
Tumor cells evade the immune system early on: Newly discovered mechanism could significantly improve cancer immunotherapies
Tumors actively prevent the formation of immune responses by so-called cytotoxic T cells, which are essential in combating cancer. Researchers at the Technical University of Munich (TUM) and the Ludwig-Maximilians-Universität München (LMU) Hospital have now uncovered for the first time how this exactly happens. The study in the journal Nature provides rationales for new cancer immunotherapies and could make existing treatments more effective. A second paper in Nature confirms the findings.
In cancer, tumors often impair the body's immune response. For example, they can prevent immune cells from perceiving cancer cells as a threat or render them inactive. Immunotherapies aim to overcome these mechanisms and stimulate the immune system, in particular the T cells. However, such therapies do not work for a large number of cancer patients. Researchers around the world are looking for the causes and new counter-strategies.
Messenger substance stops effector development of T cells in tumors
A team led by Dr. Jan Böttcher, research group leader at the Institute of Molecular Immunology at TUM, and Prof. Sebastian Kobold, Deputy Director of the Department of Clinical Pharmacology at LMU Klinikum München, has now discovered that tumors use a messenger substance to influence immune cells in an early phase of the immune response. Many cancer cells show increased secretion of the messenger substance prostaglandin E2. The researchers were able to show that prostaglandin E2 binds to EP2 and EP4, two receptors on the surface of certain immune cells.
These so-called stem-like T cells migrate from other areas of the body into the tumor. If the immune response is successful, they multiply in the tumor and develop into cytotoxic T cells that attack the cancer. "This whole process is strongly limited when tumors secrete prostaglandin E2 and this factor binds to EP2 and EP4 receptors," says Jan Böttcher. "The T cell response collapses and the tumor can progress." If the researchers prevented the interaction of messenger substance and receptor in tumor models, the immune system was able to fight tumors effectively.
Current therapies address a later point of the immune response
"We have discovered a mechanism that influences the body's immune response in a crucial phase," says Jan Böttcher. "Many tumors prevent the stem-like T cells from generating cytotoxic T cells in the tumor that could attack the cancer."
Current immunotherapies aim to prevent the cancer from switching off immune responses at a later phase. Checkpoint inhibitor therapies, for example, aim to release the blockade of fully differentiated cytotoxic T cells and "switch them back on." Before the dreaded T cell exhaustion sets in, which other researchers are trying to prevent, differentiated T cells must also be present.
Increase the effectiveness of existing therapies
"Current treatment approaches would probably be more effective if the effects of prostaglandin E2 on stem-like T cells is blocked to enable their unhindered differentiation within tumor tissue," says Sebastian Kobold.
This similarly applies to recent approaches that rely on the protein IL-2 to stimulate T cells. The current study shows that as soon as the prostaglandin E2 binds to the two receptors, T cells can no longer respond to IL-2. "We suspect that even the body's own IL-2 signals may be sufficient to enable T cells to successfully fight cancer once the effects of prostaglandin E2 have been stopped," says Sebastian Kobold.
Second study in "Nature" confirms results
A second research publication in Nature investigates the effects of prostaglandin E2 on the immune system. For this study, the authors, researchers from the University Hospital of Lausanne, collaborated with the Munich team. In their laboratory, they among other things examined T cells from human tumor tissue. When they blocked the release of prostaglandin E2 in cancer tissue, the T cells showed better expansion and were thus able to fight human cancer cells more effectively.
Search for counter-strategies begins
"We now have a concrete starting point for significantly improving immunotherapies," says Jan Böttcher. "Researchers around the world must now develop strategies to overcome the tumors' defense. We need to stop the effects of prostaglandin E2 -- either by preventing tumors from producing the molecule or by making immune cells resistant to it."
- Immune System
- Brain Tumor
- Prostate Cancer
- Lung Cancer
- Skin Cancer
- Chemotherapy
- Stem cell treatments
- Colorectal cancer
- Immune system
- Breast cancer
- Prostate cancer
- Mammography
Story Source:
Materials provided by Technical University of Munich (TUM) . Note: Content may be edited for style and length.
Journal References :
- Sebastian B. Lacher, Janina Dörr, Gustavo P. de Almeida, Julian Hönninger, Felix Bayerl, Anna Hirschberger, Anna-Marie Pedde, Philippa Meiser, Lukas Ramsauer, Thomas J. Rudolph, Nadine Spranger, Matteo Morotti, Alizee J. Grimm, Sebastian Jarosch, Arman Oner, Lisa Gregor, Stefanie Lesch, Stefanos Michaelides, Luisa Fertig, Daria Briukhovetska, Lina Majed, Sophia Stock, Dirk H. Busch, Veit R. Buchholz, Percy A. Knolle, Dietmar Zehn, Denarda Dangaj Laniti, Sebastian Kobold, Jan P. Böttcher. PGE2 limits effector expansion of tumour-infiltrating stem-like CD8+ T cells . Nature , 2024; DOI: 10.1038/s41586-024-07254-x
- Matteo Morotti, Alizee J. Grimm, Helen Carrasco Hope, Marion Arnaud, Mathieu Desbuisson, Nicolas Rayroux, David Barras, Maria Masid, Baptiste Murgues, Bovannak S. Chap, Marco Ongaro, Ioanna A. Rota, Catherine Ronet, Aspram Minasyan, Johanna Chiffelle, Sebastian B. Lacher, Sara Bobisse, Clément Murgues, Eleonora Ghisoni, Khaoula Ouchen, Ribal Bou Mjahed, Fabrizio Benedetti, Naoill Abdellaoui, Riccardo Turrini, Philippe O. Gannon, Khalil Zaman, Patrice Mathevet, Loic Lelievre, Isaac Crespo, Marcus Conrad, Gregory Verdeil, Lana E. Kandalaft, Julien Dagher, Jesus Corria-Osorio, Marie-Agnes Doucey, Ping-Chih Ho, Alexandre Harari, Nicola Vannini, Jan P. Böttcher, Denarda Dangaj Laniti, George Coukos. PGE2 inhibits TIL expansion by disrupting IL-2 signalling and mitochondrial function . Nature , 2024; DOI: 10.1038/s41586-024-07352-w
Cite This Page :
Explore More
- Humans and Earth's Deep Subsurface Fluid Flow
- Holographic Displays: An Immersive Future
- Harvesting Energy Where River Meets Sea
- Making Diamonds at Ambient Pressure
- Eruption of Mega-Magnetic Star
- Clean Fuel Generation With Simple Twist
- Bioluminescence in Animals 540 Million Years Ago
- Fossil Frogs Share Their Skincare Secrets
- Fussy Eater? Most Parents Play Short Order Cook
- Precise Time Measurement: Superradiant Atoms
Trending Topics
Strange & offbeat.

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

Cancer research highlights from 2023
Share this:.
By Mayo Clinic staff
Researchers at Mayo Clinic Comprehensive Cancer Center spent 2023 studying the biology of cancer and new ways to predict, prevent, diagnose and treat the disease. Their discoveries are creating hope and transforming the quality of life for people with cancer today and in the future. Here are some highlights from their research over the past year:
Mayo Clinic researchers link ovarian cancer to bacteria colonization in the microbiome.
A specific colonization of microbes in the reproductive tract is commonly found in people with ovarian cancer, according to a study from the Mayo Clinic Center for Individualized Medicine . Published in Scientific Reports and led by Marina Walther-Antonio, Ph.D. , a Mayo Clinic researcher, and Abigail Asangba, Ph.D., the discovery strengthens the evidence that the bacterial component of the microbiome — a community of microorganisms that also consists of viruses, yeasts and fungi — is an important indicator for early detection, diagnosis and prognosis of ovarian cancer . The study also suggests that a higher accumulation of pathogenic microbes plays a role in treatment outcomes and could be a potential indicator for predicting a patient's prognosis and response to therapy. Read more .
Artificial intelligence is forging a new future for colorectal cancer and other digestive system diseases.
Colonoscopy remains the gold standard in detecting and preventing colorectal cancer , but the procedure has limitations. Some studies suggest that more than half of post-colonoscopy colon cancer cases arise from lesions missed at patients' previous colonoscopies. In 2022, Michael Wallace, M.D. , a Mayo Clinic gastroenterologist, published the results of an international, multicenter study testing the impact of adding artificial intelligence (AI) to routine colonoscopies. His team, including James East, M.D. , a Mayo Clinic gastroenterologist, and other researchers from the U.S., the U.K., Italy, Germany and Ireland, found that incorporating AI into colonoscopies reduced the risk of missing polyps by 50%. Read more .
A big step forward: Bringing DNA sequencing data to routine patient care.
The Tapestry study , an extensive genomic sequencing clinical research study, aims to complete exome sequencing (sequencing the protein-coding regions of a genome) for 100,000 Mayo Clinic patients. The results will be integrated into patients’ electronic health records for three hereditary conditions, and the amassed data will contribute to a research dataset stored within the Mayo Clinic Cloud on the Omics Data Platform. The overall hope of Tapestry is to accelerate discoveries in individualized medicine to tailor prevention, diagnosis and treatment to a patient's unique genetic makeup. It is poised to advance evidence that exome sequencing, when applied to a diverse and comprehensive general population, can proficiently identify carriers of genetic variants that put them at higher risk for a disease, allowing them to take preventive measures. Read more .
Patients with multiple tumors in one breast may not need a mastectomy.
Patients who have multiple tumors in one breast may be able to avoid a mastectomy if surgeons can remove the tumors while leaving enough breast tissue, according to research led by the Alliance in Clinical Trials in Oncology and Mayo Clinic Comprehensive Cancer Center . Patients would receive breast-conserving therapy — a lumpectomy followed by whole-breast radiation therapy — rather than mastectomy . The study is published in the Journal of Clinical Oncology . Historically, women with multiple tumors in one breast have been advised to have a mastectomy. Now, patients can be offered a less invasive option with faster recovery, resulting in better patient satisfaction and cosmetic outcomes, says Judy Boughey, M.D. , lead author, Mayo Clinic breast surgical oncologist and the W.H. Odell Professor of Individualized Medicine. Read more .
Staging pancreatic cancer early with minimally invasive surgery shows positive results in patient prognosis.
A study published in the Journal of the American College of Surgeons reveals that performing a minor surgical procedure on patients newly diagnosed with pancreatic cancer helps to identify cancer spread early and determine the stage of cancer. The researchers add that the surgery ideally should be performed before the patient begins chemotherapy. "This is an important study because it supports that staging laparoscopy may help determine a patient's prognosis and better inform treatment so that patients avoid unhelpful or potentially harmful surgical therapy," says Mark Truty, M.D. , a Mayo Clinic surgical oncologist who led the research. Read more .
Mayo Clinic study reveals proton beam therapy may shorten breast cancer treatment.
In a trial published in The Lancet Oncology , Mayo Clinic Comprehensive Cancer Center researchers uncovered evidence supporting a shorter treatment time for people with breast cancer . The study compared two separate dosing schedules of pencil-beam scanning proton therapy , known for its precision in targeting cancer cells while preserving healthy tissue to reduce the risk of side effects. The investigators found that both 25-day and 15-day proton therapy schedules resulted in excellent cancer control while sparing surrounding non-cancerous tissue. Further, complication rates were comparable between the two study groups. "We can now consider the option of 15 days of therapy for patients based on the similar treatment outcomes observed," says Robert Mutter, M.D. , a Mayo Clinic radiation oncologist and physician-scientist. Read more .
Harnessing the immune system to fight ovarian cancer.
Mayo Clinic research is biomanufacturing an experimental, cell-based ovarian cancer vaccine and combining it with immunotherapy to study a "one-two punch" approach to halting ovarian cancer progression. This research begins with a blood draw from people with advanced ovarian cancer whose tumors have returned after standard surgery and chemotherapy. White blood cells are extracted from the blood, biomanufactured to become dendritic cells and returned to the patient. Dendritic cells act as crusaders that march through the body, triggering the immune system to recognize and fight cancer. "We're building on an earlier phase 1 clinical trial that showed promising results in terms of survival after the dendritic cell-based vaccine," says Matthew Block, M.D., Ph.D. , co-principal investigator and Mayo Clinic medical oncologist. "Of the 18 evaluable patients in the phase 1 study, 11 had cancer return, but seven of them — 40% — have been cancer-free for almost 10 years. We typically expect 90% of patients in this condition to have the cancer return." Read more .
New gene markers detect Lynch syndrome-associated colorectal cancer.
Researchers from Mayo Clinic Comprehensive Cancer Center and Mayo Clinic Center for Individualized Medicine have discovered new genetic markers to identify Lynch syndrome-associated colorectal cancer with high accuracy. Studies are underway to determine if these genetic markers are in stool samples and, if so, how this could lead to a non-invasive screening option for people with Lynch syndrome . The research was published in Cancer Prevention Research , a journal of the American Association for Cancer Research. "This is an exciting finding that brings us closer to the reality that clinicians may soon be able to offer a non-invasive cancer screening option to patients with the highest risk of getting cancer," says Jewel Samadder, M.D. , co-lead author of the paper and a Mayo Clinic gastroenterologist. Read more .
Mayo Clinic prepares to biomanufacture a new CAR-T cell therapy for B-cell blood cancers.
Mayo Clinic research has developed a new type of chimeric antigen receptor-T cell therapy (CAR-T cell therapy) aimed at killing B-cell blood cancers that have returned and are no longer responding to treatment. This pioneering technology, designed and developed in the lab of Hong Qin, M.D., Ph.D. , a Mayo Clinic cancer researcher, killed B-cell tumors grown in the laboratory and tumors implanted in mouse models. The preclinical findings are published in Cancer Immunology, Immunotherapy . "This study shows our experimental CAR-T cell therapy targets several blood cancers, specifically chronic lymphocytic leukemia," says Dr. Qin. "Currently, there are six different CAR-T cell therapies approved for treatment of relapsed blood cancers. While the results are impressive, not everyone responds to this treatment. Our goal is to provide novel cell therapies shaped to each patient's individual need." Read more .
Related Posts

Richard Vile, Ph.D., is leading research into genetically engineered viruses called oncolytic viruses for cancer treatment at Mayo Clinic.

After receiving CAR-T cell therapy at Mayo Clinic, Welsh-born John Cadwallader achieved remission and found new hope. He now receives care in the U.K. and is monitored by Mayo in the U.S. and London.

