
Vitamin D News
Top headlines, latest headlines.
- Vitamin D and Risk of Atrial Fibrillation
- Vitamin D Alters Developing Neurons
- Taking Vitamin D Could Help Prevent Dementia
- Vitamin D Levels and Melanoma Risk
- Arsenic in Drinking Water? Vitamin D3 Might Help
- Microparticle to Cut Vitamin A Deficiency
- Vitamin K: Lower Bone Fracture Risk Later
- Statin-Linked Muscle Pain: No Help from ...
- Vitamin D Deficiency Linked to Premature Death
- Vitamin D May Help With Depression
Earlier Headlines
Thursday, september 29, 2022.
- Cystic Fibrosis Patients Can Benefit from Vitamin Supplements, Research Shows
Sunday, August 7, 2022
- Down on Vitamin D? It Could Be the Cause of Chronic Inflammation
Wednesday, August 3, 2022
- Vitamin K Prevents Cell Death: New Function for a Long-Known Molecule
Tuesday, July 19, 2022
- Vitamin B6 Supplements Could Reduce Anxiety and Depression
Wednesday, July 6, 2022
- Differentiation of Rickets and Classic Metaphyseal Lesions on Radiographs
Tuesday, July 5, 2022
- Taking Vitamin D During Pregnancy Could Lower the Risk of Eczema in Babies
Tuesday, June 14, 2022
- Vitamin D Deficiency Can Lead to Dementia
Tuesday, March 8, 2022
- Placenta Plays Active Part in Transferring Vitamin D to Fetus During Pregnancy
Friday, February 25, 2022
- Study Questions the Role of Vitamin D2 in Human Health but Its Sibling, Vitamin D3, Could Be Important for Fighting Infections
Thursday, February 17, 2022
- Study Strengthens Case That Vitamins Cannot Treat COVID-19
Sunday, February 6, 2022
- Pre-Infection Deficiency of Vitamin D Is Associated With Increased Disease Severity and Mortality Among Hospitalized COVID-19 Patients
Wednesday, January 5, 2022
- Taking High-Dose Vitamin D Supplements for Five Years Did Not Affect the Incidence of Cardiovascular Disease or Cancer
Wednesday, December 8, 2021
- Sunshine May Shield Children, Young Adults from MS
Monday, December 6, 2021
- The Sunshine Vitamin That ‘D’elivers on Cardio Health
Wednesday, November 10, 2021
- Plant-Based Gummy Candy Helps Vegans and Vegetarians Get Their Vitamins
Monday, September 27, 2021
- Sunlight Exposure Guidelines May Need to Be Revised
Wednesday, September 15, 2021
- New Findings on Ambient UVB Radiation, Vitamin D, and Protection Against Severe COVID-19
Tuesday, August 17, 2021
- Vitamin D May Protect Against Young-Onset Colorectal Cancer
Monday, August 16, 2021
- New Analysis of Landmark Scurvy Study Leads to Update on Vitamin C Needs
Monday, August 9, 2021
- Growing Evidence of Vitamin K Benefits for Heart Health
Friday, August 6, 2021
- Do Vitamin D Supplements Offer Kidney-Related Benefits for Individuals With High Diabetes Risk?
Thursday, August 5, 2021
- Vitamin D Reduces the Need for Opioids in Palliative Cancer
Tuesday, July 27, 2021
- Black American Women With Vitamin D Insufficiency More Likely to Test Positive for COVID-19, Study Finds
Friday, June 11, 2021
- Vitamin D Deficiency May Increase Risk for Addiction to Opioids and Ultraviolet Rays
Tuesday, June 1, 2021
- Vitamin D May Not Provide Protection from COVID-19 Susceptibility or Disease Severity, Study Suggests
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- Ozone Removes Mating Barriers Between Fly ...
- Parkinson's: New Theory On Origins and Spread
- Clash of Stars Solves Stellar Mystery
- Secure Quantum Computing at Home
- Ocean Currents: Collapse of Antarctic Ice ...
- Pacific Cities Much Older Than Previously ...
- The Milky Way in Ancient Egyptian Mythology
- Physical Activity Best in the Evening
- How the Body Switches out of 'Fight' Mode
- New Drug Prevents Flu-Related Lung Damage
Trending Topics
Strange & offbeat.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Women rarely die from heart problems, right? Ask Paula.

When will patients see personalized cancer vaccines?
A molecular ‘warhead’ against disease
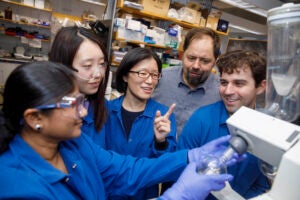
While some of the vitamin D we need is made in the body from sunlight, vitamin D deficiencies are often treated with supplementation.
Helin Loik-Tomson/iStock by Getty Images
Vitamin D benefits linked to body weight
Brigham and Women’s Communications
Study looks at correlation between positive health outcomes from vitamin D and a person’s BMI
New research finds vitamin D may metabolize differently in those considered overweight, resulting in diminished health benefits.
The study, which appears in JAMA Network Open , is a new analysis of data from the VITAL trial, a large nationwide clinical trial led by Brigham and Women’s Hospital researchers that investigated whether taking vitamin D or marine omega-3 supplements could reduce the risk of developing cancer, heart disease, or stroke.
“The analysis of the original VITAL data found that vitamin D supplementation correlated with positive effects on several health outcomes, but only among people with a BMI under 25,” said first author Deirdre K. Tobias, an associate epidemiologist in Brigham’s Division of Preventive Medicine . “There seems to be something different happening with vitamin D metabolism at higher body weights, and this study may help explain diminished outcomes of supplementation for individuals with an elevated BMI.”
Vitamin D is an essential nutrient involved in many biological processes, most notably helping our body absorb minerals, such as calcium and magnesium. While some of the vitamin D we need is made in the body from sunlight, vitamin D deficiencies are often treated with supplementation. Evidence from laboratory studies, epidemiologic research and clinical research has also suggested that vitamin D may play a role in the incidence and progression of cancer and cardiovascular disease, and it was this evidence that prompted the original VITAL trial.
The VITAL trial was a randomized, double-blind, placebo-controlled trial in 25,871 U.S. participants, which included men over the age of 50 and women over the age of 55. All participants were free of cancer and cardiovascular disease at the time of enrollment. While the trial found little benefit of vitamin D supplementation for preventing cancer, heart attack, or stroke in the overall cohort, there was a statistical correlation between BMI and cancer incidence, cancer mortality, and autoimmune disease incidence. Other studies suggest similar results for Type 2 diabetes.
“This study sheds light on why we’re seeing 30 to 40 percent reductions in cancer deaths, autoimmune diseases, and other outcomes with vitamin D supplementation among those with lower BMIs but minimal benefit in those with higher BMIs …” JoAnn E. Manson, chief of the Division of Preventive Medicine at the Brigham
The new study aimed to investigate this correlation. The researchers analyzed data from 16,515 participants from the original trial who provided blood samples at baseline (before randomization to vitamin D), as well as 2,742 with a follow-up blood sample taken after two years. The researchers measured the levels of total and free vitamin D, as well as many other novel biomarkers for vitamin D, such as its metabolites, calcium, and parathyroid hormone, which helps the body utilize vitamin D.
“Most studies like this focus on the total vitamin D blood level,” said senior author JoAnn E. Manson, chief of the Division of Preventive Medicine at the Brigham and principal investigator of VITAL. “The fact that we were able to look at this expanded profile of vitamin D metabolites and novel biomarkers gave us unique insights into vitamin D availability and activity, and whether vitamin D metabolism might be disrupted in some people but not in others.”
The researchers found that vitamin D supplementation increased most of the biomarkers associated with vitamin D metabolism in people, regardless of their weight. However, these increases were significantly smaller in people with elevated BMIs.
“We observed striking differences after two years, indicating a blunted response to vitamin D supplementation with higher BMI,” Tobias said. “This may have implications clinically and potentially explain some of the observed differences in the effectiveness of vitamin D supplementation by obesity status.”
“This study sheds light on why we’re seeing 30 to 40 percent reductions in cancer deaths, autoimmune diseases, and other outcomes with vitamin D supplementation among those with lower BMIs but minimal benefit in those with higher BMIs, suggesting it may be possible to achieve benefits across the population with more personalized dosing of vitamin D,” said Manson. “These nuances make it clear that there’s more to the vitamin D story.”
The authors conclude that the VITAL findings are a call to action for the research community to continue exploring the potential benefits of vitamin D supplementation for preventing cancer and other diseases and to take BMI into account when evaluating the supplement’s health impacts.
Disclosures: Co-author Julie Buring reported that her spouse was on the scientific advisory board of Pharmavite, which provided vitamin D and placebo. Additional disclosures can be found in the JAMA Network O pen publication.
Funding: The Vitamin D and Omega-3 Trial was supported by grant RO1ATO11729 from the National Center for Complementary and Integrative Health and, during the intervention phase, was supported by grants U01 CA138962 and R01 CA138962 from the National Cancer Institute; National Heart, Lung, and Blood Institute; Office of Dietary Supplements; National Institute of Neurological Disorders and Stroke; and the National Center for Complementary and Integrative Health. The ancillary studies are supported by grants from multiple institutes, including the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; the National Institute on Aging; the National Institute of Arthritis and Musculoskeletal and Skin Diseases; the National Institute of Mental Health; and others. Pharmavite LLC of Northridge, California (vitamin D) and Pronova BioPharma of Norway and BASF (Omacor fish oil) donated the study agents, matching placebos, and packaging in the form of calendar packs. Quest Diagnostics measured serum 25-hydroxyvitamin D, parathyroid hormone, and other biomarkers at no cost to the study. Dr LeBoff reported grants from National Institute of Arthritis and Musculoskeletal and Skin Diseases RO1 AR070854 and grants from National Institute of Arthritis and Musculoskeletal and Skin Diseases R01 ARO59775.
Share this article
You might like.
New book traces how medical establishment’s sexism, focus on men over centuries continues to endanger women’s health, lives

Sooner than you may think, says researcher who recently won Sjöberg Prize for pioneering work in field
Approach attacks errant proteins at their roots
Harvard announces return to required testing
Leading researchers cite strong evidence that testing expands opportunity
Yes, it’s exciting. Just don’t look at the sun.
Lab, telescope specialist details Harvard eclipse-viewing party, offers safety tips
For all the other Willie Jacks
‘Reservation Dogs’ star Paulina Alexis offers behind-the-scenes glimpse of hit show, details value of Native representation
A monthly newsletter from the National Institutes of Health, part of the U.S. Department of Health and Human Services
Search form
Print this issue
Digging Into Vitamin D
All About the “Sunshine” Vitamin
Getting enough vitamins and minerals is important for your health, and there’s a long list of essential ones. Vitamin D is one you may hear a lot about. It helps your body absorb calcium, a mineral your body needs to build strong bones. Your heart, muscles, and nerves also need vitamin D. Even your immune system The system that protects your body from invading viruses, bacteria, and other microscopic threats. uses vitamin D to fight off germs. But just how much do you need?
“We actually need only small to moderate amounts of vitamin D, not mega-doses,” says Dr. JoAnn Manson, a vitamin D expert at Brigham and Women’s Hospital and Harvard University.
Current guidelines recommend adults get 600 to 800 IUs (international units) of vitamin D each day. Those amounts are very important. Not getting enough can lead to serious health issues. Children’s bones can’t develop properly without enough vitamin D. In adults, a long-term deficiency can lead to fragile bones, or osteoporosis.
It’s important to make sure you get enough vitamin D. But scientists are finding that more isn’t always better.
Where to Get It
You can get vitamin D from the sun and from your diet. Your body makes vitamin D when your skin is exposed to the sun, which gives off UVB light.
But many people don’t go outside enough to get all the vitamin D they need this way. Other factors, such as clothing and sunscreen, can block how much vitamin D your skin makes when you’re in the sun.
How much melanin you have also plays a role. Melanin is a pigment that gives your skin color. Higher melanin levels cause darker skin complexions. The more melanin you have, the less vitamin D you can make from sunlight. This may put you at potential risk for vitamin D deficiency.
Sunlight exposure isn’t the only way to get vitamin D. Vitamin D is found naturally in some foods, like fatty fish. It’s also added to many dairy products and other fortified foods (see the Wise Choices box).
With so many potential sources, most people in the U.S. aren’t at risk for vitamin D deficiency. But getting enough vitamin D from foods can be difficult for some. These can include breastfed infants and people with certain gut problems that limit how nutrients are absorbed.
Older adults can be at risk of vitamin D deficiency, too. “As we age, our ability to make vitamin D in the skin declines,” says Dr. Sarah Booth, a nutrition researcher at Tufts University. Older adults may also be less likely to get outdoors.
Experts don’t recommend screening healthy people for vitamin D. But if you’re in a high-risk group, talk with a health care professional. Vitamin D levels can be measured with a blood test. Vitamin D supplements are sometimes recommended for very low levels.
Is More Better?
Although most people get enough vitamin D to avoid deficiencies, researchers have long wondered if adding extra vitamin D could be good for overall health. Many studies have linked higher levels of vitamin D in the blood with healthier outcomes.
Manson and her team conducted a large clinical trial, called VITAL, to see whether vitamin D supplements could lower risk for some health problems. They compared health outcomes for over 25,000 people in the U.S. Participants were randomly assigned to two groups: half were given vitamin D supplements and half were given a placebo (an inactive pill that looked similar).
After five years, both groups had the same risk for most of the health problems studied. These problems included heart disease, cancer, depression, and bone fractures.
“So, the vast majority of healthy people did not benefit from vitamin D supplements,” Manson says. “But we didn’t find any risk from the 2000 IUs per day that we tested.”
Other studies have also shown that taking moderate doses daily is safe over the long term. “However, at higher doses you’re going to have to start to worry about risks,” Manson warns. The upper daily limit for vitamin D is 4,000 IUs daily. Consuming more can lead to side effects like kidney stones, nausea, vomiting, and muscle weakness.
Too much vitamin D is almost always a result of taking too many supplements. But for people who can’t get enough vitamin D from the sun or their diet, vitamin D dietary supplements in moderation can help prevent a deficiency.
Finding New Uses
Scientists continue to study how vitamin D can help people, since it plays a role in many of the body’s functions.
Manson’s team is following up on their findings in VITAL that suggest taking vitamin D supplements may lower the risk for developing an autoimmune disease A condition in which the body’s disease defense system mistakenly attacks the body’s own cells and tissues. or advanced cancer. They’re also testing whether vitamin D can reduce the risk of COVID-19 infection, severe COVID symptoms, and Long COVID.
Booth and her team recently found that older adults with more vitamin D in their brains had a lower risk of dementia. But the study couldn’t tell whether vitamin D caused the lower risk. Her team is now doing more research to better understand how vitamin D affects brain health.
She thinks the answer is likely to be complicated. “Vitamin D is important,” Booth says. “But there’s no evidence that a single nutrient will slow cognitive Related to the ability to think, learn, and remember. decline or prevent Alzheimer’s disease.”
Another research team, led by Dr. Sushil Jain at Louisiana State University, is investigating the connection between diabetes, vitamin D, and a molecule called glutathione. Glutathione helps the body use vitamin D efficiently.
Black Americans have a relatively high risk of both vitamin D deficiency and diabetes. They’re also more likely to have low levels of glutathione. Jain’s team is testing if boosting both glutathione and vitamin D levels can help prevent diabetes in Black study participants.
For now, most people concerned about vitamin D would get the greatest benefit from living a healthy lifestyle, Manson explains. This includes getting outside, being physically active, not smoking, and eating a variety of healthy foods rich in vitamin D.
“A dietary supplement will never be a substitute for a healthy diet or a healthy lifestyle,” she says.
Related Stories

Sore, Scratchy Throat?

Testing an mRNA Vaccine to Treat Pancreatic Cancer

Living With Gout

COVID-19 Disrupts Gut Microbes
NIH Office of Communications and Public Liaison Building 31, Room 5B52 Bethesda, MD 20892-2094 [email protected] Tel: 301-451-8224
Editor: Harrison Wein, Ph.D. Managing Editor: Tianna Hicklin, Ph.D. Illustrator: Alan Defibaugh
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov .
For wellness toolkits, visit www.nih.gov/wellnesstoolkits .

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- News and Events
- < Back To All News
Vitamin D for heart health: where the benefits begin and end

High-dose supplements don’t help the hearts of most adults any more than modest doses do, but researchers say there’s still more to learn about the value of this essential vitamin
It’s a workhorse nutrient that strengthens bones, supports immune function, helps the heart , and powers the body in many other ways. But recent findings about vitamin D are clear: High doses do not improve heart and circulatory health for most adults any more than modest doses do. “It takes only small-to-moderate amounts of vitamin D to have optimal cardiovascular function,” said JoAnn E. Manson M.D., Dr.P.H., a study author and chief of the division of preventive medicine at Brigham and Women’s Hospital and Harvard Medical School. “More is not better,” she explained. Through ongoing research, Manson has found that adults who take either moderate or high-dose daily vitamin D supplements of at least 1,000 IU haven’t had a reduced risk for having a heart attack, stroke, or cardiovascular-related death compared to adults taking a placebo without vitamin D. This research, which has been supported by the NIH-funded Vitamin D and Omega-3 Trial (VITAL), aligns with recommendations released in June by the U.S. Preventive Services Task Force , which cited insufficient evidence to recommend adults take vitamin D or any other supplement to prevent cardiovascular disease. These findings also add to mounting evidence that vitamin D supplements are not the panacea many thought they were for a host of health problems. VITAL and other randomized trials have found, for example, that higher intakes haven’t prevented cancer, bone fractures, or falls, nor have they alleviated knee pain, cognitive decline, or atrial fibrillation – among other conditions. It is why researchers have begun shifting their focus to other more nuanced questions about the vitamin. For example, why do some people benefit from it more than others? Could supplements benefit specific populations, such as those with increased risks for heart disease? And given that VITAL showed high-dose vitamin D supplements reduced risks for autoimmune conditions, could they also help reduce the severity of COVID-19 ?
Vitamin D: Get enough, but not too much
While researchers sort through these questions, the guidelines that have been in place for years still apply. The National Academy of Medicine recommends a daily intake of 600 IU of vitamin D (mostly from foods) for people ages 1-70 and 800 IU for adults ages 71 and older. However, Manson notes it is reasonable for adults concerned about not getting enough vitamin D to take a daily supplement of 1,000-2,000 IU during the pandemic. She cautions against taking more. Consuming more than 4,000 IU daily, the upper daily limit, is considered mega-dosing and could lead to adverse effects, including high calcium levels in the blood or kidney stones.
So, what’s the best way to get vitamin D?
Getting incidental sun exposure, such as by being physically active outdoors, and eating vitamin D-rich foods , including fatty fish, fortified dairy products and cereals, and certain mushrooms, such as those exposed to ultraviolet light, are good places to start, Manson explained. Reading nutrition labels can also help people assess how much vitamin D they consume through food. After that, supplements can provide a boost for people concerned about getting too little. Or directly exposing the skin to sunlight for 15 minutes a few times each week will get you there, too, Manson said. But when it comes to vitamin D and the prevention of heart disease, Manson said “all you need is to get into that middle range where you’re not deficient.”
Understanding vitamin D and heart health
The idea that higher vitamin D intake could improve heart health emerged years ago when observational studies found people with higher blood levels of vitamin D had lower rates of cardiovascular disease. To see if vitamin D drove this effect or was just a marker of risk, researchers conducted randomized, controlled trials , including VITAL. In 2011-2013, more than 25,000 adults enrolled in VITAL, which found that high-dose vitamin D supplements did not prevent cardiovascular events. And Manson, a study director for VITAL, also conducted a meta-analysis about this topic. After reviewing 21 randomized trials related to vitamin D and cardiovascular disease, she found that “not a single one showed clear benefits of vitamin D supplements in preventing heart disease or stroke.” “In observational research, correlation does not prove causation,” she explained, underscoring the need for randomized, controlled trials. Multiple factors could explain why adults with higher vitamin D levels have been less likely to have cardiovascular disease in observational studies, Manson said. Exercise is one. People who spend more time outdoors engaged in physical activity, which supports heart and vascular health, may have higher vitamin D levels from incidental sun exposure. Diet is another. Fish and other nutrient-dense meals support heart health and tend to be higher in vitamin D. Inflammation is a third, she said. Levels of inflammation can serve as signals of disease. And since vitamin D can bind to a protein that’s more likely to be depleted from inflammation, lower levels may be a marker, as opposed to a causal factor, for chronic conditions like heart disease. However, once adults have sufficient vitamin D levels, the benefits plateau, Manson explained. “You don’t have further cardiovascular disease risk reductions with higher intake or blood levels of vitamin D.”
The future of vitamin D research
Researchers, including those leading VITAL, are now turning their attention to how vitamin D supplements may help people in other ways. Some are looking at how high-dose vitamin D supplements may support immune function in people with autoimmune conditions, including rheumatoid arthritis, lupus, and psoriasis. In this case, the results appear promising. Adults who took a high-dose vitamin D supplement for five years had a 22% reduced risk for having an autoimmune condition. Other researchers, including Manson, are studying if vitamin D can reduce the severity of COVID-19 infections, shorten recovery, and lower the risk of long COVID. Looking at how vitamin D may help people living with type 2 diabetes and cancer are the anchors of other studies. While vitamin D supplementation hasn’t prevented cancer , Manson and other VITAL researchers are studying if higher intake may slow its progression and reduce cancer-related deaths. Alvin A. Chandra, M.D., a VITAL researcher and assistant professor in the division of cardiology at the University of Texas Southwestern Medical Center, is also curious if a parallel relationship exists with vitamin D and heart disease. “There may be subgroups of patients who are at higher risk for adverse cardiovascular outcomes who may benefit from vitamin D supplementation,” he said. This could include people who have had a heart attack, stroke, or heart failure. And if there are benefits, either for vitamin D and/or omega-3 supplements, Chandra said he wants to know what levels would provide a protective effect. VITAL researchers are also studying mechanisms that may influence or indicate how easily vitamin D can be absorbed and used by the body. These variables may help explain why about one in every four to five Americans is at risk for having inadequate levels of vitamin D. Darker skin color can affect skin synthesis of vitamin D from sun exposure, for instance. According to the 2011-2014 National Health and Nutrition Examination Survey , about one in six Black children or adults was at risk for having a vitamin D deficiency compared to one in 13 Asian Americans, one in 17 Hispanics, and one in 40 whites. Aging, allergies, and underlying conditions, including Crohn’s disease and celiac disease, can also impair absorption and have other effects, as can limited sun exposure, dietary restrictions, and extended breastfeeding. How vitamin D interacts with other nutrients, such as magnesium and vitamin K, and impacts its absorption and biological actions are topics of other studies, Manson added. Researchers are also studying genetic links that may explain differences in how the vitamin is metabolized and binds to receptors. The result, she explained, could lead to personalized vitamin D requirements. Particular groups that benefit most from supplementation could also be identified and helped. “This is all part of precision prevention,” she explained.
Resources
- To learn about vitamin D, https://ods.od.nih.gov/factsheets/VitaminD-Consumer .
- To learn about heart health, visit https://www.nhlbi.nih.gov/health/heart-healthy-living .
- To learn about VITAL research, visit https://www.vitalstudy.org/index.html .
Related Health Topics
Related news & features.
- Share full article
Advertisement
Supported by
Study Finds Another Condition That Vitamin D Pills Do Not Help
The vitamin pills do not prevent bone fractures in most people or protect against many other diseases, adding to questions about medical guidance many now take for granted.

