

Patient Case #1: 19-Year-Old Male With ADHD
- Craig Chepke, MD, DFAPA, FAPA
- Andrew J. Cutler, MD
Stephen Faraone, PhD, presents the case of a 19-year-old male with ADHD.

EP: 1 . Prevalence of Adult ADHD
Ep: 2 . diagnosis and management of adults adhd compared to children.
EP: 3 . Diagnosing Adults With ADHD Based on Patient Presentation

EP: 4 . Unmet Needs in the Treatment of Adult ADHD

EP: 5 . Efficacy and Safety of Treatment Options Utilized in Adult ADHD
Ep: 6 . future of adult adhd, ep: 7 . patient case #1: 19-year-old male with adhd.

EP: 8 . Patient Case #1: Prompting an ADHD Consultation
Ep: 9 . patient case #1: differentiating between adhd and other psychiatric comorbidities, ep: 10 . patient case #1: co-managing adhd, ep: 11 . patient case #1: dealing with treatment delay in adult adhd, ep: 12 . patient case #2: a 23-year-old patient with adhd, ep: 13 . patient case #2: impressions and challenges in adult adhd, ep: 14 . patient case #2: dealing with comorbidities in adult adhd, ep: 15 . patient case #2: addressing non-adherence and stigma of adult adhd, ep: 16 . patient case #2: importance of an integrative approach in adult adhd, ep: 17 . case 3: 24-year-old patient with adhd, ep: 18 . case 3: treatment goals in adult adhd, ep: 19 . case 3: factors driving treatment selection in adult adhd, ep: 20 . implications of pharmacogenetic testing in adhd, ep: 21 . novel drug delivery systems in adhd and take-home messages.
Stephen Faraone, PhD: That's a good one, yes, I'd like that, it's a very creative one, thank you, thank you. OK, let's move on to the case presentation. This first patient is a 19-year-old male, who presented to his psychiatrist after being referred by his primary care provider, PCP for ADHD consultation, during the interview, he noted he was a sophomore in college and is taking 17 credits. This semester chief complaint includes a lack of ability to focus in class as well as struggling with time management. He complained that every time he's in class, he finds himself thinking about many other responsibilities he must complete at home and feels that he cannot control it. He has had this complaint for the past 6 years, but refused to seek help, because he feared being put on medication. In high school, he was assigned a counselor who taught him behavior techniques such as making a schedule, and going on walks, which he found to be very effective. However, these techniques were less effective once he started college. His symptoms tend to get worse before exams, he often feels very anxious, leading to horrible performance on exams, he claimed that he has been this anxious since he took his LSAT tests. Currently, he is on academic probation, and is not allowed to be part of the Student Work Program, which was his only source of income. The patient has no history of substance abuse, no history of taking any medications for his symptoms, and no history of suicidal thoughts.
Transcript edited for clarity
The Week in Review: March 11-15

Treating ADHD in Children: Concerns, Controversies, Safety Measures
Are We Over-Diagnosing ADHD Based on “Hyperactivity"?

ADHD in Older Adults
From the Pages of Psychiatric Times: February 2024

The Week in Review: February 12-16
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

A CASE STUDY
Observations of a student with ADHD over a 3-week time span.
Student X is a 14 year-old male in a 9 th Grade English class. He is average height and build. He has no physical disabilities, but suffers from a mental disorder – ADHD. He often makes careless mistakes in schoolwork. He does not pay attention to detail. He has trouble staying focused while reading long texts. He also has difficulty staying still during a lecture. He fidgets and shakes his legs uncontrollably when seemingly annoyed or anxious. He has trouble turning in homework on time and meeting deadlines in general. He frequently does not respond when spoken to directly and appears to be distracted even though he is performing no obvious task. He lets his mind wander and appears to daydream often. When he does respond and participate, he is usually off topic. Overall, he appears uninterested and aloof. One might say that the behavior is defiant – a consciously overt reluctance to participate in school. However, this student has been diagnosed by a physician as being ADHD. He has an involuntary learning disability which requires support, therapy, social skills training and/or medication.
Ready to Make a Change?
Educating children with ADHD is no easy task. Know that you are not alone. Please enlist the help of our school to find the right plan and solution for your child.

The Palgrave Handbook of Male Psychology and Mental Health pp 291–307 Cite as
Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions
- Bijal Chheda-Varma 5
- First Online: 02 March 2019
3167 Accesses
The male to female ratio of ADHD is 4:1. This chapter on ADHD provides a wide perspective on understanding, diagnosis and treatment for ADHD. It relies on a neurodevelopmental perspective of ADHD. Signs and symptoms of ADHD are described through the DSM-V criteria. A case example (K, a patient of mine) is illustrated throughout the chapter to provide context and illustrations, and demonstrates the relative merits of “doing” (i.e. behavioural interventions) compared to cognitive insight, or medication alone. Finally, a discussion of the Cognitive Behavioral Modification Model (CBM) for the treatment of ADHD provides a snapshot of interventions used by clinicians providing psychological help.
- Neuro-developmental disorders
- Behaviour modification
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Alderson, R. M., Hudec, K. L., Patros, C. H. G., & Kasper, L. J. (2013). Working memory deficits in adults with attention-deficit/hyperactivity disorder (ADHD): An examination of central executive and storage/rehearsal processes. Journal of Abnormal Psychology, 122 (2), 532–541. http://dx.doi.org/10.1037/a0031742 .
Arcia, E., & Conners, C. K. (1998). Gender differences in ADHD? Journal of Developmental and Behavioral Pediatrics, 19 (2), 77–83. http://dx.doi.org/10.1097/00004703-199804000-00002 .
Barkley, R. A. (1990). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment . New York: Guildford.
Google Scholar
Barkley, R. A. (1997). ADHD and the nature of self-control . New York: Guilford Press.
Barkley, R. A. (2000). Commentary on the multimodal treatment study of children with ADHD. Journal of Abnormal Child Psychology, 28 (6), 595–599. https://doi.org/10.1023/A:1005139300209 .
Article Google Scholar
Barkley, R., Knouse, L., & Murphy, K. Correction to Barkley et al. (2011). Psychological Assessment [serial online]. June 2011; 23 (2), 446. Available from: PsycINFO, Ipswich, MA. Accessed December 11, 2014.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders . New York, NY: International Universities Press.
Brown, T. E. (2005). Attention deficit disorder: The unfocused mind in children and adults . New Haven, CT: Yale University Press.
Brown, T. (2013). A new understanding of ADHD in children and adults . New York: Routledge.
Chacko, A., Kofler, M., & Jarrett, M. (2014). Improving outcomes for youth with ADHD: A conceptual framework for combined neurocognitive and skill-based treatment approaches. Clinical Child and Family Psychology Review . https://doi.org/10.1007/s10567-014-0171-5 .
Chronis, A., Jones, H. A., Raggi, V. L. (2006, August). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Clinical Psychology Review, 26 (4), 486–502. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2006.01.002 .
Curatolo, P., D’Agati, E., & Moavero, R. (2010). The neurobiological basis of ADHD. Italian Journal of Pediatrics, 36 , 79. http://doi.org/10.1186/1824-7288-36-79 . http://www.sciencedirect.com/science/article/pii/S0272735806000031 .
Curtis, D. (2010). ADHD symptom severity following participation in a pilot, 10-week, manualized, family-based behavioral intervention. Child & Family Behavior Therapy, 32 , 231–241. https://doi.org/10.1080/07317107.2010.500526 .
De Young, R. (2014). Using the Stroop effect to test our capacity to direct attention: A tool for navigating urgent transitions. http://www.snre.umich.edu/eplab/demos/st0/stroopdesc.html .
Depue, B. E., Orr, J. M., Smolker, H. R., Naaz, F., & Banich, M. T. (2015). The organization of right prefrontal networks reveals common mechanisms of inhibitory regulation across cognitive, emotional, and motor processes. Cerebral Cortex (New York, NY: 1991), 26 (4), 1634–1646.
D’Onofrio, B. M., Van Hulle, C. A., Waldman, I. D., Rodgers, J. L., Rathouz, P. J., & Lahey, B. B. (2007). Causal inferences regarding prenatal alcohol exposure and childhood externalizing problems. Archives of General Psychiatry, 64, 1296–1304 [PubMed].
DSM-V. (2013). Diagnostic and statistical manual of mental disorders . American Psychological Association.
Eisenberg, D., & Campbell, B. (2009). Social context matters. The evolution of ADHD . http://evolution.binghamton.edu/evos/wp-content/uploads/2012/02/eisenberg-and-campbell-2011-the-evolution-of-ADHD-artice-in-SF-Medicine.pdf .
Gizer, I. R., Ficks, C., & Waldman, I. D. (2009). Hum Genet, 126 , 51. https://doi.org/10.1007/s00439-009-0694-x .
Hinshaw, S. P., & Scheffler, R. M. (2014). The ADHD explosion: Myths, medication, money, and today’s push for performance . New York: Oxford University Press.
Kapalka, G. M. (2008). Efficacy of behavioral contracting with students with ADHD . Boston: American Psychological Association.
Kapalka, G. (2010). Counselling boys and men with ADHD . New York: Routledge, Taylor & Francis Group.
Book Google Scholar
Knouse, L. E., et al. (2008, October). Recent developments in psychosocial treatments for adult ADHD. National Institute of Health, 8 (10), 1537–1548. https://doi.org/10.1586/14737175.8.10.1537 .
Laufer, M., Denhoff, E., & Solomons, G. (1957). Hyperkinetic impulse disorder in children’s behaviour problem. Psychosomatic Medicine, 19, 38–49.
Raggi, V. L., & Chronis, A. M. (2006). Interventions to address the academic impairment of children and adolescents with ADHD. Clinical Child and Family Psychology Review, 9 (2), 85–111. https://doi.org/10.1007/s10567-006-0006-0 .
Ramsay, J. R. (2011). Cognitive behavioural therapy for adult ADHD. Journal of Clinical Outcomes Management, 18 (11), 526–536.
Retz, W., & Retz-Junginger, P. (2014). Prediction of methylphenidate treatment outcome in adults with attention deficit/hyperactivity disorder (ADHD). European Archives of Psychiatry and Clinical Neuroscience . https://doi.org/10.1007/s00406-014-0542-4 .
Safren, S. A., Otto, M. W., Sprich, S., Winett, C. L., Wilens, T. E., & Biederman, J. (2005, July). Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms. Behaviour Research and Therapy, 43 (7), 831–842. ISSN 0005-7967. http://dx.doi.org/10.1016/j.brat.2004.07.001 . http://www.sciencedirect.com/science/article/pii/S0005796704001366 .
Sibley, M. H., Kuriyan, A. B., Evans, S. W., Waxmonsky, J. G., & Smith, B. H. (2014). Pharmacological and psychosocial treatments for adolescents with ADHD: An updated systematic review of the literature. Clinical Psychology Review, 34 (3), 218–232. https://doi.org/10.1016/j.cpr.2014.02.001 .
Simchon, Y., Weizman, A., & Rehavi, M. (2010). The effect of chronic methylphenidate administration on presynaptic dopaminergic parameters in a rat model for ADHD. European Neuropsychopharmacology, 20 (10), 714–720. ISSN 0924-977X. https://doi.org/10.1016/j.euroneuro.2010.04.007 . http://www.sciencedirect.com/science/article/pii/S0924977X10000891 .
Swanson, J. M., & Castellanos, F. X. (2002). Biological bases of ADHD: Neuroanatomy, genetics, and pathophysiology. In P. S. Jensen & J. R. Cooper (Eds.), Attention deficit hyperactivity disorder: State if the science, best practices (pp. 7-1–7-20). Kingston, NJ: Civic Research Institute.
Toplak, M. E., Connors, L., Shuster, J., Knezevic, B., & Parks, S. (2008, June). Review of cognitive, cognitive-behavioral, and neural-based interventions for attention-deficit/hyperactivity disorder (ADHD). Clinical Psychology Review, 28 (5), 801–823. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2007.10.008 . http://www.sciencedirect.com/science/article/pii/S0272735807001870 .
Wu, J., Xiao, H., Sun, H., Zou, L., & Zhu, L.-Q. (2012). Role of dopamine receptors in ADHD: A systematic meta-analysis. Molecular Neurobiology, 45 , 605–620. https://doi.org/10.1007/s12035-012-8278-5 .
Download references
Author information
Authors and affiliations.
Foundation for Clinical Interventions, London, UK
Bijal Chheda-Varma
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
UCL, London, UK
John A. Barry
Norfolk and Suffolk NHS Foundation Trust, Wymondham, UK
Roger Kingerlee
Change, Grow, Live, Dagenham/Southend, Essex, UK
Martin Seager
Community Interest Company, Men’s Minds Matter, London, UK
Luke Sullivan
Rights and permissions
Reprints and permissions
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter.
Chheda-Varma, B. (2019). Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions. In: Barry, J.A., Kingerlee, R., Seager, M., Sullivan, L. (eds) The Palgrave Handbook of Male Psychology and Mental Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-04384-1_15
Download citation
DOI : https://doi.org/10.1007/978-3-030-04384-1_15
Published : 02 March 2019
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-04383-4
Online ISBN : 978-3-030-04384-1
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

ADHD Coaching: 5 Case Studies and 10 Common Challenges
A short definition of adhd coaching followed by real, relatable stories from our shimmer members.

We get this question all the time: can you give me examples of how others use coaching? Finally, we’ve surveyed 5 Shimmer members and their coaches to understand their situations, coaching plan, and results more in depth. The full list of our testimonials if you’re curious is here .
In this article, we'll explore what ADHD coaching is, real case studies of Shimmer members and the coaching plans that were developed to address their challenges, and other common challenges that members come to Shimmer ADHD Coaches with.
ADHD Coaching, defined
In short, ADHD coaching is a partnership between someone with ADHD and an expert ADHD coach, where they work together to bridge the gap between where the client is, and where they want to be. The coach helps the client to set goals, re-ignite a sense of hope, identify their strengths and weaknesses, and overcome ADHD-related challenges to reach their goals. The more obvious benefits include improvement in executive function and achievement of goals but the more nuanced benefits include things like improved self esteem and general feeling of support and understanding.
The ADHD coaching process generally starts with vision setting & goal setting, arriving at a shared understanding of the client’s situation and what has worked or not work before, and an understanding of mutual working styles. Then, they will develop a personalized coaching plan that will play out out over weeks to months of working together. Each week, they will meet to keep accountable, reflect on progress, celebrate wins, and problem solve around challenges. Over the course of the coaching journey, the coaching partnership with experiment with various methods, explore skills & strategies, and eventually land on a system that works uniquely for the client.
For a full comparison of ADHD treatment methods, check out our Head ADHD Coach, Noelle’s blog post “ ADHD Treatment Options: Medication vs Coaching vs Therapy ”
Shimmer member case studies
Cases below are inspired by Shimmer members—however, they are altered for brevity and anonymity. These cases are specific to each member & their life, and we try to include sufficient details and rationale, so you can apply similar methodologies to your challenges, but you’ll likely end up with a different solution! Feel free to ask your coach for support here!
Case Study 1: Impulsivity in relationship
Situation : Member was struggling was impulsivity at home. They would frequently say things to their partner that they later regretted.
Coaching plan : Member & coach jointly embarked on a multi-step, CBT-based plan
- Week 1: Journal each time impulsive action came up and afterwards, write down what a better action would have been. Together in session, member & coach debriefed situations and looked for patterns
- Week 2: On 1 sticky note per common situation member was impulsive on, they wrote out a short bullet point script on what they should say instead. They put it visible in front of their computer screen and silently rehearsed it 2x/day, pushing it into muscle memory
- Week 3+: Member replaced stickies with new situations and celebrated when 1 needed to get “tossed away” because it was in their muscle memory
Final outcome : Member had far less situations where they said impulsive things to their partner, and their partner gained empathy & respect for the amount of work they were putting in to address this important issue
Case Study 2: Job Hunting with ADHD
Situation : Member just finished school and was applying to jobs . The task was large & daunting, and the member wanted to make sure they were taking the right steps.
Coaching plan : Member created a career vision, explored ADHD-fit career types, and broke career tasks into chunks to stay accountable with coach
- Career vision : Member journaled about their vision as to what a perfect career and job would look like, and dug into the “why” behind it. This exercise involved reflecting on what jobs were energizing & not in the past, and what learnings to bring forward
- ADHD-fit career types : Member & coach explored together career types better fit for people with ADHD (and why).
- Member: “It was incredible! I never knew there were certain jobs more fit for my ADHD than others, and how to think about accommodations.”
- Breaking tasks into chunks : Each week, the member set goals as to what was needed to be accomplished in the job hunting process (e.g. portfolio, research on companies, networking events, etc.) and stayed accountable with their coach
Final outcome : In 2 months, member secured a dream job! We wish them the best as we continue to watch their growth in other domains :)
Case Study 3: Working deeper, and more strategically
Situation : Member never had enough time to do deeper, strategic & creative work that was required for them to be considered for their next promotion. Their calendar was peppered with calls, and they could never get into “flow state” long enough without being distracted
Coaching plan : Member & coach designed a 3x weekly deep work block, plan for distractions, and moved around call slots to work FOR the member
- 3x weekly deep work block : Coach asked questions to get to the root of member’s issue, that there was never long enough blocks of time that was protected. Together, they came up with a realistic 3x/week block, decided on the exact days & time, accompanying ritual (a special coffee), and reward (pre-cut watermelon)
- Coach also shared “time blocking” resource by Cal Newport
- TimeBlockPlanner.pdf
- Plan for distractions : Member identified things that could potentially come up and pro-actively designed mitigation strategies for each of them.
- (1) A customer could call → auto-forward to co-worker during those designated times,
- (2) A thought or notification could distract → created special distraction log on a sticky note that is on the table, and carve out time at the end of the deep work block to attend to them
- New calendar / call system : Member identified it was difficult to get anything done in 15-30 min blocks between calls, over 50% of their day was “dead” time. Together, they blocked the calendar so calls were stacked in the mornings only for Mon/Wed/Fri, and afternoons only for Tue/Thu. This gave flexibility for other parties to book calls but carved out dedicated “work time” for the member
Final outcome : Member’s work was noticeably more creative and “out of the box”, and several colleagues mentioned and praised them! They also had an easier time getting in and out of “work” zone and “call” zone each day.
Case Study 4: Following through on daily to-do lists
Situation : Member was struggling to complete their daily to-do lists . They were confident the right things were on them, but couldn’t follow through
Coaching plan : Member & coach jointly embarked on a multi-step journaling & awareness plan
- Week 1: Journal each time member actually felt motivated, indicating if the source of motivation was (1) accountability, (2) novelty, (3) personal interest, or (4) other. The goal was to identify which drivers were THEIR personal drivers.
- Week 2: Together in session, they discovered accountability as the biggest driver, with novelty as a close 2nd. Then, they brainstormed specific ways the member could inject accountability into mundane, non-urgent tasks. This week, the member sent their “mundane” list to a coworker in the morning, and looped back each afternoon with the outcome
- Week 3: Next up, they brainstormed ways the member could inject novelty into specific tasks. They came up with a specific playlist and new location (outside the office) they would do these tasks, to make it feel “fresh” in other ways
- Week 4+: When certain strategies & systems were getting stale, they brainstormed other ways that fell in the 2 buckets of accountability & novelty
Final outcome : Member had a long list of 8-10 strategies on their office wall that they could draw on to pump their own personal motivation factors (novelty + accountability) into
Case Study 5: Self esteem issues from lifetime of criticisms
Situation : Member identified general self esteem issues paired with impulsive behaviors. Throughout their life, they had faced criticisms like “lazy”, “not living up to potential”, and generally felt misunderstood
Coaching plan : Coach and member took a CBT-based approach starting with psycho-education
- Psycho-education on emotions and identifying specific feelings as a starting point
- Tracked negative thoughts/behaviors and examining underlying beliefs behind them
- Identified cognitive distortions and actively challenging them through CBT
Final outcome : Member had more awareness as to where emotional outbursts were stemming from and more productive conversations with partner to address issues appropriately
Other common ADHD coaching topics
Don’t see your situation? Here are some other common topics members come to Shimmer ADHD Coaches with. This list is not ordered nor exhaustive. We encourage you to take time to reflect which topics are most important and helpful for you to explore, and the list below is simply inspiration!
- Feeling overwhelmed, paralyzed, unable to turn brain off
- Issues with self-esteem and negative self-talk
- Inability to focus during working hours leading to a disrupted sleep routine and lack of self care
- Holding themselves accountable to changes, needing help challenging “excuse” thoughts on why things can wait
- Creating routines & schedules (e.g. morning/night)
- Paying attention in conversations and perspective taking
- Missing work deadlines, falling behind in projects
- Task initiation & task switching
- Being more productive (particularly when working from home or running own business)
- Job hunting (and the lack of structure when between jobs)
If you're interested in working with a Shimmer ADHD Coach, visit our website to learn more about our coaching services and how to get started.
Interested in more content like this?
Explore more.

