantially to the pathogenesis of MDD and that measuring of these elements and minerals may be an effective tool for depression risk prognosis. [NPID: micronutrients, nutritional supplements, MDD, major depressive disorder, depression, calcium, magnesium, macro-minerals, copper, iron, manganese, selenium, zinc]
Evaluation of some trace elements and vitamins in Major Depressive Disorder patients: A case-control study
This 2019 study recruited 60 patients with MDD and 60 individuals for control, matched by age and gender, and investigated the relationship between trace elements and vitamins with depressive disorders. The participants were examined on Cu, Zn, Ni, Cr, Mn, Mg, and Al serum levels (determined by atomic absorption spectrometry) and vitamin (E & A) concentrations (using high-performance liquid chromatography). Cu, Cr, and Al readings were found to be significantly higher in MDD patients than control, while the levels of Zn, Ni, Mn, Mg, vitamin E, and vitamin A were significantly lower in individuals diagnosed with depression. Finally, the ratio of Cu/Zn was high among depressed patients, which may have an important role in diagnosing and monitoring MDD. The results also suggest that disturbances in the level of trace elements and vitamins (E and A) are significantly related with MDD, studying Cu and Zn may be crucial in accumulating knowledge on the pathogenesis of depressive disorders, and that vitamin E deficiency may heighten the risk of developing MDD. Apparently, further exploration into trace element supplementation is required. [NPID: micronutrients, nutritional supplements, depression, Cu, Zn, Ni, Cr, Mn, Mg, Al, vitamin E, vitamin A, MDD, major depressive disorder]
The role and the effect of magnesium in mental disorders: A systematic review
While levels of magnesium are believed to be lower in patients with mental disorders, especially depression, this 2020 systematic review aimed to analyze the literature from 2010 to March of 2020 regarding the micronutrient in psychiatric disorders, in order to determine magnesium’s relationship with psychiatric pathology and its effectiveness as a therapeutic supplement. Thirty-two relevant articles were identified, consisting of 18 Depressive Disorders (DD), 4 Anxiety Disorders (AD), 4 Attention Deficit Hyperactivity Disorder (ADHD), 3 Autism Spectrum Disorder (ASD), 1 Obsessive–Compulsive Disorder (OCD), 1 Schizophrenia (SCZ) and 1 Eating Disorders (ED). Botturi et al. (2020) mainly found positive results with respect to depressive symptoms in 12 studies, with 7 indicating a significant association between lower serum magnesium levels and depression (measured with psychometric scales), 2 papers showing better depression-related outcomes following magnesium intake, and another 2 demonstrating the improvement of depressive symptoms in participants taking magnesium as an adjuvant treatment with antidepressants, all compared with control. Moreover, 2 more papers reported an association between low magnesium concentration with ADHD, while 2 other papers reported correlations of higher magnesium levels with lower Hamilton Anxiety Rating Scale (HAM-A) scores among depressed individuals and discovered the ideal levels in stressed patients. Magnesium was not significantly connected with panic or Generalized Anxiety Disorder (GAD), associations with ED and SCZ were inconsistent, and only one of three papers found lower levels in ASD. This review judges magnesium supplementation as having beneficial and potentially therapeutic effects, and believes there is reason to demand clinical trials investigating the efficacy of magnesium as single or adjuvant therapy to confirm its appropriate clinical use. [NPID: micronutrients, nutritional supplements, magnesium, mental disorders, depression, autism, ASD, ADHD, OCD, schizophrenia, SCZ, eating disorders]
Evaluation of serum amino acids and non-enzymatic antioxidants in drug-naïve first-episode major depressive disorder
To examine the serum levels of amino acids and non-enzymatic antioxidants in major depressive disorder (MDD) and study its interaction with depression, Islam et al. (2020) gathered 247 patients with MDD and 248 healthy controls (HCs) matched by age and sex, and employed the HPLC system (for amino acids, vitamin A and E), UV-spectrophotometer (to assess vitamin C) and Hamilton Depression Rating Scale (Ham-D, to measure severity of depression). It was revealed that subjects with MDD had significantly lower readings of the four amino acids (methionine, phenylalanine, tryptophan, and tyrosine) and of the three non-enzymatic antioxidants (vitamin A, E, and C), relative to healthy controls. In addition, lower methionine and tyrosine concentrations were linked with higher Ham-D scores. These findings suggest that lower methionine, phenylalanine, tryptophan, tyrosine, and non-enzymatic antioxidant levels in the blood are connected with depression, and may have been a contributing factor in the development of major depression among MDD patients. [NPID: micronutrients, nutritional supplements, non-enzymatic antioxidants, major depressive disorder, MDD, depression, amino acids, vitamin A, vitamin E, vitamin C, methionine, phenylalanine, tryptophan, tyrosine]
Vitamin B-6 and depressive symptomatology, over time, in older Latino adults
Since the association between low vitamin B6 levels and increased risk of depression has been documented but mostly in non-Hispanic white populations, Arévalo et al. (2019) recruited older adults of Puerto Rican descent, a population that has been previously reported to possess higher susceptibility to develop symptoms of depression, and tested the relationship between vitamin B6 status and depressive symptomatology longitudinally, at 3 different stages over ~ 5–7 years (baseline, after 2 years, and after 5 years). The participants’ plasma concentrations of pyridoxyl-5’-phosphate (PLP), which is a time-varying predictor of vitamin B6 levels, was determined to be significantly associated with depressive symptomatology. The data showed higher prevalence of depressive symptoms in the subjects deficient in PLP compared with those with highest levels, at baseline and over time also, even after controlling for multiple factors (age, sex, education, BMI, smoking and alcohol use, nutrition, perceived stress, stressful life events, allostatic load, use of antidepressants). But PLP levels were not linked with the rate of change in depressive symptomatology over time. The identification and treatment of people with vitamin B6 deficiency may be an effective preventative approach particularly among those of Puerto Rican descent since suboptimal concentrations of PLP was linked with higher depressive symptomatology among this study population and this relationship continued over time. [NPID: micronutrients, nutritional supplements, depression, Puerto Rico, vitamin B6, pyridoxyl-5’-phosphate, stress, allostatic load]
Greater circulating copper concentrations and copper/zinc ratios are associated with lower psychological distress, but not cognitive performance, in a sample of Australian older adults
Since the dyshomeostasis of copper and zinc is connected with neurodegeneration, Mravunac et al. (2019) set out to explore the relationship between copper and zinc serum levels, copper/zinc ratio, cognitive function, and signs of depression and anxiety among 139 Australian adults. Along with blood concentrations of zinc and copper, neurotrophic factors such as brain-derived neurotrophic factor (BDNF), vascular endothelial growth factor, and insulin-like growth factor-1 were assessed, while the Hospital Anxiety and Depression Scale and the Cogstate battery and the Behavior Rating Inventory (BRI) of Executive Function (Adult version) allowed evaluation of the participants’ anxiety and depressive symptoms, respectively. Associations with lower depressive symptoms were found for copper and copper/zinc ratio but not for cognition. Also, plasma copper was positively correlated with BDNF while zinc was not associated with any of the outcomes. To summarize, higher blood copper levels and copper/zinc ratios were related to lower depressive symptoms, and copper was also positively associated with BDNF concentrations among an older population in Australia. [NPID: micronutrients, nutritional supplements, zinc, neurodegeneration, copper, zinc, cognitive function, BDNF, anxiety, depression, executive function, Australia]
Palmitoylethanolamide counteracts brain fog improving depressive-like behaviour in obese mice: Possible role of synaptic plasticity and neurogenesis
Palmitoylethanolamide (PEA), known for its metabolic and neuroprotective effects, was investigated here by Lama et al. (2020) on its impact on the monoamine system and synaptic plasticity. In this preclinical study C57Bl/6J male mice were fed high-fat diet (HFD) for 12 weeks, before continuing in this trial being fed either 30 mg·kg-1 daily of ultra-micronized PEA or vehicle (control) for 7 weeks alongside a HFD. The study documented the depressive- and anhedonic-like behaviour, and cognitive performances of the mice, as well as performed monoamine analyses on the nucleus accumbens (Nac), prefrontal cortex (PFC), and hippocampus, and checked markers of synaptic plasticity and neurogenesis. The results showed few depressive- and anhedonic-like behaviour and reduced cognitive deficit induced by the HFD in the PEA-fed mice. Those given PEA also exhibited higher levels of 5-HT in the PFC, less dopamine and 5-HT replacement in the Nac and PFC, respectively, while their dopamine concentrations in the hippocampus and PFC also increased. Moreover, PEA seemed to improve synaptic plasticity, by restoring brain-derived neurotrophic factor signalling pathways in the hippocampus and PFC. The researchers highlighted PEA’s ability to promote neurogenesis, indicated by the reversal of the reduced glutamatergic synaptic density induced by HFD in the stratum radiatum of the CA1 of the hippocampus. PEA’s influence in monoamine homeostasis, synaptic plasticity and neurogenesis are evident, which imply its potential as an adjuvant therapy for suppressing depression-like behavior and reducing memory deficit. [NPID: micronutrients, nutritional supplements, PEA, Palmitoylethanolamide, monoamine system, synaptic plasticity, animal, cognition, depression, neurogenesis, anhedonia, nucleus accumbens, prefrontal cortex, hippocampus, memory]
Is there a relationship between chocolate consumption and symptoms of depression? A cross-sectional survey of 13,626 US adults.
To assess the relationship between chocolate consumption and depressive symptoms, this 2019 study applied the data of 13,626 adults (≥20 years) participating in the National Health and Nutrition Examination Survey between 2007-08 and 2013-14, deriving daily chocolate intake (no chocolate, non-dark chocolate, dark chocolate) and quantity of chocolate consumed (g/day) from two 24-hr dietary recalls and using the Patient Health Questionnaire (PHQ-9) to determine clinically relevant depressive symptoms (scores ≥10). Following the exclusion of diabetics, the consumption of any chocolate was reported in 11.1% of the population, while 1.4% revealed eating dark chocolate. Although the intake of dark chocolate was not significantly associated with depressive symptoms (OR=0.30), those participants who consumed dark chocolate were found to have lower odds of developing clinically relevant depressive symptoms. Moreover, the subjects in the highest quartile for chocolate consumption (104-454 g/day) were 57% less likely to develop signs of depression when compared with those who did not eat any chocolate (OR = 0.43) and after adjusting for dark chocolate consumption. These results suggest the relevance of consuming chocolates, particularly dark chocolate, in enhancing the odds of avoiding depressive symptoms, although additional longitudinal studies and further long-term investigation of chocolate consumption will be required to explain the causality of this relationship and confirm these conclusions. [NPID: micronutrients, nutritional supplements, depression, chocolate]
Association between tea consumption and depressive symptom among Chinese older adults
This 2019 paper studied the relationship between frequency and duration of drinking tea with depressive symptoms among a set of Chinese seniors, assessing whether the interaction varies by gender or age. The data used was from 2005, 2008/2009, 2011/2012 and 2014 waves of Chinese Longitudinal Healthy Longevity Survey (CLHLS). There was a correlation between consistent and frequent tea drinking with significantly fewer prevalence of depressive symptoms, while socioeconomic status, health-related behavior, physical health, cognitive function, and social engagement mediated this relationship. Although this association was only significant for males and the oldest groups, and not among women or younger elders, these findings support the consistent and frequent tea-drinking may effectively reduce the Chinese elderly population’s chances of developing depressive symptoms. In China, continuing the tradition of drinking tea may promote healthy aging in a cost-effective way. [NPID: micronutrients, nutritional supplements, tea, China, elderly, depression, socioeconomic status, cognitive function]
Association of dietary phytochemical index and mental health in women: A cross-sectional study
This 2019 study focused on the possible relationship between dietary phytochemical index (DPI) and symptoms of depression, anxiety and psychological distress among 488 Iranian women (aged 20-50). The DPI was estimated using the formula: (daily energy derived from phytochemical-rich foods (kJ)/total daily energy intake (kJ))×100. Questionnaires were used to assess diet (validated and reliable FFQ) and symptoms of depression, anxiety and psychological distress (validated depression, anxiety, stress scales). The study participants were recruited from health centres in the south of Tehran, and averaged 31·9 (sd 7·7) years in age. Signs of depression, anxiety and psychological stress were seen in 34·6, 40·6 and 42·4 % (respectively) of the studied population. Results showed women in the highest tertile of DPI had 78%, 67% and 70% lower risks in developing depression, anxiety and psychological stress, respectively, compared with those in the lowest tertile. Although this study showcases the significant association between DPI and mental health in Iranian women, prospective studies are required for further confirmation. [NPID: micronutrients, nutritional supplements, depression, anxiety, psychological distress, anxiety, stress, women, female, Iran]
Effect of green tea phytochemicals on mood and cognition
As matcha tea gains popularity and has been found to contain higher amounts of green tea phytochemicals compared to regular green tea, this 2017 review focuses on the tea constituents caffeine, L-theanine, and epigallocatechin gallate (EGCG) and its widely reported beneficial impact on mood and cognitive performance. This review aimed to summarize the acute psychoactive effects of these tea components by evaluating 49 human intervention studies. Since a limited number of intervention studies on EGCG was discovered its effects were inconclusive. But enhanced alertness, arousal and vigor were reported with caffeine, as well as better performance on time-consuming and demanding cognitive tasks, even at doses as low as 40mg. Caffeine in combination with L-theanine especially increased alertness and raised performance levels in attention-switching tasks, but to a lesser extent than caffeine alone. Even L-theanine alone, starting at 200mg, improved relaxation, tension, and calmness. These studies demonstrate the positive influences of L-theanine and caffeine on avoiding distractions and maintaining attention and memory, and the relaxing effect of L-theanine (through reduction of caffeine-induced arousal). [NPID: micronutrients, nutritional supplements, green tea, phytochemicals, caffeine, L-theanine, and epigallocatechin gallate (EGCG), cognitive performance, alertness, arousal, vigor, relaxation, tensin, calmness, attention, memory]
The relationship between dietary vitamin K and depressive symptoms in late adulthood: A cross-sectional analysis from a large cohort study
This 2019 study assessed the correlation between dietary vitamin K intake (data collected through a semi-quantitative food frequency questionnaire) and depressive symptoms [diagnosed using the 20-item Center for Epidemiologic Studies-Depression (CES-D) ≥ 16] among 4,375 adult participants (aged 45-79) from North America. Around 10% (n=437) of the subjects exhibited symptoms of depression. After adjusting for potential confounders in the logistic regression analysis, those adults with the highest vitamin k intake were associated with lower incidences of depressive symptoms (OR = 0.58; 95%CI: 0.43–0.80), although this observation only applied to subjects not taking vitamin D supplements. Since this study provides evidence on the relevance of higher dietary vitamin K with lower appearance of depressive symptoms, further research is encouraged, especially to inspect the directionality of this association. [NPID: micronutrients, nutritional supplements, vitamin K, depression, vitamin D]
Nutritional interventions in clinical depression
Rechenberg (2016) describes the lower quality of life, rise in comorbidity and increased mortality associated with depression, and the availability of a treatment option with a better safety profile than the well-established psychotherapy and pharmacotherapy used for clinical depression. Nutritional supplements are proposed as a means of reducing depressive symptoms and can be adopted as adjuvant therapy alongside pre-existing regimens, or as sole therapies. While there has been no shortage of interest in omega-3 fatty acids, B-vitamins (folate, vitamin B12, and vitamin B6), S-adenosylmethionine (SAMe), 5-hydroxytryptophan (5-HTP), and magnesium in the management of depression, this article explores the clinical data on these nutritional interventions and reviews its relevance to the pathophysiology and epidemiology of clinical depression. [NPID: micronutrients, nutritional supplements, copper, selenium, manganese, iodine, vanadium, depression, anxiety, enzymes]
Essential elements in depression and anxiety. Part II
This 2015 paper analyzes the micronutrients copper, selenium, manganese, iodine and vanadium and their roles in depression and anxiety. Młyniec et al. (2015) discuss potential mechanisms in which these elements may be linked with either depression or anxiety, including possible interactions between some of these micronutrients with enzymes that are involved in the pathophysiology of mental disorders. Furthermore, the authors inspect the dynamic between these elements and depression/anxiety, even the quantity of an element in the diet or in the blood associated with the symptoms of these disorders. [NPID: micronutrients, nutritional supplements, copper, selenium, manganese, iodine, vanadium, depression, anxiety]
The role of elements in anxiety
This 2017 review summarizes the most valuable current evidence on the roles of zinc, magnesium, copper, lithium, iron, and manganese, and the deficiencies of these micronutrients, in the pathophysiology and treatment of anxiety. [NPID: micronutrients, nutritional supplements, magnesium, copper, lithium, iron, manganese, anxiety]
Diet-induced hypothalamic dysfunction and metabolic disease, and the therapeutic potential of polyphenols
This 2019 review summarizes the influence that polyphenols can have on the neural inflammation and mitochondrial dysfunction aspects of diet-induced hypothalamic dysfunction. Polyphenols were seen to help reduce oxidative stress and inflammation within the hypothalamus, enhancing leptin signaling and mitochondrial biogenesis in the process. The role of polyphenols in reducing the production of reactive oxygen species and in augmenting the natural oxidative defense systems also assists the prevention of neurodegeneration. Samodien et al. (2019) appreciate polyphenols as nutraceuticals with excellent potential as they have shown protective qualities against hypothalamic inflammation, mitochondrial dysfunction, and neurodegeneration. As hypothalamic inflammation spreads as an individual ages, polyphenol’s ability to possibly increase longevity should be studied, along with its therapeutic value in the management of mental health disorders since they are characterized too by advanced neuroinflammation. [NPID: micronutrients, nutritional supplements, polyphenols, neural inflammation, mitochondria, hypothalamic dysfunction, hypothalamus, oxidative stress, neurodegeneration, nutraceuticals, neuroinflammation, inflammation]
Dietary total antioxidant capacity as a preventive factor against depression in climacteric women
This 2019 study explored the potential correlation between dietary total antioxidant capacity (DTAC) and nutritional parameters with prevalence of depression among a female sample from Southern Brazil. The Beck Depression Inventory (BDI) helped analyze severity of depressive symptoms, while a 24-hour dietary recall allowed the monitoring of the women’s diet. The DTAC of the population ranged from 435.60 to 4502.62 mg VCE/day and depression was reported in 44% of all participants. Coffee was identified as the most consumed antioxidant food/beverage, while polyphenols were directly linked to the antioxidant capacity of fresh foods. Furthermore, women with depression were found to consume less polyphenols (p=0.022; Cohen's d=0.80), vitamin B6 (p=0.038; Cohen's d=0.65), vitamin A (p=0.044; Cohen's d =0.63), and vitamin C (p=0.050; Cohen's d =0.61). Lower BDI scores were also related with decreased polyphenol intake. This study hopefully provides helpful information on the recommended dietary antioxidant intake to support the prevention of depression among women. [NPID: micronutrients, nutritional supplements, antioxidant, depression, Brazil, coffee, polyphenols, vitamin C, women, female]
The efficacy and safety of nutrient supplements in the treatment of mental disorders: A meta-review of meta-analyses of randomized controlled trials
This 2019 meta-review appraised all the meta-analyses conducted on randomized controlled trials (RCTs) investigating the efficacy and safety of nutrient supplements in common and severe mental disorders. The 33 meta-analyses identified by a systematic search produced outcome data of 10,951 participants. While early evidence suggests polyunsaturated fatty acids (PUFAs) may have positive impacts on attention-deficit/hyperactivity disorder, there is greater support for the use of PUFAs, and particularly eicosapentaenoic acid, in the treatment of depression. While folate-based supplementation in patients with depression and schizophrenia has been explored, high-dose methylfolate and its positive influence on major depressive disorder was highlighted. In addition, back-up for N-acetylcysteine as an adjunctive treatment in mood disorders and schizophrenia is increasing. All the nutrient supplements had good safety profiles, with no adverse effects or contraindications with psychiatric medication reported. It is therefore important that clinicians note the nutrients that are well established in their efficacy, and also be mindful of those lacking in evidence. Next research should look into the population that would benefit the most from these supplements, developing our understanding of the underlying mechanisms in the process. [NPID: micronutrients, nutritional supplements, PUFAs, ADHD, eicosapentaenoic acid, folate, depression, schizophrenia, methylfolate, major depressive disorder, MDD, depression]
Zinc, magnesium, selenium and depression: A review of the evidence, potential mechanisms and implications
Wang et al. (2018) reviewed the evidence on the association between the micronutrients zinc, magnesium and selenium, with depression, and also overviewed the potential mechanisms of action behind the interactions. Empirical data seems to strongly suggest the positive association between zinc deficiency with risk of depression, and the inverse dynamic between zinc supplementation and depressive symptoms. Research surrounding the relationship between low magnesium and selenium intake with depression was lacking and inconclusive. The mechanisms of action of these micronutrients could involve the HPA axis, glutamate homeostasis and inflammatory pathways. This review highly regards the importance of consuming adequate servings of micronutrients in supporting good mental health, and provides the readers with the most common dietary sources for zinc and various other micronutrients. The safety and efficacy of supplementation with these micronutrients, used to potentially treat depression, should be investigated more thoroughly, while prospective data on the relationship between micronutrient levels and depression remain desired. [NPID: micronutrients, nutritional supplements, zinc, magnesium, selenium, depression, HPA, HPA axis, glutamate, inflammation]
Higher vitamin B6 intake is associated with lower depression and anxiety risk in women but not in men: A large cross-sectional study
This 2020 study explored the correlation between intake of vitamin B6 with depression and anxiety among 3362 adults. Kafashani et al. (2020) used a validated 106 item self-administered Willett-format dish-based semi quantitative food-frequency questionnaire (DFQ) and an Iranian validated version of the Hospital Anxiety and Depression Scale (HADS) questionnaire to obtain data on the participants’ diet and mental health. The results exposed the significantly lower consumption of vitamin B6 in anxious and depressed individuals, compared to healthy subjects. After making adjustments for potential confounders, less vitamin B6 in the diet of the women and of the whole sample population was associated with increased risk in developing depression (OR = 1.41, P < 0.001. OR = 1.33, P = 0.02, respectively) and higher odds of suffering from anxiety (OR = 2.30, P < 0. 001, OR = 2.30, P = 0.04). This data provides further evidence of the association between lower vitamin B6 intake and increased prevalence of depression and anxiety. Enhancing nutritional status is thought to help cut down on these disorders, but further research, particularly robust randomized controlled trials, are necessary to provide more proof. [NPID: micronutrients, nutritional supplements, vitamin B6, depression, anxiety, Iran, B6]
Association between lower intake of minerals and depressive symptoms among elderly Japanese women but not men: Findings from Shika study
Nguyen et al. (2019) analyzed the mineral intake (sodium, potassium, calcium, magnesium, phosphorus, iron, zinc, copper and manganese) of 1423 Japanese elderly people (aged 65+) and examined its relationship with depressive symptoms. The mineral intake of the Japanese adults were reported through a validated and brief self-administered diet history questionnaire, while the Geriatric Depression Scale was employed to measure their depressive symptoms. Those subjects with depressive symptoms were found to have taken in less minerals than those without symptoms, considering all minerals except sodium and manganese. Among the males, the level of minerals in the diet did not vary between those showing depressive symptoms and those without signs of depression, but this did not hold true for the females. Mineral intake was significantly lower in female participants with depressive symptoms, compared to those without such symptoms; the minerals potassium, calcium, magnesium, phosphorus, iron, zinc, and copper were significantly and negatively correlated with depressive symptoms among the women, but not men. The results suggested that the deficiencies in mineral intake may be related to depressive symptoms, especially in women, among this Japanese elderly population. [NPID: micronutrients, nutritional supplements, sodium, potassium, calcium, magnesium, phosphorus, iron, zinc, copper, manganese, Japan, depression, women, female]
Dietary creatine intake and depression risk among U.S. adults
Bakian et al. (2020) examined the association between dietary creatine and depression in U.S. adults, using the data dietary creatine intakes and patient health questionnaires obtained by the 2005 to 2012 National Health and Nutrition Examination Survey (NHANES) on its 22,692 participants (aged ≥20 years). This study compared the depression prevalence in the subjects in the lowest quartile of dietary creatine intake (rate of 10.23/100) to occurrence in those in the highest quartile of creatine consumption (5.98/100 persons). While an inverse association was confirmed between dietary creatine and depression [adjusted odds ratio (AOR) = 0.68], the strongest correlations were seen in females (AOR = 0.62) and participants not taking antidepressant/anxiolytic medication (AOR = 0.58). These results highlighted a significant negative relationship between creatine intake and depression in a nationally representative cohort. This leaves the role that creatine plays in depression among women and across the lifespan to be investigated in the future. [NPID: micronutrients, nutritional supplements, creatine, depression, anxiolytic medication, women, female]
A systematic review and meta-analysis of B vitamin supplementation on depressive symptoms, anxiety, and stress: effects on healthy and 'at-risk' individuals
This 2019 systematic review and meta-analysis was undertaken to examine and quantify the effects of B vitamin supplementation on mood in both healthy and 'at-risk' populations. The review accumulated 18 articles (2015 participants) including 16 randomized controlled trials involving daily supplementation with 3 or more B group vitamins with an intervention period of at least 4 weeks. Eleven of the 18 articles reported a positive effect for B vitamins over a placebo for overall mood or a facet of mood, while 5 out of the 8 studies in “at-risk” cohorts saw significant improvements in mood. B vitamin supplementation had a positive impact on stress, while it had no effect on anxiety and its beneficial effect on depression did not reach significance level. This review implies B vitamin supplementation can effect positive changes in healthy and at-risk populations for stress, but not for depressive symptoms or anxiety, and suggests its usefulness particularly in people who are at risk due to poor nutrient status or poor mood status. [NPID: micronutrients, nutritional supplements, B vitamins, B12, B6, stress, anxiety, depression]
The association between dietary intake of magnesium and psychiatric disorders among Iranian adults: A cross-sectional study
The purpose of this 2018 study was to explore the association between magnesium uptake from diet and psychiatric disorders among a large group of Iranian adults (n=3172; age 18-55). Dietary consumption was documented with a validated dish-based 106-item semi-quantitative food frequency questionnaire, while depression and anxiety, and psychological distress were evaluated using an Iranian validated version of the Hospital Anxiety and Depression Scale, and the General Health Questionnaire. The results demonstrated a significant inverse correlation between magnesium intake and depression among normal-weight men (OR 0·45) and overweight women (OR 0·45). Low Mg intake was also connected with higher prevalence of anxiety among all women (OR 1·80) and normal-weight women (OR 1·73). While women in the highest quartile of Mg intake were 39% less likely to experience anxiety, compared with those in the lowest quartile. Even in unadjusted analyses, higher dietary Mg intake was associated with lower odds of anxiety among women (OR 0·61). Anjom-Shoae et al. (2018) were able to find evidence that dietary intake of magnesium was inversely associated with depression and anxiety but not with psychological distress. [NPID: magnesium, depression, anxiety, distress, Mg]
Nutrient and genetic biomarkers of nutraceutical treatment response in mood and psychotic disorders: A systematic review
Van der Burg and others (2019) conducted this systematic review of nutraceutical clinical trials in mood and psychotic disorders (major depression, bipolar disorder, schizophrenia) in the hope of discovering the most useful nutrient and genetic biomarkers for predicting nutraceutical response in people with these disorders. The team identified 35 studies (totalling 3836 participants) with baseline and endpoint blood nutrient markers and/or genetic polymorphisms. One of the most prominent findings was the strong association between polyunsaturated fatty acid concentrations (mostly EPA and DHA) and psychiatric outcomes observed in 10 out of 11 omega-3 studies, although the exact nature of the correlation varied between studies and diagnoses. No consistent evidence could be determined for levels of other nutrients (including Vitamin D, SAM/SAH ratios, carnitine, folate and vitamin B12) relating to treatment response, nor for the associations between one-carbon cycle genotypes (e.g. MTHFR C677 T, MTR and FOLH1) and treatment response. The available data therefore supported omega-3 indices as biomarkers of response to omega-3 treatments in mood disorders, although the researchers mention that larger population studies examining combinations of polymorphisms are required to determine if any genetic factors influence nutraceutical response in mood and psychotic disorders. [NPID: micronutrients, nutritional supplements, nutraceuticals, major depressive disorder, MDD, depression, bipolar, schizophrenia, genetic polymorphisms, EPA, DHA, vitamin D, SAM, SAH, carnitine, folate, vitamin B12, omega-3s]
The purpose of this 2018 study was to explore the association between magnesium uptake from diet and psychiatric disorders among a large group of Iranian adults (n=3172; age 18-55). Dietary consumption was documented with a validated dish-based 106-item semi-quantitative food frequency questionnaire, while depression and anxiety, and psychological distress were evaluated using an Iranian validated version of the Hospital Anxiety and Depression Scale, and the General Health Questionnaire. The results demonstrated a significant inverse correlation between magnesium intake and depression among normal-weight men (OR 0·45) and overweight women (OR 0·45). Low Mg intake was also connected with higher prevalences of anxiety among all women (OR 1·80) and also normal-weight women (OR 1·73). While women in the highest quartile of Mg intake were 39% less likely to experience anxiety, compared with those in the lowest quartile. Even in unadjusted analyses, higher dietary Mg intake was associated with lower odds of anxiety among women (OR 0·61). Anjom-Shoae et al. (2018) were able to find evidence that dietary intake of magnesium was inversely associated with depression and anxiety but not with psychological distress. [NPID: micronutrients, nutritional supplements, magnesium, psychiatric disorders, depression, anxiety, psychological distress]
The impact of essential fatty acid, B vitamins, vitamin C, magnesium and zinc supplementation on stress levels in women: A systematic review
Since women undertaking multiple roles in today’s society are increasingly experiencing psychological stress, this 2017 systematic review was designed to determine the effects of specific dietary supplements such as essential fatty acids (EFAs), B vitamins, vitamin C, magnesium and/or zinc in managing stress and anxiety in ladies. The search was for studies that recruited women aged 18 or above and that assessed stress and anxiety, including randomized controlled and pseudo-randomized trials. Due to the heterogeneity of the 14 included studies, narrative synthesis was performed. Essential fatty acids were found to be effective in various scenarios: alleviating anxiety in both premenstruation and during menopause in the absence of depression (ineffective after removing depression status); and reducing perceived stress and salivary cortisol levels during pregnancy. Also if disregarding the hormonal phase, EFAs were ineffective in reducing stress or anxiety in four groups of women. When magnesium supplementation was combined with vitamin B6, a reduction in premenstrual anxiety was seen but no effect was found with single supplementations, and when combined or not no impact was observed for stress in women suffering from dysmenorrhea. Other findings included older women experienced anxiety reduction using vitamin B6, but not folate or vitamin B12, while high-dose sustained-release vitamin C reduced anxiety and blood pressure in response to stress. To summarize, EFAs may be effective in reducing prenatal stress and salivary cortisol and may reduce anxiety during premenstrual syndrome and during menopause in the absence of depression; magnesium and vitamin B6 may be effective in combination in reducing premenstrual stress; vitamin B6 alone may reduce anxiety effectively in older women; and high-dose sustained-release vitamin C may reduce anxiety and mitigate increased blood pressure in response to stress. McCabe et al. (2017) called for longer term studies to investigate supplementation and to include compliance testing, use inert substances as controls and reliable outcome measures. [NPID: micronutrients, nutritional supplements, psychological distress, EFAs, essential fatty acids, B vitamins, vitamin C, B6, B12, anxiety, stress, zinc, magnesium, premenstrual anxiety, menstruation, blood pressure, PMS]
Low zinc, copper, and manganese intake is associated with depression and anxiety symptoms in the Japanese working population: Findings from the eating habit and well-being study
Using the data from the Eating Habit and Well-being study in Japanese workers, Nakamura et al. (2019) analyzed the relationship between the intake of six minerals with mental disorders. Among the 2089 participants of the study, there was no history of depression but 6.9% developed mental disorders (detected by Kessler's six-item psychological distress scale using a cut-off score of 12/13). The subjects’ dietary mineral intakes were estimated with the validated food frequency questionnaires, revealing the association between mental disorders with the lowest quartiles of zinc, copper, and manganese consumption. Whereas, the lowest quartiles of calcium, magnesium, and iron intake did not correlate with mental disorders. Also, combination analysis of high (≥median) or low ( Database analysis of depression and anxiety in a community sample—response to a micronutrient intervention Kimball et al. (2018) investigated the impact of a nutrition intervention program aimed at optimizing people’s vitamin D levels, on depression and anxiety by collecting data from 16,020 participants. The self-reported health measures of depression and anxiety were evaluated [using European Quality of Life Five Dimensions (EQ-5D) and Targeted Symptoms List (TSL)] as part of a community-based program focused on optimizing overall health through nutritional supplementation, education and lifestyle advice. The EQ-5D revealed that elevated levels of depression and anxiety were reported at baseline by more than 56% of the sample, but 49.2% (n = 7878) of those who reported any degree of depression or anxiety at baseline improved upon the first year in the program. Moreover, 97.2% of the 829 individuals who reported severe or extreme depression at baseline also showed improvements after one year. The better outcomes for depression and anxiety were significantly linked with higher vitamin D status (>100 nmol/L) and more strenuous physical activity, as observed in the regression analyses. This study concludes that those who suffer from mood and anxiety issues may benefit from nutritional supplements. [NPID: micronutrients, nutritional supplements, vitamin D, depression, anxiety] Association of total zinc, iron, copper and selenium intakes with depression in the US adults Li et al. (2018) studied the relationship between the total consumptions of zinc, iron, copper and selenium, with depression. This cross-sectional study extracted the data of 14,834 adults (18+ years, 7399 male: 7435 female) from the National Health and Nutrition Examination Survey (NHANES) 2009-2014. In unadjusted model and age- and gender-adjusted models, total zinc, iron, copper and selenium intakes were inversely associated with depression; when the highest quartile of copper and selenium intakes were compared to the lowest quartile, the multivariate adjusted odds ratios (ORs) of depression was recorded as 0.68 and 0.46, respectively. In addition, when quartile 3 for total zinc and iron consumption was compared to the lowest quartile, the inverse associations of depression were statistically significant, with OR of 0.7 for zinc and 0.66 for iron. Furthermore, those adults who met the Recommended Dietary Allowances (RDAs) for zinc (OR: 0.74), copper (OR: 0.68) and selenium (OR: 0.52) had significantly lower odds of depression, compared to those below the RDA. These results suggest inverse associations between total zinc, iron, copper and selenium intakes with depression. [NPID: micronutrients, zinc, iron, copper, selenium, depression] Rongo o te wā.News and Events

