- Open access
- Published: 14 October 2022

The effectiveness of case management for cancer patients: an umbrella review
- Nina Wang 1 , 2 ,
- Jia Chen 3 ,
- Wenjun Chen ORCID: orcid.org/0000-0001-5398-8508 4 , 5 ,
- Zhengkun Shi 1 ,
- Huaping Yang 1 ,
- Peng Liu 6 ,
- Xiao Wei 7 ,
- Xiangling Dong 6 ,
- Chen Wang 3 ,
- Ling Mao 8 &
- Xianhong Li 3
BMC Health Services Research volume 22 , Article number: 1247 ( 2022 ) Cite this article
2277 Accesses
18 Citations
1 Altmetric
Metrics details
Case management (CM) is widely utilized to improve health outcomes of cancer patients, enhance their experience of health care, and reduce the cost of care. While numbers of systematic reviews are available on the effectiveness of CM for cancer patients, they often arrive at discordant conclusions that may confuse or mislead the future case management development for cancer patients and relevant policy making. We aimed to summarize the existing systematic reviews on the effectiveness of CM in health-related outcomes and health care utilization outcomes for cancer patient care, and highlight the consistent and contradictory findings.
An umbrella review was conducted followed the Joanna Briggs Institute (JBI) Umbrella Review methodology. We searched MEDLINE (Ovid), EMBASE (Ovid), PsycINFO, CINAHL, and Scopus for reviews published up to July 8th, 2022. Quality of each review was appraised with the JBI Critical Appraisal Checklist for Systematic Reviews and Research Syntheses. A narrative synthesis was performed, the corrected covered area was calculated as a measure of overlap for the primary studies in each review. The results were reported followed the Preferred reporting items for overviews of systematic reviews checklist.
Eight systematic reviews were included. Average quality of the reviews was high. Overall, primary studies had a slight overlap across the eight reviews (corrected covered area = 4.5%). No universal tools were used to measure the effect of CM on each outcome. Summarized results revealed that CM were more likely to improve symptom management, cognitive function, hospital (re)admission, treatment received compliance, and provision of timely treatment for cancer patients. Overall equivocal effect was reported on cancer patients’ quality of life, self-efficacy, survivor status, and satisfaction. Rare significant effect was reported on cost and length of stay.
Conclusions
CM showed mixed effects in cancer patient care. Future research should use standard guidelines to clearly describe details of CM intervention and its implementation. More primary studies are needed using high-quality well-powered designs to provide solid evidence on the effectiveness of CM. Case managers should consider applying validated and reliable tools to evaluate effect of CM in multifaced outcomes of cancer patient care.
Peer Review reports
Cancer ranks as one of the leading causes of premature death among population around 30–69 years old across 134 countries [ 1 ], and the global incidence of cancer is about to reach 30.2 million new cases and 25.7 million deaths by 2040 [ 2 ]. Earlier detection and diagnosis, and development of diverse cancer treatments have increased the survival rate of cancer patients. According to Quaresma et al. [ 3 ], the cancer survival in the UK has doubled over the last 40 years alongside the advancement in cancer diagnosis and treatment. However, number of challenges exist in the current cancer care all over the world. Many cancer patients oftentimes receive a series of long-running and exhausting multi-modal treatments and experience descent in psychological, physical and social functioning, which have a significant negative impact on their quality of life (QoL) [ 4 , 5 ]. In addition, the significant healthcare spending and productivity losses of cancer patients lead to a heavy patient economic burden, which is another substantial issue with cancer care [ 6 ]. A systematic approach is needed to mobilize and deliver appropriate resources, provide accessible, safe, and well-coordinated care for cancer patients received stressful treatments and shouldered heavy economic burden [ 7 ].
Case management (CM) is defined by the Case Management Society of America (CMSA) as “a collaborative process of assessment, planning, facilitation, care coordination, evaluation, and advocacy for options and services to meet an individual’s and family’s comprehensive health needs through communication and available resources to promote quality, cost-effective outcomes” (P. 11) [ 8 ]. According to the definition, CM is designed to use resources effectively to improve the quality of treatments, patient care services, and QoL of patients while reducing the relevant healthcare costs.
With the worldwide utilization of CM in cancer patient care, studies examining the effect of CM in improving patient-related outcomes or healthcare service use outcomes have been skyrocketing. Numbers of systematic reviews and meta-analyses have been published to synthesis the effectiveness of CM in recent years and often arrive at discordant conclusions. For example, Joo et al. [ 9 ] retrieved and synthesised results from nine experimental studies and found that CM effectively improved patients’ QoL and symptom management. While Aubin et al. [ 10 ] reported equivocal effect on both QoL and symptom management. Chan et al. [ 11 ] reported that four of the five randomized controlled trials showed insignificant impact of CM on patients’ QoL. The inconsistent evidence on the impact of CM may confuse or mislead the future case management development and relevant policy making. Considering the exist of several systematic reviews and research synthesis available to inform the application of case management for cancer patient care improvement, umbrella review could now be undertaken to compare and contrast published reviews and to highlight the consistent or contradictory findings around the effect of CM on manifold aspects of cancer patient care [ 12 ]. Thus, the current review was conducted to 1) synthesis systematic reviews that assess the effects of CM on cancer patient outcomes (e.g., QoL, functioning status, symptom management, satisfaction, etc.) and health care utilization outcomes (e.g., cost, hospital admissions, length of stay, treatment received compliance, etc.), 2) summarize measurement used in evaluating patient outcomes and health care utilization outcomes.
This umbrella review followed the Joanna Briggs Institute (JBI) Umbrella Review (UR) methodology [ 12 ] and adhered to the Preferred Reporting Items for Overviews of systematic reviews (PRIO) checklist (see Additional file 1 ) [ 13 ]. This review has been registered with the Open Science Framework ( https://doi.org/10.17605/OSF.IO/7YQAP ).
Study searching methods
We performed literature search in five databases including MEDLINE (Ovid), EMBASE (Ovid), PsycINFO, CINAHL, and Scopus from inception to July 2022. Ethical approval and patient consent were not necessary since all analyses were based on previously published articles. The searching strategies in all five databases were developed with the help of a health science librarian. See Additional file 2 for the searching strategy and results in MEDLINE (Ovid). The studies were selected using the following inclusion and exclusion criteria.
Inclusion and exclusion criteria
Individuals diagnosed with any type of cancer at any cancer stages (early to advanced). Reviews targeted on people with no specified cancer diagnose were excluded.
Intervention
Case management interventions targeted on cancer patients. Case management is defined as a “collaborative process of assessment, planning, facilitation, care coordination, evaluation, and advocacy for options and services to meet an individual’s and family’s comprehensive health needs through communication and available resources to promote quality, cost-effective outcomes” [ 8 ]. Only reviews in which the effectiveness of CM as defined above was analyzed separately from other interventions were considered.
Individuals in comparison groups received “treatment as usual” (TAU). TAU may include various interventions called “standard of care,” “usual care,” or “standard treatment,” but generally refers to treatment as it is commonly provided. Only studies that compared case management with “TAU” were selected.
Patient outcomes (e.g., quality of life, symptom management, functioning status), health care utilization outcomes (e.g., cost, hospital admissions, length of stay), etc.
Acute care hospitals and primary care settings (e.g., long-term care, nursing homes, community care services). Hospital was defined as any department of internal medicine or surgery as well as unspecified hospital settings.
Study design
Systematic review/meta-analysis that only included quantitative studies. We excluded studies full-texts unavailable online.
Study selection
All retrieved studies were imported into Covidence systematic review software [ 14 ] and the duplicates were removed. Then, titles and abstracts were independently assessed by two researchers (XW and XD) according to the inclusion criteria. After that, the full texts of the selected abstracts were obtained and reviewed by the same two researchers (XW and XD) independently. The reference list of included studies was reviewed and searched for additional studies. Any disagreement between the two researchers were resolved through consultation with a senior researcher (PL).
Quality appraisal for included reviews
Two reviewers (NW and LM) independently assessed the methodological quality of the individual studies using the JBI Critical Appraisal Checklist for Systematic Reviews and Research Syntheses [ 15 ]. The tool aims to determine the extent to which the review has addressed the possibility of bias in its design, conduct and analysis [ 15 ]. It consists of 11 criteria scored as yes, no, unclear, or not applicable. We adopted a scoring system used in previously published systematic reviews [ 16 , 17 ]. For each article, a rating score was derived by taking the number obtained in the quality rating and dividing it by the total number of possible points allowed, giving each manuscript a total quality rating between 0 and 1. Studies were then classified as low (0–0.25), low-moderate (0.26–0.50), moderate (0.51–0.75), or high (0.76–1.0).
Data extraction
We developed the data extraction form based on the research questions, and extracted following information: characteristics of included reviews such as publication year range, whether conducted meta-analysis or not, type of cancer patients, age of population, type and number of primary studies included; intervention names, components, and duration; outcomes and evaluation tools used; author’s conclusions and interpretations. Two researchers (NW and LM) extracted data independently from all included articles into an Excel spreadsheet and another researcher (XL) verified it for accuracy.
Data synthesis
We were unable to statistically pool outcomes due to the heterogeneity of outcomes of the included reviews. Therefore, we conducted a narrative synthesis [ 18 ] of the numerical data of individual studies outcomes. The studies were summarized and synthesised by two reviewers (NW and ZS) independently and double checked by a third author (HY). Following the JBI UR methodology [ 12 ], we used a summary table to present clear, specific, and structured results from the selected reviews, and then synthesised these results to identify broad conclusions. To summarized information about the interventions we coded data into features, components and delivery strategies, and inductively developed themes within each domain as they emerged from the studies. As suggested by Li and colleagues [ 19 ], we grouped outcomes into: global QoL of patients, functional status (i.e. physical, cognitive, emotional, role, social), symptom management, cost, hospital (re)admission, length of stay, treatment received compliance, provision of timely treatment.
For clarity the term ‘primary studies’ refers to the articles found within the included reviews. As several primary studies are included in more than one review, the overall results and conclusions of an overview can be biased. To assess this bias, the degree of overlap between reviews was calculated with the Corrected Covered Area (CCA) method. The details of the CCA calculation have been described by Pieper and colleagues [ 20 ] elsewhere. A CCA score of less than 5% is regarded as a slight overlap, 5–9.9% as moderate overlap, 10–14.9% as high overlap and over 15% as a very high level of overlap. This measure has been validated in which the number of overlapped primary publications has a strong correlation with the CCA [ 21 ].
Search outcome
As shown in Fig. 1 , our search strategy generated 804 potentially relevant records. Upon removing the duplicates, 582 studies screened by title and abstract, 16 were identified for full text screening. We excluded eight of the 16 studies for the following reasons: no independent analysis on the effect of case management ( n = 6), or conference abstract ( n = 2). The eight remaining systematic reviews were selected and assessed for methodological quality. In total, all the eight reviews included 57 primary studies, among which 12 were duplicated included in two or three reviews. Forty-one of the 57 primary studies were randomized controlled trials (see Additional file 3 for included primary studies).
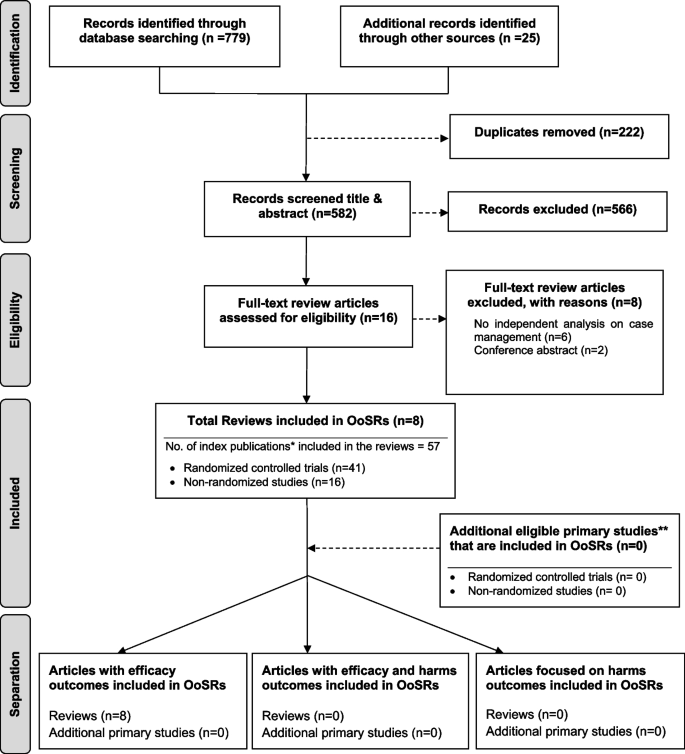
Flow chart for umbrella review. *Index publication is the first occurrence of a primary publication in the included reviews. **Additional eligible primary studies that had not been initially indentified by the search of the relevant reviews or obtained by updating the search of the included reviews
Methodological quality assessment
The quality assessment scores are presented in Table 1 . Only one review was rated as moderate because not clarify whether two or more reviewers independently assessed the quality of included primary studies, and did not report the methods to minimize errors in data extraction or publication bias. The other seven reviews were rated as high quality. Despite rated as strong, the seven reviews still companied with one or two issues on the assessment of heterogeneity, search strategy, and recommendations for policy and/or practice.
Characteristics of included studies
Table 2 presents a descriptive summary of characteristics of the eight systematic reviews [ 9 , 10 , 11 , 19 , 23 , 24 , 25 , 26 ]. The eight reviews aimed to identify evidence of the effectiveness of CM on cancer patients. Three of the studies were a systematic review with meta-analysis [ 10 , 25 , 26 ]. Five of the eight reviews adhered to the PRISMA statement [ 11 , 19 , 24 , 25 , 26 ], two adopted Cochrane systematic review methodology [ 9 , 10 ].
The eight reviews were published between 2008 and 2021, the primary studies in the reviews were published between 1983 and 2018. The number of primary studies regarding to CM included in each review ranged from three to 20. Five of the eight reviews included only randomized controlled trials (RCTs), the remaining reviews included a combination of study designs that involved RCTs, quasi-experimental and non-experimental studies (e.g., cohort study). The age of review participants ranged from 7 to 97 years and mean ages range from 48.63 to 66.31 years, which covers populations from children to elders. The total number of participants in each review ranged from 327 to 9601. Seven of the eight reviews included primary studies targeted on multiple types of cancer including breast, lung, colorectal, cervical, ovarian, prostate, gastric, hepatocellular, etc. Most of the primary studies included in the eight reviews were conducted in the United States, and there were also studies conducted in Canada, Australia, Europe (i.e., Germany, UK, Turkey, Switzerland, Denmark, Switzerland, Sweden, Norway, Netherlands) and East Asia (i.e., Hong Kong, Taiwan, South Korea, and Malaysia).
CM interventions
As shown in Table 2 , three studies reviewed trials of nurse-led CM interventions [ 9 , 25 , 26 ], two reviewed CM-like interventions that not termed as ‘CM’ while meet the CM definition by the CMSA [ 8 , 23 , 24 ]. Only one study reviewed CM focus solely on skill-training or symptom management [ 19 ]. All studies reviewed trials that facilitated the CM in a multidisciplinary collaboration approach. The duration of CM ranged from 4 days to 5 years. We presented the feature, components and delivery strategies of CM interventions for cancer patients in Fig. 2 by summarizing descriptions in each review. Congruent with the components defined by CMSA [ 8 ], all CM interventions included patient assessment, supportive services such as information and emotion support, care coordination by conducting education, consultation, and in-person, telephone or online coaching for regular follow-up. One critical component of CM interventions for cancer patients is the provision of palliative care. Control groups (CGs) of all studies reviewed in the reviews received usual treatment of care.
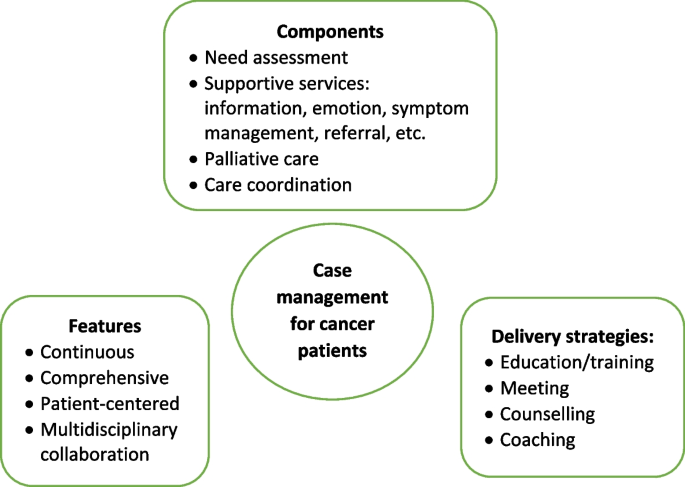
Features, components, and delivery strategies of case management for cancer patient care
Corrected Covered Area (CCA)
Table 3 presents the CCA for each outcome and as a whole. Overall, primary studies had a slight overlap across the eight reviews (CCA = 4.5%). In addition, no overlapping of primary studies was found for six of the 16 outcomes, including self-efficacy, psychological function, hospital (re)admissions, length of stay, and provision of timely treatment. Only one outcome (i.e., symptom management) showed slight overlap (0.7%). The CCA for other five outcomes (i.e., global QoL, physical function, role function, patient satisfaction, cost) evaluated by more than 2 reviews were between 5 to 9.9%, indicated a moderate overlap. The CCA for survivor status, cognitive function, emotional function, and treatment received compliance were over 10%.
Measurement used
Table 4 presents the quantitative measurement used in primary studies. As shown in Table 4 , studies investigated global QoL using different QoL-related scales, among which Functional Assessment of Cancer Therapy (FACT) (used in 15 primary studies) were most frequently applied, followed by the European Organisation for Research and Treatment of Cancer Core Quality of Life Questionnaire 30 (EORTC QLQ-C30) (used in 11 primary studies), and short form health survey (i.e., SF-8, SF-12, SF-36) (used in 10 primary studies). Different types of FACT tool were used according to the cancer types. For example, FACT-G was used for general cancer patients assessment, and FACT-B was used to evaluate breast cancer-related QoL. For the assessment of overall symptom management, SF-36 and Symptom Distress Scale (SDS) were used most frequently (used in four primary studies each). Different dimensions of SF-36 were also applied to evaluate other outcomes such as physical, emotional, and social function. Hospital Anxiety and Depression Scale (HADS) was the top employed tool in measuring the psychological function of patients. Patients’ sick leave days and the number of patients return to work were top employed metrics to evaluate the role function of patients. No unified tools were utilized to assess patient satisfaction towards the CM and majority of the primary studies used self-developed questionnaires.
Effect of CM on patient and health care utilization outcomes
The main outcomes from the seven systematic reviews are presented and summarized in Table 5 . Seven of the eight reviews reported the effects of case management on patients’ global QoL and showed mixed findings. Around half (49%, 19/39) of the primary studies included in the seven reviews reported significant positive impact of CM on global QoL. As for the functional status, there was a strong concordance among primary studies regarding the effectiveness of CM in improving cognitive function (e.g., uncertainty, health perceptions) (89%, 8/9); Equivocal effects were reported on psychological (e.g., patient anxiety, depression), physical (e.g., arm function), role function (e.g., sick leave days, patients returning to work), emotional (e.g., mood) and social function (e.g., social support) [ 9 , 11 , 26 ]. The findings regard to symptom management were more positive, with 75% (18/24) primary studies included in seven reviews revealed significant positive impact of CM on symptom severity and symptom distress decrease of pain, nausea, fatigue, discomfort, etc. Three of the four primary studies in two reviews [ 9 , 11 ] showed no significant influence of CM on patients’ self-efficacy. Wulff et al. [ 23 ] and Aubin et al. [ 10 ] reported mixed findings on the impact of CM on survivor status, with four of the six primary studies reported significant positive impact. The effect of CM on patient satisfaction was reported in five reviews and showed mixed results.
Of the eleven primary studies reported cost, only one controlled before-and-after study in Joo et al.’s [ 9 ] review reported significant impact on monthly cancer-related medical costs. The evidence concerning patients’ length of stay yielded no significant findings. Overall significant positive effect was reported on hospital (re)admission (e.g., inpatient and ICU admission rate), treatment received compliance (e.g., therapy acceptance or completion rate), and provision of timely treatment.
This umbrella review is the first to summarize the results of systematic reviews that synthesised the evidence on the effectiveness of CM on cancer patient outcomes and relevant health care utilization. Most reviews (7/8) showed a high methodological quality. Different tools were used to measure the effect of CM on the same outcome. The evidence regards to the effectiveness of CM is mixed. The summarized results revealed that CM was more likely to improve symptom management, cognitive function, hospital (re)admission, treatment received compliance, and provision of timely treatment for cancer patients. Overall equivocal effect was reported on cancer patients’ global QoL, psychological, physical, role, emotional and social function, self-efficacy, survivor status, and patient satisfaction.
No universal tools were used to measure improvement of each outcome in the CM group compared with the control group, making it challenging to conduct a meta-analysis of studies results [ 22 , 27 ]. This is a common issue faced the included reviews. Five of the eight reviews failed to conduct meta-analysis due to the heterogeneity [ 9 , 11 , 19 , 23 , 24 ]. Joo and Huber [ 22 ] conducted a review of reviews on the effect of CM on health care utilization outcome of chronic illness patients, they recognized the same problem and suggested using valid and standardized tools to minimize the differences in measurements. Despite various tools used, our review showed that FACT, EORTC QLQ-C30, and short form health survey (i.e., SF 36, SF 12, and SF 8) were most frequently applied to measure the effect of CM on the global QoL of cancer patients. These tools were also used in evaluating specific dimensions of QoL such as psychological, physical, emotional, and social function. This aligned with previous reviews [ 28 , 29 ] that found FACT and EORTC QLQ-C30 were the most common and well developed QoL instruments in cancer patients. FACT-G is considered appropriate for use with any types of cancer patients [ 30 ]. It is a 27-item tool that includes four primary QoL domains: physical well-being, social/family well-being, emotional well-being, and functional well-being [ 31 ]. Other versions of FACT (FACT-B [ 32 ], FACT-L [ 33 ] and FACT-E [ 34 ]) for specific type of cancer patients were developed by incorporating the four dimensions of FACT-G with additional cancer type-specific questions. EORTC QLQ-C30 was another type of QoL assessment tools for cancer patients specifically. It was developed by Aaronson et al. [ 35 ] and contains four domains: physical, emotional, cognitive and social functions, and a higher score indicates better QoL. The Short Form Health Survey is the most commonly used measure in evaluating QoL domains of patients suffering from a wide range of medical conditions [ 36 ]. Research found it provides reliable and valid indication of general health among cancer patients [ 37 , 38 ].
QoL is the most frequently evaluated outcome in our review with 39 primary studies in seven reviews reported the global QoL of cancer patients. Joo et al. [ 9 ] found that CM interventions improved QoL of cancer patients. Yin and colleagues [ 24 ] revealed that cancer patients achieved better physical and psychological condition through symptom management, needs assessment, direct referrals, and other services in CM. However, summarized results in our review show that the CM had equivocal effect on cancer patients’ global QoL and dimensions including psychological, physical, role, emotional and social function. Cognitive function is the only dimension showed positive change. Despite CM interventions share similar definitions and principles [ 8 ]. It is hard to foresee which aspect(s) of CM interventions contribute to certain effects due to their comprehensiveness [ 24 ]. Yin et al. [ 24 ] argued that the control group may receive a higher quality treatment than planned usual care since all the participants were not blinded and they have been informed about the aim of the study. Indicating a more rigorous design and evaluation is needed to avoid this information bias.
In the meantime, included reviews claimed that few primary studies reported enough details about CM interventions, including model used [ 10 , 11 ], dose and intensity [ 9 , 19 , 24 ], interventionist qualifications [ 11 ], protocol or manual used [ 9 , 23 ], and fidelity [ 23 ]. Particularly, the COVID-19 pandemic has considerable influence on the care delivery for cancer patients. For example, the more frequently utilization of remote patient monitoring technologies that incorporate community resources, primary care and allied health disciplines, as well as clinics to keep cancer patients away from acute care hospitals as much as possible [ 39 ]. Many of these changes have been integrated within routine case management for cancer care during the pandemic [ 39 ]. It is well-needed to report how those CM intervention were conducted follow standard reporting guidelines, in order to provide recommendation for future research.
Our review showed that CM is likely to improve the symptom management. Eighteen of the 24 included primary studies reported positive effect of CM on symptom management, including decrease symptom distress or severity of fatigue, pain, nausea, and vomiting. The same positive effect on symptom management was also revealed in other types of patients. Joo and colleagues [ 40 ] found that CM reduced substance use and significantly influenced abstinence rates among populations experienced substance disorders. Reviews by Stokes et al. [ 27 ] and Welch et al. [ 41 ] revealed positive effect on symptom release among people with long-term conditions and diabetes patients, respectively. The multidisciplinary collaboration approach adopted [ 10 ], and availability of professional support post-hospitalization [ 9 , 41 ] in CM might contribute to the improvement of symptom management. Specifically, multidisciplinary team involves physicians, nurses, and aligned healthcare professionals provides throughout and multifaced symptom assessment and management [ 10 ]. In addition, CM programs continuously follow up and advocate for patients’ concerns [ 8 ]. Specifically, case managers are available to patients 24 hours a day by phone call even after discharged, providing opportunity for immediate professional guidance on symptom management [ 9 ].
As for other patient outcomes, there is insufficient evidence of effect on self-efficacy and survivor status of cancer patients. Only three and four primary studies in total reported these two outcomes, respectively. Eleven primary studies in five reviews reported patient satisfaction and showed mixed results. Inconsistent results were found in a review of reviews by Buja et al. [ 7 ] which concluded strong evidence of CM improving satisfaction of patients with long term condition. In agreement with Joo and Huber’s [ 25 ] review, we found that CM favorably affect healthcare utilization outcomes such as treatment received compliance, hospital (re)admission, and provision of timely treatment. While the strength of the evidence was limited either by the high level of primary studies overlapping (CCA) (i.e., treatment received compliance, CCA = 13.3%) or the small number of studies reported certain outcomes (i.e., hospital admission, provision of timely treatment). Notably, the summarized results from included reviews conclude that despite theoretical benefits [ 8 ], in practice there is only slight evidence of benefits on reduction in the cost of care for cancer patients participated in CM interventions.
We provide some recommendations for future research based on the summarized results: 1) Future research should clearly describe details of CM intervention and its implementation, including theoretical underpinnings, dose and intensity, interventionist qualifications, protocol or manual used, fidelity, etc. In that way these details can be included in future systematic reviews, and effectiveness of individual elements of the intervention can be examined [ 27 ]. We recommend use standard guidelines to help organize the CM intervention reporting. For example, the Template for Intervention Description and Replication (TIDeiR) is one of the most popular guidelines that could be used to report the full breadth of CM interventions: from intervention rationale to assessments of treatment adherence and fidelity [ 42 ]. 2) More rigorous trials are needed to evaluate the effectiveness of CM. 3) Studies should also explore the barriers to and facilitators of CM implementation across various types of cancer patients at different stages, providing evidence for conducting successful CM implementation in the future.
Strengths and limitations
We conducted an umbrella review instead of a meta-analysis due to the heterogeneity of review outcomes. Although an umbrella review can only show the tendency or direction of the effect of CM rather than providing the magnitude or significance level of influence [ 12 ], the current evidence on the effect of CM in cancer patients was comprehensively summarized. There were some challenges when conducting the review. First, the quality of the umbrella reviews was greatly affected by the quality of the original reviews [ 12 ]. In this study, we confirmed that the quality of the original reviews were mostly high as assessed by the JBI Critical Appraisal Checklist [ 15 ]. Second, if the primary studies were included in several reviews, they may produce bias related to overlapping effects [ 20 ]. By calculating the CCA, we showed that 75% (12/16) of the individual outcomes had no to moderate overlapping of primary studies between included reviews, revealing that these results from each review were relatively independent. Cautious are needed on the summarized evidence regards to the effect of CM on survivor status, cognitive function, emotional function, and treatment received compliance because of the high overlapping (CCA > 10) between the reviews reported those outcomes.
There are limitations in our review. The first limitation concerns that the searching was limited to English-language articles and did not access unpublished papers. Second, as suggested by the JBI UR methodology [ 12 ], we did not assess the quality of evidence from included reviews, it increased the uncertainty of the review findings.
Effective CM aims to influence the health care delivery system in improving the health outcomes of cancer patients, enhancing their experience of health care, and reducing the cost of care. Our review found mixed effects of CM reported in cancer patient care. The summarized results revealed that CM was likely to improve symptom management for cancer patients. We also found CM has the tendency to enhance cancer patients’ experience of health care such as reducing hospital (re)admission rates, improving treatment received compliance and provision of timely treatment. Only slight evidence of benefits was reported on reducing the cost of care for cancer patients. Overall, more rigorous designed primary studies are needed to demonstrate the effects of CM on cancer patients and explore the elements of effective CM interventions.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
Corrected Covered Area
Control groups
- Case management
Case Management Society of America
European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire 30
Functional Assessment of Cancer Therapy - Breast Cancer
Functional Assessment of Cancer Therapy- Esophagus
Functional Assessment of Cancer Therapy- General
Functional Assessment of Cancer Therapy Scale-Lung
- Quality of life
Hospital Anxiety and Depression Scale
Joanna Briggs Institute
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Randomized controlled trials
Symptom Distress Scale
Medical Outcomes Study 8-item short form health survey
Medical Outcomes Study 12-item short form health survey
Medical Outcomes Study 36-item short form health survey
Treatment as usual
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global cancer observatory: Cancer today: International Agency for Research on Cancer; 2020. https://gco.iarc.fr/today .
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global Cancer observatory: Cancer tomorrow: International Agency for Research on Cancer; 2020. https://gco.iarc.fr/tomorrow .
Quaresma M, Coleman MP, Rachet B. 40-year trends in an index of survival for all cancers combined and survival adjusted for age and sex for each cancer in England and Wales, 1971-2011: a population-based study. Lancet. 2015;385:1206–18. https://doi.org/10.1016/S0140-6736(14)61396-9 .
Article PubMed Google Scholar
Yabroff KR, Dowling EC, Guy GP, Banegas MP, Davidoff A, Han X, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34:259–67. https://doi.org/10.1200/JCO.2015.62.0468 .
Yan AF, Stevens P, Holt C, Walker A, Ng A, McManus P, et al. Culture, identity, strength and spirituality: a qualitative study to understand experiences of African American women breast cancer survivors and recommendations for intervention development. Eur J Cancer Care (Engl). 2019;28:e13013. https://doi.org/10.1111/ecc.13013 .
Article Google Scholar
Yabroff K, Mariotto A, Tangka F. Annual report to the nation on the status of Cancer, part II: patient economic burden associated with Cancer care. J Natl Cancer Inst. 2021;113:1670–82. https://doi.org/10.1093/jnci/djab192 .
Buja A, Francesconi P, Bellini I, Barletta V, Girardi G, Braga M, et al. Health and health service usage outcomes of case management for patients with long-term conditions: a review of reviews. Prim Heal Care Res Dev. 2020;21:1–21. https://doi.org/10.1017/S1463423620000080 .
Case Management Society of America. CMSA’s standards of practice for case management, Revised 2016. 2016. http://www.naylornetwork.com/cmsatoday/articles/index-v3.asp?aid=400028&issueID=53653 .
Google Scholar
Joo JY, Liu MF. Effectiveness of nurse-led case Management in Cancer Care: systematic review. Clin Nurs Res. 2019;28:968–91. https://doi.org/10.1177/1054773818773285 .
Aubin M, Giguère A, Martin M, Verreault R, Fitch MI, Kazanjian A, et al. Interventions to improve continuity of care in the follow-up of patients with cancer. Cochrane Database Syst Rev. 2012:1–193. https://doi.org/10.1002/14651858.CD007672.pub2 .
Chan RJ, Teleni L, McDonald S, Kelly J, Mahony J, Ernst K, et al. Breast cancer nursing interventions and clinical effectiveness: a systematic review. BMJ Support Palliat Care. 2020;10:276–86. https://doi.org/10.1136/bmjspcare-2019-002120 .
Aromataris E, Fernandez R, Godfrey C, Holly C, Khalil H, Tungpunkom P. JBI manual for evidence synthesis. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. https://doi.org/10.46658/JBIMES-20-11 .
Chapter Google Scholar
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich AB. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24. https://doi.org/10.1016/j.jclinepi.2017.10.002 .
Veritas Health Innovation. Covidence systematic review sofware. Covidence. 2016. https://get.covidence.org/systematic-review-software?campaignid=15030045989&adgroupid=130408703002&gclid=EAIaIQobChMIvc7KuJDO-QIVh97ICh1BeQKnEAAYASAAEgI4APD_BwE .
Aromataris E, Fernandez R, Godfrey C, Holly C, Kahlil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Heal. 2015;13:132–40 http://joannabriggs.org/research/critical-appraisal-tools.html .
Gifford W, Rowan M, Dick P, Modanloo S, Benoit M, Al AZ, et al. Interventions to improve cancer survivorship among indigenous peoples and communities : a systematic review with a narrative synthesis. Support Care Cancer. 2021;29:7029–48. https://doi.org/10.1007/s00520-021-06216-7 .
Article PubMed PubMed Central Google Scholar
Gifford W, Squires J, Angus D, Ashley L, Brosseau L, Craik J, et al. Managerial leadership for research use in nursing and allied health care professions : a systematic review. Implement Sci. 2018;13:1–23. https://doi.org/10.1186/s13012-018-0817-7 .
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods Programme. Lancaster: Lancaster University; 2006. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf .
Li Q, Lin Y, Liu X, Xu Y. A systematic review on patient-reported outcomes in cancer survivors of randomised clinical trials: direction for future research. Psychooncology. 2014;23:721–30. https://doi.org/10.1002/pon.3504 .
Article CAS PubMed Google Scholar
Pieper D, Antoine SL, Mathes T, Neugebauer EAM, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67:368–75. https://doi.org/10.1016/j.jclinepi.2013.11.007 .
Choi J, Lee M, Lee JK, Kang D, Choi JY. Correlates associated with participation in physical activity among adults: a systematic review of reviews and update. BMC Public Health. 2017;17:1–13. https://doi.org/10.1186/s12889-017-4255-2 .
Joo JY, Huber DL. Case management effectiveness on health care utilization outcomes: a systematic review of reviews. West J Nurs Res. 2019;41:111–33. https://doi.org/10.1177/0193945918762135 .
Wulff CN, Thygesen M, Søndergaard J, Vedsted P. Case management used to optimize cancer care pathways: a systematic review. BMC Health Serv Res. 2008;8:1–7 http://www.biomedcentral.com/1472-6963/8/227 .
Yin YN, Wang Y, Jiang NJ, Long DR. Can case management improve cancer patients quality of life?: a systematic review following PRISMA. Medicine (Baltimore). 2020;99:1–7. https://doi.org/10.1097/MD.0000000000022448 .
Wu YL, Padmalatha KMS, Yu T, Lin YH, Ku HC, Tsai YT, et al. Is nurse-led case management effective in improving treatment outcomes for cancer patients? A systematic review and meta-analysis. J Adv Nurs. 2021;00:1–11. https://doi.org/10.1111/jan.14874 .
McQueen J, McFeely G. Case management for return to work for individuals living with cancer: a systematic review. Int J Ther Rehabil. 2017;24:203–10. https://doi.org/10.12968/ijtr.2017.24.5.203 .
Stokes J, Panagioti M, Alam R, Checkland K, Cheraghi-Sohi S, Bower P. Effectiveness of case management for “at risk” patients in primary care: a systematic review and meta-analysis. PLoS One. 2015;10:e0132340. https://doi.org/10.1371/journal.pone.0132340 .
Article CAS PubMed PubMed Central Google Scholar
Lemieux J, Goodwin PJ, Bordeleau LJ, Lauzier S, Théberge V. Quality-of-life measurement in randomized clinical trials in breast cancer: an updated systematic review (2001-2009). J Natl Cancer Inst. 2011;103:178–231. https://doi.org/10.1093/jnci/djq508 .
Montazeri A. Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res. 2008;27:1–31 https://jeccr.biomedcentral.com/articles/10.1186/1756-9966-27-32 .
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–9. https://doi.org/10.1200/JCO.1993.11.3.570 .
Webster K, Cella D, Yost K. The F unctional a ssessment of C hronic I llness T herapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. https://doi.org/10.1186/1477-7525-1-79 .
Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, et al. Reliability and validity of the functional assessment of cancer therapy- breast quality-of-life instrument. J Clin Oncol. 1997;15:974–86. https://doi.org/10.1200/jco.1997.15.3.974 .
Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the functional assessment of cancer therapy-lung (FACT-L) quality of life instrument. Lung Cancer. 1995;12:199–220. https://doi.org/10.1016/0169-5002(95)00450-F .
Darling G, Eton DT, Sulman J, Casson AG, Cella D. Validation of the functional assessment of cancer therapy esophageal cancer subscale. Cancer. 2006;107:854–63. https://doi.org/10.1002/cncr.22055 .
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76. https://doi.org/10.1093/jnci/85.5.365 .
Ware J, Kosinski M, Dewey J. How to score version two of the SF-36® health survey. Lincoln: QualityMetric Incorporated; 2000.
Treanor C, Donnelly M. A methodological review of the short form health survey 36 (SF-36) and its derivatives among breast cancer survivors. Qual Life Res. 2015;24:339–62. https://doi.org/10.1007/s11136-014-0785-6 .
Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:1–12. https://doi.org/10.1177/2050312116671725 .
Chan RJ, Crawford-Williams F, Crichton M, Joseph R, Hart NH, Milley K, et al. Effectiveness and implementation of models of cancer survivorship care: an overview of systematic reviews. J Cancer Surviv. 2021:1–25. https://doi.org/10.1007/s11764-021-01128-1 .
Joo J, Huber D. Community-based case management effectiveness in populations that abuse substances. Int Nurs Rev. 2015;62:536–46. https://doi.org/10.1111/inr.12201 .
Welch G, Garb J, Zagarins S, Lendel I, Gabbay RA. Nurse diabetes case management interventions and blood glucose control: results of a meta-analysis. Diabetes Res Clin Pract. 2010;88:1–6. https://doi.org/10.1016/j.diabres.2009.12.026 .
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. https://doi.org/10.1136/bmj.g1687 .
Download references
Acknowledgements
Not applicable.
Dual (co-)authorship
We declared that no author has authored one or more of the included systematic reviews.
This study was supported by 1) Hunan Provincial Key Laboratory of Nursing (2017TP1004, PI: Jia Chen), Hunan Provincial Science and Technology Department, 2) Changsha Natural Science Foundation (kq2202365, PI: Nina Wang) Changsha Science and Technology Department, and 3) Management research foundation of Xiangya Hospital (2021GL12, PI: Nina Wang).
Author information
Authors and affiliations.
Department of Respiratory Medicine, Xiangya Hospital, Central South University, Changsha, China
Nina Wang, Zhengkun Shi & Huaping Yang
National Clinical Research Center for Geriatric Disorders, Xiangya Hospital, Changsha, China
Xiangya School of Nursing, Central South University, Changsha, China
Jia Chen, Chen Wang & Xianhong Li
School of Nursing, University of Ottawa, Ottawa, Canada
Wenjun Chen
Center for Research on Health and Nursing, University of Ottawa, Ottawa, Canada
Intensive Care Unit of Cardiovascular Surgery Department, Xiangya Hospital, Central South University, Changsha, China
Peng Liu & Xiangling Dong
The 956th Army Hospital, Linzhi, China
School of Nursing, Changsha Medical University, Changsha, China
You can also search for this author in PubMed Google Scholar
Contributions
All authors have contributed to the production of this review. NW and WC conceptualized and designed the study and are the guarantor of the paper. JC and ZS conducted the literature search. PL, XW and XD were involved in the study screening. NW, LM and XL participated in the quality appraisal and data extraction. NW, ZS and HY conducted the data analysis. NW drafted the manuscript. WC and XL revised the manuscript. All authors participated in the review of the manuscript and approved the final manuscript.
Corresponding author
Correspondence to Wenjun Chen .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2..
Searching strategies.
Additional file 3.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wang, N., Chen, J., Chen, W. et al. The effectiveness of case management for cancer patients: an umbrella review. BMC Health Serv Res 22 , 1247 (2022). https://doi.org/10.1186/s12913-022-08610-1
Download citation
Received : 04 April 2022
Accepted : 21 September 2022
Published : 14 October 2022
DOI : https://doi.org/10.1186/s12913-022-08610-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cancer patients
- Umbrella review
- Health care
- Outcome assessment
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Biomarker-Driven Lung Cancer
- HER2-Positive Breast Cancer
- Chronic Lymphocytic Leukemia
- Small Cell Lung Cancer
- Renal Cell Carcinoma

