Advantages and Disadvantages of Vaccination
Introduction.
Over the past few years, there has been an increase in the number of diseases that affect human beings. As such, researchers and medical experts have dedicated most of the available resources to ensure that both preventive and curative measures are put in place in a bid to avoid the further spread of the various diseases that pose a serious risk to the human race. The major challenge being faced globally is creating awareness of the diseases and controlling or containing their spread. A good example that validates this statement would be the swine flu outbreak that has caused major panic throughout the world since 2009. As such governments in association with medical care providers have put in place strategies to ensure that everyone is vaccinated against this killer virus.

Thesis statement
The effectiveness of the H1N1 vaccination continues to be a highly debated topic in the medical and social community; although each side has raised genuine arguments, there are PROS and CONS to each side of the debate. This paper shall focus on these concerns all the while analyzing the advantages and disadvantages of this vaccine from each side’s point of view. As a result of this, a detailed debate shall ensue to determine whether the vaccination is necessary, beneficial or harmful to society. Recommendations shall also be made relating to the hard decisions that have to be made for the good of all humanity.
A brief history of the swine flu
Influenza viruses are a strain of viruses that infect most mammals including humans. The infected person displays symptoms such as fever, cold, cough muscular pains and fatigue. The original strand of the H1N1 virus was discovered in Lowa 1918 at the Cedar Rapids swine show. It is believed that the virus mutates rapidly and mixes with other forms of influenza viruses to come up with a new strand. As such it is very difficult to come up with the ultimate cure or even an accurate vaccine. According to Conlin (2009), the virus quickly spread in areas where there is a high population of people and domestic animals and this is why the 2009 outbreak began in Mexico and spread through America and later other countries in the world.
Problem statement
The swine flu is a killer disease that is transmitted to humans by pigs. Its symptoms are similar to those of the seasonal flu and could therefore be easily taken for granted. After it affects a human being, it spreads very fast as it can be transferred from one person to another through the same mediums as the common cold. During the 2009 outbreak, the virus had already spread before the government and medical society realized what it was. By the time they decided to take preventive measures such as quarantine and banning the importation or exportation of pork, the flu was beyond containment. Since then, most governments are insisting that everyone gets vaccinated against this deadly flu as a preventive measure while the medical facilities concentrate on containing and curing the already infected people. However the necessity of the vaccine continues to be highly debated among the communities.
Medical argument
According to statistics provided by the CDC, an estimated 36,000 Americans die each year as a result of the seasonal flu. In addition to this, the CDC claims that even if the current strain of swine flu has a lower death rate than the seasonal flu, preventive measures should be taken to ensure that the numbers do not go higher. Also they say that the current strain is more dangerous and that it poses a high risk to the young especially those born after 1957. The vaccines would be very beneficial to young children who are susceptible to various diseases because their immune systems are still developing and therefore weak. Kolata (2001) acclaims that if the world felt the full impact of the swine flu as experienced in 1918 where more than 40 million people died overnight then we would have the greatest loss of all times. This statement just goes to show how important it is to prevent such pandemics from happening further proving the importance of this vaccine. Additionally, the population levels have increased greatly over the past few decades. However, the number of medical experts is still very low in relation to the total population globally. In the event that a full blow outbreak occurs, little can be done to contain it since the required manpower would be unfairly overwhelmed and therefore the global inoculation would reduce these odds in the event that this actually happens.
Another reason why the medical community is pushing for this vaccination is because of the alarming rates at which flu rates are being reported globally. CDC claims that since April 2009, 98% of all flu cases reported in America have traces of the H1N1 virus. Within the same period, they have received a total of 274 pediatric deaths related to the 2009 H1N1 virus. This shows that the virus is beyond containment and preventive measures should be employed to avoid further spread. As a result the medical societies in conjunction with the various governments are advocating that pregnant women, the elderly and the young be vaccinated against this killer disease.
On the other hand, there are some medical professionals that are against this vaccine. According to Bauer (2009), the vaccine contains some elements which may cause differentiated health complications such as autism in children. In addition to this there is no clear information as yet pertaining to the various side effects that may come with the vaccine. This information is crucial to the public especially the old and the pregnant women as it may as well define their survival. Other medical experts insist that other prevention measures be considered before deciding on vaccination. Bauer (2009) says that maintaining high personal hygiene, proper meat inspection and availing the necessary information about the disease to the public would have a more positive effect on the prevention process than vaccination. This is because every body would exercise a certain level of caution and would therefore be less likely to contract the virus no matter how much it mutates. On the other hand, a vaccine is made specially to combat a particular disease. In the event that the virus mutates which in most cases is likely, the vaccine is rendered useless leaving the person vulnerable to the new strand. Also continuous use of drugs has been known to weaken the body’s immune system because the body becomes dependent on the drugs and cannot protect itself naturally against infections. In an era whereby everyone is required to be vaccinated against almost every illness, adding more drugs to the list makes the whole situation even worse.
Social argument
According to Balduci (2008), the vaccine may have some diverse effects on many people. It could lead to some blood disorders in the elderly and according to data provided after a series of testing, it was discovered that most old people could not produce antibodies against the H1N1 virus even after vaccination. In addition to this, many people have expressed deep concerns about the presence of thimerosal in the vaccine. Thimerosal is a preservative that contains mercury which is believed to cause autism in children and as such, many parents are hesitating to take their children for the shots. Additionally, medical experts released information stating that there is a likely chance that the vaccine may increase the risk of getting a mental disorder called the Guillain-Barré syndrome.
Also due to the time frame between the outbreak and the development of the vaccine, many people feel like the drug has not been properly tested. This is also backed by the fact that there is a lack of information pertaining to the vaccine. Many people feel that massive information campaigns should be conducted so that the public can be reassured and have a clue of what to expect from the vaccine. Up to date, most people do not understand how vaccines work and the little they know instills fear making them opt not to get vaccinated.
From the discussion above, we see that both sides have valid reasons to support their decision. However a consensus needs to be reached in order to determine the next course of action. From society’s point of view, they are reluctant because they do not understand the vaccine and as a result they fear that it may bring further complications to their lives. Also, the governments are making the vaccination process seem mandatory and as such the public sees this move as an invasion of their rights and freedom of choice. On the other hand, the medical community has good intentions when it comes to the inoculation process. They have a clear understanding of what may happen if preventive measures are not implemented as soon as possible and that is why they are insisting that at least everybody gets vaccinated against this life threatening virus.
Wise men always said that prevention is better than cure. On this note I feel that the vaccination against the H1N1 virus is indeed necessary. This decision can best be supported by weighing the advantages and disadvantages that come with the vaccination against the Swine flu. As is with any other crucial decision, the main focus of this whole decision making structure should be what is best for humanity.
Advantages of vaccinations
The first notable advantage of the swine flu vaccine is its admission methods. The vaccine can be administered in two ways; injection or as a nasal spray. This is very considerate as it factors in the age and physical well being of the patients ensuring comfort to all that use it. In addition to this, the vaccine is free in most countries and readily available to all in others. Since it is a government duty to promote health to its citizens, many governments have taken upon themselves the duty to ensure that the drugs are readily available to all their citizens for example.
In addition to this, the main reason for the production of any vaccine is the prevention of diseases. It is very difficult to prevent people from socializing, travelling and even germs but preventive measures such as vaccinations can be implemented to reduce the risk of getting sick from these sources. The swine flu infection can easily be passed among people especially children and vaccination would help reduce the chances of this happening.
According to Kolata (2001), viruses are notorious when it comes to mutation. If a vaccine is created and introduced into the body, the virus mutates into a more complex and dangerous strain rendering the vaccine useless. The H1N1 virus mutates very easily into more dangerous strains. This fact makes viruses the deadliest disease causing agents ever discovered. However if a person is vaccinated and the swine flu virus mutates, the effects of the new strain would not be as bad as when a person is not vaccinated. In addition to this, some vaccines have been known t boost the overall immune system thereby preventing other diseases from attacking the person. Vaccination has also saved millions of lives globally over the decades. The eradication of small pox whooping cough can all be attributed to vaccines. Even the less developed countries have felt the impacts of vaccination despite their poor development. Therefore vaccination has helped in improving the value and quality of life.
Disadvantages of vaccinations
Vaccination has also had its challenges over the past decades. Bauer (2009) literates that the general lack of vaccination medicines and facilities has been the major cause of pediatric deaths in most countries. Kolata (2001) further strengthens this point by saying that if people are not vaccinated against influenza, it may cause fatalities in all age brackets, disabilities and a pandemic outbreak if not contained. She continues by saying that most vaccines display side effects similar to the symptoms of the original disease but these symptoms disappear after a while.
Additionally, it has been discovered that there is a likelihood of developing complications from the vaccine if there is a history of autism in a particular family. Thimerosal, which is a preservative used in the manufacturing of the swine flu vaccine has been known to trigger autism and other mental problems especially in children due to the fact that it contains traces of mercury in it.
Another disadvantage is the fact that as years go by, more and more drugs are being developed in a bid to promote health. Due to the extensive marketing and advertisements, people end up taking almost all the drugs and in the process weaken their immune system. Balducci acclaims that constant use of drugs leads to dependency which cripples he body’s natural ability to fight infections (2008).as a result of this, in America everyone is expected to get two influenza shots for swine flu and the seasonal flu. In addition to this, the children have multiple other preventive shots lined up.
Also recent information suggests that there could be an increase in the number of brain disorders called Guillain-Barré syndrome which may be triggered by the vaccine. From these statements we see that the vaccine has not been fully tested on a mass scale in order to fully understand its effects to the various classes in society. As a result of this, the drug may be more harmful than it would be beneficial.
Due to the fact that there has been no adequate time to test the vaccine, there are major concerns from both the medical community and society about the nature of the vaccine. Many people fear that it may be a repeat of the 1976 incidence whereby the swine flu vaccine actually killed more people than the virus itself leading to major pay offs and unrest in American society back then.
Recommendations
From the discussion above, it is clear that there is a need to employ preventive measures to curb this deadly virus. The opinions of the important parties to this debate have been weighed and the advantages and disadvantages of the situation analyzed. It is therefore safe to say that the vaccination process is not only necessary but should actually be mandated all across the globe. This is because the swine flu is posing a serious threat to the existence of humanity and given its history, it may as well be the ultimate doom to our existence. As such, every thing should be done to ensure that the disease is not given a chance and if this means losing a few people to save millions more then it would be indeed a worthy cause. There are other measures that should be taken upon by each individual on a personal level. Everyone must ensure they follow the basic sanitation rules during their day to day activities such as washing hands before meals and after, seeking medical attention as soon as any symptom of influenza is visible, passing information to others about how the disease can be spread and avoided and finally, ensure that meat products that we consume are of good quality and certified by the FDA.
Vaccinations have been in use for a very long time now and they have helped save million of lives and changed the endings of many life stories. A brief history has been provided in this paper to help understand the source of the problem. In addition to this, a detailed debate has been offered as to why different people are for or against the new swine flu vaccine. The advantages and disadvantages of this vaccine have been mentioned and explained. Recommendations have been made as to why vaccination is a necessity in today’s world. If the recommendations are adhered to then we as the human race might just as well have given our existence another chance.
Balducci, L, Ershler, W & De Gaetano, G. (2008). Blood disorders in the elderly. Cambridge University Press.
Bauer, B. (2009). Parents weigh pros, cons of H1N1 vaccine. Web.
Cbs4. (2009). H1N1 Vaccine Sparks Debate Among Parents. Web.
cdc. 2009 H1N1 Flu: Situation Update . Web.
Conlin, J, R. (2009). The American Past: A Survey of American History. Cengage Learning
Kolata, G. (2001). Flu: the story of the great influenza pandemic of 1918 and the search for the virus that caused it. Simon & Schuster.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, March 21). Advantages and Disadvantages of Vaccination. https://studycorgi.com/advantages-and-disadvantages-of-vaccination/
"Advantages and Disadvantages of Vaccination." StudyCorgi , 21 Mar. 2022, studycorgi.com/advantages-and-disadvantages-of-vaccination/.
StudyCorgi . (2022) 'Advantages and Disadvantages of Vaccination'. 21 March.
1. StudyCorgi . "Advantages and Disadvantages of Vaccination." March 21, 2022. https://studycorgi.com/advantages-and-disadvantages-of-vaccination/.
Bibliography
StudyCorgi . "Advantages and Disadvantages of Vaccination." March 21, 2022. https://studycorgi.com/advantages-and-disadvantages-of-vaccination/.
StudyCorgi . 2022. "Advantages and Disadvantages of Vaccination." March 21, 2022. https://studycorgi.com/advantages-and-disadvantages-of-vaccination/.
This paper, “Advantages and Disadvantages of Vaccination”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: September 28, 2023 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
Jump to navigation
- Bahasa Malaysia