School of Psychology, Speech and Hearing
Te kura mahi ā-hirikapo.
If you’re interested in human health and behaviour and want to make a meaningful, tangible difference to people’s lives, UC's School of Psychology, Speech and Hearing is the place to start. Check it out.
Welcome to Te Kura Mahi ā-Hirikapo | School of Psychology, Speech and Hearing. If you’re interested in human health and behaviour and want to make a meaningful, tangible difference to people’s lives – this is the place to start.
We offer a range of undergraduate and postgraduate options which are highly regarded by our industries.
Our research receives national and international attention and is making a real difference to peoples' lives – from new speech therapy techniques for stroke patients to ground-breaking science into diet and mental health. We’re also home to several on-site clinics and pioneering research centres, attracting academics and specialists from all over the world.
Study in the School of Psychology, Speech and Hearing
We offer a wide range of highly regarded courses, qualifications and research opportunities in the fields of psychology , speech and language pathology , and audiology .
Our Speech and Language courses are accredited by Te Kāhui Kaiwhakatikatika Reo Kōrero o Aotearoa | New Zealand Speech-language Therapists’ Association.
We have a new Bachelor of Psychological Sciences degree or alternatively you can study psychology as part of a Bachelor of Science , Arts or Health Science .
We also have a range of postgraduate options for prospective students from a Master in Psychology, or Audiology.
Our research
UC is home to many world-leading research centres, institutes and on-site clinics. This provides students with first-hand experience in real-world research and clinical environments.
With a burgeoning post-graduate programme and new doctoral-level faculty in diverse areas of psychology, communication disorders, audiology, swallowing rehabilitation and stroke recovery, our research profile is rapidly expanding.
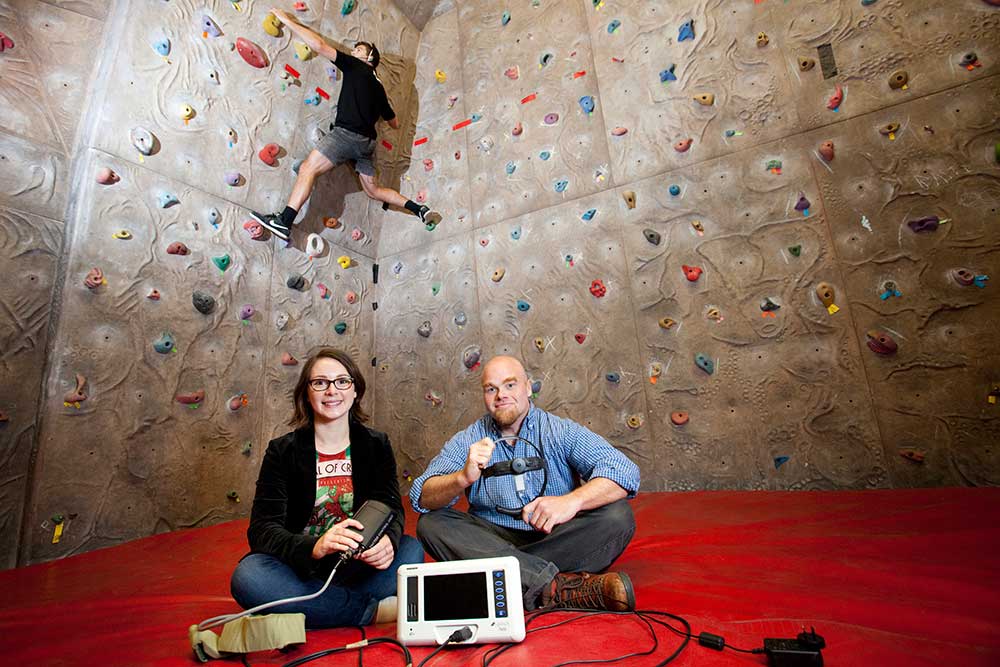
Our world-leading experts are collaborating on ground-breaking research and development work. Find out what we are working on.
The Psychology Centre
"He aha te mea nui o te ao? He tangata, he tangata, he tangata". What is the most important thing in the world? It is people, it is people, it is people.
The Psychology Centre is the clinical psychology training and research centre for UC's Clinical Psychology Programme. We offer students an opportunity to participate in a wide range of psychological assessments and treatments as part of their practicum course, working alongside senior clinical psychologists. Check out our Psychology Centre services.
CLOSED - REFERRALS FOR THERAPY
OPEN - SELF-COMPASSION COURSE
ASSESSMENTS – referrals open Monday 1st April 2024. Please note that we will NOT accespt referrals prior to the listed date.
All referrals received will be triaged to see if suitable for our student clinics.

