Amazon Prime includes:
Fast, FREE Delivery is available to Prime members. To join, select "Try Amazon Prime and start saving today with Fast, FREE Delivery" below the Add to Cart button.
- Cardmembers earn 5% Back at Amazon.com with a Prime Credit Card.
- Unlimited Free Two-Day Delivery
- Streaming of thousands of movies and TV shows with limited ads on Prime Video.
- A Kindle book to borrow for free each month - with no due dates
- Listen to over 2 million songs and hundreds of playlists
- Unlimited photo storage with anywhere access
Important: Your credit card will NOT be charged when you start your free trial or if you cancel during the trial period. If you're happy with Amazon Prime, do nothing. At the end of the free trial, your membership will automatically upgrade to a monthly membership.

Buy new: $746.00
Return this item for free.
Free returns are available for the shipping address you chose. You can return the item for any reason in new and unused condition: no shipping charges
- Go to your orders and start the return
- Select the return method

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player

Research Anthology on Mental Health Stigma, Education, and Treatment, VOL 1
Purchase options and add-ons.
- ISBN-10 1668433346
- ISBN-13 978-1668433348
- Publisher Medical Information Science Reference
- Publication date March 31, 2021
- Language English
- Dimensions 8.5 x 1 x 11 inches
- Print length 456 pages
- See all details

Product details
- Publisher : Medical Information Science Reference (March 31, 2021)
- Language : English
- Hardcover : 456 pages
- ISBN-10 : 1668433346
- ISBN-13 : 978-1668433348
- Item Weight : 2.94 pounds
- Dimensions : 8.5 x 1 x 11 inches
Customer reviews
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
No customer reviews
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Start Selling with Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Host an Amazon Hub
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices

About database About data repository
Research Anthology on Mental Health Stigma, Education, and Treatment
For full functionality of this site it is necessary to enable JavaScript. Here are the instructions how to enable JavaScript in your web browser .
This site uses cookies to make them easier to browse. Learn more about how we use cookies .
Advertisement
Interventions to Reduce Stigma Related to Mental Illnesses in Educational Institutes: a Systematic Review
- Review Article
- Open access
- Published: 05 May 2020
- Volume 91 , pages 887–903, ( 2020 )
Cite this article
You have full access to this open access article
- Ahmed Waqas ORCID: orcid.org/0000-0002-3772-194X 1 ,
- Salma Malik 2 ,
- Ania Fida 3 ,
- Noureen Abbas 4 ,
- Nadeem Mian 5 ,
- Sannihitha Miryala 6 ,
- Afshan Naz Amray 7 ,
- Zunairah Shah 8 &
- Sadiq Naveed 9
21k Accesses
40 Citations
7 Altmetric
Explore all metrics
This investigation reviews the effectiveness of anti-stigma interventions employed at educational institutes; to improve knowledge, attitude and beliefs regarding mental health disorders among students. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist guidelines were followed and protocol was registered in PROSPERO (CRD42018114535). Forty four randomized controlled trials were considered eligible after screening of 104 full-text articles against inclusion and exclusion criteria.
Several interventions have been employed to tackle stigma toward psychiatric illnesses, including education through lectures and case scenarios, contact-based interventions, and role-plays as strategies to address stigma towards mental illnesses. A high proportion of trials noted that there was a significant improvement for stigma (19/25, 76%), attitude (8/11, 72%), helping-seeking (8/11, 72%), knowledge of mental health including recognition of depression (11/14, 78%), and social distance (4/7, 57%). These interventions also helped in reducing both public and self-stigma. Majority of the studies showed that the anti-stigma interventions were successful in improving mental health literacy, attitude and beliefs towards mental health illnesses.
Similar content being viewed by others

Promoting Gender Equality: A Systematic Review of Interventions
Michaela Guthridge, Maggie Kirkman, … Melita J. Giummarra

Insiders’ Insight: Discrimination against Indigenous Peoples through the Eyes of Health Care Professionals
Lloy Wylie & Stephanie McConkey

What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review
Antonia Aguirre Velasco, Ignacio Silva Santa Cruz, … Sarah Rowe
Avoid common mistakes on your manuscript.
Introduction
Mental health disorders are prevalent worldwide, with detrimental personal, social and financial consequences [ 1 ]. It is estimated that adult mental and substance disorders account for 7% of all global burden of diseases and 19% of all years lived with disability [ 2 ]. Overall, mental health illnesses account for 16% of the global burden of disease and injury in people aged 10–19 years, with suicide being the third leading cause of deaths in adolescence [ 2 ]. Adolescents with behavioral disorders are particularly vulnerable to social exclusion and stigma, educational difficulties, overall poor health and risk-taking behaviors (e.g. sexual risk taking, substance use and aggression) [ 3 ]. Despite their presentation as a major public health concern, these conditions often go undetected and untreated. And individuals with mental health disorders report distress and poor access to healthcare due to fear of stigma, prejudice and discrimination in the society [ 3 ]. Among adolescents especially, the prevalent stigma in the educational setting, can exacerbate loneliness and isolation, often associated with suicidal behaviors [ 3 ].
Stigma, in general, is conceptualized as a feeling of disgrace, shame, and self-blame that results in social exclusion, isolation, and embarrassment [ 4 ]. Elliot et al., report that branding of individuals with mental illnesses is often associated with deviance, dangerousness and social illegitimacy [ 5 ]. These individuals, therefore, experience “label avoidance” restricting help-seeking and fearing negative reactions from others [ 4 ]. These stigmatizing perceptions toward individuals with mental illnesses can manifest in discriminatory forms such as withholding access to care, coercive treatment, avoidance, and segregated institutions ( structural stigma ) [ 6 ]. Thus, these individuals are burdened by the distress of their symptoms and the distress of the stigma.
The stigma is often divided in two forms; public stigma and self-stigma [ 6 ]. Public stigma is described as the attitude and reaction of general population towards people with mental illnesses while self-stigma corresponds to the internalized shame, guilt and poor self-image caused by acceptance of the societal prejudice [ 6 ]. Unfortunately, stigma towards mental illnesses is prevalent among all strata of our society including medical professionals [ 6 ]. This stigma is often aggravated by the stereotypical and prejudiced portrayal of mental illnesses in the media. Empirical investigations on media reporting suggest that individuals with mental illnesses are shown as deviants: “homicidal maniacs”, weaker individuals, and one with childlike perceptions [ 6 ]. Mental health illnesses and associated stigma lead to a vicious cycle resulting in poor access to mental and physical healthcare, decreased life expectancy, social exclusion in form of academic termination, unemployment, poverty, homelessness, and contact with criminal justice systems [ 7 ].
The issue of stigma toward mental illnesses is even more complex among adolescents- According to De-Luca, research in this domain is scarce (accounting for 3% of research) [ 8 ]. It is important to understand it among youth, delineate processes and barriers especially mental health attitudes and knowledge and help-seeking behaviors [ 8 ]. This is especially important because adolescence is a crucial period in an individual’s psychosocial and emotional development. At this age, the need for peer approval and inclusive social networks dictate how an adolescent cope with the double burden of mental health problems and rejection from classmates [ 8 ]. Understanding the dynamics of stigma and effects of peer perception in educational settings on identity development of the youth with mental illnesses is particularly important. This has been found to be a significant barrier in over 68% of the countries globally in a survey conducted by the World Health Organization (WHO) [ 8 ].
The WHO explicitly recommends developing programs to improve stigma and psychiatric outcomes. Recent reviews examining anti-stigma interventions in high-income countries, have shown short-term improvement in knowledge, awareness and in attitude towards mental health illnesses [ 9 ]. Studies measuring long-term effectiveness (beyond four weeks) suggested improvement in attitude and knowledge but these benefits could not translate into improvement in behavioral outcomes [ 9 ]. However, there have been fewer to no evidence synthesis efforts for educational institute -based interventions especially in the low- and middle-income countries (LMIC). Therefore, to address this paucity of data, the present review aims to summarize evidence pertaining to anti-stigma interventions for mental illnesses in educational institutes.
This systematic review follows the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist [ 10 ]. Its protocol was registered apriori in PROSPERO (CRD42018114535).
Operational Definitions
Using the framework of consensus study report on The Evidence for Stigma Change , we defined public stigma as societal reaction to an individual’s mental illness [ 11 ]. We included evidence pertaining to all the societal groups irrespective of education, socioeconomic strata or occupation. Self-stigma was defined as internalized feelings of shame, guilt and worthlessness in reaction to societal stigma [ 11 ].
Search Process
To gain an understanding of these interventions in a broader scope, we did not limit ourselves to specific psychiatric diagnoses, and made use of general search terms pertaining to psychiatric illnesses. However, we also included several terms pertaining to common mental disorders among adults and pediatric population to ensure none of the disorders important in the context of global mental health are missed. Eight academic databases including CINAHL, PubMed, Cochrane Library, Global Health Library, Virtual Health Library, POPLINE, Psycarticles, and Psycinfo and Web of Science, were searched on September 17th, 2018, using search terms noted in Table 1 . No restrictions or database filters were applied regarding language, time period or publication year. The database search was also augmented by manual searching of bibliography of eligible studies.
Study Selection
After automated removal of duplicates from bibliographic records using Endnote, we scrutinized their titles and abstracts against our pre-specified inclusion and exclusion criteria. The full texts of eligible titles identified in this phase were further scrutinized against the eligibility criteria. This phase was performed by two reviewers working independently from one another, under supervision of a senior reviewer.
We included all randomized controlled trials (RCTs) assessing the effectiveness of interventions or campaigns in educational institutions (schools, colleges, universities), that were primarily aimed to reduce stigma related to psychiatric disorders. No restriction of age, language, race, gender, ethnicity, geographic location, publication year will be applied. We did not consider any interventions which were not conducted in context of academic institutions.
Data Extraction & Analysis
Data extraction pertaining to eligible studies was performed using a standardized template by one reviewer, including bibliographic details, institutional and regional affiliations, characteristics of the study sample, and characteristics of interventions. Characteristics of study sample included the characteristics of the population of interest, age and geographical scope. While the characteristics of intervention focused on the targeted diagnosis, names of scales utilized to assess stigmatizing attitudes toward mental illnesses, and the primary outcomes measured. The interventions were stratified in three groups, according to their deliver agents: medical doctors, nurses, and psychology professionals. We also classified the interventions according to their theoretical orientations and noted the content of interventions. Later, a careful analysis of the theoretical orientation and content of interventions by the senior authors, based on an adapted version of matching and distillation framework. This enabled us to unpack these interventions into common elements or strategies employed.
Risk of bias in the studies was assessed using the Cochrane’s tool for assessment of risk of bias in RCTs across several matrices: a) randomization procedure b) allocation concealment c) blinding of participants and personnel d) blinding of outcome assessors e) attrition bias f) Other biases. Data extraction and quality assessment were performed by two independent reviewers and any disagreement were resolved by discussion or the guidance of senior reviewer. Unfortunately, due to methodological and statistical heterogeneity, we deferred the application of meta-analysis, to yield the pooled effectiveness of these interventions in reduction of stigma towards mental illnesses.
Our academic searches yielded a total number of 978 non-duplicate references, which were screened for eligibility based on their titles and abstracts. Out of these, 104 full texts were retained after exclusion of 868 citations. Thereafter, 44 RCTs s were deemed eligible after a careful review of their full texts, against the inclusion and exclusion criteria set apriori. Detailed results have been presented in PRISMA flow diagram (Fig. 1 ).
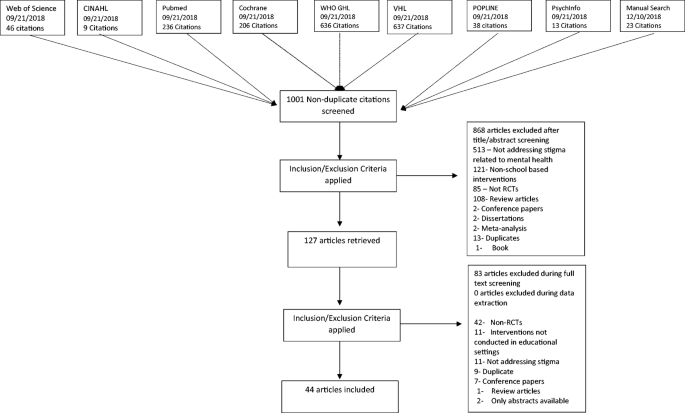
PRISMA Flow Diagram
Study Characteristics
The eligible publications were published between the years 1998 and 2018. A majority of these interventions were conducted in high income countries and regions including USA ( n = 15), Australia ( n = 7), Greece ( n = 4), UK ( n = 3), Germany (n = 1), Canada (n = 1), Portugal (n = 1), Taiwan (n = 1), Hong Kong (n = 1), Spain (n = 1), Japan ( n = 2), and Korea (n = 1). While only 6 studies were conducted in upper and lower middle-income countries including China (n = 2), Russia ( n = 2) Nigeria (n = 1) and Brazil (n = 1). Low income countries did not contribute to any RCTs in this domain.
Setting & Delivery of Interventions
Most of the evidence was from RCTs conducted in the context of urban settings ( n = 27), followed by mixed settings ( n = 5), suburban (n = 4), and rural (n = 1). The geographical region was unspecified in seven studies. A higher proportion of interventions ( n = 20) were conducted in school settings (primary school, secondary schools, high school). This was followed by graduate schools/university setting ( n = 6), undergraduate and graduate students enrolled in psychology courses (n = 5), non-psychology undergraduate setting ( n = 3), and adult schools (n = 2). Six studies were conducted in medical schools (n = 3) and nursing schools (n = 3). Among these studies, 25 were conducted in adults or predominantly adult population, 18 in adolescents or predominantly adolescent population, and one in children. The age ranged varied widely with lowest mean age of 13 years [ 12 ] and highest was 43.1 years [ 13 ].
Quality Rating
Random sequence generation was at a high/unclear risk of bias among 22 trials and allocation concealment (29 RCTs). Frequencies of studies reporting a high risk/unclear across other domains of Cochrane risk of bias tool were: blinding of outcome assessors ( n = 35), blinding of participants and personnel ( n = 31), attrition bias ( n = 14), other sources of bias ( n = 5), and selective reporting ( n = 1). A total of 35 studies were rated as having a high risk of overall bias i.e. ≥ 3 matrices of risk of bias tool were rated as having unclear or high risk of bias for these studies (Figs. 2 and 3 ). Figure 2 presents a clustered bar chart exhibiting frequencies of high, unclear and low risk bias across all matrices of Cochrane risk of bias tool.

Risk of Bias Graph

Mental health conditions targeted in stigma reduction interventions
Mental Health Conditions
Mental health illnesses, in general, were the target of these interventions in 24 studies whereas six studies targeted depression. Other targeted diagnoses were psychosis and schizophrenia ( n = 6), autism spectrum disorder ( n = 2), anxious-ambivalent attachment ( n = 1), anorexia nervosa (n = 1), and suicide (n = 1). One study focused on both depression and Tourette syndrome whereas one study addressed depression and schizophrenia. One intervention addressed engagement in psychotherapy treatment. A summary of mental health condition targeted is mentioned in fig. 3 .
Intervention Characteristics
Delivery agents of interventions included researchers ( n = 17), specialist psychiatrists, and psychologists ( n = 7), trained mental health professionals (n = 6), school teachers/course instructors ( n = 4), graduate students ( n = 2), and peers with lived experiences (n = 2) and researchers and teachers as delivery agent (n = 1). This information was missing for five studies. Numbers of sessions ranged from 1 to 8 sessions where a high proportion of interventions ( n = 25) were delivered in only one session. The numbers of sessions were unspecified in seven studies. Studies delivered the following number of interventions: two sessions(n = 4), three session (n = 4), four sessions (n = 1) and six sessions (n = 2) and eight sessions (n = 1). The duration for whole program was categorized into studies with duration of one day ( n = 11), one day to one week ( n = 8), one to four weeks ( n = 3), and longer than one month ( n = 20). The duration was not mentioned in one study [ 14 ] while another study had mixed duration depending on the type of intervention employed [ 15 ]. The longest duration of an intervention was 48 weeks [ 16 ]. The duration for each session varied from 20 min to 12 h.
Strategies & Elements of Interventions
These stigma reduction interventions constituted several different strategies as summarized in fig. 4 , most common of which were psychoeducation through lectures and discussion with mental health professionals and use of case vignettes and scenario-based interventions. Psychoeducation was also delivered via online platforms including website messages, video-based instructions, and educational short messaging service (SMS). Another important strategy highlighted in this review was contact-based learning where two most important intervention elements were role play and contact-based learning with individuals struggling with mental illnesses. The included interventions used either one teaching method or a mix of the above-mentioned.