What are the benefits and risks of vaccines for preventing COVID-19?
Key messages
– Most vaccines reduce, or probably reduce, the number of people who get COVID-19 disease and severe COVID-19 disease.
– Many vaccines likely increase number of people experiencing events such as fever or headache compared to placebo (sham vaccine that contains no medicine but looks identical to the vaccine being tested). This is expected because these events are mainly due to the body's response to the vaccine; they are usually mild and short-term.
– Many vaccines have little or no difference in the incidence of serious adverse events compared to placebo.
– There is insufficient evidence to determine whether there was a difference between the vaccine and placebo in terms of death because the numbers of deaths were low in the trials.
– Most trials assessed vaccine efficacy over a short time, and did not evaluate efficacy to the COVID variants of concern.
What is SARS-CoV-2 and COVID-19?
SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) is the virus that causes COVID-19 disease. Not everyone infected with SARS-CoV-2 will develop symptoms of COVID-19. Symptoms can be mild (e.g. fever and headaches) to life-threatening (e.g. difficulty breathing), or death.
How do vaccines prevent COVID-19?
While vaccines work slightly differently, they all prepare the body's immune system to prevent people from getting infected with SARS-CoV-2 or, if they do get infected, to prevent severe disease.
What did we want to find out?
We wanted to find out how well each vaccine works in reducing SARS-CoV-2 infection, COVID-19 disease with symptoms, severe COVID-19 disease, and total number of deaths (including any death, not only those related to COVID-19).
We wanted to find out about serious adverse events that might require hospitalization, be life-threatening, or both; systemic reactogenicity events (immediate short-term reactions to vaccines mainly due to immunological responses; e.g. fever, headache, body aches, fatigue); and any adverse events (which include non-serious adverse events).
What did we do?
We searched for studies that examined any COVID-19 vaccine compared to placebo, no vaccine, or another COVID-19 vaccine.
We selected only randomized trials (a study design that provides the most robust evidence because they evaluate interventions under ideal conditions among participants assigned by chance to one of two or more groups). We compared and summarized the results of the studies, and rated our confidence in the evidence based on factors such as how the study was conducted.
What did we find?
We found 41 worldwide studies involving 433,838 people assessing 12 different vaccines. Thirty-five studies included only healthy people who had never had COVID-19. Thirty-six studies included only adults, two only adolescents, two children and adolescents, and one included adolescents and adults. Three studied people with weakened immune systems, and none studied pregnant women.
Most cases assessed results less than six months after the primary vaccination. Most received co-funding from academic institutions and pharmaceutical companies. Most studies compared a COVID-19 vaccine with placebo. Five evaluated the addition of a 'mix and match' booster dose.
Main results
We report below results for three main outcomes and for 10 World Health Organization (WHO)-approved vaccines (for the remaining outcomes and vaccines, see main text). There is insufficient evidence regarding deaths between vaccines and placebo (mainly because the number of deaths was low), except for the Janssen vaccine, which probably reduces the risk of all-cause deaths.
People with symptoms
The Pfizer, Moderna, AstraZeneca, Sinopharm-Beijing, and Bharat vaccines produce a large reduction in the number of people with symptomatic COVID-19.
The Janssen vaccine reduces the number of people with symptomatic COVID-19.
The Novavax vaccine probably has a large reduction in the number of people with symptomatic COVID-19.
There is insufficient evidence to determine whether CoronaVac vaccine affects the number of people with symptomatic COVID-19 because results differed between the two studies (one involved only healthcare workers with a higher risk of exposure).
Severe disease
The Pfizer, Moderna, Janssen, and Bharat vaccines produce a large reduction in the number of people with severe disease.
There is insufficient evidence about CoronaVac vaccine on severe disease because results differed between the two studies (one involved only healthcare workers with a higher risk of exposure).
Serious adverse events
For the Pfizer, CoronaVac, Sinopharm-Beijing, and Novavax vaccines, there is insufficient evidence to determine whether there was a difference between the vaccine and placebo mainly because the number of serious adverse events was low.
Moderna, AstraZeneca, Janssen, and Bharat vaccines probably result in no or little difference in the number of serious adverse events.
What are the limitations of the evidence?
Most studies assessed the vaccine for a short time after injection, and it is unclear if and how vaccine protection wanes over time. Due to the exclusion criteria of COVID-19 vaccine trials, results cannot be generalized to pregnant women, people with a history of SARS-CoV-2 infection, or people with weakened immune systems. More research is needed comparing vaccines and vaccine schedules, and effectiveness and safety in specific populations and outcomes (e.g. preventing long COVID-19). Further, most studies were conducted before the emergence of variants of concerns.
How up to date is this evidence?
The evidence is up to date to November 2021. This is a living systematic review. Our results are available and updated bi-weekly on the COVID-NMA platform at covid-nma.com.
Compared to placebo, most vaccines reduce, or likely reduce, the proportion of participants with confirmed symptomatic COVID-19, and for some, there is high-certainty evidence that they reduce severe or critical disease. There is probably little or no difference between most vaccines and placebo for serious adverse events. Over 300 registered RCTs are evaluating the efficacy of COVID-19 vaccines, and this review is updated regularly on the COVID-NMA platform ( covid-nma.com ).
Implications for practice
Due to the trial exclusions, these results cannot be generalized to pregnant women, individuals with a history of SARS-CoV-2 infection, or immunocompromized people. Most trials had a short follow-up and were conducted before the emergence of variants of concern.
Implications for research
Future research should evaluate the long-term effect of vaccines, compare different vaccines and vaccine schedules, assess vaccine efficacy and safety in specific populations, and include outcomes such as preventing long COVID-19. Ongoing evaluation of vaccine efficacy and effectiveness against emerging variants of concern is also vital.
Different forms of vaccines have been developed to prevent the SARS-CoV-2 virus and subsequent COVID-19 disease. Several are in widespread use globally.
To assess the efficacy and safety of COVID-19 vaccines (as a full primary vaccination series or a booster dose) against SARS-CoV-2.
We searched the Cochrane COVID-19 Study Register and the COVID-19 L·OVE platform (last search date 5 November 2021). We also searched the WHO International Clinical Trials Registry Platform, regulatory agency websites, and Retraction Watch.
We included randomized controlled trials (RCTs) comparing COVID-19 vaccines to placebo, no vaccine, other active vaccines, or other vaccine schedules.
We used standard Cochrane methods. We used GRADE to assess the certainty of evidence for all except immunogenicity outcomes.
We synthesized data for each vaccine separately and presented summary effect estimates with 95% confidence intervals (CIs).
We included and analyzed 41 RCTs assessing 12 different vaccines, including homologous and heterologous vaccine schedules and the effect of booster doses. Thirty-two RCTs were multicentre and five were multinational. The sample sizes of RCTs were 60 to 44,325 participants. Participants were aged: 18 years or older in 36 RCTs; 12 years or older in one RCT; 12 to 17 years in two RCTs; and three to 17 years in two RCTs. Twenty-nine RCTs provided results for individuals aged over 60 years, and three RCTs included immunocompromized patients. No trials included pregnant women. Sixteen RCTs had two-month follow-up or less, 20 RCTs had two to six months, and five RCTs had greater than six to 12 months or less. Eighteen reports were based on preplanned interim analyses.
Overall risk of bias was low for all outcomes in eight RCTs, while 33 had concerns for at least one outcome.
We identified 343 registered RCTs with results not yet available.
This abstract reports results for the critical outcomes of confirmed symptomatic COVID-19, severe and critical COVID-19, and serious adverse events only for the 10 WHO-approved vaccines. For remaining outcomes and vaccines, see main text. The evidence for mortality was generally sparse and of low or very low certainty for all WHO-approved vaccines, except AD26.COV2.S (Janssen), which probably reduces the risk of all-cause mortality (risk ratio (RR) 0.25, 95% CI 0.09 to 0.67; 1 RCT, 43,783 participants; high-certainty evidence).
Confirmed symptomatic COVID-19
High-certainty evidence found that BNT162b2 (BioNtech/Fosun Pharma/Pfizer), mRNA-1273 (ModernaTx), ChAdOx1 (Oxford/AstraZeneca), Ad26.COV2.S, BBIBP-CorV (Sinopharm-Beijing), and BBV152 (Bharat Biotect) reduce the incidence of symptomatic COVID-19 compared to placebo (vaccine efficacy (VE): BNT162b2: 97.84%, 95% CI 44.25% to 99.92%; 2 RCTs, 44,077 participants; mRNA-1273: 93.20%, 95% CI 91.06% to 94.83%; 2 RCTs, 31,632 participants; ChAdOx1: 70.23%, 95% CI 62.10% to 76.62%; 2 RCTs, 43,390 participants; Ad26.COV2.S: 66.90%, 95% CI 59.10% to 73.40%; 1 RCT, 39,058 participants; BBIBP-CorV: 78.10%, 95% CI 64.80% to 86.30%; 1 RCT, 25,463 participants; BBV152: 77.80%, 95% CI 65.20% to 86.40%; 1 RCT, 16,973 participants).
Moderate-certainty evidence found that NVX-CoV2373 (Novavax) probably reduces the incidence of symptomatic COVID-19 compared to placebo (VE 82.91%, 95% CI 50.49% to 94.10%; 3 RCTs, 42,175 participants).
There is low-certainty evidence for CoronaVac (Sinovac) for this outcome (VE 69.81%, 95% CI 12.27% to 89.61%; 2 RCTs, 19,852 participants).
Severe or critical COVID-19
High-certainty evidence found that BNT162b2, mRNA-1273, Ad26.COV2.S, and BBV152 result in a large reduction in incidence of severe or critical disease due to COVID-19 compared to placebo (VE: BNT162b2: 95.70%, 95% CI 73.90% to 99.90%; 1 RCT, 46,077 participants; mRNA-1273: 98.20%, 95% CI 92.80% to 99.60%; 1 RCT, 28,451 participants; AD26.COV2.S: 76.30%, 95% CI 57.90% to 87.50%; 1 RCT, 39,058 participants; BBV152: 93.40%, 95% CI 57.10% to 99.80%; 1 RCT, 16,976 participants).
Moderate-certainty evidence found that NVX-CoV2373 probably reduces the incidence of severe or critical COVID-19 (VE 100.00%, 95% CI 86.99% to 100.00%; 1 RCT, 25,452 participants).
Two trials reported high efficacy of CoronaVac for severe or critical disease with wide CIs, but these results could not be pooled.
Serious adverse events (SAEs)
mRNA-1273, ChAdOx1 (Oxford-AstraZeneca)/SII-ChAdOx1 (Serum Institute of India), Ad26.COV2.S, and BBV152 probably result in little or no difference in SAEs compared to placebo (RR: mRNA-1273: 0.92, 95% CI 0.78 to 1.08; 2 RCTs, 34,072 participants; ChAdOx1/SII-ChAdOx1: 0.88, 95% CI 0.72 to 1.07; 7 RCTs, 58,182 participants; Ad26.COV2.S: 0.92, 95% CI 0.69 to 1.22; 1 RCT, 43,783 participants); BBV152: 0.65, 95% CI 0.43 to 0.97; 1 RCT, 25,928 participants). In each of these, the likely absolute difference in effects was fewer than 5/1000 participants.
Evidence for SAEs is uncertain for BNT162b2, CoronaVac, BBIBP-CorV, and NVX-CoV2373 compared to placebo (RR: BNT162b2: 1.30, 95% CI 0.55 to 3.07; 2 RCTs, 46,107 participants; CoronaVac: 0.97, 95% CI 0.62 to 1.51; 4 RCTs, 23,139 participants; BBIBP-CorV: 0.76, 95% CI 0.54 to 1.06; 1 RCT, 26,924 participants; NVX-CoV2373: 0.92, 95% CI 0.74 to 1.14; 4 RCTs, 38,802 participants).
For the evaluation of heterologous schedules, booster doses, and efficacy against variants of concern, see main text of review.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
An Overview of the Vaccine Debate
Looking at Both Sides of the Argument
There is a wealth of research demonstrating the efficacy and safety of vaccines —including how some have virtually eradicated infectious diseases that once killed millions. However, this has done little to sway those who believe that untold harms are being hidden from the American public.
The vaccine debate—including the argument as to whether vaccines are safe, effective, or could cause conditions like autism —has received a lot of attention from the media in recent years. With so much conflicting information being publicized, it can be a challenge to discern what is true and what is not. Therefore, it is important to learn the facts before making health decisions.
Claims and Controversy
Those who are part of the anti-vaccination movement include not only non-medical professionals but several scientists and healthcare providers who hold alternative views about vaccines and vaccination in general.
Some notable examples include:
- British healthcare provider Andrew Wakefield, who in 1998 published research linking the MMR vaccine and autism . That study has since been retracted, and he was later removed from the medical registry in the United Kingdom for falsifying scientific data.
- Pediatrician Bob Sears, who wrote the bestseller "The Vaccine Book: Making the Right Decision for your Child ," which suggested that many essential childhood vaccines were "optional." However, he was subsequently put on probation by the Medical Review Board of California in 2018 for alleged medical negligence and the inappropriate writing of medical exemptions for vaccinations.
- Dr. Jane M. Orient, director of the Association of American Healthcare Providers and Surgeons, who was among the leading opponents of the COVID-19 vaccine and one of the leading proponents of using hydroxychloroquine to treat COVID-19 during the pandemic.
These opposing views and claims, along with other information promoted by the news and social media, have led some people to question whether they know everything they need to know about vaccines.
Common Concerns Regarding Vaccines
The arguments made against vaccines are not new and have been made well before the first vaccine was developed for smallpox back in the 18th century.
The following are some of the common arguments against vaccines:
- Vaccines contain "toxic" ingredients that can lead to an assortment of chronic health conditions such as autism.
- Vaccines are a tool of "Big Pharma," in which manufacturers are willing to profit off of harm to children.
- Governments are "pharma shills," meaning they are bought off by pharmaceutical companies to hide cures or approve drugs that are not safe.
- A child’s immune system is too immature to handle vaccines , leading the immune system to become overwhelmed and trigger an array of abnormal health conditions.
- Natural immunity is best , suggesting that a natural infection that causes disease is "better" than receiving a vaccine that may cause mild side effects.
- Vaccines are not tested properly , suggesting a (highly unethical) approach in which one group of people is given a vaccine, another group is not, and both are intentionally inoculated with the same virus or bacteria.
- Infectious diseases have declined due in part to improved hygiene and sanitation , suggesting that hand-washing and other sanitary interventions are all that are needed to prevent epidemics.
- Vaccines cause the body to "shed" virus , a claim that is medically true, although the amount of shed virus is rarely enough to cause infection.
The impact of anti-vaccination claims has been profound. For example, it has led to a resurgence of measles in the United States and Europe, despite the fact that the disease was declared eliminated in the U.S. back in 2000.
Studies have suggested that the anti-vaccination movement has cast doubt on the importance of childhood vaccinations among large sectors of the population. The added burden of the COVID-19 pandemic has led to further declines in vaccination rates.
There is also concern that the same repercussions may affect COVID-19 vaccination rates—both domestically and abroad. Ultimately, vaccine rates must be high for herd immunity to be effective.
According to a study from the Centers for Disease Control and Prevention (CDC), the rate of complete recommended vaccination among babies age 5 months has declined from 66.6% in 2016 to 49.7% by May 2020. Declines in vaccination coverage were seen in other age groups as well.
Benefits of Vaccination
Of the vaccines recommended by the CDC, the benefits of immunization are seen to overwhelmingly outweigh the potential risks. While there are some people who may need to avoid certain vaccines due to underlying health conditions, the vast majority can do so safely.
According to the U.S. Department of Health and Human Services, there are five important reasons why your child should get the recommended vaccines:
- Immunizations can save your child’s life . Consider that polio once killed up to 30% of those who developed paralytic symptoms. Due to polio vaccination, the disease is no longer a public health concern in the United States.
- Vaccination is very safe and effective . Injection site pain and mild, flu-like symptoms may occur with vaccine shots. However, serious side effects , such as a severe allergic reaction, are very rare.
- Immunization protects others . Because respiratory viruses can spread easily among children, getting your child vaccinated not only protects your child but prevents the further spread of disease.
- Immunizations can save you time and money . According to the non-profit Borgen Project, the average cost of a measles vaccination around the world is roughly $1.76, whereas the average cost of treating measles is $307. In the end, the cost of prevention is invariably smaller than the cost of treatment.
- Immunization protects future generations . Smallpox vaccinations have led to the eradication of smallpox . Rubella (German measles) vaccinations have helped eliminate birth defects caused by infection of pregnant mothers in the developed world. With persistence and increased community uptake, measles could one day be declared eliminated (again) as well.
A Word From Verywell
If you have any questions or concerns about vaccinations, do not hesitate to speak with your healthcare provider or your child's pediatrician.
If a vaccine on the immunization schedule has been missed, speak to a healthcare provider before seeking the vaccination on your own (such as at a pharmacy or clinic). In some cases, additional doses may be needed.
Vaccines Healthcare Provider Discussion Guide
Get our printable guide for your next healthcare provider's appointment to help you ask the right questions.
Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life.
Thank you, {{form.email}}, for signing up.
There was an error. Please try again.
Eggerton L. Lancet retracts 12-year-old article linking autism to MMR vaccines . CMAJ . 2010 Mar 9; 182(4):e199-200. doi:10.1503/cmaj.109-3179
Park A. Doctor behind vaccine-autism link loses license . Time .
Offit PA, Moser CA. The problem with Dr Bob's alternative vaccine schedule . Pediatrics. 2009 Jan;123 (1):e164-e169. doi:10.1542/peds.2008-2189
Before the Medical Board of California, Department of Consumer Affairs, State of California. In the Matter of the Accusation Against Robert William Sears, M.D., Case No. 800-2015-012268 .
Stolberg SG. Anti-vaccine doctor has been invited to testify before Senate committee . The New York Times.
Wolfe RM, Sharp LK. Anti-vaccinationists past and present . BMJ. 2002;325(7361):430-2. doi:10.1136/bmj.325.7361.430
Agley J, Xiao Y. Misinformation about COVID-19: Evidence for differential latent profiles and a strong association with trust in science . BMC Public Health. 2021;21:89. doi:10.1186/s12889-020-10103-x
Centers for Disease Control and Prevention. Measles history .
Hussain A, Ali S, Ahmed M, Hussain S. The anti-vaccination movement: a regression in modern medicine . Cureus . 2018;10(7): e2919. doi:10.7759/cureus.2919
Bramer CA, Kimmins LM, Swanson R, et al. Decline in child vaccination coverage during the COVID-19 pandemic — Michigan Care Improvement Registry, May 2016–May 2020 . MMWR. 2020 May;69(20):630-1. doi:10.15585/mmwr.mm6920e1
Centers for Disease Control and Prevention. Why vaccinate .
Centers for Disease Control and Prevention. Poliomyelitis .
Centers for Disease Control and Prevention. Making the vaccine decision .
Borgen Project. What is the cost of measles in the developed world? .
By Vincent Iannelli, MD Vincent Iannelli, MD, is a board-certified pediatrician and fellow of the American Academy of Pediatrics. Dr. Iannelli has cared for children for more than 20 years.
Image adapted from: Engin Akyurt / Unsplash; CC0
- People & medicine
Should I get a COVID-19 vaccine? How to weigh up your risks and benefits
Your decision to get vaccinated matters
13 July 2021
Understanding both the risks and benefits of vaccination (and how we think about risk) can help you make the right decision for you or your family about having a COVID-19 vaccine.
But if you’re generally fit and healthy and living somewhere with very few or no cases of COVID-19 in your community, you might wonder—is getting the vaccine worth the potential side effects if the severe impacts of the disease don’t feel like a threat to you? Or what about pre-existing health conditions—do they increase your risk of experiencing more severe side effects?
How do we think about risks and benefits?
We make decisions every day about risk without thinking about it. But when the decision is more important, like whether to get a COVID-19 vaccine, understanding how our unconscious thinking patterns and biases affect our decision-making can help us make good choices. Human brains use mental shortcuts (called ‘ heuristics ’) all the time to enable quick decision-making. However, these shortcuts can skew our perception of how risky an activity is, or how likely a certain outcome might be.
Here are some examples:
- Overestimating risk: we often over-estimate the chances that a rare, but serious, event might occur. If that rare event is all over the media—like cases of TTS, the blood clotting syndrome linked to the AstraZeneca vaccine —we tend to overestimate those chances even more.
- Choosing to do nothing : sometimes people want to avoid a sense of regret (‘what if I make the wrong choice?’) and are more willing to accept an outcome if it’s the result of doing nothing (‘if I avoid the vaccine, I know I might catch COVID-19’), rather than a result of taking action (‘if I get the vaccine, I might have a severe side effect such as the clotting syndrome’). We are extra-cautious if we think there’s a lot of uncertainty involved.