AuDHD: Autism and ADHD Comorbidity

The Science of Slumber: Delving into Why We Sleep

0203 326 9160
Childhood ADHD – Luke’s story
Posted on Thursday, 05 April 2018, in Child & Teen ADHD
In the final part of her ADHD series, Dr Sabina Dosani, Child and Adolescent Psychiatrist and Clinical Partner London, introduces Luke, a patient she was able to help with his ADHD.
ADHD is one of the most common diagnoses for children in the UK and it is thought that 1 in 10 children will display some signs. For some children, their ADHD is severe and can have a huge impact on their ability to engage in school and to build and sustain relationships. Left untreated, evidence shows that those with ADHD are more likely to get into car accidents, engage in criminal activity and may struggle to keep a job or maintain relationships.
Luke, aged six, gets into trouble a lot at school. His mother gets called by his teacher three or four times a week for incidents of fighting, kicking and running in corridors. He is unable to finish his work and becomes quickly distracted. At home, he seems unable to sit still for any length of time, has had several falls when climbing trees and needs endless prompts to tidy his toys.
At school, he annoys his classmates by his constant interruptions, however if he has one-to-one attention from a student teacher who happens to be in his class on a placement he is able to settle and finish the work set. His father was said to have been a ‘lively’ child, then a ‘bright underachiever’ who occasionally fell foul of the law.
The school thought a visit to the GP might be a good idea. At the GP surgery, Luke ran and jumped about making animal noises. He swung on the back legs of a chair and took the batteries out of an ophthalmoscope. He was referred to a me for an assessment.
After a careful assessment, which included collecting information from school, questionnaires and observations of Luke, a diagnosis of ADHD was made. Following a discussion of the treatment options, the family decided they did not want any medication.
The first-line treatment for school‑age children and young people with severe ADHD and severe impairment is drug treatment. If the family doesn’t want to try a pharmaceutical, a psychological intervention alone is offered but drug treatment has more benefits and is superior to other treatments for children with severe ADHD.
Luke's mother was asked to list the behaviours that most concern her. She was encouraged to accept others like making noises or climbing as part of Luke’s development as long as it is safe.
Now, when Luke fights, kicks others or takes risks like running into the road he is given “time-out” which isolates him for a short time and allows him and his parents or teacher to calm down. To reduce aggression and impulsivity, Luke is taught to respond verbally rather than physically and channel energy into activities such as sports or energetic percussion playing.
Over time, Luke’s parents have become skilled at picking their battles. Home is more harmonious. They fenced their garden, fitted a childproof gate and cut some branches off a tree preventing him climbing it. His parents are concerned about Luke’s use of bad language. They have been supported to allow verbal responses as a short-term interim. Whilst these might be unacceptable in other children they are preferable to physical aggression.
At school, Luke is less aggressive, has a statement of special educational need and now works well with a classroom assistant. He has been moved to the front of the class, where the teacher can keep a close eye on him, and given one task at a time. He is given special tasks, like taking the register to the school office, so he can leave class without being expected to sit still for long periods.
Through parental training, Luke’s parents have been able to help Luke work with his challenges to better manage them. As Luke grows and develops and as he faces new challenges in life, Luke may need to revisit the efficacy of ADHD medication. His parents now feel a lot more confident in being able to help Luke and he is a happier child and more settled.
Dr Sabina Dosani Consultant Child & Adolescent Psychiatrist
Dr Sabina Dosani is a highly experienced Consultant Psychiatrist currently working for the Anna Freud Centre looking after Children and Adolescents. She has a Bachelor of Medicine and Bachelor of Surgery as well as being a member of the Royal College of Psychiatrists . Dr Dosani also has a certificate in Systemic Practice (Family Therapy).
Related Articles
- The real reason you need to take adult ADHD seriously
- 10 signs your child might have ADHD
- What causes ADHD?
- Why is ADHD in women undiagnosed so often?
- Anxiety & Stress (14)
- Behavioural Issues (5)
- Bipolar Disorder (3)
- Child Autism (14)
- Child & Teen ADHD (7)
- Child & Teen Anxiety (12)
- Child & Teen Depression (3)
- Depression (3)
- Eating Disorders (2)
- Education & Mental Health (2)
- Maternal Health (2)
- Parenting & Families (16)
- Treatments & Therapy (20)
Already a patient?
Sign in to manage your care
Learn more and see openings
Work with us as a clinician?
Sign in to your clinician portal
- Research article
- Open access
- Published: 04 September 2012
A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment
- Monica Shaw 1 ,
- Paul Hodgkins 2 ,
- Hervé Caci 3 ,
- Susan Young 4 ,
- Jennifer Kahle 5 ,
- Alisa G Woods 6 &
- L Eugene Arnold 7
BMC Medicine volume 10 , Article number: 99 ( 2012 ) Cite this article
70k Accesses
429 Citations
168 Altmetric
Metrics details
In childhood, attention deficit/hyperactivity disorder (ADHD) is characterized by age-inappropriate levels of inattentiveness/disorganization, hyperactivity/impulsiveness, or a combination thereof. Although the criteria for ADHD are well defined, the long-term consequences in adults and children need to be more comprehensively understood and quantified. We conducted a systematic review evaluating the long-term outcomes (defined as 2 years or more) of ADHD with the goal of identifying long-term outcomes and the impact that any treatment (pharmacological, non-pharmacological, or multimodal) has on ADHD long-term outcomes.
Studies were identified using predefined search criteria and 12 databases. Studies included were peer-reviewed, primary studies of ADHD long-term outcomes published between January 1980 to December 2010. Inclusion was agreed on by two independent researchers on review of abstracts or full text. Published statistical comparison of outcome results were summarized as poorer than, similar to, or improved versus comparators, and quantified as percentage comparisons of these categories.
Outcomes from 351 studies were grouped into 9 major categories: academic, antisocial behavior, driving, non-medicinal drug use/addictive behavior, obesity, occupation, services use, self-esteem, and social function outcomes. The following broad trends emerged: (1) without treatment, people with ADHD had poorer long-term outcomes in all categories compared with people without ADHD, and (2) treatment for ADHD improved long-term outcomes compared with untreated ADHD, although not usually to normal levels. Only English-language papers were searched and databases may have omitted relevant studies.
Conclusions
This systematic review provides a synthesis of studies of ADHD long-term outcomes. Current treatments may reduce the negative impact that untreated ADHD has on life functioning, but does not usually 'normalize' the recipients.
Peer Review reports
In childhood, attention deficit/hyperactivity disorder (ADHD) is a psychiatric condition characterized by age-inappropriate levels of inattention, hyperactivity-impulsiveness or a combination of these problems [ 1 , 2 ]. The symptoms of ADHD often lead to functional impairment in multiple domains and lower quality of life. Therefore, in recent years the focus of intervention has expanded from ameliorating immediate symptoms of ADHD to improving functionality in several life domains. Moreover, although traditionally regarded as a childhood disorder, it is now clear that ADHD affects both children and adults. The worldwide prevalence of ADHD has been estimated at 5.29% [ 3 , 4 ] with approximately 4% prevalence in adults [ 5 , 6 ]. According to one meta-analysis, ADHD persists in about 65% of adults diagnosed as children if ADHD in partial remission is included [ 7 ], and in about 50% of adults originally diagnosed as children according to a separate estimate [ 8 ]. Persistence of ADHD may be related to ADHD symptom severity, number of symptoms, ADHD symptom subtype, ADHD in relatives, psychosocial adversity, psychiatric comorbidities, and/or parental psychopathology [ 8 – 15 ]. Many adults with ADHD are undiagnosed and untreated. Research on ADHD in adulthood is relatively sparse [ 16 ] despite being recognized in adults as early as 1968 as 'minimal brain dysfunction' [ 17 ] and in 1972 as 'hyperkinetic disorder' [ 18 ]. Thus the negative outcomes reported by most follow-up studies may be a consequence of untreated symptoms.
The short-term effect of ADHD treatment on symptoms is well characterized. Beyond this, the longer-term consequences have been the focus of numerous individual studies but comprehensive synthesis of the available data has yet to be conducted, thus the present systematic review was performed, focusing on comprehensive summary of long-term outcomes of ADHD. Short-term studies have demonstrated decreases in core symptoms with pharmacotherapy, but there is less evidence for longer-term benefits. Poor adherence and persistence on therapy, comorbidities, poor follow-up and difficulty in accessing consistent medication management from the healthcare system may contribute to difficulty in measuring long-term effects of medication [ 19 , 20 ]. Non-pharmacological interventions such as specialized training for parents of children with ADHD and cognitive behavioral therapy (CBT) for adults also reduce symptoms, and a multimodal approach may have greater effect [ 16 , 21 ]. Both non-pharmacological (that is, psychological, social, and educational) and pharmacological treatments for ADHD are recommended by the National Institute for Health and Clinical Excellence (NICE) guidelines [ 22 ] with treatment selection depending on the age of the individual and ADHD severity. Recently published European adult guidelines for the treatment of ADHD indicate that both medications and non-pharmacological interventions may be effective for adults with ADHD, although more research specifically in adults is needed [ 23 ].
The importance of long-term studies has been recognized for more than a decade [ 24 ]. ADHD treatment guidelines as well as conclusions drawn by health technology assessment agencies recognize that ADHD is potentially a lifelong condition with a profound effect on quality-of-life [ 22 , 25 – 32 ]. Several of these organizations recognize a need for further study of the long-term consequences of ADHD and of its treatment [ 22 , 29 , 30 , 32 , 33 ]. For example, the NICE guidelines state that 'More research is needed on the influences on eventual outcome, and should include enquiry about the possible benefits (and risks) of early diagnosis and treatment' [ 22 ]. Guidelines from the Oregon Health and Science University propose that 'Good-quality evidence on the use of drugs to affect outcomes relating to global academic performance, consequences of risky behaviors, social achievements, etc. is lacking'. [ 34 ]. Because many studies of long-term outcomes (LTOs) have in fact been conducted [ 35 ], these statements may be more reflective of the quality and variability of data, rather than a lack of ADHD LTO studies. Comprehensive analysis of all available data would therefore be of value, and such an analysis is the purpose of the present review.
The National Institute of Health in the US funded the Multimodal Treatment Study of Children with ADHD (MTA); this is one of the largest independent trials examining the effects on ADHD symptoms and long-term outcomes of different ADHD treatments including: intensive behavioral intervention, medication, these two treatments combined, or routine community care [ 36 ]. In the primary intent-to-treat analyses, outcomes in this study were not significantly different for pharmacological treatment alone versus combined treatment after correction for multiple tests, but the combined group allowed as good a result with significantly lower dose of medication (methylphenidate). In two secondary analyses compositing several outcome measures, combined treatment was significantly better than pharmacological treatment alone [ 36 – 38 ]. An 8-year follow-up for this trial failed to differentiate the four treatment groups, demonstrating that regardless of treatment, participants showed improved outcomes (delinquency rating, reading and overall academic performance, and social skills) compared with baseline (pretreatment) [ 39 ]. The reasons why the original differences between groups disappeared after 8 years has been extensively debated, with arguments on opposite sides that medication was no longer effective or that all participants improved from treatment and the improvement was sustained or that the natural course of the disorder accounted for the improvement. The best interpretation may be that the data were confounded and conclusions difficult to draw [ 39 – 41 ]. The MTA study is the best-known study of the long-term outcomes of ADHD, including the early impact of treatment on later outcomes.
Based on the potential for long-term persistence of ADHD into adulthood and equivocal reports on treatment, we initiated this evidence-based systematic review to understand the long-term outcomes of ADHD with emphasis on a comprehensive synthesis of published data. Given the large differences in study design and measurements used, we decided that using a binary feature common to all the studies ('significantly different' and 'not significantly different') to define outcome results for LTOs would allow us to summarize all the included studies in a non-statistical fashion. Binary variables are used to simplify data in clinical trials for ADHD quite frequently (for example, Clinical Global Impression-Improvement (CGI-I), ADHD Rating Scale (ADHD-RS) responder analyses). 'Long term' was defined as 2 years or more and 'outcomes' were defined as life consequences, distinct from symptoms.
Our analysis sought to answer the research question: what are the long-term outcomes in participants with ADHD compared to baseline or controls and do long-term outcomes of ADHD improve with treatment (including pharmacological, non-pharmacological and multimodal)?
Studies included in this review examined outcomes of (1)participants with untreated ADHD, and (2) participants with treated ADHD. Studies that only examined symptoms (as opposed to life-consequence outcomes) were excluded. The dataset comprised studies published between January 1980 to December 2010, including longitudinal studies with prospective follow-up or retrospective measures of 2 years or more; cross-sectional studies comparing two ages differing by 2 years or more; and single cross-sectional studies of participants age 10 years or older. Age 10 was chosen as the age limit in single cross-sectional studies, based on the Diagnostic and Statistical Manual of Mental Disorders fourth edition, text revision (DSM-IV-TR) diagnosis criteria that symptoms be present before age 7 years. Examining outcomes at age 10 years or older, would conservatively allow at least 2 years to pass before outcomes were assessed, in line with our definition of 'long term' as 2 years or more. All studies were peer-reviewed, primary research articles in the English language with full text available. Studies for which all participants were less than 2 years old were excluded. Meta-analyses, case studies, and literature reviews were excluded.
The search methods for identification of studies are summarized below. More specific details of the search methods are provided in Additional File 1 . The following inclusionary terms and subterms were included: (1) names of the condition; attention deficit disorder (captured all versions of ADHD), hyperkinesis, TDAH (trouble déficit de l'attention/hyperactivité in French, or trastorno por déficit de atención con hiperactividad in Spanish), DAH (déficit de l'attention/hyperactivité in French, or déficit de atención con hiperactividad in Spanish), DAA (déficit de l'attention/activité in French, or déficit de atención y actividad in Spanish), (2) long-term outcomes; long-term, longitudinal, education, degree, socioeconomic, salary, divorce, relationship, hobbies, criminality, arrest, incarceration, automobile, car, driving, citation, weight, obesity, suicide, drug abuse, addiction, substance abuse, alcoholism, and (3) comparator condition or group; control, proband, placebo, untreated, no treatment, pretreatment, comparator, follow-up, normal. The following exclusionary terms were included: (1) developmental, causal, or symptom as subject terms (not general text words); neuroanatomy, neuropathology, molecular, gene, development, etiology, preclinical, dose-finding, reaction time, and (2) publication types; reprint, review, conference presentation.
The country of origin of each study was noted. For some analyses, studies were grouped by world region (Northern America and the Rest of the World, as defined by the United Nations GeoScheme). Studies from Northern America included those from Canada and the USA. Northern America was identified as a comparator because of the high percentage of participants who are treated for ADHD in these two countries.
To assess risk of bias, we considered search bias, researcher bias, bias of individual research groups and bias due to changes in diagnostic criteria over time.
In the analysis of outcome results, outcomes were considered different between study groups if they were reported to be statistically significantly different in the study or were presented by the study authors as obviously different so as to not require statistical comparison (for example, a study in Norway found that 80% of the study sample with ADHD were unemployed, while the unemployment rate in Norway was 3.5% at the time.) Outcomes that were not statistically significantly different were considered 'similar' to the comparator. We summarized number of outcomes as one measurement and number of studies as a separate measurement, because some studies reported more than one outcome. A list of all the studies included in the final analysis is detailed in a separate publication [ 35 ].
Data collection and analysis
Our search method has been described in a previous publication [ 35 ]. To identify as many published studies as possible, 12 databases were searched: Academic Search Premier, CINAHL, Cochrane CRCT (including EMBASE), Criminal Justice Abstracts, ERIC, MEDLINE, Military & Government collection, NHS Economic Evaluation database, PsycARTICLES, PsycINFO, SocINDEX, and Teacher Reference Center. MEDLINE was searched using two different search engines. Duplicates were eliminated electronically and manually, yielding 5,467 studies.
Based primarily on title and abstract, these studies were reviewed manually and inclusion was agreed on by two researchers. This yielded 351 studies for inclusion in the analysis. A list of all studies included in the analysis has been published [ 35 ].
All disagreements between researchers on study inclusion were resolved by examining the full text of the study. Studies included participants who were diagnosed with ADHD or symptomatic presentation of ADHD as reported by the authors of each study. Only those studies in which ADHD was the primary disorder under study were included. Studies included both naturalistic examination of ADHD course (vs non-ADHD controls or start-of-study baseline) and/or treated ADHD (vs ADHD natural course, pretreatment baseline, or non-ADHD controls). Treatments included pharmacological, non-pharmacological, and/or multimodal treatment.
Data from each study was manually extracted from the full text of the study to a database, including: (1) study location, (2) study sample size, (3) study length, (4) participant age range, (5) study support, (6) diagnostic criteria, (7) study type (longitudinal, cross-sectional, prospective, retrospective), (8) outcome measures, (9) outcome results, (10) comparator type, (11) treatment type, and (12) treatment duration. Outcome results were measured by dichotomizing all results into a binary variable of either 'poorer' or 'similar' outcomes, and with respect to outcomes with treatment, either 'benefit' or 'no benefit' with treatment. Many studies (44%) reported more than one outcome result, thus the number of outcome results is more than the number of studies. While the outcomes may be the item of interest, the number of studies from which these outcomes are derived is also informative and so is also reported.
Outcome groups
Outcome measures were compiled into nine major groups based on commonality of outcome characteristics (Figure 1 ). This grouping of outcomes has also been described in a prior publication [ 35 ]. These groups included: (1) non-medicinal drug use/addictive behavior (for example, use, abuse, and dependence on alcohol, cigarettes, marijuana, stimulants, or illicit drugs; age at first use; multiple substance use; gambling), (2) academic (for example, achievement test scores, grade point average, repeated grades, years of schooling, degrees earned), (3) antisocial behavior (for example, school expulsion, delinquency, self-reported crimes, arrests, detainment, incarceration, repeat convictions), (4) social function (for example, relationships, peer nomination scores, marital status, multiple divorces, activities, hobbies), (5) occupation (for example, employment, military service, job changes, occupation level, socioeconomic status), (6) self-esteem (for example, self-esteem scales, self-perception, suicide ideation, suicide attempts, suicide rate) (7) driving (for example, accidents, traffic violations, license suspensions, driving record), (8) services use (for example, justice system, emergency health care, financial assistance), and (9) obesity (body mass index (BMI), weight).
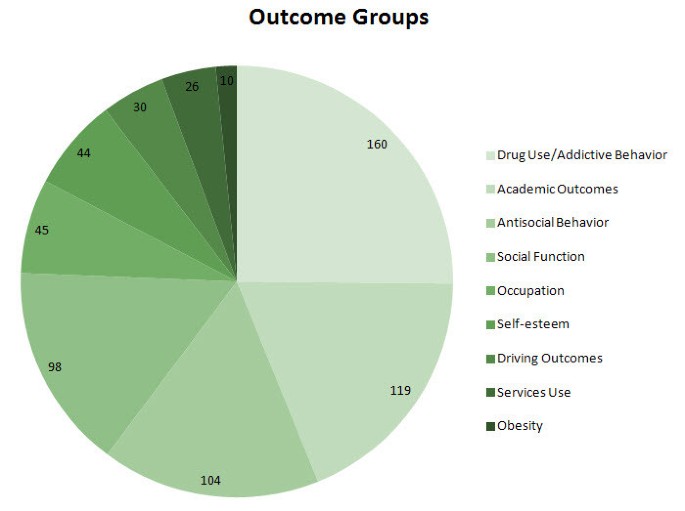
Number of outcome results by group . The pie chart shows the number of outcome results by outcome group. Note that the number of outcomes exceeds the number of studies included, because some studies examined more than one outcome. The greatest number of outcomes was measured for drug use/addictive behavior, followed by academic, antisocial behavior, social function, occupation, self-esteem, driving, services use, and obesity outcomes.
Outcome result frequency
The number of outcome results in each outcome group can be seen in Figure 1 . Drug use/addictive behavior was the most-studied outcome (160 outcome results), followed by academic (119 outcome results), antisocial behavior (104 outcome results), social function (98 outcome results), occupation (45 outcome results) self-esteem (44 outcome results), driving (30 outcome results), and services use (26 outcome results). Obesity was the least studied outcome (ten outcome results). Note that the total number of outcomes results (636) is greater than the total number of studies (351) because some studies reported more than a single outcome result.
Figure 2 shows the total number of studies published per year. There was a noticeable rise in studies of long-term outcomes of ADHD published worldwide between 1980 and 2008. The number of long-term outcome studies published at the peak in 2008 was 42 studies, dropping back to 28 in 2009 and 2010. The mean study length varied little by year, with a total mean of 9 years for which researchers collected data for each subject and range of 2 to 40 years for which researchers collected data for each subject. Data collection refers either to follow-up measures in the case of prospective studies or analysis of past records or reports in the case of retrospective studies.
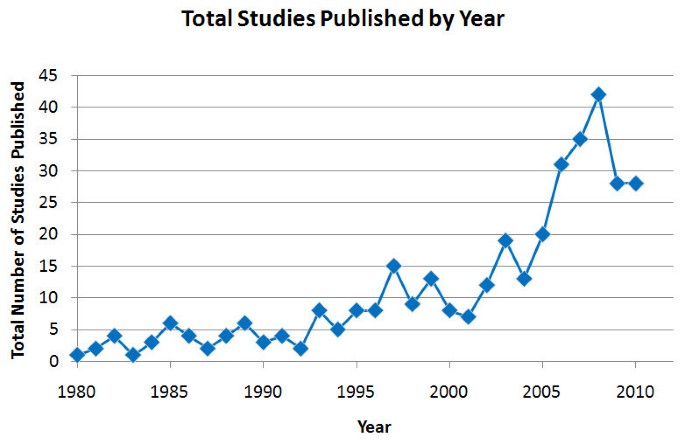
Total number of studies of long-term outcomes of attention deficit hyperactivity disorder (ADHD) published by year .
Participant ages
The ages of the participants were examined by studies of specific outcomes (Figure 3A ). Studies of children with a mid-range or mean age of 6 to 12 years measured services use, self-esteem, social function, academic outcomes, obesity, antisocial behavior, and drug use/addictive behavior, in that order of frequency. All nine outcome groups were measured in adults and adolescents. Within age categories (Figure 3B ), social function and academic outcomes comprised the largest proportion of children outcomes (53%), while drug use/addictive behavior and antisocial behavior comprised the largest proportion of adult and adolescent outcomes (43 and 46%, respectively). A substantial proportion of outcomes in children and adolescents together were self-esteem and social function outcomes (28%).
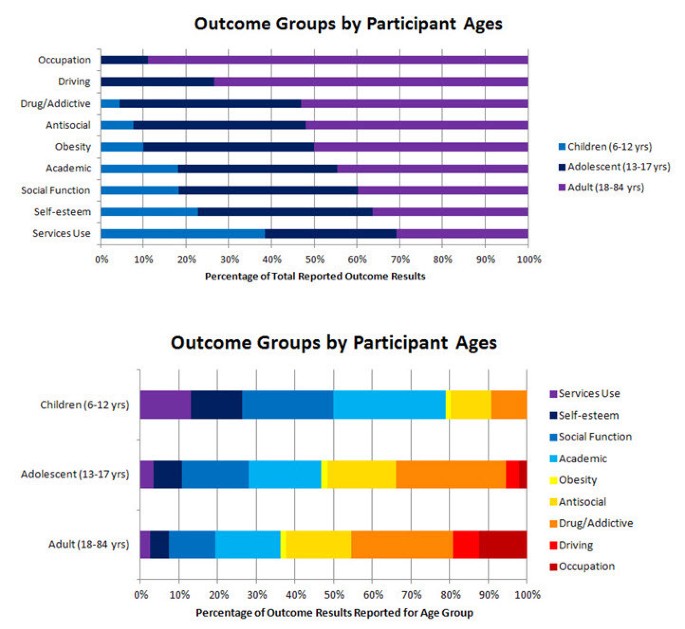
Outcome groups by ages . (A) This graph shows the mid-range/mean ages of the participants measured in studies of specific outcomes. The light blue portion of the bars represent children 6 to 12 years old, the dark blue bars represent adolescents (13 to 17 years) and the violet bars represent adults (18 to 84 years). The greatest proportion of outcomes examined in children can be seen on the bottom (services use), whereas a greater proportion of outcomes examined in adults can be seen on the top (occupation). (B) This graph shows the proportion of outcomes reported within each age category. Each colored section corresponds to the outcomes reported for each outcome group as a proportion of the total number of outcomes reported for that age category.
Outcomes with untreated ADHD
Poorer outcomes were generally observed in untreated participants with ADHD (Figure 4 ). In all, 89 studies showed that people with untreated ADHD had outcomes not substantially different from controls (26% of outcome results), whereas 244 studies showed that untreated participants with ADHD experienced poorer long-term outcomes (74% of outcome results). Note that more outcomes were observed than studies because some studies reported more than one outcome. There were a few studies (6) that reported outcomes (6) for participants with untreated ADHD that were significantly better than non-ADHD controls. The derived or reported effect sizes were not large, and these few outcomes were included in the outcomes that were 'similar' to controls. No single outcome group was represented; the outcomes varied among drug use/addictive behavior, occupation, self-esteem, and social function outcomes.
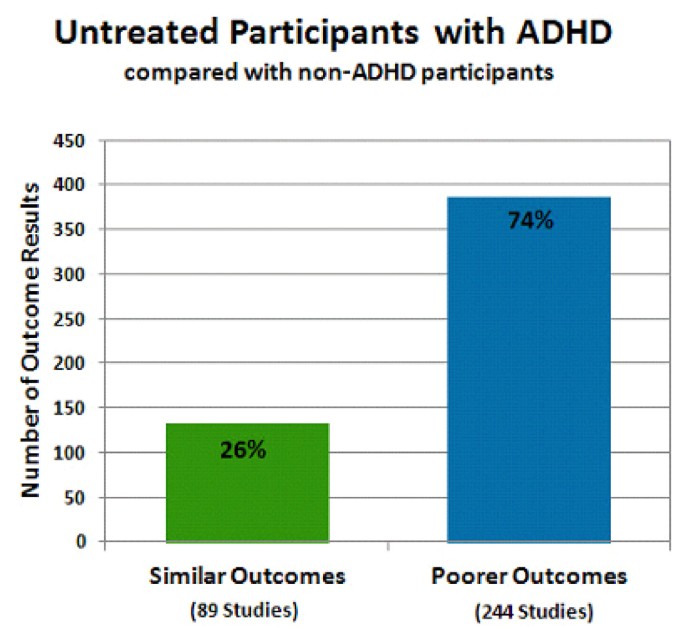
Untreated participants with attention deficit hyperactivity disorder (ADHD) compared with non-ADHD controls . The percentage of the total number of outcomes is provided for each bar. The total number of studies represented in each bar is shown in parentheses. The green bar shows the percentage of outcome results reported as similar (26% of outcomes; 89 studies) in untreated participants with ADHD compared with non-ADHD participants. The blue bar shows the percentage of outcome results reported as poorer (74% of outcomes; 244 studies) in untreated participants with ADHD compared with non-ADHD participants. The sum of the numbers of studies shown under each bar does not equal the total number of studies represented in this figure; several studies reported some outcomes that were similar to control and some outcomes that were poorer than controls. Therefore these studies are represented in both types of outcome.
Also found in the search were five studies that followed untreated participants with ADHD over 2 to 9 years and compared the long-term outcomes with the participants' status at baseline [ 42 – 46 ]. Four of these studies reported a significant deterioration from baseline without treatment [ 42 – 45 ]. Of these four, three reported a deterioration in academic outcomes (increased number of failing grades over 2 years and decline in math and reading scores over 9 years) [ 42 – 44 ] and one [ 45 ] reported a worsening in tobacco use outcomes (levels of salivary cotinine measured daily rose in untreated participants with ADHD over 2 years. Cotinine is an alkaloid from tobacco and a metabolite from nicotine, used as a measure of the number of tobacco cigarettes smoked per day). One study followed untreated participants with ADHD for 8 years into adolescence and reported an improvement in social function compared with the participant's baseline measured at the beginning of the study, although function remained significantly poorer than non-ADHD control levels [ 46 ].
Many studies did not report effect size, and effect sizes varied among studies that did report it. For example, a study of driving outcomes reported a small effect size with a Cohen's d of 0.33 ( P = 0.04) for the difference in the number of traffic accidents in the last 6 months for participants with ADHD (0.29 ± 0.73 accidents) compared with non-ADHD controls (0.15 ± 0.43 accidents), albeit this small effect size represented almost twice the rate of accidents for the ADHD group [ 47 ]. Another study of social function reported a large effect size with a Cohen's d of 1.03 ( P < 0.001) for the difference in the parent-reported peer rejection scores for children with ADHD (0.45 ± 0.55) compared with non-ADHD controls (0.07 ± 0.23), while controlling for conduct disorder as a comorbidity [ 48 ]. It is possible in studies of smaller sample size that there may have been small effects that were not reported as differences, because statistical significance was not demonstrable due to the small sample size. For the purposes of the present analysis, to provide an overall comprehensive synthesis of reported study results, all results were analyzed as reported without additional interpretive changes on our part. Inclusion in this regard was limited by the report having passed through the peer-review process.
Outcomes with ADHD treatment
Treated ADHD versus untreated ADHD was compared in 48 studies with 76 outcomes (Figure 5 ). 'Untreated ADHD' comparators included both pretreatment baseline comparisons and comparison with an untreated group of participants with ADHD. Overall, treatment of ADHD resulted in favorable outcomes for most outcomes reported (55 of 76 outcome results; 72%). Three types of outcome results for which treatment was considered beneficial were: (1) improvement compared with participants with untreated ADHD (38% outcome results), (2) improvement compared with pretreatment baseline (22% outcome results), and (3) stabilization compared with pretreatment baseline (12% outcome results). Stabilization compared to pretreatment baseline was considered a benefit of treatment because it indicated that treatment may have alleviated the natural-course deterioration in outcomes over time that has been observed in separate study samples of untreated ADHD [ 42 , 43 , 45 , 46 ]. None of the studies reporting stabilization compared with pretreatment baseline also included an untreated ADHD group, therefore this is an across-study sample comparison, subject to limitations. Three types of outcome results for which there was considered no benefit with treatment were: (1) no difference compared with participants with untreated ADHD (25% outcome results), (2) poorer outcomes compared with participants with untreated ADHD (1.5% outcomes results), and (3) poorer outcomes compared with pretreatment baseline (1.5% outcomes results). In outcomes for which there was no difference compared with participants with untreated ADHD, while there was no benefit to treatment, there was also no detriment either, such as increased incidence of substance use disorder or increased rate of suicide. No significantly increased incidence of substance abuse disorders or suicide rate compared with participants with untreated ADHD (or compared with pretreatment baseline either) was reported in any study included in this analysis. There was a single outcome following treatment that was worse for participants with untreated ADHD (increased experimentation with cocaine). A single outcome was reported to be worse than pretreatment baseline (greater percentage of study participants with decreased grade point average).
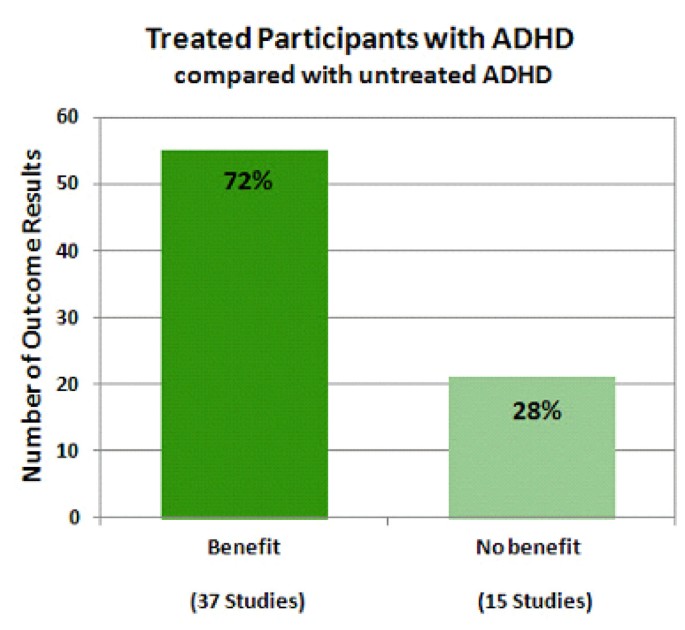
Treated participants with attention deficit hyperactivity disorder (ADHD) compared with untreated ADHD . The percentage of the total number of outcome results is provided for each bar. The total number of studies represented in each bar is shown in parentheses. The dark green bar shows the percentage of outcome results reported as exhibiting benefit (72% of outcomes; 37 studies) in treated participants with ADHD compared with untreated ADHD. The light green bar shows the percentage of outcome results reported as exhibiting no benefit (28% of outcomes; 15 studies) in treated participants with ADHD compared with untreated ADHD. Similar to Figure 4, the sum of the numbers of studies shown under each bar does not equal the total number of studies of this type, because several studies have reported some outcomes that exhibited benefit from treatment and some that did not and so these studies are represented in both types of outcome.
In 42 studies, the outcome results (n = 76) of participants with treated ADHD were compared with the outcomes of non-ADHD controls. Again, more outcomes were observed than studies because some studies reported more than one outcome. Most such studies did not show normalization with treatment. Only 18 outcomes in 16 studies were similar for participants with treated ADHD versus non-ADHD controls. A total of 58 outcomes (76% of outcomes) in 35 studies, poorer outcomes were observed for participants with treated ADHD relative to non-ADHD controls.
Benefit with treatment was analyzed according to specific outcome group for participants with treated versus untreated ADHD (Figure 6 ). Note that this analysis involved the same 48 studies and 76 outcomes in the analysis shown in Figure 5 , with the same 3 conditions considered as beneficial with treatment and the same 3 considered to exhibit no benefit with treatment. For 100% of driving and obesity outcomes reported, treatment of ADHD was beneficial. For 90% of self-esteem outcomes, 83% of social function outcomes, 71% of academic outcomes, 67% of drug use/addictive behavior outcomes, 50% of antisocial behavior outcomes, 50% of services use outcomes and 33% of occupation outcomes, treatment was reported to be beneficial. In the case of services use, less use of services (for example, emergency room visits, financial assistance) was considered to be an improvement with treatment.
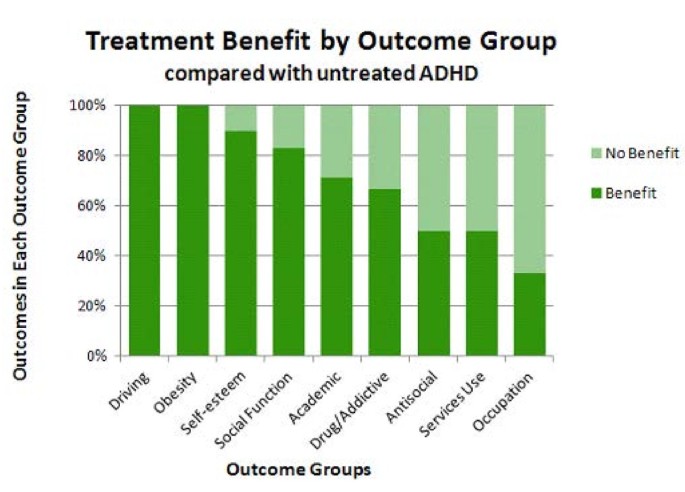
Benefit and no benefit with treatment by outcome group . This graph shows benefit (dark green bars) or no benefit (light green bars) by outcome group in treated participants with attention deficit hyperactivity disorder (ADHD) versus untreated ADHD. Improvement was reported most often in studies of driving and obesity outcomes (left side), with a greater proportion of outcomes reported to exhibit no benefit following treatment compared with no treatment in studies of occupation (right side). An intermediate proportion of studies of self-esteem, social function, academic, drug use/addictive behavior, antisocial behavior, and services use outcomes reported benefit with treatment.
Four of the nine outcome groups exhibited a substantial percentage of no benefit with treatment. These four outcome groups were drug use/addictive behavior, antisocial behavior, services use, and occupation. A subanalysis of these four outcomes examined the post-hoc hypothesis that less aggressive/consistent treatment of ADHD in the rest of the world compared with Northern America (based in part on stricter diagnosis criteria for the International Classification of Diseases , tenth edition (ICD-10) versus the DSM-IV-TR [ 49 , 50 ]) may account for the rate of reported treatment benefit observed in these four outcome groups in Figure 6 . Thus, treatment outcome by region for this subgroup of outcomes was examined (Figure 7 ). For these 4 outcome groups, studies performed in Northern America were evenly split in reporting outcome results exhibiting treatment benefit versus no benefit (11 outcome results each, 50% each). In contrast, studies performed in countries in the rest of the world (all from Europe, in this case) reported a higher percentage of outcome results exhibiting treatment benefit (six of seven outcome results; 86%, four of which were improvement in drug use/addictive behavior outcomes) versus no benefit with treatment (one of seven outcome results; 14%) (Figure 7 ). This result clearly shows that reported results of treatment in the rest of the world do not underlie the higher percentage of outcome results exhibiting no benefit with treatment for these four outcomes. On the contrary, studies from the rest of the world reported a larger percentage of outcomes exhibiting treatment benefits.
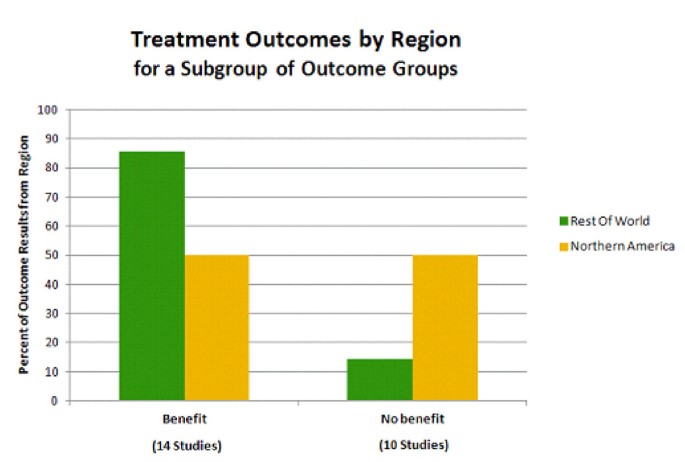
Treatment results by region for a subgroup of outcomes . Outcomes exhibiting benefit versus no benefit with treatment are shown for Northern America (yellow bars) versus the rest of the world (green bars). Note that Northern America includes Canada and the USA, and Rest of World, in this case, consists of countries in Europe. The response to treatment for four outcome groups was included: drug use/addictive behavior, antisocial behavior, services use, and occupation outcomes. The percentage of studies reporting benefit with treatment for these outcomes is greater for the rest of the world compared with Northern America. As in Figure 5, the sum of the numbers of studies shown under each bar does not equal the total number of studies of this type, because a single study reported an outcome that exhibited benefit from treatment and one that did not, and so this study is represented in both types of outcome.
Further analysis of the results observed in Figure 7 showed that this result did not appear to be associated with types of treatment, comparator groups, or outcome groups of interest in Europe compared with Northern America [ 35 ]. A greater percentage, however, of these outcome results from the rest of the world were reported in retrospective studies of adults (3 of 4 studies; 75%) compared with those from Northern America (2 of 19 studies; 11%). The majority of these outcomes from Northern America were reported in prospective studies of various age groups (15 of 19 studies; 79%). Thus, differences in study design may underlie the result shown in Figure 7 . The various treatment types mentioned in all the studies are listed in Additional File 2 . Of the 130 studies that mention treatment, 120 (92%), 49 (38%), and 24 (18%) studies mentioned pharmacological treatment, non-pharmacological treatment, and/or multimodal treatment, respectively.
Overall, the results of the present study show that the long-term outcomes for participants with ADHD when left untreated were poor compared with non-ADHD controls, and that treatment of ADHD improved long-term outcomes, but usually not to the point of normalization. The outcomes that were studied (with ADHD symptoms deliberately excluded as an outcome) most often included drug use/addictive behavior, academic, and antisocial behavior. This was followed by social function, self-esteem, occupation, driving, services use, and obesity outcomes. These trends may reflect what is of most immediate interest to society in a given time period. For example, obesity, the least-studied outcome, has come into interest only recently, likely due to the increasing obesity epidemic in developed countries. Increasing interest in the epidemiology of obesity, led to the report of an association between obesity and ADHD in 2002 [ 51 ]. Our data also indicate that there are specific geographical trends, with academic outcomes being of greater interest for study in the US and Canada and antisocial behaviors of greater interest in Europe. This difference of interest may be a function of only more severe cases, likely to have oppositional-defiant or conduct disorder comorbidity, being diagnosed outside Northern America. These trends have been described in more detail in a separate publication [ 35 ].
The number of studies of long-term outcomes of ADHD has risen noticeably over the last 30 years, especially since 2000. This corresponds to a trend in awareness of the consequences of ADHD by clinicians, which appears to be on the rise [ 52 ].
Treatment resulted in beneficial effects for many of the outcomes reported (72% of outcome results). These beneficial effects were observed as either significant improvement over pretreatment baseline, in comparison to untreated ADHD participants, or stabilization of the outcomes (that is, prevention of the deterioration over time from baseline reported with untreated ADHD [ 43 – 46 ]). Driving and obesity outcomes were the most often reported to be responsive to treatment. Of course, a decrease in obesity may be due to an appetite suppressant effect of stimulants and atomoxetine. The relatively small number of studies of these two outcomes (two studies each) comparing treated with untreated ADHD and the consistently positive response to treatment support further investigation in these areas. Three other outcomes that were often reported to be responsive to treatment were self-esteem, social function, and academic outcomes. These results are supported by a relatively large number of studies (10, 12, and 21 studies, respectively) comparing participants with treated ADHD with participants with untreated ADHD. These outcomes may be more closely related to symptom relief. The outcomes reported are not independent of one another and changes in one may reflect changes in others. The wider effects of response to treatment in these two areas may warrant further investigation.
The four remaining outcomes that appeared to be least responsive to treatment were drug use/addictive behavior, antisocial behavior, services use, and occupation, with 67%, 50%, 50%, and 33% of reported outcome results demonstrating a benefit of treatment, respectively. Persistence in these cases may have to do with the existence of comorbidities, such as conduct disorder, which has for example, been associated with increased substance use disorders [ 53 ]. Oppositional defiant disorder or conduct disorder, may contribute to long-term outcomes in people with ADHD, specifically crime and substance use [ 54 – 56 ], and thus may affect the response observed for these outcomes with treatment for ADHD. Other comorbidities, such as depression, obsessive-compulsive disorder, or autism may have similarly influenced the results we observed.
Services use may persist due to the incomplete amelioration of ADHD symptoms and impairments, possibly because although ADHD symptoms (like outcomes) respond to treatment, they are not completely normalized. Finally, continued impairment in occupation despite treatment may reflect the cumulative effects of ADHD symptoms and dysfunctioning over the lifespan. For example, low academic grades may later restrict employment or opportunities, impaired social function may precipitate extra friction with employers. The differential responsiveness of different outcomes to treatment is an intriguing area for future study.
It should be mentioned that if we had categorized the study outcomes by age, such as 5 to 17 and over 18, we may have observed different areas of improvement depending on the age group. In combining the groups it is possible that this distinction is lost. One also needs to consider however, that certain categories such as occupation would not be as relevant to the 5 to 17 age group as opposed to academic achievement, which would apply to all groups.
Even with treatment, worse outcomes were often reported for the ADHD group than for people without ADHD. This is not surprising, because although behavioral and drug treatment have been demonstrated to improve ADHD symptoms, these treatments do not necessarily normalize behavior to control levels [ 35 , 57 – 61 ].
For example, in one study of the effect of methylphenidate treatment on classroom measures, a 20 mg dose produced normalization in 30% to 60% of participants, (depending on the measurement used) although 53% to 94% showed improvement [ 58 ]. Many studies (42) in our analysis evaluated treatment effects only against non-ADHD controls, as opposed to pretreatment baseline or any untreated state. In these studies, only 24% of outcomes were reported to be similar for treated ADHD and non-ADHD controls. For all the other outcomes reported (76%), the outcomes remained worse than non-ADHD controls, and there was no mechanism with this study design by which to measure improvement with treatment that did not completely 'normalize' the outcome. In studies with other study designs (comparing participants with treated ADHD and participants with untreated ADHD or pretreatment baseline), benefit with treatment was reported for 72% of the outcomes. These study designs allowed the improvement with treatment to be demonstrated, even though the outcome may not have 'normalized'. When considering the effects of treatment reported in any one study, the comparator group used to evaluate the effectiveness of ADHD treatment is particularly important.
The results of four studies included in this analysis that used both types of comparators within the same study ((1) non-ADHD controls and (2) untreated ADHD participants or ADHD participant's pretreatment baseline) were consistent with the present overall observations that there was clear improvement or stabilization with treatment of ADHD for social function, antisocial behavior, and academic outcomes, but not to the extent that non-ADHD control outcomes were matched [ 13 , 39 , 48 , 62 ]. This general pattern was noticed in the earliest of the four studies, as the authors conclude in their 12-year follow-up study that 'The most striking finding of the study is the repetitive pattern of finding significant differences between the stimulant-treated hyperactives and their control group (with the control group almost invariably doing better). However, there are several areas in which the stimulant-treated hyperactives seem to do better than their untreated counterparts' (referring to academic, driving, self-esteem, and social function outcomes) [ 13 ]. This pattern was also found in an 8-year follow-up study of a different sample 'despite overall maintenance of improvement in functioning relative to baseline (pretreatment), the MTA group as a whole was functioning significantly less well than the non-ADHD classmate sample' [ 39 ]. In the present study, this pattern was broadly replicated across the outcome groups when analyzed individually. Comparisons against non-ADHD controls only, may mask improvements with treatment.
It should be noted that ADHD Rating Scale IV total scores decline (improve) between ages 5 to 7 and ages 14 to 18 in both Caucasians and African-Americans (although in Latinos they actually increase during these time periods). Hyperactivity-impulsivity scores, especially, decline from ages 4 to 7 to age 14 and older in both boys and girls [ 63 ]. Therefore, we cannot discount that natural decline in symptoms (and possibly other dysfunctions) occurring over time also contributes to the improvement in outcomes observed with treatment, although this idea contradicts the reported worsening of functional domains in untreated ADHD. According to one paper, symptoms and functioning are related. With full symptom remission, illicit drug use and antisocial behaviors become similar to non-ADHD controls, but while social function improves, it does not reach non-ADHD levels [ 64 ].
Finally, we observed that treatment outcomes for the subgroup of domains that exhibit lower percentages of outcomes that benefit from treatment (drug use/addictive behavior, antisocial behavior, services use, and occupation) were differentially improved when studies from Northern America were compared with those from the rest of the world (in this case, all 'Rest of World' studies were from Europe). Based on this analysis there appears to be a geographical bias with regard to how responsive these four outcome group results are reported to be with treatment, a result that may be accounted for by regional differences in study design along with the resulting study population age, or diagnostic practices. In this very specific comparison, the numbers of studies from 'Rest of World' countries are low (four studies, seven outcome results), thus as further investigation of these outcomes around the world are published, the results of this comparison may be clarified.
Limitations and possible sources of bias
Several possible risks of bias and limitations need to be considered regarding the included studies. First, a publication and cultural bias could have resulted from including only studies that were published in English. In addition, the analysis excluded unpublished studies that might have been presented at conferences, for example. Also, our search relied on search engines for 'peer reviewed' status. Moreover, by strictly adhering to Cochrane systematic review guidelines and only including studies that were identified in our original electronic search, it is possible that some relevant studies may have been missed, introducing a search engine and literature database bias. This bias was reduced by extensive searching of 12 databases. Nonetheless, we are aware of four studies that would have met inclusion criteria, but were not identified by the search engines due to a technical limitation or inadvertent search string exclusion. Examination of these studies shows that the reported results are consistent with the overall results of the present analysis. The results of these four studies are summarized briefly here. One study reported poorer outcomes for participants with ADHD versus non-ADHD controls with regard to academic achievement, occupational adjustment, antisocial behavior, relationships, and substance use [ 65 ]. A second study found a high incidence of ADHD (65%) in 23 adolescents who attempted suicide [ 66 ]. A third study reported that by young adulthood, participants with ADHD were similar to non-ADHD controls in minor aspects of social and occupational outcomes (e.g., time socializing with friends and with hobbies), but had poorer outcomes in major aspects of these outcomes (e.g., had many more offspring and most were not living with them) [ 67 ]. A fourth study found that stimulant treatment in children with ADHD significantly improved reading scores and decreased grade retention [ 68 ]. The results of these studies are consistent with our overall finding that untreated ADHD is associated with poor long-term outcomes and that these outcomes improve with treatment.
Researcher bias could also be a possible source of bias in this analysis, however, this was reduced by having two researchers independently agree on the articles included and strict, simple inclusion criteria were established prior to searching.
Other sources of bias could include biases of individual research groups, which was eliminated by including only electronically identified studies (as mentioned above) and not selectively including the studies of specific groups and omitting others. As observed, different study designs may also lead to different conclusions and taking comparators into consideration is critical. We included studies of various designs, which may minimize such bias.
A further possible bias could arise from changes over time in diagnostic criteria or discrepancy between classification systems, specifically differences in the definition of hyperkinetic disorder (ICD-9 or ICD-10) versus ADHD (DSM-III/DSM-III-R/DSM-IV). Differences are less likely within classification systems [ 3 ]. One study found that 93% of children diagnosed with ADHD using DSM-III-R diagnosis also received a DSM-IV ADHD diagnosis, indicating good correspondence between classification systems [ 69 ]. Rediagnosis of the MTA sample by ICD criteria, however, resulted in only 25% of the DSM-IV-diagnosed MTA sample of combined-type ADHD qualifying as having hyperkinetic disorder or hyperkinetic conduct disorder by ICD-10 criteria [ 69 ].
The present analysis supports the premise that without treatment, people with ADHD often experience poorer long-term outcomes and that treatment may improve the long-term outcomes of ADHD for some individuals, but not necessarily to the degree of healthy controls. Further analyses of the present data set will more comprehensively examine the impact of treatment on specific outcomes, as well as the impact of specific types of treatment modalities. The question remains as to whether the short-term benefits demonstrated by short-term drug or non-pharmacological treatment studies translate directly into long-term outcomes. Associations between specific short-term symptoms need to be examined as possible predictors for long-term outcomes, particularly because long-term studies are not always feasible. Future research should focus on the association between short-term symptom relief and long-term consequences and include longer-term follow-up of the consequences of childhood ADHD into the adult years.
Authors' information
MS was previously International Medical Director Clinical Development at Shire Pharmaceuticals and is currently Development Therapy Area Director at Norgine Pharmaceuticals. PH is Senior Director Global Health Economics & Outcomes Research at Shire Development LLC. HC is a Child and Adolescent Psychiatrist at Hôpitaux Pédiatriques de Nice CHU Lenval. SY is a Senior Lecturer in Forensic Clinical Psychology at King's College London, Institute of Psychiatry. JK is Founder and Chief Editor at BPS, International in San Diego, California. AGW is a consultant for BPS International, was formerly a consultant for Shire Development LLC, and is currently a Research Assistant Professor of Chemistry and Biomolecular Science, at Clarkson University in Potsdam, New York. LEA is a Child Psychiatrist, Educator, Professor Emeritus of Psychiatry, and a Principal Investigator in the Psychopharmacology and Related Research Program at the Ohio State University Nisonger Center.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders. 2000, Arlington, VA: American Psychiatric Association, text revision, 4
Google Scholar
World Health Organization: International Classification of Diseases. 1992, Geneva, Switzerland: WHO, 10
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA: The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007, 164: 942-948. 10.1176/appi.ajp.164.6.942.
Article PubMed Google Scholar
Polanczyk G, Rohde LA: Epidemiology of attention-deficit/hyperactivity disorder across the lifespan. Curr Opin Psychiatry. 2007, 20: 386-392. 10.1097/YCO.0b013e3281568d7a.
Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, De Girolamo G, Haro JM, Karam EG, Lara C, Lépine JP, Ormel J, Posada-Villa J, Zaslavsky AM, Jin R: Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007, 190: 402-409. 10.1192/bjp.bp.106.034389.
Article CAS PubMed Google Scholar
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM: The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006, 163: 716-723. 10.1176/appi.ajp.163.4.716.
Article PubMed PubMed Central Google Scholar
Faraone SV, Biederman J, Mick E: The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006, 36: 159-165.
Lara C, Fayyad J, de Graaf R, Kessler RC, Aguilar-Gaxiola S, Angermeyer M, Demytteneare K, de Girolamo G, Haro JM, Jin R, Karam EG, Lépine JP, Mora ME, Ormel J, Posada-Villa J, Sampson N: Childhood predictors of adult attention-deficit/hyperactivity disorder: results from the World Health Organization World Mental Health Survey Initiative. Biol Psychiatry. 2009, 65: 46-54. 10.1016/j.biopsych.2008.10.005.
Biederman J, Faraone S, Milberger S, Curtis S, Chen L, Marrs A, Ouellette C, Moore P, Spencer T: Predictors of persistence and remission of ADHD into adolescence: results from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1996, 35: 343-351. 10.1097/00004583-199603000-00016.
Biederman J, Petty CR, Clarke A, Lomedico A, Faraone SV: Predictors of persistent ADHD: an 11-year follow-up study. J Psychiatr Res. 2011, 45: 150-155. 10.1016/j.jpsychires.2010.06.009.
Gittelman R, Mannuzza S, Shenker R, Bonagura N: Hyperactive boys almost grown up. I. Psychiatric status. Arch Gen Psychiatry. 1985, 42: 937-947. 10.1001/archpsyc.1985.01790330017002.
Hart EL, Lahey BB, Loeber R, Applegate B, Frick PJ: Developmental change in attention-deficit hyperactivity disorder in boys: a four-year longitudinal study. J Abnorm Child Psychol. 1995, 23: 729-749. 10.1007/BF01447474.
Hechtman L, Weiss G, Perlman T: Young adult outcome of hyperactive children who received long-term stimulant treatment. J Am Acad Child Psychiatry. 1984, 23: 261-269. 10.1016/S0002-7138(09)60501-X.
Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M: Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry. 1993, 50: 565-576. 10.1001/archpsyc.1993.01820190067007.
Weiss G, Hechtman L, Milroy T, Perlman T: Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Psychiatry. 1985, 24: 211-220. 10.1016/S0002-7138(09)60450-7.
Young S, Amarasinghe JM: Practitioner review: non-pharmacological treatments for ADHD: a lifespan approach. J Child Psychol Psychiatry. 2010, 51: 116-133. 10.1111/j.1469-7610.2009.02191.x.
Hartocollis P: The syndrome of minimal brain dysfunction in young adult patients. Bull Menninger Clin. 1968, 32: 102-114.
CAS PubMed Google Scholar
Arnold LE, Strobl D, Weisenberg A: Hyperkinetic adult. Study of the "paradoxical" amphetamine response. JAMA. 1972, 222: 693-694. 10.1001/jama.1972.03210060047012.
Gilchrist RH, Arnold EL: Long-term efficacy of ADHD pharmacotherapy in children. Pediatr Ann. 2008, 37: 46-51. 10.3928/00904481-20080101-05.
Young S, Murphy CM, Coghill D: Avoiding the 'twilight zone': guidance and recommendations on ADHD and the transition between child and adult services. BMC Psychiatry. 2011, 11: 174-10.1186/1471-244X-11-174.
Emilsson B, Gudjonsson G, Sigurdsson JF, Baldursson G, Einarsson E, Olafsdottir H, Young S: Cognitive behaviour therapy in medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. BMC Psychiatry. 2011, 11: 116-10.1186/1471-244X-11-116.
National Institute for Health and Clinical Excellence: Attention deficit hyperactivity disorder: the NICE guideline on diagnosis and management of adhd in children, young people and adults. 2009, Leicester, UK: The British Psychological Society and The Royal College of Psychiatrists
Kooij SJ, Bejerot S, Blackwell A, Caci H, Casas-Brugué M, Carpentier PJ, Edvinsson D, Fayyad J, Foeken K, Fitzgerald M, Gaillac V, Ginsberg Y, Henry C, Krause J, Lensing MB, Manor I, Niederhofer H, Nunes-Filipe C, Ohlmeier MD, Oswald P, Pallanti S, Pehlivanidis A, Ramos-Quiroga JA, Rastam M, Ryffel-Rawak D, Stes S, Asherson P: European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD. BMC Psychiatry. 2010, 10: 67-10.1186/1471-244X-10-67.
Agency for Healthcare Research and Quality: Treatment of Attention-Deficit/Hyperactivity Disorder. 1999, Rockville, MD: US Department of Health and Human Services, 11.
American Academy of Pediatrics: Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000, 105: 1158-1170.
Article Google Scholar
Canadian Attention Deficit Hyperactivity Disorder Resource Alliance: Canadian ADHD Practice Guidelines (CAP-Guidelines). 2011, Toronto, Canada: Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA)
Coghill D, Danckaerts M, Sonuga-Barke E, Sergeant J: Practitioner review: quality of life in child mental health--conceptual challenges and practical choices. J Child Psychol Psychiatry. 2009, 50: 544-561. 10.1111/j.1469-7610.2009.02008.x.
Ebert D, Krause J, Roth-Sackenheim C: ADHD in adulthood--guidelines based on expert consensus with DGPPN support [in German]. Nervenarzt. 2003, 74: 939-946.
National Health and Medical Research Council: Australian Guidelines on Attention Deficit Hyperactivity Disorder (ADHD). 2009, Sydney, Australia: The Royal Australasian College of Physicians
Nutt DJ, Fone K, Asherson P, Bramble D, Hill P, Matthews K, Morris KA, Santosh P, Sonuga-Barke E, Taylor E, Weiss M, Young S, British Association for Psychopharmacology: Evidence-based guidelines for management of attention-deficit/hyperactivity disorder in adolescents in transition to adult services and in adults: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2007, 21: 10-41.
Pliszka S: Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007, 46: 894-921.
Scottish Intercollegiate Guidelines Network: Management of attention deficit and hyperkinetic disorders in children and young people: a national clinical guideline. 2009, Edinburgh, UK: Scottish Intercollegiate Guidelines Network
Canadian Agency for Drugs and Technologies in Health: Quality Assessment of the Canadian Attention Deficit Hyperactivity Disorder Resource Alliance ADHD Practice Guidelines in Adults with ADHD. 2011, Toronto, Canada: Canadian Agency for Drugs and Technologies in Health
McDonagh M, Christensen V, Peterson K, Thakurta S: Pharmacologic treatments for attention deficit hyperactivity disorder. Drug class review. 2009, Portland, OR: Oregon Health & Science University
Hodgkins P, Arnold LE, Shaw M, Caci H, Kahle J, Woods AG, Young S: A systematic review of global publication trends regarding long-term outcomes of ADHD. Front Psychiatry. 2011, 2: 84.
PubMed Google Scholar
MTA: A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999, 56: 1073-1086. 10.1001/archpsyc.56.12.1073.
Conners CK, Epstein JN, March JS, Angold A, Wells KC, Klaric J, Swanson JM, Arnold LE, Abikoff HB, Elliott GR, Greenhill LL, Hechtman L, Hinshaw SP, Hoza B, Jensen PS, Kraemer HC, Newcorn JH, Pelham WE, Severe JB, Vitiello B, Wigal T: Multimodal treatment of ADHD in the MTA: an alternative outcome analysis. J Am Acad Child Adolesc Psychiatry. 2001, 40: 159-167. 10.1097/00004583-200102000-00010.
Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, Clevenger W, Davies M, Elliott GR, Greenhill LL, Hechtman L, Hoza B, Jensen PS, March JS, Newcorn JH, Owens EB, Pelham WE, Schiller E, Severe JB, Simpson S, Vitiello B, Wells K, Wigal T, Wu M: Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2001, 40: 168-179. 10.1097/00004583-200102000-00011.
Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Epstein JN, Hoza B, Hechtman L, Abikoff HB, Elliott GR, Greenhill LL, Newcorn JH, Wells KC, Wigal T, Gibbons RD, Hur K, Houck PR, MTA Cooperative Group: The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009, 48: 484-500. 10.1097/CHI.0b013e31819c23d0.
Banaschewski T, Buitelaar J, Coghill DR, Sergeant JA, Sonuga-Barke E, Zuddas A, Taylor E: The MTA at 8. J Am Acad Child Adolesc Psychiatry. 2009, 48: 1120-1121. 10.1097/CHI.0b013e3181bac557.
Pliszka SR: The MTA at 8. J Am Acad Child Adolesc Psychiatry. 2009, 48: 1122-10.1097/CHI.0b013e3181ba3dd9.
Powers RL, Marks DJ, Miller CJ, Newcorn JH, Halperin JM: Stimulant treatment in children with attention-deficit/hyperactivity disorder moderates adolescent academic outcome. J Child Adolesc Psychopharmacol. 2008, 18: 449-459. 10.1089/cap.2008.021.
Schultz BK, Evans SW, Serpell ZN: Preventing failure among middle school students with attention deficit hyperactivity disorder: a survival analysis. School Psych Rev. 2009, 38: 14-27.
Weithorn CJ, Marcus M: High-active children and achievement tests: a two-year follow-up. Psychol Schools. 1985, 449-458.
Whalen CK, Jamner LD, Henker B, Gehricke JG, King PS: Is there a link between adolescent cigarette smoking and pharmacotherapy for ADHD?. Psychol Addict Behav. 2003, 17: 332-335.
Fischer M, Barkley RA, Fletcher KE, Smallish L: The stability of dimensions of behavior in ADHD and normal children over an 8-year followup. J Abnorm Child Psychol. 1993, 21: 315-337. 10.1007/BF00917537.
Thompson AL, Molina BS, Pelham W, Gnagy EM: Risky driving in adolescents and young adults with childhood ADHD. J Pediatr Psychol. 2007, 32: 745-759. 10.1093/jpepsy/jsm002.
Bagwell CL, Molina BSG, Pelham WE, Hoza B: Attention-deficit hyperactivity disorder and problems in peer relations: predictions from childhood to adolescence. J Am Acad Child Adolesc Psychiatry. 2001, 40: 1285-1292. 10.1097/00004583-200111000-00008.
European Medicines Agency: Guideline on the clinical investigation of medicinal products for the treatment of attention deficit hyperactivity disorder (ADHD). 2010, London, UK: European Medicines Agency
Lange KW, Reichl S, Lange KM, Tucha L, Tucha O: The history of attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2010, 2: 241-255. 10.1007/s12402-010-0045-8.
Altfas JR: Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry. 2002, 2: 9-10.1186/1471-244X-2-9.
Schonwald A, Lechner E: Attention deficit/hyperactivity disorder: complexities and controversies. Curr Opin Pediatr. 2006, 18: 189-195. 10.1097/01.mop.0000193302.70882.70.
Carpentier PJ, Knapen LJ, van Gogh MT, Buitelaar JK, De Jong CA: Addiction in developmental perspective: influence of conduct disorder severity, subtype, and attention-deficit hyperactivity disorder on problem severity and comorbidity in adults with opioid dependence. J Addict Dis. 2012, 31: 45-59. 10.1080/10550887.2011.642756.
Fergusson DM, Boden JM, Horwood LJ: Classification of behavior disorders in adolescence: scaling methods, predictive validity, and gender differences. J Abnorm Psychol. 2010, 119: 699-712.
Gudjonsson GH, Sigurdsson JF, Sigfusdottir ID, Young S: An epidemiological study of ADHD symptoms among young persons and the relationship with cigarette smoking, alcohol consumption, and illicit drug use. J Child Psychol Psychiatry. 2012, 53: 304-312. 10.1111/j.1469-7610.2011.02489.x.
Gudjonsson GH, Sigurdsson JF, Sigfusdottir ID, Young S: A national epidemiological study of offending and its relationship with ADHD symptoms, co-morbid psychological problems, conduct disorder, peer delinquency and illicit drug use. J Atten Disord.
Abikoff H, Gittelman R: Does behavior therapy normalize the classroom behavior of hyperactive children?. Arch Gen Psychiatry. 1984, 41: 449-454. 10.1001/archpsyc.1984.01790160035003.
Rapport MD, Denney C, DuPaul GJ, Gardner MJ: Attention deficit disorder and methylphenidate: normalization rates, clinical effectiveness, and response prediction in 76 children. J Am Acad Child Adolesc Psychiatry. 1994, 33: 882-893. 10.1097/00004583-199407000-00015.
MTA Cooperative Group: National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: changes in effectiveness and growth after the end of treatment. Pediatrics. 2004, 113: 762-769.
MTA Cooperative Group: National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: 24-month outcomes of treatment strategies for attention-deficit/hyperactivity disorder. Pediatrics. 2004, 113: 754-761.
Jensen PS, Arnold LE, Swanson JM, Vitiello B, Abikoff HB, Greenhill LL, Hechtman L, Hinshaw SP, Pelham WE, Wells KC, Conners CK, Elliott GR, Epstein JN, Hoza B, March JS, Molina BS, Newcorn JH, Severe JB, Wigal T, Gibbons RD, Hur K: 3-year follow-up of the NIMH MTA study. J Am Acad Child Adolesc Psychiatry. 2007, 46: 989-1002. 10.1097/CHI.0b013e3180686d48.
Molina BS, Flory K, Hinshaw SP, Greiner AR, Arnold LE, Swanson JM, Hechtman L, Jensen PS, Vitiello B, Hoza B, Pelham WE, Elliott GR, Wells KC, Abikoff HB, Gibbons RD, Marcus S, Conners CK, Epstein JN, Greenhill LL, March JS, Newcorn JH, Severe JB, Wigal T: Delinquent behavior and emerging substance use in the MTA at 36 months: prevalence, course, and treatment effects. J Am Acad Child Adolesc Psychiatry. 2007, 46: 1028-1040. 10.1097/chi.0b013e3180686d96.
DuPaul GJ, Power TJ, Anastopoulos AD, Reid R: ADHD rating scale-IV: checklists norms and interpretations. 1998, New York, NY: The Guilford Press
Young S, Gudjonsson GH: Growing out of ADHD: the relationship between functioning and symptoms. J Atten Dis. 12: 162-169.
Young S, Toone B, Tyson C: Comorbidity and psychosocial profile of adults with Attention Deficit Hyperactivity Disorder. Personal Individ Diff. 2003, 35: 743-755. 10.1016/S0191-8869(02)00267-2.
Manor I, Gutnik I, Ben-Dor DH, Apter A, Sever J, Tyano S, Weizman A, Zalsman G: Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents - a pilot study. Eur Psychiatry. 2010, 25: 146-150.
Fischer M, Barkley R: Young adult outcomes of children with hyperactivity: leisure, financial, and social activities. Internat J Disabil Devel Educ. 2006, 53: 229-245. 10.1080/10349120600716182.
Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ: Long-term school outcomes for children with attention-deficit/hyperactivity disorder: a population-based perspective. J Dev Behav Pediatr. 2007, 28: 265-273. 10.1097/DBP.0b013e31811ff87d.
Santosh PJ, Taylor E, Swanson J, Wigal T, Chuang S, Davies M, Greenhill L, Newcorn J, Arnold LE, Jensen P, Vitiello B, Elliott G, Hinshaw S, Hechtman L, Abikoff H, Pelham W, Hoza B, Molina B, Wells K, Epstein J, Posner M: Refining the diagnoses of inattention and overactivity syndromes: a reanalysis of the multimodal treatment study of attention deficit hyperactivity disorder (ADHD) based on ICD-10 criteria for hyperkinetic disorder. Clinical Neurosci Res. 2005, 5: 307-314. 10.1016/j.cnr.2005.09.010.
Shaw M, Caci H, Hodgkins P, Kahle J, Callamaras N, Woods A: Review of studies of ADHD: long-term outcomes with and without treatment. Eur Psychiatry. 2011, 26 (Suppl 1): 579.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1741-7015/10/99/prepub
Download references
Acknowledgements
The authors would like to thank Dr. Nicholas Callamaras for help with identifying included studies, analyses, and drafting figures, Dr. Amina Elsner for comments on the manuscript, and Anne Thomson for extensive assistance with reference retrieval.
Author information
Authors and affiliations.
Clinical Development & Medical Affairs, Shire Pharmaceuticals, Ltd, Basingstoke, UK
Monica Shaw
Global Health Economics & Outcomes Research, Shire Development LLC, 725 Chesterbrook Boulevard, Wayne, PA, 19087, USA
Paul Hodgkins
Child and Adolescent Psychiatry Hôpitaux Pédiatriques de Nice CHU Lenval, 57, Avenue de la Californie, F-06200, Nice, France
King's College London, Institute of Psychiatry, De Crespigny Park, London, SE5 8AF, UK
Susan Young
BPS International, 3830 Valley Centre #705 PMB503, San Diego, CA, 92130, USA
Jennifer Kahle
Biochemistry and Proteomics Laboratory, Chemistry and Biomolecular Science, Science Center, Room 158, Clarkson University, Potsdam, New York, 13699, USA
Alisa G Woods
Research Unit on Pediatric Psychopharmacology, 207 McCampbell Hall, Ohio State University, Ohio, 43219-1257, USA
L Eugene Arnold
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Paul Hodgkins .
Additional information
Competing interests.
MS was an employee of Shire Pharmaceuticals, Ltd. when this analysis was conducted and when this manuscript was drafted. PH is an employee of Shire Development LLC, owns Shire stock and has stock options. HC has received consulting fees from Shire (nothing for contributing to this article). SY has received research funding or consulting fees from Janssen-Cilag, Eli-Lilly, Novatis, Flynn-Pharma and Shire (nothing for contributing to this article). She was a member of the UK NICE Guideline Development Group for ADHD. JK is owner of BPS International. BPS International received funding from Shire Development LLC to perform this analysis and participate in writing this manuscript. AGW is a consultant for BPS International and has been a consultant for Shire Development LLC. LEA has received research funding or consulting fees from Astrazeneca, Biomarin, Curemark, Lilly, Novartis, Noven, Seaside Therapeutics, and Shire (nothing for contributing to this article). Funded by Shire Development LLC, Wayne PA. An earlier version of this analysis was presented as a poster [ 70 ].
Authors' contributions
All authors participated in designing and interpreting this analysis. JK, MS, and AW oversaw the literature search and analysis. All authors participated in writing portions of this manuscript and in reviewing and approving all manuscript drafts.
Monica Shaw, Paul Hodgkins contributed equally to this work.
Electronic supplementary material
