HJF Medical Research International
Participants at HJF Medical Research International in Abuja, Nigeria, have been vaccinated in the first Phase 2 clinical trial of a Lassa fever virus (LASV) vaccine candidate to date, according to IAVI, a nonprofit scientific research organization and the trial sponsor. The study ( IAVI C105/PREVAIL15 ) is funded by CEPI , an innovative global partnership working to accelerate the development of vaccines against epidemic and pandemic threats.
Maurice is one of many who have benefited from PEPFAR’s promise to deliver quality healthcare in remote communities through a mobile clinic outreach program. Before the mobile clinic, members of Maurice’s community would have to travel to Tanzania by foot - an eight-day journey in territory inhabited by wild animals and warring clans, to receive health services. “Some people would die there, and it was hard,” Maurice says.

When Edith Okafor, a 50-year-old widow and caregiver of four boys, walked into the Clinical Training and Research Centre (CTRC), 44 Nigerian Army Reference Hospital Kaduna (NARHK) to begin antiretroviral therapy in April 2007, she had no idea that that encounter would become the beacon of hope in her state of despair.

Geoffrey Mwakyusa (49), a resident of the Kyela District Council in the Mbeya Region, is among hundreds of thousands of people in the area who have connected with Community-based HIV Service Providers (CBHSP) to find out their HIV status through the distribution of HIV self-testing kits.
Ahead of the October 20 Mashujaa Day celebrations in Kericho, Kenya’s Deputy President H.E. Rigathi Gachagua, EGH, visited the Kericho, Kenya Medical Research Institute (KEMRI)/ Walter Reed Project (WRP) Clinical Research Center (CRC), where he inaugurated the biosafety level 3 tuberculosis (TB) Reference Laboratory.

The African Cohort Study (AFRICOS) celebrated its 10th Anniversary on Wednesday 1st November, 2023, with a Research Symposium to review key findings from the study, share ongoing analyses, and discuss plans under the theme titled, “Progress and Future Directions.”

In 2007, Joyce, David and their two children were featured on the cover of PEPFAR’s annual report to Congress, but their story about how PEPFAR transformed their lives began in 2005. David and Joyce were expecting their second child in 2005 when David discovered he was living with HIV. The next day, David brought his wife, Joyce, to Kericho District Hospital to get tested.
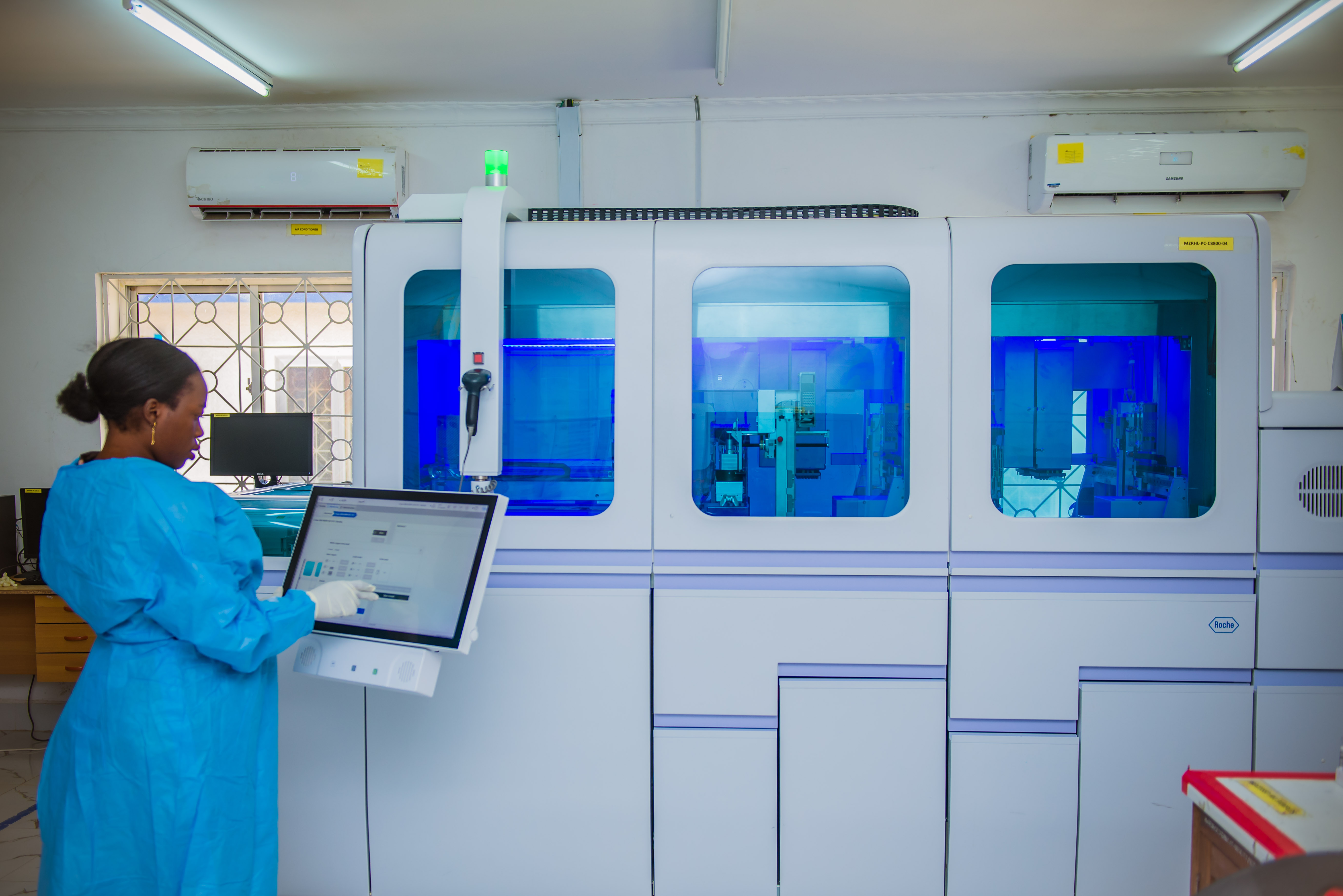
September 28, 2023, marked a significant milestone, as HJF Medical Research International Ltd/Gte. (HJFMRI Ltd/Gte.) celebrated the grand opening of its new laboratories and office complex in Abuja, Nigeria.
Deborah is one of the oldest stories of PEPFAR’s impact in Kenya and is a true testament to the purpose and mission of PEPFAR. More than 20 years ago, Deborah was diagnosed with HIV.

HJFMRI helped coordinate entomology surveillance teams to quickly gather data in a race against emerging dengue and yellow fever outbreaks in Kenya.


HJFMRI develops partnerships, infrastructure, and expertise around the world to help researchers solve complex challenges in global health. Learn more about us.
HJFMRI Focus Areas
HJFMRI has decades of experience supporting partners in a wide range of complex research endeavors. Our multidisciplinary team of experts works to implement flexible, comprehensive approaches to vaccine development, clinical research, infectious disease surveillance and therapeutics, global health program implementation, capacity building, and military-military health initiatives.
HJFMRI's Services
HJFMRI facilitates medical research by providing a range of responsive, flexible services to support clinical testing and global health program implementation around the world. We provide support services in protocol planning, site development, research operations, data collection and analysis, regulatory compliance, and international program staffing and contracts.

HJFMRI is proud to partner with organizations from across the globe to advance global health, including host country governments, public institutions, private entities, universities, and foundations.

Maseno University and School of Medicine, Kenya

Site Director

Prof. Collins Ouma is the Program Leader, Health Challenges and Systems within the African Population and Health Research Center (APHRC), where he leads amongst other things translation of research evidence to policy. His research focuses on public health, genetic, and environmental factors that predisposes the human populations to both infectious and non-infectious diseases in sub-Saharan Africa.

Dr. Samuel Bonuke Anyona , Lecturer, Medical Biochemistry, Maseno University [email protected]
Dr. Anyona is a faculty member in the Department of Medical Biochemistry, School of Medicine, Maseno University and a post-doctoral fellow under the career development (K43) grant award. His research activities focus on pediatric populations living under intense malaria transmission in western Kenya, a region holoendemic for Plasmodium falciparum. Dr. Anyona acquired hands-on experience with various techniques including; molecular genetics, molecular biology (including cloning and construct designs), biochemical and immunofluorescence analyses (both by flow cytometry and microscopy), bioinformatics, and statistics. Dr. Anyona is an alumnus of the HBNU Fogarty Global Health Fellowship Program.

Dr. Ayodo is a basic science researcher trained in genetic epidemiology of infectious diseases but now focusing on applied epidemiology and implementation research. The focus of his work is to develop community intervention models to eliminate or sustain low transmission of infectious diseases. I am also actively involved in understanding the origin of man in attempt to understand the biology of diseases of conditions such as sickle cell disease.
Dr. Kiprotich Chelimo , Senior Lecturer of Biomedical Sciences and Technology, Maseno University [email protected]
Dr. Chelimo is involved in a number of long-term active and ongoing training and research collaborations with several international institutions including: University of New Mexico-USA (current institution ofaffiliation for Dr. Perkins), University of Massachussets Medical School (MA-USA), Case Western Reserve University (Ohio-USA), Kenya Medical Research Institute (KEMRI, Centre for Global Health Research), and International Cancer Institute (Kenya). His current focus in these collaborations is to work closely with other expert scientist in supporting and nurturing a crop of upcoming scientists in my area of expertise. To date, as a senior Faculty at Maseno University in Kenya, he has mentored over 12 postgraduate students to completion.
Dr. Michael Gicheru , Associate Professor of Immunology, Kenyatta University [email protected]
Dr. Gicheru has long-term active and ongoing collaborations with Kenya Medical Research Institute (KEMRI, Centre for Global Health Research), Maseno University, University of New Mexico-USA (current institution of affiliation for Dr. Perkins), and several other institutions with current common interests in Africa with the main aim of forming a consortium to effectively mentor endemic area scientists. To date, as a senior Faculty at Kenyatta University in Kenya, he has mentored over 90 postgraduate students to completion. Dr. Gicheru has contributed to the development of vervet monkey model for leishmaniasis and evaluation of leishmania vaccine candidates in nonhuman primate model.
Dr. John Michael Ong’echa , Principal Research Officer, Kenya Medical Research Institute
Dr. Ong’echa is a Principal Research Officer with the Kenya Medical Research Institute (KEMRI) and a Senior Research Fellow at the Centre for Research in Therapeutic Sciences (CREATES), Strathmore University, Kenya. He has significant experience working on the genetics and immunology of infectious diseases. His training in immunology and genetics and many years working on Dr. Perkins’ NIH-funded project entitled “Genetic Basis of Severe Malarial Anemia – R01 AI051305” and my FIC funded R01 (Global Research Initiative Program (GRIP) – R01 TW007631) titled ‘Molecular Immunologic Role of Cytokines in the Development of Malarial Immunity’ (2007-2011) has given him adequate experience in conducting field studies. In addition, through Dr. Perkins’ D43 training grant (D43 TW005884) where I served as the Program Co-Director, he has been able to successfully mentor a large number of African scientists, most of whom have now developed independent careers in research. Dr. Ong’echa has also been involved in other additional multi-country and multi-institutional training programs.

Dr. Evans Raballah , Senior Lecturer, Department of Medical Laboratory Sciences, Masinde Muliro University of Science and Technology [email protected]
Dr. Raballah is a Senior Lecturer in the Department of Medical Laboratory Sciences. He holds a doctorate degree in Immunology, specializing in Immunogenetics of infectious diseases. His academic and research interests are in the fields of malaria, bacteremia, HIV and COVID-19. His major scholarly contribution was defining the CD4+ cells and their intracellular IFN-g and IL-17 cytokines in severe malarial anemia in a pediatric population of western Kenya. He has further published over 25 manuscripts in peer reviewed refereed journals. In 2016, he received the Junior Researcher of the year award of Masinde Muliro University of Science and Technology. He currently serves as the Co-ordinator of Medical Biotechnology program in the department of Medical Laboratory sciences and a member of the departmental postgraduate committee. Dr. Raballah is an alumnus of the HBNU Fogarty Global Health Fellowship Program.

+254 709 983000/ +254 709 983676
Our History
Our policies, partnerships and collaborators, major research themes, research platforms, scientific departments.
- Policy Briefs
- Publications
- Capacity Strengthening
- Data Access

Established in 1989
Who is KEMRI Wellcome Trust?
The KEMRI Wellcome Trust Research Programme (KWTRP) is based within the KEMRI Centre for Geographic Medical Research – (Coast). Our core activities are funded by the Wellcome Trust. We conduct integrated epidemiological, social, laboratory and clinical research in parallel, with results feeding into local and international health policy. Our research platforms include state-of-the-art laboratories, a demographic surveillance system covering a quarter of a million residents, partnership with Kilifi County Hospital in health care and hospital surveillance, a clinical trials facility, a vibrant engagement programme and a dedicated training facility.
The KWTRP leadership includes the Ag. Executive Director Edwine Barasa, the KEMRI Centre Director Dr. Joseph Mwangangi, Deputy Director George Warimwe and the Chief Operating Officer Catherine Kenyatta.
- Our mission
To undertake cutting-edge and novel research relevant to national, regional and global needs.
To conduct high quality, purposeful, and relevant research in human health, building sustainable research capacity and leadership.
- To conduct research to the highest international scientific and ethical standards on the major causes of morbidity and mortality in the region in order to provide the evidence base to improve health.
- To train an internationally competitive cadre of Kenyan and African research leaders to ensure the long term development of health research in Africa

The Kenyan Medical Research Institute (KEMRI) was established through the Science and Technology (Amendment) Act of 1979, which has since been amended to Science, Technology and Innovation Act, 2013 with the mandate to carry out health science research in Kenya. The Kilifi-based Centre for Geographic Medicine Coast (CGMR-C) is among the 12 KEMRI centers.
The Wellcome Trust was established in 1936 by an endowment left by Henry Wellcome in his will. Henry Wellcome was a rich businessman and philanthropist in the UK. He also travelled in Sudan and Egypt, where he took an interest in malaria control and commissioned a floating laboratory on the Nile. The Wellcome Trust continues to support research in Africa and was one of the first research institutions to partner with the new independent Government of Kenya in 1964, creating the Wellcome Trust Research Laboratories in Nairobi. In the 1980s a few Wellcome Trust funded scientists including Stephen Oppenheimer and Bill Watkins began working in Kilifi District Hospital in collaboration with KEMRI. In 1989 the KEMRI-Wellcome Trust Research Programme (KWTRP) was formed, led by Kevin Marsh and Norbert Peshu. Due to the continued growth of research activities in Kilifi, in 1995 KEMRI granted the Kilifi Station a full Centre status as “KEMRI Centre for Geographic Medicine Research – Coast (KEMRI CGMRC).
Finding ways to beat malaria; Initial work focused on malaria, a devastating disease that was causing the deaths of many children. Working closely with colleagues in the Ministry of Health, researchers conducted studies on insecticide-treated bed nets, antimalarial drugs to prevent malaria in pregnant women and descriptions of severe malaria. Over the last 15 years there has been impressive improvements in malaria control across Africa with Kilifi registering 90 percent drop in malaria cases. Today KWTRP continues to build on its early success in bed net trials with work led from Nairobi that provides information and advice to the national malaria control Programme’s of 14 countries, supported by statistical models to generate maps of malaria risk.
In Kilifi Hospital, KWTRP facilitated the creation of a High Dependency Paediatric Unit where severely sick children had intensive monitoring and treatment. The first studies on clinical definitions of severe malaria in children were based on simple observation by the bedside. Work on severe malaria continues today with increasingly sophisticated laboratory work, DNA sequencing and retinal imaging, and clinical trials that have informed the use of anti-epilepsy drugs and fluids in severely unwell children.
As the Programme developed it was apparent that malaria was just one of a host of health problems confronting children on the coast and that often these problems were interrelated. The focus therefore expanded to include work including pneumonia, meningitis, HIV and malnutrition. Other studies included social science and health systems perspectives, as well as research on community involvement.
In early studies KWTRP engaged shopkeepers with a training programme to ensure they gave anti-malarials at the correct dose. If done well this prevents the need for hospital admissions. These successes have been built on in recent times, with KWTRP studies now showing that SMS messages can help doctors and patients to use anti-malarials correctly. KWTRP has also shown how training and support packages can help doctors and nurses in hospital to improve their patient care. These interventions result in patients getting the correct treatment and saving lives.
The cornerstone of research success is community involvement. This is done through regular interactions with opinion leaders and a network of community representatives, the Schools Engagement Programme, social media and regular open days. The programme builds mutual understanding between researchers and the community, and ensures that research is responsive to community views and interests. This research findings have done much to improve the health of the partnering community in Kilifi, and health around Africa. The work has been enhanced by modern technology which now includes online interaction with secondary schools.
Apart from conducting the highest quality research, one of the objectives is to support the development of scientific leadership in Kenya through deliberate capacity building initiatives. KWTRP has a particular focus on building links with schools in the community, which involves promoting better understanding of science and research. In addition, it has a structured internship programme for introducing Kenyan graduates to research training master’s degree and PhD students. Young researchers are supported through a system of career development to join other research institutions in the region or to develop careers with the programme.
The Kenya Medical Research Institute is a national body mandated by an Act of Parliament to provide overall leadership and guidance for health research in Kenya. The KEMRI-Wellcome Trust Research Programme is embedded within the KEMRI Centre for Geographic Medicine Research-Coast as one of the KEMRI center’s in Kenya.
Wellcome Trust
The Wellcome Trust is an independent charity funding research to improve human and animal health. Established in 1936 and with an endowment of around 13 billion, it is the UK’s largest non-governmental source of funds for biomedical research. As a privately endowed charity, it is independent from governments, from industry and from donors.
The governing document of the Wellcome Trust is its constitution. This represents an updated version of the will of Sir Henry Wellcome, through which the Wellcome Trust was established in 1936. Ultimate responsibility for all activities lies with the Board of Governors.
The Wellcome Trust has since 1989 funded the Core activities of the KEMRI|Wellcome Trust research programme. Which includes administrative support, and support of the key platforms of clinical services, community engagement, Laboratory’s and the Kilifi Health Demographic Surveillance system. This has over time ensured continuation of the research work undertaken by the Programme.
The University of Oxford is internationally renowned for the quality and diversity of its research, with over 3000 academic staff and 3000 postgraduate students working on research. The university’s position as a centre of excellence is enhanced by the ongoing development of interdisciplinary research centers, and collaboration with international academic and industrial partners. The University has a critical mass of supported researchers both local and international, who work within the Programme. This collaboration has also resulted into a well-defined research capacity building platform for researchers in Africa.
The Department of Health in the County provides overall leadership in health service delivery, and facilitates a cordial co-existence with our research centre. Medical staff from the county and periphery health facilities participates in research activities, including clinical research.
The Nairobi programme has close working relations with the Nairobi county health department working closely with the various health institutions under its mandate to facilitate the research work done. Focus is mainly on policy and improving of health care systems. This has over time been extended to include research in key populations in the city.
In Nairobi, the Programme has forged strong links with the Ministries of Health and Education, with several of the Programme researchers acting as technical advisers to the Kenyan Government departments and playing a major part in the development of national strategies.
A series of clinical trials focusing on in-patient hospital care have led to collaborations in Eastern Uganda, notably in Soroti and Mbale District Hospitals. Mbale Clinical Research Unit has been founded on the grounds of Mbale District Hospital and includes a collaboration with Busitema University.
The work of the KEMRI-Wellcome Trust Research Programme is also based on other partnerships. Key researchers hold academic positions at a number of institutions including the universities of Oxford and Warwick, the Liverpool School of Tropical Medicine, London School of Hygiene and Tropical Medicine, Imperial College, and the Institute of Child Health in London.
KWTRP Researchers are also committed to engaging with the local community, to discuss their research and to build mutual understanding and trust between researchers and the community by responding to various concerns. By developing such strong links, the Programme can ensure that its activities are accepted and approved by local communities – a prerequisite for its long-term studies. Moreover, the close juxtaposition of research and application can help ensure that its activities are focused on delivering practical benefits.
And finally, in a national and international context, the key relationships with policy makers and health officials help to ensure that important research findings make a difference to medical care – and thus have an influence far beyond the geographic areas in which the team works.

The Programme has two main bases in Kenya but works in many other parts of the country and is increasingly involved in regional collaborations to support research in neighbouring countries.
The Ugandan unit is based in Mbale town within the Mbale Regional Referral Hospital and was founded in 2008 in response to the need for evidenced based clinical guidelines.

- Civil Society
- Document Centre
- Education NGOs and CSOs
- Education Suppliers
- Government Agencies
- Independent Schools
- Other Organisations
- Research Institutes
- Universities
- Universities and Colleges
Research Institutes in Kenya
The Kenya Medical Research Institute is one of East Africa’s leading medical research centres and is the national body responsible for carrying out health science research in Kenya. The Kenya Institute of Education promotes development and delivery of relevant, high-quality, affordable education and training programmes, materials and services. The Kenya Agricultural Research Institute has the objective of food security through improved productivity and environmental conservation.