Summary of strategies employed in stigma reduction interventions
Psychoeducation
Psychoeducation was employed in 25 studies using a variety of delivery techniques, mostly based on etiological models of psychiatric illnesses. These interventions educated participants about different attributes of mental health disorders such as epidemiological factors, clinical features, course of illnesses, and available treatment options. They were delivered through didactic lectures [ 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ], photographic images of billboard messages [ 14 ], short educational messages [ 25 , 26 ], video messages [ 27 ], structured courses and workshops for students [ 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ], and distribution of booklets and slideshows [ 29 ]. Some of authors utilized a multimodal approach for delivering their interventions, for instance, Papish et al. (2013) structured a course on different mental illnesses using teaching methods such as didactic teaching, case-based teaching with group discussions, and an optional movie night [ 28 ]. Pereira and colleagues (2014) used a mixed approach by using tutorials, videos, interactive discussion, web conference, and written text support to educate participants [I3]. A few of these interventions provided an overview of etiology of mental health disorders; biogenetic, biochemical, neurobiological, biopsychosocial, and contextual factors. Banntanye et al. [ 17 ] formulated an educational intervention based on genetic and heritability of mental health disorders as well as a biopsychosocial model involving a complex interplay of biological, social, and psychological factors [ 17 ]. Two more models were part of several interventions, for instance, the contextual model linked complicated life situations with etiology of mental health disorders and biomedical factors where neurochemical changes in the brain were studied as a cause of psychiatric disorders [ 30 ]. Using a similar model, Han and colleagues presented neurobiological factors as a cause of mental health disorders, in their interventions [ 19 ].
Bespoke Multimodal Stigma Reduction Interventions
Three studies used Mental Health First Aid (MHFA) [ 31 , 32 , 33 ] as a structured training module to address risk factors and clinical features of common mental health disorders including depression, anxiety, substance use disorders, psychosis, and eating disorders. This intervention program also educated participants on strategies to assist someone experiencing mental health crises. Two interventions tested the effectiveness of health education tools, the fotonovlea or Secret Feelings that addressed misconceptions and stigmatizing attitudes through posed photographs, captions, and soap opera narratives [ 34 , 35 ]. The Same or Not Same intervention focused on education about schizophrenia followed by an opportunity to contact with individuals struggling with schizophrenia. In the Video-Education Intervention, a video was followed by educational message. In this intervention, there was information about the cause, timeline, course of illness, and different myths [ 36 ]. In a classroom-based intervention used in two studies, projective cards were used to understand misperceptions about mental illnesses and discussion to overcome these misperceptions was carried out. In last part, patient’s narratives and role of media were also added [ 37 , 38 ].
Case vignettes or scenario-based techniques were employed in six interventions to enhanced understanding of different aspects of mental health disorders [ 15 , 39 , 40 , 41 , 42 , 43 ]. Mann et al. evaluated change in stigmatizing attitudes by comparing scenario-based teaching to provide an opportunity to read education material on mental illnesses [ 15 ]. Similar intervention was carried out by using case vignettes [ 40 ] and documentary film [ 42 ] to address stigma. In another intervention, participants were delivered a lecture on schizophrenia whereas second group had a scenario-based activity of four individuals with schizophrenia in remission [ 39 ]. It highlights the living arrangements, daily activities, needs, interests and social support system of individuals with schizophrenia [ 39 ]. Nam and colleagues (2015) used documentary to create stigma manipulating scenarios among college students with anxious-ambivalent attachment [ 42 ]. In another study, the intervention group received didactic lectures regarding factual knowledge about mental health and illness followed by case vignettes. The myths associated with mental illness, positive attitudes toward persons with mental illness, and resources to receive mental health care were examined during a group activity [ 43 ].
Contact-based interventions were assessed in 10 studies by using direct interaction with patients [ 12 , 44 , 45 , 46 , 47 , 48 , 49 , 50 ] and filmed or video techniques [ 12 , 45 , 48 , 51 , 52 ]. In an intervention, two service users on DVD described personal view of mental health and stigma followed by fact-based experience in nine key areas related to mental health disorders [ 45 ]. In Live intervention group, this exercise was conducted in live sessions whereas the control interventions delivered information about mental health and related stigma through a lecture [ 45 ]. In Our Own Voice (IOOV) , two group facilitators with history of mental health disorders addressed five components including “Dark Days, Acceptance, Treatment, Coping Mechanism, and Success. It also had corresponding videotaped sessions for each component [ 46 , 47 ]. The eBridge intervention was structured on personalized feedback about symptoms in individuals with history of suicidal behaviors along with access to resources based on the principles of motivational interviewing [ 53 ]. Self-affirmation psychotherapy was provided in a study by Lannin and colleagues [ 54 ]. In this program, an individual with mental illness is advised to repeat a positive statement or set of such statements about the self on a regular basis to inspire positive view of the self and reduce negative thinking, or low self-esteem [ 54 ]. Chisholm and colleagues (2016) work especially among adolescents concluded that educational interventions provide far more promising results than contact-based interventions [ 44 ]. Although not consistent with previous literature reporting this comparison [ 44 ], Chrisholm et al., argue for a different teaching approach for adolescents keeping in view their level of maturation, influence of the media, and that the information processing and understanding of mental illnesses differ among adolescents, as proposed in several conceptual frameworks [ 44 ].
The eligible studies reported effectiveness of these intervention on a heterogeneous body of scales, which measured stigma toward psychiatric illnesses, pre and post knowledge among participants, attitudinal and intentional changes, and recognition of psychiatric symptomatology. Moreover, help-seeking practices were also measured in these interventions. A lot of importance was placed on public stigma rather than self-stigma. The most frequent outcome was stigma ( n = 25), followed by changes in knowledge levels (n = 25), attitude ( n = 11), help-seeking (n = 11), social distance ( n = 9), and recognition and literacy regarding depression ( n = 5). Majority of studies reported an improvement in stigmatizing attitudes towards mental health disorders with improvement in both public and self-stigma (Fig. 5 ).
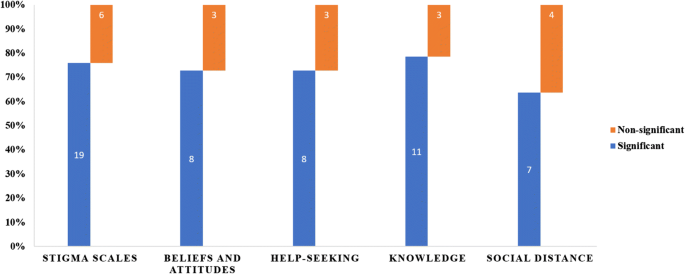
Proportion of studies demonstrating reduction in stigma related outcomes
Among 25 studies addressing stigma, where a higher proportion ( n = 19) studies reported a significant improvement in stigma levels at the study endpoint. In a study, comparing biogenetic intervention with a multifactorial intervention, there was no difference among both intervention groups from baseline line to study endpoint [ 17 ]. However, there was a significant improvement among these intervention groups from the control group. While deciphering between personal and public stigma, five studies reported stigma-related outcomes for these two concepts (personal = 3, public = 2) with only one study showing non-significant improvement [ 33 ]. Another study saw improvement at the first timepoint, but it failed to last until second visit. Out of five studies showing non-significant or no improvement, three reported non-significant change [ 14 , 26 , 40 ] whereas two reported no change from baseline to study endpoint [ 23 , 47 ].
The study on biological anti stigma intervention by Boucher and colleagues (2014) attributed non-significant improvement in stigma scores to the conceptualization of depression in as a brain disease whereas depression results from various biolopsychological factors [ 14 ]. Two studies using psychoeducation as a tool of change pointed out that lack of significant improvement in stigma is possibly due to sole use of educational interventions [ 23 , 26 ]. Pinto-Foltz and colleagues had a smaller sample size resulting in the lack of significant improvement in stigma scores [ 47 ].
Beliefs and Attitudes
The attitude was reported in 11 studies with improvement in eight studies at the study endpoint compared to baseline. One study reported improvement in authoritarianism and social restrictiveness (sub-scales of Community Attitudes Toward Mental Illness scale) while benevolence and community mental health ideology subscales failed to show significant improvements [ 42 ]. In remaining three studies, there was non-significant or lack of improvement. The duration of program has limited impact on the favorable results as one intervention had duration of three days [ 43 ]. The two other studies had duration of one [ 24 ] and eight weeks [ 32 ]. Winkle et al. (2017) reported small effect size for flyer or control group and medium effect size for the experimental group [ 22 ]. After a psychiatry clerkship, medical students reported improvement in stigmatizing attitudes but there was no improvement in attributions regarding responsibility and readiness to provide care to patients with mental illnesses [ 50 ]. Moreover, the lack of educational intervention may not be sufficient to change beliefs [ 26 , 36 ]. This underscores the need to strengthen medical school clerkships as well as enhancing the ways to interact with this patient population.
Help-Seeking
Intention and attitude to seek help were reported in 11 studies with improvement in eight studies. One study reported similar improvement among the intervention and control groups because the control group also received psychoeducation through brochures on depression [ 35 ]. In remaining three studies, there was non-significant or lack of improvement post-intervention [ 23 ]. In a rural-area based study, there was improvement in stigma and attitudes but it failed to materialize this change into help-seeking behaviors [ 23 ]. It is worth noting that adolescents in rural areas were more likely to turn to family and friends than seeking help from professionals such as school counselors [ 23 ]. In another study, the lack of improvement was regarded to inadequate dosage or duration of the program among adolescents [ 29 ]. The causation of depression as “neurological disease” was also a barrier and may have prevented college students from seeking help [ 14 ].
Knowledge of Mental Health Disorders and Treatment
The knowledge of mental health disorder and treatment was assessed in nine studies and depression literacy in five studies. Out of these 14 studies, 11 reported significant improvement in help-seeking with no improvement in three studies. It is interesting to note that two studies reported improvement in knowledge regarding depressive disorders and relevant treatment but engagement in these treatments was non-satisfactory, with a drop rate exceeding 44% [ 23 , 29 ]. The lack of improvement in three studies was reported due to lack of past experience or contact with individuals with mental illnesses [ 33 , 47 ]. In study by Pinto-Foltz, the improvement was more noticeable at 4 and 8-week timepoints among intervention group, owing to past exposure of participants in control group to mental health information [ 4 ]. For Depression Fotonovela intervention, lack of difference in improvement among both experimental and control groups was due to ceiling effect and higher baseline knowledge scores [ 34 ].
Social Distance
The social distance was assessed in seven studies with four studies reporting favorable results. Majority of the studies with favorable results had two important components including opportunity to contact with individuals with mental illness ( n = 3) and participants with a background in medicine or nursing ( n = 4). In one of these studies, a combination of two education strategies didactic education and video group fared better than the education group alone. Three of the studies reported a non-significant outcome; these studies lacked contact with individuals diagnosed with mental health disorders. Moreover, participants in these interventions were adult individuals with no background in relevant professions [ 34 ], middle school students, or students enrolled in psychology courses [ 55 ].
This article reviews the evidence for various aspects of stigma towards mental health disorders in educational settings. These interventions were carried out in university, college, and school settings, targeting a wide range of mental health disorders. Duration of intervention varied widely with most of the interventions lasting for more than four weeks. For outcome measure, majority of studies reported significant improvement for stigma (19/25, 76%), attitude (8/11, 72%), help-seeking (8/11, 72%), knowledge of mental health including recognition of depression (11/14, 78%), and social distance (4/7, 57%). It is worthwhile to appreciate that all these outcomes measure are intercalated and have a directional effect on each other.
Most of the studies included in this review focused on reduction of public stigma rather than self-stigma, two different yet highly intercalated concepts. The reviewed interventions targeted one or more of the core stigmatizing behaviors especially fear and exclusion and authoritarianism that people with mental illnesses face and inspire benevolence and compassion among the intervention recipients [ 56 ]. This was done through different strategies, most frequently being psychoeducation through didactic lectures. Other strategies were contact-based interventions, and role-plays to address stigma towards mental illnesses. Reduction of self-stigma was done through a specialized program of self-affirmation therapy, to inspire moral and adaptive adequacy of the self, with a main aim to inspire positive view of self [ 54 ].
All of these interventions followed the recommendations proposed by Corrigan et al., who recommended three ways to combat public stigma: protest, education, and contact to combat the existing stigma [ 56 ]. The latter approaches were employed frequently, however, protest in response to the stigmatizing environment propagated by public statements, media reports, and advertisements was absent in these initiatives [ 56 ]. In addition, it is also imperative to engage health care providers, stakeholders, policymakers, for development of campus-based policies combating stigma [ 57 ]. We did not find any interventions designed at the policy level as well as the system level or reporting their effectiveness and wide-ranging implications and socioeconomic benefits.
A plethora of research in recent decades has shown that stigmatizing attitudes toward mental illnesses are strongly driven by sociocultural and religious factors, as well as individual factors especially empathy and experience and education levels [ 58 , 59 , 60 , 61 ]. This is particularly relevant in context of low- and middle-income countries where such attitudes and beliefs toward mental illnesses are prevalent even among the learned. For instance, the belief in djinni possession, black magic and divine punishment as causes of mental illnesses are rampant in the Indian subcontinent. This requires the development of very culture specific interventions in these countries. And yet only one of the interventions targeting stigma toward mental illnesses has been developed in these countries [ 62 ]. This is a major gap that must be addressed by development of interventions that aim to mitigate negative cultural and social norms as well as inspire benevolence toward people with mental illnesses. It can be argued that development, testing and implementation of relevant interventions in poorer nations can foster an alternative and correct view of mental illness resulting in improved knowledge and linkage to services.
This systematic review has several strengths. An electronic search of academic databases combined with manual searching for references provides an exhaustive search for relevant evidence. It provides an overview of RCTs of interventions targeting stigma towards mental health in educational settings as well as the strategies used in each intervention and different components of these interventions. Combined with a qualitative assessment of the theoretical orientation of these intervention as well as assessment of risk of bias, makes this review an important source for development and testing of future interventions in this area. However, this review also has several limitations. Due to heterogeneity, varying intervention design, and different outcome measures, meta-analysis could not be performed. It is also important to consider the higher risk of bias in included studies while interpreting the results of these studies. These interventions were important in challenging the stereotypes and prejudice by providing an opportunity of social contact with individuals with mental illnesses, engaging in myth-busting, and increasing awareness of mental illnesses through education via text, lecture, or film [ 7 ]. However, due to lack of meta-analytic evidence, it is difficult to ascertain if a single component intervention is any better than its multi-component counterparts such as DVD or direct contact group work better than other. Although, generally a greater improvement was reported with comprehensive approaches to combat stigma [ 45 ].
This review provides some promising empirical support for anti-stigma interventions regarding mental health disorders aimed at students. These interventions were somewhat successful in reducing both self and public stigma. This highlights the need for progressively thorough, better-quality evaluations conducted with more diverse samples of the population. As it appears that short-term interventions often only have a transient effect, the implication is that researchers should study longer term interventions and to use the intervening time and outcome data to improve the interventions along the way. Future research should explore to what extent changes in students’ knowledge, attitudes, and beliefs can result in earlier help seeking.
Sickel AE, Seacat JD, Nabors NA. Mental health stigma: impact on mental health treatment attitudes and physical health. J Health Psychol. 2019;24(5):586–99.
PubMed Google Scholar
Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21(2):10.
World Health Organization. (2019). Adolescent mental health. Retrieved 15 December 2019, from https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
Schomerus G, Stolzenburg S, Freitag S, Speerforck S, Janowitz D, Evans-Lacko S, et al. Stigma as a barrier to recognizing personal mental illness and seeking help: a prospective study among untreated persons with mental illness. Eur Arch Psychiatry Clin Neurosci. 2019;269(4):469–79.
Elliott GC, Ziegler HL, Altman BM, Scott DR. Understanding stigma: dimensions of deviance and coping. Deviant Behav. 1982;3(3):275–300.
Google Scholar
Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16–20.
PubMed PubMed Central Google Scholar
Gronholm PC, Henderson C, Deb T, Thornicroft G. Interventions to reduce discrimination and stigma: the state of the art. Soc Psychiatry Psychiatr Epidemiol. 2017;52(3):249–58.
World Health Organization. Department of Mental Health, Substance Abuse, World Psychiatric Association, International Association for Child, Adolescent Psychiatry, & Allied Professions. (2005). Atlas: child and adolescent mental health resources: global concerns, implications for the future. World Health Organization.
Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387(10023):1123–32.
A. Liberati, D. G. Altman, J. Tetzlaff, C. Mulrow, P. C. Gøtzsche, J. P. Ioannidis, ... & D Moher. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Annals of internal medicine, 151(4), W-65.
National Academies of Sciences, Engineering, and Medicine. Ending discrimination against people with mental and substance use disorders: the evidence for stigma change: National Academies Press; 2016.
Ranson NJ, Byrne MK. Promoting peer acceptance of females with higher-functioning autism in a mainstream education setting: a replication and extension of the effects of an autism anti-stigma program. J Autism Dev Disord. 2014;44(11):2778–96.
Pereira CA, Wen CL, Miguel EC, Polanczyk GV. A randomised controlled trial of a web-based educational program in child mental health for schoolteachers. Eur Child Adolesc Psychiatry. 2015;24(8):931–40.
Boucher LA, Campbell DG. An examination of the impact of a biological anti-stigma message for depression on college students. J Coll Stud Psychother. 2014;28(1):74–81.
Mann CE, Himelein MJ. Putting the person back into psychopathology: an intervention to reduce mental illness stigma in the classroom. Soc Psychiatry Psychiatr Epidemiol. 2008;43(7):545–51.
Yamaguchi S, Koike S, Ojio Y, Shimada T, Watanabe KI, Ando S. Filmed social contact v. internet self-learning to reduce mental health-related stigma among university students in Japan: a randomized controlled trial. Early intervention in psychiatry, 8. 2014.
Bannatyne A, Stapleton P. Educating medical students about anorexia nervosa: a potential method for reducing the volitional stigma associated with the disorder. Eat Disord. 2015;23(2):115–33.
Giannakopoulos G, Assimopoulos H, Petanidou D, Tzavara C, Kolaitis G, Tsiantis J. Effectiveness of a school-based intervention for enhancing adolescents' positive attitudes towards people with mental illness. Ment Illn. 2012;4(2):79–83.
Han DY, Chen SH. Reducing the stigma of depression through neurobiology-based psychoeducation: a randomized controlled trial. Psychiatry Clin Neurosci. 2014;68(9):666–73.
Kosyluk KA, Al-Khouja M, Bink A, Buchholz B, Ellefson S, Fokuo K, et al. Challenging the stigma of mental illness among college students. J Adolesc Health. 2016;59(3):325–31.
Sakellari E, Lehtonen K, Sourander A, Kalokerinou-Anagnostopoulou A, Leino-Kilpi H. Greek adolescents' views of people with mental illness through drawings: mental health education's impact. Nurs Health Sci. 2014;16(3):358–64.
Winkler P, Janoušková M, Kožený J, Pasz J, Mladá K, Weissová A, et al. Short video interventions to reduce mental health stigma: a multi-Centre randomised controlled trial in nursing high schools. Soc Psychiatry Psychiatr Epidemiol. 2017;52(12):1549–57.
Swartz K, Musci RJ, Beaudry MB, Heley K, Miller L, Alfes C, et al. School-based curriculum to improve depression literacy among US secondary school students: a randomized effectiveness trial. Am J Public Health. 2017;107(12):1970–6.
Sharp W, Hargrove DS, Johnson L, Deal WP. Mental health education: an evaluation of a classroom based strategy to modify help seeking for mental health problems. J Coll Stud Dev. 2006;47(4):419–38.
Finkelstein J, Lapshin O, Wasserman E. Randomized study of different anti-stigma media. Patient Educ Couns. 2008;71(2):204–14.
Kashihara J. Examination of stigmatizing beliefs about depression and stigma-reduction effects of education by using implicit measures. Psychol Rep. 2015;116(2):337–62.
Esters IG, Cooker PG, Ittenbach RF. Effects of a unit of instruction in mental health on rural adolescents' conceptions of mental illness and attitudes about seeking help. Adolescence. 1998;33(130):469–76.
CAS PubMed Google Scholar
Papish A, Kassam A, Modgill G, Vaz G, Zanussi L, Patten S. Reducing the stigma of mental illness in undergraduate medical education: a randomized controlled trial. BMC Med Educ. 2013;13(1):141.
Perry Y, Petrie K, Buckley H, Cavanagh L, Clarke D, Winslade M, et al. Effects of a classroom-based educational resource on adolescent mental health literacy: a cluster randomised controlled trial. J Adolesc. 2014;37(7):1143–51.
Rusch LC, Kanter JW, Brondino MJ. A comparison of contextual and biomedical models of stigma reduction for depression with a nonclinical undergraduate sample. J Nerv Ment Dis. 2009;197(2):104–10.
Burns S, Crawford G, Hallett J, Hunt K, Chih HJ, Tilley PM. What’s wrong with John? A randomised controlled trial of mental health first aid (MHFA) training with nursing students. BMC Psychiatry. 2017;17(1):111.
Hart LM, Morgan AJ, Rossetto A, Kelly CM, Mackinnon A, Jorm AF. Helping adolescents to better support their peers with a mental health problem: a cluster-randomised crossover trial of teen mental health first aid. Australian & New Zealand Journal of Psychiatry. 2018;52(7):638–51.
Lipson SK, Speer N, Brunwasser S, Hahn E, Eisenberg D. Gatekeeper training and access to mental health care at universities and colleges. J Adolesc Health. 2014;55(5):612–9.
Cabassa LJ, Oh H, Humensky JL, Unger JB, Molina GB, Baron M. Comparing the impact on Latinos of a depression brochure and an entertainment-education depression fotonovela. Psychiatr Serv. 2015;66(3):313–6.
Unger JB, Cabassa LJ, Molina GB, Contreras S, Baron M. Evaluation of a fotonovela to increase depression knowledge and reduce stigma among Hispanic adults. J Immigr Minor Health. 2013;15(2):398–406.
Chan JY, Mak WW, Law LS. Combining education and video-based contact to reduce stigma of mental illness:“the same or not the same” anti-stigma program for secondary schools in Hong Kong. Soc Sci Med. 2009;68(8):1521–6.
Economou M, Louki E, Peppou LE, Gramandani C, Yotis L, Stefanis CN. Fighting psychiatric stigma in the classroom: the impact of an educational intervention on secondary school students’ attitudes to schizophrenia. Int J Soc Psychiatry. 2012;58(5):544–51.
Economou M, Peppou LE, Geroulanou K, Louki E, Tsaliagkou I, Kolostoumpis D, et al. The influence of an anti-stigma intervention on adolescents' attitudes to schizophrenia: a mixed methodology approach. Child Adolesc Mental Health. 2014;19(1):16–23.
Chung KF, Chan JH. Can a less pejorative Chinese translation for schizophrenia reduce stigma? A study of adolescents’ attitudes toward people with schizophrenia. Psychiatry Clin Neurosci. 2004;58(5):507–15.
Howard KA, Griffiths KM, McKetin R, Ma J. Can a brief biologically-based psychoeducational intervention reduce stigma and increase help-seeking intentions for depression in young people? A randomised controlled trial. J Child Adolesc Ment Health. 2018;30(1):27–39.
Nam SK, Choi SI, Lee SM. Effects of stigma-reducing conditions on intention to seek psychological help among Korean college students with anxious-ambivalent attachment. Psychol Serv. 2015;12(2):167–76.
Vila-Badia R, Martínez-Zambrano F, Arenas O, Casas-Anguera E, García-Morales E, Villellas R, et al. Effectiveness of an intervention for reducing social stigma towards mental illness in adolescents. World journal of psychiatry. 2016;6(2):239–47.
Oduguwa AO, Adedokun B, Omigbodun OO. Effect of a mental health training programme on Nigerian school pupils’ perceptions of mental illness. Child Adolesc Psychiatry Ment Health. 2017;11(1):19.
Chisholm K, Patterson P, Torgerson C, Turner E, Jenkinson D, Birchwood M. Impact of contact on adolescents’ mental health literacy and stigma: the SchoolSpace cluster randomised controlled trial. BMJ Open. 2016;6(2):e009435.
Clement S, van Nieuwenhuizen A, Kassam A, Flach C, Lazarus A, De Castro M, et al. Filmed v. live social contact interventions to reduce stigma: randomised controlled trial. Br J Psychiatry. 2012;201(1):57–64.
Corrigan PW, Rafacz JD, Hautamaki J, Walton J, Rüsch N, Rao D, et al. Changing stigmatizing perceptions and recollections about mental illness: the effects of NAMI’s in our own voice. Community Ment Health J. 2010;46(5):517–22.
Pinto-Foltz MD, Logsdon MC, Myers JA. Feasibility, acceptability, and initial efficacy of a knowledge-contact program to reduce mental illness stigma and improve mental health literacy in adolescents. Soc Sci Med. 2011;72(12):2011–9.
Staniland JJ, Byrne MK. The effects of a multi-component higher-functioning autism anti-stigma program on adolescent boys. J Autism Dev Disord. 2013;43(12):2816–29.
Campbell M, Shryane N, Byrne R, Morrison AP. A mental health promotion approach to reducing discrimination about psychosis in teenagers. Psychosis. 2011;3(1):41–51.
Chung KF. Changing the attitudes of Hong Kong medical students toward people with mental illness. J Nerv Ment Dis. 2005;193(11):766–8.
Gonçalves M, Moleiro C, Cook B. The use of a video to reduce mental health stigma among adolescents. Adolesc Psychiatry. 2015;5(3):204–11.
Koike S, Yamaguchi S, Ojio Y, Ohta K, Shimada T, Watanabe K, et al. A randomised controlled trial of repeated filmed social contact on reducing mental illness-related stigma in young adults. Epidemiol Psychiatr Sci. 2018;27(2):199–208.
King CA, Eisenberg D, Zheng K, Czyz E, Kramer A, Horwitz A, et al. Online suicide risk screening and intervention with college students: a pilot randomized controlled trial. J Consult Clin Psychol. 2015;83(3):630–6.
Lannin DG, Guyll M, Vogel DL, Madon S. Reducing the stigma associated with seeking psychotherapy through self-affirmation. J Couns Psychol. 2013;60(4):508–19.
Woods DW, Marcks BA. Controlled evaluation of an educational intervention used to modify peer attitudes and behavior toward persons with Tourette’s syndrome. Behav Modif. 2005;29(6):900–12.
Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. Eur Psychiatry. 2005;20(8):529–39.
Byrne P. Stigma of mental illness and ways of diminishing it. Adv Psychiatr Treat. 2000;6(1):65–72.
Waqas A, Zubair M, Ghulam H, Ullah MW, Tariq MZ. Public stigma associated with mental illnesses in Pakistani university students: a cross sectional survey. PeerJ. 2014;2:e698.
Haddad M, Waqas A, Qayyum W, Shams M, Malik S. The attitudes and beliefs of Pakistani medical practitioners about depression: a cross-sectional study in Lahore using the revised depression attitude questionnaire (R-DAQ). BMC Psychiatry. 2016;16(1):349.
Haddad M, Waqas A, Sukhera AB, Tarar AZ. The psychometric characteristics of the revised depression attitude questionnaire (R-DAQ) in Pakistani medical practitioners: a cross-sectional study of doctors in Lahore. BMC Res Notes. 2017;10(1):333.
Waqas A, Naveed S, Makhmoor A, Malik A, Hassan H, Aedma KK. Empathy, experience and cultural beliefs determine the attitudes towards depression among Pakistani medical students. Community Ment Health J. 2020;56(1):65–74.
Choudhry FR, Mani V, Ming LC, Khan TM. Beliefs and perception about mental health issues: a meta-synthesis. Neuropsychiatr Dis Treat. 2016;12:2807–18.
Download references
Author information
Authors and affiliations.
Institute of Population Health Sciences, University of Liverpool, Liverpool, UK
Ahmed Waqas
Program Director: Child and Adolescent Psychiatry Fellowship, Institute of Living/Hartford Healthcare, Hartford, CT, USA
Salma Malik
King Edward Medical University, Lahore, Pakistan
FMH College of Medicine & Dentistry, Lahore, Pakistan
Noureen Abbas
Mental Health Counselor, PICACS, Washington, USA
Nadeem Mian
Integrated Psychiatric Consultants, Kansas, KS, USA
Sannihitha Miryala
Dow University of Health Sciences, Karachi, Pakistan
Afshan Naz Amray
Weiss Memorial Hospital, Illinois, Chicago, USA
Zunairah Shah
Psychiatry and Behavioral Sciences, University of Kansas Medical Center, Kansas, USA
Sadiq Naveed
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ahmed Waqas .
Ethics declarations
Disclosure of potential conflicts of interest.
The authors declare that they have no conflict of interests.
Research Involving Human Participants and/or Animals
This information is not applicable because this is a review article.
Informed Consent
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Waqas, A., Malik, S., Fida, A. et al. Interventions to Reduce Stigma Related to Mental Illnesses in Educational Institutes: a Systematic Review. Psychiatr Q 91 , 887–903 (2020). https://doi.org/10.1007/s11126-020-09751-4
Download citation
Published : 05 May 2020
Issue Date : September 2020
DOI : https://doi.org/10.1007/s11126-020-09751-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Institutions
- Mental health
- Interventions
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Strategies to Reduce Mental Illness Stigma: Perspectives of People with Lived Experience and Caregivers
Associated data.
The datasets generated and/or analysed during the current study are not publicly available due institutional policy but are available from the corresponding author upon reasonable request.
Background: Reducing the stigma surrounding mental illness is a global public health priority. Traditionally, anti-stigma campaigns were led by mental health professionals/organisations and had an emphasis on increasing mental health literacy. More recently, it has been argued that people with lived experience have much to contribute in terms of extending and strengthening these efforts. The purpose of this paper was to elicit views and suggestions from people with lived experience (PWLE) as well as from informal caregivers of people with mental health conditions, on effective strategies to combat the stigma surrounding mental illness. Methods: Six focus group discussions (FGDs) were carried out with PWLE recruited at outpatient services at the Institute of Mental Health, Singapore, and five FGDs were carried out with informal caregivers who responded to advertisements for the study between March and November 2018. In all, the sample comprised 42 PWLE and 31 caregivers. All the FGDs were transcribed verbatim and were analysed using thematic analysis. A pragmatic approach was adopted for the study, and the researchers did not assume any particular philosophical orientation. Results: Four overarching themes depicting strategies to combat stigma were identified through thematic analysis. They were (1) raising mental health awareness, (2) social contact, (3) advocacy by influential figures or groups, and (4) the legislation of anti-discriminatory laws. Conclusions: These strategies were in line with approaches that have been used internationally to disrupt the process of stigma. Our study has further identified nuanced details on how these strategies can be carried out as well as possible areas of priority in the Singapore landscape.
1. Introduction
The stigma of living with a mental health condition has been described as being worse than the experience of the illness itself [ 1 ]. The aversive reactions that members of the general population have towards people with mental illness is known as public stigma and can be understood in terms of (i) stereotypes, (ii) prejudice, and (iii) discrimination [ 2 ]. Common stereotypes associated with people with mental health conditions are that they are dangerous, incompetent, and weak in character. Prejudice refers to the agreement with these stereotypes, while discrimination refers to behavioural reactions to these prejudices [ 3 ].
Beyond the interpersonal manifestations of public stigma towards people with mental health conditions, societal-level conditions such as institutional policies and practices and cultural norms have also been found to be biased against people with mental health conditions, resulting in a lack of opportunities and resources being afforded to them [ 4 ]. These socio-political disinclinations, known as structural stigma, result in people with mental health conditions being excluded from employment, living in unstable and unsafe conditions, being disqualified from health insurance, and being subjected to coercive hospitalisation and treatment [ 5 , 6 ]. The deprivation of opportunities and poor-quality resources provided to those with mental health conditions have severe bearings, as evidenced by the gross overrepresentation of individuals with mental health conditions in the criminal justice system and among those living in poverty [ 7 ]. People with mental health conditions also have significantly higher morbidity and mortality rates [ 8 ], and consequent to all the above, have a lower quality of life compared to the general population [ 9 , 10 ].
Through repeated encounters with public and structural stigma, individuals with mental health conditions are inclined to internalise these reactions, a phenomenon known as self-stigma. A systematic review found that exposure to public stigma predicts self-stigma at a later time [ 11 , 12 ]. A person’s own stigmatizing views towards mental illness is associated with lower readiness to appraise his or her own symptoms as potentially indicating a mental health problem and thus reduces help-seeking behaviour [ 13 ]. This could be because the individual seeks to avoid the label of mental illness for him- or herself [ 14 ], fathomably to guard themselves against the negative self-perceptions associated with it and the potential consequences of shame and reduced empowerment [ 15 ]. Indeed, self-stigma decreases one’s self-esteem and self-efficacy, leading to the “why try effect”, where people with mental health conditions question their worthiness and capability to pursue personal goals [ 16 , 17 ], leading to a loss of self-respect and increased shame and hopelessness [ 18 , 19 ]. Over time, higher levels of self-stigma have been found to be associated with suicidal ideation [ 18 , 20 ].
Due to these adverse effects of stigma, stigma-reduction is seen as a global public health priority [ 21 , 22 , 23 , 24 ]. Anti-stigma programmes were traditionally conducted by or in substantial consultation with groups representing psychiatric expertise [ 25 ]. However, several criticisms have been raised towards this approach in the recent years. First, the emphasis on medical understandings of mental health problems and the importance of adhering to psychiatric interventions have been criticised as fulfilling the psychiatric services agenda rather than the interest of people with mental health conditions and eclipsing inputs from other standpoints [ 3 , 26 ]. Next, mental health professionals have been found to be just as likely to stigmatise those with mental health conditions [ 27 , 28 , 29 ]. Thus, is has been argued that the professional expertise that mental health professionals have in providing mental health services may be insufficient in impacting the social spheres in which stigma operate, and it may be timely for them to move to a supporting role [ 30 ].
In recent years, anti-stigma programmes have involved people with lived experience to allow direct or parasocial interactions between target audiences and people with mental health conditions. Contact-based interventions have demonstrated the clearest evidence in reducing stigmatising attitudes, desire for social distancing and discrimination [ 31 , 32 , 33 ]. Contact-based interventions typically involve brief contact between members of a majority group and a stranger representing the stigmatized population who is quite different from a naturally occurring contact. Stigma is reduced by providing an opportunity for interpersonal contact between people who have mental illness and individuals who may hold stigma towards them. A key ingredient of contact-based interventions is the delivery of testimonies by service users [ 34 ]. The efficacy of contact-based education has led to calls for collaborations with individuals with mental health conditions to offer their experiential wisdom in challenging stigma, representing the voice of those who struggle with mental health difficulties and shedding light on blind spots and gaps in previous strategies [ 3 , 35 ]. Corrigan asserted that just as disability rights groups have adopted the slogan of “no policy or action should be taken about a group without full participation of that group”, the same should be applied to alleviate mental health stigma [ 30 ]. Additionally, while we have thus far described the negative processes that arise from stigma, there are people with mental health conditions who do not agree with the hackneyed stereotypes and respond with indignation that seems to empower and energise them to advocate for changes to the ways in which they are treated [ 2 ]. Their inputs towards initiatives that are aimed at improving service delivery and de-stigmatisation programmes have been found to lead to novel results and have been described as a strength of those programmes [ 35 , 36 ].
Singapore is a small, highly urbanised, multi-cultural country located at the Southern tip of the Malayan Peninsula. The resident population is made up of 75.9% Chinese, 15.0% Malay, 7.5% Indian, and 1.6% other ethnicities [ 37 ]. A developed country, the culture of Singapore can be described as a combination of Eastern and Western cultures, and English is the primary language of instruction. Stigma towards mental illness remains prevalent in Singapore today. An earlier nationwide survey revealed that 38.3% of the population believed that people with mental illness are dangerous, and 49.6% felt that people need to be protected from psychiatric patients [ 38 ]. A decade later, another population survey, which used a vignette-based approach, reported that 50.8% of respondents indicated that mental illness was a sign of personal weakness, 42.8% were unwilling to work closely with a person with mental health conditions on a job, and 70.2% were unwilling to have a person with mental health conditions marry into their family [ 39 ]. A recent qualitative study of daily encounters of personal stigma reported themes such as social exclusion, subjection to contemptuous treatment, and rejection by employers following the declaration of a mental health condition [ 40 ].
Anti-stigma activities in Singapore have been conducted by the state psychiatric institution, the Institute of Mental Health (IMH), the National Council of Social Service, the Health Promotion Board (statutory boards), and non-profit organisations such as the Singapore Association for Mental Health and Silver Ribbon Singapore, who have the collective aims of improving mental health literacy, access to mental health care, and improving the reintegration of people with mental health conditions into the community [ 41 , 42 ]. However, the involvement of individuals with mental health conditions in anti-stigma campaigns is lacking. The purpose of this paper was thus to elicit views and suggestions from people with lived experience (PWLE) and informal caregivers of people with mental health conditions on effective strategies to combat stigma.
The present study is part of a larger study that aimed to examine the nature of mental illness stigma in Singapore from the perspectives of five stakeholder groups, namely PWLE, informal caregivers, members of the general public, professionals working in mental health settings, and policy makers. The main purpose of this research was to provide actionable knowledge. It took a pragmatic approach common in health services research and did not assume any particular methodological orientation [ 43 ]. Only data from PWLE and caregivers were used in this analysis. The study was approved by the institutional ethics committee, the National Healthcare Group Domain Specific Review Board. Written informed consent was obtained from all participants before initiating study related procedures.
2.1. Participants
PWLE and caregivers were recruited through referrals by their clinicians or self-referral by learning about the study though poster advertisements placed in waiting areas at the IMH outpatient clinics. The IMH is Singapore’s largest provider of mental health care, providing pharmacological and psychosocial treatments as well as psychosocial rehabilitation for a range of subspecialties, including child and adolescent psychiatry, affective disorders, and psychosis. It has also spearheaded mental health education and anti-stigma events for the public. All the participants were required to be Singapore citizens and permanent residents, aged 21 years old and above, and could not be a student or professional from the mental health field.
PWLE recruitment was limited to two types of psychiatric diagnoses, mood and psychotic disorders, to attain a more homogenous account of encounters with stigma. The groups were also separated by diagnosis to facilitate the identification of members in a group with each other and to provide comfort when expressing themselves. In all, six Focus Group Discussions (FGD) were conducted with PWLE between March to May 2018 (three with individuals with mood disorders, three with those with psychosis-related disorders). Referred and self-referred PWLE were deemed clinically stable by their treating clinicians and were able to provide informed consent.
Although the poster advertisements indicated that the study sought caregivers of individuals with psychosis-related or mood disorders, no attempt was made to confirm the diagnosis of their care recipients with the treating clinicians. The caregiver group was independent of the PWLE group. Unlike the PWLE FGDs, the caregivers were not separated based on the diagnosis of their care recipient. As the initial FGDs did not identify any issue with this approach, the team carried out the rest of the FGDs in a similar manner. In all, five FGDs were conducted with caregivers between June and November 2018.
The PWLE FGDs ranged from 5–8 participants, while the caregiver FGDs ranged from 4–9 participants. The sociodemographic profiles of the PWLE and caregiver participants are presented in Table 1 . Participants received an inconvenience fee at the end of the FGD. All FGDs were conducted in English.
Sociodemographic characteristics.
# 1 missing PWLE response for Highest Completed Education.
2.2. Data Collection
The FGDs were conducted in a closed room that was relatively free from distractions in a community club, which was chosen because it is a neutral venue. Each FGD was conducted by two study team members, who served as the facilitator or the note taker for the day. The facilitators (either MS or SS) were trained and experienced in qualitative research methodologies. CMJG, OWJ, GTTH, SS, and MS took turns as note-takers in the different FGDs.
After individual consent was taken to participate in the research and to audio-record the session, each participant filled out a sociodemographic form that collated information about age, gender, education level, ethnicity, and brief information about their illness (for PWLE) or caregiving relationship (for caregivers), and the completed form was returned to the facilitator. Participants were assured that all of the data collected from them would be kept confidential, the transcripts would be de-identified such that names and other identifying features would be omitted, the audio-recording would be deleted after transcription, and that there were no correct or incorrect answers before the discussion commenced.
The experienced facilitators used a topic guide comprising open-ended questions that had been developed by the research team so that the data collected across the various FGDs would be as uniform as possible. Few specific questions were designed to elicit information that could be best addressed by a particular target group. The topic guide covered areas of mental illness stigma such as encounters of stigma and reasons for stigma. The team formulated the questions in a manner similar to that recommended by Krueger et al. [ 44 ], the recommendations of whom comprised the following: The questions should elicit information that directly relates to the study’s objectives. The questions should be easy for the participants to understand and should be phrased in a neutral manner so as not to bias participant responses. The questions can be answered by all the participants. Questions should be open-ended and not answered with a “yes” or “no” to facilitate descriptive responses. The questions should not make the participants uncomfortable when answering, and they should not trigger defensive responses. The team brainstormed the questions to answer the objectives of the research, and one researcher drafted the questioning route, rephrased, and reordered the questions to form a logical flow. The draft was circulated to the rest of the team, and suggestions were incorporated. The team aimed to keep the final total number of questions between 10–12. Decisions to omit questions were based on importance in addressing the research objectives, with final decisions being made by the lead investigator (MS). The questions were then tested out, using the first focus group as a pilot. The items that were used to elicit responses to the research question addressed in this paper was from the final segment of the topic guide: “How do you think stigma towards people with mental illness can be reduced” and “Have you heard of campaigns to reduce stigma towards those with mental illness? Is there anything that can be done better?”. The facilitator probed for range and depth of responses and sought clarification for responses that were unclear using neutral questions. Attempts were made to encourage responses from all members. The entire duration of each FGD lasted between 1.5–2 h. FGDS were carried out one at a time, first with the PWLE and then with the caregivers. At the end of each FGD, there was a debrief between the facilitator and note-taker, and a comprehensive summary was provided to the rest of the research team soon after to reflect on each session, to ensure that any problems were identified early and addressed, and emerging themes and unique points that had been raised were discussed. The FGDs were later transcribed verbatim for analysis. The decision was made by the team to cease data collection for PWLE and the caregiver groups when no new themes were identified, i.e., when data saturation was reached.
2.3. Analysis
The data were analysed using an inductive thematic analysis method [ 45 ]. Transcripts were first distributed amongst five study team members (SS, CMJG, GTTH, OWJ, and MS) for familiarisation with the collected data. Subsequently, each study team member independently identified preliminary codes from their respective transcripts. The study team members then came together, and through an iterative process of comparing the codes and combining, discarding, and redefining the codes, collaboratively decided on the final list of codes. A codebook was developed by the coders (SS, CMJG, GTTH, OWJ, and MS), in which each code was characterised by a description, inclusion and exclusion criteria, and typical and atypical exemplars to guide the coding process. To ensure coding consistency among the study team members, one transcript was first coded to establish inter-rater reliability. The study team continued to discuss, refine the codebook, and repeat the coding with another transcript until a satisfactory inter-rater reliability score was achieved (Cohen’s Kappa score > 0.75). Transcripts were then distributed among the study team members for coding. Data analysis was completed with Nvivo Version 11.0. (QSR International Pty Ltd. Hawthorn East, Australia).
After coding all transcripts, the codes were sorted such that similar codes were grouped together to form potential themes. Codes that did not seem to fit into any theme at first were revisited as the themes were gradually refined. Relationships between these themes were also examined, and different levels (main theme and sub-themes) were identified. Any remaining codes were compared against the revised themes to determine fit. The initial themes were drafted by SS, JCMG, GTTH, OWJ, and MS and presented to CSA for further refinement before finalisation.
Strategies to ensure the quality of the findings recommended by Anney [ 46 ] were exercised in this research. Data were triangulated from two different informant sources: patients and caregivers. The transcripts were read and re-read by five researchers independently. The interpretations were compared, and regular meetings were held to discuss differences until a consensus was reached. These informant and researcher triangulations aimed to increase the credibility of the findings. To ensure transferability, the participants were sampled in such a way that there was good distribution by age, gender, education level, and ethnicity, and for the caregivers, relationship with the care-recipient. Finally, for confirmability, intentional record keeping of summaries and reflections after each FGD as well as decisions made during the coding and analysis were documented to maintain an audit trail.
Four overarching themes depicting the strategies to combat stigma were identified. They included (1) raising mental health awareness, (2) social contact, (3) advocacy by influential figures or groups, and (4) legislation of anti-discriminatory laws. It was not uncommon for participants to refer to two or more approaches in a single quote. While we have selected quotes to illustrate the main theme, they may cross-cover other themes to some degree. To ensure that standard usage of English was maintained, minimally corrected verbatim of quotes are presented.
3.1. Raising Mental Health Awareness
There were two subthemes pertaining to the strategy of raising mental health awareness, which can be described as the “who and how” and “what” of this approach.