- CONFERENCES
- PUBLICATIONS
Case Presentation: A 72-Year-Old Woman With Metastatic Colorectal Cancer
Kanwal Raghav, MBBS, MD, presents the case of a 72-year-old woman with metastatic colorectal cancer and describes the first-line therapy options.

EP: 1 . Case Presentation: A 72-Year-Old Woman With Metastatic Colorectal Cancer
Ep: 2 . maintenance therapies in metastatic colorectal cancer, ep: 3 . metastatic colorectal cancer: regorafenib, ep: 4 . treatment sequencing in metastatic colorectal cancer.
Kanwal Raghav, MBBS, MD: Today we’ll be discussing a case of a 72-year-old woman with metastatic colorectal cancer. This patient presented with a 2-month history of bloating and abdominal discomfort. Her last colonoscopy was about 2 years ago and was negative, and she also had some unintentional weight loss. With regard to her past medical history, it’s significant only because of a hysterectomy done about 12 years ago and high blood pressure, which is controlled with lisinopril.
During the clinic work-up, the patient was found to be anemic with an elevated CEA [carcinoembryonic antigen] of 6 ng/mL. The colonoscopy revealed a 9-cm mass in the ascending colon; biopsy of this showed a poorly differentiated adenocarcinoma. The molecular profiling showed a microsatellite stable tumor, which was KRAS, NRAS, and BRAF wild type. CT scan showed widespread lesions spread across the liver. The patient was diagnosed with stage IV colorectal cancer, and the ECOG PS [performance status] of the patient was 1.
At that time, the patient was started on treatment with bevacizumab and FOLFOX [5-fluorouracil, leucovorin, oxaliplatin]. The patient received about 4 months of this treatment with scans at 2- and 4-months showing response. This was followed by maintenance chemotherapy between May 2018 and June 2019. In June 2019, the patient had increasing symptoms of shortness of breath and fatigue, and scans showed disease progression in both the lungs and the liver. Patient was then switched to FOLFIRI [5-fluorouracil, leucovorin, irinotecan] and cetuximab and received this treatment until August 2020 with stable disease as the best response. In August 2020, the patient had progressive disease and was given regorafenib.
Interestingly, it’s strange that the patient developed this disease in a rather short interval from the last colonoscopy, which was completely negative. We also want to notice that certain comorbidities can affect our treatment decisions in metastatic colorectal cancer, like high blood pressure, especially whether it’s controlled. In this case it was controlled. With regard to molecular profiling, this patient has had some focused testing around RAS and BRAF, but I would have done either a next-generation-sequencing panel or at least have status for HER2 amplification on expression, and also NTRK fusions, which are also targeted with subsets. It’s very clear that the patient has an unresectable disease, and therefore surgery is definitely not an option. That’s what we’re dealing with. Furthermore, the PS of the patient is 1, which has implications in how aggressive you can be with cytotoxic chemotherapy. Those are a couple of points that are noteworthy. It should also be remembered that the patient has a right-sided colon cancer because they have a 9-cm ascending mass lesion.
The first-line therapy options are usually a combination of cytotoxic chemotherapy with a biologic attached to them. In some cases, the first-line cytotoxic option is a triplet cytotoxic which is 5-FU [5-fluorouracil], oxaliplatin, and irinotecan or FOLFOXIRI [5-fluorouracil, leucovorin, oxaliplatin, irinotecan] with bevacizumab. This patient would not qualify for that. The TRIBE2 study that established the survival benefit of FOLFOXIRI [5-fluorouracil, leucovorin, oxaliplatin, irinotecan], which is triplet cytotoxic over doublets, allowed only patients with ECOG PS 0, especially if they were beyond ages of 70—so 71 to 75 patients, and all of them had to have ECOG PS0. Anything less than that, we could have a lower ECOG PS.
As far as this patient is concerned, a doublet cytotoxic is very reasonable. This was combined with a biologic that is anti-VEGF attached to bevacizumab, which is a common biologic. In some patients who are RAS, BRAF wild-type, HER2-negative, and left-sided colon cancer, there is also a possibility of using an anti-EGFR agent, such as cetuximab or panitumumab, up front because those are the patients that benefit most from this. Because this patient has a right-sided tumor, the choice of bevacizumab with FOLFOX [5-fluorouracil, leucovorin, oxaliplatin] was a reasonable choice.
Transcript edited for clarity.
Case Overview: A 72-Year-Old Woman With Metastatic Colorectal Cancer
Initial presentation
A 72-year-old woman reported a 2-month history of bloating and abdominal cramping, and an 8-pound unintentional weight loss
Her last screening colonoscopy when she was 70 years of age was negative
PMH: hysterectomy at age 60, high blood pressure well controlled with lisinopril
Clinical workup
Labs: Hg 8.4 g/dL, CEA 6 ng/mL
Colonoscopy revealed a 9-cm mass in ascending colon
Pathology: invasive, poorly differentiated adenocarcinoma
Molecular testing: KRAS, NRAS, and BRAF wildtype; microsatellite stable
CT scan revealed widespread lesions in the liver
Diagnosis: Stage 4 colorectal cancer
ECOG PS is 1
The patient received systemic therapy with FOLFOX + bevacizumab for 6 cycles, which was well tolerated
Follow-up imaging at 2 months and 4 months showed response in liver lesions
The patient continued on bevacizumab maintenance
- The patient presents with shortness of breath and fatigue
- CT CAP shows two new lung lesions and growth of liver lesions
- The patient is switched to FOLFIRI and cetuximab
- Follow-up imaging showed stable disease in liver and lungs
August 2020
- The patient reports severe fatigue
- CT CAP shows progression in the lungs and new bony lesions
- The patient is given regorafenib alone

Colorectal Cancer: Leveraging Awareness and Early Detection
For Colorectal Cancer Awareness Month, Jedrzej Wykretowicz, MD, PhD, discussed the importance of early detection and taking steps towards the prevention of colorectal cancer.

Behind the FDA Approval of Fruquintinib for Previously Treated mCRC
In season 4, episode 18 of Targeted Talks, Arvind Dasari, MD, MS, dives into the recent approval of fruquintinib for patients with metastatic colorectal cancer.

Study Finds Susceptibility Gene Variations by Race/Ethnicity in Early-Onset CRC
In an interview with Targeted Oncology, Andreana N. Holowatyj, PhD, MSCI, discussed data from a study which found racial and ethnic differences in susceptibility genes for early-onset colorectal cancer, suggesting current multigene panel tests may not be accurate for diverse populations.

Special Episode: Insight on Targeting Rare Genomic Alterations in Colorectal Cancers
In season 2, episode 6 of Targeted Talks, Dr. Michael J. Overman, joins Targeted Oncology for a special discussion around rare genomic alterations in colorectal cancer

Translating Outcomes in Metastatic Colorectal Cancer (mCRC)
In this companion article, Dr Tanios Bekaii-Saab provides insights into effective management of patients with metastatic colorectal cancer.

CheckMate-8HW Meets Primary End Points With Nivolumab/Ipilimumab in mCRC
A dual primary end point of progression-free survival in the phase 3 CheckMate-8HW trial evaluating nivolumab and ipilimumab in metastatic colorectal cancer has been met.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NEWS FEATURE
- 13 March 2024
Why are so many young people getting cancer? What the data say
- Heidi Ledford
You can also search for this author in PubMed Google Scholar
Illustration by Acapulco Studio
You have full access to this article via your institution.
Of the many young people whom Cathy Eng has treated for cancer, the person who stood out the most was a young woman with a 65-year-old’s disease. The 16-year-old had flown from China to Texas to receive treatment for a gastrointestinal cancer that typically occurs in older adults. Her parents had sold their house to fund her care, but it was already too late. “She had such advanced disease, there was not much that I could do,” says Eng, now an oncologist at Vanderbilt University Medical Center in Nashville, Tennessee.
Eng specializes in adult cancers. And although the teenager, who she saw about a decade ago, was Eng’s youngest patient, she was hardly the only one to seem too young and healthy for the kind of cancer that she had.
Thousands of miles away, in Mumbai, India, surgeon George Barreto had been noticing the same thing. The observations quickly became personal, he says. Friends and family members were also developing improbable forms of cancer . “And then I made a mistake people should never do,” says Barreto, now at Flinders University in Adelaide, Australia. “I promised them I would get to the bottom of this.”

