- Healthcare Services
- Find a Doctor
- Patient Portal
- Research and Education


Your recent searches
- Find a Location
- Nursing Careers
- Physical Therapy Careers
- Medical Education
- Research & Innovation
- Pay My Bill
- Billing & Insurance Questions
- For Healthcare Professionals
- News & Publications
- Classes & Events
- Philanthropy
Gender Affirmation Surgery
Browse this page

If you’re transgender, you may pursue hormone therapy or gender reassignment surgery to help align your body with your gender identity. Some transgender individuals also choose to pursue surgery to help reduce or enhance secondary sexual characteristics. For transgender men, this may include surgery to reduce breast size or remove the ovaries. Transgender women may elect for breast augmentation or facial feminization surgery to meet their needs. At MedStar Health, we offer the following procedures to help you be comfortable in your own skin. Types of gender reassignment surgery:
Feminizing vaginoplasty : Reconstructive surgery procedure that alters the structure of the genitals to create a vagina using penile or colon tissue. Dr. Del Corral uses a one-stage procedure, revisions can be necessary to enhance the final surgical result
Revision vaginoplasty (after loss of depth) : A secondary procedure allowing for revisions to the urethra, neovaginal canal, labia minora, and majora addressing asymmetries within the vagina, and scar revisions to help functionality. MedStar Center for Gender Affirmation specializes in revisional procedures after complications from primary vaginoplasty
Colon vaginoplasty : A different approach to an original vaginoplasty. The colon or small bowel can be used to line the vaginal wall to create depth, dilation, and providing a natural source of lubrication. At the MedStar Center for Gender Affirmation, we use a robotic-assisted approach to minimize incisions in the abdomen, and faster recovery while providing better access for the revision
Masculinizing phalloplasty/scrotoplasty : Reconstructive surgery that creates a penis using a free flap or pedicled flap of skin. These sections of the skin can be taken from the arm (radial forearm free-flap, RFF) or thigh (anterior lateral thigh pedicled flap phalloplasty, ALT). These procedures are performed in a combined team that include a reconstructive urologist and plastic surgeons
Metoidioplasty : The use of local tissue to create an enlargement to the penile area (clitoral release/enlargement, may include urethral lengthening)
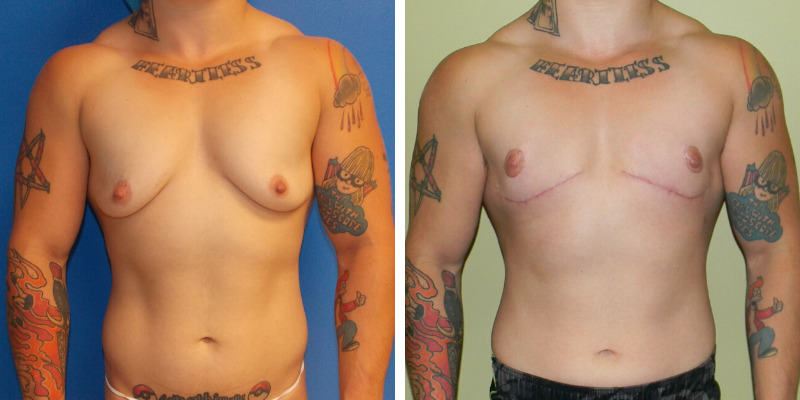
Masculinizing chest surgery (“top” surgery) : Breast tissue is removed and the nipples and areolae are altered to help masculinize the chest
Facial feminization : Reconstructive surgery procedures that alters the shape and size of facial features to make them closer to typical female facial features — this may include a brow lift, forehead re-contouring, hairline correction, and rhinoplasty (nose reshaping)
Facial masculinization : Reconstructive surgery that alters the shape and size of facial features to make them more masculine — this may include forehead lengthening and augmentation, cheek augmentation, chin re-contouring, jaw contouring, thyroid cartilage enhancement (Adam’s apple surgery), and rhinoplasty (nose reshaping)
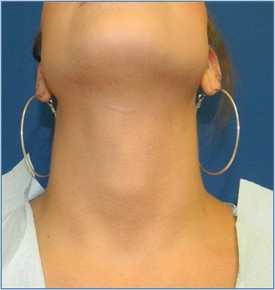
Reduction thyrochondroplasty (thyroid cartilage shave) : Reconstructive surgery that reduces the size of the thyroid cartilage, also known as the “Adam’s apple.” It is shaved down to create a more feminine appearance
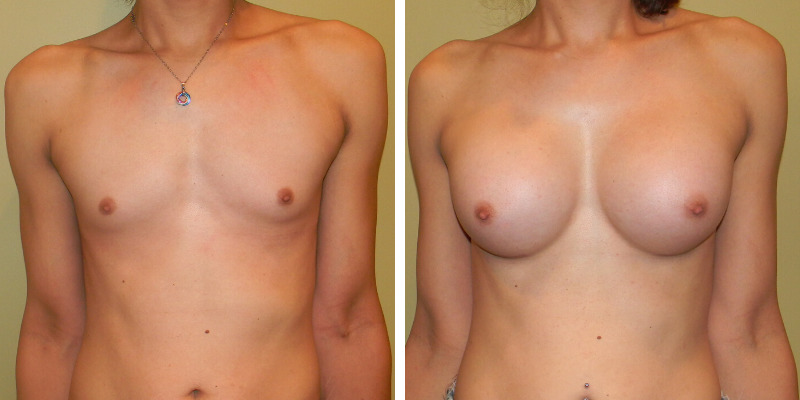
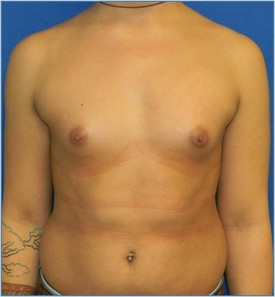
Breast augmentation mammoplasty : Surgery to reshape, enlarge, and modify the breasts and achieve a more desired shape and look to the chest
Hysterectomy with bilateral salpingo-oophorectomy : Surgical removal of the uterus, cervix, ovaries, fallopian tubes, and surrounding structures
Orchiectomy : Reconstructive surgery to remove the testicles
Vaginectomy : Reconstructive surgery to remove all parts of the vagina
Gender surgery planning and recovery
What to expect.
You may need to meet a few requirements before qualifying for certain gender affirming procedure(s) at MedStar Health. The exact requirements will depend on your insurance coverage and may include one or more letters of referral from qualified mental health professionals, well-documented gender dysphoria, and/or one year of continuous hormone therapy. Procedures that are considered strictly cosmetic by your insurance plan will have fewer requirements.
After properly qualifying for surgery, you’ll meet with one of our surgeons. They will examine you and ask questions to determine if you physically qualify for surgery. If you qualify, you’ll discuss any risks and potential complications and walk through the steps involved. You’ll be given specific instructions to follow prior to your surgery.
On the day of surgery, your surgeon may use a variety of leading-edge techniques to achieve the best results, such as minimally invasive surgery to significantly reduce scarring.
Recovery from surgery
It’s important to follow your surgeon’s instructions for proper care of your body after surgery. You may have specific directions about taking medications and how to clean and care for the surgical site. Healing may take several weeks as swelling decreases.
Why choose us?
MedStar Health is the largest health care system in Maryland and the Washington, D.C., region. When you choose us for care, you’ll have access to our network of 10 hospitals and a team of more than 3,000 physicians and specialists.
If you choose MedStar Health for a breast augmentation or reduction procedure, you’ll be choosing to work with a nationally recognized leader in breast surgeries. Our breast surgeons have years of experience working exclusively in breast procedures and have developed their own techniques to help patients recover faster and have better results.
Our providers
Location: Change location Enter your location
Gabriel Alfonso Del Corral, MD
Microvascular Plastic Surgery, Gender Surgery, Reconstructive Plastic Surgery & Plastic Surgery
Laura Tom, MD
Microvascular Plastic Surgery, Breast Surgery & Plastic Surgery
Our locations
Distance from Change location Enter your location
MedStar Health: Plastic Surgery at MedStar Washington Hospital Center
106 Irving St. NW POB North Ste. 3400 Washington, D.C., 20010
MedStar Franklin Square Medical Center
9000 Franklin Square Dr. Baltimore, MD 21237
Frequently asked questions
Do I need a referral?
If you’re exploring options for insurance coverage, you may need to request a referral from your primary care doctor, depending on your health insurance plan. Check with your carrier to see if medical coverage is an option for you and, if so, whether a referral is required.
How should I prepare?
Before surgery, you may be asked to get blood tests and take or adjust medications — this may include temporarily stopping hormone therapy. If you smoke, quitting will help you heal faster and avoid possible complications. You’ll also need to arrange for transportation to and from the hospital and for someone to stay with you the night after the surgery.
For more information visit Patient Resources or Preparing for Surgery
Dr. Gabriel Del Corral's Philosophy of Care

MedStar Center for Gender Affirmation: Vaginoplasty

Related services
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
Your Journey Starts Here!
There’s so much to consider when looking for a surgeon to perform your gender-affirming surgery: experience with the procedure, geographic location and the types of insurance they accept are all primary concerns. Before getting bogged down with too many details, start your journey by searching for surgeons that offer the procedures that you’re interested in. All set? Let’s go!
Search Surgeons by U.S. State
Search surgeons by country, search surgeons by name.

Global Surgeon Maps
Visually search for surgeons by geographic location.
- FFS Surgeons Map
- Vaginoplasty Surgeons Map
- Top Surgery Surgeons Map
- Metoidioplasty Surgeons Map
- Phalloplasty Surgeons Map
- Hysterectomy Surgeons Map
Featured Surgeons
Dr. manish champaneria.

Dr. Manish Champaneria is a board certified plastic surgeon with extensive training and experience in plastic surgery and microsurgery. He has a special focus on gender-affirming chest and facial procedures. Dr. Champaneria is based in San Diego, California.
Dr. Cassie Nghiem

Dr. Nghiem is an Ivy League-educated, fellowship-trained plastic surgeon in Washington, D.C. who specializes in transgender surgery, including Chest Masculinization and Breast Augmentation. She believes in a shared vision and works closely with her patients to deliver the best quality care that is in line with their needs. Known for her surgical skill and artistry, Dr. Nghiem’s patients also love her kind and caring demeanor.
Dr. Drew Marano

Dr. Marano is a highly skilled plastic and reconstructive surgeon in New York City specializing in Gender Affirmation Surgery. Dr. Marano is fellowship-trained in gender-affirming facial, chest and genital surgeries, including Phalloplasty and Vaginoplasty. He is passionate about gender-affirming care and committed to providing a comfortable and supportive environment for his patients.
Dr. Michael S. Beckenstein

Dr. Beckenstein is a double-board-certified Plastic Surgeon in Birmingham who is pleased to offer his expertise and skills in cosmetic and reconstructive surgery to the transgender community in Alabama and throughout the Southeast. Dr. Beckenstein has performed transgender chest/breast surgeries for over 15 years and also specializes in Hair Restoration.
Dr. Dev Gurjala

Dr. Gurjala joined Align Surgical Associates in 2019, after five years of performing gender surgery, microsurgery, and general reconstructive and aesthetic surgery in the Kaiser Permanente healthcare network. He works exclusively with trans women, trans men and non-binary patients seeking gender-affirming surgeries, including Phalloplasty, Vaginoplasty and Facial Feminization.
Dr. Christopher Salgado

Dr. Salgado is a board-certified plastic surgeon with deep expertise in gender-affirming procedures. In fact, he is one of the most experienced gender surgeons in the world. In practice for more than 20 years, Dr. Salgado performs all aspects of transgender surgeries, from Facial Feminization and Top Surgery, to complex genital procedures such as Vaginoplasty and Phalloplasty.
- Online Giving
- Pay Your Bill
- Patient Portal
- Make an Appointment

Plastic Surgery: Transgender/Gender Affirmation Surgery
Schedule a consultation.
To learn more about any of these procedures, or to schedule a consultation, please contact us at (202) 741-2365 or Book an Appointment Now with Dr. Jerry Chao. Dr. Chao will review pre and post-op pictures with you at your consultation. We accept many insurance plans, and your gender affirming surgery may be a covered benefit.
At The GW Medical Faculty Associates, we understand and respect how critical each surgical step is in your transition. Our mission is to help you feel comfortable as the person you were meant to be born as. During your initial consultation, Dr. Jerry Chao will make a meticulous analysis in order to develop an individually tailored treatment plan. As a faculty member at The George Washington University School of Medicine and Health Sciences, Dr. Chao is actively involved in clinical research to advance transgender surgical care. Dr. Chao works closely with regional centers including Whitman-Walker Health to coordinate and optimize your care.
Dr. Chao will review pre and post-op pictures with you at your consultation, and discuss what results can be expected. We accept many insurance plans, and your gender affirming surgery may be a covered benefit. Please call (202) 741-2365 to schedule a consultation.
Facial Feminization Surgery
When we see someone, it takes only a split second for our brain to process hundreds of visual cues to decide a person’s gender, age, and mood. Facial feminization surgery (FFS) serves to modify the underlying facial bone structure in order to change masbculine cues to feminine cues. Fellowship-trained in craniofacial surgery, Dr. Chao is uniquely equipped and qualified to analyze and correct your underlying facial bone structure with the utmost care, skill, and safety.
Breast Augmentation
While hormone therapy allows for some degree of breast development, that often ends up simply not being enough. Those patients are often excellent candidates for breast augmentation surgery. This is done as an outpatient surgery with breast implants, which are filled with either saline or silicone gel. During your consultation Dr. Chao will review in depth with you your choices, goals, expectations, and recovery in helping you achieve the look you want.
Chest Masculinization
Chest masculinization surgery, or “top surgery”, involves removal of the breast tissue, and repositioning/reshaping of the nipple and areola. Dr. Chao performs circumareolar (scar hidden around the areola) as well as double incision surgery and will discuss in depth with you what surgery is the most appropriate for your individual body type.

