- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
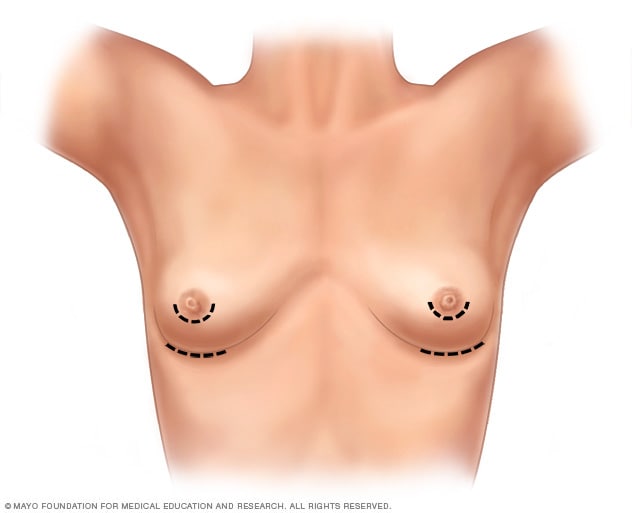
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
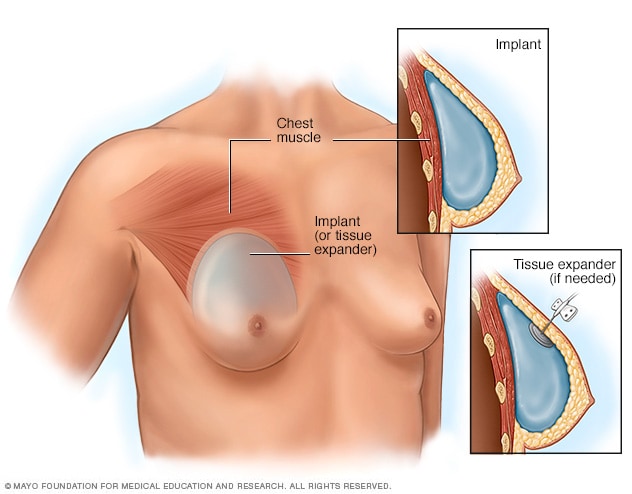
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
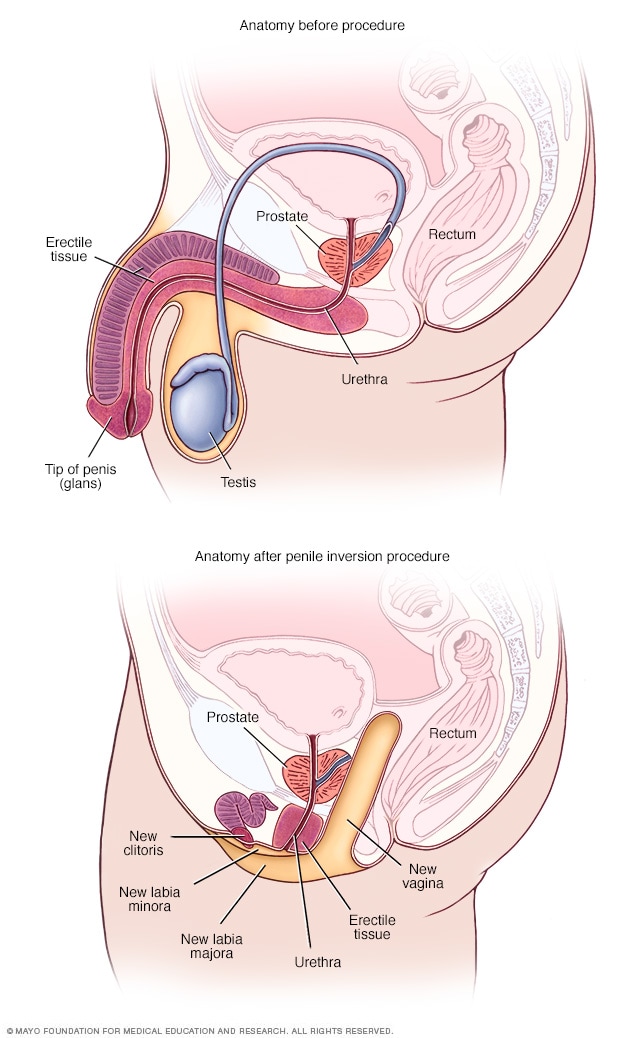
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
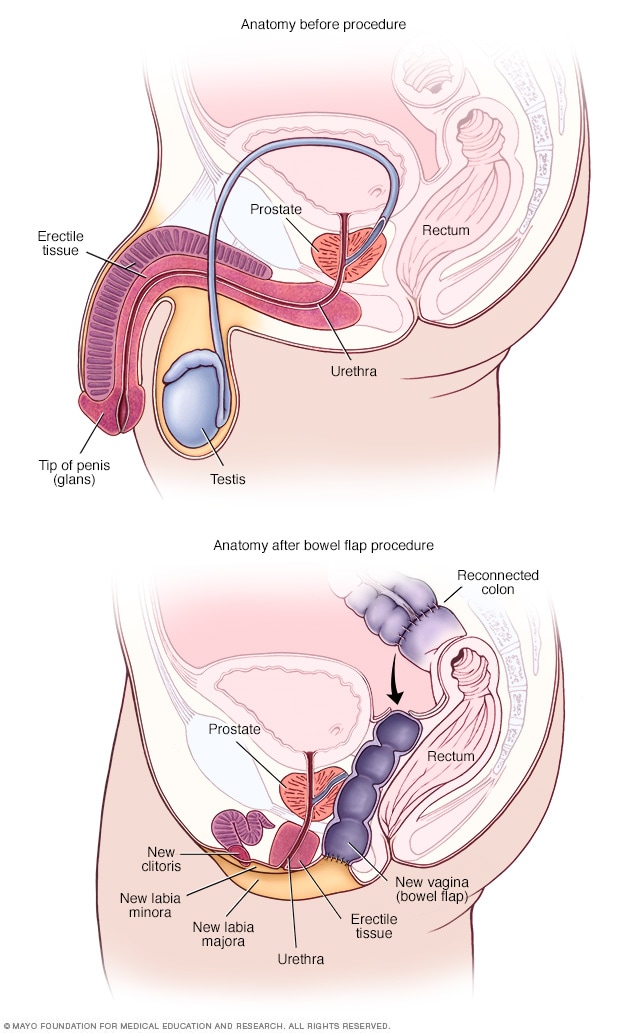
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
- Search Close Search submit
Accommodation bookings for the World Congress 2024 are offered only through direct bookings on our website. Beware of scams!
Female to Male Gender Reassignment Surgery (FTM GRS)
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia composed of the penis and scrotum.
The patient who is fit for this surgery must strictly follow the standard of care set by the World Professional Association of Transgender Healthcare (WPATH) or equivalent criteria; Express desire or live in another gender role (Female gender) long enough, under hormonal replacement therapy, evaluated and approved by a psychiatrist or other qualified professional gender therapist.
Apart from genital surgery, the patient would seek other procedures to allow them to live as males smoothly such as breast amputation, facial surgery, body surgery, etc.
Interested in having this procedure?
Useful Information
Ensure you consider all aspects of a procedure. You can speak to your surgeon about these areas of the surgery in more detail during a consultation.
The surgery is very complicated and only a handful of surgeons are able to perform this procedure. It is a multi-staged procedure, the first stage is the removal of the uterus, ovary, and vagina. The duration of the procedure is 2-3 hours. The second and later stages are penis and scrotum reconstruction which is at least 6 months later. There are several techniques for penile reconstruction depending on the type of tissue such as skin/fat of the forearm, skin/fat of the thigh, or adjacent tissue around the clitoris. This second stage of surgical time is between 3-5 hours. A penile prosthesis can be incorporated simultaneously or at a later stage. The scrotal prosthesis is also implanted later.
The procedure is done under general anesthesia and might be combined with spinal anesthesia for faster recovery by reducing the usage of anesthetic gas.
Inpatient/Outpatient
The patient will be hospitalized as an in-patient for between 5-7 days for each stage depending on the technique and surgeon. The patient will have a urinary catheter at all times in the hospital.
Additional Information
What are the risks.
The most frequent complication of FTM GRS is bleeding, wound infection, skin flap or graft necrosis, urinary stenosis and fistula, unsightly scar, etc. The revision procedure is scar revision, hair transplant, or tattooing to camouflage unsightly scars.
What is the recovery process?
During hospitalization, the patient must be restricted in bed continuously or intermittently for several days between 3-5 days. After release from the hospital, the patients return to their normal lives but not having to do physical exercise during the first 2 months after surgery. The patient will have a urinary catheter continuously for several weeks to avoid a urinary fistula. If the patient has a penile prosthesis, it would need at least 6 months before sexual intimacy.
What are the results?
With good surgical technique, the result is very satisfying with an improved quality of life. The patient is able to live in a male role completely and happily either on their own or with their female or male partners.
- Patient Information
- Global Statistics
- Media Centre
- World Congress
- Global Sponsors
- Privacy Policy
19 Mantua Road, Mount Royal, NJ 08061 United States
Registration number: 0330131
US Office: +1-603-643-2325
UK Office: +44 20 7038 7812
© 2022 International Society of Aesthetic Plastic Surgery. All Rights Reserved.
- Create an account
Log into My ISAPS
Forgot your password? Reset it here
Join the ISAPS Community
All members will continue to receive information relevant to their membership and ISAPS events.
I confirm by clicking below I would like to receive information about:
Welcome to the ISAPS community
By creating an account, you can:.
- Register for events
- Update your personal details
- Gain access to ISAPS publications and video library
- Become a member (explore our memberships here)
ISAPS Members can also:
- Access your member benefits
- Secure discounted member rates for events
- Read the Aesthetic Plastic Surgery Journal
- Gain full access to the video library
- View the Members Directory
- Update your 'Find a Surgeon' profile details
- Renew/Upgrade your Membership
The first step to becoming a part of the community is creating an account, so join us!
How Gender Reassignment Surgery Works (Infographic)
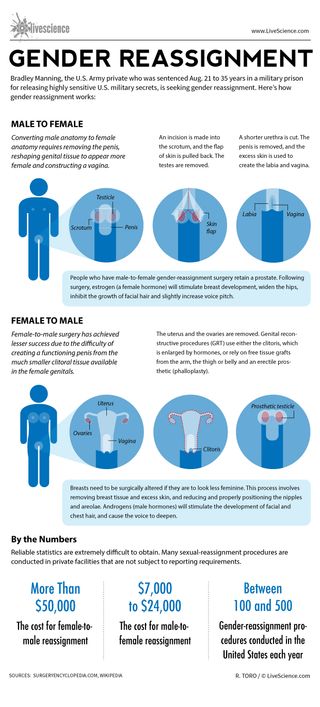
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
Space photo of the week: James Webb telescope reveals surprising starburst in ancient galaxy
Most Popular
By Anna Gora December 27, 2023
By Anna Gora December 26, 2023
By Anna Gora December 25, 2023
By Emily Cooke December 23, 2023
By Victoria Atkinson December 22, 2023
By Anna Gora December 16, 2023
By Anna Gora December 15, 2023
By Anna Gora November 09, 2023
By Donavyn Coffey November 06, 2023
By Anna Gora October 31, 2023
By Anna Gora October 26, 2023
- 2 James Webb telescope confirms there is something seriously wrong with our understanding of the universe
- 3 'You could almost see and smell their world': Remnants of 'Britain's Pompeii' reveal details of life in Bronze Age village
- 4 Amazfit Balance review
- 5 9,000-year-old rock art discovered among dinosaur footprints in Brazil
- 2 How much does Earth weigh?
- 3 Tardigrade proteins could slow aging in humans, small cell study finds
- 4 'Novel' swine flu virus sickens Pennsylvania child in 1st case of the year
MTFsurgery .net
- Orchiectomy
- Penile Inversion Vaginoplasty
- Peritoneal Vaginoplasty
- Rectosigmoid Vaginoplasty
- Vulvoplasty
- Non-Binary Bottom Surgery
- Facial Feminization Surgery
- Breast Augmentation
- Breast Augmentation w/ Fat Transfer
- Body Feminization
- What Is Board Certification?
- Getting Surgery In Thailand
- Vaginoplasty Hair Removal
- Follicular Cautery vs. Hair Removal
- Vaginal Stenosis After Vaginoplasty
- Importance of Dilation
- Breast Aug & Surgeon Experience
- Browse All Surgeons
Orchiectomy Surgeons
Vaginoplasty Surgeons
FFS Surgeons
- Breast Augmentation Surgeons
- Body Feminization Surgeons
- MTF Breast Augmentation
- MTF Vaginoplasty
MTF Surgery Guide

