- Introduction
- Conclusions
- Article Information
A, The size of the circles denotes the contribution of participants in each intervention and the thickness of the lines between circles represents the contribution of studies comparing the two interventions. B, The bar graph shows the probability of the 6 interventions ranking from best to worst based on their effectiveness. IA indicates intra-articular.
eTable 1. Explanation of the Components of the GRADE Tool and How They Were Assessed
eTable 2. Risk of Bias Assessments
eTable 3. Results of Comparisons of Interventions Assessed by Fewer Than 3 Studies and Were Not Pooled Qualitatively or Quantitatively
eTable 4. Results of Grading of the Certainty of Evidence According to the GRADE Tool for Each Comparison of Interventions
eTable 5. Results of Statistical Inconsistency Assessment for Each Pairwise Meta-analysis
eFigure 1. Results of Pairwise Meta-analyses with Respective Mean Differences for Early Short-term Outcomes
eFigure 2. Results of Pairwise Meta-analyses With Respective Mean Differences for Late Short-term Outcomes
eFigure 3. Results of Pairwise Meta-analyses With Respective Mean Differences for Mid-term Outcomes
eFigure 4. Results of Pairwise Meta-analyses With Respective Mean Differences for Function
eFigure 5. TSA Results for IA Corticosteroid vs No Treatment or Placebo for Early Short-term Pain
eFigure 6. TSA Results for IA Corticosteroid vs No Treatment or Placebo for Late Short-term Pain
eFigure 7. Network Forest Plots With Consistency Test for Late Short-term Pain
eFigure 8. Network Forest Plots With Consistency Test for Mid-term Pain

See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Challoumas D , Biddle M , McLean M , Millar NL. Comparison of Treatments for Frozen Shoulder : A Systematic Review and Meta-analysis . JAMA Netw Open. 2020;3(12):e2029581. doi:10.1001/jamanetworkopen.2020.29581
Manage citations:
© 2024
- Permissions
Comparison of Treatments for Frozen Shoulder : A Systematic Review and Meta-analysis
- 1 Institute of Infection, Immunity and Inflammation, College of Medicine, Veterinary and Life Sciences, University of Glasgow, Scotland, United Kingdom
Question Are any treatment modalities for frozen shoulder associated with better outcomes than other treatments?
Findings In this meta-analysis of 65 studies with 4097 participants, intra-articular corticosteroid was associated with increased short-term benefits compared with other nonsurgical treatments, and its superiority appeared to last for as long as 6 months. The addition of a home exercise program and/or electrotherapy or passive mobilizations may be associated with added benefits.
Meaning The results of this study suggest that intra-articular corticosteroid should be offered to patients with frozen shoulder at first contact.
Importance There are a myriad of available treatment options for patients with frozen shoulder, which can be overwhelming to the treating health care professional.
Objective To assess and compare the effectiveness of available treatment options for frozen shoulder to guide musculoskeletal practitioners and inform guidelines.
Data Sources Medline, EMBASE, Scopus, and CINHAL were searched in February 2020.
Study Selection Studies with a randomized design of any type that compared treatment modalities for frozen shoulder with other modalities, placebo, or no treatment were included.
Data Extraction and Synthesis Data were independently extracted by 2 individuals. This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline. Random-effects models were used.
Main Outcomes and Measures Pain and function were the primary outcomes, and external rotation range of movement (ER ROM) was the secondary outcome. Results of pairwise meta-analyses were presented as mean differences (MDs) for pain and ER ROM and standardized mean differences (SMDs) for function. Length of follow-up was divided into short-term (≤12 weeks), mid-term (>12 weeks to ≤12 months), and long-term (>12 months) follow-up.
Results From a total of 65 eligible studies with 4097 participants that were included in the systematic review, 34 studies with 2402 participants were included in pairwise meta-analyses and 39 studies with 2736 participants in network meta-analyses. Despite several statistically significant results in pairwise meta-analyses, only the administration of intra-articular (IA) corticosteroid was associated with statistical and clinical superiority compared with other interventions in the short-term for pain (vs no treatment or placebo: MD, −1.0 visual analog scale [VAS] point; 95% CI, −1.5 to −0.5 VAS points; P < .001; vs physiotherapy: MD, −1.1 VAS points; 95% CI, −1.7 to −0.5 VAS points; P < .001) and function (vs no treatment or placebo: SMD, 0.6; 95% CI, 0.3 to 0.9; P < .001; vs physiotherapy: SMD 0.5; 95% CI, 0.2 to 0.7; P < .001). Subgroup analyses and the network meta-analysis demonstrated that the addition of a home exercise program with simple exercises and stretches and physiotherapy (electrotherapy and/or mobilizations) to IA corticosteroid may be associated with added benefits in the mid-term (eg, pain for IA coritocosteriod with home exercise vs no treatment or placebo: MD, −1.4 VAS points; 95% CI, −1.8 to −1.1 VAS points; P < .001).
Conclusions and Relevance The findings of this study suggest that the early use of IA corticosteroid in patients with frozen shoulder of less than 1-year duration is associated with better outcomes. This treatment should be accompanied by a home exercise program to maximize the chance of recovery.
Adhesive capsulitis, also known as frozen shoulder, is a common shoulder concern manifesting in progressive loss of glenohumeral movements coupled with pain. 1 It is a fibroproliferative tissue fibrosis, and although the immunobiological advances in other diseases have helped dissect the pathophysiology of this condition, overall, the molecular mechanisms underpinning it remain poorly understood. 2 - 5
Frozen shoulder manifests clinically as shoulder pain with progressive restricted movement, both active and passive, along with normal radiographic scans of the glenohumeral joint. 6 It classically progresses prognostically through 3 overlapping stages of pain (stage 1, lasting 2-9 months), stiffness (stage 2, lasting 4-12 months), and recovery (stage 3, lasting 5-24 months). 7 However, this is an estimated time frame, and many patients can still experience symptoms at 6 years. 8 A primary care–based observational study estimated its incidence as 2.4 per 100 000 individuals per year, 9 with prevalence varying from less than 1% to 2% of the population. 10
A true evidence-based model for its medical management has not been defined, with a wide spectrum of operative and nonoperative treatments available. From the international to departmental level, management strategies vary widely, reflecting the lack of good-quality evidence. 11 The British Elbow and Shoulder Society/British Orthopaedic Association (BESS/BOA) has published recommendations in a patient care pathway for frozen shoulder, with a step-up approach in terms of invasiveness advised. 12 The UK Frozen Shoulder Trial, a randomized parallel trial comparing the clinical and cost-effectiveness of early structured physiotherapy, manipulation under anesthetic (MUA), and arthroscopic capsular release (ACR) is currently under way. 13 The aim of this systematic review is to present the available evidence relevant to treatment and outcomes for frozen shoulder with the ultimate objective of guiding clinical practice, both in primary and secondary care.
The present systematic review has been conducted and authored according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline. 14 Our patient, intervention, comparison, and outcome (PICO) was defined as follows: patients, patients with frozen shoulder of any etiology, duration, and severity; intervention, any treatment modality for frozen shoulder; comparison, any other treatment modality, placebo, or no treatment; and outcome, pain and function (primary outcomes) and external rotation range of movement (ER ROM) (secondary outcome) in the short term, midterm, or long term.
Included studies had a randomized design of any type and compared treatment modalities for frozen shoulder with other treatment modalities, placebo, or no treatment. Additionally, at least 1 of our preset outcome measures needed to be included in the study. Studies that compared different types, regimens, dosages, or durations of the same intervention were excluded (eg, different doses of corticosteroid or different exercise types). Those assessing the effectiveness of the same modality applied in different anatomical sites (eg, subacromial vs intra-articular [IA] corticosteroid) were included. Participants had to be older than 18 years with a clinical diagnosis of adhesive capsulitis. No formal diagnostic criteria were used to define frozen shoulder; however, the use of inappropriate or inadequate diagnostic criteria was taken into account in risk-of-bias assessments. Duration of the condition was not a criterion nor were previous treatments and follow-up. Inclusion of patients with specific conditions (eg, diabetes) was not an exclusion criterion, and it was not taken into account in analyses, provided that their proportion in the treatment groups was comparable.
Nonrandomized comparative studies, observational studies, case reports, case series, literature reviews, published conference abstracts, and studies published in languages other than English were excluded. Studies including patients with the general diagnosis of shoulder pain were also excluded even if a proportion of them had frozen shoulder. Studies assessing the effectiveness of different types of physiotherapy-led interventions, exercise, or stretching regimens were also excluded.
A thorough literature search was conducted by 3 of us (D.C., M.B., and M.M.) via Medline, EMBASE, Scopus, and CINAHL in February 2020, with the following Boolean operators in all fields: ( adhesive capsulitis OR frozen shoulder OR shoulder periarthritis ) AND ( treatment OR management OR therapy ) AND randomi* ). Relevant review articles were screened to identify eligible articles that may have been missed at the initial search. Additionally, reference list screening and citation tracking in Google Scholar were performed for each eligible article.
From a total of 73 299 articles that were initially identified, after exclusion of duplicate and noneligible articles, title and abstract screening, and the addition of missed studies identified subsequently, 65 studies were found to fulfil the eligibility criteria. Figure 1 illustrates the article screening process.
The internal validity (freedom from bias) of each included study was assessed with the Cochrane Collaboration’s tool for assessing risk of bias in randomized trials separately by 2 of us (D.C. and M.B.), and a third independent opinion (M.M.) was sought when disagreements existed. 15 Studies were characterized as having low, high, or unclear overall risk of bias based on the following formula: low overall risk studies had high risk of bias in 2 or fewer domains; high overall risk studies had high risk of bias in more than 2 domains; unclear overall risk studies had unclear risk of bias in more than 2 domains, unless they also had high risk of bias in more than 2 domains, in which case they were labeled as high overall risk. Risk of bias was assessed separately for outcome measures that included patient reporting (pain, function) and those that did not (ROM); all studies with nonmasked participants were labeled as high risk in the masking of outcome measures domain for patient-reported outcomes given that the assessors were the participants themselves.
Certainty of evidence was graded with the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) tool (eTable 1 in the Supplement ). 16 The scale starts with high, and depending on how many of the 5 possible limitations used in the GRADE tool were present in each comparison, the study could be downgraded to moderate, low, and very low. Grading of evidence was performed by 2 authors (D.C. and M.B.) independently and any disagreements were resolved by discussion and involvement of a third assessor (M.M.). Each outcome measure within each comparison had its own evidence grade. Our recommendations for clinical practice were based on results of either high or moderate quality evidence with both clinical and statistical significance.
Two of us (D.C. and M.B.) performed data extraction. The key characteristics of each eligible article were extracted and inserted in tables in Microsoft Word version 16.43 (Microsoft Corp) to facilitate analysis and presentation. For missing data, attempts were made to contact the original investigators for included studies published less than 10 years ago.
For the presentation of results, outcomes were divided into short-term (≤12 weeks), mid-term (>2 weeks to ≤12 months), and long-term (>12 months) follow-up. When sufficient data existed, short-term follow-up was subdivided into early short-term (2-6 weeks) and late short-term (8-12 weeks). All short-term follow-up points were converted to weeks, and all mid-term follow-up points to months for consistency and easier analysis.
Comparisons of interventions reported by fewer than 3 studies were included in the supplementary results table and were not analyzed or included in the article. When 3 or more studies contributed data for outcome measures at similar follow up times (ie, 2-6 weeks, 8-12 weeks, and 4-6 months), pairwise meta-analyses were conducted. Raw mean differences (MDs) with their accompanying 95% CIs were calculated and used in the tests for each comparison of pain and ER ROM because the tools used across studies were the same. Standardized mean differences (SMDs) were used for function because different functional scores were used.
When pain results were reported in different settings (eg, at rest, at night, with activity) in studies, only pain at rest was used in results. When both active and passive ROM were used as outcome measures, passive ROM was used in our results to increase homogeneity given that most studies used passive ROM. Results for the following outcome measures were recorded in tables and combined qualitatively only based on direction of effect to yield an overall effect for each comparison: abduction ROM, flexion ROM, and quality of life. However, these were not included in the results nor was the quality of the relevant evidence graded.
Additionally, comparisons that yielded both clinically and statistically significant results (ie, greater than or equal to the minimal clinically relevant difference and P < .05) underwent trial sequential analysis (TSA) to rule out a type I error and further reinforce our recommendations for clinical practice. TSA is a quantitative method applying sequential monitoring boundaries to cumulative meta-analyses in a similar fashion as the application of group sequential monitoring boundaries in single trials to decide whether they could be terminated early because of a sufficiently small P value. TSA is considered an interim meta-analysis; it helps control for type I and II errors and clarifies whether additional trials are needed by considering required information size. 17 The TSA graph includes 2 horizontal lines, representing the conventional thresholds for statistical significance ( Z = 1.96; P < .05); 1 vertical line, representing required information size; a curved red line, representing the TSA boundaries (ie, thresholds for statistical significance); and a blue line showing the cumulative amount of information as trials are added. A significant result is denoted by a crossing of the curved blue and red lines.
Finally, a network meta-analysis was conducted for treatments used by 3 or more studies for the primary outcome (pain) at late short-term (8-12 weeks) and mid-term (4-6 months) follow-up. Both direct and indirect comparisons were included in the model, and treatment rank probabilities were produced for the 2 follow-up time periods. The certainty of evidence deriving from network meta-analyses was not graded. Subgroup analyses for the effect of home exercise, different physiotherapy interventions, and chronicity of frozen shoulder were conducted when possible.
The term physiotherapy was used for any supervised, physiotherapist-led, noninvasive treatment (mobilizations, application of ice and heat, diathermy, electrotherapy modalities). These were grouped and analyzed together. Exercises and stretching that were performed by the participants at home (home exercise program) or under a physiotherapist’s supervision were not included in physiotherapy. Acupuncture and extracorporeal shock wave therapy (ESWT) were regarded as a separate intervention to physiotherapy. Interventions that had accompanying physiotherapy were grouped and analyzed separately from those that did not, regardless of intensity and frequency. For example, studies with a treatment group who received IA corticosteroid plus physiotherapy (eg, ice packs and diathermy) were included in the intervention category IA corticosteroid plus physiotherapy; those with a treatment group receiving only IA corticosteroid (with or without a home exercise program) were included in the IA corticosteroid category. Patients in the following groups were considered control groups and were analyzed together: no treatment, placebo, sham procedures, IA normal saline or lidocaine, simple analgesia, and home exercise alone.
The following tools and questionnaires that were found in included studies represented our function outcome measure: Shoulder Pain and Disability Index, American Shoulder and Elbow Surgeons shoulder score, Constant-Murley, and the Strengths and Difficulties Questionnaire. All patient-reported pain and function scales were uniformly converted to a scale from 0 to 10 and a scale from 0 to 100, respectively.
The Review Manager version 5 (RevMan) software was used for pairwise meta-analyses and their accompanying forest plots and heterogeneity tests (χ 2 and I 2 ). TSA software version 0.9β (Copenhagen Trial Unit) was used for TSAs; random-effect models with 5% type I error and 20% power and O’Brien-Fleming α-spending function were used for all TSA analyses. The required information size was estimated by the software based on the power (20%), mean difference, variance, and heterogeneity. Stata version 16.1 (StataCorp) with the mvmeta extension (multivariate random-effects meta-regression) was used for network meta-analyses (frequentist approach). 18
When exact mean and SD values were not reported in the included articles, approximate values (to the nearest decimal place) were derived from the graphs. When only interquartile ranges (IQRs) were reported, the SD was calculated as IQR divided by 1.35. When only the median was reported, the mean was assumed to be the same. When CIs of means were reported, SDs were calculated by dividing the length of the CI by 3.92 and then multiplying by the square root of the sample size. When SEs of mean were given, these were converted to SDs by multiplying them by the square root of the sample size. In studies in which only means and the population were given, the SD was imputed using the SDs of other similar studies using the prognostic method (ie, calculating the mean of all SDs). 19 Pooled means were calculated by adding all the means, multiplied by their sample size, and then dividing this by the sum of all sample sizes. Pooled SDs were calculated with the following formula: SD pooled = √(SD 1 2 [ n 1 -1]) + (SD 2 2 [ n 2 -1]) + … + (SD k 2 [ n k -1]) / ( n 1 + n 2 + … + n k – k ), where n indicates sample size and k , the number of samples. The following formula was used for the sample size calculation as part of GRADE’s assessment for imprecision 20 :
In which N indicates the sample size required in each of the groups; ( x 1 – x 2 ) indicates the minimal clinically relevant difference (MCRD), defined as 1 point for VAS pain, effect size of 0.45 for functional scores, and 10° for ER ROM; SD 2 indicates the population variance, calculated using pooled SD from our treatment groups; a = 1.96, for 5% type I error; and b = 0.842, for 80% power.
The MCRD for function on functional scales would have been set at 10 points. However, because SMDs were used, which produce effect sizes, rather than MDs, the 10 points were divided by the population SD (ie, 22) that was used to calculate the optimal information size (effect sizes can be converted back to functional scores when multiplied by SD).
Potential publication bias was evaluated by Egger test for asymmetry of the funnel plot in comparisons including more than 10 studies. Expecting wide-range variability in studies’ settings, a random-effects metasynthesis was employed in all comparisons.
Subgroup analyses were conducted with independent samples t tests in Graphpad version 8 (Prism) comparing pooled means and SDs. All statistical significance levels were set at P < .05, tests were 2-tailed, and clinical significance was defined as a MD or SMD being equal or higher than our predefined MCRD.
Of the 65 eligible studies, a total of 34 studies 21 - 54 were included in pairwise meta-analyses with a total of 2402 participants with frozen shoulder. Duration of symptoms ranged from 1 month to 7 years and length of follow-up from 1 week to 2 years, with most follow-up occurring at 6 weeks, 12 weeks, and 6 months.
Table 1 summarizes the main characteristics of the included studies. 21 - 87 eTable 2 in the Supplement shows the results of the risk-of-bias assessment.
Table 2 summarizes the findings of the present review. Where feasible (ie, results at similar follow-up times in at least 3 studies), pairwise meta-analyses were conducted. The results of abduction ROM, flexion ROM, and quality of life were pooled only based on direction of effect, and their certainty of evidence was not graded. eTable 3 in the Supplement summarizes the results of comparisons reported by 1 or 2 studies only. eTable 4 in the Supplement demonstrates how the strength of evidence for each outcome measure within each comparison was derived for all follow-up time categories, per GRADE. eTable 5 in the Supplement shows the heterogeneity for each comparison ( I 2 statistic) and where studies were removed to reduce heterogeneity based on sensitivity analyses.
We conducted pairwise meta-analysis comparing the effectiveness of each intervention with other interventions (or placebo/no treatment) in the short-term (early, 2-6 weeks; late, 8-12 weeks) and mid-term (4-6 months). Data for long-term follow-up (>12 months) were inadequate for analyses. Numerical data are only presented for the statistically significant comparisons; those for nonsignificant comparisons appear in the forest plots (eFigure 1, eFigure 2, and eFigure 3 in the Supplement ).
IA corticosteroid appeared to be associated with superior outcomes compared with control for early short-term pain (moderate certainty; MD, −1.4 visual analog scale [VAS] points; 95% CI, −1.8 to −0.9 VAS points; P < .001), ER ROM (high certainty; MD, 4.7°; 95% CI, 2.7° to 6.6°; P < .001), and function (high certainty; SMD, 0.6; 95% CI, 0.3 to 0.9; P < .001) and late short-term pain (moderate certainty; MD, −1.0 VAS points; −1.5 to −0.5 VAS points; P < .001), ER ROM (high certainty; MD, 6.8°; 95% CI, 3.4° to 10.2°; P < .001), and function (moderate certainty; SMD, 0.6; 95% CI, 0.3 to 0.8; P < .001).
IA corticosteroid was associated with better outcomes than control only for function (moderate certainty; SMD, 0.3; 95% CI, 0.1 to 0.5; P = .01). However, effects for pain and ER ROM were similar (moderate certainty for both).
Physiotherapy was found to be associated with improved outcomes compared with control in the early short-term for ER ROM (moderate certainty; MD, 11.3°; 95% CI, 8.6°-14.0°; P < .001). Data for other follow-up time periods were insufficient for quantitative analysis.
Combined treatment with IA corticosteroid plus physiotherapy was associated with superior outcomes vs control for early short-term ER ROM (high certainty; MD, 17.9°; 95% CI, 12.1°-23.7°; P < .001). Data for other follow-up periods were insufficient for quantitative analysis.
IA corticosteroid was associated with significant benefits compared with physiotherapy for early short-term function (moderate certainty; MD, 0.5; 95% CI, 0.2 to 0.7; P < .001) and late short-term pain (high certainty; MD, −1.1 VAS points; 95% CI, −1.7 to −0.5 VAS points; P < .001) only. Differences for early short-term pain (moderate certainty), late short-term function (moderate certainty), and early and late short-term ER ROM (moderate and high certainty, respectively) were insignificant.
IA corticosteroid was associated with better outcomes than physiotherapy for ER ROM (moderate certainty; MD, 4.6°; 95% CI, 0.7°-8.6°; P = .02). However, no significant differences in pain (low certainty) or function (moderate certainty) were observed.
Compared with IA corticosteroid alone, combined treatment with IA corticosteroid plus physiotherapy was only associated with superior outcomes for early short-term ER ROM (moderate certainty; MD, 11.6°; 95% CI, 3.7°-19.4°; P = .004). Pain and function in the early short-term (moderate and low certainty, respectively) and late short-term function (high certainty) were similar between groups.
No significant differences were found between the groups in pain, function, or ER ROM. These results had high, moderate, and high certainty, respectively.
Combined therapy with IA corticosteroid plus physiotherapy was associated with significant benefits compared with physiotherapy alone only for early short-term function (low certainty; SMD, 0.7; 95% CI, 0.3-1.0; P < .001). Differences for early short-term pain and ER ROM and late short-term function were not significant (moderate certainty for all).
No significant differences were found between the groups for pain, function, or ER ROM. These comparisons had moderate, low, and high certainty, respectively.
Compared with subacromial administration, administering corticosteroid intra-articularly was only associated with superior outcomes for early short-term pain (moderate certainty; MD, −0.6 VAS points; 95% CI, −1.1 to −0.1 VAS points; P = .02) and late short-term function (moderate certainty; SMD, 0.3; 95% CI, 0 to 0.6; P = .03). Improvements in late short-term pain (moderate certainty) and ER ROM (high certainty) and early short-term function (high certainty) were similar with the 2 interventions.
No significant differences were found between the groups for pain or ER ROM. These comparisons had moderate and high certainty, respectively.
Adding arthrographic distension to IA corticosteroid appeared to be associated with greater improvements in early and late short-term pain (early: high certainty; MD, −0.9 VAS points; −1.3 to −0.4 VAS points; P < .001; late: high certainty; MD, −0.8 VAS points; 95% CI, −1.1 to −0.5 VAS points; P < .001). Early and late short-term function (moderate and high certainty, respectively) and early and late short-term ER ROM (high certainty for both) were similar with or without distension.
No differences were found with the addition of acupuncture to physiotherapy for early short-term pain and ER ROM. These comparisons had low and high certainty, respectively.
Despite several statistically significant differences in pairwise comparisons, most did not reach the threshold for MCRD. Only IA corticosteroid vs no treatment or placebo for early and late short-term pain and function, physiotherapy with and without IA corticosteroid vs no treatment or placebo for early short-term ER ROM, IA corticosteroid vs physiotherapy for early short-term function and late short-term pain, and combination therapy with IA corticosteroid plus physiotherapy compared with IA corticosteroid for early short-term ER ROM and with physiotherapy for early short-term function reached MCRD.
For the primary outcome measure, the clinically and statistically significant results underwent TSA, which confirmed the results ruling out a type I error in 2 comparisons (IA corticosteroid vs no treatment or placebo for early and late short-term pain) but not in the comparison of IA corticosteroid vs physiotherapy for late short-term pain. This suggests that more studies may be needed to confirm the benefit of IA corticosteroid compared with physiotherapy with more confidence.
eFigures 1 to 3 in the Supplement illustrate the results of the pairwise meta-analyses and associated forest plots for early short-term, late short-term, and mid-term follow up for pain and ER ROM. eFigure 4 in the Supplement illustrates the forest plots for function, and eFigure 5 and eFigure 6 in the Supplement illustrate the TSA graphs.
Figure 2 and Figure 3 show the network maps and treatment rank probabilities for the primary outcome measure (pain) for late short-term (8-12 weeks) and mid-term (4-6 months) follow-up, respectively. eFigure 7 and eFigure 8 in the Supplement illustrates the network forests with their consistency tests.
In the late short-term, arthrographic distension plus IA corticosteroid had the highest probability (96%) of being the most effective treatment. IA corticosteroid had the highest probability (85%) of being the second most effective. Physiotherapy was the least effective treatment, followed by no treatment or placebo. No data existed in the late short-term for combined treatment with IA corticosteroid plus physiotherapy ( Figure 2 B).
In the mid-term, combined treatment with IA corticosteroid plus physiotherapy had the highest probability (43%) of being the best treatment with physiotherapy. IA corticosteroid had the highest probability (34%) of being the second best treatment. No treatment or placebo followed by subacromial corticosteroid had the highest probability of being the worst interventions ( Figure 3 B).
The potential benefit of home exercise was assessed by comparing the mean improvement in pain in patients who received (1) IA corticosteroid plus a home exercise program vs IA corticosteroid without home exercise, and (2) no treatment or placebo plus home exercise vs no treatment/placebo without home exercise. For the first comparison, a statistically significant (but clinically small) mean benefit of home exercise on pain improvement was identified at 8 to 12 weeks (MD, −0.5 VAS points; 95% CI, −0.9 to −0.1 VAS points; P = .01). The benefit of home exercise was much more substantial (clinically and statistically) in those receiving no treatment or placebo (MD, −1.4 VAS points; 95% CI, −1.8 to −1.1 VAS points; P < .001). Both results are based on 10 studies 22 , 24 , 25 , 28 , 42 , 43 , 45 , 46 , 48 , 49 with low overall risk of bias.
Similarly, we assessed for an effect of IA placebo by comparing samples who received IA placebo and no treatment from the IA corticosteroid vs no treatment or placebo comparison. Both subgroups received a home exercise program. Based on 9 studies 22 , 24 , 25 , 28 , 42 , 43 , 45 , 46 , 49 with high overall risk of bias, IA placebo was associated with statistically and clinically significant effects on pain compared with no treatment (MD, −1.6 VAS points; 95% CI, −2.1 to −1.1 VAS points; P < .001).
There was insufficient data for a similar subgroup analysis at mid-term follow-up. Subgroup analyses for the effect of chronicity on the effectiveness of treatment modalities could not be evaluated because studies including patients with mixed stages and chronicity of frozen shoulder did not include subgroup data. Finally, subgroup analyses according to physiotherapeutic interventions were not possible because of high clinical heterogeneity (various combinations of modalities and treatment durations used). Most studies used electrotherapy modalities (transcutaneous electrical nerve stimulation, therapeutic ultrasound, diathermy) combined with mobilizations, stretching, or exercises with or without heat and ice packs.
To our knowledge, this is the first systematic review and network meta-analysis to comprehensively analyze all nonsurgical randomized clinical trials pertaining to the treatment of frozen shoulder as well as the largest systematic review ever published in the field. Based on the available evidence, it appears that the use of an IA corticosteroid for patients with frozen shoulder of duration less than 1 year is associated with greater benefits compared with all other interventions, and its benefits may last as long as 6 months. This has important treatment ramifications for the general and specialist musculoskeletal practitioner, providing them with an accessible, cost-effective, 88 and evidence-based treatment to supplement exercise regimes, which we anticipate will inform national guidelines on frozen shoulder treatments moving forward.
In the short-term, IA corticosteroid appeared to be associated with better outcomes compared with no treatment in all outcome measures. Adding arthrographic distension to IA corticosteroid may be associated with positive effects that last at least as long as 12 weeks compared with IA corticosteroid alone; however, these benefits are probably not clinically significant. Compared with physiotherapy, IA corticosteroid seemed to be associated with better outcomes, with clinically significant differences. Combination therapy with IA corticosteroid plus physiotherapy may be associated with significant benefits compared with IA corticosteroid alone or physiotherapy alone for ER ROM and function, respectively, at 6 weeks. Compared with control, combined IA corticosteroid plus physiotherapy appeared to be associated with an early benefit in ER ROM (as long as 6 weeks), with clinical significance. Subacromial administration of corticosteroid appeared to be as efficacious as IA administration. The addition of acupuncture to physiotherapy did not seem to be associated with any added benefits. Based on the network meta-analysis, arthrographic distension with IA corticosteroid was probably the most effective intervention for pain at 12 weeks follow-up. IA corticosteroid alone ranked second, and as demonstrated by the pairwise meta-analysis, the benefit of adding distension appeared clinically nonsignificant.
Most compared interventions appeared to be associated with similar outcomes at 6-month follow up, without significant differences. The only intervention that was associated with mid-term statistically significant benefits compared with control and physiotherapy (without reaching clinical significance) was IA corticosteroid for function and ER ROM. No mid-term data exist assessing the effectiveness of adding arthrographic distension to IA corticosteroid and acupuncture to physiotherapy or comparing physiotherapy (with or without IA corticosteroid) with no treatment. Our network meta-analysis found that combined therapy with IA corticosteroid and physiotherapy, physiotherapy alone, and IA corticosteroid alone were the most effective interventions for pain at 6 months follow-up. However, according to our pairwise meta-analyses, their clinical benefit compared with other treatments (or even no treatment) appeared very small.
A home exercise program with simple ROM exercises and stretches administered with or without IA corticosteroid appeared to be associated with short-term pain benefits. This was statistically significant but clinically nonsignificant compared with no treatment when accompanied by IA corticosteroid. It was both clinically and statistically significant on its own.