- All member countries
- Our network:
- Commonwealth Education Online
- Commonwealth Governance Online
- Commonwealth Health Online
PUBLICATIONS, NEWS & EVENTS
Find a mentor.
All publications resulting from the research or research training supported by this award must acknowledge FIC and all co-funders with the following or comparable footnote: This project was supported by NIH Research Training Grant D43TWW009345 funded by the Fogarty International Center, the NIH Office of the Director Office of AIDS Research, the NIH Office of the Director Office of Research on Women's Health, The National Heart, Lung and Blood Institute, the National Institute of Mental Health and the National Institute of General Medical Sciences.
The content of this website is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the academic institutions affiliated with this program.
Kenya has hosted more NPGH Fogarty Fellows than any other country, so previous projects have covered a wide range of topics: everything from shock-related mortality in pediatric patients to STI modeling in non-human primates . Though much research has focused on HIV/AIDS, there have been many different approaches including the effect of hormonal birth control on HIV risk , partner notification in serodiscordant couples , and the interplay between iron deficiency, malaria, and HIV . Dr. Bukusi, Co-Director of the Research Care and Treatment Program at the Kenya Medical Research Institute, gave an interview about her career as an HIV/AIDS researcher on our blog , and Fan Lee, a 2014-2015 Fogarty Scholar also wrote about her experiences at the start of her fellowship.
For a list of projects in Kenya: click here -->
Affiliated Institutions
KEMRI conducts research from 12 research centers that focus on different areas of national and strategic importance: Centre for Biotechnology Research and Development (CBRD); Centre for Clinical Research (CCR); Centre for Geographic Medicine Research-Coast (CGMR-C); Centre for Global Health Research (CGHR); Centre for Infectious and Parasitic Diseases Control Research (CIPDCR); Centre for Microbiology Research (CMR); Centre for Public Health Research (CPHR); Centre for Respiratory Diseases Research (CRDR); Centre for Traditional Medicine and Drug Research (CTMDR); Centre for Virus Research (CVR); The Eastern and Southern Africa Centre of International Parasite Control (ESACIPAC). KEMRI also has a graduate school known as the KEMRI Graduate School of Health Sciences (KGSHS), a Health Safety and Environment Program, and a production centre.
KEMRI Centre for Global Health Research (CGHR): CGHR is located in Kisumu City, western Kenya, an area that is endemic for major infectious diseases such as malaria and HIV/AIDs. Research conducted in CGHR focuses on infectious diseases of medical importance. Specifically, the Centre has carried out cutting-edge research focusing on trials on the efficacy of drugs, emergence of drug and vector resistance, epidemiology, immunology, molecular biology, vector biology, climate and human health, characterization of malaria vaccine candidate antigens, malaria vaccine trials, malaria in pregnancy and interaction of malaria and human immunodeficiency virus (HIV), schistosomiasis, intestinal helminthes, HIV/AIDS and its impact on the community, HIV interaction with other infectious diseases, tuberculosis and reproductive health.
The Center consists of two administrative buildings, an entomology building, two refurbished laboratory blocks, a new state-of-the-art multidisciplinary laboratory complex and a clinic. The administrative blocks houses the Center Director’s office, offices for senior scientists, collaborating scientists and visiting scientists, senior administrators, a data section, a computer room, a library, storage facilities and 5 modern seminar rooms for training, meetings and holding seminars, with seating capacity ranging from 8 to 40 people. The seminar rooms are equipped with modern audio-visual (AV) equipment including LCDs, permanent and portable screens, TVs and VCRs. Two of the seminar rooms are also equipped with video-conference facilities. The laboratory facilities consist of separate well-equipped rooms for basic laboratory diagnostics, immunology and molecular biology laboratories, parasite cultures and drug sensitivity testing, a clinical hematology and biochemistry laboratory, an insectary and insecticide-testing huts. The current laboratory equipment in the Centre include a modern compound, inverted and fluorescent microscopes, differential Coulter counters, multiparameter biochemistry machines, Hb electrophoresis equipment, refrigerated bench-top centrifuges, multifunctional ELISA readers and automated washers, twin CO2 conventional incubators, liquid scintillation counters, level II biosafety cabinets, FACS count, four and five-color FACSCaliburs and FACScan, PCR enclosures and high capacity PCR machines, real-time PCR machines, 377 and 3100 ABI gene sequencers, UVP gel imaging systems, and nanopure water purification systems. There are numerous -70 ultra-freezers and several bulk liquid nitrogen tanks for sample storage.
The center has recently installed a liquid nitrogen generator with capacity to produce 500 liters of liquid nitrogen per day. In addition to the above facilities, there are several facilities for conducting hospital-based clinical studies. The biggest of these is a stand-alone Clinical Research Centre located at the New Nyanza Provincial Hospital in Kisumu City. It consists of a pediatric ward, clinical laboratory, offices and HIV counseling facilities. Plans are at an advanced stage to convert part of this facility into a vaccine trial site. This will be in addition to an already existing state-of-the-art and well-equipped vaccine and drugs trial site with capacity to conduct GCP/GLP compliant trials at Kombewa, situated about 30 kilometers from Kisumu City. Read more…
The hospital’s mission is to “provide accessible specialized quality health care, facilitate medical training, research; participate in national health planning and policy,” and its mandate includes providing facilities for medical education and research, as well as participating in national health planning. As a regional referral hospital, there is a wealth of data that can be utilized to inform and improve health care provision within and outside Kenya, especially around HIV care and treatment. KNH provides HIV care for thousands of inpatients each month and sees hundreds of HIV-infected adults and children each day at the HIV Comprehensive Care Center (CCC). The CCC has >5,000 HIV-infected adults registered in outpatient follow-up and >700 HIV-infected children enrolled in care. Eighty-one percent of these adults are currently on ART and 467 new patients were initiated during the last 6 months of 2011 alone. In the inpatient setting, KNH has implemented routine provider-initiated HIV testing (PITC), successfully testing approximately 1,000 patients monthly and finding prevalence to be >6% in this population.
The KNH Department of Research Chair Dr. Nelly Mugo, and Vice-Chair Dr. John Kinuthia, who both earned MPH degrees at UW with Fogarty funding, have identified implementation science as their current research priority and this has been endorsed at meetings with the hospital’s Deputy CEO as recently as May 2012 when Dr. Carey Farquhar met with KNH leadership to discuss research directions for the institution and future collaborations.
AIDS International Research Training Program (AIRTP): Since 1985 when Drs. Joan Kreiss and King Holmes began working in Nairobi in collaboration with the University of Nairobi and Kenyatta National Hospital, UW faculty have conducted several hundred research projects on HIV prevention, treatment and pathogenesis. This longstanding partnership between UW and KNH, and the solid research foundation that has been built over more than two decades, can be readily leveraged to focus on implementation science training relevant to the HIV care cascade. More than 450 papers have been published with AITRP trainees as first or co-authors and this number has steadily increased by 20-30 publications each year for the last 5 years. All of these publications address HIV and a significant proportion have been led by Kenyan investigators and have Kenyans as first authors, including several papers in high-profile journals such as the Lancet and JAMA. Major research projects that have been completed or are ongoing are included below to demonstrate the ability of the UW/Kenya collaboration to absorb new trainees. Those based at KNH will also build capacity for research at the institution. All will provide rich opportunities for trainees in the proposed program to conduct research in a rigorous manner with strong mentorship by experienced U.S. and Kenyan investigators. Read more…
Primary Faculty
Research themes.
- Shock-related mortality in pediatrics
- STI modeling in non-human primates
- Effects of hormonal birth control on HIV risk
- Partner notification in serodiscordant couples
- Interplay between iron deficiency, malaria, and HIV
For a list of projects in Kenya: click here
Current Fogarty Trainees
Past fogarty trainees.
- COSMAS GITOBU
- FLORENCE JAGUGA
- JEPCHIRCHIR KIPLAGAT
- DIANA MARANGU
- JAMES KANGETHE
- SIGRID COLLIER
- GRANT CALLEN
- DICKENS ONYANGO
- ASHLEY KARCZEWSKI
- NEIL SIRCAR
- SUSAN JACOB
- IRENE MUKUI
- MICHAEL SCANLON
- NICOLE YOUNG
- JERRY ZIFODYA
- NANCY NGUMBAU
- GEORGE OMONDI PAUL
- ALIZA MONROE-WISE
- EHETE BAHIRU
- ANNE KAGGIAH
- ANJULI WAGNER
- MACKENZIE FLYNN
- ODESSA LACSINA
- GEORGE AYODO
- ERIC MURIUKI
- JENNIFER MARK
- LINNET MASESE
- MARILYN KIOKO
- CYRUS AYIEKO
- DANIEL CHIVATSI
- ELIZABETH IRUNGU
- KAREN HAMRE
- BARTHOLOMEW ONDIGO
- FRANKLINE ONCHIRI
- JOHN CRANMER
- ROSE BOSIRE
Recent and Ongoing Projects
Collaborating institutions.
All publications resulting from the research or research training supported by this award must acknowledge FIC and all co-funders with the following or comparable footnote: This project was supported by NIH Research Training Grant # D43 TW009345 funded by the Fogarty International Center, the NIH Office of the Director Office of AIDS Research, the NIH Office of the Director Office of Research on Women's Health, The National Heart, Lung and Blood Institute, the National Institute of Mental Health and the National Institute of General Medical Sciences
© University of Washington, 2024

