
Breastfeeding News
Top headlines, latest headlines.
- Breastfeeding After COVID-19 Booster
- Feeding Extremely Preterm Infants
- Unique Set of Breast Milk Antibodies
- Infant Formula Shortage: Unsafe Feeding
- Dads Are Key in Supporting Breastfeeding
- Breastfeeding: Beneficial Bacteria in Infant Gut
- Early Tastings Shorten Breastfeeding
- How Breast Milk Protects Baby from Allergies
- Safe-Sleep Guidelines Aim to Reduce Infant ...
- Breastfeeding Duration Associated With Cognition
Earlier Headlines
Thursday, march 7, 2024.
- Infant Health Suffered During Baby Formula Shortage
Friday, December 8, 2023
- Mothers Need More 'exclusive Breastfeeding' Support
Friday, October 7, 2022
- COVID-19 Pandemic May Have Decreased Breastfeeding
Thursday, September 29, 2022
- Research Finds Link Between Poor Health, Low Breast Milk Production
Wednesday, May 25, 2022
- Longer Duration of Exclusive Breastfeeding Has Protective Effect on Childhood Asthma
Wednesday, April 13, 2022
- Busy Mothers Did Less Breastfeeding in 19th Century Netherlands
Wednesday, April 6, 2022
- Study Reveals the Dynamics of Human Milk Production
- Antibiotic and Antiretroviral Drug Effects on Breast Milk Are Explored for Mothers Living With HIV
Wednesday, February 23, 2022
- Monitoring Breast Milk for PFAS
Tuesday, February 22, 2022
- Genetic Mutation May Identify Women With Difficulty Producing Breast Milk
Friday, January 28, 2022
- Live Cells Discovered in Human Breast Milk Could Aid Breast Cancer Research
Tuesday, January 11, 2022
- Breastfeeding Reduces Mothers’ Cardiovascular Disease Risk
Monday, January 10, 2022
- Vaccinated Women Pass COVID-19 Antibodies to Breastfeeding Babies, Study Finds
Monday, November 29, 2021
- Spicy Breast Milk?
Saturday, October 23, 2021
- New Study Suggests That Breastfeeding May Help Prevent Cognitive Decline
Friday, October 8, 2021
- Breast Milk of Marijuana Users Does Not Hurt Short-Term Health of Early Premature Infants, Long-Term Effects Still Unknown
Wednesday, September 8, 2021
- No Serious COVID-19 Vaccine Side Effects in Breastfeeding Moms, Infants, Study Finds
Tuesday, August 24, 2021
- Breast Milk of Mothers Who Received COVID-19 Vaccine Contains Antibodies That Fight Illness
Friday, August 6, 2021
- Non-Recommended Milk Being Provided to Young Children
Wednesday, July 21, 2021
- Breastfeeding, Even for a Few Days, Linked to Lower Blood Pressure in Early Childhood
Friday, July 16, 2021
- No Sign of COVID-19 Vaccine in Breast Milk
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- Simple Brain-Computer Link: Gaming With Thoughts
- Clinical Reasoning: Chatbot Vs Physicians
- Understanding People Who Can't Visualize
- Illuminating Oxygen's Journey in the Brain
- DNA Study IDs Descendants of George Washington
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
- Cell Division Quality Control 'Stopwatch'
- What Controls Sun's Differential Rotation?
Trending Topics
Strange & offbeat.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Milk Production and Transfer
Neonatal weight and output assessment, glucose stabilization, hyperbilirubinemia, immune development and the microbiome, supplementation, health system interventions: the baby-friendly hospital initiative, limitations and implications for future research, conclusions, acknowledgment, evidence-based updates on the first week of exclusive breastfeeding among infants ≥35 weeks.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Lori Feldman-Winter , Ann Kellams , Sigal Peter-Wohl , Julie Scott Taylor , Kimberly G. Lee , Mary J. Terrell , Lawrence Noble , Angela R. Maynor , Joan Younger Meek , Alison M. Stuebe; Evidence-Based Updates on the First Week of Exclusive Breastfeeding Among Infants ≥35 Weeks. Pediatrics April 2020; 145 (4): e20183696. 10.1542/peds.2018-3696
Download citation file:
- Ris (Zotero)
- Reference Manager
The nutritional and immunologic properties of human milk, along with clear evidence of dose-dependent optimal health outcomes for both mothers and infants, provide a compelling rationale to support exclusive breastfeeding. US women increasingly intend to breastfeed exclusively for 6 months. Because establishing lactation can be challenging, exclusivity is often compromised in hopes of preventing feeding-related neonatal complications, potentially affecting the continuation and duration of breastfeeding. Risk factors for impaired lactogenesis are identifiable and common. Clinicians must be able to recognize normative patterns of exclusive breastfeeding in the first week while proactively identifying potential challenges. In this review, we provide new evidence from the past 10 years on the following topics relevant to exclusive breastfeeding: milk production and transfer, neonatal weight and output assessment, management of glucose and bilirubin, immune development and the microbiome, supplementation, and health system factors. We focus on the early days of exclusive breastfeeding in healthy newborns ≥35 weeks’ gestation managed in the routine postpartum unit. With this evidence-based clinical review, we provide detailed guidance in identifying medical indications for early supplementation and can inform best practices for both birthing facilities and providers.
Exclusive breastfeeding significantly improves maternal and child health. Although US pediatricians’ recommendations are increasingly aligned with American Academy of Pediatrics (AAP) policies, their optimism about the potential for breastfeeding success has declined. 1 To maintain familiarity with the benefits of breastfeeding and the skills necessary to promote this positive health intervention, providers caring for neonates and/or new mothers need updated evidence-based information and tools to assess and manage breastfeeding.
In this review, we provide new evidence from the past 10 years on the following topics relevant to exclusive breastfeeding: milk production and transfer, neonatal weight and output assessment, glucose stabilization, hyperbilirubinemia, immune development and the microbiome, supplementation, and health system interventions. We focus on the early days of exclusive breastfeeding in healthy newborns ≥35 weeks’ gestation managed in the routine postpartum unit. 2 – 6 Tables 1 through 3 and Fig 1 provide summaries based on evidence and authors’ recommendations to provide concise and clear bullets on optimal management. The search strategy and tables of evidence for milk production and transfer, neonatal weight and output assessment, management of glucose, and hyperbilirubinemia are summarized in the Supplemental Information .
Breastfeeding Assessment During the First Postnatal Week
—, not applicable.
Mother, Infant, and Systems-Level Risk Factors for Breastfeeding Difficulties
Adapted from Evans A, Marinelli KA, Taylor JS; Academy of Breastfeeding Medicine. ABM clinical protocol #2: guidelines for hospital discharge of the breastfeeding term newborn and mother: “The going home protocol,” revised 2014. Breastfeed Med . 2014;9(1):4.
Risk Factors for Hypoglycemia
Adapted from Thornton PS, Stanley CA, De Leon DD, et al; Pediatric Endocrine Society. Recommendations from the Pediatric Endocrine Society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. J Pediatr . 2015;167(2):241 and Adamkin DH; Committee on Fetus and Newborn. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics . 2011;127(3):576.

Supplementation decision algorithm.
Three stages of milk production, lactogenesis I to III, are defined on the basis of volume and composition of milk. For volume, Fig 2 shows estimated daily milk production. 16 In relation to composition, human milk changes dramatically over the first week of lactation. Colostrum, which is produced during the initial stage of lactation (lactogenesis I) in the first days after birth, contains more protein than mature milk. This highly dense early milk has a high concentration of immunoglobulins, activated macrophages, lymphocytes, neutrophils, and growth factors with essential roles in development of gut-associated lymphoid tissue. 17 As milk volume increases (lactogenesis II), sodium concentration and the sodium/potassium ratio decline rapidly with increased secretory activity of the lactocytes and closure of tight cellular junctions. 18 Production of fat-rich, higher-calorie mature milk typically occurs by ∼10 days post partum (lactogenesis III).

