
- Previous Article
- Next Article

Acknowledgments
Connected content.
In a special series of the ADA Journals' podcast Diabetes Core Update , host Dr. Neil Skolnik interviews special guests and authors of this clinical compendium issue. Listen now at Special Podcast Series: Focus on Diabetes or view the interviews on YouTube at A Practice Guide to Diabetes-Related Eye Care .
Summary and Conclusion
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Thomas W. Gardner; Summary and Conclusion. ADA Clinical Compendia 1 July 2022; 2022 (3): 20. https://doi.org/10.2337/db20223-20
Download citation file:
- Ris (Zotero)
- Reference Manager
Diabetes is a multifactorial disease process, and its long-term management requires the active involvement of people with diabetes and their families, as well as a large multidisciplinary care team to ensure optimal health, quality of life, and productivity. Keeping up with new medications, emerging technology, and evolving treatment recommendations can be challenging, and the language and care processes commonly used by practitioners in one discipline may be less familiar to other diabetes care professionals.
In the realm of diabetes-related eye care, our ability to prevent the progression of diabetes-related retinal disease and thereby preserve vision has never been greater. However, far too many people with diabetes still are not receiving appropriate screening to identify eye disease early and ensure its timely treatment.
It is our hope that this compendium has provided information and guidance to improve communication and encourage collaboration between eye care professionals and other diabetes health care professionals and allow them to more effectively cooperate to reduce barriers to care and improve both the ocular and systemic health of their shared patients.
Editorial and project management services were provided by Debbie Kendall of Kendall Editorial in Richmond, VA.
Dualities of Interest
B.A.C. is a consultant for Genentech and Regeneron. S.A.R. is a speaker for Allergan, Inc., and VSP Vision Care. No other potential conflicts of interest relevant to this compendium were reported.
Author Contributions
All authors researched and wrote their respective sections. Lead author T.W.G. reviewed all content and is the guarantor of this work.
The opinions expressed are those of the authors and do not necessarily reflect those of VSP Vision Care, Regeneron, or the American Diabetes Association. The content was developed by the authors and does not represent the policy or position of the American Diabetes Association, any of its boards or committees, or any of its journals or their editors or editorial boards.
Email alerts
- Online ISSN 2771-6880
- Print ISSN 2771-6872
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Reflections on the state of diabetes research and prospects for treatment
- Review Article
- Published: 07 September 2022
- Volume 14 , pages 21–31, ( 2023 )
Cite this article
- Domenico Accili ORCID: orcid.org/0000-0002-6874-3949 1 ,
- Takumi Kitamoto 2 ,
- Taiyi Kuo 3 ,
- Wendy McKimpson 1 ,
- Yasutaka Miyachi 4 ,
- Maria Mukhanova 1 ,
- Jinsook Son 1 ,
- Liheng Wang 1 &
- Hitoshi Watanabe 1
462 Accesses
Explore all metrics
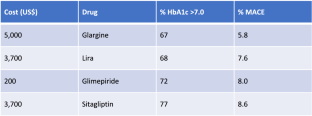
Research on the etiology and treatment of diabetes has made substantial progress. As a result, several new classes of anti-diabetic drugs have been introduced in clinical practice. Nonetheless, the number of patients achieving glycemic control targets has not increased for the past 20 years. Two areas of unmet medical need are the restoration of insulin sensitivity and the reversal of pancreatic beta cell failure. In this review, we integrate research advances in transcriptional regulation of insulin action and pathophysiology of beta cell dedifferentiation with their potential impact on prospects of a durable “cure” for patients suffering from type 2 diabetes.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Targeting pancreatic β cells for diabetes treatment
Chirag Jain, Ansarullah, … Heiko Lickert
The new biology of diabetes
Utpal B. Pajvani & Domenico Accili

Targeted pharmacological therapy restores β-cell function for diabetes remission
Stephan Sachs, Aimée Bastidas-Ponce, … Heiko Lickert
IDF. IDF Diabetes Atlas, 10th edn. In: Federation ID (eds). IDF Diabetes Atlas. Brussels: International Diabetes Federation, 2021
Taylor SI, Yazdi ZS, Beitelshees AL. Pharmacological treatment of hyperglycemia in type 2 diabetes. J Clin Invest. 2021;131:e142243
Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999–2018. N Engl J Med. 2021;384:2219–28.
Article Google Scholar
Kernan WN, Viscoli CM, Furie KL, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374:1321–31.
Article CAS Google Scholar
Ferrannini E, DeFronzo RA. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J. 2015;36:2288–96.
Holst JJ. From the incretin concept and the discovery of GLP-1 to today’s diabetes therapy. Front Endocrinol (Lausanne). 2019;10:260.
Frias JP, Fernandez Lando L, Brown K. Tirzepatide versus semaglutide once weekly in type 2 diabetes. Reply N Engl J Med. 2022;386: e17.
Drucker DJ. GLP-1 physiology informs the pharmacotherapy of obesity. Mol Metab. 2022;57: 101351.
Zinman B, Nauck MA, Bosch-Traberg H, et al. Liraglutide and glycaemic outcomes in the LEADER trial. Diabetes Ther. 2018;9:2383–92.
Home PD, Ahren B, Reusch JEB, et al. Three-year data from 5 HARMONY phase 3 clinical trials of albiglutide in type 2 diabetes mellitus: long-term efficacy with or without rescue therapy. Diabetes Res Clin Pract. 2017;131:49–60.
Cai J, Wang Y, Baser O, Xie L, Chow W. Comparative persistence and adherence with newer anti-hyperglycemic agents to treat patients with type 2 diabetes in the United States. J Med Econ. 2016;19:1175–86.
Mody R, Huang Q, Yu M, et al. Adherence, persistence, glycaemic control and costs among patients with type 2 diabetes initiating dulaglutide compared with liraglutide or exenatide once weekly at 12-month follow-up in a real-world setting in the United States. Diabetes Obes Metab. 2019;21:920–9.
Karam JH, Sanz N, Salamon E, Nolte MS. Selective unresponsiveness of pancreatic beta-cells to acute sulfonylurea stimulation during sulfonylurea therapy in NIDDM. Diabetes. 1986;35:1314–20.
Jones AG, McDonald TJ, Shields BM, et al. Markers of beta-cell failure predict poor glycemic response to GLP-1 receptor agonist therapy in type 2 diabetes. Diabetes Care. 2016;39:250–7.
Rasouli N, Younes N, Utzschneider KM, et al. Association of baseline characteristics with insulin sensitivity and beta-cell function in the glycemia reduction approaches in diabetes: a comparative effectiveness (GRADE) study cohort. Diabetes Care. 2021;44:340–9.
Taylor SI. The high cost of diabetes drugs: disparate impact on the most vulnerable patients. Diabetes Care. 2020;43:2330–2.
Barbetti F, Rapini N, Schiaffini R, Bizzarri C, Cianfarani S. The application of precision medicine in monogenic diabetes. Expert Rev Endocrinol Metab. 2022;17:111–29.
Yamagata K, Furuta H, Oda N, et al. Mutations in the hepatocyte nuclear factor-4alpha gene in maturity-onset diabetes of the young (MODY1). Nature. 1996;384:458–60.
Taylor SI, Arioglu E. Syndromes associated with insulin resistance and acanthosis nigricans. J Basic Clin Physiol Pharmacol. 1998;9:419–39.
Fajans SS, Bell GI. MODY: history, genetics, pathophysiology, and clinical decision making. Diabetes Care. 2011;34:1878–84.
Sarhangi N, Sharifi F, Hashemian L, et al. PPARG (Pro12Ala) genetic variant and risk of T2DM: a systematic review and meta-analysis. Sci Rep. 2020;10:12764.
Florez JC, Udler MS, Hanson RL. Genetics of Type 2 Diabetes. In: rd, Cowie CC, Casagrande SS, et al., eds. Diabetes in America. Bethesda (MD), 2018
Kuo T, Kraakman MJ, Damle M, Gill R, Lazar MA, Accili D. Identification of C2CD4A as a human diabetes susceptibility gene with a role in beta cell insulin secretion. Proc Natl Acad Sci USA. 2019;116:20033–42.
Gaulton KJ, Ferreira T, Lee Y, et al. Genetic fine mapping and genomic annotation defines causal mechanisms at type 2 diabetes susceptibility loci. Nat Genet. 2015;47:1415–25.
Guo S, Dai C, Guo M, et al. Inactivation of specific beta cell transcription factors in type 2 diabetes. J Clin Invest. 2013;123:3305–16.
Talchai SC, Accili D. Legacy effect of Foxo1 in pancreatic endocrine progenitors on adult beta-cell mass and function. Diabetes. 2015;64:2868–79.
Cinti F, Bouchi R, Kim-Muller JY, et al. Evidence of beta-cell dedifferentiation in human type 2 diabetes. J Clin Endocrinol Metab. 2016;101:1044–54.
Sun J, Ni Q, Xie J, et al. Beta cell dedifferentiation in T2D patients with adequate glucose control and non-diabetic chronic pancreatitis. J Clin Endocrinol Metab. 2018;104:83.
Pasquali L, Gaulton KJ, Rodriguez-Segui SA, et al. Pancreatic islet enhancer clusters enriched in type 2 diabetes risk-associated variants. Nat Genet. 2014;46:136–43.
Tennant BR, Robertson AG, Kramer M, et al. Identification and analysis of murine pancreatic islet enhancers. Diabetologia. 2013;56:542–52.
Kitamura YI, Kitamura T, Kruse JP, et al. FoxO1 protects against pancreatic beta cell failure through NeuroD and MafA induction. Cell Metab. 2005;2:153–63.
Talchai C, Xuan S, Lin HV, Sussel L, Accili D. Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure. Cell. 2012;150:1223–34.
Warton K, Foster NC, Gold WA, Stanley KK. A novel gene family induced by acute inflammation in endothelial cells. Gene. 2004;342:85–95.
Yamauchi T, Hara K, Maeda S, et al. A genome-wide association study in the Japanese population identifies susceptibility loci for type 2 diabetes at UBE2E2 and C2CD4A-C2CD4B. Nat Genet. 2010;42:864–8.
Grarup N, Overvad M, Sparso T, et al. The diabetogenic VPS13C/C2CD4A/C2CD4B rs7172432 variant impairs glucose-stimulated insulin response in 5,722 non-diabetic Danish individuals. Diabetologia. 2011;54:789–94.
Mehta ZB, Fine N, Pullen TJ, et al. Changes in the expression of the type 2 diabetes-associated gene VPS13C in the beta-cell are associated with glucose intolerance in humans and mice. Am J Physiol Endocrinol Metab. 2016;311:E488-507.
Kim-Muller JY, Fan J, Kim YJ, et al. Aldehyde dehydrogenase 1a3 defines a subset of failing pancreatic beta cells in diabetic mice. Nat Commun. 2016;7:12631.
Ishihara H, Wang H, Drewes LR, Wollheim CB. Overexpression of monocarboxylate transporter and lactate dehydrogenase alters insulin secretory responses to pyruvate and lactate in beta cells. J Clin Invest. 1999;104:1621–9.
Buteau J, Shlien A, Foisy S, Accili D. Metabolic diapause in pancreatic beta-cells expressing a gain-of-function mutant of the forkhead protein Foxo1. J Biol Chem. 2007;282:287–93.
Mousavy Gharavy SN, Owen BM, Millership SJ, et al. Sexually dimorphic roles for the type 2 diabetes-associated C2cd4b gene in murine glucose homeostasis. Diabetologia. 2021;64:850–64.
Kim-Muller JY, Kim YJ, Fan J, et al. FoxO1 deacetylation decreases fatty acid oxidation in beta-cells and sustains insulin secretion in diabetes. J Biol Chem. 2016;291:10162–72.
Ido-Kitamura Y, Sasaki T, Kobayashi M, et al. Hepatic FoxO1 integrates glucose utilization and lipid synthesis through regulation of Chrebp O-glycosylation. PLoS ONE. 2012;7: e47231.
Kim-Muller JY, Zhao S, Srivastava S, et al. Metabolic inflexibility impairs insulin secretion and results in MODY-like diabetes in triple FoxO-deficient mice. Cell Metab. 2014;20:593–602.
Sun J, Ni Q, Xie J, et al. beta-cell dedifferentiation in patients with T2D with adequate glucose control and nondiabetic chronic pancreatitis. J Clin Endocrinol Metab. 2019;104:83–94.
Kuo T, Damle M, Gonzalez BJ, Egli D, Lazar MA, Accili D. Induction of alpha cell-restricted Gc in dedifferentiating beta cells contributes to stress-induced beta-cell dysfunction. JCI Insight. 2019;5:e128351
Kuo T, Du W, Miyachi Y, et al. Antagonistic epistasis of Hnf4alpha and FoxO1 metabolic networks through enhancer interactions in beta-cell function. Mol Metab. 2021;53:101256.
Chung WK, Erion K, Florez JC, et al. Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43:1617–35.
Skyler JS, Bakris GL, Bonifacio E, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. 2017;66:241–55.
Petersen MC, Shulman GI. Mechanisms of insulin action and insulin resistance. Physiol Rev. 2018;98:2133–223.
Weyer C, Hanson RL, Tataranni PA, Bogardus C, Pratley RE. A high fasting plasma insulin concentration predicts type 2 diabetes independent of insulin resistance: evidence for a pathogenic role of relative hyperinsulinemia. Diabetes. 2000;49:2094–101.
Weyer C, Bogardus C, Mott DM, Pratley RE. The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J Clin Invest. 1999;104:787–94.
Ferrannini E, Natali A, Muscelli E, et al. Natural history and physiological determinants of changes in glucose tolerance in a non-diabetic population: the RISC Study. Diabetologia. 2011;54:1507–16.
Haeusler RA, McGraw TE, Accili D. Biochemical and cellular properties of insulin receptor signalling. Nat Rev Mol Cell Biol. 2018;19:31–44.
Nolan JJ, Ludvik B, Beerdsen P, Joyce M, Olefsky J. Improvement in glucose tolerance and insulin resistance in obese subjects treated with troglitazone [see comments]. N Engl J Med. 1994;331:1188–93.
Rosen CJ. Revisiting the rosiglitazone story–lessons learned. N Engl J Med. 2010;363:803–6.
Davidson MA, Mattison DR, Azoulay L, Krewski D. Thiazolidinedione drugs in the treatment of type 2 diabetes mellitus: past, present and future. Crit Rev Toxicol. 2018;48:52–108.
Leahy JL. Thiazolidinediones in prediabetes and early type 2 diabetes: what can be learned about that disease’s pathogenesis. Curr DiabRep. 2009;9:215–20.
CAS Google Scholar
Kraakman MJ, Liu Q, Postigo-Fernandez J, et al. PPARgamma deacetylation dissociates thiazolidinedione’s metabolic benefits from its adverse effects. J Clin Invest. 2018;128:2600–12.
Liu L, Fan L, Chan M, et al. PPARgamma deacetylation confers the antiatherogenic effect and improves endothelial function in diabetes treatment. Diabetes. 2020;69:1793–803.
Gavin JR 3rd, Roth J, Neville DM Jr, de Meyts P, Buell DN. Insulin-dependent regulation of insulin receptor concentrations: a direct demonstration in cell culture. Proc Natl Acad Sci USA. 1974;71:84–8.
Ferrannini E, Muscelli E, Natali A, et al. Association of fasting glucagon and proinsulin concentrations with insulin resistance. Diabetologia. 2007;50:2342–7.
Poy MN, Yang Y, Rezaei K, et al. CEACAM1 regulates insulin clearance in liver. Nat Genet. 2002;30:270–6.
Olefsky JM. Decreased insulin binding to adipocytes and circulating monocytes from obese subjects. J Clin Invest. 1976;57:1165–72.
Freidenberg GR, Reichart D, Olefsky JM, Henry RR. Reversibility of defective adipocyte insulin receptor kinase activity in non-insulin-dependent diabetes mellitus. Effect of weight loss. J Clin Invest. 1988;82:1398–406.
Tsuchiya K, Tanaka J, Shuiqing Y, et al. FoxOs integrate pleiotropic actions of insulin in vascular endothelium to protect mice from atherosclerosis. Cell Metab. 2012;15:372–81.
Dong XC, Copps KD, Guo S, et al. Inactivation of hepatic Foxo1 by insulin signaling is required for adaptive nutrient homeostasis and endocrine growth regulation. Cell Metab. 2008;8:65–76.
Kubota N, Kubota T, Itoh S, et al. Dynamic functional relay between insulin receptor substrate 1 and 2 in hepatic insulin signaling during fasting and feeding. Cell Metab. 2008;8:49–64.
Accili D. Insulin action research and the future of diabetes treatment: The 2017 Banting Medal for Scientific Achievement lecture. Diabetes. 2018;67:1701–9.
Golay A, DeFronzo RA, Ferrannini E, et al. Oxidative and non-oxidative glucose metabolism in non-obese type 2 (non-insulin-dependent) diabetic patients. Diabetologia. 1988;31:585–91.
Kelley DE, Mandarino LJ. Fuel selection in human skeletal muscle in insulin resistance: a reexamination. Diabetes. 2000;49:677–83.
Nandi A, Kitamura Y, Kahn CR, Accili D. Mouse models of insulin resistance. Physiol Rev. 2004;84:623–47.
McGarry JD. What if Minkowski had been ageusic? An alternative angle on diabetes. Science. 1992;258:766–70.
Haeusler RA, Accili D. The double life of Irs. Cell Metab. 2008;8:7–9.
Brown MS, Goldstein JL. Selective versus total insulin resistance: a pathogenic paradox. Cell Metab. 2008;7:95–6.
Bergman RN, Iyer MS. Indirect regulation of endogenous glucose production by insulin: the single gateway hypothesis revisited. Diabetes. 2017;66:1742–7.
Biddinger SB, Hernandez-Ono A, Rask-Madsen C, et al. Hepatic insulin resistance is sufficient to produce dyslipidemia and susceptibility to atherosclerosis. Cell Metab. 2008;7:125–34.
Inagaki T, Dutchak P, Zhao G, et al. Endocrine regulation of the fasting response by PPARalpha-mediated induction of fibroblast growth factor 21. Cell Metab. 2007;5:415–25.
Qiang L, Accili D. FGF21 and the second coming of PPARgamma. Cell. 2012;148:397–8.
Kharitonenkov A, Shiyanova TL, Koester A, et al. FGF-21 as a novel metabolic regulator. J Clin Invest. 2005;115:1627–35.
Haeusler RA, Pratt-Hyatt M, Welch CL, Klaassen CD, Accili D. Impaired generation of 12-hydroxylated bile acids links hepatic insulin signaling with dyslipidemia. Cell Metab. 2012;15:65–74.
Langlet F, Haeusler RA, Linden D, et al. Selective inhibition of FOXO1 activator/repressor balance modulates hepatic glucose handling. Cell. 2017;171(824–835): e818.
Google Scholar
Lee YK, Diaz B, Deroose M, et al. FOXO1 inhibition synergizes with FGF21 to normalize glucose control in diabetic mice. Mol Metab. 2021;49: 101187.
Cerasi E, Luft R. Insulin response to glucose infusion in diabetic and non-diabetic monozygotic twin pairs. Genetic control of insulin response? Acta Endocrinol (Copenh). 1967;55:330–45.
Consortium R. Lack of durable improvements in beta-cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care. 2019;42:1742–51.
Rahier J, Guiot Y, Goebbels RM, Sempoux C, Henquin JC. Pancreatic beta-cell mass in European subjects with type 2 diabetes. Diabetes Obes Metab. 2008;10(Suppl 4):32–42.
Trico D, Natali A, Arslanian S, Mari A, Ferrannini E. Identification, pathophysiology, and clinical implications of primary insulin hypersecretion in nondiabetic adults and adolescents. JCI Insight. 2018;3:e124912
Brunzell JD, Robertson RP, Lerner RL, et al. Relationships between fasting plasma glucose levels and insulin secretion during intravenous glucose tolerance tests. J Clin Endocrinol Metab. 1976;42:222–9.
Matschinsky FM. Glucokinase as glucose sensor and metabolic signal generator in pancreatic beta-cells and hepatocytes. Diabetes. 1990;39:647–52.
Greeley SA, Tucker SE, Worrell HI, Skowron KB, Bell GI, Philipson LH. Update in neonatal diabetes. Curr Opin Endocrinol Diabetes Obes. 2010;17:13–9.