Country Selection
Regulatory Authority
Scope of assessment, regulatory fees, ethics committee, scope of review, ethics committee fees, oversight of ethics committees.
Clinical Trial Lifecycle
Submission Process
Submission content, timeline of review, initiation, agreements & registration, safety reporting, progress reporting.
Sponsorship
Definition of Sponsor
Site/investigator selection, insurance & compensation, risk & quality management, data & records management, personal data protection.
Informed Consent
Documentation Requirements
Required elements, participant rights, emergencies, vulnerable populations, children/minors, pregnant women, fetuses & neonates, mentally impaired.
Investigational Products
Definition of Investigational Product
Manufacturing & import, quality requirements, product management, definition of specimen, specimen import & export, consent for specimen, requirements, additional resources.
Quick Facts
Clinical research in Kenya is regulated and overseen by the Pharmacy and Poisons Board (PPB) and the National Commission for Science, Technology and Innovation (NACOSTI) .
Pharmacy and Poisons Board
As per the PPA , the CTRules , and the G-KenyaCT , Kenya’s PPB is the regulatory authority responsible for clinical trial approvals, oversight, and inspections. As described in KEN-21 , the PPB and its Expert Committee on Clinical Trials (ECCT) evaluate all matters relating to clinical trials and grant permission for clinical trials to be conducted in Kenya. See KEN-20 , KEN-21 , and KEN-16 for more information about PPB.
Per the PPA and the CTRules , the PPB is authorized to undertake various mandated duties regarding regulation of medicines including (Note: the requirements provide overlapping and unique elements so each of the items listed below will not necessarily be in each source):
- Advise the government in all matters relating to the safety, packaging, labelling, distribution, and disposal of medicines
- Ensure that all medicinal products manufactured in, imported into, or exported from the country conform to prescribed standards of quality, safety, and efficacy
- Ensure that the personnel, premises, and practices employed in the manufacture, storage, marketing, distribution, and sale of medicinal substances comply with the defined codes of practice and other prescribed requirements
- Grant or revoke licenses for the manufacture, importation, exportation, distribution, and sale of medicinal substances
- Maintain a register of all authorized medicinal substances
- Publish, at least once every three (3) months, lists of authorized or registered medicinal substances and lists of products with marketing authorizations
- Regulate narcotic, psychotropic substances, and precursor chemical substances
- Consider applications for approval and alterations of dossiers intended for use in marketing authorization of medical products and health technologies
- Inspect and license all manufacturing premises, importing and exporting agents, wholesalers, distributors, pharmacies (including those in hospitals and clinics), and other retail outlets
- Prescribe a system for sampling, analysis, and other testing procedures of finished medicinal products released into the market to ensure compliance with the labeled specifications
- Conduct post-marketing surveillance of safety and quality of medical products
- Monitor the market for the presence of illegal or counterfeit medicinal substances
- Regulate the promotion, advertising, and marketing of medicinal substances in accordance with approved product information
- Approve the use of any unregistered medicinal substance for purposes of clinical trials, compassionate use, and emergency use authorization during public health emergencies
- Approve and regulate clinical trials on health products
- Disseminate information on medical products to health professionals and to the public to promote their rational use
- Collaborate with other national, regional, and international institutions on medicinal substances regulation
- Advise the Cabinet Secretary on matters relating to control, authorization, and registration of medicinal substances
- Implement any other function relating to the regulation of medicinal substances
Please note: Kenya is party to the Nagoya Protocol on Access and Benefit-sharing ( KEN-3 ), which may have implications for studies of investigational products developed using certain non-human genetic resources (e.g., plants, animals, and microbes). For more information, see KEN-15 .
National Commission for Science, Technology and Innovation
As delineated in the STI-Act and G-ECBiomedRes , in addition to obtaining the PPB’s permission to conduct research in Kenya, the principal investigator or the head of a research institution must obtain a favorable opinion from an ethics committee accredited by NACOSTI and a NACOSTI research license prior to initiating a study. NACOSTI’s role is to regulate and ensure quality in the science, technology, and innovation sector, and to advise the Kenyan government on related matters. According to Part II of the STI-Act , NACOSTI has specific research coordination and oversight functions, and it liaises with the National Innovation Agency and the National Research Fund to ensure funding and implementation of prioritized research programs. See KEN-32 for more information about NACOSTI’s mandate and functions.
Contact Information
According to the G-KenyaCT and KEN-22 , the PPB contact information is as follows:
Pharmacy and Poisons Board P.O. Box 27663 - 00506 Lenana Road Opp. DOD Nairobi, Kenya
Telephone: (+254) 02 3562107/2716905/6; (+254) 733 884411 / 720 608811; and ( +254) 709 770 100 or (+254) 709 770 xxx (where xxx represents the extension of the officer or office) Fax: +254-02-2713431
Email: [email protected] or [email protected] For Clinical Trials Inquiries: [email protected]
According to KEN-29 , the NACOSTI contact information is as follows:
National Commission for Science, Technology and Innovation off Waiyaki, Upper Kabete P. O. Box 30623 00100 Nairobi, Kenya
Phone (landline): (+254) 020 4007000, (+254) 020 8001077 Phone (mobile): 0713 788 787 / 0735 404 245
Email: [email protected] or [email protected]
In accordance with the PPA , the CTRules , the G-KenyaCT , and KEN-21 , Kenya’s Pharmacy and Poisons Board (PPB) , together with its Expert Committee on Clinical Trials (ECCT), is responsible for reviewing, evaluating, and approving applications for clinical trials using registered or unregistered investigational products (IPs). The G-KenyaCT specifies that the scope of the PPB’s assessment includes all clinical trials (Phases I-IV). As delineated in the CTRules , the G-KenyaCT , and KEN-21 , the PPB review and approval process may not be conducted in parallel with the ethics committee (EC) review. Rather, EC approval must be obtained prior to applying for PPB approval. As delineated in the STI-Act and G-ECBiomedRes , the principal investigator or the head of a research institution must obtain a favorable opinion from an EC accredited by the National Commission for Science, Technology and Innovation (NACOSTI) and a NACOSTI research license prior to initiating a study.
Clinical Trial Review Process
Per the CTRules and the G-KenyaCT , the PPB, through the ECCT, communicates the decision to approve, request additional information, or reject the application to the sponsor or the representative in writing within 30 working days of receiving a valid application. The G-KenyaCT indicates that in the case of rejection, the applicant may appeal and provide additional information to satisfy PPB requirements. In specific cases, the PPB may decide to refer the matter to external experts for recommendation.
As specified in the G-KenyaCT , each ECCT member, prior to reviewing the application, will declare any conflict of interest in the study and should have no financial or personal interests, which could affect their impartiality. During the protocol review, the reviewers must use the standard criteria (including available clinical and non-clinical data etc.) defined by the PPB. Confidentiality must be maintained during the review. Per the CTRules and the G-KenyaCT , the PPB/ECCT’s review must consider:
- The reliability and robustness of the data generated in the clinical trial, taking account statistical approaches, design of the clinical trial, and methodology, including sample size and randomization, comparator, and endpoints
- Compliance with the requirements concerning the manufacturing and import of IPs and auxiliary medicinal products
- Compliance with the labelling requirements
- The completeness and adequateness of the investigator's brochure
Regarding protocol amendments, the CTRules and the G-KenyaCT stipulate that any new information affecting the conduct/management of the trial, safety of the participants, and manufacture of the IP necessitating changes to the protocol, consent form, and trial sites require immediate submission of the amended documents to PPB for review and approval. Arrangements must be in place to take appropriate urgent safety measures to protect participants against any immediate hazard where new events relating to the conduct of the trial, or the development of the IP are likely to affect the safety of the participants. A copy of a favorable opinion letter from the EC on record must be submitted with the request for approval of a proposed amendment to the PPB. PPB approval must be obtained for all substantial amendments. Minor amendments or administrative changes may be implemented after getting the EC’s approval, but a record of these amendments must be kept for possible inspection by the PPB. See Submission Process and Submission Content sections for additional details on amendment submissions. Also, see the G-KenyaCT for examples of substantial amendments.
In addition, per the G-KenyaCT , the sponsor or the representative is required to request approval annually from the PPB at least six (6) weeks prior to the expiration of the previous approval.
Per the CTRules and the G-KenyaCT , the PPB may withdraw the authorization to conduct a clinical trial if it finds that the safety of the participants in the trial is compromised or that the scientific reasons for conducting the trial have changed. Additionally, per the CTRules , the PPB may revoke the approval if it determines that the IP has expired or is not usable.
As delineated in the G-KenyaCT , the PPB may inspect clinical trial sites to ensure that the generally accepted principles of good clinical practice (GCP) are met. The objectives of the inspection are to:
- Ensure that participants are not subjected to undue risks and that their rights, safety, and wellbeing are protected
- Validate the quality of the data generated
- Investigate complaints
- Verify the accuracy and reliability of clinical trial data submitted to the PPB in support of research or marketing applications
- Assess compliance with PPB guidelines and regulations governing the conduct of clinical trials
- Provide real-time assessment of ongoing trials
Per CRO-Inspect , the PPB is responsible for inspecting clinical trial and bioequivalence study sites that generate data for registration of medicines. The PPB requires that these sponsor and contract research organization sites comply with applicable good practices, including GCP, good laboratory practice (GLP), and good documentation practices. Based on risk assessments, the PPB will determine compliance with generally accepted good practice through inspections and, where appropriate, document reviews. In addition, see Cert-Emrgcy for information about GCP and good manufacturing practice certifications during emergencies.
Special Circumstances and Public Health Emergencies
The CTRules delineates that the PPB may, in special circumstances, authorize the conduct of a clinical trials under fast-track procedures or non-routine procedures. PPB may recognize and use clinical trial decisions, reports, or information from other competent authorities authorizing fast-track clinical trials. The special circumstances may include:
- A public health emergency
- The rapid spread of an epidemic disease
- Any other circumstance as may be determined by the PPB
The G-KenyaCT outlines PPB’s scope of assessment of a clinical trial application during a public health emergency. The PPB will conduct an expedited review and liaise with relevant stakeholders (including relevant ECs and other oversight bodies) to facilitate a holistic review of an application in a fast-track manner. The following prioritization criteria must be applied in the selection of applications for expedited review:
- Epidemiology of the emergency
- Morbidity and mortality associated with the emergency and/or condition under study
- Supporting scientific data/information available for the IP at the time of submission
- Feasibility of the implementation of the trial design within the context of the emergency
- Benefit impact of the intervention and/or trial design
In addition, PPB’s assessment will consider the following:
- The research does not compromise the response to an outbreak or appropriate care
- Studies are designed to yield scientifically valid results under the challenging and often rapidly evolving conditions of disasters and disease outbreak
- The research is responsive to the health needs or priorities of the disaster victims and affected communities and cannot be conducted outside a disaster situation
- The participants are selected fairly and adequate justification is given when particular populations are targeted or excluded, for example, health workers
- The potential burdens and benefits of research participation and the possible benefits of the research are equitably distributed
- The risks and potential individual benefits of experimental interventions are assessed realistically, especially when they are in the early phases of development
- Communities are actively engaged in study planning to ensure cultural sensitivity, while recognizing and addressing the associated practical challenges
- The individual informed consent of participants is obtained from individuals capable of giving informed consent
- Research results are disseminated, data are shared, and any effective interventions developed or knowledge generated are made available to the affected communities
STI-Act stipulates that NACOSTI issues research licenses if it finds that the conduct of the research is beneficial to the country and will not adversely affect any aspect of the nature, environment, or security of the country. The license issued will have NACOSTI’s seal and will indicate the commencement and expiration of the research. In addition, NACOSTI maintains a register of all persons granted a license, which is available for public inspection during normal working hours free of charge.
KEN-31 states that if a research license application does not meet the conditions required under the STI-Act , NACOSTI must reject the application and communicate the reasons to the applicant. Any person may appeal NACOSTI’s decision to the Cabinet Secretary within 30 days of being notified of the decision. For approved research, NACOSTI may conduct an evaluation to assess compliance with the conditions of the license. If the research project has not been completed within the stipulated period, the researcher may apply for renewal of the license and pay the requisite fee. The researcher is expected to apply for renewal by attaching a progress report instead of a proposal. KEN-31 indicates that the duration of the research license is one (1) year.
Per the PPA and the G-KenyaCT , the sponsor or the representative is responsible for paying a fee to the Pharmacy and Poisons Board (PPB) to submit a clinical trial application for authorization. The PPB currently requires a non-refundable application fee of $1,000 USD, or the equivalent in Kenya Shillings at the prevailing bank rates.
Payment Instructions
As stated in Annex 2 of the G-KenyaCT , payment is to be made by a bank check payable to the “Pharmacy and Poisons Board” and presented to the PPB’s accounts office upon submitting the application.
Payment can also be made by electronic fund transfer (EFT) to the PPB Bank account, if required. The sponsor or the representative is responsible for all bank charges associated with the EFT. Details of the EFT payment should be obtained from the PPB prior to initiating such a transaction.
As delineated in KEN-31 , the National Commission for Science, Technology and Innovation (NACOSTI) charges a fee that varies depending on the applicant’s status as Kenyan or non-Kenyan, and standing as a researcher (i.e., student, public/private institution, private company). The fees are non-refundable and apply for research license renewals. Details on additional requirements are provided in the Submission Content section.
- Student, Undergraduate/Diploma: East African Community (EAC) Countries – 100 Kenya Shillings; Kenyan Citizens – 100 Kenya Shillings; Rest of Africa – 200 Kenya Shillings; Non-Africans - $150 USD
- Research (Masters): EAC Countries – 1,000 Kenya Shillings; Kenyan Citizens – 1,000 Kenya Shillings; Rest of Africa – 2,000 Kenya Shillings; Non-Africans - $350 USD
- Research (PhD): EAC Countries – 2,000 Kenya Shillings; Kenyan Citizens – 2,000 Kenya Shillings; Rest of Africa – 4,000 Kenya Shillings; Non-Africans - $400 USD
- Post-Doctoral: EAC Countries – 5,000 Kenya Shillings; Kenyan Citizens – 5,000 Kenya Shillings; Rest of Africa – 10,000 Kenya Shillings; Non-Africans - $500 USD
- Public Institutions: Kenyan Citizens – 10,000 Kenya Shillings
- Private Institutions, Commercial/Market Research, Companies: Kenyan Citizens – 20,000 Kenya Shillings
KEN-31 indicates that the applicant must submit the research license application online through the Research Information Management System (RIMS) ( KEN-24 ). Applicants should pay the applicable fee through mobile money transfer or direct bank deposit.
As per KEN-31 , East African citizens have two (2) options for payment to the Kenya Shillings Account: 1) mobile money transfer or 2) direct bank deposit.
Mobile money transfer payments should be made via Mpesa Express. Payment using this method will be made after initiating the application process. The system will prompt the applicant to make the payment.
Direct bank deposits should be made to:
Kenya Commercial Bank Branch: Kipande House Account Name: National Commission for Science, Technology and Innovation Account Number: 1104162547 Swift Code: KCBLKENX Transaction Description: Research License Fee
Non-Kenyans should use the following U.S. Dollar Account:
NCBA Bank Branch: City Centre Account Name: National Commission for Science, Technology and Innovation Account Number: 2904970067 Swift Code: CBAFKENX Transaction Description: Research License Fee
As per the G-KenyaCT , the G-ECBiomedRes , and KEN-30 , Kenya requires an independent review of research through a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC) in one (1) of the local institutions charged with the responsibility of conducting research in human participants. KEN-25 provides a list of the accredited institutional ECs.
Ethics Committee Composition
As delineated in the G-ECAccred , institutional ECs should consist of at least seven (7) members, or an odd number above seven (7). The G-ECBiomedRes states that these members should be multidisciplinary and multisectoral in composition, collectively encompass relevant scientific expertise, balanced age and gender distribution, and include laypersons representing community interests and concerns. Per the G-ECAccred , the composition should meet the following requirements:
- At least one (1) member with knowledge and understanding of Kenyan law
- At least one-third of the members must be female, and one-third must be male
- At least one (1) member who is unaffiliated with the institution
- At least two (2) members must have research expertise and experience, one (1) of whom must be in the health field
- At least one (1) member must be a lay member
- For ECs reviewing clinical research, at least two (2) members must be clinicians, one (1) of whom is currently in active practice or clinical research
- Reflect the regional and ethnic diversity of the people of Kenya
The chairperson must also have some basic training and/or experience in bioethics and leadership. All EC appointments are the responsibility of the institution’s administrative head. See the G-ECAccred and the G-ECBiomedRes for detailed institutional EC requirements.
Terms of Reference, Review Procedures, and Meeting Schedule
Per G-ECBiomedRes , ECs need to have independence from political, institutional, professional, and market influences. As delineated in the G-ECAccred , the G-ECBiomedRes , and the STI-Regs , institutional ECs must operate within written standard operating procedures (SOPs) which delineate the EC’s process for conducting reviews. Per the G-ECAccred , SOPs should include but are not limited to information on EC scope, responsibility, and objectives, institutions served, committee functions, terms and conditions of member appointment, business procedures including meeting schedules and types of reviews, documentation, recordkeeping, and archiving procedures, quorum requirements, communication procedures, and complaint process and dispute resolution procedures. Per the G-ECAccred and the STI-Regs , these documents must be provided to NACOSTI.
Per the G-ECAccred , the quorum for NACOSTI-accredited EC meetings must be:
- At least 50 percent of the membership must form the quorum
- A lay person must be present in all meetings
- For ECs reviewing clinical research, at least two (2) members must be clinicians, one (1) of whom is currently in active practice or clinical research.
The G-ECBiomedRes also defines quorum requirements:
- The minimum number of members required to compose a quorum (e.g., more than half the members)
- The professional qualifications requirements (e.g., physician, lawyer, statistician, paramedical, or layperson) and the distribution of those requirements over the quorum; no quorum should consist entirely of members of one (1) profession or one (1) gender; a quorum should include at least one (1) member whose primary area of expertise is in a non-scientific area, and at least one (1) member who is independent of the institution/research site
Per G-ECBiomedRes , EC member terms of appointment should be established that include the duration of an appointment, the policy for the renewal of an appointment, the disqualification procedure, the resignation procedure, and the replacement procedure. A statement of the conditions of appointment should be drawn up that includes the following:
- A member should be willing to publicize their full name, profession, and affiliation
- All reimbursement for work and expenses, if any, within or related to an EC should be recorded and made available to the public upon request
- A member should sign a confidentiality agreement regarding meeting deliberations, applications, information on research participants, and related matters
Regarding training, EC members should have initial and continued education regarding the ethics and science of biomedical research. The conditions of appointment should indicate the availability and requirements of introductory training, as well as on-going continuing education. This education may be linked to cooperative arrangements with other ECs in the area, country, and region.
For detailed institutional EC requirements and information on other administrative processes, see the G-ECAccred and the G-ECBiomedRes . See KEN-17 and KEN-26 for examples of accredited EC submission and review guidelines.
According to G-ECBiomedRes , the primary scope of information assessed by the institutional ethics committees (ECs) relates to maintaining and protecting the dignity and rights of research participants and ensuring their safety throughout their participation in a clinical trial. The G-ECAccred further states that the National Commission for Science, Technology and Innovation (NACOSTI) accredits ECs in order to uphold the standard of ethics review in the country; develop public confidence and trust in the national research system; facilitate equitable access to research and human health records in health facilities; and facilitate coordination and collaboration among ECs. See the G-ECAccred and the G-ECBiomedRes for detailed ethical review guidelines.
Role in Clinical Trial Approval Process
As per the G-KenyaCT and KEN-21 , the Pharmacy and Poisons Board (PPB) ’s review and approval of a clinical trial application is dependent upon obtaining approval by an accredited institutional EC. Consequently, the PPB and EC reviews may not be conducted in parallel.
As set forth in the G-ECBiomedRes , ECs must be constituted to ensure an independent and competent review and evaluation of all ethical aspects of clinical trials. ECs must review research involving human participants to ensure they meet these ethical principles:
- Respect for persons, including respect of autonomy, protection of vulnerable groups, and protection of privacy and confidentiality
- Beneficence
- Justice, which in research means equitable distribution of the benefits and the burdens
For additional details on the principles and benchmarks for ethical review, see G-ECBiomedRes .
Per the G-ECBiomedRes , expedited review may be permitted for protocols involving no more than minimal risk to research participants.
The G-ECBiomedRes indicates that all ECs should carry out regular monitoring of approved protocols involving human participants. In case of any adverse events, the EC should report this immediately to Kenya’s National Bioethics Committee (NBC).
Per the G-ECBiomedRes , with collaborative research projects, the collaborating investigators, institutions, and countries must function as equal partners with safeguards to avoid exploitation of local researchers and participants. An external sponsoring agency should submit the research protocol to their country’s EC, as well as the Kenyan EC where the research is to be conducted. Further, this research must be responsive to the health needs of Kenya and reasonably accessible to the community in which the research was conducted. Consideration should be given to the sponsoring agency agreeing to maintain health services and faculties established for the purposes of the study in Kenya after the research has been completed. Such collaborative research must have a local/Kenyan co-principal investigator.
As per the G-KenyaCT , G-ECBiomedRes , and KEN-30 , Kenya requires an independent review of research through a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC) in one (1) of the local institutions charged with the responsibility of conducting research in human participants. The EC fee to review a clinical trial application will vary depending on the institution. See KEN-25 for a list of NACOSTI-accredited institutional ECs. For an example of institutional fee requirements charged by the Scientific and Ethics Review Unit (SERU) at the Kenya Medical Research Institute (KEMRI) , see KEN-27 .
As set forth in the STI-Act and KEN-32 , the National Commission for Science, Technology and Innovation (NACOSTI) is the central body responsible for the oversight, promotion, and coordination of research. NACOSTI’s role is to regulate and ensure quality in the science, technology, and innovation sector, and to advise the Kenyan government on related matters. As per the G-ECAccred , NACOSTI has delegated the task of reviewing research proposals for ethical clearance to accredited institutional ethics committees (ECs) to ensure that research conducted in the country observes high research ethics standards.
Per the G-ECBiomedRes , Kenya's National Bioethics Committee (NBC) advises NACOSTI on research ethics. In addition, NBC offers dispute resolution if an applicant is dissatisfied with the decision of an EC. Finally, the NBC must terminate research at any stage if it is found to be harmful to the participants.
Registration, Auditing, and Accreditation
As per the STI-Regs and the G-ECAccred , NACOSTI is responsible for accrediting institutional ECs. Per the G-ECAccred , the application requirements for accreditation are:
- A completed application form ( KEN-10 or Annex III of the G-ECAccred )
- Copy of the standard operating procedures (SOPs)
- Copies of abridged curriculum vitaes (CVs) (no more than four (4) pages) for each member of the proposed EC (including the training attended)
- Profile of the organization/institution detailing the areas of competence (no more than four (4) pages)
Per the G-ECAccred , NACOSTI issues a certificate of accreditation to accredited institutional ECs, which is valid for three (3) years from the date of NACOSTI’s notification. All accredited ECs must submit annual reports to NACOSTI by July 31st for review and monitoring. Applications for renewal of accreditation should be made six (6) months before expiry of the accreditation period. Failure to renew accreditation or failure to maintain the appropriate standards for continuity of accreditation will mean that the accredited status of the EC will lapse at the end of the current accreditation period. Accreditation must be terminated if the accredited committee fails to maintain the required standards. For re-accreditation review purposes, ECs must provide the SOPs under which they will operate. The SOPs are not required as part of the annual reporting process, unless they have been amended, but are required to be stated/included for the reaccreditation review process (every three (3) years). See the G-ECAccred for additional details on the accreditation process.
In accordance with the PPA , the STI-Act , the CTRules , the G-KenyaCT , the G-ECBiomedRes , KEN-21 , and KEN-16 , Kenya requires the sponsor or the representative to obtain clinical trial authorization from the Pharmacy and Poisons Board (PPB) ’s Expert Committee on Clinical Trials (ECCT) and an independent ethics review through a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC) in a local institution. In addition, the STI-Act and KEN-31 specify that applicants must obtain a research license from NACOSTI prior to initiating a study. The G-KenyaCT also states that the PPB review and approval process may not be conducted in parallel with the EC review. EC approval must be obtained prior to applying for PPB approval.
Regulatory Submission
As described in the G-KenyaCT and KEN-16 , the sponsor or the representative is expected to submit the clinical trial application electronically via the PPB online system ( KEN-16 ). The clinical trial application form is available in the online system ( KEN-16 ). Per the G-KenyaCT , in the event of a multicenter clinical trial, the sponsor should only file one (1) application to the PPB. According to KEN-34 , all application documents should be signed, dated, and version referenced, if applicable, and should be in English. See Annex 7 of the G-KenyaCT to view a flowchart of the submission and approval process.
The G-KenyaCT indicates that when an application for a clinical trial is accepted, an acknowledgement of receipt will be issued with a reference number for each application. This PPB/ECCT reference number must be quoted in all correspondence concerning the application in the future. This will be communicated through email to the applicant or through KEN-16 .
Per the G-KenyaCT , sponsors (applicants) can request pre-submission meetings with the PPB to discuss pertinent issues prior to formal submissions. The request must be made in an official letter and include the following information:
- Background information on the disease to be treated
- Background information on the product
- Quality development
- Non-clinical development
- Clinical development
- Regulatory status
- Rationale for seeking advice
- Proposed questions and applicant’s positions
In addition, the letter must be addressed to the Chief Executive Officer of the PPB and sent to [email protected] and copied to [email protected] . The request for a meeting should propose two (2) different dates for the meeting with the proposed dates being at least three (3) weeks away.
Per G-KenyaCT , any new information that affects the conduct/management of the trial, safety of the participants, and manufacture of the product necessitating changes to the protocol, consent form, and trial sites, etc. will require immediate submission of the amended documents to the PPB for review and approval. Minor amendments or administrative changes may be implemented after getting the EC’s approval, but a record of these amendments must be kept for possible inspection by the PPB.
National Commission for Science, Technology and Innovation
Per KEN-31 , an application for a NACOSTI research license should be submitted online via the Research Information Management System (RIMS) ( KEN-24 ).
Ethics Review Submission
Each institutional EC has its own required submission procedures, which can differ significantly regarding the application format and number of copies. See KEN-17 for an example of a NACOSTI-accredited EC’s guidelines.
Regulatory Authority Requirements
As per the CTRules , the G-KenyaCT , and KEN-34 , the following documentation must be submitted (signed, dated, and version referenced) to the Pharmacy and Poisons Board (PPB) (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source):
- Cover letter
- Study protocol
- Proof of study registration in the Pan African Clinical Trials Registry ( KEN-19 )
- Patient information leaflet and informed consent form (ICF)
- Investigators brochure (IB) and package inserts
- Investigational Medicinal Product Dossier (IMPD), including stability data for the investigational product (IP)
- Adequate data and information on previous studies and phases to support the current study
- Good manufacturing practice (GMP) certificate of the IP from the site of manufacture issued by a competent health authority in the manufacturer’s jurisdiction of origin
- Certificate of analysis of the IP
- Pictorial sample of the IPs, including the labeling text
- Signed investigator(s) curriculum vitae(s) (CV(s)), including that of the study pharmacist (the CV should include the current workload of the principal investigator (PI))
- Evidence of contractual agreement between the relevant parties
- Evidence of recent good clinical practice (GCP) training of the core study staff
- Data and Safety Monitoring Board (DSMB) information, including the charter, composition, and meeting schedule
- Detailed study budget
- Financial declaration by the sponsor and PI ( KEN-2 and Annex 5 of the G-KenyaCT )
- No conflict of interest declaration by the sponsor and PI
- Signed declarations by the sponsor, PI, and the monitor that the study will be carried out according to the protocol and applicable laws, regulations, and GCP requirements ( KEN-1 and Annex 4 of the G-KenyaCT )
- Indemnity cover for PI, investigators, and study pharmacist
- Clinical trials insurance cover for the study participants
- Copy of favorable opinion letter from local ethics committee (EC)
- Copy of current practice licenses for the investigators and study pharmacist
- Copy of approval letter(s) from collaborating institutions or other regulatory authorities, if applicable
- For multicenter/multi-site studies, an addendum for each of the proposed sites including, among other things, the sites’ capacity to carry out the study (e.g., personnel, equipment, laboratory)
- A signed statement by the applicant indicating that all information contained in, or referenced by, the application is complete and accurate, and is not false or misleading (Annex 4 of the G-KenyaCT )
- Payment of fees
- Statistical analysis plan
- A signed checklist ( KEN-34 and Annex 2 of the G-KenyaCT )
Per the G-KenyaCT , a request for approval of an amendment must include a summary of the proposed amendments; the reason for the amendment; the impact of the amendment on the original study objectives; the impact of the amendments on the study endpoints and data generated; and the impact of the proposed amendments on the safety and wellbeing of study participants.
KEN-35 describes the submission content for requesting annual approval from the PPB.
Per the STI-Regs and KEN-31 , non-Kenyan applicants must be affiliated with a Kenyan institution. Per KEN-31 , applicants must apply online through National Commission for Science, Technology and Innovation (NACOSTI) ’s Research Information Management System (RIMS) website ( KEN-24 ) and upload the following:
- Passport size color photo in JPG or PNG format
- Scanned ID/passport in PDF format
- Introductory letter from relevant institution signed by an authorized officer
- Affiliation letter from relevant local institution for foreigners signed by an authorized officer and valid for one (1) year
- Grant letter from the funding agency to support the amount indicated for the research’s funding
- PPB clinical trial approval
- Prior Informed Consent (PIC), Mutually Agreed Terms (MAT), or Material Transfer Agreement (MTA) where applicable, for applications to conduct research on genetic resources and derivatives
- Approved research proposal in PDF format
- Certificate of ethical clearance of the research (see list of accredited ECs in KEN-25 )
- Evidence of payment as the last page of the uploaded proposal
Per KEN-31 , the following conditions apply to the research license:
- The research license is valid for the proposed research, site, and specified period
- Both the research license and any rights thereunder are non-transferable
- NACOSTI may monitor and evaluate the research
- The licensee must inform the relevant County Director of Education, County Commissioner, and County Governor before research commencement
- Excavation, filming, and collection of specimens are subject to further permissions from relevant government agencies
- The research license does not give authority to transfer research materials
- The licensee shall submit one (1) hard copy and upload a soft copy of their final report within one (1) year of completion of the research
- NACOSTI reserves the right to modify the conditions of the research license including its cancellation without prior notice
KEN-31 states that if the research is not completed within the stipulated period, the applicant may apply for renewal of the research license and pay the requisite fee. A progress report should be submitted with the request for renewal instead of a proposal. The progress report must indicate the objectives and activities that have been accomplished, as well as the research work that has yet to be undertaken. KEN-31 further indicates that submissions requesting renewal should be made at least 30 days prior to the expiration of the approval period.
Ethics Committee Requirements
EC requirements vary depending on the specific EC. Examples of NACOSTI-accredited EC requirements are delineated in the Ethics and Research Application Form ( KEN-9 ) used by the Kenyatta National Hospital-University of Nairobi (KNH-UoN) Ethics and Research Committee and the Kenya Medical Research Institute (KEMRI) . As specified in KEN-9 , the following documentation is required to obtain ethics approval from these two (2) ECs:
- Three (3) copies of the application form (including at least one (1) copy with original linked signatures)
- Three (3) copies of relevant documentation (ICFs, questionnaires, data instruments, drug information summary, data collection forms, debriefing statements, advertisements, etc.)
- Three (3) copies of protocol and grant/contract
- One (1) copy of protocol and IB for trials
- Three (3) copies of thesis/dissertation proposal, where applicable to students
- PI name and contact information
- Project title
- Research personnel
- Funding information
- Project description
- Methodology and procedures
- Participants description (e.g., selection/withdrawal criteria and treatment)
- Risk benefits and adverse events (See Safety Reporting section for additional information)
- Research data confidentiality
- Consent/assent forms and waiver
As set forth in the G-ECBiomedRes , a foreign sponsoring agency must also submit its research protocol for ethics review according to its own country’s standards. This research must be responsive to the health needs of Kenya and reasonably accessible to the community in which the research was conducted.
Clinical Protocol
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). The CTRules the G-KenyaCT , the G-ECBiomedRes , and KEN-14 outline the key elements of a research protocol in Kenya (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source.):
- A project title that adequately captures the essence of the study
- The names, addresses, signatures, and updated abridged curriculum vitae of the investigators
- Evidence that the PI has prior training in good clinical practice
- Contact information for the EC and collaborating institutions
- A summary of the project
- Introduction, background, and literature review, including nonclinical data
- Study objectives, rationale, questions, and hypothesis/es
- Study site, design, and methodology
- Ethical considerations
- Role of investigators
- Publication policy
- Consent explanation - elements of consent explanations
- ICF with signature provisions for participants and the PIs
- Risks and benefits
- Mode of assessment of the safety and efficacy of the IP
- Mode of collecting, analyzing, and reporting the statistics of the clinical trial
- Source data documents of the clinical trial
- Quality control and quality assurance
- Confidentiality
- Recruitment, selection, treatment, and withdrawal of participants
- Compensation and post-trial access program
- Undue inducement and coercion
- Voluntariness
- Alternative treatment(s) if available
- Storage of specimens
- MTA, where applicable
- Data management and statistical analysis
In addition, per the G-KenyaCT , the protocol should have a clear description of study stoppage rules indicating reasons, who makes the decision, and how the decision will be communicated to the PPB and the EC.
Based on the CTRules and the G-KenyaCT , the Pharmacy and Poisons Board (PPB) 's review and approval of an application to conduct a clinical trial is dependent upon obtaining ethics approval from a National Commission for Science, Technology and Innovation (NACOSTI) -accredited ethics committee (EC) . Therefore, the PPB and EC reviews may not be conducted in parallel. In addition, the STI-Act and KEN-31 specify that all applicants must obtain a research license from NACOSTI prior to initiating a study.
Regulatory Authority Approval
Per the G-KenyaCT , sponsors (or applicants) can request pre-submission meetings to discuss pertinent issues prior to formal submissions. The request must be made in an official letter addressed to the Chief Executive Officer of the PPB and sent to [email protected] and copied to [email protected] . The request for a meeting should propose two (2) different dates for the meeting with the proposed dates being at least three (3) weeks away. (See Submission Process section for details on the content of request.)
Per the G-KenyaCT , upon receipt of a clinical trial application, the PPB’s Clinical Trial Directorate of Medicines Information and Pharmacovigilance screens the application package for completeness, which takes five (5) days. If accepted, the sponsor or the representative is issued an acknowledgement of receipt. If additional information is needed, the sponsor will have 10 days to respond. The PPB aims to respond to applications within 30 working days. The sponsor or the representative must reference the PPB/Expert Committee on Clinical Trials (ECCT) number in all future application-related correspondence. The application is then evaluated by the ECCT and PPB staff according to their respective standard operating procedures. The PPB/ECCT’s decision to approve, request additional information, or reject the application is communicated to the sponsor or the representative in writing within 30 days of receiving a valid application. If additional information is requested, the sponsor has 90 days to respond after which the PPB has 15 days to issue a final decision. In certain cases, the PPB may refer the application to external experts for their recommendation.
Per the G-KenyaCT , the sponsor or the representative is also required to request approval annually from the PPB at least six (6) weeks prior to the expiration of the previous approval. Refer to the Checklist for Submitting a Request for Annual Approval ( KEN-35 ) for relevant documentation requirements.
Per KEN-5 and KEN-31 , the timeline for NACOSTI’s license application process is 30 days.
KEN-31 states that if a research license application does not meet the conditions required under the STI-Act , NACOSTI must reject the application and communicate the reasons to the applicant. Any person may appeal NACOSTI’s decision to the Cabinet Secretary within 30 days of being notified of the decision.
