- Utility Menu

harvardchan_logo.png

Harvard T.H. Chan School of Public Health Case-Based Teaching & Learning Initiative
Teaching cases & active learning resources for public health education, case library.
The Harvard Chan Case Library is a collection of teaching cases with a public health focus, written by Harvard Chan faculty, case writers, and students, or in collaboration with other institutions and initiatives.
Use the filters at right to search the case library by subject, geography, health condition, and representation of diversity and identity to find cases to fit your teaching needs. Or browse the case collections below for our newest cases, cases available for free download, or cases with a focus on diversity.
Using our case library
Access to cases.
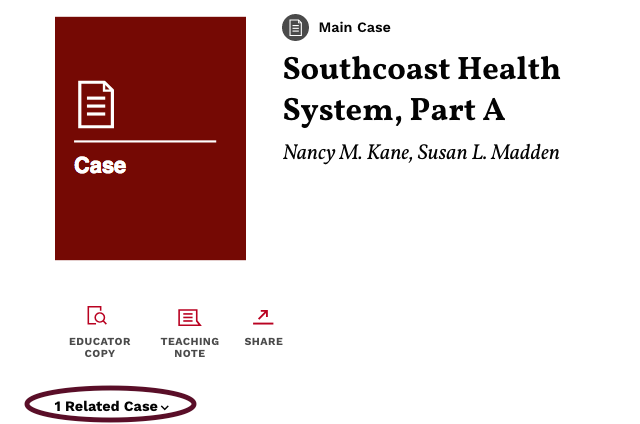
Many of our cases are available for sale through Harvard Business Publishing in the Harvard T.H. Chan case collection . Others are free to download through this website .
Cases in this collection may be used free of charge by Harvard Chan course instructors in their teaching. Contact Allison Bodznick , Harvard Chan Case Library administrator, for access.
Access to teaching notes
Teaching notes are available as supporting material to many of the cases in the Harvard Chan Case Library. Teaching notes provide an overview of the case and suggested discussion questions, as well as a roadmap for using the case in the classroom.
Access to teaching notes is limited to course instructors only.
- Teaching notes for cases available through Harvard Business Publishing may be downloaded after registering for an Educator account .
- To request teaching notes for cases that are available for free through this website, look for the "Teaching note available for faculty/instructors " link accompanying the abstract for the case you are interested in; you'll be asked to complete a brief survey verifying your affiliation as an instructor.
Using the Harvard Business Publishing site
Faculty and instructors with university affiliations can register for Educator access on the Harvard Business Publishing website, where many of our cases are available . An Educator account provides access to teaching notes, full-text review copies of cases, articles, simulations, course planning tools, and discounted pricing for your students.
What's New
Atkinson, M.K. , 2023. Organizational Resilience and Change at UMass Memorial , Harvard Business Publishing: Harvard T.H. Chan School of Public Health. Available from Harvard Business Publishing Abstract The UMass Memorial Health Care (UMMHC or UMass) case is an examination of the impact of crisis or high uncertainty events on organizations. As a global pandemic unfolds, the case examines the ways in which UMMHC manages crisis and poses questions around organizational change and opportunity for growth after such major events. The case begins with a background of UMMHC, including problems the organization was up against before the pandemic, then transitions to the impact of crisis on UMMHC operations and its subsequent response, and concludes with challenges that the organization must grapple with in the months and years ahead. A crisis event can occur at any time for any organization. Organizational leaders must learn to manage stakeholders both inside and outside the organization throughout the duration of crisis and beyond. Additionally, organizational decision-makers must learn how to deal with existing weaknesses and problems the organization had before crisis took center stage, balancing those challenges with the need to respond to an emergency all the while not neglecting major existing problem points. This case is well-suited for courses on strategy determination and implementation, organizational behavior, and leadership.
The case describes the challenges facing Shlomit Schaal, MD, PhD, the newly appointed Chair of UMass Memorial Health Care’s Department of Ophthalmology. Dr. Schaal had come to UMass in Worcester, Massachusetts, in the summer of 2016 from the University of Louisville (KY) where she had a thriving clinical practice and active research lab, and was Director of the Retina Service. Before applying for the Chair position at UMass she had some initial concerns about the position but became fascinated by the opportunities it offered to grow a service that had historically been among the smallest and weakest programs in the UMass system and had experienced a rapid turnover in Chairs over the past few years. She also was excited to become one of a very small number of female Chairs of ophthalmology programs in the country.
Dr. Schaal began her new position with ambitious plans and her usual high level of energy, but immediately ran into resistance from the faculty and staff of the department. The case explores the steps she took, including implementing a LEAN approach in the department, and the leadership approaches she used to overcome that resistance and build support for the changes needed to grow and improve ophthalmology services at the medical center.
This case describes efforts to promote racial equity in healthcare financing from the perspective of one public health organization, Community Care Cooperative (C3). C3 is a Medicaid Accountable Care Organization–i.e., an organization set up to manage payment from Medicaid, a public health insurance option for low-income people. The case describes C3’s approach to addressing racial equity from two vantage points: first, its programmatic efforts to channel financing into community health centers that serve large proportions of Black, Indigenous, People of Color (BIPOC), and second, its efforts to address racial equity within its own internal operations (e.g., through altering hiring and promotion processes). The case can be used to help students understand structural issues pertaining to race in healthcare delivery and financing, to introduce students to the basics of payment systems in healthcare, and/or to highlight how organizations can work internally to address racial equity.
Kerrissey, M.J. & Kuznetsova, M. , 2022. Killing the Pager at ZSFG , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract This case is about organizational change and technology. It follows the efforts of one physician as they try to move their department past using the pager, a device that persisted in American medicine despite having long been outdated by superior communication technology. The case reveals the complex organizational factors that have made this persistence possible, such as differing interdepartmental priorities, the perceived benefits of simple technology, and the potential drawbacks of applying typical continuous improvement approaches to technology change. Ultimately the physician in the case is not able to rid their department of the pager, despite pursuing a thorough continuous improvement effort and piloting a viable alternative; the case ends with the physician having an opportunity to try again and asks students to assess whether doing so is wise. The case can be used in class to help students apply the general concepts of organizational change to the particular context of technology, discuss the forces of stasis and change in medicine, and to familiarize students with the uses and limits of continuous improvement methods.
Yatsko, P. & Koh, H. , 2021. Dr. Joan Reede and the Embedding of Diversity, Equity, and Inclusion at Harvard Medical School , Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract For more than 30 years, Dr. Joan Reede worked to increase the diversity of voices and viewpoints heard at Harvard Medical School (HMS) and at its affiliate teaching hospitals and institutes. Reede, HMS’s inaugural dean for Diversity and Community Partnership, as well as a professor and physician, conceived and launched more than 20 programs to improve the recruitment, retention, and promotion of individuals from racial and ethnic groups historically underrepresented in medicine (UiMs). These efforts have substantially diversified physician faculty at HMS and built pipelines for UiM talent into academic medicine and biosciences. Reede helped embed the promotion of diversity, equity, and inclusion (DEI) not only into Harvard Medical School’s mission and community values, but also into the DEI agenda in academic medicine nationally. To do so, she found allies and formed enduring coalitions based on shared ownership. She bootstrapped and hustled for resources when few readily existed. And she persuaded skeptics by building programs using data-driven approaches. She also overcame discriminatory behaviors and other obstacles synonymous with being Black and female in American society. Strong core values and sense of purpose were keys to her resilience, as well as to her leadership in the ongoing effort to give historically marginalized groups greater voice in medicine and science.
Cases Available for Free Download
Johnson, P. & Gordon, R. , 2014. Dr. Sam Thenya: A Women's Health Pioneer , Harvard University: Global Health Education and Learning Incubator. Access online Abstract This case tracks Dr. Sam Thenya’s challenges in establishing and sustaining two Kenyan health organizations for women’s health. Thenya founded the Gender Violence Recovery Centre (GVRC) and the Nairobi Women’s Hospital (NWH) Medical Training College. In particular, the case focuses on the choices made as he expanded these two closely connected enterprises even though the GVRC was a non-profit enterprise while the NWH was a for-profit enterprise. Students consider how he led change to improve women’s health at both the population and system levels. They reflect on his leadership and lessons learned as he sought to change the face of women’s health care in Kenya and shift societal attitudes about gender-based violence (GBV). Students analyze how Dr. Thenya scaled up his innovative model, and the subsequent decisions he made to sustain his enterprise. They consider the ways in which he adapted his vision in order to provide GBV services free of charge and expand the reach of these services. This case also provides a Kenyan context in which to discuss health care delivery, and explores general attitudes and issues surrounding GBV.
Gordon, R. & Moon, S. , 2014. Haiti in the Time of Cholera , Harvard University: Global Health Education and Learning Incubator. Access online Abstract This case examines the United Nations' reactions to the cholera epidemic in Haiti and illuminates contemporary gaps in global governance. In January, 2010, an earthquake devastated Haiti, the poorest country in the Western Hemisphere. The public health community anticipated Haiti to be at risk for many health threats, but did not consider a cholera outbreak a likely possibility. However, in October of that year, the first case of cholera in more than 100 years was reported, sparking a cholera epidemic in Haiti. Scientific evidence later linked the original source of the cholera to poor sanitation management practices at a United Nations (UN) peacekeepers camp run by Nepal. However, the UN refused to acknowledge any responsibility for causing the cholera outbreak. Readers of this case consider the role of global governance and accountability, especially in an environment with a weak nation state.
Weinberger, E. , 2015. Weighing the Evidence: One University Takes a Hard Look at Disordered Eating Among Athletes , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract Colburn University is the largest private university in the fictitious state of Columbia and is often recognized by people from distant parts of the country for its award-winning Division I athletic teams. That’s why when athletic director Harry Ritchie makes an offhanded comment about Colburn student-athletes with eating disorders, the press pounces. This incident coupled with a complaint from a parent draws the attention of Dean Francis Reilly, who finds himself needing to peel back some of the layers embedding college athletics on the issue of eating disorders among athletes. Throughout the narrative, different perspectives on sports and eating disorders are revealed from top-level administrators, like Dean Reilly, to the student-athletes themselves. As the story concludes, the conversation about eating disorders has begun, but questions still remain on how to make Colburn University a healthy environment for its student-athletes. Intermediate and advanced level teaching notes available for faculty/instructors .
Weed, L., Lipsitch, M. & Kane, N.M. , 2010. Protecting the Population from the 2009 Pandemic H1N1 Virus , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Download free of charge Abstract Dale Morse, MD, MS, could feel the tension rising in the room. He was chair of a special meeting of the Advisory Committee on Immunization Practices (ACIP) called for July, 2009, that would make recommendations to the Centers for Disease Control (CDC) on whether to prioritize vaccine distribution to protect the population against a possible H1N1 influenza pandemic in the fall. Dr. Morse was particularly concerned that if ACIP did not set priorities now, he and other state and local public health officials could be faced with a vaccine shortage amid high demand—a situation he described as a potential public health disaster.
Elizabeth, a middle-aged African American woman living in Minnesota, develops chest pain and eventually presents to a local emergency room, where she is diagnosed with stress-related pain and given Vicodin. Members of a non-profit wellness center where she is also seen reflect on the connection between her acute chest pain and underlying stress related to her socioeconomic status. On a larger level, how much of her health is created or controlled by the healthcare system? What non-medical policy decisions impacted Elizabeth such that she is being treated with Vicodin for stress?
Focus on Diversity, Equity, and Inclusion
Weinberger, E. , 2017. Coloring the Narrative: How to Use Storytelling to Create Social Change in Skin Tone Ideals , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract Many millions of people around the world experience the pervasive, and often painful, societal messages of colorism, where lighter skin tones are asserted to be more attractive and to reflect greater affluence, power, education, and social status. Even in places where the destructive effects of colorism are fairly well understood, far less is known about the problem of skin-lightening (really, it’s “skin bleaching”) creams and lotions, and the health risks that consumers assume with these products. In this teaching case, the protagonists are two women who have recently immigrated to the United States from Nigeria and Thailand, both with a life-time of experience with these products like many of the women of their home countries. As the story unfolds, they struggle along with the rest of the characters to copy with the push and pull of community norms vs. commercial influences and the challenge of promoting community health in the face of many societal and corporate obstacles. How can the deeply ingrained messages of colorism be effectively confronted and transformed to advance social change without alienating the community members we may most want to reach? Teaching note and supplemental slides available for faculty/instructors .
Al Kasir, A., Coles, E. & Siegrist, R. , 2019. Anchoring Health beyond Clinical Care: UMass Memorial Health Care’s Anchor Mission Project , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract As the Chief Administrative Officer of UMass Memorial Health Care (UMMHC) and president of UMass Memorial (UMM) Community Hospitals, Douglas Brown had just received unanimous and enthusiastic approval to pursue his "Anchor Mission" project at UMMHC in Worcester, Massachusetts. He was extremely excited by the board's support, but also quite apprehensive about how to make the Anchor Mission a reality. Doug had spearheaded the Anchor Mission from its earliest exploratory efforts. The goal of the health system's Anchor Mission-an idea developed by the Democracy Collaborative, an economic think tank-was to address the social determinants of health in its community beyond the traditional approach of providing excellent clinical care. He had argued that UMMHC had an obligation as the largest employer and economic force in Central Massachusetts to consider the broader development of the community and to address non-clinical factors, like homelessness and social inequality that made people unhealthy. To achieve this goal, UMMHC's Anchor Mission would undertake three types of interventions: local hiring, local sourcing/purchasing, and place-based community investment projects. While the board's enthusiasm was palpable and inspiring, Doug knew that sustaining it would require concrete accomplishments and a positive return on any investments the health system made in the project. The approval was just the first step. Innovation and new ways of thinking would be necessary. The bureaucracy behind a multi-billion-dollar healthcare organization would need to change. Even the doctors and nurses would need to change! He knew that the project had enormous potential but would become even more daunting from here.
This teaching case study examines psychological trauma in a community context and the relevance, both positive and negative, of social determinants of health. Healthy People 2020 views people residing in communities with large-scale psychological trauma as an emerging issue in mental health and mental health disorders (Healthy People, 2016). The case study, which focuses on Newark, New Jersey, addresses three of the five key determinants of health: social and community context, health and health care, and neighborhood and built environment. The three key determinants are addressed using psychological trauma as an exemplar in the context of trauma-informed systems. The social and community context is addressed using concepts of social cohesion, civic participation, and discrimination. Access to health and health care are addressed with discussion of access to mental health and primary care services, health literacy, and the medical home model. Neighborhood and built environment are viewed through the lens of available government and NGO programs and resources to improve the physical environment with a focus on quality of housing, crime and violence, and environmental conditions. Upstream interventions designed to improve mental health and well-being that support trauma-informed systems are analyzed. The use of Newark as the case study setting allows a real-life exploration of each of these three key determinants of health.
This case study has four sections – introduction, case study, side bar, and vignettes. Learners should work through the case, access appropriate resources, and work in a team for successful completion.
Jessie Gaeta, the chief medical officer for Boston Health Care for the Homeless Program (BHCHP), learned on April 7, 2020 that the City of Boston needed BHCHP to design and staff in 48 hours one half of Boston Hope, a 1,000-bed field hospital for patients infected with COVID-19. The mysterious new coronavirus spreading around the world was now running rampant within BHCHP's highly vulnerable patient population: people experiencing homelessness in Boston. A nonprofit community health center, BHCHP for 35 years had been the primary care provider for Boston's homeless community. Over the preceding month, BHCHP's nine-person incident command team, spearheaded by Gaeta and CEO Barry Bock, had spent long hours reorganizing the program. (See Boston Health Care for the Homeless (A): Preparing for the COVID-19 Pandemic.) BHCHP leaders now confronted the most urgent challenge of their long medical careers. Without previous experience in large-scale disaster medicine, Gaeta and her colleagues had in short order to design and implement a disaster medicine model for COVID-19 that served the unique needs of people experiencing homelessness.
This case study recounts the decisive actions BHCHP leaders took to uncover unexpectedly widespread COVID-19 infection among Boston's homeless community in early April 2020. It details how they overcame their exhaustion to quickly design, staff, and operate the newly erected Boston Hope field hospital for the city's homeless COVID-19 patients. It then shows how they adjusted their disaster medicine model when faced with on-the-ground realities at Boston Hope regarding patients' psychological needs, limited English capabilities, substance use disorders, staff stress and burnout, and other issues.
Filter cases
Author affiliation.
- Harvard T.H. Chan School of Public Health (98) Apply Harvard T.H. Chan School of Public Health filter
- Harvard Business School (22) Apply Harvard Business School filter
- Global Health Education and Learning Incubator at Harvard University (12) Apply Global Health Education and Learning Incubator at Harvard University filter
- Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED) (11) Apply Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED) filter
- Social Medicine Consortium (8) Apply Social Medicine Consortium filter
- Harvard Kennedy School of Government (1) Apply Harvard Kennedy School of Government filter
- Harvard Malaria Initiative (1) Apply Harvard Malaria Initiative filter
- Women, Gender, and Health interdisciplinary concentration (1) Apply Women, Gender, and Health interdisciplinary concentration filter
Geographic focus
- United States (63) Apply United States filter
- Massachusetts (14) Apply Massachusetts filter
- International/multiple countries (11) Apply International/multiple countries filter
- California (6) Apply California filter
- Mexico (4) Apply Mexico filter
- India (3) Apply India filter
- Israel (3) Apply Israel filter
- New York (3) Apply New York filter
- Bangladesh (2) Apply Bangladesh filter
- Colorado (2) Apply Colorado filter
- Guatemala (2) Apply Guatemala filter
- Haiti (2) Apply Haiti filter
- Japan (2) Apply Japan filter
- Kenya (2) Apply Kenya filter
- South Africa (2) Apply South Africa filter
- Uganda (2) Apply Uganda filter
- United Kingdom (2) Apply United Kingdom filter
- Washington state (2) Apply Washington state filter
- Australia (1) Apply Australia filter
- Cambodia (1) Apply Cambodia filter
- China (1) Apply China filter
- Connecticut (1) Apply Connecticut filter
- Egypt (1) Apply Egypt filter
- El Salvador (1) Apply El Salvador filter
- Honduras (1) Apply Honduras filter
- Liberia (1) Apply Liberia filter
- Louisiana (1) Apply Louisiana filter
- Maine (1) Apply Maine filter
- Michigan (1) Apply Michigan filter
- Minnesota (1) Apply Minnesota filter
- New Jersey (1) Apply New Jersey filter
- Nigeria (1) Apply Nigeria filter
- Pakistan (1) Apply Pakistan filter
- Philippines (1) Apply Philippines filter
- Rhode Island (1) Apply Rhode Island filter
- Turkey (1) Apply Turkey filter
- Washington DC (1) Apply Washington DC filter
- Zambia (1) Apply Zambia filter
Case availability & pricing
- Available for purchase from Harvard Business Publishing (73) Apply Available for purchase from Harvard Business Publishing filter
- Download free of charge (50) Apply Download free of charge filter
- Request from author (4) Apply Request from author filter
Case discipline/subject
- Healthcare management (55) Apply Healthcare management filter
- Social & behavioral sciences (41) Apply Social & behavioral sciences filter
- Health policy (35) Apply Health policy filter
- Global health (28) Apply Global health filter
- Multidisciplinary (16) Apply Multidisciplinary filter
- Child & adolescent health (15) Apply Child & adolescent health filter
- Marketing (15) Apply Marketing filter
- Environmental health (12) Apply Environmental health filter
- Human rights & health (11) Apply Human rights & health filter
- Social innovation & entrepreneurship (11) Apply Social innovation & entrepreneurship filter
- Women, gender, & health (11) Apply Women, gender, & health filter
- Finance & accounting (10) Apply Finance & accounting filter
- Population health (8) Apply Population health filter
- Social medicine (7) Apply Social medicine filter
- Epidemiology (6) Apply Epidemiology filter
- Nutrition (6) Apply Nutrition filter
- Technology (6) Apply Technology filter
- Ethics (5) Apply Ethics filter
- Life sciences (5) Apply Life sciences filter
- Quality improvement (4) Apply Quality improvement filter
- Quantative methods (3) Apply Quantative methods filter
- Maternal & child health (1) Apply Maternal & child health filter
Health condition
- Cancer (3) Apply Cancer filter
- COVID-19 (3) Apply COVID-19 filter
- Obesity (3) Apply Obesity filter
- Breast cancer (2) Apply Breast cancer filter
- Disordered eating (2) Apply Disordered eating filter
- Ebola (2) Apply Ebola filter
- Influenza (2) Apply Influenza filter
- Injury (2) Apply Injury filter
- Malaria (2) Apply Malaria filter
- Alcohol & drug use (1) Apply Alcohol & drug use filter
- Asthma (1) Apply Asthma filter
- Breast implants (1) Apply Breast implants filter
- Cardiovascular disease (1) Apply Cardiovascular disease filter
- Cervical cancer (1) Apply Cervical cancer filter
- Cholera (1) Apply Cholera filter
- Food poisoning (1) Apply Food poisoning filter
- HPV (1) Apply HPV filter
- Malnutrition (1) Apply Malnutrition filter
- Meningitis (1) Apply Meningitis filter
- Opioids (1) Apply Opioids filter
- Psychological trauma (1) Apply Psychological trauma filter
- Road traffic injury (1) Apply Road traffic injury filter
- Sharps injury (1) Apply Sharps injury filter
- Skin bleaching (1) Apply Skin bleaching filter
Diversity and Identity
- Female protagonist (13) Apply Female protagonist filter
- Health of diverse communities (11) Apply Health of diverse communities filter
- Protagonist of color (5) Apply Protagonist of color filter
Supplemental teaching material
- Teaching note available (70) Apply Teaching note available filter
- Multi-part case (18) Apply Multi-part case filter
- Additional teaching materials available (12) Apply Additional teaching materials available filter
- Simulation (2) Apply Simulation filter
- Teaching pack (2) Apply Teaching pack filter
- Teaching example (1) Apply Teaching example filter
Browse our case library
Datar, S.M., Cyr, L. & Bowler, C.N. , 2018. Innovation at Insigne Health , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract Insigne Health is a for-profit, integrated health insurer/health care provider whose leadership believes that by shifting members' focus from "sickness" to "well-being" it could increase the overall health of its insured population and decrease the resources it spends each year on delivering care. The case puts students in the role of design researcher charged with understanding the member segment about which Insigne Health leadership is most concerned: The "silent middle." This cohort represents 70% of membership and is "neither sick nor well." Without changes in a range of behaviors, these members may be quietly developing conditions that will evolve into costly chronic diseases. From interviews included in the case, students uncover insights into member behavior and, based on these insights, generate and develop concepts to help members change behaviors and lead healthier lives.
Cash, R., et al. , 2009. Casebook on ethical issues in international health research , World Health Organization. Publisher's Version Abstract This casebook published by the World Health Organization contains 64 case studies, each of which raises an important and difficult ethical issue connected with planning, reviewing, or conducting health-related research. Available for download free of charge from the World Health Organization in English, Arabic, Russian, and Spanish.
When Dr. Marwan started as director of Ramses Hospital in Cairo in 2008, charged by the Minister of Health with improving performance, he found the hospital had been neglected for decades. A Ministry of Health quality audit had recently given the hospital the worst score of the five hospitals designated as critical to the greater Cairo area.
Dr. Marwan vowed that Ramses Hospital would come in first in the next round of quality audits. Without improving its quality scores, the hospital would be unable to pass the accreditation process required for hospital participation in a new universal social health insurance scheme. In addition—and just as critically—Dr. Marwan needed to develop a longer-term strategy for obtaining the considerable additional resources required to upgrade the long-neglected facility.
Quelch, J.A. & Rodriguez, M. , 2015. Carolinas HealthCare System: Consumer Analytics , Harvard Business Publishing. Available from Harvard Business Publishing Abstract In 2014, Dr. Michael Dulin, chief clinical officer for analytics and outcomes research and head of the Dickson Advanced Analytics (DA2) group at Carolinas HealthCare System (CHS), successfully unified all analytics talent and resources into one group over a three year period. Rapid increases in computing power and decreases in data storage costs had enabled DA2's data architects to build predictive models incorporating complex clinical, financial, demographic, and claims data that would have been impossible to create only a few years before. However, in 2014, both Apple and Google announced features in their new mobile operating systems that collected and displayed output from various health-wearables (like heart-rate monitors or step-counters), as well as electronic medical record (EMR) data. Their expertise in analytics, access to demographic and location data, as well as large consumer bases, led Dulin to consider which players consumers would trust to integrate their healthcare data in the future and what role DA2 could play.
Guerra, I., et al. , 2019. SALUDos: Healthcare for Migrant Seasonal Farm Workers , Harvard University: Social Medicine Consortium. Download free of charge Abstract The SALUDos program began in 2008 as a response to an influx of migrant seasonal farm workers (MSFWs) at a mobile medical unit serving homeless persons in Santa Clara County in Northern California. The program offered patients free and low-cost primary care services, linkage to resources, and advocacy. As the farm workers involved in this program became more involved in their primary care, they advocated for evening hours, transportation, linkage to coverage programs, and health education resources to better understand their medical and psychological conditions. During continual modifications of the SALUDos program, the team sought to understand and address large-scale social forces affecting migrant health through interventions to mitigate health inequities. Teaching note available for faculty/instructors.
Weinberger, E. , 2015. Full of Surprises: Dietary Supplements and the Gym, or, a Tale of Corporate Social Responsibility , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract Working out at the gym is a healthy endeavor, but many gyms endorse unhealthful practices. They may advertise or sell dietary supplements for weight loss or muscle building that not only fail to do what they promise, but contain potentially dangerous ingredients. Callie Guertin is a primary care physician in Hamilton, in the fictitious U.S. state of Columbia, and a daily gym-goer who is slowly awakening to the fact that her chosen new gym, MuscleTone, sells weight-loss supplements at its welcome desk. She wants them to stop; but what can she do on her own? With some guidance from a young activist, Stacie Lubin, and her sympathetic personal trainer, Rudi, Guertin learns skills of coalition building to pressure the MuscleTone chain to change its practices. Perhaps, using principles of corporate social responsibility, or CSR, MuscleTone can be made to realize that abandoning sales and advertising of supplements can produce a good result for everybody—healthier customers, of course, but also a new marketing campaign touting MuscleTone as the gym for “healthy living”? Guertin and her allies are working on MuscleTone to make just this case. Teaching note available for faculty/instructors .
- Technical Support
- Find My Rep
You are here
Case Studies in Community Health
- Jo Fairbanks - University of New Mexico, School of Public Administration, Centennial Group, Latin America
- Judith Candelaria - New Mexico Department of Health
- Description
Case Studies in Community Health presents 14 classroom-tested case study scenarios, including background information and discussion questions. Written for students in public health and community health courses, these cases help integrate the basic concepts of public health into an applied setting. The case studies provide an opportunity for students to apply those basic concepts to a "real-life" situation. The overall purpose of the book is to help students understand that public health practice occurs in a social context and therefore is subject to all the complexities of a social environment. The cases explore a broad range of topics in three critical areas of public health: epidemiology, health administration, and health program planning.
This text will be of interest students and professionals in family studies, family therapy, gerontology, health communication, medical sociology, nursing, nursing administration, nursing health, nursing research and theory, patient care, public administration, public health, quantitative research and methods, school counseling, social work, and sociology.
See what’s new to this edition by selecting the Features tab on this page. Should you need additional information or have questions regarding the HEOA information provided for this title, including what is new to this edition, please email [email protected] . Please include your name, contact information, and the name of the title for which you would like more information. For information on the HEOA, please go to http://ed.gov/policy/highered/leg/hea08/index.html .
For assistance with your order: Please email us at [email protected] or connect with your SAGE representative.
SAGE 2455 Teller Road Thousand Oaks, CA 91320 www.sagepub.com
For instructors
Select a purchasing option.

