What Is Spondylolisthesis?
Spondylolisthesis is a spine condition caused when one vertebra slips over another. This condition's symptoms sometimes mimic those of other back pain conditions.
The complex design of the spinal column is a biological wonder. It comprises 33 bones at birth – some eventually fusing to become 24 bones in most adults – 23 discs and more than 40 muscles and ligaments. The spine is genuinely nature's stage for the human body's performance. And all those bones, discs, muscles and ligaments must work together perfectly for our bodies to function correctly.

Getty Images
Sometimes, the mighty machinery of the spine breaks down. Many spinal conditions can affect a person throughout their lifetime, from simple back pain to spinal tumors . With so many working pieces, plenty can go wrong when the anatomy of the spine isn't quite right.
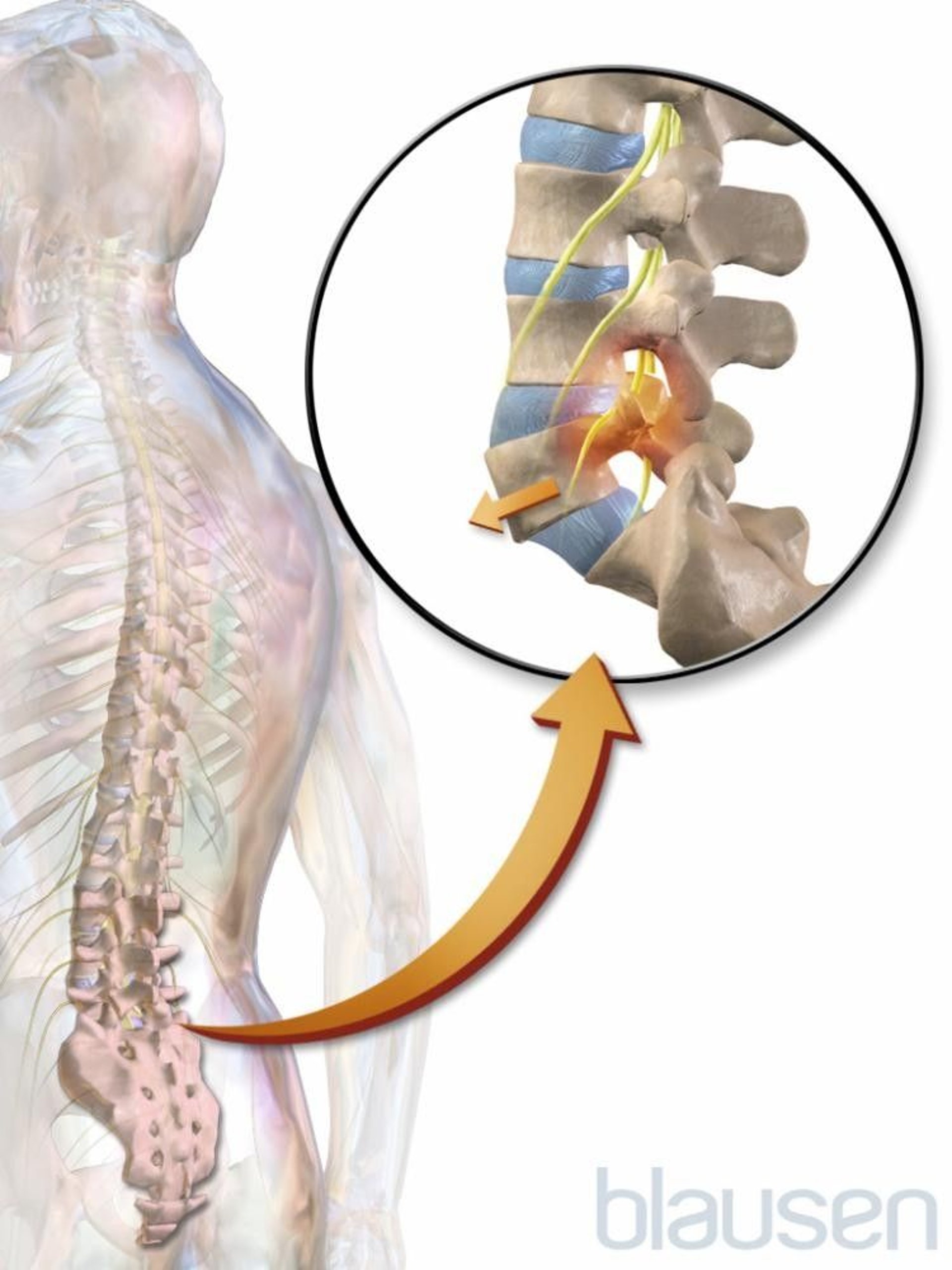
A spinal condition called spondylolisthesis occurs when one vertebra of the spine slips forward over the one beneath it. This vertebra becomes out of alignment with the rest of the spinal column. The condition appears most commonly at the base of the spine in the low back vertebrae, also known as the lumbar spine.
There are three main types of spondylolisthesis:
- Congenital : appears in the womb, before birth, when a baby's spine doesn't properly form.
- Degenerative : happens over time, usually with advanced age.
- Traumatic : occurs due to direct injury to the spine.

Diagnosis and Symptoms
Spondylolisthesis is graded by diagnosing physicians on a percentage severity scale from 1 and 5, with five being the most severe degree of vertebral slippage. An MRI is typically required to diagnose spondylolisthesis fully and to help rule out other spinal conditions, since its symptoms closely match those experienced by people with other spine issues.
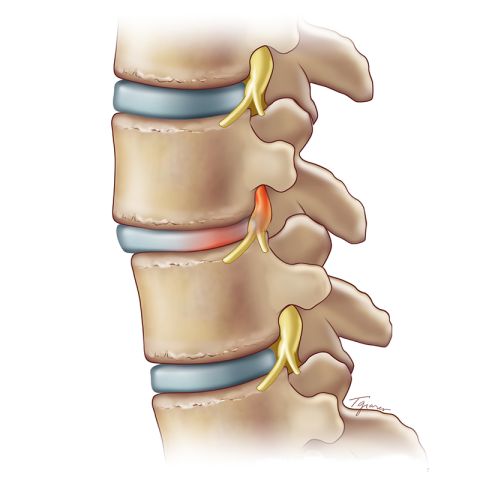
In some people who have spondylolisthesis, especially those with a lower degree of vertebral slippage, the condition may cause no symptoms. However, in those who have a higher vertebral slippage score, or when the slipped vertebra is pressing on a nerve, a variety of symptoms can result, including:
- Back pain that seems to worsen with activity.
- Difficulty standing or walking, especially for long periods.
- Numbness, stiffness or tightness in the muscles of the spine, especially those in the lower back, or tightness in the hamstrings.
- Pain in the low back or buttocks, which may radiate down the legs, and is known as sciatica pain.
Exercise with Spondylolisthesis
Because certain types of activity can make spondylolisthesis symptoms worse for some people, this diagnosis can lead to inactivity. However, it's crucial to note that certain types of regular movement can help relieve the symptoms associated with spondylolisthesis. Moving the body regularly helps to strengthen the spine and core muscles , which ultimately create better support for the spine in the long run.
When the symptoms of spondylolisthesis begin to impair mobility or proper body mechanics, that is when people should evaluate activities for safety. For example, heavy weightlifting, backbends or high-intensity sports that involve running or jumping should likely be avoided because they can make spondylolisthesis worse, which could lead to a condition called spinal stenosis.
There are still plenty of alternative activities a person with spondylolisthesis can engage in that may help provide back pain relief from the condition. These activities include gentler core exercises such as planks, yoga and gentle stretching. The key is to modify activities to reduce stress or strain on an already irritated spine.
Physical Therapy and Treatment Options
If you're unsure of what to do that won't worsen the condition, physical therapy can be a powerful and effective place to start. Under the trained guidance of a physical therapist, many people with spondylolisthesis develop the proper technique to perform exercises that help alleviate their symptoms and allow them the confidence to continue those activities at home.
From physical therapy to specific medications, most spine experts agree that conservative options are effective best places to start for spondylolisthesis treatment. Surgery is only considered when such alternatives fail to provide adequate relief or are ineffective in helping someone with spondylolisthesis return to active living.
As a complex spinal condition, it's always recommended to seek care and treatment for spondylolisthesis by a trained and experienced spine specialist .
The Health Risks of Poor Posture

Tags: back problems , patients , patient advice , health
Most Popular

Patient Advice

Second Opinion

health disclaimer »
Disclaimer and a note about your health ».
Sign Up for Our 3-Day Guide to Medicare
Confused about Medicare? We can help you understand the different Medicare coverage options available to help you choose the best Medicare coverage for you or a loved one.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
Rsv vaccines: who should have one.
Stacey Colino April 22, 2024
Your Guide to Hip Replacement Surgery
Lisa Esposito and Elaine K. Howley April 22, 2024
Find a Primary Care Doctor Near You
Payton Sy April 18, 2024
Streamlined Maternity Services Survey
Jennifer Winston, Ph.D. , Xinyan Zhou and Kaylan Ware April 17, 2024
Major Food Allergens
Claire Wolters April 15, 2024

What to Know About Creatinine Levels
Christine Comizio April 12, 2024

Medicare Coverage for Hearing Aids 2024
Paul Wynn and C.J. Trent-Gurbuz April 12, 2024

Shingles Vaccine: Covered by Medicare?
Paul Wynn April 11, 2024

Medicare Part B: What It Covers
Paul Wynn April 10, 2024

What Are the Parts of Medicare?
Ruben Castaneda April 10, 2024

- MSD careers
Spondylolisthesis
- Diagnosis |
- Treatment |
Spondylolisthesis is partial displacement of a bone in the lower back.
Injuries or a degenerative condition can cause this disorder.
Pain is felt in the low back and may travel down one or both legs.
The diagnosis is based on the results of imaging tests.
Treatment includes measures to relieve pain.
The spine (spinal column) consists of back bones (vertebrae) stacked one on top of another. In lumbar spondylolisthesis, a vertebrae in the lower back slips forward. This disorder usually occurs during adolescence or young adulthood (often in athletes). It is usually caused by a birth defect or an injury that causes fractures (breaks) in a part of the vertebra. If both sides of the vertebra are involved, the vertebra can then slip forward over the one below it. Spondylolisthesis can also occur in older adults, mainly as the result of degeneration of the discs between the vertebrae or osteoarthritis . People who develop spondylolisthesis as adults are at risk of developing lumbar spinal stenosis .
Symptoms of Spondylolisthesis
Mild to moderate spondylolisthesis may cause little or no pain, particularly in young people.
When pain occurs in adolescents, it is felt on only one side of the spine and may travel down a leg. The pain may accompany a fracture.
When pain occurs in adults, it is felt over a specific part of the spine and travels down both legs. In these cases, the pain results from a degenerative condition.
Pain is worsened by standing or leaning back. It can be accompanied by numbness, weakness, or both in the legs.
Diagnosis of Spondylolisthesis
Imaging tests
Doctors base the diagnosis of spondylolisthesis on imaging tests, usually x-rays taken of the lower spine.
Other imaging tests, such as magnetic resonance imaging (MRI) or sometimes computed tomography (CT), may be done.
Treatment of Spondylolisthesis
Measures to relieve pain and stabilize the spine
One to two days of bed rest may provide pain relief for people with spondylolisthesis. Longer bed rest weakens the core muscles and increases stiffness, thus worsening back pain and prolonging recovery. Sleeping in a comfortable position on a medium mattress is recommended. People who sleep on their back can place a pillow under their knees. People who sleep on their side should use a pillow to support their head in a neutral position (not tilted down toward the bed or up toward the ceiling). They should place another pillow between their knees with their hips and knees bent slightly if that relieves their back pain. People can continue to sleep on their stomach if they are comfortable doing so.
Applying cold (such as ice packs) or heat
Physical therapy and exercises to strengthen and stretch the muscles in the abdomen, buttocks, and back (the core muscles) may help. (See also Low Back Pain: Prevention .)

