
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics

Obesity Research
Language switcher.
Over the years, NHLBI-supported research on overweight and obesity has led to the development of evidence-based prevention and treatment guidelines for healthcare providers. NHLBI research has also led to guidance on how to choose a behavioral weight loss program.
Studies show that the skills learned and support offered by these programs can help most people make the necessary lifestyle changes for weight loss and reduce their risk of serious health conditions such as heart disease and diabetes.
Our research has also evaluated new community-based programs for various demographics, addressing the health disparities in overweight and obesity.
NHLBI research that really made a difference
- In 1991, the NHLBI developed an Obesity Education Initiative to educate the public and health professionals about obesity as an independent risk factor for cardiovascular disease and its relationship to other risk factors, such as high blood pressure and high blood cholesterol. The initiative led to the development of clinical guidelines for treating overweight and obesity.
- The NHLBI and other NIH Institutes funded the Obesity-Related Behavioral Intervention Trials (ORBIT) projects , which led to the ORBIT model for developing behavioral treatments to prevent or manage chronic diseases. These studies included families and a variety of demographic groups. A key finding from one study focuses on the importance of targeting psychological factors in obesity treatment.
Current research funded by the NHLBI
The Division of Cardiovascular Sciences , which includes the Clinical Applications and Prevention Branch, funds research to understand how obesity relates to heart disease. The Center for Translation Research and Implementation Science supports the translation and implementation of research, including obesity research, into clinical practice. The Division of Lung Diseases and its National Center on Sleep Disorders Research fund research on the impact of obesity on sleep-disordered breathing.
Find funding opportunities and program contacts for research related to obesity and its complications.
Current research on obesity and health disparities
Health disparities happen when members of a group experience negative impacts on their health because of where they live, their racial or ethnic background, how much money they make, or how much education they received. NHLBI-supported research aims to discover the factors that contribute to health disparities and test ways to eliminate them.
- NHLBI-funded researchers behind the RURAL: Risk Underlying Rural Areas Longitudinal Cohort Study want to discover why people in poor rural communities in the South have shorter, unhealthier lives on average. The study includes 4,000 diverse participants (ages 35–64 years, 50% women, 44% whites, 45% Blacks, 10% Hispanic) from 10 of the poorest rural counties in Kentucky, Alabama, Mississippi, and Louisiana. Their results will support future interventions and disease prevention efforts.
- The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is looking at what factors contribute to the higher-than-expected numbers of Hispanics/Latinos who suffer from metabolic diseases such as obesity and diabetes. The study includes more than 16,000 Hispanic/Latino adults across the nation.
Find more NHLBI-funded studies on obesity and health disparities at NIH RePORTER.

Read how African Americans are learning to transform soul food into healthy, delicious meals to prevent cardiovascular disease: Vegan soul food: Will it help fight heart disease, obesity?
Current research on obesity in pregnancy and childhood
- The NHLBI-supported Fragile Families Cardiovascular Health Follow-Up Study continues a study that began in 2000 with 5,000 American children born in large cities. The cohort was racially and ethnically diverse, with approximately 40% of the children living in poverty. Researchers collected socioeconomic, demographic, neighborhood, genetic, and developmental data from the participants. In this next phase, researchers will continue to collect similar data from the participants, who are now young adults.
- The NHLBI is supporting national adoption of the Bright Bodies program through Dissemination and Implementation of the Bright Bodies Intervention for Childhood Obesity . Bright Bodies is a high-intensity, family-based intervention for childhood obesity. In 2017, a U.S. Preventive Services Task Force found that Bright Bodies lowered children’s body mass index (BMI) more than other interventions did.
- The NHLBI supports the continuation of the nuMoM2b Heart Health Study , which has followed a diverse cohort of 4,475 women during their first pregnancy. The women provided data and specimens for up to 7 years after the birth of their children. Researchers are now conducting a follow-up study on the relationship between problems during pregnancy and future cardiovascular disease. Women who are pregnant and have obesity are at greater risk than other pregnant women for health problems that can affect mother and baby during pregnancy, at birth, and later in life.
Find more NHLBI-funded studies on obesity in pregnancy and childhood at NIH RePORTER.
Learn about the largest public health nonprofit for Black and African American women and girls in the United States: Empowering Women to Get Healthy, One Step at a Time .
Current research on obesity and sleep
- An NHLBI-funded study is looking at whether energy balance and obesity affect sleep in the same way that a lack of good-quality sleep affects obesity. The researchers are recruiting equal numbers of men and women to include sex differences in their study of how obesity affects sleep quality and circadian rhythms.
- NHLBI-funded researchers are studying metabolism and obstructive sleep apnea . Many people with obesity have sleep apnea. The researchers will look at the measurable metabolic changes in participants from a previous study. These participants were randomized to one of three treatments for sleep apnea: weight loss alone, positive airway pressure (PAP) alone, or combined weight loss and PAP. Researchers hope that the results of the study will allow a more personalized approach to diagnosing and treating sleep apnea.
- The NHLBI-funded Lipidomics Biomarkers Link Sleep Restriction to Adiposity Phenotype, Diabetes, and Cardiovascular Risk study explores the relationship between disrupted sleep patterns and diabetes. It uses data from the long-running Multiethnic Cohort Study, which has recruited more than 210,000 participants from five ethnic groups. Researchers are searching for a cellular-level change that can be measured and can predict the onset of diabetes in people who are chronically sleep deprived. Obesity is a common symptom that people with sleep issues have during the onset of diabetes.
Find more NHLBI-funded studies on obesity and sleep at NIH RePORTER.

