An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results
Gabriel veber moisés da silva.
1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
Maria Inês Rodrigues Lobato
2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
Dhiordan Cardoso Silva
Karine schwarz, anna martha vaitses fontanari, angelo brandelli costa.
3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Patric Machado Tavares
Antonio rebello horta gorgen, renan desimon cabral, tiago elias rosito, associated data.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

The initial circumferential subcoronal incision.

The de-gloved penis being passed through the scrotal opening.

The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.

The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

The inverted penile skin flap.

The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.

The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
Patient demographics.
HIV, human immunodeficiency virus .
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
Ethics statement.
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
- Open access
- Published: 03 August 2020
Quality of life in people with transsexuality after surgery: a systematic review and meta-analysis
- Mehrdad Eftekhar Ardebili 1 ,
- Leila Janani 2 ,
- Zaher Khazaei 3 ,
- Yousef Moradi ORCID: orcid.org/0000-0002-2936-5930 4 &
- Hamid Reza Baradaran 5 , 6
Health and Quality of Life Outcomes volume 18 , Article number: 264 ( 2020 ) Cite this article
16k Accesses
14 Citations
119 Altmetric
Metrics details
Several reports have demonstrated varying results on the quality of life (QoL) of the transgender population. Therefore, the aim of this study was to conduct a systematic review and meta-analysis about the quality of life (QoL) of individuals during the post transsexual surgery period.
We searched major biomedical electronic databases, including Scopus, Google Scholar, Psychological Information Database (PsycInfo), Web of Science, PubMed, Excerpta Medica dataBASE (EMBASE), and ProQuest, for all relevant literature published in English up to December 2019. The included papers required to be cross sectional studies that reported quality of life in people with transsexuality post surgery. After selecting eligible studies, 2 authors extracted data of each study independently and resolved any inconsistency by consensus with the third reviewer. The risk of bias was assessed by 2 independent research experts by the Newcastle-Ottawa Scale (NOS).
In this study, out of 497 articles extracted from the initial investigation, 8 articles with 1099 patients were ultimately selected for meta-analysis. The pooled mean of quality of life in transsexual individuals was obtained to be 70.45 (95%CI 55.87–85.03) and 59.17 (95%CI 48.59–69.74), based on World Health Organization Quality of Life (WHOQoL-BREF) and The 36-item short form of the Medical Outcomes Study questionnaire (SF36), respectively. Also, the results of the subgroup analysis for the weighted mean quality of life in male to female and female to male showed that the mean quality of life in female to male was 57.54 (95%CI 42.24–72.84) and it was 62.47 (95%CI 45.94–79.00) in male to female, based on SF36 questionnaire. Moreover, the weighted mean quality of life in female to male was 69.99 (95%CI 43.76, 96.23) and it was 70.65 (95%CI 53.11, 88.19) in male to female, based on WHOQoL-BREF questionnaire.
The results of this systematic review may support the approaches to transsexuality that facilitates sex reassignment. In this review, the means of quality of life after surgery were not compared to the means of quality of life before surgery or even before hormonal therapy which was due to inadequate number of primary studies.
Introduction
Every individual has a significant part of identity called gender identity. It is also one of the most important aspects of human identity including a sense of self and a self-image that every person has it as a man or woman [ 1 ]. Whether a human is called a woman or a man is the most important means of identifying and valuing any individual by him/herself and the environment around him/her, which encourages him to strengthen his/her gender-specific behaviors. However, this natural process, which is successful in most cases, may go through a different path in some cases, so that a child doubts about belonging to one of the 2 sexes or completely associate him/herself with the opposite sex. In this situation, s/he suffers from a sexual identity disorder, which is called transsexuality [ 2 ].
To date, no clear explanation has been provided for the etiology of transsexuality, although some speculations have been made by physicians, psychiatrists, and biologists. In this regard, the role of biological and psychological factors, such as inheritance, prenatal stress, parental sexual relations, genetic disorders, hormone structure, neurological and central nervous system problems, and some environmental factors, should be taken into consideration [ 3 , 4 ]. The prevalence of transsexuality is more common among men, with reports of 1 per 30,000, but it is 1 per 100,000 in women. According to the reported statistics, the prevalence of transsexuality is 6 per 100,000 people worldwide [ 5 , 6 ].
Although the phenomenon of transsexuality seems to be a personal matter, it has consequences in terms of its formation aspects and sociocultural dimensions [ 7 ]. Even though the number of people with transsexuality is low compared to those suffering from other diseases, but it can convert to a source of identity crisis due to the transsexuality effects on the personality and behavioral system of the individuals as well as their social adjustment [ 8 , 9 ].