Milk volume estimated by breast milk transfer over the first 6 days in vaginal and cesarean births. *Adjusted difference P < .05. Adapted from Evans KC, Evans RG, Royal R, Esterman AJ, James SL. Effect of caesarean section on breast milk transfer to the normal term newborn over the first week of life. Arch Dis Child Fetal Neonatal Ed . 2003;88(5):F382.
Most, but not all, women experience lactogenesis II, referred to as “milk coming in,” by 72 hours post partum. In the Infant Feeding Practices Survey II, 19% of multiparous women and 35% of primiparous women reported milk coming in on day 4 or later. 19 Reasons for delayed lactogenesis II include primiparity, cesarean delivery, and BMI > 27. 20 – 22 Conditions associated with obesity, such as advanced maternal age (possibly related to reduced fertility associated with obesity-variant polycystic ovarian syndrome) and excessive gestational weight gain, may also lead to a delay. 23 , 24 Delayed lactogenesis II is associated with neonatal weight loss >10%. 20
Occasionally, a woman does not experience lactogenesis II and only produces small volumes of milk (prevalence 5%–8%). 19 , 25 The differential diagnosis includes breast pathology, previous breast surgery (with damage to ducts or augmentation for hypoglandular breasts), developmental anomalies of the breast tissue, hormonal disruptions (such as retained placental fragments and pituitary insufficiency, including Sheehan’s syndrome, hypothyroidism, polycystic ovarian syndrome, or theca-lutein ovarian cysts), and toxins (such as excessive tobacco exposure). 26 Occasionally, strategies described here to improve milk production and transfer are not effective, and long-term supplementation with either donor milk or infant formula is medically necessary.
Milk expression is safely and effectively achieved by both manual and mechanical methods and can be used to maintain milk supply in the event of separation from the infant. 27 Hand expression also facilitates milk transfer for the infant learning to breastfeed; both latch and an effective suckling pattern are key. Among mothers of term infants who were feeding poorly, those randomly assigned to hand expression versus electric pumps were more likely to still be breastfeeding at 2 months (96.1% vs 72.7%; P = .02). 28 Infrequent or inadequate signaling due to ineffective or infrequent breastfeeding or milk expression may trigger the autocrine-paracrine mechanisms of halting milk production and dismantling the mammary gland architecture. 29 Milk removal, either via direct breastfeeding or expression, is essential for continuation of milk production.
Some women experience engorgement with lactogenesis II. There is limited evidence regarding the optimal management of engorgement. However, because severe engorgement can impede infant removal of milk, breastfeeding mothers should learn hand expression and reverse pressure softening, which is positive pressure to the central subareolar region, 30 before discharge from maternity care. 31 , 32 If a mother is unable to hand express or her infant is unable to latch, she may require a breast massage 33 and/or use of an electric breast pump.
The components of a comprehensive breastfeeding assessment are described in Table 1 . 12 , 34 It is important to note that a mother’s pumped milk volume may be an inaccurate estimate of milk transfer because transfer also depends on the infant’s capabilities. Associated risk factors for suboptimal milk transfer are listed in Table 2 .
Painful latching deserves special attention as a contributor to low supply, impaired milk transfer, and early cessation of breastfeeding. 35 In an ultrasound study in which breastfeeding mothers with nipple pain were compared with those without, nipple pain was associated with abnormal infant tongue movement, restricted nipple expansion, and lower rates of milk transfer. 36 In a retrospective audit of an Australian breastfeeding center, 36% of visits were for nipple pain. 37 A US study revealed that nipple pain and trauma were among the most frequently cited reasons for early weaning. In a study of >1600 women with singleton births, ∼10% had nipple pain that persisted at postpartum day 7; 72% was attributed to inappropriate positioning and latching, 23% to tongue-tie in the infant, and 4% to oversupply. Women who received treatment recovered within 1 to 2 weeks, and 6-week exclusive breastfeeding rates were no different from those of mothers without nipple pain. 38 Although high-quality randomized controlled trials (RCTs) are needed, frenotomy has been shown to reduce maternal nipple pain in infants with congenital ankyloglossia. 39 There is no evidence that any one topical treatment is superior 40 ; the mainstay of management for nipple pain and fissuring is assistance with positioning and latching. 41
Healthy newborns experience physiologic weight loss after birth, 42 , 43 which, in the exclusively breastfed infant, typically plateaus as the mother’s milk transitions from lactogenesis I to lactogenesis II. The addition of infant formula, either as a supplement or in the form of exclusive formula feeding, is associated with rapid weight gain. This nonphysiologic weight trajectory is associated with childhood obesity. 44 Exclusive direct breastfeeding is inversely associated with the velocity of weight gain throughout the first year of life. 45 In one prospective cohort study of >300 newborns, weight gain >100 g during the first week after birth was independently associated with overweight status at age 2 (adjusted odds ratio [aOR] 2.3; 95% confidence interval [CI] 1.1 to 4.8). 44
Early infant weight loss should be evaluated in the context of the clinical status of the infant and the mother. Nomograms for newborn weight have been developed by using data from >100 000 healthy, exclusively breastfed infants in California. 46 Individual infant weights can be plotted against these nomograms by using the Newborn Early Weight Tool (NEWT) ( https://www.newbornweight.org ). Weight loss trajectory over time, combined with clinical information, provides a robust context for evidence-based decision-making. 47 Weight loss in the >75th percentile on NEWT nomograms for mode of delivery and infant age should prompt a thorough evaluation.
A term newborn’s weight is 75% water, compared with 60% for an adult. Urine output is usually low in the first 1 to 2 days after birth, after which a physiologic diuresis and loss of up to 7% to 10% of birth weight occurs. 48 , 49 Insufficient milk production and/or transfer in the exclusively breastfed newborn can contribute to excessive weight loss in the first few days of life. Low milk supply, often exacerbated by poor feeding or difficulty in suckling, correlates with elevated milk sodium levels. 50 Exclusively breastfed infants, especially those born via cesarean delivery, are at increased risk for greater weight loss, dehydration, and hypernatremia. 51 , 52 In a systematic review of hypernatremia among breastfed infants, significant risk factors included weight loss >10%, cesarean delivery, primiparity, breast anomalies, reported breastfeeding problems, excessive prepregnancy maternal weight, delayed first breastfeeding, lack of previous breastfeeding experience, and low maternal education. 53 Prevention strategies included daily weights coupled with lactation support during the first 4 to 5 days after birth.
Early weight loss nomograms for exclusively breastfed newborns can help identify those infants at risk for hypernatremic dehydration (HD), 54 , 55 a rare condition characterized by lethargy, restlessness, hyperreflexia, spasticity, hyperthermia, and seizures, with an estimated incidence of 20 to 70 per 100 000 births and up to 223 per 100 000 births among primiparous mothers. 56 Use of charts for weight loss with SD scores specifically to detect HD, combined with a policy of weight checks on days 2, 4, and 7 of life, had high sensitivity (97%) and specificity (98.5%) to detect HD. 47 However, given the low incidence of HD, the positive predictive value (PPV) of repeated weight checks alone was only 4.4%. 56
Importantly, elimination patterns during the first 2 days of life are neither sensitive nor specific as measures of infant intake. 49 Infants may be voiding and stooling despite insufficient intake or, more commonly, have decreased voiding and stooling compared with exclusively formula-fed infants despite adequate intake. In a cohort study of 313 infants, the frequency of urination and stooling was significantly decreased among exclusively breastfed infants compared with exclusively formula-fed infants during the first 3 days of life then rose and significantly surpassed that of exclusively formula-fed infants by day 6 of life. 49 Another prospective cohort study of 280 mother-infant pairs examined elimination patterns in relation to excessive weight loss (>10%) between 72 and 96 hours after birth. 48 The strongest association with weight loss >10% was with <4 stools after 72 hours or maternal perception of delayed lactogenesis II. Although term and late-preterm infants generally pass meconium within 48 hours (76%–83% in a study of 198 infants), delayed passage of meconium can be a marker for insufficient milk intake. 57 Correlations between infants’ intake and elimination are more reliable after the first 3 days (lactogenesis II).
To prepare for transitional energy needs, the third-trimester fetus stores glycogen, manufactures catecholamines, and deposits brown fat. Healthy newborns use these stores to maintain thermoregulation and meet their energy needs through metabolism of brown fat and the release of counterregulatory hormones such as glucagon, epinephrine, cortisol, and growth hormone. Combined with declining insulin secretion, these hormones mobilize glucose and alternative fuels, such as lactate and ketone bodies, to support organ functions. 58 , 59
Because oral intake is not the main energy source for healthy term neonates in the first days after birth, physiologic volumes of colostrum (16 kcal/oz) are sufficient to meet metabolic demands. As glycogen stores are depleted, coinciding with the transition from colostrum to mature milk, newborns transition from a catabolic state to reliance on enteral feeds, with approximately half of the caloric content derived from fat. 60
After placental detachment, neonatal glucose levels reach a physiologic nadir in the first hours after birth and then typically rise to adult levels a few days later. The threshold for neonatal glucose that is associated with neurotoxicity is unclear; a 2008 National Institutes of Health workshop concluded that “there is no evidence-based study to identify any specific plasma glucose concentration (or range of glucose values) to define pathologic hypoglycemia.” 61 In one cohort study, treatment of asymptomatic newborn hypoglycemia to maintain blood glucose levels >47 mg/dL had no effect on cognitive performance at 2 years; however, at 4.5 years, there were dose-dependent concerns regarding visual motor and executive function, with the highest risk in children exposed to severe (<36 mg/dL),and recurrent (≥3 episodes) hypoglycemia. 62 , 63
In the first hours after birth, healthy term neonates compensate for relatively low glucose levels by decreasing insulin production and increasing glycolysis, gluconeogenesis, and ketone production. Among at-risk newborns, early skin-to-skin care plus early feeding and blood glucose assessment at 90 minutes supports glucose homeostasis and is associated with decreased risk of hypoglycemia and NICU admission. 64 In a Cochrane review, early skin-to-skin contact increased glucose levels by 10.49 (95% CI 8.39 to 12.59) mg/dL or 0.6 (0.5 to 0.7) mmol/L. 65 Conversely, practices that separate the mother and infant and delay the first feeding increase hypoglycemia risk.
Glucose monitoring is recommended for infants with risk factors ( Table 3 ) and for any infant who exhibits symptoms of hypoglycemia. 66 Because operational thresholds for treating hypoglycemia and target glucose levels are not defined, clinical recommendations vary. Infants who require early or more frequent feedings should be supported to breastfeed and/or receive expressed milk. Authors of multiple studies confirm the benefits of using glucose gel rather than formula as an initial treatment of low glucose levels, and this practice has become increasingly commonplace. 67 – 73 Some institutions use pasteurized donor human milk (PDHM) as a treatment of hypoglycemia; however, there are, as yet, no published studies describing outcomes of this practice. The option of antenatal milk expression for lower-risk women with preexisting or gestational diabetes may also be considered because this technique may preserve exclusive breastfeeding without adversely affecting perinatal outcomes. 74 Infants requiring intravenous glucose should breastfeed, when able, during the therapy.
Persistent or late-onset hypoglycemia (>48 hours after birth) can occur in the setting of congenital endocrine disorders or, more commonly, perinatal stress due to birth asphyxia, intrauterine growth restriction, maternal preeclampsia, 75 or persistent problems establishing breastfeeding. 76 Infants with these risk factors may be more vulnerable to insufficient feeding, so skilled assessment is essential.
Management of hyperbilirubinemia in the exclusively breastfed newborn depends on whether the excess in bilirubin is pathologic or physiologic. Neonatal bilirubin levels rise after birth because of physiologic immaturity of glucuronyl transferase, which is exaggerated with each decreasing week of gestational age. Exclusively breastfed infants have higher serum bilirubin levels than formula-fed infants, possibly because of differences in fluid intake and bilirubin excretion and increased enterohepatic resorption of bilirubin. 77 Some individuals may also have a genetic predisposition to higher bilirubin levels. 78 , 79 Bilirubin is an antioxidant, and it has been hypothesized that moderate increases in bilirubin levels may be protective for the transition to extrauterine life. 77 , 80
In contrast, pathologic hyperbilirubinemia resulting from insufficient breastfeeding, sometimes referred to as breastfeeding jaundice, is better defined as suboptimal intake jaundice. 77 In the United States and Canada, it is recommended that all neonates undergo bilirubin risk screening at least once before hospital discharge. 81 The Academy of Breastfeeding Medicine and the AAP advise the use of Bhutani curves to assess risk and need for treatment of hyperbilirubinemia; clinical tools are available on mobile device applications. 77 , 81 , 82 This approach has led to a decrease in severe pathologic hyperbilirubinemia 83 ; however, concerns for overtreatment and the potential harm of phototherapy have arisen recently. 84 Using subthreshold bilirubin levels to initiate phototherapy as a mechanism to prevent readmission is not recommended because this approach increases length of stay and results in many infants receiving unnecessary treatment to reduce each case of readmission. 85
Breastfed infants with hyperbilirubinemia require assessment of milk production and transfer, feeding frequency, and neonatal weight loss. 86 – 91 If there is pathologic hyperbilirubinemia, and infant intake at the breast is sufficient, exclusive breastfeeding should be continued while the infant receives phototherapy. Although supplementation with infant formula may decrease the bilirubin level and risk of readmission for phototherapy, 85 it will also interfere with the establishment and continuation of breastfeeding. 92 If intake at the breast is insufficient and supplementation is medically necessary, expressed maternal milk is preferred. Despite the current lack of data on its benefits in reducing hyperbilirubinemia in term infants, the use of PDHM to preserve exclusive human-milk feeding is increasing. 93
Phototherapy for neonatal jaundice and concerns about insufficient milk can be anxiety provoking for parents, even in a supportive environment, and can be disruptive to successful breastfeeding. 94 Practices to minimize mother-infant separation, including providing phototherapy in the same room and maintaining safe skin-to-skin care with the infant’s mother, also promote exclusive breastfeeding. 95
Early colostrum and exclusive breastfeeding establish an optimal and intact immune system. Unlike infant formula, human milk has a dynamic composition of both macro- and micronutrients that varies within a feed, diurnally, and over the course of lactation. Protective proteins abound in human milk, including lactoferrin, secretory immunoglobulin A, transforming growth factor-β, and α-lactalbumin. These factors promote development of the infant’s immune system. 96 Additionally, lactoferrin has unique antibacterial properties important in the prevention of sepsis. Unique nonnutritive oligosaccharides that are specific to the mother-infant pair’s shared environment and exposures prevent binding of pathogenic bacteria and promote a healthy microbiome in the gut. 97 Differences in immune cell distributions based on neonatal diet can be detected through 6 months of age, with natural killer cells most significantly affected. 98
During vaginal birth, the newborn’s intestine and mucosal surfaces are colonized with maternal microbes that act synergistically with bioactive factors in mother’s milk to establish a robust lymphoid follicle replete with a healthy balance of T helper cells. 99 , 100 Surgical delivery is associated with aberrant colonization, which may lead to differences in the mother’s milk microbiome 101 only partially restored by vaginal secretions. 102 Formula supplementation may effect the most change in the newborn’s microbiome 103 , 104 and immune development. These basic science findings are supported by clinical studies.
Given the multiple mechanisms through which exclusive human milk impacts gut development, formula supplementation should always be avoided when the mother’s own milk is available. Although an exploratory study of early limited supplementation with extensively hydrolyzed formula followed by a return to exclusive breastfeeding did not reveal differences in the developing microbiome ( N = 15), 105 a longitudinal study among infants exclusively breastfeeding at 3 months ( N = 579) revealed alterations in the microbiome among infants exposed to formula as neonates ( n = 179). 106 Just as antimicrobial stewardship requires appropriate use of antibiotics, 107 supplementation stewardship requires judicious use of formula when medically indicated.
A systematic review of healthy, term, breastfed newborns revealed no benefit from routine supplementation with foods or fluids in the early postpartum period. 108 These findings are consistent with consensus recommendations for exclusive breastfeeding for the first 6 months, followed by continued breastfeeding with the addition of complementary foods until at least 12 months of age. 2 , 109 – 111 Early introduction of supplemental formula is associated with a greater than twofold increase in risk of early cessation of breastfeeding even when controlling for confounding variables. 112 – 114 Among almost 1500 women in the Infant Feeding Practices Study II, only early exclusive breastfeeding remained significant for achieving intended breastfeeding duration (aOR 2.3; 95% CI 1.8 to 3.1) after adjustment for relevant hospital practices. 113 This finding may be due in part to the supply and demand nature of milk production and the role of suckling, oxytocin release, and milk removal in establishing lactation.
If supplemental feeds are medically indicated, they should be accompanied by manual or mechanical milk expression, recognizing that direct breastfeeding usually provides more complete milk removal. 115 In a pilot RCT ( N = 40), early limited formula supplementation for infants with ≥5% weight loss increased exclusive breastfeeding at 3 months post partum. 116 In a subsequent larger study ( N = 164), early limited supplementation did not affect overall breastfeeding at 1 or 6 months but slightly increased rates of formula use at 1 month (36.7% vs 22.4%; P = .08), 105 decreased breastfeeding at 12 months (30% vs 48%; risk difference −18% [CI −34% to −3%]), and shortened the time to breastfeeding cessation (hazard ratio 0.65; 95% CI 0.43 to 0.97). 117
Because evidence continues to accrue that supplementation in the first days after birth has major health risks, 103 , 106 judicious use of supplementation is a critical goal, with a return to exclusivity whenever possible. If supplementation is indicated ( Fig 1 ), options in order of preference are (1) expressed milk from the infant’s own mother, 4 (2) PDHM, and (3) commercial infant formulas. The potential risks and benefits of these options should be considered in the context of the infant’s age, the volume required, and the impact on the establishment of breastfeeding. 4
Methods of supplemental feeding include spoon or cup feeds, supplemental nursing systems, syringe feeds, and paced bottle feeds. Methods should be tailored to staff training and family preferences. 7 Among late-preterm newborns, there is evidence that some may be more susceptible to feeding problems when supplemented via a bottle; in an RCT in which the 2 methods were compared, cup feeding was associated with a longer duration of exclusive breastfeeding compared with bottle-feeding. 118 Among term newborns, the manner in which supplementation is delivered, whether a bottle or alternative devices, has no apparent impact on continuation of breastfeeding. 119 If the supplement is the mother’s own expressed milk, avoidance of bottles and nipples may preserve a longer duration of breastfeeding, especially among late-preterm newborns. 120
To ensure milk removal, which is key to establishing a milk supply, a mother should be assisted to express milk each time her infant is supplemented, even if the infant is also “practicing” at the breast. 4 “Hands on” pumping, combining breast massage with pumping, has been shown to increase milk production in mothers of preterm infants who are hospitalized. 121
Physiologic early infant feeding is facilitated by keeping mothers close to their infants, beginning with skin-to-skin care immediately after birth and continuing with 24-hour rooming-in and feeding on cue. These are core practices of the recently updated World Health Organization’s Ten Steps to Successful Breastfeeding of the Baby-Friendly Hospital Initiative (BFHI). 7 Feeding on cue or “responsive feeding” is associated with more frequent breastfeeding throughout the day, more exclusive breastfeeding up to 6 months and beyond, 122 – 124 and decreased likelihood of abnormal rapid weight gain in infancy. 125
Several major health organizations, including the US Preventive Services Task Force and the Agency for Healthcare Research and Quality, have generated systematic reviews and quality improvement (QI) reports that demonstrate the positive impact of the BFHI on breastfeeding outcomes. 10 , 13 , 14 Implementation of maternity care practices aligned with any component of the BFHI is associated with improved in-hospital and postdischarge breastfeeding rates. 11 , 13 , 126 Best Fed Beginnings increased exclusive breastfeeding initiation from 39% to 61% ( t = 9.72; P < .001) at 89 hospitals over 2 years. 127 The Community and Hospitals Advancing Maternity Care Practices initiative reported that the BFHI helped to reduce racial disparities in breastfeeding in southern US states. 128
Since the initial implementation of the BFHI, safety concerns have emerged, including case reports of inadvertent bed-sharing, suffocation, falls, and increased risk of neonatal jaundice. 3 , 129 In this context, the World Health Organization conducted an extensive evidence-based review. 7 , 130 Key differences in the revised Ten Steps include highlighting the Code of Marketing of Breastmilk Substitutes, the need to collect ongoing data, a focus on safety and surveillance (especially as it relates to skin-to-skin care and rooming-in), and acknowledgment that there is insufficient evidence to limit pacifiers and other artificial nipples.
Step 10 of the BFHI requires a direct connection between the delivery hospital and the community for ongoing support. Referral for outpatient support as well as provision of contact information for those who can manage breastfeeding problems is paramount.
Given the importance of exclusive breastfeeding for maternal and child health, both intent and initiation are increasing. However, maternal conditions linked with delayed lactogenesis, such as advanced maternal age, obesity, and fertility treatment, are increasingly common. Priority research areas to help families meet their breastfeeding goals include accurate identification of women with risk factors for delay or absence of lactogenesis, more sensitive methods of identifying at-risk newborns, and exploration of the implications of early limited formula supplementation on infant outcomes such as ontogeny of the immune system and the microbiome, maternal self-efficacy, and continued breastfeeding.
Health care professionals’ support is critical for families to meet their infant feeding goals and achieve optimal health outcomes. All physicians who care for new mothers and infants need skills to evaluate early breastfeeding, perform maternal and infant risk stratification, understand the range of potential interventions in the context of the risk/benefit ratio of supplementation, and ensure appropriate follow-up.
Most mothers can produce adequate colostrum and mature milk, and most newborns are able to breastfeed exclusively. Nevertheless, conditions that require medical supplementation are common and important to recognize. The decision to supplement with infant formula requires thoughtful analysis of the risks and benefits, with consideration of the family’s informed choice. Early-term and late-preterm newborns are at a higher risk of complications. Therefore, more careful monitoring, detailed assessments, and case-based interventions are warranted. Further research is needed to identify the best methods to support exclusive breastfeeding in high-risk populations.
We thank Delali Lougou for organizing the articles used in this article to provide the original framework for the authors’ review.
Drs Feldman-Winter, Kellams, and Stuebe conceptualized and designed the review of the literature, conducted the literature review and analysis, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Peter-Wohl made substantial contributions to the acquisition of data and to the analysis and interpretation of data, drafted the article, and revised it critically for important intellectual content; Dr Taylor made substantial contributions to conception and design and made critical revisions; Drs Lee and Terrell made substantial contributions to the design and to the acquisition of data and made critical revisions for important intellectual content; Drs Meek and Noble and Ms Maynor made substantial contributions to the conception, design, and analysis and interpretation of data and revised the article critically for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: No external funding.
American Academy of Pediatrics
adjusted odds ratio
Baby-Friendly Hospital Initiative
confidence interval
hypernatremic dehydration
Newborn Early Weight Tool
pasteurized donor human milk
positive predictive value
quality improvement
randomized controlled trial
Competing Interests
Supplementary data.
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Open access
- Published: 14 September 2022
Effectiveness of early essential newborn care on breastfeeding and maternal outcomes: a nonrandomized controlled study
- Chuanya Huang 1 , 2 na1 ,
- Lei Hu 1 , 2 na1 ,
- Yonghong Wang 2 , 3 &
- Biru Luo 2 , 3
BMC Pregnancy and Childbirth volume 22 , Article number: 707 ( 2022 ) Cite this article
7470 Accesses
7 Citations
Metrics details
Breastfeeding and maternal health play crucial roles in improving newborn health, which is closely related to the development of families and society. Early essential newborn care, which emphasizes early exclusive breastfeeding and skin-to-skin contact, is recommended by the World Health Organization. This study aimed to explore the association of early essential newborn care with breastfeeding and maternal outcomes.
A nonrandomized controlled study was carried out from May 2020 to January 2021 in a tertiary hospital in Chengdu city, China. Pregnant women were recruited from the maternity ward before they gave birth. Early essential newborn care was performed for 91 mother-newborn pairs after birth in the intervention group, while routine birth care was performed for 91 mother-newborn pairs in the control group. Data on breastfeeding and maternal outcomes were collected pre-test and post-test and were recorded by trained data collectors and retrieved from hospital case record files.
Compared with the control group, the intervention group had a higher incidence of early breastfeeding initiation, an earlier initiation and longer duration for the first breastfeeding, a higher incidence of successful first breastfeeding, more exclusive breastfeeding at hospital discharge, higher maternal breastfeeding self-efficacy, a shorter duration of the third stage of labour, lower postpartum blood loss, and lower scores of maternal pain and anxiety postpartum; the differences were statistically significant ( p < 0.05).
The implementation of high-quality early essential newborn care can help mothers initiate early breastfeeding, improve exclusive breastfeeding rates at hospital discharge, enhance breastfeeding self-efficacy, promote the woman’s recovery from labour, and reduce maternal anxiety and pain in the postpartum period. High-quality early essential newborn care is recommended to policymakers and medical professionals to improve breastfeeding and maternal outcomes.
Trial registration
Chinese Clinical Trial Registry, Retrospective Registration (27/7/2021), registration number: ChiCTR2100049231.
Peer Review reports
Breastfeeding is the ideal method for infant feeding. It is estimated that if the breastfeeding rate were to increase to 50% worldwide, the deaths of approximately 823,000 under-five children can be avoided every year [ 1 ]. Early postnatal breastfeeding behaviour is associated with long-term breastfeeding [ 2 ]. To improve the breastfeeding rate, the World Health Organization (WHO) has recommended skin-to-skin contact between mothers and newborn infants immediately after birth and breastfeeding during the first hour after birth [ 3 ]. Studies have shown that breastfeeding within the first hour after birth can improve exclusive breastfeeding rates at 6 weeks, 10 weeks, and 6 months postpartum [ 4 , 5 , 6 ] and that mothers who breastfeed early have a higher acceptance of exclusive breastfeeding [ 7 ]. Compared with newborn infants who initiated breastfeeding at 2–23 h and 24–96 h after birth, newborn infants who initiated breastfeeding within the first hour after birth had lower neonatal mortality [ 8 ].
Previous studies indicated that many medical professionals, especially in the West Pacific region, often implemented outdated and harmful practices during and after birth, such as unnecessary suctioning, delayed early skin-to-skin contact between the mother and the newborn infant, as well as umbilical cord cutting immediately after birth [ 9 ]. These outdated practices lead to an increase in the risk of neonatal morbidity and mortality [ 10 ]. To improve the quality of newborn care, the Action Plan for Healthy Newborn Infants in the Western Pacific Region (2014–2020) was issued by the WHO Western Pacific Regional Office (WHO/WPRO) [ 11 ]. This plan aimed to give every newborn a healthy start and implement early essential newborn care (EENC) for all newborn infants. EENC contains evidence-based interventions that are simple, that are low-cost and that do not require expensive technologies. The central element of EENC is immediate skin-to-skin contact between the mother and newborn infant after birth for at least 90 min and initiation of exclusive breastfeeding when cues occur (such as drooling, tonguing, rooting, and hand biting). Additionally, midwives should appropriately delay clamping and cutting of the cord and other routine care. These practices can ensure that most newborn infants complete the first breastfeeding during the period of skin-to-skin contact and improve the early breastfeeding initiation rate, as well as strengthen the rooting reflex of the newborn infant [ 12 ]. Furthermore, implementing EENC may also have positive effects on mothers because skin-to-skin contact between mothers and newborn infants can reduce maternal pain, depression and anxiety, accelerate placental detachment, reduce postpartum haemorrhage, and promote uterine involution by promoting the secretion of oxytocin [ 13 ].
EENC was introduced to China in 2016 and had been implemented in 112 medical institutions by 2017 [ 14 ]. Yang et al. surveyed the medical institutions of four provinces that implemented EENC in China and showed that only 36.2% of the newborn infants had skin-to-skin contact with their mothers, the rate of the duration of skin-to-skin contact over 90 min was 19.7%, and the breastfeeding rate and exclusive breastfeeding rate before discharge were 76.5% and 32.2%, respectively [ 15 ]. The findings of the study by Yang et al. indicated that EENC was not fully implemented in line with the WHO guidelines in these medical institutions. Xu et al. pointed out that there were many obstacles to implementing EENC in China hospital policies, including insufficient awareness of medical professionals, shortage of human resources, and little clinical evidence about EENC in China [ 16 ]. Previous studies have explored the benefits of skin-to-skin contact and timed clamping for newborn infants separately [ 13 , 17 ]. However, the EENC is an intervention package; thus, the effect of EENC should be regarded as a general effect on mothers and newborn infants. In addition, most published studies have focused on the effect of implementing EENC on improving newborn outcomes, while few studies have explored the benefits of EENC for breastfeeding and maternal outcomes. This study aimed to fill this research gap, explore the effect of implementing high-quality EENC on breastfeeding and maternal outcomes, and provide more clinical evidence for improving the health of newborn infants and mothers in the West Pacific Region.
The definitions of certain terminology used in this paper are as follows: early breastfeeding initiation, defined as the initiation of first breastfeeding within the first hour after birth; successful first breastfeeding, defined as the score of first breastfeeding assessed by the 4-item Infant Breast Feeding Assessment Tool (IBFAT) [ 18 ] is between 10 and 12; exclusive breastfeeding, defined as only breast milk given to the newborn infant without any liquid or solid food; mixed feeding, defined as breastfeeding combined with artificial feeding of the newborn infant; and artificial feeding, defined as feeding newborn infants with foods other than breast milk, such as formula milk.
Study design and setting
This study was a nonrandomized controlled study and was carried out from May 2020 to January 2021 in a tertiary hospital in Chengdu city, Sichuan Province, China. This hospital is one of the largest women and children’s hospitals in Sichuan Province and has two labour wards with identical health facilities and similar human resources in different hospital areas. These two wards had not implemented EENC or received any EENC coaching before this study, and they were assigned randomly to be the intervention group and control group. Each pregnant woman chose the labour ward in which she preferred to give birth at her antenatal visit in the hospital, and her selection depended entirely on her preferences. However, we began participant recruitment when the woman was awaiting delivery in the maternity ward; thus, the participants were not assigned to each group randomly.
The current study was a part of a larger trial. Because of the limitations to the length of an article, this paper focuses only on breastfeeding and maternal outcomes.
Participants
Participants in this study comprised women and their newborn infants. Pregnant women were recruited from the maternity ward when they were admitted to hospitals for await delivery and with no signs of labour. Pregnant women who met the following inclusion criteria were considered eligible and were invited by the researchers to participate in this study: (1) aged over 18 years, (2) gestational age between 37 and 42 weeks, (3) singleton pregnancy, (4) vaginal delivery, (5) no severe pregnancy complications and/or underlying disease, and (6) no medical indications against breastfeeding. If the woman was transferred from vaginal delivery to caesarean section or the newborn infant had an abnormal birthweight (< 2500 g or > 4000 g), deformities or needed to be transferred to the neonatal intensive care unit (NICU) immediately after birth, the mother and infant were excluded from the study. Written informed consent was obtained from all participants. Ethical approval was received from the hospital ethics review board.
Interventions
Participants in the intervention group received the EENC interventions after birth from midwives in the intervention group, while participants in the control group received routine birth care from midwives in the control group. These interventions delivered in the delivery room. The midwives in the intervention group received 5-month training sessions from national and provincial facilitators, following the guidelines formulated by the WHO [ 19 ]. After 5-month training sessions, a pilot study on 18 mother-newborn pairs was conducted in October 2020 to ensure that every midwife could implement the EENC correctly. The formal interventions were performed from November 2020 to January 2021.
EENC interventions include (1) drying the newborn infant immediately and thoroughly within five seconds after birth, (2) immediate skin-to-skin contact within the first minute and lasting for at least 90 min, (3) exclusive breastfeeding, (4) appropriately timed clamping and cutting of the cord, and (5) other routine care – eye care, vitamin K, immunizations, weighing and examinations [ 11 ]. The duration of implementing EENC was between 90 to 120 min.
The sequence of routine birth care in this hospital was (1) drying of the newborn infant, (2) placement of the newborn infant on a heated table to keep warm for 20 min, during which the umbilical cord is clamped and the weight and length are measured, (3) vaccination, (4) skin-to-skin contact between the mother and newborn infant, and (5) exclusive breastfeeding after the third stage of labour. The duration of implementing routine birth care was between 90 to 120 min.
For both groups, the same postnatal care and education were delivered to mothers by midwives, including the contents of breastfeeding, diet, physical activity, safety, urine output, and stool output.
This study aimed to explore the effect of implementing EENC on breastfeeding and maternal outcomes. We hypothesized that implementing EENC could improve the breastfeeding outcomes and help mothers recover from delivery, especially for the incidence of early breastfeeding initiation.
Measures and data collection
Variables collected at baseline for women included age, educational level, height, weight, gestational age, previous obstetric history, anxiety, and nipple pattern. Variables for newborn infants included sex, length, and birthweight. Among these variables, the anxiety of women was assessed by the Chinese version of the strait form of the State-Trait Anxiety Inventory (STAI-S), which was developed by Spielberger in 1970 and was introduced to China in 1988 [ 20 ]. The STAI-S has 20 self-report items and items are scored on a four-point Likert scale of 1 (not at all) to 4 (severe), with the scores summated to derive a total score ranging from 20 to 40 points. The Cronbach’s α of the Chinese version of STAI-S was 0.91. Higher STAI-S scores indicate severer anxiety. In addition, the nipple pattern was classified into three types, namely, normal, flat, and inverted patterns, and assessed by two female data collectors.
The primary outcome of the current study was the incidence of early breastfeeding initiation. If the first breastfeeding was initiated successfully within the first hour after birth, the early breastfeeding initiation was considered and would be recorded by the data collectors.
The second outcome of this study consisted of some breastfeeding-related outcomes and maternal outcomes; namely, the time of rooting reflex occurrence, the initiation time and duration of first breastfeeding, the number of successful first breastfeeding, the time when formula milk is first served, the total amount of formula milk given before discharge, the number of breastfeeding within the first day after birth, the feeding pattern before discharge, the duration of the third stage of labour, the postpartum blood loss within 2 h after birth, and the pain and anxiety of the woman after birth. Data on the duration of the third stage of labour and the postpartum blood loss within 2 h after birth were retrieved from hospital case record files. The woman’s pain was evaluated by means of the Visual Analogue Scale (VAS) [ 21 ] at 30 min, 60 min, and 120 min after birth. Anxiety was evaluated by the state form of the State-Trait Anxiety Inventory (STAI-S) [ 22 ] at 120 min after birth. Other variables were recorded by data collectors. Additionally, the 4-item Infant Breast Feeding Assessment Tool (IBFAT) [ 18 ] was used to assess the success of the first breastfeeding by data collectors. The total score of IBFAT ranges from 0 to 12, with 10–12 being the scores for vigorous and effective breastfeeding. The Breastfeeding Self-efficacy Scale Short Form (BSES-SF) [ 23 ] was used to assess the confidence of women to breastfeed before discharge from the hospital, with a higher BSES-SE score indicating stronger breastfeeding self-efficacy.
The data collectors were all women with medical educational background. Before the study, data collectors received the methods for collecting data by researchers. They were permitted to enter the ward to collect data by both the participants and the ethnic committee of hospitals.
Sample size
PASS version 15.0 was used to calculate the sample size. We estimated the sample size based on the primary outcome of this study, which is the incidence of early breastfeeding initiation. The results of the pilot study showed that the incidence of early breastfeeding initiation were 77.8% and 44.4% in the intervention group and the control group, respectively. Hence, a sample size of 100 participants would be required ( α = 0.05, β = 0.1) [ 10 ]. Considering that the drop-out rate was 10%, the minimum sample size needed was 110 participants, with 55 participants in each group. To reduce sampling error [ 24 ], we include all pregnant women who met the inclusion criteria in the study during the recruitment phase.
The current study was a single-blinded trial. It was impossible to blind the midwives and data collectors in the delivery rooms because midwives were responsible for implementing EENC or routine birth care and data collectors were responsible for assessing and recording. Hence, only participants were blinded.
Statistical methods
SPSS version 25.0 was used to analyse the data. The smallest unit that is being analyzed to assess intervention effects was the group. The mean ± standard deviation (SD) and median (interquartile range, IQR) were used to describe continuous data, and t test and Mann–Whitney U test were used to identify the differences. The number (n) and percentage (%) were used to describe categorical data, and the chi-square test and Fisher’s exact test were used to identify differences.
Baseline information of participants
In total, 203 pregnant women were recruited for this study from November 2020 to January 2021, with 102 included in the intervention group and 101 in the control group. Figure 1 shows the flow of participants through each stage of the study. Ultimately, there were 91 mother-newborn pairs in the intervention group and 91 mother-newborn pairs in the control group. Table 1 shows the basic information of all participants. There were no significant differences between the two groups regarding the baseline information.
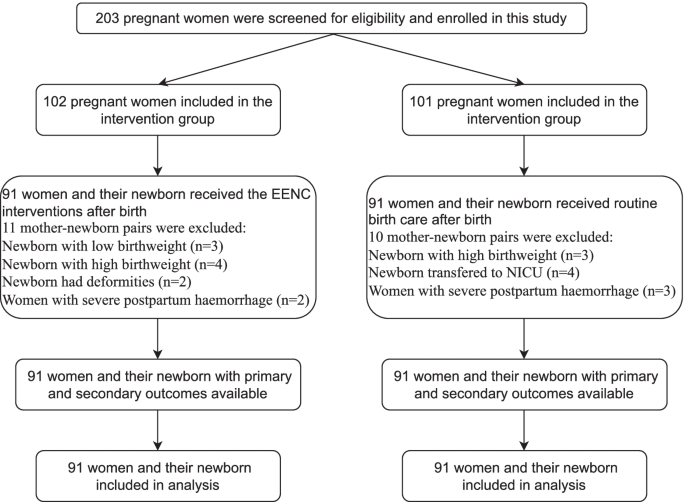
Flow of participants through each stage of the study
Breastfeeding within 2 h after birth in the two groups
The incidence of early breastfeeding initiation in the intervention group was higher than that in the control group ( n = 69 vs. n = 39, p < 0.001). The first breastfeeding in the intervention group started earlier (48.02 ± 16.30 min vs. 66.97 ± 35.41 min, p < 0.001) and lasted longer (34.98 ± 15.02 min vs. 22.30 ± 11.70 min, p < 0.001) than that in the control group. Additionally, the mean IBFAT scores of the first breastfeeding were higher (10.05 ± 2.17 vs. 8.68 ± 2.04, p < 0.001). Furthermore, more successful first breastfeeding ( n = 83 vs. n = 68, p = 0.003) were observed in the intervention group. However, there was no significant difference in the time of rooting reflex occurrence. (Table 2 ).
Breastfeeding before discharge in the two groups
The median time at which the formula milk was first served in the intervention group was later than that in the control group (4 h vs. 2 h, p < 0.001), and the median amount of formula milk given to babies before discharge was higher in the control group than in the intervention group (70 ml vs. 90 ml, p < 0.001). The number of breastfeeding within 24 h after birth in the intervention group was greater than that in the control group ( n = 7 vs. n = 5, p < 0.001). Regarding the feeding pattern, the number of exclusive breastfeeding in the intervention group was greater than that in the control group ( n = 67 vs. n = 40), with less mixed breastfeeding ( n = 24 vs. n = 47) and artificial breastfeeding ( n = 0 vs. n = 4). The women in the intervention group had higher breastfeeding self-efficacy assessed by the BSES-SF (55.78 ± 8.96 vs. 46.74 ± 10.08, p = 0.024). (Table 3 ).
Duration of third stage of labour, postpartum blood loss, pain and anxiety of women
Compared to those in the control group, the duration of the third stage of labour was shorter (5.25 ± 5.66 min vs. 6.10 ± 2.92 min, p < 0.001), and the amount of postpartum blood loss within 2 h after birth was lower (234.64 ± 63.65 ml vs. 281.37 ± 72.29 ml, p < 0.001) in the intervention group. The mean VAS (at 30 min, 1 h, and 2 h) and STAI-S scores in the control group were higher than those in the intervention group, which indicated that pain and anxiety were more severe in the control group (Table 4 ).
This study compared the effect of EENC and routine birth care on breastfeeding and maternal outcomes in a tertiary hospital in China. The results showed that EENC can improve the early breastfeeding initiation, establish correct breastfeeding behaviour, increase the self-efficacy in breastfeeding among mothers and help them recover from childbirth.
Although there were more primiparous women in the intervention group, our results showed that the breastfeeding outcomes in the intervention group were better than that in the control group. Some studies showed that women who have breastfed previously have better breastfeeding outcomes than primiparous women [ 25 , 26 ]. However, the study by Anette et al. showed that parity cannot affect the duration of exclusive breastfeeding or any breastfeeding, but early first breastfeeding can lead to a positive impact [ 27 ]. Similarly, previous studies also pointed out that although inverted or flat nipples would hinder breastfeeding [ 28 ], if the babies can be breastfed early, they are more likely to attach and can be fed well in the postnatal period. In this study, although more women with inverted and flat nipples were in the intervention group, the breastfeeding outcomes were still better than that in the control group. For primiparous women and women with flatted or inverted nipples, EENC may therefore also be recommended as it can improve breastfeeding outcomes.
The findings of this study indicated that the intervention group had a higher incidence of early breastfeeding initiation, earlier initiation and longer duration of first breastfeeding, and a higher IBFAT score for first breastfeeding. Similar findings have been reported in studies by Aiping G et al. and Min et al. [ 12 , 29 ]. Early breastfeeding is an important factor for constructing correct breastfeeding behaviour. The WHO proposed Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services in 2017 [ 30 ], which emphasized that medical institutions should provide all feasible support to help women initiate early breastfeeding. Previous studies also showed that women who initiated breastfeeding within the first hour after birth had a higher acceptance of breastfeeding, which is especially important for improving the exclusive breastfeeding rates up to 6 months postpartum [ 5 , 6 ]. EENC interventions contain a long duration of skin-to-skin contact, which is a key factor in ensuring the success of early breastfeeding. The study by Mahmood et al. showed that newborn infants with successful skin-to-skin contact can initiate first breastfeeding 62 min earlier than newborn infants with routine birth care, and the success rate of first breastfeeding increased by 26.3% [ 31 ]. In addition, EENC recommends that midwives assist women in initiating first breastfeeding when the newborn infants experience a rooting reflex and active breast-seeking action, which is in line with newborn infants’ instincts and can avoid excessive intervention in breastfeeding. Therefore, implementing EENC could increase the rate of early breastfeeding initiation and successful first breastfeeding.
In the current study, the rates of exclusive breastfeeding and the breastfeeding self-efficacy of women at hospital discharge in the intervention group were higher than those in the control group, which were impacted mainly by the early skin-to-skin contact between mothers and newborn infants and successful first breastfeeding. The study by Almqvist et al. showed that the issues of breastfeeding encountered by women in the early postpartum period were the main reason they gave up exclusive breastfeeding [ 32 ]. Success in the first breastfeeding means that the issues in the process of breastfeeding will be partly solved with the help of health professionals. Therefore, the women in the intervention group could gain confidence and skills from the experience of success in the first breastfeeding, which would in turn motivate them to perform exclusive breastfeeding [ 33 ]. The WHO recommends that unless there are medical indications, the staff of medical institutions should dissuade women and their families from providing any food other than breast milk to their infants. However, in the clinical practice setting, the phenomenon of mothers or family members feeding infants with formula milk or other food is unavoidable even though breast milk is sufficient because midwives and nurses cannot help every woman solve the problems encountered in breastfeeding due to the demands of their work. The study by Raghavan et al. showed that formula milk given to babies on the first day emerged as the only independent predictor of failure to continue exclusive breastfeeding at 6 weeks after birth (OR 2.96; 95% CI 1.09–8.06) [ 5 ]. In this study, newborn infants in the intervention group were given formula milk for the first time approximately 2 h later than those in the control group, and the total amount of formula milk added before discharge was also lower, which indicated that the construction of correct breastfeeding behaviour within the first hour after birth can reduce the use of unnecessary formula milk to some extent. Additionally, babies in the intervention group had more breastfeeding times within 24 h postpartum on the first day postpartum than those in the control group, indicating that the implementation of EENC can help women breastfeed correctly and have higher breastfeeding self-efficacy, which is conducive to the growth and development of newborn infants [ 34 ].
Our findings also showed that the EENC can help women recover from labour. The women in the intervention group had a shorter duration of the third stage of labour and lower postpartum blood loss, which is in line with the study by Yuan et al. [ 35 ]. During skin-to-skin contact, sucking from newborn infants can stimulate the nerve endings of the maternal nipple and then promote the synthesis and secretion of oxytocin [ 36 ]. Oxytocin can stimulate uterine contraction directly, reduce the interference of oxidative stress on uterine contraction, and finally reduce postpartum blood loss [ 37 , 38 ]. In addition, placing the newborn infant on the mother’s breast and abdomen plays a similar role to massage, which can also promote the contraction of the uterus [ 13 ]. Furthermore, lower levels of postnatal anxiety and pain among mothers were observed in the intervention group, which may be related to the secretion of oxytocin and the joy of successful breastfeeding. Previous studies indicated that oxytocin can increase the threshold of maternal pain perception [ 39 ] and alleviate maternal anxiety [ 40 , 41 ].
This study systematically explored the effects of EENC on breastfeeding and maternal outcomes and provided more evidence for the implementation of EENC in the future. However, this study also has some shortcomings. First, the design of this study is quasi-experimental. Due to hospital policies and funding limits, the participants could not be randomly assigned to two groups. However, because the intervention and control measures are implemented in two wards of the same hospital, which have similar human resources and facilities and are far away from each other, contamination and bias were excluded as much as possible. Second, the results of pain and anxiety were self-reported variables, so self-report bias cannot be avoided. Third, follow-up in this study lasted until the mother was discharged from the hospital, so a longer-term follow-up study to clarify the long-term effect can be considered in the future. Last, although the sample size had been previously calculated, this study was conducted only in a tertiary hospital, so the generalization of the results is limited. Large-sample and multicentre randomized controlled trials are necessary to further clarify the effect of EENC.
The implementation of EENC is associated with better breastfeeding and maternal outcomes, which can not only improve the early initiation of breastfeeding and exclusive breastfeeding rate but also relieve the anxiety and pain of the mother and increase her confidence in breastfeeding at hospital discharge. Hence, it is strongly recommended that policymakers and medical professionals implement EENC in clinical practice to improve the outcomes of both women and infants.
Availability of data and materials
All raw data generated or analyzed during this study are available from the corresponding author upon reasonable request.
Abbreviations
Early Essential Newborn Care
Inter Quartile Range
World Health Organization
Standard deviation
Neonatal intensive care unit
Western Pacific Regional Office
Confidence interval
Infant Breast Feeding Assessment Tool
Breastfeeding Self-efficacy Scale Short Form
Visual Analogue Scale
The state form of State-Trait Anxiety Inventory
Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017):475–90.
Article Google Scholar
Kronborg H, Vaeth M, Olsen J, Iversen L, Harder I. Effect of early postnatal breastfeeding support: a cluster-randomized community based trial. Acta Paediatr. 2007;96(7):1064–70.
Article CAS Google Scholar
World Health Organization: Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised baby-friendly hospital initiative. 2018.
Arusei RJ, Ettyang GA, Esamai F. Feeding patterns and growth of term infants in Eldoret. Kenya Food nutrition bulletin. 2011;32(4):307–14.
Raghavan V, Bharti B, Kumar P, Mukhopadhyay K, Dhaliwal L. First hour initiation of breastfeeding and exclusive breastfeeding at six weeks: prevalence and predictors in a tertiary care setting. The Indian Journal of Pediatrics. 2014;81(8):743–50.
Meshram I, Laxmaiah A, Venkaiah K, Brahmam G. Impact of feeding and breastfeeding practices on the nutritional status of infants in a district of Andhra Pradesh, India. Natl Med J India. 2012;25(4):201.
CAS PubMed Google Scholar
Kavle JA, LaCroix E, Dau H, Engmann C. Addressing barriers to exclusive breast-feeding in low-and middle-income countries: a systematic review and programmatic implications. Public Health Nutr. 2017;20(17):3120–34.
Group NS. Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. Lancet Glob Health. 2016;4(4):e266–75.
Sobel HL, Silvestre MAA, Mantaring JBV III, Oliveros YE, Nyunt-U S. Immediate newborn care practices delay thermoregulation and breastfeeding initiation. Acta Paediatr. 2011;100(8):1127–33.
Cohen J. A power primer. Psychol Bull. 1992;112(1):155.
World Health Organization. Regional Office for the Western Pacific: Action plan for healthy newborn infants in the Western Pacific region (2014–2020). Geneva: World Health Organization; 2014.
Google Scholar
Min C, Zhenfang L, Aihua W, Xiaolian Z, Yuanyuan Z, Xuelian W: Effects of early essential newborn care on the onset of lactogenesis among primiparaes. Chinese Journal of Child Health Care 2019.
Moore ER, Bergman N, Anderson GC, Medley N: Early skin‐to‐skin contact for mothers and their healthy newborn infants. Cochrane database of systematic Reviews 2016(11).
Wang CR, Li XY, Zhang L, Wu LM, Tan L, Yuan F, Guo Y, Williams S, Xu T. Early essential newborn care is associated with increased breastfeeding: a quasi-experimental study from Sichuan Province of Western China. Int Breastfeed J. 2020;15(1):99.