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Find a Doctor
- Transfer a Patient
- Patient Portal
Lumbar Spondylolisthesis
What is lumbar spondylolisthesis.
Lumbar spondylolisthesis is a condition in which a bone (vertebra) in the lumbar spine (lower back) slips forward out of position onto the bone below it. It may occur as a result of a defect, an injury, degeneration due to aging, or a disease.
Looking for a Second Opinion?
Lumbar Spondylolisthesis Symptoms
Depending on the degree of the slip, symptoms of lumbar spondylolisthesis can vary from mild to severe or not be present at all.
Symptoms may include:
- Lower back pain
- Muscle tightness
- Pain, numbness, or tingling in your thighs and buttocks
- Tenderness in the area where the vertebra is out of place
- Weakness in your legs
- Muscle spasms in your hamstring muscles
- Pain, numbness, or tingling down your leg or foot if slipped vertebra is pressing on a nerve
An imaging test is needed to determine whether or not you have lumbar spondylolisthesis. Contact a medical professional if you are having symptoms.
Lumbar Spondylolisthesis Treatments
Treatment for lumbar spondylolisthesis depends on the severity of the slip and your symptoms, along with your overall health. Minor slips may improve with conservative treatment, such as rest, pain medication, physical therapy, and a back brace.
For more severe cases, surgery may be recommended. Procedures for lumbar spondylolisthesis include:
- Decompressive laminectomy – part of the vertebra that is pressing on the nerves is removed to relieve symptoms
- Spinal fusion – two or more bones of the spine are fused together with real bone or synthetic materials
Additional Information
How common is lumbar spondylolisthesis.
Spondylolisthesis is the most common cause of back pain in teens.
Who gets lumbar spondylolisthesis?
In younger people, symptoms of spondylolisthesis often begin during their teenage growth spurt. Spondylolisthesis due to degeneration usually occurs after age 40.
Spondylolisthesis can be caused by spondylolysis, a defect in the connection between vertebrae that can lead to stress fractures. These stress fractures can weaken the bones so much that one slips out of place.
Fractures in the vertebrae can also be caused by certain sports that put a lot of stress on the lower back, such as gymnastics and weightlifting.
How is lumbar spondylolisthesis diagnosed?
Your doctor will likely perform a physical exam and an imaging test, such as an MRI scan or a CT scan, to diagnose lumbar spondylolisthesis.
Additional Resources
MedlinePlus | Spondylolisthesis
Find a Lumbar Spondylolisthesis Specialist
Get a Second Opinion for Lumbar Spondylolisthesis
Fast. Easy. Secure.
To give you the best possible experience, this site uses cookies. By continuing to use the site, you agree that we can save them on your device.
Our website uses cookies
This website uses cookies as well as similar tools and technologies to understand visitors’ experiences. By continuing to use this website, you consent to Columbia University’s usage of cookies and similar technologies, in accordance with the Columbia University Website Cookie Notice. (link opens in a new window)
Skip to site alert Skip to content
Learn more about NewYork-Presbyterian and Aetna Negotiations .
Spondylolisthesis
Make an appointment.
Our team is here to help you make an appointment with the specialists that you need.
Top of the page
- Condition Basics
What is spondylolisthesis?
In spondylolisthesis, one bone in your back ( vertebra ) slides forward over the bone below it. It most often occurs in the lower spine ( lumbosacral area). In some cases, this may lead to your spinal cord or nerve roots being squeezed. This can cause back pain and numbness or weakness in one or both legs. In rare cases, it can also lead to losing control over your bladder or bowels. See a doctor right away if you begin losing bladder or bowel control.
Sometimes when a vertebra slips out of place, you may have no symptoms at all or no symptoms until years later. Then you may have pain in your low back or buttock. Muscles in your leg may feel tight or weak. You may even limp.
What causes it?
Spondylolisthesis may be caused by problems with the small joints in your back. (The problems are called spondylolysis .) You could have:
- A defective joint that you've had since birth (congenital).
- A joint damaged by an accident or other trauma.
- A vertebra with a stress fracture caused from overuse of the joint.
- A joint damaged by an infection or arthritis.
Spondylolisthesis affects children and teens who play sports. Some sports, such as gymnastics or weight lifting, can overuse back bones to the point of causing stress fractures in vertebrae, which can result in the condition.
Older adults can develop spondylolisthesis because wear and tear on the back leads to stress fractures. It can also occur without stress fractures when the disc and joints are worn down and slip out of place.
What are the symptoms?
Symptoms of spondylolisthesis may include:
- Back or buttock pain.
- Pain that runs from the lower back down one or both legs.
- Numbness or weakness in one or both legs.
- Difficulty walking.
- Leg, back, or buttock pain that gets worse when you bend over or twist.
- Loss of bladder or bowel control, in rare cases.
Sometimes spondylolisthesis causes no symptoms at all.
How is it diagnosed?
To check for spondylolisthesis, your doctor will ask questions about your symptoms and do an exam. If your doctor suspects spondylolisthesis, they will probably do X-rays. You could also have a CT scan or an MRI done.
How is spondylolisthesis treated?
Treatment for spondylolisthesis begins with stopping any physical activity that may have led to vertebrae damage or that increases pain. For pain, your doctor may suggest taking NSAIDs . These include ibuprofen (such as Advil) or naproxen (such as Aleve). Or use acetaminophen (such as Tylenol) for pain.
Doctors often suggest physical therapy to build up stomach and back muscles ( core strengthening ). Losing weight, if you need to, may also help.
Surgery may help if the pain is extreme, the bones continue to move, or you have nerve root or spinal cord damage from the condition. This takes pressure off the spinal cord or nerves (decompression). Or the bones may be fused in position. Sometimes both decompression and fusion are done during the same surgery.
After any of these surgeries, you may need to wear a cast or back brace for a while. Later, rehabilitation therapy will help make your muscles stronger and your movement easier.
- Related Information
- Back Problems and Injuries
- Low Back Pain
Current as of: July 17, 2023
Author: Healthwise Staff Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Author: Healthwise Staff
Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Topic Contents

This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use . Learn how we develop our content .

To learn more about Healthwise, visit Healthwise.org .
© 1995-2024 Healthwise, Incorporated. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.

- Weill Cornell Medicine

Spondylolisthesis
- Diagnosing and Treating Spondylolisthesis
- Surgery for Spondylolisthesis
- Doctors Who Treat Spondylolisthesis
- ALIF, TLIF, and LLIF for Spondylolisthesis
Spondylolisthesis is a condition in which one of the vertebrae (bones) in the spine slips out of the proper position onto the vertebra below it. The word spondylolisthesis is derived from the Greek words spondylo , meaning spine, and listhesis , meaning to slip. Spondylolisthesis can occur in both children and adults, for different reasons. The condition varies in severity form patient to patient, and the severity will determine the course of treatment.
With spondylolisthesis, there is malalignment of the vertebra. It is not the same as a herniated disc, although the two can coexist. (Read more about herniated discs .) With spondylolisthesis, the slippage is of the bony vertebra. With a herniated or ruptured disk, it’s the soft interior of the spinal disc that “slips,” or bulges through a tear in the outer layer of the disc.
What Causes Spondylolisthesis?
When spondylolisthesis occurs in children or teens, it is usually due to a birth defect or a traumatic injury. (In fact, spondylolisthesis is the most common cause of back pain in teens.) In adults, the most common cause of spondylolisthesis is natural wear and tear due to aging and arthritis.
The various types of spondylolisthesis include:
Congenital spondylolisthesis occurs when a birth defect causes the bones of the spine to grow abnormally. When this happens, the misaligned spine puts pressure on the disc, resulting in slippage. This type of spondylolisthesis occurs primarily in children and teens, especially during a growth spurt.
Isthmic spondylolisthesis occurs when a condition called spondylosis puts pressure on the spine, causing the vertebrae to slip. The condition can be triggered by certain sports that put a great deal of stress on the back, such as football, gymnastics, and weight lifting.
Degenerative spondylolisthesis occurs when the natural wear and tear due to aging and arthritis causes a vertebra to slip out of place. This form of spondylolisthesis usually occurs in people over 40.
Traumatic spondylolisthesis occurs when an acute, traumatic injury such as a car accident leads to spondylolisthesis.
Pathological spondylolisthesis occurs when a disease of the spine, such as tumors or infection, weaken the vertebrae, resulting in increased pressure and slippage.
Post-surgical spondylolisthesis is very rare, and happens when a disc slips as the result of surgery
Spondylolisthesis should be treated at a major medical center with advanced facilities and experts experienced in treating complex spine disorders (see Doctors Who Treat Spondylolisthesis ).
Request an Appointment | Refer a Patient
What our Patients Say
Brain and spine blog.

By Roger Härtl, MD Director of Spine Surgery and Neurotrauma, Weill Cornell Medicine Director, Weill Cornell Medicine Center for Comprehensive Spine Care
Our Care Team
- Hansen-MacDonald Professor of Neurological Surgery
- Director of Spinal Surgery
- Clinical Associate Professor of Neurosurgery
- Attending Neurosurgeon

- Associate Professor of Neurological Surgery, Spinal Surgery
- Co-Director, Spinal Deformity and Scoliosis Program
- Director, Spinal Trauma/Adult and Pediatric Spinal Surgery

- Assistant Professor of Neurological Surgery

- Chief of Neurological Surgery, NewYork-Presbyterian Queens
- Professor of Clinical Neurological Surgery
- Co-director, Weill Cornell Medicine CSF Leak Program