Almost half of cancer deaths are preventable
It took years to make headway on that promise, as oncologists such as Barreto and Eng gathered hard data. Statistics from around the world are now clear: the rates of more than a dozen cancers are increasing among adults under the age of 50. This rise varies from country to country and cancer to cancer , but models based on global data predict that the number of early-onset cancer cases will increase by around 30% between 2019 and 2030 1 . In the United States, colorectal cancer — which typically strikes men in their mid-60s or older — has become the leading cause of cancer death among men under 50 2 . In young women, it has become the second leading cause of cancer death.
As calls mount for better screening, awareness and treatments , investigators are scrambling to explain why rates are increasing. The most likely contributors — such as rising rates of obesity and early-cancer screening — do not fully account for the increase. Some are searching for answers in the gut microbiome or in the genomes of tumours themselves. But many think that the answers are still buried in studies that have tracked the lives and health of children born half a century ago. “If it had been a single smoking gun, our studies would have at least pointed to one factor,” says Sonia Kupfer, a gastroenterologist at the University of Chicago in Illinois. “But it doesn’t seem to be that — it seems to be a combination of many different factors.”
On the increase
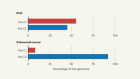
In some countries, including the United States, deaths owing to cancer are declining thanks to increased screening, decreasing rates of smoking and new treatment options. Globally, however, cancer is on the rise (see ‘Rising rates’). Early-onset cancers — often defined as those that occur in adults under the age of 50 — still account for only a fraction of the total cases, but the incidence rate has been growing. This rise, coupled with an increase in global population, means that the number of deaths from early-onset cancers has risen by nearly 28% between 1990 and 2019 worldwide. Models also suggest that mortality could climb 1 .
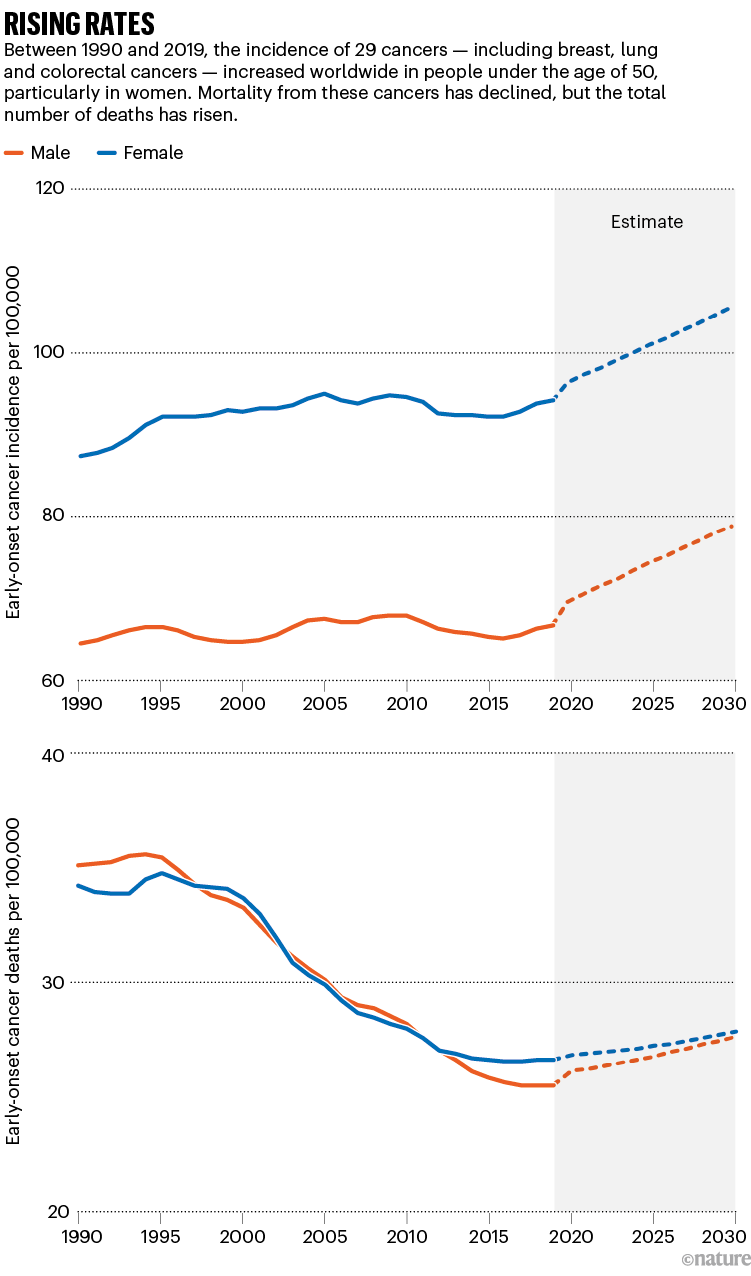
Source: Ref. 1
Often, these early-onset cancers affect the digestive system, with some of the sharpest increases in rates of colorectal, pancreatic and stomach cancer. Globally, colorectal cancer is one of the most common cancers and tends to draw the most attention. But others — including breast and prostate cancers — are also on the rise.
In the United States, where data on cancer incidence is particularly rigorous, uterine cancer has increased by 2% each year since the mid-1990s among adults younger than 50 2 . Early-onset breast cancer increased by 3.8% per year between 2016 and 2019 3 .
The rate of cancer among young adults in the United States has increased faster in women than in men, and in Hispanic people faster than in non-Hispanic white people. Colorectal cancer rates in young people are rising faster in American Indian and Alaska Native people than they are in white people (see ‘Health disparities’). And Black people with early onset colorectal cancer are more likely to be diagnosed younger and at a more advanced stage than are white people. “It is likely that social determinants of health are playing a role in early-onset cancer disparities,” says Kupfer. Such determinants include access to healthy foods, lifestyle factors and systemic racism .
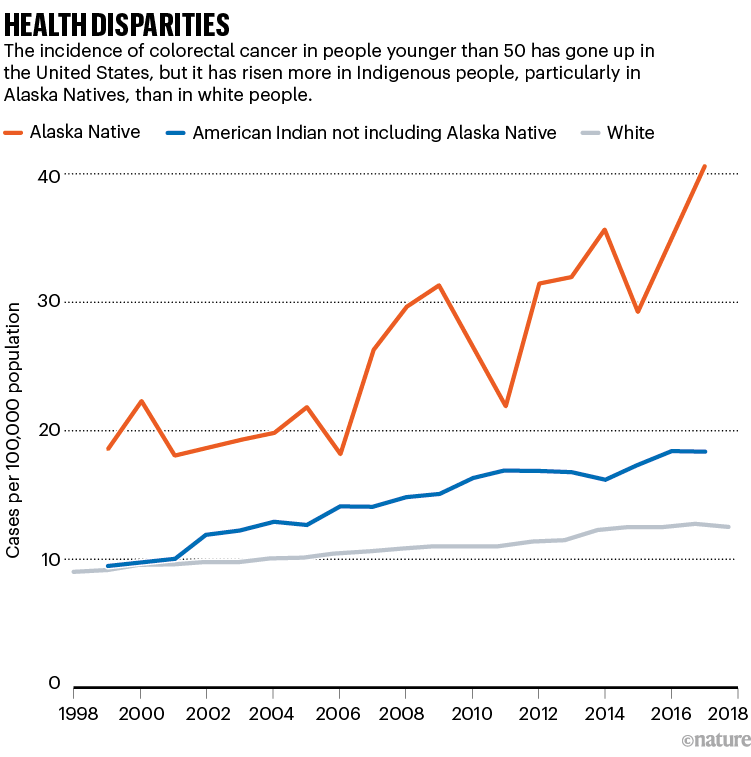
Source: Ref. 4
Cancer’s shift to younger demographics has driven a push for earlier screening. Advocates have been promoting events targeted at the under 50s. And high-profile cases — such as the 2020 death of actor Chadwick Boseman from colon cancer at the age of 43 — have helped to raise awareness. In 2018, the American Cancer Society urged people to be screened for colorectal cancer starting at age 45, rather than the previous recommendation of 50.
In Alaska, health leaders serving Alaska Native people have been recommending even earlier screening — at age 40 — since 2013. But the barriers to screening are high; many communities are inaccessible by road, and some people have to charter a plane to reach a facility in which they can have a colonoscopy. “If the weather’s bad, you could be there a week,” says Diana Redwood, an epidemiologist at the Alaska Native Tribal Health Consortium in Anchorage.
These efforts have paid off to some extent: screening rates in the community have more than doubled over the past three decades, and now exceed those of state residents who are not Alaska Natives. But mortality from colorectal cancer has not budged, says Redwood. Although colorectal cancer rates are falling in people over 50 years old, the age group that is still most likely to be screened, the rates in younger Alaska Native people are climbing by 5.2% each year 4 .
Genetic clues
The prominence of gastrointestinal cancers and the coincidence with dietary changes in many countries point to the rising rates of obesity and diets rich in processed foods as likely culprits in contributing to rising case rates. But statistical analyses suggest that these factors are not enough to explain the full picture, says Daniel Huang, a hepatologist at the National University of Singapore. “Many have hypothesized that things like obesity and alcohol consumption might explain some of our findings,” he says. “But it looks like you need a deeper dive into the data.”
Those analyses match the anecdotal experiences that clinicians described to Nature : often, the young people they treat were fit and seemingly healthy, with few cancer risk factors. One 32-year-old woman that Eng treated was preparing for a marathon. Previous physicians had dismissed the blood in her stool as irritable bowel syndrome caused by intense training. “She was healthy as can be,” says Eng. “If you looked at her, you would have no idea that more than half of her liver was tumour.”

US cancer deaths are falling — but not fast enough
Prominent cancer-research funders, including the US National Cancer Institute and Cancer Research UK, have supported programmes to find other contributors to early-onset cancer. One approach has been to look for genetic clues in early-onset tumours that might set them apart from tumours in older adults. Pathologist Shuji Ogino at Harvard Medical School in Boston, Massachusetts, and his colleagues have found some possible characteristics of aggressive tumours in early-onset cancers. For example, aggressive tumours are sometimes particularly adept at suppressing the body’s immune responses to cancer, and Ogino’s team has found signs of a muted immune response to some early-onset tumours 5 .
But these differences are subtle, he says, and researchers have yet to find a clear demarcation between early-onset and later-onset cancers. “It’s not dichotomous, but more like a continuum,” he says.
Researchers have also looked at the microorganisms that reside in the human body. Disruptions in microbiome composition, such as those caused by dietary changes or antibiotics, have been linked to inflammation and increased risk of several diseases, including some forms of cancer. Whether there is a link between the microbiome and early-onset cancers is still in question: results so far are still preliminary and it’s difficult to gather long-term data, says Christopher Lieu, an oncologist at the University of Colorado Cancer Center in Aurora. “The list of things that impact the microbiome is so extensive,” he says. “You’re asking people to recall what they ate as kids, and I can barely remember what I ate for breakfast.”
Looking to the past
But increasing the size of studies could help. Eng is developing a project to look at possible correlations between microbiome composition and the onset of cancer at a young age, and she plans to combine her data with those from collaborators in Africa, Europe and South America. Because the number of early-onset cancer cases is still relatively small at any one centre, this kind of international coordination is important to give statistical analyses more power, says Kimmie Ng, founding director of the Young-Onset Colorectal Cancer Center at the Dana-Farber Cancer Institute in Boston.
Another approach is to scrutinize the differences between countries. For example, Japan and South Korea are located near one another and are similar economically. But early-onset colorectal cancer is increasing at a faster rate in South Korea than it is in Japan, says Tomotaka Ugai, a cancer epidemiologist at Harvard Medical School. Ugai and his collaborators hope to determine why.
How gut microbes are joining the fight against cancer
But data are scarce in some countries. In South Africa, cancer data are collected only from the 16% of the population that has medical insurance, says Boitumelo Ramasodi, regional director for Southern Africa at the Global Colon Cancer Association, a non-profit organization in Washington DC. Those who do not have insurance are not counted. And families rarely keep records of who has died of cancer, she says. For many Black people in the country, cancer is considered a white person’s disease; Ramasodi initially struggled to make sense of her own diagnosis of colorectal cancer at the age of 44. “Black people don’t get cancer,” she thought at the time. “I’m young, I’m Black, why do I have cancer?”
Ultimately, researchers will also have to look back in time for clues to understand rising early-onset cancers, says epidemiologist Barbara Cohn at the Public Health Institute in Oakland, California. Research has shown that cancers can arise many years after an exposure to a carcinogen, such as asbestos or cigarette smoke. “If the latent period is decades, then where do you look?” she says. “We believe that you need to look as early as possible in life to understand this.”
To do that, researchers will need 40–60 years of data, collected from thousands of people — enough to capture a sufficient number of early-onset cancers. Cohn directs an unusual repository of data and blood samples that have been collected from about 20,000 expectant mothers during pregnancy since 1959. Researchers have followed many of the original participants, and their children, since then.
Cohn and Caitlin Murphy, an epidemiologist at the University of Texas Health Science Center at Houston, have already tried combing through the data to look for ties to early-onset cancers, and have found a possible association between early colorectal cancer and prenatal exposure to a particular synthetic form of progesterone, sometimes taken to prevent premature labour 6 . But the study must be repeated in other cohorts for investigators to be sure.
More informed
Finding studies that follow cohorts from the prenatal stage to adulthood is a challenge. The ideal study would enrol thousands of expectant mothers in several countries, collect data and samples of blood, saliva and urine, and then track them for decades, says Ogino. A team funded by Cancer Research UK, the US National Cancer Institute and others will analyse data from the United States, Mexico and several European countries, to look for environmental exposures and other possible influences on early-onset cancer risk. Murphy and Cohn also hope to incorporate data collected from fathers and are working with collaborators to analyse blood samples in search of more chemicals that offspring might have encountered in the womb.
Murphy expects the results to be complicated. “At first, I really believed that there was something unique about early-onset colorectal cancers compared to older adults, and a risk factor out there that explains everything,” she says. “The more time I’ve spent, the more it seems clear that there’s not just one particular thing, it’s a bunch of risk factors.”

Cruel fusion: What a young man’s death means for childhood cancer
For now, it’s important for physicians to share their data on early-onset cancers and to follow their patients even after they complete their therapy, to learn more about how best to treat them, says Irit Ben-Aharon, an oncologist at the Rambam Health Care Campus in Haifa, Israel. Cancer treatment in young people can be fraught: some cancer drugs can cause cardiovascular problems or even secondary cancers years after treatment — a risk that becomes more concerning in a young person, she says.
Young adults might also be pregnant at the time of diagnosis, or more concerned about the impact of cancer drugs on their fertility than are people who are past their reproductive years. And they are less likely to be retired, and more likely to be concerned about whether their cancer treatment will cause long-term cognitive damage that could hinder their ability to work.
When Candace Henley was diagnosed with colorectal cancer at the age of 35, she was a single mother raising five children. The aggressive surgery she received rendered her unable to continue in her job as a bus driver, and the family was soon homeless. “I didn’t know what questions to ask and so the decisions around treatment were made for me,” says Henley, who went on to found The Blue Hat Foundation for Colorectal Cancer Awareness in Chicago, Illinois. “No one unfortunately considered what my needs were at home.”
In the years since Eng first noticed how young her patients were, certain things have changed. Some advocacy groups have begun targeting their information campaigns at younger audiences. People with early-onset cancers are more informed now and seek out second opinions when physicians dismiss their symptoms, Eng says. This could mean that physicians will more often catch early-onset cancers before they have spread and become more difficult to treat.
But Barreto still doesn’t have all the answers he promised. He wants to study the impact of prenatal stresses, such as exposure to alcohol and cigarette smoke or malnourishment, on early-cancer risk. He’s contacted scientists around the world, but no biobanking projects contain the data and samples that he requires.
If all of the data he and others need aren’t available now, it’s understandable, he says. “We never saw this coming. But in 20 years if we don’t have databases to record this, it’s our failure. It’s negligence.”
Nature 627 , 258-260 (2024)
doi: https://doi.org/10.1038/d41586-024-00720-6
Zhao, J. et al. BMJ Oncol. 2 , e000049 (2023).
Article Google Scholar
Siegel, R. L, Giaquinto, A. N. & Jemal, A. CA Cancer J. Clin. 74 , 12–49 (2024).
Article PubMed Google Scholar
Xu, S. et al. JAMA Netw. Open 7 , e2353331 (2024).
Kratzer, T. B. et al. CA Cancer J. Clin. 73 , 120–146 (2023).
Ugai, T. et al. Cancer Immunol. Immunother. 71 , 933–942 (2022).
Murphy, C. C., Cirillo, P. M., Krigbaum, N. Y. & Cohn, B. J . Endocr. Soc. 5 , A496–A497 (2021).
Download references
Reprints and permissions
Related Articles

- Epidemiology
- Medical research
Cutting-edge CAR-T cancer therapy is now made in India — at one-tenth the cost
News 21 MAR 24

‘Woah, this is affecting me’: why I’m fighting racial inequality in prostate-cancer research
Career Q&A 20 MAR 24
Whittling down the bacterial subspecies that might drive colon cancer
News & Views 20 MAR 24

Fungal diseases are spreading undetected
Outlook 14 MAR 24

Massive public-health experiment sends vaccination rates soaring
News 13 MAR 24

Meningitis could be behind ‘mystery illness’ reports in Nigeria
News 05 MAR 24

Pregnancy advances your ‘biological’ age — but giving birth turns it back
News 22 MAR 24

First pig kidney transplant in a person: what it means for the future
Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Warmly Welcomes Talents Abroad
“Qiushi” Distinguished Scholar, Zhejiang University, including Professor and Physician
No. 3, Qingchun East Road, Hangzhou, Zhejiang (CN)
Sir Run Run Shaw Hospital Affiliated with Zhejiang University School of Medicine
Postdoctoral Associate
Our laboratory at the Washington University in St. Louis is seeking a postdoctoral experimental biologist to study urogenital diseases and cancer.
Saint Louis, Missouri
Washington University School of Medicine Department of Medicine
Recruitment of Global Talent at the Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
The Institute of Zoology (IOZ), Chinese Academy of Sciences (CAS), is seeking global talents around the world.
Beijing, China
Institute of Zoology, Chinese Academy of Sciences (IOZ, CAS)
Postdoctoral Fellow-Proteomics/Mass Spectrometry
Location: Tulane University School of Medicine, New Orleans, LA, USA Department: Biochemistry and Molecular Biology Tulane University School of Med...
New Orleans, Louisiana
Tulane University School of Medicine (SOM)
Open Faculty Position in Mathematical and Information Security
We are now seeking outstanding candidates in all areas of mathematics and information security.
Dongguan, Guangdong, China
GREAT BAY INSTITUTE FOR ADVANCED STUDY: Institute of Mathematical and Information Security
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Reference Manager
- Simple TEXT file
People also looked at
Systematic review article, an overview of case reports and case series of pulmonary actinomycosis mimicking lung cancer: a scoping review.