Learn about a recent study that supports the need for healthy sleep habits from birth: Study finds link between sleep habits and weight gain in newborns .
Obesity research labs at the NHLBI
The Cardiovascular Branch and its Laboratory of Inflammation and Cardiometabolic Diseases conducts studies to understand the links between inflammation, atherosclerosis, and metabolic diseases.
NHLBI’s Division of Intramural Research , including its Laboratory of Obesity and Aging Research , seeks to understand how obesity induces metabolic disorders. The lab studies the “obesity-aging” paradox: how the average American gains more weight as they get older, even when food intake decreases.
Related obesity programs and guidelines
- Aim for a Healthy Weight is a self-guided weight-loss program led by the NHLBI that is based on the psychology of change. It includes tested strategies for eating right and moving more.
- The NHLBI developed the We Can! ® (Ways to Enhance Children’s Activity & Nutrition) program to help support parents in developing healthy habits for their children.
- The Accumulating Data to Optimally Predict obesity Treatment (ADOPT) Core Measures Project standardizes data collected from the various studies of obesity treatments so the data can be analyzed together. The bigger the dataset, the more confidence can be placed in the conclusions. The main goal of this project is to understand the individual differences between people who experience the same treatment.
- The NHLBI Director co-chairs the NIH Nutrition Research Task Force, which guided the development of the first NIH-wide strategic plan for nutrition research being conducted over the next 10 years. See the 2020–2030 Strategic Plan for NIH Nutrition Research .
- The NHLBI is an active member of the National Collaborative on Childhood Obesity (NCCOR) , which is a public–private partnership to accelerate progress in reducing childhood obesity.
- The NHLBI has been providing guidance to physicians on the diagnosis, prevention, and treatment of obesity since 1977. In 2017, the NHLBI convened a panel of experts to take on some of the pressing questions facing the obesity research community. See their responses: Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents (PDF, 3.69 MB).
- In 2021, the NHLBI held a Long Non-coding (lnc) RNAs Symposium to discuss research opportunities on lnc RNAs, which appear to play a role in the development of metabolic diseases such as obesity.
- The Muscatine Heart Study began enrolling children in 1970. By 1981, more than 11,000 students from Muscatine, Iowa, had taken surveys twice a year. The study is the longest-running study of cardiovascular risk factors in children in the United States. Today, many of the earliest participants and their children are still involved in the study, which has already shown that early habits affect cardiovascular health later in life.
- The Jackson Heart Study is a unique partnership of the NHLBI, three colleges and universities, and the Jackson, Miss., community. Its mission is to discover what factors contribute to the high prevalence of cardiovascular disease among African Americans. Researchers aim to test new approaches for reducing this health disparity. The study incudes more than 5,000 individuals. Among the study’s findings to date is a gene variant in African Americans that doubles the risk of heart disease.
Explore more NHLBI research on overweight and obesity
The sections above provide you with the highlights of NHLBI-supported research on overweight and obesity . You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity
Affiliations.
- 1 Centre for Software Technology and Management, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia.
- 2 Centre for Software Technology and Management, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia. Electronic address: [email protected].
- 3 RIADI Laboratory, University of Manouba, Manouba, Tunisia; College of Computer Science and Engineering, Taibah University, Medina, Saudi Arabia.
- 4 Center for Artificial Intelligence Technology, Faculty of Information Science and Technology, Universiti Kebangsaan Malaysia (UKM), Bangi, 43600, Selangor, Malaysia.
- PMID: 34426171
- DOI: 10.1016/j.compbiomed.2021.104754
Obesity is considered a principal public health concern and ranked as the fifth foremost reason for death globally. Overweight and obesity are one of the main lifestyle illnesses that leads to further health concerns and contributes to numerous chronic diseases, including cancers, diabetes, metabolic syndrome, and cardiovascular diseases. The World Health Organization also predicted that 30% of death in the world will be initiated with lifestyle diseases in 2030 and can be stopped through the suitable identification and addressing of associated risk factors and behavioral involvement policies. Thus, detecting and diagnosing obesity as early as possible is crucial. Therefore, the machine learning approach is a promising solution to early predictions of obesity and the risk of overweight because it can offer quick, immediate, and accurate identification of risk factors and condition likelihoods. The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this study initially recognized the significant potential factors that influence and cause adult obesity. Next, the main diseases and health consequences of obesity and overweight are investigated. Ultimately, this study recognized the machine learning methods that can be used for the prediction of obesity. Finally, this study seeks to support decision-makers looking to understand the impact of obesity on health in the general population and identify outcomes that can be used to guide health authorities and public health to further mitigate threats and effectively guide obese people globally.
Keywords: Diseases; Machine learning; Obesity; Overweight; Risk factors.
Copyright © 2021 The Author(s). Published by Elsevier Ltd.. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Systematic Review
- Machine Learning
- Metabolic Syndrome*
- Obesity* / epidemiology
- Risk Factors
- Open access
- Published: 21 June 2021
The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies
- Emma Farrell ORCID: orcid.org/0000-0002-7780-9428 1 ,
- Marta Bustillo 2 ,
- Carel W. le Roux 3 ,
- Joe Nadglowski 4 ,
- Eva Hollmann 1 &
- Deirdre McGillicuddy 1
Systematic Reviews volume 10 , Article number: 181 ( 2021 ) Cite this article
6077 Accesses
9 Altmetric
Metrics details
Obesity is a prevalent, complex, progressive and relapsing chronic disease characterised by abnormal or excessive body fat that impairs health and quality of life. It affects more than 650 million adults worldwide and is associated with a range of health complications. Qualitative research plays a key role in understanding patient experiences and the factors that facilitate or hinder the effectiveness of health interventions. This review aims to systematically locate, assess and synthesise qualitative studies in order to develop a more comprehensive understanding of the lived experience of people with obesity.
This is a protocol for a qualitative evidence synthesis of the lived experience of people with obesity. A defined search strategy will be employed in conducting a comprehensive literature search of the following databases: PubMed, Embase, PsycInfo, PsycArticles and Dimensions (from 2011 onwards). Qualitative studies focusing on the lived experience of adults with obesity (BMI >30) will be included. Two reviewers will independently screen all citations, abstracts and full-text articles and abstract data. The quality of included studies will be appraised using the critical appraisal skills programme (CASP) criteria. Thematic synthesis will be conducted on all of the included studies. Confidence in the review findings will be assessed using GRADE CERQual.
The findings from this synthesis will be used to inform the EU Innovative Medicines Initiative (IMI)-funded SOPHIA (Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy) study. The objective of SOPHIA is to optimise future obesity treatment and stimulate a new narrative, understanding and vocabulary around obesity as a set of complex and chronic diseases. The findings will also be useful to health care providers and policy makers who seek to understand the experience of those with obesity.
Systematic review registration
PROSPERO CRD42020214560 .
Peer Review reports
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health and quality of life, increases the risk of long-term medical complications and reduces lifespan [ 1 ]. Operationally defined in epidemiological and population studies as a body mass index (BMI) greater than or equal to 30, obesity affects more than 650 million adults worldwide [ 2 ]. Its prevalence has almost tripled between 1975 and 2016, and, globally, there are now more people with obesity than people classified as underweight [ 2 ].
Obesity is caused by the complex interplay of multiple genetic, metabolic, behavioural and environmental factors, with the latter thought to be the proximate factor which enabled the substantial rise in the prevalence of obesity in recent decades [ 3 , 4 ]. This increased prevalence has resulted in obesity becoming a major public health issue with a resulting growth in health care and economic costs [ 5 , 6 ]. At a population level, health complications from excess body fat increase as BMI increases [ 7 ]. At the individual level, health complications occur due to a variety of factors such as distribution of adiposity, environment, genetic, biologic and socioeconomic factors [ 8 ]. These health complications include type 2 diabetes [ 9 ], gallbladder disease [ 10 ] and non-alcoholic fatty liver disease [ 11 ]. Excess body fat can also place an individual at increased cardiometabolic and cancer risk [ 12 , 13 , 14 ] with an estimated 20% of all cancers attributed to obesity [ 15 ].
Although first recognised as a disease by the American Medical Association in 2013 [ 16 ], the dominant cultural narrative continues to present obesity as a failure of willpower. People with obesity are positioned as personally responsible for their weight. This, combined with the moralisation of health behaviours and the widespread association between thinness, self-control and success, has resulted in those who fail to live up to this cultural ideal being subject to weight bias, stigma and discrimination [ 17 , 18 , 19 ]. Weight bias, stigma and discrimination have been found to contribute, independent of weight or BMI, to increased morbidity or mortality [ 20 ].
Thomas et al. [ 21 ] highlighted, more than a decade ago, the need to rethink how we approach obesity so as not to perpetuate damaging stereotypes at a societal level. Obesity research then, as now, largely focused on measurable outcomes and quantifiable terms such as body mass index [ 22 , 23 ]. Qualitative research approaches play a key role in understanding patient experiences, how factors facilitate or hinder the effectiveness of interventions and how the processes of interventions are perceived and implemented by users [ 24 ]. Studies adopting qualitative approaches have been shown to deliver a greater depth of understanding of complex and socially mediated diseases such as obesity [ 25 ]. In spite of an increasing recognition of the integral role of patient experience in health research [ 25 , 26 ], the voices of patients remain largely underrepresented in obesity research [ 27 , 28 ].
Systematic reviews and syntheses of qualitative studies are recognised as a useful contribution to evidence and policy development [ 29 ]. To the best of the authors’ knowledge, this will be the first systematic review and synthesis of qualitative studies focusing on the lived experience of people with obesity. While systematic reviews have been carried out on patient experiences of treatments such as behavioural management [ 30 ] and bariatric surgery [ 31 ], this review and synthesis will be the first to focus on the experience of living with obesity rather than patient experiences of particular treatments or interventions. This focus represents a growing awareness that ‘patients have a specific expertise and knowledge derived from lived experience’ and that understanding lived experience can help ‘make healthcare both effective and more efficient’ [ 32 ].
This paper outlines a protocol for the systematic review of qualitative studies based on the lived experience of people with obesity. The findings of this review will be synthesised in order to develop an overview of the lived experience of patients with obesity. It will look, in particular, at patient concerns around the risks of obesity and their aspirations for response to obesity treatment.
The review protocol has been registered within the PROSPERO database (registration number: CRD42020214560) and is being reported in accordance with the reporting guidance provided in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement [ 33 , 34 ] (see checklist in Additional file 1 ).
Information sources and search strategy
The primary source of literature will be a structured search of the following electronic databases (from January 2011 onwards—to encompass the increase in research focused on patient experience observed over the last 10 years): PubMed, Embase, PsycInfo, PsycArticles and Dimensions. There is no methodological agreement as to how many search terms or databases out to be searched as part of a ‘good’ qualitative synthesis (Toye et al. [ 35 ]). However, the breadth and depth of the search terms, the inclusion of clinical and personal language and the variety within the selected databases, which cover areas such as medicine, nursing, psychology and sociology, will position this qualitative synthesis as comprehensive. Grey literature will not be included in this study as its purpose is to conduct a comprehensive review of peer-reviewed primary research. The study’s patient advisory board will be consulted at each stage of the review process, and content experts and authors who are prolific in the field will be contacted. The literature searches will be designed and conducted by the review team which includes an experienced university librarian (MB) following the methodological guidance of chapter two of the JBI Manual for Evidence Synthesis [ 36 ]. The search will include a broad range of terms and keywords related to obesity and qualitative research. A full draft search strategy for PubMed is provided in Additional file 2 .
Eligibility criteria
Studies based on primary data generated with adults with obesity (operationally defined as BMI >30) and focusing on their lived experience will be eligible for inclusion in this synthesis (Table 1 ). The context can include any country and all three levels of care provision (primary, secondary and tertiary). Only peer-reviewed, English language, articles will be included. Studies adopting a qualitative design, such as phenomenology, grounded theory or ethnography, and employing qualitative methods of data collection and analysis, such as interviews, focus groups, life histories and thematic analysis, will be included. Publications with a specific focus, for example, patient’s experience of bariatric surgery, will be included, as well as studies adopting a more general view of the experience of obesity.
Screening and study selection process
Search results will be imported to Endnote X9, and duplicate entries will be removed. Covidence [ 38 ] will be used to screen references with two reviewers (EF and EH) removing entries that are clearly unrelated to the research question. Titles and abstracts will then be independently screened by two reviewers (EF and EH) according to the inclusion criteria (Table 1 ). Any disagreements will be resolved through a third reviewer (DMcG). This layer of screening will determine which publications will be eligible for independent full-text review by two reviewers (EF and EH) with disagreements again being resolved by a third reviewer (DMcG).
Data extraction
Data will be extracted independently by two researchers (EF and EH) and combined in table format using the following headings: author, year, title, country, research aims, participant characteristics, method of data collection, method of data analysis, author conclusions and qualitative themes. In the case of insufficient or unclear information in a potentially eligible article, the authors will be contacted by email to obtain or confirm data, and a timeframe of 3 weeks to reply will be offered before article exclusion.
Quality appraisal of included studies
This qualitative synthesis will facilitate the development of a conceptual understanding of obesity and will be used to inform the development of policy and practice. As such, it is important that the studies included are themselves of suitable quality. The methodological quality of all included studies will be assessed using the critical appraisal skills programme (CASP) checklist, and studies that are deemed of insufficient quality will be excluded. The CASP checklist for qualitative research comprises ten questions that cover three main issues: Are the results of the study under review valid? What are the results? Will the results help locally? Two reviewers (EF and EH) will independently evaluate each study using the checklist with a third and fourth reviewer (DMcG and MB) available for consultation in the event of disagreement.
Data synthesis
The data generated through the systematic review outlined above will be synthesised using thematic synthesis as described by Thomas and Harden [ 39 ]. Thematic synthesis enables researchers to stay ‘close’ to the data of primary studies, synthesise them in a transparent way and produce new concepts and hypotheses. This inductive approach is useful for drawing inference based on common themes from studies with different designs and perspectives. Thematic synthesis is made up of a three-step process. Step one consists of line by line coding of the findings of primary studies. The second step involves organising these ‘free codes’ into related areas to construct ‘descriptive’ themes. In step three, the descriptive themes that emerged will be iteratively examined and compared to ‘go beyond’ the descriptive themes and the content of the initial studies. This step will generate analytical themes that will provide new insights related to the topic under review.
Data will be coded using NVivo 12. In order to increase the confirmability of the analysis, studies will be reviewed independently by two reviewers (EF and EH) following the three-step process outlined above. This process will be overseen by a third reviewer (DMcG). In order to increase the credibility of the findings, an overview of the results will be brought to a panel of patient representatives for discussion. Direct quotations from participants in the primary studies will be italicised and indented to distinguish them from author interpretations.
Assessment of confidence in the review findings
Confidence in the evidence generated as a result of this qualitative synthesis will be assessed using the Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research (GRADE CERQual) [ 40 ] approach. Four components contribute to the assessment of confidence in the evidence: methodological limitations, relevance, coherence and adequacy of data. The methodological limitations of included studies will be examined using the CASP tool. Relevance assesses the degree to which the evidence from the primary studies applies to the synthesis question while coherence assesses how well the findings are supported by the primary studies. Adequacy of data assesses how much data supports a finding and how rich this data is. Confidence in the evidence will be independently assessed by two reviewers (EF and EH), graded as high, moderate or low, and discussed collectively amongst the research team.
Reflexivity
For the purposes of transparency and reflexivity, it will be important to consider the findings of the qualitative synthesis and how these are reached, in the context of researchers’ worldviews and experiences (Larkin et al, 2019). Authors have backgrounds in health science (EF and EH), education (DMcG and EF), nursing (EH), sociology (DMcG), philosophy (EF) and information science (MB). Prior to conducting the qualitative synthesis, the authors will examine and discuss their preconceptions and beliefs surrounding the subject under study and consider the relevance of these preconceptions during each stage of analysis.
Dissemination of findings
Findings from the qualitative synthesis will be disseminated through publications in peer-reviewed journals, a comprehensive and in-depth project report and presentation at peer-reviewed academic conferences (such as EASO) within the field of obesity research. It is also envisaged that the qualitative synthesis will contribute to the shared value analysis to be undertaken with key stakeholders (including patients, clinicians, payers, policy makers, regulators and industry) within the broader study which seeks to create a new narrative around obesity diagnosis and treatment by foregrounding patient experiences and voice(s). This synthesis will be disseminated to the 29 project partners through oral presentations at management board meetings and at the general assembly. It will also be presented as an educational resource for clinicians to contribute to an improved understanding of patient experience of living with obesity.