With this in mind, let’s consider some of the other risks and benefits of COVID-19 vaccination.
What are your risk factors for COVID-19—and what about vaccines?
Many pre-existing health conditions and other factors can increase your risk of becoming severely ill or dying from COVID-19, or experiencing long-lasting impacts. The risk depends on many factors, such how much disease is circulating in the community and which COVID-19 strains are prevalent, but also on your individual circumstances. Apart from increasing age, common risk factors include diabetes, obesity, certain heart or lung conditions, chronic inflammatory conditions, or having an immune deficiency. The risk of severe illness also increases as you get older, especially for people over the age of 70 years, and is higher for Aboriginal and Torres Strait Islander peoples, or people who smoke.
People who become severely ill have a greater risk of dying from COVID-19 or experiencing permanent disability if they recover. For those who do recover, some may experience ongoing symptoms of ‘long COVID’ such as chronic fatigue, shortness of breath, muscle pain and neurological problems for three months or more.
To weigh up the benefits and risks of getting a vaccine, consider:
- What are your chances of getting sick from COVID-19 without the vaccine and, based on that, what benefit does the vaccine offer to you in preventing severe disease?
- What are the risks or chances of experiencing side effects or complications if you have the vaccine?
Benefits of the vaccine
When there is very little or no COVID-19 disease in the community, people aren’t so concerned about getting sick. But outbreaks of COVID-19 can arise quickly. In a matter of days, COVID-19 can be in a place that has previously had low or no community transmission of the virus. Vaccination rollouts are hard to stop and start: they take time, planning and resources—and no one can predict when, or where, another outbreak might occur. That's why timely vaccination prior to outbreaks is so important.
When restrictions start to lift and our borders open up, the risk of getting COVID-19 is likely to increase again. We all need to be prepared and make sure we have the best possible protection against future infection. Vaccines can help us return to a more normal way of life and provide protection for everyone in our communities, especially the most vulnerable.