This title is also available on SAGE Knowledge , the ultimate social sciences online library. If your library doesn’t have access, ask your librarian to start a trial .
- Research article
- Open access
- Published: 01 April 2021
Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters
- Tamar Wyte-Lake ORCID: orcid.org/0000-0001-8449-7701 1 , 2 ,
- Susan Schmitz 1 ,
- Reginald J. Kornegay 3 ,
- Felix Acevedo 4 &
- Aram Dobalian 1 , 5
BMC Public Health volume 21 , Article number: 639 ( 2021 ) Cite this article
2236 Accesses
1 Citations
Metrics details
Community disaster resilience is comprised of a multitude of factors, including the capacity of citizens to psychologically recover. There is growing recognition of the need for public health departments to prioritize a communitywide mental health response strategy to facilitate access to behavioral health services and reduce potential psychological impacts. Due to the US Department of Veterans Affairs’ (VA) extensive experience providing trauma-informed behavioral healthcare to its Veterans, and the fact that VA Medical Centers (VAMCs) are located throughout the United States, the VA is well situated to be a key partner in local communities’ response plans. In this study we examined the role the VA can play in a community’s behavioral health response using case studies from three disasters.
This study investigated experiences of VA employees in critical emergency response positions ( N = 17) in communities where disasters occurred between 2017 and 2019. All respondents were interviewed March–July 2019. Data were collected via semi-structured interviews exploring participants’ experiences and knowledge about VA activities provided to communities following the regional disasters. Data were analyzed using thematic and grounded theory coding methods.
Respondents underscored VA’s primary mission after a disaster was to maintain continuity of care to Veterans. The majority also described the VA supporting community recovery. Specifically, three recent events provided key examples of VA’s involvement in disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships as well as prioritization from VA leadership to engage in humanitarian missions. The behavioral health interventions were provided by behavioral health teams integrated into disaster assistance centers and non-VA hospitals, VA mobile units deployed into the community, and VA telehealth services.
Conclusions
Recent disasters have revealed that coordinated efforts between multidisciplinary agencies can strengthen communities’ capacity to respond to mental health needs, thereby fostering resilience. Building relationships with local VAMCs can help expedite how VA can be incorporated into emergency management strategies. In considering the strengths community partners can bring to bear, a coordinated disaster mental health response would benefit from involving VA as a partner during planning.
Peer Review reports
Disaster behavioral health
The current COVID-19 pandemic, while still underway, has already demonstrated the need for psychological interventions to manage the isolation, stress, and trauma stemming from the ongoing disaster [ 1 , 2 , 3 , 4 , 5 ]. While the scale of the event is unprecedented, interest in understanding the psychological consequences of disasters is not unique to the pandemic [ 6 , 7 , 8 , 9 , 10 ]. Generally, studies exploring the impacts of disasters on behavioral health have found increases in psychological distress in the short term, with the potential for some individuals to experience long-term psychiatric disorders such as posttraumatic stress disorder, depression, and anxiety [ 6 , 7 , 8 , 9 , 10 ].
To ameliorate the potential negative health effects to impacted populations, numerous early interventions have been explored [ 7 , 11 , 12 , 13 , 14 ]. Some countries such as the Netherlands and Iceland use federally structured plans to implement disaster behavioral health interventions [ 12 , 15 ]. And countries like New Zealand have invested heavily in developing extensive mental health programs in response to large scale disaster events [ 16 , 17 ]. In the United States, federal entities strive to create resources and guidance on implementing behavioral health services after disaster, however, interventions are generally managed and delivered by state, territory, and local agencies [ 14 , 18 , 19 ]. Often, after federally declared disasters, the US Federal Government additionally provides funding through the Crisis Counseling Assistance and Training Program (CCP) to community behavioral health programs [ 8 , 13 , 20 ]. Yet the structure and content of interventions are left to the discretion of the implementing agency.
Regardless of the services provided, having a plan in place prior to a disaster can facilitate implementation [ 8 , 11 , 12 , 13 , 19 , 21 , 22 ]. Few publications detail the creation of a local disaster behavioral health response plans [ 15 , 18 , 20 ] or describe the process in which interventions were deployed following an incident [ 7 , 10 , 15 , 20 , 23 , 24 ]. Common themes arising in studies exploring disaster behavioral health plans or interventions are the need for interdisciplinary teams and interagency collaboration [ 8 , 12 , 18 , 19 , 20 ] and strong community response [ 16 ].
The United States Department of Veterans Affairs
One interagency partner often overlooked in the United States is the U.S. Department of Veterans Affairs (VA) Veterans Health Administration (VHA). Previous publications on VHA’s participation in collaborative disaster planning and preparedness efforts with local communities identified barriers to its involvement [ 25 , 26 ]. One such barrier is that the community, and sometime even VHA employees, are unaware that VHA is tasked with planning for and acting to support “national, state, and local emergency management, public health, safety and homeland security efforts” [ 9 , 27 ]. This responsibility to contribute to community efforts is called the VA’s Fourth Mission and is in addition to VHA’s duty to ensure continuity of services to veterans after a disaster.
The expertise of VHA’s 322,030 healthcare professionals and support staff who provide a range of services at its 1255 healthcare facilities spread throughout the U.S. and its territories makes VHA a valuable potential partner in disaster response [ 28 ]. In addition to inpatient and ambulatory medical care, VHA provides a variety of reintegration programs including trauma recovery and behavioral health services for Veterans and their families at its facilities and through community-based care at Vet Centers, Mobile Vet Centers, and college and university campuses [ 29 ]. How these services are applied in community response efforts has been detailed in the grey literature [ 28 , 30 , 31 , 32 ].
This study highlights the potential role of local VA facilities in supporting local behavioral health activities after a disaster, and specifically, presents three exemplars of VHA integrating into communities’ disaster behavioral health response and providing behavioral health support to non-Veterans. The three VA facilities and the events they responded to are: (1) VA Pacific Island Healthcare System (VAPIHC), which is based in Honolulu, Hawaii but provides care to Veterans throughout numerous Pacific Islands. On October 24th, 2018, Super Typhoon Yutu made direct landfall on the Mariana Islands, a US Commonwealth with a nascent established VA tele-mental health clinic on the island of Tinian. This was the strongest typhoon ever recorded to strike the area, severely damaging or destroying many buildings and much of the critical infrastructure of Tinian [ 33 ]; (2) Orlando VA Healthcare System, which serves east central Florida, and encompasses 7 counties. On June 12, 2016, a domestic terrorist attack [ 34 ], targeted hate crime, and one of the deadliest mass shootings in the U.S. occurred at a local establishment, Pulse Nightclub. In a matter of hours, 49 people were killed and 53 were wounded before law enforcement breached the building and ended the violence [ 35 ]; and (3) VA Southern Nevada HCS (VASNHCS), located in and providing care throughout Las Vegas, Nevada. On October 1, 2017, the worst mass shooting in modern history took place at the Route 91 Harvest Music Festival on the downtown Las Vegas Strip. A gunman opened fire on a crowd of more than 22,000, killing 58 people and wounding 413 [ 36 ]. These cases provide examples of interagency partnerships and the implementation of collaborative responses for communities developing their own plans to address the behavioral health needs of their citizens during disasters, including the ongoing COVID-19 pandemic.
Study design
The results presented in this paper stem from a larger study broadly examining the role of local VA facilities in responding to regional large-scale disasters. This study used qualitative interview methods to elicit study participants’ experiences during disasters impacting the U.S. between 2016 and 2018 (see Table 1 for the full list of the disasters covered in the study, the impacted US states and territories, and VA entities affiliated with the impacted areas). Findings on disaster behavioral health functions were pulled as a subset of data and analyzed. The VA Greater Los Angeles Healthcare System Institutional Review Board (Los Angeles, California USA) approved this study.
Setting and sample
The full study sample was purposively chosen to represent individuals with emergency response roles critical to coordinating VA’s local response to disasters. Emergency management personnel at various levels of the VA were the first point of contact and, when applicable, identified additional individuals with critical response roles to interview. Additional respondents were recruited independently by the project team These facilities made up the broad recruitment sample. Due to some respondents covering multiple disasters or being deployed to disasters outside their normal service region, not all entities were included in the final sample.
Data collection methods
Data were collected through semi-structured, 60-min telephone interviews between March–August 2019, using an interview guide developed for this study (see Additional file 1 ). Interviews were conducted individually with each respondent and led jointly by at least two of the authors. Interviews explored participants’ experiences and knowledge about VA activities in the community, specifically focusing on how VA networked and coordinated with non-VA community agencies. Interviews were audio-recorded, although one respondent declined to be recorded.
Analysis plan
A total of 17 individuals were interviewed. However, five interviews did not indicate collaborating with non-VA entities and were therefore not included in the analysis. Due to their involvement in multiple disasters, two respondents were interviewed twice. At completion of the interviews, this resulted in 13 interview recordings being transcribed, and one set of interview notes (due to interviewee declining to be recorded), resulting in a total of 14 interviews that were analyzed with Atlas.ti (v.7) using a grounded theory approach. In phase one of analysis, one author reviewed all 14 interviews, using inductive coding to identify emergent themes in the data, and informed by extensive conversations about project findings held by the project team at the conclusion of each interview [ 37 ]. As a product of this process, a significant emergent theme [ 37 ] was the presence of interagency partnerships implementing collaborative responses to address the behavioral health needs of local citizens during disasters. A decision was made by the project team to narrow the focused coding analyses [ 37 ] to the way local VA facilities engaged in a behavioral response within their local community, in response to their respective large-scale disaster events.
In phase two of the analysis, the initial codes identified by SS were reviewed by TWL for consistency and agreement. Codes not deemed consistent to the focus topic were dropped. Additional grounded themes were confirmed by the team and applied to the data set [ 37 ]. Consensus on final codes was achieved, and one code list was finalized. In phase three of the analysis, the final code list was applied across all relevant interviews. The final code list had a focus on behavioral health response, including behavioral health activities, method of delivery, reactions of staff, and types of impacted community populations, but also included an identification of high level themes across all disasters, including VA expertise, integrating into local, established response activities, identification of local needs, and logistical challenges. Authors TWL and SS then independently coded each interview and resolved discrepancies by consensus.
All respondents played a substantial role in VA’s activities following the respective disasters. However, only 12 participants indicated the VAMC they supported collaborated with non-VA partners during the event in question. Included disasters ranged from widespread to geographically contained; weather-related to acts of violence; and direct impact on VA facilities ranged from none to significant. Though not all respondents described intensive engagement with the community following the event, all respondents described the importance of integrating into local, established response activities. This translated into involvement in community-wide drills and planning committees and following the lead of local incident command. Respondents indicated one of the areas where the VA could provide support to the community was in disaster behavioral health relief operations.
Activities described by respondents were often centered around tasks where the VA could reduce the caseload of other community agencies by identifying Veterans obtaining services in the community and meeting their needs regardless if they were previously enrolled in VA benefits. One key activity described by several respondents included outreach into local shelters. As one respondent explained, VA staff at shelters “[distribute] fliers [that] outline that our counselors are experts in trauma, loss, and in readjustment. They also provide referrals to Veterans for a variety of services, including housing and employment. We also offered free counseling for all community members impacted .”
Identifying where shelters were established and receiving authorization to deploy VA assets to those locations required coordination with local authorities. Multiple respondents mentioned connecting with emergency management running relief efforts to describe available VA resources and detail the services available to both Veterans and the community at large. In some of the events explored in this study, the non-VA authorities were unaware of what the VA could offer while others had pre-existing relationships that allowed for more transparent understanding of how the VA could support response efforts. One respondent went on to describe how the disaster that impacted their VAMC led to additional outreach to local jurisdictions and shelter coordinating agencies (e.g., the American Red Cross) to build relationships and understanding specifically of the behavioral health services the VA could deploy, if needed and approved.
Respondents noted there were specific benefits to conducting outreach in locations where other agencies provided services to the people impacted such as shelters and Local Assistance Centers. They noted that VA staff could more easily reach Veterans to enroll them, if eligible, into VA services and offer care to those who usually used non-VA health and mental health facilities, thereby supporting local agencies by reducing potential patient loads elsewhere. Additionally, by positioning resources at a central location, VA could more readily offer community members services as an extension of their work with Veterans. One specific resource identified as useful for Veteran and community support was Mobile Vet Centers, which have the primary goal of providing social work and mental health services to Veterans. In cases where respondents mentioned this resource, they underscored that non-Veteran community members who requested services in the first days after the disaster were never turned away.
Three community profiles
Three disaster events described by respondents distinctly highlighted cases where the VA was deeply involved in the local community’s disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships, as well as prioritization from VA leadership to engage in humanitarian missions to support the community.
Telehealth in Tinian, Mariana Islands
Prior to Super Typhoon Yutu impacting the Mariana Islands, the VA Pacific Island Healthcare System (VAPIHC) established tele-mental health services on the island of Tinian. These services were located at a non-VA owned healthcare clinic using pre-positioned VA telemedicine equipment and coordinated with the clinic director and staff. Typhoon Yutu devastated the island and led to many Tinian healthcare clinic employees losing their homes. The clinic with VA tele-mental health equipment became a temporary housing site for staff as it was undamaged by the storm. The clinic director realized that in addition to sheltering needs, employees also experienced significant trauma. However, there were limited mental health resources on the island. Once VA became aware of the need, it worked with other federal agencies to manage the logistics of implementing services that took advantage of pre-positioned VA resources.
“… it was a relationship that we had with [the US Department of Health and Human Services] (HHS) and a relationship that we had with the folks on Guam and Saipan … we have a lot of relationships going on. So, we knew that we had that telehealth equipment. We also knew that Tinian was … hit pretty hard. And that there was a lot of grief. And so I can’t say how it totally emerged, but there’s so many relationships and there’s so much communication during an emergency.”
Respondents reported it was initially challenging to identify whether VA could provide mental health services in the community and how the services would be funded. Staff at all levels of the VA worked with the Federal Emergency Management Agency (FEMA) and HHS to get official authorization as well as receive federal funding for VAPIHC to provide time limited tele-mental health interventions to clinic staff on Tinian. VAPIHC Tele-mental Health Hub coordinated with the local clinic director to inform employees about available services and utilized technology onsite to provide weekly support groups for 13 health center employees.
Director’s 50 in Orlando, Florida and the pulse nightclub shooting
The Orlando VA Healthcare System (OVAHCS) houses a unique emergency response team “The Director’s 50.” Made up of multi-disciplinary VA healthcare workers, including mental health professionals (i.e. psychologists, psychiatrists, mental health nurses), the Director’s 50 can deploy a team of up to 50 volunteers within 2 hours to areas throughout the region when authorized by the Orlando VAMC Director. As described by one respondent, the mission of the team is,
“to provide an immediate gap fill to an emergency before VA can get its assets organized and into a formal support and response role. So the team is multi-disciplinary and multi-functional with its capabilities, so that it can immediately address the needs of the emergency response until VA can formalize how it’s going to provide their support to the community.”
The Director’s 50 includes interdisciplinary clinical and service support training for all members such as triage and treatment services, mental health intervention, peer counseling, and psychological support to trauma. Through participation in community-wide exercises and drills, the Director’s 50 has built versatile capabilities and strong relationships with local emergency management agencies and area hospitals.
In response to the Pulse Nightclub Shooting, VA Central Office requested OVAHCS to deploy the Director’s 50 to provide VA resources and support the community’s response. The team activated their mass notification system to alert their nearly 100 volunteer members and quickly assembled an initial response team of about 15 clinical, mental health, and support professionals within 1 hour. Respondents noted having internal approval can speed up the process of deploying teams. In general, to distribute VA resources into the community, a federal disaster declaration is required to initiate the Robert T. Stafford Disaster Relief and Emergency Assistance Act or where the HHS Secretary has activated the National Disaster Medical System, both of which grant VA the ability to provide assistance. Therefore, respondents noted a need to balance expectations of leadership to help quickly, while also ensuring VA resources were legally allowed to be used in the response.
One thing that facilitated OVAHCS’s integration into the local response system was a pre-existing relationship with the City of Orlando’s Office of Emergency Management and the Central Florida Medical Disaster Coalition, which facilitated the Director’s 50 integration into the city’s response and allowed them to report to the victim reunification center. The team was tasked.
“to be the initial communication to the family members for those victims that actually passed away. So, 49 victims, our team was assigned to go ahead and be the initial contact to let them know that their loved ones had passed, and to begin the coordination for services, grief counseling and victim advocacy, you know, to help them prepare the initial points of piecing together their lives after being notified of such tragic events.”
Accordingly, the initial multi-disciplinary team narrowed its focus to mainly members with mental health expertise. Over the next 2 weeks, the team worked with the community, helping to manage vigils and gatherings for the public, and continuing grief counseling and mental health support for the whole community, including providing peer behavioral health support to municipal first responders. Since this act of violence targeted people who were Lesbian Gay Bisexual Transgender Queer (LGBTQ) frequenting Pulse Nightclub, not only were relatives of victims or survivors from inside the building affected, but the entire LGBTQ community felt the traumatic impact of the shooting. One respondent described the importance of providing mental health support from multiple community agencies when a disaster of this magnitude occurs,
“And they [the people who were at the shooting] truly needed a place, and this is why we were there for greater than just the 24-48 hours of initially identifying the people who was killed during the shooting, you had everyone that was inside of the club who were seeking a place where they could go and receive the care and support that they needed as well. And obviously, you know, this is something that is an endemic issue with healthcare as a whole, is the access to mental health counseling and services. So VA, as well as some other partnering mental health organizations were able to supply that need right there at the site where they were doing victim notification or victim reunification and family support. We were able to do that.”
One respondent noted a key point to remember about the Director’s 50, “they are all volunteers...And these people will go—you know, 24 hours a day, day in and day out, to execute that mission. And we have to think about team resiliency.” This included caring for team member’s well-being by rotating staff and providing and attending to the mental heath of one another. As described by one respondent,
“Because when it was all said and done, the team was very affected by what they had to do. You know, just imagine hearing—you know, overwhelming grief for every one of the 49 victims’ families that would show up. And the team took that burden on … and I will tell you, to this day, it still affects the people who went and supported that mission. And they really—those who supported that mission have a greater reverence for what we do now, as a team. So you’d never have to ask them to—whether they are going to support anything related to the Director’s 50. That comradery that’s there, they won’t let their own kind of—go into the bowels of despair like that, alone.”
Integrating into community response in Las Vegas, Nevada after the route 91 harvest festival shooting
As a large city with many national and international visitors, respondents described Las Vegas as having a very centralized emergency response structure. Relationships between VA Southern Nevada HCS (VASNHCS) and local response agencies and area hospitals were described as “tightknit” with great working relationships where organizations plan and prepare for disasters together. As one respondent put it,
“what I do know is my community. I know my community partners. I know what they have, what they don’t have, they know what I have, what I don’t have. And that’s what makes us so resilient. That’s community.”
Although located too far away from the Las Vegas Strip to actively receive injured victims when the shooting occurred at the Route 91 Harvest Music Festival, VASNHCS activated its Hospital Incident Command System so it could actively participate in the community’s response and organize efforts. A Multi-Agency Coordination Center (MACC) organized the response activities, and respondents underscored the value of both pre-existing relationships and an understanding of the county’s emergency response structure. As explained by a respondent,
“You can’t wait for your community to ask you. You have to be on the forefront and know what they need. And you only do that by knowing your community. You know, I spent probably as much time in my community as I do in my medical center. A lot of the time, it’s my own time, but again, it builds that relationship that when they’re updating their mass casualty plan, one of the people they’re calling is [me].”
This previous collaboration, as well as being present at the MACC, allowed VASNHCS to identify community needs that it could address.
As news of the shooting spread, VA leadership tasked VASNHCS with deploying staff into the community. However, it was challenging to balance the push from VA to deploy with continuing to respect established local coordination structures. VASNHCS maintained a presence within the Medical Area Surge Command of the MACC to offer resources and expertise, waiting for requests, instead of directly deploying assets outside of the established system.
In the immediate response, VASNHCS assisted with managing fatalities. It offered morgue space to the county and initiated the mass fatality plan to increase morgue capacity. This provided the county and partner hospitals space for victims until they could be processed, and families could claim them. Additionally, VASNHC offered a Psychological First Aid (PFA) team.
Initially, VASNHCS deployed their PFA team to the community’s family reunification center. The team was composed of social workers, psychologists, psychiatrists, administrators (as support staff), canteen services (for water and snacks to sustain clients and staff), and the medical center’s Chief of Staff. As the situation evolved, the MACC received requests from local agencies for psychological assistance and VASNHCS transitioned to directly integrating into area hospitals.
Three Las Vegas hospitals received the bulk of the injured or dead and recognized the need for psychological interventions with their staff. Due to their close relationships with other hospitals, one respondent explained that they were familiar with the Employee Assistance Program (EAP) at these hospitals. The respondent knew it would take time for the EAP to arrive onsite and they would most likely focus on clinical staff involved in directly treating the injured. Therefore, VASNHCS developed a three-pronged approach to complement EAP services at the receiving hospitals. Firstly, the PFA team provided what one respondent called “ trauma therapy ” to hospital staff, regardless whether they worked the night of the shooting. The assistance extended beyond clinical staff to non-clinical departments, such as environmental services/housekeeping, whose staff were also impacted through their response roles.
Respondents reported one of the reasons their response in the hospitals was so successful was that the team was multidisciplinary, allowing staff from different departments to talk to people in similar positions, which was valued by the recipients.
“So for example, we have a nurse that’s trained in trauma, psychological first aid. So they want the nurses at [the hospital with a patient surge], they want to talk to our team. They were still processing. But when we brought our nurse into the ward, they were more than willing to open up to her, because she was one of them. She was part of their tribe. So we try to match our tribe to their tribe, and that’s why we were successful.”
Secondly, the VASNHCS team worked with victims of the shooting, providing PFA and social work services. Thirdly, they integrated with family members of patients at the hospitals and provided them items that they did not otherwise have because they were visitors to Las Vegas. Examples included coordinating free transportation to and from hospitals and hotels, connecting them to local mortuary services, and providing information about how to access services when they returned home.
The PFA team ran for 24 h a day, for 7 days in those three impacted hospitals. To balance VA patient care with the community response mission, VASNHCS staff volunteered shifts outside of their normal work hours. One respondent described the overwhelming desire of VA staff to help their community.
“And while it didn’t impact our staff or our clinics, or our patients, it impacted our community. I think another thing that still amazes me to this day, was the outpour of our staff and what I mean by that is they were coming out of the woodwork to support. We had more volunteers working an eight-hour shift and then coming in [to volunteer] at five o’clock or four o’clock and working to midnight to two in the morning and not go home until four or five in the morning, and then go to work the next day, because we didn’t want to impact our patient care. And they were doing this out of their—you know, because they care. They care about the community, they care about the event, they care about the people. And then at the end of the day, you know, we had more volunteers than we had placements, because we did not want to overwhelm the health systems with all of these VA personnel.”
However, with new volunteers each shift, a key lesson learned was to have a daily team debrief. As people changed daily, a debrief provided key information and a running tally of support being provided to save time and avoid reinventing the wheel identifying contacts or systems already developed.
Another lesson was that preparedness requires ongoing maintenance. The importance of ongoing preparedness was underscored when VASNHCS realized that leading up to the shooting, they had reduced their focus on PFA training. As described by one respondent, “ We noticed that we need that continuous [psychological first aid] training, that we need continuous exercising, and it’s not an easy fit, to send a bunch of people to someone else’s hospital or an area to do that kind of service .” They also realized the first wave of personnel went into community hospitals without basic supplies they needed to provide services, including basic items such as pens, PFA guides, and informational brochures.
Three months following the shooting, the VASNHCS Emergency Manager, working with the Chief of Social Work hosted a lunch for staff who volunteered to thank them for their involvement. During that event, they realized volunteers were not only impacted by the event itself, but also by their time providing support in the community. They therefore created a forum to again gather staff who had deployed at the 6 month and 9 month marks to eat and talk about the impact of the event on the healthcare system and themselves. On the 1 year anniversary, management had a special event for the volunteers,
“we actually had people from the community that we supported coming in and they broke bread with our team and what they did was, they talked about what the impact of the VA Southern Nevada Healthcare System was going into that event, and how we helped them bridge the gap [of mental health support] that was crucial at that time, and how appreciative they were to our cause and our Clark County Office of Emergency Management gave all our staff that responded T-shirts that said Vegas Strong, because they wanted them to know that we—they appreciated the work that we did for them to support our community.”
The need for attention to the psychological well-being of individuals during and after a disaster has been well proven as disasters have been found to be associated with both short and long-term symptoms and disorders [ 6 , 7 , 8 , 9 , 10 , 38 ]. Although in some parts of the world there are federally structured plans to implement disaster behavioral health interventions, in the United States there is a patchwork system that often relies on support and resource allocation from a multitude of agencies [ 8 , 13 , 14 , 18 , 19 , 20 ]. In this study we examined the role the VA can play in a community’s disaster relief effort and highlighted the opportunity for VA to support behavioral health response focusing specifically on case studies from three disasters.
Essential to effective emergency management is an understanding of, and engagement with, available resources in a local community. This is of particular importance when considering complex individual and group needs such as behavioral health support. VA Medical Centers can be seen as challenging partners to work with because they are both a federal entity and a local healthcare facility [ 26 ]. However, in the case of Super Typhoon Yutu, the federal positioning of the VA and its connection with HHS and FEMA facilitated the deployment of VAPIHC virtual resources. The regional respondents who supported the VA disaster mission in Tinian described how preexisting relationships with federal partners facilitated authorization and funding.
Another potential challenge to incorporating the VA into response efforts is that prior to offering services, VA leadership must balance the mission of the agency with community needs, without contradicting the restrictions of the Stafford Act. In all three presented cases, VA’s behavioral health support was not formally included in a city or county response plan, and yet pre-existing relationships between key stakeholders facilitated the provision of VA behavioral health services to support identified community needs. Respondents also described participating in interagency coordinating groups, response trainings, and exercises before the disaster. These activities aided in a deeper understanding of the response structures each partner operated under and encouraged strong rapport between agencies.
Relationships between VA emergency management and local emergency management proved invaluable as VA staff understood that services should not be provided without first engaging local response coordinators. All VA facility leadership and emergency managers are required to be trained in the Incident Command System (ICS) and National Incident Management System (NIMS), which are the coordinating structures all U.S. response agencies work within [ 39 ]. As a health care provider at a national level, VHA falls within the operations section Essential Support Function (ESF) 8: Public Health and Medical Services to support the Department of Health and Human Services [ 40 ]. Local jurisdictions may also connect with VAMCs through ESF 8 representation. For example, the VA has provided significant support to communities impacted by COVID-19. As of July 8, 2020, VA provided more than 330,000 pieces of Personal Protective Equipment (PPE) in support of the Fourth Mission, as well as hand sanitizer, laundry support, test kits and testing support, and webcams for use with existing equipment to state and local facilities. In addition, VA has admitted 279 non-Veterans to VA Medical Centers because of the pandemic [ 27 ]. Much of this coordination was done through ESF 8 coordination at a local or national level.
While respondents did not go into detail about their participation in the emergency management structure, some participants described their VA’s roles within emergency operations as liaisons. Groups such as this could report to either the planning, operations, or command sections within the ICS. Group supervisors would most commonly report to the operations section chief, likely through branch directors, given that the focus of the work would be more on specialized functions as needed for tactical operations. Regardless of where they fit, their presence at emergency operations centers and command posts facilitated communication to allow for VA’s integration into incident action plans. Particularly during the response to mass casualty events in Orlando and Las Vegas, understanding the local response network and then proffering available services was essential to avoid confusion or duplication of activities. By working within the established coordination centers, VA’s efforts were effectively integrated into the greater community behavioral health response and were deployed to points of greatest need. Although a detailed understanding of the integration of VA activities into ICS structures fell outside of the scope of this work, future assessment of the integration of VA representatives into local, state, and/or regional ICS structures could help clarify roles and identify which section liaisons best support (e.g., operations, planning, logistics) [ 40 ].
VA is increasingly strengthening partnerships with agencies that provide behavioral health services to Veterans and their families who use non-VA community-based care [ 41 ]. In each case example, the primary support provided by VA to the community was the provision of behavioral health services in response to an identified need. Respondents described this as being due, in large part, to the recognition of VA’s expertise in trauma and post-trauma treatment, thereby allowing these resources to come to the forefront. While not mentioned by the respondents, an additional value that VA providers add to disaster behavioral health responses is their exposure to and understanding of the unique needs of various populations throughout their communities. In addition to ensuring care is culturally competent to the unique identity of being a Veteran, VA staff must respect the diversity of Veterans themselves. Just like the U.S. population at large, Veterans represent a range of ages, races, genders, sexual orientations, socioeconomic statuses, etc. and mental health services must be considerate of this diversity. The VA recognizes this and offers training to providers to understand and respect their patients’ unique needs [ 42 ]. Working with a variety of populations preposition VA staff to have a deeper understanding of the post-disaster needs of the wider community.
Two of the case examples described in this study especially bring to the forefront the importance of disaster behavioral health response planning and implementation teams understanding unique experiences of community members. Super Typhoon Yutu directly impacted an archipelago housing a majority Asian and/or Pacific Island population. The Pulse Nightclub shooting, while a terrorist event, was a targeted hate crime intended to inflict violence on the LGBTQ community. Disaster behavioral health interventions for these affected groups not only need to take into consideration the importance of cultural competency but also the potential of re-traumatization and distinct population mental health needs.
In the Northern Mariana Islands, while there is a mix of ethnic groups (Filipino, Chamorro, Chinese, Carolinian, Korean, Palauan, etc.), many either identify as or are categorized more broadly as Asian and/or Pacific Islanders. Although there are more than 1.4 million people who are considered Pacific Islanders living the in the U.S., there is a dearth of information on the mental health of this population [ 43 ]. Similarly, the prevalence and incidence rates of mental illness in the Mariana Islands is not well studied [ 44 ]. Some sources attribute this lack of understanding to a disproportionate underuse of mental health services [ 43 ]. However, Asian and Pacific Islanders within the U.S. and those territories affiliated with it often experience transgenerational trauma, discrimination, continued loss from colonization, historical trauma, and mental health stigma which can impact psychological wellbeing and help seeking behavior. Additionally, cultural elements (collectivism, reverence for the past, hierarchical social order, etc.) of this population are important to understand when providing behavioral health services [ 43 , 45 ]. One of the reasons respondents indicated that the VA was asked to provide assistance following Typhoon Yutu was the lack of availability of mental health services in Tinian. The established VA telehealth technology increased accessibility to behavioral practitioners from VAPIHC who most likely were experienced working with Asian and Pacific Island populations since more than 55,000 Veterans who identify as this ethnicity live in Island Areas or Hawaii [ 46 , 47 ].
The Pulse Nightclub Shooting was a terrorist driven hate crime targeting individuals who identified as LGBTQ. Members of this group often experience discrimination, stigma, and trauma throughout their lives. Discrimination and heterocentric health and mental health practices can marginalize this population and impact help seeking behavior [ 48 , 49 ]. This is of particular concern as individuals who are LGBTQ face numerous mental health disparities with a higher likelihood of experiencing depression, anxiety, substance misuse, and suicide attempts. The shooting not only targeted LGBTQ people but it also took place during Latin Pride Night meaning many of the victims and casualties were LGBTQ Latinx. The resulting psychological impacts of the Pulse Nightclub shooting on those directly impacted, people who are LGBTQ Latinx, and individuals in the wider LGBTQ community have been investigated and show experiences of trauma and impacts on perceived safety [ 50 ]. At the time of the shooting, the Orlando VAMC had established relationships with LGBTQ local mental health services and had staff knowledgeable in the needs of this community [ 51 ]. In fact, in the recent past, the VA has increased its efforts to ensure Veterans who are LGBTQ receive the highest quality patient-centered care possible [ 52 ]. Mental health services in particular have bolstered recognition of the complex needs of these Veterans [ 52 ].
All three cases demonstrate innovative ways VA can provide behavioral health support outside of their facilities, i.e., via telehealth capabilities across an ocean and into a healthcare clinic, teams of mobile units reaching directly into the community to support victims, victims’ families, and the community at large, and finally by incorporating PFA teams directly into hospitals to support staff, patients, and patients’ families. This flexibility across sites to address different needs and populations while using varying available infrastructure support, is paramount to any local jurisdiction’s ability to meet on the ground needs following a disaster. It demonstrates the variability between VAMCs and the importance of local disaster behavioral health planning teams to pre-identify resources to assess local capacity. Plans can then be developed that access and deploy the tools/skills of interdisciplinary and interagency teams. Building processes to deploy local health and mental health practitioners can lead to more rapid implementation of interventions and help ensure the diversity of the impacted community is recognized and respected. Additional studies focused on how communities develop disaster behavioral health plans could provide insight into which agencies are involved and how they collaborate. It may also be useful to assess whether and how these plans are implemented to identify best practices.
In addition to the people directly impacted by disasters, respondents underscored the importance of offering support to responders as well. There is growing recognition that health care workers are themselves front-line response workers who may be psychologically impacted when caring for others, leading to a growing emphasis on the importance of selfcare and employee wellbeing [ 39 , 40 , 41 , 42 ]. In all three case studies, behavioral health support was, at least in part, directed toward healthcare workers. In the case of Las Vegas, a respondent highlighted the advantage of having behavioral health support come from individuals who understood the culture of the population they were helping, e.g., nurses supporting nurses. Further, respondents in Las Vegas and Orlando highlighted the importance of supporting deployed behavioral health team members. They detailed actions to maintain staff well-being by having rotating shifts, encouraging peer support, and facilitating gatherings for staff to publicly thank them for their efforts and allow them to address their experiences together as a group. Understanding the needs of healthcare and behavioral health personnel and building support networks into response frameworks can help better sustain and strengthen the overall response process.
A primary limitation of this study is that interviews were conducted up to one and a half years after the disasters described, potentially impacting recall. However, multiple interviewees corroborated the information presented for each of the case studies. Another limitation is that this study focused exclusively on the experiences of VA employees fulfilling mission requirements and their description of instances where VA acted in support of the Fourth Mission. Very few of the respondents directly provided the behavioral health interventions. These perspectives could provide deeper understanding of the interventions themselves as well as the impacts they may have on practitioners. Neither community members nor coalition partners were interviewed in this study. Future research would benefit from both interviewing non-VA participants to explore additional perspectives and gain greater insight on how local jurisdictions experienced collaborating with VA representatives and exploring alternative approaches to mental health units within and outside VA to examine whether and when different approaches may be preferable.
As the largest integrated healthcare system in the United States, VA can play an important role in disaster response across the country. As recognition of VA’s expertise in behavioral health grows, particularly around trauma and post-trauma treatment, VA should be considered a strong potential partner in behavioral health responses. Local VAMC staff are part of the community in which they live and the Veterans they serve are a microcosm of the larger population of the U.S. As the respondents in this study showed, there is a deep desire by VA staff to provide support following a disaster if they are able. Anticipating potential behavioral health concerns, and having a plan to address them, can foster community disaster resilience. While these plans may be different for each jurisdiction, they can be strengthened by identifying and incorporating a range of partners. Having preexisting relationships where VA’s capabilities are known before a disaster occurs can facilitate the rapid deployment of VA resources into identified areas of community need. The case studies presented demonstrate the flexible nature of these resources. By extending knowledge about innovative ways to share behavioral health and other resources in a disaster response, communities and healthcare coalitions can be better prepared to engage collectively and rapidly mobilize essential assets to support the wellbeing of those who need it most.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Crisis Counseling Assistance and Training Program
U.S. Department of Veterans Affairs
Veterans Health Administration
VA Medical Center
VA Pacific Island Healthcare System
VA Southern Nevada HCS
Veterans Health Administration Health Care System
Veterans Integrated Service Network
Office of Emergency Management
US Department of Health and Human Services
Federal Emergency Management Agency
Lesbian Gay Bisexual Transgender Queer
Multi-Agency Coordination Center
Psychological First Aid
Employee Assistance Program
Personal Protective Equipment
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. https://doi.org/10.1016/S0140-6736(20)30460-8 .
Article CAS PubMed PubMed Central Google Scholar
Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1):e32. https://doi.org/10.1192/j.eurpsy.2020.35 .
Article CAS PubMed Google Scholar
Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510–2. https://doi.org/10.1056/NEJMp2008017 .
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213 .
Article PubMed PubMed Central Google Scholar
Vigo D, Patten S, Pajer K, Krausz M, Taylor S, Rush B, et al. Mental health of communities during the COVID-19 pandemic. Can J Psychiatr. 2020. https://doi.org/10.1177/0706743720926676 .
Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716–22. https://doi.org/10.1192/bjp.2018.210 .
Article PubMed Google Scholar
Beinecke R, Raymond A, Cisse M, Renna K, Khan S, Fuller A, et al. The mental health response to the Boston bombing: a three-year review. Int J Ment Health. 2017;46(2):89–124. https://doi.org/10.1080/00207411.2017.1294969 .
Article Google Scholar
Beinecke RH. Addressing the mental health needs of victims and responders to the Boston Marathon bombings. Int J Ment Health. 2014;43(2):17–34. https://doi.org/10.2753/IMH0020-7411430202 .
Dobalian A, Callis R, Davey VJ. Evolution of the Veterans Health Administration’s role in emergency management since September 11, 2001. Disaster Med Public Health Prep. 2011;5(S2):S182–4. https://doi.org/10.1001/dmp.2011.61 .
Heslin KC, Stein JA, Dobalian A, Simon B, Lanto AB, Yano EM, et al. Alcohol problems as a risk factor for postdisaster depressed mood among U.S. veterans. Psychol Addict Behav. 2013;27(1):207–13. https://doi.org/10.1037/a0030637 .
Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, et al. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry. 2007;70(4):283–337. https://doi.org/10.1521/psyc.2007.70.4.283 .
Jacobs J, Oosterbeek M, Tummers LG, Noordegraaf M, Yzermans CJ, Duckers MLA. The organization of post-disaster psychosocial support in the Netherlands: a meta-synthesis. Eur J Psychotraumatol. 2019;10(1):1544024. https://doi.org/10.1080/20008198.2018.1544024 .
North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310(5):507–18. https://doi.org/10.1001/jama.2013.107799 .
Watson PJ, Ruzek JI. Academic/state/federal collaborations and the improvement of practices in disaster mental health services and evaluation. Admin Pol Ment Health. 2009;36(3):215–20. https://doi.org/10.1007/s10488-009-0212-4 .
Thordardottir EB, Gudmundsdottir B, Petursdottir G, Valdimarsdottir UA, Hauksdottir A. Psychosocial support after natural disasters in Iceland-implementation and utilization. Int J Disaster Risk Reduction. 2018;27:642–8. https://doi.org/10.1016/j.ijdrr.2017.11.006 .
Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry. 2014;71(9):1025–31. https://doi.org/10.1001/jamapsychiatry.2014.652 .
Gray L, MacDonald C, Mackie B, Paton D, Johnston D, Baker MG. Community responses to communication campaigns for influenza A (H1N1): a focus group study. BMC Public Health. 2012;12(1):1–12.
Compton MT, Cibulas BK, Gard B, Kaslow NJ, Kotwicki RJ, Reissman DB, et al. Incorporating community mental health into local bioterrorism response planning: experiences from the DeKalb County Board of Health. Community Ment Health J. 2005;41(6):647–63. https://doi.org/10.1007/s10597-005-8846-5 .
Pfefferbaum B, Flynn BW, Schonfeld D, Brown LM, Jacobs GA, Dodgen D, et al. The integration of mental and behavioral health into disaster preparedness, response, and recovery. Disaster Med Public Health Prep. 2012;6(1):60–6. https://doi.org/10.1001/dmp.2012.1 .
Elrod CL, Hamblen JL, Norris FH. Challenges in implementing disaster mental health programs: state program directors’ perspectives. Ann Am Acad Pol Soc Sci. 2016;604(1):152–70.
Gil-Rivas V, Kilmer RP. Building community capacity and fostering disaster resilience. J Clin Psychol. 2016;72(12):1318–32. https://doi.org/10.1002/jclp.22281 .
Melmer P, Carlin M, Castater CA, Koganti D, Hurst SD, Tracy BM, et al. Mass casualty shootings and emergency preparedness: a multidisciplinary approach for an unpredictable event. J Multidiscip Healthc. 2019;12:1013–21. https://doi.org/10.2147/JMDH.S219021 .
Naturale A, Lowney LT, Brito CS. Lessons learned from the Boston Marathon bombing victim services program. Clin Soc Work J. 2017;45(2):111–23. https://doi.org/10.1007/s10615-017-0624-7 .
Reifels L, Pietrantoni L, Prati G, Kim Y, Kilpatrick DG, Dyb G, et al. Lessons learned about psychosocial responses to disaster and mass trauma: an international perspective. Eur J Psychotraumatol. 2013;4.
Dobalian A. The US Department of veterans affairs and sustainable health care coalitions. Disaster Med Public Health Prep. 2015;9(6):726–7. https://doi.org/10.1017/dmp.2015.136 .
Schmitz S, Wyte-Lake T, Dobalian A. Facilitators and barriers to preparedness partnerships: a veterans affairs medical center perspective. Disaster Med Public Health Prep. 2018;12(4):431–6. https://doi.org/10.1017/dmp.2017.92 .
VA Fourth Mission Summary [ https://www.va.gov/health/coronavirus/statesupport.asp ].
Office of Public and Intergovernmental Affairs [ https://www.va.gov/opa/pressrel/searchResults.cfm ].
Affairs USDoV: VA Office of mental health and suicide prevention guidebook. 2018.
Google Scholar
Lawrence Q. VA secretary Wilkie: ‘We are the surge force’. In: The coronavirus crisis: NPR. NPR.org ; 2020.
Services UDoHH. HHS, FEMA, DOD and VA continue to provide sustained and critical medical care support for Puerto Rico as part of Trump Administration response to Hurricane Maria. In . HHS.gov News: US Department of Health & Human Services; 2017.
Steinhauer J. The V.A. Prepares to back up a health care system threatened by coronavirus: The New York Times; 2020.
Agency FEM. Super typhoon Yutu: one year later: FEMA; 2019.
Foundation NP: After-action review of the orlando fire department response to the attack at pulse nightclub. 2018.
Investigation FBo: Active shooter incidents in the United States in 2016 an 2017. 2018.
Department LVMP: 1 October after action review. 2018.
Charmaz K, Belgrave LL. Grounded theory: The Blackwell Encyclopedia of Sociology; 2007. https://doi.org/10.1002/9781405165518.wbeosg070 .
Lowe SR, Galea S. The mental health consequences of mass shootings. Trauma Violence Abuse. 2017;18(1):62–82. https://doi.org/10.1177/1524838015591572 .
Department of Veterans Affairs. National incident management system compliance: VHA Directive 0320.12(1): Administration VH. Washington, DC; 2021.
Veterans Health Administration. COVID-19 response plan: Management OoE; 2020.
US Department of Defense DoVA, Department of Health & Human Services. Interagency task force on military and veterans mental health; 2017. p. 1–31.
National Academies of Sciences E, and Medicine, Health and Medicine Division, Board on Health Care Services, Committee to Evaluate the Department of Veterans Affairs Mental Health Services. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies Press (US); 2018.
Subica AM, Aitaoto N, Link BG, Yamada AM, Henwood BF, Sullivan G. Mental health status, need, and unmet need for mental health services among U.S. Pacific islanders. Psychiatr Serv. 2019;70(7):578–85. https://doi.org/10.1176/appi.ps.201800455 .
Buettner K, Sablan J, Funk M, Arriola, J, Price, S, Sugiura, K, Diminic S, Drew N. WHO profile on mental health in development (WHO proMIND): Commonwealth of the Northern Mariana Islands. Geneva, World Health Organization; 2013. https://apps.who.int/iris/bitstream/handle/10665/85304/9789241505741_eng.pdf;jsessionid=A222F532F705877A650948706A437484 . Accessed 26 Mar 2021.
Mental health in the Asian Americans/Pacific Islander Community [ https://www.amsa.org/2020/09/04/mental-health-in-the-asian-americans-pacific-islander-community/#:~:text=Mental%20Health%20of%20Pacific%20Islanders&text=According%20to%20a%202019%20study%20for%20the%20general%20US%20population ].
Alessi EJ. Acknowledging the impact of social forces on sexual minority clients: introduction to the special issue on clinical practice with LGBTQ populations: Springer; 2013.
Veteran Population [ https://www.va.gov/vetdata/veteran_population.asp ].
Ussher JM. Heterocentric practices in health research and health care: implications for mental health and subjectivity of LGBTQ individuals. Fem Psychol. 2009;19(4):561–7. https://doi.org/10.1177/0959353509342933 .
LGBTQI [ https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/LGBTQI ].
Stults CB, Kupprat SA, Krause KD, Kapadia F, Halkitis PN. Perceptions of safety among LGBTQ people following the 2016 pulse nightclub shooting. Psychol Sex Orientat Gend Divers. 2017;4(3):251–6. https://doi.org/10.1037/sgd0000240 .
Lesbian, Gay, Bisexual and Transgender Veteran Care [ https://www.orlando.va.gov/services/lgbt/index.asp ].
National Academies of Sciences E, and Medicine. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies of Sciences E, and Medicine; 2018.
Download references
Acknowledgements
Not applicable.
This work was supported by the US Department of Veterans Affairs, Veterans Health Administration, Office of Emergency Management and the Office of Population Health. The views expressed in this presentation are those of the author and do not necessarily reflect the position or policy of the VA or the US government.
Author information
Authors and affiliations.
Department of Veterans Affairs, Veterans Emergency Management Evaluation Center (VEMEC), 16111 Plummer St. MS-152, North Hills, CA, 91343, USA
Tamar Wyte-Lake, Susan Schmitz & Aram Dobalian
Department of Family Medicine, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, Portland, OR, 97239, USA
Tamar Wyte-Lake
Orlando VA Medical Center, 13800 Veterans Way, Orlando, FL, 32728, USA
Reginald J. Kornegay
VA Southern Nevada Healthcare System, 6900 N. Pecos Road, North Las Vegas, NV, 89086, USA
Felix Acevedo
Division of Health Systems Management and Policy, University of Memphis School of Public Health, Memphis, TN, USA
Aram Dobalian
You can also search for this author in PubMed Google Scholar
Contributions
TWL and SS planned the study, including instrumentation, conducted the data analysis, and wrote the paper. RJK and FA supported the qualitative analysis and contributed to revising the paper. AD helped to plan the study and contributed to revising the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Tamar Wyte-Lake .
Ethics declarations
Ethics approval and consent to participate.
The Greater Los Angeles VA Healthcare System Institutional Review Board (Los Angeles, CA USA) approved this study. As the research presented no more than minimal risk of harm to subjects and involved no procedures for which written consent would be normally required outside of the research context, the study received a waiver for documentation of consent from the Institutional Review Board, and verbal, recorded audio consent was approved.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
2017 Disaster Qualitative Study: Collaboration Project Interview Guide. Interview guide utilized during project’s semi-structured interviews.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wyte-Lake, T., Schmitz, S., Kornegay, R.J. et al. Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters. BMC Public Health 21 , 639 (2021). https://doi.org/10.1186/s12889-021-10650-x
Download citation
Received : 05 August 2020
Accepted : 18 March 2021
Published : 01 April 2021
DOI : https://doi.org/10.1186/s12889-021-10650-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency preparedness
- Behavioral health; disaster response
- US Department of Veterans Affairs
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
OPINION article
Community case study article type: criteria for submission and peer review.

