
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- Health Topics
- < Back To How the Heart Works
- How Blood Flows through the Heart
- What the Heart Looks Like
- How the Heart Beats
MORE INFORMATION

How the Heart Works How Blood Flows through the Heart
Language switcher.
Arteries and veins link your heart to the rest of the circulatory system. Veins bring blood to your heart. Arteries take blood away from your heart. Your heart valves help control the direction the blood flows.
Heart valves
Heart valves control the flow of blood so that it moves in the right direction. The valves prevent blood from flowing backward.
The heart has four valves.
- The tricuspid valve separates the right atrium and right ventricle.
- The mitral valve separates the left atrium and left ventricle.
- The pulmonary valve separates the right ventricle and the pulmonary artery.
- The aortic valve separates the left ventricle and aorta.
The valves open and shut in time with the pumping action of your heart's chambers. The opening and closing involve a set of flaps called cusps or leaflets. The cusps open to allow blood to flow out of a chamber and close to allow the chamber to refill with blood. Heart valve diseases can cause backflow or slow the flow of blood through the heart.
Learn about what the valves of the heart look like and do. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Adding oxygen to blood
Oxygen-poor blood from the body enters your heart through two large veins called the superior and inferior vena cava. The blood enters the heart's right atrium and is pumped to your right ventricle, which in turn pumps the blood to your lungs.
The pulmonary artery then carries the oxygen-poor blood from your heart to the lungs. Your lungs add oxygen to your blood. The oxygen-rich blood returns to your heart through the pulmonary veins. Visit our How the Lungs Work page to learn more about what happens to the blood in the lungs.
The oxygen-rich blood from the lungs then enters the left atrium and is pumped to the left ventricle. The left ventricle generates the high pressure needed to pump the blood to your whole body through your blood vessels.
When blood leaves the heart to go to the rest of the body, it travels through a large artery called the aorta. A balloon-like bulge, called an aortic aneurysm , can sometimes occur in the aorta.
Learn about how your heart circulates blood to your lungs and throughout your body. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Supplying oxygen to the heart’s muscle
Like other muscles in the body, your heart needs blood to get oxygen and nutrients. Your coronary arteries supply blood to your heart. These arteries branch off from the aorta so that oxygen-rich blood is delivered to your heart as well as the rest of your body.
- The left coronary artery delivers blood to the left side of your heart, including your left atrium and ventricle and the septum between the ventricles.
- The circumflex artery branches off from the left coronary artery to supply blood to part of the left ventricle.
- The left anterior descending artery also branches from the left coronary artery and provides blood to parts of both the right and left ventricles.
- The right coronary artery provides blood to the right atrium and parts of both ventricles.
- The marginal arteries branch from the right coronary artery and provide blood to the surface of the right atrium.
- The posterior descending artery also branches from the right coronary artery and provides blood to the bottom of both ventricles.
Your coronary arteries supply oxygen to your body. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Some conditions can affect normal blood flow through these heart arteries. Examples include:
- Heart attack
- Coronary heart disease
The coronary veins return oxygen-low blood from the heart's muscles back to the right atrium so it can be pumped to the lungs. They include:
- The anterior cardiac veins
- The great cardiac vein
- The middle cardiac vein
- The small cardiac vein
Vasculature of the Heart
Written by Sophie Stanley
Last updated January 8, 2024 • 56 Revisions •
The entire body must be supplied with nutrients and oxygen via the circulatory system and the heart is no exception. The coronary circulation refers to the vessels that supply and drain the heart. Coronary arteries are named as such due to the way they encircle the heart, much like a crown.
This article will outline the naming, distribution, and clinical relevance of vessels in the coronary circulation .
Premium Feature
Coronary arteries.
There are two main coronary arteries which branch to supply the entire heart. They are named the left and right coronary arteries, and arise from the left and right aortic sinuses within the aorta.
The aortic sinuses are small openings found within the aorta behind the left and right flaps of the aortic valve . When the heart is relaxed, the back-flow of blood fills these valve pockets, therefore allowing blood to enter the coronary arteries.
The left coronary artery (LCA) initially branches to yield the left anterior descending (LAD), also called the anterior interventricular artery. The LCA also gives off the left marginal artery (LMA) and the left circumflex artery (Cx). In ~20-25% of individuals, the left circumflex artery contributes to the posterior interventricular artery (PIv).
The right coronary artery (RCA) branches to form the right marginal artery (RMA) anteriorly. In 80-85% of individuals, it also branches into the posterior interventricular artery (PIv) posteriorly.
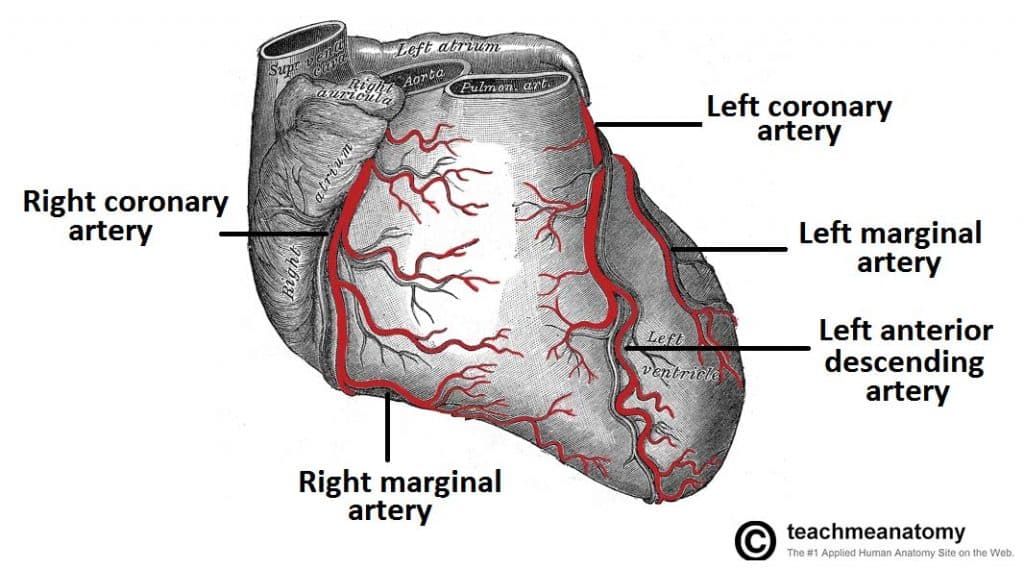
Fig 1 Anterior view of the arterial supply to the heart.