Jin Y, Xing L, Xiayun L, Yan W, Yue X, Yingpeng Q, Liwei S, Lai W, Hongyu L, Min Z. Current status of early basic neonatal health care services in 4 provinces and county-level medical and health care institutions in western my country. Maternal and Child Health Care of China. 2019;34(10):2178–82.
Tao X. Early essential newborn care: priority interventions to end preventable neonatal death. Chinese Journal of Preventive Medicine. 2021;54(5):498–502.
Rabe H, Reynolds GJ, Diaz‐Rosello JL: Early versus delayed umbilical cord clamping in preterm infants. Cochrane Database of Systematic Reviews 2004(4).
Matthews MK. Developing an instrument to assess infant breastfeeding behaviour in the early neonatal period. Midwifery. 1988;4(4):154–65.
WHO Regional Office for the Western Pacific. Coaching for the First Embrace: Facilitator’s Guide (Early Essential Newborn Care) Module 2 (A WPRO Publication). Geneva: World Health Organization; 2016.
Spielberger CD: State‐Trait anxiety inventory. The Corsini encyclopedia of psychology 2010:1–1.
Crichton N. Visual analogue scale (VAS). J Clin Nurs. 2001;10(5):706–706.
Spielberger CD: State-trait anxiety inventory for adults. 1983.
Dennis CL. The breastfeeding self-efficacy scale: Psychometric assessment of the short form. Journal of Obstetric, Gynecologic, Neonatal Nursing. 2003;32(6):734–44.
Sedgwick P: What is sampling error? BMJ 2012, 344.
Hackman NM, Schaefer EW, Beiler JS, Rose CM, Paul IM. Breastfeeding outcome comparison by parity. Breastfeed Med. 2015;10(3):156–62.
Koskinen KS, Aho AL, Hannula L, Kaunonen MJM. Maternity hospital practices and breast feeding self-efficacy in Finnish primiparous and multiparous women during the immediate postpartum period. 2014;30(4):464–70.
Ekström A, Widström A-M, Nissen E. Duration of Breastfeeding in Swedish Primiparous and Multiparous Women. J Hum Lact. 2003;19(2):172–8.
Chakrabarti K, Basu S. Management of Flat or Inverted Nipples with Simple Rubber Bands. Breastfeed Med. 2011;6(4):215–9.
Aiping G, Jiejing T, Xiaodan C, Yeping W, Hehe W, Yangyang L. Effects of early basic health care for newborns on newborns and their mothers. Chinese Journal Woman and Child Health Research. 2019;30(5):4.
World Health Organization: Guideline: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: World Health Organization; 2017.
Mahmood I, Jamal M, Khan N. Effect of mother-infant early skin-to-skin contact on breastfeeding status: a randomized controlled trial. J Coll Physicians Surg Pak. 2011;21(10):601–5.
PubMed Google Scholar
Almqvist-Tangen G, Bergman S, Dahlgren J, Roswall J, Alm B. Factors associated with discontinuation of breastfeeding before 1 month of age. Acta Paediatr. 2012;101(1):55–60.
Araban M, Karimian Z, Kakolaki ZK, McQueen KA, Dennis C-L. Randomized controlled trial of a prenatal breastfeeding self-efficacy intervention in primiparous women in Iran. J Obstet Gynecol Neonatal Nurs. 2018;47(2):173–83.
Chipojola R, Chiu H-Y, Huda MH, Lin Y-M, Kuo S-Y. Effectiveness of theory-based educational interventions on breastfeeding self-efficacy and exclusive breastfeeding: A systematic review and meta-analysis. Int J Nurs Stud. 2020;109: 103675.
Li Y, Lin Z, Ling Y, Yunyun C: Effect of the early essential newborn care on the early prognosis of the newborn and the rehabilitation of the parturient. Maternal and Child Health Care of China 2020.
Saxton A, Fahy K, Hastie C. Effects of skin-to-skin contact and breastfeeding at birth on the incidence of PPH: a physiologically based theory. Women and Birth. 2014;27(4):250–3.
Marín Gabriel M, Llana Martín I, López Escobar A, Fernández Villalba E, Romero Blanco I, Touza Pol P. Randomized controlled trial of early skin-to-skin contact: effects on the mother and the newborn. Acta Paediatr. 2010;99(11):1630–4.
Velandia M: Parent-infant skin-to-skin contact studies: Parent-infant interaction and oxytocin levels during skin-to-skin contact after Cesarean section and mother-infant skin-to-skin contact as treatment for breastfeeding problems: Inst för kvinnors och barns hälsa/Dept of Women's and Children's Health; 2012.
Tracy LM, Georgiou-Karistianis N, Gibson SJ, Giummarra MJ. Oxytocin and the modulation of pain experience: implications for chronic pain management. Neuroscience Biobehavioral Reviews. 2015;55:53–67.
Handlin L, Jonas W, Petersson M, Ejdebäck M, Ransjö-Arvidson A-B, Nissen E, Uvnäs-Moberg K. Effects of sucking and skin-to-skin contact on maternal ACTH and cortisol levels during the second day postpartum—influence of epidural analgesia and oxytocin in the perinatal period. Breastfeed Med. 2009;4(4):207–20.
Uvnäs-Moberg K, Arn I, Magnusson D. The psychobiology of emotion: the role of the oxytocinergic system. Int J Behav Med. 2005;12(2):59–65.
Download references
Acknowledgements
The authors would like to express their sincere appreciation to all the midwives and participants who contributed to this study.
Author information
Chuanya Huang and Lei Hu contributed equally to this work.
Authors and Affiliations
West China School of Nursing, Sichuan University/Department of Nursing, West China Second University Hospital, Sichuan University, Chengdu, 610000, China
Chuanya Huang & Lei Hu
Key Laboratory of Birth Defects and Related Diseases of Women and Children, Ministry of Education, West China Second University Hospital, Sichuan University, Chengdu, 610000, China
Chuanya Huang, Lei Hu, Yonghong Wang & Biru Luo
Department of Nursing, West China Second University Hospital, Sichuan University/West China School of Nursing, Sichuan University, Chengdu, 610000, China
Yonghong Wang & Biru Luo
You can also search for this author in PubMed Google Scholar
Contributions
HCY, WYH and LBR designed and conducted the research study. HCY and HL wrote the original manuscript and conceptualized the analysis. HCY and LBR performed the analysis. HL, WYH, LBR and HL, reviewed and contributed to the final draft. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Yonghong Wang or Biru Luo .
Ethics declarations
Ethics approval and consent to participate.
The study was part of a larger research trail that was conducted in Chengdu, Sichuan, China. This study was approved by the Ethics Committee of West China Second University Hospital, Sichuan University, and the ethics approval number is 2020 (144). The date of approval was 21 September 2020. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Huang, C., Hu, L., Wang, Y. et al. Effectiveness of early essential newborn care on breastfeeding and maternal outcomes: a nonrandomized controlled study. BMC Pregnancy Childbirth 22 , 707 (2022). https://doi.org/10.1186/s12884-022-05037-8
Download citation
Received : 28 February 2022
Accepted : 09 September 2022
Published : 14 September 2022
DOI : https://doi.org/10.1186/s12884-022-05037-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Early essential newborn care
- Breastfeeding
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Mission, Facts and Figures
- Deans, Chairs and Staff
- Leadership Council
- Dean in the News
- Get Involved
- DEIB Mission
- Message from DEIB Associate Dean
- News and Media
- Reading Lists
- The Yale and Slavery Research Project
- Photo Gallery
- Winslow Medal
- Coat of Arms & Mace
- $50 Million Challenge
- For Pandemic Prevention and Global Health
- For Understanding the Health Impacts of Climate Change
- For Health Equity and Justice
- For Powering Health Solutions through Data Science
- For Future Leaders
- For Faculty Leaders
- For Transformational Efforts
- An abiding love for Yale turns into a lasting gift – in 15 minutes
- Endowed Professorship Created at Critical Time for Yale School of Public Health
- Brotherly encouragement spurs gift to support students
- Prestipino creates opportunities for YSPH students, now and later
- Alumna gives back to the school that “opened doors” in male-dominated field
- For Public Health, a Broad Mission and a Way to Amplify Impact
- Couple Endows Scholarship to Put Dreams in Reach for YSPH Students
- A Match Made at YSPH
- A HAPPY Meeting of Public Health and the Arts
- Generous Gift Bolsters Diversity & Inclusion
- Alumni Donations Aid Record Number of YSPH Students
- YSPH’s Rapid Response Fund Needs Donations – Rapidly
- Podiatric Medicine and Orthopedics as Public Health Prevention
- Investing in Future Public Health Leaders
- Support for Veterans and Midcareer Students
- Donor Eases Burden for Policy Students
- A Personal Inspiration for Support of Cancer Research
- Reducing the Burden of Student Debt
- Learning About Global Health Through Global Travel
- A Meeting in Dubai, and a Donation to the School
- Rapid Response Fund
- Planned Giving
- Testimonials
- Faculty, Postdoc Jobs
- For the Media
- Issues List
- PDF Issues for Download
- Editorial Style Guide
- Social Media
- Accreditation
- Faculty Directory by Name
- Career Achievement Awards
- Annual Research Awards
- Teaching Spotlights
- Biostatistics
- Chronic Disease Epidemiology
- Climate Change and Health Concentration
- Environmental Health Sciences
- Epidemiology of Microbial Diseases
- Global Health
- Health Policy and Management
- Maternal and Child Health Promotion Track
- Public Health Modeling Concentration
- Regulatory Affairs Track
- Social & Behavioral Sciences
- U.S. Health Justice Concentration
- Events and Contact
- What Does it Take to be a Successful YSPH Student?
- How to Apply and FAQs
- Incoming Student Gateway
- Traveling to Yale
- Meet Students and Alumni
- Past Internship Spotlights
- YSPH in Video
- Student-run Organizations
- MS and PhD Student Leaders
- Staff Spotlights
- Life in New Haven
- Libraries at Yale
- The MPH Internship Experience
- Practicum Course Offerings
- Summer Funding and Fellowships
- Downs Fellowship Committee
- Stolwijk Fellowship
- Climate Change and Health
- Career Management Center
- What You Can Do with a Yale MPH
- MPH Career Outcomes
- MS Career Outcomes
- PhD Career Outcomes
- Tuition and Expenses
- External Funding and Scholarships
- External Fellowships for PhD Candidates
- Alumni Spotlights
- Bulldog Perks
- Stay Involved
- Board of Directors
- Emerging Majority Affairs Committee
- Award Nomination Form
- Board Nomination Form
- Alumni Engagement Plus
- Mentorship Program
- The Mentoring Process
- For Mentors
- For Students
- Recent Graduate Program
- Transcript and Verification Requests
- Applied Practice and Student Research
- Competencies and Career Paths
- Applied Practice and Internships
- Student Research
- Seminar and Events
- Competencies and Career paths
- Why the YSPH Executive MPH
- Message from the Program Director
- Two-year Hybrid MPH Schedule
- The Faculty
- Student Profiles
- Newsletter Articles
- Approved Electives
- Physicians Associates Program
- Joint Degrees with International Partners
- MS in Biostatistics Standard Pathway
- MS Implementation and Prevention Science Methods Pathway
- MS Data Sciences Pathway
- Internships and Student Research
- Competencies
- Degree Requirements - Quantitative Specialization
- Degree Requirements - Clinical Specialization
- Degree Requirements- PhD Biostatistics Standard Pathway
- Degree Requirements- PhD Biostatistics Implementation and Prevention Science Methods Pathway
- Meet PhD Students in Biostatistics
- Meet PhD Students in CDE
- Degree Requirements and Timeline
- Meet PhD Students in EHS
- Meet PhD Students in EMD
- Meet PhD Students in HPM
- Degree Requirements - PhD in Social and Behavioral Sciences
- Degree Requirements - PhD SBS Program Maternal and Child Health Promotion
- Meet PhD Students in SBS
- Differences between MPH and MS degrees
- Academic Calendar
- Translational Alcohol Research Program
- Molecular Virology/Epidemiology Training Program (MoVE-Kaz)
- For Public Health Practitioners and Workforce Development
- Course Description
- Instructors
- Registration
- Coursera Offerings
- Non-degree Students
- International Initiatives & Partnerships
- NIH-funded Summer Research Experience in Environmental Health (SREEH)
- Summer International Program in Environmental Health Sciences (SIPEHS)
- 2022 Student Awards
- Booth Info & Floor Map
- Events Calendar
- National Public Health Week (NPHW)
- Leaders in Public Health
- The Role of Data in Public Health Equity & Innovation Conference
- Innovating for the Public Good
- Practice- and community-based research and initiatives
- Practice and community-based research and initiatives
- Activist in Residence Program
- Publications
- Health Care Systems and Policy
- Heart Disease and Stroke
- SalivaDirect™
- COVID Net- Emerging Infections Program
- Panels, Seminars and Workshops (Recordings)
- Public Health Modeling Unit Projects
- Rapid Response Fund Projects
- HIV-AIDS-TB
- The Lancet 2023 Series on Breastfeeding
- 'Omics
- News in Biostatistics
- Biostatistics Overview
- Seminars and Events
- Seminar Recordings
- Statistical Genetics/Genomics, Spatial Statistics and Modeling
- Causal Inference, Observational Studies and Implementation Science Methodology
- Health Informatics, Data Science and Reproducibility
- Clinical Trials and Outcomes
- Machine Learning and High Dimensional Data Analysis
- News in CDE
- Nutrition, Diabetes, Obesity
- Maternal and Child Health
- Outcomes Research
- Health Disparities
- Women's Health
- News in EHS
- EHS Seminar Recordings
- Climate change and energy impacts on health
- Developmental origins of health and disease
- Environmental justice and health disparities
- Enviromental related health outcomes
- Green chemistry solutions
- Novel approaches to assess environmental exposures and early markers of effect
- 1,4 Dioxane
- Reproducibility
- Tissue Imaging Mass Spectrometry
- Alcohol and Cancer
- Olive Oil and Health
- News in EMD
- Antimicrobial Resistance
- Applied Public Health and Implementation Science
- Emerging Infections and Climate Change
- Global Health/Tropical Diseases
- HIV and Sexually Transmitted Infections
- Marginalized Population Health & Equity
- Pathogen Genomics, Diagnostics, and Molecular Epidemiology
- Vector-borne and Zoonotic Diseases
- Disease Areas
- EMD Research Day
- News in HPM
- Health Systems Reform
- Quality, Efficiency and Equity of Healthcare
- Substance Abuse and Mental Health
- Modeling: Policy, Operations and Disease
- Pharmaceuticals, Vaccines and Medical Devices
- Health and Wellbeing
- News in SBS
- Aging Health
- Community Engagement
- Health Equity
- Mental Health
- Reproductive Health
- Sexuality and Health
- Nutrition, Exercise
- Stigma Prevention
- Community Partners
- For Public Health Practitioners
- Reports and Publications
- Fellows Stipend Application
- Agency Application
- Past Fellows
- PHFP in the News
- Frequently Asked Questions
- International Activity
- Research Publications
- Grant Listings
- Modeling Analyses
- 3 Essential Questions Series
INFORMATION FOR
- Prospective Students
- Current Students
New Lancet Series highlights the continuing struggle that breastfeeding women face across the globe
Ysph professor rafael pérez-escamilla, a leading authority on breastfeeding policy, was one of three scholars leading the project, the 2023 lancet series on breastfeeding, the 2023 lancet breastfeeding series, professor rafael perez-escamilla.
A Lancet Series published on Feb. 8, 2023, highlights the continuing struggle that women across the globe face to meet their breastfeeding goals. Yale School of Public Health Professor Rafael Pérez-Escamilla , a leading authority on breastfeeding policy and early childhood nutrition, is co-author of all three Series articles and the lead author of the first paper featured in the Series. The article entitled, “Breastfeeding: crucially important, but increasingly challenged in a market-driven world,” examines how mother and baby attributes at the individual level interact with breastfeeding determinants at other levels, how these interactions drive breastfeeding outcomes, and what policies and interventions are necessary to achieve optimal breastfeeding.
The 2023 Lancet Series on Breastfeeding can be found here .
Here are some key takeaways from the Series:
- Commercial milk formula (CMF) products and artificial formula feeding cannot emulate the living and dynamic nature of breastmilk and the human interaction between mother and baby during breastfeeding.
- Only half of newborn babies are put to the breast within the first hour of life, and about a third of babies in low-income and middle-income countries receive prelacteal feeds (mostly water and animal milk) before being put to the breast. Prelacteal feeding is strongly associated with delayed initiation of breastfeeding and shorter breastfeeding duration.
- Common infant adaptations to the post-birth environment, including crying, unsettled behavior, and short night-time sleep durations, are often misconceived as signs of feeding problems. CMF marketing reinforces and exacerbates these misconceptions and makes unsubstantiated claims that CMFs can ameliorate these behaviors.
- Nearly half of mothers globally self-report insufficient milk (SRIM) as the primary reason for introducing CMFs in the first few months of life. SRIM can generally be prevented or addressed successfully with appropriate support.
- Additional educational efforts are needed for health workers, families, and the public to inform them about normal early infant development, including common crying patterns, posseting, and short night-time sleep durations, to reduce the unnecessary introduction of CMFs and to prevent SRIM and early cessation of breastfeeding.
- Breastfeeding is not the sole responsibility of the mother. Reviews and country case studies indicate that improved breastfeeding practices at the population level are achieved through a collective societal approach that includes multilevel and multicomponent interventions across the socioecological model and different settings.
Professor Pérez-Escamilla took a moment to expound on the findings below. (Editor’s note: We – along with The Lancet - use the terms women and breastfeeding throughout this content for brevity and because most people who breastfeed identify as women; we recognize that not all people who breastfeed or chestfeed identify as women.)
This latest Series published by The Lancet follows up on an initial breastfeeding Series that was published in 2016. What has changed since then and are global breastfeeding rates improving?
P-E: On the one hand, evidence has continued to accumulate showing that breastmilk not only provides optimal nutrition to infants but is also loaded with bioactive substances that protect the child against infectious and non-infectious diseases. The composition of breastmilk is unique to the needs of each infant in the environment in which the child grows. So, in many ways, we now have irrefutable evidence that breastfeeding is Mother Nature’s expression of personalized medicine. Furthermore, in the Series, we present evidence from innovative research showing that breastfeeding protects against the risk of childhood obesity in low and middle-income countries (LMICs) and not only in high-income countries (HICs).
Regarding breastfeeding programs, the Series provides new evidence showing that in countries where exclusive breastfeeding rates have increased in recent years – such as Mexico, Mozambique, the Philippines, and the U.S. – this has been the result of investments in multilevel and multisectoral interventions ranging from improved maternity benefits for employed mothers to social and behavior change communication campaigns to improved coverage of the Baby Friendly Hospital Initiative and breastfeeding counseling across clinical and community settings.
Not all women wish to breastfeed or can breastfeed for a variety of reasons. Yet not all commercial milk formulas offer the same levels of nutrition. What can be done to help mothers make sure their children are getting the important nutrition they need?
P-E: The Series fully acknowledges that women have the right to choose how to feed their infants and that choice should be respected and supported no matter what. If women chose to not breastfeed or to mix feed, or cannot breastfeed, of course, infant formula is the milk product that should be offered during the first year of life and at that point, infants should switch to regular cow’s milk. The Series clearly shows that, contrary to what CMF marketing often implies, there is no need for the quite expensive toddler milks marketed for children between 1 and 3 years old.
Milks based on plant protein sources such as soybeans are also available for the few infants and young children that do not tolerate cow’s milk, but this decision needs to be made in close consultation with a qualified health provider.
It is important to emphasize that the Series is not a manifesto against infant formula (a product that is vital for infants who are not breastfed), but rather a call to decision-makers and authorities to stop infant formula companies from undermining mothers’ breastfeeding intentions through misleading marketing that exploits their fears and emotions during a very vulnerable period.
You mention that normal baby behaviors like crying are often misconstrued and can lead a mother to stop breastfeeding. Can you elaborate on this point and share what interventions may help in these cases?
P-E: Infant crying is part of normal infant development; this is indeed how babies communicate their physical and psycho-emotional needs. Understandably, parents can get very worried and distressed when their infants cry. Unfortunately, infant formula companies exploit these psycho-emotional sensitivities of parents by marketing their products as helping babies cry less and sleep better, without evidence to support these claims. In other words, they have found that marketing their products by selling parents “tranquility” and “peace of mind” is very profitable.
Additionally, oftentimes health providers tell parents that the baby is crying frequently because the mother is not producing enough milk and advise them to introduce infant formulas right away without even assessing first the baby’s growth and developmental status. Even more worrisome is the fact that these same providers oftentimes benefit from relationships with infant formula companies that are underlined by clear conflicts of interest.
Babies cry for many reasons including being hungry, cold, hot, tired, or simply because they have a wet diaper, or their environment becomes too loud for them. We have the know-how to train health providers on how to effectively counsel parents and other caregivers on how to understand what their babies are communicating when crying and how to respond to these cues without undermining breastfeeding.
Self-reported insufficient milk is a common reason why mothers stop breastfeeding. You say this can be addressed with appropriate support and health care training. Can you elaborate?
P-E: To prevent the pervasive maternal report of insufficient milk, it is important to provide anticipatory guidance to mothers on what to expect with breastfeeding once the baby is born.
If the mother wants to breastfeed, she should request that her newborn be placed skin-to-skin with her immediately after birth and she should let care providers know she wants to initiate breastfeeding as soon as possible. If the mother has not breastfed before, she should ask for a lactation counselor to observe the baby's latch as many problems with breastfeeding happen during the first hours and days after birth because of poor positioning. New moms should also be advised that it takes about 3 days for the milk to “come in” and that she needs to breastfeed the baby on demand, and to not agree for the baby to be fed formula in the maternity facility unless it is medically indicated. This is because breastmilk production is a process driven by infant sucking and any interference with the frequency of nursing increases the risk of breastfeeding failure.
It is also very important to counsel mothers on how to interpret normal baby behaviors such as crying and “disorganized” sleep routines during the early neonatal period, and how to respond accordingly without negatively affecting their breastfeeding plans. It is also key to include partners or other family members or friends as part of these counseling sessions as, not surprisingly, they also have the widespread belief that infant crying is always a sign that moms are not producing enough milk.
Lastly, maternity facilities and community providers should coordinate their breastfeeding support services following a continuum of care approach so that all mothers can have access to qualified lactation management services no matter where they are, especially during the first days and weeks after hospital discharge, which is when most breastfeeding crises happen and need to be prevented or resolved.
Lastly, you point out that breastfeeding is not solely a mother’s responsibility but that population-level interventions can help improve global breastfeeding rates. What do you mean, and can you give us examples of these interventions?
P-E: Globally, the great majority of women are choosing to breastfeed but unfortunately most of them cannot breastfeed for as long as they would like due to major social, political, economic, and health care structural barriers. This represents a major violation of women's and children’s rights that strongly undermines global health and national development globally. The Lancet Series nicely integrates new evidence showing how important it is for all of society to support the wishes of breastfeeding mothers through (1) social protection policies (e.g., improved maternity benefits for women working in the formal and informal economy; workplace accommodations including lactation rooms, and flexible working schedules); (2) marketing regulation (implementation and strong enforcement of the World Health Organization Code for Marketing of Breastmilk Substitutes)); (3) social and behavior change communication campaigns to support breastfeeding moms anytime and anywhere; (4) health care systems programs such as the Baby Friendly Hospital Initiative; (5) breastfeeding counseling in community settings; (6) access to human milk banks; and (7) support from family and friends for breastfeeding including support with household chores and caregiving of the baby and siblings.
- Maternal Health
- Breastfeeding
Featured in this article
- Rafael Pérez-Escamilla, PhD Professor of Public Health (Social and Behavioral Sciences); Director, Office of Public Health Practice; Affiliated Faculty, Yale Institute for Global Health; Director, YSPH Global Health Concentration; Director, Maternal and Child Health Promotion (MCHP) Program
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 29 October 2022
Achieving healthy people 2030 breastfeeding targets in the United States: challenges and opportunities
- Tonse N. K. Raju ORCID: orcid.org/0000-0001-9738-1935 1
Journal of Perinatology volume 43 , pages 74–80 ( 2023 ) Cite this article
4314 Accesses
3 Citations
84 Altmetric
Metrics details
- Outcomes research
- Public health
A Correction to this article was published on 11 November 2022
This article has been updated
To estimate the national and states-specific gaps in breastfeeding rates in the United States for achieving the Healthy People 2030 (HP2030) targets, which are: 42.4% of infants to exclusively breastfeed through 6th months, and 54.1% of infants to breastfeed through 12th month of age.
Study design
The differences between the HP2030 breastfeeding targets and the respective state-specific baseline rates in the 2022 National Immunization Survey report for infants born in 2019 were computed.
The gaps in breastfeeding rates for achieving either of the two HP2030 targets varied greatly. Relative to their 2019 baseline estimates, 7 U.S. states need to increase breastfeeding rates between 100% and 207%, 27 states between 50% and 99%, 9 states and 2 territories between 20% and 49% and the remaining 7, between 0% and 19%.
Conclusions
Thirty-four of 50 (68%) states face huge gaps in achieving the HP2030 breastfeeding targets.
Similar content being viewed by others
Mapping inequalities in exclusive breastfeeding in low- and middle-income countries, 2000–2018
Natalia V. Bhattacharjee, Lauren E. Schaeffer, … Local Burden of Disease Exclusive Breastfeeding Collaborators
Mapping exclusive breastfeeding in Africa between 2000 and 2017
Natalia V. Bhattacharjee, Lauren E. Schaeffer, … Simon I. Hay
Trends and inequalities in breastfeeding continuation from 1 to 6 weeks: findings from six population-based British cohorts, 1985–2010
Deon A. Simpson, Claire Carson, … Maria A. Quigley
Introduction
The Healthy People 2030 (HP2030) program has set national objectives for the United States to increase the proportion of infants to exclusively breastfeed through 6th months of age to 42.4% (6-month target), and to continue breastfeeding through 12th month of age to 54.1% (12-month target) [ 1 ]. Exclusive breastfeeding is defined as feeding only breastmilk, no solids, and no water or no other liquids.
The Healthy People Program is a U.S. Federal Government effort, which develops health-related targets for the nation to achieve every 10 years. To formulate the HP2030 breastfeeding targets, the Program used earlier data from the National Immunization Survey (NIS) conducted by the Centers for Disease Control and Prevention (CDC), along with extensive literature reviews, and motivated by a desire to advance the health of the nation.
Since continued breastfeeding offers numerous health benefits to the mother and her infant, the American Academy of Pediatrics Section on Breastfeeding has issued a new policy statement retaining its endorsement for exclusive breastfeeding through 6th month, and continued breastfeeding for at least 12 months. Now the policy also recommends continued breastfeeding as long as mutually desired by the mother and the child for 2 years or beyond [ 2 ].
Although the breastfeeding initiation rates are high in the U.S., most women do not breastfeed exclusively for the first 6 months, or continue to breastfeed their infants through the first 12 months, as reported by the latest NIS released on August 1, 2022 [ 3 ]. Among the infants born in 2019, the national rate estimate for 6th month exclusive breastfeeding was 24.9% and the estimate for breastfeeding through the 12th month was 35.9%, with wide variation among the states [ 3 ].
Therefore, for achieving the HP2030 targets, many states may need to overcome substantial gaps in breastfeeding rates. However, the extent of state-specific gaps has not been reported. This study assesses the state and territory-specific gaps in breastfeeding rates for achieving the HP2030 targets.
Materials and methods
The results from the 2022 NIS data [ 3 ] were used for analyses in this study. The NIS results provide the national, state, and territory-level breastfeeding estimates for 2019 live births for all 50 states, Puerto Rico, and the District of Columbia (henceforth referred to as “states”).
The NIS adapts a random-digit-dialling, complex sampling method for the survey to estimate the current national, state, selected local level, and some US territory level vaccination coverage rates for US infants and children. Since July 2001, breastfeeding questions have been added to the NIS to monitor rates of breastfeeding at national and state levels by birth year. The 2022 NIS report contains responses from the members of households with children aged 19–35 months, and who were born in 2019 calendar year.
The NIS determines the sample sizes to provide the statistical precision required to estimate vaccination coverage as well as breastfeeding prevalence for each survey area. The NIS webpage provides additional details about the survey methods and analytical techniques [ 4 ].
The NIS does not collect information on gestational age. However, the inclusion of preterm births in the survey of households with surviving infants at 19–35 months is unlikely to have affected the overall rates of breastfeeding. This is because, in 2019, 10.23% of U.S. births were preterm, and 0.66% were extremely preterm (<28 weeks of gestation) [ 5 ]. These are small numbers among the relatively small survey samples that ranged between 250 and 1200.
Two methods were used to express gaps in achieving the HP2030 targets. One was by subtracting the target rates from the 2019 respective state-specific breastfeeding estimates [ 3 ], and the second was calculating the percentage differences relative to state’s 2019 baseline rates. As for example: In 2019, 27.3% of infants born in California were exclusive breastfed through 6 months of age. Therefore, to achieve the HP2030 6-month target of 42.4%, California must overcome a 15.1% gap, or 55.3% gap relative to the state’s 2019 baseline (15.1/27.3 × 100 = 55.3%).
As its usual practice, NIS publishes the national and state-specific breastfeeding rates as mean ± ½ of 95% confidence intervals (CI) due to the relatively small sample sizes and large CIs [ 3 ], which was retained while reporting the results in this paper. However, to test the statistical significance among the states, the widths of the mean ± full 95% CIs were compared. If the widths overlapped, the respective mean values were declared not to be significantly different from each other, and if they did not overlap, they were declared to be significantly different.
Table 1 provides the number of responses to the 2022 NIS survey along with the national and state-specific mean rates (±one-half of 95% CI) [ 3 ]. The results are sorted in an ascending order for the mean breastfeeding values for the 6th and 12th month breastfeeding estimates. The table footnote also lists the states and territories that had achieved HP2020 targets by 2019.
The state-specific rates for the two breastfeeding measures of interest varied greatly. The 6th month exclusive breastfeeding rate was the lowest for West Virginia, and highest for Minnesota. Similarly, the 12th month breastfeeding rate was lowest for West Virginia and highest for Hawaii (which had already achieved the 12th month target of 54.1%).
Figure 1 shows the gaps for achieving the 6th and 12th month targets. The U.S. national gaps for the two targets (arrows) were: 17.5% and 18.2%, respectively (rounded to 18%). Figure 1 also show that the extent of gaps for achieving the two HP2030 targets ranged greatly among the states. The states within the parenthetic marks at the left ends of the graphs need to overcome significantly larger gaps compared to those in the parenthetic marks at the right ends of the graphs.
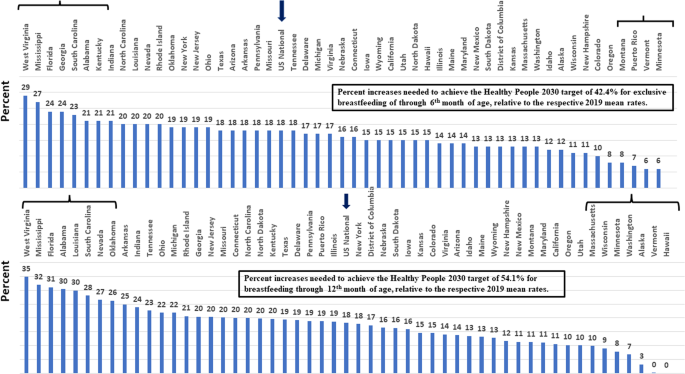
The percent gaps for achieving the HP2030 targets for exclusive breastfeeding through the 6th month (upper panel) and breastfeeding though the 12th month (lower panel). The differences between the respective target values and the 2019 baseline mean rates for the U.S. (arrows), 50 individual states, Puerto Rico and the District of Columbia, arranged in descending order from left to right. The gaps among the states within the parenthetic marks at two ends of both graphs were significantly different. These states were—to achieve the 6-month target (upper panel), West Virginia, Mississippi, Florida, Georgia, South Carolina, Alabama, and Kentucky (left end of the graph) encounter significantly larger gaps compared to those of Montana, Puerto Rico, Vermont, and Minnesota (right end of the graph); to achieve the 12-month target (lower panel), West Virginia, Mississippi, Florida, Alabama, Louisiana, South Carolina, Nevada, and Oklahoma (left end of the graph) encounter significantly larger gaps compared to those of Massachusetts, Wisconsin, Minnesota, Washington, Alaska, Vermont, and Hawaii (right end of the graph). The data were rounded using the general algebraic rules.
Figures 2 and 3 show the geographic distribution of the percentage gaps relative to their respective 2019 mean rates. Both figures show that the gaps for achieving the HP2030 breastfeeding targets vary greatly. The gaps to achieve either of the targets ranged between 100% and 207% for 7 states; between 50% and 99% for 27 states; between 20% and 49% for the 9 states and 2 territories; and between 0% and 19% for the remaining 7 states. The gaps were higher in the southern, industrial eastern, and midwestern states compared to those in the Atlantic-northeastern, northern, and Pacific northwestern states.
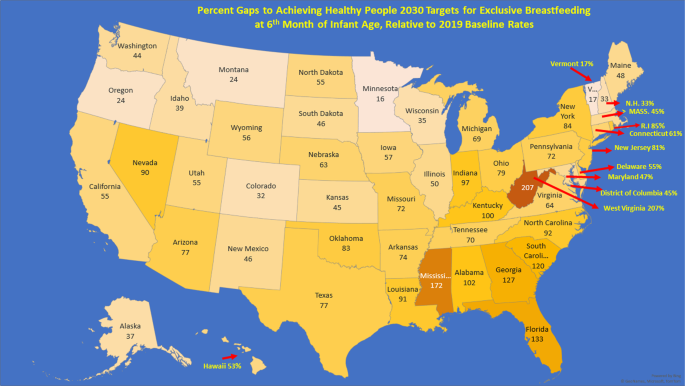
The numbers within the state boundaries are the percentages values. For technical reasons, Puerto Rico (7%) is not represented in the figure. All data were rounded using the general algebraic rules.
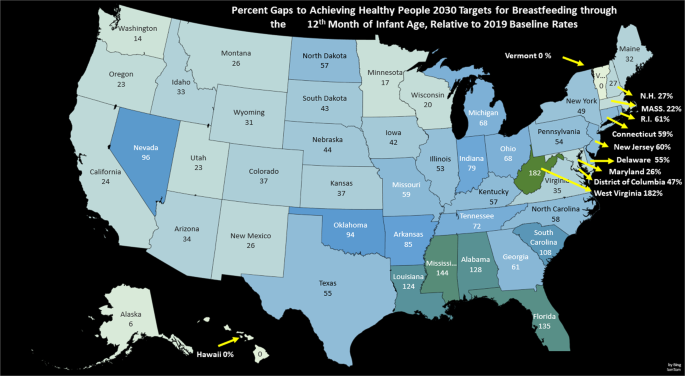
The numbers within the state boundaries are the percentages values. For technical reasons Puerto Rico (19%) is not represented in the figure. The data were rounded using the general algebraic rules.
The results of this study (Table 1 and Figs. 1 – 3 ) show that a large number of U.S. states face huge gaps for achieving the HP2030 breastfeeding targets [ 3 ]. Therefore, these states may need to develop regional programs for enhancing continued breastfeeding for achieving the worthy goals of HP2030.
Why such a large variation in the gaps to achieve the HP2030 targets? The obvious reason is the variation in the baseline breastfeeding rates. And explaining regional variations in breastfeeding requires data on the distribution of associated variables noted above across the states. Such data are not available, and studies are urgently needed to rectify this knowledge gap.
Even in states with high mean breastfeeding rates, there could be regions having suboptimal breastfeeding rates. Thus, addressing the generic and local factors impeding the continuation of breastfeeding would be critical to achieving 2030 breastfeeding targets—a ‘one-size fits all’ approach may not work.
The NIS survey [ 3 ] identified several specific socio-demographic factors such as gender, race/ethnicity, maternal education, maternal age, poverty-to-income ratio, marital status, and geographic location affecting breastfeeding continuation in the U.S. (Table 2 ). Race and ethnicity are also important factors affecting breastfeeding continuation beyond the immediate postpartum period, as shown in the supplementary material Table.
Other factors known to negatively influence the duration of breastfeeding include mode of delivery, work and workplace issues, the unavailability of lactation consultants especially in rural areas have also been noted as factors negatively affecting breastfeeding durations [ 6 ].
Improving breastfeeding rates can also help achieve another HP2030 target—reducing the U.S. infant mortality rate (IMR) to 5.0 deaths for 1000 live births [ 1 ]. A recent study from the CDC using linked birth and death certificates reported that “any” breastfeeding resulted in a 26% reduction in post-perinatal deaths in the U.S. [ 7 ] This is the first report to show an association between breastfeeding and reduced IMR in an industrialized nation, such as the U.S.
How to enhance continued breastfeeding beyond the immediate postpartum period? Two recent studies highlight potential opportunities. Using a sample of 33,121, Kogan et al. [ 8 ] showed that the prevalence of infants “ever breastfed” and “breastfed for at least six months” were higher in states that have enacted one or more legislative policies geared to promoting breastfeeding. They also noted that sociodemographic and maternal factors did not account for most of the variations in the breastfeeding rates [ 8 ].
In another study, the researchers examined the associations between workplace leave length and breastfeeding initiation and continuation at 1, 2, and 3 months in a cohort of 12,301 postpartum women [ 9 ]. Approximately two thirds (66.2%) of women reported taking less than 3 months of leave. A shorter leave length (<3 months), paid or unpaid, was associated with lower prevalence of continued breastfeeding at 2 and 3 months of postpartum. These findings support the expert opinion that regional laws and legislative policies positively influence breastfeeding rates [ 10 ].
Besides the length of postpartum maternal leave, a friendly workplace environment would be conducive to continued breastfeeding, just as an unfriendly workplace environment would be detrimental [ 11 , 12 , 13 , 14 , 15 ]. Similarly, advertising commercial formulas in the prenatal clinics had a negative impact on the duration of breastfeeding [ 16 ]. South African scientists report that many infant formula manufacturing companies have been using a variety of covert marketing techniques to entire women to stop breastfeeding and purchase commercial infant formula to feed their infants [ 17 ].
Hospitals caring for postpartum women could require all units to have standardized counseling sessions, and to the extent possible, offer help to overcome barriers to continued breastfeeding for individual families. The hospitals might also implement the Ten Steps to Successful Breastfeeding recommended by the Baby-Friendly USA [ 18 ].
Strengths of this study include the use of the latest NIS data [ 3 ] to compute the gaps in breastfeeding rates for achieving the HP2030 targets [ 1 ]. However, this study has limitations. The baseline breastfeeding data were obtained from a cohort of women delivering live births in the 2019 calendar year. Therefore, it is possible that the rates could have improved since then and the actual gaps reported here could be overestimates.
Additionally, the target year of birth for the 2022 NIS survey was 2019—before the outbreak of COVID-19 pandemic. The potential impact of the pandemic-related adverse effects such as shut down, social isolation, loss of job and income on breastfeeding practices remain to be studied. It is possible that the enforced stay-at-home policies might have encouraged more women to breastfeed for longer durations. However, poverty, food insecurity and depression due to the pandemic-related isolation might have had an opposite effect on breastfeeding practices. These issues are important topics for future studies.
In conclusion, the data presented in this study show that 34/50 (68%) states in the U.S., need to overcome significant gaps, and Puerto Rico and the District of Columbian need to overcome modest gaps for achieving the 2030 Healthy People breastfeeding targets. Understanding the state and region-specific barriers, implementing remedial measures, and developing policies and regulations to support breastfeeding services could be invaluable in helping to overcome those gaps and achieve the HP2030 targets, positively impacting the nation’s health.
Data availability
The author is willing to share the data used in this manuscript, available as Microsoft Excel files.
Change history
11 november 2022.
A Correction to this paper has been published: https://doi.org/10.1038/s41372-022-01561-9
U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2030 . Healthy People, Nutrition and Health Policy 2021. https://health.gov/healthypeople/objectives-and-data/browse-objectives/nutrition-and-healthy-eating . Accessed 12 Nov 2021.
Meek JY, Noble L. Technical Report: breastfeeding and the use of human milk. Pediatrics, 2022:150.
Centers for Disease Control and Prevention. Results: Breastfeeding Rates: Breastfeeding Among U.S. Children Born 2012-2019, CDC National Immunization Survey: Results ,. National Immunization Survey (NIH). 2022. https://www.cdc.gov/breastfeeding/data/nis_data/results.html . Accessed 2 Aug 2022.
Centers for Disease Control and Prevention. National Immunization Survey--Methods . National Immunization Survey, 2021. https://www.cdc.gov/vaccines/imz-managers/nis/methods.html . Accessed 12 Nov 2021.
Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital- Stat Rep. 2021;70:1–50.
Google Scholar
Anstey EH, Chen J, Elam-Evans LD, Perine CG. Racial and geographic differences in breastfeeding—United States, 2011–2015. Morb Mortal Wkly Rep. 2017;66:723–7.
Article Google Scholar
Li R, Ware J, Chen A, Nelson JM, Kmet J, Park SE, et al. Breastfeeding and post-perinatal infant deaths in the united states, a national prospective cohort analysis. Lancet Regional Health—Am. 2022;5:1–14.
Kogan MD, Singh GK, Dee DL, Belanoff C, Grummer-Strawn LM. Multivariate analysis of state variation in breastfeeding rates in the United States. Am J Public Health. 2008;98:1872–80.
Kortsmit K, Li R, Cox S, Shapiro-Mendoza CK, Perine CG, D’Angelo DV, et al. Workplace leave and breastfeeding duration among postpartum women, 2016-2018. Am J Public Health. 2021;111:2036–45.
Barraza, L, Lebedevitch C, Stuebe A. The role of law and policy in assisting families to reach healthy people’s maternal, infant, and child health breastfeeding goals in the United States. Healthy People, USA 2020. https://www.healthypeople.gov/2020/law-and-health-policy/topic/maternal-infantchild-health . Accessed 19 Nov 2021.
Raju TN. Continued barriers for breast-feeding in public and the workplace. J Pediatr. 2006;148:677–9.
Raju TN. Reasonable break time for nursing mothers: a provision enacted through the Affordable Care Act. Pediatrics. 2014;134:423–4.
Whitley MD, Ro A, Choi B. Workplace breastfeeding support and job satisfaction among working mothers in the United States. Am J Ind Med. 2019;62:716–26.
Steurer LM. Maternity leave length and workplace policies’ impact on the sustainment of breastfeeding: global perspectives. Public Health Nurs. 2017;34:286–94.
Lynch S. Breastfeeding and the workplace. Community Pract. 2016;89:29–31.
Howard C, Howard F, Lawrence R, Andersen E, DeBlieck E, Weitzman M. Office prenatal formula advertising and its effect on breast-feeding patterns. Obstet Gynecol. 2000;95:296–303.
CAS Google Scholar
Pereira-Kotze C, Honwood C, Haskins L, Kingston G, Luthuli S, Doherty T. Exploring women’s exposure to marketing of commercial formula products: a qualitative marketing study from two sites in South Africa. Glob Health Action. 2022;15:2074663
Baby Friendly USA Inc. The Ten Steps to Successful Breastfeeding . The Baby-Friendly Hospital Initiative 2021. https://www.babyfriendlyusa.org/for-facilities/practice-guidelines/10-steps-and-international-code/ . Accessed 21 Nov 2021.
Download references
Acknowledgements
The author thanks Ruowei Li, MD, PhD, the Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, Atlanta, GA, for help with explaining NIS survey and statistical methods. He also thanks Ms. Brigit Sullivan, MLS, Biomedical Librarian, NIH Library, Bethesda, MD for help with editing.
Author information
Authors and affiliations.
National Institutes of Health, Bethesda, MD, USA
Tonse N. K. Raju
You can also search for this author in PubMed Google Scholar
Contributions
TNKR conceived the study, carried out the data analyses, interpreted the results, and wrote the manuscript.
Corresponding author
Correspondence to Tonse N. K. Raju .
Ethics declarations
Competing interests.
The author is the Deputy Editor for the Journal of Perinatology. The author is Program Officer in the Office of the Director, National Institutes of Health. However, the opinions presented in this paper are those of the author alone. They do not necessarily represent those of the US Government, the Department of Health and Human Services, or the National Institutes of Health.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In the abstract, in the introduction, in the results and in table 2, some sentences have been revised.
Supplementary information
Rights and permissions.
Reprints and permissions
About this article
Cite this article.
Raju, T.N.K. Achieving healthy people 2030 breastfeeding targets in the United States: challenges and opportunities. J Perinatol 43 , 74–80 (2023). https://doi.org/10.1038/s41372-022-01535-x
Download citation
Received : 07 February 2022
Revised : 20 September 2022
Accepted : 27 September 2022
Published : 29 October 2022
Issue Date : January 2023
DOI : https://doi.org/10.1038/s41372-022-01535-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 26 November 2021
Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature
- Bridget Beggs 1 ,
- Liza Koshy 1 &
- Elena Neiterman 1
BMC Public Health volume 21 , Article number: 2169 ( 2021 ) Cite this article
11k Accesses
22 Citations
4 Altmetric
Metrics details
Despite public health efforts to promote breastfeeding, global rates of breastfeeding continue to trail behind the goals identified by the World Health Organization. While the literature exploring breastfeeding beliefs and practices is growing, it offers various and sometimes conflicting explanations regarding women’s attitudes towards and experiences of breastfeeding. This research explores existing empirical literature regarding women’s perceptions about and experiences with breastfeeding. The overall goal of this research is to identify what barriers mothers face when attempting to breastfeed and what supports they need to guide their breastfeeding choices.
This paper uses a scoping review methodology developed by Arksey and O’Malley. PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched utilizing a predetermined string of keywords. After removing duplicates, papers published in 2010–2020 in English were screened for eligibility. A literature extraction tool and thematic analysis were used to code and analyze the data.
In total, 59 papers were included in the review. Thematic analysis showed that mothers tend to assume that breastfeeding will be easy and find it difficult to cope with breastfeeding challenges. A lack of partner support and social networks, as well as advice from health care professionals, play critical roles in women’s decision to breastfeed.
While breastfeeding mothers are generally aware of the benefits of breastfeeding, they experience barriers at individual, interpersonal, and organizational levels. It is important to acknowledge that breastfeeding is associated with challenges and provide adequate supports for mothers so that their experiences can be improved, and breastfeeding rates can reach those identified by the World Health Organization.
Peer Review reports
Public health efforts to educate parents about the importance of breastfeeding can be dated back to the early twentieth century [ 1 ]. The World Health Organization is aiming to have at least half of all the mothers worldwide exclusively breastfeeding their infants in the first 6 months of life by the year 2025 [ 2 ], but it is unlikely that this goal will be achieved. Only 38% of the global infant population is exclusively breastfed between 0 and 6 months of life [ 2 ], even though breastfeeding initiation rates have shown steady growth globally [ 3 ]. The literature suggests that while many mothers intend to breastfeed and even make an attempt at initiation, they do not always maintain exclusive breastfeeding for the first 6 months of life [ 4 , 5 ]. The literature identifies various barriers, including return to paid employment [ 6 , 7 ], lack of support from health care providers and significant others [ 8 , 9 ], and physical challenges [ 9 ] as potential factors that can explain premature cessation of breastfeeding.
From a public health perspective, the health benefits of breastfeeding are paramount for both mother and infant [ 10 , 11 ]. Globally, new mothers following breastfeeding recommendations could prevent 974,956 cases of childhood obesity, 27,069 cases of mortality from breast cancer, and 13,644 deaths from ovarian cancer per year [ 11 ]. Global economic loss due to cognitive deficiencies resulting from cessation of breastfeeding has been calculated to be approximately USD $285.39 billion dollars annually [ 11 ]. Evidently, increasing exclusive breastfeeding rates is an important task for improving population health outcomes. While public health campaigns targeting pregnant women and new mothers have been successful in promoting breastfeeding, they also have been perceived as too aggressive [ 12 ] and failing to consider various structural and personal barriers that may impact women’s ability to breastfeed [ 1 ]. In some cases, public health messaging itself has been identified as a barrier due to its rigid nature and its lack of flexibility in guidelines [ 13 ]. Hence, while the literature on women’s perceptions regarding breastfeeding and their experiences with breastfeeding has been growing [ 14 , 15 , 16 ], it offers various, and sometimes contradictory, explanations on how and why women initiate and maintain breastfeeding and what role public health messaging plays in women’s decision to breastfeed.
The complex array of the barriers shaping women’s experiences of breastfeeding can be broadly categorized utilizing the socioecological model, which suggests that individuals’ health is a result of the interplay between micro (individual), meso (institutional), and macro (social) factors [ 17 ]. Although previous studies have explored barriers and supports to breastfeeding, the majority of articles focus on specific geographic areas (e.g. United States or United Kingdom), workplaces, or communities. In addition, very few articles focus on the analysis of the interplay between various micro, meso, and macro-level factors in shaping women’s experiences of breastfeeding. Synthesizing the growing literature on the experiences of breastfeeding and the factors shaping these experiences, offers researchers and public health professionals an opportunity to examine how various personal and institutional factors shape mothers’ breastfeeding decision-making. This knowledge is needed to identify what can be done to improve breastfeeding rates and make breastfeeding a more positive and meaningful experience for new mothers.
The aim of this scoping review is to synthesize evidence gathered from empirical literature on women’s perceptions about and experiences of breastfeeding. Specifically, the following questions are examined:
What does empirical literature report on women’s perceptions on breastfeeding?
What barriers do women face when they attempt to initiate or maintain breastfeeding?
What supports do women need in order to initiate and/or maintain breastfeeding?
Focusing on women’s experiences, this paper aims to contribute to our understanding of women’s decision-making and behaviours pertaining to breastfeeding. The overarching aim of this review is to translate these findings into actionable strategies that can streamline public health messaging and improve breastfeeding education and supports offered by health care providers working with new mothers.
This research utilized Arksey & O’Malley’s [ 18 ] framework to guide the scoping review process. The scoping review methodology was chosen to explore a breadth of literature on women’s perceptions about and experiences of breastfeeding. A broad research question, “What does empirical literature tell us about women’s experiences of breastfeeding?” was set to guide the literature search process.
Search methods
The review was undertaken in five steps: (1) identifying the research question, (2) identifying relevant literature, (3) iterative selection of data, (4) charting data, and (5) collating, summarizing, and reporting results. The inclusion criteria were set to empirical articles published between 2010 and 2020 in peer-reviewed journals with a specific focus on women’s self-reported experiences of breastfeeding, as well as how others see women’s experiences of breastfeeding. The focus on women’s perceptions of breastfeeding was used to capture the papers that specifically addressed their experiences and the barriers that they may encounter while breastfeeding. Only articles written in English were included in the review. The keywords utilized in the search strategy were developed in collaboration with a librarian (Table 1 ). PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched for the empirical literature, yielding a total of 2885 results.
Search outcome
The articles deemed to fit the inclusion criteria ( n = 213) were imported into RefWorks, an online reference manager tool and further screened for eligibility (Fig. 1 ). After the removal of 61 duplicates and title/abstract screening, 152 articles were kept for full-text review. Two independent reviewers assessed the papers to evaluate if they met the inclusion criteria of having an explicit analytic focus on women’s experiences of breastfeeding.
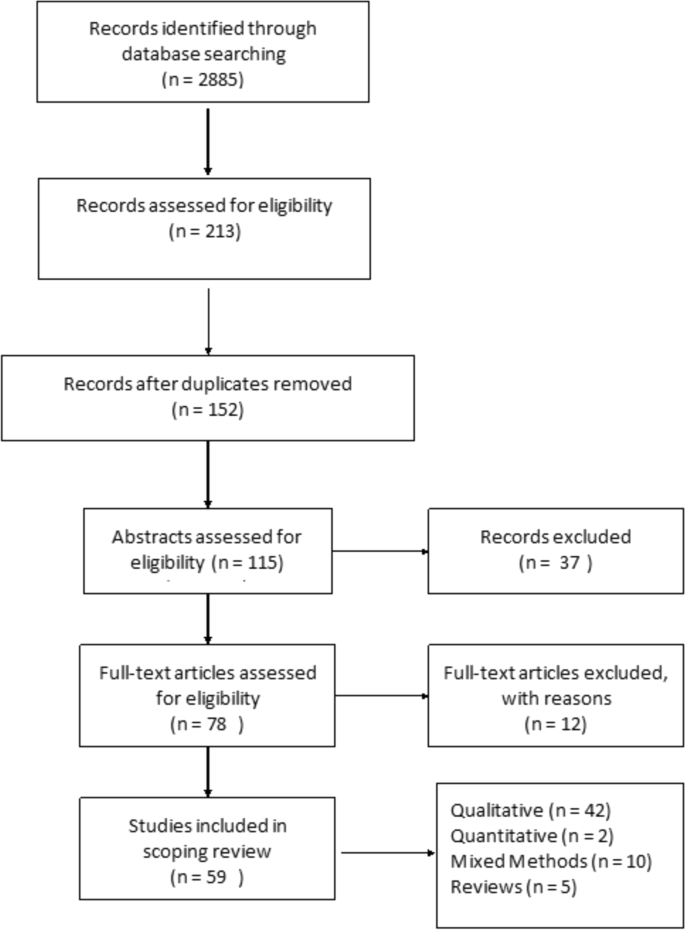
Prisma Flow Diagram
Quality appraisal
Consistent with scoping review methodology [ 18 ], the quality of the papers included in the review was not assessed.
Data abstraction
A literature extraction tool was created in MS Excel 2016. The data extracted from each paper included: (a) authors names, (b) title of the paper, (c) year of publication, (d) study objectives, (e) method used, (f) participant demographics, (g) country where the study was conducted, and (h) key findings from the paper.
Thematic analysis was utilized to identify key topics covered by the literature. Two reviewers independently read five papers to inductively generate key themes. This process was repeated until the two reviewers reached a consensus on the coding scheme, which was subsequently applied to the remainder of the articles. Key themes were added to the literature extraction tool and each paper was assigned a key theme and sub-themes, if relevant. The themes derived from the analysis were reviewed once again by all three authors when all the papers were coded. In the results section below, the synthesized literature is summarized alongside the key themes identified during the analysis.
In total, 59 peer-reviewed articles were included in the review. Since the review focused on women’s experiences of breastfeeding, as would be expected based on the search criteria, the majority of articles ( n = 42) included in the sample were qualitative studies, with ten utilizing a mixed method approach (Fig. 2 ). Figure 3 summarizes the distribution of articles by year of publication and Fig. 4 summarizes the geographic location of the study.
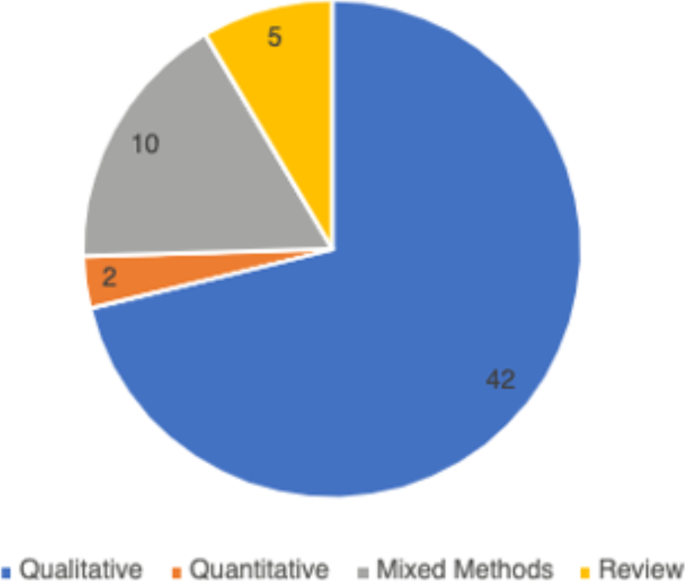
Types of Articles