GENDER REASSIGN
GENDER REASSIGN FTM TOP SURGERY
GENDER REASSIGN MTF BREAST AUGMENTATION
GENDER REASSIGNMENT MTF TOP SURGERY

GENDER REASSIGN MTF TRACHEAL SHAVE
GENDER REASSIGN MTF TOP SURGERY
A CONSULTATION
What our clients say.
Great work and results. Friendly doctor with nice treatment. Highly educated with great experience. He coordinates with his staff to stay communicated with their patients before or after surgery. You can’t feel afraid during the surgery time. I would also recommend him for plastic surgery for both genders of people.
Great office staff. Dr. Singh is truly amazing at what he does. I had a great experience with my Lipo 360. I’m currently 5 days post op and I’m loving my results.
My experience with Dr. Singh and the entire staff was exceptional! He was extremely thorough and very patient. The staff was awesome too! They were kind and always had such a wonderful attitude! I’m extremely happy with my results! Highly recommend!
Dr. Singh does amazing work. All his staff are very knowledgeable and professional. I highly recommend him.
Amazing doctor! Excellent staff. Dr. Singh is a doctor that shows you that there are still excellent doctors around. He gives you great ideas and he gives you the most bang for your buck and takes your budget seriously. I am going back soon!
The purpose of my review is to highly recommend Dr. Singh for plastic surgery. I couldn’t be more pleased with his surgical skill. His office staff was incredibly helpful as well. They are approachable and well informed. I researched several surgeons in the DC metro area and visited with three. Dr. Singh was the second surgeon I visited and when I left his office, I knew he was the best surgeon for me. He understood the results I was hoping for and he was honest with me about what I should expect. His demeanor is calm, collected, and confident. His staff is truly phenomenal. I asked them a million questions and to them there wasn’t a question too personal or too mundane. They really helped me be at ease with what I was planning to do and they walked me through every step of the procedure so I knew what to expect from surgery and during the recovery process.
WOW! Dr. Singh and his staff were wonderful. After meeting him, I was no longer nervous and very excited. They made the whole process comfortable and non-scary. The results were spectacular. I looked and felt great. I got my confidence back! I was treated great and came back for the second procedure. This is the place to go! You will be happy with the quality of work and the personalized service. Thanks so much guys!!!!
Dr. Singh is absolutely amazing at his job! I’ve been his patient for about 6 years now and I continue to use his services not only because of his expertise and meticulously high standards, but also his integrity. All of the staff are professional, kind and attentive. They truly are the best in the area!
Dr. Singh and his staff are absolutely phenomenal. I am a male diagnosed with Poland’s Syndrome. I chose to have a pec implant surgery, and I could not have been happier with my results. Stunning. No longer do I feel I have to hide my abnormality with jackets and oversized shirts. I feel I have obtained a second family with the staff. I cannot say enough…simply. From recluse to social butterfly!
Washingtonian Plastic Surgery was a great place for me to get my breast augmentation done because Dr. Navin Singh is an excellent doctor and was very upfront and honest with his opinion on what would best fit me and would look as natural as possible. I am happy with my results and totally recommend anyone who wants to become a newer and better version of themselves to go here! Very comfortable environment with great customer service from the ladies at the front desk. You won’t regret it!
I was truly impressed with your nice facility, the caring staff, and friendly attitudes and smiles. The office was furnished with style and class. The doctor I saw, Dr. Navin Singh, is TRULY AMAZING, as well as the front desk staff. It was good to be treated with professionalism and care. I appreciated their follow-up and willingness to answer questions as well. All this adds up to fabulous customer service, which can be hard to come by. THANK YOU ALL SO VERY MUCH!!! You have a customer for life.
At fifty-nine (59), I had contemplated eyelid surgery for years. My upper eyelids grossly sagging & my under-eye puffiness covered an area 2″ x 2″ under the eyes. Dr. Navin Singh’s superior excellence to detail & perfection changed my life! Dr Navin Singh is the Dr’s, the patient’s & the only choice.
Dr Singh and his staff are so professional and is always available to be in contact with, not like most doctor offices around. He was very honest and made me feel very comfortable. I’m three days into my tummy tuck procedure and I will say he explained and went over everything as they would happen. I can’t yet tell my results but it’s a noticeable change. I will definitely recommend and go back for more procedures!
I know the decision to have cosmetic surgery is a big one. It can be costly, and it carries some risk, but it will change your life for the better. I used this site a lot when making my decision and I had consultations with several surgeons. I took a methodical approach, weighed all my options carefully, and I can say with full confidence that if you’re looking for a procedure that Dr. Singh performs, you should go with him, or at least have a consultation. He’s an amazing doctor and just a great person in general. His staff is as kind, patient, thorough, and knowledgeable as he is, and all of that makes a huge difference.
Dr. Singh is AMAZING!!!! I have nothing but wonderful things to say about him and his team. He is so personable and I loved that he and his team made sure that all my questions and concerns were addressed and answered. I started my journey with Dr. Singh in 2010 with a breast augmentation. I did 500cc saline, filled to 550cc. He and his staff were so supportive and helpful before, during, and after surgery. My breasts look so nature and look fantastic!!! I was so happy with my results and Dr. Singh that I went back to him for a tummy tuck with muscle repair in 2012 and now I’m going back for liposuction!
The mini-tummy tuck turned out even better than I expected
Dr. Singh, In two weeks, I didn’t have any bruising, swelling is gone, it looks so natural. I just got engaged and I look so good in my pictures. Thanks so much.
You are a VERY special man. You & Nicolette have changed my life. THANK YOU!! 🙂

7601 Lewinsville Road, Suite 300 McLean, VA 22102 (703) 345-4377
11490 Commerce Park Drive, Suite 430 Reston, VA 20191 (703) 636-9296
Fields marked * are required
Appointments: 1-888-884-BEAR (2327)

- Gender Development Program
- Meet the Team
- Support Group for Children
- Parent Support Group
- Online Support Group for Parents
- FAQs About the Gender Development Program
Family Resources
Some young people feel, sense or know they are a gender different than the one they were assumed at birth. They may live and dress in ways typical of another gender (gender non-conformity), and some may experience the need to live and be affirmed as this gender in some or all settings. This can be an urgent need, or for others, there may be experimentation and exploration. There are also some young people who show gender non-conformity in their everyday behaviors, but may not yet have the self-advocacy skills to discuss their gender identity and their gender-related needs.
The Gender Development Program at Children's National recognizes that each child's gender journey is unique. Our team has been supporting the gender needs of youth and their families for the past 20 years, providing essential care at a time they need it most.
Our Providers
Our pediatric specialists provide personalized care for your child’s physical, mental and emotional health needs.
Contact Information
For appointments, please call 1-888-884-BEAR (2327) and for information, call 202-476-5744.
Programs Related to Gender Development
We collaborate with departments throughout Children's National to provide the best possible care to children with gender development needs.
- Gender and Autism Program
- Positive Reevaluation of Urogenital Differences (PROUD) Clinic
- Youth Pride Clinic
Caring for Gender-Diverse Youth and Their Families
Our multidisciplinary Gender Development Program team understands that the gender development of a child may be confusing to parents and families, providers and sometimes young people themselves. Parents may wonder:
- How can my child's gender-related needs best be supported?
- How do we navigate our child's gender diversity in everyday life (e.g., with family, in school, when moving into adulthood, etc.)?
- Is my child transgender?
- Will my child's gender and gender-related needs change over time?
The needs of gender-diverse youth are often complex, requiring a multidisciplinary team approach and ongoing care supports over time.
As one of the earliest founded youth gender programs, we are a multidisciplinary team of specialists who work in the assessment and broad care needs of youth on the gender spectrum and their families. We also conduct cutting-edge research to move forward our understanding of youth gender development and ways to best support gender-diverse and transgender youth. Research findings inform all of our clinical care.
We work with gender exploring, gender non-conforming, gender dysphoric, gender non-binary, transgender and gender-questioning young people, and we see children and adolescents of all ages. We also work with youth who have genetic and other conditions in which gender variation is common.
Personalized Evaluations and Tailored Care
This includes evaluation of your child's gender development and needs in the real world. Throughout care with us, your child will receive supports tailored to their unique needs, in coordination with an existing community of professionals your child already sees to ensure continuity and consistency of care.
Comprehensive Services and Collaboration with Multiple Specialties
From initial and ongoing evaluation and support to specialists in medical treatments such as Veronica Gomez-Lobo, M.D. , a pediatric gynecologist who provides medical interventions such as puberty suppression or hormone therapy, the program offers a full spectrum of care options based on the needs of each young person.
Unique Programs for Diverse Needs
- Children and teens who have both autism spectrum characteristics (or related conditions) and gender dysphoria have access to a support program designed specifically for them: the Gender and Autism Program led by John Strang, Psy.D . Many providers refer patients to our program to access these services, which may not be offered elsewhere.
- The Gender Development Program works closely with the Youth Pride Clinic , which offers primary and specialty care services to LGBTQ (lesbian, gay, bisexual, transgender and questioning/queer) patients.
Evaluation and Ongoing Supports
Your child’s care will start with an initial evaluation by our team. During this two to three-hour visit, you will meet the team together with your child and also separately. The goals of these visits vary from family to family and may include:
- Understanding the various aspects of your child’s gender development
- Screening for any mental health concerns/risks
- Support for parenting a gender diverse child
- Support for families navigating issues related to siblings, friends, school, etc.
We may ask you and your child to return for periodic follow-up visits. These visits can help us make a more extended evaluation. Your team also may suggest treatments or supportive services through Children’s National or in the community such as:
- Individual supports for youth and/or parents
- Family-specific supports
- School supports/interventions
- Support groups for you and/or your child
Recognized for Excellence
Our colleagues and peers have recognized the important care our Gender Development Program provides. Our advocacy and education efforts have been honored with the following national awards recognizing our commitment to providing compassionate, patient- and family-centered care:
- The Skylight Project Ma Vie En Rose Children’s Advocate Award, San Francisco, California
- The D.C. Youth Pride Alliance's 10 Year Anniversary Award
- The Stuart Nichols Award for outstanding achievements in gay, lesbian, bisexual and transgender community mental health
Frequently Asked Questions About Our Gender Development Program
At Children’s National, we understand that families have many questions about their child’s condition and care. Review our frequently asked questions regarding the Gender Development Program to learn more.

Main Hospital
- Specialty Care

Montgomery County
Learn about the support groups we offer for parents and children, and explore our other family resources.