12916_2012_589_moesm1_esm.doc.
Additional file 1: Search strategy details. These are the specific details of the search strategy used in this systematic review. (DOC 88 KB)
12916_2012_589_MOESM2_ESM.DOC
Additional file 2: Treatment types reported in the included studies. This list includes all the treatments mentioned in any study. Often a treatment may have been listed in the Methods of a study but no details were provided about dose or duration or age of treatment or frequency of treatment or separate connection to a specific outcome result, for example. It was possible to group treatment types by large category (pharmacological, non-pharmacological, or MMT) and pool the reported outcomes in these categories. (DOC 26 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, authors’ original file for figure 7, rights and permissions.
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Shaw, M., Hodgkins, P., Caci, H. et al. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Med 10 , 99 (2012). https://doi.org/10.1186/1741-7015-10-99
Download citation
Received : 16 July 2012
Accepted : 04 September 2012
Published : 04 September 2012
DOI : https://doi.org/10.1186/1741-7015-10-99
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Study Protocol
- Open access
- Published: 12 March 2024
The short- and longer-term effects of brief behavioral parent training versus care as usual in children with behavioral difficulties: study protocol for a randomized controlled trial
- Roos S. van Doornik 1 , 2 ,
- Saskia van der Oord 3 ,
- Joli Luijckx 4 ,
- Annabeth P. Groenman 1 , 2 , 5 ,
- Patty Leijten 5 ,
- Marjolein Luman 6 , 7 ,
- Pieter J. Hoekstra 1 , 2 ,
- Barbara J. van den Hoofdakker 1 , 2 , 8 na1 &
- Tycho J. Dekkers 1 , 10 , 2 , 7 , 9 na1
BMC Psychiatry volume 24 , Article number: 203 ( 2024 ) Cite this article
150 Accesses
Metrics details
The access to and uptake of evidence-based behavioral parent training for children with behavioral difficulties (i.e., oppositional, defiant, aggressive, hyperactive, impulsive, and inattentive behavior) are currently limited because of a scarcity of certified therapists and long waiting lists. These problems are in part due to the long and sometimes perceived as rigid nature of most evidence-based programs and result in few families starting behavioral parent training and high dropout rates. Brief and individually tailored parenting interventions may reduce these problems and make behavioral parent training more accessible. This protocol paper describes a two-arm, multi-center, randomized controlled trial on the short- and longer-term effectiveness and cost-effectiveness of a brief, individually tailored behavioral parent training program for children with behavioral difficulties.
Parents of children aged 2–12 years referred to a child mental healthcare center are randomized to (i) three sessions of behavioral parent training with optional booster sessions or (ii) care as usual. To evaluate effectiveness, our primary outcome is the mean severity of five daily ratings by parents of four selected behavioral difficulties. Secondary outcomes include measures of parent and child behavior, well-being, and parent–child interaction. We explore whether child and parent characteristics moderate intervention effects. To evaluate cost-effectiveness, the use and costs of mental healthcare and utilities are measured. Finally, parents’ and therapists’ satisfaction with the brief program are explored. Measurements take place at baseline (T0), one week after the brief parent training, or eight weeks after baseline (in case of care as usual) (T1), and six months (T2) and twelve months (T3) after T1.
The results of this trial could have meaningful societal implications for children with behavioral difficulties and their parents. If we find the brief behavioral parent training to be more (cost-)effective than care as usual, it could be used in clinical practice to make parent training more accessible.
Trial registration
The trial is prospectively registered at ClinicalTrials.gov (NCT05591820) on October 24th, 2022 and updated throughout the trial.
Behavioral difficulties, including oppositional, defiant, aggressive, hyperactive, impulsive, and inattentive behavior, are one of the most common reasons for referral to mental healthcare among children and adolescents [ 1 , 2 ]. When left untreated, problems may exacerbate and put children at risk of adverse outcomes later on in life, such as school dropout, delinquency, substance use and depression [ 3 , 4 ]. Ideally, treatment should prevent this escalation of problems, reduce the need for long and intensive treatments, and lower societal costs [ 5 ]. Behavioral parent training is the first psychosocial treatment of choice for reducing behavioral difficulties in preschool and school aged children [ 6 , 7 , 8 , 9 , 10 , 11 , 12 ]. However, its use in clinical practice is limited by a scarcity of certified therapists, long waiting lists, and the typically long and sometimes perceived as rigid nature of behavioral parent training programs, which may lead to parents not starting or finishing behavioral parent training [ 13 , 14 , 15 ]. To reduce these barriers, this study evaluates a brief and individually tailored behavioral parent training program for children with behavioral difficulties (the “ PAINT-GGZ ” program, developed by the Psychosocial ADHD & disruptive behavior INTerventions [PAINT] consortium). The brief training includes optional booster sessions for families who need additional support [ 16 ].
In behavioral parent training, parents are taught techniques to curtail children’s behavioral difficulties by avoiding or breaking coercive parent–child interactions [ 17 ]. Parenting programs have moderate short-term effects on child conduct problems [ 18 ], oppositional behavior [ 19 , 20 ], inattentive and hyperactive/impulsive behavior [ 21 , 22 ], and parenting [ 23 ]. The longer-term effects of behavioral parent training are less consistent: A meta-analysis on behavioral parent training for children with attention deficit/hyperactivity disorder (ADHD) found mostly sustained effects five months to one year after the intervention [ 24 ], while a meta-analysis on behavioral parent training for children with disruptive behaviors (e.g., tantrums, arguing, rule-breaking) shows a large heterogeneity in results, with some studies showing sustained effects and other studies showing fade-out effects or sleeper effects three years after the intervention [ 25 ]. Overall, the evidence base of behavioral parent training is well-established.
However, a scarcity of certified therapists, long waiting lists, and the typically long and sometimes perceived as rigid nature of behavioral parent training programs undermine the use of parenting interventions in clinical practice. That is, only a minority of families who seek treatment actually receive parent training, because there is a lack of certified therapists who can provide behavioral parent training and waiting lists for parenting interventions are common [ 15 ]. Also, clinicians sometimes do not recommend parent training, but rather redirect children towards medication [ 26 ]. Additionally, behavioral parent training programs are typically long (8 to 12 sessions [ 14 ],) and generally not tailored to the specific behavioral difficulties that parents seek help for [ 27 ]. This is problematic, as behavioral parent training programs are more likely to be effective when their content is tailored to the specific problems parents encounter in daily life [ 14 ]. The perceived rigidity and length of programs may lead to parents not starting or completing behavioral parent training [ 15 , 28 ]. That is, at least 25% of parents who are eligible to participate in scientific studies and qualify for behavioral parent training do not enroll in a parenting program and another 26% terminate the training prematurely [ 13 ]. Brief and individually tailored behavioral parent training programs may reduce these problems, but the few existing brief programs are barely provided and mainly evaluated in prevention settings [ 29 , 30 ]. There is thus an urgent need for evidence-based, brief and individually tailored programs.
To address this need, this randomized controlled trial evaluates the effectiveness of a brief and individually tailored behavioral parent training program with optional booster sessions for children with behavioral difficulties. The program is based on intervention elements that were effective in reducing children’s behavioral difficulties in the broader literature and our earlier work: antecedent techniques (i.e., stimulus control techniques) and consequent techniques (i.e., contingency management techniques) [ 22 , 31 , 32 ]. Antecedent techniques are aimed at changing child behavior by manipulating the antecedents of this behavior (e.g., by setting clear rules and providing structure) and consequent behavioral techniques are aimed at changing child behavior by manipulating their consequences (e.g., by praising desired behavior and ignoring undesired behavior). In a recent microtrial in which we evaluated the efficacy of antecedent and consequent techniques, both sets of techniques were found to reduce behavioral problems of children with ADHD in brief (i.e., two sessions) behavioral parent training, of which antecedent techniques were especially effective in decreasing inattention [ 33 ]. This microtrial also showed that the magnitude of effects of a brief program (i.e., medium-sized effects) was similar to those of traditional, longer programs on reducing child behavioral difficulties [ 23 , 33 , 34 ].
Building upon the findings of our microtrial, the brief behavioral parent training of the present trial consists of two sessions in which antecedent and consequent techniques are combined and a third session aimed at the evaluation and maintenance of applying the learned techniques. To prevent relapse and the possible use of other, more intensive and expensive treatments, parents can receive booster sessions in the first year after the brief training. Similar to the microtrial, the behavioral parent training is individually tailored by letting parents select four target behaviors they want to address in the training and by creating an individually tailored intervention plan based on the functional analysis (see [ 33 ]). A non-randomized pilot study ( N = 28) preceding the present trial indicated a relatively low dropout rate (14.2%), high treatment feasibility and parent and clinician satisfaction, and a reduction of children’s behavioral difficulties from pre to post intervention [ 35 ].
Objectives and hypotheses
The first objective of this study is to examine the short- and longer-term (i.e., one year) effectiveness of the brief and individually tailored behavioral parent training program with optional booster sessions compared to care as usual (CAU) on daily measured child behavioral difficulties (primary outcome) and on a range of secondary outcomes (see Outcomes). Additionally, we will explore whether a number of general demographic and clinical characteristics, parental attachment, parental psychopathology, parental reward responsivity, and reward and punishment sensitivity of the child moderate the short- and longer-term intervention effects on our primary outcome. The second objective is to investigate the cost-effectiveness of the program compared to CAU. As we assess cost-effectiveness based on measures at baseline and one year after the intervention, we can only draw conclusions about the cost-effectiveness on the longer term.
Based on our earlier work [ 33 , 35 ], we hypothesize that the brief behavioral parent training with booster sessions will be more effective than CAU in reducing children’s behavioral difficulties. Consequently, we expect parents who receive the brief behavioral parent training to use less subsequent care and thus hypothesize the brief training to be more cost-effective than CAU on the longer term.
Study design
In this two-arm multi-center randomized controlled trial, parents of children who experience behavioral difficulties in the home setting and were referred to a child mental healthcare center, are randomly assigned (1:1 ratio) to either (a) three sessions of brief behavioral parent training with optional booster sessions, or (b) CAU, as regularly provided by the involved mental healthcare centers. There are no restrictions regarding the type (e.g., psychoeducation, parent counseling and support, individual child therapy, medication) or duration of CAU, only the brief parent training investigated in this trial is not allowed. Both parents and children in the brief behavioral parent training group are not allowed to receive CAU until the first posttreatment assessment (T1). After that, CAU is allowed and parents can also make use of booster sessions with the therapist who provided the training.
Study setting
To ensure our findings reflect the real-world impact of brief behavioral parent training (i.e., to test effectiveness rather than efficacy), the trial is fully embedded in routine mental healthcare. The participating centers are academic and non-academic youth mental healthcare centers of various sizes. Therapists who provide the brief behavioral parent training have a master’s degree in psychology or child, family and education studies and have had postmaster education in cognitive behavioral therapy (at least 50 h) or have a registered higher vocational education degree as social worker in cognitive behavioral therapy. The therapists are trained in the brief parent training by supervisors qualified in cognitive behavior therapy during a one-day training of seven hours, in which therapists practice the parent training by roleplay and evaluate on their performance. Therapists also receive weekly supervision by these qualified supervisors when providing the brief parent training. Additionally, the supervisors provide feedback to each therapist on the audio-taped first session regarding protocol fidelity, intervention integrity, and the process of providing the training (e.g., engaging parents, didactic skills). There are no in- or exclusion criteria for clinicians in the CAU condition. To prevent contamination of the two research arms, therapists never provide both the brief behavioral parent training and CAU to parents participating in this study and are instructed not to share information about the contents of the brief training.
Stakeholder involvement: parent advisory board
For this trial we have installed a parent advisory board (four members, one of them [co-author JL] represents “ Balans ”, a Dutch association for parents of children with developmental problems). The board is involved in this trial since the grant application. They provided feedback and ideas for the current project and meet biannually in the first and last year of the project and annually in years two, three, and four. In the last year, they will be asked to give their ideas about the interpretation of the results. During the writing of the grant application, the parent advisory board indicated that targeting individual needs is crucial for parents and that booster sessions may be very important and helpful, as some parents may experience relinquishing of their parenting skills after finishing behavioral parent training (e.g., in stressful times). The board also tested the suitability of the measures: they considered the time investment of the questionnaires to be acceptable and indicated to use audiotapes rather than videotapes as observational measurement, as parents may perceive audiotapes as less invasive and interfering with their privacy. The members of the board receive reimbursements for all meetings.
Eligibility criteria
Families eligible for the trial must meet the following inclusion criteria:
The child is aged between 2 and 12 years;
Parents have to identify at least four behavioral difficulties of the child that occur in the home setting and that they want to target in the training, using an adapted version of a list of target behaviors [ 33 , 36 ]. This list contains 29 behaviors that can be targeted in the training, such as hyperactive, impulsive, inattentive, oppositional and defiant behavior. The items are derived from target problems that parents mentioned in previous behavioral parent training groups and concern child behaviors that are commonly targeted in behavioral parent training in clinical practice, confirming ecological validity [ 36 ].
Exclusion criteria are:
The child uses psychotropic medication (currently or in the month before the screening);
The child has at any time received a diagnosis of autism spectrum disorder (ASD) in clinical practice, as (parents of) children with ASD may have different needs and therefore may require different treatments than children with behavioral difficulties without ASD;
The child has a known IQ-score below 70, as (parents of) children with intellectual disabilities may have different needs and therefore may require different treatments than children with behavioral difficulties and typical intellectual abilities;
Parents received behavioral parent training aimed at reducing the behavioral difficulties of the concerned child in the year prior to the start of the study;
It is not a suitable period for the parents and/or the child to participate in the study (e.g., moving, divorce);
The child is not living in the same household as the parent(s) who participate(s) in the trial during at least four weekdays (to ensure that our primary outcome can be reported by the same informant(s) and that parents can apply the intervention plans at home).
Interventions
The parent training program includes the behavioral techniques that were identified as effective for reducing behavioral difficulties (i.e., oppositional, defiant, aggressive, hyperactive, impulsive, and inattentive behavior) in a preceding microtrial [ 33 ] and in the broader literature [ 22 , 23 , 31 , 32 , 34 ]. Importantly, all behavioral techniques are explained to parents and based on a functional analysis, the most suitable techniques are selected and tailored to the specific problem behaviors that parents experience with their child and to the home context. Prior to the brief training, with a researcher parents choose four daily occurring target behaviors from the list of target behaviors (see Primary Outcome) that they prefer to work on in the training [ 33 , 36 , 37 ]. For each of the four behaviors, parents also indicate in which situation the behavior occurs, using the situations that are included in the Home Situation Questionnaire [ 37 ]. The therapist providing the brief training receives a list of the chosen four behaviors in specific situations before the training.
In the first session, parents are briefly educated about supposed underlying mechanisms of behavioral difficulties in children. They learn that children with behavioral difficulties may have problems in executive functioning, such as inhibition or working memory, which may influence the way they process environmental information and exert control over their behavior [ 38 , 39 ]. Parents are taught how they can use antecedent techniques (i.e., setting rules, giving clear instructions, structuring situations, discussing situations in advance) to support their child’s executive functioning and elicit more desirable and prosocial behaviors. Parents are also taught that children with behavioral difficulties may show altered sensitivity to reinforcement and punishment, which may influence how children learn from rewards and negative consequences and the way in which their behavior is shaped by environmental consequences as provided by parents [ 40 , 41 , 42 , 43 , 44 ]. Their altered reinforcement sensitivity may lower the likelihood that children change behavior in response to corrective reactions and result in behaviors that are reward-oriented on the short term [ 40 , 43 ]. The therapist explains that consequent techniques (i.e., reinforcement [e.g., praise], planned ignoring, non-violent discipline techniques [e.g., correction, natural consequences]) are important to deal with these sensitivities, while emphasizing that the majority of the used consequent techniques should concern reinforcement. In their explanations, therapists also stress parents that the psycho-education is based on research involving many children and could therefore not directly apply to the situation of their child. After this psycho-education, the parents and therapist select a first target problem behavior along with the specific situation in which this behavior occurs daily. This behavior is chosen from the four behaviors in specific situations that parents selected beforehand with a researcher to target in the training. Together, the parents and therapist make a functional analysis of the selected behavior and create an individually tailored intervention plan. This plan contains the most suitable of the four antecedent techniques and one consequent technique (i.e., praise). The techniques are selected according to the functional analysis and adapted to the abilities and needs of the child and parents. Parents write down their intervention plan with the therapist and receive a handout with explanations of the techniques. Directly after each session, parents carry out their intervention plan at home the next week.
In the second session, the first plan is evaluated and adapted if necessary. The parents and therapist briefly recapitulate the psycho-education and intervention plan of the first session and discuss a second target problem behavior in the same way as the first problem behavior. They make an individually tailored intervention plan for the second target behavior, which again includes the most suitable techniques of all discussed antecedent and consequent techniques, based on the functional analysis of the second target behavior. Based on the results of our microtrial that antecedent techniques are effective sooner after the training (i.e., immediately) and are more effective in decreasing symptoms of inattention than consequent techniques [ 33 ], the intervention plan of the first session mainly contains antecedent techniques, while the intervention plan of the second session includes both antecedent and consequent techniques. The consequent techniques always include forms of reinforcement (e.g., praise, rewards) and can optionally include ignoring or mild negative consequences. In the third session, the second intervention plan is evaluated and adapted if necessary. Maintenance training is provided by encouraging parents to think about how the techniques can be used for other problems. Furthermore, during this session parents rehearse and practice designing an intervention plan accordingly for possible new behavior problems.
In the optional booster sessions, parents can discuss either the same or new target behaviors and create or adapt an intervention plan with the antecedent and consequent techniques that are taught in the earlier sessions. Parents are stimulated by the therapist to use the steps they have learned in the earlier sessions. Parents implement new or adapted intervention plans directly after the session. Booster sessions are not meant as prolongation of the brief training, but as stand-alone sessions to support parents in refreshing and maintaining to apply the learned techniques. Booster sessions can be combined with any CAU.
Parents in the control arm receive CAU, which in Dutch mental healthcare typically consists of psychoeducation, parent counseling and support, medication, longer behavioral parent training programs, family therapy, support at school, and/or cognitive behavior therapy or other therapy or support for the child.
Treatment fidelity
Intervention fidelity (i.e., the percentage of items covered in each session) is assessed with a fidelity checklist using an adapted version of the procedures of Abikoff and colleagues [ 45 , 46 ]. This implies that all intervention sessions (including the booster sessions) are audiotaped. The audiotapes of 20% randomly selected sessions will be scored on intervention fidelity by independent evaluators. After each session, therapists also have to complete a fidelity checklist in which they are asked which items they covered.
Recruitment
Parents of children with behavioral difficulties who are referred to one of the participating Dutch mental healthcare centers are recruited by clinicians within these centers. After the diagnostic assessment of the child and before any treatment has started, the clinicians involved in the diagnostic assessments inform parents of children who seem eligible about the study and hand out an information letter. Clinicians provide researchers with contact information of parents that have consented to sharing information and are interested in participation. The researchers then further inform parents about the trial through telephone contact. If parents want to participate, the researchers ask both parents, or other legal caretakers of the child, to provide informed consent. By default, parents have 14 days to decide upon participation and ask the researchers any questions. If needed, parents can ask for more time to decide upon participation. Once parents have provided consent, the researchers screen whether families are eligible for the study and inform parents whether they can participate.
Allocation to study arms
Randomization is performed with an online generated randomization schedule [ 47 ], using blocks of six participants for each healthcare center to ensure equal allocations to both arms within and across centers. The randomization schedule is only known and administered by independent researchers who are not involved in the trial in any other way. When participants can be randomized, the independent researchers are informed at which healthcare center the parents are participating and asked to inform the responsible researchers about which condition has been randomly assigned to these parents. Randomization occurs directly after the baseline measurement (T0).
Parents in the brief behavioral parent training arm receive three sessions of behavioral parent training. The first two sessions take 120 min each and are planned one or two weeks apart. The third session takes 60 min and is planned one week after the second session. To take parents’ and therapists’ availability into account, some flexibility in planning is allowed as long as all three sessions are planned within six weeks with at least one week between two consecutive sessions. After the third session, parents wishing to receive additional support can receive CAU and/or booster sessions. The booster sessions take 60 min each and can be provided maximally once every four weeks up to one year after the last session of the brief behavioral parent training program. Booster sessions can be suggested by the therapist who provided the brief behavioral parent training or by other involved clinicians, or requested by parents themselves.
The trial contains four measurement occasions, see Fig. 1 for the participant timeline. T0 takes place after parents provide consent and are found eligible for participation, before randomization. The first posttreatment measurement (T1) takes place one week after the third session for parents in the brief behavioral parent training arm and eight weeks after T0 for parents in the CAU arm. The second posttreatment measurement (T2) takes place six months after T1 and the third posttreatment measurement (T3) takes place twelve months after T1. Participation in the trial therefore takes approximately 14 months in total. The care families receive at the child mental healthcare center may terminate sooner if they do not need or want care anymore.
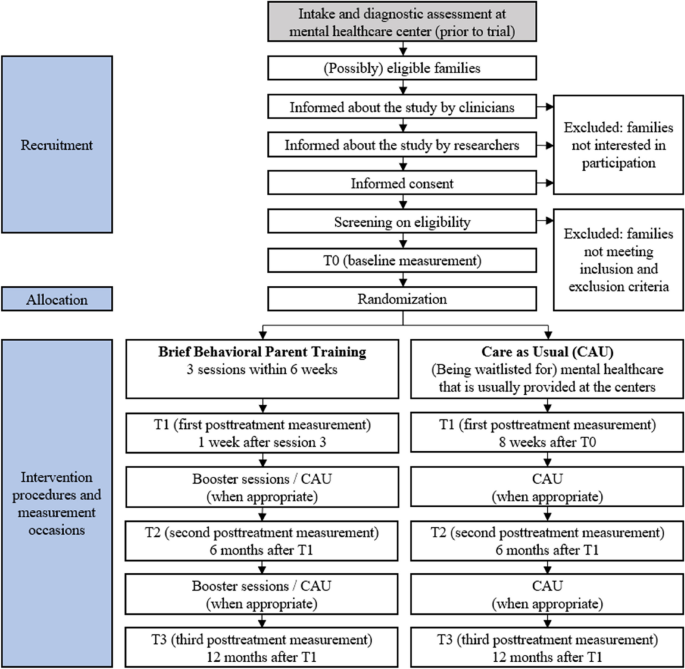
Participant Timeline
The outcomes are measured with questionnaires, audiotapes, and short daily phone calls. Completing the questionnaires (including those measuring moderator variables) takes 30 to 45 min per measurement occasion, making the audiotapes takes about 30 min per measurement occasion (i.e., two recordings of 15 min each), and making the phone calls takes two to three minutes each. Furthermore, parents in the behavioral parent training arm fill out the ECBI-I questionnaire at the beginning of and two weeks after each booster session, which takes a couple of minutes.
Demographic information and clinical characteristics
Parents will provide information on children’s age and gender, on their own and children’s ethnicity, educational background, and household composition, and on children’s previous and ongoing pharmacological and non-pharmacological treatments, medical conditions, and clinical diagnoses (e.g., ADHD, oppositional defiant disorder [ODD], conduct disorder [CD]).
Primary outcome
Individually determined daily ratings of behavioral difficulties.
The primary outcome is the mean severity of parents’ daily ratings of four selected target behaviors in specific home situations. On the adapted version of the list of target behaviors [ 33 , 36 ], parents indicate whether the 29 behaviors occur daily ( yes/no ). For the behaviors scored as yes, parents rate the severity on a 5-point Likert scale ranging from 1 ( not severe ) to 5 ( extremely severe ). Behaviors scored as no are coded 0. With a researcher, parents choose four daily occurring target behaviors from this list that they prefer to work on in the training. Parents also indicate in which situation these behaviors occur, using the situations that are included in the Home Situation Questionnaire [ 37 ].
For each measurement occasion, during preferably five but at least four consecutive weekdays, short daily phone calls with parents are made to evaluate whether the four selected target behaviors occurred in the past 24 h in the selected situation ( yes/no ). Items scored as no are rated 0 and items scored as yes are rated on a 5-point Likert scale ranging from 1 ( not severe ) to 5 ( extremely severe ). This outcome is measured at all timepoints (T0-T3). For each timepoint, the average score of all four behaviors on all weekdays is used as outcome measure.
Secondary outcomes
Parent-reported behavioral difficulties.
Children's behavioral difficulties are assessed with the Intensity scale of the Eyberg Child Behavior Inventory (ECBI-I) [ 48 ]. The Intensity scale consists of 36-items for parents of children aged 2 to 16 and measures the frequency of specific problem behavior on a 7-point Likert scale from 1 ( never ) to 7 ( always ). The convergent and divergent validity and the reliability of the ECBI-I are well established [ 49 ]. This outcome is measured at all timepoints, and at the beginning of and two weeks after each booster session for parents who receive the brief behavioral parent training.
Child well-being
Child well-being is assessed with the Health-Related Quality of Life Questionnaire (KINDL-R) [ 50 ]. Parents rate their children's quality of life on 20 items regarding emotional well-being, self-esteem, family functioning, social contacts, and school, of which the total score will be used. Parents rate the items on a Likert scale ranging from 1 ( never ) to 5 ( all the time ). The KINDL-R has revealed sufficient internal consistency (α = 0.82) [ 51 ]. This outcome is measured at all timepoints.
Parenting behaviors
Parenting behaviors are assessed with the Alabama Parenting Questionnaire (APQ; [ 52 ]). The APQ is a 42-item parent-report measure assessing five categories of parenting practices (involvement, positive parenting, poor monitoring/supervision, inconsistent discipline, and corporal punishment), of which the total score will be used. Parents rate their parenting on a 5-point scale ranging from 1 ( never ) to 5 ( always ), with higher scores representing higher levels of the particular parenting category. The reliability and validity of the APQ are well established [ 52 ]. This outcome is measured at all timepoints.
Observed parent and child behaviors
To include an observational measurement of parent and child behaviors, parents are asked to audio record their mealtime routines for at least 15 min on two different weekdays. Mealtimes are notoriously busy times in family lives and thus well suited as a setting for an ecologically valid measure. The recordings of mealtime routines are a masked measure (i.e., assessors are not aware of the intervention condition), based on the method that was used by Herbert et al. [ 53 ]. Using the recordings, the following behaviors will be scored with a global coding system: parental behavior (both supportive and non-supportive parenting), child misbehavior, and emotional talk. A subsample of recordings will be double coded until sufficient interrater reliability is established. This outcome is measured at all timepoints except T2, to minimize the burden for families.
Parenting stress
Parenting stress is assessed with the Parental Stress Scale (PSS; [ 54 ]). The PSS is an 18-item parent report scale that measures positive (e.g., emotional benefits) and negative (e.g., restrictions) aspects of parenting, of which the total score will be used. Parents have to agree or disagree with statements concerning parenting on a 5-point scale ranging from 1 ( strongly disagree ) to 5 ( strongly agree ). The adequate reliability (α = 0.83) and validity of the PSS have been demonstrated [ 54 ]. This outcome is measured at all timepoints.
Parenting self-efficacy
Parenting self-efficacy is measured with the subscale Efficacy of the Parenting Sense of Competence Scale (PSOC; [ 55 ]). On the eight items of this subscale, parents rate their capability level and problem-solving ability regarding their parental role on a 6-point scale, ranging from 1 ( strongly disagree ) to 6 ( strongly agree ). The internal consistency (α = 0.76) of the subscale Efficacy has been established [ 55 ]. This outcome is measured at all timepoints.
Quality of the parent–child relationship
The quality of the parent–child relationship is measured with the parent version of the Parent–Child Interaction Questionnaire-Revised (PACHIQ-R; [ 56 ]). On 21 items, parents rate their relationship with their child on a 5-point scale, ranging from 1 ( strongly disagree ) to 5 ( strongly agree ), of which the total score will be used. The PACHIQ-R has been demonstrated to have high internal consistency (ranging between α = 0.79 and α = 0.93) [ 56 ]. This outcome is measured at all timepoints.
Utilities, also called preferred health states, are assessed using quality-adjusted life years (QALYs). QALYs range between 0 and 1, where 0 represents death and 1 perfect health. QALYs are calculated based on the EuroQol-5D-5L (EQ-5D) questionnaire [ 57 , 58 ], which parents fill out about their child. The EuroQol-5D-5L measures the child’s health with five items (mobility, self-care, daily activities, pain, and anxiety/depression) on 5-level categorical scales. EQ-5D responses will be transferred into QALYs based on the Dutch EQ-5D-5L tariff for adults [ 59 ], as a tariff for Dutch children is not yet available. The content and face validity of the EuroQol-5D-5L are well established [ 58 ]. This outcome is measured at T0 and T3.
Use of healthcare
Use of mental healthcare within the organization where the child is treated is measured by drawing up an inventory (based on patient records) of the type of care (brief behavioral parent training, booster sessions, CAU) that is used and the duration (in minutes) of this care between T0 and T3 in both arms. The broader use of healthcare within and outside the mental healthcare centers is assessed with the Vragenlijst Intensieve Jeugdzorg , a Dutch questionnaire on intensive youth care [ 60 ]. This questionnaire assesses the use of a wide variety of healthcare (e.g., contact with general practitioner or medical professionals, use of social services or (alternative) medicines), along with the child’s use of education, contact with judicial authorities, and losses in the productivity of parents. Parents complete this questionnaire about the use and intensity of healthcare of both the child and themselves in the past three months. This outcome is measured at T0 and T3. Both measures of healthcare use (i.e., inventory of care and questionnaire) will be combined to obtain a complete image of all used care.
Costs of healthcare
Healthcare costs are estimated from a societal perspective [ 5 ]. Costs of mental healthcare are estimated by multiplying the used care by the reference prices provided in the Cost Manual of the Dutch National Health Care Institute. Costs of medication are estimated by using prices provided by the Dutch National Health Care Institute [ 61 ]. Costs in other sectors (e.g., education, justice) are estimated by using reference prices provided in the Manual Intersectoral Costs and Benefits [ 62 ]. All costs are estimated after families’ participation in the study, when their healthcare use is fully measured.
Candidate moderators
In addition to the general demographic and clinical characteristics and some baseline characteristics such as the severity of behavioral problems, the following variables are included to explore whether they moderate the short- (T1) and longer-term (T2, T3) intervention effects: parental attachment as measured with the 12-item version of the Revised Experiences in Close Relationship questionnaire (ECR-R; [ 63 , 64 ]),parental psychopathology as measured with the 25 items of the Strengths and Difficulties Questionnaire (SDQ) for adults [ 65 ], parental reward responsivity as measured with the 8-item Reward Responsiveness (RR) questionnaire [ 66 ], and child reward responsivity and punishment sensitivity as measured with the Punishment Sensitivity and Reward Responsivity subscales (combined 22 items) of the Sensitivity to Punishment and Sensitivity to Reward Questionnaire for Children (SPSRQ-C; [ 67 ]). All candidate moderators are measured at T0 only and reported by parents.
Parent and therapist satisfaction
Parents’ satisfaction with the brief behavioral parent training.
Satisfaction with the brief behavioral parent training of parents who received the intervention are measured in two ways. First, parents are asked to fill out a self-developed satisfaction questionnaire, which is based on questions of the Parent Satisfaction Questionnaire [ 68 ], the Therapy Attitude Inventory [ 69 ], and the satisfaction questionnaire that was used in Breider et al. [ 70 ]. Parents who received the brief behavioral parent training answer 13 questions about their satisfaction with the brief behavioral parent training at T1 and three questions about their satisfaction with the booster sessions (if used) at T3 on a 5-point scale ranging from 1 ( strongly disagree ) to 5 ( strongly agree ). Parents also grade the brief behavioral parent training generally between 1 ( very bad ) and 10 ( excellent ). Second, one or multiple focus group(s) will be organized with a small number of parents. In the focus group(s), the new program will be qualitatively evaluated and information about feasibility and barriers and facilitators for the implementation of the training in clinical settings will be gathered. The focus group(s) will be held after the inclusion of parents is finished, which is anticipated to be at the beginning of 2025.
Therapists’ satisfaction with the brief behavioral parent training
Therapists' satisfaction and opinion about the intervention are measured in two ways. First, therapists will be asked to fill in a self-developed satisfaction questionnaire, which is based on questions of the Parent Satisfaction Questionnaire [ 68 ], the Therapy Attitude Inventory [ 69 ], and the satisfaction questionnaire that was used in Breider et al. [ 70 ]. Therapists have to answer seven questions on a 5-point scale ranging from 1 ( strongly disagree ) to 5 ( strongly agree ) and give the brief behavioral parent training a general grade between 1 ( very bad ) and 10 ( excellent ). Second, one or multiple focus group(s) will be organized with a selection of therapists from different healthcare centers who provided the brief parent training and range in years of work experience and to how many families they have provided the brief behavioral parent training. In the focus group(s), important barriers and facilitators for the implementation of the program will be identified. Both outcomes will be measured after the trial is finished, which is anticipated to be at the beginning of 2026.
Adverse reactions
Adverse reactions are measured with a self-developed questionnaire. These reactions involve negative experiences of parents and/or children that are, according to parents, related to the care they received either in the brief parent training treatment arm or in the CAU arm. The questionnaire consists of six questions that ask parents whether they experience a decline in their trust in healthcare, (anxiety of) negative reactions from others (i.e., stigma), mental health issues, difficulties in relationships and activities, or any other difficulties or concerns that could be related to the care they received during the trial. For each question that applies to them, we ask parents to shortly elaborate on their experiences and indicate when these experiences happened. These answer options are based on the Medical and Psychological Events and Difficulties (MAPED) questionnaire that was used in the Online Parent Training for The Initial Management of ADHD referrals (OPTIMA) trial [ 71 ]. This outcome is measured at T3.
Sample size calculation
Based on our previous study that found medium-sized short term effects on daily ratings of behavioral difficulties compared to waitlist (range of Cohen’s d = 0.35 to d = 0.66, [ 33 ]) and studies showing medium-sized parenting intervention effects on behavioral difficulties using parent-report rating scales [ 19 , 20 , 25 , 36 , 72 ], we estimate the effect of our brief behavioral parent training program as compared to CAU to be at least small ( d = 0.25).
A power analysis has been performed using G*Power software [ 73 ]. Based on an effect size of d = 0.25 ( f = 0.125), two groups and three repeated measures (T0, T1, T2 for short term effectiveness), with r = 0.60 between-measurement relation, a power of 0.80 and α = 0.05, we need at least 42 participants per group, resulting in a total of 84 participants. Given that the data are clustered, we increased the sample size with 10% [ 74 ], resulting in a total of 93 participants. This is in line with the number of participants in similar studies comparing behavioral treatments to CAU (e.g., [ 36 ]).
Statistical analysis
Data will be analyzed on an intention-to-treat basis. To examine the effects of the intervention on the primary and secondary outcomes, we will conduct multilevel analyses (mixed modeling), taking missing data into account [ 75 ]. Depending on the fit of the models, up to four hierarchical levels will be distinguished: outcomes (level 1), nested within children (level 2), nested within therapists (level 3), nested within healthcare centers (level 4). Random intercepts at the subject level, therapist level and healthcare center level will be included only if the Likelihood Ratio Test shows a significant improvement of the model fit. Time will be included as short-term (T1) and longer-term (T2, T3) within-subjects factors and condition (brief parent training vs. CAU) as between-subjects factor. The interaction between time and condition will be examined to interpret changes over time between conditions. To examine whether the candidate moderator variables moderate the intervention effects, these variables will also be added as interaction effects to the multilevel analyses.
To assess the cost-effectiveness of the brief behavioral parent training compared to CAU, we will calculate the Incremental Cost Effectiveness Ratio (ICER) from a societal perspective. We will perform both a cost-utility analysis (based on QALYs) and cost-effectiveness analyses (based on the daily ratings of behavioral difficulties and based on ECBI-I scores). An ICER is calculated by dividing the difference in the total costs by the difference in the total effect (either QALYs or the daily ratings of behavioral difficulties and ECBI-I scores, respectively). In these analyses, the costs of healthcare will be used and interpolated to the previous 12 months. We will compare each ICER based on relevant willingness to pay thresholds. Bootstrapping will be used to calculate the reliability of our estimates.
Trial duration
October 2022 – December 2026.
Data management
Digital data, both raw and processed data are stored at a study specific secured folder within the network of Accare, the institution at which the research is carried out. This study specific folder can only be accessed by authorized personnel, who are involved in this study. All questionnaire data and processed audio files are stored in one, pseudonymized file, that is accompanied by a 'readme' text file that contains a code book explaining the meaning of all variables. A separate logbook-file will be created documenting all decisions that are made during the process from raw to processed data. Raw data containing identifiable information is kept strictly separate from the processed data and can only be accessed by two of the supervisors (BJvdH, TJD), research assistants and PhD candidate (RSvD). After the research project will be completed (i.e., data collection, data analysis and publishing of research articles), all digital data will be transferred to a study specific folder for long-term storage. The folder can only be accessed by authorized personnel. All research data will be stored for at least 15 years after the data collection has been completed. Upon request, the processed, pseudonymized data will be available for fellow researchers and made available (restricted access) for use in future research projects, to which all participants have consented before enrolling in the study. Requests for re-use of data will be evaluated to check whether the research question falls within the scope of the informed consent.
Ethics and dissemination
This study has been granted a non-WMO statement from the Medical Ethics Review Committee (METc) of the University Medical Center Groningen, meaning that the study does not meet the conditions of the Medical Research Involving Human Subjects Act. Ethics approval has been obtained from the Scientific and Ethical Review Board (VCWE) of the Vrije Universiteit (VU) Amsterdam (VCWE-2022–124). Approval to participate in this study has been obtained from all research partners. The results of this study will be submitted for publication in peer-reviewed journals. In addition, findings will be presented at scientific conferences and shared with stakeholders (e.g., parents, clinicians), for instance on our website ( https://www.paint-studies.nl/ ) and social media channels. Regarding clinical practice, findings will be shared with parents and mental healthcare institutions, partly in collaboration with Balans (e.g., vlogs, flyers, presentations, newsletters). If the brief behavioral parent training with booster sessions is more effective than CAU in reducing children’s behavioral difficulties, the brief training can be implemented in clinical practice.
This study protocol describes a multi-center randomized controlled trial investigating the short- and longer-term effectiveness and the cost-effectiveness of a brief, individually tailored behavioral parent training program that aims to reduce children’s behavioral difficulties. Although behavioral parent training is an evidence-based psychosocial treatment for reducing children’s behavioral difficulties, few families currently receive the intervention. This may be due to, among other reasons, a shortage of certified therapists, long waiting lists, and a perceived rigidity and length of behavioral parent training programs. Brief and individually tailored parenting interventions may reduce these problems and could therefore be a promising way to make behavioral parent training more accessible for parents.
We anticipate multiple challenges that the trial could face. For instance, clinicians’ policies and attitudes towards parent training may complicate the enrollment of eligible families in clinical practice [ 26 ]. Clinicians might be used to their work routines and experience resistance or difficulty getting acquainted with the trial, for instance because they do not feel sufficiently knowledgeable about the contents and effects of the brief behavioral parent training or feel uncertain about the procedures and administration that come with families’ participation in the trial, or because families may express hesitation about participating in a trial. As a result, clinicians may not refer eligible families or (intuitively) recommend usual care (e.g., other parent training programs or parent support, child treatments, medication) rather than the trial. We aim to tackle this hindrance by making clinicians aware that participation in this trial is in line with the stepped-care approach as delineated in international and Dutch treatment guidelines for children with ADHD and for children with disruptive behavior disorders, which suggest offering non-pharmacological treatment that includes psycho-education and practical advices, such as the brief behavioral parent training, before starting more intensive treatment or medication [ 6 , 8 , 10 , 12 ].
Other challenges concern potential hindrances for parents to participate. For instance, parents might find it difficult to complete all measurements during four occasions over an extended period of time (i.e., approximately 14 months). For several reasons, it can be difficult to stay dedicated to participate (e.g., motivational issues, time constraints). Besides, parents presumably take part in the trial hoping to receive the brief parent training and might therefore be disappointed when they are randomized into the CAU arm, which can cause their motivation for participation to decline. This might make parents who receive CAU more likely to drop out of the study. We anticipate this challenge by keeping parents involved in the measurements through frequent reminders, expressing the value of parents’ participation and thanking parents after each completed measurement. We also offer parents who consider quitting the study options to reduce the burden of the measurements (e.g., four instead of five daily phone calls, making less or no audio recordings) to possibly keep them involved for a longer period of time.
The results of the trial could have meaningful societal implications for children with behavioral difficulties and their parents. If we find the brief behavioral parent training to be more (cost-)effective than CAU, the treatment could be used in clinical practice to make parent training more accessible.
Quotient; EQ-5D-5L: EuroQol-5 Dimension 5-Level; KINDL-R: Health-Related Quality of Life Questionnaire (German abbreviation); MAPED: Medical and Psychological Events and Difficulties; METc: Medical Ethics Review Committee; ODD: Oppositional Defiant Disorder; PACHIQ-R: Parent–Child Interaction Questionnaire-Revised; PSOC: Parenting Sense of Competence Scale; PSS: Parental Stress Scale; QALYs: quality-adjusted life years; RR: Reward Responsiveness Questionnaire; SDQ: Strengths and Difficulties Questionnaire; SPSRQ-C: Sensitivity to Punishment and Sensitivity to Reward Questionnaire for Children; VCWE: Scientific and Ethical Review Board; V31, U: Vrije Universiteit Amsterdam.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
Attention-Deficit/Hyperactivity Disorder
Alabama Parenting Questionnaire
Autism Spectrum Disorder
Care as usual
Conduct Disorder
Eyberg Child Behavior Inventory Intensity scale
Experiences in Close Relationship Questionnaire Revised
EuroQol-5 Dimension 5-Level
Incremental Cost Effectiveness Ratio
Intelligence Quotient
Health-Related Quality of Life Questionnaire (German abbreviation)
Medical and Psychological Events and Difficulties
Medical Ethics Review Committee
Oppositional Defiant Disorder
Parent-Child Interaction Questionnaire-Revised
Parenting Sense of Competence Scale
Parental Stress Scale
Quality-adjusted life years
Reward Responsiveness Questionnaire
Strengths and Difficulties Questionnaire
Sensitivity to Punishment and Sensitivity to Reward Questionnaire for Children
Scientific and Ethical Review Board
Vrije Universiteit Amsterdam
Antshel KM. Psychosocial Interventions in Attention-Deficit/Hyperactivity Disorder. Child and Adolesce Psychiatr Clin N Am. 2015;24(1):79–97. https://doi.org/10.1016/j.chc.2014.08.002 .
Article Google Scholar
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual Research Review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–65. https://doi.org/10.1111/jcpp.12381 .
Article PubMed Google Scholar
Franke B, Michelini G, Asherson P, Banaschewski T, Bilbow A, Buitelaar JK, Cormand B, Faraone SV, Ginsberg Y, Haavik J, Kuntsi J, Larsson H, Lesch K-P, Ramos-Quiroga JA, Réthelyi JM, Ribases M, Reif A. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol. 2018;28(10):1059–88. https://doi.org/10.1016/j.euroneuro.2018.08.001 .
Article CAS PubMed Central PubMed Google Scholar
Reef J, Diamantopoulou S, van Meurs I, Verhulst FC, van der Ende J. Developmental trajectories of child to adolescent externalizing behavior and adult DSM-IV disorder: results of a 24-year longitudinal study. Soc Psychiatry Psychiatr Epidemiol. 2011;46(12):1233–41. https://doi.org/10.1007/s00127-010-0297-9 .
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th ed. Oxford: Oxford University Press; 2015.
Google Scholar
Akwa GGZ. Zorgstandaard ADHD [Dutch ADHD guidelines]. 2019. Retrieved December 2023 from https://www.ggzstandaarden.nl/zorgstandaarden/adhd/samenvatting .
Brestan EV, Eyberg SM. Effective psychosocial treatments of conduct-disordered children and adolescents: 29 years, 82 studies, and 5,272 kids. J Clin Child Psychol. 1998;27(2):180–9. https://doi.org/10.1207/s15374424jccp2702_5 .
Article CAS PubMed Google Scholar
National Institute for Health and Care Excellence. Antisocial behaviour and conduct disorders in children and young people: recognition and management (NICE guideline 158). 2017. Retrieved December 2023 from www.nice.org.uk/guidance/cg158 .
Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J Clin Child Adolesc Psychol. 2008;37(1):215–37. https://doi.org/10.1080/15374410701820117 .
Nederlandse Vereniging voor Psychiatrie. Oppositionele stoornis en gedragsstoornis. 2013. Retrieved December 2023 from https://richtlijnendatabase.nl/richtlijn/oppositionele_stoornis_en_gedragsstoornis/oppositionele_stoornis_-_startpagina.html .
Kaminski JW, Claussen AH. Evidence Base Update for Psychosocial Treatments for Disruptive Behaviors in Children. J Clini Child Adolesc Psychol. 2017;46(4):477–99. https://doi.org/10.1080/15374416.2017.1310044 .
National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder: Diagnosis and management (NICE guideline 87). 2019. Retrieved December 2023 from https://www.nice.org.uk/guidance/ng87 .
Chacko A, Jensen SA, Lowry LS, Cornwell M, Chimklis A, Chan E, Lee D, Pulgarin B. Engagement in Behavioral Parent Training: Review of the Literature and Implications for Practice. Clin Child Fam Psychol Rev. 2016;19(3):204–15. https://doi.org/10.1007/s10567-016-0205-2 .
Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-Based Psychosocial Treatments for Children and Adolescents With Attention Deficit/Hyperactivity Disorder. J Clin Child Adolesc Psychol. 2018;47(2):157–98. https://doi.org/10.1080/15374416.2017.1390757 .
Weisenmuller C, Hilton D. Barriers to access, implementation, and utilization of parenting interventions: Considerations for research and clinical applications. Am Psychol. 2021;76(1):104–15. https://doi.org/10.1037/amp0000613 .
Hoekstra PJ, van den Hoofdakker BJ, Rosenau PT, Dietrich A, Leijten P, Groenman AP, et al. We need better long-term intervention programs in mental health care for children and young people with chronic vulnerabilities. Eur Child Adolesc Psychiatry. 2023;32(9):1525–7. https://doi.org/10.1007/s00787-023-02281-x .
McMahon RJ, Forehand RL. Helping the Noncompliant Child: Family-based treatment for oppositional behavior. 2nd ed. New York: The Guilford Press; 2003.
Leijten P, Scott S, Landau S, Harris V, Mann J, Hutchings J, Beecham J, Gardner F. Individual Participant Data Meta-analysis: Impact of Conduct Problem Severity, Comorbid Attention-Deficit/Hyperactivity Disorder and Emotional Problems, and Maternal Depression on Parenting Program Effects. J Am Acad Child Adolesc Psychiatry. 2020;59(8):933–43. https://doi.org/10.1016/j.jaac.2020.01.023 .
Bakker MJ, Greven CU, Buitelaar JK, Glennon JC. Practitioner Review: Psychological treatments for children and adolescents with conduct disorder problems - a systematic review and meta-analysis. J Child Psychol and Psychiatry. 2017;58(1):4–18. https://doi.org/10.1111/jcpp.12590 .
Article CAS Google Scholar
McCart MR, Priester PE, Davies WH, Azen R. Differential Effectiveness of Behavioral Parent-Training and Cognitive-Behavioral Therapy for Antisocial Youth: A Meta-Analysis. J Abnorm Child Psychol. 2006;34(4):525–41. https://doi.org/10.1007/s10802-006-9031-1 .
Daley D, van der Oord S, Ferrin M, Cortese S, Danckaerts M, Doepfner M, van den Hoofdakker BJ, Coghill D, Thompson M, Asherson P, Banaschewski T, Brandeis D, Buitelaar J, Dittmann RW, Hollis C, Holtmann M, Konofal E, Lecendreux M, Rothenberger A, Sonuga-Barke EJ. Practitioner review: Current best practice in the use of parent training and other behavioural interventions in the treatment of children and adolescents with attention deficit hyperactivity disorder. J Child Psychol Psychiatry. 2017;59(9):932–47. https://doi.org/10.1111/jcpp.12825 .
Hornstra R, Dekkers TJ, Bosmans G, van den Hoofdakker B, van der Oord S. Attachment Representation Moderates the Effectiveness of Behavioral Parent Training Techniques for Children with ADHD: Evidence from a Randomized Controlled Microtrial. Res Child Adolesc Psychopathology. 2022;50(9):1151–64. https://doi.org/10.1007/s10802-022-00921-5 .
Dekkers TJ, Groenman AP, Wessels L, Kovshoff H, Hoekstra PJ, van den Hoofdakker BJ. Which factors determine clinicians’ policy and attitudes towards medication and parent training for children with Attention-Deficit/Hyperactivity Disorder? Eur Child Adolesc Psychiatry. 2022;31(3):483–93. https://doi.org/10.1007/s00787-021-01735-4 .
Doffer DPA, Dekkers TJ, Hornstra R, van der Oord S, Luman M, Leijten P, Hoekstra PJ, van den Hoofdakker BJ, Groenman AP. Sustained Improvements by Behavioural Parent Training for Children with Attention-Deficit/Hyperactivity Disorder: A Meta-Analytic Review of Longer-Term Child and Parental Outcomes. 2023. Retrieved December 2023 from https://psyarxiv.com/cymva/ .
Van Aar J, Leijten P, Orobio de Castro B, Overbeek G. Sustained, fade-out or sleeper effects? A systematic review and meta-analysis of parenting interventions for disruptive child behavior. Clin Psychol Rev. 2017;51:153–63. https://doi.org/10.1016/j.cpr.2016.11.006 .
Dekkers TJ, Hornstra R, van der Oord S, Luman M, Hoekstra PJ, Groenman AP, van den Hoofdakker BJ. Meta-analysis: Which Components of Parent Training Work for Children With Attention-Deficit/Hyperactivity Disorder? J Am Acad Child Adolesc Psychiatry. 2022;61(4):478–94. https://doi.org/10.1016/j.jaac.2021.06.015 .
DuPaul GJ, Evans SW, Mautone JA, Owens JS, Power TJ. Future Directions for Psychosocial Interventions for Children and Adolescents with ADHD. J Clin Child Adolesc Psychol. 2020;49(1):134–45. https://doi.org/10.1080/15374416.2019.1689825 .
Joseph HM, Farmer C, Kipp H, Kolko D, Aman M, McGinley J, Arnold LE, Gadow KD, Findling RL, Molina BSG. Attendance and engagement in parent training predict child behavioral outcomes in children pharmacologically treated for attention-deficit/hyperactivity disorder and severe aggression. J Child Adolesc Psychopharmacol. 2019;29(2):90–9. https://doi.org/10.1089/cap.2018.0119 .
Kolko DJ, Lindhiem O. Introduction to the Special Series on Booster Sessions and Long-Term Maintenance of Treatment Gains. J Abnorm Child Psychol. 2014;42(3):339–42. https://doi.org/10.1007/s10802-013-9849-2 .
Article PubMed Central PubMed Google Scholar
Tully LA, Hunt C. Brief Parenting Interventions for Children at Risk of Externalizing Behavior Problems: A Systematic Review. J Child Fam Stud. 2016;25(3):705–19. https://doi.org/10.1007/s10826-015-0284-6 .
Kaminski J, Valle LA, Filene JH, Boyle CL. A Meta-analytic Review of Components Associated with Parent Training Program Effectiveness. J Abnorm Child Psychol. 2008;36(4):567–89. https://doi.org/10.1007/s10802-007-9201-9 .
Leijten P, Gardner F, Melendez-Torres GJ, van Aar J, Hutchings J, Schulz S, Knerr W, Overbeek G. Meta-Analyses: Key Parenting Program Components for Disruptive Child Behavior. J Am Acad Child Adolesc Psychiatry. 2019;58(2):180–90. https://doi.org/10.1016/j.jaac.2018.07.900 .
Hornstra R, van der Oord S, Staff AI, Hoekstra PJ, Oosterlaan J, van der Veen-Mulders L, Luman M, van den Hoofdakker BJ. Which Techniques Work in Behavioral Parent Training for Children with ADHD? A Randomized Controlled Microtrial. J Clin Child Adolesc Psychol. 2021;50(6):888–903. https://doi.org/10.1080/15374416.2021.1955368 .
Hornstra R, Groenman AP, van der Oord S, Luman M, Dekkers TJ, van der Veen-Mulders L, Hoekstra PJ, van den Hoofdakker BJ. Review: Which components of behavioral parent and teacher training work for children with ADHD? – a metaregression analysis on child behavioral outcomes. In Child and Adolescent Mental Health: John Wiley and Sons Inc.; 2022. https://doi.org/10.1111/camh.12561 .
Book Google Scholar
Nijboer M, van Doornik R, Groenman A, van der Oord S, Hornstra R, van den Hoofdakker B, et al. Brief Behavioural Parent Training for Children with Impairing ADHD Characteristics: a Pilot Study. 2024. Retrieved February 2024 from https://osf.io/preprints/psyarxiv/ahkev .
Van den Hoofdakker BJ, van der Veen-Mulders L, Sytema S, Emmelkamp PMG, Minderaa RB, Nauta MH. Effectiveness of behavioral parent training for children with ADHD in routine clinical practice: A randomized controlled study. J Am Acad Child Adolesc Psychiatry. 2007;46(10):1263–71. https://doi.org/10.1097/chi.0b013e3181354bc2 .
Breen MJ, Altepeter TS. Factor Structures of the Home Situations Questionnaire and the School Situations Questionnaire. J Pediatr Psychol. 1991;16(1):59–67. https://doi.org/10.1093/jpepsy/16.1.59 .
Lipszyc J, Schachar R. Inhibitory control and psychopathology: A meta-analysis of studies using the stop signal task. J Int Neuropsychol Soc. 2010;16(6):1064–76. https://doi.org/10.1017/S1355617710000895 .
Noordermeer SDS, Luman M, Buitelaar JK, Hartman CA, Hoekstra PJ, Franke B, Faraone SV, Heslenfeld DJ, Oosterlaan J. Neurocognitive Deficits in Attention-Deficit/Hyperactivity Disorder With and Without Comorbid Oppositional Defiant Disorder. J Atten Disord. 2020;24(9):1317–29. https://doi.org/10.1177/1087054715606216 .
Matthys W, Vanderschuren LJMJ, Schutter DJLG, Lochman JE. Impaired Neurocognitive Functions Affect Social Learning Processes in Oppositional Defiant Disorder and Conduct Disorder: Implications for Interventions. Clin Child Fam Psychol Rev. 2012;15(3):234–46. https://doi.org/10.1007/s10567-012-0118-7 .
Johansen EB, Killeen PR, Russell VA, Tripp G, Wickens JR, Tannock R, Williams J, Sagvolden T. Origins of altered reinforcement effects in ADHD. In Behavioral and Brain Functions. 2009;5:7. https://doi.org/10.1186/1744-9081-5-7 .
Luman M, Tripp G, Scheres A. Identifying the neurobiology of altered reinforcement sensitivity in ADHD: A review and research agenda. Neurosci Biobehav Rev. 2010;34(5):744–54. https://doi.org/10.1016/j.neubiorev.2009.11.021 .
Marsh AA, Blair RJR. Deficits in facial affect recognition among antisocial populations: A meta-analysis. Neurosci Biobehav Rev. 2008;32(3):454–65. https://doi.org/10.1016/j.neubiorev.2007.08.003 .
Van der Oord S, Tripp G. How to Improve Behavioral Parent and Teacher Training for Children with ADHD: Integrating Empirical Research on Learning and Motivation into Treatment. Clin Child Fam Psychol Rev. 2020;23(4):577–604. https://doi.org/10.1007/s10567-020-00327-z .
Abikoff H, Gallagher R, Wells KC, Murray DW, Huang L, Lu F, Petkova E. Remediating organizational functioning in children with ADHD: Immediate and long-term effects from a randomized controlled trial. J Consult Clin Psychol. 2013;81(1):113–28. https://doi.org/10.1037/a0029648 .
Abikoff H, Thompson M, Laver-Bradbury C, Long N, Forehand RL, Miller Brotman L, Klein RG, Reiss P, Huo L, Sonuga-Barke E. Parent training for preschool ADHD: a randomized controlled trial of specialized and generic programs. J Child Psychol Psychiatry. 2015;56(6):618–31. https://doi.org/10.1111/jcpp.12346 .
Sealed Envelope Ltd. Create a blocked randomisation list. 2022. Retrieved September 27, 2022 from https://www.sealedenvelope.com/simple-randomiser/v1/lists .
Eyberg SM, Ross AW. Assessment of child behavior problems: The validation of a new inventory. J Clin Child Psychol. 1978;7(2):113–6. https://doi.org/10.1080/15374417809532835 .
Abrahamse ME, Junger M, Leijten PHO, Lindeboom R, Boer F, Lindauer RJL. Psychometric Properties of the Dutch Eyberg Child Behavior Inventory (ECBI) in a Community Sample and a Multi-Ethnic Clinical Sample. J Psychopathol and Behav Assess. 2015;37(4):679–91. https://doi.org/10.1007/s10862-015-9482-1 .
Ravens-Sieberer U, Bullinger M. Assessing health-related quality of life in chronically ill children with the German KINDL: first psychometric and content analytical results. Qual Life Res. 1998;7(5):399–407. https://doi.org/10.1023/A:1008853819715 .
Bullinger M, Brütt AL, Erhart M, Ravens-Sieberer U. Psychometric properties of the KINDL-R questionnaire: results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17(S1):125–32. https://doi.org/10.1007/s00787-008-1014-z .
Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. J Clin Child Psychol. 1996;25(3):317–29. https://doi.org/10.1207/s15374424jccp2503_8 .
Herbert SD, Harvey EA, Roberts JL, Wichowski K, Lugo-Candelas CI. A Randomized Controlled Trial of a Parent Training and Emotion Socialization Program for Families of Hyperactive Preschool-Aged Children. Behav Ther. 2013;44(2):302–16. https://doi.org/10.1016/j.beth.2012.10.004 .
Berry JO, Jones WH. The Parental Stress Scale: Initial Psychometric Evidence. J Soc Pers Relat. 1995;12(3):463–72. https://doi.org/10.1177/0265407595123009 .
Johnston C, Mash EJ. A Measure of Parenting Satisfaction and Efficacy. J Clin Child Psychol. 1989;18(2):167–75. https://doi.org/10.1207/s15374424jccp1802_8 .
Lange A, Evers A, Jansen H, Dolan C. PACHIQ-R: The Parent-Child Interaction Questionnaire-Revised. Fam Process. 2002;41(4):709–22. https://doi.org/10.1111/j.1545-5300.2002.00709.x .
EuroQol Research Foundation. EQ-5D-5L UserGuide. 2019. Retrieved December 2023 from https://euroqol.org/publications/user-guides .
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36. https://doi.org/10.1007/s11136-011-9903-x .
Versteegh MM, Vermeulen KM, Evers SMAA, de Wit GA, Prenger R, Stolk EA. Dutch Tariff for the Five-Level Version of EQ-5D. Value Health. 2016;19(4):343–52. https://doi.org/10.1016/j.jval.2016.01.003 .
Bouwmans CAM, Schawo SJ, Jansen DEMC, Vermeulen K, Reijneveld M, Hakkaart-van Roijen L. Handleiding Vragenlijst Intensieve Jeugdzorg: Zorggebruik en productieverlies. Erasmus MC. 2012. Retrieved December 2023 from https://hdl.handle.net/11370/54c0b532-1301-4a38-9094-1936e11343a4 .
Zorginstituut Nederland. 2020. Medicijnkosten.nl. 2020. Retrieved December 2023 from https://www.medicijnkosten.nl/ .
Drost RMWA, Paulus ATG, Ruwaard D, Evers SMAA. Handleiding intersectorale kosten en baten van (preventieve) interventies. Classificatie, identificatie en kostprijzen. Maastricht: Maastricht University; 2014.
Kooiman CG, Klaassens ER, van Heloma Lugt JQ, Kamperman AM. Psychometrics and validity of the Dutch Experiences in Close Relationships-Revised (ECR–r) in an outpatient mental health sample. J Pers Assess. 2013;95(2):217–24. https://doi.org/10.1080/00223891.2012.740540 .
Wei M, Russell DW, Mallinckrodt B, Vogel DL. The Experiences in Close Relationship Scale (ECR)-Short Form: Reliability, Validity, and Factor Structure. J Pers Assess. 2007;88(2):187–204. https://doi.org/10.1080/00223890701268041 .
Youth in Mind. Self-report SDQ for 17+ years. 2020. Retrieved December 2023 from https://www.sdqinfo.org/py/sdqinfo/b3.py?language=Dutch .
Van den Berg I, Franken IHA, Muris P. A New Scale for Measuring Reward Responsiveness. Front Psychol. 2010;1:239. https://doi.org/10.3389/fpsyg.2010.00239 .
Luman M, van Meel CS, Oosterlaan J, Geurts HM. Reward and Punishment Sensitivity in Children with ADHD: Validating the Sensitivity to Punishment and Sensitivity to Reward Questionnaire for Children (SPSRQ-C). J Abnorm Child Psychol. 2012;40(1):145–57. https://doi.org/10.1007/s10802-011-9547-x .
Bearss K, Lecavalier L, Minshawi N, Johnson C, Smith T, Handen B, Sukhodolsky DG, Aman MG, Swiezy N, Butter E, Scahill L. Toward an exportable parent training program for disruptive behaviors in autism spectrum disorder. Neuropsychiatry. 2013;3(2):169–80. https://doi.org/10.2217/npy.13.14 .
Eyberg SM, Johnson SM. Multiple assessment of behavior modification with families: Effects of contingency contracting and order of treated problems. J Consult Clin Psychol. 1974;42(4):594–606. https://doi.org/10.1037/h0036723 .
Breider S, de Bildt A, Nauta MH, Hoekstra PJ, van den Hoofdakker BJ. Self-directed or therapist-led parent training for children with attention deficit hyperactivity disorder? A randomized controlled non-inferiority pilot trial. Internet Interv. 2019;18:100262. https://doi.org/10.1016/j.invent.2019.100262 .
Kostyrka-Allchorne K, Ballard C, Byford S, Daley D, Downs J, French B, et al. Online Parent Training for The Initial Management of ADHD referrals (OPTIMA): the protocol for a randomised controlled trial of a digital parenting intervention implemented to support parents and children on a treatment waitlist. Trials. 2022;23(1):1003. https://doi.org/10.21203/rs.3.rs-2119453/v1 .
Daley D, van der Oord S, Ferrin M, Danckaerts M, Doepfner M, Cortese S, Sonuga-Barke EJS. Behavioral Interventions in Attention-Deficit/Hyperactivity Disorder: A Meta-Analysis of Randomized Controlled Trials Across Multiple Outcome Domains. J Am Acad Child Adolesc Psychiatry. 2014;53(8):835-847.e5. https://doi.org/10.1016/j.jaac.2014.05.013 .
Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91. https://doi.org/10.3758/BF03193146 .
Twisk JWR. Practical guides to biostatistics and epidemiology: Applied multilevel analysis: A practical guide for medical researchers: A practical guide. Cambridge University Press. 2010. https://doi.org/10.1017/cbo9780511610806 .
Twisk J, de Boer M, de Vente W, Heymans M. Multiple imputation of missing values was not necessary before performing a longitudinal mixed-model analysis. J Clin Epidemiol. 2013;66(9):1022–8. https://doi.org/10.1016/j.jclinepi.2013.03.017 .
Download references
Acknowledgements
We would like to express our gratitude to Tess Praamstra and Nienke Markensteijn, two research assistants who have made a major contribution in preparing the practical aspects for the data collection (e.g., thinking along in the logistics of the data collection, preparing the questionnaires for and phone calls to parents) and are actively involved in the execution of the data collection. We would also like to express our gratitude to Marjan Houwing, a research assistant who has set up a database in preparation of the data collection and manages the randomization of participants. We would furthermore like to express our gratitude to the parent advisory board for their involvement in the project.
This randomized controlled trial is funded by ZonMw (dossier number 60–63600-98–1151, third cash flow) in the Dutch subsidy round “ Klinisch toegepast onderzoek in de geestelijke gezondheidszorg ronde 2 ”. The funding source was not involved in the design of this trial and will not be involved in the conduct (data collection, analyses, interpretation of results) and reporting (decision to submit results, manuscript writing, dissemination of results, implementation) of the trial.
Author information
Barbara J. van den Hoofdakker and Tycho J. Dekkers contributed equally to this work.