Obesity is a complex chronic disease which increases the risk of long-term medical complications and a reduced quality of life. It affects a significant proportion of the world’s population and is a major public health concern. Obesity is the result of a complex interplay of multiple factors including genetic, metabolic, behavioural and environmental factors. In spite of this complexity, obesity is often construed in simple terms as a failure of willpower. People with obesity are subject to weight bias, stigma and discrimination which in themselves result in increased risk of mobility or mortality. Research in the area of obesity has tended towards measurable outcomes and quantitative variables that fail to capture the complexity associated with the experience of obesity. A need to rethink how we approach obesity has been identified—one that represents the voices and experiences of people living with obesity. This paper outlines a protocol for the systematic review of available literature on the lived experience of people with obesity and the synthesis of these findings in order to develop an understanding of patient experiences, their concerns regarding the risks associated with obesity and their aspirations for response to obesity treatment. Its main strengths will be the breadth of its search remit—focusing on the experiences of people with obesity rather than their experience of a particular treatment or intervention. It will also involve people living with obesity and its findings disseminated amongst the 29 international partners SOPHIA research consortium, in peer reviewed journals and at academic conferences. Just as the study’s broad remit is its strength, it is also a potential challenge as it is anticipated that searchers will generate many thousands of results owing to the breadth of the search terms. However, to the best of the authors’ knowledge, this will be the first systematic review and synthesis of its kind, and its findings will contribute to shaping the optimisation of future obesity understanding and treatment.
Availability of data and materials
Not applicable.
Abbreviations
Body mass index
Critical appraisal skills programme
Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research
Innovative Medicines Initiative
Medical Subject Headings
Population, phenomenon of interest, context, study type
Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. Can Med Assoc J. 2020;192(31):E875–91. https://doi.org/10.1503/cmaj.191707 .
Article Google Scholar
World Health Organisation. Fact sheet: obesity and overweight. Geneva: World Health Organisation; 2020.
Google Scholar
Mechanick J, Hurley D, Garvey W. Adiposity-based chronic disease as a new diagnostic term: the American Association of Clinical Endocrinologists and American College Of Endocrinology position statement. Endocrine Pract. 2017;23(3):372–8. https://doi.org/10.4158/EP161688.PS .
Garvey W, Mechanick J. Proposal for a scientifically correct and medically actionable disease classification system (ICD) for obesity. Obesity. 2020;28(3):484–92. https://doi.org/10.1002/oby.22727 .
Article PubMed Google Scholar
Biener A, Cawley J, Meyerhoefer C. The high and rising costs of obesity to the US health care system. J Gen Intern Med. 2017;32(Suppl 1):6–8. https://doi.org/10.1007/s11606-016-3968-8 .
Article PubMed PubMed Central Google Scholar
Department of Health and Social Care. Healthy lives, healthy people: a call to action on obesity in England. London: Department of Health and Social Care; 2011.
Di Angelantonio E, Bhupathiraju SN, Wormser D, Gao P, Kaptoge S, de Gonzalez AB, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86. https://doi.org/10.1016/S0140-6736(16)30175-1 .
Sharma AM. M, M, M & M: a mnemonic for assessing obesity. Obesity Reviews. 2010;11(11):808–9. https://doi.org/10.1111/j.1467-789X.2010.00766.x .
Article PubMed CAS Google Scholar
Asnawi A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract 2010;89:309-19. Diab Res Clin Pract. 2010;89:309–19.
Dagfinn A, Teresa N, Lars JV. Body mass index, abdominal fatness and the risk of gallbladder disease. 2015;30(9):1009.
Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20(9).
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. 2003;289(2):187-193.
Grover SA, Kaouache M, Rempel P, Joseph L, Dawes M, Lau DCW, et al. Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: a modelling study. 2015;3(2):114-122.
Ackerman S, Blackburn O, Marchildon F, Cohen P. Insights into the link between obesity and cancer. Curr Obes Rep. 2017;6(2):195–203. https://doi.org/10.1007/s13679-017-0263-x .
Wolin K, Carson K, Colditz G. Obesity and cancer. Oncol. 2010;15(6):556–65. https://doi.org/10.1634/theoncologist.2009-0285 .
Resolution 420: Recognition of obesity as a disease [press release]. 05/16/13 2013.
Brownell KD. Personal responsibility and control over our bodies: when expectation exceeds reality. 1991;10(5):303-10.
Puhl RM, Latner JD, O'Brien K, Luedicke J, Danielsdottir S, Forhan M. A multinational examination of weight bias: predictors of anti-fat attitudes across four countries. 2015;39(7):1166-1173.
Browne NT. Weight bias, stigmatization, and bullying of obese youth. 2012;7(3):107-15.
Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. 2015;26(11):1803-11.
Thomas SL, Hyde J, Karunaratne A, Herbert D, Komesaroff PA. Being “fat” in today’s world: a qualitative study of the lived experiences of people with obesity in Australia. 2008;11(4):321-30.
Ogden K, Barr J, Rossetto G, Mercer J. A “messy ball of wool”: a qualitative study of the dimensions of the lived experience of obesity. 2020;8(1):1-14.
Ueland V, Furnes B, Dysvik E, R¯rtveit K. Living with obesity-existential experiences. 2019;14(1):1-12.
Avenell A, Robertson C, Skea Z, Jacobsen E, Boyers D, Cooper D, et al. Bariatric surgery, lifestyle interventions and orlistat for severe obesity: the REBALANCE mixed-methods systematic review and economic evaluation. 2018;22(68).
The PLoS Medicine Editors. Qualitative research: understanding patients’ needs and experiences. Plos Med. 2007;4(8):1283–4.
Boulton M, Fitzpatrick R. Qualitative methods for assessing health care doi:10.1136/qshc.3.2.107. Qual Health Care. 1994;3:107–13.
Johnstone J, Herredsberg C, Lacy L, Bayles P, Dierking L, Houck A, et al. What I wish my doctor really knew: the voices of patients with obesity. Ann Fam Med. 2020;18(2):169–71. https://doi.org/10.1370/afm.2494 .
Brown I, Thompson J, Tod A, Jones G. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract. 2006;56(530):666–72.
PubMed PubMed Central Google Scholar
Brown I, Gould J. Qualitative studies of obesity: a review of methodology. Health. 2013;5(8A3):69–80.
Garip G, Yardley L. A synthesis of qualitative research on overweight and obese people’s views and experiences of weight management. Clin Obes. 2011;1(2-3):10–126.
Coulman K, MacKichan F, Blazeby J, Owen-Smith A. Patient experiences of outcomes of bariatric surgery: a systematic review and qualitative synthesis. Obes Rev. 2017;18(5):547–59. https://doi.org/10.1111/obr.12518 .
European Patients’ Forum. “Patients’ Perceptions of Quality in Healthcare”: Report of a survey conducted by EPF in 2016 Brussels: European Patients’ Forum; 2017.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349(jan02 1):g7647. https://doi.org/10.1136/bmj.g7647 .
Toye F, et al. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol. 2014;14(80).
Lockwood C, Porrit K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, et al. Chapter 2: Systematic reviews of qualitative evidence. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis: JBI; 2020, doi: https://doi.org/10.46658/JBIMES-20-03 .
Methley AM, et al. PICO, PICOS and SPIDER: a comparison study of spcificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Services Res. 2014;14.
Covidence. Cochrane Community; 2020. Available from: https://www.covidence.org .
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. https://doi.org/10.1186/1471-2288-8-45 .
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13(1):2. https://doi.org/10.1186/s13012-017-0688-3 .
Download references
Acknowledgements
Any amendments made to this protocol when conducting the study will be outlined in PROSPERO and reported in the final manuscript.
This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking (JU) under grant agreement No 875534. The JU receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA and T1D Exchange, JDRF and Obesity Action Coalition. The funding body had no role in the design of the study and will not have a role in collection, analysis and interpretation of data or in writing the manuscript.
Author information
Authors and affiliations.
School of Education, University College Dublin, Belfield, Dublin 4, Ireland
Emma Farrell, Eva Hollmann & Deirdre McGillicuddy
University College Dublin Library, Dublin, Ireland
Marta Bustillo
Diabetes Complications Research Centre, University College Dublin, Dublin, Ireland
Carel W. le Roux
Obesity Action Coalition, Tampa, USA
Joe Nadglowski
You can also search for this author in PubMed Google Scholar
Contributions
EF conceptualised and designed the protocol with input from DMcG and MB. EF drafted the initial manuscript. EF and MB defined the concepts and search items with input from DmcG, CleR and JN. MB and EF designed and executed the search strategy. DMcG, CleR, JN and EH provided critical insights and reviewed and revised the protocol. All authors have approved and contributed to the final written manuscript.
Corresponding author
Correspondence to Emma Farrell .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:..
PRISMA-P (Preferred Reporting Items for Systematic review and Meta-Analysis Protocols) 2015 checklist: recommended items to address in a systematic review protocol*.
Additional file 2: Table 1
. Search PubMed search string.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Farrell, E., Bustillo, M., le Roux, C.W. et al. The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies. Syst Rev 10 , 181 (2021). https://doi.org/10.1186/s13643-021-01706-5
Download citation
Received : 28 October 2020
Accepted : 14 May 2021
Published : 21 June 2021
DOI : https://doi.org/10.1186/s13643-021-01706-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lived experience
- Patient experience
- Obesity treatment
- Qualitative
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Prevention, prevention, prevention.
Losing weight is hard to do.
In the U.S., only one in six adults who have dropped excess pounds actually keep off at least 10 percent of their original body weight. The reason: a mismatch between biology and environment. Our bodies are evolutionarily programmed to put on fat to ride out famine and preserve the excess by slowing metabolism and, more important, provoking hunger. People who have slimmed down and then regain their weight don’t lack willpower—their bodies are fighting them every inch of the way.
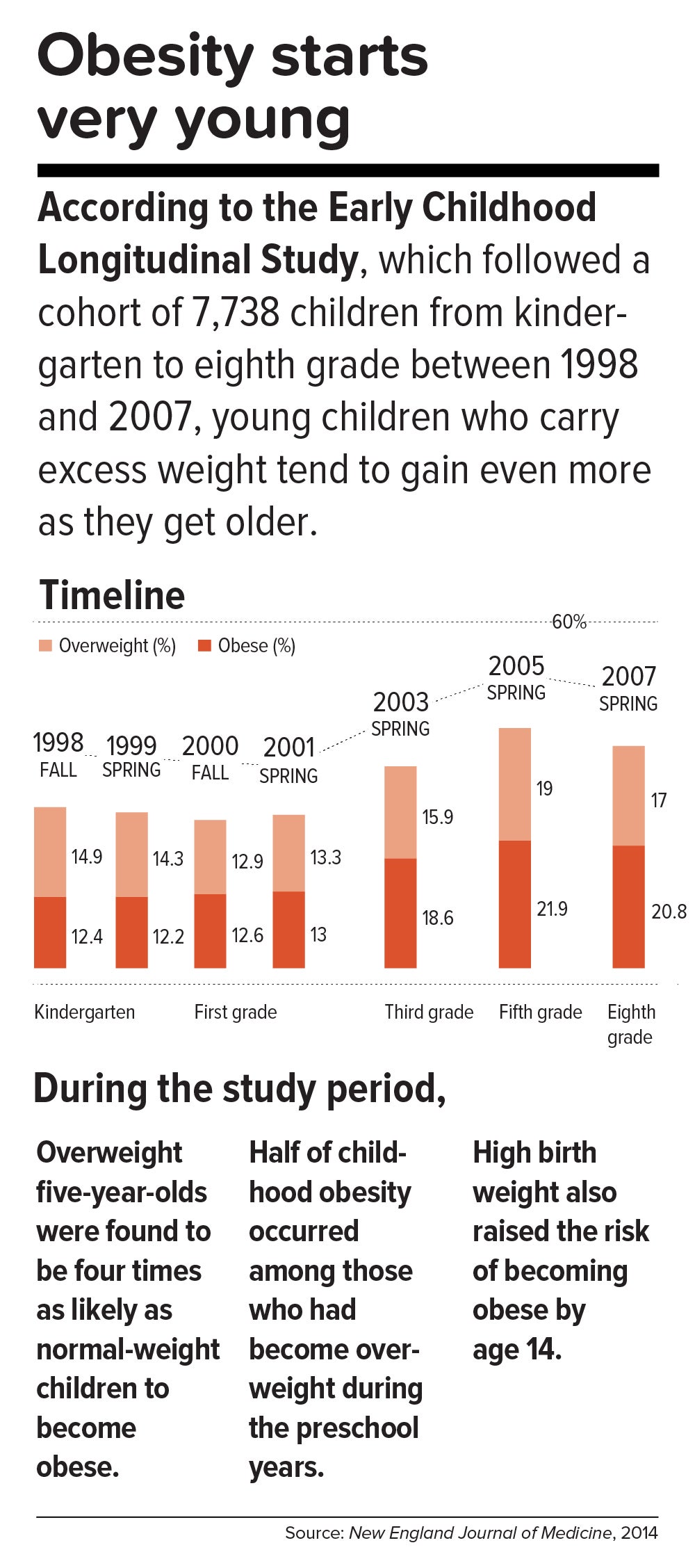
This inborn predisposition to hold on to added weight reverberates down the life course. Few children are born obese, but once they become heavy, they are usually destined to be heavy adolescents and heavy adults. According to a 2016 study in the New England Journal of Medicine , approximately 90 percent of children with severe obesity will become obese adults with a BMI of 35 or higher. Heavy young adults are generally heavy in middle and old age. Obesity also jumps across generations; having a mother who is obese is one of the strongest predictors of obesity in children.
All of which means that preventing child obesity is key to stopping the epidemic. By the time weight piles up in adulthood, it is usually too late. Luckily, preventing obesity in children is easier than in adults, partly because the excess calories they absorb are minimal and can be adjusted by small changes in diet—substituting water, for example, for sugary fruit juices or soda.
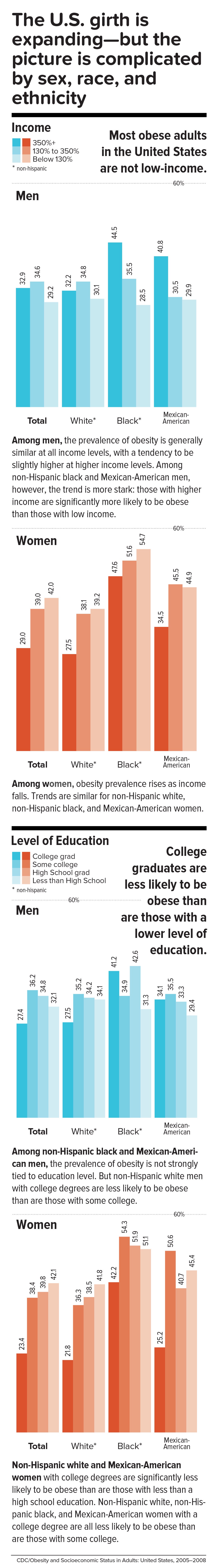
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, “Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55. During this time, people gain fat mass, not muscle mass. When they reach age 55 or so, they begin to lose their existing muscle mass and gain even more fat mass. That’s when all the metabolic problems appear: insulin resistance, high cholesterol, high blood pressure.”
Adds Walter Willett, Frederick John Stare Professor of Epidemiology and Nutrition at Harvard Chan, “The first 5 pounds of weight gain at age 25—that’s the time to be taking action. Because someone is on a trajectory to end up being 30 pounds overweight by the time they’re age 50.”
The most realistic near-term public health goal, therefore, is not to reverse but rather to slow down the trend—and even this will require strong commitment from government at many levels. In May 2017, the Trump administration rolled back recently-enacted standards for school meals, delaying a rule to lower sodium and allowing waivers for regulations requiring cafeterias to serve foods rich in whole grains. If recent expansions in food entitlements and school meals are undermined, “It would be a ‘disaster,’ to use the president’s word,” says Marlene Schwartz, director of the Rudd Center for Obesity & Food Policy at the University of Connecticut. “The federal food programs are incredibly important, not just because of the food and money they provide families, but because supporting better nutrition in child care, schools, and the WIC [Women, Infants, and Children] program has created new social norms. We absolutely cannot undo the progress that we’ve made in helping this generation transition to a healthier diet.”
Get the science right.
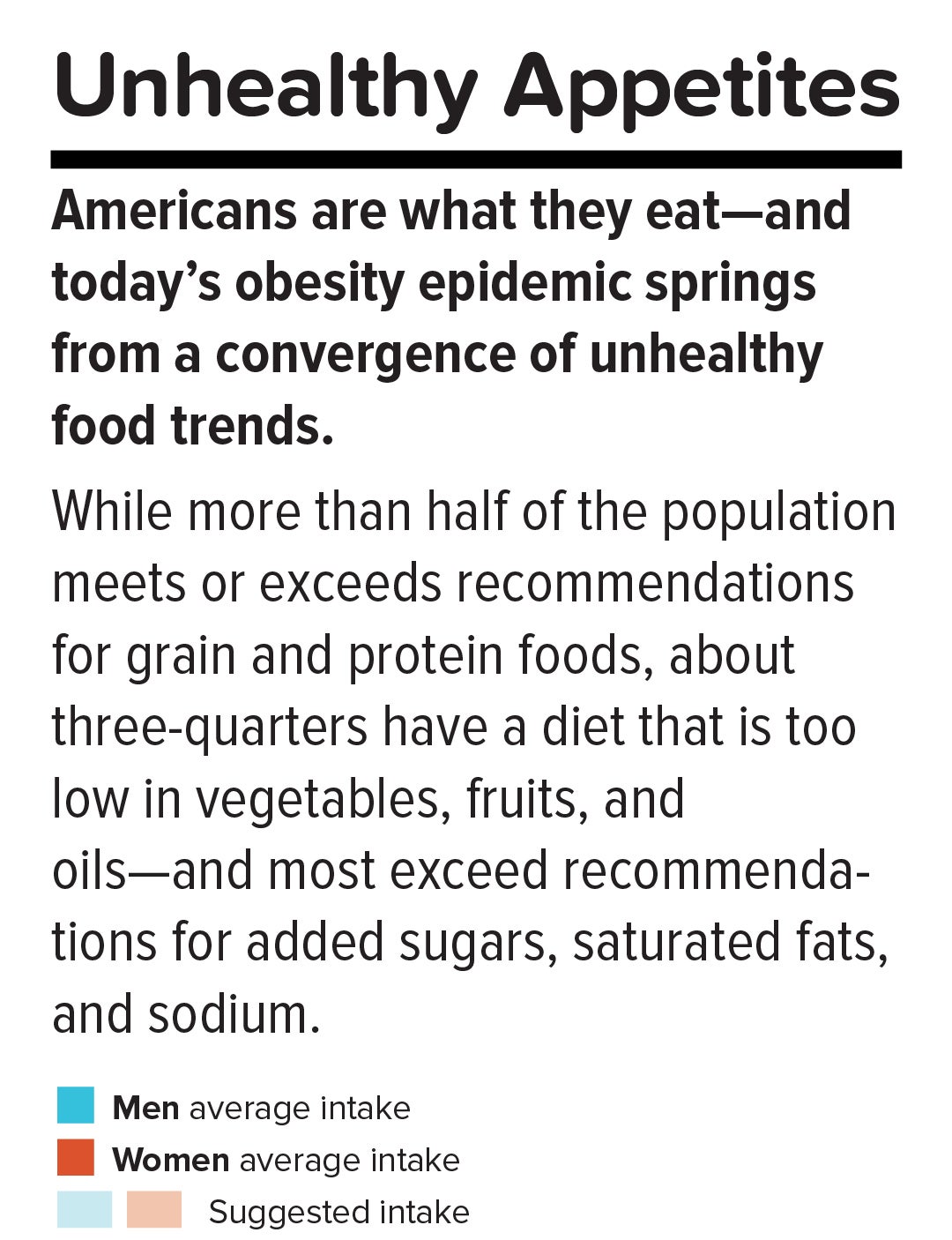
It is impossible to prescribe solutions to obesity without reminding ourselves that nutrition scientists botched things decades ago and probably sent the epidemic into overdrive. Beginning in the 1970s, the U.S. government and major professional groups recommended for the first time that people eat a low-fat/high-carbohydrate diet. The advice was codified in 1977 with the first edition of The Dietary Goals for the United States , which aimed to cut diet-related conditions such as heart disease and diabetes. What ensued amounted to arguably the biggest public health experiment in U.S. history, and it backfired.
At the time, saturated fat and dietary cholesterol were believed to be the main factors responsible for cardiovascular disease—an oversimplified theory that ignored the fact that not all fats are created equal. Soon, the public health blitz against saturated fat became a war on all fat. In the American diet, fat calories plummeted and carb calories shot up.
“We can’t blame industry for this. It was a bandwagon effect in the scientific community, despite the lack of evidence—even with evidence to the contrary,” says Willett. “Farmers have known for thousands of years that if you put animals in a pen, don’t let them run around, and load them up with grains, they get fat. That’s basically what has been happening to people: We created the great American feedlot. And we added in sugar, coloring, and seductive promotion for low-fat junk food.”
Scientists now know that whole fruits and vegetables (other than potatoes), whole grains, high-quality proteins (such as from fish, chicken, beans, and nuts), and healthy plant oils (such as olive, peanut, or canola oil) are the foundations of a healthy diet.
But there is also a lot scientists don’t yet know. One unanswered question is why some people with obesity are spared the medical complications of excess weight. Another concerns the major mechanisms by which obesity ushers in disease. Although surplus body weight can itself directly cause problems—such as arthritis due to added load on joints, or breast cancer caused by hormones secreted by fat cells—in general, obesity triggers myriad biological processes. Many of the resulting conditions—such as atherosclerosis, diabetes, and even Alzheimer’s disease—are mediated by inflammation, in which the body’s immune response becomes damagingly self-perpetuating. In this sense, today’s food system is as inflammagenic as it is obesigenic.
Scientists also need to ferret out the nuanced effects of particular foods. For example, do fermented products—such as yogurt, tempeh, or sauerkraut—have beneficial properties? Some studies have found that yogurt protects against weight gain and diabetes, and suggest that healthy live bacteria (known as probiotics) may play a role. Other reports point to fruits being more protective than vegetables in weight control and diabetes prevention, although the types of fruits and vegetables make a difference.
A 2017 article in the American Journal of Clinical Nutrition showed that substituting whole grains for refined grains led to a loss of nearly 100 calories a day—by speeding up metabolism, cutting the number of calories that the body hangs on to, and, more surprisingly, by changing the digestibility of other foods on the plate. That extra energy lost daily—by substituting, say, brown rice for white rice or barley for pita bread—was equivalent to a brisk 30-minute walk. One hundred calories a day, sustained over years, and multiplied by the population is one mathematical equivalent of the obesity epidemic.
A companion study found that adults who ate a whole-grain-rich diet developed healthier gut bacteria and improved immune responses. That particular foods alter the gut microbiome—the dense and vital community of bacteria and other microorganisms that work symbiotically with the body’s own digestive system—is another critical insight. The microbiome helps determine weight by controlling how our bodies extract calories and store fat in the liver, and the microbiomes of obese individuals are startlingly efficient at harvesting calories from food. [To learn more about Harvard Chan research on the gut microbiome, read “ Bugs in the System .”] The hormonal effects of sleep deprivation and stress—two epidemics concurrent and intertwined with the obesity trend—are other promising avenues of research.
And then there are the mystery factors. One recent hypothesis is that an agent known as adenovirus 36 partly accounts for our collective heft. A 2010 article in The Royal Society described a study in which researchers examined samples of more than 20,000 animals from eight species living with or around humans in industrialized nations, a menagerie that included macaques, chimpanzees, vervets, marmosets, lab mice and rats, feral rats, and domestic dogs and cats. Like their Homo sapiens counterparts, all of the study populations had gained weight over the past several decades—wild, domestic, and lab animals alike. The chance that this is a coincidence is, according to the scientists’ estimate, 1 in 10 million. The stumped authors surmise that viruses, gene expression changes, or “as-of-yet unidentified and/or poorly understood factors” are to blame.
Master the art of persuasion.
A 2015 paper in the American Journal of Public Health revealed the philosophical chasm that hampers America’s progress on obesity prevention. It found that 72 to 98 percent of obesity-related media reports emphasize personal responsibility for weight, compared with 40 percent of scientific papers.
A recent study by Drexel University researchers also quantified the political polarization around public health measures. From 1998 through 2013, Democrats voted in line with recommendations from the American Public Health Association 88.3 percent of the time, on average, while Republicans voted for the proposals just 21.3 percent of the time.
Clearly, we can’t count on bipartisan goodwill to stem the obesity crisis. But we can ask what kinds of messages appeal to politically divergent audiences. A stealth strategy may be to avoid even uttering the word “obesity.” On January 1 of this year, Philadelphia’s 1.5-cents-per-ounce excise tax on sugar-sweetened and diet beverages took effect. When Philadelphia Mayor Jim Kenney lobbied voters to approve the tax, his bid centered not on improving health—the unsuccessful pitch of his predecessor—but on raising $91 million annually for prekindergarten programs.
“That’s something lots of people care about and can get behind—it’s a feel-good policy, and it makes sense,” says psychologist Christina Roberto, assistant professor of medical ethics and health policy at the University of Pennsylvania, and a former assistant professor of social and behavioral sciences and nutrition at Harvard Chan. The provision for taxing diet beverages was also shrewd, she adds, because it spread the tax’s pain; since wealthier people are more likely than less-affluent individuals to buy diet drinks, the tax could not be slapped with the label “regressive.”
But Roberto sees a larger lesson in the Philadelphia story. Public health messaging that appeals to values that transcend the individual is less fraught, less stigmatizing, and perhaps more effective. As she puts it, “It’s very different to hear the message, ‘Eat less red meat, help the planet’ versus ‘Eat less red meat, help yourself avoid saturated fat and cardiovascular disease.’”
Supermarket makeovers
Supermarket aisles are other places where public health can shuffle a deck stacked against healthy consumer choices.
With slim profit margins and 50,000-plus products on their shelves, grocery stores depend heavily on food manufacturers’ promotional incentives to make their bottom lines. “Manufacturers pay slotting fees to get their products on the shelf, and they pay promotion allowances: We’ll give you this much off a carton of Coke if you put it on sale for a certain price or if you put it on an end-of-aisle display,” says José Alvarez, former president and chief executive officer of Stop & Shop/Giant-Landover, now senior lecturer of business administration at Harvard Business School. Such promotional payments, Alvarez adds, often exceed retailers’ net profits.
Healthy new products—like flash-frozen dinners prepared with heaps of vegetables and whole grains, and relatively little salt—can’t compete for prized shelf space against boxed mac and cheese or cloying breakfast cereals. One solution, says Alvarez, is for established consumer packaged goods companies to buy out what he calls the “hippie in the basement” firms that have whipped up more nutritious items. The behemoths could apply their production, marketing, and distribution prowess to the new offerings—and indeed, this has started to happen over the last five years.
