An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World Psychiatry
- v.18(3); 2019 Oct

The assessment and management of insomnia: an update
Andrew d. krystal.
1 Department of Psychiatry, University of California San Francisco School of Medicine, San Francisco, CA, USA
2 Department of Neurology, University of California San Francisco School of Medicine, San Francisco, CA, USA
Aric A. Prather
Liza h. ashbrook.
Insomnia poses significant challenges to public health. It is a common condition associated with marked impairment in function and quality of life, psychiatric and physical morbidity, and accidents. As such, it is important that effective treatment is provided in clinical practice. To this end, this paper reviews critical aspects of the assessment of insomnia and the available treatment options. These options include both non‐medication treatments, most notably cognitive behavioral therapy for insomnia, and a variety of pharmacologic therapies such as benzodiazepines, “z‐drugs”, melatonin receptor agonists, selective histamine H1 antagonists, orexin antagonists, antidepressants, antipsychotics, anticonvulsants, and non‐selective antihistamines. A review of the available research indicates that rigorous double‐blind, randomized, controlled trials are lacking for some of the most commonly administered insomnia therapies. However, there are an array of interventions which have been demonstrated to have therapeutic effects in insomnia in trials with the above features, and whose risk/benefit profiles have been well characterized. These interventions can form the basis for systematic, evidence‐based treatment of insomnia in clinical practice. We review this evidence base and highlight areas where more studies are needed, with the aim of providing a resource for improving the clinical management of the many patients with insomnia.
Insomnia is defined as a complaint of difficulty falling or staying asleep which is associated with significant distress or impairment in daytime function and occurs despite an adequate opportunity for sleep 1 , 2 . It is a common condition, with an approximate general population point prevalence of 10% 3 , 4 , 5 , 6 .
In the vast majority of cases, insomnia co‐occurs with psychiatric or physical conditions. Although it had long been believed that, when this was the case, insomnia was a symptom of those conditions, the available evidence suggests that the relationship between such conditions and insomnia is complex and sometimes bidirectional 7 , 8 , 9 , 10 . In fact, insomnia is a risk factor for major depression, anxiety disorders, substance use disorders, suicidality, hypertension and diabetes 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 . On this basis, as well as due to the fact that insomnia is associated with impairments in quality of life and an increased risk for accidents and falls, it is recommended that treatment be targeted specifically to addressing insomnia whenever it is present, including when it occurs along with physical or psychiatric conditions 24 , 25 .
For those who meet the diagnostic criteria for insomnia, a number of empirically supported treatments are available. These include non‐medication therapies as well as medication options 25 , 26 , 27 , 28 . The public health impact of this condition in terms of prevalence, morbidity and consequences on health and quality of life highlights the need to effectively diagnose and treat it in clinical practice. This paper reviews the state of the art for optimally diagnosing and treating insomnia based on the available research evidence.
DIAGNOSTIC CRITERIA FOR INSOMNIA
The clinical diagnosis of insomnia is based on the complaint of trouble falling asleep, trouble staying asleep, or early morning awakening, and resultant daytime dysfunction 1 , 2 .
This daytime dysfunction can manifest in a wide range of ways, including fatigue, malaise; impairment in attention, concentration or memory; impaired social, family, occupational or academic performance; mood disturbance, irritability, sleepiness, hyperactivity, impulsivity, aggression, reduced motivation, proneness for errors, and concerns about or dissatisfaction with sleep 2 .
The sleep disturbance must occur despite adequate opportunity for sleep in a safe, dark environment. Duration is also key to the diagnosis: to meet criteria for chronic insomnia according to the third edition of the International Classification of Sleep Disorders (ICSD‐3) or for persistent insomnia according to the DSM‐5, symptoms must be present at least three days per week for at least three months. Short term insomnia (ICSD‐3) or episodic insomnia (DSM‐5) has the same criteria as chronic insomnia, but lasts for fewer than three months.
If the sleep complaints are completely explained by another physical, psychiatric or sleep disorder, the patient does not meet diagnostic criteria for insomnia. However, insomnia is not solely a symptom of other mental disorders as was once thought 29 . Even if another disorder was the trigger or is present some of the time, if insomnia is sufficiently severe to warrant independent clinical attention, it should be recognized as a separate, comorbid disorder.
Previously, both the ICSD and the DSM described various subtypes of insomnia. These included psychophysiologic insomnia, paradoxical insomnia, idiopathic insomnia, behavioral insomnia of childhood, insomnia due to a mental disorder, insomnia due to a medical disorder, and insomnia due to a drug or substance. However, the mechanism of insomnia is poorly understood, and the various subtypes are difficult to differentiate in clinical practice 30 . Therefore, the subtypes were consolidated into chronic insomnia (ICSD‐3) and persistent insomnia disorder (DSM‐5) in the most recent editions of the manuals.
A subtype of insomnia with objectively short sleep has been described and stands out for its probable association with increased morbidity. These individuals meet criteria for chronic insomnia and, by objective measure, sleep on average less than six hours per night. This combination of insomnia with short sleep duration has been linked to hypertension, type 2 diabetes, and worse neurocognitive function 17 , 31 , 32 . Therefore, this may ultimately become a separate category in future versions of insomnia classifications.
DEMOGRAPHICS OF INSOMNIA
Symptoms of insomnia are common, with about one in three people reporting some symptoms in the previous year 33 , 34 . The point prevalence of a formal diagnosis of insomnia is 6‐15%, though occurrence rates vary by definition used 35 .
When looking at only nighttime complaints, rates are far higher. In a large population sample in France, 57% complained of trouble falling asleep, 53% of trouble staying asleep, and 41% of non‐restorative sleep, though only 19% met DSM‐IV criteria of at least one complaint three times per week for one month 36 .
For many, insomnia is a persistent condition, with 74% reporting symptoms for at least one year 37 . Persistence is more common in women, the elderly, and those with more severe insomnia. In a 3‐year study, over half of participants did remit, but there was a 27% relapse rate 37 . Family history of insomnia is also common, occurring in 35% of individuals 38 .
Women more commonly report symptoms of insomnia and daytime consequences, and are more likely to be diagnosed with insomnia than men. The male‐to‐female ratio is 1:1.4 for insomnia symptoms and 1:2 for insomnia diagnosis 5 . In both men and women, the prevalence of insomnia increases with age 5 , 39 , 40 .
Insomnia is associated with lower income, lower education, and being divorced or widowed 5 , 36 , 41 . It is also strongly associated with physical disorders, with half of those with insomnia also reporting multiple physical problems 34 , 41 . People with insomnia are more likely to rate their health poorly 42 , 43 .
Insomnia is very strongly associated with mental disorders, most commonly depression, anxiety and post‐traumatic stress disorder. Across cultures, most people with major depression report insomnia 44 , and those with insomnia are more likely to have depressed mood 42 , 43 , 45 , 46 , 47 . Insomnia is also a predictor for developing mental health problems, including depression, anxiety, bipolar disorder and suicide 45 .
CLINICAL ASSESSMENT OF INSOMNIA
Chief complaint.
The chief complaint for those with insomnia is typically difficulty initiating or maintaining sleep, early morning awakening or simply unrefreshing sleep. Early morning awakening is waking at least 30 minutes prior to the desired time, accounting for habitual bedtime, total sleep time, and premorbid pattern.
The specific complaint may vary over time and often includes more than one sleep concern. The duration, frequency and severity of this concern should be elucidated as well as exacerbating and relieving factors. Complaints of insomnia often arise only when probed during evaluation of another disorder, despite the impact of insomnia on multiple health issues.
Current sleep history
A good current sleep history is essential to confirm the diagnosis and determine the best treatment for a patient with insomnia. This includes sleep/wake schedule, bedtime routine, nocturnal behavior, and daytime dysfunction.
Sleep/wake schedule
A detailed account of time to bed, time to sleep, frequency of night awakenings, time to return to sleep, time waking in the morning, and time out of bed should be obtained.
What the patient does when not falling asleep is also important. For example, a patient who gets out of bed and eats ice cream or watches a favorite show when not sleeping is providing positive reinforcement for being awake, which is counterproductive. This can be a behavior to target and eliminate during treatment.
The sleep/wake schedule should be obtained for both work/school days and weekends or vacations. A large variation may signal a circadian rhythm disorder and serve as a target for intervention.
Does the patient nap during the day? If taking a nap later in the day, this may be decreasing sleep drive in the evening and can also be a target for intervention. If the patient reports a strong propensity to fall asleep during the daytime, this raises concern for another sleep disorder.
Bedtime routine
It is important to have the right conditions to ensure proper sleep. While someone with true insomnia will not be effectively treated by simply providing a dark, quiet environment, the clinician – in order to confirm the diagnosis – must ensure that poor sleep is not due to poor sleep conditions.
Detailing the bedtime routine may also highlight areas for intervention during the treatment phase. For example, mobile phone use is associated with shorter sleep duration 22 .
Nocturnal behavior
What does the patient do when not sleeping at night? Are there other behaviors overnight, such as snoring or leg kicking, that may signal alternative or concomitant diagnoses?
Input from a bed partner can also be helpful. In a patient who reports being awake the entire night, a bed partner often observes long periods of sleep, suggesting there may be some sleep state misperception.
Daytime dysfunction
Daytime dysfunction is part of the formal criteria for insomnia and must be assessed. This includes worsened quality of life, concerns about memory, fatigue, mood, and success at work or school.
The 3P model
The 3P model, a behavioral model of insomnia developed by Spielman 48 , can help the clinician focus a sleep history 49 . The model highlights why insomnia occurs in certain individuals and what allows acute insomnia to become chronic insomnia.
The three Ps occur in temporal order: factors predisposing an individual to insomnia, factors precipitating an acute episode of insomnia, and factors perpetuating the insomnia from acute to chronic. Predisposing factors include genetic and personality traits leading to physiologic and cognitive hyperarousal 50 , 51 . Precipitating factors are the triggers after which the insomnia cycle begins and are typically stressful events, though they can be positive, ranging from the loss of a loved one to retirement or marriage. Perpetuating factors allow the insomnia to continue, even when the trigger is removed. These factors include behaviors and thought structures that may appear to offer short‐term relief yet cause long‐term harm, such as increasing time in bed and reducing daytime activity.
Past medical history
There is a large interplay between many physical or psychiatric conditions and insomnia, and typically it is thought that a bidirectional relationship exists in which the physical or psychiatric condition exacerbates insomnia and vice versa. A huge range of physical comorbidities – including pulmonary, cardiac, gastrointestinal, endocrine, neurological, musculoskeletal and genitourinary – can contribute.
It is important to ensure that the management of these comorbid conditions is optimized when treating insomnia.
Medications
Numerous medications can impact sleep, and a thorough medication list, including over‐the‐counter medications and substances of abuse, should be elicited.
Antidepressants such as selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs) and monoamine oxidase inhibitors (MAOIs) can cause sedation or stimulation, with individual variability. Therefore, a patient may consider moving a daily dose from morning to evening or vice versa to determine how this impacts sleep.
Over‐the‐counter allergy medications often contain stimulants such as pseudoephedrine or phenylephrine, and patients may not realize that this can contribute to insomnia. Withdrawal can also contribute, such as from alcohol, benzodiazepines or opioids. Pulmonary medications, including albuterol and theophylline, can cause insomnia as well.
While insomnia is reported as a side effect of antihypertensive medications, and beta‐blockers are known to reduce melatonin levels, there is mixed evidence about the direct impact of these medications on sleep 5 , 52 , 53 .
Social history
Occupation is key to the sleep history, to ensure driving safety in patients reporting daytime sleepiness. Work or school hours are also important, as variation in these hours, shift work, and frequent travel across time zones can all disturb sleep.
Use of nicotine, caffeine, alcohol and other substances should also be noted.
Physical examination
Insomnia is not associated with any specific features on physical or mental status examination. The examination can, however, provide information about alternative diagnoses and comorbid conditions. Assessments to consider include body mass index, neck circumference and airway exam for obstructive sleep apnea 54 .
Differential diagnosis
Three criteria must be met for a diagnosis of insomnia: complaint of trouble falling or staying asleep, adequate opportunity for sleep, and daytime dysfunction. If a patient reports trouble sleeping for the expected 7‐8 hours but does not have daytime consequences, he/she may be a short sleeper. On the other hand, if there are insufficient hours of sleep and daytime dysfunction, but the patient is able to sleep when provided opportunity, this is likely to be behaviorally induced insufficient sleep. Function during vacations and weekends can be helpful to differentiate these.
Other sleep disorders that can present with the complaint of insomnia include circadian rhythm sleep‐wake disorders, restless leg syndrome, periodic leg movement disorder, and obstructive sleep apnea.
Helpful questions to distinguish circadian disorders include the time to bed and awake on weekends, holidays and vacations in contrast to work or school days and whether there is a normal duration of refreshing sleep once the patient does fall asleep. If sleeping from 3 am to 10 am provides refreshing sleep and yet the patient gets in bed at midnight and hopes to rise at 7 am, but cannot fall asleep for several hours, a delayed sleep‐wake phase disorder may be involved and the misaligned internal rhythm should be the target for treatment.
Symptoms of restless leg syndrome include an urge to move the legs at least partially relieved by moving them, typically preceded by an abnormal leg sensation, and typically occurring during times of rest at the end of the day. As the syndrome can cause trouble falling asleep, it should be ruled out or treated directly.
Obstructive sleep apnea can present with symptoms of insomnia, more commonly in women than men. Presence of snoring, frequent awakenings, witnessed apneas should be discussed and, if concern is present, polysomnography should be performed 55 , 56 .
Insomnia assessment tools
Sleep diary.
Sleep diary is a form compiled by the patient, usually for at least two consecutive weeks, in which he/she notes down the time that he/she went to bed, the time of lights out, time to sleep, time and duration of awakenings overnight, time awake in the morning, time out of bed, naps, perceived duration of sleep, and sometimes quality and depth of sleep. The use of sleep aids and alcohol is sometimes included.
This can be very useful for the diagnosis of insomnia and is core to the treatment, because it helps to characterize the specific nature of the sleep problem, delineate maladaptive behaviors and provide an indicator of treatment outcome. If a circadian rhythm disorder is being considered, a sleep diary can be very useful for making the correct diagnosis.
Actigraphy is a device, typically worn on the wrist, that records movement and employs an algorithm to estimate sleep and wake periods.
It has satisfactory reliability with the “gold standard” polysomnography in good sleepers who spend little time awake and still, but not in those with sleep difficulties where significant periods of waking stillness occur 57 , 58 , 59 , 60 . It is often combined with a light sensor to provide an estimate of the latency from lights out to sleep onset.
Actigraphy is not required in the evaluation of insomnia, but it can be useful for a patient whose sleep log or history is not reliable or when circadian disorders are suspected.
Personal monitoring devices
Commercially available devices that purport to measure sleep, often differentiating between light and deep sleep, are increasingly available. There are little published data indicating the performance of nearly all of these consumer devices and thus the accuracy of the information regarding sleep and wake periods is unknown.
Limited data suggest that some of these monitors do not accurately reflect sleep architecture, sleep efficiency or sleep latency, and tend to overestimate sleep duration in normal sleepers with far worse accuracy in insomnia patients 61 , 62 . Therefore, these devices are not recommended to make clinical decisions until there are rigorous studies establishing validity and reliability. The ease of use and consumer enthusiasm, however, does suggest that these devices may play an increasing role in evaluation and treatment moving forward.
Polysomnography
Polysomnography is the gold standard to distinguish sleep from wake. It is not needed for the diagnosis of insomnia, which is based on patient self‐report. This is because indices traditionally derived from polysomnographic data do not reflect the sleep problems reported by approximately 40% of insomnia patients 63 .
Polysomnography can be helpful to rule out other possible explanations for poor sleep, such as sleep apnea or periodic leg movement disorder. Therefore, it may be indicated when there is concern for sleep apnea or when a patient is not responding to treatment as expected.
Questionnaires
There are multiple questionnaires that can aid in the evaluation of insomnia.
In many sleep clinics, every patient completes the Epworth Sleepiness Scale 64 , given the safety concern of daytime sleepiness when driving or operating heavy machinery. The Insomnia Severity Index 65 is commonly used in research as an outcome measure. The Dysfunctional Beliefs and Attitudes about Sleep 66 can help provide additional information to guide treatment. The Pittsburgh Sleep Quality Index 67 is also commonly used to collect information about self‐perceived sleep quality.
MANAGEMENT OF INSOMNIA
When a patient is diagnosed with insomnia, treatment may be initiated with one of a number of available interventions. These can be broadly categorized as non‐medication treatments and pharmacological therapies. In the sections below we review these interventions, focusing on the available evidence from blinded controlled trials indicating their efficacy and adverse effects.
Non‐medication treatments
There are several different non‐pharmacological treatment regimens that have been tested and implemented to treat insomnia. Here, we review the components and evidence supporting the non‐medication treatment with the best empirical background and most widespread use, i.e. cognitive behavioral therapy for insomnia (CBT‐I).
Employed in a variety of formats, CBT‐I has been found to be effective in reducing insomnia and improving sleep across a wide array of clinical populations 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 . Consequently, the American College of Physicians has recommended this intervention as the first line treatment for adults with insomnia 74 .
CBT‐I has been found to be as effective in the short term as pharmacological treatments, with better long‐term persistence of benefit after the end of treatment 72 . Further, unlike nearly all medications, this therapy has relatively minimal side effects. Here, we provide a clinical review of the components of CBT‐I followed by evidence of its efficacy, including its effectiveness among patients with comorbidities, and its use across different treatment modalities.
CBT‐I is typically delivered over roughly four to seven sessions. It is unclear how many sessions confer optimal benefit, though evidence suggests that fewer than four sessions are not generally sufficient 69 , 78 .
Educational components of CBT‐I
While most patients with insomnia are likely aware of some of the behaviors that fall into the sleep hygiene category, it is important to provide them with the relevant education. This includes the importance of establishing a conducive sleep environment by keeping the bedroom dark, quiet and cool.
Patients should also be reminded not to consume sleep disturbing substances, such as caffeine, nicotine and alcohol, particularly close to bedtime. Similarly, vigorous exercise three to four hours prior to bedtime should be avoided.
Additionally, a wind down routine can be helpful in readying a patient for bed. This should include discontinuation of arousing activities, including exposure to bright light (e.g., computer screen), which can negatively affect one's circadian rhythms.
Behavioral components of CBT‐I
Stimulus control.
Conditioned arousal is one of the key factors implicated in the pathogenesis of insomnia. Repeated pairing of the bed/bedroom and experiences of physiologic arousal, fear, anxiety and frustration leads to the bed serving as a learned cue or conditioned stimulus for arousal, which is incompatible with sleep onset and maintenance.
In order to eliminate this conditioned response, patients are recommended to remove themselves from the bed and bedroom if not sleepy and sit somewhere quiet until the feeling of sleepiness returns. Similarly, at bedtime, the patients are recommended not to go to bed unless they feel sleepy. Use of the bed and bedroom is restricted to sleep and sex, which means that patients are recommended not to do other activities in bed, including read or watch television. Additionally, patients are recommended to wake up the same time each morning, seven days per week, and get out of bed within 10 to 15 minutes upon awakening.
Sleep restriction
Another common contributor to the development and preservation of insomnia is the tendency for patients to spend excess time in bed. On the surface, this makes reasonable sense given that the patients yearn to “catch” sleep whenever they can. Unfortunately, excess time in bed results in conditioned arousal and fragmented sleep.
In order to effectively carry out this technique, patients should provide at least one week of sleep diaries (though two weeks are preferred). The goal is to reduce a patient's time in bed to the reported total sleep time. For instance, if a patient's diary report indicated an average total sleep time of six hours but a time in bed of nine hours (bedtime 9 pm and wake time 6 am), the new sleep schedule would provide a time in bed of six hours (bedtime midnight and wake time 6 am).
Importantly, patients are recommended to not go to sleep until the new prescribed bedtime and only when sleepy. In choosing the sleep opportunity window, it is important to take into account the patient's chronotype.
Due to safety concerns related to sleep restriction (e.g., cognitive deficits, drowsy driving), a minimum time in bed of five hours has been used in the literature 79 . In addition, sleep restriction may exacerbate comorbidities. For instance, sleep restriction has been shown to lower seizure thresholds, increase pain sensitivity, and precipitate mania in patients with bipolar disorder 80 , 81 , 82 .
Patients are recommended to complete sleep diaries throughout treatment. Their time in bed schedule should be reviewed in each subsequent CBT‐I session, with sessions occurring every one to two weeks. The sleep diaries allow the clinician to calculate their average sleep efficiency, which is the percentage of time a patient is asleep given his/her time in bed. We recommend 85% or higher in average sleep efficiency as a metric for “good” sleep quality and a threshold to be met prior to adjusting the time in bed recommendation.
Once it is established that a patient's sleep efficiency is sufficiently high, the clinician can begin to increase the time in bed, typically by altering the prescribed bedtime by 15 min each time and tracking the patient's improvement in subjective sleep quality and daytime sleepiness.
Sleep restriction is typically the aspect of CBT‐I that suffers the most from non‐adherence. In the event that a patient is unable or unwilling to carry out the prescribed time in bed, sleep compression can also be used. This technique consists of slowly decreasing time in bed over time in order to meet the original prescribed time, and may be more palatable to patients, particularly those with significant anxiety about losing further sleep opportunity.
Relaxation and paradoxical intention
These behavioral techniques complement stimulus control and sleep restriction by providing the patient with tools for decreasing arousal prior to bedtime and in the event of nighttime awakenings.
Relaxation techniques vary, but typically include diaphragmatic breathing, the tensing and relaxing of muscle groups, and possibly visual imagery. Paradoxical intention is premised on the idea that anxiety about falling asleep is inhibiting sleep onset. Using this technique, patients are asked to stay awake as long as possible, which leads to reduced anxiety and easier sleep onset.
Cognitive components of CBT‐I
Maladaptive beliefs and thoughts about sleep are typically addressed throughout treatment. It is important for a clinician to attend to sleep‐related worries, as they tend to drive the inappropriate behaviors that perpetuate insomnia. Unrealistic expectations about sleep and catastrophic thinking about the consequences of sleep loss are among these worries.
One technique for countering catastrophic thoughts is by examining evidence from the patient's experience. For instance, if a patient has the belief that a poor night of sleep will leave him/her unable to be effective in his/her job, a clinician could help the patient identify instances when he/she was able to perform sufficiently despite a poor night of sleep. Additionally, providing patients with tools to reduce worry at bedtime can be helpful.
Another technique, known as a constructive worry exercise, requires patients to list in the early evening three or more problems that they believe will likely keep them up at night. For each problem, patients list the next step towards a solution. The exercise is folded and put away and, if patients awake during the night, they are to remind themselves that they have already taken the necessary step towards resolving that problem at their “problem‐solving best” (i.e., not in the middle of the night).
Evidence of efficacy of CBT‐I
Several meta‐analytic reviews support the efficacy of CBT‐I compared to active control conditions and usual care 68 , 69 , 70 , 72 , 78 , 79 , 80 , 81 . In a recent meta‐analysis, van Straten et al 68 pooled data from 87 randomized controlled studies that used at least one component of CBT‐I, which included 3,724 patients and 2,579 non‐treated controls. The strongest effects were improvements in insomnia symptoms, as measured using the Insomnia Severity Index (Hedges’ g=0.98), sleep efficiency (g=0.71), wake after sleep onset (g=0.63), sleep onset latency (g=0.57), and subjective sleep quality (g=0.40). A small effect was observed for changes in total sleep time (g=0.16).
Further, data suggest that CBT‐I is effective among individuals with psychiatric and physical comorbidities 70 , with some accruing evidence that it may have positive effects on comorbid outcomes 82 , 83 . CBT‐I benefits are stronger for psychiatric than physical comorbidities 70 .
CBT‐I has been delivered using a number of different formats, including face‐to‐face individual, group and digitally delivered therapy. In addition, self‐help manuals, books and videos have been developed, which allow patients to carry out treatment on their own. In general, all modalities are effective, though there is some evidence to suggest that face‐to‐face therapy outperforms self‐help. Digitally delivered CBT‐I appears to produce effects comparable to in‐person therapy 84 , 85 ; however, it is likely that in‐person supervision may be required for more complicated cases 86 .
Pharmacological therapies
A number of medications from several different classes have undergone randomized, double‐blind, placebo‐controlled trials in patients with insomnia. Those for which a statistically significant therapeutic effect compared with placebo was reported appear in Tables Tables1 1 and and2. 2 . In addition, there are a number of medications commonly used to treat insomnia that have not been demonstrated to have efficacy in at least one double‐blind, randomized, placebo‐controlled trial. These appear in Table Table3 3 .
Double‐blind placebo‐controlled trials demonstrating efficacy in the treatment of younger adults with insomnia
BDZ – benzodiazepine
Double‐blind placebo‐controlled trials demonstrating efficacy in the treatment of older adults with insomnia
Medications used to treat insomnia not demonstrated to have efficacy in at least one double‐blind placebo‐controlled trial in insomnia patients
FDA – US Food and Drug Administration
In this section we review the characteristics of all of these medications (benzodiazepines, “z‐drugs”, melatonin receptor agonists, selective histamine H1 antagonists, orexin antagonists, antidepressants, antipsychotics, anticonvulsants, and non‐selective antihistamines) and present the available evidence regarding their efficacy and safety as a basis for clinical decision making.
Benzodiazepines
Benzodiazepines are a group of compounds with a similar chemical structure. Their sleep enhancing effect is a result of positive allosteric modulation of the gamma‐aminobutyric acid (GABA) type A receptor 138 , 139 . These agents exert this modulation by binding to a specific site on the GABA‐A receptor complex (referred to as the benzodiazepine binding site), thereby changing the conformation of the receptor constituent proteins, which leads to an enhancement of the inhibition occurring when GABA binds to these receptors 140 , 141 . This enhancement of inhibition is associated with a broad set of dose‐dependent clinical effects, including sedation, anxiety reduction, seizure inhibition and myorelaxation 139 , 140 , 142 .
Of the benzodiazepine medications, triazolam, flurazepam, temazepam, quazepam and estazolam have been demonstrated to have therapeutic effects on both sleep onset and maintenance in double‐blind, placebo‐controlled trials in younger adults (Table (Table1). 1 ). In older adults, triazolam and flurazepam have been found to have therapeutic effects on sleep onset and maintenance in double‐blind, placebo‐controlled trials, whereas temazepam has been demonstrated to have therapeutic effects on sleep maintenance only (Table (Table2 2 ).
For many years the prevailing view of these medications, and medications used for the treatment of insomnia in general, was that they were inevitably associated with tolerance (i.e., loss of therapeutic benefit over time) and dependence (i.e., withdrawal symptoms upon discontinuation) when used nightly on a long‐term basis 143 . Until relatively recently, little data were available to actually assess whether this was the case 25 . As data have become available, it has been clear that tolerance and dependence do not inevitably occur and are not characteristic of long‐term nightly insomnia pharmacotherapy.
However, data on long‐term treatment are only available for some medications, and the available information leaves open the possibility that dependence does occur in some individuals 25 . This limitation is particularly notable for benzodiazepines: the longest nightly treatment study of a benzodiazepine was an 8‐week trial of temazepam, where dependence was not observed 126 . Studies of 2‐4 weeks duration were carried out with triazolam (three trials) and flurazepam (one trial), without evidence of dependence occurring 87 , 121 , 122 .
The adverse effects of benzodiazepines are dose‐dependent and reflect their broad central nervous system inhibitory activity. They include sedation, psychomotor impairment, and potential for abuse by a small subset of the population 143 . The anxiolytic and myorelaxant effects can be useful in those with comorbid anxiety or pain.
Among the available options, these agents are relatively effective at treating sleep onset problems and, as a result, may be needed in some individuals with this type of sleep problem. The only relative contraindication to their use is a history of polysubstance abuse or a specific predisposition to benzodiazepine abuse.
“Z‐drugs”
These agents are an unrelated group of compounds which act by the same mechanism as benzodiazepines, but do not share the benzodiazepine chemical structure 138 , 139 , 140 , 141 , 142 . There is some evidence that they may differ somewhat from benzodiazepines in that their action is relatively restricted to subsets of GABA‐A receptors. As a result, they may have less broad clinical effects 25 , 138 , 139 , 140 , 141 , 142 .
Double‐blind, placebo‐controlled trials demonstrate the efficacy of zaleplon for sleep onset, and of zolpidem extended‐release, zopiclone and eszopiclone (the S isomer of zopiclone) for sleep onset and maintenance in both younger and older adults. Zolpidem has a documented efficacy for sleep onset and maintenance problems in younger adults, but for sleep onset problems only in older adults (Tables (Tables1 1 and and2 2 ).
More data on long‐term treatment are available for “z‐drugs” than for benzodiazepines. The sustained efficacy of eszopiclone and zolpidem has been demonstrated in studies of nightly dosing up to one year in duration without any evidence of dependence occurring, nor was dependence found in a 6‐month study of non‐nightly treatment with extended‐release zolpidem 102 , 106 , 107 .
The potential adverse effects of the “z‐drugs” are the same as the benzodiazepines. Because of the relatively narrower effects of some of these agents, they may not be as helpful as benzodiazepines in addressing concomitant anxiety or pain. This appears to be the case for zolpidem. However, eszopiclone and zolpidem extended‐release have been found to have therapeutic effects on pain, anxiety and depression concomitant with insomnia 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 .
Like benzodiazepines, these agents are relatively more effective than other options in treating problems with sleep maintenance, and may be problematic in those predisposed towards substance abuse.
Melatonin receptor agonists
There are two melatonin receptor agonists used in the treatment of insomnia: melatonin and ramelteon.
Melatonin is a hormone that is taken by many individuals with insomnia. Normally, it is released by the pineal gland during the dark period of the day. It binds predominantly to the MT1 and MT2 receptors, though the mechanism by which this might enhance sleep is not well understood 152 .
No clear dose‐response relationship has been established for the use of melatonin for treating insomnia, and there is some evidence that sleep enhancement may depend on the time of day and may not occur until 3‐4 hours after administration 153 , 154 , 155 .
A substantial number of studies have evaluated the effects of a variety of dosages, administration times, and both immediate and prolonged release formulations of melatonin in individuals with sleep problems 156 , 157 . The available evidence suggests that this agent has a clear therapeutic effect in individuals with delayed sleep‐phase syndrome, that it has an excellent safety profile, and that there may be a modest therapeutic effect on sleep onset latency in individuals with insomnia (although it remains unclear whether this effect is of clinical significance). Some preliminary evidence supports the use of melatonin to treat sleep problems in children with neurodevelopmental disorders, in whom this agent has been established to have an excellent safety profile 158 , 159 , 160 , 161 , 162 , 163 .
The most common adverse effect of melatonin is headache, and slowing of reaction time and sedation can occur during the day. Melatonin is without abuse potential, so it could be administered to abuse‐prone individuals with insomnia. Because it is a hormone that regulates reproductive function, when taken in higher dosages it can in theory impair fertility. Therefore, it has been recommended that it not be taken in those attempting to conceive 164 , 165 , 166 , 167 .
Like melatonin, ramelteon is an agonist at MT1 and MT2 receptors. However, it is a substantially more potent agonist at these receptors than melatonin. Double‐blind, placebo‐controlled trials demonstrate the efficacy of ramelteon for sleep onset insomnia in both younger and older adults (Tables (Tables1 1 and and2). 2 ). Efficacy has been more consistently found with polysomnographic measures than self‐report measures of sleep onset. Nightly treatment for six months was evaluated and no evidence of dependence phenomena was reported 111 .
Ramelteon has a relatively benign profile of adverse effects, among which the most commonly reported are headache, sedation, fatigue and nausea. It does not have significant abuse potential and could be used for abuse‐prone individuals with sleep onset problems, though no studies have evaluated its therapeutic effects in this population. Due to its good safety profile, it may be considered for use in individuals with difficulty in sleep onset only.
Selective H1 antagonists
The only highly selective histamine H1 receptor antagonist that has been systematically studied is doxepin in the 3‐6 mg dosage range 25 .
Doxepin, originally developed as an antidepressant in dosages of 75‐150 mg/day, has H1 antagonism as its most potent pharmacological effect 168 . As a result, as the dosage is decreased, this agent becomes an increasingly specific H1 antagonist 168 .
Double‐blind, placebo‐controlled trials carried out in both younger and older adults, using both self‐report and polysomnographic endpoints, demonstrate the sleep maintenance efficacy of this medication in the 3‐6 mg range (Tables (Tables1 1 and and2). 2 ). It is notable that the therapeutic effects appear to be largest towards the end of the night, without increasing morning impairment. As such, this agent appears to be uniquely well suited for use in individuals waking up towards the end of the night and having difficulty returning to sleep. Studies of up to 3‐month duration of nightly treatment have been carried out without dependence occurring 136 .
The most common adverse effect reported in younger adults is daytime sedation. However, in older adults there were no adverse effects reported more frequently with doxepin 3 mg compared to placebo. As such, older adults with early morning awakening would be a particularly appropriate group to treat with this medication. Also, given its potent H1 antagonism, doxepin could also be considered for use in people with insomnia occurring with allergy symptoms. As this agent is without abuse potential, it could also be used in patients with sleep maintenance problems who are prone to abuse, although no data exist on its use in this population.
Orexin receptor antagonists
The name “orexins” was given to two peptides that were relatively recently discovered to arise from the neurons of the lateral hypothalamus and to promote wakefulness/arousal 118 , 119 , 120 . Agents which are orexin receptor antagonists are sleep promoting, owing to their ability to block the arousal mediated by the orexins.
Suvorexant is an agent which blocks both types of orexin receptors (orexin A and B) and has been demonstrated in double‐blind placebo‐controlled trials to have therapeutic effects on sleep onset and maintenance (including in the last third of the night) in both younger and older insomnia patients, at dosages from 10 to 40 mg (Tables (Tables1 1 and and2). 2 ). This includes a placebo‐controlled trial of nightly treatment for a year, which demonstrated sustained therapeutic effects and no significant rebound insomnia on discontinuation 120 .
The adverse effect of suvorexant that is of most importance is daytime sedation. Available studies suggest that this agent is associated with some abuse potential that is roughly comparable to that of zolpidem, so that it is probably best avoided in people predisposed to abuse.
Suvorexant is the only agent with therapeutic effects in the last third of the night without substantially increasing morning sedation that also has a robust therapeutic effect on sleep onset. As such, it could be considered for use in those patients with both sleep onset difficulties and early morning awakening.
Antidepressants
There are several medications originally developed for the treatment of major depressive disorder that are commonly used for treating insomnia. These agents may produce sleep enhancing effects by blocking the receptors for neurotransmitters that are wake enhancing, such as norepinephrine, histamine, acetylcholine and serotonin 25 .
The antidepressants most commonly used to treat insomnia are trazodone 50‐150 mg, doxepin 10‐75 mg, mirtazapine 15 mg, and amitriptyline 10‐100 mg 25 . Of these agents, only doxepin 25‐50 mg has been demonstrated to have therapeutic effects in insomnia patients in at least one placebo‐controlled, double‐blind, randomized trial, and this study was small (N=47) (Table (Table1 1 ).
Although trazodone is widely prescribed in the treatment of insomnia, it has not been found to have therapeutic effects in insomnia patients in any randomized, double‐blind, placebo‐controlled trial. It was evaluated in one such trial in younger adults, but significant effects compared with placebo were not found 97 . This should not be interpreted as definitive evidence that it lacks therapeutic effects in insomnia. In fact, that study evaluated only one dose of trazodone (50 mg), whereas clinically a range of doses from 50 to 150 mg is prescribed 25 .
There are data available on the efficacy and side effects of the S isomer of mirtazapine, which is not currently available for prescription. S‐mirtazapine, like doxepin, is a selective H1 antagonist and has been evaluated in a dosing range far below the antidepressant dosage, at which it is expected to have only H1 antagonist effects of clinical significance 169 , 170 , 171 . Placebo‐controlled, randomized, double‐blind trials carried out with this agent suggest that, like doxepin, it has robust effects on sleep maintenance, with less pronounced therapeutic effects on sleep onset 169 , 170 , 171 .
The adverse effects of the antidepressants used to treat insomnia vary. All of them can cause daytime sedation, and most may cause orthostatic hypotension. The tricyclic antidepressants doxepin (25‐50 mg) and amitriptyline can cause dry mouth, constipation, blurred vision, urinary retention, cognitive impairment, arrhythmias, and increased appetite/weight gain 25 . Mirtazapine's most important adverse effects tend to be sedation and increased appetite/weight gain. Trazodone's most important adverse effects include sedation and orthostatic hypotension; it may also induce priapism 25 .
As none of these agents has significant abuse potential, they can be considered in people with a predisposition to substance abuse. They can also be considered for use in patients who fail usual therapy or have concomitant conditions such as mood, anxiety or pain difficulties, owing to their broad pharmacological effects 25 . Doxepin and amitriptyline should be used with caution in individuals prone to cognitive impairment, urinary obstruction or glaucoma. The use of all these agents is problematic in patients with bipolar depression, because of the risk of precipitating mania 172 .
Antipsychotics
Antipsychotics are a group of medications developed for treatment of psychotic conditions that are sometimes used in clinical practice to treat insomnia, generally at a dosage lower than that typically used to treat individuals with psychosis 25 . These agents may have therapeutic effects in insomnia due to their broad antagonism of wake promoting neurotransmitter receptors, such as dopamine, histamine, serotonin, cholinergic and adrenergic receptors.
The antipsychotic medications that are most commonly used to treat insomnia in clinical practice are quetiapine 25‐250 mg and olanzapine 2.5‐20 mg. There are no rigorous double‐blind, randomized, placebo‐controlled trials demonstrating the efficacy of any antipsychotic medication for the treatment of insomnia.
A few small studies of quetiapine have been carried out. This agent was reported to improve wake time after sleep onset as compared to placebo in a trial of 20 patients with alcohol use disorder in recovery and sleep disturbance 173 . A double‐blind, randomized, placebo‐controlled trial of quetiapine 25 mg was also carried out in 13 patients with primary insomnia and demonstrated an advantage for quetiapine on sleep latency and total sleep time, although neither reached statistical significance 174 .
The primary side effects of these agents include sedation, orthostatic hypotension, dry mouth, tachycardia, increased appetite/weight gain, agitation, dizziness, constipation and akathisia. More concerning, though far less common, is the risk of tardive dyskinesia. The increased risk of cerebrovascular events in patients with dementia should also be taken into account.
As these agents are without abuse potential, they can be considered for use in people who are abuse‐prone. They are best suited, however, for insomnia occurring in patients with psychosis or bipolar disorder.
These agents should be used with caution in those with dementia, hypotension or at risk for myocardial infarction, closed‐angle glaucoma, constipation or urinary retention.
Non‐selective antihistamines
Non‐selective antihistamines that are often used to treat insomnia include diphenhydramine and doxylamine, which are ingredients in many over‐the‐counter insomnia therapies. Both of these agents have, in addition to H1 antagonism, clinically relevant M1 muscarinic cholinergic antagonism.
There are highly limited data establishing the insomnia efficacy of these drugs. A therapeutic effect of diphenhydramine 50 mg on self‐reported number of awakenings, but not sleep quality, total sleep time or sleep onset latency, was reported in a placebo‐controlled cross‐over study in 20 older primary insomnia patients 175 . Diphenhydramine 25 mg was also evaluated in a parallel‐group study along with a combination of valerian and hops in 184 insomnia patients, and found to have a significant effect vs. placebo on self‐reported sleep efficiency, but not self‐reported or polysomnographic sleep onset latency, total sleep time, or polysomnographic sleep efficiency 176 .
The most important adverse effects of these medications are sedation, dizziness, psychomotor impairment, cognitive impairment, dry mouth, blurred vision, constipation, urinary retention and weight gain. Less common side effects of diphenhydramine include agitation and insomnia, whereas doxylamine has been linked in case reports to coma and rhabdomyolysis 177 .
As these agents do not have significant abuse potential, they can, in theory, be considered for use in substance abuse‐prone insomnia patients. They are best suited for use in those with insomnia occurring in the setting of allergy symptoms or upper respiratory infections. They are best avoided in those with closed‐angle glaucoma, decreased gastrointestinal motility, urinary retention, asthma and chronic obstructive pulmonary disease.
Anticonvulsants
Some agents originally developed for treatment of seizures are at times used in the management of insomnia. They include gabapentin and pregabalin, whose potential therapeutic effects in insomnia are ascribed to a decreased release of glutamate and norepinephrine through binding to the alpha‐2‐delta subunit of N‐type voltage‐gated calcium channels 178 , 179 .
There are no double‐blind, randomized, placebo‐controlled trials evaluating the efficacy of these agents in insomnia patients. Two double‐blind, randomized, placebo‐controlled trials were carried out evaluating the effects of gabapentin 250‐500 mg on sleep disturbance created by putting people to bed five hours earlier than usual (five‐hour phase advance model). They reported that this agent significantly improved both self‐reported and polysomnographic wake time after sleep onset and total sleep time compared with placebo, but not sleep onset latency 180 , 181 .
Therapeutic effects of gabapentin and pregabalin on sleep disturbance have also been reported in studies of patients with pain, restless legs syndrome, generalized anxiety disorder, and epilepsy 182 , 183 , 184 , 185 .
The most important side effects of gabapentin are sedation, dizziness, ataxia and diplopia, whereas the most important adverse effects of pregabalin include sedation, dizziness, dry mouth, cognitive impairment and appetite increase. Pregabalin appears to have some abuse potential, whereas this is not the case for gabapentin 186 .
These agents could be considered for use in insomnia occurring in patients with pain, partial seizures or restless legs syndrome. There is some evidence supporting the use of pregabalin to treat insomnia occurring in those with alcohol use disorder 187 , 188 . Both of these medications should be avoided in patients with impaired renal function.
UNMET NEEDS
Insomnia is a common and often debilitating disorder that is associated with significant adverse consequences for physical health and well‐being. Fortunately, there are behavioral and pharmacological treatments available for treating this condition. In this paper we reviewed the evidence base for those treatments in order to provide a resource for practitioners, with the hope that this would improve the clinical management of insomnia. However, our review also illustrates that there are a number of important gaps in the research carried out to date.
We lack information on the specific effects of the various components of CBT‐I which might allow greater treatment efficiency and tailoring. While meta‐analyses demonstrate the value of CBT‐I, they also note significant heterogeneity. Variability in CBT‐I components across trials makes it difficult to determine which aspects are most responsible for the observed benefits. As such, there is a need for studies aimed at providing this information.
There are also a number of key gaps related to pharmacotherapy. The most glaring one is that we lack any double‐blind, placebo‐controlled, randomized trial demonstrating the efficacy of any pharmacological treatment for insomnia in children or adolescents. There is clearly an urgent need to carry out these studies in order to guide effective clinical practice in younger individuals with insomnia.
Another gap in insomnia pharmacotherapy research is that we lack rigorous double‐blind, placebo‐controlled trials of a number of agents commonly used to treat this condition in clinical practice. This includes agents such as trazodone, quetiapine and gabapentin. It would be of great value to those clinicians who tend to prescribe these medications if they had data delineating their risks and benefits to help guide their clinical decision making.
We also lack studies of the pharmacological treatment of insomnia in the setting of several key conditions where this treatment is very often needed, such as dementia, mild cognitive impairment and substance use disorders.
A final critical gap in our knowledge base reflected in our review is that we lack research to help guide personalization of therapy. The vast majority of studies carried out evaluate a single therapy vs. a placebo or another control intervention. More trials are needed comparing effective treatments and aimed at optimally matching treatments to specific patient types, so that we can move to greater personalization in clinical practice.
Advertisement
Trends in insomnia research for the next decade: a narrative review
- Review Article
- Published: 06 April 2020
- Volume 18 , pages 199–207, ( 2020 )
Cite this article
- Daniel Ruivo Marques 1 , 2 ,
- Ana Allen Gomes 2 , 3 ,
- Vanda Clemente 2 , 4 ,
- José Moutinho dos Santos 4 ,
- Joana Serra 4 &
- Maria Helena Pinto de Azevedo 5
605 Accesses
10 Citations
Explore all metrics
Insomnia disorder has known striking developments over the last few years. Partly due to advances in neuroimaging techniques and brain sciences, our understanding of insomnia disorder has become more fine-tuned. Besides, developments within psychological and psychiatric fields have contributed to improve conceptualization, assessment, and treatment of insomnia. In this paper, we present a list of promising 10 key “hot-topics” that we think in the next 10 years will continue to stimulate researchers in insomnia’s domain: increasing of systematic reviews and meta-analyses; improvement of existing self-report measures; increasing of genetic and epigenetic investigation; research on new pharmacological agents; advances in neuroimaging studies and methods; new psychological clinical approaches; effectiveness studies of e-treatments and greater dissemination of evidence-based therapies for insomnia; call for integrative models; network approach using in insomnia; and assessment of insomnia phenotypes. The breadth of all these topics demands the collaboration of researchers from different scientific fields within sleep medicine. In summarizing, in the next decade, it is predictable that insomnia’s research still benefit from different scientific disciplines.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways
Philip R. Jansen, Kyoko Watanabe, … Danielle Posthuma