By Gina Kolata
The idea made so much sense it was almost unquestioningly accepted: Vitamin D pills can protect bones from fractures. After all, the body needs the vitamin for the gut to absorb calcium, which bones need to grow and stay healthy.
But now, in the first large randomized controlled study in the United States, funded by the federal government, researchers report that vitamin D pills taken with or without calcium have no effect on bone fracture rates. The results, published Thursday in The New England Journal of Medicine , hold for people with osteoporosis and even those whose blood tests deemed them vitamin D deficient.
These results followed other conclusions from the same study that found no support for a long list of purported benefits of vitamin D supplements.
So, for the millions of Americans who take vitamin D supplements and the labs that do more than 10 million vitamin D tests each year, an editorial published along with the paper has some advice: Stop.
“Providers should stop screening for 25-hydroxyvitamin D levels or recommending vitamin D supplements and people should stop taking vitamin D supplements in order to prevent major diseases or extend life,” wrote Dr. Steven R. Cummings, a research scientist at the California Pacific Medical Center Research Institute, and Dr. Clifford Rosen, a senior scientist at the the MaineHealth Institute for Research. Dr. Rosen is an editor at The New England Journal of Medicine.
There are exceptions, they say: People with conditions like celiac or Crohn’s disease need vitamin D supplements, as do those who live in conditions where they are deprived of sunshine and may not eat enough foods that are routinely supplemented with vitamin D, such as cereals and dairy products to help them absorb calcium.
Getting into such a severe vitamin D-deprived state is “very hard to do in the general population,” Dr. Cummings said.
The two scientists know that in making such strong statements they are taking on vitamin sellers, testing labs and advocates who have claimed that taking vitamin D, often in huge amounts, can cure or prevent a wide variety of ailments and even help people live longer.
Doctors often check for vitamin D levels as part of routine blood tests.
The study involved 25,871 participants — men aged 50 and older and women 55 and older — who were assigned to take 2,000 international units of vitamin D each day or a placebo.
The research was part of a comprehensive vitamin D study called VITAL. It was funded by the National Institutes of Health and began after an expert group convened by what is now the National Academy of Medicine, a nonprofit organization, examined the health effects of vitamin D supplements and found little evidence. The expert group’s members were supposed to come up with a minimum daily requirement for the vitamin but found that most clinical trials that had studied the subject were inadequate, making them ask if there was any truth to the claims that vitamin D improved health.
The prevailing opinion at the time was that vitamin D was likely to prevent bone fractures. Researchers thought that as vitamin D levels fell, parathyroid hormone levels would increase at a detriment to bones.
Dr. Rosen said those concerns led him and the other members of the National Academy of Medicine’s expert group to set what he called an “arbitrary value” of 20 nanograms per milliliter of blood as the goal for vitamin D levels and to advise people to get 600 to 800 international units of vitamin D supplements to achieve that goal.
Labs in the United States then arbitrarily set 30 nanograms per milliliter as the cutoff point for normal vitamin D levels, a reading so high that almost everyone in the population would be considered vitamin D deficient.
The presumed relationship between vitamin D and parathyroid levels has not held up in subsequent research, Dr. Rosen said. But uncertainty continued, so the National Institutes of Health funded the VITAL trial to get some solid answers about vitamin D’s relationship to health.
The first part of VITAL, previously published, found that vitamin D did not prevent cancer or cardiovascular disease in trial participants. Nor did it prevent falls , improve cognitive functioning , reduce atrial fibrillation , change body compositio n, reduce migraine frequency , improve stroke outcomes , protect against macular degeneration or reduce knee pain .
Another large study, in Australia, found that people taking the vitamin did not live longer .
Dr. JoAnn Manson, chief of preventive medicine at Brigham and Women’s Hospital in Harvard Medical School and the leader of the main VITAL trial, said the study was so large it included thousands of people with osteoporosis or with vitamin D levels in a range considered low or “insufficient.” That allowed the investigators to determine that they also received no benefit for fracture reduction from the supplement.
“That will surprise many,” Dr. Manson said. “But we seem to need only small-to-moderate amounts of the vitamin for bone health. Larger amounts do not confer greater benefits.”
The bone study’s first author and principal investigator, Dr. Meryl S. LeBoff, an osteoporosis expert at Brigham and Women’s Hospital, said she was surprised. She had expected a benefit.
But she cautioned that the study did not address the question of whether people with osteoporosis or low bone mass just short of the condition should be taking vitamin D and calcium, along with osteoporosis medications. Professional guidelines say they should take vitamin D and calcium, and she will continue to adhere to them in her own practice.
Dr. Dolores Shoback, an osteoporosis expert at the University of California, San Francisco, also will continue to advise patients with osteoporosis and low bone mass to take vitamin D and calcium.
It is “a simple intervention and I will continue to prescribe it,” she said.
Others go a bit further.
Dr. Sundeep Khosla, a professor of medicine and physiology at the Mayo Clinic, said that since vitamin D “will do little or no harm and may have benefits,” he would continue to advise his patients with osteoporosis to take it, recommending the 600 to 800 units a day in the National Academy of Medicine report.
“I will still tell my family and friends who don’t have osteoporosis to take a multivitamin a day to make sure they don’t get vitamin D deficient,” he said.
Dr. Khosla follows that advice himself. Many multivitamin tablets now contain 1,000 units of vitamin D, he added.
But Dr. Cummings and Dr. Rosen remain firm, even questioning the very idea of a vitamin D deficiency for healthy people.
“If vitamin D doesn’t help, what is a vitamin D deficiency?” Dr. Cummings asked. “That implies you should take vitamin D.”
And Dr. Rosen, who signed off on the National Academy of Medicine report, has become a vitamin D therapeutic nihilist.
“I don’t believe any more in 600 units,” he said. “I don’t believe you should do anything.”
Gina Kolata writes about science and medicine. She has twice been a Pulitzer Prize finalist and is the author of six books, including “Mercies in Disguise: A Story of Hope, a Family's Genetic Destiny, and The Science That Saved Them.” More about Gina Kolata
A Guide to Supplements
Surveys suggest that more than half of americans use some kind of supplement. but how effective are all those pills, powders and tinctures.
Several companies are now selling bovine colostrum as a supplement for humans, claiming several health benefits. Here’s what experts say .
Research suggests that a daily multivitamin can improve cognition. But that doesn’t mean everyone should take one .
Proponents of castor oil claim it can improve vision, reduce wrinkles, boost hair growth and more. Can it really do all that ?
Some manufacturers claim that certain supplements can help you focus. Here is what the experts say .
Melatonin tricks your body into feeling like it’s time for bed, but it isn’t a sleeping pill. Here’s how to use it and why it might be tricky for regular users to fall asleep without it .
Can you distinguish the good supplements from the harmful or useless ones? Take our quiz .
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Vitamin D...
Vitamin D supplementation and major cardiovascular events: D-Health randomised controlled trial
- Related content
- Peer review
- Bridie Thompson , research officer 1 ,
- Mary Waterhouse , statistician epidemiologist 1 ,
- Dallas R English , professor 2 ,
- Donald S McLeod , senior research officer 1 ,
- Bruce K Armstrong , professor 3 ,
- Catherine Baxter , project manager 1 ,
- Briony Duarte Romero , research assistant 1 ,
- Peter R Ebeling , professor 4 ,
- Gunter Hartel , head of statistics 5 ,
- Michael G Kimlin , professor 6 ,
- Sabbir T Rahman , research officer 1 ,
- Jolieke C van der Pols , associate professor 7 ,
- Alison J Venn , professor 8 ,
- Penelope M Webb , professor 1 ,
- David C Whiteman , professor 1 ,
- Rachel E Neale , professor 1
- 1 Population Health Program, QIMR Berghofer Medical Research Institute, Herston, Queensland, Australia
- 2 Melbourne School of Population Health, University of Melbourne, Carlton, Victoria, Australia
- 3 School of Public Health, The University of Sydney, Sydney, New South Wales, Australia
- 4 Department of Medicine, School of Clinical Sciences, Monash University, Clayton, Victoria, Australia
- 5 Statistics Unit, QIMR Berghofer Medical Research Institute, Herston, Queensland, Australia
- 6 School of Biomedical Science, Faculty of Health, Queensland University of Technology, Kelvin Grove, Queensland, Australia
- 7 School of Exercise and Nutrition Sciences, Faculty of Health, Queensland University of Technology, Kelvin Grove, Queensland, Australia
- 8 Menzies Institute for Medical Research, University of Tasmania, Hobart, Tasmania, Australia
- Correspondence to: R Neale rachel.neale{at}qimrberghofer.edu.au
- Accepted 18 May 2023
Objective To investigate whether supplementing older adults with monthly doses of vitamin D alters the incidence of major cardiovascular events.
Design Randomised, double blind, placebo controlled trial of monthly vitamin D (the D-Health Trial). Computer generated permuted block randomisation was used to allocate treatments.
Setting Australia from 2014 to 2020.
Participants 21 315 participants aged 60-84 years at enrolment. Exclusion criteria were self-reported hypercalcaemia, hyperparathyroidism, kidney stones, osteomalacia, sarcoidosis, taking >500 IU/day supplemental vitamin D, or unable to give consent because of language or cognitive impairment.
Intervention 60 000 IU/month vitamin D 3 (n=10 662) or placebo (n=10 653) taken orally for up to five years. 16 882 participants completed the intervention period: placebo 8270 (77.6%); vitamin D 8552 (80.2%).
Main outcome measures The main outcome for this analysis was the occurrence of a major cardiovascular event, including myocardial infarction, stroke, and coronary revascularisation, determined through linkage with administrative datasets. Each event was analysed separately as secondary outcomes. Flexible parametric survival models were used to estimate hazard ratios and 95% confidence intervals.
Results 21 302 people were included in the analysis. The median intervention period was five years. 1336 participants experienced a major cardiovascular event (placebo 699 (6.6%); vitamin D 637 (6.0%)). The rate of major cardiovascular events was lower in the vitamin D group than in the placebo group (hazard ratio 0.91, 95% confidence interval 0.81 to 1.01), especially among those who were taking cardiovascular drugs at baseline (0.84, 0.74 to 0.97; P for interaction=0.12), although the P value for interaction was not significant (<0.05). Overall, the difference in standardised cause specific cumulative incidence at five years was −5.8 events per 1000 participants (95% confidence interval −12.2 to 0.5 per 1000 participants), resulting in a number needed to treat to avoid one major cardiovascular event of 172. The rate of myocardial infarction (hazard ratio 0.81, 95% confidence interval 0.67 to 0.98) and coronary revascularisation (0.89, 0.78 to 1.01) was lower in the vitamin D group, but there was no difference in the rate of stroke (0.99, 0.80 to 1.23).
Conclusions Vitamin D supplementation might reduce the incidence of major cardiovascular events, although the absolute risk difference was small and the confidence interval was consistent with a null finding. These findings could prompt further evaluation of the role of vitamin D supplementation, particularly in people taking drugs for prevention or treatment of cardiovascular disease.
Trial registration ACTRN12613000743763
Introduction
Coronary heart disease and stroke are the leading causes of death globally. 1 The risk of these events increases with age, and they are more prevalent in men than women. 2 The number of cardiovascular disease events will probably continue to increase in developed countries as populations age, and in low to middle income countries as non-communicable diseases become dominant. 3 Vitamin D has biological effects which suggest it could influence cardiovascular disease. The vitamin D receptor is expressed in cells throughout the vascular system; many of these also express 1α-hydroxylase, and are therefore able to convert 25-hydroxyvitamin D (25(OH)D) to calcitriol, the active form of vitamin D. Calcitriol reduces inflammation, regulates the renin-angiotensin-aldosterone system, and inhibits proliferation of vascular smooth muscle. 4
Meta-analyses of observational studies have found inverse associations between serum 25(OH)D concentration and risk of cardiovascular disease. 5 6 7 8 9 However, these findings might be due to reverse causality or uncontrolled confounding. Of three Mendelian randomisation studies, which largely overcome these biases, one reported an inverse association between genetically predicted 25(OH)D concentration up to 50 nmol/L and cardiovascular disease. 10 The other studies found no association, but did not allow for nonlinear effects. 11 12 A meta-analysis of randomised controlled trials concluded that vitamin D supplementation does not prevent cardiovascular events. 13 However, 45% of the 83 291 participants included in the meta-analysis were from the Women’s Health Initiative Trial, which was restricted to women, used a low dose of vitamin D, and had relatively low compliance. 14 Cardiovascular disease was the primary outcome of the Vitamin D Assessment (ViDA) study 15 and the Vitamin D and Omega 3 trial (VITAL). 16 Despite different outcome definitions, both randomised controlled trials found that vitamin D supplementation had no effect on cardiovascular disease, 15 16 but VITAL excluded people with a history of cardiovascular disease and the ViDA study had relatively few events.
We launched the D-Health Trial to determine if monthly vitamin D supplementation can improve health outcomes in the older general population. It was a large intermittent dosing trial of vitamin D supplementation (n=21 315). Previous analysis of the D-Health cohort found that vitamin D supplementation did not reduce all cause mortality (the primary outcome of the overall trial) or mortality due to cardiovascular disease, 17 but the effect on the incidence of major cardiovascular events has not been analysed.
For the current study we analysed data from the D-Health Trial to examine whether supplementing Australians aged ≥60 years with monthly doses of 60 000 IU of vitamin D altered the incidence of major cardiovascular events.
Study design, recruitment, and participants
The D-Health Trial was a randomised, double blind, placebo controlled trial with two parallel arms. 18 Between January 2014 and May 2015, randomly selected adults, aged 60-79 years, were invited from all Australian states and territories (except the Northern Territory) using a population register, the Commonwealth Electoral Roll, as the sampling frame (in Australia it is compulsory to register to vote). Volunteers aged 60-84 years were also recruited via media stories and contacts of participants. Exclusion criteria included a history of hypercalcaemia, hyperparathyroidism, kidney stones, osteomalacia, sarcoidosis, or daily intake of >500 IU of supplemental vitamin D. The full trial protocol is available online ( https://dhealth.qimrberghofer.edu.au/page/Publications/ ).
Randomisation and blinding
We used computer generated permuted block randomisation, stratified by age, sex, and state of residence, to randomly allocate participants in a 1:1 ratio to 60 000 IU of vitamin D 3 (cholecalciferol) or placebo tablets, taken as monthly oral doses. Vitamin D 3 and placebo tablets were identical in appearance. Participants, staff, and investigators were blinded to study group allocation during the intervention. Participants were notified of their allocation in March 2020. Staff and investigators remained blinded until the analyses of all cause mortality 17 were finalised. We wrote the statistical code for the current analysis blind to study group using a dataset from which the allocation variable had been removed and participants were randomly assigned to two groups of equal size. After the statistical code for prespecified analyses was finalised, we implemented it on the original dataset.
Intervention
Each year, participants were sent 12 study tablets. We reminded participants to take one tablet at the beginning of each month through text message, email, or automated landline message. The intervention period ended at five years after randomisation, or on 1 February 2020 for the 507 participants randomised after February 2015.
Baseline information
Participants completed a baseline questionnaire in which they reported sociodemographic and lifestyle factors, pre-existing health conditions, and intake of food and supplements containing vitamin D. We calculated body mass index by dividing self-reported weight (kg) by height squared (m 2 ). Serum 25(OH)D concentration was not measured at baseline; rather we developed and internally validated a model to predict deseasonalised baseline serum 25(OH)D concentration using data and serum 25(OH)D measures collected from a random subset of participants in the placebo group during the trial. 19
Adherence and adverse event reporting
Annually, participants were asked to report the number of study tablets taken and their use of any other supplements containing vitamin D not related to the study. We calculated adherence by dividing the number of tablets taken by the number they would have taken had they been fully adherent (60, except for those who died during the trial). We encouraged participants to minimise the use of off-trial vitamin D supplements, but allowed them to remain in the trial provided they took no more than 2000 IU/day. This strategy ensured participants remained below the tolerable upper intake level of 4000 IU, enabled us to capture information about off-trial vitamin D intake, and minimised missing participant reported outcome information.
Each year, we randomly selected approximately 800 participants (stratified by study group, age, sex, state, and month of recruitment) and asked them to provide blood samples for measurement of serum 25(OH)D concentration.
Participants were asked to contact the trial helpline if they experienced any health events; these were coded using the Medical Dictionary for Regulatory Activities. Diagnoses of kidney stones, hypercalcaemia, and hyperthyroidism were also captured in annual surveys.
Determination of major cardiovascular events
Cardiovascular events were a prespecified tertiary outcome of the D-Health Trial. Our published statistical analysis plan included 45 tertiary outcomes. 20 In the statistical analysis plan for the current study, we prespecified that the main outcome for this analysis was first major cardiovascular event, defined as any of myocardial infarction, stroke, or coronary revascularisation. We prespecified the first of myocardial infarction, stroke (total, ischaemic, and haemorrhagic), and coronary revascularisation separately as secondary outcomes.
We used linked hospital admissions data, Medicare Benefits Schedule records, and mortality data to determine major cardiovascular events. Medicare is Australia’s universal health insurance system, and procedures that take place outside public hospitals are recorded in the Medicare Benefits Schedule dataset. Hospital admissions data were available from each state, but not from the Northern Territory or Australian Capital Territory. Admissions to private hospitals were not available from Tasmania or South Australia. Supplementary table 1 shows the principal diagnosis codes (international classification of diseases 10th revision), procedure codes, and Medicare Benefits Schedule item numbers used to determine events. If a death from myocardial infarction or stroke occurred, with no previous hospital admission for these conditions or for coronary revascularisation, the date of major cardiovascular event was considered to be the date of death. Determination of cause of death is described elsewhere. 17
Use of cardiovascular drugs at baseline
The Pharmaceutical Benefits Scheme captures information about prescription drugs dispensed to Australian citizens and permanent residents. We used linked Pharmaceutical Benefits Scheme data to determine use of statins (Anatomical Therapeutic Chemical code C10) and other cardiovascular drugs (codes C01-C09). Use within three months after randomisation indicated baseline use. For people who did not consent to linkage with the Pharmaceutical Benefits Scheme (n=1812), we used self-reported treatment at baseline for hypercholesterolaemia and hypertension; agreement between self-reported drug use and Pharmaceutical Benefits Scheme data was high (supplementary tables 2a and 2b).
Sample size and power
The sample size for the D-Health Trial was chosen to enable 80% power to detect a difference of 9% in the mortality rate with a type 1 error rate of 0.05. 18 We estimated that given the sample size available for this analysis (n=21 302) we would have 80% power to detect a difference of 16% in the incidence of first major cardiovascular event (based on VITAL data 16 from which we estimated that 508 events would be expected in the placebo group). This effect size calculation was performed before starting analyses (before knowing the actual number of events).
Statistical analysis
Analyses followed the intention-to-treat principle and were conducted in SAS version 9.4 (SAS Institute, Cary, North Carolina, USA), R version 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria), and Stata version 17 (Stata Corp, Texas, USA). The D-Health Trial statistical analysis plan has been published previously. 20 The detailed plan for this analysis is available at https://dhealth.qimrberghofer.edu.au/page/Publications/ . Although this is one of several outcomes analysed, we have not adjusted for multiple testing.
For each outcome, follow-up began at randomisation and ended at the earliest of first major cardiovascular event of interest; last known date alive; five years and one month after randomisation; or 31 December 2019 (the date to which hospital data were provided for all states). We used Aalen-Johansen methods to plot the cause specific cumulative incidence of an outcome according to randomisation group. We used flexible parametric survival models to estimate the effect of vitamin D supplementation on outcomes. To estimate an overall hazard ratio, we used a flexible parametric survival model without any time varying coefficients. To allow the hazard ratio to vary with time, we fitted a second flexible parametric survival model that included an interaction between randomisation group and time since randomisation. We used flexible parametric survival models to estimate the difference in cause specific standardised cumulative incidence, treating death without previous major cardiovascular event as a competing risk. All flexible parametric survival models included the randomisation stratification variables of age, sex, and state of residence at baseline. Additional details of the flexible parametric survival models are included in the supplementary methods.
We assessed whether the effect of vitamin D supplementation on major cardiovascular events was modified by the following prespecified baseline characteristics: age (<70, ≥70 years); sex (men, women); body mass index (<25, ≥25); predicted deseasonalised serum 25(OH)D concentration (<50 nmol/L, ≥50 nmol/L) 19 ; statin use; and use of (non-statin) cardiovascular drugs. Participants missing data for a stratifying variable were excluded from the relevant analysis.
In prespecified sensitivity analyses, we excluded people who did not have Pharmaceutical Benefits Scheme data from the subgroup analyses by statin use and cardiovascular drug use (rather than using self-reported use of these drugs). We have not shown the data because this exclusion made no meaningful difference to the results.
In exploratory analyses (performed after the prespecified results were available) we estimated the overall effect of vitamin D supplementation on total major cardiovascular events within subgroups defined according to use of statins and non-statin cardiovascular drugs versus no use of these drugs (as opposed to use or non-use of each of these drug classes separately); and myocardial infarction and coronary revascularisation within stratums defined according to use of statins and cardiovascular drugs at baseline.
Patient and public involvement
The public were not involved in the design or reporting of this study. A participant committee contributed to the design of the participant information sheet, surveys, and newsletters.
Between January 2014 and May 2015 we invited 421 207 people to participate in the D-Health Trial. From 38 928 people who expressed interest and an additional 1896 volunteers, we recruited 21 315 eligible people ( fig 1 ). Five participants subsequently requested that their data be destroyed and eight had incomplete hospital data, leaving 21 302 in this analysis (vitamin D, n=10 658; placebo, n=10 644).

Participant flow for analyses of major cardiovascular events (Consolidated Standards of Reporting Trials—CONSORT flow diagram). *People with self-reported history of hypercalcaemia, kidney stones, hyperarathyroidism, osteomalacia, or sarcoidosis, or those taking >500 IU/day of supplemental vitamin D were ineligible. †Withdrew consent to link to health registers
- Download figure
- Open in new tab
- Download powerpoint
For the trial overall, 16 822 (79%) participants (vitamin D, n=8552 (80%); placebo, n=8270 (78%)) were still taking tablets at the end of five years; 866 people died before they completed the intervention period. The median treatment duration was five years and more than 80% of participants reported taking at least 80% of the study tablets (vitamin D, n=9006 (84%); placebo, n=8783 (82%)). During the intervention, the mean serum 25(OH)D concentration was 77 nmol/L (standard deviation 25) in the placebo group and 115 nmol/L (standard deviation 30) in the vitamin D group. The incidence of adverse events was similar in the two groups. 17
Baseline characteristics of participants included in the current analysis, including use of statins and cardiovascular drugs, were well balanced between groups ( table 1 , supplementary table 3). Fifty four per cent of participants were men and the mean age was 69 years (standard deviation 5). The median follow-up was five years.
Baseline characteristics according to randomisation group
- View inline
Major cardiovascular events
There were 1336 major cardiovascular events during follow-up (vitamin D, n=637 (6.0%); placebo, n=699 (6.6%)). Compared with the placebo group, the rate of major cardiovascular events was lower in the vitamin D group (hazard ratio 0.91, 95% confidence interval 0.81 to 1.01), although the upper bound of the confidence interval is consistent with there being no effect ( fig 2 , table 2 ). The hazard ratio did not change with time (supplementary fig 1, supplementary table 4). The difference in the standardised cause specific cumulative incidence at five years was −5.8 events per 1000 participants (95% confidence interval −12.2 to 0.5 per 1000 participants), resulting in a number needed to treat to avoid one major cardiovascular event of 172.