Speech and Hearing Clinic
UC's Speech and Hearing Clinic offers a comprehensive range of professional services for people with communication difficulties and swallowing problems. Students enrolled in our Speech and Language Pathology and Audiology programmes attend appointments and are supervised by qualified clinicians. Learn more about the UC Speech and Hearing Clinic.
Engagement and careers
Science outreach for schools.
UC's science outreach programme inspires and supports future scientists, problem solvers, and innovators. We work with teachers and scientists to enhance science education in schools, give students real world experiences, and show the exciting career opportunities possible with science. Learn about UC's science outreach for schools.

What can I do with my degree?
Search the University of Canterbury | Te Whare Wānanga o Waitaha website.
Level 1, Psychology Building
Related content
Useful links, news and events from the school of psychology, speech and hearing, new uc research into children born to mothers on methadone, 07 november 2019.
Children born to mothers treated with methadone during pregnancy are experiencing educational challenges, according to a new paper by University of Canterbury (UC) Psychology researcher Dr Samantha Lee.

Call for New Zealand specific autism research
09 june 2022.
Autistic people need to be actively involved in future research and don’t want it to focus on a cure or behaviour management.

Grant enables new programme for children living with anxiety
11 august 2022.

UC professors’ exceptional contribution recognised
04 november 2022.
Outstanding professors who have retired from the University of Canterbury (UC) over the past year but continue to contribute and inspire have been acknowledged at a celebration event.

Babies’ balance tested in new research
31 may 2021.
A new study will explore for the first time whether babies with hearing loss could also benefit from being tested for balance problems at an early age.

Innovative $2.4m research into microplastics, Antarctic predators, respiratory function
27 october 2022.
Three innovative, groundbreaking University of Canterbury researchers have been awarded $800,000 Rutherford Discovery Fellowships announced today by the Royal Society Te Apārangi.

UC entrants win all three HealthTech Awards for Best Research
23 june 2021.
University of Canterbury (UC) innovators and their health technology solutions are the winners of 2021 HealthTech awards announced at a ceremony in Auckland last night.
Unique child/family psychology training celebrates 20 years
30 september 2022.
The University of Canterbury (UC) celebrates 20 years of the Child and Family Psychology programme today. The sought-after qualification trains psychologists specifically to work with children, adolescents and families, and remains unique in Aotearoa.

Reputation is key for award-winning Canterbury psychologist
23 november 2023.
Would you rather plunge your hand into a bucket of wriggling worms or experience damage to your reputation?
In this section:
By clicking "Accept All Cookies", you agree to the storing of cookies on your device to enhance site navigation, analyse site usage, and assist in our marketing efforts.
General enquiries
0800 827 748 (within NZ) +64 3 369 3999
info@canterbury.ac.nz
International enquiries
+64 3 364 3443
Ask a question
More contact details
See all contacts
Emergency contact details
Ext: 92111 (from a campus landline) Direct dial: 0800 823 637
Emergency information
University of Canterbury | A Fair Trade University
- Frontiers in Nutrition
- Nutrition, Psychology and Brain Health
- Research Topics
Microbiome-Gut-Brain Axis Crosstalk and Clinical Outcomes
Total Downloads
Total Views and Downloads
About this Research Topic
Over 2000 years ago, the Greek physician Hippocrates of Kos said, “All disease begins in the gut.” The gut is the most important barrier for environmental factors to interact with our body, knowing that food brings nutrition as well as waste and toxicity. In the mid-19th century, a gastroenterology patient ...
Keywords : Microbiome-gut-brain axis, nutrition, behaviors, mental diseases, mental health, neurodevelopment, aging, cognitive impairment
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Is Seafood Good for Your Brain?
Fish and seafood are called brain food for good reason. Research suggests that improved memory is just one of many brain-boosting benefits associated with eating more fish and seafood, a dietitian explains.
This article is based on reporting that features expert sources.
Brain Health Benefits of Seafood