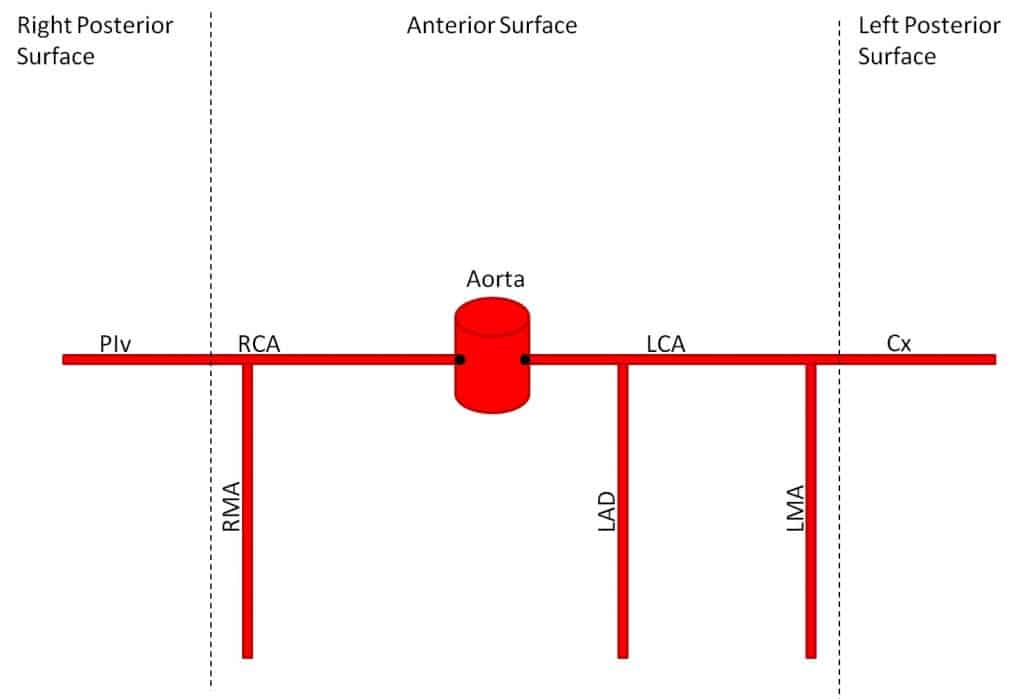
Fig 2 Overview of the branching structure of the coronary arteries.
Cardiac Veins
The venous drainage of the heart is mostly through the coronary sinus – a large venous structure located on the posterior aspect of the heart. The cardiac veins drain into the coronary sinus, which in turn, empties into the right atrium. There are also smaller cardiac veins which pass directly into the right atrium.
The main tributaries of the coronary sinus are:
- Great cardiac vein (anterior interventricular vein) – the largest tributary of the coronary sinus. It originates at the apex of the heart and ascends in the anterior interventricular groove. It then curves to the left and continues onto the posterior surface of the heart. Here, it gradually enlarges to form the coronary sinus.
- Small cardiac vein – located on the anterior surface of the heart, in a groove between the right atrium and right ventricle. It travels within this groove onto the posterior surface of the heart, where it empties into the coronary sinus.
- Middle cardiac vein (posterior interventricular vein) – begins at the apex of the heart and ascends in the posterior interventricular groove to empty into the coronary sinus.
- Posterior cardiac vein – located on the posterior surface of the left ventricle. It lies to the left of the middle cardiac vein and empties into the coronary sinus.
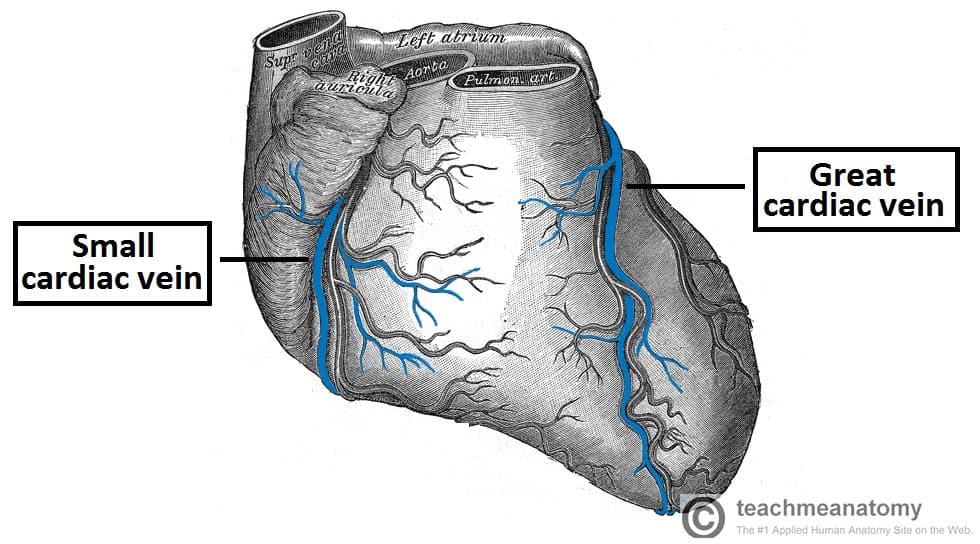
Fig 3 Anterior view of the venous drainage of the heart. Supplied by the great and small cardiac veins
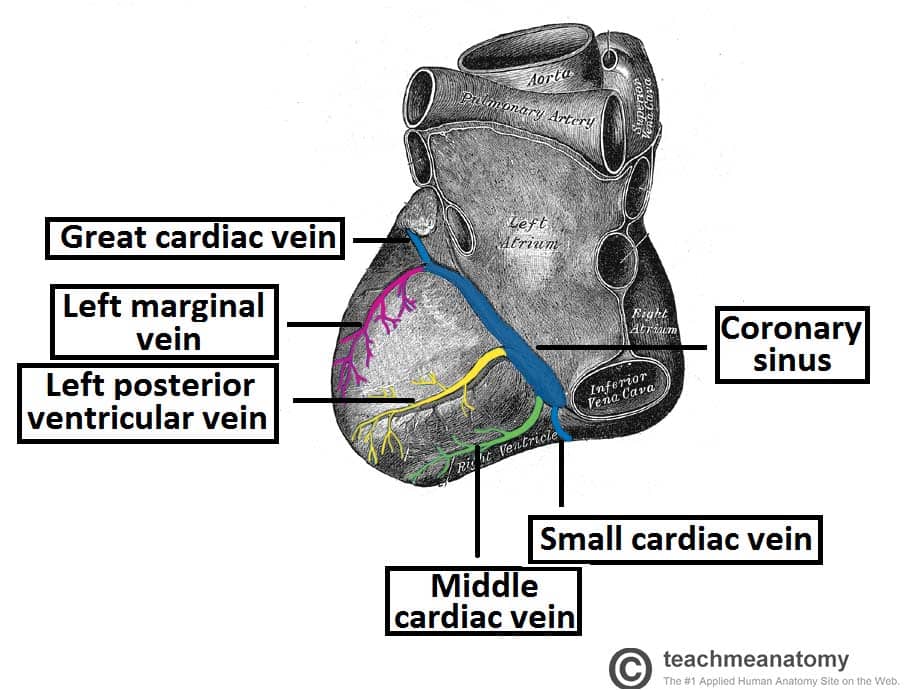
Fig 4 Posterior view of the heart, showing the venous drainage.
Dissection Images

Distribution of the Coronary Arteries
In general, the area of the heart which an artery passes over will be the area that it perfuses. The following describes the anatomical course of the coronary arteries. See Appendix A for a tabular overview of the arterial distribution.
The RCA passes to the right of the pulmonary trunk and runs along the coronary sulcus before branching. The right marginal artery arises from the RCA and moves along the right and inferior border of the heart towards the apex . The RCA continues to the posterior surface of the heart, still running along the coronary sulcus . The posterior interventricular artery then arises from the RCA and follows the posterior interventricular groove towards the apex of the heart.
The LCA passes between the left side of the pulmonary trunk and the left auricle . The LCA divides into the anterior interventricular branch and the circumflex branch. The anterior interventricular branch (LAD) follows the anterior interventricular groove towards the apex of the heart where it continues on the posterior surface to anastomose with the posterior interventricular branch. The circumflex branch follows the coronary sulcus to the left border and onto the posterior surface of the heart. This gives rise to the left marginal branch which follows the left border of the heart.