Remedi MS, Nichols CG. Chronic antidiabetic sulfonylureas in vivo: reversible effects on mouse pancreatic beta-cells. PLoS Med. 2008;5: e206.
Seino S, Sugawara K, Yokoi N, Takahashi H. beta-Cell signalling and insulin secretagogues: a path for improved diabetes therapy. Diabetes Obes Metab. 2017;19(Suppl 1):22–9.
Dor Y, Brown J, Martinez OI, Melton DA. Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature. 2004;429:41–6.
Xuan S, Kitamura T, Nakae J, et al. Defective insulin secretion in pancreatic beta cells lacking type 1 IGF receptor. J Clin Invest. 2002;110:1011–9.
Gregg BE, Moore PC, Demozay D, et al. Formation of a human beta-cell population within pancreatic islets is set early in life. J Clin Endocrinol Metab. 2012;97:3197–206.
Halban PA, Polonsky KS, Bowden DW, et al. beta-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. Diabetes Care. 2014;37:1751–8.
Savage PJ, Bennion LJ, Flock EV, et al. Diet-induced improvement of abnormalities in insulin and glucagon secretion and in insulin receptor binding in diabetes mellitus. J Clin Endocrinol Metab. 1979;48:999–1007.
Taylor R, Adamson AJ, Sattar N, Lean MEJ, Mathers JC. Di Rt. VLCD for weight loss and remission of type 2 diabetes?—Authors’ reply. Lancet. 2018;392:1307.
Fiori JL, Shin YK, Kim W, et al. Resveratrol prevents beta-cell dedifferentiation in nonhuman primates given a high-fat/high-sugar diet. Diabetes. 2013;62:3500–13.
Blum B, Roose AN, Barrandon O, et al. Reversal of beta cell de-differentiation by a small molecule inhibitor of the TGFbeta pathway. eLife. 2014;3:e02809.
Chera S, Baronnier D, Ghila L, et al. Diabetes recovery by age-dependent conversion of pancreatic delta-cells into insulin producers. Nature. 2014;514:503–7.
Lenz A, Toren-Haritan G, Efrat S. Redifferentiation of adult human beta cells expanded in vitro by inhibition of the WNT pathway. PLoS ONE. 2014;9: e112914.
Wang Z, York NW, Nichols CG, Remedi MS. Pancreatic beta cell dedifferentiation in diabetes and redifferentiation following insulin therapy. Cell Metab. 2014;19:872–82.
Sheng C, Li F, Lin Z, et al. Reversibility of beta-cell-specific transcript factors expression by long-term caloric restriction in db/db mouse. J Diabetes Res. 2016;2016:6035046.
Van de Casteele M, Leuckx G, Baeyens L, et al. Neurogenin 3+ cells contribute to beta-cell neogenesis and proliferation in injured adult mouse pancreas. Cell Death Dis. 2013;4: e523.
Berkowitz K, Peters R, Kjos SL, et al. Effect of troglitazone on insulin sensitivity and pancreatic beta-cell function in women at high risk for NIDDM. Diabetes. 1996;45:1572–9.
Brand MD. Mitochondrial generation of superoxide and hydrogen peroxide as the source of mitochondrial redox signaling. Free Radic Biol Med. 2016;100:14.
Fan J, Du W, Kim-Muller JY, et al. Cyb5r3 links FoxO1-dependent mitochondrial dysfunction with beta-cell failure. Mol Metab. 2020;34:97–111.
Amo-Shiinoki K, Tanabe K, Hoshii Y, et al. Islet cell dedifferentiation is a pathologic mechanism of long-standing progression of type 2 diabetes. JCI Insight. 2021;6:e143791
Md Moin AS, Dhawan S, Cory M, Butler PC, Rizza RA, Butler AE. Increased frequency of hormone negative and polyhormonal endocrine cells in lean individuals with type 2 diabetes. J Clin Endocrinol Metab. 2016;101:3628–36.
Son J, Ding H, Farb TB, et al. BACH2 inhibition reverses beta cell failure in type 2 diabetes models. J Clin Invest. 2021;131:e153876
Ahuja M, Ammal Kaidery N, Yang L, et al. Distinct Nrf2 signaling mechanisms of fumaric acid esters and their role in neuroprotection against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced experimental Parkinson’s-like disease. J Neurosci. 2016;36:6332–51.
Download references
Acknowledgements
This review is intended to summarize work in the Authors’ laboratory. The reference list reflects this limitation, with apologies to the many colleagues whose contributions could not be cited. This work has been supported by grants from NIH (DK64819, DK57539, DK58282, DK63608, HL87123), Astra-Zeneca, Merck, Takeda, Servier, and the JPB Foundation.
Author information
Authors and affiliations.
Department of Medicine and Berrie Diabetes Center, Vagelos College of Physicians and Surgeons of Columbia University, New York, NY, 10032, USA
Domenico Accili, Wen Du, Wendy McKimpson, Maria Mukhanova, Jinsook Son, Liheng Wang & Hitoshi Watanabe
Department of Endocrinology, Hematology and Gerontology, Chiba University Graduate School of Medicine, Chiba, Chiba, 260-8670, Japan
Takumi Kitamoto
Department of Neurobiology, Physiology, and Behavior, University of California at Davis, Davis, CA, 95616, USA
Department of Medicine and Bioregulatory Science, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Fukuoka, Japan
Yasutaka Miyachi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Domenico Accili .
Ethics declarations
Conflict of interest.
The authors declare no conflict of interest relevant to the material covered in this review.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Accili, D., Du, W., Kitamoto, T. et al. Reflections on the state of diabetes research and prospects for treatment. Diabetol Int 14 , 21–31 (2023). https://doi.org/10.1007/s13340-022-00600-2
Download citation
Received : 27 June 2022
Accepted : 02 August 2022
Published : 07 September 2022
Issue Date : January 2023
DOI : https://doi.org/10.1007/s13340-022-00600-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Metabolic disease
- New generation therapies
- Insulin action
- Dedifferentiation
- Drug target
- Selective insulin sensitizer
- Find a journal
- Publish with us
- Track your research
357 Diabetes Essay Topics & Examples
When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task.
🏆 Best Diabetes Essay Examples & Topics
⭐ most interesting diabetes research paper topics, ✅ simple & easy diabetes essay topics, 🎓 good research topics about diabetes, 💡 interesting topics to write about diabetes, 👍 good essay topics on diabetes, ❓ diabetes research question examples.
- Type 2 Diabetes The two major types of diabetes are type 1 diabetes and type 2 diabetes. Doctor: The first step in the treatment of type 2 diabetes is consumption of healthy diet.
- Living With a Chronic Disease: Diabetes and Asthma This paper will look at the main effects of chronic diseases in the lifestyle of the individuals and analyze the causes and the preventive measures of diabetes as a chronic disease.
- Leadership in Diabetes Management Nurses can collaborate and apply evidence-based strategies to empower their diabetic patients. The involvement of all key stakeholders is also necessary.
- Relation Between Diabetes And Nutrition Any efforts to lessen and eliminate the risk of developing diabetes must involve the dietary habit of limiting the consumption of carbohydrates, sugar, and fats. According to Belfort-DeAguiar and Dongju, the three factors of obesity, […]
- Diabetes Mellitus: Symptoms, Types, Effects Insulin is the hormone that controls the levels of glucose in the blood, and when the pancreas releases it, immediately the high levels are controlled, like after a meal.
- Diabetes Issues: Insulin Price and Unaffordability According to the forecast of researchers from Stanford University, the number of people with type 2 diabetes who need insulin-containing drugs in the world will increase by about 79 million people by 2030, which will […]
- Diabetes Mellitus Management in the Elderly Diabetes mellitus is a health complication involving an increase in the concentration in the concentration of blood sugar either due to a failure by cells to effectively respond to the production of insulin in the […]
- Type 2 Diabetes as a Public Health Issue In recent years, a steady increase in the incidence and prevalence of diabetes is observed in almost all countries of the world.
- Diabetes Self-Management: Evidence-Based Nursing The article by Seley and Weinger, improving diabetes self management attempts to address the possible barriers to patient education and the role of the nurse in assisting the patient to manage diabetes.
- Diabetes Mellitus Type 2: Pathophysiology and Treatment The primary etiologies linked to the patient’s T2DM condition include morbid obesity and family history. The genetic factors implicated in T2DM pathogenesis relate to a family history of the disease.
- The Aboriginal Diabetes Initiative in Canada The ADI’s goal in the CDS was to raise type 2 diabetes awareness and lower the incidence of associated consequences among Aboriginal people.
- Case Study of Patient with DKA and Diabetes Mellitus It is manifested by a sharp increase in glucose levels and the concentration of ketone bodies in the blood, their appearance in the urine, regardless of the degree of violation of the patient’s consciousness.
- Diabetes and Its Economic Effect on Healthcare For many years, there has been an active increase in the number of cases of diabetes of all types among the global population, which further aggravates the situation.
- Nursing Care For the Patient With Diabetes The right diagnosis of a patient’s condition also helps in the administering of the right medication. In this case, the doctor would keep the goal of administering the right medication to the patient.
- The Minority Diabetes Initiative Act’s Analysis The bill provides the right to the Department of Health and Human Services to generate grants to public and nonprofit private health care institutions with the aim of providing treatment for diabetes in minority communities.
- Diabetes Patients’ Long-Term Care and Life Quality Since insulin resistance can be lowered through weight reduction which, in turn, decreases the severity of the condition, it is also often incorporated into the long-term care of patients with Type 2 diabetes.
- Gestational Diabetes in a 38-Year-Old Woman The concept map, created to meet B.’s needs, considers her educational requirements and cultural and racial hurdles to recognize her risk factors and interventions to increase her adherence to the recommended course of treatment.B.said in […]
- Type 2 Diabetes Mellitus and Its Implications You call an ambulance and she is taken in to the ED. Background: Jean is still very active and works on the farm 3 days a week.
- Development of Comprehensive Inpatient and Outpatient Programs for Diabetes Overcoming the fiscal and resource utilization issues in the development of a comprehensive diabetes program is essential for the improvement of health and the reduction of treatment costs.
- Healthcare Cost Depending on Chronic Disease Management of Diabetes and Hypertension A sufficient level of process optimization and the presence of a professional treating staff in the necessary number will be able to help improve the indicators.
- Improving Glycemic Control in Black Patients with Type 2 Diabetes Information in them is critical for answering the question and supporting them with the data that might help to acquire an enhanced understanding of the issue under research. Finally, answering the PICOT question, it is […]
- Shared Decision-Making That Affects the Management of Diabetes The article by Peek et al.is a qualitative study investigating the phenomenon of shared decision-making that affects the management of diabetes. The researchers demonstrate the racial disparity that can arise in the choice of approaches […]
- Managing Obesity as a Strategy for Addressing Type 2 Diabetes When a patient, as in the case of Amanda, requires a quick solution to the existing problem, it is necessary to effectively evaluate all options in the shortest possible time.
- Tests and Screenings: Diabetes and Chronic Kidney Disease The test is offered to patients regardless of gender, while the age category is usually above 45 years. CDC1 recommends doing the test regardless of gender and is conducted once or twice to check the […]
- Obesity Management for the Treatment of Type 2 Diabetes American Diabetes Association states that for overweight and obese individuals with type 2 diabetes who are ready to lose weight, a 5% weight reduction diet, physical exercise, and behavioral counseling should be provided.
- COVID-19 and Diabetes Mellitus Lim et al, in their article, “COVID-19 and diabetes mellitus: from pathophysiology to clinical management”, explored how COVID-19 can worsen the symptoms of diabetes mellitus.
- The Importance of Physical Exercise in Diabetes II Patients The various activities help to improve blood sugar levels, reduce cardiovascular cases and promote the overall immunity of the patient. Subsequently, the aerobic part will help to promote muscle development and strengthen the bones.
- Diabetes Education Workflow Process Mapping DSN also introduces the patient to the roles of specialists involved in managing the condition, describes the patient’s actions, and offers the necessary educational materials.
- Diabetes: Treatment Complications and Adjustments One of the doctor’s main priorities is to check the compatibility of a patient’s medications. The prescriptions of other doctors need to be thoroughly checked and, if necessary, replaced with more appropriate medication.
- The Type 2 Diabetes Mellitus PICOT (Evidence-Based) Project Blood glucose levels, A1C, weight, and stress management are the parameters to indicate the adequacy of physical exercise in managing T2DM.
- Chronic Disease Cost Calculator (Diabetes) This paper aims at a thorough, detailed, and exhaustive explanation of such a chronic disease as diabetes in terms of the prevalence and cost of treatment in the United States and Maryland.
- Diabetes Mellitus Epidemiology Statistics This study entails a standard established observation order from the established starting time to an endpoint, in this case, the onset of disease, death, or the study’s end. It is crucial to state this value […]
- Epidemiology: Type II Diabetes in Hispanic Americans The prevalence of type II diabetes in Hispanic Americans is well-established, and the search for inexpensive prevention methods is in the limelight.
- Diabetes: Risk Factors and Effects Trends in improved medical care and the development of technology and medicine are certainly contributing to the reduction of the problem. All of the above indicates the seriousness of the problem of diabetes and insufficient […]
- Barriers to Engagement in Collaborative Care Treatment of Uncontrolled Diabetes The primary role of physicians, nurses, and other healthcare team members is to provide patients with medical treatment and coordinate that care while also working to keep costs down and expand access.
- Hereditary Diabetes Prevention With Lifestyle Modification Yeast infections between the fingers and toes, beneath the breast, and in or around the genital organs are the common symptoms of type 2 diabetes.
- Health Equity Regarding Type 2 Diabetes According to Tajkarimi, the number of research reports focusing on T2D’s prevalence and characteristics in underserved minorities in the U. Adapting the program’s toolkits to rural Americans’ eating and self-management habits could also be instrumental […]
- Diabetes Mellitus: Treatment Methods Moreover, according to the multiple findings conducted by Park et al, Billeter et al, and Tsilingiris et al, bariatric surgeries have a positive rate of sending diabetes into remission.
- Diagnosing Patient with Insulin-Dependent Diabetes The possible outcomes of the issues that can be achieved are discussing the violations with the patient’s family and convincing them to follow the medical regulations; convincing the girl’s family to leave her at the […]
- Human Service for Diabetes in Late Adulthood The mission of the Georgia Diabetic Foot Care Program is to make a positive difference in the health of persons living with diabetes.
- Diabetes: Symptoms and Risk Factors In terms of the problem, according to estimates, 415 million individuals worldwide had diabetes mellitus in 2015, and it is expected to rise to 642 million by the year 2040.
- Diabetes: Types and Management Diabetes is one of the most prevalent diseases in the United States caused when the body fails to optimally metabolize food into energy.
- Type 2 Diabetes’ Impact on Australian Society Consequently, the most significant impact of the disease is the increased number of deaths among the population which puts their lives in jeopardy. Further, other opportunistic diseases are on the rise lowering the quality of […]
- Epidemiology of Diabetes and Forecasted Trends The authors note that urbanization and the rapid development of economies of different countries are the main causes of diabetes. The authors warn that current diabetes strategies are not effective since the rate of the […]
- Communicating the Issue of Diabetes The example with a CGM sensor is meant to show that doctors should focus on educating people with diabetes on how to manage their condition and what to do in extreme situations.
- Obesity and Diabetes Mellitus Type 2 The goal is to define the features of patient information to provide data on the general course of the illness and its manifestations following the criteria of age, sex, BMI, and experimental data.
- The Prevention of Diabetes and Its Consequences on the Population At the same time, these findings can also be included in educational programs for people living with diabetes to warn them of the risks of fractures and prevent them.
- Uncontrolled Type 2 Diabetes and Depression Treatment The data synthesis demonstrates that carefully chosen depression and anxiety treatment is likely to result in better A1C outcomes for the patient on the condition that the treatment is regular and convenient for the patients.
- Type 2 Diabetes: Prevention and Education Schillinger et al.came to the same conclusion; thus, their findings on the study of the Bigger Picture campaign effectiveness among youth of color are necessary to explore diabetes prevention.
- A Diabetes Quantitative Article Analysis The article “Correlates of accelerometer-assessed physical activity and sedentary time among adults with type 2 diabetes” by Mathe et al.refers to the global issue of the prevention of diabetes and its complications.
- A Type 2 Diabetes Quantitative Article Critique Therefore, the main issue is the prevention of type 2 diabetes and its consequences, and this paper will examine one of the scientific studies that will be used for its exploration.
- The Diabetes Prevention Articles by Ford and Mathe The main goal of the researchers was to measure the baseline MVPA of participants and increase their activity to the recommended 150 minutes per week through their participation in the Diabetes Community Lifestyle Improvement Program.
- Type 2 Diabetes in Hispanic Americans The HP2020 objectives and the “who, where, and when” of the problem highlight the significance of developing new, focused, culturally sensitive T2D prevention programs for Hispanic Americans.
- Diabetes Mellitus as Problem in US Healthcare Simultaneously, insurance companies are interested in decreasing the incidence of diabetes to reduce the costs of testing, treatment, and provision of medicines.
- Diabetes Prevention as a Change Project All of these queries are relevant and demonstrate the importance of including people at high risk of acquiring diabetes in the intervention.
- Evidence Synthesis Assignment: Prevention of Diabetes and Its Complications The purpose of this research is to analyze and synthesize evidence of good quality from three quantitative research and three non-research sources to present the problem of diabetes and justify the intervention to address it.
- Diabetes Mellitus: Causes and Health Challenges Second, the nature of this problem is a clear indication of other medical concerns in this country, such as poor health objectives and strategies and absence of resources.
- Diabetes in Adults in Oxfordshire On a national level, Diabetes Research and Wellness Foundation aims to prevent the spread of the decease through research of the causes and effective treatment of diabetes 2 type.
- Diabetes Mellitus (DM) Disorder Case Study Analysis Thus, informing the patient about the importance of regular medication intake, physical activity, and adherence to diet in maintaining diabetes can solve the problem.
- Diabetes Mellitus in Young Adults Thus, programs for young adults should predominantly focus on the features of the transition from adolescence to adulthood. As a consequence, educational programs on diabetes improve the physical and psychological health of young adults.
- A Healthcare Issue of Diabetes Mellitus Diabetes mellitus is seen as a primary healthcare issue that affects populations across the globe and necessitates the combination of a healthy lifestyle and medication to improve the quality of life of people who suffer […]
- Control of LDL Cholesterol Levels in Patients, Gestational Diabetes Mellitus In addition, some patients with hypercholesterolemia may have statin intolerance, which reduces adherence to therapy, limits treatment efficacy, and increases the risk of CVD.
- Exploring Glucose Tolerance and Gestational Diabetes Mellitus In the case of a glucose tolerance test for the purpose of diagnosing GDM type, the interpretation of the test results is carried out according to the norms for the overall population.
- Type 2 Diabetes Health Issue and Exercise This approach will motivate the patient to engage in exercise and achieve better results while reducing the risk of diabetes-related complications.
- Diabetes Interventions in Children The study aims to answer the PICOT Question: In children with obesity, how does the use of m-Health applications for controlling their dieting choices compare to the supervision of their parents affect children’s understanding of […]
- Diabetes Tracker Device and Its Advantages The proposed diabetes tracker is a device that combines the functionality of an electronic BGL tester and a personal assistant to help patients stick to their diet plan.
- Disease Management for Diabetes Mellitus The selection of the appropriate philosophical and theoretical basis for the lesson is essential as it allows for the use of an evidence-based method for learning about a particular disease.
- Latino People and Type 2 Diabetes The primary aim of the study is to determine the facilitators and barriers to investigating the decision-making process in the Latin population and their values associated with type 2 diabetes.
- Diabetes Self-Management Education and Support Program The choice of this topic and question is based on the fact that despite the high prevalence of diabetes among adolescents in the United States, the use of DSMES among DM patients is relatively low, […]
- Diabetes Mellitus Care Coordination The aim is to establish what medical technologies, care coordination and community resources, and standards of nursing practice contribute to the quality of care and safety of patients with diabetes.
- Healthy Lifestyle Interventions in Comorbid Asthma and Diabetes In most research, the weight loss in cases of comorbid asthma and obesity is reached through a combination of dietary interventions and physical exercise programs.
- PDSA in Diabetes Prevention The second step in the “Do” phase would be to isolate a few members of the community who are affected by diabetes voluntarily.