- 1 Department of Health Promotion and Behavior, College of Public Health, The University of Georgia, Athens, GA, USA
- 2 Department of Health Promotion and Community Health Sciences, Texas A&M Health Science Center School of Public Health, College Station, TX, USA
- 3 College of Social Work, University of South Carolina, Columbia, SC, USA
The Importance of Case Studies in Public Health Education and Promotion
Health programs and practices are often conceived and delivered by community-based practitioners to address specific community health education and promotion needs ( 1 ). Although, initially untested, such programs can provide important lessons for researchers and practitioners, alike. Given the growing emphasis on community-based participatory research (CBPR) approaches ( 2 ), it is especially important for researchers to build upon findings from CBPR studies, which can contribute to the development of evidence-based programs and practices for widespread dissemination ( 3 ).
While a community case study can take many forms ( 4 , 5 ), we are defining it as a description of, and reflection upon, a program or practice geared toward improving the health and functioning of a targeted population. We utilize the term “community” in contrast to “clinical” studies, but it is important to note that a community can be defined in terms of geographic boundaries as well as demographic characteristics, common settings, and/or affiliations.
Typically, a community case study documents a local experience about delivering services to meet an identified need. Community-based studies often rely on community engagement principles, which are not typically incorporated in the more traditional science-based approach to evidence-based program development (e.g., CBPR, action research, and community-engaged research). The community case study that documents early experiences can contribute to programmatic development as well as to the future development of evidence-based practice. This has been referred to as the “practice to science” approach to the development of evidence-based practices ( 6 ). The community case study can also represent activities at later development stages, for example, documenting the experience of implementing an evidence-based program or practice in a different context (e.g., different culture, different population, and different setting) from that in which it was first developed [“from science to practice” ( 6 )]. The lessons learned from such community case studies are essential for adaptation, replication, and eventual widespread dissemination and sustainability of innovations across a wide range of settings and populations.
Although case studies are a recognized form of research ( 5 ), the criteria for evaluating the quality of such efforts necessarily differs from empirical research articles where there is less attention to the local experience and context in which the intervention occurs, and more emphasis is given to the use of standardized research designs, measures, and analyses.
Key Components of a Community Case Study
Under this article type, Frontiers in Public Health Education and Promotion will accept a broad spectrum of manuscripts that describe interventions, including programs and services, which promote public health education, practice, research, and/or policy. Such public health interventions can be implemented at the behavioral, organizational, community, environmental, and/or policy level(s). Articles require a description of the nature of the problem being addressed and rationale for the proposed intervention, the context (setting and population) in which the intervention is being implemented, and sufficient detail to allow replication of key programmatic elements. Reflections about public health impact as well as what works and what does not work should be highlighted. Additionally, submissions will require a discussion section that shares practical implications, lessons learned for future applications, and acknowledgment of any conceptual or methodological constraints. Articles should not exceed 5,000 words and include a maximum of five tables/graphs. Evaluation criteria for this article type are outlined below:
We recommend that community case study article submissions address the following issues (if relevant).
□ What is the problem? Whom does it affect?
□ What are the gaps about what is known or done currently?
□ What is the setting? Who are the key stakeholders? Who is the target population or participants?
□ With whom did you work or collaborate? Are there any unique characteristics of the team who worked to implement the solution?
□ What is the solution described by this community case study?
□ Is this solution innovative/novel in terms of content, format, and/or delivery? If yes, why?
□ What are the essential elements of the solution? Could this community case study be replicated? Include sufficient detail that the reader would know if replication would be feasible in his/her own context.
□ What are the barriers and facilitators to the development, implementation, and/or dissemination of the intervention?
□ What are the major successes of the solution? What are the promising results to date? Include data and/or evaluation results, if available.
□ How does this improve public health education, practice, research, and/or policy? What are the broader implications of this work?
□ Recommendations for those who want to replicate this in other settings, populations, or over time.
Criteria for Review (Template for Review Editors to Complete for Each Manuscript)
Indicate what the community case study describes (check all that apply)
__an education effort
__a health promotion program
__a health promotion service
__an environmental change taking place in the community
__a technological change taking place in the community
__a policy change taking place in the community
__a community partnership
__others. Please specify: _____________________
__none of the above (i.e., inappropriately categorized for submission as a community case study article).
Indicate the target audience for the case study (check all that apply)
__educators
__community professionals
__health-care professionals
__lay public
__policy makers
__other. Please specify: _____________________
Mandatory Sections and Associated Criteria
A community case study article has the following mandatory sections: abstract, introduction, background and rationale, description of the case, methodological aspects (including targeted population and setting), discussion, and lessons learned/recommendations. Are all sections present?
• Is the abstract written in a clear and comprehensive way?
• Does the abstract reflect major conclusions articulated in the case study?
Introduction
• Does the introduction present the problem in an appropriate context?
• Other comments on introduction.
Background and Rationale
• Is the intent of the case study adequately described?
• Is a justification made for the innovation/novelty of proposed case in content, format, and/or delivery?
• Are the questions asked by the case study most essential to the success of the initiative?
• Other comments on background and rationale.
Essential Elements of the Intervention
• Is the intervention adequately described (e.g., development, previous findings if any, components, and format/design)?
• Is the intervention described in sufficient detail to understand the essential elements?
• Are the implementation procedures adequately described (e.g., how is the intervention being implemented in a particular setting, population, and/or partnerships; are any adaptations needed from prior work)?
• Are the target setting(s) and population(s) adequately described so that context for the case study is clearly understood?
• Is this a single community or multiple community study?
• Is there an overall conceptual model or framework for understanding the importance of the problem and selection of intervention elements?
• Is it clear whether the emphasis is on furthering knowledge about the process and/or outcome of the case study? If focus is on process, is there attention to key elements of implementation such as reach, reproducibility, scalability, or sustainability? If on outcomes, are the metrics of success (outcome indicators) clearly articulated?
• Is the generalizability of findings/lessons learned addressed?
• Other comments on methods.
• Are findings/lessons learned accurately reported from data presented?
• Is the level of detail of the results appropriate (too much, too little, or about right)?
• Is any essential information missing?
• Other comments on results.
• Are the reported findings/lessons learned summarized briefly and described within the context of what is currently known about the public health issue(s) or problem(s) being addressed?
• Does the article conclude with practical recommendations for others who might replicate this intervention/program (or similar interventions/programs)?
• Does the article conclude with applied recommendations for those in the field who might deliver this intervention/program (or similar interventions/programs) in their communities/settings?
• Does the case study contribute concrete recommendations for delivering and/or improving the intervention for future applications (directed toward educators, researchers, or practitioners, as appropriate)?
• Does the article address any conceptual or methodological limitations for future implementation, dissemination, and sustainability?
• Other comments on discussion.
• Are the conclusions justified?
• Overall, does the article contribute to building evidence-based practice and/or policy?
• Is prior work, if any, properly and fully cited?
Article Length
• A case study article should not exceed 5,000 words. Should any part of the article be shortened? If yes, please specify which part should be shortened.
• A case study article should not include more than five tables/figures. If there are more tables/figures included, please specify if you believe tables can be combined, condensed, or eliminated.
Language and Grammar
• Are the language and grammar correct?
• Should the paper be sent to an expert in English language and scientific writing?
Other Comments
• Please add any further comments you have regarding this manuscript.
Reviewer Ratings
• Significance of issue being addressed by the case study: scored out of a maximum of 10 points
• Description of essential elements of the case study: scored out of a maximum of 10 points
• Appropriateness of the context (population and setting) in addressing the public health issue/problem described in the case study: scored out of a maximum of 10 points
• Sufficient conceptual and methodological detail describing why and how the intervention was implemented: scored out of a maximum of 10 points
• Reflections on what worked and did not work in the design, implementation, and/or dissemination of the program: scored out of a maximum of 10 points
• Quality of the writing: scored out of a maximum of 10 points
• Quality of the figure(s) and table(s): scored out of a maximum of 10 points
• Significance of the findings/lessons learned: scored out of a maximum of 10 points
• Could this intervention be replicated by other educators, researchers, or practitioners?
Author Contributions
All authors were integral in formulating and drafting the manuscript and associated criteria.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Ory MG, Smith MLS, Howell D, Zollinger A, Quinn C, Swierc S, et al. The conversion of a practice-based lifestyle enhancement program into a formalized, testable program: from texercise classic to texercise select. Front Public Health (2015) 2 :291. doi: 10.3389/fpubh.2014.00291
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health: From Process to Outcomes . John Wiley & Sons (2011).
Google Scholar
3. Ory MG, Smith ML. Research, practice, and policy perspectives on evidence-based programing for older adults. Front Public Health (2015) 3 :136. doi:10.3389/fpubh.2015.00136
CrossRef Full Text | Google Scholar
4. Soy SK. The Case Study as a Research Method. Unpublished Paper . Austin: University of Texas (1997).
5. Yin RK. Case Study Research: Design and Methods . Thousand Oaks, CA: Sage publications (2013).
6. Chen H, Levkoff S, Kleinman A. Contextual knowledge: from global aging to globalization. Can J Sociol (2014) 39 (2):141–58.
Keywords: case study, review criteria, article type, intervention, evaluation criteria
Citation: Smith ML, Levkoff SE and Ory MG (2016) Community Case Study Article Type: Criteria for Submission and Peer Review. Front. Public Health 4:56. doi: 10.3389/fpubh.2016.00056
Received: 06 November 2015; Accepted: 14 March 2016; Published: 14 April 2016
Reviewed by:
Copyright: © 2016 Smith, Levkoff and Ory. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthew Lee Smith, health@uga.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