After undergoing genetic screening as part of a research study, Tammy LeDoux learned she had Lynch syndrome, which put her at high risk of cancer.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cancer Control
- v.28; Jan-Dec 2021
Cancer Biology, Epidemiology, and Treatment in the 21st Century: Current Status and Future Challenges From a Biomedical Perspective
Patricia piña-sánchez.
1 Oncology Research Unit, Oncology Hospital, Mexican Institute of Social Security, Mexico
Antonieta Chávez-González
Martha ruiz-tachiquín, eduardo vadillo, alberto monroy-garcía, juan josé montesinos, rocío grajales.
2 Department of Medical Oncology, Oncology Hospital, Mexican Institute of Social Security, Mexico
Marcos Gutiérrez de la Barrera
3 Clinical Research Division, Oncology Hospital, Mexican Institute of Social Security, Mexico
Hector Mayani
Since the second half of the 20th century, our knowledge about the biology of cancer has made extraordinary progress. Today, we understand cancer at the genomic and epigenomic levels, and we have identified the cell that starts neoplastic transformation and characterized the mechanisms for the invasion of other tissues. This knowledge has allowed novel drugs to be designed that act on specific molecular targets, the immune system to be trained and manipulated to increase its efficiency, and ever more effective therapeutic strategies to be developed. Nevertheless, we are still far from winning the war against cancer, and thus biomedical research in oncology must continue to be a global priority. Likewise, there is a need to reduce unequal access to medical services and improve prevention programs, especially in countries with a low human development index.
Introduction
During the last one hundred years, our understanding of the biology of cancer increased in an extraordinary way. 1 - 4 Such a progress has been particularly prompted during the last few decades because of technological and conceptual progress in a variety of fields, including massive next-generation sequencing, inclusion of “omic” sciences, high-resolution microscopy, molecular immunology, flow cytometry, analysis and sequencing of individual cells, new cell culture techniques, and the development of animal models, among others. Nevertheless, there are many questions yet to be answered and many problems to be solved regarding this disease. As a consequence, oncological research must be considered imperative.
Currently, cancer is one of the illnesses that causes more deaths worldwide. 5 According to data reported in 2020 by the World Health Organization (WHO), cancer is the second cause of death throughout the world, with 10 million deaths. 6 Clearly, cancer is still a leading problem worldwide. With this in mind, the objective of this article is to present a multidisciplinary and comprehensive overview of the disease. We will begin by analyzing cancer as a process, focusing on the current state of our knowledge on 4 specific aspects of its biology. Then, we will look at cancer as a global health problem, considering some epidemiological aspects, and discussing treatment, with a special focus on novel therapies. Finally, we present our vision on some of the challenges and perspectives of cancer in the 21 st century.
The Biology of Cancer
Cancer is a disease that begins with genetic and epigenetic alterations occurring in specific cells, some of which can spread and migrate to other tissues. 4 Although the biological processes affected in carcinogenesis and the evolution of neoplasms are many and widely different, we will focus on 4 aspects that are particularly relevant in tumor biology: genomic and epigenomic alterations that lead to cell transformation, the cells where these changes occur, and the processes of invasion and metastasis that, to an important degree, determine tumor aggressiveness.
Cancer Genomics
The genomics of cancer can be defined as the study of the complete sequence of DNA and its expression in tumor cells. Evidently, this study only becomes meaningful when compared to normal cells. The sequencing of the human genome, completed in 2003, was not only groundbreaking with respect to the knowledge of our gene pool, but also changed the way we study cancer. In the post-genomic era, various worldwide endeavors, such as the Human Cancer Genome Project , the Cancer Genome ATLAS (TCGA), the International Cancer Genome Consortium, and the Pan-Cancer Analysis Working Group (PCAWG), have contributed to the characterization of thousands of primary tumors from different neoplasias, generating more than 2.5 petabytes (10 15 ) of genomic, epigenomic, and proteomic information. This has led to the building of databases and analytical tools that are available for the study of cancer from an “omic” perspective, 7 , 8 and it has helped to modify classification and treatment of various neoplasms.
Studies in the past decade, including the work by the PCAWG, have shown that cancer generally begins with a small number of driving mutations (4 or 5 mutations) in particular genes, including oncogenes and tumor-suppressor genes. Mutations in TP53, a tumor-suppressor gene, for example, are found in more than half of all cancer types as an early event, and they are a hallmark of precancerous lesions. 9 - 12 From that point on, the evolution of tumors may take decades, throughout which the mutational spectrum of tumor cells changes significantly. Mutational analysis of more than 19 000 exomes revealed a collection of genomic signatures, some associated with defects in the mechanism of DNA repair. These studies also revealed the importance of alterations in non-coding regions of DNA. Thus, for example, it has been observed that various pathways of cell proliferation and chromatin remodeling are altered by mutations in coding regions, while pathways, such as WNT and NOTCH, can be disrupted by coding and non-coding mutations. To the present date, 19 955 genes that codify for proteins and 25 511 genes for non-coding RNAs have been identified ( https://www.gencodegenes.org/human/stats.html ). Based on this genomic catalogue, the COSMIC (Catalogue Of Somatic Mutations In Cancer) repository, the most robust database to date, has registered 37 288 077 coding mutations, 19 396 fusions, 1 207 190 copy number variants, and 15 642 672 non-coding variants reported up to August 2020 (v92) ( https://cosmic-blog.sanger.ac.uk/cosmic-release-v92/ ).
The genomic approach has accelerated the development of new cancer drugs. Indeed, two of the most relevant initiatives in recent years are ATOM (Accelerating Therapeutics for Opportunities in Medicine), which groups industry, government and academia, with the objective of accelerating the identification of drugs, 13 and the Connectivity Map (CMAP), a collection of transcriptional data obtained from cell lines treated with drugs for the discovery of functional connections between genes, diseases, and drugs. The CMAP 1.0 covered 1300 small molecules and more than 6000 signatures; meanwhile, the CMAP 2.0 with L1000 assay profiled more than 1.3 million samples and approximately 400 000 signatures. 14
The genomic study of tumors has had 2 fundamental contributions. On the one hand, it has allowed the confirmation and expansion of the concept of intratumor heterogeneity 15 , 16 ; and on the other, it has given rise to new classification systems for cancer. Based on the molecular classification developed by expression profiles, together with mutational and epigenomic profiles, a variety of molecular signatures have been identified, leading to the production of various commercial multigene panels. In breast cancer, for example, different panels have been developed, such as Pam50/Prosigna , Blue Print , OncotypeDX , MammaPrint , Prosigna , Endopredict , Breast Cancer Index , Mammostrat, and IHC4 . 17
Currently, the genomic/molecular study of cancer is more closely integrated with clinical practice, from the classification of neoplasms, as in tumors of the nervous system, 18 to its use in prediction, as in breast cancer. 17 Improvement in molecular methods and techniques has allowed the use of smaller amounts of biological material, as well as paraffin-embedded samples for genomic studies, both of which provide a wealth of information. 19 In addition, non-invasive methods, such as liquid biopsies, represent a great opportunity not only for the diagnosis of cancer, but also for follow-up, especially for unresectable tumors. 20
Research for the production of genomic information on cancer is presently dominated by several consortia, which has allowed the generation of a great quantity of data. However, most of these consortia and studies are performed in countries with a high human development index (HDI), and countries with a low HDI are not well represented in these large genomic studies. This is why initiatives such as Human Heredity and Health in Africa (H3Africa) for genomic research in Africa are essential. 21 Generation of new information and technological developments, such as third-generation sequencing, will undoubtedly continue to move forward in a multidisciplinary and complex systems context. However, the existing disparities in access to genomic tools for diagnosis, prognosis, and treatment of cancer will continue to be a pressing challenge at regional and social levels.
Cancer Epigenetics
Epigenetics studies the molecular mechanisms that produce hereditable changes in gene expression, without causing alterations in the DNA sequence. Epigenetic events are of 3 types: methylation of DNA and RNA, histone modification (acetylation, methylation, and phosphorylation), and the expression of non-coding RNA. Epigenetic aberrations can drive carcinogenesis when they alter chromosome conformation and the access to transcriptional machinery and to various regulatory elements (promoters, enhancers, and anchors for interaction with chromatin, for example). These changes may activate oncogenesis and silence tumor-suppressor mechanisms when they modulate coding and non-coding sequences (such as micro-RNAs and long-RNAs). This can then lead to uncontrolled growth, as well as the invasion and metastasis of cancer cells.
While genetic mutations are stable and irreversible, epigenetic alterations are dynamic and reversible; that is, there are several epigenomes, determined by space and time, which cause heterogeneity of the “epigenetic status” of tumors during their development and make them susceptible to environmental stimuli or chemotherapeutic treatment. 22 Epigenomic variability creates differences between cells, and this creates the need to analyze cells at the individual level. In the past, epigenetic analyses measured “average states” of cell populations. These studies revealed general mechanisms, such as the role of epigenetic marks on active or repressed transcriptional states, and established maps of epigenetic composition in a variety of cell types in normal and cancerous tissue. However, these approaches are difficult to use to examine events occurring in heterogeneous cell populations or in uncommon cell types. This has led to the development of new techniques that permit marking of a sequence on the epigenome and improvement in the recovery yield of epigenetic material from individual cells. This has helped to determine changes in DNA, RNA, and histones, chromatin accessibility, and chromosome conformation in a variety of neoplasms. 23 , 24
In cancer, DNA hypomethylation occurs on a global scale, while hypermethylation occurs in specific genomic loci, associated with abnormal nucleosome positioning and chromatin modifications. This information has allowed epigenomic profiles to be established in different types of neoplasms. In turn, these profiles have served as the basis to identify new neoplasm subgroups. For example, in triple negative breast cancer (TNBC), 25 and in hepatocellular carcinoma, 26 DNA methylation profiles have helped to the identification of distinct subgroups with clinical relevance. Epigenetic approaches have also helped to the development of prognostic tests to assess the sensitivity of cancer cells to specific drugs. 27
Epigenetic traits could be used to characterize intratumoral heterogeneity and determine the relevance of such a heterogeneity in clonal evolution and sensitivity to drugs. However, it is clear that heterogeneity is not only determined by genetic and epigenetic diversity resulting from clonal evolution of tumor cells, but also by the various cell populations that form the tumor microenvironment (TME). 28 Consequently, the epigenome of cancer cells is continually remodeled throughout tumorigenesis, during resistance to the activity of drugs, and in metastasis. 29 This makes therapeutic action based on epigenomic profiles difficult, although significant advances in this area have been reported. 30
During carcinogenesis and tumor progression, epigenetic modifications are categorized by their mechanisms of regulation ( Figure 1A ) and the various levels of structural complexity ( Figure 1B ). In addition, the epigenome can be modified by environmental stimuli, stochastic events, and genetic variations that impact the phenotype ( Figure 1C ). 31 , 32 The molecules that take part in these mechanisms/events/variations are therapeutic targets of interest with potential impact on clinical practice. There are studies on a wide variety of epidrugs, either alone or in combination, which improve antitumor efficacy. 33 However, the problems with these drugs must not be underestimated. For a considerable number of epigenetic compounds still being under study, the main challenge is to translate in vitro efficacy of nanomolar (nM) concentrations into well-tolerated and efficient clinical use. 34 The mechanisms of action of epidrugs may not be sufficiently controlled and could lead to diversion of the therapeutic target. 35 It is known that certain epidrugs, such as valproic acid, produce unwanted epigenetic changes 36 ; thus the need for a well-established safety profile before these drugs can be used in clinical therapy. Finally, resistance to certain epidrugs is another relevant problem. 37 , 38

Epigenetics of cancer. (A) Molecular mechanisms. (B) Structural hierarchy of epigenomics. (C) Factors affecting the epigenome. Modified from Refs. 31 and 32 .
As we learn about the epigenome of specific cell populations in cancer patients, a door opens to the evaluation of sensitivity tests and the search for new molecular markers for detection, prognosis, follow-up, and/or response to treatment at various levels of molecular regulation. Likewise, the horizon expands for therapeutic alternatives in oncology with the use of epidrugs, such as pharmacoepigenomic modulators for genes and key pathways, including methylation of promoters and regulation of micro-RNAs involved in chemoresponse and immune response in cancer. 39 There is no doubt that integrated approaches identifying stable pharmagenomic and epigenomic patterns and their relation with expression profiles and genetic functions will be more and more valuable in our fight against cancer.
Cancer Stem Cells
Tumors consist of different populations of neoplastic cells and a variety of elements that form part of the TME, including stromal cells and molecules of the extracellular matrix. 40 Such intratumoral heterogeneity becomes even more complex during clonal variation of transformed cells, as well as influence the elements of the TME have on these cells throughout specific times and places. 41 To explain the origin of cancer cell heterogeneity, 2 models have been put forward. The first proposes that mutations occur at random during development of the tumor in individual neoplastic cells, and this promotes the production of various tumor populations, which acquire specific growth and survival traits that lead them to evolve according to intratumor mechanisms of natural selection. 42 The second model proposes that each tumor begins as a single cell that possess 2 functional properties: it can self-renew and it can produce several types of terminal cells. As these 2 properties are characteristics of somatic stem cells, 43 the cells have been called cancer stem cells (CSCs). 44 According to this model, tumors must have a hierarchical organization, where self-renewing stem cells produce highly proliferating progenitor cells, unable to self-renew but with a high proliferation potential. The latter, in turn, give rise to terminal cells. 45 Current evidence indicates that both models may coexist in tumor progression. In agreement with this idea, new subclones could be produced as a result of a lack of genetic stability and mutational changes, in addition to the heterogeneity derived from the initial CSC and its descendants. Thus, in each tumor, a set of neoplastic cells with different genetic and epigenetic traits may be found, which would provide different phenotypic properties. 46
The CSC concept was originally presented in a model of acute myeloid leukemia. 47 The presence of CSCs was later proved in chronic myeloid leukemia, breast cancer, tumors of the central nervous system, lung cancer, colon cancer, liver cancer, prostate cancer, pancreatic cancer, melanoma, and cancer of the head and neck, amongst others. In all of these cases, detection of CSCs was based on separation of several cell populations according to expression of specific surface markers, such as CD133, CD44, CD24, CD117, and CD15. 48 It is noteworthy that in some solid tumors, and even in some hematopoietic ones, a combination of specific markers that allow the isolation of CSCs has not been found. Interestingly, in such tumors, a high percentage of cells with the capacity to start secondary tumors has been observed; thus, the terms Tumor Initiating Cells (TIC) or Leukemia Initiating Cells (LIC) have been adopted. 46
A relevant aspect of the biology of CSCs is that, just like normal stem cells, they can self-renew. Such self-renewal guarantees the maintenance or expansion of the tumor stem cell population. Another trait CSCs share with normal stem cells is their quiescence, first described in chronic myeloid leukemia. 49 The persistence of quiescent CSCs in solid tumors has been recently described in colorectal cancer, where quiescent clones can become dominant after therapy with oxaliplatin. 50 In non-hierarchical tumors, such as melanoma, the existence of slow-cycling cells that are resistant to antimitogenic agents has also been proved. 51 Such experimental evidence supports the idea that quiescent CSCs or TICs are responsible for both tumor resistance to antineoplastic drugs and clinical relapse after initial therapeutic success.
In addition to quiescence, CSCs use other mechanisms to resist the action of chemotherapeutic drugs. One of these is their increased numbers: upon diagnosis, a high number of CSCs are observed in most analyzed tumors, making treatment unable to destroy all of them. On the other hand, CSCs have a high number of molecular pumps that expulse drugs, as well as high numbers of antiapoptotic molecules. In addition, they have very efficient mechanisms to repair DNA damage. In general, these cells show changes in a variety of signaling pathways involved in proliferation, survival, differentiation, and self-renewal. It is worth highlighting that in recent years, many of these pathways have become potential therapeutic targets in the elimination of CSCs. 52 Another aspect that is highly relevant in understanding the biological behavior of CSCs is that they require a specific site for their development within the tissue where they are found that can provide whatever is needed for their survival and growth. These sites, known as niches, are made of various cells, both tumor and non-tumor, as well as a variety of non-cellular elements (extracellular matrix [ECM], soluble cytokines, ion concentration gradients, etc.), capable of regulating the physiology of CSCs in order to promote their expansion, the invasion of adjacent tissues, and metastasis. 53
It is important to consider that although a large number of surface markers have been identified that allow us to enrich and prospectively follow tumor stem cell populations, to this day there is no combination of markers that allows us to find these populations in all tumors, and it is yet unclear if all tumors present them. In this regard, it is necessary to develop new purification strategies based on the gene expression profiles of these cells, so that tumor heterogeneity is taken into account, as it is evident that a tumor can include multiple clones of CSCs that, in spite of being functional, are genetically different, and that these clones can vary throughout space (occupying different microenvironments and niches) and time (during the progression of a range of tumor stages). Such strategies, in addition to new in vitro and in vivo assays, will allow the development of new and improved CSC elimination strategies. This will certainly have an impact on the development of more efficient therapeutic alternatives.
Invasion and Metastasis
Nearly 90% of the mortality associated with cancer is related to metastasis. 54 This consists of a cascade of events ( Figure 2 ) that begins with the local invasion of a tumor into surrounding tissues, followed by intravasation of tumor cells into the blood stream or lymphatic circulation. Extravasation of neoplastic cells in areas distant from the primary tumor then leads to the formation of one or more micrometastatic lesions which subsequently proliferate to form clinically detectable lesions. 4 The cells that are able to produce metastasis must acquire migratory characteristics, which occur by a process known as epithelial–mesenchymal transition (EMT), that is, the partial loss of epithelial characteristics and the acquirement of mesenchymal traits. 55