Transsexuality changes the individual’s life path in the following ways: causing many problems in physical, psychological, social, economic, and family aspects; increasing the feeling of dependence, depression, and isolation; decreasing self-confidence and social capital; and increasing the sense of vulnerability in the patients, which leads to disturbances in daily functions, social activities, and peace of mind. Moreover, transsexuality causes the patients to depend on others and be unable to participate in common social activities. All of these problems, along with various treatments, complications, and high costs of treatments, reduce the quality of life transsexual individuals [ 10 , 11 , 12 ]. Defining quality of life is difficult, as it is a broad and complex concept which is recognized by the feeling of satisfaction and happiness. The subjective nature of quality of life addresses people’s own perceptions of their lifestyles rather than reports by others [ 13 , 14 ]. Therefore, transsexual individuals with similar problems may have different opinions about their quality of life and report it differently [ 14 ]. Various studies have been done on the quality of life of transsexual individuals [ 15 , 16 , 17 , 18 ]. Changing gender is a complex phenomenon that remarkably affects the individuals’ health and social performance and also their identities [ 19 ]. It also changes the circle of the individuals’ social roles. Due to their special conditions, people who undergo gender reassignment have less successful communications with different individuals and social groups than ordinary people. Therefore, their social capital is lower than that of ordinary people, so that they sometimes face limitations in meeting their basic needs, such as education, job seeking, marriage, housing, and the need for safety, affection, and communication with others [ 7 ].
Transsexuality may affect various dimensions of the individuals’ health in their personal and social lives. Exclusion and isolation from family, friends and relatives, homelessness, and poverty are among the problems that transsexual individuals often encounter, which can reduce their quality of life [ 19 , 20 ]. Various studies reported that undergoing surgeries for gender change may improve quality of life in several areas, among which is the quality of their social life [ 21 , 22 , 23 ]. Therapeutic hormones and surgical procedures can harmonize the biological sex and the identity of the individuals, and thus improving their satisfaction and self-confidence [ 8 , 16 , 24 ]. Based on a recent report by Nobili et al., quality of life in transgender people was lower than the general population, but in their review, the authors measured quality of life (QoL) based on all types of questionnaires in general [ 25 ]. All tools and instruments can assess the impact of the disease, but cannot measure the quality of life per se, which has been aptly described as “the missing measurement in health”. WHO (The World Health Organization) has developed and designed The World Health Organization Quality of Life Brief Version (WHOQOL-BREF), which is a measure of quality of life based on a subjective, generic, and cross-cultural evaluation. This scale with The 36-item short form of the Medical Outcomes Study questionnaire (SF36) is a specific tool for measuring quality of life (QoL) and can help researchers to provide a measure of the impact of disease and quality of life [ 26 ]. Although the number of people with sexual dissatisfaction is lower compared to patients suffering from other illnesses, its impact on the cognitive and behavioral systems of individuals and on their quality of life is highly important and may become a source of identity crisis. Considering surgery for this group as one the treatment modality regarding that there are several reports with varied results about the impact of surgery on quality of life (QoL) in this group, this study was conducted to perform a systematic review and meta-analysis to measure the quality of life of individuals post transsexual surgery.
This systematic review was reported according to the Meta-Analyses of Observational Studies in Epidemiology (MOOSE) [ 27 ].

Search strategy and time period
We searched all relevant literature published up to December 2019 in major biomedical electronic databases, including Scopus, Google Scholar, Psychological Information Database (PsycInfo), Web of Science, PubMed, Excerpta Medica dataBASE (EMBASE), and ProQuest. Researchers performed a search of these databases, with hand searching through the reference lists and grey literature. The key search terms were as follow: “Transsexual Individual”, “Transsexual Individuals”, “Transsexualism”, “Female to Male (FTM)”, “Male to Female (MTF)”, “ Gender Dysphonia”, “Gender Incongruence”, “Gender Identity Disorder”, “Quality of Life”, “QoL”, “ Health-Related Quality of Life”, “Surgery”, “ Operative Therapy”, “Operative Procedures”, and “Invasive Procedures” . The final phrases for the search included these terms and their synonyms/various forms linked with appropriate hyphens and as sensitive as possible for any relevant article, according to the instructions of the database of interest. Moreover, we manually reviewed the references of the most relevant articles for any potential study that might have been initially missed while searching the electronic information sources.
We exported the search outputs into the End-Note software version 8 and deleted duplicate studies. Two independent researchers (MY and BH) reviewed the primary search results based on inclusion and exclusion criteria and eliminated some of the articles after reviewing the titles and an abstracts. Then, we investigated the search results and excluded some studies after conducting full-text review (Fig. 1 ). In case of any disagreements about the inclusion/exclusion criteria and data extraction, the third reviewer (EM) assessed the articles for inclusion in the meta-analysis.