Ethics Committee Approval
The EC review and approval process timeline will vary by institution.
In accordance with the PPA , the STI-Act , the G-KenyaCT , the G-ECBiomedRes , KEN-21 , and KEN-16 , a clinical trial can only commence after the sponsor or the representative receives authorization from Kenya’s Pharmacy and Poisons Board (PPB) , and ethics committee (EC) approval from an institutional EC that has been accredited by the National Commission for Science, Technology and Innovation (NACOSTI) prior to initiating a study. ECs are accredited pursuant to the requirements delineated in the G-ECAccred . The G-KenyaCT specifies that the PPB review and approval process may not be conducted in parallel with the EC review. In addition, the STI-Act and KEN-31 state that all applicants must obtain a research license from NACOSTI prior to initiating a study. No waiting period is required following the applicant’s receipt of these approvals.
As per the PPA and the G-KenyaCT , the sponsor or the representative is required to obtain an import license for the shipment of an investigational product to be used in the trial. (See the Manufacturing & Import section for additional information).
As stated in the G-KenyaCT , Kenyan clinical trials should be conducted in compliance with the International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ).
Clinical Trial Agreement
Prior to initiating the trial, the G-KenyaCT requires that the sponsor agree with investigator(s) on the definition, establishment, and assignment of responsibilities specified in the protocol. These responsibilities include conduct of the trial in compliance with KEN-14 and the approved protocol; data management; unblinding of treatment codes; statistical considerations; and preparation of the final clinical report. The sponsor, in a written document, may agree to transfer all related activities of the clinical trial to designated research institutions. However, all responsibility for the trial lies with the sponsor. Prior to the initiation of the clinical trial, the agreement between the sponsor and investigators should be in writing as part of the protocol submitted for PPB approval or in a separate agreement. The sponsor and investigators must sign and date the protocol of the trial to confirm the agreement.
Clinical Trial Registration
As per the G-KenyaCT , all clinical trials taking place in Kenya must be registered in the PPB’s Online Clinical Trials Registry System ( KEN-16 ). The principal investigator is required to log in and set up an account to register a study.
In addition, as required by KEN-34 , all clinical trials taking place in Kenya must be registered in the Pan African Clinical Trials Registry ( KEN-19 ).
Safety Reporting Definitions
According to the CTRules and the G-KenyaCT , the following definitions provide a basis for a common understanding of Kenya’s safety reporting requirements:
- Adverse Event (or Adverse Experience) (AE) – Any untoward medical occurrence in a participant in a clinical investigation study or intervention product, and which does not necessarily have a causal relationship with the treatment
- Adverse Drug Reaction (ADR) – All noxious and unintended responses to a clinical trial study or interventional product related to any dose or all unintended noxious responses to a registered medicinal product which occurs at doses normally used in humans for prophylaxis, diagnosis, or therapy of diseases or for modification of physiological function
- Serious Adverse Event (SAE) – Any untoward medical occurrence that at any dose: results in death, is life threatening, requires hospitalization or prolongation of existing hospitalization, results in persistent or significant disability/incapacity, or is a congenital anomaly/birth defect
- Suspected Unexpected Serious Adverse Reaction (SUSAR) – A serious adverse reaction that is not identified in practice, severity, or frequency by the referenced safety information
Safety Reporting Requirements
Investigator Responsibilities
Per G-KenyaCT , the investigator must ensure that all SAEs are reported promptly to Kenya’s Pharmacy and Poisons Board (PPB) within the mandated timelines, as described below. Proper protection procedures or treatments should be administered to trial participants with SAEs.
Sponsor Responsibilities
As indicated in the CTRules and the G-KenyaCT , the sponsor should report to the PPB and all relevant institutions, all SAEs and SUSARs occurring during the course of the trial. The G-KenyaCT specifies that the sponsor should expedite reporting all SAEs to the PPB and the ethics committee (EC), and the sponsor and investigators should immediately undertake appropriate and necessary measures and treatment to protect the trial participants. The CTRules delineates that where a sponsor conducts a clinical trial on the same health product or active pharmaceutical substance in another country, the sponsor must submit a report of any SUSAR or SAE that occurs in that other clinical trial to the PPB. Per the CTRules and the G-KenyaCT , a sponsor must submit a report of an initially fatal or life-threatening SUSAR or SAE as soon as it occurs but, in any case, not later than seven (7) days after the occurrence of the event. The G-KenyaCT indicates that if the initial report is incomplete, the sponsor must submit a completed report based on the initial information within an additional eight (8) days. As required in the CTRules and the G-KenyaCT , a report of the occurrence of a SUSAR or SAE must specify whether the SUSAR or SAE is related to the clinical trial.
As indicated in the CTRules and the G-KenyaCT , other important considerations and timelines include the following (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source.):
- The sponsor must notify all the investigators involved in ongoing clinical trials of the investigational product (IP) of all SAEs and SUSARs within 15 calendar days
- Any IP-related SAE must receive immediate medical attention and be reported to the PPB
- SAE report form must be completed (including lab results) and submitted to enable causality assessment
- All fatal cases must be accompanied by a formal autopsy report, and a verbal autopsy report should be submitted in those exceptional cases where a formal autopsy is not possible
- Any frequent IP related AE/ADR must receive immediate medical attention and be reported to the PPB within seven (7) days
- The sponsor must submit a report on a SUSAR that is not fatal or life-threatening within 15 days after the occurrence of the event
- The principal investigator (PI) is required to submit follow-up information as soon as it becomes available
- All additional information should be clearly marked as updated and must include the Protocol Number and Participant Number
- Foreign regulatory decisions that affect the safety or use of the product under study must be reported to the PPB within seven (7) days through a detailed report
- Literature reports that have implications for the safety of the IP must be submitted within 15 days with a detailed report and a copy of the publication
- New information or notification of change in nature, severity, or frequency of risk factors for the product under study or conduct of trial must be submitted within 15 days
Other Safety Reports
The G-ECBiomedRes indicate that ECs should monitor research, and will report to the National Bioethics Committee upon notification of an AE.
The CTRules and the G-KenyaCT state that the sponsor must also submit a safety report to the PPB once a year throughout the clinical trial, or upon request. The purpose of the annual safety report is to briefly describe all new safety information relevant to one (1) or more clinical trial(s), and to assess the safety conditions of the participants enrolled in these trial(s). The safety report must include a log of SAE and SUSAR events. The SAE and SUSAR log should include the following:
- Patient Identification
- Date of recruitment into the study
- Type of SAE or SUSAR
- SAE or SUSAR start and end dates
- Reason for reporting the event as an SAE or SUSAR
- Relation to IP
- SAE or SUSAR outcome
Note that the PPB may require more frequent reporting of the safety reports depending on the nature of the clinical trial being implemented. When this is the case, the PPB must communicate the required frequency to the PI and sponsor in writing.
Form Completion & Delivery Requirements
As per the G-KenyaCT and KEN-16 , all SAEs and SUSARs must be reported to the PPB via the Pharmacovigilance Electronic Reporting System (PvERS) ( KEN-6 ).
Interim and Annual Progress Reports
As stated in the G-KenyaCT , the sponsor and/or the principal investigator (PI) is required to send progress reports to the Pharmacy and Poisons Board (PPB) on an annual basis from the date of the trial’s initiation. The progress report should contain the following:
- Current status of the study
- Summary of the participants screened (e.g., failed screenings, participants enrolled, withdrawn, or lost to follow-up, and other challenges)
- Summary of protocol deviations and violations
- Updated investigational product Investigator’s Brochure
- Drug Safety Update Report
- Copy of the latest Data Safety Management Board report
- Copy of favorable opinion from the ethics committee (EC) on record
- Copy of annual practice license for the investigators and pharmacists
- Suspected, Unexpected, Serious Adverse Event (SUSAR) and Serious Adverse Event (SAE) Log
For multisite trials, per the G-KenyaCT , the sponsor or the representative must submit a summarized report for all of the sites and include the information listed above.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As per KEN-14 , the investigator should promptly provide written reports to the sponsor and the institutional EC on any changes significantly affecting the conduct of the trial, and/or increasing the risk to participants.
According to the G-KenyaCT , for annual renewal of the study, the sponsor or the representative must submit a copy of the progress report including the documents listed above. The request must also be accompanied by copies of annual practice licenses for the investigators and pharmacists, and a copy of valid insurance coverage for the participants. All documents must be submitted using the PPB’s Online Clinical Trials Registry System ( KEN-16 ). The sponsor or the representative must receive an acknowledgement of this submission before proceeding with the study. These documents must be submitted to the PPB at least six (6) weeks prior to the expiration of the previous approval.
Pursuant to KEN-14 , the investigator should submit written summaries of the trial status to the institutional EC annually, or more frequently, if requested.
Final Report
Per the G-KenyaCT , the sponsor must notify the PPB of the end of a clinical trial taking place at a Kenyan site within 15 days from the end of the clinical trial at the site. After the trial has been conducted and closed, the applicant must submit an executive summary report of the study within 30 days. This should be followed by a clinical study report within 180 days of the study closure unless otherwise justified. The report must comply with the International Council for Harmonisation's ICH E3 format ( KEN-13 ). The report must include a short but comprehensive summary of the trial’s essential findings and methodology and should also contain a layman’s summary. Additionally, the sponsor must inform the PPB of any results that will be publicly released at least 14 days before release. In addition, upon completion of the trial, as delineated in KEN-14 , the investigator is required to submit a final report to the institutional EC summarizing the trial’s outcome.
For multi-site research, the G-ECBiomedRes requires all parties to decide on procedures for drafting a common final report and publication at the onset of the research. Individual sites or institutions must not publish any data until the appropriate authorities accept the combined report.
KEN-31 further indicates that the research license applicant must submit one (1) hard copy and upload a soft copy of the final research report to the National Commission for Science, Technology and Innovation (NACOSTI) within one (1) year of the research’s completion.
As per the G-KenyaCT , a sponsor is defined as an individual, a company, an institution, or an organization who takes legal responsibility for the initiation, management, and financing of a trial. According to the G-KenyaCT , a sponsor, in a written document, may agree to transfer all related activities of the clinical trial to designated research institutions. However, all responsibility for the trial lies with the sponsor. The G-ECBiomedRes indicates that sponsors may be foreign, but must comply with certain conditions including affiliating themselves to institutions recognized in Kenya.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). In accordance with KEN-14 , Kenya permits a sponsor to transfer any or all of its trial-related duties and functions to a contract research organization (CRO) and/or institutional site(s). However, the ultimate responsibility for the trial data’s quality and integrity always resides with the sponsor. Any trial-related responsibilities transferred to a CRO should be specified in a written agreement. The CRO should implement quality assurance and quality control.
The G-KenyaCT , which requires sponsors to follow the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), states that the sponsor is responsible for selecting the investigator(s) and the institution(s) for the clinical trial and for ensuring that the investigator(s) are qualified by education, training, and experience.
Per the CTRules and the G-KenyaCT , investigators must also meet the following requirements (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source):
- Provide evidence of their qualifications and experience through an up-to-date curriculum vitae (CV)
- Have a current practice license from the Kenya Medical Practitioners and Dentist Board
- Be familiar with the characteristics and appropriate use of the investigational product (IP) as described in the protocol, current investigator’s brochure (IB), in the product information, and in other information sources
- Have a clear understanding and willingness to obey the ethical, good clinical practice (GCP) and legal requirements in the conduct of the trial
- Permit monitoring and auditing of the trial and inspection by the Pharmacy and Poisons Board (PPB) or appointed representatives
- Keep a list of appropriately qualified persons to whom the investigator has delegated significant trial-related duties
- The principal investigator (PI) must be an appropriately qualified and competent person having practical experience within the relevant professional area and who is responsible for the conduct of the clinical trial at a clinical site
- The PI must have a degree in medicine, pharmacy, pharmacology, toxicology, biochemistry, dentistry, or a related discipline from a university recognized in Kenya
- The PI must have a valid practice license from the relevant regulatory authority
- The PI must have a valid professional indemnity cover
- The PI must be a citizen of Kenya or a permanent resident in Kenya
- A PI must have had previous experience as a co-investigator in at least two (2) trials in the relevant professional area
- Have adequate time and resources to carry out the study (See Annex 6 of the G-KenyaCT for the PPB’s recommended format to document the investigator’s workload)
Further, the G-KenyaCT states that sponsors must ensure that investigators have had formal training in GCPs with proof that a GCP course was attended within the last two (2) years. If training has not been completed, it is the responsibility of the sponsor to organize this training prior to initiating the study. The investigators will need to provide evidence of having obtained this training. As delineated in KEN-14 , prior to entering into an agreement with the investigator(s) and the institution(s) to conduct a study, the sponsor should provide the investigator(s) with the protocol and an IB. Furthermore, the sponsor must sign an agreement or contract with the participating institution(s). Additionally, the sponsor must define and allocate all study related duties and responsibilities to the relevant parties participating in the study. (See the Submission Content section for additional information on clinical trial application requirements.)
Foreign Sponsor Responsibilities
The G-ECBiomedRes requires that with collaborative research projects, the collaborating investigators, institutions, and countries must function as equal partners with safeguards to avoid exploitation of local researchers and participants. An external sponsoring agency should submit the research protocol to their country’s EC, as well as the Kenyan EC where the research is to be conducted. Further, this research must be responsive to the health needs of Kenya and reasonably accessible to the community in which the research was conducted. Consideration should be given to the sponsoring agency agreeing to maintain health services and faculties established for purposes of the study in Kenya after the research has been completed. Such collaborative research must have a local/Kenyan co-principal investigator.
Data and Safety Monitoring Board
The G-KenyaCT indicates that the PPB recommends establishing a Data and Safety Monitoring Board (DSMB) to monitor trials in the following types of studies:
- Where the endpoint is such that a highly favorable or unfavorable result, or even a finding of futility at an interim analysis, might ethically require the trial to be terminated early
- When there are safety concerns due to the use of a particularly invasive treatment
- Where there is prior information suggesting the possibility of serious toxicity with the study treatment
- Where the participants involved represent a vulnerable population (e.g., children, pregnant women, elderly, terminally ill, or mentally incapacitated)
- When the participants represent a population at higher risk of death or other serious outcomes
- When the study is large, of long duration, and multi-center
KEN-14 states that a DSMB may be established to assess the progress of a clinical trial, including the safety data and the critical efficacy endpoints at intervals, and to recommend to the sponsor whether to continue, modify, or stop a trial.
Per the G-KenyaCT , the DSMB must provide the following documentation to the PPB:
- DSMB composition
- Copy of DSMB charter
- DSMB reports to be submitted to the PPB within two (2) weeks of its deliberations and in the request for annual approval
For multicenter trials, the G-ECBiomedRes requires that centralized data management and analysis should be planned as per G-WHO-DSMB .
Multicenter Studies
Per the G-KenyaCT , for multicenter studies in Kenya, the coordinating investigator should be a Kenyan resident and should assume full responsibility for the trial.
The G-ECBiomedRes requires that multicenter trials conducted simultaneously by several investigators at different sites follow the same protocol. Ideally, these trials should be initiated at the same time at all sites. The sponsor must provide the protocol to the investigators, who will accept the protocol in writing. If approved by the EC of the local host institution, the protocol may be modified to suit the local conditions. Meetings should be organized at the initial and intermediate stages of the trial to ensure uniform procedures at all sites. All sites and parties should also agree on procedures for publication of a final report. Research staff should receive training at every trial site on the uniform procedures. In addition, research staff at all sites should implement standard methods for recruitment and evaluation/monitoring of laboratory procedures and conduct of trial. There must be monitoring to ensure the sites are following the protocol, which must include measures to terminate the participation of some sites, if necessary. Finally, centralized data management and analysis should be planned as per G-WHO-DSMB .
Additional multicenter guidance is delineated in KEN-14 :
- All investigators conduct the trial in strict compliance with the protocol agreed to by the sponsor, and, if required, by the PPB, and given EC approval
- The case report forms (CRFs) are designed to capture the required data at all multicenter trial sites
- Investigator responsibilities are documented prior to the start of the trial
- All investigators are given instructions on following the protocol, complying with a uniform set of standards to assess clinical and laboratory findings, and completing the CRFs
- Communication among investigators is facilitated
Institutional Registration
The STI-Act and the STI-Regs require research institutions to register with the National Commission for Science, Technology and Innovation (NACOSTI) and obtain a Certificate of Registration. For detailed guidance on the vetting and approval process, see the STI-Regs and the G-InstitutionRegistration . The application for registration of research institutions is provided in KEN-11 , and the reporting tool for registered research institutions is provided in KEN-36 .
As set forth in the G-KenyaCT and the G-ECBiomedRes , the sponsor must provide insurance cover for the study participants and ensure that the clinical trial institution, contract research organization (CRO), and researchers have sufficient insurance cover for the clinical trial. Per the G-KenyaCT , the sponsor’s policies and procedures should address the costs of treatment of trial participants in the event of trial-related injuries, and the sponsor should submit this information as part of the clinical trial application (see KEN-34 ). In addition, a no-fault insurance cover must be obtained for all controlled human infection studies. The International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ) guides sponsors on providing insurance. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
For all sponsor-initiated studies, insurance coverage must be provided by an insurer registered by Kenya’s Insurance Regulatory Authority (IRA) , and a valid insurance certificate must be issued by the IRA prior to the trial’s initiation and cover the duration of the study. The insurance certificate must be submitted as evidence to the Pharmacy and Poisons Board (PPB) . The certificate must be properly executed by an insurance company under a valid insurance policy which makes explicit reference to the proposed study. In addition, the policy must grant coverage for any participant injury that is causally linked to trial activities. The policy must also cover the investigator(s)’ and the sponsor(s)’ liability in the trial, without excluding any damage which may be attributed to negligence. Moreover, self-insurance of the participants by other entities, such as the National Health Insurance Fund , will not be sufficient.
Further, per the G-KenyaCT , the sponsor must ensure that the investigators and CROs have professional indemnity insurance coverage for the period of the trial. The host institution must also have in place sufficient insurance to meet the potential liability of its investigators, those acting on behalf of the investigators, and its research members.
Compensation
Injury or Death
As specified in the G-KenyaCT and the G-ECBiomedRes , the sponsor is responsible for providing compensation to research participants and/or their legal heirs in the event of trial-related injuries or death. Per the G-ECBiomedRes , participants are entitled to such financial or other assistance as would compensate them equitably for any temporary or permanent impairment or disability. In the case of adverse events, there should be proper assessment, evaluation, and compensation. The G-ECBiomedRes also indicates that when investigational vaccines contain active or live-attenuated micro-organisms, should participants in the control group contract the disease for which a vaccine is being tested, free treatment must be provided.
In addition, the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ) provides guidance for sponsors on providing compensation to research participants in the event of trial-related injuries or death. The sponsor must explain to participants the compensation and/or treatment available to them in the event of trial-related injuries.
Trial Participation
The G-ECBiomedRes defines compensation to include offers to participants, monetary or otherwise, to offset the time and inconvenience for participating in research.
Post-Trial Access
Per the G-KenyaCT , the sponsor must put in place measures to ensure that the study participants have access to successful investigational products for their disease condition before the products have received a marketing authorization in Kenya, especially for the Phase III clinical trials. The G-ECBiomedRes indicates that when investigational vaccines contain active or live-attenuated micro-organisms, post-trial access to the vaccine should be available to the control group.
Quality Assurance/Quality Control
As stated in the CTRules and the G-KenyaCT , the sponsor is responsible for maintaining quality assurance (QA) and quality control (QC) systems with written standard operating procedures (SOPs) to ensure that trials are conducted and data are generated, recorded, and reported in compliance with the protocol, the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), the STI-Regs , and other applicable regulatory requirements. QC should be applied to each stage of data handling to ensure that all data are reliable and have been correctly processed. In addition, per the STI-Regs , all persons and research institutions (i.e., sponsors) undertaking research in Kenya must ensure the highest standards and quality of research for the realization of institutional mandates and national priorities.
In addition to complying with KEN-14 , the G-KenyaCT indicates QA processes should be developed to ensure:
- Regular and continuous monitoring of the study and the implementation of monitoring reports’ recommendations
- Submission of the study monitoring plan to the Pharmacy and Poisons Board (PPB) during the initial submission of the application
- The clinical trials research site must have valid registrations and approvals
- Patient safety and confidentiality are not compromised
- Analysis or evaluation of samples is performed in accordance with the protocol and good clinical practice (GCP) principles and, where applicable, the contract/agreement, the work instruction, and associated methods
- Adherence to the laboratories’ policies and SOPs
- Trial data is recorded and reported accurately, legibly, completely, and in a timely manner
- Trial data is archived
- Preparation of a work instruction detailing the procedures that will be used to conduct the analysis or evaluation prior to the initiation of sample analysis or evaluation, as necessary
- Be built or adapted for the purpose
- Have automated equipment for routine hematology, biochemistry, and serology tests
- Have procedures for analyzer calibration and quality control
- Regular maintenance of all the equipment, including point-of-care equipment
- Have a procedure for transporting samples safely and quickly from clinical areas to the laboratory
- Have written procedures for all assays, and to validate the assays
- Reagents and consumables are used within their expiry dates based on a stock control procedure
- Records are kept, including source documents and final reports
- Have a procedure for authorizing and releasing results
- Have a procedure for ‘flagging’ and notifying medical staff of abnormal results
- Have a laboratory information management system, and validate and back up the system
- Protective clothing and safety equipment are provided for staff
- Have a central alarm system for all fridges and freezers
- Have an internal audit program
Per KEN-14 , the sponsor should implement a system to manage quality throughout all stages of the trial process, focusing on trial activities essential to ensuring participant protection and the reliability of trial results. The quality management system should use a risk-based approach that includes:
- During protocol development, identify processes and data that are critical to ensure participant protection and the reliability of trial results
- Identify risks to critical trial processes and data
- Evaluate the identified risks against existing risk controls
- Decide which risks to reduce and/or which risks to accept
- Document quality management activities and communicate to those involved in or affected by these activities
- Periodically review risk control measures to ascertain whether the implemented quality management activities are effective and relevant
- In the clinical study report, describe the quality management approach implemented in the trial and summarize important deviations from the predefined quality tolerance limits and remedial actions taken
Per the G-KenyaCT protocol violations and protocol deviations must be reported to the PPB within seven (7) days of the principal investigator (PI) becoming aware of them. The details to be reported must include:
- Date of the deviation/violation
- Study participant(s) affected
- Name of the treating physician
- Detailed description of the deviation/violation
- Indication whether the study participants were adversely affected by the deviation/violation
- Explanation of why the deviation/violation occurred
- Measures taken to address the deviation/violation
- Measures taken to preclude future recurrence of the deviation/violation
In addition, see G-KenyaCT for information about medical care of trial participants during and following the clinical trial.
Controlled Human Infection Studies
The G-KenyaCT also provides detailed information on controlled human infection studies (CHIS) requirements to ensure investigator/study personnel compliance with GCP and other QA/QC requirements, including the following:
- The well characterized strain of an infectious agent should be administered at a controlled dose and by a specific route to carefully selected adult volunteers
- The studies require safe and accurate microbiology, good clinical facilities, careful recruitment, and monitoring
- Participants must be monitored for evidence of carriage or infection under medical supervision to anticipate or manage symptoms of disease and adverse events
- The value of the information to be gained should clearly justify the risks and the study must have a risk mitigation plan
- The investigators should be adequately qualified, trained, and experienced in the conduct of CHIS as well as treating patients with the infectious disease being investigated
For the complete list of requirements, see the G-KenyaCT .
The G-ECBiomedRes provides additional considerations when investigational vaccines contain active or live-attenuated micro-organisms:
- The participant to be vaccinated should be given adequate information about the adverse effects.
- Should participants in the control group contract the disease for which a vaccine is being tested, free treatment must be provided.
- Because the risks associated with vaccines produced by recombinant DNA techniques are not completely known, PPB guidelines must be strictly followed.
- Post-trial access to the vaccine should be available to the control group.
Monitoring Requirements
As part of its QA system, the G-KenyaCT requires the sponsor to develop an internal audit program. The G-KenyaCT defines an audit as a systematic examination, carried out independently of those directly involved in the trial, to determine whether the conduct of a trial complies with the agreed study protocol and whether data reported are consistent with those on record at the site. Further, the sponsor is required to obtain agreement from all involved parties to ensure direct access to all trial related sites, source data/documents, reports for monitoring and auditing purposes, and inspection by domestic and foreign regulatory authorities An investigator must, upon request from any properly authorized officer or employee of PPB, at reasonable times, permit such officer or employee to have access to, and copy and verify any records or reports made by the investigator.
Per KEN-14 , the sponsor should develop a systematic, prioritized, risk-based approach to monitoring clinical trials. The extent and nature of monitoring is flexible and permits varied approaches that improve effectiveness and efficiency. The sponsor may choose onsite monitoring, a combination of onsite and centralized monitoring, or, where justified, centralized monitoring. The sponsor should document the rationale for the chosen monitoring strategy (e.g., in the monitoring plan).
KEN-31 indicate that the National Commission for Science, Technology and Innovation (NACOSTI) may conduct an evaluation, or cause an evaluation to be conducted, of a research study to assess and evaluate compliance with the conditions of the applicable research license.
Premature Study Termination/Suspension
The G-KenyaCT states that if a trial is terminated by the PI or the sponsor, the PI or the sponsor must inform the PPB not later than 15 days following the termination date. The co-investigators must also be informed as soon as possible and should be advised in writing of potential risks to the research participants, and they must ensure that patients continue to receive medical care. The PPB must be provided with reason(s) for the termination and its impact on the proposed or ongoing trials with respect to the IP, including issues relating to IP accountability and disposal as well as record(s) maintenance. In addition, the PPB may withdraw the authorization to conduct a clinical trial if it finds that the safety of the participants is compromised or that the scientific reasons for conducting the trial have changed.
According to KEN-14 , if it is discovered that noncompliance significantly affects or has the potential to significantly affect participant protection or reliability of trial results, the sponsor should perform a root cause analysis and implement appropriate corrective and preventive actions. Further, the EC should also be informed promptly and provided the reason(s) for the termination or suspension by the sponsor.
Public Health Emergencies
The CT-Emrgcy provides guidance to sponsors, PIs, and institutions on the conduct of clinical trials during public health emergencies to maximize the safety of research participants, minimize risks to participants and the community, and ensure the integrity of the clinical trials. See CT-Emrgcy for details on a range of issues, including contingency planning, communications with participants, changes to studies, protocol deviations, reporting, and supply of investigational products (IPs) during a public health emergency.
Electronic Data Processing System
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As per KEN-14 , when using electronic trial data processing systems, the sponsor must ensure that the electronic data processing system conforms to the sponsor’s established requirements for completeness, accuracy, reliability, and consistency of intended performance. Per KEN-14 , the sponsor should base their approach to validate such systems on a risk assessment that takes into consideration the intended use and the potential of the system to affect participant protection and reliability of trial results. In addition, the sponsor should maintain standard operating procedures (SOPs) for the systems that cover setup, installation, and use. The responsibilities of the sponsor, investigator, and other parties should be clear, and the system users should be provided with training. Refer to KEN-14 for additional information.
Records Management
According to the G-KenyaCT , it is the responsibility of the investigator and the sponsor to archive safely all trial-related documentation. All Kenyan trial site-related documentation must be archived within the country and not exported. Additionally, the sponsor/applicant must inform the Pharmacy and Poisons Board (PPB) ’s Expert Committee on Clinical Trials (ECCT) in writing prior to destroying any trial documents. The notification must include the protocol number, date started and ended, and the license number.
The G-KenyaCT states that study documents must be archived for a minimum of 10 years from the end of the study. Also, records must be made available to the PPB within three (3) days if there is a concern regarding the use of a clinical trial drug and/or a risk to the health of the clinical trial participant. In any other case, records must be provided within seven (7) days of request.
Per the STI-Regs , sponsors should store research findings and information regarding research systems in a designated location with clear labels of the subject area. Research findings must be documented in bound books or documents with the research title, author, year, and other relevant information clearly printed on the cover page. A report of research work by staff and the research institution must be submitted to the National Commission for Science, Technology and Innovation (NACOSTI) within two (2) months after publication or compilation of the research report.
In addition, KEN-14 states that the sponsor and investigator/institution should maintain a record of the location(s) of their respective essential documents including source documents. The storage system used during the trial and for archiving (irrespective of the type of media used) should allow for document identification, version history, search, and retrieval. The sponsor should ensure that the investigator has control of and continuous access to the data reported to the sponsor. The investigator/institution should have control of all essential documents and records generated by the investigator/institution before, during, and after the trial.
Responsible Parties
For the purposes of data protection requirements, DPA delineates that the sponsor acts as the “data controller” in relation to research data. This is because the sponsor determines the purpose and means of processing personal data. The "data processor" processes personal data on behalf of the data controller. Data controllers and processors must be registered with the Kenya Data Commissioner. Per the DataProtect , an application for registration of a data controller or data processor must be on Form DPR1 (found in the First Schedule of DataProtect ) with supporting materials and the required registration fees as specified in the Second Schedule. See the DataProtect for additional details on registration requirements.
Data Protection
Per the DPA , the data controller (sponsor) must ensure that personal data is:
- Processed in accordance with the right to privacy of the data subject
- Processed lawfully, fairly, and in a transparent manner in relation to any data subject
- Collected for explicit, specified, and legitimate purposes and not further processed in a manner incompatible with those purposes
- Adequate, relevant, and limited to what is necessary in relation to the purposes for which it is processed
- Collected only where a valid explanation is provided whenever information relating to family or private affairs is required
- Accurate and, where necessary, kept up to date, with every reasonable step being taken to ensure that any inaccurate personal data is erased or rectified without delay
- Kept in a form that identifies the data subjects for no longer than is necessary for the purposes for which it was collected
- Not transferred outside Kenya, unless there is proof of adequate data protection safeguards or consent from the data subject
The DataProtect , which implements the DPA , requires data controllers and data processors to develop, publish, and regularly update a policy on their personal data handling practices. The policy should include the nature of personal data collected and held, how a data subject may access their personal data, complaints handling mechanisms, the lawful purpose for processing personal data, and requirements for when personal data is to be transferred outside Kenya. Regarding cross-border transfers of data, a data controller or data processor who is a transferring entity must (before transferring personal data out of Kenya) ascertain that the transfer is necessary. This necessity decision should be based on considerations such as data protection safeguards, an adequacy decision made by the Data Commissioner, and if there is consent of the data subject.
Per the DataProtect , data controllers and/or data processors must retain personal data processed for a lawful purpose and only as long as may be reasonably necessary for the purpose for which the personal data is processed. A data controller or data processor must establish a personal data retention schedule with appropriate time limits and periodic reviews. When the retention period has ended, the personal data must be erased, anonymized, or pseudonymized.
See DataProtect for additional details on data protection, including data subject rights, data protection design and principles, notification of breaches, impact assessments, and exemptions.
See Parts IV-VII of the DPA for detailed requirements on data processing, sensitive personal data, exemptions, and transfer of personal data outside of Kenya. The G-ECBiomedRes requires compliance with the DPA .
Consent for Processing Personal Data
Per the DPA , the data controller (sponsor) or data processor must bear the burden of proof for establishing a data subject’s consent to the processing of their personal data for a specified purpose. For the purposes of processing personal data, consent means any manifestation of express, unequivocal, free, specific, and informed indication of the data subject’s wishes by a statement or by a clear affirmative action, signifying agreement to the processing of personal data relating to the data subject. Unless otherwise provided under the DPA , a data subject has the right to withdraw consent at any time. The withdrawal of consent must not affect the lawfulness of processing based on prior consent before its withdrawal.
The DataProtect requires data controllers and data processors to ensure that a data subject has the capacity to consent and voluntarily gives consent. In seeking consent (prior to the processing), the data subject should be informed of:
- The identity of the data controller or data processor
- The purpose of each of the processing operations for which consent is sought
- The type of personal data that is collected and used
- Information about the use of the personal data for automated decision-making, where relevant
- The possible risks of data transfers due to absence of an adequacy decision or appropriate safeguards
- Whether the personal data processed will be shared with third parties
- The right to withdraw consent
- The implications of providing, withholding, or withdrawing consent
Per the DataProtect , this information may be presented to the data subject through a written notice, oral statement, audio or video message. The data controller or a data processor must ensure that the data subject has the capacity to voluntarily give consent that is specific to the purpose of processing .
The DPA indicates that in cases where the data subject is a minor, a person who has parental authority or a guardian may exercise personal data protection rights conferred on the subject. With regard to data processing, the DPA requires that every data controller (sponsor) or data processor must not process personal data relating to a child unless consent is given by the child's parent or guardian and the processing is in a manner that protects and advances the rights and best interests of the child. A data controller or data processor must incorporate appropriate mechanisms for age verification and consent to process personal data of a child, including available technology, volume of personal data processed, proportion of such personal data likely to be that of a child, possibility of harm to a child arising out of processing of personal data, and other factors as may be specified by the Kenya Data Commissioner.
The DPA indicates that in cases where the data subject has a mental or other disability, a person duly authorized to act as the participant’s guardian or administrator may exercise personal data protection rights conferred on the subject.
Obtaining Consent