Genome-wide meta-analysis of insomnia prioritizes genes associated with metabolic and psychiatric pathways
Kyoko Watanabe, Philip R. Jansen, … Danielle Posthuma
American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual. 3rd ed. Westchester: American Academy of Sleep Medicine; 2014.
Google Scholar
American Psychiatric Association. Diagnostic and statistical manual of mental disorders-5. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Book Google Scholar
Baglioni C, Regen W, Teghen A, Spiegelhalder K, Feige B, Nissen C, Riemann D. Sleep changes in the disorder of insomnia: a meta-analysis of polysomnographic studies. Sleep Med Rev. 2014;18(3):195–21313. https://doi.org/10.1016/j.smrv.2013.04.001 .
Article PubMed Google Scholar
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. https://doi.org/10.1016/S1389-9457(00)00065-4 .
Berman M, Jonides J, Nee D. Studying mind and brain with fMRI. Soc Cogn Affect Neurosci. 2006;1(2):158–61. https://doi.org/10.1093/scan/nsl019 .
Article PubMed PubMed Central Google Scholar
Bheemsain T, Kar S. An overview of insomnia management. Delphi Psychiatry J. 2012;15(2):294–301.
Blanken T, Benjamins J, Borsboom D, Vermunt J, Paquola C, Ramautar J, Van Someren E. Insomnia disorder subtypes derived from life history and traits of affect and personality. Lancet Psychiatry. 2019;6(2):151–63. https://doi.org/10.1016/S2215-0366(18)30464-4 .
Borsboom D, Cramer A. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9(1):91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608 .
Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. https://doi.org/10.1002/wps.20375 .
Bragantini D, Sivertsen B, Gehrman P, Lydersen S, Güzey IC. Genetic polymorphisms associated with sleep-related phenotypes; relationships with individual nocturnal symptoms of insomnia in the HUNT study. BMC Med Genet. 2019;20(1):179. https://doi.org/10.1186/s12881-019-0916 .
Broomfield N, Espie C. Towards a valid, reliable measure of sleep effort. J Sleep Res. 2005;14(4):401–7. https://doi.org/10.1111/j.1365-2869.2005.00481.x .
Busto U, Sykora K, Sellers E. A clinical scale to assess benzodiazepine withdrawal. J Clin Psychopharmacol. 1989;9(6):412–6. https://doi.org/10.1097/00004714-198912000-00005 .
Article CAS PubMed Google Scholar
Buysse D, Ancoli-Israel S, Edinger J, Lichstein K, Morin C. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29(9):1155–73. https://doi.org/10.1093/sleep/29.9.1155 .
Buysse D, Germain A, Hall M, Monk T, Nofzinger E. A neurobiological model of insomnia. Drug Discov Today Dis Models. 2011;8(4):129–37. https://doi.org/10.1016/j.ddmod.2011.07.002 .
Buysse D, Harvey A. Insomnia: recent developments and future directions. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 757–760.
Chapter Google Scholar
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–21313. https://doi.org/10.1016/0165-1781(89)90047-4 .
Cassano GB, Petracca A, Cesana BM. A new scale for the evaluation of benzodiazepine withdrawal symptoms: sessb. Curr Therapeutic Res. 1994;55(3):275–89. https://doi.org/10.1016/s0011-393x(05)80171-7 .
Article Google Scholar
Dekker K, Blanken T, Van Someren E. Insomnia and personality: a network approach. Brain Sci. 2017;7(3):28. https://doi.org/10.3390/brainsci7030028 .
Article PubMed Central Google Scholar
Edinger J, Leggett M, Carney C, Manber R. Psychological and behavioral treatments for insomnia II: implementation and specific populations. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 814–831.
Eisai Global. U.S. FDA approves Eisai’s Dayvigo TM (Lemborexant) for treatment of insomnia in adult patients. 2019. https://www.eisai.com/news/2019/news201993.html . Accessed 31 Jan 2020.
Espie C, Kyle S, Williams C, Ong J, Douglas N, Hames P, Brown J. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35(6):769–81. https://doi.org/10.5665/sleep.1872 .
Fernandez-Mendoza J. The insomnia with short sleep duration phenotype: an update on it’s importance for health and prevention. Curr Opin Psychiatry. 2017;30(1):56–63. https://doi.org/10.1097/YCO.0000000000000292 .
Field A, Gillett R. How to do a meta-analysis. Br J Math Stat Psychol. 2010;63:665–94. https://doi.org/10.1348/000711010X502733 .
Gehrman P, Pfeiffenberger C, Byrne E. The role of genes in the insomnia phenotype. Sleep Med Clin. 2013;8(3):323–31. https://doi.org/10.1016/j.jsmc.2013.04.005 .
Gilbert P. The origins and nature of compassion focused therapy. Br J Clin Psychol. 2014;53(1):6–41. https://doi.org/10.1111/bjc.12043 .
Gregory AM, Rijsdijk FV, Eley TC, Buysse DJ, Schneider MN, Parsons M, Barclay NL. A longitudinal twin and sibling study of associations between insomnia and depression symptoms in young adults. Sleep. 2016;39(11):1985–92. https://doi.org/10.5665/sleep.6228 .
Hadian S, Jabalameli S. The effectiveness of compassion-focused therapy (CFT) on rumination in students with sleep disorders: a quasi-experimental research, before and after. J Urmia Univ Med Sci. 2019;30(2):86–96.
Hein M, Lanquart J-P, Loas G, Hubain P, Linkowski P. Similar polysomnographic pattern in primary insomnia and major depression with objective insomnia: a sign of common pathophysiology?. BMC Psychiatry. 2017. https://doi.org/10.1186/s12888-017-1438-4
Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, Baglioni C. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43:96–105. https://doi.org/10.1016/j.smrv.2018.10.006 .
Jansen P, Watanabe K, Stringer S, Skene N, Bryois J, Posthuma D. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat Genet. 2019;51:394–403. https://doi.org/10.1038/s41588-018-0333-3 .
Jones S, van Hees V, Mazzotti D, Marques-Vidal P, Sabia S, van der Spek A, Wood A. Genetic studies of accelerometer-based sleep measures in 85,670 individuals yield new insights into human sleep behaviour. Nat Commun. 2018;10(1):1585. https://doi.org/10.1038/s41467-019-09576-1 .
Article CAS Google Scholar
Kobayashi M, Okajima I, Narisawa H, Kikuchi T, Matsui K, Inada K, Inoue Y. Development of a new benzodiazepine hypnotics withdrawal symptom scale. Sleep Biol Rhythm. 2018;16(3):263–71. https://doi.org/10.1007/s41105-018-0151-0 .
Lane J, Jones S, Dashti H, Wood A, Aragam K, Saxena R. Biological and clinical insights from genetics of insomnia symptoms. Nat Genet. 2019;51:387–93. https://doi.org/10.1038/s41588-019-0361-7 .
Article CAS PubMed PubMed Central Google Scholar
Lilenfeld S. What is “evidence” in psychotherapies? World Psychiatry. 2019;18(3):245–6. https://doi.org/10.1002/wps.20654 .
Lind MJ, Gehrman PR. Genetic pathways to insomnia. Brain Sci. 2016;6(4):64. https://doi.org/10.3390/brainsci6040064 .
Article CAS PubMed Central Google Scholar
Ma Z-R, Shi L-J, Deng M-H. Efficacy of cognitive behavioral therapy in children and adolescents with insomnia: a systematic review and meta-analysis. Braz J Med Biol Res. 2018;51(6):e7070. https://doi.org/10.1590/1414-431X20187070 .
Marques D. Do we need neuroimaging to treat insomnia effectively? Sleep Med. 2019;53:205. https://doi.org/10.1016/j.sleep.2017.08.005 .
Marques D. “Time to relax”: considerations on relaxation training for insomnia disorder. Sleep Biol Rhythm. 2019;17(2):263–4. https://doi.org/10.1007/s41105-018-00203-y .
Marques D. Self-report measures as complementary exams in the diagnosis of insomnia. Revista Portuguesa de Investigação Comportamental e Social. 2020. [Accepted for publication] .
Marques D, Azevedo MH. Potentialities of network analysis for sleep medicine. J Psychosom Res. 2018;111:89–90. https://doi.org/10.1016/j.jpsychores.2018.05.019 .
Marques D, Clemente V, Gomes A, Azevedo MH. Profiling insomnia using subjective measures: where are we and where are we going. Sleep Med. 2018;43:103–4. https://doi.org/10.1016/j.sleep.2017.12.006 .
Marques D, Gomes A, Azevedo MH. Utility of studies in community-based populations. 2019. [Manuscript submitted for publication] .
Marques D, Gomes A, Caetano G, Castelo-Branco M. Insomnia disorder and brain’s default-mode network. Curr Neurol Neurosci Rep. 2018;18(8):45. https://doi.org/10.1007/s11910-018-0861-3 .
Marques D, Gomes A, Clemente V, Santos J, Castelo-Branco M. Default-mode network activity and its role in comprehension and management of psychophysiological insomnia: a new perspective. New Ideas Psychol. 2015;36:30–7. https://doi.org/10.1016/j.newideapsych.2014.08.001 .
Marques D, Gomes A, Clemente V, Santos J, Duarte I, Caetano G, Castelo-Branco M. Unbalanced resting-state networks activity in psychophysiological insomnia. Sleep Biol Rhythm. 2017;15(2):167–77. https://doi.org/10.1007/s41105-017-0096-8 .
Marques D, Gomes AA, Clemente V, Moutinho J, Caetano G, Castelo-Branco M. An overview regarding insomnia disorder: conceptualization, assessment and treatment. In: Columbus AM, editor. Advances in psychology research. New York: Nova Science Publishers Inc; 2016. p. 81–116.
Marques D, Gomes A, Clemente V, Santos J, Caetano G, Castelo-Branco M. Neurobiological correlates of psychological treatments for insomnia: a review. Eur Psychol. 2016;21(3):195–205. https://doi.org/10.1027/1016-9040/a000264 .
McNally R. Can network analysis transform psychopathology? Behav Res Ther. 2016;86:95–104. https://doi.org/10.1016/j.brat.2016.06.006 .
Morales-Lara D, De-la-Peña C, Murillo-Rodríguez E. Dad’s snoring may have left molecular scars in your DNA: the emerging role of epigenetics in sleep disorders. Mol Neurobiol. 2018;55(4):2713–24. https://doi.org/10.1007/s12035-017-0409-6 .
Morin C. Contributions of cognitive-behavioral approaches to the clinical management of insomnia. Prim Care Companion J Clin Psychiatry. 2002;4(1):21–6.
Morin C, Vallières A, Ivers H. Dysfunctional Beliefs and Attitudes about Sleep (DBAS): validation of a brief version (DBAS-16). Sleep. 2007;30(11):1547–54. https://doi.org/10.1093/sleep/30.11.1547 .
Ong J, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt J. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37(9):1553–63. https://doi.org/10.5665/sleep.4010 .
Owen M, Cardno A, O’Donovan M. Psychiatric genetics: back to the future. Mol Psychiatry. 2000;5(1):22–31. https://doi.org/10.1038/sj.mp.4000702 .
Päivi L, Sitwat L, Harri O-K, Joona M, Raimo L. ACT for sleep—internet-delivered self-help ACT for sub-clinical and clinical insomnia: a randomized controlled trial. J Context Behav Sci. 2019;12:119–27. https://doi.org/10.1016/j.jcbs.2019.04.001 .
Palagini L, Biber K, Riemann D. The genetics of insomnia–evidence for epigenetic mechanisms? Sleep Med Rev. 2014;18(3):225–35. https://doi.org/10.1016/j.smrv.2013.05.002 .
Perlis M, Ellis J, Kloss J, Riemann D. Etiology and pathophysiology of insomnia. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 769–784.
Perlis M, Shaw P, Cano G, Espie C. Models of insomnia. In: Kryger M, Roth T, Dement W, editors. Principles and practice of sleep medicine. 5th ed. Missouri: Elsevier Saunders; 2011. p. 850–865.
Qureshi I, Mehler M. Epigenetics of sleep and chronobiology. Curr Neurol Neurosci Rep. 2014;14(3):432. https://doi.org/10.1007/s11910-013-0432-6 .
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis J, Spiegelhalder K. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. https://doi.org/10.1111/jsr.12594 .
Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14(1):19–311. https://doi.org/10.1016/j.smrv.2009.04.002 .
Riemann D, Spiegelhalder K, Nissen C, Hirscher V, Baglioni C, Feige B. REM sleep instability: a new pathway for insomnia? Pharmacopsychiatry. 2012;45(5):167–76. https://doi.org/10.1055/s-0031-1299721 .
Rodriguez M, Maeda Y. Meta-analysis of coefficient alpha. Psychol Methods. 2006;11(3):306–22. https://doi.org/10.1037/1082-989X.11.3.306 .
Schulz H, Salzarulo P. The development of sleep medicine: a historical sketch. J Clin Sleep Med. 2016;12(7):1041–52. https://doi.org/10.5664/jcsm.5946 .
Siddaway A, Wood A, Hedges L. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019;70:747–70. https://doi.org/10.1146/annurev-psych-010418-102803 .
Sirois F, Nauts S, Molnar D. Self-compassion and bedtime procrastination: an emotion regulation perspective. Mindfulness. 2019;10(3):434–45. https://doi.org/10.1007/s12671-018-0983-3 .
Spiegelhalder K, Regen W, Baglioni C, Nissen C, Riemann D, Kyle S. Neuroimaging insights into insomnia. Curr Neurol Neurosci Rep. 2015;15(3):9. https://doi.org/10.1007/s11910-015-0527-3 .
Stein M, McCarthy M, Chen C, Jain S, Gelernter J, He F, Ursano R. Genome-wide analysis of insomnia disorder. Mol Psychiatry. 2018;23(11):2238–50. https://doi.org/10.1038/s41380-018-0033-5 .
Stepanski E. Behavioral sleep medicine: a historical perspective. Behav Sleep Med. 2003;1(1):4–21. https://doi.org/10.1207/S15402010BSM0101_3 .
Tam V, Patel N, Turcotte M, Bossé Y, Paré G, Meyre D. Benefits and limitations of genome-wide association studies. Nat Rev Genet. 2019;20(8):467–84. https://doi.org/10.1038/s41576-019-0127 .
Tolin D, McKay D, Forman E, Klonsky E, Thombs B. Empirically supported treatment: recommendations for a new model. Clin Psychol Sci Pract. 2015;22(4):317–38. https://doi.org/10.1111/cpsp.12122 .
Trauer J, Qian M, Doyle J, Rajaratnam S, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191–204. https://doi.org/10.7326/M14-2841 .
van Dalfsen J, Markus C. The involvement of sleep in the relationship between the serotonin transporter gene-linked polymorphic region (5-HTTLPR) and depression: a systematic review. J Affect Disord. 2019;256:205–12. https://doi.org/10.1016/j.jad.2019.05.047 .
van Straten A, van der Zweerde T, Kleiboer A, Cuijpers P, Morin C, Lancee J. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. 2018;38:3–16. https://doi.org/10.1016/j.smrv.2017.02.001 .
Walsh J, Roth T. Pharmacologic treatment of insomnia: benzodiazepine receptor agonists. In: Kryger M, Roth T, Dement W, editors. Principles and practices of sleep medicine. 6th ed. Philadelphia: Elsevier; 2017. p. 832–841.
Wang Y, Wang F, Zheng W, Zhang L, Ng C, Unqvari G, Xiang Y. Mindfulness-based interventions for insomnia: A meta-analysis of randomized controlled trials. Behav Sleep Med. 2018. https://doi.org/10.1080/15402002.2018.1518228 [Epub ahead of print] .
Whitfield-Gabrieli S, Ford J. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49–76. https://doi.org/10.1146/annurev-clinpsy-032511-143049 .
Wilson B. Cutting edge developments in neuropsychological rehabilitation and possible future directions. Brain Impair. 2011;12(1):33–42. https://doi.org/10.1375/brim.12.1.33 .
Wilson B. Neuropsychological rehabilitation: state of the science. S Afr J Psychol. 2013;43(3):267–77. https://doi.org/10.1177/0081246313494156 .
Winkler A, Rief W. Effect of placebo conditions on polysomnographic parameters in primary insomnia: a meta-analysis. Sleep. 2015;38(6):925–31. https://doi.org/10.5665/sleep.4742 .
Wittchen H, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, Steinhausen H. The size and burden of mental disorders and other disorders of the brain in Europe. Eur Neuropsychopharmacol. 2011;21(9):655–79. https://doi.org/10.1016/j.euroneuro.2011.07.018 .
Download references
Acknowledgements
The authors would like to express their gratitude to the reviewers for their important comments and suggestions.
Author information
Authors and affiliations.
Department of Education and Psychology, University of Aveiro, Campus Universitário de Santiago, 3810-193, Aveiro, Portugal
Daniel Ruivo Marques
Faculty of Psychology and Educational Sciences, CINEICC-Center for Research in Neuropsychology and Cognitive Behavioral Intervention, University of Coimbra, Coimbra, Portugal
Daniel Ruivo Marques, Ana Allen Gomes & Vanda Clemente
Faculty of Psychology and Educational Sciences, University of Coimbra, Rua Do Colégio Novo, 3000-115, Coimbra, Portugal
Ana Allen Gomes
Sleep Medicine Centre, Coimbra University Hospital Centre (CHUC), Coimbra, Portugal
Vanda Clemente, José Moutinho dos Santos & Joana Serra
Faculty of Medicine, University of Coimbra, Rua Larga, 3004-504, Coimbra, Portugal
Maria Helena Pinto de Azevedo
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Daniel Ruivo Marques .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Marques, D.R., Gomes, A.A., Clemente, V. et al. Trends in insomnia research for the next decade: a narrative review. Sleep Biol. Rhythms 18 , 199–207 (2020). https://doi.org/10.1007/s41105-020-00269-7
Download citation
Received : 20 August 2019
Accepted : 28 March 2020
Published : 06 April 2020
Issue Date : July 2020
DOI : https://doi.org/10.1007/s41105-020-00269-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sleep disorder
- Find a journal
- Publish with us
- Track your research
ORIGINAL RESEARCH article
The different faces of insomnia.