Authors and Affiliations
Accare Child Study Center, Groningen, The Netherlands
Roos S. van Doornik, Annabeth P. Groenman, Pieter J. Hoekstra, Barbara J. van den Hoofdakker & Tycho J. Dekkers
Department of Child and Adolescent Psychiatry, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands
Clinical Psychology, KU Leuven, Louvain, Belgium
Saskia van der Oord
Balans, National Parent Association, Bunnik, The Netherlands
Joli Luijckx
Research Institute of Child Development and Education, University of Amsterdam, Amsterdam, The Netherlands
Annabeth P. Groenman & Patty Leijten
Department of Clinical, Neuro- and Developmental Psychology, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands
Marjolein Luman
Department of Complex Behavioral Disorders and Forensic Youth Psychiatry, Levvel, Amsterdam, The Netherlands
Marjolein Luman & Tycho J. Dekkers
Department of Clinical Psychology and Experimental Psychopathology, University of Groningen, Groningen, The Netherlands
Barbara J. van den Hoofdakker
Department of Child and Adolescent Psychiatry, Amsterdam University Medical Center (AUMC), Amsterdam, The Netherlands
Tycho J. Dekkers
Department of Psychology, University of Amsterdam, Amsterdam, The Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
BJvdH, SvdO, APG, PJH, ML, PL, JL, and TJD prepared the grant application to obtain funding for the trial. RSvD prepared the body, figure, references and formatting of the present manuscript. BJvdH, SvdO, and TJD supervised RSvD in preparing the trial and writing the manuscript. BJvdH, SvdO, TJD, APG, PL, ML, and PJH contributed to preparing the body of the manuscript. JL reviewed the contents of the manuscript on behalf of the parent advisory board.
Corresponding author
Correspondence to Roos S. van Doornik .
Ethics declarations
Ethics approval and consent to participate.
The Medical Ethics Review Committee (METc) of the University Medical Center Groningen has granted this trial a non-WMO statement on April 21st, 2022, meaning that the study does not meet the conditions of the Medical Research Involving Human Subjects Act. The Scientific and Ethical Review Board (VCWE) of the Vrije Universiteit (VU) Amsterdam, the Netherlands, has given approval for this trial on September 20th, 2022 (VCWE-2022–124). All research partners have given consent to collaborate in this trial. Before deciding upon participation, legal caretakes are informed about the study in detail, both through an information letter and through telephone calls with a researcher. All parents provide written informed consent during the recruitment.
Consent for publication
Not applicable.
Competing interests
BJvdH and SvdO were involved in the development and evaluation of several Dutch parent and teacher training programs, among which the brief behavioral parent training that is being investigated in this trial, and are both involved in the training and supervision of therapists who deliver the brief behavioral parent training. BJvdH, SvdO and TJD also provide the brief behavioral parent training to participants themselves. ML has co-developed teacher training programs and other behavioral treatments. BJvdH, SvdO and ML have been advisors of Dutch ADHD guideline groups and BJvdH and SvdO are also members of the European ADHD Guidelines Group (EAGG). SvdO is on the higher health council in Belgium, an advisory committee about ADHD to the minister of health in Belgium and is on the board of trustees of “ Zit Stil ”; the ADHD advocacy organization in Flanders. BJvdH is an advisor of the Dutch Knowledge Centre for Child and Adolescent Psychiatry. BJvdH, SvdO, ML, PL, APG, PJH and TJD have received research grants from ZonMw. SvdO has also received several research grants from FWO (Flanders Research Foundation). JL is member of the parent advisory board that is involved in this trial. RSvD, APG, PL and PJH have no non-financial conflict of interest.
BJvdH receives royalties as one of the editors of “ Sociaal Onhandig ” (published by Van Gorcum), a Dutch book for parents that can be used in parent training. SvdO declares a financial honorarium and reimbursement for travel expenses from MEDICE for being a speaker on non-pharmacological treatments of ADHD. The other authors have no financial conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
van Doornik, R.S., van der Oord, S., Luijckx, J. et al. The short- and longer-term effects of brief behavioral parent training versus care as usual in children with behavioral difficulties: study protocol for a randomized controlled trial. BMC Psychiatry 24 , 203 (2024). https://doi.org/10.1186/s12888-024-05649-8
Download citation
Received : 21 February 2024
Accepted : 01 March 2024
Published : 12 March 2024
DOI : https://doi.org/10.1186/s12888-024-05649-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Behavioral difficulties
- Behavioral parent training
- Individually tailored
- Psychosocial intervention
- Randomized controlled trial
- Effectiveness
- Cost-effectiveness
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
NIH Researchers Identify Brain Connections Associated With ADHD in Youth
Large study finds atypical interactions between the frontal cortex and information processing centers deep in the brain
March 13, 2024 • Media Advisory
Researchers at the National Institutes of Health (NIH) have discovered that symptoms of attention-deficit/hyperactivity disorder (ADHD) are tied to atypical interactions between the brain’s frontal cortex and information processing centers deep in the brain. The researchers examined more than 10,000 functional brain images of youth with ADHD and published their results in the American Journal of Psychiatry . The study was led by researchers at NIH’s National Institute of Mental Health (NIMH) and National Human Genome Research Institute.
Luke Norman, Ph.D., a staff scientist in the NIMH Office of the Clinical Director, and colleagues analyzed brain images supplied by more than 8,000 youth with and without ADHD sourced from six different functional imaging datasets. Using these images, the researchers examined associations between functional brain connectivity and ADHD symptoms.
They found that youth with ADHD had heightened connectivity between structures deep in the brain involved in learning, movement, reward, and emotion (caudate, putamen, and nucleus accumbens seeds) and structures in the frontal area of the brain involved in attention and control of unwanted behaviors (superior temporal gyri, insula, inferior parietal lobe, and inferior frontal gyri).
While neuroscience researchers have long suspected that ADHD symptoms result from atypical interactions between the frontal cortex and these deep information-processing brain structures, studies testing this model have returned mixed findings, possibly due to the small nature of the studies, with only 100 or so subjects. Researchers suggest that the smaller studies may not have been able to reliably detect the brain interactions leading to the complex behaviors seen in ADHD.
The findings from this study help further our understanding of the brain processes contributing to ADHD symptoms—information that can help inform clinically relevant research and advancements.
Luke Norman, Ph.D., staff scientist in the NIMH Office of the Clinical Director and lead author of the paper
Norman, L. J., Sudre, G., Price, J., & Shaw, P. (2024). Subcortico-cortical dysconnectivity in ADHD: A voxel-wise mega-analysis across multiple cohorts. American Journal of Psychiatry . https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.20230026
About the National Institute of Mental Health (NIMH): The mission of the NIMH is to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery and cure. For more information, visit the NIMH website .
About the National Institutes of Health (NIH) : NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit the NIH website .
NIH…Turning Discovery Into Health ®