This supplement is sponsored by the American Academy of Family Physicians. The project has been made possible with funding from Bristol Myers Squibb.
BRIAN FORREST, MD, CASEY WILLIAMS, MD, MARSHA BROUSSARD, DrPH, MPH, TIFFANY HILL, MD, WHITNEY KIRKMAN, PBT-ASCP, MA, AND RAJANI BHARATI, PhD, MPH
Fam Pract Manag. 2023;30(2):29-34
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity in the United States. 1 Approximately one in five deaths is due to CVD, and the United States spends around $229 billion each year on CVD-related care and productivity losses. 2 Though the mortality rate due to CVD is decreasing, racial disparities in outcomes have persisted, mainly driven by the complex interplay of social determinants of health (SDoH) and structural racism. 3 , 4
Beginning in March 2021, the American Academy of Family Physicians (AAFP) implemented a two-year project to address cardiovascular disparities in African American communities, with a focus on atrial fibrillation (AFib). The project utilized a clinic-community partnership model within which family physicians and their health care teams explored the needs of their communities and leveraged the resulting information to foster innovative ideas and work with community partners to reduce cardiovascular disparities.
Three family medicine practices participated in the project:
Access Healthcare, a direct primary care (DPC) clinic in Apex, North Carolina
DePaul Community Health Centers (DCHC), a federally qualified health center (FQHC) network in New Orleans, Louisiana
Trenton Medical Center dba Palms Medical Group, an FQHC in Trenton, Florida
A physician expert and the Prevention Institute trained the participating family physicians and their care teams on topics such as AFib detection and management; disparities in cardiovascular care and outcomes; SDoH and health equity; and community engagement. Applying insights from this training, each practice used patient surveys and in-depth interviews to assess their community's needs. They also conducted environmental scans to identify existing community resources (e.g., community needs assessment reports, community health improvement plans) and possible public health partners. An action planning workshop was held in collaboration with the University of Kansas to help practices develop interventions based on their assessment findings. The practices subsequently implemented these interventions. The AAFP assisted with the institutional review board (IRB) application, design of data collection instruments, and data analysis.
The project was completed in February 2023. While the full impact of this project has not yet been evaluated, the following case studies describe each participating practice's experiences and what they learned on their unique journey from needs assessment to interventions.
CASE STUDY 1:
Access healthcare, brian forrest, md, and whitney kirkman, pbt-ascp, ma.
Access Healthcare is a DPC safety-net practice, and 40% of our patients are uninsured. Between April and May of 2022, we surveyed 58 patients and conducted in-depth interviews with three patients. It was challenging to get people to complete a patient survey and even more challenging to engage them in lengthy interviews, but it was heartening to get positive feedback about our practice. Through the assessment, we learned that our patients' biggest concern about getting cardiovascular care was out-of-pocket costs for labs, visits, and medication. During interviews, our patients also described the bias they experienced in other health care settings. Learning about ways that discrimination, bias, and lack of food and transportation resources impacted patients' access to care changed our perspective.
We also conducted interviews with local community leaders from the African Methodist Episcopal (AME) Church, the North Carolina Medical Society, and an Alliance for Health Equity Grant organization, as well as with insurance company executives and hospital system CEOs. These interviews focused on finding out how we could more effectively improve health equity and decrease disparities. Fixing a problem starts with innovation, so the ideas generated for this project were aimed at improving in three focus areas.
Improve the structural determinants of health, such as inequities in power or status: For this focus area, we reimagined and redirected health care media content, such as Access Health Radio, a live AM/FM radio show and podcast focused on cardiovascular topics. To improve health literacy through education, we made this programming available through more accessible platforms. We also convened community-driven educational sessions to increase health literacy and awareness of CVD. For example, we partnered with AME Church leaders to broadcast live question-and-answer sessions on CVD that were available to the public across our state. Additionally, we identified and addressed patients' barriers to accessing transportation, food, and exercise resources by creating a set of standardized screening questions for use during check-in at our practice.
Advocate for policies across all settings that advance greater health equity: These policies were aimed at increasing awareness and education regarding SDoH and inequities in our community, as well as addressing these issues. We worked with policymakers at the North Carolina Leadership Forum to identify solutions to alleviate inequities, with a focus on food deserts, transportation problems, barriers to access to expanded Medicaid and insurance options, and caps on Supplemental Nutrition Assistance Program (SNAP) benefits for healthy food options. We also advocated for resources to support community-driven transportation solutions, such as free public transportation or rideshare vouchers.
Target service disparities and inequities in health care access and quality: We started by routinely assessing the affordability of medications and follow-up care and intervening when necessary, and we applied Plan-Do-Study-Act (PDSA) quality improvement cycles to see what impact we were having. One of our ideas was partnering with a national mail-order pharmacy to create a program that offers a $30 monthly cap on all generic medication shipped at no cost to our patients. This program is now available nationwide for practices that want to participate. We also created a $35 subscription plan in the DPC model 5 , 6 for patients with AFib and CVD. All coagulation testing and visits and consultations with an in-house clinical practicing pharmacist (PharmD) were made available at no additional charge for medical optimization. We also advocated for lower costs and improved access and quality for all patients, and we continue to look for ways to accomplish these goals.
Through this project, we learned the importance of meeting people where they are rather than where we expect them to be. We also learned that the process of working with community leaders and bridging ideological gaps was more productive than we expected. New legislation, policies, and grant programs are likely to improve CVD disparities. We are now developing a systematic program to assess discrimination bias in health care facilities and reduce it through peer-to-peer coaching and PDSA initiatives that are being funded jointly by Bristol Myers Squibb and Pfizer. We hope to create a self-sustaining nonprofit to offer these assessments and interventions to practices willing to embrace the challenge.
CASE STUDY 2:
Depaul community health centers, casey williams, md, and marsha broussard, drph, mph.
DePaul Community Health Centers is an FQHC network with ten locations in the New Orleans metropolitan area that serve ten distinct communities. With an enrollment of over 50,000 patients, DCHC provides a comprehensive range of services for all ages, including prevention and primary health care, prenatal and pediatric care, dental and optometry care, and mental and behavioral health care. We also administer the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) for families with food insecurity. DCHC serves some of the city's most vulnerable patients, including a majority African American population that experiences disparities in CVD treatment and outcomes. With its focus on reducing AFib health disparities, this project gave DCHC the opportunity to obtain feedback from our affected population and work with colleagues across the country to explore innovations in primary prevention.
Our project began with a community needs assessment that was conducted at one of the DCHC locations and included three components:
A survey of patients experiencing cardiovascular health issues: The primary objective of the survey was to obtain feedback from our cardiovascular patients regarding the quality of care at DCHC, barriers to accessing care, and concerns regarding their medications. The survey also collected demographic information (e.g., income, education, employment) to inform our analysis.
Interviews of patients with cardiovascular health issues: A DCHC physician conducted these interviews with his patients to delve deeper into cultural and environmental factors that influence patients' health conditions.
Interviews of community organizations with a mission to address the need for healthy food and promote physical activity: Two of the project coordinators conducted interviews with seven community agencies to create understanding, promote alignment, and identify local resources available to help DCHC patients improve their cardiovascular health.
The survey showed that our patients' primary concerns in getting cardiovascular care were appointment scheduling issues and out-of-pocket costs for labs/visits, medication, and transportation. The interview findings were very interesting because patients in different age groups had varied perspectives. For instance, patients in their 40s were concerned with the interventions necessary to improve health and prolong longevity. They wanted improvements in neighborhood walkability and access to local parks for exercise. Patients in their 60s had concerns related to navigating the health care system. In particular, they noted that insurance determines what options are available for medical devices (e.g., hearing aids), and there can be drastic differences in the quality of these options. Patients in this age group were also concerned about how the expansion of medical facilities would affect the character of their neighborhood. They wondered how these facilities would benefit the area's long-term residents before and after establishing their presence and whether interventions would be implemented equitably. Patients in their 80s expressed concern about their neighborhood's changing demographics and the impacts of gentrification. Specifically, they mentioned that the types of vendors and options available locally had changed over time, as well as citing increased food prices and a lack of places to park.
Based on our assessments of needs and feasibility, we offered a series of three educational sessions to provide information on the prevention of AFib, which has some modifiable risk factors. We offered information on AFib risk factors, epidemiology, symptoms, and prevention. To support lifestyle interventions, we engaged with several community organizations: the American Heart Association for educational resources; New Orleans Recreation Development Commission for access to exercise facilities; and Sankofa Community Development Corporation for healthy food options, such as fresh produce. Based on the individual patient's determination of their concerns and needs, we provided contact information so they could pursue the opportunities these community resources offered to optimize heart health. We faced some timing and location challenges when executing our educational events. In consideration of accessibility and patients' schedules, we offered the sessions at the end of the day at our clinic facility. However, the topics and concerns covered could have been more conveniently addressed via a virtual health meeting. In the future, we may implement this change in how we deliver and design our outreach programs for CVD prevention.
We plan to provide more information about the medication assistance we offer and to do more outreach with our health coach program and chronic care management (CCM) team. Steps we have taken to identify patients who may benefit from our health coaches and CCM program include identifying SDoH and overutilization of emergency department services. To sustain our model for the practice, we plan to have sessions that recur monthly/quarterly to reinforce and remind our population about the importance of AFib prevention and the availability of existing community resources.
CASE STUDY 3:
Trenton medical center dba palms medical group, tiffany hill, md.
Palms Medical Group is an FQHC with 12 locations throughout northeast Florida, including Trenton Medical Center, which is located on the outskirts of Jacksonville, Florida. The center provides a full range of medical services to patients with commercial and public insurance and to patients who are uninsured. When this project began, the medical group had a partnership with Orange Park Family Medicine Residency Program, and I had dual responsibility as both a clinician at Trenton Medical Center and faculty for the residency program. My interest in participating in this project stemmed from my desire for both academic development and attainment of a more tangible approach to addressing the community's medical needs.
Assessment of our African American patients' perception of health care was obtained via qualitative measures (i.e., in-depth interviews) and quantitative measures (i.e., survey accessed via QR code) during April and May of 2022. Although the patient survey had a low response rate, we obtained comprehensive perspective through our in-depth patient interviews. As an FQHC, we can provide affordable medications to our uninsured patients through the 340B Drug Pricing Program. But despite measures in place to help them overcome financial obstacles, an overwhelming number of surveyed patients reported that out-of-pocket cost of medication was one of their primary concerns about getting cardiovascular-related care. Additionally, almost 40% of the surveyed patients stated that concern about adverse effects was a barrier to taking medications. The qualitative data revealed that our African American patients want to focus on mitigating CVD through a healthy diet and physical activity and showed how structural determinants (e.g., community context, living or working conditions) affect their ability to adopt a healthy lifestyle.
In-person interviews offered a useful perspective on the large impact relationships can have on health care. Patients were more inclined to participate and engage with physicians they trusted. Numerous patients repeated the themes of community and education. Motivated by altruism, they wanted to empower other African American individuals. Specifically, they expressed the importance of instilling awareness of early CVD detection and preventive care. For example, one patient with a history of CVD explained their impetus for participating in the interview by saying, “I want to help someone know what to look for before something like that happens, so they don't have to go through what I have.” Additionally, the interviewees emphasized the significance of family history, advocacy, and accountability.
Unfortunately, our momentum came to a halt when the relationship between Orange Park Family Medicine Residency Program and Palms Medical Group dissolved, but the project was transitioned to the residency program. To expand our outreach to the African American community, we have partnered with a new free clinic that provides sexually transmitted infection (STI) testing in the inner city of Jacksonville. We will provide screenings for risk factors of CVD, hypertension, diabetes, and hyperlipidemia. Patients will be connected with an insurance broker to help them obtain affordable insurance.
Partnering with local food banks and urban farms will help us facilitate lifestyle changes that can reduce cardiovascular risk. Additionally, we will identify patients whose passion for health and community engagement aligns with ours, and they will serve as liaisons by providing outreach via community events and social media. We hope this will improve trust and intracommunity education. Further education on CVD will occur through small groups conducted by family medicine residents. The residency program has implemented a lifestyle medicine residency curriculum that gives residents the necessary tools for educating and guiding patients.
We did encounter some challenges in strategizing and finding ways to create more community engagement. Development of partnerships and solutions that would create a sustainable construct to address the community's needs did not align with my clinic's goals. Despite my personal passion for this project's focus, organizational buyin was lacking. However, the formation of a new partnership allowed me to achieve project aims.
KEY TAKEAWAYS
Make an impact on improving health equity by reducing barriers created by SDoH.
Identify your community's needs and explore community resources in your area. Counties often already have community needs assessment reports and community health improvement plans.
Connect with patients and listen to their input. It can be an enlightening experience.
Form community partnerships or engage in existing community coalitions to link your patients with resources.
Meet members of your community where they are. It is not productive to provide information and patient education via formats or platforms that your patients do not use or see.
Offer information in a variety of ways (e.g., audiovisual content, paper packets, internet links, text messages) to improve access and maintain awareness.
Be mindful of patient concerns about access and expense. Modify management based on need, if necessary.
Establish organizational goals that align with a commitment to building sustainable relationships within the community.
Be innovative and customize solutions that meet the needs of your community and practice. You can improve the care you provide and your patients' outcomes by improving health literacy, increasing access to affordable care and medications, and advocating locally for policy solutions to help ameliorate the impacts of SDoH. Keep in mind that the same solutions may not work in all locations.
CDC – Office of Minority Health & Health Equity (OMHHE)
This project has been made possible with funding from Bristol Myers Squibb. | © 2023 American Academy of Family Physicians. All rights reserved.
HOP22121387
Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation . 2021;143(8):e254-e743.
Center for Disease Control and Prevention. Heart disease facts. October 14, 2022. Accessed November 18, 2022. https://www.cdc.gov/heartdisease/facts.htm
Mazimba S, Peterson PN. JAHA spotlight on racial and ethnic disparities in cardiovascular disease. J Am Heart Assoc . 2021;10(17):e023650.
Singh GK, Siahpush M, Azuine RE, et al. Widening socioeconomic and racial disparities in cardiovascular disease mortality in the United States, 1969–2013. Int J MCH AIDS . 2015;3(2):106-118.
Sprey E. New practice models are gaining acceptance in primary care. Physicians Practice. August 20, 2014. Accessed December 13, 2022. https://www.physicianspractice.com/view/new-practice-models-are-gaining-acceptance-primary-care
Forrest B. New primary-care models can change the way you practice medicine. Physicians Practice. December 7, 2011. Accessed December 13, 2022. https://www.physicianspractice.com/view/new-primary-care-models-can-change-way-you-practice-medicine
Continue Reading
More in FPM
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

