- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Cancer Treatments and Research
Learn more about the progress made in improving cancer survival rates
Cancer Treatment Development
Radiotherapy, immunotherapy, targeted therapy.
- Combination Therapies
Diagnostics
Considerable progress has been made in reducing cancer rates and improving cancer survival in the United States since the 1990s. A greater understanding of the immune system , genetics , and cancer pathology has opened the doors to an ever-increasing range of new cancer treatments and diagnostic tools.
Advances in cancer care have been highly specific in terms of the diagnostic and treatment modalities that are recommended for each type of cancer. This article will describe these key treatments as well as the process of cancer treatment development.
sanjeri / Getty Images
Throughout the years, there have been discoveries of drugs and treatment methods that prove to be more successful or reliable than previous ones. These treatment methods are discovered in different ways.
Some are found in nature through the testing and studying of plants, fungi, and animals. Others are found through the study of cancer cells and existing drugs or procedures. But before any type of treatment method is used on patients, there is an important process that ensures its safety and effectiveness.
New cancer drugs typically go through stages of clinical research. These stages are:
- Preclinical research : Preclinical research aims to ensure a form of treatment is safe for human use. Laboratory studies that include animal research and in vitro studies , or experiments usually done in test tubes and Petri dishes, are common in this research stage.
- Clinical research : After preclinical research is successful, clinical research focuses on testing the form of therapy on humans. This clinical research stage can be lengthy (up to 10 years or more) as the discovered treatment goes through phases of clinical trials .
- Post-clinical research : Post-clinical research involves studying a therapy that has gone through the clinical research phase and received approval for human use. This involves collecting data on effectiveness and safety in real-world use.
Advances in and refinement of cancer surgery—including the use of targeted drugs and other medications before and after surgery—that can improve outcomes for cancer patients continue to emerge.
Studies comparing the outcomes of different surgical methods have helped guide doctors in selecting the technique that is most likely to result in a better long-term prognosis.
Video-Assisted Thoracoscopic Surgery (VATS) Lobectomy for Lung Cancer
During a lobectomy , a portion of a lobe of a lung that is affected by cancer is removed.
The minimally invasive technique known as VATS lobectomy, done with general anesthesia , often involves a shorter recovery time than open surgery for lung cancer . The American College of Chest Physicians identifies VATS lobectomy as the preferred method for treating early-stage lung cancer.
During the procedure, a thoracoscope, which is a small tube with a light and camera attached to the end, is inserted between the ribs through a small incision. The affected lung tissue is then removed using special tools.
Open Surgery for Cervical Cancer
In a clinical trial between 2008 and 2013, 631 women were enrolled to compare the efficacy of open surgery with that of minimally invasive surgery for the treatment of cervical cancer .
Postoperative quality of life for both groups was similar. But open surgery resulted in lower rates of cancer recurrence and higher disease-free survival.
Another study found that patients with early-stage cervical cancer who had minimally invasive surgery experienced higher recurrence rates than those who had open surgery, making open surgery a better option for some patients.
Radiation therapy is used as an adjunct to cancer treatment. More effective and targeted radiotherapies are being used to treat early and advanced cancers.
Stereotactic Ablative Radiotherapy (SABR) for Metastatic Cancer
A study demonstrated that patients receiving SABR in addition to standard of care showed improved survival compared with patients receiving palliative standard of care.
SABR for Inoperable Early-Stage Lung Cancer
For patients who are not surgical candidates, SABR offers an alternative. This approach was shown to have excellent local control and well tolerated in a cohort of 273 patients.
Immunotherapy uses the body's immune system to fight cancer. Immunotherapy can boost or change how the immune system works so it can find and attack cancer cells.
Molecular testing, which can help select patients most suitable for immunotherapy, has opened the door to this newer form of treatment. Some of the early and commonly used immunotherapy agents are vaccines, including the first FDA-approved cancer vaccine, sipuleucel-T, for prostate cancer .
Below are some breakthrough agents grouped by category:
- Monoclonal antibodies , such as Trodelvy for metastatic triple-negative breast cancer
- Oncolytic virus therapy , including Imlygic for inoperable melanoma
- CAR T-cell therapy , such as CD22 for acute lymphoblastic leukemia relapse
- Cancer vaccines , such as Provenge for prostate cancer
Targeted therapy is when drugs are directed at specific proteins or genes that promote cancer cell growth. It is designed to attack cancer cells directly.
Some of the targeted drugs commonly used to treat cancer are Tagrisso (osimertinib), Tarceva (erlotinib), and Iressa (gefitinib) for lung cancer, and Kadcyla (ado-trastuzumab), Tykerb (lapatinib), and Afinitor (everolimus) for breast cancer.
Kinase Inhibitors
Dysregulation of protein kinases is involved in many types of cancer, and this protein is the target of several cancer drugs.
Drugs like Rozlytrek (entrectinib) and Tabrecta (capmatinib) are used to treat metastatic non-small cell lung cancer .
- Rozlytrek (entrectinib) is used to treat non-small cell lung cancer that is positive for ROS1 and the neurotrophic receptor tyrosine kinases (NTRK) fusion-positive solid tumors. It inhibits cell-proliferation while targeting ROS1, a receptor tyrosine kinase.
- Tabrecta (capmatinib) is a tyrosine kinase inhibitor that can help to shrink tumors involving a MET mutation. The MET gene produces a receptor tyrosine kinase, which is involved in cell proliferation and cell survival.
Kinase Inhibitor
Our bodies contain enzymes called kinases, which help to regulate functional processes such as cell signaling and cell division. A kinase inhibitor blocks the action of kinases.
PARP Inhibitors
Drugs, such as Zejula, are used to treat ovarian cancer . The drug inhibits the enzymatic activity of enzyme poly (ADP-ribose) polymerase (PARP). In a study of 533 patients who had recurring ovarian cancer, Zejula increased the time experienced without symptoms compared with standard therapy.
Combination Therapies
Combination therapy means using two forms of cancer therapy in conjunction. Newer classes of drugs are being combined with traditional chemotherapy to improve outcomes. This approach becoming the standard of care for treating some types of cancer.
One recent example is the combination of Tecentriq and Avastin in the treatment of liver cancer.
It is an ongoing area of critical research to develop better and more accurate diagnostic and screening techniques. Below are some next-generation technologies that are being developed. However, keep in mind these techniques (aside from ctDNA) have yet to be approved by the FDA.
Artificial Intelligence Mammograms
In a study that involved 28,296 independent interpretations, AI performance was comparable to radiologists' diagnostic ability for detecting breast cancer.
Liquid Biopsy for Breast Cancer
A liquid biopsy can detect circulating levels of cell-free DNA (cfDNA) and circulating tumor DNA (ctDNA).
In a meta-analysis that included 69 published research studies. with 5,736 breast cancer patients, researchers determined that the status of ctDNA mutation predicts disease recurrence and adverse survival results. They also found that the levels of cfDNA can predict metastasis of the axillary lymph node.
Monarch Robotic Endoscopy for Lung Cancer
This may be advantageous for patients with external lung lesions that need biopsy prior to surgery, radiation, targeted therapies, or immunotherapy.
Genomic Cancer Screening in Embryos
A polygenic risk score used by genomic prediction accurately distinguished which person in a set of siblings will inherit a medical condition. The accuracy was cited between 70% and 90%, depending upon the condition.
At-Home Urine Test for Prostate Cancer
A convenient, at-home urine test can be used to detect extracellular vesicle-derived RNA to provide prognostic information for men under active surveillance for prostate cancer.
A Word From Verywell
Cancer research that is investigating better treatments and diagnostic tools is ongoing. Even if you have advanced metastatic cancer, it may be comforting to know that newer treatments are being studied and approved every year. As treatments become better and better, your chances of survival and remission will also improve. If you have been diagnosed with cancer, it may also help to seek a cancer support group to boost your mental well-being and resilience.
American Society of Clinical Oncology: Cancer.Net. How are cancer drugs discovered and developed .
Cancer.net Improvements in Surgery for Cancer: The 2020 Advance of the Year.
Berfield KS, Farjah F, Mulligan MS. Video-assisted thoracoscopic lobectomy for lung cancer . Ann Thorac Surg. 2019 Feb;107(2):603-609. doi: 10.1016/j.athoracsur.2018.07.088
Frumovitz M, Obermair A, Coleman RL, Pareja R, Lopez A, Ribero R. Quality of life in patients with cervical cancer after open versus minimally invasive radical hysterectomy (Lacc): a secondary outcome of a multicentre, randomised, open-label, phase 3, non-inferiority trial . Lancet Oncol . 2020 Jun;21(6):851-860. doi: 10.1016/S1470-2045(20)30081-4
Kim SI, Cho JH, Seol A, et al. Comparison of survival outcomes between minimally invasive surgery and conventional open surgery for radical hysterectomy as primary treatment in patients with stage IB1-IIA2 cervical cancer . Gynecol Oncol . 2019;153(1):3-12. doi:10.1016/j.ygyno.2019.01.008
Palma DA, Olson R, Harrow S, Gaede S, Louie A, Haasbeek C. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (Sabr-comet): a randomised, phase 2, open-label trial. Lancet. 2019 May 18;393(10185):2051-2058. doi: 10.1016/S0140-6736(18)32487-5
Murray L, Ramasamy S, Lilley J, et al. Stereotactic Ablative Radiotherapy (SABR) in Patients with Medically Inoperable Peripheral Early Stage Lung Cancer: Outcomes for the First UK SABR Cohort . Clin Oncol (R Coll Radiol) . 2016;28(1):4-12. doi:10.1016/j.clon.2015.09.007
American Cancer Society. Immunotherapy .
Sastre J, Sastre-Ibañez M. Molecular diagnosis and immunotherapy . Curr Opin Allergy Clin Immunol . 2016 Dec;16(6):565-570. doi: 10.1097/ACI.0000000000000318
Vansteenkiste JF, Van De Kerkhove C, Wauters E, Van Mol P. Capmatinib for the treatment of non-small cell lung cancer. Expert Rev Anticancer Ther . 2019;19(8):659-671. doi:10.1080/14737140.2019.1643239
Matulonis UA, Walder L, Nøttrup TJ, et al. Niraparib Maintenance Treatment Improves Time Without Symptoms or Toxicity (TWiST) Versus Routine Surveillance in Recurrent Ovarian Cancer: A TWiST Analysis of the ENGOT-OV16/NOVA Trial . J Clin Oncol . 2019;37(34):3183-3191. doi:10.1200/JCO.19.00917
Breast Cancer Research Foundation. How Combination Therapies Are Changing the Landscape of Breast Cancer Care .
Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma . N Engl J Med . 2020;382(20):1894-1905. doi:10.1056/NEJMoa1915745
Rodriguez-Ruiz A, Lång K, Gubern-Merida A, et al. Stand-Alone Artificial Intelligence for Breast Cancer Detection in Mammography: Comparison With 101 Radiologists . J Natl Cancer Inst . 2019;111(9):916-922. doi:10.1093/jnci/djy222
Alimirzaie S, Bagherzadeh M, Akbari MR. Liquid biopsy in breast cancer: A comprehensive review . Clin Genet . 2019 Jun;95(6):643-660. doi: 10.1111/cge.13514
Murgu SD. Robotic assisted-bronchoscopy: technical tips and lessons learned from the initial experience with sampling peripheral lung lesions. BMC Pulm Med. 2019 May 9;19(1):89. doi: 10.1186/s12890-019-0857-z
Lello L, Raben TG, Hsu SDH. Sibling validation of polygenic risk scores and complex trait prediction. Sci Rep 10 , 13190 (2020). doi.org/10.1038/s41598-020-69927-7
Connell SP, Hanna M, McCarthy F, et al. A Four-Group Urine Risk Classifier for Predicting Outcome in Prostate Cancer Patients [published online ahead of print, 2019 May 20]. BJU Int . 2019;124(4):609-620. doi:10.1111/bju.14811
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
February 27, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
New drug could unlock benefits of immunotherapy for more patients
by Institute of Cancer Research
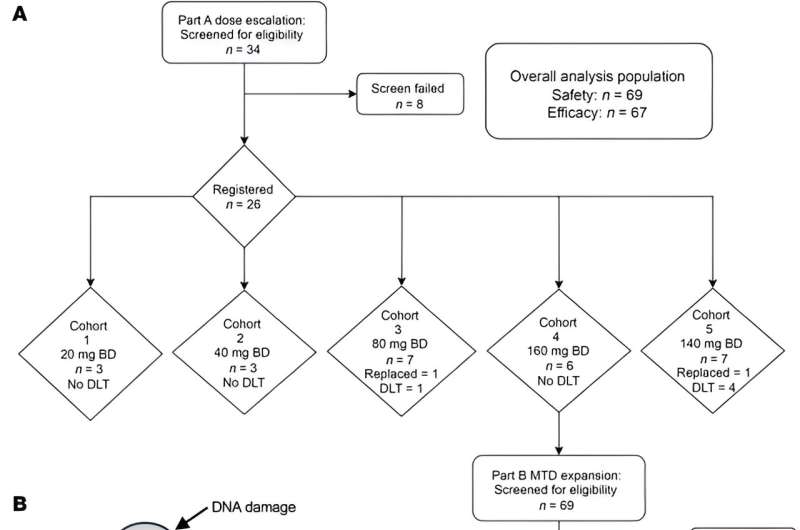
A new drug could offer a powerful way to sensitize tumors to immunotherapy, a new trial suggests. The results have been published in the Journal of Clinical Investigation .
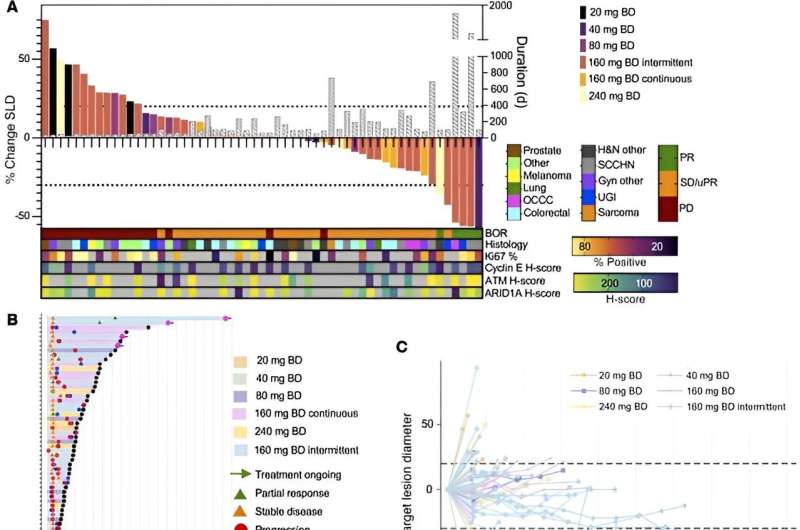
Ceralasertib showed promise for patients no longer responding to current cancer treatments in an early clinical trial. Given on its own, the drug stabilized the growth of tumors in more than half of patients who received it, with one patient seeing benefits for more than five years.
Prime tumors to be more responsive to immunotherapy
Researchers found that ceralasertib, a drug that targets cancer's ability to repair its DNA by blocking a key protein called ATR, also profoundly increased immune activity in some patient's tumors—changes which could leave them much more susceptible to immunotherapy treatments.
The study opens exciting new avenues for future trials which would use ceralasertib to prime tumors to be more responsive to immunotherapies, potentially unlocking their benefits for a wider group of patients.
A team at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust led the phase I PATRIOT trial. Researchers treated 67 patients with very advanced solid tumors with ceralasertib on its own. For these patients, other treatments had stopped working and their tumors were continuing to grow.
Tumor biopsies showed immune response
Ceralasertib, which can be taken as a pill, stopped tumors growing in more than half of patients—34 out of 66 patients whose treatment response could be measured. In five patients, the drug shrank their tumors. Of the 39 patients who benefited from the drug, 68% saw no progression of their disease for at least four months.
One patient with advanced ovarian cancer, whose tumor had faults in the key DNA repair gene ARID1A, responded remarkably well to ceralasertib, seeing their tumor continue to shrink over a period of more than five years. Researchers at The Institute of Cancer Research (ICR) previously identified the ARID1A gene as a marker of sensitivity to ATR inhibitors such as ceralasertib.
In the current study, the scientists compared tumor biopsies taken before and after treatment with ceralasertib to understand the underlying biology behind the drug's effects.
They were excited to observe that the drug on its own caused profound changes in patients' immune systems, both in their blood and within their tumors, in addition to its impact on DNA repair.
Giving ceralasertib led to increases in a type of immune cell that seeks out and kills cancer cells in the blood, alongside increased infiltration of immune cells into the tumors. These are signs that tumors are under attack and would be responsive to a range of immunotherapies—drugs which harness the body's own immune system to fight cancer.
Critical biological insights
Clinical trials have already shown that ceralasertib is effective when used in combination with the most common type of immunotherapy, known as PDL-1 inhibitors, but the current study is the first to prove that ceralasertib modulates the immune system in its own right.
The researchers have gained critical insight into the way in which the drug primes tumors to respond to immunotherapies. They hope this will lead to even better combinations of the drug with immunotherapy—a cutting-edge class of drugs which currently only works for a minority of patients.
Since the PATRIOT trial launched, other clinical trials led by the ICR and The Royal Marsden have begun—investigating the use of ceralasertib in combination with other drugs which prevent DNA from repairing itself, such as the PARP inhibitor olaparib.
Study leader Dr. Magnus Dillon, Clinician Scientist at The Institute of Cancer Research, London, and Clinical Consultant at The Royal Marsden NHS Foundation Trust, said, "This is the largest clinical trial of an ATR inhibitor, and it's encouraging to see that on its own ceralasertib can keep cancer from progressing and even shrink patients' tumors for an impressive time, giving some patients precious extra years of living well. It has also given us a clue as to the biological markers which may predict who could benefit from this drug in future.
"Excitingly, this trial provides us with the biological insights for how best to combine this drug with an immunotherapy and generate an even more powerful cancer treatment for people who have exhausted other options."
Dr. Anna Kinsella, Science Engagement Manager at Cancer Research U.K., said, "This is the largest study to date showing the potential of a class of drugs called ATR inhibitors in treating cancer when used alone. While there is still a long way to go before ceralasertib can be used in the clinic, it's always exciting to see new approaches showing potential in early-stage clinical trials.
"These promising results lay the foundations for future clinical trials and offer scientists and doctors new avenues of research. We look forward to seeing how this work drives further progress."
Explore further
Feedback to editors