Several systematic reviews have been published assessing the effectiveness of therapeutic interventions for frozen shoulder. Sun et al 89 looked at the effectiveness if IA corticosteroid by comparing it with no treatment, and their findings were similar to ours, reporting that IA corticosteroid may be associated with benefits on pain, function, and ROM that are most pronounced in the short-term and can last as long as 6 months. The systematic review of both randomized and observational studies by Song et al 90 is also in agreement with our results, showing a possible early benefit of IA corticosteroid, which likely diminishes in the mid-term. An earlier systematic review by Maund et al, 88 which was only based on limited evidence (meta-analyses of 2 and 3 studies), was largely inconclusive, demonstrating possible benefits of IA corticosteroid (with and without physiotherapy) in conjunction with a home exercise program. A Cochrane review on arthrographic distension 91 was also in agreement with our results, showing that arthrographic distension with IA corticosteroid may be associated with short-term benefits in pain, ROM, and function. Their comparison of combined treatment vs IA corticosteroid alone yielded no significant differences; however, it was only based on 2 studies. A 2018 systematic review by Saltychev et al 92 also supports our findings, having demonstrated a small but clinically insignificant benefit of the addition of arthrographic distension to IA corticosteroid. In their systematic review, Catapano et al 93 reported that the addition of arthrographic distension to IA corticosteroid may be associated with a clinically significant benefit at 3 months; however, no quantitative analyses were conducted. Finally, a Cochrane review investigating the effects of manual therapy and exercise 94 concluded that they are probably associated with worse outcomes compared with IA corticosteroid in the short-term, which is in accordance with the findings of the present review, and another study 95 investigating the effectiveness of electrotherapy modalities was inconclusive because of lack of sufficient evidence.
In this review we aimed to assess the comparative effectiveness of all interventions for frozen shoulder, both surgical and nonsurgical; however, conclusions on the former could not be reached given that included studies did not assess the same interventions, which precluded pooling their results. The existing literature is conflicting regarding the superiority of arthroscopic capsular release (ACR) over nonoperative modalities; De Carli et al 62 reported no short-term or long-term benefits of ACR plus MUA compared with IA corticosteroid plus physiotherapy in function or ROM. Conversely, Mukherjee et al 75 found that ACR was associated with significant improvements in pain, function, and ROM compared with IA corticosteroid in the short-term and mid-term. Gallacher et al 63 demonstrated mixed results, concluding that compared with IA corticosteroid plus arthrographic distension, combined treatment with ACR and IA corticosteroid may be associated with improved function, external rotation, and flexion ROM but not quality of life and abduction ROM in the short-term and mid-term. The risk of complications, where reported, was not higher in the surgical groups. 63 The existing evidence on MUA, which is not a surgical procedure per se although it is administered under general anesthesia, is more consistent, suggesting its lack of long-term superiority compared with other commonly used nonsurgical treatments or even no treatment. 65 , 71 , 76
Because of the paucity of robust evidence, no firm recommendations exist for clinical practice. The National Institute of Health and Care Excellence (NICE) guidelines, 96 influenced in turn by the BESS/BOA recommendations, recommend a stepped approach, starting with physiotherapy and only considering IA corticosteroid if there is no, or slow, progress. 96 With our review, we provide convincing evidence that IA corticosteroid is associated with better short-term outcomes than other treatments, with possible benefits extending in the mid-term; therefore, we recommend its early use with an accompanying home exercise program. This can be supplemented with physiotherapy to further increase the chances of resolution of symptoms by 6 months.
Most patients in the included studies had duration of symptoms of less than 1 year; therefore, our management recommendations are strongest for this subgroup, which includes patients most commonly encountered in clinical practice. Based on the underlying pathophysiology of the condition, usual practice is to only administer IA corticosteroid in the painful and not freezing phase (also advised by NICE guidance 95 ); however, this is not backed up by evidence. In our review, studies that included patients with symptoms for more than 1 year reported equally substantial improvements in outcome measures including ROM and function; therefore, the benefits of corticosteroids may also apply to the freezing phase of frozen shoulder. 48 , 79
Despite the comprehensiveness and rigor of our methods, which include thorough risk of bias assessments and grading of evidence, we do recognize its limitations. Frozen shoulder of all chronicity was analyzed together; therefore; conclusions about specific stages and their most effective management could not be drawn. Most studies included a home exercise program, but its frequency, intensity, and duration were not taken into account in comparisons nor were separate analyses made adjusting for it. Finally, physiotherapy interventions, regardless of nature and duration, were grouped and analyzed together to minimize imprecision; in reality, some might be more effective than others. However, we only present findings that derived from thorough quantitative analyses, which were in turn substantially reinforced by the TSA, minimizing the risk for type I errors; most previous similar meta-analyses did not use TSA. Additionally, we present the first network meta-analysis including all conservative treatments for frozen shoulder. Furthermore, we based our recommendations on both statistically and clinically significant results.
Based on the findings of the present review, we recommend the use of IA corticosteroid for patients with frozen shoulder of duration less than 1 year because it appeared to have earlier benefits than other interventions; these benefits could last as long as 6 months. We also recommend an accompanying home exercise program with simple ROM exercises and stretches. The addition of physiotherapy in the form of an electrotherapy modality and supervised mobilizations should also be considered because it may add mid-term benefits and can be used on its own, especially when IA corticosteroid is contra-indicated. Implicated health care professionals should always emphasize to patients that frozen shoulder is a self-limiting condition that usually lasts for a few months but can sometimes take more than 1 year to resolve and its resolution may be expedited by IA corticosteroid. This should be offered at first contact, and an informed decision should be made by the patient after the risks and alternative therapies are presented to them. In the future, other interventions that have shown promising results and currently have inadequate evidence for definitive conclusions (eg, MUA, ACR, specific types of electrotherapy and mobilizations) should be assessed with large, well-designed randomized studies. Finally, future studies should include subgroup analyses assessing the effectiveness of specific interventions on frozen shoulder of different chronicity and stage.
Accepted for Publication: October 22, 2020.
Published: December 16, 2020. doi:10.1001/jamanetworkopen.2020.29581
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2020 Challoumas D et al. JAMA Network Open .
Corresponding Author: Neal L. Millar, MD, PhD, Institute of Infection, Immunity, and Inflammation, College of Medicine, Veterinary and Life Sciences University of Glasgow, 120 University Ave, Glasgow G12 8TA, United Kingdom ( [email protected] ).
Author Contributions: Dr. Challoumas had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Challoumas, McLean, Millar.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: Challoumas, Millar.
Statistical analysis: Challoumas.
Obtained funding: Millar.
Administrative, technical, or material support: Challoumas, McLean.
Supervision: Challoumas, Millar.
Conflict of Interest Disclosures: None reported.
Funding/Support: This work was funded by grant MR/R020515/1 from the Medical Research Council UK.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
Frozen shoulder
- Related content
- Peer review
- Marta Karbowiak , trauma and orthopaedics core trainee 1 ,
- Thomas Holme , trauma and orthopaedics registrar 2 ,
- Maisum Mirza , general practitioner 3 ,
- Nashat Siddiqui , consultant orthopaedic and upper limb surgeon 2
- 1 Royal Hampshire County Hospital, Winchester, UK
- 2 Kingston Hospital NHS Foundation Trust, Kingston upon Thames, UK
- 3 Warlingham Green Medical Practice, Warlingham, UK
- Correspondence to M Karbowiak mkarbowiak{at}doctors.org.uk
What you need to know
Patients with diabetes are at higher risk of developing frozen shoulder and having bilateral symptoms than the general population
Recovery times vary, but can be years, and some patients are left with residual pain or functional impairment
Physiotherapy is the most commonly used intervention and can be supplemented by intra-articular steroid injections
Treatments offered in secondary care include joint manipulation under anaesthesia, arthroscopic capsular release, and hydrodilatation
The UK FROST trial compared manipulation under anaesthetic, arthroscopic capsular release, and early structured physiotherapy with intra-articular corticosteroid injections, and found that none of the interventions were clinically superior
Frozen shoulder is a common and often debilitating condition that lacks a clear consensus on management, partly owing to a lack of high quality evidence on the various treatments options. In this clinical update, we offer an overview of the latest evidence on management of frozen shoulder, incorporating the clinical implications of recently published research, including the UK FROST study—the largest randomised controlled trial in this field to date, which compares surgical treatments with early structured physiotherapy and intra-articular corticosteroid injections.
What is frozen shoulder?
Frozen shoulder is a condition that results in development of thickened, fibrosed joint capsule, contraction of the joint, and reduced intra-articular volume. 1 The exact cause of these changes is unknown, with several possible processes suggested in the literature. 1 Over the years, uncertainty has surrounded the definition and classification of this condition, leading to inconsistencies in both clinical practice and scientific studies. 2 This is partially owing to the wide spectrum of clinical presentations, with patients experiencing different levels and combinations of symptoms. This also means their lives can be affected in many different ways, depending on the severity of the condition and their daily activities.
Who gets it?
The age of onset is usually in the fifth decade of life, with peak incidence between the ages of 40 and 60. 3 Women are more commonly affected than men, with one study reporting the incidence as 3.38 and 2.36 per 1000 person years, respectively. 4
Patients with diabetes have a 10% to 20% lifetime risk of developing frozen shoulder, 5 6 and are more likely to have bilateral shoulder involvement than the general population. 7 Frozen shoulder has been linked to conditions such as hypothyroidism, hypercholesterolaemia, and heart disease, although evidence is insufficient to determine whether these associations are independent. 8
How is it diagnosed?
Frozen shoulder is primarily a clinical diagnosis ( box 1 ). Patients can present with a range of symptoms related to the shoulder, although pain is often the initial trigger for presentation. Three distinct phases are commonly described, 11 with each phase typically lasting several months:
Diagnosis of frozen shoulder 9
History—insidious onset of shoulder pain, often anterolateral initially; pain at night; sometimes minimal trauma associated around time of onset
Examination—painful movement restriction, passive external rotation less than 30°, passive elevation less than 100°; cases where the disease affects the posterior capsule more than the anterior can present with reduction in internal rotation
Investigations—plain radiographs are useful to check for arthritic changes in the glenohumeral joint and are recommended by the British Elbow and Shoulder Society 10 ; ultrasound and magnetic resonance imaging may be considered depending on the clinical features and differential diagnoses
Freezing/proliferative phase—stiffness with progressively worsening pain (usually constant but exacerbated by movement)
Frozen/adhesive phase—ongoing stiffness with improved pain levels, reduction in range of motion, in particular on external rotation
Thawing/resolution phase—gradual improvement in range of motion.
The clinical course can be variable 2 and not all people with frozen shoulder will experience all three of these stages. Pain at night is a common feature, often causing considerable disruption to sleep. Patients can also experience sudden jerking movements associated with pain. 2 Diagnostic pointers for frozen shoulder are summarised in box 2 , and differential diagnoses are listed in table 1 .
When to refer to secondary care
British Elbow and Shoulder Society guidelines 10 advise to refer:
Cases of atypical presentation or marked functional limitation
Persistence of pain despite primary care interventions beyond three months
American Family Physician guidelines recommend referral to a shoulder specialist if no improvement is seen with physiotherapy and corticosteroid injections after three months 12
Differential diagnoses
- View inline
What is the clinical course of frozen shoulder?
Frozen shoulder is often described in literature as a “self-limiting” condition, and patients typically experience resolution of symptoms without or regardless of any treatment. 13 Most people with the condition make a full recovery, although recovery time tends to be slow—between one and three years. 14 15 Some experience residual symptoms: the original prospective study on frozen shoulder from 1975 found that half of patients had residual clinical restriction in range of movement after 5-10 years, and 7% had ongoing functional limitation. 11 Similar rates were reported in more recent literature, with one study 6 of patients under the care of a specialist shoulder clinic followed up at average 52 months finding that 41% reported residual symptoms. Recurrence of primary frozen shoulder after the initial resolution of symptoms is poorly reported in literature, but in our experience is rare. Up to 20% of patients can develop the condition on the opposite side. 5 Patients with diabetes generally have poorer response to treatment and, with interventions such as manipulation under anaesthetic, are at higher risk of requiring further procedures. 16
How is frozen shoulder managed?
After establishing a clinical diagnosis of frozen shoulder, explain the typical progression of the condition. Discuss the range of available management options and the risks associated with each intervention ( table 2 ). An individual approach involving exploring the extent of functional limitation and establishing treatment goals can aid in deciding the appropriate treatment.
Summary of treatment options
Advise patients to continue to use the arm as pain allows. 9 Over-the-counter or prescription painkillers can help to alleviate pain, which is often the most debilitating symptom experienced in the early stages and can limit engagement with physiotherapy. Sleeping on the unaffected side or using pillows for support in bed can help with night time pain. Heat or ice packs over the affected area can be used for additional pain relief. Shoulder stiffness can lead to other musculoskeletal symptoms, most commonly neck and lower back pain, which can also be targeted with physiotherapy. In the early stages, we recommend patients try simple home exercises such as placing things higher up to encourage reaching, gentle stretching, and pendulum exercises. 17
Physiotherapy
The main role of physiotherapy is in the frozen/adhesive phase (when the initial symptoms of pain have subsided) with stretches and strengthening exercises. This should be sustained with additional resistance based exercises in the thawing/resolution phase. 18 Structured approaches include group or individual physiotherapy, with formal range of motion exercises, soft tissue massage, and trigger point release. 19 The recommended initial treatment course is six to 12 weeks. 5
Corticosteroid injections
Corticosteroid injections can help in reducing pain and improving range of movement, particularly in the early stages of the condition and when combined with physiotherapy. A 2020 systematic review and meta-analysis on the management of frozen shoulder assessed the effectiveness of available treatment strategies across 65 studies with 4097 patients. 20 The authors found that intra-articular (IA) corticosteroid injections were associated with short term improvement in external rotation and pain compared with no treatment or placebo. IA corticosteroid injections with physiotherapy were found to be superior to IA corticosteroid injections alone for early range of motion only. Physiotherapy with IA corticosteroid injections was found to be superior to physiotherapy alone for short term outcomes using several symptom and functional scoring systems, but not for range of motion or medium term function.
IA steroid injections are associated with better pain relief compared with subacromial injections. 21 Interestingly, a 2021 clinical trial found that, even though ultrasound guided IA injections were associated with greater accuracy than blind IA injections, no difference was seen between them in pain and functional outcome scores. 22
Corticosteroid injections are generally considered safe and are associated with mild side effects only. In one study, three of 58 patients (5.2%) reported mild self-limiting nausea and dizziness. 23 Another reported that, of 133 participants, one patient (0.7%) experienced prolonged pain at the injection site, and three patients (2.3%) developed transient facial flushing. 24 Steroid injections can affect blood glucose control in patients with diabetes, particularly in the first day after the intervention. 25
Surgical options—arthroscopic capsular release and manipulation under anaesthetic
Arthroscopic capsular release (ACR) is a surgical procedure carried out under general or regional anaesthesia. The shoulder capsule is divided using arthroscopic instruments and the shoulder is re-examined to confirm optimal release. Manipulation under anaesthetic (MUA) is a procedure where the shoulder is manipulated by the surgeon to stretch and tear the joint capsule. It is carried out under general or regional anaesthesia.
The recently published UK FROST study compared ACR, MUA, and early structured physiotherapy with intra-articular corticosteroid injection. 26 The study is the largest randomised controlled trial of these interventions to date, with 503 participants recruited across 35 UK hospitals. In UK FROST, short term outcomes of ACR at three months were overall worse compared with physiotherapy with corticosteroid injection or MUA. However, at 12 months ACR was found to be associated with better functional scores (Oxford Shoulder Score, OSS) compared with both MUA and physiotherapy (OSS difference 2.01 and 3.06, respectively), although this was less than the clinically important effect size of 4-5 OSS points. The study authors concluded that none of the three interventions was clinically superior, but that ACR carried higher risks (3.9% in this cohort had a serious adverse event compared with 1% of those who had MUA), and MUA was the most cost effective intervention.
One weakness of UK FROST is that it was unable to determine to what extent the improvements in outcomes were the result of the interventions rather than the natural course of the condition. A randomised controlled trial of 125 patients in Finland 17 comparing MUA with supportive treatment (home exercises) found no difference in terms of pain levels or functional ability between the two groups at 12 month follow-up; minimal differences were noted in range of motion in favour of the MUA group. Another smaller RCT comparing ACR with supportive care did not find any significant differences between the two in functional outcome scores. 27
MUA is generally associated with low rates of adverse events—UK FROST 26 recorded two serious (1%) and 15 non-serious (7.5%) adverse events for 201 patients. These were largely minor reactions such as residual stiffness, nerve pain, and paraesthesia. One case (0.5%) of septic joint arthritis was recorded, and three patients (1.5%) experienced postoperative worsening of shoulder pain. MUA was found to be cost effective as functional improvement was seen sooner, meaning less need for prolonged physiotherapy and follow-up.
Hydrodilatation
Hydrodilatation involves injecting fluid into the shoulder joint to disrupt the capsular adhesions, and is usually performed in a clinic setting. Solutions used and volumes injected vary in literature, but most clinicians use normal saline with local anaesthetic and corticosteroid. 28 Hydrodilatation was not included in the UK-FROST study as it was not widely available until recently. It has since become a common management option alongside MUA and ACR in many UK secondary care centres.
A 2008 Cochrane review 29 noted hydrodilatation was associated with short term improvement in pain, function, and range of motion. However, a more recent 2018 systematic review and meta-analysis 28 found that the procedure had an overall insignificant effect on clinical outcomes—the authors noted minimal improvement in pain and range of motion (number needed to treat of 12) with no significant improvement in disability. One small randomised controlled trial 30 comparing MUA and hydrodilatation found that functional scores were significantly better in the hydrodilatation cohort with higher patient satisfaction rates, although the study was conducted in a small patient cohort (38 joints in total). At present, comparisons with surgical treatments are difficult owing to a lack of high quality evidence. A Delphi study 31 backed by the British Elbow and Shoulder Society is under way to help inform future directions of research. Adverse events reported with the use of hydrodilatation include pain, flushing, syncopal episodes, and one case of glenohumeral joint infection. 28
Education into practice
How might you explain the different stages of frozen shoulder to a patient first presenting with the condition?
What strategies could be used in the community to widen the access to physiotherapy for patients?
How patients were involved in the creation of this article
A patient with experience of the condition reviewed a draft of the manuscript. In response to their feedback, we developed the section on management to include more detail about analgesia and adjuncts to physiotherapy.
How this article was created
We conducted a Medline search using the terms “frozen shoulder” and “adhesive capsulitis” to identify the relevant references and review the latest published evidence. We also searched the Cochrane library and consulted the British Elbow and Shoulder Society website for current guidelines.
Information resources for patients
British Elbow & Shoulder Society Website: advice on common shoulder conditions, when to seek medical advice, and recommended self-care measures: https://bess.ac.uk
Patient.info: information about the condition and management: https://patient.info/bones-joints-muscles/frozen-shoulder-leaflet
American Academy of Orthopaedic Surgeons: resource outlining treatment options and home exercises: https://orthoinfo.aaos.org/en/diseases--conditions/frozen-shoulder/
The Chartered Society of Physiotherapy: information on managing shoulder pain and recommended exercises: https://www.csp.org.uk/publications/shoulder-pain-exercises
We have read and understood the BMJ policy on declaration of interests and declare the following interests: none.
Provenance and peer review: commissioned, based on an idea from the author; externally peer reviewed.
- Peloquin C ,
- Robinson CM ,
- Clipsham K ,
- Bridgman JF
- Guyver PM ,
- Goodchild L ,
- Brownson P ,
- Siegel LB ,
- Klinger HM ,
- von Knoch M
- Levine WN ,
- Kashyap CP ,
- Blaine TA ,
- Bigliani LU
- Macfarlane RJ ,
- Loganathan K
- Kivimäki J ,
- Pohjolainen T ,
- Malmivaara A ,
- Russell S ,
- Jariwala A ,
- Richards J ,
- Challoumas D ,
- Brealey SD ,
- UK FROST Study Group
- Smitherman JA ,
- Cricchio M ,
- Saltychev M ,
- Virolainen P ,
- Fredericson M
- Buchbinder R ,
- Johnston RV ,
- Quraishi NA ,
- Johnston P ,
- Chakrabarti AJ
- Brealey S ,
- Research article
- Open access
- Published: 04 April 2022
Living with a frozen shoulder – a phenomenological inquiry
- Suellen Anne Lyne 1 , 2 ,
- Fiona Mary Goldblatt 1 , 2 &
- Ernst Michael Shanahan ORCID: orcid.org/0000-0001-8309-3289 1 , 2
BMC Musculoskeletal Disorders volume 23 , Article number: 318 ( 2022 ) Cite this article
8347 Accesses
12 Citations
13 Altmetric
Metrics details
Frozen shoulder (adhesive capsulitis) is an inflammatory condition affecting the capsule of the glenohumeral joint. It is characterised by a painful restricted range of passive and active movement in all planes of motion. The impact of frozen shoulder on affected individuals remains poorly characterised. In this study we sought to better understand the lived experience of people suffering from frozen shoulder to characterise the physical, psychological and socioeconomic impact of the condition.
A qualitative study using a phenomenological approach was undertaken. Purposeful sampling was used to identify individuals for interview. Semi-structured interviews were performed and continued until saturation was achieved. A biopsychosocial framework was used during the analysis in order to generate themes which best described the phenomenon and reflected the lived experience of individuals’ suffering from this condition.
Ten interviews were conducted, and five main themes emerged including; the severity of the pain experience, a loss of independence, an altered sense of self, the significant psychological impact, and the variable experience with healthcare providers.
Conclusions
These findings offer an insight into the lived experience of individuals with frozen shoulder, both on a personal and sociocultural level. The pain endured has profound impacts on physical and mental health, with loss of function resulting in a narrative reconstruction and altered sense of self. Our findings illustrate that frozen shoulder is much more than a benign self-limiting musculoskeletal condition and should be managed accordingly.
Trial registration
ANZCTR 12620000677909 Registered 28/04/2020 https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=379719&isReview=true
Peer Review reports
Frozen shoulder is often poorly diagnosed and inadequately managed, and this study adds important insights on the lived experience of individuals suffering from frozen shoulder.
The severity and pervasiveness of the pain endured, a loss of independence and patients’ altered sense of self are profound representations of living with a frozen shoulder.
This study challenges us to reconsider whether our current treatment targets for frozen shoulder are appropriate.
An emphasis on early and effective pain management and on managing the psychological sequelae of the disease emerge from this study as key treatment targets.
Frozen shoulder is a common but often under-recognised condition. It is an inflammatory and fibrosing condition affecting the glenohumeral joint capsule, characterised by shoulder pain and stiffness with significant resultant disability [ 1 , 2 ]. The aetiology is unknown, however a number of risk factors have been identified including diabetes and shoulder trauma [ 1 , 3 ]. Frozen shoulder is considered primary if it occurs spontaneously, or secondary if there is an antecedent event such as trauma. The combined prevalence is estimated between 3 and 5% in the general population, but rates as high as 20% are reported in people with diabetes [ 4 , 5 ]. Peak age of onset is 40–60 years and women are affected slightly more often than men [ 6 , 7 ]. Given frozen shoulder typically affects those of working age, there are resultant economic impacts, both on a personal and societal level [ 8 ].
Frozen shoulder is predominantly a clinical diagnosis. Restriction of movement occurs in all planes of motion, both passive and active, and there is insufficient joint degeneration to account for the restricted movement [ 9 ]. The pathognomonic feature is almost complete loss of external rotation [ 7 ]. Additional investigations are usually non-contributory but can be useful in ruling out other pathologies. The natural history of frozen shoulder remains poorly understood [ 10 ], but the most commonly accepted description of disease progression is defined by three overlapping clinical phases. Phase one manifests as severe shoulder pain, typically worse at night, with concurrent progressive loss of motion. This phase can last 2–9 months and is known as the painful phase . Phase two, the frozen phase , lasts 4–12 months and is characterised by gradual reduction in pain, but persistent and considerable restriction in movement. Phase three, termed the resolution or thawing phase, and can last 12–36 months [ 3 ]. Few effective treatments are available which significantly alter the natural history of disease [ 2 ]. The extent of recovery is variable, with some reporting persistent pain and residual limitation of movement. In one large case series 35% of people had mild to moderate and 6% had severe symptoms, at a mean follow up of 4.4 years [ 11 ]. Recurrence is uncommon, although the contralateral shoulder can become affected in 6–17% of patients within the first 5 years [ 11 ]. In current practice the management of frozen shoulder has been primarily undertaken by orthopaedic surgeons and physical therapists who emphasise biomechanics and restoration of range of motion. This approach has tended to shape our understanding of the condition and influence treatment targets.
The clinical picture of frozen shoulder is well described but the impact on individual suffering is poorly characterised. Some people describe difficulties with basic activities of daily living, such as showering, dressing and cooking [ 8 ]. The pain is reported to interfere with sleep, which further intensifies the pain and impacts one’s ability to engage with domestic, social and occupational activities [ 12 , 13 ]. What remains poorly described is the experience of protracted and debilitating shoulder pain which has the potential for profound physical, psychological and socioeconomic consequences [ 14 ]. A recent systematic review of patients’ experiences with shoulder disorders in general concluded that patients contend with considerable disruption to their lives, impacting sleep, cognitive function and emotional wellbeing [ 12 ]. However, there is very limited data reporting the impact of frozen shoulder. One paper focused on patients’ experiences with conventional care pathways [ 8 ] and another examined patients’ experience of a specific treatment, Bowen’s technique [ 15 ]. To our knowledge, there have been no papers describing a holistic exploration of the lived experience of frozen shoulder.
Despite its prevalence, treatment outcomes for frozen shoulder continue to be modest [ 2 ]. Given this reality, it is important to ask why our treatments appear to be missing the mark. Is it possible our therapeutic targets are not the most appropriate for this poorly understood condition? Little is reported about the experience of individuals suffering from frozen shoulder, so in this paper we set out to better understand the lived experience. We believe this work to be important in helping to better manage this common medical condition. By improving understanding of the impact on the individual, we aim to increase practitioner awareness of the disease and its severity, facilitate earlier diagnosis and better design therapies which improve outcomes that are important to patients [ 16 ].
A qualitative study using a phenomenological approach was employed to explore the lived experience of a group of individuals suffering from frozen shoulder. Participants were identified from a group of patients with a recent diagnosis of frozen shoulder based on assessment by a specialist Rheumatologist. Inclusion criteria included male and female participants, aged over 18 years. There were no exclusion criteria. Patients were referred to the Southern Adelaide Local Health Network (SALHN) rheumatology outpatient clinic from community and hospital settings, including general practice, physiotherapists and specialty services, with the exception of one participant who was not previously known to the service. Purposive sampling was used to select individuals for interview. Patients who reported significant psychosocial impact from their frozen shoulder were invited to participate.
Interviews took place either in person at the rheumatology outpatient clinic or via audio and video telehealth, between June and August 2020. In-depth, semi-structured interviews were conducted using an interview guide (Supplementary File 1 ) Following an introduction to orientate participants, the interviewer asked the interviewee to describe the impact of the frozen shoulder on their life. Questions were “directed to the participants’ experiences, feelings, beliefs and convictions about the theme in question” [ 17 ]. An iterative approach was used for the interviews, meaning that knowledge acquired in each interview helped guide questioning for interviews of subsequent participants and enabled identification of emergent themes [ 18 ]. The audio-recorded interviews were transcribed and data de-identified. Each transcript was given to the respective interviewee to read, and an opportunity provided to amend or add any material they felt relevant. Interviews were conducted by a single researcher, SL, who had no involvement in the participants’ medical care prior to study commencement, minimising risk of bias. SL is a rheumatologist who had professional knowledge of the condition and was trained in qualitative interview techniques. Interviewing was continued until saturation was achieved, that is until interviewees introduced no new perspectives, no new themes emerged, and no further coding was possible [ 19 , 20 ]. The SALHN Human Research Ethics Committee approved the study (OFR number: 81.20, ANZCTR 12620000677909).
A phenomenological approach was deemed the most appropriate enquiry method because the research sought to understand the participants’ conscious experience; their judgments, perceptions and emotions [ 21 , 22 , 23 ]. The philosophy of Husserl and methods described by Colaizzi were applied to analyse the interviews [ 21 , 24 ]. This involves reading the interviews in their entirety, repeatedly if necessary, in order to become familiar with the data set and develop a holistic sense of the interview, the “gestalt” [ 25 ]. The researchers attempt to bracket out their own prejudices and presuppositions to avoid prejudging the data and therefore allow true realisation of the essence of the experience in order to “enter the unique world of the informant/participant” [ 26 , 27 ]. Coding was conducted using NVivo 12 Qualitative Data Analysis Software [ 28 ]. Coding was performed by the three authoring researchers and all interviews were at least dual coded. The authors are rheumatologists with experience in qualitative research. Codes were collated and sorted, and units of meaning delineated, taking into account the literal content, the number of times the unit of meaning arose, and how the meaning was delivered. Themes were derived from the data rather than being identified in advance. Themes emerged as units of meaning were clustered, bringing together recurrent experience and its variant manifestations, in order to get to the essence of the phenomenon and elucidate the “lived experience” [ 29 , 30 ].
Of the 16 individuals invited, ten agreed to participate (Eight female and two male, age range 32–72). No participants were excluded, and all provided written informed consent. Four did not respond to our invitation and two others expressed interest but we not formally recruited before saturation was achieved. Nine interviewees had recovered from their frozen shoulder, having been diagnosed within the preceding 2 years, while one was still in the resolution phase. Two participants had suffered two frozen shoulders, affecting each shoulder at different time points, whereas the remainder had only one arm affected. Data analysis resulted in identification of five main themes; the severity of the pain experience, a loss of independence, an altered sense of self, the significant psychological impact, and the variable experience with healthcare providers.
The severity of the pain experience
The intractable nature and intensity of the pain dominated the participants’ experience of frozen shoulder. The pain was severe and the timing unpredictable, although most often precipitated by movement. Participants used vivid descriptors of pain, such as “horrible”, “excruciating”, “debilitating” and “unbearable” to illustrate their experience.