Looking for a Surgeon To Perform Your MTF Gender Reassignment Surgery? MTF Surgery's partner surgeons offer the full spectrum of male-to-female surgeries, including:
- Rectosigmoid Vaginoplasty & Sigma-Lead
- Body Sculpting / Body Feminization
Find a Surgeon »
Non-binary options for bottom surgery.

The Role of Fat Transfer in Breast Augmentation

Vaginal Stenosis and Robotic Peritoneal Flap Revision

Use It or Lose It: The Importance of Dilation Following Vaginoplasty

A Patient's Guide to Pre-Operative Hair Removal for Vaginoplasty

Board Certified: What Does It Mean?

Introduction to Gender Reassignment Surgery in Thailand

Featured Surgeons
Dr. Dany Hanna
Fellowship-trained Gender Surgeon based in Dallas who works exclusively with trans and non-binary people, offering gender-affirming genital surgeries.
Dr. Scott Mosser
Dr. Mosser is a highly experienced gender surgeon based in San Francisco who specializes in Breast Augmentation and Body Feminization.
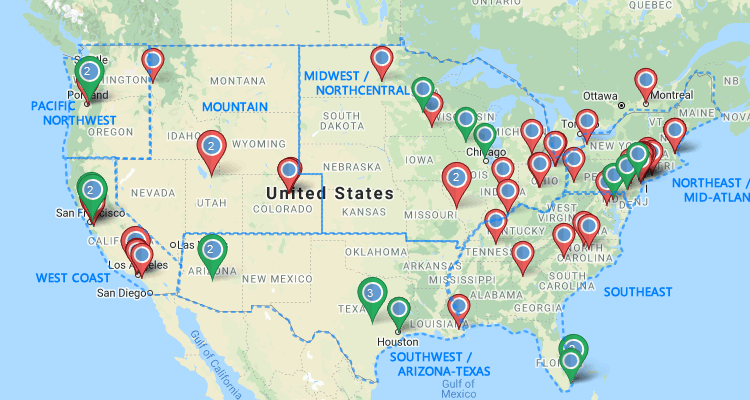
Map of Vaginoplasty Surgeons
Surgery Spotlight: Orchiectomy

What Patients Need To Know Before Choosing a Vaginoplasty Technique

Vulvoplasty: Assessing an Alternative to Vaginoplasty

Old Approach, New Application: Peritoneal Pull-Through Vaginoplasty
Dr. Thomas Satterwhite
Board-certified plastic surgeon in San Francisco who works exclusively with trans and non-binary patients.

Dr. Drew Marano
Fellowship-trained gender surgeon in New York City who is passionate about Robotic Vaginoplasty and providing stellar care.
Dr. Hope Sherie
Dr. Sherie is a board-certified surgeon who has extensive training in MTF surgery procedures, including Orchiectomy. Based in Charlotte.
Dr. John Whitehead
Experienced Vaginoplasty surgeon known for his exceptional surgical skills as well as his great bedside manner and communication style.
Breast Augmentation 101

Why Your Surgeon Needs Experience With Trans Breast Augmentation
There are significant differences between trans and cis chest measurements that have implications concerning breast implant selection and surgical approach, underlying the importance of selecting a surgeon who has experience specifically with Trans Breast Augmentation. Read more »
Dr. Amir Dorafshar
Dr. Dorafshar is an internationally distinguished craniofacial surgeon who specializes in gender-affirming facial surgery and is based in Chicago.
Dr. Praful Ramineni
With more than 15 years of working as a plastic surgeon, Dr. Ramineni is an experienced choice for natural-looking Facial Feminization outcomes.
Breast / Body Feminization Surgeons
Dr. Laurel Chandler
Dr. Chandler is a Harvard fellowship-trained plastic surgeon who has received specialty training in gender-affirming breast and facial surgery.
Dr. Walter Lin
Dr. Lin is a fellowship-trained Plastic Surgeon who performs gender-affirming Breast Augmentation for at the Buncke Clinic/San Francisco Transgender Institute.
Surgeons in Thailand
Dr. Kamol Pansritum
Dr. Kamol is recognized as one of the most experienced GRS Surgeons in the world. He currently performs more than 200 MTF reassignment surgeries a year. Bangkok, Thailand.
Dr. Pichet Rodchareon
Dr. Pichet is a board-certified plastic surgeon in Bangkok who is considered one of top SRS and FFS surgeons in Thailand. His training includes cranio and maxillo facial surgery.

Gender reassignment surgery: an overview
Affiliation.
- 1 Gender Surgery Unit, Charing Cross Hospital, Imperial College NHS Trust, 179-183 Fulham Palace Road, London W6 8QZ, UK.
- PMID: 21487386
- DOI: 10.1038/nrurol.2011.46
Gender reassignment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics. Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female-to-male transsexuals, are the core procedures in gender reassignment surgery. Nongenital procedures, such as breast enlargement, mastectomy, facial feminization surgery, voice surgery, and other masculinization and feminization procedures complete the surgical treatment available. The World Professional Association for Transgender Health currently publishes and reviews guidelines and standards of care for patients affected by gender dysphoria, such as eligibility criteria for surgery. This article presents an overview of the genital and nongenital procedures available for both male-to-female and female-to-male gender reassignment.
Publication types
- Plastic Surgery Procedures / methods*
- Plastic Surgery Procedures / psychology
- Postoperative Complications / prevention & control
- Postoperative Complications / psychology
- Sex Reassignment Surgery / methods*
- Sex Reassignment Surgery / psychology
- Transsexualism / diagnosis
- Transsexualism / psychology
- Transsexualism / surgery*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Anaesthesiol Intensive Ther
- v.53(4); 2021 Oct
- PMC10165989