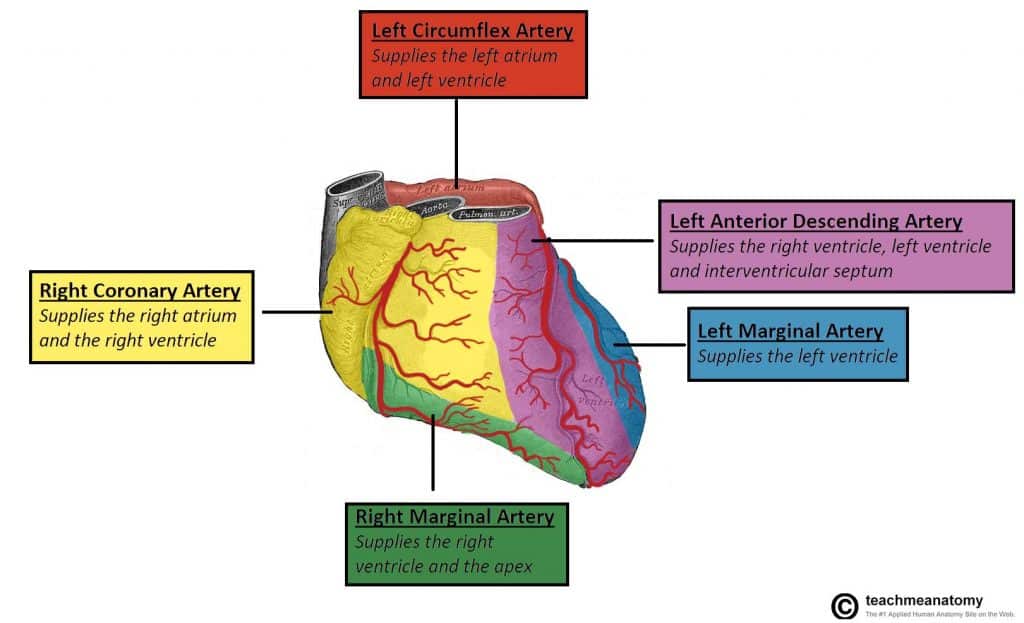
Fig 4 Anterior view of territorial arterial supply to the heart.
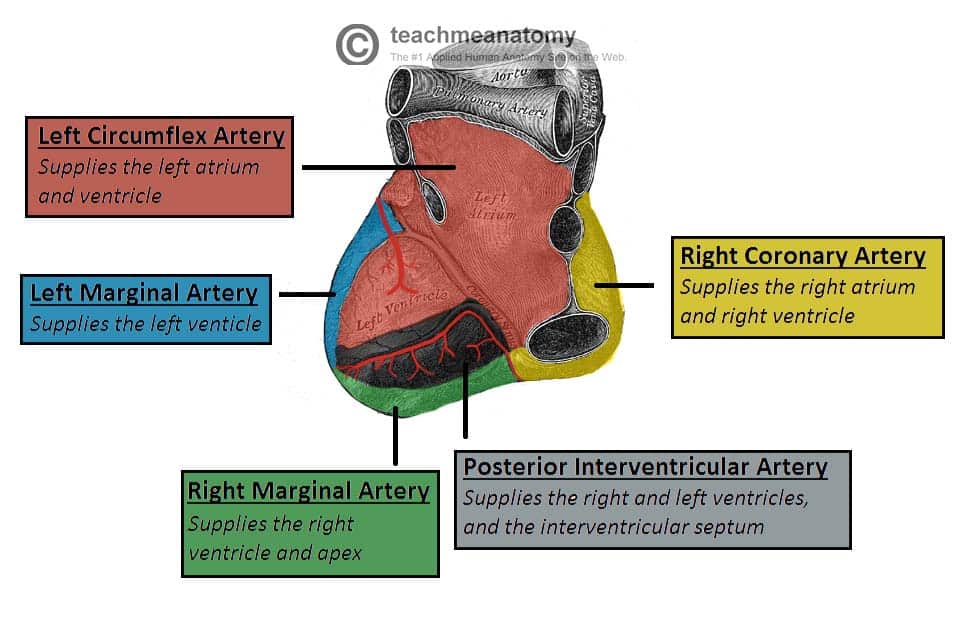
Fig 5 Posterior view of territorial arterial supply to the heart.
Clinical Relevance
Coronary artery disease.
Coronary artery disease or coronary heart disease (CHD) is a leading cause of death, both in the UK and worldwide. It describes a reduction in blood flow to the myocardium and has several causes and consequences.
CHD can result in reduced blood flow to the heart as a result of narrowing or blockage of the coronary arteries. This may be due to atherosclerosis , thrombosis, high blood pressure, diabetes or smoking. All these factors lead to a reduced flow of blood to the heart through physical obstruction or changes in the vessel wall.
Angina pectoris is one consequence of CHD. Angina pectoris describes the transient pain a person may feel on exercise as a result of lack of oxygen supplied to the heart. This pain is felt across the chest but is quickly resolved upon rest. Exercise is a trigger for angina as the coronary arteries fill during the diastolic period of the cardiac cycle. On exercising, the diastolic period is shortened meaning that there is less time for blood flow to overcome a blockage in one of the coronary vessels in order to supply the heart.
If left untreated, angina can soon progress to more severe consequences, such as a myocardial infarction . The sudden occlusion of an artery results in infarction and necrosis of the myocardium. This means a section of the heart is unable to beat (which part of the heart depends on which artery has become occluded). The ECG leads on which an MI change appears can be used to locate the artery that had been occluded as shown in the table.
Diagnosis and Treatment of Coronary Artery Disease
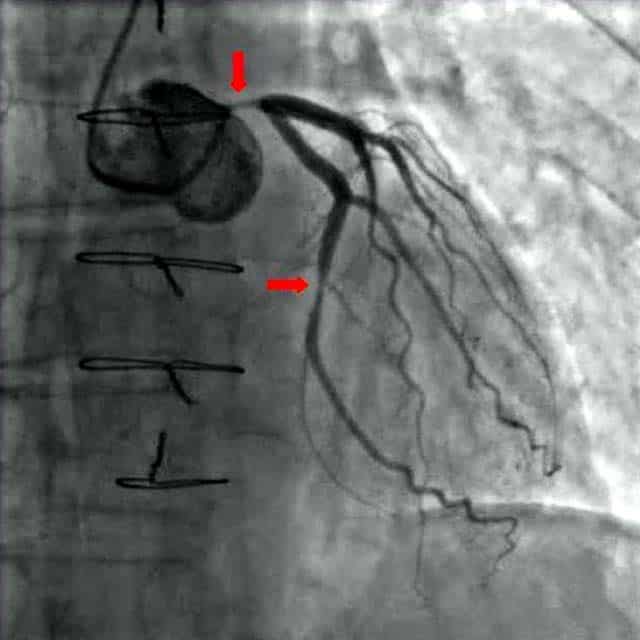
Fig 1.6 A coronary angiogram. Two critical narrowings have been labelled.
A blockage in a coronary artery can be rapidly identified by performing a coronary angiogram . The imaging modality involves the insertion of a catheter into the aorta via the femoral artery . A contrast dye is injected into the coronary arteries and x-ray based imaging is then used to visualise the coronary arteries and any blockage that may be present.
Immediate treatment of a blockage can be performed by way of a coronary angioplasty, which involves the inflation of a balloon within the affected artery. The balloon pushes aside the atherosclerotic plaque and restores the blood flow to the myocardium. The artery may then be supported by the addition of an intravascular stent to maintain its volume.
Appendix A – Tabular Overview of the Vasculature of the Heart
Recommended reading, forgot password.
Please enter your username or email address below. You will receive a link to create a new password via emai and please check that the email hasn't been delivered into your spam folder.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Report question, rate this article.
BLOOD SUPPLY OF THE HEART
Aug 04, 2014
220 likes | 564 Views
BLOOD SUPPLY OF THE HEART. Dr Jamila EL medany. &. Dr Essam Salama. Objectives. At the end of the lecture the student should be able to know about; The arterial supply of the cardiac muscle regarding (origin, course, distribution and branches). The coronary anastmosis.