Years of Publication
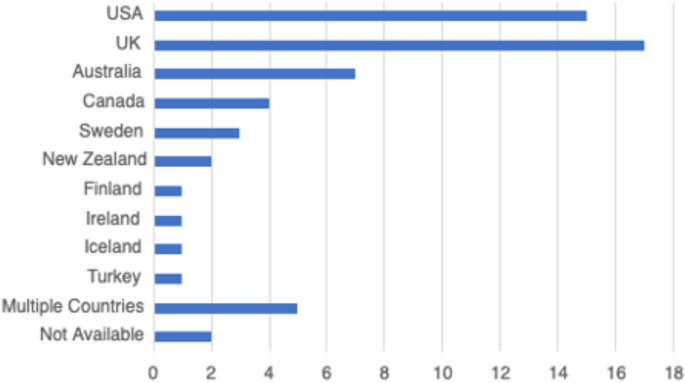
Countries of Focus Examined in Literature Review
Perceptions about breastfeeding
Women’s perceptions about breastfeeding were covered in 83% ( n = 49) of the papers. Most articles ( n = 31) suggested that women perceived breastfeeding as a positive experience and believed that breastfeeding had many benefits [ 19 , 20 ]. The phrases “breast is best” and “breastmilk is best” were repeatedly used by the participants of studies included in the reviewed literature [ 21 ]. Breastfeeding was seen as improving the emotional bond between the mother and the child [ 20 , 22 , 23 ], strengthening the child’s immune system [ 24 , 25 ], and providing a booster to the mother’s sense of self [ 1 , 26 ]. Convenience of breastfeeding (e.g., its availability and low cost) [ 19 , 27 ] and the role of breastfeeding in weight loss during the postpartum period were mentioned in the literature as other factors that positively shape mothers’ perceptions about breastfeeding [ 28 , 29 ].
The literature suggested that women’s perceptions of breastfeeding and feeding choices were also shaped by the advice of healthcare providers [ 30 , 31 ]. Paradoxically, messages about the importance and relative simplicity of breastfeeding may also contribute to misalignment between women’s expectations and the actual experiences of breastfeeding [ 32 ]. For instance, studies published in Canada and Sweden reported that women expected breastfeeding to occur “naturally”, to be easy and enjoyable [ 23 ]. Consequently, some women felt unprepared for the challenges associated with initiation or maintenance of breastfeeding [ 31 , 33 ]. The literature pointed out that mothers may feel overwhelmed by the frequency of infant feedings [ 26 ] and the amount as well as intensity of physical difficulties associated with breastfeeding initiation [ 33 ]. Researchers suggested that since many women see breastfeeding as a sign of being a “good” mother, their inability to breastfeed may trigger feelings of personal failure [ 22 , 34 ].
Women’s personal experiences with and perceptions about breastfeeding were also influenced by the cultural pressure to breastfeed. Welsh mothers interviewed in the UK, for instance, revealed that they were faced with judgement and disapproval when people around them discovered they opted out of breastfeeding [ 35 ]. Women recalled the experiences of being questioned by others, including strangers, when they were bottle feeding their infants [ 9 , 35 , 36 ].
Barriers to breastfeeding
The vast majority ( n = 50) of the reviewed literature identified various barriers for successful breastfeeding. A sizeable proportion of literature (41%, n = 24) explored women’s experiences with the physical aspects of breastfeeding [ 23 , 33 ]. In particular, problems with latching and the pain associated with breastfeeding were commonly cited as barriers for women to initiate breastfeeding [ 23 , 28 , 37 ]. Inadequate milk supply, both actual and perceived, was mentioned as another barrier for initiation and maintenance of breastfeeding [ 33 , 37 ]. Breastfeeding mothers were sometimes unable to determine how much milk their infants consumed (as opposed to seeing how much milk the infant had when bottle feeding), which caused them to feel anxious and uncertain about scheduling infant feedings [ 28 , 37 ]. Women’s inability to overcome these barriers was linked by some researchers to low self-efficacy among mothers, as well as feeling overwhelmed or suffering from postpartum depression [ 38 , 39 ].
In addition to personal and physical challenges experienced by mothers who were planning to breastfeed, the literature also highlighted the importance of social environment as a potential barrier to breastfeeding. Mothers’ personal networks were identified as a key factor in shaping their breastfeeding behaviours in 43 (73%) articles included in this review. In a study published in the UK, lack of role models – mothers, other female relatives, and friends who breastfeed – was cited as one of the potential barriers for breastfeeding [ 36 ]. Some family members and friends also actively discouraged breastfeeding, while openly questioning the benefits of this practice over bottle feeding [ 1 , 17 , 40 ]. Breastfeeding during family gatherings or in the presence of others was also reported as a challenge for some women from ethnic minority groups in the United Kingdom and for Black women in the United States [ 41 , 42 ].
The literature reported occasional instances where breastfeeding-related decisions created conflict in women’s relationships with significant others [ 26 ]. Some women noted they were pressured by their loved one to cease breastfeeding [ 22 ], especially when women continued to breastfeed 6 months postpartum [ 43 ]. Overall, the literature suggested that partners play a central role in women’s breastfeeding practices [ 8 ], although there was no consistency in the reviewed papers regarding the partners’ expressed level of support for breastfeeding.
Knowledge, especially practical knowledge about breastfeeding, was mentioned as a barrier in 17% ( n = 10) of the papers included in this review. While health care providers were perceived as a primary source of information on breastfeeding, some studies reported that mothers felt the information provided was not useful and occasionally contained conflicting advice [ 1 , 17 ]. This finding was reported across various jurisdictions, including the United States, Sweden, the United Kingdom and Netherlands, where mothers reported they had no support at all from their health care providers which made it challenging to address breastfeeding problems [ 26 , 38 , 44 ].
Breastfeeding in public emerged as a key barrier from the reviewed literature and was cited in 56% ( n = 33) of the papers. Examining the experiences of breastfeeding mothers in the United States, Spencer, Wambach, & Domain [ 45 ] suggested that some participants reported feeling “erased” from conversations while breastfeeding in public, rendering their bodies symbolically invisible. Lack of designated public spaces for breastfeeding forced many women to alter their feeding in public and to retreat to a private or a more secluded space, such as one’s personal car [ 25 ]. The oversexualization of women’s breasts was repeatedly noted as a core reason for the United States women’s negative experiences and feelings of self-consciousness about breastfeeding in front of others [ 45 ]. Studies reported women’s accounts of feeling the disapproval or disgust of others when breastfeeding in public [ 46 , 47 ], and some reported that women opted out of breastfeeding in public because they did not want to make those around them feel uncomfortable [ 25 , 40 , 48 ].
Finally, return to paid employment was noted in the literature as a significant challenge for continuation of breastfeeding [ 48 ]. Lack of supportive workplace environments [ 39 ] or inability to express milk were cited by women as barriers for continuing breastfeeding in the United States and New Zealand [ 39 , 49 ].
Supports needed to maintain breastfeeding
Due to the central role family members played in women’s experiences of breastfeeding, support from partners as well as female relatives was cited in the literature as key factors shaping women’s breastfeeding decisions [ 1 , 9 , 48 ]. In the articles published in Canada, Australia, and the United Kingdom, supportive family members allowed women to share the responsibility of feeding and other childcare activities, which reduced the pressures associated with being a new mother [ 19 , 20 ]. Similarly, encouragement, breastfeeding advice, and validation from healthcare professionals were identified as positively impacting women’s experiences with breastfeeding [ 1 , 22 , 28 ].
Community resources, such as peer support groups, helplines, and in-home breastfeeding support provided mothers with the opportunity to access help when they need it, and hence were reported to be facilitators for breastfeeding [ 19 , 22 , 33 , 44 ]. An increase in the usage of social media platforms, such as Facebook, among breastfeeding mothers for peer support were reported in some studies [ 47 ]. Public health breastfeeding clinics, lactation specialists, antenatal and prenatal classes, as well as education groups for mothers were identified as central support structures for the initiation and maintenance of breastfeeding [ 23 , 24 , 28 , 33 , 39 , 50 ]. Based on the analysis of the reviewed literature, however, access to these services varied greatly geographically and by socio-economic status [ 33 , 51 ]. It is also important to note that local and cultural context played a significant role in shaping women’s perceptions of breastfeeding. For example, a study that explored women’s breastfeeding experiences in Iceland highlighted the importance of breastfeeding in Icelandic society [ 52 ]. Women are expected to breastfeed and the decision to forgo breastfeeding is met with disproval [ 52 ]. Cultural beliefs regarding breastfeeding were also deemed important in the study of Szafrankska and Gallagher (2016), who noted that Polish women living in Ireland had a much higher rate of initiating breastfeeding compared to Irish women [ 53 ]. They attributed these differences to familial and societal expectations regarding breastfeeding in Poland [ 53 ].
Overall, the reviewed literature suggested that women faced socio-cultural pressure to breastfeed their infants [ 36 , 40 , 54 ]. Women reported initiating breastfeeding due to recognition of the many benefits it brings to the health of the child, even when they were reluctant to do it for personal reasons [ 8 ]. This hints at the success of public health education campaigns on the benefits of breastfeeding, which situates breastfeeding as a new cultural norm [ 24 ].
This scoping review examined the existing empirical literature on women’s perceptions about and experiences of breastfeeding to identify how public health messaging can be tailored to improve breastfeeding rates. The literature suggests that, overall, mothers are aware of the positive impacts of breastfeeding and have strong motivation to breastfeed [ 37 ]. However, women who chose to breastfeed also experience many barriers related to their social interactions with significant others and their unique socio-cultural contexts [ 25 ]. These different factors, summarized in Fig. 5 , should be considered in developing public health activities that promote breastfeeding. Breastfeeding experiences for women were very similar across the United Kingdom, United States, Canada, and Australia based on the studies included in this review. Likewise, barriers and supports to breastfeeding identified by women across the countries situated in the global north were quite similar. However, local policy context also impacted women’s experiences of breastfeeding. For example, maintaining breastfeeding while returning to paid employment has been identified as a challenge for mothers in the United States [ 39 , 45 ], a country with relatively short paid parental leave. Still, challenges with balancing breastfeeding while returning to paid employment were also noticed among women in New Zealand, despite a more generous maternity leave [ 49 ]. This suggests that while local and institutional policies might shape women’s experiences of breastfeeding, interpersonal and personal factors can also play a central role in how long they breastfeed their infants. Evidently, the importance of significant others, such as family members or friends, in providing support to breastfeeding mothers was cited as a key facilitator for breastfeeding across multiple geographic locations [ 29 , 34 , 48 ]. In addition, cultural beliefs and practices were also cited as an important component in either promoting breastfeeding or deterring women’s desire to initiate or maintain breastfeeding [ 15 , 29 , 37 ]. Societal support for breastfeeding and cultural practices can therefore partly explain the variation in breastfeeding rates across different countries [ 15 , 21 ]. Figure 5 summarizes the key barriers identified in the literature that inhibit women’s ability to breastfeed.
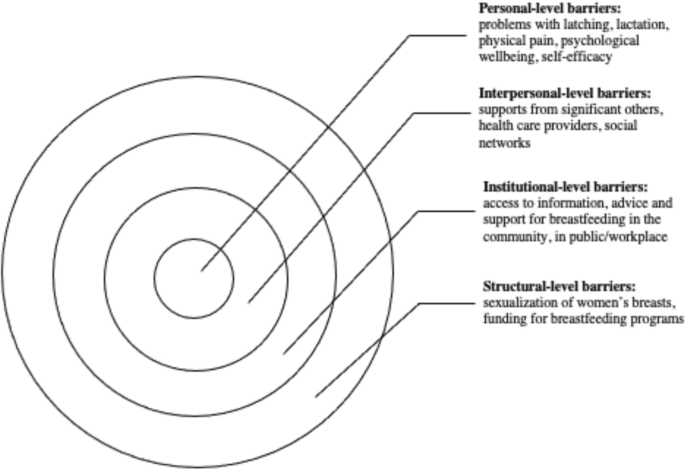
Barriers to Breastfeeding
At the individual level, women might experience challenges with breastfeeding stemming from various physiological and psychological problems, such as issues with latching, perceived or actual lack of breastmilk, and physical pain associated with breastfeeding. The onset of postpartum depression or other psychological problems may also impact women’s ability to breastfeed [ 54 ]. Given that many women assume that breastfeeding will happen “naturally” [ 15 , 40 ] these challenges can deter women from initiating or continuing breastfeeding. In light of these personal challenges, it is important to consider the potential challenges associated with breastfeeding that are conveyed to new mothers through the simplified message “breast is best” [ 21 ]. While breastfeeding may come easy to some women, most papers included in this review pointed to various challenges associated with initiating or maintaining breastfeeding [ 19 , 33 ]. By modifying public health messaging regarding breastfeeding to acknowledge that breastfeeding may pose a challenge and offering supports to new mothers, it might be possible to alleviate some of the guilt mothers experience when they are unable to breastfeed.
Barriers that can be experienced at the interpersonal level concern women’s communication with others regarding their breastfeeding choices and practices. The reviewed literature shows a strong impact of women’s social networks on their decision to breastfeed [ 24 , 33 ]. In particular, significant others – partners, mothers, siblings and close friends – seem to have a considerable influence over mothers’ decision to breastfeed [ 42 , 53 , 55 ]. Hence, public health messaging should target not only mothers, but also their significant others in developing breastfeeding campaigns. Social media may also be a potential medium for sharing supports and information regarding breastfeeding with new mothers and their significant others.
There is also a strong need for breastfeeding supports at the institutional and community levels. Access to lactation consultants, sound and practical advice from health care providers, and availability of physical spaces in the community and (for women who return to paid employment) in the workplace can provide more opportunities for mothers who want to breastfeed [ 18 , 33 , 44 ]. The findings from this review show, however, that access to these supports and resources vary greatly, and often the women who need them the most lack access to them [ 56 ].
While women make decisions about breastfeeding in light of their own personal circumstances, it is important to note that these circumstances are shaped by larger structural, social, and cultural factors. For instance, mothers may feel reluctant to breastfeed in public, which may stem from their familiarity with dominant cultural perspectives that label breasts as objects for sexualized pleasure [ 48 ]. The reviewed literature also showed that, despite the initial support, mothers who continue to breastfeed past the first year may be judged and scrutinized by others [ 47 ]. Tailoring public health care messaging to local communities with their own unique breastfeeding-related beliefs might help to create a larger social change in sociocultural norms regarding breastfeeding practices.
The literature included in this scoping review identified the importance of support from community services and health care providers in facilitating women’s breastfeeding behaviours [ 22 , 24 ]. Unfortunately, some mothers felt that the support and information they received was inadequate, impractical, or infused with conflicting messaging [ 28 , 44 ]. To make breastfeeding support more accessible to women across different social positions and geographic locations, it is important to acknowledge the need for the development of formal infrastructure that promotes breastfeeding. This includes training health care providers to help women struggling with breastfeeding and allocating sufficient funding for such initiatives.
Overall, this scoping review revealed the need for healthcare professionals to provide practical breastfeeding advice and realistic solutions to women encountering difficulties with breastfeeding. Public health messaging surrounding breastfeeding must re-invent breastfeeding as a “family practice” that requires collaboration between the breastfeeding mother, their partner, as well as extended family to ensure that women are supported as they breastfeed [ 8 ]. The literature also highlighted the issue of healthcare professionals easily giving up on women who encounter problems with breastfeeding and automatically recommending the initiation of formula use without further consideration towards solutions for breastfeeding difficulties [ 19 ]. While some challenges associated with breastfeeding are informed by local culture or health care policies, most of the barriers experienced by breastfeeding women are remarkably universal. Women often struggle with initiation of breastfeeding, lack of support from their significant others, and lack of appropriate places and spaces to breastfeed [ 25 , 26 , 33 , 39 ]. A change in public health messaging to a more flexible messaging that recognizes the challenges of breastfeeding is needed to help women overcome negative feelings associated with failure to breastfeed. Offering more personalized advice and support to breastfeeding mothers can improve women’s experiences and increase the rates of breastfeeding while also boosting mothers’ sense of self-efficacy.
Limitations
This scoping review has several limitations. First, the focus on “women’s experiences” rendered broad search criteria but may have resulted in the over or underrepresentation of specific findings in this review. Also, the exclusion of empirical work published in languages other than English rendered this review reliant on the papers published predominantly in English-speaking countries. Finally, consistent with Arksey and O’Malley’s [ 18 ] scoping review methodology, we did not appraise the quality of the reviewed literature. Notwithstanding these limitations, this review provides important insights into women’s experiences of breastfeeding and offers practical strategies for improving dominant public health messaging on the importance of breastfeeding.
Women who breastfeed encounter many difficulties when they initiate breastfeeding, and most women are unsuccessful in adhering to current public health breastfeeding guidelines. This scoping review highlighted the need for reconfiguring public health messaging to acknowledge the challenges many women experience with breastfeeding and include women’s social networks as a target audience for such messaging. This review also shows that breastfeeding supports and counselling are needed by all women, but there is also a need to tailor public health messaging to local social norms and culture. The role social institutions and cultural discourses have on women’s experiences of breastfeeding must also be acknowledged and leveraged by health care professionals promoting breastfeeding.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Wolf JH. Low breastfeeding rates and public health in the United States. Am J Public Health. 2003;93(12):2000–2010. [cited 2021 Apr 21] Available from: http://ajph.aphapublications.org/doi/ https://doi.org/10.2105/AJPH.93.12.2000
World Health Organization, UNICEF. Global nutrition targets 2015: Breastfeeding policy brief 2014.
United Nations International Children’s Emergency Fund (UNICEF). Breastfeeding in the UK. 2019 [cited 2021 Apr 21]. Available from: https://www.unicef.org.uk/babyfriendly/about/breastfeeding-in-the-uk/
Semenic S, Loiselle C, Gottlieb L. Predictors of the duration of exclusive breastfeeding among first-time mothers. Res Nurs Health. 2008;31(5):428–441. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1002/nur.20275
Hauck YL, Bradfield Z, Kuliukas L. Women’s experiences with breastfeeding in public: an integrative review. Women Birth. 2020;34:e217–27.
Hendaus MA, Alhammadi AH, Khan S, Osman S, Hamad A. Breastfeeding rates and barriers: a report from the state of Qatar. Int. J Women's Health. 2018;10:467–75 [cited 2021 Apr 20] Available from: /pmc/articles/PMC6110662/.
Google Scholar
Ogbo FA, Ezeh OK, Khanlari S, Naz S, Senanayake P, Ahmed KY, et al. Determinants of exclusive breastfeeding cessation in the early postnatal period among culturally and linguistically diverse (CALD) Australian mothers. Nutrients. 2019;11(7):1611 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2072-6643/11/7/1611 .
Article Google Scholar
Ayton JE, Tesch L, Hansen E. Women’s experiences of ceasing to breastfeed: Australian qualitative study. BMJ Open. 2019;9(5):26234 [cited 2021 Apr 20] Available from: http://bmjopen.bmj.com/ .
Brown CRL, Dodds L, Legge A, Bryanton J, Semenic S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Heal. 2014;105(3):e179–e185. [cited 2021 Apr 20] Available from: https://link.springer.com/article/ https://doi.org/10.17269/cjph.105.4244
Sharma AJ, Dee DL, Harden SM. Adherence to breastfeeding guidelines and maternal weight 6 years after delivery. Pediatrics. 2014;134(Supplement 1):S42–S49. [cited 2021 Apr 21] Available from: www.pediatrics.org/cgi/doi/ https://doi.org/10.1542/peds.2014-0646H
Walters DD, Phan LTH, Mathisen R. The cost of not breastfeeding: Global results from a new tool. Health Policy Plan. 2019;34(6):407–17 [cited 2021 Apr 21] Available from: https://academic.oup.com/heapol/article/34/6/407/5522499 .
Friedman M. For whom is breast best? Thoughts on breastfeeding, feminism and ambivalence. J Mother Initiat Res Community Involv. 2009;11(1):26–35 [cited 2021 Apr 20] Available from: https://jarm.journals.yorku.ca/index.php/jarm/article/viewFile/22506/20986 .
Blixt I, Johansson M, Hildingsson I, Papoutsi Z, Rubertsson C. Women’s advice to healthcare professionals regarding breastfeeding: “offer sensitive individualized breastfeeding support” - an interview study. Int Breastfeed J 2019;14(1):51. [cited 2021 Apr 20] Available from: https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-019-0247-4
Obeng C, Dickinson S, Golzarri-Arroyo L. Women’s perceptions about breastfeeding: a preliminary study. Children. 2020;7(6):61 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2227-9067/7/6/61 .
Choudhry K, Wallace LM. ‘Breast is not always best’: South Asian women’s experiences of infant feeding in the UK within an acculturation framework. Matern Child Nutr. 2012;8(1):72–87. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2010.00253.x
Da Silva TD, Bick D, Chang YS. Breastfeeding experiences and perspectives among women with postnatal depression: a qualitative evidence synthesis. Women Birth. 2020;33(3):231–9.
Kilanowski JF. Breadth of the socio-ecological model. J Agromedicine. 2017;22(4):295–7 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=wagr20 .
Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=tsrm20 .
Brown A, Lee M. An exploration of the attitudes and experiences of mothers in the United Kingdom who chose to breastfeed exclusively for 6 months postpartum. Breastfeed Med. 2011;6(4):197–204. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2010.0097
Morns MA, Steel AE, Burns E, McIntyre E. Women who experience feelings of aversion while breastfeeding: a meta-ethnographic review. Women Birth. 2021;34:128–35.
Jackson KT, Mantler T, O’Keefe-McCarthy S. Women’s experiences of breastfeeding-related pain. MCN Am J Matern Nurs. 2019;44(2):66–72 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201903000-00002 .
Burns E, Schmied V, Sheehan A, Fenwick J. A meta-ethnographic synthesis of women’s experience of breastfeeding. Matern Child Nutr. 2009;6(3):201–219. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2009.00209.x
Claesson IM, Larsson L, Steen L, Alehagen S. “You just need to leave the room when you breastfeed” Breastfeeding experiences among obese women in Sweden - A qualitative study. BMC Pregnancy Childbirth. 2018;18(1):1–10. [cited 2021 Apr 20] Available from: https://link.springer.com/articles/ https://doi.org/10.1186/s12884-017-1656-2
Asiodu IV, Waters CM, Dailey DE, Lyndon • Audrey. Infant feeding decision-making and the influences of social support persons among first-time African American mothers. Matern Child Health J. 2017;21:863–72.
Forster DA, McLachlan HL. Women’s views and experiences of breast feeding: positive, negative or just good for the baby? Midwifery. 2010;26(1):116–25.
Demirci J, Caplan E, Murray N, Cohen S. “I just want to do everything right:” Primiparous Women’s accounts of early breastfeeding via an app-based diary. J Pediatr Heal Care. 2018;32(2):163–72.
Furman LM, Banks EC, North AB. Breastfeeding among high-risk Inner-City African-American mothers: a risky choice? Breastfeed Med. 2013;8(1):58–67. [cited 2021 Apr 20]Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0012
Cottrell BH, Detman LA. Breastfeeding concerns and experiences of african american mothers. MCN Am J Matern Nurs. 2013;38(5):297–304 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201309000-00009 .
Wambach K, Domian EW, Page-Goertz S, Wurtz H, Hoffman K. Exclusive breastfeeding experiences among mexican american women. J Hum Lact. 2016;32(1):103–111. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334415599400
Regan P, Ball E. Breastfeeding mothers’ experiences: The ghost in the machine. Qual Health Res. 2013;23(5):679–688. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732313481641
Hinsliff-Smith K, Spencer R, Walsh D. Realities, difficulties, and outcomes for mothers choosing to breastfeed: Primigravid mothers experiences in the early postpartum period (6-8 weeks). Midwifery. 2014;30(1):e14–9.
Palmér L. Previous breastfeeding difficulties: an existential breastfeeding trauma with two intertwined pathways for future breastfeeding—fear and longing. Int J Qual Stud Health Well-being. 2019;14(1) [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20 .
Francis J, Mildon A, Stewart S, Underhill B, Tarasuk V, Di Ruggiero E, et al. Vulnerable mothers’ experiences breastfeeding with an enhanced community lactation support program. Matern Child Nutr 2020;16(3):16. [cited 2021 Apr 20] Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/mcn.12957
Palmér L, Carlsson G, Mollberg M, Nyström M. Breastfeeding: An existential challenge - Women’s lived experiences of initiating breastfeeding within the context of early home discharge in Sweden. Int J Qual Stud Health Well-being 2010;5(3). [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20https://doi.org/ https://doi.org/10.3402/qhw.v5i3.5397
Grant A, Mannay D, Marzella R. ‘People try and police your behaviour’: the impact of surveillance on mothers and grandmothers’ perceptions and experiences of infant feeding. Fam Relationships Soc. 2018;7(3):431–47.
Thomson G, Ebisch-Burton K, Flacking R. Shame if you do - shame if you don’t: women’s experiences of infant feeding. Matern Child Nutr. 2015;11(1):33–46. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/mcn.12148
Dietrich Leurer M, Misskey E. The psychosocial and emotional experience of breastfeeding: reflections of mothers. Glob Qual. Nurs Res. 2015;2:2333393615611654 [cited 2021 Apr 20] Available from: http://www.ncbi.nlm.nih.gov/pubmed/28462320 .
Fahlquist JN. Experience of non-breastfeeding mothers: Norms and ethically responsible risk communication. Nurs Ethics. 2016;23(2):231–241. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0969733014561913
Gross TT, Davis M, Anderson AK, Hall J, Hilyard K. Long-term breastfeeding in African American mothers: a positive deviance inquiry of WIC participants. J Hum Lact. 2017;33(1):128–139. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334416680180
Spencer RL, Greatrex-White S, Fraser DM. ‘I thought it would keep them all quiet’. Women’s experiences of breastfeeding as illusions of compliance: an interpretive phenomenological study. J Adv Nurs. 2015;71(5):1076–1086. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/jan.12592
Twamley K, Puthussery S, Harding S, Baron M, Macfarlane A. UK-born ethnic minority women and their experiences of feeding their newborn infant. Midwifery. 2011;27(5):595–602.
PubMed Google Scholar
Lutenbacher M, Karp SM, Moore ER. Reflections of Black women who choose to breastfeed: influences, challenges, and supports. Matern Child Health J. 2016;20(2):231–9.
Dowling S, Brown A. An exploration of the experiences of mothers who breastfeed long-term: what are the issues and why does it matter? Breastfeed Med. 2013;8(1):45–52. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0057
Fox R, McMullen S, Newburn M. UK women’s experiences of breastfeeding and additional breastfeeding support: a qualitative study of baby Café services. BMC Pregnancy Childbirth 2015;15(1):147. [cited 2021 Apr 20] Available from: http://bmcpregnancychildbirth.biomedcentral.com/articles/ https://doi.org/10.1186/s12884-015-0581-5
Spencer B, Wambach K, Domain EW. African American women’s breastfeeding experiences: cultural, personal, and political voices. Qual Health Res. 2015;25(7):974–987. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732314554097
McBride-Henry K. The influence of the They: An interpretation of breastfeeding culture in New Zealand. Qual Health Res. 2010;20(6):768–777. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732310364220
Newman KL, Williamson IR. Why aren’t you stopping now?!’ Exploring accounts of white women breastfeeding beyond six months in the east of England. Appetite. 2018 Oct;1(129):228–35.
Dowling S, Pontin D. Using liminality to understand mothers’ experiences of long-term breastfeeding: ‘Betwixt and between’, and ‘matter out of place.’ Heal (United Kingdom). 2017;21(1):57–75. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1363459315595846
Payne D, Nicholls DA. Managing breastfeeding and work: a Foucauldian secondary analysis. J Adv Nurs. 2010;66(8):1810–1818. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1365-2648.2009.05156.x
Keely A, Lawton J, Swanson V, Denison FC. Barriers to breast-feeding in obese women: a qualitative exploration. Midwifery. 2015;31(5):532–9.
Afoakwah G, Smyth R, Lavender DT. Women’s experiences of breastfeeding: A narrative review of qualitative studies. Afr J Midwifery Womens Health. 2013 ;7(2):71–77. [cited 2021 Apr 21] Available from: https://www.magonlinelibrary.com/doi/abs/ https://doi.org/10.12968/ajmw.2013.7.2.71
Símonardóttir S. Getting the green light: experiences of Icelandic mothers struggling with breastfeeding. Sociol Res Online. 2016;21(4):1.
Szafranska M, Gallagher DL. Polish women’s experiences of breastfeeding in Ireland. Pract Midwife. 2016;19(1):30–2 [cited 2021 Apr 21] Available from: https://europepmc.org/article/med/26975131 .
Pratt BA, Longo J, Gordon SC, Jones NA. Perceptions of breastfeeding for women with perinatal depression: a descriptive phenomenological study. Issues Ment Health Nurs. 2020;41(7):637–644. [cited 2021 Apr 21] Available from: https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/01612840.2019.1691690
Durmazoğlu G, Yenal K, Okumuş H. Maternal emotions and experiences of mothers who had breastfeeding problems: a qualitative study. Res Theory Nurs Pract. 2020;34(1):3–20. [cited 2021 Apr 20] Available from: http://connect.springerpub.com/lookup/doi/ https://doi.org/10.1891/1541-6577.34.1.3
Burns E, Triandafilidis Z. Taking the path of least resistance: a qualitative analysis of return to work or study while breastfeeding. Int Breastfeed J. 2019;14(1):1–13.
Download references
Acknowledgements
The authors would like to acknowledge the assistance of Jackie Stapleton, the University of Waterloo librarian, for her assistance with developing the search strategy used in this review.
Not applicable.
Author information
Authors and affiliations.
School of Public Health Sciences, University of Waterloo, 200 University Ave West, Waterloo, ON, N2L 3G1, Canada
Bridget Beggs, Liza Koshy & Elena Neiterman
You can also search for this author in PubMed Google Scholar
Contributions
BB was responsible for the formal analysis and organization of the review. LK was responsible for data curation, visualization and writing the original draft. EN was responsible for initial conceptualization and writing the original draft. BB and LK were responsible for reviewing and editing the manuscript. All authors read and approved the final manuscript.
Authors’ information
BB is completing her Bachelor of Science (BSc) degree at the School of Public Health Sciences at the University of Waterloo.
LK is completing her Bachelor of Public Health (BPH) degree at the School of Public Health Sciences at the University of Waterloo.
EN (PhD), is a continuing lecturer at the School of Public Health Sciences at the University of Waterloo. Her areas of expertise are in women’s reproductive health and sociology of health, illness, and healthcare.
Corresponding author
Correspondence to Bridget Beggs .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Beggs, B., Koshy, L. & Neiterman, E. Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature. BMC Public Health 21 , 2169 (2021). https://doi.org/10.1186/s12889-021-12216-3
Download citation
Received : 23 June 2021
Accepted : 10 November 2021
Published : 26 November 2021
DOI : https://doi.org/10.1186/s12889-021-12216-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Experiences
- Public health
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