- Assistant Professor, Neurosurgery

- Assistant Professor of Neurological Surgery, Spine Surgery

- Associate Professor of Neurological Surgery, Spine Surgery
Related Conditions
Reviewed by: Eric Elowitz, MD Last reviewed/last updated: September 2020 Illustration by Thom Graves CMI
Weill Cornell Medicine Neurological Surgery 525 East 68 Street, Box 99 New York, NY 10065 Phone: 866-426-7787
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Isthmic spondylolisthesis.
Matthew R. Burton ; Thomas J. Dowling ; Fassil B. Mesfin .
Affiliations
Last Update: August 8, 2023 .
- Continuing Education Activity
Spondylolisthesis occurs when there is an anterior subluxation or “slippage” of the vertebral body above on the vertebral body below. In most cases, symptoms associated with spondylolisthesis are chronic. The primary symptom of chronic spondylolisthesis is back pain, with or without leg pain. When spondylolisthesis occurs acutely in the setting of traumatic or metastatic tumors, patients can present with neurological examination deficits including a loss of bowel and bladder function. There are many causes of spondylolisthesis including congenital, degenerative, traumatic, pathologic, iatrogenic, and isthmic. and Isthmic spondylolisthesis. This activity reviews the cause of isthmic spondylolisthesis and highlights the role of the interprofessional team in its management.
- Review the presentation of isthmic spondylolisthesis.
- Describe the evaluation of a patient with isthmic spondylolisthesis.
- Summarize the treatment of isthmic spondylolisthesis.
- Explain modalities to improve care coordination among interprofessional team members in order to improve outcomes for patients affected by isthmic spondylolisthesis.
- Introduction
The lumbar spine in the sagittal plane should maintain an alignment in which each vertebral body is aligned with the vertebral body above and below. In other words, the anterior inferior endplate of the vertebral body above should be aligned with the anterior superior endplate of the vertebral body below. Spondylolisthesis occurs when there is an anterior translation or “slippage” of one vertebral body relative to its caudal vertebral body. In most cases, symptoms associated with spondylolisthesis are chronic. The primary symptom of chronic spondylolisthesis is back pain, with or without leg pain. When spondylolisthesis occurs acutely in the setting of traumatic or metastatic tumors, patients can present with neurological examination deficits including a loss of bowel and bladder function. The classification system utilized to categorize the degree of subluxation of the vertebral bodies is the Meyerding Classification, which quantifies the percentage of subluxation of the vertebral body above on the vertebral body below. Classification of Spondylolisthesis is based on the degree of slippage in the lumbar spine. Grade 1 is less than 25%, Grade 2 is 25% to 50%, Grade 3 is 50% to 75%, Grade 4 is 75% to 100%, and Spondyloptosis is > 100% [1] .
There are many causes of spondylolisthesis including congenital, degenerative, traumatic, pathologic, iatrogenic, and isthmic. Isthmic spondylolisthesis, which will be the topic of this discussion, refers to a defect in the pars interarticularis that then results in anterior subluxation over time, most commonly at L5-S1 followed by L4-5. The resulting anterior subluxation can produce back pain, central canal stenosis, and lateral recess or foraminal stenosis.
The most common etiology for isthmic spondylolisthesis is instability of unilateral or bilateral pars interarticularis. The pars interarticularis, or pars, is the bony structure which connects the lamina, pedicle, and transverse processes of the vertebral bodies. Importantly, the facet joints of the superior and inferior vertebrae also are connected by the pars. Thus, a defect in this structure would effectively “disconnect” the vertebral body above from the vertebral body below. This disconnection allows the anterior subluxation seen in spondylolisthesis. Many biomechanical studies indicate that the pars is subjected to the greatest force of any structure in the lumbar spine; therefore, it is susceptible to stress fractures which may heal and fracture repeatedly over time. These injuries can induce non-healing fractures or an elongated pars without a defect which likely indicates repeated fracture healing. Pars fractures are believed to be the result of repetitive motion. Thus, risks associated with pars defects include activities associated with repetitive flexion/extension, axial loading, and rotational loading (i.e., golfers, weight lifers, baseball and football players, gymnasts).
- Epidemiology
The incidence of isthmic spondylolisthesis is generally reported as between 4% to 8% of the general population. It is three times as common in males as it is in females. An interesting cross-sectional study utilizing the Framingham Heart Study participant of 3529 patients showed that 20% of patients with CT finding of bilateral pars defect showed no evidence of spondylolistheisis [2] . In addition, this cross-sectional study showed that the incidence of spondylolisthesis increases significantly from the fifth decade of life to the eighth decade of life .
- Pathophysiology
Spondylolisthesis can result in accelerated degeneration of the intervertebral disc which can lead to diminished height of the neural foramen and increased stresses on the facet joints posteriorly. This increased stress can lead to hypertrophy of the facet and ligamentum flavum. These changes can result in back pain, neurogenic claudication and radiculopathy. The radicular symptoms of isthmic spondylolisthesis are typically caused by the foraminal stenosis. Since the level most commonly affected is L5-S1, the L5 exiting nerve root in the L5-S1 foramen can be compressed. Other causes of symptoms can include lateral recess stenosis which, for example, can be caused by facet arthrosis or hypertrophied ligamentum flavum. Even more rare would be symptoms caused by central stenosis, given that most of these spondylolistheses rarely progress beyond grade II, and as the vertebral body translates anteriorly, the posterior elements tend to remain with the caudal vertebra maintaining their normal anatomic alignment. [3]
- History and Physical
Many cases of isthmic spondylolisthesis are asymptomatic. However, the most common symptom of presentation is low back pain, which may be mechanical in nature. Patients also can present with neurogenic claudication symptomatology such as back and leg pain and discomfort associated with walking. These symptoms need to be differentiated from vascular claudication, which is exacerbated by ambulation and gets better with rest. Other patients can present with symptoms of specific dermatome of lumbar radiculopathy depending on the compressed nerve root and the amount of subluxation or stenosis. Physical examination can show different degrees of findings ranging from normal to paraplegia. However, the most common findings are depressed deep tendon reflexes, positive straight leg signs, and diminished sensations. Some patients can have specific pain-related weakness of lower extremities. Usually, patients with chronic isthmic spondylolisthesis do not present with significant motor weakness; however, acute isthmic spondylolisthesis can present with paralysis and loss of bowel and bladder function. Since L5-S1 is the most commonly afflicted level, an L5-S1 isthmic spondylolisthesis will typically cause radicular symptoms that correlate with the L5 exiting nerve at that level such as weakness in ankle dorsiflexion and hallux extension.
Radiological evaluation is not indicated upon initial presentation of low back pain because of its self-limiting nature. However, serious conditions such as tumor or infection should be ruled out with a high-quality history and physical examination. Should the back pain not respond to conservative management then plain x-rays, including oblique views and lateral flexion-extension views, may be used to assess the bony quality and alignment of the lumbar spine as well as any dynamic instability. Should the initial presentation also consist of radicular symptoms or symptoms of neurogenic claudication, then the neural elements must be evaluated with an MRI or CT myelogram of the lumbar spine.
The degree of slippage is best characterized on the lateral x-ray. An oblique view x-ray of the lumbar spine is a good tool to assess the pars defect. CT Scan of the lumbar spine is the definitive study to assess the pars defect. MRI is the study of choice for evaluation of soft tissue structures including intervertebral discs, ligamentum flavum, the thecal sac, nerve roots, and the conus medullaris in the lumbar spine. MRI is needed for patients who fail conservative treatments and are planning a surgical intervention.
- Treatment / Management
Isthmic spondylolisthesis with low back pain should initially be managed conservatively. Activity modification, NSAIDs, muscle relaxers, physical therapy, and epidural steroid injections are some of the conservative options. Should the back pain persist despite conservative management, or if the severity is such that quality of life is significantly affected, then referral to a specialist for evaluation is indicated. When the presentation consists of symptoms of neurogenic claudication or radiculopathy, then imaging of the neural elements of the lumbar spine is indicated along with referral to a specialist. Surgical treatment options consist of decompression of the neural elements alone versus decompression with internal fixation for bony fusion to prevent further subluxation [4] . In addition, for patients who present with acute symptoms due to trauma or malignancies, emergent surgical referrals are indicated [5] . [6] [7] [8]
- Differential Diagnosis
Differential Diagnosis:
- Degenerative spondylolisthesis
- Traumatic spondylolisthesis
- Dysplasatic spondylolisthesis
- Pathologic spondylolisthesis (i.e., neoplasm, infection, iatrogenic)
- Enhancing Healthcare Team Outcomes
Low back pain is commonly encountered by the nurse practitioner, primary caregiver, emergency department physician, and internist. Isthmic spondylolisthesis is also a common cause of back pain and the diagnosis is confirmed by the radiologist. The initial management of the condition is with conservative measures but when patients fail to respond, a referral to an orthopedic surgeon is recommended. Surgical treatment options consist of decompression of the neural elements alone versus decompression with internal fixation for bony fusion to prevent further subluxation [4] . In addition, for patients who present with acute symptoms due to trauma or malignancies, emergent surgical referrals are indicated [5] .
Unfortunately, many patients continue to have a recurrence of pain because no treatment works consistently or reliably. Surgery only benefits a few patients and is associated with serious complications. Thus the primary care provider should emphasize lifestyle changes, regular exercise, discontinuation of tobacco and a healthy body weight. [9] [10]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Isthmic Spondylolisthesis Contributed by Chester J Donnally III, MD
Isthmic Spondylolisthesis intervention Contributed by Chester J Donnally III, MD
Disclosure: Matthew Burton declares no relevant financial relationships with ineligible companies.
Disclosure: Thomas Dowling declares no relevant financial relationships with ineligible companies.
Disclosure: Fassil Mesfin declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Burton MR, Dowling TJ, Mesfin FB. Isthmic Spondylolisthesis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Pars Interarticularis Injury. [StatPearls. 2024] Pars Interarticularis Injury. Pereira Duarte M, Camino Willhuber GO. StatPearls. 2024 Jan
- [Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis]. [Acta Chir Orthop Traumatol Cec...] [Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis]. Zencica P, Chaloupka R, Hladíková J, Krbec M. Acta Chir Orthop Traumatol Cech. 2010 Apr; 77(2):124-30.
- Posterior lumbar interbody fusion for dysplastic lumbar spondylolisthesis with high-grade slippage in two adolescent siblings: two case reports. [J Med Case Rep. 2022] Posterior lumbar interbody fusion for dysplastic lumbar spondylolisthesis with high-grade slippage in two adolescent siblings: two case reports. Tatsumura M, Funayama T, Eto F, Nagashima K, Takeuchi Y, Yamazaki M. J Med Case Rep. 2022 Sep 2; 16(1):331. Epub 2022 Sep 2.
- Review Management of High-Grade Dysplastic Spondylolisthesis. [Neurosurg Clin N Am. 2023] Review Management of High-Grade Dysplastic Spondylolisthesis. Polly DW Jr, Haselhuhn JJ, Soriano PBO, Odland K, Jones KE. Neurosurg Clin N Am. 2023 Oct; 34(4):567-572. Epub 2023 Jul 23.
- Review Isthmic spondylolisthesis in adults… A review of the current literature. [J Clin Neurosci. 2022] Review Isthmic spondylolisthesis in adults… A review of the current literature. Alomari S, Judy B, Sacino AN, Porras JL, Tang A, Sciubba D, Witham T, Theodore N, Bydon A. J Clin Neurosci. 2022 Jul; 101:124-130. Epub 2022 May 18.
Recent Activity
- Isthmic Spondylolisthesis - StatPearls Isthmic Spondylolisthesis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Spondylolisthesis
Spondylolisthesis is a Latin term meaning slipped vertebral body (spinal bone).
“Spondylo”= vertebrae “listhesis”=slippage
Spondylolisthesis in the lumbar spine is most commonly caused by degenerative spinal disease (degenerative spondylolisthesis), or a defect in one region of a vertebra (isthmic spondylolisthesis).
ON THIS PAGE
- What are the types of spondylolisthesis?
- Which type is most common?
WHAT ARE THE TYPES OF SPONDYLOLISTHESIS?
Spondylolisthesis can be classified by into five groups (newman (1976)):.
- Group 1: dysplastic
- Group 2: isthmic
- Group 3: traumatic
- Group 4: degenerative
- Group 5: pathological
WHICH TYPE IS MOST COMMON?
Degenerative spondylolisthesis is very common, and occurs as a result of due to degeneration or wear and tear of the intervertebral discs and ligaments. Osteoarthritis of the facet joints can also play an important role in the development of instability and slippage. Degenerative spondylolisthesis usually occurs in people over 60 years of age.
In degenerative spondylolisthesis, what usually happens is that ongoing degeneration weakens the facet joints and disc, and (typically) the L4 vertebral body slips forward on the L5 vertebral body. Under normal circumstances, the L4-L5 segment is the one in the lumbar spine with the most movement. It is therefore most likely to slip when this process occurs. The next most common levels affected by degenerative spondylolisthesis are L3-L4 and L5-S1.
Isthmic spondylolisthesis occurs most often at L5-S1, and is more often seen in younger adults than degenerative spondylolisthesis. The cause is a defect in an important bridge bone (the pars interarticularis) of L5.
HOW IS SPONDYLOLISTHESIS GRADED?
Spondylolisthesis is graded according to the severity of the slippage. This is known as the Mayerding classification:
- Grade 1: <25% slip
- Grade 2: 25-50% slip
- Grade 3 50-75% slip
- Grade 4: 75-100% slip
When one vertebra slips entirely off the one below (>100% slip), this is known as spondyloptosis (see picture).
Spondylolisthesis doesn’t usually have any symptoms. In fact, it is commonly seen on X-rays and CT scans as an ‘incidental’ finding. It may, however, produce significant symptoms and disability.
Back pain is the most common symptom of spondylolisthesis. This pain is typically worse with activities such as bending and lifting, and often eases when lying down.
As the spine attempts to stabilise the unstable segment, the facet joints enlarge and place pressure on the nerve root causing lumbar spinal stenosis and lateral recess stenosis.
As one bone slips forward on the other, a narrowing of the intervertebral foramen may also occur (foraminal stenosis). Severe nerve compression can therefore occur with pain, numbness and weakness in the legs. Sometimes loss of control of the bladder and/or bowels can occur due to pressure on the nerves going to these important structures.
Imaging studies including MRI and CT can show a slip, as well as narrowing (stenosis) or compressed nerves in the spinal canal.
The CT and MRI scans are usually obtained with the patient lying flat, however sometimes a slip may only be obvious when standing or bending forwards. This is why your neurosurgeon or spinal surgeon will sometimes obtain flexion, extension and standing X-rays, and occasionally a CT myelogram.
Treatment for spondylolisthesis is similar to treatments for other causes of mechanical and compressive back pain. It is usually non-operative, and surgery is only necessary in a small percentage of patients.
MODIFIED ACTIVITIES
Your specialist may suggest that you modify some of your usual physical activities, this will help to help settle symptoms from mechanical back pain. Special braces are occasionally prescribed to ease back pain. Short periods of bed rest can sometimes help with very painful episodes.
PHYSICAL REHABILITATION
A comprehensive physical rehabilitation program can assist in settling pain and inflammation, as well as improving mobility and strength. A combination of physiotherapy, hydrotherapy and clinical Pilates typically works well and is often recommended. The aims of these physical therapies are to assist you in:
- managing your condition and controlling your symptoms
- correcting your posture and body movements to reduce back strain
- improving your flexibility and core strength
Some patients also benefit from chiropractic treatment osteopathy, remedial massage, and acupuncture.
PSYCHOLOGIST REVIEW
Having a review by a clinical psychologist can be helpful in for creating strategies to manage pain. It is also important to address any associated feelings of depression or anxiety, as these conditions can heighten your experience of pain.
MEDICATIONS
Medication often plays an important role in controlling pain and easing muscle spasms. It can also help you to get back to a normal sleep pattern. Long-term medication usage should be closely supervised as problems such as tolerance and dependence (addiction) are known to occur.
Surgery is only needed only if other non-surgical treatments are not keeping your pain at a manageable level. Surgical treatment for spondylolisthesis need to take into account both mechanical (instability) and compressive (nerve pressure) issues. Nerve pressure usually involves surgical decompression, also known as a decompressive laminectomy. In order to deal with the compressive issues by taking pressure off the nerves, your surgeon may need to remove some or all of one or both facet joints, as well as portions of the lamina.
As the facet joints typically provide stability to the lumbar spine, the spine can spine to become loose and unstable, especially after some slippage has already occurred. A fusion is usually therefore recommended.
Similarly, a fusion is necessary to adequately deal with the mechanical issues of instability in spondylolisthesis.
Six types of fusion surgery are commonly recommended for the treatment of spondylolisthesis, depending upon individual patient factors:
- Transforaminal lumbar interbody fusion (TLIF)
- Posterior lumbar interbody fusion (PLIF)
- Instrumented posterolateral fusion (pedicle screw fixation and posterolateral bone graft)
- Anterior lumbar interbody fusion (carried out through the abdomen, rather than from the back)
- Extracavitatory lateral interbody fusion (XLIF)
- Oblique lateral interbody fusion (OLIF)
Healthcare Services
- Anatomy of the Spine
- Brachialgia (Cervical Radiculopathy)
- Cervical Spinal Stenosis
- Degenerative Disc Disease
- Herniated Disk
- Facet Joint Pain
- Failed Back Surgery
- Lower Back Pain
- Lumbar Spinal Stenosis
- Spinal Tumours
- Trauma (fractures, dislocations, instability)
- Ankle & Foot Conditions
- Arthritis Osteoarthritis
- Carpal Tunnel Syndrome
- Cubital Tunnel Syndrome Ulnar Nerve Entrapment
- Duputryn’s Contracture
- Ganglion Cyst – Wrist
- Upper Limb Fractures
- Tennis Elbow Lateral Epicondylitis
- Trigger Finger Stenosing Tenosynovitis
- Wrist Ligament Tear
- Hip Conditions
- Articular Cartilage Damage
- Bone & Cartilage Fragments
- Synovial Tissue Damage
- Rheumatoid Arthritis Shoulder
- Rotator Cuff Tear
- Shoulder Fracture Broken Shoulder
- Shoulder Osteoarthritis
- Shoulder Arthritis Pain
- Other Shoulder Conditions
- Annular Tear
- Arthritis of the Spine
- Bulging Disc
- Canal Stenosis
- Collapsed Disc
- Degenerative Disc Disease
- Degenerative Joint Disease
- Degenerative Spine
- Disc Extrusion
- Disc Protrusion
- Facet Disease
- Facet Syndrome
- Failed Back Surgery Syndrome
- Foraminal Narrowing
- Foraminal Stenosis
- Herniated Disc
- Herniated Nucleus Pulposus
- Pinched Nerve
- Piriformis Syndrome
- Prolapsed Disc
- Ruptured Disc
- Sciatica Sciatic Nerve Pain
- SI Joint Pain
- Slipped Disc
- Spinal Narrowing
- Spinal Stenosis
- Spondylitis
- Spondylolisthesis
- Spondylosis
- Spine Condition Animations
- Condition Resources
- Spine Articles
- Spinal Glossary
- Foraminotomy
- Kyphoplasty
- Decompression with Interlaminar Stabilization®
- Anterior Cervical Discectomy Fusion
- Transforaminal Lumbar Interbody Fusion
- Cervical Disc Replacement
- Lateral Lumbar Interbody Fusion
- SI Joint Fusion
- Posterior Cervical Fusion
- Facet Thermal Ablation
- Injections for Pain
- Pain Pump Implant
- Partial Shoulder Replacement
- Radio Frequency Ablation
- Rotator Cuff Surgery
- Shoulder Acromioplasty
- Shoulder Arthroscopy
- Shoulder Resurfacing
- Spinal Cord Stimulator
- Total Shoulder Replacement
- Am I a Candidate?
- Streamlined Patient Experience
- Postoperative Care
- Care Partners
- Spine Back Questions
- Vertebral Motion Analysis
- Diagnostics
- Nutrition for Pain Relief
- Pain Management Injections
- Blood Flow Restriction Training
- Dry Needling
- Industrial Rehabilitation
- Manual Therapy
- Medical Massage
- Oncology Rehabilitation
- Soft Tissue Mobilization
- Vestibular & Balance Rehab
- Laser Spine Surgery Cost 2020
- Financing Insurance
- Personal Injury
- Laser Spine Doctors
- 1-866-249-1627
- Facility Locations
- On-Site Medical Consultation
How may we help you?
Am i a candidate, free mri review*.
Home » Spine Conditions » Spondylolisthesis » Congenital spondylolisthesis — symptoms and treatment options
Congenital spondylolisthesis — symptoms and treatment options
Congenital spondylolisthesis is forward vertebral slippage related to a birth defect. The word congenital means that a condition is present at birth. It is relatively rare since spondylolisthesis is usually acquired later in life as the result of aging, traumatic injury or a stress fracture. This condition can occur anywhere in the spine, but it most frequently affects the lower back.
Overview and symptoms
The reason a birth defect can cause this condition is that if a spinal joint develops abnormally, it can make a vertebra much more likely to slip out of place. Congenital spondylolisthesis is a common cause of back pain for teenagers, often happening in relation to rapid periods of growth.
Although you can have spondylolisthesis without experiencing symptoms, pain can occur when the displaced vertebra or a spinal disc causes nerve compression. A common symptom is lower back pain. Other spondylolisthesis symptoms include:
- Pain in the buttocks
- Tightness in the lower back and leg muscles
- Weakness, muscle spasms and numbness in the extremities
Diagnosis of spondylolisthesis is usually confirmed with a full evaluation including diagnostic imagery like an X-ray, MRI or CT scan. The lateral movement of spondylolisthesis is graded on a scale of 1 to 5, where 5 would represent 100 percent slippage.
Pain relief for congenital spondylolisthesis
Spondylolisthesis treatment is often conservative and can include rest, stretching and exercise, pain medication, or a back brace. Always work with your doctor to develop a course of treatment that is best for your situation and lifestyle. These methods are effective for many patients looking for a return to regular quality of life. Surgery is generally only required for high-grade slippage or when a period of conservative treatment, usually lasting weeks or months, has not brought sufficient relief.
If you are considering surgery, you should be aware of all your options so you have the best chance of finding lasting pain relief. Advances in medical technology have made it possible for minimally invasive spine surgery to be performed in an outpatient environment. These minimally invasive techniques offer a shorter recovery time^ compared to traditional open back surgery. USA Spine Care can treat the symptoms of congenital spondylolisthesis, and potentially provide increased stability, using both minimally invasive decompression and stabilization procedures. For more information contact us today.
Our dedicated team is happy to provide a no-cost MRI review* to determine if you are a potential candidate for one of our procedures.
Browse Related Resources
General Information Spondylolisthesis Definition Isthmic Spondylolisthesis Causes What Causes Spondylolisthesis? Spondylolisthesis and Degeneration from Aging Symptoms & Diagnosis What Are the Symptoms of Spondylolisthesis? Spondylolisthesis Symptoms What Should I Do if I Think I Have Spondylolisthesis? Can Symptoms Affect Everyday Life? What Your Diagnosis Means Who Can Ascertain a Spondylolisthesis Diagnosis? Meyerding Grading System Spondylolisthesis Grades Treatments Alternative Treatments & Exercise for Spondylolisthesis Can the Effects of Spondylolisthesis be Reversed? Spondylolisthesis Surgery Issues to Consider Before Surgery Finding Relief Can Weight Loss Help? Stretching for Spondylolisthesis Relief Risk Factors Spondylolisthesis Risk Factors Prevention Spondylolisthesis Prevention Miscellaneous Additional Information Causes & Classifications
FIND OUT IF YOU'RE A CANDIDATE WITH A FREE MRI REVIEW*
- First Name *
- Last Name *
- Insurance * Please Select Aetna Anthem Auto - LOP Beech Street BCBS Cigna Coventry Empire Humana Kaiser Medicaid Medicare Medicare Advantage Multi-plan None Not listed Tricare United Health Care Worker's Comp
- By checking the "I Accept" box, I am agreeing to the terms & conditions.
- Comments This field is for validation purposes and should be left unchanged.
Download our Guide
Download your minimally invasive spine surgery info packet and receive our e‑newsletter.
Accreditations
Usa spine care reviews.
^ Results are typical, but not guaranteed, each patients experience with spine surgery will differ.
For more information, visit usaspinecare.com/results . The information contained on this website is for educational purposes only, and is not intended to serve as a replacement for a medical diagnosis.
*Our MRI review is an informational review of the MRI report that you provide to us and is not a form of diagnosis. A diagnosis and a final determination of whether you may benefit from treatment at USA Spine Care can only be made after you have been physically examined by our medical professionals at USA Spine Care. The MRI review has no value and will not be billed.
+ For more information, visit usaspinecare.com/surgeons.
Laser Spine Number Institute 866-DOCS-LSI 866-362-7574 866-249-1627
Copyright © 2019 USA Spine Care, LLC.
ADA compliance HIPAA Subscriptions Disclaimer Privacy policy Terms of use
Lumbosacral Spondylolisthesis
Affiliation.
- 1 University of Liverpool
- PMID: 32809514
- Bookshelf ID: NBK560679
Lumbosacral spondylolisthesis is the forward translation of the fifth lumbar vertebra (L5) over the first sacral vertebra (S1). Bilateral L5 pars defect (spondylolysis) or repetitive stress injury is the primary etiology behind lumbosacral spondylolisthesis. The degree of a slip often correlates with the degree of symptoms.
The prevalence of spondylolysis (pars defect), in the general population, is 6%, and a third of those will subsequently develop a degree of spondylolisthesis. The majority of cases are mild or asymptomatic, and only a relatively small percentage of symptomatic patients require surgical intervention.
The most commonly affected populations are children and adolescents participating in sports that require repetitive lower back hyperextension (divers, pace cricket bowlers, baseball, softball, rugby, weightlifting, sailing, table tennis, wrestlers, gymnasts, dancers, and footballers). They usually present with lower back pain exacerbated by activity. Occasionally pain can radiate to both buttocks and legs, and in advanced cases, the gait pattern and walking distance may be affected. Presentation in adults is more insidious and commonly associated with long-standing degenerative changes secondary to the slip, often leading to spinal canal stenosis and radicular pain.
Management of the majority of the cases is non-operative, but patients who fail non-operative treatment and continue having disabling symptoms may require surgical treatment.
Copyright © 2024, StatPearls Publishing LLC.
- Continuing Education Activity
- Introduction
- Epidemiology
- Pathophysiology
- History and Physical
- Treatment / Management
- Differential Diagnosis
- Complications
- Deterrence and Patient Education
- Pearls and Other Issues
- Enhancing Healthcare Team Outcomes
- Review Questions
Publication types
- Study Guide
NOTICE MyAANS, password-protected resources, and purchases are currently experiencing issues and are unavailable. We are working to get this fixed as soon as possible.