Active military service may heighten women's risk of having low birthweight babies
13 hours ago

Significant global variation in COVID-19 guidelines: Most countries recommend at least one treatment that doesn't work

Study connects enjoyment of nature to lower inflammation levels
14 hours ago

Bacteria in the intestine that change in response to inflammation could have an impact on our immune system
15 hours ago

Researchers develop deep-learning model capable of predicting cardiac arrhythmia 30 minutes before it happens

Improving cancer immunotherapy by prolonging T-cell survival

Eye-opener: Pupils enlarge when people focus on tasks
16 hours ago

Study finds COVID-19 pandemic led to some, but not many, developmental milestone delays in infants and young children

Common antibiotic may be helpful in fighting respiratory viral infections

In psychedelic therapy, clinician-patient bond may matter most
Related stories.

Clinical trial shows durvalumab plus ceralasertib boosted immune response in lung cancer patients
Feb 13, 2024

Olaparib plus ceralasertib may benefit pediatric cancer patients with DNA-repair-deficient tumors
Apr 18, 2023

Immune system link with rare ovarian cancer could guide future treatment
Oct 14, 2021

Immunotherapy plus an investigational cancer drug improves anti-tumor effects
Nov 8, 2023

Investigators profile three treatment response trajectories to close in on triple-negative breast cancer
Jan 8, 2024

Cancer drug that targets two immune-evading tumor tactics performs well in early clinical trial
Oct 19, 2023
Recommended for you

Study identifies signs of repeated blast-related brain injury in active-duty United States Special Operations Forces
17 hours ago

Hitchhiking of synthetic antigen stimulates antibody production against cancer cells
21 hours ago

Researchers find obese people and tall, centrally obese people are more likely to get colorectal cancer
22 hours ago

Genetically engineering a treatment for incurable brain tumors

New study furthers understanding of lung regeneration
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
April 16, 2024
10 min read
New Prostate Cancer Treatments Offer Hope for Advanced Cases
Major discoveries during the past 10 years have transformed prostate cancer treatment, enabling it to proceed even for the most advanced form of the disease
By Marc B. Garnick
David Cheney
D eciding how to diagnose and treat prostate cancer has long been the subject of controversy and uncertainty. A prime example involves prostate-specific antigen (PSA) testing, a blood test for a telltale protein that can reveal cancer even when the patient has no symptoms. After its introduction in the early 1990s, PSA testing was widely adopted—millions of tests are done in the U.S. every year. In 2012, however, a government task force indicated that this test can lead to overtreatment of cancers that might have posed little danger to patients and so might have been best left alone.
While arguments for and against PSA testing continue to seesaw back and forth, the field has achieved a better grasp on what makes certain prostate cancers grow quickly, and those insights have paved the way for better patient prognoses at every stage of the disease, even for the most advanced cases. A prostate cancer specialist today has access to an enhanced tool set for treatment and can judge when measures can be safely deferred.
The importance of these advances cannot be overstated. Prostate cancer is still one of the most prevalent malignancies. Aside from some skin cancers, prostate cancers are the most common cancers among men in the U.S. Nearly 270,000 people in America will be diagnosed with prostate cancer this year, and it is the fourth most common cancer worldwide. Fortunately, the vast majority of patients will live for years after being diagnosed and are more likely to die of causes unrelated to a prostate tumor.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
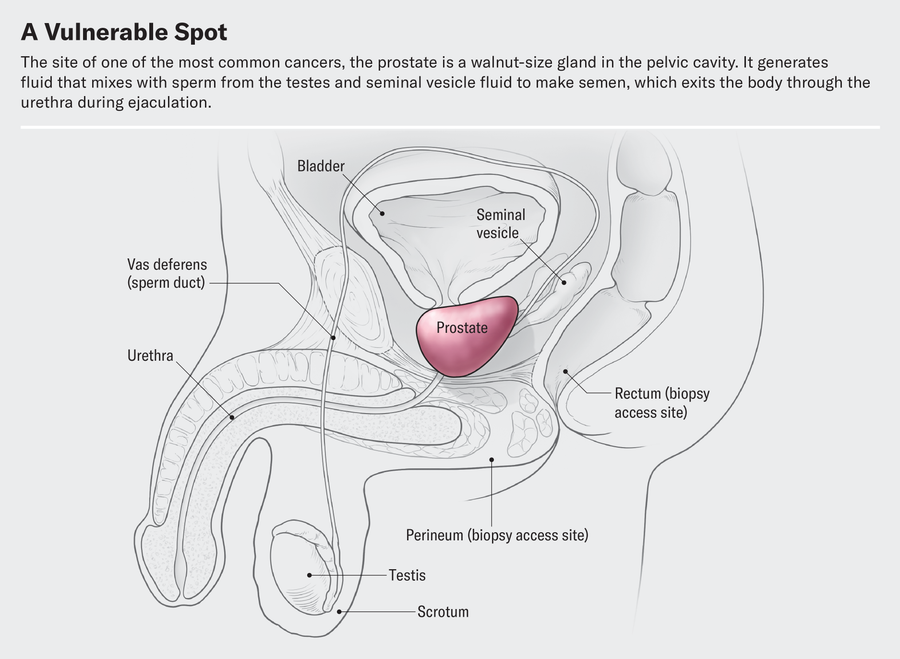
At its most basic level, prostate cancer is a malignancy that occurs in the prostate gland, which produces fluid that mixes with sperm from the testicles to make semen. The prostate is located in front of the rectum, below the bladder and above the penis, and cancer in the gland has four major stages.
Early on, localized tumors show no evidence of extension beyond the prostate gland. A second, “regionally advanced” form of the disease remains close to the prostate. Then there are metastatic prostate cancers, which spread outside the gland to other parts of the body. Treatment of tumors in this category has benefited from improved diagnostic imaging tests. In fact, with these tests, cancer specialists have characterized the fourth category, oligometastatic prostate cancer, a disease stage on a continuum between localized prostate cancer and more broadly dispersed metastatic disease. Major discoveries in the past 10 years have transformed the way we approach each type of prostate cancer, and these advances are likely to continue for decades to come.
The first treatment steps for people with localized cancer involve risk stratification. Through this process, a physician gauges the likelihood of a cancer’s being eliminated or cured by local treatment (usually surgery or radiation) and, if it does abate, of its returning. A physician determines the risk based on PSA results, physical examination of the prostate gland and inspection of cells from the biopsied tumor.
The right course of action for a patient with elevated PSA levels continues to undergo constant revision. Until five to seven years ago, a physician evaluated a person with high PSA by feeling their prostate gland for potentially cancerous abnormalities. Invariably, the next step would be a needle biopsy—an uncomfortable procedure in which the physician obtains snippets of prostate tissue through the rectum.
But we now have a way to biopsy through the perineum—the area between the back of the scrotum and the anal-rectal area. Thanks to technical improvements, it can be done in an outpatient setting without general anesthesia or sedation. The technique reduces the patient’s risk of infection and need for antibiotics because it doesn’t disrupt the bacterial flora in the rectum. In a recent study, researchers compared outcomes in patients who underwent a transrectal biopsy and received antibiotics with those for people who had a transperineal biopsy with minimal to no antibiotics. They found the two approaches comparable in terms of complications from infections.
Even more exciting is the prospect of eliminating biopsies altogether. When a patient has an abnormal PSA value but their rectal examination shows no obvious evidence of cancerous deposits, physicians can now use magnetic resonance imaging (MRI) to look at the prostate and surrounding tissue. MRI scans are best for identifying clinically significant cancers—those that, if left untreated or undiagnosed, could eventually spread. MRI can also uncover more extensive cancer spread or tumors in unusual locations such as the front of the prostate.
Another benefit of MRI procedures is that they identify fewer clinically insignificant cancers—those that are unlikely to cause problems and might best be left alone. In this case, failure to detect certain cancers is a good thing because it spares people unnecessary treatment. In some medical centers in the U.S. and many in Europe, a physician will perform a biopsy only if the MRI scan does reveal evidence of clinical significance. Studies that have compared the two diagnostic approaches—routine biopsy for all patients with elevated PSA levels versus biopsies based on abnormal MRI findings—found they are similarly effective at detecting clinically significant cancers.
Once a patient is diagnosed with prostate cancer, what happens next? For decades the debate over treatment has been just as contentious as the debate over diagnosis. Fortunately, new research from the U.K. has provided some clarity. Investigators there studied several thousand people with elevated PSA levels whose prostate biopsies showed cancer. These patients were randomized to receive surgical removal of the cancerous gland, radiation treatments or no active treatment at all. At the end of 15 years of comprehensive follow-up, about 3 percent of patients in each group had died of prostate cancer, and nearly 20 percent in each group had died of unrelated causes.
Based on the results of this study and others, more people are now being offered “active surveillance” after a prostate cancer diagnosis, in which treatment is either delayed or avoided altogether. Careful monitoring of patients who have not undergone surgery or radiation is becoming more common; it is now being extended even to those with more worrisome tumors. The monitoring involves a range of measures: PSA testing every three to six months, physical examination of the prostate gland and assessment of the patient’s urinary symptoms. Those tests are followed by repeat biopsies at increasing intervals, as long as there are no significant pathological changes.
If a cancer is identified as having either intermediate- or high-risk features, doctors need to track its progression, usually with bone scans using radiopharmaceuticals and with abdominal-pelvic computed tomography (CT) scans, which may show any spread in the areas to which prostate cancer most often metastasizes. Unfortunately, these techniques are not sensitive enough to reliably detect cancer in structures less than a centimeter in diameter, such as lymph nodes. Consequently, small areas of metastatic disease may go undetected. These cases are said to be “understaged.”
Understaging can now be studied through more precise diagnostic testing. Typically patients whose disease is understaged are not treated until the cancer becomes detectable through symptoms such as urination problems or pain. The disease then may require intensive therapies, and there is less of a chance of long-term remission. One technology that can help address understaging is advanced scanning that combines radiodiagnostic positron-emission tomography (PET) with CT.
These scans can detect molecules commonly found in prostate cancer cells, such as prostate-specific membrane antigen (PSMA). If PSMA is present outside the prostate gland, such as in pelvic lymph nodes, the affected areas can be identified, and a plan can be made for targeted radiation treatments or surgical removal.
Let’s consider how PET-CT scanning can be used in clinical practice. One of my patients, a 68-year-old man, was diagnosed with prostate cancer that was localized but had high-risk features. The traditional diagnostic bone and CT scans did not show any evidence of cancer spread outside the prostate. A PET-CT scan for PSMA, however, did reveal the presence of several small deposits of cancer cells in well-defined areas of the pelvis, indicating the cancer had spread to the lymph nodes. This finding prompted treatment that included radiation therapy in the prostate gland and the cancerous lymph nodes, as well as androgen-deprivation therapy (ADT), a treatment that reduces levels of testosterone, the hormone that enables prostate cancer to grow and progress.
The more precise identification of small tumor deposits in a limited number of pelvic lymph nodes—diagnosed as oligometastatic prostate cancer—enabled a new use for an old technology in oncology called metastasis-directed therapy (MDT), which targets cancer-containing lymph nodes or bony areas with radiation. At times, surgical removal of the abnormal lymph nodes may also be incorporated into MDT. Recently published studies on the use of MDT in conjunction with conventional treatments show, in some cases, long-term remission lasting through years of follow-up. Until recently, such a scenario was unthinkable for people whose prostate cancer had spread to their lymph nodes. My patient had the PSMA scan and MDT, as well as a relatively short course of ADT. He is cancer-free for now.
Precise identification of small metastatic deposits has other positive benefits. ADT has for decades been the mainstay for treating many forms of prostate cancer. Patients must continue the therapy for years, sometimes for the rest of their lives. Side effects of ADT are similar to those experienced during menopause. In fact, “andropause” is the term that captures the effects of ADT. Lower levels of testosterone are accompanied by a multitude of symptoms, including but not limited to loss of libido, erectile dysfunction, weight gain, hot flashes, bone loss, cognitive impairment, mood changes, diminished energy, and worsening of preexisting heart and vascular problems.
Studies of MDT for oligometastatic prostate cancer have raised the question of whether ADT could be delayed, administered for a shorter duration or even omitted in patients who otherwise would have required it. By strategically deploying traditional forms of localized treatment—usually surgery to remove the prostate gland or radiation—with added MDT for oligometastatic disease, doctors can significantly shorten the duration of ADT or potentially eliminate it. Such an approach would have been difficult to imagine five years ago. Longer-term follow-up studies will help scientists determine whether some people diagnosed in this fashion can go into an extended remission.
F or advanced forms of prostate cancer that have spread to other parts of the body, ADT has been the main treatment. Physicians historically have generally recommended surgical removal of the testicles—the primary source of testosterone—or the administration of other hormones that block the production and action of testosterone. In the mid-1980s I was involved with research on drugs called luteinizing hormone–releasing hormone analogues that lowered testosterone by shutting off the signal in the brain that instructs the testicles to make testosterone. Today newer agents have been added that further lower and block testosterone’s action.
The goal of prostate cancer treatment at later stages is to eliminate multiple sources of testosterone. As noted earlier, testosterone in the body comes predominantly from the testicles; the adrenal glands also produce a small amount. But prostate cancer cells can evolve to produce their own androgens. Testosterone and its active form, dihydrotestosterone (DHT), traverse the membranes of prostate cancer cells and interact with androgen receptors in the cytoplasm, a cell’s liquid interior. The receptors then transport DHT to the nucleus, where it instructs the cancer cell to grow, replicate and spread.
Traditional ADT does little to affect either the production of testosterone by the adrenal glands or androgen-producing prostate cancer cells, and it doesn’t block the activity of androgen receptors. But new approaches to ADT may address these shortcomings. Drug combinations that affect all these processes have substantially improved survival in people with metastatic prostate cancer—and, more important, patients are able to tolerate these more intensive treatment programs.
Instead of just one drug to decrease testosterone, new standards for treatment prescribe combinations of two or even three drugs. In addition to traditional ADT, there are medications such as docetaxel, a chemotherapy, and other new drugs that can block the production of testosterone by the adrenal glands or cancer cells or stop it by interfering with the activity of androgen receptors. All these drug combinations have resulted in meaningful improvements in survival.
Yet another therapy for advanced disease involves the identification of PSMA-expressing cancer cells that can be targeted with pharmaceuticals designed to deliver radioactive bombs. An injectable radiopharmaceutical can be delivered selectively to these cells, leaving healthy cells mostly unaffected. This therapy, lutetium-177-PSMA-617 (marketed as Pluvicto), has been approved by the U.S. Food and Drug Administration for the treatment of prostate cancer that has become resistant to other forms of ADT and chemotherapy. It is likely to become an important therapy for even earlier stages of prostate cancer.
Genetics and genomic testing of patients and cancers have also helped in the quest for improvement of symptoms and longer survival. Some genetic mutations that are known to increase the risk of breast and ovarian cancer have also been associated with a heightened risk of prostate cancer. Testing for such mutations is becoming much more common, and patients who have them can be treated with specific therapies that block their deleterious effects, leading to better outcomes.
An understanding of the type of mutation is also critical—for both patients and their family members. Germline mutations are inherited from a patient’s biological parents by every cell in the body. These mutations can be passed along to the patient’s children. A somatic mutation, in contrast, is not inherited but develops in the cancer itself. Targeted therapies designed specifically to correct the effects of either germline or somatic mutations have produced significant improvements in patient longevity. Some of the most commonly recognized cancer mutations—either somatic or germline—are those in BRCA genes, which have been associated with early-onset breast and ovarian cancer.
When researchers studied cancer in families with BRCA mutations, they uncovered many cases of prostate cancer. This finding led to the discovery that BRCA mutations appeared in both men and women in these families. The mutations change the way DNA is repaired, introducing defects that can result in cancer formation. Drugs have now been developed that treat cancers linked to the BRCA mutations. Several such drugs—those in a class called poly(ADP-ribose) polymerase (PARP) inhibitors—have recently received FDA approval for use as a treatment in people with these mutations. This research has led to more widespread genetic testing of patients with prostate cancer and, when germline mutations are found, family genetic counseling.
All these advances have occurred over the past decade—an incredibly short interval in the context of cancer oncology. Current options for early-stage prostate cancer enable physicians and patients to feel more at ease with conservative choices rather than immediate interventions with negative side effects. For patients whose cancers are advanced at initial diagnosis or progress and become metastatic, the treatment of oligometastases now often leads to long-term remission and requires fewer treatments with harmful systemic side effects. For those with more widespread metastatic disease, their cancer can now be managed with improved therapeutics based on a better understanding of disease biology. These new strategies have begun to transform this once rapidly fatal disease into a chronic condition that people can live with for years or even for their full life expectancy.
Marc B. Garnick is Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center in Boston. He is editor in chief of Harvard Medical School’s 2024–2025 Report on Prostate Diseases.
Cancer patients can now be 'matched' to best treatment with DNA and lab-dish experiments
Identifying the most effective cancer treatment for a given patient from the get-go can help improve outcomes.