Share Presentation
- right coronary artery
- venous blood
- heart chambers
- left margin
- anterior interventricular a

Presentation Transcript
BLOOD SUPPLY OF THE HEART Dr Jamila EL medany & Dr Essam Salama
Objectives • At the end of the lecture the student should be able to know about; • The arterial supply of the cardiac muscle regarding (origin, course, distribution and branches). • The coronary anastmosis. • The arterial supply to the conducting system of the heart. • The venous drainage of the heart regarding (origin, tributaries and termination).
Arterial Supply The arterial supply of the heart is provided by Coronary Arteries : Right Coronary artery & Left Coronary artery They are distributed over the cardiac surface, within the subepicadium connective tissue. L Coronary artery
Origin of Coronary Arteries LCA RCA • Fromthe initial part of theAscendingAorta. (Immediately above the aortic valve). AA
Right Coronary Artery Arises from the anterior aortic sinus of the ascending aorta. Descends in the right atrioventricular groove between the Right Auricle and the Pulmonary trunk. At the inferior border of the heart it continuous posterioly to anastomose with the left coronary.
(RCA ) Supplies: • Right atrium, • Right ventricle, • part of Left Atrium, • Left ventricle & Atrioventricular septum.
Branches • (1) Right Conus artery: • To the infundibulum and the upper part of the anterior wall of the right ventricle. • (2)Anterior Ventricular arteries • To the anterior surface of the right ventricle. • The Marginal arteryis the largest branch. Ca
(3) Posterior ventricular arteries: • To the diaphragmatic surface of the right ventricle. • (4) Atrial branches: • To the right atrium . • The Artery of the SAN.
(5) Posterior Interventricular A: • Supplies: • a.Diaphragmatic surface of the R & L Ventricles. • b. Posterior part of the IVS Excluding its Apex. • C. Septal branch to the AVN.
Left Coronary Artery The Larger of the two coronaries. Arises from the left posterior aortic sinus of the ascending aorta. Descends: Between the pulmonary trunk and the left auricle. In the IV groove to the apex of the heart. Divides into two branches: (Anterior IV & Circumflex) .
Left Coronary Artery • It anastomoses with the right coronary inthe posterior IV groove (in 2/3 of people) • It Supplies: • Greater part of Left Atrium, • Left Ventricle and Ventricular Septum
Branches • Ventricular branches to both ventricles and the IV septum. Circumflex artery gives : Left Marginal to the left margin of the LV tillthe apex. Anterior Interventricular A gives: • Left (Lateral) diagonal • Anterior & • Posterior ventricular to (LV) • Atrial to ( LA)
Variations of the Coronary Arteries • Right dominance: • In (90 %) of population, the Posterior Interventricular artery is a branch of the Right Coronary. • Left dominance: • In the rest (10%), the Posterior Interventricular artery arises from the Circumflex branch of the Left Coronary A
Coronary Anastomosis Anastomoses between terminal branches of the right and left coronaries exist but not large enough to provide adequate blood supply.
Arterial Supply ofConducting System • SAN, AVN & AVB are usually supplied by Right coronary. • RBB of (AVB) is supplied by Left coronary • LBB of (AVB) is supplied by both right and left coronaries
Venous Drainage • 1. Anterior cardiac veins: • Open directly into the Right Atrium. • 2. Venae Cordis minime • Open into the heart chambers. • 3. Coronary sinus
Coronary Sinus • Drains most of the venous blood of the heart. • Lies in the posterior part of the AV groove. • Origin : • It is the direct continuation of the Great Cardiac Vein. • Tributaries: • (1) Cardiac Veins: • A. Great. • B. Middle. • C. Small. • (2) Oblique vein of left atrium.
It empties into Right Atrium. • Its opening is inferior & to the left of the IVC opening. • It is guarded by a valve.
- More by User
CNS Blood Supply
CNS Blood Supply. Nabeel Kouka, MD, DO, MBA www.brain101.info. Spinal Cord Vascular Supply. Arterial Supply - Spinal Arteries Anterior (1) & Posterior (2) Spinal Artery from Vertebral artery
2.51k views • 57 slides
Blood Supply of Spinal Cord
The spinal cord is supplied by 1. Anterior spinal artery 2. Posterior spinal artery 3. Spinal branch from the 1st intercostal artery 4. Spinal branch from the 11th intercostal arteryBranches of the vertebral, deep cervical, intercostal, and lumbar arteries contribute to three arteries that ru
3.15k views • 10 slides
Path of Blood Through The Heart
Path of Blood Through The Heart. Heart Chambers and Valves. Atria or Atrium Auricles Ventricles Interatrial Septum Interventricular septum Atrioventricular Orifice. Heart Chambers and Valves. Atrioventricular Valve (A-V valve) Sulci Atrioventricular (coronary) Sulcus
389 views • 15 slides
Coronary heart disease (CHD) is a narrowing of the small blood vessels that supply blood and oxygen to the heart.
Coronary heart disease (CHD) is a narrowing of the small blood vessels that supply blood and oxygen to the heart. .
312 views • 11 slides
Blood supply
Vascular Supply. About 18% of the total blood volume in the body circulates in the brain, which accounts for about 2% of the body weight. The blood transports oxygen, nutrients, and other substances necessary for proper functioning of the brain tissues and carries away metabolites. Loss of conscio
497 views • 26 slides

The Path of Blood Through the Heart
The Path of Blood Through the Heart. Part I All the blood from the body travels through veins back to the heart. The blood from the head and neck enter the heart through the superior vena cava . Most of the blood from the rest of body enters the heart through the inferior vena cava .
530 views • 5 slides
Blood supply of Brain
Blood supply of Brain. Essam Ealdin Abdelhady Salama. Arterial supply of the brain . Four arteries enter into the cranial cavity to supply the brain; Two vertebral arteries. Two internal carotid arteries. Vertebral arteries. Aries from 1 st part of the subclavian artery.
824 views • 30 slides
UNDERSTANDING THE BLOOD FLOW OF THE HEART
UNDERSTANDING THE BLOOD FLOW OF THE HEART. Rheede Hopgood . Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium.
295 views • 8 slides
Blood Supply of the Upper Limb
Blood Supply of the Upper Limb. Dr: Yasser Seddeg. Arteries of Upper Limb. Axillary Artery. Continuation of subclavian artery at lateral border of first rib Becomes brachial artery at lower border of teres major Divided into three parts by overlying pectoralis minor. teres major.
2.1k views • 17 slides
Blood supply of the Brain
Blood supply of the Brain. Arterial Blood Supply. Arterial blood supply of the brain Brain is supplied by pairs of internal carotid artery and vetebral artery. . Internal Carotid Artery.
820 views • 18 slides
Blood Supply of the Upper Limb. Dr. Sama-ul-Haque. Objectives. Objectives. Axillary Artery. Begins at the lateral border of 1 st rib as a continuation of subclavian artery . Ends at the lower border of teres major muscle by continuing as brachial artery .
1.78k views • 62 slides
Blood Supply
Blood Supply. Human Neurobiology ANHB 2217 Avinash Bharadwaj Semester 1, 2006 Week 2. Blood Vessels of CNS. Nervous tissue – high metabolic needs One-fiftieth of body weight One-sixth of circulating blood volume One-fifth of oxygen consumption Extreme sensitivity to reduction or loss
443 views • 15 slides
BLOOD FLOW through the HEART
BLOOD FLOW through the HEART. Biology Version:. The right and left sides of the heart work together Right Side Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium. Left Side
870 views • 55 slides
Blood supply of the Heart
Blood supply of the Heart. Dr. Sama ul Haque Dr Rania Gabr. Objectives. Enlist the arteries and veins supplying heart. Describe the origin and branches of the right and left coronary arteries. Define coronary artery anastomosis.