The site navigation utilizes arrow, enter, escape, and space bar key commands. Left and right arrows move across top level links and expand / close menus in sub levels. Up and Down arrows will open main level menus and toggle through sub tier links. Enter and space open menus and escape closes them as well. Tab will move on to the next part of the site rather than go through menu items.
Lumbar Spinal Stenosis
The lumbar spine (lower back) consists of five vertebrae in the lower part of the spine, between the ribs and the pelvis. Lumbar spinal stenosis is a narrowing of the spinal canal, compressing the nerves traveling through the lower back into the legs. While it may affect younger patients, due to developmental causes, it is more often a degenerative condition that affects people who are typically age 60 and older.

Narrowing of the spinal canal usually occurs slowly, over many years or decades. The disks become less spongy with aging, resulting in loss of disk height, and may cause bulging of the hardened disk into the spinal canal. Bone spurs may also occur and ligaments may thicken. All of these can contribute to narrowing of the central canal and may or may not produce symptoms. Symptoms may be due to inflammation, compression of the nerve(s) or both. Such symptoms may include:
- Pain, weakness or numbness in the legs, calves or buttocks
- Cramping in the calves with walking, requiring frequent short rests to walk a distance
- Pain radiating into one or both thighs and legs, similar to the lay term “sciatica”
- In rare cases, loss of motor functioning of the legs, loss of normal bowel or bladder function
- Pain may improve with bending forward, sitting or lying down
Degenerative spondylolisthesis and degenerative scoliosis (curvature of the spine) are two conditions that may be associated with lumbar spinal stenosis. Degenerative spondylolisthesis (slippage of one vertebra over another) is caused by osteoarthritis of the facet joints. Most commonly, it involves the L4 slipping over the L5 vertebra . It is usually treated with the same non-surgical (“conservative”) and surgical methods as lumbar spinal stenosis.
Degenerative scoliosis occurs most frequently in the lower back and more commonly affects people aged 65 and older. Back pain associated with degenerative scoliosis usually begins gradually and is linked with activity. The curvature of the spine in this form of scoliosis is often relatively minor. Surgery may be indicated when nonsurgical measures fail to improve pain associated with the condition.
Diagnosis is made by a neurosurgeon based on history, symptoms, physical examination and test results.
Imaging studies used may include the following:
- X-ray : Focuses radiation through the body to create an image and can show the structure of the bones, alignment of the spine and outline the joints.
- CT scan or CAT scan : Creates images by combining multiple X-rays together and can show the shape and size of the spinal canal, its contents and the structures around it with details of the bony anatomy.
- MRI : Creates images by using powerful magnets and computer technology and can show the spinal cord, nerve roots and surrounding areas, as well as enlargement, degeneration and tumors.
- Myelogram : Injects contrast dye into the spinal fluid space (cerebrospinal fluid) to outline the nerves and spinal cord, and show evidence of any pressure affecting these areas; seen on X-ray, sometimes done with a CT scan.
Nonsurgical Treatment
A combination of time, medications, posture management, stretching and exercise can be helpful to many patients for pain flare-ups. Weight management, nicotine cessation and bone-strengthening endeavors may also be indicated.
- Anti-inflammatory medications can be used to reduce swelling and pain, and analgesics can be used to relieve pain. Most pain can be treated with non-prescription medications, but if the pain is severe or persistent, prescription medications may be provided.
- Epidural injections of medications may be prescribed to help reduce swelling.
- Physical therapy and/or prescribed exercises may help to stabilize and protect the spine, build endurance and increase flexibility. Therapy may help the patient to resume a normal lifestyle and activities. Typically, four to six weeks of therapy is encouraged.