Getty Images
Rumor has it that one of the oldest known recipes in the Mediterranean – found in "Deipnosophistae" by the ancient Greek Athenaeus – is a recipe for fish ( grilled fish sprinkled with grated cheese). For millennia, seafood has played an important role in Mediterranean cuisine, health and culture. In fact, nutrition research over the last 20 years has revealed the increasing importance of including fish and seafood in an overall healthy diet . This was evident when a nutrition science panel met in 2008 to update Oldways’ original Mediterranean Diet Pyramid.
“One of the most notable updates was to make fish and seafood more prominent on the Mediterranean diet pyramid,” explains Oldways President Sara Baer-Sinnott.
Today, nutrition researchers recognize seafood as a staple food group in brain-healthy diets like the MIND diet and the Mediterranean diet. But what exactly does the research us about the link between seafood, cognition, mood and brain structure?
Omega-3s for Brain Health
DHA, or docosahexaenoic acid, is an omega-3 fatty acid that is a building block of our brain. In other words, just as calcium is to our bones, DHA is to our brains.
“The foods we eat become who we are by changing the composition of our brains,” explains Dr. Joseph Hibbeln, a psychiatrist with Barton Health and omega-3 expert.
Seafood is the main source of DHA in the diet, so it’s not surprising that scientists are making note of links between eating seafood and brain health. Seafood also contains protein, essential vitamins and minerals, and EPA, or eicosapentaenoic acid, another type of omega-3 fatty acid that supports brain health.
A body of research has found that EPA and DHA reduce small proteins in the brain that promote inflammation and are associated with depression, Alzheimer’s disease and cognitive decline. Another study , in the American Journal of Preventive Medicine, found that people who regularly eat fish have more voluminous brains than those who do not. This study found that eating fish – baked or broiled – is associated with larger gray matter volumes in brain areas responsible for memory and cognition in healthy elderly people.
Eating fish at least twice a week may shield delicate blood vessels in the brain from subtle damage that can lead to mild cognitive impairment, dementia or stroke, according to research published in Neurology in 2021, adding to the growing evidence that seafood supports brain health.
Omega-3 levels can be measured in the body as a marker of how much seafood and/or omega-3 supplements people consume.
“Higher levels of omega-3 measured in plasma or red blood cells are associated with lower risk for developing Alzheimer’s and dementia ,” explains William Harris, president of the Fatty Acid Research Institute. His research quantifies these relationships in large cohort studies . While there hasn’t yet been a large randomized-controlled trial measuring seafood intake or omega-3 fatty acid intake as a way to prevent dementia , Harris explains that at this point, given the consistency of the evidence, “to withhold omega-3 fatty acids would not be ethical in a randomized controlled trial.”
Mental Health Benefits of Seafood
“The most pressing and immediate thing in peoples live is the behaviors and emotions that emerge when brain is deficient and critical nutrients,” says Hibbeln. In other words, keeping our brains nourished is just as important for our mental health as it is for our cognitive health.
An analysis of double-blind randomized controlled trials encompassing more than 10,000 patients across 35 studies found that giving patients EPA-predominant omega-3 fatty acids was able to produce significant clinical effects that were, in some cases, greater than what you would see from antidepressant medications .
Nearly 20 years ago, the American Psychiatric Association concluded that omega-3 fatty acids EPA and DHA have a protective effect in mood disorders like major depressive disorder and bipolar disorder . And yet still today, Hibbeln says that “the mental health benefits of omega-3 fatty acids are underknown, underutilized and under implemented” within the greater medical community.
Mercury Concerns
The Dietary Guidelines for Americans recommend that adults eat at least 8 ounces of seafood per week, but emphasize that pregnant or breastfeeding individuals should not exceed 12 ounces per week of a variety of seafood from choices that are lower in methylmercury. However, in the more than 20 years since cautionary advice on mercury and seafood was first issued in the U.S., dozens of studies have started to paint a more nuanced picture of this relationship.
Methylmercury was recognized as a neurotoxin when dangerously high levels from industrial contamination events in the 20th century were linked to overt, damaging effects on the brain and nervous system, particularly in young children. While overt harm from extreme exposures have not been reported again, considerable research has been conducted since then to better understand the relationship between seafood consumption during pregnancy, exposure from normal background levels of methylmercury in that seafood and neurodevelopment in children.
Over 30 such studies have now analyzed data from more than 200,000 mother-child pairs . The studies have found little evidence of harm to neurodevelopment associated with that consumption. Instead, the research points to over 50 incidences of benefits to children’s neurodevelopment, including improvements to IQ, from the women’s consumption of seafood as compared to children whose mothers ate less or no seafood during pregnancy.
In other words, the benefits of eating seafood outweigh any potential risks.
“What we see consistently in those studies is that over 12 ounces per week tends to be better than under 12 (ounces per week),” says Philip Spiller, former director of the then-Office of Seafood within the United States Food and Drug Administration and lead author of a recently published study that analyzed the research results. “The evidence is robust enough that messaging to pregnant women should emphasize the likelihood of benefits to their children’s neurodevelopment, that more is better than less, and should no longer emphasize cautionary behavior to avoid risk that the studies have not found.”
As it stands, nearly 90% of Americans are falling short of recommended seafood amounts according to the Dietary Guidelines for Americans.
“If you obsess on mercury you’re missing the big picture,” says Tom Brenna, PhD, professor of pediatrics, of chemistry, and of nutrition at the Dell Medical School and the College of Natural Sciences at the University of Texas at Austin, and Professor Emeritus at Cornell University. “The studies overall show great benefit, so the risk is not eating enough seafood.”
Buying and Cooking Seafood
Seafood cooks quicker than chicken, and yet this brain-healthy food group is surprisingly underutilized in home kitchens. At the supermarket, seafood can be found in fresh, frozen and canned forms – all of which can be used in delicious and nutritious meals. For people who are new to seafood, or any food for that matter, remember that taste preferences aren’t set in stone. Making an effort to try seafood often and in different forms is a great way to nurture a taste for this popular protein source.
When identifying seafood options higher in omega-3 content, Harris suggests remembering the acronym SMASH, which stands for salmon, mackerel, anchovies, sardines and herring. “Twice a week, eat a meal with one of these,” recommends Harris, noting that salmon is one of his go-to choices.
Baer-Sinnott suggests taking a cue from heritage diets, like the Mediterranean diet , to experience how seafood fits into healthy eating patterns rooted in tradition and culture. “Eating fish and seafood twice a week is good for your health and it is also easy and delicious,” says Baer-Sinnott. “With all of this evidence, why wouldn’t you?”
“Pick a fillet, throw some olive oil right in the pan and cook it a little bit on each side. Don’t overthink it,” assures Brenna. A sea of culinary possibility awaits.
7 Signs of Vitamin B12 Deficiency

The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Baer-Sinnott is president of Oldways, a nonprofit food and nutrition organization helping people live healthier, happier lives through cultural food traditions and lifestyles.
Brenna is a professor of pediatrics at Dell Medical School at the University of Texas in Austin. He is a former professor of human nutrition, chemistry, chemical biology and food science at Cornell University in Ithaca, New York.
Harris is president of the Fatty Acid Research Institute in South Dakota. He is also founder of OmegaQuant Analytics, LLC and the developer of the Omega-3 Index blood test.
Hibbeln is a board-certified psychiatrist with Barton Health in California, a nutritional neuroscientist and omega-3 expert.
Spiller is the former director of the Office of Seafood for the Center for Food Safety and Applied Nutrition, U.S. Food and Drug Administration.
Tags: brain health , diet and nutrition , food and drink
Most Popular

health disclaimer »
Disclaimer and a note about your health », you may also like, colon cancer diet.
Ruben Castaneda and Shanley Chien March 20, 2024

Health Benefits and Recipes for Beans
Janet Helm March 15, 2024

Worst Foods for Gut Health
Ruben Castaneda and Elaine K. Howley March 12, 2024

Best Foods for Gut Health

Is Mushroom Coffee Good for You?
Keri Gans March 11, 2024
6 to 1 Grocery Shopping Method
Toby Amidor March 11, 2024
12 Best Superfoods for Older Adults
Christine Comizio and Elaine K. Howley March 7, 2024

Best Frozen Meals
Joan Salge Blake March 6, 2024

Healthiest Olive Oil
Claire Wolters March 6, 2024
How Many Calories Per Day to Lose Weight
Paul Wynn March 5, 2024


Parents Are Paying More For Mental Health Care For Their Kids—And That Needs to Change
New research highlights the financial burden receiving mental health care can be on a family.
U.S. Surgeon General Dr. Vivek Murthy, MD, MBA , emphasized the increase in depression, anxiety, and suicidal ideation symptoms in children and adolescents in 2021. He then issued an advisory pointing to social media as a catalyst for the youth mental health crisis in 2023. A recent study is now calling attention to the price families are paying to help their children with mental health care —a price not every family can afford.
The study by researchers from virtual mental health care provider Brightline and published in JAMA Network Open found that families with a child or adolescent with a mental health condition paid $4,361 more toward medical spending for the child, a 31.1% uptick from 2017. Additionally, families with a child or adolescent with a mental health condition spent $2,337 more for family members, and study authors say that caregiver mental health care may be a reason for the cost.
“Our study highlights the rise in mental health conditions among children is a growing concern, with far-reaching impacts beyond the child,” says Theoren Loo , a clinical data scientist at Brightline and the study's co-author. “This study suggests that child and family member mental health are connected, not only by clinical symptoms but also by increased medical spending.”
The increased costs come at an increasingly challenging time to be a child or teen in the world, and experts are concerned.
“Compared to when I was a child, it is much more difficult to grow up in this era,” says Julian C. Lagoy, MD , a board-certified psychiatrist with Mindpath Health. “ Suicide, depression, and anxiety are much more prevalent now than when I was a child. If we do not correct this soon, we will continue to see rises in suicide and depression in our children. There will be a lot more adults with mental health problems in the future.”
This can also compound and have a ripple effect on the next generation of children. Parents spoke with experts about the potential reasons for the increased costs, their concerns, and how parents can afford crucial mental healthcare for their children and teens.
Why are Mental Health Care Costs for Pediatrics Rising?
Experts say numerous factors are likely contributing to the rise in mental healthcare costs for pediatric patients. However, Loo says there’s an important caveat.
“It’s worth noting that not all mental health spending is bad,” Loo says. “In fact, the increase in cost may be attributed to an increase in accessibility and utilization of mental health services, which in turn may be driven by the adoption of telehealth services, decrease in stigma around mental health, and legislative support for behavioral health services...However, some costs reflect the need for improved prevention and treatment of pediatric mental healthcare.”
Understanding the reasons can help parents feel less alone and hopefully drive change.
The pandemic
The research went live on March 11, 2024, the fourth anniversary of the World Health Organization declaring COVID-19 a global pandemic . While large-scale gatherings and in-person learning have resumed, experts say families are still grappling with mental health issues, such as anxiety, depression, and suicidal behavior.
Some suggest an uptick in mental health issues related to the pandemic.
“The pandemic has intensified mental health issues among children due to isolation, disruption of routines, and increased stress,” says Daniel Rinaldi, MA , a therapist, and founder of MNTL Town , a digital platform where parents can request videos featuring puppets tailored to their child's specific needs. “These factors have contributed to the rise in healthcare spending on pediatric mental health.”
Social media
Dr. Murthy specifically called out social media in a sobering warning last year . One expert who works closely with youth says platforms have created and exacerbated a myriad of issues.
“First, it’s created a culture of comparison, in which kids evaluate their worth according to how closely they live up to unrealistic, curated lifestyles and beauty standards,” Maggie C. Vaughan, LMFT, PhD , a psycholgist and the Head of Youth Transformation at Tapouts says. “Second, with apps like Snapchat and Instagram, kids know where their friends are at all times and therefore know when they’ve been left out.”
In short? The always-connected nature means kids can’t catch a break from feeling left out or less-than.
Therapist shortage
The decreasing stigma around mental health has prompted a higher demand for services—that’s not a bad thing, as people need help. Unfortunately, while advice to get a child struggling with mental health issues is well-meaning and spot-on, the supply of therapists is not there. Nearly half (47%) of Americans are living in an area with a shortage of mental health professionals.
“We know there are not enough therapists to meet the level of pediatric mental health needs we are seeing,” says Myra Altman, PhD , Brightline’s Chief Clinical Officer and a study co-author. “This results in long wait times and a lack of access to high-quality care, which can exacerbate costs because kids and families aren’t getting the support they need when they need it. Instead, many families don’t receive care until they are in crisis, such as going to an emergency room, which leads to higher costs.”
Insurance has in-network providers. However, not everyone has insurance.
“Many American families, especially those in marginalized communities, live paycheck to paycheck and oftentimes don't carry health insurance that covers the cost of receiving mental health care services,” Dr. Lagoy says. “When you add increasing costs of child mental health care, this increases stress on the family and makes it more difficult to make a living, leading to increased risk of anxiety and depression.”
It’s a vicious and unfair cycle. Children in families facing socioeconomic inequalities were more likely to experience mental health challenges during the COVID-19 pandemic, according to some.
“This can be devastating for marginalized communities who already suffer from large mental health inequalities due to inaccessibility to high-quality mental healthcare, cultural stigma, language barriers, and discrimination,” says Loo, who hopes the new research calls attention to this concern and breaks down access barriers.
Further, even if you do have insurance that covers mental health services, many mental health providers don't take insurance.
Affording Mental Health Care for Your Child
Loo notes it is helpful if families can access and afford care for a child before they are in crisis. But how? Experts share advice for families on how to afford mental health care for children (and access it in the first place).
Start with the school
Schools may have resources like a social worker or psychologist families can tap into, especially if they are struggling to find a private practitioner without a wait list for new patients. Dr. Vaughan says seeing the person regularly is typically best. However:
“Even short, routine check-ins can make a huge difference,” she adds. “See if the school can provide referrals to external low-cost providers or volunteer child mentors.”
Check out SAMHSA
The Substance Abuse and Mental Health Services Administration (SAMHSA) , an agency within the Department of Health and Human Services (HHS), is a national service focused on behavioral health. It can help families tap into resources they may not have found through Google searches or pediatrician/school referrals, including local ones.
“SAMHSA explains the offerings of and links to helplines, substance abuse programs, mental health programs, and disaster support,” Dr. Vaughan says. “SAMHSA staff are available by phone if you can’t find what you need through their site.”
Insurance coverage
Rinaldi encourages families with access to insurance to take advantage of their plans when trying to access affordable mental healthcare.
“You can always call the insurance company and ask about the benefits, and many of the benefits should be available online, too,” Rinaldi says. “However, if you have any questions, call the insurance provider and ask specifically for a therapist who would be covered. Some insurance providers may even cover online therapy, so it's worth an ask.”
Rinaldi also suggests comparing plans during open enrollment to see which ones offer the most mental healthcare services.
Look for reduced fees and sliding scales
Mental health providers may offer lower fees for people who need them.
“Conduct a search for low-fee and reduced-fee mental health centers,” Dr.Vaughan says. “Many agencies offer sliding-scale services, with fees determined according to your particular financial situation.”
Dr. Vaughan says people can also call individual therapists and ask if they offer sliding-scale fees.
Group therapy or workshops
One-on-one talk therapy can be beneficial. However, if no one in your area is accepting new patients, Rinaldi says group therapy and workshops can also provide support.
“Typically, group sessions or workshops can be more affordable than individual therapy and offer social support from peers facing similar challenges,” Rinaldi says. “Check out local group sessions, and ask parents and community members if they know of any groups, workshops, or sessions.”
For more Parents news, make sure to sign up for our newsletter!
Read the original article on Parents .

New England Journal of Medicine Series: Wearable Digital Health Technologies
Courtesy of the researchers
by Rosalind W. Picard
March 18, 2024
- #wearable computing
- #technology
- #cognitive science
- #mental health
- #public health
- Rosalind W. Picard Professor of Media Arts and Sciences
- Media Lab Research Theme: Life with AI
- Media Lab Research Theme: Connected Mind + Body
Share this post
Researchers in the Affective Computing group at the MIT Media Lab have been invited to edit a series of articles on the topic of Wearable Digital Health Technologies in the New England Journal Medicine ; the series includes articles related to epilepsy, depression, diabetes, and cardiovascular disease, among other areas.
Peruse the articles in this series below!