“You see the Western movies [where] they forge the steel and … plunge it into the cold water … that’s what it feels like, hot, molten lava encapsulated by metal, dragging your shoulder down”
The pain affected all facets of life, impacting work, sleep, personal hygiene, interpersonal relationships and independence. The prolonged duration and inescapable nature of the pain made it both debilitating and demoralising. It was consistently recognised that above all else, participants wanted the pain to go away. Pain was the priority and was considered far more significant than the loss of movement:
“All I wanted was for the pain to go away”.
Resolution of the pain had a major positive psychological impact on participants:
“Once the pain was alleviated, then I could cope with everything else”.
Improvement in pain enabled participants to engage more effectively in physical therapies and begin their recovery.
A loss of Independence
The degree and impact of the disability and loss of independence was another prominent theme. There were implications both at home and in the workplace. Activities such as dressing, driving, shopping and personal hygiene were limited, or near impossible for some, occasionally with resultant loss of income. This was particularly evident for those whose dominant arm was affected.
“It's hard to describe how much it limits you. You can't do anything”.
Many participants felt that the severity of their illness and consequent disability was underappreciated by others due to the ‘invisible’ nature of frozen shoulder. Often a sense of stoicism was expressed as people tried to cope as though nothing was wrong, while simultaneously becoming frustrated by others’ inability to appreciate their incapacity. Many struggled to accept their disability, and were reluctant to rely on others:
“I felt like I was abusing my friends … to ask them again or to rely on them again, that was stupid”.
Meanwhile, others exhibited a greater sense of acceptance and self-kindness. There was an apparent sense of fear associated with loss of independence; fear of being judged, of being a burden, of resentment, and of loss of income. This fear was compounded by social isolation and a sense of hopelessness, particularly for those with limited social supports and inadequate access to services.
An altered sense of self
The loss of independence, in combination with intractable pain, prompted an identity narrative reconstruction for some participants, resulting in an altered sense of self. In the context of the severe pain and physical limitation, individuals struggled to meet their own expectations, and also the expectations of those around them.
“I was supposed to be the one that could cope and do everything”
This resulted in a growing separation between their private sense of self and their public social identity, causing a paradigm shift in their self-concept [ 30 , 31 , 32 ]. Pain was a constant reminder of disability. Their disability prevented them for undertaking activities of daily living, as well as activities that brought joy, such as sport and playing with children or grandchildren. Inability to drive or catch public transport caused their world to shrink. Interrupted sleep caused fatigue and irritability, as well as an inability to function at full capacity at work. The fear of being a burden and lack of understanding from others resulted in social isolation:
I didn't want anybody around me because I didn't want anybody to see me the way I was”
Cumulatively, these factors challenged the sufferers’ perception of self and often resulted in social withdrawal. For some, this altered sense of self was enduring, and in others it was transient. Resilience and strong supportive social networks were recognised as important factors in preventing such a loss in sense of self.
The psychological impact
Living with a frozen shoulder often had profound psychological effects including anxiety, irritability, depression and even the contemplation of suicide. The unrelenting pain, as well as interrupted sleep, were key determinants of mood:
“When the world is crumbling and you’re in pain … it’s a dark time”
Furthermore, patients often felt they weren’t believed about the severity of their pain, with a lack of empathy and understanding emanating from family, friends, colleagues and members of the medical profession. People reported feeling frustrated at their lost independence and lack of understanding from others. This frustration manifest itself as irritability.
“people see me as more cantankerous than they’d ever been seen before.”
Depression was frequently reported.
“I’d had enough, I couldn’t handle it and my depression got really bad”
Two participants had even contemplated suicide as a means of ending their pain.
“had I woken up the next morning … still in the same sort of pain, then yes, I may not still be here”
A lack of recognition of the individuals’ mental health issues by treating health professionals was reported, and may have contributed to the psychological impacts being poorly managed.
The healthcare approach
Medical and allied health professionals often appeared to lack awareness of this condition. At times, this resulted in prolonged delays to diagnosis, inappropriate investigation and inadequate treatment.
“I’d seen 3 or 4 GP’s up to that point and none of them, they’re all sending me off to have an ultrasound for bursitis and no one, and I’d even mentioned frozen shoulder and, and they were all like “No we don’t think it’s that” you know, and so I felt very disempowered from the medical profession and very not understood.”
There were many differing interpretations by the health professionals of what “frozen shoulder” actually meant and why people get it. On reflection, participants became aware of this knowledge gap over time. An apparent lack of compassion and empathy was sometimes noted as members of the healthcare team trivialised the severity of symptoms and failed to acknowledge their impact.
“[They] never ever asked me how things, how was I managing at home”
The severity of the pain was also underappreciated by certain practitioners, as demonstrated by the lack of compassion when asked to perform exercises:
“She grabbed my arm, and she used all her force to pull my arm all the way up, I screamed like you had no idea.”
Participants expressed concerns about the overall knowledge and experience of many of their healthcare providers and suggested a need to improve this through further education. In contrast, participants described a sense of relief when a health practitioner was able to identify and confidently manage their frozen shoulder. The knowledge of being understood provided a sense of relief, and instilled patients with new hope.
“I almost burst into tears. I can feel it now. I was like
Oh my God, someone understands me”
The formation of a therapeutic relationship and established treatment targets was evidently important in the overall healing process.
To our knowledge, this is the first qualitative study to describe the phenomenon of living with a frozen shoulder. Jones et al. explored the perceptions of people living with frozen shoulder and their priorities for treatment [ 8 ] however, while this work emphasised the loss of function and unacceptable delays to treatment, there was little evaluation of the subjective experience and psychological impact of the pain.
The aetiology and pathophysiology of frozen shoulder remains poorly understood and is postulated by some to be an algoneurodystrophic process, on the same spectrum as chronic regional pain syndrome [ 33 , 34 ]. It is difficult to delineate the role of tissue damage and nociceptive stimulation in perception of pain from frozen shoulder. According to Moseley, pain experience does not correlate directly with the state of the tissues and many factors across somatic, psychological and social domains influence pain modulation [ 35 ]. In the absence of a clear pathological process and inadequate direction from health practitioners, the sufferer’s consciousness is held accountable for their own condition [ 36 , 37 ]. The complexity of musculoskeletal pain has been extensively studied and there is an ever-growing body of evidence which explores the modern concept of chronic pain [ 35 , 38 , 39 , 40 ]. It has been consistently demonstrated that expectations and pre-existing personality traits influence one’s experience of pain. For example, catastrophising and health-related anxiety are associated with heightened pain experience, whereas resilience and strong social supports help ameliorate pain [ 40 , 41 ]. Given the burden of psychological distress expressed by some of our participants, it is imperative that patient expectations, social isolation and health related anxiety be acknowledged and addressed early when managing frozen shoulder.
Physical therapy is considered by many as first line therapy for frozen shoulder despite multiple studies and a recent Cochrane review demonstrating little evidence to support physical therapy [ 34 , 42 , 43 , 44 ]. Our work has highlighted that the patients’ priority is pain management, above all else. Patient-centred care involves listening to patients’ priorities [ 16 ] and empowering patients to effectively critique and provide feedback on the quality and appropriateness of healthcare services [ 45 ]. In our study, pain management clearly was prioritised by the patients over range of movement. By treating the pain effectively, participants said that they would be better able to cope psychologically with their incapacity and engage better with physical therapies.
Our data showed that being understood by healthcare professionals and others also played a therapeutic role. Participants reported feeling frustrated and disempowered by the lack of understanding and empathy offered by health professionals. This sentiment has been echoed by other qualitative work exploring chronic pain, even in specialist pain clinics, where it seems the clinician’s ability to truly understand the patients’ experience is “outside their lexicon of knowledge” [ 8 , 14 ]. If a patient’s experience is misrepresented or trivialised by the health practitioner, this may propagate a negative self-image with resultant shame, distress and altered sense of self [ 46 ]. Such feelings promote resentment and helplessness and are counterproductive to the therapeutic relationship, while also increasing risk of anxiety and depression [ 38 ]. This in turn magnifies the individual’s experience of pain. Conversely, if a patient feels their struggle is understood, there are profound positive impacts. It validates the individual’s experience, which instils a sense of relief and hope, reaffirms their functioning as a social individual and diminishes their sense of spoiled identity [ 14 ]. There is a large body of evidence which supports the need for a strong therapeutic alliance when managing chronic musculoskeletal pain, based on a shared understanding of the symptomatology and treatment targets, and the management of frozen shoulder is no different [ 47 , 48 ].
The findings in this research have allowed us to reconceptualise the treatment targets for frozen shoulder and a number of issues have been identified which may improve patient care. Firstly, a clearer focus on early and effective pain management is imperative, as is improved management of the psychological sequelae. These findings align with an increasing body of evidence that explores the impact of pain and pain-related behaviours on outcomes in frozen shoulder [ 49 , 50 , 51 ]. Treatment of chronic musculoskeletal pain is complex, requiring a multifaceted biopsychosocial approach. While targeting nociceptive signals with analgesia and neural blockade may be helpful, educating patients about the mechanisms of chronic musculoskeletal pain is also of great importance [ 52 ]. Enquiring about a patient’s coping strategies and acknowledging their struggle are simple measures to provide improved psychological support. In Australia, there is a paucity of services available for patients with short term incapacity, however, referral to a psychologist and advocating for access to community support services may be beneficial. Education is required to enable practitioners to better recognise and manage frozen shoulder. Equally, the language chosen by clinicians needs to be reconsidered in order to foster a constructive therapeutic alliance [ 53 ]. Given that frozen shoulder is so painful and slow to improve, early patient education is critical to ameliorate apprehension and help formulate realistic treatment targets [ 4 ]. We believe that addressing the above short fallings will reduce pain severity, lessen the sense of spoiled identity and help minimise rates of anxiety and depression.
There are a number of strengths to our study. The use of bracketing and dual coding has minimised potential bias. Employing phenomenology as the methodology in this study has allowed the voice of individuals’ experiences to be clear. Some limitations to this study also need to be considered. Participants’ experiences were historical, having recovered from their frozen shoulder some weeks or months prior and it is therefore possible that themes may have differed in participants with active disease. Recall bias must also be taken into consideration. Because of public health restriction in place at the time of our study, interviews were conducted in person, and via audio and video telehealth. Use of different communication platforms may have impacted rapport and limit translatability. Furthermore, this was a small study which included mostly patients from a single tertiary centre and limited geographical area.
This study has focused on the experience of living with a frozen shoulder. It has provided new insight into the severity of the pain and the subsequent impact on physical and mental health, with loss of function resulting in a narrative reconstruction and altered sense of self. Insights from this research align with recent studies that emphasise the importance of pain-perception and pain-related behaviours in patients with frozen shoulder. Increased practitioner awareness of patient experience helps facilitate earlier diagnosis and refocuses treatment approaches based on patient priorities. A clearer emphasis on early and effective pain management and on managing the psychological sequelae of the disease are two clear opportunities which emerge from this study.
Availability of data and materials
De identified original interviews available from the corresponding author upon reasonable request.
Hochberg MGE, Silman A, Smolen J, Weinblatt M, Weismanet M. Rheumatology: the shoulder. 7th ed. USA: Elsevier; 2018.
Google Scholar
Challoumas D, Biddle M, McLean M, Millar NL. Comparison of treatments for frozen shoulder: a systematic review and Meta-analysis. JAMA Netw Open. 2020;3(12):e2029581.
Article PubMed PubMed Central Google Scholar
Brun SP. Idiopathic frozen shoulder. Aust J Gen Pract. 2019;48(11):757–61.
Article PubMed Google Scholar
Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1(3–4):180–9.
Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016;6(1):26–34.
Ramirez J. Adhesive capsulitis: diagnosis and management. Am Fam Physician. 2019;99(5):297–300.
PubMed Google Scholar
Dias R, Cutts S, Massoud S. Frozen shoulder. Bmj. 2005;331(7530):1453–6.
Jones S, Hanchard N, Hamilton S, Rangan A. A qualitative study of patients' perceptions and priorities when living with primary frozen shoulder. BMJ Open. 2013;3(9):e003452.
Kelley MJ, Shaffer MA, Kuhn JE, Michener LA, Seitz AL, Uhl TL, et al. Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther. 2013;43(5):A1–31.
Lewis J. Frozen shoulder contracture syndrome - Aetiology, diagnosis and management. Man Ther. 2015;20(1):2–9.
Maund E, Craig D, Suekarran S, Neilson A, Wright K, Brealey S, et al. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2012;16(11):1–264.
Article CAS PubMed PubMed Central Google Scholar
Page MJ, O'Connor DA, Malek M, Haas R, Beaton D, Huang H, et al. Patients' experience of shoulder disorders: a systematic review of qualitative studies for the OMERACT shoulder Core domain set. Rheumatology. 2019;58(8):1410–21.
Longo UG, Facchinetti G, Marchetti A, Candela V, Risi Ambrogioni L, Faldetta A, et al. Sleep disturbance and rotator cuff tears: a systematic review. Medicina (Kaunas). 2019;55(8):453. https://doi.org/10.3390/medicina55080453 .
Harding G, Parsons S, Rahman A, Underwood M. "it struck me that they didn't understand pain": the specialist pain clinic experience of patients with chronic musculoskeletal pain. Arthritis Rheum. 2005;53(5):691–6.
Carter B. Clients' experiences of frozen shoulder and its treatment with Bowen technique. Complement Ther Nurs Midwifery. 2002;8(4):204–10.
Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100–3.
Welman J, Kruger F. Research methodology for the business and adminstrative sciences. Cape Town: Oxford University Press; 1999.
McGrath C, Palmgren PJ, Liljedahl M. Twelve tips for conducting qualitative research interviews. Med Teach. 2019;41(9):1002–6.
Easton KL, McComish JF, Greenberg R. Avoiding common pitfalls in qualitative data collection and transcription. Qual Health Res. 2000;10(5):703–7.
Article CAS PubMed Google Scholar
Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18:59–82.
Article Google Scholar
Colaizzi P. In: RVaM K, editor. Psychological research as a phenomenologist views it. Existential phenomenological alternatives for psychology. New York: Oxford University Press; 1978.
Creswell J. In: Oaks T, editor. Qualitative inquiry and research design: choosing among five approaches. 3rd ed: Sage Publications; 2012.
Cohen L, Manion L, Morrison K. Research methods in education. 5th ed. London: Routledge Falmer; 2000.
Hycner R. Some guidelines for the phenomenological analysis of interview data. Hum Stud. 1985;8:279–303.
Flick U. An introduction to qualitative research. 4th ed. London: Sage Publications; 2009.
Groenewald T. A phenomenological research design illustrated. Int J Qual Methods. 2004;3(1):42–55.
Moustakas C. Phenomenological research methods. London: Sage Publications; 1994.
Book Google Scholar
QSR International Pty Ltd. NVivo (released in 2018). 2018.
Dowling M, Cooney A. Research approaches related to phenomenology: negotiating a complex landscape. Nurse Res. 2012;20(2):21–7.
Nowell LSNJ, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16:1–13.
Kelly M. Self, identity and radical surgery. Sociol Health Illn. 1992;14:390–415.
Yoshinda K. Reshaping of self: a pendular reconstruction of self and identity among adults with traumatic spinal cord injury. Sociol Health Illn. 1993;15:217–45.
Müller LP, Müller LA, Happ J, Kerschbaumer F. Frozen shoulder: a sympathetic dystrophy? Arch Orthop Trauma Surg. 2000;120(1–2):84–7.
Le HV, Lee SJ, Nazarian A, Rodriguez EK. Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow. 2017;9(2):75–84.
Moseley G. Reconceptualising pain according to modern pain science. Phys Ther Rev. 2007;12:169–78.
Eccleston C, Williams AC, Rogers WS. Patients' and professionals' understandings of the causes of chronic pain: blame, responsibility and identity protection. Soc Sci Med. 1997;45(5):699–709.
Kugelmann R. The psychology and management of pain. Theory Pscyhol. 1997;7:43–65.
Smith J, Osborn M. Pain as an assault on the self: an interpretive phenomenological analysis of the psychological impact of chronic benign low back pain. Psychol Health. 2007;24:517–34.
Eccleston C. A normal psychology of chronic pain. Psychologist. 2011;24:422–5.
Morley S. Psychology of pain. Br J Anaesth. 2008;101(1):25–31.
Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17(1):52–64.
Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003;2003(2):Cd004258.
PubMed Central Google Scholar
Page MJ, Green S, Kramer S, Johnston RV, McBain B, Chau M, et al. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014;(8):CD011275. https://doi.org/10.1002/14651858.CD011275 .
Ryans I, Montgomery A, Galway R, Kernohan WG, McKane R. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology (Oxford). 2005;44(4):529–35.
Article CAS Google Scholar
Pulvirenti M, McMillan J, Lawn S. Empowerment, patient centred care and self-management. Health Expect. 2014;17(3):303–10.
Lewis H. Shame - the 'sleeper' in psychopathology: the role of shame in symptom formation. Hillsdale: Lawrence Erlbaum Associates; 1987.
Lin I, Wiles L, Waller R, Caneiro JP, Nagree Y, Straker L, et al. Patient-centred care: the cornerstone for high-value musculoskeletal pain management. Br J Sports Med. 2020;54(21):1240–2.
Geenen R, Overman CL, Christensen R, Åsenlöf P, Capela S, Huisinga KL, et al. EULAR recommendations for the health professional's approach to pain management in inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77(6):797–807.
De Baets L, Matheve T, Dierickx C, Bijnens E, Jans D, Timmermans A. Are clinical outcomes of frozen shoulder linked to pain, structural factors or pain-related cognitions? An explorative cohort study. Musculoskelet Sci Pract. 2020;50:102270.
De Baets L, Matheve T, Traxler J, Vlaeyen J, Timmermans A. Pain-related beliefs are associated with arm function in persons with frozen shoulder. Shoulder Elbow. 2020;12(6):432–40.
Chiaramonte R, Bonfiglio M, Chisari S. A significant relationship between personality traits and adhesive capsulitis. Rev Assoc Med Bras. 1992;66(2):166–73.
Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. J Pain. 2015;16(9):807–13.
Roter D, Hall J. Doctors talking with patients/patients talking with doctors: improving communication in medical visits. Santa Barbara: Praeger; 2006.
Download references
Acknowledgements
The authors would like to thank all the patients who participated in the interview process. We would also like to thank Narelle Goldie, who transcribed the audio-recordings and Liz Briggs who assisted with patient recruitment.
No external funding.
Author information
Authors and affiliations.
Rheumatology Department, Level 2, Flinders Medical Centre, Flinders Drive, 5042, Adelaide, South Australia
Suellen Anne Lyne, Fiona Mary Goldblatt & Ernst Michael Shanahan
College of Medicine and Public Health, Flinders University, Adelaide, South Australia
You can also search for this author in PubMed Google Scholar
Contributions
The manuscript has been read and approved by all the authors. Contributions for each author are as follows; S.A.L. responsible for participant recruitment, conducting interviews, data analysis through coding and authorship of article; F. M G. responsible for dual coding of interviews and co-authorship; E.M.S. who is the principal investigator, responsible for study design, patient recruitment, dual coding of interviews and co-authorship. The final manuscript has been read and approved by all authors.
Corresponding author
Correspondence to Ernst Michael Shanahan .
Ethics declarations
Ethics approval and consent to participate.
The Southern Adelaide Local Health Network Human Research Ethics Committee approved the study (OFR number: 81.20,) All participants gave written informed consent to participate.
Consent for publication
Not applicable.
Competing interests
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lyne, S.A., Goldblatt, F.M. & Shanahan, E.M. Living with a frozen shoulder – a phenomenological inquiry. BMC Musculoskelet Disord 23 , 318 (2022). https://doi.org/10.1186/s12891-022-05251-7
Download citation
Received : 09 August 2021
Accepted : 21 March 2022
Published : 04 April 2022
DOI : https://doi.org/10.1186/s12891-022-05251-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adhesive capsulitis
BMC Musculoskeletal Disorders
ISSN: 1471-2474
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Adhesive capsulitis (frozen shoulder)
Citation, doi, disclosures and case data.
At the time the case was submitted for publication Domenico Nicoletti had no recorded disclosures.
Presentation
55-year-old female with decreased range of motion and left shoulder pain increasing over the last 2 months.
Patient Data
Sagittal T1-weighted sequences show the complete obliteration of subcoracoid fat triangle and distinct fatty tissue surrounding the coracohumeral ligament as having disappeared, and the coracohumeral ligament cannot be measured. The coronal T2-weighted fat-suppressed image demonstrates an abnormally thickened inferior glenohumeral ligament and the axillary pouch is contracted and poorly distended. There is also supraspinatus tendinopathy without tear.
Annotated images of adhesive capsulitis.
Case Discussion
Adhesive capsulitis is a self-limited clinical syndrome characterized by painful, gradual loss of active and passive glenohumeral motion. Replacement of the fat in the rotator interval with the abnormal soft tissue that can encase the biceps anchor ( subcoracoid triangle sign ), can be classified on a sagittal T1-weighted image as (A) absent, (B) partial, (C) complete.
1 article features images from this case
- Subcoracoid triangle sign
11 public playlists include this case
- CTMRI Viva by Rudolf Kuhn
- Shoulder by Dr Sunaina Arora
- MSK by Joshua Taylor
- Msk2 by Kevin Sheng
- Mixed Films 2021 by Varsha Kumar
- FMH2 - Osteo by Guillaume Fahrni
- Adhesive capsulitis by dao van ly
- msk by Mihir Desai
- MSK VIVA 5 by Maria Kirkinis
- shoulder2 by Noor Abbas Hummadi Fayadh
- MSK VIVA by Michael Le ◉
Related Radiopaedia articles
- Adhesive capsulitis of the shoulder
Promoted articles (advertising)
How to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Adhesive capsulitis: a case study
Affiliation.
- 1 Brooke Army Medical Center at Fort Sam, Houston, TX, USA.
- PMID: 20016342
- DOI: 10.1097/NOR.0b013e3181c01227
Adhesive capsulitis (AC), also known as frozen shoulder, is a common and painful musculoskeletal disorder. The shoulder is a complex joint comprising 3 bones and multiple muscle groups, ligaments, and tendons. Accompanying the inflammation of the joint is stiffness that greatly restricts the patient's motion and strength. AC is a treatable condition requiring months of daily physical therapy. The reports that 1 in 7 Americans has a musculoskeletal impairment including shoulder problems that accounted for 14 million visits to physicians' offices in 2003. It is imperative that practitioners accurately assess and diagnose the patient with shoulder pain to facilitate an appropriate plan of care. This paper will discuss the case of a patient with AC including differential diagnoses, pathophysiology, and treatment options.
Publication types
- Case Reports
- Bursitis / diagnosis*
- Bursitis / rehabilitation
- Diagnosis, Differential
- Education, Continuing
- Middle Aged
- Physical Examination
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Treatment of eight patients with frozen shoulder: a case study series

2005, Journal of Bodywork and Movement Therapies
Related Papers
Physical Therapy
Background and PurposeThe purpose of this study was to compare the use of 3 mobilization techniques—end-range mobilization (ERM), mid-range mobilization (MRM), and mobilization with movement (MWM)—in the management of subjects with frozen shoulder syndrome (FSS).SubjectsTwenty-eight subjects with FSS were recruited.MethodsA multiple-treatment trial on 2 groups (A-B-A-C and A-C-A-B, where A=MRM, B=ERM, and C=MWM) was carried out. The duration of each treatment was 3 weeks, for a total of 12 weeks. Outcome measures included the functional score and shoulder kinematics.ResultsOverall, subjects in both groups improved over the 12 weeks. Statistically significant improvements were found in ERM and MWM. Additionally, MWM corrected scapulohumeral rhythm significantly better than ERM did.Discussion and ConclusionIn subjects with FSS, ERM and MWM were more effective than MRM in increasing mobility and functional ability. Movement strategies in terms of scapulohumeral rhythm improved after 3 ...
International Journal of Recent Innovations in Medicine and Clinical Research
Background: The term "capsulitis" or "frozen shoulder" refers to a common shoulder condition characterized by the global restriction in the shoulder range of motion in a capsular pattern. The capsular pattern in the shoulder is characterized by most limitation of passive lateral rotation and abduction. Aim: To determine the recent research evidences for the effectiveness of mobilization along with conventional therapy in frozen shoulder patients. Method: This review includes randomized controlled trails (RCTs). Searching done by Google Scholar, PubMed and Pedro from 2010 to 2019. We used terms like-frozen shoulder, mobilization, manipulation, exercise, shoulder pain and physiotherapy management. Result: Present outcomes shows that mobilization along with conventional therapy is effective technique in reducing pain and increasing Range of motion (ROM) in frozen shoulder patients without adverse effects. The search resulted in 50 articles but only 05 articles were selected for the study based on criteria. Conclusion: Mobilization program with conventional therapy designed for frozen shoulder treatment can be more effective in increasing shoulder ROM and reducing pain.
Medicina (Kaunas, Lithuania)
Jelena Sokk
Clinical Rehabilitation
Sylwia Mętel
Objective: To compare the short- and long-term effects of a structural-oriented (convential) with an activity-oriented physiotherapeutic treatment in patients with frozen shoulder. Design: Double-blinded, randomized, experimental study. Setting: Outpatient clinic. Subjects: We included patients diagnosed with a limited range of motion and pain in the shoulder region, who had received a prescription for physiotherapy treatment, without additional symptoms of dizziness, a case history of headaches, pain and/or limited range of motion in the cervical spine and/or temporomandibular joint. Interventions: The study group received treatment during the performance of activities. The comparison group was treated with manual therapy and proprioceptive neuromuscular facilitation (conventional therapy). Both groups received 10 days of therapy, 30 minutes each day. Main measures: Range of motion, muscle function tests, McGill pain questionnaire and modified Upper Extremity Motor Activity Log wer...
Journal of Orthopaedic & Sports Physical Therapy
Brian Leggin
Journal of emerging technologies and innovative research
Sakshi Sadhu
Background: Frozen shoulder is the most common self limiting disability which affects about 2-5% of the population with the females being more prone. It’s having three phases and the treatment depends upon the phases. The best treatment choice should be started from the conservative treatment then proceed to invasive. Frozen shoulder case is clinically diagnosed and requires minimal investigations as there is complete restriction in the passive and active range of motion. Objective: The objective of this case study was to provide the relief to the patient in terms of pain as well increase the range of motion which helps in enhancing the functional activities. This case study evaluates the effect of combined treatment methods used in the physiotherapy. Case Description: A 48 year female visited OPd with the complaints of pain and restricted active and passive range of motion in the left shoulder. The shoulder disability index of the patient was approximately 90% and the severity of t...
smita kanase
Introduction: Frozen Shoulder describes the clinical entity in which person has restricted passive mobility at Glenohumeral joint, which causes functional limitations.Diabetes mellitus patients are more affected by this condition. Many techniques are found effective in treating frozen shoulder. The present study was done in frozen shoulder patients with diabetes mellitus with the aim to find out additional effect of Kinesiotaping along with Maitland mobilization in managing frozen shoulder. Objectives: To study and compare effectiveness of Maitland mobilization and kinesiotaping on functional outcome in frozen shoulder. Method: 32 subjects were divided in 2 Groups. GROUP A (experimental Group) treated with Maitland mobilization and Kinesiotaping and GROUP B (control Group) treated with Maitland mobilization. Both the Groups were initially treated with hot moist packs for 20 min and Ultrasound for 5 min. Exercises were advised. Subjects received 4 weeks intervention for 3 days/ week....
Journal of Shoulder and Elbow Surgery
Jim Richards
www.rphsonline.com
Research in Pharmacy and Health Sciences
Background: Frozen shoulder is disorder of the connective tissue that limits the normal Range of motion of the shoulder in diabetes, frozen shoulder is thought to be caused by changes to the collagen in the shoulder joint as a result of long term Hypoglycemia. Mobilization is a therapeutic movement of the joint. The goal is to restore normal joint motion and rhythm. The use of mobilization with movement for peripheral joints was developed by mulligan. This technique combines a sustained application of manual technique "gliding" force to the joint with concurrent physiologic motion of joint, either actively or passively. This study aims to find out the effects of mobilization with movement and end range mobilization in frozen shoulder in Type I diabetics. Materials and Methods: 30 subjects both male and female, suffering with shoulder pain and clinically diagnosed with frozen shoulder was recruited for the study and divided into two groups with 15 patients each based on convenient sampling method. Group A patients received mobilization with movement and Group B patients received end range mobilization for three weeks. The outcome measurements were SPADI, Functional hand to back scale, abduction range of motion using goniometer and VAS. Results: The mean values of all parameters showed significant differences in group A as compared to group B in terms of decreased pain, increased abduction range and other outcome measures. Conclusion: Based on the results it has been concluded that treating the type 1 diabetic patient with frozen shoulder, mobilization with movement exercise shows better results than end range mobilization in reducing pain and increase functional activities and mobility in frozen shoulder.
Dr. Maryam Imdad, Dr. Nimra Aslam, Dr Raees Sabir, Dr. Hareem Aslam, Dr. Ayesha Niaz, Dr. Muhammad Waqar Younas
Editor iajps
Background: Frozen shoulder, also known as adhesive capsulitis, is a painful condition associated with fibrosis, progressive pain, decreased range of motion (ROMs) which leads towards severe shoulder pain, stiffness and infirmity. Most common in diabetic patients. Adhesive capsulitis is a clinical problem as well as a combination of psychological, physical and social factors that can lead to disability, may contribute to other conditions such as neck pain, chest pain. To deal with these complications Physical Therapy can play an important role. Aims and Objectives: Therefore, this study is designed to see the effectiveness of these Physical Therapy Treatments (METs, Joint Mobilization, hot pack) for pain and decreased ROM in the patients of frozen shoulder. Methodology: A sample size of 30 subjects was collected from four clinical settings of Faisalabad, divided into treatment and Control group through randomization. Outcomes of attentiveness are pain, ROM and disability. Universal Goniometer and NPRS was used for outcome measures. SPADI for shoulder disability. SPSS version 20 was used for statistical analysis and conclusion was made accordingly. Results: Joint Mobilization showed significant results in frozen shoulder. Conclusion: Joint mobilization with METs and hot pack are the potential treatment option for patients of frozen shoulder in all adult population regardless of harms and side effects. However a bigger sample size and a longer duration of the study are needed. The conclusion appeared as, the joint mobilization shows more significant effects when use with METs and hot pack.