- Diabetes: Statistics, Disparities, Therapies The inability to produce adequate insulin or the body’s resistance to the hormone is the primary cause of diabetes. Diabetes is a serious health condition in the U.S.and the world.
- Type 2 Diabetes Prescriptions and Interventions The disadvantage is the difficulty of obtaining a universal model due to the complexity of many factors that can affect the implementation of recommendations: from the variety of demographic data to the patient’s medical history.
- Health Education for Female African Americans With Diabetes In order to address and inform the public about the challenges, nurses are required to intervene by educating the population on the issues to enhance their understanding of the risks associated with the conditions they […]
- Diabetes Risk Assessment and Prevention It is one of the factors predisposing patients suffering from diabetes to various cardiovascular diseases. With diabetes, it is important to learn how to determine the presence of carbohydrates in foods.
- Diabetes Mellitus: Preventive Measures In addition to addressing the medical specialists who will be of service in disease prevention, it will emphasize the intervention programs required to help control the spread of the illness.
- “The Diabetes Online Community” by Litchman et al. The researchers applied the method of telephone interviews to determine the results and effectiveness of the program. The study described the value of DOC in providing support and knowledge to older diabetes patients.
- Mobile App for Improved Self-Management of Type 2 Diabetes The central focus of the study was to assess the effectiveness of the BlueStar app in controlling glucose levels among the participants.
- Type 2 Diabetes in Minorities from Cultural Perspective The purpose of this paper is to examine the ethical and cultural perspectives on the issue of T2DM in minorities. Level 2: What are the ethical obstacles to treating T2DM in ethnic and cultural minorities?
- Ethics of Type 2 Diabetes Prevalence in Minorities The purpose of this article analysis is to dwell on scholarly evidence that raises the question of ethical and cultural aspects of T2DM prevalence in minorities.
- Type 2 Diabetes in Minorities: Research Questions The Level 2 research questions are: What are the pathophysiological implications of T2DM in minorities? What are the statistical implications of T2DM in minorities?
- Improving Adherence to Diabetes Treatment in Primary Care Settings Additionally, the patients from the intervention group will receive a detailed explanation of the negative consequences of low adherence to diabetes treatment.
- An Advocacy Tool for Diabetes Care in the US To ensure the implementation and consideration of my plea, I sent a copy of the letter to the government officials so it could reach the president.
- Diabetes and Allergies: A Statistical Check The current dataset allowed us to test the OR for the relationship between family history of diabetes and the presence of diabetes in a particular patient: all variables were dichotomous and discrete and could take […]
- Type 2 Diabetes in Adolescents According to a National Diabetes Statistics Report released by the Centers for Disease Control and Prevention, the estimated prevalence of the disease was 25 cases per 10,000 adolescents in 2017. A proper understanding of T2D […]
- Analysis of Diabetes and Its Huge Effects In the US, diabetes is costly to treat and has caused much physical, emotional and mental harm to the people and the families of those who have been affected by the disease.
- Nursing: Self-Management of Type II Diabetes Sandra Fernandes and Shobha Naidu’s journal illustrates the authors’ understanding of a significant topic in the nursing profession.”Promoting Participation in self-care management among patients with diabetes mellitus” article exposes readers to Peplau’s theory to understand […]
- The Impact of Vegan and Vegetarian Diets on Diabetes Vegetarian diets are popular for a variety of reasons; according to the National Health Interview Survey in the United States, about 2% of the population reported following a vegetarian dietary pattern for health reasons in […]
- “Diabetes Prevention in U.S. Hispanic Adults” by McCurley et al. This information allows for supposing that face-to-face interventions can be suitable to my practicum project that considers measures to improve access to care among African Americans with heart failure diseases. Finally, it is possible to […]
- Diabetes Disease of the First and Second Types It is a decrease in the biological response of cells to one or more effects of insulin at its average concentration in the blood. During the first type of diabetes, insulin Degludec is required together […]
- The Trend of the Higher Prevalence of Diabetes According to the CDC, while new cases of diabetes have steadily decreased over the decades, the prevalence of the disease among people aged below twenty has not.
- Person-Centered Strategy of Diabetes and Dementia Care The population of focus for this study will be Afro-American women aged between sixty and ninety who have diabetes of the second type and dementia or are likely to develop dementia in the future.
- Video Consultations Between Patients and Clinicians in Diabetes, Cancer, and Heart Failure Services For example, during one of my interactions with the patient, I was asked whether the hospital had the policy to avoid face-to-face interaction during the pandemic with the help of video examinations.
- Diets to Prevent Heart Disease, Cancer, and Diabetes In order to prevent heart disease, cancer, and diabetes, people are required to adhere to strict routines, including in terms of diet. Additionally, people wanting to prevent heart disease, cancer, and diabetes also need to […]
- The Centers for Diabetes’ Risks Assessment In general, the business case for the Centers for Diabetes appears to be positive since the project is closely aligned with the needs of the community and the targets set by the Affordable Care Act.
- Diabetes Management: Case Study Type 1 and Type 2 diabetes contrast based on their definitions, the causes, and the management of the conditions. Since the CDC promotes the avoidance of saturated fat and the increase of fiber intake for […]
- Intervention Methods for Type 2 Diabetes Mellitus An individual should maintain a regulated glycemic control using the tenets of self-management to reduce the possibility of complications related to diabetes.
- Diabetes Mellitus as Leading Cause of Disability The researchers used data from the Centers for Disease Control and Prevention, where more than 12% of older people in the US live with the condition.
- Depression in Diabetes Patients The presence of depression concomitant to diabetes mellitus prevents the adaptation of the patient and negatively affects the course of the underlying disease.
- The Relationship Between Diabetes and COVID-19 After completing the research and analyzing the articles, it is possible to suggest a best practice that may be helpful and effective in defining the relationship between diabetes and COVID-19 and providing a way to […]
- Pre-diabetes and Urinary Incontinence Most recent reports indicate that a physiotherapy procedure gives a positive result in up to 80% of patients with stage I or SUI and mixed form and 50% of patients with stage II SUI.
- Type 1 Diabetes: Recommendations for Alternative Drug Treatments Then, they have to assess the existing levels of literacy and numeracy a patient has. Tailoring educational initiatives to a person’s unique ethnic and cultural background is the basis of cultural competence in patient education.
- Type 2 Diabetes: A Pharmacologic Update Diabetes presents one of the most common diagnoses in causes of ED visits among adults and one of the leading causes of death in the United States.
- Type 2 Diabetes and Its Treatment The main difference in type 2 diabetes is the insensitivity of the body’s cells to the action of the hormone insulin and their insulin resistance.
- Diabetes: Vulnerability, Resilience, and Care In nursing care, resilience is a critical concept that shows the possibility of a person to continue functioning and meeting objectives despite the existing challenges.
- Diabetes Prevention in the United States The analysis of these policies and the other strategies provides the opportunity to understand what role they might play in the improvement of human health. NDPP policy, on the other hand, emphasizes the role of […]
- Teaching Experience: Diabetes Prevention The primary objective of the seminar is to reduce the annual number of diabetes cases and familiarize the audience with the very first signs of this disease.
- Summary of Type 2 Diabetes: A Pharmacologic Update The authors first emphasize that T2D is one of the most widespread diseases in the United States and the seventh leading cause of death.
- Insulin Effects in a Diabetes Person I will use this source to support my research because the perception of diabetes patients on insulin therapy is essential for understanding the impact they cause on the person.
- Diabetes and Medical Intervention In the research conducted by Moin et al, the authors attempted to define the scope of efficiency of such a tool as an online diabetes prevention program in the prevention of diabetes among obese/overweight population […]
- Diabetes Mellitus Type 2 and a Healthy Lifestyle Relationship The advantage of this study over the first is that the method uses a medical approach to determining the level of fasting glucose, while the dependences in the study of Ugandans were found using a […]
- Diabetes: Epidemiological Analysis I would like to pose the following question: how can epidemiology principles be applied to these statistics for further improvements of policies that aim to reduce the impact of diabetes on the U.S.population? The limited […]
- Pathogenesis and Prevention of Diabetes Mellitus and Hypertension The hormone is produced by the cells of the islets of Langerhans found in the pancreas. It is attributed to the variation in the lifestyle of these individuals in these two geographical zones.
- Parental Intervention on Self-Management of an Adolescent With Diabetes Diabetes development and exposure are strongly tied to lifestyle, and the increasing incidents rate emphasizes the severity of the population’s health problem.
- Addressing the Needs of Hispanic Patients With Diabetes Similarly, in the program at hand, the needs of Hispanic patients with diabetes will be considered through the prism of the key specifics of the community, as well as the cultural background of the patients.
- Diabetes: Epidemiologic Study Design For instance, the range of their parents’ involvement in the self-management practices can be a crucial factor in treatment and control.
- What to Know About Diabetes? Type 1 diabetes is caused by autoimmune reaction that prevent realization of insulin in a body. Estimated 5-10% of people who have diabetes have type 1.
- Diabetes in Saudi Arabia It is expected that should this underlying factor be discovered, whether it is cultural, societal, or genetic in nature, this should help policymakers within Saudi Arabia create new governmental initiatives to address the problem of […]
- “Medical Nutrition Therapy: A Key to Diabetes Management and Prevention” Article Analysis In the process of MNT application, the dietitian keeps a record of the changes in the main components of food and other components of the blood such as blood sugars to determine the trend to […]
- Nutrition and Physical Activity for Children With a Diabetes When a child understands that the family supports him or her, this is a great way to bring enthusiasm in dealing with the disease.
- Global and Societal Implications of the Diabetes Epidemic The main aim of the authors of this article seems to be alerting the reader on the consequences of diabetes to the society and to the whole world.
- Diabetes and Hypertension Avoiding Recommendations Thus, the promotion of a healthy lifestyle should entail the encouragement of the population to cease smoking and monitor for cholesterol levels.
- Pregnant Women With Type I Diabetes: COVID-19 Disease Management The grounded theory was selected for the given topic, and there are benefits and drawbacks of utilizing it to study the experiences of pregnant women with type I diabetes and COVID-19.
- Current Recommendations for the Glycemic Control in Diabetes Management of blood glucose is one of the critical issues in the care of people with diabetes. Therefore, the interval of the A1C testing should also depend on the condition of the patient, the physician’s […]
- Diabetes Mellitus: Types, Causes, Presentation, Treatment, and Examination Diabetes mellitus is a chronic endocrinologic disease, which is characterized by increased blood glucose concentration.
- Diabetes Problem at Country Walk Community: Intervention and Evaluation This presentation develops a community health nursing intervention and evaluation tool for the diabetes problem affecting Country Walk community.
- Communication Challenges Between Nurses and Patients With Type 2 Diabetes According to Pung and Goh, one of the limitations of communication in a multicultural environment is the language barrier that manifests itself in the direct interaction of nurses with patients and in the engagement work […]
- Diabetes Type 2 from Management Viewpoint Demonstrate the effects of type 2 diabetes and provide background information on the disease; Discuss the management plans of diabetes centers and critically analyze the frameworks implemented in the hospitals; Examine the existing methodology models […]
- Nursing Plan for the Patient with Diabetes Type 2, HTN, and CAD The health of the population is the most valuable achievement of society, so the preservation and strengthening of it is an essential task in which everyone should participate without exception.
- Diagnosis and Classification of Diabetes Mellitus Diabetes is a serious public health concern that introduces a group of metabolic disorders caused by changes in the sugar blood level.
- Diabetes Mellitus Type II: A Case of a Female Adult Patient In this presentation, we are going to develop a care plan for a 47-year-old woman with a 3-year-old history of Diabetes Mellitus Type 2 (also known as Type II DM).
- Diabetes Insipidus: Disease Process With Implications for Healthcare Professionals This presentation will consider the topic of Diabetes Insipidus (DI) with a focus on its etiology and progress.
- The Nature of Type 1 Diabetes Mellitus Type 1 diabetes mellitus is a chronic autoimmune disease that has an active genetic component, which is identified by increased blood glucose levels, also known as hyperglycemia.
- A Study of Juvenile Type 1 Diabetes in the Northwest of England The total number of children under seventeen years living with type 1 diabetes in North West England by 2009 was 2,630.
- Imperial Diabetes Center Field Study The purpose is to examine the leadership’s practices used to maintain and improve the quality and safety standards of the facility and, using the observations and scholarly research, offer recommendations for improvement.
- Diabetes Risk Assessment After completing the questionnaire, I learned that my risk for the development of diabetes is above average. Modern risk assessment tools allow identifying the current state of health and possibilities of developing the disease.
- The Role of Telenursing in the Management of Diabetes Type 1 Telemedicine is the solution that could potentially increase the coverage and improve the situation for many t1DM patients in the world.
- Health Issues of Heart Failure and Pediatric Diabetes As for the population, which is intended to participate in the research, I am convinced that there is the need to specify the patients who should be examined and monitored.
- Juvenile Diabetes: Demographics, Statistics and Risk Factors Juvenile diabetes, also referred to as Type 2 diabetes or insulin-dependent diabetes, describes a health condition associated with the pancreas’s limited insulin production. The condition is characterized by the destruction of the cells that make […]
- Diabetes Mellitus: Pathophysiologic Processes The main function of insulin produced by cells within the pancreas in response to food intake is to lower blood sugar levels by the facilitation of glucose uptake in the cells of the liver, fat, […]
- Type 2 Diabetes Management in Gulf Countries One such study is the systematic review on the quality of type 2 diabetes management in the countries of the cooperation council for the Arab states of the Gulf, prepared by Alhyas, McKay, Balasanthiran, and […]
- Patient with Ataxia and Diabetes Mellitus Therefore, the therapist prioritizes using the cushion to the client and persuades the patient to accept the product by discussing the merits of the infinity cushion with a low profile in enabling the customer to […]
- Diabetes Evidence-Based Project: Disseminating Results In this presentation, the involvement of mentors and collaboration with administration and other stakeholders are the preferred steps, and the idea to use social networking and web pages has to be removed.
- The Problem of Diabetes Among African Americans Taking into consideration the results of the research and the information found in the articles, the problem of diabetes among African Americans has to be identified and discussed at different levels.
- Childhood Obesity, Diabetes and Heart Problems Based on the data given in the introduction it can be seen that childhood obesity is a real problem within the country and as such it is believed that through proper education children will be […]
- Hypertension and Antihypertensive Therapy and Type 2 Diabetes Mellitus In particular, Acebutolol impairs the functions of epinephrine and norepinephrine, which are neurotransmitters that mediate the functioning of the heart and the sympathetic nervous system.
- Adult-Onset Type 2 Diabetes: Patient’s Profile Any immediate care as well as post-discharge treatment should be explained in the best manner possible that is accessible and understandable to the patient.
- Diabetes: Diagnosis and Treatment The disease is characterized by the pancreas almost not producing its own insulin, which leads to an increase in glucose levels in the blood.
- How to Manage Type 2 Diabetes The article is significant to the current research problem as the researchers concluded that the assessment of metabolic processes in diabetic patients was imperative for adjusting in the management of the condition.
- Type 2 Diabetes Analysis Thus, type 2 diabetes has medical costs, or the difficulties of coping up with the illness, economic ones, which are the financial costs of managing it, and the organizational ones for the healthcare systems.
- Clinical Trial of Diabetes Mellitus On the other hand, type II diabetes mellitus is caused by the failure of the liver and muscle cells to recognize the insulin produced by the pancreatic cells.
- Diabetes: Diagnosis and Related Prevention & Treatment Measures The information presented on the articles offers an insight in the diagnosis of diabetes among various groups of persons and the related preventive and treatment measures. The study identified 3666 cases of initial stages of […]
- Reinforcing Nutrition in Schools to Reduce Diabetes and Childhood Obesity For example, the 2010 report says that the rates of childhood obesity have peaked greatly compared to the previous decades: “Obesity has doubled in Maryland over the past 20 years, and nearly one-third of youth […]
- The Connection Between Diabetes and Consuming Red Meat In light of reporting the findings of this research, the Times Healthland gave a detailed report on the various aspects of this research.
- Synthesizing the Data From Relative Risk Factors of Type 2 Diabetes Speaking of such demographic factors as race, the white population suffers from it in the majority of cases, unlike the rest of the races, the remaining 0.
- Using Exenatide as Treatment of Type 2 Diabetes Mellitus in Adults Kendal et al.analyzed the effects of exenatide as an adjunct to a combination of metformin and sulfonylurea against the combination of the same drugs without the adjunct.
- Enhancing Health Literacy for People With Type 2 Diabetes Two professionals, Andrew Long, a professor in the school of heath care in the University of Leeds, and Tina Gambling, senior lecturer in the school of health care studies from the University of Cardiff, conducted […]
- The Scientific Method of Understanding if Coffee Can Impact Diabetes The hypothesis of the experiment ought to be straightforward and understandable. The control group and the experiment group for the test are then identified.
- Gestational Diabetes Mellitus: Review This is because of the current patterns that show an increase in the prevalence of diabetes in offspring born to mothers with GDM.
- Health Service Management of Diabetes
- Necrotizing Fasciitis: Pathophysiology, Role of Diabetes
- The Benefits of Sharing Knowledge About Diabetes With Physicians
- Gestational Diabetes Mellitus – NSW, Australia
- Health and Wellness: Stress, Diabetes and Tobacco Related Problems
- 52-Year-Old Female Patient With Type II Diabetes
- Healthy People Project: Personal Review About Diabetes
- Nursing Diagnosis: Type 1 Diabetes & Hypertension
- Nursing Care Development Plan for Diabetes and Hypertension
- Coronary Heart Disease Aggravated by Type 2 Diabetes and Age
- Diabetes as the Scourge of the 21st Century: Locating the Solution
- Psychosocial Implications of Diabetes Management
- Gestational Diabetes in a Pregnant Woman
- Diabetes Mellitus: Prominent Metabolic Disorder
- Holistic Approach to Man’s Health: Diabetes Prevention
- Holistic Image in Prevention of Diabetes
- Educational Strategies for Diabetes to Patients
- Diabetes and Obesity in the United Arab Emirates
- Epidemiological Problem: Diabetes in Illinois
- Diabetes as a Chronic Condition
- Managing Diabetes Through Genetic Engineering
- Diabetes, Functions of Insulin, and Preventive Practices
- Treating of Diabetes in Adults
- Counseling and Education Session in Type II Diabetes
- Diabetes II: Reduction in the Incidence
- Community Health Advocacy Project: Diabetes Among Hispanics
- Community Health Advocacy Project: Hispanics With Diabetes
- Hispanics Are More Susceptible to Diabetes That Non-Hispanics
- Rates Diabetes Between Hispanics Males and Females
- Diabetes Mellitus and HFSON Conceptual Framework
- Prince Georges County Community Health Concern: Diabetes
- Fats and Proteins in Relation to Type 2 Diabetes
- Alcohol Interaction With Medication: Type 2 Diabetes
- Diabetes Management and Evidence-Based Practice
- Critical Analysis of Policy for Type 2 Diabetes Mellitus in Australia
- The Treatment and Management of Diabetes
- Obesity and Diabetes: The Enemies Within
- Impact of Diabetes on the United Arab Emirates’ Economy
- Childhood Obesity and Type 2 Diabetes
- Health Nursing and Managing Diabetes
- Diabetes Management: How Lifestyle, Daily Routine Affect Blood Sugar
- Diabetes Management: Diagnostics and Treatment
- Diabetes Mellitus Type 2: The Family Genetic History
- Diabetes Type II: Hormonal Mechanism and Intracellular Effects of Insulin
- Social, Behavioral, and Psychosocial Causes of Diseases: Type 2 Diabetes
- Supportive Intervention in the Control of Diabetes Mellitus
- Enhancing Foot Care Practices in Patients With Diabetes
- Community Health Promotion: The Fight Against Diabetes in a Community Setting
- Diabetes in Australia and Saudi Arabia
- Diabetes: The Advantages and Disadvantages of Point of Care Testing
- Diabetes Mellitus Type 2 or Non-Insulin-Dependent Diabetes Mellitus
- Qualitative Research in Diabetes Management in Elderly Patient
- Diabetes Prevention Measures in the Republic of the Marshall Islands
- Impact of Diabetes on Healthcare
- Gestational Diabetes: American Diabetes Association Publishers
- Health Promotion: Diabetes Mellitus and Comorbidities
- Gestational Diabetes: Child Bearing Experience
- Diabetes Mellitus Effects on Periodontal Disease
- Diabetes Type II Disease in the Community
- The Relationship of Type 2 Diabetes and Depression
- Glycemic Control in Individuals With Type 2 Diabetes
- The Diagnosis of Diabetes in Older Adults and Adolescents
- Physical Activity in Managing Type-2 Diabetes
- High Risk of Developing Type 1 and Type 2 Diabetes Mellitus
- Children With Type 1 Diabetes in Clinical Practice
- Type 2 Diabetes Treatment Analysis
- Type 2 Diabetes Mellitus: Revealing the Diagnosis
- The Type 2 Diabetes Prevention: Lifestyle Choices
- Indigenous and Torres Strait Population and Diabetes
- Interpretation of the Diabetes Interview Transcript
- Type 1 Diabetes: Using Glucose Monitoring in Treatment
- Managing Type 2 Diabetes Patients’ Blood Sugar Prior to and After Surgical Procedures
- Dubai Diabetes… We Care: Leaflet Review
- Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes: Medical Terminology Definition
- Modern Diabetes Treatment Tools
- Diabetes: Encapsulation to Treat a Disease
- Current Dietary for the Treatment of Diabetes
- Diabetes: Discussion of the Disease
- Stranahan on Diabetes Impairs Hippocampal Function
- A Clinical-Based Study of Young Adults Who Have Diabetes
- Panax Ginseng for Diabetes Treatment
- Depression and Diabetes Association in Adults
- Is There Anu Cure For Diabetes?