Another approach is to make nutritious foods more convenient to eat. “We have all of these cooking shows and upscale food magazines, but most people don’t have the time or inclination—or the skills, quite frankly—to cook,” says Alvarez. “Instead, we should focus on creating high-quality, healthy, affordable prepared foods.”
An additional model is suggested by Jeff Dunn, a 20-year veteran of the soft drink industry and former president of Coca-Cola North America, who went on to become an advocate for fresh, healthy food. Dunn served as president and chief executive officer of Bolthouse Farms from 2008 to 2015, where he dramatically increased sales of baby carrots by using marketing techniques common in the junk food business. “We operated on the principles of the three 3 A’s: accessibility, availability, and affordability,” says Dunn. “That, by the way, is Coke’s more-than-70-year-old formula for success.”
Show them the money.
Obesity kills budgets. According to the Campaign to End Obesity, a collaboration of leaders from industry, academia, public health, and policymakers, annual U.S. health costs related to obesity approach $200 billion. In 2010, the nonpartisan Congressional Budget Office reported that nearly 20 percent of the rise in health care spending from 1987 to 2007 was linked to obesity. And the U.S. Centers for Disease Control and Prevention (CDC) found that full-time workers in the U.S. who are overweight or obese and have other chronic health conditions miss an estimated 450 million more days of work each year than do healthy employees—upward of $153 billion in lost productivity annually.
But making the money case for obesity prevention isn’t straightforward. For interventions targeting children and youth, only a small fraction of savings is captured in the first decade, since most serious health complications don’t emerge for many years. Long-term obesity prevention, in other words, doesn’t fit into political timetables for elected officials.
Yet lawmakers are keen to know how “best for the money” obesity-prevention programs can help them in the short run. Over the past two years, Harvard Chan’s Steve Gortmaker and his colleagues have been working with state health departments in Alaska, Mississippi, New Hampshire, Oklahoma, Washington, and West Virginia and with the city of Philadelphia and other locales, building cost-effectiveness models using local data for a wide variety of interventions—from improved early child care to healthy school environments to communitywide campaigns. “We collaborate with health departments and community stakeholders, provide them with the evidence base, help assess how much different options cost, model the results over a decade, and they pick what they want to work on. One constant that we’ve seen—and these are very different political environments—is a strong interest in cost-effectiveness,” he says.
In a 2015 study in Health Affairs , Gortmaker and colleagues outlined three interventions that would more than pay for themselves: an excise tax on sugar-sweetened beverages implemented at the state level; elimination of the tax subsidy for advertising unhealthy food to children; and strong nutrition standards for food and drinks sold in schools outside of school meals. Implemented nationally, these interventions would prevent 576,000, 129,100, and 345,000 cases of childhood obesity, respectively, by 2025. The projected net savings to society in obesity-related health care costs for each dollar invested: $31, $33, and $4.60, respectively.
Gortmaker is one of the leaders of a collaborative modeling effort known as CHOICES—for Childhood Obesity Intervention Cost-Effectiveness Study—an acronym that seems a pointed rebuttal to the reflexive conservative argument that government regulation tramples individual choice. Having grown up not far from Des Plaines, Illinois, site of the first McDonald’s franchise in the country, he emphasizes to policymakers that at this late date, America cannot treat its way out of obesity, given current medical know-how. Only a thoroughgoing investment in prevention will turn the tide. “Clinical interventions produce too small an effect, with too small a population, and at high cost,” Gortmaker says. “The good news is that there are many cost-effective options to choose from.”
While Gortmaker underscores the importance of improving both food choices and options for physical activity, he has shown that upgrading the food environment offers much more benefit for the buck. This is in line with the gathering scientific consensus that what we eat plays a greater role in obesity than does sedentary lifestyle (although exercise protects against many of the metabolic consequences of excess weight). “The easiest way to explain it,” Gortmaker says, “is to talk about a sugary beverage—140 calories. You could quickly change a kid’s risk of excess energy balance by 140 calories a day just by switching from a sugary drink a day to water or sparkling water. But for a 10-year-old boy to burn an extra 140 calories, he’d have to replace an hour-and-a-half of sitting with an hour-and-a-half of walking.”
Small tweaks in adults’ diets can likewise make a big difference in short order. “With adults, health care costs rise rapidly with excess weight gain,” Gortmaker says. “If you can slow the onset of obesity, you slow the onset of diabetes, and potentially not only save health care costs but also boost people’s productivity in the workforce.”
One of Gortmaker’s most intriguing calculations spins off of the food industry’s estimated $633 million spent on television marketing aimed at kids. Currently, federal tax treatment of advertising as an ordinary business expense means that the government, in effect, subsidizes hawking of junk food to children. Gortmaker modeled a national intervention that would eliminate this subsidy of TV ads for nutritionally empty foods and beverages aimed at 2- to 19-year-olds. Drawing on well-delineated relationships between exposure to these advertisements and subsequent weight gain, he found that the intervention would save $260 million in downstream health care costs. Although the effect would probably be small at the individual level, it would be significant at the population level.
Level the playing field through taxes and regulation.
When public health took on cigarette smoking, starting in the 1960s, it did so with robust policies banning television ads and other marketing, raising taxes to increase prices, making public places smoke-free, and offering people treatment such as the nicotine patch. In 1965, the smoking rate for U.S. adults was 42.2 percent; today, it is 16.8 percent.
Similarly, America reduced the rate of deaths caused by motor vehicle accidents—a 90 percent decrease over the 20th century, according to the CDC—with mandatory seat belt laws, safer car designs, stop signs, speed limits, rumble strips, and the stigmatization of drunk driving.
Change the product. Change the environment. Change the culture. That is also the policy recipe for stopping obesity.
Laws that make healthy behaviors easier are often followed by positive changes in those behaviors. And people who are trying to adopt healthy behaviors tend to support policies that make their personal aspirations achievable, which in turn nudges lawmakers to back the proposals.
One debate today revolves around whether recipients of federal Supplemental Nutrition Assistance Program (SNAP) benefits (formerly known as food stamps) should be restricted from buying sodas or junk food. The largest component of the USDA budget, SNAP feeds one in seven Americans. A USDA report, issued last November, found that the number-one purchase by SNAP households was sweetened beverages, a category that included soft drinks, fruit juices, energy drinks, and sweetened teas, accounting for nearly 10 percent of SNAP money spent on food. Is the USDA therefore underwriting the soda industry and planting the seeds for chronic disease that the government will pay to treat years down the line?
Eric Rimm, a professor in the Departments of Epidemiology and Nutrition at the Harvard Chan School, frames the issue differently. In a 2017 study in the American Journal of Preventive Medicine , he and his colleagues asked SNAP participants whether they would prefer the standard benefits package or a “SNAP-plus” that prohibited the purchase of sugary beverages but offered 50 percent more money for buying fruits and vegetables. Sixty-eight percent of the participants chose the healthy SNAP-plus option.
“A lot of work around SNAP policy is done by academics and politicians, without reaching out to the beneficiaries,” says Rimm. “We haven’t asked participants, ‘What’s your say in this? How can we make this program better for you?’” To be sure, SNAP is riddled with nutritional contradictions. Under current rules, for example, participants can use benefits to buy a 12-pack of Pepsi or a Snickers bar or a giant bag of Lay’s potato chips but not real food that happens to be heated, such as a package of rotisserie chicken. “This is the most vulnerable population in the country,” says Rimm. “We’re not listening well enough to our constituency.”
Other innovative fiscal levers to alter behavior could also drive down obesity. In 2014, a trio of strong voices on food industry practices—Dariush Mozaffarian, DrPH ’06, dean of Tufts University’s Friedman School of Nutrition Science and Policy and former associate professor of epidemiology at the Harvard Chan School; Kenneth Rogoff, professor of economics at Harvard; and David Ludwig, professor in the Department of Nutrition at Harvard Chan and a physician at Boston Children’s Hospital—broached the idea of a “meaningful” tax on nearly all packaged retail foods and many chain restaurants, with the proceeds used to pay for minimally processed foods and healthier meals for school kids. In essence, the tax externalizes the social costs of harmful individual behavior.
“We made a straightforward proposal to tax all processed foods and then use the income to subsidize whole foods in a short-term, revenue-neutral way,” explains Ludwig. “The power of this idea is that, since there is so much processed food consumption, even a modest tax—in the 10 to 15 percent range—is not going to greatly inflate the cost of these foods. Their price would increase moderately, but the proceeds would not disappear into government coffers. Instead, the revenue would make healthy foods affordable for virtually the entire population, and the benefits would be immediately evident. Yes, people will pay moderately more for their Coke or for their cinnamon bear claw but a lot less for nourishing, whole foods.”
Another suggestion comes from Sandro Galea, dean of the Boston University School of Public Health, and Abdulrahman M. El-Sayed, a public health physician and epidemiologist. In a 2015 issue of the American Journal of Public Health , they called for “calorie offsets,” similar to the carbon offsets used to mitigate environmental harm caused by the gas and oil industries. A “calorie offset” scheme could hand the food and beverage industries a chance at redemption by inviting them to invest in such undertakings as city farms, cooking classes for parents, healthy school cafeterias, and urban green spaces.
These ambitious proposals face almost impossibly high hurdles. Political battle lines typically pit public health against corporations, with Big Food casting doubt on solid nutrition science, deeming government regulation a threat to free choice, and making self-policing pledges that it has never kept. On the website for the Americans for Food and Beverage Choice, a group spearheaded by the American Beverage Association, is the admonition: “[W]hether it’s at a restaurant or in a grocery store, it’s never the government’s job to decide what you choose to eat and drink.”
Yet surprisingly, many public health professionals are convinced that the only way to stop obesity is to make common cause with the food industry. “This isn’t like tobacco, where it’s a fight to the death. We need the food industry to make healthier food and to make a profit,” says Mozaffarian. “The food industry is much more diverse and heterogeneous than tobacco or even cars. As long as we can help them—through carrots and sticks, tax incentives and disincentives—to move towards healthier products, then they are part of the solution. But we have to be vigilant, because they use a lot of the same tactics that tobacco did.”
Sow what we want to reap.
Americans overeat what our farmers overproduce.
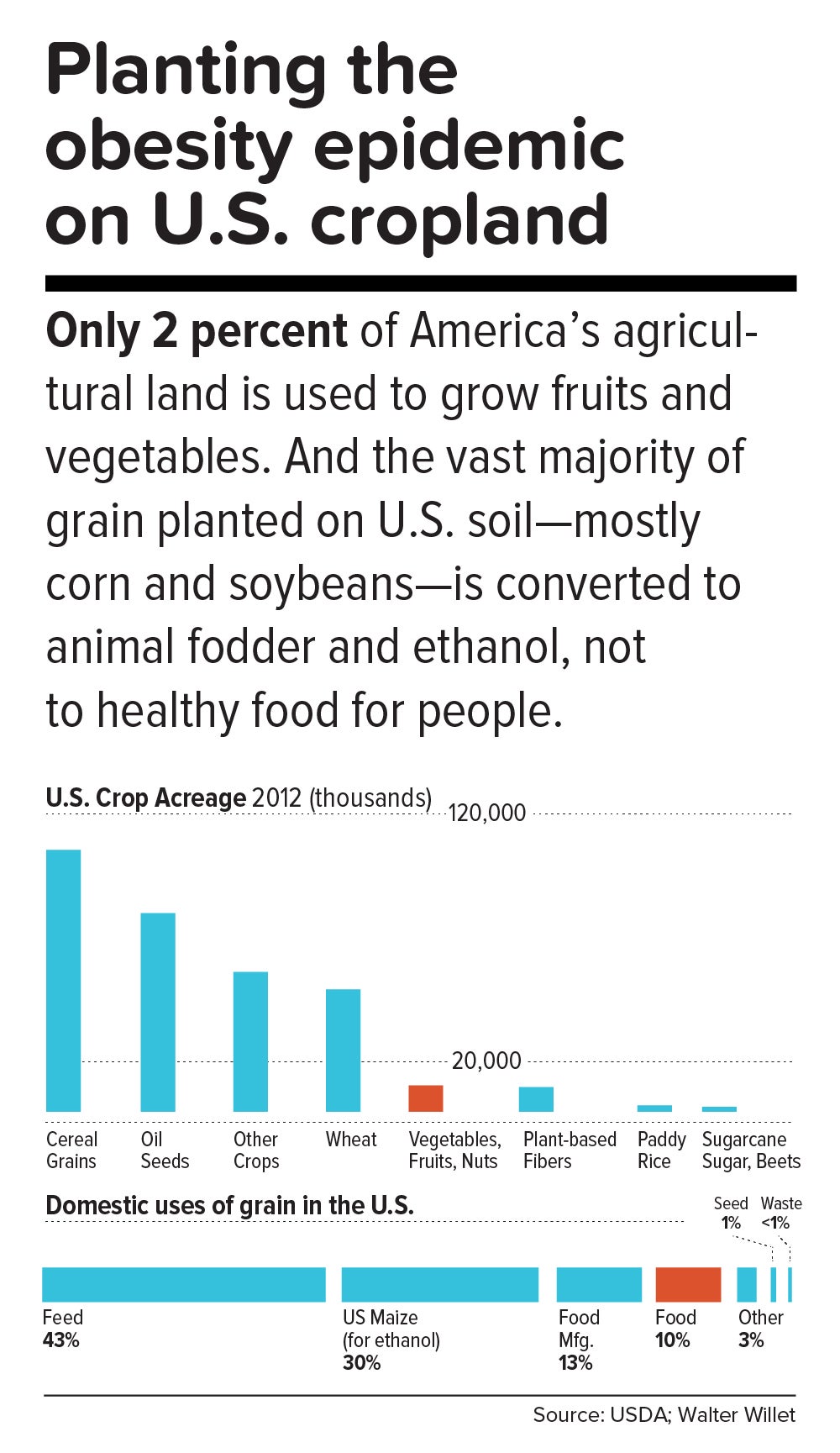
“The U.S. food system is egregiously terrible for human and planetary health,” says Walter Willett. It’s so terrible, Willett made a pie chart of American grain production consumed domestically. It shows that most of the country’s agricultural land goes to the two giant commodity crops: corn and soy. Most of those crops, in turn, go to animal fodder and ethanol, and are also heavily used in processed snack foods. Today, only about 10 percent of grain grown in the U.S. for domestic use is eaten directly by human beings. According to a 2013 report from the Union of Concerned Scientists, only 2 percent of U.S. farmland is used to grow fruits and vegetables, while 59 percent is devoted to commodity crops.
Historically, those skewed proportions made sense. Federal food policies, drafted with the goal of alleviating hunger, preferentially subsidize corn and soy production. And whereas corn or soybeans could be shipped for days on a train, fruits and vegetables had to be grown closer to cities by truck farmers so the produce wouldn’t spoil. But those long-ago constraints don’t explain today’s upside-down agricultural priorities.
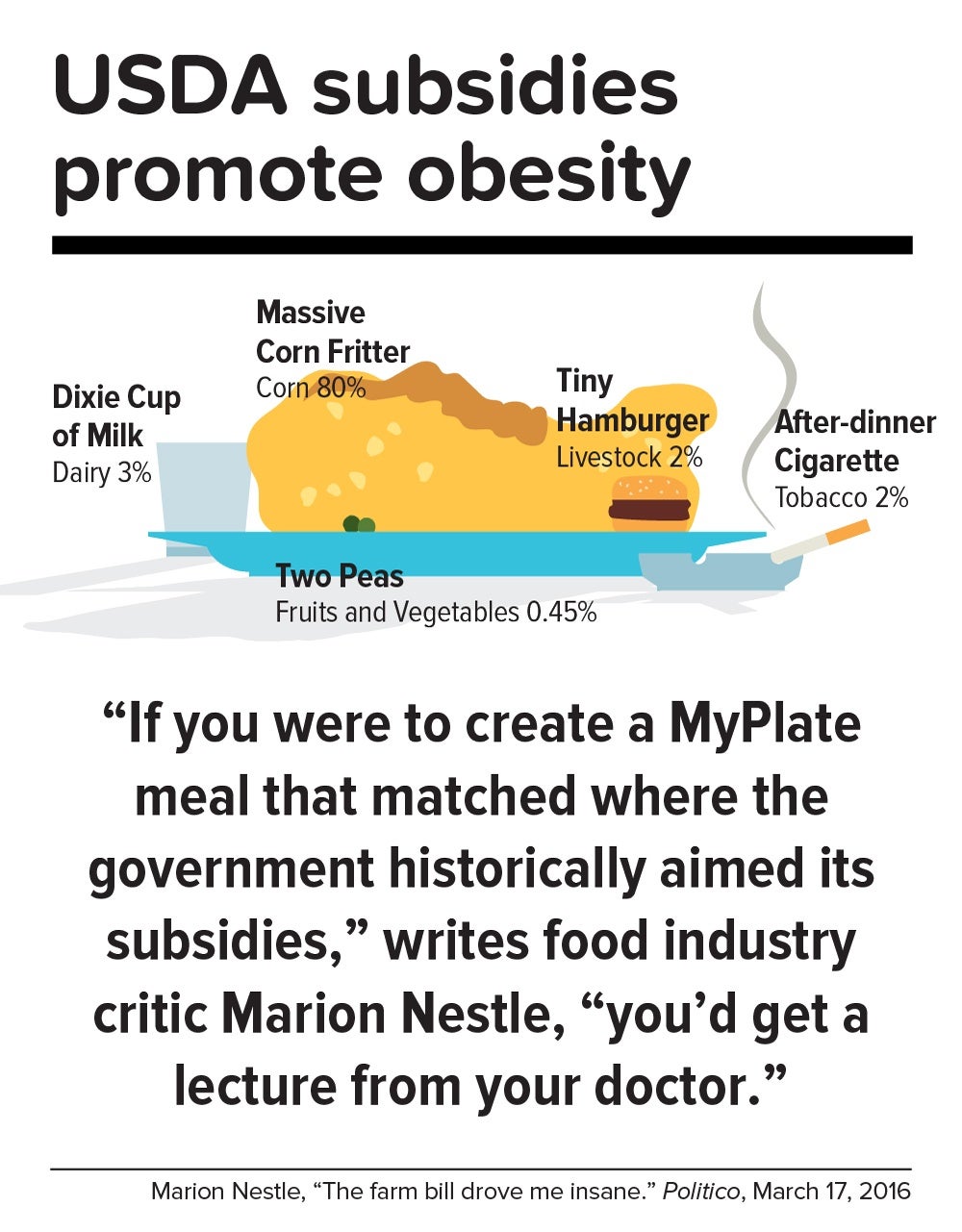
In a now-classic 2016 Politico article titled “The farm bill drove me insane,” Marion Nestle illustrated the irrational gap between what the government recommends we eat and what it subsidizes: “If you were to create a MyPlate meal that matched where the government historically aimed its subsidies, you’d get a lecture from your doctor. More than three-quarters of your plate would be taken up by a massive corn fritter (80 percent of benefits go to corn, grains and soy oil). You’d have a Dixie cup of milk (dairy gets 3 percent), a hamburger the size of a half dollar (livestock: 2 percent), two peas (fruits and vegetables: 0.45 percent) and an after-dinner cigarette (tobacco: 2 percent). Oh, and a really big linen napkin (cotton: 13 percent) to dab your lips.”
In this sense, the USDA marginalizes human health. Many of the foods that nutritionists agree are best for us—notably, fruits, vegetables, and tree nuts—fall under the bureaucratic rubric “specialty crops,” a category that also includes “dried fruits, horticulture, and nursery crops (including floriculture).” Farm bills, which get passed every five years or so, fortify the status quo. The 2014 Farm Bill, for example, provided $73 million for the Specialty Crop Block Grant Program in 2017, out of a total of about $25 billion for the USDA’s discretionary budget. (The next Farm Bill, now under debate, will be coming out in 2018.)
By contrast, a truly anti-obesigenic agricultural system would stimulate USDA support for crop diversity—through technical assistance, research, agricultural training programs, and financial aid for farmers who are newly planting or transitioning their land into produce. It would also enable farmers, most of whom survive on razor-thin profit margins, to make a decent living.
In the early 1970s, Finland’s death rate from coronary heart disease was the highest in the world, and in the eastern region of North Karelia—a pristine, sparsely populated frontier landscape of forest and lakes—the rate was 40 percent worse than the national average. Every family saw physically active men, loggers and farmers who were strong and lean, dying in their prime.
Thus was born the North Karelia Project, which became a model worldwide for saving lives by transforming lifestyles. The project was launched in 1972 and officially ended 25 years later. While its initial goal was to reduce smoking and saturated fat in the diet, it later resolved to increase fruit and vegetable consumption.
The North Karelia Project fulfilled all of these ambitions. When it started, for example, 86 percent of men and 82 percent of women smeared butter on their bread; by the early 2000s, only 10 percent of men and 4 percent of women so indulged. Use of vegetable oil for cooking jumped from virtually zero in 1970 to 50 percent in 2009. Fruit and vegetables, once rare visitors to the dinner plate, became regulars. Over the project’s official quarter-century existence, coronary heart disease deaths in working-age North Karelian men fell 82 percent, and life expectancy rose seven years.
The secret of North Karelia’s success was an all-out philosophy. Team members spent innumerable hours meeting with residents and assuring them that they had the power to improve their own health. The volunteers enlisted the assistance of an influential women’s group, farmers’ unions, homemakers’ organizations, hunting clubs, and church congregations. They redesigned food labels and upgraded health services. Towns competed in cholesterol-cutting contests. The national government passed sweeping legislation (including a total ban on tobacco advertising). Dairy subsidies were thrown out. Farmers were given strong incentives to produce low-fat milk, or to get paid for meat and dairy products based not on high-fat but on high-protein content. And the newly established East Finland Berry and Vegetable Project helped locals switch from dairy farming—which had made up more than two-thirds of agriculture in the region—to cultivation of cold-hardy currants, gooseberries, and strawberries, as well as rapeseed for heart-healthy canola oil.
“A mass epidemic calls for mass action,” says the project’s director, Pekka Puska, “and the changing of lifestyles can only succeed through community action. In this case, the people pulled the government—the government didn’t pull the people.”
Could the United States in 2017 learn from North Karelia’s 1970s grand experiment?
“Americans didn’t become an obese nation overnight. It took a long time—several decades, the same timeline as in individuals,” notes Frank Hu. “What were we doing over the past 20 years or 30 years, before we crossed this threshold? We haven’t asked these questions. We haven’t done this kind of soul-searching, as individuals or society as a whole.”
Today, Americans may finally be willing to take a hard look at how food figures in their lives. In a July 2015 Gallup phone poll of Americans 18 and older, 61 percent said they actively try to avoid regular soda (the figure was 41 percent in 2002); 50 percent try to avoid sugar; and 93 percent try to eat vegetables (but only 57.7 percent in 2013 reported they ate five or more servings of fruits and vegetables at least four days of the previous week).
Individual resolve, of course, counts for little in problems as big as the obesity epidemic. Most successes in public health bank on collective action to support personal responsibility while fighting discrimination against an epidemic’s victims. [To learn more about the perils of stigma against people with obesity, read “ The Scarlet F .”]
Yet many of public health’s legendary successes also took what seems like an agonizingly long time to work. Do we have that luxury?
“Right now, healthy eating in America is like swimming upstream. If you are a strong swimmer and in good shape, you can swim for a little while, but eventually you’re going to get tired and start floating back down,” says Margo Wootan, SD ’93, director of nutrition policy for the Center for Science in the Public Interest. “If you’re distracted for a second—your kid tugs on your pant leg, you had a bad day, you’re tired, you’re worried about paying your bills—the default options push you toward eating too much of the wrong kinds of food.”
But Wootan has not lowered her sights. “What we need is mobilization,” she says. “Mobilize the public to address nutrition and obesity as societal problems—recognizing that each of us makes individual choices throughout the day, but that right now the environment is stacked against us. If we don’t change that, stopping obesity will be impossible.”
The passing of power to younger generations may aid the cause. Millennials are more inclined to view food not merely as nutrition but also as narrative—a trend that leaves Duke University’s Kelly Brownell optimistic. “Younger people have been raised to care about the story of their food. Their interest is in where it came from, who grew it, whether it contributes to sustainable agriculture, its carbon footprint, and other factors. The previous generation paid attention to narrower issues, such as hunger or obesity. The Millennials are attuned to the concept of food systems.”
We are at a public health inflection point. Forty years from now, when we gaze at the high-resolution digital color photos from our own era, what will we think? Will we realize that we failed to address the obesity epidemic, or will we know that we acted wisely?
The question brings us back to the 1970s, and to Pekka Puska, the physician who directed the North Karelia Project during its quarter-century existence. Puska, now 71, was all of 27 and burning with big ideas when he signed up to lead the audacious effort. He knows the promise and the perils of idealism. “Changing the world may have been utopic,” he says, “but changing public health was possible.”
News from the School