In all Kenyan clinical trials, a freely given informed consent must be obtained from each participant in accordance with the requirements set forth in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). (Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .) The informed consent form (ICF) is viewed as an essential document that must be reviewed and approved by a National Commission for Science, Technology and Innovation (NACOSTI) -accredited institutional ethics committee (EC). The ICF must be provided to the Pharmacy and Poisons Board (PPB) with the clinical trial application. (See the Required Elements section for details on what should be included in the form.)
The CTRules , the G-KenyaCT , and the G-ECBiomedRes state that the investigator, or the designated representative, must provide detailed research study information to the participant and/or the legal representative(s) or guardian(s). Per G-ECBiomedRes , all individual consent must be written and, in no case, should collective community agreement or the consent of a community leader or other authority substitute for an individual informed consent. The G-KenyaCT and the G-ECBiomedRes also specify that the oral and written information concerning the trial, including the ICF, should be easy to understand and presented without coercion or unduly influencing a potential participant to enroll in the clinical trial. None of the oral and written information concerning the research study, including the written ICF, should contain any language that causes the participant and/or the legal representative(s) and/or guardian(s) to waive or to appear to waive the legal rights, or that releases or appears to release the investigator(s), the institution, the sponsor, or the representatives from their liabilities for any negligence. The participant, and the legal representative(s) or guardian(s), should also be given adequate time to consider whether to participate.
According to the CTRules , the G-KenyaCT , and KEN-14 , any change in the ICF due to a protocol modification should be approved by the EC before such changes are implemented. The participant and/or the legal representative(s) or guardian(s) will also be required to re-sign the revised ICF and receive a copy of any amended documentation.
Language Requirements
As stated in the CTRules and the G-KenyaCT , the ICF content should be presented in either English or Kiswahili, and the local spoken language of the area, where applicable. Copies of the English ICF should be submitted to the PPB and to the EC.
Documenting Consent
The CTRules and the G-KenyaCT state that the participant and/or the legal representative(s) or guardian(s), and the person who conducted the informed consent discussion should sign and personally date the ICF. Where the participant is illiterate, and/or the legal representative(s) or guardian(s) is illiterate, verbal consent should be obtained in the presence of and countersigned by an impartial witness. Before participating in the study, the participant should receive a copy of the signed and dated ICF, and any other written information provided during the informed consent process. The participant and/or the legal representative(s) or guardian(s) should also receive a copy of any updates to the signed and dated ICF.
According to KEN-14 , where the participant is illiterate and/or the legal representative(s) and/or guardian(s) is illiterate, an impartial witness should be present during the entire informed consent discussion. The witness should sign and date the ICF after the following steps have occurred:
- The written ICF and any other written information to be provided to the participant is read and explained to the participant and the legal representative(s) and/or guardian(s)
- The participant and the legal representative(s) and/or guardian(s), have orally consented to the participant’s involvement in the trial, and has signed and dated the ICF, if capable of doing so
Before participating in the study, the participant or the legal representative(s) and/or guardian(s) should receive a copy of the signed and dated ICF.
Waiver of Consent
No information is available.
Based on the CTRules , the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), the informed consent form (ICF) should include the following statements or descriptions, as applicable (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source):
- Title of the project and that the study involves research and an explanation of its nature and purpose
- The expected duration of the participant’s participation
- The participant’s responsibilities in participating in the trial
- Experimental aspects of the study
- Approximate number of participants involved in the trial
- Trial treatment schedule and the probability for random assignment to each treatment
- Principal investigator(s), institution, and ethics committee (EC) contact information, the person(s) to contact for further information regarding the trial and the rights of trial participants, and whom to contact in the event of trial-related injury
- Any foreseeable risks or discomforts to the participant, and when applicable, to an embryo, fetus, or nursing infant
- Any expected benefits or prorated payment to the participant; if no benefit is expected, the participant should also be made aware of this
- Alternative procedures or treatment that may be available to the participant, including a statement on disclosure of appropriate alternative procedures or courses of treatment that might be advantageous to participants when the research involves non-validated procedures, devices, or therapies
- Compensation and/or medical treatment available to the participant or the family or dependents in the event of a trial-related injury
- Any additional costs to the participant that may result from participation in the research
- The extent to which confidentiality records identifying the participant will be maintained, and if the results of the trial are published, the participant’s identity will remain confidential
- That the Pharmacy and Poisons Board (PPB) will be granted direct access to the participant’s original medical records to verify clinical trial procedures and/or data without violating the participant’s confidentiality
- The details on storage and exportation of biological samples, if applicable
- The details on storage and ownership of personal data
- Information about unblinding, if applicable
- The extent of the investigator’s responsibility, if any, to provide medical services to the participant
- That therapy will be provided free of charge for specified types of research-related injury, including the investigators’ responsibilities in this regard
- That participation is voluntary, the participant may withdraw at any time, and refusal to participate will not involve any penalty or loss of benefits, or reduction in the level of care to which the participant is otherwise entitled
- That the participant will be informed about the dissemination of findings and about any publication of the participant’s medical information, including photographs and pedigree charts
- Foreseeable circumstances under which the investigator(s) may remove the participant without consent
- That the participant and/or the legal representative(s) or guardian(s) will be notified in a timely manner if significant new findings develop during the study which may affect the participant’s willingness to continue
- Consent to incomplete disclosure, for example, if it is necessary to inform participants that some information is being withheld deliberately and the reasons for that decision; an offer to disclose the purpose at the conclusion of the study can be made
Note that per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
In addition, the CTRules delineates that if the potential participant is a child, the ICF must also contain these elements:
- The pathophysiology of the disease or subject of the clinical trial
- The methods of diagnosis
- The currently available treatment or prevention strategy in the pediatric population
- The incidence and prevalence of the disease or subject of the clinical trial in the overall population and in the pediatric population
- The evidence and assumptions on key differences between the disease or subject of the clinical trial in the overall population and the pediatric population
In accordance with the Declaration of Helsinki ( KEN-33 ) principles upheld in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), Kenya’s ethical standards promote respect for all human beings and safeguard the rights of research participants. A participant’s rights must also be clearly addressed in the informed consent form (ICF) and during the informed consent process. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
The Right to Participate, Abstain, or Withdraw
As set forth in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and KEN-14 , a participant and/or the legal representative(s) or guardian(s) should be informed that participation is voluntary, that the participant may withdraw from the research study at any time, and that refusal to participate will not involve any penalty or loss of benefits to which the participant is otherwise entitled.
The Right to Information
As delineated in the CTRules , the G-KenyaCT , the G-ECBiomedRes , and KEN-14 , a potential research participant and/or the legal representative(s) or guardian(s) has the right to be informed about the nature and purpose of the research study, its anticipated duration, study procedures, any potential benefits or risks, any compensation for participation or injury/treatment, and any significant new information regarding the research study.
The DPA further indicates that data subjects have a right to:
- Be informed of how their personal data is to be used
- Access their personal data in custody of the data controller (sponsor) or data processor
- Object to the processing of all or part of their personal data
- Correct false or misleading data
- Delete false or misleading data about them
The Right to Privacy and Confidentiality
As per the G-KenyaCT , the G-ECBiomedRes , and KEN-14 , all participants must be afforded the right to privacy and confidentiality, and the ICF must provide a statement that recognizes this right.
The Right of Inquiry/Appeal
The G-KenyaCT , KEN-14 , and the G-ECBiomedRes state that the research participant and/or the legal representative(s) or guardian(s) should be provided with contact information for the sponsor and the investigator(s) to address trial-related inquiries. Further, the G-ECBiomedRes requires that the ethics committee contact information also be provided.
The Right to Safety and Welfare
The G-ECBiomedRes and KEN-14 state that a research participant’s right to safety and the protection of the participant’s health and welfare must take precedence over the interests of science and society. KEN-14 upholds the Declaration of Helsinki ( KEN-33 ). (See the Required Elements and Vulnerable Populations sections for additional information regarding requirements for participant rights.)
The G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), make provisions to protect the rights of a research participant during the informed consent process when the procedure is complicated by emergencies. Per the G-KenyaCT , research must be conducted in accordance with KEN-14 . As delineated in the G-KenyaCT and the G-ECBiomedRes , in an emergency, if the signed informed consent form (ICF) cannot be obtained from the research participant, the consent of the legal representative(s) or guardian(s) should be obtained. If the prior consent of the participant or the legal representative(s) or guardian(s) cannot be obtained, the participant’s enrollment should follow measures specified in the protocol, and/or elsewhere, to ensure compliance with ethics committee (EC) and the Pharmacy and Poisons Board (PPB) requirements. The G-ECBiomedRes requires that the principle of clinical equipoise be applied, which essentially means the participant is not any worse off by enrolling.
During a public health emergency, the G-KenyaCT stipulates that the informed consent of participants must be obtained in individuals capable of giving informed consent. The CT-Emrgcy includes safeguards to protect clinical trial participants during a public health emergency, including the recommendation to reconsent if there are amendments as a result of the emergency.
Per KEN-14 , in an emergency, if the signed ICF has not been obtained from the research participant and/or the legal representative(s) or guardian(s), or if an effective treatment is lacking but the investigational product could address the participant’s emergency needs, the clinical trial may be conducted. However, the method used on the participant must be explained clearly in the trial protocol, and the EC must approve the protocol in advance. The participant and/or the legal representative(s) or guardian(s) should be informed about the trial as soon as possible, and consent to continue and other consent should be requested, as appropriate.
As per the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), in all Kenyan clinical trials, research participants selected from vulnerable populations must be provided additional protections to safeguard their health and welfare during the informed consent process. Vulnerable populations include those participants with diminished autonomy whose decision to participate in a clinical trial may be unduly influenced by the expectation of benefits associated with participation or by coercion. This may include, but is not limited to, children/minors, pregnant women, neonates, fetuses, medical students, members of the uniformed forces, prisoners, orphans, homeless populations, unemployed, internally displaced persons, economically or educationally disadvantaged persons, marginalized social groups, individuals with terminal illnesses, and the mentally challenged. KEN-14 also includes members of a group with a hierarchical structure, such as medical, pharmacy, dental, and nursing students, subordinate hospital and laboratory personnel, employees of the pharmaceutical industry, members of the armed forces, and persons kept in detention. Other vulnerable subjects include persons in nursing homes, patients in emergency situations, ethnic minority groups, homeless persons, nomads, refugees, minors, and those incapable of giving consent. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .
Elderly Persons
The G-ECBiomedRes defines an elderly/senior citizen as a person who has attained the age of 65 years. Their physical or mental state may affect their ability to make voluntary decisions regarding their participation in research projects. Such research involving elderly/senior citizens must comply with the following requirements:
- Strict adherence to ethical principles
- The risk-benefit ratio must be favorable to the research participant
- The participants must be protected from gross violation of human rights
Persons in Dependent Groups
Per the G-ECBiomedRes , research involving data collection by superiors on their subordinates involves relationships such as employer-employee, teacher-students, supervisor-staff, sponsor-dependent, and parent-children. This relationship impairs independent consent by the participants leading to complacency. Therefore, research involving the superior/subordinate relationships must fulfill the following requirements:
- The superior must strictly follow ethical principles to avoid undue pressure
- Subordinates must be protected from gross violation of human rights
- The trial design must be based on a need-to-know principle and improve the conditions of the participants
Persons in Low-Resource Communities
The G-ECBiomedRes provides the following requirements related to conducting research on participants in low-resource settings:
- Persons in such settings should not be involved in research that could be carried out reasonably well in developed communities
- The research should be responsive to the health needs and priorities of the community in which it is to be implemented
- Undue inducement to participate in the research must be avoided at all costs
Armed Forces
The G-ECBiomedRes stipulates that research involving the members of the armed forces may be vulnerable because of the conditions of their service, which may affect their ability to make voluntary decisions regarding their participation in research. Such research must be conducted to ensure that:
- Participants are protected from gross violations of human rights
- There is strict adherence to ethical principles
- There is at least one (1) member of the ethics committee approving such research who is an enlisted and authoritative member of the armed forces
Terminally Ill
Per the G-ECBiomedRes , research involving participants who are terminally ill with an incurable medical condition are vulnerable. Their state may affect their ability to make voluntary decisions regarding their participation in research. Such research can only be conducted when:
- The objectives of the project(s) cannot be achieved using another non-vulnerable group
- The risk-benefit ratio should be favorable to the research participant
See the Children/Minors; Pregnant Women, Fetuses & Neonates; Prisoners; and Mentally Impaired sections for additional information about these vulnerable populations.
According to the G-KenyaCT , a minor is someone under 18 years of age. As set forth in the G-KenyaCT , the G-ECBiomedRes , and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), when the research participant is a minor, informed consent should be obtained from the legal representative(s) or guardian(s). Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 . The informed consent forms, assent forms, and the patient information sheets should be in a language that the parent or legal representative clearly understand. All pediatric participants should be fully informed about the trial and its risks and benefits in a language and terms that they are easily able to understand.
Per the G-KenyaCT , a minor should take part in the informed consent procedure in a way tailored to their age and mental maturity. If capable, the participant should sign and personally date the written informed consent. In addition, consent given by pediatric participants should not be considered valid without prior approval by the ethics committee (EC).
The CTRules , the G-ECBiomedRes , and the G-KenyaCT state that a study may only be conducted on minors if several conditions are fulfilled including (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source):
- Pediatric participants will not be involved in research that might be equally carried out in adults
- The purpose of the research is to generate knowledge relevant to the health needs of children
- The legal representative(s) or guardian(s) must provide proxy consent and ensure assent has been obtained to the extent of the child’s capabilities. However, if the minor refuses to participate after proxy consent is given, the minor’s refusal must be respected unless there is no other medical alternative from which the minor could benefit
- The risk presented by interventions not intended to benefit the minor is low and commensurate with the importance of the knowledge to be gained
- Interventions that are intended to provide therapeutic benefit are likely to be at least as advantageous to the individual child as any available alternative
- No incentives or financial inducements are given to the participant or the legal representative(s) or guardian(s) except to provide compensation for expenses and loss of earnings directly related to the participation in the trial
Additionally, per the G-KenyaCT , the trial should also address the following considerations:
- Provide useful answers to the study population
- The medicine satisfies a need for the population being studied
- Children are adequately monitored and protected
- If there is no direct benefit to the child, or there is no more than minimal risk to the participant(s)
- Trial results will be published
- End-of-trial treatment provisions will be made
Assent Requirements
As delineated in the G-KenyaCT , before undertaking research involving children, the investigator must ensure that the agreement (assent) of each child has been obtained to the extent of the child’s capabilities, and a child’s refusal to participate or continue in the research must be respected. Assent is defined as a child’s affirmative agreement to participate in research, where the child is below the age of the majority but old enough to understand the proposed research in general, its expected risks and possible benefits, and the activities expected of them as participants. The G-ECBiomedRes provides that in children above seven (7) years and below 18 years where the parent(s) or the legal guardian(s) gives proxy consent, assent must be obtained from the child.
For an example of an accredited EC’s assent requirements, see the Kenyatta National Hospital-University of Nairobi (KNH-UoN) Ethics and Research Committee ’s sample minor assent form ( KEN-17 ).
Per the G-KenyaCT , research must be conducted in accordance with the requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). In accordance with KEN-14 , informed consent requirements for conducting clinical trials with pregnant or nursing women or fetuses follow the general requirements listed in the Required Elements section . Specifically, the informed consent form should include a statement on the reasonably foreseeable risks or inconveniences to the participant, and when applicable, to an embryo, fetus, or nursing infant.
As per the G-ECBiomedRes , research involving pregnant, lactating, and breastfeeding women may pose compromised long-term outcomes for the child. In addition, potential parent(s) can make decisions on behalf of the fetus(es), embryo(s), and zygote(s).
For fetal, embryo, and zygote(s) cases, research should be limited as follows:
- Cases that present no harm or offer assistance to the life system of the participants
- No procedures should be permitted that are likely to harm them
- A fetus ex-utero and alive, embryo, and zygote must not be involved in research unless it is intended to enhance the life of that fetus, embryo, and zygote or unless the research involves no risk to them
The following guidelines must be followed for research involving pregnant, lactating, and breastfeeding women:
- The research carries no more than minimal risk to the fetuses or nursing infants
- Pregnant or nursing women should generally not be clinical trial participants except where such trials are designed to protect or advance the health of the pregnant/nursing women or fetuses/nursing infants, and for which women who are not pregnant or nursing would not be suitable participants
- The justification for such research should be that participants must not be arbitrarily deprived of the opportunity to benefit from investigational drugs, vaccines, or other agents that promise therapeutic or preventive benefits
Per the G-ECBiomedRes and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), prisoners are considered vulnerable because incarceration could affect their ability to make a voluntary decision regarding participation in research. (Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 ). A research study involving prisoners should ensure that these prospective participants are informed and given the opportunity to make their own decisions without any interference or reprisals from a higher authority. The ethics committee must also ensure that the study will be independently monitored to assure the dignity and rights of the prisoners involved in the research.
As per the G-ECBiomedRes and the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), an ethics committee (EC) within the relevant institution must approve the participation of adult research participants who are incapable by reason of physical and mental capacity to give consent. (Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in KEN-14 .)
In addition, as delineated in the G-ECBiomedRes , a research study may involve participants with mental incapacities or behavioral disorders under the following conditions:
- Such research could not be carried out equally well with individuals who are in possession of their full mental faculties
- The knowledge gained would be relevant to the health needs of persons with mental or behavioral disorders
- The participant’s consent has been obtained to the extent of the participant’s capabilities, and a prospective participant’s refusal to participate is always respected
- In the case of incompetent individuals, informed consent shall be obtained from a legal guardian or other duly authorized person
- The degree of risk attached to the intervention not intended to benefit the individual participant is low and commensurate with the importance of knowledge to be gained
- Interventions that are intended to provide therapeutic benefit are likely to be at least as advantageous to the individual participant as any alternative
As delineated in the G-KenyaCT , an investigational product is also referred to as an investigational new drug (IND) in Kenya. Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). The G-KenyaCT and KEN-14 define an IND as a pharmaceutical form of an active ingredient or placebo being tested or used as a reference in a clinical trial. This includes a product with a marketing authorization when it is used or assembled (formulated or packaged) in a different way from the approved form, when used for an unapproved indication, or when used to gain further information about an approved use.
Manufacturing
According to the PPA and the G-KenyaCT , the Pharmacy and Poisons Board (PPB) is responsible for authorizing the manufacture of all drug products, including investigational products (IPs) in Kenya. Per the CTRules and the G-KenyaCT , an IP must be manufactured in accordance with the requirements of good manufacturing practice (GMP). The CTRules requires a sponsor to immediately notify the PPB in writing when a pharmaceutical or chemical alteration may affect the quality, safety, or efficacy of the IP product during an ongoing clinical trial. The G-KenyaCT states that the sponsor must submit the IP dossier directly to the PPB or may submit it through the principal investigator. The IP dossier must be prepared as per the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), which is required per G-KenyaCT . The manufacture of IPs may be subject to GMP inspection by the PPB in the same way as the case of marketed drug products. See the G-KenyaCT for detailed chemistry and manufacturing information to be provided to the PPB if the IP has not been registered with the PPB.
KEN-14 also requires IPs to be manufactured, handled, and stored in accordance with applicable GMPs and used in accordance with the approved protocol.
Per t he PPA , the PPB is authorized to regulate the manufacturing of medicine, including:
Per the PPA and the ImpExp , the PPB is authorized to regulate the import and export of health products and technologies, including IPs. As per the ImpExp and the G-KenyaCT , to obtain an import permit for a clinical trial, the sponsor or investigator must submit an application online to the Kenya Trade Network Agency’s Kenya TradeNet Single Window System ( KEN-28 ). The following documents must be submitted (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source):
- The proforma invoice or invoice
- The ethics committee favorable opinion letter
- The Expert Committee on Clinical Trials approval letter from the PPB
- Registration of the institution where the research is being undertaken
The G-KenyaCT states that the sponsor must submit to the PPB a copy of the endorsed clinical trial import permit and/or evidence of delivery to the approved investigator(s)/trial center(s) on importation and supply of each consignment of the product. The product must only be supplied to the investigator(s) at the trial site(s) named in the clinical trial import license application for the purpose and use as stated in the said application. Prior PPB notification and approval is required for changes in the investigator, trial site, or protocol. The sponsor must inform PPB of any change in information, or any information received that casts doubt on the continued validity of the data, which was submitted with, or in connection with the application for the import permit. The sponsor must also inform the PPB of any decision to discontinue the trial to which the permit relates and state the reason for the decision. See KEN-8 for additional details on the procedures for obtaining an import license.
Per the CTRules , the import of an IP must comply with the applicable regulatory requirements to ensure integrity and accountability of the products. The PPB may revoke or suspend an import permit if the IP was manufactured in conditions not consistent with GMP; if the clinical trial was discontinued; or if the sponsor provided false information.
Please note: Kenya is party to the Nagoya Protocol on Access and Benefit-sharing ( KEN-3 ), which may have implications for studies of IPs developed using certain non-human genetic resources (e.g., plants, animals, and microbes). For more information, see KEN-15 .
Investigator’s Brochure
In accordance with the CTRules and the G-KenyaCT , the sponsor must provide an up-to-date investigator’s brochure (IB). An updated IB and Drug Safety Update Report (DSUR) must be submitted whenever available but at least once year as a notification to the Pharmacy and Poisons Board (PPB) or when there are substantial changes to the previous version.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As specified in the G-KenyaCT and KEN-14 , the IB must provide coverage of the following areas:
- Physical, chemical, and pharmaceutical properties
- The pharmacological aspects including its metabolites in all animal species tested
- The pharmacokinetics and metabolism including its biological transformation in all animal species tested
- Toxicological effects in any animal species tested under a single dose study, a repeated dose study, or a special study
- Results of clinical pharmacokinetic studies
- Information regarding safety, pharmacodynamics, efficacy, and dose responses that were obtained from previous clinical trials in humans
The G-KenyaCT indicates that the sponsor must also follow the guidance contained in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ).
Quality Documentation
In accordance with the G-KenyaCT , a good manufacturing practice (GMP) certificate must be provided by a competent authority from the country of manufacture to the PPB in the clinical trial application. At a minimum, the GMP certificate should include the competent authority’s name and contact details, address of the manufacturing site, date of inspection, and validity period. Certificates of Analysis (CoAs) must also be provided to the PPB for all investigational products (IPs) and comparator products. Per KEN-14 , the sponsor must maintain a CoA to document the identity, purity, and strength of the IP(s) to be used in the clinical trial.
See the G-KenyaCT for detailed chemistry and manufacturing information to be provided to the PPB if the IP has not been registered with the PPB. In addition, see Cert-Emrgcy for information about good clinical practice (GCP) and GMP certifications during emergencies.
(See Product Management section for additional information on sponsor requirements).
Per the G-KenyaCT , investigational products (IPs) used in Kenyan clinical trials must be properly labelled. A final copy/version of the labelling must be submitted to the Pharmacy and Poisons Board (PPB) for approval and should contain the following minimum information:
- Statement indicating that the product is for “clinical trial purpose only”
- Recommended storage conditions
- Protocol code or identification
- Name, address, and telephone number of the sponsor, contract research organization, or investigator (the main contact for information on the product, clinical trial, and emergency unblinding)
- Pharmaceutical dosage form, route of administration, quantity of dosage units, and in the case of open trials, the name/identifier and strength/potency
- The batch and/or code number to identify the contents and packaging operation
- A trial reference code allowing identification of the trial, site, investigator, and sponsor, if not given elsewhere
- The trial participant identification number/treatment number and, where relevant, the visit number
- The name of the investigator (if not included above)
- Directions for use (reference may be made to a leaflet or other explanatory document intended for the trial participant or person administering the product)
- Period of use (use-by date, expiry date, or re-test date as applicable), in month/year format and in a manner that avoids any ambiguity
- The complete physical address of the manufacturing site
As indicated in the G-KenyaCT , it is recommended that an IP is not re-labeled wherever possible. It is, however, accepted that in certain cases it is necessary to re-label and the PPB will review applications for the extension of expiration dates based on sufficient evidence being provided by the applicant that an extended expiration date is warranted. A written justification and evidence should be provided to the PPB. Any re-labelling of remaining IPs from previously manufactured batches must be performed in accordance with good manufacturing practice (GMP) principles and is limited to an extension of the expiration date where sufficient evidence is available to support such extension. Any request for re-labelling should be accompanied by a certificate of analysis of the product from a PPB-recognized laboratory or World Health Organization (WHO) prequalified laboratories ( KEN-18 ). After approval, the re-labelling must be carried out under the supervision of a pharmaceutical inspector on the ground. In case of use-date extension, an additional label should be affixed to the IP to indicate the new use date and repeat the batch number. It may be superposed on the old use date, but not on the original batch number. PPB will not approve re-labelling of product if the proposed additional label obscures the original labelling. At all times, the original label should be visible. This operation may be performed on site by the clinical trial monitor(s) or the clinical trial site pharmacist, in accordance with specific and standard operating procedures. The operation should be checked by a second person. Documented evidence of this additional labelling should be available in the trial documentation and in the batch records. KEN-34 indicates that all documents submitted to the PPB in a clinical trial application should be in English, including a pictorial sample of the IP with the labeling text.
The International Council for Harmonisation’s Guideline for Good Clinical Practice E6(R2) ( KEN-14 ), which the G-KenyaCT requires following, states that the IP must be coded and labeled in a manner that protects the blinding, if applicable. The IPs must also be suitably packaged in a manner that will prevent contamination and unacceptable deterioration during transport and storage.
Supply, Storage, and Handling Requirements
Per the PPA , the Pharmacy and Poisons Board (PPB) is responsible for the regulation of investigational products (IPs), including all matters relating to the safety, packaging, and distribution of medicines. The PPB must ensure that all medicinal products manufactured in, imported into, or exported from the country conform to prescribed standards of quality, safety, and efficacy. Further, the PPB must ensure that the personnel, premises, and practices employed in the manufacture and storage of IPs complies with prescribed requirements.
Per the G-KenyaCT , research must be conducted in accordance with requirements set forth in the International Council for Harmonisation's Guideline for Good Clinical Practice E6(R2) ( KEN-14 ). As defined in the G-KenyaCT and KEN-14 , the sponsor must ensure the following (Note: the sources provide overlapping and unique elements so each of the items listed below will not necessarily be in each source):
- Timely delivery of IPs to the investigator(s)
- Records that document shipment, receipt, disposition, return, and destruction of the IPs are maintained
- A system for retrieving IPs and documenting this retrieval is maintained
- A system for the disposition of unused IPs is maintained
- Steps taken to ensure that the IPs are stable over the period of use
- Sufficient quantities of the IPs used in the trials are maintained
To the extent stability permits, samples should be retained either until the analyses of the trial data are complete or as required by the applicable regulatory requirement(s), whichever represents the longer retention period.
As defined in the G-KenyaCT and KEN-14 , the sponsor must also supply the investigator(s)/institution(s) with the IPs, including the comparator(s) and placebo, if applicable. The sponsor or the representative should not supply either party with the IP(s) until approval from the PPB and a favorable opinion letter from the local and national ethics committees (ECs) are obtained. In addition, the G-KenyaCT requires the following supply, storage, and handling processes:
- Analysis or evaluation of samples is performed in accordance with the protocol and, where applicable, the contract/agreement, the work instruction, and associated methods
- Adherence to the laboratories, policies, and standard operating procedures (SOPs)
- Prior to the initiation of sample analysis or evaluation, it is often necessary to prepare a work instruction detailing the procedures, which will be used to conduct the analysis or evaluation
- Regularly maintain all the equipment, including point-of-care equipment
- Have written procedures for all assays, and validate the assays
- Have a stock control procedure to make sure that reagents and consumables are used within their expiry dates
- Keep records, including source documents and final reports
- Have a laboratory information management system, and validate and backup the system
- Provide protective clothing and safety equipment for staff
The G-KenyaCT also states that the sponsor must submit to the PPB a copy of the endorsed Clinical Trial Import License and/or evidence of delivery to the approved investigator(s)/institution(s) upon importing and supplying each product consignment. In addition, the IP must only be supplied to the investigator(s)/institution(s) named in the application for the Clinical Trial Import License/Clinical Trial Exemption for the purpose and use specified. The sponsor must inform the PPB in the event of any information changes including:
- Information the sponsor receives that casts doubt on the continued validity of the submitted data
- Information associated with the Clinical Trial Import License
See the G-KenyaCT for additional information on principal investigator requirements relating to the Clinical Trial Import License.
Record Requirements
As per the G-KenyaCT , the sponsor is required to maintain records that document IP(s) shipment, receipt, disposition, return, and destruction. The sponsor must also maintain a system for retrieving IPs and documenting this retrieval, and maintain a system for the disposition of unused IPs.
According to the G-KenyaCT , IP manufacturers or importers must also retain samples for each batch of bulk product, and the packaging components used for each finished batch, for at least two (2) years following the trial. The sponsor should maintain sufficient samples from each batch and keep a record of their analyses and characteristics for reference so that, if necessary, an independent laboratory could reconfirm the same data.
Specimens are not defined in the Kenyan regulations. However, per KEN-26 , the Kenya Medical Research Institute (KEMRI) identifies biological samples and specimens as including, but not limited to, blood samples, saliva, breast milk samples, mosquito parts samples, biological cultures, tissue and tissue samples, hair samples, human stool, and environmental samples used in human health research.
Import/Export
Per the G-ECBiomedRes , biological material must not be imported nor exported without proper justification and authorization, which includes a signed material transfer agreement (MTA) approved by the relevant institutions and deposited with the National Commission for Science, Technology and Innovation (NACOSTI) . For exports, a Kenyan investigator must be included in the team that is conducting the research in the recipient country. All biological samples and data collected during research belong to the local participating institutions and country.
In addition, KEN-37 has indicated that Kenya’s Pharmacy and Poisons Board (PPB) will approve of an export for overseas research if the following requirements are met:
- PPB initial approval letter or annual approval letter
- Ethics committee (EC) approval letter
- Study protocol with a summary justification for the participants' sample exportation
- Informed consent form that highlights the areas where study participants are informed about the exportation of their samples
The G-KenyaCT states that in the case of transfer of materials during research involving children, the sponsor or the representative or the principal investigator should provide to the EC an MTA including, but not limited to, the following information:
- Identification of the provider and recipient
- Definition of the trial and how the material will and will not be used
- Maintenance of confidentiality of background of supporting data or information, if any
- Indemnification and insurance
In addition, KEN-26 provides an example of the Kenya Medical Research Institute (KEMRI) 's procedures for handling requests to ship biological samples or specimens. KEN-17 also provides an example of an MTA form from the Kenyatta National Hospital-University of Nairobi (KNH-UoN) Ethics and Research Committee .
Detailed information is currently unavailable regarding Kenya’s Pharmacy and Poisons Board (PPB) ’s requirements for obtaining informed consent from participants prior to collecting, storing, or using their biological sample(s). However, the G-KenyaCT , states that for research involving children, the sponsor or the representative or the principal investigator should provide examples of patient information leaflets and informed consent forms (ICF) to the ethics committee (EC) for any proposed archiving of biological specimens for later research, or for genetics research.
The G-ECBiomedRes requires that participants are made aware of the use of personal data through informed consent, including secondary data and biological material in biobanks. The secondary use of data requires approval by an accredited EC. The investigator must obtain consent from the participants for the new study. For situations where this is not practicable, the relevant accredited EC can approve a waiver of individual consent following confirmation that the participants had previously consented to storage of the biological samples/data, and that this data is delinked from personal identifiers. In cases where the sample is stored in a foreign institution, the collaborating EC should also conduct its own deliberation. Researchers sending samples abroad must ensure that consent for transfer of materials was obtained during collection of the samples and that the collaborating EC gave approval.
See KEN-4 for Kenya Medical Research Institute (KEMRI) 's sample ICF that includes guidance on specimens. As another example, see KEN-17 for the Kenyatta National Hospital-University of Nairobi (KNH-UoN) Ethics and Research Committee ’s form and guidance on genetic research and biobanking.
See the Required Elements and Participant Rights sections for additional information on informed consent.
Country Announcement
See the Kenya updates page for details on recent revisions to the profile.
COUNTRY NEWS (Information Not Yet Incorporated Into Country Profile):
New Pharmacy and Poisons Board GMP Guidelines The Pharmacy and Poisons Board recently published online the Kenya Good Manufacturing Practices Guidelines , which went into effect on April 28, 2023, and contains multiple World Health Organization (WHO) technical guidelines.
New NACOSTI E-Citizen Platform Effective November 17, 2023, all research licencing services were migrated to the E-Citizen Platform following the Presidential Directive on the digitalization of payment for government services. See the Research Information Management System (RIMS) website for more details.
New Pharmacy and Poisons Board Guidelines The Pharmacy and Poisons Board recently posted online the Guidelines on Benefit-Risk Assessment of Health Products and Technologies (January 2023). The guidance provides sponsors and researchers with a framework to assess, report, and convey the benefits and risks of a medicinal product in a standard format.