3.1.1. Target Groups/Setting and Methods
Anti-stigma awareness initiatives for the general population were frequently suggested by participants, and they recommended outreach through both traditional and social media as well as popular mass events such as marathons and festivals in order to reach a wide range of members of the public from the young to the old. They also emphasised that these efforts should be carried out repeatedly, reasoning that increased exposure to the topic will lead to greater familiarity and with time, greater acceptance of this taboo subject.
You all have to do a lot of campaigns, running it tends to stick in their minds (Male, 37 years, Psychosis-related disorder, PWLE FGD 5)
Educating the public because it is very important. More on media because there are many people on the internet or computer, TV and all sorts ah, newspaper of course, articles, so that more people will come to know so that lesser, I mean to accept slowly. The stigma will grow weaker and weaker, not that strong. (Female, 65 years, Caregiver FGD 3)
With regards to media portrayal, the participants discouraged the use of drama in and of itself as a means of education. They asserted that such media forms tend to sensationalise mental illness through negative characterizations that further reinforce existing stereotypes. Instead, they prefer coverage through documentaries and talk shows.
I think drama is not a good way to go to raise awareness of mental illness because in drama, it’s drama what. You have to be dramatic, and you have to be dramatic you have to sensationalise. But maybe talk shows are better. Talk show where they invite celebrities together with professionals and then they talk it out. (Male, 28 years, Psychosis-related disorder, PWLE FGD 5)
Raising mental health awareness in two specific target groups was frequently brought up. The first group that the participants wanted to increase mental health awareness in was among school students. The participants rationalised that it would be easier to influence young people whose attitudes are more malleable. They also voiced concerns that youth are a vulnerable group due the heightened challenges they face such as intense academic pressures and societal expectations. Thus, they would benefit from literacy-based interventions to facilitate early recognition and help-seeking behaviours. Some of the participants suggested an incremental approach whereby younger primary school-age students could be primed with information on mental well-being before being introduced to more serious topics on mental health conditions.
Education from, it’s ok for those who are already old enough like us, we can’t like, some people we can’t really unlearn what we learn so we have to teach the new generation and input in what are the more important things, like for example, the major concerns as of now and like how important is mental health so that they won’t grow up to be like their parents or like whoever. So, I think it starts from the younger ones la they will receive fresh information and they won’t have any judgement against us (Female, 22 years, Mood disorder, PWLE FGD 2)
I think it should start across Singapore, like for example, starting from schools, starting from workplaces, meeting the employers you know, the teachers, the, the facilitators, starting from there you know. So, when you have that well-established, designed activities you know, I mean the initiative, we have that initiative to go to, to the schools you know, at a younger age when they already start to understand, so when they come to work, as an maybe an employer, so they can understand further what happens to the subordinates, what happens to the employees who have mental illness. (Female, 48 years, Caregiver FGD 5)
The second target group was employers. The participants commented that in contrast to the recent advances in efforts to raise mental health awareness, workplaces were especially lagging in this regard, and overt stigmatisation continues to occur in workplaces. Legislative measures were also recommended to combat stigma and discrimination in this setting (this will be further elaborated in the fourth theme).
Essentially run multiple small campaigns across companies so we start from the top tier and then you go down to the middle tier and then into the SME like a small, very small enterprises and things like that to do awareness campaign with all their HR [Human Resource], their ops [operations] department and things like that so that they learn. So at least if the managers learn, hopefully they’ll pass that on, not always. It will not always happen, but it might you know, so at least there’s a trickle-down effect and it last longer (Male, 28 years, Mood disorder, PWLE FGD 6)
I think the Singapore government is very effective, and they are respectable, so Ministry of Health or IMH organize talk to the employers, to the unions, trade unions. (Male, 64 years, Caregiver FGD 5)
3.1.2. Types of Content
The participants recommended that messages pertaining to the prevalence of mental illness debunking common myths about mental illness and likening it instead to other chronic illnesses could reduce stigma and demystify mental illness. The participants also recommended disseminating information on where and how mental illness can be managed as well as the efficacy of treatments to emphasise the treatability of mental illnesses.
Get the MP [member of parliament] come and talk, share with them, share with the population, mental illness is common. Especially depression, 1 in 5, in the population will get depression, or even now, now 1 in 4. (Male, 64 years, Caregiver FGD 5)
To me education is the best way to, to erase all these myths (Male, 49 years, Psychosis-related disorder, PWLE FGD 4)
Let them know, no big deal. It is just like any other chronic illness. I say in your whole lifetime anyone can suffer some from of mental illness. (Female, 65 years, Caregiver FGD 3)
The PWLE cautioned that anti-stigma messages should not result in “over-normalisation” or careless over-identification of mental illness and trivialisation among lay members of the public, as it makes light of the disruptions to the lives of those who have been diagnosed with them and the suffering they bring.
You don’t want to reduce stigma so much to the point when somebody likes oh I like to put my water bottle on the right side, oh I’m OCD. You know. Or like oh I had a negative thought that came in, oh I have schizophrenia. You don’t want people to like over-normalise it, cause that does happen in these days. Like when just somebody likes to be neat, they consider themselves OCD. Yeah, it’s so frustrating. The definition of mental illness is it’s supposed to disrupt your natural life. If it doesn’t disrupt your life in any way, it’s not supposed to be considered a mental illness. So, when people are like oh I’m very OCD, or like oh I have depression. Yeah, everybody has depression. (Female, 23 years, Psychosis related disorder, PWLE FGD 5)
They also did not wish for others to take pity on them or treat them differently on account of their mental illness but to instead be supportive in their recovery.
You shouldn’t get them to sympathize with you, more like to understand them. Rather than like say that okay you must be careful of this people, you must just give them information you know (Male, 24 years, Mood disorder, PWLE FGD 6)
We would educate them on how to less stigma, how to know about our condition, then how to actually support us in the recovery process (Female, 34 years, Psychosis-related disorder, PWLE- FGD 4)
3.2. Social Contact
Three kinds of social contact were raised by the participants: celebrity disclosures, testimonies of success stories by people with mental health conditions and opportunities to interact with them.
3.2.1. Celebrity Disclosures
The participants exemplified that the disclosure of mental health struggles by local celebrities as being particularly impactful. They reasoned that Singapore has a celebrity culture in which celebrities have a large following and influence. Sharing their mental health difficulties would drive the message that mental illness does not discriminate, debunk certain stereotypes associated with mental illness, validate the experiences of those coming to terms with their illness, and encourage open and honest discussion about mental illness.
I think it’s good if you can get someone, well known in Singapore, to share about their family members having mental illness or they themselves having mental illness. (Female, 51 years, Caregiver FGD 5)
In Singapore, there is a podcast. That is actually supposed to be a comedy podcast, but every now and then it gets a bit real. And they talk about themselves. So, I think, I don’t know if you guys know Nathan Hartono? He runs a podcast with his friend named Jon Kensey who’s also based in Singapore. He’s Filipino but he’s based in Singapore. He does comedy shows, he does, he’s a comedian. He does all these funny little things but every now and then when we write in, and we are allowed to write in to them it’ll just be like an idea of what would you suggest if we are going through this thing. So, he actually openly talks about his depression. So, he’ll share experiences, he’ll share what he would do, he would make things very clear that it’s not supposedly the only way or the best way to do things but that’s how he would have done it. Yeah, and the thing these little things help knowing that even people who are supposedly seen on a higher pedestal is also facing the same things as you are. Yeah, really changes a lot (Male, 23 years, Mood disorder, PWLE FGD 1)
3.2.2. Sharing Inspirational Recovery Stories
Apart from celebrity figures, the PWLE suggested that inspiring recovery stories of people with lived experiences can be included in anti-stigma efforts. They reasoned that these stories illustrate that mental illness does not need to be a barrier to attaining a meaningful life, that people with mental health conditions could be productive members of society, an embodiment of strength and courage despite adversity, and give hope to those worried about their or their loved one’s future.
I remember that time I was watching the news about lady, she suffered from mental illness but she… she see doctors, follows up regularly, she is recovered in that sense. She secured a job as a lecturer in one of the local polytechnic. She wrote a book. She was very frank with her employer, that was good, and they accept her as she is but she still go back to the hospital like every several months for follow-up and stuff like that. So I find that very enlightening. That there is such people who actually like make good head way in their life despite having mental illness. So I think if you can find more of such people and interview them highlight to the public that is actually… we can also be successful in their own way, it will be good. (Female, 44 years, Psychosis-related disorder, PWLE FGD 3)
3.2.3. Opportunities for Social Contact
The participants opined that it would be beneficial for those without mental illnesses to have opportunities for direct social contact with PWLE. They identified the benefits of this strategy as allowing people to relate to PWLE on a more personal level and debunk extreme examples of mental illness. They added that such a first-hand experience would be more compelling than didactic approaches.
( Another participant: Education is important) And exposure, I think. Because education is like you are telling people you know? But I think exposure for them to experience it, interaction with people with mental illness. It really speaks more than words. How they… because people always have this misconception ‘oh ok, mental illness, violence, negative, crazy, talking to yourself…’ But in fact, in fact most mental patients are not like that, they don’t behave that way. (Female, 39 years, Caregiver FGD 1)
I would emphasize priorities on interaction between the regular population and those with illness. To let them realize there’s no big difference. (Male, 24 years, Mood disorder, PWLE FGD 6)
3.3. Advocacy by Influential Figures or Groups
The participants felt that the question of “who” leads the de-stigmatisation efforts matters. Some participants suggested that mental health experts should partner with organisations that have larger influence, while others asserted that the efforts should be helmed by organisations other than psychiatric experts.
Because like even in my head, the assumption is it’ll probably come from IMH. Which to me is not the most effective method of campaigning because then everybody would be like, yeah they would do this, of course they would do this. So, I think, no. (Male, 23 years, Mood disorder, PWLE FGD 1)
They identified individuals and groups with political affiliations as being particularly suited due to their authoritative influence, networks, and access to funds.
To be effective it has to be nationwide, government-led initiative. It cannot be a little bit here and there, by IMH or by Caregiver Alliance, it doesn’t really work. It has to be nationwide and it has to have the support of the government. First, they have the resources and as what (another FGD participant) said uh, they can be very effective if they are very serious in wanting this campaign to be successful, they can do it. (Female, 51 years, Caregiver FGD 5)
3.4. Legislation of Anti-Discriminatory Laws
3.4.1. removal of declaration of mental illness in job application and scholarship forms.
In virtually all the FGDs, the participants called for the removal of the declaration of mental illness from job application and scholarship application forms. They regarded this requirement as being both irrelevant and discriminatory and believed that their unsuccessful applications were directly due to their disclosure.
Now we talk about the functional ability of a mental illness person, we talk about work. When you work, you need to fill in a lot of forms. There are a lot of things that…why must there be a declaration by the organisation? Why? Why? That is not good, that is not fair. In school, in army or in certain big organisation, there is always a declare, “Are you mentally ill? Do you have a mental problem?” Why is that in the form? It should be out. (Male, 62 years, Caregiver FGD 1)
I hope like whenever you’re applying for a job then you do not need to tick off the, “Do you have a mental illness?” that... that column. But maybe being open about it and talk about it would make the person understand in your shoes (Female, 25 years, Mood disorder, PWLE FGD 6)
3.4.2. Policies That Encourage Employers to Hire and Support PWLE in Workplaces
Although the participants called for the removal of mental illness declarations on application forms, they preferred to be truthful about their condition, as they feared being discovered if they had lied to increase their chances of employment. They also found that concealing their condition and their medical appointments was burdensome. The PWLE suggested that apart from raising awareness among employers, governmental support could be given to encourage employers to hire individuals with known mental health conditions.
The government could perhaps encourage their employers to take on mental patients who are willing to disclose their conditions of their job contracts. I stay in (name of a sheltered home) and the practice of their employment specialist is to have a very honest declaration. Just help… just say we have, this person who is going to help work has a mental condition. So they say that is why I follow them because they do it on a clean cut basis but I feel very upset because I follow suit, I declare my condition, and I loss so many chances of being employed. So government can do, I think government has yet to, have a lot to do. (Female, 55 years, Psychosis-related disorder, PWLE FGD 3)
In line with my unemployment, no money, and at the same time, I feel like I can contribute la to the greater society, ah you know what I’m saying? So that maybe in the future, people will say okay never mind you can work but then like you know, every year got psychiatric evaluation you know that’s even better, you know. A company that’s accepting of your condition. (Male, 24 years, Mood disorder, PWLE FGD 6)
Lastly, several participants shared being caught in awkward situations upon disclosure and the found reactions by their superiors inappropriate. Thus, they suggested that guidelines can be put in place to inform employers on how to respond sensitively to those who choose to disclose.
Maybe you can suggest to MOM [Ministry of Manpower] to remove the questions about health conditions. Have some regulations or advice to employers about how they can react to people who declare or maybe even take it out from the application form. For example, in the US [United States], you’re not actually, it’s kind of discriminatory, you’re not allowed to. It’s against the law to discriminate people based on their orientation or whatever, their conditions. So maybe in Singapore, we can move ahead in that regard. (Male, 28 years, -Psychosis-related disorder, PWLE FGD 5)
4. Discussion
The suggestions by the PWLE and caregivers in tackling stigma can be classified broadly as raising awareness through education, social contact, advocacy, and legislative reform. These strategies are in line with the approaches that have been used internationally to disrupt the process of stigma. Corrigan et al. [ 47 ] have suggested three approaches: education, protest, and contact, while Arboleda-Florez and Stuart [ 22 ] extended Corrigan’s typography with three additional strategies: legislative reform, advocacy, and stigma self-management. Our study has further identified nuanced details on how this can be carried out in the Singapore landscape.
Raising awareness through public education was the most suggested strategy. It is appealing, as it targets lack of awareness and misinformation with the provision of information. Young people in particular were identified as a target group for educational intervention due to the burgeoning pressure they face, the potential they have in changing the future, and the opportunities that school settings have to deliver interventions using a literacy approach, points that have also been described previously [ 48 , 49 ] in the literature. School-friendly literacy approaches have been shown to be effective in improving knowledge about mental health conditions [ 50 ].
The participants suggested various ways of raising awareness for the general population and drew particular attention to the potential problems of media strategies due to their tendency towards presenting stories in a sensational manner. Gottipatti et al. [ 51 ] explored local media portrayals of people with mental disorders in Singapore’s largest media organisations, Singapore Press Holdings and MediaCorp, and reported that mental health-related articles in Singapore were primarily negative in sentiment, with crime-related news accounting for 40% of the corpus. Moreover, mental health experts had unwittingly used stigmatising terms in interviews. The authors suggested that media professionals and editors can also be enlisted to play a more proactive gatekeeping role and to counteract the largely negative portrayal of mental illness by providing articles on well-being and recovery. They also proposed a rule-based solution model based on text mining and natural language processing (NLP) techniques that can automatically identify aspects of stigma in media articles for editing before publication [ 51 ]. Similarly, Stout, Villeges, and Jennings [ 52 ] suggested for informational and educational activities to be arranged for journalists that teach techniques to report on mental health stories in a balanced and responsible way. Other strategies that have been used include SANE Australia’s (a charitable advocacy group) StigmaWatch program, which monitors and responds to the inaccurate or inappropriate media portrayal of mental illness. If problematic reporting is not remedied, then the group may consider taking public action [ 35 ].
The participants also cautioned that messaging should not result in benevolent stigma—an unintended consequence of well-intentioned approaches, where people with mental illness are treated as being unable to competently handle life’s demands and need a benevolent authority to make decisions for them [ 30 ]. This kind of messaging is stigmatizing, as is perpetuates power imbalances by appealing to the public to do good for a seemingly weak, pitiful subordinate group [ 53 ]. Such a response disempowers people with mental health conditions and stunts opportunities for personal growth. The participants in our study, as Corrigan had pointed out, wished for empathy cultivation leading to being treated with parity rather than pity. They also cautioned that efforts at normalising mental illness should not result in the trivialisation of the disorder. Research has suggested that those who accept their mental illness as part of their identity, overcome the challenges of stigma, and who remain resilient, may feel a sense of pride in being able to do so [ 30 ]. Thus, symptoms that are “undeserving” of the diagnosis may be viewed as discrediting their strength and authenticity.
The second theme that the participants identified was an opportunity for members of the general public to have social contact with a PWLE. They believed that many members of the public had never had personal interactions with a person with mental illness and formed attitudes towards people with mental health conditions based on stereotypes. In line with Allport’s [ 54 ] intergroup contact strategy, they proposed that personal contact with individuals with mental health conditions would reduce prejudice towards them. Purely naturalistic contact in everyday settings, however, does not reduce stigma [ 55 ], as high rates of stigma persist amongst mental health service staff who are in contact with individuals with mental health conditions on a daily basis [ 56 ]. Effective contact-based strategies are planned interactions with certain conditions in place. Some of these conditions relate to the credibility of the speaker, the local relevance to the audience, the disclosure of personal struggles due to the illness and “on the way up stories” describing successes in areas of living independently, employment and in having quality relationships [ 21 , 25 , 31 , 57 ] A local study examining the impact of a combined education and face-to-face contact intervention with university students showed that the intervention significantly improved stigma, reduced the desire for social distancing, and improved attitudes towards help-seeking [ 32 , 33 , 58 ]. However, the effects of this intervention was short-term, highlighting our participants’ assertion as well as supporting literature that stigma-reduction efforts should be continuous [ 57 ].
While such planned interactions can be logistically challenging and encumber continuity of exposure, the evidence suggests that non-face-to-face contact can also deliver notable results [ 59 ]. Schiappa et al.’s [ 60 ] “parasocial contact theory”, which was built upon Allport’s hypothesis proposes that sustained mass-mediated contact with a media figure engenders a parasocial relationship where the viewer feels a real, emotional connection with the figure that is akin to that with a close friend. Thus, the revelation of a stigmatised identity from the celebrity with whom a parasocial bond already exists has a greater potential to reduce stigma than an encounter with someone new who reveals the same stigmatised identity [ 61 ]. Indeed, an experimental study among undergraduate students showed that exposure to a video of popular pop singer, Demi Lovato, disclosing her experience with bipolar disorder (BD) significantly reduced negative stereotypes towards BD, and the higher the level of parasocial relationship, the lower their negative stereotypes of people with BD were [ 59 ]. There is also potential for repeated exposure to mass-mediated content to effect long-term change, as demonstrated in a longitudinal study in which college students who were presented with filmed social contact every 2 months over a 12-month period showed significantly positive long-term outcomes (24 months follow-up) in terms of their behavioural intentions for social contact with PWLE compared to the control groups [ 62 ]. Participants highlighted that this approach could serve well in a society such as Singapore, which has a celebrity culture.
The third and fourth themes relate to advocacy by influential figures/groups and the legislation of anti-discriminatory laws. Legislative reform is designed to prohibit discrimination on any grounds, improve the protection of people with mental illness, and offer reasonable accommodations in areas such as employment, education, and housing. Advocacy is designed to ensure that people with mental illness enjoy the rights and freedom offered by legislation and provide avenues of redress for inequitable policies and procedures [ 22 ]. Discussions among participants on these themes highlighted the importance of governmental organisations, grassroots leaders, and other public figures who carry the clout to push for changes in policy and practices to create an environment that is more inclusive and supportive of people with mental health conditions. They argued that mental health experts are not the best people for this task, alluding to the fact that it could be perceived as an act of self-interest to promote the importance of their profession—a point also identified by Clement et al. [ 63 ]. Corrigan [ 30 ] contrasted the service agenda in targeting stigma with the rights agenda, where the former is aimed at removing barriers to professional care, while the latter replaces disenfranchisement with affirming attitudes and behaviours. These agendas, which have different purposes and processes, may compete, and choices need to be made in allocating resources to work towards the chosen endpoint [ 30 ].
The participants in the study commented that mental health awareness has increased in Singapore in the past couple of years, but these advancements have not caught on as quickly, particularly in workplaces. A significant proportion of PWLE remain unemployed despite their desire and ability to work [ 64 ]. At the time when the data were collected, mental illness declarations were still a part of job application processes. In the FGDs, the participants zealously urged for this practice to be put to an end, as it impeded their employability and career ambitions. Further to the removal of this declaration, they suggested that support schemes should be offered to employers for hiring people with mental illnesses. A systematic review of anti-stigma interventions in workplaces showed that targeted interventions could lead to improved employee knowledge and supportive behaviour towards people with mental health problems [ 65 ]. However, due to the methodological shortcomings of the included studies, the heterogeneity of the intervention content and other issues, no efficacious intervention element could be identified. The current evidence suggests that specific workplace messages are more influential than more general workplace messages, and these messages should also be tailored for different stakeholders within the workplace (e.g., supervisors vs. employees) [ 66 ]. Corrigan recommended that identifying specific stigma change goals can be undertaken through a needs assessment conducted together with the target group [ 67 ]. One component of stigma change identified in this study was the inclusion of practice guidelines on responding to disclosure appropriately, fairly, and sensitively in workplaces.
Several mental illness de-stigmatisation endeavours, some of which have incorporated the suggestions identified in this research, have occurred in Singapore. First, Singapore launched its first long-running anti-stigma campaign called Beyond the Label in September 2018, with PWLE fronting the campaign and a strong social media presence. In January 2019, the first insurance policy that covers common mental illnesses, the AIA Beyond Critical Care, was launched by AIA Singapore. In December of the same year, the Tripartite Alliance for Fair and Progressive Employment Practices declared that asking job applicants about their mental health condition without good reason was discriminatory and that employers who do not abide by the updated guidelines may be liable to enforcement actions. As one of the PWLE in our FGD summarised,
“It’s moving, it’s slow…but it is gaining momentum…This is the best time for the mentally ill. People are more able to speak up for themselves even as patients and that is a wonderful thing”.
There are a few limitations to this study. First, the participants were recruited on a voluntary basis. Thus, the findings may not reflect the broader views of PWLE and caregivers. Two FGDs had only four and five participants, which may have made the dynamics of that group different from the larger-sized ones although the analyses did not suggest any specific themes coming up or being omitted in those FGDs. Second, as the researchers were from the IMH, participants have may withheld their critical views of the mental health system and suggestions to improve it, as it was possible that they did not want to offend the researchers affiliated with the institution. Third, the data were analysed from the lens of the researchers—the PWLE and caregivers were not part of the team analysing the data.
Notwithstanding these limitations, this study is one of a few studies in Singapore to have obtained inputs on stigma reduction from the perspectives of those who have been stigmatised. While several positive steps have been taken towards de-stigmatisation, evaluation efforts for these initiatives are currently lacking. It is recommended that scientifically rigorous evaluations of these efforts be undertaken so that outcomes can be tested, and the initiatives can be continually improved. Further, PWLE should be included in future anti-stigma research as well as in the evaluation of these campaigns and programmes.
5. Conclusions
The PWLE and caregivers highlighted that careful deliberation is needed when crafting messages to raise awareness about mental illnesses to avoid the unintended effects of trivialisation of these illnesses and the generation of sympathy. The research also identified how individuals such as community leaders and media figures are in advantageous positions to reduce stigma and advocate for better support for people with mental health conditions. The continued evaluation of new anti-stigma strategies is important to informing the impact of these efforts as well as to fine-tune future initiatives.
Acknowledgments
We would like to thank the participants for sharing their perspectives and making this work possible.
Author Contributions
Project administration, investigation, formal analysis, writing—original draft: S.S.; project administration, investigation, formal analysis, writing—review and editing: C.M.J.G.; investigation; formal analysis, writing—review and editing: G.T.H.T.; investigation, formal analysis, writing—review and editing: W.J.O.; funding acquisition, conceptualization, writing—review and editing: S.A.C.; conceptualization, methodology, investigation, formal analysis, supervision, writing—review and editing: M.S. All authors have read and agreed to the published version of the manuscript.
The study was supported by Tote Board (Singapore) under the Tote Board Strategic Initiative on Mental Health. The funding body of the study had no involvement with the design of the study, collection, data analysis and interpretation, or in the writing of manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by National Healthcare Group Domain Specific Review Board (DSRB Reference No. 2017/01175).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
ORIGINAL RESEARCH article
Treatment-seeking threshold and accessibility of psychiatric outpatient services in switzerland: the relationship with stigma and self-esteem.