Visiting Children's National
We’re here to help make your trip to Children’s National as easy as possible. Discover information about transportation and parking, visiting hours, where to stay during your visit, spending the night at the hospital and things to do in the area.
MTFsurgery .net
- Orchiectomy
- Penile Inversion Vaginoplasty
- Peritoneal Vaginoplasty
- Rectosigmoid Vaginoplasty
- Vulvoplasty
- Non-Binary Bottom Surgery
- Facial Feminization Surgery
- Breast Augmentation
- Breast Augmentation w/ Fat Transfer
- Body Feminization
- What Is Board Certification?
- Getting Surgery In Thailand
- Vaginoplasty Hair Removal
- Follicular Cautery vs. Hair Removal
- Vaginal Stenosis After Vaginoplasty
- Importance of Dilation
- Breast Aug & Surgeon Experience
- Browse All Surgeons
- Orchiectomy Surgeons
Vaginoplasty Surgeons
- FFS Surgeons
- Breast Augmentation Surgeons
- Body Feminization Surgeons
- MTF Breast Augmentation
- MTF Vaginoplasty
MTF Surgery » Surgeons
Surgeons Who Perform Gender-Affirming Surgery
Trans feminine Gender Affirming Surgery is becoming more and more common, but it can still be tough to find the right surgeon. The surgeons listed below are highly qualified plastic, reconstructive, urological and cosmetic surgeons who regularly perform gender-affirming procedures for those on the trans feminine spectrum. When choosing a surgeon, look for board certification, experience with transgender surgery, and a someone you feel confident and comfortable with.
Also see: Vaginoplasty Surgeons , Orchiectomy Surgeons
Featured Surgeons
Dr. Kathy Rumer
Dr. Kathy Rumer is an expert in transgender surgery, performing 200-250 MTF gender reassignment surgeries per year. Dr. Rumer also directs a 1-year gender surgery fellowship program. She offers the full range of male to female surgery procedures, including Vaginoplasty, Facial Feminization Surgery and Breast Augmentation. Read more »
Dr. Scott Mosser
Dr. Scott W. Mosser is a board certified and award-winning surgeon based in San Francisco who specializes in MTF/N Breast Augmentation and Body Feminization. He has worked with the transgender community for more than 10 years. Dr. Mosser is co-founder of the American Society of Gender Surgeons (ASGS), and Medical Director of the Gender Institute at Saint Francis Memorial Hospital. Read more »
Dr. Gabriel Del Corral
Dr. Del Corral is a double board-certified plastic and reconstructive surgeon who offers Vaginoplasty and other gender-affirming procedures at the Medstar Center for Gender Affirmation in Washington D.C. and Baltimore, Maryland. Fellowship trained in microsurgery, Dr. Del Corral also has expertise in reconstructive surgery, maxillofacial surgery and cosmetic surgery. He specializes in Gender Affirmation Surgery and has a particular interest in Vaginoplasty and Facial Feminization. More »
Dr. Scott W. Mosser is a board certified and award-winning surgeon based in San Francisco who specializes in MTF/N Breast Augmentation and Body Feminization. He has worked with the transgender community for more than 10 years. Dr. Mosser is co-founder of the American Society of Gender Surgeons (ASGS), and Medical Director of the Gender Institute at Saint Francis Memorial Hospital. More »
Dr. Danny Hanna
Dr. Hanna is a fellowship-trained Gender Surgeon based in Dallas, Texas. At the Hanna Gender Center, Dr. Hanna works exclusively with transgender and non-binary patients, offering gender-affirming genital surgeries as well as Breast Augmentation, Body Sculpting and Hair Grafting. More »
Newly Added Surgeons
Dr. Kenan Celtik
Dr. Celtik is a Reconstructive Urologist who specializes in gender-affirming Vaginoplasty. He is fellowship-trained in Gender Surgery and has completed 15 years of advanced medical education, including rigorous training in female pelvic reconstruction, robotic surgery and neurourology. Dr. Celtik's deep expertise and commitment to providing exceptional care and surgical outcomes make him a great choice of Vaginoplasty surgeon. He joined the Crane Center for Transgender Surgery in 2023 and is based in the San Francisco area. More »
Dr. Drew Marano
Dr. Marano is a fellowship-trained plastic and reconstructive surgeon in New York City who has deep expertise in Gender Affirmation Surgery. Dr. Marano is fellowship-trained in the full spectrum of gender-affirming procedures and is particularly passionate about Robotic Vaginoplasty and Facial Feminization Surgery. Dr. Marano's extensive training and dedication to provide the highest level of care make him a sound choice of surgeon in the New York metropolitan area. More »
Dr. Aneesh Gupta
Dr. Gupta is a triple board-certified cosmetic surgeon in Philadelphia who offers Breast Augmentation and Body Feminization surgery. Dr. Gupta's experience with gender-affirming care has informed how Jazzi Cosmetic Surgery has created a welcoming environment for all patients. Throughout your surgical journey, you can expect everyone you interact with at Jazzi to be friendly and professional. More »
Facial Feminization Experts
Dr. Gerhard Mundinger
Dr. Mundinger is a board-certified plastic surgeon with broad training and expertise in craniofacial and gender-affirming surgery. Dr. Mundinger joined the Austin branch of the Crane Center for Transgender Surgery in 2021, where he offers Facial Feminization Surgery, Vaginoplasty and Breast Augmentation. More »
Dr. Amir Dorafshar
Dr. Dorafshar is a highly distinguished plastic, reconstructive and craniofacial surgeon who specializes in gender-affirming facial surgery. Based in Chicago, Dr. Dorafshar formerly served as the Division Chief of Plastic & Reconstructive Surgery and the Program Director of the Plastic & Reconstructive Surgery Fellowship at Rush University Medical Center. He is now in private practice in Chicago. More »
Dr. Thomas Satterwhite
Dr. Satterwhite is a Plastic Surgeon in San Francisco works exclusively with transgender and non-binary patients. Dr. Satterwhite performs Facial Feminization Surgery, Vaginoplasty, Breast and Buttock Augmentation, and Body Sculpting. More »
Dr. Josef Hadeed
Dr. Hadeed is a board certified, Duke University-trained surgeon who offers gender-affirming feminizing surgery in Beverly Hills, California and Miami, Florida. Dr. Hadeed's surgical offerings include Orchiectomy, Facial Feminization, Breast Augmentation and Body Sculpting. More »
Dr. Alexander Facque
Dr. Facque is a board-certified plastic surgeon in San Francisco, California who joined the Gender Confirmation Center's team in September 2020 as a full-time Associate Surgeon with deep expertise in Facial Gender Confirmation Surgery, Breast Augmentation and Body Sculpting. Dr. Facque was introduced to gender-affirming care in 2012 and now works exclusively with transgender and non-binary patients. More »
Dr. Drew Schnitt
Dr. Schnitt is a board certified cosmetic, plastic, reconstructive and craniofacial surgeon. In practice since 2002, Dr. Schnitt's extensive experience in cosmetic and craniofacial surgery make him a great choice for Facial Feminization Surgery in Florida, as well as Breast Augmentation, and Body Sculpting. More »
Dr. Toby Meltzer
Dr. Meltzer is a plastic and reconstructive surgeon who is widely recognized as one of the leading surgeons in the field of Gender Reassignment Surgery. Dr. Meltzer has been performing MTF Surgery since 1993 and has completed over 4000 gender affirming surgeries. He performs about 200 gender reassignment surgery cases per year in Scottsdale, Arizona. More »
Dr. Christopher Salgado
Dr. Salgado is a board-certified plastic surgeon in Florida who has deep expertise in Gender Affirming Surgery. In practice for more than 20 years, Dr. Salgado performs all aspects of male-to-female surgery, from Facial Feminization and Breast Augmentation to Vaginoplasty, giving patients the opportunity to experience a continuity of care throughout their surgical transition. After many years in academic practice, Dr. Salgado opened his private practice in Miami in 2019. More »
Dr. Eric Bensimon
Dr. Bensimon has dedicated his career to helping trans women seeking FFS. With over 15 years experience in FFS, Dr. Eric Bensimon is one of the world's most experienced surgeons practicing Facial Feminization Surgery. Dr. Bensimon is based in Montreal, Canada. More »
Dr. Praful Ramineni
Dr. Ramineni is a highly experienced, board-certified plastic and reconstructive surgeon who specializes in gender-affirming top and bottom surgeries. Dr. Ramineni has more than 15 years of experience as a surgeon and performs at least 600 procedures a year. He's known for not just his exceptional surgical skills and natural-looking results, but also for his caring bedside manner and great communication style. More »
Dr. Daniel J. Freet
Dr. Freet is a board certified Plastic and Reconstructive Surgeon who offers the full spectrum of MTF Surgery procedures at the University of Texas in Houston. Leading a multidisciplinary gender surgery team, Dr. Freet performs Gender Reassignment Surgery (Vaginoplasty), as well as Facial Feminization and Breast Augmentation. More »
Dr. Angela Rodriguez
Dr. Rodriguez is a board-certified plastic surgeon in San Francisco who is dedicated full time to providing surgical care for transgender patients. She is highly proficient in gender-affirming Vaginoplasty and has a special interest in Facial Feminization. Her commitment to transforming lives and passion for social justice drove her pursuance to master transgender surgery, but it's Dr. Rodriguez's surgical skills, bedside manner and results that patients love. More »
Dr. Curtis Crane
Dr. Crane is a board-certified plastic surgeon in Austin, Texas who has deep experience with the full spectrum of male-to-female Gender Reassignment Surgery procedures. Dr. Crane and his team perform approximately 130 Vaginoplasty surgeries every year, as well as Vulvoplasty, Facial Feminization and Breast Augmentation. More »
Dr. Richard Santucci
Dr. Santucci, who spent 18 years as one of the nation's most distinguished academic Reconstructive Urologists, hasn't looked back since turning his focus to Gender Affirming Surgery. Before joining the Crane Center for Transgender Surgery, Dr. Santucci served as the Director of the Center for Urologic Reconstruction and the Specialist-in-Chief for Urology at the Detroit Medical Center. Dr. Santucci's years of experience with complex genitourinary surgery uniquely qualifies him to excel at gender-affirming genital reconstruction. More »
Dr. Ashley DeLeon
Dr. DeLeon is a board-certified surgeon who specializes exclusively in Gender Affirmation Surgery. Dr. DeLeon was fellowship trained in gender-affirming procedures by Dr. Curtis Crane. Dr. DeLeon practices in Austin, Texas at the Crane Center for Transgender Surgery, one of the busiest gender surgery practices in the world. Dr. DeLeon's special focus is on male-to-female bottom surgery procedures: Orchiectomy, Vulvoplasty and Vaginoplasty. More »
Dr. Dev Gurjala
Dr. Gurjala is a board-certified plastic surgeon in San Francisco who offers the full array of male-to-female surgery. Prior to joining Align Surgical Associates in 2019, Dr. Gurjala performed gender surgery, microsurgery, and general reconstructive and aesthetic surgery for five years in the Kaiser Permanente system in California. More »
Dr. Michael Safir
Dr. Safir is a board-certified urologist in Los Angeles who specializes exclusively in gender-affirming bottom surgery procedures. With sub-specialty certification in Female Pelvic Medicine and Reconstructive Surgery (FPM-RS), Dr. Safir is one of a handful of urologists in the world with individual fellowship training and experience in both male and female genital reconstruction. He gained signicant experience performing gender-affirming genital procedures for five years at one of the highest volume gender surgery centers in the world. More »
Dr. John Henry Pang
Dr. Pang is a double board-certified plastic and reconstructive surgeon who has also completed fellowship training in Gender Affirming Surgery. Before joining Align Surgical Associates in San Francisco, Dr. Pang completed the Transgender Surgery training program at Mount Sinai in New York City. His practice is dedicated to providing the highest level of care for his transgender and non-binary patients. More »
Dr. Heidi Wittenberg
Dr. Wittenberg is an experienced Urogynecologist in San Francisco who works exclusively with trans and non-binary patients. Dr. Wittenberg is the director of MoZaic Care, which specializes in gender affirming genital and pelvic surgeries, and a Founder Surgeon and Co-Director for the first SRC accredited Center of Excellence in Gender Confirmation Surgery, at Greenbrae Surgery Center. More »
Dr. Adam Bonnington
Dr. Bonnington is a Gender Surgeon in San Francisco who has focused his career on working with underrepresented patient populations. He joined Dr. Heidi Wittenberg at MoZaic Care as a Surgical Associate in 2020 where he works exclusively with transgender and non-binary individuals. Dr. Bonnington performs Orchiectomy and Vaginoplasty. More »
Dr. Loren Schechter
Dr. Schechter is one of the country's foremost experts on gender-affirming surgery. He is the Medical Director of the Gender Affirmation Surgery Program at Rush University Medical Center in Chicago. Dr. Schechter's outstanding surgical skills and more than 20 years experience with transgender surgery have made him an in-demand surgeon. He offers the full spectrum MTF Gender Confirmation procedures, including Breast Augmentation, single-stage Vaginoplasty, and FFS. More »
Dr. Ellie Zara Ley
Dr. Ley is a board-certified plastic surgeon who had over 15 years of training and experience in plastic surgery, craniofacial surgery and microsurgery before completing Gender Surgery training. Now based in San Francisco, Dr. Ley provides superb surgical care for those seeking Vaginoplasty, Facial Feminization and other feminizing surgeries. More »
Dr. Kathy Rumer is an expert in transgender surgery, performing 200-250 MTF gender reassignment surgeries per year. Dr. Rumer also directs a 1-year gender surgery fellowship program. She offers the full range of male to female surgery procedures, including Vaginoplasty, Facial Feminization Surgery and Breast Augmentation. More »
Dr. John Whitehead
Dr. Whitehead offers gender affirming male-to-female surgery in Florida. Dr. Whitehead was trained in the art of gender reassignment surgery by Dr. Harold Reed, the now-retired urologist who practiced at The Reed Center for decades. Dr. Whitehead offers Orchiectomy, Vaginoplasty and Vulvoplasty. More »
Dr. Dmitriy Nikolavsky
Dr. Nikolavsky is a highly regarded Reconstructive Urologist and Gender Surgeon at SUNY Upstate Medical University in Syracuse NY. In addition to offering primary Vaginoplasty surgery, Dr. Nikolavsky is also an expert at treating post-operative urinary complications and provides long term follow-up care for patients who have had Vaginoplasty. Read more »