Invasion and metastasis cascade. Invasion and metastasis can occur early or late during tumor progression. In either case, invasion to adjacent tissues is driven by stem-like cells (cancer stem cells) that acquire the epithelial–mesenchymal transition (EMT) (1). Once they reach sites adjacent to blood vessels, tumor cells (individually or in clusters) enter the blood (2). Tumor cells in circulation can adhere to endothelium and extravasation takes place (3). Other mechanisms alternative to extravasation can exist, such as angiopelosis, in which clusters of tumor cells are internalized by the endothelium. Furthermore, at certain sites, tumor cells can obstruct microvasculature and initiate a metastatic lesion right there. Sometimes, a tumor cells that has just exit circulation goes into an MET in order to become quiescent (4). Inflammatory signals can activate quiescent metastatic cells that will proliferate and generate a clinically detectable lesion (5).
Although several of the factors involved in this process are currently known, many issues are still unsolved. For instance, it has not yet been possible to monitor in vivo the specific moment when it occurs 54 ; the microenvironmental factors of the primary tumor that promote such a transition are not known with precision; and the exact moment during tumor evolution in which one cell or a cluster of cells begin to migrate to distant areas, is also unknown. The wide range of possibilities offered by intra- and inter-tumoral heterogeneity 56 stands in the way of suggesting a generalized strategy that could resolve this complication.
It was previously believed that metastasis was only produced in late stages of tumor progression; however, recent studies indicate that EMT and metastasis can occur during the early course of the disease. In pancreatic cancer, for example, cells going through EMT are able to colonize and form metastatic lesions in the liver in the first stages of the disease. 52 , 57 Metastatic cell clusters circulating in peripheral blood (PB) are prone to generate a metastatic site, compared to individual tumor cells. 58 , 59 In this regard, novel strategies, such as the use of micro-RNAs, are being assessed in order to diminish induction of EMT. 60 It must be mentioned, however, that the metastatic process seems to be even more complex, with alternative pathways that do not involve EMT. 61 , 62
A crucial stage in the process of metastasis is the intravasation of tumor cells (alone or in clusters) towards the blood stream and/or lymphatic circulation. 63 These mechanisms are also under intensive research because blocking them could allow the control of spreading of the primary tumor. In PB or lymphatic circulation, tumor cells travel to distant parts for the potential formation of a metastatic lesion. During their journey, these cells must stand the pressure of blood flow and escape interaction with natural killer (NK) cells . 64 To avoid them, tumor cells often cover themselves with thrombocytes and also produce factors such as VEGF, angiopoietin-2, angiopoietin-4, and CCL2 that are involved in the induction of vascular permeability. 54 , 65 Neutrophils also contribute to lung metastasis in the bloodstream by secreting IL-1β and metalloproteases to facilitate extravasation of tumor cells. 64
The next step in the process of metastasis is extravasation, for which tumor cells, alone or in clusters, can use various mechanisms, including a recently described process known as angiopellosis that involves restructuring the endothelial barrier to internalize one or several cells into a tissue. 66 The study of leukocyte extravasation has contributed to a more detailed knowledge of this process, in such a way that some of the proposed strategies to avoid extravasation include the use of integrin inhibitors, molecules that are vital for rolling, adhesion, and extravasation of tumor cells. 67 , 68 Another strategy that has therapeutic potential is the use of antibodies that strengthen vascular integrity to obstruct transendothelial migration of tumor cells and aid in their destruction in PB. 69
Following extravasation, tumor cells can return to an epithelial phenotype, a process known as mesenchymal–epithelial transition and may remain inactive for several years. They do this by competing for specialized niches, like those in the bone marrow, brain, and intestinal mucosa, which provide signals through the Notch and Wnt pathways. 70 Through the action of the Wnt pathway, tumor cells enter a slow state of the cell cycle and induce the expression of molecules that inhibit the cytotoxic function of NK cells. 71 The extravasated tumor cell that is in a quiescent state must comply with 2 traits typical of stem cells: they must have the capacity to self-renew and to generate all of the cells that form the secondary tumor.
There are still several questions regarding the metastatic process. One of the persisting debates at present is if EMT is essential for metastasis or if it plays a more important role in chemoresistance. 61 , 62 It is equally important to know if there is a pattern in each tumor for the production of cells with the capacity to carry out EMT. In order to control metastasis, it is fundamental to know what triggers acquisition of the migratory phenotype and the intrinsic factors determining this transition. Furthermore, it is essential to know if mutations associated with the primary tumor or the variety of epigenetic changes are involved in this process. 55 It is clear that metastatic cells have affinity for certain tissues, depending on the nature of the primary tumor (seed and soil hypothesis). This may be caused by factors such as the location and the direction of the bloodstream or lymphatic fluid, but also by conditioning of premetastatic niches at a distance (due to the large number of soluble factors secreted by the tumor and the recruitment of cells of the immune system to those sites). 72 We have yet to identify and characterize all of the elements that participate in this process. Deciphering them will be of upmost importance from a therapeutic point of view.
Epidemiology of Cancer
Cancer is the second cause of death worldwide; today one of every 6 deaths is due to a type of cancer. According to the International Agency for Research on Cancer (IARC), in 2020 there were approximately 19.3 million new cases of cancer, and 10 million deaths by this disease, 6 while 23.8 million cases and 13.0 million deaths are projected to occur by 2030. 73 In this regard, it is clear the increasing role that environmental factors—including environmental pollutants and processed food—play as cancer inducers and promoters. 74 The types of cancer that produce the greatest numbers of cases and deaths worldwide are indicated in Table 1 . 6
Total Numbers of Cancer Cases and Deaths Worldwide in 2020 by Cancer Type (According to the Global Cancer Observatory, IARC).
Data presented on this table were obtained from Ref. 6.
As shown in Figure 3 , lung, breast, prostate, and colorectal cancer are the most common throughout the world, and they are mostly concentrated in countries of high to very high human development index (HDI). Although breast, prostate, and colorectal cancer have a high incidence, the number of deaths they cause is proportionally low, mostly reflecting the great progress made in their control. However, these data also reveal the types of cancer that require further effort in prevention, precise early detection avoiding overdiagnosis, and efficient treatment. This is the case of liver, lung, esophageal, and pancreatic cancer, where the difference between the number of cases and deaths is smaller ( Figure 3B ). Social and economic transition in several countries has had an impact on reducing the incidence of neoplasms associated with infection and simultaneously produced an increase in the types related to reproductive, dietary, and hormonal factors. 75