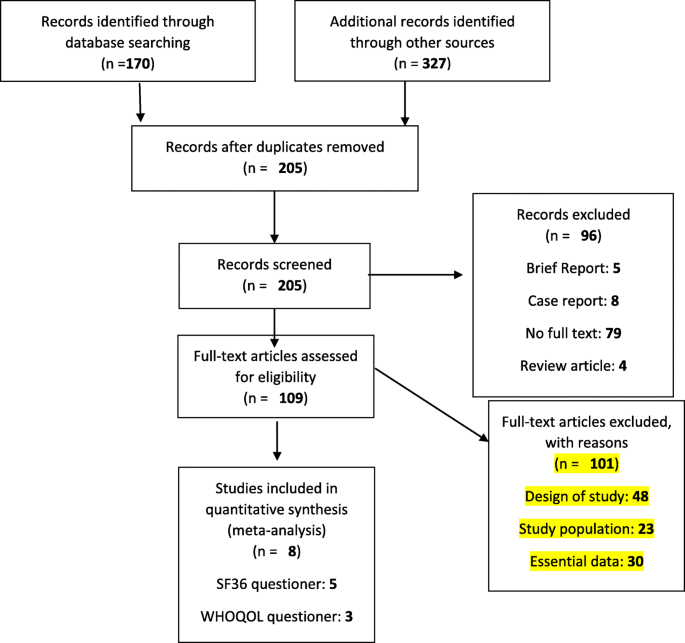
Flow diagram of the literature search and study selection
Inclusion and exclusion criteria
After initial screening, all manuscripts were evaluated thoroughly by reaching and reading their full-texts. Inclusion criteria were as follow:
Study Design: The included studies required to be cross sectional.
Participants: The included study populations were transsexual individuals, those with gender dysphoria and transsexualism, and those with previous diagnoses according to International Classification of Diseases (ICD) or Diagnostic and Statistical Manual of Mental Disorders (DSM) or self-defined as a transgender.
Language: The main articles were required to be in English.
Assessment Method: Studies were eligible for inclusion if they had used SF36 and WHOQoL-BREF questionnaires to evaluate quality of life in individuals post transsexual surgery. The SF-36 consists of 36 questions grouped into 8 domains: physical function (domain 1), social function (domain 2), role physical (domain 3), role emotional (domain 4), mental health (domain 5), vitality (domain 6), body pain (domain 7), and general health (domain 8). A score ranging from 0, indicating the worst health status, to 100, indicating the best health status, is assigned for each domain [ 28 ]. The WHOQOL-BREF, a 26-item instrument, measures the following broad domains: physical health, psychological health, social relationships, and environment [ 29 , 30 ]. It contains 2 items on “overall QoL and general health and 24 items on satisfaction, which are evaluated in 4 domains: physical health, (7 items), psychological health (6 items), social relationships (3 items), and environmental health (8 items). Each item is scored on a 5-point Likert scale from 1 to 5, scored in a positive direction, with lower scores denoting a lower QoL, and transformed to a 4–20 score [ 31 ].
Summary Measures: The selected articles required to report at least the main outcome measurements of interest according to our research questions: quality of life in patients after surgery.
Other study types, including clinical trials, letters, cohorts, case controls, case series, and case reports were excluded. Also, articles that did not report quality of life by WHOQoL-BREF or SF36 were excluded from analysis.
Data extraction
After eligible manuscripts were selected, 2 independent reviewers (MY and JL) extracted data inconsistencies and corrected and resolved them by consensus and consultation with the third reviewer (BH). Moreover, after sorting out the list of included studies, we performed cross-checking by the first author’s name and year of publication to consider any possibility of data overlap. During the entire data collection, any discrepancy in the procedures was resolved by further assessments and discussions with the third researcher.
Risk of Bias
Two research experts (MY and KHZ) assessed the quality assessment of eligible remained papers independently by the Newcastle-Ottawa Scale (NOS) [ 32 , 33 ]. This scale has been adapted from the Newcastle-Ottawa Quality Assessment Scale for cohort and case-control studies to perform quality assessments on cross sectional studies for the systematic reviews. This scale is a modified version of the NOS scale and has been used by several other researchers who felt the need to adapt the NOS scale to appropriately assess the quality of cross sectional studies. We did a comprehensive search of the literature and found that a study with a NOS score of 7 or more can be considered a good study [ 34 ]. In addition, quality of included studies assessed by general information about sample representativeness, study participants, sample size, study participants and setting, data analysis, measurement, and confounding factors/subgroups. In this study, Cohen’s kappa statistic was used to determine the agreement between the results of quality assessment of the 2 experts, which was found to be 0.92.