- Diabetes Type 2 in Children: Causes and Effects
- Type 1 Diabetes Mellitus Case
- Health, Culture, and Identity as Diabetes Treatment Factors
- Diabetes Prevention in Chinese Elderly in Hunan
- “Experiences of Patients With Type 2 Diabetes Starting Insulin Therapy” by Phillips
- Type 2 Diabetes: Nursing Change Project
- Diabetes and Health Promotion Concepts
- Type 2 Diabetes Project Results Dissemination
- Type 2 Diabetes in Geriatric Patients
- Type 2 Diabetes and Geriatric Evidence-Based Care
- Cultural Empowerment. Diabetes in Afro-Americans
- Diabetes Self-Management: Relationships & Expectations
- Diagnosis and Classification of Diabetes Mellitus
- Improving Comprehensive Care for Patients With Diabetes
- Diabetes Impact on Cardiovascular and Nervous Systems
- Side Effects of Metformin in Diabetes Treatment
- Type 2 Diabetes and Drug Treatments
- Diabetes Mellitus and Health Determinants
- Nursing Leadership in Diabetes Management
- Diabetes Education for African American Women
- Latent Autoimmune Adult Diabetes
- Obesity: Epidemiology and Health Consequences
- Diabetes in Urban Cities of United States
- Diabetes in Australia: Analysis
- Type 2 Diabetes in the Afro-American Bronx Community
- Type 2 Diabetes From Cultural and Genetic Aspects
- Type 2 Diabetes in Bronx: Evidence-Based Practice
- Type 2 Diabetes in Bronx Project for Social Change
- Cardiovascular Care in Type 2 Diabetes Patients
- Ambition Diabetes and Diet on Macbeths’ Example
- Diabetes as Community Health Issue in the Bronx
- Diabetes Management Plan: Diagnosis and Development
- Diabetes Treatment and Care
- Transition from Pediatric to Adult Diabetes Care
- Diabetes Awareness Program and Strategic Planning
- Diabetes: Disease Control and Investigation
- Diabetes Pain Questionnaire and Patient Feedback
- Perception of Diabetes in the Hispanic Population
- Clinical Studies of Diabetes Mellitus
- Diabetes Mellitus and Problems at Work
- Diabetes in the US: Cost Effectiveness Analysis
- Diabetes Investigation in Space Flight Research
- Diabetes Care Advice by Food and Drug Administration
- Artificial Intelligence for Diabetes: Project Experiences
- Chronic Care Model for Diabetes Patients in the UAE
- Diabetes Among British Adults and Children
- Endocrine Disorders: Diabetes and Fibromyalgia
- Future Technologies: Diabetes Treatment and Care
- Epidemiology of Type 1 Diabetes
- Diabetes: Treatment Technology and Billing
- Pathophysiology of Mellitus and Insipidus Diabetes
- Cure for Diabetes: The Impossible Takes a Little Longer
- Stem Cell Therapy as a Potential Cure for Diabetes
- Stem Cell Therapy and Diabetes Medical Research
- Type II Diabetes Susceptibility and Socioeconomic Status
- Obesity and Hypertension in Type 2 Diabetes Patients
- Strongyloides Stercoralis Infection and Type 2 Diabetes
- Socioeconomic Status and Susceptibility to Type II Diabetes
- Diabetes Mellitus: Differential Diagnosis
- Diabetes Disease in the USA Adults
- Education for African Americans With Type 2 Diabetes
- Diabetes Treatment and Funding in Fulton County
- Diabetes Care: Leadership and Strategy Plan
- Diabetes Mellitus’ New Treatment: Principles and Process
- Diet and Nutrition: European Diabetes
- Preventing the Proliferation Diabetes
- Diabetes: Symptoms, Treatment, and Prevention
- Diabetes and Cardiovascular Diseases in Medicine
- Ecological Models to Deal with Diabetes in Medicine
- Different Types of Diabetes Found in Different Countries
- Analysis of Program “Prevent Diabetes Live Life Well”
- The Effect of Physical, Social, and Health Variables on Diabetes
- Micro and Macro-Cosmos in Medicine and Care Models for Prevention of Diabetes
- Why Qualitative Method Was Chosen for Diabetes Program Evaluation
- Humanistic Image of Managing Diabetes
- Diabetes mellitus Education and hemoglobin A1C level
- Obesity, Diabetes and Heart Disease
- Illuminate Diabetes Event Design
- Cause and Diagnosis of Type 2 diabetes
- Patient Voices: Type 2 Diabetes. Podcast Review
- Type I Diabetes: Pathogenesis and Treatment
- Human Body Organ Systems Disorders: Diabetes
- Age Influence on Physical Activity: Exercise and Diabetes
- Hemoglobin A1C Test for Diabetes
- Why Injury and Diabetes Have Been Identified as National Health Priority?
- What Factors Are Involved in the Increasing Prevalence of Type II Diabetes in Adolescents?
- Does the Socioeconomic Position Determine the Incidence of Diabetes?
- What Are the Four Types of Diabetes?
- How Fat and Obesity Cause Diabetes?
- How Exercise Affects Type 2 Diabetes?
- How Does the Treatment With Insulin Affect Type 2 Diabetes?
- How Diabetes Does Cause Depression?
- Does Diabetes Prevention Pay For Itself?
- How Does Snap Participation Affect Rates of Diabetes?
- Does Overeating Sugar Cause Diabetes, Cavities, Acne, Hyperactivity and Make You Fat?
- Why Diabetes Mellitus and How It Affects the United States?
- Does Alcohol Decrease the Risk of Diabetes?
- How Does a Person With Diabetes Feel?
- Does Periodontal Inflammation Affect Type 1 Diabetes in Childhood and Adolescence?
- How Can the Paleolithic Diet Control Type 2 Diabetes?
- How Does Insulin Help Diabetes Be Controlled?
- Does Economic Status Matter for the Regional Variation of Malnutrition-Related Diabetes?
- How Can Artificial Intelligence Technology Be Used to Treat Diabetes?
- What Are the Main Causes and Treatments of Diabetes?
- What Evidence Exists for Treatments Depression With Comorbid Diabetes Using Traditional Chinese Medicine and Natural Products?
- Why Was Qualitative Method Chosen for Diabetes Program Evaluation?
- What Are the Three Types of Diabetes?
- How Does Poverty Affect Diabetes?
- What Is the Leading Cause of Diabetes?
- How Is Diabetes Diagnosed?
- What Are the Main Symptoms of Diabetes?
- How Diabetes Adversely Affects Your Body?
- What Are the Most Common Symptoms of Undiagnosed Diabetes?
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 25). 357 Diabetes Essay Topics & Examples. https://ivypanda.com/essays/topic/diabetes-essay-examples/
"357 Diabetes Essay Topics & Examples." IvyPanda , 25 Feb. 2024, ivypanda.com/essays/topic/diabetes-essay-examples/.
IvyPanda . (2024) '357 Diabetes Essay Topics & Examples'. 25 February.
IvyPanda . 2024. "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
1. IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
Bibliography
IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
- Disease Questions
- Health Promotion Research Topics
- Metabolism Research Topics
- Healthcare Questions
- Obesity Ideas
- Heart Failure Titles
- Childhood Obesity Research Ideas
- Epigenetics Essay Titles
- Alcohol Abuse Paper Topics
- Pathogenesis Research Ideas
- Therapeutics Research Ideas
- Hypertension Topics
- Osteoarthritis Ideas
- Cardiomyopathy Titles
- Malnutrition Titles
This paper is in the following e-collection/theme issue:
Published on 2.4.2024 in Vol 26 (2024)
The Impact of Digital Self-Monitoring of Weight on Improving Diabetes Clinical Outcomes: Quasi-Randomized Study
Authors of this article:

Original Paper
- Yifat Fundoiano-Hershcovitz 1 , PhD ;
- Marilyn D Ritholz 2 , PhD ;
- David L Horwitz 3 , MD, PhD ;
- Ephraim Behar 1 , MSc ;
- Omar Manejwala 1 , MD ;
- Pavel Goldstein 4 , PhD
1 Dario Health, Caesarea, Israel
2 Joslin Diabetes Center, Harvard Medical School, Boston, MA, United States
3 DLH Biomedical Consulting, Las Vegas, NV, United States
4 School of Public Health, University of Haifa, Haifa, Israel
Corresponding Author:
Yifat Fundoiano-Hershcovitz, PhD
Dario Health
Caesarea, 3079821
Phone: 972 525296979
Email: [email protected]
Background: The management of type 2 diabetes (T2D) and obesity, particularly in the context of self-monitoring, remains a critical challenge in health care. As nearly 80% to 90% of patients with T2D have overweight or obesity, there is a compelling need for interventions that can effectively manage both conditions simultaneously. One of the goals in managing chronic conditions is to increase awareness and generate behavioral change to improve outcomes in diabetes and related comorbidities, such as overweight or obesity. There is a lack of real-life evidence to test the impact of self-monitoring of weight on glycemic outcomes and its underlying mechanisms.
Objective: This study aims to assess the efficacy of digital self-monitoring of weight on blood glucose (BG) levels during diabetes management, investigating whether the weight changes may drive glucose fluctuations.
Methods: In this retrospective, real-world quasi-randomized study, 50% of the individuals who regularly used the weight monitoring (WM) feature were propensity score matched with 50% of the users who did not use the weight monitoring feature (NWM) based on demographic and clinical characteristics. All the patients were diagnosed with T2D and tracked their BG levels. We analyzed monthly aggregated data 6 months before and after starting their weight monitoring. A piecewise mixed model was used for analyzing the time trajectories of BG and weight as well as exploring the disaggregation effect of between- and within-patient lagged effects of weight on BG.
Results: The WM group exhibited a significant reduction in BG levels post intervention ( P <.001), whereas the nonmonitoring group showed no significant changes ( P =.59), and both groups showed no differences in BG pattern before the intervention ( P =.59). Furthermore, the WM group achieved a meaningful decrease in BMI ( P <.001). Finally, both within-patient ( P <.001) and between-patient ( P =.008) weight variability was positively associated with BG levels. However, 1-month lagged back BMI was not associated with BG levels ( P =.36).
Conclusions: This study highlights the substantial benefits of self-monitoring of weight in managing BG levels in patients with diabetes, facilitated by a digital health platform, and advocates for the integration of digital self-monitoring tools in chronic disease management. We also provide initial evidence of testing the underlying mechanisms associated with BG management, underscoring the potential role of patient empowerment.
Introduction
People with type 2 diabetes (T2D) face challenging self-management regimens to improve glycemia and decrease morbidity and mortality while often dealing with high costs of care [ 1 ]. Obesity is one of the most common, serious, and costly medical condition in the United States, with a prevalence of 41.9% from 2017 to 2020 [ 2 ]. After a dramatic increase in its prevalence over several decades, obesity has become a major public health crisis in the United States [ 3 ]. Obesity has become one of the leading causes of death, as it is known to be the main risk factor for several noncommunicable diseases, particularly T2D [ 4 ]. It is crucial to take effective and decisive actions to hinder both the rise in the prevalence of obesity and the prevention and treatment of obesity and other obesity-related comorbidities. Approximately 80% to 90% of patients with T2D have overweight or obesity, which imposes a considerable burden on individuals, families, communities, and the health system [ 5 , 6 ].
Obesity and overweight are considered the primary accelerators for the T2D inflammatory component inducing progressive loss of beta cell insulin secretion with coexisting insulin resistance [ 7 - 9 ]. In addition, the expansion of white adipose tissue is related to a changed microenvironment in obesity, which impairs insulin signaling, reduces insulin-stimulated glucose transport activity, and accelerates beta cell dysfunction [ 10 ].
Previous studies have shown the beneficial effect of weight-lowering treatment on diabetes outcomes [ 11 ].
Healthful weight reduction in patients with obesity can improve glucose metabolism [ 12 ]. Weight reduction via carbohydrate-restricted nutritional intervention in patients with preobesity or obesity and prediabetes or T2D may contribute to improvement or remission in diabetes mellitus [ 13 ].
Antiobesity therapies for the treatment of patients with obesity and T2D include those that reduce body weight and improve glucose levels and other metabolic parameters. Considering the prevalence of obesity-related conditions such as adiposopathy and the fact that a significant portion of patients in cardiovascular outcomes trials for T2D had overweight or obesity, there is support for the “treat obesity first” therapeutic approach [ 13 ]. It is recommended in the guidelines for obesity that appropriate 5% to 10% weight loss can achieve significant metabolic improvement [ 14 ]. For the prevention of T2D, even modest weight reduction as little as 5%, can significantly reduce diabetes-associated complications [ 15 , 16 ]. Previous studies have shown that changes in various indexes such as blood lipid, blood glucose (BG), and insulin improved when weight loss reached 15% [ 14 ]. Furthermore, long-term tight weight control resulted in significant glycemic improvement, particularly demonstrated in the overweight population with T2D [ 17 , 18 ].
One of the goals of chronic condition management is to increase awareness and generate behavioral change to improve clinical outcomes. Behavior change for effective self-management was proven to improve health outcomes and quality of life in people living with chronic conditions such as obesity, T2D, and heart disease [ 19 ]. Underlying well-intentioned lifestyle messages is the assumption that if people deem health important, are aware of exercise and nutrition guidelines, and have access to healthy options to maintain proper levels of nutrition, diet, and exercise, then they will make healthier choices [ 20 ]. The American Diabetes Association guidelines state that lifestyle management should be intensive and involve frequent follow-ups [ 21 ].
Despite these recommendations, data from the National Health and Nutrition Examination Survey indicate that only 54.6% of patients reported receiving any diabetes education and only 13.4% had received an educational visit of any kind [ 16 ]. Earlier studies showed that helping participants with goal setting and self-monitoring of behavior, for instance, using a logbook and receiving feedback on the outcome of behavior, was associated with better intervention effects [ 22 ].
Facilitating behavior change involves using a series of strategies aimed at empowering patients, enabling them to take increasing control of their condition. This includes setting clear, achievable, and personalized goals, as well as enhancing self-efficacy [ 23 - 25 ]. The timing of health information and feedback focuses on when health behavior messages are delivered to people with diabetes. As diabetes care visits usually take place every 3 months, there can be a significant gap between these appointments and the daily engagement in desired behaviors. This gap makes it challenging to offer timely behavioral prompts or reinforcement [ 26 ].
In fact, patients’ mindset may modulate health outcomes, including glucose levels, in patients with diabetes [ 27 ]. Indeed, increasing perceived self-monitoring would be expected to result in subsequent health benefits [ 28 ], including glucose control in diabetes [ 29 ]. Individuals possess significant psychological influence over their health [ 30 ].
Currently, traditional health care models are being revamped with digital technologies. Digital platforms have the potential to improve our ability to enhance the delivery of health care for individual patients as well as empower patients to have more control over, and make better-informed decisions about, their health. Treatment optimization through digital health could enhance users’ alertness to their health condition through real-time monitoring, leading to effective treatments that build awareness of their daily health-related behaviors and promote increased engagement with those behaviors [ 31 - 34 ]. Technology-driven solutions can help people with diabetes build awareness of their daily health-related behaviors and promote increased engagement with those behaviors [ 32 - 34 ].
Communication of test results has been shown to be highly desired by people who have overweight, and lifestyle-focused educational messages providing advice, motivational reminders, and support have also been shown to be effective in improving chronic conditions [ 35 ]. Using a mobile platform for self-management purposes could facilitate individuals with chronic conditions in gaining insight into and controlling their BG and weight levels. Self-monitoring is a core component of behavioral obesity treatment; however, it is unknown how digital health has been used for self-monitoring and what engagement rates are achieved in these interventions [ 36 ].
Mobile apps have been shown to improve diabetes outcomes via education and support for adherence to evidence-based recommendations [ 37 - 40 ]. Mobile technology has emerged as a potentially useful platform to facilitate weight management [ 41 ]. Mobile apps for weight management typically offer similar features, including self-monitoring of diet and physical activity. Users can set goals within specified time frames and input data into the app, often receiving reminders or text messages. These apps have shown promising results [ 41 ]. Numerous digital health technologies have been developed to support the self-management of single chronic diseases, primarily diabetes. These technologies provide timely feedback, enhance patient education, and support the behavioral changes necessary for effective weight management. Recent research has indicated that digital self-monitoring tools can significantly influence health behaviors in patients with T2D, leading to better management of their condition [ 42 , 43 ]. However, given the rise in the number of people managing multiple chronic conditions, it is imperative to design and implement digital health technologies to deal with the additional complexities of multiple chronic conditions, such as the management of multiple symptoms and self-management tasks, avoiding further burden or inconvenience to the user [ 44 - 46 ]. Integrating the management of multiple conditions onto a single platform, where users can monitor their measurements and relevant lifestyle parameters, interact with all their data, share their data, and receive educational support, could help to minimize the known burden of multimorbidity self-management [ 47 - 49 ].
However, there is limited research on platforms that have been implemented to tackle multimorbidity or evaluated over longitudinal periods [ 45 ]. Specifically, the current literature is missing rigorous real-life studies to test the role of a simple self-monitoring of weight and diabetes management platform to better understand the direct association between weight monitoring and glycemic outcomes. Mainly, data are lacking on whether more frequent self-monitoring of those 2 conditions (weight and glycemia) has any impact on body weight and glycemic control in real-world clinical practice among patients with T2D and obesity [ 50 ]. In addition, many of these exclusively weight loss programs are time consuming and costly [ 51 ].
Our study seeks to address this gap by exploring the efficacy of digital self-monitoring of weight in managing BG levels in patients with T2D who are also managing their weight. We used a retrospective analysis of a home-use digital platform containing a diabetes BG meter and weight monitoring system with full longitudinal data capture using a supportive mobile platform among people with T2D and overweight levels. We followed users for 6 months before and 6 months after using the app for self-monitoring of weight and compared them with a matched control group that never used weight monitoring on the platform. We hypothesized that self-monitoring of weight would result in a significant improvement in BG levels. Moreover, weight monitoring (WM) will be associated with a reduction in weight levels. We also hypothesized a linkage between the changes in weight levels and the reduction in BG levels.
This study used the Dario Health digital therapeutics solution for chronic conditions to support the self-management of BG and weight levels. The platform combines an innovative meter with a phone app that is available for both Android and iOS devices. The glucose meter consists of a small pocket-sized holder for strips, a lancet, and the meter. The meter is removed from the holder and plugged directly into a cell phone, effectively converting the cell phone into the display screen for the meter. Weight level monitoring data are logged manually into the app on a special data entry screen ( Figure 1 ).
Connecting the BG meter directly to the phone and adding weight levels improves the quality of data collection. Additional information for weight measurement includes an informative color scale of weight ranges reflecting the Centers for Disease Control and Prevention definitions for BMI (kg/m 2 ) interpretation: <18.5 is underweight, 18.5 to 24.9 is healthy weight, 25.0 to 29.9 is overweight, and ≥30.0 is obese [ 52 ]. All information is stored in the users’ logbook in the app “attached” to the specific BG or weight reading. Data are uploaded to the cloud for backup and further analysis. Digital platform functions include interface design elements as well as specific educational content, wording, or digital interventions that affect the users’ choices in the digital environment; these functions provide personal health information and prompt feedback.