Despite many efforts to find better, more effective ways to treat cancer, it remains a leading cause of death by disease among children in the U.S.
Cancer patients are also getting younger. Cancer diagnoses among those under 50 has risen by about 80% worldwide over the past 30 years. As of 2023, cancer is the second-leading cause of death both in the U.S. and around the world. While death rates from cancer have decreased over the past few decades, about 1 in 3 patients in the U.S. and 1 in 2 patients worldwide still die from cancer.
Despite advances in standard cancer treatments, many cancer patients still face uncertain outcomes when these treatments prove ineffective. Depending on the stage and location of the cancer and the patient's medical history, most cancer types are treated with a mix of radiation, surgery and drugs. But if those standard treatments fail, patients and doctors enter a trial-and-error maze where effective treatments become difficult to predict because of limited information on the patient's cancer.
My mission as a cancer researcher is to build a personalized guide of the most effective drugs for every cancer patient. My team and I do this by testing different medications on a patient's own cancer cells before administering treatment, tailoring therapies that are most likely to selectively kill tumors while minimizing toxic effects.
In our newly published results of the first clinical trial combining drug sensitivity testing with DNA testing to identify effective treatments in children with cancer, an approach called functional precision medicine , we found this approach can help match patients with more FDA-approved treatment options and significantly improve outcomes.
What is functional precision medicine?
Even though two people with the same cancer might get the same medicine, they can have very different outcomes. Because each patient's tumor is unique, it can be challenging to know which treatment works best.
To solve this problem, doctors analyze DNA mutations in the patient's tumor, blood or saliva to match cancer medicines to patients. This approach is called precision medicine . However, the relationship between cancer DNA and how effective medicines will be against them is very complex. Matching medications to patients based on a single mutation overlooks other genetic and nongenetic mechanisms that influence how cells respond to drugs.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
How to best match medicines to patients through DNA is still a major challenge. Overall, only 10% of cancer patients experience a clinical benefit from treatments matched to tumor DNA mutations.
Functional precision medicine takes a different approach to personalizing treatments. My team and I take a sample of a patient's cancer cells from a biopsy, grow the cells in the lab and expose them to over 100 drugs approved by the Food and Drug Administration. In this process, called drug sensitivity testing , we look for the medications that kill the cancer cells.
New clinical trial results
Providing functional precision medicine to cancer patients in real life is very challenging. Off-label use of drugs and financial restrictions are key barriers. The health of cancer patients can also deteriorate rapidly, and physicians may be hesitant to try new methods.
But this is starting to change. Two teams in Europe recently showed that functional precision medicine could match effective treatments to about 55% of adult patients with blood cancers such as leukemia and lymphoma that did not respond to standard treatments.
Most recently, my team's clinical trial focused on childhood cancer patients whose cancer came back or didn't respond to treatment. We applied our functional precision medicine approach to 25 patients with different types of cancer.

Our trial showed that we could provide treatment options for almost all patients in less than two weeks. My colleague Arlet Maria Acanda de la Rocha was instrumental in helping return drug sensitivity data to patients as fast as possible. We were able to provide test results within 10 days of receiving a sample, compared with the roughly 30 days that standard genomic testing results that focus on identifying specific cancer mutations typically take to process.
Most importantly, our study showed that 83% of cancer patients who received treatments guided by our approach had clinical benefit, including improved response and survival.
Expanding into the real world
Functional precision medicine opens new paths to understanding how cancer drugs can be better matched to patients. Although doctors can read any patient's DNA today, interpreting the results to understand how a patient will respond to cancer treatment is much more challenging. Combining drug sensitivity testing with DNA analysis can help personalize cancer treatments for each patient.
I, along with colleague Noah E. Berlow , have started to add artificial intelligence to our functional precision medicine program. AI enables us to analyze each patient's data to better match them with tailored treatments and drug combinations. AI also allows us to understand the complex relationships between DNA mutations within tumors and how different treatments will affect them.
— 'Very concerning': Microplastics can accumulate in cancer cells and may help them spread, study hints
— Gut bacteria linked to colorectal cancer in young people
— New mRNA 'cancer vaccine' trial launches in UK
My team and I have started two clinical trials to expand the results of our previous studies on providing treatment recommendations through functional precision medicine. We're recruiting a larger cohort of adults and children with cancers that have come back or are resistant to treatment.
The more data we have, the easier it will become to understand how to best treat cancer and ultimately help more patients access personalized cancer treatments.
This edited article is republished from The Conversation under a Creative Commons license. Read the original article .

Diana Azzam is an Assistant Professor and Research Director of the newly established Center for Advancing Personalized Cancer Treatments (CAPCT) at Florida International University. She has a Masters in Biochemistry from the American University of Beirut, Lebanon and a PhD in Biochemistry & Molecular Biology from the University of Miami, Florida. Her lab focuses on implementing functional precision medicine (FPM) approaches in adult and pediatric cancer patients that have run out of treatment options. Working with local hospitals including Nicklaus Children's Hospital and Cleveland Clinic Florida, her lab delivers individualized treatment plans based on a patient's cancer genomic profile and ex vivo drug response. She is currently engaged in two clinical studies to assess feasibility and clinical utility of FPM in relapsed/refractory patients with childhood cancer (ClinicalTrials.gov registration: NCT05857969) and adult cancer (ClinicalTrials.gov registration: NCT06024603). She is working on setting up the first CLIA-certified lab in the State of Florida dedicated for functional cancer drug testing. Her goal is to launch large-scale prospective multi-center randomized clinical trials to better assess efficacy of FPM approaches in the treatment of refractory/relapsed cancers. In parallel, she is working on utilizing FPM as a tool to reduce health disparities in childhood cancer patients from minority populations. She is also integrating a novel machine learning approach to identify specific biomarkers among minority populations that can be targeted using FDA-approved drugs. Her lab also investigates cancer stem cells and how they may result from chronic environmental exposures to toxic metals such as arsenic.
Detecting cancer in minutes possible with just a drop of dried blood and new test, study hints
Catherine, Princess of Wales, announces cancer diagnosis
Massive heat wave and a supercell thunderstorm caused deadly, baseball-sized hailstones to rain down on Spain
Most Popular
- 2 Giant, 82-foot lizard fish discovered on UK beach could be largest marine reptile ever found
- 3 Nightmare fish may explain how our 'fight or flight' response evolved
- 4 Lyrid meteor shower 2024: How to watch stunning shooting stars and 'fireballs' during the event's peak this week
- 5 Why do cats' claws retract but dogs' claws don't?
- 2 'Uncharted territory': El Niño to flip to La Niña in what could be the hottest year on record
- 3 Rare 'porcelain gallbladder' found in 100-year-old unmarked grave at Mississippi mental asylum cemetery
- 4 'I nearly fell out of my chair': 1,800-year-old mini portrait of Alexander the Great found in a field in Denmark
- 5 NASA reveals 'glass-smooth lake of cooling lava' on surface of Jupiter's moon Io
Genetically engineering a treatment for incurable brain tumors
Purdue researchers develop fully off-the-shelf, stem cell-derived, natural killer cells against glioblastoma.
Purdue University researchers are developing and validating a patent-pending treatment for incurable glioblastoma brain tumors. Glioblastomas are almost always lethal with a median survival time of 14 months. Traditional methods used against other cancers, like chemotherapy and immunotherapy, are often ineffective on glioblastoma.
Sandro Matosevic, associate professor in the Department of Industrial and Molecular Pharmaceutics in Purdue's College of Pharmacy, leads a team of researchers that is developing a novel immunotherapy to be used against glioblastoma. Matosevic is also on the faculty of the Purdue Institute for Cancer Research and the Purdue Institute for Drug Discovery.
The Matosevic-led research has been published in the peer-reviewed journal Nature Communications .
The Purdue glioblastoma treatment
Matosevic said traditional cell therapies have almost exclusively been autologous, meaning taken from and returned to the same patient. Blood cells from a patient are engineered to better recognize and bind to proteins on cancer cells, then given back to the same patient to bind to and attack cancer cells. Unfortunately, these therapies have limited to no effect on glioblastoma.
"By contrast, we are developing immunotherapy based on novel, genetically engineered, fully off-the-shelf or allogeneic immune cells. Allogeneic cells are not sourced from the same patient, but rather another source," Matosevic said. "In our study, we sourced -- or rather engineered -- cells from induced pluripotent stem cells. So we eliminated the need for blood and instead differentiated stem cells into immune cells, or natural killer cells, and then genetically engineered those."
Matosevic said novel Purdue immunotherapy can be considered to have a true off-the-shelf source.
"We can envision having unlimited supplies of these stem cells ready to be engineered," Matosevic said. "This does not require blood to be sourced. And because these are human cells, they are directly usable in human patients."
Validation and next development steps
The research team tested its treatment by conducting animal studies with mice bearing human brain tumors, which were treated by direct injection of the newly engineered immune cells.
"Our preclinical studies showed these immune cells to be particularly remarkable in targeting and completely eliminating the growth of the tumors," Matosevic said. "We found that we can engineer these cells at doses suitable for clinical use in humans. This is significant because one of the major hurdles to clinical translation of cell-based therapies to humans has been the poor expansion and lack of potency of cells that were sourced directly from patients. Using an off-the-shelf, fully synthetic approach breaks down significant barriers to the manufacturing of these cells."
Matosevic said the next step to develop the glioblastoma treatment is to conduct clinical trials to treat patients with brain tumors, including those that were not successfully eliminated by surgery.
"Our ultimate goal is to bring this therapy to patients with brain tumors," Matosevic said. "These patients urgently deserve better, and more effective, treatment options. We believe there is true potential for this therapy, and we have the motivation and capacity to bring it to the clinic.
"We are working with neurosurgical clinician collaborators to not only obtain funding, but also initiate clinical protocols," he added. "We are also open to and always seeking new collaborations and partnerships with those who have interest in supporting our mission to translate this therapy to the clinic, where it is needed the most."
Matosevic disclosed the innovative glioblastoma treatment to the Purdue Innovates Office of Technology Commercialization, which has applied for a patent from the U.S. Patent and Trademark Office to protect the intellectual property.
Matosevic and the research team received funding from the National Institutes of Health, the V Foundation for Cancer Research, the Purdue Institute for Cancer Research and industry partners.
- Brain Tumor
- Immune System
- Brain-Computer Interfaces
- Neuroscience
- Brain tumor
- Esophageal cancer
- Hodgkin's lymphoma
- Colorectal cancer
- Malignant melanoma
- Acupuncture
- Traditional Chinese medicine
Story Source:
Materials provided by Purdue University . Original written by Steve Martin. Note: Content may be edited for style and length.
Journal Reference :
- Kyle B. Lupo, Xue Yao, Shambhavi Borde, Jiao Wang, Sandra Torregrosa-Allen, Bennett D. Elzey, Sagar Utturkar, Nadia A. Lanman, MacKenzie McIntosh, Sandro Matosevic. synNotch-programmed iPSC-derived NK cells usurp TIGIT and CD73 activities for glioblastoma therapy . Nature Communications , 2024; 15 (1) DOI: 10.1038/s41467-024-46343-3
Cite This Page :
Explore More
- This Alloy Is Kinky
- Giant Galactic Explosion: Galaxy Pollution
- Flare Erupting Around a Black Hole
- Two Species Interbreeding Created New Butterfly
- Warming Antarctic Deep-Sea and Sea Level Rise
- Octopus Inspires New Suction Mechanism for ...
- Cities Sinking: Urban Populations at Risk
- Puzzle Solved About Ancient Galaxy
- How 3D Printers Can Give Robots a Soft Touch
- Combo of Multiple Health Stressors Harming Bees
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cancers (Basel)