Dr. Jonathan Keith
Dr. Keith is a fellowship-trained Plastic Surgeon in New Jersey with expertise in Gender Reassignment Surgery. In 2018, Dr. Keith co-founded the first multidisciplinary clinical program for transgender patients in New Jersey. He is the first surgeon in New Jersey to offer the full range of gender-affirming procedures, including Facial Surgery, Vaginoplasty and Breast Augmentation. More »
Dr. Nick Esmonde
Dr. Esmonde is a Gender Surgeon in Portland, Oregon who has impeccable training in Gender Affirmation Surgery and whose practice is almost exclusively focused on helping transgender and non-binary patients. Dr. Esmonde offers the full spectrum of feminizing surgeries, from Facial Feminization to Vaginoplasty. More »
Dr. Christopher McClung
Dr. McClung is a board-certified urologist in Columbus, Ohio who specializes in gender-affirming Vaginoplasty. Dr. McClung's deep experience with complex urological reconstructions provided an ideal background for becoming a Gender Surgeon. He has now performed over 200 feminizing bottom surgeries and his practice is fully dedicated to providing gender-affirming surgical care. In addition to his urology and reconstructive expertise, Dr. McClung's patients also appreciate his gentle bedside manner. More »
Dr. Min Jun
Dr. Min Jun is an exceptionally trained Reconstructive Urologist and Gender Surgeon in San Francisco who specializes in Robotic Peritoneal Flap Vaginoplasty. Dr. Jun has completed fellowship training in both Reconstructive Urology and Gender Affirming Surgery. He worked with the Crane Center for Transgender Surgery in 2020-2023 and now has his own practice in San Francisco. More »
Surgeons in Thailand
Dr. Pichet Rodchareon
Dr. Pichet Rodchareon is a board-certified plastic surgeon in Bangkok who has extensive experience performing male-to-female Gender Reassignment Surgery. Dr. Pichet is considered one of top SRS surgeons in Thailand. His training includes plastic surgery, hand surgery, craniofacial and maxillofacial surgery. More »
Dr. Kamol Pansritum
Dr. Kamol Pansritum is recognized as one of the most experienced GRS Surgeons in the world, having completed over 5,000 gender reassignment surgeries, and more than 10,000 related surgical procedures for trans women since 1997. Dr. Kamol currently performs more than 200 MTF reassignment surgeries a year at his private hospital in Bangkok, Thailand. More »
More MTF Surgeons
Dr. E. Antonio Mangubat
Dr. E. Antonio Mangubat is the Pacific Northwest's most sought-after surgeon for transgender surgery, with more than 20 years of experience performing procedures for trans women, including Facial Feminization, MTF Breast Augmentation, Body Sculpting and Hair Restoration. More »
Dr. Alvina Won
Dr. Won is a board-certified Cosmetic Surgeon who is committed to providing the highest level of compassionate care in a welcoming environment for all patients. Dr. Won gained significant experience with gender-affirming surgery during a year-long cosmetic surgery fellowship with Dr. Tony Mangubat, a 20+ year veteran of transgender surgery. Based in the Seattle area, just north of Seattle, Dr. Won now devotes part of her practice to performing MTF Breast Augmentation, Buttock Augmentation and Body Sculpting. More »
Dr. Laurel Chandler
Dr. Chandler is a Harvard fellowship-trained plastic surgeon who has received specialty training in gender-affirming breast surgery. During both her residency and fellowship training, Dr. Chandler worked with established gender surgeons to learn the aesthetic nuances of transgender Breast Augmentation. Dr. Chandler provides individualized care for a diverse range of patients, up to 90% of whom are transgender and non-binary. More »
Dr. Russell Sassani
Dr. Russell Sassani is a board certified plastic and reconstructive surgeon who has quickly become one of the most popular surgeons in the Southeastern United States for trans women. He performs Breast Augmentation, Facial Feminization and Body Sculpting in the Mami/Fort Lauderdale area. More »
Dr. Mark Youssef
Dr. Mark Youssef, Director of the Transgender Surgery Institute of Southern California, is a Cosmetic Surgeon in Santa Monica who helps clients on the trans feminine spectrum with Breast Augmentation, Body Feminization and Facial Feminization surgeries. He operates at his private surgery center, Younique Surgery Center in Santa Monica. More »
Dr. Hope Sherie
Dr. Hope Sherie is a board-certified cosmetic surgeon who has extensive training in MTF surgery procedures. Dr. Sherie offers trans women the highest level of surgical care at her practice in Charlotte, North Carolina. Procedures available include Orchiectomy and Breast Augmentation. More »
Dr. Javad Sajan
Voted #1 Best Surgeon in Seattle in 2016 and 2017, Dr. Sajan is an internationally recognized Cosmetic & Reconstructive Plastic Surgeon whose specializations include Facial Feminization and Breast Augmentation. Dr. Sajan enjoys providing gender-affirming surgical care and is honored to play a role in his patients' transitions. More »
Dr. Daniel Jacobs
Dr. Jacobs is a board-certified plastic surgeon in San Francisco, California who joined the Gender Confirmation Center in July 2022. With more than 30 years of plastic experience and a practice that's dedicated to gender-affirming care, Dr. Jacobs is a sound choice for transfeminine and non-binary individuals seeking Breast Augmentation surgery. More »
Dr. Daniel Crane
Dr. Crane is a plastic surgeon in the Miami area who has expertise in breast, body and facial surgeries. He was one of only 30 residents selected from across the country to participate in a highly specialized aesthetic fellowship training program. In 2022, Dr. Crane joined Dr. Drew Schnitt's Inspire Aesthetics.. His unique training in plastic and aesthetic surgery provides him with the knowledge and experience to help you achieve your surgery goals. More »
Dr. Charles Lee
Dr. Charles Lee is a board-certified plastic and reconstructive surgeon who has deep expertise in microsurgery and breast surgery. In practice since 2003, Dr. Lee offers MTF Top Surgery at Crane Center for Transgender Surgery in San Francisco. More »
Dr. Alan Dulin
Dr. Alan Dulin is a board-certified surgeon who has many years of experience performing Male-to-Female Surgery in the Dallas area. Dr. Dulin offers transgender women Breast Augmentation & Body Contouring, Facial Feminization Surgery and Orchiectomy. More »
Dr. Scott Harris
Dr. Scott Harris is a board-certified Surgeon with years of experience performing Male to Female Surgery in Texas. Known for his meticulous attention to detail, Dr. Harris offers a number of feminizing surgeries for trans women, including Facial Feminization Surgery, Breast Augmentation and Body Sculpting procedures. More »
Dr. Cassie Nghiem
Dr. Nghiem is an Ivy League-educated, fellowship-trained plastic surgeon in Washington, D.C. who specializes in Gender-Affirming Surgery, including Breast Augmentation and Facial Feminization. She works closely with her patients to deliver the best quality care that is aligned with their goals. Known for her advanced surgical skills, Dr. Nghiem's patients also love her friendly personality and kind demeanor. More »
Dr. Manish Champaneria
Dr. Manish Champaneria is a board-certified surgeon with extensive training and experience in plastic surgery and a special focus on reconstructive breast procedures and Facial Feminization. Dr. Champaneria practices in San Diego, California. More »
Dr. Walter Lin
Dr. Walter Lin is a fellowship-trained Plastic Surgeon in San Francisco who performs Breast Augmentation for transfeminine individuals. Dr. Lin's expertise in the areas of microsurgical reconstruction of the extremities, breast, and lymphatic systems has greatly contributed to his skill with gender-affirming Breast Augmentation. Dr. Lin joined the staff of Buncke Clinic and the San Francisco Transgender Institute in 2017. More »
Dr. Michelle Lee
Dr. Lee is a board-certified and fellowship-trained plastic surgeon with high proficiency in aesthetic and reconstructive procedures for the breast and face. Widely regarded as being one of the finest plastic surgeons in the Los Angeles area, Dr. Lee possesses the perfect combination of skill, artistry, experience and compassion, which makes her ideally suited to performing gender-affirming surgery. More »
Dr. Dustin Reid
Dr. Dustin Reid is a double board-certified plastic surgeon in Austin who offers Breast Augmentation, Body Feminization and Hair Restoration. Dr. Reid is committed to providing expert surgical care and guidance throughout your surgery experience. More »
Dr. Daniel Medalie
Dr. Daniel Medalie is a board certified plastic and reconstructive surgeon who has been performing gender-affirming surgeries since 1996. Based in the Cleveland area, he offers Breast Augmentation and Tracheal Shave procedures for transfeminine individuals. More »
Dr. Jeffrey Marvel
Dr. Marvel is a board-certified cosmetic surgeon who has developed a great reputation in Nashville and Central Tennessee for his technical skills, attention to detail and natural-looking results. Since 1997, Dr. Marvel and Marvel Cosmetic Surgery's dedicated staff have offered top-notch hospitality and care for patients seeking a wide range of cosmetic procedures, including Facial Feminization, Breast Augmentation and Hair Grafting. More »
Dr. Eric Emerson
Dr. Eric Emerson is a Board-Certified Plastic Surgeon with over 20 years experience specializing in breast surgery, body contouring and facial surgery. Dr. Emerson is a sound choice for trans women seeking breast augmentation and body and facial feminization surgery in the Carolinas and eastern United States. More »
Dr. Gregory Swank
Dr. Gregory Swank a board-certified, Duke University-trained surgeon who offers male-to-female surgery in North Carolina. Dr. Swank's surgical offerings for trans women include Breast Augmentation, and Body and Facial Feminization. More »
Dr. Michael Beckenstein
Dr. Michael Beckenstein is a double-board-certified Plastic Surgeon in Birmingham who is pleased to offer his expertise and skills in cosmetic and reconstructive surgery to the MTF community in Alabama and throughout the Southeast. Dr. Beckenstein specializes in Breast Augmentation as well as Hair Restoration. More »
Dr. Helena Guarda
Dr. Helena Guarda is a board-certified Plastic and Reconstructive Surgeon who is committed to offering Breast Augmentation and Feminization Surgeries as part of her LGBT-friendly practice in Suffolk, Virginia. Dr. Guarda is excited to work with patients from all parts of Virginia, as well as those coming from nearby states such as North Carolina, Maryland, West Virginia, Tennessee, and Kentucky. More »
Dr. Elliot Jacobs
Dr. Jacobs is a nationally-recognized, board-certified plastic surgeon in Boca Raton, Florida with more than 30 years of experience in breast and facial surgeries. Dr. Jacobs offers MTF Surgery procedures at his private, modern and fully accredited surgical suite. More »
Dr. Rex Moulton-Barrett
Dr. Rex Moulton-Barrett is a double board certified cosmetic, plastic and reconstructive surgeon in the San Francisco Bay Area who has been performing MTF Breast Augmentation surgery since 2010. Read more »
Dr. Vartan Mardirossian
Dr. Vartan Mardirossian is a surgeon in South Florida who specializes in Facial Feminization Surgery. Dr. Mardirossian has extensive training and experience performing Facial Feminization procedures, including 7 years of training under renowned FFS surgeon Dr. Jeffrey Spiegel . Read more »
Last updated: 02/21/24

DC Orders Insurers to Cover Sex-Change Surgery
Published february 27, 2014 • updated on february 27, 2014 at 8:26 pm.
Insurance companies in the District of Columbia have been ordered to stop denying coverage to transgender residents seeking gender-reassignment surgery. Mayor Vincent Gray says the new rules will end health-care discrimination against the transgender population and put "the district at the forefront of advancing the rights of transgender individuals.'' A bulletin issued Thursday by the city's Department of Insurance, Securities and Banking says that gender dysphoria is a recognized medical condition. It says the various forms of treatment for that condition, including sex-change procedures, are covered benefits. Gray says people with gender dysphoria, also known as gender identity disorder, "should not have to pay exorbitant out-of-pocket expenses for medically necessary treatment.''
Allowing transition-related care is absolutely vital to allow transgender people to live full, good lives," said activist Andy Bowen of the National Center for Transgender Equality. The city already has laws banning discrimination against transgender people. Health care is as vital as efforts to curb violence against transgender people, according to the Gray administration.
Mara Keisling, who runs the National Center for Transgender Equality, told News4's Tom Sherwood there are still other areas of discrimination, like in employment, but access to health care is vital.
Costs for counseling, medicines and gender surgeries can total tens of thousands of dollars, an especially large burden for lower-income people facing job discrimination.
DC orders transgender health care coverage

Washington D.C. will require insurance companies to provide health coverage to trans residents, including gender reassignment surgery.
Mayor Vincent Gray announced the change in policy Thursday, saying in a statement, “This action places the District at the forefront of advancing the rights of transgender individuals.” Washington D.C. has laws that ban discrimination against transgender people.
The D.C. Department of Insurance, Securities and Banking issued a bulletin Thursday noting that not only does D.C. law prohibit “discrimination in health insurance against people based on gender identity or expression,” but that surgery must be covered as well.
“[I]t is the position of the Department that treatment for gender dysphoria, including gender reassignment surgeries, is a covered benefit, and individuals diagnosed with gender dysphoria are entitled to receive medically necessary benefits and services under individual and group health insurance policies covering medical and hospital expenses,” the bulletin read .
Only a small handful of states have laws protecting transgender rights where health insurance is concerned, and without insurance coverage, medically necessary measures such as hormone therapy and different surgeries can be prohibitively expensive.
Transgender people, "should not have to pay exorbitant out-of-pocket expenses for medically necessary treatment,” Mayor Gray said in his statement.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Transl Med
- v.9(7); 2021 Apr