Cause specific cumulative incidence of major cardiovascular events according to randomisation group and time since randomisation. Curves estimated using Aalen-Johansen methods, treating death without previous major cardiovascular event as a competing risk. Hazard ratio (vitamin D v placebo) was estimated using a flexible parametric survival model that included randomisation group, age, sex, and state of residence at baseline. 95% CI=95% confidence interval; MACE=major cardiovascular event
Hazard ratios for vitamin D in relation to major cardiovascular events
No effect modification was found according to baseline age, sex, or body mass index ( fig 3 , supplementary figs 2-7). The hazard ratio was lower in people with predicted baseline 25(OH)D concentration ≥50 nmol/L than in those with predicted baseline 25(OH)D <50 nmol/L (hazard ratio 0.87, 95% confidence interval 0.76 to 0.98 v 1.04, 0.84 to 1.27; P for interaction=0.14; fig 3 , supplementary figs 8 and 9). The hazard ratio was also lower in people using statins at baseline versus those who were not (0.83, 0.71 to 0.97 v 0.98, 0.84 to 1.13; P for interaction=0.14), and in those who were using cardiovascular drugs at baseline versus those who were not (0.84, 0.74 to 0.97 v 1.01, 0.84 to 1.20; P for interaction=0.12; fig 3 , supplementary figs 10-13). In exploratory analyses within subgroups defined according to use of statins or cardiovascular drugs at baseline versus no use, similar patterns were observed (supplementary table 5). In an exploratory analysis requested by reviewers, we performed analyses within subgroups defined by self-report of a major cardiovascular event before baseline. In contrast to the above findings, the effect was stronger in people who did not report a history of major cardiovascular event (0.89, 0.78 to 1.01) versus those who did report an event (0.95, 0.79 to 1.15; supplementary table 5). However, the confidence interval for those reporting an event was wide and the P value for interaction high (0.53).

Effect of vitamin D supplementation on incidence of major cardiovascular events for all participants and by selected baseline characteristics. Hazard ratios (vitamin D v placebo) were estimated using flexible parametric survival models. All models included randomisation group, age, sex, and state of residence at baseline. Models producing estimates by levels of age, sex, body mass index, predicted 25-hydroxyvitamin D (25(OH)D) concentration, use of statins, and use of (non-statin) cardiovascular drugs include the characteristic of interest and an interaction between randomisation group and the characteristic of interest. P value for interaction is from a likelihood ratio test comparing models with and without the interaction term. 95% CI=95% confidence interval
Specific cardiovascular events
The cumulative incidence and hazard of myocardial infarction were lower in the vitamin D group (hazard ratio 0.81; 95% confidence interval 0.67 to 0.98; table 2 , supplementary figs 14 and 15). The same was true of coronary revascularisation, although the confidence interval for the hazard ratio included the null (0.89, 0.78 to 1.01; table 2 , supplementary figs 16 and 17). There was no interaction with elapsed time for these outcomes (supplementary figs 15 and 17). The intervention had no apparent effect on stroke (0.99, 0.80 to 1.23; table 2 , supplementary fig 18-23). In exploratory analyses of myocardial infarction and coronary revascularisation, we did not find evidence of interactions with baseline statin and other cardiovascular drug use (supplementary table 6).
Principal findings
In this analysis of data from the D-Health Trial we found some evidence that supplementation with 60 000 IU of vitamin D 3 per month for up to five years reduced the incidence of major cardiovascular events, particularly myocardial infarction and coronary revascularisation. The absolute differences were small, and the confidence intervals for total major cardiovascular events and coronary revascularisation were consistent with null findings. For total major cardiovascular events, there was some indication of a stronger effect in those who were using statins or other cardiovascular drugs at baseline, or who had higher predicted vitamin D status, although the interaction terms were not statistically significant. We found no evidence of interaction with age, sex, or body mass index.
Strengths and limitations
The D-Health Trial has several strengths. Over 21 000 people were recruited from the general population and supplemented for five years, with extremely high retention and adherence. 17 Determination of cardiovascular events and mortality outcomes was achieved through comprehensive data linkage to population based administrative data sources. The lack of private hospital data for South Australia and Tasmania would have resulted in a small underestimate of events. However, the underestimation would have been low because only a quarter of participants came from these states, we captured public hospital data, and procedures were able to be identified through Medicare Benefits Schedule data. Importantly, any underestimate would probably not have differed between the study groups.
Comparison with other studies
A meta-analysis of randomised controlled trials, including the VITAL and ViDA studies that had major cardiovascular events or cardiovascular disease as the primary outcome, concluded that vitamin D supplementation does not prevent cardiovascular events. 13 VITAL did not observe a protective effect for overall major cardiovascular events (including myocardial infarction, stroke, death from cardiovascular causes, and coronary revascularisation; hazard ratios ranged from 0.95 to 0.96). 16 Similarly, the ViDA study concluded that vitamin D supplementation was not protective against total cardiovascular disease (hazard ratio 1.02, 95% confidence interval 0.87 to 1.20) or stroke (0.95, 0.55 to 1.62). 15 The hazard ratio for myocardial infarction was similar to the D-Health Trial findings, although the confidence interval was wide (0.90, 0.54 to 1.50). The D-Health Trial has multiple outcomes, increasing the likelihood of chance findings. However, if the effect on myocardial infarction observed in the D-Health Trial is a true effect, and not due to chance, the reasons for the lack of consistency across studies are unclear. The discrepancy with VITAL might partly be caused by differences in study design and adherence. For example, VITAL excluded people with a history of cardiovascular disease (other than hypertension), and the cohort was more racially diverse. Whereas we used linked data to capture major cardiovascular events, VITAL captured events through participant report in annual surveys, followed by verification of reported events. Differential reporting between study groups might have masked any protective effect of vitamin D. Further, unlike D-Health and ViDA, VITAL used a daily dosing regimen of 2000 IU/day. While evidence is emerging to suggest that daily dosing is of greater benefit for health outcomes such as cancer mortality and infection, the monthly dosing regimen might have led to higher adherence in D-Health than in VITAL; in D-Health 80% of participants reported taking approximately 80% of study tablets, whereas in VITAL around 80% reported taking two thirds of study tablets. 16
We did not observe a protective effect of vitamin D on stroke. However, the number of stroke events was relatively low, particularly when haemorrhagic stroke, which has different pathophysiology, was excluded; therefore, the confidence intervals were wide and consistent with benefit or harm. Moreover, there are several examples where associations with myocardial infarction and stroke differ, 21 22 23 so this finding is not entirely unexpected.
In prespecified subgroup analyses, we observed an effect of vitamin D on major cardiovascular events in people who were taking statins or cardiovascular drugs at baseline, but not in those who were not taking these drugs. The interactions were not significant at P<0.05, and it is plausible that these are chance findings. Nevertheless, given the lower power to detect interactions compared with main effects, and the observed strong protective effect in those taking these drugs, these interactions are of interest. There was high concurrent use of statins and other cardiovascular drugs (supplementary table 7), and the interaction could reflect an effect in people who are already at high risk of experiencing a cardiovascular event, rather than a synergistic effect between vitamin D and a particular drug. However, the exploratory analysis by self-reported history of major cardiovascular events was inconsistent with this hypothesis, and it is plausible that there is an interaction between vitamin D and the drugs examined. For example, a number of commonly used statins depend on the enzyme CYP3A4 for activation, and the CYP3A4 gene is responsive to calcitriol, suggesting that vitamin D might alter the effect of statin use. 24 Further investigation of these potential interactions is warranted.
Although we observed a protective effect for vitamin D on major cardiovascular events among people predicted to be vitamin D sufficient at baseline, but not on those predicted to be insufficient, this finding needs to be interpreted with caution because we used predicted rather than measured vitamin D status. Because of the relatively low positive predictive value of the model (0.23), a considerable proportion of those predicted to be in the low group will have been vitamin D replete. While it is plausible that vitamin D supplementation becomes protective at higher serum 25(OH)D concentrations, we found that the 25(OH)D concentration attained in the vitamin D group was only slightly higher in those with predicted deseasonalised baseline serum 25(OH)D concentration ≥50 nmol/L than in those predicted to be deficient (supplementary fig 24).
Generalisability of findings
We need to consider whether the D-Health findings are generalisable to the broader population. A direct comparison with Australian rates of myocardial infarction or major cardiovascular events is not possible because national statistics report myocardial infarction and angina as a single entity. The incidence rates for stroke were a little lower in the D-Health Trial cohort (Australia: 360/100 000 v D-Health: 302/100 000 person years), 2 probably reflecting the better overall health of D-Health participants, who were less likely to report having poor overall health, and less likely to be current smokers. 25 D-Health participants were also less likely to be statin users (35% v 44%), 26 suggesting that if our findings of a more marked effect in statin users at baseline is real, a greater effect might be expected in the Australian population.
The mean 25(OH)D concentration of the D-Health placebo participants throughout the trial, probably indicative of baseline concentration in the cohort, was 76 nmol/L, and the proportion with 25(OH)D <50 nmol/L was 13%. 17 These figures are reasonably representative of the Australian population; in 2011-12 the mean serum 25(OH)D concentration was 69 nmol/L and 16% of people aged ≥65 years had 25(OH)D concentration <50 nmol/L. 27 However, the findings cannot be generalised to populations with a greater prevalence of vitamin D deficiency.
Conclusions
In conclusion, these findings indicate that vitamin D supplementation might reduce the incidence of major cardiovascular events, particularly myocardial infarction and coronary revascularisation. This protective effect could be more marked in those taking statins or other cardiovascular drugs at baseline. Subgroup analyses in other large trials might help to clarify this issue. In the meantime, these findings suggest that conclusions that vitamin D supplementation does not alter risk of cardiovascular disease are premature.

What is already known on this topic
Observational studies have consistently shown inverse associations between 25-hydroxy vitamin D concentration and cardiovascular disease
Randomised controlled trials have not shown that vitamin D supplementation reduces the incidence of major cardiovascular events, although most trials were not adequately powered to investigate this issue
What this study adds
Vitamin D supplementation might reduce the risk of major cardiovascular events, although the absolute risk difference was small and the confidence interval was consistent with a null finding
Further evaluation is warranted, particularly in people taking statins or other cardiovascular disease drugs
Ethics statements
Ethical approval.
The D-Health Trial was approved by the QIMR Berghofer Medical Research Institute Human Research Ethics Committee and was monitored by an external data and safety monitoring board. The following committees additionally approved the data linkage components: ACT Health Human Research Ethics Committee, NSW Population and Health Services Research Ethics Committee, Department of Health WA Human Research Ethics Committee. All participants provided informed consent (electronic or written).
Data availability statement
Anonymised data can be made available upon reasonable request, with appropriate human research ethics approvals and data transfer agreements in place. Data provided by external registers will not be made available, but derived variables can be shared.
Acknowledgments
We acknowledge the D-Health Trial staff and members of the Data and Safety Monitoring Board (Patricia Valery, Ie-Wen Sim, Kerrie Sanders); Services Australia for supplying Medicare Benefits Schedule data and Pharmaceutical Benefits Scheme data; D-Health Trial participants who took part in this research; The State and Territory health departments (Western Australia, Victoria, South Australia & Northern Territory, New South Wales, Queensland, and Tasmania) for the provision of inpatient hospital data, the State Registries of Births, Deaths and Marriages for death data and State and Territory Data Linkage Units for undertaking linkage of these datasets; Victorian Department of Justice and National Coronial Investigation System as joint custodians of the Cause of Death Unit Record File which was used to identify participants who had died of a major cardiovascular event.
Contributors: BT and MW are joint first authors of this paper. BT, MW, and REN drafted the paper. REN, DCW, DRE, PMW, DSM, PRE, BKA, and AJV obtained funding and provided oversight. BT, MW, and STR performed analyses. REN, DCW, DRE, PMW, DSM, MGK, JvdP, BKA, and AJV participated in trial conception and development of research methods. All authors provided final approval of the version to be published. REN is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: The D-Health Trial is funded by National Health and Medical Research Council (NHMRC) project grants (GNT1046681, GNT1120682). REN, PMW, DCW, and PRE are/were supported by fellowships from the NHMRC (GNT1060183, GNT1173346, GNT1155413, GNT1197958). DSM is supported by a Metro North Clinician Research Fellowship and a Queensland Advancing Clinical Research Fellowship. The vitamin D assays were performed at the University of Western Australia, supported by infrastructure funding from the Western Australian State Government in partnership with the Australian Federal Government, through Bioplatforms Australia and the National Collaborative Research Infrastructure Strategy. The funding sources played no role in the conduct or reporting of the D-Health Trial or in the decision to submit the manuscript for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from National Health and Medical Research Council, Metro North, Queensland Health, University of Western Australia, Western Australian State Government, Australian Federal Government, Bioplatforms Australia, National Collaborative Research Infrastructure Strategy for the submitted work. PMW has funding from AstraZeneca for an unrelated study of ovarian cancer; PRE reports grants and other from Amgen, grants from Sanofi, and grants from Alexion; REN has funding from Viatris for an unrelated study of pancreatic cancer. All other authors declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
The lead author (the manuscript’s guarantor) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Findings from this study will be disseminated to the trial participants through a plain language summary included in the trial newsletter. Following the embargo, the results will be publicised through mainstream media, and the social media platforms of the institute through which the trial was conducted. The work will be presented at specialist clinical meetings and conferences.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ World Health Organization. The top 10 causes of death. Geneva: World Health Organization, 2020. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death .
- ↵ Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. Canberra: AIHW, 2023. https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/all-heart-stroke-and-vascular-disease .
- ↵ World Health Organization. Noncommunicable diseases country profiles 2018. Geneva: WHO, 2018. https://www.who.int/publications/i/item/9789241514620 .
- von Essen MR ,
- Gholami F ,
- Manson JE ,
- Elamin MB ,
- Abu Elnour NO ,
- Elamin KB ,
- Kariuki M ,
- Selvanayagam JB ,
- Timofeeva MN ,
- China Kadoorie Biobank Collaborative Group
- Barbarawi M ,
- Jackson RD ,
- LaCroix AZ ,
- Women’s Health Initiative Investigators
- Stewart AW ,
- VITAL Research Group
- Duarte Romero B ,
- Armstrong BK ,
- Waterhouse M ,
- English DR ,
- Borges MC ,
- Schmidt AF ,
- Jefferis B ,
- UCLEB Consortium**
- Colantonio LD ,
- Bittner V ,
- Safford MM ,
- ↵ Australian Institue of Health and Welfare. Older Australians. Canberra: AIHW, 2021. https://www.aihw.gov.au/reports/older-people/older-australians .
- Ofori-Asenso R ,
- Ilomäki J ,
- Curtis AJ ,
- Zoungas S ,
- Malacova E ,
- Cheang PR ,
Scientists Reveal New Findings About Older Adults Who Take Vitamin D
Research suggests that supplementing with vitamin D may reduce the risk of heart attacks and other cardiovascular events.

We've been independently researching and testing products for over 120 years. If you buy through our links, we may earn a commission. Learn more about our review process.
- Vitamin D is widely known for its role in supporting immunity and bone health.
- New research suggests that supplementing with vitamin D may reduce the risk of heart attacks and other cardiovascular events.
Vitamin D is a unique nutrient in that it comes from the food we eat and is a hormone that our bodies make. The fat soluble vitamin has a slew of important functions and vitamin D health benefits , from supporting immunity and healthy bones to improving mood. But new research shows that it may have other protective benefits for older adults.
A recent study published in the British Medical Journal , looked at a large sample of older adults ages 60 to 84. Participants were divided into two groups – one was given a placebo, while the other was given a vitamin D supplement of 60,000 IU a month (which averages out to about 2,000 IU a day) for up to five years. At the end of the study, data was analyzed from over 16,800 participants who were still taking the tablets.
During the trial, there were about 1,336 major cardiovascular events (i.e. heart attack, stroke and procedures to treat coronary artery disease). But compared with the placebo group, the rate of major heart problems was slightly lower in the vitamin D group, especially for those who were already taking heart medicines like statins at the beginning of the study.
Although the results are compelling, the findings were not statistically significant and prior research has shown no association with vitamin D supplementation and major heart problems. Ultimately, the best strategies to support heart health and reduce risk of heart disease include eating a healthy balanced diet , staying physically active , quitting smoking, reducing alcohol consumption, keeping blood pressure under control and checking your cholesterol levels. It's also important to take your medicines as directed and attend regular check-ups with your health care team.
GHI Top Vitamin D Picks

MegaFood Vitamin D3
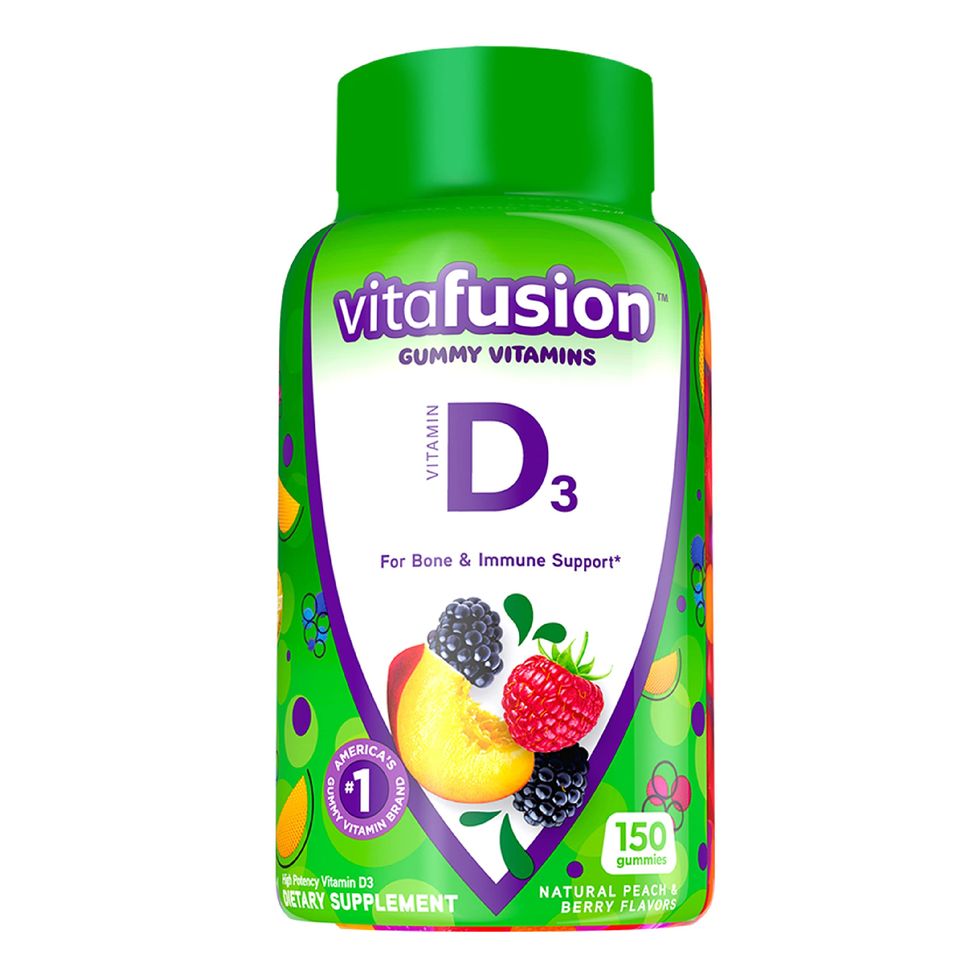
Vitafusion Vitamin D3

NOW Vitamin D-3
But that doesn't mean that vitamin D isn't important for heart health. In fact, vitamin D is needed to support blood vessels and normal blood pressure. What's more, a vitamin D deficiency has been associated with elevated levels of lipids (a.k.a fats) in your blood, as well as vascular dysfunction and arterial stiffening. Research has also linked a lower vitamin D status to an increased risk of ischemic stroke , heart attack and heart disease .
How much vitamin D do I need?
Older adults need about 600 – 800 IU of vitamin D daily, depending on their age. You can get this through a combination of sun exposure and vitamin-D rich foods , which include salmon, eggs, sardines, liver, white mushrooms and fortified foods.
But supplementing with more isn't always better. Since vitamin D is a fat-soluble vitamin, too much can put you at serious risk for toxicity including adverse side effects like kidney stones and high calcium levels in the blood. Our experts say that it is best not to consume more than 4,000 IU daily, which is the tolerable upper intake level.
Signs of vitamin D deficiency
We recommend speaking with your healthcare provider if you suspect a vitamin D deficiency, as they can take bloodwork and then recommend the appropriate supplementation dosage based on your current levels. Some common signs of vitamin D deficiency include:
- Mood changes
- Muscle pain and weakness
- Reduced immune function
- Increased inflammation
- Frequent infections
- Rickets (in children)
- Bone disorders
What should I look for in a vitamin D supplement?
Since the U.S. Food and Drug Administration (FDA) does not approve dietary supplements for safety and effectiveness prior to going to market, it's incredibly important to thoroughly research each supplement you add to your regimen and speak with your healthcare provider before doing so. Look for options that have been tested for purity, potency and safety by a credible third-party organization.
Our team of registered dietitians spent months analyzing dozens of vitamin D supplements to bring you our top-tested recommendations for the best vitamin D supplements on the market.
The bottom line: New research suggests that supplementing with vitamin D may reduce the risk of heart attacks, but the results were not statistically significant and more research is needed. That being said, vitamin D does play a role in supporting a healthy heart, blood vessels and normal blood pressure. If you suspect a deficiency, speak with your healthcare provider who can take bloodwork and determine the appropriate supplement dose for you. The best strategies to support heart health include eating a healthy balanced diet, staying physically active, quitting smoking, reducing alcohol consumption and keeping blood pressure under control.
Stefani (she/her) is a registered dietitian, a NASM-certified personal trainer and the director of the Good Housekeeping Institute Nutrition Lab, where she handles all nutrition-related content, testing and evaluation. She holds a bachelor’s degree in nutritional sciences from Pennsylvania State University and a master’s degree in clinical nutrition from NYU. She is also Good Housekeeping’s on-staff fitness and exercise expert. Stefani is dedicated to providing readers with evidence-based content to encourage informed food choices and healthy living. She is an avid CrossFitter and a passionate home cook who loves spending time with her big fit Greek family.