Physical Activity and Cancer Care—A Review
Weronika misiąg.
1 Student Research Club No. 180, Faculty of Medicine, Wroclaw Medical University, 50-367 Wroclaw, Poland
Anna Piszczyk
Anna szymańska-chabowska.
2 Department of Internal Medicine, Occupational Diseases, Hypertension and Clinical Oncology, Wroclaw Medical University, 50-556 Wroclaw, Poland
Mariusz Chabowski
3 Department of Nursing and Obstetrics, Faculty of Health Science, Wroclaw Medical University, 51-618 Wroclaw, Poland
4 Department of Surgery, 4th Military Teaching Hospital, 50-981 Wroclaw, Poland
Associated Data
All the data analysed during the current study are available from the corresponding author upon reasonable request.
Simple Summary
The aim of this paper is to outline the role and potential benefits of physical activity for cancer patients. We present a review of publications on the subject in order to compare the findings reported in the literature and draw general conclusions that could help clinicians who provide cancer care to develop a more comprehensive treatment approach. This review may also help patients overcome barriers and become more motivated to take up physical activity, which would improve their quality of life. We wish to demonstrate to patients that physical activity should not be regarded as a burdensome medical recommendation but rather as a factor that can reduce the risk of cancer mortality and recurrence.
In 2020, 19.3 million new cancer cases were diagnosed, and almost 10 million deaths from cancer were recorded. Cancer patients may experience fatigue, depression, anxiety, reduced quality of life and sleep problems. Cancer treatments cause numerous side effects and have a negative impact on all body systems. Physical activity is important for cancer patients. The aim of this review is to analyse recent studies on the role of physical activity in cancer patients and emphasize its importance. The review included 36 papers published in English between 2017 and 2021. The findings from these studies show that physical activity decreases the severity of side effects of cancer treatment, reduces fatigue, improves quality of life, has a positive impact on mental health and improves aerobic fitness in cancer patients. Moreover, it reduces the risk of cancer recurrence and death. Physical activity is recommended for patients with any type of cancer and at all stages of treatment. The type of physical activity should depend on the condition of the individual patient. It is extremely difficult to determine what type, intensity and duration of physical activity is likely to have the greatest effect.
1. Introduction
In 2020, 19.3 million new cancer cases were diagnosed, and almost 10 million deaths from cancer were recorded [ 1 ]. Cancer patients may experience fatigue, depression, anxiety, reduced quality of life (QoL) and sleep problems [ 2 , 3 , 4 ].
Cancer treatments have many side effects. They exert a negative impact on: the cardiovascular system, the endocrine system, the digestive system, the immune system, the nervous system, the respiratory system, systemic symptoms such as fatigue, which can persist for many years after treatment, and lymphedema [ 5 ].
Physical activity (PA) is important for cancer patients. The World Health Organization distinguishes between two types of physical activity: aerobic physical activity and anaerobic physical activity. Physical activity can be classified according to intensity as: light-intensity physical activity, 1.5–3 metabolic equivalents of task (METs), which does not result in a significant increase in heart rate or respiratory rate (one example of light-intensity physical activity is slow walking); moderate-intensity physical activity, 3–6 METs; and vigorous-intensity physical activity, more than 6 METs [ 6 ].
PA improves QoL, increases aerobic fitness, has a positive influence on mental health and reduces the side effects of cancer treatment, fatigue and mortality in cancer patients [ 2 , 3 , 7 , 8 , 9 ]. The type of physical activity should depend on the condition of the individual patient. A patient’s response to a given physical activity stimulus may vary due to the side effects of treatment, demographic factors (age), mobility restrictions or comorbidities [ 10 ]. However, patients should undertake physical activity unless the disturbances are severe enough to prevent them from exercising [ 11 ]. Moreover, a patient’s ability to tolerate exercise may vary during a disease. This is caused by the variability in the intensity of the symptoms [ 5 ].
With patients facing a life-threatening illness, recommending additional physical activity may seem to be unnecessarily burdensome or too simplistic, as it would require an investment of time and energy from the patient [ 10 ].
Although there are many research papers about the benefits of physical activity in cancer patients, in practice combining PA with treatment is rare. In 2020, as many as 35.5% of the cancer survivors aged 18 years and older reported physical inactivity [ 12 ]. Only 7% of cancer patients perform adequate exercises [ 13 ]. This manuscript analyses the recent studies from the last five years on the role of physical activity in cancer patients under active treatment and cancer survivors and emphasize its importance. The review summarizes the results gathered from 36 articles and presents the influence of PA in cancer care for different types of tumour and patient groups.
The aim of the study is to present the impact of physical activity on cancer patients and cancer survivors in order to reach the largest possible group of readers, both among healthcare professionals and oncological patients.
2. Material and Methods
We conducted a search of articles in the PubMed, Web of Science and EBSCO Information Services using the following keywords: cancer care, physical activity, survivors, quality of life, QoL. The inclusion criteria were as follows: articles in English, publication between 2017 and 2022. A total of 971 records were initially identified. We removed 381 duplicates and excluded articles to which we had no access, articles in a language other than English and articles not directly related to the subject of the review ( n = 326). During the eligibility assessment, we also excluded articles concerning cancer prevention, since the aim of this review was to evaluate the role of physical activity in patients already diagnosed with cancer, as well as articles with insufficient data ( n = 228). Thirty-six articles were ultimately identified as eligible for inclusion. These publications were meta-analyses, systematic reviews and randomised controlled trials. The identification process of eligible studies is shown in Figure 1 . Patient-reported outcomes were assessed using Functional Assessment of Cancer Therapy Scale (FACT) with a subscale for fatigue (FACT-F) [ 8 ]. The FACT Measurement System consists of over 250 questions, and it measures health-related QoL in patients with cancer and other chronic diseases. Patients are asked to answer about 60 questions, based on the general version FACT-G, then new questions could be added to focus specifically on the problems of a given disease [ 14 , 15 , 16 ].

Identification of studies via databases.
We carried out a review of 36 systematic reviews, meta-analyses and randomised controlled trials concerning physical activity and cancer care. The studies included in the review investigated the effects of physical activity, as measured by a number of questionnaires assessing the type, frequency and duration of particular activities. We presented the results in Table 1 . This table compares the influence of physical activity on cancer patients: both survivors and patients under active oncology treatment. It shows results depending on: the type of cancer, type of intervention and its intensity and the frequency and duration of PA. The main findings in Table 1 describes if the cancer care with PA is superior to the usual care of these patients. This paper presents the findings from studies investigating the impact of physical activity on particular areas of life in cancer patients, such as: QoL, mental health, physical fitness, muscle strength and impact on body weight. The survey describes the impact of PA on side effects, fatigue, mortality, survival and recurrence of cancer. A summary of the key points is presented in Figure 2 .
Comparison of the influence of physical activity on cancer survivors.
PA—physical activity; CARE—Combined Aerobic and Resistance Exercise; DELCaP—Diet, Exercise, Lifestyle and Cancer Prognosis Study; PAGA—Physical Activity Guidelines for Americans; RPA—recreational physical activity; MET—metabolic equivalent of task (minutes/hours); PCa—prostate cancer; PCSM—prostate-cancer-specific mortality; CRF—cancer-related fatigue.