Global Reach
For more 50 than years, the U.S. military has maintained a substantial program for infectious disease research in Kenya. These collaborations have expanded to eight countries under the U.S. Army Medical Research Directorate–Africa (USAMRD-A), which is headquartered on the campus of the Kenya Medical Research Institute (KEMRI) in Nairobi.
WRAIR helped establish the KEMRI-Kericho Clinical Research Centre (CRC) 1999 in collaboration with KEMRI and HJF, and a new CRC opened in 2012 where more than 50 clinical studies have been completed. The Kericho CRC has conducted randomized, double-blind, placebo-controlled and IND/FDA-regulated studies from Phase I to IV.
- Vaccines against HIV, Ebola and polio; therapeutics against HIV, diarrhea, tuberculosis and opportunistic diseases/ malignancies
- Chosen by several Shigella vaccine manufacturers to conduct three large scale multivalent Shigella vaccine trials
- NIH Networks – Part of National Institutes of Health Division of AIDS/AIDS Clinical Trials Group (ACTG) and IMPAACT, the maternal/child HIV treatment and prevention research network funded by the National Institute of Child Health and Human Development

Kenya Research
In 1999, MHRP launched an international HIV vaccine research program in collaboration with the Kenya Medical Research Institute ( KEMRI) based in Kericho, Kenya. The program has developed expertise and infrastructure to support HIV vaccine, therapeutic and other infectious disease research. MHRP also works with a KEMRI satellite clinic, the Kombewa Clinical Research Centre, in Kisumu County . These programs are known locally as the Walter Reed Program-Kenya. The Moi University Clinical Research Centre in Eldoret is also part of MHRP's NIH-funded Clinical Trials Unit.
Kericho Clinical Research Center
The KEMRI Walter Reed Project Clinical Research Center, which opened in Kericho 2012, has successfully conducted more than 52 studies, ranging from clinical trials of therapeutics and vaccines to cohort studies. The Kericho CRC is part of MHRP’s NIAID Clinical Trials Unit networks, and maintains the high caliber standards and accreditations required for those activities :
- AIDS Clinical Trials Group ( ACTG )
- International Maternal, Pediatric, Adolescent, AIDS Clinical Trials ( IMPAACT ) Network
- HIV Vaccine Trials Network ( HVTN )
- COVID-19 Prevention Network ( CoVPN )
HIV Vaccine Research
The CRC has conducted three HIV vaccine trials and an HIV vaccine trial, RV460, completed vaccination in 2023 and analysis is ongoing. This was a randomized, double blind comparative adjuvant study for a DNA/ Protein Prime/Boost HIV Vaccine using gp145, which was developed by MHRP. One of the adjuvants being evaluated in this study is the MHRP-created ALF product .
Therapeutic studies have also been conducted at the CRC related to HIV/AIDS care and treatment and associated opportunistic infections such as tuberculosis, malignancies (Kaposi’s sarcoma) and malaria.
Cohort Studies
Over a period of nearly 10 years (2009-2018), the CRC carried out a large prospective acute infection cohort study, RV217 . The Kericho site enrolled more than 900 volunteers in the study for twice-weekly blood collections with 34 incident acute HIV infections observed. The high rate of volunteer visit compliance was key to study success.
Kericho continues to support the PEPFAR-funded African Cohort Study (AFRICOS) , a 15-year cohort longitudinal study that evaluates the impact of clinical, biological and socio-behavioral issues on HIV infection and disease progression. The Kericho site is also an implementer of the PEPFAR program in the region, so the surrounding community is assured access to HIV care, including antiretroviral therapy. The MOCHI cohort study began in 2022.
Other Infectious Diseases Research
The site has also conducted Ebola and polio vaccine trials. Additionally, the site has one Shigella vaccine trial in review, with two others under development. Plans for a yellow fever vaccine trial and a COVID-19 vaccine trial are also in the works.
Kombewa Clinical Research Centre, Kisumu
A KEMRI satellite clinic, the Kombewa Clinical Research Centre in Kisumu County participates in the African Cohort Study and other PEPFAR-supported research for the optimization of HIV prevention and treatment services. Current public health research is being conducted in collaboration with the Kenya Defense Force to investigate factors associated with virologic suppression and drug resistance in HIV positive children and adolescents on ART in Kenya (RV518).
Previously, Kisumu sites also participated in Phase 2 trials to assess a candidate Ebola vaccine regimen, Ad26.ZEBOV and/or MVA-BN-Filo.
Moi University Clinical Research Centre, Eldoret
Moi University Clinical Research Centre (MUCRC) is located at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya. MRHP has worked with the site since 2008, the same year it was selected as a Clinical Research Site for the AIDS Clinical Trials Group (ACTG) Network. As part of that network, the site's work with MHRP is primarily in the area of HIV therapeutics and co-morbidity research.
U.S. Army Medical Research Directorate–Africa
The U.S. Department of Defense has conducted research in Kenya at the invitation of the Kenyan government since 1969. All MRHP activities in Kenya are conducted under the U.S. Army Medical Research Directorate–Africa (USAMRD-A), which is on the campus of the Kenyan Medical Research Institute (KEMRI) in Nairobi.