Incidence and mortality for some types of cancer in the world. (A) Estimated number of cases and deaths in 2020 for the most frequent cancer types worldwide. (B) Incidence and mortality rates, normalized according to age, for the most frequent cancer types in countries with very high/& high (VH&H; blue) and/low and middle (L&M; red) Human Development Index (HDI). Data include both genders and all ages. Data according to https://gco.iarc.fr/today , as of June 10, 2021.
In the past 3 decades, cancer mortality rates have fallen in high HDI countries, with the exception of pancreatic cancer, and lung cancer in women. Nevertheless, changes in the incidence of cancer do not show the same consistency, possibly due to variables such as the possibility of early detection, exposure to risk factors, or genetic predisposition. 76 , 77 Countries such as Australia, Canada, Denmark, Ireland, New Zealand, Norway, and the United Kingdom have reported a reduction in incidence and mortality in cancer of the stomach, colon, lung, and ovary, as well as an increase in survival. 78 Changes in modifiable risk factors, such as the use of tobacco, have played an important role in prevention. In this respect, it has been estimated that decline in tobacco use can explain between 35% and 45% of the reduction in cancer mortality rates, 79 while the fall in incidence and mortality due to stomach cancer can be attributed partly to the control of Helicobacter pylori infection. 80 Another key factor in the fall of mortality rates in developed countries has been an increase in early detection as a result of screening programs, as in breast and prostate cancer, which have had their mortality rates decreased dramatically in spite of an increase in their incidence. 76
Another important improvement observed in recent decades is the increase in survival rates, particularly in high HDI countries. In the USA, for example, survival rates for patients with prostate cancer at 5 years after initial diagnosis was 28% during 1947–1951; 69% during 1975–1977, and 100% during 2003–2009. Something similar occurred with breast cancer, with a 5-year survival rate of 54% in 1947–1951, 75% in 1975–1977, and 90% in 2003–2009. 81 In the CONCORD 3 version, age-standardize 5-year survival for patients with breast cancer in the USA during 2010–2014 was 90%, and 97% for prostate cancer patients. 82 Importantly, even among high HDI countries, significant differences have been identified in survival rates, being stage of disease at diagnosis, time for access to effective treatment, and comorbidities, the main factors influencing survival in these nations. 78 Unfortunately, survival rates in low HDI countries are significantly lower due to several factors, including lack of information, deficient screening and early detection programs, limited access to treatment, and suboptimal cancer registration. 82 It should be noted that in countries with low to middle HDI, neoplasms with the greatest incidence are those affecting women (breast and cervical cancer), which reflects not only a problem with access to health services, but also a serious inequality issue that involves social, cultural, and even religious obstacles. 83
Up to 42% of incident cases and 47% of deaths by cancer in the USA are due to potentially modifiable risk factors such as use of tobacco, physical activity, diet, and infection. 84 It has been calculated that 2.4 million deaths by cancer, mostly of the lung, can be attributed to tobacco. 73 In 2020, the incidence rate of lung cancer in Western Africa was 2.2, whereas in Polynesia and Eastern Asia was 37.3 and 34.4, respectively. 6 In contrast, the global burden of cancer associated with infection was 15.4%, but in Sub-Saharan Africa it was 30%. 85 Likewise, the incidence of cervical cancer in Eastern Africa was 40.1, in contrast with the USA and Canada that have a rate of 6.2. This makes it clear that one of the challenges we face is the reduction of the risk factors that are potentially modifiable and associated with specific types of cancer.
Improvement of survival rates and its disparities worldwide are also important challenges. Five-year survival for breast cancer—diagnosed during 2010-2014— in the USA, for example, was 90%, whereas in countries like South Africa it was 40%. 82 Childhood leukemia in the USA and several European countries shows a 5-year survival of 90%, while in Latin-American countries it is 50–76%. 86 Interestingly, there are neoplasms, such as pancreatic cancer, for which there has been no significant increase in survival, which remains low (5–15%) both in developed and developing countries. 82
Although data reported on global incidence and mortality gives a general overview on the epidemiology of cancer, it is important to note that there are great differences in coverage of cancer registries worldwide. To date, only 1 out of every 3 countries reports high quality data on the incidence of cancer. 87 For the past 50 years, the IARC has supported population-based cancer registries; however, more than one-third of the countries belonging to the WHO, mainly countries of low and middle income (LMIC), have no data on more than half of the 18 indicators of sustainable development goals. 88 High quality cancer registries only cover 4% of the population in Africa, 8% in Asia, and 7% in Latin America, contrasting with 83% in the USA and Canada, and 33% in Europe. 89 In response to this situation, the Global Initiative for Cancer Registry Development was created in 2012 to generate improved infrastructure to permit greater coverage and better quality registries, especially in countries with low and middle HDI. 88 It is expected that initiatives of this sort in the coming years will allow more and better information to guide strategies for the control of cancer worldwide, especially in developing regions. This will enable survival to be measured over longer periods of time (10, 15, or 20 years), as an effective measure in the control of cancer. The WHO has established as a target for 2025 to reduce deaths by cancer and other non-transmissible diseases by 25% in the population between the ages of 30–69; such an effort requires not only effective prevention measures to reduce incidence, but also more efficient health systems to diminish mortality and increase survival. At the moment, it is an even greater challenge because of the effects of the COVID-19 pandemic which has negatively impacted cancer prevention and health services. 90
Oncologic Treatments
A general perspective.
At the beginning of the 20th century, cancer treatment, specifically treatment of solid tumors, was based fundamentally on surgical resection of tumors, which together with other methods for local control, such as cauterization, had been used since ancient times. 91 At that time, there was an ongoing burst of clinical observations along with interventions sustained on fundamental knowledge about physics, chemistry, and biology. In the final years of the 19 th century and the first half of the 20th, these technological developments gave rise to radiotherapy, hormone therapy, and chemotherapy. 92 - 94 Simultaneously, immunotherapy was also developed, although usually on a smaller scale, in light of the overwhelming progress of chemotherapy and radiotherapy. 95
Thus began the development and expansion of disciplines based on these approaches (surgery, radiotherapy, chemotherapy, hormone therapy, and immunotherapy), with their application evolving ever more rapidly up to their current uses. Today, there is a wide range of therapeutic tools for the care of cancer patients. These include elements that emerged empirically, arising from observations of their effects in various medical fields, as well as drugs that were designed to block processes and pathways that form part of the physiopathology of one or more neoplasms according to knowledge of specific molecular alterations. A classic example of the first sort of tool is mustard gas, originally used as a weapon in war, 96 but when applied for medical purposes, marked the beginning of the use of chemicals in the treatment of malignant neoplasms, that is, chemotherapy. 94 A clear example of the second case is imatinib, designed specifically to selectively inhibit a molecular alteration in chronic myeloid leukemia: the Bcr-Abl oncoprotein. 97
It is on this foundation that today the 5 areas mentioned previously coexist and complement one another. The general framework that motivates this amalgam and guides its development is precision medicine, founded on the interaction of basic and clinical science. In the forecasts for development in each of these fields, surgery is expected to continue to be the fundamental approach for primary tumors in the foreseeable future, as well as when neoplastic disease in the patient is limited, or can be limited by applying systemic or regional elements, before and/or after surgical resection, and it can be reasonably anticipated for the patient to have a significant period free from disease or even to be cured. With regards to technology, intensive exploration of robotic surgery is contemplated. 98
The technological possibilities for radiotherapy have progressed in such a way that it is now possible to radiate neoplastic tissue with an extraordinary level of precision, and therefore avoid damage to healthy tissue. 99 This allows administration of large doses of ionizing radiation in one or a few fractions, what is known as “radiosurgery.” The greatest challenges to the efficacy of this approach are related to radio-resistance in certain neoplasms. Most efforts regarding research in this field are concentrated on understanding the underlying biological mechanisms of the phenomenon and their potential control through radiosensitizers. 100
“Traditional” chemotherapy, based on the use of compounds obtained from plants and other natural products, acting in a non-specific manner on both neoplastic and healthy tissues with a high proliferation rate, continues to prevail. 101 The family of chemotherapeutic drugs currently includes alkylating agents, antimetabolites, anti-topoisomerase agents, and anti-microtubules. Within the pharmacologic perspective, the objective is to attain a high concentration or activity of such molecules in specific tissues while avoiding their accumulation in others, in order to achieve an increase in effectiveness and a reduction in toxicity. This has been possible with the use of viral vectors, for example, that are able to limit their replication in neoplastic tissues, and activate prodrugs of normally nonspecific agents, like cyclophosphamide, exclusively in those specific areas. 102 More broadly, chemotherapy also includes a subgroup of substances, known as molecular targeted therapy, that affect processes in a more direct and specific manner, which will be mentioned later.
There is no doubt that immunotherapy—to be explored next—is one of the therapeutic fields where development has been greatest in recent decades and one that has produced enormous expectation in cancer treatment. 103 Likewise, cell therapy, based on the use of immune cells or stem cells, has come to complement the oncologic therapeutic arsenal. 43 Each and every one of the therapeutic fields that have arisen in oncology to this day continue to prevail and evolve. Interestingly, the foreseeable future for the development of cancer treatment contemplates these approaches in a joint and complementary manner, within the general framework of precision medicine, 104 and sustained by knowledge of the biological mechanisms involved in the appearance and progression of neoplasms. 105 , 106
Immunotherapy
Stimulating the immune system to treat cancer patients has been a historical objective in the field of oncology. Since the early work of William Coley 107 to the achievements reached at the end of the 20 th century, scientific findings and technological developments paved the way to searching for new immunotherapeutic strategies. Recombinant DNA technology allowed the synthesis of cytokines, such as interferon-alpha (IFN-α) and interleukin 2 (IL-2), which were authorized by the US Food and Drug Administration (FDA) for the treatment of hairy cell leukemia in 1986, 108 as well as kidney cancer and metastatic melanoma in 1992 and 1998, respectively. 109
The first therapeutic vaccine against cancer, based on the use of autologous dendritic cells (DCs), was approved by the FDA against prostate cancer in 2010. However, progress in the field of immunotherapy against cancer was stalled in the first decade of the present century, mostly due to failure of several vaccines in clinical trials. In many cases, application of these vaccines was detained by the complexity and cost involved in their production. Nevertheless, with the coming of the concept of immune checkpoint control, and the demonstration of the relevance of molecules such as cytotoxic T-lymphocyte antigen 4 (CTLA-4), and programmed cell death molecule-1 (PD-1), immunotherapy against cancer recovered its global relevance. In 2011, the monoclonal antibody (mAb) ipilimumab, specific to the CTLA-4 molecule, was the first checkpoint inhibitor (CPI) approved for the treatment of advanced melanoma. 110 Later, inhibitory mAbs for PD-1, or for the PD-1 ligand (PD-L1), 111 as well as the production of T cells with chimeric receptors for antigen recognition (CAR-T), 112 which have been approved to treat various types of cancer, including melanoma, non-small cell lung cancer (NSCLC), head and neck cancer, bladder cancer, renal cell carcinoma (RCC), and hepatocellular carcinoma, among others, have changed the paradigm of cancer treatment.
In spite of the current use of anti-CTLA-4 and anti-PD-L1 mAbs, only a subgroup of patients has responded favorably to these CPIs, and the number of patients achieving clinical benefit is still small. It has been estimated that more than 70% of patients with solid tumors do not respond to CPI immunotherapy because either they show primary resistance, or after responding favorably, develop resistance to treatment. 113 In this regard, it is important to mention that in recent years very important steps have been taken to identify the intrinsic and extrinsic mechanisms that mediate resistance to CPI immunotherapy. 114 Intrinsic mechanisms include changes in the antitumor immune response pathways, such as faulty processing and presentation of antigens by APCs, activation of T cells for tumor cell destruction, and changes in tumor cells that lead to an immunosuppressive TME. Extrinsic factors include the presence of immunosuppressive cells in the local TME, such as regulatory T cells, myeloid-derived suppressor cells (MDSC), mesenchymal stem/stromal cells (MSCs), and type 2 macrophages (M2), in addition to immunosuppressive cytokines.
On the other hand, classification of solid tumors as “hot,” “cold,” or “excluded,” depending on T cell infiltrates and the contact of such infiltrates with tumor cells, as well as those that present high tumor mutation burden (TMB), have redirected immunotherapy towards 3 main strategies 115 ( Table 2 ): (1) Making T-cell antitumor response more effective, using checkpoint inhibitors complementary to anti-CTLA-4 and anti-PD-L1, such as LAG3, Tim-3, and TIGT, as well as using CAR-T cells against tumor antigens. (2) Activating tumor-associated myeloid cells including monocytes, granulocytes, macrophages, and DC lineages, found at several frequencies within human solid tumors. (3) Regulating the biochemical pathways in TME that produce high concentrations of immunosuppressive molecules, such as kynurenine, a product of tryptophan metabolism, through the activity of indoleamine 2,3 dioxygenase; or adenosine, a product of ATP hydrolysis by the activity of the enzyme 5’nucleotidase (CD73). 116
Current Strategies to Stimulate the Immune Response for Antitumor Immunotherapy.
Abbreviations: TME, tumor microenvironment; IL, interleukin; TNF, Tumor Necrosis Factor; TNFR, TNF-receptor; CD137, receptor–co-stimulator of the TNFR family; OX40, member number 4 of the TNFR superfamily; CD27/CD70, member of the TNFR superfamily; CD40/CD40L, antigen-presenting cells (APC) co-stimulator and its ligand; GM-CSF, granulocyte-macrophage colony-stimulating factor; IFN, interferon; STING, IFN genes-stimulator; RIG-I, retinoic acid inducible gene-I; MDA5, melanoma differentiation-associated protein 5; CDN, cyclic dinucleotide; ATP, adenosine triphosphate; HMGB1, high mobility group B1 protein; TLR, Toll-like receptor; HVEM, Herpes virus entry mediator; GITR, glucocorticoid-induced TNFR family-related gene; CTLA4, cytotoxic T lymphocyte antigen 4; PD-L1, programmed death ligand-1; TIGIT, T-cell immunoreceptor with immunoglobulin and tyrosine-based inhibition motives; CSF1/CSF1R, colony-stimulating factor-1 and its receptor; CCR2, Type 2 chemokine receptor; PI3Kγ, Phosphoinositide 3-Kinase γ; CXCL/CCL, chemokine ligands; LFA1, lymphocyte function-associated antigen 1; ICAM1, intercellular adhesion molecule 1; VEGF, vascular endothelial growth factor; IDO, indolamine 2,3-dioxigenase; TGF, transforming growth factor; LAG-3, lymphocyte-activation gene 3 protein; TIM-3, T-cell immunoglobulin and mucin-domain containing-3; CD73, 5´nucleotidase; ARs, adenosine receptors; Selectins, cell adhesion molecules; CAR-T, chimeric antigen receptor T cell; TCR-T, T-cell receptor engineered T cell.
Apart from the problems associated with its efficacy (only a small group of patients respond to it), immunotherapy faces several challenges related to its safety. In other words, immunotherapy can induce adverse events in patients, such as autoimmunity, where healthy tissues are attacked, or cytokine release syndrome and vascular leak syndrome, as observed with the use of IL-2, both of which lead to serious hypotension, fever, renal failure, and other adverse events that are potentially lethal. The main challenges to be faced by immunotherapy in the future will require the combined efforts of basic and clinical scientists, with the objective of accelerating the understanding of the complex interactions between cancer and the immune system, and improve treatment options for patients. Better comprehension of immune phenotypes in tumors, beyond the state of PD-L1 and TME, will be relevant to increase immunotherapy efficacy. In this context, the identification of precise tumor antigenicity biomarkers by means of new technologies, such as complete genome sequencing, single cell sequencing, and epigenetic analysis to identify sites or subclones typical in drug resistance, as well as activation, traffic and infiltration of effector cells of the immune response, and regulation of TME mechanisms, may help define patient populations that are good candidates for specific therapies and therapeutic combinations. 117 , 118 Likewise, the use of agents that can induce specific activation and modulation of the response of T cells in tumor tissue, will help improve efficacy and safety profiles that can lead to better clinical results.
Molecular Targeted Therapy
For over 30 years, and based on the progress in our knowledge of tumor biology and its mechanisms, there has been a search for therapeutic alternatives that would allow spread and growth of tumors to be slowed down by blocking specific molecules. This approach is known as molecular targeted therapy. 119 Among the elements generally used as molecular targets there are transcription factors, cytokines, membrane receptors, molecules involved in a variety of signaling pathways, apoptosis modulators, promoters of angiogenesis, and cell cycle regulators. 120
Imatinib, a tyrosine kinase inhibitor for the treatment of chronic myeloid leukemia, became the first targeted therapy in the final years of the 1990s. 97 From then on, new drugs have been developed by design, and today more than 60 targeted therapies have been approved by the FDA for the treatment of a variety of cancers ( Table 3 ). 121 This has had a significant impact on progression-free survival and global survival in neoplasms such as non-small cell lung cancer, breast cancer, renal cancer, and melanoma.
FDA Approved Molecular Targeted Therapies for the Treatment of Solid Tumors.
Abbreviations: mAb, monoclonal antibody; ALK, anaplastic lymphoma kinase; CDK, cyclin-dependent kinase; CTLA-4, cytotoxic lymphocyte antigen-4; EGFR, epidermal growth factor receptor; FGFR, fibroblast growth factor receptor; GIST, gastrointestinal stroma tumor; mTOR, target of rapamycine in mammal cells; NSCLC, non-small cell lung carcinoma; PARP, poli (ADP-ribose) polimerase; PD-1, programmed death protein-1; PDGFR, platelet-derived growth factor receptor; PD-L1, programmed death ligand-1; ER, estrogen receptor; PR, progesterone receptor; TKR, tyrosine kinase receptors; SERM, selective estrogen receptor modulator; TKI, tyrosine kinase inhibitor; VEGFR, vascular endothelial growth factor receptor. Modified from Ref. [ 127 ].
Most drugs classified as targeted therapies form part of 2 large groups: small molecules and mAbs. The former are defined as compounds of low molecular weight (<900 Daltons) that act upon entering the cell. 120 Targets of these compounds are cell cycle regulatory proteins, proapoptotic proteins, or DNA repair proteins. These drugs are indicated based on histological diagnosis, as well as molecular tests. In this group there are multi-kinase inhibitors (RTKs) and tyrosine kinase inhibitors (TKIs), like sunitinib, sorafenib, and imatinib; cyclin-dependent kinase (CDK) inhibitors, such as palbociclib, ribociclib and abemaciclib; poli (ADP-ribose) polimerase inhibitors (PARPs), like olaparib and talazoparib; and selective small-molecule inhibitors, like ALK and ROS1. 122
As for mAbs, they are protein molecules that act on membrane receptors or extracellular proteins by interrupting the interaction between ligands and receptors, in such a way that they reduce cell replication and induce cytostasis. Among the most widely used mAbs in oncology we have: trastuzumab, a drug directed against the receptor for human epidermal growth factor-2 (HER2), which is overexpressed in a subgroup of patients with breast and gastric cancer; and bevacizumab, that blocks vascular endothelial growth factor and is used in patients with colorectal cancer, cervical cancer, and ovarian cancer. Other mAbs approved by the FDA include pembolizumab, atezolizumab, nivolumab, avelumab, ipilimumab, durvalumab, and cemiplimab. These drugs require expression of response biomarkers, such as PD-1 and PD-L1, and must also have several resistance biomarkers, such as the expression of EGFR, the loss of PTEN, and alterations in beta-catenin. 123
Because cancer is such a diverse disease, it is fundamental to have precise diagnostic methods that allow us to identify the most adequate therapy. Currently, basic immunohistochemistry is complemented with neoplastic molecular profiles to determine a more accurate diagnosis, and it is probable that in the near future cancer treatments will be based exclusively on molecular profiles. In this regard, it is worth mentioning that the use of targeted therapy depends on the existence of specific biomarkers that indicate if the patient will be susceptible to the effects of the drug or not. Thus, the importance of underlining that not all patients are susceptible to receive targeted therapy. In certain neoplasms, therapeutic targets are expressed in less than 5% of the diagnosed population, hindering a more extended use of certain drugs.
The identification of biomarkers and the use of new generation sequencing on tumor cells has shown predictive and prognostic relevance. Likewise, mutation analysis has allowed monitoring of tumor clone evolution, providing information on changes in canonic gene sequences, such as TP53, GATA3, PIK3CA, AKT1, and ERBB2; infrequent somatic mutations developed after primary treatments, like SWI-SNF and JAK2-STAT3; or acquired drug resistance mutations such as ESR1. 124 The study of mutations is vital; in fact, many of them already have specific therapeutic indications, which have helped select adequate treatments. 125
There is no doubt that molecular targeted therapy is one of the main pillars of precision medicine. However, it faces significant problems that often hinder obtaining better results. Among these, there is intratumor heterogeneity and differences between the primary tumor and metastatic sites, as well as intrinsic and acquired resistance to these therapies, the mechanisms of which include the presence of heterogeneous subclones, DNA hypermethylation, histone acetylation, and interruption of mRNA degradation and translation processes. 126 Nonetheless, beyond the obstacles facing molecular targeted therapy from a biological and methodological point of view, in the real world, access to genomic testing and specific drugs continues to be an enormous limitation, in such a way that strategies must be designed in the future for precision medicine to be possible on a global scale.
Cell Therapy
Another improvement in cancer treatment is the use of cell therapy, that is, the use of specific cells as therapeutic agents. This clinical procedure has 2 modalities: the first consists of replacing and regenerating functional cells in a specific tissue by means of stem/progenitor cells of a certain kind, 43 while the second uses immune cells as effectors to eliminate malignant cells. 127
Regarding the first type, we must emphasize the development of cell therapy based on hematopoietic stem and progenitor cells. 128 For over 50 years, hematopoietic cell transplants have been used to treat a variety of hematologic neoplasms (different forms of leukemia and lymphoma). Today, it is one of the most successful examples of cell therapy, including innovative modalities, such as haploidentical transplants, 129 as well as application of stem cells expanded ex vivo . 130 There are also therapies that have used immature cells that form part of the TME, such as MSCs. The replication potential and cytokine secretion capacity of these cells make them an excellent option for this type of treatment. 131 Neural stem cells can also be manipulated to produce and secrete apoptotic factors, and when these cells are incorporated into primary neural tumors, they cause a certain degree of regression. They can even be transfected with genes that encode for oncolytic enzymes capable of inducing regression of glioblastomas. 132
With respect to cell therapy using immune cells, several research groups have manipulated cells associated with tumors to make them effector cells and thus improve the efficacy and specificity of the antitumor treatment. PB leckocytes cultured in the presence of IL-2 to obtain activated lymphocytes, in combination with IL-2 administration, have been used in antitumor clinical protocols. Similarly, infiltrating lymphocytes from tumors with antitumor activity have been used and can be expanded ex vivo with IL-2. These lymphocyte populations have been used in immunomodulatory therapies in melanoma, and pancreatic and kidney tumors, producing a favorable response in treated patients. 133 NK cells and macrophages have also been used in immunotherapy, although with limited results. 134 , 135
One of the cell therapies with better projection today is the use of CAR-T cells. This strategy combines 2 forms of advanced therapy: cell therapy and gene therapy. It involves the extraction of T cells from the cancer patient, which are genetically modified in vitro to express cell surface receptors that will recognize antigens on the surface of tumor cells. The modified T cells are then reintroduced in the patient to aid in an exacerbated immune response that leads to eradication of the tumor cells ( Figure 4 ). Therapy with CAR-T cells has been used successfully in the treatment of some types of leukemia, lymphoma, and myeloma, producing complete responses in patients. 136