Case Study: Johns Hopkins Community Health Partnership: A model for transformation
Collaborators.
- J-CHiP Program : Eric B Bass , William Baumgartner , Michele Bellantoni , Scott A Berkowitz , Romsai Tony Boonyasai , Daniel Brotman , Patricia Brown , Amy Deutschendorf , Linda Dunbar , Samuel C Durso , Anita Everett , Michael Fingerhood , Kevin Frick , Peter Greene , Lindsay Hebert , David Hellmann , Debra Hickman , Douglas E Hough , Eric Howell , Xuan Huang , Chidinma Ibe , Sarah Kachur , Anne Langley , Diane Lepley , Curtis Leung , Constantine Lyketsos , Yanyan Lu , Shannon Murphy , Mary Myers , Tracy Novak , Kymberlee Olson , Leon Purnell , Stephanie Reel , Judy Reitz , Melissa Richardson , Regina Richardson , Mike Rogers , Paul Rothman , Carol Sylvester , Martha Sylvia , Albert W Wu , Hunter Young , Roy Ziegelstein , Ray Zollinger
Affiliations
- 1 Johns Hopkins University School of Medicine, United States. Electronic address: [email protected].
- 2 Johns Hopkins Healthcare, United States.
- 3 Johns Hopkins University School of Medicine, United States.
- 4 Johns Hopkins Health System, United States.
- 5 Sisters Together and Reaching, United States.
- 6 Men and Families Center, United States.
- 7 Johns Hopkins Community Physicians, United States.
- PMID: 27693204
- DOI: 10.1016/j.hjdsi.2016.09.001
To address the challenging health care needs of the population served by an urban academic medical center, we developed the Johns Hopkins Community Health Partnership (J-CHiP), a novel care coordination program that provides services in homes, community clinics, acute care hospitals, emergency departments, and skilled nursing facilities. This case study describes a comprehensive program that includes: a community-based intervention using multidisciplinary care teams that work closely with the patient's primary care provider; an acute care intervention bundle with collaborative team-based care; and a skilled nursing facility intervention emphasizing standardized transitions and targeted use of care pathways. The program seeks to improve clinical care within and across settings, to address the non-clinical determinants of health, and to ultimately improve healthcare utilization and costs. The case study introduces: a) main program features including rationale, goals, intervention design, and partnership development; b) illness burden and social barriers of the population contributing to care challenges and opportunities; and c) lessons learned with steps that have been taken to engage both patients and providers more actively in the care model. Urban health systems, including academic medical centers, must continue to innovate in care delivery through programs like J-CHiP to meet the needs of their patients and communities.
Copyright © 2016 Elsevier Inc. All rights reserved.
- Academic Medical Centers*
- Community Health Planning*
- Community Health Services
- Cooperative Behavior*
- Delivery of Health Care / economics
- Delivery of Health Care / organization & administration*
- Hospitals, Urban
- Middle Aged
- Organizational Case Studies*
- Patient-Centered Care
- Primary Health Care
- Urban Health Services
Community Engagement in Health-Related Research: A Case Study of a Community-Linked Research Infrastructure, Jefferson County, Arkansas, 2011–2013
COMMUNITY CASE STUDY — Volume 12 — July 23, 2015
M. Kathryn Stewart, MD, MPH; Holly C. Felix, PhD, MPA; Mary Olson, DMin; Naomi Cottoms, MA; Ashley Bachelder, MPH, MPS; Johnny Smith; Tanesha Ford, MA; Leah C. Dawson, MS; Paul G. Greene, PhD
Suggested citation for this article: Stewart MK, Felix HC, Olson M, Cottoms N, Bachelder A, Smith J, et al. Community Engagement in Health-Related Research: A Case Study of a Community-Linked Research Infrastructure, Jefferson County, Arkansas, 2011–2013. Prev Chronic Dis 2015;12:140564. DOI: http://dx.doi.org/10.5888/pcd12.140564 external icon .
PEER REVIEWED
Community Context
Interpretation, acknowledgments, author information.
Underrepresentation of racial minorities in research contributes to health inequities. Important factors contributing to low levels of research participation include limited access to health care and research opportunities, lack of perceived relevance, power differences, participant burden, and absence of trust. We describe an enhanced model of community engagement in which we developed a community-linked research infrastructure to involve minorities in research both as participants and as partners engaged in issue selection, study design, and implementation.
We implemented this effort in Jefferson County, Arkansas, which has a predominantly black population, bears a disproportionate burden of chronic disease, and has death rates above state and national averages.
Building on existing community–academic partnerships, we engaged new partners and adapted a successful community health worker model to connect community residents to services and relevant research. We formed a community advisory board, a research collaborative, a health registry, and a resource directory.
Newly formed community–academic partnerships resulted in many joint grant submissions and new projects. Community health workers contacted 2,665 black and 913 white community residents from December 2011 through April 2013. Eighty-five percent of blacks and 88% of whites were willing to be re-contacted about research of potential interest. Implementation challenges were addressed by balancing the needs of science with community needs and priorities.
Our experience indicates investments in community-linked research infrastructure can be fruitful and should be considered by academic health centers when assessing institutional research infrastructure needs.
Racial disparities in health and health care quality are well documented (1). An important barrier to addressing such disparities is low levels of research participation among those groups that experience disparities in illness and death rates (2). This imbalance in research creates challenges in understanding and developing strategies to address the causes of disparities (3). Multiple factors have been identified as affecting minority participation in research, including lack of trust, power differences, limited access to health care and research opportunities, participant burden, and lack of perceived relevance (2–6). Community engagement has been identified as a way to address these factors. True engagement of underrepresented communities is facilitated by intentional structural supports such as establishing community advisory boards, developing financial and other resources, involving minority researchers, hiring community health workers, sharing resources with community partners, and using community-based participatory research approaches (7–9). We describe an enhanced model of community engagement in which we developed a community-linked research infrastructure to involve minorities in research both as participants and as partners engaged in issue selection, study design, and implementation.
This community-linked research infrastructure (infrastructure) was implemented in Jefferson County, Arkansas, which has a predominantly black population (55.6%), bears a disproportionate burden of chronic illness, and has disease and death rates exceeding state and national averages ( Table 1 ).
The infrastructure, funded from 2010 through 2013 by the National Institute on Minority Health and Health Disparities, deployed intentional structural supports identified in the literature as facilitating true community engagement (7,8). An existing long-term community–academic partnership between the Fay W. Boozman College of Public Health (the College), University of Arkansas for Medical Sciences (UAMS), and Tri-County Rural Health Network (Tri-County) developed the grant proposal to build community infrastructure for engaging minorities in research. As such, all infrastructure activities focused on this overall community engagement goal rather than on engagement in a specific program to address a particular health issue.
Intentional structural supports designed for the infrastructure consisted of an implementation team; a community advisory board to advise on infrastructure activities; the Community Health and Research Connector Program (connector program) staffed by local community health workers, called “connectors,” to address cultural, social, and community factors affecting access to and use of health-related resources (eg, social services, medical care, research opportunities); a health registry to provide the community advisory board with input from a large segment of the community regarding health needs and use of health-related resources; a resource directory to facilitate community access to health-related resources; and a research collaborative to solicit ideas on research priorities from community organizations. Tri-County conducted community forums to engage communities in dialogue about research relevant to health disparities. Forums and community advisory board meetings identified concerns about disparities in chronic disease, lack of health resources, and sociocultural barriers to health care and health care use that defined the focus of the infrastructure. The Figure illustrates the contributions the implementation team made to develop and deliver the main components of the infrastructure and the associated outcomes that the components were conceptualized to affect. The UAMS institutional review board reviewed all infrastructure activities and determined that the service activities of the connector program did not constitute research.
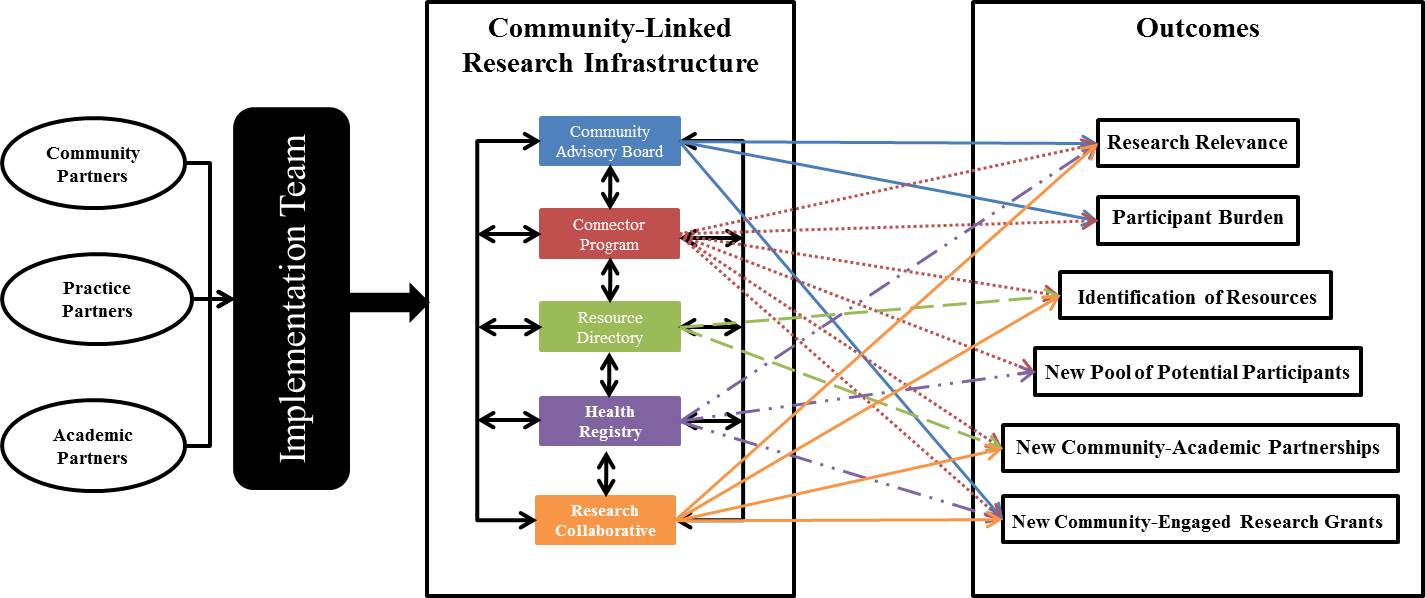
Figure. Conceptual framework of the infrastructure. [A text version of this figure is also available.]
The figure presents a conceptual framework to depict 1) the composition of the implementation team, 2) components of the infrastructure, and 3) which outcomes each component was to contribute to and influence. The figure shows these 3 sections, respectively, from left to right with arrows between each. Section 1 shows 3 circles labelled Community Partners, Practice Partners, and Academic Partners with an adjoining line and arrow that points to a box labeled Implementation Team. The Implementation Team box connects to Section 2. Section 2 is titled Community-Linked Research Infrastructure and lists the following infrastructure components, each in a different box, in a vertical line. From top to bottom they read: Community Advisory Board, Connector Program, Resource Directory, Health Registry, and Research Collaborative. Each component is connected by 2-sided arrows that draw a line between all the components to illustrate their interconnectedness and to signify that they all function at the same time. Each component also has 2 to 5 matching 1-sided arrows that point to the right to various outcomes listed in Section 3. Community Advisory Board arrows connect to Research Relevance, Participant Burden, and New Community-Engaged Research Grants. Connector Program arrows connect to Research Relevance, Participant Burden, Identification of Resources, New Pool of Potential Participants, New Community–Academic Partnerships, and New Community-Engaged Research Grants. Resource Directory arrows connect to Identification of Resources and New Community–Academic Partnerships. Health Registry arrows connect to Research Relevance, New Pool of Potential Participants, and New Community-Engaged Research Grants. Research Collaborative arrows connect to Research Relevance, Identification of Resources, New Community–Academic Partnerships, and New Community-Engaged Research Grants. Section 3 is titled Outcomes and lists the following outcomes in boxes in a vertical line. From top to bottom they read: Research Relevance, Participant Burden, Identification of Resources, New Pool of Potential Participants, New Community–Academic Partnerships, and New Community-Engaged Research Grants. The arrows in Section 2 indicate an influence and association with the infrastructure components.
The objectives of the infrastructure were to hire and train local community health workers, contact at least 1,200 community residents, document residents’ health concerns and conditions, assess residents’ interest in health-related service programs and research projects, link residents to health-related resources, and facilitate minority community–academic research partnerships. We report on challenges addressed and short-term successes in designing and deploying this community engagement infrastructure.
Intentional structural supports
Implementation team. The implementation team of grassroots, academic, and health practice community members included representatives from Tri-County, Shiloh Baptist Church, the College, and the UAMS South Central Regional Program in Jefferson County (South Central) ( Table 2 ). In addition to managing overall efforts, the team facilitated community-partnered research by introducing community partners to noninfrastructure researchers with expertise related to health issues prioritized by the community and by soliciting interest from researchers with expertise in responding to community concerns.
Community advisory board. The 8-member community advisory board was established to integrate the voice of the grassroots community into infrastructure design and implementation. Community partners on the implementation team invited selected community residents and representatives of community organizations with personal experience and knowledge of health and social issues in Jefferson County to serve on the community advisory board. Advisory board members received training on community-based participatory research and health disparities before being asked to sign a memorandum of understanding outlining their commitment to the infrastructure and the benefits of participation. Members were paid an honorarium to recognize their contributions in quarterly meetings.
Community Health and Research Connector Program. The connector program was designed as a public service provided by connectors to directly engage community residents and facilitate their access to and use of health-related resources, including both services and research opportunities. This program was adapted from another community health worker program, called the Community Connector Program, which successfully promoted use of community-based long-term care services as a cost-effective alternative to institutional care (12).
The connector program aimed to serve 1,200 minority and low-income community residents. Research participation was not required for assistance from connectors. Connectors were responsible for administering the registry questionnaire to document health needs and research interests, sustaining contact with community residents to develop trust and bi-directional interaction, facilitating connections to needed resources, providing follow-up, establishing liaisons with referral sites, entering data into an electronic database, and conducting quality control procedures to maintain data integrity.
Black residents of Jefferson County were hired as connectors. Tri-County employed the connectors rather than UAMS because employment by a community organization was seen as representing community interests and built trust with community residents. This strategy allowed us to allocate salary support for connectors to the Tri-County subcontract consistent with efforts to build financial support for community organizations and jobs to strengthen the local economy.
Community and academic partners shared responsibility for training the connectors. Tri-County assumed primary responsibility for training on civic rights and responsibilities, leadership, interpersonal communication, first impressions, understanding and processes for reaching the community, cultural and linguistic competence, safety, needs assessments, conducting forums, and developing resource directories. Researchers from the College took the lead in training on community-based participatory research and health disparities and on data collection, data entry, and quality control. Connectors also became certified in Human Subjects Protection in Research through the Office for Human Research Protections of the US Department of Health and Human Services and the Health Insurance Portability and Accountability Act (HIPAA).
Connectors engaged community members by helping them access community services: primary and specialty care, prescription assistance, and post-hospitalization follow-up; financial support for utilities, food, and housing; and assistance with re-entry into society from prison. Connectors primarily made contact with community members through regular visits to offices of health and social services, churches, community events, and through formal referral agreements with specific providers. For example, the connector program had an agreement with South Central to allow connectors to staff a desk in the clinic’s waiting room, providing community members with direct access to connector services. In this context of service, connectors collected community members’ contact and basic demographic information, invited them to complete the registry health questionnaire, and elicited community interest in research by asking community members whether they would be willing to be contacted about research opportunities.
Health registry. A health registry was designed to collect contact information, to monitor the health needs and interests of people served by the Connector program, to provide the community advisory board with community input regarding health status and use of health-related resources, and to monitor the connector program. Connectors collected data using both paper and electronic records. Forums and community advisory board meetings initially identified a broad scope of issues for potential inclusion in the registry health questionnaire. Academic partners selected items from validated instruments to assess these issues. Community partners reviewed proposed items and helped select those that best captured community concerns while minimizing participant burden. These items were incorporated into a draft presented to the community advisory board in a discussion of survey research methods followed by a group cognitive interviewing exercise. After input from connectors and the implementation team, the community advisory board’s feedback was incorporated into a revised version, which included 119 closed-ended items and 1 open-ended question about health concerns ( Table 3 ).
Resource directory. The resource directory developed by the connectors contained information about health and social services and research opportunities. Connectors developed relationships with the staff of organizations providing services and documented information in the directory to which they referred when linking community residents to needed services.
Research collaborative. We formed the research collaborative to facilitate communication, resource development, and community-engaged research. Tri-County’s executive director and South Central’s administrator co-chaired the collaborative. Other members represented the regional hospital, the local public health unit, Blue Cross Blue Shield of Arkansas, the Arkansas Department of Corrections, Shiloh Baptist Church, and the College.
New community–academic research partnerships
The implementation team was successful in engaging minority community representatives as partners in research. The College’s researchers made introductions and invited noninfrastructure researchers to team meetings and community advisory board meetings in the community, and Tri-County followed up to explore collaborative opportunities. Eighteen researchers assisted by the infrastructure were sent a brief survey by email to assess their experiences. All reported positive interactions with the infrastructure. They had varying levels of engagement ranging from assistance in grant planning to implementation of community-engaged research. Researchers also reported how they had benefited from networking facilitated by the infrastructure and from Tri-County staff or the community advisory board chair and how connectors assisted in recruiting volunteers for their studies. Researchers reported that infrastructure community partners consulted with them about their ongoing or potential future community-engaged research projects, contributed to the development of funding proposals, and served as community co-investigators on funded grants. Connectors also served on numerous community advisory boards for researchers.
As of August 2014, the infrastructure facilitated submission of 23 grants involving more than 100 community partners and collaborating organizations and 46 researchers from 9 academic institutions. One example that included minority community partners and minority researchers introduced through the infrastructure focused on measuring trust. Other studies growing out of new partnerships involved the faith community’s work on mental health (16,17). Other research topics in grants submitted were substance abuse, social networks, sexual violence, pesticide exposure, and health literacy.
Community advisory board
The community advisory board played an active role in establishing the infrastructure’s focus on facilitating research addressing health disparities, creating the registry questionnaire, and testing use of an electronic audience response system for group administration of the questionnaire to community residents. Community advisory board members reviewed aggregated registry data to assist with data interpretation, clarify needed services, identify research issues for further study, and express concerns about risks to participants or the community.
Some community advisory board members had severe health problems that sometimes affected their level of engagement. The connector program was a critical component, because connectors often helped them meet their needs. In one case, clinicians on the implementation team and community advisory board helped a member access badly needed surgical care.
Community Health and Research Connector Program
The opportunity to link residents to services was fulfilling for those employed as connectors. However, salary support based on grant funding and an emphasis on defined procedures for data collection created challenges in retaining qualified connectors. We learned we needed to hire connectors who understood the value of research and had a strong commitment to the infrastructure. For example, one connector had had a very positive research experience herself, which enabled her to explain on a personal level why research participation is important.
The regulatory training was a challenge for some connectors who had little or no previous experience with online training. Connectors who completed the training without difficulty served as role models and tutors.
Connectors exceeded service goals by serving 2,665 black and 913 white community residents from December 2011 through April 2013. Among these residents, 85% of blacks and 88% of whites were willing to be contacted again about research that might be of interest to them.
Health registry
Barriers to completing the health questionnaire were tensions between community concerns about survey length and wording of standardized items and researchers’ interest in covering common causes of disease and death and using validated questions for comparison purposes. These tensions were addressed by facilitating community advisory board and connector input in the design phase, incorporating community-generated questions, and allowing connectors the flexibility of collecting only contact information and ascertaining community residents’ willingness to be re-contacted with or without the shorter questionnaire sections on health concerns and medical history.
Resource directory
Connectors were successful in developing relationships with referral agencies potentially able to provide residents with needed resources. Resources with the potential to influence interest in and access to preventive health care and research were assistance with rent and utility bills and enrollment in Medicaid and pharmacy assistance programs.
Transportation between Jefferson County and Little Rock, where more clinical studies are conducted, was a barrier to research participation, and although we engaged many investigators in community research partnerships, we were less successful in finding clinical studies focused on diseases of interest to community residents (eg, lupus).
Research collaborative
Research collaborative members met regularly to discuss organizational issues and concerns related to health disparities. For example, representatives from the Arkansas Department of Corrections described high rates of pregnancy among newly released female inmates, which led to collaborative efforts between the Arkansas Department of Corrections, the Jefferson County health unit of the Arkansas Department of Health, the South Central Clinic, and the connectors to facilitate access to family planning services in the community before release. In addition, regional hospital representatives discussed concerns about avoidable hospital readmissions and the possibility of a study to test use of connectors to help reduce readmissions. Toward that aim, connectors and hospital administrators established HIPAA-compliant procedures to refer patients to connectors as a routine component of hospital discharge to facilitate connector assistance.
This article describes a community engagement effort to increase involvement of minorities as research partners and to identify minorities in the community interested in learning about opportunities to participate in research. By implementing intentional structural supports (ie, community–academic partnerships, community advisory board, community health worker model, health registry, resource directory, research collaborative), we were able to engage the broader community in research and successfully reach populations with disproportionate health burdens. UAMS investigators, including black, white, and other minority researchers, have engaged with community organizations, and black community residents now serve as community co-investigators on new studies focused on issues of importance to the community (16,17). The adaptation of the Community Connector Program (12), the integration of institutional providers’ assistance with referrals and connections, and the community engagement approach of the infrastructure created a context in which access was increased and minorities were engaged who often are not represented in research.
Our work is instructive in the context of the efforts of others to increase minority research engagement. Chadiha et al have also reported the use of community-based participatory research, including a community advisory board, to build a research volunteer registry of senior urban blacks (18). They were able to enroll 1,273 volunteers in the registry over 7 years by recruiting at events sponsored by the health research center. At least 9 researchers successfully used their registry to recruit study participants over 5 years. In comparison, the infrastructure was able to engage a larger population of potential research participants in a shorter period, perhaps because it was more community-driven, hired local connectors through a community organization instead of relying on volunteers, and targeted both community organizations and individual residents for engagement.
The connectors were able to engage and provide information to a predominantly minority population often underrepresented in research, which encouraged the population’s interest in learning about research opportunities. Eighty-five percent of blacks and 88% of whites were willing to be contacted again about research that might be of interest to them. This finding is consistent with the review conducted by Wendler et al of 20 studies reporting consent rates by race or ethnicity. That review found few differences between blacks and whites in their willingness to participate in research and suggested that access is a greater barrier than attitudes (6).
A survey of community health worker programs in 2011 found that three-fourths of respondents were involving community health workers in research activities; 39% of respondents reported involvement of community health workers in research recruitment (19). A more recent multisite study conducted by Cottler and colleagues at 7 Clinical and Translational Science Award (CTSA) Sentinel Network sites found blacks were more willing than other racial groups to participate in research, even when it required obtaining blood samples (20). That study, like the infrastructure, hired community health workers to engage residents directly, and the authors concluded that the workers were crucial to research success. The community health workers were hired by the institutional members of the CTSA Sentinel Network and focused on direct engagement of potential participants rather than building partnerships with the organizations by which they are served to be sure they did not “bypass the input of community members or inadvertently privilege the perceptions of community leaders and service providers” (20). Although this approach may be effective in recruiting people for clinical trials and avoiding censoring and interpretation of community residents’ research interests by organizational gatekeepers, engagement at both individual and organizational levels allowed the infrastructure to facilitate development of new community–academic partnered studies and programs and engage minority investigators in community-engaged research while also identifying individual-level interest in research.
Although both the infrastructure and the Sentinel Network successfully engaged minorities in research through the work of community health workers, sustainability of interventions employing community health workers has traditionally been a challenge. Research infrastructure funding, such as CTSA resources or research center grants, is potentially an ideal source of support for community health workers. Although the grant period that supported the development of the infrastructure is complete, Tri-County managed to continue support for some of their connectors through grants on which they are partners. New organizational partnerships facilitated through the infrastructure will likely continue well into the future. We believe our experience with the infrastructure indicates that investments in community-based research infrastructure should be considered by academic health centers when assessing institutional research infrastructure needs.
The authors thank the connectors, the members of the research collaborative and of the community advisory board, and the technical support of the registry received from the UAMS Translational Research Institute’s Comprehensive Informatics Resource Center. We also express our appreciation to Dr Robert Price, Assistant Director of Regional Programs for Research, for his support as our practice partner in the infrastructure. This work was supported by NIH grant no. A1-37154-01, NIH CTSA grant no. 8UL1TR000039, and Arkansas Prevention Research Center, Center for Disease Control and Prevention Grant no. U48 DP001943.
Corresponding Author: M. Kathryn Stewart, MD, MPH, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, 4301 West Markham St, Slot 820, Little Rock, AR 72205. Telephone: 501-526-6625. Email: [email protected] .
Author Affiliations: Holly C. Felix, Ashley Bachelder, Leah C. Dawson, Paul G. Greene, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, Little Rock, Arkansas; Mary Olson, Naomi Cottoms, Tri County Rural Health Network, Inc, Helena, Arkansas; Johnny Smith, Shiloh Baptist Church and Ten Thousand Black Men, Pine Bluff, Arkansas; Tanesha Ford, University of Arkansas at Pine Bluff, Pine Bluff, Arkansas.
- Agency for Healthcare Research and Quality. 2013 National Healthcare Disparities Report. Rockville (MD): US Department of Health and Human Services; 2014. AHRQ Publication No. 12-0006. http://www.ahrq.gov/research/findings/nhqrdr/nhdr13/2013nhdr.pdf. Accessed November 26, 2014.
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health 2006;27:1–28. CrossRef external icon PubMed external icon
- Branson RD, Davis K Jr, Butler KL. African Americans’ participation in clinical research: importance, barriers, and solutions. Am J Surg 2007;193(1):32–9; discussion 40. CrossRef external icon PubMed external icon
- Braunstein JB, Sherber NS, Schulman SP, Ding EL, Powe NR. Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine (Baltimore) 2008;87(1):1–9. CrossRef external icon PubMed external icon
- Russell KM, Maraj MS, Wilson LR, Shedd-Steele R, Champion VL. Barriers to recruiting urban African American women into research studies in community settings. Appl Nurs Res 2008;21(2):90–7. CrossRef external icon PubMed external icon
- Wendler D, Kington R, Madans J, Van Wye G, Christ-Schmidt H, Pratt LA, et al. Are racial and ethnic minorities less willing to participate in health research? PLoS Med 2006;3(2):e19. CrossRef external icon PubMed external icon
- Terpstra J, Coleman KJ, Simon G, Nebeker C. The role of community health workers (CHWs) in health promotion research: ethical challenges and practical solutions. Health Promot Pract 2011;12(1):86–93. CrossRef external icon PubMed external icon
- Minkler M, Wallerstein N, editors. Community-based participatory research for health: from process to outcomes. 2nd edition. San Francisco (CA): Jossey-Bass; 2008.
- Shalowitz MU, Isacco A, Barquin N, Clark-Kauffman E, Delger P, Nelson D, et al. Community-based participatory research: a review of the literature with strategies for community engagement. J Dev Behav Pediatr 2009;30(4):350–61. CrossRef external icon PubMed external icon
- US Census Bureau. American Community Survey; 2013. http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. Accessed February 23, 2015.
- Centers for Disease Control and Prevention, National Center for Health Statistics. CDC WONDER: about underlying cause of death 1999–2013. http://wonder.cdc.gov/ucd-icd10.html. Accessed February 23, 2015.
- Felix HC, Mays GP, Stewart MK, Cottoms N, Olson M. The care span: Medicaid savings resulted when community health workers matched those with needs to home and community care. Health Aff (Millwood) 2011;30(7):1366–74. CrossRef external icon PubMed external icon
- Stewart MK, Felix HC, Cottoms N, Olson M, Shelby B, Huff A, et al. Capacity building for long-term community-academic health partnership outcomes. Int Public Health J 2013;5(1):115–28. PubMed external icon
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System, 2012. http://www.cdc.gov/brfss/. Accessed June 16, 2015.
- National Cancer Institute. Health Information National Trends Survey. http://hints.cancer.gov/. Accessed June 16, 2015.
- Sullivan G, Hunt J, Haynes TF, Bryant K, Cheney AM, Pyne JM, et al. Building partnerships with rural Arkansas faith communities to promote veterans’ mental health: lessons learned. Prog Community Health Partnersh 2014;8(1):11–9. CrossRef external icon PubMed external icon
- Yeary K, Bryant K, Haynes T, Turner J, Smith J, Kuo D, et al. Community exchange of “best practices” to conduct a multi-level, mixed methods health assessment across two counties: Faith-Academic Initiative for Transforming Health (FAITH) in the Delta. Proceedings of the 2014 Annual Meeting of the American Public Health Association, New Orleans, Louisiana, November 15–19, 2014.
- Chadiha LA, Washington OGM, Lichtenberg PA, Green CR, Daniels KL, Jackson JS. Building a registry of research volunteers among older urban African Americans: recruitment processes and outcomes from a community-based partnership. Gerontologist 2011;51(Suppl 1):S106–15. CrossRef external icon PubMed external icon
- Felix HC, Lee D, Stewart MK, Greene PG. Engagement of community health workers in the research enterprise: a survey of organizations and the research roles given CHWs. Journal of Community Engagement and Higher Education 2013;5(1):13–23.
- Cottler LB, McCloskey DJ, Aguilar-Gaxiola S, Bennett NM, Strelnick H, Dwyer-White M, et al. Community needs, concerns, and perceptions about health research: findings from the clinical and translational science award sentinel network. Am J Public Health 2013;103(9):1685–92. CrossRef external icon PubMed external icon
Table 1. Sociodemographic Characteristics and Selected Health Indicators, Jefferson County, Arkansas, Arkansas State, and United States
Table 2. implementation team, case study of a community-linked research infrastructure, jefferson county, arkansas, december 2011–april 2013, table 3. health registry questionnaire, case study of a community-linked research infrastructure, jefferson county, arkansas, december 2011–april 2013.
Abbreviation: BRFSS, Behavioral Risk Factor Surveillance System.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Urban Greening as a Response to Societal Challenges. Toward Biophilic Megacities (Case Studies of Saint Petersburg and Moscow, Russia)
- First Online: 17 March 2023
Cite this chapter
- Diana Dushkova 8 ,
- Maria Ignatieva 9 &
- Irina Melnichuk 10
Part of the book series: Cities and Nature ((CITIES))
680 Accesses
The population density in megacities is continuously increasing, resulting in a reduction of green spaces and a deterioration in the urban environment quality. Urban green is often being replaced by parking places, shopping centers, and service enterprises. This chapter examines the efforts of two megacities in Russia—Moscow and Saint Petersburg—to organize sustainable greening solutions for their residential areas using new achievements in landscape design theory and practice, such as the concept of the biophilic city. The chapter analyzes the history of greening strategies and discusses the concept of urban green infrastructure and its implementation in both Russian megacities. The chapter presents an assessment of the current state of urban green spaces and the most recent master plans and how these cities are facing and responding to modern societal challenges. The results of an analytical review of the most successful urban greening projects in Moscow and Saint Petersburg are presented as well. The economic and climatic features of the urban green areas and their architectural and planning features are considered, along with strategies for further development of the urban green spaces in both cities, aiming to address the new principles of biophilic cities.
- Urban green spaces
- Greening strategies
- Biophilic cities
- Societal challenges
- Saint Petersburg
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Aleksandrova S (2013) Sustainability principles for St. Petersburg landscape with Scandinavian experience in mind: application of Swedish green space research result of “the eight characteristics”. Master’s thesis, 30 hec, Advanced level, A2E Landscape Architecture—master’s programme, Alnarp
Google Scholar
Archive Buro of Moscow (2018) Holiday of liberated labor: the first subbotniks in the capital. https://www.mos.ru/news/item/9998073/ . Accessed 10 Jan 2019
Archive Committee of Saint Petersburg (2019) Archive Committee of Saint Petersburg. https://spbarchives.ru/ . Accessed 10 Jan 2019
Beatley T (2010) Biophilic Cities: Integrating Nature into Urban Design and Planning. Island Press, Washington, DC
BioDAT (2005) Moscow—the Lotten capital of the XXI century. http://biodat.ru/db/birds/sol2005.htm . Accessed 10 Jan 2019
Breuste JH, Qureshi S, Xue F (2015) Urban ecosystems: functions, services and sustainable management. Ecocity Green Build 42–52
Bunin AV (1953) Istoriya gradostroitelnogo iskusstva (History of urban planning). Gosudarstvennoje Izdatel’stvo Literatury po stroitel’stvu i Arhitekture. Moscow (in Russian)
Bunin AV, Ilyin LA, Polyakov NH, Shkarikov VA (1945) Gradostroitel’stvo (Urban planning). Izda-tel’stvo Akademii Arhitektury SSSR, Mosow (in Russian)
DEMP – Department for Environmental Management and Protection (2018) Norms and rules for the design of objects of non-traditional types of gardening in the city of Moscow (un-published). Available at: http://www.dpioos.ru/eco/ru/activity/n_160/o_13279 . Accessed 20 Oct 2018
Dushkova D, Krasovskaya T (2018) Post-Soviet single-industry cities in northern Russia: movement towards sustainable development. A case study of Kirovsk. Belgeo (on-line). Revue Belge De Géographie 4:1–25. https://doi.org/10.4000/belgeo.27427
Article Google Scholar
Dushkova D, Haase D, Haase A (2016) Urban green space in transition: historical parks and Soviet heritage in Arkhangelsk, Russia. Crit Housing Anal 3(2):61–70. https://doi.org/10.13060/23362839.2016.3.2.300
Federal Russian Government (1995) Federal Law of Russia No. 33 “On specially protected natural territories” from 14.03.1995. www.oopt.info . Accessed 21 Dec 2018 (in Russian)
Genplan Moskvy (Masterplan Moscow) (1935) O generalnom plane rekonstrukcii Moskvy (About the general plan for the reconstruction of Moscow). Partizdat, Moscow (in Russian)
Goretskaya A (2017) Toporina V (2017) The ecological framework of the city. Three pillars of landscape architecture: design, planning and management. New visions. In: Ignatieva M, Melnichuk I (eds) Conference proceedings. Saint-Petersburg State Polytechnic University, Polytechnic University Publishing House, Saint-Petersburg, pp 23–24
Haase D (2017) Urban ecosystem, their services and town planning. Crit Reflecti Sel Shortcomings. URBANISTICA 159:90–94
Haase D, Dushkova D, Haase A, Kronenberg J (in press) Green infrastructure in post-socialist cities: evidence and experiences from Russia, Poland and Eastern Germany. In: Tuvikene T, Sgibnev W, Neugebauer CS (eds) Post-socialist urban infrastructures. Taylor & Francis/Routledge, UK
Ignatieva M (1997) The mystery of ancient Russian gardens. Lustgarden. J Swedish Soc Dendrol Park Cult 69–78
Ignatieva M (2010) Design and future of urban biodiversity. In: Müller N, Werner P, Kelcey J (eds) Urban biodiversity and design. Wiley-Blackwell, Oxford, pp 118–144
Chapter Google Scholar
Ignatieva M (2013) Historic gardens—where nature meets culture—can be urban biodiversity hotspots. The nature of cities. https://www.thenatureofcities.com/2013/01/27/historic-gardens-where-nature-meets-culture-can-be-urban-biodiversity-hotspots/ . Accessed 22 Oct 2018
Ignatieva M, Ahrné K (2013) Biodiverse green infrastructure for the 21st century: from “green desert” of lawns to biophilic cities. J Archit Urban 37(1):1–9
Ignatieva M, Konechnaya G, Stewart G (2011a) St. Petersburg. In: Kelcey J, Müller N (eds) Plants Habitats Eur Cities. Springer Science & Business Media, pp 407–452
Ignatieva M, Stewart GH, Meurk C (2011b) Planning and design of ecological networks in urban areas. Landscape Ecol Eng 7:17–25
Ignatieva M, Murray R, Waldenström H (2015) Can large parks be urban green saviors? The nature of cities. https://www.thenatureofcities.com/2015/12/03/can-large-parks-be-urban-green-saviors/ . Accessed 28 Oct 2018
Ignatieva M, Golosova E, Melnichuk I, Smertin V (2018) Development of biophilic cities in Russia: from ideal scientific town and Ecopolis to the green strategy of the modern mega-polis. In: IFLA World Congress Singapore proceedings, Singapore, 2018. http://www.ifla2018.com/eproceedings
Kabisch N, Korn H, Stadler J, Bonn A (2017) Nature-based solutions to climate change adaptation in urban areas. Springer International Publishing, Cham. https://doi.org/10.1007/978-3-319-56091-5
Kartinki24.ru (2019) Vasily Polenov. Moscow courtyard. http://www.kartinki24.ru/kartinki/art/16906-vasiliy-polenov-moskovskiy-dvorik.html . Accessed 10 Jan 2019
Khodakov Y (1986) Gorodskoje Ozelenenije (The urban greenery). Lenisdat, Leningrad (in Russian)
Klimanova OA, Kolbovsky EY (2013) Protected areas in the system of territorial planning and functional zoning of the Moscow city. Regional Geoecol Issues 177–180 (in Russian)
Kochurov BI, Ivashkina IV (2015) Urban Landscapes of Moscow and their spatial transformation. Ecol Urban Areas 2:48–54
Korzhev MP (ed) (1954) Ozelenenije sovetskih gorodov: Posobie po Projektirovaniju (Greening of Soviet cities: Green projects Manual). Gosudarstvennoje Isdatelstvo literaturi po stroitelstvu i architecture, Moscow (in Russian)
Melnichuk I (2017) St. Petersburg green infrastructure and methods of its formation. In: Igna-tieva M, Melnichuk I (eds) Three pillars of landscape architecture: design, planning and management. New visions. Conference proceedings, Saint-Petersburg State Polytechnic University, 2017. Polytechnic University Publishing House, Saint-Petersburg, pp 105–112
Minin AA (2014) Sustainable development and ecosystem services of natural areas of Moscow. Bulletin Towards Sustain Devel Russia 69:2–9
Moscow city council (1999, with modifications of 2014) Moscow law on the protection of green areas. http://docs.cntd.ru/document/901734936 . Accessed 21 Dec 2018 (in Russian)
Mosecomonitoring (2017) The state reports of department of environmental management and environmental protection of Moscow for 2016. Mosecomonitoring, Moscow. http://mosecom.ru/reports/2014/report2014.pdf . Accessed 28 Oct 2018 (in Russian)
Mosgorstat Moscow (2018) Moscow city committee of statistics by Russian Federal State statistics service. About demographic, economic and social situation in Moscow in 2018. http://moscow.gks.ru/wps/wcm/connect/rosstat_ts/moscow/ru/statistics/population/ . Accessed 26 Oct 2018 (in Russian)
Müller N, Werner P (2010) Urban biodiversity and the case for implementing the convention on biological diversity in towns and cities. In: Müller N, Werner P, Kelcey (eds) Urban biodiversity and design. Blackwell Publishing, pp 1–33. https://doi.org/10.1002/9781444318654.ch1
Nilsson K, Åkerlund U, Konijnendijk van den Bosch C, Alekseev A, Caspersen O, Guldager S, Kuznetsov E, Mezenko A, Selikhovkin A (2007) Implementing urban greening aid projects—the case of St. Petersburg Russia. Urban for Urban Green 6:93–101. https://doi.org/10.1016/j.ufug.2007.01.004
Pauleit S, Olafsson AS, Rall E, van der Jagt A, Ambrose-Oji B, Andersson E, Anton B, Buijs A, Haase D, Elands B, Hansen R, Kowarik I, Kronenberg J, Mattijssen T (2018) Urban green infrastructure in Europe—status quo, innovation and perspectives. Urban for urban green. Rosstat 2017. Federal State statistics service. Russia 2016—Statistical pocketbook, Moscow
Petrostat (2018) Department of Federal State Statistics Service of St. Petersburg and Leningrad region. About demographic, economic and social situation in Saint Petersburg in 2018. http://petrostat.gks.ru/wps/wcm/connect/rosstat_ts/petrostat/ru/statistics/Sant_Petersburg/ . Accessed 26 Oct 2018 (in Russian)
Research and Project Institute of Moscow City Master plan (2018) Research and Project Institute of Moscow City Master plan. https://genplanmos.ru . Accessed 10 Jan 2019
Seto K, Reenberg A (eds) (2014) Rethinking global land use in an urban era. Struengmann forum reports, vol 14. Julia Lupp, series editor, MIT Press, Cambridge, MA
Shumilova OV (2016) Methods of St. Petersburg Green Infrastructure formation. St. Petersburg State Forest Techical University, St. Petersburg (in Russian)
St. Petersburg city council (2004, with modifications of 2010) St. Petersburg law on the protection of green areas. http://pravo.gov.ru/proxy/ . Accessed 05 Jan 2019 (in Russian)
State Research and design center of Saint Petersburg Masterplan (2018) State Research and design center of Saint Petersburg Masterplan. http://www.gugenplan.spb.ru . Accessed 10 Jan 2019
Totalarch (2019) Regular gardens of Peter's time. Regular style evolution and later baroque mid-18th century. http://landscape.totalarch.com/russian_gardens/baroque . Accessed 10 Jan 2019
Vasenev I, Dovletyarova E, Chen Z, Valentini R (2017) Megacities 2050: Environmental con-sequences of urbanization. In: Proceedings of the VI international conference on landscape architecture to support city sustainable development. Springer International Publishing. https://doi.org/10.1007/978-3-319-70557-6
Weiner DR (2002) A little corner of freedom: Russian nature protection from Stalin to Gorbachev. University of California Press
WHO—World Health Organisation (2017) Urban green space interventions and health: a review of impacts and effectiveness. Full report. WHO Regional Office for Europe, Copenhagen. http://www.euro.who.int/__data/assets/pdf_file/0010/337690/FULL-REPORT-for-LLP.pdf?ua=1 . Accessed 20 Dec 2018
Yanitsky O, Usacheva O (2017) History of the “Green City” in Russia. J Culture Art Res 6(6):125–131. https://doi.org/10.7596/taksad.v6i6.1330
Zemvopros.ru (2019) The master plan of St. Petersburg 2015–2025. Functional area map. https://www.zemvopros.ru/genplan.php . Accessed 10 Jan 2019
Download references
Acknowledgements
This work was supported by the Russian Foundation for Basic Research (RFBR) project “Mathematical-cartographic assessment of medico-ecological situation in cities of European Russia for their integrated ecological characteristics” (2018–2020) under Grant number No 18-05-406 00236/18 and by the Horizon 2020 Framework Program of the European Union project “Connecting Nature” under Grant Agreement No 730222.
Author information
Authors and affiliations.
Department Urban and Environmental Sociology, Helmholtz Centre for Environmental Research - UFZ, Permoserstraße 15, Leipzig, 04318, Germany
Diana Dushkova
School of Design, University of Western Australia, Stirling Highway 35, Perth, 6001, Australia
Maria Ignatieva
Faculty of Landscape Architecture, Saint Petersburg State Forest Technical University, Institutskij pereulok 5, St.-Petersburg, 194021, Russia
Irina Melnichuk
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Diana Dushkova .
Editor information
Editors and affiliations.
Department of Geography and Geology, University of Salzburg, Salzburg, Austria
Jürgen Breuste
Landscape Change and Management, Leibniz Institute of Ecological Urban and Regional Development, Dresden, Sachsen, Germany
Martina Artmann
Center for Environmental Research and Impact Studies, University of Bucharest, Bucharest, Romania
Cristian Ioja
Department of Geography (Landscape Ecology), Humboldt University of Berlin, Berlin, Germany
Salman Qureshi
Rights and permissions
Reprints and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Dushkova, D., Ignatieva, M., Melnichuk, I. (2023). Urban Greening as a Response to Societal Challenges. Toward Biophilic Megacities (Case Studies of Saint Petersburg and Moscow, Russia). In: Breuste, J., Artmann, M., Ioja, C., Qureshi, S. (eds) Making Green Cities. Cities and Nature. Springer, Cham. https://doi.org/10.1007/978-3-030-73089-5_25
Download citation
DOI : https://doi.org/10.1007/978-3-030-73089-5_25
Published : 17 March 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-73088-8
Online ISBN : 978-3-030-73089-5
eBook Packages : Earth and Environmental Science Earth and Environmental Science (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
https://www.nist.gov/baldrige/2017-arroyo-fresco-community-health-center-case-study
Baldrige Performance Excellence Program
2017 arroyo fresco community health center case study.