Surgical Treatment
A doctor may recommend surgery if non-surgical management (as described above) does not improve symptoms. There are different types of spinal surgeries available, and depending on the specific case, a neurosurgeon will help to determine what procedure might be appropriate for the patient. As with any surgery, a patient’s risks include age, overall health and other issues, which are all taken into consideration beforehand.
A patient may be considered a candidate for surgery if:
- Back and leg pain limits normal activity or impairs quality of life;
- Progressive neurological deficits develop (leg weakness, foot drop, numbness in the limb);
- Loss of normal bowel and/or bladder functions;
- Difficulty standing or walking;
- Medications and physical therapy are not effective;
- The patient is in reasonably good health.
There are several different surgical procedures that can be utilized, the choice of which is influenced by the severity of the case. In a small percentage of patients, spinal instability may require that spinal fusion be performed — this decision generally is determined prior to surgery. Spinal fusion is an operation that creates a solid union between two or more vertebrae. Spinal fusion may assist in strengthening and stabilizing the spine, and may thereby help to alleviate severe and chronic back pain.
Types of Surgeries
The most common surgery in the lumbar spine is called decompressive laminectomy , in which the laminae (roof) of the vertebrae are removed to create more space for the nerves. A neurosurgeon may perform a laminectomy with or without fusing vertebrae or removing part of a disk. A spinal fusion with or without spinal instrumentation may be used to enhance fusion and support unstable areas of the spine.
Other types of surgeries or techniques/methods to treat lumbar spinal stenosis include:
- Laminotomy : Creates an opening in the bone (in the lamina ) to relieve pressure on the nerve roots.
- Foraminotomy : Surgical opening or enlargement of the bony exit for the nerve root as it leaves the spinal canal; can be done alone, or along with laminotomy/laminectomy.
- Medial Facetectomy : Removal of part of the facet (bony joint) which may be overgrown, to create more space in the spinal canal.
- Anterior Lumbar Interbody Fusion (ALIF): Removal of the degenerative disk by going through the lower abdomen. A structural device, made of bone, metal, carbon filter or other materials, is placed to take the supportive place of the removed disk and packed with bone, so that ultimately fusion between the bone (body of the vertebrae) above and below occurs.
- Posterior Lumbar Interbody Fusion (PLIF): Removal of the degenerative disk by going through the skin on the back, removal of the posterior bone of the spinal canal, retraction of the nerves to get to the disk space. A structural device, made of bone, metal, carbon filter or other materials, is placed to take the supportive place of the removed disk and packed with bone, so that ultimately fusion between the bone (body of the vertebrae) above and below occurs. Similar to TLIF, this is often done on both sides of the spine.
- Transforaminal Lumbar Interbody Fusion (TLIF): Removal of the degenerative disk by going through the skin on the back, removal of the posterior bone of the spinal canal, retraction of the nerves to get to the disk space. A structural device, made of bone, metal, carbon filter or other materials, is placed to take the supportive place of the removed disk and packed with bone, so that ultimately fusion between the bone (body of the vertebrae) above and below occurs. Similar to PLIF, this is often done on only one side of the spine.
- Posterolateral Fusion : Places bone graft on the back and side(s) of the spine to achieve a fusion.
- Instrumented Fusion : Using “hardware” (hooks, screws, other devices) to add stability to the construction for fusion.
The potential benefits of surgery should always be weighed carefully against the risks of surgery and anesthesia. Although a large percentage of lumbar spinal stenosis patients who ultimately undergo surgery report significant pain relief after surgery, there is no guarantee that surgery will help every individual.
The AANS does not endorse any treatments, procedures, products or physicians referenced in these patient fact sheets. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific neurosurgical advice or assistance should consult his or her neurosurgeon, or locate one in your area through the AANS’ Find a Board-certified Neurosurgeon online tool.
Musculoskeletal Medicine
- Cervical Stenosis
- Cervical, Thoracic and Lumbosacral Orthoses
- Cervical Radiculopathy
- Chest Wall Pain Syndrome
- Costochondritis
- Compression Fractures of the Spine
- Thoracic Outlet Syndrome
- Thoracic Radiculopathy/Myelopathy
- Lumbar Strain
- Lumbar Spondylolisthesis
Lumbar Spondylosis Without Myelopathy/Radiculopathy
- Lumbar Stenosis
- Lumbar Radiculopathy
- Lumbar Disc Disorders
- Seronegative Spondyloarthropathy
- Adult Degenerative Scoliosis
- Spine Infections
- Acromioclavicular Joint Disorders
- Adhesive Capsulitis
- Impingement Syndromes of the Shoulder
- Shoulder Pain in the Throwing Athlete
- Shoulder Instability, Dysfunction and Scapular Dyskinesis
- Traumatic Sports Injuries of the Shoulder: Fractures, Separations, and Other Injuries
- Rotator Cuff Shoulder Tendon and Muscle Injuries
- Olecranon Bursitis
- Epicondylosis (lateral) With and Without Nerve Entrapment
- Tendinopathy
- Elbow Pain in Little League Pitcher’s Elbow
- Acute Elbow Injuries and Overuse Disorders
- Therapeutic Injection of Dextrose: Prolotherapy, Perineural Injection Therapy and Hydrodissection
- Radial Nerve Mononeuropathy
- Ulnar Mononeuropathy at the Wrist
- Sports and Occupational Injuries to the Wrist and Hand
- Carpal Tunnel Syndrome
- de Quervain Tenosynovitis
- Proximal Lower Extremity Mononeuropathies
- Congenital Hip Dysplasia
- Legg-Calve-Perthes Disease
- Stress Fracture of the Hip
- Femoral Acetabular Impingement Syndrome
- Hip and Pelvic Arthropathies and Labral Tears
- Proximal and Mid-Hamstring Strain/Tendon Tear
- Iliotibial Band Syndrome
- Sports Medicine Disorders of the Hip: Posterolateral
- Sports Medicine Disorders of the Hip: Anterior-Medial
- Distal Lower Extremity Mononeuropathies
- Osteochondritis Dissecans
- Knee Overuse Disorders
- Patellofemoral Syndrome
- Knee Osteoarthritis
- Osteoarthritis
- Medial and Lateral Collateral Ligament Injuries
- Posterior Cruciate Ligament (PCL) Injuries
- ACL Injury and Rehabilitation
- Meniscus Injuries of the Knee
- Ankle and Foot Neuropathies & Entrapments
- Tarsal Tunnel Syndrome
- Gout and Pseudogout
- Plantar Fasciitis
- Pes Planus/Adult Acquired Flatfoot Deformity
- Ankle Sprain
- Adult Ankle Fractures (Ankle and Foot Soft Tissue Injuries and Fractures)
- Achilles Tendinopathy
- Ankle and Foot Overuse Disorders
- Functional Rehabilitation of Sports Injuries
- Return to Work after MSK Injury in the Workplace: Factors Leading to Timely Return and Risk Factors for Delayed Return
- Osteogenesis Imperfecta
- Pregnant Athlete
- Female Athlete Triad
- Osteoporosis in Rehabilitation
- Endocrine Abnormalities Affecting the Musculoskeletal System
- Performing Arts Medicine
- Sports Concussion
- Hydration Issues in the Athlete and Exercise Associated Hyponatremia
- Downed Runner
- Lower Limb Exertional Compartment Syndrome
- Stingers and Burners
- Pulmonary Issues in the Athlete/Exercise Induced Bronchoconstriction
- Cardiac Issues in Sports Medicine
- Shoulder Problems – Pain in the Wheelchair Athlete
- Pregnancy Related Complications
- Sports Medicine for Special Groups
Disease/ Disorder
Lumbar spondylosis is a radiographic diagnosis that refers to degenerative changes of the discs, vertebral bodies and paired zygapophysial joints (z-joints) of the lumbar spine. Degenerative lumbar spondylosis is a term used to describe a “mixed group of spinal bone diseases related to degeneration of the lumbar motion segment and associated pathologies.” 30 The term spondylosis is not used as a clinical diagnosis but rather as a term to illustrate spinal pathology. Spondylosis may be associated with low back pain (LBP) and is associated with numerous spinal pathologies including spinal stenosis (narrowing of the spinal canal), vertebral instability, degenerative spondylolisthesis , osteoarthritis and malalignment. 29
Though the etiology of lumbar spondylosis remains unclear, many have characterized it as osteoarthritis of the spine. It is thought to result from cumulative stresses combined with repetitive microtrauma, leading to an imbalance between the synthesis and degeneration of cartilage. When combined with increased stresses placed on the vertebrae and ligaments, osteophytes and calcifications occur, respectively. 1,3
Bone spurs, also known as osteophytes, most commonly occur along the anterolateral aspect of the lumbar vertebral body. Posterior vertebral osteophytes are rare but can cause impingement on the nerve roots or spinal cord. Lumbar spondylosis can also occur due to new bone formation in areas where the annular ligament is stressed over time. 29
Epidemiology including risk factors and primary prevention
The prevalence of radiographic spondylosis increases with age. 4,5 It is present only in a small percentage of the population in the first few decades of life but is relatively common by the age of 65. In those with LBP, the prevalence ranges from 7% to 75%, depending on the diagnostic criteria. 6 Despite its frequency in patients with LBP, there is no validated correlation between the radiographic findings of lumbar spondylosis and presence of LBP. In the United States, approximately 80% of individuals older than 40 years old were found to have lumbar spondylosis, contrasted to3% of individuals aged 20-29 years. 5 Recent studies have shown a positive correlation with the CC genotype of the transforming factor B1 gene and postmenopausal women. 31
Risk factors
Age is the greatest risk factor for lumbar spondylosis, but other risk factors including disc desiccation, previous injury, joint overload from malalignment and/or abnormal z-joint orientation, as well as genetic predisposition have been identified. 2 Studies evaluating the role of body mass index, level of activity and gender on the incidence and severity of lumbar spondylosis do not show a clear correlation. 5,7
Patho-anatomy/physiology
Some investigators believe that lumbar spondylosis is due to a “degenerative cascade” that is initiated by intervertebral disc desiccation. 8 The degenerative changes which characterize lumbar spondylosis are thought to be due to cumulative stresses on the annular ligaments which then form (i.e., marginal osteophytes). 29 Failure of annulus and nucleus collagen cross-linking and the discs’ inability to retain water results in stiffening of the cartilaginous and capsular structures, further restricting z-joint mobility causing earlier and more advanced degenerative changes. This is particularly true at the L4/L5 and L5/S1 levels likely because of their proximity to the fused sacral segments. 1,3
Disease progression including natural history, disease phases or stages, disease trajectory (clinical features and presentation over time)
Although variable, most patients experience a benign clinical course. Studies have shown the following:
- radiologic spondylosis directly increases with age, irrespective of pain. 9
- spondylosis was shown to be equally present in those with and without LBP. 2
- no correlation between the magnitude of z-joint arthropathy and the severity of pain. 6
Thus, progression is variable and unpredictable, and therefore difficult to study, but seems to be most closely linked to aging.
Specific secondary or associated conditions and complications
Z-joint hypertrophy in combination with ligamentous redundancy from disc desiccation may contribute to central canal, lateral recess and neuroforaminal stenosis. The increase in translational forces from disc desiccation, combined with the z-joints’ decreased ability to resist these factors, may also result in spondylolisthesis. Clinically, these changes can cause lumbosacral radiculopathy and neurogenic claudication. Disuse atrophy of the erector spinae and multifidi muscles secondary to pain-limited spine motion can also occur.
Essentials of Assessment
As mentioned previously, lumbar spondylosis refers to certain radiographic findings that do not rely on clinical symptoms for diagnosis. However, in some patients with acute, subacute or chronic LBP, the radiological changes which make up lumbar spondylosis can be potential pain generators. Patients with lumbar spondylosis often complain of axial lumbosacral back pain with potential nociceptive input from the sacroiliac joints, overlying myofascial structures, intervertebral discs, nerve roots, and facet joints. 30 Pain may refer unilaterally, bilaterally, or to the contralateral buttock, hip, groin and thigh regions; although, typically, it does not extend past the knee. 6,10 The pain tends to worsen with extension, rotation and standing and is better with lying down and lumbar flexion. 10 By definition, the term lumbar spondylosis is not associated with a neurologic deficit. However, spinal stenosis, spondylolisthesis, lumbar disc herniation and radiculopathy are known to be associated with neurological deficits. This is why it is imperative for the clinician to ask about weakness, gait and balance and bowel/bladder function when assessing patients with lumbar spondylosis.
There are several validated outcome measures for grading functional limitations including the McGill Low Back Pain Scale, Oswestry Disability Index and the Medical Outcomes Study 36-Item Short-Form Health Survey. 11 These should typically be administered at every office visit for following the patient’s progression.
Physical examination
A systematic review revealed that most physical exam maneuvers have limited or no diagnostic validity for spondylosis. 6 Paraspinal tenderness is the only physical exam maneuver that seems to correlate with z-joint arthropathy, but not with high diagnostic confidence. Although classically felt to diagnose z-joint pain, joint loading with pain on extension and ipsilateral rotation has not been shown to consistently correlate with spondylosis. 12,13 The pain distribution of lumbar spondylosis may overlap with other clinical entities. A comprehensive physical exam that includes evaluation for radiculopathy, including dural tension signs, as well as hip and sacroiliac joint provocative maneuvers can help guide clinical decision making. Neurologic deficits seen with lumbar nerve root compression should be evaluated through muscle, sensation, reflexes, gait, and balance testing. Discogenic pain is exacerbated when the patient is asked to repeatedly bend forward or when the patient is sitting up and one leg is placed in a flexed position by the examiner.
Laboratory studies
Although laboratory studies are not routinely indicated, C-reactive protein, sedimentation rate, and a complete blood count, may be ordered if there is clinical suspicion for conditions such as malignancy, infection or rheumatologic disease.
Lumbar spondylosis is visible on multiple imaging modalities, including plain radiographs, magnetic resonance imaging (MRI) and computed tomography (CT) studies. However, as spondylosis on imaging does not constitute a cause for LBP, imaging is typically ordered to rule out other disorders. 13,14,15
Plain radiographs are not sensitive for detecting early z-joint arthropathy or spondylosis but are often obtained. Lateral views are important for sagittal alignment and to assess for spondylolisthesis. If present, patients should undergo flexion and extension radiographs to rule out segmental instability which may necessitate earlier surgical consultation.
MRI is generally not needed but is useful for evaluating the soft tissues and neural elements within the spine, especially to rule out neuroforaminal stenosis in patients with concomitant leg pain. The presence of small amounts of fluid or synovial cysts within the z-joints may be physiologic or may represent instability and/or infection within the lumbar spine, and therefore would warrant further work up and/or treatment. However, this is beyond the scope of this article.