Bethany Kotlar, PhD '24, studies how children fare when they're born to incarcerated mothers

Soccer, truffles, and exclamation points: Dean Baccarelli shares his story

Health care transformation in Africa highlighted at conference

COVID, four years in


Obesity: The Journal of The Obesity Society
Seeking groundbreaking scientific information on obesity? Looking for leading-edge, peer-reviewed research? Then Obesity is your essential source.
By reading Obesity , the official journal of The Obesity Society, you will stay informed about vital developments in this quickly evolving field. You will also get the latest reviews and commentaries from colleagues around the globe, representing a range of interests, ideas and viewpoints.
You can receive access to Obesity as a member of The Obesity Society.* Non-members can view abstracts of recent articles and full text of articles older than 12 months.
Access Obesity now!
*ALSO NOTE: Student and early career members do not automatically receive access to Obesity . These members are able to receive online and/or print access to Obesity for additional fees. Visit our membership page for more information.
Having Obesity login issues? Please call 301-563-6526 or email [email protected] .
Submit your research to Obesity today!
Submit your best research and join the community of thought leaders in the fight against obesity. Read more about Obesity .
Obesity editorial staff
Editor-in-Chief : Michael Jensen, MD Associate Editor-In-Chief : Leanne Redman, PhD
Obesity Journal Symposium
Leading papers from the journal are presented at the annual Obesity Journal Symposium at ObesityWeek® each November. You can review these papers in the December issue of Obesity and read papers from previous competitions.
Thank you for your interest in joining a TOS Committee.
Your request has been sent..
Cookies on Obesity.org
By using Obesity.org, you agree to our use of cookies. We use cookies to provide you with a great experience and to help our website run effectively.
Your payment has been processed successfully!
We’re sorry. we could not process your payment..
MINI REVIEW article
This article is part of the research topic.
Understanding Obesity to Determine the Best Therapeutic Option: From Lifestyle Interventions to Therapies
The effect of intermittent fasting on microbiota as a therapeutic approach in obesity Provisionally Accepted