A graphical abstract summarizing the presented results.
3.1. Side Effects of Cancer Treatment
Chemotherapy and radiotherapy inhibit physical activity due to their side effects, such as severe fatigue, lack of energy as well as hair loss and mental health problems [ 17 ]. Chemotherapy is more likely than chemoradiotherapy to cause fatigue and reduce motivation to exercise. While chemoradiotherapy involves a more intensive treatment schedule, it is better tolerated by patients [ 18 ]. Physical activity has been shown to reduce the side effects of treatment and fatigue in cancer patients. The reduction was seen in those patients who, despite the side effects of treatment, underwent physical activity [ 7 ]. Studies report that regular PA reduces disease-specific side effects in patients with MM [ 19 , 20 ]. However, there is no evidence that physical activity mitigates the cardiotoxicity induced by cytostatic drugs [ 21 ].
3.2. Fatigue
One study included in the review found that regular physical activity combined with an appropriate diet (the patients completed 71% of the aerobic exercise sessions of 41 ± 25 min and 58% of the resistance exercise sessions planned as part of the intervention) reduced the fatigue resulting from intensive cancer treatment. The QoL was improved as well as lower limb muscle mass and endurance in breast cancer patients undergoing chemotherapy or radiotherapy. An important finding from the study was that the beneficial effect on QoL and fatigue persisted one year after the intervention [ 2 ]. Combined aerobic and resistance exercise has been found to reduce fatigue in patients with breast cancer [ 8 ]. In a study by Singh et al. [ 3 ], analysing the findings from 19 clinical trials, physical activity was observed to have a significant effect on fatigue in patients with colorectal cancer as compared with usual cancer care. Physical activity reduces the level of fatigue in cancer patients. The association between exercise and reduced fatigue has been demonstrated in patients with breast, prostate, colon and lung cancers [ 4 ]. Moreover, moderate-intensity physical activity has been found to reduce cancer-related fatigue in patients with colorectal cancer [ 22 ].
3.3. Quality of Life
Physical activity improves physical and social QoL and reduces anxiety and depression in cancer patients [ 2 , 3 ]. Unlike moderate to vigorous intensity physical activity, sedentary time negatively affects QoL and wellbeing of cancer patients [ 4 ]. Findings from one randomised controlled trial showed that aerobic and resistance exercise improves QoL by reducing depression, fatigue and physical deconditioning, which are the most common symptoms reported by breast cancer survivors [ 23 ]. Combined aerobic and resistance exercise performed during chemotherapy results in better longer-term QoL outcomes in breast and colorectal cancer patients, improving sleep quality, reducing anxiety and depression and having a positive impact on happiness [ 3 , 8 ]. Our review also included studies investigating the effects of physical activity on QoL in paediatric cancer patients with the use of the Paediatric Quality of Life Inventory. The studies showed that exercise interventions significantly improved QoL in the patients [ 24 , 25 , 26 , 27 ], even patients with haematological malignancies such as multiple myeloma [ 28 , 29 , 30 ]. Physical activity has also been shown to improve QoL and reduce anxiety and depression in ovarian cancer patients [ 27 ]. The findings from one study indicated that physical activity improves QoL in cancer patients despite the bothersome side effects of cancer treatment [ 7 ].
3.4. Mental Health
Physical activity has a positive impact on the mental health of cancer patients and adds positivity to their daily life [ 7 ]. One study showed that aerobic, resistance and flexibility exercises undertaken by prostate cancer patients with bone metastases for 3 months resulted in self-reported improvements in physical functioning, which had a positive influence on the mental health of the patients studied [ 31 ]. Another study found that an 8-week exercise intervention programme consisting of twice-per-week sessions of 60 min of resistance, flexibility and cardiorespiratory exercises performed by patients with different types of cancer improved the capability of the patients to express positive emotions, improved their functional capacity and had a positive influence on their mental health [ 32 ].
3.5. Physical Fitness, Muscle Strength, Impact on Body Weight
Studies have shown that exercise improves aerobic fitness and upper-body strength and reduces BMI and body fat in colorectal cancer patients. The results of a meta-analysis conducted by Singh et al. showed a greater effect for exercise interventions lasting over 12 weeks and interventions conducted during chemotherapy in patients with colorectal cancer [ 3 ]. Combined aerobic and resistance exercise has been found to be associated with superior upper and lower body muscle endurance in breast cancer patients [ 8 ].
3.6. Mortality and Longer Survival
There is an association between greater physical activity and reduced mortality in colorectal, breast and prostate cancer patients, with 40–50% risk reductions observed among individuals undertaking physical activity [ 33 ]. A study by Palesh et al. found that engaging in moderate physical activity was associated with longer survival and reduced hazard of cancer-related mortality in patients with advanced breast cancer [ 34 ]. In their study, Di Maso et al. noted that only vigorous physical activity had the advantage over inactivity in terms of reduced risks of cardiovascular and cancer mortality [ 35 ]. The cohort studies referred to by the authors reported approximately 40% reduction in mortality from prostate cancer in physically active men. Physical activity has also been found to reduce the risk of mortality in breast and colorectal cancer patients [ 36 ]. Barnard et al. [ 37 , 38 ] reported that intense physical activity reduces insulin resistance and insulin levels, with greater effects observed for a combination of intense physical activity and a low-fat, high-fibre diet. One study reported that breast cancer patients who met the minimum physical activity guidelines (PAGAs) had lower hazards of mortality compared with physically inactive patients (HR = 0.74, 95%, CI = 0.56 to 0.96; HR—hazard ratio; CI—confidence interval) [ 9 ]. A cohort study carried out by Wang et al. [ 39 ] that investigated the effects of recreational physical activity in patients with non-metastatic prostate cancer found that engaging in ≥17.5 MET-h/week of recreational physical activity, compared with 3.5 ≤ 8.75 MET-h/week of recreational physical activity, was associated with a 31% lower risk of prostate cancer-specific mortality (HR 0.69, CI 95%, p = 0.006), with no differences between the TNM stage of a tumour.
3.7. Recurrence
Combined aerobic and resistance exercise reduces the incidence of metabolic syndrome in cancer survivors, particularly breast cancer survivors. Metabolic syndrome is a risk factor for breast cancer recurrence [ 23 , 40 ]. A randomised controlled trial conducted among 100 breast cancer survivors, assigned either to exercise or usual care, showed an improvement in BMI and levels of circulating biomarkers, i.e., insulin, IGF-1, adiponectin and leptin, in the exercise group after the exercise intervention. An improvement in all metabolic syndrome variables persisted at the 3-month follow-up in the exercise group. Another study found that breast cancer patients meeting the minimum PAGAs both before and after their diagnosis had >50% reduced hazards of recurrence in comparison with patients not meeting this minimum at either time point. The study also found reduced hazards of recurrence for patients not meeting the minimum physical activity guidelines prior to diagnosis but who reported meeting the guidelines after their treatment (2-year follow-up) [ 9 ].
4. Discussion
A diagnosis of cancer has a profound impact on the life of the patient. The fear of cancer progression, metastases and side effects of systemic treatment affects the quality of life as well as the mental and physical health of cancer patients. The anxiety, depression and bothersome somatic symptoms, such as fatigue, nausea, vomiting and hair loss, experienced by cancer patients significantly inhibit their physical activity. The barriers to undertaking physical activity faced by cancer patients are a very complex issue. They are associated with a number of factors. The nature, type and extent of cancer; the presence of metastases; cancer treatment and its side effects; the patient’s attitude to their illness and their coping strategy, as well as social and family support, have an enormous impact on the patient’s motivation and quality of life and thus their attempt to undertake regular physical activity. Moreover, cancer patients are often concerned that physical activity could have a negative impact on their illness, especially patients with diagnosed multiple myeloma, whom have the highest physical and mental impairments and a low QoL [ 20 , 45 ]. Furthermore, they are less willing to include exercise in their standard cancer treatment because of the fear that it will make them feel worse and due to a lack of knowledge of the benefits of physical activity. However, numerous studies have reported that standard cancer care combined with physical activity is superior to standard pharmacological care. Physical activity improves the daily functioning of cancer patients, reduces fatigue, side effects of intensive treatments, anxiety and depression and improves muscle endurance and mass, thereby allowing patients to perform their daily activities without difficulty. Moreover, the findings from the studies showed that physical activity is associated with a reduced risk of cancer of the breast, colon, stomach and endometrium (10–20% risk reduction). The studies manifest that PA reduces the risk of mortality by 40–50% for breast, colon and prostate cancers [ 33 ].
Cancer-related fatigue is a serious and complex problem that affects the quality of life and daily activities of cancer patients. Although, based on the results in the studies [ 2 , 3 , 4 ], it can be concluded that there is a correlation between fatigue and a tendency to have less PA, it cannot be considered as an unequivocal cause of decline in PA. Nevertheless, fatigue has a major impact on the functioning of cancer patients, and clinicians should aim to reduce fatigue levels. Numerous studies have shown that physical activity is associated with a significant reduction in fatigue in breast, colorectal, ovarian and prostate cancer patients and multiple myeloma patients [ 3 , 8 , 19 , 22 , 27 , 31 , 43 ]. A systematic review by Cataldi et al. found that aerobic exercise is more effective than other treatments in reducing cancer-related fatigue. Their review suggested that exercise should be performed at least 2 days per week for at least 8 weeks in order to achieve the best results and showed that the effects of low- to medium-intensity exercise did not differ between women and men [ 46 ].
According to the National Comprehensive Cancer Network (NCCN) and the American College of Sports Medicine (ACSM) (2018), physical activity improves QoL and physiological and psychological fitness in cancer patients [ 46 ].
Chemotherapy and radiotherapy have a negative impact on many aspects of the lives of cancer patients, reducing their interest in physical activity and decreasing the effectiveness of exercise. The side effects of treatment are bothersome, especially for patients with MM, and their intensity is much higher than people with other haematological cancers [ 20 , 47 ]. One study revealed that cancer patients found it very difficult to engage in physical activity in public places due to the side effects of their treatment, such as hair loss, as well as the fear of overheating and infection [ 17 ]. However, physical activity has been shown to reduce the side effects of cancer treatment. Importantly, the beneficial effect of an intervention involving physical activity in reducing such side effects of cancer treatment as fatigue persisted one year after the intervention [ 2 ]. Chemotherapy not only affects QoL and causes bothersome side effects, but it also has a direct impact on the patient’s physiology. It reduces mitochondrial function by impairing oxidative phosphorylation, resulting in sarcopenia. Moreover, it may reduce lung function [ 43 , 48 ]. It has been shown that aerobic exercise mitigates the impact of cancer treatment on physiological functions. Physical activity helps increase blood flow, activates the sympathetic nervous system, regulates the endocrine system and mobilises cytotoxic lymphocytes and NK cells, thus exerting antitumor effects. Moreover, it reduces the levels of lactate, which are a factor in promoting tumour growth [ 49 , 50 ].
The results from a study by Cannioto et al. [ 9 ] showed that breast cancer patients meeting the minimum guidelines for physical activity both before and after diagnosis had >50% reduced hazards of cancer recurrence and mortality. These findings are of great importance for the development of clinical oncology, as they suggest that clinicians should advise their patients to increase their physical activity immediately after a diagnosis, which would result in significant benefits. However, the benefits of regular engagement in physical activity are not only directly associated with cancer care but also translate into a reduced risk of comorbidities, improved cardiovascular function and physical fitness and thus improved wellbeing and better daily functioning.
Physical activity can improve immune system function by mobilizing leukocytes with increased functional capacities into the circulation. It helps with the elimination of dysfunctional T cells and improves the abundance of some T cell populations. PA may have an impact on CTLA-4 (inhibitory immune checkpoint) and provide to better response to immunotherapy in cancer patients [ 51 , 52 ].
As for incorporating exercise into cancer care and improving treatment outcomes, it is crucial to understand the role of the intensity, dose and mode of exercise in cancer patients. It is necessary to consider the individual needs of patients, the type of cancer they have as well as their treatment and health history. It has been found that the sooner physical activity is incorporated into a patient’s treatment plan after diagnosis, the more effective it is [ 53 ]. High-intensity exercise is not contraindicated for all cancer patients. Therefore, patients should not be restricted to exercise of low intensity. High-intensity exercise should be avoided by those who suffer from nausea and vomiting as well as those who have a blood clot related to a peripheral central catheter [ 54 ]. Positive effects of exercise are observed with sessions of at least 20 min on most days of the week (accounting for planned days of rest and unplanned days of inactivity [ 55 ] due to one of the following barriers: fatigue, pain, lack of motivation [ 54 ]). Recommendations from the ACSM, the NCCN and the Clinical Oncology Society of Australia (COSA) recommend participation in 150 min of moderate-intensity aerobic exercise, 3–5 sessions per week, as well as resistance training at least 2 days per week as part of a programme lasting 6–12 weeks [ 56 , 57 , 58 ]. It is also recommended that exercise interventions should, at least initially, be supervised by exercise trainers or physical therapists [ 59 ]. Cataldi et al. recommend increasing the quantity and quality of exercise in cancer patients by monitoring all parameters during exercise sessions. Persons responsible for cancer care should take into consideration the outcomes of studies on this subject, so as to best plan the intensity and volume of exercise for their patients [ 46 ]. Similarly, the World Cancer Research Fund (WCRF) and the American Institute for Cancer Research (AICR) recommend participation in at least 150 min of moderate-intensity exercise per week, including strength training exercises at least twice a week [ 60 ].
A major challenge for cancer patients is the very initiation of regular physical activity. This, in turn, is influenced by their strategy for coping with the illness. Strategies for coping with cancer can be constructive (e.g., fighting spirit, positive redefinition) or destructive (e.g., helplessness, hopelessness, anxious preoccupation). Choosing a constructive strategy will help initiate and maintain physical activity, whereas destructive strategies are a major barrier to the initiation of physical activity. The helplessness and anxiety associated with a diagnosis of cancer result in the patient giving in to the illness. This reduces the patient’s QoL, making it more difficult for them to maintain motivation for engaging in physical activity [ 61 ]. Other barriers to participation in physical activity reported by cancer patients include: fatigue, business and the associated lack of time [ 62 ], severe pain and social and environmental barriers—lack of an exercise partner, lack of exercise facilities, fear of injury, lack of willpower, lack of interest, lack of equipment and lack of experience [ 63 , 64 ]. A relatively large proportion of patients (approximately 17.9%) cite the lack of access to information about how to exercise and what type of exercise would be best for them as the reason for which they do not engage in physical activity [ 64 ]. Another reason why patients do not initiate physical activity is their concern that a given type of exercise is contraindicated for them due to their illness.
It is very difficult for patients to maintain the appropriate intensity of exercise, especially if they suffer from chronic comorbidities or experience bothersome side effects of cancer treatment. The occurrence of comorbidities such as hypertension, kidney disease, diabetes, liver disease or obesity is increasing in cancer survivors [ 65 ]. Obesity, which occurs particularly in colorectal and breast cancer survivors, increases the risk of heart diseases and hypercholesterolemia and has an influence on survival [ 66 ]. Attempts are being made to determine what training intensity would be most beneficial for such patients in terms of improving their QoL and maintaining their motivation for participating in physical activity. All members of the cancer care team should promote physical activity at all stages of cancer treatment. Exercise should be individualised, planned and tailored to the individual patient and adjusted to a specific type of cancer, as it offers major potential for reducing cancer morbidity and mortality [ 67 ]. Studies show that flexible time for PA sessions, low-cost and close location to home met with highest interest from patients and better compliance [ 20 ]. The literature discussed above suggests that physical activity has a significant multidimensional impact on the quality of life of cancer patients and plays a major role in improving cancer care, treatment outcomes, increasing survival time and reducing mortality in cancer patients. Therefore, it is important that clinical recommendations focus on educating patients and attempting to change their attitude to exercise [ 62 ]. It is extremely hard to find the best way to encourage patients to start and maintain physical activities. Nevertheless, the healthcare providers should aim to encourage patients to exercise. An adequate education and demonstration PA advantages may be the first step to motivate them. Healthcare professionals should devote their time to patients, list the barriers the cancer patients and cancer survivors are struggling with and should try to find a solution to reduce the barriers and recommend an appropriate intervention. Psychological help could be invaluable. The results presented in this study may be helpful to convince patients that PA can offer them many benefits for their QoL, everyday functioning and survival time.
5. Limitations
The study has potential limitations. The first limitation is the selection of articles only in English, which introduces a language bias. The reason for this limitation is the insufficient knowledge of other languages to discuss the results in the study with appropriate precision. The second limitation is exclusion of the papers which the authors had no access to, which may potentially have impact on the results. The third limitation is the lack of an unequivocal way to encourage patients to start and maintain PA. Our purpose is to motivate the authors of future studies to search for an effective method encouraging patients to exercise.
6. Conclusions
Physical activity improves quality of life, increases survival and reduces mortality, fatigue, side effects of treatment and the risk of recurrence.
Physical activity should be selected individually, depending on the type of cancer, treatment and comorbidities.
It is extremely difficult to determine what type, intensity and duration of physical activity is likely to have the greatest effect.
Funding Statement
This research received no external funding.

Author Contributions
W.M. wrote the manuscript; A.P. reviewed and drafted the manuscript; A.S.-C. analysed the data and supervised the manuscript; M.C. participated in supervision and project administration. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 25 March 2020
How cancer genomics is transforming diagnosis and treatment
- Bianca Nogrady 0
Bianca Nogrady is a freelance science writer in Sydney, Australia.
You can also search for this author in PubMed Google Scholar
DNA sequencing allows oncologists to characterize tumours on the basis of genetic mutations. Credit: KTSDESIGN/SPL
When cancer was first described by the ancient Greek physician Hippocrates, he identified just two forms: the non-ulcer-forming carcinos and the ulcer-forming carcinoma. In the late nineteenth century, physicians found, with the help of the microscope, that cancer had multiple cellular forms.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 579 , S10-S11 (2020)
doi: https://doi.org/10.1038/d41586-020-00845-4
This article is part of Nature Outlook: Cancer diagnosis , an editorially independent supplement produced with the financial support of third parties. About this content .
Schmitz, R. et al. N. Engl. J. Med. 378 , 1396–1407 (2018).
Article PubMed Google Scholar
van der Velden, D. L. et al. Nature 574 , 127–131 (2019).
Berland, L. et al. J. Thorac. Dis. 11 , S71–S80 (2019).
Download references
Related Articles

- Health care

AI traces mysterious metastatic cancers to their source
News 17 APR 24

Biological age surges in survivors of childhood cancer
Research Highlight 11 APR 24
How to supercharge cancer-fighting cells: give them stem-cell skills
News 10 APR 24

Dozens of genes are linked to post-traumatic stress disorder
Research Highlight 22 APR 24

Cell-type-resolved mosaicism reveals clonal dynamics of the human forebrain
Article 10 APR 24

AI can help to tailor drugs for Africa — but Africans should lead the way
Comment 09 APR 24
More work is needed to take on the rural wastewater challenge
Correspondence 23 APR 24

What toilets can reveal about COVID, cancer and other health threats
News Feature 17 APR 24

Smoking bans are coming: what does the evidence say?
Postdoctoral Position - Synthetic Cell/Living Cell Spheroids for Interactive Biomaterials
Co-assembly of artificial cells and living cells to make co-spheroid structures and study their interactive behavior for biomaterials applications.
Mainz, Rheinland-Pfalz (DE)
University of Mainz
2024 Recruitment notice Shenzhen Institute of Synthetic Biology: Shenzhen, China
The wide-ranging expertise drawing from technical, engineering or science professions...
Shenzhen,China
Shenzhen Institute of Synthetic Biology
Recruitment of Global Talent at the Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
The Institute of Zoology (IOZ), Chinese Academy of Sciences (CAS), is seeking global talents around the world.
Beijing, China
Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
Research Associate - Brain Cancer
Houston, Texas (US)
Baylor College of Medicine (BCM)
Senior Manager, Animal Care
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Cancer treatment research: Innovative insights towards a cure

In this guide
- Importance of studying tumors and clinical trial designs
The importance of cancer treatment research
What role do physicians play in cancer research studies.
- The latest technologies in cancer cell treatment research
- Future cell and gene therapies
How to keep up with cancer treatment research?
Importance of studying tumors and clinical trial designs .
Cancer remains one of the leading causes of death globally 1 . In the past couple of decades cancer research has received a lot of attention. Researchers have dedicated time and effort towards studies on causes, disease progression and pathophysiology, detection methods, treatments and palliative care. While some studies have led nowhere, some have been impactful and yielded innovative breakthroughs. For instance, studies have led to a deeper understanding of tumor progression and this has been helpful in designing more precise therapies.
Continuous efforts are still required for better cancer prevention, diagnosis, and cure. Physicians definitely play a significant role in cancer research study. According to a Sermo poll, 63% of physicians had participated in a cancer research study and 69% of physicians indicated interest in participating or conducting a cancer research study. Perhaps, you are also interested in contributing to malignant tumor studies but not sure what role best suits you as a physician.
This article focuses on how physicians can participate, keep up with advancements, and the future of cancer cell investigation.