REGISTERED RESEARCH INSTITUTIONS IN KENYA
We use cookies, privacy overview.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Bull World Health Organ
- v.98(10); 2020 Oct 1

Language: English | French | Spanish | Arabic | Chinese | Russian
Legal and institutional foundations for universal health coverage, Kenya
Fondements juridiques et institutionnels pour l'instauration d'une couverture maladie universelle au kenya, fundamentos jurídicos e institucionales de la cobertura sanitaria universal en kenia, الأسس القانونية والمؤسسية للتغطية الصحية الشاملة، كينيا, 肯尼亚:全民健康覆盖的法律和体制基础, Правовые и институциональные основы всеобщего охвата услугами здравоохранения, Кения, regina mbindyo.
a World Health Organization Country Office, UN Complex Gigiri, Block U3, UN Gigiri Avenue, Nairobi, Kenya.
Jackson Kioko
b Kenya Health Professions Oversight Authority, Nairobi, Kenya.
c Pharmacy and Poisons Board, Nairobi, Kenya.
Stephen Cheruiyot
d Ministry of Health, Nairobi, Kenya.
Mary Wangai
Joyce onsongo, annette omwoyo.
e Kenya Law Reform Commission, Nairobi, Kenya.
Christine Kisia
Koome miriti.
f Kenya National Commission on Human Rights, Nairobi, Kenya.
Kenya’s Constitution of 2010 triggered a cascade of reforms across all sectors to align with new constitutional standards, including devolution and a comprehensive bill of rights. The constitution acts as a platform to advance health rights and to restructure policy, legal, institutional and regulatory frameworks towards reversing chronic gaps and improving health outcomes. These constitutionally mandated health reforms are complex. All parts of the health system are transforming concurrently, with several new laws enacted and public health bodies established. Implementing such complex change was hampered by inadequate tools and approaches. To gain a picture of the extent of the health reforms over the first 10 years of the constitution, we developed an adapted health-system framework, guided by World Health Organization concepts and definitions. We applied the framework to document the health laws and public bodies already enacted and currently in progress, and compared the extent of transformation before and after the 2010 Constitution. Our analysis revealed multiple structures (laws and implementing public bodies) formed across the health system, with many new stewardship structures aligned to devolution, but with fragmentation within the regulation sub-function. By deconstructing normative health-system functions, the framework enabled an all-inclusive mapping of various health-system attributes (functions, laws and implementing bodies). We believe our framework is a useful tool for countries who wish to develop and implement a conducive legal foundation for universal health coverage. Constitutional reform is a mobilizing force for large leaps in health institutional change, boosting two aspects of feasibility for change: stakeholder acceptance and authority to proceed.
Résumé
Adoptée en 2010, la Constitution du Kenya a entraîné une série de réformes dans tous les secteurs afin de les adapter aux nouvelles normes constitutionnelles, notamment à la décentralisation et à une charte détaillée des droits. La Constitution sert de tremplin pour faire progresser les droits en matière de santé et restructurer les cadres politiques, juridiques, institutionnels et réglementaires en vue de réduire les disparités chroniques et d'améliorer les résultats cliniques. Toutefois, ces réformes de santé prévues dans la Constitution sont complexes. Toutes les composantes du système de santé évoluent en même temps, de nombreuses lois inédites sont promulguées et des organismes de santé publique sont créés. L'emploi d'approches et d'outils inadaptés a entravé la mise en œuvre de ces changements si complexes. Pour mieux appréhender l'étendue des réformes de santé entreprises au cours des 10 premières années de la Constitution, nous avons développé un cadre sanitaire sur mesure, inspiré des concepts et définitions de l'Organisation mondiale de la Santé. Nous avons appliqué ce cadre afin de récolter des données sur les organismes publics et les lois relatives à la santé qui ont d'ores et déjà été édictées ou sont en cours d'élaboration, et avons comparé l'ampleur des transformations avant et après la Constitution de 2010. Notre analyse a révélé de multiples structures (lois et organes publics de mise en œuvre) réparties dans l'ensemble du système de santé, avec plusieurs nouvelles structures de gestion conformes à la décentralisation mais une fragmentation au niveau de la sous-fonction de régulation. En décomposant les fonctions normatives du système de santé, le cadre a permis d'établir une cartographie globale des différentes caractéristiques de ce système (fonctions, lois et organes de mise en œuvre). Nous sommes convaincus que notre cadre représente un outil utile pour les pays qui souhaitent développer et instaurer des bases juridiques propices à la création d'une couverture maladie universelle. La réforme constitutionnelle possède un pouvoir de mobilisation capable de faire progresser le changement institutionnel dans le domaine de la santé. Et ce, en renforçant deux aspects qui favorisent sa réalisation: l'acceptation de la part des intervenants, et l'autorité nécessaire pour agir.
La Constitución de Kenia de 2010 generó una serie de reformas en todos los sectores para ajustarse a los nuevos estándares constitucionales, incluida la transmisión y una amplia carta de derechos. La constitución representa una plataforma para promover los derechos sobre la salud y reestructurar los marcos jurídicos, institucionales y normativos con el fin de revertir las deficiencias crónicas y mejorar los resultados de la salud. Estas reformas de la salud, establecidas por mandato constitucional, son complejas. Asimismo, todas las áreas del sistema de salud se están transformando de manera simultánea, ya que se han promulgado varias leyes nuevas y se han establecido organismos de salud pública. Sin embargo, la falta de herramientas y métodos adecuados limitó la implementación de estos cambios tan complejos. Se elaboró un marco adaptado del sistema sanitario, que se guía por los conceptos y las definiciones de la Organización Mundial de la Salud, para tener una idea del alcance de las reformas sanitarias en los primeros 10 años de la constitución. En este contexto, se aplicó el marco para documentar las leyes sanitarias y los organismos públicos ya promulgados y en curso, en el que se comparó el grado de transformación antes y después de la Constitución de 2010. El análisis realizado reveló que se habían formado múltiples estructuras (leyes y organismos públicos de ejecución) en todo el sistema sanitario, que tenían muchas estructuras de gestión nuevas alineadas con la transmisión, pero que estaban fragmentadas dentro de la subfunción de reglamentación. Al desestructurar las funciones normativas del sistema sanitario, el marco permitió realizar un mapeo completo de los diversos atributos del sistema sanitario (funciones, leyes y organismos de ejecución). Se considera que el marco que se propone aquí es un instrumento útil para los países que quieren elaborar e implementar un fundamento jurídico propicio para la cobertura sanitaria universal. La reforma constitucional es una fuerza de movilización que permite obtener importantes avances en el cambio institucional del sector sanitario, lo que fomenta dos aspectos de la viabilidad del cambio: la aceptación de las partes interesadas y la autoridad para proceder.
ملخص
أطلق الدستور الكيني لعام 2010 سلسلة من الإصلاحات عبر كل القطاعات للتوافق مع المعايير الدستورية الجديدة، بما في ذلك انتقال السلطة ووثيقة شاملة للحقوق. يعمل الدستور كمنصة للنهوض بالحقوق الصحية وإعادة هيكلة أطر العمل السياسية والقانونية والمؤسسية والتنظيمية بهدف رأب الفجوات المزمنة وتحسين النتائج الصحية. إن هذه الإصلاحات الصحية التي يفرضها الدستور تتسم بالتعقيد. تتغير جميع أطراف النظام الصحي بشكل متزامن، إلى جانب العديد من القوانين الجديدة التي تم سنها، وهيئات الصحة العامة التي تم إنشاؤها. وقد تعرض تنفيذ مثل هذا التغيير المعقد للتعويق بسبب الأدوات والأساليب غير الملائمة. للحصول على صورة لمدى الإصلاحات الصحية خلال السنوات العشر الأولى من تطبيق الدستور، قمنا بوضع إطار عمل معدّل للنظام الصحي، في ضوء مفاهيم وتعريفات منظمة الصحة العالمية. قمنا بتطبيق إطار عمل لتوثيق القوانين الصحية والهيئات العامة التي تم تنفيذها بالفعل، والتي هي قيد التنفيذ، وقمنا بمقارنة مدى التحول قبل وبعد دستور 2010. كشف تحليلنا عن العديد من الهياكل (القوانين والهيئات العامة المنفذة) التي تشكلت عبر النظام الصحي، مع العديد من هياكل الإشراف الجديدة المتوافقة مع انتقال السلطة، ولكن مع التجزئة داخل الوظيفة الفرعية التنظيمية. من خلال تفكيك وظائف النظام الصحي المعيارية، قام إطار العمل بتمكين رسم خرائط شاملة لمختلف سمات النظام الصحي (الوظائف والقوانين والهيئات المنفذة). نحن مؤمن بأن إطار عملنا هو أداة مفيدة للبلدان التي تريد وضع وتنفيذ أساس قانوني ملائم للتغطية الصحية الشاملة. الإصلاح الدستوري هو قوة دفع لتحقيق قفزات واسعة في التغيير المؤسسي الصحي، مما يعزز جانبين من جدوى التغيير: قبول أصحاب المصلحة وسلطة المضي قدما.
摘要
2010 年《肯尼亚宪法》推动了各部门的一系列改革,以遵循新宪法标准,包括权力下放和全面的人权法案。《宪法》为促进卫生权和调整政策、法律、体制和监管框架提供了一个平台,从而扭转长期差距,改善卫生成效。这些宪法规定的卫生改革很复杂。卫生体系的所有部门同时转型,颁布了若干新准则,并建立了公共卫生机构。此类复杂变革的实施受到了举措和方法不充足的阻碍。为了解该宪法前 10 年卫生改革的程度,我们根据世界卫生组织理念和界定,制定了一个合适的卫生体系框架。我们利用此框架记录已设立并正在实施的卫生法和公共机构,并对比了 2010 年《肯尼亚宪法》实施前后的改革程度。我们的研究结果表明,整个卫生体系形成多重结构(准则和实施中的公共机构),其中许多新的管理结构与权力下放一致,但在下级监管方面存在分歧。通过解析卫生体系标准职责,该框架提供了各种卫生体系属性的详细信息(职责,准则和实施机构)。我们认为,我们的框架有助于为某些国家实现全民健康覆盖打下坚实的法律基础并赋予实施。宪法改革可推动卫生体制取得突破性变革,增强了变革可行性的两个方面:利益相关者的接受程度和实施授权。
Резюме
Конституция Кении от 2010 года инициировала комплекс реформ во всех секторах, чтобы привести их в соответствие с новыми конституционными стандартами, включая передачу полномочий и всеобъемлющий билль о правах. Конституция действует в качестве платформы для продвижения прав в области здравоохранения и реструктуризации политической, правовой, институциональной и нормативной базы для устранения хронических пробелов и улучшения результатов в отношении здоровья. Эти обусловленные конституцией реформы в сфере здравоохранения являются сложносоставными. Трансформация всех частей системы здравоохранения происходит одновременно, поэтому было принято несколько новых законов и были созданы органы общественного здравоохранения. Реализации таких сложных изменений препятствовали ненадлежащие инструменты и подходы. Для получения представления о масштабах реформ в сфере здравоохранения за первые 10 лет действия конституции авторы разработали адаптированную рамочную структуру для системы здравоохранения, руководствуясь концепциями и определениями Всемирной организации здравоохранения. Эту структуру применили, чтобы документально фиксировать, какие законы уже приняты и какие органы уже функционируют, а какие только находятся в процессе создания, и сравнили степень преобразований до и после принятия Конституции 2010 года. Как показал анализ, в системе здравоохранения существует множество структур (законов и исполнительных государственных органов), при этом большое количество новых надзорных структур связано с делегированием полномочий, но внутри регулятивной подфункции существует значительная раздробленность. Путем деконструкции нормативных функций системы здравоохранения рамочная структура позволила выполнить всеобъемлющее картирование различных атрибутов системы здравоохранения (функций, законов и исполнительных органов). Авторы считают, что такая рамочная структура является полезным инструментом для стран, которые хотят разработать и внедрить благоприятную правовую основу для всеобщего охвата услугами здравоохранения. Конституционная реформа — это движущая сила для значительного продвижения в институциональных изменениях в сфере здравоохранения, которая усиливает два аспекта осуществимости изменений: принятие заинтересованными сторонами и полномочия на выполнение.
Introduction
The constitution of a country is its supreme law, which underpins all other laws as well as citizens’ pursuit of peace, justice and human development. 1 Explicit constitutional provisions on the right to health exist in 28 of 47 Member States of the World Health Organization (WHO) African Region. 1 Yet there is limited knowledge about country experiences with constitutionally mandated health reforms, particularly in low- and middle-income countries.
Kenya’s 2010 Constitution 2 replaced the constitution adopted when the country gained independence in 1963, creating new normative, structural, institutional, policy and administrative standards. The 2010 Constitution provides important opportunities for fundamental reform, through key reform agents such as independent commissions and a restructured judiciary and parliament, among other core institutions, agencies and organs in government. 3 A key constitutional standard requires the state to take policy, legislative and other measures to fulfil its obligations in respect of health. Consequently, in 2010 the Government of Kenya embarked on a reform of health policies, legislation and institutions. The health reforms are complex, with several multistakeholder processes running concurrently, developing various laws and detailing the formation or restructuring of various bodies. The reforms resonate with the United Nations high-level declaration on universal health coverage (UHC), which includes a commitment to strengthen legislative and regulatory frameworks for UHC. 4 In this respect, measuring change in Kenya’s health reforms would contribute knowledge to advance UHC.
On the 10th anniversary of the constitution, we describe our efforts to review the status of these health reforms. The Health Systems Governance Collaborative, 5 in efforts to simplify governance to improve its understanding and applicability, has outlined a three-level approach for assessing the different elements and levels of governance: structural, process and outcome. Our paper focuses on structural measures, specifically the national laws and governance entities – the public implementing organizations and formal groupings across the entire health system. The aim of this article is to demonstrate an approach to measurement of health-system structure, and to apply that approach to analyse gaps and generate evidence for action to strengthen the structural capabilities in the Kenya health system.
In the following sections we first outline our theoretical framework on structural reforms in health systems. We then describe the background to Kenya’s health-system reforms and the adapted health-system framework that we developed to analyse the multi-institutional reforms. Finally, we present our analysis and lessons learnt.
Theoretical framework
There is considerable evidence associating the constitutional right to health with better health outcomes. 6 , 7 A significant association has been found between a right to health in a national constitution and reductions in infant and under-five mortality rates. 6 Other researchers found that institutional environments shaped by a right to health encourage more and better delivery of health services and can partly account for a positive impact on health outcomes. 7 In this section we highlight some key linkages across health rights, health law, health institutions and health outcomes.
The rule of law is increasingly recognized as a determinant of health, and pivotal to health and development. WHO has observed that most public health challenges have a legal component and that the concept of public health law “includes the legal powers that are necessary for the State to discharge its obligation to realize the right to health for all members of the population.” 8 Further, it has been argued that the rule of law is a largely unacknowledged prerequisite for a well-functioning health system. 9 The law can translate vision into action on sustainable development, strengthen the governance of national and global health institutions and implement fair, evidence-based health interventions. 10 The law can be an effective tool to harmonize the mandates of public agencies, clarify functions and promote multiagency cooperation; to designate the responsible agency to resolve a particular issue; and to create new entities to coordinate activities across multiple agencies. 10 WHO notes that countries that have achieved UHC have built it on legal foundations, underscoring that developing and implementing a legal environment conducive to UHC is a critical investment. 11 WHO highlights three critical elements to assess country contexts on whether UHC law reform is feasible: (i) whether there is acceptance of (or opposition to) the proposed reform; (ii) whether there is authority to proceed (especially authority from political decision-makers); and (iii) whether the country has the ability to complete the work (the capacity to make, implement and administer laws). 12 Using the context of Kenya, we aim to demonstrate the extent of feasibility of UHC law reform, and to contribute lessons on the systematic assessment of legal and regulatory frameworks for UHC.
Effective health reforms should include reforming and restructuring the institutions through which health policies are implemented. 13 One author has described institutions as the rules of the game – the formal and informal rules and norms that structure citizens’ rights, entitlements, opportunities and voices. 14 A distinction can be drawn between organizations and institutions. Organizations (public or private) are created to perform defined functions. Organizations are primarily the agent for institutional change with the emphasis on the interaction between the rules of the game (institutions) and the players of the game (organizations). 14 Formal institutions, the focus of this article, include the written constitution, laws, policies, rights and regulations enforced by official authorities (public organizations or agencies). 15 An analysis of institutional change includes considering whether a particular function is necessary or not (for example, the need for an agency or new patterns of service delivery by organizations). Organizational change, however, focuses on internal capacities (for example, automation of business processes or upgrading equipment). 16 Institutional change analysis must be driven by a focus on desired outcomes: in the case of health, multiple outcomes relating to UHC. Appropriate approaches and tools are needed to analyse and diagnose gaps and to predict further institutional change to strengthen the health system for UHC. 16 We describe an approach to analyse concurrent change to multiple health laws and public organizations.
We also consider social science theories related to advocacy and policy change efforts. 17 Among these, the large-leaps theory posits that “when conditions are right, change can happen in sudden, large bursts that represent a significant departure from the past, as opposed to small incremental changes over time that usually do not reflect a radical change from the status quo.” 17 In Kenya, the 2010 Constitution created a major shift in feasibility for health law reforms, which triggered large changes in policies, laws, institutional and regulatory frameworks. In Fig. 1 , we illustrate a theoretical connection between constitutional standards and long-term health-system goals, via analysing institutional change, optimizing the interconnected health outcomes, and rationalizing their assignment to health actors (public and private).

Theory of change on translating constitutional standards to health goals
Background to reforms
The key aspects of Kenya’s 2010 Constitution in relation to health were twofold: devolution of power to 47 county governments; and explicit provisions on the right to health. The extent of devolution of administrative functions varies across sectors. The health functions are extensively devolved: the national government is assigned health policy, national referral services and capacity-building for counties; county governments are assigned person-based and public health services within their jurisdictions. 18 – 20 The constitution prescribed mechanisms and timelines for implementation of the various constitutional changes, including a time-limited independent body to oversee the transition to devolved government. This process entailed the development of enabling legislation and institutions for devolution, including intergovernmental relations, applicable to all sectors. The constitution triggered a large number of public-sector reforms and energized political commitment to reforms, including initiatives to streamline the governance of public agencies in all sectors, and to prioritize government investments and reforms in UHC, agriculture and nutrition, housing and manufacturing. 21 , 22
To guide the transformation in the health sector, the Kenya Health Policy (2012–2030) was formulated 23 with policy priorities structured around WHO’s six key components of a well-functioning health system: (i) leadership and governance; (ii) service delivery; (iii) health system financing; (iv) health workforce; (v) medical products, vaccines and technologies; and (vi) health information systems. 24 – 26 This six-component structure was adapted for Kenya by highlighting additional policy issues and areas for investment. The policy proposed to overhaul the health legal framework by installing a new general health law and specific laws to restructure each component. This comprehensive legal framework incorporated health infrastructure as a seventh component ( Fig. 2 ). After the county governments were elected in 2013, the health policy was validated and updated to the Kenya Health Policy (2014–2030), 27 and health research was added as an eighth component. At various stages, the health ministry established ad hoc technical working groups and formal advisory panels. These groups act as the primary platforms for elaborating the needed change within the various reform initiatives and for facilitating broad stakeholder engagement and external technical support. 28 , 29

Comprehensive health legal framework for Kenya
Conceptual and analytical framework
A major challenge in analysing the multi-institutional change in Kenya was the lack of a uniform and coherent approach. The use of simplistic tools to analyse complex health systems often contributes to interventions that upset the equilibrium of the system, which can lead to policy resistance from stakeholders. 30 To align the health sector with the 2010 constitutional standards, Kenya’s health policy prescribed specific laws to transform multiple parts of the system, but lacked detail on the overall structural design, offering no rationale on the configuration of health functions or the implementing organizations envisioned to optimize health outcomes across the devolved system. Therefore, to analyse what has changed since 2010, we deconstructed the health legal (and institutional) framework, component-by-component and function-by-function, guided by WHO concepts and definitions.
WHO describes a health system as a set of interconnected parts that have to function together to be effective, consisting of all the organizations, institutions, resources and people whose primary purpose is to improve health. 31 , 32 The WHO framework for health-systems performance assessment identifies four basic health-system functions through which health investments flow: (i) stewardship; (ii) resource generation; (iii) service provision; and (iv) financing. In this respect, a health system would be considered well performing when all the relevant organizations, institutions, resources and people are functioning together and contributing optimally to attaining three intrinsic goals or outcomes: health; responsiveness; and fair financial contribution. 33 Consequently, health institutional reforms would be expected to optimize institutional capabilities to achieve the intrinsic health outcomes by transforming health functions component-by-component.
We developed an approach – the adapted health-system framework – which enables a structured, all-inclusive framing of health functions, and promotes uniform and coherent analysis to identify structural gaps across the health system. We superimposed the core eight components of the Kenya Health Policy 2014–2030 and the four basic health-system functions described above. In this way, we created a grid with each cell representing a distinct health function. Our framework allows structure and function to converge, giving a perspective of the health system’s foundational elements and acting as a tool to visualize change. We used the framework to systematically document the national health laws and public bodies (those already enacted and those in progress) to assess the extent of change, diagnose gaps and identify corrective adjustments. Hence, this article is not concerned with monitoring constitutional implementation, 34 , 35 or assessing whether specific health-system functions or accountability mechanisms are achieving desired outcomes (such as access to medicines 36 or immunization coverage 37 ).
Other authors have observed that stewardship is usually the most neglected function within health systems, yet it “anchors health to the wider society, comprising three broad tasks: providing vision and direction, collecting and using intelligence, and exerting influence through regulation and other means.” 38 The sub-function of regulation has been discussed when describing the complex health-care regulatory system in the United States of America. Seven distinct areas of regulatory focus were identified, 39 all addressing three competing health outcomes (access, quality and costs). These seven regulatory spheres are essentially a subset of our adapted framework since they relate to WHO’s concept of health stewardship, and they align with WHO’s six core health-system components. The spheres exclude health leadership (responsible for overall stewardship), and the other five components are subdivided and expanded to distinguish the perspectives relating to health regulation. Thus, health business relationships, public health and health research are distinct regulatory components. Our discussion will therefore highlight two stewardship sub-functions: overall system design and regulation.
Assessment methods
We obtained empirical evidence for this assessment from two primary sources. First, all the authors were closely involved in the health reform processes in various capacities, either as government planning experts or as technical advisors, engaging through the technical working groups and advisory panels. Second, we analysed various documents including national policies, legislative instruments (laws, executive orders, legal notices and legislative bills). We identified all the instruments enacted for purposes relating to health, as published in the official Kenyan Government website. 40 We then compiled a chronological list of these legislative instruments from 1921 to June 2020. For each instrument listed, we reviewed the legal text and identified two attributes: public body created and health function assigned. We then mapped all the bodies onto the adapted framework according to assigned function to see which governing entities and implementing organizations are in place and functional. We created two profiles: pre-constitution and post-constitution. Similarly, we mapped the initiatives that were in progress by June 2020 (technical working groups, advisory panels or parliamentary bills). To assess the extent of change in the regulatory sub-functions, we also extracted the data on the regulatory bodies formed to date (enacted and in-progress) and mapped these onto the seven regulatory spheres. 39
Legal and institutional changes
Before the 2010 Constitution, Kenya’s health system was managed centrally by two health ministries and governed through the Public Health Act of 1921 and other statutes governing specific functions. A total of 28 public bodies existed (in the statutes), although three of these were not currently operating, and we could not ascertain whether they had ever been constituted ( Table 1 ). Shortcomings of the pre-constitution health structures were that institutional change was largely aligned to vertical public health programmes or to health professions. In particular, health professional bodies regulated most aspects of health in a cadre-centric model, creating a disproportionate focus on professional practice, with virtually no balancing laws or independent authorities to safeguard consumer interests (such as safety, pricing and confidentiality).
NA: not applicable.
Notes: Cells of the adapted health-system framework show public health-sector bodies (and year of enactment) created before the 2010 Constitution of Kenya. Core components are based on World Health Organization’s (WHO) Key components of a well functioning health system , 2010. 24 Functions are based on WHO’s framework for health systems performance assessment, 1999. 33 In some cases we could not ascertain the reasons why a body was non-operational.
In the period since the 2010 Constitution was adopted there has been a large increase in the number of health bodies. This transformation has included enactment of eight laws and creation of 65 new bodies (16 national, two intergovernmental and 47 county health departments). Seven additional reforms were in progress by June 2020 ( Table 2 ).
Notes: Cells of the adapted health-system framework show public health-sector bodies (and year of enactment) created after the 2010 Constitution of Kenya up to June 2020. Core components are based on the World Health Organization’s (WHO) Key components of a well functioning health system , 2010. 24 Functions are based on WHO’s framework for health systems performance assessment, 1999. 33
Of the new laws, the Health Act, 2017 was the first major post-independence health legislation, delineating multiple health functions at the national, intergovernmental and county levels, establishing new bodies and mandating others to be enacted. The Act signalled a fundamental shift towards cadre-neutral health stewardship bodies (professions, products and institutions) and a greater focus on consumer aspects within health functions. These multiple reform initiatives demonstrate significant feasibility for health reforms. By prioritizing UHC reforms, political decision-makers have signalled authority to proceed, and broad acceptance by stakeholders. The multiple stakeholder engagement mechanisms led by the health ministry (technical working groups and advisory panels) enable the articulation of specific reforms within functions, facilitate consensus-building and isolate contentious issues to be resolved. Parliament is actively (but independently) engaged, including sponsoring bills in some priority areas (blood services, food and drug regulation), which creates pressure on health stakeholders to fast-track any related reform initiatives. These multiple forces are driving the large-leaps change to a new state of governance arrangements for health, aligned to devolution, and to broader government policies (such as governance of state agencies).
The function of health stewardship has shown the greatest transformation, with the creation of a steward of stewards (the national health ministry) and delineated stewardship sub-functions across the devolved system. Of the 65 new bodies created, 59 have stewardship mandates (the other six are concerned with creating resources). Of the seven reforms in progress, six involve elaborating stewardship sub-functions (the other reform is concerned with a financing function). This considerable change would be expected to enhance system capabilities in providing vision and direction, collecting and using intelligence, and exerting influence, all contributing to the achievement of desired health outcomes.
The seven distinct regulatory components are at varying stages of transformation ( Table 3 ). Two new regulators have been formed (concerning health professionals and health research); two new regulators are mandated to be formed (for drugs and devices, and health-care institutions); three initiatives are in progress (concerning public health, financing arrangements and business relationships). However, two regulatory areas remain fragmented (public health and health-care professionals). For professions, five new cadre-centric bodies were created, resulting in a total number of 12 bodies ( Table 2 ).
a See also Table 1; Table 2.
b A key recommendation of Kenya’s Presidential Task Force on Parastatal Reforms is the de-linking (from government ownership) of all bodies that are funded through members’ fees (member organizations) in all sectors. In the health sector, all the 12 cadre-centric boards and councils fall into this category, but the recommended de-linking has not yet been done.
Notes: We based the regulatory areas on the seven spheres of regulatory authority described by Field, 2007. 39 The listed structures might not cover all the needed regulatory activities. In some cases we could not ascertain the reasons why a body was non-operational.
Overall, our analysis revealed structural gaps or inconsistencies across many health functions. We noted that, when the new laws and bodies were created, all the pre-constitution laws and bodies (including non-operational bodies) remained unchanged. Except for two merged health ministries, and minor amendments to other laws, these pre-existing structures were not eliminated or consolidated. The inherent fragmentation has therefore become entrenched in the system, with the attendant inefficiencies (gaps, duplication, overlaps and conflicts of mandates). A corrective action is therefore needed to rationalize and consolidate health functions, especially the regulation of public health and health-care professionals.
Conclusion and lessons learnt
Our approach has enabled us to measure institutional change, diagnose gaps and generate evidence for predicting further change across the entire health system of Kenya. Overall, the multiple gaps identified across the health-system components demonstrate the multiple opportunities to streamline health functions across the system. To identify strategic options for further institutional change, a systematic review of the evidence is needed, function-by-function, focused on defined outcomes. However, because a national health system is one system with multiple interconnected parts, any predictions about change in one function require a holistic vision of the overall design of the health system, describing each distinct element, and how the various parts should operate together. By mapping backward from the overall health system goals, we need to define the desired outcomes relating to the distinct health functions, then identify actions that are needed to optimize these outcomes across the interconnected parts of the health system.
We believe our adapted health-system framework is a useful tool for countries needing an all-inclusive framing of health-system structural elements to envision the overall design (future), analyse gaps (current) and predict the needed institutional change. In this respect, the grid is a versatile tool, to create context-specific frameworks, according to the health system attribute(s) mapped onto the cells (laws, bodies, gaps, outcomes). The various mappings can create multiple platforms for engagement, facilitating a holistic approach to health reforms.
The framework could be a useful tool for countries wishing to develop and implement a conducive legal environment for UHC. We have been able to quantify the extent of institutional change in Kenya’s health system and to diagnose gaps for corrective action to strengthen health functions, but we did not focus on the effects or impact of these changes. We encourage further studies to assess the adequacy of laws enacted and the capabilities or actual performance of the bodies created. We have learnt that a national constitutional reform is a mobilizing force for large-leaps institutional change in health, boosting two aspects of feasibility of conducting health reforms for UHC: acceptance by stakeholders; and authority to proceed from political decision-makers. 12 The third aspect of feasibility – capability – requires capacity enhancement and interdisciplinary collaboration (health, legal and human rights), which promotes mutual learning and uniformity of actions. Priorities for capacity enhancement include technical framing of reform issues and formulating health law that is compliant with UHC. Implementing health institutional change requires a holistic, big-picture perspective, envisioning the overall health-system design as it should be, including the spatial arrangement of health functions and the corresponding outcomes. It is then possible to systematically analyse the structural elements to diagnose gaps and to predict change.
Acknowledgements
We thank: Lucy Musyoka, Pacifica Onyancha, Charles Kandie, Mercy Mwangangi, Jared Nyakiba and Mohamed Sheick, all Ministry of Health, Kenya; Njeri Githanga of the National Council for Law Reporting (Kenya Law); Gilbert Kokwaro of Strathmore Business School, Strathmore University, Kenya; Elizabeth Kamundia of Kenya National Commission on Human Rights; Helen Kariuki of University of Nairobi, Kenya; and Nollascus Ganda of WHO Kenya.
Competing interests:
None declared.