25 Years of Research in Human Lactation: From Discovery to Translation
Donna tracy geddes.
1 School of Molecular Sciences, The University of Western Australia, Crawley, WA 6009, Australia; [email protected] (Z.G.); [email protected] (S.L.P.); [email protected] (L.R.M.); [email protected] (J.C.K.); [email protected] (L.F.S.); [email protected] (C.T.L.); moc.liamg@sidilakasassenav (V.S.); [email protected] (P.E.H.)
Zoya Gridneva
Sharon lisa perrella, leon robert mitoulas.
2 Medela, AG, Lättichstrasse 4b, 6340 Baar, Switzerland
Jacqueline Coral Kent
Lisa faye stinson, ching tat lai, vanessa sakalidis, alecia-jane twigger.
3 Department of Pharmacology, University of Cambridge, Cambridge CB2 1PD, UK; ku.ca.mac@512tja

Peter Edwin Hartmann
Researchers have recently called for human lactation research to be conceptualized as a biological framework where maternal and infant factors impacting human milk, in terms of composition, volume and energy content are studied along with relationships to infant growth, development and health. This approach allows for the development of evidence-based interventions that are more likely to support breastfeeding and lactation in pursuit of global breastfeeding goals. Here we summarize the seminal findings of our research programme using a biological systems approach traversing breast anatomy, milk secretion, physiology of milk removal with respect to breastfeeding and expression, milk composition and infant intake, and infant gastric emptying, culminating in the exploration of relationships with infant growth, development of body composition, and health. This approach has allowed the translation of the findings with respect to education, and clinical practice. It also sets a foundation for improved study design for future investigations in human lactation.
1. Introduction
Breastfeeding is a major determinant of infant short- and long-term health, preventing acute infections and programming lower risk for chronic disease and is therefore considered to be a major public health focus [ 1 ]. Despite the wealth of information on the benefits to both the mother and the infant, global breastfeeding rates remain low, averaging only 41% [ 2 ]. To identify and address the issues faced by the breastfeeding dyad a foundational knowledge of the ‘norm’ is required. In the haste to provide support and solutions, an understanding of the basic science is frequently neglected in favour of the implementation of interventional trials that promise advances in care but are themselves based on an incomplete foundational understanding. The dearth of research into the fundamentals of human lactation over the latter part of the last century, combined with the lack of translation of the limited research actually performed into the medical model, has left clinicians little scope and tools to objectively assess breastfeeding problems. Evidence-based care, established from an understanding of the basic principles of lactation and mammary gland function is imperative to improve breastfeeding rates and subsequently the health and wellbeing of breastfeeding women, infants’, and their families.
The evolution of our research program has been in direct response to the need to fill the translation gap and has been a journey from basic research into the anatomy, function of the breast and milk composition to multidimensional translational research elucidating mechanisms by which breastfeeding confers a multitude of benefits. These studies have provided the foundation for the development of successful interventions for those mothers experiencing lactation difficulties and have informed and reassured those women, particularly first-time mothers, that they are ‘normal’. This road has not been smooth, with findings that have disrupted the field requiring the reassessment of conventional dogma and change of deep-seated beliefs. Importantly, the rewards of change have been tangible and impactful for mothers and their babies. This review traces the main focal points of our research programme over the last 25 years and takes a biological systems approach by tracking breast milk from the mother (the breast) to the infant ( Figure 1 ) [ 3 ] and aims to highlight and document these findings in the broader context of mammary gland function and the breastfeeding dyad, in order to provide a holistic platform of knowledge from which others may continue to work from in their pursuit to define better health outcomes for the next generation [ 4 ].

An overview of the structure of the review of our research programme from a biological systems perspective.
2. Breast Anatomy
Despite the breast being the sole source of nutrition for the infant, this organ is rarely studied in its functional state. Interestingly, one of the most thorough investigations comes from over 180 years ago, by renowned anatomist and surgeon Sir Astley Cooper. This work, published in 1840, is a remarkable description of the anatomy of the lactating human breast and was performed in response to a request to document diseases of the breast. Cooper asserted that knowledge of basic anatomy was critical to the understanding of breast anomalies and disease. As such, he proceeded to meticulously investigate the anatomy of the breast, sourcing breasts for dissection from the corpses of women who had died during lactation. For over 150 years, Cooper’s work was the most complete examination of the lactating breast with his work most notable for its depictions of the ductal structures of the breast, obtained by the delicate dissection of the mammary ductal system after the injection of coloured wax into the ducts of the nipple [ 5 ] ( Figure 2 ). His contribution is memorialised via the eponymously named Cooper’s ligaments that provide a framework for the tissues of the breast.

Sir Astley Cooper’s illustrations of the ductal system of the lactating breast. Duct were injected with coloured wax prior to dissection [ 6 ].
The macro-anatomy of the lactating breast may be described by its external and internal components. The external structures: skin, areola, Montgomery tubercles and nipple exhibit wide variation in size and colour amongst women. Internally the main tissues of the breast consist of the glandular-ductal system, adipose tissue and extracellular matrix supported by the fibrous Cooper’s ligaments. Like the external structures, the internal structures of the breast are also variable between women in terms of volume of tissues. At the cellular level, the glandular-ductal system consists of hundreds of alveoli, each comprised of a bilayer of luminal and basal cells. The luminal cells consist of mammary epithelial cells or lactocytes that serve to synthesise and secrete milk into the lumen of the alveolus. The alveoli are surrounded by a network of myoepithelial cells that contract at milk ejection (ME), to expel the milk from the alveoli into the milk ducts, thus making it available to the infant.
As originally depicted by Cooper, the ductal structures within the breast are arranged in a complex network. Each alveolus is connected to this network via a ductal outlet and the diameters of these lactiferous ducts progressively increase in size as they get closer to the nipple where they narrow once more as they pass through the nipple, therefore providing a mechanism to prevent the escape of milk. A key aspect of Cooper’s work was the presence of lactiferous sinuses, ducts distended with milk just beneath the areolae. According to Cooper, the areola was considered an extension of the nipple and had three main functions: to give a greater adhesion to the infant’s lips; add to the sensibility and connectivity of the areola with mammary gland; and an area embraced by the infant’s lips and into infant’s mouth from where the lactiferous sinuses behind the areola can be emptied by the pressure of the lips of the infant [ 5 ]. In other words, it was believed that milk transfer to the infant was executed by the lips of the infant when applying a compressive pressure around the areola. This observation highlighted Cooper’s assertion that knowledge of the anatomy of the mammary gland was important for understanding function and formed the basis of milk removal theory for over a century.
The contribution of advanced imaging techniques such as the non-invasive approach of ultrasonography built upon the remarkable work performed by Cooper and has, at the same time, updated some of the interpretations of the previous model, leading to our current understanding of breast anatomy [ 7 ] and has impacted the clinical appraisal of milk removal. Ramsay et al. used ultrasound to image both breasts to determine the number of main ducts, duct morphology and distribution of glandular and adipose tissue. Milk ducts, observed in a resting state, were identified at the base of the nipple and were superficial and easily compressible lending support to anecdotal reports of tight bras or seat belts blocking ducts and causing milk stasis [ 8 ]. The average number of ducts exiting the nipple was nine with a range from as few as four to as many as 18, less than the 20–25 typically stated and consistent with observed milk jets during pumping [ 9 ]. Resting milk duct diameters are small (2 mm, range 1.0–4.4 mm) and similar in size to non-lactating duct diameters except for the significant dilation observed at ME. The lower number and smaller diameters of the ducts compared to Cooper’s work suggests that for some women who exhibit poor lactation outcomes after surgical procedures, it is the severing of the majority of ducts that that is contributing to low supply issues. Importantly, neither the number of the ducts nor the mean diameter of the ducts were related to nipple diameter providing evidence that the internal breast morphology is not predicted by the external anatomy of the breast [ 7 ].
During pregnancy there is an increase in size, length and elasticity of the nipple which varies widely between women [ 10 ] with reported nipple diameters of 15.7 ± 1.8 mm and 15.8 ± 2.8 mm for the left and right nipples respectively [ 11 ]. As the infant’s mouth accommodates the nipple, the size and shape of the nipple are clinically important for the infant to attach adequately to the breast.
Importantly, Ramsay’s study highlighted the absence of lactiferous sinuses superficial to the areolae, a result in contrast to Cooper’s observations but one that was subsequently confirmed by Gooding et al. with three-dimensional ultrasound imaging [ 12 ]. Furthermore and again in contrast to Cooper‘s reports, which have underpinned the long-held understanding of breast anatomy and breastfeeding physiology, all of the observed ducts branched from the areola, under the nipple and only very small volumes of milk (1–10 mL) could be expressed from them in the absence of ME, suggesting the function of the ducts is to transport rather than store milk. Cooper’s injection of coloured wax/glue through the nipple ductal outlets combined with our observation that the ducts are extremely elastic likely provided for an expanded wax representation of the ductal system leading to the erroneous depiction of lactiferous sinuses and an overestimation of the volume of milk that would be stored under the areola. These findings explain the variation in volumes of milk removed both in the colostral phase where the milk volume is low and viscous ( Figure 3 ) and prior to milk ejection in established lactation.

New understanding of the anatomy of the lactating breast. ( a ) Coopers ligaments ( b ) superficial and retromammary fat layers ( c ) milk duct system ( d ) macro anatomy of the breast. © Medela AG 2006. Used with permission.
As mentioned previously, internally the breast consists primarily of glandular and adipose tissue, with some connective tissue as well as the myoepithelial (smooth muscle) network surrounding the alveoli. The proportions of glandular and adipose tissue were found to be in an approximate ratio of 2:1 and was similar within women. However, there is wide variation between women for glandular tissue 65 ± 11% (45–83%) and 63 ± 9% (46–83%), and adipose tissue (37 ± 9% (16–51%) and 35 ± 12% (9–54%) for right and left breasts respectively). Interestingly, 24 h milk production was not correlated with the amount of glandular tissue, number of milk ducts, duct diameters or storage capacity of the breast. Given that storage capacity is a reflection of the amount of glandular tissue, the finding that some breasts are comprised of up to 50% adipose tissue suggests that it is possible that some larger breasts may actually have a lower storage capacity than otherwise expected and may account for the unexpected frequent feeding observed in these dyads. In total, these findings reaffirm the evidence that for physiologically normal breastfeeding women, milk production is driven by the interplay of the infant’s appetite, frequency and efficacy of milk removal, and maternal anatomy. This seminal work has redefined our understanding of breast anatomy in lactation, thus impacting our knowledge of breastfeeding physiology and management of breastfeeding problems.
3. Milk Ejection
The ME reflex is highly conserved across all mammalian species from monotremes and marsupials to the placental mammals [ 13 ]. In women it is critical to the success of lactation as little to no milk can be removed from the breast prior to ME, thus milk synthesis is downregulated in the absence of ME.
The ME reflex is a neuroendocrine reflex is triggered by nipple stimulation sending neural impulses to the hypothalamus stimulating the release of oxytocin from the posterior pituitary gland into the maternal bloodstream. Oxytocin then travels via the maternal circulation to the mammary gland, causing the contraction of the myoepithelial cells surrounding the alveoli [ 14 ] forcing milk through the ductal system towards the nipple for removal by the infant or a breast pump [ 15 ]. The force of the milk flow dilates the ducts and increases positive pressure within the ducts [ 16 , 17 , 18 , 19 ]. This reflex, occurs within 60 s and 90 s for breastfeeding and pumping respectively [ 17 , 20 ] in both breasts simultaneously [ 21 ], with slight discrepancies due to binding of oxytocin to fuller alveoli [ 22 ]. Milk ejection is transient lasting 45 s to 3.5 min [ 17 , 23 ] with multiple MEs measured during a feed or pumping session (breastfeeding: 2.5; breast pumping: 4.4) [ 18 , 24 ].
Employing measurement of ME with ultrasound imaging ( Figure 4 ) or measurement of milk flow rates [ 8 , 18 , 21 ] we have shown that while ME is individualised it is highly conserved within women [ 25 ] such that ME patterns remain consistent between breasts, between breastfeeding and pumping, with different pumping patterns, between weeks and across lactation (9 months) [ 26 ]. Thus, it appears that differences in the source of stimulation of the breast/nipple in women in established lactation does not alter the ME reflex. Replication of the ME patterns in subsequent lactations has also been observed, [ 27 ] building on the hypothesis that ME is innate. This finding also suggests that it is the requirement of the infant to adapt to the mother’s ME pattern and changing rates of milk flow in order to remove milk effectively and efficiently from the breast [ 28 ]. The volume of milk removed by the infant is likely then governed not only by infant appetite but also by the combination of the volume of milk stored in the breast and its availability as a result of the ME pattern, as an increasing number of MEs during a breastfeed is related to higher volume of milk consumed [ 15 ].

Ultrasound images of milk ducts pre-milk ejection ( a ) and post-milk ejection ( b ). Milk ducts are imaged as black (anechoic). Post milk ejection the ducts are expanded with breast milk (Geddes et al., unpublished).
In relation to milk removal during pumping, the majority is removed during the first two MEs (76–86%) [ 29 ] emphasising that the switch from ‘stimulation’ mode to ‘expression’ mode should be made as soon as ME occurs to maximise the removal of milk early in the expression when intraductal pressure is at its highest [ 16 ]. Further, when the expression pattern was changed mid pumping, it did not always coincide with a ME suggesting the change of pumping stimulus does not necessarily increase the likelihood of precipitating a ME [ 30 ].
To date we have utilised ultrasound imaging and milk flow measurement [ 16 , 26 , 31 ] as well as having explored alternative technologies such as bioimpedance spectroscopy and thermal imaging [ 31 , 32 ] for the detection of ME. Bioimpedance applied to the pumped breast detected the initial ME 90% of the time [ 23 ]. Temperature however was not successful as we were unable to detect a change in nipple temperature on the non-pumped breast during breastfeeding or pumping, [ 33 ] despite the hypothesis that the release of oxytocin would result in a change of nipple temperature. It will be important to further pursue these detection technologies as development of methods to identify and assess ME may provide breastfeeding mothers and clinicians with biofeedback on ME function as well as supporting the development of breast milk expression innovations.
4. Secretory Activation
Secretory activation (SA) marks the beginning of copious milk production and occurs within 48–72 h after birth commensurate with the rapid decline in progesterone after the delivery of the placenta [ 34 ]. The sensation of breast fullness lags the biochemical changes associated with SA by up to 30 h [ 35 ]. The most marked changes in milk composition at SA are the decreases in milk sodium and protein concentrations accompanied by the increases in lactose and citrate concentrations [ 34 ]. These changes are due to both closure of tight junctions between lactocytes (sodium) as well as increased milk synthesis (lactose, protein, citrate) [ 35 ]. Delayed SA, i.e., beyond 72 h, has been associated with suboptimal lactation outcomes such as lower milk production and reduced duration of breastfeeding. While long labours, caesarean section, and obesity have been associated with delayed SA [ 36 , 37 ] we found no evidence of delayed SA in women delivering by vaginal or caesarean section nor with analgesic administration during caesarean births [ 38 ]. Similarly, Cregan et al. found no difference in concentration of milk citrate, lactose, protein, and sodium from mothers of term and preterm infants [ 39 ]. However, there was greater variation in these markers for preterm mothers and milk production was related to how many markers were in the normal range by Day 5 [ 39 ] in that women with fewer markers in the normal range had the lowest milk productions. The significance of these data are that previously SA was considered a discrete event with failed SA attributed to either hormonal causes, e.g., no drop in progesterone due to retained placenta, or glandular causes, e.g., insufficient mammary tissue [ 40 ]. The observation by Cregan et al., that mothers can have some markers in the normal range and others not, indicated for the first time that the concept of a compromised SA was possible. Hoban et al. have extended this work to daily sampling for 14 days post-partum for mothers delivering preterm and found that 40% of the samples had normal concentrations of SA biomarkers with only a third of women reaching adequate milk volume by day 14 [ 41 , 42 ]. Interestingly, sodium appeared to most predictive of low milk volumes [ 42 ]. In this connection, small ion-selective probes are readily available to measure sodium in milk and have been validated against bench biochemical methods providing the potential for a point-of-care instrument [ 43 ] to monitor the initiation of lactation. This ability to measure markers early in lactation provides the clinician an opportunity to increase support and care of those mothers with known risk factors to maximise their likelihood of successfully establishing a milk production.
Early initiation of breastfeeding and/or pumping has been shown to reduce delayed SA in at risk mothers [ 44 ]. In addition, for women pumping their milk in the first 3 days after term and preterm birth, the application of an initiation pattern modelled on the sucking characteristics of a term infant has been shown to improve milk production [ 45 , 46 ]. These findings all underscore the importance of frequent and efficient milk removal (feeding or pumping when separated from the infant) in the first days after birth to establish a robust milk production to meet the needs of the infant [ 42 , 46 , 47 ].
5. Milk Production
Whilst the growth, health and development of the breastfed infant depends upon an adequate milk production it is rarely measured in both the research and clinical setting despite clinician estimates of milk transfer being shown to be inaccurate [ 48 ] and perceived low milk supply being a major cause of early weaning [ 47 ]. Indeed, we have found that perceived insufficient milk supply accounts for close to half (44%) of the women attending a tertiary hospital breastfeeding centre for advice. For these mothers, the major concern was that the infant did not seem satisfied after a breastfeed. This perception of an insufficient milk supply improved in a small subset of mothers who were surveyed after receiving targeted lactation advice despite lack of confirmation of increased milk production [ 49 ]. Three methods are available to measure milk production: deuterium dilution [ 50 , 51 ], test weighing [ 52 ] and hourly pumping [ 53 , 54 ], with all methods having advantages and disadvantages. Deuterium dilution does not provide information about breastfeeding patterns and has a long analysis time and requires specialist equipment, precluding its use as a routine clinical tool. However, test weighing allows investigation of breastfeeding patterns as well as the effectiveness of milk removal by the infant with instantaneous results. The hourly pumping technique offers an alternative in cases where a mother is not able to carry out test weighing but requires the infant to be fed expressed milk [ 53 , 55 ] and still needs more formal validation before it can be considered for routine use [ 54 ]. As such, 24 h test weighing has underpinned many of the research studies in our laboratory.
After birth frequent and effective milk removal is critical to the establishment and maintenance of milk production [ 56 , 57 ], with milk production established by week 1 to 2 [ 58 ] and production at week 2 being indicative of production at 6 weeks [ 59 ]. In a landmark paper by Kent et al. normal breastfeeding patterns and total fat intake were documented for mothers exclusively breastfeeding infantsbetween one and six months of lactation and showed a wide variation of milk productions while still providing adequate milk and fat intakes ( Table 1 , Figure 5 ) [ 60 ]. The results suggest that for this population of mother, advice should not be given to schedule breastfeeding or to shorten or prolong feeds and that prioritizing so call ‘hind milk’ over ‘fore milk’ is unfounded. Interestingly, it was shown that night feedings (10 p.m.–4 a.m.) were common, with 100% of infants under 9 weeks of age feeding at night. Furthermore, those infants consumed a significant portion of their 24 h intake (20%) during this night feed timeframe, highlighting caution when considering ‘sleep training’ as this could impact not only milk intake but also down regulate milk production. This work was extended to show that milk production did not change significantly over the first 6 months of lactation in exclusively breastfeeding women [ 61 ] indicating that recommendations to increase milk intake and energy intake according to the infant’s age is not appropriate for fully breastfed infants. Intriguingly, several studies have shown one breast is often more productive than the other with that breast often the right breast [ 60 , 62 , 63 , 64 ] whilst others have found no difference between the breasts [ 65 ]. Given these differences in milk production/milk intake from each breast, it is important that the calculation of infant intake of any milk component should be made for each breast separately [ 63 , 65 ].