3.89k views • 27 slides

Blood/Heart
Blood/Heart. Heart Facts. The heart you see drawn on the average Valentine is only a rough representation Of the actual structure of the heart. Your heart is actually shaped more like an Upside down pear. Crazy Fact.
535 views • 18 slides
BLOOD SUPPLY OF THE HEART. Dr Jamila EL medany. &. Dr Essam Salama. Objectives. At the end of the lecture the student should be able to know about; The arterial supply of the cardiac muscle regarding (origin, course, distribution and branches). The coronary anastmosis .
410 views • 18 slides
Liver Blood Supply
Management of Adult Patients With Ascites Due to Cirrhosis AASLD 2004 Guideline Ahmed Mayet, Pharm.D. Liver Blood Supply. 75% blood supply by portal and hepatic veins 25% by hepatic arteries. Hepatocytes function as detoxification of toxic substances and synthesizer of proteins,
1.78k views • 123 slides
BLOOD SUPPLY OF BRAIN
BLOOD SUPPLY OF BRAIN. BY: DR. IBRAR AHMED HASHMI. ARTERIAL SUPPLY OF BRAIN. COMMON CAROTID ARTERY 70% blood is delivered to ICA
1.81k views • 49 slides
Blood supply of the Brain. Arterial Blood Supply. Arterial blood supply of the brain Brain is supplied by pairs of internal carotid artery and vetebral artery. Internal Carotid Artery.
608 views • 57 slides
289 views • 18 slides
Blood supply of the Heart & Conduction System
Blood supply of the Heart & Conduction System. Dr. Nabil Khouri. Arterial supply of Heart. Right coronary artery Left coronary artery. Introduction:. Coronary arteries - VASAVASORUM arising from aortic sinuses of Valsalva of Ascending aorta Rt CA - from Rt aortic sinus (ant)
512 views • 37 slides

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
Blood supply of the Heart
Published by Aubrey Young Modified over 8 years ago
Similar presentations
Presentation on theme: "Blood supply of the Heart"— Presentation transcript:
Thorax Unit Lecture 5 & 6 د. حيدر جليل الأعسم
A. location of heart (p.530) in thorax, in inferior mediastinum

Internal features of Heart Dr. Sama ul Haque Dr Rania Gabr.
Internal features of Heart
LECTURE 39 Dr. REHAN.
Anatomy of the Heart DR.SANAA AL-SHAARAWI DR.SAEED VOHRA.

THORACIC CAVITY HEART.
Portland Community College
HEART, ITS BLOOD SUPPLY & PERICARDIUM
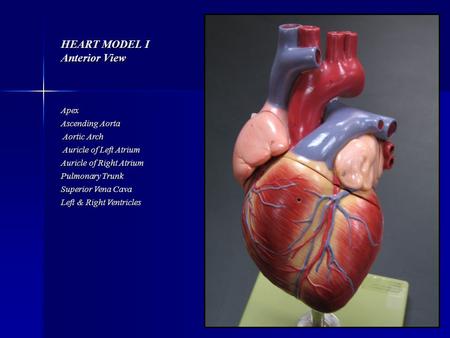
HEART MODEL I Anterior View
Mediastinum and Heart Sanjaya Adikari Department of Anatomy.
Coronary Arteries , Veins & Lymphatic components Salah Tarabsheh
Biology 323 Human Anatomy for Biology Majors Lecture 10 Dr. Stuart S. Sumida Heart: Structure, Function, Development.
Exercise 35 Anatomy of the Heart.
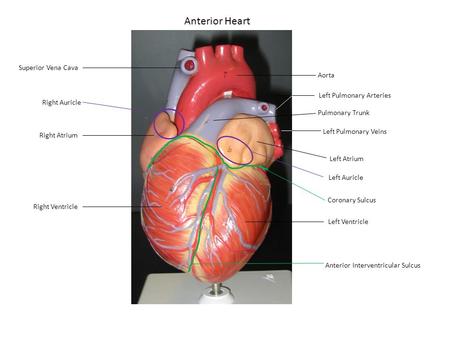
Anterior Heart Superior Vena Cava Aorta Left Pulmonary Arteries
C h a p t e r 20 The Heart PowerPoint® Lecture Slides prepared by Jason LaPres Lone Star College - North Harris Copyright © 2009 Pearson Education, Inc.,
Anatomy of cardiovascular system
By Prof. Saeed Abuel Makarem
Arteries & Veins To Know For Practical
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Coronary artery disease.
Rai Dilawar Shahjehan ; Beenish S. Bhutta .
Affiliations
Last Update: August 17, 2023 .
- Continuing Education Activity
Coronary artery disease is a common heart condition that involves atherosclerotic plaque formation in the vessel lumen. This leads to impairment in blood flow and thus oxygen delivery to the myocardium. It is a cause of major morbidity and mortality in the US and worldwide. To avoid the high morbidity and mortality associated with this condition, it must be promptly diagnosed and treated. This activity illustrates the evaluation, diagnosis, and management of coronary artery disease and highlights the role of the healthcare team in evaluating and treating patients with this condition.
- Identify the etiology of coronary artery disease.
- Outline the evaluation of coronary artery disease.
- Discuss the management options available for coronary artery disease.
- Introduction
Coronary artery disease is a condition in which there is an inadequate supply of blood and oxygen to the myocardium. It results from occlusion of the coronary arteries and results in a demand-supply mismatch of oxygen. It typically involves the formation of plaques in the lumen of coronary arteries that impede blood flow. It is the major cause of death in the US and worldwide. At the beginning of the 20th century, it was an uncommon cause of death. Deaths due to CAD peaked in the mid-1960s and then decreased however, it still is the leading cause of death worldwide. [1]
Coronary artery disease is a multifactorial phenomenon. Etiologic factors can be broadly categorized into non-modifiable and modifiable factors. Non-modifiable factors include gender, age, family history, and genetics. Modifiable risk factors include smoking, obesity, lipid levels, and psychosocial variables. In the Western world, a faster-paced lifestyle has led people to eat more fast foods and unhealthy meals which has led to an increased prevalence of ischemic heart diseases. In the US, better primary care in the middle and higher socioeconomic groups has pushed the incidence towards the later part of life. Smoking remains the number one cause of cardiovascular diseases. In 2016, the prevalence of smoking among the United States among adults was found to be at 15.5 %. [2]
The male gender is more predisposed than the female gender. Hypercholesterolemia remains an important modifiable risk factor for CAD. Increased low-density lipoproteins (LDL) increased the risk for CAD and elevated high-density lipoproteins (HDL) decrease the incidence of CAD. An individual's 10-year risk of atherosclerotic cardiovascular disease can be calculated using the ASCVD equation available online on the American Heart Association portal. Markers of inflammation are also strong risk factors for coronary artery disease. High sensitivity CRP (hsCRP) is thought to be the best predictor of coronary artery disease in some studies although uses for it in a practical setting are controversial. [3]
- Epidemiology
Coronary artery disease is very common in both developed and developing worlds. In one study, it was estimated that CAD represented 2.2% of the overall global burden of disease and 32.7% of cardiovascular diseases. It costs over 200 billion dollars annually to the health care system in the United States. It is estimated that 7.6% of men and 5.0% of women in the US lived with coronary artery disease from 2009 to 2012 based on the national health survey done by the American Heart Association (AHA). This amount to 15.5 million Americans afflicted with the disease during this time. [4] [5]
The incidence of CAD is observed to rise with age, regardless of gender. In the ONACI registry in France, the incidence of CAD was about 1% in the 45 to 65 age group, which increased to about 4% as the age group reached 75 to 84 years. [6]
- Pathophysiology
The hallmark of the pathophysiology of CAD is the development of atherosclerotic plaque. Plaque is a build-up of fatty material that narrows the vessel lumen and impedes the blood flow. The first step in the process is the formation of a "fatty streak." Fatty streak is formed by subendothelial deposition of lipid-laden macrophages, also called foam cells. When a vascular insult occurs, the intima layer breaks, and monocytes migrate into the subendothelial space where they become macrophages. These macrophages take up oxidized low-density lipoprotein (LDL) particles, and foam cells are formed. T cells get activated, which releases cytokines only to aid in the pathologic process. Growth factors released activate smooth muscles, which also take up oxidized LDL particles and collagen and deposit along with activated macrophages and increase the population of foam cells. This process leads to the formation of subendothelial plaque.