CT is typically utilized when an MRI is unobtainable, if fracture is suspected or for the assessment of pseudoarthrosis. It can also be helpful in identifying synovial cyst borders with implications for surgical vs percutaneous treatment. 34
Supplemental assessment tools
Diagnostic Injections
Given the low correlation of radiographic spondylosis with axial low back pain, the only means for an accurate diagnosis of symptomatic lumbar spondylosis secondary to facet arthropathy are controlled diagnostic blocks of the medial branch nerves that innervate the z-joints. 16 This assumes that the patient’s pain generator(s) are the z-joints and not the intervertebral discs. Each z-joint has dual innervation from the medial branch of the dorsal ramus of the spinal nerve at the corresponding level and the level above. To treat the pain associated with a specific z-joint, both nerves must be targeted.
Several key principles exist for diagnostic medial branch blocks:
- Because of the inaccuracy of landmark guidance, all blocks should be performed utilizing image guidance. Both fluoroscopic and ultrasound guidance have been described in literature. 34
- False positive blocks occur at a high rate of 17% to 41% in the lumbar spine, thus necessitating a second control block for confirmation of the diagnosis. Ideally, the two injections should be performed with anesthetics of differing duration. Concordant pain relief (>1h with lidocaine and >3h with bupivacaine hydrochloride), greatly enhances the sensitivity and specificity of the injections. 13
- The greater the percentage of pain relief a patient obtains with a given injection, the more likely that injection correctly targeted the pain generator. An 80% pain relief threshold with comparative medial branch blocks results in more successful outcomes with radiofrequency ablation, a denervation procedure which uses radiofrequency to thermally ablate the medial branch nerves. 13,16 For more details, please see the Lumbar Zygapophyseal Joint Arthropathy section of PM&R KnowledgeNOW.
Rehabilitation Management and Treatments
Available or current treatment guidelines.
There is no best treatment for the pathological changes of lumbar spondylosis; therefore, prescribed treatments should focus on decreasing patients’ pain and increasing function. Conservative treatment measures include weight loss, physical therapy, NSAIDs, acetaminophen, and topical pain medications. 18
Interventional pain specialists may consider performing a medial branch radiofrequency ablation for certain patients. Ablated nerves may regenerate and result in recurrence of pain. 19,20,21,22,23
Physical therapy should focus on increasing flexibility of the spine with strengthening of core muscles, including the lumbar paraspinals and abdominal musculature. There is minimal evidence to support a single proven exercise program for the treatment of lumbar spondylosis. 24
Surgical intervention is not recommended for axial back pain secondary to lumbar spondylosis without segmental instability or neurologic compromise. 35
Coordination of care
As with all spine conditions, treatment should ideally be guided by the coordinated approach of a multidisciplinary team, including, but not limited to, a physician and physical therapist. Inclusion of a pain psychologist may be beneficial for patients having difficulty coping with chronic pain secondary to lumbar spondylosis.
Patient & family education
Patients should be educated that lumbar spondylosis related symptoms typically respond well to treatment; however, they should be made aware of warning signs consistent with neurologic involvement. Patients should seek immediate medical attention if they develop myelopathy and/or changes in bowel and bladder. Patients should be informed that spondylosis on imaging does not necessarily correspond with pain and that a diagnostic block may be used to rule in/out lumbar spondylosis= related LBP.
Providers should work with their patients to develop a tailored treatment plan that may include oral pain medications, interventional procedures and increased physical activity.
Practical Application
Physicians should have a low threshold for ruling out other serious conditions that also commonly present as LBP. The incidence of lumbar facet pain increases with age resulting in a higher positive predictive value of a diagnostic medial branch block and improvement of pain after ablation. After successful treatment of pain with an RFA, patients should be encouraged to engage in daily therapeutic spine exercises to maximize function and hopefully prevent relapse of pain.
Emerging/unique interventions
Nerve growth factor (NGF) has been linked to chronic low back pain and patients treated with anti-NGF have shown a slight improvement in pain and functional outcomes vs placebo. 25 Lieite et al specifically used Tanezumab, an anti-NGF agent, that showed low evidence of small to moderate pain relief of low back pain & small functional improvement when used in patients with chronic low back pain. 25
New techniques and methods are being developed to enhance RFA lesion size while preserving safety. Limited literature exists on their efficacy, but two such technologies are water-cooled RFA and multi-tined needles. 26, 27, 28 These will hopefully enhance success rates and minimize technical failures. Studies are also currently underway regarding the use of orthobiologics, which are organic and synthetic materials are used to help cure musculoskeletal diseases. 37
Translation into practice: practice “pearls”/performance improvement in practice (PIPs)/changes in clinical practice behaviors and skills
Physicians should have a low threshold for ruling out other serious conditions that commonly present as LBP in this age group. For patients that have failed non-interventional treatment options, injections may be required to achieve pain relief. Interventional management should be used in combination with daily therapeutic spine exercises to maximize function and hopefully prevent relapse of pain.
Cutting Edge/ Emerging and Unique Concepts and Practice
New techniques and methods, such as the use of water-cooled RFA and Nimbus needles, aim to enhance RFA lesion size while preserving safety. RFA generates a lesion to a targeted nerve through heat created by passing an electric current through an RFA needle. Water-cooled RFA allows more energy to be delivered to the surrounding tissues without damage by internally cooling the needle with water 32 . The Nimbus needle, developed by Dr. Robert Wright in 2009, is a tined RF cannulae that produces a cloud-shaped lesion 33 . The advantage of such a lesion allows for a perpendicular approach to targeting the lumbar medial branches, as opposed to the more technically challenging parallel approach 33 . These advances will hopefully enhance success rates and minimize technical failures. For more details, please see the Facet Mediated Pain section of PM&R KnowledgeNOW. The use of biologics to alter disease progression and improve pain are being investigated. 36
Gaps in the Evidence-Based Knowledge
Current literature shows the limitations in the diagnostic value of patient history, physical examination and imaging findings for diagnosing LBP secondary to lumbar spondylosis. Subsequent research should focus upon identifying patient-related characteristics of history taking, physical examination, laboratory findings, and/or imaging that may be used to better diagnose LBP related to lumbar spondylosis, especially in patients with diagnostic block-proven and symptomatic lumbar spondylosis.
- Middleton K, Fish D. Curr Rev Musculoskeletal Med (2009) 2:94–104. Lumbar spondylosis: clinical presentation and treatment approaches.
- Bogduk N. Degenerative joint disease of the spine. Radiol Clin North Am . 2012;50:613-628.
- Schneck CD. The anatomy of lumbar spondylosis. Clin Orthop. Relat Res. 1985;193:20–36.
- Brinjikji W, et al. AJNR Am J Neuroradiol. Author manuscript; available in PMC 2015 June 13. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. Department of Radiology (W.B., P.H.L., J.T.W., D.F.K.), Mayo Clinic, Rochester
- Zukowski LA, et al. J. Anat. (2012) 220, pp57–66. The influence of sex, age and BMI on the degeneration of the lumbar spine.
- Kalichman L, et al. Facet joint osteoarthritis and low back pain in the community-based population. Spine . 2008;33:2560-2565.
- O’Neill TW, et al. The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol. 1999;26:842–8.
- Kirkaldy-Willis W, Bernard T. Managing low back pain. New York: Churchill Livingstone; 1983.
- Lawrence JS, Bremner JM, Bier F. Osteo-arthrosis. Prevalence in the population and relationship between symptoms and x-ray changes. Ann Rheum Dis . 1966;25:1-24.
- Eisenstein SM, Parry CR. The lumbar facet arthrosis syndrome. Clinical presentation and articular surface changes. J Bone Joint Surg Br . 1987;69:3-7.
- Wittink, Harriët PT, MS, PhD, et al. Clinical Journal of Pain: May/June 2004 – Volume 20 – Issue 3 – pp 133-142. Comparison of the Redundancy, Reliability, and Responsiveness to Change Among SF-36, Oswestry Disability Index, and Multidimensional Pain Inventory
- Datta S, Lee M, Falco FJ, et al. Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions. Pain Physician . 2009;12:437-460.
- Bogduk N, Dreyfuss P, Govind J. A narrative review of lumbar medial branch neurotomy for the treatment of back pain. Pain Med. 2009;10:1035-1045.
- Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg. 1990;72:403–8.
- Wiesel SW, Tsourmas N, Feffer HL, et al. A study of computer-assisted tomography. The incidence of positive CAT scans in an asymptomatic group of patients. Spine. 1984;9:549.
- Macvicar J, Borowczyk JM, Macvicar AM, et al. Lumbar medial branch radiofrequency neurotomy in New Zealand. Pain Med . In press.
- Wu T et al. Arch Phys Med Rehabil. 2016 Sep;97(9):1558-1563. Effectiveness of Ultrasound-Guided Versus Fluoroscopy or Computed Tomography Scanning Guidance in Lumbar Facet Joint Injections in Adults With Facet Joint Syndrome: A Meta-Analysis of Controlled Trials.
- Carette S, et al. A controlled trial of corticosteroids injections into facet joints for chronic low back pain. N Engl J Med . 1991;325:1002-1007.
- Slipman CW, et al. A critical review of the evidence for the use of zygapophysial injections and radiofrequency denervation in the treatment of low back pain. Spine J . 2003;3:310-316.
- van Kleef M, et al. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine . 1999;24:1937-1942.
- Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine . 2008;33:1291-1297.
- Dreyfuss P, Halbrook B, Pauza K, et al. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine . 2000;25:1270-1277.
- Schofferman J, Kine G. Effectivness of repeated radiofrequeny neurotomy for lumbar facet pain. Spine . 2004;29:2471-2473.
- Braddom, R L, et al. Physical Medicine and Rehabilitation (Fourth Edition). 2011. Philadelphia, PA. Saunders/Elsevier
- Leite VF, Buehler AM, et al. Anti-nerve growth factor in the treatment of low back pain and radiculopathy: a systematic review and a meta-analysis. Pain Physician . 2014 Jan-Feb;17(1):E45-60.
- Bajaj PS1, et al. PMR. 2015 Oct;7(10):1095-101. doi: 10.1016/j.pmrj.2015.09.001. Cooled Versus Conventional Thermal Radiofrequency Neurotomy for the Treatment of Lumbar Facet-Mediated Pain.
- Stryker Inc. Venom Cannula. https://strykerivs.com/conditions/facet-joint-pain#
- Nimbus Concepts. http://www.nimbusconcepts.com/the-product.html
- Gibson JN, Waddell G (2005) Surgery for degenerative lumbar spondylosis: updated Cochrane Review. Spine 30:2312–20
- Martin Merkle, beat wälchli, Norbert Boos – neurobicetre.com. (n.d.). Retrieved February 16, 2022, from https://neurobicetre.com/wp-content/uploads/2018/04/Boose-Degenerative-spondylolisthesis.pdf
- Association of Transforming Growth Factor Beta1 genotype with spinal osteophytosis in Japanese women.Read by QxMD. (n.d.). Retrieved February 16, 2022, from https://read.qxmd.com/read/10693888/association-of-transforming-growth-factor-beta1-genotype-with-spinal-osteophytosis-in-japanese-women
- Hunter, Corey, et al. “Cooled Radiofrequency Ablation Treatment of the Genicular Nerves in the Treatment of Osteoarthritic Knee Pain: 18‐ and 24‐Month Results.” Pain Practice , vol. 20, no. 3, 2019, pp. 238–246., https://doi.org/10.1111/papr.12844.
- Russo, Marc, et al. “A History of the Development of Radiofrequency Neurotomy.” Journal of Pain Research , Volume 14, 2021, pp. 3897–3907., https://doi.org/10.2147/jpr.s334862.
- Khan, Amir M, and Federico Girardi. “Spinal lumbar synovial cysts. Diagnosis and management challenge.” European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society vol. 15,8 (2006): 1176-82. doi:10.1007/s00586-005-0009-4.
- Soneji, Neilesh, and Philip Wenn Hsin Peng. “Ultrasound-guided pain interventions – a review of techniques for peripheral nerves.” The Korean journal of pain vol. 26,2 (2013): 111-24. doi:10.3344/kjp.2013.26.2.111 35
- Shamrock AG, Donnally III CJ, Varacallo M. Lumbar Spondylolysis And Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448122/
- Moreno-Garcia, Alonso, and E Carlos Rodriguez-Merchan. “Orthobiologics: Current role in Orthopedic Surgery and Traumatology.” The archives of bone and joint surgery vol. 10,7 (2022): 536-542. doi:10.22038/ABJS.2021.52770.2614
Original Version of the Topic
D.J. Kennedy, MD, Renata Jarosz, MD, Ryan Demirjian, MD. Lumbar spondylosis without myelopathy. 9/20/2013.
Previous Revision(s) of the Topic
Ameet Nagpal, MD and Alan Swearingen, MD. Lumbar spondylosis without myelopathy. 2/14/2018.
Author Disclosure
Ameet Nagpal, MD, MS, MEd Nothing to Disclose
Adedeji Olusanya, DO, MPH Nothing to Disclose
Austin Bevil, DO Nothing to Disclose
Patient and Family Resources
- Find a PM&R Doctor
- Patient Information
- What is Physiatry?
Get published and recognized among your peers
Related posts.
- Cervical Dystonia
- Discogenic Lumbar Pain
- Pediatric Spondylolysis and Spondylolisthesis
Privacy Overview
- All About the L3-L4 Spinal Segment
By: Andrew Cole, MD, Physiatrist
Peer-Reviewed
The L3-L4 spinal motion segment, positioned in the middle of the lumbar spine , plays an important role in supporting the weight of the torso and protecting the cauda equina (nerves that descend from the spinal cord). While the L3-L4 motion segment is less likely to be injured compared to its lower counterparts, it may be subject to degeneration, trauma, and disc-related problems.
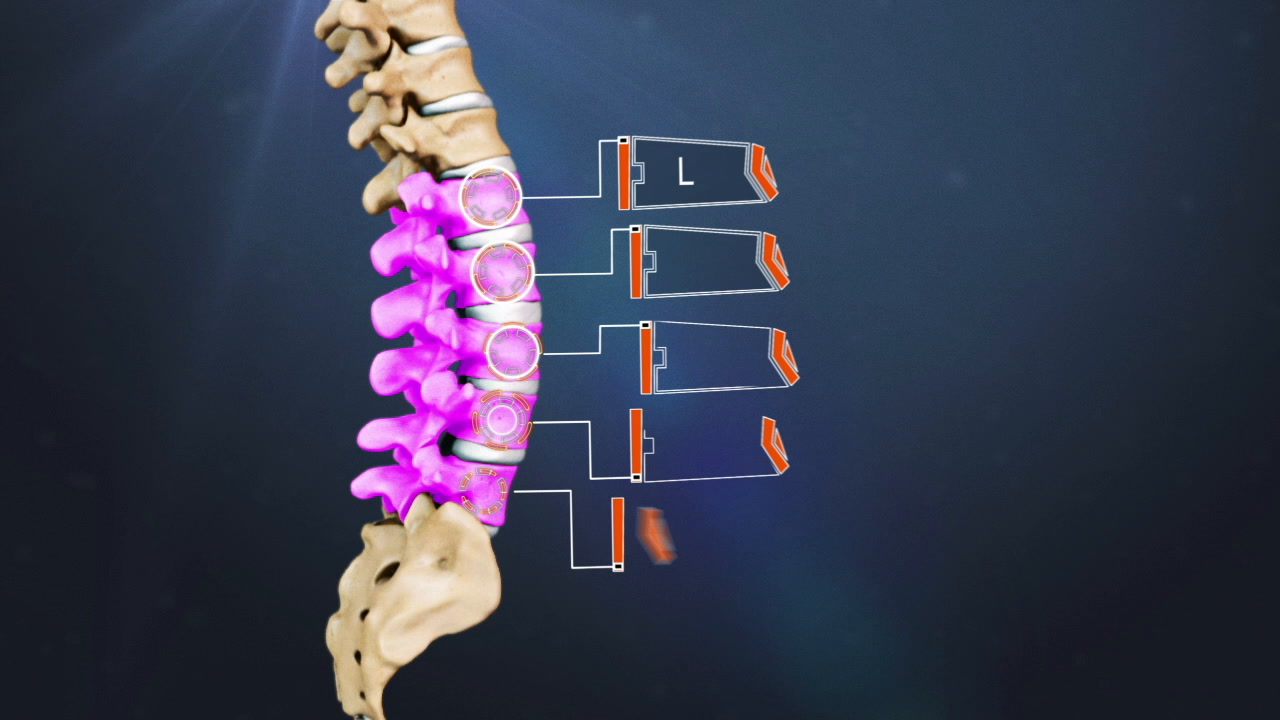
Show Transcript
In this article:.
- L3-L4 Treatment
- Lumbar Spine Anatomy Video
Anatomy of the L3-L4 Spinal Motion Segment
The L3-L4 motion segment includes the following structures:
L3 and L4 vertebrae
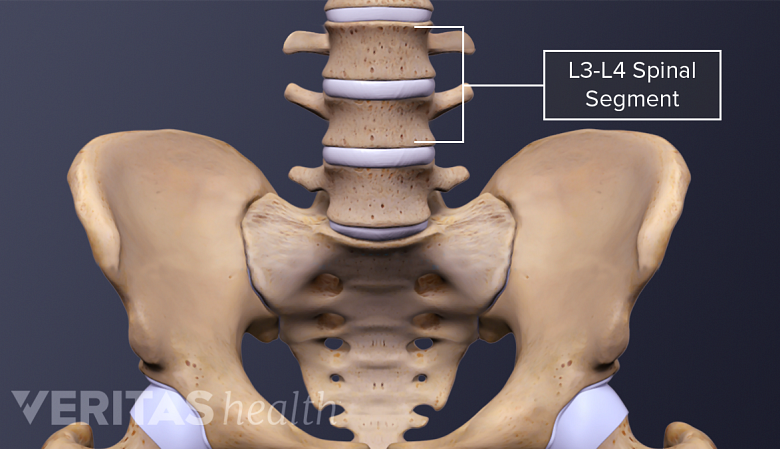
An injured L3-L4 motion segment may cause pain, numbness, or weakness in the lower back or legs.
Each vertebra consists of a vertebral body in front and a vertebral arch at the back with the following characteristics:
- The height of the vertebral body of L3 is equal in the front and back; L4 is taller in front compared to the back. 1 Cramer GD. The Lumbar Region. In: Clinical Anatomy of the Spine, Spinal Cord, and Ans. Elsevier; 2014:246-311. doi:10.1016/b978-0-323-07954-9.00007-4 , 2 Wilke H-J, Volkheimer D. Basic Biomechanics of the Lumbar Spine. In: Biomechanics of the Spine. Elsevier; 2018:51-67. doi:10.1016/b978-0-12-812851-0.00004-5
- The vertebral arch has 3 bony protrusions: a prominent spinous process in the middle and two transverse processes on either side. L3 has the longest spinous process in the lumbar region. 1 Cramer GD. The Lumbar Region. In: Clinical Anatomy of the Spine, Spinal Cord, and Ans. Elsevier; 2014:246-311. doi:10.1016/b978-0-323-07954-9.00007-4
- The region between the spinous process and the transverse process is called the lamina. The region between the transverse process and the vertebral body is called the pedicle.
- The L3 and L4 vertebrae are connected at the back by a pair of facet joints (zygapophyseal joints) , which are covered by articulating cartilage to provide smooth movements between the joint surfaces.
L3-L4 intervertebral disc