CAR-T cell therapy. (A) T lymphocytes obtained from cancer patients are genetically manipulated to produce CAR-T cells that recognize tumor cells in a very specific manner. (B) Interaction between CAR molecule and tumor antigen. CAR molecule is a receptor that results from the fusion between single-chain variable fragments (scFv) from a monoclonal antibody and one or more intracellular signaling domains from the T-cell receptor. CD3ζ, CD28 and 4-1BB correspond to signaling domains on the CAR molecule.
Undoubtedly, CAR-T cell therapy has been truly efficient in the treatment of various types of neoplasms. However, this therapeutic strategy can also have serious side effects, such as release of cytokines into the bloodstream, which can cause different symptoms, from high fever to multiorgan failure, and even neurotoxicity, leading to cerebral edema in many cases. 137 Adequate control of these side effects is an important medical challenge. Several research groups are trying to improve CAR-T cell therapy through various approaches, including production of CAR-T cells directed against a wider variety of tumor cell-specific antigens that are able to attack different types of tumors, and the identification of more efficient types of T lymphocytes. Furthermore, producing CAR-T cells from a single donor that may be used in the treatment of several patients would reduce the cost of this sort of personalized cell therapy. 136
Achieving wider use of cell therapy in oncologic diseases is an important challenge that requires solving various issues. 138 One is intratumor cell heterogeneity, including malignant subclones and the various components of the TME, which results in a wide profile of membrane protein expression that complicates finding an ideal tumor antigen that allows specific identification (and elimination) of malignant cells. Likewise, structural organization of the TME challenges the use of cell therapy, as administration of cell vehicles capable of recognizing malignant cells might not be able to infiltrate the tumor. This results from low expression of chemokines in tumors and the presence of a dense fibrotic matrix that compacts the inner tumor mass and avoids antitumor cells from infiltrating and finding malignant target cells.
Further Challenges in the 21st Century
Beyond the challenges regarding oncologic biomedical research, the 21 st century is facing important issues that must be solved as soon as possible if we truly wish to gain significant ground in our fight against cancer. Three of the most important have to do with prevention, early diagnosis, and access to oncologic medication and treatment.
Prevention and Early Diagnosis
Prevention is the most cost-effective strategy in the long term, both in low and high HDI nations. Data from countries like the USA indicate that between 40-50% of all types of cancer are preventable through potentially modifiable factors (primary prevention), such as use of tobacco and alcohol, diet, physical activity, exposure to ionizing radiation, as well as prevention of infection through access to vaccination, and by reducing exposure to environmental pollutants, such as pesticides, diesel exhaust particles, solvents, etc. 74 , 84 Screening, on the other hand, has shown great effectiveness as secondary prevention. Once population-based screening programs are implemented, there is generally an initial increase in incidence; however, in the long term, a significant reduction occurs not only in incidence rates, but also in mortality rates due to detection of early lesions and timely and adequate treatment.
A good example is colon cancer. There are several options for colon cancer screening, such as detection of fecal occult blood, fecal immunohistochemistry, flexible sigmoidoscopy, and colonoscopy, 139 , 140 which identify precursor lesions (polyp adenomas) and allow their removal. Such screening has allowed us to observe 3 patterns of incidence and mortality for colon cancer between the years 2000 and 2010: on one hand, an increase in incidence and mortality in countries with low to middle HDI, mainly countries in Asia, South America, and Eastern Europe; on the other hand, an increase in incidence and a fall in mortality in countries with very high HDI, such as Canada, the United Kingdom, Denmark, and Singapore; and finally a fall in incidence and mortality in countries like the USA, Japan, and France. The situation in South America and Asia seems to reflect limitations in medical infrastructure and a lack of access to early detection, 141 while the patterns observed in developed countries reveal the success, even if it may be partial, of that which can be achieved by well-structured prevention programs.
Another example of success, but also of strong contrast, is cervical cancer. The discovery of the human papilloma virus (HPV) as the causal agent of cervical cancer brought about the development of vaccines and tests to detect oncogenic genotypes, which modified screening recommendations and guidelines, and allowed several developed countries to include the HPV vaccine in their national vaccination programs. Nevertheless, the outlook is quite different in other areas of the world. Eighty percent of the deaths by cervical cancer reported in 2018 occurred in low-income nations. This reveals the urgency of guaranteeing access to primary and secondary prevention (vaccination and screening, respectively) in these countries, or else it will continue to be a serious public health problem in spite of its preventability.
Screening programs for other neoplasms, such as breast, prostate, lung, and thyroid cancer have shown outlooks that differ from those just described, because, among other reasons, these neoplasms are highly diverse both biologically and clinically. Another relevant issue is the overdiagnosis of these neoplasms, that is, the diagnosis of disease that would not cause symptoms or death in the patient. 142 It has been calculated that 25% of breast cancer (determined by mammogram), 50–60% of prostate cancer (determined by PSA), and 13–25% of lung cancer (determined by CT) are overdiagnosed. 142 Thus, it is necessary to improve the sensitivity and specificity of screening tests. In this respect, knowledge provided by the biology of cancer and “omic” sciences offers a great opportunity to improve screening and prevention strategies. All of the above shows that prevention and early diagnosis are the foundations in the fight against cancer, and it is essential to continue to implement broader screening programs and better detection methods.
Global Equity in Oncologic Treatment
Progress in cancer treatment has considerably increased the number of cancer survivors. Nevertheless, this tendency is evident only in countries with a very solid economy. Indeed, during the past 30 years, cancer mortality rates have increased 30% worldwide. 143 Global studies indicate that close to 70% of cancer deaths in the world occur in nations of low to middle income. But even in high-income countries, there are sectors of society that are more vulnerable and have less access to cancer treatments. 144 Cancer continues to be a disease of great social inequality.
In Europe, the differences in access to cancer treatment are highly marked. These treatments are more accessible in Western Europe than in its Eastern counterpart. 145 Furthermore, highly noticeable differences between high-income countries have been detected in the cost of cancer drugs. 146 It is interesting to note that in many of these cases, treatment is too costly and the clinical benefit only marginal. Thus, the importance of these problems being approached by competent national, regional, and global authorities, because if these new drugs and therapeutic programs are not accessible to the majority, progress in biomedical, clinical and epidemiological research will have a limited impact in our fight against cancer. We must not forget that health is a universal right, from which low HDI countries must not be excluded, nor vulnerable populations in nations with high HDI. The participation of a well-informed society will also be fundamental to achieve a global impact, as today we must fight not only against the disease, but also against movements and ideas (such as the anti-vaccine movement and the so-called miracle therapies) that can block the medical battle against cancer.
Final Comments
From the second half of the 20th century to the present day, progress in our knowledge about the origin and development of cancer has been extraordinary. We now understand cancer in detail in genomic, molecular, cellular, and physiological terms, and this knowledge has had a significant impact in the clinic. There is no doubt that a patient who is diagnosed today with a type of cancer has a better prospect than a patient diagnosed 20 or 50 years ago. However, we are still far from winning the war against cancer. The challenges are still numerous. For this reason, oncologic biomedical research must be a worldwide priority. Likewise, one of the fundamental challenges for the coming decades must be to reduce unequal access to health services in areas of low- to middle income, and in populations that are especially vulnerable, as well as continue improving prevention programs, including public health programs to reduce exposure to environmental chemicals and improve diet and physical activity in the general population. 74 , 84 Fostering research and incorporation of new technological resources, particularly in less privileged nations, will play a key role in our global fight against cancer.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Hector Mayani https://orcid.org/0000-0002-2483-3782
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
After 40 years of smoking, she survived lung cancer thanks to new treatments

Yuki Noguchi

Denise Lee on her last day of chemo. In addition to chemo and surgery, she was treated with immunotherapy. She's currently in remission. Denise Lee hide caption
Denise Lee on her last day of chemo. In addition to chemo and surgery, she was treated with immunotherapy. She's currently in remission.
Denise Lee grew up in Detroit in the mid-1970s and went to an all-girls Catholic high school. She smoked her first cigarette at age 14 at school, where cigarettes were a popular way of trying to lose weight.
Instead, her nicotine addiction lasted four decades until she quit in her mid-50s.
"At some point it got up as high as 2.5 packs a day," Lee, 62, recalls.
Yet she didn't think about lung cancer risk — until she saw a billboard urging former smokers to get screened. Lee, a retired lawyer living in Fremont, Calif., used to drive past it on her way to work.
"The thing that caught my attention was the fact that it was an African American female on the front," she recalls.

Shots - Health News
The american cancer society says more people should get screened for lung cancer.
She eventually got the low-dose CT scan recommended for current and former smokers. When doctors found an early, but dangerous, tumor, Lee cried and panicked. Her mother had cared for her father, who'd died of prostate cancer. "My biggest concern was telling my mom," she says.
But that was six years ago, and Lee is cancer free today. Surgery removed the 2-inch tumor in her lung, then new treatments also boosted her immune system, fighting off any recurrence.
Lung cancer remains the most lethal form of the disease, killing about 135,000 Americans a year – more than breast, prostate and colon cancer combined – which is why many people still think of a diagnosis as synonymous with a death sentence. But with new treatments and technology, the survival rates from lung cancer are dramatically improving, allowing some patients with relatively late-stage cancers to live for years longer.
"If you're gonna have lung cancer, now is a good time," Lee says of the advances that saved her.

Denise Lee has been cancer-free for six years. She says she's grateful she got screened and caught her lung cancer early enough that treatment has been effective. Denise Lee hide caption
Denise Lee has been cancer-free for six years. She says she's grateful she got screened and caught her lung cancer early enough that treatment has been effective.
The key breakthrough, says Robert Winn, a lung cancer specialist at Virginia Commonwealth University, is the ability to better pinpoint the mutations of a patient's particular form of cancer. In the past, treatments were blunt tools that caused lots of collateral damage to healthy parts of the body while treating cancer.
"We've gone from that to molecular characterization of your lung cancer, and it has been a game changer," Winn says. "This is where science and innovation has an impact."
One of those game-changing treatments is called targeted therapy . Scientists identify genetic biomarkers in the mutated cancer cells to target and then deliver drugs that attack those targets, shrinking tumors.