Risks of the vaccine
Consider this scenario: if 100,000 people receive the AstraZeneca vaccine, what are the chances of experiencing side effects or complications as a result?
Common side effects from COVID-19 vaccines include pain at the injection site, headaches, fatigue, or feeling flu-like symptoms. This is normal and indicates the vaccine is working. In a group of 100,000 people , we would expect just under 50,000 people to experience side effects because they are so common.
Severe side effects: we would also expect to see 1 to 2 people experience a severe complication like TTS. The risks of TTS are higher for younger people, especially those under 60 years. Anyone who develops severe headaches and tiredness up to 30 days after the first dose should seek medical help immediately. It’s important to know that even if someone becomes ill with TTS, doctors now have a better understanding of the condition. It’s much easier to diagnose and get the right treatment , so the chances of recovery are higher than they were before.
Case study: why Kathie changed her mind
Kathie, 56, lives in a small rural town in Victoria. At first, she didn't see a strong need to get a COVID-19 vaccine.
‘I was slightly nervous about getting sick from the injection, and the stories of the risks of blood clotting [from the AstraZeneca vaccine] made me think twice,’ she says.
However, an outbreak in Melbourne changed her mind. After seeing the rapid rise in new cases of COVID-19, Kathie realised the risk factors of getting the AstraZeneca vaccine were ‘so minimal’ compared to the spread of the disease. ‘I wanted to do anything I could to stop the spread and the impact of COVID-19,’ she says.
‘So I got my AstraZeneca shot at my doctor's surgery. It wasn't painful; it felt similar to the flu shot,’ she says. ‘I had a slight temperature and felt a bit achy the next morning, and felt a bit tired for a couple of days.’
She now hopes that more people will roll up their sleeves to raise the number of vaccinated people in Australia and prevent the spread of COVID-19. ‘We all have to do our part.’
Looking out for your friends, family and community
When you are vaccinated against COVID-19, you not only protect yourself, but also those around you. Even if you are fit and healthy and have a lower risk of becoming severely ill from COVID-19, you might pass the virus on to a more vulnerable person if you become infected. You may not know which people in your life are more vulnerable to disease and death from COVID-19: an elderly parent or a friend undergoing chemotherapy are obviously at higher risk, but we don’t always know what risk factors affect others. Getting vaccinated helps keep your friends and family safe.
As more people get vaccinated, everyone is better protected against future outbreaks. Everyone can help reduce the impact and spread of COVID-19. Your decision to get vaccinated matters.
- vaccination
- public health
- immunisation
DHEC is Restructuring
On July 1, 2024, the South Carolina Department of Health and Environmental Control (DHEC) becomes two separate agencies — the South Carolina Departments of Environmental Services (SCDES) and Public Health (DPH). Additionally, DHEC's retail food program and milk and dairy lab will merge with the South Carolina Department of Agriculture . See our DHEC Restructuring page to learn more.
Search DHEC
Benefits and risks of vaccines.
All medications and vaccines have potential risks that must be carefully weighed against the benefits that medications and vaccines offer to prevent illness. Vaccination is one of the most successful public health interventions in reducing disease spread, preventing complications and even deaths from vaccine preventable diseases. The success of vaccines in reducing disease should not suggest that vaccine preventable diseases are no longer a threat. Even though immunizations have significantly reduced vaccine preventable diseases, there were nearly 7,800 reports of vaccine preventable diseases in South Carolina in 2016. Of the 238 disease outbreak investigations that DHEC conducted, 29% of them were outbreaks of influenza, many of which occurred in school and nursing home settings affecting populations of people who are vulnerable to complications from the flu. In fact the age groups with the highest rates of hospitalizations from the flu include those 0 to 4 years of age and those older than 65. There have been 94 deaths from the flu reported in South Carolina during the current flu season.
No vaccine offers 100% protection and vaccine efficacy meaning how well a vaccine prevents illness among those vaccinated varies from one type of vaccine to the next and how well a vaccine works also depends on the health status of the person vaccinated. For example, the flu vaccine does not protect the elderly against catching the flu as well as it does in younger people. But very importantly, several studies suggest that elderly people vaccinated against the flu have less severe disease, are less likely to be hospitalized and are less likely to die. We continue to see preventable illness, hospitalizations and unfortunately deaths in South Carolina from influenza, whooping cough, meningitis, hepatitis B, and other diseases. We also continue to see travelers import diseases like measles that are no longer common here but that cause outbreaks in communities with low vaccination rates. Vaccines do have some risk for adverse reaction, the most common being redness and soreness at the injection site or fever and allergic reactions. More serious complications like seizures and the neurologic condition Guillian-Barre are also reported but occur very rarely and far less commonly than the complications and deaths from vaccine preventable diseases.
Related Resources
Sc immunization data, measles (rubeola).
June 22, 2020
The Risks of Rushing a COVID-19 Vaccine
Telescoping testing time lines and approvals may expose all of us to unnecessary dangers
By William A. Haseltine
Mladen Antonov Getty Images
The excitement and enthusiasm for a COVID-19 vaccine by the end of 2020 is both palpable and understandable. We all hope for a rapid end to the pandemic and an effective vaccine would be a surefire solution. But there are risks that come with a fast-tracked vaccine delivered end of this year, not the least of which are the risks related to the safety of the vaccine itself.
Telescoping testing timelines and approvals may expose all of us to unnecessary dangers related to the vaccine. While preclinical trials to evaluate the potential safety and efficacy of vaccine candidates are likely to include tens of thousands of patients, it is still unclear whether that number will be large enough and a trial will last long enough to evaluate safety for a drug that would be administered to so many. The US alone plans to vaccinate hundreds of millions of people with the first successful candidate. One serious adverse event per thousand of a vaccine given to 100 million people means harm to 100,000 otherwise healthy people.
Aside from questions of safety that attend any vaccine, there are good reasons to be especially cautious for COVID-19. Some vaccines worsen the consequences of infection rather than protect, a phenomenon called antibody-dependent enhancement (ADE). ADE has been observed in previous attempts to develop coronavirus vaccines. To add to the concern, antibodies typical of ADE are present in the blood of some COVID-19 patients. Such concerns are real. As recently as 2016, Dengavxia, intended to protect children from the dengue virus, increased hospitalizations for children who received the vaccine.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Questions also arise around the efficacy of a potential vaccine. The little we know of the current generation of COVID-19 vaccines raises serious questions regarding their ability to protect people from infection. We know all the candidates tested to date in non-human primates failed to protect any of the monkeys from infection of the nasal passages, the primary route of human infection. Failure to protect entirely from infection fits with all we know about attempts to protect monkeys from two other deadly coronaviruses, those that cause SARS and MERS.
On a brighter note, at least some of the candidate vaccines did raise significant immune responses. How that translates to protection of humans is uncertain though as monkeys do not become noticeably ill or exhibit many of the life-threatening consequences of COVID-19, even when exposed to high doses of the virus via the nose, lung, and rectum simultaneously. As many of the most serious COVID symptoms do not appear until late in the disease course, sometimes four to five weeks following exposure, there is a possibility that we will not have sufficient time to judge efficacy of a new vaccine, even by the lower standard of symptom amelioration.
An effective COVID-19 vaccine also faces several hurdles beyond our control. The older we get the poorer our ability to respond to vaccines. Resistance to vaccination begins early at age 30 and becomes progressively more profound with time. That is especially troubling as those over 60 are the population most at risk. Vaccination of the elderly may sometimes succeed by administering repeated doses and by increasing the potency of the vaccine with powerful adjuvants. But these adjuvants can be especially risky for the very old.
It seems a folly then to rush our way towards a vaccine in 2020 if it is likely to have only limited benefit to the population most in need and may put otherwise healthy people at risk. The risk goes far beyond the dangers a COVID vaccine alone may hold. Public support for vaccines in general is already an issue. Trust in other lifesaving vaccines will be eroded even further if a COVID vaccine goes wrong and many more people—children especially—will be at risk if vaccination rates fall.
Yes, we are all increasingly longing for an end to the outbreak. But a safe vaccine, effective for all those at risk, is worth the wait, especially when we have other solutions in hand. We already know from the experience of countries in Asia that the epidemic can be stopped in its tracks with basic public health measures: widespread testing, contact tracing, and mandatory controlled quarantine—not necessarily in a dismal public health facility as many imagine, but in our own homes with virtual supervision or in a hotel environment. These efforts alone could bring new infections down to almost zero within just weeks.
In addition, I believe it will be possible before the end of this year to protect those most at risk from exposure with combinations of monoclonal antibodies or with truly effective antiviral drugs . These drugs could treat those who were ill and prevent further infection. In addition to pursuing a vaccine within a realistic timeframe, we should also be throwing our weight behind these other types of medical solutions which have historically been much quicker to bring to market safely.
There is no doubt we need an urgent end to the pandemic. Economies around the world are crashing. Governments are piling up trillions of dollars in debt. And, in the US alone, tens of millions are without work or income. But there are still costs that are too great, even when compared to such numbers. When we have solutions to the pandemic in hand we cannot risk the potential lives lost of rushing a COVID vaccine to market. We must hold dear the central dictum of the medical community, first, do no harm. Trust that given the time science will deliver a medical solution in the form of a vaccine or a chemoprophylactic drug treatment, and in the meantime let us immediately implement the public health strategies that we know will work today to drive new infections down to nothing.
Read more about the coronavirus outbreak from Scientific American here . And read coverage from our international network of magazines here .
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 27, Issue 6
- Balancing benefits and potential risks of vaccination: the precautionary principle and the law of unintended consequences
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-3140-3278 David Robert Grimes 1 , 2
- 1 Dublin City University , Dublin , Ireland
- 2 Department of Oncology , University of Oxford , Oxford , UK
- Correspondence to Dr David Robert Grimes, Dublin City University, Dublin, Ireland; davidrobert.grimes{at}dcu.ie
Vaccination is a life-saving endeavour, yet risk and uncertainty are unavoidable in science and medicine. Vaccination remains contentious in the public mind, and vaccine hesitancy is a serious public health issue. This has recently been reignited in the discussion over potential side effects of COVID-19 vaccines, and the decision by several countries to suspend measures such as the AstraZeneca vaccine. In these instances, the precautionary principle has often been invoked as a rationale, yet such heuristics do not adequately weigh potential harms against real benefits. How we analyse, communicate and react to potential harms is absolutely paramount to ensure the best decisions and outcomes for societal health, and maintaining public confidence. While balancing benefits and risks is an essential undertaking, it cannot be achieved without due consideration of several other pertinent factors, especially in the context of vaccination, where misguided or exaggerated fears have in the past imperilled public health. While well meaning, over reactions to potential hazards of vaccination and other health interventions can have unintended consequences, and cause lingering damage to public trust. In this analysis, we explore the challenges of assessing risk and benefit, and the limitations of the precautionary principle in these endeavours. When risk is unclear, cautious vigilance might be a more pragmatic and useful policy than reactionary suspensions.
- public health
- risk management
- vaccine-preventable diseases
https://doi.org/10.1136/bmjebm-2021-111773
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
The advent of several effective vaccines against the scourge of COVID-19, created in record time, is a towering medical and scientific triumph. These interventions have the collective ability to stem the deadly tide of COVID-19, and ultimately to banish the sheer misery the pandemic has wrought. Yet optimism has been somewhat marred by reports of an unusual type of blood clot associated with both the AstraZeneca vaccine (Vaxzevria) and the Johnson & Johnson’s Janssen vaccine.
This phenomenon, currently dubbed vaccine-induced thrombosis and thrombocytopaenia (VITT), 1 has dominated discourse on vaccine safety worldwide. This has been especially pronounced in Europe, with several European nations opting to temporality suspend the AstraZeneca vaccine in March 2021. Following the European Medicine’s Agency clarification that ‘ benefits of Vaxzevria outweigh its risks in adults of all age groups ’ , 2 suspensions were reversed in many countries, but a sense of scepticism remains. In several states, reintroduction came with additional restrictions, including France, Spain, Finland, Sweden and Germany, limited to only older groups. It remains suspended in Denmark and Norway.
In the USA, Johnson & Johnson’s similar offering was also temporarily suspended by the FDA, based on similar rare reports, and born of what the FDA described as an ‘ abundance of caution’, with use of the vaccine since been resumed. In both the USA and Europe, however, opinion on the wisdom of these suspensions has been polarised, with many regulatory bodies quite reasonably insisting that investigatory pauses are vital to maintain safety standards and public confidence. The opposite, equally reasonable position, argues that suspensions based on such limited data were damaging over-reactions to events which occur at most a handful of times per million.
Vaccine safety itself is a topic long contentious in the public mind. It is also impossible to consider the issue divorced from the deadly reality of COVID-19. This ongoing debate is a microcosm of how we deal with risk and uncertainty - and one from which it is vital we draw some important lessons.
Emergent risks and uncertain data
A total of 252 cases of thrombotic events with low platelet counts following Vaxzevria vaccination were reported by 28 April 2021 in the UK, 3 of which 93 were cerebral venous sinus thrombosis (CVST). With 22.6 million doses given by the same date, this suggests an incidence of approximately 11.15 cases per million people vaccinated (4.12 cases CVST per million vaccinated). Estimated background incidence of CVST ranges from 5 to 15 cases per million people per year, 4 this in isolation might seem to imply no obvious elevation due to the vaccine. But emergent cases of postvaccination CVST coincide with low platelet count, an unusual combination potentially hinting at a deeper association. Interpretation, however, is complicated by the fact that there is only limited data on the incidence of CVSTs occurring with thrombocytopaenia. 3
The ongoing situation is a perfect exemplar of the difficulties of making decisions when data is limited and in rapid flux; both typical CVST and VITT are vanishingly rare, and even a handful of recorded events can skew interpretations. This renders estimates of true incidence intrinsically uncertain, compounded by the fact that CVST incidence itself varies with age, sex and other risk factors—the conceptive pill, for instance, is associated with a sevenfold increase in CVST risk for women aged 15–50. 5 And while COVID-19 infection itself is associated with both substantially increased risk of CVST 6 and reduced platelet count, 7 the available evidence to date suggests that the specific combination of thrombotic events and concurrent thrombocytopaenia is not a common feature of COVID-19 infection. 3
Available data on VITT too are transient and subject to change: initially, it was hypothesised that condition might only affect females, but this position has evolved with growing evidence. Risk, however, does appear elevated in younger cohorts—UK data to date suggests that the incidence in those aged 18–39, the risk of these side effects could be as high as 1 in 50 000—roughly double that of other age cohorts. 3 Yet making a causal connection is a fraught affair, and it remains unclear whether the association is due to the vaccine platform, some unknown immunological mechanism or even whether the relationship is spurious.
The precautionary principle
It would of course be completely remiss if national health bodies failed to react to evidence of harm, regardless of how rare or evanescent this signal might be. For regulators across Europe, the decision to suspend AstraZeneca’s offering was justified by invocation of the precautionary principle. This concept itself originated in 1970s German law as the Vorsorgeprinzip, or the principle of foresight, with the laudable aim of regulating potential hazards from air pollution. What exactly it entails, however, is not always clear, as there is no universally accepted definition of the precautionary principle, 8 rendering interpretations of the principle somewhat nebulous. Broadly speaking, variants of the principle can be categorised as either ‘weak’ or ‘Strong’, with some common variants given in box 1 .
Weak and strong formulations of the precautionary principle
Weak (or minimal) interpretations of the principle maintain that scientific uncertainty does not justify inaction, and legislation or safety measures may be warranted despite an absence of complete scientific or medical evidence concerning specific hazards. Variations include:
‘Where there are threats of serious or irreversible damage, lack of full scientific certainty shall not be used as a reason for postponing cost-effective measures to prevent environmental degradation’—Rio Declaration (1992)
‘When human activities may lead to morally unacceptable harm that is scientifically plausible but uncertain, actions shall be taken to avoid or diminish that harm’—UNESCO (2005)
Strong (or maximal) interpretations, by contrast, reverse the burden of proof for harm, and insist that scientific uncertainty necessitates legislation or suspension until the absence of hazard has been proven. Formulations include
‘ When an activity raises threats of harm to human health or the environment, precautionary measures should be taken even if some cause and effect relationships are not established scientifically. In this context the proponent of the activity, rather than the public, should bear the burden of proof.’—Wingspan declaration (1998)
‘[When] potential adverse effects are not fully understood, the activities should not proceed’—United Nations World Charter for Nature (1992)
Weak formulations of the precautionary principle are rarely controversial, and widely practised: very few of us would object to wearing a seat belt to mitigate against the low but plausible risk of being in a car accident, for instance. In this respect, the weak formulation has even been described by some authors as a truism. 9 Strong variations illicit far more criticism; one recurring criticism has been that these formulations are inherently one sided, making no attempt to balance risk and benefit. Other authors have argued the principle is entirely logically inconsistent. 10 Sunstein points out that the principle in this formulation is self-defeating, noting that there are ‘ risks of one kind or another are on all sides of regulatory choices, and it is therefore impossible, in most real-world cases, to avoid running afoul of the principle ’ 9 in its strong formulation.
It is important to note that the principle itself is designed solely when considering plausible threats in an environment of uncertainty. The European commission suggest that ‘… recourse to the precautionary principle presupposes that potentially dangerous effects deriving from a phenomenon, product or process have been identified, and that scientific evaluation does not allow the risk to be determined with sufficient certainty. ’ 11 Crucially, the precautionary principle only applies to uncertainty, for situations when an activity poses a plausible risk of harm and when the extent of that harm is unknown. It explicitly does not apply in situations where the risk of harm can be accurately quantified, and a desired level of protection defined. It is mistaken to conflate risk and uncertainty in applications of the principle, as it only applies reasonably to the latter scenario.
Balancing risk and benefit
where E is the exposure to COVID-19 in a particular grouping, presuming that VITT is a direct consequence of vaccination. This calculation however is not trivial, because one’s exposure risk to COVID-19 is highly dynamic and dependent on several factors, chiefly population incidence and the rate eligible people are vaccinated in that population. In the extreme situation where everyone in the younger cohort was instantaneously vaccinated, this would imply four deaths per million from VITT, if no risk mitigation for thrombotic events was undertaken. At the opposite extreme, if an entire young population were infected at once with no vaccination, one would expect about 400 deaths per million from COVID-19, a figure two orders of magnitude greater. Neither situation is of course realistic, because the dynamics of those infected and vaccinated vary with time. Additionally, VITT risk, when pre-empted, can be mitigated against. Even in populations at potentially elevated risk of adverse effect, high rate of vaccination remains the optimum scenario for the well-being of the entire cohort until incidence of COVID-19 in the population is extremely low.
Public perception and the law of unintended consequences
Faced with a non-zero risk of harm, it was understandable that some regulators moved to suspend the AstraZeneca vaccine. But while understandable and well meaning, this was not a zero-risk strategy. The first reason is pragmatic; suspensions of an effective vaccine inevitably leave vulnerable people unprotected from the virus, prolonging the pandemic. Nor do suspensions mitigate the spread of COVID-19, or stem the tide of hospital admissions and needless deaths the vaccine prevents. This harm becomes even more severe when we consider ramifications beyond the calculus of risk and benefit. Public confidence and perception of risk are not mere functions of the data, but reflect broader media, psychological and communication influences.
The controversy over this vaccine highlights a glaring problem in modern science: the disconnect between scientific and public understanding of adverse effects. In our hyperconnected world, misleading narratives can quickly take hold, to our detriment. Reporting of the hypothetical risks of the vaccine tended towards hyperbole, and frequently did not give sufficient context for a reader to infer that benefits outweighed potential risks . This feeds into a spiral of mistrust where harms are perceived as amplified while benefits are side lined in discourse over interventions like vaccination. This is not unexpected—public perception is inherently affected by regulatory action and skewed reporting examples of which are given in box 2 .
Vaccination confidence crises and unintended consequences
Measles-mumps-rubella (MMR) (UK, Samoa): In 1998, physician Andrew Wakefield asserted a fraudulent and now debunked link between MMR vaccination and autism. These claims were prominent in UK media in the early 2000s, and led to increased vaccine hesitancy, with MMR vaccine uptake declining from 92% in 1996 to 84% in 2006, and as low as 61% in parts of London in 2003, and numerous continuing avoidable outbreaks worldwide. 18 In 2018, the accidental death of two children in Samoa led to mass rejection of the MMR vaccine, stoked by antivaccine campaigners, driving vaccination rates to lows of 31%. A single case of measles that August ultimately led to over 5700 cases and 83 deaths by early 2020 in a country of just over 200 000 people. 19
Human papilloma virus (HPV) (Japan, Denmark, Ireland): Japan’s Ministry of Health, Labor and Welfare temporarily suspend government recommendations for the HPV vaccination in 2013, following sensational media reports of women harmed by the vaccine. Even though these ostensible adverse effects were shown to have no causal relationship with the vaccine, uptake plummeted from 70% to less than 1% in a year. 13 20 Despite efforts to rebuild public confidence, uptake of the genital cancer-preventing HPV vaccine in Japan remains abysmal, estimated to cost over 11 000 lives in future. 21 Similar fears (perpetuated by antivaccine activists and eventually echoed by politicians and broadcasters) in Denmark in 2014 saw uptake collapse from 79% to 17%. 22 The following year, Ireland was hit by similar disinformation which saw uptake fall from highs of 87%–51% within a year. Ireland was able to reverse this trend thanks to sustained efforts from the government, health service, physicians, scientists and patient advocates. 23 24
Pertussis (UK): Press coverage of a 1974 report ascribing 36 reactions to the pertussis vaccine and suggestions by physician Gordon Stewart that the vaccine risks outweighed benefits initiated a scare, driving vaccine uptake down from 81% to 31%. A spate of pertussis epidemics and deaths ensued, despite mainstream medical opinion at the time being clear on the benefits of vaccination. Public confidence was only restored after the publication of a national reassessment of vaccine efficacy, which eventually saw uptake increase above 90%. 25
Vaccine hesitancy is a spectrum, 12 and while vaccine suspensions are carried out by regulators in good faith, it takes very little effort for bad-faith actors to present this as unassailable evidence of harm to an unsuspecting audience, nudging people away from vaccination. This effectively means that laudable attempts to be transparent with potential risk with the aim of reassuring can be weaponised into achieve the precise opposite—a grim example of the law of unintended consequences. Even before the pandemic began, antivaccine propaganda was a serious threat to public health. 13 Exposure to antivaccine conspiracy theories had a marked negative impact on parental intention to vaccinate, 14 and a dark renaissance of once virtually conquered diseases across the world led the WHO to declare vaccine hesitancy a top 10 threat to public health in 2019. Antivaccine myths have undergone an alarming resurgence online, with a staggering rise in targeted disinformation and conspiracy theories propagated about the vaccine. 15 It is thus crucial that decisions and communication on vaccine safety are taken with full cognisance of how they could be perceived by vested interests, and effects this might have on wider public perception. As Heidi Larson noted, vaccine confidence is not down solely to trust in the medical and scientific professions, but ‘… trust in government and the policies they create is essential, along with the government’s own trust in science to inform their policy decisions .’ 16
Responding to future risk and uncertainty
While it is crucial to accurately convey risk and uncertainty in all health endeavours, Voltaire’s famous dictum about ‘the perfect being the enemy of the good’ is sometimes unfortunately realised in health settings, to our collective detriment. it is imperative that risks and benefits are carefully weighed up and contrasted, adjusted as the data becomes more robust. Moreover, it is critical to be cognisant of how public health actions might be perceived. When confronted with uncertainty, reacting before ample reflection is ill advised for two reasons. First, it increases the likelihood of making a poor judgement. Second, actions taken without full consideration of context and related issues can fall victim to unintended consequences and subpar outcomes. In the case of vaccination, this can manifest not only as temporarily diminished public health responses, but lingering damage to public confidence and increased vaccine hesitancy; as the adage reminds us, the road to hell is paved with good intentions, and an oversensitivity to ostensible side effects can lead to long-term confidence problems.
With regard to COVID-19 vaccination specifically, it is likely that potential harms were somewhat ameliorated by the existence of alternative mRNA vaccines. But future situations will arise when an inoculation or health measure does not have a ready alternate, as has happened historically ( box 2 ). How we best navigate these scenarios in future is something with urgent relevance. The precautionary principle, while commonly invoked as a rationale for action, is only truly appropriate when risk cannot be quantified. Despite its frequent invocation, it is not an ideal heuristic to assess or respond to potential vaccination risks; weak formulations are unobjectionable but do not lead to any clear course of action. Strong formulations, by contrast, would insist that vaccination be suspended indefinitely, without consideration of the risks and harms of suspending a life-saving programme. More subtly, the precautionary principle is inappropriate when risk can be accurately quantified and should be applied only to uncertainty itself. When risk can be broadly quantified, then Risk-Benefit analysis 17 is more informative than more vague approaches.
So how might we proceed in future? Suspensions might be an over-reaction to small signals of harm, but conversely it would be irresponsible to ignore simply because it is small. But it is a false dichotomy to suppose the only choices are to continue haphazardly or outright suspend; perhaps a more pragmatic approach is the fusion of both schools; a cautious vigilance where vaccinated individuals are monitored for warning signs of rare side effects so that ill effects can be circumvented without impeding vaccine drives. Aided by mathematical modelling and constant monitoring, approaches should be flexible, and the risk–benefit balance constantly updated so that maximum benefit can be derived. How this is communicated too is of paramount importance—full transparency must be maintained in how decisions are made, lest adjustments in the light of new data are misinterpreted as the censoring of vaccine risks, which could inadvertently play in the narrative of antivaccine activists. This invokes the deeper question of how the reporting of adverse effects impacts public understanding, a complex question beyond the scope of this analysis. Even so, a cognisance of this dimension is vital on the part of policy-makers.
The inescapable reality is that while risks can be reduced, they can never be eliminated. Measures that mitigate one risk must be balanced with competing hazards, and the net benefit or harms considered; your car seat belt may decapitate you in an accident, but it is far more likely to save your life. Abstract and nebulous as risk can be, it is vital that perspective is maintained, and that positions evolve with emerging evidence. While true of all medical interventions, this is especially resonant with vaccination, which, despite incredible life-saving efficacy, remains contentious in the public mind. While striving to ensure safety, we should not overlook the fact that over-reactions to phantom safety signals in the past have inflicted lingering damage on public trust and health. To circumvent this, we must ensure decisions are evidence-based, can strike a considered balance between risk and benefit.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study does not involve human participants.
- Greinacher A ,
- Warkentin TE , et al
- European Medicines Agency
- Public Health England
- Castelli GP ,
- Pognani C ,
- Sozzi C , et al
- Amoozegar F ,
- Ronksley PE ,
- Sauve R , et al
- Naazie IN ,
- Elsayed N , et al
- Bhattacharjee S ,
- European Commission, Environment Directorate-General, University of the West of England B
- Sunstein CR
- European Parliamentary Research Service,
- Heywood AE ,
- Hanley SJB ,
- Yoshioka E ,
- Ito Y , et al
- Smith MA , et al
- Suppli CH ,
- Hansen ND ,
- Rasmussen M , et al
- Corcoran B ,
Twitter @drg1985
Contributors DRG has international expertise in the spread of health disinformation and public trust in science. He also advises internationally on science and health policy, chiefly on vaccination and public understanding. DRG is the guarantor of this article.
Funding This study was funded by Wellcome Trust (214461/Z/18/Z).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
You are using an outdated browser. Please upgrade your browser to improve your experience.