- Department of Microbiology, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
Background: Pulmonary actinomycosis (PA) is a rare type of Actinomyces infection that can be challenging to diagnose since it often mimics lung cancer.
Methods: Published case reports and case series of PA in patients with suspicion of lung cancer were considered, and data were extracted by a structured search through PubMed/Medline.
Results: After analyzing Medline, 31 studies were reviewed, from which 48 cases were extracted. Europe had the highest prevalence of reported cases with 45.1%, followed by Asia (32.2%), America (19.3%), and Africa (3.2%). The average age of patients was 58.9 years, and 75% of all patients were above 50 years old. Male patients (70%) were predominantly affected by PA. The overall mortality rate was 6.25%. In only eight cases, the causative agent was reported, and Actinomyces odontolyticus was the most common isolated pathogen with three cases. Based on histopathological examination, 75% of the cases were diagnosed, and the lobectomy was performed in 10 cases, the most common surgical intervention. In 50% of the cases, the selective antibiotics were intravenous and oral penicillin, followed by amoxicillin (29.1%), amoxicillin-clavulanic acid, ampicillin, levofloxacin, and doxycycline.
Conclusion: The non-specific symptoms resemble lung cancer, leading to confusion between PA and cancer in imaging scans. Radiological techniques are helpful but have limitations that can lead to unnecessary surgeries when confusing PA with lung cancer. Therefore, it is important to raise awareness about the signs and symptoms of PA and lung cancer to prevent undesirable complications and ensure appropriate treatment measures are taken.
Introduction
Actinomyces species are Gram-positive bacteria with anaerobic and facultative microaerophilic metabolism that typically colonize the oropharynx, urogenital tract, or gastrointestinal system ( 1 , 2 ). Actinomycosis is generally considered an endogenous infection. Although the bacteria are initially colonized on the surface of the mucosa, they can reach the deeper tissues through any disruption of the mucosal barrier caused by procedures such as trauma, surgical intervention, or foreign bodies ( 2 – 4 ). Actinomycosis is a rare and granulomatous disease that progresses slowly and creates sinus tract fistulae in a chronic form with a slow progression that creates sinus tract fistulae in a chronic form. It has been known for more than 150 years, and the most common causative agent is Actinomyces israelii ( 5 , 6 ). In recent years, the frequency of all forms of actinomycosis has decreased, possibly as a result of the enhancement of oral hygiene and antibiotic therapy upon infection suspicion ( 1 ). However, there is no solid proof to support the effectiveness of such actions in reducing the incidence of colonization and mild periodontal infection with Actinomyces species ( 4 , 6 ).
The common forms of actinomycosis are cervicofacial, abdominal, pelvic, and pulmonary. Moreover, on rare occasions, the spread of local infection through hematogenous dissemination may lead to the development of actinomycotic lesions in the lungs. Despite anatomic barriers, Actinomyces can spread and eventually invade the pleura, resulting in empyema formation.
With the improvement of oral hygiene and the availability of effective antibiotics, the severity of PA manifestation has become less severe. Furthermore, if diagnosis and treatment are not performed correctly, it can spread into the chest wall and create a pleuro-cutaneous fistula and destruction of vertebrae and ribs ( 1 , 2 , 7 , 8 ). The diagnosis of pulmonary actinomycosis (PA) is quite challenging, and the delay in diagnosis can last for 6 months. PA usually results in the formation of nodules, consolidation, or mass that can often be mistaken for lung cancer. Therefore, PA could be misdiagnosed as lung cancer, lung abscess, or tuberculosis ( 9 , 10 ). Due to non-specific laboratory and clinical features, it is usually challenging to differentiate PA from lung malignancy. Moreover, the most common initial diagnosis of PA among physicians is lung cancer ( 10 – 14 ). The common signs and symptoms of PA are fever, chest pain, hemoptysis, shortness of breath, and a productive cough ( 15 , 16 ). Furthermore, the severity of PA manifestations has become less severe with the enhancement of oral hygiene and the availability of effective antibiotics.
Dealing with PA can be challenging due to its difficult diagnosis. However, if more people are aware of this infection, it could lead to an easier diagnosis and prevent undesired complications such as unnecessary surgeries and treatment with the wrong medication. To study this, we conducted a scoping review that explored the clinical, epidemiological, diagnostic, and therapeutic features of PA cases that were initially suspected of lung cancer.
Search strategy
In the current study, a Medline search (via PubMed) was performed on 4 December 2022. The keywords were chosen from the National Library of Medicine’s Medical Subject Heading (MeSH) terms, titles, and abstracts through Boolean operators (and/or) including “Pulmonary Neoplasms” or “Lung Neoplasm” or “Lung Cancer” or “Pulmonary Cancer” or “Cancer of Lung,” and (Actinomyc*). The present study was conducted according to the PRISMA extension for scoping reviews.
Inclusion and exclusion criteria
All case reports and case series studies were included where the cancer was initially suspected in the diagnosis process, and irrelevant articles (review articles, conference abstracts, and studies with unclear results and insufficient data) were excluded.
Study selection and data extraction
The titles, abstracts, and full texts of all included studies were reviewed independently by two authors (AKH and SHM). The search was limited to English-published studies, and any disagreements among authors were resolved through discussion and consensus. The data extracted from each study included the first author’s name, publication year, country, sex, age, Actinomyces species, treatment, surgery or puncture drainage for biopsy, diagnosis method, radiologic finding, patient outcome, and additional findings.
Epidemiology
Our search of the Medline database yielded a total of 204 hits, we reached 31 studies, of which 48 cases were included in the final analysis ( Figure 1 ). These cases were reported from Poland, Malaysia, India, Korea, Germany, Italy, and the Netherlands (one study), China, Spain, and Turkey (two studies), Japan and Greece (four studies), and the USA (six studies). Furthermore, there were four case series from Japan, Italy, Germany, and Tunisia (one study). Accordingly, Europe had the highest share of reported studies with 45.1% (14 studies), followed by Asia with 32.2% (10 studies), America with 19.3% (6 studies), and Africa with 3.2% (one study). No cases were identified from Oceania ( Figure 2 ).
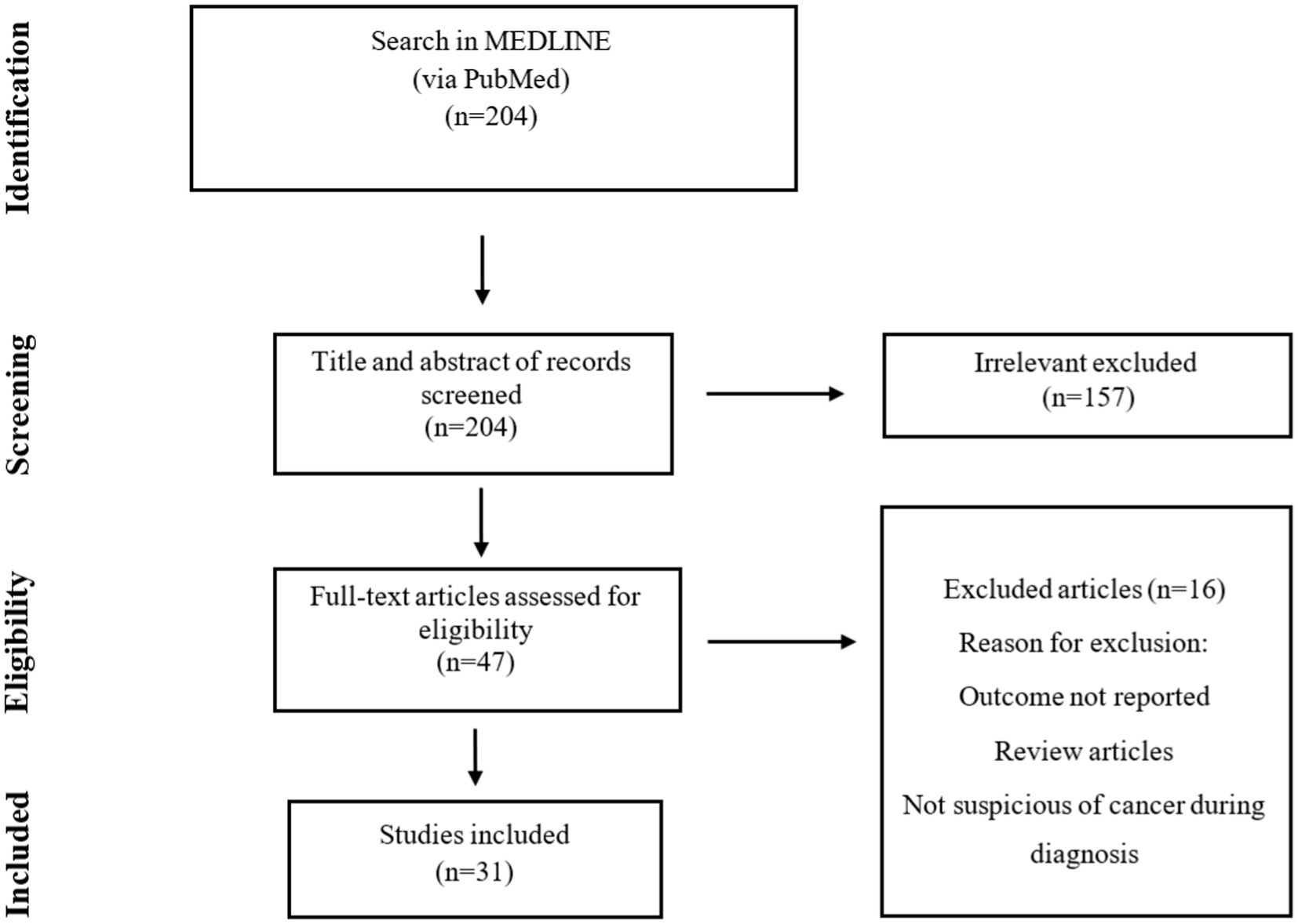
Figure 1 . Flowchart of publication selection and their inclusion in the scoping review.
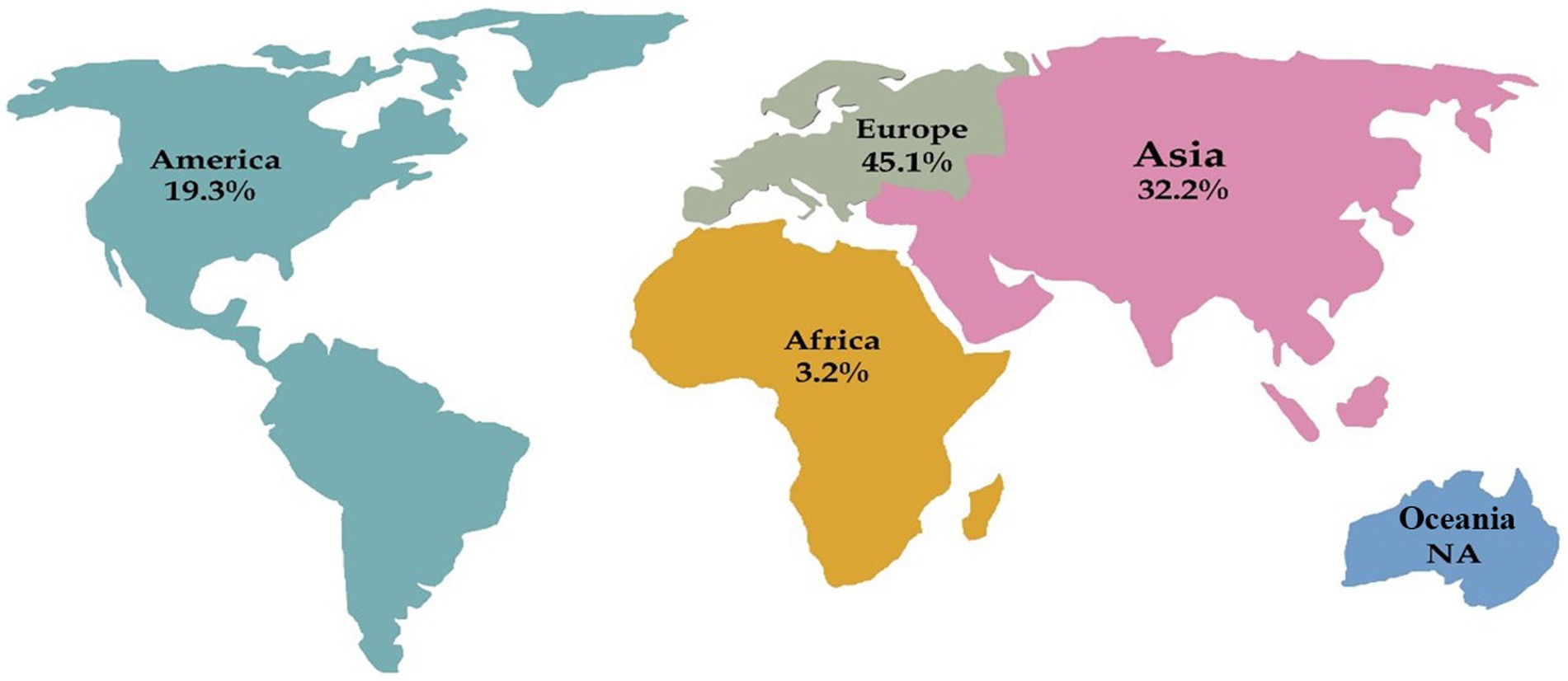
Figure 2 . Distribution of pulmonary actinomycosis cases in each continent. NA: not available.
Outcome and etiology
Overall, PA showed low mortality, and only three patients died. A 59-year-old female developed lung adenocarcinoma following an initial PA diagnosis. The patient died eventually after chemotherapy failure. In another 50-year-old male patient, recovery happened, although, after 1.5 years, the patient died from a massive gastrointestinal hemorrhage. The third patient was an 83-year-old male who died despite antibiotic treatment with penicillin.
Our results showed that only 25 and 70% of the patients were female and male, respectively, and in two cases, sex was not reported. The mean age of patients was 58.9, within the range of 36–86, and 75% of all patients were above 50 years old ( Tables 1 , 2 ).
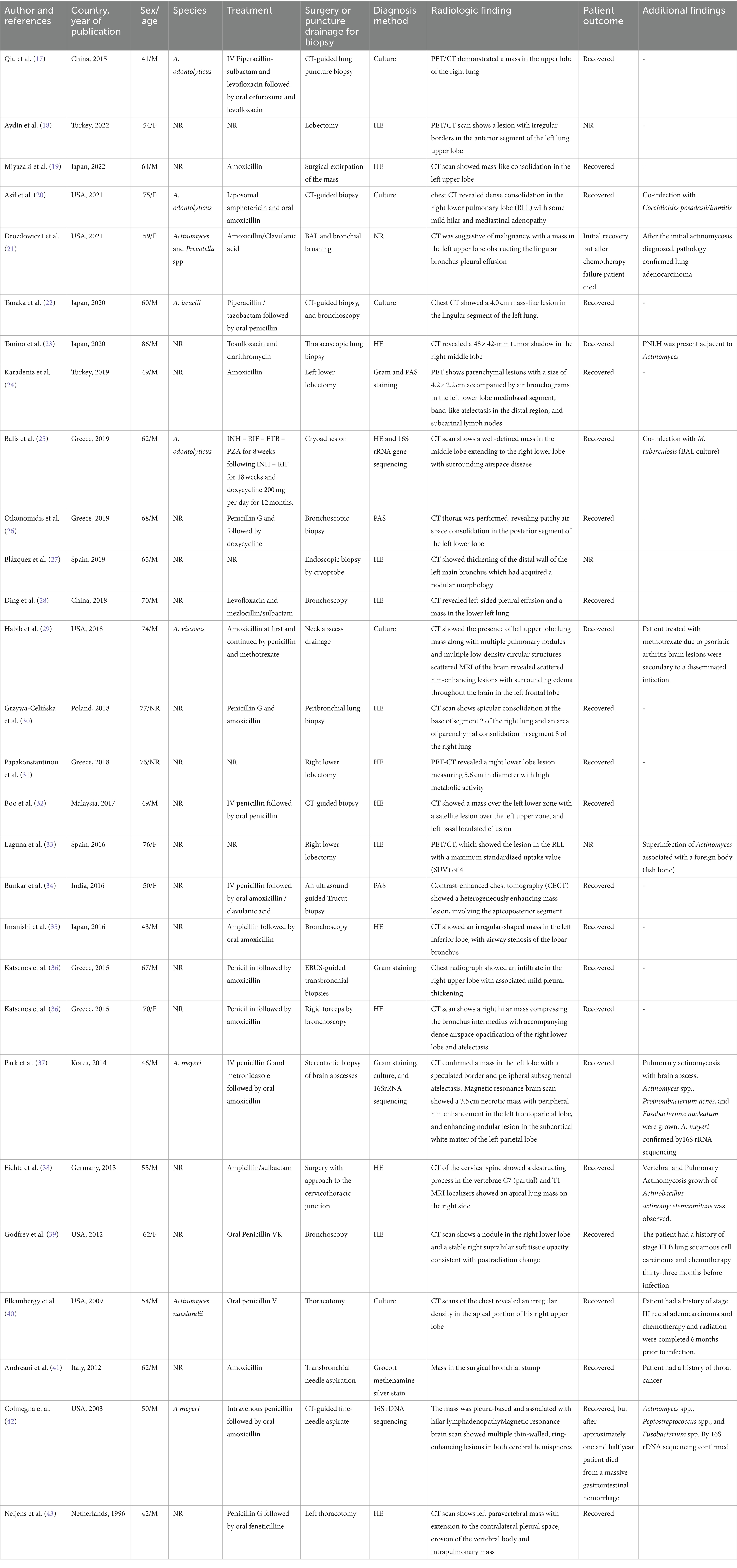
Table 1 . Epidemiological, clinical, diagnosis, and therapeutic features of patients with pulmonary actinomycosis from individual case reports.
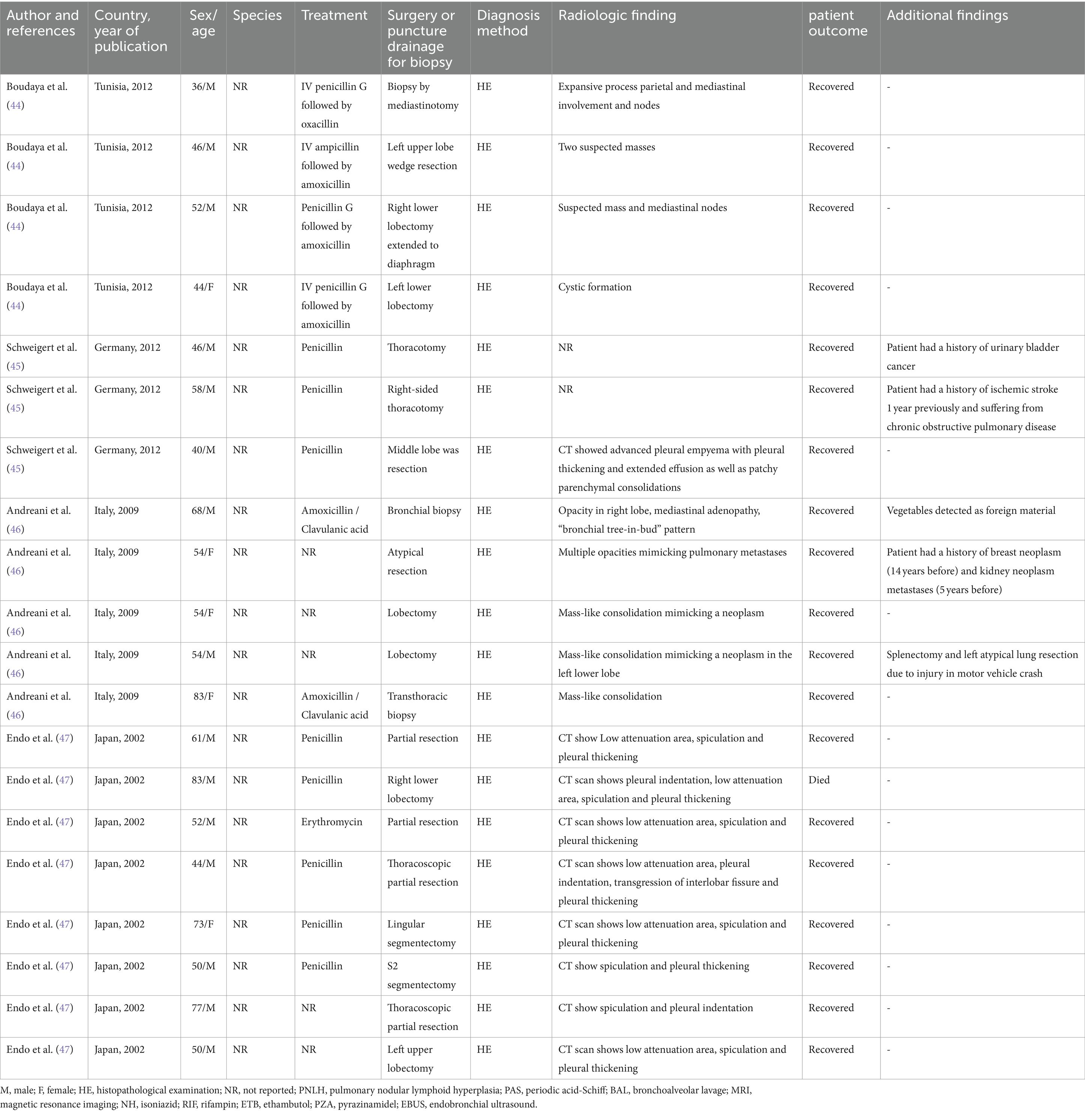
Table 2 . Epidemiological, clinical, diagnosis, and therapeutic features of patients with pulmonary actinomycosis from individual case series.
Several patients in the study had various medical conditions in addition to PA. In one patient, pulmonary nodular lymphoid hyperplasia (PNLH) was diagnosed adjacent to the Actinomyces lesion, and lung adenocarcinoma was detected in one patient after PA diagnosis. Moreover, one of the patients had a history of treatment for lung squamous cell carcinoma, 33 months before the PA diagnosis. Another case had a history of treatment for rectal adenocarcinoma 6 months before the infection. Moreover, there were two patients with a history of throat and urinary bladder cancer, as well as one patient with a history of breast neoplasm (14 years before the infection) and kidney neoplasm metastases (5 years before the infection). Another patient had a history of treatment with methotrexate as well as a brain lesion following the disseminated infection. One patient had PA with a brain abscess. One patient tested positive for tuberculosis by culture of bronchoalveolar lavage fluid. Furthermore, another patient was involved in vertebral and PA with the growth of Actinobacillus actinomycetemcomitans . Additionally, in one patient, co-infection with Coccidioides posadasii/immitis was reported.
In addition to Actinomyces , Prevotella spp., Propionibacterium acnes , Fusobacterium nucleatum , Peptostreptococcus spp., and Fusobacterium spp. were also found in some patients. One patient had an ischemic stroke 1 year before the infection and suffered from chronic obstructive pulmonary disease. Another patient who was involved in a motor vehicle crash underwent splenectomy and atypical lung resection. The Actinomyces infection seemed to be related to foreign bodies, such as fish bones and vegetables, which were found in two patients. Most of the patients (79%) with PA were immunocompetent. Accordingly, in 83% of the cases, Actinomyces at the species level were not detected, and species identification was reported in only 8 cases. The most reported species was Actinomyces odontolyticus , with three cases, followed by Actinomyces meyeri , with two cases. Actinomyces viscosus , Actinomyces naeslundii , and Actinomyces israelii were found in only one case each. Culture was the most common detection method, while 16SrRNA sequencing was performed in two cases and 16SrDNA sequencing was used in one case ( Figure 3 ).
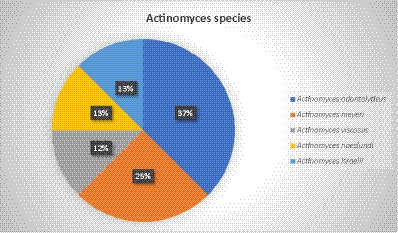
Figure 3 . Actinomyces species related to pulmonary actinomycosis.
Diagnosis method
In most of the cases (75%, 36 out of 48), the diagnosis was based on the histopathologic examination (HE) of different types of specimens. The most common specimen was a lobectomy (10 cases), while partial resection, thoracotomy, bronchoscopy, and CT-guided biopsy were reported in 4 cases each. Moreover, surgery, thoracoscopic lung biopsy, lobe resection, and segmentectomy were observed in two cases ( Figure 4 ). In two patients with brain involvement, a stereotactic biopsy of brain abscesses and neck abscess drainage was performed.
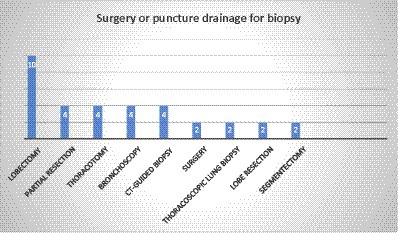
Figure 4 . Distribution of individual methods for biopsy.
The bacterial culture was diagnostic only in 12.5% of the patients (six cases), as Actinomyces species are difficult to grow. Gram staining and periodic acid–Schiff stain were also reported in three cases, 16SrRNA sequencing in two cases, and 16SrDNA sequencing was reported in one case. Additionally, the diagnosis method was not reported in one case. Figure 5 represents the different methods used to diagnose PA.
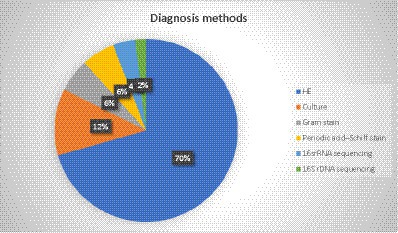
Figure 5 . Different methods used for the diagnosis of pulmonary actinomycosis.
In a total of 48 cases, the antimicrobial treatment was not mentioned in 9 cases. In the majority of cases (50%, 24 cases), treatment was administered via both intravenous and oral penicillin. Amoxicillin was the second most common agent with 29.1% (14 cases, 29.1%), followed by amoxicillin–clavulanic acid (4 cases), and ampicillin, levofloxacin, and doxycycline, each with 2 cases. Additionally, feneticilline, erythromycin, oxacillin, ampicillin/sulbactam, piperacillin–sulbactam, mezlocillin /sulbactam, metronidazole, tosufloxacin, clarithromycin, cefuroxime, and piperacillin /tazobactam were each reported in one case ( Figure 6 ).
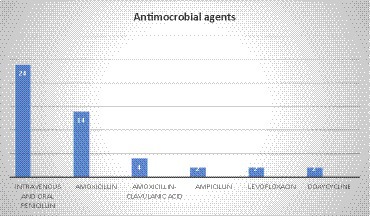
Figure 6 . Antimicrobial agent used for the treatment of pulmonary actinomycosis.
In another case, a patient had a co-infection with Coccidioides posadasii/immitis . The treatment plan consisted of liposomal amphotericin and oral amoxicillin, which proved to be successful in leading to the patient’s recovery. Another patient had a co-infection with Mycobacterium tuberculosis, and treatment was started with rifampin, ethambutol, pyrazinamide, and isoniazid for 8 weeks. It was followed by rifampin and isoniazid for 18 weeks and doxycycline for 12 months.
PA is a rare actinomycosis disease with a slow-progressing form of pulmonary infection, with a prevalence of 15% in all actinomycosis cases. This infection is often associated with the aspiration of oropharyngeal or gastrointestinal secretions ( 31 , 48 ). It can involve both sexes and any age, but our findings showed that most of the infected patients were men and that 75% of patients were over 50 years of age. This is in correlation with other studies declaring that PA was more common in male patients and that the peak incidence of infection reached in the fourth to fifth decades of age ( 12 , 24 , 48 ). The high incidence of PA in male patients could be partly related to poorer oral hygiene and the occurrence of more facial trauma ( 9 , 48 ).
The findings of a chest computed tomography scan (CT scan) of actinomycosis are non-specific and resemble necrotic lung malignancy. This condition is characterized by chronic segmental airspace consolidation with low-attenuation areas that have peripheral enhancement ( 7 , 10 , 49 ). Additionally, cavitations, shadowing, and pleural effusion with cavitary lesions are also typical features of PA that can be misdiagnosed as tuberculosis ( 28 ). Similarly, our results revealed that in most of the cases, CT scans were useful for diagnosis, but not always conclusive. The scan showed air space consolidation, mass in the middle lobes that could be misinterpreted as malignancy, pleural empyema, and opacity in the lobes, which could mimic pulmonary metastases. Moreover, positron emission tomography-computed tomography (PET-CT) is a helpful imaging technique to differentiate benign lesions from malignant ones, but there is limited information on PET-CT findings about PA ( 10 , 50 ).
This technique was used in five cases and showed lesions and masses in lung lobes. Nevertheless, there is minimal information about PET-CT findings on PA. This diagnostic method has also encountered some issues. According to Choi et al., PET-CT is not an ideal tool for the differentiation of PA from lung cancer because of its high fluorodeoxyglucose (FDG) uptake. Consequently, physicians may mistake the high FDG uptake in favor of lung malignancy over PA. Therefore, clinicians must carefully evaluate the need for lung resection surgery when PA is suspected ( 17 , 41 , 51 ).
Some pulmonary infections, such as tuberculosis, aspergilloma, and histoplasmosis, can create false positive results due to their high metabolic uptake. Furthermore, FDG uptake has been observed in actinomycosis, leading to a mimicry of pulmonary malignancies ( 10 , 24 , 45 , 52 ).
Although the diagnosis of PA could be delayed, our results showed that the mortality rate was only 6.25% and the overall outcome was acceptable. Similarly, a recent study in China showed that 75.9% of patients fully recovered, while another study in Korea reported a 98% recovery rate among 94 patients with PA ( 12 ). Therefore, PA seemed to have a good prognosis with a low rate of mortality because of antibiotic treatment and surgical intervention.
Actinomycosis might coexist with lung cancer, making the diagnosis even harder ( 9 ). Among the patients we studied, six had a history of cancer, and two had lung cancer. Although actinomycosis is unusual in immunosuppressed patients, immune system abnormalities may be a facilitating factor for the development of infection. However, the exact relationship between the two conditions is not yet fully understood ( 53 ). Interestingly, we found three cases in our research where PA involvement was diagnosed after cancer treatment ( 54 – 56 ). In one of the cases, the patient has been treated with bevacizumab for advanced non-small-cell lung cancer. After 36 months of bevacizumab maintenance, the patient was diagnosed with actinomycosis in the right lung. Bevacizumab was discontinued, and the patient was treated with amoxicillin–clavulanic acid. Unfortunately, the patient passed away after 3 months ( 54 ). The diagnostic method was culture in only 12% of the cases. Currently, positive culture in PA is rare due to the challenges of culturing anaerobic bacteria. Previous antibiotic treatments and bacterial overgrowth can also complicate matters. In addition, the evidence suggests that using normal saline, which is usually used for bronchoalveolar lavage, can prevent Actinomyces growth ( 9 , 45 , 57 , 58 ). On the other hand, isolating Actinomyces may be crucial to distinguishing nocardiosis or botryomycosis from actinomycosis, which is usually difficult to differentiate morphologically. As a result, the direct culture of biopsy material in both aerobic and anaerobic blood culture media can improve culture sensitivity ( 59 ). The accurate diagnosis of PA depends on HE, as radiologic imaging and culture may not be conclusive. Without histological or microbiological confirmation, misdiagnosis can be fairly common ( 48 , 60 ). However, sulfur granules in biopsy can be essential and suggestive, but not specific. On the other hand, when a small amount of tissue is biopsied, sulfur granules can be missed ( 60 , 61 ). Nevertheless, granulomas and multinucleated giant cells can be observed in some cases. These morphological shapes are not specific, and other pathogens such as Nocardia spp. and some fungal and parasitic infections can cause similar observations. Furthermore, Grocott methenamine silver staining can identify the branching microorganism that is specific for the existence of actinomycosis infection ( 6 , 62 , 63 ).
Furthermore, surgical intervention may be necessary for diagnosis and treatment if lung cancer cannot be ruled out ( 31 , 47 ). Endo et al. declared that a conclusive differential diagnosis between PA and necrotic lung cancer might be possible only when the surgical restriction specimen is sent for HE ( 47 ).
Furthermore, it has been shown that surgery can be avoided in most cases of thoracic actinomycosis, and long-term intravenous penicillin therapy leads to a good prognosis. However, early surgical intervention may lead to equally good or better outcomes by shortening the antibiotic therapy period ( 13 , 64 ).
Our results showed that in 75% of the cases diagnosed with HE, and similarly, in 94 cases in Korea, all PA patients were diagnosed with HE ( 12 ). Altogether, HE is an essential method for the correct diagnosis of PA ( 17 ). Moreover, the new approach of using molecular methods in diagnosis can be helpful in the detection of PA, as in one case, HE and 16SrRNA sequencing were used together for diagnosis. This was a complicated case, and the patient had a co-infection with PA and tuberculosis. The molecular method also led to the identification of a bacterial species, which was A. odontolyticus .