Could ADHD drugs reduce the risk of early death? Unpacking the findings from a new Swedish study
A ttention-deficit hyperactivity disorder (ADHD) can have a considerable impact on the day-to-day functioning and overall well-being of people affected. It causes a variety of symptoms including difficulty focusing, impulsivity and hyperactivity.
For many, a diagnosis of ADHD, whether in childhood or adulthood, is life changing. It means finally having an explanation for these challenges, and opens up the opportunity for treatment, including medication.
Although ADHD medications can cause side effects, they generally improve symptoms for people with the disorder, and thereby can significantly boost quality of life.
Now a new study has found being treated for ADHD with medication reduces the risk of early death for people with the disorder. But what can we make of these findings?
A large study from Sweden
The study, published this week in JAMA , was a large cohort study of 148,578 people diagnosed with ADHD in Sweden. It included both adults and children.
In a cohort study, a group of people who share a common characteristic (in this case a diagnosis of ADHD) are followed over time to see how many develop a particular health outcome of interest (in this case the outcome was death).
For this study the researchers calculated the mortality rate over a two-year follow up period for those whose ADHD was treated with medication (a group of around 84,000 people) alongside those whose ADHD was not treated with medication (around 64,000 people). The team then determined if there were any differences between the two groups.
What did the results show?
The study found people who were diagnosed and treated for ADHD had a 19% reduced risk of death from any cause over the two years they were tracked, compared with those who were diagnosed but not treated.
In understanding this result, it's important—and interesting—to look at the causes of death. The authors separately analyzed deaths due to natural causes (physical medical conditions) and deaths due to unnatural causes (for example, unintentional injuries, suicide, or accidental poisonings).
The key result is that while no significant difference was seen between the two groups when examining natural causes of death, the authors found a significant difference for deaths due to unnatural causes.
So what's going on?
Previous studies have suggested ADHD is associated with an increased risk of premature death from unnatural causes, such as injury and poisoning.
On a related note, earlier studies have also suggested taking ADHD medicines may reduce premature deaths. So while this is not the first study to suggest this association, the authors note previous studies addressing this link have generated mixed results and have had significant limitations.
In this new study, the authors suggest the reduction in deaths from unnatural causes could be because taking medication alleviates some of the ADHD symptoms responsible for poor outcomes—for example, improving impulse control and decision-making. They note this could reduce fatal accidents.
The authors cite a number of studies that support this hypothesis, including research showing ADHD medications may prevent the onset of mood, anxiety and substance use disorders , and lower the risk of accidents and criminality. All this could reasonably be expected to lower the rate of unnatural deaths.
Strengths and limitations
Scandinavian countries have well-maintained national registries that collect information on various aspects of citizens' lives, including their health. This allows researchers to conduct excellent population-based studies.
Along with its robust study design and high-quality data, another strength of this study is its size. The large number of participants—almost 150,000—gives us confidence the findings were not due to chance.
The fact this study examined both children and adults is another strength. Previous research relating to ADHD has often focused primarily on children.
One of the important limitations of this study acknowledged by the authors is that it was observational. Observational studies are where the researchers observe and analyze naturally occurring phenomena without intervening in the lives of the study participants (unlike randomized controlled trials).
The limitation in all observational research is the issue of confounding. This means we cannot be completely sure the differences between the two groups observed were not either partially or entirely due to some other factor apart from taking medication.
Specifically, it's possible lifestyle factors or other ADHD treatments such as psychological counseling or social support may have influenced the mortality rates in the groups studied.
Another possible limitation is the relatively short follow-up period. What the results would show if participants were followed up for longer is an interesting question, and could be addressed in future research.
What are the implications?
Despite some limitations, this study adds to the evidence that diagnosis and treatment for ADHD can make a profound difference to people's lives. As well as alleviating symptoms of the disorder, this study supports the idea ADHD medication reduces the risk of premature death.
Ultimately, this highlights the importance of diagnosing ADHD early so the appropriate treatment can be given. It also contributes to the body of evidence indicating the need to improve access to mental health care and support more broadly.
This article is republished from The Conversation under a Creative Commons license. Read the original article .
Provided by The Conversation

Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Hosted content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- New entity of adult ultra-short coeliac disease: the first international cohort and case–control study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5528-917X Suneil A Raju 1 , 2 ,
- http://orcid.org/0000-0002-0707-4059 Emily A Greenaway 1 , 2 ,
- http://orcid.org/0000-0002-8493-7698 Annalisa Schiepatti 3 , 4 ,
- Giovanni Arpa 5 , 6 ,
- Nicoletta Vecchione 7 ,
- Chao LA Jian 8 ,
- Charlotte Grobler 9 ,
- Margherita Maregatti 10 ,
- Olivia Green 1 , 2 ,
- Freya J Bowker-Howell 1 , 2 ,
- http://orcid.org/0000-0002-2713-8355 Mohamed G Shiha 1 , 2 ,
- Hugo A Penny 1 , 2 ,
- Simon S Cross 2 ,
- http://orcid.org/0000-0002-7426-1145 Carolina Ciacci 7 ,
- http://orcid.org/0000-0002-2114-2353 Kamran Rostami 11 ,
- Shokoufeh Ahmadipour 12 ,
- Afshin Moradi 13 ,
- Mohammad Rostami-Nejad 14 ,
- Federico Biagi 3 , 4 ,
- Umberto Volta 15 ,
- Michelangelo Fiorentino 15 ,
- Benjamin Lebwohl 16 ,
- Peter HR Green 16 ,
- Suzanne Lewis 16 ,
- Javier Molina-Infante 17 , 18 ,
- Pilar Mata-Romero 18 ,
- http://orcid.org/0000-0003-4416-6216 Valentina Vaira 19 , 20 ,
- http://orcid.org/0000-0002-0873-0759 Luca Elli 10 ,
- Irfan Soykan 21 ,
- Arzu Ensari 22 ,
- David S Sanders 1 , 2
- 1 Academic Unit of Gastroenterology , Sheffield Teaching Hospitals NHS Foundation Trust , Sheffield , UK
- 2 Division of Clinical Medicine, Faculty of Medicine and Population Health , The University of Sheffield Medical School , Sheffield , UK
- 3 Gastroenterology Unit of Pavia Institute , Istituti Clinici Scientifici Maugeri IRCCS , Pavia , Italy
- 4 Department of Internal Medicine and Medical Therapy , University of Pavia , Pavia , Italy
- 5 Department of Molecular Medicine, Fondazione IRCCS Policlinico San Matteo , University of Pavia , Pavia , Italy
- 6 Anatomical Pathology Unit of Pavia Institute , Istituti Clinici Scientifici Maugeri IRCCS , Pavia , Italy
- 7 Department of Medicine, Surgery, Dentistry , University of Salerno , Fisciano , Italy
- 8 Gastroenterology and Hepatology , MidCentral District Health Board , Palmerston North , New Zealand
- 9 Medlab Central Limited , Palmerston North , New Zealand
- 10 Center for Prevention and Diagnosis of Celiac Disease , Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico , Milan , Italy
- 11 Department of Gastroenterology , MidCentral District Health Board , Palmerston North , New Zealand
- 12 Hepatitis ResearcH Center , Lorestan University of Medical Sciences , Khoram-Abad , Iran (the Islamic Republic of)
- 13 School of Medicine, Department of Pathology , Shahid Beheshti University of Medical Sciences , Tehran , Iran (the Islamic Republic of)
- 14 Celiac Disease and Gluten Related Disorders Research Center , Shahid Beheshti University of Medical Sciences , Tehran , Iran (the Islamic Republic of)
- 15 Department of Medical and Surgical Sciences , University of Bologna , Bologna , Italy
- 16 Celiac Disease Center , Columbia University Medical Center , New York , New York , USA
- 17 Department of Gastroenterology , Centro de Investigación Biomédica en Red , Madrid , Spain
- 18 Department of Gastroenterology , Hospital Universitario de Caceres , Caceres , Spain
- 19 Department of Pathophysiology and Transplantation , University of Milan , Milano , Italy
- 20 Division of Pathology , Fondazione IRCCS Ca’ Granda-Ospedale Maggiore Policlinico , Milano , Italy
- 21 Department of Gastroenterology , Ankara University Faculty of Medicine , Ankara , Turkey
- 22 Department of Pathology , Ankara University Faculty of Medicine , Ankara , Turkey
- Correspondence to Dr Suneil A Raju, Academic Unit of Gastroenterology, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield S10 2JF, UK; suneilraju{at}gmail.com
Background Ultra-short coeliac disease (USCD) is defined as villous atrophy only present in the duodenal bulb (D1) with concurrent positive coeliac serology. We present the first, multicentre, international study of patients with USCD.
Methods Patients with USCD were identified from 10 tertiary hospitals (6 from Europe, 2 from Asia, 1 from North America and 1 from Australasia) and compared with age-matched and sex-matched patients with conventional coeliac disease.
Findings Patients with USCD (n=137, median age 27 years, IQR 21–43 years; 73% female) were younger than those with conventional coeliac disease (27 vs 38 years, respectively, p<0.001). Immunoglobulin A-tissue transglutaminase (IgA-tTG) titres at index gastroscopy were lower in patients with USCD versus conventional coeliac disease (1.8×upper limit of normal (ULN) (IQR 1.1–5.9) vs 12.6×ULN (IQR 3.3–18.3), p<0.001).
Patients with USCD had the same number of symptoms overall (median 3 (IQR 2–4) vs 3 (IQR 1–4), p=0.875). Patients with USCD experienced less iron deficiency (41.8% vs 22.4%, p=0.006).
Both USCD and conventional coeliac disease had the same intraepithelial lymphocytes immunophenotype staining pattern; positive for CD3 and CD8, but not CD4.
At follow-up having commenced a gluten-free diet (GFD) (median of 1181 days IQR: 440–2160 days) both USCD and the age-matched and sex-matched controls experienced a similar reduction in IgA-tTG titres (0.5 ULN (IQR 0.2–1.4) vs 0.7 ULN (IQR 0.2–2.6), p=0.312). 95.7% of patients with USCD reported a clinical improvement in their symptoms.
Interpretation Patients with USCD are younger, have a similar symptomatic burden and benefit from a GFD. This study endorses the recommendation of D1 sampling as part of the endoscopic coeliac disease diagnostic workup.
- coeliac disease
- gluten free diet
- gluten sensitive enteropathy
- celiac disease
Data availability statement
Data are available on reasonable request.
https://doi.org/10.1136/gutjnl-2023-330913
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
The first study of ultra-short coeliac disease in adults in 2016 identified patients with villous atrophy confined to the duodenal bulb with positive coeliac serology.
Systematic review and meta-analyses suggest that taking a duodenal bulb biopsy can increase the diagnostic yield of adult coeliac disease by 8%.
There are limited further studies and no data on how these patients respond to treatment.
WHAT THIS STUDY ADDS
Our study provides the first international data of patients with ultra-short coeliac disease.
At presentation, adult patients with ultra-short coeliac disease are significantly younger, have a similar symptomatic burden but lower serological titres.
Adult patients with ultra-short coeliac disease improve both clinically and serologically when on a gluten-free diet.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our data support adherence to undertaking a bulb biopsy.
Once identified these patients can be treated effectively with a gluten-free diet.
Introduction
Coeliac disease is a common autoimmune disorder that affects individuals worldwide, with a global prevalence between 0.7% and 1.4%. 1 Despite being an increasingly significant global health problem, a significant proportion of individuals with coeliac disease remain undiagnosed (5%–76%). 2 3 There is a global delay in diagnosing coeliac disease which is reported to be between 9.7 and 13.3 years. 4–6 Furthermore, 5%–12.4% of patients have had a previous gastroscopy (where no biopsies were taken) prior to their diagnosis representing a missed opportunity to diagnose coeliac disease. 7 8 A gluten-free diet (GFD) remains the only treatment, and adherence improves quality of life for the individual and potentially reduces the burden to the healthcare system. 9 10
The conventional form of coeliac disease is characterised by villous atrophy (VA) and crypt hyperplasia in the second part of the duodenal mucosa (D2) with concurrent positive coeliac serology ( figure 1 ). 11 Historical early reports of the value of acquiring biopsies from the duodenal bulb (D1) were disregarded in favour of biopsies from the distal duodenum as it was suggested that histological interpretation was potentially impaired by the presence of Brunner’s glands, gastric heterotropia and duodenitis. 12 Ultra-short coeliac disease (USCD) is defined as patients with VA only present in the duodenal bulb (D1) and concurrent positive coeliac serology ( figure 1 ). This term was coined in 2016 and systematic review and meta-analyses suggest that taking a duodenal bulb biopsy can increase the diagnostic yield of adult coeliac disease by 8%. For paediatric populations, this was shown to be 4% (95% CI 1% to 9%; p<0.001). 12
- Download figure
- Open in new tab
- Download powerpoint
Subtypes of coeliac disease divided by extent of villous atrophy.
Subsequently, the American College of Gastroenterology and British Society of Gastroenterology (BSG) now recommend bulb biopsy as standard practice when an upper endoscopy is undertaken to assess for ‘suspected coeliac disease/malabsorption’. However, adherence to biopsy protocols is low (37.0%–39.5%). 11 13–15 One reason for this may be a perceived increase in cost or alternatively a perception that a patient with histological changes confined to the bulb may not benefit from a GFD. 7 The value of taking D1 biopsies remains controversial and there is only a single centre study of 26 adult patients from the UK describing the clinical presentation of VA confined to D1. 11 14–17
Understanding the phenotype and therapeutic outcomes of patients with USCD is crucial for optimising diagnostic approaches and treatment strategies, as well as improving overall patient care and long-term health outcomes. There is a paucity of data regarding the phenotype of patients with USCD by comparison to conventional coeliac disease. Furthermore, there are limited data on the benefit of a GFD in patients with USCD. To address this, we present the first, multicentre, international study of patients with USCD.
The study was proposed after the 19th International Society for the Study of Celiac Disease Conference, Sorrento, October 2022, as an international, multicentre, observational cohort study enrolling all patients with USCD between 2009 and 2022. Patient data were collected from hospital databases that prospectively record information about patients with coeliac disease. One centre collected information retrospectively from hospital records based on positive histological findings. Ten tertiary coeliac disease centres participated in the study: Sheffield, UK; Caceres, Spain; New York City, USA; Palmerston North, New Zealand; Ankara, Turkey; Bologna, Pavia, Milan and Salerno, Italy; Tehran, Iran.
Group 1: For this cohort study, adult (≥16 years) patients were identified from 10 tertiary hospitals between January 2009 and December 2022. Patients were defined as having USCD if they had a combination of positive serological markers (immunoglobulin A-tissue transglutaminase (IgA-tTG) or immunoglobulin A-endomysial antibody (IgA-EMA)) and histologically confirmed VA confined to D1 while on a gluten containing diet. D2 biopsies were architecturally non-diagnostic of coeliac disease (Marsh grades 0–2) and diagnoses were made locally by gastroenterologists with expertise in coeliac disease.
Group 2: For the age-matched and sex-matched case-control study, controls were identified from databases of adult patients with coeliac disease diagnosed in each centre. Each age-matched and sex-matched control was from the same centre as the patient with USCD. Age-matched and sex-matched adult coeliac disease controls were then randomly selected using IBM SPSS V.27.0 (IBM) case control matching function.
Both USCD and age-matched and sex-matched controls had D1 and D2 biopsies.
Data were collected following assessment by a clinician with a special interest in coeliac disease at each centre. Data were reviewed in case notes, endoscopy records and the referral. Data were collected on presenting symptoms, serology at time of presentation (including haemoglobin, vitamin B 12 , folate, iron, vitamin D, IgA-tTG and IgA-EMA), human leucocyte antigen (HLA) typing and histology of duodenal biopsies. Patients with USCD and the case–control patients were then followed up to determine the effects of a GFD on their serological markers and symptoms. All patients were assessed for commonly occurring symptoms in coeliac disease both at presentation and follow-up.
In order to assess for any potential differences between USCD and conventional coeliac disease when specifically considering age and sex at presentation, a further analysis was undertaken comparing all patients with USCD (n=137) to those with conventional coeliac disease from the Sheffield, UK coeliac database (n=434).
IgA-tTG antibody levels were measured by different ELISA kits (Aeskulisa Diagnostics (Wendelsheim, Germany), ELiA Celikey (Thermo Fisher, Freiburg, Germany), ARUP Laboratories (Utah, USA), QuantaLite (Inova Diagnostics, San Diego, California), Eu-tTG (Eurospital, Italy) and Euroimmune (Luebeck, Germany)). Therefore, levels were standardised using the upper limit of normal (ULN) based on the manufacturer’s supplied reference ranges. IgA-EMA was detected by immunofluorescence on primate oesophagus sections (Binding Site, Birmingham, UK). The normal ranges of blood tests differed by centre, and therefore, to allow for direct comparison, the lower limit of normal (LLN) was used for ferritin, vitamin B 12 , folic acid and vitamin D based on the manufacturer’s supplied reference ranges of each test. All blood tests were complete prior to endoscopy as part of the referral process.
HLA typing was performed for HLA-DQ2 and DQ8 at six centres and full genomic HLA typing at three. One centre did not perform HLA typing ( table 1 ).
- View inline
Number of cases of ultra-short coeliac disease from each centre
Biopsies and histology
Multiple biopsies were taken in D1 and quadrantic biopsies in D2 and the most severe histological findings used for diagnosis and analysis. The biopsy specimens were first preserved in formalin and then embedded in paraffin wax. Afterwards, they were thinly sliced into sections measuring 3 µm in thickness. These sections were subsequently stained using H&E. Duodenal biopsies were assessed by experienced histopathologists with an interest in gastroenterology. The biopsies were all orientated by experienced biomedical scientists in the histopathology laboratory and three levels were cut from each specimen. This ensured that in at least some of the levels there were full length villi present and the interpreting histopathologists looked for the longest villi that were present in all three levels. Grading was completed using the modified Marsh criteria: Marsh 1 lesions demonstrated increased intraepithelial lymphocytes (IEL), Marsh 2 lesions demonstrated crypt hyperplasia and Marsh 3 lesions demonstrated VA. 18
CD3 antibody was measured using streptavidin biotin peroxidase method by automated Ventana Benchmark XT system (Roche, Ventana Medical Systems, Tucson), Clone:LN10: Leica Concentrate and immunohistochemistry anti-human Cd3 Dako or GenScript. CD8 antibody was measured with clone: C8/44B; Dako RTU Link and CD4 with clone:4B12; Dako RTU Link. An average of two biopsies was tested for both D1 and D2.
Follow-up data were collected in each centre based on clinical improvement (Likert scale) divided into four categories: ‘symptoms worse’, ‘symptoms the same’, ‘symptoms improved’ and ‘symptoms completely resolved’ after clinical assessment as part of routine care. Serological follow-up was completed using the blood tests as described above. The length of follow-up varied based on the time the patient was known to the centre.
Statistical analysis
Data handling was completed using Microsoft Excel (2016); statistical analysis was conducted in IBM SPSS V.27.0 (IBM).
The prevalence of each presenting symptom was compared between cohorts using χ 2 test of two proportions where there was adequate sample size and if not, Fisher’s exact test was used. 19 Shapiro-Wilk test was used to assess for Gaussian distribution of continuous data such as age and IgA-tTG titre. Where normally distributed and no outliers, a t-test was used, otherwise the Mann-Whitney U test used. A p<0.05 was considered statistically significant.
Role of the funding source
No funding was acquired to complete this study.
When comparing age and sex between individuals diagnosed with conventional coeliac disease (n=434), and USCD, it was observed that those with USCD presented at a younger age (27 years (IQR 21–43 years) vs 38 years (IQR 26–53 years), p<0.001) but no difference in sex ratio (66.6% vs 73.7% females, respectively, p=0.12).
For other comparisons, group 1 patients with USCD (n=137) were compared with group two patients with conventional coeliac disease (n=137) ( table 1 ). Group 1 patients were referred from primary care, were self-referring, referred from other departments within the same hospital (with symptoms or positive coeliac disease serology) or referred from other hospitals (68%, 19%, 10%, 3%, respectively).
Patients with USCD (group 1) when compared with age-matched and sex-matched conventional coeliac disease (group 2) had the same number of symptoms overall (median 3 (IQR 2–4) vs 3 (IQR 1–4), p=0.875).
The most common presenting symptoms for patients with USCD were abdominal pain, diarrhoea and bloating ( table 2 ). When compared with age-matched and sex-matched patients with conventional coeliac disease, patients with USCD had more flatulence (13.1% vs 5.1%, p=0.021). Patients with conventional coeliac disease also demonstrated more iron deficiency (41.8% vs 22.4%, p=0.006). Patients with USCD had higher index ferritin levels than age-matched and sex-matched patients with conventional coeliac disease (2.5×LLN (IQR 1.0 x-5.8xLLN) vs 1.2xLLN (IQR 0.6×−2.7xLLN), p<0.001) though there was no difference in iron deficiency anaemia (p=0.181).
Presentation of patients with ultra-short coeliac disease (USCD) and age-matched and sex-matched patients with conventional coeliac disease
In total, 65.3% of patients had HLA typing complete. More patients with USCD were HLA-DQ2 homozygous than patients with conventional coeliac disease (40.4% vs 25.8%, p=0.038) ( table 2 ). Patients with USCD also had lower IgA-tTG titres compared with patients with conventional coeliac disease (1.8×ULN (IQR 1.1–5.9) vs 12.6×ULN (IQR 3.3–18.3), p<0.001). Similarly, a lower proportion of patients with USCD tested positive for IgA-EMA (76.5% vs 89.2%, p=0.043) ( figure 2 ).
Comparison of serological markers in coeliac disease at baseline and follow-up. Serological comparisons made between patients with ultra-short coeliac disease and age-matched and sex-matched controls at baseline and follow-up for: (A) immunoglobulin A—tissue transglutaminase titre, (B) ferritin, (C) folate, (D) vitamin B 12 , (E) vitamin D, (F) immunoglobulin A—endomysial antibody. LLN, lower limit of normal; ULN, upper limit of normal.
Biopsy findings
Patients with USCD had a similar number of biopsies taken compared with patients with conventional coeliac disease from D2 (4 (IQR 4–4) vs 4 (IQR 4–4), p=0.870) and D1 (2 (IQR 1–2) vs 2 (IQR 1–2), p=0.164). In total, 16.8% of patients with USCD had a previous gastroscopy of which only 45.5% had a previous D1 biopsy taken. In patients diagnosed with USCD, biopsies from D2 were histologically normal in 41.6% of cases, Marsh grade 1 in 41.6% of cases and Marsh grade 2 in 16.8% of cases. In the age-matched and sex-matched controls, 94.6% had VA in D1.
The immunophenotype of the intraepithelial lymphocytes was the same in both D1 and D2 with all the intraepithelial lymphocytes staining with CD3 and CD8, but not with CD4 ( figure 3 ).
Biopsies of D2 and D1 from a patient with ultra-short coeliac disease. In the H&E-stained sections of D2 (A) there is a normal villous height, no significant crypt hyperplasia but there is an increased number of intraepithelial lymphocytes. In the H&E-stained sections of D1 (E) there is complete villous atrophy, gross crypt hyperplasia and an increased number of intraepithelial lymphocytes. The immunophenotype of the intraepithelial lymphocytes is the same in both sites with all the intraepithelial lymphocytes staining with CD3 (B, F) and CD8 (D, H) but none of them stain with CD4 (C, G).
Serological and clinical assessment occurred after a median of 1181 days (IQR 440–2160 days). Following recommendation of a GFD patients with both USCD and the age-matched and sex-matched controls experienced a similar reduction in IgA-tTG titres (0.5 ULN (IQR 0.2–1.4) vs 0.7 ULN (IQR 0.2–2.6), p=0.312) and similar levels of IgA-EMA positivity (26.9% vs 23.1%, p=0.598) ( figure 2 ). Levels of vitamin B 12 , iron, folate and vitamin D all improved after undertaking a GFD ( figure 2 ). Symptomatic improvement occurred in both patients with USCD and in the age-matched and sex-matched controls (95.7% vs 89.1%, p=0.115). In total, 16.1% of patients with USCD had complete resolution of their symptoms, 79.6% reported a partial improvement, 3.2% reported no change in their symptoms and 1.1% reported symptoms to be worse after following a GFD.
This is the first multicentre international study of USCD. We have demonstrated that patients with USCD are younger than those with conventional coeliac disease and have lower IgA-tTG titres. Despite only having VA in the duodenal bulb patients with USCD are both symptomatic and derive benefit from a GFD. This study endorses the recommendation of taking samples from D1 as a mandatory component of coeliac disease diagnostic workup.
A single-centre study (n=26) from our centre previously identified patients with USCD as younger and having lower IgA-tTG titres. Furthermore, this work demonstrated that an additional D1 biopsy can increase the diagnostic yield by 9.7%. 16 Despite endorsement from the American College of Gastroenterology and BSG, the adherence to biopsy protocols in general remains low (37.0%–39.5%). 11 13–15 As a result, there remains a global delay in diagnosing coeliac disease between 9.7 and 13.3 years. 4–6 Of the patients with USCD, 41.6% and 16.8% had Marsh 1 and Marsh 2 lesions in D2, respectively, therefore, if only D2 biopsies were taken, these patients may have been incorrectly diagnosed as having potential coeliac disease. 11 The implications for both the patient and the clinical recommendation to follow a GFD are different in ‘real-world’ practice when faced with a patient with potential coeliac disease by comparison to VA (Marsh 3) confirmed coeliac disease. The BSG guidelines have made no recommendation for the role of a GFD in patients with ‘potential coeliac disease’.
Conversely in a prospective randomised controlled study of 23 patients with potential coeliac disease (Marsh grades 1–2, raised IEL only or raised IEL and crypt hyperplasia but no VA) individuals who were randomised to commence a GFD showed both symptomatic benefit and a reduction in their tTG titres. 20 In this historical study from 2003 to 2008, none of the patients had a duodenal bulb biopsy. It could be suggested that these patients may have had USCD.
It is perceived that a bulb biopsy strategy may increase healthcare utilisation costs. This may be due to the use of a second histopathology pot (for the bulb biopsy), processing costs and increased pathology reporting time. This may explain some of the reluctance to take biopsies, however, adequate duodenal biopsy strategies potentially avoid diagnostic delays for patients with undiagnosed adult coeliac disease and are a cost-effective approach in improving the quality-adjusted life-years of patients with coeliac disease. 21 22
It may be possible to place D1 and D2 biopsy samples in the same histopathology pot. A historical paediatric study (n=198) found that ‘intraepithelial lymphocytosis was easily recognised in bulb biopsies, and that although the normal villous-to-crypt ratio is lower in the bulb than in the more distal duodenum, significant VA was usually apparent’. When samples were reviewed by experienced histopathologists, the changes of coeliac disease were still identifiable and the risk of interobserver variability was low. 23
We found that patients with conventional coeliac disease were more likely to have iron deficiency than those with USCD, which may correlate with more extensive mucosal inflammation and impaired absorptive capacity of the duodenum in the former. Interestingly, there was no difference in iron deficiency anaemia.
When considering the paediatric population, in a study of 834 paediatric patients diagnosed with coeliac disease, 11% were diagnosed with USCD, these USCD paediatric patients were also found to have lower tissue transglutaminase antibody titres and less iron deficiency than patients with conventional coeliac disease. 24 This suggests that the paediatric and adult USCD cases are similar. This is corroborated by capsule endoscopy studies that demonstrate an association between iron deficiency anaemia, increased age and extent of disease in conventional coeliac disease. 25
Our study demonstrates that HLA DQ2 homozygosity is more common in conventional CD by comparison to USCD (40.4% vs 25.8% p=0.038). This could suggest that the HLA genotype may have a quantitative relationship between the DQ heterodimer and phenotype. Supporting this, a study of seven patients with USCD that found the HLA-DQ2 haplotype to be less common in patients with USCD and no difference in HLA-DQ8 haplotype. 26 However, all these findings are based on small sample sizes and further investigation is required to determine the significance of a possible different HLA haplotype in USCD.
A limitation of this study is that histology samples could be affected by interindividual variability between histopathologists, however, as all histopathologists have a specialist interest in coeliac disease the risk of this is reduced. It is uncertain how this would translate to ‘real-world’ clinical practice beyond centres with an interest in coeliac disease.
Another limitation is the lack of a central reference lab so there was no standardisation between IgA-tTG assays; to address this, the results were evaluated in relation to the ULN as stated by the manufacturer for each assay. Centres involved have a special interest in coeliac disease, and therefore, there may be a referral bias.
In conclusion, this is the first multicentre international study to evaluate the new entity of USCD. Patients with USCD are younger than those with conventional coeliac disease and have lower serological markers of coeliac disease. Despite only having VA in the duodenal bulb, patients with USCD are both symptomatic and derive benefit from a GFD. This study endorses the recommendation of taking samples from D1 as a mandatory component of coeliac disease diagnostic workup.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
All clinical data were anonymised prior to analysis. Patients underwent clinical tests and assessments as part of their routine care. The Sheffield UK Coeliac Research Database was approved by the Yorkshire and the Humber Sheffield Research Ethics Committee, under registration number 14/YH/1216 renewed 19/YH/0095. The database is used to identify efficiently and comprehensively patients eligible for a specific healthcare intervention in order to help recruitment into trials, and for using routine clinical data to study the course of disease and effectiveness of healthcare used in daily coeliac clinical practice. Where necessary, all data collection was approved locally by research and development/audit departments within the country of collection. The study protocol was approved by the ethical committee of the Research Institute for Gastroenterology and Liver Disease, Shahid Beheshti University of Medical Science Tehran (protocol IR.SBMU.RIGLD.REC.1395.87), the local research committee at Palmerston North Hospital, the Columbia University Irving Medical Center Institutional Review Board (protocol IRB-AAAB0960), the local Institution Review Board of Caceres or the Ethics Committee of IRCCS Pavia, ICS Maugeri, Pavia, Italy (protocol number CE2381).
Acknowledgments
We would like to thank Dr Nuria Fernandez-Gonzalez for preparing the histological samples.
- Strand TA , et al
- Lionetti E ,
- Balanzoni L , et al
- Ramakrishna BS ,
- Makharia GK ,
- Chetri K , et al
- Norström F ,
- Lindholm L ,
- Sandström O , et al
- Violato M ,
- Cranney A ,
- Zarkadas M ,
- Graham ID , et al
- Taylor MA ,
- Blanshard RJ ,
- Naylor G , et al
- Lebwohl B ,
- Markoff S , et al
- Sanders DS ,
- Collin P , et al
- Ludvigsson JF ,
- Biagi F , et al
- McCarty TR ,
- O’Brien CR ,
- Gremida A , et al
- Neugut AI , et al
- Rubio-Tapia A ,
- Semrad C , et al
- Mooney PD ,
- Evans KE , et al
- Cross SS , et al
- Oberhuber G ,
- Granditsch G ,
- Vogelsang H
- Hollander M ,
- A. Wolfe D ,
- Viljamaa M , et al
- Matalon S ,
- Kriger-Sharabi O , et al
- Greenaway EA ,
- Glickman JN ,
- Roiff T , et al
- Ben-Tov A , et al
- Chetcuti Zammit S ,
- Mata-Romero P ,
- Martín-Holgado D ,
- Ferreira-Nossa HC , et al
Twitter @DrSunnyR, @Mo_Shiha
Contributors SAR, EAG and DSS conceptualised and designed the study with comments from AS, GA, NV, CLAJ, CG, MM, OG, FJB-H, MGH, HAP, SSC, CC, KR, SA, AM, MR-N, FB, UV, MF, BL, PHRG, SL, JM-I, PMR, VV, LE, IS and AE. Data were collected by all authors and collated by SAR. Data analysis was completed by SAR and interpreted by all authors. Writing of the manuscript was completed by SAR and edited initially by DSS and then all authors. DSS is the guarantor. The final version was approved by all authors.
Funding DSS has previously received an educational grant from Dr Schaer (a gluten‐free food manufacturer). Dr Schaer has no involvement in this study. HAP funded by a Clinical Lecturers grant (CL-2021-04-002) from the NIHR.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
The lived experiences of adults with attention-deficit/hyperactivity disorder: A rapid review of qualitative evidence
Callie m. ginapp.
1 Yale School of Medicine, Yale University, New Haven, CT, United States
Grace Macdonald-Gagnon
2 Department of Psychiatry, Yale School of Medicine, New Haven, CT, United States
Gustavo A. Angarita
3 Connecticut Mental Health Center, New Haven, CT, United States
Krysten W. Bold
Marc n. potenza.
4 Connecticut Council on Problem Gambling, Wethersfield, CT, United States
5 Child Study Center, Yale School of Medicine, New Haven, CT, United States
6 Department of Neuroscience, Yale University, New Haven, CT, United States
7 Wu Tsai Institute, Yale University, New Haven, CT, United States
Associated Data
Attention-deficit/hyperactivity disorder (ADHD) is a common condition that frequently persists into adulthood, although research and diagnostic criteria are focused on how the condition presents in children. We aimed to review qualitative research on lived experiences of adults with ADHD to characterize potential ADHD symptomatology in adulthood and provide perspectives on how needs might be better met. We searched three databases for qualitative studies on ADHD. Studies ( n = 35) in English that included data on the lived experiences of adults with ADHD were included. These studies covered experiences of receiving a diagnosis as an adult, symptomatology of adult ADHD, skills used to adapt to these symptoms, relationships between ADHD and substance use, patients’ self-perceptions, and participants’ experiences interacting with society. Many of the ADHD symptoms reported in these studies had overlap with other psychiatric conditions and may contribute to misdiagnosis and delays in diagnosis. Understanding symptomatology of ADHD in adults may inform future diagnostic criteria and guide interventions to improve quality of life.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) has an estimated prevalence of 7% among adults globally ( 1 ). ADHD has historically been considered a disorder of childhood; however, 40–50% of children with ADHD may meet criteria into adulthood ( 2 ). Diagnostic criteria for ADHD include symptoms of inattention, hyperactivity, and impulsiveness present since childhood ( 3 ). These criteria are largely based on presentations in children, although diagnostic criteria have changed over time to better but not completely encompass considerations of experiences of adults ( 3 , 4 ).
Although adult ADHD is highly treatable with stimulant medication ( 5 ), adults with ADHD often have unmet needs. Substance use disorders (SUDs) are approximately 2.5-fold more prevalent among adults with versus without ADHD ( 6 , 7 ). Adults with ADHD are particularly likely to be incarcerated, with 26% of people in prison having ADHD ( 8 ). As diagnosis of ADHD has increased considerably in recent decades ( 9 ), there are likely many adults with ADHD who were not originally diagnosed as children. In more recent years, ADHD is still frequently underdiagnosed or misdiagnosed as other psychiatric conditions such as mood or personality disorders ( 10 ). Even when patients are diagnosed with ADHD as children, many patients lose access to resources when transitioning from child to adult health services ( 11 ) which may contribute to less than half of people with ADHD adhering to stimulant medication ( 12 ).
Non-pharmacological interventions such as cognitive behavioral therapy (CBT) have shown promise with helping adults manage their ADHD symptoms, although such symptoms are not completely ameliorated by therapy ( 13 – 15 ). A more thorough understanding of the symptoms adults with ADHD experience and the effects that these symptoms have on their lives may allow for more efficacious or targeted therapeutic interventions.
Qualitative research may provide insight into lived experiences, and findings from such studies may direct future research into potential symptoms and therapeutic interventions. The aim of this review is to describe the current qualitative literature on the lived experiences of adults with ADHD. This review may provide insight into the symptomatology of adult ADHD, identify areas where patient needs could be better met, and define gaps in understanding.
Search strategy
Using rapid review methodology ( 16 ), PubMed, PsychInfo, and Embase were searched on October 11th, 2021 with no date restrictions. The search terms included “ADHD” and related terms as well as “qualitative methods” present in the titles or abstracts. The full search ( Supplementary Appendix 1 ) was conducted with the help of a clinical librarian. The search yielded 417 articles which were uploaded to Endnote X9 where 111 duplicates were removed. The remaining 307 articles were uploaded to Covidence Systematic Review Management Software for screening, with one additional duplicate removed. The search also yielded a previous review on the lived experiences of adults with ADHD ( 17 ). The ten articles present in this review were also uploaded to Covidence where two duplicates were removed resulting in 314 unique articles.
Study selection
Studies reporting original peer-reviewed qualitative data on the lived experience of adults with ADHD, including mixed-methods studies, were eligible for inclusion. “Adult” was defined as being 18 years of age or older; studies that included adolescent and young adult participants were only included if results were reported separately by age. Studies that included some participants without ADHD were included if results were reported separately by diagnosis. Any studies with adult participants who were exclusively reflecting on their childhood experiences with ADHD were considered outside this study’s scope, as were studies on family members, medical providers, or other groups commenting on adults with ADHD. Articles could be from any country, but needed to have been published in English. Individual case studies were not included due to concerns with generalizability.
Twenty percent of titles and abstracts were screened by two reviewers for meeting the inclusion criteria. Studies were not initially excluded based on participants’ ages as many titles and abstracts did not specify age. One reviewer screened the remaining abstracts; a second reviewer screened all excluded abstracts. For full-text screening, ten articles were screened by both reviewers to ensure consistency. One reviewer screened the remaining articles; a second reviewer screened all excluded articles.
Quality appraisal
Quality appraisal was completed by one reviewer using the Joanna Briggs Institute critical appraisal checklist for qualitative research ( 18 ). Half of included studies did not state philosophical perspectives, two-thirds did not locate researchers culturally or theoretically, nearly one-third did not include specific information about ethics approval, and only two studies commented on reflexivity ( Supplementary Appendix 2 ). Given the varied quality appraisal results and the small body of literature, all studies were included regardless of methodological rigor.
Data extraction
Data extracted included general study characteristics and methodology, participant characteristics (sample size, demographics, and country of residence), study aims, and text excerpts of qualitative results. Study characteristics were entered into a Google Sheets document. PDFs of all studies were uploaded into NVivo 12, and results sections were coded using grounded theory ( 19 ). One reviewer extracted and coded data; a second reviewed extracted data for thematic consistency.
Study characteristics
One-hundred-and-seventy-three articles were deemed relevant in title and abstract screening. Of these, 35 were included after the full-text review ( Figure 1 ). Articles were published between 2005 and 2021, and methodology mostly consisted of individual interviews (91%), with other studies utilizing focus groups (14%). Eight studies focused on young adults (18–35 years), and three were specific to older adults (>50 years). Two had exclusively male participants, and three had exclusively female participants. Nineteen were conducted in Europe, nine in North America, and three in Asia. No studies included participants from Africa, South America, or Oceania. In six studies, participants had current or prior SUDs, six studies focused on college students, four included participants diagnosed in adulthood, and two included highly educated/successful participants ( Table 1 ).