- 1 Universitäre Psychiatrische Kliniken (UPK) Basel, Klinik für Erwachsene, University of Basel, Basel, Switzerland
- 2 Faculty of Psychology, Division of Clinical Psychology and Epidemiology, University of Basel, Basel, Switzerland
- 3 Institute for Evaluation Research, Universitäre Psychiatrische Kliniken (UPK) Basel, University of Basel, Basel, Switzerland
Perceived stigmatization and low self-esteem are linked to poorer mental health outcomes, but their impact on treatment-seeking thresholds and the importance of outpatient service location remain unclear. The study included 525 outpatients of the University Psychiatric Clinic (UPK) Basel, Switzerland, of whom 346 were treated at inner city services and 179 at services located on the main site of the UPK at the outer city limits. Perceived discrimination and devaluation (PDD), self-esteem (SE), treatment-seeking threshold (TST), and accessibility were measured via a self-reported questionnaire. The PDD consisted of 12 items evaluating beliefs about the level of stigma towards individuals with mental illness in the general population on a 5-point Likert scale. SE, TST and accessibility were assessed through single-item 7-point Likert scales. PDD and SE were positively correlated ( p < 0.001), suggesting that lower perceived stigma was linked to higher self-esteem, and were not associated with TST. The relationship between PDD and SE remained consistent after controlling for age, gender, and nationality. Age was negatively correlated with TST ( p = 0.022), while gender did not significantly influence any of the variables. There was little variation regarding PDD, with emergencies at the site of the psychiatric clinic and substance use disorder (SUD) patients reporting higher levels of stigmatization. Emergency patients and those with SUD and personality disorder reported the lowest SE ratings. TST showed a broad range and was highest for emergency services and transcultural psychiatry patients. Differences in accessibility were mainly linked to the location, with outpatient service users in the inner city reporting better accessibility ( p < 0.001) and higher SE ( p = 0.009). In comparison to patients using services with planned contacts only, patients in emergency settings differed by higher TST ( p = 0.018) and better ratings of accessibility ( p = 0.004). In conclusion, there was a relevant amount of stigmatization, impaired self-esteem, and, for some outpatient services, high thresholds to seek treatment. Future research should explore other factors influencing TST. The findings highlight the need to address stigmatization and accessibility when planning mental health services.
To this day, suffering from a mental illness means a double burden for those affected due to the illness itself and the stigmatization of mentally ill people ( 1 , 2 ). Despite the availability of effective treatments, a substantial number of individuals with mental illness continue to experience barriers in seeking and receiving appropriate care ( 3 – 5 ). Only about one third of individuals with mental illnesses actually seek mental health treatment ( 6 ).
One critical factor contributing to this treatment-seeking threshold is perceived stigma of mental illness, including both what an individual thinks most people believe about the stigmatized group in general and how the individual thinks society views him or her personally as a member of the stigmatized group ( 7 ). Negative and discriminatory prejudices toward people with mental illness that are frequently endorsed in society include perceptions of decreased trustworthiness and professional skills ( 8 ). Perception of public stigma is seen as the initial step toward developing self-stigma, which involves internalizing negative beliefs about oneself due to one’s mental health condition ( 8 – 14 ). At the same time, perceived stigma represents a major source of maintaining self-stigma ( 9 , 15 ).
Perceived public stigma and self-stigma have been found to impact attitudes toward seeking psychological help ( 16 – 18 ). These factors also influence perceived need for help and the desire to self-manage mental health issues, potentially delaying or preventing help-seeking behavior ( 18 – 20 ).
Being an important barrier affecting an individual’s decision to seek care for mental health problems, perceived and self-stigma have been linked to adverse outcomes, including worsened mental health symptoms, treatment avoidance, poorer treatment adherence and higher suicide risk ( 21 – 25 ).
Individuals who internalize negative stereotypes about mental illness may experience feelings of shame, guilt, hopelessness, decreased self-esteem and lower self-efficacy, impacting their quality of life ( 15 , 26 – 29 ). Perceived and self-stigma may lower an individual’s self-esteem by labeling themselves as socially unacceptable when seeking psychological help ( 16 ). In contrast, high self-esteem may play a significant role in mitigating the impact of perceived stigma on an individual’s well-being and improving motivation to seek treatment ( 15 , 30 , 31 ). In our study, we therefore expect to find significant correlations between perceived discrimination and devaluation (PDD), self-esteem (SE), and treatment-seeking threshold (TST).
While the link between mental illness stigma, self-esteem, and treatment-seeking threshold has gained considerable empirical attention, relatively less focus has been directed towards investigating the potential influence of the accessibility of psychiatric outpatient treatment sites in this context. Accessibility refers to the extent to which mental health services are readily available, physically reachable, affordable, and socially acceptable to individuals in need. Several factors can contribute to treatment site accessibility, including proximity, transportation options, cost, and cultural acceptability. Often, outpatient services are strategically placed at highly frequented and easy to reach local venues (e.g., in the city center or in proximity of a train station) to increase accessibility. On the other hand, economic considerations favor integrating integration of outpatient services with inpatient mental health clinics, which are often not optimized for accessibility and tend to be more stigmatized ( 32 – 34 ). For example, in the canton of Basel, the Psychiatric University Clinic operates multiple specialized outpatient services, some of which are within the inpatient mental health clinic perimeter, while others are strategically placed within the inner city limits. However, it is unclear if these different settings address patient populations with different help-seeking thresholds, and how they influence perceived stigma and self-esteem. Thus, regarding the potential impact of accessibility, we will explore the hypothesis that patients receiving treatment at psychiatric outpatient services in the inner city exhibit significantly different levels of perceived discrimination and devaluation (PDD), self-esteem (SE), treatment-seeking threshold (TST), and accessibility compared to the main site of the psychiatric university hospital at the outer city limits.
Other factors that affect the stigmatization of patients are the diagnosis and the type of service sought. Seeking help at psychiatric emergency services, often associated with severe mental illness, aggressive and self-harming behavior, can lead to heightened stigmatization ( 35 ). Thus, we will investigate whether the type of contact (planned contacts only versus unplanned emergency contacts) has a significant impact on perceived discrimination and devaluation (PDD), self-esteem (SE), and treatment-seeking threshold (TST).
Patients with substance use disorders, psychotic illnesses and personality disorders often face discrimination and devaluation due to prevailing societal prejudices against these specific conditions ( 36 – 39 ). For instance, patients with psychotic illnesses are seen as more dangerous and unpredictable compared to other mental illnesses ( 40 , 41 ). Individuals with personality disorders are perceived as untreatable, manipulative and challenging in relationships ( 42 , 43 ). Addiction disorders are frequently assumed to be self-inflicted resulting from a lack of discipline and are also more often associated with self-neglect and criminal behavior ( 37 , 44 , 45 ). Research has demonstrated that these particularly stigmatized patient groups have lower self-esteem compared to other mental health conditions ( 39 , 46 – 49 ). Thus, regarding the treatment focus of the psychiatric outpatient service, we assume that there will be significant differences in perceived discrimination and devaluation (PDD), self-esteem (SE), and treatment-seeking threshold (TST).
Furthermore, gender, age, and cultural factors such as nationality and ethnicity can influence an individual’s experience of stigma and treatment-seeking behavior. According to previous studies, males are more likely to experience both public and self-stigma associated with psychological help-seeking in comparison to females, and women tend to show fewer stigmatizing attitudes ( 50 – 53 ). Aging, for instance, may influence perceived stigma and willingness to seek treatment, with older individuals showing lower stigma scores and more positive attitudes toward help-seeking ( 54 ). Ethnic minorities and migrant populations may face increased stigma and barriers to seeking help ( 55 – 57 ). At the same time, these groups seem to be more vulnerable to mental disorders, with a higher prevalence compared to the general population ( 58 , 59 ). Thus, we hypothesize that the gender, age, and nationality of the participants have an influence on perceived discrimination and devaluation (PDD), self-esteem (SE), and treatment-seeking threshold (TST).
Aims of the study
The current paper aims to examine if psychiatric outpatient treatment sites are addressing different patient groups regarding perceived stigma, self-esteem, and treatment-seeking threshold depending on their accessibility, and to explore the relationship between perceived stigma, self-esteem, and treatment-seeking threshold.
The University Psychiatric Clinic (UPK) Basel is the only psychiatric university clinic in Northwestern Switzerland and serves a catchment area of about 200,000 persons in the canton of Basel-Stadt and the surrounding area. It provides psychiatric emergency care and basic psychiatric diagnostics and treatment for this population, but also maintains highly specialized services (e.g., for non-organic sleep disorders) for a larger catchment area. In 2018, 14 outpatient treatment services were available at the UPK Basel. Some of the services were located at the main site of the psychiatric clinic (Wilhelm Klein-Strasse 27, CH-4056 Basel) at the outer city limits, some were located within the inner city limits (Kornhausgasse 7, CH-4051 Basel), and one outpatient service was located within the inner city limits directly at the somatic university hospital (Spitalstrasse 2, CH-4056 Basel). Figure 1 gives an overview on these geographic locations.