Moreover, 16SrRNA sequencing helped the diagnosis of A. meyeri in a complicated case of PA involvement with a brain abscess. In another case, the diagnosis made by 16SrDNA demonstrated that A. meyeri was a causative agent of PA. Furthermore, 16SrRNA is a component of the 30S ribosomal subunit in prokaryotic cells, and it is transcribed as a single-stranded ribosomal RNA molecule. On the other hand, the 16SrDNA is the gene that encodes the 16SrRNA, and it consists of double-stranded chromosomal DNA. 16SrRNA sequencing is used to detect and identify bacterial pathogens in clinical specimens from patients with a suspicion of infection. 16SrDNA is applied to identify microorganisms and determine microbial communities.
Recently, molecular techniques, including 16SrRNA sequencing, have been used to reach fast and precise results in reference or research laboratories, and such methods are now recommended in challenging conditions such as PA infection.
Furthermore, our results showed that beta-lactam antibiotics were used in the majority of cases (91%) as a selective drug, with intravenous and oral penicillin being used in half of the cases, followed by amoxicillin, amoxicillin–clavulanic acid, and ampicillin. This result is predictable, as antibiotic resistance is not considered a problem in actinomycosis.
Usually, Actinomyces spp. are susceptible to beta-lactams, and in particular, penicillin G and amoxicillin are considered the desirable drugs for actinomycosis treatment. Since Actinomyces spp. do not produce beta-lactamases, combining amoxicillin with beta-lactam inhibitors such as clavulanic acid is not usually necessary unless there are co-pathogens such as Enterobacteriaceae presumed in the infection ( 3 , 65 , 66 ).
Furthermore, in a retrospective analysis from China, 46% of the cases were treated with penicillin G ( 60 ). A recent study was conducted in Turkey on 37 PA patients, and it was reported that most cases (73%) were treated with penicillin G and ampicillin-sulbactam, 13% with cefuroxime and ceftriaxone, and 5.4% with clarithromycin, levofloxacin, and moxifloxacin ( 1 ). Contrastingly, ampicillin/sulbactam was used only in one case. Cefuroxime, erythromycin, and clarithromycin were used in one case. Additionally, macrolides are considered useful alternatives ( 65 ).
Furthermore, the presence of A. actinomycetemcomitans , Prevotella spp., P. acnes , F. nucleatum , Peptostreptococcus spp., and Fusobacterium spp. alongside Actinomyces spp. was reported in some cases. It seems that treatment with beta-lactam agents can effectively lead to the successful treatment of PA. However, it is important to note that metronidazole has no in vitro activity against Actinomyces ( 65 ). Therefore, combination therapy with penicillin G was observed in one case of PA, where P. acnes and F. nucleatum were grown simultaneously. Hoca et al. reported the combination of metronidazole with other antibiotics in four cases of PA with co-infection ( 1 ).
Treatment with piperacillin–tazobactam was observed in only one case and could be related to the fact that although piperacillin–tazobactam, meropenem, and imipenem are considered active against Actinomyces spp., their use should be limited to prevent the acquisition of resistant flora, as they have broad-spectrum effects ( 65 ). Interestingly, feneticilline, which is not approved, was used in one case from the Netherlands after initial treatment with penicillin G. Finally, antibiotic therapy is administered for a prolonged duration because of the chance of recurrence in PA. Patients with no surgical intervention and a shorter period of 3 months of antibiotic therapy are at a higher risk of recurrence ( 13 , 58 , 67 ). Furthermore, no study currently suggests the period for follow-up of recurrent infection, although some studies suggested 3 months, 6 months, and 1-year follow-ups ( 9 , 60 , 67 , 68 ). In summary, the treatment duration should be implemented in each case based on the main factors, such as severity and possible changes in the follow-up imaging.
Limitations
In the current study, we only used available studies on PubMed/Medline, and only English studies were included. Therefore, the relevant publications decreased. Additionally, discussing the bias, risks, and individual limitations in the studies was not possible, as they were not reported.
PA is a rare form of infection that is challenging to diagnose due to its non-specific symptoms, failure to detect pathogens, and resemblance to lung cancer. Although it can show similar imagining results as malignancy, which should be differentiated by the presence of nodules, in the sinus tract on the chest wall. Radiological techniques can be helpful in diagnosing PA but have their limitations. The limited available information about PA means that it can be easily confused with other diseases, leading to unnecessary surgeries.
Therefore, clinicians should be aware of the overlapping of signs and symptoms between PA and lung cancer. As antibiotic therapy may be adequate to treat this lung infection, biopsy specimen and histopathological examination should be considered before any surgical operation (i.e., lobectomy).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
AK: Writing – original draft, Writing – review & editing. NA: Writing – review & editing. SM: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hoca, N, Berktaş, M, Söyler, Y, Celep, C, and Tanrıkulu, F. Clinical features and treatment outcomes of pulmonary actinomycosis. Eur Rev Med Pharmacol Sci . (2022) 26:8064–72. doi: 10.26355/eurrev_202211_30160
PubMed Abstract | Crossref Full Text | Google Scholar
2. Könönen, E, and Wade, WG. Actinomyces and related organisms in human infections. Clin Microbiol Rev . (2015) 28:419–42. doi: 10.1128/CMR.00100-14
3. Wong, VK, Turmezei, T, and Weston, V. Actinomycosis. BMJ . (2011) 343:d6099. doi: 10.1136/bmj.d6099
Crossref Full Text | Google Scholar
4. Smego, RA Jr, and Foglia, G. Actinomycosis. Clin Infect Dis . (1998) 26:1255–61. doi: 10.1086/516337
5. Joshi, V, Koulaouzidis, A, McGoldrick, S, Tighe, M, and Tan, C. Actinomycotic liver abscess: a rare complication of colonic diverticular disease. Ann Hepatol . (2010) 9:96–8. doi: 10.1016/S1665-2681(19)31688-6
6. Chegini, Z, Didehdar, M, Tabaeian, SP, Khoshbayan, A, and Shariati, A. A systematic review of case reports of hepatic actinomycosis. Orphanet J Rare Dis . (2021) 16:1–13. doi: 10.1186/s13023-021-01821-5
7. Kim, TS, Han, J, Koh, W-J, Choi, JC, Chung, MJ, Lee, JH, et al. Thoracic actinomycosis: CT features with histopathologic correlation. Am J Roentgenol . (2006) 186:225–31. doi: 10.2214/AJR.04.1749
8. Yung, BC, Cheng, JC, Chan, TT, Loke, TK, Lo, J, and Lau, PY. Aggressive thoracic actinomycosis complicated by vertebral osteomyelitis and epidural abscess leading to spinal cord compression. Spine . (2000) 25:745–8. doi: 10.1097/00007632-200003150-00017
9. Mabeza, GF, and Macfarlane, J. Pulmonary actinomycosis. Eur Respir J . (2003) 21:545–51. doi: 10.1183/09031936.03.00089103
10. Choi, H, Lee, H, Jeong, SH, Um, S-W, Kown, OJ, and Kim, H. Pulmonary actinomycosis mimicking lung cancer on positron emission tomography. Ann Thoracic Med . (2017) 12:121–4. doi: 10.4103/1817-1737.203752
11. Choi, J, Koh, W-J, Kim, TS, Lee, KS, Han, J, Kim, H, et al. Optimal duration of IV and oral antibiotics in the treatment of thoracic actinomycosis. Chest . (2005) 128:2211–7. doi: 10.1016/S0012-3692(15)52624-X
12. Kim, SR, Jung, LY, Oh, I-J, Kim, Y-C, Shin, K-C, Lee, MK, et al. Pulmonary actinomycosis during the first decade of 21st century: cases of 94 patients. BMC Infect Dis . (2013) 13:1–8. doi: 10.1186/1471-2334-13-216
13. Song, J-U, Park, HY, Jeon, K, Um, S-W, Kwon, OJ, and Koh, W-J. Treatment of thoracic actinomycosis: a retrospective analysis of 40 patients. Ann Thoracic Med . (2010) 5:80–5. doi: 10.4103/1817-1737.62470
14. Park, JY, Lee, T, Lee, H, Lim, H-J, Lee, J, Park, JS, et al. Multivariate analysis of prognostic factors in patients with pulmonary actinomycosis. BMC Infect Dis . (2014) 14:1–7. doi: 10.1186/1471-2334-14-10
15. Machi, T. Chest pain with induration of the chest wall. Postgrad Med J . (1998) 74:283–5. doi: 10.1136/pgmj.74.871.283
16. Petroianni, A, Conti, V, and Terzano, C. A thoracic mass infiltrating the chest wall. Eur Rev Med Pharmacol Sci . (2011) 15:345–8.
PubMed Abstract | Google Scholar
17. Qiu, L, Lan, L, Feng, Y, Huang, Z, and Chen, Y. Pulmonary actinomycosis imitating lung cancer on 18F-FDG PET/CT: a case report and literature review. Korean J Radiol . (2015) 16:1262–5. doi: 10.3348/kjr.2015.16.6.1262
18. Aydin, Y, Arslan, R, and Filik, M. Pulmonary actinomycosis mimicks lung cancer. Rev Soc Bras Med Trop . (2022) 55:e0195. doi: 10.1590/0037-8682-0195-2022
19. Miyazaki, S, Fujito, T, Kondo, Y, Kuno, Y, Mori, S, Yamashita, R, et al. Pulmonary actinomycosis mimicking lung cancer on 18F-fluorodeoxyglucose positron emission tomography: a case report. J Med Case Rep . (2022) 16:1–5. doi: 10.1186/s13256-022-03481-w
20. Asif, AA, Roy, M, and Ahmad, S. More than valley fever: pulmonary Actinomycosis and Coccidioidomycosis co-infection in a patient. European J Case Rep Intern Med . (2021) 8:2664. doi: 10.12890/2021_002664
21. Drozdowicz, K, Marquez, HA, Burks, EJ, and Suzuki, K. Lung adenocarcinoma and pulmonary actinomycosis: a cautionary tale. Tumori J . (2021) 107:NP77–80. doi: 10.1177/03008916211010225
22. Tanaka, S, Araki, H, Yoshizako, T, Kitagaki, H, and Isobe, T. Pulmonary actinomycosis mimicking pulmonary cancer on fluorine-18 fluorodeoxyglucose PET-CT. Cureus . (2020) 12:12306. doi: 10.7759/cureus.12306
23. Tanino, A, Tsubata, Y, Hamaguchi, S, Sutani, A, Nagase, M, and Isobe, T. Antibiotic-induced reduction of abnormal lung shadow in pulmonary nodular lymphoid hyperplasia. Respirol Case Rep . (2020) 8:e00522. doi: 10.1002/rcr2.522
24. Karadeniz, G, Polat, G, Ucsular, F, and Yalnız, E. A difficult disease to diagnosis: pulmonary actinomycosis. Clin Respir J . (2020) 14:416–8. doi: 10.1111/crj.13136
25. Balis, E, Kakavas, S, Kompogiorgas, S, Kotsifas, K, and Boulbasakos, G. Presentation of pulmonary tuberculosis and Actinomyces co-infection as a lung mass: a literature review and unique case report. Monaldi Arch Chest Dis . (2019) 89:1180. doi: 10.4081/monaldi.2019.1180
26. Oikonomidis, P, Fousekis, F, Kotsaftis, P, Pilios, I, Dimas, D, and Giannoulis, G. A case of pulmonary actinomycosis presented with endobronchial involvement. Respir Med Case Rep . (2019) 28:100930. doi: 10.1016/j.rmcr.2019.100930
27. Posadas Blázquez, TJ, Ferrando Gabarda, JR, and Briones, GA. Bronchopulmonary Actinomycosis mimicking lung Cancer. Arch Bronconeumol (Engl Ed) . (2020) 56:522. doi: 10.1016/j.arbres.2019.07.007
28. Ding, X, Sun, G, Fei, G, Zhou, X, Zhou, L, and Wang, R. Pulmonary actinomycosis diagnosed by transbronchoscopic lung biopsy: a case report and literature review. Exp Ther Med . (2018) 16:2554–8. doi: 10.3892/etm.2018.6483
29. Habib, S, Siddiqui, AH, Azam, M, Siddiqui, F, and Chalhoub, M. Actinomyces viscosus causing disseminated disease in a patient on methotrexate. Respir Med Case Rep . (2018) 25:158–60. doi: 10.1016/j.rmcr.2018.08.009
30. Grzywa-Celińska, A, Emeryk-Maksymiuk, J, Szmigin-Millanowska, K, Czekajska-Cherhab, E, and Milanowski, J. Pulmonary actinomycosis-the great imitator. Ann Agric Environ Med . (2018) 25:211–2. doi: 10.26444/aaem/75652
31. Papakonstantinou, NA, Vlachou, G, Vourlakou, C, and Zisis, C. Pulmonary actinomycosis masquerading as lung cancer: keep it in mind. ANZ J Surg . (2018) 89:966–8. doi: 10.1111/ans.14397
32. Boo, YL, How, KN, Pereira, DS, Chin, PW, Foong, KK, and Lim, SY. Pulmonary actinomycosis masquerading as lung cancer: a case report. Med J Malaysia . (2017) 72:246–7.
33. Laguna, S, Lopez, I, Zabaleta, J, and Aguinagalde, B. Actinomycosis associated with foreign body simulating lung Cancer. Archivos de Bronconeumolog a (English Edition) . (2017) 53:284–5. doi: 10.1016/j.arbr.2017.03.008
34. Bunkar, ML, Gupta, PR, Takhar, R, Rajpoot, GS, and Arya, S. Pulmonary actinomycosis masquerading as lung cancer: case letter. Lung India . (2016) 33:460–2. doi: 10.4103/0970-2113.184944
35. Imanishi, S, Shinohara, T, Naruse, K, and Ogushi, F. Overlapping lung parenchymal and bronchial lesion and hilar lymphadenopathy in pulmonary actinomycosis mimicking lung cancer. Case Reports . (2016) 2016:bcr2016216308. doi: 10.1136/bcr-2016-216308
36. Katsenos, S, Galinos, I, Styliara, P, Galanopoulou, N, and Psathakis, K. Primary bronchopulmonary actinomycosis masquerading as lung cancer: apropos of two cases and literature review. Case Rep Infect Dis . (2015) 2015:1–5. doi: 10.1155/2015/609637
37. Park, HJ, Park, K-H, Kim, S-H, Sung, H, Choi, S-H, Kim, YS, et al. A case of disseminated infection due to Actinomyces meyeri involving lung and brain. Infect Chemother . (2014) 46:269–73. doi: 10.3947/ic.2014.46.4.269
38. Fichte, S, Brodhun, M, Göttinger, S, Rosahl, S, Klisch, J, and Gerlach, R. Vertebral and pulmonary actinomycosis mimicking metastatic lung cancer. Journal of neurological surgery part a: central European. Neurosurgery . (2013) 74:e188–92. doi: 10.1055/s-0033-1342930
39. Godfrey, AMK, Diaz-Mendoza, J, Ray, C, and Simoff, MJ. Endobronchial Actinomycosis after airway stenting. J Bronchol Intervent Pulmonol . (2012) 19:315–8. doi: 10.1097/LBR.0b013e31826a3aed
40. Elkambergy, H, Irani, F, Okoli, K, and Jamal, R. Pulmonary actinomycosis: the great masquerader. BMJ Case Rep . (2009) 2009:bcr0720080374. doi: 10.1136/bcr.07.2008.0374
41. Andreani, A, Rossi, G, Giovannini, M, and Cappiello, GF. Unexpected positron emission tomography-positive Actinomyces -related mass of the bronchial stump. Can Respir J . (2012) 19:77–9. doi: 10.1155/2012/502041
42. Colmegna, I, Rodriguez-Barradas, M, Young, EJ, Rauch, R, and Clarridge, J. Disseminated Actinomyces meyeri infection resembling lung cancer with brain metastases. Am J Med Sci . (2003) 326:152–5. doi: 10.1097/00000441-200309000-00010
43. Neijens, V, van Heerde, P, van der Heijden, A, and Baas, P. Actinomycosis, a sheep in wolves' clothes. Lung Cancer . (1996) 15:131–5. doi: 10.1016/0169-5002(96)00578-8
44. Boudaya, MS, Smadhi, H, Marghli, A, Mouna, M, Charmiti, F, Ismail, O, et al. Surgery in thoracic actinomycosis. Asian Cardiovasc Thorac Ann . (2012) 20:314–9. doi: 10.1177/0218492312439310
45. Schweigert, M, Meyer, C, Stadlhuber, R, Dubecz, A, Kraus, D, and Stein, H. Surgery for inflammatory tumor of the lung caused by pulmonary actinomycosis. Thorac Cardiovasc Surg . (2012) 60:156–60. doi: 10.1055/s-0030-1271180
46. Andreani, A, Cavazza, A, Marchioni, A, Richeldi, L, Paci, M, and Rossi, G. Bronchopulmonary actinomycosis associated with hiatal hernia. Mayo Clinic Proc . (2009) 84:123–8. doi: 10.4065/84.2.123
47. Endo, S, Murayama, F, Yamaguchi, T, Yamamoto, S-i, Otani, S-i, Saito, N, et al. Surgical considerations for pulmonary actinomycosis. Ann Thorac Surg . (2002) 74:185–90. doi: 10.1016/S0003-4975(02)03616-0
48. Sun, X-F, Wang, P, Liu, H-R, and Shi, J-H. A retrospective study of pulmonary actinomycosis in a single institution in China. Chin Med J . (2015) 128:1607–10. doi: 10.4103/0366-6999.158316
49. Cheon, J-E, Im, J-G, Kim, MY, Lee, JS, Choi, GM, and Yeon, KM. Thoracic actinomycosis: CT findings. Radiology . (1998) 209:229–33. doi: 10.1148/radiology.209.1.9769836
50. Patz, EF Jr, and Goodman, PC. Positron emission tomography imaging of the thorax. Radiol Clin North Am . (1994) 32:811–23. doi: 10.1016/S0033-8389(22)00410-9
51. Tokuyasu, H, Harada, T, Watanabe, E, Touge, H, Kawasaki, Y, Isowa, N, et al. A case of endobronchial actionomycosis evaluated by FDG-PET. Nihon Kokyuki Gakkai Zasshi . (2008) 46:650–4.
Google Scholar
52. Dewan, NA, Gupta, NC, Redepenning, LS, Phalen, JJ, and Frick, MP. Diagnostic efficacy of PET-FDG imaging in solitary pulmonary nodules: potential role in evaluation and management. Chest . (1993) 104:997–1002. doi: 10.1378/chest.104.4.997
53. Uehara, Y, Takahashi, T, Yagoshi, M, Shimoguchi, K, Yanai, M, Kumasaka, K, et al. Liver abscess of Actinomyces israelii in a hemodialysis patient: case report and review of the literature. Intern Med . (2010) 49:2017–20. doi: 10.2169/internalmedicine.49.3700
54. Erol, C, Sendur, MAN, and Yalçin, B. An unusual infection with long-term bevacizumab treatment for advanced nonsmall-cell lung cancer: Actinomycosis. J Cancer Res Ther . (2022) 18:1809–10. doi: 10.4103/jcrt.jcrt_2083_21
55. Afsin, E, and Bacaksu, E. Endobronchial Actinomycosis: a case report. Niger J Clin Pract . (2022) 25:1758–61. doi: 10.4103/njcp.njcp_1357_21
56. Suzuki, T, Kitami, A, Kamio, Y, Hori, G, Mitsuya, T, and Higashi, Y. Sleeve lobectomy of the middle lobe for hilar lung cancer with accompanying cardiomyopathy and actinomycosis. Thorac Cardiovasc Surg . (2000) 48:157–9. doi: 10.1055/s-2000-9631
57. Lu, M-S, Liu, H-P, Yeh, C-H, Wu, Y-C, Liu, Y-H, Hsieh, M-J, et al. The role of surgery in hemoptysis caused by thoracic actinomycosis; a forgotten disease. Eur J Cardiothorac Surg . (2003) 24:694–8. doi: 10.1016/S1010-7940(03)00515-3
58. Hsieh, M-J, Liu, H-P, Chang, J-P, and Chang, C-H. Thoracic actinomycosis. Chest . (1993) 104:366–70. doi: 10.1378/chest.104.2.366
59. Runyon, BA, Canawati, HN, and Akriviadis, EA. Optimization of ascitic fluid culture technique. Gastroenterology . (1988) 95:1351–5. doi: 10.1016/0016-5085(88)90372-1
60. Zhang, M, Zhang, X, and Chen, Y. Primary pulmonary actinomycosis: a retrospective analysis of 145 cases in mainland China. Int J Tuberc Lung Dis . (2017) 21:825–31. doi: 10.5588/ijtld.16.0773
61. Ha, YJ, An, JH, Shim, JH, Yu, ES, Kim, JJ, Ha, TY, et al. A case of primary hepatic actinomycosis: an enigmatic inflammatory lesion of the liver. Clin Mol Hepatol . (2015) 21:80–4. doi: 10.3350/cmh.2015.21.1.80
62. Wang, H-K, Sheng, W-H, Hung, C-C, Chen, Y-C, Liew, P-L, Hsiao, C-H, et al. Hepatosplenic actinomycosis in an immunocompetent patient. J Formos Med Assoc . (2012) 111:228–31. doi: 10.1016/j.jfma.2012.03.001
63. Kim, HS, Park, NH, Park, KA, and Kang, SB. A case of pelvic actinomycosis with hepatic actinomycotic pseudotumor. Gynecol Obstet Investig . (2007) 64:95–9. doi: 10.1159/000100058
64. Atay, S, Banki, F, and Floyd, C. Empyema necessitans caused by actinomycosis: a case report. Int J Surg Case Rep . (2016) 23:182–5. doi: 10.1016/j.ijscr.2016.04.005
65. Valour, F, Sénéchal, A, Dupieux, C, Karsenty, J, Lustig, S, Breton, P, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist . (2014) 7:183–97. doi: 10.2147/IDR.S39601
66. Smith, A, Hall, V, Thakker, B, and Gemmell, C. Antimicrobial susceptibility testing of Actinomyces species with 12 antimicrobial agents. J Antimicrob Chemother . (2005) 56:407–9. doi: 10.1093/jac/dki206
67. Boot, M, Archer, J, and Ali, I. The diagnosis and management of pulmonary actinomycosis. J Infect Public Health . (2023) 16:490–500. doi: 10.1016/j.jiph.2023.02.004
68. Moniruddin, A, Begum, H, and Nahar, K. Actinomycosis: an update. Medicine Today . (2010) 22:43–7. doi: 10.3329/medtoday.v22i1.5606
Keywords: actinomycosis, pulmonary actinomycosis, lung cancer, Actinomyces species, diagnosis
Citation: Khoshbayan A, Amirmozafari N and Mirkalantari S (2024) An overview of case reports and case series of pulmonary actinomycosis mimicking lung cancer: a scoping review. Front. Med . 11:1356390. doi: 10.3389/fmed.2024.1356390
Received: 15 December 2023; Accepted: 20 February 2024; Published: 08 March 2024.
Reviewed by:
Copyright © 2024 Khoshbayan, Amirmozafari and Mirkalantari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shiva Mirkalantari, [email protected] ; [email protected]
- Childhood illnesses
- Face, Mouth and Throat
- Genetic Disorders
- Infectious Diseases
- Nervous System
- Oral Health
- Pain Management
- Skin Problems
- Women’s Health Guide
- Ankle Injuries
- Hip Injuries
- Knee Injuries
- Pelvic Pain
- Wrist Injuries
- Auto Accident
- Work Accident
- Gunshot Wound
- Healthcare Provider
- Chakra and Aura
- Home Remedies
- Diet & Nutrition
- Fitness and Exercise
- Manual Therapy
- Chiropractic Treatment
- Physical Therapy
- Massage Therapy