Wearable Digital Health Technology for Epilepsy
Elizabeth Donner, Orrin Devinsky, and Daniel Friedman; guest editors Stephen H. Friend, Geoffrey S. Ginsburg, Rosalind W. Picard, Jeffrey M. Drazen. "Wearable Digital Health Technology for Epilepsy." New England Journal of Medicine 2024; 390:736-745. DOI: 10.1056/NEJMra2301913
Wearable Digital Health Technologies for Monitoring in Cardiovascular Medicine
Erica S. Spatz, Geoffrey S. Ginsburg, John S. Rumsfeld, and Mintu P. Turakhia; guest editors Stephen H. Friend, Geoffrey S. Ginsburg, Rosalind W. Picard, Jeffrey M. Drazen. "Wearable Digital Health Technologies for Monitoring in Cardiovascular Medicine." New England Journal of Medicine 2024; 390:346-356. DOI: 10.1056/NEJMra2301903
Wearable technology in clinical practice for depressive disorder
Fedor, S., Lewis, R., Pedrelli, P., Mischoulon, D., Curtiss, J., & Picard, R. W. (2023). Wearable technology in clinical practice for depressive disorder. New England Journal of Medicine, 389(26), 2457-2466.
Digital Technology for Diabetes
Michael S. Hughes, Ananta Addala, and Bruce Buckingham; guest editors Stephen H. Friend, Geoffrey S. Ginsburg, Rosalind W. Picard, Jeffrey M. Drazen. "Digital Technology for Diabetes." New England Journal of Medicine 2023; 389:2076-2086. DOI: 10.1056/NEJMra2215899
Wearable Digital Health Technology
Friend, Stephen H., Geoffrey S. Ginsburg, and Rosalind W. Picard. "Wearable Digital Health Technology." New England Journal of Medicine 389.22 (2023): 2100-2101.
AI and Accountability: Who is responsible for managing AI?
On the Technically Optimistic podcast, Prof. Rosalind Picard and others discuss the challenges of accountability and responsibility in AI.
Scientist and Engineer Rosalind Picard Is Transforming Digital Health with Wearable AI
Rosalind Picard’s unique technology is revolutionizing digital health.
Research Group Overview: Affective Computing
Advancing human wellbeing by developing new ways to communicate, understand, and respond to emotion
Alcohol Use Disorder
- Binge Drinking
- Drinking Problem
Illegal Drug Addiction
Prescriptions.
- Benzodiazepines
- Antidepressants
- Inpatient Rehab
- Residential Rehab

Alcohol Rehab
- Methadone Clinics
- Sober Living
- Family Therapy
Recovery Programs
- 12-Step Programs
- SMART Recovery
- Families of Addicts
Early Recovery
- Stages of Change
- Handle Triggers
- Rehab Insights
Sustained Recovery
- Sober Curious Life
Long-Term Recovery
- Jellinek Curve
- Life After Rehab
Find Treatment
- Find Addiction Center
- Find Suboxone Center
2024 Addiction Statistics: Accurate Data on Substance Abuse in the US

In This Article
The United States faces a complex and evolving crisis when it comes to substance use disorders (SUDs). These disorders affect people across demographics. It destroys lives and strains families, communities, and healthcare systems.
Understanding the shocking scale of this problem, along with its risk factors, is crucial for creating prevention and treatment programs that save lives.
- Nearly 50 million Americans experienced a substance use disorder in the past year.
- Despite the widespread need, only a tiny fraction (9.1%) of those with co-occurring mental health issues and SUDs receive treatment for both conditions.
- Over 70% of individuals with alcohol abuse or dependence never receive treatment.
- Suicidal thoughts are alarmingly common, affecting over 13 million US adults and 3.4 million adolescents in the past year.
- Addiction doesn't discriminate: heroin use has increased across all income levels in recent years.
This article draws on the most recent and reliable data sources available. By focusing on up-to-the-minute information, we gain the clearest possible picture of the challenges and the best ways to address them.
Prevalence of Substance Use Disorders by Drug Type
Substance use disorders (SUDs) affect a significant portion of the US population. In 2022, the numbers reveal the varying prevalence of different substance-related disorders:
Overall Substance Use Disorders
- An estimated 48.7 million Americans aged 12 or older had a substance use disorder (SUD) in the past year.
Alcohol Use Disorder (AUD)
- Alcohol use disorders were the most common, affecting 29.5 million people.
Drug Use Disorder (DUD)
- 27.2 million people had a drug use disorder.
- Of those with DUD, 8.0 million also had an alcohol use disorder, highlighting the overlap between the two.
Illicit Drug Use
- Around 70.3 million people aged 12 or older used illicit drugs in the past year.
- Marijuana was the most common illicit drug, used by 61.9 million people (22.0% of those aged 12+).
Mental Health & Substance Use
- Mental health issues are closely linked to SUDs. Nearly 1 in 4 adults (59.3 million) experienced any mental illness (AMI) in the past year.
- Among adolescents (12-17), 19.5% (4.8 million) experienced a major depressive episode (MDE) in the past year.
Suicidal Thoughts & Behaviors
Suicidal thoughts are concerningly common, especially linked to mental health struggles:
- 1 in 20 US adults (13.2 million) had serious suicidal thoughts in the past year.
- Over 1 in 8 adolescents (13.4% or 3.4 million) had serious suicidal thoughts in the past year.
These statistics show the widespread impact of substance use disorders. It's crucial to address both substance use and mental health needs, as they often go hand-in-hand.
Age and Gender Differences in Addiction Rates
Substance use and addiction rates vary significantly based on both age and gender. Here's a breakdown of the key trends:
Gender Differences
Males vs. females.
Generally, men are more likely to use illicit drugs and have higher rates of alcohol use/dependence. However:
- Women are equally likely to develop substance use disorders (SUDs).
- Women may be more prone to cravings and relapse, impacting their recovery process.
Specific Substances
- Marijuana: Use is lower among females, but they may experience different effects.
- Alcohol: Men have historically had higher AUD rates, but this gap is narrowing.
- Prescription Drugs: Women are more likely to overdose or seek emergency care due to prescription drug misuse.
- Stimulants: Abuse rates are similar, but women may start using earlier and experience stronger cravings.
Age Differences
- Adolescents: Alcohol use rates are surprisingly similar for boys and girls aged 12-17.
- Young Adults: Females aged 12-20 may have slightly higher rates of alcohol misuse than males.
- Older Adults: Women 65+ have significantly higher rates of prescription painkiller addiction than their male peers.
Treatment & Recovery Considerations
- Gender-Specific Care: Treatment programs tailored to the unique needs of men or women can be more effective.
- Telescoping Effect: Women often progress from substance use to dependence more quickly than men, impacting treatment approaches.
Online Therapy Can Help
Over 3 million people use BetterHelp. Their services are:
- Professional and effective
- Affordable and convenient
- Personalized and discreet
- Easy to start
Answer a few questions to get started

Socioeconomic Factors and Addiction Risk
Socioeconomic status plays a significant role in addiction risk. Here's how factors like income, education, and social circumstances contribute:
Income & Addiction
- Smoking is much more common among low-income individuals than those with high incomes.
- Contrary to stereotypes, higher income levels are linked to increased alcohol and drug use among teens and young adults.
Education & Parental Influence
- Low parental education levels correlate with an increased risk of heroin use in children.
- Students who skip school (truancy) are far more likely to experiment with or become addicted to heroin.
Socioeconomic Disparities
- People in the lowest income brackets are more likely to report problems associated with substance abuse.
- Lower socioeconomic status dramatically increases the risk of alcohol-related death and opioid addiction.
Unexpected Trends
- Heroin use has increased across all income groups in the US.
- Upper-middle-class youth face a surprisingly high risk of drug and alcohol addiction.
Poverty, Marginalization, & Substance Use
- Poverty and social disadvantage create a cycle where substance use becomes both a cause and a consequence of hardship.
Addiction doesn't discriminate based on socioeconomic status. Effective prevention and treatment must address the unique challenges faced by people from all backgrounds.
Get Professional Help
BetterHelp can connect you to an addiction and mental health counselor.

Co-occurring Mental Health Disorders and Addiction
People can struggle with both substance use disorders (SUDs) and mental health conditions, known as co-occurring disorders or dual diagnoses. Here's a look at how prevalent this is:
Prevalence of Co-occurring Disorders
- 7.7 million US adults experience co-occurring mental health and substance use disorders.
- Of adults with SUDs, 37.9% also have a mental illness. Among adults with a mental illness, 18.2% have a co-occurring SUD.
- Over 60% of teens in substance use treatment programs also meet the criteria for a mental health disorder.
Treatment & Barriers
- Only 9.1% of people with co-occurring disorders receive treatment for both conditions.
- Common reasons for not seeking help include cost (cited by 52.2% of those needing mental health care) and not being ready to stop using substances (38.4%).
Specific Conditions
- SUDs frequently co-occur with anxiety disorders like generalized anxiety, panic disorder, and PTSD.
- Depression, bipolar disorder, and other mood disorders are also highly prevalent alongside substance use disorders.
Additional Statistics
- Co-occurring serious mental illness (SMI) and SUDs in young adults (18-25) rose from 1.7% in 2015 to 2.8% in 2019.
- Of those with heroin use disorder, over 66% are nicotine-dependent, and significant percentages struggle with alcohol or cocaine addiction.
- People with co-occurring disorders are much more likely to be arrested, highlighting the complex challenges they face.
Global Perspective
- Studies across cultures show high rates (50-80%) of psychiatric conditions among people with drug use disorders.
The significant overlap between mental health and addiction underscores the need for treatment that addresses both conditions simultaneously.
Treatment Rates and Barriers to Accessing Care
Despite the importance of treatment, many individuals with mental health and substance use disorders never receive the help they need. Here's a look at the numbers:
Treatment Rates
- Co-occurring Disorders: Only 9.1% of the 7.7 million adults with co-occurring disorders receive treatment for both conditions.
- Substance Use Disorders (SUDs): Treatment gaps are wide, with the vast majority (78.1%) of individuals with alcohol abuse/dependence going untreated.
- Mental Health Disorders: Over half of people with conditions like depression, anxiety disorders, and bipolar disorder do not receive treatment.
Barriers to Accessing Care
There are various barriers to accessing proper care for SUD treatment. Closing the treatment gap requires addressing these obstacles:
- Cost & Insurance: High costs and inadequate insurance coverage prevent many from seeking care (37% for mental health, 31% for SUD treatment).
- Provider Shortages: Lack of mental health professionals, especially in rural areas, limits access.
- Stigma: Fear of judgment or confidentiality concerns deter individuals from seeking help.
- Lack of Awareness: People may not know what resources exist or how to recognize signs of needing help.
- Systemic Issues: Long waitlists, fragmented care systems, and socioeconomic factors like poverty create additional barriers.
Phone, Video, or Live-Chat Support
BetterHelp provides therapy in a way that works for YOU. Fill out the questionnaire, get matched, begin therapy.

Substance use disorders (SUDs) are a widespread problem in the US. It affects nearly 50 million people. This crisis cuts across all demographics and has devastating consequences for individuals, families, and communities.
Alarmingly, despite the need, treatment rates remain low. Only a tiny fraction receive help, especially for co-occurring mental health issues.
We must strive for improved access to treatment programs that address both substance use and mental health needs. Considering the unique challenges different populations face will lead to more effective solutions.
What's Next?
- What Is Rehab Like?
- Why Call an Addiction Hotline?
- How to Sober Up
- Tapering off of alcohol
Get matched with an affordable mental health counselor

Related Articles

Fentanyl Statistics 2024: Up-to-Date Facts on Abuse and Overdose
Medically Reviewed by: Annamarie Coy
- Baptiste-Roberts K., & Hossain, M. “Socioeconomic Disparities and Self-reported Substance Abuse-related Problems.” PubMed, 2018.
- “Common Comorbidities with Substance Use Disorders Research Report.” Nih.gov; National Institutes on Drug Abuse (US), 2020.
- “Comorbidities in drug use disorders.” UNODC.
- “Exploring Barriers to Mental Health Care in the U.S.” Research and Action Institute, 2022.
- Fonseca et al. “A Gender Perspective of Addictive Disorders.” Current Addiction Reports, 2021.
- “Gender Differences in Substance Use, Treatment and Recovery.” Partnership to End Addiction, 2023.
- Gerra et al. “Socioeconomic Status, Parental Education, School Connectedness and Individual Socio-Cultural Resources in Vulnerability for Drug Use among Students.” International Journal of Environmental Research and Public Health, 2020.
- “HHS, SAMHSA Release 2022 National Survey on Drug Use and Health Data.” Samhsa.gov, 2023.
- “Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health.” Samhsa.gov, 2019.
- Kohn et al. “The treatment gap in mental health care.” Bulletin of the World Health Organization, 2019.
- “More than 4 in 10 U.S. Adults Who Needed Substance Use and Mental Health Care Did Not Get Treatment.” National Council for Mental Wellbeing, 2022.
- “Comorbidity: Substance Use and Other Mental Disorders.” National Institute on Drug Abuse, 2018.
- “Sex and Gender Differences in Substance Use | National Institute on Drug Abuse.” National Institute on Drug Abuse, 2022.
- “Part 1: The Connection Between Substance Use Disorders and Mental Illness.” National Institute on Drug Abuse, 2022.
- Patrick et al. “Socioeconomic Status and Substance Use Among Young Adults: A Comparison Across Constructs and Drugs.” Journal of Studies on Alcohol and Drugs, 2012..
- “Poverty and Marginalization Remains Key Factors for Substance Use.” United Nations: Office on Drugs and Crime, 2021.
- McHugh et al. “Sex and gender differences in substance use disorders.” Clinical Psychology Review, 2018.
- “Socioeconomic Status and Drug Use.” Turnbridge, 2017./
- “More Than 1 in 9 Adults With Co-Occurring Mental Illness and Substance Use Disorders Are Arrested Annually. ” The Pew Charitable Trusts, 2023.
- “The Socioeconomic Impact on Addiction.” Townsendla.com, 2023.