RELATED PAPERS
Carlos San Juan Mesonada
Dr.usama S Soliman , Ayman Khalil
The Semantic Web–ISWC 2010
SOUVIK KUNDU 15BEC0849
Fernanda De Negri
Journal of SAFOG
Preet Agarwal
… de Andalucía 2002
Oriol Vicente Campos
Journal of Scientific Research and Reports
NGOZI UZOR UDEH
PEOPLE: International Journal of Social Sciences
ratana daungkaew
Berliner Journal für Soziologie
Jürgen Mackert
Frontiers in Neuroanatomy
Angel Rodriguez
Neurocybernetyka teoretyczna
Ryszard Tadeusiewicz
Journal of Insect Behavior
jean-pierre lumaret
Revista Colombiana De Sociologia
Julián Seguel González
Daniel Rivera García
UMROH CIREBON
umroh cirebon
Special Care in Dentistry
Anastasia Kossioni
Khan Marwat
Alianza Editorial
Leandro Pereira Gonçalves
Clinical lymphoma & myeloma
Sheila Piva
African Journal of Biomedical Research
Emmanuel Acheampong
Daniel C.W. Ho
hjjhgj kjghtrg
GeroScience
Swathi HEMACHANDRA
Humanismus in der deutschen Literatur des Mittelalters und der Frühen Neuzeit
Beate Kellner
Oxford Music Online
Rosemary Firman
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Patient Care & Health Information
- Diseases & Conditions
- Frozen shoulder
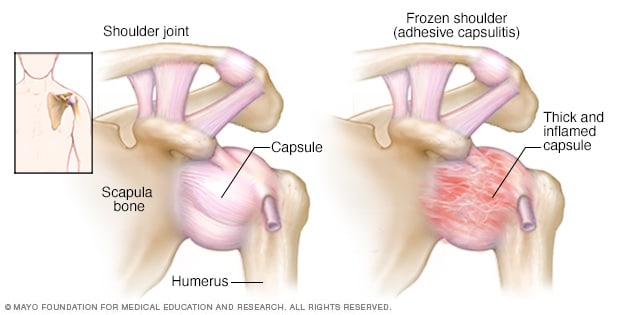
Frozen shoulder occurs when the connective tissue enclosing the joint thickens and tightens.
Frozen shoulder, also called adhesive capsulitis, involves stiffness and pain in the shoulder joint. Signs and symptoms typically begin slowly, then get worse. Over time, symptoms get better, usually within 1 to 3 years.
Having to keep a shoulder still for a long period increases the risk of developing frozen shoulder. This might happen after having surgery or breaking an arm.
Treatment for frozen shoulder involves range-of-motion exercises. Sometimes treatment involves corticosteroids and numbing medications injected into the joint. Rarely, arthroscopic surgery is needed to loosen the joint capsule so that it can move more freely.
It's unusual for frozen shoulder to recur in the same shoulder. But some people can develop it in the other shoulder, usually within five years.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Mayo Clinic Sports Medicine
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Products for Daily Living from Mayo Clinic Store
Frozen shoulder typically develops slowly in three stages.
- Freezing stage. Any movement of the shoulder causes pain, and the shoulder's ability to move becomes limited. This stage lasts from 2 to 9 months.
- Frozen stage. Pain might lessen during this stage. However, the shoulder becomes stiffer. Using it becomes more difficult. This stage lasts from 4 to 12 months.
- Thawing stage. The shoulder's ability to move begins to improve. This stage lasts from 5 to 24 months.
For some people, the pain worsens at night, sometimes disrupting sleep.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The shoulder joint is enclosed in a capsule of connective tissue. Frozen shoulder occurs when this capsule thickens and tightens around the shoulder joint, restricting its movement.
It's unclear why this happens to some people. But it's more likely to happen after keeping a shoulder still for a long period, such as after surgery or an arm fracture.
Risk factors
Certain factors may increase the risk of developing frozen shoulder.
Age and sex
People 40 and older, particularly women, are more likely to have frozen shoulder.
Immobility or reduced mobility
People who've had to keep a shoulder somewhat still are at higher risk of developing frozen shoulder. Restricted movement can be the result of many factors, including:
- Rotator cuff injury
- Recovery from surgery
Systemic diseases
People who have certain diseases appear more likely to develop frozen shoulder. Diseases that might increase risk include:
- Overactive thyroid (hyperthyroidism)
- Underactive thyroid (hypothyroidism)
- Cardiovascular disease
- Parkinson's disease
One of the most common causes of frozen shoulder is not moving a shoulder while recovering from a shoulder injury, broken arm or stroke. If you've had an injury that makes it difficult to move your shoulder, talk to your health care provider about exercises that can help you maintain your ability to move your shoulder joint.
- McMahon PJ, et al., eds. Sports medicine: Upper extremity. In: Current Diagnosis & Treatment in Orthopedics. 6th ed. McGraw Hill; 2021. https://accessmedicine.mhmedical.com. Accessed June 18, 2022.
- Frozen shoulder. American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/diseases--conditions/frozen-shoulder. Accessed June 14, 2022.
- Prestgaard TA. Frozen shoulder (adhesive capsulitis). https://www.uptodate.com/contents/search. Accessed June 14, 2022.
- Challoumas D, et al. Comparison of treatments for frozen shoulder: A systematic review and meta-analysis. JAMA Network Open. 2020; doi:10.1001/jamanetworkopen.2020.29581.
- Kim YJ. Acupuncture management for acute frozen shoulder: A case report. Clinical Case Reports. 2021; doi:10.1002/ccr3.5055.
- Shoulder exercises
Associated Procedures
- Cortisone shots
News from Mayo Clinic
- Mayo Clinic Minute: Tips to help a frozen shoulder Dec. 06, 2023, 06:01 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

Case Study: Frozen Shoulder Success

28 Jan Case Study: Frozen Shoulder Success
Disclaimer: The pathologies “adhesion” and “scar tissue” are used interchangeably here in our discussion of frozen shoulder. In medical terms, the only difference between the two is that an “adhesion” implies connective tissue build up without trauma while “scar tissue” implies with trauma.
I’ve already written how I don’t care about your herniated disc and the truth about plantar fasciitis .
Now, it’s time to write about something else I don’t care about.
Your frozen shoulder diagnosis. And a real case study to prove results!
The patient to the right, Jeff, was diagnosed with a “frozen shoulder”, also known as “ adhesive capsulitis ” (wikipedia). He experienced this condition as “stiffness and tightness” in his right shoulder that began over 18 months before his first visit with Barefoot Rehab .
Previously, Jeff had undergone “physical therapy” treatment for 2 months, starting 15 months before his first visit with Barefoot Rehab . Traditional physical therapy uses many modalities such as ultrasound, electronic stimulation, different variations of massage, and strengthening work. Jeff noted that the “physical therapy” consisted mainly of exercises.
Here, we can assume based on his past treatment that “weakness” was the primary pathology being treated by the previous physical therapists, then “strengthening” would be the primary solution.
Remember, we always have to match up the pathology with the correct treatment for that pathology.
- Pathology –> Solution
- Nail –> Hammer (metaphor for using the proper tool for the proper problem)
- Screw –> Screwdriver
- Weakness –> Strengthening or “Physical Therapy”
He noted this treatment made his range “somewhat better”, but he still couldn’t reach overhead. In the picture above, notice his right arm in front of his ear. He couldn’t lift it any higher than that position and he felt a “soft, bouncy” stop at the top of his range of motion.
His range was far from normal.
Enter: Barefoot Rehab
At his first visit with us, Jeff was able to reach his shoulder about 140 degrees from his side with intense effort.
After palpating (fancy doctor word for “feeling”) various shoulder tissues including infraspinatus, teres minor, subscapularis, and the posterior-inferior shoulder capsule, we were able to determine that Jeff’s primary issue was “Adhesion/Scar tissue in the right rotator cuff muscles.”
- Adhesion –> Adhesion manipulation
Upon further examination of his history, it was determined that Jeff makes relative good lifestyle choices: he consumes alcohol minimally, does not smoke cigarettes, eats his vegetables, has effective stress management techniques, and has a regular exercise routine. In other words, these common pathologies were minimized as problems for Jeff.
The only contributing factor to his diagnosis was his occupation, which causes him to sit at a desk for eight hours/day. This was explained to Jeff. We included in Jeff’s treatment plan overhead movements such as a strict press and yoga movements such as downward dog to assist in maintaining full shoulder flexion.
- Sedentary job –> 2 minute microbreaks for every 30 minutes of sitting consisting of walking, lunging, shoulder circles.
After 16 visits, Jeff was able to reach his shoulder 180 degrees from his side, almost touching his ear. This is just shy of what a normal, healthy range would be (his arm in contact his ear).
He noted that it felt easy and he had no stiffness or tightness.

How Will Your Flexibility Change Each Visit? (another case study video)
Below is a woman who had 10 years of frozen shoulder and 2 surgeries. The treatment was not recorded. She was 90% better after 7 treatments.
But you can clearly see how her flexibility and range of motion changes after each visit.
You can even hear her friend’s surprise at how well she is moving!
Other Important Notes on the Frozen Shoulder Diagnosis
Jeff responded extremely well to our treatment ( manual adhesion release ) of one pathology (adhesion).
In true frozen shoulder cases, this is rare.
Frozen shoulder can involve several other dysfunctions that are important to point out:
- Structural dysfunction – ie. labral tears, internal disc derangements or other disc pathology of the cervical spine.
- Metabolic dysfunction – ie. micronutrient deficiencies, food allergies/intolerances, under-the-radar medical conditions, or other immune-comprised problems
- Stress dysfunction – too much sympathetic nervous system overload.
- Emotional dysfunction – ie. an emotional story that necessitates possible Freudian intervention or another therapy of the sort.
In addressing the above list, it’s important to be mindful of non-musculoskeletal caues for a diagnosis like “frozen shoulder”. Only by identifying all non-normal variations from the norm when it comes to our individual health and happiness can we get rid of chronic pain.

Case Study: Frozen Shoulder Success | Primal Docs
[…] Case Study: Frozen Shoulder Success […]
Charlene henry
So you’re stating he was “lazy” and that’s how he developed frozen shoulder?? What about the majority of us who develop it because we are the complete opposite? I do triple as much as I’m suppose to do daily and have always lifted and carried way more than my little body should handle. That was why I was told I developed it and why I am having trouble in BOTH shoulders at the same time. I’m confused on this article…
Hi Charlene,
Where did you deduce that Jeff was “lazy”? I did say that he has a desk job, where he sits 8 hours/day. But I also mentioned that he has a regular exercise routine. I’m suggesting that he developed frozen shoulder as a result of overuse with adhesion being laid down, tightening his tissue and range of motion. Exactly what caused the overuse is hard to say given this data.
If you overused your rotator cuff musculature and didn’t give your muscles a chance to recover, that’s a really good environment to develop “frozen shoulder” or adhesion in your rotator cuff. Have you been undergoing treatment for them? Is it working? If you want to take a picture/video of your range of motion, I can look at it.
Let me know if this helps to clarify. Let’s have a dialogue and I can help you figure out a diagnosis.
kaleem mohd
Evidence for physiotherapy to manage true frozen shoulder have been conflicting over the years. As a physical therapist at healthclues, Hyderabad In my experience, in the early stages of the condition, physiotherapy can be extremely useful for pain reduction. However, the movement often remains restricted. There is, however, research supporting physiotherapy in the middle to late stages of the condition as well as after more invasive input. After such a long period of immobility, the shoulder needs lots of encouragement and muscle patterning retraining to rehabilitate back to full function.
Thank you for the perspective Kaleem.
Aubrey Corcoran
I’m a middle aged female Crossfitter who developed frozen shoulder a full 14 months ago. I suffered through 5 months of 2x weekly physical therapy before insurance would cover an MRI. Once I had a correct diagnosis (no tears, but I did have adhesive capsulitis) I had a recommendation from my orthopedic surgeon to try a different PT clinic. Within 2 months of 2 hours, 2x week (so a total of 32 hours) of PT, which included adhesion release (manipulation, extremely uncomfortable) I had significant measurable success. I am now at full ROM and have resumed pull ups and overhead presses. I am still not up to my previous level of strength, and I do have a twinge of tightness in my affected shoulder, but the adhesions HAD to be broken to get where I am. So thankful for my surgeon’s advice.
Beautiful Aubrey. This is what success looks like. Yes, thank God for your surgeon. : )
Brittany Jennings
Thank you for posting
You’re welcome Brittany!
REVIEW article
A new perspective of frozen shoulder pathology; the interplay between the brain and the immune system.

- 1 Department of Physical Therapy, Faculty of Health Sciences, Campus of Melilla, University of Granada, Melilla, Spain
- 2 University Chair in Clinical Psychoneuroimmunology, University of Granada and PNI Europe, Melilla, Spain
- 3 Clinical Medicine and Public Health PhD Program, Faculty of Health Sciences, University of Granada, Granada, Spain
Frozen shoulder (FS), also known as adhesive capsulitis of the shoulder (FS), is a fibrotic inflammatory process of unknown etiology whose main symptoms are pain, stiffness and the loss of joint mobility. These symptoms may be associated with pathologies such as diabetes, Dupuytren’s syndrome and the prevalence of today’s sedentary lifestyle. This literature review provides an overview of the epidemiology and pathogenesis of this pathology, as well as the mechanisms of lowgrade chronic inflammation and infection, insulin resistance, and omics-science associated with it. We also propose a new hypothesis related to the possibility that the GABAergic system could play a decisive role in the development of frozen shoulder and that therefore diabetes type 1, endocrinological autoimmune disorders and frozen shoulder are connected by the same pathophysiological mechanisms. If that is true, the combined presence of psycho-emotional stress factors and pathogenic immune challenges could be the main causes of frozen shoulder syndrome. Finally, we propose a series of possible intervention strategies based on a multifactorial etiological and mechanistic concept.
1 Introduction
Frozen shoulder (FS) or adhesive capsulitis of the shoulder (FS) is a disorder characterized by its inflammatory and fibrotic process ( Pietrzak, 2016 ). Codman first included the term “frozen shoulder” in 1934 ( Dias et al., 2005 ). The predominant symptoms of this pathology in people suffering from it are stiffness, pain and a limitation in the range of active and passive mobility of the glenohumeral joint ( Hannafin and Chiaia, 2000 ; Hagiwara et al., 2018 ). These symptoms have impact on personal and professional life and disturb people from performing their normal daily activities, affecting their quality of life ( Chen et al., 2017 ). The disability in the shoulder can last over a period of one or more years during which range of motion is slowly restored in 60% of the affected population ( Sarasua et al., 2021 ).
The other 40% of patients develop a chronic disorder ( Buchbinder et al., 2007 ) and become increasingly more limited in their daily functions ( Walmsley et al., 2014a ; Chen et al., 2017 ). Interesting is that the quality of life seems to be solely related with purely the loss of motion of the affected shoulder and as such a successful treatment would improve both physical performance and quality of life ( Fernandes, 2015 ).
It is of outmost importance to understand the reasons why FS resolves in 60% and persist in 40% of affected patients. Several factors seem to operate simultaneously in patients in which FS does not resolve and are of psychological, functional, etiological, and biological character. A retrospective study concerning the success rate of arthroscopic capsular release and relationship with functional and psychological factors showed that traumatic etiology, depression and anxiety decreased success rate after operation ( Galasso et al., 2023 ). Another study with 210 patients (F/M = 130/80), investigated the outcome of consecutive physiotherapy, cortisone injection and, when necessary, arthroscopic release, in patients with FS and the impact of diabetes and obesity on that outcome ( Barbosa et al., 2019 ). Interestingly, the study showed no association of BMI and successful outcome of FS treatments whereas patient with diabetes showed worse results when treated with physiotherapy and cortisone injection. The authors of this study refer to diabetes as a known risk factor for FS and conclude that mechanistic prove still lacks to explain the significant impact of diabetes on onset and resolve of FS ( Barbosa et al., 2019 ). They refer to the fact that glycosylated Hb does not seem related with FS and so glycation and the forming of advanced glycolated end products cannot explain mechanistically the relationship between FS and persistent FS. Other explanations are therefore needed. Later we will describe a new hypothesis about the way FS develops and persists.
The common opinion about the pathophysiology of FS is based on a “inflammation-fibrotic cascade’ theory, characterized by fibroproliferative tissue fibrosis, whereby fibroblasts, producing predominantly type I and type III collagen and transform into myofibroblasts (a smooth muscle phenotype). This process is further accompanied by inflammation, neoangiogenesis and neoinnervation ( Millar et al., 2022 ). Neoinnervation and the change of tissue morphology could explain the main hallmarks of FS, meaning pain and loss of range of motion ( Akbar et al., 2019a ). Epidemiological data reflect a prevalence of FS of 3%–5% in the general population ( Sarasua et al., 2021 ).
The syndrome consists of three phases ( Walmsley et al., 2014a ; Cho et al., 2018 ): i) the painful freezing phase in which pain precedes a loss of range of motion lasting 10–36 weeks ( Walmsley et al., 2014b ; Zhang et al., 2021 ); ii) the state of freezing or adhesive phase, lasting 4–12 months where pain gradually reduces while the range of motion stays impaired ( Walmsley et al., 2014b ; Zhang et al., 2021 ); and iii) the thawing or regression phase where range of motion improves progressively ( Walmsley et al., 2014b ; Zhang et al., 2021 ). However, 40% of patients do not recover normal range of motion and keep experiencing symptoms and that makes this classification still contentious ( Millar et al., 2022 ).
The course of FS and its impact on physical wellbeing, mental health, together with a sustained loss of productivity and global economy has been shown ( Bouaicha et al., 2020 ). Although a common opinion about the pathophysiology exists (the above-mentioned cascade), the disparity of results observed in the literature regarding the etiology of FS, suggests that there remain mechanistic lagunes in the pathophysiology and etiology of FS ( Austin et al., 2014 ).
New insights about the possible etiology of FS come from a recent study ( de Mello et al., 2023 ) that shows a significant increase of FS cases during the COVID-19 pandemic. They investigated retrospectively 1.983 patients that suffered from FS and compared the number of patients that became affected from March 2019 to February 2020 and from March 2020 to February 2021 ( de Mello et al., 2023 ). During the pandemic the incidence of FS was 2.41-fold higher compared to the previous year ( de Mello et al., 2023 ). Data that confirmed the results of other epidemiological studies were related with a 4-fold increase of FS in patients suffering from diabetes ( Whelton and Peach, 2018 ). The same holds for the possible association between hypothyroidism and the incidence of FS which in this study shows a 5-fold increase, again in coherence with earlier published data ( Cohen et al., 2020 ).
The new findings are mainly related with psycho-emotional factors. The individuals that suffered from depression and anxiety had, respectively, 8.8 ( p < 0.001) and 14 ( p < 0.001) times and significant greater risk on the development of FS ( Whelton and Peach, 2018 ). The results of an earlier systematic review ( Brindisino et al., 2022 ) already emphasized on the impact of depression and anxiety on physical dimensions such as shoulder pain, range of motion and pain perception. These data suggest that ‘toxic’ emotions and ‘toxic’ thoughts ( Pruimboom, 2023 ) could be part of the multifactorial etiology of FS and further research should elicit possible mechanisms of how exactly these ‘yellow flag’ factors could cause FS.
Genetic susceptibility as risk factor for FS is also proposed and suggested by results of a genome-wide association study by Scott et al. ( Scott-solomon et al., 2022 ). Three polymorphisms of genetic loci related with cell proliferation and production of extracellular matrix and collagen fibers seem to be as associated with FS, diabetes and hypothyroidism and so genetic susceptibility should be included in the list of possible risk factors ( Scott-solomon et al., 2022 ). One of the loci as a risk factor for FS is the Wnt gene ( Scott-solomon et al., 2022 ). A polymorphism of the Wnt gene has also been found in people suffering from morbus Dupuytren, giving a possible explanation for the relationship between morbus Dupuytren and FS ( Dolmans et al., 2011 ).
Further confusion about the definite causes of FS and the mechanisms behind it is caused by the fact that there exists a great disparity in success rates by interventions based on the known epidemiologic, etiological and mechanistic data known thus far ( Cohen et al., 2016 ; Cho et al., 2019 ; Mertens et al., 2022 ). These disparities make it legitimate to state that the best way to treat people with FS is primary prevention.
Psychological factors were already identified as risk factors for the development of FS and for worse outcome in patients who underwent chirurgical repair of a rotator cuff injury ( Aïm et al., 2022 ). The authors of the latter study conclude that although significant worse outcome was measured for patients suffering from anxiety and depression, it was not clear if the psychological state was cause or consequence ( Aïm et al., 2022 ). Anxiety, depression and pain, the latter a hallmark of FS, do not only share psychological characteristics, but also biological ones.
Spontaneous pain, as initiating symptom for idiopathic FS, is often part of a cluster of syndromes including depression, pain and chronic fatigue ( Mokhtari et al., 2019 ). Several pathways have been described to explain the comorbidity between the three syndromes, although the common opinion about the connections is mostly based on the presence of a chronic neuroinflammation causing hippocampal atrophy, accompanied with decreased neurogenesis, decreased neuroplasticity and less presence of neurotrophic factors ( Raison et al., 2006 ; Jain et al., 2011 ; Mokhtari et al., 2019 ). Causes of neuroinflammation range from endotoxemia ( De and Pruimboom, 2015 ; Mohammad and Thiemermann, 2021 ), and metabolic syndrome ( Van Dyken and Lacoste, 2018 ) via acute brain trauma and stroke ( Leung et al., 2007 ) to sleep disturbances ( Zhu et al., 2012a ) and high calorie diet ( Robbins and Solito, 2022 ). Stroke and acute brain trauma have also been associated with FS ( Leung et al., 2007 ) and the same holds for sleep disturbances ( Jankowska-Polańska et al., 2021 ). Overall, psychological and immunological factors are related with onset and prognosis of FS and so treatment should account interventions improving functioning of the brain, the immune system and the shoulder.
If we could identify the sum of non-confounding risk factors as cause of FS than the use of for instance lifestyle medicine would be indicative. Primary prevention is more than early detection of a disease. Nevertheless, measurements that help to recognize the disease in its early stage before symptoms appear and fibrosis sets in, helps to slow the development of FS and supports faster healing ( Pietrzak, 2016 ). In this regard, metabolic factors (diabetes mellitus and thyroid disorders, metabolic syndrome), autonomic symptoms and pain sensitivity may contribute to the prognosis in terms of shoulder pain, disability, and quality of life in patients with FS ( Nathan, 2002 ). Therefore, inflammation control has been proposed to be the best option when the etiology of a pathology is unknown ( Hand et al., 2008 ). The diagnosis of frozen shoulder is classified into primary and secondary. Primary FS is characterized by a progressive and painful loss of the active and passive mobility range in the shoulder with its causes being unknown ( Walmsley et al., 2014b ); secondary FS is of a known intrinsic or extrinsic cause with stiffness in the shoulder being established for instance after surgery ( Hannafin and Chiaia, 2000 ).
The care of musculoskeletal health is often based on the recognition of patient-reported findings, physical examination and evidence of an initial inflammatory state leading to fibrosis ( Hand et al., 2008 ).
However, some patients with FS (between 7% and 50%) have symptoms for a long period of time with 6% having them for more than 7 years ( Eljabu et al., 2016 ), which again can be explained by an incomplete understanding of frozen shoulder’s etiology ( Mertens et al., 2022 ). In this sense, FS is currently understood in a multifactorial way, in which chronic low-grade inflammation (LGI), alterations in glucose metabolism (especially insulin resistance with compensatory hyperinsulinemia), chronic ischemia and endotoxemia are important factors of great scientific interest. Perhaps adding omics sciences could shed light on the understanding of the mechanisms and causes that lead to FS and we will therefore add some data related with metabolomics and proteomics ( Nathan, 2002 ; de la Serna et al., 2021 ). We will further propose a new perspective of the etiology and possible treatment of patients suffering from FS through the description of the interplay of the brain and immune system in people suffering from FS, diabetes type 1 and even morbus Hashimoto.
2 Epidemiology
The prevalence of FS in the entire population is 2%–5% ( Dias et al., 2005 ; Hand et al., 2008 ; Austin et al., 2014 ). Most patients suffering from FS are women (70%) ( Hannafin and Chiaia, 2000 ) with the most frequent age range being between 40 and 60 ( Hand et al., 2008 ). Although the exact etiology is unknown, the risk factors are: diabetes, Dupuytren’s syndrome, heart and neck surgery, Parkinson’s disease, smoking, thyroid disease and chronic regional pain syndrome ( Bridgman, 1972 ; Hannafin and Chiaia, 2000 ; Thomas et al., 2007 ; Chan et al., 2017 ).
FS has been clearly demonstrated to be associated with diabetes ( Thomas et al., 2007 ; Austin et al., 2014 ; Chan et al., 2017 ), with type 1 diabetes being the most frequent risk factor for its development. Its incidence in the diabetic population is 10%–36% higher than in the general population, which indicates that poor glucose control is related to the development of FS in the long term ( Thomas et al., 2007 ). A key factor in this association is the level of hemoglobin ( Bridgman, 1972 ). In the literature, there is a hypothesis which suggests that hyperglycemic levels associated with diabetes can incite changes in the collagen of the joints thereby unleashing fibrotic and inflammatory variations, and these changes in the joint have been observed in pathological studies of the disease ( Austin et al., 2014 ). Chronic hyperglycemic levels increase the possibility of the production of advanced glycation end products which are known to cause cross linking of collagen fibers that can result in fibrosis of the capsules of the shoulder ( Li et al., 2015 ). One of the most susceptible substances for glycation caused by chronic hyperglycemia is hemoglobin ( Malka et al., 2016 ) and therefore HbAc1 could be a valid parameter of AGE products as part of the etiology of FS. A relevant study including 201,531 patients with diabetes of which 1,150 suffered from frozen shoulder did not support any association of HbAc1 with the incidence of FS ( Yian et al., 2012 ). This study confirms that people suffering from diabetes have an increased risk for FS but glycation of HbAc1 does not seem to have influence on that risk ( Yian et al., 2012 ). It is surprising that people suffering from diabetes type 1 are at greater risk for suffering FS than patients suffering from diabetes type 2 ( Thomas et al., 2007 ). Both groups of patients show repetitive hyperglycemia periods and both show signs from inflammation and metabolic disturbances at the level of lipid physiology including LDL, VLDL and triglycerides values in the bloodstream ( Razi et al., 2017 ; Tell et al., 2020 ). Dyslipidaemia is part of the pathophysiological changes in FS and therefore the metabolic state resulting from diabetes one and two could explain partly the association between diabetes and FS. What it does not explain is the difference between the impact of diabetes type 1 and 2 on FS. COVID-19 has perhaps given a new perspective to explain this difference. FS is also associated with axial spondylarthritis (axSA), according to a study investigating 2,859 patients suffering from axSA ( Huang et al., 2020 ). SA is associated with increased risk and early onset in patients human leukocyte antigen B27 (HLA-B27)-positive ( Huang et al., 2020 ). A recent meta-analysis and systematic review found that FS is also strongly associated with the presence of HLA-B27 ( Prodromidis and Charalambous, 2016 ). These findings further support the possibility that FS has an auto-immune origin or shares certain pathophysiological mechanisms with all the auto-immune diseases with which FS risk is associated.
One of those mechanisms could be related with the GABA-ergic dependent nervous system. Diabetes type 1 is considered an autoimmune disease and the main autoimmune response is against glutamic acid decarboxylase (GAD65) ( Towns and Pietropaolo, 2011 ). GAD65 is a super autoantigen with high level of presence in the brain ( Nataf, 2017 ).
GAD65 is a synaptic enzyme that catalyzes y-aminobutyric acid (GABA) from glutamate. Its expression in inhibitory terminals is essential for functioning of the GABAergic system ( Mende et al., 2016 ). The immune reaction against GAD65 resulting in the production of antibodies is not only evidenced in diabetes type 1 but also in several central nervous system disorders grouped as GAD-antibody spectrum disorders ( Tsiortou et al., 2021 ). These disorders are characterized by severe anxiety, depressed mood, and specifically anxiety and phobias for physical challenges ( Tsiortou et al., 2021 ). The study of Pires ( de Mello et al., 2023 ) showed that anxiety and depression during the COVID-19 pandemic increases the risk for FS with a factor 8.8 which is even greater than other associations ( de Mello et al., 2023 ). GAD65 antibodies that can lead to diabetes type 1 and central nervous disorders are often a consequence of two synergistic risk factors, according to Nataf ( Nataf, 2017 ). The simultaneous exposure of an immune challenge combined with psycho-emotional stress increases the risk of T cell priming against GAD65 and this can produce both diabetes type 1 and central nervous system disorders ( Nataf, 2017 ). SARS-COV-2 has brought fear, anxiety an depression to many affected and non affected COVID-19 individuals ( Kupcova et al., 2023 ), and these psycho-emotion state in combination with viral challenges could be responsible for an increases of antoantibodies GAD65 in persons already suffering from diabetes type 1. It is even possible that COVID-19 can elicit diabetes type 1 according to a case study by Genç ( Genç et al., 2021 ). During the pandemic cases of hyperglycemia, diabetic ketoacidosis and diabetes type 1 increased and so SARS-CoV-2 seems to trigger or unmask DM1 ( Wang et al., 2013 ). Could autoantibodies against GAD65, which are associated with diabetes type 1, brain disorders, anxiety, and depression, also have a significant role in the development of Frozen Shoulder (FS), especially considering its higher occurrence in patients with hypothyroidism and Hashimoto’s disease ( Brindisino et al., 2022 ), and the elevated risk of endocrinological autoimmune diseases related to these autoantibodies ( Gambelunghe et al., 2000 )? The GABAergic system has multiple functions related with hallmarks of inflammatory diseases such as rheumatoid arthritis ( Shan et al., 2023 ), pain ( Jasmin et al., 2004 ), and GABA-disorders as seen in people suffering from autoimmune activity against GAD65 develop a stiff body disease ( Tsiortou et al., 2021 ). These data, although speculative, support the development of the hypothesis that FS related with diabetes type 1 is of autoimmune origin. Antibody spreading is a known mechanism in autoimmune diseases and spreading of GAD65 has been evidenced in people suffering from diabetes type 1, although the level of auto-antibodies was not high enough to predict auto-reactivity in the infiltrated tissues ( Söhnlein et al., 2000 ). Nevertheless, disturbances of the GABA-system could lead to fear of physical challenges and movement neglect is one of the evidenced risk factors for the development of FS ( de la Serna et al., 2021 ) ( Figure 1 ).