2017 Arroyo Fresco Community Health Center Case Study Part One PDF (Covers, Contents, Eligibility Certification Form, Organization Chart, Page A-1 Award Application Form, Glossary, Organization Profile) Part Two PDF (Responses Addressing Criteria Categories 1-6 Items) Part Three PDF (Responses Addressing Criteria Category 7 Results Items) 2017 Arroyo Fresco Community Health Center Feedback Report PDF Baldrige Excellence Framework (Health Care)
Case study resources illustrate the Baldrige Award application and evaluation process. These resources include
- a case study, which is a sample Baldrige Award application showing a fictitious organization's responses to the requirements of the Baldrige Excellence Framework
- a feedback report modeled on the report received by actual Baldrige Award applicants; this feedback report is based on the scorebook produced by a team of Baldrige examiners who evaluated the fictitious application against the Criteria
Case studies show you the format and general content of a Baldrige Award application. However, because the primary purpose of the case study is to provide learning opportunities for Baldrige examiners and others, the case study purposely does not address all Criteria requirements or demonstrate role-model responses in all areas. See the case study scorebook and feedback report to learn how the fictitious organization scored and to see its strengths and opportunities for improvement.
The 2017 Baldrige case study depicts a nonprofit, community health center serving western Arizona from 11 clinics and 4 mobile service vans. Created by volunteer Baldrige alumni examiners Kay Kendall, Joe Muzikowski, and Glenn Bodinson, the fictitious Arroyo Fresco was written to represent community health centers, which were established over the past 50 years in underserved areas in all 50 states. (The case study was reviewed by Baldrige alumni examiners Beth Katzenberg and Steve Bonk.) Fast-growing communities along the U.S.-Mexican border, as well as Native American and retiree populations, are represented in the case study. Barriers to care include lower levels of prevention screening, less efficient and effective detection and management of chronic disease, large incidences of diabetes and diabetes-related mortality, and other chronic health problems, such as asthma, cardiovascular disease, depression, obesity, and substance abuse and other addictive behavior. To address these, Arroyo Fresco has developed core competencies in providing culturally competent, patient-centered care; expertise in the treatment of diseases prevalent within its patient population; and collaborative relationships that increase access to specialty care and other services. “Enabling services” the organization provides its patients include transportation, translation, health education, and home visitation. Arroyo Fresco Community Health Center uses the Baldrige Excellence Framework to guide its strategy, leadership and management systems, knowledge management system, and performance improvement.
The Arroyo Fresco Case Study is based on the 2017–2018 Baldrige Excellence Framework (Health Care) .
Baldrige Materials Archive (Previous Case Study Packets) Applying for the Award
- Baldrige Customer Service [email protected] (301) 975-2036 NIST/BPEP 100 Bureau Drive, M/S 1020 Gaithersburg, MD 20899-1020
This paper is in the following e-collection/theme issue:
Published on 1.4.2024 in Vol 10 (2024)
Using Project Extension for Community Healthcare Outcomes to Enhance Substance Use Disorder Care in Primary Care: Mixed Methods Study
Authors of this article:

Original Paper
- MacKenzie Koester, MPH ;
- Rosemary Motz, MPH, MA, RDN ;
- Ariel Porto, MPH ;
- Nikita Reyes Nieves, MPH ;
- Karen Ashley, EdD
Weitzman Institute, Moses Weitzman Health System, Washington, DC, United States
Corresponding Author:
MacKenzie Koester, MPH
Weitzman Institute
Moses Weitzman Health System
1575 I Street Northwest
Washington, DC, 20005
United States
Phone: 1 8603476971
Email: [email protected]
Background: Substance use and overdose deaths make up a substantial portion of injury-related deaths in the United States, with the state of Ohio leading the nation in rates of diagnosed substance use disorder (SUD). Ohio’s growing epidemic has indicated a need to improve SUD care in a primary care setting through the engagement of multidisciplinary providers and the use of a comprehensive approach to care.
Objective: The purpose of this study was to assess the ability of the Weitzman Extension for Community Healthcare Outcomes (ECHO): Comprehensive Substance Use Disorder Care program to both address and meet 7 series learning objectives and address substances by analyzing (1) the frequency of exposure to the learning objective topics and substance types during case discussions and (2) participants’ change in knowledge, self-efficacy, attitudes, and skills related to the treatment of SUDs pre- to postseries. The 7 series learning objective themes included harm reduction, team-based care, behavioral techniques, medication-assisted treatment, trauma-informed care, co-occurring conditions, and social determinants of health.
Methods: We used a mixed methods approach using a conceptual content analysis based on series learning objectives and substances and a 2-tailed paired-samples t test of participants’ self-reported learner outcomes. The content analysis gauged the frequency and dose of learning objective themes and illicit and nonillicit substances mentioned in participant case presentations and discussions, and the paired-samples t test compared participants’ knowledge, self-efficacy, attitudes, and skills associated with learning objectives and medication management of substances from pre- to postseries.
Results: The results of the content analysis indicated that 3 learning objective themes—team-based care, harm reduction, and social determinants of health—resulted in the highest frequencies and dose, appearing in 100% (n=22) of case presentations and discussions. Alcohol had the highest frequency and dose among the illicit and nonillicit substances, appearing in 81% (n=18) of case presentations and discussions. The results of the paired-samples t test indicated statistically significant increases in knowledge domain statements related to polysubstance use ( P =.02), understanding the approach other disciplines use in SUD care ( P =.02), and medication management strategies for nicotine ( P =.03) and opioid use disorder ( P =.003). Statistically significant increases were observed for 2 self-efficacy domain statements regarding medication management for nicotine ( P =.002) and alcohol use disorder ( P =.02). Further, 1 statistically significant increase in the skill domain was observed regarding using the stages of change theory in interventions ( P =.03).
Conclusions: These findings indicate that the ECHO program’s content aligned with its stated learning objectives; met its learning objectives for the 3 themes where significant improvements were measured; and met its intent to address multiple substances in case presentations and discussions. These results demonstrate that Project ECHO is a potential tool to educate multidisciplinary providers in a comprehensive approach to SUD care.
Introduction
In the United States, overdose deaths continue to be a major cause of injury-related deaths. Since the onset of the COVID-19 pandemic, numbers have only accelerated, and the state of Ohio has led the nation in high substance use disorder (SUD) rates, including drug use and prescription drug use. The Centers for Disease Control and Prevention ranks the state among the top 5 across the United States with the highest rates of opioid overdose deaths [ 1 ]. While research has shown an increase in the number of people enrolled in substance use treatment in Ohio between 2015 and 2019 there was still a notable high increase in the annual average prevalence of past-year illicit drug use disorder in Ohio (3.6%) compared to the regional average (3%) and the national average (2.9%) [ 2 ]. In addition, past-month alcohol use disorder (9.3%), cannabis use disorder (5.8%), and tobacco use disorder (35.2%) were higher than the national average among young adults aged 18-25 years [ 2 ]. Ohio’s growing epidemic has highlighted the need to improve SUD care in a primary care setting by training providers to better address differences in care and social determinants of health through the use of behavioral techniques, harm-reduction philosophy of care, medication management, and a team-based care approach.
Weitzman Extension for Community Healthcare Outcomes: Comprehensive Substance Use Disorder Care Program
Beginning in 2021, Buckeye Health Plan and Ohio University Heritage College of Osteopathic Medicine have partnered with the Weitzman Institute (WI), a national primary care research, policy, and education institute, to provide targeted support and education to Ohio primary care medical and behavioral health providers working with underserved patients, especially those in the rural, southeastern Appalachian region, using the evidence-based Project Extension for Community Healthcare Outcomes (ECHO) learning model. Project ECHO uses frequent videoconference sessions to connect a target audience of learners with subject matter experts for didactic and case-based instruction and engaged discussion [ 3 ]. Through regular attendance at these sessions, Project ECHO aims to equip learners with the knowledge, confidence, and skills to better manage complex cases.
WI has over 11 years of experience in developing and delivering Project ECHO programs to meet the needs of providers working in resource-limited settings. As an early adopter of the model in 2012, Weitzman ECHO programs have been offered in 22 topic areas to over 8000 health care professionals across all 50 states, Washington D.C., and Puerto Rico. Working in collaboration, Buckeye Health Plan and Ohio University aimed to leverage this expertise and offer multiple Project ECHO programs each year for providers in topics of the greatest need and interest.
As described, one of Ohio’s most dire population health needs is to improve outcomes for patients experiencing addiction. Thus, SUD was selected as the second ECHO program developed through this partnership. More specifically, opioids are a heightened concern throughout both Ohio and the United States, and the opioid epidemic has spurred significant funding allocations, such as the Biden Administration’s US $1.5 billion award to states and territories to end the epidemic [ 4 ]. However, there are many additional substances of concern, both illicit and nonillicit, such as alcohol, tobacco, cannabis, methamphetamine, and cocaine [ 5 ], which may receive less attention given the directed funding for opioids. For this reason, it was decided that the ECHO would address not only opioids, or any one substance, but rather be designed to provide techniques to help providers address SUD overall through a comprehensive, team-based lens and a harm reduction philosophy of care. Reflecting this broad topical approach, the program was titled the Weitzman ECHO: Comprehensive Substance Use Disorder Care (CSUDC ECHO) program.
CSUDC ECHO consisted of 24 twice-monthly sessions held between July 2021 and July 2022. Each 1-hour session included a 20- to 25-minute didactic presentation followed by 1 patient case submitted by a participant before the session and discussed live for the remaining 35-40 minutes. Textbox 1 outlines the didactic presentation topics for each session. A multidisciplinary core faculty facilitated each session and was comprised of 1 physician with dual board certification in family medicine and addiction medicine and experienced in treating SUDs at federally qualified health centers; 1 nurse practitioner who developed and leads a federally qualified health center medication-assisted treatment (MAT) program; 1 supervisory licensed counselor; and 1 population health expert. Together, the faculty built a 12-month curriculum covering diverse topics such as medication management, team-based care, trauma-informed care, stages of change and motivational interviewing, polysubstance use and co-occurring conditions, and coordinating levels of care.
Session and didactic topic
- Philosophy of care (no case presentation).
- Harm reduction strategies.
- Principals of medication management.
- Team-based care: care provision partners.
- Trauma-informed care: an overview.
- Motivational interviewing.
- Stages of change for addiction.
- Assessing stages of change and stage-based interventions.
- Medications for opioid use disorder basics.
- Behavioral health and primary care coordination.
- Transitions of care.
- Polysubstance use.
- Social determinants of health including barriers or challenges (no case presentation).
- Adverse childhood experiences.
- Legal factors and access.
- Mental health crisis and coordination of care.
- Medication-assisted treatment for alcohol and tobacco use disorders.
- Self-determination and strength-based approaches.
- Contingency management for substance use disorder.
- HIV and hepatitis C virus in patients with substance use disorder.
- Screening, brief intervention and referral to treatment into primary care.
- Stimulant use disorder treatment and medication management.
- Co-occurring mental health substance use disorder.
- Tobacco cessation for polysubstance patients.
Participants were recruited by email blasts targeted to each partner’s network of Ohio primary care providers and other members of the care team. A total of 109 participants attended at least one session, 16 participants attended between 7 and 11 sessions, and 23 participants attended over 12 (half) of the sessions. On average, there were 32 attendees at each session. Continuing education credits were offered to medical providers, behavioral health providers, and nurses.
Purpose of Study
The purpose of this study was to assess the ability of CSUDC ECHO to both address and meet 7 learning objectives ( Textbox 2 ) and address multiple substances by analyzing (1) the frequency of exposure to the learning objective topics and substance types during case discussions and (2) participants’ knowledge, self-efficacy, skills, and attitudes related to the treatment of SUDs pre- to postprogram.
- Project a harm reduction philosophy of care into your treatment of patients experiencing substance use disorders and explain this concept to peers.
- Use the care team more effectively to improve the management of patients experiencing substance use disorders.
- Use motivational interviewing and other behavioral techniques to improve patient outcomes related to substance use disorders.
- Better differentiate and implement medication management strategies for patients experiencing substance use disorders.
- Illustrate trauma-informed practices in the screening, assessment, and treatment of patients experiencing substance use disorders.
- Describe and manage common co-occurring conditions and polysubstance use more effectively in patients experiencing substance use disorders.
- Distinguish and address factors related to social determinants of health faced by specific populations experiencing substance use disorders.
Study Design and Data Collection
This study used a mixed methods design, using a conceptual content analysis [ 6 ] analyzing ECHO participant-led case presentations, as well as a 2-tailed paired-samples t test of participant self-reported learner outcomes. All ECHO attendees who registered and attended the Project ECHO CSUDC sessions are included in the deductive content analysis. All ECHO attendees who registered before and through the first session of the series were invited to complete a preseries survey (n=106) via Qualtrics survey software (Qualtrics). The preseries survey remained open for 3 weeks from June 25, 2021, to July 18, 2021. A total of 79 responses were received (n=79) for a response rate of 75%. Upon completion of the ECHO series, active attendees (ie, those that were still active at the conclusion of the series and did not officially drop from the series, as well as those who enrolled throughout the series) were invited to complete a postseries survey via Qualtrics Survey Software (n=90). The postseries survey remained open for 4 weeks from July 7, 2022, to August 2, 2022. A total of 25 responses were received (n=25) for a response rate of 28%. A total of 16 consented participants completed both the preseries and postseries surveys (n=16) and are included in the paired-samples t tests statistical analysis.
Ethical Considerations
This study was approved by the Community Health Center, Inc, Institutional Review Board (IRB; 1190) on January 6, 2022. Informed consent was accounted for by the authors through the administration of a consent form on the postseries survey gathering participant consent to use their deidentified survey data for the paired-samples t test analysis. The deductive content analysis was considered a secondary analysis and was given exempt status. All data used in this study were deidentified, accounting for privacy and confidentially. No compensation for participation in this study was deemed necessary by the IRB.
Survey Tools
The preseries and postseries surveys were internally created and based on the Consolidated Framework for Implementation Research (CFIR) [ 7 ] and Moore’s Model of Outcomes Assessment Framework [ 8 ]. The specific CFIR domains assessed for include intervention characteristics, outer setting, inner setting, characteristics of individuals, and process [ 7 ]. Additionally, the levels of Moore’s Model of Outcomes Assessment Framework assessed for include level 2 (satisfaction), level 3a (declarative knowledge), level 3b (procedural knowledge), level 4 (competence), level 5 (performance), and level 6 (patient health) [ 8 ]. The surveys assessed changes in participants’ self-reported knowledge, attitudes, self-efficacy, and skills through statements centered on the series’ learning objectives. The preseries survey also collected participant characteristics including provider type and years of experience working with patients diagnosed with SUDs, as well as team-based care practices. Additionally, the postseries survey collected information on engagement and practice changes. The preseries survey instrument is presented in Multimedia Appendix 1 and the postseries survey instrument is presented in Multimedia Appendix 2 .
While the preseries survey and postseries survey tools were based on CFIR [ 7 ] and Moore’s Model of Outcomes Assessment Framework [ 8 ], both surveys were internally designed. The internal research and evaluation and CSUDC ECHO programmatic teams created the survey tools through several iterations of the internal review, which also consisted of selecting the appropriate domain (ie, knowledge, attitudes, self-efficacy, and skills) to assess each series’ learning objective. Each domain used a 5-point Likert scale to assess responses. The surveys were then presented to the CSUDC ECHO series stakeholders and faculty for review and approval before administering the surveys to the ECHO attendees. See Multimedia Appendices 1 and 2 for the domain placement of learning objectives and the 5-point Likert scales.
Conceptual Content Analysis
To further evaluate Weitzman ECHO CSUDC aims, researchers conducted a conceptual content analysis [ 6 ] using a set of a priori themes extracted from the series’ learning objectives. Series’ learning objectives are detailed in Textbox 2 . To establish a priori themes, researchers met before the launch of the ECHO to examine the series’ 7 learning objectives and extracted 7 themes for the content analysis. The themes were: harm reduction, team-based care, behavioral techniques, MAT, trauma-informed care, co-occurring conditions, and social determinants of health. To assess the frequency to which multiple substances were discussed, the themes also included 5 illicit and nonillicit substances of concern: alcohol, stimulants, opioids, cannabis, tobacco, or nicotine, plus polysubstance use when any 2 or more of these substances were identified. A conceptual analysis approach was used to gauge the dose and frequency of all learning objective themes and selected illicit and nonillicit substances. The content analysis aimed to confirm the discussion of the series’ learning objectives during case presentations and to determine to what extent multiple substances were able to be addressed.
Researchers evaluated all 22 participant-led ECHO case presentations and discussions for the presence of the selected themes in the prepared participant cases, faculty recommendations, and participant recommendations. Case presentations and discussions consisted of participants independently preparing a patient case to present and receive participant and faculty guidance for a patient treatment plan. Case presentations were recorded and transcribed using Zoom videoconferencing software (Zoom Video Communications, Inc). The transcriptions were then used for the conceptual content analysis.
To ensure coding accuracy, 4 researchers independently coded 27% (n=6) of the case presentations and met to reconcile discrepancies and better establish coding parameters. After reconciling discrepancies, 1 researcher coded the remaining 16 case presentations and discussion transcripts. The content analysis themes and descriptions are presented in Table 1 .
Paired-Samples t Test
To determine if Project ECHO CSUDC affected participant learner outcomes, researchers calculated mean scores reported on a Likert scale of 1 to 5 and conducted a paired-samples t test to compare pre- and postseries scores at a .05 significance level. The surveys consisted of matching statements assessing knowledge, self-efficacy, attitudes, and skills associated with the series’ learning objectives. The data were assessed for normality and homogeneity of variance and the assumptions were met. The data analysis was conducted using SPSS Statistics for Windows (version 26.0; IBM Corp).
Participant Characteristics
CSUDC ECHO participants were asked to report their role type on the preseries survey. Of the participants that responded to the survey items (n=79), a majority were other care team members (n = 32; 41%) followed by behavioral health providers (n = 30; 38%) and medical providers (n = 16; 21%). Additionally, participants were asked to indicate their years of experience working with SUDs. Most participants had between 1 and 5 years of experience (n=23; 29%) followed by 6-10 years (n=15; 19%), 11-20 years (n=14; 18%), less than 1 year (n=13; 16%), 7 participants indicated they do not work directly with patients (n=7; 9%), 21-30 years (n=4; 5%), 31-40 years (n=2; 3%), and more than 40 years of experience (n=1; 1%). Full participant characteristics of the entire CSUDC ECHO attendees, excluding the paired-samples t test sample, the paired-samples t test sample only, and all combined CSUDC ECHO attendees are provided in Table 2 .
The attendance data of participants included in the paired-samples t test analysis were analyzed. Further, 6 (n=6; 38%) of the paired-samples t test participants attended 1% (n=1) to 25% (n=6) of the 24 CSUDC ECHO sessions, 3 (n = 3; 19%) attended 26% (n=7) to 49% (n=11) of the sessions, 4 (n = 4; 25%) attended 50% (n=12) to 75% (n=18) of the sessions, and 3 (n = 3; 19%) attended 76% (n=19) to 100% (n=24) of the sessions.
a ECHO: Extension for Community Healthcare Outcomes.
b CSUDC: Comprehensive Substance Use Disorder Care.
c SUD: substance use disorder.
The conceptual content analysis indicated that all of the a priori themes relating to the learning objectives resulted in high frequencies and doses, appearing in a majority of case presentations and discussions. Further, 3 themes appeared in 100% (n = 22) of case presentations and discussions, including team-based care at a frequency of 156, followed by harm reduction at a frequency of 152, and social determinants of health at a frequency of 135. In total, 4 themes appeared in less than 100% (n=22) of case presentations and discussions, but above 81% (n=18), including co-occurring conditions with a frequency of 118 and appearing in 95% (n = 21) of case presentations and discussions, followed by behavioral techniques at a frequency of 108 and appearing in 91% (n = 20) of case presentations and discussions, MAT at a frequency of 89 and appearing in 86% (n = 19) of case presentations and discussions, and trauma-informed care at a frequency of 79 and appearing in 82% (n=18) case presentations and discussions. Additionally, multiple substances were represented but at differing frequencies. The substance that resulted in the highest frequency and dose was alcohol at a frequency of 64 and appeared in 81% (n = 18) of case presentations and discussions, followed by stimulants at a frequency of 55 and 77% (n=17) of case presentations and discussions, opioids at a frequency of 49 and 59% (n = 13) of case presentations and discussions. Cannabis resulted with a frequency of 38 but appeared in 64% (n = 14) of case presentations and discussions. Finally, tobacco and nicotine resulted in the lowest frequency at 11 and dose appearing in 27% (n = 6) of case presentations and discussions. When evaluating polysubstance use, which was limited to the use of two or more of the listed substances, we found a dose of 95% (n = 21) of case presentations and discussions. The frequency of polysubstance use was not included in the conceptual content analysis since it was not a learning objective theme and the emphasis of the conceptual content analysis was focused on the specific illicit and nonillicit substance types. The results of the conceptual content analysis are presented in Table 3 .
a MAT: medication-assisted treatment.
b —: not available.
In total, 4 knowledge domain statements resulted in statistically significant increases: understanding polysubstance use in patients experiencing SUD ( P =.02), understanding the approach colleagues in other disciplines use to address SUD ( P =.02), knowledge of medication management strategies for nicotine use disorder ( P =.03), and knowledge of medication management strategies for opioid use disorder (OUD; P =.003). Additionally, all knowledge domain statements resulted in an increased change in mean score from preseries to postseries. The results of the knowledge domain preseries and postseries scores are presented in Table 4 .
No attitudes domain statements resulted as statistically significant. All attitudes domain statements resulted in an increased change in mean score from preseries to postseries except the statement about a treatment plan for a patient experiencing an illicit SUD only being successful if abstinence is maintained, which resulted in a negative change in mean score. The negative change in mean score from preseries to postseries was the appropriate direction of change for alignment with promoting a harm reduction philosophy. The results of the attitudes domain preseries and postseries scores are presented in Table 5 .
Self-Efficacy
In total, 2 self-efficacy statements resulted in statistically significant increases: choosing a medication management strategy for nicotine use disorder ( P =.002) and alcohol use disorder ( P =.02). Additionally, all self-efficacy domain statements resulted in an increased change in mean score from preseries to postseries. The results of the self-efficacy domain preseries and postseries scores are presented in Table 6 .
a SMART: specific, measurable, achievable, relevant, timely.
In total, 1 skill domain statement resulted in a statistically significant increase: using the stages of change theory to provide stage-based interventions to patients experiencing SUDs ( P =.03). Additionally, all skill domain statements resulted in an increased change in mean score from preseries to postseries. The results of the skill domain preseries and postseries scores are presented in Table 7 .
a IOP: intensive outpatient.
Principal Findings
Ohio’s annual average prevalence of tobacco use, heroin use, use of prescription pain relievers, OUDs, illicit drug use disorder, and SUD have been higher compared to both regional and national averages [ 2 ]. Considering the need to address this public health concern, CSUDC ECHO was implemented to train Ohio providers and care team members in substance use care. CSUDC ECHO enhanced the Project ECHO work in this field by focusing content and learning objectives on a comprehensive, team-based lens and a harm reduction philosophy of care to address multiple illicit and nonillicit substances including opioids, alcohol, nicotine, cannabis, and stimulants. To assess the ability of the CSUDC ECHO program to meet its 7 program learning objectives ( Textbox 2 ) and address multiple substances, this study analyzed (1) the frequency of exposure to learning objective themes and substance types during case presentations and discussions and (2) participating providers’ change in knowledge, attitudes, self-efficacy, and skills related to the treatment of SUDs.
Study results demonstrate that all 7 learning objectives were frequently addressed in the content of case presentations and discussions throughout the program, with team-based care being the most frequently mentioned, 3 objectives appearing in 100% (n=22) of case discussions (eg, team-based care, harm reduction, and co-occurring conditions), and all 7 objectives appearing in >81% (n=18) of all cases discussed. This may have resulted in the learner outcome improvement pre- to postprogram for multiple learner domains (eg, knowledge, self-efficacy, and skill) for the following themes: team-based care, MAT, polysubstance use, and behavioral techniques. No pattern emerged among the participants included in the paired-samples t test analysis exposure to didactic topics and changes in learner outcomes.
Alcohol, stimulants, opioids, cannabis, and nicotine were addressed in the content of case presentations and discussions throughout CSUDC ECHO with alcohol being the most frequently mentioned and most common substance appearing in cases, 4 substances appearing in >59% (n=13) of case discussions (eg, alcohol, stimulants, opioid, and cannabis), and all coded substances appearing in at least a quarter of cases. The dialogue about these substances during case discussions likely resulted in improvements to the following learner outcomes related to medication management: alcohol use disorder, OUD, and nicotine use disorder. Medication management of cannabis use disorder was not assessed in the pre- to postsurveys. Additionally, the didactic presentation topics that centered on alcohol, opioid, and nicotine use disorder resulted in a higher attendance rate with about 40% (n=6) to 50% (n=8) of the participants included in the paired-samples t test analysis attending the sessions, as compared to only 20% (n=3) of the aforementioned participant sample having attended the session centered on stimulant use disorder.
These findings indicate that the ECHO program’s content aligned with its stated learning objectives; met its learning objectives for the 3 themes where significant improvements were measured; and met its intent to address multiple substances in case presentations and discussions. While case presentations and discussions comprise from half to the majority of content in the sessions (30-35 minutes of a 60-minute session), content during sessions also includes faculty didactic presentations (20-25 minutes), which also addresses these 7 learning objectives and various substances but was not a part of the content analysis. Therefore, learner outcome improvements may also be a result of content addressed in didactic presentations.
While the Project ECHO model has been shown to be effective in training the primary care workforce [ 9 ], specifically on OUD [ 10 , 11 ] and addiction medicine [ 12 , 13 ], there has been no documentation, to our knowledge, of the ability of a team-based, comprehensive SUD and polysubstance-focused Project ECHO designed to improve learner outcomes (eg, knowledge, self-efficacy, and skills). Although Komaromy and colleagues [ 14 ] investigated the frequency of cases presented based on substance type in a comprehensive SUD-focused ECHO, a content analysis of the case presentation and discussion transcripts was not analyzed to either assess the frequency of substances or learning objectives. Furthermore, to our knowledge, this process has not been combined in a mixed method approach to compare learner outcomes with a content analysis to gauge the ability of an SUD-focused Project ECHO program to meet its stated learning objectives. Our results reported here align with this literature and expand to demonstrate that Project ECHO is a potential tool to effectively educate multidisciplinary providers in a comprehensive approach to SUD care.
This study has several strengths which promote the ability of the Project ECHO model in enhancing health care providers’ knowledge, self-efficacy, and skill associated with comprehensive SUD care. The focus of this study is unique as there is minimal research exploring the benefits and training ability of Project ECHO with a comprehensive SUD care focus. This study’s noteworthy strength is the use of a mixed methods design that presents a comprehensive evaluation correlating the content addressed in the case presentations and discussions to statistically significant learner outcomes to demonstrate how this telementoring continuing education series improved provider’s knowledge, skills, and self-efficacy to benefit participating providers and their practices.
Limitations
This study faced several limitations during data collection and analysis. The first limitation of this study was the limited sample size and low response rate. There was a decline between the number of participants who completed the preseries survey and postseries survey, resulting in a low comparative sample, which restricted the options for statistical analysis. Another limitation was generalizability; the results of this Project ECHO are limited to the target audience of medical providers, behavioral health providers, and care team members from the state of Ohio, which is not a representative sample of broader populations nationally. Additionally, participants self-selected to take part in the Project ECHO series, which presents the potential for self-selection bias. Another limitation this study faced was the lack of available or reliable data on Project ECHO and its ability to meet learning objectives and address multiple substances through providers’ knowledge, self-efficacy, skill, and attitudes. Furthermore, self-reported data to assess knowledge and skills, and self-reported data in general, could present participant biases and is difficult to corroborate with outcomes. The use of internally designed survey instruments instead of using validated instruments presents as a limitation. In light of these limitations, future studies in this subject matter should include a larger data set. Additionally, future studies using a nested analysis approach might provide more insight into how the learning objective themes coincide with the various illicit and nonillicit substance types and would be a useful analysis to contribute to the knowledge base. Another recommendation for future studies in this subject matter should include a deeper analysis of attendance dose and exposure to didactic topics to better understand the impact on changes in learner outcomes. Future research with greater validity will contribute to the significant gaps in literature regarding this subject.
Conclusions
The purpose of this research study was to assess the ability of CSUDC ECHO to both address and meet 7 learning objectives ( Textbox 2 ) and address multiple substances by analyzing (1) the frequency of exposure to the learning objective topics and substance types during case presentations and discussions and (2) participants’ knowledge, self-efficacy, skills, and attitudes related to the treatment of SUDs from pre- to postprogram. The results of this study indicate that CSUDC ECHO was able to both address and meet its learning objectives while addressing multiple substances, as demonstrated by improvements in learner knowledge, self-efficacy, and skills. All learning objective themes resulted in high frequencies and doses, appearing in a majority of case presentations throughout the series. These promising results suggest that Project ECHO is a potential tool to educate primary care providers, behavioral health providers, and care team members in a comprehensive approach to SUD assessment and treatment through complex case discussions combined with didactic learning for certain settings. As Project ECHO programs continue to be established globally and existing programs strengthen, further research examining the model’s ability to achieve positive learning outcomes and factors that may contribute to these outcomes (eg, frequency of topic dose) is needed to confirm the outcomes in larger population samples, additional topics of focus, and other geographical settings.
Acknowledgments
The authors would like to acknowledge our partners at Buckeye Health Plan and Ohio University Heritage College of Osteopathic Medicine. We would like to thank our funders, Centene Corporation through its subsidiary, Buckeye Health Plan; without their financial support, this work would not have been possible. We would like to thank the faculty that led the ECHO sessions, delivered didactic presentations, and provided high-quality case recommendations, including core faculty members Dana Vallangeon, doctor of medicine, Tracy Plouck, master of public administration, Amy Black, master of science in nursing, advanced practice registered nurse, nurse practitioner-certified, Ericka Ludwig, licensed professional clinical counselors applying for training supervision designation, licensed independent chemical dependency counselor, as well as guest faculty members. We would also like to thank our Weitzman Institute colleagues who helped with the content analysis: Zeba Kokan, Claire Newby, and Reilly Orner. To learn more about Weitzman Extension for Community Healthcare Outcomes programs, visit their website [ 15 ]. This project was supported by Buckeye Health Plan, a subsidiary of Centene Corporation. The views, opinions, and content expressed in this paper do not necessarily reflect the views, opinions, or policies of Buckeye Health Plan or Centene Corporation. The authors did not use generative artificial intelligence in any portion of this paper.
Data Availability
The data sets generated and analyzed during this study are not publicly available due to a portion of the data being deemed as exempt by the institutional review board and the institutional review board approving a waiver of informed consent for the exempt data, as well as the sensitive nature of the data, but are available from the corresponding author on reasonable request.
Authors' Contributions
MK wrote this paper, reviewed this paper, designed the evaluation plan, and performed the qualitative and statistical analyses. AP wrote this paper, reviewed this paper, and assisted with the evaluation design and approval. RM wrote this paper, reviewed this paper, performed the literature review, and assisted with the evaluation design and approval. NRN wrote this paper, reviewed this paper, and performed the literature review. KA critically reviewed this paper.
Conflicts of Interest
None declared.
Weitzman Extension for Community Healthcare Outcomes: Comprehensive Substance Use Disorder Care preseries survey instrument.
Weitzman Extension for Community Healthcare Outcomes: Comprehensive Substance Use Disorder Care postseries survey instrument.
- Drug overdose mortality by state. Centers for Disease Control and Prevention. 2023. URL: https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_mortality/drug_poisoning.htm [accessed 2023-01-30]
- Behavioral health barometer: Ohio, Volume 6: indicators as measured through the 2019 national survey on drug use and health and the national survey of substance abuse treatment services. Substance Abuse and Mental Health Services Administration. 2020. URL: https://www.samhsa.gov/data/sites/default/files/reports/rpt32852/Ohio-BH-Barometer_Volume6.pdf [accessed 2023-01-30]
- Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199-2207. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fact sheet: Biden-Harris administration announces new actions and funding to address the overdose epidemic and support recovery. The White House. 2022. URL: https://www.whitehouse.gov/briefing-room/statements-releases/2022/09/23/fact-sheet-biden-harris-administration-announces-new-actions-and-funding-to-address-the-overdose-epidemic-and-support-recovery/ [accessed 2023-01-27]
- Key substance use and mental health indicators in the United States: results from the 2019 national survey on drug use and health. Substance Abuse and Mental Health Services Administration. 2020. URL: https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf [accessed 2023-01-25]
- Abroms LC, Padmanabhan N, Thaweethai L, Phillips T. iPhone apps for smoking cessation: a content analysis. Am J Prev Med. 2011;40(3):279-285. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Moore DE, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 2009;29(1):1-15. [ CrossRef ] [ Medline ]
- Zhou C, Crawford A, Serhal E, Kurdyak P, Sockalingam S. The impact of project ECHO on participant and patient outcomes: a systematic review. Acad Med. 2016;91(10):1439-1461. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tofighi B, Isaacs N, Byrnes-Enoch H, Lakew R, Lee JD, Berry C, et al. Expanding treatment for opioid use disorder in publicly funded primary care clinics: exploratory evaluation of the NYC health + hospitals buprenorphine ECHO program. J Subst Abuse Treat. 2019;106:1-3. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alford DP, Zisblatt L, Ng P, Hayes SM, Peloquin S, Hardesty I, et al. SCOPE of pain: an evaluation of an opioid risk evaluation and mitigation strategy continuing education program. Pain Med. 2016;17(1):52-63. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sagi MR, Aurobind G, Chand P, Ashfak A, Karthick C, Kubenthiran N, et al. Innovative telementoring for addiction management for remote primary care physicians: a feasibility study. Indian J Psychiatry. 2018;60(4):461-466. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Englander H, Patten A, Lockard R, Muller M, Gregg J. Spreading addictions care across Oregon's rural and community hospitals: mixed-methods evaluation of an interprofessional telementoring ECHO program. J Gen Intern Med. 2021;36(1):100-107. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Komaromy M, Duhigg D, Metcalf A, Carlson C, Kalishman S, Hayes L, et al. Project ECHO (Extension for Community Healthcare Outcomes): A new model for educating primary care providers about treatment of substance use disorders. Subst Abus. 2016;37(1):20-24. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Weitzman Institute. URL: https://www.weitzmaninstitute.org/education/weitzman-echo/ [accessed 2024-03-12]
Abbreviations
Edited by T de Azevedo Cardoso; submitted 12.04.23; peer-reviewed by A Arbabisarjou, J Ford Ii; comments to author 12.09.23; revised version received 06.11.23; accepted 29.02.24; published 01.04.24.
©MacKenzie Koester, Rosemary Motz, Ariel Porto, Nikita Reyes Nieves, Karen Ashley. Originally published in JMIR Medical Education (https://mededu.jmir.org), 01.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Medical Education, is properly cited. The complete bibliographic information, a link to the original publication on https://mededu.jmir.org/, as well as this copyright and license information must be included.
- Our Story at 100 Promoting human progress since 1924, expanding equity and opportunity today
- Our Staff Our work is made possible by a staff of mission-driven professionals
- Diversity, Equity and Inclusion Central to how we operate and fund, we center DEI in all we do
- Careers Check for new openings and learn about working at The Kresge Foundation
- Board of Trustees Leaders who provide governance, expertise and support to our work
- Press Room Resources and information for commnunications professional
- How We Operate
- American Cities Effective, inclusive community development in U.S. cities
- Arts & Culture Positioning culture and creativity as drivers of more just communities
- Detroit Expanding long-term, equitable opportunity in our hometown
- Education Addressing postsecondary attainment and closing equity gaps
- Environment Helping cities with equitable climate resilience strategies
- Health Building equity-focused systems of health to achieve well-being
- Human Services Increasing social-economic mobility for people with low incomes
- Social Investment Practice Unlocking capital for community development
- Strategic Learning, Research & Evaluation Building a culture of learning across the organization and support community learning priorities
- Initiatives Our time-bound funding programs can bring multiple Kresge teams together to co-create strategies
- Grants Awarded A database of grants dating back to 2009
- Social Investments Made A database of PRIs, guarantees and other investments
- Current Funding Opportunities All open funding opportunities are listed by program
- How to Apply Details on eligibility, FAQs, Fluxx guidance and more
- For Current Grantees FAQs for partners, communicating about your work and more
- News & Views
Decarbonizing community facilities: case studies
Environment, Social Investment Practice
Many community facilities operated by nonprofits can benefit from going solar. The influx of federal funds through the Inflation Reduction Act and the Greenhouse Gas Reduction Fund makes 2024 a ripe moment to explore solar options, including solar+storage. Co-developing organizations are intermediaries well-versed in the solar installation and financing process. They can be productive partners for nonprofits, as they have specialized in working with nonprofit community facilities that serve specific sectors. This series of case studies will showcase examples from across the country and through various community facility types of solar projects implemented with the assistance of a co-developer. The goal of this series is to help building operators see examples to follow and make the case that they can’t afford to wait to begin to go solar.
Community facility type: Nonprofit
- Organization : United Parents Against Lead (UPAL)
- Place: Petersburg, Virginia
- System Type: Rooftop mounted
- System size: 33 kW
- Technical Assistance : Clean Energy Group
Community facility type: Community Action Agency
- Organization : Greater Bergen Community Action
- Place: Bergen County New Jersey
- System size: 3 sites, 118KW total
- Co-developer : Cap Solar