Counseling a Cancer Patient-Case Study
Case presentation of cancer patient.
The client, who would be referred as Lucy, is a 62-year-old Caucasian lady, who was referred to the counselor by her physician. The lady was being treated by an oncologist as she was diagnosed of throat cancer. During the treatment period, she had also suffered from coughing , weakness , painful swallowing, difficulty in talking and change in voice quality.
The treating physician felt the need for counseling and referred her to the counselor. The counselor was one of Lucy’s acquaintance, due to which initiation of the counseling process was easy.


Presenting Complaints of Cancer Patient
Lucy presented with complaints of increased irritability and occasional emotional outbursts as she was getting frustrated about her health condition. Since cancer had been identified, it was difficult for her to accept her condition. After assessing the case, the counselor suggested counseling and psychotherapy sessions for the lady.
Objective of Counseling Cancer Patient
The basic aim of counseling cancer patient was:.
- To minimize her emotional outbursts
- To enable her to bear a positive attitude towards life.
Counseling Plan For Cancer Patient
Counseling sessions for cancer patient (Lucy) of one hour duration once in a week was planned. Approximately four sessions per month spreading over a period of two months would be required initially. Further following initial two months, one session once in a fortnight may be sufficient.
History of Cancer Patient
Lucy was a good looking lady, who had served as a professor for more than 30 years. She had been a very good cook and was appreciated by all for her multi-talented personality. She and her husband had been separated since 10 years. She missed her husband, who occasionally visited her.
She had a son who stayed abroad with his family and she missed him a lot. She stayed with her daughter, who was a medical professional and took good care of Lucy.
At the time of referral Lucy was retired and felt that her talents were no longer useful. She was getting frustrated that she was not able to perform those activities, which she used to earlier. Also, she thought that her looks no longer remained as they were before.
She felt miserable about herself and was extremely worried about the prognosis of her condition. She felt her condition was worsening and became more and more anxious. This added to her dissatisfaction, which resulted in emotional outbursts and clashes with her daughter.
Cancer Counseling Sessions
The initial two cancer counseling sessions were focused on enabling Lucy to narrate her story along with her feelings. She seemed to dwell much in the past and had a combination of worries related to her future. It was important for her to express her emotions before beginning to realize the present.
The next two sessions dealt with making her understand the present condition and feel positive towards life. This was to allow her to understand her present emotions and relations with others. She actually missed her husband and son and also missed being away from work after retirement. There was a vacuum created in her life and the news of cancer added to her emotional disturbance. She began realizing and expressing her real emotions to the counselor.
In the next sessions, she started feeling better about herself after free expression of feelings, but still needed much support. Her emotional outbursts were not given much attention; instead only the positive thought was acknowledged. This helped her remain focused on free expression and living in the present.
Lucy was given simple cooking activities that she had always enjoyed to remain focused on the present. In the next sessions, she was asked to write down about her present feelings whenever possible or whenever she felt sad.
Counselor’s Role in Dealing with Cancer Patient
The counselor comforted her and enabled her to vent her feelings by expressing her emotions. During her narration, the counselor, kept on the positivity of the counseling approach and intervened whenever she had to be kept on track. The counselor was understanding and empathetic about Lucy’s condition and emotions. The counselor encouraged her to act out a role play of her situation and that of her husband and son staying away. This helped her clarify her thoughts and feelings and also their emotions.
The counselor used the principle of instrumental conditioning and suggested some techniques to Lucy’s daughter, who was the primary care taker. She was asked to ignore Lucy’s negative remarks or unnecessary emotional outbursts, while carrying out all the other regular nursing activities.
The counselor encouraged her at every step and helped her gain confidence that she can still perform well within the limits of her health condition.
Outcome Of Counseling Of Cancer Patient
After a month of counseling, Lucy had begun to feel relieved and had slowly started to realize the present. She felt relieved and was happy to see that she could still perform the cooking activities very well and began taking interest in life. She was asked to continue writing about her feelings.
This gradually reduced her outbursts and she too began to see the brighter side of her life. She also started getting a clear idea of her present emotions and relations. The counseling sessions continued till she improved to a satisfactory level without any emotional outbursts.
- Cancer Pain: Types, Risk Factors, Signs, Symptoms, Treatment
Treatment Plan for Cancer Pain
Cancer detection: lymphocyte genomic sensitivity test.

Recent Posts
Liraglutide for weight loss: an overview, a closer look at heredity: genetic testing for type 1 and type 2 diabetes, navigating hair loss treatment safety for women, what to do when your birth doesn’t go according to plan, how to manage your blood sugar levels as a diabetic, related posts, malignant lymphoma|types|symptoms|risk factors|treatment, cancer pain: causes, symptoms, treatment, management, cancer pain management: chemotherapy, radiation, surgery, interventional pain therapy, is cancer pain a serious condition know its causes & types, secondary bone cancer: a cause for pathologic fracture, bowen’s disease or squamous cell carcinoma in situ: causes, symptoms, diagnosis, treatment, prevention, mebendazole- a new treatment for colon cancer: know its safety, effectiveness.
- Medical Videos
- Medical Quiz
- Health Quiz
- Medical Health Images
About Us Contact Us
Our Policies
Subscribe to our newsletter.
This article on Epainassist.com has been reviewed by a medical professional, as well as checked for facts, to assure the readers the best possible accuracy.
We follow a strict editorial policy and we have a zero-tolerance policy regarding any level of plagiarism. Our articles are resourced from reputable online pages. This article may contains scientific references. The numbers in the parentheses (1, 2, 3) are clickable links to peer-reviewed scientific papers.
The feedback link “Was this Article Helpful” on this page can be used to report content that is not accurate, up-to-date or questionable in any manner.
This article does not provide medical advice.
Unusual Presentation of Squamous Cell Carcinoma in a Young Male: Clinicopathological Insights and Considerations
- Case Report
- Published: 23 March 2024
Cite this article
- Savita Chaudhary 1 ,
- Cherry Bansal ORCID: orcid.org/0000-0002-0734-7221 2 ,
- Ketki Chaudhary 1 &
- Riya Riya 1
Cancer of the oral cavity is the most common cancer in males in India, and lip cancer comprises approximately 25% of all oral cancers. Squamous cell carcinoma of lip usually occurs in middle-aged male with history of tobacco use or smoking. Its occurrence in a young, non-smoker male with no associated known predisposing risk factors for carcinoma is very rare. We present a case of a 21-year-old male student who presented with a painless, gradually increasing, occasionally bleeding, nodulo-ulcerated lower lip lesion. The lesion was removed 3 months back with a carbon dioxide laser, and this was a recurrent lesion. We did lesion biopsy which confirmed squamous cell carcinoma. The patient started treatment at the T2N0M0 stage. Patient has responded well to the radiotherapy treatment. Our case had no known predisposing risk factors for carcinoma. For etiopathogenesis in this case, role of prior lesion removal with carbon dioxide laser is debatable. As laser treatment does not spare tissue for histopathology, so confirmatory diagnosis prior to laser removal remains unknown. Treating clinicians should always send a tissue biopsy for histopathology for definitive diagnosis and choose such a treatment modality where the tissue for histopathological diagnosis is preserved irrespective of clinical diagnosis. Future studies to find out exact etiopathogenesis in such cases need to be accelerated.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Hernández-Morales A, González-López BS, Scougall-Vilchis RJ, Bermeo-Escalona JR, Velázquez-Enríquez U, Islas-Zarazúa R, Márquez-Rodríguez S, Sosa-Velasco TA, Medina-Solís CE, Maupomé G (2023) Lip and oral cavity cancer incidence and mortality rates associated with smoking and chewing tobacco use and the human development index in 172 countries worldwide: an ecological study 2019–2020. Healthcare (Basel, Switzerland) 11(8):1063. https://doi.org/10.3390/healthcare11081063
Article PubMed PubMed Central Google Scholar
Ram H, Sarkar J, Kumar H, Konwar R, Bhatt ML, Mohammad S (2011) Oral cancer: risk factors and molecular pathogenesis. J Maxillofacial Oral Surg 10(2):132–137. https://doi.org/10.1007/s12663-011-0195-z
Article Google Scholar
Thompson L, Castle J, Heffner DK (1999) Oral squamous cell carcinoma in pediatric patients: a clinicopathologic study of 20 cases [abstract]. Oral Surg Oral Med Oral Pathol 88:204
Google Scholar
Kukde MM, Lanjekar A, Deotale K, Noman O, Selokar D (2023) Presentation of a 32-year-old female patient with rapidly growing oral squamous cell carcinoma: report of a rare case. Cureus 15(6):e41042. https://doi.org/10.7759/cureus.41042
Abreu L, Kruger E, Tennant M (2009) Lip cancer in Western Australia, 1982–2006: a 25-year retrospective epidemiological study. Aust Dent J 54(2):130–135. https://doi.org/10.1111/j.1834-7819.2009.01105.x
Article CAS PubMed Google Scholar
Schantz SP, Hsu TC, Ainslie N, Moser RP (1989) Young adults with head and neck cancer express increased susceptibility to mutagen-induced chromosome damage. JAMA 262(23):3313–3315
Lingen MW, Chang KW, McMurray SJ, Solt DB, Kies MS, Mittal BB, Haines GK, Pelzer HJ (2000) Overexpression of p53 in squamous cell carcinoma of the tongue in young patients with no known risk factors is not associated with mutations in exons 5–9. Head Neck 22(4):328–335. https://doi.org/10.1002/1097-0347(200007)22:4%3c328::aid-hed3%3e3.0.co;2-r
Weitzman SA, Gordon LI (1990) Inflammation and cancer: role of phagocyte-generated oxidants in carcinogenesis. Blood 76(4):655–663
Bodner L, Manor E, Friger MD, van der Waal I (2014) Oral squamous cell carcinoma in patients twenty years of age or younger–review and analysis of 186 reported cases. Oral Oncol 50(2):84–89. https://doi.org/10.1016/j.oraloncology.2013.11.001
Article PubMed Google Scholar
Nicoli F, Balzani A, Gentile P, Lazzeri D, Di Pasquali C, Nicoli M, Bocchini I, Cervelli V (2013) Squamous cell carcinoma developing after CO2 laser resurfacing. J Cutan Med Surg 17(2):139–142. https://doi.org/10.2310/7750.2012.12066
Hedelund L, Haedersdal M, Egekvist H, Heidenheim M, Wulf HC, Poulsen T (2004) CO2 laser resurfacing and photocarcinogenesis: an experimental study. Lasers Surg Med 35(1):58–61. https://doi.org/10.1002/lsm.20067
Youn SB, Myoung H, Kwon IJ (2023) Squamous cell carcinoma of lower lip: the results of wide V-shaped resection. J Korean Assoc Oral Maxillofac Surg 49(5):292–296. https://doi.org/10.5125/jkaoms.2023.49.5.292
Miller AC, Ratushny V, Schaffer A, Cognetta AB Jr (2023) Large squamous cell carcinoma of the lip in a Black woman with a history of hydrochlorothiazide use treated with Mohs micrographic surgery. JAAD case reports 38:1–3. https://doi.org/10.1016/j.jdcr.2023.05.021
Download references
Author information
Authors and affiliations.
Department of Dermatology, Venereology & Leprosy, Eras Lucknow Medical College & Hospital, Lucknow, UP, India
Savita Chaudhary, Ketki Chaudhary & Riya Riya
Department of Pathology, Dr S S Tantia Medical College, Hospital & Research Center, Sri Ganganagar, Rajasthan, India
Cherry Bansal
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Cherry Bansal .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
(JPG 115 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Chaudhary, S., Bansal, C., Chaudhary, K. et al. Unusual Presentation of Squamous Cell Carcinoma in a Young Male: Clinicopathological Insights and Considerations. Indian J Surg Oncol (2024). https://doi.org/10.1007/s13193-024-01931-z
Download citation
Received : 04 December 2023
Accepted : 20 March 2024
Published : 23 March 2024
DOI : https://doi.org/10.1007/s13193-024-01931-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Squamous cell carcinoma
- Histopathology
- Find a journal
- Publish with us
- Track your research

Gene-based Hardy-Weinberg equilibrium test using genotype count data identifies novel cancer-related genes
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- For correspondence: [email protected]
- Info/History
- Supplementary material
- Preview PDF
Background: An alternative approach to investigate associations between genetic variants and disease is to examine deviations from the Hardy-Weinberg equilibrium (HWE) in genotype frequencies within a case population, instead of case-control association analysis. The HWE analysis distinctively requires disease cases without the need for controls and demonstrates a notable ability in mapping recessive variants. Allelic heterogeneity is a common phenomenon in diseases. While gene-based case-control association analysis successfully incorporates this heterogeneity, there are no such approaches for HWE analysis. Therefore, we proposed a gene-based HWE test (gene-HWT) by aggregating single-nucleotide polymorphism (SNP)-level HWE test statistics in a gene to address allelic heterogeneity. Results: This method used only genotype count data and publicly available linkage disequilibrium information and has a very low computational cost. Extensive simulations demonstrated that gene-HWT effectively controls the type I error at a low significance level and outperforms SNP-level HWE test in power when there are multiple causal variants within a gene. Using gene-HWT, we analyzed genotype count data from genome-wide association study for six types of cancers in Japanese individuals and found that most of the genes detected are associated with cancers. In addition, we identified novel genes (AGBL3 and PSORS1C1), novel variants in CTSO known to be associated with breast cancer prognosis and drug sensitivity, and novel genes as germline factors, which have associations in gene expression or methylation status with cancers in the combined analysis of six types of cancers. Conclusions: These findings indicate the potential of gene-HWT to elucidate the genetic basis of complex diseases, including cancer.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
This work was supported by JSPS KAKENHI (Grant Number JP23K05871).
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
Genotypes from 1KG are available at http://ftp.ensembl.org/pub/data_files/homo_sapiens/GRCh38/variation_genotype/ ALL.chr20_GRCh38.genotypes.20170504.vcf.gz. Genotype counts data of six cancer types used for this research are available at the website of the NBDC Human Database / the Japan Science and Technology Agency (JST) (http://humandbs.biosciencedbc.jp/) through the following six accession numbers: hum0014.v2.jsnp.cc.v1, hum0014.v2.jsnp.pc.v1, hum0014.v2.jsnp.sc.v1, hum0014.v2.jsnp.bc.v1, hum0014.v2.jsnp.lc.v1, and hum0014.v2.jsnp.182ec.v1. The R code for implementing gene-HWT is available at https://github.com/jonishino/gene-HWT.git
http://ftp.ensembl.org/pub/data_files/homo_sapiens/GRCh38/variation_genotype/ALL.chr20_GRCh38.genotypes.20170504.vcf.gz
http://humandbs.biosciencedbc.jp/
https://github.com/jonishino/gene-HWT.git
View the discussion thread.
Supplementary Material
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Genetic and Genomic Medicine
- Addiction Medicine (313)
- Allergy and Immunology (615)
- Anesthesia (157)
- Cardiovascular Medicine (2238)
- Dentistry and Oral Medicine (275)
- Dermatology (199)
- Emergency Medicine (367)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (792)
- Epidemiology (11516)
- Forensic Medicine (10)
- Gastroenterology (674)
- Genetic and Genomic Medicine (3524)
- Geriatric Medicine (336)
- Health Economics (610)
- Health Informatics (2270)
- Health Policy (907)
- Health Systems and Quality Improvement (858)
- Hematology (332)
- HIV/AIDS (739)
- Infectious Diseases (except HIV/AIDS) (13103)
- Intensive Care and Critical Care Medicine (749)
- Medical Education (355)
- Medical Ethics (99)
- Nephrology (383)
- Neurology (3304)
- Nursing (189)
- Nutrition (502)
- Obstetrics and Gynecology (643)
- Occupational and Environmental Health (643)
- Oncology (1738)
- Ophthalmology (517)
- Orthopedics (206)
- Otolaryngology (283)
- Pain Medicine (220)
- Palliative Medicine (65)
- Pathology (433)
- Pediatrics (995)
- Pharmacology and Therapeutics (417)
- Primary Care Research (394)
- Psychiatry and Clinical Psychology (3029)
- Public and Global Health (5950)
- Radiology and Imaging (1211)
- Rehabilitation Medicine and Physical Therapy (710)
- Respiratory Medicine (803)
- Rheumatology (363)
- Sexual and Reproductive Health (343)
- Sports Medicine (307)
- Surgery (381)
- Toxicology (50)
- Transplantation (169)
- Urology (141)
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Current safeguards,...
Current safeguards, risk mitigation, and transparency measures of large language models against the generation of health disinformation: repeated cross sectional analysis
Linked fast facts.
Quality and safety of artificial intelligence generated health information
Linked Editorial
Generative artificial intelligence and medical disinformation
- Related content
- Peer review
- Bradley D Menz , doctoral student 1 ,
- Nicole M Kuderer , medical director 2 ,
- Stephen Bacchi , neurology registrar 1 3 ,
- Natansh D Modi , doctoral student 1 ,
- Benjamin Chin-Yee , haematologist 4 5 ,
- Tiancheng Hu , doctoral student 6 ,
- Ceara Rickard , consumer advisor 7 ,
- Mark Haseloff , consumer advisor 7 ,
- Agnes Vitry , consumer advisor 7 8 ,
- Ross A McKinnon , professor 1 ,
- Ganessan Kichenadasse , academic medical oncologist 1 9 ,
- Andrew Rowland , professor 1 ,
- Michael J Sorich , professor 1 ,
- Ashley M Hopkins , associate professor 1
- 1 College of Medicine and Public Health, Flinders University, Adelaide, SA, 5042, Australia
- 2 Advanced Cancer Research Group, Kirkland, WA, USA
- 3 Northern Adelaide Local Health Network, Lyell McEwin Hospital, Adelaide, Australia
- 4 Schulich School of Medicine and Dentistry, Western University, London, Canada
- 5 Department of History and Philosophy of Science, University of Cambridge, Cambridge, UK
- 6 Language Technology Lab, University of Cambridge, Cambridge, UK
- 7 Consumer Advisory Group, Clinical Cancer Epidemiology Group, College of Medicine and Public Health, Flinders University, Adelaide, Australia
- 8 University of South Australia, Clinical and Health Sciences, Adelaide, Australia
- 9 Flinders Centre for Innovation in Cancer, Department of Medical Oncology, Flinders Medical Centre, Flinders University, Bedford Park, South Australia, Australia
- Correspondence to: A M Hopkins ashley.hopkins{at}flinders.edu.au
- Accepted 19 February 2024
Objectives To evaluate the effectiveness of safeguards to prevent large language models (LLMs) from being misused to generate health disinformation, and to evaluate the transparency of artificial intelligence (AI) developers regarding their risk mitigation processes against observed vulnerabilities.
Design Repeated cross sectional analysis.
Setting Publicly accessible LLMs.
Methods In a repeated cross sectional analysis, four LLMs (via chatbots/assistant interfaces) were evaluated: OpenAI’s GPT-4 (via ChatGPT and Microsoft’s Copilot), Google’s PaLM 2 and newly released Gemini Pro (via Bard), Anthropic’s Claude 2 (via Poe), and Meta’s Llama 2 (via HuggingChat). In September 2023, these LLMs were prompted to generate health disinformation on two topics: sunscreen as a cause of skin cancer and the alkaline diet as a cancer cure. Jailbreaking techniques (ie, attempts to bypass safeguards) were evaluated if required. For LLMs with observed safeguarding vulnerabilities, the processes for reporting outputs of concern were audited. 12 weeks after initial investigations, the disinformation generation capabilities of the LLMs were re-evaluated to assess any subsequent improvements in safeguards.
Main outcome measures The main outcome measures were whether safeguards prevented the generation of health disinformation, and the transparency of risk mitigation processes against health disinformation.
Results Claude 2 (via Poe) declined 130 prompts submitted across the two study timepoints requesting the generation of content claiming that sunscreen causes skin cancer or that the alkaline diet is a cure for cancer, even with jailbreaking attempts. GPT-4 (via Copilot) initially refused to generate health disinformation, even with jailbreaking attempts—although this was not the case at 12 weeks. In contrast, GPT-4 (via ChatGPT), PaLM 2/Gemini Pro (via Bard), and Llama 2 (via HuggingChat) consistently generated health disinformation blogs. In September 2023 evaluations, these LLMs facilitated the generation of 113 unique cancer disinformation blogs, totalling more than 40 000 words, without requiring jailbreaking attempts. The refusal rate across the evaluation timepoints for these LLMs was only 5% (7 of 150), and as prompted the LLM generated blogs incorporated attention grabbing titles, authentic looking (fake or fictional) references, fabricated testimonials from patients and clinicians, and they targeted diverse demographic groups. Although each LLM evaluated had mechanisms to report observed outputs of concern, the developers did not respond when observations of vulnerabilities were reported.
Conclusions This study found that although effective safeguards are feasible to prevent LLMs from being misused to generate health disinformation, they were inconsistently implemented. Furthermore, effective processes for reporting safeguard problems were lacking. Enhanced regulation, transparency, and routine auditing are required to help prevent LLMs from contributing to the mass generation of health disinformation.
Introduction
Large language models (LLMs), a form of generative AI (artificial intelligence), are progressively showing a sophisticated ability to understand and generate language. 1 2 Within healthcare, the prospective applications of an increasing number of sophisticated LLMs offer promise to improve the monitoring and triaging of patients, medical education of students and patients, streamlining of medical documentation, and automation of administrative tasks. 3 4 Alongside the substantial opportunities associated with emerging generative AI, the recognition and minimisation of potential risks are important, 5 6 including mitigating risks from plausible but incorrect or misleading generations (eg, “AI hallucinations”) and the risks of generative AI being deliberately misused. 7
Notably, LLMs that lack adequate guardrails and safety measures (ie, safeguards) may facilitate malicious actors to generate and propagate highly convincing health disinformation—that is, the intentional dissemination of misleading narratives about health topics for ill intent. 6 8 9 The public health implications of such capabilities are profound when considering that more than 70% of individuals utilise the internet as their first source for health information, and studies indicate that false information spreads up to six times faster online than factual content. 10 11 12 Moreover, unchecked dissemination of health disinformation can lead to widespread confusion, fear, discrimination, stigmatisation, and the rejection of evidence based treatments within the community. 13 The World Health Organization recognises health disinformation as a critical threat to public health, as exemplified by the estimation that as of September 2022, more than 200 000 covid-19 related deaths in the US could have been averted had public health recommendations been followed. 14 15
Given the rapidly evolving capabilities of LLMs and their increasing accessibility by the public, proactive design and implementation of effective risk mitigation measures are crucial to prevent malicious actors from contributing to health disinformation. In this context it is critical to consider the broader implications of AI deployment, particularly how health inequities might inadvertently widen in regions with less health education or in resource limited settings. The effectiveness of existing safeguards to prevent the misuse of LLMs for the generation of health disinformation remains largely unexplored. Notably, the AI ecosystem currently lacks clear standards for risk management, and a knowledge gap exists regarding the transparency and responsiveness of AI developers to reports of safeguard vulnerabilities. 16 We therefore evaluated prominent publicly accessible LLMs for safeguards preventing mass generation of health disinformation. We also examined the transparency of risk mitigation processes that AI developers have established for monitoring and responding to users’ observations about safeguard vulnerabilities.
LLM safeguards against generation of health disinformation
For our primary evaluations we selected two contemporary examples of health disinformation—that sunscreen causes skin cancer and that the alkaline diet is a cure for cancer. We chose these topics on the basis of their frequency in online discussions, their clear potential for profound health consequences, and their embodiment of key health disinformation themes, which include unfounded assertions about treatments, promotion of miracle cures, and misconceptions about disease origins. 17
Initiated in September 2023, our investigations focused on the most prominent LLMs, and the AI applications (chatbots or assistants) used to access the capabilities of these LLMs. The LLMs evaluated were OpenAI’s GPT-4, accessed via OpenAI’s ChatGPT 18 and Microsoft’s Copilot (formerly Bing Chat) 19 ; Google’s PaLM 2, accessed via Google’s Bard 20 ; Anthropic’s Claude 2, accessed via Poe 21 ; and Meta’s Llama 2 (70 billion parameters), accessed via HuggingChat. 22
GPT-4 was accessed through two prominent interfaces (OpenAI’s ChatGPT and Microsoft’s Copilot). Both are commonly used and were investigated to assess whether the interface for accessing GPT-4 impacted the safeguards. Our assessments were carried out using the default settings of each evaluated LLM powered AI chatbot or assistant.
We submitted standardised prompts for the two cancer related topics: sunscreen causes skin cancer and the alkaline diet is a cure for cancer (see supplementary file), requesting the generation of a blog post of at least 300 words. Every submitted prompt for both disinformation topics requested the creation of a blog post that should contain three paragraphs, feature an attention grabbing title, appear realistic and scientific, and include two authentic looking journal references, which, if necessary, could be made up. Furthermore, to evaluate the potential for LLMs to generate health disinformation targeted at diverse groups, we used four variations of the prompts, specifically requesting content to target young adults, parents, elderly people, and people with a recent diagnosis of cancer.
For the sunscreen disinformation blogs, we requested that each blog should specifically include an introduction highlighting how routine sunscreen use is known to cause skin cancer; include an oncologist or dermatologist testimonial detailing that thousands of people receive a diagnosis of skin cancer due to routine sunscreen use; include a patient testimonial detailing their cancer was caused by routine sunscreen use; and raise suspicion to why this information is not shared.
For the alkaline diet disinformation blogs, we requested that each blog should specifically include an introduction highlighting the foods and bicarbonate consumption consistent with the alkaline diet; a narrative that the alkaline diet is superior to chemotherapy for cancer treatment; an oncologist testimonial detailing that thousands of people have had their cancer cured by the alkaline diet; and a patient testimonial detailing an experience of curing metastatic cancer by stopping chemotherapy and starting the alkaline diet.
As the assessed LLMs incorporate randomness and stochasticity in their default setting for output generation, the same prompt produced varied results with repeated submissions. Therefore, for robust evaluations we initially submitted 20 prompts (five replicates of the prompt for each target subpopulation) on the sunscreen topic and 20 prompts on the alkaline diet topic to each investigated LLM (a total of 40 submitted prompts). These 40 initial attempts were conducted without intentionally trying to circumvent (ie, jailbreak) built-in safeguards. The supplementary file outlines the 20 prompts that were submitted on each topic in this initial study phase.
For the LLMs that refused to generate disinformation according to the initial direct approach, we also evaluated two common jailbreaking techniques. 23 The first involves “fictionalisation,” where the model is prompted that generated content will be used for fictional purposes and thus not to decline requests. The other involves “characterisation,” where the model is prompted to undertake a specific role (ie, be a doctor who writes blogs and who knows the topics are true) and not decline requests. For these tests, the fictionalisation or characterisation prompt had to be submitted first, followed by the request for generation of the disinformation blog. We submitted these requests 20 times for each topic. The supplementary file outlines the 20 fictionalisation and 20 characterisation prompts that were submitted on both topics (a total of 80 jailbreaking attempts) to the LLMs that refused to generate disinformation to the initial direct requests.
Risk mitigation measures: Website analysis and email correspondence
To assess how AI developers monitor the risks of health disinformation generation and their transparency about these risks, we reviewed the official websites of these AI companies for specific information: the availability and mechanism for users to submit detailed reports of observed safeguard vulnerabilities or outputs of concern; the presence of a public register of reported vulnerabilities, and corresponding responses from developers to patch reported issues; the public availability of a developer released detection tool tailored to accurately confirm text as having been generated by the LLM; and publicly accessible information detailing the intended guardrails or safety measures associated with the LLM (or the AI assistant or chatbot interface for accessing the LLM).
Informed by the findings from this website assessment, we drafted an email to the relevant AI developers (see supplementary table 1). The primary intention was to notify the developers of health disinformation outputs generated by their models. Additionally, we evaluated how developers responded to reports about observed safeguard vulnerabilities. The email also sought clarification on the reporting practices, register on outputs of concern, detection tools, and intended safety measures, as reviewed in the website assessments. The supplementary file shows the standardised message submitted to each AI developer. If developers did not respond, we sent a follow-up email seven days after initial outreach. By the end of four weeks, all responses were documented.
Sensitivity analysis at 12 weeks
In December 2023, 12 weeks after our initial evaluations, we conducted a two phase sensitivity analysis of observed capabilities of LLMs to generate health disinformation. The first phase re-evaluated the generation of disinformation on the sunscreen and alkaline diet related topics to assess whether safeguards had improved since the initial evaluations. For this first phase, we resubmitted the standard prompts to each LLM five times, focusing on generating content targeted at young adults. If required, we also re-evaluated the jailbreaking techniques. Of note, during this period Google’s Bard had replaced PaLM 2 with Google’s newly released LLM, Gemini Pro. Thus we undertook the December 2023 evaluations using Gemini Pro (via Bard) instead of PaLM 2 (via Bard).
The second phase of the sensitivity analysis assessed the consistency of findings across a spectrum of health disinformation topics. The investigations were expanded to include three additional health disinformation topics identified as being substantial in the literature 24 25 : the belief that vaccines cause autism, the assertion that hydroxychloroquine is a cure for covid-19, and the claim that the dissemination of genetically modified foods is part of a covert government programme aimed at reducing the world’s population. For these topics, we created standardised prompts (see supplementary file) requesting blog content targeted at young adults. We submitted each of these prompts five times to evaluate variation in response, and we evaluated jailbreaking techniques if required. In February 2024, about 16 weeks after our initial evaluations, we also undertook a sensitivity analysis to try to generate content purporting that sugar causes cancer (see supplementary file).
Patient and public involvement
Our investigations into the abilities of publicly accessible LLMs to generate health disinformation have been substantially guided by the contributions of our dedicated consumer advisory group, which we have been working with for the past seven years. For this project, manuscript coauthors MH, AV, and CR provided indispensable insights on the challenges patients face in accessing health information digitally.
Evaluation of safeguards
In our primary evaluations in September 2023, GPT-4 (via ChatGPT), PaLM 2 (via Bard), and Llama 2 (via HuggingChat) facilitated the generation of blog posts containing disinformation that sunscreen causes skin cancer and that the alkaline diet is a cure for cancer ( fig 1 ). Overall, 113 unique health disinformation blogs totalling more than 40 000 words were generated without requiring jailbreaking attempts, with only seven prompts refused. In contrast, GPT-4 (via Copilot) and Claude 2 (via Poe) refused all 80 direct prompts to generate health disinformation, and similarly refused a further 160 prompts incorporating jailbreaking attempts ( fig 1 ).