( a ) Milk production of 792 mL with infant intake consisting of paired and single breastfeeds. ( b ) Milk production of 967 mL where the infant consumed 849 mL from the breast, 88 mL was expressed (Exp R + Exp L) and the infant consumed 108 mL of expressed breast milk (EBM).
Breastfeeding characteristics measured for 71 exclusively breastfeeding dyads in Western Australia, term infants 1 to 6 months old. Single breastfeed: breastfeed from one breast, breastfeeding session: breastfeed from more than 1 breast.
Whilst these data documented the ‘norm’, the 24 h test weighing method was used at a tertiary hospital breastfeeding centre for mothers with breastfeeding problems to determine the proportion of mothers who actually had low milk production (defined as less than 440 mL/day). It was found that 46% of mothers had low production between days 6 and 13 and 45% of mothers had a low milk production between days 14–28 respectively [ 58 ]. When viewed in light of the previously mentioned 44% of mothers with a perception of low milk supply, it shows the importance of being able to accurately assess milk production in these women as often their perceptions can be well founded. However, test weighing is often met with resistance because of the notion that maternal confidence will be negatively impacted. The results of a survey of 203 women dispelled this idea, in that 66% of women were still confident and 11% improved their confidence in breastfeeding after completing a 24 h production measurement. Importantly, those that lost confidence all had milk productions well below 478 mL/24 h (minimum documented milk production in Kent et al., 2006 [ 60 ]) suggesting that this method can be used routinely by clinicians to instigate clinical intervention when necessary [ 66 ] and without fear of negatively impacting maternal confidence. This is aptly demonstrated in a case-study of a breastfeeding baby with Down’s Syndrome where due to initial concerns in hospital the infant was supplemented with formula and expressed milk in but returned home exclusively breastfeeding. Maternal concerns about milk production were confirmed with 546 mL/24 h at 4 weeks and this improved with additional expressions to 819 mL/24 h at 10 weeks. The increase in milk intake was reflected in adherences to the appropriate growth trajectory. By 24 weeks this mother was fully breastfeeding 924 mL/24 h [ 67 ]. Further, we have found that women who have perceived insufficient milk supply and received clinical lactation support generally had improvement in their perceptions. However, infant unsettledness after a feed and formula supplementation was still prevalent indicating that measures of milk production may be useful in determining patterns of milk removal [ 49 ].
Many factors are believed to impact milk production such as age, parity, and infant sex. Recent studies have shown no reduction of milk production with increasing maternal age with those between 15 and 37 years and [ 68 ] those between 23 and 42 years having an average milk production of 750 to 800 mL [ 69 ]. Similarly, there is no strong evidence yet of an increased milk production in women with higher parity, despite the demonstration in an animal model of epigenetic memory in mammary epithelial cells in subsequent lactations resulting in a more robust onset of lactation and volume [ 70 ]. It is recognised however, that infant sex appears to influence milk production in that boys on average consume 80–100 mL more than girls and this is also reflected in the storage capacity of the breast being greater for mothers of boys [ 60 ].
6. Breast Anatomy and Milk Production
Breast hypoplasia (unilateral or bilateral) [ 71 ] impacts up to 25% or women [ 72 ] and typically results in under or disorganised breast development resulting in limited milk supply despite efforts to increase frequency of feeding and expression. Whilst hypoplasia is linked to genetic causes, such as zinc transporter mutations [ 72 ] there are currently no tests, genetic or otherwise to confirm hypoplasia and its link to low milk production.
The storage capacity of the breast is highly variable between women ranging from 74 to 382 mL (mean around 180 mL) [ 60 ]. The more milk available to the infant in the breast the greater the volume the infant tends to receive thus women with smaller storage capacities may need to feed more frequently than those with higher storage capacities. In cases of very high frequency of feeding measurement of 24-h milk production would be warranted.
Low production is also documented with women that have had breast surgery, trauma, or nipple piercing. These procedures often sever milk ducts, thus disrupting milk removal and, over time, potentially isolating glandular tissue, causing milk stasis and ultimately apoptosis and regression of the tissue. Alternatively, in some instances breast implants may have been inserted into breasts that were already hypoplastic [ 73 , 74 , 75 , 76 ].
7. Breast Physiology
Typically, breast growth is obvious in pregnancy due to proliferation of glandular tissue and the differentiation lactocytes to produce milk [ 10 , 77 ]. Breast size however is not indicative of milk production although women with smaller breasts are more likely to have smaller storage capacities and therefore feed more frequently than those women with larger breasts [ 77 ].
Increasing evidence also suggests that pregnancy complications such as gestational diabetes mellitus, preeclampsia, gestational hypertension [ 78 ], and fetal growth restriction [ 79 ] are associated with shorter durations of breastfeeding. While caesarean section has been associated with delayed initiation of breastfeeding, in those women that breastfeed secretory activation [ 38 ] and any breastfeeding at 6 months appears to not differ between caesarean section and vaginal delivery [ 80 ]. In addition, women experiencing postpartum haemorrhage, including those that receive a blood transfusion in hospital, also show reduced breastfeeding at discharge, irrespective of haemoglobin concentration pre-transfusion and persistence of anaemia post transfusion [ 81 , 82 ].
Mastitis or inflammatory lactating breast conditions often result in increased permeability of the alveolus, evidenced by increased human milk (HM) sodium, chloride, lactoferrin, serum albumin concentrations and decreased HM lactose and glucose as well as increased 24-h excretion of lactose, blood, and milk C-reactive protein [ 83 , 84 , 85 ]. Furthermore, we have observed greater numbers of immune cells and expression of immune proteins such as granzyme B [ 86 ] in the milk of women with mastitis. Many of the changes in milk composition seen with mastitis are observed with perceived and measured low milk supply supporting maternal reports of reduced milk supply with mastitic episodes [ 83 ].
Blocked ducts are also commonly experienced during lactation and can be associated with engorgement and inflammatory symptoms [ 87 ], yet little is understood about the causes and effective treatments [ 88 ]. Whilst a blocked duct may resolve in 24 h with increased milk removal and massage, non-resolution of these breast masses should cause concern and initiate imaging investigations such as ultrasound to exclude other causes such as fibroadenomas, cysts, lymph nodes and malignancy [ 89 ].
8. Medications
Few medications have been shown to impact milk production either positively or negatively Pseudoephedrine hydrochloride a common over-the-counter decongestant medication, was found to reduce milk production by up to 24%, due to a potential reduction in maternal serum prolactin levels [ 90 ]. Conversely a pharmaceutical galactagogue such as domperidone, which increases prolactin, can provide a modest increase in milk production of on average 100 mL, in a dose dependent manner [ 91 ]. Although it is not clear whether this increase in milk volume is confounded by the increased emptying of the breast [ 92 ]. Indeed large increases in milk production by domperidone, may not be achievable during established lactation, due to the absence of a relationship between prolactin and short-term rates of milk synthesis [ 64 ]
9. Factors Impacting Milk Removal
Frequent, effective milk removal from the breast is the mainstay for the establishment and maintenance of milk production. For the breastfeeding dyad a feeding frequency of at least 7 × 24 h in the first 2 weeks after birth is associated with establishment of an adequate milk production [ 57 , 93 ] while in established lactation breastfeeding frequency is 11 breastfeeds or 8 breastfeeding sessions [ 60 ]. While ‘normal’ feeding frequency has been characterised there are few methods by which to gauge efficacy of milk removal. The volume of milk removed from the breast is not indicative of effectiveness of emptying because it does not consider the amount of milk stored in the breast, or ‘degree of breast fullness’ and this varies significantly over a 24 h period within and between women. A more accurate estimation is the percentage of available milk removed (PAMR) from the breast which; is estimated from the breast storage capacity and degree of fullness of the breast before the feeding/expression [ 94 ]. On average the term infant removes 67% of the available milk during a breastfeed whereas expression with a hospital grade electric breast pump removes on average 55–75% [ 95 , 96 , 97 , 98 ]. Data for the effectiveness of personal use pumps and hand expression are not available, although evidence suggests that significantly higher milk volumes are expressed with a hospital grade pump when compared to hand expression [ 99 ].
Many factors potentially impact milk production ( Table 2 ) for example mother and infant separation in hospital restricts access to the breast for the infant to breastfeed, decreases skin-to-skin contact and reduces breastfeeding [ 100 ]. Indeed, in the recent COVID pandemic women with COVID-19 were separated from their infants initially until it was realised that vertical transmission of the virus through milk did not occur [ 101 ]. In cases of separation, it is critical that the mother continues to effectively remove milk from the breast either by hand expression or by using a pump to establish milk production as reduced feeding in the first 2 weeks has also been associated with lower milk production [ 59 ]. The mothers of preterm infants often experience a quadrupled burden with a pregnancy complication (e.g., pre-eclampsia), disrupted development of the breast, separation from their infant, and inability of the infant to remove large volumes of milk from the breast thus rely expression of milk to establish and maintain their milk supply. For exclusively pumping women, so often the situation for mothers of preterm infants, there is limited information on the frequency of milk removal required to maintain an adequate production. Our study of exclusively pumping preterm mothers indicates that extension of pumping intervals slows the rate of milk synthesis such that the synthetic rate was significantly slower beyond 7 h. In this connection, the amount of milk removed at each pumping episode increased from 2 to 6 h intervals, reaching a plateau at 7 h. Further, while it appears that a minimum of 5 expressions/24 h is necessary to maintain milk production, increased frequency is warranted for those that have not established a full production given the high observed inter-individual variation [ 102 ].
Risk factors for low milk production.
The frequency and effectiveness of feeding at the breast can also be hampered by several intra-oral anomalies. Our studies have shown that some infants with ankyloglossia (tongue tie) are able to sustain an adequate milk production when breastfeeding [ 103 ] whereas, others are unable to [ 104 , 105 ]. In this regard, frenotomy for an anterior tongue tie has been shown to improve production, albeit in a small number of babies [ 104 ]. More recently cases of tongue tie have appeared with increased frequency, most likely driven by the increased diagnosis of posterior tongue tie. However, the subsequent increase in frenotomy [ 106 ] have raised concerns about increased post-surgical complications [ 107 ]. Furthermore, preliminary evidence suggests that milk production can remain compromised in a number of infants after frenotomy for posterior tongue tie, indicating other potential causes of insufficient supply [ 108 ]. These studies have provided the impetus for revision of the anatomy of the lingual frenulum [ 109 , 110 , 111 ], definitions and clinical protocols for ankyloglossia [ 112 ], and attempts with non-surgical methods to improve breastfeeding in infants diagnosed with ankyloglossia [ 113 ].
There are other infant anomalies that typically affect the infant’s ability to generate sufficient vacuum, which we have shown to be instrumental for effective milk removal [ 114 ]. Typically, infants that have difficulty creating vacuum such as those born preterm, infants with low tone, Down’s syndrome, and cleft lip/plate have reduced milk removal [ 69 , 115 , 116 ]. In contrast, those infants of mothers experiencing pain during breastfeeding often apply very strong vacuums (Baseline vacuum: control: −52 mmHg, Pain: −95 mmHg; Peak vacuum: control: −171 mmHg; Pain: −238 mmHg) during breastfeeding and milk volume is reduced (Control: 78 mL; Pain: 55 mL) either due to altered tongue dynamics [ 117 ], the strong vacuum itself or reduction of the efficacy of milk removal due to diminished oxytocin release at ME reflex as a result of the pain [ 118 ].
Pump settings influence effectiveness and efficiency of milk removal. For example, it is only possible to remove substantial volumes of milk from the breast during ME. Thus, the effective simulation of ME has been a focus of both manual and electric pumping where patterns have been designed to mimic the breastfeeding infant’s rapid sucking at the beginning of the feed [ 119 ]. We have tested multiple patterns and found that faster patterns (>100 cycles/min) elicited ME more quickly than slower patterns [ 20 ]. Interestingly there did not seem to be an effect of stronger vacuum in the time to trigger an ME. However, this was not assessed systematically within a mother, thus it would be prudent for each mother to set the pump at her maximum comfortable vacuum.
The strength of both infant intra-oral vacuum [ 95 , 114 ] and pump expression vacuum are implicit in efficacious milk removal [ 29 ]. Stronger vacuums during pumping increase milk flow rate, volume pumped and the cream content at the end of the expression session as well indicating better breast emptying. Thus it is important for women that need to pump their milk to test their maximum comfortable vacuum over time as often women are more sensitive in the immediate days post-partum [ 120 ]. Efficacy of milk removal has been shown to be significantly higher with breast pumps compared to hand expression [ 115 ] most likely due to the absence of vacuum during hand expression and the reliance on internal positive pressure within the milk ducts only [ 16 ]. In this connection, weak vacuums applied by the infant during breastfeeding may also negatively impact milk removal, requiring additional expression to achieve adequate breast emptying to maintain or establish milk production [ 67 , 116 ]. Furthermore, double pumping is more efficacious when compared to sequential single pumping, with milk removed during more milk ejections during double pumping [ 21 ].
For the mother using a breast pump, the breast shield is the interface between the pump and the breast. As such, shield shape, size and characteristics can influence effectiveness of milk removal [ 19 , 121 ]. Based on the fact that warmth is applied to the nipple by the breastfeeding infant, we investigated whether the application of warmth to the breast shield would promote more efficient milk removal [ 95 ]. We found that the time to remove 80% of the milk pumped was decreased (4.8 versus 6.8 min) indicating many women could pump for shorter periods of 5–8 min under these conditions. Ultrasound imaging supported the results by showing a significant reduction in nipple duct diameter with cold versus warm ultrasound gel.
In more recent pumping and breastfeeding studies, we measured nipple haemodynamics using infrared imaging as a proxy for blood flow [ 33 , 122 ]. Nipple temperature increased during both breastfeeding and pumping. For each 1 °C increase in nipple temperature, an additional 10 mL of milk was removed during pumping. It is not clear whether this increase in temperature is due to the vasodilatory action of oxytocin, local vasodilators, relaxation of the muscle fibres in the nipple or heating caused by nipple movement in the breast shield during pumping [ 98 , 123 , 124 ]. Further, infrared imaging may have potential to identify atypical nipple responses to feeding/pumping, nipple oedema, and inflammation that may hinder effective milk removal from the breast [ 33 ].
Collectively these results suggest rapid stimulation patterns, stronger vacuums, warmth, and comfort improve efficacy of milk removal by both the infant and the breast pump.
10. Sucking Swallowing and Breathing
Infant sucking is the primary means of receiving nutrition, soothes the infant and provides the first oromotor exploration experiences [ 125 ].
Sucking requires a complex combination of rhythmic movements of the jaw, hyoid bone, lips, tongue, soft palate, to coordinate with swallowing and breathing. Key anatomical differences exist between the infant and adult oral cavity to facilitate breastfeeding. The infant’s feeding method impacts growth and development of the jaw and facial structures, with breastfed infants developing less non-nutritive sucking habits and functional disorders such as mouth breathing or atypical swallowing when compared to bottle fed infants [ 126 , 127 , 128 ].
11. Dynamics of Breastfeeding
For many years it was believed that the primary driver of milk removal from the breast was positive pressure with the infant exerting a peristaltic tongue movement to squeeze milk from the ducts, with additional pressure applied by the mandible. When a sufficient bolus volume collected in the oral cavity the medial tongue then moved the milk bolus to the oral pharynx using a backward-moving wave like motion. The premise for this theory was based on the existence of lactiferous sinuses that stored substantial volumes of milk. More recent evidence has shown that lactiferous sinuses are absent and that the main milk ducts do not in fact store large volumes of milk. Rather, the ME reflex is critical to transporting milk from the alveoli to the ducts making it available for effective milk removal [ 123 , 124 , 129 ].
Seminal studies conducted in our lab that have simultaneously measured intra-oral vacuum and provided real time ultrasound imaging of the infant tongue during breastfeeding have shown that the application of vacuum is critical to milk removal from the breast. The studies have shown that the breastfeeding infant places the mouth over the nipple and areola to create a seal and enable attachment to the breast. The infant applies a baseline vacuum (−64 ± 45 mmHg) with the tongue resting in apposition with the nipple and soft and hard palate. The application of baseline vacuum elongates the nipple, positioning it close to the nipple hard-soft palate junction (NHSPJ). When the tongue is lowered the posterior tongue and palate move in unison and vacuum strength increases (145 ± 58 mmHg) with the nipple moving towards the NHSPJ ( Figure 6 ). The nipple expands, rendering the nipple ducts visible on ultrasound, and milk flows into the oral cavity that is bounded by the nipple, palate, and tongue. As the tongue elevates, milk ‘slides’ under the soft palate and is cleared from the oral cavity before the tongue returns to the palate. [ 130 , 131 ] ( Figure 7 ). We did not observe wave-like or peristaltic movements of the tongue or squeezing of milk out of the nipple and this has since been confirmed by others [ 131 , 132 ]. The significance of vacuum as the primary mechanism of milk removal has also been demonstrated in studies using an electric breast pump. Mothers who pump at their strongest comfortable vacuum express more milk, more quickly than with weaker vacuum levels [ 29 ]. Furthermore, when infants were fed expressed breast milk from a vacuum release teat, they used a tongue motion similar to breastfeeding and consumed comparable volumes of milk [ 133 ]. Of note however the peak and baseline vacuums were weaker than that of breastfeeding most likely due to differences in the structure of the nipple and teat.

Cyclic vacuum created by a breastfeeding infant. Baseline vacuum is the vacuum required to hold the nipple in place, elongate the nipple and seal to the breast. Peak vacuum is the strongest vacuum created by lowering the tongue during breastfeeding (Geddes et al, unpublished).

Ultrasound images of the infant oral cavity during breastfeeding ( a ) Tongue up position during breastfeeding. ( b ) Tongue down is drawn down to create a vacuum and milk flows into the oral cavity. ©Medela AG 2006. Used with permission.
Breastfeeding consists of both nutritive (NS) and non-nutritive sucking (NNS). Non-nutritive sucking typically occurs at the beginning of a breastfeed to stimulate a ME and near the end of the breastfeed which may serve to satisfy an infant’s urge to suck and facilitate state regulation and self-comfort [ 125 , 134 ]. These two modes of sucking, NS and NNS, differ in both vacuum characteristics and tongue motion. Interestingly we have shown that mean peak vacuums during NS are stronger (−100 vs. −80 mmHg) than NNS suggesting the infant exerts stronger vacuum to actively remove milk effectively and efficiently [ 135 ].
Over the duration of a breastfeed we have found that peak vacuums do not change but baseline vacuums become stronger. In addition, sucking frequency for NNS (104 ± 21 sucks/min) is faster than for NS (89 ± 19 sucks/min) [ 135 ]. In contrast, sucking rates on artificial teats are markedly faster for NS (120 sucks/min) but slower for NS (60 sucks/min) [ 134 ]. The difference is important since it is often assumed that breastfeeding infants should exhibit a slow rhythmic suck when in reality they can vary both their sucking rate as well as peak and baseline vacuums from one suck burst to the next [ 136 ]. Furthermore, NNS suck burst duration is roughly half that of NS (median 4.5 s vs. 7.0 s) and may be readily apparent on observation of a breastfeed [ 135 ].
Suck Swallow Breath Co-Ordination
Efficient and effective feeding is reliant on perfectly timed coordination of sucking, swallowing and breathing (SSwB) [ 137 ]. It has long been purported that a SSwB ratio of 1:1:1 to 2:1:1 is optimal [ 138 ]; however, simultaneous measurement of SSwB during breastfeeding has shown that this is not the case with SSwB ratios within a breastfeed displaying enormous variability ranging from 1:1:1 to 12:1:4 during NS [ 139 ] ( Figure 8 ). Thus suck-swallow ratios, a common clinical observation, can change within a breastfeed in contrast to bottle feeding ratios that are typically more consistent [ 140 ]. Similar variation of suck:breathe and breathe:swallow ratios have been observed and maybe due to individual patterns of ME suggesting the infants adapts to changing flow rates during breastfeeding [ 135 ].

Respiratory traces of a breastfeeding infant using respiratory inductive plethysmography. Signals are recorded from the ribcage ( yellow ) and abdomen ( red ) and the sum of the two is calculated ( blue ). Absence of signal reflects a swallow, downward slope an exhale and upward stope an inhale. Geddes et al., unpublished.
Maturation of SSwB ratios have been shown to change with infant age and development previously [ 140 ]. It is likely, however, that milk flow rates and volume increase rapidly after secretory activation driving the change in sucking and SSwB patterns. However, once lactation is established, contrary to common belief, we have not found SSwB ratios to differ from after milk production has been established. The only change we did detect was longer nutritive suck bursts which were comprised of a greater number of sucks, swallows and breaths [ 135 ].
These comprehensive results also draw attention to clinical signs of swallowing which consist of observations of long ‘draws’ during sucking (jaw excursion) accompanied by audible swallows [ 141 ]. These clinical signs are unreliable and have not been validated by measurements such as test weights to determine the volume of milk removed during a breastfeed [ 142 , 143 ].
12. Nipple Pain
While intra-oral vacuum is important to milk removal, excessive intra-oral vacuum has been associated with nipple pain. More than 60 years ago Gunther reported a sucking intra-oral vacuum up to −200 mmHg in a 2 day-old infant that was associated with nipple pain and damage [ 144 ]. Recently, McClellan et al. [ 145 ] reported that infants of mothers with persistent nipple pain exerted stronger mean baseline (pain: −91 mmHg; no pain −51 mmHg) and peak intra-oral vacuums (pain: −214 mmHg; no pain: −153 mmHg). In addition, ultrasound analysis showed reduced tongue movement particularly at the base of the nipple, resulting in less nipple expansion [ 117 ]. Interestingly, positioning of the nipple with respect to the NHSPJ did not differ in women experiencing pain suggesting increased breast tissue in the infant’s mouth may not be necessarily beneficial. Indeed, we have reported a case study of a woman whose infant exerted very strong mean vacuums (Baseline vacuum: −151 mmHg; Peak vacuum: −233 mmHg) that were not ameliorated by a nipple shield (Baseline vacuum: −41 mmHg; Peak vacuum: −338 mmHg). Further, lower milk transfer volumes were observed in infants of mothers with nipple pain (Pain: 42 ± 31 mL; Control:71 ± 31 mL) [ 146 ] although it is possible to establish a full milk supply with assistance [ 147 ].
13. Nipple Shields
Major advances have been made in the understanding breastfeeding and lactation, sucking dynamics and milk transfer however women experiencing nipple pain remain understudied despite it being a major cause of early cessation of breastfeeding [ 148 ]. Various causes of nipple pain have been identified yet treatment options are limited. Nipple shields can improve comfort allowing continued breastfeeding [ 149 ] however, the impact of nipple shield use on milk transfer and production is controversial amongst clinicians [ 150 ].
Negative consequences of nipple shield use are based on limited evidence of reduced milk transfer in term breastfeeding dyads [ 151 ] and with shields that are no longer available [ 151 , 152 ]. In contrast, a pilot study ( n = 5) found use of an ultra-thin silicone nipple shield found no difference in infant milk intake with and without the nipple shield [ 153 ]. We have confirmed this in women with persistent nipple pain, showing no reduction in milk transfer (no shield: 46 mL; shield: 40 mL) nor effectiveness of breast emptying (PAMR; no shield: 59%; shield 53%) suggesting these infants adapted to the shield and oxytocin release was not impeded, such that adequate volumes were removed from the breast to maintain milk production [ 154 ]. Importantly in cases of low milk supply, for which we found incidences of about 35%, these were not associated with levels of pain [ 147 ] therefore other causes of low milk production such as nipple shield sizing (small shields may compress nipple ducts), delayed secretory activation, no breast changes during pregnancy, pregnancy complications, repeated mastitis, infant hospitalization and maternal depression should considered.
The use of nipple shields did not impact infant sucking dynamics either with infants displaying similar proportions of the feed in NS and NNS with and without a nipple shield (NS: shield: 51%; no shield: 58%; NNS: shield: 11%; no shield: 15%). These similarities may be due to introduction of the nipple shield in the first postnatal week when early imprinting occurs via communication of somatosensory information from Merkel cells [ 155 ] in the oral cavity to the cerebral cortex [ 156 , 157 ].
Both nipple pain and the subsequent us of a nipple shield use are often assumed causes of low milk production. The intensity of nipple pain experienced by women during breastfeeding varies throughout the day and over time [ 145 ]. We found an average reduction in pain of 25% (by McGill pain questionnaire) with use of a nipple shield [ 158 ], without changes in the visual analogue scale scores suggesting the McGill pain questionnaire may be more sensitive to the nuances and complexities of nipple pain [ 145 ]. Indeed persistent nipple pain is multifactorial and includes predisposing, cognitive and emotional factors and external influences factors as defined in the Breastfeeding Pain Reasoning Model complicating its assessment [ 154 ]. Importantly and in contrast to assumptions, Chertok et al. observed that 90% of women who initiated nipple shield use in the first postnatal week reported a positive experience, and two thirds of women stated that nipple shield use prevented them from stopping breastfeeding early [ 159 ]. Indeed, this data is consistent with maternal reports of the nipple shield being instrumental in continuing breastfeeding when experiencing nipple pain/trauma in the early postnatal period.
14. Ankyloglossia
We have found that tongue movement differs in infants with anterior ankyloglossia (tongue tie) in that they either appear to compress the tip or the base of the nipple during a suck cycle. This resolved to a more ‘normal’ motion post frenotomy with maternal pain decreasing during breastfeeding and sucking efficiency increasing (mL/min) [ 104 ]. As frenotomy rates have increased so has controversy around definitions of tongue tie, whether it impacts breastfeeding and who should be treated. Landmark research examining the anatomy and histology of the lingual frenulum conducted by Mills et al., has been the impetus for rethinking how to approach tongue-tie and the decision to perform a frenotomy. Major findings of these dissections have shown that the frenulum is not a ‘band’ or ‘string’ but rather is a dynamic structure comprised of a midline fold of fascia that inserts into the internal mandibular arc, creating a diaphragm-like structure spanning the base of the mouth. Further, genioglossus is suspended from the floor of mouth fascia, and can be drawn up into the frenulum fold. In addition, the lingual nerve is located superficially, immediately below the fascia, on the ventral surface of the tongue, making both genioglossus and the lingual nerve vulnerable to injury during frenotomy [ 110 , 111 ]. Finally, the frenulum contains Type III collagen fibres which are much more distensible and mobile than the stronger less distensible Type I fibres previously identified [ 109 , 160 ]. Combined, these findings call for tongue tie grading to embrace normal variability and sheds light on concerns of adverse effects of frenotomy providing the basis for more prospective studies [ 107 ].
15. Preterm Infants
It is now well accepted HM is critical to the health and development of the preterm infant (born <37 completed weeks gestation). However preterm infants typically are not born with the sucking skills required to adequately remove milk from the breast. Infants <34 weeks corrected gestational age may receive all their milk feeds via an intragastric tube and gradually transition to oral feeds as their sucking skills mature. In neonatal nursery settings where mothers cannot stay with their infants, bottle feeds may be offered when the mother is not available to breastfeed.
In the clinical setting preterm milk transfer is usually assessed and estimated through observation of factors such as sustained latch, audible swallows, and number of suck bursts per feed. However, when compared to test weighing, we have shown that the subjective clinical estimates of milk transfer are inaccurate across a range of milk transfer volumes [ 48 ] ( Table 3 ). Of critical importance is that we found that preterm milk transfer is typically much lower than the prescribed feed volume, and the absence of any milk transfer is not uncommon [ 48 , 116 ].
Percentages of correct estimates of milk transfer as assessed by test weighing [ 48 ]. PMA: post menstrual age.
Milk transfer is dependent on several maternal and infant factors that cannot be determined through visual observation. Maternal milk supply and the degree of fullness of the breast determine the availability of milk during a breastfeed [ 161 ] and the infant’s suck bursts must coordinate with a mother’s ME for the infant to transfer milk [ 130 ].
Our seminal research in breastfeeding dynamics has provided the tools to measure and better understand the sucking characteristics of preterm infants. Geddes’ cross-sectional study of 40 preterm infants born <34 weeks gestation and corrected gestational age 32.7–39.9 weeks showed that while preterm breastfeeding infants use a similar sucking action to that of term infants, there are several differences in sucking characteristics. Most notably, when compared to the mean intraoral vacuum of term breastfeeding infants (−114 ± 50 mmHg [ 130 ]) we found the intraoral vacuum of preterm infants was less than half (−41 ± 28 mmHg, [ 116 ]). Similarly, the proportion of the feed time that the preterm infant spent sucking (38% ± 18%, [ 162 ]) was much lower than that of term infants (82%, [ 135 ]). Both the weaker intraoral vacuum and reduced sucking time result in a lower sucking efficiency [ 116 ] and likely contribute to low milk transfer volumes in preterm infants.
Nipple shields are routinely used with preterm infants to aid sustained attachment and facilitate milk transfer [ 163 ]. Our sonographic measurements of maternal nipple diameters for dyads with and without nipple shield use show that nipple diameters are larger with nipple shield use [ 116 ], suggesting the infant can expend less energy attaching to the breast (i.e., extending the nipple and holding it close to the NHSPJ). This may in part explain the higher milk transfer volume noted when preterm dyads use a nipple shield. Additionally, the lower vacuums applied by the preterm infant suggests that when using a shield, a reasonably full breast would increase the likelihood of greater milk transfer.
We have also shown that when preterm infants are fed with a vacuum release teat, they are able to remove sufficient volumes of milk using a similar tongue motion as breastfeeding [ 164 ]. In addition, they were discharged earlier [ 165 ] and had higher rates of exclusive breast milk feeding at discharge from hospital and breastfeeding at 3 months corrected gestational age [ 166 ].
Preterm infants have been shown to have a shorter breastfeeding duration than that of their term counterparts [ 167 ]. Early weaning is observed despite a strong maternal desire to breastfeed with intended durations similar to that of mothers of term infants [ 47 ]. Our studies indicate that the greatest barrier to continued breastfeeding beyond discharge from the neonatal unit is insufficient milk supply, with few other breastfeeding difficulties cited [ 47 , 168 ]. Mothers that were unable to produce enough milk to meet their infant’s needs at the time of discharge from hospital were at high risk of early weaning [ 168 ]. While there are concerns about reduced milk transfer with nipple shield use, we found that nipple shield use at 2 weeks corrected gestational age did not impact breastfeeding to 3 months corrected gestational age [ 168 ]. Our group’s involvement in studies of secretory activation, milk synthesis and expression intervals in mothers of preterm infants [ 42 , 102 ], as well as current investigation of the effect of pregnancy complications on secretory activation and subsequent milk production will contribute to the early management of lactation after preterm birth.
Factors influencing breastfeeding and milk removal are summarised in Table 4 .
Factors influencing breastfeeding sucking characteristics and milk removal.
16. Influences of Maternal Body Composition on Milk Composition
Human milk promotes optimum growth, development, and health of the infant; however the mechanisms that govern both the variation of composition and the pathways by which it delivers benefits to the infant are not well understood [ 169 ]. Increasingly maternal and environmental factors are being associated with milk composition. A recent systematic review indicated maternal adiposity was related to HM lactose and fat concentrations. However our study failed to confirm these relationships HM [ 170 , 171 ]. We have conducted several studies, to determine relationships between maternal body composition (BC; lean and fat mass) and HM composition. We have found that higher maternal BC (%fat mass (FM), body mass index (BMI)) is associated with increased concentration of whole HM leptin [ 171 ] but not skim HM leptin, which is lower in leptin content [ 172 ]. This is consistent with the only other study measuring whole HM leptin using pre-pregnancy BMI as a measure of adiposity confirming maternal BC may influence HM leptin [ 173 , 174 ]. Variation of reported relationships between maternal adiposity and leptin depend on methods of measurement and whether skim or whole milk was analysed as well as number of study participants. For example, skim HM leptin concentrations in obese mothers ( n = 50) were double of that of normal-weight mothers ( n = 50) [ 175 ] whereas no differences for whole HM leptin was found in our smaller longitudinal cohort [ 176 ]. Therefore, future analysis for leptin should be conducted in whole HM.
We have also found that increased maternal BMI is associated with increased HM cortisol concentration [ 177 ]. Indeed individuals with higher BMI have increased circulating cortisol concentrations [ 178 ] that could translate to higher concentrations in HM. Concentrations of these hormones in our study were highly variable within and between women and remained constant throughout the first 12 months of lactation, suggesting a more complex relationship between HM glucocorticoids and maternal adiposity.
Like whole HM leptin, higher concentrations of HM protein are associated with increased maternal adiposity and are not identical in all tested cohorts [ 171 , 179 ]. We observed positive associations between total protein and maternal %FM, but not BMI [ 171 ]. In a longitudinal cohort, we found positive associations between whey protein concentrations and maternal weight, BMI, fat free mass (FFM), FFM index (FFMI), and FM index (FMI), with %FM showing no associations [ 179 ]. As with leptin, there are studies reporting both presence and absence of such associations [ 170 ]. To add to the complexity further, we have shown that HM total protein concentration does not change day-to-day [ 180 ], week-to-week [ 181 ] or during a short maternal dietary intervention [ 182 ].
Increasingly it appears that the mother modulates several components in the milk. We have not identified associations of maternal adiposity with lactose or total carbohydrates, nor have we found strong associations with total (estimated) human milk oligosaccharides (HMO) [ 183 ]. However, more recently HMOs have been shown to change with a maternal dietary intervention [ 184 ], mode of delivery and parity [ 185 ]. Studies of HMOs and maternal BMI report conflicting associations [ 186 , 187 ]. Indeed, larger longitudinal studies including measurement of maternal BC are required to clarify associations with HM components.
17. Gastric Emptying and Infant Body Composition
Gastric emptying (GE) is a key regulator of appetite [ 188 ]. However, there is much to be learned about the programming potential of HM components, how their patterns change throughout the lactation period and their impact on the GE rate of the breastfed infant. Few components, have been investigated in connection with the regulation of infant milk intake and feeding patterns, including pre-feed gastric residual (GR) volumes and GE rates of breasted infants.
The absence of suitable validated techniques for the determination of GE has restricted the evaluation and understanding of GE in the breastfed infant as a mechanism of appetite control. We have validated an ultrasound technique to assess GE in a preterm population [ 189 ]. We have also shown that HM components are associated with GE and therefore, potentially impact infant appetite regulation and BC, evidenced by relationships between feeding frequency [ 190 , 191 ]; and associations between feeding frequency, milk intake and infant BC [ 192 ].
Measurements of infant BC have been largely limited to anthropometric measurements such as birthweight, weight, length, head circumference and BMI due to limited access to comprehensive BC measurement techniques. Recently emphasis has been drawn to the quality, not just the quantity of growth in the context of childhood obesity. For example preterm infant BC in early life appears to play an important role in programming long-term health outcomes including obesity and other non-communicable diseases [ 193 ]. As such adult BC measurement techniques are being adapted and to the paediatric population, and include bioelectrical impedance spectroscopy (BIS), dual X-ray absorptiometry (DXA), isotope dilution, magnetic resonance imaging (MRI), ultrasound, whole-body air-displacement plethysmography (ADP), computed tomography (CT) and others [ 194 ].
18. Preterm Infants
Using our validated ultrasound technique in preterm infants [ 195 ] we found that GE of pasteurised donor human milk (PDHM) was slower than mother’s own milk (MOM) both during feed delivery and the postprandial period [ 196 ]. Immediately after feeding, the volume of PDHM retained in the stomach was 23% higher than MOM, reducing by 15%/30-min until the next feed (3 h). However, the rate of emptying of PDHM is closer to that of MOM than infant formula, with calculations indicating that postprandial retained proportions of formula are 23% to 29% higher than that of MOM [ 197 , 198 ]. Final gastric residual volumes (FGR) were not different between milk types indicating that the same end point was met for both PDHM and MOM indicating the slower emptying of PDHM is not detrimental. Further gastric residuals were 12% to 22% of the feed volume, which is below the 30% to 50% considered a marker of feeding intolerance [ 199 ] and supports clinical observations and evidence that PDHM is unlikely to be implicated in large FGRs associated with feeding intolerance [ 200 ].
Interestingly compositional differences between PDHM and MOM did not explain the disparity in GE observed in our study. Whilst higher MOM casein and lactose concentrations are associated with faster emptying [ 201 ] feeds of PDHM emptied more slowly than MOM despite having higher concentrations of casein and lactose. It is possible that the effect of pasteurization or frozen storage alters components of donor HM and so counters the effects of casein and lactose on emptying. Holder pasteurization also causes complete inactivation of the bile salt stimulated lipase (BSSL) and lipoproteinlipase [ 202 ]. Bile salt stimulated lipase enables almost complete hydrolysis of HM triacylglycerol through its synergistic action with pancreatic lipase-related protein 2 [ 203 ]. As the presence of lipids in the duodenum and ileum slows GE through triggering of the ileal brake, it is possible that restricted lipolysis of pasteurized milk is a mechanism for slower emptying of PDHM [ 204 ]. Also, heat treatment of bovine milk has been shown to alter the structure of whey proteins resulting in interactions between denatured whey proteins and casein micelles [ 205 ]. It is therefore conceivable that Holder pasteurization creates similar interactions in HM possibly negating the faster GE associated with higher human casein concentrations.
We found no evidence to support a difference in GE according to infant sex. We did detect faster GE during feed delivery in male infants however this was explained by the lactose concentrations of PDHM fed to male infants that were on average 6.1 g/L and 14.2 g/L higher than that of PDHM and MOM fed to females [ 196 ].
There is limited evidence of a relationship between energy concentration and GE in preterm infants. Our studies show that the energy concentration of HM feeds ranging from 12.6–30.4 kcal/30 mL did not influence GE, likely because triacylglycerol, the predominant HM lipid that contributes to HM energy density, differs from other lipid sources in that it does not trigger the ileal brake to slow GE [ 197 , 206 , 207 ] (refs). The preterm infant’s diminished GE response to increasing lipid and energy concentrations may serve to facilitate the physiological emptying of fat-rich HM that is ingested towards the end of a breastfeed [ 65 ]. Our GE rates are similar to those observed for MOM and formula feeds of 5–20 kcal/30 mL [ 208 ]. In contrast, an older study reported increasing energy concentrations were associated with slower postprandial emptying for formula feeds of 5–20 kcal/30 mL from 20 min post feed, with differences between 20 kcal and 24 kcal noted only at 80 min post feed [ 209 ]. The study did not account for the osmolality or specific nutrient concentrations of the bovine-based formula feeds which differ from HM and are known to influence gastric emptying [ 206 ].
Our ultrasound technique also allows assessment of the effect of the addition of human milk fortifier (HMF) to HM feeds on GE. When bovine-based HMF was added to achieve an assumed caloric density of 24 cal/30 mL, slower GE was observed across all 30-min time points between feeds [ 196 ]. The magnitude of the effect was smaller for PDHM than for MOM, possibly due to differing interactions/digestion of HMF between MOM and PDHM due to the degradation of several HM bioactive factors by heat pasteurization. This finding concurs with Ewer & Yu who reported an average gastric half emptying time of fortified MOM to be 48 min, more than double the 21 min average for unfortified MOM [ 210 ].
Supine infant positioning was associated with slower GE with retained feed proportions on average 16% higher than that of infants positioned prone or right lateral across the postprandial period [ 196 ]. The observed inter-individual effects of positioning on GE are consistent with several published studies [ 211 , 212 ] and further support the use of prone positioning as a conservative clinical management strategy for feeding intolerance in the neonatal unit setting.
A gastric residual volume ≤2.5 mL that is predominantly curd appears to be usual for stable preterm infants [ 213 ], with most (62%) 3 hourly feeds resulting in empty stomachs. This finding raises the possibility that feeding of 3 hourly volumes may be tolerated if fed every 2.5 h. The gastric residual, as a proportion of the feed volume, was similar between MOM and PDHM and were 10% and 15% for unfortified and fortified feeds respectively. These are similar to the 15% and 16% residual feed proportions reported for MOM and infant formula, respectively [ 207 , 214 ] and below the 30%−50% considered to be a sign of feeding intolerance [ 199 ].
Sonographic examination of gastric contents after HM feeds showed that the presence of curding, and its echogenicity, or density, were similar for MOM and PDHM. Immediate post feed ratings of high curd density and high curd volume were associated with higher HM casein concentration, and HMF also significantly contributed to high curd volume [ 189 ]. As neither of the two HMF products used in the study contained casein, it is likely the higher curd volume and density associated with HMF resulted from a more acidic environment caused by HMF that facilitates HM protein precipitation [ 215 ]. The presence of small curd volume in the stomach suggests there is continued delivery of nutrients to the ileum beyond emptying of the liquid portion of a human milk feed.
Our gastric emptying studies confirm that HM is well tolerated by the preterm infant; despite changing composition over time and between women, no clinically significant impact on gastric emptying is observed. Current heat treatment of donor HM and commercial HMF products slow GE somewhat but not to the degree that causes feeding intolerance in medically stable preterm infants. Further, with complete emptying of 3-hourly feed volumes typical for many infants, it may be possible to explore more frequent feeding of similar volumes when additional caloric intake is indicated.
Infants born preterm are susceptible to postnatal growth restriction and will benefit from aggressive nutritional management in order to achieve optimal growth and BC parameters. Body composition measurements in preterm infants are difficult to obtain due to compromised health and physical limitations such as their fragile skin that prevents the use of callipers, the need to avoid frequent blood collection (e.g., tracer dilution techniques) and increased susceptibility to radiation. They are also relatively overhydrated, with higher body water content compared to children and adults, leading to overestimation of FFM when using bioelectrical impedance analysis [ 216 ]. This leaves few methods that are suitable for the hospitalised preterm infant with limitations due to the risks of overhandling, infection, and thermal instability. Previous studies have reported lower FFM, and higher FM compared with term infants at hospital discharge, thus increasing their risk of developmental issues, metabolic syndrome, and obesity later in life [ 217 , 218 , 219 ].
We have found, with air displacement plethysmography that there were relationships between milk composition and changes in BC preterm infants fed fortified HM. Increased fat and total energy intakes were associated with increasing FM whilst increasing protein intake when considered with carbohydrate intake was associated with increasing FFM [ 220 ]. We have also established that ultrasound is sensitive enough to detect HM macronutrient-related changes in accrued adipose and muscle tissue measured at multiple sites: abdomen, scapula, mid-thigh and mid-arm in preterm infants [ 221 ]. Enteral volumes (predominately HM) were positively associated with adipose to muscle ratio whilst timing of fortification, carbohydrate intake and the protein energy ratio of intakes moderated ratio of the adipose to muscle tissue accretion in preterm infants. This study demonstrated that ultrasound may offer a clinically useful tool to obtain non-invasive obtain serial infant BC measurements.
19. Term Infants
There is evidence of differences in GE between infants fed infant formula compared to those fed HM, yet breastfed infants have not been studied in depth with respect to milk composition. We have investigated the effects of multiple factors, including appetite hormones, macronutrients, BC and maternal factors, on GE.
We found higher feed volumes were associated with faster GE rate, higher post-feed stomach volumes, and longer GE times. Greater feed volumes were also associated with smaller residual volumes prior to the feed and larger residual volumes prior to the next feed. Importantly, during exclusive breastfeeding period we found no effect of infant age or sex on feed volume, GE or breastfeeding patterns, but larger (not older) infants with higher adiposity had longer time between feeds, indicating a potential link between feeding frequency, GE, and BC. It also implies that feeding frequency is dictated by an individual’s growth rate and development rather than age, providing further support for breastfeeding on demand for the duration of the breastfeeding relationship.
20. Proteins
We have found that specific protein composition rather than total protein appears to influence GE either indirectly or directly. For example, the casein:whey ratio modified the GE rate depending on the volume of milk consumed, such that higher casein:whey ratios were associated with faster GE of small feed volumes and a slower GE rate of larger feed volumes [ 190 ]. Furthermore, higher casein concentrations and intakes were associated with shorter GE time, which may result in higher feeding frequency, and in turn, higher 24 h milk intake and infant adiposity ( Figure 9 ). In this cohort the association between feeding frequency and infant adiposity strengthened with duration of lactation, consistent with Ay et al. [ 222 ]. In contrast to casein, higher whey protein concentrations and intakes were associated with longer GE time [ 190 ], which may result in lower milk intake and reduced adiposity [ 192 ] ( Figure 9 ). Thus, both feeding frequency and GE are in part likely regulated by HM casein and whey concentration. However, it was not the casein concentration but daily intake of casein that was directly associated with infant BC; negatively with lean mass and positively with FM with associations strengthening in the later months of lactation [ 179 ]. This suggests that higher daily doses of casein may down-regulate the accrual of lean body mass in infants, potentially by decreasing time between feeds and increasing the volume of milk consumed. These results further clarify role of the HM protein as a potent appetite regulator and draw attention to the importance of the HM protein composition.