@media(max-width: 64rem){.css-o9j0dn:before{margin-bottom:0.5rem;margin-right:0.625rem;color:#ffffff;width:1.25rem;bottom:-0.2rem;height:1.25rem;content:'_';display:inline-block;position:relative;line-height:1;background-repeat:no-repeat;}.loaded .css-o9j0dn:before{background-image:url(/_assets/design-tokens/goodhousekeeping/static/images/Clover.5c7a1a0.svg);}}@media(min-width: 48rem){.loaded .css-o9j0dn:before{background-image:url(/_assets/design-tokens/goodhousekeeping/static/images/Clover.5c7a1a0.svg);}} Diet & Nutrition

The 101 on High-Protein Vegetables

If You Have High Cholesterol, Try This Supplement

Our Guide to the Healthiest Starbucks Drinks

Is Oat Milk Really a Scam? Not Exactly

13 Foods That'll Help You Sleep Through the Night

4 Health-Focused Smoothies To Brighten Your Day

What to Eat for Healthy Hair

The Best Multivitamins for Women

Good Housekeeping Dietary Supplements Methodology

Top Health Benefits of Coconut Water

Get Cooking With Celebrity Chef Jason Roberts

Vitamin D is both a nutrient we eat and a hormone our bodies make. It is a fat-soluble vitamin that has long been known to help the body absorb and retain calcium and phosphorus ; both are critical for building bone. Also, laboratory studies show that vitamin D can reduce cancer cell growth, help control infections and reduce inflammation. Many of the body’s organs and tissues have receptors for vitamin D, which suggest important roles beyond bone health, and scientists are actively investigating other possible functions.
Few foods naturally contain vitamin D, though some foods are fortified with the vitamin. For most people, the best way to get enough vitamin D is taking a supplement because it is hard to eat enough through food. Vitamin D supplements are available in two forms: vitamin D2 (“ergocalciferol” or pre-vitamin D) and vitamin D3 (“cholecalciferol”). Both are also naturally occurring forms that are produced in the presence of the sun’s ultraviolet-B (UVB) rays, hence its nickname, “the sunshine vitamin,” but D2 is produced in plants and fungi and D3 in animals, including humans. Vitamin D production in the skin is the primary natural source of vitamin D, but many people have insufficient levels because they live in places where sunlight is limited in winter, or because they have limited sun exposure due to being inside much of the time. Also, people with darker skin tend to have lower blood levels of vitamin D because the pigment (melanin) acts like a shade, reducing production of vitamin D (and also reducing damaging effects of sunlight on skin, including skin cancer).
Recommended Amounts
The Recommended Dietary Allowance for vitamin D provides the daily amount needed to maintain healthy bones and normal calcium metabolism in healthy people. It assumes minimal sun exposure.
RDA: The Recommended Dietary Allowance for adults 19 years and older is 600 IU (15 mcg) daily for men and women, and for adults >70 years it is 800 IU (20 mcg) daily.
UL: The Tolerable Upper Intake Level is the maximum daily intake unlikely to cause harmful effects on health. The UL for vitamin D for adults and children ages 9+ is 4,000 IU (100 mcg).
Many people may not be meeting the minimum requirement for the vitamin. NHANES data found that the median intake of vitamin D from food and supplements in women ages 51 to 71 years was 308 IU daily, but only 140 IU from food alone (including fortified products). [1] Worldwide, an estimated 1 billion people have inadequate levels of vitamin D in their blood, and deficiencies can be found in all ethnicities and age groups. [2-4] In the U.S., about 20% of White adults and 75% of Black adults have blood levels of vitamin D below 50 nmol/L. [83] In industrialized countries, doctors are seeing the resurgence of rickets, the bone-weakening disease that had been largely eradicated through vitamin D fortification. [5-7] There is scientific debate about how much vitamin D people need each day and what the optimal serum levels should be to prevent disease. The Institute of Medicine (IOM) released in November 2010 recommendations increasing the daily vitamin D intake for children and adults in the U.S. and Canada, to 600 IU per day. [1] The report also increased the upper limit from 2,000 to 4,000 IU per day. Although some groups such as The Endocrine Society recommend 1,500 to 2,000 IU daily to reach adequate serum levels of vitamin D, the IOM felt there was not enough evidence to establish a cause and effect link with vitamin D and health benefits other than for bone health. Since that time, new evidence has supported other benefits of consuming an adequate amount of vitamin D, although there is still not consensus on the amount considered to be adequate.
Vitamin D and Health
The role of vitamin D in disease prevention is a popular area of research, but clear answers about the benefit of taking amounts beyond the RDA are not conclusive. Although observational studies see a strong connection with lower rates of certain diseases in populations that live in sunnier climates or have higher serum levels of vitamin D, clinical trials that give people vitamin D supplements to affect a particular disease are still inconclusive. This may be due to different study designs, differences in the absorption rates of vitamin D in different populations, and different dosages given to participants. Learn more about the research on vitamin D and specific health conditions and diseases:
Several studies link low vitamin D blood levels with an increased risk of fractures in older adults. Some studies suggest that vitamin D supplementation in certain amounts may prevent such fractures, while others do not. [8-11]
- A meta-analysis of 12 randomized controlled trials that included more than 42,000 people 65+ years of age, most of them women, looked at vitamin D supplementation with or without calcium, and with calcium or a placebo. Researchers found that higher intakes of vitamin D supplements—about 500-800 IU per day—reduced hip and non-spine fractures by about 20%, while lower intakes (400 IU or less) failed to offer any fracture prevention benefit. [12]
- A systematic review looked at the effect of vitamin D supplements taken with or without calcium on the prevention of hip fractures (primary outcome) and fractures of any type (secondary outcome) in older men and postmenopausal women 65+ years of age. It included 53 clinical trials with 91,791 participants who lived independently or in a nursing home or hospital. It did not find a strong association between vitamin D supplements alone and prevention of fractures of any type. However, it did find a small protective effect from all types of fractures when vitamin D was taken with calcium. All of the trials used vitamin D supplements containing 800 IU or less. [13]
- The VITamin D and OmegA-3 TriaL (VITAL) double-blind placebo-controlled randomized trial of 25,871 women and men, 55+ years and 50+ years of age, respectively, did not find a protective effect from vitamin D supplements on bone fractures. [81] The participants were healthy at the start of the study—representative of the general population and not selected based on low bone mass, osteoporosis, or vitamin D deficiency—and were given either 2,000 IU of vitamin D or a placebo taken daily for about five years. Vitamin D did not lower the incidence of total bone fractures or fractures of the hip or spine.
Vitamin D may help increase muscle strength by preserving muscle fibers, which in turn helps to prevent falls, a common problem that leads to substantial disability and death in older people. [14–16] A combined analysis of multiple studies found that taking 700 to 1,000 IU of vitamin D per day lowered the risk of falls by 19%, but taking 200 to 600 IU per day did not offer any such protection. [17] However, the VITAL trial following healthy middle-aged men and women did not find that taking 2,000 IU of vitamin D daily compared with a placebo pill reduced the risk of falls. [82]
Though taking up to 800 IU of vitamin D daily may benefit bone health in some older adults, it is important to be cautious of very high dosage supplements. A clinical trial that gave women 70+ years of age a once-yearly dosage of vitamin D at 500,000 IU for five years caused a 15% increased risk of falls and a 26% higher fracture risk than women who received a placebo. [18] It was speculated that super-saturating the body with a very high dose given infrequently may have actually promoted lower blood levels of the active form of vitamin D that might not have occurred with smaller, more frequent doses. [13]
JoAnn Manson, MD, DrPH , leader of the main VITAL trial and coauthor of the report on fracture, commented:
“We conclude that, in the generally healthy U.S. population of midlife and older adults, vitamin D supplementation doesn’t reduce the risk of fractures or falls. This suggests that only small-to-moderate amounts of vitamin D are needed for bone health and fall prevention, achieved by most community-dwelling adults. Of course, vitamin D deficiency should always be treated and some high-risk patients with malabsorption syndromes, osteoporosis, or taking medications that interfere with vitamin D metabolism will benefit from supplementation.”
Nearly 30 years ago, researchers noticed an intriguing relationship between colon cancer deaths and geographic location: People who lived at higher latitudes, such as in the northern U.S., had higher rates of death from colon cancer than people who lived closer to the equator. [19] Many scientific hypotheses about vitamin D and disease stem from studies that have compared solar radiation and disease rates in different countries. These studies can be a good starting point for other research but don’t provide the most definitive information. The sun’s UVB rays are weaker at higher latitudes, and in turn, people’s vitamin D blood levels in these locales tend to be lower. This led to the hypothesis that low vitamin D levels might somehow increase colon cancer risk. [3]
Animal and laboratory studies have found that vitamin D can inhibit the development of tumors and slow the growth of existing tumors including those from the breast, ovary, colon, prostate, and brain. In humans, epidemiological studies show that higher serum levels of vitamin D are associated with substantially lower rates of colon, pancreatic, prostate, and other cancers , with the evidence strongest for colorectal cancer. [20-32]
However, clinical trials have not found a consistent association:
The Women’s Health Initiative trial, which followed roughly 36,000 women for an average of seven years, failed to find any reduction in colon or breast cancer risk in women who received daily supplements of 400 IU of vitamin D and 1,000 mg of calcium, compared with those who received a placebo. [33,34] Limitations of the study were suggested: 1) the relatively low dose of vitamin D given, 2) some people in the placebo group decided on their own to take extra calcium and vitamin D supplements, minimizing the differences between the placebo group and the supplement group, and 3) about one-third of the women assigned to vitamin D did not take their supplements. 4) seven years may be too short to expect a reduction in cancer risk. [35,36]
A large clinical trial called the VITamin D and OmegA-3 TriaL (VITAL) followed 25,871 men and women 50+ years of age free of any cancers at the start of the study who took either a 2,000 IU vitamin D supplement or placebo daily for a median of five years. [37] The findings did not show significantly different rates of breast, prostate, and colorectal cancer between the vitamin D and placebo groups. The authors noted that a longer follow-up period would be necessary to better assess potential effects of supplementation, as many cancers take at least 5-10 years to develop.
Although vitamin D does not seem to be a major factor in reducing cancer incidence, evidence including that from randomized trials suggests that having higher vitamin D status may improve survival if one develops cancer. In the VITAL trial, a lower death rate from cancer was observed in those assigned to take vitamin D, and this benefit seemed to increase over time since starting on vitamin D. A meta-analysis of randomized trials of vitamin D, which included the VITAL study, found a 13% statistically significant lower risk of cancer mortality in those assigned to vitamin D compared to placebo. [38] These findings are consistent with observational data, which suggest that vitamin D may have a stronger effect on cancer progression than for incidence.
The heart is basically a large muscle, and like skeletal muscle, it has receptors for vitamin D. [39] Immune and inflammatory cells that play a role in cardiovascular disease conditions like atherosclerosis are regulated by vitamin D. [40] The vitamin also helps to keep arteries flexible and relaxed, which in turn helps to control high blood pressure. [41]
In the Health Professionals Follow-up Study nearly 50,000 healthy men were followed for 10 years. [42] Those who had the lowest levels of vitamin D were twice as likely to have a heart attack as men who had the highest levels. Meta-analyses of epidemiological studies have found that people with the lowest serum levels of vitamin D had a significantly increased risk of strokes and any heart disease event compared with those with the highest levels. [40;43-46]
However, taking vitamin D supplements has not been found to reduce cardiovascular risk. A meta-analysis of 51 clinical trials did not demonstrate that vitamin D supplementation lowered the risk of heart attack, stroke, or deaths from cardiovascular disease. [47] The VITamin D and OmegA-3 TriaL (VITAL) came to the same conclusion; it followed 25,871 men and women free of cardiovascular disease who took either a 2,000 IU vitamin D supplement or placebo daily for a median of five years. No association was found between taking the supplements and a lower risk of major cardiovascular events (heart attack, stroke, or death from cardiovascular causes) compared with the placebo. [37]
Vitamin D deficiency may negatively affect the biochemical pathways that lead to the development of Type 2 diabetes (T2DM), including impairment of beta cell function in the pancreas, insulin resistance, and inflammation. Prospective observational studies have shown that higher vitamin D blood levels are associated with lower rates of T2DM. [48]
More than 83,000 women without diabetes at baseline were followed in the Nurses’ Health Study for the development of T2DM. Vitamin D and calcium intakes from diet and supplements were assessed throughout the 20-year study. [49] The authors found that when comparing the women with the highest intakes of vitamin D from supplements with women with the lowest intakes, there was a 13% lower risk of developing T2DM. The effect was even stronger when vitamin D was combined with calcium: there was a 33% lower risk of T2DM in women when comparing the highest intakes of calcium and vitamin D from supplements (>1,200 mg, >800 IU daily) with the lowest intakes (<600 mg, 400 IU).
A randomized clinical trial gave 2,423 adults who had prediabetes either 4000 IU of vitamin D or a placebo daily for two years. The majority of participants did not have vitamin D deficiency at the start of the study. At two years, vitamin D blood levels in the supplement versus placebo group was 54.3 ng/mL versus 28.2 ng/mL, respectively, but no significant differences were observed in rates of T2DM at the 2.5 year follow-up. [50] The authors noted that a lack of effect of vitamin D may have been due to the majority of participants having vitamin D blood levels in a normal range of greater than 20 ng/mL, which is considered an acceptable level to reduce health risks. Notably, among the participants who had the lowest blood levels of vitamin D at the beginning of the study, vitamin D supplementation did reduce risk of diabetes. This is consistent with the important concept that taking additional vitamin D may not benefit those who already have adequate blood levels, but those with initially low blood levels may benefit.
Vitamin D’s role in regulating the immune system has led scientists to explore two parallel research paths: Does vitamin D deficiency contribute to the development of multiple sclerosis, type 1 diabetes, and other so-called “autoimmune” diseases, where the body’s immune system attacks its own organs and tissues? And could vitamin D supplements help boost our body’s defenses to fight infectious disease, such as tuberculosis and seasonal flu?
Multiple Sclerosis The rate of multiple sclerosis (MS) is increasing in both developed and developing countries, with an unclear cause. However, a person’s genetic background plus environmental factors including inadequate vitamin D and UVB exposure have been identified to increase risk. [51] Vitamin D was first proposed over 40 years ago as having a role in MS given observations at the time including that rates of MS were much higher far north (or far south) of the equator than in sunnier climates, and that geographic regions with diets high in fish had lower rates of MS. [52] A prospective study of dietary intake of vitamin D found women with daily intake above 400 IU had a 40% lower risk of MS. [53] In a study among healthy young adults in the US, White men and women with the highest vitamin D serum levels had a 62% lower risk of developing MS than those with the lowest vitamin D levels. [54] The study didn’t find this effect among Black men and women, possibly because there were fewer Black study participants and most of them had low vitamin D levels, making it harder to find any link between vitamin D and MS if one exists. Another prospective study in young adults from Sweden also found a 61% lower risk of MS with higher serum vitamin D levels; [55] and a prospective study among young Finnish women found that low serum vitamin D levels were associated with a 43% increased risk of MS. [56] In prospective studies of persons with MS, higher vitamin D levels have been associated with reduced disease activity and progression. [57,58] While several clinical trials are underway to examine vitamin D as a treatment in persons with MS, there are no clinical trials aimed at prevention of MS, likely because MS is a rare disease and the trial would need to be large and of long duration. Collectively, the current evidence suggests that low vitamin D may have a causal role in MS and if so, approximately 40% of cases may be prevented by correcting vitamin D insufficiency. [59] This conclusion has been strengthened substantially by recent evidence that genetically determined low levels of vitamin D predict higher risk of multiple sclerosis.
Type 1 Diabetes Type 1 diabetes (T1D) is another disease that varies with geography—a child in Finland is about 400 times more likely to develop T1D than a child in Venezuela. [60] While this may largely be due to genetic differences, some studies suggest that T1D rates are lower in sunnier areas. Early evidence suggesting that vitamin D may play a role in T1D comes from a 30-year study that followed more than 10,000 Finnish children from birth: Children who regularly received vitamin D supplements during infancy had a nearly 90% lower risk of developing type 1 diabetes than those who did not receive supplements. [61] However, multiple studies examining the association between dietary vitamin D or trials supplementing children at high risk for T1D with vitamin D have produced mixed and inconclusive results [62] Approximately 40% of T1D cases begin in adulthood. A prospective study among healthy young adults in the US found that White individuals with the highest levels of serum vitamin D had a 44% lower risk of developing T1D in adulthood than those with the lowest levels. [63] No randomized controlled trials on vitamin D and adult onset T1D have been conducted, and it is not clear that they would be possible to conduct. More research is needed in this area.
Flu and the Common Cold The flu virus wreaks the most havoc in the winter, abating in the summer months. This seasonality led a British doctor to hypothesize that a sunlight-related “seasonal stimulus” triggered influenza outbreaks. [64] More than 20 years after this initial hypothesis, several scientists published a paper suggesting that vitamin D may be the seasonal stimulus. [65] Among the evidence they cite:
- Vitamin D levels are lowest in the winter months. [65]
- The active form of vitamin D tempers the damaging inflammatory response of some white blood cells, while it also boosts immune cells’ production of microbe-fighting proteins. [65]
- Children who have vitamin D-deficiency rickets are more likely to get respiratory infections, while children exposed to sunlight seem to have fewer respiratory infections. [65]
- Adults who have low vitamin D levels are more likely to report having had a recent cough, cold, or upper respiratory tract infection. [66]
A randomized controlled trial in Japanese school children tested whether taking daily vitamin D supplements would prevent seasonal flu. [67] The trial followed nearly 340 children for four months during the height of the winter flu season. Half of the study participants received pills that contained 1,200 IU of vitamin D; the other half received placebo pills. Researchers found that type A influenza rates in the vitamin D group were about 40% lower than in the placebo group; there was no significant difference in type B influenza rates.
Although randomized controlled trials exploring the potential of vitamin D to prevent other acute respiratory infections have yielded mixed results, a large meta-analysis of individual participant data indicated that daily or weekly vitamin D supplementation lowers risk of acute respiratory infections. [68] This effect was particularly prominent for very deficient individuals.
The findings from this large meta-analysis have raised the possibility that low vitamin D levels may also increase risk of or severity of novel coronavirus 2019 (COVID-19) infection. Although there is no direct evidence on this issue because this such a new disease, avoiding low levels of vitamin D makes sense for this and other reasons. Thus, if there is reason to believe that levels might be low, such as having darker skin or limited sun exposure, taking a supplement of 1000 or 2000 IU per day is reasonable. This amount is now part of many standard multiple vitamin supplements and inexpensive.
More research is needed before we can definitively say that vitamin D protects against the flu and other acute respiratory infections. Even if vitamin D has some benefit, don’t skip your flu shot. And when it comes to limiting risk of COVID-19, it is important to practice careful social distancing and hand washing.
Tuberculosis Before the advent of antibiotics, sunlight and sun lamps were part of the standard treatment for tuberculosis (TB). [69] More recent research suggests that the “sunshine vitamin” may be linked to TB risk. Several case-control studies, when analyzed together, suggest that people diagnosed with tuberculosis have lower vitamin D levels than healthy people of similar age and other characteristics. [70] Such studies do not follow individuals over time, so they cannot tell us whether vitamin D deficiency led to the increased TB risk or whether taking vitamin D supplements would prevent TB. There are also genetic differences in the receptor that binds vitamin D, and these differences may influence TB risk. [71] Again, more research is needed.
Other A utoimmune Conditions The Vitamin D and Omega 3 trial (VITAL), a randomized double-blind placebo-controlled trial following more than 25,000 men and women ages 50 and older, found that taking vitamin D supplements (2,000 IU/day) for five years, or vitamin D supplements with marine omega-3 fatty acids (1,000 mg/day), reduced the incidence of autoimmune diseases by about 22%, compared with a placebo. Autoimmune conditions observed included rheumatoid arthritis, psoriasis, polymyalgia rheumatica, and autoimmune thyroid diseases (Hashimoto’s thyroiditis, Graves’ disease). [80] The doses in these supplements are widely available and generally well-tolerated. The authors recommended additional trials to test the effectiveness of these supplements in younger populations and those at high risk of developing autoimmune diseases.
- A promising report in the Archives of Internal Medicine suggests that taking vitamin D supplements may reduce overall mortality rates: A combined analysis of multiple studies found that taking modest levels of vitamin D supplements was associated with a statistically significant 7% reduction in mortality from any cause. [72] The analysis looked at the findings from 18 randomized controlled trials that enrolled a total of nearly 60,000 study participants; most of the study participants took between 400 and 800 IU of vitamin D per day for an average of five years. Keep in mind that this analysis has several limitations, chief among them the fact that the studies it included were not designed to explore mortality in general, or explore specific causes of death. A recent meta-analysis suggests that this reduction in mortality is driven mostly by a reduction in cancer mortality. [38] More research is needed before any broad claims can be made about vitamin D and mortality. [73]
- A large cohort study of more than 307,000 White European participants found a 25% increased risk of premature deaths from any cause in those who had vitamin D blood levels of 25 nmol/L (10 ng/ml), compared with those who had 50 nmol/L (20 ng/ml) (the National Academy of Medicine cites a vitamin D blood level of 50 nmol/L as adequate for most people). [74] Similar increases in risks were seen for deaths due to cardiovascular disease, cancer, and respiratory disease, and risks increased sharply among those with even lower levels of vitamin D. Although the numbers of non-White participants were small, the findings were similar in this group. The study used Mendelian randomization, which measured genetic variations to confirm these findings. This confirmation is important because it documents that the adverse health outcomes among people with low levels of vitamin D represent a causal relationship between vitamin D deficiency and premature death. Specifically, this method removed potential confounding by factors such as obesity, smoking, and alcohol intake.
In an analysis of more than 427,000 White European participants using Mendelian randomization, a 54% higher risk of dementia was seen among participants with low vitamin D blood levels of <25 nmol/L compared with those having adequate levels of 50 nmol/L. [75]
Food Sources
Few foods are naturally rich in vitamin D3. The best sources are the flesh of fatty fish and fish liver oils. Smaller amounts are found in egg yolks, cheese, and beef liver. Certain mushrooms contain some vitamin D2; in addition some commercially sold mushrooms contain higher amounts of D2 due to intentionally being exposed to high amounts of ultraviolet light. Many foods and supplements are fortified with vitamin D like dairy products and cereals.
- Cod liver oil
- Orange juice fortified with vitamin D
- Dairy and plant milks fortified with vitamin D
- Fortified cereals