Health & Nursing
Courses and certificates.
- Bachelor's Degrees
- View all Business Bachelor's Degrees
- Business Management – B.S. Business Administration
- Healthcare Administration – B.S.
- Human Resource Management – B.S. Business Administration
- Information Technology Management – B.S. Business Administration
- Marketing – B.S. Business Administration
- Accounting – B.S. Business Administration
- Finance – B.S.
- Supply Chain and Operations Management – B.S.
- Accelerated Information Technology Bachelor's and Master's Degree (from the School of Technology)
- Health Information Management – B.S. (from the Leavitt School of Health)
Master's Degrees
- View all Business Master's Degrees
- Master of Business Administration (MBA)
- MBA Information Technology Management
- MBA Healthcare Management
- Management and Leadership – M.S.
- Accounting – M.S.
- Marketing – M.S.
- Human Resource Management – M.S.
- Master of Healthcare Administration (from the Leavitt School of Health)
- Data Analytics – M.S. (from the School of Technology)
- Information Technology Management – M.S. (from the School of Technology)
- Education Technology and Instructional Design – M.Ed. (from the School of Education)
Certificates
- View all Business Degrees
Bachelor's Preparing For Licensure
- View all Education Bachelor's Degrees
- Elementary Education – B.A.
- Special Education and Elementary Education (Dual Licensure) – B.A.
- Special Education (Mild-to-Moderate) – B.A.
- Mathematics Education (Middle Grades) – B.S.
- Mathematics Education (Secondary)– B.S.
- Science Education (Middle Grades) – B.S.
- Science Education (Secondary Chemistry) – B.S.
- Science Education (Secondary Physics) – B.S.
- Science Education (Secondary Biological Sciences) – B.S.
- Science Education (Secondary Earth Science)– B.S.
- View all Education Degrees
Bachelor of Arts in Education Degrees
- Educational Studies – B.A.
Master of Science in Education Degrees
- View all Education Master's Degrees
- Curriculum and Instruction – M.S.
- Educational Leadership – M.S.
- Education Technology and Instructional Design – M.Ed.
Master's Preparing for Licensure
- Teaching, Elementary Education – M.A.
- Teaching, English Education (Secondary) – M.A.
- Teaching, Mathematics Education (Middle Grades) – M.A.
- Teaching, Mathematics Education (Secondary) – M.A.
- Teaching, Science Education (Secondary) – M.A.
- Teaching, Special Education (K-12) – M.A.
Licensure Information
- State Teaching Licensure Information
Master's Degrees for Teachers
- Mathematics Education (K-6) – M.A.
- Mathematics Education (Middle Grade) – M.A.
- Mathematics Education (Secondary) – M.A.
- English Language Learning (PreK-12) – M.A.
- Endorsement Preparation Program, English Language Learning (PreK-12)
- Science Education (Middle Grades) – M.A.
- Science Education (Secondary Chemistry) – M.A.
- Science Education (Secondary Physics) – M.A.
- Science Education (Secondary Biological Sciences) – M.A.
- Science Education (Secondary Earth Science)– M.A.
- View all Technology Bachelor's Degrees
- Cloud Computing – B.S.
- Computer Science – B.S.
- Cybersecurity and Information Assurance – B.S.
- Data Analytics – B.S.
- Information Technology – B.S.
- Network Engineering and Security – B.S.
- Software Engineering – B.S.
- Accelerated Information Technology Bachelor's and Master's Degree
- Information Technology Management – B.S. Business Administration (from the School of Business)
- View all Technology Master's Degrees
- Cybersecurity and Information Assurance – M.S.
- Data Analytics – M.S.
- Information Technology Management – M.S.
- MBA Information Technology Management (from the School of Business)
- Full Stack Engineering
- Web Application Deployment and Support
- Front End Web Development
- Back End Web Development
3rd Party Certifications
- IT Certifications Included in WGU Degrees
- View all Technology Degrees
- View all Health & Nursing Bachelor's Degrees
- Nursing (RN-to-BSN online) – B.S.
- Nursing (Prelicensure) – B.S. (Available in select states)
- Health Information Management – B.S.
- Health and Human Services – B.S.
- Psychology – B.S.
- Health Science – B.S.
- Healthcare Administration – B.S. (from the School of Business)
- View all Nursing Post-Master's Certificates
- Nursing Education—Post-Master's Certificate
- Nursing Leadership and Management—Post-Master's Certificate
- Family Nurse Practitioner—Post-Master's Certificate
- Psychiatric Mental Health Nurse Practitioner —Post-Master's Certificate
- View all Health & Nursing Degrees
- View all Nursing & Health Master's Degrees
- Nursing – Education (BSN-to-MSN Program) – M.S.
- Nursing – Leadership and Management (BSN-to-MSN Program) – M.S.
- Nursing – Nursing Informatics (BSN-to-MSN Program) – M.S.
- Nursing – Family Nurse Practitioner (BSN-to-MSN Program) – M.S. (Available in select states)
- Nursing – Psychiatric Mental Health Nurse Practitioner (BSN-to-MSN Program) – M.S. (Available in select states)
- Nursing – Education (RN-to-MSN Program) – M.S.
- Nursing – Leadership and Management (RN-to-MSN Program) – M.S.
- Nursing – Nursing Informatics (RN-to-MSN Program) – M.S.
- Master of Healthcare Administration
- MBA Healthcare Management (from the School of Business)
- Business Leadership (with the School of Business)
- Supply Chain (with the School of Business)
- Back End Web Development (with the School of Technology)
- Front End Web Development (with the School of Technology)
- Web Application Deployment and Support (with the School of Technology)
- Full Stack Engineering (with the School of Technology)
- Single Courses
- Course Bundles
Apply for Admission
Admission requirements.
- New Students
- WGU Returning Graduates
- WGU Readmission
- Enrollment Checklist
- Accessibility
- Accommodation Request
- School of Education Admission Requirements
- School of Business Admission Requirements
- School of Technology Admission Requirements
- Leavitt School of Health Admission Requirements
Additional Requirements
- Computer Requirements
- No Standardized Testing
- Clinical and Student Teaching Information

Transferring
- FAQs about Transferring
- Transfer to WGU
- Transferrable Certifications
- Request WGU Transcripts
- International Transfer Credit
- Tuition and Fees
- Financial Aid
- Scholarships
Other Ways to Pay for School
- Tuition—School of Business
- Tuition—School of Education
- Tuition—School of Technology
- Tuition—Leavitt School of Health
- Your Financial Obligations
- Tuition Comparison
- Applying for Financial Aid
- State Grants
- Consumer Information Guide
- Responsible Borrowing Initiative
- Higher Education Relief Fund
FAFSA Support
- Net Price Calculator
- FAFSA Simplification
- See All Scholarships
- Military Scholarships
- State Scholarships
- Scholarship FAQs
Payment Options
- Payment Plans
- Corporate Reimbursement
- Current Student Hardship Assistance
- Military Tuition Assistance
WGU Experience
- How You'll Learn
- Scheduling/Assessments
- Accreditation
- Student Support/Faculty
- Military Students
- Part-Time Options
- Virtual Military Education Resource Center
- Student Outcomes
- Return on Investment
- Students and Gradutes
- Career Growth
- Student Resources
- Communities
- Testimonials
- Career Guides
- Skills Guides
- Online Degrees
- All Degrees
- Explore Your Options
Admissions & Transfers
- Admissions Overview
Tuition & Financial Aid
Student Success
- Prospective Students
- Current Students
- Military and Veterans
- Commencement
- Careers at WGU
- Advancement & Giving
- Partnering with WGU
The Risks and Benefits of Vaccination
- See More Tags

How do vaccines work?
Nobody likes getting shots, but at the end of the day vaccines and shots save lives. The diseases that vaccines prevent can be deadly, and these shots work with the body’s natural defense to develop immunity to these deadly diseases.
When bacteria or viruses invade your body, they attack and multiply. This is called an infection, and it’s what causes illnesses. Our immune system then fights this infection, and has a supply of cells or antibodies that remember the infection and can fight that disease in the future.
The vaccines we get can help our bodies develop immunity, as tiny doses of the disease are introduced to our body, without causing illness. It helps the immune system develop the same response as a real infection, so you can develop antibodies and fight it in the future.
Some people argue that natural immunity is best for your body. While this is true, many immune systems can't handle the virus that comes, and things like measles, polio, and smallpox can kill children or leave devastating results like paralysis or neurological damage. Immunizations are a much safer way to help immune systems create the antibodies needed to fight these diseases.
Registered nurses or other educated healthcare professionals ones who administer vaccines . These nurses are trained in school about the proper ways to administer vaccines, what reactions to watch out for, and can explain vaccine safety to help ensure you are educated and comfortable.
As more health professionals enter the field, there are more trained experts to help with vaccine safety.
Risks of vaccination.