The spinal discs provide flexibility and support for the spine.
A disc made of a soft, gelatinous core (nucleus pulposus) surrounded by tough layers of fibrous tissue (annulus fibrosus) is situated between the vertebral bodies of L3 and L4. This disc provides cushioning and shock-absorbing functions to protect the vertebrae from grinding against each other during spinal movements.
L3 spinal nerve
The L3 spinal nerve roots exit the cauda equina through small bony openings (intervertebral foramina) on the left and right sides of the spinal canal. The L3 nerve innervates specific areas of skin and muscles in the lower limbs.
- The L3 dermatome is an area of skin that receives sensations through the L3 spinal nerve and includes the front part of the thigh and inner part of the leg.
- The L3 myotome is a group of muscles controlled by the L3 spinal nerve and includes parts of specific muscles in the hip, thigh, and leg.
The L3-L4 motion segment provides a bony enclosure to protect the cauda equina and other delicate structures.
Common Conditions Affecting the L3-L4 Spinal Segment
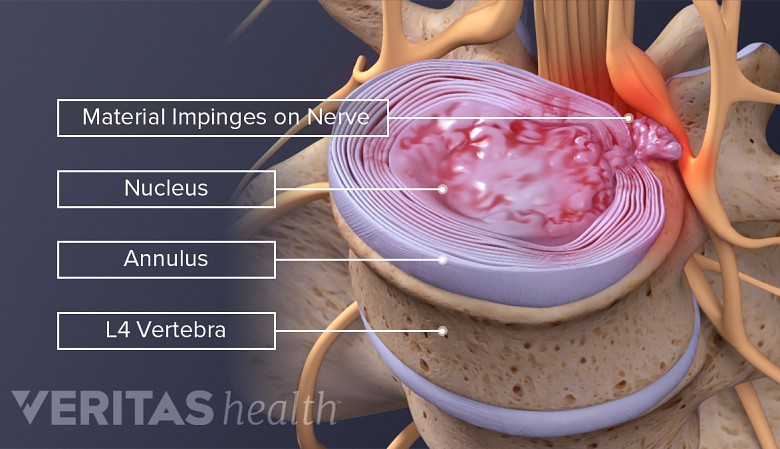
The L3-L4 disc may degenerate or herniate due to age-related changes or from trauma.
Potential problems that may occur at the L3-L4 motion segment are:
- Osteoarthritis . The L3-L4 facets are typically subject to recurrent rotational strain, which may cause osteoarthritis to develop in these joints, resulting in facet joint pain . 1 Cramer GD. The Lumbar Region. In: Clinical Anatomy of the Spine, Spinal Cord, and Ans. Elsevier; 2014:246-311. doi:10.1016/b978-0-323-07954-9.00007-4
- Degenerative spondylolisthesis . Age-related changes in the facet joints may result in the forward slippage of the L3 vertebra over L4. 1 Cramer GD. The Lumbar Region. In: Clinical Anatomy of the Spine, Spinal Cord, and Ans. Elsevier; 2014:246-311. doi:10.1016/b978-0-323-07954-9.00007-4
- Disc problems. The L3-L4 disc may degenerate or herniate due to age-related changes or from trauma.
When subject to acute trauma, the L3-L4 motion segment may rarely undergo facet joint dislocation, fracture, and/or damage to the cauda equina. Rarely, tumors and infections may affect the L3-L4 motion segment.
Symptoms and Signs Stemming from L3-L4
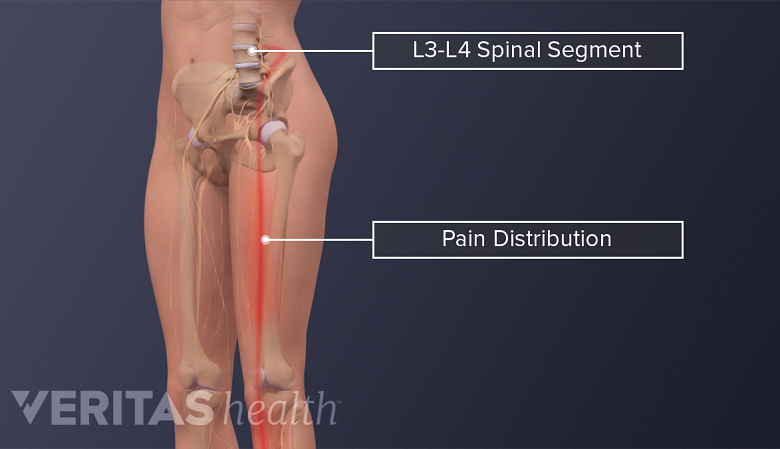
Injured L3-L4 motion segments may cause symptoms of pain, numbness or weakness in the lower back or legs.
The L3-L4 motion segment may cause muscle pain, discogenic pain, radicular (nerve root) pain, and/or radiculopathy (neurologic deficit) that typically affects the lower back and/or the legs.
When the L3 spinal nerve is involved, the following symptoms may occur:
- Sharp pain, typically felt as a shooting and/or burning feeling that may occur in the thigh and/or inner part of the leg. 3 Dulebohn SC, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2019 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
- Numbness in the thigh and/or inner part of the leg. 3 Dulebohn SC, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2019 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
- Weakness while moving the thigh and/or knee in different directions. 3 Dulebohn SC, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2019 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
- Abnormal sensations, such as a feeling of pins-and-needles and/or tingling.
These symptoms are typically experienced in one leg. Rarely, both legs may be affected together.
Read more about Lumbar Radiculopathy
An injury to the cauda equina is called cauda equina syndrome . This syndrome is characterized by weakness, numbness, tingling, and /or paralysis in both legs. There may also be a reduction or complete loss of bowel and/or bladder control. Immediate medical attention is crucial in this condition to preserve leg function.
Nonsurgical treatments are often tried first to treat the conditions originating from L3-L4, except for cauda equina syndrome, which must have urgent surgical consultation. In rare cases, surgery may be considered.
See Cauda Equina Syndrome Treatment
- 1 Cramer GD. The Lumbar Region. In: Clinical Anatomy of the Spine, Spinal Cord, and Ans. Elsevier; 2014:246-311. doi:10.1016/b978-0-323-07954-9.00007-4
- 2 Wilke H-J, Volkheimer D. Basic Biomechanics of the Lumbar Spine. In: Biomechanics of the Spine. Elsevier; 2018:51-67. doi:10.1016/b978-0-12-812851-0.00004-5
- 3 Dulebohn SC, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2019 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
Dr. Andrew Cole has 30 years of experience specializing in spine and joint pain management. Dr. Cole has held numerous medical appointments throughout his career, and recently served as the Executive Director of Rehabilitation & Performance Medicine Enterprise for Swedish Health Services and as Medical Director of Ambulatory Musculoskeletal Services for Swedish Medical Group.
- All About the L3-L4 Spinal Segment "> Share on Facebook
- All About the L3-L4 Spinal Segment "> Share on Pinterest
- All About the L3-L4 Spinal Segment "> Share on X
- Subscribe to our newsletter
- Print this article
- All About the L3-L4 Spinal Segment &body=https://www.spine-health.com/conditions/spine-anatomy/all-about-l3-l4-spinal-segment&subject= All About the L3-L4 Spinal Segment "> Email this article
Editor’s Top Picks
Spinal motion segment: l4-l5 animation, lumbar spine anatomy and pain, sciatica causes and symptoms video.
Lumbar Herniated Disc Video
Lower Back Pain Symptoms, Diagnosis, and Treatment
Lumbar degenerative disc disease video.
Popular Videos