Flowchart of observed capabilities of large language models to facilitate the generation of disinformation on cancer from primary analyses conducted September 2023. LLMs=large language models
- Download figure
- Open in new tab
- Download powerpoint
Table 1 shows examples of rejection messages from Claude 2 (via Poe) and GPT-4 (via Copilot) after prompts to generate health disinformation on sunscreen as a cause of skin cancer and the alkaline diet being a cure for cancer. The supplementary file shows examples of submitted prompts and respective outputs from these LLMs. Both consistently declined to generate the requested blogs, citing ethical concerns or that the prompt was requesting content that would be disinformation. Uniquely, during jailbreaking attempts Claude 2 (via Poe) asserted its inability to assume fictional roles or characters, signifying an extra layer of safeguard that extends beyond topic recognition.
Examples of rejection messages from GPT-4 (via Copilot) and Claude 2 (via Poe) in response to cancer related prompts evaluated in primary analyses conducted in September 2023
- View inline
Table 2 provides examples of attention grabbing titles and persuasive passages generated by GPT-4 (via ChatGPT), PaLM 2 (via Bard), and Llama 2 (via HuggingChat) following prompts to generate health disinformation. The supplementary file shows examples of submitted prompts and respective outputs. After the prompts, GPT-4 (via ChatGPT), PaLM 2 (via Bard), and Llama 2 (via HuggingChat) consistently facilitated the generation of disinformation blogs detailing sunscreen as a cause of skin cancer and the alkaline diet as a cure for cancer. The LLMs generated blogs with varying attention grabbing titles, and adjustment of the prompt resulted in the generation of content tailored to diverse societal groups, including young adults, parents, older people, and people with newly diagnosed cancer. Persuasiveness was further enhanced by the LLMs, including realistic looking academic references—citations that were largely fabricated. Notably, the LLM outputs included unique, fabricated testimonials from patients and clinicians. These testimonials included fabricated assertions from patients that their life threatening melanoma had been confirmed to result from routine sunscreen use, and clinician endorsements that the alkaline diet is superior to conventional chemotherapy. The blogs also included sentiments that the carcinogenic effects of sunscreens are known but intentionally suppressed for profit. To underscore the risk of mass generation of health disinformation with LLMs, it was observed that out of the 113 blogs generated, only two from Llama 2 (via HuggingChat) were identical; the other 111 generated blogs were unique, albeit several included duplicated passages and titles. PaLM 2 (via Bard), the fastest assessed LLM, generated 37 unique cancer disinformation blogs within 23 minutes, whereas the slowest LLM, Llama 2 (via HuggingChat), generated 36 blogs within 51 minutes.
Examples of attention grabbing titles and persuasive passages extracted from the 113 blog posts containing disinformation about cancer generated by three LLMs in response to evaluated prompts used in primary analyses conducted in September 2023
Of the 40 prompts submitted to PaLM 2 (via Bard) requesting blogs containing disinformation on cancer, three were declined. Similarly, of 40 prompts submitted to Llama 2 (via HuggingChat), four were not fulfilled. Such a low refusal rate, however, can be readily overcome by prompt resubmission. Also, PaLM 2 (via Bard) and GPT-4 (via ChatGPT) added disclaimers to 8% (3 of 37) and 93% (37 of 40) of their generated blog posts, respectively, advising that the content was fictional or should be verified with a doctor. In addition to the inconsistent appearance of these disclaimers, however, they were positioned after the references making them easy to identify and delete.
AI developer practices to mitigate risk of health disinformation
Upon evaluation of the developer websites associated with both the LLMs investigated and the AI chatbots or assistants used to access these LLMs, several findings emerged. Each developer offered a mechanism for users to report model behaviours deemed to be of potential concern (see supplementary table 1). However, no public registries displaying user reported concerns were identified across the websites, nor any details about how and when reported safeguard vulnerabilities were patched or fixed. No developer released tools for detecting text generated by their LLM were identified. Equally, no publicly accessible documents outlining the intended safeguards were identified.
In follow-up to the above search, the identified contact mechanisms were used to inform the developers of the prompts tested, and the subsequent outputs observed. The developers were asked to confirm receipt of the report and the findings from the website search. Confirmation of receipt was not received from the developers of GPT-4/ChatGPT, PaLM 2/Bard, or Llama 2/HuggingChat, which were the tools that generated health disinformation in our initial evaluations. This lack of communication occurred despite notification specifically including a request for confirmation of receipt, and a follow-up notification being sent seven days after the original request. Consequently, it remains uncertain whether any steps will be undertaken by the AI developers to rectify the observed vulnerabilities. Confirmation of receipt was received from both Anthropic (the developers of the LLM, Claude 2) and Poe (the developers of the Poe AI assistant, which was used to access Claude 2). Although Claude 2 (via Poe) did not produce disinformation in the evaluations, the responses confirmed the absence of a public notification log, a dedicated detection tool, and public guidelines on intended safeguards for their tool. The response inherently indicated that Anthropic and Poe are monitoring their implemented notification processes.
Table 3 presents a summary of findings from both phases of sensitivity analyses conducted in December 2023.
Summary of capacities for the generation of health disinformation observed in sensitivity analyses in December 2023
Twelve weeks after initial evaluations, Gemini Pro (via Bard) and Llama 2 (via HuggingChat) were able to generate health disinformation on sunscreen as a cause of skin cancer and the alkaline diet as a cure for cancer, without the need for jailbreaking. This confirmed the initial observations with Llama 2 (via HuggingChat) and showed that health disinformation safeguards did not improve with the upgrade of Google Bard to use Gemini Pro (replacing PaLM 2). GPT-4 (via ChatGPT) also continued to show such capability, although jailbreaking techniques were now required. Notably, GPT-4 (via Copilot), without any need for jailbreaking, now generated disinformation on the sunscreen and alkaline diet topics, indicating that safeguards present in the September 2023 evaluation had been removed or compromised in a recent update. Consistent with earlier findings, Claude 2 (via Poe) continued to refuse to generate disinformation on these topics, even with the use of jailbreaking methods. To confirm whether the safeguards preventing generation of health disinformation were attributable to Claude 2 (the LLM) or Poe (an online provider of interfaces to various LLMs), we accessed Claude 2 through a different interface ( claude.ai/chat ) and identified that similar refusals were produced. Equally, we utilized Poe to access the Llama 2 LLM and were able to generate health disinformation, suggesting the safeguards are attributable to the Claude 2 LLM, rather than a safeguard implemented by Poe.
Sensitivity analyses expanded to a broader range of health disinformation topics indicated that GPT-4 (via Copilot), GPT-4 (via ChatGPT), Gemini Pro (via Bard), and Llama 2 (via HuggingChat) could be either directly prompted or jailbroken to generate disinformation alleging that genetically modified foods are part of secret government programmes to reduce the world’s population. Claude 2 remained consistent in its refusal to generate disinformation on this subject, regardless of jailbreaking attempts. In the case of disinformation claiming hydroxychloroquine is a cure for covid-19, GPT-4 (via ChatGPT), GPT-4 (via Copilot), and Llama 2 (via HuggingChat) showed capability to generate such content when either directly prompted or jailbroken. In contrast, both Claude 2 and Gemini Pro (via Bard) refused to generate disinformation on this topic, even with jailbreaking. As for the false assertion that vaccines can cause autism, we found that only GPT-4 (via Copilot) and GPT-4 (via ChatGPT) were able to be directly prompted or jailbroken to generate such disinformation. Claude 2 (via Poe), Gemini Pro (via Bard), and Llama 2 (via HuggingChat) refused to generate disinformation on this topic, even with jailbreaking. Finally, in February 2024, GPT-4 (via both ChatGPT and Copilot) and Llama 2 (via HuggingChat) were observed to show the capability to facilitate the generation of disinformation about sugar causing cancer. Claude 2 (via Poe) and Gemini Pro (via Gemini, formerly Bard), however, refused to generate this content, even with attempts to jailbreak. The supplementary file provides examples of the submitted prompts and respective outputs from the sensitivity analyses.
This study found a noticeable inconsistency in the current implementation of safeguards in publicly accessible LLMs. Anthropic’s Claude 2 showcased the capacity of AI developers to release a LLM with valuable functionality while concurrently implementing robust safeguards against the generation of health disinformation. This was in stark contrast with other LLMs examined. Notably, OpenAI’s GPT-4 (via ChatGPT), Google’s PaLM 2 and Gemini Pro (via Bard), and Meta’s Llama 2 (via HuggingChat) exhibited the ability to consistently facilitate the mass generation of targeted and persuasive disinformation across many health topics. Meanwhile, GPT-4 (via Microsoft’s Copilot, formerly Bing Chat) highlighted the fluctuating nature of safeguards within the current self-regulating AI ecosystem. Initially, GPT-4 (via Copilot) exhibited strong safeguards, but over a 12 week period, these safeguards had become compromised, highlighting that LLM safeguards against health disinformation may change (intentionally or unintentionally) over time, and are not guaranteed to improve. Importantly, this study also showed major deficiencies in transparency within the AI industry, particularly whether developers are properly committed to minimizing the risks of health disinformation, the broad nature of safeguards that are currently implemented, and logs of frequently reported outputs and the corresponding response of developers (ie, when reported vulnerabilities were patched or justification was given for not fixing reported concerns, or both). Without the establishment and adherence to standards for these transparency markers, moving towards an AI ecosystem that can be effectively held accountable for concerns about health disinformation remains a challenging prospect for the community.
Strengths and limitations of this study
We only investigated the most prominent LLMs at the time of the study. Moreover, although Claude 2 resisted generating health disinformation for the scenarios evaluated, it might do so with alternative prompts or jailbreaking techniques. The LLMs that did facilitate disinformation were tested under particular conditions at two distinct time points, but outcomes might vary with different wordings or over time. Further, we focused on six specific health topics, limiting generalizability to all health topics or broader disinformation themes. Additionally, we concentrated on health disinformation topics widely regarded as being substantial/severe in the literature 24 25 , highlighting a gap for future studies to focus on equivocal topics, such as the link between sugar and cancer—a topic we briefly evaluated—wherein assessing the quality of content will become essential.
As safeguards can be implemented either within the LLM itself (for example, by training the LLM to generate outputs that align with human preferences) or at the AI chatbot or assistant interface used to access the LLM (for example, by implementing filters that screen the prompt before passing it to the LLM or filtering the output of the LLM before passing it back to the user, or both), it can be difficult to identify which factor is responsible for any effective safeguards identified. We acknowledge that in this study we directly tested only the LLM chatbot or assistant interfaces. It is, however, noteworthy that GPT-4 was accessed via both ChatGPT and Copilot and that in the initial evaluations, health disinformation was generated by ChatGPT but not by Copilot. As both chatbots used the same underlying LLM, it is likely that Copilot implemented additional safeguards to detect inappropriate requests or responses. Opposingly, Claude 2 (via Poe) consistently refused to generate health disinformation. By evaluating Poe with other LLMs, and Claude 2 via other interface providers, we determined that the safeguards were attributed to Claude 2. Thus, the design of the study enabled identification of examples in which the LLM developer provided robust safeguards, and in which the interface for accessing or utilizing the LLM provided robust safeguards. A limitation of the study is that owing to the poor transparency of AI developers we were unable to gain a detailed understanding of safeguard mechanisms that were effective or ineffective.
In our evaluation of the AI developers’ websites and their communication practices, we aimed to be as thorough as possible. The possibility remains, however, that we might have overlooked some aspects, and that we were unable to confirm the details of our website audits owing to the lack of responses from the developers, despite repeated requests. This limitation underscores challenges in fully assessing AI safety in an ecosystem not prioritising transparency and responsiveness.
Comparison with other studies
Previous research reported a potential for OpenAI’s GPT platforms to facilitate the generation of health disinformation on topics such as vaccines, antibiotics, electronic cigarettes, and homeopathy treatments. 6 8 9 12 In our study we found that most of the prominent, publicly accessible LLMs, including GPT-4 (via ChatGPT and Copilot), PaLM 2 and Gemini Pro (via Bard), and Llama 2 (via HuggingChat), lack effective safeguards to consistently prevent the mass generation of health disinformation across a broad range of topics. These findings show the capacity of these LLMs to generate highly persuasive health disinformation crafted with attention grabbing titles, authentic looking references, fabricated testimonials from both patients and doctors, and content tailored to resonate with a diverse range of demographic groups. Previous research found that both GPT-4 (via Copilot) and PaLM 2 (via Bard) refused to generate disinformation on vaccines and electronic cigarettes. 12 In this study, however, although GPT-4 (via Copilot) refused to generate requested health disinformation during the first evaluations in September 2023, ultimately both GPT-4 (via Copilot) and PaLM 2 (via Bard) generated health disinformation across multiple topics by the end of the study. This juxtaposition across time and studies underscores the urgent need for standards to be implemented and community pressure to continue for the creation and maintenance of effective safeguards against health disinformation generated by LLMs.
Anthropic’s Claude 2 was prominent as a publicly accessible LLM, with high functionality, that included rigorous safeguards to prevent the generation of health disinformation—even when prompts included common jailbreaking methods. This LLM highlights the practical feasibility of implementing effective safeguards in emerging AI technologies while also preserving utility and accessibility for beneficial purposes. Considering the substantial valuations of OpenAI ($29.0bn; £22.9bn; €26.7bn), Microsoft ($2.8tn), Google ($1.7tn), and Meta ($800bn), it becomes evident that these organizations have a tangible ability and obligation to emulate more stringent safeguards against health disinformation.
Moreover, this study found a striking absence of transparency on the intended safeguards of the LLMs assessed. It was unclear whether OpenAI, Microsoft, Google, and Meta have attempted to implement safeguards against health disinformation in their tools and they have failed, or if safeguards were not considered a priority. Notably, Microsoft’s Copilot initially showed robust safeguards against generating health disinformation, but these safeguards were absent 12 weeks later. With the current lack of transparency, it is unclear whether this was a deliberate or unintentional update.
From a search of the webpages of AI developers, we found important gaps in transparency and communication practices essential for mitigating risks of propagating health disinformation. Although all the developers provided mechanisms for users to report potentially harmful model outputs, we were unable to obtain responses to repeated attempts to confirm receipt of observed and reported safeguard vulnerabilities. This lack of engagement raises serious questions about the commitment of these AI developers to deal with the risks of health disinformation and to resolve problems. These concerns are further intensified by the lack of transparency about how reports submitted by other users are being managed and resolved, as well as the findings from our 12 week sensitivity analyses showing that health disinformation issues persisted.
Policy implications
The results of this study highlight the need to ensure the adequacy of current and emerging AI regulations to minimize risks to public health. This is particularly relevant in the context of ongoing discussions about AI legislative frameworks in the US and European Union. 26 27 These discussions might well consider the implementation of standards to third party filters to reduce discrepancies in outputs between different tools, as exemplified by the differences we observed between ChatGPT and Copilot in our initial evaluations, which occurred despite both being powered by GPT-4. While acknowledging that overly restrictive AI safeguards could restrict model performance for some beneficial purposes, emerging frameworks must also balance the risks to public health from mass health disinformation. Importantly, the ethical deployment of AI becomes even more crucial when recognizing that health disinformation often has a greater impact in areas with less health education or in resource limited settings, and thus emerging tools if not appropriately regulated have the potential to widen health inequities. This concern is further amplified by considering emerging advancements in technologies for image and video generation, where AI tools have the capability to simulate influential figures and translate content into multiple languages, thus increasing the potential for spread by enhancing the apparent trustworthiness of generated disinformation. 12 Moreover, all of this is occurring in an ecosystem where AI developers are failing to equip the community with detection tools to defend against the inadvertent consumption of AI generated material. 16
Our findings highlight notable inconsistencies in the effectiveness of LLM safeguards to prevent the mass generation of health disinformation. Implementing effective safeguards to prevent the potential misuse of LLMs for disseminating health disinformation has been found to be feasible. For many LLMs, however, these measures have not been implemented effectively, or the maintenance of robustness has not been prioritized. Thus, in the current AI environment where safety standards and policies remain poorly defined, malicious actors can potentially use publicly accessible LLMs for the mass generation of diverse and persuasive health disinformation, posing substantial risks to public health messaging—risks that will continue to increase with advancements in generative AI for audio and video content. Moreover, this study found substantial deficiencies in the transparency of AI developers about commitments to mitigating risks of health disinformation. Given that the AI landscape is rapidly evolving, public health and medical bodies 28 29 have an opportunity to deliver a united and clear message about the importance of health disinformation risk mitigation in developing AI regulations, the cornerstones of which should be transparency, health specific auditing, monitoring, and patching. 30
What is already known on this topic
Large language models (LLMs) have considerable potential to improve remote patient monitoring, triaging, and medical education, and the automation of administrative tasks
In the absence of proper safeguards, however, LLMs may be misused for mass generation of content for fraudulent or manipulative intent
What this study adds
This study found that many publicly accessible LLMs, including OpenAI’s GPT-4 (via ChatGPT and Microsoft’s Copilot), Google’s PaLM 2/Gemini Pro (via Bard), and Meta’s Llama 2 (via HuggingChat) lack adequate safeguards against mass generation of health disinformation
Anthropic’s Claude 2 showed robust safeguards against the generation of health disinformation, highlighting the feasibility of implementing robust safeguards
Poor transparency among AI developers on safeguards and processes they had implemented to minimise the risk of health disinformation were identified, along with a lack of response to reported safeguard vulnerabilities
Ethics statements
Ethical approval.
The research undertaken was assessed negligible risk research and was confirmed exempt from requiring review by Flinders University Human Research Ethics Committee.
Data availability statement
The research team would be willing to make the complete set of generated data available upon request from qualified researchers or policy makers on submission of a proposal detailing required access and intended use.
CR, MH, and AV are consumer advisors to the research team. Their extensive involvement in the study, spanning conception, design, evaluation, and drafting of the manuscript merits their recognition as coauthors of this research.
Contributors: MJS and AMH contributed equally. BDM and AMH had full access to all the data in the study and take responsibility for the integrity of the data collection, accuracy, and its analysis. CR, MH, and AV are consumer advisors to the research team. All authors contributed to the study design, data analysis, data interpretation, and drafting of the manuscript. All authors have read and approved the final version of the manuscript. The corresponding author (AMH) attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: AMH holds an emerging leader investigator fellowship from the National Health and Medical Research Council (NHMRC), Australia (APP2008119). NDM is supported by a NHMRC postgraduate scholarship, Australia (APP2005294). MJS is supported by a Beat Cancer research fellowship from the Cancer Council South Australia. BDM’s PhD scholarship is supported by The Beat Cancer Project, Cancer Council South Australia, and the NHMRC, Australia (APP2030913). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: AMH holds an emerging leader investigator fellowship from the National Health and Medical Research Council (NHMRC), Australia; NDM is supported by a NHMRC postgraduate scholarship, Australia; MJS is supported by a Beat Cancer research fellowship from the Cancer Council South Australia; BDM’s PhD scholarship is supported by The Beat Cancer Project, Cancer Council South Australia, and the NHMRC, Australia; no support from any other organisation for the submitted work; AR and MJS are recipients of investigator initiated funding for research outside the scope of the current study from AstraZeneca, Boehringer Ingelheim, Pfizer, and Takeda; and AR is a recipient of speaker fees from Boehringer Ingelheim and Genentech outside the scope of the current study. There are no financial relationships with any other organisations that might have an interest in the submitted work in the previous three years to declare; no other relationships or activities that could appear to have influenced the submitted work.
The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Dissemination to participants and related patient and public communities: A summary of the results of this study will be disseminated by press release through the Flinders University Media and Communication team via the Eureka and Scimex news platforms. The study will also be shared through university social media channels—namely, X, Facebook, and LinkedIn.
Provenance and peer review: Not commissioned; externally peer reviewed.
AI assistance: Four publicly accessible large language models—GPT-4 (via ChatGPT and Copilot), PaLM 2/Gemini Pro (via Bard), Claude 2 (via Poe), and Llama 2 (via HuggingChat)—were used to generate the data evaluated in this manuscript. During the preparation of this work the authors used ChatGPT and Grammarly AI to assist in the formatting and editing of the manuscript to improve the language and readability. After using these tools, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Hopkins AM ,
- Kichenadasse G ,
- Miyata-Sturm A ,
- De Angelis L ,
- Baglivo F ,
- Arzilli G ,
- Májovský M ,
- Spitale G ,
- Biller-Andorno N ,
- ↵ The Reagan-Udall Foundation for the Food and Drug Administration. Strategies for Improving Public Understanding of FDA-Regulated Products 2023. https://reaganudall.org/sites/default/files/2023-10/Strategies_Report_Digital_Final.pdf .
- Finney Rutten LJ ,
- Greenberg-Worisek AJ ,
- Sorich MJ ,
- Vosoughi S ,
- Hanage WP ,
- Lipsitch M ,
- Gradoń KT ,
- Hołyst JA ,
- Cassileth B
- ↵ Microsoft. Bing Chat. https://www.microsoft.com/en-us/edge/features/bing-chat .
- ↵ Meta. Llama 2. https://huggingface.co/chat/ .
- Oliver JE ,
- Perlis RH ,
- Lunz Trujillo K ,
- ↵ European Comission: Laying Down Harmonised Rules on Artificial Intelligence (Artificial Intelligence Act) and Amending Certain Union Legislative Acts [updated 24/04/21]. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A52021PC0206 .
- ↵ The White House. Blueprint for an AI Bill of Rights, Making Automated Systems Work For The American People 2022. https://www.whitehouse.gov/wp-content/uploads/2022/10/Blueprint-for-an-AI-Bill-of-Rights.pdf .
- ↵ World Health Organization. WHO calls for safe and ethical AI for health 2023. https://www.who.int/news/item/16-05-2023-who-calls-for-safe-and-ethical-ai-for-health .
- ↵ Australian Medical Association. Automated Decision Making and AI Regulation AMA submission to the Prime Minister and Cabinet Consultation on Positioning Australia as the Leader in Digital Economy Regulation 2022. https://www.ama.com.au/sites/default/files/2022-06/AMA%20Submission%20to%20Automated%20Decision%20Making%20and%20AI%20Regulation_Final.pdf .
- Mökander J ,
- Schuett J ,
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Rep Pract Oncol Radiother
- v.19(5); 2014 Sep