- 1 Department of Internal Medicine and Dermatology, Interdisciplinary Center of Sleep Medicine, Charité - Universitätsmedizin Berlin, Berlin, Germany
- 2 Department of Behavioral Therapy and Psychosomatic Medicine, Rehabilitation Center Seehof, Federal German Pension Agency, Seehof, Germany
- 3 Department of Biology, Saratov State University, Saratov, Russia
Objectives: The identification of clinically relevant subtypes of insomnia is important. Including a comprehensive literature review, this study also introduces new phenotypical relevant parameters by describing a specific insomnia cohort.
Methods: Patients visiting the sleep center and indicating self-reported signs of insomnia were examined by a sleep specialist who confirmed an insomnia diagnosis. A 14-item insomnia questionnaire on symptoms, progression, sleep history and treatment, was part of the clinical routine.
Results: A cohort of 456 insomnia patients was described (56% women, mean age 52 ± 16 years). They had suffered from symptoms for about 12 ± 11 years before seeing a sleep specialist. About 40–50% mentioned a trigger (most frequently psychological triggers), a history of being bad sleepers to begin with, a family history of sleep problems, and a negative progression of insomnia. Over one third were not able to fall asleep during the day. SMI (sleep maintenance insomnia) symptoms were most frequent, but only prevalence of EMA (early morning awakening) symptoms significantly increased from 40 to 45% over time. Alternative non-medical treatments were effective in fewer than 10% of cases.
Conclusion: Our specific cohort displayed a long history of suffering and the sleep specialist is usually not the first point of contact. We aimed to describe specific characteristics of insomnia with a simple questionnaire, containing questions (e.g., ability to fall asleep during the day, effects of non-medical therapy methods, symptom stability) not yet commonly asked and of unknown clinical relevance as yet. We suggest adding them to anamnesis to help differentiate the severity of insomnia and initiate further research, leading to a better understanding of the severity of insomnia and individualized therapy. This study is part of a specific Research Topic introduced by Frontiers on the heterogeneity of insomnia and its comorbidity and will hopefully inspire more research in this area.
Introduction
Insomnia is one of the most frequent sleep disorders with continuously increasing prevalence. About 30–50% of the US adult population exhibit insomnia symptoms, 15–20% display a short-term insomnia of <3 months, and 5–15% display a chronic insomnia of >3 months ( 1 – 3 ). Common diagnostic manuals include the ICSD-3 (International Classification of Sleep Disorders, 3 rd Edition, American Academy of Sleep Medicine 2014) and the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5 th Edition, American Psychiatric Association 2013) ( 4 , 5 ). Main characteristics of insomnia include dissatisfaction with sleep quantity and quality with one or more of the following symptoms: difficulties initiating sleep, difficulties maintaining sleep (frequent or prolonged awakenings with problems returning to sleep again), and early morning awakening (occurring earlier than desired after a total sleep time of only 3–5 h with the inability to return to sleep). The disturbed sleep is associated with stress, psychological strain and suffering, as well as impairment in social, occupational, and other important areas of functioning. Complaints include fatigue, exhaustion, lack of energy, daytime sleepiness, cognitive impairment (e.g., attention, concentration, and memory), mood swings (e.g., irritability, dysphoria), impaired occupational functioning and impaired social functioning. The symptoms occur for at least 3 nights per week for at least 3 months and occur despite an adequate sleep environment.
Previous dichotomization of insomnia in primary and secondary (or comorbid) insomnia has been abandoned with the new editions of the DSM-5 and ICSD-3. Currently, insomnia is mostly characterized by the common phenotypes of sleep onset insomnia (SOI insomnia, difficulty falling asleep), sleep maintenance insomnia (SMI insomnia, difficulty staying asleep), early morning awakenings insomnia (EMA insomnia), and a combination of those. Another categorization follows the timeframe of being an acute (<1 month), subacute (1–3 months), and chronic insomnia (>3 months) ( 4 , 5 ). While other sleep disorders (e.g., sleep apnea) are categorized by severity into mild, moderate, or severe, which has important implications for the choice of therapy, insomnia still lacks such a classification. The Insomnia Severity Index (ISI) is the only instrument currently in use that allows for severity classification: no insomnia (score 0–7), subclinical insomnia (score 8–14), or moderate to severe insomnia (score 15–28) ( 6 ).
The characterization of different phenotypes is important to establish clinically relevant subtypes of insomnia. It may help to reduce the heterogeneity of insomnia and facilitate cause identification and personalized treatments. Yet there are not many standardized instruments of insomnia diagnosis allowing for phenotyping. However, there has been evidence that insomniacs with a total sleep time of <6 h suffer a more severe insomnia than insomniacs with a total sleep time of 6 h or more ( 7 ). They display mental and psychological impairment compared to patients with average or longer than average sleep. However, mortality is increased for insomniacs with longer total sleep time ( 8 ). The sleep duration with the 6-h distinction also influences the therapy outcome, success of cognitive-behavioral therapy (CBT), and the relation to comorbid bipolar disorder ( 9 , 10 ). Recently, a study investigated subtypes of insomnia according to psychological stress ( 11 ). Questioning 2,224 volunteers with an ISI score of at least 10 and a control group of 2,098 volunteers with an ISI score below 10, five insomnia subtypes were identified: highly distressed, moderately distressed but sensitive to positive reinforcement (accepting of positive emotions), moderately distressed insensitive to positive reinforcement, slightly distressed with a high reactivity to their environment and life circumstances, and slightly distressed with low reactivity. The results showed a high stability of the classification over the 5-year investigation. The psychological categorization is clinically relevant as there were clear differences identified between the subtypes regarding development, therapy success, presence of electroencephalogram (EEG) biomarker, and the risk for depression. This was a first approach to subtyping insomnia patients according to psychological health. The exact effect of psychological health, family history, comorbidity, personality, environment and sleep quality on insomnia is still unclear. Similar symptom clusters have been discussed for other disorders including depression ( 12 ).
Our study is part of the specific Research Topic introduced by Frontiers on the heterogeneity of insomnia and its comorbidity. We aim to encourage and further the discussion on insomnia heterogeneity and the need for possible phenotyping, we do not intend to provide a complete list of phenotypes or possible clusters. The study picked up the approach of subtyping insomnia by collecting a short questionnaire during anamnesis on possible related symptoms, onset and course of insomnia. We described phenotypical traits of insomniacs with a cohort of sleep disturbed patients from a specialized outpatient clinic for sleep disorders.
Participants and Recruitment
Since 2018, a specialized 14-item insomnia questionnaire has formed part of the clinical routine at the outpatient clinic of the Interdisciplinary Center of Sleep Medicine, Charité—Universitätsmedizin Berlin ( Figure 1 ). The questionnaire is the result of literature research, clinical experience, and consensus of psychologists, neurologist, psychiatrists, and sleep physicians within the sleep center. Patients who visited the outpatient clinic between 01/2019 and 02/2020 and indicated self-reported symptoms presenting a suspicion of insomnia (e.g., difficulties initiating sleep, maintaining sleep, or early morning awakening) according to ICSD-3 criteria were recruited and completed the questionnaire. In total, 486 patients were examined by a physician specializing in sleep disorders and insomnia who confirmed an insomnia diagnosis. The questionnaire did not contain any identifying information. As the questionnaire is part of the clinical routine and the de-identified data has been analyzed retrospectively, ethical review and approval was not required in accordance with the local legislation and institutional requirements. As part of the clinical routine, patients signed informed consent forms allowing de-identified data of their patient file, including the insomnia questionnaire, to be used for research purposes.
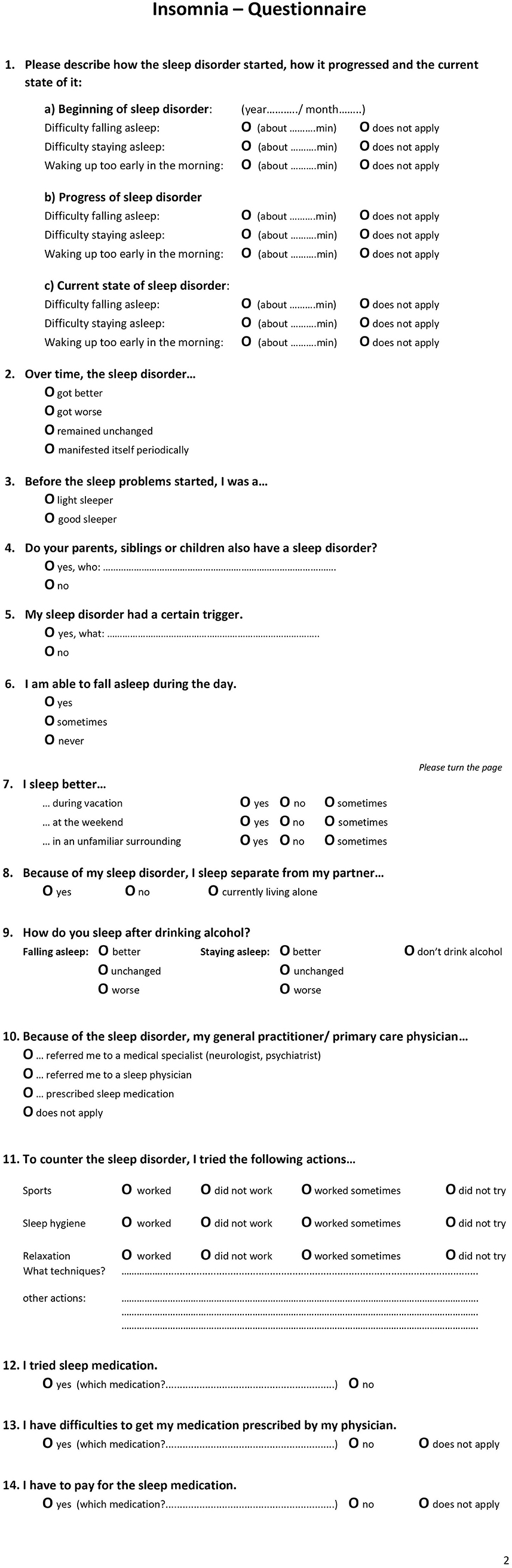
Figure 1 . The English translation of the 14-item Insomnia Questionnaire with page 1 and page 2.
Questionnaire
The insomnia questionnaire consisted of 14 items ( Figure 1 presents an English translation of the questionnaire). These included questions related to (1) type of insomnia (SOI—sleep onset insomnia, SMI—sleep maintenance insomnia, EMA—early awakening insomnia, multiple answers possible) at three points in time (start of disorder, progression, current state), (2) progression of insomnia, (3) sleep history of being a light or good sleeper, (4) relatives with sleep disorder, (5) triggers, (6) daytime sleep, (7) sleeping in different environments, (8) sleeping arrangement with partner, (9) alcohol as a sleep aid, (10) referral/ recommendation of general practitioner (multiple answer options), (11) alternative sleep treatments, and (12–14) sleep medication.
Procedure of the examination was standardized and performed by the same physician: On arrival, patients received several sleep questionnaires including the 14-item insomnia questionnaire. They were asked to complete these questionnaires before seeing the physician. During the following in-person consultation, the physician completed a full anamnesis (a patient-reported medical history) and confirmed a diagnosis of a primary insomnia according to ICSD-3 criteria. Next, the questions of the insomnia questionnaire were evaluated. Certain questions were clarified, and missing information added. For example, for question 3, light sleeper was defined. Light sleeper includes patients with a regular bedtime but whose sleep is sensitive to light, temperature, and noise. They need a specific degree of sleep comfort and sleep worse in an unfamiliar environment. These patients can nap during the day and sleep better during vacation and time off (e.g., weekends). They perceive their sleep as non-restorative. They also do not meet the diagnostic criteria of insomnia. The question refers to the time before the insomnia started, mostly referring to childhood / adolescence. For question 6, it was clarified that daytime napping included a daytime situation that explicitly allows for napping. For question 7, it was explained that “weekend” also included the days off work.
Sample size was calculated based on prevalence data and the estimated number of insomnia patients: ca. 30–50% of 328.2 million people (US population estimate 2019) result in about 98.5–164.1 million patients ( 13 ). With an accepted error rate of maximum 5% and a confidence interval of 95%, the sample size was set to at least 400 questionnaires in order to detect sufficiently powerful effects. Statistical analysis was performed using SPSS (IBM SPSS Statistics, Version 20). The patient cohort was described using a descriptive analysis with numbers and percentages ( Table 1 ). In order to investigate possible insomnia subgroups based on phenotypes/characteristics, we compared items with dichotomous answers. Item 7 (sleeping in different environments), item 9 (alcohol as a sleep aid), and item 11 (alternative sleep treatments) each had several subcategories which were consolidated into one overall category. For the text answer of item 5 (trigger) we performed a qualitative data analysis by subjectively grouping the text data and visually presenting the categories. A t-test was used for group comparisons of continuous variables (e.g., age), the chi-square test for dichotomous variables. Significance level was set at 0.05.
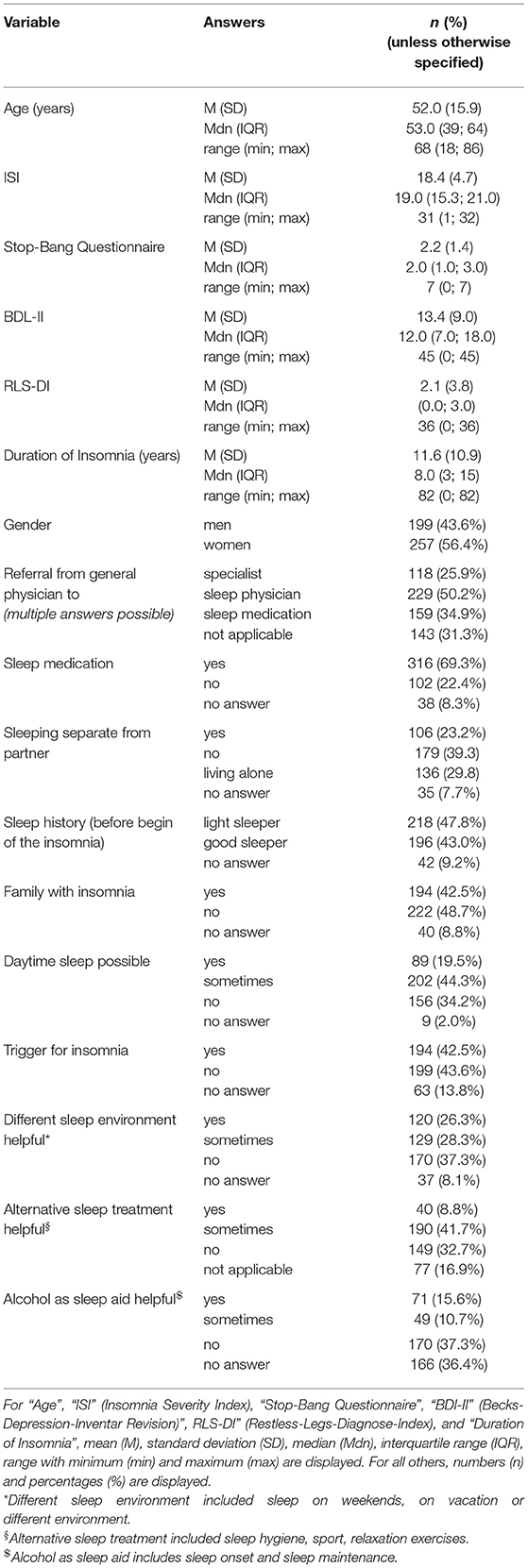
Table 1 . Sample description ( n = 456 patients).
Patient Description
Due to missing information that could also not be completed during the in-person consultation with the physician, 30 questionnaires were removed from analysis. The remaining 456 questionnaires were de-identified and analyzed. The patient cohort ( Table 1 ) reported having sleep problems for an average of 11.6 ± 10.9 years (range: 0–82 years, where 0 means the symptoms just started within the past month). The cohort consisted of slightly more female insomniacs (56%) and had an average age of 52.0 ± 15.9 years (range: 18–86 years). More than half of the patients reported having a partner and not living alone (63%), and of those 37% slept in a separate room due to the sleep disorder. If the patient went to a general physician first, 50% were referred to a sleep specialist and 26% to another specialist (neurologist, psychiatrist etc.). In 35% of those cases, the general physician initiated a therapy with sleep medication. In general, 69% of the patients reported having used sleep medication, 23% indicated that they had not. Only 9% mentioned that it was difficult to get sleep medication. While 26% stated they had to pay for sleep medication, 37% said they did not. In Germany, sleep medication for primary insomnia covered by insurance only includes melatonin (only for patients over 55 years) and z-drugs (only for the acute therapy of 4 weeks).
Sleep Characteristics
About 43% of the patients indicated that they had a history of being good sleepers before the insomnia onset, while 48% mentioned that they have always been light sleepers. Forty-three percent reported having a family member with sleep problems. Despite insomnia symptoms, 20% of patients indicated that they were able to fall asleep during the day and 44% sometimes. While 43% of patients reported a trigger for the sleep problems, 42% reported no trigger ( Table 1 ). Figure 2 presents a categorization of the reported triggers. The most frequent triggers were of psychological nature (22%) including depression, anxiety, post-traumatic stress disorder, death of a family member, trauma, rape, psychotherapy etc. Stress was listed as a separate category but is to be considered as a subcategory of psychological triggers (additional 11%). Work related triggers including change or loss of job, freelance work, work problems, shift work, long work hours, workload, mobbing/ bulling etc. accounted for 15%.
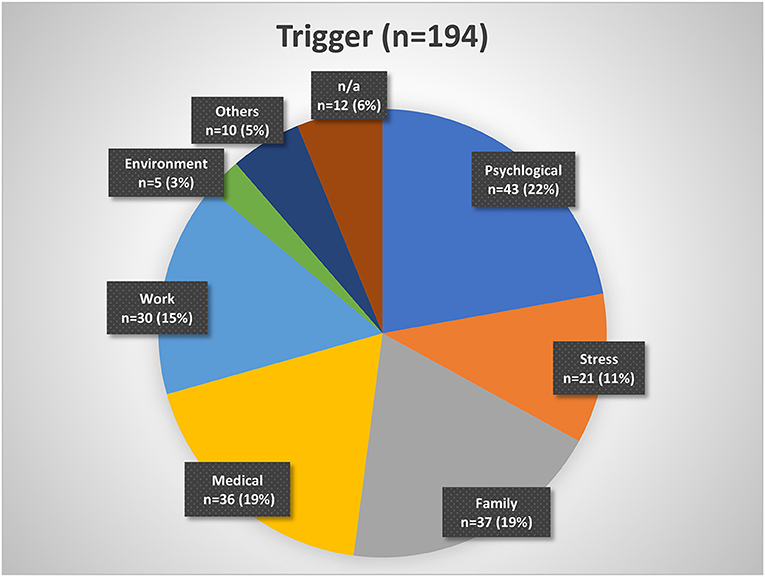
Figure 2 . Insomnia triggers organized by categories. Psychological triggers include depression, fear, trauma, etc. Stress may be considered a subgroup of psychological triggers. Family triggers include birth, children, marriage, divorce, etc. Medical triggers include sickness, operations, etc. Work triggers include mobbing, loss of job, change of job, workload, etc. Environment triggers include noise, lighting, neighborhood, etc. Other triggers include smoking, attitude, etc. n/a, not available.
The question about sleep in a different environment (item 7 of the questionnaire) included three subcategories: sleep during vacation, sleep at weekends, and sleep in unfamiliar surroundings. Sleep during vacation was perceived as better by 21% ( n = 84), sometimes better by 30% ( n = 121), and not at all better by 49% ( n = 198). Sleep at the weekend was perceived as better by 18% ( n = 70), sometimes better by 26% ( n = 103), and not at all better by 56% ( n = 224). Sleep in unfamiliar surroundings was perceived as better by 5% ( n = 19), sometimes better by 17% ( n = 68), and not at all better by 78% ( n = 304). We consolidated the subcategories in one general environment variable. First, sleep in a different environment (in general) was considered better if a patient answered “yes (sleep better)” to at least one of the subgroups. The remaining patients were categorized into the sometimes group if they answered “sometimes” to at least one of the subcategories. Then, the remaining patients were categorized into the “no (do not sleep better)” or “no answer” category. In general, 26% indicated that they sleep better in different environments, 28% sometimes, and 37% not at all ( Table 1 ).
The question for alternative non-medical treatments (item 11) also included three subcategories: sport, sleep hygiene, and relaxation techniques. Sport only helped in 7% ( n = 26), helped sometimes in 32% ( n = 130), and did not help in 46% ( n = 185). Sleep hygiene helped in 5% ( n = 18), helped sometimes in 29% ( n = 103), and did not help in 43% ( n = 154). Relaxation techniques helped in 5% ( n = 19), helped sometimes in 32% ( n = 117), and did not help in 38% ( n = 142). We combined the subcategories into one overall variable of non-medical treatment in the same way as for item 7. In general, 9% of the patients indicated that an alternative treatment helps, 42% mentioned it helped sometimes, and 33% reported it did not help at all ( Table 1 ).
Alcohol as a sleep aid (item 9) included two subcategories: alcohol as a sleep aid for sleep onset and alcohol as a sleep aid for sleep maintenance. While 40% ( n = 112) indicated alcohol helps with SOI symptoms, it did not change sleep onset in 41% ( n = 116) and symptoms got worse in 19% ( n = 54). Alcohol helped with SMI symptoms in 11% ( n = 31), did nothing in 46% ( n = 123), and got worse in 43% ( n = 116). We also consolidated this variable. Alcohol as a sleep aid in general helped, if a patient answered “sleep got better” to at least one of the two subcategories (without a “sleep got worse” for the other category). Alcohol worsened sleep if a patient answered at least once “got worse” (without a “got better” for the other category). We added the answer option “alcohol helps sometimes” for patients that answered “got better” to one of the categories and “got worse” to the other. The remaining patients were categorized as “no change” or “no answer.” In general, alcohol helped in 16%, helped sometimes in 11%, and did not help (or even got worse) in 37% ( Table 1 ).
Table 2 presents a further description of insomnia subtypes based on these sleep characteristics. We dichotomized the answers into yes/no in order to create a more equal group distribution for comparison. Patients with a sleep history of being light sleepers even before insomnia onset, had significantly longer insomnia symptoms than patients with a sleep history of being good sleepers ( p < 0.05). Patients with a family history of sleep problems were significantly more frequently female ( p < 0.05), had suffered from insomnia symptoms significantly longer ( p < 0.01), and presented significantly more EMA symptoms ( p < 0.05) than patients without a family history of sleep problems. Patients who were able to sleep during the day were significantly more frequently male ( p = 0.001) and displayed fewer SOI ( p < 0.001) and fewer EMA symptoms ( p < 0.01) than patients who could not sleep during the day. Patients with no trigger displayed a tendency to having a longer insomnia duration than patients with a trigger ( p = 0.05). Patients who were able to sleep better in different environments were significantly younger ( p < 0.001) and showed a tendency to shorter insomnia duration ( p = 0.05) than patients who did not sleep better in another environment. Patients for whom alcohol helped as a sleep aid were significantly younger ( p < 0.001) and presented significantly more SOI symptoms ( p < 0.001).
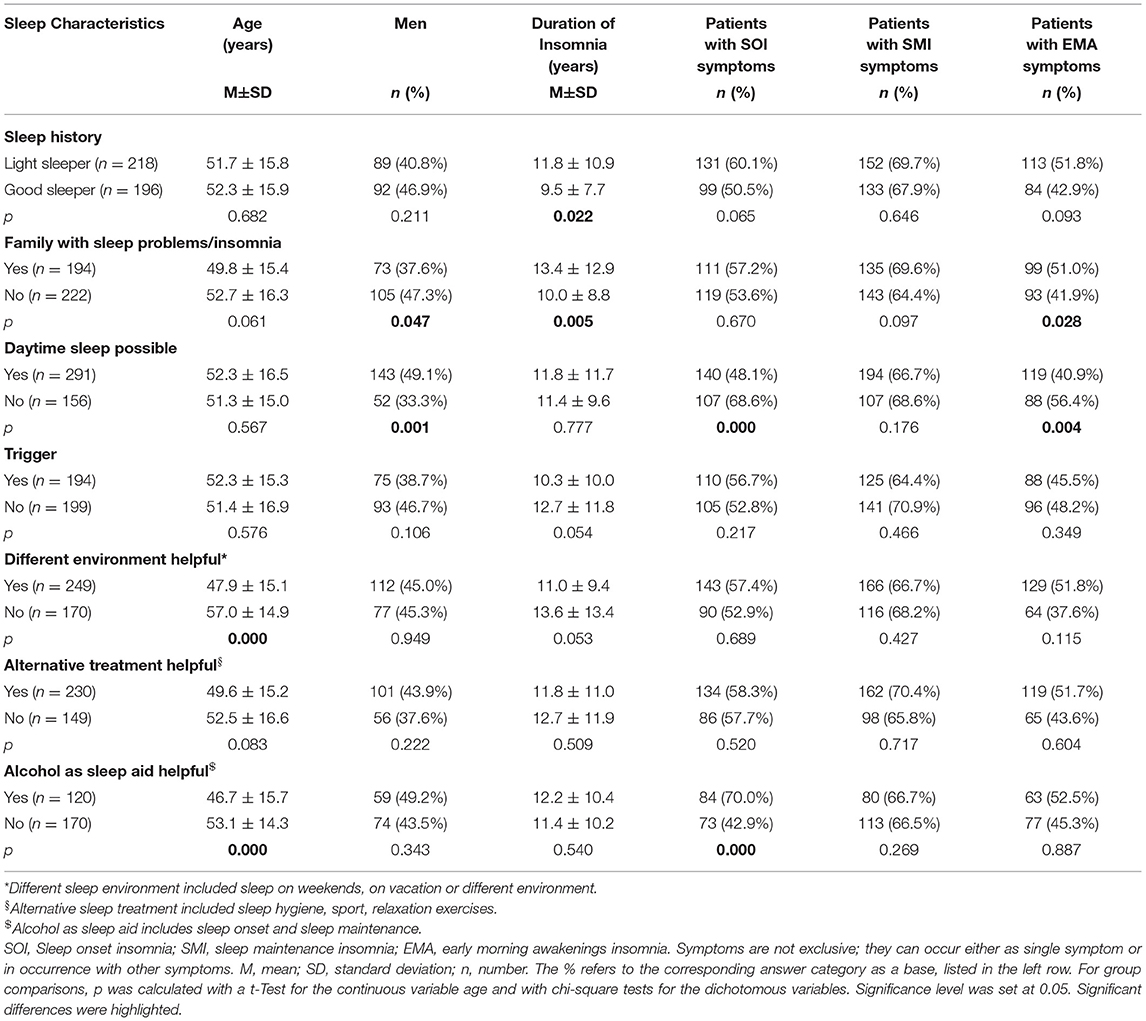
Table 2 . Description of possible insomnia phenotype subgroups based on sleep characteristics.
Insomnia Symptom Subtypes and Progression
At time of visit, 54% of patients presented SOI symptoms, 66% SMI symptoms, and 45% EMA symptoms ( Table 3 ). In 57% of the patients, there was a combination of those symptoms. Patients with SOI symptoms reported on average that they needed 85.6 ± 55.0 min to fall asleep. Patients with SMI symptoms reported waking up for about 79.0 ± 58.2 min after sleep onset. And patients with EMA symptoms reported that they woke up on average 79.0 ± 56.5 min too early in the morning. Patients with EMA symptoms (not exclusively, combination of symptoms possible) had the shortest history of sleep problems (10.2 ± 9.1 years, range: 0–44 years) compared to patients with SOI symptoms (12.0 ± 9.8 years, range: 0–82 years) and patients with SMI symptoms (11.5 ± 10.6 years, range: 0–82 years). Differences were not significant.
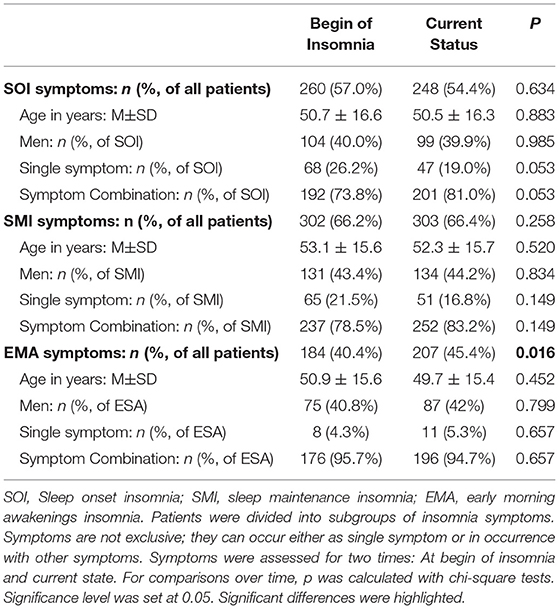
Table 3 . Patient description by insomnia subgroups based on symptoms over time.
Table 3 presents the possible change of sleep symptoms over time by type of sleep symptoms. There was no significant change in SOI or SMI symptoms. Only EMA symptoms significantly increased over time ( p = 0.016). Figure 3 presents the progression in severity of the sleep disorder. Fewer than 10% reported an improvement of symptoms, while in 41% the sleep disorder got worse. In 20% the symptoms showed a periodic pattern. The progression was independent of current symptoms.
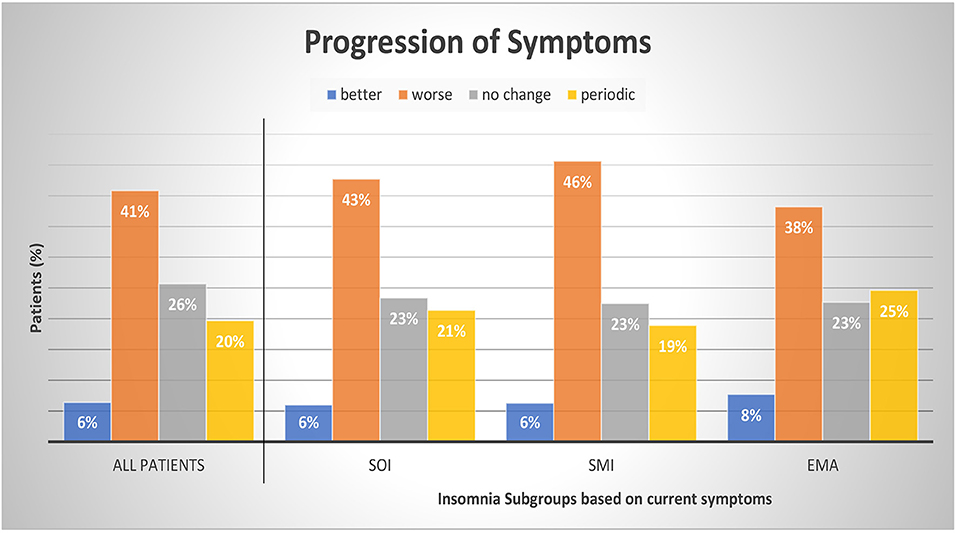
Figure 3 . Progression of symptoms by insomnia subgroups. Patients were divided into subgroups of current insomnia symptom. Symptoms are not exclusive, they can occur either as single symptom or in occurrence with other symptoms. SOI, Sleep onset insomnia; SMI, sleep maintenance insomnia; EMA, early morning awakenings insomnia. A patient with a periodic pattern of insomnia experiences weeks or months long periods with insomnia symptoms alternating with symptom free periods. For comparisons between symptom groups, p was calculated with chi-square tests. Results were not significant at a 0.05 level. The sum of the subcategories does not add up to 100% as we refrained from displaying the category “missing data and multiple answers” (7% All patients, 7% SOI, 6% SMI, and 7% EMA).
A distinct cohort of insomnia patients that reported to a special outpatient clinic for sleep disorders revealed that about 40–50% of the patients mentioned a trigger for the sleep problems, were not good sleepers to begin with (light sleepers), had a family history of sleep problems, and had a progressive course of insomnia. Over one third were not able to fall asleep during the day. Insomnia with SMI symptoms was most frequent, as well as a psychological trigger. Over time, EMA symptoms increased. Alternative non-medical treatments were only lastingly effective in fewer than 10%. Over two thirds of the patients (69%) had tried sleep medication. One of the unique traits of our cohort is the duration of the sleep problem before the visit to a specialist (over 11 years). For most, the sleep specialist/clinic is not the first point of contact. Thus, our patient cohort is not comparable to one from a general physician or population-based cohort.
Our results emphasize the insomnia heterogeneity and the need for phenotyping. Following, we will first discuss the characteristics assessed with our questionnaire starting with some new aspects that are currently not commonly asked (history of being a light sleeper, daytime sleep, effects of alternative treatments, alcohol, temporal stability/change of insomnia symptoms). Then, we will review the current literature for further possible phenotypes. Table 4 presents an overview.
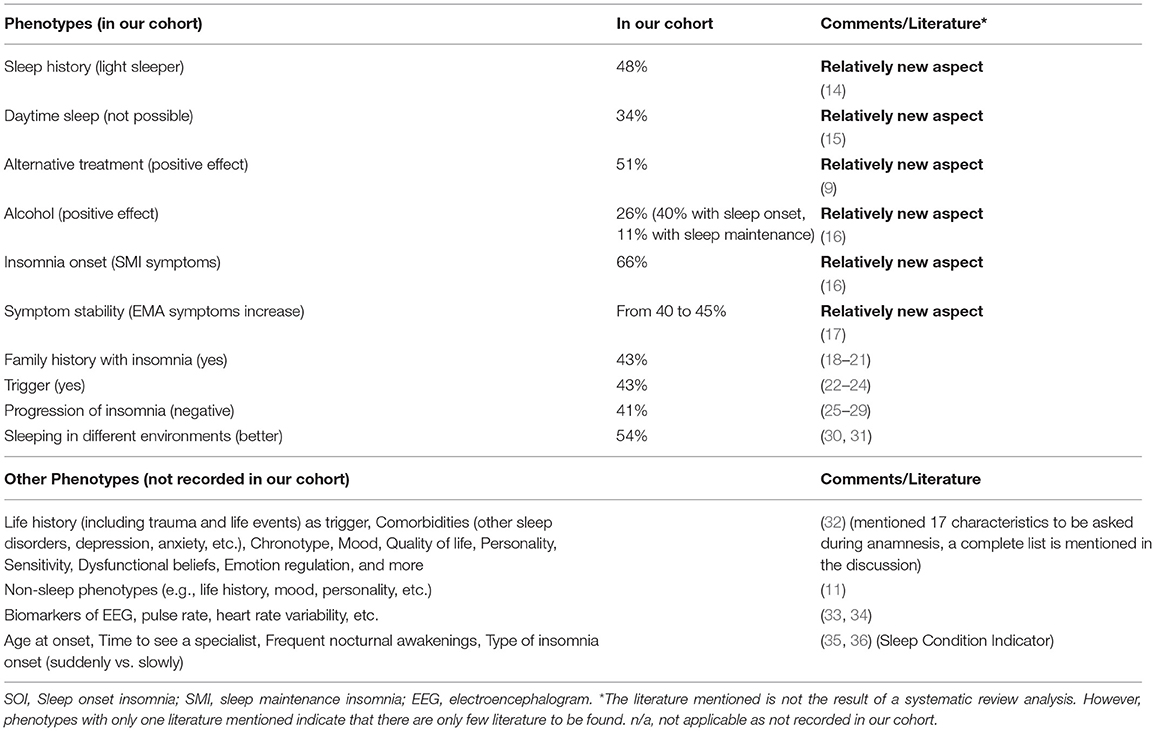
Table 4 . Overview of discussed phenotypes.
Phenotypes—Based on Our Cohort
Sleep history.
Almost half of our cohort (48%) presented a bad sleep history, indicative of an idiopathic insomnia.
There are no clear biomarkers or diagnostic criteria to distinguish between psychophysiological and idiopathic (chronic) insomnia ( 14 ). In order to identify idiopathic insomnia, we ask the patient for their sleep history, specifically before insomnia onset. Did the patient always experience poor (light) sleep, or were they a fairly good sleeper? We assume that light sleep is the pre-stage of insomnia, but not every light sleeper needs to develop insomnia, indicating that these variables are not predictors for differentiating between psychophysiological and idiopathic insomnia. Whether this distinction of good and bad sleep before developing insomnia influences therapy will need to be further investigated. Also, the term “light (bad)” sleep needs to be clearly defined and standardized.
Daytime Sleep
Using our questionnaire, we found in our cohort that 34% of patients reported not being able to take a nap during the daytime despite being tired and despite having the explicit opportunity of taking a nap. Those patients were predominantly women with more SOI and more EMA symptoms compared to patients who were able to fall asleep during the day. They did not differ regarding the duration of their insomnia symptoms.
Currently, it is not common during insomnia diagnosis to ask whether a patient is able to fall asleep during the day or to conduct a Multiple Sleep Latency Test (MSLT) for objective assessment. Our own experience with insomnia patients, however, showed how important this question is. We experienced that patients who sleep poorly at night and are tired during the day, but cannot sleep in the day either, usually have a higher degree of insomnia. They tend to suffer for more nights a week and are more resistant to therapy. In contrast, the possibility of falling asleep during the day, in front of the television, in the car, on public transport, in a meeting, or in other quiet surroundings, seems to be a sign of a lower degree of insomnia.
The ability to nap during the day has also been a criterion for other indications in the literature. The Hyperarousal Scale by Regestein et al. ( 37 ) provides indirectly a reference to the degree of alertness during the day and thus to the inability to fall asleep. Khassawneh et al. ( 38 ) used the scale together with the patient's subjective statement that they cannot nap during the day and found that patients with hyperarousal and short sleep duration have more cognitive deficits in memory tests. Li et al. ( 39 ) used the MSLT with a threshold value of 14 min to define hyperarousal. Drake et al. ( 40 ) also used the MSLT and investigated sleep disturbances due to commonly experienced stressful situations to identify factors representing the construct of “stress-related” vulnerability to sleep disturbance. Subjects with a high Ford Insomnia Response to Stress Test (FIRST) score had poorer sleep quality at night and higher latencies of sleep in the MSLT. Roehrs et al. ( 15 ) performed the MSLT in 95 patients with primary insomnia (32–64 years) and in 55 healthy sleepers and found a higher sleep latency in insomniacs (13.2 ± 4.65 min vs. 11.0 ± 4.93 min). However, the difference is small and the variability among insomniacs is high (between 2 and 20 min). The MSLT is still a questionable method for diagnosing insomnia, but it may be a possible tool for subtyping insomnia with regard to the ability to fall asleep during daytime. Espie et al. ( 41 ) examined daytime symptoms of 11,129 participants with ( n = 5,083) and without insomnia, coming from different backgrounds. Of the analyzed items (energy, concentration, relationships, ability to stay awake, mood, and ability to get through work), the items “energy” and “mood” turned out to be the two most important parameters for insomniacs, but not the item “ability to stay awake.” The importance of the criterion daytime sleepiness and/or ability to stay awake seems therefore recognized, but not yet uniformly defined and requires further research.
Alternative Treatment (Behavioral Therapy)
In our cohort, about 83% of the patients have tried at least one of these alternative non-medical behavioral treatments: sport, sleep hygiene, and/or relaxation techniques. In one third of the patients (33%) these techniques did not help. There were no significant age, gender, or symptom differences between patients with effective alternative treatments and patients where it was not effective. However, we did not investigate the severity of insomnia and it may be possible that patients where the alternative treatments did not show a positive effect may be patients with more severe insomnia.
Therapy recommendations for insomnia include a multi-modal behavioral therapy including psychological elements (e.g., CBT) as the first therapeutic step which many patients do complete, most commonly even before they arrange a visit to a specialist ( 42 ). This is also what we found in our cohort. Most of our patients have tried to educate themselves on their sleep problems, have tried to improve their sleep hygiene, have tried alternative non-medical treatments (e.g., sport, relaxation, etc.), and already went to either a natural health practitioner, homeopath, psychologist or psychotherapist. Currently, CBT is not yet good enough established in Germany as a definite treatment for insomnia. Studies have shown that CBT had less of an effect on insomniacs with short sleep duration ( 9 ). We assume that this also applies to patients with a more severe insomnia. However, severity has yet to been clearly defined. Patients will most likely show a similar reaction to phytopharmacology or alternative “smart” therapy (e.g., acoustic or electrical stimulation). A future quality check and standardization of CBT methods may be helpful in order to use the success of alternative treatment/behavioral therapy as a phenotypical criterion. We hypothesize that successful CBT is mainly linked to mild insomnia. For moderate to severe insomnia, CBT should be a necessary concomitant therapy.
In our cohort, only about 26% mentioned that alcohol helps with sleep problems in general. Patients for whom alcohol helped were significantly younger and presented more SOI symptoms. A more detailed analysis showed that alcohol helped especially with sleep onset (40%), less with sleep maintenance (only 11%). In 43% of our patients, alcohol even worsened sleep maintenance, which other studies confirmed ( 16 ). However, in almost half of our patients, alcohol showed no change.
Alcohol is a widely used sleep aid. Asking for the soporific effect of alcohol should become standard during insomnia anamnesis, as well as asking for the soporific effect of drugs (CBD, cannabis, etc.) which have become more and more a topic of sleep research ( 43 ). It is surprising that in our cohort many patients reported a lack of positive effect of alcohol as a sleep aid. It may be that the alcohol amount consumed was not high enough, as we did not ask for specifics.
Symptoms at Time of Insomnia Onset
In our cohort, 57% had SOI symptoms when the insomnia started (in 74% as a combination with other symptoms), 66% had SMI symptoms at the beginning (in 79% as a combination of symptoms), and 40% started with EMA symptoms (in 96% with other symptoms). The majority had a combination of several symptoms. Hence, in most cases of insomnia the sleep disorder started with SMI symptoms (either as single symptom or in combination). We found that patients with single SOI or single EMA were significantly younger than patients with a SOI combination (single: age 47 ± 17 years, combination: age 52 ± 16 years; p < 0.01) or EMA combination (single: age 39 ± 13 years, combination: age 51 ± 15 years; p < 0.01), respectively.
Bjorøy et al. ( 16 ) also investigated subtypes of insomnia in an extensive web-based survey with 64,503 patients who had displayed insomnia for >6 months. Here, 60% of the younger insomniacs (on average 37 years) showed SOI symptoms, either as a combination with SMI and/or EMA symptoms or as a single symptom. Confirming our own results, Bjorøy et al. ( 44 ) also found that SOI as a single symptom was more frequent in younger insomniacs, a SOI symptom combination more frequent in older insomniacs. They revealed further predictors for a symptom combination including female gender, evening chronotype, less education, and being single. While we do not assess aspects such as chronotype, they are important. Literature has shown that there is a higher insomnia prevalence in general in people with an evening chronotype. Insomniacs with a symptom combination also showed a higher comorbidity with depression, anxiety, and a higher use of alcohol and sleeping pills ( 16 ).
Symptom Stability Over Time
Not just the severity, but also the symptoms can change over time. In our cohort, prevalence of SOI and SMI symptoms did not change; EMA symptoms, however, significantly increased from 40 to 45% from first noticing those symptoms to the present (visit to a sleep specialist). Patients with SOI symptoms showed a tendency of an increase of SOI in symptom combination instead of as a single symptom (from 74 to 81%).
An early study of Hohagen et al. ( 17 ) also investigated the progression of insomnia symptoms and possible temporal stability of different patterns in 328 patients (18–65 years). In only 4 months, they discovered a >50% change in SOI, SMI, and EMA symptoms. Only in rare cases did a specific and single symptom insomnia (either SOI, SMI, or EMA) change from one to another single symptom. However, in many single symptom insomnia cases another symptom occurred over time while the first symptom stayed dominant. This tendency was also seen in our cohort regarding the SOI symptoms.
Family History
Almost half of our patient cohort (43%) reported a family history of disturbed sleep/insomnia. These patients were foremost female and presented more EMA symptoms than patients without a family history present.
A specific gene for insomnia is not known but a genetic predisposition cannot be completely ruled out ( 18 , 19 ). A twin study of children revealed a moderate inheritability of insomnia, and another study reported 35% inheritability ( 20 , 21 ).
In our cohort, almost every second patient (43%) reported a trigger. Patients with or without a trigger in our cohort did not differ regarding age, gender, and insomnia symptoms. However, those patients with no triggers showed a tendency to longer insomnia duration then the ones with a trigger. Here, it may be possible that the start of the trigger (whether sudden or slowly, unconsciously developing) may have an impact on the perception of insomnia as a chronic condition. Within our cohort, most frequently named were psychological triggers (e.g., depression, anxiety, trauma, burnout), family triggers (e.g., birth, divorce, custody battles), and medical/biological triggers including surgery and other illnesses. Work triggers (e.g., mobbing/ bulling, job loss) and stress as a separate psychological trigger came next.
Triggers are part of Spielman's theoretical model (1987) of factors causing chronic insomnia. The 3Ps consist of predisposing factors, precipitating factors which trigger acute insomnia, and perpetuating factors ( 22 , 23 ). Triggers would belong to the precipitating factors and may lead to a chronic insomnia. For a working patient, work related stress and job strain may play a bigger role as a trigger and moderator of the insomnia than for those patients that are not working ( 24 ). However, whether the existence of a trigger influences the progression or therapy of insomnia still needs to be further investigated.
Progression of Insomnia
Our patients reported most frequently a negative progression of insomnia (41%); in 26% there were no changes, and only in 7% was there an improvement. On average, the patients suffered from insomnia symptoms for about 11.6 years (range 0–82 years) before seeing a sleep specialist. Patients with predominantly EMA symptoms showed the shortest sleep problem history with 10.2 years (range 0–44 years) compared to patients with SOI or SMI symptoms. About 20% of our patients reported a periodic pattern of symptom severity.
The periodic pattern may be indicative of a non-24 h disorder ( 25 ). A patient with a periodic pattern of insomnia experiences weeks or months long periods with insomnia symptoms alternating with symptom free periods. Green et al. ( 26 ) also investigated the progression of insomnia for over 20 years in 5-year intervals. Patterns included: healthy pattern, episodic pattern, chronic pattern, and a pattern with the development of symptoms in the follow-up period. Chronic insomnia was linked to older women and the working class. It showed that social factors do affect the progression of a sleep disorder, a fact also indicated by Patel et al. ( 27 ) and Arber et al. ( 28 ). There is another distinction of insomnia subtypes by progression introduced by Wu et al. ( 29 ): persistent insomnia, remission, or relapse.
Sleep in Different Environments
Over half of our patients (54%) reported sleeping better in a different environment, including weekends/days with time off from work (51%), vacation (44%), and unfamiliar surroundings in general (22%). The category “unfamiliar surroundings” received the lowest number. Patients may have included job related hotel stays and therefore increased stress level, which may account for the lower number. Patients stating they slept better in a different environment were predominantly younger members of our cohort.
If patients reported sleeping better at weekends or on vacation, this may be an indication that the sleep disorder was caused by work stress or daily routine. In the literature, this is called behavioral induced insufficient sleep ( 30 , 31 ). As only few insomniacs are able to quit their job or family, this category may represent a specific insomnia phenotype. For those, specific interventions are possible including the end of shift work, change to home office work, change from full-time to part-time work, etc.
Further Discussion of Phenotypes
Studies suggest that insomnia is a heterogenic disorder and the identification of different phenotypes or comorbidities is important for personalized treatments ( 45 ). In our study, we presented some new aspects on what insomniacs should be asked during anamnesis and what should be considered during phenotyping. Benjamin et al. ( 32 ) already proposed the following characteristics: (1) life history including demographics, mental and physical health, trauma and life events. This study showed that more women than men and more older people than younger people suffer from insomnia and life events are usually triggers. Such triggers are mostly to be found at home, in health or at work/school, as could also be confirmed with our patients. But who reacts to such a negative trigger with insomnia and why, when, at what age, is not yet known and may possibly have a genetic reason. Further characteristics included (2) subjective sleep quality, (3) fatigue, sleepiness, hyperarousal in the daytime, (4) other sleep disorders, (5) lifetime sleep history, (6) chronotype, (7) depression, anxiety, mood, (8) quality of life, (9) personality, (10) worry, rumination, self-consciousness, sensitivity, (11) dysfunctional beliefs, (12) self-conscious emotion regulation and coping, (13) nocturnal mentation, (14) wake resting state mentation, (15) lifestyle including physical activity and food intake, (16) body temperature, and (17) hedonic evaluation. Other possible non-sleep phenotypes included: MRI, cognition, mood, traits, history of life events, family history, PSG, sleep microstructure, genetics. Blanken et al. ( 11 ) distinguished insomnia subtypes according to the so-called non-sleep categories of life history, mood perception, and personality. Miller et al. ( 33 ) presented an insomnia cluster analysis based on neurocognitive performance, sleep-onset measures of qualitative EEG, and heart rate variability (HRV). They identified two main clusters, depending on duration of sleep (<6 h vs. >6 h). The HRV changes during falling asleep may also play a role, as may the spectral power of the sleep EEG, and parameters from the sleep hypnogram such as sleep onset latency and wake after sleep onset. In one of our own studies, we were able to demonstrate that the increased nocturnal pulse rate and vascular stiffness in insomniacs with low sleep efficiency (<80%) represented an early sign of elevated cardiovascular risk, and thus presented a useful tool for phenotyping insomnia ( 34 ). In the future, other objective characteristics may include biomarkers or radiological features ( 46 , 47 ).
Further characteristics that may play a role but have not yet been mentioned or investigated are the age of the patient during insomnia onset, frequent nocturnal awakenings, the time it takes to see a specialist, and the kind of insomnia onset, slowly progressing or suddenly unexpected. There is no defined age at which the likelihood of insomnia increases, but we know that menopause is a major trigger for women. Grandner et al. ( 35 ) were able to show that getting older alone is not a predictor of insomnia, it rather includes multifactorial events. The question of how long it takes to see a specialist is also part of the Sleep Condition Indicator (SCI) by Espie et al. ( 36 ). They asked whether the insomnia had lasted longer than a year, 1–2, 3–6, or 7–12 months. We can easily agree with such a classification in terms of content. Many patients who wake up frequently at night consider this an insomnia with SMI symptoms. Frequent nocturnal awakenings, but with the ability to fall asleep again straight away, are according to the definition not considered a SMI insomnia. We did not address this in the present study, which presents a limitation. While it is mentioned in the DSM-5 as an independent sign of insomnia, patients affected by frequent nocturnal but subjectively normal sleep lengths and still restful sleep do not (yet) have insomnia. Whether it is an independent phenotype or a preliminary stage of a SMI insomnia should be further examined and defined. It also needs to be clarified whether devices for sleep registration help us with phenotyping. Polysomnography is certainly a very strong phenotypic feature when sleep time is very short, wake times after sleep onset is high and deep and/or dream sleep and sleep efficiency are not optimal. However, the current status is such that it is not suitable for diagnosis ( 48 ). In the near future, technical advances will help to provide objective, long-term sleep data, which are important for diagnosis, subtyping, and therapy for different types of insomnia.
Currently, questionnaires have been used to assess insomnia. The most known questionnaires include the ISI and the Pittsburgh Sleep Quality Index (PSQI). These are valid instruments ( 6 , 49 ). However, there are a number of other questionnaires used for insomnia such as the Amsterdam Resting-State Questionnaire (ARSQ), Dysfunctional Beliefs and Attitudes About Sleep Scale (DBAS), Sleep-Related Behaviors Questionnaire (SRBQ), Sleep Functional Impact Scale (SFIS), Leeds Sleep Evaluation Questionnaire (LSEQ), Glasgow Sleep Effort Scale (GSES) ( 50 – 55 ). In 2014, Espie et al. ( 36 ) introduced the SCI which presented a good instrument for identifying the presence of insomnia and also allowed for time differentiation. Also, the short version with only 2 questions seems valid, where questions are asked about the number of nights in the past month with poor sleep and about the trouble in general caused by sleep ( 56 ). Kalmbach et al. ( 57 ) presented a differentiation between good and bad sleepers based on the Presleep Arousal Scale—Cognitive (PSAS-C) and—Somatic (PSAS-S). People with a high PSAS-C have higher sleep latency and wake times after sleep onset, as well as higher MSLT latency and lower sleep efficiency and total sleep time. The PSAS-C in particular seems to be a good measure of the hyperarousal state. Research and official expert recommendations will show which questionnaires should be favored in clinical practice.
Limitations
Our study intended to encourage and further the discussion on insomnia heterogeneity and the need for possible phenotyping. While we introduced some new aspects of phenotyping, we neither provided a complete list of possible phenotypes nor defined specific clusters. Limitations of our study include the fact that further important aspects (e.g., comorbidity, employment, having children, chronotype, employment etc.) may need consideration. Also, some aspects of the questionnaire will need a more precise definition (e.g., light sleeper, daytime napping, weekend/vacation, alternative treatment, alcohol use), patients were not differentiated regarding sleep duration (<6 h vs. >6 h), and the progression of insomnia was observed retrospectively and not investigated prospectively. While our study was performed with patients of a sleep center, there is also need for phenotyping and thorough assessment of those phenotype characteristics in patients of a primary care setting.
As part of a specific Research Topic introduced by Frontiers on the heterogeneity of insomnia, our study provides further ideas on the already existing approaches to phenotyping insomnia patients. The aim of our study was not to examine all conceivable phenotypic features of insomnia, but to help document specific characteristics with simple questions about the onset and course of insomnia during anamnesis. While the clinical relevance of some of those possible phenotypes is not yet clear (e.g., sleep history, trigger, daytime sleep, sleep in a different environment, alternative treatment, insomnia progression/symptom stability etc.), they should play a role in future research and medical care of insomnia patients. We would like to give an impulse for further research in this area, in order to better differentiate insomnia, thus leading to more effective individualized therapy.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