Figure 1 Locations of psychiatric outpatient services of the UPK Basel. Source: Statistical Office of the Canton of Basel-Stadt (Statistisches Amt des Kantons Basel-Stadt) https://www.basleratlas.ch .
The UPK Basel routinely conducts anonymous patient satisfaction surveys as part of its quality management procedures. For the current paper, data from the patient survey conducted in 2018 were available. No ethics committee vote was necessary for the analysis and publication of this anonymously collected routine quality management data. This was confirmed by the responsible ethics committee (Ethics Committee of Northwestern Switzerland; EKNZ; Req-2023-01405).
Participants and procedures
All patients who had at least one contact with a psychiatric outpatient service at the UPK Basel between 26 th March 2018 and 25 th June 2018 (cut-off date of the survey) and had a place of residence in Switzerland were invited to participate. A total of 2,203 patients were sent self-report questionnaires via standard mail within Switzerland. The questionnaires were provided in German. Due to organizational reasons, the questionnaires were not sent abroad. Participants were informed about the purpose and methodology of the survey and were assured of the confidentiality and anonymity of their responses. There was no time limit imposed on completing the questionnaires. A stamped return envelope was enclosed.
Data entry was performed by the Institute for Evaluation Research, Basel, a separate entity from the UPK Basel, to further ensure confidentiality. Paper questionnaires were scanned, data was converted into an electronic format, checked for plausibility and, if necessary, post-processed using Remark Office OMR, V8.0 ( 60 ). The data entry process involved assigning numerical codes to responses, thereby assuring anonymity of the participants, and then double-checking for data accuracy and completeness.
Assessments
Perceived stigma was measured using the Perceived Discrimination Devaluation Scale (PDD), developed by Link ( 8 ), which consists of twelve items measuring respondents’ beliefs about the extent to which ‘most people’ would discriminate against and devalue individuals with a history of psychiatric treatment. The PDD, also known as ‘stereotype awareness’, evaluates individuals’ recognition of the negative views held by the general population towards those with mental illness ( 15 ).
Responses indicate the level of agreement with each statement, rated on a 5-point Likert scale ranging from 1 (“statement does not apply”) to 5 (“statement applies fully”). A low level of perceived stigma against people with mental illness is indicated by agreement with six positively poled items (e.g. “Most people would treat a former mental patient just as they would treat anyone.”) and disagreement with six negatively poled ones (e.g. “Most people think less of a person who has been in a mental hospital.”). The scale demonstrated sufficient global internal consistency of α = 0.84 ( 61 ).
For the purpose of this study, the German translation of the PDD was used ( 62 ). To facilitate statistical analysis, the six negatively worded items of the PDD were reversed so that higher values corresponded to lower perceived stigma. Then, a total PDD mean score was calculated by summing the values of all twelve items and dividing by twelve. As a result of reversing the negatively worded items, the final PDD mean score ranged from 1 (strongly perceived stigma) to 5 (low perceived stigma).
To assess self-esteem, the Single-Item Self-Esteem Scale ( 63 ) was utilized. Participants were instructed to rate their agreement with the statement “I have high self-esteem” on a 7-point Likert scale ranging from 1 (Not very true of me) to 7 (Very true of me). The Single-Item Self-Esteem Scale offers a test-retest reliability of 0.75 ( 63 ) according to the Heise procedure ( 64 ).
Treatment-seeking threshold (TST) was self-reported using a single item (“I had inhibitions about seeking treatment at the outpatient service.”) 7-point Likert scale ranging from 1 to 7 with higher values indicating a higher threshold. The item referred to the first contact to the outpatient service.
The accessibility of the treatment site was equally assessed through a self-report single item (“The outpatient treatment service was easily accessible for me.”) on a 7-point Likert scale where higher values were synonymous with greater ease of accessibility.
Age, gender and nationality of participants were recorded using free text fields.
Data analysis
Descriptive statistics and Mann-Whitney U tests ( 65 ) were used to compare mean values for perceived discrimination and devaluation, self-esteem, treatment-seeking threshold, and accessibility between psychiatric outpatient clinics that were located within the inner city or on the main site of the psychiatric university hospital at the outer city limits.
Shapiro-Wilk ( 66 ) and Levene ( 67 ) tests were conducted to assess normal distribution and variances, respectively. A Kruskal-Wallis test ( 68 ) was used to analyze differences based on the psychiatric service visited.
To examine the correlation between PDD, SE, and TST, Pearson’s correlation analysis was performed. Correlation analyses were calculated for the whole sample and for the subgroups of outpatient services located inside and outside the inner city limits. A significance level of p < 0.05 was used to determine the statistical significance of the correlation coefficient.
Partial correlations were performed to test whether gender, age and nationality of the subjects could be potential confounding variables. For the partial correlation analysis of nationality, participants’ countries of origin were grouped into regional categories due to some foreign nationalities being represented by one person. Nationality was used for descriptive statistics only because of uneven group sizes.
Confidence intervals with a coverage probability of 95% were calculated for the mean values and correlation coefficients to estimate the uncertainty surrounding the obtained results ( 69 ).
Any missing values were excluded pairwise. As this was an exploratory study aimed at generating new hypotheses, no correction for multiple testing was performed. Data were analyzed using IBM SPSS Statistics 27.0 ( 70 ).
Table 1 provides information on the catchment area, type of contacts available, and spectrum of diagnoses treated in the different outpatient services. While most outpatient services have planned contacts, the walk-in outpatient service (inner city) and the patient admission/emergencies service (outer city) provide emergency services and unplanned appointments. Most services have the canton of Basel-Stadt and its surrounding regions as catchment area. The outpatient service for non-organic sleep disorders, however, serves a supracantonal catchment area.
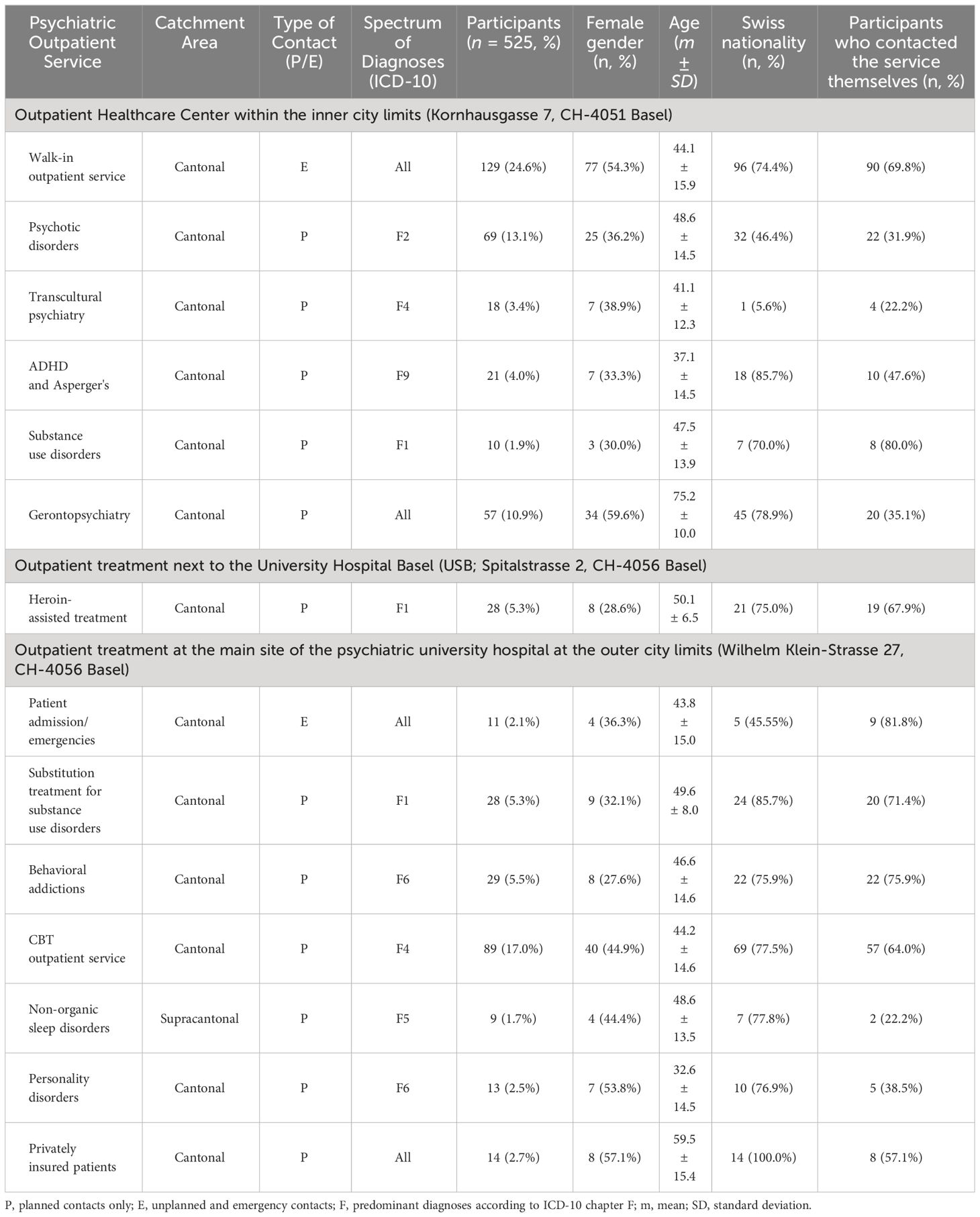
Table 1 Psychiatric outpatient service characteristics and patient samples.
In addition, Table 1 lists information on the number of participants from each outpatient service as well as descriptive statistics on gender, age, nationality and the percentage of participants who had contacted the service themselves. A final sample of 525 participants answered the survey, resulting in a response rate of 23.8% (for an overview on the distribution across outpatient services, please cf. Table 1 ). The response rates of the psychiatric outpatient clinics were at least 15.6% (substitution treatment for substance disorders) and a maximum of 42.4% (privately insured patients).
63.2% of the survey participants were patients from outpatient services located within the inner city, and 36.8% were from services located in the outer city limits. 44.6% of the participants were female. The participants were aged between 18 and 99 years with a mean (m) of 48.8, a standard deviation (SD) of 17.1 and a 95% confidence interval (CI) ranging from 47.2 to 50.3 years. 371 (70.7%) were Swiss citizens, 23 (4.4%) had the Swiss and a foreign nationality. Participants of foreign nationality were predominantly German (23; 4.4%), Italian (18; 3.4%), or Turkish (9; 1.7%). 8 (1.5%) participants were from other Western European countries, 13 (2.5%) from Eastern Europe and 1 (0.2%) participant was from mixed European descent. Outside of Europe, 7 (1.3%) participants were from Eastern Asia, 5 (1.0%) from the Middle East, 5 (1.0%) from African countries and 1 (0.2%) participant was from the USA. 41 (7.8%) participants did not specify their nationality.
296 (56.4%) participants had contacted the outpatient service themselves. 173 (33.0%) had started treatment in 2018. 106 (20.2%) out of 471 participants had already finished their treatment at the time of the survey, while 365 (69.5%) were still in treatment.
Descriptive statistics for perceived discrimination and devaluation (PDD), self-esteem (SE), treatment-seeking threshold (TST), and accessibility of each outpatient service are shown in Table 2 .
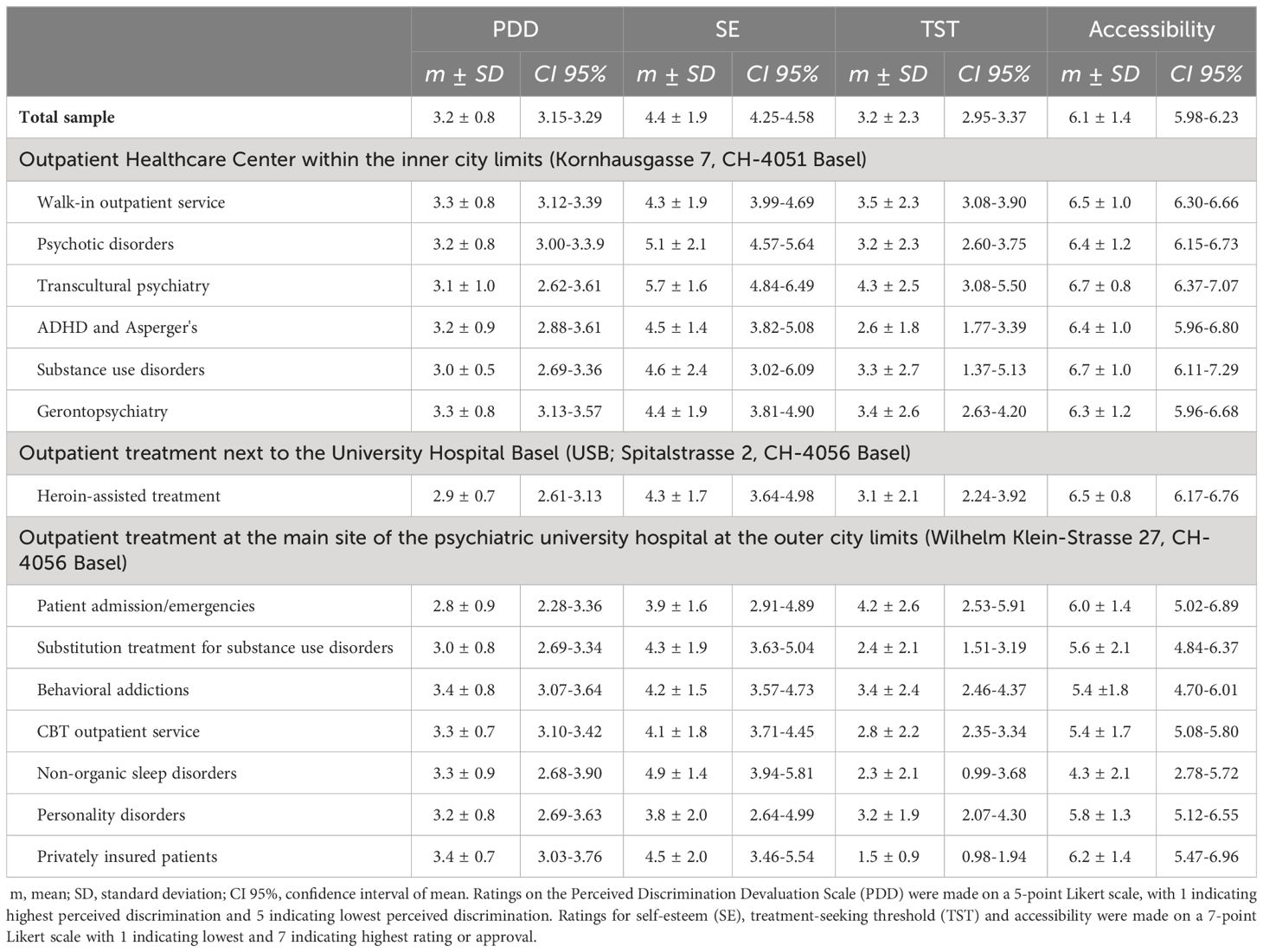
Table 2 Clinical data of psychiatric services and perceived discrimination and devaluation (PDD), self-reported self-esteem (SE), threshold to seek treatment (TST) and accessibility of site by survey participants.
In the total sample of n = 525, PDD was reported at a considerable level by all patients (mean of 3.2) with little variation (SD=0.8, CI 3.15-3.29). SE had a mean score of 4.4 ± 1.9 (CI 4.25-4.58). TST was generally low to medium with a mean of 3.2 ± 2.3 (CI 2.95-3.37). For all psychiatric services, accessibility was rated high with 6.1 ± 1.4 (CI 5.98-6.23).
Correlation analyses revealed a significant association between perceived discrimination and devaluation and self-esteem ( r = 0.244, CI 0.156-0.329, p < 0.001) with a small effect size. Higher PDD scores indicating less stigma were associated with higher SE. Regarding TST, no significant correlation to PDD ( r = -0.081, CI [-0.173] – [0.014], p = 0.093) or SE ( r = -0.018, CI [-0.112] – [0.077], p = 0.712) was found in the total sample.
The data for SE, TST, and service location accessibility were not normally distributed ( p < 0.001), while PDD was approximately normally distributed ( p = 0.014). Levene’s test showed significant inequality of error variances ( p < 0.001) when conducting an ANCOVA test with PDD as an independent variable. Due to violation of homogeneity of variances assumption, Kruskal-Wallis tests were used to analyze group differences among the 14 psychiatric outpatient services. Significant differences were found in SE (H(13) = 23,675, p = 0.034) and location accessibility (H(13) = 56,474, p < 0.001), but not in PDD (H(13) = 15,147, p = 0.298) or TST (H(13) = 21,574, p = 0.062). Further analysis was conducted through descriptive statistics and Mann-Whitney U tests.
346 participants from seven psychiatric outpatient services in the inner city, at either Kornhausgasse or Spitalstrasse, had an average PDD score of 3.2 (SD ± 0.8, CI 3.14-3.31), SE score of 4.6 ± 1.9 (CI 4.35-4.79), TST of 3.3 ± 2.3 (CI 3.01-3.53) and rated accessibility at 6.5 ± 1.1 (CI 6.33-6.57).
179 participants from seven outpatient services located at the psychiatric university hospital main site on the outer city limits had an average PDD score of 3.2 ± 0.8 (CI 3.09-3.33), SE score of 4.1 ± 1.7 (CI 3.88-4.40), TST score of 2.9 ± 2.2 (CI 2.58-3.29), and rated accessibility of treatment service at 5.4 ± 1.8 (CI 5.19-5.72).
Mann-Whitney U tests assessed differences in PDD, SE, TST, and accessibility of treatment location by outpatient service location. Patients at inner city services rated their accessibility significantly better than those treated at Wilhelm Klein-Strasse ( z = -6.85, p < 0.001, r = 0.308). Inner city patients also had significantly higher SE ( z = -2.62, p = 0.009, r = 0.123), but no significant differences were found in PDD ( z = 0.19, p = 0.851) or TST ( z = -1.39, p = 0.163) between groups. Positive correlations were found between PDD and SE for both inner city ( r = 0.211, CI 0.099-0.318, p < 0.001) and Wilhelm Klein-Strasse ( r = 0.314, CI 0.168-0.447, p < 0.001) patients. No significant correlations were found for TST and PDD ( r = -0.051, CI [-0.213] – [0.114], p = 0.545) or SE ( r = -0.111, CI [-0.267] – [0.050], p = 0.176) in either group.
The following analysis compares the ratings for PDD, SE, and TST for all 14 psychiatric outpatient services.
The highest levels of perceived stigma were reported by emergency patients (2.8 ± 0.9, CI 2.28-3.36) and patients with substance use disorders from three different outpatient services (2.9 ± 0.7, CI 2.61-3.13, 3.0 ± 0.5, CI 2.69-3.36 and 3.0 ± 0.8, CI 2.69-3.34) while patients from the behavioral addictions outpatient service (3.4 ± 0.8, CI 3.07-3.64) and privately insured patients (3.4 ± 0.7, CI 3.03-3.76) had the lowest PDD ratings.
Self-esteem ratings varied across services, with personality disorder, with patients using services for personality disorder (3.8 ± 2.0, CI 2.64-4.99), substance use disorder (4.3 ± 1.7, CI 3.64-4.98 and 4.3 ± 1.9, CI 3.63-5.04) and emergency services (3.9 ± 1.6, CI 2.91-4.89 and 4.3 ± 1.9, CI 3.99-4.69) having the lowest SE ratings. Patients from the transcultural psychiatry service (5.7 ± 1.6, CI 4.84-6.49), the psychosis outpatient service (5.1 ± 2.1, CI 4.57-5.64), and the outpatient service for non-organic sleep disorders (4.9 ± 1.4, CI 3.94-5.81) reported the highest SE ratings.
The lowest TST were reported by privately insured patients (1.5 ± 0.9, CI 0.98-1.94), patients from the service for non-organic sleep disorders (2.3 ± 2.1, CI 0.99-3.68), and patients receiving substitution treatment for substance use disorders (2.4 ± 2.1, CI 1.51-3.19). In addition, patients seeking diagnostic evaluation for ADHD and Asperger’s (2.6 ± 1.8, CI 1.77-3.39), and patients from the cognitive behavioral therapy outpatient service (2.8 ± 2.2, CI 2.35-3.34) had a relatively low TST. The highest TST were reported by emergency patients (4.2 ± 2.6, CI 2.53-5.91) at the main psychiatric hospital site and patients from the transcultural psychiatry service (4.3 ± 2.5, CI 3.08-5.50).
The emergency service at the main site of the clinic and the walk-in outpatient service in the inner city were compared with 12 services for planned contacts only using a Mann-Whitney U test. Significant differences were found for TST ( z = [- 2.37], p = 0.018, r = 0.111) and accessibility ( z = [- 2.90], p = 0.004, r = 0.131). Emergency patients showed a higher TST with a mean of 3.5 ± 2.3 (CI 3.1-3.9) in comparison to patients with planned appointments (3.0 ± 2.3, CI 2.8-3.3). The accessibility of the location was rated significantly better by emergency patients (6.5 ± 1.0, CI 6.3-6.6) than by patients in the planned setting (6.0 ± 1.5, CI 5.8-6.1). No significant differences emerged for PDD ( z = [- 0.46], p = 0.643) and SE ( z = [- 0.78], p = 0.434).
Partial correlations with gender, age distribution and nationality as possible confounding variables showed no change in effect size or direction of the correlations between perceived stigma and self-esteem.
Gender and age were tested for bivariate correlations with PDD, SE and TST. Between the age of the participants and TST, there was a significant negative relationship ( r = -0.111, CI [-0.203] - [-0.016], p = 0.022). Gender was not significantly related to any of the examined variables.
This study examined the association of outpatient services location with patients’ self-reported perceived stigma, self-esteem, treatment-seeking threshold, and service accessibility, and explored the association between perceived stigma, self-esteem, and treatment-seeking threshold in psychiatric outpatients. The adequately sized survey sample stems from a large university psychiatry tertiary care service provider covering all adult psychiatric diagnosis groups. Outpatient services ranged from emergency services and specialized outpatient services for specific diagnosis or age groups to outpatient services dedicated to privately insured patients. Half of the services were from outpatient services located in the inner city (with about two thirds of the participants), half were located at the outer city limit at the location of the main psychiatric hospital (with about one third of the participants). Thus, the current survey covered a broad and diverse range of outpatient services and allowed for a comparison of two geographical locations.
Concerning the relationship between perceived stigma, self-esteem, and treatment-seeking threshold, we found a positive correlation between low perceived discrimination/devaluation and self-esteem, which is in accordance with the published literature ( 15 , 29 , 71 , 72 ). However, no significant correlations between perceived stigmatization and treatment-seeking threshold emerged in our sample. In addition, no significant correlations between self-esteem and treatment-seeking threshold were found. While this result certainly has to be replicated in future studies, it indicates that other factors might be relevant for the threshold to seek treatment. According to the majority of empirical evidence, both perceived and self-stigma is associated with a negative attitude towards treatment ( 73 – 75 ). However, the systematic review and meta-analysis by Schnyder and colleagues (2017) found that participants’ own negative attitudes toward seeking mental health help and their stigmatizing attitudes toward people with mental illness were stronger associated with lower active help-seeking whereas perceived stigma did not prove to be a significant predictor ( 76 ). Other studies that focused on the role of perceived stigma also failed to demonstrate its influence as a correlate of treatment seeking ( 77 ). Instead, other factors like lack of knowledge about mental illnesses and their treatments, negative attitudes toward mental health treatment and a preference for self-reliance might have a greater influence on treatment uptake ( 23 , 31 ). In their study on individuals with major depression, the research group of Schomerus (2013) found that older age, higher education level, high conscientiousness, low resilience, social support, childhood abuse, and more severe depression were linked with help-seeking ( 78 ). In our study, we identified the type of contact as a potential factor influencing the treatment-seeking threshold, with significantly higher treatment-seeking thresholds observed in emergency patients compared to patients with scheduled appointments. This is consistent with the findings of negative stereotypes and higher stigma toward psychiatric emergency departments. Increasing knowledge on the topic of treatment-seeking threshold might mean having a possibility to reduce this threshold and help getting more persons in need into treatment.
In regards to the impact of location of psychiatric outpatient treatment sites on perceived stigma, self-esteem, treatment-seeking threshold and accessibility from the service user’s perspective, significant differences were discovered in favor of the inner city services for self-esteem and accessibility.
When comparing the services at both locations separately, it was found that the accessibility ratings for services in the inner city were relatively similar, while those on the outer city limit exhibited greater variance. The highest rating for accessibility for the psychiatric services at the outer city limits came from privately insured patients and was only slightly lower than the accessibility of the seven services in the city center. For these patients, being located in a more remote location might even be considered as an advantage to maintain privacy. Conversely, the non-organic sleep disorder service with a larger catchment area received the lowest accessibility ratings, which may correspond to the longer distances patients have to take into account to reach the service from their place of living.
The comparison between services for unplanned emergencies versus planned contact only unveiled distinct differences between location accessibility and the treatment-seeking threshold. Emergency services, where reaching the location quickly may not be a priority due to the urgent nature of the mental health issue, were rated highly in terms of accessibility. This outcome could potentially indicate lower expectations from emergency patients or higher demands from patients with scheduled appointments. It is plausible that patients with scheduled appointments may receive treatment over an extended period, making the accessibility of the location a more crucial factor than for a one-time appointment. The threshold for seeking treatment was found to be significantly higher for emergency patients, particularly for those seeking help at the main psychiatric hospital site. These pronounced inhibitions among emergency patients align with prior research ( 35 ).
In relation to the impact of treatment focus of the psychiatric service, only self-esteem and accessibility showed significant variation. Here, the findings were different for the individual outpatient services, with patients receiving treatment at emergency services, services for substance use disorder and services aimed at personality disorders having the lowest ratings for self-esteem. This is in line with the existing literature ( 35 , 43 , 79 ). Patients from the outpatient service for non-organic sleep disorders had a relatively high self-esteem, which corresponds to low ratings for perceived stigma and to the relatively good acceptance of this field of mental health problems in society ( 80 , 81 ). However, and contra intuitively ( 36 , 39 , 82 , 83 ), patients from the psychosis outpatient service and from the transcultural psychiatry service reported the highest self-esteem ratings. In line with the aforementioned studies, we would have expected lower self-esteem in patients who are or have been treated in the transcultural psychiatric services and in the service specialized on psychosis treatment. We speculate that in these services, there might have been a response bias filtering out the more impaired patients with potentially lower self-esteem.
Lastly, there were no significant differences between inner city and outer city services regarding perceived discrimination and threshold to seek treatment. Perceived discrimination was considerable for all patients with little variation. Patients receiving treatment from the behavioral addictions outpatient service and privately insured patients reported the least perceived stigmatization, while emergency patients at the site of the psychiatric hospital and patients with substance use disorders rated perceived stigma highest. This is also compatible with the published literature ( 35 , 84 , 85 ). The threshold to seek treatment varied from low to medium, with privately insured patients, those from the cognitive-behavioral therapy (CBT) outpatient ( 86 , 87 ), patients with non-organic sleep disorders ( 81 ), and those seeking diagnostic evaluation of ADHD and Asperger’s ( 88 , 89 ) reported the lowest treatment-seeking thresholds.
Contrary to the established pattern of SUD services having patients with the highest perceived stigmatization and lowest self-esteem, patients receiving substitution treatment for substance use disorders reported a relatively low threshold to seek treatment. This patient group tends to have a long-standing therapeutic relationship with multiple daily visits to the outpatient service to receive their medication, which might help explain this finding. Aside from emergency patients, the highest treatment-seeking threshold was reported by patients of the transcultural psychiatry service. In contrast to the high self-esteem, the high treatment-seeking threshold of patients in the transcultural outpatient service is consistent with previous findings ( 55 , 57 , 90 , 91 ). Probable explanations for the increased treatment-seeking threshold in transcultural outpatients could be explained, among other things, by language barriers, and depending on the cultural background, by negative stereotypes of mental illness and psychiatric treatment and preference for help from family members or traditional health services.
Regarding potential confounding variables, such as gender, age, and nationality, we did not find the effect of gender found in other studies, according to which men and women differ in their help-seeking behavior for mental problems by public stigma and self-stigma, in the present sample. We also found no evidence of increased treatment inhibition among males in the gender distribution of the study participants. In our sample, the gender ratios were almost equally distributed. This means that about as many men as women sought therapeutic support in the 14 psychiatric outpatient clinics of the UPK Basel and took part in our patient survey. On the other hand, not all studies found gender differences for the perception of stigma ( 92 ).
Age seemed to have a significant influence and their perception and handling of barriers towards treatment seeking. This is consistent with other research that has also found lower inhibitions to therapeutic treatment in older individuals ( 54 ).
Nationality did not change the important link between stigma and self-esteem in the actual correlation. However, the variable was not appropriate for a bivariate correlation with stigma, self-esteem, and threshold due to the significantly different group sizes and low representation of ethnic minorities. Although nationality was recorded in our sample, no information was provided on the countries where the participants had resided in their lifetime, and thus it is unclear which cultures may have influenced them. Cultural factors other than nationality that could potentially influence perceived stigma and treatment-seeking threshold were not part of our study and could be subject of future research. These factors could include cultural differences in the frequency and prevalence of mental illnesses, perception and expression of mental illness symptoms, understanding of mental illness treatment, attitudes towards traditional and alternative treatment approaches, religious and spiritual beliefs, and coping with mentally ill family members ( 57 , 91 , 93 ).
Limitations
It is important to acknowledge certain limitations of this study. First, although the total sample size of 525 participants is adequate for our analyses, our survey may be underpowered to detect differences between outpatient services with small participant numbers. In addition, even with an adequate response rate of about 24%, a large percentage of patients did not take part in this survey. Especially patients with high perceived discrimination and low self-esteem and individuals with a high treatment-seeking threshold might not have responded. Directly examining patients during their stay at the outpatient service could help to avoid this limitation in future research, though some patients may still choose not to answer questionnaires.
The low number of cases in some outpatient clinics impairs the statistical calculations and interpretability of the results. The width of the confidence intervals indicates which mean values should be interpreted with caution.
In addition, the use of self-report measures introduces potential biases due to social desirability and individual differences in introspection. Self-esteem, threshold to seek treatment, and service accessibility were each surveyed using only a single item ( 33 ). Although this is intended to ensure the cost- and time-effectiveness of the questionnaire, it may mean that not all aspects of these complex constructs were mapped. The application of a single item self-esteem scale has, however, been shown to be a valid, reliable, and economical instrument ( 94 , 95 ).
Clinical data like patient’s diagnosis, severity and course of illness were not available. Therefore, the treatment focus of the outpatient clinic had to be used as a proxy.
We only performed analyses using the total PDD score and did not examine the individual twelve items of the PDD scale. It is possible that certain items, such as agreeing to let mentally ill individuals care for children, employment opportunities, or challenges in forming and maintaining friendships, may have been rated differently and correlated differently with self-esteem and treatment-seeking threshold.
The sample primarily included Swiss citizens and residents of other European countries. The participants’ nationality was only used in the descriptive statistics and partial correlation analysis due to the uneven distribution of groups. While the Swiss group was sizable with 371 individuals, the groups of participants from other nationalities, typically consisting of fewer than 20 people per country or region, were too small to draw conclusive findings.
The study only contains answers of people with mental illnesses who sought help and in that process found access to the treatment site or might have overcome inhibitions towards treatment. There is no information on the general population’s perception of accessibility of treatment at the mentioned treatment sites nor on people with mental illnesses who did not find access to treatment. It would be interesting to compare the values of the surveyed sample, particularly self-esteem and perceived stigma, with a population without mental illness.
Conclusion and recommendations for future research
We showed significant correlation of perceived discrimination and devaluation and self-esteem, whereas there was no significant association between these variables with threshold to seek treatment. It was evident that many patients experienced stigmatization, impaired self-esteem, underlining the importance of research in this area. On the other hand, threshold to seek treatment was reported low to medium in the whole sample, with patients from some outpatient services reporting higher thresholds.
For future research, it would be beneficial to explore various forms of stigma, and to incorporate longitudinal research methods. It is recommended to consider temporal criteria, such as the frequency and number of appointments at psychiatric outpatient services, in future surveys. Additionally, studying whether perceived stigma, treatment-seeking threshold, and accessibility to locations are influenced by the frequency of appointments at outpatient clinics could provide valuable insights.
Previous studies indicate that individuals’ own stereotypes and negative attitudes towards mental health treatment may have a stronger influence on the decision to seek treatment than perceived stigma. Therefore, it is important to include these variables in future studies. Factors like socio-economic status, employment status, and education level of participants could help explain variations in assessments of stigma, self-esteem, and treatment-seeking threshold.
Future research should consider potential confounders that may affect the outcomes being studied. For instance, treatment satisfaction was not taken into account in the analysis of this study. Given that treatment satisfaction can impact perceived stigma, self-esteem, and treatment-seeking threshold ( 96 – 98 ), further studies could focus on patients’ evaluations of treatment and their interactions with the variables studied here. Investigating whether factors that improve treatment satisfaction like treatment type, care continuity and involvement of patients ( 98 ), influence stigmatization and enhance the willingness to seek treatment, could be of interest. On the other hand, factors that diminish treatment satisfaction like issues with finances and accommodation, physical health needs and a high percentage of occupied beds ( 98 ) could also lead to an increase in self-stigma and reduce motivation for help-seeking in the future.
Other factors such as diagnosis, illness severity, coping mechanisms, social support, personality traits, and cultural aspects should also be explored for their associations with perceived stigmatization and treatment-seeking threshold.
Differences in accessibility were mainly linked to location, with outpatient services in inner cities being significantly more accessible. However, the perception of accessibility also depends on the needs of patient groups addressed. These results should remind authorities responsible for planning mental health services that it is important to lower the treatment-seeking threshold to seek treatment and to focus on the service users’ perspective.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Northwestern Switzerland. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