CRISPR gene-editing may boost cancer immunotherapy, new study finds
Another is immunotherapy, usually taken as a pill, which stimulates the body's own defense system to identify foreign cells, then uses the immune system's own power to fight the cancer as if it were a virus.
As scientists identify new cancer genes, they're creating an ever-broader array of these drugs.
Combined, these treatments have helped increase national survival rates by 22% in the past five years – a rapid improvement over a relatively short time, despite the fact that screening rates are very slow to increase. Winn says as these treatments get cheaper and readily available, the benefits are even reaching rural and Black populations with historic challenges accessing health care.
The most remarkable thing about the drugs is their ability to, in some cases, reverse late-stage cancers. Chi-Fu Jeffrey Yang, a thoracic surgeon at Massachusetts General Hospital and faculty at Harvard Medical School, recalls seeing scans where large dark shadows of tumor would disappear: "It was remarkable to see the lung cancer completely melting away."
To Yang, such progress feels personal. He lost his beloved grandfather to the disease when Yang was in college. If he were diagnosed today, he might still be alive.
"Helping to take care of him was a big reason why I wanted to be a doctor," Yang says.
But the work of combating lung cancer is far from over; further progress in lung cancer survival hinges largely on getting more people screened.
Low-dose CT scans are recommended annually for those over 50 who smoked the equivalent of a pack a day for 20 years. But nationally, only 4.5% of those eligible get those scans , compared to rates of more than 75% for mammograms.
Andrea McKee, a radiation oncologist and spokesperson for the American Lung Association, says part of the problem is that lung cancer is associated with the stigma of smoking. Patients often blame themselves for the disease, saying: "'I know I did this to myself. And so I don't I don't think I deserve to get screened.'"
McKee says that's a challenge unique to lung cancer. "And it just boggles my mind when I hear that, because, of course, nobody deserves to die of lung cancer."
Denise Lee acknowledges that fear. "I was afraid of what they would find," she admits. But she urges friends and family to get yearly scans, anyway.
"I'm just so grateful that my diagnosis was early because then I had options," she says. "I could have surgery, I could have chemotherapy, I could be a part of a clinical trial."
And all of that saved her life.
- lung cancer screening
- immunotherapy
- lung cancer
Advances in Melanoma and Other Skin Cancers Research
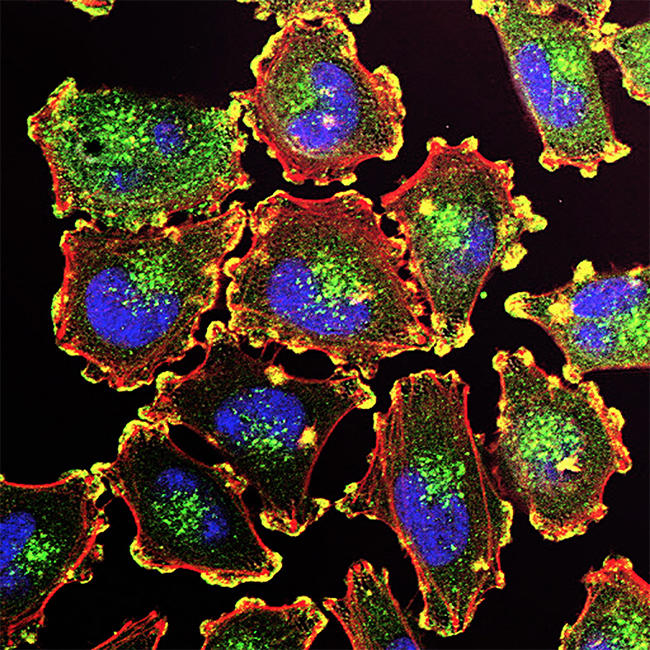
Metastatic melanoma cells.
NCI-funded researchers are working to advance our understanding of how to treat melanoma and other skin cancers. Much progress has been made in treating people with melanoma that has spread in their bodies ( metastatic melanoma). Yet many people still don't benefit from the newest drugs, and others may relapse after initially successful treatment.
This page highlights some of the latest research in treatment for melanoma and other skin cancers, including clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and current research findings from recent studies.
Melanoma Treatment
Surgery remains the standard treatment for early-stage melanoma and may also be used as part of therapy for more advanced disease. However, researchers are now focusing on developing treatments that directly target specific mutations in melanoma cells or that harness the body’s immune system to attack melanoma.
Both of these approaches— targeted therapies and immunotherapies —have led to dramatic improvements in survival for patients with advanced melanoma over the last decade. Researchers are continuing to explore ways to make these treatments more effective for more patients.
Targeted therapies
Targeted therapies use drugs or other substances to attack specific types of cancer cells with less harm to normal cells. About half of people with melanoma that has metastasized or can’t be removed with surgery ( unresectable melanoma) have mutations in the BRAF gene . These mutations result in abnormal B-Raf proteins that can cause uncontrolled growth of melanoma cells.
Drugs have been developed that block the effects of these altered B-Raf proteins. Other new drugs block proteins that work together with altered B-Raf proteins to promote cancer cell growth. These include proteins produced by the MEK genes. The combination of blocking both B-Raf and MEK has been found to be particularly successful in treating melanoma that has a mutation in the BRAF gene. Three such combinations are approved for people with metastatic or unresectable melanoma that has mutations in the BRAF gene:
- dabrafenib (Tafinlar) and t rametinib (Mekinist)
- encorafenib (Braftovi) and b inimetinib (Mektovi)
- vemurafenib (Zelboraf) and c obimetinib (Cotellic)
However, although these drug combinations may be effective initially, most people develop resistance to them within a year. Researchers are studying how melanoma cells manage to grow in the presence of these targeted therapies, with the goal of finding ways to overcome resistance. Ideas being tested include new drug combinations and drugs that target the B-Raf pathway in different ways than existing drugs.
Immune checkpoint inhibitors
Immunotherapies are treatments that help the body’s immune system fight cancer more effectively. Melanoma tends to have a relatively high number of genetic mutations that can be recognized by the immune system compared with other cancer types. This makes it more likely that melanoma will respond to immunotherapy.
One type of immunotherapy, called immune checkpoint inhibition , has shown impressive results in some people with advanced melanoma. Four immune checkpoint inhibitors are now approved for the treatment of melanoma that can’t be removed with surgery or that has metastasized:
- i pilimumab (Yervoy)
- pembrolizumab (Keytruda)
- nivolumab (Opdivo)
- atezolizumab (Tecentriq) , when used in combination with two targeted drugs
The combination of ipilimumab and nivolumab is also approved for some patients with metastatic or unresectable melanoma. In the study that led to its approval, more than half of the people who received the combination were alive 5 years after treatment . Another clinical trial showed that this combination can also shrink melanoma that has spread to the brain in some patients.
The combination of nivolumab with a new type of immune checkpoint inhibitor called relatlimab also improved the amount of time people with advanced melanoma lived without their cancer getting worse . This combination received FDA approval in 2022, under the name Opdualag , for people aged 12 or older with untreated melanoma that can't be removed surgically or has spread within the body.
Scientists are looking for ways for more people to have success with these drugs. Unfortunately, even when used in combination, immune checkpoint inhibitors don't work for all patients with metastatic or unresectable melanoma. However, patients whose tumors do shrink or disappear often have responses that last for years. Researchers are now testing ways to increase the number of people with melanoma who benefit from this type of treatment, such as these below.
- Combining immune checkpoint inhibitors with immunostimulant s. Immunostimulants produce a type of chemical alarm in the body that tells the immune system that a threat exists. In a small clinical trial that combined pembrolizumab with an immunostimulant, tumors shrank in almost 80% of people who received the two treatments together . Larger trials of this and other combinations of immunotherapy drugs are underway.
- Testing new and existing immune checkpoint inhibitors in combination with targeted therapies and other types of drugs.
- Changing people’s gut microbes before treatment with an immune checkpoint inhibitor. For example, a study led in part by NCI researchers found that changing some people’s gut microbes could make their melanoma more likely to shrink during treatment with an immune checkpoint inhibitor.
Learning what treatments to give first
Melanoma researchers are also looking to understand how best to use existing therapies. One pressing question had been whether it is better for people who have advanced melanoma with mutations in the BRAF gene to receive targeted drugs or immune checkpoint inhibitors first.
An NCI-sponsored trial, DREAMseq, has helped answer this question. Patients with advanced melanoma were randomly assigned to receive either a combination of targeted drugs or a combination of immune checkpoint inhibitors. When their cancer recurred, they received the other combination. The study found that more people who received the immune checkpoint inhibitor combination first were still alive 2 years later than people who received the combination of the targeted drugs first.
Researchers are also searching for biomarkers in melanoma that can predict which tumors might respond to other immunotherapies or drug combinations.
Harnessing the body’s immune cells
Adoptive cell therapy. Another type of immunotherapy, called adoptive cell therapy (ACT), is also being tested in patients with metastatic melanoma. In ACT, T cells (a type of immune cell) are given to a patient to help the body fight diseases, such as cancer.
In a small, early-phase clinical trial of ACT, about half of patients with metastatic melanoma saw their tumors shrink, and a quarter remained in remission for as long as the study tracked them—in some cases for up to a decade. But the procedure is complicated and expensive, and half of people do not benefit from the treatment at all or experience dangerous or even fatal side effects. Researchers are looking for ways to make ACT work for more patients such as the examples below.
- One idea being tested is the use of immune cells that have been collected from patients, altered to make them better at killing cancer cells, and then infused back into patients. Such therapies include CAR T cells, a type of treatment where a patient's T cells are changed in the lab so they will attack cancer cells . Researchers are also testing other ways to boost the ability of T cells to kill tumor cells.
- Another idea is to find common proteins that are present in many people's tumors. This could allow for the creation of “off-the-shelf” T-cell therapies that don’t have to be made on a custom basis for each patient.
Immunotherapy following surgery for advanced melanoma
Adjuvant therapy is additional cancer treatment given after primary surgical treatment. Nivolumab, ipilimumab, and pembrolizumab have all been approved as adjuvant therapies for melanoma that has spread to nearby lymph nodes but can be removed with surgery. In clinical trials, all three immune checkpoint inhibitors reduced the risk of recurrence for some patients when given after surgery, although many patients experienced serious side effects.
Another study tested pembrolizumab in patients with early-stage melanoma that has not spread to the lymph nodes but had a high risk of doing so. It found that giving pembrolizumab after surgery reduced the chance of the cancer coming back or spreading elsewhere in the body . However, the treatment can cause significant side effects. More studies are needed to understand how to identify the people with this type of high-risk, early-stage melanoma who would benefit the most from such treatment.
Researchers are also exploring whether immune checkpoint inhibitors might be more effective if given before surgery. One NCI-sponsored trial compared the outcomes of patients with melanoma at high risk of recurring who receive pembrolizumab both before and after surgery with those in patients who receive the drug only after surgery. That trial found that people who received the drug both before and after surgery had a substantially lower risk of their cancer coming back than those who only received adjuvant treatment.
Rare Melanoma Types
Some rare types of melanoma have lagged behind melanoma of the skin in terms of advances in treatment. These include intraocular (uveal) melanoma , which starts in the eye; desmoplastic melanoma , a rare form of melanoma of the skin; and mucosal melanoma, which begins in the mucosal membranes , such as the linings of the nose and mouth.
However, recent small clinical trials suggest that these types of melanoma may also respond to immunotherapies. One NCI-sponsored trial tested pembrolizumab in people with desmoplastic melanoma . Initial results from this trial showed that the drug shrinks both tumors that can be removed surgically and those that cannot. The trial participants are still being tracked to see if pembrolizumab improves how long they live overall.
Immune checkpoint inhibitors have been less effective in intraocular melanoma than in other types of melanoma. However, a different type of immunotherapy called a bispecific fusion protein has shown promise for treating this rare cancer. These drugs bind to melanoma cells and the body’s own immune cells at the same time, to bring them together. This allows the immune cells to kill the melanoma cells. In a clinical trial, one such drug, called tebentafusp, became the first drug to show an improvement in overall survival for patients with metastatic intraocular melanoma.
Merkel Cell Carcinoma
Another rare type of skin cancer, called Merkel cell carcinoma (MCC), has been shown to be the most sensitive of any tumor type to treatment with a single immune checkpoint inhibitor. In 2017, an immunotherapy called avelumab (Bavencio) received the first-ever FDA approval for a drug to treat MCC. In addition, more than half of patients with MCC in a small clinical trial had their tumors shrink or disappear during treatment with pembrolizumab, which received FDA approval for the treatment of MCC in 2018.
In 2023, a third immunotherapy drug called retifanlimab (Zynyz) received FDA approval for the treatment of MCC that has recurred or spread elsewhere in the body. Other immunotherapy drugs are currently being tested in this rare cancer type.
Treatment for Advanced Basal Cell Carcinoma and Squamous Cell Carcinoma
Basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) of the skin are the most common cancers in the United States. They rarely spread to other organs and are seldom fatal. However, every year many people are diagnosed with advanced BCC or SCC.
Recent breakthroughs in targeted therapies and immunotherapies have changed the way people with advanced BCC and SCC are treated. Ongoing research seeks to build on these breakthroughs such as:
- The targeted drugs sonidegib (Odomzo) and vismodegib (Erivedge) which can control tumors for a long time in some people with BCC. However, resistance often develops. In addition, side effects can cause some patients who need to take the drugs for a long time to stop taking them. Researchers are now looking for ways to change when and how much of these drugs are given, both to delay the development of resistance and to make them easier to tolerate.
- cemiplimab (Libtayo) for some people with metastatic or locally advanced SCC that can't be removed with surgery. Cemiplimab is also being tested as a treatment given before surgery for some people whose cancer can be removed.
- pembrolizumab for some people with recurrent or metastatic SCC
- cemiplimab for some people with advanced BCC whose tumors have become resistant to targeted therapy
New clinical trials are now testing other immunotherapy drugs and combinations in SCC and BCC.
For people whose BCC or SCC has not spread, surgery remains the mainstay of treatment. But less-intensive versions of radiation therapy have been developed for people who can’t tolerate surgery for larger tumors, such as the frail elderly.
NCI-Supported Research Programs
Many NCI-funded researchers at the NIH campus, and across the United States and world, are seeking ways to address melanoma and other skin cancers more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some is more clinical, seeking to translate this basic information into improving patient outcomes. The programs listed below are a small sampling of NCI’s research efforts for melanoma and other skin cancers.
Scientists in the Division of Cancer Epidemiology and Genetics (DCEG) study families in which multiple members have developed certain cancers. In collaboration with the Melanoma Genetics Consortium (GenoMEL), DCEG researchers are searching for new genes in both melanoma-prone families and through a genome-wide association study to find genes that may increase the risk of melanoma.
The Skin Specialized Programs of Research Excellence (Skin SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Skin SPORE program’s main focus is on melanoma research activities, but it also includes projects in other skin cancer types, such as cutaneous T-cell lymphoma.
NCI's National Clinical Trials Network (NCTN) is a collection of organizations and clinicians that coordinates and supports cancer clinical trials at more than 3,000 sites across the United States and Canada. NCTN currently has a variety of trials testing treatments for skin cancer .
The Division of Cancer Control and Population Sciences (DCCPS) oversees the Cancer Trends Progress Report, an online report that tracks the nation's progress against cancer from prevention through end of life. Topics in the report that inform melanoma and skin cancer research are sun-protective behavior , indoor and outdoor tanning , and sunburn . The division’s Health Behaviors Research Branch (HBRB) supports research in the area of sun protection and reducing indoor tanning practices, through both measurement and intervention studies.

Clinical Trials
NCI funds and oversees both early- and late-stage clinical trials to develop new treatments and improve patient care. Trials are available for melanoma prevention and treatment and non-melanoma skin cancer prevention and treatment .
Melanoma and Other Skin Cancers Research Results
The following are some of our latest news articles about research on melanoma and other skin cancers:
- First Cancer TIL Therapy Gets FDA Approval for Advanced Melanoma
- Rare Melanoma Very Likely to Respond to Treatment with Pembrolizumab
- Immunotherapy before Surgery Appears Effective for Some with Melanoma
- Androgen Receptor May Explain Sex Differences in Melanoma Treatment Response
- Study Adds to Debate about Screening for Melanoma
- Opdualag Becomes First FDA-Approved Immunotherapy to Target LAG-3
View the full list of Melanoma and Other Skin Cancers Research Results and Study Updates .
Detecting cancer in minutes possible with just a drop of dried blood and new test, study hints
Early tests suggest that a new tool that requires only a single drop of blood could detect three of the deadliest forms of cancer.