Over time, this plaque could grow in size or become stable if no further insult occurs to the endothelium. If it becomes stable, a fibrous cap will form, and the lesion will become calcified over time. As time passes, the lesion can become hemodynamically significant enough that not enough blood would reach the myocardial tissue at the time of increased demands, and angina symptoms would occur. However, symptoms would abate at rest as the oxygen requirement comes down. For a lesion to cause angina at rest, it must be at least 90% stenosed. Some plaques can rupture and lead to exposure of tissue factor, which culminates in thrombosis. This thrombosis could cause subtotal or total occlusion of the lumen and could result in the development of acute coronary syndrome (ACS) in the form of unstable angina, NSTEMI, or STEMI, depending on the level of insult. [7]
Classification of coronary artery disease is typically done as under:
- Stable ischemic heart disease (SIHD)
- ST-elevation MI (STEMI)
- Non-ST elevation MI (NSTEMI)
- Unstable angina
- History and Physical
It is very important to take a detailed history and physical examination before proceeding towards further workup. Coronary artery disease could manifest as stable ischemic heart disease (SIHD) or acute coronary syndrome (ACS). It can further progress into congestive heart failure (CHF) if not controlled. Patients should be asked about chest pain, its relation to physical activity, and radiation of the pain into the jaw, neck, left arm, or into the back. Dyspnea should be evaluated for rest and also on activity. The patient should also be asked about syncope, palpitations, tachypnea, lower extremity edema, orthopnea, and exercise capacity. A family history of ischemic heart diseases should be obtained along with dietary, smoking, and lifestyle habits.
Physical examination should include inspection, palpation, and auscultation. One should inspect for any acute distress, jugular venous distention, and peripheral edema. In palpation, one should palpate for fluid thrill and heave. The extent of peripheral edema if present should be evaluated. The distension of the jugular vein should be measured. In auscultation, the heart should be auscultated in all four locations and lungs should also be auscultated with a special focus on the lower zones.
There are several modalities to evaluate for coronary artery disease including EKG, Echo, CXR, Stress test, cardiac catheterization, and blood work to name the main ones. These tests are done depending on the context in which patients are presenting. The following are details on different diagnostic modalities we have available for the evaluation of coronary artery disease:
Electrocardiogram (EKG)
EKG is a very basic yet enormously helpful test in the evaluation of coronary artery disease. It measures electrical activity in the cardiac conduction system and is measured by 10 leads attached to the skin at standardized locations. It provides information about both the physiology and anatomy of the heart. It typically has 12 leads on the paper that is printed once the test is performed and each lead correlates with the specific location of the heart. Important information to notice on an EKG is a heart's rate, rhythm, and axis. After that, information regarding acute and chronic pathologic processes can be obtained. In acute coronary syndrome, one can see ST-segment changes and T wave changes. If an ACS has degenerated into arrhythmias, that can also be seen. In chronic settings, EKG can show information like axis deviation, bundle branch blocks, and ventricular hypertrophy. EKG is also a cost-effective and readily available testing modality that is not user-dependent.
Echocardiography
Echocardiography is an ultrasound of the heart. It is a useful and non-invasive mode of testing that is performed in both acute and chronic and inpatient and outpatient settings. In acute settings, it could tell about wall motion, valvular regurgitation and stenosis, infective or autoimmune lesions, and chamber sizes. It also is useful in the diagnosis of acute pulmonary pathologies like pulmonary embolism. It also evaluates the pericardial cavity. In chronic settings, it can be done to see the same information mentioned above and also a response to the therapy. It also is used in an outpatient setting as part of stress testing. In addition to diagnostics, it also has a role in therapeutics for example, pericardiocentesis could be performed with the needle-guided by echocardiography. This test is user-dependent and could be costly compared to EKG. [8]
Stress Test
The stress test is a relatively non-invasive test to evaluate for coronary artery disease. It is used in the setting of suspected angina or angina equivalent and is helpful in ruling in or out coronary pathology when interpreted in an appropriate setting. During the test, the heart is artificially exposed to stress and if the patient gets certain abnormal EKG changes in ST segments or gets symptoms of angina, the test is aborted at that point and coronary artery disease is diagnosed. EKGs are obtained before, during, and after the procedure, and the patient is continuously monitored for any symptoms. There are mainly two types of stress tests; exercise stress test and pharmacologic stress test. In exercise stress tests, the patient has to run on a treadmill until he achieves 85% of the age-predicted maximal heart rate. If a patient develops exertional hypotension, hypertension (>200/110 mmHg), ST-segment elevations or depression, or ventricular or supraventricular arrhythmias. [9]
Chest X-ray
Chest X-ray is an important component of the initial evaluation of cardiac disease. The standard imaging films include standing posteroanterior (PA) and left lateral decubitus. Sometimes, anteroposterior (AP) projection is obtained especially in inpatient settings with the patient lying down, however, this interpretation of AP films is significantly limited. Proper analysis of PA and AP views provides useful and cost-effective information about the heart, lungs, and vasculature. Interpretation should be done in a stepwise pattern so that important information is not overlooked.
Blood work aids in establishing the diagnosis and assessing therapeutic responses. In acute settings, cardiac enzymes and B-type natriuretic peptides are often done along with complete blood counts and metabolic panels. BNP provides information about volume overload of cardiogenic origin however it has its limitations. It can be falsely elevated in kidney diseases and falsely low in obesity. Cardiac enzymes like CK and troponin provide information about an acute ischemic event. In chronic settings, lipid panel provides important prognostic information. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) aid in assessing disease like acute pericarditis. Liver function tests (LFT) can be done to evaluate for an infiltrative process that can affect the liver and heart simultaneously like hemochromatosis. Liver tests are also done to assess increased right heart pressures, especially in chronic settings.
Cardiac Catheterization
Cardiac catheterization is the gold standard and most accurate modality to evaluate ischemic coronary heart disease. It is however an invasive procedure with associated complications. Not everyone is a candidate for the procedure. In non ACS settings, patients with intermediate pretest probability for CAD are usually the right candidates for it. In the ACS setting, all STEMI patients and selected NSTEMI patients get an emergent cardiac catheterization. This procedure is done in a cardiac catheterization lab, is expertise dependent, and is done under moderate sedation. There is contrast exposure in the procedure which could cause serious allergic reactions and kidney injury.