PRISMA flow diagram showing the search strategy for identifying qualitative studies on the lived experience of adult attention-deficit/hyperactivity disorder (ADHD).
Article characteristics of included studies.
1 Ages not reported consistently across studies.
2 Substance use disorder.
An overview of the identified themes is described in Figure 2 , and Table 2 provides a summary of main findings. Several of the themes overlap with each other, and such areas are identified in the main text.

Schematic diagram of the domains of features linked to the lived experiences of adults with ADHD.
Summary of results.
Adult diagnosis
Assessment and diagnosis of adult ADHD were reported as laborious and included prior misdiagnoses ( 20 – 22 ), lack of psychiatric resources ( 23 ), and physicians’ stigma regarding adult ADHD ( 24 ). Participants were often diagnosed only after their children were diagnosed ( 23 , 24 ). However, after receiving a diagnosis, relief was commonly reported initially. Adults noted that receiving a diagnosis helped explain previously seemingly inexplicable symptoms and feelings of being different, and allowed for participants to blame themselves less for perceived shortcomings ( 24 – 31 ).
Identity changes were another reported finding after diagnosis, both positive and negative. Some participants reported experiencing existential questioning of their identities ( 25 , 26 ); others reported feeling increased levels of self-awareness ( 26 , 28 ). Some participants reported having initial doubts about the validity of their diagnoses ( 26 , 28 ). Some reported experiencing emotional turmoil and concerns about the future ( 25 , 26 , 29 ). A commonly reported late step involved acceptance, both of themselves and their diagnoses, sometimes coupled with increased interest in researching ADHD ( 24 , 25 , 28 , 29 , 32 ). A ubiquitous finding was participant regret that they had not been diagnosed earlier, largely because of the many years they had gone without understanding their condition or receiving treatment ( 22 , 24 , 26 – 30 ). In one study, participants who had been diagnosed as children had better emotional control and self-esteem ( 33 ). No studies reported participant regret about their ADHD diagnosis.
Symptomatology of attention-deficit/hyperactivity disorder
Inattention, impulsivity, and hyperactivity.
Consistent with current diagnostic conceptualizations, difficulties with attention and concentration were described. These difficulties hindered completion of daily life tasks at home, school, and work ( 24 , 27 , 28 , 32 , 34 – 37 ). Some participants reported not experiencing a pervasive deficit of attention, but rather only struggling when the topic was not of personal interest and could sustain attention on interesting tasks for long periods of time ( 33 , 38 – 42 ). Attention could be influenced by the environment; for example, attention worsened in distracting environments or improved in intense, stimulating environments ( 40 , 41 ).
Impulsivity was widely reported and reflected in risk-taking including reckless driving, unprotected sex, and extreme sports ( 20 , 24 , 28 , 33 , 36 , 43 ). Impulsive spending was noted ( 20 , 36 – 38 , 44 ). Impulsive speech (“blurting out”) was common and often led to strained interpersonal relationships ( 24 , 32 , 33 , 36 , 37 , 40 ).
Fewer studies described participants’ struggles with hyperactivity, such as with staying still or not being constantly busy ( 24 , 34 , 36 ). Hyperactivity was reported as an internal symptom by some participants, noted as inner feelings of restlessness ( 22 , 36 , 37 , 39 ), or described as resulting in excessive talking ( 36 ). This more subtle hyperactivity was mostly reported by women or older adults.
Chaos, lack of structure, and emotions
Living in chaos was often reported, whether involving internal feelings of being unsettled ( 28 ), or external aspects such as turbulent schedules or disorganized living spaces ( 22 , 24 , 27 , 36 ). Participants often struggled with maintaining structure in daily routines, resulting in irregular sleeping and eating, difficulty completing household tasks, and strained social lives ( 36 – 38 , 43 , 44 ). Increased autonomy in adulthood was often perceived as difficult to manage compared to more highly structured childhoods.
Although lacking from current diagnostic criteria, emotional dysregulation was often noted. Participants reported experiencing extreme emotional reactions to interpersonal conflicts such as terminations of romantic relationships or receiving negative feedback at work ( 24 , 34 , 38 , 40 ). Negative feelings of anxiety and agitation were common ( 22 , 24 , 29 , 31 , 33 , 34 , 36 , 38 , 44 ), as was difficulty with controlling, recognizing, naming, and managing emotions ( 30 , 40 , 41 , 44 ). One study noted that emotional lability has positive aspects since participants’ emotional highs were higher ( 45 ).
Positive aspects of attention-deficit/hyperactivity disorder
Not all aspects of ADHD were perceived as negative. Impulsivity was reported by some as fun and spontaneous ( 26 , 37 , 45 ), struggles with attention were reported as promoting creativity and motivating focus on details ( 21 , 33 , 40 , 41 , 45 ), and hyperactivity was described as providing energy to pursue one’s passions ( 40 , 45 ). Learning to live with ADHD-related impairments was reported as promoting resilience and humanity ( 45 ), and increased tendencies to keep calm in chaotic settings ( 40 ). Ability to maintain focus for extended periods on topics of personal interest was sometimes seen as helpful, although unpredictable ( 33 ).
Adapting to symptoms
Coping skills.
Participants reported compensatory organizational strategies that increased structure in their daily lives. Creating regimented sleeping, eating, working, and relaxing schedules ( 30 , 35 , 42 , 44 , 46 ), and keeping to-do lists or using reminder apps ( 24 , 32 , 37 , 40 , 42 , 46 ) were frequently-reported strategies. Some participants reported thriving without formal structure while working from home since they were able to maintain daily routines and were free from distractions ( 34 ).
Participants reported being able to adjust their environment to best suit their needs, whether that be decreasing distracting stimulation ( 32 , 46 ) or cultivating a highly stressful and stimulating environment ( 39 ). Creating space for physical activity was reported as a helpful outlet for hyperactivity ( 24 , 33 , 39 , 43 , 46 ). Having awareness of their diagnosis allowed newly-diagnosed participants to attribute their symptoms to their disorder, thereby decreasing self-blame ( 24 , 26 , 32 ). In one study, participants engage in self-talk to modify their behavior ( 32 ). Participants reported implementing social skills to prevent interrupting others and adjusting their social circles to accommodate their symptoms ( 24 , 35 , 46 ).
Substance use was also described as a coping strategy, although there were also drawbacks associated with using substances. Such findings are discussed under “substance use.”
Stimulant medications were commonly used to help manage ADHD symptoms; participants reported that stimulants facilitated task prioritization, goal achievement, and productivity often to “life-changing” extents ( 22 , 24 – 27 , 29 , 32 , 35 , 40 , 46 – 48 ). Stimulants were sometimes reported as assisting with social and emotional functioning by promoting calmness ( 22 , 24 , 30 , 40 ). Some participants took their medications on an as-needed basis, choosing to take them only when they had much work ( 20 , 27 , 32 , 33 , 47 ). In one study, participants reported feeling pressured to sell their medication, and in another, participants reported increasing their dosages to stay up all night in order to better complete school work ( 27 , 47 ).
Participant ambivalence or hesitation to take stimulants was reported due to therapeutic and adverse effects. Reported adverse effects included “not feeling like oneself,” resulting in difficulties with socializing and creativity ( 22 , 27 , 35 , 40 , 47 ), somatic effects such as appetite suppression and insomnia ( 22 , 27 , 35 , 40 , 47 ), unpleasant emotions including irritability and numbness ( 35 , 40 , 47 ), and rebound symptoms and withdrawal side effects when the medications wore off ( 29 , 47 ).
Outside support
Studies noted participants adapting to living with their symptoms by receiving formal accommodations at work and school. Reported workplace accommodations included reduction of auditory distractions and bosses who would provide organizational advice or extra reminders about due dates ( 24 , 25 , 40 ). Reported accommodations in college consisted of separate testing environments and extra time on examinations. However, inaccessibility of disability offices, limited willingness of professors to comply with accommodations, and lack of participant engagement with accommodations due to not wanting to seem different resulted in many participants not utilizing such resources ( 27 , 32 ).
Individual therapy was reported as helpful for managing symptoms and acquiring self-knowledge, especially therapeutic interventions designed for ADHD and CBT ( 22 , 23 , 27 , 41 ). However, some participants reported minimal benefits from seeing therapists who did not specialize in ADHD, and CBT was reported to need improvement to be specially tailored to adults with ADHD such as being more engaging or being reframed as ADHD coaching ( 22 , 27 , 33 ). Community care workers added structure to some participants’ lives and aided with motivation in one study ( 42 ).
In some studies, participants expressed desires to be involved with support groups for adults with ADHD in order to learn new coping skills and find community, but not knowing where to access such services ( 28 , 40 ). Those who had participated in ADHD support or focus groups reported feeling validated and less isolated, as well leaving with improved strategies for symptom management ( 24 , 31 , 41 , 49 ). Support was also reported in personal relationships. Having a supportive partner often helped participants tremendously with organization and life tasks, especially for men married to women ( 24 , 43 ). A close friend or family member encouraging accountability and creating a sense of togetherness was viewed as advantageous ( 32 , 42 ).
Substance use and addiction
Reasons for substance use.
The SUDs were commonly reported among adults with ADHD and often seen as a form of self-medication. In every study that discussed self-medication, participants reported using substances to feel calm and relaxed; substances included nicotine/tobacco, alcohol, marijuana, cocaine, and methamphetamine ( 20 , 24 , 32 , 46 , 50 – 52 ). Nicotine/tobacco, marijuana, ecstasy (MDMA), and methamphetamine were used to help improve focus, particularly before diagnosis and subsequent to stimulant treatment ( 20 , 24 , 32 , 51 , 52 ). Participants also reported using substances to help feel “normal” as they facilitated social interactions and helped complete activities of daily life ( 20 , 50 , 52 ). One study described college males’ experiences with video game addictions which resulted in neglecting schoolwork ( 32 ).
The tendencies of people with ADHD to make impulsive decisions were suggested as linking ADHD and substance use ( 20 , 52 ). Substance use worsened ADHD symptoms, most notably impulsivity ( 44 , 52 ). One study attributed high rates of substance use to participants with ADHD being less fearful and more rebellious than individuals without ADHD ( 50 ).
Although discontinuing substance use was regarded as a difficult process with frequent relapses, participants considered their quality of life to improve after quitting ( 30 , 44 , 53 ). Nicotine withdrawal was reported to worsen ADHD symptoms, and participants desired smoking-cessation programs specifically tailored for those with ADHD ( 53 ). Even after discontinuation of substance use, participants reported difficulties accessing stimulant medication due to their substance-use histories ( 52 ).
Stimulants and use of other substances
Findings relating stimulant use and use of other substances were mixed. Prescription stimulant usage was reported as a protective factor against use of other substances. Participants who had previously been self-medicating reported that when they had been on stimulants, they did not need other substances to help them feel calm and focused ( 46 , 47 , 50 , 52 ). Stimulants were reported to decrease cigarette cravings ( 50 ). In one study, a participant commented that her stimulant prescription generated a hatred of taking pills, which she reported subsequently prevented her from using drugs ( 54 ).
Some participants reported stimulant prescriptions as increasing risk of substance use. Some reported that stimulants directly increased nicotine cravings ( 50 ). Indirect connections were reported, such as feelings of social exclusion due to being labeled as medicated or due to participants feeling used to taking drugs since childhood ( 54 ). Other participants reported no connection between stimulant medication and use of other substances ( 50 , 54 ).
Perceptions of self and diagnosis
Self-esteem.
Participants often reported experiencing low self-esteem which they attributed to feeling unable to keep up with work or school, being told they were not good enough by others, and frequently failing at life goals ( 24 , 27 – 29 , 33 , 36 , 37 , 41 , 43 ). Low self-image was typically worse in childhood and improved over time, especially after receiving a diagnosis ( 28 , 36 , 43 ). In one study, some participants did not see themselves as having any flaws despite repeatedly being told otherwise, possibly due to being distracted from the emotional impact of these remarks ( 29 ).
Views of attention-deficit/hyperactivity disorder
Some participants viewed ADHD as a personality trait or difference as opposed to a disorder or disability ( 31 , 32 , 39 , 41 , 45 ). Some participants reported finding the ADHD diagnosis limiting and not wanting the disorder to define who they were ( 27 , 28 ). When asked if they would want their ADHD “cured” in one study, participants’ responses ranged from “definitively yes” to “definitely no.” Many reported feeling ambivalent as they described both positive and negative aspects of ADHD ( 20 ).
Interactions with society
Relationships with others.
Difficulties building and maintaining relationships with others were regularly reported. Participants reported that impulsivity hindered their social interactions due to their tendencies to make inappropriate remarks, engage in reckless behaviors, and agree to engagements without thinking through consequences, resulting in being associated with people to whom they did not want to be linked ( 20 , 22 , 32 , 33 , 36 , 43 ). Reported organizational struggles contributed to participants frequently being late and having cluttered living spaces ( 24 , 38 ). Participants reported misunderstanding social norms and hierarchies and being hesitant about starting conversations ( 28 , 30 , 40 , 43 ). They reported feeling overwhelmed by others’ emotions and unsure how to respond to them ( 44 ). Some participants reported choosing to hide their ADHD diagnoses, and the resultant barrier made socializing feel exhausting ( 24 ). Participants reported that these factors made sustaining long-term relationships especially difficult ( 22 , 31 , 38 , 43 ).
Feeling different from others was widely reported, most notably in childhood ( 20 , 24 , 27 , 29 , 31 , 32 ). This experience was described as feeling misunderstood, like a misfit, abnormal, and/or like there was something wrong with them ( 20 , 24 , 27 , 29 , 33 , 43 , 45 , 50 ). Participants reported consciously pretending to be normal as an attempt to fit in ( 28 , 41 ). Some participants reported seeing themselves as more brave or rebellious than their peers, which sometimes resulted in positive self-images ( 24 , 36 , 50 ). A strong desire to advocate for “the underdog” in interpersonal relationships was described by some women ( 31 ). In one study, most participants did not describe feeling different from others, but reported having felt misunderstood as children ( 36 ).
Participants with ADHD who also had children diagnosed with ADHD reported that their approaches to their children’s diagnoses were shaped by their own ADHD experiences. Parents reported uniform support of diagnostic testing, although the best time for testing was not agreed-upon ( 26 , 48 ). Opinions on starting their children on stimulants varied, ranging from enthusiastic support to viewing medication as a last resort, even among participants who had responded positively to stimulants themselves ( 48 ). Most participants reported supporting shared decision-making with the child.
Outside perceptions of attention-deficit/hyperactivity disorder
Participants reported their social networks often expressed preconceived notions about the diagnosis, such as ADHD being “fake” or restricted to children ( 27 – 29 , 37 , 41 ). Stigma about ADHD was reported as having prevented many from disclosing their diagnosis both personally and professionally ( 24 , 26 , 28 , 29 , 32 ). Increased awareness and education about ADHD were desired by participants to help them function better in society ( 28 , 41 ).
Societal expectations
Some studies discussed participants’ difficulties with meeting societal expectations. Participants reported struggling to keep up with daily tasks such as maintaining their living spaces, paying bills and remembering to eat ( 28 , 33 , 35 , 41 ). These difficulties were reported to result in exasperation, low self-esteem, and exhaustion ( 29 , 33 ).
Education and occupation
Academic underachievement was widely reported; most studies focused on postsecondary education. Some participants reported having to try harder than their peers for the same results ( 28 , 35 ), while others reported that they fell behind due to not putting in much effort ( 24 , 27 ). Reports of low motivation to complete assignments until the last minute, as it then became easier to focus, led to missed deadlines ( 32 , 35 , 38 ). Participants reported difficulties paying attention in class ( 24 , 27 , 32 , 35 ), struggling with reading comprehension ( 27 , 32 ), and needing extra tutoring ( 24 , 28 ). Participants reported these difficulties prevented them from “reaching their potential” as they were unable to complete advanced courses or degrees necessary for their careers of choice ( 20 , 22 , 31 , 37 , 39 ). A third of participants in one study noted that they did not struggle academically ( 31 ). Reported coping mechanisms for mitigating academic impairment included medications ( 35 , 47 ), active engagement with materials facilitated by small class sizes or study groups ( 23 , 35 ), and studying from home with fewer distractions ( 34 ). Formal academic accommodations are discussed under the outside support subheading of adapting to symptoms.
Occupational struggles were commonly reported, with many studies detailing participant underemployment or unemployment and high job-turnover rates ( 22 , 31 , 33 , 37 , 41 , 43 ). Difficulties with punctuality and keeping up with tasks and deadlines were reported to generate tensions in the workplace ( 20 , 22 , 24 , 33 , 35 , 39 ), and participants reported frequently being bored and unable to stay focused on their responsibilities, with noisy workplaces promoting distractibility ( 20 , 24 , 33 , 35 , 39 , 40 ). Some studies noted difficulties understanding and navigating social hierarchies in the workplace ( 20 , 40 ). In one study, participants reported feeling unable to maintain work-life balance, overworking until they felt burnt out ( 36 ). Working in fields of intrinsic interest, multitasking, and self-employment were reported strategies used to achieve occupational success ( 24 , 31 , 40 ). Having an understanding employer who could assist with task delegation and understand their needs was described as promoting positive workplace dynamics ( 25 , 33 , 40 ). Clearly defied roles and working with others helped some participants remain engaged in work ( 42 ). College students often reported part-time jobs as rewarding, with responsibilities helping them manage their academic pursuits ( 35 ).
Accessing services
Adults described difficulties accessing healthcare for ADHD. Most reported having to fight to receive a diagnosis and medication due to perceptions of stigma from physicians about adult ADHD ( 22 ). After diagnosis, participants often felt they did not receive adequate counseling or follow-up, especially when seeing general practitioners ( 22 , 26 ). Many participants reported not seeing physicians regularly for medication management due to bureaucratic difficulties ( 21 ); college students reported often having their former pediatricians refill prescriptions without regular appointments ( 47 ). Many participants in one study had little knowledge of ADHD services available to them despite regular appointments ( 32 ).
This review characterizes the current literature on the lived experiences of adults with ADHD. This includes experiences of having been diagnosed as an adult, symptomatology of adult ADHD, skills used to adapt to ADHD symptoms, relationships between ADHD and substance use, individual perceptions of self and of having received ADHD diagnoses, and social experiences interacting in society.
Similar themes were noted in a previous review on lived experiences of adults with ADHD consisting of ten studies, three of which were included here ( 17 ). Such themes included participants feeling different from others, perceiving themselves as creative, and implementing coping skills. There were also other similar findings from a review of eleven studies on the experiences of adolescents with ADHD ( 55 ). Overlapping themes included participants feeling that ADHD symptomatology has some benefits, experiencing difficulties with societal expectations, emotions and interpersonal conflicts, struggling with identity and stigma, and having varying experiences with stimulants. The overlaps in findings from these two reviews suggest there are shared experiences between adolescents and adults with ADHD. Unique from previous reviews on lived experiences of people with ADHD are the present qualitative findings of experiences of having received diagnoses in adulthood, reflections on ADHD and substance use, occupational struggles, attention dysregulation, and emotional symptoms of ADHD.
The relationship between ADHD effects and poor occupational performance has been previously described. People with ADHD often struggle with unemployment and underemployment and functional impairment at work ( 56 – 58 ). The findings of this review suggest that adults with ADHD may benefit from workplace accommodations and from decreased stigma around adult ADHD.
Findings suggest that people with ADHD often experience attention dysregulation as opposed to attention deficits, per se . This notion builds on previous clinical observations ( 59 ) and quantitative literature ( 60 , 61 ) documenting that adults with ADHD may hyperfocus on tasks of interest. These findings suggest that inattention does not fully capture the attentional symptoms of the condition and suggest a possible need for updated diagnostic criteria.
Emotional dysregulation was described by many studies in this review, and there were no studies in which participants denied struggling with emotions. These findings provide support for a conceptual model of ADHD that presents emotional dysregulation as a core feature of ADHD, as opposed to models stating that emotional dysregulation is a subtype of ADHD or simply that the domains are correlated ( 62 ). Debates exist regarding whether or not specific clinical aspects of disorders constitute core or diagnostic features ( 63 ). The DSM-5 and ICD-11 have viewed differently the criteria for specific disorders, including with respect to engagement for emotional regulation or stress-reduction purposes [e.g., behavioral addictions like gambling and gaming disorders, and other behaviors relating to compulsive sexual engagement ( 3 , 64 , 65 )]. Because emotional dysregulation is often overlooked as being associated with ADHD, patients experiencing such symptoms may be mistaken for having other conditions such as mood or personality disorders. Appreciating the emotional symptoms of ADHD may help psychiatrists, psychologists, and social workers more accurately diagnose ADHD in adults and decrease misdiagnosis.
The recurrent themes of difficulty naming and recognizing emotions found here suggest that ADHD may be associated with alexithymia. One study found that 22% of adults with ADHD were highly alexithymic but their mean scores on the rating scale for alexithymia were not significantly different from controls ( 66 ). Parenting style, attachment features, and ADHD symptoms have been found to predict emotional processing and alexithymia measures among adults with ADHD ( 67 ). More research is needed into the relationship between ADHD symptoms and alexithymia.
There was considerable heterogeneity in wishes regarding cures for ADHD (suggesting both perceived benefits and detriments) and stimulant use being association with SUDs. From a clinical perspective, both points will be important to understand better. With regard to the latter, ADHD and SUDs frequently co-occur; one meta-analysis found that 23% of people with SUDs met criteria for ADHD ( 68 ). Furthermore, youth with ADHD are seven-fold more likely than those without to experience/develop SUDs; however, early treatment with stimulants appeared to decrease this risk ( 69 ). Understanding better motivations for substance use in adults with ADHD as may be gleaned through considering lived experiences may help decrease ADHD/SUD co-occurrence and improve quality of life.
This review highlights gaps in the qualitative literature on adult ADHD. Nearly all included studies took place in Europe, North America or Asia; there is a dearth of qualitative research on ADHD in the Global South. Although most studies did not report race, those that did often had a majority of White participants. Racial/ethnic disparities in ADHD diagnosis may contribute to the relatively low diversity of study participants ( 9 ), and such disparities are further reason to expand research focused on non-White individuals with ADHD. Most studies focused on young or middle-aged adults and most participants were male; more research is needed on how ADHD may impact older adults and other gender identities. Although long considered to disproportionately affect male children at approximately 3:1 ( 70 ), ADHD in adults has been reported to have gender ratios of 1.5:1 ( 71 ). Among the adult psychiatric population, some studies have found no gender difference in prevalence or up to a 2.5:1 female predominance ( 72 ). This finding suggests that women often may not receive diagnoses until adulthood and there may be strong links with other psychopathologies in women. The lived experience of women with ADHD should be further examined; this insight may help to understand why women often go undiagnosed and experience other psychiatric concerns.
Future qualitative studies should explore how ADHD symptoms change over the lifespan as this was not addressed in any of the included studies. There were very few findings relating to how adults with ADHD conceptualize the condition and how their diagnosis interacts with their identities. Some studies reported on difficulties adults with ADHD have with accessing services; further exploration is needed into how the medical community can better meet the needs of this population. Findings from this review may be used to inform future ADHD screening tools. The Adult ADHD Self-Report Scale (ASRS) is a widely used screening tool that covers symptoms of inattention, impulsivity, and hyperactivity ( 73 ). This review suggests that symptoms may be more expansive than what is included in the ASRS and that questions on attentional dysregulation and hyperfocusing, emotional dysregulation, internal chaos, low self-esteem, and strained interpersonal relationships could be tested for validity for inclusion. The Conners’ Adult ADHD Rating Scales (CAARS) includes questions on emotional lability and low self-esteem in addition to symptoms covered by the ASRS ( 74 ), although the scale has been found to have high false-positive and false-negative rates ( 75 ). Further studies are needed to develop screening tools that capture the lived experience of adults with ADHD while maintaining appropriate sensitivity and specificity. This review may also inform tailoring CBT and other therapeutic interventions for ADHD. For example, CBT may help develop skills for volitional hyperfocusing on productive tasks instead of feeling pulled away from daily activities.
This study has limitations. Being a rapid review, it was not an exhaustive search of the available literature and may have missed some relevant studies that would have been identified by a systematic search. The search strategy consisted of ADHD and qualitative research methods; studies that did not include “qualitative” in their titles or abstracts may not have been identified. This may explain why the previous review on the lived experiences of adults with ADHD ( 17 ) included studies not identified by this search. Although a formal quality appraisal was completed, all studies were included regardless of the quality assessment as to not further narrow the review. For example, studies were not excluded based on how they verified ADHD diagnosis as many studies did not specify if or how this was completed. Although restricting studies based on quality metrics may have made the present findings more robust, the amount of data that would have been excluded would have been considerable and may have resulted in omitting important findings. These variable quality metrics not only limit the findings of the present review, but also speak to limitations in the methodological rigor of qualitative research on adult ADHD.
Attention-deficit/hyperactivity disorder is a relatively common diagnosis among adults. Exploration of the lived experiences of adults with ADHD may illuminate the breadth of symptomatology of the condition and should be considered in the diagnostic criteria for adults. Understanding symptomatology of adults with ADHD and identifying areas of unmet need may help guide intervention development to improve the quality of life of adults with ADHD.
Author contributions
CG and MP contributed to the conception of the review. CG and GM-G performed the abstract and full text screening. CG performed the data synthesis and wrote the first draft of the manuscript. GM-G, GA, KB, and MP contributed to the revising and editing the manuscript. All authors read and approved the submitted version.
Acknowledgments
We would like to express gratitude to clinical librarian Courtney Brombosz for her assistance in developing the search strategy.
This work was supported by the Yale School of Medicine Office of Student Research One-Year Fellowship and the K12 DA000167 grant.
Conflict of interest
MP has consulted for and advised Opiant Pharmaceuticals, Idorsia Pharmaceuticals, BariaTek, AXA, Game Day Data, and the Addiction Policy Forum; has been involved in a patent application with Yale University and Novartis; has received research support from the Mohegan Sun Casino and Connecticut Council on Problem Gambling; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; and has consulted for law offices and gambling entities on issues related to impulse control or addictive disorders. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.949321/full#supplementary-material
The heat index -- how hot it really feels -- is rising faster than temperature
A 3 degree f rise in temperature due to global warming may seem endurable, but it can actually feel like 10 degrees f.
Texans have long endured scorching summer temperatures, so a global warming increase of about 3 degrees Fahrenheit (1.5 Celsius) might not sound like much to worry about.
But a new study concludes that the heat index -- essentially how hot it really feels -- has increased much faster in Texas than has the measured temperature: about three times faster.
That means that on some extreme days, what the temperature feels like is between 8 and 11 F (5 to 6 C) hotter than it would without climate change.
The study, using Texas data from June, July and August of 2023, highlights a problem with communicating the dangers of rising temperatures to the public. The temperature alone does not accurately reflect the heat stress people feel. Even the heat index itself, which takes into account the relative humidity and thus the capacity to cool off by sweating, gives a conservative estimate of heat stress, according to study author David Romps, a professor of earth and planetary science at the University of California, Berkeley.
In 2022, Romps co-authored a paper pointing out that the way most government agencies calculate the heat index is inaccurate when dealing with the temperature and humidity extremes we're seeing today. This leads people to underestimate their chances of suffering hyperthermia on the hottest days and of their chances of dying.
Texas is not an outlier. Last week, Arizona's most populous county, covering most of Phoenix, reported that heat-associated deaths last year were 50% higher than in 2022, rising from 425 in 2022 to 645 in 2023. Two-thirds of Maricopa County's heat-related deaths in 2023 were of people 50 years or older, and 71% occurred on days when the National Weather Service had issued an excessive heat warning, according to the Associated Press.
"I mean, the obvious thing to do is to cease additional warming, because this is not going to get better unless we stop burning fossil fuels," Romps said. "That's message No. 1, without doubt. We have only one direction we can really be taking the planet's average temperature, and that's up. And that's through additional burning of fossil fuels. So that's gotta stop and stop fast."
The reason that it feels much hotter than you'd expect from the increase in ambient temperature alone is that global warming is affecting the interplay between humidity and temperature, he said. In the past, relative humidity typically dropped when the temperature increased, allowing the body to sweat more and thus feel more comfortable.
But with climate change, the relative humidity remains about constant as the temperature increases, which reduces the effectiveness of sweating to cool the body.
To deal with the irreversible temperature increases we already experience, people need to take precautions to avoid hyperthermia, Romps said. He advised that, for those in extreme heat situations and unable to take advantage of air conditioning, "you can use shade and water as your friends.
"You can coat yourself in water. Get a wet rag, run it under the faucet, get your skin wet and get in front of a fan. As long as you are drinking enough water and you can keep that skin wetted in front of the fan, you're doing a good thing for yourself."
Romps' study was published March 15 in the journal Environmental Research Letters ( ERL ).
It's the humidity
Romps, an atmospheric physicist, got interested several years ago in how the human body responds to global warming's increased temperatures. Although the heat index, defined in 1979, is based on the physiological stresses induced by heat and humidity, he noted that the calculations of the heat index did not extend to the extremes of heat and humidity experienced today. Romps and graduate student and now postdoctoral fellow Yi-Chuan Lu extended the calculation of the heat index to all combinations of temperature and humidity, enabling its use in even the most extreme heat waves, like those that buffeted Texas in the summer of 2023.
Over the decades, the nation's major weather forecaster, the National Oceanic and Atmospheric Administration's (NOAA) National Weather Service, has dealt with the lack of calculated values for high heat and humidity by extrapolating from the known values. Romps and Lu found, however, that the commonly used extrapolation falls far short when conditions of temperature and humidity are extreme. Although the heat index has now been calculated for all conditions using the underlying physiological model, those values have not yet been adopted by NOAA.
After Lu spent a sweltering summer in Texas last year, Romps decided to take the state as a case study to determine how global warming has affected the perceived heat stress represented by the corrected heat index.
"I picked Texas because I had seen some high heat index values there that made me think, OK, this is a state that this summer is probably experiencing combinations of heat and humidity that are not being captured properly by NOAA's approximation to the heat index," he said.
He found that, while temperatures peaked at various places and times around the state last summer, one place, Houston's Ellington Airport, stood out. On July 23, 2023, he calculated that the heat index was 75 C, or 167 F. Global warming accounted for 12 F (6 C) of that heat index, he said.
"It sounds completely insane," Romps said. "It's beyond the physiological capacity of a young, healthy person to maintain a standard core temperature. We think it's hyperthermic, but survivable."
The fact that people can survive such temperatures is a testament to the power of evaporative cooling to cool the body, though intense sweating requires the heart to pump more blood to the skin to shed heat, which is part of heat stress. In a 2023 paper, Romps and Lu argued that what many have referred to as the maximum survivable temperature, a wet bulb temperature of 35 C (equivalent to a skin temperature when sweating of 95 F, close to the average person's core body temperature), would actually rarely lead to death in a young and healthy adult, though it would cause hyperthermia. The wet bulb temperature is what a thermometer measures when a wet rag is wrapped around it, so it takes account of the cooling effects of sweat.
"Heat index is very much like the wet bulb thermometer, only it adds the metabolic heat that a human has that a thermometer does not have," Romps said. "We think if you kept your skin wet and you were exposed to 167 degrees, even though we're approaching something like a setting on the oven, you'd still be alive. Definitely not happy. But alive."
While the current study didn't try to predict when, in the future, heat waves in Texas might generate a heat index high enough to make everyone hyperthermic, "we can see that there are times when people are getting pushed in that direction," he said. "It's not terribly far off."
Romps plans to look at other regions in light of the improved heat index scale he and Lu have proposed and expects to find similar trends.
"If humanity goes ahead and burns the fossil fuel available to it, then it is conceivable that half of Earth's population would be exposed to unavoidably hyperthermic conditions, even for young, healthy adults," Romps said. "People who aren't young and healthy would be suffering even more, as would people who are laboring or are out in the sun -- all of them would be suffering potentially life-threatening levels of heat stress."
- Severe Weather
- Global Warming
- Environmental Issues
- Environmental Policy
- Environmental Awareness
- IPCC Report on Climate Change - 2007
- Atmospheric circulation
- Mantle plume
- Mount Rainier
Story Source:
Materials provided by University of California - Berkeley . Original written by Robert Sanders. Note: Content may be edited for style and length.
Journal Reference :
- David M Romps. Heat index extremes increasing several times faster than the air temperature . Environmental Research Letters , 2024; 19 (4): 041002 DOI: 10.1088/1748-9326/ad3144
Cite This Page :
Explore More
- Metamaterial: An Endless Domino Effect
- Quantum Tornado and Black Holes
- First Neolithic Boats in Mediterranean
- Heat Index Is Rising Even Faster Than Temps
- Clear Evidence Climate Change Is Human-Caused
- Crave Snacks After Eating? Food-Seeking Neurons
- Microplastics in Remote Marine Protected Areas
- 'Fairy Circles' Made by Plant Water Stress
- Rise in Global Fungal Drug-Resistant Infections
- AI Can Help Tell When Humans Are Lying
Trending Topics
Strange & offbeat.
- Best Of The Best
- Alcohol News
- Animal & Wildlife News
- Astronomy News
- Beauty News
- Cancer News
- Children News
- Drug & Medication News
- Education News
- Environment News
- Exercise News
- Happiness News
- Historical News
- Intelligence
- Law Enforcement
- Longer Life News
- Marijuana News
- Mobile Phones News
- Parenting News
- Psychological News
- Social Media News
- Sports News
- Weight Loss News
- Workplace News
© 2024 41 Pushups, LLC