Is There a Difference Between Vitamin D3 and Vitamin D2 Supplements?
Ultraviolet light.
Vitamin D3 can be formed when a chemical reaction occurs in human skin, when a steroid called 7-dehydrocholesterol is broken down by the sun’s UVB light or so-called “tanning” rays. The amount of the vitamin absorbed can vary widely. The following are conditions that decrease exposure to UVB light and therefore lessen vitamin D absorption:
- Use of sunscreen; correctly applied sunscreen can reduce vitamin D absorption by more than 90%. [78]
- Wearing full clothing that covers the skin.
- Spending limited time outdoors.
- Darker skin tones due to having higher amounts of the pigment melanin, which acts as a type of natural sunscreen. [79]
- Older ages when there is a decrease in 7-dehydrocholesterol levels and changes in skin, and a population that is likely to spend more time indoors.
- Certain seasons and living in northern latitudes above the equator where UVB light is weaker. [78] In the northern hemisphere, people who live in Boston (U.S.), Edmonton (Canada), and Bergen (Norway) can’t make enough vitamin D from the sun for 4, 5, and 6 months out of the year, respectively. [78] In the southern hemisphere, residents of Buenos Aires (Argentina) and Cape Town (South Africa) make far less vitamin D from the sun during their winter months (June through August) than they can during their spring and summer months. [78] The body stores vitamin D from summer sun exposure, but it must last for many months. By late winter, many people in these higher-latitude locales are deficient. [79]
Note that because ultraviolet rays can cause skin cancer, it is important to avoid excessive sun exposure and in general, tanning beds should not be used.
Signs of Deficiency and Toxicity
Vitamin D deficiency may occur from a lack in the diet, poor absorption, or having a metabolic need for higher amounts. If one is not eating enough vitamin D and does not receive enough ultraviolet sun exposure over an extended period (see section above), a deficiency may arise. People who cannot tolerate or do not eat milk, eggs, and fish, such as those with a lactose intolerance or who follow a vegan diet, are at higher risk for a deficiency. Other people at high risk of vitamin D deficiency include:
- People with inflammatory bowel disease (ulcerative colitis, Crohn’s disease) or other conditions that disrupt the normal digestion of fat. Vitamin D is a fat-soluble vitamin that depends on the gut’s ability to absorb dietary fat.
- People who are obese tend to have lower blood vitamin D levels. Vitamin D accumulates in excess fat tissues but is not easily available for use by the body when needed. Higher doses of vitamin D supplementation may be needed to achieve a desirable blood level. Conversely, blood levels of vitamin D rise when obese people lose weight.
- People who have undergone gastric bypass surgery, which typically removes the upper part of the small intestine where vitamin D is absorbed.
Conditions resulting from prolonged vitamin D deficiency:
- Rickets: A condition in infants and children of soft bones and skeletal deformities caused by failure of bone tissue to harden.
- Osteomalacia: A condition in adults of weak and softened bones that can be reversed with supplementation. This is different than osteoporosis, in which the bones are porous and brittle and the condition is irreversible.
Vitamin D toxicity most often occurs from taking supplements. The low amounts of the vitamin found in food are unlikely to reach a toxic level, and a high amount of sun exposure does not lead to toxicity because excess heat on the skin prevents D3 from forming. It is advised to not take daily vitamin D supplements containing more than 4,000 IU unless monitored under the supervision of your doctor.
Symptoms of toxicity:
- Weight loss
- Irregular heart beat
- Hardening of blood vessels and tissues due to increased blood levels of calcium, potentially leading to damage of the heart and kidneys
Did You Know?
Catching the sun’s rays in a sunny office or driving in a car unfortunately won’t help to obtain vitamin D as window glass completely blocks UVB ultraviolet light.
Vitamins and Minerals
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, D.C.: National Academies Press, 2010. https://www.ncbi.nlm.nih.gov/books/NBK56070/
- Holick MF. Vitamin D deficiency. New England Journal of Medicine . 2007 Jul 19;357(3):266-81.
- Gordon CM, DePeter KC, Feldman HA, Grace E, Emans SJ. Prevalence of vitamin D deficiency among healthy adolescents. Archives of pediatrics & adolescent medicine . 2004 Jun 1;158(6):531-7.
- Lips PT. Worldwide status of vitamin D nutrition. The Journal of steroid biochemistry and molecular biology . 2010 Jul 1;121(1-2):297-300.
- Robinson PD, Högler W, Craig ME, Verge CF, Walker JL, Piper AC, Woodhead HJ, Cowell CT, Ambler GR. The re-emerging burden of rickets: a decade of experience from Sydney. Archives of Disease in Childhood . 2006 Jul 1;91(7):564-8.
- Kreiter SR, Schwartz RP, Kirkman Jr HN, Charlton PA, Calikoglu AS, Davenport ML. Nutritional rickets in African American breast-fed infants. The Journal of pediatrics . 2000 Aug 1;137(2):153-7.
- Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics . 2008 Aug 1;122(2):398-417.
- Boonen S, Lips P, Bouillon R, Bischoff-Ferrari HA, Vanderschueren D, Haentjens P. Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials. The Journal of Clinical Endocrinology & Metabolism . 2007 Apr 1;92(4):1415-23.
- Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. Jama . 2005 May 11;293(18):2257-64.
- Cauley JA, LaCroix AZ, Wu L, Horwitz M, Danielson ME, Bauer DC, Lee JS, Jackson RD, Robbins JA, Wu C, Stanczyk FZ. Serum 25-hydroxyvitamin D concentrations and risk for hip fractures. Annals of internal medicine . 2008 Aug 19;149(4):242-50.
- Cauley JA, Parimi N, Ensrud KE, Bauer DC, Cawthon PM, Cummings SR, Hoffman AR, Shikany JM, Barrett-Connor E, Orwoll E. Serum 25-hydroxyvitamin D and the risk of hip and nonspine fractures in older men. Journal of Bone and Mineral Research . 2010 Mar;25(3):545-53.
- Bischoff-Ferrari HA, Willett WC, Wong JB, Stuck AE, Staehelin HB, Orav EJ, Thoma A, Kiel DP, Henschkowski J. Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Archives of internal medicine . 2009 Mar 23;169(6):551-61.
- Avenell A, Mak JC, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database of Systematic Reviews . 2014(4).
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, Wong JB. Effect of vitamin D on falls: a meta-analysis. Jama . 2004 Apr 28;291(16):1999-2006.
- Broe KE, Chen TC, Weinberg J, Bischoff-Ferrari HA, Holick MF, Kiel DP. A higher dose of vitamin D reduces the risk of falls in nursing home residents: a randomized, multiple-dose study. Journal of the American Geriatrics Society . 2007 Feb;55(2):234-9.
- Bischoff-Ferrari HA, Orav EJ, Dawson-Hughes B. Effect of cholecalciferol plus calcium on falling in ambulatory older men and women: a 3-year randomized controlled trial. Archives of internal medicine . 2006 Feb 27;166(4):424-30.
- Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ . 2009 Oct 1;339:b3692.
- Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, Nicholson GC. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. Jama . 2010 May 12;303(18):1815-22.
- Garland CF, Garland FC. Do sunlight and vitamin D reduce the likelihood of colon cancer?. International journal of epidemiology . 1980 Sep 1;9(3):227-31.
- Garland CF, Gorham ED, Mohr SB, Garland FC. Vitamin D for cancer prevention: global perspective. Annals of epidemiology . 2009 Jul 1;19(7):468-83.
- McCullough ML, Zoltick ES, Weinstein SJ, Fedirko V, Wang M, Cook NR, Eliassen AH, Zeleniuch-Jacquotte A, Agnoli C, Albanes D, Barnett MJ. Circulating vitamin D and colorectal cancer risk: an international pooling project of 17 cohorts. JNCI: Journal of the National Cancer Institute . 2019 Feb 1;111(2):158-69.
- Yin L, Grandi N, Raum E, Haug U, Arndt V, Brenner H. Meta-analysis: longitudinal studies of serum vitamin D and colorectal cancer risk. Alimentary pharmacology & therapeutics . 2009 Jul;30(2):113-25.
- Wu K, Feskanich D, Fuchs CS, Willett WC, Hollis BW, Giovannucci EL. A nested case–control study of plasma 25-hydroxyvitamin D concentrations and risk of colorectal cancer. Journal of the National Cancer Institute . 2007 Jul 18;99(14):1120-9.
- Gorham ED, Garland CF, Garland FC, Grant WB, Mohr SB, Lipkin M, Newmark HL, Giovannucci E, Wei M, Holick MF. Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. American journal of preventive medicine . 2007 Mar 1;32(3):210-6.
- Giovannucci E. Epidemiological evidence for vitamin D and colorectal cancer. Journal of Bone and Mineral Research . 2007 Dec;22(S2):V81-5.
- Lin J, Zhang SM, Cook NR, Manson JE, Lee IM, Buring JE. Intakes of calcium and vitamin D and risk of colorectal cancer in women. American journal of epidemiology . 2005 Apr 15;161(8):755-64.
- Huncharek M, Muscat J, Kupelnick B. Colorectal cancer risk and dietary intake of calcium, vitamin D, and dairy products: a meta-analysis of 26,335 cases from 60 observational studies. Nutrition and cancer . 2008 Dec 31;61(1):47-69.
- Bertone-Johnson ER, Chen WY, Holick MF, Hollis BW, Colditz GA, Willett WC, Hankinson SE. Plasma 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D and risk of breast cancer. Cancer Epidemiology and Prevention Biomarkers . 2005 Aug 1;14(8):1991-7.
- Garland CF, Gorham ED, Mohr SB, Grant WB, Giovannucci EL, Lipkin M, Newmark H, Holick MF, Garland FC. Vitamin D and prevention of breast cancer: pooled analysis. The Journal of steroid biochemistry and molecular biology . 2007 Mar 1;103(3-5):708-11.
- Lin J, Manson JE, Lee IM, Cook NR, Buring JE, Zhang SM. Intakes of calcium and vitamin D and breast cancer risk in women. Archives of Internal Medicine . 2007 May 28;167(10):1050-9.
- Robien K, Cutler GJ, Lazovich D. Vitamin D intake and breast cancer risk in postmenopausal women: the Iowa Women’s Health Study. Cancer causes & control . 2007 Sep 1;18(7):775-82.
- Freedman DM, Chang SC, Falk RT, Purdue MP, Huang WY, McCarty CA, Hollis BW, Graubard BI, Berg CD, Ziegler RG. Serum levels of vitamin D metabolites and breast cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiology and Prevention Biomarkers . 2008 Apr 1;17(4):889-94.
- Wactawski-Wende J, Kotchen JM, Anderson GL, Assaf AR, Brunner RL, O’sullivan MJ, Margolis KL, Ockene JK, Phillips L, Pottern L, Prentice RL. Calcium plus vitamin D supplementation and the risk of colorectal cancer. New England Journal of Medicine . 2006 Feb 16;354(7):684-96.
- Chlebowski RT, Johnson KC, Kooperberg C, Pettinger M, Wactawski-Wende J, Rohan T, Rossouw J, Lane D, O’Sullivan MJ, Yasmeen S, Hiatt RA. Calcium plus vitamin D supplementation and the risk of breast cancer. JNCI: Journal of the National Cancer Institute . 2008 Nov 19;100(22):1581-91.
- Holick MF. Calcium plus vitamin D and the risk of colorectal cancer. N Engl J Med . 2006; 354:2287-8; author reply 2287-8.
- Giovannucci E. Calcium plus vitamin D and the risk of colorectal cancer. N Engl J Med . 2006; 354:2287-8; author reply 2287-8.
- Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, Gibson H, Gordon D, Copeland T, D’Agostino D, Friedenberg G. Vitamin D supplements and prevention of cancer and cardiovascular disease. New England Journal of Medicine . 2019 Jan 3;380(1):33-44.
- Keum N, Lee DH, Greenwood DC, Manson JE, Giovannucci E. Vitamin D supplementation and total cancer incidence and mortality: a meta-analysis of randomized controlled trials. Annals of Oncology . 2019 May 1;30(5):733-43.
- Giovannucci E. Expanding roles of vitamin D. J Clin Endocrinol Metab . 2009; 94:418-20.
- Norman PE, Powell JT. Vitamin D and cardiovascular disease. Circulation research . 2014 Jan 17;114(2):379-93.
- Holick MF. The vitamin D deficiency pandemic and consequences for nonskeletal health: mechanisms of action. Molecular aspects of medicine . 2008 Dec 1;29(6):361-8.
- Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Archives of internal medicine . 2008 Jun 9;168(11):1174-80.
- Pilz S, März W, Wellnitz B, Seelhorst U, Fahrleitner-Pammer A, Dimai HP, Boehm BO, Dobnig H. Association of vitamin D deficiency with heart failure and sudden cardiac death in a large cross-sectional study of patients referred for coronary angiography. The Journal of Clinical Endocrinology & Metabolism . 2008 Oct 1;93(10):3927-35.
- Pilz S, Dobnig H, Fischer JE, Wellnitz B, Seelhorst U, Boehm BO, März W. Low vitamin D levels predict stroke in patients referred to coronary angiography. Stroke . 2008 Sep 1;39(9):2611-3.
- Booth TW, Lanier PJ. Vitamin D deficiency and risk of cardiovascular disease. Circulation Res117. 2008;503:511.
- Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, Kinkeldei J, Boehm BO, Weihrauch G, Maerz W. Independent association of low serum 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality. Archives of internal medicine . 2008 Jun 23;168(12):1340-9.
- Elamin MB, Abu Elnour NO, Elamin KB, Fatourechi MM, Alkatib AA, Almandoz JP, Liu H, Lane MA, Mullan RJ, Hazem A, Erwin PJ. Vitamin D and cardiovascular outcomes: a systematic review and meta-analysis. The Journal of Clinical Endocrinology & Metabolism . 2011 Jul 1;96(7):1931-42.
- Mitri J, Pittas AG. Vitamin D and diabetes. Endocrinol Metab Clin North Am . 2014 Mar;43(1):205-32.
- Pittas AG, Dawson-Hughes B, Li T, Van Dam RM, Willett WC, Manson JE, Hu FB. Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes care . 2006 Mar 1;29(3):650-6.
- Pittas AG, Dawson-Hughes B, Sheehan P, Ware JH, Knowler WC, Aroda VR, Brodsky I, Ceglia L, Chadha C, Chatterjee R, Desouza C, Dolor R, Foreyt J, Fuss P, Ghazi A, Hsia DS, Johnson KC, Kashyap SR, Kim S, LeBlanc ES, Lewis MR, Liao E, Neff LM, Nelson J, O’Neil P, Park J, Peters A, Phillips LS, Pratley R, Raskin P, Rasouli N, Robbins D, Rosen C, Vickery EM, Staten M; D2d Research Group. Vitamin D Supplementation and Prevention of Type 2 Diabetes. N Engl J Med . 2019 Aug 8;381(6):520-530
- Dobson R, Giovannoni G. Multiple sclerosis–a review. European journal of neurology . 2019 Jan;26(1):27-40.
- Goldberg P. Multiple sclerosis: vitamin D and calcium as environmental determinants of prevalence: (A viewpoint) part 1: sunlight, dietary factors and epidemiology. International Journal of Environmental Studies . 1974 Jan 1;6(1):19-27.
- Munger KL, Zhang SM, O’reilly E, Hernan MA, Olek MJ, Willett WC, Ascherio A. Vitamin D intake and incidence of multiple sclerosis. Neurology . 2004 Jan 13;62(1):60-5.
- Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. Jama . 2006 Dec 20;296(23):2832-8.
- Salzer J, Hallmans G, Nyström M, Stenlund H, Wadell G, Sundström P. Vitamin D as a protective factor in multiple sclerosis. Neurology . 2012 Nov 20;79(21):2140-5.
- Munger KL, Hongell K, Åivo J, Soilu-Hänninen M, Surcel HM, Ascherio A. 25-Hydroxyvitamin D deficiency and risk of MS among women in the Finnish Maternity Cohort. Neurology . 2017 Oct 10;89(15):1578-83.
- Ascherio A, Munger KL, White R, Köchert K, Simon KC, Polman CH, Freedman MS, Hartung HP, Miller DH, Montalbán X, Edan G. Vitamin D as an early predictor of multiple sclerosis activity and progression. JAMA neurology . 2014 Mar 1;71(3):306-14.
- Fitzgerald KC, Munger KL, Köchert K, Arnason BG, Comi G, Cook S, Goodin DS, Filippi M, Hartung HP, Jeffery DR, O’Connor P. Association of vitamin D levels with multiple sclerosis activity and progression in patients receiving interferon beta-1b. JAMA neurology . 2015 Dec 1;72(12):1458-65.
- Ascherio A, Munger KL. Epidemiology of multiple sclerosis: from risk factors to prevention—an update. InSeminars in neurology 2016 Apr (Vol. 36, No. 02, pp. 103-114). Thieme Medical Publishers.
- Gillespie KM. Type 1 diabetes: pathogenesis and prevention. Cmaj . 2006 Jul 18;175(2):165-70.
- Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. The Lancet . 2001 Nov 3;358(9292):1500-3.
- Rewers M, Ludvigsson J. Environmental risk factors for type 1 diabetes. The Lancet . 2016 Jun 4;387(10035):2340-8.
- Munger KL, Levin LI, Massa J, Horst R, Orban T, Ascherio A. Preclinical serum 25-hydroxyvitamin D levels and risk of type 1 diabetes in a cohort of US military personnel. American journal of epidemiology . 2013 Mar 1;177(5):411-9.
- Hope-Simpson RE. The role of season in the epidemiology of influenza. Epidemiology & Infection . 1981 Feb;86(1):35-47.
- Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, Madronich S, Garland CF, Giovannucci E. Epidemic influenza and vitamin D. Epidemiology & Infection . 2006 Dec;134(6):1129-40.
- Ginde AA, Mansbach JM, Camargo CA. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Archives of internal medicine . 2009 Feb 23;169(4):384-90.
- Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. The American journal of clinical nutrition . 2010 May 1;91(5):1255-60.
- Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ . 2017 Feb 15;356:i6583.
- Zasloff M. Fighting infections with vitamin D. Nature medicine . 2006 Apr;12(4):388-90.
- Nnoaham KE, Clarke A. Low serum vitamin D levels and tuberculosis: a systematic review and meta-analysis. International journal of epidemiology . 2008 Feb 1;37(1):113-9.
- Chocano-Bedoya P, Ronnenberg AG. Vitamin D and tuberculosis. Nutrition reviews . 2009 May 1;67(5):289-93.
- Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Archives of internal medicine . 2007 Sep 10;167(16):1730-7.
- Giovannucci E. Can vitamin D reduce total mortality?. Archives of Internal Medicine . 2007 Sep 10;167(16):1709-10.
- Sutherland JP, Zhou A, Hyppönen E. Vitamin D Deficiency Increases Mortality Risk in the UK Biobank: A Nonlinear Mendelian Randomization Study. Annals of Internal Medicine . 2022 Oct 25.
- Navale SS, Mulugeta A, Zhou A, Llewellyn DJ, Hyppönen E. Vitamin D and brain health: an observational and Mendelian randomization study. The American Journal of Clinical Nutrition . 2022 Apr 22.
- Tripkovic L, Lambert H, Hart K, Smith CP, Bucca G, Penson S, Chope G, Hyppönen E, Berry J, Vieth R, Lanham-New S. Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. The American journal of clinical nutrition . 2012 Jun 1;95(6):1357-64.
- Wilson LR, Tripkovic L, Hart KH, Lanham-New SA. Vitamin D deficiency as a public health issue: using vitamin D 2 or vitamin D 3 in future fortification strategies. Proceedings of the Nutrition Society . 2017 Aug;76(3):392-9.
- Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr . 2004; 79:362-71
- Holick MF. Vitamin D deficiency. N Engl J Med . 2007; 357:266-81.
- Hahn J, Cook NR, Alexander EK, Friedman S, Walter J, Bubes V, Kotler G, Lee IM, Manson JE, Costenbader KH. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ . 2022 Jan 26;376:e066452.
- LeBoff MS, Chou SH, Ratliff KA, et al. Supplemental Vitamin D and Incident Fractures in Midlife and Older Adults. N Engl J Med . 2022 Jul 28;387:299-309.
- LeBoff MS, Murata EM, Cook NR, Cawthon P, Chou SH, Kotler G, Bubes V, Buring JE, Manson JE. VITamin D and OmegA-3 TriaL (VITAL): effects of vitamin D supplements on risk of falls in the US population. The Journal of Clinical Endocrinology & Metabolism . 2020 Sep;105(9):2929-38.
- Ames BN, Grant WB, Willett WC. Does the high prevalence of vitamin D deficiency in African Americans contribute to health disparities?. Nutrients . 2021 Feb 3;13(2):499. *W.B.G. receives funding from Bio-Tech Pharmacal, Inc. (Fayetteville, AR). The other authors have no conflicts of interest to declare.
Last reviewed March 2023
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 10, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Research suggests probiotics plus vitamin D supplements may benefit people with schizophrenia

Previous studies have questioned whether gut microbe imbalances and vitamin D deficiency may be linked to schizophrenia.
New research published in Neuropsychopharmacology Reports now indicates that taking probiotics plus vitamin D supplements may improve cognitive function in individuals with the disease.
For the study, 70 adults with schizophrenia were randomized to take a placebo or probiotic supplements plus 400 IU vitamin D daily for 12 weeks. Severity of the disease and cognitive function were evaluated by tests called the Positive and Negative Syndrome Scale (PANSS) and the 30-point Montreal Cognitive Assessment (MoCA), respectively.
A total of 69 patients completed the study. The MoCA score increased by 1.96 units in the probiotic-containing supplement group compared with the placebo group . Also, the percentage of patients with MoCA scores of 26 or higher (indicating normal cognition) rose significantly in the intervention group. Between-group differences in PANSS scores were not significant.
"Probiotics may be a novel way to treat mental disorders by regulating gut microbiota ," said corresponding author Gita Sadighi, MD, of the University of Social Welfare and Rehabilitation Sciences, in Iran.
Explore further
Feedback to editors

Study improves understanding of effects of household air pollution during pregnancy
4 minutes ago

Wearable sensors for Parkinson's can improve with machine learning, data from healthy adults
51 minutes ago

New insights on B cells: Researchers explore building better antibodies and curbing autoimmune diseases

Grieving pet owners comforted by 'supernatural' interactions

Study shows AI improves accuracy of skin cancer diagnoses

Cell's 'garbage disposal' may have another role: Helping neurons near skin sense the environment

Chlamydia vaccine shows promise in early trial

Researchers find no link between COVID-19 virus and development of asthma in children

Pandemic drinking hit middle-aged women hardest, study finds

Researchers shed light on the molecular causes of different functions of opioid receptors
Related stories.

Sex differences seen in cognitive impairment for tardive dyskinesia in schizophrenia
May 19, 2023

Is a commonly-used screening tool for cognitive impairment accurate in diverse populations?
Jan 10, 2024

Details of Montreal Cognitive Assessment widely publicized
Jul 24, 2018

Fiber supplements could improve brain function in seniors, study says
Mar 23, 2024

Dementia screening test adapted for people with hearing problems
Mar 3, 2023

Cognitive impairment predicts outcomes for ICU survivors
Jul 1, 2022
Recommended for you

Study finds that dopamine projections to the amygdala contribute to encoding identity-specific reward memories
7 hours ago

Scientists uncover a missing link between poor diet and higher cancer risk
4 hours ago

PFAS exposure from high-seafood diets may be underestimated, finds study
8 hours ago

First national study of Dobbs ruling's effect on permanent contraception among young adults
2 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- News, Analysis & Insights on Nutrition, Supplements, and Health
Vitamin D reduces menstrual pain and medication use: Review
10-Apr-2024 - Last updated on 10-Apr-2024 at 08:14 GMT
- Email to a friend

Writing in the journal Nutrients , researchers from Taiwan evaluated the effect of vitamin D supplementation in 687 menstruating females across 11 studies by measuring pain score reduction. They then conducted trial sequential analysis (TSA) to assess the statistical power and precision of the meta-analysis and identify the ‘true’ intervention effect.
“In the pooled analyses, we found that vitamin D supplementation significantly decreased the pain intensity of dysmenorrhoea, and the cumulative power supports a ‘true’ treatment response,” they wrote, concluding that vitamin D reduced prostaglandin levels (lipids with a role in menstruation) and inflammation.
A common condition, significant burden
Dysmenorrhoea, characterized by painful menstrual periods , is a common condition that affects 45% to 95% of females.
It can be classified into ‘primary’ dysmenorrhoea, defined as painful menstruation in the absence of pelvic pathology, or ‘secondary’ dysmenorrhoea, which is characterized by painful menses due to pelvic pathology or a recognized medical condition.
"Dysmenorrhoea represents a significant global health burden that requires attention," the researchers wrote. "Healthcare costs for patients with dysmenorrhoea are 2.2 times those for the general population. Additionally, in some countries, the annual cost associated with dysmenorrhoea treatment is 25 million USD."
The Taiwanese researchers, however, noted that some studies have reported limited effects, with variations in supplementation levels and dosages.
Vitamin D for menstrual pain
The review collected studies through a systematic search of the Cochrane Library, Embase, Google Scholar, Medline and Scopus databases, from inception up until Dec. 30, 2023.
Studies were included if they were randomized controlled trials, involved women who had regular menstruation, compared vitamin D supplementation with placebo or other active treatments before and after their use, and assessed pain severity using a validated tool.
Primary and secondary outcomes were measured by the changes in pain intensity and rescue analgesic use, respectively.
The assessment showed that vitamin D supplementation significantly decreased pain intensity in patients with dysmenorrhoea compared with controls, and subgroup analysis revealed that vitamin D supplementation reduced primary dysmenorrhoea pain but not secondary dysmenorrhoea pain.
The authors noted that while one study suggested an association between underlying vitamin D concentration and various pain-related conditions, the specific mechanism of vitamin D on dysmenorrhoea remains unclear.
They hypothesized that as vitamin D receptors are found in the ovaries, uterus, placenta and pituitary gland, vitamin D could suppress the expression of inflammation-induced markers and contractile-associated factors in uterine myometrial smooth-muscle cells by interacting with these receptors.
Additionally, in the studies included, a decrease in serum vitamin D (25(OH)D) levels was observed in the luteal phase of the menstrual cycle, which the authors suggested could stimulate an increase in inflammatory cytokines and prostaglandins, exacerbating the pain intensity of dysmenorrhoea.
They noted that due to the inter-study heterogeneity, the results should be interpreted with caution, and further large-scale high-quality studies are necessary to confirm the findings.
Journal: Nutrients doi: 10.3390/nu16071089 “Vitamin D Supplementation for Patients with Dysmenorrhoea: A Meta-Analysis with Trial Sequential Analysis of Randomised Controlled Trials” Authors: Kan-Chu Lin et al.
Related products

Pycnogenol® for healthy hair and beautiful skin during menopause
Content provided by Horphag Research | 08-Mar-2024 | White Paper
Like other symptoms related to menopause, some women will experience noticeable changes to hair quality and density during this transition phase.