- 1 Centro de Investigación Genética y Genómica, Facultad de Ciencias de la Salud Eugenio Espejo, Universidad UTE, Quito, Ecuador, Ecuador
- 2 Centro de Investigación de Salud Pública y Epidemiología Clínica (CISPEC), Universidad UTE., Ecuador
The final, formatted version of the article will be published soon.
Obesity, a public health challenge, arises from a complex interplay of factors such as dietary habits and genetic predisposition. Alterations in gut microbiota, characterized by an imbalance between Firmicutes and Bacteroidetes, further exacerbate metabolic dysregulation, promoting inflammation and metabolic disturbances. Intermittent fasting (IF) emerges as a promising dietary strategy showing efficacy in weight management and favoring fat utilization. Studies have used mice as animal models to demonstrate the impact of IF on gut microbiota composition, highlighting enhanced metabolism and reduced inflammation. In humans, preliminary evidence suggests that IF promotes a healthy microbiota profile, with increased richness and abundance of beneficial bacterial strains like Lactobacillus and Akkermansia. However, further clinical trials are necessary to validate these findings and elucidate the long-term effects of IF on microbiota and obesity. Future research should focus on specific tissues and cells, the use of advanced -omics techniques, and exploring the interaction of IF with other dietary patterns, to analyze microbiota composition, gene expression, and potential synergistic effects for enhanced metabolic health. While preliminary evidence supports the potential benefits of IF in obesity management and microbiota regulation, further research with diverse populations and robust methodologies is necessary to understand its implications and optimize personalized dietary interventions.This review explores the potential impact of IF on gut microbiota and its intricate relationship with obesity. Specifically, we will focus on elucidating the underlying mechanisms through which IF affects microbiota composition, as well as its subsequent effects on obesity.
Keywords: Obesity, microbiota, intermittent fasting, Diet, dietary habits
Received: 28 Feb 2024; Accepted: 15 Apr 2024.
Copyright: © 2024 Cadena-Ullauri, Guevara-Ramírez, Ruiz-Pozo, Tamayo-Trujillo, Paz Cruz, Simancas-Racines and Zambrano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Mx. Ana Karina Zambrano, Centro de Investigación Genética y Genómica, Facultad de Ciencias de la Salud Eugenio Espejo, Universidad UTE, Quito, Ecuador, Quito, Pichincha, Ecuador
People also looked at
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Research articles
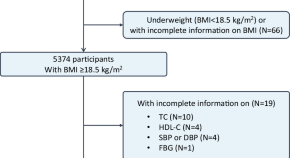
Association between BMI-based metabolic phenotypes and prevalence of intracranial atherosclerotic stenosis: a cross-sectional study
- Xinsheng Han
Genetic evidence for involvement of β2-adrenergic receptor in brown adipose tissue thermogenesis in humans
- Yuka Ishida
- Mami Matsushita
- Kazuhiro Nakayama
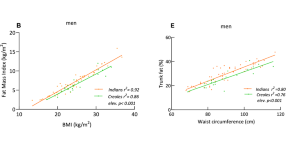
Visceral-to-peripheral adiposity ratio: a critical determinant of sex and ethnic differences in cardiovascular risks among Asian Indians and African Creoles in Mauritius
- Vinaysing Ramessur
- Sadhna Hunma
- Abdul G. Dulloo
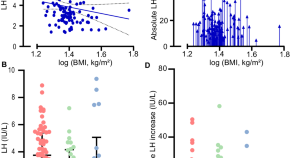
The influence of body composition on the response to dynamic stimulation of the endocrine pituitary-testis axis
- Julie Abildgaard
- Anne Kirstine Bang
- Niels Jørgensen
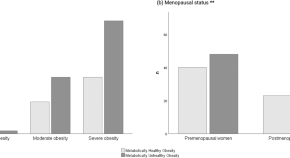
Distinguishing health-related parameters between metabolically healthy and metabolically unhealthy obesity in women
- Fernando Mendonça
- Pietra Soares
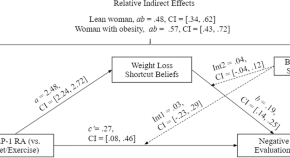
The effect of GLP-1 receptor agonist use on negative evaluations of women with higher and lower body weight
- Stacy M. Post
- Susan Persky

Association of body-mass index with physiological brain pulsations across adulthood – a fast fMRI study
- Lauri Raitamaa
- Joona Kautto
- Vesa Kiviniemi
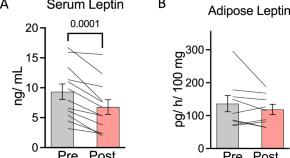
Calorie restriction-induced leptin reduction and T-lymphocyte activation in blood and adipose tissue in men with overweight and obesity
- Rebecca L. Travers
- William V. Trim
- Dylan Thompson

Effects of prenatal THC vapor exposure on body weight, glucose metabolism, and feeding behaviors in chow and high-fat diet fed rats
- Catherine Hume
- Samantha L. Baglot
- Matthew N. Hill
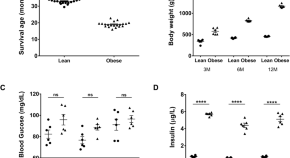
Obesity-related glomerulopathy is associated with elevated WT1 expression in podocytes
- Sneha Jakhotia
- Rajesh Kavvuri
- G. Bhanuprakash Reddy
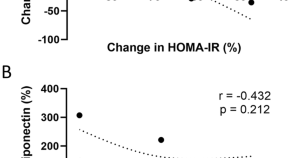
Identification of circulating apolipoprotein M as a new determinant of insulin sensitivity and relationship with adiponectin
- Laurie Frances
- Mikaël Croyal
- Nathalie Viguerie

Sex differences in adipose insulin resistance are linked to obesity, lipolysis and insulin receptor substrate 1
- Peter Arner
- Daniel Peter Andersson
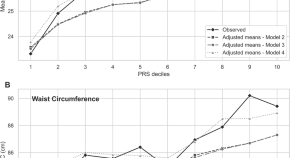
Obesity risk in young adults from the Jerusalem Perinatal Study (JPS): the contribution of polygenic risk and early life exposure
- Hagit Hochner
- Rachely Butterman
- Michal Linial

Serum IL-36β levels are associated with Insulin sensitivity in paediatric patients with obesity
- Paloma Narros-Fernández
- Andrew O’Donnell
- Patrick T. Walsh
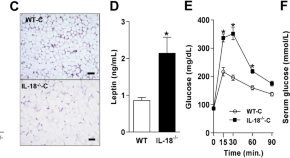
Role of IL-18 in adipose tissue remodeling and metabolic dysfunction
- Jaqueline Pereira Lana
- Marina Chaves de Oliveira
- Adaliene Versiani Matos Ferreira
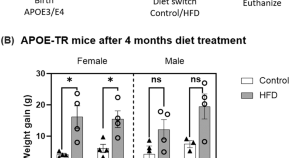
Obesity affects brain cortex gene expression in an APOE genotype and sex dependent manner
- Harshul Pandit
- Nahdia S. Jones
- G. William Rebeck

miR-548ag promotes DPP4 expression in hepatocytes through activation of TLR(7/8)/NF-κB pathway
- Jianyu Xiong
- Chaoyue Sun
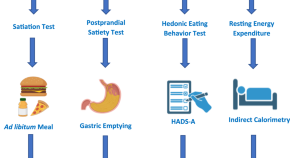
Cumulative effect of obesity phenotypes on body weight and body mass index
- Wissam Ghusn
- Lizeth Cifuentes
- Andres Acosta
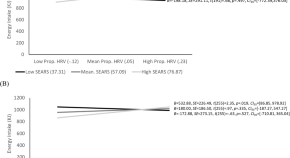
The effects of acute social ostracism on subsequent snacking behavior and future body mass index in children
- Aimee E. Pink
- Bobby K. Cheon
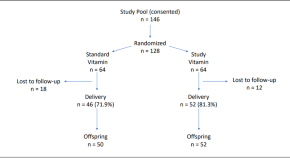
Supplementation with antioxidant micronutrients in pregnant women with obesity: a randomized controlled trial
- Sarbattama Sen
- Sara Cherkerzian
- Simin N. Meydani
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Guidance on energy and macronutrients across the lifespan
In the long history of recommendations for nutritional intake, current research is trending toward the concept of "food as medicine" -- a philosophy in which food and nutrition are positioned within interventions to support health and wellness. In the paper -- "Guidance on Energy and Macronutrients Across the Lifespan" -- by Pennington Biomedical Research Center's Dr. Steven Heymsfield, he shares the latest clarity and recommendations in the rich and storied history of energy and macronutrient intake.
The research paper by Dr. Heymsfield and colleague Dr. Sue Shapses, Professor of Nutritional Sciences at Rutgers University and Director of the Next Center at the New Jersey Institute for Food, Nutrition and Health, was recently published in the New England Journal of Medicine , showcasing recommendations with increased clarity for protein, fat, carbohydrates, fiber and water intake at various stages in the human lifespan.
"Couple with the amount and pattern of the foods people eat, the primary macronutrients of protein, carbohydrates and fat can shape the major determinates of health throughout the lifespan," said Dr. Heymsfield, who is a professor of Metabolism & Body Composition at Pennington Biomedical. "Even considering the incredible diversity of traits and nutritional needs across the global population, we can potentially provide effective care for all patients, including the growing number of patients with diet-related diseases, so long as we recognize the subtle effects of the key macronutrients."
Throughout the research document, the authors frequently reference the original, historic research for which they are providing the latest incarnation and related knowledge. Focusing primarily on energy and three macronutrients -- protein, carbohydrates and fat, and their subsequent substrates -- amino acids, glucose and free fatty acids, the paper shows how these can fuel growth and maintenance throughout life. For optimal health, the study provides dietary reference intakes for the three micronutrients at various stages: 0 to 6 months, 7 months to slightly less than a year old, one year to three, four to eight years, nine to 13 years, 14 to 18 years, over 19 years, and then additional recommendations for pregnancy and lactation.
The research goes on to provide recommendations to patients and caregivers on healthy eating patterns consistent with the energy and macronutrient guidelines and includes an online calculator. While the energy requirements and variable needs for the three main macronutrients and multiple micronutrients vary across the nine life stage groups, there are overarching nutritional goals for patients when choosing healthy food patterns. A variety of healthy meal pattern examples are available, but reoccurring components feature the inclusion of vegetables of all types, whole fruits, fat-free or low-fat dairy, lean meats, seafood, eggs, beans, and nuts, plant- and seafood-based oils, and grains, with at least half of those being whole grains.
The need to incorporate the three main macronutrient groups and micronutrients into the diets of the various life stage groups is a matrix that is further complicated as varying financial resources, personal preferences, cultural backgrounds and ethnic food traditions are accounted for. The paper structures a priority framework, offering better insights into those diets that can be tailored for specific diet-related chronic conditions, such as obesity or type 2 diabetes.
"The legacy of research into dietary nutrition continues to refine what we know about our bodies and the capacity for a tailored diet, featuring key macronutrients to support our long-term health," said Dr. John Kirwan, Executive Director of Pennington Biomedical Research Center. "Dr. Heymsfield's recent paper in the New England Journal of Medicine is the latest contribution to this research history of contributing to the knowledge base, and further promotes the notion of 'food as medicine' -- delivering the potential to improve health across the lifespan with bespoke, nutrient-rich diets."
- Diet and Weight Loss
- Staying Healthy
- Agriculture and Food
- Food and Agriculture
- Healthy diet
- Epidemiology
- Chinese food therapy
- Food groups
Story Source:
Materials provided by Pennington Biomedical Research Center . Note: Content may be edited for style and length.
Journal Reference :
- Steven B. Heymsfield, Sue A. Shapses. Guidance on Energy and Macronutrients across the Life Span . New England Journal of Medicine , 2024; 390 (14): 1299 DOI: 10.1056/NEJMra2214275
Cite This Page :
Explore More
- Two Species Interbreeding Created New Butterfly
- Warming Antarctic Deep-Sea and Sea Level Rise
- Octopus Inspires New Suction Mechanism for ...
- Cities Sinking: Urban Populations at Risk
- Puzzle Solved About Ancient Galaxy
- How 3D Printers Can Give Robots a Soft Touch
- Combo of Multiple Health Stressors Harming Bees
- Methane Emission On a Cold Brown Dwarf
- Remarkable Memories of Mountain Chickadees
- Predicting Future Marine Extinctions
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob Pediatr Health
Childhood and Adolescent Obesity in the United States: A Public Health Concern
Adekunle sanyaolu.
1 Federal Ministry of Health, Abuja, Nigeria
Chuku Okorie
2 Essex County College, Newark, NJ, USA
3 Saint James School of Medicine, Anguilla, British West Indies
Jennifer Locke
Saif rehman.
Childhood and adolescent obesity have reached epidemic levels in the United States. Currently, about 17% of US children are presenting with obesity. Obesity can affect all aspects of the children including their psychological as well as cardiovascular health; also, their overall physical health is affected. The association between obesity and other conditions makes it a public health concern for children and adolescents. Due to the increase in the prevalence of obesity among children, a variety of research studies have been conducted to discover what associations and risk factors increase the probability that a child will present with obesity. While a complete picture of all the risk factors associated with obesity remains elusive, the combination of diet, exercise, physiological factors, and psychological factors is important in the control and prevention of childhood obesity; thus, all researchers agree that prevention is the key strategy for controlling the current problem. Primary prevention methods are aimed at educating the child and family, as well as encouraging appropriate diet and exercise from a young age through adulthood, while secondary prevention is targeted at lessening the effect of childhood obesity to prevent the child from continuing the unhealthy habits and obesity into adulthood. A combination of both primary and secondary prevention is necessary to achieve the best results. This review article highlights the health implications including physiological and psychological factors comorbidities, as well as the epidemiology, risk factors, prevention, and control of childhood and adolescent obesity in the United States.
Introduction
Childhood and adolescent obesity have reached epidemic levels in the United States, affecting the lives of millions of people. In the past 3 decades, the prevalence of childhood obesity has more than doubled in children and tripled in adolescents. 1 The latest data from the National Health and Nutrition Examination Survey show that the prevalence of obesity among US children and adolescents was 18.5% in 2015-2016. Overall, the prevalence of obesity among adolescents (12-19 years; 20.6%) and school-aged children (6-11 years; 18.4%) was higher than among preschool-aged children (2-5 years; 13.9%). School-aged boys (20.4%) had a higher prevalence of obesity than preschool-aged boys (14.3%). Adolescent girls (20.9%) had a higher prevalence of obesity than preschool-aged girls (13.5%; Figure 1 ). 1 Moreover, the rates of obesity have been steadily rising from 1999-2000 through 2015-2016 ( Figure 2 ). 1 According to Ahmad et al, 80% of adolescents aged 10 to 14 years, 25% of children younger than the age of 5 years, and 50% of children aged 6 to 9 years with obesity are at risk of remaining adults with obesity. 2

Prevalence of obesity among children and adolescents aged 2 to 19 years, by sex and age: the United States, 2015-2016.

Trends in obesity prevalence among children and adolescents aged 2 to 19 years: the United States, 1999-2000 through 2015-2016.
Obesity can affect all aspects of children and adolescents including but not limited to their psychological health and cardiovascular health and also their overall physical health. 3 The association between obesity and morbid outcomes makes it a public health concern for children and adolescents. 4 Obesity has an enormous impact on both physical and psychological health. Consequently, it is associated with several comorbidity conditions such as hypertension, hyperlipidemia, diabetes, sleep apnea, poor self-esteem, and even serious forms of depression. 5 In addition, children with obesity who were followed-up to adulthood were much more likely to suffer from cardiovascular and digestive diseases. 3 The increase in body fat also exposes the children to increase in the risk of numerous forms of cancers, such as breast, colon, esophageal, kidney, and pancreatic cancers. 6
Due to its public health significance, the increasing trend in childhood obesity needs to be closely monitored. 7 However, these trends have proved to be challenging to quantify and compare. While there are many factors and areas to consider when discussing obesity in children and adolescents, there are a few trends that are evident in recent studies. For example, the prevalence of obesity varies among ethnic groups, age, sex, education levels, and socioeconomic status. A report published by the National Center for Health Statistics using data from the National Health and Nutrition Examination Survey provides the most recent national estimates from 2015 to 2016 on obesity prevalence by sex, age, race, and overall estimates from 1999-2000 through 2015-2016. 1 Prevalence of obesity among non-Hispanic black (22.0%) and Hispanic (25.8%) children and adolescents aged 2 to 19 years was higher than among both non-Hispanic white (14.1%) and non-Hispanic Asian (11.0%) children and adolescents. There were no significant differences in the prevalence of obesity between non-Hispanic white and non-Hispanic Asian children and adolescents or between non-Hispanic black and Hispanic children and adolescents. The pattern among girls was similar to the pattern in all children and adolescents. The prevalence of obesity was 25.1% in non-Hispanic black, 23.6% in Hispanic, 13.5% in non-Hispanic white, and 10.1% in non-Hispanic Asian girls. The pattern among boys was similar to the pattern in all children and adolescents except that Hispanic boys (28.0%) had a higher prevalence of obesity than non-Hispanic black boys (19.0%; Figure 3 ). 1 This review article is aimed at studying the health implications including physical and psychological factors and comorbidities, as well as the epidemiology, risk factors, prevention, and control of childhood and adolescent obesity in the United States.