Gender reassignment surgery – a narrative overview of anaesthetic considerations and implications
Priyanka mishra.
1 Department of Anaesthesia, All India Institute of Medical Sciences, Rishikesh, India
Amborish Nath
2 Department of Burns and Plastic Surgery, AIIMS Rishikesh, India
Ashutosh Kaushal
3 Department of Anaesthesia, AIIMS Bhopal, India
Rakesh Kain
4 Department of Burns and Plastic Surgery, VMMC Safdarjung Hospital, India
The twenty-first century, with its transforming ideology and rising acceptance, is witnessing an increased number of transgender people applying for gender reassignment surgery (GRS). The procedure of GRS is a lengthy and complex one involving the active collaboration of multiple disciplines including psychology, psychiatry, family medicine, plastic surgery, endocrinology, otolaryngology, urology, gynaecology, maxillofacial surgery, and anaesthesiology. The considerable paucity of literature regarding the management of patients presenting for GRS places health care providers at a disadvantage. It is imperative to cautiously regard the specific medical, emotional, social, and economic concerns regarding these patients. Health care providers need to be trained well to deal empathetically with such patients. The present literature about GRS deals mainly with the surgeon’s perspective, while the anaesthetist’s approach remains hazy. This is because GRS imposes the need for anaesthesiologists to search for better and more efficient modes of anaesthesia so as to improve prognosis and minimize the associated morbidity. Anaesthetists should understand the associated psychological aspects and effects of hormone therapy while performing an extensive and informative pre-operative evaluation to formulate an effective strategy. Providing the optimal modes for anaesthesia and keeping a cautious watch for complications along with timely intervention in the advent of the same comprise the approach for high-quality anaesthetic care. This review aims to provide a detailed overview of significant considerations and competent peri-operative outcomes in patients presenting for GRS.
The right to gender identity is one that amounts to contouring an individual’s personality. The present hour calls for an understanding of the meaning that the term transgender holds. It needs to be recognized that sex and gender although often used interchangeably are quite distinct. Sex refers to the physical characteristics (e.g. reproductive organs, chromosomes, hormones) employed to assign people to be female, male, or intersex. However, gender is more of a social construct, sprouting from cultural expectations that shape an individual’s external appearance and conduct [ 1 ]. Gender identity disorders have been frowned upon throughout their existence, making their treatment quite controversial. Gender dysphoria, earlier known as gender identity disorder, describes a heterogeneous group of individuals having the desire to possess secondary sexual characteristics of the opposite sex and possessing varying degrees of dissatisfaction regarding their anatomical gender [ 2 ]. Gender reassignment surgery (GRS) has proven to be a revolutionary intervention for patients with gender dysphoria, hence playing a pivotal role in alleviating their psychological discomfort. GRS is a multidisciplinary endeavour requiring a collaborative effort of psychology, psychiatry, family medicine, plastic surgery, endocrinology, otolaryngology, urology, gynaecology, maxillofacial surgery, and, last but not least, anaesthesiology.
Though GRS is becoming popular and more acceptable, there is still a relative lack of awareness of the process and its associated challenges amongst healthcare professionals. GRS has been performed with various approaches, single and multiple settings, hence imposing the need for anaesthetists to search for better and more efficient modes of anaesthesia to improve prognosis and minimize the associated morbidity. Just as surgeons develop areas of specialization to better care for their patients, anaesthesiologists have specialized in out- and inpatient surgery, both cosmetic and reconstructive.
The vanishing stigma, increasing demographic and acceptance of transgender and gender non-binary (TGNB) individuals calls for the field of medicine to catch up too. Hence, it is only discerning to expect that in coming times, they will present more frequently in general surgical settings and as they do, we would be well prepared to provide them high-quality peri-operative care. The ardent need to review this topic is rooted in the acknowledgement that although there are articles discussing the surgical and peri-operative outlooks of this procedure, there is scarce literature about the role, considerations, and strategies for anaesthesia in these procedures. This substantial shortfall in the published literature regarding the holistic concerns of GRS demands further strategies to be explored. We have discussed the anaesthetist strategy governed by consideration of the psychological aspects, effects of hormone therapy, optimal modes for anaesthesia and cautious watch for complications along with timely intervention for handling the same for providing high-quality anaesthetic care. In this article, we aim to analyse, understand, and formulate an approach for the entire procedure from an anaesthesiologist’s perspective.
RESEARCH METHODS
For this review, we retrieved data by a systematic literature search carried out in the research databases including PubMed, EMBASE, and Google Scholar. We included review articles, original studies, and case reports in our search.
History and current scenario
Dr Alan L. Hart, a TB specialist in the US, became one of the first female-to-male transgender persons who underwent gonadectomy and hysterectomy for his gender dysphoria in 1917 [ 3 ]. According to the 2018 census, nearly 0.6% of adults in the United States, or 1.5 million individuals, make up the transgender community. The estimated transgender population worldwide in the 2018 census ranged between 1% and 2% of the total population, which is nearly 900 million people. The American Society for Plastic Surgeons (ASPS) has reported an expeditious rise in GRS of up to 155% within the span of 2016 to 2017 [ 4 ]. With the legalization of transgender in most of the countries throughout the globe, the curve of GRS surgery is probably going to run further upslope.
OVERVIEW OF THE PROCEDURE
As already described, GRS requires a multidisciplinary approach. To begin with, the guidelines for the Recommendation of GRS indicate that the patient should be physically and psychologically prepared for surgery and should have a clear perception of the interventions to be performed along with the risks and possible complications [ 5 ]. Preparation for GRS is a multistage process that includes an elaborate psychological and wellbeing assessment of the patient. This may take nearly 12 months for complete psychosocial preparation of the patient to deal with the transition. Psychological evaluation is then followed by feminizing or masculinizing hormone replacement therapy (HRT) prescribed by a consulting endocrinologist. There should be documented “real-life experience in the desired role” for at least a whole year [ 5 ]. GRS ensues at the end of this process. The algorithm for the entire procedure is summarized in Figure 1 .

Algorithm for the procedure of gender reassignment surgery
INITIAL EVALUATION
What is required is having an elaborate understanding and assessment of the patient’s psychological, medical, legal, and social concerns. In developing countries, a substantial proportion of this relates to social and psychological aspects. The mental wellbeing assessment aims at evaluating and treating the mental health issues, offering suggestions with peer support with or without family therapy, assessing the gender expression level and the readiness of the patient for fully or partially reversible and irreversible interventions [ 6 ]. A reassuring and sensitive attitude towards the patient affirming that they would receive the best available care without any judgment aids in alleviating their anxiety and concerns. A holistic approach to assessment involves the multidisciplinary effort of various medical teams.
ANAESTHETIC PLAN OF CARE
Pre-operative assessment.
Apart from the routine preoperative assessment as for any other surgery, here we need to address specific history, examination, and investigations. The aim should be at the optimization of the patient care through risk reduction and informed consent [ 7 ]. It also caters to efficiently preparing the patient for surgery and anaesthesia while encouraging their compliance and participation.
- The biological sex and current gender identity of the patient should be noted.
- In the absence of specific gender assignment, measurements and calculations with gender specificity become tricky, e.g. ideal body weight, target-controlled propofol infusion using Schneider mode [ 8 ].
- Medical concerns.
- Patient’s preferred form of address (i.e., title, name, pronouns).
- History of use of anti-depressants, anti-anxiety, and other psychotropic drugs should be derived.
- Higher risk of tobacco, substance abuse, and sexually transmitted diseases (STDs) should be taken into consideration [ 9 ]. The prevalence of HIV was found to be 8.2% in the Indian transgender community as compared to 0.31% national HIV prevalence in India [ 10 ].
- History of multiple silicone injections can cue towards the existence of granulomatous disease, pneumonitis, organ failure, and infection [ 11 , 12 ].
- Masculinizing or feminizing therapy with a detailed description of drugs.
- Duration of therapy.
- Should be done with due respect to the privacy and dignity of the patient while maintaining professionalism.
- A chaperone of the gender of the patient’s choice should be present during physical examination.
- Should include assessment of any restrictive lung disease (common in female-to-male [FTM] chronic chest binders) [ 8 ].
- Most of the parameters should be evaluated as per the patient’s biological sex.
- However, for patients who have received HRT for more than six months, it has been suggested to compare the laboratory values to their cis-counterparts rather than their biological sex [ 13 ].
- There is still limited evidence regarding interpretations in different stages of gender transition.
Investigations to evaluate effects of HRT:
- complete lipid profile to screen for dyslipidaemias;
- liver function assessment to screen for any liver dysfunction;
- complete coagulation profile;
- screening for thromboembolism, breast and endometrial malignancy [ 15 , 16 ].
- Recognition and management of depression, anxiety, and regret.
- Advice on quitting smoking and explanation of its implications.
- Discontinuation of HRT for nearly 2-4 weeks before surgery in consultation with the endocrinologist and surgeon, keeping in consideration that prolonged withdrawal of hormones may culminate in the reversal of desirable effects [ 17 ].
- Considering the use of low-dose aspirin along HRT to reduce the risk of thromboembolism.
- Patients should be well informed regarding the overall cost, duration of hospitalization, surgical and anaesthetic options, complications, and post-operative care, and consent should be obtained.
Anaesthetic implications and concerns of HRT
It is not only relevant but imperative for an anaes-thesiologist to be aware of the various effects of HRT as it can guide the formulation of an efficient plan for anaesthesia. The various medications given in feminizing hormonal therapy include gonadotropin-releasing hormone agonists such as leuprolide and goserelin, spironolactone (androgen blockers), oral, parenteral or transdermal oestrogens and 5-α-reductase inhibitors such as finasteride. These medications can pose a higher risk of endocrine (e.g., diabetes) and cardiovascular (e.g., hypertension, venous thromboembolism [VTE]) implications. Testosterone therapy has been associated with derangements in liver function, which in turn complicate the drug metabolism. These risks are higher in the patients receiving oral formulations, hence necessitating the discontinuation of HRT for a few weeks prior to the surgery [ 16 ]. However, the withdrawal of hormone therapy can potentially make these patients more emotional, with rapid mood swings. This in turn can pose certain challenges for the anaesthetist in patient handling in the perioperative window ( Table 1 ). Incidence of postoperative delirium and post-operative nausea and vomiting (PONV) has also been found to be higher in patients on HRT. Some cases have revealed the occurrence of migraines in patients on anti-androgens. It is important to remember that in many cases these patients require lifelong administration of HRT unless curtailed by severe adverse effects.
Anaesthetic implications and concerns of hormone replacement therapy
Intra-operative considerations
The intra-operative care of these patients is distinctive as it needs the discernment of special anatomical, psychological, physiological, and pharmacological issues as numerated in Figure 2 . An anaesthesiologist needs to pay close attention to the following considerations:

Intra-operative considerations of gender reassignment surgery
- There should be clear instructions to the peri-operative team to maintain minimum traffic within the operating room (OR), particularly when the surgery involves exposure of the chest and/or genital regions.
- The patient’s preferred pronouns should be known and used at all times by the peri-operative staff when addressing the patient and any unnecessary questions should be discouraged.
Modes of anaesthesia
CSE – combined spinal-epidural, GA – general anaesthesia, LA – local anaesthesia, PNB – peripheral nerve block, PONV – post-operative nausea and vomiting, PACU – post-anaesthesia care unit, HRT – hormone replacement therapy.
- Transfer and positioning of the transgender patients who have undergone external body contouring procedures can be challenging and needs to be done with utmost caution.
- FTM transgenders may be using chest wraps and breast binders that need to be removed beforehand. Though there is still insufficient literature on the topic, chronic use of these tight chest binders can pose the risk of a restrictive respiratory pattern [ 14 ].
- Interestingly, even the most routine procedure of urinary catheterization can get tricky and challenging in the patients who have already had GRS concerning the urethra done, e.g. metoidioplasty with urethral lengthening, phalloplasty, or vaginoplasty.
- Patients who have recently had various facial aesthetic procedures such as rhinoplasty or jaw reconstruction may pose a challenge during bag and mask ventilation and should be handled with care and caution.
- Patients who have had previous voice pitch altering surgery such as chondroplasty or laryngoplasty may present as a difficult airway scenario as they pose the risk of tracheal stenosis or perforation, vocal cord damage, and dysphagia. Hence, a difficult airway cart should be kept ready [ 22 ].
- It needs to be taken into consideration that transgender women suffer from higher rates of HIV infection and might be on anti-retroviral therapy (ART). The various sedatives, anxiolytics, hypnotics, and antibiotics may present significant interactions with antiretroviral agents and result in altered drug metabolism [ 23 ].
- As these patients have been off steroid therapy for few weeks, they might experience steroid withdrawal syndrome. This can be prevented by administering a steroid bolus of 100-200 mg hydrocortisone intra-operatively.
- An anaesthetist needs to be vigilant for elevated intraoperative risks due to the possible existing respiratory, renal, cardiovascular, and hepatic compromise of the patient.
- VTE is a major perioperative concern due to the use of HRT medications and needs to be looked out for and relevant preventive interventions should be adopted. Cautious haemodynamic monitoring needs to be done for the early identification and management of this dreaded complication. Intraoperative prophylaxis should be provided with subcutaneous heparin and graded compression devices.
- Higher incidence of stroke has been linked to greater erythropoietin production and haematocrit and hence increased blood viscosity, attributed to parenteral testosterone therapy. Therefore, adequate hydration should be maintained for the patient [ 24 ].
- Considering the extensive nature of surgery, efficient pain control is imperative.
COMPLICATIONS
GRS presents with its arena of complications to be looked out for and dealt with. Amongst them, certain complications demand the anaesthesiologist’s ardent attention ( Table 3 ). These patients may be suffering from anaemia owing to the multiple and prolonged operations they undergo over some time. This needs to be taken care of by adopting appropriate pre-operative optimizing and perioperative blood loss reducing strategies. Two of the dreaded complications that the patients on oestrogen therapy should be monitored for are pulmonary embolism (PE) and deep vein thrombosis (DVT) [ 25 ]. These haematological events are attributed to peri-operative immobility, but due to the thrombotic effects of transgender HRT, there is a considerably higher risk of the same in these patients. The range of occurrence of VTE in transgender women on oestrogen therapy is from 0% to 6% [ 26 ]. The hypercoagulable state resulting due to HRT medications (both male-to-female and FTM) can precipitate cerebrovascular accidents and myocardial infarction and also aggravate any pre-existing coronary disease. This in turn warrants maintenance of adequate hydration at all times along with utmost care during all the phases of anaesthesia, supplemented by cautious intra-operative monitoring.
Complications in gender reassignment surgery, associated risk factors and preventive measures
The extensive wound surface, adverse effects of steroid therapy, and repeated surgery make these patients more susceptible to various infections, necrotizing fasciitis, and septicaemia [ 27 ]. The various other surgical complications include gastrointestinal events (e.g., rectal injury and rectovaginal fistula) and urinary tract complications (e.g., urethral stricture, fistula, and incontinence). Some unspecific events such as inguinal hernia, compartment syndrome, and asymmetry can also be witnessed after the surgery.
POSTOPERATIVE CONSIDERATIONS
The challenges continue after the completion of surgery, as the post-operative period in these patients has its concerns of postoperative pain, anxiety, depression, withdrawal, and at times regret [ 28 ]. Amongst the other parts of a detailed handover to the post-operative care team, one of the most important is validation of the patient’s preferred pronoun and name to avoid any unnecessary and repeated questioning [ 8 ]. It should be ensured that there is a multi-pronged approach with optimal analgesic strategies to manage post-operative pain. This can include epidural anaesthesia, intravenous analgesics, peripheral nerve blocks, parenteral therapy, and patient-controlled analgesia (PCA). There should be a collaborative approach to tend to the patient’s mental health, as well as social and spiritual needs. Canner et al . [ 29 ] reported that transgender patients require a higher level of care, highlighting the significance of formal training of health care providers for best practices to encourage and achieve a respectful and holistic approach towards anaesthesia delivery. Early implementation of social work and community support in the postoperative period plays a major part to smoothen the process of discharge while assisting the transition to patient recovery.
IMPORTANCE OF TEAMWORK AND COLLABORATION
As already mentioned, the complex procedure of gender reassignment involves a multidisciplinary effort of psychology, psychiatry, family medicine, plastic surgery, endocrinology, otolaryngology, urology, gynaecology, maxillofacial surgery, and anaesthesia. Evaluation by mental health professionals for eligibility criteria is a precondition for GRS as it can be a physically, emotionally, financially, and socially overwhelming procedure. The plastic surgeons, otolaryngologists, urologists and all other contributing surgeons need to have clear and competent participation in this long-term therapy. The surgeon and endocrinologist should also collaborate in optimizing HRT withdrawal and restart in the peri-operative period. The current state of affairs is still lacking such a closed loop inter-disciplinary approach. Hence, an efficient and especially dedicated team can help in achieving the ultimate goal of quality management to harness favourable outcomes for the patient.
CONCLUSIONS
Various parts of the world still suffer through an under-representation of the transgender community which stays confined to the margins of society. However, there is no denying the fact that with the changing tide and rising acceptability of transgender persons, the field of medicine is going to be presented with an increased proportion of these patients. The specific emotional, physiological, and pharmacological concerns coupled with the collaborative interplay of multiple disciplines make this class of patients a challenging lot. It is the attitude, preparedness and prudence of the medical team that can bring about a favourable outcome. Proper training of various health care professionals appears imperative here to empathetically handle and efficiently treat these patients. We would not be wrong in believing that the quality care provided before, during and after surgery has a substantial impact on patient outcomes after GRS. This simultaneously deserves acknowledgement of the fact that extensive studies and evidence are needed to understand and define better strategies for perioperative care in patients presenting for GRS.
ACKNOWLEDGEMENTS
Financial support and sponsorship, conflict of interest.
- FIND A PROVIDER
I'm a Candidate
I'm a Provider
Log In / Sign Up
I'm a candidate
Provider login
I'm a provider
List your practice
FTM Gender Confirmation: Genital Construction
The specifics, the takeaway.
Download the app
As part of a transgender individual’s transition, genital reassignment surgery alters female genitalia into male genitalia.
Written By: Erin Storm, PA-C
Published: October 07, 2021
Last updated: February 18, 2022
- Procedure Overview
- Ideal Candidate
- Side Effects
- Average Cost
thumbs-up Pros
- Can Help Complete A Gender Affirmation Journey
thumbs-down Cons
- Potentially Cost Prohibitive
Invasiveness Score
Invasiveness is graded based on factors such as anesthesia practices, incisions, and recovery notes common to this procedure.
Average Recovery
Application.
Surgical Procedure
$ 50000 - $ 100000
What is a female to male (FTM) gender reassignment surgery?
Female to male (FTM) gender reassignment surgery is also known as sex reassignment surgery (SRS), genital construction, and generally as gender confirmation surgery. These plastic surgery procedures are used by transgender patients to remove and alter female genitalia into traditional male genitalia.
Plastic surgeons will usually perform a hysterectomy and salpingo-oophorectomy to remove the uterus and ovaries. A vaginoplasty or vaginectomy will close the vagina, the erectile tissue of the clitoris is released and with the mons portion of the pubic area a neo-phallus is created (phalloplasty or metoidioplasty). The labia majora then become the scrotum (scrotoplasty), bilateral testicular implants are placed, and finally the urethra is lengthened through the newly created penile tissue.
Typically gender reassignment surgery is performed as a last step in a transgender individuals transition journey. Guidelines on standards of care from The World Professional Association for Transgender Health (WPATH) state candidates must have letters of recommendation from their mental health professional and healthcare provider, have been living full time as a man for one year, and have completed one year of hormonal therapy to be eligible.
Information on facial masculinization surgeries, top surgeries (like a mastectomy), and other female to male gender affirming surgeries as part of a gender transition for transmen can be found in our comprehensive guide to FTM gender affirmation solutions .
What concerns does a FTM gender reassignment surgery treat?
- Transmasculine Bottom Surgery & Genital Construction : Female to male gender reassignment surgery creates male genitalia that are aesthetically authentic and functional.
Who is the ideal candidate for a FTM gender reassignment surgery?
The ideal candidate for FTM gender reassignment surgery is a transgender man seeking to complete his physical embodiment of his gender identity. This reconstructive genital surgery creates functioning male genitalia. FTM gender reassignment surgery is not recommended for those who have not been on hormone therapy for one year, have not been living full time as a man for one year, do not have letters of recommendation from their mental health provider and physician, children under the age of 18, and those with certain chronic medical conditions.
What is the average recovery associated with a FTM gender reassignment surgery?
Most patients experience four to six weeks of recovery time following a FTM gender reassignment surgery. Patients can expect bruising, swelling, and tenderness following the procedure. A urinary catheter is typically used for two to three weeks.
What are the potential side effects of a FTM gender reassignment surgery?
Possible side effects following a FTM gender reassignment surgery include bleeding, swelling, bruising, incision site infection, altered sensation, difficulty urinating due to strictures, difficulty with sexual function, prolonged edema, and complications from anesthesia or the procedure.
What can someone expect from the results of a FTM gender reassignment surgery?
The results of FTM gender reassignment surgery are permanent. This procedure creates functional male genitalia and removes all female genitalia.
What is the average cost of a FTM gender reassignment surgery?
What to expect.
A FTM gender reassignment surgery creates male genitalia. Here is a quick guide for what to expect before, during, and after a FTM gender reassignment surgery:
Before Surgery
- Prophylactic antibiotics or antivirals may be prescribed
- Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol, Aspirin, and prescription anticoagulants
- Stop smoking four weeks prior to the procedure and continue cessation for four weeks post op
- No alcohol two days prior to the procedure
- Do not eat or drink six hours before
During Surgery
- General anesthesia
- A hysterectomy, oophorectomy, and vaginoplasty are performed
- The clitoris is released from suspensory ligaments
- The neo-phallus and scrotum are created with existing tissues
- Testicular implants are placed - The urethra is lengthened
Immediately After Surgery
- Swelling, bruising, and tenderness
1 - 30 Days After Treatment & Beyond
- Resume most activities after a few days
- Swelling typically resolves within a few weeks
- Avoid strenuous activity for two to four weeks
- Remove urinary catheter after two to three weeks
Result Notes
- Results are permanent
- Proper aftercare will ensure optimal results
- Any revisions needed are typically not performed until six months after the initial procedure
Gender confirmation surgeries for transgender individuals are an important component of transgender health and in creating an embodied gender identity. Gender reassignment surgery allows transgender men who feel it is a part of their transition to more fully embrace their gender identity.
To learn more about our content creation practices, visit our Editorial Process page .
Source List
AEDIT uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- American Society of Plastic Surgeons Gender Confirmation Surgeries plasticsurgery.org
- Karel E Y Claes Chest Surgery for Transgender and Gender Nonconforming Individuals PubMed.gov ; 2018-07-02
Related Procedures