Related Pages
- Fentanyl Statistics 2024: Up-to-Date Facts on Abuse and Overdose The United States is in the middle of a devastating...
Evidence Based
Who answers.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- BMJ NPH Collections
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Apple cider vinegar for weight management in Lebanese adolescents and young adults with overweight and obesity: a randomised, double-blind, placebo-controlled study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-0214-242X Rony Abou-Khalil 1 ,
- Jeanne Andary 2 and
- Elissar El-Hayek 1
- 1 Department of Biology , Holy Spirit University of Kaslik , Jounieh , Lebanon
- 2 Nutrition and Food Science Department , American University of Science and Technology , Beirut , Lebanon
- Correspondence to Dr Rony Abou-Khalil, Department of Biology, Holy Spirit University of Kaslik, Jounieh, Lebanon; ronyaboukhalil{at}usek.edu.lb
Background and aims Obesity and overweight have become significant health concerns worldwide, leading to an increased interest in finding natural remedies for weight reduction. One such remedy that has gained popularity is apple cider vinegar (ACV).
Objective To investigate the effects of ACV consumption on weight, blood glucose, triglyceride and cholesterol levels in a sample of the Lebanese population.
Materials and methods 120 overweight and obese individuals were recruited. Participants were randomly assigned to either an intervention group receiving 5, 10 or 15 mL of ACV or a control group receiving a placebo (group 4) over a 12-week period. Measurements of anthropometric parameters, fasting blood glucose, triglyceride and cholesterol levels were taken at weeks 0, 4, 8 and 12.
Results Our findings showed that daily consumption of the three doses of ACV for a duration of between 4 and 12 weeks is associated with significant reductions in anthropometric variables (weight, body mass index, waist/hip circumferences and body fat ratio), blood glucose, triglyceride and cholesterol levels. No significant risk factors were observed during the 12 weeks of ACV intake.
Conclusion Consumption of ACV in people with overweight and obesity led to an improvement in the anthropometric and metabolic parameters. ACV could be a promising antiobesity supplement that does not produce any side effects.
- Weight management
- Lipid lowering
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjnph-2023-000823
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Recently, there has been increasing interest in alternative remedies to support weight management, and one such remedy that has gained popularity is apple cider vinegar (ACV).
A few small-scale studies conducted on humans have shown promising results, with ACV consumption leading to weight loss, reduced body fat and decreased waist circumference.
WHAT THIS STUDY ADDS
No study has been conducted to investigate the potential antiobesity effect of ACV in the Lebanese population. By conducting research in this demographic, the study provides region-specific data and offers a more comprehensive understanding of the impact of ACV on weight loss and metabolic health.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The results might contribute to evidence-based recommendations for the use of ACV as a dietary intervention in the management of obesity.
The study could stimulate further research in the field, prompting scientists to explore the underlying mechanisms and conduct similar studies in other populations.
Introduction
Obesity is a growing global health concern characterised by excessive body fat accumulation, often resulting from a combination of genetic, environmental and lifestyle factors. 1 It is associated with an increased risk of numerous chronic illnesses such as type 2 diabetes, cardiovascular diseases, several common cancers and osteoarthritis. 1–3
According to the WHO, more than 1.9 billion adults were overweight worldwide in 2016, of whom more than 650 million were obese. 4 Worldwide obesity has nearly tripled since 1975. 4 The World Obesity Federation’s 2023 Atlas predicts that by 2035 more than half of the world’s population will be overweight or obese. 5
According to the 2022 Global Nutrition Report, Lebanon has made limited progress towards meeting its diet-related non-communicable diseases target. A total of 39.9% of adult (aged ≥18 years) women and 30.5% of adult men are living with obesity. Lebanon’s obesity prevalence is higher than the regional average of 10.3% for women and 7.5% for men. 6 In Lebanon, obesity was considered as the most important health problem by 27.6% and ranked fifth after cancer, cardiovascular, smoking and HIV/AIDS. 7
In recent years, there has been increasing interest in alternative remedies to support weight management, and one such remedy that has gained popularity is apple cider vinegar (ACV), which is a type of vinegar made by fermenting apple juice. ACV contains vitamins, minerals, amino acids and polyphenols such as flavonoids, which are believed to contribute to its potential health benefits. 8 9
It has been used for centuries as a traditional remedy for various ailments and has recently gained attention for its potential role in weight management.
In hypercaloric-fed rats, the daily consumption of ACV showed a lower rise in blood sugar and lipid profile. 10 In addition, ACV seems to decrease oxidative stress and reduces the risk of obesity in male rats with high-fat consumption. 11
A few small-scale studies conducted on humans have shown promising results, with ACV consumption leading to weight loss, reduced body fat and decreased waist circumference. 12 13 In fact, It has been suggested that ACV by slowing down gastric emptying, might promote satiety and reduce appetite. 14–16 Furthermore, ACV intake seems to ameliorate the glycaemic and lipid profile in healthy adults 17 and might have a positive impact on insulin sensitivity, potentially reducing the risk of type 2 diabetes. 8 10 18
Unfortunately, the sample sizes and durations of these studies were limited, necessitating larger and longer-term studies for more robust conclusions.
This work aims to study the efficacy and safety of ACV in reducing weight and ameliorating the lipid and glycaemic profiles in a sample of overweight and obese adolescents and young adults of the Lebanese population. To the best of our knowledge, no study has been conducted to investigate the potential antiobesity effect of ACV in the Lebanese population.
Materials and methods
Participants.
A total of 120 overweight and obese adolescents and young adults (46 men and 74 women) were enrolled in the study and assigned to either placebo group or experimental groups (receiving increasing doses of ACV).
The subjects were evaluated for eligibility according to the following inclusion criteria: age between 12 and 25 years, BMIs between 27 and 34 kg/m 2 , no chronic diseases, no intake of medications, no intake of ACV over the past 8 weeks prior to the beginning of the study. The subjects who met the inclusion criteria were selected by convenient sampling technique. Those who experienced heartburn due to vinegar were excluded.
Demographic, clinical data and eating habits were collected from all participants by self-administered questionnaire.
Study design
This study was a double-blind, randomised clinical trial conducted for 12 weeks.
Subjects were divided randomly into four groups: three treatment groups and a placebo group. A simple randomisation method was employed using the randomisation allocation software. Groups 1, 2 and 3 consumed 5, 10 and 15 mL, respectively, of ACV (containing 5% of acetic acid) diluted in 250 mL of water daily, in the morning on an empty stomach, for 12 weeks. The control group received a placebo consisting of water with similar taste and appearance. In order to mimic the taste of vinegar, the placebo group’s beverage (250 mL of water) contained lactic acid (250 mg/100 mL). Identical-looking ACV and placebo bottles were used and participants were instructed to consume their assigned solution without knowing its identity. The subject’s group assignment was withheld from the researchers performing the experiment.
Subjects consumed their normal diets throughout the study. The contents of daily meals and snacks were recorded in a diet diary. The physical activity of the subjects was also recorded. Daily individual phone messages were sent to all participants to remind them to take the ACV or the placebo. A mailing group was also created. Confidentiality was maintained throughout the procedure.
At weeks 0, 4, 8 and 12, anthropometric measurements were taken for all participants, and the level of glucose, triglycerides and total cholesterol was assessed by collecting 5 mL of fasting blood from each subject.
Anthropometric measurements
Body weight was measured in kg, to the nearest 0.01 kg, by standardised and calibrated digital scale. Height was measured in cm, to the nearest 0.1 cm, by a stadiometer. Anthropometric measurements were taken for all participants, by a team of trained field researchers, after 10–12 hours fast and while wearing only undergarments.
Body mass indices (BMIs) were calculated using the following equation:
The waist circumference measurement was taken between the lowest rib margin and the iliac crest while the subject was in a standing position (to the nearest 0.1 cm). Hip circumference was measured at the widest point of the hip (to the nearest 0.1 cm).
The body fat ratio (BFR) was measured by the bioelectrical impedance analysis method (OMRON Fat Loss Monitor, Model No HBF-306C; Japan). Anthropometric variables are shown in table 1 .
- View inline
Baseline demographic, anthropometric and biochemical variables of the three apple cider vinegar groups (group 1, 2 and 3) and the placebo group (group 4)
Blood biochemical analysis
Serum glucose was measured by the glucose oxidase method. 19 Triglyceride levels were determined using a serum triglyceride determination kit (TR0100, Sigma-Aldrich). Cholesterol levels were determined using a cholesterol quantitation kit (MAK043, Sigma-Aldrich). Biochemical variables are shown in table 1 .
Statistical methods and data analysis
Data are presented as mean±SD. Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software (version 23.0). Significant differences between groups were determined by using an independent t-test. Statistical significance was set at p<0.05.
Ethical approval
The study protocol was reviewed and approved by the research ethics committee (REC) of the Higher Centre for Research (HCR) at The Holy Spirit University of Kaslik (USEK), Lebanon. The number/ID of the approval is HCR/EC 2023–005. The participants were informed of the study objectives and signed a written informed consent before enrolment. The study was conducted in accordance to the International Conference and Harmonisation E6 Guideline for Good Clinical Practice and the Ethical principles of the Declaration of Helsinki.
Sociodemographic, nutritional and other baseline characteristics of the participants
A total of 120 individuals (46 men and 74 women) with BMIs between 27 and 34 kg/m 2 , were enrolled in the study. The mean age of the subjects was 17.8±5.7 years and 17.6±5.4 years in the placebo and experimental groups respectively.
The majority of participants, approximately 98.3%, were non-vegetarian and 89% of them reported having a high eating frequency, with more than four meals per day. Eighty-seven per cent had no family history of obesity and 98% had no history of childhood obesity. The majority reported not having a regular exercise routine and experiencing negative emotions or anxiety. All participants were non-smokers and non-drinkers. A small percentage (6.7%) were following a therapeutic diet.
Effects of ACV intake on anthropometric variables
The addition of 5 mL, 10 mL or 15 mL of ACV to the diet resulted in significant decreases in body weight and BMI at weeks 4, 8 and 12 of ACV intake, when compared with baseline (week 0) (p<0.05). The decrease in body weight and BMI seemed to be dose-dependent, with the group receiving 15 mL of ACV showing the most important reduction ( table 2 ).
Anthropometric variables of the participants at weeks 0, 4, 8 and 12
The impact of ACV on body weight and BMI seems to be time-dependent as well. Reductions were more pronounced as the study progressed, with the most significant changes occurring at week 12.
The circumferences of the waist and hip, along with the Body Fat Ratio (BFR), decreased significantly in the three treatment groups at weeks 8 and 12 compared with week 0 (p<0.05). No significant effect was observed at week 4, compared with baseline (p>0.05). The effect of ACV on these parameters seems to be time-dependent with the most prominent effect observed at week 12 compared with week 4 and 8. However it does not seem to be dose dependent, as the three doses of ACV showed a similar level of efficacy in reducing the circumferences of the waist/hip circumferences and the BFR at week 8 and 12, compared with baseline ( table 2 ).
The placebo group did not experience any significant changes in the anthropometric variables throughout the study (p>0.05). This highlights that the observed improvements in body weight, BMI, waist and hip circumferences and Body Fat Ratio were likely attributed to the consumption of ACV.
Effects of ACV on blood biochemical parameters
The consumption of ACV also led to a time and dose dependent decrease in serum glucose, serum triglyceride and serum cholesterol levels. ( table 3 ).
Biochemical variables of the participants at weeks 0, 4, 8 and 12
Serum glucose levels decreased significantly by three doses of ACV at week 4, 8 and 12 compared with week 0 (p<0.05) ( table 3 ). Triglycerides and total cholesterol levels decreased significantly at weeks 8 and 12, compared with week 0 (p<0.05). A dose of 15 mL of ACV for a duration of 12 weeks seems to be the most effective dose in reducing these three blood biochemical parameters.
There were no changes in glucose, triglyceride and cholesterol levels in the placebo groups at weeks 4, 8 and 12 compared with week 0 ( table 3 ).
These data suggest that continued intake of 15 mL of ACV for more than 8 weeks is effective in reducing blood fasting sugar, triglyceride and total cholesterol levels in overweight/obese people.
Adverse reactions of ACV
No apparent adverse or harmful effects were reported by the participants during the 12 weeks of ACV intake.
During the past two decades of the last century, childhood and adolescent obesity have dramatically increased healthcare costs. 20 21 Diet and exercise are the basic elements of weight loss. Many complementary therapies have been promoted to treat obesity, but few are truly beneficial.
The present study is the first to investigate the antiobesity effectiveness of ACV, the fermented juice from crushed apples, in the Lebanese population.
A total of 120 overweight and obese adolescents and young adults (46 men and 74 women) with BMIs between 27 and 34 kg/m 2 , were enrolled. Participants were randomised to receive either a daily dose of ACV (5, 10 or 15 mL) or a placebo for a duration of 12 weeks.
Some previous studies have suggested that taking ACV before or with meals might help to reduce postprandial blood sugar levels, 22 23 but in our study, participants took ACV in the morning on an empty stomach. The choice of ACV intake timing was motivated by the aim to study the impact of apple cider vinegar without the confounding variables introduced by simultaneous food intake. In addition, taking ACV before meals could better reduce appetite and increase satiety.
Our findings reveal that the consumption of ACV in people with overweight and obesity led to an improvement in the anthropometric and metabolic parameters.
It is important to note that the diet diary and physical activity did not differ among the three treatment groups and the placebo throughout the whole study, suggesting that the decrease in anthropometric and biochemical parameters was caused by ACV intake.
Studies conducted on animal models often attribute these effects to various mechanisms, including increased energy expenditure, improved insulin sensitivity, appetite and satiety regulation.
While vinegar is composed of various ingredients, its primary component is acetic acid (AcOH). It has been shown that after 15 min of oral ingestion of 100 mL vinegar containing 0.75 g acetic acid, the serum acetate levels increases from 120 µmol/L at baseline to 350 µmol/L 24 ; this fast increase in circulatory acetate is due to its fast absorption in the upper digestive tract. 24 25
Biological action of acetate may be mediated by binding to the G-protein coupled receptors (GPRs), including GPR43 and GPR41. 25 These receptors are expressed in various insulin-sensitive tissues, such as adipose tissue, 26 skeletal muscle, liver, 27 and pancreatic beta cells, 28 but also in the small intestine and colon. 29 30
Yamashita and colleagues have revealed that oral administration of AcOH to type 2 diabetic Otsuka Long-Evans Tokushima Fatty rats, improves glucose tolerance and reduces lipid accumulation in the adipose tissue and liver. This improvement in obesity-linked type 2 diabetes is due to the capacity of AcOH to inhibit the activity of carbohydrate-responsive, element-binding protein, a transcription factor involved in regulating the expression of lipogenic genes such as fatty acid synthase and acetyl-CoA carboxylase. 26 31 Sakakibara and colleagues, have reported that AcOH, besides inhibiting lipogenesis, reduces the expression of genes involved in gluconeogenesis, such as glucose-6-phosphatase. 32 The effect of AcOH on lipogenesis and gluconeogenesis is in part mediated by the activation of 5'-AMP-activated protein kinase in the liver. 32 This enzyme seems to be an important pharmacological target for the treatment of metabolic disorders such as obesity, type 2 diabetes and hyperlipidaemia. 32 33
5'-AMP-activated protein kinase is also known to stimulate fatty acid oxidation, thereby increasing energy expenditure. 32 33 These data suggest that the effect of ACV on weight and fat loss may be partly due to the ability of AcOH to inhibit lipogenesis and gluconeogenesis and activate fat oxidation.
Animal studies suggest that besides reducing energy expenditure, acetate may also reduce energy intake, by regulating appetite and satiety. In mice, an intraperitoneal injection of acetate significantly reduced food intake by activating vagal afferent neurons. 32–34 It is important to note that animal studies done on the effect of acetate on vagal activation are contradictory. This might be due to the site of administration of acetate and the use of different animal models.
In addition, in vitro and in vivo animal model studies suggest that acetate increases the secretion of gut-derived satiety hormones by enter endocrine cells (located in the gut) such as GLP-1 and PYY hormones. 25 32–35
Human studies related to the effect of vinegar on body weight are limited.
In accordance with our study, a randomised clinical trial conducted by Khezri and his colleagues has shown that daily consumption of 30 mL of ACV for 12 weeks significantly reduced body weight, BMI, hip circumference, Visceral Adiposity Index and appetite score in obese subjects subjected to a restricted calorie diet, compared with the control group (restricted calorie diet without ACV). Furthermore, Khezri and his colleagues showed that plasma triglyceride and total cholesterol levels significantly decreased, and high density lipoprotein cholesterol concentration significantly increased, in the ACV group in comparison with the control group. 13 32–34
Similarly, Kondo and his colleagues showed that daily consumption of 15 or 30 mL of ACV for 12 weeks reduced body weight, BMI and serum triglyceride in a sample of the Japanese population. 12 13 32–34
In contrast, Park et al reported that daily consumption of 200 mL of pomegranate vinegar for 8 weeks significantly reduced total fat mass in overweight or obese subjects compared with the control group without significantly affecting body weight and BMI. 36 This contradictory result could be explained by the difference in the percentage of acetate and other potentially bioactive compounds (such as flavonoids and other phenolic compounds) in different vinegar types.
In Lebanon, the percentage of the population with a BMI of 30 kg/m 2 or more is approximately 32%. The results of the present study showed that in obese Lebanese subjects who had BMIs ranging from 27 and 34 kg/m 2 , daily oral intake of ACV for 12 weeks reduced the body weight by 6–8 kg and BMIs by 2.7–3.0 points.
It would be interesting to investigate in future studies the effect of neutralised acetic acid on anthropometric and metabolic parameters, knowing that acidic substances, including acetic acid, could contribute to enamel erosion over time. In addition to promoting oral health, neutralising the acidity of ACV could improve its taste, making it more palatable. Furthermore, studying the effects of ACV on weight loss in young Lebanese individuals provides valuable insights, but further research is needed for a comprehensive understanding of how the effect of ACV might vary across different age groups, particularly in older populations and menopausal women.
The findings of this study indicate that ACV consumption for 12 weeks led to significant reduction in anthropometric variables and improvements in blood glucose, triglyceride and cholesterol levels in overweight/obese adolescents/adults. These results suggest that ACV might have potential benefits in improving metabolic parameters related to obesity and metabolic disorders in obese individuals. The results may contribute to evidence-based recommendations for the use of ACV as a dietary intervention in the management of obesity. The study duration of 12 weeks limits the ability to observe long-term effects. Additionally, a larger sample size would enhance the generalisability of the results.
Ethics statements
Patient consent for publication.
Consent obtained from parent(s)/guardian(s)
Ethics approval
This study involves human participants and was approved by the research ethics committee of the Higher Center for Research (HCR) at The Holy Spirit University of Kaslik (USEK), Lebanon. The number/ID of the approval is HCR/EC 2023-005. Participants gave informed consent to participate in the study before taking part.
- Pandi-Perumal SR , et al
- Poirier P ,
- Bray GA , et al
- World Health Organization
- Global Nutrition Report
- Geagea AG ,
- Jurjus RA , et al
- Liao H-J , et al
- Serafin V ,
- Ousaaid D ,
- Laaroussi H ,
- Bakour M , et al
- Halima BH ,
- Sarra K , et al
- Fushimi T , et al
- Khezri SS ,
- Saidpour A ,
- Hosseinzadeh N , et al
- Montaser R , et al
- Hlebowicz J ,
- Darwiche G ,
- Björgell O , et al
- Santos HO ,
- de Moraes WMAM ,
- da Silva GAR , et al
- Pourmasoumi M ,
- Najafgholizadeh A , et al
- Walker HK ,
- Sanyaolu A ,
- Qi X , et al
- Nosrati HR ,
- Mousavi SE ,
- Sajjadi P , et al
- Johnston CS ,
- Quagliano S ,
- Sugiyama S ,
- Fushimi T ,
- Kishi M , et al
- Hernández MAG ,
- Canfora EE ,
- Jocken JWE , et al
- Le Poul E ,
- Struyf S , et al
- Goldsworthy SM ,
- Barnes AA , et al
- Priyadarshini M ,
- Fuller M , et al
- Karaki S-I ,
- Hayashi H , et al
- Karaki S-I , et al
- Yamashita H ,
- Fujisawa K ,
- Ito E , et al
- Sakakibara S ,
- Yamauchi T ,
- Oshima Y , et al
- Schimmack G ,
- Defronzo RA ,
- Goswami C ,
- Iwasaki Y ,
- Kim J , et al
Supplementary materials
- Press release
Contributors RA-K: conceptualisation, methodology, data curation, supervision, guarantor, project administration, visualisation, writing–original draft. EE-H: conceptualisation, methodology, data curation, visualisation, writing–review and editing. JA: investigation, validation, writing–review and editing.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests No, there are no competing interests.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Urban Health
- v.94(3); 2017 Jun