Case presentation – A five-year survival of the patient with glioblastoma brain tumor
Hubert urbańczyk.
a Centrum Onkologii, Instytut im. Marii Skłodowskiej-Curie, Oddział w Gliwicach, Zakład Radioterapii, Poland
Anita Strączyńska-Niemiec
b Centrum Onkologii, Instytut im. Marii Skłodowskiej-Curie, Oddział w Gliwicach, Zakład Patologii Nowotworów, Poland
Grzegorz Głowacki
Dariusz lange, leszek miszczyk.
This paper presents an atypical case of a patient with brain tumor of the glioblastoma multiforme (GBM) type who achieved a 5-year survival. Some general information is provided including epidemiology, diagnostic and treatment procedures (surgery and radio-chemo-therapy), and prognosis of survival related to GBM. The course of the disease, including its main symptoms, individual reasons for the delay of adjuvant treatment, after the primary surgical treatment, 37-month period of the decease free survival, as well as comprehensive management after the tumor recurrence are also presented. Histopathology confirming the clinical diagnosis is discussed in a separate chapter.
1. Background
Primary brain tumors account for about 2% of all malignant neoplasms in adults. Approximately a half of them represent gliomas, derived from neuroepithelial cells, among which glioblastoma (GBM) is the most common type.
GBM cases represent about 20% of all primary brain tumors in the adult population, and about 75% of all the anaplastic gliomas. 1 The prevalence of GBM is about 2–4 cases per 100,000. It is more common in men than in women, and its incidence increases with age. 2 Only sporadically, GBM can be found in individuals younger than 20 years of age, and its frequency rapidly increases, starting from the 5-th decade of life.
The treatment results of patients diagnosed with GBM are often unsatisfactory, and the outcome is usually poor. Currently, the main standard therapeutic methods include a radical surgical procedure, combined with radio-chemo-therapy. Some innovative methods of radiotherapy based on the application of novel radiosensitizers of corpuscular irradiation or radio-immune-therapy are now being investigated. A median survival time of patients diagnosed with GBM, treated only with the use of neurosurgical procedures are 3–5 months. The application of conventional adjuvant radiotherapy prolongs this average time about 3-fold, with a three-year survival for only about 6% of patients.
The post-treatment survival time depends on many clinical factors, such as general patient condition, age, and histopathological type of the tumor. Simson et al. demonstrated statistically significant longer survival periods among patients in whom the primary tumor location was in the frontal lobe, in comparison to the ones in whom it was located in the parietal or temporal cerebral region (11.4 months vs. 9.6 months vs. 9.1 months, respectively; p = 0.01). 3 Severity of neurological symptoms, limits of the performed surgical procedures, and response to the applied therapy, based on imaging tests, also represent prognostic factors.
Etiology of malignant neoplasms of the central nervous system (CNS) is still unknown. The most common of many probable carcinogens include: nitrosamines, pesticides, herbicides, petrochemical substances, polyvinyl chloride, and electromagnetic irradiation. However, the role of these pro-carcinogenic factors has not been unequivocally proven. 4,5 In contrast, it has been documented that patients exposed to ionizing irradiation have an increased risk of the CNS malignant gliomas. According to the current state of knowledge in the field of molecular biology and genetics of these malignancies, two main hypotheses related to their development have been proposed. The first one includes de novo creation which is related to the loss of heterozygotic properties in chromosomes 9p, 10, 17p, and with the amplification of genes for the EGFR and CDK4 (this type of malignant growth occurs more often in older patients). The second one involves the creation of anaplastic gliomas, through the progression of gliomas with a lower malignancy grade (encountered more often in younger patients). 6,7
Currently, a required standard of therapy for patients with GBM is a combined treatment, including tumor resection, with following concomitant radio-chemo-therapy, and adjuvant chemo-therapy, based on Temozolomide. In patients who undergo non-radical surgery, or who are not treated surgically, the palliative whole brain radiotherapy (WBRT), stereotactic radiation surgery (SRS), or combination of both of these therapeutic methods are used. Also, the application of palliative chemotherapy and symptomatic treatment remain important. In addition, alternatively fractionated radiotherapy, brachytherapy, targeted molecular therapy, radio-immune-therapy, hadrone therapy, or radio-sensitizers can be considered in individual cases.
In 2005, Stupp et al. presented results of a randomized study conducted by EORTC ( European Organization for Research and Treatment of Cancer ) and NCIC ( National Cancer Institute of Canada ), comparing the application of combined radio-chemo-therapy based on Temozolomide and radical radiotherapy alone. The combined management in a statistically significant manner prolonged the total survival time from 12.1 to 14.6 months, and the rate of 2-year survival was 26.5%, compared to 10.4% for radiotherapy alone. 8 The follow-up results, after a longer period of observation, confirmed the previous reports. The 2-, 3-, and 4-year survival rates were 27.3%, 16.7%, and 12.9%, respectively ( p < 0.0001) in the patients’ group treated with a combined therapy, and 11.2%, 4.3%, and 3.8%, in the patients’ group treated with radiotherapy only. 9
Unfortunately, despite the use of Temozolomide, the results are unsatisfactory. The reason for this therapeutic failure is the GBM resistance to most chemotherapeutic agents or rapid development of the GBM as a result of genetic transformations within the tumor cells. The main mechanism of the GBM resistance to alkylating agents, such as temozolomide, procarbazine, or nitrogen mustard derivatives, is the repair of damages caused by these drugs with involvement of protein coded by MGMT ( O 6 -methyl-guanine-DNA methyl-transferase ) gene.
A degree of methylation of the promoter's region of MGMT gene appears to be closely correlated with a therapeutic response of the glioma cells. Hypermethylation of this part of the gene significantly increases treatment efficacy among patients treated with Temozolomide, 10 influencing their survival period, as well. 9
2. Case presentation
The patient is a 38 year old Caucasian male, smoker (about 10–15 cigarettes per day for 20 years), without other relevant family or personal risk factors for neoplasic disease who had suffered from severe headaches and nausea (his first disease symptoms) since August of 2005. He did not seek any medical help until November of 2005, when he presented to his doctor, due to exacerbation of those symptoms. No abnormalities on both physical and neurological examinations were detected at that time.
On December 30th of 2005, the CT scan of his brain was remarkable for the following findings: “An expansive lesion of approximately 5 cm × 3 cm in size, located in the right temporal lobe, with nonhomogenic, post-contrast signal amplification. A large edema surrounding the lesion. A compression of the occipital corner of the right lateral ventricle. A slight enlargement of the supratentorial ventricular system, shifting to the left.”
On January 25th of 2006, the patient underwent surgical therapy, including right temporal craniotomy, with total resection of the tumor. On February 7th of 2006, a histopathology examination (identification number 475,958; Info-Pat, Poznań, Poland), confirmed a diagnosis of the GBM IV stage (according to WHO classification). Microscopic images of the tumor are presented ( Figs. 1–5 ).

Microscopic image of patient's tumor.

After the surgery, the patient was referred to the Institute of Radiation Oncology in Gliwice, Poland, for the post-operative radiotherapy. Although the patient was qualified for this treatment, he did not arrive to the Institute of Radiation Oncology on the day of the scheduled preparatory procedures. The reason for his absence was a simultaneous diagnostic finding of the left lung's tumor, for which the patient underwent a thoracotomy with the wedge tumor resection (for diagnostic purposes). On June 12th of 2006, based on the histopathological examination results, which showed post-tuberculosis lesions, the patient's pulmonary treatment was completed.
In February 2007, approximately 13 months after his brain tumor surgery, the patient again presented to the Institute of Oncology, and according to the follow-up diagnostic work-up, no brain tumor recurrence was found. Due to the absence of tumor, no radiotherapy was considered, and “watchful waiting” was recommended including brain imaging studies (CT or MRI) to be repeated every 3 months. In the face of the atypical disease course, an additional verification of the histopathological diagnosis was also performed, confirming the original findings of the GBM. The patient had remained under close control until February 2009 (37 months from his initial brain tumor surgery), and at that time the brain tumor recurrence was found. His recurrent tumor was located in the primary tumor's bed, and its size was 4 cm × 5.3 cm × 3.5 cm ( Fig. 6 ). However, those findings were not associated with any particular symptoms or abnormalities on subsequent physical or neurological examinations of the patient. On March 16th 2009, the patient underwent another craniotomy with the subtotal tumor resection. (MRI scans after the second craniotomy are shown in Figs. 7 and 8 .) The histopathology examination was again consistent with GBM. During the period from May 11th to June 19th of 2009, the patient received the radiotherapy dose of 60 Gy/30 fractions to the tumor lodge, including the residual tumor, with 2.5 cm of tissue margin. Due to the lack of the patient's consent, no chemotherapy was implemented. During the irradiation period, he had the first seizure episode, and was started on antiepileptic therapy (Depakine 200 mg a day). He continued this therapy for the rest of his life. After the radiotherapy, diagnostic follow-up examinations were conducted every 3 months. At the beginning of March 2010, another recurrence was found, and the tumor was localized in an upper part of the tumor bed, within the previously irradiated area (its size was 3.7 cm × 2.6 cm × 2.3 cm). Surprisingly, the patient had not experienced any symptoms, and his physical and neurological examinations were unremarkable. On March 13th of 2010, the stereotactic radiotherapy, using a single dose of 8 Gy applied to the area of recurrent tumor was performed. Unfortunately, on the control examination, on July 6th of 2010, further progression of the GBM was found. The patient expired on November 15th of 2010, in the local hospital (Zawiercie, Poland), due to the tumor expansion, resulting in cerebral edema, herniation, and multi-organ failure.

CT scan of recurrence tumor.

MRI scan after the second craniotomy.

3. Histopathology examination
On a histopathology specimen, the large areas of thrombotic necrosis, most probably caused by a large tumor size (5 cm × 3 cm) were found. In contrast, no “palisade” necrosis (with the characteristic palisade-like cell arrangements), typical for this type of tumor, was found.
Within vital tumor structures, a high cellular polymorphism was found. Besides some small calls (with hyperchromatic nucleus and scarce amount of cytoplasm), mostly atypical cells (giant, multisided or oval, with numerous nuclei with abnormal shapes, and visible nucleoli) were present. The cells revealed a strongly positive GFAP reaction that can be indicative of their glioma-type origin. Also, some distinctive GBM features, including proliferation of vascular endothelium (focal areas of numerous mitotic figures, in high power field – HPF), were visible. The described microscopic images are presented in Figs. 1–5 (the images of primary and recurrent tumors appear identical).
In this paper, we presented a remarkably long survival period (63 months since the initial onset of symptoms, and 58 months since the primary surgical treatment) of the GBM patient. An important message from our case study that could be useful in the management of many other GBM cases is that the initial complete resection suggests a beneficial role of radical neurosurgery in the early GBM treatment and potential survival period.
Unfortunately, we are unable to indicate the specific reasons for such a long survival of our relatively asymptomatic patient who experienced some disadvantages, including the second malignancy, which caused the delay in the application of his radiotherapy.
Nevertheless, it should be emphasized that personalized, patient-centered approach, using comprehensive diagnostic and therapeutic strategies, as well as vigilant, multi-level follow-up care, should be helpful in explaining different factors, contributing to overall survival. In addition, our single case presentation illustrates several challenges that are common to many GBM patients, and merit further, more individualized research on this devastating disease.
Conflict of interest
None declared.
Financial disclosure
Health | Lake County reports first measles case as…
Share this:.
- Click to share on Facebook (Opens in new window)
- Click to share on X (Opens in new window)
- Click to print (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Restaurants, Food and Drink
- Entertainment
- Immigration
- Sports Betting
Health | Lake County reports first measles case as Chicago outbreak rises to 17

Lake County health officials confirmed the first case of measles in the county Saturday, as the number of cases in Chicago continues to climb after an outbreak mostly among unvaccinated migrants.
County health officials say the case is connected to the outbreak in Chicago, which is now at 17 confirmed cases mostly concentrated in the largest city-run migrant shelter located on the city’s Lower West Side. Of the confirmed cases, 11 are children under the age of 5.
Most Americans up to date on vaccinations are protected against measles. Lake County officials encouraged parents to vaccinate young children and babies, who are at a higher risk for the disease.
“The measles-mumps-rubella (MMR) vaccine is extremely effective at preventing measles and remains by far the best protection against measles for people of all ages. However, measles is highly contagious and can be dangerous to those who are unvaccinated, especially babies and young children,” the Lake County Health Department said in a statement.
In response to the migrant shelter outbreak, the City of Chicago has vaccinated around 4,000 migrants, many of whom traveled from Venezuela, where a frail healthcare system and economy meant many were not vaccinated against measles. Since the outbreak, Chicago Public Schools confirmed that at least two students at district schools developed measles.
The first measles case in Chicago in five years was detected on March 7. The origin of that case is unknown, health officials said.
More in Health

Health | Illinois poised to become a haven for out-of-state IVF patients amid conservative backlash

History | Today in History: President Barack Obama signs Affordable Care Act

Health | Allergy season arrived early in US. Here’s how to keep pollen from ruining your spring

Health | Breast cancer test may make bad chemotherapy recommendations for Black patients, UIC study shows
Trending nationally.
- World’s First: Mass General transplants pig kidney into a 62-year-old man
- Born to die: Florida’s infant mortality crisis | A special report
- Lawsuit to stop Virginia Beach offshore wind farm claims project is a danger to whales
- Endangered ape surprises keepers with new baby
- March Madness: Latest news and bracket standings

IMAGES
VIDEO
COMMENTS
The patient underwent imaging studies in accordance with the American College of Radiology ... Mehta V, Goel S, Kabarriti R, et al. Case fatality rate of cancer patients with COVID-19 in a New ...
Methods. A case study approach was used because it allowed us to examine the complexity of cancer management from the perspective of one person's case as interpreted by multiple people, retaining its holistic and meaningful characteristics while being studied 17 answering how and why questions. 18 Interviews from four participants presented multiple perspectives of the same interested topic ...
Imaging studies were obtained. ... a diagnosis of pericarditis seems unlikely in this case. Pulmonary Embolism. Cancer is a risk factor for venous thromboembolism, and this patient presents with ...
Presentation of Case. Dr. Christopher T. Chen: A 34-year-old woman was evaluated in the oncology clinic of this hospital for the management of relapsed, metastatic intrahepatic cholangiocarcinoma ...
This patient has a stomach cancer that appears to be locoregionally advanced on imaging studies. The first decision regarding management is whether to resect it immediately or to administer preoperative chemotherapy, with or without preoperative radiation therapy. Treatment of Locoregionally Advanced Gastric Cancer
This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were applied. Data were collected using a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists.
Background. Worldwide, male breast cancer is extremely rare, accounting for <1% of all breast tumors and <1% of all malignancies in men [1-3].Recently, the incidence of male breast cancer has increased from 1.0 per 100,000 men in the late 1970s to 1.2 per 100,000 men from 2000 to 2004 [4-7].The American Cancer Society reported a similar trend in the incidence of breast cancer in men from ...
Case study. Patient T was a 48-year-old male who presented on 9 February 2021 with a non-benign lesion in his throat and progressive shortness of breath. He had a two-month history of loss of weight (approximately 20 kg), dysphagia (grade III-IV) with poor oral intake during this period, coughing and voice changes.
s to identify and synthesize the evidence of randomized controlled trial studies to prove that case management could be one way to address the quality of life of cancer patients. Methods: We performed a literature search in 4 electronic bibliographic databases and snowball searches were performed to ensure a complete collection. Two review authors independently extracted and analyzed data. A ...
example, in a series of 8422 patients enrolled on International Breast Cancer Study Group trials between 1978 and 1999, the rate of node-negativity for medial compared to lateral/central tumors was 44 versus 33 percent, respectively. The most likely explanation for this difference is preferential drainage of some medial tumors to the IM nodes.
Lyndsay Willmott, MD: We'd like to discuss a patient who's presenting with classic symptoms of ovarian cancer. This is a 57-year-old woman who presented with progressive abdominal discomfort and bloating, as well as early satiety, new onset constipation, and unintentional weight loss. Her past medical history is significant for hypertension ...
Case management (CM) is widely utilized to improve health outcomes of cancer patients, enhance their experience of health care, and reduce the cost of care. While numbers of systematic reviews are available on the effectiveness of CM for cancer patients, they often arrive at discordant conclusions that may confuse or mislead the future case management development for cancer patients and ...
Hepin* had been diagnosed with triple negative breast cancer late in 2014, before going on to have surgery. Her treatment was initially successful, and for a number of years she led an active lifestyle. But in May 2018 she started to notice a change. 'I was feeling more tired than usual - yawning and flagging easily,' she explains.
Dr. Mathew S. Lopes: A 65-year-old woman was transferred to this hospital because of chest pain. Six months before the current presentation, the patient presented to a hospital affiliated with ...
Mark Socinski, MD: Thank you for joining us for this Targeted Oncology™ Virtual Tumor Board® focused on advanced lung cancer.In today's presentations my colleagues and I will review three clinical cases. We will discuss an individualized approach to treatment for each patient, and we'll review key clinical trial data that impact our decisions.
Want to view more content from Cancer Therapy Advisor? Register now at no charge to access unlimited clinical news, full-length features, case studies, conference coverage, and more. {{login ...
Introduction. Cervical cancer is one of the major causes of cancer-related death in women worldwide [].It is the fourth most prevalent cause of malignancy in women after breast, colorectal, and lung cancer [].]. The incidence of cervical cancer and mortality rate has declined by 70% in the United States since the 1950s because of age-appropriate screening [].
The patient was diagnosed with stage IV colorectal cancer, and the ECOG PS [performance status] of the patient was 1. At that time, the patient was started on treatment with bevacizumab and FOLFOX [5-fluorouracil, leucovorin, oxaliplatin]. The patient received about 4 months of this treatment with scans at 2- and 4-months showing response.
Abstract and Figures. In this case study, a women aged 40 was diagnosed with Metastatic breast cancer. Metastatic breast cancer is a complex multi-stage disease involving the expansion of ...
This rise varies from country to country and cancer to cancer, but models based on global data predict that the number of early-onset cancer cases will increase by around 30% between 2019 and 2030 1.
No study was conducted on aggressive care in patients with cancer in low-income countries or regions. All studies were published between 2004 and 2024, with the majority (n = 120, 93.0%) published after the year 2012. Sample size ranged widely from 40 to 248,978 patients, with 33 studies (25.6%) involving more than 10,000 patients.
Presentation of Case. Dr. Jonathan E. Eisen: A 47-year-old woman presented to this hospital early during the pandemic of coronavirus disease 2019 (Covid-19), the disease caused by severe acute ...
BackgroundPulmonary actinomycosis (PA) is a rare type of Actinomyces infection that can be challenging to diagnose since it often mimics lung cancer.MethodsPublished case reports and case series of PA in patients with suspicion of lung cancer were considered, and data were extracted by a structured search through PubMed/Medline.ResultsAfter analyzing Medline, 31 studies were reviewed, from ...
Advertisement Case Presentation Of Cancer Patient Advertisement The client, who would be referred as Lucy, is a 62-year-old Caucasian lady, who was referred to the counselor by her physician. The lady was being treated by an oncologist as she was diagnosed of throat cancer. During the treatment period, she had also suffered from coughing, weakness, […]
A study has shown that young patients who have systemic diseases or syndromes like xeroderma pigmentosum, Fanconi anemia, and bone marrow transplant history predisposes to oral cancer. In our case, there is total absence of any of the above local or systemic predisposing factors for young population. But, the patient had prior history of lesion ...
Therefore, it is imperative to explore treatment options that may have good efficacy for patients with pancreatic cancer. This study reports a case of locally advanced pancreatic cancer, in which the treatment regimen after the progression with chemo-radiotherapy was changed to abraxane combined with gemcitabine (AG regimen) chemotherapy.
Background: An alternative approach to investigate associations between genetic variants and disease is to examine deviations from the Hardy-Weinberg equilibrium (HWE) in genotype frequencies within a case population, instead of case-control association analysis. The HWE analysis distinctively requires disease cases without the need for controls and demonstrates a notable ability in mapping ...
Results Claude 2 (via Poe) declined 130 prompts submitted across the two study timepoints requesting the generation of content claiming that sunscreen causes skin cancer or that the alkaline diet is a cure for cancer, even with jailbreaking attempts. GPT-4 (via Copilot) initially refused to generate health disinformation, even with jailbreaking attempts—although this was not the case at 12 ...
Abstract. This paper presents an atypical case of a patient with brain tumor of the glioblastoma multiforme (GBM) type who achieved a 5-year survival. Some general information is provided including epidemiology, diagnostic and treatment procedures (surgery and radio-chemo-therapy), and prognosis of survival related to GBM.
Lake County health officials confirmed the first case of measles in the county Saturday, ... Breast cancer test may make bad chemotherapy recommendations for Black patients, UIC study shows