FTM Gender Confirmation Solutions

Adam’s Apple Enhancement

FTM Gender Confirmation: Facial Masculinization

FTM Gender Confirmation: Transmasculine Top & Bottom Surgeries
View all procedures
Learn More About FTM Gender Confirmation: Genital Construction in The AEDITION

Gender Transitioning And Skincare: Taking Care Of Your Changing Face
Side effects of hormone therapy often show up on the skin in the form of acne, pigmentation, and uneven skin texture. Here’s what you need to know about the most common skin concerns and treatment options.

Everything You Need To Know About Clavicle Surgery
Clavicle (a.k.a. collarbone) surgery is growing in popularity among patients seeking to change the length and prominence of the bone, enhance their décolleté, and improve the overall proportion of the body.

Finding The Right Plastic Surgeon, Dermatologist, Or Cosmetic Dentist
When considering a cosmetic procedure, it is so important to find the right doctor for you.
Discover more articles

‘Try on’ aesthetic procedures and instantly visualize possible results with AEDIT and our patented 3D aesthetic simulator.
Find Top Aesthetic Providers Near You
Providers by locations.
- Alpharetta, GA Providers
- Cockeysville, MD Providers
- Fall River, MA Providers
- Lone Tree, CO Providers
- Metairie, LA Providers
- Minneapolis, MN Providers
- More Locations
- New Haven, CT Providers
- Scottsdale, AZ Providers
- Skokie, IL Providers
- Southfield, MI Providers
- Springdale, AR Providers
- Tampa, FL Providers
- Torrance, CA Providers
- Washington, DC Providers
Providers by Specialties
- Cosmetic Dentistry Providers
- Cosmetic Dermatology Providers
- Cosmetic Surgery Providers
- Dermatologic Surgery Providers
- Dermatology Providers
- Facial Plastic and Reconstructive Surgery Providers
- General Surgery Providers
- Hair Restoration Surgery Providers
- Head and Neck Surgery Providers
- Medspa Providers
- More Procedures
- Oculoplastic Surgery Providers
- Plastic and Reconstructive Surgery Providers
- Vaginal Rejuvenation Providers
Providers by Procedures
- Acne Scar Treatment Providers
- Acne Treatment Providers
- Birthmark Removal Providers
- Blepharoplasty Providers
- Botox Providers
- Brow Lift Providers
- Buccal Fat Removal (Cheek Reduction) Providers
- Cheek Augmentation (Cheek Implants) Providers
- Cheek Surgery Providers
- Chemical Peels Providers
- Chin Surgery (Mentoplasty) Providers
- Dental Treatments Providers
- Dermabrasion Treatment Providers
- Dermal Fillers & Injectables Providers
- More Specialties
Wyoming passes bill to halt gender transition in minors

Mehaniq | Shutterstock
The State of Wyoming officially passed a law that bans the use of gender transitioning surgeries and puberty blockers on minors. Passed by the state’s senate on March 22 and signed into law by Governor Mark Gordon, the installation of Senate File 99 (SF99) brings the number of states with such protections to children at 24.
According to local Wyoming outlet WYO4 News , the law is known as the “children gender change prohibition.” In a press release, Gov. Gordon explained his choice to sign the bill:
“I signed SF99 because I support the protections this bill includes for children. However, it is my belief that the government is straying into the personal affairs of families,” Gordon added. “Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others.”
The law states that “gender transitioning and reassignment procedures are grounds for suspension or revocation of a physician’s or health care provider’s license …” It does, however, include exceptions in cases of a child “born with a medically verifiable genetic disorder of sex development.”
The law makes it clear that any exception to the rule must be conducted only with the consent of parents or guardians. The law does not prevent minors from pursuing mental health professionals for care , but it does prevent mental health workers from proposing gender transitioning surgery or medication.
On the same day, Governor Gordon vetoed House Bill 148: Regulation of Abortions. The governor’s office noted that this bill was originally designed to properly regulate abortions within the state, but was rejected due to amendments. Gov. Gordon believed that these amendments would have opened the law up to legal challenges. He said that the passage of a bill with such holes “would, in my mind, be derelict and would have only sacrificed additional unborn lives in Wyoming.”
Read more comments from Governor Gordon at WYO4 News .