There are some very rare and very mild side effects that can be the result of vaccinations. These side effects completely depend on the immunization you got, and how your specific body will react to it. While there are side effects, as with any medication, it’s important to note that unvaccinated children run the risk of spreading diseases or catching a deadly disease themselves.
Mild side effects.
There are sometimes very mild side effects from getting a vaccine. As the vaccine enters your body and is pretending to be the infection, you may get some of the symptoms of that disease like a cold symptoms, or a slight fever that shows your body is fighting the infection. There may be soreness of muscles or redness at the injection site. All of these very mild side effects go away in a couple of days.
Rare side effects.
There is a very rare chance you or your child could have more severe side effects that come from vaccines. High fevers, rashes, or neurological episodes are these very rare side effects. Medical professionals are trained to deal directly with these kinds of side effects, and each of them is extremely rare— more rare than getting the disease that is being immunized against.
Rarely, individuals will be allergic to vaccinations and can have reactions to their shots. While allergic reactions can be very dangerous, again, they are extremely rare. The CDC reports that in 2015, only 33 people had a serious allergic reaction out of 25 million vaccines given. Many people have genetic indications that they could be allergic to vaccines and are able to work with health professionals to stay safe.
Benefits of vaccinations.
Disease control..
Vaccines are extremely effective at controlling or eliminating dangerous diseases. The World Health Organization reports that the measles vaccine has prevented more than 20 million deaths since 2000.
Smallpox has been completely eradicated thanks to vaccinations, and polio is not far behind. Polio vaccines are still given to help keep control of the disease until it has been globally removed.
Immunizations have a direct impact on disease and virus control in the United States, and across the globe. Immunizations have turned deadly, devastating diseases into preventable diseases that are no longer life-threatening.
Herd immunity.
When more people have vaccinations, it makes everyone less likely to get the disease that is vaccinated against. This control of diseases is called herd immunity, and benefits the entire community.
For example, routine measles vaccines are high in the United States, with 91% of preschool children vaccinated. Measles has an extremely low occurrence rate as a result. But as specific areas dip in the number of vaccines, outbreaks have been seen. In 2018, 17 measles outbreaks impacting more than 370 people were confirmed. This is a direct result of localized areas opting out of vaccines.
When more people decide not to vaccinate, the diseases they prevent against have the potential to flare up or even get out of control. This is why research on vaccine safety is crucial; health professionals want to explain the slight risks of vaccines, and share how the benefits outweigh any risk because of things like herd immunity, that keep everyone safe.
Vaccines have been a hot topic for debate as research has come out about them. Many controversial studies, like the research about vaccines causing autism, have since been discredited. It’s important to look to health professionals as you research and learn about vaccinations and how they can benefit your family.
Ready to Start Your Journey?
HEALTH & NURSING
Recommended Articles
Take a look at other articles from WGU. Our articles feature information on a wide variety of subjects, written with the help of subject matter experts and researchers who are well-versed in their industries. This allows us to provide articles with interesting, relevant, and accurate information.
{{item.date}}
{{item.preTitleTag}}
{{item.title}}
The university, for students.
- Student Portal
- Alumni Services
Most Visited Links
- Business Programs
- Student Experience
- Diversity, Equity, and Inclusion
- Student Communities
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection
- PMC10127050

Learning from five bad arguments against mandatory vaccination
Maxwell j. smith.
a Faculty of Health Sciences and Rotman Institute of Philosophy, Western University, 1151, Richmond Street, London, Ontario N6A 5B9, Canada
Ezekiel J. Emanuel
b Perelman School of Medicine and The Wharton School, University of Pennsylvania, 423, Guardian Drive, Blockley Hall, Philadelphia, PA 19104-4884, USA
Associated Data
No data was used for the research described in the article.
1. Introduction
The suboptimal uptake of COVID-19 vaccines in many parts of the world has prompted unprecedented public debate concerning the ethics of mandatory vaccination [1] . It is imperative we learn lessons from this debate so we are better positioned to navigate policy proposals for mandatory vaccination in the future. Specifically, we should aim to dispense with unsophisticated ethical claims that distract from or otherwise parody more nuanced and forceful arguments and which overshadow other important ethical concerns that have by comparison received little attention. To this end, we identify five ethical objections to mandatory vaccination that are of poor quality but have been frequently raised during the COVID-19 pandemic, including that mandatory vaccination violates the Nuremberg Code, that it is coercive, that it violates informed consent, that it is discriminatory, and that it infringes civil liberties. We argue that, presented as such, each ought to be rejected, allowing future consideration of mandatory vaccination to be focused on concerns more worthy of ethical scrutiny.
2. Mandatory vaccination violates the Nuremberg code
The Nuremberg Code is a set of principles for the ethics of human experimentation delineated in the 1947 Nazi doctor case of United States v. Brandt et al. [2] . Principle one emphasizes that voluntary consent is essential for human participation in research. Vaccination mandates violate the Nuremberg Code because COVID-19 vaccines are ‘experimental’ and because mandates undermine the voluntariness of informed consent.
2.2. Response
COVID-19 vaccines used in practice and involved in vaccination mandates are either authorized or fully approved by national regulatory authorities. Hence, they are not experimental and not part of research, and thus not covered by the Nuremberg Code. Taking approved medicines prescribed or used as a matter of regular medical or public health practice does not constitute an experiment or research in any common understandings of the terms.
But what of the fact that COVID-19 vaccines are still being studied? All medicines undergo on-going study without being considered experimental. The study of medicines does not cease once evidence regarding their safety and efficacy has met the standards of regulatory approval and are used in regular clinical and public health practice. For instance, a drug’s effectiveness is often compared to other interventions. But this does not render those medicines ‘experimental’ and subject to regulations for human subjects research.
Ultimately, whether something is called ‘experimental’ is arguably irrelevant and unhelpful when evaluating the ethics of vaccination mandates because this is a term that could include everything from first-in-human use to off-label use to medicines authorized for emergency use. Each of these has different evidentiary standards, requiring different forms of ethical scrutiny, and so should be assessed accordingly. The mere charge of being ‘experimental’ is therefore of little or no moral importance; instead, what should matter from a moral perspective is whether there is sufficient causal evidence and a positive risk-benefit ratio to justify the use of the medicine in practice [3] . In practical terms, approval or authorization by a national regulatory authority indicate when this condition has been satisfied.
Finally, this objection seems to be confused because no country has in fact legally recognized the Nuremberg Code for the ethical conduct of research. Consequently, a ‘violation’ of the Nuremberg Code would represent a violation of principles of historical ethical importance, not a violation of a law or regulation (e.g., actual regulations governing research or laws concerning informed consent for vaccination).
3. Mandatory vaccination is coercive
Coercive policies use force or threats to compel individuals to do something they would not otherwise do [4] . Mandatory vaccination compels people to get vaccinated by, for instance, threatening them with job loss or a fine if they aren’t vaccinated, and are thus coercive, and hence, unethical.
3.2. Response
People are routinely compelled to do things they would not otherwise do under threat of punishment, including paying taxes, heeding speed limits, and showing up to work on time. If one considers these to be examples of coercion, then the power wielded by governments and employers is commonly ‘coercive’ power. Consequently, the mere charge of coercion is not enough to conclude that an activity is necessarily ethically wrong. Instead, opponents of vaccination mandates should explain why the use of coercion is unjustified, for example because it is not necessary or proportionate to achieve an important objective, because the ethical costs of coercion outweigh the goods that can be achieved through its use, or because its consequences would be so severe as to negate meaningful choice [5] .
Conversely, ethicists sometimes define coercion more narrowly as a state of affairs where people are made worse off no matter which choice they take (where ‘worse off’ may be understood both in terms of becoming materially worse off or becoming worse off by virtue of interference with one’s rights, but not simply disliking one’s choices) [4] , [5] . The classic example is the thief with a gun demanding “your money or your life.” If one believes people are not worse off for having obeyed tax policies, speed limits, and work requirements, or because such activities are justified by people’s consent to the overall scheme of society, one might conclude these cases do not actually constitute coercion. This is reflected in the claim that “if the mafia threatens to destroy your property if you fail to pay protection money, this threat will count as coercive; but if the just, well-regulated state threatens to confiscate your property unless you pay taxes, this threat is arguably not coercive.” [6] . Hence, on this account, mandatory vaccination would be coercive only if people were made worse off no matter which option they choose. Consequently, on this view, opponents of mandatory vaccination should show why all options they are presented with, including being vaccinated with all accommodations or exemptions for medical or religious reasons, makes people worse off (appreciating that no policies, e.g., tax policies, speed limits, etc., carry no burden at all). And as previously noted, even if one is successful in arguing that mandatory vaccination is coercive, one must still argue why that use of coercion is ethically objectionable, and hence, unjustified.
4. Mandatory vaccination violates informed consent
Vaccination is a medical intervention for which there is an ethical and legal requirement to obtain informed consent, which must be given voluntarily. Mandatory vaccination violates informed consent because the consent is not voluntary.
4.2. Response
Mandatory vaccination and laws requiring informed consent have co-existed for decades, strongly suggesting that mandatory vaccination does not, or at least need not, undermine legal requirements of informed consent. Mandatory vaccination would be involuntary if it were truly compulsory; that is, a forced injection. But typically, mandatory vaccination policies tend to require that one be vaccinated as a condition of work or to use a service. Do these conditions undermine the voluntariness of informed consent?
Requirements to get a medical intervention exist in many situations without violating informed consent. As an extreme example, doctors staying the winter at an Australian Antarctic station are required to prophylactically have their appendix removed [7] . In some instances, organ transplant patients are required to have various vaccines, such as the hepatitis B vaccine. While these examples share few features with vaccination employment conditions, they are analogous insofar as they illustrate how requirements to get a medical intervention as a condition to do something else, like work in a particular setting, need not vitiate the voluntariness of informed consent. By making a voluntary decision to stay the winter at an Australian Antarctic station or get a transplant, a person has made a choice to accept the associated required medical intervention. There is no requirement to get an organ transplant or stay at an Australian Antarctic station. While there may be compelling reasons to do so, a patient remains free to refuse consent to those conditions.
The important moral sense in which informed consent to be vaccinated is voluntary is if one is able to visit a vaccination clinic, experience no pressure to be vaccinated, and be free to walk away at any point without getting vaccinated. That one has a compelling reason to visit the vaccination clinic and get vaccinated does not necessarily mean the voluntariness of their consent has been undermined.
5. Mandatory vaccination is discriminatory
Mandatory vaccination imposes restrictions or sanctions on individuals who are unwilling to be vaccinated. This discriminates against people just because they are unvaccinated.
5.2. Response
Differential treatment is not inherently discriminatory in the important moral sense of the term. For example, employment conditions routinely impose requirements of education, skills, or medical procedures. These lead to the unequal treatment of people who belong to different groups. But this does not necessarily constitute discrimination that is morally objectionable, and hence, prohibited by law—that is, wrongfully imposed disadvantageous treatment—because the distinction is not arbitrarily related to a characteristic the person does not control or that is unrelated to job performance, such as sex, race, sexual orientation, or religion. Employment conditions become discriminatory when they make distinctions between people on grounds that are unrelated to job performance or occupational health and safety. Vaccination status on its own is not considered discriminatory because it is modifiable and can reflect a bona fide requirement of occupational health and safety.
Where vaccination status could be construed as discriminatory in the important moral and legal senses is when it is meaningfully connected to grounds otherwise protected from discrimination, such as disability or religion [8] . Consequently, vaccination mandates typically provide reasonable accommodations to avoid discrimination on these protected grounds. But this obligation is not absolute. If the accommodation puts others at risk of harm, the duty to accommodate may be limited. This is why some jurisdictions, like the state of Mississippi, maintain that “exemption from required immunizations for religious, philosophical, or conscientious reasons is not allowed.” [9] . Moreover, some human rights agencies have noted that while discrimination based on religious beliefs (i.e., ‘creed’) is prohibited on human rights grounds, personal preferences or singular beliefs about vaccination do not amount to a creed and thus do not constitute a protected ground upon which discrimination is prohibited [8] .
6. Mandatory vaccination infringes civil liberties
The imposition of direct or indirect restrictions or sanctions via vaccination mandates interferes with civil liberties, including the right to liberty, privacy, and bodily integrity, which renders them unethical.
6.2. Response
Civil liberties are not absolute and can be justifiably limited. This is reflected in the adage “my right to swing my fist ends where your nose begins.” This idea is also commonly enshrined in law and constitutions, where a balance is effected between the rights of the individual and the interests of society by permitting limits to be placed on guaranteed civil liberties. Consequently, the mere charge that vaccination mandates infringe civil liberties is not enough to conclude they are necessarily ethically wrong. In fact, mandatory vaccination could in some cases advance civil liberties. As the American Civil Liberties Union argues: “Far from compromising civil liberties, vaccine mandates actually further civil liberties. They protect the most vulnerable among us, including people with disabilities and fragile immune systems, children too young to be vaccinated and communities of color hit hard by the disease.” [10] . Opponents of vaccination mandates should instead argue how vaccination mandates are more than minimally impairing of rights and that the overall impact on a person’s rights is unnecessary or disproportionate to achieve the stated objectives of the mandate [11] .
7. Conclusions
The COVID-19 pandemic has taught the world many lessons, including about the ethics of mandatory vaccination. Many of the arguments frequently raised against mandatory vaccination represent unsophisticated claims that, if not significantly modified to engage the ethical contours related to the approval of medicines, coercion, informed consent, discrimination, and civil liberties, should not be taken seriously. Moreover, we should not accept these unsophisticated claims as ‘shorthands’ for more sophisticated ones, whereby we are expected to ‘fill in the blanks’ about how, for example, one’s mere charge of coercion or discrimination entails the sorts of arguments that may give that charge greater moral force. Such arguments must be made explicit. To be clear, the five arguments against mandatory vaccination presented in this paper are bad arguments (but are nonetheless common). They can be improved to become more forceful. But as presented, they do not supply the necessary elements to be convincing, and thereby distract from more nuanced arguments that carry greater force and overshadow other important ethical concerns that have by comparison received little attention, such as concerns related to the potential negative impacts vaccination mandates may have on equity and public trust and how those impacts might be mitigated. [1] It would be a shame if when the next pandemic occurs the world rejects the possibility of vaccination mandates on the basis of the superficial claims identified in this paper rather than engaging with more sophisticated arguments for and against their use.
8. Author statement
All authors attest they meet the ICMJE criteria for authorship.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: MJS is an uncompensated Expert Advisory Member of the World Health Organization (WHO) COVID-19 Ethics & Governance Working Group, WHO Expert Group on Ethical Considerations of Social Listening and Infodemic Management, Public Health Agency of Canada Public Health Ethics Consultative Group, and Ontario Public Health Emergencies Science Advisory Committee, and from 2020-2021 served as a compensated member of Ontario’s COVID-19 Vaccine Distribution Task Force. EJE reports the following: UNESCO Global Conference uncompensated speaker; School of Pharmaceutical & Biotech Business uncompensated speaker; NIH Demystifying Medicine Series uncompensated speaker; ASPO 45th Annual Meeting uncompensated speaker; Blue Cross Blue Shield uncompensated speaker; National Health Equity Summit uncompensated speaker; The Galien Foundation uncompensated speaker; Temple Shalom Chicago speaker series uncompensated speaker; AIFA Italian Medical Agency uncompensated speaker; Rainbow Push Coalition/CEF uncompensated speaker; IDSA uncompensated speaker, personal fees from Rise Health, travel fees from The Galien Foundation; Vin Future uncompensated speaker; personal fees from Well Sky; personal fees from Rightway; Brown University uncompensated speaker; personal fees from Signature Healthcare Foundation; Organisation for Economic Cooperation & Development uncompensated speaker, personal fees from Healthcare Leaders of New York; 21st Population Health Colloquium uncompensated speaker; personal fees from Medimpact; American Academy of Arts & Sciences uncompensated speaker; Village MD uncompensated speaker; The Galien Foundation uncompensated speaker; University of Sydney Australia uncompensated speaker; personal fees from Massachusetts Association of Health Plans; Virtahealth uncompensated speaker; Tel Aviv University uncompensated speaker; American Philosophical Society uncompensated speaker; personal fees from Princeton University; personal fees from Philadelphia Committee on Foreign Relations; Health Action Alliance uncompensated speaker; personal fees from Yale University Grand Rounds; personal fees from Hartford Medical Society; UCSF uncompensated speaker; Ichan School of Medicine uncompensated speaker; University of Minnesota uncompensated speaker; IPHS Addis Conference uncompensated speaker; personal fees from AAHC Global Innovation Forum; personal fees from HMSA & Queens Health System; Faith Health Alliance Project uncompensated speaker; travel fees from Macalester College; CDC Learning event uncompensated speaker; travel fees from Oak CEO Summit; American Academy of Political & Social Science uncompensated speaker; Primary Care Transformation Summit uncompensated speaker; 16th World Congress of Bioethics uncompensated speaker; Blue Cross Blue Shield Research Health Alliance uncompensated speaker; personal fees from Advocate Aurora Health Summit, travel fees from DPharm Conference; personal fees from UPMC Shadyside Medical Center; ASCO Quality Care Symposium uncompensated speaker; travel fees from UCSF Department of Urology Grand Rounds; personal fees from Advocate Aurora Health; personal fees from Cain Brothers Conference; personal fees from Bowdoin College; Brookings Institution uncompensated moderator; travel fees from Galien Jerusalem Ethics Forum; non-financial support from HLTH 2022 Las Vegas; National Academies Forum on Microbial Threats uncompensated speaker; National University of Singapore uncompensated speaker; Williams College uncompensated speaker; NIH Grand Rounds uncompensated discussant, travel fees from HMSA; Stanford Graduate School of Business uncompensated speaker; World Bank uncompensated panelist; travel fees from Tel Aviv University; Serving on the following boards: Board of Advisors Cellares; Advisor Clarify Health; Unpaid External Advisory Board Member Village MD; Occasional Advisor Notable; Advisory Board Member JSL Health; Advisory Board Member Peterson Center on Healthcare; Special Advisor to Director General WHO; Expert Advisory Member WHO COVID-19 Ethics & Governance Working Group; Advisory Board Member Biden's Transition COVID-19 Committee; Advisory Board Member HIEx Health Innovation Exchange Partnership sponsored by the UN Geneva.
Data availability
The pros and cons of compulsory vaccination
Government reviewing policy to mandate Covid vaccines for frontline NHS staff
- Newsletter sign up Newsletter