Sexual Identity, Stigma, and Depression: the Role of the “Anti-gay Propaganda Law” in Mental Health among Men Who Have Sex with Men in Moscow, Russia
Emily hylton.
1 Center for Public Health and Human Rights, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St., Room E7141, Baltimore, MD 21205 USA
Andrea L. Wirtz
Carla e. zelaya, carl latkin.
2 Department of Health, Behavior and Society, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD USA
Alena Peryshkina
3 AIDS Infoshare, Moscow, Russian Federation
Vladmir Mogilnyi
Petr dzhigun, irina kostetskaya.
4 Department of Statistics, The University of Haifa, Mt Carmel, Israel
Chris Beyrer
Associated data.
Depression is a major public health problem in the Russian Federation and is particularly of concern for men who have sex with men (MSM). MSM living in Moscow City were recruited via respondent-driven sampling and participated in a cross-sectional survey from October 2010 to April 2013. Multiple logistic regression models compared the relationship between sexual identity, recent stigma, and probable depression, defined as a score of ≥23 on the Center for Epidemiological Studies Depression scale. We investigated the interactive effect of stigma and participation in the study after the passage of multiple “anti-gay propaganda laws” in Russian provinces, municipalities, and in neighboring Ukraine on depression among MSM. Among 1367 MSM, 36.7% ( n = 505) qualified as probably depressed. Fifty-five percent identified as homosexual ( n = 741) and 42.9% identified as bisexual ( n = 578). Bisexual identity had a protective association against probable depression (reference: homosexual identity AOR 0.71; 95%CI 0.52–0.97; p < 0.01). Those who experienced recent stigma (last 12 months) were more likely to report probable depression (reference: no stigma; AOR 1.75; 95%CI 1.20–2.56; p < 0.01). The interaction between stigma and the propaganda laws was significant. Among participants with stigma, probable depression increased 1.67-fold after the passage of the anti-gay laws AOR 1.67; 95%CI 1.04–2.68; p < 0.01). Depressive symptoms are common among MSM in Russia and exacerbated by stigma and laws that deny homosexual identities. Repeal of Russia’s federal anti-gay propaganda law is urgent but other social interventions may address depression and stigma in the current context.
Electronic supplementary material
The online version of this article (doi:10.1007/s11524-017-0133-6) contains supplementary material, which is available to authorized users.
Introduction
Depression and other mental health disorders represent a large proportion of the global burden of disease and are the second leading cause of global disability [ 1 , 2 ]. In the Russian Federation, this trend is consistent, if not magnified, among men. Here, the prevalence of depressive symptoms in men residing in urban areas has been reported as high as 23% in 1999–2000, as defined by a score of ≥16 on the Center for Epidemiological Studies Depression (CES-D) scale [ 3 ]. As of 2011, the suicide rate among Russian men was estimated at 35.1 per 100,000 persons—one of the highest in the world. [ 4 ] Global reports suggest that men who have sex with men (MSM) often have higher prevalence of depression than heterosexual men [ 5 ], and the little research that has been conducted in Russia on the topic suggests that such patterns may persist among MSM [ 6 ]. Analysis of HIV-infected MSM found that over one-third have reported symptomology indicative of probable depression and more than half of MSM in Moscow have reported hazardous or harmful levels of alcohol abuse that may be related to depression [ 7 ].
Across settings, research among MSM has shown that homophobia and social stigma may contribute to depression [ 8 ]. While less is known from the Russian Federation, research from similar epidemiologic settings in Central Asia has provided some insight, demonstrating that even where homosexuality has been decriminalized, stigmatization of homosexuality persists [ 9 ], and MSM who regularly practice the receptive role during anal intercourse experience increased levels of stigma [ 10 ]. Social stigma in Central Asia has been associated with reduced access to health and social services among MSM [ 9 , 11 ], including key HIV prevention and treatment services [ 9 ]. Depressive symptoms among MSM in Central Asia has been explained in part by high prevalence of community-level stigma [ 9 ]. Research from other countries with similar contexts in which homosexuality is decriminalized but where there is no legal protection for MSM against discrimination [ 12 ] have demonstrated the association between increased levels of perceived and experienced stigma and depression among MSM [ 13 , 14 ] and inconsistent use of condoms and depression among MSM [ 15 ]. Social support [ 16 ] and social cohesion [ 13 ] within the MSM community, however, appear to have a protective effect against depression among MSM in these countries.
Recent events within Russia provide context and rationale for understanding the factors associated with poor mental health outcomes among MSM. In June 2013, the Russian government issued the “anti-gay propaganda law,” a national ban on “propaganda for non-traditional sexual relations” that criminalized the sharing of information related to same sex practices. The law effectively legitimized public stigma and violence against lesbian, gay, bisexual, and transgender people (LGBT) in Russia [ 17 , 18 ]. This came on the heels of similar laws in the City of St. Petersburg (March 2012) that would fine individuals up to 500,000 rubles (approximately $17,000 USD) for spreading “homosexual propaganda,” as well as other related legislation in multiple oblasts (administrative divisions) across the Russian Federation, and a widely praised draft law in neighboring Ukraine (October 2012) that would impose up to 5 years imprisonment for spreading “propaganda of homosexuality [ 19 ].” While Russia’s national anti-gay propaganda law was not passed until 2013, the St. Petersburg, other provincial laws, and Ukraine bill (subsequently revoked in 2015 after the conclusion of this study) [ 20 ] received heavy media attention at the time, prompted considerable political and social discussion around the acceptance of homosexuality in Russia, and built substantial support for a possible federal law in Russia. Subsequently, a poll conducted by the Pew Research Center in 2013 found that nearly three in four Russians believed that society should not accept homosexuality [ 21 ]. Political analysts have since suggested that Russian President Vladimir Putin’s stance that homosexuality is a threat to Russian society [ 17 ] is part of a political narrative that deliberately links non-traditional sexualities to an imperialistic West [ 18 ]. Given related literature [ 22 ] and current events in Russia, this research sought to assess the level of depression among MSM in Moscow, Russia, explore the relationship between sexual identity and depressive symptoms among MSM in Russia, and explore the role of environmental changes in acceptance of homosexuality in the Russian Federation as it relates to depression.
The data for this analysis was gathered through a cross-sectional, NIH-funded study conducted in Moscow, Russia, between October 2010 and April 2013. The research was a collaborative effort conducted jointly by Johns Hopkins University and AIDS Infoshare, a local non-governmental organization that provides anonymous HIV testing and counseling and STI screening and treatment in an LGBT-friendly context in Moscow. All sampling, data collection, and biologic testing methods have been previously described [ 7 , 23 ].
Participants
Inclusion criteria required participants to be fluent in Russian, assigned male at birth, aged 18 years or older, currently reside in Moscow, report anal sex with a man in the past 12 months, and provide verbal informed consent. Participants were recruited via respondent-driven sampling (RDS), a chain recruitment method that is used to reach hidden or hard-to-reach populations [ 24 ]. Participants were provided 1000 rubles (approximately $40 USD) as reimbursement for their participation in the study and 500 rubles ($20 USD) for each peer recruited into the study. Thirty-one waves of recruitment produced a sample of 1367 participants for the analysis [ 23 ].
Informed by formative research [ 25 ], cognitive testing [ 26 ], and pilot testing methods, the structured survey was designed to gather information on sociodemographic characteristics, sexual practices and identity, substance use, experienced and perceived stigma, and mental health symptoms. Depression symptoms were the outcome of interest and sexual identity, stigma, and other known correlates [ 13 , 15 , 27 – 30 ] of depression were covariates of interest for this analysis. Measures of sexual identity and practices were adapted from the US CDC’s National Health Behavior Survey [ 31 ] and included questions about sexual identity (“heterosexual,” “homosexual,” “bisexual,” or “other”) and about the sex of the respondent’s sexual partners in the last 12 months (male or female).
The CES-D scale [ 32 ] was used as a screening tool for current (past 7 days) depressive symptomology (Cronbach’s α 0.889). The CES-D score was stratified into three categories: “unlikely to be depressed” (CES-D <16), “possibly depressed” (CES-D 16–22), and “probably depressed” (CES-D ≥23) [ 32 ]. Given that 36.7% endorsed a score of probably depressed ( n = 505) and 11% of the sample scored in the possibly depressed range ( n = 121), coupled with our interest in understanding the factors that were correlated with greater probability of depression [ 33 ], scores were transformed to a binary variable: “unlikely or possibly depressed” (CES-D <23) and probably depressed (CES-D ≥23).
A five-item scale was used to identify recent (last 12 months) experienced stigma (Cronbach’s α 0.713). This was a subscale of a larger stigma scale that had been developed from qualitative research [ 25 ], underwent cognitive testing [ 26 ] among MSM participants for further refinement, and were reviewed by MSM participants to assess face validity. The experienced stigma subscale included experience of public mocking, poor treatment by family members, experience of physical assault, being forced to move accommodation, and experiencing poor treatment within healthcare facilities due to sexual preferences. A positive indication for any one of these five variables was defined as a recent experience of stigma. The alcohol use disorders identification test (AUDIT), a validated scale in Russia, was included in the survey for identification of alcohol use in the last 12 months (Cronbach’s α = 0.80) [ 34 ]. AUDIT scores were stratified into three groups: a score <8 representing abstinence or low use, 8–15 “hazardous use,” and ≥16 “harmful use,” including those with potential alcohol dependency (score of 20 or higher), according to WHO categories [ 35 ].
Statistical Analysis
Survey data were analyzed using the STATA version 14 statistical software (Stata Corporation, College Station, USA). Depression, measured by the CES-D score, was the primary outcome of interest. Descriptive analysis was performed using Pearson’s chi-squared test. Sensitivity analyses were performed first using binary logistic analysis with unlikely to be depressed and a combined “possibly or probably depressed” and then using ordered logistic analysis with all three categories. A final sensitivity analysis was performed to test whether the model results changed with the inclusion of bisexual behavior (reporting both male and female sex partners) in place of bisexual identity.
Data collected via RDS recruitment are often weighted during statistical analysis to provide population prevalence estimates. Population estimates for the population characteristics and depression were calculated using the RDS-II estimator (Volz-Heckathorn) and bootstrapping with 1000 iterations to produce 95% confidence intervals (95%CI) [ 36 ]. Both crude sample proportions and RDS-weighted population prevalence estimates are provided in Appendix .
On exploratory analysis, the linear relationship between CES-D scores and time in which participants were surveyed was evaluated given increasing homophobia and the ultimate passage of the propaganda law. This relationship was significant, thus, we included the date of when participants completed the survey as a covariate in the model. This was transformed to a binary variable with March 7, 2012 as a breakpoint: the date in which the governor of St. Petersburg signed a law banning the sharing of homosexual propaganda [ 37 ]. While our study took place in Moscow City, political and media attention to the St. Petersburg law created an atmosphere of increased violence and discrimination against the LGBT population across Russia. The category for participation in the survey after the passage of the law is also inclusive of other key time periods that signify the deteriorating climate for LGBT populations, including the passage of the draft Ukraine law that received wide support and discussion in Russia (October 2012) and the date when the anti-gay propaganda law was introduced to the Russian Parliament (January 2013) [ 38 ]. Our model tests for an increase in the odds of probable depressive symptoms before and after the St. Petersburg law as a binary variable and as an interaction term with experienced stigma.
Variables known to be associated with depression symptoms (income, sexual identity, experience of stigma, social connectedness, alcohol use) [ 13 , 15 , 27 – 30 ] or with a p value of p < 0.10 in bivariate analysis were included in the multivariable model. The Furnival-Wilson leaps-and-bounds algorithm was used to perform variable selection on a wide array of models with depression as the outcome of interest and socioeconomic, demographic, experiential, and behavioral factors as predictor variables. Akaike’s information criteria were used to select the best model, and multiple logistic regression was used to obtain adjusted odds ratios (AOR) for the variables in the selected model. Collinearity for the model was checked using variance inflation factors (VIFs). While the VIF for the interaction between survey date and experience of stigma was 2.88, all other VIFs were well under 2.0, indicating that collinearity is not of concern. Pearson’s goodness-of-fit test was used to check model fit.
Ethical Review
The study was approved by both the Ethics Committee of the State Medical University, IP Pavlov, St. Petersburg, Russia, and the Johns Hopkins Bloomberg School of Public Health Institutional Review Board, Baltimore, Maryland.
A total of 1376 MSM with a median age of 30 years [IQR 24–36] were enrolled in the study, 85.7% of whom were born within Russia. Over half (55%) identified as homosexual, 42.9% identified as bisexual, and 2.1% identified as other sexual identities, including heterosexual. By contrast, 64.6% reported only male sexual partners, while 35.4% reported both male and female partners in the last 12 months. Thirty-six percent reported experiencing stigma due to their sexual preferences. Over one-third (36.7%) qualified as probably depressed ( n = 505), 11% as possibly depressed ( n = 151), and 52.3% unlikely to be depressed according to the CES-D ( n = 720).
Table Table1 1 presents the participant demographic and behavioral characteristics stratified by depression symptomatology. Appendix Table 1 presents the RDS-weighted estimates stratified by depression symptomatology. Those with symptoms indicating probable depression (CESD ≥23) were more likely to have full-time employment (59.7%) than those with symptoms indicating unlikely or possible depression (CESD <23; 51.4%, p = 0.03). MSM in the probable depression group were more likely to identify as homosexual (64.7% vs. 49.5, p < 0.001) and less likely to report feeling comfortable with their sexual orientation (86.5 vs. 93.2%; p value <0.001) than those in the unlikely/possible depression group. Those with probable depression scores reported higher levels of experienced stigma (62.7 vs. 39.4%; p value <0.001) than those who were possibly/unlikely depressed. A larger proportion of those with probable depression had been detained in jail or prison (8.6%) than those with unlikely/possible depression (4.6%; p value <0.01). A greater proportion of those in the group with probable depression participated in the survey after the “propaganda law” was signed into law in St. Petersburg (61.4%) compared to those in the unlikely/possibly depressed group (48.7%; p value <0.001).
Demographic and behavioral characteristics of MSM in Moscow, Russia, by depression symptomatology from 2010 to 13 ( N = 1376)
Table Table2 2 displays the bivariate and multivariable logistic regression analyses of sexual identity, stigma, passage of the anti-gay propaganda laws, and other correlates with probable depression. After controlling for other confounders, the odds of probable depression was 29% lower among those identifying as bisexual (AOR 0.71 95%CI 0.52–0.97; p = 0.03) as compared to those reporting homosexual identity. The adjusted odds of depression was nearly twice as high for those who reported experiencing stigma in the last 12 months (ref: little/no stigma; AOR 1.75; 95%CI 1.20–2.56; p < 0.01). Those who reported discomfort with their sexual identity had almost sixfold increased odds of depression relative to those who reported feeling comfortable with their sexual identity (AOR 5.85; 95%CI 2.71–12.64; p < 0.001). A history of jail or detention was associated with a nearly twofold increased odds of probable depression (AOR 1.78; 95%CI 1.00–3.17; p = 0.05) compared to those who did not have a history of detention. Probable depression was also 35% lower for those with five or more sexual partners in the last 6 months (ref: ≤1 partner; AOR 0.54; 95%CI 0.37–0.81; p < 0.01).
Crude and adjusted relative odds of depression ( N = 1376)
a Adjusted model includes income, marriage to a woman, sexual identity, comfort with sexual preference, number of sexual partners, experience of stigma, social connectedness to gay space, alcohol use, history of detention in jail or prison, date of taking survey, and time-stigma interaction
Prior to including the interaction between time and experienced stigma in the multivariable model, the adjusted odds of depression for those who were surveyed after the signing of the St. Petersburg propaganda law was 1.5-fold greater than that of participants who were surveyed before the approval of the law (AOR 1.65, 95%CI 1.23–2.22; p = 0.001). After including the interaction between time and experience of stigma in the final model, the adjusted odds of depression associated with the survey date was no longer significant (AOR 1.34, 95%CI 0.95–1.91; p = 0.10). The interaction itself, however, was significant, and computed estimates for the combination with the interaction were highly significant. In this case, among people with experienced stigma, depression increased twofold after the passage of the St. Petersburg law (ref: participation prior to the law; AOR 2.24; 95%CI 1.49–3.39; p < 0.001). Finally, in the period after the law was passed, the odds of probable depression among people with experienced stigma were almost threefold that of those without experienced stigma (AOR 2.92; 95%CI 2.02–4.24; p < 0.001).
A sensitivity analysis was performed with the same multivariable model but including the variable measuring behavioral bisexuality in terms of the gender of reported sex partners in the last 12 months (in lieu of bisexual identity). Here, the association became stronger as the adjusted odds ratio dropped from 0.71 (95%CI 0.52–0.97, p = 0.03) in the previous model to 0.58 (95%CI 0.42–0.81; p < 0.01).
Depression is common in the Russian Federation, and particularly so for MSM. Over a third of MSM in this sample qualified with “probable depression” according to the CES-D scale, and nearly half scored high enough to qualify as at least “possibly depressed.” These estimates for MSM in Russia exceed the general estimates of 23% for possible depression (CES-D cutoff of 16) in men in urban areas of Russia [ 3 ]. While methodological differences and temporal effects may play a role, differences may also be explained, in part, by the high prevalence of experienced stigma and its strong relationship with depressive symptoms.
Evidence has shown that sexual identity may be a correlate of depression and other mental health outcomes. In this study, bisexual identity appears to provide a protective effect against depression among MSM in Russia. Discomfort with sexual identity was also strongly associated with depressive symptoms. The protective relationship between bisexual identity and depression contradicts the general body of research, which predominantly originates from the USA, that has demonstrated increased risk for poor mental health outcomes with bisexual identity and similarly high risk for poor social wellbeing compared to those who identify as homosexual or heterosexual [ 22 ].
One reason for this surprising discrepancy may be the context of increasing and state-sanctioned homophobia in Russia. In a country that has criminalized information related to same sex behaviors, and ultimately criminalized LGBT visibility, the political and social environment has become increasingly hostile towards MSM. The discourse around the anti-gay movement has promoted traditional morals, masculinity, and traditional sexual relations and has been associated with increased violence towards LGBT populations and may decrease individual comfort with one’s sexual identity [ 18 ]. It is possible that endorsing a level of opposite-sex attraction in addition to same-sex attraction allows a degree of psychological refuge from feelings of exclusion, self-stigma, and experiences of violence. Discomfort with sexual identity may further be measuring underlying, internalized homophobia, which has demonstrated significant impact on mental health, including anxiety and depression [ 39 ].
The experience of detention in jail or prison also had a strong relationship with depressive symptoms. While we did not collect information about the reason for imprisonment, it would be interesting to know if sexual identity played either a real or perceived role in the justification for imprisonment.
Several factors limit the inferences of this study. The study was cross-sectional, limiting our ability to determine the temporal relationship between sexual identity and depression and prevents causal association. However, the use of recall periods for experiences of stigma (past 12 months) and depression (past 7 days) allows some interpretation of temporality. We utilized a tool to measure depression symptoms rather than depression diagnosed by a mental health professional, which may potentially misclassify participants; however, the CES-D has been well-established and validated in the Russian context. Enrollment and testing methods, criteria for study inclusion, and financial incentives may have influenced our sample. It is also possible that RDS did not reach particular subgroups within the MSM community. However, this study is unusual in its success of recruiting a large number of MSM (31 waves and over 1300 MSM) in a highly stigmatized setting. Despite potential limitations, RDS seems to have been one of the most productive pathways of recruiting MSM in this context [ 23 ].
Our results show that homosexual identity, experience of stigma, and experience of imprisonment are all associated with depressive symptoms in MSM in Russia. The passing of anti-gay propaganda laws in the region in 2012 and in the Russian Federation in 2013 [ 40 ], which effectively criminalizes information related to homosexual and bisexual identity, further modifies the relationship between stigma and depression among MSM. Because social support has been shown to be protective against depression in MSM in this context [ 41 ], interventions that build social support in the MSM community in Russia and enable access to non-stigmatizing mental health services may help to combat the negative effects of stigma and help protect against depression in this population.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(DOCX 35 kb)
Acknowledgements
We wish to thank SANAM clinic and Tatiana Bondarenko for insight, support, and use of the SANAM clinic for conduct of qualitative research and the Be Safe study. We appreciate the efforts put forth by Irina Deobald and Konstantin Dyakonov in the formative phases of this project. We are deeply thankful to the participants who contributed their time and personal experiences to this study.
Authors’ Contributions
CB, ALW, CEZ, NG, VM, AP, and CL collaborated in the design and oversight of the overall study. PD and KI collected data. EH conducted data analysis. ALW reviewed and provided input to the statistical analysis. EH and ALW wrote the initial drafts of this manuscript. All authors had full access to the data, reviewed and edited the manuscript, and all take responsibility for its integrity as well as the accuracy of the analysis.
Compliance with Ethical Standards
Funding for this study came from the National Institute of Mental Health (NIMH R01 MH085574-01A2) “High Risk Men: Identity, Health Risks, HIV and Stigma” funded from 2009 to 2014. Drs. Wirtz, Latkin, Galai, and Beyrer are also supported by the Johns Hopkins University Center for AIDS Research (P30AI094189).