- Treatment / Management
Coronary artery disease could present either as stable ischemic heart disease (SIHD) or acute coronary syndrome (ACS). The former present in a chronic setting while the latter presents more in an acute setting. The management depends on the particular disease type. We will discuss the management of each subtype separately:
Stable Ischemic Heart Disease
Stable ischemic heart disease presents as stable angina. Stable angina typically presents as substernal chest pain or pressure that worsens with exertion or emotional stress and gets relieved with rest or nitroglycerin and is of 2 months duration. It is important to know that classic anginal symptoms could be absent and it could present differently with atypical symptoms and exertional dyspnea instead in certain demographic groups including women, elderly age, and diabetics. Management of SIHD includes both non-pharmacologic and pharmacologic interventions. Lifestyle modifications include smoking cessation, regular exercise, weight loss, good control of diabetes and hypertension, and a healthy diet. Pharmacologic interventions include cardioprotective and antianginal medications.
Every patient should get guideline-directed medical therapy (GDMT) which includes low dose aspirin, beta-blocker, as-needed nitroglycerin, and moderate to high-intensity statin. If symptoms are not controlled with this, beta-blocker therapy should be titrated up to heart rates 55-60, and the addition of calcium channel blocker and long-acting nitrates should be considered. [10] Ranolazine could also be added to relieve refractory anginal symptoms. If maximal GDMT has failed to relive angina, cardiac catheterization should be done to visualize the coronary anatomy and a decision should be made for percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) based on the patient profile. [11]
Acute Coronary Syndrome
The acute coronary syndrome presents as sudden onset substernal chest pain or pressure typically radiating to the neck and left arm and may be accompanied by dyspnea, palpitations, dizziness, syncope, cardiac arrest, or new-onset congestive heart failure. Prompt EKG is necessary for all patients with ACS to assess for STEMI and typically is done pre-hospital by an emergency medical services crew. STEMI is recognized by the presence of ST elevation in contiguous leads of 1 mm in limb leads or precordial leads excepting V2 and V3. In V2 and V3, men need to have 2 mm elevations and women 1.5 mm to qualify for STEMI diagnosis. New-onset left bundle branch block (LBBB) is also considered a STEMI equivalent. If STEMI is present, emergency PCI is warranted in a PCI capable facility or if a PCI facility is available within 2 hours distance. If the PCI capable facility is more than 2 hours away, intravenous thrombolytic therapy is indicated after making sure there are no contraindications to it.
It is important to differentiate a true STEMI from other conditions that mimic STEMI on EKG like acute pericarditis, Brugada syndrome, early repolarization changes, and LVH associated changes. All patients should get a full dose of sublingual aspirin (324 mg) upon presentation. Nitrates should be given for pain relief after making sure there are no contraindications to nitrates like hypotension, RV failure, and consumption of phosphodiesterase inhibitors in the past 24-48 hours. High-dose statin therapy and beta-blockers should also be initiated early. P2Y12 inhibitors (prasugrel, ticagrelor, or prasugrel) should be started based on the patient profile. Patients who have NSTE ACS should get anticoagulation, typically heparin or enoxaparin are used. For NSTEMI, early invasive therapy within 24 hours is advised for patients with intermediate to high TIMI scores (>2). [12] [13]
Regular visits with cardiologists and family physicians are key to good long term management of coronary artery disease. Medication adherence and lifestyle modification are important.
- Differential Diagnosis
Coronary artery disease has a wide range of differential diagnoses because of the proximity of the heart with adjacent organs, including the lungs, stomach, big vessels, and musculoskeletal organs. Acute anginal chest pain could mimic acute pericarditis, myocarditis, prinzmetal angina, pericardial effusion, acute bronchitis, pneumonia, pleuritis, pleural effusion, aortic dissection, GERD, peptic ulcer disease, esophageal motility disorders, and costochondritis. Stable ischemic heart disease could also mimic GERD, Peptic ulcer disease, costochondritis, and pleuritis. History, physical examination, and diagnostic studies should be carefully carried out to narrow down the differential diagnosis and reach an accurate diagnosis.
- Toxicity and Adverse Effect Management
Both medical and surgical management for ischemic heart disease is associated with their side effects and complications. These undesirable effects could be mitigated by careful selection, physician expertise, and patient education. Aspirin therapy is associated with bleeding, idiosyncratic, and allergic drug reactions. [14] Statin therapy can cause myalgias, diarrhea, and arthralgias among side effects. [15]
Beta-blockers could cause bradycardia and hypotension. ACEIs could result in hypotension, dizziness, creatinine elevation, cough, and allergic reactions including angioedema. [16] PCI can possibly cause coronary artery perforation, stent thrombosis in an acute setting, and in-stent restenosis on chronic basis. [17] CABG can have its own complications including but not limited to arrhythmias, cardiac tamponade, post-op bleeding, infection, renal impairment, and phrenic nerve injury.
The prognosis of the disease depends on multiple factors some of which could be modified while others are non-modifiable. Patient's age, gender, family history and genetics, ethnicity, dietary and smoking habits, medication compliance, availability of healthcare and financial status, and the number of arteries involved are some of the factors. Comorbid conditions including diabetes mellitus, hypertension, dyslipidemia, and chronic kidney disease also have a role in the overall outcome. [18]
- Complications
Arrhythmias, acute coronary syndrome, congestive heart failure, mitral regurgitation, ventricular free wall rupture, pericarditis, aneurysm formation, and mural thrombi are the main complication associated with coronary artery disease. [19] [20] [10]
- Deterrence and Patient Education
Coronary artery disease is caused by a combination of modifiable and nonmodifiable factors. Primary care providers should focus on the modifiable risk factor modification on each routine visit. Tight control of diabetes, hypertension and lipid levels in addition to smoking cessation, weight loss and exercise can make a huge difference. Since it is a global public health concern, in school curriculums and different avenues of media, more awareness needs to be created.
- Pearls and Other Issues
Several landmark trials were done over the past few decades which have totally changed the way we care for coronary artery disease patients. It is beyond the scope of this article to discuss individual trial results, however, the following are the names of some important studies. ISIS-2, CURE, CLARITY-TIMI 28, TIRTON-TIMI 38, PLATO, and CURRENT-OASIS 7 trials were done regarding guidelines for antiplatelet medications. [21] SYNERGY, ACUITY, ExTRACT-TIMI 25, OASIS-5, and ATLAS ACS/ TIMI 52 were done about the use of anticoagulation. ADMIRAL, ACUITY, ISAR-REACT 3, and HORIZONS-AMI are famous trials regarding GpIIb/IIIa use, COMMIT for beta-blockers while SHOCK, DANAMI-2, BASKET-LATE, TIMACS, and BASKET-PROVE are about PCI and CABG. MIRACL trial was done about statin use.
- Enhancing Healthcare Team Outcomes
Evaluation of ischemic heart disease can frequently present a diagnostic dilemma. Such patients can present non-specific symptoms like chest pain or shortness of breath. The cause of chest pain or shortness of breath could be due to a myriad of diseases including gastrointestinal, cardiac, musculoskeletal, psychological, and pulmonary causes. While a cardiologist is often involved as a central player, it is important to take other team members on board as indicated including a gastroenterologist, pulmonologist, and psychiatrist. Radiologists also are an important resource in the whole process. Nurses are a very important part of the diagnostic and therapeutic workup as well as they provide key bedside information not witnessed by the physicians in their short encounters.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Classification of CAD. Image created by the author Rai Dilawar Shahjehan, MD.
Disclosure: Rai Dilawar Shahjehan declares no relevant financial relationships with ineligible companies.
Disclosure: Beenish Bhutta declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Shahjehan RD, Bhutta BS. Coronary Artery Disease. [Updated 2023 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Instantaneous Wave-Free Ratio. [StatPearls. 2024] Instantaneous Wave-Free Ratio. Soos MP, Gonzalez-Morales D, McComb D. StatPearls. 2024 Jan
- Review The epidemic of the 20(th) century: coronary heart disease. [Am J Med. 2014] Review The epidemic of the 20(th) century: coronary heart disease. Dalen JE, Alpert JS, Goldberg RJ, Weinstein RS. Am J Med. 2014 Sep; 127(9):807-12. Epub 2014 May 5.