A new AI-powered test could one day be used to accurately and quickly detect three major types of cancer using only a single spot of dried blood.
In preliminary experiments, the tool was able to distinguish between patients with diagnosed pancreatic, gastric or colorectal cancer and people without cancer — and the analysis took just minutes. By detecting certain chemicals in blood, the test could identify when a patient had cancer around 82% to 100% of the time, researchers say.
The new tool uses machine learning, a type of artificial intelligence (AI), to analyze by-products of metabolism, or metabolites, in blood samples. These metabolites — which are found in the liquid portion of blood known as serum — act as "biomarkers" that can potentially flag cancer's presence in the body.
Screening for these blood biomarkers has been proposed as a potential way to diagnose cancer at earlier stages of the disease, when survival rates are higher and patients may have no telltale symptoms. Despite being some of the world's deadliest cancers , pancreatic , colorectal and gastric cancers currently have no standalone blood tests that are accurate enough to diagnose the diseases on their own. Instead, doctors usually rely on imaging or surgical procedures to detect cancerous tissue.
Related: Cancer patients can now be 'matched' to best treatment with DNA and lab-dish experiments
The new test would theoretically require less than 0.05 milliliters of blood to diagnose these diseases. That's according to the scientists in China who developed the test and described their findings in a paper published Monday (April 22) in the journal Nature Sustainability .
Compared to liquid blood, dried serum can be "collected, stored and transported at much lower cost and with much simpler equipment," said Dr. Chaoyuan Kuang , an assistant professor at the Albert Einstein College of Medicine and an oncologist at Montefiore Health System who was not involved in the research.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Because of the ease of storing dried blood, "this could help democratize the availability of cancer early detection testing across the world," Kuang told Live Science in an email.
However, the new cancer-detecting test likely won't enter use for a long time, he added. "We are most likely still years away from being able to offer this test to patients in a widespread fashion," Kuang said.
In the new study, the researchers ran several proof-of-concept tests that demonstrated the tool could accurately differentiate between blood donors with cancer versus those without it. They also showed that dried blood worked as well as traditional liquid blood-based tests. For example, in one experiment, using the dried blood spots enabled them to detect 81.2% of cases of pancreatic cancer, compared to 76.8% using liquid blood samples.
In the U.S., only one biomarker is currently approved by the Food and Drug Administration to diagnose pancreatic cancer. It's known as CA19-9, and current tests that detect the metabolite are around 80% accurate at identifying symptomatic cases of the disease. However, they flag only 13% of cases in which patients have no symptoms, so they're not as useful for super-early cancer detection.
The scientists behind the new test say that, if used in large cancer screening programs, their test could make a huge difference. Based on modeling they performed, they reported the new tool could reduce the estimated proportion of undiagnosed cases of pancreatic, gastric and colorectal cancers by about 20% to 50% if it was used for population-level cancer screening in rural China.
The new paper is a "great start," Kuang said. However, validating the new tool will require more testing, especially in large, diverse populations, he said. The study only tested a few hundred samples of blood, so it's unclear how well the findings will apply to other groups. The researchers also only tested the machine learning model on people who were already known to have cancer; they've yet to test its utility as a true diagnostic tool.
A blood test like this would need to go through "extensive clinical trials" with thousands of patients and regulatory review, Dr. Michael Cecchini , co-director of the colorectal program at the Center for Gastrointestinal Cancers at the Yale Cancer Center who was not involved in the research, told Live Science in an email.
— 'Very concerning': Microplastics can accumulate in cancer cells and may help them spread, study hints
— Gut bacteria linked to colorectal cancer in young people
— New mRNA 'cancer vaccine' trial launches in UK
Nevertheless, the tool's potential is "immense," Kuang said. With further development, it could theoretically be used for the early detection of other types of cancer or for other diseases, or to monitor the progression of disease in patients who have already been diagnosed, he said.
By 2030, scientists estimate that around 75% of cancer deaths will occur in low- and middle-income countries, where people face disproportionately-high barriers to medical care . The new tool, in part because it uses dried blood, could help improve access to tests in remote areas where resources are limited, the study authors wrote in their report.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun ? Send us your questions about how the human body works to [email protected] with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking journalism training. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. ( [email protected] )
Cancer patients can now be 'matched' to best treatment with DNA and lab-dish experiments
Catherine, Princess of Wales, announces cancer diagnosis
Chemo side effect caused man's eyelash growth to go haywire
admin said: Early tests suggest that a new tool that requires only a single drop of blood could detect three of the deadliest forms of cancer. Detecting cancer in minutes possible with just a drop of dried blood and new test, study hints : Read more
- View All 1 Comment
Most Popular
- 2 Giant, 82-foot lizard fish discovered on UK beach could be largest marine reptile ever found
- 3 Global 'time signals' subtly shifted as the total solar eclipse reshaped Earth's upper atmosphere, new data shows
- 4 Rare 'porcelain gallbladder' found in 100-year-old unmarked grave at Mississippi mental asylum cemetery
- 5 'I nearly fell out of my chair': 1,800-year-old mini portrait of Alexander the Great found in a field in Denmark
- 2 'We were in disbelief': Antarctica is behaving in a way we've never seen before. Can it recover?
- 3 George Washington's stash of centuries-old cherries found hidden under Mount Vernon floor
- 4 Scientists create 'toxic AI' that is rewarded for thinking up the worst possible questions we could imagine
- 5 5 catastrophic megathrust earthquakes led to the demise of the pre-Aztec city of Teotihuacan, new study suggests
Canadian doctors are using ’outdated’ guidelines to screen for cancer, experts warn
Canada's national guidelines recommend against breast cancer screening for women in their 40s, despite growing evidence in favour of it. A group of experts say the Canadian Task Force on Preventive Health Care's recommendations are outdated and lagging behind what other jurisdictions are doing to detect various forms of cancer early.
Photo: Associated Press / Torin Halsey
Cancer experts say current recommendations use old data, lack expert advice and are too slow to update
Carolyn Holland can't help wondering how many years of her life she's lost because her breast cancer was diagnosed late.
The Ottawa mom first discovered lumps in her breasts while in the shower. At 43 years old, she'd never had a mammogram.
After seeing her doctor, she was sent for a scan, which confirmed the cancer. But at that point it had already advanced. Holland needed two types of chemotherapy, radiation, the removal of her lymph nodes and a double mastectomy.
This shouldn't happen to other women. It's preventable, Holland said.
Holland's doctors told her that her treatment could have been less drastic had the cancer been detected sooner. But Canada's national guidelines do not recommend routine breast cancer screening for women under the age of 50.
Had I been able to access screening at 40, this wouldn't have been my outcome, she said.
A group of medical experts say Canadian lives are at risk because family doctors are using outdated guidelines to decide whether, and when, to send their patients for routine cancer screenings.
The guidelines are issued by the Canadian Task Force on Preventive Health Care (new window) , an arms-length panel of 15 doctors and other primary care providers set up by the federal government. The independent volunteer panel examines the research on screening and preventing various illnesses, including cancer.
These guidelines impact millions of Canadians. The consequences are grim. Current task force guidelines often limit access to critical life-saving screening, said Dr. Shiela Appavoo, an Edmonton-based radiologist.
She's with the Coalition for Responsible Healthcare Guidelines, a group of cancer specialists, family doctors and patients calling for changes to how the guidelines are created.
The coalition says the task force is using outdated research, doesn't properly take in the advice of experts and is far too slow to update its recommendations.
Family doctors taught to follow national guidelines
The task force's breast cancer screening guidelines are set to be updated next month. The current recommendations (new window) , last updated in 2018, recommend against broad screening of women in their 40s.
The Canadian Cancer Society withdrew its support for the guidelines in December 2022, citing concerns that they were not keeping pace with new research, in particular the growing incidence of cancer (new window) in younger populations around the world. The latest statistics (new window) show the cancer most commonly diagnosed in Canadians aged 30 to 49 is breast cancer.
WATCH | Cancer screening guidelines are out of date, experts say:
Canada’s cancer screening guidelines are out of date, doctors say
A group of cancer experts say Canadian national screening guidelines are a decade out of date, which is leading to people getting diagnosed later, when they are more difficult to treat.
Many provinces have ignored the task force guidelines by lowering the age when they offer breast cancer screening to include women in their 40s.
British Columbia (new window) , Nova Scotia (new window) , P.E.I (new window) . and Yukon (new window) all allow women to access routine mammograms in their 40s. Alberta (new window) and the Northwest Territories (new window) start screenings at 45. Ontario will start covering screening mammograms (new window) for women in their 40s this fall.
- Self-referral mammograms for women in their 40s coming to N.B. (new window)
- Sask. announces creation of breast health centre in Regina, expansion of screening eligibility (new window)
While some provinces have expanded screening eligibility to younger women, many doctors still might not send their patients for the test because the national guidelines recommend against it, Appavoo said.
Unfortunately, a lot of family physicians are taught and trained to follow the task force guidelines, Appavoo said.
That's a problem, she said, because a patient is most likely to go for cancer screening if their doctor recommends it.
So it is really important to give family doctors appropriate and adequate information on who to screen and when to screen, Appavoo said.
- Just Asking wants to know: What questions do you have about cancer screening in Canada? Are the current guidelines adequately serving you? Fill out the details on this form (new window) and send us your questions ahead of our show on April 27.
The lack of leadership on national guidelines has also led to piecemeal coverage across the country, she said, because some Canadians have access to cancer screening sooner than others.
Cancer research from 1960s still being used
Dr. Anna Wilkinson saw firsthand the impact of those guidelines she was taught to follow. As an Ottawa family physician who treats oncology patients, she's worked with many women in their 40s dying of breast cancer.
They asked for a mammogram and they were told, 'No, you don't need one because you're in your 40s,' Wilkinson said. It's heartbreaking.
That prompted Wilkinson to co-author a study (new window) that compared breast cancer statistics from provinces that screened women in their 40s to stats from provinces that followed the task force guidelines. Her study found that earlier screening led to significantly improved survival rates.
- AUDIOWomen take on the fight for earlier breast cancer screening (new window)
- Canada should follow U.S. call to screen for breast cancer at 40, doctors and patients say (new window)
Despite new evidence from Canada and around the world about the benefits of screening women at younger ages, Wilkinson said the task force continues to weigh outdated data when making its recommendations.
The task force is still using data from a 1963 trial to determine whether women should be screened today, she said.
That is completely irrelevant at this point, Wilkinson said. There is nothing about the way that breast cancer screening was done or treatment was done in the 60s that reflects today's practices.
Other cancer guidelines out of date, experts say
The task force screening guidelines for several other types of cancer also lag behind what many experts, cancer organizations and other jurisdictions recommend.
They are harming Canadians because they are leading us to diagnose cancers at a later stage when we know survival is worse and when the costs of treatment are more, Wilkinson said.
The guidelines for cervical cancer haven't been updated since 2013 and aren't due to be revisited until 2025.
The task force currently recommends against screening for HPV (new window) , citing concerns the research is too premature. HPV is the virus that causes most cases of cervical cancer and it can be detected much sooner than a Pap test detects changes in cervical cells.
By comparison, the U.K.'s screening (new window) advisory body began recommending HPV screening in 2016 while Australia replaced routine Pap tests (new window) with HPV screening in 2017. Many provinces have begun screening for HPV (new window) , despite the national guidelines.
The task force's guidelines for lung cancer screening (new window) were last updated in 2016 and are not due to be revamped until 2026. The task force gives what it calls a weak recommendation to screen heavy tobacco users with low-dose CT scans, despite research (new window) that has found CT scans help to detect lung cancer early and decrease the number of deaths.
Half of the time when we diagnose people with lung cancer, it's already Stage 4, which is incurable, said Dr. Paul Wheatley-Price, who leads the lung cancer program at the Ottawa Hospital Cancer Care Centre.
He said the amount of time it takes the task force to update its guidelines is baffling.
- Her mom's lung cancer was caught too late. It's part of a pattern in Nunavik (new window)
- One hospital's push to bring genetic cancer testing to more Black women (new window)
The task force's guidelines on prostate cancer (new window) , which won't be updated until 2026, recommend against prostate specific antigen (PSA) blood tests. The Canadian Urological Association has criticized that advice (new window) since it was issued in 2014; it argues that trials show screening reduces prostate cancer deaths by up to 44 per cent.
Those (task force) guidelines are about 10 years old and we've made a huge amount of progress, said Dr. Fred Saad, director of prostate cancer research at the Montreal Cancer Institute. The input that came from experts was basically ignored.
The Canadian Cancer Society also recommends (new window) that men consider having a PSA test done starting at age 50, and that Black men begin testing at 45.
The task force also doesn't offer different guidelines for screening based on a patient's ethnicity, despite research that shows some populations are diagnosed with certain cancers at earlier ages. Inuit, for example, are more than twice as likely as the rest of the population to be diagnosed with lung cancer, according to the Canadian Partnership Against Cancer. (new window)
The risk of 'over-diagnosis'
New studies are coming out all the time, said task force member Dr. Eddy Lang — but they don't always offer enough evidence for the panel to change its recommendations.
Our system is arguably in crisis and it may not be the best use of resources to be detecting things early, Lang said, who works as an emergency room physician in Calgary.
While the task force does consult with cancer experts, Lang said, those experts don't get to set the guidelines — and there's a good reason for that.
A mammogram is shown here, which is an x-ray picture of the breast that is used to screen for cancer.
Photo: (CBC News)
Someone who's been researching and advocating in the breast cancer or prostate cancer field for their whole career might have a different view than a neutral group that is trying to make recommendations for family doctors, he said.
Experts in the area will often focus a bit more on the benefits of screening and may not have as much attuned understanding or awareness of the harms that [are] often seen more at the primary care level, and that is our audience.
Lang said the task force needs to factor in the risks associated with over-diagnosis — of subjecting patients to cancer treatments that can be more harmful than the cancer itself, or of treating a cancer that never would have caused a problem in the first place.
I thought it was common knowledge, you screened for cancer, you catch it early, you nip it in the bud. But when I joined the task force and started looking at the evidence, I was actually blown away at how significant the harms can be of early detection, he said.
But cancer survivor Carolyn Holland said Canadians have the right to know if they have cancer, and then make informed decisions about treatment.
What I would tell the task force is, you are not saving us from harm, she said. You're actually putting us in harm's way by denying us screening, by denying us the chance to catch cancers early.
Marina von Stackelberg (new window) · CBC News

Taps will be turned off if water rules are defied: Merritt mayor Taps will be turned off if water rules are defied: Merritt mayor. Posted: 8 hours ago.
Merritt imposes strict water limitations months early amid extreme drought

Table set for Honda’s massive bet on Canada’s electric vehicle sector Table set for Honda’s massive bet on Canada’s electric vehicle sector. Posted: 8 hours ago.
What to watch for as Honda announces its new presence in Canada's EV industry

Mexican farmers take on avocado growers in fight for water during drought Mexican farmers take on avocado growers in fight for water during drought. Posted: 9 hours ago.
Mexico has received roughly half of its usual rainfall over the past year

U.K. tabloids abuzz with Canadians’ ’Loch Ness monster' photo U.K. tabloids abuzz with Canadians’ ’Loch Ness monster' photo. Posted: 9 hours ago.
Moving object was 'bigger than a Sasquatch but smaller than Ogopogo,' B.C. man jokes