Prevalence of obesity among children and adolescents aged 2 to 19 years, by sex and race and Hispanic origin: the United States, 2015-2016.
Methodology
We performed a literature search using online electronic databases (PubMed, MedlinePlus, Mendeley, Google Scholar, Research Gate, Global Health, and Scopus) using the keywords “childhood,” “adolescents,” “obesity,” “BMI,” and “overweight.” Articles were retrieved and selected based on relevance to the research question.
Ethical Approval and Informed Consent
Ethics approval and informed consent were not required for this narrative review.
Definition of Childhood Obesity
Defining obesity requires a suitable measurement of body fat and an appropriate cutoff range. 8 Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared, rounded to 1 decimal place. Obesity in children and adolescents was defined as a BMI of greater than or equal to the age- and sex-specific 95th percentile and overweight with a BMI between the 85th and 95th percentiles of the 2000 Centers for Disease Control and Prevention (CDC) growth charts. 9
However, the use of the BMI percentile according to the age/sex of the CDC growth charts for very high BMIs can result in estimates that differ substantially from those that are observed, 10 , 11 and this constrains the maximum BMI that is attainable at given sex and age. 12 , 13 These limitations have resulted in the classification of severe obesity as a BMI ≥120% of the 95th percentile rather than a percentile greater than the 95th percentile. 11 , 14 A BMI of 120% of the 95th percentile corresponds to a BMI of ~35 among 16 to 18 year olds.
Physiology of Energy Regulation and Obesity
Obesity is a chronic multifactorial disease, characterized by an excessive accumulation of adipose tissue, commonly as a result of excessive food intake and/or low energy expenditure. Obesity can be triggered by genetic, psychological, lifestyle, nutritional, environmental, and hormonal factors. 15
Obesity is found in individuals that are susceptible genetically and involves the biological defense of an elevated body fat mass, the mechanism of which could be explained in part by interactions between brain reward and homeostatic circuits, inflammatory signaling, accumulation of lipid metabolites, or other mechanisms that impair hypothalamic neurons. 16
Normal energy regulation physiology is under tight neurohormonal control. The neurohormonal control is performed in the central nervous system through neuroendocrine connections, in which circulating peripheral hormones, such as leptin and insulin, provide signals to specialized neurons of the hypothalamus reflecting body fat stores and induces appropriate responses to maintain the stability of these stores. The hypothalamic region is where the center of the regulation of hunger and satiety is located. Some of them target the activity of endogenous peptides, such as ghrelin, pancreatic polypeptide, 17 peptide YY, and neuropeptide Y, 18 as well as their receptors.
The physiology of energy regulation may result in obesity in susceptible people when it goes awry from genetic and environmental modulators. There is strong evidence of the majority of obesity cases that are associated with central resistance to both leptin and insulin actions. 19 , 20 The environmental modulators equally play critical roles in obesity. Changes in the circadian clock are associated with temporal alterations in feeding behavior and increased weight gain. 21 Stress interferes with cognitive processes such as executive function and self-regulation. Second, stress can affect behavior by inducing overeating and consumption of foods that are high in calories, fat, or sugar; by decreasing physical activity; and by shortening sleep. Third, stress triggers physiological changes in the hypothalamic-pituitary-adrenal axis, reward processing in the brain, and possibly the gut microbiome. Finally, stress can stimulate the production of biochemical hormones and peptides such as leptin, ghrelin, and neuropeptide Y. 17
The lateral hypothalamus (LH) plays a fundamental role in regulating feeding and reward-related behaviors; however, the contributions of neuronal subpopulations in the LH are yet to be identified thoroughly. 22 The LH has also been associated with other aspects of body weight regulation, such as physical activity and thermogenesis. 23 The LH contains a heterogeneous assembly of neuronal cell populations, in which γ-aminobutyric acid (GABA) neurons predominate. 23 LH GABA neurons are known to mediate multiple behaviors important for body weight regulation, thus altering energy expenditure. 23
Etiology and Risk Factors
Excess body fat is a major health concern in childhood and adolescent populations. The dramatic increase in childhood obesity foreshadows the serious health consequences of their adult life. As obesity begins from childhood and spans through adult life, it becomes increasingly more difficult to treat successfully. Being able to identify the risk factors and potential causes of childhood obesity is one of the best strategies for preventing the epidemic. 24
According to the Morbidity and Mortality Weekly Report released in 2011, there is an acceptance that there is no single cause of childhood obesity and that energy imbalance is just a part of the numerous factors. 25 Many children have a discrepancy between what is taken in and what is expended. 26 For example, children with obesity consume approximately 1000 calories more than what is necessary for their body to function healthily and to be able to participate in regular physical activities. Over 10 years, there will be an excess of 57 pounds of unnecessary weight. With excessive caloric intake, as well as sedentary lifestyles, childhood obesity will continue to rise if no changes are implemented. Adding daily physical activity, better sleep patterns, as well as dietary changes can help decrease the number of excess calories and help with obesity-related problems in the future.
Also, during childhood, excess fat accumulates when the increase in caloric intake exceeds the total energy expenditure. 26 Furthermore, children living in the United States today compared with children living in the 1900s are participating in more than 6 hours per day activities on social media. This includes but is not limited to traditional television, video gaming, and blogging/Facebook activities. An additional economic rationalization for the increase in childhood obesity is technology. In other words, Americans can now eat more in less time.
In a study, Cutler et al found that an increase in consumption of food tends to be related to technology innovation in food production and transportation. Technology has thus made it increasingly possible for firms to mass prepare food and ship to consumers for ready consumption, thereby taking advantage of scale economies in food preparation. The result of this change has been a significant reduction in the time costs for food production. These lower time costs have led to increased food consumption and, ultimately, increased weights. 27 Eliminating the time cost of food preparation disproportionately increases consumption for hyperbolic discounters because time delay is a particularly important mechanism for discouraging those individuals from consuming. 27 Society today prefers immediate satisfaction with regard to food and convenience over the long-term goals of living a long, healthy life. The availability of high-caloric, less-expensive food coupled with the extensive advertisement and easy accessibility of these foods has contributed immensely to the rising trend of obesity. 28 For example, there have been reductions in the price of McDonalds and Coca-Cola (5.44% and 34.89%, respectively) between 1990 and 2007, while there was about a 17% increase in the price of fruits and vegetables between 1997 and 2003. 29
Likewise, only 16% of children walk or bike to school today as compared with 42% in the late 1960s. However, the distance, convenience, weather, scanty sidewalks, and anxiety about crimes against children could all contribute to this difference. Furthermore, with elementary, middle, and high school combined, only 13.8% of these schools provide adequate daily physical education classes for at least 4 hours a week. 30
Some other potential risk factors have been reported through research studies that involve issues that affect the child in utero and childhood. Table 1 represents potential risk factors and confounders of childhood obesity. 31
Potential Risk Factors of Childhood Obesity.
Abbreviations: BMI, body mass index; SES, socioeconomic status.
Catalano et al argues that maternal BMI before conception, independent of maternal glucose status or birth weight, is a strong predictor of childhood obesity. 32 Infants at the highest quarter for weight at 8 and 18 months are more likely to become children with obesity at age 7, than children in the lower quarters. Certain behaviors have been linked to childhood obesity and overweight; these are a lack of physical activity and unhealthy eating patterns (eating more food away from home, drinking more sugar-sweetened drinks, and snacking more frequently), resulting in excess energy intake. 22 , 31 In addition, when one parent presents with obesity, there is an increased potential for the child to become obese over the years. Naturally, the risk is higher for the children when both parents present with obesity. Furthermore, a study that followed children over time observed that children who got less sleep <10.5 hours at age 3 were 45% more likely to be children with obesity at the age of 7, than children who got greater than 12 hours of sleep during their first 3 years of life. 33 , 34
While all the above-mentioned factors are informative, there is still the need for further research concerning childhood and adolescent obesity and obesity in general. Risk factors for obesity in childhood are still somewhat uncertain, and evidence-based research for preventative strategies is lacking. Moreover, effective action to prevent the childhood obesity epidemic requires evidence-based on early life risk factors, and this evidence, unfortunately, is still incomplete. Furthermore, a research study has attempted to capture the complete picture of childhood obesity early life course risk factors. In the study, they identified that parental BMI and gestational weight gain among other factors should be considered in prevention programs. 35
Health Effects of Childhood Obesity
Childhood obesity is known to have a significant impact on both physical and psychological health. Sahoo et al stated that “childhood obesity can profoundly affect children’s physical health, social and emotional well-being, as well as self-esteem.” They associated poor academic performance and a lower quality of life experienced by the child with childhood obesity. They also stated that “metabolic, cardiovascular, orthopedic, neurological, hepatic, pulmonary, and menstrual disorders among others are consequences of childhood obesity.” 36 There are many health consequences of childhood obesity, and three of the more common ones are sleep apnea, diabetes, and cardiovascular diseases. 36
Psychological Consequences of Obesity
Several studies related to childhood and adolescent obesity have focused primarily on physiological consequences. Other studies have been conducted regarding the association between psychiatric disorders and obesity; these have resulted in conflict due to obesity being found to be an insignificant factor for psychopathology. However, a comparative study by Britz et al found that high rates of mood, anxiety, somatoform, and eating disorders were detected among children with obesity. The study also observed that most psychiatric disorders began after the onset of obesity. In this large population-based study, it was found that a staggering 60% of females and 35% of males reported that they have engaged in binge eating and expressed a lack of control over their diet. 37
Goldfield et al conducted a study among 1400 adolescents with obesity, overweight, and normal weight in grades 7 to 12. Their BMIs, as determined by the International Obesity Task Force, were the criteria used to define each group. Each participant completed a questionnaire on body images, eating behaviors, and moods. Adolescents with obesity reported significantly higher body dissatisfaction, social isolation, depression symptoms, anhedonia, and negative self-esteem than those of normal weight. 38 There is widespread stigmatization of people with obesity that causes harm rather than the intention to motivate people to lose weight. Stigma contributes to behaviors such as binge eating, social isolation, avoidance of health care services, decreased physical activity, and increased weight gain, which worsens obesity and creates additional barriers to healthy behavior change. 39 Weight-based bullying in youth is considered a common, serious problem in many countries. 40 In a study conducted by O’Brien et al, to test whether the association between weight stigma experiences and disordered eating behaviors, that is, emotional eating, uncontrolled eating, and loss-of-control eating, are mediated by weight bias internalization and psychological distress among 634 undergraduate university students, and results of statistical analyses showed that weight stigma was significantly associated with all measures of disordered eating, and with weight bias internalization and psychological distress. 41
Asthma and Obesity
There is mounting evidence that childhood obesity is a risk factor for the development of asthma. 42 A research study was conducted by Belamarich et al to investigate 1322 children aged 4 to 9 years with asthma. Obesity, as defined by the CDC, is the BMI, with weight and height being greater than the 95th percentile. This was the criteria used to identify the 249 children with obesity, while the BMI between the 5th and 95th percentile identified the children who were not obese. After a baseline assessment was done, the 9-month study found that the children with obesity had a higher number of days of wheezing over 2 weeks (4.0 vs 3.4) and as well had more unscheduled emergency hospital visits (39% vs 31%). 42
Obesity directly correlates with the severity of asthma, as well as poor response to corticosteroids. 43 In fact, children with obesity who also have a history of asthma are more challenging to control and linked to worse quality of life. 44 A prospective trial found that weight loss in patients with obesity and a history of asthma can significantly aid them to control the asthma attacks. 43
Chronic Inflammation and Childhood Obesity
Lumeng and Saltiel reported that obesity in children affects multiple organ systems and predisposes them to diseases. The effect of obesity on the tissue can manifest in the development of insulin-resistant type 2 diabetes, the risk of cancer, and pulmonary diseases. 45
The inflammatory response to obesity triggers pathogens, systematic increases in circulatory inflammatory cytokines, and acute-phase reactants (eg, C-reactive proteins), which inflames the tissues. This is often caused by the activation of tissue leukocytes. Chronic inflammation in children with obesity can induce meta-inflammation that is unique when compared with other inflammatory paradigms (eg, infection, autoimmune diseases). 45 Researchers have reported that children with obesity are at risk of lifelong meta-inflammation. In these children, the inflammatory markers are elevated as early as in the third year of life. 45 , 46 This has been linked to heart disease later in life. 19 The long-term consequences of such findings can cause cumulative vascular damage that correlates with the increased weight status. 47
The short-term and long-term effects of obesity on the health of children is a significant concern because of the negative psychological and health consequences. 46 The potential negative psychological outcomes are depressive symptoms, poor body image, low self-esteem, a risk for eating disorders, and behavior and learning problems. Additional negative health consequences include insulin resistance, type 2 diabetes, asthma, hypertension, high total, and low-density lipoprotein cholesterol and triglyceride levels in the blood, low high-density lipoprotein cholesterol levels in the blood, sleep apnea, early puberty, orthopedic problems, and nonalcoholic steatohepatitis 46 , 47 ( Figure 4 ). Children with obesity are more likely to become adults with obesity, thus increasing their risk for several diseases before they even reach their teen years. 48