JB: Formal analysis, Writing – original draft. LI: Writing – review & editing. CR: Writing – review & editing. JM: Writing – review & editing. UL: Writing – review & editing. CH: Formal analysis, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author CH declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Huber CG, Sowislo JF, Schneeberger AR, Flury B, Lang UE. Empowerment – ein Weg zur Entstigmatisierung. Schweizer Archiv Für Neurol Und Psychiatr . (2015) 166:224–31. doi: 10.4414/sanp.2015.00359
CrossRef Full Text | Google Scholar
2. Shalbafan M, El Hayek S, de Filippis R. Editorial: Mental-health-related stigma and discrimination: Prevention, role, and management strategies. Front Psychiatry . (2023) 14:1136995. doi: 10.3389/fpsyt.2023.1136995
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Huber CG, Steiger S, Möller J, Lang UE. The attitude of the public concerning coercive measures in psychiatric patients. Fortschr Der Neurol Psychiatr . (2022). doi: 10.1055/a-2036-7780
4. Steiger S, Moeller J, Sowislo JF, Lieb R, Lang UE, Huber CG. Approval of coercion in psychiatry in public perception and the role of stigmatization. Front Psychiatry . (2022) 12:819573. doi: 10.3389/fpsyt.2021.819573
5. Steiger S, Moeller J, Sowislo JF, Lieb R, Lang UE, Huber CG. General and case-specific approval of coercion in psychiatry in the public opinion. Int J Environ Res Public Health . (2023) 20:2081. doi: 10.3390/ijerph20032081
6. Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, et al. Prevalence and treatment of mental disorders 1990 to 2003. New Engl J Med . (2005) 352:2515–23. doi: 10.1056/nejmsa043266
7. LeBel TP. Perceptions of and responses to stigma. Sociology Compass . (2008) 2:409–32. doi: 10.1111/j.1751-9020.2007.00081.x
8. Link BG. Understanding labeling effects in the area of mental disorders: an assessment of the effects of expectations of rejection. Am Sociological Rev . (1987) 52:96–112. doi: 10.2307/2095395
9. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry . (2002) 1:16–20.
PubMed Abstract | Google Scholar
10. Corrigan PW, Morris S, Larson J, Rafacz J, Wassel A, Michaels P, et al. Self-stigma and coming out about one’s mental illness. J Community Psychol . (2010) 38:259–75. doi: 10.1002/jcop.20363
11. Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 european countries. Psychol Med . (2012) 42(8):1741–52. doi: 10.1017/S0033291711002558
12. Hinshaw SP, Stier A. Stigma as related to mental disorders. Annu Rev Clin Psychol . (2008) 4:367–93. doi: 10.1146/annurev.clinpsy.4.022007.141245
13. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol . (2001) 27(1):363–85.
Google Scholar
14. Lucksted A, Drapalski AL. Self-stigma regarding mental illness: Definition, impact, and relationship to societal stigma. Psychiatr Rehabil J . (2015) 38(2):99–102. doi: 10.1037/prj0000152
15. Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: Implications for self-esteem and self-efficacy. J Soc Clin Psychol . (2006) 25:875–84. doi: 10.1521/jscp.2006.25.8.875
16. Vogel DL, Wade NG, Haake S. Measuring the self-stigma associated with seeking psychological help. J Couns Psychol . (2006) 53:325–37. doi: 10.1037/0022-0167.53.3.325
17. Pattyn E, Verhaeghe M, Sercu C, Bracke P. Public stigma and self-stigma: Differential association with attitudes toward formal and informal help seeking. Psychiatr Serv . (2014) 65:232–8. doi: 10.1176/appi.ps.201200561
18. Jennings KS, Cheung JH, Britt TW, Goguen KN, Jeffirs SM, Peasley AL, et al. How are perceived stigma, self-stigma, and self-reliance related to treatment-seeking? A three-path model. Psychiatr Rehabil J . (2015) 38:109–16. doi: 10.1037/prj0000138
19. Andrade LH, Alonso J, Mneimneh Z, Wells JE, Al-Hamzawi A, Borges G, et al. Barriers to mental health treatment: Results from the WHO World Mental Health surveys. psychol Med . (2014) 44:1303–17. doi: 10.1017/S0033291713001943
20. Préville M, Tahiri SDM, Vasiliadis HM, Quesnel L, Gontijo-Guerra S, Lamoureux-Lamarche C, et al. Association between perceived social stigma against mental disorders and use of health services for psychological distress symptoms in the older adult population: Validity of the STIG scale. Aging Ment Health . (2015) 19:464–74. doi: 10.1080/13607863.2014.944092
21. Thornicroft G. Stigma and discrimination limit access to mental health care. Epidemiologia e Psichiatria Sociale . (2008) 17:14–9. doi: 10.1017/S1121189X00002621
22. Corrigan PW, Mittal D, Reaves CM, Haynes TF, Han X, Morris S, et al. Mental health stigma and primary health care decisions. Psychiatry Res . (2014) 218:35–8. doi: 10.1016/j.psychres.2014.04.028
23. Britt TW, Jennings KS, Cheung JH, Pury CLS, Zinzow HM. The role of different stigma perceptions in treatment seeking and dropout among active duty military personnel. Psychiatr Rehabil J . (2015) 38:142–9. doi: 10.1037/prj0000120
24. de Filippis R, Menculini G, D’Angelo M, Carbone EA, Tortorella A, De Fazio P, et al. Internalized-stigma and dissociative experiences in bipolar disorder. Front Psychiatry . (2022) 13:953621. doi: 10.3389/fpsyt.2022.953621
25. Masoomi M, Hosseinikolbadi S, Saeed F, Sharifi V, Jalali Nadoushan AH, Shoib S. Stigma as a barrier to suicide prevention efforts in Iran. Front Public Health . (2023) 10:1026451. doi: 10.3389/fpubh.2022.1026451
26. Markowitz FE. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav . (1998) 39:335–47. doi: 10.2307/2676342
27. Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res . (2004) 129:257–65. doi: 10.1016/j.psychres.2004.08.003
28. Van Brakel WH, Anderson AM, Mutatkar RK, Bakirtzief Z, Nicholls PG, Raju MS, et al. The Participation Scale: Measuring a key concept in public health. Disability Rehabil . (2006) 28:193–203. doi: 10.1080/09638280500192785
29. Yanos PT, DeLuca JS, Roe D, Lysaker PH. The impact of illness identity on recovery from severe mental illness: A review of the evidence. Psychiatry Res . (2020) 288:112950. doi: 10.1016/j.psychres.2020.112950
30. Kleim B, Vauth R, Adam G, Stieglitz RD, Hayward P, Corrigan P. Perceived stigma predicts low self-efficacy and poor coping in schizophrenia. J Ment Health . (2008) 17:482–91. doi: 10.1080/09638230701506283
31. Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. psychol Sci Public Interest Supplement . (2014) 15:37–70. doi: 10.1177/1529100614531398
32. Sowislo JF, Gonet-Wirz F, Borgwardt S, Lang UE, Huber CG. Perceived dangerousness as related to psychiatric symptoms and psychiatric service use-a vignette based representative population survey. Sci Rep . (2017) 8:1–7. doi: 10.1038/srep45716
33. Sowislo JF, Lange C, Euler S, Hachtel H, Walter M, Borgwardt S, et al. Stigmatization of psychiatric symptoms and psychiatric service use: a vignette-based representative population survey. Eur Arch Psychiatry Clin Neurosci . (2017) 267:351–7. doi: 10.1007/s00406-016-0729-y
34. Steiger S, Sowislo JF, Moeller J, Lieb R, Lang UE, Huber CG. Personality, self-esteem, familiarity, and mental health stigmatization: a cross-sectional vignette-based study. Sci Rep . (2022) 12. doi: 10.1038/s41598-022-14017-z
35. da Silva AG, Baldaçara L, Cavalcante DA, Fasanella NA, Palha AP. The impact of mental illness stigma on psychiatric emergencies. Front Psychiatry . (2020) 11:573. doi: 10.3389/fpsyt.2020.00573
36. Brohan E, Elgie R, Sartorius N, Thornicroft G. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: The GAMIAN-Europe study. Schizophr Res . (2010) 122:232–8. doi: 10.1016/j.schres.2010.02.1065
37. Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: A review of population studies. Alcohol Alcoholism . (2011) 46:105–12. doi: 10.1093/alcalc/agq089
38. Sheehan L, Dubke R, Corrigan PW. The specificity of public stigma: A comparison of suicide and depression-related stigma. Psychiatry Res . (2017) 256:40–5. doi: 10.1016/j.psychres.2017.06.015
39. Vass V, Sitko K, West S, Bentall RP. How stigma gets under the skin: the role of stigma, self-stigma and self-esteem in subjective recovery from psychosis. Psychosis . (2017) 9:235–44. doi: 10.1080/17522439.2017.1300184
40. Durand-Zaleski I, Scott J, Rouillon F, Leboyer M. A first national survey of knowledge, attitudes and behaviours towards schizophrenia, bipolar disorders and autism in France. BMC Psychiatry . (2012) 12. doi: 10.1186/1471-244X-12-128
41. Colizzi M, Ruggeri M, Lasalvia A. Should we be concerned about stigma and discrimination in people at risk for psychosis? A systematic review. psychol Med . (2020) 50:705–26. doi: 10.1017/S0033291720000148
42. Aviram RB, Brodsky BS, Stanley B. Borderline personality disorder, stigma, and treatment implications. Harvard Rev Psychiatry . (2006) 14:249–56. doi: 10.1080/10673220600975121
43. Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep . (2016) 18:1–7. doi: 10.1007/s11920-015-0654-1
44. Earnshaw V, Smith L, Copenhaver M. Drug addiction stigma in the context of methadone maintenance therapy: an investigation into understudied sources of stigma. Int J Ment Health Addict . (2013) 11:110–22. doi: 10.1007/s11469-012-9402-5
45. Matthews S, Dwyer R, Snoek A. Stigma and self-stigma in addiction. J Bioethical Inq . (2017) 14:275–86. doi: 10.1007/s11673-017-9784-y
46. Rüsch N, Hölzer A, Hermann C, Schramm E, Jacob GA, Bohus M, et al. Self-stigma in women with borderline personality disorder and women with social phobia. J Nervous Ment Dis . (2006) 194:766–73. doi: 10.1097/01.nmd.0000239898.48701.dc
47. Trucco EM, Connery HS, Griffin ML, Greenfield SF. The relationship of self-esteem and self-efficacy to treatment outcomes of alcohol-dependent men and women. Am J Addict . (2007) 16:85–92. doi: 10.1080/10550490601184183
48. Morgades-Bamba CI, Fuster-Ruizdeapodaca MJ, Molero F. The impact of internalized stigma on the well-being of people with Schizophrenia. Psychiatry Research 271(December . (2019) 2018):621–7. doi: 10.1016/j.psychres.2018.12.060
49. Chebli H, Azraf F, Berrada H, Sabir M, Omari F. Self-esteem and addictions. SAS J Med . (2023) 09:941–4. doi: 10.36347/sasjm.2023.v09i09.007
50. Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. Am Psychol . (2003) 58:5–14. doi: 10.1037/0003-066X.58.1.5
51. Hackler A, Vogel D, Wade N. Attitudes toward seeking professional help for an eating disorder: The role of stigma and anticipated outcomes. J Couns Dev . (2010) 88:424–31. doi: 10.1002/j.1556-6678.2010.tb00042.x
52. Topkaya N. Psikolojik yardi{dotless}m almaya ilişkin tutumu yordamada cinsiyet, psikolojik yardi{dotless}m alma nedeniyle kendini damgalama ve sosyal damgalanma. Kuram ve Uygulamada Egitim Bilimleri . (2014) 14:480–7. doi: 10.12738/estp.2014.2.1799
53. Ruiz JC, Fuentes-Durá I, López-Gilberte M, Dasí C, Pardo-García C, Fuentes-Durán MC, et al. Public stigma profile toward mental disorders across different university degrees in the University of Valencia (Spain). Front Psychiatry . (2022) 13:951894. doi: 10.3389/fpsyt.2022.951894
54. Mackenzie CS, Heath PJ, Vogel DL, Chekay R. Age differences in public stigma, self-stigma, and attitudes toward seeking help: A moderated mediation model. J Clin Psychol . (2019) 75:2259–72. doi: 10.1002/jclp.22845
55. Amri S, Bemak F. Mental health help-seeking behaviors of Muslim immigrants in the United States: Overcoming social stigma and cultural mistrust. J Muslim Ment Health . (2012) 7:43–63. doi: 10.3998/jmmh.10381607.0007.104
56. Nasser A. Factors affecting attitudes toward seeking and using formal mental health and psychological services among Arab-Muslims population. J Muslim Ment Health . (2014) 3:243–67. doi: 10.1080/15564900802487675
57. Byrow Y, Pajak R, McMahon T, Rajouria A, Nickerson A. Barriers to mental health help-seeking amongst refugee men. Int J Environ Res Public Health . (2019) 16:2634. doi: 10.3390/ijerph16152634
58. Blomstedt Y, Johansson SE, Sundquist J. Mental health of immigrants from the former Soviet Bloc: A future problem for primary health care in the enlarged European Union? A cross-sectional study. BMC Public Health . (2007) 7:1–12. doi: 10.1186/1471-2458-7-27
59. Close C, Kouvonen A, Bosqui T, Patel K, O’Reilly D, Donnelly M. The mental health and wellbeing of first generation migrants: A systematic-narrative review of reviews. Globalization Health . (2016) 12:1–13. doi: 10.1186/s12992-016-0187-3
60. Gravic Inc. Remark office OMR, V8.0 . Malvern, PA, USA: Gravic Inc. (2010).
61. Link BG, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: can negative consequences of mental illness labeling be avoided? J Health Soc Behav . (1991) 32:302–20. doi: 10.2307/2136810
62. Matschinger H, Angermeyer MC, Link BG. [Variation of response structures in relation to degree of personal involvement–a methodologic study exemplified by the “Discrimination Devaluation Scale”]. Psychotherapie Psychosomatik Medizinische Psychol . (1991) 41:278—283.
63. Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: Construct validation of a single-item measure and the Rosenberg Self-Esteem Scale. Pers Soc Psychol Bull . (2001) 27:151–61. doi: 10.1177/0146167201272002
64. Heise DR. Separating reliability and stability in test-retest correlation. Am Sociological Rev . (1969) 34:93–101. doi: 10.2307/2092790
65. Mann HB, Whitney DR. On a test of whether one of two random variables is stochastically larger than the other. Ann Math Stat . (1947) 18(1):50–60. doi: 10.1214/aoms/1177730491
66. Shapiro SS, Wilk MB. An analysis of variance test for normality (Complete samples). Biometrika . (1965) 52:591–611. doi: 10.1093/biomet/52.3-4.591
67. Levene H. Robust tests for equality of variances. Contributions to Probability Stat . (1960) 278–92.
68. Kruskal WH, Wallis WA. Use of ranks in one-criterion variance analysis. J Am Stat Assoc . (1952) 47:583–621. doi: 10.1080/01621459.1952.10483441
69. Bender R, Lange S. What is a confidence interval? Deutsche Medizinische Wochenschrift . (2007) 132:17–8. doi: 10.1055/s-2007-959031
70. IBM. SPSS Statistics (27.0) . Armonk, NY, USA: IBM Corp (2020).
71. Ilic M, Reinecke J, Bohner G, Röttgers HO, Beblo T, Driessen M, et al. Belittled, avoided, ignored, denied: assessing forms and consequences of stigma experiences of people with mental illness. Basic Appl Soc Psychol . (2013) 35:31–40. doi: 10.1080/01973533.2012.746619
72. Mashiach-Eizenberg M, Hasson-Ohayon I, Yanos P, Lysaker P, Roe D. Internalized stigma and quality of life among persons with severe mental illness: The mediating roles of self-esteem and hope. Psychiatry Res . (2013) 208:15–20. doi: 10.1016/j.psychres.2013.03.013
73. Feldhaus T, Falke S, von Gruchalla L, Maisch B, Uhlmann C, Bock E, et al. The impact of self-stigmatization on medication attitude in schizophrenia patients. Psychiatry Res . (2018) 261:391–9. doi: 10.1016/j.psychres.2018.01.012
74. Guarneri JA, Oberleitner DE, Connolly S. Perceived stigma and self-stigma in college students: A literature review and implications for practice and research. Basic Appl Soc Psychol . (2019) 41:48–62. doi: 10.1080/01973533.2018.1550723
75. Tao TJ, Hui CLM, Ho ECN, Hui PWM, Suen YN, Lee EHM, et al. Correlates and predictors of perceived stigma and self-stigma in Chinese patients with psychosis. Early Intervention Psychiatry . (2022) 16:1075–84. doi: 10.1111/eip.13251
76. Schnyder N, Panczak R, Groth N, Schultze-Lutter F. Association between mental health-related stigma and active help-seeking: Systematic review and meta-analysis. Br J Psychiatry . (2017) 210:261–8. doi: 10.1192/bjp.bp.116.189464
77. Golberstein E, Eisenberg D, Gollust SE. Perceived stigma and mental health care seeking. Psychiatr Serv . (2008) 59:392–9. doi: 10.1176/appi.ps.59.4.392
78. Schomerus G, Appel K, Meffert PJ, Luppa M, Andersen RM, Grabe HJ, et al. Personality-related factors as predictors of help-seeking for depression: A population-based study applying the Behavioral Model of Health Services Use. Soc Psychiatry Psychiatr Epidemiol . (2013) 48:1809–17. doi: 10.1007/s00127-012-0643-1
79. Rüsch N, Lieb K, Bohus M, Corrigan PW. Self-stigma, empowerment, and perceived legitimacy of discrimination among women with mental illness. Psychiatr Serv . (2006) 57:399–402. doi: 10.1176/appi.ps.57.3.399
80. Sutton EL. Insomnia. Ann Internal Med . (2021) 174:ITC33–48. doi: 10.7326/AITC202103160
81. He S, Ke XJ, Wu Y, Kong XY, Wang Y, Sun HQ, et al. The stigma of patients with chronic insomnia: a clinical study. BMC Psychiatry . (2022) 22:1–10. doi: 10.1186/s12888-022-04091-y
82. Gary FA. Stigma: Barrier to mental health care among ethnic minorities. Issues Ment Health Nurs . (2005) 26:979–99. doi: 10.1080/01612840500280638
83. Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: Internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophr Bull . (2007) 33:192–9. doi: 10.1093/schbul/sbl016
84. Yang LH, Wong LY, Grivel MM, Hasin DS. Stigma and substance use disorders: An international phenomenon. Curr Opin Psychiatry . (2017) 30:378–88. doi: 10.1097/YCO.0000000000000351
85. Crapanzano K, Hammarlund R, Ahmad B, Hunsinger N, Kullar R. The association between perceived stigma and substance use disorder treatment outcomes: a review. Substance Abuse and Rehabilitation . Subst Abuse Rehabil . (2018) 10:1–12. doi: 10.2147/sar.s183252
86. Miles H, Peters E, Kuipers E. Service-user satisfaction with CBT for psychosis. Behav Cogn Psychother . (2007) 35:109–16. doi: 10.1017/S1352465806003158
87. Beehler GP, Loughran TA, King PR, Dollar KM, Murphy JL, Kearney LK, et al. Patients’ perspectives of brief cognitive behavioral therapy for chronic pain: Treatment satisfaction, perceived utility, and global assessment of change. Families Systems Health . (2021) 39:351–7. doi: 10.1037/fsh0000606
88. Young Z, Tickle A, Gillott A, Groom M. Psychological impact of an adult ADHD diagnosis: “A blessing and a curse?” Life Span Disability . (2019) 22:173–203.
89. Huang Y, Trollor JN, Foley KR, Arnold SRC. “I’ve spent my whole life striving to be normal”: internalized stigma and perceived impact of diagnosis in autistic adults. Autism Adulthood . (2023) 5:423–36. doi: 10.1089/aut.2022.0066
90. McCrone P, Bhui K, Craig T, Mohamud S, Warfa N, Stansfeld SA, et al. Mental health needs, service use and costs among Somali refugees in the UK. Acta Psychiatrica Scandinavica . (2005) 111:351–7. doi: 10.1111/j.1600-0447.2004.00494.x
91. Aloud N, Rathur A. Factors affecting attitudes toward seeking and using formal mental health and psychological services among Arab Muslim populations. J Muslim Ment Health . (2009) 4:79–103. doi: 10.1080/15564900802487675
92. Patten SB, Williams JVA, Lavorato DH, Bulloch AGM, Charbonneau M, Gautam M, et al. Perceived stigma among recipients of mental health care in the general Canadian population. Can J Psychiatry . (2016) 61:480–8. doi: 10.1177/0706743716639928
93. Piwowarczyk L, Bishop H, Yusuf A, Mudymba F, Raj A. Congolese and Somali beliefs about mental health services. J Nervous Ment Dis . (2014) 202:209–16. doi: 10.1097/NMD.0000000000000087
94. Robins RW, Trzesniewski KH, Tracy JL, Gosling SD, Potter J. Global self-esteem across the life span. Psychol Aging . (2002) 17:423–34. doi: 10.1037/0882-7974.17.3.423
95. Brailovskaia J, Margraf J. How to measure self-esteem with one item? Validation of the German single-item self-esteem scale (G-SISE). Curr Psychol . (2020) 39:2192–202. doi: 10.1007/s12144-018-9911-x
96. Cloninger CR. The science of well being: An integrated approach to mental health and its disorders. Psychiatria Danubina . (2006) 18:218–24.
97. Verhaeghe M, Bracke P, Christiaens W. Stigma and client satisfaction in mental health services. J Appl Soc Psychol . (2010) 40:2295–318. doi: 10.1111/j.1559-1816.2010.00659.x
98. Stamboglis N, Jacobs R. Factors associated with patient satisfaction of community mental health services: A multilevel approach. Community Ment Health J . (2020) 56:50–64. doi: 10.1007/s10597-019-00449-x
Keywords: social stigma, stereotyping, patient satisfaction, self report, mental health, community mental health services, ambulatory care, health services research
Citation: Billian J, Imfeld L, Roth CB, Moeller J, Lang UE and Huber CG (2024) Treatment-seeking threshold and accessibility of psychiatric outpatient services in Switzerland: the relationship with stigma and self-esteem. Front. Psychiatry 15:1377971. doi: 10.3389/fpsyt.2024.1377971
Received: 28 January 2024; Accepted: 19 March 2024; Published: 12 April 2024.
Reviewed by:
Copyright © 2024 Billian, Imfeld, Roth, Moeller, Lang and Huber. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christian G. Huber, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Vax1 Pennmedicine
Global Summit Convenes to Address Mental Health Crisis Amidst Pandemic Fallout
Amidst the lingering fallout of the COVID-19 pandemic and its profound impacts on mental well-being, leaders and experts from around the world have gathered at a global summit to address the escalating mental health crisis. With mental health disorders on the rise and millions of individuals experiencing heightened levels of stress, anxiety, and depression, urgent action is needed to prioritize mental health support, raise awareness, and implement holistic strategies for mental well-being.
The international summit, attended by heads of state, mental health professionals, policymakers, advocates, and representatives from civil society organizations, aims to catalyze a coordinated response to the mental health challenges exacerbated by the pandemic and address the systemic issues contributing to the global mental health crisis. Discussions at the summit encompass a wide range of topics, including mental health care delivery, stigma reduction, community support systems, and the integration of mental health into public health agendas.
The COVID-19 pandemic has had far-reaching effects on mental health, exacerbating existing vulnerabilities and creating new challenges for individuals, families, and communities worldwide. Lockdowns, social isolation, economic hardship, and uncertainty about the future have taken a toll on mental well-being, leading to an increase in mental health disorders, substance abuse, and suicidal behavior.
Key priorities of the summit include:
- Scaling Up Mental Health Services: Participants are focusing on strategies to expand access to mental health services and support, particularly in underserved communities and low-resource settings. Investments in mental health infrastructure, telemedicine platforms, and community-based services are essential in ensuring that individuals in need receive timely and appropriate care.
- Promotion of Mental Health Literacy: Efforts to raise awareness and promote mental health literacy are prioritized to reduce stigma and discrimination associated with mental illness and encourage help-seeking behaviors. Public education campaigns, school-based mental health programs, and workplace mental health initiatives are essential in promoting understanding, empathy, and support for individuals living with mental health challenges.
- Integration of Mental Health into Health Systems: The integration of mental health into primary health care and community health systems is underscored as a key priority in improving access to mental health services and reducing treatment gaps. Task-sharing approaches, collaborative care models, and digital mental health solutions are promoted to strengthen the capacity of health systems to deliver comprehensive, person-centered mental health care.
- Support for Vulnerable Populations: Participants are advocating for targeted interventions to address the mental health needs of vulnerable populations, including children and adolescents, older adults, refugees, and frontline workers. Trauma-informed care, psychosocial support programs, and culturally sensitive interventions are essential in meeting the diverse and complex mental health needs of marginalized and at-risk groups.
- Investment in Research and Innovation: Investments in mental health research, innovation, and evidence-based interventions are essential in advancing knowledge, identifying effective strategies, and driving progress in mental health promotion and treatment. Multidisciplinary research collaborations, technology-enabled solutions, and data-driven approaches are promoted to generate insights and inform policy and practice in the field of mental health.
As the summit progresses, there is a shared commitment among participants to prioritize mental health as a global public health priority and accelerate efforts to address the mental health crisis comprehensively. By working together to implement holistic and integrated strategies, promote awareness, reduce stigma, and expand access to mental health services, global leaders aim to create a world where mental well-being is valued, supported, and prioritized for all.
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to take your pulse
- How to measure your respiratory rate
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Mental health advocates push for less stigma, more help in Michigan
Despite the flurry of post-pandemic headlines about the mental health crisis enveloping our nation, folks who could benefit from getting help are often not doing so because of a powerful six-letter word: stigma.
There’s a double standard when it comes to getting help for physical illnesses like diabetes or heart issues (which most folks would think ludicrous to not do so) versus mental illnesses, which encompasses hundreds of diseases, from depression to schizophrenia to anxiety. Many with mental illness suffer in silence, embarrassed to talk about it or ask for help, even though statistics show people can live fuller and happier lives with it.
“While post-pandemic we are talking more about mental illness and the importance of valuing and protecting our mental health, mental illness is a crisis in America,” said Kevin Fischer, executive director of National Alliance on Mental Illness, Michigan chapter . “Just talking about it is not enough; we need action. We have an annual national “ Stand Up to Cancer ” event that broadcasts across multiple TV networks but no “Stand Up to Stigma.” Far more people are diagnosed with mental illness than cancer each year. Why no outcry for us?“
The mental health crisis is impacting business, too: “Companies lose almost $200 billion in lost earnings each year in employee absenteeism and productivity in the U.S. alone due to mental health issues involving themselves or taking care of a family member,” Fischer said.
When you consider one out of every five adults experiences some sort of mental illness during the course of a year, according to NAMI, it’s a conversation that should be happening more often.
Emily Sexton, CEO of Henry Ford Health’s Behavioral Health Hospital opening on the campus of the Henry Ford Hospital on Maple Road in West Bloomfield later this year, has been focusing on it. Sexton is a registered nurse who specialized in infectious diseases 20 years ago when she began. In recent years, mental health has been part of her job, too.
“We know when a person suffers from mental health issues, it can impact so many facets of their lives,” she said. “We want to help ensure anyone who deals with these serious issues never gets to that point.”
The 192-bed in-patient behavioral health hospital is a partnership between Henry Ford and Acadia Healthcare. The hospital will offer behavioral health services and serve as an academic site, too, educating the next generation of behavioral health care providers, including psychiatry residents, medical students and nurses.
“New and groundbreaking research, technology, quality programs, innovation, access and brand-new facilities like the one we are building in West Bloomfield are starting to reveal the breadth of what’s possible,” she said.
“The enduring stigma surrounding both mental health and substance use can cause serious delays in seeking care,” Sexton said. “This may be due to fears of judgment, unequal treatment or fear of losing their livelihood. Societal efforts to destigmatize mental health care and fostering open dialogue are commendable, yet there remains a pressing need to establish inclusive environments where those suffering can access care without fear of prejudice or harm.”
Eric Hipple, former Detroit Lions All-Star quarterback, has been sharing his story to let people know help is at hand.
Hipple began suffering from depression while a star quarterback at Utah State University in the late 1970s. It came and went during his NFL playing days but became more pronounced after he hung up his cleats in the late 1980s.
Hipple has been through a lot as he dealt with his own depression and his family’s: His beloved son, Jeff Hipple, lost his life to the disease when he was 15 years old; he died by suicide in 2000.
Since then, Hipple has become an advocate and in-demand powerful speaker for schools, veterans groups and organizations. He’s worked with the NFL, the University of Michigan, Blue Cross Blue Shield of Michigan and organizations including BeNICE.org , which has worked with over 150 Michigan schools and 30,000 high school coaches, Hipple said.
The topic of opening up about mental health is resonating with younger folks.
“I believe the youth of today understands the language and symptoms better and accepts mental health as a real illness and are not afraid to tell someone or ask for help,” Hipple said.
U.S. Sen. Debbie Stabenow is another longtime champion for mental health. Her father suffered from bipolar disorder, which had been misdiagnosed and caused issues in her family growing up. While a student at Michigan State University in the 1970s, she happened to learn about a new drug, lithium, being used to treat the disease and told her family about it. Her father got the help he needed, which made a world of difference.
“We’ve taken steps to reduce the stigma around mental health but there is more work to be done,” Stabenow said. “We are changing the behavioral health care system in our country and moving towards treating health care above the neck the same as health care below the neck. This transformation, in addition to more people telling their stories about themselves and their loved ones, means more people can see that they are not alone.”
Elizabeth Hertel, director of the Michigan Department of Health and Human Services, has been waving the flag to help, particularly young people which is when most mental illness surfaces.
“We need to talk openly about mental health and the fact any of us could use support or services at one time or another during our lives,” Hertel said. "We need to normalize having a mental health checkup, just like we do getting regular health screenings.”
She said the state has invested more than $360 million in community behavioral services the past two years to ensure “families can receive services when and where they need them.”
That said, more help is needed in the state as it faces an ongoing need of mental health professionals .
NAMI Michigan’s Fischer, whose son Dominique died by suicide, told me he didn’t know much about mental illness until Dominique began having issues in college.
“Mental illness doesn’t discriminate,” said Fischer, who is celebrating his 10 th anniversary on the job . “We need to do a better job of raising awareness and telling people it’s OK to ask for help.”
If you or someone you know is in immediate mental health crisis, or considering suicide, call the Suicide and Crisis Lifeline at 988.
More: 3 metro Detroit leaders help those with special needs — off the clock. Here's how
More: Ford family on path to help other families: Here's how
Contact Carol Cain: 248-355-7126 or [email protected] . She is senior producer/host of “Michigan Matters,” which airs 5:30 a.m. Sundays on CBS Detroit and noon Sundays on Detroit 50 WKBD. See MEDC CEO Quentin Messer Jr., Rochester Hills Mayor Bryan Barnett and Chris Holman of Michigan Business Network on this Sunday’s show. "Michigan Matters" can also be found on those stations’ listings on FUBO, Pluto TV, Youtube.com . It is streamed 9 p.m. weeknights.
- UB Directory
- Office of the Provost >
- Academic & Administrative Units >
SUNY funding to boost mental health services at UB
'embedded' counselors to join the school of social work and other academic units this summer.