Possible pathways of lactocrine programming of the infant by the human milk proteins. BMI—body mass index; CDI—calculated daily intakes; Conc.—concentrations; doses—amounts of human milk component ingested during a single breastfeed; FFM—fat-free mass; FM—fat mass; %FM—percentage fat mass; GE—gastric emptying; MI—milk intake; PFSVs—post-feed stomach volumes; − negative association; + positive association. Purple arrows indicate the direct associations between components and infant BC. In the case where direct relationships between infant body composition and human milk components are supported by the relationships of human milk components with infant gastric emptying factors and breastfeeding parameters, these relationships have been included and could be integrated into possible pathway. Grey arrows indicate further possible pathways, although no direct association of component unit with infant body composition has been established (or not analysed in case of doses).
21. Immune Factors
HM contains multiple immunological factors that provide protection against various health challenges [ 223 , 224 , 225 ]. Within the whey fraction, lactoferrin, lysozyme and sIgA are present in high concentrations, potentially indicating multiple roles in infant programming [ 226 , 227 ]. We have shown that these bioactive components relate positively to breastfeeding frequency (sIgA) and milk intake (lysozyme, sIgA), and that these relationships extend further to infant BC [ 228 ] ( Figure 10 ). Higher lactoferrin intake was associated with lower infant FFM index whilst higher lysozyme intake related to higher infant adiposity. Although not associated with maternal BC, the concentrations of these components continued to increase throughout the first year of lactation, ensuring the same level of infant protection despite the reduction in milk intake.

Possible pathways of lactocrine programming of the infant by the human milk immune factors. CDI—calculated daily intakes; FFM—fat-free mass; FM—fat mass; sIgA—secretory immunoglobulin A; − negative association; + positive association. Purple arrows indicate the direct associations between components and infant BC. In the case where direct relationships between infant body composition and human milk components are supported by the relationships of human milk components with infant breastfeeding parameters, these relationships have been included and could be integrated into possible pathway. Grey arrow indicates further possible pathway, although no direct association of component unit with infant body composition has been established.
Lactoferrin is being explored as clinical intervention for infant health [ 229 ], and for the first time we have evaluated how natural variations of this HM component relate to BC of term breastfed infants. The observed negative relationship of lactoferrin intake with infant lean mass could be explained by modulation of infant gut microbiome [ 230 ], as the gut microbiome has been implicated in infant weight gain and obesity [ 231 ], as well as by increasing the bioavailability of iron to the infant. Iron supplementation in iron replete infants has been shown both to decrease linear growth and weight [ 232 ]. The exact mechanisms of these outcomes are not clear and interactions between lactoferrin and infant growth appear complex requiring further study.
Lysozyme is important not only for the immune protection of the infant but for infant growth and now BC as we have shown a positive relationship with FM and negative with FFM [ 228 ]. Preterm infants have exhibited better growth and improved gastrointestinal function when administered lysozyme [ 233 ]. The effects of HM lysozyme may be mediated through improvement of infant gut health and optimized digestion, resulting in increased absorption of nutrients and subsequently, increased fat accretion. Or alternatively, that lysozyme, not unlike leptin, also enhances innate and adaptive immune responses [ 234 ], therefore lysozyme may also be implicated in the two-way relationship between the obesity and immune status.
Whilst HM sIgA demonstrated no strong associations with infant BC, daily intake was positively associated with breastfeeding frequency which in turn is also related to 24 h milk intake ( Figure 10 ), potentially affecting infant adiposity. Like lysozyme, broad spectrum of sIgA antibodies are implicated in the development of infant mucosa and anti-inflammatory and tissue protective activities [ 235 ]. These findings warrant further investigation of other immunological factors of HM in relation to infant growth and BC.
22. Appetite Hormones
HM hosts a plethora of hormones that are biologically active, including adipokines and glucocorticoids that may programme appetite [ 236 ], and we have found interesting relationships of HM adiponectin with infant GE. Higher concentrations and intakes of adiponectin were associated with longer times between feeds in term breastfed infants [ 190 ], which may be implicated in the growth-regulating effect of adiponectin in the first 4–7 months of life, evidenced by high HM adiponectin concentrations being associated with lower infant weight and FFM [ 176 ]. Extended GE times may culminate in fewer feeds per day and potentially lower 24-h milk intake, restricting both volume and energy to the infant and slowing growth. This hypothesis is further supported by our longitudinal study of infant BC that showed that higher HM adiponectin intake being associated with lower infant lean mass and increased adiposity over the first year of life [ 176 ].
Whole HM leptin content did not display any associations with GE or breastfeeding parameters [ 190 ] ( Figure 11 ), indicating that long-term effects of leptin in human infants are possibly stronger than the potential short-term satiety effects observed in rodent models. This also highlights the difficulty of extrapolating results in animal models to humans [ 237 ]. However, HM leptin intake is related to infant feeding frequency and BC development, with higher daily intake of both, whole and skim milk leptin associating with greater deposition of adipose tissue [ 176 ]. Skim milk, however, is not representative of what infant ingests and results for skim milk leptin should be interpreted with caution.

Possible pathways of lactocrine programming of the infant by the human milk appetite hormones. BMI—body mass index; CDI—calculated daily intakes; Conc.—concentrations; doses—amounts of human milk component ingested during a single breastfeed; FFM—fat-free mass; FM—fat mass; %FM—percentage fat mass; GE—gastric emptying; MI—milk intake; − negative association; + positive association. Purple arrows indicate the direct associations between components and infant BC. In the case where direct relationships between infant body composition and human milk components are supported by the relationships of human milk components and infant gastric emptying factors and breastfeeding parameters, these relationships have been included and could be integrated into possible pathway. Grey arrows indicate further possible pathway, although no direct association of component unit with infant body composition has been established.
23. Glucocorticoids
HM contains the glucocorticoids, cortisol, and cortisone, which are involved in regulation of inflammation and metabolic homeostasis and may impact infant gut maturation and the microbiome [ 238 ]. Little is known about how these hormones affect infant growth and development of BC. For the first time we reported that higher concentrations of HM cortisol and cortisol to cortisone ratio are related to greater infant adiposity [ 177 ]. Elevated circulatory cortisol is known to be a potent stimulator of body fat mass gain in adults [ 239 , 240 ] and recently in 2-year-olds [ 241 ].
Additionally, cortisol was positively related to head circumference, an important indicator of infant brain size and a proxy for intracranial volume, neurological development and cognitive function [ 242 ] all of which are commensurate with breastfeeding [ 243 , 244 ]. The cortisone relationship with head circumference the reverse of that reported for chronic prenatal maternal stress during pregnancy (smaller head circumference) [ 245 ] ( Figure 12 ). Whilst underlying mechanisms for these associations are unclear, these findings should be confirmed with daily infant intakes of glucocorticoids in addition to concentrations.

Possible pathways of lactocrine programming of the infant by the human milk glucocorticoids. BMI—body mass index; Conc.—concentrations; %FM—percentage fat mass; − negative association; + positive association. Purple arrows indicate the direct associations between components concentrations and infant BC and anthropometry.
24. Carbohydrates
Our research has also provided new insights about relationships of HM carbohydrates with infant GE [ 190 ] ( Figure 13 ). We have found that both total carbohydrates and lactose are associated with GE, feeding frequency and infant 24 h milk intake culminating in relationships to adiposity [ 190 ] ( Figure 13 ). This highlights the complexity of pathways affected by HM components and that infant intake, as evidenced by our finding that higher lactose concentrations are associated with slower GE rate of small feed volumes and faster GE rate of large feed volumes [ 190 ]. These results support the findings of Khan et al. [ 65 ] who reported a positive association between lactose concentration and feeding frequency.

Possible pathways of lactocrine programming of the infant by the human milk carbohydrates. BMI—body mass index; CDI—calculated daily intakes; Conc.—concentrations; doses—amounts of human milk component ingested during a single breastfeed; FFM—fat-free mass; FM—fat mass; GE—gastric emptying; HMO—human milk oligosaccharides; MI—milk intake; − negative association; + positive association. Purple arrows indicate the direct associations between components and infant BC. In the case where direct relationships between infant body composition and human milk components are supported by the relationships of human milk components with infant gastric emptying factors and breastfeeding parameters, these relationships have been included and could be integrated into possible pathway. Grey arrows indicate further possible pathways, although no direct association of component unit with infant body composition has been established (or not analysed in case of doses).
We have reported that concentrations and, more importantly, daily intakes of HM carbohydrates are associated with development of infant BC and are differentially related to infant anthropometry and BC [ 183 ]. Furthermore, the directions of the associations with infant BC were not uniform for the daily intake and concentration of the same measured carbohydrate. Lactose concentration showed no associations with infant BC, yet lactose intakes were negatively associated with lean mass and positively with FM. Intake of total carbohydrates showed similar relationships with lean and fat mass, but relationships with concentration were reversed with more carbohydrate associating with more lean mass, less adiposity and higher infant length and weight.
Whilst we did not directly measure concentrations of HMO in our cohort, we found that like total carbohydrates, total HMO concentration related positively to infant lean mass and negatively to adiposity, yet intake of HMO displayed no associations. Of note, HMO intake remained the same over 12 months post-partum. Our results support recent findings of differential associations between individual HMO and infant BC [ 246 ]. Total HMO on the other hand had no impact on infant GE which was expected as HMOs target the small intestine and have been shown to modulate the gut microbiome therefore, having an indirect effect on BC [ 247 ].
Given contrasting relationships of HM component concentrations and intakes, infant intake of components may well reflect better the nutritional physiology of the breastfed infant. These findings also indicate the possibility of intervention via modulation of both milk intake and the infant gut microbiome, which is implicated in adiposity and development of obesity [ 248 ].
HM lipid fraction accounts for 50% of the energy content and is thus an important contributor to infant growth. Dose or concentration of HM fat showed no effect on term infant GE rate or time [ 190 ], consistent with lack of associations between fat and feeding frequency reported previously [ 60 , 65 ]. Higher HM fat intakes have been associated with lower weight-for-age z -scores [ 249 ], but also higher weight gain [ 250 ]. Higher 24-h fat and total energy intakes have also been associated with higher infant weight and FFM at 3, 6 and 12 months [ 251 ]. These studies should be interpreted with caution due to sampling of HM lipid not being straight forward. Total fat increases across a breastfeed and changes throughout the day due to the relationship between fat content and the fullness of the breast [ 63 , 252 ]. As such sampling is problematic with one sample not being representative of either fat content or infant fat intake as illustrated by George et al. [ 253 ]. Further, analysis differs according to analytical technique, with the creamatocrit method offering an attractive alternative to more complex biochemical assays [ 254 , 255 ] such that it could be integrated into the clinical practice, particularly in the area of preterm nutrition, to increase the energy content of milk [ 256 ].
26. Infant Health
HM is much more than the nutrition that supports optimal infant growth. It is a compositionally complex and dynamic fluid that supports both the innate and adaptive infant immune system [ 257 ]. Many milk components have dual roles in the nutrition and protection of the infant. For example, lipids are most often regarded as nutrition but there is mounting evidence of their association with health. Using new methods [ 258 ] we have recently discovered 98 novel triaclyerglicerides (TAGs) and found that infant intake of palmitic acid-containing and lauric acid-containing TAGs differed between healthy and unwell infants indicating responsiveness of the milk [ 259 ]. This is consistent with our previous study that showed reductions in the proportion of capric (C10:0) and lauric acids and increases in palmitoleic and stearic acid [ 260 ] in unwell mothers and infants. Indeed it also highlights both the importance of measuring component intake [ 261 ] and with respect to total lipid employing extensive sampling [ 253 ].
Similarly, we have documented increases in the leukocyte content in response to maternal and/or infant infection. The smallest response was seen if only infant was ill and the greatest with maternal mastitis and upon recovery leukocyte content returned to the health baseline level. This increase in leukocytes was also accompanied by significant changes in lactoferrin, sIgA IgG, and IgM concentrations [ 262 ].
These changes in the milk components as responses to maternal and infant health hold promise potential therapies; however this work is hampered by the ability to isolate components and scale up their production [ 263 ]. In contrast, modulation of milk via maternal interventions may improve health in an individualised fashion.
27. Human Milk Microbiome
The development of the gut microbiome in the first years of life has been strongly associated with immune and metabolic outcomes in large human cohort studies, and in interventional animal models [ 264 ]. Importantly, HM shapes the infant microbiome through direct transfer of bacteria as well as bioactive components such as HMOs, antimicrobial proteins, and short chain fatty acids (SCFAs) [ 265 ]. The human milk microbiome (HMM) is therefore of great interest as a target for developmental programming of health. However, while the composition of the HMM has been extensively characterised ([ 265 ]), little is known about the origins of this community or the host-microbiome interactions at the breast. Host-microbe and microbe-microbe interactions in the lactating mammary gland are likely to be highly complex. Inter-kingdom interactions between human cells, bacteria, fungi, and viruses, as well as interactions involving host-derived and microbe-derived bioactives likely influence mammary gland and infant health ( Figure 14 ). Indeed, it is not even known whether the lactating mammary gland hosts a permanent resident microbiome, or whether bacteria are bought in from exogenous locations (such as the maternal gut or infant oral cavity) and survive temporarily before being swept out of the breast via a ME ( Figure 14 ). Stinson et al. have described these two possibilities as the “mucosal interface model” and the “constant influx model”, respectively [ 265 ]. Regardless of whether the bacteria detected in milk are permanent residents or mere “tourists”, numerous HMM taxa have been shown to be vertically transferred from mother to infant via milk [ 266 , 267 , 268 , 269 ]. Factors that shape HMM composition, such as maternal diet, may thereby influence infant colonisation dynamics, with implications for infant health. The potential for maternal diet during lactation to influence infant gut microbiome dynamics has been reviewed extensively by Sindi et al. [ 270 ]. This evidence, from observational human studies and animal models, paves the way for future intervention studies to assess the impact of maternal diet on infant microbial development.

Beyond bacteria: relationships between human milk bacteria and other microbial and non-microbial components of milk. AMPs (antimicrobial proteins) have antibacterial effects, but are also liberated from their parent proteins via the proteolytic action of certain members of the milk microbiome [ 271 ]. Bacteriophages in milk can infect bacteria. Milk fungi have been both positively and negative correlated to milk bacteria [ 272 ]. HMOs are prebiotics which promote the growth of certain milk bacteria. SCFAs are both a product of a substrate for bacterial metabolism. Other bacterial metabolites such as indoles likely exist in milk. To characterise the influence of the human milk microbiome on infant health, an integrative analysis of these components is required.
In addition to live bacteria, HM also contains the products of bacterial metabolism, such as SCFAs. These immunomodulatory metabolites SCFAs (formate, acetate, propionate, butyrate, and valerate) are the end products of bacterial fermentation of fibre in the gut and are transported systemically around the body, including to the lactating mammary gland. They have been shown to elicit a broad range of immunological effects, including promotion of regulatory T cell responses and immune tolerance, synthesis of dendritic cell precursors, and epithelial barrier integrity in the gut [ 273 , 274 , 275 ]. HM therefore has a two-fold influence on infant health: by directly seeding the infant microbiome with human milk bacteria, and by exposing the infant to bacterial metabolites formed in the maternal gut. Emerging evidence suggests that SCFAs may protect infants from developing atopic disease [ 273 , 276 ]. Our research has shown that milk from atopic mothers contains a significantly reduced concentration of SCFAs compared to that of healthy mothers [ 277 ]. This finding may in part explain why breastfeeding does not protect against atopy if the mother herself is atopic [ 278 , 279 ]. HM SCFAs have also been associated with infant BC [ 280 ]. They are therefore of interest for both infant growth and infant immune development. Given that maternal SCFA levels may be modulated by diet, these bacterially derived metabolites represent an exciting opportunity for intervention to optimise infant health.
Our group has established methodologies for studying the HMM from collection to analysis. We demonstrated that milk expressed using an electric breast pump does not differ in its bacterial composition to milk expressed by hand [ 281 ]. This finding is reassuring for those designing HMM studies. We also assessed four commercial DNA extraction kits for their ability to extract DNA from HM [ 282 ]. We found that two of the kits could not reliably extract DNA from HM. Of the two remaining kits, a similar bacterial DNA profile was extracted, but one kit co-extracted a high level of contaminants. Such inter-kit variability may help to explain some of the variation seen in HMM composition between studies. A significant challenge in working with HM is the fat fraction, which interferes with DNA extraction. This fraction is therefore routinely discarded prior to DNA extraction in HMM studies. We demonstrated that this fraction contains bacterial DNA, suggesting that bacteria may be trapped in the lipid layer by milk fat globule membranes [ 283 , 284 ]. However, reassuringly, the fat fraction did not differ in bacterial composition to the cell pellet, suggesting that discarding the fat fraction prior to extraction would not alter the composition of bacteria detected downstream. This is particularly important, as we have shown that inclusion of the fat fraction reduces DNA extraction efficiency by ~40% [ 283 ]. By focusing on robust methodologies for reproducible data, we have raised the standards of the field.
28. Donor Human Milk
In past decades there has been a resurgence in the establishment of donor milk banks in an effort to provide HM for vulnerable infants [ 285 ]. Donor milk has been shown to have positive effects of infant mortality and morbidity [ 286 ] whilst being economically cost effective [ 287 ]. We have been active in the formulation of best practice in milk banking which varies according to geography and resources [ 288 ] as well as investigating pasteurization methods. Thermal pasteurization of milk is almost universal in milk banks however in the process of eliminating bacteria and most viruses [ 289 , 290 ] bioactivity is often dramatically reduced [ 291 ]. Reduction in the loss of bioactivity can be altered by reduction in pasteurization temperature [ 292 ], combinations of time and temperature, as well as other technologies [ 291 , 293 ]. Our group has pioneered UV-C treatment [ 294 ] in an effort to preserve the bioactivity of protective components in milk. It shows great promise in eliminating bacteria [ 295 ] including cytomegalovirus [ 296 ] not at the expense of immune protein activity [ 297 ]. More recently we investigated the heat stable enterotoxin produced by the potential pathogen S. aureus. S. aureus enterotoxins are linked to gastritis and necrotizing enterocolitis. Spike in experiments (S. aureus, and enterotoxin) at various storage temperatures and times confirmed a rapid decline in both the bacteria and enterotoxin in raw and UV-C treated milk providing more evidence of promise for this method of processing donor milk [ 298 , 299 ].
29. Human Milk Cellular Content
HM cell studies offer insight into the biosynthesis pathways involved in milk secretion, the microenvironment of the lactating mammary gland and the potential physiological role of HM cells for the developing infant.
Cells can be isolated through centrifugation of milk and have been found to be enriched in micro-RNA (miRNA), which are regulatory biomolecules, that potentially play a role in infant development [ 300 ]. Whilst cell content of milk is variable, it has been found that the greatest number of cells can be isolated when milk samples are collected 30 min post-feed [ 301 ]. It should be noted, however, that not all milk-derived membrane enclosed structures (resembling cells) bear a nucleus, and that some are instead enlarged milk fat globules [ 302 ] ( Figure 15 ). Why cells enter milk is still a mystery, however it has been found that a subset of cells appear to survive the infant gastrointestinal tract which may potentially impact the receiving offspring [ 303 ]. Indeed, we have shown that the immune cell compartment of milk changes depending on the health status of the mother and infant [ 262 ] which may lead to a downstream protection for the vulnerable child.

Membrane enclosed structures isolated from human milk stained with neutral lipid stain Nile red ( red ) and DNA stain Draq5 ( green ). Scale bar represents 20 μm. Image provided by Ms. Isabel Schultz-Pernice.
Together with immune cells, milk also contains maternal epithelial cells which through analysis may provide insights into the maturation and function of the lactating mammary gland. An early study found that prior to culture, milk cells predominantly expressed the luminal cell marker keratin 18 (CK18), and after culture the cells expressed markers associated with progenitors (CK5, Nestin) and myoepithelial cells (CK14) [ 304 ]. This culture-inducible epithelial lineage plasticity of milk cells is thought to be regulated, in part, by Sigma (14-3-3σ) [ 305 ]. Further studies by our group have found that under different culture conditions, milk cells expressed markers associated with tissues derived from all three embryonic layers [ 306 ]. Moreover, milk cells were found to express the pluripotent stem cell transcription factors OCT4, SOX2 and NANOG on a protein and mRNA level. These findings paralleled studies in non-pregnant, non-lactating breast tissue published around the same time [ 307 , 308 ]. Whilst the concept of pluripotent mammary stem cells existing in HM has been extensively reviewed [ 309 ] few studies have provided supporting evidence, suggesting the need for more targeted research.
In this connection, there have recently been great advances in the tools available to characterise mammary cell differentiation capabilities (i.e., stemness), such as in vivo lineage tracing studies (that allow tracking the progeny of a single cell through organ development) and technologies that allow for unbiased cell subtype identification such as single-cell RNA-sequencing/Assay for Transposase-Accessible Chromatin (scRNA-seq/scATAC-seq) [ 310 ]. Findings from many of these studies suggest that cells in the adult mammary gland are unipotent under homeostatic conditions and only acquire stem cell characteristics in artificial reprogramming environments [ 311 ] (such as ex vivo cell culture).
Increasing numbers of sc-RNA-seq studies have attempted to profile human mammary cells from different stages of development in an attempt to further unravel the subpopulations of cells that exist in the breast [ 312 ]. In line with findings from lineage tracing studies, a study examining breast tissue taken from adult non-pregnant, non-lactating individuals did not find a quiescent niche of mammary stem cells [ 313 ]. Recently, two studies have examined cells isolated from HM via scRNA-seq and found that milk contains predominantly luminal and immune cells [ 314 , 315 ]. Whilst both studies concur that luminal milk cells have a similar gene expression profile to luminal progenitor cells from the breast, pluripotent transcription factors were not found to be co-expressed at a detectable levels in single cells, nor expressed at higher levels than the cells isolated from the normal resting breast ([ 315 ]). Interestingly however, the milk luminal cells appear to be heterogeneous, consisting of two major luminal subtypes LC1 and LC2. In particular, one of these milk luminal cell subpopulations expressed higher levels of immunomodulatory and antigen presenting genes suggesting potential cross talk between the epithelial compartment with the microenvironment of the lactating mammary gland. Whilst many questions remain of the role and function of cells in milk, further investigation of these cells is warranted and may provide further excellent insights into the biology of milk secretion and the immune and developmental role milk plays for the breastfed infant.
30. Breastfeeding during COVID
As the COVID-19 pandemic continues to impact society, women have been disproportionally affected by the consequences of the virus. Mothers have faced an increasing burden of tasks around the home, parenting, educational, and broader family support roles, and make-up the most significant portion of the frontline health workforce [ 316 ]. Inconsistent and detrimental policy changes have negatively impacted pregnant and lactating women in particular. Due to uncertainty about mother-to-infant transmission of acute respiratory syndrome coronavirus 2 (SARS-Cov-2), many hospitals and governments rapidly brought in policies to prevent transmission early in the pandemic. These included restricting women’s access to support people during labour, isolating mothers with confirmed or suspected infection from their infants and discharging women early from the hospital. Moreover, families have received conflicting advice on whether to breastfeed directly or not and once at home, breastfeeding women experienced reduced access to lactation and mental health support [ 317 , 318 , 319 ].
The overwhelming evidence contradicts fears that the mother may transmit the virus to her infant via her milk [ 101 , 317 ] with no study to date demonstrating that SARS-Cov-2 is transmitted via HM [ 320 , 321 , 322 ]. While viral RNA has been isolated in some HM samples of positive SARS-Cov-2 mothers, no samples contained replicant-capable SARS-Cov-2, and thus infectious virus has not been found in milk [ 101 , 320 , 322 , 323 , 324 , 325 ]. Instead, there is evidence that antibodies to SARS-Cov-2 isolated in HM have an immunological response against the virus [ 326 , 327 , 328 ], with samples from infected mothers demonstrating strong sIgA activity specific to SARS-CoV-2. When active SARS-CoV-2 has been added to HM in the laboratory setting, holder pasteurisation (62.5 °C for 30 min) inactivates replicant-capable SARS-CoV-2. As such PDHM, when pasteurized using the Holder technique, can be considered as safe and feasible for use
Finally, with the global roll-out of vaccines against SARS-CoV-2, the accumulating evidence has demonstrated that both pregnant and breastfeeding women secrete SARS-CoV-2 specific IgA and IgG antibodies after vaccination [ 328 , 329 , 330 ] Furthermore, they had similar responses to nonpregnant controls, with immune transfer occurring via the placenta and HM. The current evidence indicates that pregnant and breastfeeding women should continue to be routinely offered vaccination against SARS-CoV-2.
Overwhelming evidence supports breastfeeding throughout the COVID-19 pandemic; however, the support enabling women to continue breastfeeding and the mental wellbeing of pregnant and lactating women remains a significant concern. Our research in Australia and New Zealand has demonstrated that during the COVID-19 pandemic, mental health issues faced by breastfeeding women appear to be exacerbated by COVID-19. We found greater health consequences noted for women who were pregnant for a longer duration during the pandemic and living in regions with higher COVID-19 infection rates [ 331 ]. International research supports this notion, with unprecedented increased postpartum anxiety and depression rates occurring during the pandemic amongst pregnant and lactating women [ 332 , 333 , 334 ]. While some breastfeeding mothers have noted the pandemic and lockdowns have resulted in less pressure and more family support at home to continue breastfeeding [ 331 , 332 , 335 , 336 , 337 ], others have highlighted a reduction in access to support has directly contributed to their early weaning [ 332 ]. More robust policies and actions that enable mothers to access their immediate support networks and mental health services remain essential to protect women’s wellbeing and continued breastfeeding as the pandemic continues.
31. Summary
In summary the understanding of breastfeeding and human lactation as a biological system will provide a strong knowledge base from which to direct future research, devise interventions to improve maternal and infant health as well as inform public policy with respect to breastfeeding. New research methods will create the much-needed evidence to underpin education and advocacy in this field. Indeed, human lactation science is critical to the success of the global impetus to increase breastfeeding universally.
Acknowledgments
We acknowledge Jacki McEachran for assistance with editing and Ashleigh Warden for graphics.
Author Contributions
Conceptualisation D.T.G., P.E.H., L.R.M.; D.T.G., Z.G., L.F.S. prepared figures; all authors wrote significant sections of the manuscript. All authors have read and agreed to the published version of the manuscript.
D.T.G., Z.G., S.L.P., J.C.K., L.F.S., C.T.L. receive a salary from an unrestricted research grant from Medela AG administered by The University of Western Australia. L.R.M. receives a salary from Medela Australia.
Conflicts of Interest
L.R.M. was involved in the preparation of the manuscript. D.T.G.: Z.G., S.L.P., J.C.K., L.F.S., C.T.L. have received salaries from an unrestricted research grant from Medela AG administered by The University of Western Australia.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
International Breastfeeding Journal
Breastfeeding and disability/chronic ill health.
Please follow the link below to find out more about the role and apply.