The monthly average weight level, which was defined as the means of all of a user’s weight measurements taken over a 30-day interval, was used as the core outcome metric. The monthly average BG level, which was defined as the meaning of all of a user’s BG measurements taken over a 30-day interval, was used as another outcome metric. The mobile platform collected the following medical and sociodemographic information (by self-report) for each user: sex, age, BMI during registration, physical activity level, stress level (0=no stress and 10=very stressed), alcohol consumption (number of drinks per week), smoking (0=never and 3=yes), and added comorbidities (such as high lipids, chronic kidney disease, cardiovascular disease, sleep disorder, cancer, or stress and depression). Socioeconomic status (median household income) was matched by applying zip code data to Census [ 53 ] and app engagement (number of app sessions per month). All data were transferred and stored in compliance with the Health Insurance Portability and Accountability Act requirements using Amazon Web Services database solutions. All data were anonymized before extraction for this study.
Study Population
A retrospective data study was performed on the Dario database on individuals who used the Dario platform between 2017 and 2023. The users purchased the device via a direct-to-consumer channel. The inclusion criteria were as follows: individuals who reported in the Dario app as diagnosed with T2D with a BG level of >140 mg/100 mL and BMI >25 kg/m 2 in their first month on the platform (baseline) and weight monitoring system (WM group) and used the weight monitoring system (WM monitoring). The resulting group of users was matched through the propensity scores procedure with users with similar clinical parameters but who have not been using the weight monitoring (non–weight monitoring; [NWM] group).
Study Design
The aim of our study design was to evaluate the impact of weight monitoring on BG levels. For the WM group, it was crucial to establish a clear start point for weight monitoring to assess its effects accurately. This start point is a defined intervention onset, marking when participants began actively monitoring their weight using the digital platform.
Conversely, for the NWM group, such a start point for “nonintervention” does not inherently exist, as these participants did not engage in weight monitoring. Hence, selecting a random start point for this group was a methodological necessity. This approach ensures that any observed differences in outcomes are attributable to the act of weight monitoring itself, rather than temporal factors or external influences. Therefore, the comparison between the groups hinges on the presence or absence of weight monitoring behavior. Using this approach, we enhanced the internal validity of the study. This allowed us to isolate the effect of weight monitoring from that of other variables and assess its impact on BG levels more accurately.
Propensity Scores: Causal Inference
Propensity score matching was used in this study to address potential confounding factors and enhance the comparability of the WM and NWM groups. The rationale behind using propensity score matching lies in its ability to reduce bias and mimic the randomization process, thereby facilitating causal inference in observational studies [ 54 ].
In originally nonrandomized studies, it is common for treatment assignment (in this case, use of the weight monitoring system) to be influenced by patient characteristics and other confounding variables. These factors may introduce bias and affect the estimation of treatment effects. Propensity score matching offers a systematic approach to account for such biases and create comparable treatment and control groups [ 55 ].
The propensity score, defined as the conditional probability of receiving the treatment given a set of observed covariates, summarizes the individual’s likelihood of being assigned to the WM group. By incorporating a comprehensive set of covariates that are potential confounders, such as age, sex, initial BG and BMI levels, smoking status, alcohol consumption, stress level, comorbidities, median household income, and platform engagement, the propensity score attempts to balance the distribution of these covariates between the WM and NWM groups.
Matching participants based on their propensity scores allows a comparison between similar individuals who only differ in terms of the treatment received. This strategy helps to reduce selection bias and confounding effects, enabling a more valid estimation of the causal effect of weight monitoring on glycemic control.
The use of propensity score matching aligns with the principle of exchangeability, as it creates groups that are comparable in terms of observed characteristics. By achieving a balance on observed covariates, the propensity score matching enhances the internal validity of the study and strengthens the plausibility of causal inference from the observed associations [ 56 ].
In this study, the propensity scores were calculated for each participant using the “matchit()” function from the R package matchit , which followed a nearest-neighbor approach, and the distance metric used was based on logistic regression using a 1:1 ratio between the 2 study groups [ 57 ].
To achieve balanced groups, nearest-neighbor matching with a caliper width of 0.1 SDs of the propensity score was applied. The matching procedure aimed to identify, for each WM user, a corresponding NWM participant with the closest propensity score. Participants without suitable matches were excluded from the analysis. Figure 2 presents the efficacy of the matching procedure for balancing the groups. A caliper width of 0.05 SDs was reached for all the parameters except alcohol consumption which remained within 0.1 SDs.

Ethical Considerations
All data used for the analysis were anonymized before extraction for this study. The study received an exemption from the institutional review board under the Ethical and Independent Review Services, a professional review board, which issued the institutional review board exemption for this study (18032-06#) [ 58 ]. The users who participated in the study were provided with a Terms of Use document mentioning the legally valid consent of the end user for the company to collect and access their information. The use of the app, site, or services shall be deemed to constitute user consent to be legally bound by these Terms and the Privacy Policy. Please refer to the current “Terms-of-use” at the link [ 59 ].
Analytic Approach
Traditionally, a classical linear longitudinal model assumes a single-slope growth pattern for changes in an outcome variable over time. However, empirical data often exhibit more complex patterns that cannot be adequately captured by such a simple model. In our study, we used piecewise-based mixed-effects models to allow for greater flexibility in modeling trajectories over time [ 60 ].
The piecewise model approach offers the advantage of accommodating different linear trends in the data across distinct regions. Specifically, we used a mixed piecewise model to assess differential changes in the WM and NWM groups in the monthly average BG level in 2 segments: before and after weight monitoring use. This approach enabled us to capture the potential changes in BG trajectories associated with the introduction of the monitoring system. Using a statistical model that accounted for curvilinear changes, we were able to test the complex effects and capture the dynamics of the associated BG fluctuations.
For the analysis, the time data were centered around the beginning of the weight monitoring period. We included a 6-month timeframe before and after this point to capture the potential impact of weight monitoring use. In the NWM group, we randomly selected a cutoff point and included data collected during the 6 months before and after the simulated cutoff point. To model the temporal changes in the monthly average weight level between the WM and NWM groups, we fitted a piecewise-based mixed-effects model. The piecewise cutoff point was set at the initiation of weight monitoring, assuming a change in the time-related trajectory of the monthly average BG level between the 2 groups. We incorporated interaction terms between the time trajectories and groups to capture this differential effect. Thus, 2 time parameters (pre and postintervention) were used as covariates, the groups (WM and NWM) were considered as a factor, and the monthly number of BG measurement served as a potential confounding variable. All the tests were 2-tailed and the type 1 error was set to 5%. The model included random intercepts and random slopes for the time trajectory after the piecewise cutoff, accounting for individual variability in BG changes.
In addition, we used mixed model analysis to examine the time trajectory of BMI changes (covariate) for the initial 6 months of weight monitoring in the WM group, controlling for baseline BMI and the number of monthly BMI measures as confounding variables. These models included random intercepts and random slopes of the time trajectory to capture individual variations in weight changes over time. Unstandardized regression weights (B), test statistics ( t ), and associated significance ( P values) were reported.
Finally, the monthly BMI levels were disaggregated to separate within- and between-person variabilities using person-level centering and person-level aggregation [ 61 ]. In addition, a 1-month lagged within-person BMI was calculated. Thereafter, a mixed model was applied to test the 1-month lagged and simultaneous association of monthly within-person BMI changes and between-person BMI with the monthly average BG level. All the model predictors were defined as covariates.
In total, 1932 users were included in the study. The WM group included 50% users, and the NWM group, matched through the propensity scores procedure, included 50% users. The study cohort comprised 51.6% (997/1932) of men, and 60.82% (1175/1932) of the participants had comorbidities. The average age of the participants was 62.8 (SD 12.5) years, with an average BMI of 35.4 (SD 7.3). The median household income for the participants was US $68,200 (SD US $25,100). The distribution of the other parameters is presented in Table 1 by study group.
No differences were found between the WM and NWM groups. The study included individuals with diabetes who monitored their BG levels and weight using the Dario platform.
The distribution of various sample characteristics overall and by WM and NWM groups is presented in Table 1 , and any significant differences were shown.
a WM: weight monitoring.
b NWM: non–weight monitoring.
c BG: blood glucose.
Weight Monitoring Is Associated With BG Levels
The results from the piecewise mixed model analysis indicated a significant interaction between the time trajectory, starting weight monitoring and the group (B=3.02; t =6.03; P <.001) on BG levels ( Table 2 ). Specifically, the WM group demonstrated a significant reduction in the BG levels (B=−2.81; t =−8.88; P <.001), whereas the NWM group did not exhibit a significant time trend (B=0.21; t =0.55; P =.59; Figure 3 ). Before weight monitoring, there was no significant difference observed in BG time trends between the 2 groups (B=0.69; t =1.06; P =.29). Furthermore, we investigated the proportion of users who achieved a BG level reduction in their last month of measurement less than the average BG levels of 154 mg/100 mL, 183 mg/100 mL, and 212 mg/100 mL, equivalent to estimated glycated hemoglobin (HbA 1c ) of 7.0, 8.0, and 9.0, respectively [ 62 ]. Remarkably, of the 966 users examined per group, 45% (435/966) versus 36% (348/966), 71% (686/966) versus 59% (570/966), and 85% (821/966) versus 76% (734/966) of the WM versus NWM individuals demonstrated substantial reductions in HbA 1c levels of <154 mg/100 mL, 183 mg/100 mL, and 212 mg/100 mL, respectively ( P <.001 for all).
a BG: blood glucose.
b σ2 residual variability=843.15; τ00 UID random intercept=2099.24; τ11 UID.time2 random slope of the second slope=53.68; ρ01 UID: covariance between the random intercept and slope=−0.27; intraclass correlation=0.72.
c #BG measurements=number of BG measurements per month.
d time1represents the piecewise slopes before the weight monitoring intervention.
e NWM: non–weight monitoring.
f time2 represents the piecewise slopes after the weight monitoring intervention.

BMI Fluctuations and the Link to BG
During the weight monitoring period ( Table 3 ) of the WM group, a significant decrease in BMI was observed (B=−0.13; t =−9.35; P <.001).
Interestingly, the number of monthly measurements was negatively associated with BMI (B=−0.003; t =−2.22; P =.03). Furthermore, the findings of the lagged analysis disaggregating within- and between-person variabilities shed light on BMI as a potential mechanism driving BG ( Table 4 ). Specifically, the analysis demonstrated that an increase in within-person BMI was associated with elevated BG levels (B=4.67; t =3.47; P <.001). Similarly, an increase in between-person BMI was found to be associated with higher BG levels (B=0.61; t =2.65; P =.008). However, the 1-month lagged back BMI was not associated with BG levels (B=−0.77; t =−0.91; P =.36).
b σ2 residual variability=0.24; τ00 UID random intercept=1.29; τ11 UID.time random slope of the time=0.17; ρ01 UID covariance between the random intercept and slope=−0.25; intraclass correlation=0.93.
c time represents the slope over 6 months after the intervention.
b WM: weight monitoring.
c σ2 residual variability=464.96; τ00 UID random intercept=1684.51; τ11 UID.time random slope of the within-person BMI=325.17; ρ01 UID covariance between the random intercept and slope=−0.01; intraclass correlation=0.80.
Principal Findings
This study examined the ability of people with diabetes to regulate BG levels through simple weight monitoring. It used propensity score matching for the control group and used a piecewise mixed model as a statistical framework to describe the nonlinear behavior in BG levels, comparing 2 user cohorts over time. Our analysis indicated that before the weight monitoring phase, both groups demonstrated flat trajectories in BG levels. However, after starting the use of the self-monitoring of weight, the WM group experienced a significant reduction in BG levels, whereas the NWM group’s BG levels remained flat.
In addition, by disaggregating within- and between-person BMI variabilities, we showed an association between both BMI sources and BG levels, suggesting that general BMI levels and BMI fluctuations can potentially contribute to BG modulation. However, a lagged analysis did not find an association between within-person BMI fluctuations and next-month BG levels, which does not support the claim of BMI as a potential mechanism of BG changes.
This study demonstrates that the use of digital tools for self-monitoring of weight can significantly affect BG levels in patients with T2D. This finding offers a practical approach to enhancing T2D management, especially for the majority of patients who are also dealing with overweight or obesity issues. Given that weight loss has been consistently shown to improve glycemic control in patients with T2D, as highlighted in previous studies [ 12 - 16 , 25 ], our findings reinforce the importance of weight management as an integral part of diabetes care. Self-monitoring can enhance patient awareness and engagement in their health management, leading to better outcomes. This aligns with the growing body of evidence suggesting that patient engagement and empowerment are critical in managing chronic conditions such as T2D [ 34 , 40 , 63 , 64 ].
Self-monitoring is the centerpiece of behavioral weight loss intervention programs. A significant association between self-monitoring and weight loss was consistently reported for various health conditions; however, the level of evidence was weak due to methodological limitations [ 65 ]. The use of self-monitoring in behavioral changes has a strong theoretical foundation. Self-management was defined as “the personal application of behavior-change tactics that produces a desired change in behavior” [ 66 ]. Through self-management interventions, individuals learn to identify occurrences of their own target responding, accurately self-recording the target response, self-evaluating their behavior, and self-delivering reinforcement as a consequence [ 67 ].
Although self-monitoring has been described as the cornerstone of behavioral treatment for weight loss, there is a limited examination conducted in the literature [ 65 ]. More recently, self-weighing has been introduced as a monitoring component. Daily weighing is valuable for individuals trying to lose weight or prevent weight gain [ 68 ]. Consistent with our findings, frequent self-weighing was associated with a lower fat intake, a greater history of dieting to lose weight, and a lower current BMI [ 68 , 69 ].
Previous systematic reviews provided extensive evidence that self-monitoring via digital health, including weight, diet, and physical activity, is associated with superior weight loss [ 36 ]. It was specifically shown how distinct features of a digital therapeutic app have the potential to deliver equitable person-centric care and how digital engagement can play a key role in enhancing a person’s chronic condition self-management [ 63 , 64 , 70 , 71 ].
Self-monitoring has been shown repeatedly to be an important feature of behavioral weight loss digital programs [ 71 ]. Self-monitoring of weight and diet were positively correlated with weight loss, and the more consistently the monitoring occurred, the better the weight loss [ 72 , 73 ]. Self-monitoring is also a core component of behavioral obesity treatment, but there is limited knowledge about the efficacy of digital self-monitoring of weight in diabetes [ 36 ]. We had previously demonstrated how digital engagement and digital blood pressure monitoring may improve diabetes management [ 34 , 74 ]. Prominently, in this study, the WM and NWM groups were not different in their digital engagement. In addition, the median household income distribution of users in both groups was comparable, suggesting that the digital solution is desired and affordable across lower-, middle-, and high-income levels to enhance glycemic and weight loss outcomes. Mobile apps can successfully help patients lose weight and represent a cost-effective and accessible alternative to intensive in-person weight loss programs [ 51 ].
From a psychological perspective, it is assumed that individuals using a digital platform may develop more active roles in managing their health, and self-monitoring affects health in part or in whole via the placebo effect, initiated by mindset modulations [ 75 ]. In the realm of physical exercise, a compelling body of research highlights the remarkable impact of mindset on various health parameters. It has been demonstrated that individuals’ mindsets about stress could profoundly alter their cortisol levels and influence various hormonal and cardiovascular functions when confronted with stressful situations [ 76 ]. Levy et al [ 77 ] conducted a noteworthy study that revealed a significant association between individuals’ mindsets about aging and their cardiovascular function as well as their actual longevity. A notable example of this phenomenon is evident in the study conducted by Crum and Langer [ 28 ], who investigated the effects of mindset on hotel room attendants. These workers, upon adopting the mindset that their daily work constituted a form of beneficial exercise, experienced substantial improvements in several critical health indicators, including weight, BMI, and systolic blood pressure. The potential mechanism may include beliefs and feelings of control people have over their health [ 28 , 78 ]. Collectively, these studies illuminate the potent role of the mindset in shaping various aspects of physical health, providing a background for the potential effect of weight monitoring on BG levels through mindset changes, considering the absence of a quasi-causal association between BMI and BG levels. There is evidence supporting the idea that the placebo effect plays a role in prompting the psychological benefits associated with health-related outcomes [ 79 ]. Treatments are delivered in a context that includes social and physical signals, verbal suggestions, and clinical history. This context is actively interpreted by the brain and can elicit expectations, memories, and emotions, which in turn can influence health-related outcomes in the body [ 79 ]. Considering the absence of a quasi-causal association between BMI and BG levels, one may consider the effect of self-weighing on BG levels to be mediated by perceptional processes, including mindset modulation.
In agreement with previous studies, we found that the WM group, which monitored their weight, also improved their BMI levels over time [ 80 ]. There is strong and consistent evidence that obesity management can delay the progression from prediabetes to T2D and is highly beneficial in treating T2D [ 80 - 83 ]. A significant overlap between T2D and overweight or obesity in etiology and disease mechanisms was broadly investigated. Previous studies have shown a significant improvement in all diabetes-related outcomes, including weight reduction, in patients with T2D and those who have overweight [ 17 ]. Controlling both diseases through weight management requires an intensive multidisciplinary approach [ 84 , 85 ]. As body weight increases, patients become more insulin resistant [ 86 ], which further drives the need for higher doses of antihyperglycemic medications to keep BG levels in the target range, which then may increase weight gain [ 17 ]. It was observed that in obese individuals, adipose tissue releases increased amounts of nonesterified fatty acids, glycerol, hormones, proinflammatory cytokines, and other factors that are involved in the development of insulin resistance. Insulin resistance associated with dysfunction of pancreatic islet beta cells results in the failure to maintain BG levels within the target range [ 86 ]. Losing weight can alleviate many of these issues. While losing weight, the pancreas is better able to keep up with the body’s need for insulin. In some cases, weight loss is enough to restore BG to a normal level, which eliminates diabetes or even lowers the need for insulin therapy or other medications to control diabetes [ 87 ]. However, other important components may also play a role in weight and BG levels, and other laboratory tests may need to be performed by health care providers.
Monitoring several chronic conditions may have the potential to offer a greater means for helping people with diabetes who have overweight or obesity effectively modulate their glycemia and weight than managing each condition separately. The findings of this study suggest the need for further exploration of how digital health platforms can be effectively integrated into routine clinical practice. Future research should focus on how these tools can be optimized for individual patient needs and how they can be incorporated into broader diabetes management programs. In addition, exploring the long-term impacts of such interventions on patient outcomes and health care use will be valuable. We expect that our analytical framework will be useful for examining other chronic conditions and metabolic syndrome outcomes (eg, lipid profile).
Limitations
As in all studies involving retrospective real-world data, groups were not randomly assigned, and treatment protocols were not prescribed. The propensity score matching approach, while comprehensive, introduces potential biases due to selection methods, which may not be fully mitigated. Unobserved confounders, measurement errors, and other limitations inherent to observational studies may still impact the validity of causal inferences. Nevertheless, propensity score matching represents a rigorous analytical technique that is widely accepted and applied in observational studies to approximate the design and control of randomized controlled trials, making it a valuable tool in the pursuit of causal inference. In this study, we relied on self-reported data for measurements, including weight and BMI. Although self-reporting is a common and practical method in many observational and digital health studies, it can be subject to inaccuracies due to factors such as recall bias or the desire to present oneself in a certain light.
In this real-world data analysis, we designed our timescale to capture changes over a 6-month period both before and after the initiation of weight monitoring. Nevertheless, it is worth noting that the research question of interest in this study could potentially be explored at various temporal scales, including daily, weekly, or monthly intervals. Given the practical challenges associated with monitoring daily changes in real-world settings, most studies in this domain tend to emphasize monthly fluctuations. Moreover, while BG levels offer real-time data and are sensitive to immediate changes in diabetes management, they do not provide a comprehensive view of long-term glycemic control. In addition, longer-term weight monitoring can provide a long-term perspective on glycemic control. Monitoring HbA 1c levels over a longer period would provide additional insights into the long-term effects of self-monitoring of weight on glycemic control. However, our study was designed to assess the short-term impacts of digital self-monitoring of weight on BG levels with increased resolution compared to HbA 1c . The 6-month period was chosen as it provides a sufficient window to observe significant changes in BG levels in response to weight management, without extending to long-term effects where other variables might confound the results. In addition, the average BMI of the participants was 35.0 (SD 7.3), which is considered a unique population of obesity. Furthermore, longer-term follow-up with these participants is needed because it is not clear how long this weight loss and glycemic improvement will last and what needs to be added for increased sustainability.