Figure 1 . Social defeat and psycho-emotional distress lead to increased presentation of brain super autoantigens, which are presented to pro-inflammatory T lymphocytes present in the meninges of the brain. Immune challenges such as virus, bacteria and leaky gut, sedentary lifestyle, and obesity, produce a LGI and activity of both the innate and acquired immune system. The heightened activity of the T lymphocytes increases the susceptibility for the development of Teffector cells primed for multiple super autoantigens like GAD65. Active Teffector cells respond to GAD65 (antigen) presented by antigen presenting cells in the meninges inducing the primus movens of a possible autoimmune reaction. Teffector cells primed for GAD65, migrate to the peripheral body and specifically the pancreas, where they find a high level of GAD65 inducing a severe auto-immune response that ultimately leads to diabetes type 1. Antigen spreading to specific sites attract Teffector cells into the susceptible shoulder (non-dominant neglected), the thyroid gland, and the hand muscles, whereas immune activity in the brain causes a neuroinflammation, leading to depression, fear and anxiety.
When eliminating the difference of incidence between DM1 and FS and DM2 and FS, it seems plausible that components of the metabolic syndrome and the metabolic syndrome as part of DM1 and two are (co) responsible for increased pro-inflammatory cytokine production ( Austin et al., 2014 ), causing a state of chronic low-grade inflammation as part of the pathophysiology of FS ( Hutcheson and Rocic, 2012 ). This chronic low-grade inflammation is further related with increased oxidative stress, caused by the production of excessive reactive oxygen species (ROS) and oxidative stress is also part of FS ( Vicente, 2016 ).
2.1 A short resume of the literature related with the shoulder pathogenesis in FS
Stiffness, pain, and limited range of motion are common symptoms in people suffering from frozen shoulder (FS). The accumulation of advanced glycation end products (AGEs) in the shoulder, associated with insulin resistance, compensatory hyperinsulinemia, chronic hypoxia, and endotoxemia, are also characteristic ( Bridgman, 1972 ). Cytokines play a fundamental role in the development of the disease and could possibly be used as diagnostic markers. Interleukin cytokine IL-1 is involved in key functions such as immune cell recruitment, cell proliferation and tissue destruction ( Chen et al., 2017 ). The presence of activated mast cells, T and B lymphocytes and inflammatory mediators (including cytokines) found in synovial biopsies in patients suffering from FS, support the pathophysiological role of pro-inflammatory cytokines in FS ( Bridgman, 1972 ). These cytokines further can cause persistent capsular fibrosis and thus, the development of FS. Next to infiltrated immune cells, fibroblasts and myofibroblasts are present in great amounts ( Bunker et al., 2000 ), whose main function are the maintenance of the extracellular connective tissue matrix. Overactivation of myofibroblasts gives raise to formation of fibrotic tissue and tissue contraction, whereas they normally have an important repair function ( Ramos et al., 2004 ). When the matrix contracts, pain and stiffness occur. Myofibroblasts and immune cells influence each other and by their cytokines and growth factors ( Bunker et al., 2000 ).
3 Low grade inflammation and subclinical infection
Modern life is characterized by high calorie intake, sedentary lifestyle and many other toxic factors brought by the development of culture ( Ramos et al., 2004 ). Culture should not been seen as some reaction on evolution, it is just its logical result ( Ramos et al., 2004 ). The factors that killed humans millions of times have been responsible for the search for solutions and humans have achieved many benefits by using their intelligence. Today people in developed countries hardly die of starvation, dehydration, heat or cold because of respectively agriculture, a sanitary system, air conditioning and central heating ( Al-Amrani et al., 2021 ). Nature shaped survival strategies and intelligence and the end-result is culture. The need for physical activity is almost fully eliminated by motorizing transport, food is brought by a courier and so too much food and a chronic lack of physical activity are logical consequences of culture as a result of nature ( Ramos et al., 2004 ; Pruimboom, 2023 ). Culture, as result of nature, developed based on the ultimate law of evolution, meaning save energy for survival and reproduction ( Casanova et al., 2023 ).
Modern lifestyle is a direct cause of many detrimental health effects and that probably means we have had too much of culture ( Pruimboom et al., 2015 ). Factors such as light pollution, air pollution, sleep disturbances, alcohol abuse, smoking, sitting time, high calorie diet, increase loneliness and social defeat factors such a poverty, all produce a chronic stress response, with multiple consequences ( McEwen et al., 2015 ). Chronic stress leads to activation of the immune system. Lifestyle can also directly cause inflammation by the production of a lifestyle associated molecular pattern that consists of increased LDL and uric acid. Both are immunogenic compounds producing a pro-inflammatory state ( Zindel and Kubes, 2020 ). Chronic stress was recently defined as chronic irritation ( Navarro et al., 2023 ) and chronic irritation produces low-grade inflammation that, on its turn, increases permeability of multiple mucosal barriers including the gut ( Fasano and Shea-Donohue, 2005 ; de Punder and Pruimboom, 2015 ; Fasano, 2020 ; Zindel and Kubes, 2020 ; Navarro et al., 2023 ). The translocation of bacterial debris and other toxins to the blood stream, and present in those mucosal organs, are co-responsible for the observed low-grade inflammation ( Fasano and Shea-Donohue, 2005 ; Fasano, 2020 ). During any type of inflammation barrier break-down is observed where any form of injury can start with low-grade inflammation and may lead to systemic inflammation ( Bunker et al., 2014 ). LGI activates the stress systems chronically and cortisol, noradrenalin and pro-inflammatory cytokines can cause (severe) damage to tight junctions of systemic barriers ( de Punder and Pruimboom, 2015 ). The blood-brain barrier, the blood-retinal barrier, the blood-nerve barrier, the blood-lymph barrier and the blood-cerebrospinal fluid barrier increase their permeability or are damaged by LGI, possibly causing a systemic inflammation of all vital organs ( Bridgman, 1972 ; Rönnbäck and Hansson, 2019 ). The systemic inflammation caused by LGI can easily explain the presence of an inflammatory state in the frozen shoulder of affected people ( Hagiwara et al., 2018 ). Some cytokines, such as HMGB1, have been shown to play a role in FS pathology; they are thought to be needed for the onset and perpetuation of FS since their release during stress bolsters the inflammatory tissue response seen in patients ( Akbar et al., 2019a ; de la Serna et al., 2021 ; Millar et al., 2022 ).
LGI can be produced by many chronic stress factors of both sterile and non-sterile character. Non-sterile etiological factors for FS include possible infiltration of bacteria that normally inhabit human skin, such as Propionibacterium acne (P. acne), that recently has been identified in people suffering from FS ( Bunker et al., 2014 ; Cucchi et al., 2017 ). A recent study showed the presence of multiple alarmins (IL-33, S100A9, S100A8 and HMGB1) in the joint capsule in FS, and these alarmins are associated with an infective response against P. acne ( Cucchi et al., 2017 ; Akbar et al., 2019b ). P. acne could not only be a possible cause of FS, it is also the most frequent bacteria that causes infection in the affected shoulder after surgical procedures ( Cher et al., 2018 ). Corynebacterium propinquum and Streptococcus epidermis are commonly found in the affected shoulder and are also part of etiological factors of disc herniation as shown in several studies ( Lavergne et al., 2017 ). The postulated mechanism by which these bacteria reach the shoulder capsule is through the mouth, mainly during tooth brushing ( Bhanji et al., 2002 ; Capoor et al., 2017 ). Oral dysbiosis, which mediates local and peripheral inflammatory pathologies, can be the origin of the development of a pathological atopobiome in different tissues including the brain ( Kelly et al., 2015 ), the spine and discs ( Teichtahl et al., 2015 ) and the shoulder ( Hajishengallis, 2015 ). The way the bacteria reach the infiltrated organs is still in debate although data suggest that they migrate in an ‘invisible state of dormancy’ ( Malka et al., 2016 ). The dormant state of the bacteria prevents immune detection and facilitates migration and infiltration in organs with a low pO2 level such as the intervertebral disc and the shoulder capsule, and even more in sedentary people ( de la Serna et al., 2021 ). Therefore, a combination of low-grade inflammation and the possible presence of a subclinical infection could explain the observed inflammation-fibrotic cascade in FS.
The inflammatory phase can be considered a protective event but it can become a threat when it is exacerbated ( Potgieter et al., 2015 ); for this reason, inflammation has been linked to several degenerative diseases as well as mitochondrial alterations, with mitochondria playing an important role in pro-inflammatory signaling ( Campos et al., 2003 ). Strategies aimed at controlling excessive oxidative stress in mitochondria may represent preventive and therapeutic interventions in inflammation ( López-Armada et al., 2013 ). Impaired mitochondrial function is associated with several acute and chronic inflammatory diseases ( López-Armada et al., 2013 ). A recent review has shown how mitochondrial dysfunction can end up appearing in many different pathologies, such as fibromyalgia, chronic fatigue syndrome, diabetes, some types of cancer, and neurodegenerative diseases (e.g., Parkinson’s or Alzheimer’s). In patients with FS, it seems logical to suspect mitochondrial dysfunction as a consequence of the observed alterations in glucose metabolism, insulin resistance, lack of shoulder mobility, a low oxygen level and the level of free radicals as all known risk factors for mitochondrial dysfunction ( Casanova et al., 2023 ), as well as in chronic shoulder pain ( Hamed-Hamed et al., 2023 ).
If LGI and subclinical infection contribute to FS, interventions targeting both entities should prevail in patients suffering from FS. Although common opinion is that the use of NSAIDs as anti-inflammatory intervention could help to resolve FS, data are confounding ( Ewald, 2011 ). NSAIDs have been part of medicine since decades and their role is based on the assumption that the metabolites produced out of arachidonic acid (AA) (as part of the debris in tissue injuries) are deleterious for wound healing and cause inflammation ( Wang et al., 2021 ). NSAIDs inhibit COX-2 enzymes responsible for the production of different metabolites of AA, including prostaglandin E2 (PgE2, 82). PgE2 has long been considered a pro-inflammatory eicosanoid ( Kawahara et al., 2015 ). Studies from Hangai ( Hangai et al., 2016 ) and more recently Avramia ( Avramia et al., 2021 ) show that PgE2 should be considered an immune-suppressive damage associated molecular pattern (DAMP) and is probably therefore the most abundant eicosanoid in an acute inflammatory environment ( Hangai et al., 2016 ). The notion that inflammation is some ‘bad’ invention of evolution has been the driver of the search for anti-inflammatory drugs for decades. Serhan ( Serhan, 2017 ) warns for the possible immune-suppressive activities of anti-inflammatory drugs and its iatrogenic effect on the development of chronic inflammation by preventing resolution ( Serhan, 2017 ). Parisien et al. ( Parisien et al., 2022 ) showed the possible negative impact of NSAIDs use after acute injury on resolution and possibly causing chronic pain syndromes ( Parisien et al., 2022 ). The study performed a transcriptome-wide analysis in peripheral immune cells of 98 individuals suffering from acute low back pain, and followed up for 3 months ( Parisien et al., 2022 ). The main finding was that neutrophil activity in inflammation was protective against the development of chronic pain and thousands of genetic transcriptional changes were observed only in those participants with resolved pain and none in those with persistent pain ( Parisien et al., 2022 ). Further research elicited that mice receiving NSAIDs showed the same absence of transcriptional activity as the immune cells of the participants with persistent pain. Retrospective analysis of individuals reporting acute low back pain in the UK Biobank identified an increased risk of the development of chronic pain in patients using NSAIDs ( Parisien et al., 2022 ).
To our knowledge, there is no research done on the possible negative effects of the use of NSAIDs in persons suffering from FS. Despite pain relief at start, the use of NSAIDs and its anti-inflammatory effects could be counteractive for long outcome of FS. Already in 2011 ( Ewald, 2011 ) evidence of the use of NSAIDs in people suffering from FS was limited and hard evidence still lacks.
We propose to use a much more integrative approach in the treatment of patients suffering from FS. In line with other disciplines, it is perhaps time to recover the knowledge about the way the immune system normally solves injury and infection successful ( Truchetet and Pradeu, 2018 ).
As knowledge advances about the way fatty acids influence immune activity, new lipid formulas with beneficial effects have been developed. Those lipids are nutritionally adapted and are useful for improving inflammation-based pathologies promoting a faster recovery and reducing the use of anti-inflammatory drugs that can produce serious adverse effects ( Serhan, 2017 ). This benefit has led fatty acids, especially n-3 PUFAs and oleic, to be considered as immuno-nutrients ( Mesa et al., 2006 ). Likewise, olive oil phenolics have been shown to reduce the generation of reactive oxygen species (ROS) in phagocytic cells, in vitro , and inhibit the activity of the enzyme 5-lipoxygenase involved in pro-inflammatory events ( Shibutami and Takebayashi, 2021 ). This approach may allow for the identification of dietary biomarkers and a deeper understanding of metabolic dynamics and the resulting impact on health ( Vazquez-Aguilar et al., 2023 ). The use of omics-science could help to find the exact immunological players in people suffering from FS. The search for the presence of super autoantigens and their antibodies is needed to support our new hypothesis presented earlier in this paper.
4 Metabolomics and proteomics in pain and chronic conditions as proxy for FS
The science of metabolomics studies low molecular weight chemical compounds that exist in biological tissues or cells because of genetic changes or physiological or pathological metabolic conditions ( Cui et al., 2017 ).
Proteomics is defined as the complete evaluation of the structure and function of proteins to understand the nature of an organisms. The main purpose of proteomics is to find essential biomarkers that support mechanistic pathways in health and disease ( Al-Amrani et al., 2021 ). Proteomics provides a better understanding of the structure and the function of an organism than genomics. Nevertheless, it is much more complicated than genomics because of the immense number of estimated proteins in humans (>million) opposite to the relative small number of genes (22.000). Proteomics could be used to verify our hypothesis about why DM1 is more associated with FS than DM2. That research should find proteins of an immune reaction related with T lymphocytes and the presence of GAD65 or other super autoantigens and their antibodies. To our knowledge such research is lacking in the international scientific literature and so for now it is still speculative.
One manuscript describes the proteomics of FS in different parts of the shoulder capsule and in different types of patients ( Kawahara et al., 2015 ). Protein spectrum was measured in different compartments of the shoulder capsule in twelve patients suffering from primary FS with severe stiffness compared with seven patients presenting FS with a rotator cuff tear as the control group ( Kawahara et al., 2015 ). There were important differences found between the two groups of patients and several proteins were highlighted as clinical important ( Kawahara et al., 2015 ). Firstly, there are significant differences in presence of proteins related with P13K-Akt and PPAR signaling which are essential compounds in insulin and leptin metabolism ( Giorgino et al., 2009 ; Thon et al., 2016 ). Patients with primary FS present increased P13K-Akt and PPAR signaling compared with the rotator cuff group ( Hagiwara et al., 2018 ). Increased activity of both signaling pathways suggest greater presence/activity of insulin and leptin as part of the pathophysiology of primary FS and related with insulin and leptin resistance ( Thon et al., 2016 ; Huang et al., 2018 ). Persons with rotator cuff damage present a proteome much more related with direct damage and less with metabolic disturbances. The latter conclusion is based on the presence of proteins that signal staphylococcus aureus infection, antigen processing/presentation, and lysosome and phagosome activity ( Kawahara et al., 2015 ). Phagosome and lysosome activity elicit the presence of damage associated molecular patterns and pathogen associated molecular patterns ( Roh and Sohn, 2018 ; Khorshidian et al., 2022 ). Damage and possible pathogen infiltration by opening the blood/capsule barrier seem to be the main causes of the symptomatology of FS after rotator cuff damage. This could mean that patients suffering from primary FS need treatment much more focused on lifestyle changes and specific metabolic interventions to solve insulin and leptin resistance, whereas people with traumatic FS demand a much more orthopedic treatment. The writers of this study also conclude that primary and secondary FS show different etiology and pathophysiology, meaning that interventions should also differ ( Kawahara et al., 2015 ).
It is obvious that only one proteomics study in people suffering from FS cannot be used as golden standard. Much more studies are necessary to determine and identify the exact mechanisms and etiology of primary and secondary FS, but the first step has been made.
Not published as a proteomics research paper but as a pathology manuscript, Hand et al. ( Hand et al., 2007 ) showed the presence of multiple immune cells in the shoulder of 22 conservative therapy resistant patients suffering from primary FS. Mast cells presence was highest followed by T lymphocytes, B lymphocytes and macrophages, evidencing a state of chronic inflammation in primary FS ( Hand et al., 2007 ). Mast cells regulate fibroblast proliferation, an interaction that suggests that the inflammatory state leads to fibrosis through intermediation of mast cells ( Hand et al., 2007 ). The presence of T and B lymphocytes as part of the acquired immune system gives rise to the existence of an autoimmune reaction in the frozen shoulder against the fibrotic tissue ( Hand et al., 2007 ), although other hypotheses could be emphasized. More research will shed light on our hypothesis in which anxiety, fear and depression are related with increased risk for the activation of T lymphocytes against GAD65, diabetes type 1, Hashimoto and perhaps FS ( Nataf, 2017 ).
Proteomics science in FS is still very limited, so metabolomics can add only limited knowledge to the etiology and pathophysiology of FS. Perhaps the best way to identify biomarkers for FS is the use of metabolomics studies related with global chronic pain conditions and translate those studies in comparative pathology to FS ( Aroke and Powell-Roach, 2020 ). Mantyselka et al. observed that in a group of individuals with chronic musculoskeletal pain the circulating levels of ornithine and amino acids were increased when compared to another group where individuals reported no pain or their pain was not persistent ( Mäntyselkä et al., 2017 ). These results are consistent with a 2019 study investigating biomarkers and glutamate changes in fibromyalgia patients suffering from chronic musculoskeletal pain. The metabolites found to be altered included ornithine, L-arginine, Nε-methyl-L-lysine, L-glutamate, L-glutamine and asymmetric dimethylarginine (ADMA) ( Clos-Garcia et al., 2019 ). Moreover, metabotropic glutamate receptors could also play a role in neuropathic pain ( Osikowicz et al., 2013 ). In the study by Finco et al. higher levels of choline and phosphocholine, citrate, alanine and taurine were seen in patients with neuropathic pain when compared to patients with nociceptive pain ( Finco et al., 2016 ).
Further studies show that lipid metabolism dysregulation is involved in the persistence of pain ( Ma et al., 2022 ). The study by González et al. suggests that serum lipid markers, specifically sphingomyelins and triacylglycerols, are associated with chronic pain ( Gonzalez et al., 2022 ).
These findings could eventually be used to develop primary preventive interventions ( Teckchandani et al., 2021 ).
The evidence that idiopathic FS is associated with glucose and lipid metabolic diseases is increasing. One study observed that some proteins, such as adipokines, adiponectin, leptin and resistin, which are involved in metabolism, have been linked to the development of frozen shoulder ( Mäntyselkä et al., 2017 ).
Moreover, Bunker T. et al. focused on hyperlipidemia as a possible risk factor for frozen shoulder after observing clinical relationships between it and Dupuytren’s contracture ( Al-Amrani et al., 2021 ); this aforementioned study supports the hypothesis that elevated serum lipid levels are associated with frozen shoulder, and demonstrates that low-density hypercholesteremia and lipoprotein hypercholesteremia are progressively associated with frozen shoulder ( Al-Amrani et al., 2021 ).
Again another study found higher expression levels of TNC, which is a lipoprotein involved in cell adhesion, fibroblast migration and other processes related to tissue remodeling and wound healing, in synovial capsule samples from patients with adhesive capsulitis ( Mertens et al., 2022 ).
Molecular biology studies have shown frozen shoulder capsular changes indicating that angiogenesis, inflammatory cell infiltration and expression levels of inflammatory cytokines, such as interleukin (IL1-IL6) increase in frozen shoulder ( Hagiwara et al., 2018 ).
To the best of our knowledge, preliminary results have only been reported in one study regarding this and it showed that the serum total cholesterol level may be related to shoulder stiffness ( de La Puerta Vázquez et al., 2004 ; Sung et al., 2014 ; Lee et al., 2019 ).
Etiological and mechanistic research currently lack new hypothesis explaining the spontaneous occurrence of primary FS whereas traumatic secondary FS is much less mystical. Our new perspective of the development of FS, based on the interaction between the brain and the immune holds promise when confirmed by further investigations ( Nataf, 2017 ; Dantzer, 2018 ).
5 Proposed interventions for frozen shoulder
Current therapies for the treatment of FS are both surgical and non-surgical, although no definitive management model is available yet ( Challoumas et al., 2020 ).
Treatment choice depends mostly on expert opinions and is mostly based on qualitative experience instead of quantitative and recent research ( Bridgman, 1972 ). There is no consensus about the best common treatment for patients with FS ( Johnson et al., 2007 ) and therefore new perspectives are urgently needed.
We propose to use a drug-free treatment protocol based on the different mechanisms and etiological factors known to be part of FS. As chronic anti-inflammatory pharmacological interventions can be deleterious ( Johnson et al., 2007 ; Challoumas et al., 2020 ), the use of nutrition as medicine could provide valid effects on the inflammatory state or even on the mental state of patients suffering from FS ( Brain et al., 2019 ). Furthermore, experimental and epidemiological data indicate that changes in the source of lipids consumed in the diet can modify the fatty acid composition of many cell types, including cells involved in the development of many inflammatory and immunological diseases ( Shibutami and Takebayashi, 2021 ; Hamed-Hamed et al., 2023 ). Hence, the use of dietary strategies as part of the FS treatment could be indicated.
The use of pre- and/or certain probiotics, as remedy against disturbances of the microbiome, could provide both acute and chronic inflammatory relief ( Ho et al., 2014 ) through regulation of the immune response and increase in the production of IL-10 ( Ho et al., 2014 ). IL10 is capable of inhibition of cytokine and inflammatory chemokine production ( Akdis and Akdis, 2014 ). Lactobacillus plantarum (L. plantarum), a common used probiotic bacterial strain, inhibits the production of pro-inflammatory cytokines such as TNF- α and IL-6 ( Ahn et al., 2019 ). The possibility of infiltration of pathogenic virus or bacteria as part of the pathophysiology of FS makes it legitimate to propose the use of lactoferrin as a natural antimicrobial, anticarcinogenic, antioxidant, and anti-inflammatory substance ( Zimecki and Kruzel, 2007 ).
Other less known interventions could serve multiple purposes of which the use of therapeutic hypercapnia is perhaps the most indicated one ( Tolstun et al., 2022 ). The use of therapeutic hypercapnia, the search for short term increase of CO2 in the bloodstream up to 50 mmHG by breathing exercises or CO2 devices with a partial pressure of 60–70 mmHG, has shown surprising effects on diet related behavior, blood circulation in the brain, integrity of the blood-brain barrier and immune activity in mice and human ( Yang et al., 2019 ; Tolstun et al., 2022 ; Tzeng et al., 2022 ).
The life of the naked mole rat, known for its longevity and resistance against multiple diseases, was used as a model for life expectancy enhancing in rodents ( Tolstun et al., 2022 ). The naked mole rat lives in a natural intermittent hypoxia/hypercapnia environment. Imitating this environment, other rodents also slowed down their metabolism, presented accelerated skin wound healing and reduced their calorie intake with 30%–40% spontaneously ( Tolstun et al., 2022 ). If these results would be confirmed in human we would have a simple way to reduce over-eating as one of the most important deleterious lifestyle factors in modern life. Therapeutic hypercapnia further has profound effects on the immune system. The study of Tzeng ( Tzeng et al., 2022 ), shows that the use of therapeutic hypercapnia ameliorates acute cellular rejection in the skin of a mouse acute allograft rejection model by suppressing the expression of proinflammatory cytokines and neutrophil infiltration, inhibiting T cell activation and accumulation, and inducing Treg cell differentiation ( Tzeng et al., 2022 ). If these effects are confirmed in humans, then the use of a plastic bag rebreathing strategy could be effective to (partially) counter chronic inflammation and reduce calorie intake spontaneously. Already in 1995 ( Yang et al., 2019 ) it was shown that 1–2 min rebreathing in a plastic bag could by slightly increasing CO2 levels in the blood, improve retinal arterial obstructive diseases in young patients ( Harino et al., 1995 ).
Therapeutic and permissive hypercapnia are often used in the same context although there are important differences between them. Therapeutic hypercapnia is based on active inspiration of air with higher pCO2 than normal, whereas permissive hypercapnia is the tolerated CO2 level when lungs are less stressed ( Lee et al., 2019 ). We propose ‘plastic bag rebreathing technics’ as a simple and effective way to increase pCO2 in blood and produce the beneficial effects of hypercapnia. The possibility that this technic causes any damage when controlled for time and tolerance is minimum. Nevertheless, hypercapnia can be damaging as evidenced during the COVID-19 pandemic. During the pandemic, health professionals came in situations in which they used a plastic bag over their head to protect themselves against possible infection with SARS-CoV-2 ( Bakirtzi et al., 2016 ). This way rebreathing their own breath was forced. Three volunteers were used as a model for tolerance measurements and negative effects of forced ‘therapeutic’ hypercapnia ( Lee et al., 2020 ). CO2 levels in the bag increased almost immediately and resulted in significant hypercapnia at termination. Tolerance was reached at 5 min and was produced by breathlessness, anxiety and feelings of distress ( Lee et al., 2020 ). We propose intermittent therapeutic hypercapnia exercises with a length of 90 s and several times per day.
The proposed interventions are drug free, under control of the patients and promising when combined with knowledge transfer about pain, fear, anxiety and depression as assessed by multiple studies of the group of Lorimer Mosely and David Butler ( Moseley and Butler, 2015 ).
6 Conclusion
This study features an integrative view based on the current scientific evidence on FS pathology. Frozen shoulder has been observed to share mechanisms, such as low-grade inflammation and multiple metabolic disturbances, with pathologies such as diabetes and Hasimoto syndrome. Etiology of FS with autoimmune diseases also share essential topics such as the simultaneous presence of immune challenges and psycho-emotional distress at the start of the disease. Knowledge about the interplay between the immune system and the brain gives rise to the development of new treatments for people suffering from FS. Identification of the mechanisms that explain the association between an increased risk for the development of FS in people suffering from type 1 diabetes, Dupuytren, Hashimoto, and axial Spondylarthritis are missing, although several hypotheses have been elaborated in this review. Disorders of the GABA-ergic nervous could be (co-) responsible for the possible association between the mentioned maladies and FS risk. The COVID-19 pandemic increased the incidence of the development of FS, type 1 diabetes, Hashimoto and Dupuytren significantly ( de Mello et al., 2023 ). Fear, anxiety and depression seem were associated with the increased incidence of the mentioned maladies and all three states are related changes in the GABA-ergic nervous system ( Kupcova et al., 2023 ). A possible neurogenic background of FS has recently been elucidated in a small study with 10 patients who received a central nervous system combined treatment with significant improvement ( Mena-Del Horno et al., 2022 ). We further propose the possibility that FS, just as the associated maladies has an autoimmune background. The striking increase of FS when suffering from several autoimmune diseases, including but less mentioned axSA, suggests a possible auto-immune background for FS. Both explanations do not exclude one of them. The opposite is true. The way the brain and the immune system interplay when faced with simultaneous immune and psycho-emotional challenges increased the possibility that immune cells are primed against super-autoantigens in the brain and it are these antigens that are also present in peripheral tissues and organs. If those primed T lymphocytes can destroy Beta-cells of Langerhans, it is plausible that these Teffector cells can destroy other tissues when faced with the same antigen. There are important indications for the presence of a possible neuroimmune connection as cause for FS and several other diseases; nevertheless this new perspective about the etiology of FS has to be confirmed with new mechanistic research.