Articles like these are sponsored free for every Catholic through the support of generous readers just like you.
Help us continue to bring the Gospel to people everywhere through uplifting Catholic news, stories, spirituality, and more.
Voice Pitch Shaping and Genderization: New Needs of Cosmetic Phonoplastic Surgery
- Original Articles
- Non-Surgical Procedures
- Published: 02 April 2024
Cite this article
- Zhijin Li 1 na1 ,
- Dingyue Zhang 2 na1 ,
- Hongsai Chen 3 ,
- Ying Liu 4 &
- Hayson Chenyu Wang ORCID: orcid.org/0000-0002-2958-1588 4
Voices can convey content, emotion, and essential information about an individual’s gender and social information. Closely related to gender identification and sexual attraction, voices also positively affect many psychological factors of individuals. Surgeries have evolved from treating congenital diseases to fulfilling an individual’s aesthetic needs for voice. Voice shaping is emerging as the next cosmetic surgery hotspot after skincare and appearance and body shaping. This paper summarizes the development of voice pitch shaping and genderization procedures out of the cosmetic need.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these evidence-based medicine ratings, please refer to the Table of Contents or the online Instructions to Authors https://www.springer.com/00266 .
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
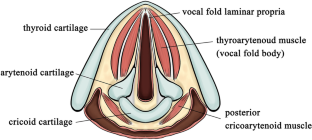
Apicella CL, Feinberg DR (2009) Voice pitch alters mate-choice-relevant perception in hunter-gatherers. Proc Biol Sci 276(1659):1077–1082
PubMed Google Scholar
Cartei V, Garnham A, Oakhill J, Banerjee R, Roberts L, Reby D (2019) Children can control the expression of masculinity and femininity through the voice. R Soc Open Sci 6(7):190656
Article PubMed PubMed Central Google Scholar
Kamachi M, Hill H, Lander K, Vatikiotis-Bateson E (2003) “Putting the face to the voice”: matching identity across modality. Curr Biol 13(19):1709–1714
Article CAS PubMed Google Scholar
Blank H, Anwander A, von Kriegstein K (2011) Direct structural connections between voice- and face-recognition areas. J Neurosci 31(36):12906–12915
Article CAS PubMed PubMed Central Google Scholar
Anderson JA (2014) Pitch elevation in trangendered patients: anterior glottic web formation assisted by temporary injection augmentation. J Voice 28(6):816–821
Article PubMed Google Scholar
Davies M (2014) Would you have surgery to change your VOICE? Rise in Chinese people undergoing radical procedures to sound deeper or more high-pitched. Daily Mail.com. http://dailym.ai/1p1j8xi
ABC News (2004) The latest in plastic surgery: the 'Voice-Lift'. ABC News.com. https://abcnews.go.com/GMA/DrJohnson/story?id=127887
Rha KH (n.d.) Plastic surgery to change not only appearance but voice. Medical Tourism Magazine. https://www.magazine.medicaltourism.com/article/plastic-surgery-to-change-not-only-appearance-but-voice .
Zhang Z (2016) Mechanics of human voice production and control. J Acoust Soc Am 140(4):2614
Gray SD, Titze IR, Alipour F, Hammond TH (2000) Biomechanical and histologic observations of vocal fold fibrous proteins. Ann Otol Rhinol Laryngol 109(1):77–85
Kim HT (2020) Vocal feminization for transgender women: current strategies and patient perspectives. Int J Gen Med 13:43–52
Hiramatsu H, Tokashiki R, Nakamura H et al (2012) Analysis of high-pitched phonation using three-dimensional computed tomography. J Voice 26(5):548–554
Hong YT, Hong KH, Jun JP, Hwang PH (2015) The effects of dynamic laryngeal movements on pitch control. Am J Otolaryngol 36(5):660–665
Roers F, Murbe D, Sundberg J (2009) Predicted singers’ vocal fold lengths and voice classification-a study of x-ray morphological measures. J Voice 23(4):408–413
Okui A, Konomi U, Kanazawa T et al (2020) Therapeutic efficacy of basic fibroblast growth factor in patients with vocal fold atrophy. Laryngoscope 130(12):2847–2852
Hodges-Simeon CR, Grail GPO, Albert G et al (2021) Testosterone therapy masculinizes speech and gender presentation in transgender men. Sci Rep 11(1):3494
Hillenbrand JM, Clark MJ (2009) The role of f(0) and formant frequencies in distinguishing the voices of men and women. Atten Percept Psychophys 71(5):1150–1166
Re DE, O’Connor JJ, Bennett PJ, Feinberg DR (2012) Preferences for very low and very high voice pitch in humans. PLoS ONE 7(3):e32719
Puts DA, Jones BC, DeBruine LM (2012) Sexual selection on human faces and voices. J Sex Res 49(2–3):227–243
Gray ML, Courey MS (2019) Transgender voice and communication. Otolaryngol Clin North Am 52(4):713–722
Brown KM, Dahl KL, Cler GJ, Stepp CE (2021) Listener age and gender diversity: effects on voice-based perception of gender. J Voice 35(5):739–745
Watt SO, Tskhay KO, Rule NO (2018) Masculine voices predict well-being in female-to-male transgender individuals. Arch Sex Behav 47(4):963–972
Leongomez JD, Pisanski K, Reby D et al (1840) Voice modulation: from origin and mechanism to social impact. Philos Trans R Soc Lond B Biol Sci 2021(376):20200386
Google Scholar
Nolan IT, Morrison SD, Arowojolu O et al (2019) The role of voice therapy and phonosurgery in transgender vocal feminization. J Craniofac Surg 30(5):1368–1375
Kitajima K, Tanabe M, Isshiki N (1979) Cricothyroid distance and vocal pitch. Experimental surgical study to elevate the vocal pitch. Ann Otol Rhinol Laryngol 88(1):52–55
Bernal GL, Morales LJ, Hernandez VJ, Beltran O (2016) Modified type IV thyroplasty (cricothyroid approximation) in a patient with androphonia. Acta Otorrinolaringol Esp 67(3):179–181
Gibbins N, Bray D, Harries ML (2011) Long-term quantitative results of an Isshiki type 4 thyroplasty-a case study. J Voice 25(3):283–287
Koufman JA, Isaacson G (1991) Laryngoplastic phonosurgery. Otolaryngol Clin North Am 24(5):1151–1177
Yang CY, Palmer AD, Murray KD, Meltzer TR, Cohen JI (2002) Cricothyroid approximation to elevate vocal pitch in male-to-female transsexuals: results of surgery. Ann Otol Rhinol Laryngol 111(6):477–485
Neumann K, Welzel C (2004) The importance of the voice in male-to-female transsexualism. J Voice 18(1):153–167
Tucker HM (1985) Anterior commissure laryngoplasty for adjustment of vocal fold tension. Ann Otol Rhinol Laryngol 94(6 Pt 1):547–549
Wagner I, Fugain C, Monneron-Girard L, Cordier B, Chabolle F (2003) Pitch-raising surgery in fourteen male-to-female transsexuals. Laryngoscope 113(7):1157–1165
Song TE, Jiang N (2017) Transgender phonosurgery: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 156(5):803–808
Mastronikolis NS, Remacle M, Biagini M, Kiagiadaki D, Lawson G (2013) Wendler glottoplasty: an effective pitch raising surgery in male-to-female transsexuals. J Voice 27(4):516–522
Remacle M, Matar N, Morsomme D, Veduyckt I, Lawson G (2011) Glottoplasty for male-to-female transsexualism: voice results. J Voice 25(1):120–123
Kim HT (2017) A new conceptual approach for voice feminization: 12 Years of experience. Laryngoscope 127(5):1102–1108
Orloff LA, Mann AP, Damrose JF, Goldman SN (2006) Laser-assisted voice adjustment (LAVA) in transsexuals. Laryngoscope 116(4):655–660
Kocak I, Akpinar ME, Cakir ZA, Dogan M, Bengisu S, Celikoyar MM (2010) Laser reduction glottoplasty for managing androphonia after failed cricothyroid approximation surgery. J Voice 24(6):758–764
Isshiki N, Taira T, Tanabe M (1983) Surgical alteration of the vocal pitch. J Otolaryngol 12(5):335–340
CAS PubMed Google Scholar
Geneid A, Rihkanen H, Kinnari TJ (2015) Long-term outcome of endoscopic shortening and stiffening of the vocal folds to raise the pitch. Eur Arch Otorhinolaryngol 272(12):3751–3756
Cartei V, Bond R, Reby D (2014) What makes a voice masculine: physiological and acoustical correlates of women’s ratings of men’s vocal masculinity. Horm Behav 66(4):569–576
Tsuji DH, Sennes LU, Imamura R, Trezza PM, Hanayama EM (2002) Cirurgia para diminuir a freqüência fundamental da voz - tireoplastia tipo III de Isshiki. Rev Brasileira de Otorrinolaringologia 68(1):133–138
Article Google Scholar
Cler GJ, McKenna VS, Dahl KL, Stepp CE (2020) Longitudinal case study of transgender voice changes under testosterone hormone therapy. J Voice 34(5):748–762
Buckley DP, Dahl KL, Cler GJ, Stepp CE (2020) Transmasculine voice modification: a case study. J Voice 34(6):903–910
Dahl KL, Francois FA, Buckley DP, Stepp CE (2022) Voice and speech changes in transmasculine individuals following circumlaryngeal massage and laryngeal reposturing. Am J Speech Lang Pathol 31(3):1368–1382
Aaron Ziegler TH, Wiedrick J, Helou LB (2018) Effectiveness of testosterone therapy for masculinizing voice in transgender patients: a meta-analytic review. Int J Transgenderism 19(1):25–45
Allen JE, Belafsky PC (2009) Botulinum toxin in the treatment of vocal fold nodules. Curr Opin Otolaryngol Head Neck Surg 17(6):427–430
Biello A, Volner K, Song SA (2022) Laryngeal botulinum toxin injection. StatPearls, Treasure Island (FL)
Whurr R, Lorch M, Fontana H, Brookes G, Lees A, Marsden CD (1993) The use of botulinum toxin in the treatment of adductor spasmodic dysphonia. J Neurol Neurosurg Psychiatry 56(5):526–530
Estes C, Sadoughi B, Coleman R, Sarva H, Mauer E, Sulica L (2018) A prospective crossover trial of botulinum toxin chemodenervation versus injection augmentation for essential voice tremor. Laryngoscope 128(2):437–446
deSilva B, Crenshaw D, Matrka L, Forrest LA (2019) Vocal fold botulinum toxin injection for refractory paradoxical vocal fold motion disorder. Laryngoscope 129(4):808–811
Cannito MP, Kahane JC, Chorna L (2008) Vocal aging and adductor spasmodic dysphonia: response to botulinum toxin injection. Clin Interv Aging 3(1):131–151
Isshiki N, Tanabe M, Ishizaka K, Broad D (1977) Clinical significance of asymmetrical vocal cord tension. Ann Otol Rhinol Laryngol 86(1 Pt 1):58–66
Bultynck C, Cosyns M, T’Sjoen G, Van Borsel J, Bonte K (2021) Thyroplasty Type III to lower the vocal pitch in trans men. Otolaryngol Head Neck Surg 164(1):157–159
Hoffman MR, Devine EE, Remacle M, Ford CN, Wadium E, Jiang JJ (2014) Combined type IIIB with bilateral type I thyroplasty for pitch lowering with maintenance of vocal fold tension. Eur Arch Otorhinolaryngol 271(6):1621–1629
Pasternak K, Francis DO (2019) An update on treatment of voice-gender incongruence by otolaryngologists and speech-language pathologists. Curr Opin Otolaryngol Head Neck Surg 27(6):475–481
Casado JC, O’Connor C, Angulo MS, Adrian JA (2016) Wendler glottoplasty and voice-therapy in male-to-female transsexuals: results in pre and post-surgery assessment. Acta Otorrinolaringol Esp 67(2):83–92
LeJeune FE, Guice CE, Samuels PM (1983) Early experiences with vocal ligament tightening. Ann Otol Rhinol Laryngol 92(5):475–477
Tucker HM (1985) Anterior commissure laryngoplasty for adjustment of vocal fold tension. Ann Otol Rhinol Laryngol 94(6):547–549
Yang CY, Palmer AD, Murray KD, Meltzer TR, Cohen JI (2002) Cricothyroid approximation to elevate vocal pitch in male-to-female transsexuals_ results of surgery. Ann Otol Rhinol Laryngol 111(6):477–485
Mora E, Cobeta I, Becerra A, Lucio MJ (2018) Comparison of cricothyroid approximation and glottoplasty for surgical voice feminization in male-to-female transsexuals. Laryngoscope 128(9):2101–2109
Donald PJ (1982) Voice change surgery in the transsexual. Head Neck Surg 4(5):433–437
Anderson J (2007) Endoscopic laryngeal web formation for pitch elevation. J Otolaryngol 36(1):6–12
Meister J, Hagen R, Shehata-Dieler W, Kuhn H, Kraus F, Kleinsasser N (2017) Pitch elevation in male-to-female transgender persons-the wurzburg approach. J Voice 31(2):e7–e15
Yilmaz T, Kuscu O, Sozen T, Suslu AE (2017) Anterior glottic web formation for voice feminization: experience of 27 patients. J Voice 31(6):757–762
Rohlfing ML, Kuperstock JE, Friedman D, Spiegel JH (2020) An ex vivo porcine model of the anterior glottoplasty for voice feminization surgery. Laryngoscope 130(4):E206–E212
Brown SK, Chang J, Hu S et al (2021) Addition of wendler glottoplasty to voice therapy improves trans female voice outcomes. Laryngoscope 131(7):1588–1593
Chang J, Brown SK, Hu S et al (2021) Effect of wendler glottoplasty on acoustic measures of voice. Laryngoscope 131(3):583–586
Titze IR, Palaparthi A, Mau T (2021) Vocal tradeoffs in anterior glottoplasty for voice feminization. Laryngoscope 131(5):1081–1087
Gross M (1999) Pitch-raising surgery in male-to-female transsexuals. J Voice 13(2):246–250
Kunachak S, Prakunhungsit S, Sujjalak K (2000) Thyroid cartilage and vocal fold reduction_ a new phonosurgical method for male-to-female transsexuals. Ann Otol Rhinol Laryngol 109(11):1082–1086
Thomas JP, Macmillan C (2013) Feminization laryngoplasty: assessment of surgical pitch elevation. Eur Arch Otorhinolaryngol 270(10):2695–2700
Download references
Acknowledgment
Author information.
Zhijin Li and Dingyue Zhang contributed equally and shared the first-authorship.
Authors and Affiliations
Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China
Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China
Dingyue Zhang
Department of Otorhinolaryngology, Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
Hongsai Chen
Department of Plastic and Reconstructive Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine, No. 639 of Zhizaoju Road, District Huangpu, Shanghai, 200011, China
Ying Liu & Hayson Chenyu Wang
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Ying Liu or Hayson Chenyu Wang .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflicts of interest to disclose.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study informed consent is not required.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Li, Z., Zhang, D., Chen, H. et al. Voice Pitch Shaping and Genderization: New Needs of Cosmetic Phonoplastic Surgery. Aesth Plast Surg (2024). https://doi.org/10.1007/s00266-024-03919-0
Download citation
Received : 18 November 2023
Accepted : 08 February 2024
Published : 02 April 2024
DOI : https://doi.org/10.1007/s00266-024-03919-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Voice pitch shaping
- Cosmetic phonosurgery
- Voice genderization
- Find a journal
- Publish with us
- Track your research