Conclusions
In summary, our study underscored the tangible benefits of self-monitoring of weight in the modulation of BG levels among people with diabetes. By leveraging an innovative analytical framework, we found that self-monitoring of weight led to significant reductions in BG levels in the WM group, despite the lack of a direct causal link between BMI fluctuations and BG changes. Drawing from extensive evidence, both historical and from our study, the act of self-monitoring seems to foster a heightened sense of agency and potentially influence health outcomes through mindset modulations.
From a practical standpoint, these findings reinforce the importance of digital health tools in chronic disease management, especially in the realms of diabetes and obesity. Digital self-monitoring platforms not only offer scalable and affordable solutions but also empower individuals to take a proactive role in their health journey. Moreover, the convergence of digital health tools with robust psychological mechanisms, such as the placebo effect and mindset modulation, paves the way for a holistic approach to health care.
This research may also open the door to a myriad of possibilities. While we have illuminated the potential effects of self-monitoring of weight on diabetes management, similar methods could be deployed to investigate the impact on other chronic conditions and metabolic syndrome outcomes. Furthermore, with advancing technology, more granular, real-time data can be leveraged to delve deeper into the daily or even hourly impacts of such interventions. Future studies should also focus on investigating the mechanisms underlying the comorbidity of diabetes and obesity and their management, identifying, and applying mediation models that drive behavioral change that goes beyond multiple chronic conditions.
In light of the significant overlap between T2D and obesity, there is an imperative need to conceptualize and design multifaceted interventions. Blending digital innovation, behavioral science, and clinical knowledge, we can usher in a new era of person-centric health care that is not only responsive but also preemptive. The journey has just begun, and the road ahead promises transformative potential for patients and health care systems alike.
Conflicts of Interest
YFH, EB, and OM are employees of Dario Health. MDR and DLH serve as Dario Health scientific advisory board members, and PG has received a consulting fee to assist with analyses but otherwise has no conflicts of interest.
- Amante DJ, Harlan DM, Lemon SC, McManus DD, Olaitan OO, Pagoto SL, et al. Evaluation of a diabetes remote monitoring program facilitated by connected glucose meters for patients with poorly controlled type 2 diabetes: randomized crossover trial. JMIR Diabetes. Mar 11, 2021;6(1):e25574. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bryan S, Afful J, Carroll M, Te-Ching C, Orlando D, Fink S, et al. National health and nutrition examination survey 2017–March 2020 prepandemic data files—development of files and prevalence estimates for selected health outcomes. Centers for Disease Control and Prevention. 2021. URL: https://www.cdc.gov/nchs/data/nhsr/nhsr158-508.pdf [accessed 2024-03-16]
- Cawley J, Biener A, Meyerhoefer C, Ding Y, Zvenyach T, Smolarz BG, et al. Direct medical costs of obesity in the United States and the most populous states. J Manag Care Spec Pharm. Mar 2021;27(3):354-366. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leitner DR, Frühbeck G, Yumuk V, Schindler K, Micic D, Woodward E, et al. Obesity and type 2 diabetes: two diseases with a need for combined treatment strategies - EASO can lead the way. Obes Facts. 2017;10(5):483-492. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nianogo RA, Arah OA. Forecasting obesity and type 2 diabetes incidence and burden: the ViLA-obesity simulation model. Front Public Health. 2022;10:818816. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ruze R, Liu T, Zou X, Song J, Chen Y, Xu R, et al. Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Front Endocrinol (Lausanne). 2023;14:1161521. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Rev Endocrinol. Jul 2020;16(7):349-362. [ CrossRef ] [ Medline ]
- American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. Jan 2019;42(Suppl 1):S13-S28. [ CrossRef ] [ Medline ]
- Versini M, Jeandel PY, Rosenthal E, Shoenfeld Y. Obesity in autoimmune diseases: not a passive bystander. Autoimmun Rev. Sep 2014;13(9):981-1000. [ CrossRef ] [ Medline ]
- Tuomi T, Santoro N, Caprio S, Cai M, Weng J, Groop L. The many faces of diabetes: a disease with increasing heterogeneity. Lancet. Mar 22, 2014;383(9922):1084-1094. [ CrossRef ] [ Medline ]
- Thom G, Messow CM, Leslie WS, Barnes AC, Brosnahan N, McCombie L, et al. Predictors of type 2 diabetes remission in the Diabetes Remission Clinical Trial (DiRECT). Diabet Med. Aug 2021;38(8):e14395. [ CrossRef ] [ Medline ]
- Bays HE. Why does type 2 diabetes mellitus impair weight reduction in patients with obesity? A review. Obes Pillars. Sep 2023;7:100076. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bays HE, Bindlish S, Clayton TL. Obesity, diabetes mellitus, and cardiometabolic risk: an obesity medicine association (OMA) clinical practice statement (CPS) 2023. Obes Pillars. Mar 2023;5:100056. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kong DX, Xiao Y, Zhang ZX, Liu YB. Study on the correlation between metabolism, insulin sensitivity and progressive weight loss change in type-2 diabetes. Pak J Med Sci. 2020;36(7):1523-1528. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Scheen AJ, Van Gaal LF. Combating the dual burden: therapeutic targeting of common pathways in obesity and type 2 diabetes. Lancet Diabetes Endocrinol. Nov 2014;2(11):911-922. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Apovian CM, Okemah J, O'Neil PM. Body weight considerations in the management of type 2 diabetes. Adv Ther. Jan 2019;36(1):44-58. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hamdy O, Ashrafzadeh S, Mottalib A. Weight management in patients with type 2 diabetes: a multidisciplinary real-world approach. Curr Diab Rep. Jul 17, 2018;18(9):66. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bolignano D, Zoccali C. Effects of weight loss on renal function in obese CKD patients: a systematic review. Nephrol Dial Transplant. Nov 2013;28 Suppl 4:iv82-iv98. [ CrossRef ] [ Medline ]
- Araújo-Soares V, Hankonen N, Presseau J, Rodrigues A, Sniehotta FF. Developing behavior change interventions for self-management in chronic illness: an integrative overview. Eur Psychol. 2019;24(1):7-25. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health. Aug 2014;104(8):e25-e31. [ CrossRef ] [ Medline ]
- Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. Dec 2018;41(12):2669-2701. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act. Mar 28, 2017;14(1):42. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Magkos F, Yannakoulia M, Chan JL, Mantzoros CS. Management of the metabolic syndrome and type 2 diabetes through lifestyle modification. Annu Rev Nutr. 2009;29:223-256. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Estabrooks PA, Nelson CC, Xu S, King D, Bayliss EA, Gaglio B, et al. The frequency and behavioral outcomes of goal choices in the self-management of diabetes. Diabetes Educ. 2005;31(3):391-400. [ CrossRef ] [ Medline ]
- Reynolds LR, Anderson JW. Practical office strategies for weight management of the obese diabetic individual. Endocr Pract. 2004;10(2):153-159. [ CrossRef ] [ Medline ]
- Hood KK, Hilliard M, Piatt G, Ievers-Landis CE. Effective strategies for encouraging behavior change in people with diabetes. Diabetes Manag (Lond). 2015;5(6):499-510. [ FREE Full text ] [ Medline ]
- Raffali A, Asraf RM. Fostering growth mindset principles in the prevention of type 2 diabetes through a narrative game. Int J Learn Teach Educ Res. 2023;22(2):244-261. [ FREE Full text ] [ CrossRef ]
- Crum AJ, Langer EJ. Mind-set matters: exercise and the placebo effect. Psychol Sci. Feb 2007;18(2):165-171. [ CrossRef ] [ Medline ]
- Park C, Pagnini F, Reece A, Phillips D, Langer E. Blood sugar level follows perceived time rather than actual time in people with type 2 diabetes. Proc Natl Acad Sci U S A. Jul 19, 2016;113(29):8168-8170. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee KS, Feltner FJ, Bailey AL, Lennie TA, Chung ML, Smalls BL, et al. The relationship between psychological states and health perception in individuals at risk for cardiovascular disease. Psychol Res Behav Manag. 2019;12:317-324. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Awad A, Trenfield SJ, Pollard TD, Ong JJ, Elbadawi M, McCoubrey LE, et al. Connected healthcare: improving patient care using digital health technologies. Adv Drug Deliv Rev. Nov 2021;178:113958. [ CrossRef ] [ Medline ]
- Cahn A, Akirov A, Raz I. Digital health technology and diabetes management. J Diabetes. Jan 2018;10(1):10-17. [ CrossRef ] [ Medline ]
- Han J, King F, Klonoff D, Drincic A, Crosby KP, Robinson T, et al. Digital diabetes congress 2019. J Diabetes Sci Technol. Sep 2019;13(5):979-989. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fundoiano-Hershcovitz Y, Hirsch A, Dar S, Feniger E, Goldstein P. Role of digital engagement in diabetes care beyond measurement: retrospective cohort study. JMIR Diabetes. Feb 18, 2021;6(1):e24030. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chow CK, Redfern J, Hillis GS, Thakkar J, Santo K, Hackett ML, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA. 2015;314(12):1255-1263. [ CrossRef ] [ Medline ]
- Patel ML, Wakayama LN, Bennett GG. Self-monitoring via digital health in weight loss interventions: a systematic review among adults with overweight or obesity. Obesity (Silver Spring). Mar 2021;29(3):478-499. [ CrossRef ] [ Medline ]
- Michie S, Yardley L, West R, Patrick K, Greaves F. Developing and evaluating digital interventions to promote behavior change in health and health care: recommendations resulting from an international workshop. J Med Internet Res. Jun 29, 2017;19(6):e232. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Offringa R, Sheng T, Parks L, Clements M, Kerr D, Greenfield MS. Digital diabetes management application improves glycemic outcomes in people with type 1 and type 2 diabetes. J Diabetes Sci Technol. May 25, 2018;12(3):701-708. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bollyky JB, Melton ST, Xu T, Painter SL, Knox B. The effect of a cellular-enabled glucose meter on glucose control for patients with diabetes: prospective pre-post study. JMIR Diabetes. Oct 07, 2019;4(4):e14799. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Osborn CY, van Ginkel JR, Rodbard D, Heyman M, Marrero DG, Huddleston B, et al. One drop | mobile: an evaluation of hemoglobin A1c improvement linked to app engagement. JMIR Diabetes. Aug 24, 2017;2(2):e21. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ghelani DP, Moran LJ, Johnson C, Mousa A, Naderpoor N. Mobile apps for weight management: a review of the latest evidence to inform practice. Front Endocrinol (Lausanne). 2020;11:412. [ FREE Full text ] [ CrossRef ] [ Medline ]
- MacPherson MM, Merry KJ, Locke SR, Jung ME. mHealth prompts within diabetes prevention programs: a scoping review. Mhealth. 2022;8:20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- MacPherson MM, Merry KJ, Locke SR, Jung ME. Effects of mobile health prompts on self-monitoring and exercise behaviors following a diabetes prevention program: secondary analysis from a randomized controlled trial. JMIR Mhealth Uhealth. Sep 05, 2019;7(9):e12956. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. Feb 14, 2013;15(2):e35. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Doyle J, Murphy E, Gavin S, Pascale A, Deparis S, Tommasi P, et al. A digital platform to support self-management of multiple chronic conditions (ProACT): findings in relation to engagement during a one-year proof-of-concept trial. J Med Internet Res. Dec 15, 2021;23(12):e22672. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ancker JS, Witteman HO, Hafeez B, Provencher T, Van de Graaf M, Wei E. "You get reminded you're a sick person": personal data tracking and patients with multiple chronic conditions. J Med Internet Res. Aug 19, 2015;17(8):e202. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Doyle J, Murphy E, Kuiper J, Smith S, Hannigan C, Jacobs A, et al. Managing multimorbidity: identifying design requirements for a digital self-management tool to support older adults with multiple chronic conditions. In: Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. 2019. Presented at: CHI '19; May 4-9, 2019;1-14; Glasgow, Scotland. URL: https://dl.acm.org/doi/10.1145/3290605.3300629
- Lim CY, Berry AB, Hartzler A, Hirsch T, Carrell DS, Bermet ZA, et al. Facilitating self-reflection about values and self-care among individuals with chronic conditions. In: Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. 2019. Presented at: CHI '19; May 4-9, 2019;1-12; Glasgow, Scotland. URL: https://dl.acm.org/doi/10.1145/3290605.3300885 [ CrossRef ]
- Caldeira C, Gui X, Reynolds TL, Bietz M, Chen Y. Managing healthcare conflicts when living with multiple chronic conditions. Int J Hum Comput Stud. Jan 2021;145:102494. [ FREE Full text ] [ CrossRef ]
- Tomah S, Mahmoud N, Mottalib A, Pober DM, Tasabehji MW, Ashrafzadeh S, et al. Frequency of self-monitoring of blood glucose in relation to weight loss and A1C during intensive multidisciplinary weight management in patients with type 2 diabetes and obesity. BMJ Open Diabetes Res Care. 2019;7(1):e000659. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ufholz K, Werner J. The efficacy of mobile applications for weight loss. Curr Cardiovasc Risk Rep. Mar 23, 2023;17(4):83-90. [ FREE Full text ] [ CrossRef ] [ Medline ]
- About adult BMI. Centers for Disease Control and Prevention. URL: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html [accessed 2022-05-03]
- Measuring America's people, places, and economy. The United States Census Bureau. URL: https://www.census.gov/ [accessed 2024-03-16]
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. May 2011;46(3):399-424. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. Mar 12, 2012;39(1):33-38. [ CrossRef ]
- Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. Feb 01, 2010;25(1):1-21. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ho D, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1-28. [ CrossRef ]
- Home page. Ethical & Independent Review Services (E&I). URL: https://eandireview.com/ [accessed 2023-06-13]
- Terms of use. DarioHealth Corp. URL: https://www.dariohealth.com/terms-of-use/ [accessed 2024-03-16]
- Kohli N, Peralta Y, Zopluoglu C, Davison ML. A note on estimating single-class piecewise mixed-effects models with unknown change points. Int J Behav Dev. Feb 15, 2018;42(5):518-524. [ CrossRef ]
- Yardley L, Morrison L, Bradbury K, Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. Jan 30, 2015;17(1):e30. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ, et al. A1c-Derived Average Glucose Study Group. Translating the A1C assay into estimated average glucose values. Diabetes Care. Aug 2008;31(8):1473-1478. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Frias J, Virdi N, Raja P, Kim Y, Savage G, Osterberg L. Effectiveness of digital medicines to improve clinical outcomes in patients with uncontrolled hypertension and type 2 diabetes: prospective, open-label, cluster-randomized pilot clinical trial. J Med Internet Res. Jul 11, 2017;19(7):e246. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shan R, Sarkar S, Martin SS. Digital health technology and mobile devices for the management of diabetes mellitus: state of the art. Diabetologia. Jun 8, 2019;62(6):877-887. [ CrossRef ] [ Medline ]
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. Jan 2011;111(1):92-102. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cooper JO, Heron TE, Heward WL. Applied Behavior Analysis. 3rd edition. Old Bridge, NJ. Pearson Prentice Hall; 2020.
- Erhard P, Wong T, Barnett M, Falcomata T, Lang R. Self-management skills and applied behavior analysis. In: Matson JL, Sturmey P, editors. Handbook of Autism and Pervasive Developmental Disorder: Assessment, Diagnosis, and Treatment. Cham, Switzerland. Springer; 2022;957-973.
- Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. Dec 2005;30(3):210-216. [ CrossRef ] [ Medline ]
- Patel ML, Hopkins CM, Brooks TL, Bennett GG. Comparing self-monitoring strategies for weight loss in a smartphone app: randomized controlled trial. JMIR Mhealth Uhealth. Feb 28, 2019;7(2):e12209. [ FREE Full text ] [ CrossRef ] [ Medline ]
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 1. improving care and promoting health in populations: standards of care in diabetes-2023. Diabetes Care. Jan 01, 2023;46(Supple 1):S10-S18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lin PH, Grambow S, Intille S, Gallis JA, Lazenka T, Bosworth H, et al. The association between engagement and weight loss through personal coaching and cell phone interventions in young adults: randomized controlled trial. JMIR Mhealth Uhealth. Oct 18, 2018;6(10):e10471. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Burke LE, Warziski M, Starrett T, Choo J, Music E, Sereika S, et al. Self-monitoring dietary intake: current and future practices. J Ren Nutr. Jul 2005;15(3):281-290. [ CrossRef ] [ Medline ]
- Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behav Ther. Jun 1993;24(3):377-394. [ CrossRef ]
- Gershoni T, Ritholz MD, Horwitz D, Manejwala O, Donaldson-Pitter T, Fundoiano-Hershcovitz Y. Glycemic management by a digital therapeutic platform across racial/ethnic groups: a retrospective cohort study. Applied Sciences. Dec 29, 2022;13(1):431. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tighe SA, Ball K, Kensing F, Kayser L, Rawstorn JC, Maddison R. Toward a digital platform for the self-management of noncommunicable disease: systematic review of platform-like interventions. J Med Internet Res. Oct 28, 2020;22(10):e16774. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Crum AJ, Salovey P, Achor S. Rethinking stress: the role of mindsets in determining the stress response. J Pers Soc Psychol. Apr 2013;104(4):716-733. [ CrossRef ] [ Medline ]
- Levy BR, Slade MD, Kunkel SR, Kasl SV. Longevity increased by positive self-perceptions of aging. J Pers Soc Psychol. Aug 2002;83(2):261-270. [ CrossRef ] [ Medline ]
- Salvia MG, Ritholz MD, Craigen KL, Quatromoni PA. Women's perceptions of weight stigma and experiences of weight-neutral treatment for binge eating disorder: a qualitative study. EClinicalMedicine. Feb 2023;56:101811. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wager TD, Atlas LY. The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci. Jul 2015;16(7):403-418. [ FREE Full text ] [ CrossRef ] [ Medline ]
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. on behalf of the American Diabetes Association. 8. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of care in diabetes-2023. Diabetes Care. Jan 01, 2023;46(Suppl 1):S128-S139. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rothberg AE, McEwen LN, Kraftson AT, Fowler CE, Herman WH. Very-low-energy diet for type 2 diabetes: an underutilized therapy? J Diabetes Complications. 2014;28(4):506-510. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garvey WT, Ryan DH, Bohannon NJ, Kushner RF, Rueger M, Dvorak RV, et al. Weight-loss therapy in type 2 diabetes: effects of phentermine and topiramate extended release. Diabetes Care. Dec 2014;37(12):3309-3316. [ CrossRef ] [ Medline ]
- Davies MJ, Bergenstal R, Bode B, Kushner RF, Lewin A, Skjøth TV, et al. NN8022-1922 Study Group. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA. Aug 18, 2015;314(7):687-699. [ CrossRef ] [ Medline ]
- Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American association of clinical endocrinologists and American college of endocrinology on the comprehensive type 2 diabetes management algorithm - 2018 executive summary. Endocr Pract. Jan 2018;24(1):91-120. [ CrossRef ] [ Medline ]
- ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. on behalf of the American Diabetes Association. 5. Facilitating positive health behaviors and well-being to improve health outcomes: standards of care in diabetes-2023. Diabetes Care. Jan 01, 2023;46(Supple 1):S68-S96. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. Dec 14, 2006;444(7121):840-846. [ CrossRef ] [ Medline ]
- Bishop S. Losing weight can have big impact on those with diabetes. Mayo Clinic News Network. URL: https://newsnetwork.mayoclinic.org/discussion/losing-weight-can-have-big-impact-on-those-with-diabetes/ [accessed 2023-08-06]
Abbreviations
Edited by G Eysenbach, T Leung; submitted 28.11.23; peer-reviewed by Y Ding, T de Azevedo Cardoso; comments to author 02.01.24; revised version received 18.02.24; accepted 22.02.24; published 02.04.24.