Community facility type: Community Health Center
- Organization : Planned Parenthood California Central Coast
- Place: Ventura and San Luis Obispo, California
- System size: 2 sites, 49KW total
- Developer : Asteri Solar LLC
- Organization : San Fernando Community Health Center
- Place: San Fernando, California
- System size: 106 kW
- Developer : Collective Energy
Related Resources
Planned parenthood of california central coast solar case study.
Environment, Health, Social Investment Practice
San Fernando Community Health Center solar case study
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Lippincott Open Access
Mortality Related to Air Pollution with the Moscow Heat Wave and Wildfire of 2010
Dmitry shaposhnikov.
From the a Institute of Economic Forecasting, Russian Academy of Sciences, Moscow, Russia; b Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden; c Centre for Occupational and Environmental Medicine, Stockholm County Council, Stockholm, Sweden; d Institute of Demography, Higher School of Economics, Moscow, Russia; and e State Environmental Protection Institution Mosecomonitoring, Moscow, Russia.
Boris Revich
Tom bellander, getahun bero bedada, matteo bottai, tatyana kharkova, ekaterina kvasha, elena lezina, eugenia semutnikova, göran pershagen.
Supplemental Digital Content is available in the text.
Background:
Prolonged high temperatures and air pollution from wildfires often occur together, and the two may interact in their effects on mortality. However, there are few data on such possible interactions.
We analyzed day-to-day variations in the number of deaths in Moscow, Russia, in relation to air pollution levels and temperature during the disastrous heat wave and wildfire of 2010. Corresponding data for the period 2006–2009 were used for comparison. Daily average levels of PM 10 and ozone were obtained from several continuous measurement stations. The daily number of nonaccidental deaths from specific causes was extracted from official records. Analyses of interactions considered the main effect of temperature as well as the added effect of prolonged high temperatures and the interaction with PM 10 .
The major heat wave lasted for 44 days, with 24-hour average temperatures ranging from 24°C to 31°C and PM 10 levels exceeding 300 μg/m 3 on several days. There were close to 11,000 excess deaths from nonaccidental causes during this period, mainly among those older than 65 years. Increased risks also occurred in younger age groups. The most pronounced effects were for deaths from cardiovascular, respiratory, genitourinary, and nervous system diseases. Continuously increasing risks following prolonged high temperatures were apparent during the first 2 weeks of the heat wave. Interactions between high temperatures and air pollution from wildfires in excess of an additive effect contributed to more than 2000 deaths.
Conclusions:
Interactions between high temperatures and wildfire air pollution should be considered in risk assessments regarding health consequences of climate change.
Heat waves and wildfires constitute important public health threats. Predictions based on climate change scenarios indicate that more intense and longer heat events are likely to become more frequent in temperate zones. 1 , 2 Acute effects of heat waves on mortality are well documented. 3 , 4 Primarily, cardiovascular mortality in the elderly population is affected, but studies have generally lacked adequate power to assess risks for other less common causes, as well as for persons of working ages. Furthermore, there is limited evidence on the interplay between heat intensity and duration regarding their adverse health effects.
Wildfire activity is also expected to be affected by climate change and leads to increased exposure to combustion-related particles. 5 There is compelling evidence linking particulate air pollution in general to total 6 and cardiovascular mortality 7 after both short- and long-term exposure. More specifically, some studies have reported associations between wildfires and increased mortality, 8 , 9 whereas others found no such relation 10 , 11 or reported weak associations, 12 which may be a result of low statistical power. Evidence is lacking on interactions between extended high temperatures and air pollution from wildfires on cause-specific mortality although these exposures often occur together. 2
The prolonged heat wave in Moscow during the summer of 2010 triggered numerous wildfires in forests and peat bogs near the city. Earlier studies in Moscow have reported both heat and particulate-related effects on mortality, although under less extreme circumstances than in 2010. 13 , 14 The initial death toll estimate for the heat wave in the summer of 2010 was around 55,000 for the European part of the Russian Federation. 15 However, data on daily mortality have not previously been available, and analyses have not been possible on daily variations in temperature, air pollution levels, and mortality. Our aim was to analyze day-to-day variations of cause-specific mortality in Moscow in relation to air pollution levels and temperature during the heat wave and wildfire period in July and August 2010.
Air Pollution and Meteorology
Daily meteorological and air pollution data from 2006 to 2010 were supplied by the State Environmental Protection Institution Mosecomonitoring, which operates the Moscow State Environmental Monitoring System. 16 , 17 Automatic air quality monitoring stations are placed in all functional zones of the city: residential zones, mixed residential/industrial zones, green areas, and near motorways. Each station continuously monitors a set of pollutants under WHO maintenance and air quality measurement guidelines. 18
PM 10 and ozone measurements are the focus of our analyses. The number of PM 10 measuring stations in Moscow increased from six in 2006 to nine in 2008. PM 10 was initially measured by Russian-made radio-isotopic devices. Between 2006 and 2008, these instruments were gradually replaced at all stations with oscillating microbalance monitors TEOM1400a (Thermo Fisher Scientific, Franklin, MA). Although PM 10 measurements for this study were obtained mostly from TEOM1400a, three stations that used radio-isotopic devices until 2008 were also included. A factor of 1.3 was used to convert TEOM1400a to reference gravimetric measurements, as recommended for Northern and Central Europe. 19 This factor was not applied during the days with maximum air temperatures above 30°C. The number of ozone-monitoring stations increased from nine in 2006 to 13 in 2010. Ozone was measured by ultraviolet fluorescence methodology and differential optical absorption spectroscopy.
Only the stations that had more than 75% of valid hourly averages during each day were included in calculations of city average pollution levels during that day. Day-to-day variations in numbers of operating stations were taken into account by a standardization procedure. Thus, each observation from a station was subtracted from that station’s annual mean and the resulting value divided by the corresponding standard deviation. Then, a common daily mean was constructed by averaging all available standardized observations for that day. Finally, this average was multiplied by the standard deviation of the most representative station, and the mean annual concentration of this station was added. Selection of the most representative station was based on the completeness of measurements during a particular year. Data from at least one PM 10 -monitoring and one O 3 -monitoring station were available for each day during the observation period.
Average daily temperatures and relative humidity were obtained by Mosecomonitoring from the Meteorological Observatory of the Moscow State University, which has data acquisition procedures complying with requirements of the World Meteorological Organization. In the calculation of heat wave threshold temperatures, data from 1980 and onward were used.
Information on daily deaths in the city of Moscow during the 5-year period 2006–2010 was based on Russian State statistics. With a population of 11.5 million in 2010, Moscow experiences about 300 deaths a day. Each death in Russia is certified by an authorized medical expert, who identifies the date, place, and primary cause of death using International Classification of Diseases, Tenth Revision ( ICD-10 ) codes. This expert issues a “medical certificate of death” that is reported to the local civil registration office. This office then makes an official record of death and reports it to the Russian State Statistical Service. No specific validation of death records was performed for this study, but the autopsy rate in Moscow is relatively high, varying from 46% in 2006 to 50% in 2009. The proportion of ill-defined and unspecified causes of death ( ICD-10 code R99) was 4–5% during this period.
Statistical Analysis
A detailed description of the statistical methodology is provided in the eAppendix ( http://links.lww.com/EDE/A778 ). Data were analyzed using two complementary approaches. In the first, we analyzed mortality from all major causes defined in the ICD-10 chapters, except for those with fewer than 100 deaths during the heat wave period (6 July to 18 August 2010). Generalized linear models with identity link and Gaussian errors were applied to estimate the expected death counts for each cause of death separately. 20 The death count during the period 2006–2009 was modeled as a function of time to predict the expected death counts during the heat wave period in 2010. In the second approach, we considered the effects of air pollution and temperature (and their interaction) on total nonaccidental mortality, using a generalized linear model with a logarithmic link function and Gaussian errors during the whole study period 2006–2010. The independent variables included long-term time trend modeled by linear and quadratic functions of day number during the study period; seasonal periodicity modeled by a restricted cubic spline for day of year; day of week introduced by indicator variables; relative humidity during the day of the outcome; average measures of PM 10 , ozone, and temperature over the day of the outcome and the previous day; average measures of PM 10 , ozone, and temperature over the time period between the 6th and the 2nd day before the outcome; an interaction term between ozone and season; and a multiplicative interaction term between PM 10 and temperature exceeding 18°C (minimum of the mortality-temperature relationship). The variables used to model the “added” effect of the number of days into the heat wave (sometimes called “wave effect”) follow the approach described by Gasparrini and Armstrong. 21
Figure Figure1 1 shows daily temperature and PM 10 levels in Moscow from 1 June to 31 August 2010, as well as total number of nonaccidental deaths. On several days, 24-hour average temperatures exceeded 30°C and PM 10 levels exceeded 300 μg/m 3 . A heat wave threshold was set at the 98th percentile of daily mean temperatures (23.6°C). Using a heat wave definition of at least three consecutive days with temperatures above this threshold, six heat waves were identified in 2006–2009 and two in 2010 (6 days in late June and 44 days between 6 July and 18 August). The latter prolonged heat wave period in 2010 is the primary focus of our analyses. We observed three episodes when daily mean PM 10 levels exceeded the 98th percentile (90 μg/m 3 ), and all are nested within the prolonged heat wave period. As seen in Figure Figure1, 1 , both temperature and air pollution levels influenced the mortality. The highest number of deaths followed the major air pollution episode in early August, during the final part of the heat wave, when daily death rates were three times higher than normal. For comparison, data on daily temperature, PM 10 levels, and mortality during the whole observation period (2006–2010) are shown in eFigure 1 ( http://links.lww.com/EDE/A778 ).

Daily nonaccidental deaths, mean temperature, and PM 10 levels in Moscow during the summer of 2010. Solid lines show observed values; dashed lines, expected values.
The Table shows observed and expected number of deaths from 6 July to 18 August 2010, according to age and major disease groups. The total number of excess deaths from nonaccidental causes during this period was 10,860. Risks were higher among those older than 65 years, although a clear increase was seen also in those of working ages. Risks were elevated for all specific causes; the greatest relative increases were observed for deaths from nervous system (relative risk [RR] = 3.07), genitourinary (RR = 2.54), cerebrovascular (RR = 2.37), ischemic heart (RR = 2.29), and respiratory (RR = 2.05) diseases. Renal diseases were responsible for most of the excess risk among the genitourinary diseases. We saw no clear sex-related differences in excess number of deaths during the heat wave (data not shown).
Observed (O) and Expected (E) Deaths During the Moscow Heat Wave from 6 June to 18 August 2010

There was a strong increase in mortality during the heat wave not explained by temperature as estimated from previous years. Figure Figure2 2 shows the main effect of temperature specified as an increase in mortality attributable to variations of daily temperatures over the preceding week, relative to the minimum of the mortality-temperature relationship. The minimum appeared at 18°C, and high temperatures in particular led to sharp increases in mortality. Figure Figure3 3 shows the effect of consecutive heat wave days (“added” effect of temperature) specified by the relative increase in mortality from nonaccidental causes modeled as a smooth function of day number starting 6 July 2010. There is a steep increase in RR during the first 2 weeks of the heat wave, up to 1.38 (95% confidence interval [CI] = 1.27–1.50), and then a gradual decrease until the end of the heat wave.

Relative increase in nonaccidental mortality 2006–2010 in Moscow related to temperature, averaged over 1 week, compared with a temperature of 18°C. The graphs indicate mean relative increase and 95% confidence interval.

Relative increase in nonaccidental mortality in Moscow between 6 July and 18 August 2010 attributable to the effect of consecutive heat wave days. The graphs indicate mean relative increase and 95% confidence interval.
The estimated relative increases in daily nonaccidental mortality attributable to temperature, air pollution, and their interaction are illustrated in Figure Figure4. 4 . The relative increases attributable to air pollution and interaction are calculated against the mean levels of PM 10 and ozone during the summers 2006–2009 (36 and 35 μg/m 3 , respectively). Each curve marks up the respective multiplier or factor: AB represents the expected death count from model (1); AC/AB is the relative increase in mortality attributable to the main effect of high temperatures; AD/AC represents the relative increase in mortality attributable to the “added” effect of prolonged high temperatures on consecutive days; AE/AD is the relative increase attributed to linear terms with air pollution; and AF/AE is the relative increase attributed to interaction between PM 10 and temperature.

Estimated contributions from temperature, air pollution, and their interaction to daily number of nonaccidental deaths in Moscow during the heat wave period in the summer of 2010. “Interaction” is between PM 10 and temperature; “pollution” is PM 10 and ozone; “added” is the heat wave effect in addition to the temperature effect; and “main” is the temperature effect.
We chose the order of explanatory variables in Figure Figure4 4 to illustrate what would happen if all pollution is taken away, leaving only temperature as a risk factor. This hypothetical situation would correspond to the area below the D line in the graph. The relative magnitude of the interaction term can be illustrated by comparing the predicted responses of total nonaccidental mortality with increases in PM 10 at varying temperatures. For example, relative increases in mortality per 10 μg/m 3 PM 10 were 0.43% (95% CI % = 0.09–0.77%) at temperature ≤18°C, 0.77% (0.40%–1.13%) at temperature equal to 22°C, and 1.44% (0.94%–1.94%) at temperature equal to 30°C. Risk coefficients for PM 10 and ozone at various time lags after the exposure are reported in the eAppendix ( http://links.lww.com/EDE/A778 ).
Three types of sensitivity analyses were performed to test the robustness of estimated risks to key assumptions of the statistical model. Regarding the method of accounting for temporal confounding, we observed a convergence of the results obtained from models with sinusoidal and restricted cubic splines of day of year. The risk coefficient for PM 10 remained fairly stable when we changed the specification of the main effect of temperature, varying the degree of residual confounding over the course of 1 week after the exposure. Regarding the choice of the heat wave threshold, it is of note that the model based on 99% percentile threshold resulted in a marked reduction in the heat-PM 10 interaction coefficient. This more strict definition led to a later start of the heat wave, a greater influence by the “added” effect of temperature, and relatively less important interaction effects. Model assumptions and results of sensitivity analyses are reported in eTable 1 ( http://links.lww.com/EDE/A778 ).
We also estimated the approximate partial contributions from several risk factors to the total nonaccidental excess mortality during the heat wave period by linearization of the multiplicative model (2). The predominant influence appeared to be from the main effect of temperature, ie, the increased risk attributable to the independent effects of daily temperature levels, which accounted for 40% of the excess number of nonaccidental deaths, corresponding to more than 4300 deaths. Air pollution and temperature-air pollution interaction (exceeding an additive effect) showed shares of 9% and 20%, respectively, corresponding to about 1000 and 2200 deaths. Both PM 10 and ozone were included under “air pollution,” with contributions of 5% and 4%, respectively, while the interaction focused on temperature and PM 10 . The total attributable proportion for temperature effects, including both main and “added” effects, as well as interactions with air pollution, amounted to 91%, whereas the corresponding proportion for air pollution was 29%.
Our study is unique in the combination of the intensity and duration of the heat wave, the high levels of air pollution from wildfires, and the large size of the affected population. These circumstances, together with the high-quality information on daily levels of air pollution and other environmental factors, as well as cause-specific mortality, made it possible to address some crucial issues for risk assessment in relation to climate change. For example, there are no previous data on combined effects on mortality by heat waves and air pollution from wildfires, although exposure to these combined factors is likely to occur more frequently with global warming. The importance of the interaction between high temperatures and air pollution in relation to mortality was highlighted for ozone during the 2003 heat wave in Europe. 22 Overall, the excess number of deaths in Moscow during the heat wave period was more than 10,000, which exceeds the number of deaths during heat waves in Chicago in 1995 23 and Paris in 2003, 24 and illustrates the public health impact of extreme weather conditions.
Most evidence on heat wave–related mortality comes from older people. 4 , 25 We found clear effects in people younger than 65 years, although stronger associations were observed in those above this age. High excess risks were seen primarily for diseases of the cardiovascular, respiratory, nervous, and genitourinary systems. Earlier evidence has pointed mainly to associations with cardiovascular and respiratory mortality, but a few studies have also reported heat wave–related excess mortality for mental and renal diseases. 26 , 27 Increased cardiovascular stress, kidney dysfunction, and disturbances of the electrolytic balance caused by dehydration contribute to the more pronounced effects for certain causes of death. We also found excess risks for other common causes of death, including cancer and diseases of the digestive system. This is probably related to poor conditions in hospitals and other treatment facilities, such as lack of air conditioning. In addition, heat wave effects on mortality are affected by both intensity and duration in a complex interplay. 3 , 21 , 28 , 29 Our findings show increasing excess risks with up to 2 weeks of prolonged high temperatures, followed by a downward trend that may indicate harvesting of the most susceptible individuals or the development of better coping strategies with time.
Several studies on particulate air pollution in cities, mainly from traffic and other sources unrelated to wildfires, indicate stronger effects by PM 10 or other measures of particulate air pollution during months with high temperatures. 30 – 32 For example, a study from Korea found a yearly excess mortality of 0.28% per 10 μg/m 3 PM 10 , which increased to 0.57% in the summer. 31 In our data, the excess mortality per 10 μg/m 3 PM 10 increased from 0.43% below 18°C to 1.44% at 30°C. Our results contribute to the available evidence on air pollution from wildfires and mortality, which is limited and inconclusive, 8 – 12 and indicate that interactions with high temperatures are of importance, similar to the situation for urban particulate air pollution. A recent report estimated the global mortality attributable to smoke from vegetation fires to more than 300,000 deaths annually. 33 Our findings provide strong evidence that interactions between high temperatures and wildfire air pollution need to be considered in health risk assessments, particularly because the two often occur together.
In conclusion, our study shows major acute effects on mortality by high temperatures and air pollution during the prolonged 2010 heat wave in Moscow. Effects were seen among the working age population as well as the older population and for causes of death in addition to cardiovascular disease. Mortality related to the prolonged heat wave increased steeply during the first 2 weeks, after which the excess risk gradually tapered off. Interaction between high temperatures and air pollution from wildfires added a substantial number of deaths.
Supported by grants from the Swedish Research Council FORMAS and the Swedish Environmental Protection Agency.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article ( www.epidem.com ). This content is not peer-reviewed or copy-edited; it is the sole responsibility of the author.
Editors' note: A commentary on this article appears on page 365.
Help | Advanced Search
Computer Science > Computation and Language
Title: distilling large language models for biomedical knowledge extraction: a case study on adverse drug events.
Abstract: Large language models (LLMs), such as GPT-4, have demonstrated remarkable capabilities across a wide range of tasks, including health applications. In this paper, we study how LLMs can be used to scale biomedical knowledge curation. We find that while LLMs already possess decent competency in structuring biomedical text, by distillation into a task-specific student model through self-supervised learning, substantial gains can be attained over out-of-box LLMs, with additional advantages such as cost, efficiency, and white-box model access. We conduct a case study on adverse drug event (ADE) extraction, which is an important area for improving care. On standard ADE extraction evaluation, a GPT-3.5 distilled PubMedBERT model attained comparable accuracy as supervised state-of-the-art models without using any labeled data. Despite being over 1,000 times smaller, the distilled model outperformed its teacher GPT-3.5 by over 6 absolute points in F1 and GPT-4 by over 5 absolute points. Ablation studies on distillation model choice (e.g., PubMedBERT vs BioGPT) and ADE extraction architecture shed light on best practice for biomedical knowledge extraction. Similar gains were attained by distillation for other standard biomedical knowledge extraction tasks such as gene-disease associations and protected health information, further illustrating the promise of this approach.
Submission history
Access paper:.
- Other Formats
References & Citations
- Google Scholar
- Semantic Scholar
BibTeX formatted citation
Bibliographic and Citation Tools
Code, data and media associated with this article, recommenders and search tools.
- Institution
arXivLabs: experimental projects with community collaborators
arXivLabs is a framework that allows collaborators to develop and share new arXiv features directly on our website.
Both individuals and organizations that work with arXivLabs have embraced and accepted our values of openness, community, excellence, and user data privacy. arXiv is committed to these values and only works with partners that adhere to them.
Have an idea for a project that will add value for arXiv's community? Learn more about arXivLabs .

IMAGES
VIDEO
COMMENTS
This teaching case study examines psychological trauma in a community context and the relevance, both positive and negative, of social determinants of health. Healthy People 2020 views people residing in communities with large-scale psychological trauma as an emerging issue in mental health and mental health disorders (Healthy People, 2016).
Case Studies in Community Health presents 14 classroom-tested case study scenarios, including background information and discussion questions. Written for students in public health and community health courses, these cases help integrate the basic concepts of public health into an applied setting. The case studies provide an opportunity for ...
In this study we examined the role the VA can play in a community's behavioral health response using case studies from three disasters. This study investigated experiences of VA employees in critical emergency response positions (N = 17) in communities where disasters occurred between 2017 and 2019.
Community Health Case Studies selected from Developing and Developed Countries - common principles for moving from evidence to action December 2008 Archives of Medical Science 4(4):358-63.
Case Study: Not mentioned: Community Health: A project was developed and implemented in primary health centers to improve young men's adherence to a teenage health care program using participatory planning techniques, and rapid assessment procedures. Process Outcome: 1) Self-assessment workshops were held with the local teams.
Takeaways from Case Studies of Community Care Hubs Joshua Breslau, Petra W. Rasmussen, Nabeel Qureshi, and Evan D. Peet RAND Health Care PR-A2895-1 September 2023 Prepared for the Office of the Assistant Secretary for Planning and Evaluation RAND's publications do not necessarily reflect the opinions of its research clients and sponsors.
Community Case Study Article Type: Criteria for Submission and Peer Review. Matthew Lee Smith 1,2* Sue E. Levkoff 3 Marcia G. Ory 2. 1 Department of Health Promotion and Behavior, College of Public Health, The University of Georgia, Athens, GA, USA. 2 Department of Health Promotion and Community Health Sciences, Texas A&M Health Science Center ...
A 3-month study in New York City Public Housing using Community Health Workers also found that they improved health care access and improved social determinants of health such as reducing food insecurity and improving ability to pay rent on time and improving access to exercise and exercising among residents . In this study we could not ...
CASE STUDY 1: Access Healthcare, Brian Forrest, MD, and Whitney Kirkman, PBT-ASCP, MA ... DePaul Community Health Centers is an FQHC network with ten locations in the New Orleans metropolitan area ...
This case study describes a comprehensive program that includes: a community-based intervention using multidisciplinary care teams that work closely with the patient's primary care provider; an acute care intervention bundle with collaborative team-based care; and a skilled nursing facility intervention emphasizing standardized transitions and ...
for Community Health Workers Scott Tornek Chief Strategy Officer of the Center for Community Health Workers Cheryl Garfield Senior Community Health Worker The Population Health Advisor team is grateful to organizations that shared their insights, analysis, and time with us. We would like to recognize the following organizations for being ...
The Importance of Case Studies in Public Health Education and Promotion. Health programs and practices are often conceived and delivered by community-based practitioners to address specific community health education and promotion needs ().Although, initially untested, such programs can provide important lessons for researchers and practitioners, alike.
Preventing Chronic Disease (PCD) is a peer-reviewed electronic journal established by the National Center for Chronic Disease Prevention and Health Promotion. PCD provides an open exchange of information and knowledge among researchers, practitioners, policy makers, and others who strive to improve the health of the public through chronic disease prevention.
This case study presents findings from a CBPR oral health project with an indigenous community in Costa Rica called La Casona. La Casona is a community within the Coto Brus Indigenous Territory which extends near the frontier between Costa Rica and Panama.
We reviewed data from the electronic health data system used by Community Health Workers (CHWs) in the Richmond/Henrico Health District of the Virginia Department of Health from January 1st 2013 to December 31st 2020, to map the Community Health Workers' impact on Social Determinants of Health. We also interviewed the CHWs to obtain demographic information and information about the ...
a unique position to address health issues in any underserved community. Their greatest asset is their ability to establish a trusting relationship with the community. Using this relationship as a foundation, a CHW can then engage both health care providers and members of the community to work towards better health outcomes.
Prepared by Health Equity Solutions State Examples of Medicaid Community Engagement Strategies: Two Case Studies Community engagement is a key component of health equity work because it fosters trust and mutual respect, unearths unforeseen or unintended barriers to health, and improves efficacy by ensuring programs respond to the
The COVID-19 pandemic and related lockdowns around the world led to a general decline in physical and mental health because of isolation, lack of social interaction, restriction of movement and travel, and dramatic lifestyle changes [].The COVID-19 pandemic also demonstrated the importance of having access to green and blue spaces for human health and well-being during pandemics [2,3,4].
A prospective study design was based on the longitudinal California Alameda County community health studies. HRQOL outcome was defined in the Moscow survey by life satisfaction, life happiness, self-rated health status, and the Alameda County Physical Health Profile, but only the distribution of physical health is reported here.
2.1 Study Area. Moscow and Saint Petersburg are among the most populous cities in Russia and in Europe and are the fastest growing cities in Russia. Between 1991 and 2018, the population increased from 9.02 to 12.56 million people in Moscow and from 5.00 to 5.35 million in Saint Petersburg (Mosgorstat Moscow 2018; Petrostat 2018).Urban areas have been continuing to expand.
Case Study homelessness community health reasoning george mayfield, 68 years old primary concept health promotion interrelated concepts (in order of emphasis)
Created by volunteer Baldrige alumni examiners Kay Kendall, Joe Muzikowski, and Glenn Bodinson, the fictitious Arroyo Fresco was written to represent community health centers, which were established over the past 50 years in underserved areas in all 50 states. (The case study was reviewed by Baldrige alumni examiners Beth Katzenberg and Steve ...
Background: Substance use and overdose deaths make up a substantial portion of injury-related deaths in the United States, with the state of Ohio leading the nation in rates of diagnosed substance use disorder (SUD). Ohio's growing epidemic has indicated a need to improve SUD care in a primary care setting through the engagement of multidisciplinary providers and the use of a comprehensive ...
This series of case studies will showcase examples from across the country and through various community facility types of solar projects implemented with the assistance of a co-developer. The goal of this series is to help building operators see examples to follow and make the case that they can't afford to wait to begin to go solar.
Heat waves and wildfires constitute important public health threats. Predictions based on climate change scenarios indicate that more intense and longer heat events are likely to become more frequent in temperate zones. 1,2 Acute effects of heat waves on mortality are well documented. 3,4 Primarily, cardiovascular mortality in the elderly population is affected, but studies have generally ...
Large language models (LLMs), such as GPT-4, have demonstrated remarkable capabilities across a wide range of tasks, including health applications. In this paper, we study how LLMs can be used to scale biomedical knowledge curation. We find that while LLMs already possess decent competency in structuring biomedical text, by distillation into a task-specific student model through self ...