Guiding the conversation—types of regret after gender-affirming surgery and their associated etiologies
Sasha karan narayan.
1 Department of Surgery, Oregon Health and Science University, Portland, OR, USA;
Rayisa Hontscharuk
2 Department of Plastic and Reconstructive Surgery, Rush University Medical Center, Chicago, IL, USA;
Sara Danker
3 Division of Plastic Surgery, University of Miami Miller School of Medicine, Miami, FL, USA;
Jess Guerriero
4 Transgender Health Program, Oregon Health & Science University, Portland, OR, USA;
Angela Carter
5 Primary Care, Equi Institute, Portland, OR, USA;
Gaines Blasdel
6 NYU Langone Health, New York, NY, USA;
Rachel Bluebond-Langner
Randi ettner.
7 University of Minnesota, Minneapolis, MN, USA;
8 Callen-Lorde Community Health Center, New York, NY, USA;
Loren Schechter
9 The University of Illinois at Chicago, Chicago, IL, USA;
10 Rush University Medical Center, Chicago, IL, USA;
11 The Center for Gender Confirmation Surgery, Weiss Memorial Hospital, Chicago, IL, USA;
Jens Urs Berli
12 Division of Plastic & Reconstructive Surgery, Oregon Health & Science University, Portland, OR, USA
Associated Data
The article’s supplementary files as
A rare, but consequential, risk of gender affirming surgery (GAS) is post-operative regret resulting in a request for surgical reversal. Studies on regret and surgical reversal are scarce, and there is no standard terminology regarding either etiology and/or classification of the various forms of regret. This study includes a survey of surgeons’ experience with patient regret and requests for reversal surgery, a literature review on the topic of regret, and expert, consensus opinion designed to establish a classification system for the etiology and types of regret experienced by some patients.
This anonymous survey was sent to the 154 surgeons who registered for the 2016 World Professional Association for Transgender Health (WPATH) conference and the 2017 USPATH conference. Responses were analyzed using descriptive statistics. A MeSH search of the gender-affirming outcomes literature was performed on PubMed for relevant studies pertaining to regret. Original research and review studies that were thought to discuss regret were included for full text review.
The literature is inconsistent regarding etiology and classification of regret following GAS. Of the 154 surgeons queried, 30% responded to our survey. Cumulatively, these respondents treated between 18,125 and 27,325 individuals. Fifty-seven percent of surgeons encountered at least one patient who expressed regret, with a total of 62 patients expressing regret (0.2–0.3%). Etiologies of regret were varied and classified as either: (I) true gender-related regret (42%), (II) social regret (37%), and (III) medical regret (8%). The surgeons’ experience with patient regret and request for reversal was consistent with the existing literature.
Conclusions
In this study, regret following GAS was rare and was consistent with the existing literature. Regret can be classified as true gender-related regret, social regret and medical regret resulting from complications, function, pre-intervention decision making. Guidelines in transgender health should offer preventive strategies as well as treatment recommendations, should a patient experience regret. Future studies and scientific discourse are encouraged on this important topic.
Introduction
Over the past several years, there has been sustained growth in institutional and social support for transgender and gender non-conforming (TGNC) care, including gender-affirming surgery (GAS) ( 1 ). The American Society of Plastic Surgeons (ASPS) estimates that in 2016, no less than 3,200 gender-affirming surgeries were performed by ASPS surgeons. This represents a 20% increase over 2015 ( 2 ) and may be partially attributable to an increase in third party coverage ( 3 , 4 ). A rare, but consequential, risk of GAS is post-operative regret that could lead to requests for surgical reversal. As the number of patients seeking surgery increases, the absolute number of patients who experience regret is also likely to increase. While access to gender-affirming health care has expanded, these gains are under continued threat by various independent organizations, religious, and political groups that are questioning the legitimacy of this aspect of healthcare despite an ever-growing body of scientific literature supporting the medical necessity of many surgical and non-surgical affirming interventions. It is therefore not surprising that studies on regret and surgical reversal are scarce compared to studies on satisfaction and patient-reported outcomes. The transgender community rightfully fears that studies on this topic can be miscited to undermine the right to access to healthcare.
The goal of this study is to assist patients, professionals, and policy makers regarding this important, albeit rare, occurrence. We do so by addressing the following:
- The current literature regarding the etiology of regret following gender-affirming surgery;
- The experience of surgeons regarding requests for surgical reversal.
Based on these results, the authors propose a classification system for both type and etiology of regret.
It is important to acknowledge that the authors identify along the gender spectrum and are experts in the field of transgender health (mental health, primary care, and surgery). We hope to facilitate discussion regarding this multifaceted and complex topic to provide a stepping-stone for future scientific discussion and guideline development. Our ultimate goal is to reduce the possibility of regret and provide clinical support to patients suffering from the sequelae of regret. We present the following article in accordance with the SURGE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-6204 ).
A 16-question survey (see Table S1 ) was developed and uploaded to the online survey platform SurveyMonkey (SurveyMonkey, Inc., San Mateo, CA, USA). This anonymous survey was e-mailed by the senior author to the 154 surgeons who registered for the 2016 World Professional Association for Transgender Health (WPATH) conference and the 2017 USPATH conference. There were no incentives offered for completing this survey. One reminder e-mail was sent after the initial invitation.
Respondents were asked to describe their practices, including: country of practice, years in practice, a range estimate of the total number of TGNC patients surgically treated, and the number of TGNC patients seen in consultation who expressed regret and a desire to reverse or remove the gendered aspects of a previous gender-affirming surgery. We limited the questions to breast and genital procedures only. Facial surgery was excluded as there are no associated WPATH criteria, so there is less standardization of patient selection for surgery. Thus, we did not feel that those patients should be pooled with those who were subject to WPATH criteria in our calculation for prevalence of regret. We did not define the term “regret” in order to capture a wide range of responses. Respondents were asked about their patients’ gender-identification, the patient’s surgical transition history, and the patient’s reasons for requesting reversal surgery. If the respondents had experience with patients seeking reversal surgery, the number of such interventions were queried to include: the initial gender-affirming procedure and the patients’ reason(s) for requesting reversal procedures. The respondents were also asked about the number of reversal procedures they had performed, and what requirements, if any, they would/did have prior to performing such procedures. Finally, respondents were asked whether they believed that the WPATH Standards of Care 8 should address this topic.
Statistical analysis
Response rate was calculated from the total number of respondents as compared to the number of unique survey invitations sent. Responses to the survey were analyzed using descriptive statistics. When survey questions offered ranges, (i.e., estimating the number of patients surgically treated), the minimum and maximum values of each of the selected answers were independently summed to report a more comprehensible view of the data. Partially completed surveys were identified individually and accounted for in analysis. Any missing or incomplete data items from the survey were excluded from the results with the denominator adjusted accordingly.
Narrative literature review
A MeSH search of the gender-affirming outcomes literature was performed on PubMed for relevant studies pertaining to regret and satisfaction. Terms included (regret) and (transgender) and (surgery) or (satisfaction) and (transgender) and (surgery). These terms included their permutations according to the PubMed search methodology. Original research and review studies whose abstracts addressed the following topics were included for full-text review: gender-affirming surgery, sex reassignment, patient satisfaction, detransition, regret. A total of 163 abstracts were reviewed and a total of 21 articles were closely read for the relevant discussion of regret and satisfaction.
Ethical statement
This study was approved by the Oregon Health & Science Institutional Review Board #17450 and was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Subjects were physicians and so gave consent through their participation in the survey. The patients who were captured in the study were not individually consented for this research as the IRB felt it to be unnecessary given the degree of separation of the study and lack of identifiers. None of the study outcomes affect future management of the patients’ care.
Survey results
Of the 154 surgeons who received the survey between December 2017 and February 2018, 46 (30%) surgeons completed the survey. The survey, including its results, can be found in Table S1 . Thirty respondents (65%) were in practice for greater than 10 years, and most (67%) practice in the United States, followed by Europe (22%). The respondents treated between 18,125 and 27,325 TGNC or gender non-conforming (TGNC) patients. Most of the respondents (72%) surgically treated over 100 TGNC patients (see Figure 1 ). Of the 46 respondents, 61% of respondents encountered either at least one patient with regret regarding their surgical transition or a patient who sought a reversal procedure—irrespective of whether their initial surgery was performed by the respondent or another surgeon. Twelve respondents (26%) encountered one patient with regret, and the remaining 12 (26%) encountered two or more patients with regret. One respondent indicated that they encountered between 10 and 20 patients who regretted their surgical gender transition. No respondent encountered more than 20 such patients (see Figure 2 ). This amounted to a total of 62 patients with regret regarding surgical transition, or a 0.2% to 0.3% rate of regret. Of these 62 patients, 13 (21%) involved chest/breast surgery and 45 (73%) involved genital surgery (see Table 1 ).

Distribution of transgender surgery experiences among respondents.

Number of transgender patients encountered who expressed regret.
Totals do not add to 100 due to incomplete responses.
Of the 62 patients who sought surgical reversal procedures, at the time of their initial gender-affirming surgery, 19 patients identified as trans-men, 37 identified as trans women, and 6 identified as non-binary. The reasons for pursuing surgical reversal were provided for 46 patients (74%) and included: change in gender identity or misdiagnosis (26 patients, 42%), rejection or alienation from family or social support (9 patients, 15%), and difficulty in romantic relationships (7 patients, 11%). In some patients, surgical complications or social factors were cited as a reason for regret and request for reversal of genital surgery—no change in the patient’s gender identity was elucidated (see Table 2 , etiologies of regret). Of the 37 trans-women seeking reversal procedures, complaints at the time of secondary surgical consultation included: vaginal stenosis (7 patients), rectovaginal fistulae (2 patients), and chronic genital pain (3 patients). Of the 19 trans-men seeking reversal procedures, complaints at the time of secondary surgical consultation included: urethral fistulae (2 patients) and urethral stricture (1 patient). A total of 36 reversal procedures were reported, with supplemental qualitative descriptions provided for only 23 procedures. The distribution of the 23 reversal procedures is found in Table 1 .
Totals exceed 100 as respondents could select multiple options.
Most respondents (91%) indicated that new mental health evaluations would be required prior to performing surgical reversal procedures. Eighty-eight percent of respondents indicated that WPATH SOC 8 should include a chapter on reversal procedures (see Figure 3 ).