IF, TP, and VK had the role of supervision and conceptualized the study. IF was responsible for data collection. NL performed data analysis. All authors were involved in visualization and writing including data interpretation, result discussion, and drafting and reviewing the manuscript.
This was not an industry supported study. The study was initiated and funded by the Charité—Universitätsmedizin Berlin owned funding.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank all the patients that participated, and Hendrik Straße and Sandra Zimmermann involved in data entry and processing.
1. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. (2002) 6:97–111. doi: 10.1053/smrv.2002.0186
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. (2006) 7:123–30. doi: 10.1016/j.sleep.2005.08.008
3. Krystal AD, Prather AA, Ashbrook LH. The assessment and management of insomnia: an update. World Psychiatry. (2019) 18:337–52. doi: 10.1002/wps.20674
CrossRef Full Text | Google Scholar
4. American Academy of Sleep Medicine. International Classification of Sleep Disorders . 3rd ed. Darien, IL: American Academy of Sleep Medicine (2014).
Google Scholar
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders – Section II: Diagnostic Criteria and Codes: Sleep-Wake Disorders . 5th ed. Arlingten, VA: American Psychiatric Association (2013).
6. Bastien CH, Vallières A, Morin CM. Validation of the nsomnia Severity Index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
7. Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev. (2013) 17:241–54. doi: 10.1016/j.smrv.2012.09.005
8. Wallace ML, Lee S, Hall MH, Stone KL, Langsetmo L, Redline S, et al. Heightened sleep propensity: a novel and high-risk sleep health phenotype in older adults. Sleep Health. (2019) 5:630–8. doi: 10.1016/j.sleh.2019.08.001
9. Bathgate CJ, Edinger JD, Krystal AD. Insomnia patients with objective short sleep duration have a blunted response to cognitive behavioral therapy for insomnia. Sleep. (2017) 40: zsw012. doi: 10.1093/sleepj/zsx050.334
10. Lewis KJS, Richards A, Karlsson R, Leonenko G, Jones SE, Jones HJ, et al. Comparison of genetic liability for sleep traits among individuals with bipolar disorder I or II and control participants. JAMA Psychiatry. (2019) 77:303–10. doi: 10.1001/jamapsychiatry.2019.4079
11. Blanken TF, Benjamins JS, Borsboom D, Vermunt JK, Paquola C, Ramautar J, et al. Insomnia disorder subtypes derived from life history and traits of affect and personality. Lancet Psychiatry. (2019) 6:151–63. doi: 10.1016/S2215-0366(18)30464-4
12. Bondar J, Caye A, Chekroud AM, Kieling C. Symptom clusters in adolescent depression and differential response to treatment: a secondary analysis of the treatment for adolescents with depression study randomised trial. Lancet Psychiatry. (2020) 7:337–43. doi: 10.1016/S2215-0366(20)30060-2
13. United States Census Bureau. Source 2019 Population Estimates . (2020). Available online at: https://data.census.gov/cedsci/all?q=Population%20estimates/ (accessed November 2, 2020).
14. Passarella S, Duong MT. Diagnosis and treatment of insomnia. Am J Health Syst Pharm. (2008) 65:927–34. doi: 10.2146/ajhp060640
15. Roehrs TA, Randall S, Harris E, Maan R, Roth T. MSLT in primary insomnia: stability and relation to nocturnal sleep. Sleep. (2011) 34:1657–52. doi: 10.5665/sleep.1426
16. Bjorøy I, Jørgensen VA, Pallesen S, Bjorvatn B. The prevalence of insomnia subtypes in relation to demographic characteristics, anxiety, depression, alcohol consumption and use of hypnotics. Front Psychol. (2020) 11:527. doi: 10.3389/fpsyg.2020.00527
17. Hohagen F, Käppler C, Schramm E, Riemann D, Weyerer S, Berger M. Sleep onset insomnia, sleep maintaining insomnia and insomnia with early morning awakening–temporal stability of subtypes in a longitudinal study on general practice attenders. Sleep. (1994) 17:551–4.
PubMed Abstract | Google Scholar
18. Jansen PR, Watanabe K, Stringer S, Skene N, Bryois J, Hammerschlag AR, et al. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat Genet. (2019) 51:394–403. doi: 10.1038/s41588-018-0333-3
19. Stein MB, McCarthy MJ, Chen CY. Genome-wide analysis of insomnia disorder. Mol Psychiatry. (2018) 23:2238–50. doi: 10.1038/s41380-018-0033-5
20. Barclay NL, Gehrman PR, Gregory AM, Eaves LJ, Silberg JL. The heritability of insomnia progression during childhood/adolescence: results from a longitudinal twin study. Sleep. (2015) 38:109–18. doi: 10.5665/sleep.4334
21. Beaulieu-Bonneau S, LeBlanc M, Mérette C, Dauvilliers Y, Morin CM. Family history of insomnia in a population-based sample. Sleep. (2007) 30:1739– 45. doi: 10.1093/sleep/30.12.1739
22. Spielman AJ, Caruso LS, Glovinsky PB. A behavioral-perspective on insomnia treatment. Psychiatr Clin North Am. (1987) 10:541–53. doi: 10.1016/S0193-953X(18)30532-X
23. Perlis ML, Corbitt CB, Kloss JD. Insomnia research: 3Ps and beyond. Sleep Med Rev. (2014) 18:191–93. doi: 10.1016/j.smrv.2014.01.003
24. Halonen JI, Lallukka T, Pentti J, Stenholm S, Rod NH, Virtanen M, et al. Change in job strain as a predictor of change in insomnia symptoms: analyzing observational data as a non-randomized pseudo-trial. Sleep. (2017) 40:zsw007. doi: 10.1093/sleep/zsw007
25. Solaiman SS, Agrawal R. Non-24-hour sleep-wake circadian rhythm disorder in a sighted male with normal functioning. J Clin Sleep Med. (2018) 14:483–4. doi: 10.5664/jcsm.7008
26. Green MJ, Espie CA, Hunt K, Benzeval M. The longitudinal course of insomnia symptoms: inequalities by sex and occupational class among two different age cohorts followed for 20 years in the west of Scotland. Sleep. (2012) 35:815–23. doi: 10.5665/sleep.1882
27. Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. (2010) 10:475. doi: 10.1186/1471-2458-10-475
28. Arber S, Bote M, Meadows R. Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc Sci Med. (2009) 68:281–9. doi: 10.1016/j.socscimed.2008.10.016
29. Wu MP, Lin HJ, Weng SF, Ho CH, Wang JJ, Hsu YW. Insomnia subtypes and the subsequent risks of stroke: report from a nationally representative cohort. Stroke. (2014) 45:1349–54. doi: 10.1161/STROKEAHA.113.003675
30. Hublin C, Sallinen M. Behaviorally induced insufficient sleep. Sleep Med Clin. (2012) 7:313–23. doi: 10.1016/j.jsmc.2012.03.008
31. Williams AB, Dzierzewski JM, Griffin SC, Lind MJ, Dick D, Rybarczyk BD. Insomnia disorder and behaviorally induced insufficient sleep syndrome: prevalence and relationship to depression in college students. Behav Sleep Med. (2020) 18:275–86. doi: 10.1080/15402002.2019.1578772
32. Benjamins JS, Migliorati F, Dekker K, Wassing R, Moens S, Blanken TF, et al. Insomnia heterogeneity: characteristics to consider for data-driven multivariate subtyping. Sleep Med Rev. (2017) 36:71–81. doi: 10.1016/j.smrv.2016.10.005
33. Miller CB, Bartlett DJ, Mullins AE, Dodds KL, Gordon CJ, Kyle SD, et al. Clusters of insomnia disorder: an exploratory cluster analysis of objective sleep parameters reveals differences in neurocognitive functioning, quantitative EEG, and heart rate variability. Sleep. (2016) 39:1993–2004. doi: 10.5665/sleep.6230
34. Laharnar N, Grote L, Zou D, Hedner J, Sommermeyer D, Straßenburger C, et al. Overnight pulse wave analysis to assess autonomic changes during sleep in insomnia patients and healthy sleepers. PLoS ONE. (2020) 15:e0232589. doi: 10.1371/journal.pone.0232589
35. Grandner MA. Sleep duration across the lifespan: implications for health. Sleep Med Rev. (2012) 16:199–201. doi: 10.1016/j.smrv.2012.02.001
36. Espie CA, Kyle SD, Hames P, Gardani M, Fleming L, Cape J. The sleep condition indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open. (2014) 4:e004183. doi: 10.1136/bmjopen-2013-004183
37. Regestein QR, Bambrosia J, Hallett M, Murawski B, Paine M. Daytime alertness in patients with insomnia. Am J Psychiatry. (1993) 150:1529–34. doi: 10.1176/ajp.150.10.1529
38. Khassawneh BY, Bathgate CJ, Tsai SC, Edinger JD. Neurocognitive performance in insomnia disorder: the impact of hyperarousal and short sleep duration. J Sleep Res. (2018) 27:e12747. doi: 10.1111/jsr.12747
39. Li Y, Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Sun Y, Zhou J, et al. Insomnia with physiological hyperarousal is associated with hypertension. Hypertension. (2015) 65:644–50. doi: 10.1161/HYPERTENSIONAHA.114.04604
40. Drake C, Richardson G, Roehrs T, Scofield H, Roth T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep. (2004) 27:285–91. doi: 10.1093/sleep/27.2.285
41. Espie CA, Kyle SD, Hames P, Cyhlarova E, Benzeval M. The daytime impact of DSM-5 insomnia disorder: comparative analysis of insomnia subtypes from the Great British Sleep Survey. J Clin Psychiatry. (2012) 73:e1478–84. doi: 10.4088/JCP.12m07954
42. Baglioni C, Altena E, Bjorvatn B, Blom K, Bothelius K, Devoto A, et al. The European academy for cognitive behavioural therapy for insomnia: an initiative of the European insomnia network to promote implementation and dissemination of treatment. J Sleep Res. (2020) 29:e12967. doi: 10.1111/jsr.12967
43. Suraev A, Grunstein RR, Marshall NS, D'Rozario AL, Gordon CJ, Bartlett DJ, et al. Cannabidiol (CBD) and Δ(9)-tetrahydrocannabinol (THC) for chronic insomnia disorder ('CANSLEEP' trial): protocol for a randomised, placebo-controlled, double-blinded, proof-of-concept trial. BMJ Open. (2020) 10:e034421. doi: 10.1136/bmjopen-2019-034421
44. Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Lahti T, Partonen T. Relation of chronotype to sleep complaints in the general Finnish population. Chronobiol Int . (2012) 29:311–7. doi: 10.3109/07420528.2012.655870
45. Bjorvatn B, Jernelöv S, Pallesen S. Insomnia – A heterogenic disorder often comorbid with psychological and somatic disorders and diseases: a narrative review with focus on diagnostic and treatment challenges. Front Psychol. (2021) 12:639198. doi: 10.3389/fpsyg.2021.639198
46. Mikoteit T, Brand S, Eckert A, Holsboer-Trachsler E, Beck J. Brain-derived neurotrophic factor is a biomarker for subjective insomnia but not objectively assessable poor sleep continuity. J Psychiatr Res. (2019) 110:103–9. doi: 10.1016/j.jpsychires.2018.12.020
47. Neumann N, Lotze M, Domin M. Sex-specific association of poor sleep quality with gray matter volume. Sleep. (2020) : zsaa035. doi: 10.1093/sleep/zsaa035
48. Collen J, York CM. Wrist wearables: more questions than answers? J Clin Sleep Med. (2019) 15:1077–78. doi: 10.5664/jcsm.7858
49. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index – a new instrument for psychiatric practice and research. Psychiat Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
50. Espie CA, Inglis SJ, Harvey L, Tessier S. Insomniacs' attributions: psychometric properties of the dysfunctional beliefs and attitudes about sleep scale and the sleep disturbance questionnaire. J Psychosom Res. (2009) 48:141–8. doi: 10.1016/s0022-3999(99)00090-2
51. Palagini L, Cellini N, Mauri M, Mazzei I, Simprage S, dell'Osso L, et al. Multiple phenotypes of resting-state cognition are altered in insomnia disorder. Sleep Health. (2016) 2:239–45. doi: 10.1016/j.sleh.2016.05.003
52. Ree MJ, Harvey AG. Investigating safety behaviours in insomnia: the development of the sleep-related behaviours questionnaire (SRBQ). Behav Change. (2004) 21:26–36. doi: 10.1375/bech.21.1.26.35971
53. Bell C, McLeod LD, Nelson LM, Fehnel SE, Zografos LJ, Bowers B. Development and psychometric evaluation of a new patient-reported outcome instrument measuring the functional impact of insomnia. Qual Life Res. (2011) 20:1457–68. doi: 10.1007/s11136-011-9885-8
54. Tarrasch R1, Laudon M, Zisapel N. Cross-cultural validation of the Leeds Sleep Evaluation Questionnaire (LSEQ) in insomnia patients. Hum Psychopharmacol. (2003) 18:603–10. doi: 10.1002/hup.534
55. Broomfield NM, Espie CA. Towards a valid, reliable measure of sleep effort. J Sleep Res. (2005) 14:401–7. doi: 10.1111/j.1365-2869.2005.00481.x
56. Luik AI, Machado PF, Siriwardena N, Espie CA. Screening for insomnia in primary care: using a two-item version of the Sleep Condition Indicator. Br J Gen Pract. (2019) 69:79–80. doi: 10.3399/bjgp19X701045
57. Kalmbach DA, Cheng P, O'Brien LM, Swanson LM, Sangha R, Sen S, et al. A randomized controlled trial of digital cognitive behavioral therapy for insomnia in pregnant women. Sleep Med. (2020) 72:82–92. doi: 10.1016/j.sleep.2020.03.016
Keywords: insomnia, phenotypes, subtypes, heterogeneity, symptom, progression, questionnaire, screening
Citation: Fietze I, Laharnar N, Koellner V and Penzel T (2021) The Different Faces of Insomnia. Front. Psychiatry 12:683943. doi: 10.3389/fpsyt.2021.683943
Received: 22 March 2021; Accepted: 24 May 2021; Published: 29 June 2021.
Reviewed by:
Copyright © 2021 Fietze, Laharnar, Koellner and Penzel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Naima Laharnar, naima.laharnar@charite.de
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 14, Issue 3
- Association between physical activity over a 10-year period and current insomnia symptoms, sleep duration and daytime sleepiness: a European population-based study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-6585-5777 Erla Bjornsdottir 1 ,
- http://orcid.org/0000-0001-6561-3746 Elin Helga Thorarinsdottir 2 , 3 ,
- Eva Lindberg 4 ,
- Bryndis Benediktsdottir 3 , 5 ,
- Karl Franklin 6 ,
- Debbie Jarvis 7 , 8 ,
- Pascal Demoly 9 ,
- http://orcid.org/0000-0001-7034-0615 Jennifer L Perret 10 ,
- Judith Garcia Aymerich 11 , 12 ,
- http://orcid.org/0000-0002-0798-2153 Sandra Dorado-Arenas 13 ,
- Joachim Heinrich 14 , 15 ,
- http://orcid.org/0000-0001-8509-7603 Kjell Torén 16 ,
- http://orcid.org/0000-0002-0003-1988 Vanessa Garcia Larsen 17 ,
- Rain Jögi 18 ,
- Thorarinn Gislason 3 , 5 ,
- http://orcid.org/0000-0001-5093-6980 Christer Janson 4
- 1 Department of psychology , Reykjavik University , Reykjavik , Iceland
- 2 Department of psychology , Heilsugæsla Höfuðborgarsvæðisins , Reykjavik , Iceland
- 3 Department of psychology, Faculty of Medicine , University of Iceland , Reykjavik , Iceland
- 4 Department of Medical Sciences: Respiratory, Allergy and Sleep Research , Uppsala University , Uppsala , Sweden
- 5 Department of Sleep , Landspítali Háskólasjúkrahús , Reykjavik , Iceland
- 6 Department of Surgical and Perioperative Sciences , Umea Universitet , Umea , Sweden
- 7 Population Health and Occupational Disease, National Heart and Lung Institute , Imperial College London School of Public Health , London , UK
- 8 Department of psychology, MRC-PHE Centre for Environment and Health , Imperial College London , London , UK
- 9 Department of psychology, University Hospital of Montpellier , University of Montpellier–INSERM UMR UA11 , Montpellier , France
- 10 Department of psychology, Melbourne Medical School , The University of Melbourne , Melbourne , Victoria , Australia
- 11 Department of psychology, Centre for Research in Environmental Epidemiology (CREAL) , ISGlobal , Barcelona , Spain
- 12 Department of psychology , Universitat Pompeu Fabra , Barcelona , Spain
- 13 Department of Pulmonology , Hospital Galdakao-Usansolo , Galdacano , Spain
- 14 Department of psychology, Institute and Clinic for Occupational, Social and Environmental Medicine , Ludwig Maximilians University Munich , Munchen , Germany
- 15 Department of psychology, Allergy and Lung Health Unit, Melbourne School of Population and Global Health, Melbourne Medical School , The University of Melbourne , Melbourne , Victoria , Australia
- 16 Occupational and Environmental Medicine, Institutionen för Medicin , Göteborgs Universitet , Göteborg , Sweden
- 17 Program in Human Nutrition, Department of International Health , Johns Hopkins University Bloomberg School of Public Health , Baltimore , Maryland , USA
- 18 Department of psychology, The Lung Clinic , Tartu University Hospital , Tartu , Estonia
- Correspondence to Dr Erla Bjornsdottir; erlabjo{at}gmail.com
Objectives To explore the relationship between physical activity over a 10-year period and current symptoms of insomnia, daytime sleepiness and estimated sleep duration in adults aged 39–67.
Design Population-based, multicentre cohort study.
Setting 21 centres in nine European countries.
Methods Included were 4339 participants in the third follow-up to the European Community Respiratory Health Survey (ECRHS III), who answered questions on physical activity at baseline (ECRHS II) and questions on physical activity, insomnia symptoms, sleep duration and daytime sleepiness at 10-year follow-up (ECRHS III). Participants who reported that they exercised with a frequency of at least two or more times a week, for 1 hour/week or more, were classified as being physically active. Changes in activity status were categorised into four groups: persistently non-active; became inactive; became active; and persistently active.
Main outcome measures Insomnia, sleep time and daytime sleepiness in relation to physical activity.
Results Altogether, 37% of participants were persistently non-active, 25% were persistently active, 20% became inactive and 18% became active from baseline to follow-up. Participants who were persistently active were less likely to report difficulties initiating sleep (OR 0.60, 95% CI 0.45–0.78), a short sleep duration of ≤6 hours/night (OR 0.71, 95% CI 0.59–0.85) and a long sleep of ≥9 hours/night (OR 0.53, 95% CI 0.33–0.84) than persistently non-active subjects after adjusting for age, sex, body mass index, smoking history and study centre. Daytime sleepiness and difficulties maintaining sleep were not related to physical activity status.
Conclusion Physically active people have a lower risk of some insomnia symptoms and extreme sleep durations, both long and short.
- sleep medicine
- epidemiology
- primary care
- public health
- sports medicine
Data availability statement
Data are available upon reasonable request.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2022-067197
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
The longitudinal study design, in which the exposure (physical activity) is measured 10 years prior to the sleep outcomes, enables an investigation into whether the consistency of physical activity over time has an impact on current symptoms of insomnia, sleep duration and daytime sleepiness.
Data were collected using standardised and validated procedures and instruments, increasing its internal validity.
Data were obtained from nine European countries, increasing the external validity of our findings.
One limitation of our study is that sleep variables are only available at the follow-up, which precluded testing their effect on baseline physical activity.
Insomnia symptoms, sleep durations and daytime sleepiness data were obtained by questionnaire and no sleep disorder diagnoses from medical providers or objective assessments were available.
Introduction
Disturbed sleep is common in the general population and impacts health and quality of life. 1–3 Chronic sleep disturbances are associated with cardiovascular disease, metabolic dysfunction, psychiatric disorders and increased mortality. 4–6
Physical activity and sleep
Regular exercise is associated with better health and several studies suggest that physical activity (PA) is beneficial to sleep and may improve symptoms of chronic insomnia. 7–10 It is, however, unclear how significant these benefits are and which factors may have a moderating effect on them. 11 The positive association between PA and sleep may be subject to multiple moderating factors such as gender, age, body mass index (BMI), fitness level, general health and the characteristics of the type of exercise in question. Therefore, sleep and PA probably influence each other through complex, reciprocal interactions including multiple physiological and psychological pathways. 7
PA and daytime sleepiness
There is evidence that more PA is associated with less daytime sleepiness. 12–17 Cross-sectional studies have shown that low PA is associated with an increased likelihood of excessive daytime sleepiness (EDS) 14–16 and that subjects participating in exercise are less likely to have EDS. 12 17 In older adults, increasing PA by doing home exercises has been shown to improve EDS and reduce the prevalence of insomnia symptoms, 13 while another study showed that increasing PA protected women from future insomnia. 18 Other studies have contradictory findings. In an epidemiological study of 4405 Koreans, daytime sleepiness was more common among those in the top quartile of PA compared with those in the lowest quartile group. 19 Among patients with obstructive sleep apnoea, increased PA was associated with a lower severity of disease and a 28% decrease in EDS. 20 The daily association between PA and sleep duration was described in 2021, based on a systematic review and meta-analysis of 33 peer-reviewed papers, which showed that, on the night following increased PA, there was a lower total sleep time. 21
Limitations of previous studies
There is a lack of epidemiological data from long-term follow-up studies of large cohorts exploring the association of PA with sleep length, daytime sleepiness and insomnia symptoms. Previous research on PA and sleep-related outcomes has several important limitations. Most studies are cross-sectional or have a short follow-up interval, preventing the possibility of elucidating whether increased PA improves sleeping outcomes or whether reduced PA is a consequence of sleep problems. Finally, the effects of PA on sleep length, daytime sleepiness and insomnia symptoms have not been studied simultaneously.
Aims of the current study
Therefore, the aim of the present study was to assess the inter-relationship between PA, based on frequency, duration and intensity, and symptoms of insomnia, self-reported sleep durations and daytime sleepiness among middle-aged subjects from 21 centres in nine countries at two moments in time, 10 years apart, providing important longitudinal follow-up data.
Materials and methods
We studied participants from the second and third follow-up surveys of the European Community Respiratory Health Survey (ECRHS II and III, www.ecrhs.org ), an international, population-based, multicentre cohort study of asthma and allergic disease, which was first carried out in 1990. Detailed descriptions of the methods used for ECRHS I and ECRHS II have been published elsewhere. 22 23 Briefly, participating centres randomly selected samples from subjects aged 20–44 in order to track them for asthma, allergy and lung disease (see: www.ecrhs.org ). Participants completed a short postal questionnaire about asthma and asthma-like symptoms and, from those who responded, a random sample was selected to undergo a more detailed clinical examination. In ECRHS II, subjects who had participated in the clinical phase of ECRHS I (performed between 1991 and 1994) were invited to participate in the follow-up study. The clinical phase of ECRHS II was carried out between 1998 and 2002. ECRHS III is the second follow-up study and was carried out from February 2011 to January 2014. 22–24 The present study is based on data from ECRHS II and III (see figure 1 for the flow chart).
- Download figure
- Open in new tab
- Download powerpoint
Flow chart of the study population in the European Community Respiratory Health Survey (ECRHS).
Health, habits and measurements
Subjects answered the core ECRHS questionnaires, which included questions on lifestyle, respiratory symptoms, smoking history and general health. ‘Current smokers’ were defined as those who smoked tobacco regularly during the last month. ‘Former smokers’ were defined as smokers who denied having smoked regularly in the month prior to the examination. Those who reported no regular smoking at the time of or prior to the examination were defined as ‘never smokers’. The participants’ height and weight were measured and their BMI was calculated. 24
Assessment of PA
PA was assessed in ECRHS II and III using replies from questionnaires. The assessment of PA in ECRHS has previously been described in detail, including how both the frequency and duration of PA were used to divide the population into categories. 22 In brief, participants were asked how often and for how many hours per week they usually exercised to the point that they became out of breath or sweaty. Participants who exercised two or more times a week, for at least 1 hour/week, were classified as physically active. Changes in activity status from baseline to follow-up were categorised into four PA groups: persistently non-active (non-active at both baseline and follow-up), became inactive (active at baseline and non-active at follow-up), became active (non-active at baseline and active at follow-up) and persistently active (active at both baseline and follow-up).
Sleep questionnaires and measurements
Sleep-related symptoms were assessed using the Basic Nordic Sleep Questionnaire, 25 where participants were asked about the frequency of insomnia symptoms. Answers were provided on a scale of 1–5: (1) never or very seldom, (2) less than once a week, (3) once to twice a week, (4) three to five times a week, (5) every day or almost every day of the week. Insomnia symptoms were defined using answers to three questions from the Basic Nordic Sleep Questionnaire: ‘I have difficulties falling asleep at night’ (difficulties initiating sleep), ‘I wake up often during the night’ (difficulties maintaining sleep) and ‘I wake up early in the morning and can’t fall back asleep’ (early morning awakenings). Those who reported these symptoms of insomnia ≥3 times a week (scores 4 and 5) were considered to have the corresponding insomnia subtype. Daytime sleepiness was evaluated using the Epworth Sleepiness Scale (ESS), a brief questionnaire that measures daytime sleepiness based on the likelihood of falling asleep in eight different situations. 26 Participants with an ESS score >10 were considered to have EDS. Participants were asked the question: how much sleep do you estimate that you get on average each night? According to their answers, they were classified as: short sleepers (≤6 hours/night), normal sleepers (6–9 hours/night) or long sleepers (≥9 hours/night).
Patient and public involvement
The study’s design did not involve patients or the general public. However, all participating patients were informed of the research objectives and their informed consent was obtained. The survey was completed by participants voluntarily and no input from patients was sought in interpreting or writing up the results. The results of the research will not be disseminated to the patients.
Statistical analysis
Data are presented as numbers and percentages or mean±SD, depending on distribution. For bivariate analysis, the χ 2 test and one-way analysis of variance were used for nominal and continuous variables. Logistic regression was used for multivariable analyses to estimate the association between PA and sleep-related outcomes. The model was adjusted for potential confounders including age, sex, BMI, smoking history and study centre. In the analysis, all variables, including study centre (n=21), were treated as fixed effects. STATA V.16 was used for all statistical analyses.
Participants and level of PA
From a total of 5850 participants in ECRHS II, we excluded those with missing data and included a total of 4339 participants (48% men) (see figure 1 ). Figure 2 shows the prevalence of insomnia symptoms, short and long sleep durations and daytime sleepiness among subjects in the different countries included in the study. From baseline to 10 years later, 36.9% of participants were persistently non-active, 17.9% became physically active at follow-up, 20.3% of participants became inactive and 24.9% were persistently active ( table 1 ). There were geographical differences in the level of PA between the ECRHS countries ( figure 3 ). Participants in Norway were most likely to be persistently active, while participants in Spain, followed by Estonia, were most likely to be persistently non-active ( figure 3 ).
Prevalence of any insomnia symptom, short sleep duration (≤6 hours/night), long sleep duration (≥9 hours/night) and daytime sleepiness (Epworth Sleepiness Scale (ESS) score >10) by country.
Activity levels by country.
- View inline
Characteristics and general health of the participants by the level of physical activity
General characteristics and health
Persistently active participants were more often men, they were younger and they had a slightly lower BMI ( table 1 ). They were also less likely to be current smokers and more likely to be currently working ( table 1 ).
Insomnia symptoms
In unadjusted analysis, there was a significant difference in reporting difficulties initiating sleep, early morning awakenings and any insomnia symptom where those persistently active were least likely to report these symptoms. Also, persistently active subjects were the least likely to report having two or three insomnia symptoms ( table 2 ). After adjusting for age, sex, BMI, smoking history and study centre, this negative association remained significant for difficulties initiating sleep (OR 0.58 (0.42–0.77)), any insomnia symptom (OR 0.78 (0.65–0.94)) and reporting two (OR 0.60 (0.43–0.82)) and three (OR 0.63 (0.41–0.98)) insomnia symptoms ( table 3 ). Additionally, in adjusted analysis, persistently active subjects were significantly less likely to report difficulties initiating sleep (OR 0.80 (0.66–0.97)) ( table 3 ). There were also independent associations between insomnia symptoms and age, female gender and BMI ( table 4 ).
Insomnia symptoms, sleep duration and daytime sleepiness by level of physical activity
Independent association between the level of physical activity and medical disorders, insomnia symptoms, daytime sleepiness and sleep duration expressed as adjusted* ORs (95% CI) with the persistently non-active group as reference
Associations between age, sex, BMI and smoking history and sleep-related symptoms
Sleep duration and daytime sleepiness
In unadjusted analysis, there was a significant difference in short and long sleep durations between levels of activity. Those who were persistently active were most likely to be normal sleepers while the persistently non-active were least likely to be in that category (70.9% vs 59.2%, respectively) ( table 2 ). After adjusting for age, sex, BMI, smoking history and study centre, these results remained significant for persistently active subjects. They were significantly more likely to be normal sleepers (OR 1.55 (1.29–1.87)) and significantly less likely to be short sleepers (OR 0.71 (0.58–0.85)) or long sleepers (OR 0.48 (0.28–0.80)) ( table 3 ). Additionally, those who became active were more likely to be normal sleepers than those who were persistently non-active (OR 1.21 (1.00–1.47)) ( table 3 ).
However, there was not a significant association between the mean ESS score or percentage with an ESS score >10 and level of PA ( tables 2 and 3 ). Daytime sleepiness was also independently associated with smoking ( table 4 ).
The main results of this study were that participants who reported being physically active at the start and end of a 10-year follow-up period were less likely to report insomnia symptoms at the follow-up. We also found that subjects who are persistently active are more likely to sleep the recommended 6–9 hours. This association remained statistically significant after adjusting for sex, age, smoking history and BMI. We also found that persistently active participants were more often men, were younger, had a slightly lower BMI and were less likely to be current smokers and more likely to be currently working.
Our results are in line with previous studies that have shown the beneficial effect of PA on symptoms of insomnia, 9 10 but the current study additionally shows the importance of consistency in exercising over time, because the association was lost for initially active subjects who became inactive. A recent meta-analysis examining the effects of acute and regular exercise on a range of sleep variables showed that acute exercise (less than 1 week of exercise) has a small beneficial effect on many objective measures of sleep, such as total sleep time, insomnia symptoms and sleep quality. 7 Furthermore, this meta-analysis found greater benefits from regular exercise for both subjective and objective sleep parameters over time. Regular exercise had small beneficial effects on total sleep time and sleep efficiency, small-to-medium beneficial effects on sleep onset latency and moderate beneficial effects on sleep quality. 7
There are two recent systematic reviews and meta-analyses on the effects of PA on sleep 7 and insomnia, 9 both substantially reviewing the same randomised controlled studies. Banno et al included nine studies with a total of 557 participants. 7 The majority of participants exercised three times or less per week and the follow-up interval was 4 months or shorter in all the studies except one. Their conclusion was that exercise could improve sleep, but that higher quality research was needed. 7 Five studies on insomnia, and, additionally, six on insomnia symptoms, showed shorter sleep latency and higher sleep efficacy, but the authors also acknowledged the small size of the literature and severe methodological limitations, often based on selection bias. 9 In addition, most previous studies are cross-sectional, which can also be considered a limitation.
Furthermore, a recent systematic review of PA and sleep showed that moderate exercise had a more promising outcome in terms of sleep quality than vigorous exercise. It is therefore important to study further the impact of the intensity of PA, in the context of age and gender, when exploring any beneficial impact on sleep. 27
This study has a long follow-up period (10 years) and indicates strongly that consistency in PA might be an important factor in optimising sleep duration and reducing the symptoms of insomnia. Most other studies have had a much shorter follow-up period, 7 which makes it more difficult to assess the consistency of activity over time.
Our results indicate that those who maintain a consistent level of PA are also less likely to be both short (<6 hours) and long sleepers (>9 hours). Those who are physically active in general are also more likely to engage in a healthier lifestyle, 28 which can likewise have an effect on sleep. Lifestyle factors, such as a healthy diet and being physically active, are probably part of a phenotype that characterises those individuals who are generally engaged in a healthy lifestyle. A recent review highlighted the importance of focusing on the combination of sleep, diet and exercise when exploring healthy longevity. 29
The three groups reporting low PA in either of the ECRHS surveys, or at both points in time, all report a very similar prevalence of insomnia symptoms, extreme sleep lengths and daytime sleepiness. This is somewhat surprising, especially given that those who were active in the follow-up survey but not at the baseline have a very similar symptom profile to those who were inactive in both surveys. Our study found that consistency in a behaviour such as PA for more than a decade is strongly related to a lower incidence of insomnia and a more ‘normal’ sleep length. Important information concerning ‘the healthy phenotype’ would be missed if the PA data were available only at baseline or at follow-up but not at both timepoints.
In a recent review based on 22 randomised controlled trials concerning the effects of regular exercise (lasting at least 2 months on a regular basis) on self-reported sleep quality, insomnia and daytime sleepiness, it was found that regular PA improved subjective sleep quality, insomnia severity and daytime sleepiness as measured with the ESS. 30 These results regarding insomnia symptoms are in line with our study, but the results on daytime sleepiness differ from our results. The reason for this discrepancy could be due to different study populations, as there were only two studies in this review that measured daytime sleepiness using the ESS; one study assessed this among the elderly, 60 years and older, 13 and the other among overweight and obese men. 31 Another recent review of 32 randomised controlled trials on the effects of exercise on improving sleep disturbances showed that exercise is beneficial in improving sleep quality, symptoms of insomnia, restless legs, sleep apnoea and daytime sleepiness. However, exercise only had significant effects on sleepiness if it had lasted for more than 12 weeks, while the exercise period did not matter in regard to the association to sleep quality and insomnia symptoms. 32
Another recent study showed that high or increasing levels of PA could protect women from future insomnia. 18 Therefore, exercise seems to have a stronger association with sleep quality and insomnia than with sleepiness, which is in line with our results. However, almost all previous studies have the limitation that the definition of sleepiness is limited to the estimate that the likelihood of falling asleep but not the general feeling of sleepiness that we have shown is also an important part of sleepiness. 33 34 Another recent review exploring the associations of exercise, sleep and cognitive function among older adults showed that PA is associated with improved cognitive function but the association of sleep and cognitive function seems to be U shaped, as too much or too little sleep is negatively associated with cognitive function. 35 We did not explore cognitive function in the current study but it would be interesting for future studies to explore further how cognitive function is affected by the association of PA and sleep.
This study has several strengths such as the population-based nature, the longitudinal study design and the large sample collected in the same manner at many centres in nine different countries. Another strength is the use of standardised and validated procedures and instruments. The long follow-up period is also a strength since data on PA are collected 10 years apart and subjects are categorised according to change in PA. This study is, however, not without limitations. It is not possible to know whether those who are active at both timepoints have been continuously physically active throughout the study period or only at these two timepoints. Furthermore, PA was only measured using a questionnaire. Another limitation of our study is that sleep variables are only available at the follow-up, and we only have information on insomnia symptoms but not the diagnosis of insomnia disorder. Sleep length and daytime sleepiness are also based on subjective data. Therefore, even though the measurement of PA is longitudinal, it may not be entirely appropriate to describe the associations between PA and sleep outcomes as longitudinal. Also, there are potential implications of residual confounders that can influence both PA and sleep which were not explored in the current study (eg, mental health, musculoskeletal disorders/chronic pain) which could influence the study findings.
In conclusion, PA over time is associated with lower prevalence of insomnia symptoms and with sleeping between 6 and 9 hours/night.
Ethics statements
Patient consent for publication, ethics approval.
This study involves human participants and ethical approval from the local research ethics committees and written consent from participants were obtained from each site. Australia: Monash University Human Research Ethics Committee (project number CF11/1818-2010001012). Belgium: Comité voor Medische Ethiek (UZA/UA 11/41/288). Denmark: De Videnskabsetiske Komiteer for Region Midtjylland (M-20110106). Estonia: Research Ethics Committee of the University of Tartu (UT REC 209T-17 and 225/M-24). France: Etude ECRHS III: Promotion CHU de Grenoble. Ethical approval from CPP Sud est V 4 mars 2011. Approval from Ministry of Health (AFSSAPS B110053-70) (Paris, Grenoble, Montpellier, Bordeaux). Germany: Ethikkommission der Bayerischen Landesärztekammer (Positive Votum: 10015). Iceland: National Bioethics Committee of Iceland (VSN-11-121-S3). Italy: Ethics Committee of IRCCS ‘San Matteo’ Hospital Foundation, University of Pavia (approval number 24215/2011) (Pavia), ‘Comitato Etico per la sperimentazione dell’Azienda Ospedaliera Universitaria Integrata di Verona’ (N Prog 1393) (Verona). Norway: Regional Ethics Committee West Norway (2010/759). Spain: Ethics Committee of the Parc de Salut Mar, Barcelona (Comité etic d’investigacio clínica, CEIC)–Parc de Salut Mar, Barcelona (approval number 2009/3500/1). Switzerland: Swiss Academy of Sciences. Sweden: Regional Ethical Review Board in Uppsala (decision number 2010/432). UK: NRES Committee London-Stanmore REC (Ref 11/LO/0965). Participants gave informed consent to participate in the study before taking part.
- Gottlieb DJ ,
- Redline S ,
- Nieto FJ , et al
- Sivertsen B ,
- Lallukka T ,
- Salo P , et al
- Gangwisch JE ,
- Heymsfield SB ,
- Boden-Albala B , et al
- Luyster FS ,
- Strollo PJ ,
- Zee PC , et al
- Taniguchi M , et al
- Kredlow MA ,
- Capozzoli MC ,
- Hearon BA , et al
- Haddock G ,
- Mulligan LD , et al
- Passos GS ,
- Poyares D ,
- Santana MG , et al
- Kelley GA ,
- Andrianasolo RM ,
- Galan P , et al
- Brandão GS ,
- Gomes GSBF ,
- Brandão GS , et al
- Chasens ER ,
- Sereika SM ,
- Weaver TE , et al
- Blazer DG ,
- McClain JJ ,
- Laposky AD , et al
- Urponen H ,
- Hasan J , et al
- Spörndly-Nees S ,
- Åsenlöf P ,
- Yi H , et al
- Iftikhar IH ,
- Youngstedt SD
- Chevance G ,
- Romain A-J , et al
- Fuertes E ,
- Carsin A-E ,
- Antó JM , et al
- Burney P , et al
- Björnsdóttir E ,
- Lindberg E , et al
- Partinen M ,
- Cobb-Clark DA ,
- Kassenboehmer SC ,
- Masanovic B ,
- Bu T , et al
- Chen XJ , et al
- Wiklund P , et al
- Mazzotti DR ,
- Keenan BT ,
- Thorarinsdottir EH , et al
- Thorarinsdottir EH ,
- Bjornsdottir E ,
- Benediktsdottir B , et al
- Mellow ML ,
- Crozier AJ ,
- Dumuid D , et al
EB and EHT are joint first authors.
TG and CJ are joint senior authors.
Contributors EHT and EB equally drafted, participated in manuscript preparation and were responsible for communications with other coauthors. TG and CJ participated in the design of the study, manuscript preparation and review of the manuscript on several stages. EHT performed the statistical analysis with help from CJ. EL, BB, KF, DJ, PD, JLP, JGA, SD-A, JH, KT, VGL and RJ participated in data collection and/or reviewing of the paper. TG is responsible for the writing of this manuscript accuracy of the data and
accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding Financial support for ECRHS III: Australia: National Health and Medical Research Council. Belgium: Antwerp South, Antwerp City: Research Foundation Flanders (FWO), grant code G041008N10 (both sites). Estonia: Tartu-SF0180060s09 from the Estonian Ministry of Education. France: (All) Ministère de la Santé, Programme Hospitalier de Recherche Clinique (PHRC) National 2010; Bordeaux: INSERM U897, Université Bordeaux Segalen; Grenoble: Comite Scientifique AGIRadom 2011; Paris: Agence Nationale de la Santé, Région Ile de France, Domaine d’intérêt majeur (DIM). Germany: Erfurt: German Research Foundation HE 3294/10-1; Hamburg: German Research Foundation MA 711/6-1, NO 262/7-1. Iceland: Reykjavik, Landspitali University Hospital Research Fund, University of Iceland Research Fund, Icelandic College of Family Physicians Research Fund, ResMed Foundation, California, USA, Orkuveita Reykjavikur (Geothermal plant), Vegagerðin (Icelandic Road Administration, ICERA), Icelandic Research Fund (grant number 173701-052). Italy: All Italian centres were funded by the Italian Ministry of Health, Chiesi Farmaceutici. In addition, Verona was funded by Cariverona Foundation, Education Ministry (MIUR). Norway: Norwegian Research Council (grant number 214123), Western Norway Regional Health Authorities (grant number 911631), Bergen Medical Research Foundation. Spain: Fondo de Investigación Sanitaria (PS09/02457, PS09/00716 09/01511, PS09/02185, PS09/03190), Servicio Andaluz de Salud, Sociedad Española de Neumología y Cirurgía Torácica (SEPAR 1001/2010); Barcelona: Fondo de Investigación Sanitaria (FIS PS09/00716); Galdakao: Fondo de Investigación Sanitaria (FIS 09/01511); Huelva: Fondo de Investigación Sanitaria (FIS PS09/02185) and Servicio Andaluz de Salud; Oviedo: Fondo de Investigación Sanitaria (FIS PS09/03190). Sweden: All centres were funded by the Swedish Heart and Lung Foundation, Swedish Asthma and Allergy Association, Swedish Association Against Lung and Heart Disease, Swedish Research Council for Health, Working Life and Welfare (FORTE); Göteborg: Also received further funding from the Swedish Council for Working Life and Social Research; Umea also received funding from Vasterbotten Country Council ALF grant. Switzerland: Swiss National Science Foundation (grant numbers 33CSCO-134276/1, 33CSCO-108796, 3247BO-104283, 3247BO-104288, 3247BO-104284, 3247-065896, 3100-059302, 3200-052720, 3200-042532, 4026-028099), Federal Office for Forest, Environment and Landscape, Federal Office of Public Health, Federal Office of Roads and Transport, Canton’s government of Aargan, Basel-Stadt, Basel-Land, Geneva, Luzern, Ticino, Valais and Zürich, Swiss Lung League, Canton's Lung League of Basel Stadt/Basel, Landschaft, Geneva, Ticino, Valais and Zurich, SUVA, Freiwillige Akademische Gesellschaft, UBS Wealth Foundation, Talecris Biotherapeutics, Abbott Diagnostics, European Commission 018996 (GABRIEL), Wellcome Trust (WT 084703MA). UK: Medical Research Council (grant number 92091). Support was also provided by the National Institute for Health Research through the Primary Care Research Network.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Here’s how you know
- U.S. Department of Health and Human Services
- National Institutes of Health
NCCIH Clinical Digest
for health professionals
Psychological and Physical Approaches for Sleep Disorders: What the Science Says
Clinical Guidelines, Scientific Literature, Info for Patients: Psychological and Physical Approaches for Sleep Disorders