Wyoming governor signs bill banning gender reassignment surgery, care
March 23 (UPI) -- Wyoming's Republican governor has signed a bill into law banning doctors in that state from performing gender transitioning and gender reassignment procedures for children.
Wyoming became the 24th state to enact similar legislation after Gov. Mark Gordon signed the bill Friday.
Legislators in both the state House and Senate passed the legislation earlier this month.
"I signed SF99 because I support the protections this bill includes for children, however it is my belief that the government is straying into the personal affairs of families," Gordon said in a statement.
"Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others," he said.
In addition to doctors, the law also subjects pharmacists and other healthcare professionals to legal penalties for providing gender-affirming care to minors, including the revocation of licenses.
"There was an opportunity to find common cause on issues we agreed with: surgery for minors is inappropriate, other healthcare options ... should remain the purview of parents and their qualified physicians," Wyoming Equality Executive Director Sara Burlingame said in a statement to WyoFile .
She said she was "dismayed" at the new law, calling it a clear case of "government overreach."
Two states, Montana and Idaho have had similar bans blocked by federal judges.
Last month, officials in Idaho asked the Supreme Court to allow the state to enforce its felony ban on minors receiving gender-affirming healthcare, calling the scope of the lower court's decision too broad.
Rates of Suicide Attempts Doubled After Gender-Reassignment Surgery: Study

Attempted suicide rates among people who identified as transgender more than doubled after receiving a vaginoplasty, according to a peer-reviewed study published in The Journal of Urology.
Researchers found the rates of psychiatric emergencies were high both before and after gender-altering surgery, with similar overall rates in both groups. However, suicide attempts were markedly higher in those who received vaginoplasties.
“In fact, our observed rate of suicide attempts in the phalloplasty group is actually similar to the general population, while the vaginoplasty group’s rate is more than double that of the general population,” the study authors wrote.
Among the 869 patients who underwent vaginoplasty, 38 patients attempted suicide—with nine attempts before surgery, 25 after surgery, and four attempts before and after surgery. Researchers found a 1.5 percent overall risk of suicide before vaginoplasty and a 3.3 percent risk of suicide after the procedure. Almost 3 percent of those who attempted suicide after undergoing vaginoplasty did not present with a risk of suicide prior to surgery.
Among the 357 biologically female patients who underwent phalloplasty, there were six suicide attempts with a 0.8 percent risk of suicide before and after surgery.

Overall, the proportion of those who experienced an emergency room and inpatient psychiatric encounter outside of suicide attempts was similar between the vaginoplasty and phalloplasty groups. Approximately 22.2 percent and 20.7 percent of patients, respectively, experienced at least one psychiatric encounter.
Suicide Rate 19-Fold Higher
“It’s hard to refute this paper because it’s a longitudinal study,” Dr. Oliva said. “In Sweden, everyone is in a database, and through diagnosis codes, they’re able to follow what happens to every citizen in terms of their medical history. They waited more than 10 years after people had surgery and found that death by suicide had an adjusted hazard ratio of 19.1.”
Surgical Procedures
A penial inversion is the most commonly performed procedure where the skin is removed from the penis and inverted to form a pouch that is inserted into the vaginal cavity created between the urethra and the rectum. Surgeons then partially remove, shorten, and reposition the urethra and create a labia majora, labia minora, and clitoris.
Another surgical method involves using a robotic system that enables surgeons to reach into the body through a small incision in the belly button to create a vaginal canal. The type of vaginoplasty performed varies among patients. For example, younger patients who have never experienced puberty may have insufficient penile skin to do a standard penile inversion.
Vaginoplasty Associated With Serious Risks
“For cosmetic surgery, if the complication rate was more than 2 percent to 3 percent, you wouldn’t have any patients,” Dr. Oliva told The Epoch Times. “These are very high percentage rates that we just accept.”
Dr. Oliva said complications with these surgical procedures are very high and he thinks this is why suicide rates are so high.
“People think this is going to solve the problem and it doesn’t,” he said.
Booster Vaccination May Affect COVID-19 Symptoms and Severity: Study

US Physicians Received Billions From Pharmaceutical and Medical Device Industry, New Research Finds

Abnormal Levels of Toxins Found in General Mills ‘LOADED’ Cereal: Report
Rates of Suicide Attempts Doubled After Gender-Reassignment Surgery: Study