Respondent’s requirements to proceed with surgical reversal.
Literature review
Overall, the incidence of regret following gender-affirming surgery has been reported to be consistently very low ( 5 - 26 ). Wiepjes et al. ( 27 ) reported an overall incidence of surgical regret in the literature in transgender men as <1% and transgender women as <2%. Landen et al. comment that outcomes following gender-affirming surgery have improved due to preoperative patient assessment, more restrictive inclusion criteria, improved surgical techniques, and attention to postoperative psychosocial guidance ( 28 ). Although retrospective, the Wiepjes et al. study is the largest series to date and included 6,793 patients over 43 years. In this study, only 14 patients were classified as regretful, and only 10 of these patients pursued procedures consistent with intent to detransition. Perhaps most importantly, the Amsterdam team categorized regret into three main subtypes: “ social regret , true regret , and feeling non - binary ”.
Many of the reviewed studies aimed to identify various variables or risk factors that may identify patients that are at risk or that may predict future postoperative regret.
Earlier studies focused on patient characteristics and identified several variables that were associated with regret in their patient populations. These variables include psychological variables ( 11 , 22 , 23 ), such as previous history of depression ( 15 , 26 ), character pathology ( 26 ) or personality disorder ( 5 , 15 ), history of psychotic disorder ( 15 , 28 ), overactive temperament ( 26 ), negative self-image ( 26 ) or other psychopathology ( 15 , 19 , 26 ), as well as various social or familial factors that include history of family trauma ( 19 , 29 ), poor family support ( 5 , 11 , 15 , 28 ), belonging to a non-core group ( 28 ), previous marriage ( 15 , 19 ), and biological parenthood ( 15 , 19 ). Landen et al. identified poor family support as the most important variable predicting future postoperative regret in transgender men and women undergoing gender-affirming surgery in Sweden between 1972–1992 ( 28 ). Defined as subsequent application for reversal surgery, the authors found that 3.8% of their study population regretted their surgery. Other factors previously associated with regret include: sexual orientation ( 5 , 7 , 15 , 19 ), impaired postoperative sexual function [most notably in transgender women; ( 29 )], previous military service ( 29 ), a physically strenuous job ( 29 ), history of criminality ( 5 ), age at time of surgery and transition [>30 year increased risk; ( 5 , 6 , 11 , 15 , 19 , 29 )], asexual or hyposexual status preoperatively ( 15 , 29 ), too much or too little ambivalence regarding prospect of surgery ( 29 ), and/or an absence of gender nonconformity in childhood ( 15 ).
Studies examining transgender women have identified postoperative sexual function to be a significant factor contributing to possible surgical regret ( 15 , 29 ). A literature review by Hadj-Moussa et al. ( 11 ) (2018) identified poor sexual function as a factor that may contribute to postoperative regret in transgender women after vaginoplasty. Lindemalm et al. ( 29 ) (1986) previously reported a rate of 30% regret in their study examining 13 transgender women in Sweden after vaginoplasty. This rate of regret is the highest reported and appears to be an outlier. In their patient population, they found that only one third had a surgically-created vagina capable of sexual intercourse. This was consistent with patient-reported poor postoperative sexual function and highlights the importance of discussing sexual function following vaginoplasty. Similarly, Lawrence et al. ( 15 ) (2003) found that occasional regret was reported in 6% of transgender women after vaginoplasty, with 8 of the 15 regretful patients identifying disappointing physical and functional outcomes after their surgery. These findings are consistent with literature reviews that have found that regret is related to unsatisfactory surgical outcomes and poor postoperative function ( 19 , 30 ).
Transgender men have been found to manifest more favorable psychosocial outcomes following surgery and are less likely to report post-surgical regret ( 26 ). These findings highlight the importance of surgical results, and their influence on surgical regret. Despite this difference between transgender men and women, overall regret continues to remain low.
While the rate of surgical regret is low, many patients can suffer from many forms of “minor regret” after surgery. Although this could skew the outcomes data ( 30 ), this is considered temporary and can be overcome with counseling. As such, this should not be calculated in assessments of true regret ( 30 ). Alternatively, lasting regret is attributed to gender dysphoria and is explicitly expressed through patient postoperative behaviors ( 30 ). Factors that have been found to contribute to “minor regret” after gender-affirming surgery include postsurgical factors such as pain during and after surgery, surgical complications, poor surgical results, loss of partners, loss of job, conflict with family, and disappointments that various expectations linked to surgery were not fulfilled ( 19 ). Previous reviews further underline the importance of following the contemporaneous WPATH Standards of Care. This is especially important regarding patient education pertaining to surgical expectations and outcomes ( 11 , 26 ). Patient education programs are thought to identify those individuals who would most benefit from surgery ( 20 ). Other issues reported to decrease postoperative regret include appropriate preoperative diagnosis ( 19 , 20 , 26 ), consistent administration of hormone therapy ( 15 ), adequate psychotherapy ( 15 ), and the extent to which a patient undergoes a preoperative “real-life test” living in their desired gender role ( 15 , 19 , 20 , 26 ).
As compared to the volume of literature regarding postoperative satisfaction following gender-affirming surgery, the literature on regret is still relatively small. However, the literature (and anecdotal surgeon reports) consistently shows low rates of regret. We juxtaposed these findings to the surgeons’ experience with patients seeking reversal surgery or verbalizing regret. We found a rate of regret between 0.2–0.3%. This is consistent with the most recent data from Wiepjes et al. who reported rates of regret of 0.3% for trans-masculine and 0.6% for trans-feminine patients ( 27 ). The question of prevalence seems relatively well-answered by the current literature.
Perhaps the most striking finding is the heterogeneity of etiologies and risk factors associated with regret. Within this context, establishing consistent definitions for both regret and its underlying etiology is essential. Furthermore, as our understanding of gender identity evolves, our definitions and understanding become more precise. We highlight the Wiepjes et al. classification as an example of how narrower definitions may preclude an understanding of evolving gender theory. This predominantly single-institution study included 6,793 individuals, and the authors classified regret into three subtypes: social regret, true regret, and feeling non-binary. They categorized patients as either trans-female or trans-male. Conversely, in the 2015 US Transgender Survey, 35% of the nearly 28,000 respondents reported a non-binary identification ( 31 ). The classification by Wiepjes et al. is important in that it recognizes that individuals may not regret “transitioning”, but rather regret specific aspects of their medical treatment. More specifically, if these individuals request a reversal procedure, they are not necessarily requesting a “reversal” of their gender identity. However, the Wiepjes et al. study does not elaborate on this topic.
Case example: a trans-masculine, non-binary individual after testosterone therapy and chest masculinization regrets having secondary sex characteristics from hormonal therapy but is highly satisfied following chest masculinization. This should be considered true gender-related regret as the individual desires, at least in part, to return to the phenotype of the sex assigned at birth (e.g., hair removal). However, the etiology regarding this type of regret can be varied. For example, the etiology may include: insufficient exploration of the individual’s gender identity [by the individual and/or mental health professional (misdiagnosis)], lack of knowledge of professionals regarding surgical options for non-binary individuals, insurance carrier mandate to undergo hormonal therapy prior to chest masculinization (healthcare stigma), etc.
Based on the reviewed literature and our consensus expert opinion, we propose the following classification of regret, examples of etiology pertaining to regret ( Table 3 ), and an overview of associated terminology regarding regret ( Table 4 ).
Regret is a general term that describes an emotional state wherein a previous decision now feels incorrect. This can be temporary (fleeting ambivalence) or permanent. Permanent regret can be divided into three forms: true gender-related regret, social regret, and medical regret.
True gender-related regret involves a person having undergone a transition in gender whether by social, medical, or surgical means, indicating a formal change in gender identity, who then desires to return to their assigned sex at birth or a different gender identity. True gender-related regret differs from other types of regret in that it implies a misdiagnosis or misinterpretation of gender incongruence at the time of transition. Based on the case example, true gender-related regret need not be related to all medical treatments, but instead may be focused on specific treatments for which the individual seeks reversal. True gender-related regret constituted 42% of the requests for surgical reversal in our study. Etiology may include: misdiagnosis, insufficient exploration of gender identity, or barriers to access for options to transition to non-binary gender expression.
Social regret refers to one’s desire to return to their sex assigned at birth to alleviate the repercussions of transitioning on their social life. The etiologies can vary widely and include feeling unsafe in public, losing partnership, feeling unable to partake in one’s community, and encountering professional barriers. An additional reason identified in this study included religious conflict, mentioned in 9% of individuals. Social regret was cited in 37.1% of the requests for surgical reversal.
Medical regret includes regret originating from a direct outcome of a surgery or an irreversible consequence thereof. This area is particularly important for the medical community as it is preventable and may increase as access to care expands. Medical regret can be further subdivided into regret secondary to medical complications, long-term functional outcomes (i.e., sexual), and preoperative decision-making.
Medical regret due to inadequate preoperative decision-making is directly related to a medical intervention, but it is not due to a change in gender identity, medical complication, functional outcome, or social stigma. Examples include choosing a simple-release metoidioplasty rather than a phalloplasty or regretting gonadal sterilization later in life ( 32 ). In these situations, individuals may not have appreciated the long-term implications at the time they underwent the procedure, may have received incomplete or inaccurate counseling, may have had a change in life goals, or may have not had access to technologies that are currently available. This form of regret may be mitigated by employing a multidisciplinary approach which includes discussions beyond surgical risks (i.e., fertility preservation, sexuality, etc.) ( 33 , 34 ). Medical regret was cited in 8% of requests for reversal, however 24% of patients were separately noted to have experienced post-operative complications.
Associated definitions
Gender fluidity is an inclusive term describing gender along a spectrum rather than a binary construct. When applied to identity, gender fluidity, sometimes called “genderqueer” ( 35 , 36 ) describes an individual who remains flexible regarding their identity and may identify differently at different times in their lives. Surgeons should work collaboratively with their mental health colleagues to help the patient understand the impact of surgery and how surgery may influence/affect future life goals. Non-identified gender fluidity can be one etiology for true gender-related regret.
Continued transition medically recognizes the concept of gender fluidity and the gender spectrum. This patient seeks additional medical treatment following their initial gender-affirming procedure(s) and may express an evolving gender identity or request further surgical consolidation of their identity. The patient need not express regret over their initial transition. An example is a patient assigned male-at-birth who takes feminizing hormones and undergoes breast augmentation. Subsequently, the patient returns to the surgeon indicating they identify as non-binary and requests implant removal. With decreased stigmatization of non-binary gender identity and ability to access non-binary affirming surgical options, this type of regret may be less common in the future.
Detransition refers to a change in gender role and/or the cessation of medical transition (e.g., hormonal treatment). This term has been used controversially and disparagingly with regards to surgical transition and fails to honor the spectrum of reasons why patients may undergo reversal surgery. However, some patients utilize this term to self-identify and to describe their experiences. This term should not be used to describe the process of surgical reversal.
Retransition is a phenomenon where a patient, following surgical reversal procedures, later feels that this reversal was wrong and seeks to re-affirm their previously expressed gender identity. A reason for retransition may include a change in societal structure that has provided a safer environment for transition. The need to distinguish continued transition from retransition results from a clash between increasing societal perception of a gender spectrum and the Western culture’s binary gender construct ( 35 ).
Fleeting ambivalence (considered short-term regret) over one’s transition is common, especially if the patient experiences initial surgical complications or loss of their support communities. The normal grief experienced as a result of trauma should not be pathologized, and the patient should be encouraged to trust in their long-standing gender identification. Some patients may desire a change in gender identify as a result of feeling unsafe due to severe social stigma. Knowing this, healthcare teams should counsel patients regarding the implications of transitioning within a given societal structure prior to surgery. This may include discussions regarding the effect of transitioning on relationships, careers, personal safety in public, sexuality, etc. These discussions are often facilitated by the patient’s mental health professional and/or primary care provider.
Special considerations
We recognize that regret and surgical reversal are complex, multifaceted phenomena without an easy treatment path. While both regret and requests for surgical reversal are rare, the need for guideline development is critical in providing high-quality care for this patient population, regardless of prevalence.
A concern expressed by both providers and patients is that discussions regarding regret and surgical reversal may be used to restrict access to affirming care. The authors believe that research including feelings of grief and regret will not only help individuals who experience severe forms of regret but will also help to refine surgical indications and procedures to minimize this already rare occurrence. Finally, and perhaps most importantly, failure to study regret and surgical reversal procedures will allow these topics to be left up to interpretation and may not reflect the actual experience of patients.
Limitations
The literature review was not performed systematically and as such is subject to selection bias. Our survey involved a survey of gender surgeons but did not include other medical or mental health professionals who may evaluate patients requesting surgical reversal. In addition, the study findings are limited by its design. Because survey studies are prone to recall bias, response bias, and selection bias, they are not well-suited for calculating the prevalence of a particular condition. For example, 89% of the respondents practice in the United States and Europe. This leaves significant areas of the world underrepresented and so does not represent the experiences or desires of all international surgeons. Furthermore, the survey was distributed in English only, as it was circulated to surgeons who attended conferences in the United States. Most notably, patients may have sought consultation from multiple surgeons resulting in an overestimation of the prevalence of regret. Conversely, patients seeking surgical reversal may not have had access to additional surgical care, causing an underestimate in the prevalence of regret. While our study findings are strengthened by external validation from other studies, the true prevalence of regret remains an estimate.
Regret after gender-affirming surgery was found to be rare, both in the literature as well as in our survey of surgeons’ experiences with this topic. Regret can be classified as true gender-related regret, social regret and medical regret from complications, function, pre-intervention decision making. Guidelines in transgender health should include both preventive strategies as well as treatment guidelines if regret occurs. Future studies and scientific discourse are encouraged on this important topic.
Supplementary
Acknowledgments.
The authors acknowledge the many surgeons who were surveyed in this work, and the community members who thusly contributed to the survey results.
This research was orally presented by Dr. Sasha Narayan at the Philadelphia Trans Wellness Conference (PTWC) August 2018 in Philadelphia, PA and at the World Professional Association for Transgender Health (WPATH) International Conference, November 2018 in Buenos Aires, Argentina. This research was orally presented by Dr. Sara Danker at Plastic Surgery, The Meeting (PSTM), October 2018 in Chicago, IL.
Funding : None.
Ethical Statement : The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Oregon Health & Science Institutional Review Board #17450. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Subjects were physicians and so gave consent through their participation in the survey. The patients who were captured in the study were not individually consented for this research as the IRB felt it to be unnecessary given the degree of separation of the study and lack of identifiers. None of the study outcomes affect future management of the patients’ care.
Provenance and Peer Review : This article was commissioned by the Guest Editors (Drs. Oscar J. Manrique, John A Persing, and Xiaona Lu) for the series “Transgender Surgery” published in Annals of Translational Medicine . The article has undergone external peer review.
Reporting Checklist : The authors have completed the SURGE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-6204
Data Sharing Statement : Available at http://dx.doi.org/10.21037/atm-20-6204
Conflicts of Interest : All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-6204 ). The series “Transgender Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. RBL reports that he serves on the standards of care committee of WPATH. No financial reward. Dr. AR reports that he serves as board member for World Professional Association for Transgender Health. This is an uncompensated position. Dr. LS reports other from Elsevier Publishing, other from Springer Publishing, outside the submitted work; and he serves on the board of WPATH (world professional association for transgender health), this is an unpaid position. Dr. JUB reports that he serves on the standards of care committee of the World professional association of transgender health. No financial reward associated with this. The authors have no other conflicts of interest to declare.