- Myocardial oxygen supply:demand ratio as reference for coronary vasodilatory drug effects in humans. [Heart. 1997] Myocardial oxygen supply:demand ratio as reference for coronary vasodilatory drug effects in humans. Vergroesen I, Kal JE, Spaan JA, Van Wezel HB. Heart. 1997 Aug; 78(2):117-26.
- Multidetector computed tomography for coronary artery disease screening in asymptomatic populations: evidence-based analysis. [Ont Health Technol Assess Ser....] Multidetector computed tomography for coronary artery disease screening in asymptomatic populations: evidence-based analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2007; 7(3):1-56. Epub 2007 May 1.
- Review Biomarkers to monitor the prognosis, disease severity, and treatment efficacy in coronary artery disease. [Expert Rev Cardiovasc Ther. 2023] Review Biomarkers to monitor the prognosis, disease severity, and treatment efficacy in coronary artery disease. Yazdani AN, Pletsch M, Chorbajian A, Zitser D, Rai V, Agrawal DK. Expert Rev Cardiovasc Ther. 2023 Jul-Dec; 21(10):675-692. Epub 2023 Oct 26.
Recent Activity
- Coronary Artery Disease - StatPearls Coronary Artery Disease - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Sathish Rajamani. The heart receives its blood supply from two coronary arteries - the right and left coronary arteries. These branch directly off the aorta. The right coronary artery supplies the right atrium and ventricle as well as parts of the left ventricle and septum. The left coronary artery is larger and supplies the left atrium and ...
Overview of the main coronary arteries and cardiac veins. Coronary arteries and cardiac veins. The heart is a muscular, four-chambered organ that is responsible for distributing blood throughout the body. The continuous activity of the heart creates a large demand for nutrients to be delivered to cardiac tissue and for waste to be removed.
The left coronary artery delivers blood to the left side of your heart, including your left atrium and ventricle and the septum between the ventricles.; The circumflex artery branches off from the left coronary artery to supply blood to part of the left ventricle. The left anterior descending artery also branches from the left coronary artery and provides blood to parts of both the right and ...
750 likes | 3.76k Views. Blood supply of the Heart. Dr. Sama ul Haque Dr Rania Gabr. Objectives. Enlist the arteries and veins supplying heart. Describe the origin and branches of the right and left coronary arteries. Define coronary artery anastomosis. Download Presentation.
Download ppt "Blood Supply of the Heart". Objectives At the end of the lecture the student should be able to know about; The arterial supply of the cardiac muscle regarding (origin, course, distribution and branches). The coronary anastomosis. The arterial supply to the conducting system of the heart.
The blood circulatory system (cardiovascular system) delivers nutrients and oxygen to all cells in the body. It consists of the heart and the blood vessels running through the entire body. The arteries carry blood away from the heart; the veins carry it back to the heart. The system of blood vessels resembles a tree: The "trunk" - the main artery (aorta) - branches into large arteries ...
Anatomy of the heart made easy along with the blood flow through the cardiac structures, valves, atria, and ventricles. Cardiovascular system animation for U...
BLOOD SUPPLY OF THE HEART Dr Jamila EL medany & Dr Essam Salama. Objectives • At the end of the lecture the student should be able to know about; • The arterial supply of the cardiac muscle regarding (origin, course, distribution and branches). • The coronary anastmosis. • The arterial supply to the conducting system of the heart. • The venous drainage of the heart regarding (origin ...
Naming Coronary Arteries. There are two main coronary arteries which branch to supply the entire heart. They are named the left and right coronary arteries, and arise from the left and right aortic sinuses within the aorta. The aortic sinuses are small openings found within the aorta behind the left and right flaps of the aortic valve.When the heart is relaxed, the back-flow of blood fills ...
23 Conducting system of Heart. S-A Node: Right coronary artery (60%) Left coronary artery (40%) A-V Node and A-V Bundle: Right coronary artery Right Bundle branch: Left coronary artery Left Bundle branch: Right & Left coronary arteries. 24 Cardiac dominance 85%-Rt dominant coronary artery 8%-.
The left coronary artery arises from the left posterior aortic sinus. It passes behind the pulmonary trunk and emerges between the left auricle and the infundibulum of the right ventricle. The left coronary is the larger of the coronary arteries. It soon divides into two terminal branches: the circumflex and anterior interventricular branches.
The cusps are pushed open to allow blood flow in one direction, and then closed to seal the orifices and prevent the backflow of blood. Backward prolapse of the cusps is prevented by the chordae tendineae-also known as the heart strings-fibrous cords that connect the papillary muscles of the ventricular wall to the atrioventricular valves.. There are two sets of valves: atrioventricular ...
The cardiovascular system provides blood supply throughout the body. By responding to various stimuli, it can control the velocity and amount of blood carried through the vessels. The cardiovascular system consists of the heart, arteries, veins, and capillaries. The heart and vessels work together intricately to provide adequate blood flow to all parts of the body. The regulation of the ...
59 likes • 22,812 views. Kaif Qureshi. Follow. BLOOD SUPPLY OF HEART anatomy 1st year. Health & Medicine. 1 of 22. Download now. Blood supply of heart - Download as a PDF or view online for free.
Presentation Transcript. BLOOD SUPPLY OF THE HEART Dr Jamila EL medany & Dr Essam Salama. Objectives • At the end of the lecture the student should be able to know about; • The arterial supply of the cardiac muscle regarding (origin, course, distribution and branches). • The coronary anastmosis. • The arterial supply to the conducting ...
Circulatory system. The circulatory system, also called cardiovascular system, is a vital organ system that delivers essential substances to all cells for basic functions to occur. Also commonly known as the cardiovascular system, is a network composed of the heart as a centralised pump, blood vessels that distribute blood throughout the body, and the blood itself, for transportation of ...
Presentation on theme: "Blood supply of the Heart"— Presentation transcript: 1 Blood supply of the Heart. Dr. Sama ul Haque. 2 Objectives Enlist the arteries and veins supplying heart. Enlist the arteries and veins supplying heart. Describe the origin and branches of the right and left coronary arteries. Define coronary artery anastomosis.
Anatomi - Free download as Powerpoint Presentation (.ppt), PDF File (.pdf), Text File (.txt) or view presentation slides online. The document discusses the arterial blood supply and venous drainage of the heart. It notes that the heart receives its arterial blood supply primarily from the right and left coronary arteries. It also describes the branches and territories supplied by each coronary ...
Summary. The cardiovascular system consists of the heart, blood vessels, and blood. Its primary function is to transport nutrients and oxygen-rich blood to all parts of the body and to carry ...
The primary function of the heart is to serve as a muscular pump propelling blood into and through vessels to and from all parts of the body. The arteries, which receive this blood at high pressure and velocity and conduct it throughout the body, have thick walls that are composed of elastic fibrous tissue and muscle cells. The arterial tree—the branching system of arteries—terminates in ...
Coronary artery disease is a condition in which there is an inadequate supply of blood and oxygen to the myocardium. It results from occlusion of the coronary arteries and results in a demand-supply mismatch of oxygen. It typically involves the formation of plaques in the lumen of coronary arteries that impede blood flow. It is the major cause of death in the US and worldwide. At the beginning ...
heart, organ that serves as a pump to circulate the blood. It may be a straight tube, as in spiders and annelid worms, or a somewhat more elaborate structure with one or more receiving chambers (atria) and a main pumping chamber (ventricle), as in mollusks. In fishes the heart is a folded tube, with three or four enlarged areas that correspond ...