.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Cognitive Behavioral Therapy for Insomnia (CBT-I)
Current clinical practice guidelines from the American Academy of Sleep Medicine (2021) recommend psychological and behavioral interventions in the treatment of chronic insomnia disorder in adults.
- The American Academy of Sleep Medicine guidelines state: “We recommend that clinicians use multicomponent cognitive behavioral therapy for insomnia (CBT-I) for the treatment of chronic insomnia disorder in adults (strong recommendation). We suggest that clinicians use relaxation therapy as a single-component therapy for the treatment of chronic insomnia disorder in adults (conditional recommendation).” The authors of the guidelines also noted that there were fewer than three studies meeting their inclusion criteria for the use of cognitive therapy, paradoxical intention, mindfulness, biofeedback, and intensive sleep retraining; as a result, no recommendations were made about these treatments.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} What Does the Research Show?
- Clinical practice guidelines issued by the American Academy of Sleep Medicine in 2021 recommend psychological and behavioral interventions for the treatment of chronic insomnia disorder in adults. The guidelines state: “We recommend that clinicians use multicomponent cognitive behavioral therapy for insomnia (CBT-I) for the treatment of chronic insomnia disorder in adults (strong recommendation).”
- A 2018 analysis of pooled data from 4 randomized controlled trials of 546 peri- and postmenopausal women with insomnia and bothersome vasomotor symptoms found that CBT-I produced the greatest reduction in Insomnia Severity Index (ISI) from baseline compared to an education control.
- A 2014 randomized controlled trial examined the comparative efficacy of cognitive behavioral therapy, tai chi, and a sleep seminar education control in 123 older adults with chronic and primary insomnia. The study found that cognitive behavioral therapy performed better than tai chi and sleep seminar education in remission of clinical insomnia. The cognitive behavioral therapy group also showed greater improvement in sleep quality, sleep parameters, fatigue, and depressive symptoms than the tai chi and sleep seminar education groups.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Safety
- CBT-I is considered safe.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Relaxation Techniques
There is a small amount of low-quality evidence that relaxation techniques by themselves can help with chronic insomnia. Relaxation techniques may be recommended in certain situations, depending on individual preferences, health provider qualifications, and treatment availability.
Current clinical practice guidelines from the American Academy of Sleep Medicine (2021) conditionally recommend relaxation therapy as a single-component therapy for the treatment of chronic insomnia disorder in adults.
- Clinical guidelines from the American Academy of Sleep Medicine (2021) made a conditional recommendation to use relaxation therapy as a single-component therapy based on “a small body of low-quality evidence from five studies showing clinically meaningful improvements in one critical outcome, consideration that some patients prefer relaxation therapy, the fact that mental health providers are trained to deliver this form of treatment, and the potential for relaxation therapy to require only limited resources.”
- A 2018 systematic review looked at 27 studies of psychological interventions to try to improve sleep. The studies involved 2,776 college students who ranged from healthy sleepers to those with a diagnosed sleep disorder. About 22 percent of the studies investigated “relaxation, mindfulness, hypnotherapy” treatments. This review recommended cognitive behavioral therapy to improve sleep in college students. The review also found that relaxation approaches helped somewhat with sleep quality and sleep problems but especially with mental health. The authors recommended that “relaxation, mindfulness, hypnotherapy” treatments be combined with cognitive behavioral therapy as a way to enhance mental health benefits.
- Relaxation therapies for insomnia are considered safe.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Yoga
Yoga has been shown to be helpful for sleep in several studies of cancer patients, women with sleep problems, and older adults and in individual studies of other population groups, including people with arthritis and women with menopause symptoms. However, a 2019 clinical practice guideline from the U.S. Department of Veterans Affairs and U.S. Department of Defense said there was insufficient evidence to recommend for or against yoga for treating insomnia.
- A 2020 systematic review and meta-analysis of 19 studies involving a total of 1,832 participants found positive effects of yoga in 16 randomized controlled trials, compared with the control group, in improving sleep quality among women using Pittsburgh Sleep Quality Index (PSQI); however, 2 studies revealed no effects of yoga compared to the control group in reducing insomnia among women using ISI. Seven studies revealed no evidence for effects of yoga compared with the control group in improving sleep quality for women with breast cancer using PSQI, while four studies revealed no evidence for the effects of yoga compared with the control group in improving the sleep quality for peri/postmenopausal women using PSQI.
- A 2020 secondary analysis of a randomized controlled trial involving 320 adults with chronic low-back pain and poor sleep quality prior to the intervention found modest but statistically significant improvements in sleep quality in the yoga (12 weekly yoga classes) and physical therapy groups.
- A 2019 systematic review of 11 studies that evaluated the use of yoga to manage stress and burnout in health care workers concluded that yoga is effective in improving physical problems and quality of sleep, as well as reducing stress levels and burnout. However, the authors of the review noted that it would be necessary to broaden the subject further and acquire more robust scientific evidence by designing and implementing research studies equipped with a solid methodological structure on bigger sample groups.
- A 2013 multicenter, randomized controlled trial evaluated the effect of yoga on sleep quality in 410 cancer survivors suffering from moderate or greater sleep disruption between 2 and 24 months after surgery, chemotherapy, and/or radiation therapy. The study found that compared with standard care, yoga participants demonstrated greater improvements in global sleep quality and subjective sleep quality, daytime dysfunction, wake after sleep onset, sleep efficiency, and medication use at postintervention.
- A 2022 randomized controlled trial investigated the effects of yoga (duration of 20 weeks) on menopausal symptoms and sleep quality across menopause statuses in 208 women. Based on participant responses to questionnaires, the study found that yoga decreased menopausal symptoms, with the strongest effects noted in postmenopausal women, followed by perimenopausal women. In addition, yoga significantly improved sleep quality in postmenopausal and perimenopausal women after controlling for social support, depression, anxiety, stress, and menopausal symptoms; however, yoga did not affect sleep quality in premenopausal women.
- Yoga is generally considered a safe form of physical activity for healthy people when performed properly, under the guidance of a qualified instructor. However, as with other forms of physical activity, injuries can occur.
- The most common injuries are sprains and strains, and the parts of the body most commonly injured are the knee or lower leg. Serious injuries are rare. The risk of injury associated with yoga is lower than that for higher impact physical activities.
- Hot yoga has special risks related to overheating and dehydration.
- Pregnant women, older adults, and people with health conditions should talk with their health care providers and the yoga instructor about their individual needs. They may need to avoid or modify some yoga poses and practices.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Tai Chi
Results of several studies, using objective and subjective measures, have shown that tai chi may be helpful for people with sleep problems. However, a 2019 clinical practice guideline from the U.S. Department of Veterans Affairs and U.S. Department of Defense said there was insufficient evidence to recommend for or against using tai chi to treat insomnia.
- A 2020 systematic review and meta-analysis of 20 randomized controlled studies from 5 countries involving a total of 1,703 patients found that compared with nontherapeutic and other active treatments, tai chi has a positive effect on improving sleep quality. An in-depth analysis showed that 24-form and 8-form Yang-style tai chi had significant positive effects on sleep quality, as assessed by the Pittsburgh Sleep Quality Index (PSQI).
- A 2021 randomized controlled trial assigned 320 participants 60 years or older and with chronic insomnia to three groups: 12-week tai chi training, 12-week conventional exercise, and no intervention control. The study found that compared with the control group, the exercise and tai chi groups showed improved sleep efficiency, reductions of wake time after sleep onset, and reduced awakenings as measured by actigraphy. However, there were no significant differences between the exercise and tai chi groups.
- Tai chi appears to be safe. A 2019 meta-analysis of 24 studies (1,794 participants) found that the frequency of adverse events was similar for people doing tai chi, another active intervention, or no intervention.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Meditation and Mindfulness Practices
A 2019 clinical practice guideline from the U.S. Department of Veterans Affairs and U.S. Department of Defense said there was not enough evidence to know whether mindfulness meditation is helpful for people with insomnia, and a 2021 clinical practice guideline from the American Academy of Sleep Medicine said there was not enough evidence to make recommendations on using mindfulness by itself for insomnia.
- A 2022 review of 20 studies and 2,890 participants found that mindfulness-based stress reduction might be ineffective for improving sleep quality in people with insomnia, but the authors noted that the studies were small and showed bias.
- A 2019 systematic review and meta-analysis of 18 studies (1,654 total participants) found that mindfulness meditation practices improved sleep quality more than education-based treatments. However, the effects of mindfulness meditation approaches on sleep quality were no different than those of evidence-based treatments such as cognitive behavioral therapy and exercise.
- Results from a 2015 randomized controlled trial involving 60 adults aged 75 years and over with chronic insomnia suggest that the mindfulness-based stress reduction program could be a useful treatment for chronic insomnia for this age group.
- Meditation and mindfulness practices usually are considered to have few risks.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Music-Based Interventions
A 2022 review of 13 studies with 1,007 adult participants found that listening to music may lead to improved reports of sleep quality among people with insomnia. However, there was not enough good-quality evidence to determine the effect of listening to music on the severity of insomnia or the number of times a person wakes up.
- A 2022 review of 13 studies with 1,007 adult participants found that listening to music may lead to improved reports of sleep quality among people with insomnia. However, there was not enough good-quality evidence to determine the effect of listening to music on the severity of insomnia or the number of times a person wakes up. The results showed that listening to music may slightly improve sleep-onset latency, sleep duration, sleep efficiency, and daytime effects.
- In general, research studies of music-based interventions do not show any negative effects. However, listening to music at too high a volume can contribute to noise-induced hearing loss.
- Because music can be associated with strong memories or emotional reactions, some people may be distressed by exposure to specific pieces or types of music.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Acupuncture
A 2019 clinical practice guideline from the U.S. Department of Veterans Affairs and U.S. Department of Defense said there was not enough evidence to recommend for or against using acupuncture for insomnia, except for a weak recommendation for auricular acupuncture, which involves specific points on the outer ear. Results from some studies suggest that auricular acupuncture may help improve insomnia; however, many of the studies conducted on acupuncture for sleep disorders are small and are of low quality.
- A 2021 review of 11 studies and 775 participants suggested that acupuncture may help improve insomnia, but the studies were small, differed from each other in many ways (e.g., treatment dosage, acupoint selection), and judged to be low quality.
- A 2019 clinical practice guideline from the U.S. Department of Veterans Affairs and U.S. Department of Defense said there was not enough evidence to recommend for or against using acupuncture for insomnia, except for a weak recommendation for auricular acupuncture, which involves specific points on the outer ear.
- A 2020 evaluation of 7 systematic reviews (10,001 participants) on auricular acupuncture for insomnia found that the reviews suggested auricular acupuncture may be beneficial, but the quality of most of the reviews was low or critically low and the quality of the studies within the reviews was poor.
- Relatively few complications from using acupuncture have been reported. However, complications have resulted from use of nonsterile needles and improper delivery of treatments. When not delivered properly, acupuncture can cause serious adverse effects, including infections, punctured organs, and injury to the central nervous system.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} References
- Cocchiara RA, Peruzzo M, Mannocci A, et al. The use of yoga to manage stress and burnout in healthcare workers: a systematic review . Journal of Clinical Medicine . 2019;8(3):284.
- Cui H, Wang Q, Pedersen M, et al. The safety of tai chi: a meta-analysis of adverse events in randomized controlled trials . Contemporary Clinical Trials . 2019;82:85-92.
- Edinger JD, Arnedt JT, Bertisch SM, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline . Journal of Clinical Sleep Medicine . 2021;17(2):255-262.
- Friedrich A, Schlarb AA. Let’s talk about sleep: a systematic review of psychological interventions to improve sleep in college students . Journal of Sleep Research . 2018;27(1):4-22.
- Guthrie KA, Larson JC, Ensrud KE, et al. Effects of pharmacologic and nonpharmacologic interventions on insomnia symptoms and self-reported sleep quality in women with hot flashes: a pooled analysis of individual participant data from four MsFLASH trials . Sleep . 2018;41(1):zsx190.
- Huang J, Shen M, Qin X, et al. Effectiveness of auricular acupuncture for insomnia: an overview of systematic reviews . Evidence-Based Complementary and Alternative Medicine. 2020;2020:6920902.
- Irwin MR, Olmstead R, Carrillo C, et al. Cognitive behavioral therapy vs. tai chi for late life insomnia and inflammatory risk: a randomized controlled comparative efficacy trial . Sleep . 2014;37(9):1543-1552.
- Jespersen KV, Pando-Naude V, Koenig J, et al. Listening to music for insomnia in adults . Cochrane Database of Systematic Reviews . 2022;8(8):CD010459.
- Li H, Chen J, Xu G, et al. The effect of tai chi for improving sleep quality: a systematic review and meta-analysis . Journal of Affective Disorders . 2020;274:1102-1112.
- Mustian KM, Sprod LK, Janelsins M, et al. Multicenter, randomized controlled trial of yoga for sleep quality among cancer survivors . Journal of Clinical Oncology . 2013;31(26):3233-3241.
- Mysliwiec V, Martin JL, Ulmer CS, et al. The management of chronic insomnia disorder and obstructive sleep apnea: synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guidelines . Annals of Internal Medicine . 2020;172(5):325-336.
- Roseen EJ, Gerlovin H, Femia A, et al. Yoga, physical therapy, and back pain education for sleep quality in low-income racially diverse adults with chronic low back pain: a secondary analysis of a randomized controlled trial . Journal of General Internal Medicine . 2020;35(1):167-176.
- Rusch HL, Rosario M, Levison LM, et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials . Annals of the New York Academy of Sciences. 2019;1445(1):5-16.
- Siu PM, Yu AP, Tam BT, et al. Effects of tai chi or exercise on sleep in older adults with insomnia: a randomized clinical trial . JAMA Network Open . 2021;4(2):e2037199.
- Susanti HD, Sonko I, Chang P-C, et al. Effects of yoga on menopausal symptoms and sleep quality across menopause statuses: a randomized controlled trial . Nursing and Health Sciences . 2022;24(2):368-379.
- Wang W-L, Chen K-H, Pan Y-C, et al. The effect of yoga on sleep quality and insomnia in women with sleep problems: a systematic review and meta-analysis . BMC Psychiatry . 2020;20(1):195.
- Zhang J-X, Liu X-H, Xie X-H, et al. Mindfulness-based stress reduction for chronic insomnia in adults older than 75 years: a randomized, controlled, single-blind clinical trial . Explore (NY). 2015;11(3):180-185.
- Zhao F-Y, Fu Q-Q, Kennedy GA, et al. Can acupuncture improve objective sleep indices in patients with primary insomnia? A systematic review and meta-analysis . Sleep Medicine . 2021;80:244-259.
NCCIH Clinical Digest is a service of the National Center for Complementary and Integrative Health, NIH, DHHS. NCCIH Clinical Digest, a monthly e-newsletter, offers evidence-based information on complementary health approaches, including scientific literature searches, summaries of NCCIH-funded research, fact sheets for patients, and more.
The National Center for Complementary and Integrative Health is dedicated to exploring complementary health products and practices in the context of rigorous science, training complementary health researchers, and disseminating authoritative information to the public and professionals. For additional information, call NCCIH’s Clearinghouse toll-free at 1-888-644-6226, or visit the NCCIH website at nccih.nih.gov . NCCIH is 1 of 27 institutes and centers at the National Institutes of Health, the Federal focal point for medical research in the United States.
Content is in the public domain and may be reprinted, except if marked as copyrighted (©). Please credit the National Center for Complementary and Integrative Health as the source. All copyrighted material is the property of its respective owners and may not be reprinted without their permission.
Subscriptions
NCCIH Clinical Digest is a monthly e-newsletter that offers evidence-based information on complementary and integrative health practices.
Clinical Digest Archive
Insomnia Research News
Top headlines, latest headlines.
- Simulated Microgravity: Gene Expression Rhythms
- Sleep Apnea Solution: Right Under Your Nose?
- Poor Sleep Linked to Migraine Attacks
- Hope for Treating Sleep Disorders: No Pills
- Distinct Sleep Types Identified
- Wrist Device: Early Warning of Alzheimer's
- Blood-Based Marker to Identify Sleep Deprivation
- Good Sleep Stimulates the Immune System
- Too Little Sleep: Risk of Type 2 Diabetes
- Sleep Apnea, Memory and Thinking Problems
Earlier Headlines
Friday, march 1, 2024.
- Healthy Sleep Needs a Healthy Day: Boost Exercise to Beat Your Bedtime Blues
Wednesday, February 28, 2024
- Neurons Help Flush Waste out of Brain During Sleep
Friday, February 23, 2024
- Hearing Relaxing Words in Your Sleep Slows Your Heart Down
Thursday, February 22, 2024
- Wake-Up Call for Us All to Establish Regular Healthy Sleeping Patterns
Monday, February 19, 2024
- Understanding the Relationship Between Our Sleep, Body Clock and Mental Health
Tuesday, February 6, 2024
- Improving Quality of Life and Sleep in People With Memory Problems Without Using Drugs
Tuesday, January 23, 2024
- One of the Keys to Healthy Sleep and Blood Sugar Has Been Found
Wednesday, January 17, 2024
- Streamlining Cognitive Behavioral Therapy for Chronic Insomnia
Thursday, January 4, 2024
- Study Reveals New Genetic Link Between Anorexia Nervosa and Being an Early Riser
- Even in Midlife, Disrupted Sleep Tied to Memory, Thinking Problems Later on
Wednesday, January 3, 2024
- Research Reveals Promising Approach to Enhance Treatment for Sleep Apnea-Related Issues
Tuesday, January 2, 2024
- Enlarged Spaces in Infant Brains Linked to Higher Risk of Autism, Sleep Problems
Thursday, December 28, 2023
- Study Identifies 'visual System' Protein for Circadian Rhythm Stability