Could ADHD Drugs Reduce The Risk Of Early Death?
Article written by hassan vally , associate professor, epidemiology, deakin university.
Attention-deficit hyperactivity disorder (ADHD) can have a considerable impact on the day-to-day functioning and overall wellbeing of people affected. It causes a variety of symptoms including difficulty focusing, impulsivity and hyperactivity.
For many, a diagnosis of ADHD, whether in childhood or adulthood, is life changing. It means finally having an explanation for these challenges, and opens up the opportunity for treatment, including medication.
Although ADHD medications can cause side effects, they generally improve symptoms for people with the disorder, and thereby can significantly boost quality of life.
Now a new study has found being treated for ADHD with medication reduces the risk of early death for people with the disorder. But what can we make of these findings?
A large study from Sweden
The study, published in JAMA (the prestigious journal of the American Medical Association), was a large cohort study of 148,578 people diagnosed with ADHD in Sweden. It included both adults and children.
In a cohort study, a group of people who share a common characteristic (in this case a diagnosis of ADHD) are followed over time to see how many develop a particular health outcome of interest (in this case the outcome was death).
For this study the researchers calculated the mortality rate over a two-year follow up period for those whose ADHD was treated with medication (a group of around 84,000 people) alongside those whose ADHD was not treated with medication (around 64,000 people). The team then determined if there were any differences between the two groups.
What did the results show?
The study found people who were diagnosed and treated for ADHD had a 19% reduced risk of death from any cause over the two years they were tracked, compared with those who were diagnosed but not treated.
In understanding this result, it’s important – and interesting – to look at the causes of death. The authors separately analyzed deaths due to natural causes (physical medical conditions) and deaths due to unnatural causes (for example, unintentional injuries, suicide, or accidental poisonings).
The key result is that while no significant difference was seen between the two groups when examining natural causes of death, the authors found a significant difference for deaths due to unnatural causes.
So what’s going on?
Previous studies have suggested ADHD is associated with an increased risk of premature death from unnatural causes, such as injury and poisoning.
On a related note, earlier studies have also suggested taking ADHD medicines may reduce premature deaths. So while this is not the first study to suggest this association, the authors note previous studies addressing this link have generated mixed results and have had significant limitations.
In this new study, the authors suggest the reduction in deaths from unnatural causes could be because taking medication alleviates some of the ADHD symptoms responsible for poor outcomes – for example, improving impulse control and decision-making. They note this could reduce fatal accidents.
The authors cite a number of studies that support this hypothesis, including research showing ADHD medications may prevent the onset of mood, anxiety and substance use disorders , and lower the risk of accidents and criminality. All this could reasonably be expected to lower the rate of unnatural deaths.
Strengths and limitations
Scandinavian countries have well-maintained national registries that collect information on various aspects of citizens’ lives, including their health. This allows researchers to conduct excellent population-based studies.
Along with its robust study design and high-quality data, another strength of this study is its size. The large number of participants – almost 150,000 – gives us confidence the findings were not due to chance.
The fact this study examined both children and adults is another strength. Previous research relating to ADHD has often focused primarily on children.
One of the important limitations of this study acknowledged by the authors is that it was observational. Observational studies are where the researchers observe and analyze naturally occurring phenomena without intervening in the lives of the study participants (unlike randomized controlled trials).
The limitation in all observational research is the issue of confounding. This means we cannot be completely sure the differences between the two groups observed were not either partially or entirely due to some other factor apart from taking medication.
Specifically, it’s possible lifestyle factors or other ADHD treatments such as psychological counselling or social support may have influenced the mortality rates in the groups studied.
Another possible limitation is the relatively short follow-up period. What the results would show if participants were followed up for longer is an interesting question, and could be addressed in future research.
What are the implications?
Despite some limitations, this study adds to the evidence that diagnosis and treatment for ADHD can make a profound difference to people’s lives. As well as alleviating symptoms of the disorder, this study supports the idea ADHD medication reduces the risk of premature death.
Ultimately, this highlights the importance of diagnosing ADHD early so the appropriate treatment can be given. It also contributes to the body of evidence indicating the need to improve access to mental health care and support more broadly.
This article is republished from The Conversation under a Creative Commons license. Read the original article .
You might also be interested in:
- Following these 8 healthy habits slows down aging by up to 6 years
- ‘Smart’ ADHD drugs like Ritalin, Adderall may actually make students less productive
- Using ‘Study Drugs’ Without ADHD Primes Brain For Substance Abuse
- Adults with ADHD 3 times more likely to develop dementia, study warns
- The Same Brain Abnormality Discovered In All Children With Language Disorders
Related Studies

Coping Saves Lives: Men Who Find Ways To Manage Stress Live Longer March 20, 2024

Sitting all day linked to an early death — and exercise won’t help March 1, 2024

This 5-Day Diet That Mimics Fasting Slows Down Aging February 20, 2024
what drugs and how much?
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
The Philippines economy in 2024: Stronger for longer?
The Philippines ended 2023 on a high note, being the fastest growing economy across Southeast Asia with a growth rate of 5.6 percent—just shy of the government's target of 6.0 to 7.0 percent. 1 “National accounts,” Philippine Statistics Authority, January 31, 2024; "Philippine economic updates,” Bangko Sentral ng Pilipinas, November 16, 2023. Should projections hold, the Philippines is expected to, once again, show significant growth in 2024, demonstrating its resilience despite various global economic pressures (Exhibit 1). 2 “Economic forecast 2024,” International Monetary Fund, November 1, 2023; McKinsey analysis.
The growth in the Philippine economy in 2023 was driven by a resumption in commercial activities, public infrastructure spending, and growth in digital financial services. Most sectors grew, with transportation and storage (13 percent), construction (9 percent), and financial services (9 percent), performing the best (Exhibit 2). 3 “National accounts,” Philippine Statistics Authority, January 31, 2024. While the country's trade deficit narrowed in 2023, it remains elevated at $52 billion due to slowing global demand and geopolitical uncertainties. 4 “Highlights of the Philippine export and import statistics,” Philippine Statistics Authority, January 28, 2024. Looking ahead to 2024, the current economic forecast for the Philippines projects a GDP growth of between 5 and 6 percent.
Inflation rates are expected to temper between 3.2 and 3.6 percent in 2024 after ending 2023 at 6.0 percent, above the 2.0 to 4.0 percent target range set by the government. 5 “Nomura downgrades Philippine 2024 growth forecast,” Nomura, September 11, 2023; “IMF raises Philippine growth rate forecast,” International Monetary Fund, July 16, 2023.
For the purposes of this article, most of the statistics used for our analysis have come from a common thread of sources. These include the Central Bank of the Philippines (Bangko Sentral ng Pilipinas); the Department of Energy Philippines; the IT and Business Process Association of the Philippines (IBPAP); and the Philippines Statistics Authority.
The state of the Philippine economy across seven major sectors and themes
In the article, we explore the 2024 outlook for seven key sectors and themes, what may affect each of them in the coming year, and what could potentially unlock continued growth.
Financial services
The recovery of the financial services sector appears on track as year-on-year growth rates stabilize. 6 Philippines Statistics Authority, November 2023; McKinsey in partnership with Oxford Economics, November 2023. In 2024, this sector will likely continue to grow, though at a slower pace of about 5 percent.
Financial inclusion and digitalization are contributing to growth in this sector in 2024, even if new challenges emerge. Various factors are expected to impact this sector:
- Inclusive finance: Bangko Sentral ng Pilipinas continues to invest in financial inclusion initiatives. For example, basic deposit accounts (BDAs) reached $22 million in 2023 and banking penetration improved, with the proportion of adults with formal bank accounts increasing from 29 percent in 2019 to 56 percent in 2021. 7 “Financial inclusion dashboard: First quarter 2023,” Bangko Sentral ng Pilipinas, February 6, 2024.
- Digital adoption: Digital channels are expected to continue to grow, with data showing that 60 percent of adults who have a mobile phone and internet access have done a digital financial transaction. 8 “Financial inclusion dashboard: First quarter 2023,” Bangko Sentral ng Pilipinas, February 6, 2024. Businesses in this sector, however, will need to remain vigilant in navigating cybersecurity and fraud risks.
- Unsecured lending growth: Growth in unsecured lending is expected to continue, but at a slower pace than the past two to three years. For example, unsecured retail lending for the banking system alone grew by 27 percent annually from 2020 to 2022. 9 “Loan accounts: As of first quarter 2023,” Bangko Sentral ng Pilipinas, February 6, 2024; "Global banking pools,” McKinsey, November 2023. Businesses in this field are, however, expected to recalibrate their risk profiling models as segments with high nonperforming loans emerge.
- High interest rates: Key interest rates are expected to decline in the second half of 2024, creating more accommodating borrowing conditions that could boost wholesale and corporate loans.
Supportive frameworks have a pivotal role to play in unlocking growth in this sector to meet the ever-increasing demand from the financially underserved. For example, financial literacy programs and easier-to-access accounts—such as BDAs—are some measures that can help widen market access to financial services. Continued efforts are being made to build an open finance framework that could serve the needs of the unbanked population, as well as a unified credit scoring mechanism to increase the ability of historically under-financed segments, such as small and medium-sized enterprises (SMEs), to access formal credit. 10 “BSP launches credit scoring model,” Bangko Sentral ng Pilipinas, April 26, 2023.
Energy and Power
The outlook for the energy sector seems positive, with the potential to grow by 7 percent in 2024 as the country focuses on renewable energy generation. 11 McKinsey analysis based on input from industry experts. Currently, stakeholders are focused on increasing energy security, particularly on importing liquefied natural gas (LNG) to meet power plants’ requirements as production in one of the country’s main sources of natural gas, the Malampaya gas field, declines. 12 Myrna M. Velasco, “Malampaya gas field prod’n declines steeply in 2021,” Manila Bulletin , July 9, 2022. High global inflation and the fact that the Philippines is a net fuel importer are impacting electricity prices and the build-out of planned renewable energy projects. Recent regulatory moves to remove foreign ownership limits on exploration, development, and utilization of renewable energy resources could possibly accelerate growth in the country’s energy and power sector. 13 “RA 11659,” Department of Energy Philippines, June 8, 2023.
Gas, renewables, and transmission are potential growth drivers for the sector. Upgrading power grids so that they become more flexible and better able to cope with the intermittent electricity supply that comes with renewables will be critical as the sector pivots toward renewable energy. A recent coal moratorium may position natural gas as a transition fuel—this could stimulate exploration and production investments for new, indigenous natural gas fields, gas pipeline infrastructure, and LNG import terminal projects. 14 Philippine energy plan 2020–2040, Department of Energy Philippines, June 10, 2022; Power development plan 2020–2040 , Department of Energy Philippines, 2021. The increasing momentum of green energy auctions could facilitate the development of renewables at scale, as the country targets 35 percent share of renewables by 2030. 15 Power development plan 2020–2040 , 2022.
Growth in the healthcare industry may slow to 2.8 percent in 2024, while pharmaceuticals manufacturing is expected to rebound with 5.2 percent growth in 2024. 16 McKinsey analysis in partnership with Oxford Economics.
Healthcare demand could grow, although the quality of care may be strained as the health worker shortage is projected to increase over the next five years. 17 McKinsey analysis. The supply-and-demand gap in nursing alone is forecast to reach a shortage of approximately 90,000 nurses by 2028. 18 McKinsey analysis. Another compounding factor straining healthcare is the higher than anticipated benefit utilization and rising healthcare costs, which, while helping to meet people's healthcare budgets, may continue to drive down profitability for health insurers.
Meanwhile, pharmaceutical companies are feeling varying effects of people becoming increasingly health conscious. Consumers are using more over the counter (OTC) medication and placing more beneficial value on organic health products, such as vitamins and supplements made from natural ingredients, which could impact demand for prescription drugs. 19 “Consumer health in the Philippines 2023,” Euromonitor, October 2023.
Businesses operating in this field may end up benefiting from universal healthcare policies. If initiatives are implemented that integrate healthcare systems, rationalize copayments, attract and retain talent, and incentivize investments, they could potentially help to strengthen healthcare provision and quality.
Businesses may also need to navigate an increasingly complex landscape of diverse health needs, digitization, and price controls. Digital and data transformations are being seen to facilitate improvements in healthcare delivery and access, with leading digital health apps getting more than one million downloads. 20 Google Play Store, September 27, 2023. Digitization may create an opportunity to develop healthcare ecosystems that unify touchpoints along the patient journey and provide offline-to-online care, as well as potentially realizing cost efficiencies.
Consumer and retail
Growth in the retail and wholesale trade and consumer goods sectors is projected to remain stable in 2024, at 4 percent and 5 percent, respectively.
Inflation, however, continues to put consumers under pressure. While inflation rates may fall—predicted to reach 4 percent in 2024—commodity prices may still remain elevated in the near term, a top concern for Filipinos. 21 “IMF raises Philippine growth forecast,” July 26, 2023; “Nomura downgrades Philippines 2024 growth forecast,” September 11, 2023. In response to challenging economic conditions, 92 percent of consumers have changed their shopping behaviors, and approximately 50 percent indicate that they are switching brands or retail providers in seek of promotions and better prices. 22 “Philippines consumer pulse survey, 2023,” McKinsey, November 2023.
Online shopping has become entrenched in Filipino consumers, as they find that they get access to a wider range of products, can compare prices more easily, and can shop with more convenience. For example, a McKinsey Philippines consumer sentiment survey in 2023 found that 80 percent of respondents, on average, use online and omnichannel to purchase footwear, toys, baby supplies, apparel, and accessories. To capture the opportunity that this shift in Filipino consumer preferences brings and to unlock growth in this sector, retail organizations could turn to omnichannel strategies to seamlessly integrate online and offline channels. Businesses may need to explore investments that increase resilience across the supply chain, alongside researching and developing new products that serve emerging consumer preferences, such as that for natural ingredients and sustainable sources.
Manufacturing
Manufacturing is a key contributor to the Philippine economy, contributing approximately 19 percent of GDP in 2022, employing about 7 percent of the country’s labor force, and growing in line with GDP at approximately 6 percent between 2023 and 2024. 23 McKinsey analysis based on input from industry experts.
Some changes could be seen in 2024 that might affect the sector moving forward. The focus toward building resilient supply chains and increasing self-sufficiency is growing. The Philippines also is likely to benefit from increasing regional trade, as well as the emerging trend of nearshoring or onshoring as countries seek to make their supply chains more resilient. With semiconductors driving approximately 45 percent of Philippine exports, the transfer of knowledge and technology, as well as the development of STEM capabilities, could help attract investments into the sector and increase the relevance of the country as a manufacturing hub. 24 McKinsey analysis based on input from industry experts.
To secure growth, public and private sector support could bolster investments in R&D and upskill the labor force. In addition, strategies to attract investment may be integral to the further development of supply chain infrastructure and manufacturing bases. Government programs to enable digital transformation and R&D, along with a strategic approach to upskilling the labor force, could help boost industry innovation in line with Industry 4.0 demand. 25 Industry 4.0 is also referred to as the Fourth Industrial Revolution. Priority products to which manufacturing industries could pivot include more complex, higher value chain electronic components in the semiconductor segment; generic OTC drugs and nature-based pharmaceuticals in the pharmaceutical sector; and, for green industries, products such as EVs, batteries, solar panels, and biomass production.
Information technology business process outsourcing
The information technology business process outsourcing (IT-BPO) sector is on track to reach its long-term targets, with $38 billion in forecast revenues in 2024. 26 Khriscielle Yalao, “WHF flexibility key to achieving growth targets—IBPAP,” Manila Bulletin , January 23, 2024. Emerging innovations in service delivery and work models are being observed, which could drive further growth in the sector.
The industry continues to outperform headcount and revenue targets, shaping its position as a country leader for employment and services. 27 McKinsey analysis based in input from industry experts. Demand from global companies for offshoring is expected to increase, due to cost containment strategies and preference for Philippine IT-BPO providers. New work setups continue to emerge, ranging from remote-first to office-first, which could translate to potential net benefits. These include a 10 to 30 percent increase in employee retention; a three- to four-hour reduction in commute times; an increase in enabled talent of 350,000; and a potential reduction in greenhouse gas emissions of 1.4 to 1.5 million tons of CO 2 per year. 28 McKinsey analysis based in input from industry experts. It is becoming increasingly more important that the IT-BPO sector adapts to new technologies as businesses begin to harness automation and generative AI (gen AI) to unlock productivity.
Talent and technology are clear areas where growth in this sector can be unlocked. The growing complexity of offshoring requirements necessitates building a proper talent hub to help bridge employee gaps and better match local talent to employers’ needs. Businesses in the industry could explore developing facilities and digital infrastructure to enable industry expansion outside the metros, especially in future “digital cities” nationwide. Introducing new service areas could capture latent demand from existing clients with evolving needs as well as unserved clients. BPO centers could explore the potential of offering higher-value services by cultivating technology-focused capabilities, such as using gen AI to unlock revenue, deliver sales excellence, and reduce general administrative costs.
Sustainability
The Philippines is considered to be the fourth most vulnerable country to climate change in the world as, due to its geographic location, the country has a higher risk of exposure to natural disasters, such as rising sea levels. 29 “The Philippines has been ranked the fourth most vulnerable country to climate change,” Global Climate Risk Index, January 2021. Approximately $3.2 billion, on average, in economic loss could occur annually because of natural disasters over the next five decades, translating to up to 7 to 8 percent of the country’s nominal GDP. 30 “The Philippines has been ranked the fourth most vulnerable country to climate change,” Global Climate Risk Index, January 2021.
The Philippines could capitalize on five green growth opportunities to operate in global value chains and catalyze growth for the nation:
- Renewable energy: The country could aim to generate 50 percent of its energy from renewables by 2040, building on its high renewable energy potential and the declining cost of producing renewable energy.
- Solar photovoltaic (PV) manufacturing: More than a twofold increase in annual output from 2023 to 2030 could be achieved, enabled by lower production costs.
- Battery production: The Philippines could aim for a $1.5 billion domestic market by 2030, capitalizing on its vast nickel reserves (the second largest globally). 31 “MineSpans,” McKinsey, November 2023.
- Electric mobility: Electric vehicles could account for 15 percent of the country’s vehicle sales by 2030 (from less than 1 percent currently), driven by incentives, local distribution, and charging infrastructure. 32 McKinsey analysis based on input from industry experts.
- Nature-based solutions: The country’s largely untapped total abatement potential could reach up to 200 to 300 metric tons of CO 2 , enabled by its biodiversity and strong demand.
The Philippine economy: Three scenarios for growth
Having grown faster than other economies in Southeast Asia in 2023 to end the year with 5.6 percent growth, the Philippines can expect a similarly healthy growth outlook for 2024. Based on our analysis, there are three potential scenarios for the country’s growth. 33 McKinsey analysis in partnership with Oxford Economics.
Slower growth: The first scenario projects GDP growth of 4.8 percent if there are challenging conditions—such as declining trade and accelerated inflation—which could keep key policy rates high at about 6.5 percent and dampen private consumption, leading to slower long-term growth.
Soft landing: The second scenario projects GDP growth of 5.2 percent if inflation moderates and global conditions turn out to be largely favorable due to a stable investment environment and regional trade demand.
Accelerated growth: In the third scenario, GDP growth is projected to reach 6.1 percent if inflation slows and public policies accommodate aspects such as loosening key policy rates and offering incentive programs to boost productivity.
Focusing on factors that could unlock growth in its seven critical sectors and themes, while adapting to the macro-economic scenario that plays out, would allow the Philippines to materialize its growth potential in 2024 and take steps towards achieving longer-term, sustainable economic growth.
Jon Canto is a partner in McKinsey’s Manila office, where Frauke Renz is an associate partner, and Vicah Villanueva is a consultant.
The authors wish to thank Charlene Chua, Charlie del Rosario, Ryan delos Reyes, Debadrita Dhara, Evelyn C. Fong, Krzysztof Kwiatkowski, Frances Lee, Aaron Ong, and Liane Tan for their contributions to this article.
Explore a career with us
Related articles.

The Philippines Growth Dialogues

What does 2023 hold for the Philippines’ economy?

On the verge of a digital banking revolution in the Philippines

IMAGES
VIDEO
COMMENTS
Case Study 1 - Jack Jack is a 7 year old male Grade 1 student who lives in Toronto with his parents. He is the only child to two parents, both of whom have completed post-graduate education. There is an extended family history of Attention Deficit/Hyperactivity Disorder (ADHD), mental health concerns as well as academic excellence.
up the case study, names those activities in brief without the full details and explicit information each client-family receives in why and how to implement the program. Go to www.handle.org for more information. The HANDLE® Institute 7 Mt. Lassen Drive, Suite B110 San Rafael, CA 94903 415-479-1800
The present study analyzes a specific case of ADHD with predominantly inattentive presentation, covering monopolar electroencephalogram recording (brain mapping called MiniQ) and intervention via neurofeedback. ... here, the values were very close. The SMR wave also increased notably, by 2.57 points at Fz and 2.89 points at Cz. In short, the ...
Case Study Details. Jen is a 29 year-old woman who presents to your clinic in distress. In the interview she fidgets and has a hard time sitting still. She opens up by telling you she is about to be fired from her job. In addition, she tearfully tells you that she is in a major fight with her husband of 1 year because he is ready to have ...
OK, let's move on to the case presentation. This first patient is a 19-year-old male, who presented to his psychiatrist after being referred by his primary care provider, PCP for ADHD consultation, during the interview, he noted he was a sophomore in college and is taking 17 credits. This semester chief complaint includes a lack of ability to ...
To address the limitations of both methods for examining short-term memory in ADHD, Gibson et al. (2017, 2018) called for a bifactor modeling approach to provide latent estimates that maximally distinguish between primary (short-term memory) and secondary memory (working memory). This is the approach used in the current study.
Despite increased awareness, Attention-deficit hyperactivity disorder (ADHD) is a chronic condition that affects 8% to 12% of school-aged children and contributes significantly to academic and social impairment. There is currently broad agreement on evidence-based best practices of ADHD identification and diagnosis, therapeutic approach, and ...
I like to participate in the foll. Case Study: Interventions 10. 3 for Personal and Social Development Completes homework (See Appendix G). 3. Attendance Record. missed 1.5 days of school and has ...
Introduction. Attention deficit hyperactivity disorder (ADHD) is a frequent mental disorder with childhood onset and a worldwide prevalence of at least 2.8% ().It is characterized by the three core symptoms of attention deficit, hyperactivity, and impulsivity manifesting since childhood ().Adult ADHD is also commonly associated with different comorbidities (3, 4), particularly obsessive ...
3.8 (2020): 23-29. Undetected Story of Adult ADHD: A Case Based Short Commentary. 27. in this case might have (mis) guided earlier psychiatrist t o prescribe clonazepam/Lorazepam every time. Being ...
Fig. 1 summarizes suggested steps in caring for adults with ADHD and can guide providers with limited experience in treating the disorder. With improved science and longer life spans, many disorders once seen only during childhood are now continuing into adulthood. ADHD is one of many disorders once thought to only occur in children and resolve as
Stimulant medications have been shown to be effective in the treatment of ADHD in both children and adults. The mechanism of action for drug therapy is believed to be linked to an increase in extracellular dopamine and norepinephrine levels in the frontal cortex by inhibiting the reuptake of these neurotransmitters (Contini et al., 2013).The overall outcome is improvement in impulsive behavior ...
A CASE STUDY. Observations of a student with ADHD over a 3-week time span. ... He has no physical disabilities, but suffers from a mental disorder - ADHD. He often makes careless mistakes in schoolwork. He does not pay attention to detail. He has trouble staying focused while reading long texts. He also has difficulty staying still during a ...
Maternal lifestyle before, during and post birth have also been indicated in brain abnormalities which lead to ADHD traits. For instance, prenatal alcohol exposure is linked with disruptive, hyperactive and impulsive behaviours (D'Onofrio et al. 2007).Hyperactive behaviours were reported in connection with maternal smoking as nicotine receptors modulate dopaminergic activity which if ...
In short, ADHD coaching is a partnership between someone with ADHD and an expert ADHD coach, where they work together to bridge the gap between where the client is, and where they want to be. ... Case Study 2: Job Hunting with ADHD. Situation: Member just finished school and was applying to jobs. The task was large & daunting, and the member ...
In adult ADHD, the symptoms may be comorbid or mimic other conditions making diagnosis and treatment difficult. Adults with ADHD require an in-depth assessment for proper diagnosis and treatment. The presentation and treatment of adults with ADHD can be complex and often requires interdisciplinary care.
For some children, their ADHD is severe and can have a huge impact on their ability to engage in school and to build and sustain relationships. Left untreated, evidence shows that those with ADHD are more likely to get into car accidents, engage in criminal activity and may struggle to keep a job or maintain relationships. Case Study
ADHD symptoms. Research in population-based samples indicates that for both sexes the hyperactive-impulsive type predominates in pre-schoolers, whereas the inattentive-type is the most common presentation from mid-to-late childhood and into adulthood [4, 21].By contrast, clinical studies typically report a greater prevalence of combined-type ADHD [5, 12, 22].
Beyond this, the longer-term consequences have been the focus of numerous individual studies but comprehensive synthesis of the available data has yet to be conducted, thus the present systematic review was performed, focusing on comprehensive summary of long-term outcomes of ADHD. Short-term studies have demonstrated decreases in core symptoms ...
5 CASE STUDY 1 Attention Defi cit Hyperactivity Disorder (ADHD) in children and young people Alison Coad. Georgia is 10 and lives with her mum, Emma, her dad, Nick and her younger brother Sam, aged 7.
A comparative study on short-term effects of methylphenidate and atomoxetine on ADHD reported significantly higher weight loss in children treated with atomoxetine . ... the precise nature of the physiological changes underlying the clinical manifestations of ADHD in each case could be slightly different, affecting the effectiveness of the ...
The access to and uptake of evidence-based behavioral parent training for children with behavioral difficulties (i.e., oppositional, defiant, aggressive, hyperactive, impulsive, and inattentive behavior) are currently limited because of a scarcity of certified therapists and long waiting lists. These problems are in part due to the long and sometimes perceived as rigid nature of most evidence ...
One recent study reported a 14% increase in ADHD stimulant prescriptions ... "This devastating reality is the case for too many Americans who need generic drugs for ADHD, cancer, and other ...
While neuroscience researchers have long suspected that ADHD symptoms result from atypical interactions between the frontal cortex and these deep information-processing brain structures, studies testing this model have returned mixed findings, possibly due to the small nature of the studies, with only 100 or so subjects.
The study, published this week in JAMA, was a large cohort study of 148,578 people diagnosed with ADHD in Sweden. It included both adults and children. It included both adults and children.
Background Ultra-short coeliac disease (USCD) is defined as villous atrophy only present in the duodenal bulb (D1) with concurrent positive coeliac serology. We present the first, multicentre, international study of patients with USCD. Methods Patients with USCD were identified from 10 tertiary hospitals (6 from Europe, 2 from Asia, 1 from North America and 1 from Australasia) and compared ...
Studies reporting original peer-reviewed qualitative data on the lived experience of adults with ADHD, including mixed-methods studies, were eligible for inclusion. "Adult" was defined as being 18 years of age or older; studies that included adolescent and young adult participants were only included if results were reported separately by age.
The study, using Texas data from June, July and August of 2023, highlights a problem with communicating the dangers of rising temperatures to the public. The temperature alone does not accurately ...
A large study from Sweden. The study, published in JAMA (the prestigious journal of the American Medical Association), was a large cohort study of 148,578 people diagnosed with ADHD in Sweden. It included both adults and children. In a cohort study, a group of people who share a common characteristic (in this case a diagnosis of ADHD) are followed over time to see how many develop a particular ...
The Philippines ended 2023 on a high note, being the fastest growing economy across Southeast Asia with a growth rate of 5.6 percent—just shy of the government's target of 6.0 to 7.0 percent. 1 "National accounts," Philippine Statistics Authority, January 31, 2024; "Philippine economic updates," Bangko Sentral ng Pilipinas, November 16, 2023. ...