1. Pro: reducing risk of infection
2. con: unnecessary interference, 3. pro: protecting the vulnerable, 4. con: staff shortages, 5. pro: a route to normality, 6. con: the omicron factor, 7. pro: conflict of freedoms, 8. con: divide society.
Ministers are meeting today to decide whether or not to scrap plans to mandate Covid vaccinations for frontline NHS staff, with the deadline for health workers to have their first jab just days away.
Unless they have a medical exemption, patient-facing health and care workers in England “risk being redeployed or losing their jobs altogether” if they have not had two doses of the vaccine by April, reported Nursing Times .
Are Covid vaccine passports legal? The government’s step-by-step plan for ‘new chapter’ of Covid Can you get Omicron twice?
With the final date for the first dose on 3 February, nursing leaders and unions have urged the government to delay the policy “amid concerns of the impact it will have on the workforce”, said the magazine.
Subscribe to The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.
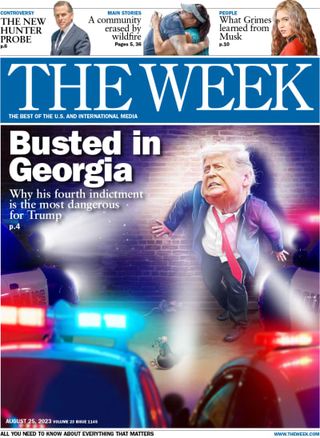
Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Last week, Health Secretary Sajid Javid said the principle of patient safety remains “unchanged” but revealed that the government is “reflecting” on its policy of compulsory Covid vaccination for NHS staff now that the Omicron variant has taken hold in the country.
“No jab, no job” rules have become commonplace in some parts of the world as countries fight Covid-19, said the i news site. Vaccine passports are also being used for international travel or for access to large events and public spaces in different nations.
Boris Johnson has previously acknowledged that there are “moral complexities, ethical problems that need to be addressed” around compulsory vaccination and certification. Here are just some of those key issues.
More than 11,600 people caught Covid in hospital and died after being admitted for a different reason, according to an exclusive report in The Telegraph last November. Jeremy Hunt, the Conservative chairman of the Health and Social Care Select Committee, said the “truly shocking” data “surely strengthens the case for mandatory vaccination for frontline healthcare staff”. An NHS spokesperson said staff had “rigorously” followed infection prevention guidance and blamed the infection rates in hospitals on the rates in the community. While vaccinated people can still spread Covid, a jab provides “some protection” against infection and transmission, according to the UK Health Security Agency . For some, this is not enough to justify enforced vaccination.
One of the biggest arguments against any form of compulsory inoculation is the idea that it represents government encroachment on personal freedoms. Human rights campaign group Liberty has urged the government to support people using education and wider access to vaccination rather than through “pressure and punishment”. Its director, Gracie Bradley, warned that a “coercive approach” will “damage trust between employers, patients and key workers”, while Liberal Democrat MP Tim Farron said mandatory shots were “utterly illiberal, utterly wrong and a challenge to our freedoms”.
Sajid Javid has said compulsory vaccination for NHS frontline workers is imperative to “avoid preventable harm and protect patients in the NHS”. Announcing the policy in November last year, he told the House of Commons: “The weight of the data shows our vaccinations have kept people safe and they have saved lives. This is especially true for vulnerable people in health and care settings.” Care home workers and volunteers are already required to show proof of full vaccination against Covid-19 unless they have a medical exemption. Johnson has previously said the idea should not feel “alien”, pointing out that surgeons are expected to have a vaccination against hepatitis B. In the BMJ , Daniel Sokol, a medical ethicist and clinical negligence barrister, said that for healthcare workers refusing the vaccine would be “contrary to the ethics of their profession”.
Health bosses are “increasingly concerned about the risk of losing a large number of staff when the NHS is struggling with both the Omicron variant and backlogs”, reported The Times . The Royal College of GPs, the Royal College of Nursing and Royal College of Midwives have called for a delay in the deadline for NHS staff to be vaccinated. The newspaper estimated that nearly 80,000 NHS staff are yet to be vaccinated, 5.4% of the total. However, in the BMJ, Sokol argued that unvaccinated healthcare workers “can also cause indirect harm from staff absences and disruption to the health service caused by severe disease”.
Vaccine passports have been touted as one way to revive sectors where it is harder to keep a social distance, such as travel and hospitality. Israel was one of the first countries to use a vaccine passport system. Its “Green Pass” permits fully vaccinated individuals to access indoor venues. Meanwhile, Emmanuel Macron’s decision in July to bring in a vaccine passport scheme in France was a “jaw-dropper”, Politico said. But it proved to be the “best moment” in the president’s handling of the coronavirus crisis – “maybe even of his tenure”, said public health consultant Martin Blachier. France, “one of the most vaccine-sceptical nations on earth”, became “one of the most vaccinated countries in the world” over the summer, said Wired . Similarly, since the consultation on the vaccine mandate for NHS staff last September, around 100,000 unvaccinated health staff have come forward for their jabs, said Nursing Times.
Last week Javid said that although the principle of patient safety remained “unchanged”, the NHS mandate was announced when Delta was the dominant variant. Now that the typically “less severe” Omicron variant accounts for “almost all cases” across the country, it is right that “we reflect on all this and keep all Covid policies properly under review”, Javid told MPs. Another argument related to Omicron is that two vaccines are now less effective than they were against Delta, although some argue that this is a reason to expand the NHS vaccine mandate to three doses.
Alberto Giubilini, an ethics researcher from the University of Oxford, suggested that there is a “conflict of freedoms” when it comes to mandatory vaccination. While people should be free to choose whether or not they receive medical intervention such as an inoculation, vulnerable people who are unable to have a jab should also have the freedom to live a normal life. “Which infringement of freedom is the largest burden and which one is justified? That’s what we should ask,” he wrote for The Conversation .
In New Zealand , where Covid policies grant more freedoms to vaccinated citizens, Prime Minister Jacinda Ardern has admitted that she has created two classes of people with different rights. The Institute for Government has warned of the “potential ethical implications” of using vaccine passes. “Passports could further exacerbate existing inequalities, particularly as vaccine take-up has varied among different groups,” said the think-tank. Internationally, entire countries may also be waiting years to travel if they are unable to access a vaccination programme.
Sign up for Today's Best Articles in your inbox
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com

Under the Radar The play will resemble the kickoff structure seen in the much-smaller XFL
By Justin Klawans, The Week US Published 3 April 24

The Week Recommends Camping, but make it glamorous — and don't forget the s'mores
By Catherine Garcia, The Week US Published 3 April 24

The Explainer The practice reduces the size of a product without lowering the price — and it's perfectly legal
By Becca Stanek, The Week US Published 3 April 24

Today's Big Question Brits suffering from both lockdown nostalgia and collective trauma that refuses to go away
By Chas Newkey-Burden, The Week UK Published 26 March 24

Opinion Remote school let kids down. It will take much more than extra tutoring for kids to recover.
By Mark Gimein Published 19 March 24
Under the radar The future is looking blurry. And very nearsighted.
By Devika Rao, The Week US Published 5 February 24

in depth Rapidly spreading new JN.1 strain is 'yet another reminder that the pandemic is far from over'
By Arion McNicoll, The Week UK Published 12 January 24
The Explainer Covid is not the only disease with a long version
By Devika Rao, The Week US Published 9 January 24

Talking Point Former PM has faced weeks of heavy criticism from former colleagues at the public hearing
By The Week Staff Published 4 December 23

The Explainer Experts warn against pushing 'pandemic panic button' following outbreak of respiratory illness
By Keumars Afifi-Sabet, The Week UK Published 27 November 23

Speed Read Then PM struggled to get his head around key terms and stats, chief scientific advisor claims
By The Week UK Published 20 November 23
- Contact Future's experts
- Terms and Conditions
- Privacy Policy
- Cookie Policy
- Advertise With Us
The Week is part of Future plc, an international media group and leading digital publisher. Visit our corporate site . © Future US, Inc. Full 7th Floor, 130 West 42nd Street, New York, NY 10036.
Appointments at Mayo Clinic
- Infant and toddler health
Childhood vaccines: Tough questions, straight answers
Do vaccines cause autism? Is it OK to skip certain vaccines? Get the facts on these and other common questions.
Part of taking care of kids is setting them up for a healthy future. Vaccines play a big part in health.
Vaccines for illnesses such as diphtheria, rotavirus, polio, tetanus, whooping cough, also called pertussis, and others are given in the first year of life. If these diseases seem uncommon it's because vaccines are doing their job.
Still, you might wonder about the benefits and risks of childhood vaccines. Here are answers to some common questions about childhood vaccines.
Is natural immunity better than vaccination?
No. In general, it is better to prevent sickness by getting vaccinated rather than getting an infection.
Getting infected with a germ may provide some people with a longer lasting immune response but at higher risk. For example, getting a Haemophilus influenzae type b (Hib) bacterial infection could lead to permanent deafness, brain damage or even death.
Childhood vaccines protect kids from serious diseases and complications. Vaccines also lower the chance of spreading a disease.
Do vaccines cause autism?
No. Vaccines do not cause autism. Researchers haven't found a connection between autism and childhood vaccines. The original study that ignited the controversy in 1998 was removed from the scientific record, also called retracted, in 2010.
Are vaccine side effects dangerous?
Most vaccine side effects are not dangerous. Any medicine, including vaccines, can cause side effects. Most of the time, these side effects are minor. Some examples are a low-grade fever, headache, fussiness or soreness at the injection site.
Rarely, a child might experience a severe side effect, such as an allergic reaction or a seizure. These are rare side effects, and caregivers and health care providers monitor for them after vaccination.
Of course, vaccines aren't given to children who have known allergies to specific parts of the vaccine. And if your child has a life-threatening reaction to one vaccine, further doses of that vaccine won't be given.
The risk of a vaccine causing serious harm or death is very small. The benefits of getting a vaccine are much greater than the possible side effects for almost all children.
Why are vaccines given so early?
Most babies are born with developing immune systems. Vaccination makes sure a baby has as much protection from disease and disease complications as is safely possible. It also helps prevent babies and children from spreading illness to others.
Vaccines for children are timed carefully. Vaccines are given when protection inherited from the mother fades and the child's immune system is ready, but before kids come in contact with the germs that cause real infections.
Is it OK to pick and choose vaccines?
It's not a good idea to skip some vaccines. That leaves your child without protection. It allows a child to spread disease to others. For some children, such as kids being treated for cancer, their main protection from disease is the immunity of the people around them.
And because diseases are still spreading in many parts of the world, skipping vaccines puts your child at risk in the future.
If you are worried about a certain vaccine, talk about your concerns with your child's health care provider. If your child falls behind the standard vaccine schedule, ask your child's health care provider how to catch up.
Have more questions? Read the vaccine guidance from Mayo Clinic.
Mayo Clinic Minute: Why and when children should be vaccinated
Elizabeth Cozine, M.D.: Vaccination prevents a child from getting an illness. It also prevents them from spreading an illness.
Jason Howland: Dr. Elizabeth Cozine, a Mayo Clinic family physician, says the Centers for Disease Control and Prevention has a standard immunization schedule for school-age children that begins with ages 4 to 6.
Dr. Cozine: …which we think of as kindergarten shots. So that's measles, mumps, rubella and varicella.
Jason Howland: She says the next set of routine immunizations is at age 11…
Dr. Cozine: …which is tetanus, diphtheria and pertussis, and the meningococcal immunization.
Jason Howland: It's also recommended every child get an annual flu shot. And HPV vaccination, which prevents cancer, can start as early as age 9. Dr. Cozine says it's important to educate families on the importance of childhood vaccinations. She likens it to seat belt safety.
Dr. Cozine: Immunizations are no different. If we have opportunities to protect our children against serious illness and potentially even death, even if the risk of that illness or the risk of death from that illness is really quite low, I'm all for it.
Jason Howland: For the Mayo Clinic News Network, I'm Jason Howland.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Children’s health information and parenting tips to your inbox.
Sign-up to get Mayo Clinic’s trusted health content sent to your email. Receive a bonus guide on ways to manage your child’s health just for subscribing. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Our e-newsletter will keep you up-to-date on the latest health information.
Something went wrong with your subscription.
Please try again in a couple of minutes
- Timing and spacing of immunobiologics. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/timing.html. Accessed Feb. 27, 2023.
- Infants and children birth through age 6. U.S. Department of Health and Human Services. https://www.hhs.gov/immunization/who-and-when/index.html. Accessed Feb. 27, 2023.
- Drutz J, et al. Autism spectrum disorder and chronic disease: No evidence for vaccines or thimerosal as a contributing factor. https://www.uptodate.com/contents/search. Accessed Feb. 27, 2023.
- Drutz J, et al. Standard immunizations for children and adolescents: Overview. https://www.uptodate.com/contents/search. Accessed Feb. 27, 2023.
- Your child's first vaccines. Centers for Disease Control and Prevention. http://www.cdc.gov/vaccines/hcp/vis/vis-statements/multi.html. Accessed Feb. 27, 2023.
- Vaccine recommendations. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/hcp/adults/for-practice/standards/recommend.html. Accessed Feb. 27, 2023.
- The editors of the Lancet. Retraction: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. The Lancet. 2010. doi:10.1016/S0140-6736(10)60175-4.
- How vaccines strengthen your baby's immune system. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/parents/why-vaccinate/strengthen-baby-immune.html. Accessed Feb. 27, 2023.
- H. influenzae: Diagnosis, treatment, and complications. Centers for Disease Control and prevention. https://www.cdc.gov/hi-disease/about/diagnosis-treatment.html. Accessed Feb. 27, 2023.
Products and Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: A Practical Guide to Help Kids of All Ages Thrive
- Car seat safety
- Car sickness in children
- COVID-19 in babies and children
- COVID-19 vaccines for kids: What you need to know
- Enterovirus D68 and parechovirus: How can I protect my child?
- Flu shots for kids
- Hand-washing tips
- Iron deficiency in children
- Language development
- Mayo Clinic Minute: Are you keeping your child as safe as possible in the car?
- Mayo Clinic Minute: Why getting vaccinated for the flu is doubly important this season
- Thermometer basics
- Thermometers: Understand the options
- Vaccine guidance from Mayo Clinic
- Vital Vaccinations
- When to Take Your Child to the E.D.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Childhood vaccines - Tough questions straight answers
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Share full article
Advertisement
Supported by
Guest Essay
I’m a Doctor. Dengue Fever Took Even Me by Surprise on Vacation.