UB will use most of its new state funding to hire seven counselors who will be embedded within the academic units. Photo: Onion Studio
Published April 11, 2024
UB is expanding mental health support for students, which includes the hiring of several new “embedded” counselors and broadening virtual or teletherapy services.
Gov. Kathy Hochul recently announced new state funding for mental health support across SUNY campuses, including $1 million at UB.
“College can be a stressful and overwhelming time and this funding will expand mental health services on college campuses so students can focus on just being students,” the governor said in a statement.
UB will use the bulk of its funding, which is recurring, to hire seven counselors. Each will be embedded within one of seven academic units: the schools of Management, Social Work, Nursing, Public Health and Health Professions, and Architecture and Planning; the Graduate School of Education; and the College of Arts and Sciences.
“Student health and wellness is a significant priority at the University at Buffalo,” says Brian Hamluk, vice president for student life. “Prioritizing embedded counselors and other mental health-related services underscores our continued commitment to the well-being of our students, ensuring they have the resources and support they need to thrive both academically and personally here at UB.”
The seven new hires will start over the summer, bringing the total number of counselors on campus to 31, says Sharon Mitchell, senior director of student wellness and director of counseling services.
“The biggest thing is the accessibility,” Mitchell says of embedded counselors. “It’s just more convenient if you don’t have to add travel time to get to and from your appointment.
“Also, it reduces stigma because it normalizes seeking help,” Mitchell says. “There’s an academic adviser in the building. There’s a success coach in the building. Now, there’s a mental health counselor in the building. These are all resources that could be of help to students.”
The Embedded Counselor Program, which recently won an award at the national conference of student affairs administrators, started at UB in 2017 with an embedded counselor in athletics. Since then, the program has added an embedded counselor in the Jacobs School of Medicine and Biomedical Sciences; the School of Law, Dental Medicine, Engineering and Applied Sciences, and most recently, Pharmacy and Pharmaceutical Sciences.
Now, with these new hirings, a counselor will be embedded within each academic unit.
“They primarily provide individual counseling,” Mitchell says. “However, we also do outreach.
“For example,” she says, “if the medical school has exams, maybe we offer an educational workshop on managing stress. What’s nice is that we can tailor the programming specifically for students of a particular academic community.”
During the five-year period prior to the pandemic, Counseling Services saw a 43% increase in the number of students seeking mental health services and a 29% increase in the number of attended counseling sessions.
Since the COVID-19 pandemic, students have requested more support on campus for their mental health.
To make an appointment with Counseling Services, students can call 716-645-2720.
In addition to the seven new counselors, the new funding will pay for:
- Expanded teletherapy services . Counseling Services will contract with a professionally licensed vendor to provide services online or over the phone. This makes counseling more accessible and convenient for students who need services outside regular business hours.
“Even though we will have more counselors we are only open until 7 p.m. two nights a week,” Mitchell says. “The teletherapy services will allow us to provide services for students whose schedules just can’t fit into that or who might do a round of treatment with us but need additional care.”
- A financial well-being program coordinator . UB students have reported that finances are among their biggest stressors and a primary factor in their academic success and retention. A financial wellness coordinator can help them with financial literacy and developing a financial plan, while guiding them toward available resources.
- A sexual and reproductive health nurse educator . Students have requested more support regarding their reproductive health, contraception and sexually transmitted infections. This position would provide students with both clinical and educational services.
- Four graduate assistants. The four new positions will increase capacity for both clinical and educational programming.
- Trauma, illness and grief training . This training, open to staff and faculty, would help grow the emotional support of the campus beyond what mental health counselors can provide during the aftermath of a traumatic experience.
Featured Centers and Institutes