Comorbidities and potential health consequences of childhood obesity. 47
Prevention and Control
There are two primary components to the prevention and control of childhood obesity.
The first is to educate parents on proper nutritional requirements for their children and the second is to implement the learned information. Educating parents on proper nutrition and dietary caloric intake requirements for their children is at the forefront for the prevention of obesity; however, the way the information is disseminated may affect the usefulness of the information. For example, one of the main limitations to the education of parents about childhood obesity is that typically written information is used as the conduit to health information and disease prevention. 49 The Growing Right Onto Wellness (GROW) trial used a systematic assessment of patient education material that was used for the prevention of childhood obesity in the low health literate population. 49 Results suggest that the average readability is of grade 6 level (SMOG [Simple Measure of Gobbledygook] Index 5.63 ± 0.76 and Fry graph 6.0 ± 0.85) and that adjustment of education material must be done for low health literate populations to adequately comprehend educational material and maintain motivation on the prevention of childhood obesity. 49 A similar study was conducted to further support this improvement when using color-coordinated diagrams to help parents visualize instead of trying to comprehend with numbers and words. It proved to be successful as parents were able to see where they were going wrong and make the necessary changes in their children’s diet. 49
Similarly, the National Institute of Child Health and Human Development Study of Early Child Care and Youth Development conducted a study on 744 adolescents and parents, and analyzed data to determine if parental (maternal and paternal, individually) reactions to children’s behavior was related to childhood obesity. 50 The study concluded that informing parents that their attitude toward their children’s behaviors will play a prominent role in preventing childhood obesity. 50 Parental education on nutrition, health, and the involvement of politicians, physicians, and school personnel are key for the prevention of childhood obesity. However, community and educational institutions have begun legislating and incorporating programs such as providing healthy foods at schools and also health information sessions directed toward young individuals, aimed at preventing childhood obesity in the United States and Canada. 51
Another effective prevention measure against childhood obesity is the awareness of parents on the meal and snack portion sizes. In a systematic review conducted on the effects of portion size manipulation with children and portion education/training interventions on dietary intake with parents, it was determined that the ability of adults to accurately estimate portion size improved following education/training. 52 Education of parents and children on diet requirements has its limitations in that the information must be easy to understand and be easily accessible in order to be practical. Making the available education materials easier to understand from just tables and numbers to more relatable aspects such as colors or figures, parents were able to visualize the changes they need to make whether it is with regard to portion sizes or even seeing how much childhood obesity is present in their family. Although much of the literature provided to parents is targeted to help those with lower numeracy skills, many parents benefited from the information being comparative from right/wrong and good/bad with regard to dieting. 49
The study recommended that proper educational materials, including useful and understandable literature, be used to control meal portion sizes and to help parents identify when children are at risk of obesity. Similarly, healthy eating practices should be taught by schools as a mandatory and essential method in the prevention of childhood obesity. 52
The implementation of healthy eating practices and adequate exercise regimes are essential in the prevention and control of childhood obesity. For example, information from systematic reviews, randomized controlled trials, and well-designed observational studies indicate that evidence-based prevention and control of childhood obesity can be accomplished with the collaboration of community/school, primary health care, and home-based/family-based interventions that involve both physical activity and dietary component. 53 In particular, the control of children with obesity is of significant value, as is the prevention of obesity. Two randomized control trials of 182 families were conducted from November 2005 to September 2007, and they studied the efficacy of US pediatric obesity treatment guidelines in children aged 4 to 9 years with a standardized BMI (ZBMI) greater than the 85 percentile. 54 Briefly, Trial 1 studied the impact on ZBMI by reducing snack foods and sugar-sweetened beverages and increasing fruits, vegetables, and low-fat dairy. 54 Trial 2 studied the impact on ZBMI by decreasing sugar-sweetened beverages and increasing physical activity and increasing low-fat milk consumption and reducing television watching. In Trial 1, the resulting ZBMI reduced within 6 months, and this was maintained through to the 12th month (ΔZBMI 0-12 months = −0.12 ± 0.22). 53 In Trial 2, the resulting ZBMI reduced within 6 months and continued to improve till the 12 months (ΔZBMI 0-12 months = −0.16 ± 0.31). 50
A similar cluster-randomized trial in England studied the effects of the reduction of carbonated beverages on the number of children with obesity in 29 classes (644 children). 51 Results indicate that a decrease of 0.6 glasses of carbonated drinks (250 mL) over three days per week decreased the number of children with obesity by 0.2%, while the control group increased by 7.5% (mean difference = 7.7%, 2.2% to 13.1%) at 12 months. However, diet control is only one component of the control and prevention of childhood obesity, while adequate exercise is another. 55
A systematic review and meta-analyses of the impact of diet and exercise programs (single or combined) was done on their effects on metabolic risk reduction in the pediatric population. 56 Analyses indicated that the addition of exercise to dietary intervention led to greater improvements in the levels of high-density lipoprotein cholesterol (3.86 mg/dL; 95% confidence interval [CI] = 2.70 to 4.63), fasting glucose (−2.16 mg/dL; 95% CI = −3.78 to −0.72), and fasting insulin (−2.75 µIU/mL; 95% CI = −4.50 to −1.00) over 6 months. 56 Diet and exercise are both important factors in the control and prevention of childhood obesity. It is our recommendation that parents and community (teachers and doctors) should be involved in identifying children at risk based on their BMI and participate in implementing practices such as good diet control through the reduction of sugary drinks, fatty foods, and also encouraging safe exercise programs to prevent and control childhood obesity in the society. 56
While all of the previous data express the more obvious prevention methods with regard to childhood obesity, it is imperative to note that ensuring that the whole family is involved in the intervention will yield the greatest results. 2 All current studies indicate that families must be included in childhood treatment of obesity. However, for the success of the child’s weight loss program, it is vital that the parents understand that the causes of obesity are often a mixture of four factors: genetic causes, parental habits, overeating, and poor exercise habits. Thus, instilling some responsibility on the parents and informing them that controlled food preparation, diet control, and family participation in physical activities will all assist in the treatment and control of obesity in their children. 2
Childhood obesity has increased significantly in recent decades and has quickly become a public health crisis in the United States and all over the world. Its increase in prevalence has provoked widespread research efforts to identify the factors that contributed to these changes. 57 Obesity starts with an imbalance between caloric intake and caloric expenditure. 58 Children with obesity are at greater risk of adult obesity; therefore, if we can educate and improve the health habits of families even before they start having children, this can help reduce the increasing rate of childhood obesity in the United States. Parents and caregivers with proper education on the causes and consequences of childhood obesity can help prevent childhood obesity by providing healthy meals and snacks, daily physical activity, and nutrition education to their family members. 59 Families need to take the approach of not adapting to their family being on a diet but more of a healthy lifestyle. A family’s home environment can influence children at a young age; therefore, making changes starting in the household early can educate and influence them to grow up healthy. Although prevention programs may be more expensive in the short term, the long-term benefits acquired through prevention are much more likely to save an even greater amount of health care costs. Not only will the children have a better childhood and self-esteem, but prevention programs can also decrease the incidence of cardiovascular diseases, diabetes, stroke, and possibly cancers in adulthood. 60 The overall need to decrease the obesity rate will help children and their families in the generations to come by building a healthy lifestyle and environment. In order to tackle the climbing obesity rate, overall health and lifestyle needs to be a priority as they balance one with the other. 49 While effective interventions to thwart childhood obesity still remain elusive, the sustainability of the interventions already in place will enable children and their families to adopt these important health behaviors as lifelong practices and improve their health. 58
Treatment of Obesity and the Physiology of Energy Regulation
As discussed previously, a variety of mechanisms participate in weight regulation and the development of obesity in children, including genetics, developmental influences (“metabolic programming” or epigenetics), individual and family health behaviors, and environmental factors. Among these potential mechanisms, only environmental factors are potentially modifiable during childhood and adolescence.
Unfortunately, despite intensive lifestyle modifications and support for healthy practices within the children’s environment, some children will continue to struggle with extreme excess weight and associated comorbidities. 61 , 62 Therefore, a combination of pharmacotherapy and lifestyle modification can be considered. 61 Overweight children should not be treated with medications unless significant, severe comorbidities persist despite lifestyle modification. The use of pharmacotherapy should also be considered in overweight children with a strong family history of type 2 diabetes or cardiovascular risk factors. Constant bidirectional communication between the brain and the gastrointestinal tract, as well as the brain and other relevant tissues (ie, adipose tissue, pancreas, and liver), ensures that the brain constantly perceives and responds accordingly to the energy status/needs of the body. This elegant biological system is subject to disruption by a toxic obesogenic environment, leading to syndromes such as leptin and insulin resistance, and ultimately further exposing individuals who are obese to further weight gain and type 2 diabetes mellitus. Currently, the only Food and Drug Administration–approved prescription drug indicated for the treatment of pediatric obesity is orlistat (Xenical; Genentech USA, Inc, South San Francisco, CA). 63 Orlistat works by inhibiting gastric and pancreatic lipases, the enzymes that break down triglycerides in the intestine. Moreover, imaging studies in humans are beginning to examine the influence that higher- order/hedonic brain regions have on homeostatic areas, as well as their responsiveness to homeostatic peripheral signals. With a greater understanding of these mechanisms, the field moves closer to understanding and eventually treating the casualties of obesity.
The number of children with obesity in the United States has increased substantially over the years; due to its public health significance, the increasing trends need to be closely monitored. While a complete picture of all the risk factors associated with obesity remains elusive, many of the studies agreed that prevention is the key strategy for controlling the current problem. Since the combination of diet, exercise, and physiological and psychological factors are all important factors in the control and prevention of childhood obesity, primary prevention methods should be aimed at educating the child and family and encouraging appropriate diet and exercise from a young age through adulthood while secondary prevention should be targeted at lessening the effect of childhood obesity by preventing the child from continuing unhealthy habits and obesity into adulthood. A combination of primary and secondary prevention is necessary to achieve the best results. Thus, a combined implementation of both types of preventions can significantly help lower the current prevalence of childhood and adolescent obesity in the United States. Failure to take appropriate actions could lead to serious public health consequences.
Author Contributions: AS: Contributed to conception and design; drafted manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
XQ: Contributed to the acquisition, analysis, and interpretation.
JL: Contributed to the acquisition, analysis, and interpretation.
SR: Contributed to the acquisition, analysis, and interpretation.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.


IMAGES
COMMENTS
Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the prevalence of 30.5% during 1999 to 2002. 2 Among those afflicted with ...
The obesity epidemic. The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a).A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2.It is well known that obesity and overweight are a growing problem globally with high rates in ...
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
1. Introduction. Obesity is a chronic disease that is increasing in prevalence and is now considered to be a global epidemic. Epidemiologic studies have revealed an association between high body mass index (BMI) and an extensive range of chronic diseases such as Non Alcoholic Fatty Liver (NAFL), cardiovascular disease , , diabetes mellitus , several malignancies , , musculoskeletal diseases ...
A. Khera and T.M. Powell-WileyN Engl J Med 2023;389:2287-2288. Overweight and obesity have reached epidemic proportions, affecting more than 70% of the U.S. adult population and more than 50% of ...
Obesity articles from across Nature Portfolio. Obesity is a condition in which excess fat has accumulated in the body, such that it can have an adverse effect on health. Obesity is defined as a ...
The findings from our approach suggest with high predictive accuracy that by 2030 nearly 1 in 2 adults will have obesity (48.9%; 95% confidence interval [CI], 47.7 to 50.1), and the prevalence ...
DOI: 10.1056/NEJMe1514957. The prevalence of severe obesity in the United States has increased dramatically, not only among adults but also among children. The increase in childhood severe obesity ...
The emergence of obesity and related chronic diseases in the 1970s [ 9] prompted a new wave of body composition research aimed at developing methods of phenotyping people for adiposity and ...
Obesity is excessive accumulation of body fat, that results from the impairment in energy balance mechanisms [ 3, 4 ]. Example of the condition edema can illustrate this point. Edema is not a ...
The NHLBI supports research on obesity and its impact on cardiovascular health, sleep, pregnancy, and health disparities. Find current studies, guidelines, and resources on obesity prevention and treatment.
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
Obesity is a prevalent, complex, progressive and relapsing chronic disease characterised by abnormal or excessive body fat that impairs health and quality of life. It affects more than 650 million adults worldwide and is associated with a range of health complications. Qualitative research plays a key role in understanding patient experiences and the factors that facilitate or hinder the ...
Remarkable recent growth in obesity research is evidenced by the increasing number of articles published on obesity and metabolic disorders, with citations doubling over the past 5 years. This surge showcases the field's dynamism and its critical integration within the broader scope of endocrine studies. Interdisciplinary research can enhance ...
Worldwide adult obesity has more than doubled since 1990, and adolescent obesity has quadrupled. In 2022, 2.5 billion adults (18 years and older) were overweight. Of these, 890 million were living with obesity. In 2022, 43% of adults aged 18 years and over were overweight and 16% were living with obesity. In 2022, 37 million children under the ...
Future childhood obesity research should evaluate the best methods for educating primary care providers in providing family-centered care and the optimal approaches to delivering this care. Acknowledgments. The authors would like to thank Dr Tom D. Thacher, Mayo Clinic Department of Family Medicine Research Chair, for support of our work. ...
Obesity is the official journal of The Obesity Society and is the premier source of information for increasing knowledge, fostering translational research from basic to population science, and promoting better treatment for people with obesity. Obesity publishes important peer-reviewed research and cutting-edge reviews, commentaries, and public ...
Statistics obscure suffering. According to 2014 national data, 35 percent of adult men and 40.4 percent of adult women are obese—that is, their body mass index, or BMI, a standard calculation of weight divided by height, is greater than or equal to 30. (Normal BMI is 18.5 to 24.9; overweight is 25 to 29.9.) Among youth 2 to 19 years old, the ...
Submit your best research and join the community of thought leaders in the fight against obesity. Read more about Obesity.. Obesity editorial staff. Editor-in-Chief: Michael Jensen, MD Associate Editor-In-Chief: Leanne Redman, PhD. Obesity Journal Symposium. Leading papers from the journal are presented at the annual Obesity Journal Symposium at ObesityWeek® each November.
This topic has sparked a diversified approach to companies' weight loss portfolios, as captured by STAT's Obesity Drug Tracker, which reflects differing views on the optimal approach to weight ...
Obesity, a public health challenge, arises from a complex interplay of factors such as dietary habits and genetic predisposition. Alterations in gut microbiota, characterized by an imbalance between Firmicutes and Bacteroidetes, further exacerbate metabolic dysregulation, promoting inflammation and metabolic disturbances. Intermittent fasting (IF) emerges as a promising dietary strategy ...
Read the latest Research articles from International Journal of Obesity. ... International Journal of Obesity (Int J Obes) ISSN 1476-5497 (online) ISSN 0307-0565 (print) nature.com sitemap ...
Obesity, mortality and BMI. Obesity, as defined by BMI (Table 1), is associated with an increased risk of all-cause mortality, with CVD and malignancy being the most common causes of death. 5 -8 A meta-analysis of 239 prospective studies involving 10.6 million individuals from Asia, Australia, New Zealand, Europe and North America found that all-cause mortality was lowest between a BMI of 20 ...
New research indicates that evening exercise may have more health benefits for people who have obesity. K.C. Alfred/Getty Images. Obesity increases a person's risk for several medical conditions ...
The research paper by Dr. Heymsfield and colleague Dr ... offering better insights into those diets that can be tailored for specific diet-related chronic conditions, such as obesity or type 2 ...
LONG BEACH, Calif.--(BUSINESS WIRE)-- Ark Clinical Research ("Ark") is advancing accessible solutions for obesity and obesity-related diseases through clinical research and a free health clinic, which administers health assessments and manages patient care.Ark is a research organization with sites in Long Beach and Fountain Valley, California. While the clinical research organization ...
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health, increases the risk of long-term medical complications and reduces lifespan. 1 Epidemiologic studies define obesity using the body mass index (BMI; weight/height 2), which can stratify obesity-related health risks at the population level.Obesity is operationally defined as a BMI exceeding 30 kg ...
Early Evidence Supports Ketogenic Diet for Mental Illness. Eve Bender. April 18, 2024. 0. The ketogenic diet shows promise in reducing the symptoms of bipolar disorder and schizophrenia and ...
Introduction. Childhood and adolescent obesity have reached epidemic levels in the United States, affecting the lives of millions of people. In the past 3 decades, the prevalence of childhood obesity has more than doubled in children and tripled in adolescents. 1 The latest data from the National Health and Nutrition Examination Survey show that the prevalence of obesity among US children and ...