Thursday, December 21, 2023
- Psychologist Publishes Most Thorough Compilation of Sleep and Emotion Research to Date
- Artery Calcification More Common in Night Owls
- Connection Between Light Levels and Mental Health -- Climate Change Could Also Have an Impact in the Future
Tuesday, December 19, 2023
- Night Sweats Reveal the Severity of Sleep Apnea
Wednesday, December 13, 2023
- Very Irregular Sleep Linked to Higher Risk of Dementia
- Rare Sleep Disorder More Prevalent Than Previously Thought
- Yoga Nidra Might Be a Path to Better Sleep and Improved Memory
- How Stress Activates Neurons That Disrupt Sleep
Wednesday, December 6, 2023
- Light Therapy May Improve Symptoms of Alzheimer's Disease
Monday, December 4, 2023
- Survey Finds Americans Struggle to Maintain Healthy Habits During the Holiday Season
Thursday, November 30, 2023
- Brain Waves Usually Found in Sleep Can Protect Against Epileptic Activity
Monday, November 20, 2023
- Poor Work Performance Among Japanese Employees Strongly Associated With Insufficient Sleep
Friday, November 17, 2023
- Ingestible Electronic Device Detects Breathing Depression in Patients
Wednesday, November 15, 2023
- People With Obesity Burn Less Energy During Day
Monday, November 13, 2023
- Shortening Sleep Time Increases Diabetes Risk in Women
- Study Finds Melatonin Use Soaring Among Youth
Tuesday, November 7, 2023
- Why We Don't All Develop Posttraumatic Stress Disorder After Trauma
Thursday, November 2, 2023
- One Sleepless Night Can Rapidly Reverse Depression for Several Days
Tuesday, October 31, 2023
- New Position Statement Supports Permanent Standard Time
Monday, October 30, 2023
- Improving Deep Sleep May Prevent Dementia, Study Finds
Wednesday, October 25, 2023
- How Sleep Disruption Can Exacerbate Pain
Friday, October 20, 2023
- Consistent Lack of Sleep Is Related to Future Depressive Symptoms
Friday, October 13, 2023
- Not Getting Enough Sleep? Your Vascular Cells Are Drowning in Oxidants
Wednesday, October 11, 2023
- Risk Factors for Dementia Vary by Ethnicity, Study Finds
Tuesday, October 10, 2023
- Extreme Sports: How Body and Mind Interact
Thursday, October 5, 2023
- Increased Deep Sleep Benefits Your Heart
Monday, October 2, 2023
- Losing Sleep? It Might Be Time to Check Your Blood Pressure
- A Surprising Way to Disrupt Sleep
Thursday, September 28, 2023
- Parkinson's: Are Our Neurons More Vulnerable at Night?
- Wearable Device Data Reveals That Reduced Sleep and Activity in Pregnancy Is Linked to Premature Birth Risk
Friday, September 15, 2023
- New Parent? Night Shift? New Analysis Suggests Ideal Nap Strategy to Survive All-Nighters
Tuesday, September 12, 2023
- Researchers Develop Novel, Automated Measure of Sleep Studies to Determine Severity of Obstructive Sleep Apnea
Monday, September 11, 2023
- 'Night Owls' More Likely Than 'early Birds' To Develop Diabetes
- Healthy Lifestyle Can Help Prevent Depression -- And New Research May Explain Why
Friday, September 8, 2023
- Sleep-Wake Therapy Gives New Hope for Teens With Depression
Thursday, September 7, 2023
- Elucidating the Mechanism of Aripiprazole Action in Treating Circadian Rhythm Sleep Disorders
Wednesday, September 6, 2023
- How Sleep Deprivation Can Harm the Brain
- Insomnia Drug Helps Prevent Oxycodone Relapse
Wednesday, August 30, 2023
- Stress and Insomnia Linked to Irregular Heart Rhythms After Menopause
Tuesday, August 29, 2023
- Sleep Data from Over 220,000 People Reveal Global Differences in Weekly Sleep Variability and Sleep Extension
- More Sleep Could Reduce Impulsive Behavior in Children
Wednesday, August 23, 2023
- A Fitness Tracker for Brain Health: How a Headband Can Identify Early Signs of Alzheimer's Disease in Your Sleep
Monday, August 21, 2023
- Intermittent Fasting Improves Alzheimer's Pathology, Study Shows
Thursday, August 17, 2023
- Lesser-Known Brain Cells May Be Key to Staying Awake Without Cost to Cognition, Health
Wednesday, August 9, 2023
- Playing Catch-Up on Weekends May Not Improve Cardiovascular Cost of Sleep Loss
Friday, August 4, 2023
- How People Feel About Their Sleep Matters to Their Well-Being, New Research Suggests
Wednesday, August 2, 2023
- Irregular Sleep Patterns Associated With Harmful Gut Bacteria
Friday, July 28, 2023
- Enhanced Light Sensitivity May Contribute to Alzheimer's 'sundowning,' Disease Progression
Saturday, July 22, 2023
- How Mother and Infant Sleep Patterns Interact During the First Two Years of Life
Friday, July 21, 2023
- Cause of Sleep Disturbance in Cardiac Disease Identified: Ganglia Play Previously Unrecognized Role
Thursday, July 13, 2023
- High-Quality Sleep Promotes Resilience to Depression and Anxiety
Tuesday, July 11, 2023
- A Neurobehavioral Signature of Risk for Mania
Friday, July 7, 2023
- Deep-Sleep Brain Waves Predict Blood Sugar Control
Wednesday, July 5, 2023
- Lack of Sleep Lessens Cognitive Benefits of Physical Activity
Friday, June 16, 2023
- Dads Are Key in Supporting Breastfeeding, Safe Infant Sleep
Tuesday, May 30, 2023
- Junk Food May Impair Our Deep Sleep
Thursday, May 25, 2023
- Researchers Identify Potential New Treatment for Those Who Act out Their Dreams While Sleeping
- Keeping Time: Understanding the Master Clock in the Brain
Tuesday, May 16, 2023
- Losing Sleep Over Losing Sleep: How Watching the Clock Impacts Insomnia, Use of Sleep Aids
Thursday, May 4, 2023
- Deep Sleep May Mitigate Alzheimer's Memory Loss
Monday, May 1, 2023
- Exposure to Airplane Noise Increases Risk of Sleeping Fewer Than 7 Hours Per Night
Wednesday, April 26, 2023
- New Research Sheds Light on How Circadian Rhythms Work
Monday, April 24, 2023
- New Machine-Learning Method Predicts Body Clock Timing to Improve Sleep and Health Decisions
Thursday, April 20, 2023
- Sleeping Pill Reduces Levels of Alzheimer's Proteins
Thursday, April 13, 2023
- Time Out: We All Need a Three-Day Weekend
Thursday, March 30, 2023
- Fluid Flow in the Brain Can Be Manipulated by Sensory Stimulation
- Do Your Headaches Happen at the Same Time of Day?
- Novel Drug Offers Hope for Heart Failure Patients
Friday, March 24, 2023
- Time of Day Matters When It Comes to Cancer Diagnosis and Treatment
Thursday, March 16, 2023
- Short Night-Time Sleep Linked With Nearly Doubled Risk of Clogged Leg Arteries
Wednesday, March 15, 2023
- Sleep Quality Is Significantly Associated With Quality of Life Indicators Over Time
Monday, March 13, 2023
- Getting a Good Night's Sleep Could Boost Your Response to Vaccination
Friday, March 10, 2023
- Dim Lights Before Bedtime to Reduce Risk of Gestational Diabetes
Wednesday, March 8, 2023
- Poor Sleep Linked to Years of Poor Cardiovascular Health
Monday, March 6, 2023
- Trouble Falling Asleep at Bedtime or in the Middle of the Night? It Could Impact Your Risk for Developing Dementia
Friday, March 3, 2023
- A Good Night's Sleep May Make It Easier to Stick to Exercise and Diet Goals
- Acid Glia in REM Sleep: Stronger Acid Response in Epileptic Mice
Friday, February 24, 2023
- Insomnia Tied to Greater Risk of Heart Attack, Especially in Women
- Getting Good Sleep Could Add Years to Your Life
Thursday, February 16, 2023
- Indicator of Early Form of Parkinson's in Stool Sample
Tuesday, February 7, 2023
- How Age and Sex Influence Our Body Clocks
Monday, February 6, 2023
- Following Healthy Lifestyle May Reduce Risk of Long COVID
Friday, February 3, 2023
- Researchers Find a Link Between Traffic Noise and Tinnitus
Tuesday, January 31, 2023
- Moderate and Intense Physical Activity Favors Good Sleep
- Do Sleep Medications Increase Your Chances of Dementia?
Monday, January 30, 2023
- Mating Causes 'jet Lag' In Female Fruit Flies, Changing Behavior
Friday, January 27, 2023
- Non-Invasive Neurotechnology Reduces Symptoms of Insomnia and Improves Autonomic Nervous System Function
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- Extremely Fast Wound Healing: New Treatment
- Micro-Lisa! Novel Nano-Scale Laser Writing
- Simple Brain-Computer Link: Gaming With Thoughts
- Clinical Reasoning: Chatbot Vs Physicians
- Understanding People Who Can't Visualize
- Illuminating Oxygen's Journey in the Brain
- DNA Study IDs Descendants of George Washington
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
Trending Topics
Strange & offbeat.
- Open access
- Published: 29 March 2024
Insomnia and creativity in Chinese adolescents: mediation through need for cognition
- Xiaoyang Ren 1 ,
- Min Shi 1 &
BMC Psychology volume 12 , Article number: 180 ( 2024 ) Cite this article
69 Accesses
Metrics details
Creativity is an essential cognitive ability that plays a crucial role in advanced thinking. While previous research has demonstrated the impact of insomnia on cognitive function, its effects on creativity in Chinese adolescents remain unclear. This study explored the relationship between insomnia (specifically, daytime and nighttime disturbances) and creativity in adolescents. Additionally, it examined the potential mediating effect of the need for cognition on this relationship.
Questionnaires were administered to 302 adolescents to measure their creativity, need for cognition, and insomnia levels using the Williams Creative Tendencies Scale, Need for Cognition Scale, and Bergen Insomnia Scale, respectively. Regression analysis was conducted to examine the direct impact of insomnia on creativity. Furthermore, a mediation model was constructed to investigate the role of the need for cognition in mediating the relationship between insomnia and creativity.
The findings of the present study indicated that insomnia had a direct impact on the creativity of adolescents, demonstrating a time-of-day effect. Daytime disturbances were found to have a positive correlation with overall creativity and imagination, whereas no significant direct effect was found between nighttime disturbances and creativity. Further analysis revealed that insomnia, specifically daytime disturbances, might influence creativity by affecting the individual’s need for cognition. However, no similar indirect effects were observed for the relationship between nighttime disturbances and creativity.
Conclusions
Our findings indicate that adolescents might experience improved creativity as a result of daytime disruptions, and the level of need for cognition could play a crucial role in understanding the link between insomnia and creativity in adolescents.
Peer Review reports
Introduction
Insomnia is a condition characterized by an individual’s self-reported difficulties in sleeping [ 1 , 2 ]. It is characterized by symptoms such as taking a long time to fall asleep, waking up frequently during the night, experiencing prolonged periods of wakefulness during sleep, and frequent brief awakenings [ 3 ]. In recent years, issues like staying up late, not getting enough sleep, and struggling to fall asleep have become increasingly prevalent among adolescents [ 4 ]. The White Paper 2023 China Youth and Children’s Sleep Index, released by the China Sleep Research Association, reveals concerning statistics about the sleep patterns of junior high school students in China. According to the report, only 18.9% of these students manage to sleep for more than 8 h, while a staggering 59.4% sleep for less than 7 h. On average, these students only get 6.82 h of sleep, indicating that the majority of them do not meet the recommended amount of sleep. A study conducted in the Shandong Province of China explored the prevalence of sleep problems among adolescents. The findings revealed that 37.44% of adolescents suffered from insufficient sleep, while 26.89% reported experiencing poor sleep quality [ 5 ]. Another meta-analysis, which included 63 studies and a total of 430,422 Chinese adolescents, discovered that 104,802 adolescents experienced sleep disturbances. The overall prevalence of sleep problems was found to be 26%, with junior high school students having a detection rate of 20% [ 6 ]. As widely known, adolescents go through a crucial stage of psychological transformation. Issues such as sleep deprivation and sleep disorders appear to have a significant influence on their mental well-being, especially in terms of cognition and personality development [ 7 , 8 ].
Can tired minds generate creative ideas? Some researchers have found that the cognitive processes utilized before sleep by individuals with insomnia, such as rehearsing, planning, and problem-solving, are similar to the stages involved in creative thinking, such as preparation and incubation [ 9 , 10 ]. As a result, a hypothesis has emerged suggesting that individuals with disrupted sleep might exhibit greater creativity. In addition, it should be noted that disrupted sleep and the widely recognized consequences of sleep deprivation are symptoms of depression and anxiety [ 11 , 12 ], while depression and anxiety have also been associated with creativity [ 13 ]. This suggests that sleep issues could have been prevalent among individuals who are highly creative. However, it is important to consider that sleep problems have been shown to negatively affect cognitive function as well. For example, a study using fMRI have demonstrated that lack of sleep reduced the communication between various brain regions such as the amygdala, dorsolateral prefrontal cortex, dorsal anterior cingulate gyrus, and right inferior frontal gyrus. This weakened functional connectivity could result in a negative bias when it comes to encoding memories [ 14 ]. Additionally, research has found that sleep deprivation could also impact the activity of brain regions involved in fearful learning, namely the prefrontal cortex, hippocampus, and amygdala [ 15 ]. Since the activity of the aforementioned brain regions is crucial for individual creativity, some researchers have also suggested that problems such as sleep deprivation and sleep disorders may produce impairments in cognition, memory, etc., which in turn interfere with creativity [ 16 ].
It is noteworthy that only two studies have delved into the connection between insomnia and creativity until now. Firstly, researchers discovered a positive correlation between insomnia and creativity by comparing the prevalence of sleep disturbances in 30 creative children versus 30 control children. Notably, the highly creative children exhibited a higher incidence of sleep disturbances than the control group [ 17 ]. Subsequently, a recent study indicated a minor direct impact of a global insomnia factor on divergent thinking, implying time-of-day effects where nighttime sleep disturbances positively predicted divergent thinking more strongly than daytime disturbances [ 18 ]. These findings suggest that sleep disturbances may possess some beneficial predictive effects on creativity among children and adolescents. However, there could be disparities in the impact of sleep disturbances during the day and night. Despite this, the majority of existing studies have focused on the influence of insomnia on creative thinking, leaving a gap in research evidence regarding its effects on creative personality. It is established that insomnia is linked to personality traits [ 19 ]. Therefore, the primary objective of this study is to investigate the relationship between adolescents’ creativity (specifically creative personality) and insomnia. Building on the outcomes of previous studies, we hypothesized that insomnia would significantly and positively predict adolescents’ creativity (creative personality).
Although a tenuous link has been established between insomnia and creativity, it is postulated that additional variables might influence this relationship. Taking these observations into account, a crucial question arises: How does insomnia impact creativity? Since coming up with original and useful ideas requires several cognitively demanding processes [ 20 , 21 ], the need for cognition may also play an important role in creativity. The need for cognition refers to an individual’s tendency to engage in and derive pleasure from tasks that require cognitive effort [ 22 ]. Individuals with a strong need for cognition are more prone to innovate and have a deeper interest in addressing challenging problems. For instance, research suggested that those with a high cognitive need were more likely to generate ideas for ambiguous scenarios [ 23 ]. Furthermore, individuals with a strong need for cognition exhibited heightened creativity in problem-solving and possessed more pronounced creative personalities [ 24 , 25 ]. Therefore, the need for cognition might serve as a significant and positive predictor of creative personality [ 26 ]. In considering the role of insomnia in creativity, it is plausible that the need for cognition could act as a mediator, influencing the association between the two variables.
However, there was evidence that insomnia could impact individuals’ willingness to invest more time and effort when faced with complex tasks. The microanalytic model of insomnia highlighted hyperarousal as a key regulatory feature, which could distort perceptions of time and exacerbate the challenges associated with falling asleep and experiencing distress. As a result, the consequences of insomnia on the following day could include fatigue, mood disturbances such as irritability, cognitive impairments, and a reduced ability to engage in or enjoy mentally demanding tasks [ 27 ]. Furthermore, the maintained cognitive model of insomnia suggested that insomniacs tend to worry excessively about sleep and its consequences. This negative cognition leaded to emotional distress, and the resulting anxiety prompted individuals to hyperfocus on internal and external cues related to sleep-related threats. Consequently, this state of anxiety could lead to a lack of interest and motivation in solving complex problems, as well as crowding out the time needed for engaging in mentally challenging tasks [ 28 ]. Supported by neuroimaging and neurobiochemistry evidence, researchers have found that individuals with insomnia often exhibit impairments in various cognitive functions, including episodic memory, working memory, and certain aspects of executive functioning [ 7 ]. Given these findings, it is likely that insomnia can reduce an individual’s cognitive engagement and motivation to seek new knowledge, thereby suppressing the anticipated effect of insomnia on creativity. Therefore, the second objective of our study was to further investigate the psychological mechanisms that underlie the impact of insomnia on creativity. Drawing from the aforementioned theoretical and empirical evidence, we hypothesized that the need for cognition played a mediating role in the relationship between insomnia and creativity.
Taking into account that previous research primarily focused on young adults or children, who exhibited distinct sleep patterns compared to adolescents, the relationship between insomnia and the creativity of adolescents, particularly their creative personality, remained enigmatic. The objective of this study was to explore the impact of insomnia on adolescents’ creativity, specifically their creative personality, and to unravel the underlying mechanisms. Drawing from existing theoretical and empirical research, we postulated that: (1) insomnia, encompassing both daytime and nighttime disturbances, was associated with creativity in adolescents, and there might exist time-of-day effects (H1); and (2) the need for cognition might serve as a mediator between insomnia and creativity (H2).
Materials and methods
After a thorough literature review and consideration of previous research, the research questions and hypotheses were formulated in January 2023. Utilizing a cross-sectional research design, questionnaires were administered to a cohort of middle school students in Jinan, Shandong Province, in April of the same year. These questionnaires aimed to capture data on all the relevant research variables, including creativity, insomnia, and the need for cognition at the same time. Subsequently, the collected data was entered into a database and subjected to rigorous checking and analysis.
Participants and procedure
To ensure the validity and relevance of our study, we collaborated closely with a local school in the recruitment process. Initially, we liaised with the school’s head to disseminate recruitment details. Leveraging the assistance of class teachers, we carefully selected participants based on the following criteria: all participants were required to be native Chinese speakers with normal or corrected vision, exhibit no signs of mental or physical health issues, possess normal intellectual development, not encounter any reading difficulties, and not consume psychotropic drugs. Only students who expressed a willingness to participate and fulfilled the study’s criteria were ultimately chosen to participate in the testing process. This meticulous approach ensured that our sample population was representative and well-suited for the objectives of our research.
In this study, 318 junior high school students participated, of whom 302 were included in the primary analysis due to having complete datasets, yielding an effective participation rate of 94.97%. Participants’ ages ranged from 12 to 14, with an average of 12.97 years ( SD = 0.49). Specifically, 41 were 12 years old, 229 were 13, and 32 were 14. 147 were females (48.7%) and 155 were males (51.3%). Regarding the parents’ educational backgrounds, the survey revealed that 31 fathers (10.3%) and 34 mothers (11.3%) held university degrees or higher qualifications. Notably, most parents had completed their education at the middle or high school level (70.2%). When it came to parental occupations, the survey found that the fathers’ top three professions were doctors (25.5%), self-employed individuals (11.6%), and drivers (8.3%). Meanwhile, for mothers, the most common occupations were self-employed (19.2%), salespeople (11.6%), and laborers (8.9%).
The Institutional Review Board of Shandong Normal University has granted approval for this study, ensuring that all measurements adhere strictly to the pertinent guidelines and regulations for psychological research. The group tests were conducted within the classroom setting, led by a psychology-major researcher as the primary tester. Initially, we secured the authorization and support of the school’s teaching department. Subsequently, we utilized the students’ self-study period to clarify the purpose of the research and underscore the principles of voluntariness, anonymity, and honesty. Ultimately, the participants were required to complete a psychological test within approximately 30 min, assessing various aspects such as creativity, need for cognition, insomnia, along with personal family information.
An adapted version of the Williams Creative Tendencies Scale (WCTS) was utilized to assess the creativity of the participants [ 29 ]. This scale was widely employed in numerous prior creativity studies and exhibited strong reliability [ 30 , 31 ]. The adapted version included 11 items to measure adventurousness, 14 items to measure curiosity, 13 items to measure imagination, and 12 items to measure challenge. Each item was rated on a Likert scale ranging from 1 (strongly disagree) to 3 (strongly agree). By compiling the total scores, we can effectively evaluate the creativity of the students. Notably, all the items demonstrated good reliability, with a Cronbach’s α value of 0.86.
- Need for cognition
The Need for Cognition Scale (NCS) [ 22 ] was employed in its shortened version to assess participants’ need for cognition. The 18-item Chinese version of the NCS was initially introduced [ 32 ] and subsequently validated as suitable for both adolescents and young adults in subsequent studies [ 33 ]. Participants were instructed to answer the questions based on their actual circumstances. Each item was rated using a Likert-type scale ranging from 1 (strongly opposed) to 5 (strongly agreed). The total score was calculated by summing up the responses to all 18 items, with higher scores indicating a stronger need for cognition. This measurement demonstrated good reliability in the current study, with a Cronbach’s α value of 0.76.
We utilized the Bergen Insomnia Scale (BIS) to assess insomnia among the participants [ 34 ]. The scale comprises six items, all aligned with the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria for clinical insomnia. The validity of these items has been confirmed through subjective reports and polysomnographic data, encompassing sleep-stage progression, limb movement, and physiological measurements of respiration during controlled laboratory sleep. Three items focus on nighttime disturbances, such as “How many days a week did it take you over 30 minutes to fall asleep after switching off the lights in the past month?”; the other three items target daytime disturbances, like “How many days a week did you feel rested upon waking up in the past month?”. Participants were asked to rate their symptoms on a weekly basis using an eight-point scale ranging from 0 to 7. The total score for the first three items represents nighttime disturbances, while the last three items reflect daytime disturbances. This measurement demonstrated strong reliability for daytime disturbances (Cronbach’s α = 0.86), nighttime disturbances (Cronbach’s α = 0.62), and the overall insomnia score (Cronbach’s α = 0.80) in the Chinese population. According to previous literature, this scale demonstrated good reliability among the Chinese population [ 35 ].
Socioeconomic status (SES)
Recognizing the challenges in precisely measuring income, domestic researchers often turn to an alternative method: assessing a family’s socioeconomic status (SES) through a detailed analysis of their parents’ occupation and education level [ 36 ]. In the present study, we utilized the SES questionnaire to gather participants’ reports on their parents’ occupational and educational backgrounds [ 37 ]. These reports were then coded and graded, following established occupational classification standards, to ensure consistency and comparability across respondents. The occupational classification system employed in this study encompassed five distinct levels: (1) those engaged in temporary, unskilled, agricultural, or non-technical work; (2) self-employed individuals, manual laborers, and technicians; (3) general management and professional technical personnel, including clerks and employees in the commercial service industry; (4) middle-level professionals, managers, and technical personnel, as well as auxiliary professionals specializing in various fields of science, technology, and enterprise work; and (5) senior professional technicians, executives, and leading cadres exercising administrative functions in government, institutions, and social organizations, as well as high- and middle-level managers in large and medium-sized enterprises and private business owners. By utilizing this graded classification system, we aimed to capture a comprehensive representation of participants’ SES backgrounds, ensuring the validity and reliability of our findings.
Furthermore, the educational attainment of parents was categorized into distinct levels:“no schooling or primary education”, “junior middle school”, “high school or technical secondary school”, “junior college”, “university (undergraduate)”, and “graduate”. Participants were required to select the most appropriate category based on their parents’ educational qualifications, and each choice was assigned a numerical score ranging from 1 to 6 during the coding process.
Ultimately, the cumulative score served as an indicator of the family’s socioeconomic status, with a potential range spanning from 4 to 22. Notably, in this research endeavor, the SES scores for both mothers and fathers were computed separately, allowing for a nuanced understanding of each parent’s contribution to the overall socioeconomic profile of the family.
Data analysis
First, we employed the Pearson correlation to assess the relationships between the research variables in the present study. To explore the direct impact of insomnia (independent variables) on creativity (dependent variables), we resorted to multiple linear regression analysis. Specifically, gender, age, socioeconomic status of both parents, and insomnia total score (or daytime and nighttime disturbances) were simultaneously entered into the regression equation. Additionally, we utilized the mediation model to delve into the intricate relationships between insomnia, need for cognition, and creativity. To validate the mediation effects, we relied on the bootstrapping method. From the data, 5000 bootstrap samples were drawn, and 95% bootstrap confidence intervals (CI) were computed. For these statistical analyses, we employed SPSS 17.0 process SPSS macro PROCESS (model 4) ( http://www.afhayes.com ) [ 38 ]. This macro has been extensively used and developed for testing complex models incorporating mediating variables [ 39 ].
Common method deviation test
While the self-report method is a popular choice for data collection, it can potentially lead to common method variance (CMV) issues. To mitigate these concerns, we implemented various control measures to safeguard participants’ anonymity. Among these measures, we ensured that the collected data was strictly limited to scientific research purposes and employed reverse expressions for certain items [ 40 ]. Additionally, to enhance the study’s precision, we utilized the Harman single factor test to process the data. Specifically, we conducted a non-rotating principal component factor analysis on the aforementioned items. The results indicated that the first factor explained only 13.66% of the variation (falling below the 40% threshold). Consequently, this study did not exhibit significant common method variance issues in the collected data.
Descriptive statistics of study variables
Table 1 presents the means, standard deviations, bivariate correlations and gender differences among study variables. The independent samples t-test results revealed that females significantly scored higher than males on measures of insomnia, daytime disturbances, and imagination. Our findings further indicated a positive correlation between insomnia and daytime disturbances with imagination, whereas a negative correlation was observed with the need for cognition. Moreover, the need for cognition demonstrated positive associations with the creativity total score, adventure, curiosity, imagination, and challenge. Mother’s socioeconomic status (SES) exhibited a positive association with imagination. The data for all variables had no outliers and were within three standard deviations. The distributions of all variables approached normality, with skewness and kurtosis ranging from − 1 to 1.
Direct effect tests
The collinearity diagnosis revealed that the tolerance values for the variables of insomnia, daytime and nighttime disturbances, and need for cognition were greater than 0.2, ranging from 0.78 to 0.98, indicating the absence of significant collinearity issues.
The regression analysis results demonstrated that insomnia ( β = 0.19, p < 0.01) and daytime disturbances ( β = 0.24, p < 0.01) positively predicted imagination when controlling for gender, age, father’s SES, and mother’s SES. However, no significant direct effect of nighttime disturbances was observed on the creativity total score, adversity, curiosity, imagination, and challenge (Tables 2 and 3 ). Therefore, H1 was supported. Based on previous research, effect sizes of 0.10, 0.30, and 0.50 are considered small, medium, and large, respectively [ 18 , 41 ]. Consequently, insomnia ( β = 0.19) and daytime disturbances ( β = 0.24) exhibited small-to-medium positive effects on creativity, particularly in terms of imagination.
Indirect effect tests
The indirect effect of need for cognition between insomnia and creativity.
Firstly, the total effect of insomnia on creativity was tested, and it was demonstrated that the path coefficient was not significant. Subsequently, the mediating variable of cognition was added to the model to obtain the path type shown in Fig. 1 . The results showed that insomnia had a direct effect on creativity, and the need for cognition played an indirect role between insomnia and creativity (Table 4 ). The bootstrap test was utilized, and 5000 repeated samples were taken to test the mediating effect and estimate the confidence interval. The absence of 0 in the 95% confidence interval suggested that the indirect effect was significant (see Table 5 ). Therefore, H2 was supported. Similar results were found for imagination, while only indirect effects were found for adventure, curiosity, and challenge. According to the recently proposed mediation effect test method [ 42 ], the indirect effect of need for cognition on the relationship between insomnia and creativity was established, which manifested suppression effects. In other words, the inclusion of the need for cognition enhanced the relationship between insomnia and creativity.
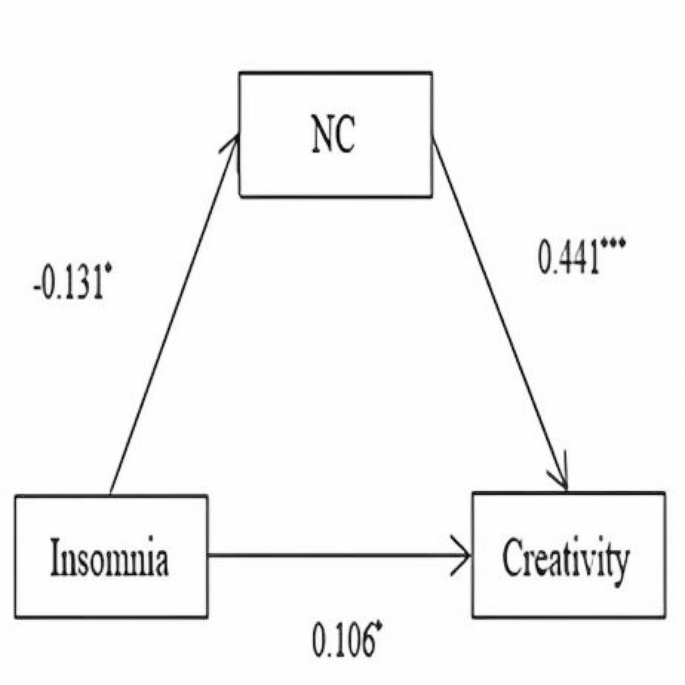
Mediation analysis model testing relationships among insomnia, need for cognition (NC) and creativity
The indirect effect of need for cognition between daytime disturbances and creativity
Similar analysis processes were also conducted to investigate the relationship between daytime disturbances and creativity. Testing the total effect of daytime disturbances on creativity revealed that the path coefficient was not significant. The mediating variable, need for cognition, was then added to the model to obtain the path type shown in Fig. 2 . The results showed that daytime disturbances had a direct effect on creativity, and the need for cognition played an indirect role in the relationship between daytime disturbances and creativity (Table 6 ). Finally, the bootstrap test was employed, and 5000 replicated samples were taken to test the mediating effect and establish the confidence interval. The exclusion of 0 from the 95% confidence interval indicated a statistically significant indirect effect (see Table 7 ). Similar results were found for imagination, while for adventure, curiosity, and challenge, only indirect effects were found. Also, the inclusion of the need for cognition enhanced the relationship between daytime disturbances and creativity.
The indirect effect of need for cognition between nighttime disturbances and creativity
Although s imilar analysis processes were also conducted to examine the relationship between nighttime disturbances and creativity, no significant direct of nighttime disturbances or indirect effects of the need for cognition were found (see Supplementary Table S1 , Table S2 ).
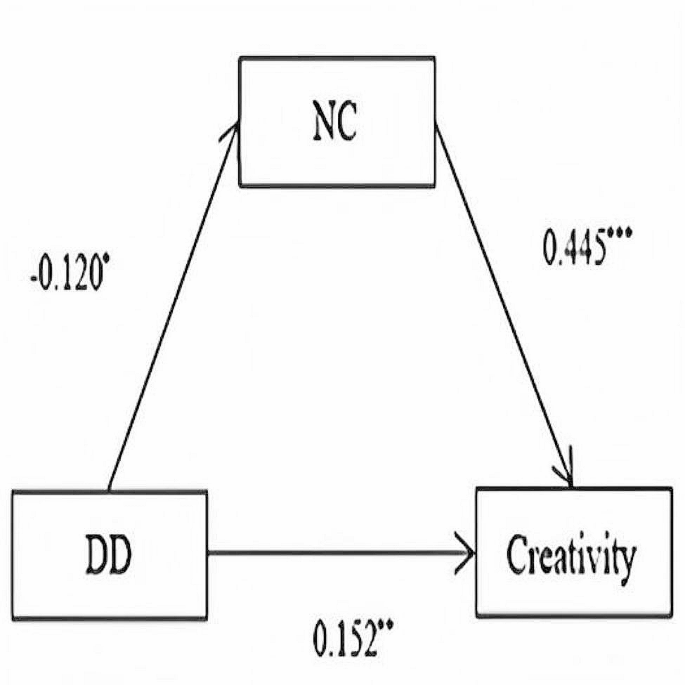
Mediation analysis model testing relationships among daytime disturbances (DD), need for cognition (NC) and creativity
Insomnia and creativity in Chinese adolescents
The current study firstly examined the direct effect of insomnia (daytime disturbances, nighttime disturbances) on adolescents’ creativity. Based on our preliminary findings, insomnia was found to have a beneficial impact on the overall creativity score and imagination, aligning with prior research (H1 was supported). Further analysis showed that there indeed existed time-of-day effects: disturbances during the day had a significant effect on imagination, whereas the effect of disturbances during the night was not significant.
It’s worth nothing that the direct impact of insomnia on creativity was limited to imagination. Imagination is the ability to imagine things that have not yet happened and speculate intuitively, transcending the boundaries of the senses and reality [ 43 ]. It is the basis of all creative activities and a crucial part of culture life [ 44 ]. In a state of insomnia, individuals’ minds may be active, which may enhance individuals’ ability to visualize and increase their openness to new ideas and perspectives.
Moreover, our findings revealed a significant direct impact of daytime disturbances solely on imagination, with no comparable effect observed for nighttime disturbances. This seemed to contrast previous research conducted on young adults, indicating that ‘evening types’ - individuals who typically prefer staying up late and waking up late - tend to perform slightly better on certain measures of creativity [ 45 ]. However, it’s crucial to note that the sleep patterns of adolescents differ from those of young adults. Even if they stay up late, adolescents have less chance of waking up late. Consequently, nighttime disturbances may not be advantageous for them. Conversely, daytime disturbances resulting in fatigue and mood swings might lead to less stringent cognitive control, fostering opportunities for unconventional thinking. Hence, it becomes evident that the investigation of insomnia’s influence on creativity should take into account the time-of-day effects. Daytime disturbances appeared to positively predict creativity more strongly than nighttime disturbances in adolescents.
Mediation of need for cognition
Although the direct impact of insomnia on creativity was notable, the majority of the observed effects were of small-to-medium magnitude. Researchers postulated the existence of a third variable that could potentially mediate the relationship between sleep and creativity [ 46 ]. To delve deeper into the influence of insomnia on creativity, we investigated the intermediary role of the need for cognition. Our findings generally indicated that insomnia might exert its influence on creativity by modulating the need for cognition (H2 was supported). The introduction of need for cognition as a variable strengthened the predictive power of insomnia-related factors (such as daytime disturbances) on creative outcomes (like imagination). These observations suggests the emergence of a suppression effect, which refers to a scenario where a third variable attenuates the relationship between an independent variable (X) and a dependent variable (Y), even when the null hypothesis is true. In psychological research, the absence of a direct relationship between X and Y often poses a challenge. The suppression effect offered a valuable framework for addressing such scenarios and elucidating why significant relationships might not be immediately apparent [ 47 ]. Similarly, our results revealed that need for cognition acted as a suppressor, mitigating the effects of insomnia on creativity.
Despite the absence of a significant direct effect of insomnia, the need for cognition was supported as an indirect influence on adventure, curiosity, and challenge. Adventurousness, curiosity, and challenge-seeking all involve cognitive endeavors such as facing failure or criticism, inquiring into the root cause of problems, engaging in confusing situations, and making order out of chaos [ 43 ]. These creative personalities are strongly influenced by their need for cognition, and insomnia may influence them indirectly by altering their need for cognition.
Limitations
Although these findings offer valuable insights, it’s important to acknowledge several limitations. Firstly, the study employed a cross-sectional design, which assessed variables simultaneously, thus lacking evidence of a temporal link between insomnia and creativity. Longitudinal studies are needed to establish a definitive cause-and-effect relationship between these variables. Secondly, the current study primarily focused on creative personality, overlooking the impact of creative cognition. Given that insomnia is a small-to-medium predictor of divergent thinking [ 18 ], it’s crucial to investigate whether the need for cognition mediates this relationship, enhancing our understanding of the factors that truly influence insomnia’s predictive power over creativity. Finally, the findings of this study have not been replicated in other samples, limiting their generalizability. Future research should aim to replicate these results in diverse enrollment groups, particularly those experiencing severe insomnia, to gain a more comprehensive understanding of the phenomenon.
Despite the limitations described, the present study has two strengths. The primary strength is to first reveal the time-of-day effect associated with insomnia and adolescents’ creativity. These preliminary findings offer profound insights into the impact of sleep disturbances on adolescents’ creativity, thereby aiding in the development of accurate sleep concepts and promoting mental well-being. Secondly, insomnia was found to be more likely to influence creativity through affecting need for cognition. These revelations contribute to establishing scientific frameworks for understanding adolescents’ sleep patterns and suggest that the need for cognition is a crucial aspect in examining the link between insomnia and creativity. Notably, the suppression effect of the need for cognition offers an explanation for the tenuous association between insomnia and creativity, providing a theoretical foundation for fostering the emergence and development of creativity among adolescents with insomnia.
Data availability
Data is provided within the manuscript.
Abbreviations
Williams Creative Tendencies Scale
Need for Cognition Scale
Bergen Insomnia Scale
Socioeconomic Status
Common Method Variance
Father Socioeconomic Status
Mother Socioeconomic Status
Daytime Disturbances
Nighttime Disturbances
Need for Cognition
Standard Error
Savard MH, Savard J, Simard S, Ivers H. Empirical validation of the insomnia severity index in cancer patients. Psychol Oncol. 2005;14(6):429–41.
Article Google Scholar
Liu S, Zhang B. Interpretation of Chinese guidelines for the diagnosis and treatment of insomnia. Chin J Mod Neurol. 2017;17(9):633–8.
Google Scholar
Sateia MJ, Doghramji K, Hauri PJ, Morin CM. Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 2000;23:243–308.
Article PubMed Google Scholar
Li L, Sun H. Review of research on bedtime procrastination. China J Health Psychol. 2020;28(2):316–20.
Pei Y, Wang X, Kong L, Ran X, Wei M, Gao J. The correlation between sleep and mental health of primary and secondary school students in Shandong Province. Chin School Health. 2023;44(11):1674–8.
Meng J, Ling G, Jing H, Gou l. Prevalence of sleep disturbances in Chinese adolescents: a systematic review and meta-analysis. PLoS ONE. 2021; 6(3), e0247333.
Fortier-Brochu É, Beaulieu-Bonneau S, Ivers H, Morin CM. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev. 2012;16(1):83–94.
Kronholm E, Puusniekka R, Jokela J, et al. Trends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011. J Sleep Res. 2015;24:3–10.
Runco MA. Problem finding, problem solving, and creativity. Norwood, NJ: Ablex; 1994.
Wallas G. The art of thought. London: J. Cape; 1926.
Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40(8):700–8.
Neckelmann D, Mykletun A, Dahl AA. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. 2007;30(7):873–80.
Article PubMed PubMed Central Google Scholar
Carson SH. Creativity and psychopathology: a shared vulnerability model. Can J Psychiatry. 2011;56(3):144–53.
Shao Y, Lei Y, Wang L et al. Altered resting-state amygdala functional connectivity after 36 hours of total sleep deprivation. PLoS ONE 2014; 9(11), e112222.
Zhang J, Zhang H, Li H, Lei Y. The effect of sleep on fear learning and its cognitive neural mechanism. Adv Psychol Sci. 2023;31(4):631–40.
Dirk DC, Renato P. Sleepy but creative? How affective commitment, knowledge sharing and organizational forgiveness mitigate the dysfunctional effect of insomnia on creative behaviors. Personnel Rev. 2020;50(1):108–28.
Healey D, Runco MA. Could creativity be associated with insomnia? Creativity Res J. 2006;18(1):39–43.
Beaty RE, Silvia PJ, Nusbaum EC, Vartanian O. Tired minds, tired ideas? Exploring insomnia and creativity. Think Skills Creativity. 2013;9:69–75.
Ma G, Cui F. Research progress on the relationship between personality traits and insomnia. Chin J Health Med. 2017;19(1):87–9.
Amabile TM. A model of creativity and innovation in organizations. In Staw BM, Cummings LL, editors. Research in organizational behavior. Greenwich. 1988, 123–167.
Mumford MD, Mobley MI, Reiter-Palmon R, et al. Process analytic models of creative capacities. Creativity Res J. 1991;4:91–122.
Cacioppo JT, Petty RE. The need for cognition. J Personal Soc Psychol. 1982;42:116–31.
Dollinger SJ. Need for uniqueness, need for cognition, and creativity. J Creative Behav. 2003;37:99–116.
Du Z, Zhang L, Wang Y. Relationship between college students cognitive need, specialty commitment and innovative personality. Chin J School Health. 2011;32(4):454–6.
Hahn MH, Lee KC. Exploring the role of self-confidence, need-for-cognition, and the degree of IT support on individual creativity: multilevel analysis approach. Curr Psychol. 2017;36:565–76.
Du Z, Zhang L, Wang Y. The relationship between college students’ cognitive needs, professional commitment and innovative personality. Chin School Health. 2011;32(4):454–6.
Morin CM. Insomnia: psychological assessment and management. Guilford Press. 1993; 56–60.
Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40(8):869–93.
Lin X, Wang M. Williams creative thinking activity manual. Taiwan: Psychology publishing house; 1997.
Li WF, Li XT, Huang LJ, et al. Brain structure links trait creativity to openness to experience. Soc Cognit Affect Neurosci. 2015;10(2):191–8.
Tang G, Zou H, Hou K, et al. The characteristics of family innovation environment and their effects on everyday creative behavior: the mediating role of personality. J Psychol Sci. 2014;37(5):1125–31.
Gao Q. Conceptualization and measurement of need for cognition. Chin J Psychol. 1994;36(1):1–20.
Yang L, Zhang Q. An experimental study on Relationship between intrinsic-extrinsic motivation and Creativity of 1-Grade Junior High School Students. J Southwest China Normal Univ (Natural Science). 2004;29(1):123–6.
Pallesen S, Bjorvatn B, Nordhus IH, et al. A new scale for measuring insomnia: the Bergen Insomnia Scale. Percept Mot Skills. 2008;107(3):691–706.
Wei S, Chen B, Zhao Q, Bai Y. Reliability and validity of the Chinese version of the Bergen Shift Sleep Questionnaire. Chin J Mod Nurs. 2018;24(29):3508–12.
Qiao N, Zhang J, Liu G, Lin C. Effects of family socioeconomic status and parental involvement on junior students’ academic achievements: the moderating role of students’ perception of teachers’ support. Psychol Dev Educ. 2013;29:507–14.
Shi B, Shen J. The relationship between family socioeconomic status, intelligence, internal motivation and creativity. Psychol Dev Educ. 2007;23:30–4.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis. New York: Guilford Press; 2013.
Carciofo R. Morningness–eveningness and affect: the mediating roles of sleep quality and metacognitive beliefs. Sleep Biol Rhythms. 2020;18(1):17–26.
Zhou H, Long L. Statistical remedies for common method biases. Adv Psychol Sci. 2004;12:942–50.
Cohen J. Statistical power for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988.
Wen Z, Ye B. Mediation effects analysis: methodology and model development. Adv Psychol Sci. 2014;22(5):731–45.
Liu C, Zhang H, Zhang L, et al. The influence of parental rearing style on students’ creativity tendency and self-efficacy. China J Health Psychol. 2013;21(4):589–91.
Vygotsky LS. Imagination and creativity in childhood. J Russian East Eur Psychol. 2004;42(1):7–97.
Giampietro M, Cavallera GM. Morning and evening types and creative thinking. Pers Indiv Differ. 2006;42:453–63.
Liu N, Yuan Y. Relationship between creativity and insomnia in children and adolescents. China J Health Psychol. 2022;30(5):790–4.
Liu Z, Liu T, Mu S. Statistical analysis framework of suppression effect and its application. Psychology: Techniques Appl. 2021;9(10):610–8.
Download references
Acknowledgements
Not applicable.
This research did not receive any specifc grant from funding agencies in the public, commercial, or not-for-proft sectors.
Author information
Authors and affiliations.
Department of Psychology, Shandong Normal University, No.88 East Wenhua Road, 250014, Jinan, China
Xiaoyang Ren, Min Shi & Si Si
You can also search for this author in PubMed Google Scholar
Contributions
Xiaoyang Ren and Si Si wrote the main manuscript text and Min Shi prepared figures and tables. All authors reviewed the manuscript.Author Contributions Statement.
Corresponding author
Correspondence to Si Si .
Ethics declarations
Ethical approval and consent.
Ethical approval for the study was provided by the Institutional Review Board of Shandong Normal University, Jinan, China. Informed consent from their legal guardian for study participation was obtained. All measurements were performed in accordance with relevant guidelines and regulations of psychological study.
Competing interests
The authors declare no competing interests.
Conflict of interest
The author declared that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Consent for publication
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ren, X., Shi, M. & Si, S. Insomnia and creativity in Chinese adolescents: mediation through need for cognition. BMC Psychol 12 , 180 (2024). https://doi.org/10.1186/s40359-024-01663-3
Download citation
Received : 03 January 2024
Accepted : 15 March 2024
Published : 29 March 2024
DOI : https://doi.org/10.1186/s40359-024-01663-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Time-of-day effect
- Indirect effect
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Could Regular Exercise Cure Your Insomnia? New Research Says Yes
By Dennis Thompson and Carole Tanzer Miller HealthDay Reporters