Statistical analysis
After data extraction, STATA version 14.0 (Stata Corp. College Station, TX, USA) was used for meta-analysis [ 35 , 36 ]. We extracted the mean and standard deviations (SD) of included articles and pooled them in the meta-analysis. According to the guidelines of WHOQoL-BREF, the raw domain scores for the WHOQOL-BREF were transformed to a score between four and 20. The scores of each domain are scaled in a positive direction (i.e., lower scores denote lower quality of life). The mean score of the items in each domain is used to calculate the domain scores, which are ultimately transformed linearly to a scale of zero (worst measured health) to 100 (best measured health) [ 37 , 38 , 39 ]. The SF-36 Health Survey contains 36 items that are scored out of eight scales: physical functioning, role limitations due to physical health problems, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems and mental health. It also includes a single item that provides an indication of perceived change in health. For each scale, a score ranging from zero (worst measured health) to 100 (best measured health) was calculated [ 40 , 41 ].
A Cochran Q test was conducted to assess heterogeneity and an I 2 statistic was calculated to estimate the percentage of total variation resulting from between-study variation (31). Low, moderate, or high degrees of heterogeneity were approximated by I 2 values of 25, 50, and 75%, respectively. If the I 2 value was larger than 50%, random-effect model was estimated. Heterogeneity was assessed by subgrouping MTF and FTM, age, domains of questionnaire, type of questionnaire, and country. Publication bias was assessed by Egger and Begg’s test, with a significance level set at p -value < 0.10. In addition, funnel plots were planned if more than 10 studies were encountered for each forest plot; however, the number of studies was not found to be adequate for such plotting.
In this study, out of 497 articles extracted from the initial investigation, 8 [ 15 , 16 , 17 , 24 , 42 , 43 , 44 , 45 ] with 1099 patients were ultimately selected for meta-analysis (Fig. 1 , Tables 1 and 2 ). The results of risk of bias assessment are presented in Table 3 .
The pooled mean of quality of life after surgery in 633 transsexual individuals was obtained to be 59.17 (95%CI 48.59–69.74) by SF36 questionnaire (Table 4 ). Also, the results of subgroup analysis for the weighted mean quality of life by MTF and FTM showed that the mean quality of life in FTM was 57.54 (95%CI 42.24–72.84) and it was 62.47 (95%CI 45.94–79.00) in MTF, with 507 and 126 transsexual patients, respectively (Table 4 ). Moreover, the physical domain had a higher weighted mean [74.53 (95%CI 59.13, 89.92)]. Patients ( N = 407) aged ≤35 had higher weighted means than patients aged > 35 ( N = 226) [60.00 (95%CI 44.36, 75.64) vs 60.21 (95%CI 43.88, 76.54)] (Table 4 ). The weighted mean of quality of life was higher in French transsexuals ( N = 164) than American transsexuals ( N = 376) [76.17 (95%CI 53.60, 88.73) vs 48.05 (95%CI 34.33, 61.76)] (Table 4 ).
The pooled mean of quality of life in transsexual individuals was obtained to be 70.45 (95%CI 55.87–85.03), with 466 transsexual patients, by WHOQoL-BREF questionnaire (Table 5 ). Furthermore, the results of subgroup analysis for the weighted mean quality of life by MTF and FTM showed that the mean quality of life in FTM was 69.99 (95%CI 43.76, 96.23) and it was 70.65 (95%CI 53.11, 88.19) in MTF, with 334 and 132 transsexual patients, respectively (Table 5 ). Also, the social domain had a higher weighted mean of quality of life [68.25 (95%CI 50.32, 86.17)]. Patients aged ≤35 ( N = 194) had higher weighted means than patients aged > 35 ( N = 372) [73.31 (95%CI 54.53, 92.09) vs 66.12 (95%CI 42.46, 99.63)] (Table 5 ).
Discussions
In the present research, 8 studies [ 15 , 16 , 17 , 24 , 42 , 43 , 44 , 45 ] were ultimately analyzed to assess the quality of life of transsexual individuals using SF-36 and WHOQoL-BREF questionnaires. The results of this study showed that the mean scores of quality of life were higher in FTMs, based on the SF36 and WHOQOL questionnaires. The results of the study by Parola et al. showed that the quality of social life as well as the quality of sexual life improved after transsexual surgery. Also, female-to-male individuals had better friendly, professional and social lifestyles than male-to-female ones [ 46 ]. Transsexual made people more engaging and active in various social activities, and caused them to have stronger social relationships and get out of social isolation. This improvement in social relationships can increase their quality of life [ 47 , 48 ]. On the other hand, Kuhn et al. showed that patients’ satisfaction was significantly lower compared to that of the control group [ 10 ]. Most studies have been performed on quality of life of clinical patients, but not enough attention has been paid to quality of life of transsexual patients. In line with our findings, Wierckx K et al. showed that the mean of quality of life increased after hormone therapy [ 24 ]. Moreover, Dhiordan et al. performed a before-after survey on sex reassignment surgery in Brazilian male-to-female transsexual individuals and found that domains II (psychological) and IV (social relationships) of the WHOQoL-BREF were improved after stereotactic radiosurgery (SRS) in patients compared after surgery compared to before surgery [ 49 ].