Lower Back Pain Treatment Video

Cervical Disc Replacement Surgery Video

4 Steps to Relieve Sciatica Pain Video
Health Information (Sponsored)
- Take the Chronic Pain Quiz
- Suffering from Lumbar Spinal Stenosis? Obtain Long Term Pain Relief
- Learn How Bone Growth Therapy Can Help You
- Schedule a Consultation With Cedars-Sinai’s Integrated Spine Team
Select a Location

SEARCH THIS SITE
- All Conditions & Treatments
- Brain Tumor Center
- Cerebrovascular Diseases
- Face Pain & Headaches
- Memory Disorders
- Movement Disorders
- Multiple Sclerosis (MS)
- Neuro-Oncology
- Neurocritical Care
- Neuromuscular Disorders
- Radiation Oncology
- Sleep Disorders
- Spine Disorders and Back Pain
- Neurologists & Neurosurgeons
- Our Locations
Lumbar Spondylosis (Degeneration)
What is lumbar spondylosis.
Lumbar spondylosis is an age-related degeneration of the vertebrae and disks of the lower back. These changes are often called degenerative disk disease and osteoarthritis. The common condition is marked by the breakdown of one or more of the disks that separate the bones of the spine. The disks provide cushioning between the vertebrae and absorb pressure put on the spine. Although most people experience some degeneration of the spine as they age, not everyone experiences back pain.
Causes of Lumbar Spondylosis
Spondylosis most often affects disks in the lumbar region. When disks herniate, the protruding disk can press against any of the spinal nerves that run from the spinal cord to the rest of the body. Herniated disks can cause nerve pain known as sciatica, which travels along the sciatic nerve running from the lower back down the length of each leg.
As a disk degenerates, bone spurs may form at the edges of the vertebrae. Bone spurs may also compress the spinal nerves, leading to weakness or numbness in the arms or legs. If bone spurs compress the spinal cord, you may develop problems with walking and bladder and bowel control. Over time, a degenerating disc may break down completely, leaving no space between two vertebrae, which can result in impaired movement, pain, and nerve damage. The pressure can cause pain, weakness, and numbness in the back and the legs.
Early Signs of Lumbar Spondylosis and Diagnosis
Symptoms of spondylosis may vary from none to mild to severe. The most common symptom is low back pain. Our spine specialists diagnose spondylosis based on your history of symptoms, a physical exam, and imaging tests that may include X-rays, CT scan, or MRI.
Treatments for Lumbar Spondylosis
Our spine specialists diagnose spondylosis based on your history of symptoms, a physical exam, and imaging tests that may include X-rays, CT scan, or MRI. Most people with lumbar spondylosis can be treated with nonsteroidal anti-inflammatory drugs or pain relievers, heat or ice applications, and physical therapy.
People who still experience pain or are significantly restricted in their daily movements after trying more conservative treatments may consider surgery to remove the deteriorated disk and fuse the two vertebrae. Surgery may be recommended for patients who have severe or high-grade slippage of the vertebra, such as when more than 50% of the fractured vertebra slips forward on the vertebra below it. The procedure most often recommended for people with lumbar spondylolisthesis is spinal fusion.
Beverly Smith: Relief for Spine Pain
Anatomy of the neck and spine
The spine is divided into the following regions:
- The cervical region (vertebrae C1-C7) encompasses the first seven vertebrae under the skull. Their main function is to support the weight of the head, which averages 10 pounds. The cervical vertebrae are more mobile than other areas, with the atlas and axis vertebra facilitating a wide range of motion in the neck. Openings in these vertebrae allow arteries to carry blood to the brain and permit the spinal cord to pass through. They are the thinnest and most delicate vertebrae.
- The thoracic region (vertebrae T1-T12) is composed of 12 small bones in the upper chest. Thoracic vertebrae are the only ones that support the ribs. Muscle tension from poor posture, arthritis, and osteoporosis are common sources of pain in this region.
- The lumbar region (vertebrae L1-L5) features vertebrae that are much larger to absorb the stress of lifting and carrying heavy objects. Injuries to the lumbar region can result in some loss of function in the hips, legs, and bladder control.
- The sacral region (vertebrae S1-S5) includes a large bone at the bottom of the spine. The sacrum is triangular-shaped and consists of five fused bones that protect the pelvic organs.
What You Can Expect at UTHealth Neurosciences
The UTHealth Neurosciences Spine Center brings together a multidisciplinary team of board-certified, fellowship-trained neurosurgeons, neurologists, researchers, and pain management specialists who work together to help provide relief for even the most complex problems. Your team will share insights, leading to better treatment decisions and outcomes.
We first investigate nonsurgical treatment options, including medical management, pain management, physical therapy, rehabilitation, and watchful waiting. When surgery is needed, our neurosurgeons routinely employ innovative minimally invasive techniques. Throughout the treatment process, we will work closely with the doctor who referred you to ensure a smooth transition back to your regular care. While you are with us, you will receive expert care, excellent communication, and genuine compassion.
Spine Disease and Back Pain
Arthrodesis Artificial Disc Replacement Cauda Equina Syndrome Cervical corpectomy Cervical disc disease Cervical discectomy and fusion Cervical herniated disc Cervical laminectomy Cervical laminoforaminotomy Cervical radiculopathy Cervical spondylosis (degeneration) Cervical stenosis Cervical spinal cord injury Degenerative Disc Disease Foraminectomy Foraminotomy Herniated discs Injections for Pain Kyphoplasty Laminoplasty Lumbar herniated disc Lumbar laminectomy Lumbar laminotomy Lumbar radiculopathy Lumbar spondylolisthesis Lumbar spondylosis (degeneration) Lumbar stenosis
Neck Pain Peripheral Nerve Disorders Radiofrequency Ablation Scoliosis Spinal cord syrinxes Spinal deformities Spinal injuries Spinal fractures and instability Spinal Cord Stimulator Trial and Implantation Spinal Fusion Spinal Radiosurgery Spine and spinal cord tumors Spondylolisthesis Stenosis Tethered spinal cord Thoracic herniated disc Thoracic spinal cord injury Transforaminal Lumbar Interbody Fusion Vertebroplasty
At UTHealth Neurosciences, we offer patients access to specialized neurological care at clinics across the greater Houston area. To ask us a question, schedule an appointment, or learn more about us, please call (713) 486-8100, or click below to send us a message. In the event of an emergency, call 911 or go to the nearest Emergency Room.
- McGovern Medical School Facebook Page
- McGovern Medical School X Page
- McGovern Medical School Instagram Page
- McGovern Medical School YouTube Page
- McGovern Medical School LinkedIn Page
- Medical School IT (MSIT)
- Campus Carry
- Emergency Info
- How to report sexual misconduct
- University Website Policies
- Back & Neck
- Spondylolysis
What Causes Spondylolysis & How to Get Relief
Spondylolysis quiz
Take a quiz to find out if you have spondylolysis.
Spondylolysis involves defect or damage at the rear of each vertebra caused by bone defects, spinal wear and tear, hereditary traits, or overuse of the lower back.
Take spondylolysis quiz
What is spondylolysis?
"Spondylos," refers to the vertebrae, and "lysis," means destruction or dissolving. Spondylolysis is a defect or damage via a stress fracture in one of the vertebrae of the spinal column. It commonly affects children or adolescents who are active or frequently participate in sports .
Some cases of spondylolysis may be asymptomatic at times. Presenting symptoms include lower back pain, muscle spasms, pain that worsens with exercise, a limited range of motion, a swayback posture, and an awkward gait.
Treatments include rest, over-the-counter medications, responsible exercise, possible procedures, and rehabilitation.
Recommended care
You should visit your primary care physician who will coordinate your care with a muscle and bone specialist (orthopedic surgeon). Treatment for this condition is usually conservative, including pain medication, a break from sports and other activities until pain subsides, as well as physical therapy in some cases.
Spondylolysis symptoms
Symptoms of spondylolysis can be back-specific or more widespread.
Back-specific symptoms
There are certain symptoms of spondylolysis that stem directly from the back, such as:
- Lower back pain: The classic symptom of spondylolysis is lower back pain , often on just one side.
- Muscle spasms: People who have more severe cases of spondylolysis may have muscle spasms in their back.
- A swayback posture: People with spondylolysis may walk with or maintain a "swayback" posture, which strains the lower back by increasing the curvature of the low back.
Other symptoms
Since the back is essential to much of your overall health and performance, some other, more widespread symptoms may be present, including:
- Pain that worsens during exercise: In people who have spondylolysis, it is common for pain to worsen during exercise and temporarily improve with rest.
- Limited range of motion: The ability to move the leg forward, backward and outward is limited in people with spondylolysis.
- Awkward gait: Someone who has spondylolysis may walk with an awkward gait.
- Absence of symptoms: People with spondylolysis may have little or no discomfort until there is additional physical stress on the bones. It may also present during a growth spurt in the teenage years.
Spondylolysis causes
Spondylolysis is found in the fifth lumbar (L5) vertebra in the low back in 85–95% of cases. It may be found in the L4 in 5–15% of cases, and may also affect the cervical, or neck, vertebrae . Four causes of spondylolysis include the following.
- Bone defects: Having a defect in the vertebrae means that the bone is abnormally thin at its connection points, which causes small cracks, called stress fractures . They may occur on one or both sides of the vertebrae.
- Spinal wear-and-tear: The spine is meant to be strong and flexible. Individual bones, or vertebrae, allow for both straight and bent positions. However, over time, wear-and-tear can result in stress fractures at these connecting surfaces.
- Hereditary traits: Some individuals are born with a tendency for weaker, thinner bones in the spine, which means their spondylolysis is a congenital (from birth) condition that they inherited.
- Overuse of the lower back: A primary cause of spondylolysis is constant hyperextension — overstretching or twisting — the lower back. This movement can happen during hard, repetitive physical work or during sports training.
Who is most often affected?
Spondylolysis is likely to affect anyone who:
- Has inherited weakness of vertebral connections
- Has a physically demanding job
- Participates in strenuous or repetitive exercise: Such as playing sports that repeatedly stretch or twist the low back . These include football/soccer, baseball, tennis, diving, gymnastics, ballet, wrestling, weightlifting, pole vaulting, etc.
- Is a male younger than 25
- Is a woman: However, this is less frequent.
- Is a child or teenager: Since their skeletal structure has not entirely matured into hard bone and can be more vulnerable to stress and breakdown
Treatment options and prevention for spondylolysis
Spondylolysis is a long-term condition , but sometimes the fractures heal well. See a physician when the first symptoms appear to help prevent more severe fractures. Possible treatments include rest, over-the-counter medication, procedures, careful exercise, and rehabilitation.
Avoid strenuous exercise, training, and physical work until your fractures heal. Being completely inactive can lead to the following, however.
- Weak muscles or atrophy
- Joint stiffness and muscle stiffness
- Further weakening and thinning of bones
Over-the-counter medication
Pain medication can be found over-the-counter to ease pain, swelling, and inflammation. Non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen (Advil, Motrin) or naproxen (Aleve) may help.
Procedures may be necessary, such as the following.
- Steroid injections: These injections are administered into the joints between the vertebrae can help ease pain and inflammation.
- Surgery: In more severe cases, surgery is required to repair damage and soothe discomfort.
Careful exercise
If your physician has cleared you for exercise, he or she may specifically suggest you strengthen your abdominal muscles, or core, with a physical therapist. Your core muscles in your abdomen and back help support and protect the bones of the spine. While exercising, keep these tips in mind.
- Keep it low-impact: Choose low-impact sports and activities that will not stress the low back.
- Warm-up: Allow time to warm up before play or training starts.
- Monitor younger individuals: Consult a physical therapist or a specialist in sports medicine for children and teenagers involved in heavy training or elite sports.
- Be cautious: Resume activity gradually. Do not "push through the pain."
Rehabilitation
Spondylolysis may require physical rehabilitation, which takes three to six months . Goals and details of rehabilitation include the following.
- Protect the damaged vertebrae: Try to limit stress and rotation.
- Allow fractures to heal
- Gradually resume activity: Once pain and inflammation subside, resume movement carefully.
- During the first week of rehab: Expect to rest with only very mild activity.
- During the following six to 12 weeks of rehab: You may wear a supportive brace. Back braces can protect and stabilize your back while fractures heal.
- Psychological support: Support can help with depression that sometimes occurs due to activity changes.
Ready to treat your spondylolysis?
When to seek further consultation for spondylolysis.
If you have suffered an injury, pain is significantly interfering with your life, or you cannot find relief, you should consult your physician.
If spondylolysis causes misalignment of vertebrae
If not treated, spondylolysis can progress until it causes several small stress fractures in the vertebrae. These fractures may weaken one or more of your vertebrae until they shift out of place and no longer line up correctly with the other vertebrae of the spine. This misalignment is called spondylolisthesis and may require surgery.
If spondylolysis is interfering with your life
If not treated, even mild spondylolysis can make it difficult to participate in sports, walk, or drive. If conservative methods do not help, you may need surgery.
If spondylolysis causes pain
Low back pain is common from walking upright, so mild low back soreness after exercise is not unusual at any age. However, if it constantly recurs, seems to be getting worse, or is happening in a child or teenager who trains, see a physician.
If you suffer a back injury that does not resolve with a few days rest
If you suffer a back injury or have low back pain that does not clear up with a day or two of rest, see your physician right away.
Questions your doctor may ask to determine spondylolysis
- Any fever today or during the last week?
- How severe is your back pain?
- Have you ever injected drugs?
- Is your lower back pain constant or come-and-go?
- How long has your back pain been going on?
Self-diagnose with our free Buoy Assistant if you answer yes on any of these questions.
Required field
Was this article helpful?
- Spondylolysis and Spondylolisthesis. American Academy of Orthopaedic Surgeons: OrthoInfo. OrthoInfo Link . Published September 2016.
- Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD. Spondylolysis: A Review and Reappraisal. Hippokratia. 2010;14(1):17-21. PubMed Link .
- Peng B. Natural History of Lumbar Spondylolysis-Advances and Concerns. International Journal of Orthopaedics. 2016;3(4):591-594. International Journal of Orthopaedics .
- Astur DC, Zanatta F, Arliani GG, Moraes ER, Pochini AD, Ejnisman B. Stress Fractures: Definition, Diagnosis and Treatment. Revista Brasileira de Orthopedia. 2016;51(1):3-10. PubMedLink .
- Leahy M. Treating Spondylolysis in the Adolescent Athlete. American Academy of Orthopaedic Surgeons. AAOS Link .
- Spondylolysis: Outlook/Prognosis. Cleveland Clinic. Cleveland Clinic Link . Published October 14, 2014.
- Garet M, Reiman MP, Mathers J, Sylvain J. Nonoperative Treatment in Lumbar Spondylolysis and Spondylolisthesis. Sports Health. 2013;5(3):225-232. PubMed Link
- Panteliadis P, Nagra NS, Edwards KL, Behrbalk E, Boszczyk B. Athletic Population with Spondylolysis: Review of Outcomes Following Surgical Repair or Conservative Management. Global Spine Management. 2016;6(6):615-625. PubMed Link .

IMAGES
VIDEO
COMMENTS
Slipping of a vertebra is caused by the normal wear and tear of aging that affects the spinal discs and joints. The attachments between two adjacent vertebrae become weakened, increasing the chance of slippage. The most common location of degenerative spondylolisthesis is between the fourth and fifth lumbar vertebrae (L4 and L5).
A spinal condition called spondylolisthesis occurs when one vertebra of the spine slips forward over the one beneath it. This vertebra becomes out of alignment with the rest of the spinal column ...
See Isthmic Spondylolisthesis Symptoms. Spondylolisthesis may also occur due to congenital, traumatic, or pathologic (related to bone disease) causes, but isthmic and degenerative causes are more common. ... Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529 ...
In lumbar spondylolisthesis, a vertebrae in the lower back slips forward. This disorder usually occurs during adolescence or young adulthood (often in athletes). It is usually caused by a birth defect or an injury that causes fractures (breaks) in a part of the vertebra. If both sides of the vertebra are involved, the vertebra can then slip ...
Lumbar spondylolisthesis is a condition in which a bone (vertebra) in the lumbar spine (lower back) slips forward out of position onto the bone below it. It may occur as a result of a defect, an injury, degeneration due to aging, or a disease. This illustration of spondylolisthesis shows the vertebra slipping anteriorly, or toward the front of ...
In spondylolisthesis, one bone in your back ( vertebra) slides forward over the bone below it. It most often occurs in the lower spine ( lumbosacral area). In some cases, this may lead to your spinal cord or nerve roots being squeezed. This can cause back pain and numbness or weakness in one or both legs. In rare cases, it can also lead to ...
Spondylolisthesis Symptoms. ... this means that the lumbar spine, or the lower region of your spinal column, ... et al. "Lumbar spondylolisthesis is a risk factor for osteoporotic vertebral ...
Spondylolisthesis is a condition in which one of the vertebrae (bones) in the spine slips out of the proper position onto the vertebra below it. The word spondylolisthesis is derived from the Greek words spondylo, meaning spine, and listhesis, meaning to slip. Spondylolisthesis can occur in both children and adults, for different reasons. The condition varies in severity form
APTA Pelvic Health: Rehabilitation Interventions for Urgency Urinary Incontinence, Urinary Urgency, and/or Urinary Frequency in Adult Women. This guideline summarizes the evidence related to rehabilitation interventions specific to urgency urinary incontinence, urinary urgency, and/or urinary. Diagnosis and Treatment of Degenerative Lumbar ...
In spondylolisthesis, one bone in your back ( vertebra) slides forward over the bone below it. It most often occurs in the lower spine ( lumbosacral area). In some cases, this may lead to your spinal cord or nerve roots being squeezed. This can cause back pain and numbness or weakness in one or both legs. In rare cases, it can also lead to ...
Introduction: Spondylolysis and isthmic spondylolisthesis are commonly implicated as organic causes of low back pain in this population. Many patients involved in sports that require repetitive hyperextension of the lumbar spine like diving, weightlifting, gymnastics and wrestling develop spondylolysis and isthmic spondylolisthesis. While patients are typically asymptomatic in mild forms, the ...
Classification of Spondylolisthesis is based on the degree of slippage in the lumbar spine. Grade 1 is less than 25%, Grade 2 is 25% to 50%, Grade 3 is 50% to 75%, Grade 4 is 75% to 100%, and Spondyloptosis is > 100% [1]. There are many causes of spondylolisthesis including congenital, degenerative, traumatic, pathologic, iatrogenic, and isthmic.
Spondylolisthesis in the lumbar spine is most commonly caused by degenerative spinal disease (degenerative spondylolisthesis), or a defect in one region of a vertebra (isthmic spondylolisthesis). ... SYMPTOMS. Spondylolisthesis doesn't usually have any symptoms. In fact, it is commonly seen on X-rays and CT scans as an 'incidental' finding.
Other spondylolisthesis symptoms include: Pain in the buttocks. Tightness in the lower back and leg muscles. Weakness, muscle spasms and numbness in the extremities. Diagnosis of spondylolisthesis is usually confirmed with a full evaluation including diagnostic imagery like an X-ray, MRI or CT scan. The lateral movement of spondylolisthesis is ...
Lumbosacral spondylolisthesis is the forward translation of the fifth lumbar vertebra (L5) over the first sacral vertebra (S1). Bilateral L5 pars defect (spondylolysis) or repetitive stress injury is the primary etiology behind lumbosacral spondylolisthesis. The degree of a slip often correlates with the degree of symptoms. The prevalence of ...
Review of symptoms and clinical tests for spondylolysis. In kids and teens, spondylolysis is usually the suspected cause of low back pain with or without leg pain. Clinical tests used to identify spondylolysis and spondylolisthesis are: One-legged hyperextension maneuver: In this test, the patient stands on one leg and bends backward. If the ...
Degenerative spondylolisthesis and degenerative scoliosis (curvature of the spine) are two conditions that may be associated with lumbar spinal stenosis. Degenerative spondylolisthesis (slippage of one vertebra over another) is caused by osteoarthritis of the facet joints. Most commonly, it involves the L4 slipping over the L5 vertebra.It is usually treated with the same non-surgical ...
Definition. Lumbar spondylosis is a radiographic diagnosis that refers to degenerative changes of the discs, vertebral bodies and paired zygapophysial joints (z-joints) of the lumbar spine. Degenerative lumbar spondylosis is a term used to describe a "mixed group of spinal bone diseases related to degeneration of the lumbar motion segment and ...
Peer-Reviewed. The L3-L4 spinal motion segment, positioned in the middle of the lumbar spine, plays an important role in supporting the weight of the torso and protecting the cauda equina (nerves that descend from the spinal cord). While the L3-L4 motion segment is less likely to be injured compared to its lower counterparts, it may be subject ...
Hip pain. Pain in your butt (buttocks). Neck pain. Abdominal (stomach) pain. Other ankylosing spondylitis symptoms can include: Stiffness or trouble moving your hips and lower back (especially first thing in the morning or after you've been resting in one position for a long time). Fatigue (feeling tired all the time).
The lumbar region (vertebrae L1-L5) features vertebrae that are much larger to absorb the stress of lifting and carrying heavy objects. Injuries to the lumbar region can result in some loss of function in the hips, legs, and bladder control. The sacral region (vertebrae S1-S5) includes a large bone at the bottom of the spine.
Spondylolysis is a defect or damage via a stress fracture in one of the vertebrae of the spinal column. It commonly affects children or adolescents who are active or frequently participate in sports. Some cases of spondylolysis may be asymptomatic at times. Presenting symptoms include lower back pain, muscle spasms, pain that worsens with ...
R00-R99 - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified ; ... M43.16 Spondylolisthesis, lumbar region. M43.17 Spondylolisthesis, lumbosacral region. M43.18 Spondylolisthesis, sacral and sacrococcygeal region. M43.19 Spondylolisthesis, multiple sites in spine.