©Yifat Fundoiano-Hershcovitz, Marilyn D Ritholz, David L Horwitz, Ephraim Behar, Omar Manejwala, Pavel Goldstein. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 02.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Research paper
Writing a Research Paper Conclusion | Step-by-Step Guide
Published on October 30, 2022 by Jack Caulfield . Revised on April 13, 2023.
- Restate the problem statement addressed in the paper
- Summarize your overall arguments or findings
- Suggest the key takeaways from your paper
The content of the conclusion varies depending on whether your paper presents the results of original empirical research or constructs an argument through engagement with sources .
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes


Table of contents
Step 1: restate the problem, step 2: sum up the paper, step 3: discuss the implications, research paper conclusion examples, frequently asked questions about research paper conclusions.
The first task of your conclusion is to remind the reader of your research problem . You will have discussed this problem in depth throughout the body, but now the point is to zoom back out from the details to the bigger picture.
While you are restating a problem you’ve already introduced, you should avoid phrasing it identically to how it appeared in the introduction . Ideally, you’ll find a novel way to circle back to the problem from the more detailed ideas discussed in the body.
For example, an argumentative paper advocating new measures to reduce the environmental impact of agriculture might restate its problem as follows:
Meanwhile, an empirical paper studying the relationship of Instagram use with body image issues might present its problem like this:
“In conclusion …”
Avoid starting your conclusion with phrases like “In conclusion” or “To conclude,” as this can come across as too obvious and make your writing seem unsophisticated. The content and placement of your conclusion should make its function clear without the need for additional signposting.
Scribbr Citation Checker New
The AI-powered Citation Checker helps you avoid common mistakes such as:
- Missing commas and periods
- Incorrect usage of “et al.”
- Ampersands (&) in narrative citations
- Missing reference entries
Having zoomed back in on the problem, it’s time to summarize how the body of the paper went about addressing it, and what conclusions this approach led to.
Depending on the nature of your research paper, this might mean restating your thesis and arguments, or summarizing your overall findings.
Argumentative paper: Restate your thesis and arguments
In an argumentative paper, you will have presented a thesis statement in your introduction, expressing the overall claim your paper argues for. In the conclusion, you should restate the thesis and show how it has been developed through the body of the paper.
Briefly summarize the key arguments made in the body, showing how each of them contributes to proving your thesis. You may also mention any counterarguments you addressed, emphasizing why your thesis holds up against them, particularly if your argument is a controversial one.
Don’t go into the details of your evidence or present new ideas; focus on outlining in broad strokes the argument you have made.
Empirical paper: Summarize your findings
In an empirical paper, this is the time to summarize your key findings. Don’t go into great detail here (you will have presented your in-depth results and discussion already), but do clearly express the answers to the research questions you investigated.
Describe your main findings, even if they weren’t necessarily the ones you expected or hoped for, and explain the overall conclusion they led you to.
Having summed up your key arguments or findings, the conclusion ends by considering the broader implications of your research. This means expressing the key takeaways, practical or theoretical, from your paper—often in the form of a call for action or suggestions for future research.
Argumentative paper: Strong closing statement
An argumentative paper generally ends with a strong closing statement. In the case of a practical argument, make a call for action: What actions do you think should be taken by the people or organizations concerned in response to your argument?
If your topic is more theoretical and unsuitable for a call for action, your closing statement should express the significance of your argument—for example, in proposing a new understanding of a topic or laying the groundwork for future research.
Empirical paper: Future research directions
In a more empirical paper, you can close by either making recommendations for practice (for example, in clinical or policy papers), or suggesting directions for future research.
Whatever the scope of your own research, there will always be room for further investigation of related topics, and you’ll often discover new questions and problems during the research process .
Finish your paper on a forward-looking note by suggesting how you or other researchers might build on this topic in the future and address any limitations of the current paper.
Full examples of research paper conclusions are shown in the tabs below: one for an argumentative paper, the other for an empirical paper.
- Argumentative paper
- Empirical paper
While the role of cattle in climate change is by now common knowledge, countries like the Netherlands continually fail to confront this issue with the urgency it deserves. The evidence is clear: To create a truly futureproof agricultural sector, Dutch farmers must be incentivized to transition from livestock farming to sustainable vegetable farming. As well as dramatically lowering emissions, plant-based agriculture, if approached in the right way, can produce more food with less land, providing opportunities for nature regeneration areas that will themselves contribute to climate targets. Although this approach would have economic ramifications, from a long-term perspective, it would represent a significant step towards a more sustainable and resilient national economy. Transitioning to sustainable vegetable farming will make the Netherlands greener and healthier, setting an example for other European governments. Farmers, policymakers, and consumers must focus on the future, not just on their own short-term interests, and work to implement this transition now.
As social media becomes increasingly central to young people’s everyday lives, it is important to understand how different platforms affect their developing self-conception. By testing the effect of daily Instagram use among teenage girls, this study established that highly visual social media does indeed have a significant effect on body image concerns, with a strong correlation between the amount of time spent on the platform and participants’ self-reported dissatisfaction with their appearance. However, the strength of this effect was moderated by pre-test self-esteem ratings: Participants with higher self-esteem were less likely to experience an increase in body image concerns after using Instagram. This suggests that, while Instagram does impact body image, it is also important to consider the wider social and psychological context in which this usage occurs: Teenagers who are already predisposed to self-esteem issues may be at greater risk of experiencing negative effects. Future research into Instagram and other highly visual social media should focus on establishing a clearer picture of how self-esteem and related constructs influence young people’s experiences of these platforms. Furthermore, while this experiment measured Instagram usage in terms of time spent on the platform, observational studies are required to gain more insight into different patterns of usage—to investigate, for instance, whether active posting is associated with different effects than passive consumption of social media content.
If you’re unsure about the conclusion, it can be helpful to ask a friend or fellow student to read your conclusion and summarize the main takeaways.
- Do they understand from your conclusion what your research was about?
- Are they able to summarize the implications of your findings?
- Can they answer your research question based on your conclusion?
You can also get an expert to proofread and feedback your paper with a paper editing service .
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
The conclusion of a research paper has several key elements you should make sure to include:
- A restatement of the research problem
- A summary of your key arguments and/or findings
- A short discussion of the implications of your research
No, it’s not appropriate to present new arguments or evidence in the conclusion . While you might be tempted to save a striking argument for last, research papers follow a more formal structure than this.
All your findings and arguments should be presented in the body of the text (more specifically in the results and discussion sections if you are following a scientific structure). The conclusion is meant to summarize and reflect on the evidence and arguments you have already presented, not introduce new ones.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Caulfield, J. (2023, April 13). Writing a Research Paper Conclusion | Step-by-Step Guide. Scribbr. Retrieved April 2, 2024, from https://www.scribbr.com/research-paper/research-paper-conclusion/
Is this article helpful?

Jack Caulfield
Other students also liked, writing a research paper introduction | step-by-step guide, how to create a structured research paper outline | example, checklist: writing a great research paper, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Endocrinol Metab
- v.25(5); Sep-Oct 2021
Quality of Life and Diabetes in India: A Scoping Review
Ramasamy aarthy.
1 Deakin University, School of Medicine, IMPACT, Institute for Innovation in Physical and Mental Health and Clinical Translation, Geelong, Australia
2 Madras Diabetes Research Foundation, Chennai, India
Antonina Mikocka-Walus
3 School of Psychology, Deakin University, Australia
Rajendra Pradeepa
Ranjit mohan anjana.
4 Dr Mohan's Diabetes Specialities Centre and Madras Diabetes Research Foundation, Chennai, India
Viswanathan Mohan
Kathryn aston-mourney.
In recent years, numerous studies have explored the quality of life (QoL) in those with diabetes mellitus. The aim of this scoping review was to explore the current state of knowledge on QoL and its various associated factors among people with diabetes in India. Three databases were searched (PubMed, Scopus, and Medline) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. A total of 41 articles were included in the review. The included studies were largely conducted in the Southern states and mainly investigated individuals with type 2 diabetes. The World Health Organization Quality of Life (WHOQOL-BREF) and Short Form Health Survey (SF-36) were the instruments used most often. In general, the studies showed that people with diabetes had poorer QoL than those without diabetes, and women with diabetes reported poorer QoL than men, consistent with findings across the world. However, the studies had significant methodological flaws which limit the validity and generalizability of the findings. Therefore, there is an urgent need to conduct high-quality QoL studies which are representative of all states of India as well as different types of diabetes in India in order to address this gap in the evidence.
I NTRODUCTION
Diabetes, a serious long-term condition, is considered one of the great global health challenges of the twenty-first century. An estimated 463 million people had diabetes in 2019, and this is expected to reach 578 million by 2030 and 700 million by 2045.[ 1 ] The countries with the highest number of adults with diabetes include China, India, and the USA.[ 1 ] Those living with diabetes are predisposed to complications such as retinopathy, neuropathy, cardiovascular disease, and diabetic foot disease. Moreover, psychological complications such as anxiety and depression are also common and impact psychosocial life and everyday functioning, contributing to poor quality of life [QoL].[ 2 ] The American Diabetes Association has classified diabetes into the following categories: 1. type 1 diabetes (T1D) “due to autoimmune beta cell destruction leading to absolute insulin deficiency” 2. type 2 diabetes (T2D) “due to progressive loss of beta-cell insulin secretion frequently on the background of insulin resistance” 3. Gestational diabetes mellitus (GDM) as “diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt diabetes prior to gestation” and 4. specific types of diabetes due to other causes (example- monogenic diabetes syndromes0).[ 3 ] It is important to understand the impact of each of these types of diabetes on QoL in order to achieve the best outcomes for all patients.
Quality of life (QoL)/Health-Related Quality of Life (HRQoL) and diabetes
The World Health Organisation (WHO) has defined QoL as “ an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.” [ 4 ] QoL is considered an important health outcome, with good quality of life representing the ultimate therapeutic goal in chronic conditions.[ 5 ] The term was first used in medical literature in the 1960s and since then has gained considerable popularity in research and clinical practice. QoL includes four main components namely physical, psychological, social relationship, and environment.[ 6 ]
The term, “Health-Related Quality of Life (HRQoL)” is an inclusive term and is defined as the “physical, psychological and social domains of health, seen as distinct areas that are influenced by a person's experiences, beliefs, expectations, and perceptions.”[ 7 ] In the current literature, QoL and HRQoL are used interchangeably although each has its own meaning. In some definitions, HRQoL reflects health status, whereas in others it goes beyond health and encompasses concepts more consistent with QoL such as the environment.[ 8 , 9 ] QoL is a broader concept and covers all aspects of life, including education and social environment which reach beyond health. HRQoL, on the other hand, is used to measure self-perceived health or disease status and to understand the distinction between aspects of life related to health.[ 8 ]
QoL is decreased in patients with diabetes and becomes even worse when complications develop, or comorbidities exist.[ 6 ] Diabetes can negatively affect physical well-being in four major ways: 1) by leading to the development of long-term complications, 2) by being associated with short-term complications, 3) through the demands imposed by various treatment regimens, and 4) by affecting psychological functioning via its impact on mood.[ 10 ] For instance, persistent fatigue and tiredness can occur due to elevated blood glucose levels. Conversely, hypoglycemia (low glucose levels) symptoms can also be exhausting and discouraging.[ 10 ] Thus, both hypo- and hyperglycemia may affect the patient's overall sense of well-being. Lastly, social wellbeing is also compromised as diabetes can affect the patient's social relationships.[ 10 ]
The significant determinants shown to affect QoL among patients with diabetes include the type of diabetes, its duration, glycemic control, gender, complications, treatment regimen, and psychosocial factors.[ 11 ]
Tools used to measure QoL/HRQoL in patients with diabetes
Both generic and diabetes-specific instruments are widely used to measure the various domains of QoL. Overall, health and comorbidities are measured by generic tools, whereas diabetes-specific tools address diabetes-related aspects and the burden and impact of diabetes on an individual's lifestyle.[ 2 ] The most popular instrument used to measure general QoL is the WHO Quality of Life (WHOQoL) questionnaire. Among the diabetes-specific tools, the Diabetes Quality of Life (DQOL) and Audit of Diabetes-Dependent Quality of Life (ADDQoL) are the most popular.[ 12 ] In a recent scoping review, theme analysis of 30 diabetes-specific tools to measure QoL was undertaken and determined that tools often measured the impact of societal attitudes, public policies, and context on QoL in addition to mental, physical, and social health components.[ 2 ]
Quality of life and diabetes in India
India is currently second in the world in diabetes prevalence, with an estimated 77 million people affected in 2019, and this number is expected to reach 101 million by 2030.[ 1 ] The Indian Council of Medical Research (ICMR) - India DIABetes (ICMR-INDIAB) study has reported diabetes prevalence in 15 of the 31 states/union territories of India completed and published to date. The average prevalence was 7.3%; however, large differences in prevalence are observed between the states, indicating epidemiological transition.[ 13 ]
The earliest studies on diabetes QoL in India were conducted among T1D patients in 2007[ 14 ] and among T2D patients in 2009.[ 15 ] Since then, QoL assessment publications have increased however they are largely reported from tertiary care hospital settings and characterized by small sample sizes. Hence, the results of the studies cannot be generalized to the larger Indian population.[ 16 ] In addition to the existing drawbacks as stated above, more QoL assessment tools are being developed,[ 17 , 18 , 19 ] increasing the complexity of generalizing from multiple QoL tools. A recent article reported a scarcity of QoL studies among diabetic patients in India as a major limitation of the current literature.[ 16 ]
Hence, better recognition of the importance of the QoL construct in managing chronic conditions is important and a review of QoL studies, timely. Therefore, this scoping review aims to explore the current state of knowledge on QoL in people with diabetes in India. This paper also attempts to study the various factors associated with QoL in those with diabetes in India.
This scoping review was based on the five stages outlined in the Arksey and O’Malley Framework[ 20 ] and guidelines from the Joanna Briggs Institute.[ 21 ] The Preferred Reporting Items for Systematic Review and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR)[ 22 ] were used. Registration on the International Prospective Register of Systematic Reviews (PROSPERO) was not possible as scoping reviews had not been accepted at the time of the review.
Stage 1: Identifying the research questions
- What are the various measurement tools used to measure QoL/HRQoL status among patients with diabetes in India?
- What are the various factors reported to be associated with quality of life and diabetes in India?
Stage 2: Identifying the relevant studies
Search strategy.
The scoping review included all original studies published in English on QoL assessment and diabetes in India. The review included all types of diabetes including T1D, T2D, gestational diabetes, and other forms of diabetes. Grey literature including conference proceedings, dissertation, and thesis reports was included. The inclusion criteria contained “observational studies” and were not restricted to any type of diabetes and included adults and children. The exclusion criteria included “intervention studies” and “nondiabetic patients.” The keywords searched consisted of “Diabetes” AND “Quality of life OR health related quality of life” AND “India.” The search terms were intentionally kept broad and sensitive enough to include all relevant studies in the review. The search strategy used in PubMed is found in Table 1 .
Search strategy used in PubMed
Databases used
The databases used for the review included PubMed, Scopus, and Medline and were searched between April and July 2020. The results were then imported to Covidence systematic review software, (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org ), a web-based platform, which helps to streamline the collection of articles. The references of identified publications were screened for any additional relevant papers.
Stage 3: Study selection
Two independent investigators were involved in the study selection process. AR ran the searches in the individual databases and screened the titles in Covidence. The full-text review was conducted independently by AR and PR and, in case of disagreement, a third reviewer (VM) was consulted as a subject expert.
Stage 4: Charting the data
A template for data extraction is presented in Table 2 .
Description of data extracted from each included study
Stage 5: Collating, summarizing, and reporting the results
A PRISMA diagram showing the screening results is shown in Figure 1 .

PRISMA flow diagram of study inclusion
General characteristics
Overall, 497 studies were imported for screening, of which 43 duplicate references were removed. A title/abstract screening of the remaining 454 articles was done, and 398 studies considered were removed due to nonrelevance of the subject to the objective of the review. After a full-text review of 56 articles, 15 studies were excluded due to having the wrong outcomes/settings and finally, 41 studies were included in the scoping review. A summary of the reviewed articles is in Appendix 1 .
Of the 41 selected studies, one study was conducted in a community setting,[ 23 ] one study was conducted at primary health care center setting,[ 24 ] and another at secondary care facility,[ 25 ] with the 38 remaining studies conducted in tertiary health care facilities. The public health care system in India is a three-tier structure comprising primary, secondary, and tertiary levels. Primary health care centers are involved in providing primary care, whereas district hospitals and sub-divisional hospitals provide secondary care. Tertiary health care is delivered by medical college hospitals. The identified studies largely come from the southern part of India (19 studies) with thirteen studies reported from the state of Karnataka.
Most of the QoL assessment studies (39 studies) among diabetes patients in India have been published within the last decade. Overall, there were 31 studies that included T2D patients, four studies on T1D patients, one study on GDM, whereas five studies did not report their diabetes classification. The reviewed studies tended to have small sample sizes with sample size justification provided in only nine studies.[ 16 , 23 , 24 , 26 , 27 , 28 , 29 , 30 , 31 ] While four studies mentioned the use of convenience sampling,[ 25 , 32 , 33 , 34 ] 28 studies did not mention their sample design.
Five case-control studies where diabetes respondents were compared with nondiabetes patients were identified,[ 26 , 35 , 36 , 37 , 38 ] whereas the remainder of studies were cross-sectional.
Quality of life and type of diabetes
There were 29 studies with QoL assessment in T2D cohorts. Four studies reported QoL assessment among T1D patients.[ 14 , 27 , 39 , 40 ] A single study reported QoL assessment among mothers with gestational diabetes mellitus.[ 41 ] Seven studies have conducted QoL assessment among both T1D and T2D patients with diabetes.[ 15 , 25 , 32 , 36 , 38 , 42 , 43 ]
Only a few studies reported the mean QoL scores among T2D patients, and the scores varied drastically among different QoL assessment tools as seen in Appendix 1. The minimum score of 38.40 was reported from using the SF-36 tool,[ 31 ] and the maximum score of 86.83 was reported by QOLID.[ 44 ] Four studies reported scores that varied between 54.8 and 57.8.[ 25 , 33 , 36 , 45 ]
Among the T1D patients, the mean DAWN QoL scores reported were 35[ 39 ] and 29.3[ 40 ] which indicated a moderate QoL. The higher DAWN scoring indicates a greater impact on QoL.[ 40 ]
Quality of life and gender
Of the reviewed studies, only 14 reported gender and QoL. Poorer QoL in women than men were reported in nine studies on T2D[ 15 , 23 , 25 , 31 , 35 , 37 , 45 , 46 , 47 ] and in one study on T1D.[ 14 ] It is of interest that three studies had reported better QoL among female respondents with diabetes when compared to their male counterparts.[ 30 , 34 , 46 ]
Poor sleep quality was frequently reported among females as compared to men with T2D, which had detrimental effects on the HRQoL assessment.[ 48 ]
Quality of life and duration of diabetes
Of the 41 reviewed studies, seven studies reported a longer duration of diabetes to be associated with poorer QoL among T2D patients.[ 24 , 26 , 29 , 37 , 49 , 50 , 51 ] However, this factor was not reported in the T1D studies.