One study found that the quality of life in such areas as public health, role limitation, and physical and personal constraints was lower 15 years after transsexual surgery [ 10 ]. In a study by Newfield et al., it was shown that the quality of life was lower in female-to-male bisexual than in male-to-female participants. Female-to-male participants who had received testosterone had a higher quality of life than non-hormone-treated patients [ 16 ]. The apparent characteristics of transsexual individuals, including their voice and face, and their friends and family members’ behaviors were effective in their post-surgery communications in the community; limitations and problems were found to be greater for male-to-female transsexual individuals [ 22 ]. In the study by Pitts et al., most of the participants assessed their health as good or very good. Bisexual people had a lower health status than normal people in Australia and New Zealand on the SF36 scale. The rate of depression among transsexual individuals was much higher than ordinary people in Australia, and biological men were twice as likely to experience depression compared to biological women [ 50 ]. As transsexualism is an unpredictable phenomenon and the negative attitude of the environment to transsexual individuals may be negative, it causes limitations for the individuals undergoing transsexualism. Limitations such as family and community disapproval may impose the risk of vulnerability to transsexual individuals, which could gradually affect their quality of life and pave the way for their depression [ 51 ].
In their study, Rezaei et al. showed that family function, emotional fusion, behavior control, and emotional responsiveness can play a significant role in helping transsexual individuals to accept their new sexual role [ 52 ].
The results of the study by Movahed et al. indicated that the mean gender identity disorder among transsexual individuals was much lower than those who did not undergo this type of surgery. A comparison between gender identity disorder in transsexual individuals before and after surgery showed that their disorder was severely reduced after surgery. In addition, the mean total index of the quality of life and level of psychological well-being was different among transsexual individuals compared to nontranssexual individuals; for example, transsexuals had a higher quality of life and mental health compared to nontranssexual individuals [ 53 ].
Rakic et al. found that hormone therapy reduced depression and identity disorder in transsexual individuals and increased their quality of life. Although surgery and hormone therapy slightly improved the quality of life of transsexual individuals, their widespread social and interpersonal problems were much more than nontranssexual individuals [ 48 ].
In a study by Rahimparvar et al., the quality of life of transsexual women was almost the same as that of nontranssexual women (Quality of life in both groups were moderate.). However, the mean total score of quality of life in transsexual women was slightly higher than that of nontranssexual women [ 17 ]. In a study by Weyers et al., the mean total score of quality of life was 73.3 ± 25.11 in transsexual women [ 18 ]. One study showed that the life quality score depended on gender, and the mean score of quality of life in women was lower than that of men (35). TS person who still has a girl’s body, even though wearing males’ clothes and having males’ behaviors, may be seen as a strong and daring girl and such masculine appearance and behavior may be perceived as a sign of reliability [ 54 ].
However, if MTF person has women-specific behaviors, he will be severely excluded from the community and will be considered a weak and womanly person. After transsexual surgeries, MTF individuals will formally and legally be in the position of women and will quite irreversibly face discrimination and limitations of women, which may gradually reduce their quality of life [ 54 ].
The results of prior studies showed that the mean score of quality of life in transsexual people decreased with age. Because when the age, physical problems and physical pain increase, their quality of life increase too [ 55 , 56 ].
The results of different studies showed that marital status affected the mean score of quality of life. Due to social and economic pressures, divorced women felt helpless and, despite governmental and nongovernmental financial support, they often had limited and painful lives, and their difficult life circumstances made them feel depressed [ 57 , 58 ]. The results of various studies showed that the mean score of TS people’s quality of life increased with higher levels of education, as educated people usually feel more psychologically secure. Also, the mean quality of life was lower in unemployed transsexual individuals than in others [ 59 ].
Results of a review by Nobili et al. showed that transsexual people have poorer mental health QoL compared to the general population. Also, QoL in participants who were exclusively post- cross-sex hormonal treatment (CHT) found no difference in mental health QoL between groups, but in our systematic review, which was based on WHOQoL-BREF questionnaire, it was found that transsexual people have poorer environmental QoL and based on SF36 have poorer role emotional QoL. In addition, the pooled weighted mean of QoL in our review had a lower heterogeneity (I2) than a recent review by Nobili et al., because we included only cross sectional studies and calculated weighted mean based on WHOQOL-BREF and SF36 questionnaire [ 25 ].
In this review, the means of quality of life of individuals before transsexual surgery were not compared to their means of quality of life before surgery or even before hormonal therapy, because the number of primary studies was inadequate.