Just bought a used car? There’s a chance it’s stolen, as thieves exploit weakness in … Just bought a used car? There’s a chance it’s stolen, as thieves exploit weakness in vehicle registrations. Posted: 12 hours ago.
Nearly 1/3 of stolen vehicles may now have been title ‘washed’ and resold
Together we are beating cancer
About cancer
Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
Cancers in general
- Clinical trials
Causes of cancer
Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
Get involved
- Make a donation
By cancer type
- Leave a legacy gift
- Donate in Memory
Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay For Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our We Are campaign
Our research
- Brain tumours
- Skin cancer
- All cancer types
By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
Funding for researchers
Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
Applying for funding
- Start your application online
- How to make a successful application
- Funding committees
- Successful applicant case studies
How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
Shop online
- Wedding favours
- Cancer Care
- Flower Shop
Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
Cancer news
- Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
ABOUT CANCER
GET INVOLVED
NEWS & RESOURCES
FUNDING & RESEARCH
You are here

Current research
Improving diagnosis of chronic lymphocytic leukaemia.
- Read more about Improving diagnosis of chronic lymphocytic leukaemia

Surgeon Mr John Findlay is developing new techniques to better predict cancer behaviour and patient outcomes from treatment.
- Read more about Developing techniques to predict oesophageal and gastric cancer behaviour
Identifying novel treatments for bowel cancer
- Read more about Identifying novel treatments for bowel cancer
AI powered tools tackling oesophageal cancer
- Read more about AI powered tools tackling oesophageal cancer
Developing techniques to predict oesophageal and gastric cancer behaviour
A new dual-action cancer-killing virus.
- Read more about A new dual-action cancer-killing virus
Combining radiotherapy, minimally invasive surgery and immunotherapy to improve treatment of people with prostate cancer
- Read more about Combining radiotherapy, minimally invasive surgery and immunotherapy to improve treatment of people with prostate cancer
Taking inspiration from nature to trap cancer cells
- Read more about Taking inspiration from nature to trap cancer cells
Can exercise help prevent bowel cancer returning?
- Read more about Can exercise help prevent bowel cancer returning?
Finding new ways to tackle bowel cancer
- Read more about Finding new ways to tackle bowel cancer
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Cancer therapy articles from across Nature Portfolio
Cancer therapy describes the treatment of cancer in a patient, often with surgery, chemotherapy and/or radiotherapy. Targeted therapies are also available for some cancer types. A cancer patient might receive many different types of therapy, including those aimed at relieving the symptoms of cancer, such as pain.

Lighting the torch: intratumoural T cell-to-stroma enrichment score as a predictor of immunotherapy response in urothelial carcinoma
T cell infiltration in the tumour microenvironment (TME) is a prerequisite for sustained antitumour immune responses. However, identifying predictive biomarkers that quantify T cell infiltration and the presence of proinflammatory TMEs associated with immune-checkpoint inhibitor (ICI) response for clinical implementation has proved challenging. Here, we highlight a study that validates a T cell-to-stroma enrichment score generated from RNA sequencing data as a novel biomarker for ICI response in patients with urothelial carcinoma.
- David H. Aggen
- Jonathan E. Rosenberg
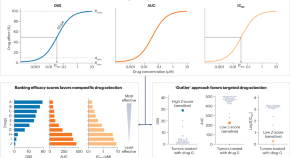
Functional precision medicine for pediatric cancers
A small, prospective clinical study shows that ex vivo drug screening of pediatric cancer samples can identify effective therapeutic options. If validated, these findings could herald a new approach to precision medicine in this setting.
- M. Emmy M. Dolman
- Paul G. Ekert
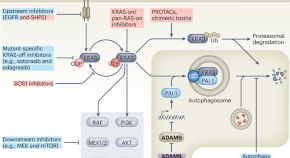
KRAS degradation averts PDAC chemoresistance
Effectively targeting deregulated KRAS signaling remains an unmet clinical need, as current approaches commonly lead to the development of chemoresistance in clinical settings. ADAM9-mediated lysosomal KRAS degradation is now shown to counteract PDAC chemoresistance independently of mutational status.
- Laura Leonhardt
- Matthias Hebrok
Related Subjects
- Cancer immunotherapy
- Cancer therapeutic resistance
- Chemotherapy
- Drug development
- Radiotherapy
- Targeted therapies
- Tumour vaccines
Latest Research and Reviews
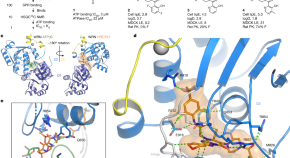
Discovery of WRN inhibitor HRO761 with synthetic lethality in MSI cancers
HRO761 is a potent, selective, allosteric WRN inhibitor that binds at the interface of the D1 and D2 helicase domains, locking WRN in an inactive conformation.
- Stephane Ferretti
- Jacques Hamon
- Marta Cortés-Cros
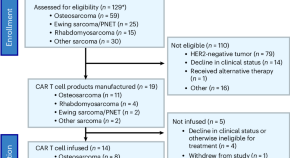
Autologous HER2-specific CAR T cells after lymphodepletion for advanced sarcoma: a phase 1 trial
In this phase 1 trial, Hegde et al. treat 13 individuals with advanced sarcoma with lymphodepletion followed by HER2-specific CAR T cells, which were found to be safe and showed antitumor activity.
- Meenakshi Hegde
- Shoba Navai
- Nabil Ahmed
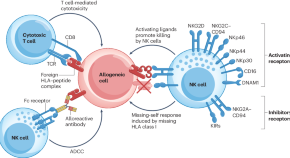
Engineering immune-evasive allogeneic cellular immunotherapies
Genome editing approaches can be used to confer immune-evasive properties to allogeneic cellular immunotherapies, with the aim of achieving persistent responses and efficiencies that are comparable to those of autologous chimeric antigen receptor T cell therapies. This Perspective discusses how current knowledge about viral or tumour immune evasion could be incorporated into the design of off-the-shelf tumour-specific T and NK cells for the production of cost-effective and scalable cancer immunotherapies.
- Karen E. Martin
- Quirin Hammer
- Karl-Johan Malmberg
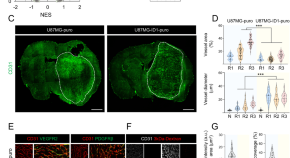
ID1 high /activin A high glioblastoma cells contribute to resistance to anti-angiogenesis therapy through malformed vasculature
- Sang-Hun Choi
- Junseok Jang
- Hyunggee Kim

Annexin A2 combined with TTK accelerates esophageal cancer progression via the Akt/mTOR signaling pathway
- Haibo Zhang

SRY-Box transcription factor 9 triggers YAP nuclear entry via direct interaction in tumors
- Chen-Hong Ding
- Wei-Fen Xie
News and Comment
Overtreatment of multiple myeloma and its precursor states: de-escalation is an urgent need in clinical practice and trials.
Certain subsets of patients with multiple myeloma or its precursor conditions are overtreated with current approaches to therapy. Herein, we highlight several key areas where we believe de-escalation of treatment is needed. Dedicated trials to assess these de-escalation approaches and urgent changes to current clinical practices are needed.
- Ghulam Rehman Mohyuddin
- Aaron M. Goodman
ALND can be safely omitted for patients with sentinel-node macrometastases
- David Killock
Afami-cel provides a novel treatment option for rare sarcoma subtypes
- Peter Sidaway
Patient-reported toxic effects of hypofractionated versus conventional RT
- Maria Chiara Masone
Safe delivery of ICI therapy through sub-urothelial injection
Transrectal prostate biopsy: easy, effective and safe.
- Romain Diamand
- Alexandre Peltier
- Simone Albisinni
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Frontiers in Genome Editing
- Genome Editing in Cancer and Immunology
- Research Topics
Insights in Genome Editing in Cancer and Immunology 2024
Total Downloads
Total Views and Downloads
About this Research Topic
We are now entering the third decade of the 21st Century, and, especially in the last years, the achievements made by scientists have been exceptional, leading to major advancements in the fast-growing field of genome editing technologies and their applications in cancer and immunology research. Frontiers has organized a series of Research Topics to highlight the latest advancements in research across the field of genome editing, with articles from the members of our accomplished Editorial Boards. This editorial initiative of particular relevance is being led by Dr. Sidi Chen, Specialty Chief Editor of the Genome Editing in Cancer and Immunology section, and Associate Editors Dr. Xiaoyu Zhou and Dr. Lei Peng, and focuses on new insights, novel developments, current challenges, latest discoveries, recent advances, and future perspectives in the field. The Research Topic solicits brief, forward-looking contributions from the editorial board members that describe the state of the art, outlining recent developments and major accomplishments that have been achieved and that need to occur to move the field forward. Authors are encouraged to identify the greatest challenges in the sub-disciplines, and how to address those challenges. The goal of this special edition Research Topic is to shed light on the progress made in the past decade in the genome editing field, and on its future challenges to provide a thorough overview of the field. This article collection will inspire, inform and provide direction and guidance to researchers in the field.
Keywords : genome editing, cancer, immunology
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, submission deadlines, participating journals.
Manuscripts can be submitted to this Research Topic via the following journals:
total views
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.

IMAGES
VIDEO
COMMENTS
Tumors actively prevent the formation of immune responses by so-called cytotoxic T cells, which are essential in combating cancer. Researchers have now uncovered for the first time how this ...
Targeted therapies have swiftly taken a prominent position in cancer research and clinical oncology in recent decades, thanks to the molecular insights into oncogenic processes and mechanisms ...
Nature Cancer publishes research, reviews and comment across the spectrum of the cancer field, from fundamental preclinical, to translational and clinical work. ... Latest Research articles
December 27, 2023. Estimated reading time: 6 minutes. By Mayo Clinic staff. Researchers at Mayo Clinic Comprehensive Cancer Center spent 2023 studying the biology of cancer and new ways to predict, prevent, diagnose and treat the disease. Their discoveries are creating hope and transforming the quality of life for people with cancer today and ...
According to the International Agency for Research on Cancer (IARC), in 2020 there were approximately 19.3 million new cases of cancer, and 10 million deaths by this disease, 6 while 23.8 million cases and 13.0 million deaths are projected to occur by 2030. 73 In this regard, it is clear the increasing role that environmental factors ...
The growing global burden of cancer is rapidly exceeding the current cancer control capacity. More than 19 million new cancer cases were diagnosed in 2020 worldwide, and 10 million people died of cancer.1 By 2040, that burden is expected to increase to around 30 million new cancer cases annually and 16 million deaths from cancer according to the Global Cancer Observatory.
The Nature Portfolio editors who handle cancer primary research, methods, protocols and reviews bring you the latest articles, covering all aspects from disease mechanisms to therapeutic ...
ACS has published Cancer Facts & Figures annually since 1951. This report provides the most current information about cancer. A unique feature of this report and its accompanying scientific article, Cancer Statistics, is the projected number of cancer cases and deaths expected nationally, and in each state, in the current year.These widely cited projections serve as a basis for research and ...
The Facts & Figures annual report provides: Estimated numbers of new cancer cases and deaths in 2021 (In 2021, there will be an estimated 1.9 million new cancer cases diagnosed and 608,570 cancer deaths in the United States.) Current cancer incidence, mortality, and survival statistics. Information on cancer symptoms, risk factors, early ...
The American Cancer Society says more people should get screened for lung cancer She eventually got the low-dose CT scan recommended for current and former smokers. When doctors found an early ...
Cancer News and Stories. Our team of experts brings you cancer-related news, features, and survivor stories. For the latest news about research we conduct and fund, see ACS Research News. Our team of expert journalists brings you all angles of the cancer story - from breaking news and survivor stories to in-depth insights into cutting-edge ...
Cancer Research publishes impactful original studies, reviews, and opinion pieces of high significance to the broad cancer research community. Cancer Research seeks manuscripts that offer conceptual or technological advances leading to basic and translational insights into cancer biology. Read More About the Journal.
Current research in childhood brain and spinal cord tumors focuses on understanding the underlying causes of these cancers, developing new treatments, and reducing the toxic effects of effective therapies. For example, ... View the full list of brain cancer research results and study updates. Reviewed: September 29, 2023;
This page highlights some of the latest research in treatment for melanoma and other skin cancers, including clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and current research findings from recent studies. ... Topics in the report that inform melanoma and skin cancer research are ...
Read the latest Research articles from Nature Cancer. ... De Blank and colleagues examine data from childhood cancer survivors diagnosed between 1970 and 1999 and find that exposure to radiation ...
In the U.S., only one biomarker is currently approved by the Food and Drug Administration to diagnose pancreatic cancer. It's known as CA19-9, and current tests that detect the metabolite are ...
By Melinda Krigel. Leading cancer researchers from UC San Francisco presented talks about advances in targeted therapy, cancer genomics, eliminating treatment disparities and other cancer research topics at this year's annual meeting of the American Association for Cancer Research (AACR) conference, which was held April 5-10 in San Diego.
The Canadian Cancer Society withdrew its support for the guidelines in December 2022, citing concerns that they were not keeping pace with new research, in particular the growing incidence of ...
We are issuing a call for research papers that utilize innovative approaches to address current challenges in cancer prevention, detection, diagnosis and treatment — both clinical trials and ...
Current research. Enable for snippets. Enable for news posts. Improving diagnosis of chronic lymphocytic leukaemia. ... Cancer Research UK is a registered charity in England and Wales (1089464), Scotland (SC041666), the Isle of Man (1103) and Jersey (247). A company limited by guarantee. Registered company in England and Wales (4325234) and the ...
Depression. Detection. Diagnosis. Diet Nutrition. Disparities. E-Cigarettes. End of Life. Exercise Physical Activity Fatigue. Get the latest cancer research news about the work of our American Cancer Society staff researchers and research grantees.
In the United States, lung cancer, colorectal cancer, pancreatic cancer and breast cancer are the four top causes of cancer deaths. A report from the American Cancer Society especially highlighted ...
Cancer therapy articles from across Nature Portfolio. Cancer therapy describes the treatment of cancer in a patient, often with surgery, chemotherapy and/or radiotherapy. Targeted therapies are ...
We are now entering the third decade of the 21st Century, and, especially in the last years, the achievements made by scientists have been exceptional, leading to major advancements in the fast-growing field of genome editing technologies and their applications in cancer and immunology research. Frontiers has organized a series of Research Topics to highlight the latest advancements in ...
A great deal of research is being done to learn more about the genetic changes inside bone cancer cells. Doctors are using what they learn to develop new targeted drugs for some types of bone cancer, as well as to test and use existing targeted drugs that focus on some of these gene changes. These drugs might change the cancer's ability to grow ...
The Upstate Cancer Center will mark the 10 th anniversary of its opening with a daylong retreat highlighting some of the cancer research being done by Upstate faculty. The retreat is set for Friday, April 26 from 8 a.m. to 6 p.m., and will be held at the CNY Biotech Accelerator, 841 East Fayette St., Syracuse.