Online Claims Misrepresent Washington Bill Aimed at Runaway Transgender Youth
By Saranac Hale Spencer
Posted on May 3, 2023
Q: Does a proposed law in Washington state say that the government can take children away from parents who don’t agree to gender transition surgery?
A: No. Under the bill, licensed youth shelters no longer have to report the location of a runaway child to the child’s parents if the child is seeking gender-affirming or reproductive care. Instead, the shelters must notify the state’s child services department.
FULL QUESTION
Is it true that SB-5599 say[s] that the government can take away minors from parents if they refuse to agree to gender Transition Surgery[?]
FULL ANSWER
A bill in the state of Washington that would allow licensed youth and homeless shelters to notify the state’s child services department in lieu of a parent in cases where a minor has left home in order to pursue gender-affirming or reproductive care is moving toward passage.
Critics say that it would interfere with parental rights, while advocates say it’s a necessary change to keep runaway minors safe and off the streets.
The bill has passed both houses of the legislature and Washington Gov. Jay Inslee, a Democrat, has signaled that he is likely to sign the legislation.
“We believe it is better to have a young person in a shelter with some adult supervision than having them out living on the streets — maybe being trafficked, sexually trafficked, maybe being exposed to drugs,” Inslee said at an April 13 press conference .
The proposed law would affect about a dozen minors each year, the office of state Sen. Marko Liias, who sponsored the bill, told us in an email.
“It’s not like kids are coming by the thousands or even by the hundreds,” Jarel Sanders — who is on the board of directors at Equal Rights Washington, which has lobbied for the bill — told FactCheck.org in a phone interview.
As it stands now , licensed shelters in Washington can contact the children’s services department instead of parents if there are “compelling reasons” to do so. The compelling reasons include circumstances in which notifying a parent would subject the minor to abuse or neglect, which is defined as sexual abuse or exploitation, injury, or negligent treatment or maltreatment.
The bill would add the pursuit of “protected health care services” to the list of “compelling reasons.” Protected health care services would include reproductive health care , meaning contraception and abortion, and gender-affirming care , which we’ll explain further below.
The law would still — as it currently does — require the children’s department to make a good faith attempt to notify a parent after a minor is referred for care and it must “offer services designed to resolve the conflict and accomplish a reunification of the family.”
That would be handled through the department’s Family Reconciliation Services , Nancy Gutierrez, a spokeswoman for the state’s Department of Children, Youth & Families, told FactCheck.org in an email.
FRS offers short-term family counseling and referrals for mental health care, among other services, with the aim of keeping families together .
“We would focus on offering services designed to resolve familial conflicts and accomplish reunification as directed by the legislation,” Gutierrez said.
Mike Faulk, a spokesman for Inslee, told us the same thing in an email.
“DCYF’s main role is to offer services designed to resolve family conflicts and accomplish a reunification of the family,” he said.
But online posts have misrepresented the proposed legislation, prompting confusion.
For example, Donald Trump Jr. wrote on Twitter , “Washington passes bill allowing the state to TAKE CHILDREN AWAY FROM PARENTS that do not consent to their child’s gender transition surgeries…”
And the conservative website 100 Percent Fed Up posted a headline claiming: “BREAKING: State of Washington Passes Bill Allowing Government to Take Minor Children Away From Parents If They Refuse To Agree to Gender Transition Surgery.” The site shared that story with its 1.5 million Facebook followers.
Those claims misleadingly exaggerate the bill’s impact.
No Change to Medical Consent Laws
The online claims suggest that the bill would create a new exception allowing minors to undergo major medical procedures without parental consent. But the bill doesn’t change the state’s medical consent laws.
Under state law , those under age 18 don’t generally have the right to make medical decisions without parental consent.
There is, however, an exception that was introduced in 2022 that allows homeless youth — as defined by the federal McKinney-Vento Homeless Assistance Act — to get consent from a school nurse, school counselor or homeless student liaison for “nonemergency, outpatient, primary care services, including physical examinations, vision examinations and eyeglasses, dental examinations, hearing examinations and hearing aids, immunizations, treatments for illnesses and conditions, and routine follow-up care customarily provided by a health care provider in an outpatient setting, excluding elective surgeries.”
Kim Justice, executive director of Washington’s Office of Homeless Youth Prevention & Protection Programs , told FactCheck.org in an email: “SB 5599 does not make any changes to the types of health care available to homeless youth or how they access that care. The bill only pertains to situations in which the Department of Children, Youth, and Families would be notified instead of a parent regarding a youth’s admission to a shelter or host home program.”
A Range of Gender-Affirming Care
A related suggestion from the online posts is the emphasis on “gender transition surgeries,” as if surgery is the primary type of treatment.
But gender-affirming care is much more encompassing than just surgery. The Washington bill uses this definition : “[A] service or product that a health care provider… prescribes to an individual to support and affirm the individual’s gender identity.”
The World Health Organization has explained that “gender-affirmative health care can include any single or combination of a number of social, psychological, behavioural or medical (including hormonal treatment or surgery) interventions designed to support and affirm an individual’s gender identity.”
In addition, gender – affirming surgery — which includes facial surgery, surgery to either reduce or augment breasts and genital surgery — is generally performed on adults .
“Although current protocols typically reserve surgical interventions for adults,” says the American Academy of Pediatrics’ policy statement on care for transgender children and adolescents, “they are occasionally pursued during adolescence on a case-by-case basis, considering the necessity and benefit to the adolescent’s overall health and often including multidisciplinary input from medical, mental health, and surgical providers as well as from the adolescent and family.”
So surgical procedures are uncommon for minors in general, and that’s expected to be the case for those who would be affected by the Washington bill.
Some medical options for gender-affirming care for minors include puberty blockers and hormone therapy, the effects of which are either reversible or partially reversible.
The most recent standards of care published in 2022 by the World Professional Association for Transgender Health advise that adolescents, their parents and their doctors should understand the evidence for both medical and surgical interventions before starting treatment.
“It seems reasonable that decisions to move forward with medical and surgical treatments should be made carefully,” the association says. “Despite the slowly growing body of evidence supporting the effectiveness of early medical intervention, the number of studies is still low, and there are few outcome studies that follow youth into adulthood.”
The Washington bill would largely provide transgender youth with doctors who offer a safe and understanding environment — calling patients by their preferred pronouns, for example — and connecting them to counselling, Sanders said.
“Surgeries are not the majority,” he said, explaining that the bill is much more about social and therapeutic services. The goal is really to reduce suicide attempts, Sanders said.
Gender-affirming care, which can reduce that risk, is supported by more than two dozen major medical organizations, including the American Medical Association , the American Psychiatric Association , the Endocrine Society and the American Academy of Pediatrics .
“Evidence has demonstrated that forgoing gender-affirming care can have tragic consequences,” the AMA wrote in a recent letter urging governors to reject bans on gender-affirming care. The letter cited heightened incidences of mental health disorders among transgender people, which, it said, “is widely thought to be a consequence of minority stress, the chronic stress from coping with societal stigma, and discrimination because of one’s gender identity and expression. Because of this stress, transgender minors also face a significantly heightened risk of suicide.”
“Transgender children, like all children, have the best chance to thrive when they are supported and can obtain the health care they need,” the letter said. “Studies suggest that improved body satisfaction and self-esteem following the receipt of gender-affirming care is protective against poorer mental health and supports healthy relationships with parents and peers. Studies also demonstrate dramatic reductions in suicide attempts, as well as decreased rates of depression and anxiety.”
Providing Safe Shelter
Another major claim in the online posts is that the bill would impact laws regarding the removal of children from their homes.
That’s not the case, said Laurie Lippold , director of public policy at Partners for Our Children , housed at the University of Washington, which researches the child welfare system.
Current state law requires Child Protective Services to initiate a process overseen by the courts to remove a child in the case of abuse or neglect.
This bill doesn’t propose changes to those laws.
It wouldn’t change any child abuse reporting laws or justification requirements for removing children from homes, Lippold said.
Rather, the bill is designed to ensure that minors who have left home have access to safe shelter.
So, the claims that Washington has passed a sweeping new bill that will result in teens being taken from their homes to undergo surgery are vastly overstating the reality. The proposed law would likely affect about a dozen vulnerable transgender minors each year by providing them with housing if they have left home in order to pursue certain types of gender-affirming or reproductive care.
Editor’s note: FactCheck.org does not accept advertising. We rely on grants and individual donations from people like you. Please consider a donation. Credit card donations may be made through our “ Donate ” page. If you prefer to give by check, send to: FactCheck.org, Annenberg Public Policy Center, 202 S. 36th St., Philadelphia, PA 19104.
Johns, Michelle M., et al. “ Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students — 19 States and Large Urban School Districts, 2017 .” Morbidity and Mortality Weekly Report. 25 Jan 2019.
Herman, Jody L., Taylor N.T. Brown and Ann P. Haas. “ Suicide Thoughts and Attempts Among Transgender Adults .” UCLA School of Law Williams Institute. Sep 2019.
Paley, Amit, et al. “ 2022 National Survey on LGBTQ Youth Mental Health .” Trevor Project. Accessed 22 Apr 2023.
Washington State Legislature. Bill Information — SB 5599 . Accessed 21 Apr 2023.
Liias, Marko and Joe Nguyen. “ What the right has wrong about caring for trans youth .” Seattle Times. Updated 24 Feb 2023.
Inslee, Jay (@GovJayInslee). “ WATCH: Governor Inslee Media Availability .” YouTube. 13 Apr 2023.
Sanders, Jarel. Board of directors, Equal Rights Washington. Telephone interview with FactCheck.org. 20 Apr 2023.
Health and Human Services, Office of Population Affairs. Gender-Affirming Care and Young People . Accessed 21 Apr 2023.
Hut Erin. Spokeswoman, Sen. Marko Liias. Email to FactCheck.org. 26 Apr 2013.
Gutierrez, Nancy. Spokeswoman, Washington Department of Children, Youth & Families. Email to FactCheck.org 1 May 2023.
Faulk, Mike. Spokesman, Gov. Jay Inslee. Email to FactCheck.org. 1 May 2023.
Cleveland Clinic. Gender Affirmation (Confirmation) or Sex Reassignment Surgery . Reviewed 3 May 2021.
Liang, Fan. “ Gender Affirmation Surgeries .” Johns Hopkins Medicine. Accessed 24 Apr 2023.
Rafferty, Jason, et al. “ Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents .” American Academy of Pediatrics. 1 Oct 2018.
Justice, Kim. Executive director, Washington’s Office of Homeless Youth Prevention & Protection Programs. Email to FactCheck.org. 1 May 2023.
Coleman, E., et al. “ Standards of Care for the Health of Transgender and Gender Diverse People, Version 8 .” International Journal of Transgender Health. 15 Sep 2022.
Smith, Timothy M. “ What to know about gender-affirming care for younger patients .” American Medical Association. 21 Dec 2021.
American Psychiatric Association. “ Position Statement on Access to Care for Transgender and Gender Diverse Individuals .” Jul 2018.
Endocrine Society. Transgender Health — An Endocrine Society Position Statement . 16 Dec 2020.
Revised Code of Washington. RCW 26.28.015 . Age of majority for enumerated specific purposes. Accessed 25 Apr 2023.
Washington State Legislature. Bill Information — SB 5883 . Accessed 25 Apr 2023.
Revised Code of Washington. RCW 7.70.065 . Informed consent—Persons authorized to provide for patients who do not have capacity—Priority—Unaccompanied homeless minors. Accessed 25 Apr 2023.
Lippold, Laurie. Director of public policy, Partners for Our Children. Telephone interview with FactCheck.org. 20 Apr 2023.
Washington State Department of Children, Youth & Families. Placement Out-of-Home and Conditions for Return Home . Updated 20 Oct 2022.
Total Joint Arthroplasties in Transgender Patients: Unique Considerations for an Emerging Patient Population
Affiliation.
- 1 From the Washington DC Veterans Affairs Medical Center, Department of Orthopedic Surgery (Harper), and Belmont Plastic Surgery, Washington, DC (Maiorino).
- PMID: 35439219
- DOI: 10.5435/JAAOS-D-21-00914
Currently, no studies exist on transgender patients undergoing orthopaedic procedures within the orthopaedic literature at large. This echoes a trend within medicine in general, where despite their unique characteristics, transgender patients are largely ignored in medical research. As gender reassignment surgery becomes more commonplace and these patients' age into joint arthroplasties, orthopaedic surgeons will rapidly be faced with treating this patient group. Unique considerations include medical comorbidities commonly associated with the patient population, deep vein thrombosis risk while on cross-gender hormone therapy, surgical positioning considerations, and social support implications after surgery. In addition, risk reductions for possible future gender reassignment surgeries include consideration for extended perioperative antibiotics and diligent surveillance for implant ingrowth issues. An emphasis is placed on being comfortable with transgender patients to ensure equal access to health care while ensuring understanding and accuracy in describing the risks of surgery that are unique to this patient population.
Copyright © 2022 by the American Academy of Orthopaedic Surgeons.
- Arthroplasty
- Delivery of Health Care
- Gender Identity
- Sex Reassignment Surgery*
- Transgender Persons*
Current Weather
Latest Weathercast
Interactive Radar
Inslee signs bill protecting minors seeking gender-affirming care from estranged parents
by ED KOMENDA Associated Press

OLYMPIA, Wash. — Minors seeking gender-affirming care in Washington will be protected from the intervention of estranged parents under a measure signed into law by Gov. Jay Inslee Tuesday afternoon.
The new law is part of a wave of legislation this year in Democratic-led states intended to give refuge amid a conservative movement in which lawmakers in other states have attacked transgender rights and limited or banned gender-affirming care for minors.
Existing Washington law generally requires licensed shelters and host homes to notify parents within 72 hours when a minor comes into their care. Under the new law, facilities can instead contact the state Department of Children, Youth and Families, which could then attempt to reunify the family if feasible. Youths will also be allowed to stay at host homes — private, volunteer homes that temporarily house young people without parental permission.
More than a half-dozen states, from New Jersey to Vermont to Colorado, have passed or are considering similar bills or executive orders around transgender health care, civil rights and other legal protections. In Michigan, Democratic Gov. Gretchen Whitmer in March signed a bill outlawing discrimination on the basis of gender identity and sexual orientation for the first time in her state.
RELATED | Washington state shields people seeking abortion, trans care
Oregon lawmakers are expected to pass a bill that would further expand insurance coverage for gender-affirming care to include things like facial hair removal and Adam's apple reduction surgery, procedures currently considered cosmetic by insurers but seen as critical to the mental health of transitioning women.
Shield protections have been enacted this year in Colorado, Illinois, New Jersey and New Mexico. California, Massachusetts and Connecticut passed their own measures last year, largely barring authorities from complying with subpoenas, arrest warrants or extradition requests from states that have banned gender-affirming treatments.
Protections in blue states are being baked into law as Republican-led states take steps to bar access to gender-affirming care for transgender minors, which for people under 18 typically involves puberty blockers or other hormone treatments. Restrictions have gone into effect in eight states this year — including conservative Utah and South Dakota — and are slated to be in at least nine more by next year.
Those who oppose gender-affirming care raise fears about the long-term effects treatments have on teens, argue research is limited and focus particularly on irreversible procedures such as genital surgery or mastectomies.
Yet those operations are rarely performed on minors. Doctors typically guide kids toward therapy or voice coaching long before medical intervention. Puberty blockers, anti-androgens that block the effects of testosterone, and hormone treatments are far more common than surgery. They have been available in the U.S. for more than a decade and are standard treatments backed by major doctors' organizations, including the American Medical Association.
In Washington, local Republican lawmakers have spent weeks railing against the legislation signed into law Tuesday. Senate GOP leader John Braun said in March that it would drive "a wedge between vulnerable kids and their parents." Online, some users have twisted the content of the measure to suggest it will see the state ripping children from their homes.
But those claims misrepresented the legislation, which is intended to keep estranged young people housed, according to experts and the lawmaker sponsoring the bill. The bill does not address custody and would not result in the state taking children away from their homes and parents.
The Washington legislation requires the state Department of Children, Youth and Families to make a "good faith attempt" to notify parents after they are contacted by shelters or host homes and offer services designed to "resolve the conflict and accomplish a reunification of the family," according to the bill text. Family reunification efforts would be pursued when possible, according to Washington state Sen. Marko Liias, a Democrat who was the bill's primary sponsor.
"If a young person is totally estranged from their parents, has no meaningful relationship, we need someone to care for that child," Inslee said at a news conference last month.