It seems that the weighted mean of QoL was better in transsexual individuals after surgery, but these results need to enough studies for compare to means of QOL before surgery with after surgery. Transsexuals remain a population at risk for low QoL and mental health. Therefore, it is suggested to pay more attention to different aspects of their treatment, including psychological and physical aspects. The main finding of this study may support the approaches to transsexuality that facilitate sex reassignment.
Availability of data and materials
The study data extracted for analyses in the current publication are available from the corresponding author upon reasonable request.
Abbreviations
Confidence Interval
Female to Male
Male to Female
Quality of Life
Transsexualism
Excerpta Medica dataBASE
Newcastle-Ottawa Scale
World Health Organization Quality of Life
The 36-item short form of the Medical Outcomes Study questionnaire
The World Health Organization
The World Health Organization Quality of Life Brief Version
The Meta-Analyses of Observational Studies in Epidemiology
Psychological Information Database
International Classification of Diseases
Diagnostic and Statistical Manual of Mental Disorders
Standard Deviations
Cross-sex Hormonal Treatment
Stereotactic Radiosurgery
Berzonsky MD. Identity style and well-being: does commitment matter? Identity. 2003;3:131–42.
Google Scholar
Di Ceglie D. Gender identity disorder in young people. Adv Psychiatr Treat. 2000;6:458–66.
Brassard A, Péloquin K, Dupuy E, Wright J, Shaver PR. Romantic attachment insecurity predicts sexual dissatisfaction in couples seeking marital therapy. J Sex Marital Ther. 2012;38:245–62.
PubMed Google Scholar
Beren SE, Hayden HA, Wilfley DE, Grilo CM. The influence of sexual orientation on body dissatisfaction in adult men and women. Int J Eat Disord. 1996;20:135–41.
CAS PubMed Google Scholar
Snyder DK, Berg P. Determinants of sexual dissatisfaction in sexually distressed couples. Arch Sex Behav. 1983;12:237–46.
Danafar A, Behian S. Gender identity disorder and social factors affecting it among Transsexualists, who referred to the social welfare organization in 2013-2015. Tolooebehdasht. 2017;16:75–87.
Mousavi SM, Habibollahi S, Ghasemnejad SM. A comparison of life quality and social adjustment among normal people and those with gender identity disorder (transsexual). J Appl Environ Biol Sci. 2015;5:19–24.
Zucker KJ, Bradley SJ. Gender identity disorder and psychosexual problems in children and adolescents. London: Guilford Press; 1995. p 3-20.
De Vries AL, Steensma TD, Doreleijers TA, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med. 2011;8:2276–83.
Kuhn A, Bodmer C, Stadlmayr W, Kuhn P, Mueller MD, Birkhäuser M. Quality of life 15 years after sex reassignment surgery for transsexualism. Fertil Steril. 2009;92:1685–9 e1683.
Fredriksen-Goldsen KI, Kim H-J, Shiu C, Goldsen J, Emlet CA. Successful aging among LGBT older adults: physical and mental health-related quality of life by age group. The Gerontologist. 2014;55:154–68.
PubMed PubMed Central Google Scholar
Yang X, Zhao L, Wang L, Hao C, Gu Y, Song W, Zhao Q, Wang X. Quality of life of transgender women from China and associated factors: a cross-sectional study. J Sex Med. 2016;13:977–87.
Schalock RL. Quality of life: application to persons with disabilities. USA: AAMR; 1996. p 50-190.
Shariati M, Nasiri Kalmarzi R, Abaei Hasani S, Goodarzi E, Hasanzadeh J, Ataee P, Rad F, Mansouri M, Khalafi B, Moradi G. The impact atopic dermatitis on the life quality of childrens 1-6 year. Int J Pediatr. 2018;6:7003–11.
Motmans J, Meier P, Ponnet K, T'Sjoen G. Female and male transgender quality of life: socioeconomic and medical differences. J Sex Med. 2012;9:743–50.
Newfield E, Hart S, Dibble S, Kohler L. Female-to-male transgender quality of life. Qual Life Res. 2006;15:1447–57.
Vasegh Rahimparvar F, Mousavi MS, Rayisi F, Khodabandeh F, Bahrani N. Comparison of quality of life in gender identity disorders after sex reassignment surgery with normal women in Tehran, Iran, 2012. Iran J Obstet Gynecol Infertil. 2013;16:10–9.
Weyers S, Elaut E, De Sutter P, Gerris J, T'sjoen G, Heylens G, De Cuypere G, Verstraelen H. Long-term assessment of the physical, mental, and sexual health among transsexual women. J Sex Med. 2009;6:752–60.
De Cuypere G, Gijs L. Care for adults with gender identity disorder; 2014.
Simon L, Zsolt U, Fogd D, Czobor P. Dysfunctional core beliefs, perceived parenting behavior and psychopathology in gender identity disorder: a comparison of male-to-female, female-to-male transsexual and nontranssexual control subjects. J Behav Ther Exp Psychiatry. 2011;42:38–45.