Author contributions
Study conception (SN-L and DH), design (SN-L and DH), acquisition of data (SN-L), analysis and interpretation of data (SN-L, DH, and LP) drafting of manuscript (SN-L, DH, and LP) and critical revision (SN-L, DH, and LP). All authors contributed to the article and approved the submitted version.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was partially funded by University Chair in Clinical Psychoneuroimmunology, University of Granada, Spain.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Ahn J. E., Kim H., Chung D. K. (2019). Lipoteichoic acid isolated from lactobacillus plantarum maintains inflammatory homeostasis through regulation of Th1- and Th2-induced cytokines. J. Microbiol. Biotechnol. 29 (1), 151–159. doi:10.4014/jmb.1809.09001
PubMed Abstract | CrossRef Full Text | Google Scholar
Aïm F., Chevallier R., Marion B., Klouche S., Bastard C., Bauer T. (2022). Psychological risk factors for the occurrence of frozen shoulder after rotator cuff repair. Orthop. Traumatology Surg. Res. 108 (2), 103212. doi:10.1016/j.otsr.2022.103212
CrossRef Full Text | Google Scholar
Akbar M., McLean M., Garcia-Melchor E., Crowe L. A., McMillan P., Fazzi U. G., et al. (2019b). Fibroblast activation and inflammation in frozen shoulder. PLoS One 14 (4), e0215301. Published 2019 Apr 23. doi:10.1371/journal.pone.0215301
Akbar M., McLean M., Garcia-Melchor E., Crowe L. A. N., McMillan P., Fazzi U. G., et al. (2019a). Fibroblast activation and inflammation in frozen shoulder. PLoS ONE 14 (4), e0215301. doi:10.1371/journal.pone.0215301
Akdis C. A., Akdis M. (2014). Mechanisms of immune tolerance to allergens: role of IL- 10 and Tregs. J. Clin. Invest. 124 (11), 4678–4680. doi:10.1172/JCI78891
Al-Amrani S., Al-Jabri Z., Al-Zaabi A., Alshekaili J., Al-Khabori M. (2021). Proteomics: concepts and applications in human medicine. World J. Biol. Chem. 12 (5), 57–69. doi:10.4331/wjbc.v12.i5.57
Aroke E. N., Powell-Roach K. L. (2020). The metabolomics of chronic pain conditions: a systematic review. Biol. Res. Nurs. 22 (4), 458–471. doi:10.1177/1099800420941105
Austin D. C., Gans I., Park M. J., Carey J. L., Kelly J. D. (2014). The association of metabolic syndrome markers with adhesive capsulitis. J. Shoulder Elb. Surg. 23 (7), 1043–1051. doi:10.1016/j.jse.2013.11.004
Avramia I., Amariei S., Ursachi F.-V. (2021). Bioactiveβ -glucans, adjuvants in SARS-CoV-2 antiviral therapy. Biomed J Sci Tech Res 33 (4). doi:10.26717/bjstr.2021.33.005431
Bakirtzi K., Law I. K., Xue X., Iliopoulos D., Shah Y. M., Pothoulakis C. (2016). Neurotensin promotes the development of colitis and intestinal angiogenesis via hif-1α-miR- 210 signaling. J. Immunol. 196 (10), 4311–4321. doi:10.4049/jimmunol.1501443
Barbosa F., Swamy G., Salem H., Creswell T., Espag M., Tambe A., et al. (2019). Chronic adhesive capsulitis (frozen shoulder): comparative outcomes of treatment in patients with diabetes and obesity. J. Clin. Orthop. Trauma 10 (2), 265–268. doi:10.1016/j.jcot.2018.02.015
Bhanji S., Williams B., Sheller B., Elwood T., Mancl L. (2002). Transient bacteremia induced by toothbrushing a comparison of the Sonicare toothbrush with a conventional toothbrush. Pediatr. Dent. 24 (4), 295–299.
PubMed Abstract | Google Scholar
Bouaicha S., Wieser K., Kriechling P., Scholz-Odermatt S. M. (2020). A large-scale assessment of the healthcare burden of adhesive capsulitis of the shoulder joint. Swiss Med. Wkly. 150, w20188. doi:10.4414/smw.2020.20188
Brain K., Burrows T. L., Rollo M. E., Chai L. K., Clarke E. D., Hayes C., et al. (2019). A systematic review and meta-analysis of nutrition interventions for chronic noncancer pain. J. Hum. Nutr. Diet. 32 (2), 198–225. doi:10.1111/jhn.12601
Bridgman J. F. (1972). Periarthritis of the shoulder and diabetes mellitus. Ann. Rheum. Dis. 31 (69), 69–71. doi:10.1136/ard.31.1.69
Brindisino F., Silvestri E., Gallo C., Venturin D., Di Giacomo G., Peebles A. M., et al. (2022). Depression and anxiety are associated with worse subjective and functional baseline scores in patients with frozen shoulder contracture syndrome: a systematic review. Arthrosc. Sports Med. Rehabil. 4 (3), e1219–e1234. Published 2022 May 21. doi:10.1016/j.asmr.2022.04.001
Buchbinder R., Youd J. M., Green S., Stein A., Forbes A., Harris A., et al. (2007). Efficacy and cost-effectiveness of physiotherapy following glenohumeral joint distension for adhesive capsulitis: a randomized trial. Arthritis Rheum. 57 (6), 1027–1037. doi:10.1002/art.22892
Bunker T. D., Boyd M., Gallacher S., Auckland C. R., Kitson J., Smith C. D. (2014). Association between Propionibacterium acnes and frozen shoulder: a pilot study. Shoulder Elb. 6 (4), 257–261. doi:10.1177/1758573214533664
Bunker T. D., Reilly J., Baird K. S., Hamblen D. L. (2000). Expression of growth factors, cytokines and matrix metalloproteinases in frozen shoulder. J. Bone Jt. Surg. Br. 82 (5), 768–773. doi:10.1302/0301-620x.82b5.9888
Campos F. G., Waitzberg D. L., Teixeira M. G., Mucerino D. R., Kiss D. R., Habr-Gama A. (2003). Pharmacological nutrition in inflammatory bowel diseases. Nutr. Hosp. 18 (2), 57–64.
Capoor M. N., Ruzicka F., Schmitz J. E., James G. A., Machackova T., Jancalek R., et al. (2017). Propionibacterium acnes biofilm is present in intervertebral discs of patients undergoing microdiscectomy. PLoS One 12 (4), e0174518. Published 2017 Apr 3. doi:10.1371/journal.pone.0174518
Casanova A., Wevers A., Navarro-Ledesma S., Pruimboom L. (2023). Mitochondria: it is all about energy. Front. Physiol. 14, 1114231. Published 2023 Apr 25. doi:10.3389/fphys.2023.1114231
Challoumas D., Biddle M., McLean M., Millar N. L. (2020). Comparison of treatments for frozen shoulder: a systematic review and meta-analysis. JAMA Netw. Open 3 (12), e2029581. Published 2020 Dec 1. doi:10.1001/jamanetworkopen.2020.29581
Chan J. H., Ho B. S., Alvi H. M., Saltzman M. D., Marra G. (2017). The relationship between the incidence of adhesive capsulitis and hemoglobin A1c. J. Shoulder Elb. Surg. 26 (10), 1834–1837. doi:10.1016/j.jse.2017.03.015
Chen W., Meng J., Qian H., Deng Z., Chen S., Xu H., et al. (2017). A study of IL-1β, MMP-3, TGF-β1, and GDF5 polymorphisms and their association with primary frozen shoulder in a Chinese han population. Biomed. Res. Int. 2017, 3681645. doi:10.1155/2017/3681645
Cher J. Z. B., Akbar M., Kitson S., Crowe L. A. N., Garcia-Melchor E., Hannah S. C., et al. (2018). Alarmins in frozen shoulder: a molecular association between inflammation and pain. Am. J. Sports Med. 46 (3), 671–678. doi:10.1177/0363546517741127
Cho C. H., Bae K. C., Kim D. H. (2019). Treatment strategy for frozen shoulder. Clin. Orthop. Surg. 11 (3), 249–257. doi:10.4055/cios.2019.11.3.249
Cho C. H., Song K. S., Kim B. S., Kim D. H., Lho Y. M. (2018). Biological aspect of pathophysiology for frozen shoulder. Biomed. Res. Int. 2018, 7274517. Published 2018 May 24. doi:10.1155/2018/7274517
Clos-Garcia M., Andrés-Marin N., Fernández-Eulate G., Abecia L., Lavín J. L., van Liempd S., et al. (2019). Gut microbiome and serum metabolome analyses identify molecular biomarkers and altered glutamate metabolism in fibromyalgia. EBioMedicine 46, 499–511. doi:10.1016/j.ebiom.2019.07.031
Cohen C., Ferreira L. M., Santoro B. P., Figueiredo E. A., Smith M. C., Andreoli C. V., et al. (2016). The roles of tenascin C and Fibronectin 1in adhesive capsulitis: a pilot gene expression study. Clin. (Sao Paulo) 71(6):325–331. doi:10.6061/clinics/2016(06)07
Cohen C., Tortato S., Silva O. B. S., Leal M. F., Ejnisman B., Faloppa F. (2020). Association between frozen shoulder and thyroid diseases: strengthening the evidences. Rev. Bras. Ortop. (Sao Paulo) 55 (4), 483–489. doi:10.1055/s-0039-3402476
Cucchi D., Marmotti A., De G. S., Costa A., D'Apolito R., Conca M., et al. (2017). Risk factors for shoulder stiffness: current concepts. Joints 5 (4), 217–223. Published 2017 Dec 11. doi:10.1055/s-0037-1608951
Cui J., Zhang T., Xiong J., Lu W., Duan L., Zhu W., et al. (2017). RNA-sequence analysis of samples from patients with idiopathic adhesive capsulitis. Mol. Med. Rep. 16 (5), 7665–7672. doi:10.3892/mmr.2017.7579
Dantzer R. (2018). Neuroimmune interactions: from the brain to the immune system and vice versa. Physiol. Rev. 98 (1), 477–504. PMID: 29351513; PMCID: PMC5866360. doi:10.1152/physrev.00039.2016
De P., Pruimboom L. (2015). Stress induces endotoxemia and low-grade inflammation by increasing barrier permeability. Front. Immunol. 6, 223. doi:10.3389/fimmu.2015.00223
de La Puerta Vázquez R., Martínez-Domínguez E., Sánchez Perona J., Ruiz- Gutiérrez V. (2004). Effects of different dietary oils on inflammatory mediator generation and fatty acid composition in rat neutrophils. Metabolism 53 (1), 59–65. doi:10.1016/j.metabol.2003.08.010
de la Serna D., Navarro-Ledesma S., Alayón F., López E., Pruimboom L. (2021). A comprehensive view of frozen shoulder: a mystery syndrome. Front. Med. (Lausanne) 8, 663703. PMID: 34046418; PMCID: PMC8144309. doi:10.3389/fmed.2021.663703
de Mello D. P. P., Corbin J. N. B., Holanda L. S., Pascarelli L., Nishimura E. M., de Almeida T. B. C. (2023). Incidence and epidemiology of adhesive capsulitis during the covid-19 pandemic. Acta Ortop. Bras. 31 (1), e261132. doi:10.1590/1413-785220233101e261132
de Punder K., Pruimboom L. (2015). Stress induces endotoxemia and low-grade inflammation by increasing barrier permeability. Front. Immunol. 6, 223. doi:10.3389/fimmu.2015.00223
Dias R., Cutts S., Massoud S. (2005). Frozen shoulder. BMJ 331 (7530), 1453–1456. doi:10.1136/bmj.331.7530.1453
Dolmans G. H., Werker P. M., Hennies H. C., Furniss D., Festen E. A., Franke L., et al. (2011). Wnt signaling and Dupuytren's disease. New Engl. J. Med. 365, 307–317. Oyang 2023. doi:10.1056/nejmoa1101029
Eljabu W., Klinger H. M., von Knoch M. (2016). Prognostic factors and therapeutic options for treatment of frozen shoulder: a systematic review. Arch. Orthop. Trauma Surg. 136 (1), 1–7. doi:10.1007/s00402-015-2341-4
Ewald A. (2011). Adhesive capsulitis: a review. Am. Fam. Physician 83 (4), 417–422.
Fasano A. (2020). All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Res 9, F1000 Faculty Rev-69. F1000 Faculty Rev-69. doi:10.12688/f1000research.20510.1
Fasano A., Shea-Donohue T. (2005). Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nat. Clin. Pract. Gastroenterol. Hepatol. 2 (9), 416–422. doi:10.1038/ncpgasthep0259
Fernandes M. R. (2015). Correlation between functional disability and quality of life in patients with adhesive capsulitis. Acta Ortop. Bras. 23 (2), 81–84. doi:10.1590/1413-78522015230200791
Finco G., Locci E., Mura P., Massa R., Noto A., Musu M., et al. (2016). Can urine metabolomics Be helpful in differentiating neuropathic and nociceptive pain? A proof-of-concept study. PLoS One 11 (3), e0150476. Published 2016 Mar 2. doi:10.1371/journal.pone.0150476
Galasso O., Mercurio M., Luciano F., Mancuso C., Gasparini G., De Benedetto M., et al. (2023). Arthroscopic capsular release for frozen shoulder: when etiology matters. Knee Surg. Sports Traumatol. Arthrosc. 31 (11), 5248–5254. doi:10.1007/s00167-023-07561-2
Gambelunghe G., Forini F., Laureti S., Murdolo G., Toraldo G., Santeusanio F., et al. (2000). Increased risk for endocrine autoimmunity in Italian type 2 diabetic patients with GAD65 autoantibodies. Clin. Endocrinol. (Oxf) 52 (5), 565–573. doi:10.1046/j.1365-2265.2000.00983.x
Genç S., Evren B., Bozbay A., Aydın E. Ş., Genç Ö., Şahin I. (2021). Could covid-19 trigger type 1 diabetes? Presentation of covid-19 case presented with diabetic ketoacidosis. Acta Endocrinol. (Buchar) 17 (4), 532–536. doi:10.4183/aeb.2021.532
Giorgino F., Leonardini A., Laviola L., Perrini S., Natalicchio A. (2009). Cross-talk between PPARgamma and insulin signaling and modulation of insulin sensitivity. PPAR Res. 2009, 818945. doi:10.1155/2009/818945
Gonzalez P. A., Simcox J., Raff H., Wade G., Von Bank H., Weisman S., et al. (2022). Lipid signatures of chronic pain in female adolescents with and without obesity. Lipids Health Dis. 21 (1), 80. Published 2022 Aug 30. doi:10.1186/s12944-022-01690-2
Hagiwara Y., Mori M., Kanazawa K., Ando A., Yabe Y., Koide M., et al. (2018). Comparative proteome analysis of the capsule from patients with frozen shoulder. J. Shoulder Elb. Surg. 27 (10), 1770–1778. doi:10.1016/j.jse.2018.03.010
Hajishengallis G. (2015). Periodontitis: from microbial immune subversion to systemic inflammation. Nat. Rev. Immunol. 15 (1), 30–44. doi:10.1038/nri3785
Hamed-Hamed D., Stryuf F., Pruimboom L., Navarro-Ledesma S. (2023). Efficacy of combined strategies of physical activity, diet and sleep disorders as treatment in patients with chronic shoulder pain, A systematic review. Front. Physiol. 14, 11221807. Published 2023 Apr 25. doi:10.3389/fphys.2023.1221807
Hand C., Clipsham K., Rees J. L., Carr A. J. (2008). Long-term outcome of frozen shoulder. J. Shoulder Elb. Surg. 17 (2), 231–236. doi:10.1016/j.jse.2007.05.009
Hand G. C. R., Athanasou N. A., Matthews T., Carr A. J., Surgery O. (2007). The pathology of frozen shoulder. J. BONE Jt. Surg. 89, 928–932. doi:10.1302/0301-620X.89B7.19097
Hangai S., Ao T., Kimura Y., Matsuki K., Kawamura T., Negishi H., et al. (2016). PGE2 induced in and released by dying cells functions as an inhibitory DAMP. Proc. Natl. Acad. Sci. U. S. A. 113 (14), 3844–3849. doi:10.1073/pnas.1602023113
Hannafin J. A., Chiaia T. A. (2000). Adhesive capsulitis. A treatment approach. Clin. Orthop. Relat. Res. 372, 95–109. doi:10.1097/00003086-200003000-00012
Harino S., Grunwald J. E., Petrig B. J., Riva C. E. (1995). Rebreathing into a bag increases human retinal macular blood velocity. Br. J. Ophthalmol. 79 (4), 380–383. PMID: 7742289; PMCID: PMC505107. doi:10.1136/bjo.79.4.380
Ho Y. H., Lu Y. C., Chang H. C., Lee S. Y., Tsai M. F., Huang Y. T., et al. (2014). Daily intake of probiotics with high IFN-γ/IL- 10 ratio increases the cytotoxicity of human natural killer cells: a personalized probiotic approach. J. Immunol. Res. 2014, 721505. doi:10.1155/2014/721505
Huang S. W., Wang J. Y., Lin C. L., Huang C. C., Liou T. H., Lin H. W. (2020). Patients with axial spondyloarthritis are at risk of developing adhesive capsulitis: real-world evidence database study in taiwan. J. Clin. Med. 9 (3), 787. Published 2020 Mar 13. doi:10.3390/jcm9030787
Huang X., Liu G., Guo J., Su Z. (2018). The PI3K/AKT pathway in obesity and type 2 diabetes. Int. J. Biol. Sci. 14 (11), 1483–1496. Published 2018 Aug 6. doi:10.7150/ijbs.27173
Hutcheson R., Rocic P. (2012). The metabolic syndrome, oxidative stress, environment, and cardiovascular disease: the great exploration. Exp. Diabetes Res. 2012, 271028. doi:10.1155/2012/271028
Jain R., Jain S., Raison C. L., Maletic V. (2011). Painful diabetic neuropathy is more than pain alone: examining the role of anxiety and depression as mediators and complicators. Curr. Diabetes Rep. 11 (4), 275–284. doi:10.1007/s11892-011-0202-2
Jankowska-Polańska B., Polański J., Dudek K., Sławuta A., Mazur G., Gajek J. (2021). The role of sleep disturbance, depression and anxiety in frail patients with AF–gender differences. J. Clin. Med. 10 (1), 11–14. doi:10.3390/jcm10010011
Jasmin L., Wu M. V., Ohara P. T. (2004). GABA puts a stop to pain. Curr. Drug Targets CNS Neurol. Disord. 3 (6), 487–505. doi:10.2174/1568007043336716
Johnson A. J., Godges J. J., Zimmerman G. J., Ounanian L. L. (2007). The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. J. Orthop. Sports Phys. Ther. 37 (3), 88–99. doi:10.2519/jospt.2007.2307
Kawahara K., Hohjoh H., Inazumi T., Tsuchiya S., Sugimoto Y. (2015). Prostaglandin E2-induced inflammation: relevance of prostaglandin E receptors. Biochim. Biophys. Acta 1851 (4), 414–421. doi:10.1016/j.bbalip.2014.07.008
Kelly J., Kennedy P., Cryan J., Dinan T., Clarke G., Hyland N. (2015). Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front. Cell. Neurosci. 9, 392. doi:10.3389/fncel.2015.00392
Khorshidian N., Khanniri E., Koushki M. R., Sohrabvandi S., Yousefi M. (2022). An overview of antimicrobial activity of lysozyme and its functionality in cheese. Front. Nutr. 9, 833618. Published 2022 Mar 9. doi:10.3389/fnut.2022.833618
Kupcova I., Danisovic L., Klein M., Harsanyi S. (2023). Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol. 11 (1), 108. Published 2023 Apr 11. doi:10.1186/s40359-023-01130-5
Lavergne V., Malo M., Gaudelli C., Laprade M., Leduc S., Laflamme P., et al. (2017). Clinical impact of positive Propionibacterium acnes cultures in orthopedic surgery. Orthop. Traumatol. Surg. Res. 103 (2), 307–314. doi:10.1016/j.otsr.2016.12.005
Lee H. J., Hong O. K., Kwak D. H., Kim Y. S. (2019). Metabolic profiling of serum and tissue from the rotator interval and anterior capsule in shoulder stiffness: a preliminary study. BMC Musculoskelet. Disord. 20 (1), 364. Published 2019 Aug 7. doi:10.1186/s12891-019-2709-7
Lee S., Li G., Tong L., Tse G. (2020). COVID-19: electrophysiological mechanisms underlying sudden cardiac death during exercise with facemasks. Med. Hypotheses 144, 110177. doi:10.1016/j.mehy.2020.110177
Leung J., Moseley A., Fereday S., Jones T., Fairbairn T., Wyndham S. (2007). The prevalence and characteristics of shoulder pain after traumatic brain injury. Clin. Rehabil. 21 (2), 171–181. doi:10.1177/0269215506070254
Li W., Lu N., Xu H., Wang H., Huang J. (2015). Case control study of risk factors for frozen shoulder in China. Int. J. Rheum. Dis. 18, 508–513. doi:10.1111/1756-185X.12246
López-Armada M. J., Riveiro-Naveira R. R., Vaamonde-García C., Valcárcel-Ares M. N. (2013). Mitochondrial dysfunction and the inflammatory response. Mitochondrion 13 (2), 106–118. doi:10.1016/j.mito.2013.01.003
Ma C., Liu M., Tian J., Zhai G., Cicuttini F., Schooneveldt Y. L., et al. (2022). Lipidomic profiling identifies serum lipids associated with persistent multisite musculoskeletal pain. Metabolites 12 (3), 206. Published 2022 Feb 25. doi:10.3390/metabo12030206
Malka R., Nathan D. M., Higgins J. M. (2016). Mechanistic modeling of hemoglobin glycation and red blood cell kinetics enables personalized diabetes monitoring. Sci. Transl. Med. 8 (359), 359ra130. doi:10.1126/scitranslmed.aaf9304
Mäntyselkä P., Ali-Sisto T., Kautiainen H., Niskanen L., Viinamäki H., Velagapudi V., et al. (2017). The association between musculoskeletal pain and circulating ornithine: a population-based study. Pain Med. 18 (6), 1145–1151. doi:10.1093/pm/pnw285
McEwen B. S., Gray J. D., Nasca C. (2015). 60 YEARS OF NEUROENDOCRINOLOGY: redefining neuroendocrinology: stress, sex and cognitive and emotional regulation. J. Endocrinol. 226 (2), T67–T83. doi:10.1530/JOE-15-0121
Mena-Del Horno S., Dueñas L., Lluch E., Louw A., Luque-Suarez A., Mertens M. G., et al. (2022). A central nervous system focused treatment program for people with frozen shoulder: a feasibility study. Int. J. Environ. Res. Public Health 19 (5), 2628. Published 2022 Feb 24. doi:10.3390/ijerph19052628
Mende M., Fletcher E. V., Belluardo J. L., Pierce J. P., Bommareddy P. K., Weinrich J. A., et al. (2016). Sensory-Derived glutamate regulates presynaptic inhibitory terminals in mouse spinal cord. Neuron 90 (6), 1189–1202. doi:10.1016/j.neuron.2016.05.008
Mertens M. G., Meeus M., Noten S., Verborgt O., Fransen E., Lluch Girbés E., et al. (2022). Understanding the clinical profile of patients with frozen shoulder: a longitudinal multicentre observational study. BMJ Open 12 (11), e056563. Published 2022 Nov 21. doi:10.1136/bmjopen-2021-056563
Mesa G. M. D., Aguilera García C. M., Gil Hernández A. (2006). Importancia de los lípidos en el tratamiento nutricional de las patologías de base inflamatoria. Nutr. Hosp. 21 (Suppl. 2), 30–43.
Google Scholar
Millar N. L., Meakins A., Struyf F., Willmore E., Campbell A. L., Akbar M., et al. (2022). Frozen shoulder. Nat. Rev. Dis. Prim. 8 (1), 59. doi:10.1038/s41572-022-00386-2
Mohammad S., Thiemermann C. (2021). Role of metabolic endotoxemia in systemic inflammation and potential interventions. Front. Immunol. 11, 594150. doi:10.3389/fimmu.2020.594150
Mokhtari T., Tu Y., Hu Li (2019). Involvement of the Hippocampus in chronic pain and depression. Brain Sci. Adv. 5 (4), 288–298. doi:10.26599/bsa.2019.9050025
Moseley G. L., Butler D. S. (2015). Fifteen years of explaining pain: the past, present, and future. J. Pain 16 (9), 807–813. doi:10.1016/j.jpain.2015.05.005
Nataf S. (2017). Evolution, immunity and the emergence of brain superautoantigens. F1000Res 6, 171. Published 2017 Feb 21. doi:10.12688/f1000research.10950.1
Nathan C. (2002). Points of control in inflammation. Nature 420 (6917), 846–852. doi:10.1038/nature01320
Navarro L. S., Hamed-Hamed D., González-Muñoz A., Pruimboom L. (2023). Effectiveness of treatments that alter metabolomics in cancer patients-A systematic review. Cancers (Basel) 15 (17), 4297. doi:10.3390/cancers15174297
Osikowicz M., Mika J., Przewlocka B. (2013). The glutamatergic system as a target for neuropathic pain relief. Exp. Physiol. 98 (2), 372–384. doi:10.1113/expphysiol.2012.069922
Parisien M., Lima L. V., Dagostino C., El-hachem N., Drury G. L., Grant A. V., et al. (2022). Acute inflammatory response via neutrophil activation protects against the development of chronic pain. Sci. Transl. Med. 2022. doi:10.1126/scitranslmed.abj9954
Pietrzak M. (2016). Adhesive capsulitis: an age related symptom of metabolic syndrome and chronic low-grade inflammation? Med. Hypotheses 88, 12–17. doi:10.1016/j.mehy.2016.01.002
Potgieter M., Bester J., Kell D. B., Pretorius E. (2015). The dormant blood microbiome in chronic, inflammatory diseases. FEMS Microbiol. Rev. 39 (4), 567–591. doi:10.1093/femsre/fuv013
Prodromidis A. D., Charalambous C. P. (2016). Is there a genetic predisposition to frozen shoulder?a systematic review and meta-analysis. JBJS Rev. 4 (2), e4. doi:10.2106/JBJS.RVW.O.00007
Pruimboom L. (2023). Psychoneuroimmunology in the daily clinic is only possible within a contextual frame. Nature . (in Press).
Pruimboom L., Raison C. L., Muskiet F. A. (2015). Physical activity protects the human brain against metabolic stress induced by a postprandial and chronic inflammation. Behav. Neurol. 2015, 569869. doi:10.1155/2015/569869
Raison C. L., Capuron L., Miller A. H. (2006). Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 27 (1), 24–31. doi:10.1016/j.it.2005.11.006
Ramos A. C., Becerril B. C., Cisneros L. J. G., MarthaMiofibroblasto M. R.El (2004). Una célula multifuncional en La patología pulmonar. Rev. Inst. Nal. Enf. Resp. Mex. Rev. 17 (3), 215–231.
Razi F., Forouzanfar K., Bandarian F., Nasli-Esfahani E. (2017). LDL-cholesterol measurement in diabetic type 2 patients: a comparison between direct assay and popular equations. J. Diabetes Metab. Disord. 16, 43. Published 2017 Nov 3. doi:10.1186/s40200-017-0326-2
Robbins J. P., Solito E. (2022). Does neuroinflammation underlie the cognitive changes observed with dietary interventions? Front. Neurosci. 16, 854050. doi:10.3389/fnins.2022.854050
Roh J. S., Sohn D. H. (2018). Damage-associated molecular patterns in inflammatory diseases. Immune Netw. 18 (4), e27. Published 2018 Aug 13. doi:10.4110/in.2018.18.e27
Rönnbäck C., Hansson E. (2019). The importance and control of low- grade inflammation due to damage of cellular barrier systems that may lead to. Syst. Inflamm. 10 (May), 1–8. doi:10.3389/fneur.2019.00533
Sarasua S. M., Floyd S., Bridges W. C., Pill S. G. (2021). The epidemiology and etiology of adhesive capsulitis in the U.S. Medicare population. BMC Musculoskelet. Disord. 22 (1), 828. doi:10.1186/s12891-021-04704-9
Scott-solomon E., Boehm E., Kuruvilla R. (2022). The sympathetic nervous system in development and disease. Nat. Rev. Neurosci. 22 (11), 685–702. doi:10.1038/s41583-021-00523-y
Serhan C. N. (2017). Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms. FASEB J. 31 (4), 1273–1288. doi:10.1096/fj.201601222R
Shan Y., Zhao J., Zheng Y., Guo S., Schrodi S. J., He D. (2023). Understanding the function of the GABAergic system and its potential role in rheumatoid arthritis. Front. Immunol. 14, 1114350. Published 2023 Feb 7. doi:10.3389/fimmu.2023.1114350
Shibutami E., Takebayashi T. (2021). A scoping review of the application of metabolomics in nutrition research: the literature survey 2000-2019. Nutrients 13 (11), 3760. Published 2021 Oct 24. doi:10.3390/nu13113760
Söhnlein P., Müller M., Syren K., Hartmann U., Böhm B. O., Meinck H. M., et al. (2000). Epitope spreading and a varying but not disease-specific GAD65 antibody response in Type I diabetes. The Childhood Diabetes in Finland Study Group. Diabetologia 43 (2), 210–217. doi:10.1007/s001250050031
Sung C. M., Jung T. S., Park H. B. (2014). Are serum lipids involved in primary frozen shoulder? A case-control study. J. Bone Jt. Surg. Am. 96 (21), 1828–1833. doi:10.2106/JBJS.M.00936
Teckchandani S., Nagana Gowda G. A., Raftery D., Curatolo M. (2021). Metabolomics in chronic pain research. Eur. J. Pain 25 (2), 313–326. doi:10.1002/ejp.1677
Teichtahl A. J., Urquhart D. M., Wang Y., Wluka A. E., Wijethilake P., Sullivan R. O., et al. (2015). Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J. 15 (7), 1593–1601. doi:10.1016/j.spinee.2015.03.039
Tell S., Nadeau K. J., Eckel R. H. (2020). Lipid management for cardiovascular risk reduction in type 1 diabetes. Curr. Opin. Endocrinol. Diabetes Obes. 27 (4), 207–214. doi:10.1097/MED.0000000000000551
Thomas S. J., McDougall C., Brown I. D., Jaberoo M. C., Stearns A., Ashraf R., et al. (2007). Prevalence of symptoms and signs of shoulder problems in people with diabetes mellitus. J. Shoulder Elb. Surg. 16 (6), 748–751. doi:10.1016/j.jse.2007.02.133
Thon M., Hosoi T., Ozawa K. (2016). Possible integrative actions of leptin and insulin signaling in the hypothalamus targeting energy homeostasis. Front. Endocrinol. (Lausanne) 7, 138. Published 2016 Oct 20. doi:10.3389/fendo.2016.00138
Tolstun D., Muradian K., Bezrukov V. (2022). Therapeutic hypercapnia. Review. Ageing Longev. 3 (3), 101–113. doi:10.47855/al9020-2022-3-5
Towns R., Pietropaolo M. (2011). GAD65 autoantibodies and its role as biomarker of type 1 diabetes and latent autoimmune diabetes in adults (LADA). Drugs Future 36 (11), 847. PMID: 22869930; PMCID: PMC3411186. doi:10.1358/dof.2011.036.11.1710754
Truchetet M. E., Pradeu T. (2018). Re-thinking our understanding of immunity: robustness in the tissue reconstruction system. Semin. Immunol. 36, 45–55. Epub 2018 Mar 15. PMID: 29550156. doi:10.1016/j.smim.2018.02.013
Tsiortou P., Alexopoulos H., Dalakas M. C. (2021). GAD antibody-spectrum disorders: progress in clinical phenotypes, immunopathogenesis and therapeutic interventions. Ther. Adv. Neurol. Disord. 14, 17562864211003486. Published 2021 Mar 30. doi:10.1177/17562864211003486
Tzeng Y.-S., Peng Y. J., Tang S. E., Huang K. L., Chu S. J., Wu S. Y., et al. (2022). Intermittent exposure of hypercapnia suppresses allograft rejection via induction of Treg differentiation and inhibition of neutrophil accumulation. Biomedicines 10, 836. doi:10.3390/biomedicines10040836
Van Dyken P., Lacoste B. (2018). Impact of metabolic syndrome on neuroinflammation and the blood–brain barrier. Front. Neurosci. 12, 930. doi:10.3389/fnins.2018.00930
Vazquez-Aguilar A., Sanchez-Rodriguez E., Rodriguez-Perez C., Rangel-Huerta O. D., Mesa M. D. (2023). Metabolomic-based studies of the intake of virgin olive oil: a comprehensive review. Metabolites 13 (4), 472. Published 2023 Mar 25. doi:10.3390/metabo13040472
Vicente P. J. M. (2016). Hombro doloroso e incapacidad temporal. El retorno al trabajo tras larga baja por hombro doloroso: causalidad del trabajo en el hombro doloroso. Med. Segur. Trab. 62 (245), 337–359.