WEDNESDAY, March 27, 2024 (HealthDay News) -- Folks who consistently work out two to three times a week are less likely to suffer from insomnia, a new study says.
That sort of long-term commitment to exercise also helps people get the recommended amount of sleep each night, according to findings published March 26 in the journal BMJ Open .
The paper “indicates strongly that consistency in [physical activity] might be an important factor in optimizing sleep duration and reducing the symptoms of insomnia,” concluded the research team led by Icelandic psychologists Erla Bjornsdottir and Elin Helga Thorarinsdottir .
For the study, researchers tracked the exercise habits and sleep quality of nearly 4,400 middle-aged adults from 21 hospitals in nine European countries.
U.S. Cities With the Most Homelessness

Participants were specifically asked how often they exercise to the point that they become out of breath or sweaty.
Researchers found that people who persistently worked out at least a few times a week -- totaling at least one hour of exercise weekly -- were:
42% less likely to find it difficult to fall asleep
22% less likely to suffer any symptoms of insomnia
40% less likely to suffer more than one insomnia symptom
Symptoms of insomnia include taking a long time to go to sleep, waking in the night and feeling excessively sleepy during the day.
People who consistently exercised also were 55% more likely to get the normal, recommended amount of shut-eye, between 6 and 9 hours a night, researchers found.
They were 29% less likely to have short sleep less than 6 hours, and 52% less likely to have long sleep of 9 hours or more, results show.
In addition, folks who became active during the course of the decade-long study were 21% more likely to become normal sleepers than those who remained inactive.
These results jibe with other studies that have linked regular exercise with sound sleep, researchers said in a journal news release.
People who work out not only make their bodies tired enough to get good sleep, but they also are more likely to follow a healthy lifestyle, the researchers noted.
More information
Johns Hopkins Medicine has more on exercising for better sleep .
SOURCE: BMJ , news release, March 26, 2024
Copyright © 2024 HealthDay . All rights reserved.
Join the Conversation
Tags: exercise and fitness , sleep disorders
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Florida High Court OKs Abortion Vote
Lauren Camera April 1, 2024