Innovation in convenient formats: vegan gummies
Content provided by Cambridge Commodities | 05-Mar-2024 | Product Brochure
Supplements and vitamins in pill form have been around for decades, but consumers are now seeking alternatives that fit with their busy lifestyles and...

Step into the colorful world of Care4U® botanicals
Content provided by IFF | 14-Feb-2024 | Product Catalog
At IFF, we have been harvesting the best of what nature has to offer for more than 50 years and it’s just the beginning.
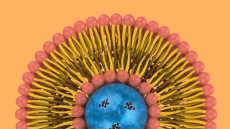
Discover Maximum Nutrient Delivery. Try the PureWay™ Range
Content provided by LEHVOSS Nutrition | 23-Jan-2024 | White Paper
When exploring the world of liposomal ingredients, finding the right one is key. Our PureWay™ range stands out by utilising a genuine liposomal technology,...
Related suppliers
- Cambridge Commodities
- HP Ingredients
- Pycnogenol® for healthy hair and beautiful skin during menopause Horphag Research | Download Technical / White Paper
- Innovation in convenient formats: vegan gummies Cambridge Commodities | Download Product Brochure
- Healthy ageing: a food supplement from Biofarma Group Biofarma Group | Download Technical / White Paper
- Innovation in Stress and Sleep Management: Holixer Natural Remedies Private Limited | Download Technical / White Paper
- Krill oil supports six key areas of healthy aging Aker BioMarine | Download Technical / White Paper
- In Weight Management Go Beyond with Slendacor® PLT Health Solutions | Download Technical / White Paper
Upcoming supplier webinars
- 23 Apr 2024 Tue How does Keratin hydrolysate improve Skin, hair, and nails beauty?
- 24 Apr 2024 Wed How to reduce crosslinking and ensure fast dissolution in soft caps
On-demand webinars
- Mitigating safety: Challenges in pet food manufacturing Webinar
- Premium categories: Does the humanization trend still have legs? Webinar
- Sustainable sourcing: Limiting pet industry impact on ecosystems Webinar
- Mining the microbiome: Balance is everything Webinar
- Nutraceutical market trends for 2024: insights by PharmaLinea and IQVIA PharmaLinea Ltd.

Promotional Features

NutraIngredients
- Advertise with us
- Press Releases – Guidelines
- Contact the Editor
- Report a technical problem
- Subscription Benefits
- Why Register
- Whitelist our newsletters
- Editorial Calendar
- Event Calendar
- TODAY Plaza
- Share this —

- Watch Full Episodes
- Read With Jenna
- Inspirational
- Relationships
- TODAY Table
- Newsletters
- Start TODAY
- Shop TODAY Awards
- Citi Music Series
- Listen All Day
Follow today
More Brands
- On The Show
Do you need vitamin D supplements? New study casts doubt on benefits
A new study casts doubt on the widespread use of high-dose vitamin D supplements, suggesting that the pills do not actually prevent bone fractures in healthy adults without vitamin D deficiencies.
The debate about the effectiveness of vitamin pills and supplements for the general population is not new. Despite the $150 billion-dollar industry 's best efforts, research continues to show that the vitamin pills many of us think are doing our bodies good aren't actually doing much to make us healthier, TODAY previously reported .
“Vitamin D is really important for bone health, and (together) with calcium, it's incredibly important in terms of preventing osteoporosis,” NBC News medical contributor Dr. Natalie Azar said on TODAY Thursday. However, people without a vitamin D deficiency may not get added bone health benefits from high-dose daily supplement pills, according to a new study led by scientists at Harvard Medical School .
New study looks at benefits of vitamin D supplements for healthy people
In the large randomized controlled trial, researchers tested whether 2000 IU (international units) per day of vitamin D3 supplements by itself would result in a lower risk of bone fractures compared to a placebo.
The study included over 25,800 participants, all over the age of 50, who were generally healthy. Participants were not selected for vitamin D deficiency, low bone mass, or osteoporosis, the authors wrote.
After following these participants for over five years, researchers found that vitamin D3 supplements "did not result in a significantly lower risk of fractures than (the) placebo among generally healthy midlife and older adults," the study authors wrote.
“This was a study done in people who weren’t selected for vitamin D deficiency, so it’s not unusual that you wouldn’t find an effect of vitamin D supplements,” said Azar.
Most people in the U.S. have adequate blood levels of vitamin D, but nearly one out of four people have levels that are inadequate or too low for bone and overall health, according to the NIH .
Easy sources of vitamin D
Vitamin D not only keeps bones strong and healthy — it’s also important for immune function, muscle function and brain health, Azar said. We get vitamin D from four main sources, she added.
- Sunlight: Vitamin D is produced in the body when ultraviolet rays from sunlight strike the skin, which triggers vitamin D synthesis, according to the National Institutes of Health's Office of Dietary Supplements.
- Foods: Vitamin D-rich foods include salmon, tuna, mackerel, fish oil and cod liver oil, said Azar.
- Vitamin D-fortified foods: Fortified foods provide most of the vitamin D in American diets, according to NIH. These include milk, orange juice and fortified cereals, Azar said.
- Dietary supplements: Pills either contain vitamin D2 (plant-derived) or D3 (often derived from animals but can be from lichen), according to NIH.
"The NIH does recommend that folks do take vitamin D or at least ingest vitamin D every day," said Azar.
If someone does not get enough vitamin D from their diet or sunlight, or has a medical condition that affects vitamin D levels or bone density, they will need to take supplements. That's because not getting enough vitamin D can cause muscle weakness, bone pain, and lead to osteoporosis , which causes bones to become fragile and break more easily, according to the NIH.
Risk factors for a vitamin D deficiency include gastric bypass surgery, liver or kidney disease, malabsorption, Crohn’s disease, obesity, having darker skin and not getting enough sun exposure, said Azar.
“If you have risk factors for vitamin D deficiency or osteoporosis, you definitely should be continuing your vitamin D and calcium,” said Azar.
How much vitamin D is needed daily?
For everyone else, more vitamin D isn’t necessarily better. So how much vitamin D do healthy people need? "The dose that was used in this study (2000s IU daily) is a little bit higher than what is normally recommended for most Americans," Azar said.
These are the recommended dietary allowances for vitamin D, according to the NIH:
0–12 months: 10 mcg (400 IU)
1–13 years: 15 mcg (600 IU)
14–18 years: 15 mcg (600 IU)
19–50 years: 15 mcg (600 IU)
51–70 years: 15 mcg (600 IU)
> 70 years: 20 mcg (800 IU)
"It’s really important also to point out again (that) this study was done in normal healthy people," said Azar. So the takeaway from this study "doesn't necessarily apply to people who have risks for osteoporosis or who have low bone mass," she added.
So if you have a vitamin D deficiency, you can and should absolutely keep taking your vitamin D, said Azar. But healthy individuals may not reap as much benefit from these supplements.
Caroline Kee is a health reporter at TODAY based in New York City.