Cancer is a complex disease and has a huge burden in the United states and globally. Its incidence has been projected to increase in the near future. By 2040, the number of new cases per year is estimated to increase to 29.5 million and the number of cancer-related deaths to 16.4 million across the globe 2 .
To combat the devastating effect of growing cancer rates, the study of cancer and its treatment is important. In the last decade, we have seen ground-breaking advances that have revolutionized patient outcomes and survival rates. As researchers continuously study genetic material, cell division, and cell signals, better and more innovative treatments can be designed to fight cancer.
Cancer research is also important for improvements in diagnosis and detection methods. Conventional tumor diagnosis involves the analysis of normal tissue, disease tissue, and cytology specimens obtained through a tumor biopsy procedure to examine physical appearance and to determine whether a tumor is malignant 3 . Advancements in molecular medicine have allowed more in depth analysis of tumor markers in cancer studies.
Sophisticated technologies in ultrastructure, light microscopy, enzyme histochemistry, immunohistochemistry and molecular diagnostics have revolutionized how cancer is detected and characterized 4 . Researchers have used these technologies and have obtained deeper understanding of cancer cells and their uncontrolled proliferation.
Cancer research study can also help to identify the cause and risk factors of certain cancers. The underlying causes of many cancers remain a puzzle but thanks to research certain causes and risk factors have been established. Over the years, the understanding of cancer and its causes have improved. Several studies have revealed certain carcinogens like specific chemicals and viruses. With continuous investigation, better steps towards prevention can be taken.
Another reason why researching malignant tumors matter is to improve the management of cancer. This disease is often debilitating with severe symptoms, treatment side effects and secondary effects such as poor appetite and mental health disruptions. Better supportive and palliative care methods are needed to help patients navigate the course of the disease better. The disease can also present a huge burden on a patient’s loved ones and caretaker. There is still a need to find ways that cancer and its treatment can have less consequences for patients and their loved ones.

The most obvious role of physicians in cancer care is in diagnosis, treatment and care of patients. However, we are currently in very interesting times in cancer research that requires multidisciplinary collaborations to arrive at more innovative breakthroughs. Besides physicians’ active contribution to the diagnosis and comprehensive management of patients, physicians can participate in different capacities to support cancer research. Here are a few roles physicians and oncologists can participate in to deliver meaningful impact.
Laboratory/bench research
For physicians who enjoy discovery, they can channel their training and expertise towards significant laboratory work for cancer treatment research. Such physicians are not only essential to discovery and pre-clinical studies but also play a significant role in translational research.
Many physician scientists have contributed to interesting cancer discoveries and developments such as retroviral oncogenes and gene-targeted therapies 5 . Studying healthy cells, stem cells, DNA repairs, specific antigens, chemotherapy and other therapy efficacy and side effects all move the needle forward.
Translational research
Translational medicine involves interpreting and integrating new knowledge obtained from research into clinical practice and in the same way using observations from clinical practice to improve pre-clinical research 6 . Its bidirectional approach is necessary for development of disease-targeted therapies and for improving standard treatment efficacy.
Physicians lie at the heart of clinical investigation and clinical practice. Consequently, they are in the best position to drive translational research to promote innovation of new therapies.
Shaping and informing clinical trials
A very essential part of drug development and cancer treatment research is a clinical trial. Clinical trials are most often conducted in phases- Phase 1, Phase 2 and Phase 3. Doctors, particularly those with a specialty in oncology, can help in developing clinical trial protocols. Doctors, because of their experience and training, can help define the end-point for clinical studies and other solid tumor study designs. They can also help define the right patient population to be included in a clinical trial based on age, damaged cells, genes, tumor spread, severity of disease, and other prognostic factors.
Defining and modifying treatment recommendations
With novel breakthroughs for the treatment of cancer into clinical practice, there is a need to update the standards of care to more effective options. To bolster DNA repair, help the body work properly, and beat most cancers, it often requires combining therapies. Additionally, doctors must also consider co-existing diseases and minimize side effects.
Arriving at these recommendations requires collective research effort and collaborations of doctors. Doctors have specialized training and experience with patient-level care that enables them to make sound decisions about the most effective and safe recommendations for different patient groups regarding the person’s cancer .

Pass down clinical knowledge to young doctors and medical students
Cancer research is continuously evolving and its rapid advancement is dependent on the understanding of previous discoveries and developments. Knowledge management is a very important aspect of research and training the next generation of doctors and researchers is essential. Physicians can advance cancer investigation by educating young doctors and medical students about the latest developments in diagnosis and management.
Participate in medical research surveys
For physicians who want to contribute to cancer investigation but in a more flexible manner, medical research surveys are an excellent option. Medical industry for physicians are commonly paid online surveys . By participating in surveys, physicians with a specialty in oncology can give real-world insights from their experience with patients. These insights are valuable to pharmaceutical companies and contribute to cancer treatment analysis and development.
The latest technologies in cancer cell treatment research
The way cancer is treated has changed over the years, offering hope to patients everywhere. Advances in tech to better understand normal cell and cancer cell growth are promising. The survival rate was 49% in the mid-1970s and has since increased to 68%. Five-year survival rates have been consistently rising for even longer.
Today, we have seen breakthrough treatments that have revolutionized health care and outcomes – thanks to new technology. Here are some of the recent technology advancements in cancer treatment research.

According to a Sermo poll, 46% of Sermo physicians see CRISPR as the most important cancer research treatment technology. With CRISPR, gene editing has never been better. This sophisticated technology allows scientists to access DNA and alter pieces of DNA by deleting and/or inserting parts of the DNA in a cell. CRISPR technology is used today in cancer research and has the potential to transform cancer research and treatments. CRISPR has been used in studies on cancer for various purposes including modifying immune cells to boost the immune system to kill cancer cells. Detecting specific antigens, protein signals, and target cancer cells 7 .
Telehealth is a growing concept that allows patients access cancer treatment and care remotely. With the COVID-19 pandemic, this has become even more popular and is considered safer and more convenient for patients and doctors. Telehealth platforms have also been used for health monitoring, video consultations and in-home therapies.
Artificial intelligence
Artificial intelligence and machine learning is no new concept in our world today. It is used by many industries to improve daily activities such as online shopping, web search, cybersecurity and social media interaction. In recent times, it has been used in tumor studies to improve diagnosis, predictions and care. By inputting AI with imaging data and population-based records, researchers can analyze diagnostic results faster. They can also derive more precise predictions of cancer incidence as well as organs and cells at risk.
Cryo-electron microscopy
Continuous developments in microscope design have given birth to Cryo-EM. Cryo-EM generates high resolution images of tissue sections, cells and protein molecules. Never before could scientists visualize these molecules at such high resolutions. This allows them to analyze biological structures better and obtain a more complete understanding of how cancer progresses in the body and how cancer cells respond to chemotherapy, surgery, immunotherapy, and other first treatment options. Cryo-EM is a valuable tool in cancer research studies.
Robotic surgery
Years ago, the possibility of this happening was far-fetched but thanks to technological advancements robotic surgeries are here to stay. The major advantage of robotic surgery is that it involves less pain and less blood loss. They allow for shorter hospital stays and faster recovery. Furthermore, with the assistance of a robot, doctors can carry out surgical procedures with more precision, flexibility and control.

Future cell and gene therapies
The cancer care community worldwide has celebrated a lot of revolutionary treatments in the last few decades. Innovative therapies such as CAR-T-cell therapy, precision medicines and radiation therapy have been instrumental to improving survival outcomes significantly.
But there is still a need for new treatments especially for high risk and advanced cancers that are difficult to treat. Patients and caretakers, whose voices should be considered in cancer research, also report how much they desire cancer drugs with less side effects. Hence, drugs in the future should focus on safe and efficacy.
In the next couple of years, cancer treatment research will prioritize precision medicine. The medical community has witnessed how targeted therapies and immunotherapies have transformed cancer treatments. There is a buzzing excitement of the potential of more individualized therapies. With precision medicine, cancer treatments can be tailored to match each person’s genetic composition and history. These therapies can be more effective with less side effects than conventional treatment options 8 .
Future studies will also delve deeper into cell-based therapy, an immunotherapy strategy that positions the body’s immune cells to recognize antigen signals and attack dangeours tumors. This treatment method, also known as chimeric antigen receptor therapy, or CAR therapy, has demonstrated efficacy in treatment of blood cancers and so far six CAR T-cell therapies have been approved by the Food and Drug Administration 9 . This new paradigm of treatments can create more therapeutic options for other types of cancer including solid tumors.
Other new approaches that offer promise include drug repurposing. Common generics which are used to treat other diseases are being researched to study their effectiveness in preventing cancer. A good example is Aspirin, an anti-inflammatory drug, which has been evaluated in a number of studies for reducing the likelihood of cancer 10 . Researchers have assessed other drugs like antibiotics, non-steroidal anti-inflammatory, cardiovascular, antidepressants, and antipsychotic drugs for their anti-tumoural effect 11
Doctors who have a keen interest in oncology should keep abreast with these innovative treatment options and studies so they can give patients the best evidence-based cost effective options.
Cancer treatment research evolves very quickly and because of this, the knowledge a doctor gained during training may be outdated for today’s practice. With the influx of innovative therapies and the advancement of sophisticated technologies used in cancer study, there is a lot more to choose from than what was in the books during medical training.
Mind you, studies and clinical trials never stop. The deluge of novel treatments and tools present both an opportunity and a challenge to the medical oncology community. Doctors have to continuously stay up to date with the changes and evolution of cancer treatments so they can ensure patients get the best outcomes possible.
However, what is not commonly discussed is how doctors can continuously stay in the loop of the changes. Quite frankly, it may be difficult for physicians to stay up to date with all the changes in diagnostic methods and treatments as well as with updates in causes, risk factors and prevention.
The expectation for doctors to incorporate the rapid evolution of knowledge feels insurmountable. 73% of Sermo physicians surveyed report looking up cancer treatment research once a week and 52% of Sermo physicians refer to Medical journals/publications to find resources on cancer treatment research. Nonetheless, relying solely on reading published articles may not be the most effective method. It requires a lot of time skill in refining search on popular search engines.
More effective strategies are needed for doctors to stay updated and to disseminate information. Here are some recommendations:
Leverage the power of community
Physician community groups with common interests are a shortcut to learning what’s most important in very limited time. In such groups, physicians participate in virtual tumor boards , discuss new therapies and studies and share lessons. Sermo is a leading oncology community. You can engage with more than 1 million physicians across 150 countries. Sermo offers a unique physician-first online community that allows clinicians to communicate about critical issues to them and their patients.
If you would like to learn more about cancer treatment research and how physicians can contribute to cancer research, sign up on Sermo today for more.
Leverage on strong partnerships with bigger bodies
No man is an island they say and in cancer research this statement is even more meaningful. Bigger cancer centers and cancer-dedicated research bodies are excellent educational pools. Such centers and national institutes have more expertise than small centers and they also disseminate research findings on their platforms frequently. Some examples are National Cancer Institute , American Cancer Society, the World Health Organization’s International Agency for Research on Cancer (IARC) and the Association of Community Cancer Centers .
Another benefit of doctors partnering with such organizations is that they can easily learn about new and upcoming clinical trials. This way they can easily recognize new treatment options that may benefit their patients and enroll them in clinical studies.
Be proactive about knowledge management – hire someone!
Doctors can learn a thing or two from the legal profession and hire someone to do the research on new therapies and report succinctly to them as needed. Lawyers hire paralegals who carry out research for upcoming cases and considering the volume of information available, it makes sense to adopt this in medical oncology.
This person should have some medical training and excellent research and communication skills. By delegating this responsibility, doctors can focus more on patient satisfaction and outcomes. With this support, they can make better decisions based on recent findings in a timely and effective manner.
Use artificial intelligence
Earlier, artificial intelligence was discussed as an advanced technology that can revolutionize cancer research. Artificial intelligence can also be used in developing smarter medical information systems. Applying machine learning to AI systems to clinical knowledge improves information management and helps doctors synthesize and organize medical information faster and better.
An example of an AI system that helps oncologists stay up to date with advancements in cancer research is the MD Anderson Oncology Expert Advisor powered by IBM Watson. The Oncology Expert Advisor pools clinical data from a diverse patient population, shares updated knowledge on treatments and matches patients with clinical trials. The most attractive feature of this virtual advisor to oncologists is how it organizes and lays out literature including treatment guidelines and research findings relevant to each patient’s case. By doing this, the AI supplies physicians with the best evidence-based treatment options and supports the consideration of new treatments for improved patient outcomes.
Conferences
Attending conferences is also a way to keep up with cancer breakthroughs. Conferences like ASCO and ESMO bring together physicians, researchers, industry representatives and patient advocates to share advances in cancer treatment research amongst other cancer-related topics. It also provides an excellent avenue to network, share ideas and patient findings.
Cancer treatment research is evolving and doing so quickly. The last couple of decades has witnessed the sprout of revolutionary advancements in cancer diagnosis and treatment. But there is still a lot to do–especially as cancer cases are expected to increase. So then, all hands on deck – including physicians.
Physicians are faced with the challenge of managing cancer patients, contributing to cancer research and staying up to date with constant changes It can be really demanding but with these tips, one can forge a path forward.
Don’t go it alone. Take advantage of a community of physicians that shares experiences and actionable insights by joining Sermo. To get started, create your free Sermo account now .
- Bhutani et al
- Bhardwaj et al, 2011
- Ishida et al, 2016
- Rodrigues et al, 2022
More physician resources
A complete guide to paid physician surveys

10 best medical specialties for physicians needing a change of pace

Identifying and navigating ethical issues in healthcare
Chemotherapy to Treat Cancer