PhD Excellence Initiative
A campus-wide, student-centric effort to ensure that UB’s PhD programs remain among the strongest in the world.
Recent University News
- 4/11/24 Friday, April 12 JSMBS Bike Tune Up Event Postponed
- 4/11/24 Educating providers about female genital cutting
- 4/11/24 Time to rethink school discipline
- 4/11/24 New study probes macrophages’ role in developing pulmonary fibrosis
- 4/11/24 SUNY funding to boost mental health services at UB

IMAGES
VIDEO
COMMENTS
The Research Anthology on Mental Health Stigma, Education, and Treatment explores the latest research on the newest advancements in mental health, best practices and new research on treatment, and the need for education and awareness to mitigate the stigma that surrounds discussions on mental health. The chapters will cover new technologies ...
Research Anthology on Mental Health Stigma, Education, and Treatment, VOL 1: 9781668433348: Medicine & Health Science Books @ Amazon.com
Ageing and mental health: a psychological aspect of later life ; Chapter 34. The social mandate to deal with mental health: a comparison between interventions in a mental health center, a school, and a psychoanalytic office ; Chapter 35. Mental health education and literacy in schools: the Australian experience ; Chapter 36.
Introduction and background. Stigma, characterized by societal prejudice and discrimination, profoundly influences psychiatric care, creating barriers to the timely recognition and treatment of mental health disorders [].Deeply embedded in societal norms, stigma is a multifaceted issue permeating every level of psychiatric care, leading to delayed treatment, increased morbidity, and a ...
The Research Anthology on Mental Health Stigma, Education, and Treatment explores the latest research on the newest advancements in mental health, best practices and new research on treatment, and ...
It is time to end all forms of stigma and discrimination against people with mental health conditions, for whom there is double jeopardy: the impact of the primary condition and the severe consequences of stigma. Indeed, many people describe stigma as being worse than the condition itself. This Lancet Commission report is the result of a collaboration of more than 50 people worldwide.
The Digital and eTextbook ISBNs for Research Anthology on Mental Health Stigma, Education, and Treatment are 9781799886006, 179988600X and the print ISBNs are 9781799885443, 1799885445. Save up to 80% versus print by going digital with VitalSource.
Research Anthology on Mental Health Stigma, Education, and Treatment, 3 volume by available in Hardcover on Powells.com, also read synopsis and reviews. In times of uncertainty and crisis, the mental health of individuals become a concern as added...
Mental Health and Higher Education. Mental health issues, such as depression, anxiety, suicidal ideation, and self-injury, are prevalent among college students; in a study of thousands of college students, 32% reported symptoms consistent with at least one of these health issues (Eisenberg, Hunt, & Speer, 2013).They can affect educational outcomes and relationships and can result in death.
Mental Health Clinical Decision Support Exploiting Big Data. Research Anthology on Mental Health Stigma, Education, and Treatment. Hershey: IGI Global, 2021 - (Khosrow-Pour, M.), s. 341-359. ISBN 9781799885443 Institutional support: RVO:67985807 Keywords : big data * decision support * machine learning * supervised learning * mental health
This investigation reviews the effectiveness of anti-stigma interventions employed at educational institutes; to improve knowledge, attitude and beliefs regarding mental health disorders among students. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist guidelines were followed and protocol was registered in PROSPERO (CRD42018114535). Forty four randomized ...
Discover Research Anthology on Mental Health Stigma, Education, and Treatment, VOL 1 by Information R... Management Association and millions of other books available at Barnes & Noble. Shop paperbacks, eBooks, and more!
explores the latest research on the newest advancements in mental health, best practices and new research on treatment, and the need for education and awareness to mitigate the stigma that surrounds discussions on mental health. The chapters will cover new technologies that are impacting delivery modes for treatment, the latest methods and ...
1. Introduction. The stigma of living with a mental health condition has been described as being worse than the experience of the illness itself [].The aversive reactions that members of the general population have towards people with mental illness is known as public stigma and can be understood in terms of (i) stereotypes, (ii) prejudice, and (iii) discrimination [].
Buy Research Anthology on Mental Health Stigma, Education, and Treatment, VOL 2 by Information R Management Association (Editor) online at Alibris. We have new and used copies available, in 1 editions - starting at $750.85.
In book: Research Anthology on Mental Health Stigma, Education, and Treatment (pp.909-919)
Summary: Abstract: "This book explores the latest research on the newest advancements in mental health, best practices and new research on treatment, and the need for education and awareness to mitigate the stigma that surrounds discussions on mental health by providing chapters that cover new technologies that are impacting delivery modes for treatment, the latest methods and models for ...
Research Anthology on Mental Health Stigma, Education, and Treatment | In times of uncertainty and crisis, the mental health of individuals become a concern as added stressors and pressures can cause depression, anxiety, and stress. Today, especially with more people than ever experiencing these effects due to the Covid-19 epidemic and all that comes along with it, discourse around mental ...
Abstract. Mental health stigma can be defined as the display of negative attitudes, based on prejudice and misinformation, in response to a marker of illness. Stigma creates mental distress for ...
Estimated research findings suggest that almost two-thirds of adults with psychiatric conditions do not receive the required treatment services. ... Verma, N. (2021). Ageing and mental health: A psychological aspect of later life. In Research anthology on mental health stigma, education, and treatment (pp. 549-572). ... research findings ...
Background. To this day, suffering from a mental illness means a double burden for those affected due to the illness itself and the stigmatization of mentally ill people (1, 2).Despite the availability of effective treatments, a substantial number of individuals with mental illness continue to experience barriers in seeking and receiving appropriate care (3-5).
Promotion of Mental Health Literacy: Efforts to raise awareness and promote mental health literacy are prioritized to reduce stigma and discrimination associated with mental illness and encourage help-seeking behaviors. Public education campaigns, school-based mental health programs, and workplace mental health initiatives are essential in ...
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
This chapter takes a broader approach to understanding why these shootings may have happened by reviewing the empirical literature to identify possible correlations from childhood and adolescent trauma experiences (and subsequent mental health problems) to later adult violence. Understanding why people commit mass shootings in the United States is perplexing and discerning perpetrators ...
More: Ford family on path to help other families: Here's how. Contact Carol Cain: 248-355-7126 or [email protected]. She is senior producer/host of "Michigan Matters," which airs 5:30 a.m ...
D. Impact of structural stigma . II. Overview of SUD A. Determinants of SUD 1. Genetic factors 2. Neurobiology of substance use, misuse, and addiction as a chronic disease 3. Impact of the unequal access to any health care, lack of education, stigma, and biases on SUD and recovery B. Substances of Concern 1. Opioids 2. Stimulants 3. Depressants 4.
UB is expanding mental health support for students, which includes the hiring of several new "embedded" counselors and broadening virtual or teletherapy services. Gov. Kathy Hochul recently announced new state funding for mental health support across SUNY campuses, including $1 million at UB. "College can be a stressful and overwhelming ...