Besharat MA. Relationship of alexithymia with coping styles and interpersonal problems. Procedia Soc Behav Sci. 2010;5:614–8.
Michel A, Ansseau M, Legros J-J, Pitchot W, Mormont C. The transsexual: what about the future? European Psychiatry. 2002;17:353–62.
Parola N, Bonierbale M, Lemaire A, Aghababian V, Michel A, Lançon C. Study of quality of life for transsexuals after hormonal and surgical reassignment. Sexologies. 2010;19:24–8.
Wierckx K, Van Caenegem E, Elaut E, Dedecker D, Van de Peer F, Toye K, Weyers S, Hoebeke P, Monstrey S, De Cuypere G. Quality of life and sexual health after sex reassignment surgery in transsexual men. J Sex Med. 2011;8:3379–88.
Nobili A, Glazebrook C, Arcelus J. Quality of life of treatment-seeking transgender adults: a systematic review and meta-analysis. Rev Endocr Metab Disord. 2018;19:199–220.
Group W. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41:1403–9.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–12.
Iudici M, Cuomo G, Vettori S, Avellino M, Valentini G. Quality of life as measured by the short-form 36 (SF-36) questionnaire in patients with early systemic sclerosis and undifferentiated connective tissue disease. Health Qual Life Outcomes. 2013;11:23.
Lodhi FS, Montazeri A, Nedjat S, Mahmoodi M, Farooq U, Yaseri M, Kasaeian A, Holakouie-Naieni K. Assessing the quality of life among Pakistani general population and their associated factors by using the World Health Organization’s quality of life instrument (WHOQOL-BREF): a population based cross-sectional study. Health Qual Life Outcomes. 2019;17:9.
Malibary H, Zagzoog MM, Banjari MA, Bamashmous RO, Omer AR. Quality of life (QoL) among medical students in Saudi Arabia: a study using the WHOQOL-BREF instrument. BMC Med Educ. 2019;19:344.
Organization WH. WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment: field trial version, December 1996. Geneva: World Health Organization; 1996.
Wells G: The Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomised studies in meta-analyses. 2001. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Wells G: Shea B, O'Connell D., Peterson J, Welch V, Losos M, et al. The Newcastle Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2011.
Kremelberg D. Practical statistics: a quick and easy guide to IBM® SPSS® statistics, STATA, and other statistical software. London: SAGE publications; 2010. p 83-100.
StataCorp L. STATA finite mixture models reference manual. Release; 2017.
WHOQOL-BREF W. Introduction, administration, scoring and generic version of the assessment—field trial version. Geneva: Switzerland; 1996.
Skevington SM, Tucker C. Designing response scales for cross-cultural use in health care: data from the development of the UK WHOQOL. Br J Med Psychol. 1999;72:51–61.
Organization WH. WHOQOL user manual: Programme on mental health. Switzerland: World Health Organization; 1998.
Ware JE Jr. SF-36 health survey update. Spine. 2000;25:3130–9.
Framework IC. The MOS 36-item short-form health survey (SF-36). Med Care. 1992;30:473–83.
Başar K, Öz G, Karakaya J. Perceived discrimination, social support, and quality of life in gender dysphoria. J Sex Med. 2016;13:1133–41.
George A, Janardhana N, Muralidhar D. Quality of life of transgender older adults. Int J Soc Sci Humanit Invent. 2015;4:7–11.
Gorin-Lazard A, Baumstarck K, Boyer L, Maquigneau A, Gebleux S, Penochet JC, Pringuey D, Albarel F, Morange I, Loundou A, et al. Is hormonal therapy associated with better quality of life in transsexuals? A cross-sectional study. J Sex Med. 2012;9:531–41.
Thompson HM, Reisner SL, VanKim N, Raymond HF. Quality-of-life measurement: assessing the WHOQOL-BREF scale in a sample of high-HIV-risk transgender women in San Francisco, California. Int J Transgenderism. 2015;16:36–48.
Ainsworth TA, Spiegel JH. Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Qual Life Res. 2010;19:1019–24.
Blanchard R. Typology of male-to-female transsexualism. Arch Sex Behav. 1985;14:247–61.
Rakic Z, Starcevic V, Maric J, Kelin K. The outcome of sex reassignment surgery in Belgrade: 32 patients of both sexes. Arch Sex Behav. 1996;25:515–25.
da Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, Salvador J, Silveira E, Rosito TE, Lobato MIR. WHOQOL-100 before and after sex reassignment surgery in Brazilian male-to-female transsexual individuals. J Sex Med. 2016;13:988–93.
Pitts MK, Couch M, Mulcare H, Croy S, Mitchell A. Transgender people in Australia and New Zealand: health, well-being and access to health services. Fem Psychol. 2009;19:475–95.