Scientists Reveal New Findings About Older Adults Who Take Vitamin D
- Vitamin D is widely known for its role in supporting immunity and bone health.
- New research suggests that supplementing with vitamin D may reduce the risk of heart attacks and other cardiovascular events.
- Look for a high-quality vitamin D supplement that is third-party tested for purity, potency and safety, and speak with your healthcare provider about the right dose for you.
Vitamin D is a unique nutrient in that it comes from the food we eat and is a hormone that our bodies make. The fat soluble vitamin has a slew of important functions and vitamin D health benefits , from supporting immunity and healthy bones to improving mood. But new research shows that it may have other protective benefits for older adults.
A recent study published in the British Medical Journal , looked at a large sample of older adults ages 60 to 84. Participants were divided into two groups – one was given a placebo, while the other was given a vitamin D supplement of 60,000 IU a month (which averages out to about 2,000 IU a day) for up to five years. At the end of the study, data was analyzed from over 16,800 participants who were still taking the tablets.
During the trial, there were about 1,336 major cardiovascular events (i.e. heart attack, stroke and procedures to treat coronary artery disease). But compared with the placebo group, the rate of major heart problems was slightly lower in the vitamin D group, especially for those who were already taking heart medicines like statins at the beginning of the study.
Although the results are compelling, the findings were not statistically significant and prior research has shown no association with vitamin D supplementation and major heart problems. Ultimately, the best strategies to support heart health and reduce risk of heart disease include eating a healthy balanced diet , staying physically active , quitting smoking, reducing alcohol consumption, keeping blood pressure under control and checking your cholesterol levels. It's also important to take your medicines as directed and attend regular check-ups with your health care team.
But that doesn't mean that vitamin D isn't important for heart health. In fact, vitamin D is needed to support blood vessels and normal blood pressure. What's more, a vitamin D deficiency has been associated with elevated levels of lipids (a.k.a fats) in your blood, as well as vascular dysfunction and arterial stiffening. Research has also linked a lower vitamin D status to an increased risk of ischemic stroke , heart attack and heart disease .
How much vitamin D do I need?
Older adults need about 600 – 800 IU of vitamin D daily, depending on their age. You can get this through a combination of sun exposure and vitamin-D rich foods , which include salmon, eggs, sardines, liver, white mushrooms and fortified foods.
But supplementing with more isn't always better. Since vitamin D is a fat-soluble vitamin, too much can put you at serious risk for toxicity including adverse side effects like kidney stones and high calcium levels in the blood. Our experts say that it is best not to consume more than 4,000 IU daily, which is the tolerable upper intake level.
Signs of vitamin D deficiency
We recommend speaking with your healthcare provider if you suspect a vitamin D deficiency, as they can take bloodwork and then recommend the appropriate supplementation dosage based on your current levels. Some common signs of vitamin D deficiency include:
- Mood changes
- Muscle pain and weakness
- Reduced immune function
- Increased inflammation
- Frequent infections
- Rickets (in children)
- Bone disorders
What should I look for in a vitamin D supplement?
Since the U.S. Food and Drug Administration (FDA) does not approve dietary supplements for safety and effectiveness prior to going to market, it's incredibly important to thoroughly research each supplement you add to your regimen and speak with your healthcare provider before doing so. Look for options that have been tested for purity, potency and safety by a credible third-party organization.
Our team of registered dietitians spent months analyzing dozens of vitamin D supplements to bring you our top-tested recommendations for the best vitamin D supplements on the market.
The bottom line: New research suggests that supplementing with vitamin D may reduce the risk of heart attacks, but the results were not statistically significant and more research is needed. That being said, vitamin D does play a role in supporting a healthy heart, blood vessels and normal blood pressure. If you suspect a deficiency, speak with your healthcare provider who can take bloodwork and determine the appropriate supplement dose for you. The best strategies to support heart health include eating a healthy balanced diet, staying physically active, quitting smoking, reducing alcohol consumption and keeping blood pressure under control.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Vitamin D: What's new a year on from the COVID‐19 outbreak?
Helena gibson‐moore.
1 British Nutrition Foundation, London UK
When COVID‐19 hit the UK in early 2020, few would have envisaged that this catastrophic public health crisis would still be posing an unprecedented threat to human health, healthcare systems, public life and the economy a year on. Saving lives and slowing the worldwide pandemic remains an urgent priority. A great deal has been learnt but COVID‐19 is still a relatively new disease and research into preventative measures and treatments continues to evolve. During the pandemic, there has been an increased clinical and public interest in the role of diet and health, particularly in supporting immunity, sparking media stories suggesting that certain food components and supplements are capable of ‘boosting’ the immune system (BBC, 2020 ; Mirror, 2020 ).
No specific food or supplement can simply ‘boost’ immunity. To support normal immune function, the body requires adequate energy and nutrition (Calder, 2020 ), and specific roles have been demonstrated for a number of vitamins, trace elements, amino acids and fatty acids, which together contribute to the body's immune defences, including ability to reduce risk of infections (Calder, 2020 ). For example, the European Commission has approved health claims for vitamin A, vitamin B6, folate, vitamin B12, vitamin C, vitamin D, zinc, selenium, iron and copper recognising their contribution to the normal function of the immune system (EC, 2021 ) (see Lockyer, 2020 for more details on these nutrients and their role in immunity). However, early on in the pandemic, the spotlight landed on vitamin D presumably because vitamin D status is typically lowest in late winter when respiratory tract infections peak (Berry et al., 2011 ; Lanham‐New et al., 2020 ). Whilst this is purely an association rather than indicative of causation, interest continued to grow once it was realised that severe COVID‐19 outcomes were particularly common in those population groups known to be at greater risk of low vitamin D status, including people living with obesity and those from ethnic minorities (discussed in more detail later on) (PHE, 2020 ). Therefore, a potential beneficial effect of vitamin D in protecting against COVID‐19 infection and disease severity was considered plausible and has stimulated much research to investigate whether this is actually the case.
Vitamin D is a generic name for two different secosteroid compounds, ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3) (Buttriss et al., 2021 ). Vitamin D3 is found in a limited number of foods such as oil‐rich fish, eggs, red meat and vitamin D‐fortified products, but the main source results from synthesis in the skin following exposure to sunlight (UVB radiation at 290–315 nm), which converts 7‐dehydrocholesterol to vitamin D3. In contrast, vitamin D2 production is not triggered by sunlight in humans but can be obtained from fungi ( e.g. wild mushrooms or UVB treated cultivated mushrooms) and yeasts (Lanham‐New et al., 2020). In 1940, a mandatory requirement of vitamin D (and vitamin A) fortification of margarines was introduced, which was removed in 2013, although many fat spreads still contain vitamin D, added on a voluntary basis (Defra, 2014 ).
Vitamin D status is usually measured by the level of the circulating metabolite 25‐hydroxyvitaminD [25(OH)D], produced by hepatic hydroxylation of vitamin D sourced from either skin or the gut via oral intake (SACN, 2016 ). 25(OH)D is the most commonly used marker of vitamin D status because it has a relatively long half‐life (several weeks) and its concentration in serum/plasma reflects dietary intakes, UVB exposure and biological reserves of vitamin D (Buttriss et al., 2021 ). In the UK, a plasma or serum 25(OH)D concentration of 25 nmol/l (10 ng/ml) is considered as the minimum necessary for protecting musculoskeletal health and lowering the risk of osteomalacia (adults) and nutritional rickets (children). These conditions are characterised by pain, deformities, fractures and poor bone mineralisation, and are caused by low calcium intakes and/or vitamin D deficiency and are corrected by nutritional intervention (Buttriss et al., 2021 ; SACN, 2016 ). However, it is noteworthy that different thresholds are used to indicate risk; for example, the US Institute of Medicine set a minimum threshold of 30 nmol/l to define increased risk of deficiency and 50 nmol/l as the minimum threshold for ‘sufficiency’ (Institute of Medicine, 2011 ).
The angle of the sun determines whether skin synthesis of vitamin D is possible. So, during the winter months in areas further away from the equator (between October to March in the UK), there is insufficient solar UVB to support adequate vitamin D synthesis (Schoenmakers et al., 2016 ). During the winter months in countries such as the UK, the body is reliant on tissue stores of vitamin D as dietary intake typically does not meet the recommended vitamin D requirements [the National Diet and Nutrition Survey (NDNS) (years 2016/2017–2018/2019) suggests average vitamin D intakes from food sources only for adults aged 19–64 years is 2.9 µg/day] (PHE & FSA, 2020 ), and vitamin D status usually declines. Interestingly, the NDNS (years 2008/2009–2011/2012) that compared data for the devolved nations shows a larger proportion of individuals living in Scotland and Northern Ireland with a plasma 25(OH)D concentration below 25 nmol/l than that of the UK as a whole, and it is assumed this is because of the lower availability of UVB for vitamin D synthesis at higher latitudes (Bates et al., 2017a ; Bates et al., 2017b ). Globally, low vitamin D status is prevalent in a wide range of population groups, including those in low latitude areas ( i.e. closer to the equator) with an abundance of sunlight (Bouillon, 2019 ), and not necessarily confined to winter (Mendes et al., 2020 ). This may be due to environmental factors, such as air pollution, as well as cultural factors where skin is covered up and therefore not exposed to sunlight (Al‐Yatama et al., 2019 ). Older, housebound adults and individuals with dark skin pigment are at particular risk of vitamin D deficiency in the UK. The latter is associated with lower efficiency of cutaneous vitamin D synthesis due to the higher concentration of melanin in darker skin, but can also be exacerbated by sun avoidance and by culturally defined dress codes that require skin to be covered when outdoors (SACN, 2016 ).
In 2016, the Science Advisory Committee on Nutrition (SACN) published its Vitamin D and Health report, which reviewed the totality of the evidence at the time, and new dietary reference values were set based on protecting musculoskeletal health ( i.e. rickets, osteomalacia, falls, risk of falling and muscle strength) (SACN, 2016 ). Insufficient evidence was found for vitamin D in relation to non‐musculoskeletal outcomes (Buttriss et al., 2021 ; SACN, 2016 ). The reference nutrient intake (RNI) established for vitamin D was modelled on the basis of maintaining population protective 25(OH)D concentrations of ≥25 nmol/l, at the individual level, throughout the year; below this concentration, the risk of poor musculoskeletal health increases (Buttriss et al., 2021 ; SACN, 2016 ). The RNI was set at 10 µg/day [400 international units (IU)/day] for everyone over 4 years of age. For infants and younger children, data were insufficient to set a RNI, so instead, as a precaution, a ‘Safe Intake’ of 8.5–10 µg/day (340–400 IU) was recommended (SACN, 2016 ) (see Table Table1 1 for a summary of recent official advice in the UK on vitamin D). Prior to this in the UK, an RNI for vitamin D was set only for population groups at high risk of deficiency, for example young children, pregnant and lactating women, adults aged over 65 years and some ethnic minorities (DH, 1991 ). It was assumed that, for most people, the amount of vitamin D produced by exposure to sunlight containing UVB in the summer months would be adequate for achieving serum 25(OH)D concentrations ≥25 nmol/l during winter, but the new report recognised that this was now not the case.
Recent UK official advice on vitamin D supplements
Since SACN's report in 2016, standard government advice has been to consider taking a daily vitamin D supplement of 10 µg [400 IU] in the winter months (between October and March in the UK), since it is difficult for people to get enough vitamin D from food alone (NHS, 2020 ; SACN, 2016 ). However, in April 2020 Public Health England (PHE) reissued advice that whilst people are following recommendations to stay at home due to lockdown rules they may not be getting enough vitamin D from sunlight exposure, so everyone should additionally consider taking a daily vitamin D supplement of 10 µg in spring and summer (NHS, 2020 ). At the time, PHE emphasised that this advice was specifically to underpin musculoskeletal health, and that there was no evidence vitamin D supplementation would help to prevent COVID‐19 infection as a media story at the time had suggested (heart.co.uk, 2020 ).
Since then, more research has been published and there have been several rapid reviews on the available evidence on acute respiratory tract infections, but they have concluded that there is still insufficient reliable evidence to support taking vitamin D supplements in order to prevent or treat COVID‐19, and that more well‐designed studies are needed, particularly high‐quality randomised controlled trials (NICE, 2020a ; SACN, 2020a ; SACN, 2020b ). However, some experts argue that whilst results of clinical trials are pending, there is little to lose in recommending higher dose vitamin D supplements amidst this public health emergency, as a low‐risk nutritional intervention that is inexpensive and safe, and may have potential gains for some individuals (Lewis, 2020 ). The topic remains controversial and continues to attract media headlines (ITV News, 2021 ; The Guardian, 2021a ; The Guardian, 2021b ). This article aims to explore some of the aspects in the scientific debate on vitamin D supplementation and COVID‐19 and the public health implications, as well as providing some background on vitamin D's role in immunity.
Vitamin D and immunity
The immune system is complex and involves a network of cells, tissues and organs that work together to defend the body against a variety of assaults, including attacks from pathogens. Vitamin D has been shown to have immunoregulatory and anti‐inflammatory properties (Calder, 2020 ). Vitamin D receptors have been identified in most immune cells, including in activated T cells, antigen‐presenting cells, macrophages, monocytes and cytotoxic T cells, and some cells of the immune system ( e.g. macrophages and monocytes) can synthesise the active form of vitamin D from its precursor (Calder, 2020 ; Di Rosa et al., 2011 ). Data from in vitro studies suggest that vitamin D can increase the ability of the innate immune system to fight against viruses and defend against respiratory pathogens, as well as inhibit pulmonary inflammatory responses (Hughes & Norton, 2009 ; Sassi et al., 2018 ; Zdrenghea et al., 2017 ) and other evidence suggests vitamin D might also exert an inhibitory effect on the adaptive immune system by retarding the differentiation of B cell precursors into plasma cells and reducing the inflammatory response of T helper 1 cells (EFSA, 2010 ). Furthermore, population‐based studies have shown that serum 25(OH)D concentration is associated with improved lung function markers (Craveiro et al., 2018 ; Ganji et al., 2020 ).
Vitamin D and COVID‐19: A brief look at the evidence so far
In the spring of 2020, the available evidence linking vitamin D with upper respiratory tract infections (URTIs) was reviewed by Lanham‐New and colleagues (Lanham‐New et al., 2020). The authors concluded that there were plausible mechanisms linking vitamin D and protection against URTI, but whether these mechanisms apply with COVID‐19 is not currently known. One of the studies discussed was a systematic review and meta‐analysis of individual participant data from vitamin D supplementation randomised controlled trials (RCTs), which reported that vitamin D supplementation can reduce the incidence of acute URTIs, especially in those with vitamin D deficiency at baseline (Martineau et al., 2017 ). However, study settings, vitamin D supplemental doses, reporting and assessment of ARTIs and trial results were very heterogenous. Many of the included studies were in populations with pre‐existing respiratory disease, and the overall statistically significant result in the meta‐analysis of the 24 included trials was dependent on the inclusion of two studies undertaken in developing countries (Mongolia and Afghanistan), which may limit their applicability to the general population in the UK (Lanham‐New et al., 2020). Lanham‐New and colleagues recommended a need for appropriate vitamin D RCTs to evaluate the effects of vitamin D supplementation on COVID‐19 infections. However, until there is more robust scientific evidence for vitamin D, they strongly cautioned against the use of high vitamin D supplementation [greater than the upper limit of 4000 IU/day (100 µg/day)], and strongly endorsed avoidance of vitamin D deficiency in the population and following government advice on supplementation (10 µg/day) (Lanham‐New et al., 2020).
Observational evidence indicates that, in general, groups such as some ethnic minorities, older adults and people living with obesity, who are at greater risk of hospitalisation and mortality risk from COVID‐19 infection, also have lower vitamin D status (Lanham‐New et al., 2020). According to a PHE report looking at disparities in the risk and outcomes of COVID‐19, among those diagnosed with COVID‐19, the mortality risk (not taking into account underlying health issues) is greater in males, people aged 80 years or over, those living in deprived areas and those in Black, Asian and Minority Ethnic (BAME) population groups (PHE, 2020 ). In England up to 8 May 2020, 27% of deaths from COVID‐19 were reported among people in care homes, and obesity has also been linked to COVID‐19 infection and poorer outcomes among those infected ( i.e. hospitalisation and/or death) (PHE, 2020 ). Observational data have also shown an association between patients who have low vitamin D status and an increased risk of severe COVID‐19 infection (Liu et al., 2021 ; Panagiotou et al., 2020 ). Data from an initial analysis of the first‐reported UK Biobank COVID‐19‐positive cases [ n = 580 (included those who have been treated as a hospital inpatient as well as those who have not)] compared with negative controls ( n = 723) found, on average, serum 25(OH)D status was almost identical in those who tested positive (43.3 nmol/l) compared to those who tested negative (44.1 nmol/l) for COVID‐19. Similarly, a more recent study on the UK Biobank cohort (656 had inpatient confirmed COVID‐19 infection and 203 died of COVID‐19 infection) did not demonstrate a link between 25(OH)D concentrations and risk of severe COVID‐19 infection and mortality (Hastie et al., 2021 ). Notably, vitamin D status was assessed in the Biobank cohort a decade before the pandemic, in 2006–2010 and so may have since changed.
In June 2020, SACN published a rapid review which included the systematic review and meta‐analysis by Martineau et al. ( 2017 ) (mentioned earlier) that had reported some benefit. SACN concluded there was insufficient evidence to determine whether vitamin D supplementation could have a role in preventing respiratory tract infections (SACN, 2020a ). Subsequently, the National Institute for Health and Care Excellence (NICE), PHE and SACN convened an expert panel and published rapid guidelines in December 2020 on vitamin D for COVID‐19, under the auspices of NICE (NICE, 2020a ; see Table Table1). 1 ). The panel agreed that although low vitamin D status has been associated with more severe outcomes from COVID‐19, it was not possible to confirm causality because many of the risk factors for severe COVID‐19 outcomes are the same as the risk factors for low vitamin D status. They added that since vitamin D is a negative acute phase reactant, its serum concentration falls during a systemic inflammation such as severe COVID‐19 illness and it is difficult to know if low vitamin D levels, measured after the onset of infection, cause poor outcomes or are a result of the infection (NICE, 2020a ; SACN, 2020b ; Wise, 2020 ). It could also be possible, however, that vitamin D requirements increase as a result of infection, causing serum levels to fall, since it has been reported, for example, that epithelial cells in the lungs activate vitamin D in response to infection, leading to increased levels of the anti‐microbial peptide, cathelicidin (Laaksi, 2012 ).
Included in the NICE review was discussion of a recent systematic review and meta‐analysis by Jolliffe et al. ( 2021 ). This study reported that vitamin D supplementation reduced the risk of acute respiratory infections and that protection was associated with administration of daily doses of 10–25 µg (400–1000 IU) of vitamin D for up to 12 months, compared with placebo, despite evidence of significant heterogeneity across trials (Jolliffe et al., 2021 ). NICE highlighted a number of notable limitations with the sub‐group analyses. Protection was only seen in children (aged 1–16 years), yet poorer outcomes of COVID‐19 are generally far more common in older adults (NICE, 2020a ). Beneficial effects on acute respiratory tract infection prevention in children were associated with daily doses of 10–25 µg (400–1000 IU) of vitamin D, but not with higher doses [over 25 µg (1000 IU) daily or more], when supplementation was weekly or monthly, or in adults (NICE, 2020a ). In addition, the panel highlighted substantive limitations in the included studies with inconsistency between study results and differences in study populations and methodologies including country, latitude, age ranges, comorbidities, dosing frequency, percentage of participants with low vitamin D status (<25 nmol/l) and definitions of outcomes (including type of respiratory infection), making it difficult to draw conclusions relevant to the general population (NICE, 2020a ).
When the panel considered the evidence for treating COVID‐19 using vitamin D supplements, they were presented with evidence from the NICE evidence review of vitamin D for COVID‐19 (NICE, 2020a ), which comprised one small, very low quality, RCT in secondary care from Spain (Entrenas Castillo et al., 2020 ). The trial used a very high dose of oral calcifediol [25(OH)D], the circulating metabolite of vitamin D produced from vitamin D in the liver, which is not commonly used as a supplement in the UK. This dose was estimated to be considerably higher than UK vitamin D recommendations, equivalent to around 5000 µg (200 000 IU) of vitamin D in the first week [about 700 µg vitamin D (28 000 IU) daily] falling to 1300 µg (52 000 IU) in subsequent weeks for the duration of the study [about 200 µg vitamin D (8000 IU) daily]. The panel also had concerns about differences in comorbidities between the two comparator groups and a lack of blinding which could have resulted in biased estimates (NICE, 2020a ; Wise, 2020 ).
In relation to COVID‐19, the NICE guidance recognises that there is currently no robust evidence to recommend vitamin D supplementation specifically to prevent or treat COVID‐19 (unless as part of a clinical trial). The panel also recognised the pressing need for good quality, relevant data to ensure that guidance can be updated if necessary ( i.e . definitive large‐scale RCTs, including population groups who have higher risk of low vitamin D status and/or are disproportionally affected by COVID‐19, such as BAME groups and people living with obesity). Whilst awaiting results of such trials, the panel agreed that the UK population should be encouraged to adhere to current government guidance, that is to take a daily supplement containing 10 µg of vitamin D especially between October and early March, and all year round for those at particular risk of low vitamin D status ( e.g. those who are frail, housebound or in a care home, or those who usually wear concealing clothes outdoors). These recommendations are to support good musculoskeletal health, and the panel was aware of the updated SACN recommendation that a vitamin D intake of 10 µg/day may also provide some additional benefit in reducing the risk of acute respiratory tract infections (NICE, 2020a ). At the end of November 2020, the government announced free vitamin D supplements for those who are clinically extremely vulnerable and for care home residents for the winter months to support general health, in particular bone and muscle health (DHSC 2020). This topic is being kept under review and the panel agreed that the recommendations for COVID‐19 prevention and treatment should be considered for an update as additional evidence from trials becomes available (NICE, 2020a ). The panel acknowledged that a number of RCTs considering vitamin D supplementation in prevention and treatment COVID‐19 are known to be in progress and many of these are listed in NICE guideline NG187 (NICE, 2020a ), some of which are outlined on the next section.
Since the publication of the NICE review, and at the time of writing this article, results from some studies and trials on vitamin and COVID‐19 have become available, and mostly have demonstrated that vitamin D is not related to COVID‐19 outcomes. An RCT in Brazil aimed to investigate the effect of a single high dose of vitamin D3 on hospital length of stay in patients with COVID‐19 (Murai et al., 2021 ). The study included 240 hospitalised patients with COVID‐19 who were moderately to severely ill at the time of enrolment and were randomly assigned to receive a single oral dose of 200 000 IU (5000 µg) of vitamin D3 ( n = 120) or placebo ( n = 120). Results indicated that length of hospital stay was not significantly different between the vitamin D3 group and the placebo group, nor was in‐hospital mortality, admission to the intensive care unit or need for mechanical ventilation. The authors concluded that their findings do not support the use of a high dose of vitamin D3 for treatment of moderate to severe COVID‐19 (Murai et al., 2021 ). Several limitations have been highlighted. Firstly, the relatively low sample size means it could have been underpowered to detect small, but clinically meaningful, differences between the groups (Murai et al., 2021 ). Secondly, patients who required invasive mechanical ventilation and those admitted to the intensive care unit, in other words those who were critically ill, were excluded; therefore, the results cannot be generalised to critically ill patients. Thirdly, only 115 participants had vitamin D deficiency [25(OH)D <20 ng/ml]. Lastly, the patients were given vitamin D3 after a relatively long time from symptom onset to randomisation (mean of 10.3 days) (Murai et al., 2021 ).
An accompanying editorial stated that if this clinical trial is taken in isolation, the findings may appear ambiguous; for example, the findings do not exclude clinically important benefit (or harm) from high‐dose vitamin D3 administration in hospitalised patients with moderate to severe COVID‐19. In addition, the study did not look at use of vitamin D in patients with mild (outpatient) COVID‐19 who are early in their symptom course (Leaf & Ginde, 2021 ). Leaf and Ginde emphasised that, based on experience in the pandemic, it is likely many of the other trials currently running will also be underpowered or will not achieve target enrolment. Therefore, given the lack of highly effective therapies against COVID‐19, Leaf and Ginde conclude that it is important to remain open‐minded to emerging results from rigorously conducted studies of vitamin D, despite smaller sample sizes and important limitations of some studies (Leaf & Ginde, 2021 ). Also worthy of consideration is that differences in participants, type, dose, initial vitamin status and duration of vitamin D supplementation, study endpoints and risk of bias make interpretation of the trial evidence difficult (Vimaleswaran et al., 2021 ).
A study, yet to be peer‐reviewed at the time of writing, made headlines in The Guardian and found no evidence that vitamin D sufficiency could protect against COVID‐19 (The Guardian, 2021c ). Butler‐Laporte and colleagues used two‐sample Mendelian randomisation (MR) to assess evidence supporting a causal effect of circulating 25(OH)D levels on COVID‐19 susceptibility and severity (Butler‐Laporte et al., 2021 ). MR is a genetic epidemiological method that uses genetic variants as instrumental variables to infer the causal effect of an exposure [in this case 25(OH)D level] on an outcome (in this case, COVID‐19 susceptibility and severity) in observational data (Butler‐Laporte et al., 2021 ; Davies et al., 2018 ). The researchers used the genetic variants obtained from the largest consortium of COVID‐19 cases and controls (The COVID‐ 19 Host Genetics Initiative, 2020 ), and the largest study on genetic determinants of vitamin D levels from UK Biobank data (Manousaki et al., 2020 ), and used MR to estimate the effect of increased vitamin D on COVID‐19 outcomes, whilst limiting confounding. In multiple analyses, results showed no evidence for an association between genetically predicted vitamin D levels and COVID‐19 susceptibility, hospitalisation or severe disease. The researchers conclude that their findings suggest that other therapies should be prioritised over vitamin D for COVID‐19 trials (Butler‐Laporte et al., 2021 ).
Clinical trials on vitamin D and COVID‐19 and the impact of vaccination programmes
A number of clinical trials, looking at either the prevention or treatment of COVID‐19 with vitamin D, are currently under way, and the main results are anticipated some time in 2021. One trial looking at whether vitamin D can prevent COVID‐19 is the CORONAVIT trial, an open‐label, phase 3, RCT conducted in the UK, investigating whether implementation of a test‐and‐treat approach to correct sub‐optimal vitamin D status results in reduced risk and/or severity of COVID‐19 and other acute respiratory infections (Clinicaltrials.gov, 2020a ). The trial is designed to recruit 6200 healthy individuals aged 16 years or older, and participants in the intervention group with low vitamin D status will be offered either 20 µg/day (800 IU/day) or 80 µg/day (3200 IU/day) of vitamin D3, whilst the control group receives standard care [national recommendation of 10 µg/day (400 IU/day) vitamin D]. The primary endpoint is the proportion of participants experiencing at least one doctor‐diagnosed or laboratory‐confirmed acute respiratory infection of any cause over 6 months. The secondary endpoints include a number of COVID‐19‐related endpoints, such as requiring hospitalisation due to COVID‐19, hospitalised for COVID‐19 requiring ventilatory support, and dying of COVID‐19, as well as other endpoints such as the proportion of participants who experience influenza requiring hospitalisation, dying of any cause, dying of influenza and dying of any acute respiratory infection (Clinicaltrials.gov, 2020a ).
Other trials are looking at the therapeutic benefit of high doses of vitamin D in people with COVID‐19. The CoVitTrial is a multicentre randomised trial of high dose versus standard dose vitamin D3 in high‐risk COVID‐19 patients based in France. It is recruiting 260 patients aged 65 years or older, diagnosed with COVID‐19 infection within the preceding 3 days and seen in a hospital, clinical consultation or nursing home setting (Clinicaltrials.gov, 2020b ). The trial compares a single high oral dose of 10 000 µg (400 000 IU) of vitamin D3 with a single lower oral dose of 1250 µg (50 000 IU) of vitamin D3. The primary endpoint is death from any cause during the first 14 days; secondary endpoints include death from any cause during the first 28 days and clinical evolution over 14 days and 28 days based on the World Health Organization (WHO) Ordinal Scale for Clinical Improvement for COVID‐19 (Clinicaltrials.gov, 2020b ).
The first COVIDIOL trial in Cordoba, Spain (Entrenas Castillo et al., 2020 ), included in the recent rapid review mentioned earlier, is being followed by a trial involving 1008 patients aged 18–90 years diagnosed with either COVID‐19 and radiological image compatible with inflammatory pleuropulmonary exudate or with onset of symptoms in the last 7 days and an uncomplicated respiratory infection for outpatient follow‐up (Clinicaltrials.gov, 2020c ). The intervention group will receive the best available treatment (which will include any combination of drugs included in the current protocol of the Ministry of Health and/or complementary notes issued by the Spanish Agency of Medicines and Health Products) plus oral calcifediol [25(OH)D] [2 capsules (532 µg/21 280 IU) on day 1 and 1 capsule (266 µg/10 640 IU) on days 3, 7, 14, 21 and 28], whereas the control group will receive the best available treatment only as described earlier (Clinicaltrials.gov, 2020c ). The primary endpoints are intensive care unit (ICU) admission and death within 28 days; secondary endpoints include time until admission to ICU with mechanical ventilation, time from onset of symptoms to discharge of patients in conventional hospitalisation, and time until mechanical ventilation is removed (Clinicaltrials.gov, 2020c ).
A trial investigating both the prevention and treatment of COVID‐19 with vitamin D is the Vitamin D for COVID ‐ 19 (VIVID) trial in the US. This is recruiting 1500 newly diagnosed individuals with COVID‐19 infection, together with up to one close household contact for each COVID‐19 patient (~1200 contacts), randomised to either vitamin D3 [loading dose of 240 µg/day (9600 IU/day) for day 1 and day 2, then 80 µg/day (3200 IU/day] or placebo in a 1:1 ratio and a household cluster design (study duration of 4 weeks) (Wang et al., 2021 ). The primary outcome is the occurrence of hospitalisation and/or mortality; key secondary outcomes include symptom severity scores among cases and changes in the infection (seroconversion) status (to help identify infection rates) for their close household contacts. Changes in vitamin D 25(OH)D levels will be assessed, and their relation to study outcomes will be investigated (Wang et al., 2021 ).