Chemotherapy works against cancer by killing fast-growing cancer cells.
Chemotherapy (also called chemo) is a type of cancer treatment that uses drugs to kill cancer cells .
How chemotherapy works against cancer
Chemotherapy works by stopping or slowing the growth of cancer cells, which grow and divide quickly. Chemotherapy is used for two reasons:
- Treat cancer: Chemotherapy can be used to cure cancer, lessen the chance it will return, or stop or slow its growth.
- Ease cancer symptoms: Chemotherapy can be used to shrink tumors that are causing pain and other problems.
Which types of cancer does chemotherapy treat
Chemotherapy is used to treat many types of cancer. For some people, chemotherapy may be the only treatment you receive. But most often, you will have chemotherapy with other cancer treatments. The types of treatment that you need depend on the type of cancer you have, if it has spread and where, and if you have other health problems. To learn more about treatment for your cancer, see the PDQ® cancer treatment summaries for adult and childhood cancers .
How chemotherapy is used with other cancer treatments
When used with other treatments, chemotherapy can
- make a tumor smaller before surgery or radiation therapy (called neoadjuvant chemotherapy)
- destroy cancer cells that may remain after surgery or radiation therapy (called adjuvant chemotherapy )
- help other treatments work better
- kill cancer cells that have returned or spread to other parts of your body
Chemotherapy can cause side effects
Chemotherapy not only kills fast-growing cancer cells, but also kills or slows the growth of healthy cells that grow and divide quickly. Examples are cells that line your mouth and intestines and those that cause your hair to grow. Damage to healthy cells may cause side effects, such as mouth sores, nausea, and hair loss. Side effects often get better or go away after you have finished chemotherapy.
The most common side effect is fatigue, which is feeling exhausted and worn out. You can prepare for fatigue by
- asking someone to drive you to and from chemotherapy
- planning time to rest on the day of and day after chemotherapy
- asking for help with meals and childcare on the day of and at least one day after chemotherapy
There are many ways you can help manage chemotherapy side effects. For more information, see the section on side effects .
How much chemotherapy costs
The cost of chemotherapy depends on
- the types and doses of chemotherapy used
- how long and how often chemotherapy is given
- whether you get chemotherapy at home, in a clinic or office, or during a hospital stay
- the part of the country where you live
Talk with your health insurance company about what services it will pay for. Most insurance plans pay for chemotherapy. To learn more, talk with the business office where you go for treatment.
If you need financial assistance, there are organizations that may be able to help. To find such organizations, go to the National Cancer Institute database Organizations that Offer Support Services and search for "financial assistance." Or call toll-free 1-800-4-CANCER (1-800-422-6237) to ask for information on organizations that may help.
What to expect when receiving chemotherapy
How chemotherapy is given.
Chemotherapy may be given in many ways. Some common ways include
- oral: comes in pills, capsules, or liquids that you swallow
- intravenous (IV): goes directly into a vein
- injection: given by a shot in a muscle in your arm, thigh, or hip, or right under the skin in the fatty part of your arm, leg, or belly
- intrathecal: injected into the space between the layers of tissue that cover the brain and spinal cord
- intraperitoneal (IP): goes directly into the peritoneal cavity, which is the area in your body that contains organs such as your intestines, stomach, and liver
- intra-arterial (IA): injected directly into the artery that leads to the cancer
- topical: comes in a cream that you rub onto your skin
Of all the methods mentioned above, chemotherapy is most often given with an IV, through a thin needle that is placed in a vein on your hand or lower arm. Your nurse will put the needle in at the start of each treatment and remove it when treatment is over. IV chemotherapy may also be given through catheters or ports, sometimes with the help of a pump.
- Catheter: A catheter is a thin, soft tube. A doctor or nurse places one end of the catheter in a large vein, often in your chest area. The other end of the catheter stays outside your body. Most catheters stay in place until you have finished your chemotherapy treatments. Catheters can also be used to give you other drugs and to draw blood. Be sure to watch for signs of infection around your catheter. See the section about infection for more information.
- Port: A port is a small, round disc that is placed under your skin during minor surgery. A surgeon puts it in place before you begin your course of treatment, and it remains there until you have finished. A catheter connects the port to a large vein, most often in your chest. Your nurse can insert a needle into your port to give you chemotherapy or draw blood. This needle can be left in place for chemotherapy treatments that are given for longer than one day. Be sure to watch for signs of infection around your port. See the section about infection for more information.
- Pump: Pumps are often attached to catheters or ports. They control how much and how fast chemotherapy goes into a catheter or port, allowing you to receive your chemotherapy outside of the hospital. Pumps can be internal or external. External pumps remain outside your body. Internal pumps are placed under your skin during surgery.
How your doctor decides which chemotherapy drugs to give you
There are many different chemotherapy drugs. Which ones are included in your treatment plan depends mostly on
- the type of cancer you have and how advanced it is
- whether you have had chemotherapy before
- whether you have other health problems, such as diabetes or heart disease
Where you go for chemotherapy
You may receive chemotherapy during a hospital stay, at home, or as an outpatient at a doctor’s office, clinic, or hospital. Outpatient means you do not stay overnight. No matter where you go for chemotherapy, your doctor and nurse will watch for side effects and help you manage them. For more information on side effects and how to manage them, see the section on side effects .
How often you receive chemotherapy
Treatment schedules for chemotherapy vary widely. How often and how long you get chemotherapy depends on
- your type of cancer and how advanced it is
- cure your cancer
- control cancer's growth
- ease symptoms
- the type of chemotherapy you are getting
- how your body responds to the chemotherapy
You may receive chemotherapy in cycles. A cycle is a period of chemotherapy treatment followed by a period of rest. For instance, you might receive chemotherapy every day for 1 week followed by 3 weeks with no chemotherapy. These 4 weeks make up one cycle. The rest period gives your body a chance to recover and build new healthy cells.
Missing a chemotherapy treatment
It is best not to skip a chemotherapy treatment. But, sometimes your doctor may change your chemotherapy schedule if you are having certain side effects. If this happens, your doctor or nurse will explain what to do and when to start treatment again.
How chemotherapy may affect you
Chemotherapy affects people in different ways. How you feel depends on
- the dose of chemotherapy you are getting
- your type of cancer
- how advanced your cancer is
- how healthy you are before treatment
Since everyone is different and people respond to chemotherapy in different ways, your doctor and nurses cannot know for sure how you will feel during chemotherapy.
How will I know if chemotherapy is working?
You will see your doctor often. During these visits, they will ask you how you feel, do a physical exam , and order medical tests and scans . Tests might include blood tests. Scans might include MRI , CT , or PET scans .
You cannot tell if chemotherapy is working based on its side effects. Some people think that severe side effects mean that chemotherapy is working well, or that no side effects mean that chemotherapy is not working. The truth is that side effects have nothing to do with how well chemotherapy is fighting your cancer.
Special diet needs while on chemotherapy
Chemotherapy can damage the healthy cells that line your mouth and intestines and cause eating problems. Tell your doctor or nurse if you have trouble eating while you are receiving chemotherapy. You might also find it helpful to speak with a dietitian . For more information about coping with eating problems see the booklet Eating Hints or the section on side effects .
Working during chemotherapy
Many people can work during chemotherapy, as long as they match their work schedule to how they feel. Whether or not you can work may depend on what kind of job you have. If your job allows, you may want to see if you can work part-time or from home on days you do not feel well.
Many employers are required by law to change your work schedule to meet your needs during cancer treatment. Talk with your employer about ways to adjust your work during chemotherapy. You can learn more about these laws by talking with a social worker .
Researchers develop a new way to safely boost immune cells to fight cancer
Researchers in Virginia Tech’s College of Engineering have developed a new cancer immunotherapy to localize cancer-killing cytokines in tumors to improve treatment effectiveness.
- Hailey Wade
19 Apr 2024
- Share on Facebook
- Share on Twitter
- Copy address link to clipboard
Cancer is the monster of our society. Last year alone, more than 600,000 people in the United States died from cancer, according to the American Cancer Society . The relentless pursuit of understanding this complex disease has shaped medical progress on developing treatment procedures that are less invasive while still highly effective.
Immunotherapy is on the rise as a possible solution. Immunotherapy involves harnessing the power of the body’s immune system to fight against cancer cells. Researchers in the College of Engineering have found a way to revamp a treatment procedure into a groundbreaking practice.
Rong Tong , associate professor in chemical engineering , has teamed up with Wenjun "Rebecca" Cai , associate professor in materials science and engineering , to explore a cancer immunotherapy treatment that has long been of interest to researchers. In their newly published article in the journal Science Advances , Tong and Cai detailed their approach, which involves activating the immune cells in the body and reprogramming them to attack and destroy the cancer cells. This therapeutic method is frequently implemented with the protein cytokine. Cytokines are small protein molecules that act as intercellular biochemical messengers and are released by the body's immune cells to coordinate their response.
“Cytokines are potent and highly effective at stimulating the immune cells to eliminate cancer cells,” Tong said. “The problem is they’re so potent that if they roam freely throughout the body, they’ll activate every immune cell they encounter, which can cause an overactive immune response and potentially fatal side effects.”
Tong and Cai, in collaboration with chemical engineering and materials science and engineering graduate students, have developed an innovative approach to employ cytokine proteins as a potential immunotherapy treatment. Unlike previous methods, their technique ensures that the immune cell stimulating cytokines effectively localize within the tumors for weeks while preserving the cytokine’s structure and reactivity levels.
Combining forces to take down cancer cells
Current cancer treatments, such as chemotherapy, cannot distinguish between healthy cells and cancer cells. When someone with cancer is treated with chemotherapy, the treatment attacks all of the cells in their body, which can lead to side effects such as hair loss and fatigue. Stimulating the body’s immune system to attack tumors is a promising alternative to treat cancer. The delivery of cytokines can jump-start immune cells in the tumor, but overstimulating healthy cells can cause severe side effects.
“Scientists determined a while ago that cytokines can be used to activate and fight against tumors, but they didn’t know how to localize them inside the tumor while not exposing toxicity to the rest of the body,” said Tong. “Chemical engineers can look at this from an engineering approach and use their knowledge to help refine and elevate the effectiveness of the cytokines so they can work inside the body effectively.”
The research team’s goal is to find a balance between killing cancer cells in the body while sparing healthy cells.
To accomplish this goal, Tong and his students used their expertise to create specialized particles with distinctive sizes that help determine where the drug is going. These microparticles are designed to stay within the tumor environment after being injected into the body. Cai and her students worked on measuring these particles’ surface properties.
“In the field of materials science and engineering, we study the surface chemistry and mechanical behavior of materials, such as the specialized particle created for this project,” Cai said. “Surface engineering and characterization, along with particle size, play important roles in controlled drug delivery, ensuring prolonged drug presence and sustained therapeutic effectiveness.”
To ensure successful drug delivery, Tong and his chemical engineering students designed a novel strategy that:
- Anchors cytokines to these new microparticles, limiting the harm of cytokines to healthy cells
- Allows the newly particle-anchored cytokines to jump-start immune systems and recruit immune cells to attack cancer cells
“Our strategy not only minimizes cytokine-induced harm to healthy cells, but also prolongs cytokine retention within the tumor,” Tong said. “This helps facilitate the recruitment of immune cells for targeted tumor attack.”
The next step in the process involves combining the new, localized cytokine therapy method with commercially available, Food and Drug Administration (FDA)-approved checkpoint blockade antibodies, which reactivate the tumor immune cells that have been silenced so they can fight back the cancer cells.
“When there is a tumor inside the body, the body’s immune cells are being deactivated by the cancer cells,” Tong explained. “The FDA-approved checkpoint blocking antibody helps “take off the brakes” that tumors put on immune cells, while the cytokine molecules “step on the gas” to jump-start the immune system and get an immune cell army to fight cancer cells. These two approaches work together to activate immune cells.”
Combining the checkpoint antibodies with the particle-anchored cytokine proved to successfully eliminate many tumors in their study.
Engineering an impact on cancer treatment
Team members hope their impact on immunotherapy treatment is part of a greater movement toward cancer treatment approaches that are harmless to healthy cells. The new approach of attaching cytokines to particles also could be used in the future to deliver other types of immunostimulatory drugs, according to the team.
“Researchers are still looking for safer and more effective cancer treatments,” said Tong. “This motivation is what drives us to develop new technologies in the field. The whole class of drugs that are employed to jump-start the immune system to fight cancer cells has largely not yet succeeded. Our goal is to create novel solutions that allow researchers to test these drugs with existing FDA-approved therapeutics, ensuring both safety and enhanced efficacy.”
Cai said the nature of cancer treatment research requires expertise across engineering disciplines.
“I view this project as a perfect marriage between chemical engineering and materials science,” Cai said. “The former focuses on the synthesis and drug delivery part, the latter on applying advanced materials characterization. This collaboration not only accelerates immunotherapy research, but also has the ability to transform cancer treatment.”
Chelsea Seeber
540-231-2108
- Cancer Research
- Chemical Engineering
- College of Engineering
- Good Health and Well-Being
- Materials Science and Engineering
- One Health Frontier
- Virginia Tech Global Distinction
Related Content

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

Innovation in lung cancer screening, treatment
Share this:.
By Jason Howland
Lung cancer is the largest cancer killer of adult men and women worldwide. One of the reasons is that by the time symptoms develop, the cancer is too advanced for a cure.
The goal of lung cancer screening is to detect cancer at an earlier stage and save more lives. Smoking is the No. 1 cause of lung cancer, and it's recommended that anyone over 55 who has a significant history of smoking, even if they no longer smoke, should be screened.
Lung cancer screening, for those eligible, should be done annually, and it involves a low-dose CT scan of the lungs. Janani Reisenauer, M.D. , a thoracic surgeon and interventional pulmonologist, says Mayo Clinic is one of the pioneers in using new technology to fight the disease.
Watch this video to hear Dr. Reisenauer discuss innovation in lung cancer screening and treatment:
A lung nodule or lesion is an abnormality revealed on a CT scan that looks like a cancer. And to find out if it is cancer, doctors may recommend a technique called bronchoscopy .
"Very similar to having a colonoscopy performed where somebody is holding a scope. They're twisting the dials on that scope as they're maneuvering that scope through your airway or through your intestines for example," says Dr. Reisenauer.
That's a traditional manual bronchoscopy. Dr. Reisenauer says Mayo Clinic is one of only a handful of medical centers approved by the Food and Drug Administration to use robotic bronchoscopy.
"I would think about robotic bronchoscopy as a remote-controlled car. It doesn't go anywhere without you driving it and telling it where to go. But rather than me holding a scope that's maneuvered through a patient, the scope is docked to a robotic instrument," says Dr. Reisenauer.
Offering more precision, flexibility and control than a traditional bronchoscopy. She says it improves the ability to not only diagnose lung cancer, but now, in some cases, treat it.
"Mayo Clinic is participating in many cancer trials now, where we are treating lung nodules with a variety of ablative mechanisms. So we're either using extreme heat or cold, or even in some cases electricity. Or viruses injecting into tumors to try to reduce tumor burden or kill tumors," says Dr. Reisenauer.
Learn more about lung cancer .
Also, read these articles:
- Mayo Clinic expert on the importance of lung cancer screening
- Reducing your risk of lung cancer
- Does smoking marijuana increase lung cancer risk?
- Era of hope for patients with lung cancer
A version of this article was originally published on the Mayo Clinic News Network .
Related Posts

Dr. Jesse Bracamonte discusses the importance of cancer screenings as well as preventive screenings for diabetes and cardiovascular disease.

Dr. Janani Reisenauer talks about the importance of lung cancer screening for people with a substantial smoking history.