The Week in Cartoons April 1-5
April 1, 2024, at 3:48 p.m.

White House Easter Egg Roll
April 1, 2024
What to Know About the Easter Egg Roll
Steven Ross Johnson April 1, 2024

Jobs Back on the Radar to Start Q2
Tim Smart April 1, 2024

Biden Besting Trump in Campaign Cash
Susan Milligan and Lauren Camera March 29, 2024


Researchers May Have Found a Cure for Insomnia—and It’s So Simple
- New research links regular exercise with a lower risk of insomnia.
- This joins a growing body of evidence that supports working out for better sleep.
- Doctors say when you work out can make a difference.
Working out regularly can help boost your heart health and lower your risk of a slew of diseases, including cancer . But, new research has found that regular exercise is associated with less insomnia and better sleep.
The study, which was published in BMJ Open , analyzed data from more than 4,300 people between the ages of 39 and 67 over a 10-year period. The researchers specifically looked at physical activity and matched that with questions on insomnia symptoms, how long people slept at night, and how sleepy they felt during the day.
The data showed that people who were persistently active (meaning, they exercised for at least an hour a week) were less likely to say that they had trouble falling asleep or that they got less than six hours of sleep a night compared to those who didn’t exercise regularly. The researchers also found that those who were persistently active were 55% more likely to sleep between six to nine hours.
“Physically active people have a lower risk of some insomnia symptoms and extreme sleep durations, both long and short,” the researchers concluded.
Insomnia is a common sleep disorder that can cause people to have trouble falling asleep, staying asleep, or getting good quality sleep, according to the National Heart, Lung, and Blood Institute (NHLBI). Insomnia can happen even if you have the time and the right environment to sleep well, and it can interfere with your daily activities.
Insomnia can be short-term and caused by stress or changes in your schedule or environment, or it can be chronic, where it lasts for three or more nights a week fo rmore than three months and can't be explained by another health problem, the NHLBI says.
But why might regular exercise help with sleep, and what’s the best way to go about this? Sleep experts explain.
Why is there a link between exercise and sleep?
This study isn’t the first to find a connection between exercise and sleep. However, it adds to the current literature by showing a connection between regular activity and good sleep.
One meta-analysis of 22 randomized controlled trials published in 2021 found that people who were physically active were more likely to say that they had good sleep quality and minimal to no symptoms of insomnia. They were also more likely to report feeling awake during the daytime.
Another analysis of 34 studies found that 29 of them concluded that exercise helped improve how well people slept, as well as how long they were asleep for. And a 2023 systemic review of 23 studies found a link between regular physical activity and improved sleep quality. The researchers also discovered that physical activity showed “promise” in managing sleep disorders like insomnia.
The latest findings “are not surprising, but I like that this seems to be related more to moving your body vs. needing to join a gym,” says W. Christopher Winter, M.D. , a neurologist and sleep medicine physician with Charlottesville Neurology and Sleep Medicine and host of the Sleep Unplugged podcast.
Dr. Winter says that exercise can be such a powerful sleep aid that he usually jokes with patients that “if you’re not sleeping well, you need to exercise. And if you’re already exercising, you need to exercise more.”
There are a few reasons why exercise can be so effective for sleep, Dr. Winter says. One is that exercise can simply wear you out. “If you do a hard swimming workout, you are going to be tired when it’s time for bed,” he says. He also points out that professional baseball players he works with tend to sleep better once they start training for the season than they do during the off-season when they’re not exercising as much.
But being active can do even more for your sleep health than making you feel wiped, according to behavioral sleep medicine specialist Shelby Harris, Psy.D., a licensed clinical psychologist in private practice in White Plains, New York, and director of sleep health with Sleepopolis . “It helps you relax, sets your body's internal clock, reduces stress, and boosts your mood,” she says. It also, “makes your sleep deeper and more restful, helps you manage your weight, and keeps you healthier overall,” she adds.
How to use physical activity for sleep
Insomnia is a complicated condition, and it’s a little of a reach to say that incorporating more physical activity into your day will magically make all cases of insomnia go away. “Exercise can increase one’s drive to fall asleep,” Dr. Winter says. “But for complicated and difficult insomnia, exercise may or may not be the ticket.” Still, he says adding more movement into your day can definitely help.
At baseline, sleep medicine doctors recommend following the Activity Guidelines for Americans , which suggest trying for at least 150 minutes a week of moderate-intensity exercise or at least 75 minutes a week of vigorous-intensity exercise. It’s also recommended to get in two or more days a week of muscle-strengthening activities.
But, research has found that there are some nuances to keep in mind when you’re working out for better sleep. One analysis found that doing regular moderate-intensity physical activities is the most effective for sleep quality, while high-intensity physical activities—especially when you do them in the evening or close to bedtime—may actually cause trouble sleeping.
“If you can exercise at any time, doing it first thing in the morning is better for sleep,” Dr. Winter says. Working out at night may make you feel ramped up when you should be winding down, he points out, and exercising in the morning can signal to your body that it's time to wake up.
Evening workouts aren’t bad for everyone, though, Harris says—it ultimately depends on your body. “Consistency matters, so pick a time that fits into your schedule and stick with it,” she advises. “While some people feel relaxed after evening workouts, others find it harder to wind down for bed. Just pay attention to how your body responds and avoid intense workouts too close to bedtime for better sleep.”
But Dr. Winter says it’s best to work out whenever you can if mornings are tough for you. “Most people will be able to fall asleep at the end of a strenuous day that includes exercise,” he says.
Try 200+ at home workout videos from Men’s Health, Women’s Health, Prevention, and more on All Out Studio free for 14 days!

- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Pilot study shows ketogenic diet improves severe mental illness
A small clinical trial led by Stanford Medicine found that the metabolic effects of a ketogenic diet may help stabilize the brain.
April 1, 2024 - By Nina Bai

A study led by researchers at Stanford Medicine showed that diet can help those with serious mental illness. nishihata
For people living with serious mental illness like schizophrenia or bipolar disorder, standard treatment with antipsychotic medications can be a double-edged sword. While these drugs help regulate brain chemistry, they often cause metabolic side effects such as insulin resistance and obesity, which are distressing enough that many patients stop taking the medications.
Now, a pilot study led by Stanford Medicine researchers has found that a ketogenic diet not only restores metabolic health in these patients as they continue their medications, but it further improves their psychiatric conditions. The results, published March 27 in Psychiatry Research , suggest that a dietary intervention can be a powerful aid in treating mental illness.
“It’s very promising and very encouraging that you can take back control of your illness in some way, aside from the usual standard of care,” said Shebani Sethi , MD, associate professor of psychiatry and behavioral sciences and the first author of the new paper.
Making the connection
Sethi, who is board certified in obesity and psychiatry, remembers when she first noticed the connection. As a medical student working in an obesity clinic, she saw a patient with treatment-resistant schizophrenia whose auditory hallucinations quieted on a ketogenic diet.
That prompted her to dig into the medical literature. There were only a few, decades-old case reports on using the ketogenic diet to treat schizophrenia, but there was a long track record of success in using ketogenic diets to treat epileptic seizures.
“The ketogenic diet has been proven to be effective for treatment-resistant epileptic seizures by reducing the excitability of neurons in the brain,” Sethi said. “We thought it would be worth exploring this treatment in psychiatric conditions.”
A few years later, Sethi coined the term metabolic psychiatry, a new field that approaches mental health from an energy conversion perspective.

Shebani Sethi
In the four-month pilot trial, Sethi’s team followed 21 adult participants who were diagnosed with schizophrenia or bipolar disorder, taking antipsychotic medications, and had a metabolic abnormality — such as weight gain, insulin resistance, hypertriglyceridemia, dyslipidemia or impaired glucose tolerance. The participants were instructed to follow a ketogenic diet, with approximately 10% of the calories from carbohydrates, 30% from protein and 60% from fat. They were not told to count calories.
“The focus of eating is on whole non-processed foods including protein and non-starchy vegetables, and not restricting fats,” said Sethi, who shared keto-friendly meal ideas with the participants. They were also given keto cookbooks and access to a health coach.
The research team tracked how well the participants followed the diet through weekly measures of blood ketone levels. (Ketones are acids produced when the body breaks down fat — instead of glucose — for energy.) By the end of the trial, 14 patients had been fully adherent, six were semi-adherent and only one was non-adherent.
The participants underwent a variety of psychiatric and metabolic assessments throughout the trial.
Before the trial, 29% of the participants met the criteria for metabolic syndrome, defined as having at least three of five conditions: abdominal obesity, elevated triglycerides, low HDL cholesterol, elevated blood pressure and elevated fasting glucose levels. After four months on a ketogenic diet, none of the participants had metabolic syndrome.
On average, the participants lost 10% of their body weight; reduced their waist circumference by 11% percent; and had lower blood pressure, body mass index, triglycerides, blood sugar levels and insulin resistance.
“We’re seeing huge changes,” Sethi said. “Even if you’re on antipsychotic drugs, we can still reverse the obesity, the metabolic syndrome, the insulin resistance. I think that’s very encouraging for patients.”
The participants reported improvements in their energy, sleep, mood and quality of life.
The psychiatric benefits were also striking. On average, the participants improved 31% on a psychiatrist rating of mental illness known as the clinical global impressions scale, with three-quarters of the group showing clinically meaningful improvement. Overall, the participants also reported better sleep and greater life satisfaction.
“The participants reported improvements in their energy, sleep, mood and quality of life,” Sethi said. “They feel healthier and more hopeful.”
The researchers were impressed that most of the participants stuck with the diet. “We saw more benefit with the adherent group compared with the semi-adherent group, indicating a potential dose-response relationship,” Sethi said.
Alternative fuel for the brain
There is increasing evidence that psychiatric diseases such as schizophrenia and bipolar disorder stem from metabolic deficits in the brain, which affect the excitability of neurons, Sethi said.
The researchers hypothesize that just as a ketogenic diet improves the rest of the body’s metabolism, it also improves the brain’s metabolism.
“Anything that improves metabolic health in general is probably going to improve brain health anyway,” Sethi said. “But the ketogenic diet can provide ketones as an alternative fuel to glucose for a brain with energy dysfunction.”
Likely there are multiple mechanisms at work, she added, and the main purpose of the small pilot trial is to help researchers detect signals that will guide the design of larger, more robust studies.
As a physician, Sethi cares for many patients with both serious mental illness and obesity or metabolic syndrome, but few studies have focused on this undertreated population.
She is the founder and director of the metabolic psychiatry clinic at Stanford Medicine.
“Many of my patients suffer from both illnesses, so my desire was to see if metabolic interventions could help them,” she said. “They are seeking more help. They are looking to just feel better.”
Researchers from the University of Michigan; the University of California, San Francisco; and Duke University contributed to the study.
The study was supported by Baszucki Group Research Fund, Keun Lau Fund and the Obesity Treatment Foundation.
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care


IMAGES
VIDEO
COMMENTS
For many, insomnia is a persistent condition, with 74% reporting symptoms for at least one year. Persistence is more common in women, the elderly, and those with more severe insomnia. In a 3‐year study, over half of participants did remit, but there was a 27% relapse rate. Family history of insomnia is also common, occurring in 35% of ...
1.1. The Definition of Insomnia. This review addresses insomnia disorder (ID), by far the most common sleep disorder, as well as the second most common neuropsychiatric disorder, only outnumbered by the Diagnostic and Statistical Manual of Mental Disorders comprehensive category of all anxiety disorders (1, 2).ID is defined by symptoms that we may all have experienced: difficulties initiating ...
Insomnia. Dear readers of the Journal of Sleep Research, This virtual issue of JSR brings together ten articles published in 2019 and 2020 dealing with different aspects of insomnia. Insomnia, especially in its chronic form, is a frequent sleep disorder, probably the most frequent sleep disorder of all, afflicting approximately 10% of the adult ...
Insomnia is highly prevalent in clinical practice, occurring in up to 50% of primary care patients. Insomnia can present independently or alongside other medical conditions or mental health disorders and is a risk factor for the development and exacerbation of these other disorders if not treated. In 2016, the American College of Physicians recommended that insomnia be specifically targeted ...
Roughly 50% of those with insomnia have a psychiatric disorder, 10 most commonly a mood disorder (e.g., major depressive disorder) or an anxiety disorder (e.g., generalized anxiety disorder or ...
This article is part of the Research Topic Insomnia: A Heterogenic Disorder Often Comorbid With Other Disorders and Diseases View all 9 articles. The Epidemiology of Insomnia and Sleep Duration Across Mental and Physical Health: The SHoT Study. Børge Sivertsen 1,2,3* Mari Hysing 4 Allison G. Harvey 5 Keith J. Petrie 6.
Several decades of research produced a significant amount of knowledge on insomnia. Insomnia is clinically defined as a difficulty fall asleep, maintaining sleep, and/or waking-up before the desired time. These difficulties or insomnia episodes should be present on average three nights per week during 3 months at least.
This article is part of the Research Topic Insomnia: A Heterogenic Disorder Often Comorbid With Other Disorders and Diseases View all 9 articles. ... Insomnia research: 3Ps and beyond. Sleep Med Rev. (2014) 18:191-93. doi: 10.1016/j.smrv.2014.01.003. CrossRef Full Text | Google Scholar. 24. Halonen JI, Lallukka T, Pentti J, Stenholm S, Rod NH ...
Strategic opportunities in sleep and circadian research: report of the Joint Task Force of the Sleep Research Society and American Academy of Sleep Medicine. Sleep. 2014;37(2):219-227. Crossref Google Scholar; 74. Jackson CL, Walker JR, Brown MK, Das R, Jones NL. A workshop report on the causes and consequences of sleep health disparities. Sleep.
This article reviews the history of insomnia pharmacotherapy, documenting the evolution that has occurred over time in the increasing availability of medications with novel mechanisms of action that more specifically target the neural systems that modulate sleep/wake function. ... Research Grants: Janssen Pharmaceuticals, Axsome Pharmaceutics ...
Insomnia is the inability to fall or stay asleep, even when one has the opportunity to do so. People who suffer from insomnia may be unsatisfied with their sleep and exhibit one or more of the ...
Objectives To explore the relationship between physical activity over a 10-year period and current symptoms of insomnia, daytime sleepiness and estimated sleep duration in adults aged 39-67. Design Population-based, multicentre cohort study. Setting 21 centres in nine European countries. Methods Included were 4339 participants in the third follow-up to the European Community Respiratory ...
Purpose: Anxiety, insomnia, and physical activity (PA) are interrelated, but the bi-directional relationships between these three variables are not well understood. Less is known of these relationships in settings of disrupted daily activities and acute stress. This study aimed to characterize and examine relationships between insomnia, anxiety, and PA throughout the first year of the COVID-19 ...
This Special Issue, "New Research in Insomnia", is timely, as it will feature articles that address how insomnia develops and is maintained through cognitions, emotions and sleep dysregulation. I invite you to submit your latest innovative research on insomnia for this Special Issue. Dr. Célyne H. Bastien. Guest Editor.
Over time, exercising at least twice a week is associated with significantly fewer insomnia symptoms and better sleep duration, new research shows. The study included 4339 adults aged 39-67 years ...
The American Academy of Sleep Medicine guidelines state: "We recommend that clinicians use multicomponent cognitive behavioral therapy for insomnia (CBT-I) for the treatment of chronic insomnia disorder in adults (strong recommendation). We suggest that clinicians use relaxation therapy as a single-component therapy for the treatment of ...
Learn about insomnia, sleep deprivation and other sleep problems. See the latest research on insomnia causes, possible cures involving melatonin and other treatment options.
Insomnia: The Latest Research. If you have trouble falling asleep or staying asleep, you may have insomnia, the most common sleep disorder. Between 10% and 30% of adults have chronic insomnia, and ...
Creativity is an essential cognitive ability that plays a crucial role in advanced thinking. While previous research has demonstrated the impact of insomnia on cognitive function, its effects on creativity in Chinese adolescents remain unclear. This study explored the relationship between insomnia (specifically, daytime and nighttime disturbances) and creativity in adolescents.
HealthDay. WEDNESDAY, March 27, 2024 (HealthDay News) -- Folks who consistently work out two to three times a week are less likely to suffer from insomnia, a new study says. That sort of long-term ...
Getting active. You don't have to start running marathons to get the benefit. You just have to start, the experts said. "Even moderate-intensity exercise, such as walking or yoga, can have ...
But, new research has found that regular exercise is associated with less insomnia and better sleep. The study, which was published in BMJ Open, analyzed data from more than 4,300 people between ...
The research team tracked how well the participants followed the diet through weekly measures of blood ketone levels. (Ketones are acids produced when the body breaks down fat — instead of glucose — for energy.) By the end of the trial, 14 patients had been fully adherent, six were semi-adherent and only one was non-adherent.