Walmsley S., Osmotherly P. G., Rivett D. A. (2014a). Movement and pain patterns in early stage primary/idiopathic adhesive capsulitis: a factor analysis. Physiotherapy 100 (4), 336–343. doi:10.1016/j.physio.2014.02.001
Walmsley S., Osmotherly P. G., Rivett D. A. (2014b). Clinical identifiers for early-stage primary/idiopathic adhesive capsulitis: are we seeing the real picture? Phys. Ther. 94 (7), 968–976. doi:10.2522/ptj.20130398
Wang B., Wu L., Chen J., Dong L., Chen C., Wen Z., et al. (2021). Metabolism pathways of arachidonic acids: mechanisms and potential therapeutic targets. Signal Transduct. Target Ther. 6 (1), 94. Published 2021 Feb 26. doi:10.1038/s41392-020-00443-w
Wang K., Ho V., Hunter-Smith D. J., Beh P. S., Smith K. M., Weber A. B. (2013). Risk factors in idiopathic adhesive capsulitis: a case control study. J. Shoulder Elb. Surg. 22 (7), e24–e29. doi:10.1016/j.jse.2012.10.049
Whelton C., Peach C. A. (2018). Review of diabetic frozen shoulder. Eur. J. Orthop. Surg. Traumatol. 28 (3), 363–371. doi:10.1007/s00590-017-2068-8
Yang W. C., Wang Q., Chi L. T., Wang Y. Z., Cao H. L., Li W. Z. (2019). Therapeutic hypercapnia reduces blood-brain barrier damage possibly via protein kinase Cε in rats with lateral fluid percussion injury. J. Neuroinflammation 16 (1), 36. PMID: 30760300; PMCID: PMC6375143. doi:10.1186/s12974-019-1427-2
Yian E. H., Contreras R., Sodl J. F. (2012). Effects of glycemic control on prevalence of diabetic frozen shoulder. J. Bone Jt. Surg. Am. 94 (10), 919–923. doi:10.2106/JBJS.J.01930
Zhang J., Zhong S., Tan T., Li J., Liu S., Cheng R., et al. (2021). Comparative efficacy and patient-specific moderating factors of nonsurgical treatment strategies for frozen shoulder: an updated systematic review and network meta-analysis. Am. J. Sports Med. 49 (6), 1669–1679. doi:10.1177/0363546520956293
Zhu B., Dong Y., Xu Z., Gompf H. S., Ward S. A. P., Xue Z., et al. (2012a). Sleep disturbance induces neuroinflammation and impairment of learning and memory. Neurobiol. Dis. 48 (3), 348–355. doi:10.1016/j.nbd.2012.06.022
Zimecki M., Kruzel M. L. (2007). Milk-derived proteins and peptides of potential therapeutic and nutritive value. J. Exp. Ther. Oncol. 6 (2), 89–106.
Zindel J., Kubes P. (2020). DAMPs, PAMPs, and LAMPs in immunity and sterile inflammation. Annu. Rev. Pathol. 15, 493–518. doi:10.1146/annurev-pathmechdis-012419-032847
Keywords: frozen shoulder (adhesive capsulitis), shoulder pain, shoulder condition, autoimmune disorder, endocrinological disease, low grade inflammation, psychosocial factors
Citation: Navarro-Ledesma S, Hamed-Hamed D and Pruimboom L (2024) A new perspective of frozen shoulder pathology; the interplay between the brain and the immune system. Front. Physiol. 15:1248612. doi: 10.3389/fphys.2024.1248612
Received: 27 June 2023; Accepted: 18 March 2024; Published: 29 March 2024.
Reviewed by:
Copyright © 2024 Navarro-Ledesma, Hamed-Hamed and Pruimboom. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Santiago Navarro-Ledesma, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Open access
- Published: 21 October 2016
Intelligent framework for diagnosis of frozen shoulder using cross sectional survey and case studies
- Humaira Batool 1 ,
- M. Usman Akram 1 ,
- Fouzia Batool 2 &
- Wasi Haider Butt 1
SpringerPlus volume 5 , Article number: 1840 ( 2016 ) Cite this article
2261 Accesses
1 Citations
1 Altmetric
Metrics details
Frozen shoulder is a disease in which shoulder becomes stiff. Accurate diagnosis of frozen shoulder is helpful in providing economical and effective treatment for patients. This research provides the classification of unstructured data using data mining techniques. Prediction results are validated by K-fold cross-validation method. It also provides accurate diagnosis of frozen shoulder using Naïve Bayesian and Random Forest models. At the end results are presented by performance measure techniques.
In this research, 145 respondents (patients) with a severe finding of frozen shoulder are included. They are selected on premise of (clinical) assessment confirmed after by MRI. This data is taken from the department of Orthopedics (Pakistan Institute of Medical Sciences Islamabad and Railway Hospital Rawalpindi) between September 2014 to November 2015. Frozen shoulder is categorized on the basis of MRI result. The predictor variables are taken from patient survey and patient reports, which consisted of 35+ variables. The outcome variable is coded into numeric system of “intact” and “no-intact”. The outcome variable is assigned into numeric code, 1 for “intact” and 0 for “no-intact”. “Intact” group is used as an indication that tissue is damaged badly and “no-intact” is classified as normal. Distribution of result is 110 patients for “Intact” group and 35 patients for “No-Intact” group (false positive rate was 24 %). In this research we have utilized two methods i.e. Naive Bayes and Random Forest. A statistics regression model (Logistic regression) to categorize frozen shoulder finding into “intact” and “no-intact” classes. In the end, we validated our results by Bayesian theorem. This gives a rough estimate about the probability of frozen shoulder.
In this research, our anticipated and predictive procedures gave better outcome as compared to statistical techniques. The specificity and sensitivity ratio of predicting a frozen shoulder are better in the Naïve Bayes as compared to Random Forest. In end the likelihood ratio results are used with Bayesian theorem for final evaluation of the results, from this we conclude predictive model is valid model for classification of frozen shoulder.
Conclusions
We have used three predictive models in our study to classify frozen shoulder. Then we validated our predictive results by Bayesian theorem to give a rough estimate about the probability of occurrence of disease or not. This enhances the clinical decision making regarding frozen shoulder.
The tendons and bones that make up our shoulder joint are enclosed in a capsule of connective tissue. Whenever shoulder capsule become tightened and thick around the joint, the problem of frozen shoulder occurs (Crubbs 1993 ). Mostly frozen shoulder problem can be categorized into either primary also called unknown reason (idiopathic) or secondary (known reason) (Dias et al. 2005 ). Main signs and symptoms which lead to frozen shoulder are bad posture, post-operative (after surgery), stroke and patients suffering from diabetes (Mao et al. 1997 ). Frozen shoulder is more prone diabetics (20 %) than general population (2–5 %).Its ratio in insulin dependent patients are about 36 % (Afsar et al. 2014 ). Females are affected more than males (Manske and Prohaska 2010 ). Many treatments are available for frozen shoulder including both operative and non-operative. Operative procedures include manipulation under anesthesia and arthroscopic surgeries. Surgery reduces the severe complications of frozen shoulder. Non-operative includes pain management through different modalities (Transcutaneous electrical nerve stimulation, Short wave diathermy, Interferential therapy etc.), mobilization techniques, exercise plan and precautionary measures. All treatments just improve the functional time to recovery and increase the range of motion (Neviaser 1945 ). However, none of the treatment is authentic to totally eliminate the future chance of disease.
Main symptoms observed in frozen shoulder patients are pain, stiffness and loss of range of motion (Crubbs 1993 ). According to our knowledge, no work has been done on frozen shoulder using unstructured data (Ahmad et al. 2012 ). Only a few studies have been performed on clinical examinations and treatments with medical perspective, but no work has been done for the diagnosis of a frozen shoulder with respect to predictor values. The objective of this research is to develop reliable method for diagnosing frozen shoulder. Another significance of this study, is to analyze frozen shoulder intelligently by using unstructured data.
Physical examinations are generally considered low-cost process and results can directly be obtained at the time of the consultation. On the other hand, precision is based upon doctor’s knowledge and practice. Now a day’s frozen shoulder is diagnosed by clinical examination and imaging tests (Değerlendirmesi 2014 ). Firstly doctor diagnoses the problem by asking the patient to rotate the shoulder in a different direction. If physicians are uncertain about the problem, then formal test such as magnetic resonance imaging (MRI) can be carried out for diagnosis. Arthography is considered a standard test for the diagnosis of a frozen shoulder. It is having sensitivity 91 %, specificity 100 % and accuracy 92 %, but the test is an expensive and painful process (Ryu et al. 1993 ).
Better diagnosis and treatment plan for frozen shoulder are made through clinical findings. A lot of clinical examination methods have been developed to help in diagnosing frozen shoulder (Manske and Prohaska 2008 ). If patient is having limitations in hand elevation, then Apley scratch test is used for the diagnosis of disease. In Apley scratch test, patient is asked to put his/her arm above head and arrive at behind the neckline to touch his/her upper back. This test analyzes the rotation of upward, external and elevation (Anderson et al. 2011 ). During physical examination if the patient is having severe pain, then the physical assessment is marked positive. Previous researches showed that the ROM (range of motion) and Apley scratch test are good for diagnosing frozen shoulder (Woodward and Best 2000 ).
There is no existing fact, that any solitary check can diagnose frozen problem (Mitchell et al. 2005 ). Cost-effective treatment process is always dependent upon proper clinical assessment and diagnosis. The severity of the disease can be judged best by imaging tests as compared to clinical examination. According to the recent researches, if we make decision just on the basis of physical examination, it has sure chances that to give us false-positive ratio. Analysis made on the basis of physical examination always conflict with the imaging test. Due to this, we cannot make any decision just on the basis of clinical examination (Manske and Prohaska 2008 ; Bulgen et al. 1984 ; Clarke et al. 1974 ; Binder et al. 1984 ; Shaffer et al. 1992 ; Sharma et al. 1993 ).
This research provides a pathway towards accurate and correct diagnosis of frozen shoulder. The objective of this research is to develop reliable method for frozen shoulder. First milestone is to collect questionnaire from work related and chronic disease patients. Then on the basis of questionnaire and physical examination reports, we develop model which detect frozen shoulder category.
Identification of frozen problem by intelligence based framework is a new research area because previously it was based upon clinical examination. Clinical examination accuracy is dependent upon physician experience. Few case studies based researches have been done on clinical examination for the diagnosis of different shoulder problems but no research has been done on the correct diagnosis of shoulder problem by using intelligence framework. It may cause life time abnormality if not monitored well on time. So intelligence test should be used as a side assessment, for correct diagnosis of shoulder problem.
Data mining process is called as computational process. During computational process, software matches different patterns on the basis of logics. It classifies the huge datasets using different techniques like statistics and machine learning [ML] (Han et al. 2011 ; Bellazzi and Zupan 2008 ). This information discovery procedure turned out to be an accepted area to make inquires in diverse fields. It is being used in medical domain to discover patterns among medical variables. This also predicts disease outcomes using historical data (Bellazzi and Zupan 2008 ; Ramesh et al. 2004 ).
It is a difficult task for a doctor to properly diagnose and recommend treatment for some serious disease problems. In this context intelligent system model is considered as a useful procedure. We took information from different patients and then forecast a conclusion of interest (Bellazzi and Zupan 2008 ; Witten and Frank 2005 ). This will help us to take decision at a clinical level. Predictive methods of data mining are, Naïve Bayesian and Random Forest. These have been used most of the time to predict the conclusion of disease (Bellazzi and Zupan 2008 ; Griffith 2000 ). Some relevant studies used this concept; to provide prediction about how many patients are at high risk during anesthesia (Lin et al. 2011 ). Another study was on internal shoulder derangements (Oh et al. 1999 ).
Our main objective is to build up a procedure to diagnose frozen shoulder and to make decisions on the basis of physical information without depending on tests like MRI. Tests should only be used for detailed clinical hypothesis and only be recommended in severe and undiagnosed cases (Weinstein et al. 1980 ; Kassirer 1989 ; Pauker and Kassirer 1980 ). This study also used a predictive procedure of data mining and Chi Square test, to increase the precision of diagnosing frozen shoulder without physical examination. In this study we build a model and also made comparison among three predictive models (logistic regression, Random forest and Naïve Bayes) to categorize frozen shoulder groups on the basis of physical examination results, patient reports and survey.
Proposed methodology
This research classifies the unstructured data using data mining techniques. It also used predictive models like Naïve Bayesian and Random forest to improve the diagnosis of frozen shoulder.
Methodology comprises of feasibility study, data gathering, preprocessing, and detecting predictor attributes. Then on the basis of training data, result was graded into different meaningful classification.
Architecture
This research used three tier architecture levels for analysis of disease. Figure 1 shows the architecture.
Requirement level
This consists of collecting and finalizing data at single point. It also includes linkage of data with datasets level, to build an intelligent system for problem analysis. Requirement engineering [RE] process suggests the most common requirements according to the needs.
Datasets level
This mainly deals with database. Database consists of datasets.
Component level
This consists of framework to classify data.
Block diagram of proposed system
Figure 2 shows the block diagram of the proposed system. The data we collected from patient reports and patient survey was in an unstructured form. Unstructured data mean raw data. Almost 80 % of medical data are available in an unstructured form like patient’s reports, lab report, and doctor review. We have collected history of different patients by case study method, for the purpose to get some predictor variables. All those case studies reveal that either the frozen shoulder problem occurred due to work related problem or either it is due to disease base problem. In the second level of architecture we converted unstructured data of patients into structured form by using software. Structure data was analyzed by the software. Then preprocessing was done on a datasets it includes feature extraction. Details about feature extraction method are mentioned in below section. In the third level of architecture we have applied different predictive model to classify unstructured data. This will also help in deciding either frozen shoulder patient classifies into intact class or no-intact class.
Requirement engineering process
In our research study, we have used a well known requirement engineering process model for data preparation. Requirement engineering process is called as “The process to gather the requirements from client analyze and document them”. Data preparation output would be used for predicting result accurately and intelligently. Client involvement may be a major consideration in the development of most successful systems. The main purpose of using requirement engineering process in our study is that, the most difficult phase is to collect patient’s information and user involvement for finalizing all data at some single point. So far it is largely unexplored. Model defines the approaches and methods used to deal with difficulties.
Requirement engineering is a four step process, which includes feasibility study, requirement gathering, requirement specification, and requirement validation. Each stage has its specific tasks and outputs.
The emphasis of first step is on getting better understanding of project objectives to establish better plans to achieve business and intelligent goals. Feasibility study is an analysis of the importance of an idea. Conducting a feasibility study is a good practice to gives focuses to the project and outline alternatives. Next step includes data collection from the patient and doctors. It involves communicate with the patient and doctors to know their views about disease and to identify important features for survey. Data understanding is achieved by categorizing data into work based, disease based. After finalizing the requirements next phase of the process is requirement specification, requirement specification is same like blueprints. Framework selection according to domain is an art which can easily tie all internal factors of requirements. Framework design usually utilize the most time of the project. When business goals are settled then next step is requirement validation. Requirement validation step involves to check whether all important points are covered correctly and easily validate through alternatives. It also confirms that whether all domain requirements are accurately adjusted in a document or not.
This study was conducted with the collaboration of Pakistan Institute of Medical Science Islamabad and Railway Hospital Rawalpindi, Pakistan. A real report based data of frozen shoulder patients was used. In this study, original data set is used that was obtained from Hospitals. For the purpose of domain understating we covered different case studies. This composed data was unstructured patient’s records. First we transformed the unstructured reports/survey into planned order and then picked out important variables. By hands mean, we have selected some hidden predictive variables from the patient reports, which were obtained from the information doctor has taken during the subjective examination or history taking. We designed a patient survey with the assistance of therapeutic specialists (practitioners).Extraction of meaningful information from the survey was done very carefully. The requirement engineering process was used to decide whether the extracted attributes are sufficient and contains all the meaningful attributes or still extra information is required to get important variables. The mining (extraction) of variables is key benefit to get the knowledge of problem field plus it would assist additionally within the study. After the categorization of data, datasets was formed. Requirement analysis steps are shown in a Fig. 3 .
Requirement analysis phase
Significance of irregular (unstructured) data
In 1998, Merrill Lynch declared that a normal 80 % of all business information has it source in unstructured form (Murdoch and Detsky 2013 ). Mostly larger part of business information should came from unstructured source. As indicated by another source (Murdoch and Detsky 2013 ), around 80 % of the medical information that might be patient’s reports is in irregular form. Once the unorganized information is organized and put in database is called planned data. The planned information is easily comprehensible by computers and is used by framework for problem analysis.
We have collected meaningful information from last level which would be helpful for decision. We designed the datasets to grasp the collected variables. The patient survey data set contained different variables which were categorical, nominal and scale data. The description and values of patient’s survey variables are stated in Table 1 . The description and values of patient’s reports variables are stated in Table 2 .
Data collection procedure
In this research, 145 respondents (patients) with severe symptoms of frozen shoulder were included. They were selected on the premise of (clinical) assessment confirmed after by MRI. This data was taken from the department of Orthopedics (Pakistan Institute of Medical Sciences Islamabad and Railway Hospital Rawalpindi) between September 2014 to November 2015. Frozen shoulder was categorize on the basis of MRI result.MRI result was used a standard.
The result variable was coded into numeric system of “intact” and “no-intact”. “Intact” group incorporated that tissue has been damaged badly and “no-intact” was classified as normal tissue. The result distribution variable was 110 for “Intact” and 35 patients for “No-Intact” (False positive rate of 24 %). The judgment variable was the clinical results, which consist of 35+ variables. Apley’s Scratch Test and Resisted Tests (ROM) are common provocative tests in diagnosing frozen shoulder (Woodward and Best 2000 ). These two tests were utilized as screening/diagnostic tests in the analysis models. In this research, we have utilized three mining methods to categorize frozen shoulder (intact and no-intact classes).it includes, Naive bayes and the Random Forest and a statistics regression model (logistic regression). Dataset consisted of surveyed questions and reports. It contained all the data on the subject of abnormalities and their relation, as it is used for assessment and association purposes. However, for this study there was no availability of dataset either locally or globally. Due to this, we have collected data from different hospitals by survey method. The assessment of proposed framework of frozen shoulder patients was performed on a locally gathered dataset.
Precision in medical systems is extremely significant. We have used three tier architecture. It includes requirement level, datasets level and component level. First two levels have already been explained in the previous section. Component level includes feature extraction and classification techniques. The study also helps in comparison with different classification techniques.
This paper includes proposed framework results and details of dataset. Comparison with the other techniques is also included for the validation of proposed system. We used statistics regression model (logistic regression) to assess the outcomes (Lin et al. 2010 ; Bagley et al. 2001 ). The result of this model is then compared with other two Classification Techniques (which are Nave Bayes and Random Forest). We have used cross validation techniques for performance authentication. Verification was done by comparing the accuracy of classification models.
Feature selection
In this step unrelated variables and unnecessary information was eliminated. At the start numbers of variables were 35 + , extracted from the survey and reports. A few of the variables were unnecessary and was not helpful in decision making. Those variables were removed by feature selction method. Data preprocessing includes feature selection, which helps in decreasing the unrelated data and improves the learning effectiveness. This also increases the accuracy of models. After this procedure, resulted variables are those variables that are helpful for identification of purpose and also produce high accuracy for classification models. Feature extraction was done by T TEST technique and significance probability value was taken as 0.05.
Most of the research questions have been validated through hypothesis. The research questions are for our knowledge and therefore the statistics that comes hereafter. Whenever, we have created hypothesis test in statistics, a P value always help us to conclude the importance of our outcome. Basically hypothesis tests are used to check the strength of a claim that is made about a community. This claim is known as the null hypothesis. After the outcome, if the null hypothesis is inaccurate then we would accept the other hypothesis as true. In statistics, P value is a range among Zero and One and translated in the subsequent way:
After study if results show small P value (≤0.05), then we can easily reject the null hypothesis because smallest P value shows strong evidence against the null hypothesis.
After study if results show large P value (>0.05), then we cannot reject the null hypothesis because large P value shows weak evidence against the null hypothesis.
After study if results show P values near the cutoff (0.05), then we could go either way because results are on margin.
Component level (classification phase)
In this section, we would explain in detail about the component steps. It is used to categorize the data. We will compare different classification techniques. At the end, conclusion can be made on the basis of comparison results.
Training and testing procedure
Generally the error is related with randomness results in biasing the estimation. Cross-validation is regularly applied to minimize the error. The power of a prediction model to generalize unseen data can be frequently validated by K-fold cross validation method. All sampling data is divided into K equal size subsamples randomly, by K-fold cross-validation procedure strategy. We have used 50 % data for testing purpose and 50 % data for training purpose. The both method (training and testing) is then repeated K time. In this study, K-fold cross-validation number ten was chosen in light of the fact that numerous researches have demonstrated that ten as an ideal validation number. In the tenfold cross-approval, the method was repeated ten times with totally dissimilar training and testing datasets (Kohavi 1995 ; Bengio and Grandvalet 2004 ; Breiman et al. 1984 ).
We have additionally checked the error of different predictive models by performance measures method during comparative analysis (Delen et al. 2005 ).
We have collected data from 145 frozen shoulder patients by survey and patient’s real reports. Table 3 shows the demographic data of the patients. The majority patients were Female (71 %); the age ranges were in between 46–60 years (44.8 %).
Majority respondents were employee (44.8 %) and housewife. Majority of the patients dominant hand was right (86.9 %) and their body mass was normal (55.2 %). Majority of the patients were suffering from HBP-diabetes-depression (37.9 %).Stress level in majority of patients was high due to occupation (57.9 %). Left shoulder was involved in majority of the respondent (60.7 %).Those patients wake at night with pain ratio was (86.2 %); (53.8 %) respondents were having main complaint of the pain-stiffness. History of complain; due to work related activities were present in (43.4 %) patients. Origin of pain was sudden in (39.3 %) respondents and nearly 58.6 % of patients rated their pain as worst. The ratio of patients with no such complaint before was (72.4 %). Majority was not having any previous history of dislocation, injection in a shoulder and before history of surgery and (80 %) patients were on medication. Majority respondents told that pain interferes with their routine work (96.6 %) and also with their sports activities. (55.9 %) patients told that after heat therapy they feel better but that is just for some time. Majority said that repetitive lifting loads at their work place are main cause of pain and almost (77.2 %) were using pain killers for musculoskeletal problems (77.2 %).
Clinical examination is being done mostly on the basis of Active range of motion, internal rotation, flexion and Apley’s scratch. These are considered as standard interpreter attributes to decide the frozen shoulder. The proportions of positive finding were 97.2, 89.0, 93.1 and 89.0 % respectively. Respondent, were having negative passive range of motion, external rotation were positive 91.7 %, Abduction test were positive 42.8 as shown in Table 4 . The assessment attributes also included different kind of pain types (which are sharp, aching, throbbing, numbness, shooting, burning pain) which were then coded into two responses. The response having sharp pain was (82.1 %) and percentage of aching pain was (64.8 %).The throbbing pain was (95.9 %). Some patients had numbness (80 %), burning (77.2 %) and shooting ratio was 91.0 %.
The P value was used to look at the valuable attribute between the “intact” and “no-intact” class. Table 5 shows the valuable attribute between Intact and No-Intact class. The asterisk (*) code in a last column shows the significance of each predictor variable. Variables with **** code are the most significant ones and all others variable without any * has no significance association. Along with MRI report, we have assigned class labels to every record.
Probability method evaluated the significance of an attribute by computing the worth of P value measurement. It uses ranker search technique with threshold P ≤ 0.05. This search method gives weight and P value by their individual evaluations. Mostly P value was used to check the similarity between the Intact and No-Intact groups of each variable. Those variables which have mentioned in Table 5 with Starric (**) codes, are selected due to their P value less than 0.05. Four (****) code variables are more significant follow by three codes, two codes and one code. One (*) code is least significant due to having more P value among the other significant variables. The performance of the proposed system is evaluated on significant variables. The effective attributes are shown in Table 5 .
Firstly we separated variables against the code. According to the coding scheme, we have separately applied model on different codes and then judged the accuracy of different variable codes. We have also validated our results and calculated the accuracy by the formula given in Eq. 1 .
Models comparative analysis
We have used different prediction models for this study. Firstly, we have analyzed the data by logistic regression model. After model implementation, we have used two other classification techniques for the purpose of analysis and comparison with Logistic Regression. The following results were obtained: LR model classified data with 96.55 % accuracy during training of model. LR model gave 95.10 % accuracy during cross validation. We have applied the same steps on Naïve Bayes and Random Forest. Table 6 results show that Random Forest categorizes the data 94.48 % while training, it gives 89.81 % accuracy during cross validation time. For Naïve Bayes we achieved 99.31 % accuracy during training of model, it gives 99.29 % accuracy during cross validation. Overall results show that, Naïve Bayes model performs most excellent on our data along with other procedures and techniques. Table 6 shows the classification models results.
Table 6 shows the prediction performances measure of AUC and etc. According to the above result, each metric depicts that Naïve Bayes performance are best than other models. Naïve Bayes is with highest accuracy. Along with Naïve Bayes, LR also shows immense performance that is 95.10 %. Naive Bayes has most favorable precision (100 %), sensitivity (97.5 %), specificity (100 %), accuracy (99.29), AUC(0.99) and likelihood positive and negative ratios (40,0).Logistic Regression results were also similar to recognize frozen shoulder with sensitivity (91.67), specificity (97.7), precision (89.67), accuracy (95.1), AUC (0.96) and likelihood positive and negative ratios (11,0.04).The predictive data mining models Naïve Bayes, Logistic Regression has statistically better performances than the Random Forest.
In end we adopted the area under the receiver operating characteristics (AUROC). AUROC was used to analyze the biasness, which is basically used to differentiate those who have an Intact or who don’t. Mostly the predictive models accuracy is explained by the area under the curve. We can classify the accuracy of predictive models by matching the points. If result shows value (0.90–1) then the diagnostic test is excellent, for good its value is (0.80–0.90). Table 6 shows the predictive models along with their AUC value.
The areas under the curve for Naïve bayes is 0.99 and for logistic regression its 0.96 and for random forest its 0.89. Overall values shows this Naïve Bayes would be considered to be excellent for separating intact from no-intact group.
The study conclude this Naïve Bayes performed more accurately in TPR (Intact class and the area under curve value is = 0.99) compared to random forest TPR (Intact class area under the curve 0.89).These differences are statistically different.
Models prediction power can be judged through likelihood ratio that’s why we have summarized the likelihood ratios in Table 7 . Table 7 is showing likelihood ratio.
Discussion and conclusion
There are many reasons for musculoskeletal disability. After low back pain and neck pain, the third most common cause of musculoskeletal disability is shoulder pain. Frozen shoulder is characterized by pain, stiffness and limited range of motion in shoulder joint. Frozen shoulder condition cannot be identified through X-ray; MRI is carried out to explore this condition. The first description of primary frozen shoulder has been made 150 year ago, but only 16 limited researches has been done to diagnose the underlying cause. According to the cause’s symptoms, secondary frozen shoulder problem may occur after trauma or surgery. Little work has been made on the valuable treatment options for frozen shoulder. Due to limited knowledge about the treatment plan in literature, it’s really tough for diagnosis of the exact problem and recommendation of best treatment plan. All the treatment plans which are mentioned in a literature have a different success rates. Its estimated value in common population is 2–3 % and a 5–6 % ratio is mentioned by the orthopedics surgeons (Mitchell et al. 2005 ).
This study also verifies that the frozen shoulder problem mostly occurred in female patients. In this research our anticipated, predictive procedures performed well than the statistical techniques. The specificity and sensitivity ratio of an intelligently predicting frozen shoulder are better in the Naïve Bayes and Logistic Regression models as compared to Random Forest. Our results are similar to recent researches which shows that, mining procedures are more helpful than statistical to accurately diagnose different diseases (Wahbeh et al. 2011 ; Grossi et al. 2007 ). However, mining techniques has not been used so much by orthopedic doctors for disease prediction. This limitation enlightens that little researches and studies have been done on a predictive data mining in the field of orthopedic. Numerous orthopedic researches and studies have examined the pathology, treatment and capability of the clinical exam to properly identify frozen shoulder. Previous researches also show that there is extensive value of sensitivity (up to 20–91 %) and specificity (up to 20–100 %) for disease diagnosing by Arthography method. That is why then arthography results are compared with sonographic signs (Ryu et al. 1993 ), but no studies has examined the physical examination variable for disease diagnosing. We established that our predictive mining techniques (Naïve Bayesian and the Logistic Regression) are correct for identifying frozen shoulder. These models having specificity is 91–98 %, and sensitivity is 96–100 %, which is better than earlier researches. If the research shows high sensitivity and moderate specificity, then we can easily use the mining techniques more than statistical for identifying frozen shoulder. We can reduce the unnecessary imaging test ratio and also decrease the false positive rate by data mining procedures.