Learn if your company is eligible for NIH SBIR or STTR funding, how to apply , and what to expect during each step of the application process. Multiple registrations are required to prepare your application and apply for funding.
- Understanding SBIR and STTR
- Eligibility Criteria
- Grants Policy
- Foreign Disclosure and Risk Management
- SBIR and STTR Grants (NOFO s )
- SBIR Contract Solicitations
- Commercialization Readiness Pilot (CRP)
- Supplemental Funding to Diversify the Entrepreneurial Workforce
- How to Apply
- Transition Award (Coming Soon)
Our team can help you maximize the benefits from NIH programs and resources which help you bring your innovations to life.
- TABA Funding
- TABA Needs Assessment
- Pitch Coaching
- SOW Development
- Reimbursement
Explore the benefits of public-private partnership in NIH’s nationwide network of innovators who convert academic discoveries into healthcare solutions.
The NIH is actively turning discovery into health by helping small businesses develop innovative technologies that improve health and save lives. See how .
- Search Technologies from Academic Centers and Hubs
We value diverse perspectives in biomedical innovation and strive to empower scientists and entrepreneurs to bring their discoveries to patients.
- Contact the SEED Team
- Who to Contact and When
- HHS Small Business Program Managers

Research Evaluation and Commercialization Hubs (REACH)
Research Evaluation and Commercialization Hubs (REACH) support academic innovators to convert promising scientific discoveries into medical products while training a diverse biomedical workforce that is globally competitive in technology development and entrepreneurship.
Early consideration of the healthcare impact and commercial viability of scientific discoveries, combined with milestone-driven product development plans, results in de-risked projects primed for startup company formation or licensing.
This trans-NIH program implements the Phase 0 Proof of Concept Partnership pilot program authorized in the 2011 SBIR/STTR Reauthorization Act (P.L. 112-81) . In 2023, NIH committed $1 million per year for four years to five new REACH hubs (see the REACH Notice of Funding Opportunity ). Together, they will support academic innovators at over 75 institutions in 12 states.
CBC HITES | GCC REACH | Mid-South REACH | Rocky Mountain REACH | UM-BILD
More information about prior REACH hubs is here .
How the Programs Work

-->

Chicago Biomedical Consortium Hub of Innovative Technologies for Entrepreneurship and Science
Institutes:
- Northwestern University
- University of Illinois at Chicago
- University of Chicago
- Loyola University Chicago
- Illinois Institute of Technology
- Rush University
- Rosalind Franklin University
- Discovery Partners Institute
- Northern Illinois University
Gulf Coast Consortia REACH

- Texas A&M University Health Science Center
- University of Texas Medical Branch
- Texas Southern University
- William Marsh Rice University
- Baylor College of Medicine
- Houston Methodist Research Institute
- MD Anderson Cancer Center
- Rice University
- University of Houston
- University of Texas Health Science Center
Mid-South REACH

- Vanderbilt University
- University of Louisville
- Jackson State University
- George Mason University
- American Baptist College
- Belmont University
- Christian Brothers University
- East TN State University
- Fisk University
- Meharry Medical College
- Middle Tennessee State University
- Union University
- Tennessee Board of Regents – Community Colleges
- Tennessee State University
- Tennessee Technological University
- University of Memphis
- University of Tennessee Campuses
- Vanderbilt University Medical Center
- Mississippi State University
- University of Mississippi
- University of Southern Mississippi
- Eastern Kentucky University
- Kentucky Community & Technical College System
- Kentucky State University
- Morehead State University
- Murray State University
- Northern Kentucky University
- University of Kentucky
- Western Kentucky University
- Christopher Newport University
- James Madison University
- Longwood University
- Norfolk State University
- Old Dominion University
- Radford University
- University of Mary Washington
- University of Virginia
- Virginia Commonwealth University
- Virginia Military Institute
- Virginia State University
Rocky Mountain REACH

- University of Montana
- University of Washington
- University of Wyoming
- University of Alaska Anchorage
- Montana State University
- Montana Technological University
- Salish Kootenai College
- Flathead Valley Community College
- Boise State University
- Idaho State University
- University of Idaho
University of Maryland Baltimore Life Science Discovery
- University of Maryland Baltimore
- University of Maryland School of Medicine
- University of Maryland Baltimore County
- Morgan State University
- University of Maryland College Park
- Maryland Innovation Initiative
- Blackbird Laboratories

Stay in the Loop
Subscribe to our mailing list for updates on deadlines and important information.
- Small Business Funding
- Product Development Support
- Entrepreneurial Training
- Resources and Events
Fraud, Waste and Abuse
- Report Fraud
HHS Vulnerability Disclosure | Technical Issues: E-mail OER Webmaster


CENTRE FOR BIOTECHNOLOGY RESEARCH AND DEVELOPMENT (CBRD) NAIROBI
Staff profiles.

The Centre for Biotechnology Research and Development (CBRD) is mandated to undertake basic and biotechnology-related research on human diseases in Kenya, with the overall goal of contributing to the improvement of human health and welfare.
To improve human health and quality of life through research, capacity building innovation and service delivery
To be a leading Centre of excellence in research for human health
CBRD is mandated to undertake basic and biotechnology-related research on human diseases in Kenya, with the overall goal of contributing to the improvement of human health and welfare. The Centre’s mandates are:
- To apply modern science and biotechnology to discover, develop and improve tools and strategies for diagnosis, prevention and control of major human diseases in Kenya and the region.
- To improve basic understanding of the biology of disease-causing agents of public health importance in Kenya and the region, including their responses to intervention (e.g. drugs or vaccines), host responses and disease processes (e.g. immunity, pathogenesis, patho-physiology, host-pathogen interactions), and disease epidemiology.
- To coordinate and advise on issues related to basic biomedical and biotechnological research, pre-clinical studies, quality control and bio-safety.
- To provide specialized laboratory services and expertise to the scientific community and the general public.
- To train, mentor and supervise undergraduate and postgraduate students from local colleges and universities.
- Human DNA Identification for paternity testing and identification within the context of disasters and crime scene investigation ( Get Service )
- CD4/CD8 testing in HIV/AIDS patients as a service to the scientific community and to the general public.
- Training and mentorship of Master’s and Doctor of Philosophy degree students
- Training in flow cytometry technology
- Research training for university post-graduate students
- Training of university undergraduate and polytechnic students on industrial attachment,
- Supply vertebrate animals (mice, hamsters, guinea pigs) for research or teaching purposes to interested researchers or institutions.
Ongoing Research Activities
Stem Cell Research seeks to develop new diagnostic and therapeutic tools for cancer and diabetes with the goal of reducing the economic burden of medical care, thus making it more accessible
Malaria Research involving malaria prevalence studies and surveillance for antimalarial and insecticide efficacy and resistance in Kenya so as to inform policies on malaria control and treatment through the provision of quality data to ensure that only quality and effective antimalarials and insecticides are in use. Additional research is in the development of new malaria diagnostic tools and of novel antimalarial and insecticidal compounds.
Schistosomiasis Research involves disease surveillance to determine areas where schistosomiasis treatment coverage should be increased as well as development of new more sensitive and cost-effective tools for schistosomiasis diagnosis and control.
Lymphatic filariasis research involving epidemiological surveys on Lymphatic filariasis in Coastal Kenya to determine the impact of Mass Drug Administration (MDA) in this Lymphatic filariasis endemic area and development of a new Point of Care (POC) diagnostic kit for Lymphatic filariasis for use in the resource-limited settings.
Leishmaniasis Research includes disease surveillance and epidemiological studies with the goal of identifying new foci of leishmaniasis transmission and thus control to reduce disease transmission, evaluation of anti-leishmania activity of a novel compound in the mouse model, and in vitro and anti-leishmaniasis vaccine studies.
Forensic Research:
- Characterization of Forensic-Quality Haplotypes Representing the diversity of the Kenyan Population for the development of a Full Mitochondrial Genome Reference Database
- Testing new forensic DNA methods to enhance accountability for sexual violence in Kenya.
Get Service
Schistosomiasis Division
Among the neglected tropical parasitic diseases targeted for eradication/elimination include schistosomiasis and soil-transmitted helminthiases. Currently, 258 million of the world’s population is infected with schistosomiasis ranking it as one of the most common and difficult to control.
Immunology Division
The immunology division is mandated to carry out Stem Cell Research.
Entomology and Ecology Division
Leishmaniasis division.
Leishmania Division is involved in research in Leishmaniasis which includes disease surveillance and epidemiological studies with the goal of identifying new foci of leishmaniasis transmission.
Malaria Division/Human Identification Department (HID)
Learn more
Animal Facility

Dr. Luna Kamau
Centre director.
Dr. Luna Kamau, is a Molecular Entomology and Ecology Researcher with over 22 years of experience in research and training in vector biology and control. She has held numerous research grants in the field of molecular and population genetic studies of disease vectors, vector ecology, and behaviour, insecticide resistance, development, and testing of new tools for vector identification, analysis and control. She is widely published and has played a key role in supervised and mentored students and upcoming scientists in the field. Dr. Kamau also serves as the Deputy Director, Centre for Biotechnology Research and Development at KEMRI. Dr. Kamau is a member of the Kenya National Academy of Sciences (KNAS), a Fellow of the African Academy of Sciences, and a Fellow of The World Academy of Sciences (TWAS).
View all Staff Profiles
Contact info.
P.O. Box 54840 Nairobi-00200 Kenya
Email: gro.irmek obfsctd @DRBC
This article is free to read if you register or sign in.
Simply register at no cost.
Questions or problems? Email [email protected] or call 0711 046 000 .
700M ESTATE
Siblings tussle over father’s sh700m estate 20 years on, chepkosgei accuses her step-siblings of treating them as strangers since the death of their father..
• The former medic had property that included hundreds of acres of agricultural land and prime plots spread across Nandi, Uasin Gishu, and Kakamega counties.
• The children are now embroiled in a vicious court battle after disagreeing on how to share their father’s vast estate.
The children of a former medical doctor in Eldoret are engaged in a vicious court battle over the control of their father’s Sh700 million estate.
Siblings from the first and second wives of Vincent Kiprotich Komurgor have failed to agree on how to share his estate 20 years after his demise.
The former medic had property that included hundreds of acres of agricultural land and prime plots spread across Nandi, Uasin Gishu, and Kakamega counties.
Children of the two wives, Anne Kiprotich and Esther Cheboi (both deceased), are now embroiled in a vicious court battle after disagreeing on how to share their father’s vast estate.
Grace Chepkogei, Ben Kimutai and David Kibet from the second wife have petitioned the court to prevail upon their siblings Ignatius Rotich, Louis Rotich and Mark Rotich from the first wife to recognise them as children of Komurgor, saying they are entitled to a share of his estate.
Court documents presented before Eldoret High Court judge Reuben Nyakundi by Chepkosgei on behalf of her two siblings, claimed that despite being the biological children of Komurgor, their stepbrothers have refused to recognise them and have denied them inheritance.
When she appeared before Justice Nyakundi yesterday , Chepkosgei said they were living in destitution after their step-siblings evicted them from their father’s property in Langas estate along the Eldoret-Kapsabet highway.
“We were forcibly ejected from our late father's house in Langas estate by our step-siblings, leaving us to live in destitution because they have also excluded us from benefiting from his estate,” she said.
Chepkosgei accused her step-siblings, Ignatius, Louis and Mark of treating them as strangers since the death of their father.
To back up her claims that they were Komurgor’s biological children, Chepkosgei produced in court paternity test results as evidence.
The tests, which she claimed showed a 99.9 per cent accuracy were conducted at the Kenya Medical Research Institute (Kemri).
“My samples and that of my stepbrother, Ignatius were extracted for DNA tests and the outcome showed that we are of the same father with a 99.9 per cent accuracy,” she told the judge.
Chepkosgei said it was on these grounds they were forced to move to the court 13 years ago and obtained a court order that revoked the grant of letters of administration that had been issued to their step-siblings.
She also accused her siblings of denying them, despite being raised together by their stepmother. They said their predicament started after the death of their stepmother 15 years ago.
However, their step-siblings, led by Ignatius, vehemently denied that the petitioners were their siblings hence not beneficiaries of their father’s estate. They asked the court to order investigations into their identities.
He claimed the applicants might have forged documents they presented in court in an attempt to conceal their actual identities.
In documents presented in court, Ignatius claims their alleged stepmother was buried in her husband’s (not their father's) home in Tot, Elgeyo Marakwet county, saying this was a clear indication she was not married to their late father.
“It is not right to give access to our late parent’s house to strangers to live in because they are not beneficiaries of our late father’s estate,” Ignatius said.
It's court battle for billions of Kenya's eminent dead
Most popular, be on lookout for landslides, murang’a residents cautioned, mystery of sh600m pipeline land sold at sh7m, azimio pushing for ouko-type inquiry in ogolla's death, police prefer killing suspects to arresting them – report, key agencies flag flaws in ruto, raila iebc reforms plan, latest videos, senators call on wamatangi to sort challenges at kiambu hospital, ruto announces 50% tariff reduction for night time manufacturing, sign up for the free star email newsletter and receive the latest kenya news daily..
share this!
April 23, 2024 report
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
New evidence found for Planet 9
by Bob Yirka , Phys.org
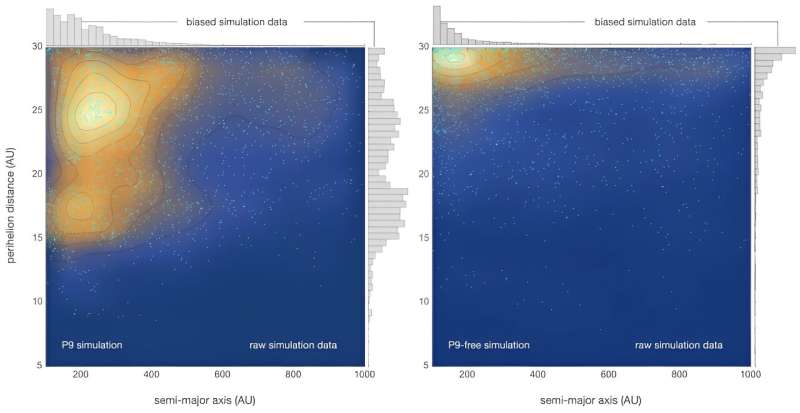
A small team of planetary scientists from the California Institute of Technology, Université Côte d'Azur and Southwest Research Institute reports possible new evidence of Planet 9. They have published their paper on the arXiv preprint server, and it has been accepted for publication in The Astrophysical Journal Letters .
In 2015, a pair of astronomers at Caltech found several objects bunched together beyond Neptune's orbit, near the edge of the solar system. The bunching, they theorized, was due to the pull of gravity from an unknown planet—one that later came to be called Planet 9.
Since that time, researchers have found more evidence of the planet, all of it circumstantial. In this new paper, the research team reports what they describe as additional evidence supporting the existence of the planet.
The work involved tracking the movements of long-period objects that cross Neptune's orbit and exhibit irregular movements during their journey. They used these observations to create multiple computer simulations , each depicting different scenarios.
In addition to factoring in the impact of Neptune's gravitational pull , the team also added data to take into account what has come to be known as the galactic tide, a combination of forces exerted by Milky Way objects beyond the solar system.
The research team found that the most plausible explanation for the behavior of the objects was interference from gravity exerted by a large distant planet. Unfortunately, the simulations were not of the type that would allow the research team to identify the location of the planet.
The team acknowledges that other forces could be at play that might explain the behavior that they simulated but suggest they are less likely. They also note that further evidence will become available as the Vera Rubin Observatory in Chile is set to begin operations sometime next year. It will be equipped, they note, to search in new ways for the planet in a rigorous assessment of its existence.
Journal information: Astrophysical Journal Letters , arXiv
© 2024 Science X Network
Explore further
Feedback to editors

Bioluminescence first evolved in animals at least 540 million years ago, pushing back previous oldest dated example

Star bars show universe's early galaxies evolved much faster than previously thought
2 hours ago

Scientists study lipids cell by cell, making new cancer research possible

Squids' birthday influences mating: Male spear squids shown to become 'sneakers' or 'consorts' depending on birth date

Study finds rekindling old friendships as scary as making new ones
5 hours ago

How light can vaporize water without the need for heat

Researchers develop eggshell 'bioplastic' pellet as sustainable alternative to plastic
6 hours ago

Previous theory on how electrons move within protein nanocrystals might not apply in every case
7 hours ago

Fruit fly pest meets its evolutionary match in parasitic wasp

World's chocolate supply threatened by devastating virus
Relevant physicsforums posts, help on essay about star formation, what did i capture, our beautiful universe - photos and videos.
12 hours ago
'Devil' comet visible tonight 21.04.24
Apr 21, 2024
Solar Activity and Space Weather Update thread
Apr 19, 2024
Will we ever communicate with extraterrestial life in a reasonable time frame?
More from Astronomy and Astrophysics
Related Stories

Japanese astrophysicists suggest possibility of hidden planet in the Kuiper Belt
Sep 1, 2023

New evidence for existence of Planet Nine
May 21, 2018

There's one last place Planet Nine could be hiding
Feb 19, 2024

If Planet 9 is out there, here's where to look
Aug 30, 2021

Evidence of Planet Nine diminishing as researchers find no evidence of clustering
Feb 17, 2021

In search of the ninth planet
Oct 17, 2017
Recommended for you

Observations explore globular cluster system in the galaxy NGC 4262

Astrophysicists work toward unification of turbulence framework—weak-to-strong transition discovered in turbulence
8 hours ago

A first glimpse at our galaxy's magnetic field in 3D
9 hours ago

New JWST observations reveal black holes rapidly shut off star formation in massive galaxies
11 hours ago

Researchers detect a new molecule in space
13 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Phys.org in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
The Kenya Medical Research Institute (KEMRI) is a State Corporation established in Kenya in 1979 through the Science and Technology (Repealed) Act, Cap 250 of the Laws of Kenya operated under the Science Technology and Innovation Act, 2013 as the national body responsible for carrying out research in human health in Kenya. Currently, KEMRI ...
Kenya Medical Research Institute (KEMRI) is a State Corporation established through the Science and Technology (Amendment) Act of 1979, which has since been amended to Science, Technology and Innovation Act 2013. The 1979 Act established KEMRI as a National body responsible for carrying out health research in Kenya. Currently, KEMRI Operates ...
The KEMRI Wellcome Trust Research Programme is a. world-renowned health research unit of excellence. The programme was formed in 1989 when the Kenya Medical Research Institute formed a partnership with the Wellcome Trust and the University of Oxford. The Programme has grown from a small group of 12 to a state of the art facility hosting over ...
The Kenya Medical Research Institute (KEMRI) is a state corporation established through the Science and Technology (Amendment) Act of 1979, (since amended to the Sciences, Technology and Innovation Act 2013), during the tenure of Nicholas Biwott as Minister of State, as the national body responsible for carrying out health research in Kenya.. KEMRI is the medical research arm of the Kenya ...
HJFMRI is proud to partner with organizations from across the globe to advance global health, including host country governments, public institutions, private entities, universities, and foundations. Where We Work. HJFMRI is an international medical research organization. We have operations in 13 countries globally and are a wholly owned ...
The Kenya Medical Research Institute (KEMRI) is a State Corporation established in Kenya in 1979 through the Science and Technology (Repealed) Act, Cap 250 of the Laws of Kenya operated under the Science Technology and Innovation Act, 2013 as the national body responsible for carrying out research in human health in Kenya. Currently, KEMRI ...
The AMPATH Kenya Research Program seeks to improve the health of the Kenyan people by answering the toughest questions our policy leaders and health care providers face. Researchers from our network of 20+ partner institutions are dedicated to strengthening health systems, informing more effective public policy, and finding insights that ...
The Centre for Global Health Research (CGHR) is a Kenya Medical Research Institute (KEMRI) facility located in western Kenya. Since it was established in 1984, the CGHR has furthered research on infectious diseases of medical importance. The CGHR has a rich history in cutting-edge research focused on clinical efficacy of drugs for the treatment of tropical diseases, emergence of drug and ...
The Kenyan Medical Research Institute (KEMRI) was established through the Science and Technology (Amendment) Act of 1979, which has since been amended to Science, Technology and Innovation Act, 2013 with the mandate to carry out health science research in Kenya. The Kilifi-based Centre for Geographic Medicine Coast (CGMR-C) is among the 12 ...
Reacting to the announcement, the Kenya Medical Research Institute Director-General Elijah Songok expressed his gratitude to the Kemri fraternity. "First, I want to thank the Board of Directors for providing the institute with leadership; and second the members of staff for working tirelessly in ensuring the dissemination of health research ...
The Kenya Medical Research Institute is one of East Africa's leading medical research centres and is the national body responsible for carrying out health science research in Kenya. The Kenya Institute of Education promotes development and delivery of relevant, high-quality, affordable education and training programmes, materials and services
Through a fruitful partnership between the Kenya Medical Research Institute and the UK's Wellcome Trust, KWTRP has made significant strides in infectious disease and public health research. You might recall hearing about their crucial role in discovering a new strain of the Ebola virus and creating a malaria vaccine.
Kenya Medical Research Institute (KEMRI)KEMRI is the principal medical research institute in Kenya and has collaborated with the UW AITRP since 1989, when the first of seven KEMRI researchers received long-term training at the UW. KEMRI conducts research from 12 research centers that focus on different areas of national and strategic importance ...
Overview. As per the G-KenyaCT, the G-ECBiomedRes, and KEN-30, Kenya requires an independent review of research through a National Commission for Science, Technology and Innovation (NACOSTI)-accredited ethics committee (EC) in one (1) of the local institutions charged with the responsibility of conducting research in human participants. KEN-25 provides a list of the accredited institutional ECs.
For more 50 than years, the U.S. military has maintained a substantial program for infectious disease research in Kenya. These collaborations have expanded to eight countries under the U.S. Army Medical Research Directorate-Africa (USAMRD-A), which is headquartered on the campus of the Kenya Medical Research Institute (KEMRI) in Nairobi.
Find 584 researchers and browse 4 departments, publications, full-texts, contact details and general information related to Kenya Medical Research Institute | Nairobi, Kenya | KEMRI
The U.S. Department of Defense has conducted research in Kenya at the invitation of the Kenyan government since 1969. WRAIR's expeditionary laboratory, the U.S. Army Medical Research Directorate-Africa (USAMRD-A), is on the campus of the Kenyan Medical Research Institute (KEMRI) in Nairobi. All MRHP activities in Africa, including PEPFAR, are ...
Kenya Medical Research Institute (KEMRI) is a State Corporation established through the Science and Technology (Amendment) Act of 1979, which has since been amended to Science, Technology and Innovation Act 2013. The 1979 Act established KEMRI as a National body responsible for carrying out health research in Kenya.
In 1999, MHRP launched an international HIV vaccine research program in collaboration with the Kenya Medical Research Institute ( KEMRI) based in Kericho, Kenya. The program has developed expertise and infrastructure to support HIV vaccine, therapeutic and other infectious disease research. MHRP also works with a KEMRI satellite clinic, the ...
Research focus or area: Category Public/Private/ International: Postal Address: Physical Address: 1. Kenya Forestry Research Institute (KEFRI) Dr. Jane Njuguna: [email protected]: Forestry and Allied Natural Resources: Public: P.O. Box 20412 - 00200, Nairobi: Muguga, Off Nairobi - Nakuru Highway, Nairobi. 2. Kenya Marine and Fisheries Research ...
• Kenya Medical Research Institute (1979) None: NA: ... (2012), created by amalgamating the Kenya Institute of Administration and three other government training institutions : None: Three successive Executive Orders on the structure of the National Government (2013, 2016 and 2018) established a single health ministry and its portfolio ...
Research Evaluation and Commercialization Hubs (REACH) support academic innovators to convert promising scientific discoveries into medical products while training a diverse biomedical workforce that is globally competitive in technology development and entrepreneurship. Early consideration of the healthcare impact and commercial viability of ...
To have a robust clinical antifungal pipeline it's essential to invest and monitor its upstream development. In November 2022 WHO released the WHO fungal priority pathogens list (FPPL), a catalogue of the 19 fungi that represent the greatest threat to public health. The list is the first global effort to systematically prioritize fungal pathogens, considering the unmet research and development ...
Kenya Medical Research Institute (KEMRI) is a State Corporation established through the Science and Technology (Amendment) Act of 1979, which has since been amended to Science, Technology and Innovation Act 2013. The 1979 Act established KEMRI as a National body responsible for carrying out health research in Kenya.
The tests, which she claimed showed a 99.9 per cent accuracy were conducted at the Kenya Medical Research Institute (Kemri). "My samples and that of my stepbrother, Ignatius were extracted for ...
A 2018 study of pain medicine curriculum in 383 medical schools internationally and found 96% of schools in the United Kingdom and United States, and nearly 80% of schools in Europe had no required dedicated teaching in pain medicine. Additionally, the study showed U.S. medical students received the lowest number of hours (fewer than 10 ...
A small team of planetary scientists from the California Institute of Technology, Université Côte d'Azur and Southwest Research Institute reports possible new evidence of Planet 9 ...