By Deborah Heaney
Dr. Heaney is a physician in Ann Arbor, Mich.
I hate mosquitoes so much that I take my own bug repellent to parties. But in early March, on a trip with my partner to the idyllic island of Curaçao off Venezuela, I was caught off guard by insect bites after our bed-and-breakfast hosts said that mosquitoes didn’t usually appear until late summer.
Near the end of the vacation, my legs began to ache. After I couldn’t keep up with my partner on a snorkeling adventure, he pulled me from the water. My ribs felt broken, as if I’d been smashed against large boulders in the sea. Later that day came intense fever, alternating with shaking chills.
Back in Michigan — weak, nauseated and dehydrated from explosive diarrhea — I ended up in the emergency department. Tests showed worrisome white blood cell levels and abnormal liver numbers. The physician assistant who saw me was perplexed; she gave me IV fluids and medication for nausea and sent me home.
A few days later I developed itching so severe that I couldn’t sleep. A bright red rash spread over both thighs and up my lower back. My brain was foggy, and my balance was so impaired that I would have failed a sobriety test. My primary care doctor had no answers. But as my head began to clear, it occurred to me to request a dengue fever test.
Two days later, the test was positive.
Despite my training in medicine, I was blindsided. Dengue, a mosquito-borne illness, is surging through Latin America and the Caribbean, including in Puerto Rico, where a public health emergency was declared last week. This year is likely to be the worst on record, in part because of El Niño-driven temperature spikes and extreme weather linked to climate change. As temperatures rise and precipitation patterns grow more erratic, the problem will get only worse.
But neither the traveling public nor our frontline health workers are prepared. Without urgent reforms to how we educate travelers, doctors, nurses and others — as well as reforms to public health surveillance and early warning systems — we will be doomed to miss textbook cases like mine. That means those infected with dengue will miss out on timely treatment, possibly even spreading the virus to areas where it was never found before.
The dengue virus, which is primarily transmitted by the Aedes aegypti mosquito, infects up to 400 million people every year in nearly every region of the world, but it is most prevalent in Latin America, South and Southeast Asia and East Africa. Most cases are asymptomatic or, like mine, are considered mild, although the aptly nicknamed breakbone fever often doesn’t feel that way. Some 5 percent of cases progress to a severe, life-threatening disease including hemorrhagic fever.
One malicious feature of dengue is that when someone is infected a second time with a different type of the virus, the risk of severe illness is higher. A vaccine exists, but the Centers for Disease Control and Prevention recommends it only for children ages 9 to 16 who had dengue before and live in places where the virus is common. That’s because, paradoxically, if you’ve never had dengue, the vaccine puts you at greater risk of severe illness your first time.
Dengue outbreaks, which, in the Americas, tend to occur every three to five years , now appear to be expanding their geographic reach as temperatures climb . The Aedes aegypti mosquito has typically had difficulty surviving and reproducing during the winter in temperate climates. But in parts of Brazil, which is experiencing a dengue emergency , the thermometer no longer dips as low in the winter as it once did, allowing the bugs to reproduce year-round. Overall, Latin America and the Caribbean have had three times the number of cases this year as reported for the same period in 2023, which was a record year. Higher temperatures are also helping the virus develop faster inside the mosquito, leading to a higher viral load and a higher probability of transmission. And mosquitoes are benefiting from standing water from rains and floods that are growing more extreme in a warming world.
As the virus spreads globally, travelers are bringing infections back to the continental United States. Based on 2024 numbers to date, this year should show a clear increase of cases here at home compared with 2023, given that the typical dengue season hasn’t even started yet. There could also be local outbreaks in places like Florida, Texas and California, which experienced small ones in the past. As Dr. Gabriela Paz-Bailey, the chief of the C.D.C.’s dengue branch, told me by email, “Increased travel to places with dengue risk could lead to more local transmission, but the risk of widespread transmission in the continental United States is low.”
But since testing is done only on a small fraction of cases, many are going uncounted. I was the one who requested that I be tested. Had I not been given a diagnosis, I would not be aware of my increased risk of severe illness if I am reinfected. Getting a diagnosis is crucial to inform those infected in areas where the Aedes mosquito lives so that the virus doesn’t spread further.
The growing risk means travelers to regions with dengue must be savvier: They can check local news and U.S. State Department advisories, bring an effective insect repellent and protective clothing and book lodging with air-conditioning or screens on the windows and doors. Though Aedes aegypti mosquitoes now live year-round in many locations and are pushing northward into new regions , thanks to climate change and other factors, there are still seasons when the risk is greater, and travelers might consider avoiding trips during those periods. Travel insurance with medical coverage may also be a useful precaution.
For medical professionals, this should be a warning. We need to start thinking about dengue as a possible diagnosis, not just a piece of textbook trivia. We should ask about recent travel when treating patients presenting with symptoms, especially symptoms not easily explained by other diagnoses.
Medical schools are gradually integrating climate change effects into curriculums . This is essential, since malaria, Lyme, West Nile and other insect-borne diseases are on the rise, as are other conditions like heat illness, asthma and allergies that are worsened by climate change. This work must accelerate, and training must include those of us who are already practicing. State medical boards should consider mandating continuing education on tropical emerging illnesses, as they do on many other pertinent topics.
After receiving my positive test result, I called the emergency department to leave a message for my previous provider about my diagnosis, assuming she had never before seen dengue. If we continue on this trajectory, I’m certain this won’t be her last case.
Deborah Heaney is a preventive, occupational and environmental health physician practicing in Ann Arbor, Mich. She also holds a master’s degree in public health.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
An earlier version of this article included an incorrect reference to the mosquitoes that spread dengue. They are members of the Aedes genus, not species.
How we handle corrections

COMMENTS
Advantages of vaccinations. The first notable advantage of the swine flu vaccine is its admission methods. The vaccine can be administered in two ways; injection or as a nasal spray. This is very considerate as it factors in the age and physical well being of the patients ensuring comfort to all that use it. In addition to this, the vaccine is ...
The vaccine will reduce loss of life and will help to recover economic loss. Since the outbreak of COVID-19, the mortality rate has been estimated to be around 2.1%, with nearly 3.5 million people dead by 25 May 2021. 13 Severe/fatal cases of COVID-19 are associated with immune hyperactivation and excessive cytokine release, leading to multiple organ failure. 14-16 It has been estimated that ...
Key messages. - Most vaccines reduce, or probably reduce, the number of people who get COVID-19 disease and severe COVID-19 disease. - Many vaccines likely increase number of people experiencing events such as fever or headache compared to placebo (sham vaccine that contains no medicine but looks identical to the vaccine being tested).
Due to polio vaccination, the disease is no longer a public health concern in the United States. Vaccination is very safe and effective . Injection site pain and mild, flu-like symptoms may occur with vaccine shots. However, serious side effects, such as a severe allergic reaction, are very rare. Immunization protects others.
Vaccination rates vary tremendously across states and communities, despite this shared history of vaccine successes, the outstanding safety and effectiveness of the available vaccines for COVID-19, and skyrocketing cases of dangerously ill people overwhelming hospitals in many parts of the US. It's disappointing, to say the least.
Advantages and Disadvantages of Vaccination. The natural world is home to a truly vast diversity of pathogenic micro-organisms, which can cause a similarly diverse range of diseases in humans, other animals, and plants. The human immune system contains a sophisticated series of defences against such infections, and generally functions ...
Typical side effects include pain at the injection site, fever, fatigue, headache, muscle pain, chills and diarrhoea. The chances of any of these side effects occurring after vaccination differ according to the specific vaccine. COVID-19 vaccines protect against the SARS-CoV-2 virus only, so it's still important to keep yourself healthy and well.
A side effect or reaction isn't necessarily all bad, by the way; it may indicate that the body is building protection against the virus. For the four vaccines listed above, common side effects include. pain at the site of the injection. painful, swollen lymph nodes in the arm where the vaccine was injected. tiredness.
Common side effects from COVID-19 vaccines include pain at the injection site, headaches, fatigue, or feeling flu-like symptoms. This is normal and indicates the vaccine is working. In a group of 100,000 people, we would expect just under 50,000 people to experience side effects because they are so common. Severe side effects: we would also ...
All medications and vaccines have potential risks that must be carefully weighed against the benefits that medications and vaccines offer to prevent illness. Vaccination is one of the most successful public health interventions in reducing disease spread, preventing complications and even deaths from vaccine preventable diseases. The success of ...
An effective COVID-19 vaccine also faces several hurdles beyond our control. The older we get the poorer our ability to respond to vaccines. Resistance to vaccination begins early at age 30 and ...
Vaccination is a life-saving endeavour, yet risk and uncertainty are unavoidable in science and medicine. Vaccination remains contentious in the public mind, and vaccine hesitancy is a serious public health issue. This has recently been reignited in the discussion over potential side effects of COVID-19 vaccines, and the decision by several countries to suspend measures such as the AstraZeneca ...
Vaccines are very effective at preventing disease, but they don't work all the time. Most of the recommended childhood immunizations are 90%-100% effective, according to the CDC.
As the vaccine enters your body and is pretending to be the infection, you may get some of the symptoms of that disease like a cold symptoms, or a slight fever that shows your body is fighting the infection. There may be soreness of muscles or redness at the injection site. All of these very mild side effects go away in a couple of days.
An additional aspect of vaccines many parents are troubled with is the increase in suggested vaccines for young children. "Today, the CDC recommends that children receive vaccines for 10 diseases — plus the flu vaccine — by age 6, which can mean up to 37 separate shots. That compares to five vaccines for the same age group in 1995 ...
01/20/2021 January 20, 2021. Vaccines are safe and save lives. The rapid development of COVID-19 vaccines has people asking questions. Here is an overview of the reactions and side effects you can ...
Discussion. Although vaccines demonstrate effectiveness against this disease, vaccine hesitancy reveals concerns towards short-term and long-term side effects or adverse reactions such as post-inoculation death. Mandatory vaccination is used to provide herd immunity, but is refutable due to infringement of human rights and autonomy.
Disadvantages of Covid-19 Vaccine Essay. This essay sample was donated by a student to help the academic community. Papers provided by EduBirdie writers usually outdo students' samples. India has been provided with and is distributing two vaccines namely OxfordAstraZeneca vaccine, known in India as Covishield, and a domestic product, Covaxin ...
3.1. Claim. Coercive policies use force or threats to compel individuals to do something they would not otherwise do [4]. Mandatory vaccination compels people to get vaccinated by, for instance, threatening them with job loss or a fine if they aren't vaccinated, and are thus coercive, and hence, unethical. 3.2.
Boris Johnson has previously acknowledged that there are "moral complexities, ethical problems that need to be addressed" around compulsory vaccination and certification. Here are just some of ...
Most vaccine side effects are not dangerous. Any medicine, including vaccines, can cause side effects. Most of the time, these side effects are minor. Some examples are a low-grade fever, headache, fussiness or soreness at the injection site. Rarely, a child might experience a severe side effect, such as an allergic reaction or a seizure.
A vaccine exists, but the Centers for Disease Control and Prevention recommends it only for children ages 9 to 16 who had dengue before and live in places where the virus is common. That's ...