All the previous studies related to medical statistics were planned to explore the analysis among group data. If requirement is to do medical diagnosis at a single level, then we cannot use the same procedure due to its limitations (Grossi et al. 2007 ; Chang 2006 ). During statistical analysis, researchers do a study on a collection of population to disclose relationships among them. Through evidence-based statistics, we can easily predict a diagnosis at an individual level. Therefore, in our study we used the intelligent data mining model, to give an answer at the specific level of classification (Grossi et al. 2007 ; Chang 2006 ; Rygielski et al. 2002 ).
We have developed an intelligent system by using clinical reports, which can be applied to every individual patient of frozen shoulder. During clinical assessments mostly doctors make diagnosis and recommend treatment on the basis of clinical examination and imaging tests. During physical assessment, doctors frequently face different type of problems. On this basis, it’s really difficult for them to determine the disease probability. The classification output of predictive mining was mostly expressed by group method. In this, each individual patient was marked just into one group without knowing that the patients are in the exact class or not. Then, we evaluated the P value against each variable. On the basis of P value results, we have ignored some irrelevant variable. After P value calculation, we used significant variables in a model to predict results and also measure model accuracy. To support our predictive results, we calculated the probability of the prediction outcome with LR (Sox and Harold 1996 ; Dujardin et al. 1994 ; Sox et al. 1988 ) and Fagan’s theorem (Deeks and Altman 2004 ; Lang and Secic 1997 ). The sensitivity and specificity of the Naïve Bayesian model were 100 and 97.5 % (as showed in Table 6 ) which has given a positive LR (LR+) of 40 and a negative LR (LR−) of 0. The sensitivity and specificity of the Logistic Regression model were 96.7 and 91.67 % (as showed in Table 6 ) which has given a positive LR (LR+) of 11 and a negative LR (LR−) of 0.04 (Table 7 ) (Deeks and Altman 2004 ; Lang and Secic 1997 ; Lu et al. 2014 ).
The positive likelihood result showed that, if a patient visits a hospital with a frozen shoulder there is 11 % time more chance that it has a positive test than those who doesn’t. On the other hand, if a patient visits without a diagnosed case of a frozen shoulder, then there is approximately 5 % times more chances that its original test will be negative. Previous studies has recommended that if any model shows its LR+ value greater than ten, there are chances that its original test would be positive. On the other hand, if model results show it LR− value less than 1, there are chances that original test would be negative (Akobeng 2007 ).
In our study, firstly we calculated the predictive model results and also calculated the likelihood ratios. At the end we have used a Bayesian standard theorem, to evaluate the possibility of presence or absent of a frozen shoulder using a prediction result (intact or no-intact) and a prior probability. On the basis of likelihood ratio, doctors can easily give a rough estimate either a patient has a severe frozen shoulder or not. This will also help to tell the severity of disease before recommending an image test (Espallardo 2003 ). In Bayesian theorem, the main purpose of likelihood ratio is to change the posterior possibility of having disease, after an outcome is well-known (Gill et al. 2005 ).
We can easily predict the posterior probability by Fagan nomogram. nomo-gram represents usually through graph, that gives the posterior ratio that a disease is exist or not on the basis of predictive results and prior ratio (Akobeng 2007 ). Fagan nomo-gram tool mark the prior probability on a left side, (a straight line start with a prior ratio of having a disease) and then moved towards the likelihood ratio and at the last intersect at the posterior ration to show ratio of having a disease. For example, if the disease prevalence ratio for a patient is 76 %, according to our Logistic Regression model the patient should be in a class of “intact” with an LR+ 11 (Table 7 ), Firstly, tool marked the prior probability ratio at the left side which is 76 % then draw a straight line (Fig. 3 ) and marked the point of LR+ 11 % that intersect at the posterior probability of 97 % (Halkin et al. 1998 ). This result shows that, when the mining model result is “Intact” then the ratio of having a frozen shoulder for this patient increase from 76 to 97 %.Conversely, when the model outcome is “no-intact” then the possibility of having the patient an intact decrease from 76 to 11 %. Hence, our model outcome help doctors in making diagnostic decision and treatment, mainly if the prior possibility ratio of a frozen shoulder is at the middle. Our model outcomes can be utilized not only to categorize a patient into the ‘‘intact’’ or ‘‘no-intact’’ class but also to change the prior possibility in a way to approximate the posterior possibility.
There are also some limitations for which future research is recommended. First, to deal with the problem which can be occurred due to sample size and also more characteristics of patients are required to deal with the generalization issue (Lawrence and Giles 2000 ). Secondly, more mining models such as SVM (support vector machine) or decision tree/neural network should also be used to discover improvement of the prediction. Thirdly, more research is needed to examine whether other medical parameters like Capsular Pattern test or the Lift-off test can be good attributes in affecting the miming model performances. Our research did not focus on a surgery or arthroscopy as main principles, although, the real finding can only be guessed by surgery results. In our study, we used MRI results as a reference standard. Instead of this, the performance and legitimacy of our prediction mining models should be further checked on those patients, who are undergoing for a surgery. Figure 4 shows the Fagan’s nomo-gram mapping.
Fagan’s nomo-gram
To our information, this study is the initial analysis on an unstructured data with numerous characteristics (age, gender) and disease information (such as disease related, work related), which potentially help the diagnosis of frozen shoulder.
Afsar SS, Gulzar M, Idrees M, Ullah Babar I (2014) Results of Intra-articular injection of methylprednisolone in idiopathic adhesive capsulitis. Pak J Surg. 30(1):45–50
Google Scholar
Ahmad S, Rafi MS, Siddiqui IA, Hamidi K, Faruq NM (2012) The frequency of adhesive capsulitis in diabetes mellitus patients. Pak J Rehabilit 1(2):49–55
Akobeng AK (2007) Understanding diagnostic tests 2: likelihood ratios, pre-and post-test probabilities and their use in clinical practice. Acta Paediatr 96(4):487–491
Article PubMed Google Scholar
Anderson BC, Anderson RJ, Fields KB, Grayzel J (2011) Evaluation of the patient with shoulder complaints. UpToDate, Waltham
Bagley SC, White H, Golomb BA (2001) Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol 54(10):979–985
Article CAS PubMed Google Scholar
Bellazzi R, Zupan B (2008) Predictive data mining in clinical medicine: current issues and guidelines. Int J Med Inform 77:81–97
Bengio Y, Grandvalet Y (2004) No unbiased estimator of the variance of k-fold cross-validation. J Machine Learn Res 5:1089–1105
MathSciNet MATH Google Scholar
Binder AI, Bulgen DY, Hazleman BL, Roberts S (1984) Frozen shoulder: a long-term prospective study. Ann Rheum Dis 43(3):361–364
Article CAS PubMed PubMed Central Google Scholar
Breiman L, Friedman J, Stone CJ, Olshen RA (1984) Classification and regression trees. CRC Press, Boca Raton
MATH Google Scholar
Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S (1984) Frozen shoulder: prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis 43(3):353–360
Chang L (2006) Applying data mining to predict college admissions yield: a case study. New Direct Institut Res 2006(131):53–68
Article Google Scholar
Clarke GR, Willis LA, Fish WW, Nichols PJR (1974) Assessment of movement at the glenohumeral joint. Orthopaedics 7(2):55–71
Crubbs N (1993) Frozen shoulder syndrome: a review of literature. J Orthop Sports Phys Ther 18(3):479–487
Deeks JJ, Altman DG (2004) Diagnostic tests 4: likelihood ratios. BMJ 329(7458):168–169
Article PubMed PubMed Central Google Scholar
Değerlendirmesi OBR (2014) Radiological assessment of the shoulder region
Delen D, Walker G, Kadam A (2005) Predicting breast cancer survivability: a comparison of three data mining methods. Artif Intell Med 34(2):113–127
Dias R, Cutts S, Massoud S (2005) Frozen shoulder. Br Med J 331(7530):1453
Dujardin B, Van den Ende J, Van Gompel A, Unger JP, Van der Stuyft P (1994) Likelihood ratios: a real improvement for clinical decision making? Eur J Epidemiol 10(1):29–36
Espallardo N (2003) Decisions on diagnosis in family practice: use of sensitivity, specificity, predictive values and likelihood ratios. Asia Pac Family Med 2(4):229–232
Gill CJ, Sabin L, Schmid CH (2005) Why clinicians are natural bayesians. Br Med J Int 330(7499):1080–1083
Griffith J (2000) Artificial neural networks: are they ready for use as clinical decision aids? Med Decis Making 20(2):243–244
Article MathSciNet CAS PubMed Google Scholar
Grossi E, Mancini A, Buscema M (2007) International experience on the use of artificial neural networks in gastroenterology. Digest Liver Dis 39(3):278–285
Article CAS Google Scholar
Halkin A, Reichman J, Schwaber M, Paltiel O, Brezis M (1998) Likelihood ratios: getting diagnostic testing into perspective. QJM 91(4):247–258
Han J, Pei J, Kamber M (2011) Data mining: concepts and techniques. Elsevier, Amsterdam
Kassirer JP (1989) Our stubborn quest for diagnostic certainty. N Engl J Med 320(22):1489–1491
Kohavi R (1995) A study of cross-validation and bootstrap for accuracy estimation and model selection. Int Joint Conference Artif Intell. 14(2):1137–1145
Lang TA, Secic M (1997) How to report statistics in medicine. American College of. Physicians, Philadelphia
Lawrence S, Giles CL (2000) Overfitting and neural networks: conjugate gradient and backpropagation. IEEE International Joint Conference on Neural networks, Proceedings of the IEEE-INNS-ENNS, vol 1. pp 114–119)
Lin CC, Ou YK, Chen SH, Liu YC, Lin J (2010) Comparison of artificial neural network and logistic regression models for predicting mortality in elderly patients with hip fracture. Injury 41(8):869–873
Lin CS, Chang CC, Chiu JS, Lee YW, Lin JA, Mok MS, Li YC (2011) Application of an artificial neural network to predict postinduction hypotension during general anesthesia. Med Decis Making 31(2):308–314
Lu HY, Huang CY, Su CT, Lin CC (2014) Predicting rotator cuff tears using data mining and bayesian likelihood ratios. PLoS ONE 9(4):e94917
Article ADS PubMed PubMed Central Google Scholar
Manske RC, Prohaska D (2008) Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskeletal Med 1(3–4):180–189
Manske RC, Prohaska D (2010) Clinical commentary and literature review: diagnosis, conservative and surgical management of adhesive capsulitis. Shoulder Elbow 2(4):238–254
Mao CY, Jaw WC, Cheng HC (1997) Frozen shoulder: correlation between the response to physical therapy and follow-up shoulder arthrography. Arch Phys Med Rehabil 78(8):857–859
Mitchell C, Adebajo A, Hay E, Carr A (2005) Shoulder pain: diagnosis and management in primary care. Br Med J 331(7525):1124–1128
Murdoch TB, Detsky AS (2013a) The inevitable application of big data to health care. JAMA 309(13):1351–1352
Murdoch TB, Detsky AS (2013b) The inevitable application of big data to health care. JAMA 309(13):1351–1352
Neviaser JS (1945) Adhesive capsulitis of the shoulder. J Bone Joint Surg Am 27(2):211–222
Oh CH, Schweitzer ME, Spettell CM (1999) Internal derangements of the shoulder: decision tree and cost-effectiveness analysis of conventional arthrography, conventional MRI, and MR arthrography. Skeletal Radiol 28(12):670–678
Pauker SG, Kassirer JP (1980) The threshold approach to clinical decision making. N Engl J Med 302(20):1109–1117
Ramesh AN, Kambhampati C, Monson JRT, Drew PJ (2004) Artificial intelligence in medicine. Ann R Coll Surg Engl 86(5):334
Rygielski C, Wang JC, Yen DC (2002) Data mining techniques for customer relationship management. Technol Soc 24(4):483–502
Ryu KN, Lee SW, Rhee YG, Lim JH (1993) Adhesive capsulitis of the shoulder joint: usefulness of dynamic sonography. J Ultrasound Med 12(8):445–449
CAS PubMed Google Scholar
Shaffer B, Tibone JE, Kerlan RK (1992) Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am 74(5):738–746
Sharma RK, Bajekal RA, Bhan S (1993) Frozen shoulder syndrome. Int Orthop 17(5):275–278
Sox MD, Harold C (1996) The evaluation of diagnostic tests: principles, problems, and new developments. Annu Rev Med 47(1):463–471
Sox HC, Blatt MA, Higgins MC, Marton KI (1988). Measuring the outcome of care. Med Decis Mak 201–237
Wahbeh AH, Al-Radaideh QA, Al-Kabi MN, Al-Shawakfa EM (2011) A comparison study between data mining tools over some classification methods. International Journal of Advanced Computer Science and Applications 8(2):18–26
Weinstein MC, Fineberg HV, Elstein AS, Frazier HS, Neuhauser D, Neutra RR, McNeil BJ (1980) Clinical Decision Analysis. WB Saunders Co., Philadelphia
Witten IH, Frank E (2005) Data mining: practical machine learning tools and techniques. Morgan Kaufmann, Burlington
Woodward TW, Best TM (2000) The painful shoulder: part I clinical evaluation. Am Fam Physician 61(10):3079–3089
Download references
Authors’ contributions
HB and MUA carried out the algorithm designing, conducted experiments, participated in the sequence alignment and drafted the manuscript. WHB and FB participated in the sequence alignment. HB, WHB and MUA participated in the design of the study and performed the statistical analysis. FB validated the algorithms from clinical perspective and provided annotations. All authors read and approved the final manuscript.
Acknowledgements
We are thankful to Pakistan Institute of Medical Sciences (PIMS) for their clinical support and help. They also helped us in gathering patient’s data.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and affiliations.
National University of Sciences and Technology, Islamabad, Pakistan
Humaira Batool, M. Usman Akram & Wasi Haider Butt
Riphah College of Rehabilitation Sciences, Riphah International University Islamabad, Islamabad, Pakistan
Fouzia Batool
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to M. Usman Akram .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Cite this article.
Batool, H., Usman Akram, M., Batool, F. et al. Intelligent framework for diagnosis of frozen shoulder using cross sectional survey and case studies. SpringerPlus 5 , 1840 (2016). https://doi.org/10.1186/s40064-016-3537-y
Download citation
Received : 13 June 2016
Accepted : 13 October 2016
Published : 21 October 2016
DOI : https://doi.org/10.1186/s40064-016-3537-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Random Forest
- Freeze Shoulder
- Unstructured Data
- Data Mining Model
- Statistic Regression Model

Frozen shoulder research may hold the key to understanding fibrosis resolution
R esearchers have identified how cells work to resolve frozen shoulder, opening up potential new targets for treatment and reducing the need for surgery.
Frozen shoulder is a painful and disabling condition affecting the ligaments that form the shoulder joint capsule. Patients experience severe stiffening of their affected shoulder which can last for several years, interfering with activities of daily life.
Frozen shoulder is a unique musculoskeletal disease as it unusually resolves spontaneously over time. This distinguishes the condition from most fibrotic (scarring) diseases that are progressive and irreversible, for example knee arthrofibrosis affecting the ligaments comprising the knee capsule after joint replacement.
Senior author Professor Stephanie Dakin, Versus Arthritis Career Development Fellow, and the team at NDORMS studied tissues collected from frozen shoulder patients undergoing surgery to improve their shoulder mobility. Their work is published in the journal Nature Communications .
"We purposefully studied tissues from patients with advanced-stage frozen shoulder to understand how the condition ultimately resolves. Using cutting-edge technologies, we identified that the shoulder capsule is predominantly comprised of fibroblasts (the major cell types that form ligaments) and macrophages, a type of immune cell.
"We discovered that distinct populations of macrophages in the shoulder capsule are enriched to resolve inflammation. We performed experiments using patient-derived cells, revealing that crosstalk between these resolving macrophages and fibroblasts reduced inflammation and promoted tissue remodeling, providing us with cellular evidence of how frozen shoulder resolves.
"We next compared the resolving macrophages identified in the shoulder capsule with the same cell population found in synovial tissues from rheumatoid arthritis patients who were in disease remission. This analysis supported the initial findings that resolving macrophages brought about resolution of inflammation in synovial tissues and resolution of fibrosis in the shoulder capsule.
"Finally, we analyzed fetal shoulder tissues, identifying resolving macrophage and fibroblast populations comparable to those in frozen shoulder. This suggests that the template to resolve fibrosis is established during shoulder development," said Dakin.
Collectively, this study identifies that targeting crosstalk between resolving cell types in the shoulder capsule could accelerate resolution of frozen shoulder, addressing an unmet clinical requirement for patients and reducing the need for surgery. Importantly, this work also provides a basis for potential therapeutic resolution of persistent fibrotic diseases beyond the shoulder joint.
More information: Michael T. H. Ng et al, A single cell atlas of frozen shoulder capsule identifies features associated with inflammatory fibrosis resolution, Nature Communications (2024). DOI: 10.1038/s41467-024-45341-9
Provided by NDORMS, University of Oxford
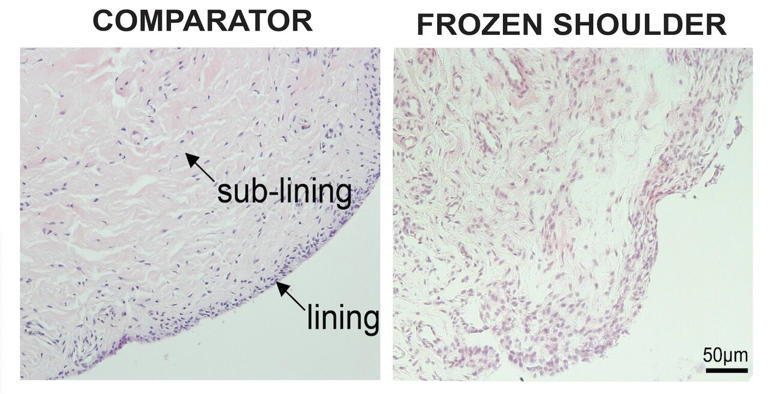
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Can Chiropr Assoc
- v.44(3); 2000 Sep
Adhesive capsulitis: a case report
Adhesive capsulitis or frozen shoulder is an uncommon entity in athletes. However, it is a common cause of shoulder pain and disability in the general population. Although it is a self limiting ailment, its rather long, restrictive and painful course forces the affected person to seek treatment. Conservative management remains the mainstay treatment of adhesive capsulitis. This includes chiropractic manipulation of the shoulder, therapeutic modalities, mobilization, exercise, soft tissue therapy, nonsteroidal anti-inflammatory drugs, and steroid injections. Manipulation under anesthesia is advocated when the conservative treatment fails. A case of secondary adhesive capsulitis in a forty-seven-year-old female recreational squash player is presented to illustrate clinical presentation, diagnosis, radiographic assessment and conservative chiropractic management. The patient’s shoulder range of motion was full and pain free with four months of conservative chiropractic care.
Full text is available as a scanned copy of the original print version. Get a printable copy (PDF file) of the complete article (2.5M), or click on a page image below to browse page by page. Links to PubMed are also available for Selected References .
Images in this article
Figure 1 on p.171
Figure 2 on p.172
Figure 3 on p.172
Click on the image to see a larger version.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Locke S, Colquhoun D, Briner M, Ellis L, O'Brien M, Wollstein J, Allen G. Squash racquets. A review of physiology and medicine. Sports Med. 1997 Feb; 23 (2):130–138. [ PubMed ] [ Google Scholar ]
- Montpetit RR. Applied physiology of squash. Sports Med. 1990 Jul; 10 (1):31–41. [ PubMed ] [ Google Scholar ]
- Silko GJ, Cullen PT. Indoor racquet sports injuries. Am Fam Physician. 1994 Aug; 50 (2):374–384. [ PubMed ] [ Google Scholar ]
- Berson BL, Rolnick AM, Ramos CG, Thornton J. An epidemiologic study of squash injuries. Am J Sports Med. 1981 Mar-Apr; 9 (2):103–106. [ PubMed ] [ Google Scholar ]
- Chard MD, Lachmann SM. Racquet sports--patterns of injury presenting to a sports injury clinic. Br J Sports Med. 1987 Dec; 21 (4):150–153. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Anton HA. Frozen shoulder. Can Fam Physician. 1993 Aug; 39 :1773–1778. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grubbs N. Frozen shoulder syndrome: a review of literature. J Orthop Sports Phys Ther. 1993 Sep; 18 (3):479–487. [ PubMed ] [ Google Scholar ]
- Wadsworth CT. Frozen shoulder. Phys Ther. 1986 Dec; 66 (12):1878–1883. [ PubMed ] [ Google Scholar ]
- Neviaser TJ. Adhesive capsulitis. Orthop Clin North Am. 1987 Jul; 18 (3):439–443. [ PubMed ] [ Google Scholar ]
- Miller MD, Wirth MA, Rockwood CA., Jr Thawing the frozen shoulder: the "patient" patient. Orthopedics. 1996 Oct; 19 (10):849–853. [ PubMed ] [ Google Scholar ]
- Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975; 4 (4):193–196. [ PubMed ] [ Google Scholar ]
- Lundberg BJ. The frozen shoulder. Clinical and radiographical observations. The effect of manipulation under general anesthesia. Structure and glycosaminoglycan content of the joint capsule. Local bone metabolism. Acta Orthop Scand Suppl. 1969; 119 :1–59. [ PubMed ] [ Google Scholar ]
- Pearsall AW, Speer KP. Frozen shoulder syndrome: diagnostic and treatment strategies in the primary care setting. Med Sci Sports Exerc. 1998 Apr; 30 (4 Suppl):S33–S39. [ PubMed ] [ Google Scholar ]
- Emig EW, Schweitzer ME, Karasick D, Lubowitz J. Adhesive capsulitis of the shoulder: MR diagnosis. AJR Am J Roentgenol. 1995 Jun; 164 (6):1457–1459. [ PubMed ] [ Google Scholar ]
- Rizk TE, Christopher RP, Pinals RS, Higgins AC, Frix R. Adhesive capsulitis (frozen shoulder): a new approach to its management. Arch Phys Med Rehabil. 1983 Jan; 64 (1):29–33. [ PubMed ] [ Google Scholar ]
- Mao CY, Jaw WC, Cheng HC. Frozen shoulder: correlation between the response to physical therapy and follow-up shoulder arthrography. Arch Phys Med Rehabil. 1997 Aug; 78 (8):857–859. [ PubMed ] [ Google Scholar ]
- Polkinghorn BS. Chiropractic treatment of frozen shoulder syndrome (adhesive capsulitis) utilizing mechanical force, manually assisted short lever adjusting procedures. J Manipulative Physiol Ther. 1995 Feb; 18 (2):105–115. [ PubMed ] [ Google Scholar ]
- Baslund B, Thomsen BS, Jensen EM. Frozen shoulder: current concepts. Scand J Rheumatol. 1990; 19 (5):321–325. [ PubMed ] [ Google Scholar ]
- Hill JJ, Jr, Bogumill H. Manipulation in the treatment of frozen shoulder. Orthopedics. 1988 Sep; 11 (9):1255–1260. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
This study presents a systemic view on the pathogenesis of frozen shoulder with the strength of evidence-based medicine as the basis of a systemic proposal for both the diagnostic and therapeutic levels. FS is a dysfunction related to pathologies such as diabetes, Parkinson's, Dupuytren's and hypothyroidism.
stiff shoulder, commonly diagnosed as frozen shoulder, is assessed without consideration of the entire shoulder complex. The biomechanics of the shoulder complex must be re-evaluated before each treatment session to determine the appropriate course of treatment. This paper presents a treatment regime for the painful, stiff shoulder.
Diercks RL, Stevens M. Gentle thawing of the frozen shoulder: a prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two years. ... a case report. J Shoulder Elbow Surg. 2011; 20 (3):e23-e26. [Google Scholar] 63.
Frozen shoulder (FS) is a relatively common condition characterized by pain and stiffness of the shoulder joint. The exact cause of primary FS is unknown and in some patients the condition can persist for several years. Treatment strategies vary depending on stage of presentation, patient factors and clinician preferences.
Key Points. Question Are any treatment modalities for frozen shoulder associated with better outcomes than other treatments?. Findings In this meta-analysis of 65 studies with 4097 participants, intra-articular corticosteroid was associated with increased short-term benefits compared with other nonsurgical treatments, and its superiority appeared to last for as long as 6 months.
Frozen shoulder is a condition that results in development of thickened, fibrosed joint capsule, contraction of the joint, and reduced intra-articular volume. 1 The exact cause of these changes is unknown, with several possible processes suggested in the literature. 1 Over the years, uncertainty has surrounded the definition and classification ...
Injecting corticosteroids into the shoulder joint might help decrease pain and improve shoulder mobility, especially if given soon after frozen shoulder begins. Hydrodilatation. Injecting sterile water into the joint capsule can help stretch the tissue and make it easier to move the joint. This is sometimes combined with a steroid injection.
Adults with a differential diagnosis of frozen shoulder were referred from a rheumatologist-run shoulder clinic. Eight patients (2 men and 6 women) consecutively seen for treatment of frozen shoulder, at Addenbrookes NHS Trust in Cambridge, UK were included in this study. All patients consented to treatment and were fully informed of the plan ...
Frozen shoulder (adhesive capsulitis) is an inflammatory condition affecting the capsule of the glenohumeral joint. It is characterised by a painful restricted range of passive and active movement in all planes of motion. The impact of frozen shoulder on affected individuals remains poorly characterised. In this study we sought to better understand the lived experience of people suffering from ...
Take the CE Test. Adhesive capsulitis (AC), also known as frozen shoulder, is a common and painful musculoskeletal disorder. The shoulder is a complex joint comprising 3 bones and multiple muscle groups, ligaments, and tendons. Accompanying the inflammation of the joint is stiffness that greatly restricts the patient's motion and strength.
Frozen shoulder is used to denote a limitation of. shoulder motion without abnormalities of the joint. surface, fracture or dislocation. The onset of frozen. shoulder is usually gradual and ...
Case Discussion. Adhesive capsulitis is a self-limited clinical syndrome characterized by painful, gradual loss of active and passive glenohumeral motion. Replacement of the fat in the rotator interval with the abnormal soft tissue that can encase the biceps anchor ( subcoracoid triangle sign ), can be classified on a sagittal T1-weighted image ...
Adhesive capsulitis (AC), is also known as frozen shoulder an insidious painful condition of the shoulder persisting more than 3 months. This inflammatory condition that causes fibrosis of the glenohumeral joint capsule is accompanied by gradually progressive stiffness and significant restriction of range of motion (typically external rotation). However, the patients may develop symptoms ...
Adhesive capsulitis (AC), also known as frozen shoulder, is a common and painful musculoskeletal disorder. The shoulder is a complex joint comprising 3 bones and multiple muscle groups, ligaments, and tendons. ... Adhesive capsulitis: a case study Orthop Nurs. 2009 Nov-Dec;28(6):279-83. doi: 10.1097/NOR.0b013e3181c01227. Author Janie M ...
Background and PurposeThe purpose of this study was to compare the use of 3 mobilization techniques—end-range mobilization (ERM), mid-range mobilization (MRM), and mobilization with movement (MWM)—in the management of subjects with frozen shoulder syndrome (FSS).SubjectsTwenty-eight subjects with FSS were recruited.MethodsA multiple-treatment trial on 2 groups (A-B-A-C and A-C-A-B, where A ...
Frozen shoulder, also called adhesive capsulitis, involves stiffness and pain in the shoulder joint. Signs and symptoms typically begin slowly, then get worse. Over time, symptoms get better, usually within 1 to 3 years. Having to keep a shoulder still for a long period increases the risk of developing frozen shoulder.
In this case report, we have used the acupoints are Zhongping, LI 14, and Ashi point. The strengths of the acupuncture management of this case and the implementation of acupuncture cause an improvement in movements of the shoulder in the patient suffering from frozen shoulder. After an acupuncture treatment 24 times, the symptoms are recovered ...
The patient to the right, Jeff, was diagnosed with a "frozen shoulder", also known as " adhesive capsulitis " (wikipedia). He experienced this condition as "stiffness and tightness" in his right shoulder that began over 18 months before his first visit with Barefoot Rehab. Previously, Jeff had undergone "physical therapy ...
1 Introduction. Frozen shoulder (FS) or adhesive capsulitis of the shoulder (FS) is a disorder characterized by its inflammatory and fibrotic process (Pietrzak, 2016).Codman first included the term "frozen shoulder" in 1934 (Dias et al., 2005).The predominant symptoms of this pathology in people suffering from it are stiffness, pain and a limitation in the range of active and passive ...
Objectives Frozen shoulder is a disease in which shoulder becomes stiff. Accurate diagnosis of frozen shoulder is helpful in providing economical and effective treatment for patients. This research provides the classification of unstructured data using data mining techniques. Prediction results are validated by K-fold cross-validation method. It also provides accurate diagnosis of frozen ...
Frozen shoulder is a painful and disabling condition affecting the ligaments that form the shoulder joint capsule. ... this study identifies that targeting crosstalk between resolving cell types ...
Among all the prevalent painful conditions of the shoulder, frozen shoulder remains one of the most debated and ill-understood conditions. ... JY, Kam M, Jung J. Association between fasting glucose levels and adhesive capsulitis in a normoglycemic population: A case-control study. Journal of Shoulder and Elbow Surgery. 2020; 29 (11):2240-2247
Nearly 50 million km2 of global land experiences seasonal transitions from predominantly frozen to thawed conditions, significantly impacting various ecosystems and hydrologic processes. In this study, we assessed the capability to retrieve surface freeze-thaw (FT) conditions using Sentinel-1 synthetic aperture radar (SAR) data time series at two agro-forested study sites, St-Marthe and St ...
Adhesive capsulitis or frozen shoulder is an uncommon entity in athletes. However, it is a common cause of shoulder pain and disability in the general population. Although it is a self limiting ailment, its rather long, restrictive and painful course forces the affected person to seek treatment. Conservative management remains the mainstay ...