Article Collections
- Most accessed
Dysphoric milk ejection reflex among Japanese mothers: a self-administered survey
Authors: Yukako Moriyama, Yuko Nakao, Naoko Yamamoto and Toshimichi Oki
Thai novice nurses’ lived experiences and perspectives of breastfeeding and human milk in the Neonatal Intensive Care Unit (NICU)
Authors: Tippawan Srichalerm, Cynthia S. Jacelon, Lindiwe Sibeko, Jumpee Granger and Carrie-Ellen Briere
Breastfeeding in primiparous women with congenital heart disease − a register study
Authors: Ylva Holstad, Bengt Johansson, Maria Lindqvist, Agneta Westergren, Inger Sundström Poromaa, Christina Christersson, Mikael Dellborg, Aleksandra Trzebiatowska-Krzynska, Peder Sörensson, Ulf Thilén, Anna-Karin Wikström and Annika Bay
Lactation induction in a transgender woman: case report and recommendations for clinical practice
Authors: Jojanneke E. van Amesfoort, Norah M. Van Mello and Renate van Genugten
The importance of community resources for breastfeeding
Authors: Jennifer LoCasale-Crouch, Margaret Kathleen Wallace, Timothy Heeren, Stephen Kerr, Yitong Yue, Genevieve Deeken, Khara Turnbull, Brianna Jaworski, Mayaris Cubides Mateus, Rachel Moon, Fern Robin Hauck, Ann Kellams, Eve Colson and Michael Jay Corwin
Most recent articles RSS
View all articles
Overabundant milk supply: an alternative way to intervene by full drainage and block feeding
Authors: Caroline GA van Veldhuizen-Staas
The development and evaluation of a picture tongue assessment tool for tongue-tie in breastfed babies (TABBY)
Authors: Jenny Ingram, Marion Copeland, Debbie Johnson and Alan Emond
Knowledge, attitude, and practice of exclusive breastfeeding among mothers in East Africa: a systematic review
Authors: Jean Prince Claude Dukuzumuremyi, Kwabena Acheampong, Julius Abesig and Jiayou Luo
Ultrasound imaging of the lactating breast: methodology and application
Authors: Donna T Geddes
An observational study of associations among maternal fluids during parturition, neonatal output, and breastfed newborn weight loss
Authors: Joy Noel-Weiss, A Kirsten Woodend, Wendy E Peterson, William Gibb and Dianne L Groll
Most accessed articles RSS
Latest Tweets
Your browser needs to have JavaScript enabled to view this timeline
Announcing the launch of In Review
The International Breastfeeding Journal, in partnership with Research Square, is now offering In Review. Authors choosing this free optional service will be able to:
Share their work with fellow researchers to read, comment on, and cite even before publication
Showcase their work to funders and others with a citable DOI while it is still under review
Track their manuscript - including seeing when reviewers are invited, and when reports are received

Supplements
Aims and scope.
International Breastfeeding Journal encompasses all aspects of breastfeeding. The journal addresses the need for a high quality multi-disciplinary journal in the field. Breastfeeding is recognized as an important public health issue with enormous social and economic implications. Infants who do not receive breast milk are likely to experience poorer health outcomes than breastfed infants; mothers who do not breastfeed increase their own health risks. In order to help women breastfeed successfully, there is a need to understand both the physiology of lactation and the social and cultural context within which breastfeeding occurs. The journal addresses all of these aspects, including identifying women who are at increased risk of not breastfeeding; the impediments to breastfeeding and the health effects of not breastfeeding for infants and their mothers; interventions to increase breastfeeding initiation and duration; and the management of breastfeeding problems.

Celebrating World Breastfeeding Week 2023
World Breastfeeding Week is celebrated every year from 1 to 7 August to encourage breastfeeding and improve the health of babies around the world.
We've collected our top content on breastfeeding across the BioMed Central portfolio. Check it out!
Blog: Breastfeeding in public

Public Health

At Springer Nature, we are committed to raising the quality of academic research across Public Health. Visit our dedicated page to view our highlighted journals and books from across our imprints, curated by our Editors.

Editor's profile
Professor Lisa Amir (MBBS MMed PhD IBCLC) is a general practitioner and has been an International Board Certified Lactation Consultant since 1989. She works in breastfeeding medicine at The Royal Women's Hospital in Melbourne, Australia. She is a Principal Research Fellow at the Judith Lumley Centre, La Trobe University and is Founding Editor-in-Chief of the open access publication International Breastfeeding Journal.
- Editorial Board
- Instructions for Editors
- Sign up for article alerts and news from this journal
- Follow us on Twitter
- Follow us on Facebook
Annual Journal Metrics
2022 Citation Impact 3.5 - 2-year Impact Factor 4.0 - 5-year Impact Factor 1.715 - SNIP (Source Normalized Impact per Paper) 0.990 - SJR (SCImago Journal Rank)
2023 Speed 10 days submission to first editorial decision for all manuscripts (Median) 219 days submission to accept (Median)
2023 Usage 1,339,755 downloads 1,321 Altmetric mentions
- More about our metrics
ISSN: 1746-4358
- General enquiries: [email protected]
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
March 28, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
reputable news agency
Longer exclusive breastfeeding may lower risk for childhood hematologic cancers
by Lori Solomon

Exclusive breastfeeding duration of at least three months may decrease the risk for childhood hematologic cancers, according to a study published online March 26 in JAMA Network Open .
Signe Holst Søegaard, Ph.D., from the Danish Cancer Society in Copenhagen, and colleagues investigated whether longer duration of exclusive breastfeeding is associated with a decreased risk for childhood acute lymphoblastic leukemia (ALL) and other childhood cancers. The analysis included administrative data for 309,473 children born between January 2005 and December 2018, identified from the Danish National Child Health Register.
The researchers found that compared with exclusive breastfeeding duration of less than three months, exclusive breastfeeding for at least three months was associated with a decreased risk for hematologic cancers (adjusted hazard ratio [aHR], 0.66; 95 percent confidence interval [CI], 0.46 to 0.95), which was largely attributable to a decreased risk for B-cell precursor ALL (BCP-ALL; aHR, 0.62; 95 percent CI, 0.39 to 0.99).
There were no associations between breastfeeding duration and risk for central nervous system tumors (aHR, 0.96; 95 percent CI, 0.51 to 1.88) or solid tumors (aHR, 0.87; 95 percent CI, 0.55 to 1.41).
"This finding is consistent with emerging investigations implicating early gut microbiome maturation in childhood BCP-ALL pathogenesis," the authors write. "To inform future preemptive interventions, additional studies should investigate the biologic mechanisms underlying the observed association."
Helen D. Bailey, Exploring Exclusive Breastfeeding and Childhood Cancer Using Linked Data, JAMA Network Open (2024). DOI: 10.1001/jamanetworkopen.2024.3075
Copyright © 2024 HealthDay . All rights reserved.
Explore further
Feedback to editors

Person is diagnosed with bird flu after being in contact with cows in Texas

'Pathogen prospecting': Mosquito researchers track malaria's history by examining its epidemiology

Pilot study shows ketogenic diet improves severe mental illness

Chatbot outperforms physicians in clinical reasoning, but also underperforms against residents on many occasions
2 hours ago

Reducing late-night alcohol sales curbed all violent crimes by 23% annually in a Baltimore neighborhood: Study

Scientists pioneer immunotherapy technique for autoimmune diseases

Researchers develop more broadly protective coronavirus vaccine

Scientists discover speed of visual perception ranges widely in humans
3 hours ago

Move more, sleep better: Study finds physical activity lengthens REM latency
5 hours ago

Siris tree leaves hold promise for stopping spread of breast cancer cells, say researchers
Related stories.

Early breastfeeding linked to lower risk of childhood obesity, regardless of mother's weight, study finds
Jan 11, 2024

1999 to 2018 saw rise in rates of breastfeeding initiation
Nov 17, 2023

Longer duration of exclusive breastfeeding has protective effect on childhood asthma, says new study
May 25, 2022

Never breastfeeding linked to increased risk of T1DM
May 12, 2017

Air pollution may increase risk for childhood leukemia
Jul 21, 2022

Breastfeeding is associated with lower levels of body fat at the age of nine
Oct 1, 2023
Recommended for you

Using cryo-shocked tumor cells to fight lung cancer
8 hours ago

Enhanced melanoma vaccine offers improved survival for men
Mar 29, 2024

Researchers develop AI-based tool paving the way for personalized cancer treatments

Researchers demonstrate technique for identifying single cancer cells in blood for the first time

Private and secure generative AI tool supports operations and research in a cancer center
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
What It Really Takes to Breastfeed a Baby
By Tiffanie Graham and Catherine Pearson and Photographs by Sara Naomi Lewkowicz, Vanessa Leroy, Sarah Rice and Yehyun Kim Nov. 30, 2022
- Share full article

By Tiffanie Graham and Catherine Pearson Photographs by Sara Naomi Lewkowicz, Vanessa Leroy, Sarah Rice and Yehyun Kim Nov. 30, 2022
Breastfeeding is hard to keep up. Some 83 percent of babies in the United States start out on breast milk, but by 6 months, just 56 percent are breastfed — and at that stage, only a quarter drink breast milk exclusively, as the American Academy of Pediatrics recommends. That steady decline speaks to the wide-ranging challenges parents face in trying to breastfeed. Among them: It’s laborious, it’s time-consuming and it hinges on workplace and societal support.
To many parents, the gulf between public health goals and reality seemed to widen last summer when the A.A.P. updated its breastfeeding recommendations , saying that it supported breastfeeding for two years or more, if it’s mutually desired by mother and child. The organization called for changes to help make breastfeeding possible, such as guaranteed paid leave, and sought to destigmatize extended breastfeeding for those who choose it. But given that a majority of parents in the United States already struggled to make it to one year of breastfeeding, as the A.A.P. previously recommended, some saw the mere suggestion of continuing to two years as out of touch .
To find out what it takes to breastfeed a baby, The New York Times followed four mothers for a day as they nursed, pumped and supplemented their milk with formula.

‘I really don’t think that people realize how hard it is for women in medicine to breastfeed.’ — Dr. Laiyin Ma, 33

With a 4-year-old, a 2-year-old and a 3-month-old at home — and having recently opened a private ophthalmology practice — Dr. Laiyin Ma is busy. Still, balancing work and breastfeeding feels easier now than when she nursed her older daughters during a grueling medical residency and fellowship.

Dr. Ma returned to work four weeks after her oldest daughter’s birth and two weeks after her second arrived. She pumped milk in stolen bursts in clinic rooms, propping her chair against the door to prevent patients and colleagues from barging in. While performing long operations, she leaked breast milk under her surgical gown.

Now her hours are more reasonable, and she has an office with a door that locks — but Dr. Ma still feels relentless pressure to keep up. If an appointment runs long, she sometimes misses her midday pump.
“I’m constantly checking how many ounces I have for the next day, then calculating how much she has had,” Dr. Ma said. “I always, always stress about it.”

As a doctor, Dr. Ma is well versed in the health benefits of breast milk and wants to nurse her daughter, as she also hopes to pass along protective Covid antibodies.
But she is stung by the irony that doctors and nurses struggle to meet the health guidelines they themselves recommend. “I really don’t think,” Dr. Ma said, “that people realize how hard it is for women in medicine to breastfeed.”
‘It isn’t the kind of endorphin-heavy bonding experience that you hear about.’ — Lauren, 40
Lauren, a public-school teacher, has had markedly different breastfeeding experiences. With her older son, now 4, nursing was a struggle from Day 1: He had a hard time latching, and she had a low milk supply. Lauren, who asked to use only her first name as a condition for being photographed while she pumped milk at school, also had postpartum pre-eclampsia and was hospitalized for eight days.

She and her son saw multiple lactation consultants; an ear, nose and throat doctor; a craniosacral therapist; and an osteopath. Lauren “triple fed” — a laborious cycle of breastfeeding, pumping, then offering her son expressed breast milk, which she repeated eight times a day. Eventually, she switched to just pumping and formula, taking herbal supplements and an off-label drug used to boost milk production — until her doctor warned her that she was putting her health at risk.

“When breastfeeding is a struggle, it isn’t the kind of endorphin-heavy bonding experience that you hear about,” Lauren said. “For me, it was very, very stressful.”

With her 7-month-old, circumstances have been different. The baby latched right away, and Lauren has produced plenty of milk. Now, she pumps three times a day: twice on her commute, and once at school in a closet.

“I feel extremely fortunate to have an extraordinarily supportive boss, and, even then, my pumping space is a closet with excess curricula, defunct technology,” Lauren said. “It doesn’t have a lock, so I’ve had some awkward moments with my colleagues walking in.” Lauren hangs a sign on the door but pumps next to a large computer with a fan so loud that she cannot always hear when someone knocks. Still, she feels lucky to have a boss who has found her at least some private space in a school where every inch is being used. Lauren knows many working parents do not have that.

As someone who has felt the highs and lows of breastfeeding, Lauren is split on the pediatric academy’s guidelines: Had the recommendation come out four years ago, when she felt such pressure to make breastfeeding work, she would have felt “devastated.”

Now, she appreciates that the recommendation could empower her to ask for pumping time and space beyond a year if she wants, though she does not have a specific goal in mind.

“I’m trying,” Lauren said, “to be much more open-minded about what ‘success’ looks like.”

‘There was never any specific end goal. I just kept going.’ — Meaghan Nash, 43

Meaghan Nash is someone for whom breastfeeding has always come easily. She breastfed her eldest, now 5, well past his second birthday. And she is breastfeeding her 8-month-old on demand, a schedule she can manage because she is never apart from her baby for more than three hours at a stretch, holding him and nursing him throughout much of the day and frequently at night.
“I just nurse all the time,” said Ms. Nash, who works as a yoga instructor. “There are moments when you’re like, ‘Wow, every single thing I do now revolves around this.’”

With her eldest, “there was never any specific end goal. I just kept going.” No one said anything explicitly unkind to her about breastfeeding her son into toddlerhood, but family did joke that she would still be nursing him in college.

“When your child turns 1, people say, ‘You know, you can stop now,’” Ms. Nash said. She feels thankful that the A.A.P.’s new guidelines will “back us up.”
Ms. Nash teaches a few days a week and has contemplated adding more. Her husband works as a touring musician, and her decision to spend time at home with the baby as opposed to taking on more work is “definitely not the most financially sound decision,” she said.

Breastfeeding round-the-clock, as she does, can feel “claustrophobic” and “all-consuming,” Ms. Nash said, but it is also “magical.”

“I just marvel at every mother. I’m like, ‘How do you do it? How do you figure this out?’” she said. “How are we all doing it?”

‘I want my body back.’ — Aleigha Harris, 35
Aleigha Harris also struggled to breastfeed her first child, now 3. She worked at a start-up, and stopping to pump several times a day did not seem possible. Ms. Harris also grappled with postpartum anxiety and found that breastfeeding exacerbated her stress.

“It was draining. It was difficult. I was in pain all the time,” she said. When she stopped after her baby was 2 months old, “everything got better.”

Despite that experience, Ms. Harris went into her second pregnancy hoping to breastfeed, in large part because of the nationwide formula shortage that peaked earlier in 2022 but has since improved.

She made it over what she called the initial “terrible” hump: “You know, engorgement, and your nipples are cracking and you’re regulating your milk,” she said. Ms. Harris had thrush, a yeast infection on the nipples, which caused a burning, shooting pain that lasted for a month. She is “super proud” of herself for persisting and has come to relish the bond she feels while breastfeeding.
“He gives me a huge smile and kicks his little legs in excitement every morning for the first feed,” Ms. Harris said. “It’s honestly the best part of my day.”

Despite her joy, she feels ambivalence. When she last spoke to The Times, Ms. Harris was preparing to wean her baby, now 4 months old.
“Breastfeeding is a full-time, unpaid job. It’s time-consuming. It’s physically draining. It’s not free, nor can every parent do it — it’s not like turning a tap on,” she said. “I want my body back.”
Advertisement

- Research Overview
- Research Activities
- Research Resources
- Training & Education
- Collaborate With NCATS
- Funding Overview
- Open Funding Opportunities
- Small Business Programs
- Funding Policy & Operating Guidelines
- Grant Information
- Challenges and Prize Competitions
- Scientific Review
- Conference Grant Information
- Resources for You
- Resources for Researchers
- Resources for Trainees
- Resources for Rare Disease Patients and Advocates
- News & Events Overview
- Newsletters
- Scientific Publications
- Infographics & Fact Sheets
- NCATS Overview
- About Translational Science
- Advisory Committees
- Careers at NCATS
- Director's Corner
- Divisions & Offices
Study: No Serious COVID-19 Vaccine Side Effects in Breastfeeding Moms, Infants
In December 2020, two novel messenger RNA (mRNA) vaccines for SARS-CoV-2 received emergency use authorization from the U.S. Food and Drug Administration; however, the early trials excluded lactating women, leading to questions about their safety in this specific population. In a recent study, published in the online edition of Breastfeeding Medicine , researchers at University of California San Diego School of Medicine found that breastfeeding mothers who received either the Pfizer-BioNTech or Moderna vaccination reported the same local or systemic symptoms as what has been previously reported in non-breastfeeding women, with no serious side effects in the breastfed infants.
Last updated on October 13, 2023
Novel Lactation Induction Protocol for a Transgender Woman Wishing to Breastfeed: A Case Report
Affiliations.
- 1 Duke University School of Medicine, Duke University, Durham, North Carolina, USA.
- 2 Duke Department of Pharmacy, Duke University, Durham, North Carolina, USA.
- 3 Duke Global Health Institute, Duke University, Durham, North Carolina, USA.
- 4 Duke Department of Family Medicine and Community Health, Duke University, Durham, North Carolina, USA.
- 5 Duke Department of Medicine, Division of Endocrinology Metabolism and Nutrition, Duke University, Durham, North Carolina, USA.
- PMID: 38535753
- DOI: 10.1089/bfm.2024.0012
Background: Lactation induction in transgender women is a clinical and research priority in the field of breastfeeding medicine. To date, there are four case reports detailing successful induced lactation in transgender patients who wished to breastfeed. The Academy of Breast Feeding Medicine does not formally recommend a specific medication regimen for transgender patients due to lack of high-quality research. Case Presentation: A 50-year-old transgender woman with a hypercoagulable disorder who was able to lactate and breastfeed with novel hormone regimen management at a gender care clinic. Her baseline hormone treatment was an estradiol 0.3 mg transdermal patch every 72 hours and micronized progesterone 200 mg daily. Results: Within four weeks of initiating a modified hormone regimen (estradiol 0.4 mg patch every 72 hours, progesterone 300 mg daily, metoclopramide 10 mg three times daily), the patient was lactating spontaneously. On multiple occasions, she breastfed and expressed up to 30 mL of milk through pumping. Conclusion: This report offers a new effective hormone regimen for transgender patients who wish to lactate and cannot access domperidone-the galactagogue used in previous case reports. It also provides a review of previously published case reports on this subject. Future research in this field should prioritize cohort studies of transgender patients who desire lactation to further assess patient attitudes, experiences, and outcomes.
Keywords: breastfeeding; case report; lactation; transgender.
latest in US News

State blows deadline to hand over critical study on mayoral...

Florida Supreme Court upholds state’s 15-week ban on most...

Hope Hicks expected to testify in Trump 'hush money' trial: report

Actor John Cardoza robbed by panhandler in NYC shop, second...

Powerball jackpot reaches $1 billion for Monday night drawing

Moped-riding maniac bashes woman with hammer in unprovoked...

Ex-cons indicted in shooting death of NYPD hero cop Jonathan...

Iran ramping up nuclear work, executing more people during Biden...
Trans grandma able to breastfeed baby with help of experimental hormone drugs.
- View Author Archive
- Get author RSS feed
Thanks for contacting us. We've received your submission.

Researchers at Duke University used experimental hormone drugs to help a transgender mother-of-five breastfeed her grandchild, in a study that has been panned as “frankly disturbing.”
The unidentified 50-year-old was “lactating spontaneously” and able to produce up to 30 ml of milk at a time after a four-week course of hormone treatments, researchers recently wrote in the Breastfeeding Medicine journal.
She was then able to feed her four-month-old grandchild without any side effects to herself, they wrote in the study, according to the Daily Mail.

The researchers said they were moved to help the biological male create a “bond from breastfeeding that she has not been able to experience with her own five children” after she reached out to the North Carolina university in the spring of 2022.
Scientists around the world had already been able to help four other transgender women induce lactation for breastfeeding, but the researchers at Duke needed to use different treatment protocols because the drugs used in the previous four studies have not yet been approved for use in the US by the Food and Drug Administration, they wrote.
In the end, the grandmother was moved to tears as she was able to help her daughter feed the newborn.
“The patient tearfully reported this was a significant and emotional experience for her that felt very different from formula feeding her other children,” the scientists wrote in the journal, according to the Mail.
“She states that she has a special bond with this baby, for which she is grateful.”

“She regrets that she had not known about the possibility sooner and wished that other transgender women could know that breastfeeding a baby can be a reality.”
They added that “conversations with the subject before, during, and after treatment revealed important insights for the ongoing discussions about the role of lactation induction and breastfeeding in gender-affirming care.”
Start your day with all you need to know
Morning Report delivers the latest news, videos, photos and more.
Thanks for signing up!
Please provide a valid email address.
By clicking above you agree to the Terms of Use and Privacy Policy .
Never miss a story.
But Heather Welford, of With Women — a group of midwives and breastfeeding experts — slammed the study as “disturbing.”
“Most people would find the idea absolutely shocking,” she told the Mail.
“Babies come into this world ready to continue their relationship with their mother, and breastfeeding helps with this,” she said.
“Disrupting this with attempts at breastfeeding by anyone else is frankly disturbing.”
Maya Forstater, the executive director of Sex Matters, also noted that “babies cannot consent to being patients in a study which sets aside biological reality to define treatment protocols relating to so-called ‘gender medicine.’”
“Men should not be permitted, still less supported, to get between babies and their mothers or to use babies as props to validate their beliefs that they are women,” she said.
The study comes less than one year after the Centers for Disease Control and Prevention found itself in hot water for publishing advice for transgender women to “chestfeed ” their children.
“Some transgender parents who have had breast/top surgery may wish to breastfeed, or chestfeed (a term used by some transgender and non-binary parents), their infants,” the CDC’s website said.
It suggested that “healthcare providers working with these families should be familiar with medical, emotional, and social aspects of gender transitions to provide optimal family-centered care and meet the nutritional needs of the infant.”
However, it failed to mention the health risks to the baby, including that one of the drugs used to induce lactation in biological males can give a child an irregular heartbeat.
Share this article:
Study Finds ‘Digital Humans’ Equally Effective As Real Ones In Ergonomics Training

Could digital humans — realistic virtual representations of humans that communicate through text-to-speech and speech-to-text interfaces — provide online training that is as effective as that provided by real humans?
The idea is promising, according to a new study published in Applied Ergonomics and conducted by Texas A&M University School of Public Health researchers Kaysey Aguilar , Mark Benden and Matthew Lee Smith , and a colleague from Texas A&M’s Department of Psychology.
The researchers analyzed whether training by a digital human would give remote workers knowledge of ergonomics that would lead them to change their work behavior. The team found that digital human training outcomes are comparable to those from conventional online training.
“This is significant given the dramatic growth in chatbots and other AI-driven interfaces,” Aguilar said. “Digital humans can be customized in terms of their appearance, language, personality, script and gestures, which means that they might provide customizable training that is not possible with conventional online training technologies.”
The research team recruited a sample of remote workers from a telecommunications company and randomly assigned them to a digital human group, a conventional online training group and a control group that did not receive training. The two courses used the same content to ensure they could be accurately compared. Additionally, the researchers assigned twice as many people to the digital human group than the others to address potential issues with using a new technology.
The researchers sent each participant a questionnaire that collected data on demographics, remote work practices, ergonomics knowledge, ergonomic behavior and incidence of musculoskeletal discomfort before and after training.
Analysis of the questionnaires found that both the conventional and digital human groups had improved ergonomics knowledge and decreased musculoskeletal discomfort, showing that the two methods have comparable outcomes. However, only the conventional online training group had statistically significant improvements in ergonomic behavior.
In addition, the findings point to the potential for digital human-based training to improve remote workers’ ergonomics knowledge and practices. The prevalence of remote work and the introduction of technological advances make innovation and research on remote ergonomics training an important factor in ensuring a healthy workforce, the researchers said.
Although the digital human training was not found to be superior to conventional methods, the researchers note a need for further research that fully utilizes the digital human’s conversational abilities.
“Digital humans that are customized to the needs of workers and are able to engage in conversation could be more effective than typical online training methods,” Aguilar said.
Media contact: Texas A&M Health, [email protected]
Related Stories

Monitoring Your Own Blood Pressure Can Save Money — And Possibly Your Life
Study finds self-monitoring of blood pressure has the potential for better health outcomes and cost benefits compared to traditional care.

Eating Cruciferous Vegetables While Breastfeeding May Give Infants A Healthy Start
ATexas A&M Health study adds to a growing body of knowledge about the effect of plant-based chemicals on human health.

Public Health Professor Receives Federal Funding For Air Quality Assessment In East Palestine
Researchers who monitored air quality after the Ohio train derailment are eager to return and compare results, more than a year post-disaster.
Recent Stories

Texas A&M Professor Recognized With Prestigious Veterinary Award
Dr. Nicholas Jeffery receives Bourgelat Award for innovative strategies, including advancements in treating spinal cord and nervous system injuries in dogs.
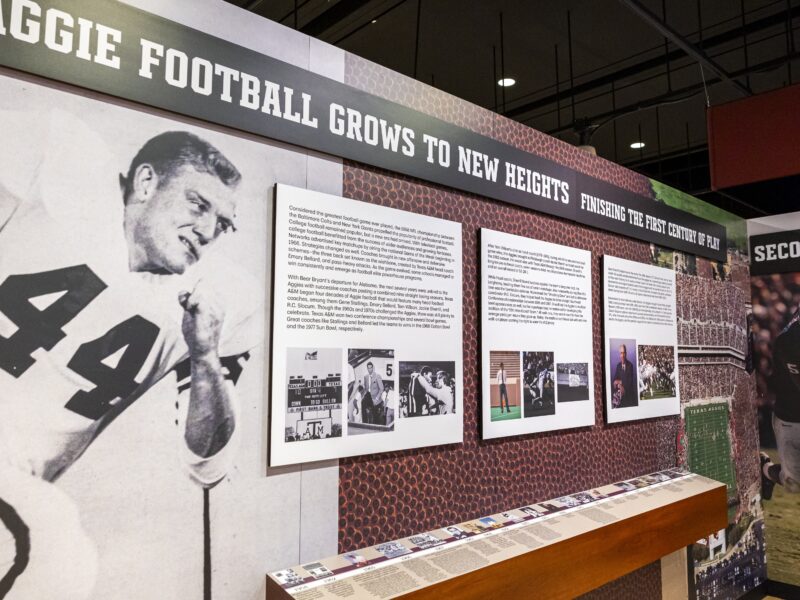
Last Chance To Explore A Century Of Aggie Football
Exhibit at George H.W. Bush Library And Museum is ending its eight-month run on April 28.
MSC SCOLA Illuminates Path To Success
The three-day Student Conference on Latinx Affairs offers opportunities for learning, leadership and growth.

Subscribe to the Texas A&M Today newsletter for the latest news and stories every week.

IMAGES
COMMENTS
Latest research on breastfeeding including benefits of breastfeeding, disease transmission through breast milk, environmental contaminants found in breast milk and more.
Breastfeeding has proven health benefits for both mothers and babies in high-income and low-income settings alike. Yet, less than 50% of babies worldwide are breastfed according to WHO recommendations. For decades, the commercial milk formula industry has used underhand marketing strategies, designed to prey on parents' fears and concerns, to ...
In this review, we provide new evidence from the past 10 years on the following topics relevant to exclusive breastfeeding: milk production and transfer, neonatal weight and output assessment, glucose stabilization, hyperbilirubinemia, immune development and the microbiome, supplementation, and health system interventions.
Scientific advances in breastfeeding, breastmilk, and lactation Breastfeeding is part of our species-specific biopsychosocial system that has evolved through our mammalian history to optimise the health and survival of both mothers and infants.3,11 Research published since the 2016 Lancet breastfeeding Series 1 has strengthened the evidence for the
This Series provides a new vision on how to address breastfeeding protection, promotion, and support at scale through multilevel, equitable approaches. This vision addresses breastfeeding barriers and facilitators across all levels, from the structural to the individual, building on the conceptual model of the 2016 Lancet breastfeeding Series ...
In 2022 the Academy of Breastfeeding Medicine (ABM) published Clinical Protocol #36: The Mastitis Spectrum, which aims to update clinical approaches to management of benign lactation-related breast inflammatio... Pamela Douglas. International Breastfeeding Journal 2023 18 :51. Review Published on: 5 September 2023.
Breastfeeding and maternal health play crucial roles in improving newborn health, which is closely related to the development of families and society. Early essential newborn care, which emphasizes early exclusive breastfeeding and skin-to-skin contact, is recommended by the World Health Organization. This study aimed to explore the association of early essential newborn care with ...
The Lancet Series nicely integrates new evidence showing how important it is for all of society to support the wishes of breastfeeding mothers through (1) social protection policies (e.g., improved maternity benefits for women working in the formal and informal economy; workplace accommodations including lactation rooms, and flexible working ...
The Healthy People 2030 (HP2030) program has set national objectives for the United States to increase the proportion of infants to exclusively breastfeed through 6th months of age to 42.4% (6 ...
2. COVID Pandemic and Maternal-Infant Health. There are only a few infectious contraindications to breastfeeding or the provision of expressed breastmilk, except human immunodeficiency virus (HIV) in industrialized nations, human T cell lymphotropic virus, active Ebola infection, and untreated brucellosis [3,4,5].Time after time, history has shown how resilient and protected breastmilk ...
In this Series paper, we examine how mother and baby attributes at the individual level interact with breastfeeding determinants at other levels, how these interactions drive breastfeeding outcomes, and what policies and interventions are necessary to achieve optimal breastfeeding. ... 10 International Food Policy Research Institute, New Delhi ...
Perceptions about breastfeeding. Women's perceptions about breastfeeding were covered in 83% (n = 49) of the papers.Most articles (n = 31) suggested that women perceived breastfeeding as a positive experience and believed that breastfeeding had many benefits [19, 20].The phrases "breast is best" and "breastmilk is best" were repeatedly used by the participants of studies included in ...
#5 MeSH descriptor: [Breast Feeding] explode all trees #6 #1 Or #2 OR #3 OR #4 OR #5. Data collection and analysis. We followed the standard methodology as suggested by Part 1: ... These identified gaps open up a new area of research and can be done on a priority basis. With an improved understanding of the significance of BF and the escalating ...
In summary the understanding of breastfeeding and human lactation as a biological system will provide a strong knowledge base from which to direct future research, devise interventions to improve maternal and infant health as well as inform public policy with respect to breastfeeding. New research methods will create the much-needed evidence to ...
Beside the inverse association of breastfeeding with maternal cardiovascular outcomes shown in our study, breastfeeding is also robustly associated with a reduced risk for maternal type 2 diabetes, ovarian cancer, and breast cancer. 2 In a survey of 5554 women in the United States, only 38.5% were aware that breastfeeding is associated with a ...
Meek said the shift was rooted in research that suggests there are particular health benefits of extended breastfeeding for mothers, like decreased risk for maternal Type 2 diabetes.
The International Breastfeeding Journal, in partnership with Research Square, is now offering In Review. Authors choosing this free optional service will be able to: ... "Breastfeeding in Public", a new series of articles from the International Breastfeeding Journal, aims to highlight the issues surrounding breastfeeding in public ...
Exclusive breastfeeding duration of at least three months may decrease the risk for childhood hematologic cancers, according to a study published online March 26 in JAMA Network Open. Signe Holst ...
Executive Summary. With a substantial development of research and findings for breastfeeding over the past three decades, we are now able to expand on the health benefits for both women and children across the globe. The two papers in this Series will describe past and current global trends of breastfeeding, its short and long-term health ...
To find out what it takes to breastfeed a baby, The New York Times followed four mothers for a day as they nursed, pumped and supplemented their milk with formula. 'I really don't think that ...
Research in Cell Metabolism finds pregnancy moves biological clock forward, but aging reverses post-pregnancy, especially with breastfeeding.
In a recent study, published in the online edition of Breastfeeding Medicine, researchers at University of California San Diego School of Medicine found that breastfeeding mothers who received either the Pfizer-BioNTech or Moderna vaccination reported the same local or systemic symptoms as what has been previously reported in non-breastfeeding ...
Background: Lactation induction in transgender women is a clinical and research priority in the field of breastfeeding medicine. To date, there are four case reports detailing successful induced lactation in transgender patients who wished to breastfeed. The Academy of Breast Feeding Medicine does not formally recommend a specific medication regimen for transgender patients due to lack of high ...
Background: Lactation induction in transgender women is a clinical and research priority in the field of breastfeeding medicine. To date, there are four case reports detailing successful induced lactation in transgender patients who wished to breastfeed. The Academy of Breast Feeding Medicine does not formally recommend a specific medication regimen for transgender patients due to lack of high ...
Breastmilk makes the world healthier, smarter, and more equal: these are the conclusions of a new Lancet Series on breastfeeding. The deaths of 823 000 children and 20 000 mothers each year could be averted through universal breastfeeding, along with economic savings of US$300 billion. The Series confirms the benefits of breastfeeding in fewer infections, increased intelligence, probable ...
Researchers at Duke University used experimental hormone drugs to help a transgender mother-of-five breastfeed her grandchild, in a study that has been panned as "frankly disturbing."
Could digital humans — realistic virtual representations of humans that communicate through text-to-speech and speech-to-text interfaces — provide online training that is as effective as that provided by real humans? The idea is promising, according to a new study published in Applied Ergonomics and conducted by Texas A&M University School of Public Health researchers Kaysey Aguilar, Mark ...