Quality of life and glycemic control
Not surprisingly, poor glycemic control was associated with impaired QoL in three studies among T2D patients.[ 30 , 34 , 37 ] Similarly, poor glycemic control was associated with poor QoL among T1D children in one article.[ 27 ]
Quality of life and diabetes-related complications
Of the 41 reviewed articles, four studies reported QoL assessment and diabetes-related complications. A cross-sectional study on QoL assessment among 382 T1D and T2D patients with different microvascular and macrovascular complications reported that diabetic complications were associated with reduced QoL. Neuropathy and nephropathy were associated with lower QoL as compared with other diabetic complications.[ 38 ]
A case-control study (100 cases and 100 controls) among T2D patients from Delhi reported lower mean values of WHO-QoL for all the domains in patients with complications of diabetes (more specific for nephropathy and neuropathy) as compared with patients without diabetes complications.[ 26 ]
Among the microvascular complications of diabetes, diabetic retinopathy (DR) and QoL assessment were reported in three studies.[ 42 , 52 , 53 ] One study reported lower QoL among patients with diabetes with diabetic retinopathy (DR) as compared to those without. The study participants included T1D and T2D patients. The lowest QOL scores were obtained from subjects with proliferative diabetic retinopathy (PDR).[ 52 ] The second was a cross-sectional study that reported poor QoL with proliferative diabetic retinopathy (PDR) as compared with nonproliferative DR (NPDR) in 250 T2D patients.[ 42 ] The third, a prospective, observational study among 189 T2D patients reported a significant reduction in HRQoL with the severity of retinopathy.[ 53 ]
Quality of life and treatment regimen
Better QoL was observed among patients receiving a single- or two-drug regimen as compared with patients receiving a combination regimen of oral hypoglycemic agents (metformin, glipizide, voglibose, repaglinide, sitagliptin, and vildaglitpin) and insulin in one study with T2D patients.[ 54 ] Treatment satisfaction of patients receiving metformin alone or in combination with glipizide was better than that of the patients receiving oral hypoglycemic agents and/or insulin.[ 54 ]
Quality of life and psychosocial factors
A study from Jaipur (n = 50) reported that more than half of patients with T2D noted impaired QoL.[ 37 ] In another cross-sectional study, among 300 T2D participants from Delhi, poor sleep quality was reported and associated with poor QoL.[ 48 ]
A case-control study showed that depression was significantly more prevalent among people with T2D than controls and was associated with poorer QoL.[ 26 ]
A study among T2D patients with and without depression reported that in the presence of depression, QOL deteriorated.[ 55 ]
Quality of life and comorbidities/metabolic syndrome
Of the 41 reviewed studies, only two assessed QoL among T2D patients with comorbidities[ 24 ] or metabolic syndrome.[ 56 ] A stroke had a high negative impact on the physical HRQoL. The presence of comorbidities affected the physical component summary (PCS) and the mental component summary (MCS) of the Short Form Health Survey-12. Subjects with visual impairment and stroke had significantly reduced quality of life.[ 24 ] Among T2D diabetes patients with metabolic syndrome, a greater significant decline is observed in PCS and MCS as compared to those without metabolic syndrome.[ 56 ]
Commonly used QoL measurement tools in Indian studies
The QoL assessment among T2D patients in India has been conducted using both generic and diabetes-specific instruments [ Table 3 ]. Among the generic tools, the WHOQoL-BREF tool was employed in eleven studies and the SF-36 V2 questionnaire in nine studies. The diabetic-specific QOLID questionnaire tool was used in eight studies. Table 3 describes the commonly used QoL assessment tools used in India identified in the review.
Commonly used QoL assessment tools used in India identified in the review
The WHOQOL-BREF (10 studies)[ 25 , 26 , 29 , 30 , 35 , 36 , 57 , 58 , 59 , 60 ] and SF 36 (eight studies)[ 15 , 23 , 31 , 32 , 41 , 45 , 47 , 56 ] are the most commonly used generic instruments among T2D subjects in India. One study used both generic and diabetes-specific tools for QoL assessment and found that both instruments are equally effective and reliable in the evaluation of QoL among diabetes patients.[ 29 ]
In recent years, the QOLID questionnaire has been increasingly used among Indian researchers.[ 16 , 27 , 38 , 42 , 44 , 49 , 51 , 54 ] QOLID is specifically designed for an Indian population and has high internal consistency of 0.894 (identified using Cronbach's alpha) and discriminant validity which makes it popular among Indian researchers. Cronbach's alpha is provided as a measure of the internal consistency and expressed as a number between 0 and 1.[ 61 ]
For QoL assessment among T1D patients, four different questionnaires were used [ Table 3 ] including Diabetes Control and Complications Trial (DCCT) (modified for the Indian context), DAWN Youth QoL, Diabetes specific quality of life score (DSQoL). In a recent study, the QOLID questionnaire mainly designed for the Indian diabetic adult population was translated into Hindi and modified with minor changes for T1D children.[ 27 ]
D ISCUSSION
The present review is the first to our knowledge to collate articles related to QoL assessment in people living with diabetes in India. The review demonstrates that most evidence on QoL in India is available in individuals with T2D patients. The QoL assessment among T1D Indian children is scarce and needs to be investigated in future studies. In addition, there is little to no evidence of QoL in the Indian population for gestational diabetes mellitus (GDM) and monogenic forms of diabetes. As five million women have GDM in India[ 62 ] and new cases of monogenic diabetes are continually being reported due to advances in the field of molecular genetics,[ 63 , 64 , 65 ] QoL assessment needs to be urgently addressed in these subtypes of diabetes in order to be able to offer more support to these groups.
The largest number of studies (19 studies) were reported from southern states of India, many from teaching tertiary hospitals/institutions, especially from Karnataka as compared to other regions (North, East, West) of the country. One of the possible reasons could be that Karnataka has the largest number of teaching medical institutions in India. Notably, only a single study was reported from community settings. In the future, QoL assessment needs to be undertaken in large community settings with a proper sample size selection to understand the QoL status at the population level, which is currently missing. The presently available studies have small sample sizes, come from hospital settings, and have a short duration which makes it difficult to generalize the findings for a larger population.
During this review, it was observed that QoL is largely reported as being better among men as compared with women with diabetes, a consistent finding with studies conducted across the world.[ 11 , 66 ] A study was done in a secondary care setting highlighted the need to improve the QoL among women with diabetes.[ 25 ] Rubin et al .[ 11 ] in their review paper stated that men with diabetes have an advantage over women in HRQoL and recommended control for gender in future studies, which would be relevant to the Indian settings as well.
Though many studies in recent years have used QOLID as a measurement tool, generic questionnaires such as WHOQOL-BREF and SF-36 V2 continue to be used in India. The WHOQOL-100 was initially developed with international consensus but more recently a short form WHOQOL-BREF, with validity and reliability similar to the longer measure, has become available.[ 12 ] Many prefer to use the WHOQOL-BREF questionnaire as it is associated with a low time burden.[ 37 ] Though not diabetes-specific, it is largely applicable to people with diabetes and has been validated in Indian languages including Hindi.[ 67 , 68 , 69 ]
The SF-36 V2 questionnaire contains two components (Physical Component Summary and Mental Component Summary) and includes eight domains.[ 12 ] The questionnaire is available in Indian languages – Hindi and Kannada.[ 15 , 23 ] The Cronbach's alpha score for Hindi version is 0.70.[ 70 ] Though this tool is popular among Indian researchers, the reviewed studies have not stated the reasons behind selecting the tool.
QOLID is a reliable and valid questionnaire developed for Indian patients with diabetes. It contains eight domains with 34 questions and takes 7 min to complete.[ 18 ] The QOLID questionnaire is also now modified to measure QoL among Indian children.[ 27 ] The questionnaire has high internal consistency, discriminant validity, and has an overall Cronbach's alpha value of 0.894. However, the tool is designed for middle- and higher-income groups, and the authors suggest that the tool should be redeveloped for wider socio-economic groups and for community settings.[ 18 ] In the future, this questionnaire should be modified and validated for the Indian population across various socio-economic status levels. Socioeconomic status is defined as “a measure of an individual or family's economic and social position in relation to others, based on various variables for that like income, education, occupation, etc.”[ 71 ]
Table 4 illustrates the various domains of the commonly used questionnaire for QoL assessment.
Various domains used in the commonly used questionnaires
Newer questionnaires have also been developed to measure QoL, including MDQoL-17 which was developed and validated in 2010 and is available in local languages.[ 17 ] Another QoL assessment questionnaire was developed only for diabetic foot ulcer patients.[ 19 ] Though it is encouraging to have newer tools for QoL assessment available, these should be properly validated before entering common use. For example, one review paper identified Short Form -12 and Appraisal of Diabetes Scale as ideal and feasible tools for QoL assessment in busy clinical settings.[ 72 ]
The following section recommends several factors to be considered for the selection of QoL assessment tools in future research.
Guidelines to select the right tool for QoL assessment
With new tools being developed for Indian settings, care should be taken to select the right tool for assessment.[ 17 , 19 ] One of the best ways to avoid the unnecessary development of new instruments is to select an existing and validated measure. It is important to understand the various domains, the questionnaire will measure. It is also important to analyze the previous validation of the questionnaire and report psychometric properties. Cronbach's alpha is the most widely used objective measure of internal reliability and the acceptable value ranges from 0.70 to 0.95.[ 61 ] The WHOQOL-BREF, Appraisal of Diabetes Scale and QOLID have Cronbach's values of 0.78, 0.80, and 0.89, respectively, showing that they are all reliable tools.
It is also important to understand the purpose of the specific tool. Was it developed for clinical, research, or community settings? Is it patient-centered, treatment-centered, or diet-centered? The questionnaire should be made culturally appropriate to include patients’ needs and perspectives. It is crucial to consider the length of the questionnaire in order to avoid “questionnaire fatigue.” It has been suggested to keep shorter questionnaires for clinical screening and longer measures for researchers to gain further insights into the assessment of QoL.[ 2 ]
In addition, a few questions can be considered while selecting an ideal QoL measure as suggested by Speight et al .[ 12 ] They include the hypothesis and objective of the study, examination of the instrument and with each item and its response options, in case of generic measures are any relevant issues missed, response acceptance by the respondents, previous validation of the questionnaire in the given population/country/language, and analysis of data. If the clinician and researchers are not confident in such analysis, they can collaborate in a multidisciplinary team with a social scientist experienced in the development, use, and interpretation of measures in diabetes.
Limitations of the study
This study has some limitations. The quality of the reported studies is largely poor, with low homogeneity, and hence it was not possible to combine them into a meta-anlysis. Except for a few studies, most lacked a robust study methodology, many have not followed a scientific approach to sampling, relying on convenience sampling. Similarly, very few studies have mentioned the rationale as to why a particular QoL assessment questionnaire was preferred. In addition, several studies have not reported a thorough data analysis and interpretation.
Therefore, it is recommended that future research on QoL assessment in India should aim for better-designed studies with greater scientific rigor. Such studies would help in a better understanding of QoL and diabetes in India.
C ONCLUSION
With the increased prevalence of diabetes in India and around the world, it is becoming even more important to assess the QoL as an outcome measure in long-term illness and management. The review is the first of its kind from India to review the various QoL assessment tools used. The current review showcased that poorer QoL was observed in people with diabetes as compared to those without diabetes. However, the reviewed studies were largely focused on T2D patients, with significant methodological issues, and small samples limiting their validity and generalizability. There is an urgent need to conduct extensive and high-quality QoL assessment studies with sample sizes representative of various groups and types of diabetes in India to address this gap in the evidence.
National recommendations are available in India for psychosocial management of diabetes, which provide practical guidelines to achieve qualitative improvement in diabetes management.[ 73 ] Similarly, a consensus statement has been issued to address the psychosocial challenges and management for South Asian women with diabetes.[ 74 ] However, as highlighted in this review, extensive research in this area is still required. Following this, further research on these guidelines should be updated to improve the psychosocial aspects of patients with diabetes in India.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Summary of the articles reviewed
Footnotes : Sample size-n; QoL- Quality of Life; S. D- Standard Deviation; QOLID- Quality of Life Instrument for Indian Diabetic Patients; DR- Diabetic Retinopathy;
a WHOQOL-BREF - is a 26-item brief questionnaire over four major domains namely physical, psychological, social relationships, and environment. The responses of the WHOQOL-BREF are scored in a Likert scale fashion from 1 to 5. The total raw scores for these five dimensions will be transformed into 0 and 100 and then the analysis of the transformed score to be done with low score indicating poor QoL.
b Health-related quality of life-EQ-5D or European Quality of Life- 5 Dimensions questionnaire consists of two parts- the first part is a health status categorized into five dimensions- mobility, self-care, usual activities, pain/discomfort, and anxiety/depression which scores from 0 (no problem) to 1 (extreme problems). The response to the first part is converted into an EQ-5D profile or EQ-5D index which ranges from -0.111 to 1, where 1 represents preferred health. The second part is a visual analog scale (VAS) to determine the overall health status and contains 20 cm scale to measure the patient's perception of quality of life on the day of the interview. The scale ranges from 0 to 100, 0 represents worst health, while 100 represents the best health.
c QOLID - developed in India consists of 34 items with eight domains on general health, role limitations due to physical health, symptom frequency, physical endurance, treatment satisfaction, financial worries, diet advice satisfaction, and mental health. The items were scored from 1 to 5, the maximum possible score is 169 and the minimum 34. The quality of life is classified into good (125-169), moderate (79-124), and poor (34-78).
d Down Quality of Life for young - is a 22-item validated questionnaire in six domains namely impact of symptoms related to diabetes, the impact of the treatment, impact on activities, parents’ issues, worry about the future, and perception of one's own health. Administered to subjects 10-18 years which each question having five possible responses ranging from ‘0’ (never) to ‘4’ (all the time) and the responses are added to get the total score for the subscale. Higher scores indicate a greater adverse impact on QoL
e SF-12 Short Form Health Survey 12 (SF-12) is a shorter version of the 36-item SF-36.
f SF-36 V2 - It consists of 36 items covering eight domains: physical functioning (PF), role limitations caused by physical health problems (RP), bodily pain (BP), perception of general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional health problems (RE) and mental health (MH). The eight domains may be further grouped into two summary measures of the physical component summary (PCS) and the mental component summary (MCS). These aggregated scores are converted into norm-based scores (mean, 50; SD, 10), and higher scores indicate a more favorable physical functioning and psychological well-being.
g ADDQoL -ADDQoL questionnaire is a third-generation individualized QoL instrument and contains 19 item domains. It evaluates the general QoL as well as the diabetes-dependent QoL. ADDQoL starts with two overview items assessing the patient's present global QoL (range + 3–−3) and the impact of diabetes on the QoL (range − 3–+3). For both items, lower scores indicate a poorer QoL. In the subsequent items, the respondent rates the impact of diabetes (range − 3 to + 3) and the importance of QoL (range 3–0) on 19 item domains.
h National Eye Institute 25- Item Visual Function Questionnaire (NEI-VFQ-25)- The NEI-VFQ-25 consists of questions related to general health and vision, difficulties with activities and response to vision problems. To calculate an overall composite score for the VFQ-25, simply average the vision-targeted subscale scores, excluding the general health rating question. By averaging the sub-scale scores rather than the individual items, we have given equal weight to each sub-scale, whereas averaging the items would give more weight to scales with more items.
i Modified Diabetes Quality of Life (MDQoL) -17- It consists of 17 questions that comprise seven domains, which include physical functioning, role limitations due to physical health problems, role limitations due to personal or emotional problems, emotional well-being, social functioning, energy/fatigue, and general health perceptions. All the contents are scored so that a high score depicts a more favorable health state. The possible scores are 0-100, 0 being the minimum and 100 being the maximum score. Scores represent the percentage of the total possible score achieved.
j Appraisal of Diabetes Scale (ADS)- is a seven-item diabetes-specific scale that attempts to assess patients’ feelings and attitudes about diabetes. It consists of items covering distress caused by diabetes, control over diabetes (two items), uncertainty due to diabetes, anticipated future deterioration, coping, and effect of diabetes on life goals. Each question in this scale uses Likert scale with five possible answers (1 - not at all, 2 - slight, 3 - moderate, 4 - very, and 5 - extremely). The total score can range from 0 (best level of health) to 35 (worst level of health). Thus, a lower score on the ADS scale suggests better QOL.
k Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES) SF - The raw scores on QLESQ-SF were converted to percentage maximum scores (QLESPER).
l DCCT- Diabetes Control and Complications Trial (DCCT) questionnaire , after deleting questions found irrelevant in Indian context and those pertaining only to type 1 diabetic subjects were used.
R EFERRENCES

IMAGES
VIDEO
COMMENTS
Summary and Conclusion. Diabetes is a multifactorial disease process, and its long-term management requires the active involvement of people with diabetes and their families, as well as a large multidisciplinary care team to ensure optimal health, quality of life, and productivity. Keeping up with new medications, emerging technology, and ...
Biomedical research continues to provide new insights in our understanding of the mechanism of diabetes development that is reviewed here. Recent studies may provide tools for the use of several genes as targets for risk assessment, therapeutic strategies and prediction of complications. ... CONCLUSION. Diabetes mellitus is the epidemic of the ...
Introduction. Insulin resistance and β-cell dysfunction are the 2 major hallmarks of type 2 diabetes mellitus (T2DM) that appear as the result of disturbed homeostasis [].Failure of β-cells (∼80% of their β-cell function) and insulin resistance in muscles and the liver is a vicious triumvirate responsible for the core physiological defects.
The research articles from 1990 onwards, a total of 111 studies were reviewed for the present study, a deep illustration about the inclusion and exclusion of studies is given in Fig. 1. Download : Download high-res image ... will be improved and can be used as used to predict cumulative risk associated with diabetes. 19. Conclusion ...
Type-2 diabetes is a major, non-communicable disease with increasing prevalence at a global level. ... In conclusion, effective lifestyle modifications including counseling on weight loss, adoption of a healthy dietary pattern like the Mediterranean diet, together with physical activity are the cornerstone in the prevention of type-2 diabetes ...
requires insulin injections for survival) and type 2 diabetes (where the body cannot properly use the insulin it produces), separate global estimates of diabetes prevalence for type 1 and type 2 do not exist. The majority of people with diabetes are affected by type 2 diabetes. This used to occur nearly entirely among adults, but
A similar conclusion can be reached about whether there is a core tissue defect at the organismal level ... As articulated in a classic essay by McGarry , ... Accili D. Insulin action research and the future of diabetes treatment: The 2017 Banting Medal for Scientific Achievement lecture. Diabetes. 2018;67:1701-9.
diabetes research and clinical practice 143 (2018) 101 - 112 105 modulate caloric intake or loss (GLP-1RAs, SGLT2b' s) [31,40] . Successful outcomes of some GLP-1RA and SGLT2b CVO Ts
Conclusion. The rising pattern of sedentary lifestyle and the higher incidence of obesity has contributed to an ever-increasing number of patients with diabetes, generating a massive demand for anti-diabetic medication and prompting companies to invest more on research and development for developing targeted formulations.
The research could lead to a better availability of beta cells for future research purposes. Type 1 and type 2 diabetes results when beta cells in the pancreas fail to produce enough insulin, the ...
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
Diabetes"5 and "Conquer Diabetes".6 One of the main goals of USDHHS's report, Healthy People 2010, is to improve the quality of life for persons with diabetes.7 Taking control of diabetes to improve quality of life has put the spotlight on the need for additional support and education for patients with type 2 diabetes.
357 Diabetes Essay Topics & Examples. Updated: Feb 25th, 2024. 25 min. When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task. We will write.
Background: The management of type 2 diabetes (T2D) and obesity, particularly in the context of self-monitoring, remains a critical challenge in health care. As nearly 80% to 90% of patients with T2D have overweight or obesity, there is a compelling need for interventions that can effectively manage both conditions simultaneously. One of the goals in managing chronic conditions is to increase ...
Conclusion: Early detection of diabetes is critical for effective therapy. Many people have no idea whether or not they have it. The full assessment of Machine learning approaches for early diabetes prediction and how to apply a variety of supervised and unsupervised machine learning algorithms to the dataset to achieve the best accuracy are addressed in this paper..
Diabetes is one of fatal, metabolic and costly disease that increases blood sugar level, affecting people of all ages. According to the Public Health Agency of Canada, between 2003-2004 and 2013 ...
Table of contents. Step 1: Restate the problem. Step 2: Sum up the paper. Step 3: Discuss the implications. Research paper conclusion examples. Frequently asked questions about research paper conclusions.
Introduction. Diabetes mellitus (DM) is probably one of the oldest diseases known to man. It was first reported in Egyptian manuscript about 3000 years ago. 1 In 1936, the distinction between type 1 and type 2 DM was clearly made. 2 Type 2 DM was first described as a component of metabolic syndrome in 1988. 3 Type 2 DM (formerly known as non-insulin dependent DM) is the most common form of DM ...
as 592 million. Diabetes is a disease caused due to the increase level of blood. glucose. This h igh blood glucose produces the symptoms of frequent urination, increased thirst, and increased ...
Please use one of the following formats to cite this article in your essay, paper or report: APA. Infante, Deliana. (2023, November 14). Trailblazing Discoveries: The Top 5 Diabetes Research ...
The Indian Council of Medical Research (ICMR) - India DIABetes (ICMR-INDIAB) study has reported diabetes prevalence in 15 of the 31 states/union territories of India completed and published to date. ... For example, one review paper identified Short Form -12 and Appraisal of Diabetes Scale as ideal and feasible tools for QoL assessment in busy ...