Nationals third baseman Nick Senzel won’t need surgery on broken right hand. Lipscomb promoted
The Associated Press
March 30, 2024, 4:04 PM
- Share This:
- share on facebook
- share on threads
- share on linkedin
- share on email
CINCINNATI (AP) — Washington’s Nick Senzel won’t require surgery on his broken right hand, and Nationals manager Dave Martinez isn’t sure when the third baseman will return.
“It comes down to pain tolerance now,” Martinez said Saturday.
Senzel fractured a bone in thumb when a ball took a bad hop during batting practice before Thursday’s opener against the Reds. He was put on the 10-day injured list, and the Nationals selected the contract of infielder Trey Lipscomb from Triple-A Rochester. Lipscomb hit .400 (20 for 50) in spring training with one homer and seven RBIs in 21 games.
The 23-year-old Lipscomb, one of Washington’s top prospects, was set to make his major league debut Saturday at third base and batting ninth.
AP MLB: https://apnews.com/hub/MLB and https://twitter.com/AP_Sports
Copyright © 2024 The Associated Press. All rights reserved. This material may not be published, broadcast, written or redistributed.
Related News

Reds and Nationals square off with series tied 1-1

Eddie Rosario’s sacrifice fly caps 3-run 9th inning off Alexis Díaz as Nationals beat Reds 7-6

Reds meet the Nationals with 1-0 series lead
Recommended.

Crews carefully start removing first piece of twisted steel from collapsed Baltimore bridge

Bruins beat the Capitals 3-2 in a shootout in a potential first-round playoff preview

Virginia adopts regulatory changes for special education amid federal review
Related categories:.
D.C. United’s Russell Canouse sidelined indefinitely with health issue

Russell Canouse , a defensive midfielder in his eighth season with D.C. United, is sidelined indefinitely with a health condition unrelated to the ankle injury that has kept him out since preseason, Coach Troy Lesesne said Thursday.
“It’s something we’re monitoring right now and we’re evaluating [and] that’s going to probably keep him out for a little bit of time,” Lesesne said. “It’s indefinite, and I don’t have a ton of information right now, but it’s noninjury related.”
Club officials said they did not want to discuss the matter, and Canouse was not available to comment.
Canouse, 28, has not trained with the team recently despite recovering from an ankle injury suffered during preseason camp in Saudi Arabia. Lesesne said Canouse’s ankle is at “full strength.”
Canouse, a native of central Pennsylvania, is second on the roster in continuous services behind captain Steven Birnbaum , who is in his 11th season. He started a career-high 27 matches last year and has made 137 regular season appearances since he arrived from German club Hoffenheim in 2017.
Steven Birnbaum still rehabbing after surgery
Birnbaum, who suffered a setback in his recovery from preseason knee surgery, continues to rehab indoors while the team practices. There is no timetable for his return, though Lesesne said the defender is “making more progress this week.”
Goalkeeper Tyler Miller , unavailable since shoulder surgery last fall, has integrated back into training with the other keepers and is a few weeks from competing fully, Lesesne said.
Rookie defender Garrison Tubbs (hamstring) will remain sidelined for a few weeks.
Four players return from international duty
Four players who missed United’s 2-2 draw at St. Louis last weekend have returned from international duty and are available for Saturday’s match against Montreal at Audi Field.
Defensive midfielder Matti Peltola played 90 minutes in Finland’s 4-1 defeat at Wales in a European Championship playoff. He then was a second-half sub during a 2-1 victory over Estonia in a home friendly but left early with a migraine. Peltola trained with United on Thursday.
Right back Aaron Herrera played 90 minutes in each of Guatemala’s friendlies against Venezuela (0-0 draw in Houston) and Ecuador (2-0 defeat in Harrison, N.J.).
Forward Kristian Fletcher went 60 minutes in the U.S. under-19 national team’s 3-2 victory over England in Morocco, then played the second half in a 1-0 defeat to Morocco. Defender Matai Akinmboni went 82 minutes in the first friendly and the last 18 in the second. …
Left back Pedro Santos is back after serving a red-card suspension.
United finalizes radio plans
Six weeks into the season, United finalized plans to resume radio broadcasts, led by play-by-play announcer Dave Johnson , who will continue his streak of team TV or radio calls to 29 seasons. Bruce Murray will rejoin him as color commentator.
Starting on Saturday, the pair can be heard on WTSD (1190 AM), WONK (104.7 FM), 101.1 on HD2 radio and the iHeartRadio streaming service. Their call is also an audio option on Apple TV’s coverage.
- D.C. United’s Russell Canouse sidelined indefinitely with health issue 3 hours ago D.C. United’s Russell Canouse sidelined indefinitely with health issue 3 hours ago
- Mallory Swanson and Catarina Macario return to USWNT after long injury absences March 26, 2024 Mallory Swanson and Catarina Macario return to USWNT after long injury absences March 26, 2024
- A joyous night for USMNT turns the page for Tyler Adams and Gio Reyna March 25, 2024 A joyous night for USMNT turns the page for Tyler Adams and Gio Reyna March 25, 2024


COMMENTS
Types of gender reassignment surgery: Feminizing vaginoplasty: Reconstructive surgery procedure that alters the structure of the genitals to create a vagina using penile or colon tissue. Dr. ... Plastic Surgery at MedStar Washington Hospital Center 106 Irving St. NW POB North Ste. 3400 . Washington, D.C., 20010 Get directions. Miles away. 202 ...
Schedule a Consultation. To learn more about any of these gender affirmation procedures, contact West End Plastic Surgery. Call us at 202-785-4187 to schedule a consultation with Dr. Ruff. Our practice serves Washington D.C. and surrounding areas.
The Johns Hopkins Center for Transgender and Gender Expansive Health offers comprehensive, evidence-based and affirming care for transgender youth and adults that is in line with the standards of care set by the World Professional Association for Transgender Health (WPATH). We offer services for children and adolescents, dermatology, facial ...
Dr. John L. Whitehead. Dr. Whitehead is a surgeon who performs gender affirming male-to-female genital surgeries, as well as FTM Top Surgery in Florida. Dr. Whitehead was trained in the art of gender reassignment surgery by Dr. Harold Reed, the now-retired urologist who performed GRS for decades in Miami. Dr.
Schedule A Consultation. (202) 741-2365 or Book an Appointment Now with Dr. Jerry Chao. Dr. Chao will review pre and post-op pictures with you at your consultation. We accept many insurance plans, and your gender affirming surgery may be a covered benefit. At The GW Medical Faculty Associates, we understand and respect how critical each ...
D.C. Child and Family Services Agency 200 I Street SE, Washington, DC 20003 (202) 442-6100 www.cfsa.dc.gov www.fosterdckids.org Facebook/CFSADC Twitter@DCCFSA ... Reassignment Surgery Policy of the DC Department of Health Care Finance, which is based in part on
You can't feel afraid during the surgery time. I would also recommend him for plastic surgery for both genders of people. 7601 Lewinsville Road, Suite 300. McLean, VA 22102. (703) 345-4377. 11490 Commerce Park Drive, Suite 430. Reston, VA 20191. (703) 636-9296.
111 Michigan Avenue, NW Washington, DC 20010. 1-888-884-2327. Emergency Department Info. Specialty Care; Montgomery County. 9850 Key West Avenue Rockville, Maryland 20850. 301-765-5400 or 800-787-0243. 301-294-0897. Specialty Care; All Gender Development Program Locations. Family Resources.
One Judiciary Square ǀ 441 4th Street, NW, Suite 900S, Washington, D.C. 20001 (202) 442-5988 Fax (202) 442-4790 GOVERNMENT OF THE DISTRICT OF COLUMBIA Department of Health Care Finance Subject: Gender Reassignment Surgery Policy Policy#: OD-001-17 Policy Scope: Gender Reassignment Surgery Policy Number of Pages: ... this policy clarifies DC
Dr. Toby Meltzer. Dr. Meltzer is a plastic and reconstructive surgeon who is widely recognized as one of the leading surgeons in the field of Gender Reassignment Surgery. Dr. Meltzer has been performing MTF Surgery since 1993 and has completed over 4000 gender affirming surgeries.
Gender-affirming surgery is a procedure that changes the look and function of your body. ... GA 30305, 404-364-7000 • Kaiser Foundation Health Plan of the Mid-Atlantic States, Inc., in Maryland, Virginia, and Washington, D.C., 2101 E. Jefferson St., Rockville, MD 20852 • Kaiser Foundation Health Plan of the Northwest, 500 NE Multnomah St ...
News4's Tom Sherwood reports. Insurance companies in the District of Columbia have been ordered to stop denying coverage to transgender residents seeking gender-reassignment surgery. Mayor ...
Washington D.C. will require insurance companies to provide health coverage to trans residents, including gender reassignment surgery. Mayor Vincent Gray announced the change in policy Thursday ...
Language assistance is available at no cost to you, 24 hours a day, 7 days a week. You can request interpreter services, materials translated into your language, or in alternative formats. Just call us at 1-800-464-4000, 24 hours a day, 7 days a week (closed holidays). TTY users, call 711.
Washington, DC. - The DC Department of Health Care Finance (DHCF) has updated Policy Number 001-17 to clarify coverage for Gender Reassignment Surgery (GRS). The policy supersedes all previous policies and is effective as of September 1, 2016. It applies to all District of Columbia Medicaid providers and managed care organizations. Gender reassignment surgery is not a covered benefit of the DC ...
Washington DC Children's National Medical Center The Gender Development Program at Children's National has been supporting the gender needs of youth and their families for the past 20 years. As one of the earliest founded youth gender programs, we are a multidisciplinary team of specialists who work in the assessment and broad care needs of ...
An April analysis of American Civil Liberties Union data by The Washington Post found at least 29 bills targeting ... cadaver to someone who wanted to reverse a gender reassignment surgery. Del.
Gender Health Case Management Program. 1-888-245-9004. [email protected]. Gender Health Appointing Line. 206-630-1929. Member Services.
Effects of adequacy of gender reassignment surgery on psychological adjustment: a follow-up of fourteen male-to-female patients. Arch Sex Behav 1989; 18:145-53. 10.1007/BF01543120 ... Washington, DC: National Center for Transgender Equality, 2016. [Google Scholar] 32. Hage JJ, van Turnhout AA. Long-term outcome of metoidioplasty in 70 female-to ...
Gender Affirmation (Confirmation) or Sex Reassignment Surgery. Reviewed 3 May 2021. ... Washington State Department of Children, Youth & Families. Placement Out-of-Home and Conditions for Return ...
1 From the Washington DC Veterans Affairs Medical Center, Department of Orthopedic Surgery (Harper), and Belmont Plastic Surgery, Washington, DC (Maiorino). PMID: 35439219 ... As gender reassignment surgery becomes more commonplace and these patients' age into joint arthroplasties, orthopaedic surgeons will rapidly be faced with treating this ...
Washington Gov. Jay Inslee signs bills at the Washington State Capitol, Tuesday, May 9, 2023, in Olympia, Wash. One of those bills was Senate Bill 5599, which was designed to protect young people ...
CINCINNATI (AP) — Washington's Nick Senzel won't require surgery on his broken right hand, and Nationals manager Dave Martinez isn't sure when the third baseman will return. "It comes down to ...
Midfielder Russell Canouse, who joined D.C. United during the 2017 season, appeared in a career-high 27 MLS matches last season. (Jonathan Newton/The Washington Post) Russell Canouse, a defensive ...
By Associated Press - Sunday, March 31, 2024. JERUSALEM — Prime Minister Benjamin Netanyahu 's office says the Israeli leader will undergo surgery on Sunday for a hernia. Netanyahu 's office ...