IMAGES
COMMENTS
A more recent explanation for the way in which our food may affect our mental wellbeing is the effect of dietary patterns on the gut microbiome—a broad term that refers to the trillions of microbial organisms, including bacteria, viruses, and archaea, living in the human gut. The gut microbiome interacts with the brain in bidirectional ways ...
A nutritional component to mental healthcare by 2030. CNP's vision for the future of mental healthcare is a one that includes the role of diet in supporting mental health. CNP is working to fill the void in our current mental healthcare model by consolidating research, developing curriculum, and creating a methodology through which we can ...
Can nutrition affect your mental health? A growing research literature suggests the answer could be yes. Western-style dietary habits, in particular, come under special scrutiny in much of this research. A meta-analysis including studies from 10 countries, conducted by researchers at Linyi People's Hospital in Shandong, China, suggests that ...
Nutrition and mental health: A review of current knowledge about the impact of diet on mental health ... In recent years, there has been a surge in research on the effects of nutrition on mental status, which may be an important aspect of the prevention of many mental disorders and, at the same time, may lead to a reduction in the proportion of ...
An increasing number of studies are revealing that diet and nutrition are critical not only for physiology and body composition, but also have significant effects on mood and mental well-being. In particular, Western dietary habits have been the object of several research studies focusing on the relationship between nutrition and mental health.
Our guest is Julia Rucklidge, Ph.D. Dr. Rucklidge is a professor of clinical psychology at the University of Canterbury in New Zealand, where she leads the Mental Health and Nutrition Research Group and serves on the Executive Committee for the International Society of Nutritional Psychiatry Research. Julia's interest in nutrition and mental ...
The CNP Micronutrients and Mental Health Research Category ... (a test of mental health) compared with the control group. The intervention group also reported being less "mentally tired" both before and after completing the cognitive demand battery. ... Rhee, Lee, and Ahn (2020) retrieved data from the Korea National Health and Nutrition ...
Diet influences numerous aspects of health, including weight, athletic performance, and risk of chronic diseases, such as heart disease and type 2 diabetes. According to some research, it may ...
This series is intended to showcase the diversity of studies being conducted in a new, rapidly emerging field of nutrition and mental health, coined by leaders in the field as nutritional psychiatry (Sarris, Logan, et al., 2015).The series begins with an article by Sánchez-Villegas, Ruiź-Canela, Gea, Lahortiga, and Martínez-González (2016) that fits into the field of nutritional ...
In 2020, the Agriculture, Nutrition and Health (ANH) Academy constituted a working group of interdisciplinary experts on mental health and food and nutrition, as well as methodologists with expertise in the design and evaluation of implementation research programmes in these fields.
The relationship between nutrition and mental health is bidirectional: the foods we eat affect our mental health, and our mental health status affects what and how well we eat. This month, the American Psychiatric Association (APA) and the American Society for Nutrition (ASN) are partnering to highlight the interconnectedness of nutrition and mental health. To learn more about how the public ...
A healthy diet includes a full range of vegetables, fruits, legumes (lentils, chickpeas, beans), sh, whole grains (rice, quinoa, oats, breads, etc.), nuts, avocados and olive oil to support a healthy brain. Sweet and fatty foods should be special treats, not the staples of your diet. People who eat a diet high in whole foods such as fruits ...
With a burgeoning post-graduate programme and new doctoral-level faculty in diverse areas of psychology, communication disorders, audiology, swallowing rehabilitation and stroke recovery, our research profile is rapidly expanding. Psychology, Speech and Hearing research. Our world-leading experts are collaborating on ground-breaking research ...
The aim of this article was to carry out a scoping review of existing research on the influence of food on mental health: (1) Background: nutrition, nutrient levels or an adequate body weight seem to influence the mental health status of individuals. The consumption of psychotropic drugs also seems to contribute to overweight; (2) Methods: fifteen previous research articles were used in the ...
According to the World Health Organization (WHO), depression is a leading cause of ill health and disability around the world. Understanding and managing mental health disorders is a public health challenge. Research continues to grow our understanding of the relationship between nutrition and the mind, and current evidence supports that diet has a role in psychological health.
Julia Rucklidge - Mental Health & Nutrition Research: Te Puna Toiora, Christchurch, New Zealand. 11,105 likes · 59 talking about this · 6 were here. University of Canterbury, Christchurch NZ....
Research about the microbiome-gut-brain axis (MGB) has accelerated at an incredible pace to expand the knowledge of the role of microbiota on the brain and behaviors, from the development of nervous system in early life to mental health and cognitive function, even health aging and longevity. This research topic aims to disseminate advanced ...
Development of Global Agendas on Mental Health and Food Security and Nutrition. We trace the progression of both mental health and FSN on the global agenda, marked by the Millennium Development Goals (MDGs) in 2000, to the SDGs in 2015 and beyond (Figure 1).The MDGs focused many of their targets and indicators on health, but linked to nutrition only though a narrow focus on hunger and ...
The article presents the chronology and results of the International Scientific and Practical Conference Commitment to Mental Health Issues, which was organized and conducted by the Department of ...
In fact, nutrition research over the last 20 years ... Hibbeln says that "the mental health benefits of omega-3 fatty acids are underknown, underutilized and under implemented" within the ...
Historically, outpatient psychiatry in Russia set the same values and goals that are currently included in the European Mental Health Action Plan (2013-20)1 and, since they were started, the community-based services were developed as highly resourced settings (ie, specialised services dedicated to specific patient groups with a variety of forms of medical care).2 The first community-based ...
New research highlights the financial burden receiving mental health care can be on a family. U.S. Surgeon General Dr. Vivek Murthy, MD, MBA, emphasized the increase in depression, anxiety, and ...
Researchers in the Affective Computing group at the MIT Media Lab have been invited to edit a series of articles on the topic of Wearable Digital Health Technologies in the New England Journal Medicine; the series includes articles related to epilepsy, depression, diabetes, and cardiovascular disease, among other areas.. Peruse the articles in this series below!
Nutrition has a role in the prevention and the treatment of behavioral health disorders. 3 Suboptimal nutrition has been implicated in the underlying pathology of behavioral health disorders because of the essential role of nutrients in the neuroendocrine system. Nutrients, including tryptophan, vitamin B 6, vitamin B 12, folic acid (folate ...
Within the Department of Precision Health, Dr. Torsten Bohn, Head of the Nutrition & Health Research Group (NUTRIHEALTH), aims, in collaboration with his team, to explore dietary patterns, their ...
Mental Health & Substance Use. Mental health issues are closely linked to SUDs. Nearly 1 in 4 adults (59.3 million) experienced any mental illness (AMI) in the past year. Among adolescents (12-17), 19.5% (4.8 million) experienced a major depressive episode (MDE) in the past year. Suicidal Thoughts & Behaviors
Associated Data. 1. Introduction. A large number of scientists and health professionals recognize that balanced nutrition is fundamental for a good state of physical health. The World Health Organization working group focused on nutrition as a key component of disease prevention, indicating that " a balanced and varied diet, composed of a ...
Background and aims Obesity and overweight have become significant health concerns worldwide, leading to an increased interest in finding natural remedies for weight reduction. One such remedy that has gained popularity is apple cider vinegar (ACV). Objective To investigate the effects of ACV consumption on weight, blood glucose, triglyceride and cholesterol levels in a sample of the Lebanese ...
The Union of Mental Health of Russia and the Journal "Mental Health" announce the I All-Russian contest of research papers on mental health for students of medical and non-medical universities pursuing psychology, psychiatry, psychotherapy, sociology, law, economics studies. ... Meeting of the United Nations Member States Group of Friends ...
Funding for this study came from the National Institute of Mental Health (NIMH R01 MH085574-01A2) "High Risk Men: Identity, Health Risks, HIV and Stigma" funded from 2009 to 2014. Drs. Wirtz, Latkin, Galai, and Beyrer are also supported by the Johns Hopkins University Center for AIDS Research (P30AI094189).