Worthy of consideration is that, since these trials were initiated, there has been a roll out of a large‐scale vaccination programme, especially in the UK in older and middle‐aged adults, and front‐line workers (NHS, 2021 ), which could potentially decrease the power of the trials by reducing the event rate (Proteomics & Metabolomics, 2021 ). However, vitamin D status has also been suggested to influence the effectiveness of vaccinations. A systematic review and meta‐analysis of nine studies (involving 2367 participants) found that individuals with low vitamin D status were less protected against two strains of influenza after having been vaccinated compared to those who had adequate vitamin D levels (Lee et al., 2018 ). Professor Adrian Martineau, Queen Mary University of London, the lead researcher of the CORONAVIT trial has said that he hopes vitamin D might improve the immune response to the COVID‐19 vaccination making it more effective, and that his team are investigating that possibility as a sub‐study within the trial (Proteomics & Metabolomics, 2021 ).
Public health implications of widespread low vitamin D status
Low vitamin D status is widespread in many countries and could be preventable by supplementation, especially in the winter months (Brenner, 2021 ; Griffin et al., 2020). In the UK, prior to SACN's advice in 2016, the government's advice was that only vulnerable groups ( e.g. young children, pregnant and lactating women, adults aged over 65 years and some ethnic minorities) should take vitamin D supplements to meet the recommended intakes set by COMA in 1991. Yet, the re‐emergence of nutritional rickets in young children in some groups of the population, as well as widespread low vitamin D status in the population as a whole, suggests that these recommendations were not being widely implemented (Buttriss, 2020 ). The most recent data published from the NDNS include the period following the new advice on vitamin D introduced in 2016 [years 9–11 of the rolling programme (2016/2017–2018/2019)]. Results show that mean vitamin D intakes from all sources (including supplements) were below the recommendations for all age groups (except for women aged 65–74 years), and that 19% of children aged 11–18 years, 16% of adults aged 19–64 years and 13% of adults aged 65 years and over, had low vitamin D status (PHE & FSA, 2020 ). However, there is some evidence of improvement in vitamin D status in children. Compared with years 7 and 8 (combined), the mean 25(OH)D concentration was 6.2 nmol/l higher in children aged 4–10 years in years 9–11 (combined). Consistent with this, the prevalence of deficiency in children aged 4–10 years was lower in years 9–11 (combined) (2%) compared with years 7 and 8 (combined) (10%), although this difference was not tested for statistical significance. There were no significant changes in mean 25(OH)D in the other age groups (PHE & FSA, 2020 ). Interestingly, women aged 65–74 years had the highest vitamin D supplement use, with 40% taking supplements compared to just 9% of children aged 11–18 years, 17% of adults aged 19–64 years and 32% of adults aged 65 years and over (PHE & FSA, 2020 ). These data suggest that people are still insufficiently aware of government advice on vitamin D supplementation and/or how to implement it (Buttriss, 2020 ).
The sample size of the NDNS is not large enough to explore sub‐group differences. However, the UK Biobank has been used to study regional, BMI‐related and ethnic minority differences in vitamin D status (Lin et al., 2021 ). The authors report that Asian ( n = 4297/8000, 53.7%) and Black ( n = 2459/7046, 34.9%) participants had a higher prevalence of vitamin D deficiency than White participants ( n = 50 920/422 907, 12%). Male sex, abnormal BMI (underweight/overweight/obese), non‐white ethnic backgrounds (Mixed/Asian/Black/Chinese/Other ethnicity), smoking, living in Scotland ( i.e . a more northerly latitude) and being more socioeconomically deprived were associated with higher risk of vitamin D deficiency (defined as <25 nmol/l) (Lin et al., 2021 ).
Although there are signs of improvement from the NDNS , compliance with current advice is far from widespread. This highlights the importance of healthcare professionals routinely raising awareness of the need for supplementation at every point of contact, especially in at‐risk groups. It has also been suggested that the need for somewhat complex and nuanced advice seems to have led to an oversimplified interpretation by some healthcare professionals, which may be leading to confusion about the detail of the government's recommendations (Buttriss, 2020 ; Buttriss et al., 2021 ). Over the past year, advice from government has become more streamlined (Table (Table1) 1 ) and this may be of help going forward. NICE's guidance on Vitamin D deficiency in adults – treatment and prevention has recently been updated which recommends that all adults living in the UK, including people at increased risk of vitamin D deficiency (NICE, 2020b ), should take a daily supplement containing 400 IU (10 µg) of vitamin D throughout the year, including in the winter months, but it is unclear if this advice is routinely given. Whilst the government has supplementation policies in place, a recent workshop concluded that there has been a lack of implementation strategies (Buttriss et al., 2021 ). Therefore, as part of a multi‐pronged approach to ensure that the government's vitamin D recommendations are actioned, it has been suggested that a fortification strategy to improve dietary intakes might be a consideration, especially if uptake of supplements remains low (Buttriss, 2020 ).
With regards to COVID‐19, some experts argue that the lack of good randomised trial data, particularly with respect to vitamin D supplementation and disease prevention, does not necessarily indicate that vitamin D supplementation should not be advised based on the precautionary principle that it does no harm, may be beneficial and improves bone health (Griffin et al., 2020; Vimaleswaran et al., 2021 ). An evidence synthesis report by The Royal Society on recommendations for vitamin D supplementation for the prevention of COVID‐19 suggests that vitamin D supplementation could be recommended based on indirect evidence just as the recommendations for social distancing and the wearing of masks have been (Griffin et al., 2020). Furthermore, even a small effect on protection from infection that may lower the COVID‐19 effective Reproduction number ( R ) from just above one (as estimated for many countries shortly before or during lockdown measures of varying intensity during most of the second half of 2020) to just below one could make the difference between further exponential growth or regression of the pandemic (Brenner, 2021 ). A position statement from the Spanish Society of Geriatrics and Gerontology on vitamin D supplementation for the prevention and treatment of COVID‐19 also recommends that its use should be standardised in clinical practice, despite the lack of evidence on specific doses of vitamin D to treat COVID‐19 in older adults. They argue that ‘… in an ideal world, health decisions must be made based on overwhelming evidence, but a time of crisis such as the current one may require a slightly different set of rules ’ (Tarazona‐Santabalbina et al., 2021 ).
Experts agree that regardless of whether vitamin D protects against COVID‐19, adequate levels are important for musculoskeletal health so current recommendations on taking vitamin D supplements should be widely promoted (Brenner, 2021 ; Griffin et al., 2020; NICE, 2020a , 2020b ). However, regarding safety, SACN reiterates the upper limits for vitamin D recommended by the European Food Safety Authority (EFSA), of 100 µg/day (4000 IU/day) for adults and children aged 11–17 years, 50 µg/day (2000 IU/day) for children aged 1–10 years and 25 µg/day (1000 IU) for infants (SACN, 2016 ).
Low vitamin D status particularly during the winter months remains commonplace around the world. This situation could be alleviated if supplementation policies designed to support musculoskeletal health were followed. It remains unclear whether vitamin D can protect against COVID‐19 although studies are exploring this hypothesis. Despite some media headlines, it is important that vitamin D (or any other nutrient, food or supplement) is never positioned as a ‘magic bullet’ against COVID‐19. During this unprecedented time, when people are constantly bombarded with information from the internet and social media and may be highly vulnerable to misinformation, it is vital that robust evidence‐based messaging is disseminated to avoid a scenario where people may be misled into believing that taking vitamin D supplements will prevent or treat COVID‐19 infection. Even if robust evidence emerges for vitamin D (or another nutrient), it should be considered in the context of the other established approaches to combat the disease, such as vaccines, social distancing, wearing of masks, keeping windows open and hygiene measures. The communication of nuanced messages, where the evidence‐base is less certain, is complex as it involves making a distinction between telling people that they should do something because it will make a difference versus telling people that they could do something that might help.
As the vaccination programme continues to be rolled out to more population groups, and is seen as a reliable action to bring an end to the pandemic, its effects could be maximised by ensuring the population has adequate nutrition and is taking vitamin D supplements as recommended, particularly those in at‐risk groups. Although, no one food or single nutrient can combat infections or support the immune system, following a healthy, dietary pattern that includes foods rich in vitamin D and other nutrients known to support the immune system, maintaining a healthy weight, as well as having a healthy lifestyle including regular physical activity, safe exposure to sunlight, stress management and adequate amounts of sleep are all important.
Conflict of interest
The authors received no direct financial contribution towards the production of this article. Funding to support the British Nutrition Foundation’s charitable aims and objectives comes from a range of sources including membership, donations and project grants from food producers and manufacturers, retailers and food service companies. Further information about the British Nutrition Foundation’s activities and funding can be found at www.nutrition.org.uk/aboutbnf/ .
- Al‐Yatama, F.I. , AlOtaibi, F. , Al‐Bader, M.D. & Al‐Shoumer, K.A. (2019) The effect of clothing on vitamin D status, bone turnover markers, and bone mineral density in young Kuwaiti females . International Journal of Endocrinology , 2019 , 1–10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bates, B. , Clifford, R. , Collins, D. , Cox, L. , Davidson, N. & Gay, C. et al. (2017b) National Diet and Nutrition Survey: results from years 1‐4 (combined) for Northern Ireland (2008/09–2011/12) . [Internet]. Available from: www.food.gov.uk/research/national‐diet‐andnutrition‐survey‐ndns/national‐diet‐and‐nutrition‐survey‐ndns‐report‐for‐northern‐ireland [Accessed 3rd March 2021]. [ Google Scholar ]
- Bates, B. , Lennox, A. , Prentice, A. , Bates, C. , Page, P. , Nicholson, S. et al. (2017a) National Diet and Nutrition Survey: results from years 1–4 (combined) for Scotland (2008/09‐2011/12) [Internet]. Available from: https://www.foodstandards.gov.scot/publicationsand‐research/publications/national‐diet‐and‐nutrition‐survey‐rolling‐programme‐results‐fromyears‐1‐4 [Accessed 3 March 2021]. [ Google Scholar ]
- BBC . (2020) Covid‐19: can ‘boosting’ your immune system protect you? By Zaria Gorvett, 9th April 2020 . Available from: https://www.bbc.com/future/article/20200408‐covid‐19‐can‐boosting‐your‐immune‐system‐protect‐you [Accessed 25 February 2021]. [ Google Scholar ]
- Berry, D.J. , Hesketh, K. , Power, C. & Hyppönen, E. (2011) Vitamin D status has a linear association with seasonal infections and lung function in British adults . British Journal of Nutrition , 106 ( 9 ), 1433–1440. [ PubMed ] [ Google Scholar ]
- Bouillon, R. (2019) Vitamin D status is worse in Africa than in other continents . Lancet , 8 , e20–e21. [ PubMed ] [ Google Scholar ]
- Brenner, H. (2021) Vitamin D supplementation to prevent COVID‐19 infections and deaths‐accumulating evidence from epidemiological and intervention studies calls for immediate action . Nutrients , 13 ( 2 ), 411. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Butler‐Laporte, G. , Nakanishi, T. , Mooser, V. , Morrison, D.R. , Abdullah, T. , Adeleyeet, O. et al. (2021) Vitamin D and COVID‐19 susceptibility and severity in the COVID‐19 Host Genetics 2 Initiative: a Mendelian randomization study . Available from: https://www.medrxiv.org/content/ 10.1101/2020.09.08.20190975v5.full.pdf [Accessed 10th March 2021]. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buttriss, J. (2020) Is a vitamin D fortification strategy needed? Nutrition Bulletin , 45 ( 2 ), 115–122. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Buttriss, J.L. , Lanham‐New, S.A. , Steenson, S. , Levy, L. , Swan, G.E. , Darling, A.L. et al. (2021) Implementation strategies for improving Vitamin D status and increasing Vitamin D intake in the UK: current controversies and future perspectives. Proceedings of the 2nd Rank Prize Funds Forum on Vitamin D . British Journal of Nutrition . Ahead of print. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Calder, P.C. (2020) Nutrition, immunity and COVID‐19 . BMJ Nutrition, Prevention & Health , 3 ( 1 ), 74–92. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Clinicaltrials.gov . (2020a) Trial of Vitamin D to reduce risk and severity of COVID‐19 and other acute respiratory infections (CORONAVIT) . Available from: https://clinicaltrials.gov/ct2/show/ {"type":"clinical-trial","attrs":{"text":"NCT04579640","term_id":"NCT04579640"}} NCT04579640 [Accessed 20th February 2021]. [ Google Scholar ]
- Clinicaltrials.gov . (2020b) COvid‐19 and Vitamin D supplementation: a multicenter randomized controlled trial of high dose versus standard dose Vitamin D3 in high‐risk COVID‐19 patients (CoVitTrial) . Available from: https://clinicaltrials.gov/ct2/show/ {"type":"clinical-trial","attrs":{"text":"NCT04344041","term_id":"NCT04344041"}} NCT04344041 [Accessed 20th February 2021]. [ Google Scholar ]
- Clinicaltrials.gov . (2020c) Prevention and treatment with calcifediol of COVID‐19 induced acute respiratory syndrome (COVIDIOL) . Available from: https://clinicaltrials.gov/ct2/show/ {"type":"clinical-trial","attrs":{"text":"NCT04366908","term_id":"NCT04366908"}} NCT04366908 [Accessed 20th February 2021]. [ Google Scholar ]
- Craveiro, V. , Cabral, M. , Araújo, J. , Falcão, H. , Guimarães, J. & Ramos, E. (2018) Association of serum 25‐hydroxyvitamin D concentration with pulmonary function in young adults . Nutrients , 10 , 1728. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Davies, N.M. , Holmes, M.V. & Davey Smith, G. (2018) Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians . British Medical Journal , 362 , k601. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Defra (Department for Environment, Food and Rural Affairs) . (2014) Consultation on revoking Regulation 4 of the Spreadable Fats (Marketing Standards) and Milk and Milk Products (Protection of Designations) (England) Regulations 2008 – margarine fortification: summary of response . Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/287673/margarine‐fortification‐sum‐resp‐201403.pdf [Accessed 11th March 2021]. [ Google Scholar ]
- DH (Department of Health) . (1991) Dietary reference values for food energy and nutrients for the United Kingdom . Report on Health and Social Subjects. Committee on Medical Aspects of Food Policy (COMA). [ PubMed ] [ Google Scholar ]
- DHSC (Department of Health and Social Care) . (2020) At‐risk groups to receive free winter supply of vitamin D . Available from: https://www.gov.uk/government/news/at‐risk‐groups‐to‐receive‐free‐winter‐supply‐of‐vitamin‐d [Accessed 20th February 2021]. [ Google Scholar ]
- Di Rosa, M. , Malaguarnera, M. , Nicoletti, F. , & Malaguarnera, L. (2011) Vitamin D3: a helpful immuno‐modulator . Immunology , 134 ( 2 ), 123–139. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- EC (European Commission) . (2021) EU Register of health claims . Available from: https://ec.europa.eu/food/safety/labelling_nutrition/claims/register/public/?event=register.home [Accessed 25th February 2021]. [ Google Scholar ]
- EFSA (European Food Safety Authority) . (2010) Scientific Opinion on the substantiation of health claims related to vitamin D and normal function of the immune system and inflammatory response (ID 154, 159), maintenance of normal muscle function (ID 155) and maintenance of normal cardiovascular function (ID 159) pursuant to Article 13(1) of Regulation (EC) No 1924/2006 . Available from: https://efsa.onlinelibrary.wiley.com/doi/ 10.2903/j.efsa.2010.1468 [Accessed 3rd March 2021]. [ CrossRef ] [ Google Scholar ]
- Entrenas Castillo, M. , Entrenas Costa, L.M. , Vaquero Barrios, J.M. , et al. (2020) “Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID‐19: A pilot randomized clinical study” . J Steroid Biochem Mol Bio , 203 , 105751. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ganji, V. , Al‐Obahi, A. , Yusuf, S. , Dookhy, Z. , & Shi, Z. (2020) Serum vitamin D is associated with improved lung function markers but not with prevalence of asthma, emphysema, and chronic bronchitis . Scientific Reports , 10 , 11542. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Griffin, G. , Hewison, M. , Hopkin, J. , Kenny, R. , Quinton, R. Rhodes, J. , Subramanian, S. , Thickett, D. (2020) Vitamin D and COVID‐19: evidence and recommendations for supplementation . R Soc Open Sci . 7 ( 12 ): 201912. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hastie, C.E. , Pell, J.P. & Sattar, N. (2021) Vitamin D and COVID‐19 infection and mortality in UK Biobank . European Journal of Nutrition , 60 ( 1 ), 545–548. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Heart.co.uk . (2020) This Morning doctor urges UK public to take Vitamin D to help fight coronavirus. 16 April 2020 . Available from: https://www.heart.co.uk/news/coronavirus/vitamin‐d‐immune‐system/ [Accessed 24th February 2021]. [ Google Scholar ]
- Hughes, D.A. & Norton, R. (2009) Vitamin D and respiratory health . Clinical & Experimental Immunology , 158 , 20–25. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- IOM (Institute of Medicine) . (2011) Dietary reference intakes for calcium and vitamin D . Washington, DC: The National Academes Press. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21796828 [Accessed 24th February 2021]. [ Google Scholar ]
- ITV News . (2021) Covid: should I take vitamin D? By Natalia Jorquera, 26 January 2021 . Available from: https://www.itv.com/news/2021‐01‐26/can‐vitamin‐d‐help‐in‐the‐fight‐against‐covid [Accessed 24th February 2021]. [ Google Scholar ]
- Jolliffe, D. , Camargo, C.A. , Sluyter, J. , Aglipay, M. , Aloia J.F., Ganmaa D. et al. (2021) Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta‐analysis of aggregate data from randomised controlled trials . Lancet Diabetes & Endocrinology , 9 ( 5 ), 276–292. [ PubMed ] [ Google Scholar ]
- Laaksi, I. (2012) Vitamin D and respiratory infection in adults . Proceedings of the Nutrition Society , 71 ( 1 ), 90–97. [ PubMed ] [ Google Scholar ]
- Lanham‐New, S.A. , Webb, A.R. , Cashman, K.D. , Buttriss, J.L. , Fallowfield, J.L. , Masud, T. et al. (2020) Vitamin D and SARS‐CoV‐2 virus/COVID‐19 disease . BMJ Nutrition, Prevention & Health , 3 ( 1 ), 106–110. 10.1136/bmjnph-2020-000089 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leaf, D.E. & Ginde, A.A. (2021) Vitamin D3 to treat COVID‐19: different disease, same answer . Journal of the American Medical Association , 325 ( 11 ), 1047–1048. 10.1001/jama.2020.26850 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee, M.‐D. , Lin, C.‐H. , Lei, W.‐T. , Chang, H.‐Y. , Lee, H.‐C. , Yeung, C.‐Y. et al. (2018) Does vitamin D deficiency affect the immunogenic responses to influenza vaccination? A systematic review and meta‐analysis . Nutrients , 10 ( 4 ), 409. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lewis, P.J. (2020) Sixty seconds on … vitamin D . British Medical Journal , 371 , m3872. [ PubMed ] [ Google Scholar ]
- Lin, L. , Smeeth, L. , Langan, S. , & Warren‐Gash, C. (2021) Distribution of vitamin D status in the UK: a cross‐sectional analysis of UK Biobank . British Medical Journal Open , 11 , e038503. 10.1136/bmjopen-2020-038503 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu, N. , Sun, J. , Wang, X. , Zhang, T. , Zhao, M. & Li, H. (2021) Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta‐analysis . International Journal of Infectious Diseases , 104 , 58–64. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lockyer, S. (2020) Effects of diets, foods and nutrients on immunity: implications for COVID‐19? Nutrition Bulletin , 45 ( 4 ), 456–473. [ Google Scholar ]
- Manousaki, D. , Mitchell, R. , Dudding, T. , Haworth, S. , Harroud, A. , Forgetta, V. et al. (2020) Genome‐wide association study for vitamin D levels reveals 69 independent loci . American Journal of Human Genetics , 106 , 327–337. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Martineau, A.R. , Jolliffe, D.A. , Hooper, R.L. , Greenberg, L. , Aloia, J.F. , Bergman, P. et al. (2017) Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta‐analysis of individual participant data . British Medical Journal , 356 , i6583. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mendes, M.M. , Charlton, K. , Thakur, S. , Ribeiro, H. & Lanham‐New, S.A. (2020) Future perspectives in addressing the global issue of vitamin D deficiency . Proceedings of the Nutrition Society , 79 ( 2 ), 246–251. [ PubMed ] [ Google Scholar ]
- Mirror . (2020) Strengthen your immune system against Covid with help of Vitamin D, zinc and pickles. By Jane Symons, 24 October 2020 . Available from: https://www.mirror.co.uk/lifestyle/health/strengthen‐your‐immune‐system‐against‐22898920 [Accessed 25th February 2021]. [ Google Scholar ]
- Murai, I.H. , Fernandes, A.L. , Sales, L.P. , Pinto, A.J. , Goessler, K.F. , Duran, C.S. et al. (2021) Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID‐19: a randomized clinical trial . Journal of the American Medical Association , 325 ( 11 ), 1053–1060. 10.1001/jama.2020.26848 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- NHS . (2020) Vitamin D . Available from: https://www.nhs.uk/conditions/vitamins‐and‐minerals/vitamin‐d/ [Accessed 9th March 2021]. [ Google Scholar ]
- NHS . (2021) Coronavirus (COVID‐19) vaccine . Available from: https://www.nhs.uk/conditions/coronavirus‐covid‐19/coronavirus‐vaccination/coronavirus‐vaccine/ [Accessed 24th February 2021]. [ Google Scholar ]
- NICE (National Institute for Health and Care Excellence) . (2020a) COVID‐19 rapid guideline: vitamin D . Available from: https://www.nice.org.uk/guidance/ng187/chapter/Context [Accessed 25th February 2021]. [ PubMed ] [ Google Scholar ]
- NICE (National Institute for Health and Care Excellence) . (2020b) Vitamin D deficiency in adults – treatment and prevention . Available at: https://cks.nice.org.uk/topics/vitamin‐d‐deficiency‐in‐adults‐treatment‐prevention/management/prevention/ [Accessed 12th March 2021]. [ Google Scholar ]
- Panagiotou, G. , Tee, S.A. , Ihsan, Y. , Athar, W. , Marchitelli, G. , Kelly, D. et al. (2020) Low serum 25‐hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID‐19 are associated with greater disease severity . Clinical Endocrinology (Oxf) , 93 ( 4 ), 508–511. 10.1111/cen.14276. Epub 2020 Aug 6. PMID: 32621392; PMCID: PMC7361912. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- PHE & FSA (Public Health England and the Food Standards Agency) . (2020) NDNS: results from years 9 to 11 (2016 to 2017 and 2018 to 2019 . Available from: https://www.gov.uk/government/statistics/ndns‐results‐from‐years‐9‐to‐11‐2016‐to‐2017‐and‐2018‐to‐2019 [Accessed 24th February 2021]. [ Google Scholar ]
- PHE (Public Health England) . (2020) Disparities in the risk and outcomes of COVID‐19 . Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/889861/disparities_review.pdf [Accessed 25th February 2021]. [ Google Scholar ]
- Proteomics & Metabolomics . (2021) Talking vitamin D and COVID‐19 with Professor Adrian Martineau . Available from: https://www.technologynetworks.com/proteomics/articles/talking‐vitamin‐d‐and‐covid‐19‐with‐professor‐adrian‐martineau‐344615 [Accessed 24th February 2021]. [ Google Scholar ]
- SACN (Scientific Advisory Committee on Nutrition) . (2016) Vitamin D and health . Available from: https://www.gov.uk/government/publications/sacn‐vitamin‐d‐and‐health‐report [Accessed 23rd February 2021]. [ Google Scholar ]
- SACN (Scientific Advisory Committee on Nutrition) . (2020b) Update of rapid review: vitamin D and acute respiratory tract infections . Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/945179/SACN_December2020_VitaminD_AcuteRespiratoryTractInfections.pdf [Accessed 24th February 2021]. [ Google Scholar ]
- SACN (Scientific Advisory Committee on Nutrition) . (2020a) Rapid review: vitamin D and acute respiratory tract infections . Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/944108/SACN_June2020_VitaminD_AcuteRespiratoryTractInfections.pdf [Accessed 25th February 2021]. [ Google Scholar ]
- Sassi, F. , Tamone, C. & D'Amelio, P. (2018) Vitamin D: nutrient, hormone, and immunomodulator . Nutrients , 10 ( 11 ), 1656. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schoenmakers, I. , Gousias, P. , Jones, K.S. & Prentice, A. (2016) Prediction of winter vitamin D status and requirements in the UK population based on 25(OH) vitamin D half‐life and dietary intake data . The Journal of steroid biochemistry and molecular biology , 164 , 218–222. [ PubMed ] [ Google Scholar ]
- Tarazona‐Santabalbina, F.J. , Cuadra, L. , Cancio, J.M. , Carbonell, F.R. , Garrote, J.M.P. , Casas‐Herrero. Á. et al. (2021) Vitamin D supplementation for the prevention and treatment of COVID‐19: a position statement from the Spanish Society of Geriatrics and Gerontology . Revista Española de Geriatría y Gerontología , 56 ( 3 ), 177–182. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- The COVID‐19 Host Genetics Initiative . (2020) The COVID‐19 Host Genetics Initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS‐CoV‐2 virus pandemic . European Journal of Human Genetics , 28 , 715–718. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- The Guardian . (2021a) Does vitamin D combat Covid? By Mattha Busby, 10 January 2021 . Available from: https://www.theguardian.com/lifeandstyle/2021/jan/10/does‐vitamin‐d‐combat‐covid [Accessed 25th February 2021]. [ Google Scholar ]
- The Guardian . (2021b) UK keeping research on link between vitamin D and Covid under review. By Mattha Busby, 5 February 2021 . Available from: https://www.theguardian.com/world/2021/feb/05/matt‐hancock‐orders‐third‐review‐on‐link‐between‐vitamin‐d‐and‐covid [Accessed 15th March 2021]. [ Google Scholar ]
- The Guardian . (2021c) Vitamin D supplements may offer no Covid benefits, data suggests. By Natalie Grover, 9 March 2021 . Available from: https://www.theguardian.com/world/2021/mar/09/vitamin‐d‐supplements‐may‐offer‐no‐covid‐benefits‐data‐suggests [Accessed 15th March 2021]. [ Google Scholar ]
- Vimaleswaran, K.S. , Forouhi, N.G. & Khunti, K. (2021) Vitamin D and covid‐19 . British Medical Journal , 372 , n544. [ PubMed ] [ Google Scholar ]
- Wang, R. , DeGruttola, V. , Lei, Q. , Mayer, K.H. , Redline, S. , Hazra, A. et al. (2021) The vitamin D for COVID‐19 (VIVID) trial: a pragmatic cluster‐randomized design . Contemporary Clinical Trials , 100 , 106176. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wise, J. (2020) Covid‐19: evidence is lacking to support vitamin D's role in treatment and prevention . British Medical Journal , 371 , m4912. [ PubMed ] [ Google Scholar ]
- Zdrenghea, M.T. , Makrinioti, H. , Bagacean, C. , Bush, A. , Johnston, S.L. & Stanciu, L.A. (2017) Vitamin D modulation of innate immune responses to respiratory viral infections . Reviews in Medical Virology , 27 , 1–3. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
An estimated one third or more of U.S. adults 60 years of age or older take vitamin D supplements, not including those who take multivitamins or other compounds containing vitamin D.1 Yet controver...
A new study finds vitamin D supplements with or without omega-3s decreased the risk of autoimmune diseases by 22 percent compared to placebo. ... VITAL is a randomized, double-blind, placebo-controlled research study of 25,871 men (age 50 and older) and women (age 55 and older) across the U.S., conducted to investigate whether taking daily ...
Feb. 25, 2022 — New research has found significant differences between the two types of vitamin D, with vitamin D2 having a questionable impact on human health. However, the study found that ...
A new meta-analysis of 52 RCTs including a total of 75,454 participants concluded that vitamin D (either vitamin D 3 or D 2) supplementation did not change mortality (RR 0.98, 95% CI 0.95-1.02 ...
Randomized clinical trials (RCTs) of vitamin D supplementation were mostly designed to test vitamin D dosage. Heaney's guidelines for clinical studies of nutrient effects 2,3 showed that vitamin ...
The novel coronavirus severe acute respiratory syndrome (SARS-CoV-2) has progressed rapidly from an outbreak to a global pandemic, with new variants rapidly emerging.Coronavirus disease 2019 (COVID-19), the disease resulting from SARS-CoV-2 infection, can lead to multiorgan damage. Due to the extremely contagious and fatal nature of the virus, it has been a priority of medical research to find ...
If these guidelines are not fulfilled in healthy children aged 4-10 years, supplementation of cholecalciferol in dose 600-1000 IU/day (15-25 µg/day) is recommended throughout the year, based on body weight and the dietary vitamin D intake. (4) In healthy children aged 1-10 years, calcifediol is not recommended. 4.3.
The second Special Issue of Nutrients dedicated to "Vitamin D, Immune Response, and Autoimmune Diseases" will include original data and recent achievements from authors who would like to participate in this research topic. Vitamin D 3 (cholecalciferol) is a secosteroid hormone that derives mostly from exposure of the body to the sun and ...
New research finds vitamin D may metabolize differently in those considered overweight, resulting in diminished health benefits. The study, which appears in JAMA Network Open, is a new analysis of data from the VITAL trial, a large nationwide clinical trial led by Brigham and Women's Hospital researchers that investigated whether taking vitamin D or marine omega-3 supplements could reduce ...
Getting enough vitamins and minerals is important for your health, and there's a long list of essential ones. Vitamin D is one you may hear a lot about. It helps your body absorb calcium, a mineral your body needs to build strong bones. Your heart, muscles, and nerves also need vitamin D. Even your immune system uses vitamin D to fight off germs.
Through ongoing research, Manson has found that adults who take either moderate or high-dose daily vitamin D supplements of at least 1,000 IU haven't had a reduced risk for having a heart attack, stroke, or cardiovascular-related death compared to adults taking a placebo without vitamin D. This research, which has been supported by the NIH ...
A study of nearly 26,000 people who were assigned to take vitamin D each day found the vitamin had no effect, even among people who had low vitamin D levels or osteoporosis. MShieldsPhotos/Alamy ...
Objective To investigate whether supplementing older adults with monthly doses of vitamin D alters the incidence of major cardiovascular events. Design Randomised, double blind, placebo controlled trial of monthly vitamin D (the D-Health Trial). Computer generated permuted block randomisation was used to allocate treatments. Setting Australia from 2014 to 2020. Participants 21 315 participants ...
New study sheds light on vitamin D's role in cardiovascular health. In a recent study published in the journal Nutrients, researchers conducted a prospective population-based analysis to ...
The fat soluble vitamin has a slew of important functions and vitamin D health benefits, from supporting immunity and healthy bones to improving mood. But new research shows that it may have other ...
Learn more about the research on vitamin D and specific health conditions and diseases: ... Lanham-New SA. Vitamin D deficiency as a public health issue: using vitamin D 2 or vitamin D 3 in future fortification strategies. Proceedings of the Nutrition Society. 2017 Aug;76(3):392-9.
New research published in Neuropsychopharmacology Reports now indicates that taking probiotics plus vitamin D supplements may improve cognitive function in individuals with the disease. For the ...
1. Introduction. Due to the interest in immune health prompted by the pandemic and its lasting effects on mental health and sleep disturbances, melatonin (N-acetyl-5-methoxytryptamine) has become a popular topic of media discussion as well as a research interest, with several publications steadily rising every year.In conjunction with the plethora of scientific discoveries, there has been ...
Vitamin D supplementation may decrease pain intensity in patients with painful menstrual cramps, according to a new systematic review and meta-analysis. Writing in the journal Nutrients , researchers from Taiwan evaluated the effect of vitamin D supplementation in 687 menstruating females across 11 studies by measuring pain score reduction.
New study looks at benefits of vitamin D supplements for healthy people. In the large randomized controlled trial, researchers tested whether 2000 IU (international units) per day of vitamin D3 ...
Over the course of three years, 8,851 schoolchildren aged 6-13 living in Mongolia received a weekly oral dose of vitamin D supplementation. 95.5% of participants had vitamin D deficiency at baseline, and study supplements were highly effective in boosting vitamin D levels into the normal range. However, they had no effect on fracture risk or on ...
New genetic study finds a direct link between dementia and a lack of vitamin D. Dementia is diminished cognitive functioning with a loss of ability to remember, think, solve problems, or make decisions — if it has progressed to the point that it interferes with doing everyday activities. It is a broad term, rather than a specific disease.
Vitamin D is widely known for its role in supporting immunity and bone health. New research suggests that supplementing with vitamin D may reduce the risk of heart attacks and other cardiovascular ...
New research published in Neuropsychopharmacology Reports now indicates that taking probiotics plus vitamin D supplements may improve cognitive function in individuals with the disease. For the study, 70 adults with schizophrenia were randomized to take a placebo or probiotic supplements plus 400 IU vitamin D daily for 12 weeks. ...
A great deal has been learnt but COVID‐19 is still a relatively new disease and research into preventative measures and treatments continues to evolve. ... The most recent data published from the NDNS include the period following the new advice on vitamin D introduced in 2016 [years 9-11 of the rolling programme (2016/2017-2018/2019)].
New research published in Neuropsychopharmacology Reports now indicates that taking probiotics plus vitamin D supplements may improve cognitive function in individuals with the disease. For the study, 70 adults with schizophrenia were randomized to take a placebo or probiotic supplements plus 400 IU vitamin D daily for 12 weeks.
4. Line 24 - It's mentioned that "several studies have found an association" but only 1 citation is listed. 5. "Not genetic mechanisms" probably should be more appropriately labeled. 6. Line 50 states "many papers have showed" but only one is cited. 7. Line 105 and 107 - I believe the abbreviation is (T2DM). 8.
There's a good bit of research to back up Dr. Serwer's recommendation to try to hit those vitamin D daily recommendations. For instance, research published in Clinical Nutrition in 2020 pointed ...