Attempted suicide rates among people who identified as transgender more than doubled after receiving a vaginoplasty, according to a peer-reviewed study published in The Journal of Urology.
The study analyzed the rates of psychiatric emergencies before and after gender-altering surgery among 869 males who underwent vaginoplasty and 357 females who underwent phalloplasty in California from 2012 to 2018.
Researchers found the rates of psychiatric emergencies were high both before and after gender-altering surgery, with similar overall rates in both groups. However, suicide attempts were markedly higher in those who received vaginoplasties.
“In fact, our observed rate of suicide attempts in the phalloplasty group is actually similar to the general population, while the vaginoplasty group’s rate is more than double that of the general population,” the study authors wrote.
Among the 869 patients who underwent vaginoplasty, 38 patients attempted suicide—with nine attempts before surgery, 25 after surgery, and four attempts before and after surgery. Researchers found a 1.5 percent overall risk of suicide before vaginoplasty and a 3.3 percent risk of suicide after the procedure. Almost 3 percent of those who attempted suicide after undergoing vaginoplasty did not present with a risk of suicide prior to surgery.
Among the 357 biologically female patients who underwent phalloplasty, there were six suicide attempts with a 0.8 percent risk of suicide before and after surgery.
Overall, the proportion of those who experienced an emergency room and inpatient psychiatric encounter outside of suicide attempts was similar between the vaginoplasty and phalloplasty groups. Approximately 22.2 percent and 20.7 percent of patients, respectively, experienced at least one psychiatric encounter.
The study found a 33.9 percent chance that a biological man undergoing vaginoplasty would experience a psychiatric encounter post-surgery compared with a 26.5 percent chance for biological women who underwent phalloplasty, if an episode had occurred before surgery. The authors stressed the importance of counseling biological males undergoing a feminizing transition with a history of prior psychiatric emergencies.
Suicide Rate 19-Fold Higher
In an interview with The Epoch Times, Dr. Alfonso Oliva, a board-certified plastic and reconstructive surgeon, said research into the psychiatric outcomes and long-term follow-up of those who have sex-reassignment surgery is lacking, but an important paper is worth mentioning. In a 2011 paper published in PLOS ONE , researchers found that people who underwent sex reassignment surgery had substantially higher rates of overall mortality, suicidal behavior, and psychiatric morbidity compared with the general population.
“It’s hard to refute this paper because it’s a longitudinal study,” Dr. Oliva said. “In Sweden, everyone is in a database, and through diagnosis codes, they’re able to follow what happens to every citizen in terms of their medical history. They waited more than 10 years after people had surgery and found that death by suicide had an adjusted hazard ratio of 19.1.”
You can “quibble” about emergency room encounters, but this study shows that for patients who had transgender surgery, their suicide rate after 10 years was 19-fold higher than the general population, Dr. Oliva said. Additionally, the study excluded people with psychiatric illnesses, so these are individuals thought to have no psychiatric illness outside of dysphoria.
Surgical Procedures
A phalloplasty is a multistep process undertaken by a biological female who wants to transition to a male, where a penis is created using tissues from the genitals and forearm or thigh. The external genitals, such as the labia or outer labia, are used to create a scrotum, and testicular implants are inserted months later along with an implant that will cause erections.
Vaginoplasty is the most commonly performed gender-reassignment surgery for those with gender dysphoria , with more than 3,000 procedures performed annually. According to Johns Hopkins Medicine, vaginoplasty is a surgical procedure that involves removing the penis, testicles, and scrotum to create a vulva and functional vagina. Surgeons typically create a vaginal canal using the skin surrounding the existing penis and scrotum or by using a skin graft from the abdomen or thigh.
A penial inversion is the most commonly performed procedure where the skin is removed from the penis and inverted to form a pouch that is inserted into the vaginal cavity created between the urethra and the rectum. Surgeons then partially remove, shorten, and reposition the urethra and create a labia majora, labia minora, and clitoris.
Another surgical method involves using a robotic system that enables surgeons to reach into the body through a small incision in the belly button to create a vaginal canal. The type of vaginoplasty performed varies among patients. For example, younger patients who have never experienced puberty may have insufficient penile skin to do a standard penile inversion.
“When you take a child who’s about to undergo puberty—and they suggest giving puberty blockers to stop puberty at age 10 to 11 1/2—and when you do that for little boys, they aren’t able to get tissue from the penis and scrotum, so creating a vagina is very difficult,” Dr. Oliva told The Epoch Times. “You have to use tissue from other areas of the body, such as the peritoneum or the colon. Some researchers in Brazil are actually looking into using tilapia fish ,” he added.
After a vaginoplasty is performed, the recovery process is extensive and vaginal dilation must be performed at varying intervals throughout the patient’s life.
Vaginoplasty Associated With Serious Risks
In addition to an increased risk of suicide, vaginoplasty is associated with numerous physical complications, including wound separation, vaginal stenosis, hematoma, rectovaginal fistulas, granulation tissue, bleeding, infection, skin or clitoral necrosis, suture line dehiscence (when the surgical incision opens), urinary retention or vaginal prolapse.
According to a 2021 paper in the International Brazilian Journal of Urology , a rectovaginal fistula is the “most devastating complication” of a vaginoplasty that can occur “despite careful technique” and without obvious injury to the rectum.
A rectovaginal fistula is an abnormal connection between the rectum and vagina that can cause fecal incontinence, hygiene issues, vaginal or anal irritation, and potentially life-threatening abscesses and fistula recurrence.
A 2021 review in Andrology found that rates of complications following penile inversion vaginoplasty ranged from 20 to 70 percent, with most of the complications occurring during the first four months following the procedure.
In a 2018 Clinical Anatomy review and meta-analysis , researchers reviewed 125 articles to assess neovaginal complications following surgery. After selecting 13 studies that included 1,684 patients, they found a complication rate of 32 percent, with a reoperation rate of 22 percent for non-esthetic reasons.
“For cosmetic surgery, if the complication rate was more than 2 percent to 3 percent, you wouldn’t have any patients,” Dr. Oliva told The Epoch Times. “These are very high percentage rates that we just accept.”
Dr. Oliva said complications with these surgical procedures are very high and he thinks this is why suicide rates are so high.
“People think this is going to solve the problem and it doesn’t,” he said.
A June 2018 paper on postoperative outcomes of 117 patients who underwent vaginoplasty published in the Journal of the American Society of Plastic Surgeons found that 26 percent of patients experienced granulation tissue, 20 percent had intravaginal scarring, and 20 percent experienced prolonged pain.
In a 2017 paper published in The Journal of Urology , researchers followed patients who underwent penile inversion vaginoplasty. Of 330 patients, 95 (29 percent), presented with postoperative complications. Three of those patients developed a rectoneovaginal fistula, and 30 patients required a second operation.
In a 2016 study published in Urology , researchers retrospectively reviewed clinical records of 69 patients who underwent vaginoplasty from January 2005 to January 2015. Although complications during surgery were not reported, 22 percent of patients experienced major postoperative complications.
“We’ve been transitioning adults in the United States since 2007, but where’s the data from gender identity clinics? Why is nothing published in the United States about long-term function? Why do we have nothing published on sexual function? We should be able to follow that and should be studying it and we’re not,” Dr. Oliva told The Epoch Times.
- Entertainment
- London / Europe
- Border / Cartel Chronicles
- Israel / Middle East
- Latin America
- On the Hill Articles
- On The Hill Exclusive Video
- Breitbart News Daily
- Newsletters
- Baltimore Bridge Collapse
- Biden Border Crisis
- Tish Shakedown
Wyoming Bans ‘Gender-Reassignment,’ Puberty Blocking Procedures for Children

The state of Wyoming has outlawed “gender-reassignment” procedures for children in an effort to ban the permanent sterilization, castration, and mutilation of minors.
Gov. Mark Gordon (R) signed SF0099 , also known as the “Children gender change prohibition,” into law on Friday. The law allows exceptions for “procedures or treatments that are performed with the consent of the child’s parent or guardian and are for a child who is born with a medically verifiable genetic disorder of sex development.”
“I signed SF99 because I support the protections this bill includes for children; however, it is my belief that the government is straying into the personal affairs of families,” Gordon said in a press release . “Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others.”
Related — Women’s Rights Activist: Never Use the Language of Trans-Activism — Don’t Give It Any Validation
The new law specifically prohibits any “surgery that sterilizes the child, including castration, vasectomy, hysterectomy, oophorectomy, metoidioplasty, orchiectomy, penectomy, phalloplasty and vaginoplasty.”
It also covers “sex-change” and puberty-blocking hormones.
The move was commended by Gays Against Groomers, an organization of gay people and other allies who advocate against child transgenderism.
🚨 BREAKING: Governor @Mark_Gordon_WY has signed SF0099 into law! Child sterilization and mutilation will be BANNED in Wyoming! Thank you to everyone who called! We did it! #StateByState https://t.co/Ba9Dp2rqbA pic.twitter.com/uKwMXbBtbq — Gays Against Groomers (@againstgrmrs) March 22, 2024
The governor vetoed HB148, also titled “Regulation of abortions,” on Friday. That bill would have placed more restrictions on Wyoming’s abortion clinics.
Gordon’s office said that the initially proposed bill “would have properly regulated surgical abortion clinics in Wyoming,” but amendments to the bill “complicated its purpose, making it vulnerable to legal challenges.”
“With the judge certifying these cases to the Wyoming Supreme Court, the state is closer than ever to a decision on the constitutionality of abortion in Wyoming,” Gordon said. “It is my opinion that HB148, as amended, had the potential to further delay the resolution of this critical issue for the unborn.”
He added that “the potential of starting over on a new course of legal arguments would in my mind be derelict, and would have only sacrificed additional unborn lives in Wyoming.”
Please let us know if you're having issues with commenting.

IMAGES
VIDEO
COMMENTS
Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too. Studies consistently show that gender affirmation surgery reduces gender dysphoria and related conditions, like anxiety and depression.
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
A 2018 study found that 94-100% of participants who had undergone gender-affirming surgery reported satisfaction with the surgical results, with the variance depending on the type of procedure.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help. Facial gender surgery can include a variety ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly ...
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person ...
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to describe people ...
Female-to-male gender reassignment surgery (FTM GRS) is a complex and irreversible genital surgery for female transsexual who is diagnosed with gender identity disorder and has a strong desire to live as male. The procedure is to remove all female genital organs including the uterus, ovaries, and vagina with the construction of male genitalia ...
Here's how gender reassignment works: Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina. An incision ...
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
His confidence in this new approach is the result of nearly three decades of expertise and innovation in SRS and urogenital reconstructive surgery, which includes 600 male-to-female vaginoplasties, 900 female-to-male metoidioplasties, 300 female-to-male phalloplasties, and the co-development of a penile disassembly technique for epispadias repair.
Breast Augmentation 101. MTF Breast Augmentation is a surgery procedure that transforms a masculine-looking chest into breasts that have a feminine shape and size. Using breast implants, MTF Breast Augmentation can provide a female breast contour when hormone replacement therapy alone has proved insufficient for breast development.
Gender reassignment surgery may also be referred to as gender-affirming or gender-confirmation surgery which is part of a treatment plan for gender identity dysphoria. Surgery includes the surgical procedures by which one's physical appearance and function of a person's existing sexual characteristics are changed to those of the other sex ...
Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female ...
The twenty-first century, with its transforming ideology and rising acceptance, is witnessing an increased number of transgender people applying for gender reassignment surgery (GRS). The procedure of GRS is a lengthy and complex one involving the active collaboration of multiple disciplines including psychology, psychiatry, family medicine ...
A FTM gender reassignment surgery creates male genitalia. Here is a quick guide for what to expect before, during, and after a FTM gender reassignment surgery: Before Surgery. Prophylactic antibiotics or antivirals may be prescribed. Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol ...
The law states that "gender transitioning and reassignment procedures are grounds for suspension or revocation of a physician's or health care provider's license …"
Later, with the advancement of gender reassignment surgery, pitch adjustment became part of a series of gender reassignment treatments and was used to give transgender groups the appropriate second sexual characteristics to their final gender . A rise has followed this need for vocal tuning of a cosmetic nature in recent years [6,7,8].
March 23 (UPI) --Wyoming's Republican governor has signed a bill into law banning doctors in that state from performing gender transitioning and gender reassignment procedures for children.Wyoming ...
Vaginoplasty is the most commonly performed gender-reassignment surgery for those with gender dysphoria, with more than 3,000 procedures performed annually. According to Johns Hopkins Medicine ...
Vaginoplasty is the most commonly performed gender-reassignment surgery for those with gender dysphoria, with more than 3,000 procedures performed annually. According to Johns Hopkins Medicine, vaginoplasty is a surgical procedure that involves removing the penis, testicles, and scrotum to create a vulva and functional vagina.
The state of Wyoming has outlawed "gender-reassignment" procedures for children in an effort to ban the permanent sterilization, castration, and mutilation of minors. Gov. Mark Gordon (R) signed SF0099, also known as the "Children gender change prohibition," into law on Friday. The law allows exceptions for "procedures or treatments ...