Nuttbrock L, Hwahng S, Bockting W, Rosenblum A, Mason M, Macri M, Becker J. Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. J Sex Res. 2010;47:12–23.
REZAEI AM, Azadi A, Ahmadi F, Vahedian AA. Comparison of depression, anxiety, stress and quality of life in dormitories students of Tarbiat Modares University; 2007.
Movahed M, Hoseynzade Kasmani M. The relation of gender identity disorder and quality of life. J Soc Welf. 2011;12:111–42.
Bauer GR, Hammond R, Travers R, Kaay M, Hohenadel KM, Boyce M. “I don't think this is theoretical; this is our lives”: how erasure impacts health care for transgender people. J Assoc Nurses AIDS Care. 2009;20:348–61.
Bayat M, Bayat M. Quality of life for women in Mashhad. In: The strategic Thoughts, Women and Families; 2012. p. 575–87.
Montazeri A, Gashtasbi A, Vahdani Nia MS. Translation, reliability and validity of the Persian standard SF36. [Article in Persian]. Payesh J. 2006;5:49–56.
Norozi E, Mostafavi F, Hassanzadeh A, MOODI M, Sharifirad G. Factors related with quality of life among postmenopausal women in Isfahan, Iran, based on behavioral analysis phase of precede model; 2011.
Hafariyan L, Aghaei A, Kajbaf M, Kamkar M, et al. Knowledge Res Appli Psychol. 2009;41:82–61.
Wai H, Tsang P. Hong Kong men with low incomes have worse health-related quality of life as judged by SF-36 scores. Hong Kong Med J. 2006;12:351–4.
Download references
Acknowledgements
This study has been supported by the Deputy of Research and Technology of Kurdistan University of Medical Sciences, Sanandaj, Iran (Ethical code: IR.MUK.REC.1398.167). Kurdistan University of Medical Sciences, Sanandaj, Iran funded this study.
Kurdistan University of Medical Sciences, Sanandaj, Iran funded this study.
Author information
Authors and affiliations.
Mental Health Research Center, Psychosocial Health Research Institute (PHRI), Iran University of Medical Science, Tehran, Iran
Mehrdad Eftekhar Ardebili
Preventive Medicine and Public Health Research Center, Psychosocial Health Research Institute (PHRI), Iran University of Medical Sciences, Tehran, Iran
Leila Janani
Department of Public Health, School of Medicine, Dezful University of Medical Sciences, Dezful, Iran
Zaher Khazaei
Social Determinants of Health Research Center, Research Institute for Health Development, Kurdistan University of Medical Sciences, Sanandaj, Iran
Yousef Moradi
Endocrine Research Center, Institute of Endocrinology and Metabolism, Iran University of Medical Sciences (IUMS), Tehran, Iran
Hamid Reza Baradaran
Ageing Clinical & Experimental Research Team, Institute of Applied Health Sciences, Aberdeen, Scotland, AB25 2ZD, UK
You can also search for this author in PubMed Google Scholar
Contributions
ME and YM conceptualized the idea for this review, formulated the review question and objectives, assisted with the development of the final search strategy, contributed to the data analysis/interpretation and writing the manuscript. HRB contributed to the conceptualization of the final review question, formulation of the review objectives, data analysis/interpretation and writing the manuscript. LJ and ZKH contributed equally to the formulation of the review question/objectives, development of the search strategy, conducting the searches, data extraction, data analysis/interpretation, and the writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yousef Moradi .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Eftekhar Ardebili, M., Janani, L., Khazaei, Z. et al. Quality of life in people with transsexuality after surgery: a systematic review and meta-analysis. Health Qual Life Outcomes 18 , 264 (2020). https://doi.org/10.1186/s12955-020-01510-0
Download citation
Received : 16 December 2018
Accepted : 24 July 2020
Published : 03 August 2020
DOI : https://doi.org/10.1186/s12955-020-01510-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Male to female
- Female to male
- Quality of life
- WHOQoL-BREF
- Transsexual individuals
Health and Quality of Life Outcomes
ISSN: 1477-7525
- Submission enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) . The authors found that GAS promotes the improvement of psychological aspects and social ...
Conclusion . This review supports the need for more sustainable and accessible gender-affirming surgery as a means for improving the mental health and overall QoL among transgender individuals and indicates the need for further research with greater methodological rigor focusing on correlates of positive gender-affirming surgical outcomes.
The pooled mean of quality of life after surgery in 633 transsexual individuals was obtained to be 59.17 (95%CI 48.59–69.74) by SF36 questionnaire (Table 4).Also, the results of subgroup analysis for the weighted mean quality of life by MTF and FTM showed that the mean quality of life in FTM was 57.54 (95%CI 42.24–72.84) and it was 62.47 (95%CI 45.94–79.00) in MTF, with 507 and 126 ...