Learn about lung cancer risk factors and what you can do to reduce your risk of developing the disease.
There’s a powerful story behind every headline at Ohio State Health & Discovery. As one of the largest academic health centers and health sciences campuses in the nation, we are uniquely positioned with renowned experts covering all aspects of health, wellness, science, research and education. Ohio State Health & Discovery brings this expertise together to deliver today’s most important health news and the deeper story behind the most powerful topics that affect the health of people, animals, society and the world. Like the science and discovery news you find here? You can support more innovations fueling advances across medicine, science, health and wellness by giving today.
BROUGHT TO YOU BY
- The Ohio State University
- College of Dentistry
- College of Medicine
- College of Nursing
- College of Optometry
- College of Pharmacy
- College of Public Health
- College of Veterinary Medicine
- Ohio State Wexner Medical Center
- Ohio State's Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute
Subscribe. The latest from Ohio State Health & Discovery delivered right to your inbox.
How tumor ablation is curing some cancer patients with less pain and decreased risk
Vascular and Interventional Radiologist, Clinical Assistant Professor Ohio State Wexner Medical Center
- Share on Facebook
- Share on Linkedin
- Share via Email
- Share this page

If there’s a sniper in cancer treatment , it’s ablation. In this minimally invasive procedure, a small needle is inserted to precisely zap a tumor — by freezing or heating it. The treatment is over 90% effective in completely curing small tumors.
This technology, which uses extreme temperatures to destroy cancer cells, represents the best of medicine. It's minimally invasive, very effective, has low risks of complications and a quick recovery.
What is tumor ablation?
With ablation treatment, we use energy to burn or freeze a tumor. The technology can be used on a cancerous (malignant) tumor or any non-cancerous (benign) tumor that is growing or causing problems.
Cryoablation is the process of using one or more probes to create an ice ball around a tumor that destroys the cancerous cells. In microwave and radiofrequency ablation, the cells heat up and burn.
Ablation can be used to treat certain liver, kidney or lung cancers. Interventional radiologists are starting to use it in other types of cancer, such as breast and prostate cancer. In bone cancer, ablation helps with pain management and gives patients relief.
The procedure can also help with pain management for nerve issues.
Some patients receive ablation as their only treatment. Others need ablation in combination with other cancer treatment options, including chemotherapy .
The benefits of ablation for tumors
Completely removing a cancerous or benign tumor in the past has usually required surgery. Now, ablation is an effective and reliable treatment option, depending on a tumor’s location and size. Patients typically go home the same day, cancer-free, with a pinhole incision and a small bandage. For patients and doctors alike, it can feel like magic.
Lung tumors
For certain lung tumors , ablation has multiple benefits over surgical treatments, including shorter recovery time, less bleeding, lower incidence of infection and a decreased rate of major complications.
Liver tumors
Ablation techniques are a promising treatment option for early-stage liver cancer because many patients aren’t eligible for surgery.
Kidney tumors
Ablation can precisely target tumor cells in kidney cancer while sparing surrounding healthy kidney tissue. This is particularly important for patients seeking to spare kidney function or those who are at high risk for surgery.
Ablation can often be repeated if new tumors develop, or if a treated tumor recurs.
How ablation works
Depending on the size and location of the tumor, ablation can cure cancer. This means a patient can come in the morning with a malignant tumor and walk out a few hours later cancer-free.
While under general anesthesia, your radiologist will place one or more very small, thin probes through the skin. Your physician will guide the probes to the exact location of the tumor and freeze or burn it using an ultrasound or CT scan to help see inside the body.
The actual freezing or heating treatment takes about 10-30 minutes, but preparation and recovery add a few hours. You’ll leave with a small bandage over the tiny insertion site.
Nothing is as rewarding in medicine as a same-day oncology treatment cure in which patients leave cancer-free without even a stitch.
Frequently asked questions about ablation
Who’s a good candidate for tumor ablation.
Depending on the stage and location of your tumor, ablation may be a good option. When it's a viable option, most patients prefer minimally invasive treatment because incisions are tiny. That means you’ll recover quicker and have less risk of complications and side effects compared to surgery.
Ablation may be the only treatment option for some patients with other health issues who aren’t candidates for traditional therapies.
Are there side effects of ablation?
After the procedure, you might experience mild to moderate pain, which can be managed with pain medication.
Less common risks are risks of infection, bleeding or injury to adjacent soft tissues. If ablation involves treating a lung tumor, you may need a chest tube for a few days afterward. It's also not uncommon to have bloody phlegm when you cough immediately after the procedure.
You may experience pink or bloody urine after the procedure on a kidney tumor.
What’s the difference between freezing and burning ablation procedures?
Ohio State offers two primary ablation techniques: cryoablation (freezing) and microwave ablation (heating). The best procedure for you depends on the tumor's size and location. The organ your doctor is treating can also affect which type of treatment to use.
Both methods have their advantages. Heating ablation requires fewer probes. Cryoablation allows the radiologist to see the ice around the tumor and avoid getting close to critical structures, such as blood vessels or organs.
We mostly use microwave ablation in the liver. We offer both in the kidney or lungs. If there are no critical structures around the tumor, your doctor will likely use heat. When a tumor has critical structures next to it or is in a small space, your doctor may use cryoablation.
Why is Ohio State a good place to get tumor ablation?
Expert interventional radiologists at Ohio State perform a large number of ablation treatments for a variety of tumors. The technique isn’t available at all hospitals and requires practice and precision. At Ohio State, radiologists manage a high volume of ablation patients, including more complicated cases.
Ablation is one of a few minimally invasive treatment options. Interventional radiologists are like the Swiss army knife of oncology — we find the right, precise tool for your condition and overall health. Together with a group of other specialists in medical, surgical and radiation oncology, we strive to provide positive treatment outcomes.
Ablation is an expanding treatment technique in oncology, and Ohio State researchers continue to study how it can benefit patients.
At The James, there is no routine cancer
Our experts develop and deliver the most advanced targeted treatments leading to better outcomes and more hope.

- Cancer Treatment ,
- Kidney Cancer ,
- Lung Cancer ,
- Ohio State Wexner Medical Center ,
- OSUCCC – James
Related websites
Articles on health.

What to know about endometrial (uterine) cancer, on the rise in the U.S.
By Casey Cosgrove, MD
The American Cancer Society projects there will be nearly 68,000 cases of uterine cancer diagnosed in the United States in 2024 and that more than 13,000 people will die of it.

Are ‘hurkle-durkling’ and ‘bed-rotting’ self-care strategies or mental health warning signs?
By Nicole Hollingshead, PhD
Hurkle-durkling and bed-rotting: Are these lounging forms of self-care healthy or harmful? An Ohio State expert discusses benefits and drawbacks.
Why is my eye twitching?
By J.P. Maszczak, OD
10 times you can head to a pharmacy before a doctor's office
By Rebecca Lahrman, PharmD, MS, BCACP
What to know about TIL therapy, a new treatment for skin cancer
By Richard C. Wu, MD, PhD
Get articles and stories about health, wellness, medicine, science and education delivered right to your inbox from the experts at Ohio State.
Required fields
Tell us more about yourself
By clicking "Subscribe" you agree to our Terms of Use . Learn more about how we use your information by reading our Privacy Policy .
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
Health Inc.
- Public Health
Oncologists' meetings with drug reps don't help cancer patients live longer
Sydney Lupkin

Drug companies often do one-on-one outreach to doctors. A new study finds these meetings with drug reps lead to more prescriptions for cancer patients, but not longer survival. Chris Hondros/Getty Images hide caption
Drug companies often do one-on-one outreach to doctors. A new study finds these meetings with drug reps lead to more prescriptions for cancer patients, but not longer survival.
Pharmaceutical company reps have been visiting doctors for decades to tell them about the latest drugs. But how does the practice affect patients? A group of economists tried to answer that question.
When drug company reps visit doctors, it usually includes lunch or dinner and a conversation about a new drug. These direct-to-physician marketing interactions are tracked as payments in a public database, and a new study shows the meetings work. That is, doctors prescribe about five percent more oncology drugs following a visit from a pharmaceutical representative, according to the new study published by the National Bureau of Economic Research this month.
But the researchers also found that the practice doesn't make cancer patients live longer.
"It does not seem that this payment induces physicians to switch to drugs with a mortality benefit relative to the drug the patient would have gotten otherwise," says study author Colleen Carey , an assistant professor of economics and public policy at Cornell University.
For their research, she and her colleagues used Medicare claims data and the Open Payments database , which tracks drug company payments to doctors.
While the patients being prescribed these new cancer drugs didn't live longer, Carey also points out that they didn't live shorter lives either. It was about equal.
The pharmaceutical industry trade group, which is known as PhRMA, has a code of conduct for how sales reps should interact with doctors. The code was most recently updated in 2022, says Jocelyn Ulrich, the group's vice president of policy and research .
"We're ensuring that there is a constant attention from the industry and ensuring that these are very meaningful and important interactions and that they're compliant," she explains.
The code says that if drug reps are buying doctors a meal, it must be modest and can't be part of an entertainment or recreational event. The goal should be education.
Ulrich also points out that cancer deaths in the U.S. have declined by 33 percent since the 1990s , and new medicines are a part of that.

IMAGES
VIDEO
COMMENTS
855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. If you have a cancer diagnosis and are weighing your treatment options, consider participating in a clinical trial. Although they may seem intimidating at first, clinical trials can be extremely beneficial no matter what type or stage of cancer you have.
The advent of targeted therapy and immunotherapy has revolutionized the treatment of cancer, especially with the development and availability of sophisticated diagnostic and molecular ...
Find research articles on cancer treatment, including news stories, clinical trials, blog posts, and descriptions of active studies. ... Researchers hope to learn more about whether people with cancer might benefit from treatments that target inflammation around tumors. Some early studies have yielded promising results and more are on the horizon.
Many newly approved cancer therapeutics offer limited clinical benefits yet are still prescribed to patients. A common-sense revolution in oncology would prioritize treatments that meaningfully ...
Selected NCI Activities in Cancer Treatment Research. For more than 50 years, NCI has played an active role in cancer drug development—from conducting preclinical studies in the laboratory to testing potential therapies in humans. NCI researchers conduct clinical trials to test cancer treatments at the National Institutes of Health in ...
Immunotherapy. Immunotherapy uses the body's immune system to fight cancer. Immunotherapy can boost or change how the immune system works so it can find and attack cancer cells. Molecular testing, which can help select patients most suitable for immunotherapy, has opened the door to this newer form of treatment.
Epidemiological research is the study of the patterns, causes, and effects of cancer in a group of people of a certain background. This research encompasses both observational population-based studies but also includes clinical epidemiological studies where the relationship between a population's risk factors and treatments are tested.
The American Cancer Society (ACS) has helped make possible almost every major cancer breakthrough since 1946. Since then, we've invested more than $5 billion in cancer research, making us the largest nonprofit funder of cancer research in the United States, outside of the federal government. We remain committed to finding more - and better ...
Immunotherapy has revolutionized cancer treatment and rejuvenated the field of tumor immunology. ... application of cytokines in cancer treatment benefits from the ... immunology research due to ...
Cancer is a global health problem responsible for one in six deaths worldwide. Treating cancer has been a highly complex process. Conventional treatment approaches, such as surgery, chemotherapy, and radiotherapy, have been in use, while significant advances are being made in recent times, including stem cell therapy, targeted therapy, ablation therapy, nanoparticles, natural antioxidants ...
April 19, 2024. Source: Virginia Tech. Summary: Researchers explore a cancer immunotherapy treatment that involves activating the immune cells in the body and reprogramming them to attack and ...
In this systematic review and meta-analysis, we show that advanced cancer patients who have exhausted standard of care treatments and participate in a randomized clinical trial with a control arm without any anticancer drug overall benefited from the experimental treatment when randomized into the experimental arms with a 42% decrease in the risk of disease progression and a 18% decrease in ...
1. Introduction. Immunotherapy harnesses a patient's immune system to target cancer and has resulted in novel therapeutic approaches and unprecedented clinical outcomes [].Although immunotherapeutic approaches have found success in a variety of cancer subtypes and clinical scenarios challenges still remain [2,3,4,5].Thus, comprehensive knowledge of how these therapies function is essential ...
Lung cancer remains the most lethal form of the disease, killing about 135,000 Americans a year - more than breast, prostate and colon cancer combined - which is why many people still think of ...
Dr. Anna Kinsella, Science Engagement Manager at Cancer Research U.K., said, "This is the largest study to date showing the potential of a class of drugs called ATR inhibitors in treating cancer ...
Initial funding for the second trial is provided by the National Cancer Institute Specialized Programs of Research Excellence (NCI SPORE). "We hope that the treatment will prolong lives for patients with glioblastoma," said Okada, who is a professor of neurosurgery at UCSF and a member of the Weill Institute for Neurosciences. "However ...
This research will help accelerate the development and delivery of novel ASO cancer therapies. ... L687 is an effective drug delivery system that may extend the benefits of ASO treatment to other ...
At its most basic level, prostate cancer is a malignancy that occurs in the prostate gland, which produces fluid that mixes with sperm from the testicles to make semen. The prostate is located in ...
Overall, only 10% of cancer patients experience a clinical benefit from treatments matched to tumor DNA mutations. Functional precision medicine takes a different approach to personalizing treatments.
Purdue University. "Genetically engineering a treatment for incurable brain tumors." ScienceDaily. ScienceDaily, 22 April 2024. <www.sciencedaily.com / releases / 2024 / 04 / 240422120626.htm ...
Simple Summary. The aim of this paper is to outline the role and potential benefits of physical activity for cancer patients. We present a review of publications on the subject in order to compare the findings reported in the literature and draw general conclusions that could help clinicians who provide cancer care to develop a more comprehensive treatment approach.
The idea, says Voest, is to give the people at the highest risk of dying from cancer access to a wider pool of potential treatments, whether these are the standard of care for a particular cancer ...
Importance of studying tumors and clinical trial designs. Cancer remains one of the leading causes of death globally 1. In the past couple of decades cancer research has received a lot of attention. Researchers have dedicated time and effort towards studies on causes, disease progression and pathophysiology, detection methods, treatments and ...
Chemotherapy works by stopping or slowing the growth of cancer cells, which grow and divide quickly. Chemotherapy is used for two reasons: Treat cancer: Chemotherapy can be used to cure cancer, lessen the chance it will return, or stop or slow its growth. Ease cancer symptoms: Chemotherapy can be used to shrink tumors that are causing pain and ...
Hormonal treatments (HT) for prostate cancer (e.g., androgen deprivation therapy) yield clinical and survival benefits, yet adverse cognitive changes may be a side effect. Since psychosocial factors are largely modifiable, interventions targeting these factors may help mitigate these adverse cognitive effects. This systematic review aimed to identify a range of psychosocial factors associated ...
Researchers in the College of Engineering explore a cancer immunotherapy treatment that involves activating the immune cells in the body and reprogramming them to attack and destroy cancer cells. This therapeutic method frequently uses cytokines, small protein molecules that act as intercellular biochemical messengers and are released by the body's immune cells to coordinate their response.
Watch this video to hear Dr. Reisenauer discuss innovation in lung cancer screening and treatment: A lung nodule or lesion is an abnormality revealed on a CT scan that looks like a cancer. And to find out if it is cancer, doctors may recommend a technique called bronchoscopy. "Very similar to having a colonoscopy performed where somebody is ...
The benefits of ablation for tumors. Completely removing a cancerous or benign tumor in the past has usually required surgery. Now, ablation is an effective and reliable treatment option, depending on a tumor's location and size. Patients typically go home the same day, cancer-free, with a pinhole incision and a small bandage.
Trained volunteers drive patients and families to hospitals and clinics for treatment. Call the American Cancer Society at 1-800-227-2345 to see whether this program is available in your area. People who have Medicaid or Medicare might be able to get help with travel to medical centers and doctors' offices for cancer treatment.
Drug company reps commonly visit doctors to talk about new medications. A team of economists wanted to know if that helps patients live longer. They found that for cancer patients, the answer is no.